

By Audience
- Therapist Toolbox
- Teacher Toolbox
- Parent Toolbox
- Explore All
By Category
- Organization
- Impulse Control
- When Executive Function Skills Impair Handwriting
- Executive Functioning in School
- Executive Functioning Skills- Teach Planning and Prioritization
- Adults With Executive Function Disorder
- How to Teach Foresight
- Bilateral Coordination
- Hand Strengthening Activities
- What is Finger Isolation?
- Occupational Therapy at Home
- Fine Motor Skills Needed at School
- What are Fine Motor Skills
- Fine Motor Activities to Improve Open Thumb Web Space
- Indoor Toddler Activities
- Outdoor Play
- Self-Dressing
- Best Shoe Tying Tips
- Potty Training
- Cooking With Kids
- Scissor Skills
- Line Awareness
- Spatial Awareness
- Size Awareness
- Pencil Control
- Pencil Grasp
- Letter Formation
- Proprioception
- How to Create a Sensory Diet
- Visual Perception
- Eye-Hand Coordination
- How Vision Problems Affect Learning
- Vision Activities for Kids
- What is Visual Attention?
- Activities to Improve Smooth Visual Pursuits
- What is Visual Scanning
- Classroom Accommodations for Visual Impairments

Fine Motor Leaft Craft
- Free Resources
- Members Club
Executive Functioning Skills
Executive function, so, what exactly is executive function, explore popular topics.
What do all these words mean?
Executive Functioning Skills guide everything we do. From making decisions, to staying on track with an activity, to planning and prioritizing a task . The ability to make a decision, plan it out, and act on it without being distracted is what allows us to accomplish the most mundane of tasks to the more complicated and multi-step actions. Children with executive functioning issues will suffer in a multitude of ways. Some kids have many deficits in EF and others fall behind in several or all areas. Everyone needs to develop and build executive functions as they grow. Functional adults may still be struggling with aspects of executive functioning skills. Executive dysfunction can interfere with independence and the ability to perform activities. The cognitive skills are an interconnected web of processing that allows for self-regulation, planning, organization, and memory.
As a related resource, try these self-reflection activities for kids .
What are executive functioning Skills?
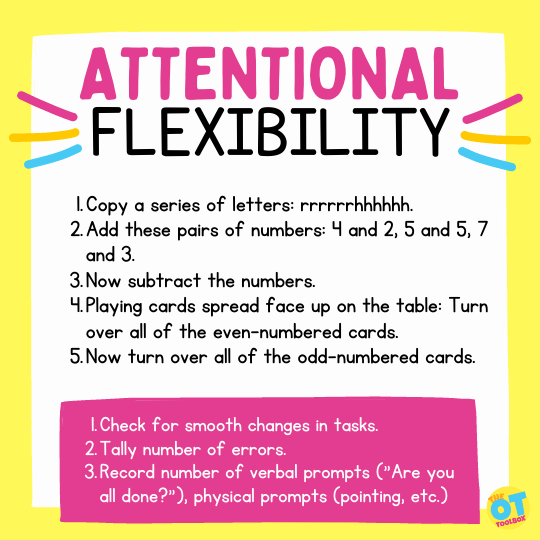
Executive functioning skill names, cognitive flexibility.
- Check for smooth changes in tasks.
- Tally number of errors.
- Record number of verbal prompts (“Are you all done?”), physical prompts (pointing, etc.)
Executive function and handwriting
How to build executive function skills:
Tools to grow executive functioning skills.
We have many resources and tools to grow executive functioning skills in functional tasks and learning. Explore the executive functioning blog posts below.
Some tools to support and grow executive functioning skills involve breaking down tasks into the components of executive functioning. By that I mean that you’ll want to focus on the specific executive functions that allow us to pay attention to instructions, plan out a task, and then recall how and why we are doing things, and then maintain the impulse control in order to sustain use of our existing skills in completing the task.
I love to provide students with specific tools to grow and nurture each of these executive functions.
We have resources and activities for the different executive functioning skills on different blog posts on this site, but one way to grow these areas is by focusing on one task and then developing tools for each aspect of that task.
For example, take on common struggle: writing down homework assignments and completing them when they are due, while managing the organization needed for the materials. You can try other tips for organizing a backpack that can help, too.
This is a common challenge for students with executive functioning that is below that of their peers. We know that executive functioning skills don’t fully develop until the early 30’s , so asking a teenager to utilize mature executive functioning skills requires tricks and practice. We can make it part of their routine rather than asking them to complete tasks on a whim with mature executive functioning.
Let’s look at the tools we can use to grow the skills needed for our homework example.
The student needs to write down their homework assignment during a busy classroom, possibly when there is a lot of other commotion going on. It seems like this is more of a challenge than it used to be because of the deceives like tablets, laptops that students use now, versus the old-fashioned paper planners that they could quickly write on and then tuck into their backpacks. Now, jotting down an assignment means pulling up a notes app or opening another program on the device. It’s not as easy for students to quickly jot down page numbers for their math homework.
We see students that believe they can remember the homework or think they can write it down when they open their laptop in their next class, but that just doesn’t happen. The attention and the distraction of this age means that the assignment is gone form their minds by the time they get that device opened back up again.
Tools to grow these skills include: using a post it note to quickly write down the assignment. This can support impulse control, attention, working memory, and organization skills.
Next, we have the home aspect. The student might not bring home all of the materials needed for the assignment. They might be left in the locker or lost somewhere along the way from school to home. We might see missing books, missing worksheets a forgotten device, or other materials that are missing or left at school. This involves organization skills, working memory, attention to detail, and impulse control.
Tools to grow this aspect might be using a check in before the student leaves school for the day. They might have a check in process in their locker in the way of a check list. You can practice this by assigning your student “homework” where they need to take home a piece of paper and bring it back to school the next day. Continue with this practice for a week so that they process of checking to make sure they have that slip of paper both in the morning and in the afternoon becomes part of the routine.
Be sure to check out all of our strategies to grow executive functioning skills by clicking through the blog posts on executive functioning skills…
Top Executive Function Blog Posts

- Executive Functioning Skills , Free Resources
Tools to Stop to Think
- Attention , Executive Functioning Skills , Occupational Therapy Activities , Sensory
Self-Reflection Activities
- Executive Functioning Skills , Free Resources , Occupational Therapy
Drawing Mind Maps
- Executive Functioning Skills , Functional Skills , Occupational Therapy Activities
Executive Function Coaching
- Executive Functioning Skills , Free Resources , Mental Health , Occupational Therapy
The Power of Yet
Breaking Down Goals
- Attention , Executive Functioning Skills , Occupational Therapy
Executive Function Tests

- Attention , Development , Executive Functioning Skills , Occupational Therapy
Spring Activities for Executive Functioning
Executive function in products.

Self Regulation Toolkit

How-to Life Sequences Made Easy – Cut & Paste
Fix the Mistakes-Fun Themes Bundle

Task Completion Cards (5 Theme Bundle)
Free Executive Function Resources

Fall Leaf Auditory Processing Activities

Pumpkin Sensory Activities
Pumpkin Deep Breathing Exercise for Halloween Mindfulness
Learning with Dyed Alphabet Pasta
Explore more tools, fine motor skills, functioning skills, handwriting, quick links, sign up for the ot toolbox newsletter.
Get the latest tools and resources sent right to your inbox!
Get Connected

- Want to read the website AD-FREE?
- Want to access all of our downloads in one place?
- Want done for you therapy tools and materials
Join The OT Toolbox Member’s Club!
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

A Problem-Based Learning Curriculum for Occupational Therapy Education

1995, American Journal of Occupational Therapy
To prepare practitioners and researchers who are well equipped to deal with the inevitable myriad changes in health care and in society coming the 21st century, a new focus is needed in occupational therapy education. In addition to proficiency in clinical skills and technical knowledge, occupational therapy graduates will need outcome competencies underlying the skills of critical reflection. In this article, the author presents (a) the rationale for the need for change in occupational therapy education, (b) key concepts of clinical reasoning and critical reflection pertaining to the outcome such change in occupational therapy education should address, (c) problem-based learning as a process and educational method to prepare occupational therapists in these competencies, and (d) the experience of the Program in Occupational Therapy at Shenandoah University in Winchester, Virginia, in implementing a problem-based learning curriculum.
Related Papers
The American Journal of Occupational Therapy
Charlotte Royeen
Objectives. Problem-based learning (PBL) is increasingly being used within health care professional educational programs to develop critical thinking skills via a learner-centered approach. However, few studies have evaluated the effect of participation in a PBL-centered curriculum on occupational therapy knowledge and skill development over time from the perspective of the students involved. This study examined student evaluations of the first three class cohorts participating in a PBL-based curriculum. Method. A participatory action design study involving qualitative, student-led focus groups was conducted with 154 students across 2 years of the education program. Fourteen focus groups were audiotaped, and those audiotapes were transcribed by an outside expert, followed by two levels of analysis by program faculty members and a member check by student participants. Results. Themes that emerged from the data analysis related to (a) defining elements of PBL, (b) the role of students...
American Journal of Occupational Therapy
Kerryellen G Vroman
Donna Wooster
Steven Whitcombe
The British Journal of Occupational Therapy
Deborah Davys
Critical thinking is a component of occupational therapy education that is often intertwined with professional reasoning, even though it is a distinct construct. While other professions have focused on describing and studying the disciplinary-specific importance of critical thinking, the small body of literature in occupational therapy education on critical thinking has not been systematically analyzed. Therefore, a systematic mapping review was conducted to examine, describe, and map existing scholarly work about critical thinking in occupational therapy education. Inclusion/exclusion criteria were set, database searches conducted, and 63 articles identified that met criteria for full review based on their abstracts. Thirty-five articles were excluded during full review, leaving 28 articles for analysis and coding using a data extraction tool. Eleven articles (39%) had a primary focus of critical thinking, and of those 11 articles, the majority were about instructional methods. Qua...
Journal of Occupational Therapy Education
Brenda Coppard
The American journal of occupational therapy : official publication of the American Occupational Therapy Association
Linda De Wet
Within occupational therapy education, there has been increased attention to curricula and courses that emphasize problem solving, clinical reasoning, and synthesis of information across traditional discipline-specific boundaries. This article describes the development, implementation, and outcomes of a problem-based learning course entitled Selected Cases in Occupational Therapy. The course was designed to help students to integrate the various elements of a specific occupational therapy curriculum and to enhance their abilities to respond to an ever-changing health care environment. An evaluation of the course by the first 11 students who completed it revealed both strengths and weaknesses. Students responded that the course enhanced their professional behavior, including interpersonal communication skills, team work, and follow-through with professional responsibilities; helped them to integrate the various elements of the total occupational therapy academic program; enhanced the...
Date Presented 4/21/2018 This study provides relevant information about what instructional methods faculty use most often and what they find valuable to successfully teach clinical reasoning. Future work needs to identify specific methods that are most effective to build the cadre of contemporary scholarship of teaching and learning for occupational therapy. Primary Author and Speaker: Whitney Henderson Additional Authors and Speakers: Brenda Coppard Contributing Authors: Youngue Qi
The Open Journal of Occupational Therapy
LaRonda Lockhart-Keene
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Occupational Therapy in Health Care
Moses Ikiugu
Journal of the Scholarship of Teaching and Learning
Helene Larin
Occupational Therapy International
Charles Juwah
Adriana Reyes Torres
British Journal of Occupational Therapy
South African Journal of Occupational Therapy
Lizelle Jacobs
The Internet Journal of Allied Health Sciences & Practice
Bill O'Dell
Christine Kroll
Hiba Zafran
Tara Cusack , Sinead McMahon
South African Journal of Physiotherapy
carina eksteen
Iranian Rehabilitation Journal (IRJ)
Steven Taff
Helen Madill
Wyona M Freysteinson, PhD, MN
Iranian Rehabilitation Journal
narges shafaroodi
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Copyright © 2024 OccupationalTherapy.com - All Rights Reserved
Cognitive Interventions In The Home: A Practical Approach For OT Professionals
Krista covell-pierson, otr/l, bcb-pmd.
- Acute Care, Community and Home Health
- Cognition and Executive Function
- Gerontology and Aging
To earn CEUs for this article, become a member.
unlimit ed ceu access | $129/year
Editor's note: This text-based course is a transcript of the webinar, Cognitive Interventions In The Home: A Practical Approach For OT Professionals, presented by Krista Covell-Pierson, OTR/L, BCB-PMD.
Learning Outcomes
- Identify four ways an OT can integrate cognition into a treatment plan.
- List four assessments for cognition that are appropriate to use in the home setting.
- Recognize four types of memory impairments and distinguish between dementia and delirium.
Introduction
Today, we will delve into cognitive interventions in the home—a practical approach tailored for occupational therapy professionals. Our profession holds significant potential to profoundly impact individuals' lives, although, at times, it may seem challenging to grasp the full scope of our role. However, during our discussion, I aim to provide you with valuable insights that you can readily integrate into your practice.
I reside in Colorado and am the proprietor of Covell Care and Rehab, a private practice where we serve a diverse patient population. The majority of our patients contend with various cognitive impairments, an aspect of care that I find particularly rewarding. Our work extends to individuals coping with conditions such as dementia, brain injuries, mild cognitive impairment, and other cognitive-related issues.
In my 22-year career as an occupational therapist, I have come to believe that, as OTs, we can enhance our approach to addressing cognition. As we embark on a deeper exploration during this hour, I encourage you to consider how you can better assist patients facing cognitive challenges.
You might wonder why this topic is of utmost importance. Given your roles as OT practitioners, you likely recognize its significance and inherent value. However, I intend to equip you with the language and rationale to explain its importance to our patients, their families, our colleagues, supervisors, and third-party payers. Effective communication, both verbally and in written documentation, is crucial. Therefore, we will touch on various aspects of this skill.
Why Is This Important?
When defining cognition, it's essential to appreciate the multifaceted nature of the concept. Several skills interplay when we consider cognition. One definition I find particularly insightful is derived from the Dementias Platform in the United Kingdom, and it reads as follows: "Cognition is a term for the mental processes that take place in the brain, such as thinking, attention, language, learning, memory, and perception." The areas are listed below.
- Skill generalization and combination
- Functional cognition
We also know as OTs that these processes are not discrete abilities, like this gentleman in his raft (Figure 1).

Figure 1. Man in a raft in the water.
Cognitive processes are intricately interconnected, akin to floating on a raft. Our objective is to equip our patients with diverse skills that harmoniously converge, enabling them to become proficient, functioning individuals, regardless of age. Therefore, when we clarify our purpose, we must emphasize that we are not solely focused on enhancing learning or memory.
Instead, our aim is for these improvements to translate into a higher quality of life. Effective communication plays a pivotal role here. While we often discuss these individual facets, it is equally essential to view the bigger picture and recognize the invaluable role that occupational therapists bring to the table.
Patients may have previously undergone neuropsychological evaluations, cognitive screenings with physicians, or worked with speech-language pathologists. Nevertheless, we can step in and comprehensively assess the array of skills listed here, aligning them with our patients' life goals. Thus, our presence within the cognitive team is highly practical.
The research underscores that when patients receive occupational therapy tailored to address functional cognition, it significantly reduces their risk of hospitalization or re-hospitalization. This outcome is compelling and resonates with various stakeholders, including third-party payers, administrators, supervisors, and, most importantly, our patients and their families. Keeping our loved ones out of the hospital is a shared priority for all.
Cognition Impacts ADLs
- Home management
- Financial management
- Community involvement
Moving beyond discussing cognition, let's look at how cognition profoundly influences our daily activities, our routines, and, ultimately, our quality of life. While it's not groundbreaking for us to acknowledge that cognitive skills impact daily living, what sets us apart is our ability to effectively communicate how we can enhance these activities.
The tasks I've outlined here serve as simple examples that can be seamlessly integrated into our therapeutic goals to demonstrate tangible improvements in function through enhanced cognition.
Is it truly impactful if someone can recall five random words when prompted? Not really, because it lacks functionality. What genuinely matters is if someone can remember five essential steps in operating their washing machine, enabling them to independently and efficiently do their laundry. The real victory lies in achieving practical, meaningful outcomes where individuals no longer require constant caregiver assistance.
Our approach involves identifying these personally significant tasks, aligning them with the cognitive processes that require improvement, and then guiding our patients through the journey of mastering these tasks. This approach benefits our patients and facilitates clearer communication in our notes and collaboration with our peers, which we will delve into further.
ADLs at Home
Figure 2 shows an infographic showing how the person, task, and environment are interconnected.
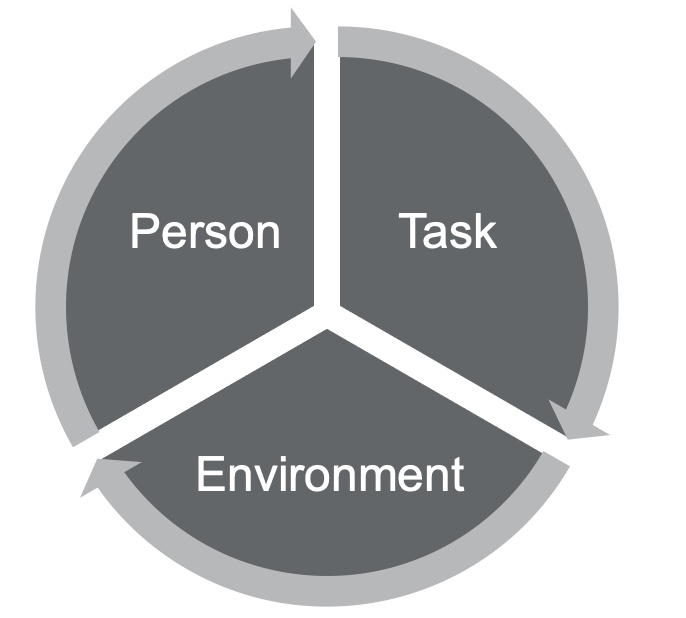
Figure 2. Person-task-environment diagram.
I frequently use diagrams like the one shown here because they align with the person-environment model, which emphasizes a holistic approach to assessing occupational performance. When working with our patients, conducting a comprehensive assessment is crucial. This assessment should encompass an examination of their skills, deficits, desires, mental and physical health, and medical needs. The goal is to develop a personal profile, recognizing that all these facets significantly impact an individual's functional cognition.
Next, we focus on identifying meaningful tasks, a process in which both the patient and their family members or caregivers play a vital role. Prioritizing tasks that resonate with the patient's motivations is imperative because intrinsic motivation is pivotal, especially when dealing with cognitive challenges. If a task isn't personally meaningful, it can be challenging to rationalize its importance, particularly for those already facing cognitive difficulties.
Additionally, it's crucial to assess how the patient perceives their skillset and compare it with our observations. Often, individuals with cognitive difficulties may overestimate their abilities. Input from loved ones and caregivers is equally valuable, as their perceptions might differ from our assessments.
A particularly rewarding aspect of our work is when we can engage with patients in their homes. This intimate setting allows us to witness their daily lives, which can be both dynamic and enlightening. Unlike a static therapy gym, homes vary, offering a unique and enjoyable challenge.
Here are two real-life examples that illustrate the diversity of environments we encounter. I had a patient who was living in a mother-in-law-type apartment above the garage. She had a huge family with members coming in and out all the time. It was distracting even for me during treatment, so I knew it was distracting for her, especially living with memory loss and cognitive fatigue related to chemotherapy treatments. I also had a patient who lived two minutes away in low-income housing. She had very limited resources and no social support system in town. Her family lived out of state, and she had no friends. She was dealing with crippling anxiety, memory loss, and decreased problem-solving skills related to years of alcohol and drug abuse. These are different people in two different environments. I can start by going into the home and looking for ideas and answers based on those environments. I can see what's meaningful to them. For example, I might see that they have a smartphone or notes next to the phone. I might see that they have their own cookbooks and like to cook. I can start using those things to make the tasks more meaningful when I'm in the environment. Working in the home setting requires flexibility and adaptability, but it's where the magic truly happens. Utilizing personal items like photographs, meaningful objects, or even the layout of their home can enhance memory recall and yield better results. Whether you're considering working in a home setting or already doing so, it's a personally rewarding endeavor. You'll find ample opportunities to connect with patients and significantly impact their lives.
Lastly, the American Occupational Therapy Association (AOTA) advocates for our role in the cognitive space. They define us as experts in measuring functional cognition, encompassing everyday task performance. Recognizing subtle cognitive impairments is crucial, as they often go untreated but can significantly impact an individual's functioning. As OTs, we treat cognitive impairments because they have the potential to compromise the safety and long-term well-being of our patients. By familiarizing yourself with AOTA's resources and language, you can strengthen your documentation and advocacy efforts, ensuring that OTs continue to play a vital role in addressing cognition and improving the lives of our patients. For additional information, refer to AOTA's resources on cognitive intervention.
Integrating Cognition Into a Treatment Plan
- Starts with chart review
- Education to patients/families of brain function as it relates to ADL at home
- Identification of areas of concern at home
- Administration of cognitive assessments at home
The integration of cognition into a treatment plan is a pivotal aspect of our occupational therapy practice. It's a process that begins with a thorough chart review, a step that some therapists may sometimes overlook in the midst of their busy daily routines. However, I want to emphasize the significance of this step. Neglecting it can potentially hinder the outcomes of your treatment plan.
A strong understanding of neuroanatomy is essential when reviewing medical records, especially in cases involving cognitive challenges. While most of us studied neuroanatomy in college, refreshing your knowledge may be a good idea, especially if it's been a while. Although we won't go into an in-depth neuroanatomy lesson, I'll touch on some key points to jog your memory. This knowledge will serve as a foundation for aligning the information you gather from chart reviews with your patient assessments. It also enables you to educate your patients, their families, and caregivers about what's happening in the brain.
You don't need to become a neurologist, but having a strategic understanding of the neurological aspects can significantly benefit your approach. For example, consider a patient who exhibits inappropriate behavior, like a previous client of mine. He would go out into public and act inappropriately, especially towards some of the women working at a local coffee shop. This gentleman was quite large, standing at 6'7", and that alone could be intimidating. Some of his inappropriate behaviors required occupational therapy intervention, but I also understood that trauma in his brain might have contributed to these behaviors. It's important to approach your work with a bit of strategy and understanding about what's going on neurologically. Knowing how specific areas of the brain might be contributing to certain behaviors can be incredibly valuable. It's all about bringing this understanding back to functional cognition.
If you find yourself without access to detailed medical records or relevant neurology reports, especially when dealing with a patient diagnosed with dementia but lacking associated medical documentation, consider requesting these records or making referrals to specialists. In some areas, neurology departments may have lengthy waitlists, so it's wise to get the process started early to ensure your patients receive timely support for their cognitive challenges.
Let's briefly review the critical regions of the brain. The frontal lobe, often referred to as our "mission control," plays a central role in cognitive functioning. It influences emotional expression, problem-solving, memory, judgment, and even sexual behaviors. Understanding this region can help us connect cognitive deficits with functional challenges. The temporal lobes are responsible for visual, olfactory, and auditory processing. These processes are vital for healthy thinking, emotional responses, and communication. The occipital lobes act as our visual hub, enabling us to interpret color, shapes, and object locations. In contrast, the insular cortex facilitates sensory processing, emotional expression, and some motor functions. The parietal lobe allows us to make sense of sensory experiences in the world, ensuring we can understand our surroundings and adapt our actions accordingly. There are also subcortical structures deep within the brain, including the diencephalon, pituitary gland, limbic structures, and basal ganglia. These structures can be likened to a "switchboard" or "mission control," simplifying complex medical concepts for our patients.
When educating patients and families about brain function in relation to activities of daily living (ADLs), consider using relatable examples and analogies. For instance, you could compare the brain to an avocado. This can make complex information more accessible and engaging.
Once you've conducted a chart review and gathered relevant information, it's an excellent time to begin educating your patients and their families about brain function and its implications for daily life. This step is crucial in building a strong foundation for your treatment plan. It helps your patients and their families understand the reasoning behind your interventions, making your approach transparent and empowering.
For instance, I once worked with an aide in an assisted living facility who had been caring for residents with different diagnoses for years but was unaware of the differences between these conditions and their effects on motor planning, cognition, and progression. Educating her about these differences transformed her perspective and improved her caregiving. Incorporate this education into your treatment plans and goals, and consider including caregiver-based goals when appropriate. By fostering understanding and collaboration, you can ensure that your interventions are effective and well-received.
Identifying areas of concern in the patient's home is the next crucial step. During evaluations, patients and their families may provide a wealth of information, but it's essential to sift through this data and prioritize. Given the pervasive influence of cognitive deficits, the list of concerns can be extensive. Start by identifying safety concerns, as these should always be addressed first.
Subsequently, focus on two to three areas that are particularly important to the patient and their family. This targeted approach allows for more manageable and effective interventions. Keep in mind that cognitive improvements in one area may have a positive ripple effect on other ADLs.
Treatment Planning Within the Home Environment
- Interpretation of results/Giving results meaning
- Identification of areas to work on
- Determining Functional Cognition!
Giving meaning to assessment scores is crucial. It's not enough to provide a number; we need to translate those scores into practical implications for the individual's daily life. This helps us pinpoint areas that require intervention and tailor our treatment plans to address specific functional challenges related to cognitive deficits.
Functional Cognition
- The cognitive ability to perform daily life tasks is conceptualized as incorporating metacognition, executive function, other domains of cognitive functioning, performance skills (e.g., motor skills that support action), and performance patterns.
- Making Functional Cognition a Professional Priority | The American Journal of Occupational Therapy | American Occupational Therapy Association (aota.org)
- Functional cognition should ONLY be evaluated in actual task performance. Home is ideal!
Functional cognition is a critical aspect of occupational therapy practice, and its definition has evolved over the years to provide a more comprehensive understanding of its role in daily life. The current definition emphasizes the integration of cognitive skills for performing activities of daily living (ADLs) and includes skills, strategies, and psychosocial elements. This updated definition acknowledges the impact of the environment, mental health, and physical health on an individual's cognitive abilities, making it a more robust framework for OTs to assess and address functional cognition in their clients.
Consideration for Functional Cognitive Treatment Planning
- Person focused
- Environment
- Emotional health
- Neurological and biological factors
In the realm of functional cognitive treatment planning, our focus naturally gravitates towards a person-centered approach. This inclination is hardly surprising, given that we, as occupational therapists, excel at catering to individual needs and aspirations. However, we may not always consider the profound impact of culture in our practice.
Culture, encompassing one's upbringing and early learning experiences, profoundly influences how individuals engage with their surroundings, perceive others, absorb and retain information, and form judgments. It's essential to recognize that these cultural nuances can vary significantly, especially when working with individuals from diverse backgrounds or those whose cultures we may not be intimately familiar with. A thoughtful exploration, whether through conversations with the patient or their family or through independent research, can unearth vital insights that should not be overlooked.
Cultural awareness aside, we must also cast our gaze upon the environmental factors that bear upon an individual's performance. Consider the case of a patient dwelling in a mother-in-law apartment, where chaos perpetually reigns. Amidst the constant juggling of pet care, from dogs to kittens and birthing cats, alongside the responsibility of caring for a boyfriend with brittle diabetes, distraction becomes a relentless companion, exhausting in its own right. Here, our task is to discern the nuances of such environments and strategize on managing their impact.
Emotional well-being is another facet deserving of our attention. A poignant quote aptly reminds us that "emotional function and cognitive function aren't unrelated to each other; they're completely intertwined." This truth is self-evident to anyone who has traversed the depths of grief, battled the shadows of depression, or grappled with the relentless grip of anxiety. When we encounter a patient navigating such emotional storms, we must acknowledge that their cognitive abilities may bear the brunt of these turbulent waters. A recently bereaved patient struggling to find equilibrium may exhibit signs of forgetfulness or cognitive struggle directly linked to their emotional state.
Lastly, we must not overlook the neurological and biological dimensions. Employing tools like brain scans and neuropsychological evaluations, we gain invaluable insights into the mind's inner workings. This knowledge becomes a cornerstone for crafting precise treatment plans and, where necessary, advocating for specialized care. Consider this parallel: just as you wouldn't prescribe the same medication for every patient with chest pain, so too should we be cautious of hastily offering psychiatric drugs without a comprehensive understanding of what's transpiring within the patient's brain. As occupational therapists, recognizing the significance of these assessments, our duty extends to educating our patients and championing their access to the expertise that can provide tailored solutions for their unique cognitive challenges.
Assessments to Use at Home
- Confusion Assessment Method: to identify patients with delirium: The_Confusion_Assessment_Method.pdf (va.gov)
- The Brief Interview for Mental Health Status
- Performance Assessment of Self-Care Skills
- Executive Function Performance Test
Let's now delve into the assessments that can be incorporated into our practice. Although some of these assessments may initially appear unconventional for occupational therapists, they offer valuable insights and are integral to comprehensive care.
The Confusion Assessment Method (CAM) and Brief Interview for Mental Health Status (BIMS) do not inherently align with traditional OT practices, but both have gained approval from Medicare for assessing cognition. CAM, for instance, aids in identifying delirium in patients. Delirium, which can range from subtle to severe, may not always be readily apparent. By conducting CAM, we ensure that cognitive assessments are appropriate, as addressing cognition when delirium is present can be counterproductive. Even if you are confident that delirium isn't a factor, utilizing CAM demonstrates a thorough approach, which can be crucial for third-party payer compliance. The Centers for Medicare and Medicaid Services (CMS) has integrated CAM into post-acute care assessments, which might already be a part of your healthcare team's protocol.
On the other hand, BIMS, another CMS-approved assessment, serves as a valuable tool for neuropsychological screening. For example, if you encounter a patient grappling with profound grief and depression, the BIMS can shed light on their mental state. It's essential to address mental health concerns before diving into cognitive evaluations. Collaborating with your healthcare team to determine who administers these assessments can streamline the process. Alternatively, you can administer them yourself; they are efficient and quick, providing a solid foundation for cognitive assessments.
Let's explore assessments that align more closely with traditional occupational therapy practices. The Performance Assessment of Self-Care Skills is a reliable, client-centered, performance-based assessment designed to measure occupational performance in daily life tasks. It can be effectively employed with adolescents, adults, and older adults, even in home settings. Comprising 26 core tasks, including mobility, basic ADLs, IADLs with a physical focus, and crucially, 14 IADL tasks related to cognition, the PASS provides a holistic view of a patient's abilities and how they navigate various tasks.
The Executive Function Performance Test examines a patient's capabilities in tasks like cooking, phone use, medication management, and bill payment within their home environment. It offers valuable insights into a patient's functional abilities and serves as an educational tool for families. Additionally, it's accessible as a free download, providing convenient access to a useful assessment tool.
Despite their initial differences from conventional OT practices, these assessments play an indispensable role in ensuring comprehensive care and tailored interventions for our patients.
Additional Assessments to Use at Home
- Fitness to Drive Screening Measure: Web-based to identify at-risk drivers
- Loewenstein Occupational Therapy Cognitive Assessment (LOTCA): Cognitive and visual perception skills in older adults are assessed
- Mini-Mental State Examination (MMSE): Measures orientation, recall, short-term memory, calculation, language, and constructability
- Cognitive-Performance Test (CPT): Explains and predicts capacity to function in various contexts and guide intervention plans
- Cognistat: Rapid testing for delirium, MCI, and dementia (can be used with teens to adults)
- Trail Making Tests A and B
Incorporating assessments into our home-based occupational therapy practice is essential for providing comprehensive care. One critical area that demands our attention is assessing a patient's fitness to drive. If you work in the community, be it outpatient, home care, or mobile outpatient services, addressing a patient's ability to drive is paramount, especially when cognitive issues are at play. However, determining whether a patient should drive requires specific skills and training. If you lack this expertise, it's crucial to connect with a Certified Driving Rehab Specialist (CDRS), often an occupational therapist or physical therapist with extensive training in driving assessments. Collaborating with CDRSs is vital, as it directly relates to public health, safety, and community well-being. The tragic example of a wrong-way driver causing a fatal accident highlights the significance of addressing driving concerns diligently.
Here are some assessments that you can integrate into your practice. The Loewenstein Occupational Therapy Cognitive Assessment, previously known as the LOTCA, assesses cognitive and visual perception skills. It aids in identifying various levels of cognitive difficulties and provides insights into a patient's learning potential and thinking strategies. This information significantly influences our treatment planning and intervention selection. Additionally, the LOTCA offers different versions tailored to different age groups, enhancing its versatility.
Mini-Mental State Examination (MMSE) assesses orientation, recall, short-term memory, calculation, language, and constructive ability. While it's commonly administered in physician's offices, you can also use it in your home-based practice. There's a similar tool called the SLUMS (Saint Louis University Mental Screening), which is a free assessment option.
The Cognitive-Performance Test (CPT) is a performance-based assessment that explains and predicts a patient's capacity to function in various contexts. It employs the Allen Cognitive Levels for rating patients, which can be shared with their families to help them understand cognitive challenges better.
Although typically used in inpatient psychiatric facilities, the Cognistat can be adapted for home-based assessments. It's a rapid test that differentiates between delirium, mild cognitive impairment, and dementia and can be applied across various age groups.
The Trail Making Tests A and B evaluate general cognitive function, including working memory, visual processing, visual-spatial skills, selective and divided attention, processing speed, and psychomotor coordination. Trail Making Test B, in particular, has been linked to poor driving performance. If a patient performs poorly on this test and intends to drive, it's advisable to refer them to a CDRS or consider pursuing CDRS certification.
These assessments, though diverse in their applications and availability, expand our toolkit for home-based occupational therapy. Some may require purchase, while others can be downloaded. Discuss the possibility of integrating these assessments into your practice with your employer to enhance the quality of care you provide during home visits.

Clinical Observations
- Errors in math
- Frustration from the patient
- Distractibility
- Difficulty focusing
- Repeated phrases
- Requires redirection
- Unable to locate items
- Impulsivity
- Reduced reciprocity
- Reduced problem-solving skills
- Delayed or absent recall
- Changes in perception
- Poor insight
- Changes in personality
- Irritability
- Safety concerns
- Increased fatigue
- Decreased organization
It's essential to emphasize the value of your clinical observations and activity analyses in your documentation. These observations, rooted in your skilled assessment and honed through clinical experience, provide crucial insights into a patient's cognitive abilities and challenges.
For instance, consider an activity as straightforward as making a peanut butter and jelly sandwich, reminiscent of college days. While occasional difficulties in locating items or lapses in focus are common and may not necessarily indicate a cognitive issue, persistent patterns of such challenges warrant attention. If you consistently encounter these issues or receive complaints from families, it's an indication that cognitive assessment and intervention may be necessary, even if your initial focus was on a different aspect of care. Your ability to recognize these signs and adapt your approach is a testament to your clinical expertise and dedication to comprehensive patient care.
Home Strategies
- Visual cues
- Automatic timers
- Lighting alternatives
- DME for fall prevention
- Reduced clutter
- Alarm/alert systems
- Phones and computers
- Routine modifications
- Mental health support/activities
- Paper calendars
- Timers for time modulation
- Caregiver education
- Driving alternatives
- Dementia education and training
- Emergency preparedness
- “Just right challenge” tasks
- Safety training
- Stress management
Working in a patient's home setting can be an incredibly rewarding experience for occupational therapists. It provides a unique opportunity to tap into our innate creativity and adaptability as professionals. Here are some strategies and interventions that can be seamlessly integrated into home-based care:
Utilizing visual cues can be highly effective. For example, consider a patient who frequently snacks on unhealthy foods. To address this issue, you can clear a designated place on the kitchen counter, place a placemat there, and instruct caregivers to set out specific healthier snacks on the placemat. This visual cue prompts the patient to choose healthier options, promoting improved dietary habits.
While automatic timers can be useful, it's crucial that the patient understands their purpose. Many patients may become confused when timers go off without clear instructions. Therefore, ensuring the patient comprehends the intended use of timers and how to respond when they activate is essential.
In cases where certain areas lack adequate illumination, such as bathrooms, adjusting the lighting can reduce patient distress and confusion, particularly for those with cognitive impairments. Ensuring a well-lit environment can enhance their comfort and safety.
Managing a patient's energy levels throughout the day is vital. Cognitive issues, from dementia to brain injuries, can lead to increased fatigue. Therefore, helping patients modulate their activity levels and prevent excessive exhaustion is integral to care planning.
Smartphones, computers, and phones can be valuable tools for patients, provided they have a basic understanding of how to use them. Caregiver education in this regard can empower patients to leverage technology for various aspects of daily life.
Stress can significantly worsen cognitive function. Implementing stress management techniques and strategies can be beneficial for patients. This may include relaxation exercises, mindfulness practices, or simple stress-reduction activities.
Although not listed, exercise plays a crucial role in maintaining and improving cognitive function. Incorporating physical activity, even in modified forms, can engage the cerebellum and contribute to clearer thinking and improved cognitive abilities.
In summary, home-based occupational therapy allows us to be creative and tailor interventions to suit each patient's unique environment and needs. Utilizing visual cues, appropriate technology, and effective energy management can enhance our patients' quality of life and well-being while addressing cognitive challenges.
Adding Goals to Treatment Plans
- Client-based
- Assist level
When formulating goals for cognitive interventions, it's beneficial to employ the COAST framework, emphasizing client-centered, occupation-based, specific, and time-bound goals. These objectives should align with the principles of functional cognition and measure improvements in functional outcomes. Here are a few practical examples:
Medication Management Goal
For this goal, the focus is on the patient's ability to manage their medications effectively. In the COAST framework, the goal is tailored to a specific patient, the occupation in focus is the proper administration of daily medications, the patient will employ learned strategies to achieve this goal, the specific objective is for the patient to take all five of their daily medications using the strategies they've acquired, and the patient is expected to reach this goal within a timeframe of three consecutive days within two weeks.
Phone Management Goal
This goal centers around a patient's capability to manage medical appointments through phone calls. In the COAST framework, the goal is customized to meet the specific patient's needs, the occupation in focus is the efficient management of medical appointments via telephone, the patient is encouraged to strive for independent management using their contact list and iPhone, the specific aim is for the patient to make two phone calls with a flawless accuracy rate to manage medical appointments, and the patient is expected to reach this goal within the span of four treatment sessions.
Meal Preparation Goal
In this scenario, the goal is to enhance a patient's ability to prepare a meal, leveraging visual cues. In the COAST framework, the goal is tailored to meet the specific patient's needs, the occupation in focus is the independent preparation of a meal, visual cues will be used to assist the patient in achieving this goal, the specific aim is for the patient to prepare a simple meal while relying on visual cues placed within the kitchen, and the patient is expected to reach this goal within a specified timeframe.
In your documentation, it's crucial to be explicit about the cognitive strategies being employed. This guides the treatment approach and sets clear expectations regarding when the patient is anticipated to succeed. By adhering to the COAST framework and focusing on measurable functional improvements, your cognitive goals will effectively address each patient's unique needs and challenges.
Challenges With Documentation
- EMR useability
- Limited resources online or with employers
- Cognitive goals can require extra time to ensure quality
- Medically necessary required for billing
- Third-party payer authorizations can be more difficult to obtain
Documenting cognitive interventions can pose challenges, particularly within electronic medical records (EMRs) that may not be tailored to occupational therapists. It's not uncommon for EMRs to be more user-friendly for physical therapists, so OTs often need to get creative in how they use these systems. This might involve finding workarounds or advocating for the necessary resources and support from employers to ensure efficient documentation.
Cognitive goals and interventions may also require additional time compared to traditional physical therapy interventions. Justifying this extended timeframe in your treatment recommendations for third-party payers is crucial. Instead of merely stating that you're working on a specific task, such as transfer training, provide a clear rationale for the prolonged duration. For instance, if you're implementing errorless learning techniques or addressing specific cognitive challenges, explain why this additional time is medically necessary for the patient's benefit.
Navigating third-party payment authorizations can be more complex when dealing with cognitive disabilities. Advocacy becomes essential in such cases. You may encounter denials, but don't hesitate to appeal these decisions. Back your appeal with well-structured documentation that educates the payer about the intricacies of cognitive impairments and their impact on the patient's daily life. Emphasize the medical necessity of your interventions. This advocacy can lead to successful outcomes, as exemplified by a case where an appeal secured additional therapy sessions for a patient who ultimately achieved her academic and career goals despite cognitive challenges.
In summary, documenting cognitive interventions may require creativity within EMRs, justification for extended treatment times, and advocacy to secure the necessary authorizations. Through clear and informed documentation, you can effectively convey the medical necessity of your interventions and advocate for the best outcomes for your patients.
Billing for Cognition
- Therapeutic interventions that focus on cognitive function (e.g., attention, memory, reasoning, executive function, problem-solving, and/or pragmatic functioning) and compensatory strategies to manage the performance of an activity (e.g., managing time or schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient contact.
- Therapeutic interventions that focus on cognitive function (e.g., attention, memory, reasoning, executive function, problem-solving and/or pragmatic functioning) and compensatory strategies to manage the performance of an activity (e.g., managing time or schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient contact.
When it comes to billing for cognitive interventions in occupational therapy, there are specific Current Procedural Terminology (CPT) codes that you should use. These codes help you accurately document and bill for the services you provide. Here's a breakdown of the relevant codes:
The 97129 code is used for the initial 15 minutes of therapeutic interventions. It's important to note that this code is the same as 97130 in terms of definition. After the initial 15 minutes, you would use the 97130 code for each additional 15-minute increment of therapeutic interventions.
It's crucial to be precise in your documentation and use the language provided in the CPT code descriptions. This helps ensure that your third-party payer understands the nature of the interventions you're providing and approves the billing accordingly. For example, if your therapy session focused on executive function tasks, make sure to explicitly mention that in your documentation. By aligning your documentation with the CPT code definitions, you provide a clear and accurate account of the services you delivered.
To stay organized and informed, consider keeping a handy reference sheet of CPT codes and their definitions, even if you're experienced in your field. This can be a valuable tool for ensuring consistency and accuracy in your billing and documentation practices.
Types of Cognitive Impairments
As we wind down, I want to talk about delirium and dementia for a second.
Delirium Vs. Dementia
Delirium is a condition that, while more commonly associated with acute care settings, can also manifest in the community or during home care visits. As occupational therapists, it's essential to be knowledgeable about delirium because of its potential severity and impact on patients. You might be the primary healthcare provider present in these situations, so identifying delirium becomes crucial.
Delirium is characterized by a sudden onset and is primarily defined by disturbances in attention and awareness. Recognizing delirium is essential because it can lead to significant complications if left unaddressed. Being vigilant and informed about delirium ensures that you can provide appropriate care and support, especially when you're working in home care or outpatient settings where immediate access to medical personnel may not be readily available.
Delirium
- Disturbance in attention and awareness developing acutely tends to fluctuate in severity
- At least one additional disturbance in cognition
- Disturbances are not better explained by dementia
- Disturbances do not occur in the context of a coma
- Evidence of an underlying organic cause
Delirium is a condition characterized by its rapid onset and varying degrees of severity. It's marked by at least one noticeable disturbance in cognition, and it's important to note that this disturbance cannot be attributed to dementia. To help identify delirium quickly, you can utilize the delirium assessment we discussed earlier, which is a fast and efficient tool. If the assessment indicates delirium, seeking immediate medical attention is crucial. While it's rare to encounter someone in a coma during home visits, delirium can manifest in various ways and usually indicates an underlying cause.
Delirium can result from factors such as medication interactions, psychiatric issues, or infections. When you're in a home care setting and observe signs of delirium, it's essential to prioritize the person's safety and well-being by promptly getting them the necessary medical care.
- Significant cognitive decline in one or more cognitive domains.
- Cognitive impairment interferes with ADL.
- Cognitive impairment does not occur exclusively in the context of delirium.
- Cognitive decline is not better explained by other medical or psychiatric conditions.
Dementia is distinguished by significant cognitive decline in one or more cognitive domains, and this decline typically interferes with a person's ability to perform daily activities. It's important to note that delirium and dementia can coexist and are not mutually exclusive conditions. While someone with dementia can experience delirium, the two are distinct.
To diagnose dementia, a physician is required as it involves a comprehensive evaluation beyond the scope of occupational therapy. It's essential to remember that dementia is not a specific disease; rather, it is an umbrella term encompassing various conditions characterized by cognitive decline. Each type of dementia, such as Alzheimer's disease, vascular dementia, or Lewy body dementia, has its unique features and progression patterns. Thus, it's crucial to recognize that not all dementias are the same, and a proper diagnosis is necessary for appropriate management and care planning.
- Vascular dementia
- Dementia with Lewy bodies
- Frontotemporal dementia
- Alzheimer’s
- Mild cognitive impairment
- Encephalopathy
It's crucial to understand that dementia is a broad category encompassing various conditions, each with its unique characteristics and underlying causes. Dementia is not a single disease but rather a term used to describe a range of cognitive impairments. Here are some types of dementia and their distinguishing features:
Vascular dementia results from impaired blood flow to the brain, leading to problems with reasoning, planning, judgment, memory, and other cognitive functions. It is often characterized by cognitive deficits that can vary in severity, as if the brain's function has "holes" due to damage from inadequate blood flow.
Dementia with Lewy bodies is a progressive dementia characterized by a decline in thinking, reasoning, and independent function. Individuals with this type of dementia commonly experience sleep disturbances, visual hallucinations, and movement disorders, such as slow movements, tremors, and rigidity. It is closely related to Parkinson's disease.
Frontotemporal dementia refers to a group of disorders caused by nerve loss in the brain's frontal and temporal lobes. It can manifest as changes in behavior, empathy, judgment, foresight, and language abilities. The specific symptoms may vary depending on the regions of the brain most affected.
Alzheimer's disease is the most common type of dementia, accounting for 60-80% of dementia cases. It is characterized by progressive cognitive decline, including memory loss, language problems, and difficulties with daily activities. Plaques and tangles in the brain are hallmarks of Alzheimer's.
Mild Cognitive Impairment (MCI) represents cognitive impairments that are more significant than expected for an individual's age and education level but do not meet the criteria for dementia. While individuals with MCI are at increased risk of developing Alzheimer's disease, not everyone with MCI progresses to dementia.
Encephalopathy refers to a broad term for brain dysfunction. It can lead to a range of cognitive difficulties, including problems with concentration, suicidal thoughts, lethargy, vision issues, swallowing difficulties, seizures, dementia-like behaviors, and more.
Understanding the specific type of dementia is essential for appropriate care and interventions, as each type may require different management strategies and approaches. Additionally, dementia is a complex condition with various underlying causes, and research continues to uncover more about its mechanisms and risk factors.
- Stanley B. Prusiner
- Florence Clark, PhD, OTR/L, FAOTA
As we conclude this session, I'd like to share some valuable insights and practical tips for addressing cognition in occupational therapy. Remember, as occupational therapy practitioners, our role is to help people live life to the fullest, providing practical solutions for success in everyday living. We can assist individuals in maximizing their function, vitality, and productivity, regardless of their cognitive impairments.
It's crucial to advocate for our patients and for the occupational therapy profession's involvement in addressing cognition. Staying informed about neuroanatomy and emerging scientific findings allows us to develop creative and effective treatment plans tailored to each patient's needs, especially when working in a home-based setting.
One essential aspect to remember is that the brain plays a central role in all bodily functions. As Thomas Edison aptly put it, "The chief function of the body is to carry the brain around." Therefore, even when working on physical aspects with our patients, we must recognize the critical importance of cognitive function.
In documenting cognitive deficits influenced by psychosocial aspects during home visits, it's essential to provide specific examples. For instance, if a patient exhibits signs of depression that impact their daily life, you can document the patient's emotional state, any refusal to participate in activities, and your efforts to address their emotional well-being. While we cannot diagnose depression, we can highlight observable signs and symptoms and collaborate with other healthcare professionals for further evaluation and intervention.
Regarding the Allen Cognitive Levels, you can access resources and printouts online. There are books available, such as "Understanding the Allen Cognitive Levels," that can serve as valuable references. These levels can be instrumental in helping patients and their families better understand cognitive impairments and manage associated behaviors effectively.
In summary, occupational therapy practitioners play a vital role in addressing cognition, and we have the tools and knowledge to make a meaningful impact on our patients' lives. By advocating for our patients, staying informed, and using evidence-based approaches, we can help individuals with cognitive impairments lead more fulfilling and independent lives.
Thank you for joining this session.
Adamit, T., Shames, J., & Rand, D. (2021). Effectiveness of the Functional and Cognitive Occupational Therapy (FaC o T) intervention for improving daily functioning and participation of individuals with mild stroke: A randomized controlled trial. International journal of environmental research and public health , 18 (15), 7988. https://doi.org/10.3390/ijerph18157988
Cognition, Cognitive Rehabilitation, and Occupational Performance. (2019). AJOT , 73 (Supplement_2), 7312410010p1–7312410010p26. https://doi.org/10.5014/ajot.2019.73S201
Edwards, D. F., Wolf, T. J., Marks, T., Alter, S., Larkin, V., Padesky, B. L., Spiers, M., Al-Heizan, M. O., & Giles, G. M. (2019). Reliability and validity of a functional cognition screening tool to identify the need for occupational therapy. AJOT , 73 (2), 7302205050p1–7302205050p10. https://doi.org/10.5014/ajot.2019.028753
Manee, F. S., Nadar, M. S., Alotaibi, N. M., & Rassafiani, M. (2020). Cognitive assessments used in occupational therapy practice: A global perspective. Occupational Therapy International , 8914372. https://doi.org/10.1155/2020/8914372
Stigen, L., Bjørk, E., & Lund, A. (2022). Occupational therapy interventions for persons with cognitive impairments living in the community. Occupational therapy in health care , 1–20. Advance online publication. https://doi.org/10.1080/07380577.2022.2056777
Covell-Pierson, K. (2023). Cognitive interventions in the home: A practical approach for OT professionals. OccupationalTherapy.com , Article 5638. Available at www.occupationaltherapy.com

Occupational therapist and entrepreneur, Krista Covell-Pierson is the founder and owner of Covell Care and Rehabilitation, LLC. Krista created Covell Care and Rehabilitation to improve the quality of services available for clients of all ages living in the community through a one-of-a-kind mobile outpatient practice which aims to improve the lives of clients and clinicians alike. Krista attended Colorado State University receiving degrees in social work and occupational therapy. She has worked in various settings including hospitals, home health, rehabilitation centers and skilled nursing. Through her private practice, Krista created a model that she teaches other therapists looking to start their own business. She has extensive experience as a fieldwork educator and received the Fieldwork Educator of the Year Award from Colorado State University. Krista served as the President of the Occupational Therapy Association of Colorado for two years. She presents to groups of professionals and community members on a regular basis and has a heart to help others become the best version of themselves.
Related Courses
Course: #5963 level: introductory 1 hour, incontinence: practical tips for the occupational therapy practitioner (part 1), course: #3609 level: intermediate 1 hour, incontinence: practical tips for the occupational therapy practitioner (part 2), course: #3610 level: intermediate 1 hour, assessing and preventing falls at home: a practical approach for the ot, course: #5413 level: intermediate 2 hours, covid-19 with older adults: an update, course: #5494 level: introductory 2.5 hours.
Our site uses cookies to improve your experience. By using our site, you agree to our Privacy Policy .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Research-based occupational therapy education: An exploration of students’ and faculty members’ experiences and perceptions
Kjersti velde helgøy.
1 Center of Diakonia and Professional Practice, VID Specialized University, Stavanger, Norway
Jens-Christian Smeby
2 Centre for the Study of Professions, OsloMet – Oslo Metropolitan University, Oslo, Norway
Tore Bonsaksen
3 Department of Health and Nursing Science, Faculty of Social and Health Sciences, Inland Norway University of Applied Science, Elverum, Norway
4 Faculty of Health Studies, VID Specialized University, Sandnes, Norway
Nina Rydland Olsen
5 Department of Health and Functioning, Faculty of Health and Social Sciences, Western Norway University of Applied Sciences, Bergen, Norway
Associated Data
In accordance with restrictions imposed by the Norwegian Data Protection Services (NSD) with ID number 8453764, data must be stored on a secure server at VID Specialized University. The contents of the etics committe`s approval resolution as well as the wording of participants` written consent do not render public data access possible. Access to the study`s minimal and depersonalized data set may be requested by contacting the project manager, KVH, email: [email protected] or the institution: on.div@tsop .
Introduction
One argument for introducing research in bachelor`s degree in health care is to ensure the quality of future health care delivery. The requirements for research-based education have increased, and research on how research-based education is experienced is limited, especially in bachelor health care education programmes. The aim of this study was to explore how occupational therapy students and faculty members experienced and perceived research-based education.
This qualitative, interpretative description consisted of three focus group interviews with occupational therapy students in their final year (n = 8, 6 and 4), and three focus group interviews with faculty members affiliated with occupational therapy programmes in Norway (n = 5, 2 and 5). Interviewing both students and faculty members enabled us to explore the differences in their experiences and perceptions.
Five integrative themes emerged from the analysis: “introducing research early”, “setting higher expectations”, “ensuring competence in research methods”, “having role models” and “providing future best practice”. Research was described as an important aspect of the occupational therapy bachelor program as it helps ensure that students achieve the necessary competence for offering future best practice. Students expressed a need to be introduced to research early in the program, and they preferred to have higher expectations regarding use of research. Competence in research methods and the importance of role models were also highlighted.
Conclusions
Undergraduate health care students are expected to be competent in using research. Findings from our study demonstrated that the participants perceived the use of research during training as important to ensure future best practice. Increasing the focus on research in the programme’s curricula and efforts to improve students’ formal training in research-specific skills could be a starting point towards increased use of research in the occupational therapy profession.
Occupational therapists have positive attitudes towards research, but implement research evidence infrequently within their daily practice [ 1 ]. Professional education is believed to play an important role in the development of positive attitudes towards evidence-based practice (EBP) skills [ 2 , 3 ]. One approach to improving evidence-based practice uptake in clinical practice is through the integration of research in education [ 4 , 5 ]. Developing student’s research skills is an important aspect of EBP [ 6 ] and participation in a research course has been found to improve nursing student’s attitudes towards research [ 7 ]. The World Federation of Occupational Therapists recommends an occupation-focused curriculum that includes critical thinking, problem-solving, EBP, research and life-long learning [ 8 , p. 6]. As such, educators in occupational therapy are advised to engage in research [ 8 , p. 53].
Several studies have explored how to link research and teaching in higher education [ 9 – 20 ]. Based on previous research [ 9 , 10 , 15 – 20 ], Huet developed a research-based education model that distinguishes between research-led teaching and research-based teaching [ 14 ]. Research-led teaching means that academics use their expertise as active researchers or use the research of others to inform their teaching. Research-based teaching means that students develop research skills by being involved in research or other inquiry-based activities. Research-led teaching and research-based teaching is interconnected, and research and teaching should be seen as interlinked [ 14 ]. One strategy for linking research and teaching is to bring research into the classroom, e.g. through academics presenting their research relevant to the subject and discussing research outcomes and methods with students [ 14 ]. In a research-based learning environment, students learn how to become critical thinkers, lifelong learners and to generate discipline-enriching knowledge [ 14 ].
Research-based education has mainly been emphasized in disciplinary university education [ 21 ]. In medical education, students’ knowledge, perceptions and attitudes towards research have been examined in several studies [ 22 – 25 ]. In their review, Chang and Ramnanan [ 22 ] found that medical students had positive attitudes towards research. Similar results emerged in Paudel et al.`s cross-sectional study [ 24 ]. Kandell and Vereijken et al. [ 25 ] found that first-year students believed that research would be important to keeping up to date in their future clinical practice.
Less research has been carried out on research-based education in bachelor’s programmes in health care, but the requirements for research-based education have also increased in these programmes [ 21 , p. 11]. Some studies have, however, investigated the attitudes, skills and use of research among nursing students [ 4 , 7 , 26 ]. In their literature reviews, Ross [ 7 ] found that nursing students have positive attitudes towards research and Ryan [ 26 ] found that nursing students are generally positive towards the use of research. Ross [ 7 ] noted that participation in research courses and research-related activity improved students’ attitudes towards nursing research. Leach et al. [ 4 ] have argued that undergraduate research education has an impact on nursing students’ research skills and use of EBP.
Students in occupational therapy and physiotherapy have been found to share positive attitudes towards research [ 27 ]. Similarly, studies have found positive attitudes towards EBP among occupational therapy students [ 28 – 31 ]. Stronge and Cahill [ 29 ] found that students were willing to practice EBP, but a lack of time and clinical instructors not practising EBP were perceived as barriers. Stube and Jedlicka [ 28 ] and Jackson [ 30 ] highlighted the importance of learning EBP through fieldwork experiences. DeCleene Huber et al. [ 31 ] found that students were least confident in EBP skills that involved using statistical procedures and statistical tests to interpret study results. These studies focused mainly on students’ attitudes and competence in EBP and research utilization (RU), and other elements of research-based education, such as student’s exposure to and engagement with research evidence were not investigated.
Few studies have explored faculty members’ perceptions of research in undergraduate education. Wilson et al. [ 32 ] found that the way in which university teachers in university disciplines translate research into learning experiences depends on their own personal perception of research. Some academics have highlighted that disciplinary content must be learned before engaging in research [ 32 ]. This idea is in accordance with the findings of Brew and Mantai [ 33 ], who also found variations in the way in which academics conceptualized undergraduate research. Experiences, attitudes and barriers towards research have been examined among the junior faculty of a medical university, and findings indicate that fewer than half of the participants in the study were involved in research at the time [ 34 ]. Ibn Auf et al. [ 35 ] found that the factors significantly influencing positive perceptions of research experience among the faculty at medical programmes were being male, having had education in research during undergraduate level, having been trained in research following graduation, and having undertaking years of research. To our knowledge, few studies have been conducted on faculty members’ perceptions of research in health care education, and we have identified only one such study related to occupational therapy education [ 36 ]. In a survey Ordinetz [ 36 ] found that the faculty members had a positive attitude towards research-related activities, and they considered research as an integral component of their role. Still, participants found research-related activities difficult to perform.
Research into how research-based education is experienced and perceived by faculty members and students is limited, especially in bachelor’s programmes in health care [ 21 , p. 11]. To gain a better understanding of the advantages or disadvantages of linking teaching and research, we therefor aimed to explore students’ and faculty members’ experiences and perceptions of research-based education in one bachelor’s programme in health care in Norway. Our specific research questions were:
- How do students and faculty members in occupational therapy programmes perceive the emphasis on research in the programme?
- How do occupational therapy students and faculty members perceive the expectations regarding research during the programme?
- What similarities and differences exist between the experiences and perceptions of students and faculty members regarding research-based education in the programme?
Context of the research
In Norway, it is required that higher education should be research-based [ 37 ]. According to the Act relating to universities and university college § 1–1 b, education must be on the cutting edge in terms of research, development work and artistic practice [ 37 ]. In a recent white paper on quality in higher education, research-based education is defined as education that is linked to a research environment; is conducted by staff who also carry out research; builds on existing research in a particular field; provides knowledge about the philosophy of science and research methods; and provides opportunities for students to learn how research is conducted from staff or students themselves conducting research as a part of their studies [ 38 ].
In Norway, six higher education institutions offer bachelor’s programmes in occupational therapy. The bachelor’s degree in occupational therapy consists of 180 European Credit Transfer and Accumulation System (ECTS) credits and covers four main areas of learning: the natural sciences, medicine, the humanities and the social sciences as described in the National Curriculum [ 39 ]. In total, clinical education consists of 60 ECTS. Philosophy of science and research methods comprise 6 ECTS, and research and development consist of 9 ECTS. The bachelor project module involves research and development work in occupational therapy and consists of 15–20 ECTS, with some variation across programmes. According to the national curriculum, the purpose of the occupational therapy education is to prepare students to be professionally up-to-date, future-oriented and research-based in their practice [ 39 ]. Students should be able to read research papers and use research results in their professional practice, and they should be able to justify their actions to users, other professionals and employers. These regulations have typically been operationalized as learning outcomes, such as: “Students will be able to apply relevant theories and research results, to understand people with activity problems as a result of somatic illness or injury, and to be able to make reasoned choices of intervention”, or “Students will be able to find and apply research to justify an intervention in occupational health” [ 40 ].
Most higher education institutions in Norway require that faculty members hold a master’s degree and many require a PhD or equivalent. It is regulated by law that at least 20% of faculty members in programmes at the bachelor’s level have PhD or equivalent according to the regulation concerning supervision of the quality of education in higher education § 2–3 (4) [ 41 ]. The amount of time that faculty members are able to use on research and development varies between institutions. The type of academic position will often influence the percentage of time for which they can apply; 20% of a full-time position for assistant professors, 30% of a full-time position for associate professors and 40% of a full-time position for full professors [ 42 ].
We used a qualitative design with empirical data from six focus group interviews, and the research strategy ‘Interpretative description’ guided the analysis. Interpretive description is an inductive approach inspired by ethnography, grounded theory and phenomenology [ 43 ], and is a research strategy suitable for studying phenomena in practical disciplines, such as nursing, teaching and management [ 44 ]. It is an approach driven by a fundamental belief in the rightness of striving to find better ways to serve one’s disciplinary purpose, and the potential of research to guide one there [ 43 , p. 12].
Participants
A purposive sample was recruited consisting of two different participant categories: final year occupational therapy students and faculty members. Participants were recruited from three different bachelor’s programmes in Norway. We contacted programme managers, who helped us recruit faculty members. We used the students’ digital learning platform to inform them about the study and students were encouraged to contact us via email should they wish to participate in the study. Focus group interviews with students were conducted after their final clinical placement, when they had just started working on their bachelor’s projects. The study sample for this project consisted of two groups: third-year occupational therapy students (n = 18), and faculty members (n = 12). In total, 30 persons between the ages of 21 and 64 participated in the study ( Table 1 ), 7 of whom were men.
| Characteristics | Students | Faculty members |
|---|---|---|
| Invited/participated | 145/18 | 30/12 |
| Number of focus group interviews | 3 | 3 |
| Sex | ||
| Men | 6 | 1 |
| Women | 12 | 11 |
| Age | ||
| 20–29 | 15 | 1 |
| 30–39 | 3 | 3 |
| 40–49 | 2 | |
| < 50 | 6 | |
| Clinical experience (years) | ||
| 0–4 | 10 | 2 |
| 5–9 | 3 | 2 |
| 10–19 | 6 | |
| < 20 | 2 | |
| Teaching experience (years) | ||
| 0–4 | 5 | |
| 5–9 | 1 | |
| 10–19 | 4 | |
| < 20 | 2 | |
| Highest degree obtained | ||
| Bachelor’s degree | 2 | |
| Master’s degree | 8 | |
| PhD or equivalent | 3 |
*Held a bachelor’s degree in other subject area before entering the bachelor’s program in occupational therapy.
Data collection
In total, we conducted six focus group interviews with occupational therapy students and faculty members from three different bachelor’s programmes. All focus groups were conducted during the spring of 2019. The focus groups with students and faculty members were conducted separatly, due to differences in expertise and power; according to Krueger [ 45 , p. 22], this is necessary to ensure that participants feel free to speak openly. The size of the focus groups ranged from two to eight participants ( Table 1 ), and they lasted between 76 and 86 minutes. A digital voice recorder was used to audiotape each session. The focus groups were held at a convenient time and location for the participants, such as meeting rooms on campus. All participants were asked to provide written consent before participating in the study, and completed a form, giving brief details about their background. A thematic interview guide was developed, based on the aim of this study and on previous research on research-based education. The following topics were covered: 1) perceptions of the term “research-based education”; 2) expectations regarding the use of research in education, including clinical placements; 3) students’ involvement in research projects and the faculty’s experiences regarding such involvement; 4) faculty’ members participation in research; 5) experiences with teaching research methods and the philosophy of science; and 6) research-based education and future professional practice. The first author developed the interview guide, drawing on previous research on the subject, and in cooperation with the three other authors. The authors are faculty members at different educational institutions. All authors were interested in the topic of research-based education, and were experienced both in teaching and supervising health care students, and conducting focus groups.
Ethical considerations
The Norwegian Data Protection Services (NSD) approved the study (ID number 845364). Participation in the study was voluntary and the participants had the opportunity to withdraw from the study at any time without consequences. All transcripts and notes were anonymous and written consent was obtained from all the participants. None of the authors conducted focus group interviews with their own colleagues.
Previous research into research-based education served as an important starting point for the interview guide and the analysis. Interpretive description guided the process of analysing the data [ 43 ]. The co-moderators took notes during the focus group interviews, and all focus group interviews were transcribed verbatim. After each focus group interview, the moderator and co-moderator engaged in a short debriefing session. The first and last author (KVH and NRO) performed the analyses, separately at first, followed by a joint analysis in which the two authors discussed and compared their interpretation of the data and agreed on patterns and themes. Word processing was used to analyse the data, and the analysis consisted of a series of operations: 1) reading the transcripts many times while being as open-minded as possible; 2) writing marginal remarks by consistently questioning the text and pointing out important points, potential themes or patterns; 3) condensing; 4) broad coding, 5) comparing and contrasting within focus groups with similar participant categories; and finally 6) comparing and contrasting focus groups compromised of different participant-categories. Comparing and contrasting within and between focus group interviews, enabled us to generate patterns and themes within the entire data set.
The analysis was characterized by a back and forth process that involved taking things apart and putting them back together again. Throughout this process, the first author frequently returned to the transcripts to ensure that the interpretations reflected the data. To ensure rigor and credibility in the analysis, the authors stepped away from the data periodically to ask questions such as: “what am I seeing?”, “why am I seeing that?”, “how else might I understand this aspect of data?”, “what might I not be seeing?” and “what are they not telling me?” [ 43 , p.174]. This approach prompted the authors to see the data through “alternative lenses” and to acknowledge that there was much else to be seen [ 43 , p. 174].
The aim of this study was to explore how occupational therapy students and faculty members experienced and perceived research-based education. Across the focus group interviews, we identified five integrative themes; “introducing research early”; “setting higher expectations”; “ensuring competence in research methods”; “having role models”, and “providing future best practice”. Students felt it was important to be introduced to research early on in the programme, meet high expectations regarding the use of research, gain competence in research methods and have role models who use research evidence during clinical education. Faculty members felt that students needed competence in research methods and they highlighted the importance of linking research to professional practice. We found the most contrasting views between students and faculty members to be related to the theme “setting higher expectations”. While the students would have liked more focus on research, the faculty members discussed whether expectations regarding the use of research were too high. Both students and faculty members across the focus group interviews believed that research-based education was important with regards to helping students achieve the necessary competences to provide future best practice.
Introducing research early
Across the focus group interviews, several students expressed the belief that focusing on research early in their education would better enable them to read and understand research during their training. Furthermore, one participant highlighted that occupational therapists are expected to integrate up-to-date research findings in their practice, and learning about research in the early stages was important in order to ensure this competence. Most students questioned the timing of when research should be introduced to students during their training. One of these students was of the opinion that learning about research should be mandatory from the start of the programme:
“I wished that teaching related to research was mandatory early in my studies. Everything you want to be good at requires practice, right? I wished that I had better research skills; [in particular concerning] searching for and using articles before we started working on our bachelor’s project.” (Student, Focus group 3)
This participant had also experienced benefits, such as higher grades, when using research articles in assignments. One of the other students highlighted that critical thinking is also part of research-based education. Students expressed a need to be critical with regard to research, and several of them wished that the curriculum had focused on how to read an article critically. Some of the participants pointed out that the use of research was not introduced until their final year, which they felt was too late.
Learning about research early on in the programme was also mentioned in one of the focus group interviews with faculty members. Some of the faculty members believed that learning to use research should be introduced at the start of the programme, as research is a natural part of academic development. For students to be able to read research articles early, they must also learn about research methods early on in the programme.
“I think it is important for [students’] academic development to start early. That they start early, and really expects that they will implement it in their first, second and third year, and that it won’t just come abruptly in third year.” (Faculty member, Focus group 6)
In contrast to this, one of the faculty members expressed that early on, some students seem more focused on understanding what it will be like to practice occupational therapy, rather than learning about research evidence:
“Of course, one must start [focusing on research], but I understand students who wish to understand what the profession is like first and foremost, right? What will my day consist of as a clinician when I graduate, that is what they want to know first, right?” (Faculty member, Focus group 6)
This faculty member felt that first-year students strived to grasp the concept of occupational therapy, and that understanding the profession is essential early on in their training. Later, students can develop their understanding and use of research evidence.
Setting higher expectations
Several students expressed that they would have preferred their teachers to have set higher expectations early on regarding the use of research during their training. They had the impression that the expectations had changed for new student cohorts, and they wished that they had been given the same opportunity. In contrast, however, one student described having been given clear expectations regarding the use of research articles during the first year, although these expectations decreased as the program progressed. This participant felt that the expectations regarding the use of research in assignments were too low, especially after the first year:
“It… seems sufficient to include a sentence from an article, and to refer to one research article in the reference list, and then it is okay in a way. I think the expectations are too low. We must include a research article, but why do we do this really? What is the point? Nothing more is required.” (Student, Focus group 2)
Some students also experienced that the expectations regarding the use of research use were too low during their clinical placements. They expressed that it was unusual to talk about theory and research during placement. As future clinical instructors, they would expect more research use from their students.
We found the most contrasting views between students and faculty members regarding this theme. While students would have liked more focus on research, the faculty members discussed whether expectations regarding the use of research were too high. In one focus group with faculty members, participants discussed how students’ motivations regarding the use of research varied. In their experience some of the students were mainly interested in hands-on practice, whereas others were more interested in research. In another focus group, faculty members indicated that they were satisfied with the requirements and expectations regarding research use among their students. They highlighted that learning about research requires maturation, and that the extent to which research can be integrated during training is limited.
Another factor that was highlighted by faculty members was a fear that the increased demand for research-based education could create a distance to professional practice. Some participants highlighted that it takes time to understand the profession and that too much emphasis on research in education could threaten this process. In one focus group interview, there was a discussion regarding how to balance the emphasis on research and profession- specific knowledge:
One participant remarked that research was too much in focus:
“In light of the national expectations regarding research-based and evidence-based practice, we need to ask ourselves, what is our profession, right? We live in a time and a society where evidence-based practice and research is almost emphasized too much.” (Faculty member, Focus group 6)
In contrast, however, one of the other faculty members in the same focus group, stated that one does not forget the importance of the occupational therapy profession when conducting research, and emphasized the importance of research in education.
In another focus group interview, some of the faculty members were concerned about the increasing demand for research competence among faculty members. They feared a situation where the majority of the faculty might have research competence, but limited clinical experience, which might affect the students’ learning of specific occupational therapy skills:
“Occasionally I fear that we have less of the experience-based knowledge in the faculty, now that faculty members are expected to have a PhD. Many [faculty members] start their career at the university colleges and universities and complete the doctoral degree, without having much clinical experience.” (Faculty member, Focus group 1)
Ensuring competence in research methods
Both students and faculty members highlighted that student’s needed competence in research methods. The students emphasized the need for more competence and skills regarding quantitative methods and statistics, to enable them to read and understand research articles. Several students stated that, while they had some knowledge about qualitative methods, they had not learned much about quantitative methods. The importance of competence in research methods was highlighted in one of the focus group interviews with students:
“If you have competence in [research] methods, then it might be easier to read and understand a research article. Often when I try to read a research article about something medical, I skip the methods section because I don’t understand it.” (Student, Focus group 2)
Students believed that reading research articles prepared them for clinical work. In fact, one participant was very aware of a lack of competence in research methods during a clinical placement and expressed this as follows:
“I experienced that clinical instructor said in the beginning of the placement “you [as a student] can use research, as you are good at it”. “This is perhaps a bit unfortunate, since we haven`t been sufficiently introduced to how to find and interpret research, and not early enough. As such, we didn’t used it [research] in the placement, because we haven’t been confident enough.” (Student, Focus group 3)
Competence in research methods was also discussed in relation to students’ bachelor’s projects. Students expressed that it was too late to start learning about research methods in the final year. If research methods were not introduced at an earlier stage, students felt unprepared for their bachelor’s project. Students stated that expectations regarding research use only took place in one exam, and they wished that they had been challenged more regarding the use of research throughout the programme. Benefits from reading research articles compared with regular textbooks were highlighted, such as learning more about the results from interventions within different patient groups. Faculty members also felt that teaching methods and the philosophy of science was not sufficiently integrated in the programme. They noted that a consequence of this was a lack of competence in research methods among students, which in turn was a challenge regarding student participation in research projects initiated by faculty members. As one participant explained:
“What I think now is that of course they have received too little teaching related to research methods to be able to contribute. I have a bad conscience that they have received too little basic knowledge to get started doing it.” (Faculty member, Focus group 5)
Having role models
Some of the students experienced working alongside role models who used research evidence, both on campus and in clinical placements. With regards to clinical instructors acting as role models, one of the students stated:
“The clinical instructors used a lot of research, so I felt that I also had to [use research evidence] to keep on track.” (Student, Focus group 2)
A student from another focus group also experienced clinical instructors as expecting students to use research, although this varied from placement to placement:
“If I had treated a patient, I had to justify this with research, but it was mostly when I had placements in hospitals, so it depended very much on the clinical placement site.” (Student, Focus group 4)
Some of the students encountered the expectation that nearly all treatments performed during their placements should be justified with research evidence, especially in hospital-based services. For example one particular student described:
“In my final clinical placement in occupational health services, it was only research that mattered. At this placement you were expected not to say anything without reading up on legislation and the latest knowledge.” (Student, Focus group 4)
In contrast to this, however, several other participants had the impression that their clinical instructors did not use much research but instead emphasized experienced-based knowledge and placed more emphasis on the students’ interaction skills. These students perceived that their clinical instructor’s decision-making was based on experience-based knowledge. One participant experienced this lack of emphasis on research in clinical placements as follows:
“My clinical instructor in my last clinical placement, started to say “I am probably not going to test you on use of research evidence, because there you are superior to me, since it has been so long since I have done that. Rather, I will keep an eye on your communication skills and how you appear.” (Student, Focus group 2)
Later in the focus group interview, the same participant stated:
“I wasn’t surprised, because this experience was similar to earlier experiences from other clinical placements: that we are not challenged on research-based stuff by the clinical instructor.” (Student, Focus group 2)
This is similar to the view of another participant who expressed that research use was not visible in any of the clinical placements. Despite or perhaps because of this experience, this participant saw the need to use research to keep-up-to date in future clinical practice.
Faculty members across the focus group interviews noted a variation regarding clinical instructors’ engagement in research evidence; however, one participant highlighted an increasing focus on research among clinicians:
“I always address [research] during clinical placement visits when clinical instructors are present, and I experience that the practice field is much more focused on research now than before. Many say that this is thanks to the students.” (Faculty member, Focus group 1)
As such, students could also influence the use of research evidence during clinical education. One of the faculty members confirmed this when noting that the students requested justifications based on research after lectures on making orthoses. This faculty member recalled that students had stated that they wished the clinician lecturer had used research evidence to better justify this type of intervention. The faculty member believed that students developed their critical thinking skills during the programme and became increasingly interested in how research supported clinical decisions. Some of the faculty members highlighted that they made an effort to stimulate students’ critical thinking skills, and that they were focused on educating students that could integrate critical thinking into their professional practice.
Students also experienced faculty members as role models in terms of using research in various ways. Some of the students described a difference between younger and more experienced faculty members. They found that younger faculty members who held a PhD and were recently hired, were more focused on research than faculty members with more clinical experience. The students described this as a generational shift that has possible led to an increased focus on research in the programme recently. Overall, the students’ impression of their teachers as active researchers varied. Some students had the impression that some of their teachers did not conduct much research, and others had the impression that all of the faculty members conducted research, that they invited students to participate in their projects, and that their research was visible both in their teaching and in reading lists:
“They talk about their research projects, so everyone as far as I know is involved in research in some way. I also see their names on research articles.” (Student, Focus group 3)
Furthermore, none of the students in the three focus group interviews remembered that teachers had focused on research during students’ clinical placements visits:
“I didn’t get any questions about research from the teacher during my placement visit. In a way I feel that everybody says that research is so important, but it feels like it is mostly experience-based.” (Student, Focus group 2)
In one of the focus group interviews with students, some participants described their uncertainly regarding whether their teachers were basing their lectures on research, as the Power Point presentations often lacked references. One student remarked:
“Since [the teachers] refer to theory using old sources, I don’t trust that they have searched for new research.” (Student, Focus group 3)
Providing future best practice
Across the focus group interviews, participants perceived that research in occupational therapy bachelor’s programmes was important with regard to helping students achieve the necessary competence to provide future best practice. Both students and faculty members expressed a need to use research as an information source to justify their professional practice to other professions and collaborators. From the students’ perspective, research can provide professional credibility and drive the profession forward. One student expressed the following:
“You… desire that the intervention or the treatment or what you provide is the most professionally credible option, and that this option will have the best possible effect.” (Student, Focus group 2)
This participant described the importance of incorporating research in training and clinical placements, to ensure that graduates integrate research in future clinical practice. Furthermore, the participant expressed a responsibility to keep-up-to date with research. One of the other participants in this focus group agreed, and emphasized that when working with patients, it is important to be familiar with the latest research evidence in a particular field.
Faculty members emphasized that graduates should have the necessary competence to be able to justify treatment choices to meet the demands of society. One of the faculty members stated that emphasis on research in the programme would probably increase the focus on research after graduation, when students would be less exposed to research than they were during their training. Another stated explicitly that being able to justify treatments using research, as opposed to using intuition only, could empower students in their future practice:
“When you work in hospital-based services, if you suggest an intervention, then you will be asked why you would do that and then you can justify it with research. And that is something I believe, the benefits of empowering our students to meet the demands of society, especially in hospital-based services.” (Faculty member, Focus group 1)
Our aim was to explore how occupational therapy students and faculty members experienced and perceived research-based education. We found that students were engaged in learning about research and they considered research to be important. Both students and faculty members perceived that research in bachelor’s programmes was important with regards to helping students achieve the necessary competence to provide future best practice in occupational therapy. Students expressed a need to be introduced to research in the early stages of the programme, and for higher expectations regarding the use of research during their education. Both students and faculty members acknowledged the need for students to gain competence in research methods, as this would enable them to read research articles and participate in research projects. Students maintained that both clinical instructors and faculty members were important role models in the use of research evidence.
In this study, students expressed that they would have preferred to learn about research earlier in their programme, and some of the faculty members highlighted that integrating research at an early stage was important for academic development. Early integration of research and enquiry has also been emphasized by Healey and Jenkins [ 15 ] and Jenkins and Healey [ 46 ]. Jenkins and Healey [ 46 ] have suggested that institutions and departments develop courses that engage students in research and enquiry from the beginning of their first year. They used the term “enquiry” to highlight the importance of curiosity, as well as critical thinking. An argument for early integration of research and enquiry is to enhance the linkage between teaching and discipline-based research [ 15 ]. Walkington et al. [ 47 ] have argued that all undergraduate geography students would benefit from early attempts to develop skills in enquiry and research. They found that students felt more prepared to undertake research independently when they were given the opportunity to practise research skills in advance [ 47 ]. This is relevant to our study findings, as the bachelor’s project in the final year in the occupational therapy programmes involves research-related tasks, but learning research methods takes time. Accordingly the students who participated in our study reported that they would have liked to learn about research methods earlier, as this would have better prepared them for undertaking their bachelor’s project.
Some of the faculty members in our study believed an early introduction to the use of research is a part of academic development and the importance of progressing in this area throughout the programme was underlined. In contrast, however, one of the faculty members expressed that, in the early stages of the programme, some students seemed to be more focused on understanding the role of the occupational therapist than learning about research. This contrasting view coincides with the findings of Wilson et al. [ 32 ], who found that some academics appear to have a hierarchical understanding of research, in which disciplinary content must be learned before engaging in research. Nevertheless, students and faculty member alike explicitly articulated the need for students to develop and learn critical thinking skills at an early stage in their programme, such as how to read an article critically. Critical thinking skills were highlighted as being both important for professional practice and research-based education. However, integrating the use of research evidence early also comes with challenges. Kyvik et al. [ 48 ] found that undergraduate professional students developed only limited understanding of research. This speak to the importance of integrating the use of research as early as possible in students’ training, as these are competences that students need in order to engage in evidence-based practice as professionals.
Most of the students experienced a lack of expectations regarding the use of research in assignments and during clinical placements, whereas some of the faculty members wondered whether the expectations were too high. Some faculty members feared that the increased demand for research-based education could widen the gap between education and professional practice. Interestingly, it appears that engaging in research and professional practice may be perceived as two separate domains, with some ambiguity concerning the role of research in the occupational therapy profession. This provides further support to Kyvik’s [ 21 , p. 142] argument that research-based education in bachelor programmes in health care should place an emphasis not just on enquiry-based learning but its relevance for professional practice.
Both students and faculty members in our study described competence in research methods among students as important. Students reported a need for competence in research methods, including quantitative methods, to be able to understand research articles. Moreover, faculty members reported that the lack of students’ competence in research methods could represent a challenge when including students in their own research projects. However, Decleene Huber et al. [ 31 ] found that students lacked confidence in using statistical procedures and statistical tests to interpret study results. Kyvik et al. [ 48 ] and Brew and Mantai [ 33 ] found that undergraduates lacked the research skills needed to be involved in faculty projects. This represent a potential challenge, as most students in our study reported that they wanting to know more about their teachers’ research and to be involved in their research projects. Students also highlighted that involvement in faculty research might be a way to inspire them to continue with research in the future. Healey and Jenkins [ 15 ] have argued that students seemed more motivated if they were integrated in their teachers’ research projects at an early stage in their studies. Moreover, Smyth et al. [ 49 ] claimed that students value research experience and experienced benefits from engaging in research such as an improved understanding of the research process, increased critical thinking and professional and practical skills. This supports the view that learning about research methods, including quantitative and statistical methods, should be integrated throughout the programme.
In our study, students highlighted the importance of role models with regards to using research, especially during clinical placements. Students reported that they were positively influenced by clinical instructors who used research in their work, and as a result, they felt obliged to use research to maintain their own professional development. Students who had experienced the opposite still reported that they had searched for and used research evidence to keep-up-to date. The importance of role models in promoting EBP and the use of research evidence has been reported in several studies [ 28 – 30 , 50 , 51 ]. Olsen et al. [ 50 ] and McCluskey [ 51 ] found that clinical instructors were important role models regarding EBP for students in clinical placements. Stube and Jedlicka [ 28 ] have suggested that educators have a role in assisting students to become scholarly consumers of evidence. In our study, most of the students had the overall impression that faculty members used research in their teaching, but the degree to which students were involved in research projects varied. In one focus group interview, students highlighted that all the faculty members were active researchers and published articles. However, students found that faculty members visiting students during placements were less inclined to focus on research. Some students also reported a focus on experienced-based knowledge more than on research-based knowledge among some clinical instructors. Closer cooperation between education and practice might be a way to increase the emphasis on research during clinical placements. Role models for use of research is of importance.
Experience with research and development work during training may enhance interest in applying research in one’s future working life [ 48 ]. Future quality health care delivery is often a main argument for integrating research in bachelors’ programme in health care education, such as occupational therapy education. In our study, both faculty members and students highlighted the importance of focusing on research in training to ensure that graduates have the necessary competence to provide future best practice. Previous research findings also indicated that students have a strong belief in the value of research for their future clinical practice [ 25 ] and desire to keep up-to-date in their field [ 23 ]. To achieve this, it is important that students start as early as possible and ideally during their formal education [ 2 ]. Deicke et al. [ 52 ] have highlighted that students need to work with actual research literature, develop research designs and undertake empirical research to increase their interest in research. Findings from our study indicate that emphasis should be placed on introducing the use of research at an early stage in the programme and higher expectations should be set for students regarding the use of research, both on campus and during clinical placements, to ensure that students achieve competence in research methods and that they are exposed to role models who use research evidence.
Occupational therapists have positive attitudes towards research, but infrequently implement research evidence in their daily practice [ 1 ]. This may be due to barriers such as lack of time to read research, insufficient facilities and difficulty understanding statistical analyses [ 53 ]. Results from our study indicate that a link between research and profession-specific knowledge is necessary for research-based education in bachelor’s programmes in health care education. Research should be integrated in teaching. Along this lines, Huet [ 14 ] has argued that faculty members need to be engaged in a scholarly manner within their disciplinary field, and has highlighted the importance of raising a culture of research and teaching as two integrated activities. Learning in a research-based education environment may ensure that students enriches the knowledge in their discipline [ 14 ]. Students need to be socialized into a culture of research. Ideally, the learning of research-specific skills should be integrated into all fields of learning in a programmes curricula and include skills in critical thinking, problem-solving, EBP and research, as emphasized by WFOT [ 8 ]. Increasing focus on research in curricula and improving the students’ formal training in research-specific skills could be a starting point towards increased use of research in the occupational therapy profession.
Limitations
This study explored the experiences and perceptions of occupational therapy students and faculty members regarding research-based education in three different occupational therapy programs in Norway. Conducting focus group interviews with both students and faculty members enabled us to explore and compare differences in perceptions and experiences. Focus groups compared to individual interviews can potentially create a synergy that is not possible in individual interviews [ 54 , p. 18]. The challenge with this method, is that there is a possibility that dominant participants can influence the results and participants tend to intellectualize [ 45 , p. 22, 13]. In our study, we did not experience dominant participants, although one of the participants in one of the focus group interviews contributed very little. We made efforts to include this participant more directly in the conversation.
This study was conducted in the early phase of third-year students’ bachelor’s projects. There is a possibility that the students were more focused on research during this phase of their training. It is also possibly that students who participated in this study could have been more interested in research-based education than students who chose not to participate. While a specific interest in research-based education may also have been the case for the faculty members who chose to participate in the study, we note that only three of the participating faculty members held a PhD or equivalent, and the majority of their experience originated from clinical practice. Thus, when considering the faculty’s views as expressed in this study, the characteristics of the group should be considered. In addition, one of the focus groups, made up of faculty members consisted of only two participants. A strenght of our study, is that two authors conducted the analysis. We considered using member checking, but decided against it, as, according to Thorne [ 43 p. 175], member checking can lead to false confidence if the participants confirm what you thought or potentially derail you from good analytic interpretations if they do not. With regards to the participants, however, we feel that including both students and faculty members as study participants represents a strength of the study. A corresponding limitations is that we are unable to assess the extent to which the study sample is representative of the population of faculty and students in occupational therapy education in Norway. However, as establishing representativity is generally not an aim of qualitative studies, and according to Thorne [ 43 , p. 105], there is no definitive rule regarding the correct sample size for an interpretive description study, we believe our findings still offer important insights for the field.
This study explored the experiences and perceptions of occupational therapy students and faculty members from three occupational therapy bachelor’s programmes in Norway regarding research-based education. Students in these programmes are expected to be competent in using research evidence. Findings from our study show that both students and faculty members perceive the use of research during training as important in order for students to provide future best practice. Furthermore, findings indicate that setting high expectations regarding the use of research early on, may be important in a bachelor’s programme in health care such as occupational therapy. Ensuring competence in research methods seems to be essential for achieving success in terms of research-based education. Moreover, clinical instructors and faculty members were highlighted as important role models in the use of research evidence. Future research is needed that focuses on the use of research by clinical instructors and their expectations of students regarding using research in clinical placements. Quantitative studies are also needed, so that a wider population can be reached, as are more focus groups among students and faculty members in other professional education programmes.
Supporting information
S1 checklist, funding statement.
The author(s) received no soecific funding for this work.
Data Availability
- PLoS One. 2020; 15(12): e0243544.
Decision Letter 0
22 Jul 2020
PONE-D-20-09978
Research-based occupational therapy education: an exploration of students` and faculty members` experiences and perceptions
Dear Dr. Helgøy,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
All reviewers pointed to main strengths of the manuscript. But they identified issues, especially at the conceptual and methodological level, that require major revisions.
Please submit your revised manuscript by Sep 05 2020 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
We look forward to receiving your revised manuscript.
Kind regards,
Sara Rubinelli
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. Please include a copy of Table 2 which you refer to in your text on page 14
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: Yes
Reviewer #3: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: N/A
Reviewer #2: N/A
Reviewer #3: N/A
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: Thank you for the opportunity to review this paper, which explores students’ and faculty members’ experiences with and perceptions of research-based occupational therapy education. The study method was described in detail and the analysis was conducted in line with the interpretative description methodology. I particularly enjoyed reading the quotes, which further demonstrated the depths of the research finding.
I have some concern with the way that ‘research-based education’ is conceptualised in the manuscript. Research-based teaching refers to teaching practice “…when academics plan, deliver and assess students’ work through their involvement in research or inquiry-based activities” (p.728, Huet, 2018 – Research-based education as a model to change the teaching and learning environment in STEM disciplines, published in the European Journal of Engineering Education, 43:5, 725-740). A similar term – ‘research-lead teaching’ – occurs when academics use their expertise as active researcher or use the research of others to inform teaching. Without knowing how the occupational therapy curriculum is structured, I find it difficult to accept that it is indeed research based. It would have been beneficial for the authors to give more detail about how the curriculum is designed and delivered and to provide a few examples of research-based learning activities. Why is occupational therapy education considered as a short professional education programme, given that it is a bachelor degree? What are the expectations placed on the lecturers teaching in the occupation therapy programme, in terms of their engagement with research? Are they all clinicians? Again, providing more information about the course structure might help reduce the confusion here.
I would have liked to see more rationale given to using interpretive description as the study methodology. What’s the advance of this approach and why is it most suitable for the current study?
Participants commented on the fear that “… the increased demand for research-based education could cause a distance to professional practice”. It would be important to discuss whether comments like this fits the overall research-based model and to provide solutions to reduce such fears. I personally think that research and teaching should not be competing against each other and that the whole premise of research-based education is to incorporate research into teaching, as a means to facilitate active inquiry and critical thinking.
Reviewer #2: 1) 1. The qualitative research in the care activities is interesting, related to the management of good health science education in explaining the views, phenomena and perceptions of both the instructor and the learner.
2. The method should be improved to give details of the research methodology to understand more clearly how to do, what to do and how to analyze in order to get reliable research results Due to a small sample number
3) 3) Summary of themes is good but should make the diagram interesting In order for readers to understand the elements discovered in quality research more clearly, will make this research suitable for dissemination that useful in occupational therapy for the publication of world-renowned journals. Should adjust the diagram to be clear
In my opinion, this paper is good for occuaptional therapy education and health science education. It can share in PLoS ONE journal to contribute around the world. I’m Ok accpet thay Minor Revision,
Best Regards
Supat Chupradit, Ph.D.
Assistant Professor in Occupational Therapy, Depaertment of Occupational Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Thailand
Reviewer #3: Exploring the perceptions of OT students and faculty regarding their experiences with receiving education about research is an important topic related to encouraging evidence-based practice in the field of OT. See attached review for detailed comments and recommendations for revision.
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: Yes: Yan Chen
Reviewer #2: Yes: Supat Chupradit
Reviewer #3: No
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Submitted filename: PLOSOne review 07 2020.docx
Author response to Decision Letter 0
29 Oct 2020
Dear Editor and Reviewers: I have incorporated all of your suggestions into my revision. They were very helpful. Thank you. Please find them adressed in a separate document.
Submitted filename: Response to Reviewers.docx
Decision Letter 1
24 Nov 2020
PONE-D-20-09978R1
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Additional Editor Comments (optional):
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #1: All comments have been addressed
Reviewer #2: All comments have been addressed
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #1: Thank you for addressing all my concerns. The revised paper reads well and I have no further comments to make.
Reviewer #2: The Occupational Therapy Education research work is extensive and quite comprehensive, this is impressive manuscript. I accept the manuscript.
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Reviewer #1: No
Reviewer #2: Yes: Assistant Professor Dr. Supat Chupradit
Department of Occupational Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, 50200, Thailand.
Email: [email protected]
ORCID https://orcid.org/0000-0002-8596-2991
Acceptance letter
10 Dec 2020
Dear Dr. Helgøy:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Sara Rubinelli

OT INTERVENTIONS
Play slideshow, occupational therapy interventions.

Occupational therapists help people participate in the things they want and need to do through the therapeutic use of everyday activities (occupations). At the core of occupational therapy is a belief in health through doing . "Doing" may range from participating in practical and leisure activities to more subtle activities such as cultivating empathy or identifying values. Psychosocial occupational therapy interventions seek to optimize human functioning using a holistic approach. Interventions may facilitate reaching a youth’s goals surrounding social skills, communication skills, decision-making, problem-solving, emotional regulation, coping strategies, healthy risk-taking, attention span and focus, intrinsic motivation, values identification, positive self-concept, time management, agency and self-efficacy. Interventions are customized to leverage a youth’s interests and strengths, facilitate optimal well-being, and to match a youth’s stage of development. OTTP occupational therapists practice client-centered, trauma-informed care. For a visual tour representing a small sampling of possible interventions, view our OT slideshow above.
Core Beliefs
• There is a positive relationship between occupation and health (physical/emotional) • ”All people need to...engage in the occupations of their need and choice , to grow through what they do, and to experience independence or interdependenc e , equality, participation, security, health and well being .” • Occupations structure daily life, are central to our identity and sense of competence, and have particular meaning and value to us. • Health and well being can be affected by environmental barriers to participation. American Occupational Therapy Association (2002). Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 56, 609-639.
Ot domain / scope of practice.
OT’s Established Body of Knowledge & Expertise
Areas of Occupation
Activities of daily living instrumental activities of daily living rest & sleep education work play leisure social participation, client factors, values, beliefs, spirituality body functions body structures , performance skills, sensory/perceptual motor & praxis emotion regulation cognitive communication / social , performance patterns, habits routines roles rituals , context & environment, cultural personal physical social temporal virtual , activity demands, objects/properties space social sequencing / timing required actions required body structures & function , american occupational therapy association (2002). occupational therapy practice framework: domain and process. american journal of occupational therapy, 56, 609-639..
Problem Solving in Occupational Therapy

- Otago Polytechnic

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Neha Malgaonkar

- Sefali Dushyant Patel

- HEALTH QUAL LIFE OUT

- Beverley Goodman

- Daphne Ari-Even Roth
- Na’ilah Suad Nasir
- Richard W. Longman

- Rosemary Hagedorn

- Christine A Mayers
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Problem-based learning in occupational therapy curriculum - implications and challenges
Affiliations.
- 1 a Department of Occupational Therapy, Sackler Faculty of Medicine , School of Health Professions, Tel Aviv University , Tel Aviv , Israel.
- 2 b Department of Occupational Science and Occupational Therapy, Faculty of Medicine , University of British Columbia , Vancouver , BC , Canada.
- PMID: 28494627
- DOI: 10.1080/09638288.2017.1325942
Purpose: Problem-based learning (PBL) is an educational method that fosters self-directed study in small groups. The purpose of this study was to describe the Tel Aviv University's occupational therapy (OT) program and the challenges implementing such program. In addition, the study compared the PBL grades obtained by students who are native Hebrew speakers with those students who are native Arabic speakers; and, assessed the correlation between the grades in the PBL course and the grades in the clinical fieldwork studies.
Method: 166-second year OT undergraduate students participated. All completed three PBL courses and seven weeks of clinical fieldwork studies. Data collection included students' grades in PBL course (based on PBL evaluation forms) and in clinical fieldwork studies (based on preceptor's evaluation and a written assignment).
Results: Pearson correlations revealed significant correlations between PBL grades and clinical fieldwork studies grades. T-test analysis between students who are native Hebrew speakers and those who are native Arabic speakers revealed significant differences in PBL grades.
Conclusions: Findings imply partial congruence between students' grades in the PBL course and their achievements in the fieldwork studies. Findings might suggest that adjustments should be made in order to assist students from minorities (challenged by language requirements) in gaining higher grades in the PBL program. Implications for Rehabilitation Problem-Based Learning (PBL) is an educational method, which fosters independent, self-directed study in small groups. PBL studies have the potential to prepare students for their clinical experience during studies. The PBL program should be adjusted for students from minorities (challenged by language requirements and different cultural backgrounds) in order to assist them in gaining more benefits from the program.
Keywords: Culture; education; program development; program evaluation; students; teaching.
PubMed Disclaimer
Similar articles
- [Introduction of a brief Problem-Based-Learning (PBL) experience in traditional medical faculty curriculum]. Heyman SN, Reches A, Safadi R, Cohen R. Heyman SN, et al. Harefuah. 2007 Jun;146(6):435-8, 502, 501. Harefuah. 2007. PMID: 17760396 Hebrew.
- Rethinking the globalisation of problem-based learning: how culture challenges self-directed learning. Frambach JM, Driessen EW, Chan LC, van der Vleuten CP. Frambach JM, et al. Med Educ. 2012 Aug;46(8):738-47. doi: 10.1111/j.1365-2923.2012.04290.x. Med Educ. 2012. PMID: 22803751
- An evaluation of a problem-based learning experience in an occupational therapy curriculum in the UK. Spalding NJ, Killett A. Spalding NJ, et al. Occup Ther Int. 2010 Jun;17(2):64-73. doi: 10.1002/oti.288. Occup Ther Int. 2010. PMID: 20146196
- Problem-based learning in physical therapy: a review of the literature and overview of the McMaster University experience. Saarinen-Rahiika H, Binkley JM. Saarinen-Rahiika H, et al. Phys Ther. 1998 Feb;78(2):195-207; discussion 207-11. doi: 10.1093/ptj/78.2.195. Phys Ther. 1998. PMID: 9474111 Review.
- Adoption of Problem-Based Learning in Medical Schools in Non-Western Countries: A Systematic Review. Chan SCC, Gondhalekar AR, Choa G, Rashid MA. Chan SCC, et al. Teach Learn Med. 2024 Apr-May;36(2):111-122. doi: 10.1080/10401334.2022.2142795. Epub 2022 Nov 29. Teach Learn Med. 2024. PMID: 36444767 Review.
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Taylor & Francis
Other Literature Sources
- scite Smart Citations
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
VIDEO
COMMENTS
Get All The CEs You Need As A Occupational Therapist With HomeCEU. Subscribe to Save More. Trusted CE Provider to Over 100,000 Healthcare Professionals. Shop OT CEU Today!
Interventions recommended by the team as the result of problem solving may include implementing alternative instructional methodologies or providing more intensive instruction, such as tutoring sessions for the problematic content area. ... education when needed. Occupational Therapy Within the RtI Model. 6 Under an RtI model, occupational ...
Problem solving is described as a series of steps including referral, data collection, assessment, problem identification, planning, intervention and evalua-tion, which is mirrored by the OT process. Additionally, there are consid-ered to be two stages (Robertson, 1996): identifying the problem (also called the occupational therapy diagnosis ...
Describes the central concepts that ground occupational therapy practice and builds a common understanding of the basic tenets and vision of the profession. ... Provide client education on the following topics: Traumatic brain injury ... Teach the client how to use a problem-solving strategy (i.e., define problem, brainstorm solutions, evaluate ...
Such occasions encourage problem solving and collaboration among the occupational therapy practitioner, the child, and the child's family members. Occupational therapy practitioners should collaborate with family to design interventions to address self-care, sleep, and social participation through the use of functional tasks, play-based ...
The Directorate of Occupational Therapy at Salford University adopted a modified problem-based learning (PBL) approach in March 2004. In recent years, PBL has received mixed reviews as a teaching ...
Occupational therapy practitioners integrate the domain-general process of the Goal-Plan-Do- Check cognitive strategy that is part of the CO-OP to mediate the problem-solving procedure by offering guidance and solution interpretations in an effort to promote learning generalization (Missiuna et al., 2001; Polatajko, 2017).
Methods. We conducted a scoping study that aimed to identify the digital learning designs used in occupational therapy (OT) education and review the effectiveness, learner perceptions, clinical skills integrated, and technology-based learning strategies used to facilitate learning. Four databases were searched using subheadings and terms ...
Problem-solving therapy teaching problem-solving skills in a structured way to enable participants to systematically identify problems, generate alternative solutions, select the best solution, develop and conduct a plan, and evaluate whether the problem is solved ... Occupational therapy education programs housed close to other vision care ...
occupational therapy graduate course. The use of peer teaching strategies, including a Fishbowl discussion and case-based problem solving, were compared to a faculty-led lecture approach to determine which approach best prepared student critical thinking. Participants included 115 first year graduate occupational therapy students.
Abstract. Background: Evidence supports the role of occupational therapy (OT) for older adults, and therapeutic use of problem solving may provide a way to improve older adult's occupational performance. Aim: To assess the effectiveness and describe the contents of OT interventions aimed at improving older adults' occupational performance by strengthening their problem-solving skills.
Strand One: The Theoretical Underpinning of Problem Solving. Strand Two: The Relationship of Problem Solving to Other Models of Reasoning. Strand Three: Using Problem Solving to Define Outcomes in Reasoning. Conclusion. References
Attention, problem solving, flexible thinking, working memory, self-control, and even emotional control are executive functioning skills that allow us to manage day-to-day tasks, stay safe, and get things done. When executive functioning is a challenge, you'll see trouble with planning, prioritization, organization, and staying on a task.
A Problem-Based Learning Curriculum for Occupational Therapy Education Charlotte Brasic Royeen Key Words: education. problem identification To prepare practitioners and researchers who are well eqUipped to deal with the inevitable myriad changes in health care and in societv comin(~ in the 21st century, a new/ocus is needed in occupational therap)) education. 1n addition to projicienC)' in ...
Editor's note: This text-based course is a transcript of the webinar, Cognitive Interventions In The Home: A Practical Approach For OT Professionals, presented by Krista Covell-Pierson, OTR/L, BCB-PMD. Learning Outcomes. After this course, participants will be able to: Identify four ways an OT can integrate cognition into a treatment plan.
If an individual's EOC is inconsistent with the profession's practice epistemology, the student or practitioner may struggle with effectively solving ill-structured occupational performance problems. The purpose of this paper is to increase awareness of the constructs of EOC, to describe its importance to occupational therapy education and ...
The World Federation of Occupational Therapists recommends an occupation-focused curriculum that includes critical thinking, problem-solving, EBP, research and life-long learning [8, p. 6]. As such, educators in occupational therapy are advised to engage in research [8, p. 53].
Occupational Therapy Interventions for Older Adults With ...
Eficient and effective occupational therapy curricular and course design is essential to develop competent and reflective practitioners. The intentional use of metacognitive strategies could improve the development of higher-order thinking and learning outcomes. The study explored the use of metacognitive strategies to improve learning and ...
Psychosocial occupational therapy interventions seek to optimize human functioning using a holistic approach. Interventions may facilitate reaching a youth's goals surrounding social skills, communication skills, decision-making, problem-solving, emotional regulation, coping strategies, healthy risk-taking, attention span and focus, intrinsic ...
Problem solving is a cognitive approach to reasoning that is. encapsulated within the occupational therapy profession by the use of the. 'OT process', which is evident in all major ...
Abstract. Purpose: Problem-based learning (PBL) is an educational method that fosters self-directed study in small groups. The purpose of this study was to describe the Tel Aviv University's occupational therapy (OT) program and the challenges implementing such program. In addition, the study compared the PBL grades obtained by students who are ...
These frameworks share in common the steps of (1) gather information; (2) identify the individuals concerned, ethical problem, values in conflict, and ethical standards at risk; (3) prioritize values, principles, and desired outcomes; (4) implement the chosen action; and (5) reflect and seek feedback. The AOTA Occupational Therapy Code of ...
Introduction. A national study from 2014 found that occupational therapists in Sweden experience increased work-related stress [Citation 1], with 60% thinking about changing their workplace and 35% thinking about changing profession altogether [Citation 2].One identified challenging aspect of working as an occupational therapist has been in the transition from being an occupational therapy ...