Home — Essay Samples — Social Issues — Euthanasia — Why Euthanasia Should Be Legal: Analysis of Arguments and Counterarguments

Why Euthanasia Should Be Legal: Analysis of Arguments and Counterarguments
- Categories: Assisted Suicide Euthanasia Right to Die
About this sample

Words: 1865 |
10 min read
Published: Aug 14, 2023
Words: 1865 | Pages: 4 | 10 min read
Table of contents
Introduction, why euthanasia should be legal, works cited, counterarguments.
- Corder, Mike. “Dutch Euthanasia Center Sees 22% Rise in Requests in 2019.” WAVY.com, 7 Feb. 2020, www.wavy.com/news/health/dutch-euthanasia-center-sees-22-rise-in-requests-in-2019/. Accessed 10 March 2020.
- Davis, Jacky. “Kevin Davis Deserved Choice.” Dignity in Dying, www.dignityindying.org.uk/story/kevin-davis/. Accessed 13 March 2020.
- De La Torre, Esther B. The Right to Assisted Suicide , www.lonestar.edu/rightto-assist-suicide.htm. Accessed 19 March 2020.
- “Euthanasia Laws - Information on the Law about Euthanasia.” Information on the Law about Euthanasia - Suicide, Life, Act, and Mercy - JRank Articles, law.jrank.org/pages/11858/Euthanasia.html. Accessed 10 March 2020.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Social Issues

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
3 pages / 1552 words
2 pages / 850 words
3 pages / 1531 words
3 pages / 1154 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Euthanasia
Euthanasia, the act of intentionally ending a person's life to relieve suffering, has been a topic of intense ethical and practical debate. While proponents argue for its legalization as a compassionate end-of-life option, this [...]
The debate surrounding euthanasia is complex and multifaceted, involving considerations of ethics, religion, personal autonomy, and the value of human life. While advocates argue that euthanasia provides relief to those [...]
Euthanasia, the practice of ending the life of a suffering patient through the use of barbiturate or paralytic injections, remains a highly controversial medical procedure. While it is legal in the majority of European Union [...]
Euthanasia, also known as mercy killing, is a highly controversial topic that has sparked heated debates across the globe. The concept of euthanasia involves deliberately ending the life of a patient who is suffering from an [...]
Imagine facing a terminal illness with no hope for recovery, only prolonged suffering and pain. In such situations, the concept of euthanasia, or assisted suicide, becomes a controversial but increasingly relevant topic. [...]
Battin, M. P., Rhodes, R., & Silvers, A. (2015). The Patient as Victim and Vector: Can Ethics Abandon the Ideal of the Autonomous Patient? The American Journal of Bioethics, 15(3), 3-14.Pereira, J. M. (2011). Legalizing [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Essay: The Quality of Mercy Killing
I f it were only a matter of law, the public would not feel stranded. He killed her, after all. Roswell Gilbert, a 76-year-old retired electronics engineer living in a seaside condominium in Fort Lauderdale, Fla., considered murdering his wife Emily for at least a month before shooting her through the head with Luger as she sat on their couch. The Gilberts had been husband and wife for 51 years. They were married in 1934, the year after Calvin Coolidge died, the year after Prohibition was lifted, the year that Hank Aaron was born. At 73, Emily had Alzheimer’s disease and osteoporosis; her spinal column was gradually collapsing. Roswell would not allow her to continue life as “a suffering animal,” so he committed what is called a mercy killing The jury saw only the killing; they felt Gilbert had mercy on himself. He was sentenced to 25 years with no chance of parole, which would make him 101 by the time he got out. The Governor has been asked to grant clemency. Most Floridians polled hope that Gilbert will go free.
Not that there ever was much of a legal or practical question involved. Imagine the precedent set by freeing a killer simply because he killed for love. Othello killed for love, though his passion was loaded with a different motive. Does any feeling count, or is kindness alone an excuse for murder? Or age: maybe someone has to be 76 and married 51 years to establish his sincerity. There are an awful lot of old people and long marriages in Florida. A lot of Alzheimer’s disease and osteoporosis as well. Let Gilbert loose, the fear is, and watch the run on Lugers.
Besides, the matter of mercy killing is getting rough and out of hand. Nobody seems to use poison anymore. In Fort Lauderdale two years ago, a 79-year-old man shot his 62-year-old wife in the stairwell of a hospital; like Emily Gilbert, she was suffering from Alzheimer’s disease. In San Antonio four years ago, a 69-year-old man shot his 72-year-old brother to death in a nursing home. Last June a man in Miami put two bullets in the heart of his three-year-old daughter who lay comatose after a freak accident. An organization that studies mercy killings says that nine have occurred this year alone. You cannot have a murder every time someone feels sorry for a loved one in pain. Any fool knows that.
Yet you also feel foolish watching a case like Gilbert’s (if any case can be said to be like another) because, while both feet are planted firmly on the side of law and common sense, both are firmly planted on Gilbert’s side as well. The place the public really stands is nowhere: How can an act be equally destructive of society and wholly human? The reason anyone would consider going easy on Gilbert is that we can put ourselves in his shoes, can sit at his wife’s bedside day after day, watching the Florida sun gild the furniture and listening to the Atlantic lick the beach like a cat. Emily dozes. He looks at her in a rare peaceful pose and is grateful for the quiet.
Or he dreams back to when such a scene would have been unimaginable: she, sharp as a tack, getting the better of him in an argument; he, strong as a bull, showing off by swinging her into the air–on a beach, perhaps, like the one in front of the condominium where old couples like themselves walk in careful slow motion at the water’s edge. Since the case became a cause, photographs of the Gilberts have appeared on television, she in formal gown, he in tails; they, older, in a restaurant posing deadpan for a picture for no reason, the way people do in restaurants. In a way the issue here is age: mind and body falling away like slabs of sand off a beach cliff. If biology declares war, have people no right to a pre-emptive strike? In the apartment he continues to stare at her who, from time to time, still believes they are traveling together in Spain.
Now he wonders about love. He loves his wife; he tells her so; he has told her so for 51 years. And he thinks of what he meant by that: her understanding of him, her understanding of others, her sense of fun. Illness has replaced those qualities in her with screams and a face of panic. Does he love her still? Of course, he says; he hates the disease, but he loves his wife. Or–and this seems hard–does he only love what he remembers of Emily? Is the frail doll in the bed an impostor? But no; this is Emily too, the same old Emily hidden somewhere under the decaying cells and in the folds of the painkillers. It is Emily and she is suffering and he swore he would always look after her.
He considers an irony: you always hurt the one you love. By what act or nonact would he be hurting his wife more? He remembers news stories he has read of distraught people in similar positions, pulling the plugs on sons and husbands or assisting in the suicides of desperate friends. He sympathizes, but with a purpose; he too is interested in precedents. Surely, he concludes, morality swings both ways here. What is moral for the group cannot always be moral for the individual, or there would be no individuality, no exceptions, even if the exceptions only prove the rule. Let the people have their rules. What harm would it do history to relieve Emily’s pain? A little harm, perhaps, no more than that.
This is what we see in the Gilbert case, the fusion of our lives with theirs in one grand and pathetic cliché in which all lives look pretty much alike. We go round and round with Gilbert: Gilbert suddenly wondering if Emily might get better, if one of those white-coated geniuses will come up with a cure. Gilbert realizing that once Emily is gone, he will go too, since her way of life, however wretched, was their way of life. He is afraid for them both. In The Merchant of Venice Portia says that mercy is “twice blessed;/ It blesses him that gives and him that takes.” The murder committed, Gilbert does not feel blessed. At best, he feels he did right, which the outer world agrees with and denies.
Laws are unlikely to be changed by such cases: for every modification one can think of, there are too many loopholes and snares. What Gilbert did in fact erodes the whole basis of law, which is to keep people humane and civilized. Yet Gilbert was humane, civilized and wrong: a riddle. In the end we want the law intact and Gilbert free, so that society wins on both counts. What the case proves, however, is that society is helpless to do anything for Gilbert, for Emily or for itself. All we can do is recognize a real tragedy when we see one, and wonder, perhaps, if one bright morning 1934 Gilbert read of a mercy killing in the papers, leaned earnestly across the breakfast table and told his new bride: “I couldn’t do that. I could never do that.” –By Roger Rosenblatt
More Must-Reads From TIME
- What Student Photojournalists Saw at the Campus Protests
- How Far Trump Would Go
- Why Maternity Care Is Underpaid
- Saving Seconds Is Better Than Hours
- Welcome to the Golden Age of Ryan Gosling
- Scientists Are Finding Out Just How Toxic Your Stuff Is
- The 100 Most Influential People of 2024
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

2.3: Euthanasia, or Mercy Killing (Nathan Nobis)
- Last updated
- Save as PDF
- Page ID 30133

- Golden West College via NGE Far Press
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
9 Euthanasia, or Mercy Killing Nathan Nobis 24
1. Introduction
Sadly, there are people in very bad medical conditions who want to die. They are in pain, they are suffering, and they no longer find their quality of life to be at an acceptable level anymore. Given all that, they want their lives to end: they want to be out of their misery. Some of these people are kept alive by machines or other medical treatments. If these machines were turned off or the medical interventions stopped, these people would die.
Can it be morally permissible , or not wrong , to turn off these machines or stop treatment and so let someone die, in circumstances like these? Many people think it can be. They believe that, morally, we do not have to do everything we can to keep someone alive, no matter their quality of life or what they want. Indeed, sometimes keeping someone alive, when they could be allowed to die, would be wrong: we really should just let them die.
Here I develop an argument for this view, that what’s usually called “passive euthanasia” can be morally permissible. More interestingly though, I explain how the reasons in favor of passive euthanasia suggest and support thinking that in some circumstances “active euthanasia” is justified, so it can be OK to actively kill some patients, for example, by giving them an overdose of drugs that will painlessly end their lives. So, I argue that if you think it can sometimes be OK and appropriate to let some patients die, then you should also think it can sometimes be OK and appropriate to actively kill some patients.
2. Definitions
Let’s begin with some definitions to better understand the issues.
First, our topic is euthanasia , which is sometimes called “mercy killing.” The word euthanasia relates to the idea of a “good death.” People typically seek euthanasia to avoid a very bad death full of agony, pain, and suffering and all that results from that: for example, people wracked with horrific pain might not be able to meaningfully experience their final days or weeks with loved ones, due to the constant agony: when you are in terrible pain, it’s hard to talk, and listen, and share.
The most common type of euthanasia involves someone euthanizing someone else. Another type involves someone performing euthanasia on themselves, or euthanizing themselves: this is a type of suicide.
Euthanasia is usually classified as three types: voluntary , non-voluntary and involuntary :
Here we will only discuss arguments about voluntary euthanasia, but readers can thoughtfully extend that discussion to the unique circumstances of non-voluntary euthanasia. Since involuntary euthanasia, passive or active, is generally wrong, it won’t be discussed further.
3. An Argument for Passive Euthanasia
‘No’ suggests that we must always do everything we can to keep someone alive, even if they are miserable, want to die, and say so. To many, that’s just cruel. If a dog or cat were in a similar condition, we would do the merciful and humane thing and put them out of their misery: this is perhaps the one way that animals are often treated better than humans.
The judgment that ‘yes, it can be OK to let someone die’ can be supported by both consequentialist (or utilitarian) and Kant-inspired moral reasoning. What Kant himself argued about these issues might be different from what’s argued here: Kant sometimes applied his own moral principles to practical issues in unconvincing ways.
For the consequentialist, the person being out of their misery is a better consequence for them, and overall, than their staying alive: killing them decreases the net unhappiness, pain, and badness in the world. For the Kantian, letting them die respects their autonomy (or personal self-governance): we should respect people’s decisions about profound issues in their own lives. Given their reasonable desires, respecting their wishes treats them as “end in themselves,” but forcing them to live in their unwanted condition treats them as a “mere means” toward our own ends, not their own.
‘Yes’ can also be supported by spelling out conditions in which it can be OK to let someone die. We begin with an ‘if’ and develop a moral principle:
If …
- someone is dying, and
- is in horrible pain and suffering, and
- that pain and suffering cannot be relieved, and
- that person wants to die and clearly says so, and
- informed, thoughtful and caring people agree that the person would be better off no longer living…,
then it can be permissible to let that person die.
To many people, a principle like this seems plausible. And it justifies passive euthanasia in many circumstances.
The details of a principle like this, however, take us to harder questions about euthanasia, harder than those that arise in most circumstances: for examples, what if someone wants to die now but isn’t currently in horrible pain and suffering, or is expecting to die, but many years later after a very slow decline? Should anyone else have “say” over your own life or judge whether some pain and suffering is “horrible enough” for you to reasonably wish to die? If so, who? What if someone isn’t dying and doesn’t even have a bad medical condition but just finds their life not worth living and so wants to die (and so, say, plans to starve themselves to death or do other things that will result in their death)? These harder questions, and others, would need to be addressed for a complete defense of this or similar principles and any arguments based on them.
In sum, a basic case for passive euthanasia can be supported by utilitarian, Kantian and common-sense moral thinking. Let’s consider two objections before moving on to the case for active euthanasia.
3.1. First, some claim that pain can always be controlled, and patients always kept comfortable, so there is never a need to let anyone die (or, of course, actively kill them).
In reply, medical professionals try their best to control pain and make patients comfortable and they often are effective. But the insistence that pain can always be made bearable for everyone is, unfortunately, not true: some patients’ pains cannot be controlled to their own satisfaction.
3.2. Second, some argue that “miracles” are always possible, so there’s always a chance that someone gets better and even survives, and so we shouldn’t let patients die.
These hopes are understandable, but there are conditions that nobody has ever recovered from, and so the chances are very slim. And we don’t usually make important decisions based on very unlikely chances: for example, you could be in an unlikely car accident where a seatbelt harms you, rather than helps you: nevertheless, wearing a seatbelt is the smart choice.
Also, no type of euthanasia, passive or active, would prevent a miracle, especially a genuine miracle involving divine intervention: turning off the machines could be the occasion for a miraculous recovery, and an overdose of painkillers could be miraculously transformed into life-saving medications. People hoping for a miracle shouldn’t forget what miracles really could be.
4. An Argument for Active Euthanasia
The basic argument for active euthanasia, that is, for intentionally killing people who, due to their medical conditions, wish to be killed and say so is fairly simple.
We begin by reflecting on the basic reasons why passive euthanasia can be OK: it gets people out their misery and respects what they want for their own lives. “Letting people die” is a means toward those ends or goals. However, these goals can be pursued more directly and immediately by actively killing patients who wish to die. Letting people die often takes a long time, and that time will often be filled with pain and suffering, which the patient wants to avoid. Killing people, when they want to be killed , achieves the goals that they want, that is, to be out of their misery, more quickly and with less pain. And that is what they want, so they get what they want, quicker.
So, the basic assumptions that less unwanted pain and suffering is typically better than more and people’s desires about profound matters affecting their own lives and deaths usually should be fulfilled sooner than later , and the fact that killing someone is often a more effective means towards those ends, justifies active euthanasia, at least in some circumstances.
5. Objections: Potentially Relevant Differences Between Active and Passive Euthanasia
There are many objections to this type of reasoning, all intended to explain why active euthanasia is wrong but passive euthanasia can be permissible. Let’s consider some of the most common.
5.1. First, some claim that it’s always wrong to intentionally kill someone, so passive euthanasia can be OK but active euthanasia is wrong.
In reply, while we should agree that it’s, at least, nearly always wrong to intentionally kill someone, we should observe that most people want to live and do not currently have lives full of pain, suffering, and misery. So, the rule against killing is good in general, but we can argue that there are justifiable exceptions to this rule and that euthanasia is one of them.
5.2. Second, some argue that allowing active euthanasia puts us on a “slippery slope” to murdering patients, and people in general, who are not in challenging medical circumstances or do not want to die. That’s wrong, so we shouldn’t allow euthanasia, which might lead to that.
In reply, we can rightly wonder why that would happen, since arguments for euthanasia are very specific on the conditions where it might be permissible. They are especially clear that if someone wants to live, they should not be euthanized.
5.3. Third, some argue there is always an important (moral) difference between “allowing” something to happen and “doing” something, and so passive euthanasia is OK but active is not.
We might wonder if there is a clear distinction here. Consider this example:
You see that someone is about to unknowingly walk and fall into a deep pit in the ground. You could easily warn them of the pit, but you keep quiet and they fall in and are seriously injured. You tell yourself that if you had pushed them into the pit, you’d be blameworthy, but since you have “done nothing” you are completely blameless.
Many would find this judgment unbelievable: you did do something: what you did was stay silent and not warn them of the pit. “Inaction” is itself an action: doing nothing is doing something . Furthermore, what you did (in “doing nothing”) was wrong. It would often be worse for you to push the person into the pit yourself (or maybe not?), but your letting them fall in was wrong: you partially caused their injury: had you acted differently, they wouldn’t have gotten hurt.
Examples like these suggest that there are not clear moral or conceptual differences between doing something and allowing something to happen . The objection above mistakenly assumes there are.
5.4. There’s an important (moral) difference between killing and letting die, and so passive euthanasia is OK but active is not.
This final objection is similar to the previous. James Rachels famously responds with an example like this:
An evil aunt will inherit lots of money if her five-year-old nephew dies. She plans to drown him in the bathtub and make it look like an accident. She will get away with it. He just started his bath and she’s on her way to the bathroom to drown him. She opens the bathroom door and is delighted to see that he has slipped in the bathtub and is drowning. She watches, ready to push him under if he steadies himself and is able to save his own life. But, as her luck would have it, he doesn’t and so he drowns. She never touches him throughout the ordeal and inherits the cash, never telling a soul what happened.
What an awful story. What an awful aunt. Her motives were awful and what she did was wrong. If she explained that she didn’t “do anything,” that she didn’t do anything wrong, that, at best, she merely “let someone die” – it’s not like she killed anyone! – she is profoundly mistaken: letting someone die can be just as bad (or nearly as bad) as killing someone. We might even say that a way to kill someone is to let them die.
The objection here depends on a clear moral distinction between killing and letting die. There is no such distinction.
5.5. Mistakes are possible, so we shouldn’t allow euthanasia.
A final objection is not to the ethics of euthanasia per se, but whether, as a social or legal policy, it should be allowed: it’s possible that we could think an action is, or can be, morally permissible, but that for various reasons, as society we shouldn’t allow it.
The concern is that where active euthanasia is allowed, some people who should not be killed could be killed. This is true: this is a possibility. It’s also true that where passive euthanasia is allowed, some people could be let die who should be kept alive. The argument is that since mistakes and wrongdoing regarding euthanasia are always possible, we should not allow it as a society. (This is consistent with thinking that euthanasia is sometimes morally permissible).
In reply, we cannot ignore the opposing truth that if euthanasia is not allowed, that would result in mistakes and wrongdoing also: people would be wrongly kept alive, and wrongly forced to endure more suffering than they can bear and their deepest desires for their own lives disrespected.
These possible mistakes, unlike the possible mistakes in allowing euthanasia, however, cannot be corrected or addressed by any safeguards or precautions, if euthanasia is not allowed. The wisest strategy then is to allow euthanasia, with limits and safeguards, and work to ensure that any mistakes and wrongdoing are minimized, and hopefully prevented completely.
6. Conclusions
There are, of course, more objections to these arguments, and other important arguments and concerns to discuss, and factual information to review, to have genuinely responsible views about these matters: this essay is just a start.
These issues of this essay are important and not just for people currently facing difficulties where euthanasia might be part of the response. These issues are important to all of us since we have no idea what will happen to us, and our loved ones, years down the road, tomorrow, or even later today: an accident or illness might befall us that forces us to ask and answer hard questions about whether our lives are still worth living. While we hope these questions aren’t forced on us, we should ask them now and work on answering them now, together and as individuals. Part of a good death is that it is an end of a good life, and an opportunity to begin a better life is always now.
James Rachels, “Active and Passive Euthanasia,” New England Journal of Medicine 1975; 292: 78-80.
For Further Reading
Young, Robert, “Voluntary Euthanasia”, The Stanford Encyclopedia of Philosophy (Spring 2019 Edition), Edward N. Zalta (ed.), forthcoming URL = < https://plato.stanford.edu/archives/spr2019/entries/euthanasia-voluntary/ >.
Cholbi, Michael, “Suicide”, The Stanford Encyclopedia of Philosophy (Fall 2017 Edition), Edward N. Zalta (ed.), URL = < https://plato.stanford.edu/archives/fall2017/entries/suicide/ >.
Woollard, Fiona and Howard-Snyder, Frances, “Doing vs. Allowing Harm”, The Stanford Encyclopedia of Philosophy (Winter 2016 Edition), Edward N. Zalta (ed.), URL = < https://plato.stanford.edu/archives/win2016/entries/doing-allowing/ >.
For Review and Discussion
1. What are the reasons someone might their life to end? Are those reasons strong enough to support their ending their life? Why or why not?
2. We regularly euthanize non-human animals, but euthanizing people is limited to certain countries (most notably The Netherlands). Is there a major difference between non-human animals and people that justifies our different use of euthanasia? Why or why not?
3. What is the strongest argument opposed to allowing active euthanasia? Is this argument stronger than the arguments in favor of active euthanasia? Why or why not?
mercy killing
Primary tabs.
A mercy killing is the intentional ending of life of a person who is suffering from a terminal, painful illness. The term–also called “right to die” –is most often used to describe voluntary euthanasia, though it is also used in reference to non-voluntary euthanasia and involuntary euthanasia.
Voluntary euthanasia is considered either passive or active. Passive voluntary euthanasia is when a person dies after refusing or withdrawing their consent for lifesaving medical intervention. This is legal in many countries, including the United States following Cruzan v. Missouri Department of Health , where the Supreme Court decided that a competent person had “ a constitutionally protected right to refuse lifesaving hydration and nutrion .” Active voluntary euthanasia, on the other hand, generally occurs when a person is administered large doses of painkilling medication. This term includes assisted suicide , where a patient is provided with the medication to end their own life. The term also includes physician assisted suicide , where a licensed medical professional administers the medication. Active voluntary euthanasia is legal in some countries, to some extent. These countries include Belgium , Canada , Colombia , Luxembourg , the Netherlands , Switzerland , and some states in Australia . In the United States, the Supreme Court refused to recognize active voluntary euthanasia as a Constitutional right in Washington v. Glucksberg . However, some states have recognized a right to active voluntary euthanasia through death with dignity statutes .
Non-voluntary euthanasia, on the other hand, involves a patient who is unable to consent to life-ending measures. Involuntary euthanasia involves a patient who does not or resists such measures. Both are illegal in all countries.
[Last updated in June of 2020 by the Wex Definitions Team ]
- ACADEMIC TOPICS
- law and medicine
- THE LEGAL PROCESS
- criminal law
- wex definitions
Mercy Killing: An Ethical Argument with Regards to the Future Term Paper
Mercy killing has been defined as the act of terminating life in a way that alleviates pain and suffering (Brill, 166). Over the years, the ethical nature of mercy killing has been largely debated.
Currently, only a few countries have legalized voluntary euthanasia. Although some people argue that mercy killing alleviates pain and is mainly a matter of choice for those requesting it, the act should be done away with since it demeans life. The future is built upon hope for better thing and mercy killing is in a form, the abandonment of hope. Mercy killing goes against all the principles of sustainability and as such should be done away with.
In order to form a valid argument it is important to understand the types of mercy killing. There are two types of mercy killing (euthanasia): Voluntary and involuntary euthanasia. Voluntary euthanasia is referred to as mercy killing by consent while involuntary occurs without the consent of the patient (Griffith and Tengnah. 356).
Under law, voluntary euthanasia is usually acceptable under certain conditions however this does not speak to the ethical nature of the act. Under close investigation, it can be proven that the act is highly unethical regardless of the type.
First, mercy killing highly depends on the mental competency of the patient. The mental competency of patients who have undergone years of pain and suffering is usually under question (Lesser, 331). Some of these patients may be under pressure from their caretakers to end their lives.
The pressure may be in the form of guilt whereby the patient feels that by committing suicide he or she may alleviate the suffering they are imposing on their love ones (Gill and Voss, 8). The act therefore may be not exclusively the wishes of the patient. Mercy killing opens pathways with which unscrupulous relatives and caregivers may put undue pressure on the patient to engage in the act.
While the patient may be able to provide the consent, the reasons behind it are questionable as they not only relate on their level of suffering or pain. Patients who are in comas may also be subject to mercy killing with the validation that they are in pain. However, it is impossible to say for certain that these patients actually feel pain and the degree of pain these patients feel. Mercy killing under this situation cannot be justified in any way.
Secondly, mercy killing might act as an obstacle to medical development due to reduced motivation. When the AIDS virus first appeared, many people thought that it was incurable. Those suffering from the virus were so scared of their impending doom that they opted for suicide. However, over the years, many medications have been developed that have made the disease manageable with patients living meaningful, long lives.
According to Brill (166), many physicians do agree that it is impossible to point out which diseases are incurable. By allowing mercy killing, people not only act impatiently but also impede the motivation behind the development of new cures and developments that may prolong life (Savage, 330). Technological development in the modern world takes place in a very fast pace.
It is impossible to say what will be developed tomorrow or the day after that may serve as a reprieve for patients from pain and suffering. Mercy killing does not focus on the future but rather on the present and mainly the past. How can something be termed as right if it negates the possibility for others to receive better treatment in the future? Regardless of personal feelings, society has a responsibility of preserving and maintaining life for as long as possible.
The invention of life support machines seeks to prolong life as long as possible while alternate cures or medical procedures are being investigated. By randomly killing those deem incurable or terminally ill, we also kill the motivation for the development of better medicines or procedures that may save people in the future or eliminate the sickness completely.
Mercy killing also promotes discrimination against those who are terminally ill and those with incurable illnesses. The government usually spends a lot of money caring for the terminally ill and those with incurable diseases. It is therefore advantageous for those who have been declared physically and mentally incurable to be allowed to die.
According to Savage (330), Mike Ervin a journalist with muscle dystrophy argued that although he requires 24 hour care every day, he is still a functioning member of society. He adds that mercy killing is demoralizing as it acts as a reminder of how the sick and those with disabilities are unwelcomed by the society.
Lesser points out that mercy killing may lead humanity to situation he terms as “the slippery slope” (332). He argues that mercy killing may be used as it was used in Nazi Germany to purify the race. If mercy killings for those who are terminally ill or with incurable diseases are allowed, who will stop the elimination of the old, mentally ill or criminally insane? Society has a lot of individuals who can be termed as socially unfit hence a liability to the society.
When mercy killing is accepted by the society, it is a matter of time before these social misfits are subjected to death under the guise of mercy killing. Those suffering from hunger and famine, unable to support themselves might soon find themselves being “put down” for their own good. The search for a pure race has always existed amongst society with people seeking for a disease free, intelligent and superior race (Lesser, 332). Mercy killing can thus serve as a starting point for the achievement of this dream in the future.
Finally, mercy killing also destroys the fabric of human civilization: the rule of law. Civilization was built upon sympathy and the respect of life. In the past, the sick and those afflicted with incurable diseases were left out to die. The rule of law was founded upon moral and ethical principles. By allowing mercy killing, however justified, the line between plain murder and “assisted” suicide can become blurred (Griffith and Tengnah, 356).
Many cases have been witnessed whereby the care takers take upon their own hands to terminate the lives of their patients. Savage (330) highlights a case where a mother shot her sons in the head as she believed that they were in too much suffering. By allowing mercy killings, cases like this can become very common. It is important to note that prolonged sickness makes it hard to distinguish who is suffering more, the caretakers or the patients themselves.
Under too much stress, the caregivers might misinterpret their own pain with that of their patients. Human beings are just evolved animals with the same urges of killing. Mercy killing may thus become a common defense against murder (Savage, 329). If voluntary mercy killing is allowed or justified by society, it can be used to take the lives of those who did not request it. Finally, people claim that everyone has a right to choose whether to live or die.
However, when the rights of one person infringe upon the rights of many, that right is negated under law. When mercy killing is allowed for one person, it may act as a precedence whereby others suffering from the same condition are persuaded to follow the same action (Brill, 166).
This is the same situation that takes place in mass suicide where people follow the teachings of one person believing it to be true and the only way. Society cannot take chance with mercy killing as the future of others depends on what is carried out by a few individuals.
Mercy killing has elicited a lot of debate on its ethical nature and legality. Some governments have allowed mercy killing on the condition that is voluntary.
However, it can be seen that mercy killing has to be stamped out completely in the world. If mercy killings are not eradicated, we might soon be living in a world whereby discrimination of the terminally ill or the disabled is rampart and the rule of law is twisted with murders being committed under the guise of mercy killings.
Developments in medicine can also be hampered living countless people suffering from conditions that could have been cured given more patience and dedication.
The main benefit of abolishing mercy killings is that life will always be valued by society. Nothing important happens when people are dead and it is only by preserving life that humanity develops and prospers. Pain and suffering is part of life, and while it is unfair for some to undergo extreme amount of these two, death can never be justified not when there are chances for a better tomorrow.
Works Cited
Brill, A. A. “Is ‘Mercy Killing’ Justified? With a Reply to Dr. Alexis Carrel,” Vital Speeches of the Day . Ed. Orgel, Samuel. New York: EBSCO publishing, 2003: 165-167
Gill, Carol and Larry Voss. “Views of Disabled People Regarding Legalized Assisted Suicide Before and After a Balanced Informational Presentation”. Journal of Disability Policy Studies 16.1 (2005): 6-15
Griffith, Richard and Cassam Tengnah. “Assisted Suicide: Increased Support for a Change in the Law.” British Journal of Community Nursing 14.8 (2010): 356-362
Lesser, Harry. “Should it be Legal to Assist Suicide?” Journal of Evaluation in Clinical Practice 16 (2010): 330-334
Savage, Teresa. “An Argument Against Mercy Killing: A response to Caitlin’s ‘Normalization, Chronic Sorrow and Murder’.” Pediatric Ethics, Issues, and Commentary 29.4 (2003): 329-330
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, September 13). Mercy Killing: An Ethical Argument with Regards to the Future. https://ivypanda.com/essays/mercy-killing-an-ethical-argument-with-regards-to-the-future/
"Mercy Killing: An Ethical Argument with Regards to the Future." IvyPanda , 13 Sept. 2018, ivypanda.com/essays/mercy-killing-an-ethical-argument-with-regards-to-the-future/.
IvyPanda . (2018) 'Mercy Killing: An Ethical Argument with Regards to the Future'. 13 September.
IvyPanda . 2018. "Mercy Killing: An Ethical Argument with Regards to the Future." September 13, 2018. https://ivypanda.com/essays/mercy-killing-an-ethical-argument-with-regards-to-the-future/.
1. IvyPanda . "Mercy Killing: An Ethical Argument with Regards to the Future." September 13, 2018. https://ivypanda.com/essays/mercy-killing-an-ethical-argument-with-regards-to-the-future/.
Bibliography
IvyPanda . "Mercy Killing: An Ethical Argument with Regards to the Future." September 13, 2018. https://ivypanda.com/essays/mercy-killing-an-ethical-argument-with-regards-to-the-future/.
- Euthanasia: Every For and Against
- Euthanasia: Moral Rationalist View
- A New Fight to Legalize Euthanasia
- Ethics in the Healthcare Delivery
- Medical Ethics: Arguments for Medical Dishonesty
- The Major Components of Bioethics in Healthcare
- Ethical and Legal Issues in Nursing Setting
- No More Abortion: Anti-Abortion Debate
Advertisement
Should Physician-Assisted Suicide or Euthanasia be Legalized in the United States? A Medically Informed Perspective
- IMPRESSIONISTIC REPORTING
- Published: 08 November 2023
- Volume 63 , pages 1058–1074, ( 2024 )
Cite this article

- W. Craig Fowler 1 , 2 &
- Harold G. Koenig ORCID: orcid.org/0000-0003-2573-6121 3 , 4 , 5 , 6
1880 Accesses
Explore all metrics
There is a pressing debate in the United States concerning the implied physicians’ obligation to do no harm and the status of legalizing physician-assisted suicide (PAS). Key issues that underpin the debate are important to consider. These include: (1) foundational medical beginnings; (2) euthanasia’s historical and legal background context; and (3) the key arguments held by those for and against legalization of PAS. This paper reviews the major claims made by proponents for the legalization of PAS and the associated complexities and concerns that help underscore the importance of conscience freedoms. Relief of suffering, respect for patient autonomy, and public policy arguments are discussed in these contexts. We argue here that the emphasis by healthcare providers should be on high quality and compassionate care for those at the end of life’s journey who are questioning whether to prematurely end their lives. If medicine loses its chief focus on the quality of caring—even when a cure is not possible—it betrays its objective and purpose. In this backdrop, legalization of PAS harms not only healthcare professionals, but also the medical profession’s mission itself. Medicine’s foundation is grounded in the concept of never intentionally to inflict harm. Inflicting death by any means is not professional or proper, and is not trustworthy medicine.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Alliance Vita.org. (2019). Euthanasia in the Netherlands: I.Summary II.Statistical Data III.Legislatioin IV.Large Number of Infringements Recorded V.Laxism of Oversight Bodies VI.Uneasiness from Medical Staff VII.Criticisms from Outside the Netherlands [Review]. Retrieved 3–13–23 from https://www.alliancevita.org/wp-content/uploads/2019/08/euthanasia-in-the-netherlands.pdf
American Academy of Medical Ethics. (2021). AAME Statement on Physician-Assisted Suicide (PAS) and Euthanasia Retrieved 3–13–23 from https://ethicalhealthcare.org/physician-assisted-suicide/
American Medical Association. (2021). Ethics: Physician-Assisted Suicide . AMA. Retrieved 3–13–23 from https://code-medical-ethics.ama-assn.org/ethics-opinions/physician-assisted-suicide
American Osteopathic Association. (2022). Policy Statement H346-A/17: Physician Assisted Death Retrieved 3–13–23 from http://policysearch.wpengine.com/wp-content/uploads/H346-A2017-PHYSICIAN-ASSISTED-DEATH.pdf
American Psychiatric Association (2023). What is depression? Retrieved on 7–22–23 from https://www.psychiatry.org/patients-families/depression/what-is-depression .
Ansseau, M., Dierick, M., Buntinkx, F., Cnockaert, P., De Smedt, J., Van Den Haute, M., & Vander Mijnsbrugge, D. (2004). High prevalence of mental disorders in primary care. Journal of Affective Disorders, 78 (1), 49–55. https://doi.org/10.1016/s0165-0327(02)00219-7
Article CAS PubMed Google Scholar
Aznar, J. (2021). Opinion of physicians and the general population on the legalization of euthanasia and assisted suicide. Cuadernos De Bioética, 32 (104), 23–36. https://doi.org/10.30444/cb.85
Article PubMed Google Scholar
Barsness, J. G., Regnier, C. R., Hook, C. C., & Mueller, P. S. (2020). US medical and surgical society position statements on physician-assisted suicide and euthanasia: A review. BMC Medical Ethics, 21 (1), 111. https://doi.org/10.1186/s12910-020-00556-5
Article PubMed PubMed Central Google Scholar
Beville, K. (2014). Dying to kill: a christian perspective on euthanasia and assisted suicide . Christian Publishing House.
Blackstone, E., & Youngner, S. J. (2018). When slippery slope arguments miss the mark: A lesson from one against physician-assisted death. Journal of Medical Ethics, 44 (10), 657–660. https://doi.org/10.1136/medethics-2018-104931
Boer, T. A. (2011). Euthanasia. In Green, J. B., Lapsley, J., Miles, R., & Verhey, A. (eds.), Dictionary of Scripture and ethics . Grand Rapids, MI: Baker Books.
Bollen, J. A. M., Ten Hoopen, R., van der Hoeven, M., Shaw, D., Brierley, J., Ysebaert, D., van Heurn, L. W. E., & van Mook, W. (2019). Organ donation after euthanasia in children: Belgian and Dutch perspectives. Archives of Disease in Childhood, 104 (9), 827–830. https://doi.org/10.1136/archdischild-2018-315560
Boudreau, J. D., & Somerville, M. (2014). Euthanasia and assisted suicide: A physician’s and ethicist’s perspectives. Medicolegal and Bioethics, 4 (1), 1–11. https://doi.org/10.2147/MB.S73197
Article Google Scholar
Bridge, J. A., Greenhouse, J. B., Ruch, D., Stevens, J., Ackerman, J., Sheftall, A. H., Horowitz, L. M., Kelleher, K. J., & Campo, J. V. (2020). Association between the release of netflix’s 13 reasons why and suicide rates in the united states: An interrupted time series analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 59 (2), 236–243. https://doi.org/10.1016/j.jaac.2019.04.020
Britannica (2022a). States with Legal Physician-Assisted Suicide. Britannica ProCon . Retrieved 3–13–23 from https://euthanasia.procon.org/states-with-legal-physician-assisted-suicide/
Britannica (2022b). Euthanasia & Physician-Assisted Suicide (PAS) around the World. Britannica ProCon . Retrieved 3–13–23 from https://euthanasia.procon.org/euthanasia-physician-assisted-suicide-pas-around-the-world/
British Medical Association. (2020). Get Informed Have Your Say: Physician-assisted dying 2020 BMA member survey [Information Pack]. Retrieved on 4–20–22 from https://www.bma.org.uk/media/2353/bma-physician-assisted-dying-info-pack-april-2020.pdf
Brown, P. J., Rutherford, B. R., Yaffe, K., Tandler, J. M., Ray, J. L., Pott, E., Chung, S., & Roose, S. P. (2016). The depressed frail phenotype: The clinical manifestation of increased biological aging. American Journal of Geriatric Psychiatry, 24 (11), 1084–1094. https://doi.org/10.1016/j.jagp.2016.06.005
CA (2023). CA to pay $300K for trying to force religious doctors to end patients' lives. Retrieved on 8–2–23 from https://adflegal.org/press-release/ca-pay-300k-trying-force-religious-doctors-end-patients-lives .
Caplan, A. L., & Curlin, F. A. (2017). Physician-Assisted Dying: The Antithesis of Medicine, Says Doc. Retrieved April 20, 2022, from https://www.medscape.com/viewarticle/874232
Chakraborty, R., El-Jawahri, A. R., Litzow, M. R., Syrjala, K. L., Parnes, A. D., & Hashmi, S. K. (2017). A systematic review of religious beliefs about major end-of-life issues in the five major world religions. Palliative & Supportive Care, 15 (5), 609–622. https://doi.org/10.1017/s1478951516001061
CMDA. (2022). Physician—Assisted Suicide. Standards 4 Life, A resource publication of Christian Medical & Dental Associations . https://cmda.org/standards-4-life/
CMDA. (2022). Right of Conscience. Standards 4 Life, A resource publication of Christian Medical & Dental Associations . https://cmda.org/standards-4-life/
Collett, T. S. (2004). Protecting the health care provider's right of conscience. Center for Bioethics and Human Dignity . http://www.cbhd.org/resources/healthcare/collett_2004-04-27
Dahlgren, J. (2015). [Christian doctors and medical students: The issue of freedom of conscience is far greater than the abortion issue]. Lakartidningen, 112 . (Kristna läkare och medicinstuderande:--Frågan om samvetsfrihet är långt större än abortfrågan.)
Dierickx, S., Deliens, L., Cohen, J., & Chambaere, K. (2015). Comparison of the Expression and Granting of Requests for Euthanasia in Belgium in 2007 vs 2013. JAMA Internal Medicine, 175 (10), 1703–1706. https://doi.org/10.1001/jamainternmed.2015.3982
Dugdale, L. S., & Callahan, D. (2017). Assisted death and the public good. Southern Medical Journal, 110 (9), 559–561. https://doi.org/10.14423/smj.0000000000000690
Dugdale, L. S., Lerner, B. H., & Callahan, D. (2019). Pros and cons of physician aid in dying. Yale Jounal of Biology and Medicine, 92 (4), 747–750. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6913818/
Google Scholar
Euthanasia. (2015). In Compton’s Encyclopedia . Compton’s Encyclopedia.
Fontalis, A., Prousali, E., & Kulkarni, K. (2018). Euthanasia and assisted dying: what is the current position and what are the key arguments informing the debate? Journal of the Royal Society of Medicine, 111 (11), 407–413. https://doi.org/10.1177/0141076818803452
Geisler, N. L. (2010). Christian ethics: Contemporary issues and options . Grand Rapids, MI: Baker Academic.
González, H. M., Vega, W. A., Williams, D. R., Tarraf, W., West, B. T., & Neighbors, H. W. (2010). Depression care in the United States: too little for too few. Archives of General Psychiatry, 67 (1), 37–46. https://doi.org/10.1001/archgenpsychiatry.2009.168
Grudem, W. (2018). Christian Ethics: An Introduction to Biblical Moral Reasoning . Crossway.
Ha, J., & Yang, H.-S. (2021). The Werther effect of celebrity suicides: Evidence from South Korea. PLoS ONE, 16 (4), e0249896–e0249896. https://doi.org/10.1371/journal.pone.0249896
Article CAS PubMed PubMed Central Google Scholar
Hagelin, J., Nilstun, T., Hau, J., & Carlsson, H. E. (2004). Surveys on attitudes towards legalisation of euthanasia: importance of question phrasing. Journal of Medical Ethics, 30 (6), 521–523. https://doi.org/10.1136/jme.2002.0025434
Humphry, D. (2011). Final Exit . Norris Lane Press/ERGO.
Jones, D. A., & Paton, D. (2015). How does legalization of physician-assisted suicide affect rates of suicide? Southern Medical Journal, 108 (10), 599–604. https://doi.org/10.14423/smj.0000000000000349
Khawaja, M., & Khawaja, A. (2021). The ethics of dying: deciphering pandemic-resultant pressures that influence elderly patients’ medical assistance in dying (MAiD) decisions. International Journal of Environmental Research and Public Health, 18 (16), 8819. https://doi.org/10.3390/ijerph18168819
Kheriaty, A. (2015). Social contagion effects of physician-assisted suicide: Commentary on “how does legalization of physician-assisted suicide affect rates of suicide?” Southern Meical Journal, 108 (10), 605–606. https://doi.org/10.14423/smj.0000000000000346
Kim, E., & Levy, R. J. (2020). The role of anaesthesiologists in lethal injection: a call to action. Lancet, 395 (10225), 749–754. https://doi.org/10.1016/s0140-6736(19)32986-1
Kirchhoffer, D. G., & Lui, C. W. (2021). Public reasoning about voluntary assisted dying: An analysis of submissions to the Queensland Parliament. Australia. Bioethics, 35 (1), 105–116. https://doi.org/10.1111/bioe.12777
Koenig, H. G. (1993). Legalizing physician-assisted suicide: Some thoughts and concerns. Journal of Family Practice, 37 (2), 171–179.
CAS PubMed Google Scholar
Kussmaul, W. G., 3rd. (2017). The slippery slope of legalization of physician-assisted suicide. Annals of Interal Medicine, 167 (8), 595–596. https://doi.org/10.7326/m17-2072
Lindblad, A., Löfmark, R., & Lynöe, N. (2009). Would physician-assisted suicide jeopardize trust in the medical services? An empirical study of attitudes among the general public in Sweden. Scandinavian Journal of Public Health, 37 (3), 260–264. https://doi.org/10.1177/1403494808098918
Lysaught, M. T., Kotva, J., Lammers, S. E., & Verhey, A. (2012). On Moral Medicine: Theological Perspectives on Medical Ethics . Wm. B. Eerdmans Publishing.
Magelssen, M., Supphellen, M., Nortvedt, P., & Materstvedt, L. J. (2016). Attitudes towards assisted dying are influenced by question wording and order: A survey experiment. BMC Medical Ethics, 17 (1), 24. https://doi.org/10.1186/s12910-016-0107-3
Manning, M. (1998). Euthanasia and Physician-Assisted Suicide : Killing or Caring? Paulist Press.
McCullough, L. B. (2018). Historical dictionary of medical ethics . Rowman & Littlefield.
Meilaender, G. (2020). Bioethics: A Primer for Christians (Fourth (Edition). William B. Eerdmans Publishing Company.
Miles, S. H. (2005). The Hippocratic Oath and the ethics of medicine . Oxford University Press.
Mitchell, A. J., Vaze, A., & Rao, S. (2009). Clinical diagnosis of depression in primary care: a meta-analysis. Lancet, 374 (9690), 609–619. https://doi.org/10.1016/s0140-6736(09)60879-5
Moreland, J.P., & Rae, S.B. (2000). Body & Soul: Human Nature & the Crisis in Ethics . Westmont, IL: IVP Academic.
Nath, U., Regnard, C., Lee, M., Lloyd, K. A., & Wiblin, L. (2021). Physician-assisted suicide and physician-assisted euthanasia: evidence from abroad and implications for UK neurologists. Practical Neurology, 21 (3), 205–211. https://doi.org/10.1136/practneurol-2020-002811
Nelson, T., & Anderson, J. K. (1997). Moral dilemmas . Nashville, Tennessee: Thomas Nelson.
Niederkrotenthaler, T., Braun, M., Pirkis, J., Till, B., Stack, S., Sinyor, M., Tran, U. S., Voracek, M., Cheng, Q., Arendt, F., Scherr, S., Yip, P. S. F., & Spittal, M. J. (2020). Association between suicide reporting in the media and suicide: systematic review and meta-analysis. British Medical Journal, 368 , m575. https://doi.org/10.1136/bmj.m575
Niederkrotenthaler, T., Kirchner, S., Till, B., Sinyor, M., Tran, U. S., Pirkis, J., & Spittal, M. J. (2021). Systematic review and meta-analyses of suicidal outcomes following fictional portrayals of suicide and suicide attempt in entertainment media. EClinicalMedicine, 36 , 100922–100922. https://doi.org/10.1016/j.eclinm.2021.100922
Oregon Public Health Division, C. F. H. S. (2022). Oregon Death with Dignity Act : 2021 Data Summary . Retrieved 3–13–23 from https://www.oregon.gov/oha/PH/PROVIDERPARTNERRESOURCES/EVALUATIONRESEARCH/DEATHWITHDIGNITYACT/Documents/year24.pdf
Pesut, B., Greig, M., Thorne, S., Storch, J., Burgess, M., Tishelman, C., Chambaere, K., & Janke, R. (2020). Nursing and euthanasia: A narrative review of the nursing ethics literature. Nursing Ethics, 27 (1), 152–167. https://doi.org/10.1177/0969733019845127
Pirkis, J., Blood, R. W., Beautrais, A., Burgess, P., & Skehans, J. (2006). Media guidelines on the reporting of suicide. Crisis, 27 (2), 82–87. https://doi.org/10.1027/0227-5910.27.2.82
Rae, S. B. (2009). Moral Choices: An Introduction To Ethics (Third (Edition). Zondervan.
Rajkumar, R. P. (2021). Physician-assisted suicide in dementia: Paradoxes, pitfalls and the need for prudence. Frontiers in Sociology, 6 , 815233. https://doi.org/10.3389/fsoc.2021.815233
Reidenberg, D., Niederkrotenthaler, T., Sinyor, M., Bridge, J. A., & Till, B. (2020). 13 Reasons why: The evidence is in and cannot be ignored. Journal of the American Academy of Child and Adolescent Psychiatry, 59 (9), 1016–1018. https://doi.org/10.1016/j.jaac.2020.01.019
Rosenstein, D. L. (2011). Depression and end-of-life care for patients with cancer. Dialogues in Clinical Neuroscience, 13 (1), 101–108. https://doi.org/10.31887/DCNS.2011.13.1/drosenstein
Sade, R. M., & Kavarana, M. N. (2017). Surgical ethics: today and tomorrow. Future Cardiology, 13 (6), 567–578. https://doi.org/10.2217/fca-2017-0057
SB 471 (2023). SB 471. Refusal of end-of-life options Act. Retrieved on 8–2–23 from https://nmlegis.gov/Legislation/Legislation?Chamber=S&LegType=B&LegNo=471&year=23 .
Schemmer, K. E. (2012). Tinkering With People: What You Need to Know About the Medical Ethics Crisis . Xulon Press.
Simpson, A. I. F. (2018). Medical assistance in dying and mental health: A legal, ethical, and clinical analysis. Canadian Journal of Psychiatry, 63 (2), 80–84. https://doi.org/10.1177/0706743717746662
Sulmasy, D. P., Finlay, I., Fitzgerald, F., Foley, K., Payne, R., & Siegler, M. (2018). Physician-assisted suicide: Why neutrality by organized medicine is neither neutral nor appropriate. Journal of General Internal Medicine, 33 (8), 1394–1399. https://doi.org/10.1007/s11606-018-4424-8
Sulmasy, D. P., Travaline, J. M., Mitchell, L. A., & Ely, E. W. (2016). Non-faith-based arguments against physician-assisted suicide and euthanasia. The Linacre Quarterly, 83 (3), 246–257. https://doi.org/10.1080/00243639.2016.1201375
Sulmasy, L. S., & Mueller, P. S. (2017). Ethics and the Legalization of Physician-Assisted Suicide: An American College of Physicians Position Paper. Annals of Internal Medicine, 167 (8), 576–578. https://doi.org/10.7326/m17-0938
Till, B., Strauss, M., Sonneck, G., & Niederkrotenthaler, T. (2015). Determining the effects of films with suicidal content: a laboratory experiment. British Journal of Psychiatry, 207 (1), 72–78. https://doi.org/10.1192/bjp.bp.114.152827
Tylee, A., & Gandhi, P. (2005). The importance of somatic symptoms in depression in primary care. Primary Care Companion to the Journal of Clinical Psychiatry, 7 (4), 167–176. https://doi.org/10.4088/pcc.v07n0405
World Medical Association. (2021). WMA declaration on euthanasia and physician-assisted suicide . World Medical Association. https://www.wma.net/policies-post/declaration-on-euthanasia-and-physician-assisted-suicide/
Zworth, M., Saleh, C., Ball, I., Kalles, G., Chkaroubo, A., Kekewich, M., Miller, P. Q., Dees, M., Frolic, A., & Oczkowski, S. (2020). Provision of medical assistance in dying: A scoping review. British Medical Journal Open, 10 (7), e036054. https://doi.org/10.1136/bmjopen-2019-036054
Download references
Acknowledgements
Both authors acknowledge that they are opposed to physician-assisted suicide (which some call voluntary euthanasia) and all other forms of euthanasia except certain forms of passive euthanasia, where the competent patient decides to refuses life-sustaining measures such as CPR, medication, food, and/or water at the end-of-life to hasten their death.
No funding has been received by either author to support the writing of this article.
Author information
Authors and affiliations.
Campbell University School of Osteopathic Medicine, Lillington, NC, USA
W. Craig Fowler
University of North Carolina School of Medicine, Chapel Hill, NC, USA
Department of Psychiatry, Duke University Medical Center, Box 3400, Durham, NC, 27710, USA
Harold G. Koenig
Department of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
Ningxia Medical University, Yinchuan, People’s Republic of China
Shiraz University of Medical Sciences, Shiraz, Iran
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Harold G. Koenig .
Ethics declarations
Competing interests.
The authors have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Fowler, W.C., Koenig, H.G. Should Physician-Assisted Suicide or Euthanasia be Legalized in the United States? A Medically Informed Perspective. J Relig Health 63 , 1058–1074 (2024). https://doi.org/10.1007/s10943-023-01939-9
Download citation
Accepted : 16 October 2023
Published : 08 November 2023
Issue Date : April 2024
DOI : https://doi.org/10.1007/s10943-023-01939-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Physician-assisted suicide
- Conscience freedoms
- Hippocratic Oath
- Palliative care
- Find a journal
- Publish with us
- Track your research

Do You Agree or Disagree With Euthanasia or Mercy Killing?
Euthanasia is the deliberate advancement of a person’s death for the benefit of that person. In most cases euthanasia is carried out because the person asks to die, but there are cases where a person can’t make such a request.
A person who undergoes euthanasia is usually terminally ill. Euthanasia can be carried out either by doing something, such as administering a lethal injection, or by not doing something necessary to keep the person alive (for example failing to keep their feeding tube going).
In my opinion it’s not moral to kill a person even if they are terminally ill because this person need a chance to live along and see his life, but there are people that disagree.
I have a debate in my college about this topic and I’d like to hear if you agree or disagree with euthanasia.
All the Yes points:
It frees up hospital beds and resources, it ends the patient life because he/she is already terminally ill, it relieves suffering, right to choose, relatives spared the agony of watching their loved ones deteriorate beyond recognition, it reduces the spread of diseases, the relationship between law and medical ethics, the ethical safeguards of pas, discrimination in palliative care and how pas can end it, how to save a life, all the no points:, it is not moral to end the patient’s life because he has the right to live longer, it is murder, sanctity of life, making the decision for yourself, or others, voluntary euthanasia gives doctors too much power, a lack of responsbility, the price they pay, the worst evil, yes because….
Terminally ill patients, or those in a permanent vegetative state, can take up valuable hospital beds for those who do want to get better. If they do not want to live, then they should not be allowed to take the beds and care of those that do. Long term palliative care for the terminally ill is a huge and ultimately wasteful drain on medical resources. Why waste these precious resources on someone who has expressed a desire to die, when they could be improving the life of someone who wants to live? In addition, these resources could be re-allocated to further the research of the specific disease the patient is suffering in order to allow future generations to either not have the disease or increase the quality level of care for future patients of this disease by alleviating the symptoms of the disease at the very least. In addition, if the patient is an organ donator and the organs are healthy, it may save up several lives which are ultimately invaluable. working in the care system with people with dementia i have to say in many cases its cruel to keep them alive, we are kinder to our pets when so ill. This is an awful disease which takes any quality of life away, One lady i know has been bed ridden for 5 years unable to communicate , move her limbs or anything if the nazis had done this to people it would be a war crime. This is not about god or any other belief its about common sense. Everyone should have the right to say while they are still of good mind if they get this or another illness at a certain stage they have their life ended, What i see every day is slow often distressing painful deaths which is no more than cruelty,we really have to change the way we think
No because…
Just because beds in hospitals are needed by others is no reason to allow a person to die! Some can be cared for at home, or in special hospices. If we stopped caring for the terminally ill at all where would we draw the line? Is treating the elderly also a waste of resources because they are nearing the end of their lives anyway? I think that to describe palliative care as a “huge and ultimately wasteful drain on medical resources” is rather harsh! I’m not sure that families of the terminally ill would agree with you there.
Terminally ill means terminally ill. This means that the patient, unless an absolute miracle happens, will die eventually regardless of how many interventions it takes to prolong his or her life expectancy. This time and money could be used to help others or cure others who aren’t mortally wounded or diseased. The rebuttal presupposes that an individual needs to wait for a hypothetical existence of a treatment being developed on an assumption that decisions that are finalized is not a justification for terminating a patient’s life at one’s explicit consent. If decisions made in your life were to be stagnated each and every time in order for an opportunity to arise everytime, the basis for this principle would not be a good one at the very least. Wait one day, wait one week, wait one month, we’ll stay back and see. An indecisiveness for something which might not exist within one’s lifetime would make a claim for which things ought to be reversible or decisions ought to be remade in order for things to be “controlled” in a manner. In this respect, of the practice of “Euthanasia”, death is the ultimate goal of avoidance and thus a finalized decision of upholding pain until the very last minute of life in respect to waiting for a treatment outweighs the ultimate outcome of death. The opposition makes a claim that reversibility of a decision that may be regretted later due to it being finalized is better on these grounds, however, if life was controllable in all aspects and under all possible circumstances, we were able to scroll back on our decisions, what meaningful would arise out of the circumstances for which our decisions are made on? What would the product of our actions, time and energy be? Aren’t these decisions philosophically what identify us as who we are even to the extent of a life or death situation? Also, even if a cure was possible, what complications will arise thereafter? What if the patient is of old age and will die anyways but has already lived a long healthy life? It cannot be justified to deem that waiting for something which might or might not exist in a future to occur outweighs the prospect of pain. Wait for a miracle “cure”, wait for a revolutionary science “discovery” to solve our problems, wait for a technological “innovation”…this line of thought may be wise in some situations but not necessarily in the case of Euthanasia.
The patient may be terminally ill but this statement aside from repeating other points discounts the possibility of new treatments being developed in time to cure the illness he or she is facing.
If a terminal patient faces a long, slow, painful death, surely it is much kinder to spare them this kind of suffering and allow them to end their life comfortably. Pain medications used to allieviate symptoms often have unpleasant side effects or may leave the patient in a state of sedation. It is not as if they are really ‘living’ during this time; they are merely waiting to die. They should have the right to avoid this kind of torturous existence and be allowed to die in a humane way. Appeal to “naturalism” is a very bad argument. We take medical pills, we put up an umbrella to avoid having rain fall on us, we try to not live in a tribal manner like our ancestors where we deem ourselves to live a civilized life where we do not simply kill eachother and rape eachother because its the “natural conclusion” of our actions. Suffering may a part of the human condition and it can be argued to be useful in preventing us from self-destructive habits, physical dismemberment or physiological damage due to negligence of the body, etc. However, does that justify that we ought to endure a pointless pain just because it must be part of life’s experience? Just because life is unfair doesn’t mean we should start treating others unfairly, or just because sex is a part of the human experience, that we have an obligation to perform intercourse. Also, if an argument of biological existence is made, then why is it limited to humans in the treatment of this manner? What is the difference between existence and living? Do people want to live in a state where they cannot progress, breathe, talk, hear, see, suffer from paralysis and slowly die? People do want to live, and merely existing is not enough. If we just had to exist, then why do we need a spectrum of other human experiences? Why do not we just limit ourselves to sleep, eat, reproduce, etc? There is more to life than existing in such a state.
There is a straight answer for this: Suffering is part of the human condition and part of life’s experience. Also medication can be improved to help a person’s quality of life and make their deaths as humane as possible. Futhermore even if a person is in a state of sedation they are still biologically existing and still have what some would say an obligation to live their life until its natural conclusion. i think that it is our fate and nothing happens in theis world just like that for no reason. Everything in this world happen for a reason that could be beneficial for that person but he or she may not realise it. You may say know that how if a person is suffering severly from ilness would that be a good thing for him or her ?? Bu toyu never know. I mean that i take as murder. We all say and agree that murder is something really bad and is not allowed so how come killing a person is the right thing?? Even if that person is suffering.What would you call it? Wouldn’t you call it killing. I will say that life is something complicated. It is not something that we could ever realise and understand 100 percent but each and every single person lives for a reason and when someone would die i definitly don’t have the choice to choose whether to kill that person or not even if he or she is suffering. Maybe yes a person would absolutely like to avoid suffering and have a relaxed life but sometimes and mostly always things don’t always turn out to be exactly like what we want. So I think it depends on how a person believes in God if he or she have faith in God then they will know that this is the will of God and will take it. We can’t say that there is a life with no suffering each and every person in his life have suffered in their life but it is how you deal with them that matters and not to run away because you’re afraid to face them or afraid that you would suffer because they alwaus say that you will always face your biggest fears in your life. So i would never kill a person and take the blame for it my entire life as i might someday sit alone and ask myself a question, did i kill my mother??
Our legal system accepts that people have a legal right to choose when to die, as demonstrated by the fact that suicide is legal. This right is denied to those who are incapable of taking their own lives unaided. Legalising euthanasia would redress this balance. Our legal system also recognises that assisting a suicide attempt is a crime. Human beings are independent biological entities, and as an adult, have the right to take and carry out decisions about themselves. A human being decides who they spend their life with, their career path, where they live, whether to bear children. So what is the harm in allowing a terminally ill patient to decide for themselves whether they die in a hospital or in their own home? Surely a terminally ill sufferer is better qualified to decide for themselves whether they are better off dead or alive? Their disease makes them so crippled they cannot commit suicide alone. A quote from The Independent in March 2002 stated that “So long as the patient is lucid, and his or her intent is clear beyond doubt, there need be no further questions” [[ The Independent” Editiorial Make euthansia available for those who can choose it http://www.independent.co.uk/opinion/leading-articles/make-euthanasia-available-for-those-who-can-choose-it-653034.html Accessed 03.09]]. Human beings should be as free as possible and unnecessary restraints on human rights are strongly discouraged. The opposition makes an arguement of inclination. However, it ought to be rejected that people, intuitions or legal entities should advocate the death of an individual. The life an individual rests in the considerations of the consequences of an individual’s actions. If we deny them this right, we make a claim that we own their life. We own the product of their time, energy and utility. This is something we must never fall into. Although it may be said from a financial sense, things aren’t good; we do attempt to put human life in an invaluable scale. It may be said that human beings are precious for various reasons, but the value of an individual’s life can never be determined by the state, another individual or entity. Even though life insurances are in place, the individual’s self-assigned worth is what gives the individual its own worth for its very own existence.
The right to choose is not something which our legal system has “accepted” we all have. This is far from the truth. Suicide was decriminalised in the UK solely for the reason that it is not a punishable offence – it is of course impossible to punish a dead person. This is by no means a reflection of the general opinion of society. Furthermore the European Court of Human Rights ruled in the case of Diane Pretty that a person does not has a recognised right to die as stated in this quote: “No right to die, whether at the hands of a third person or with the assistance of a public authority could be derived.” [[ BBC Online News “British woman denied right to die” http://news.bbc.co.uk/1/hi/health/1957396.stm%5D%5D Unfortunately giving any sort of ‘right to chose’ also denies a right to choose for others. If Euthanasia is allowed then people who are terminally ill, critically injured or simply old may well feel compelled to choose and option they don’t really want to take. If Euthanasia is allowed in some cases these people whose treatment may be costing relatives or the state a lot of money may well feel that they are not worth the cost of keeping them alive. This is not something we would want anyone to feel as in essence it takes away their freedom of choice on the matter.
A person dying from cancer feels weak; exhausted and loses the will to fight. Muscles waste away, appearance changes and the patient starts to look older. A cancer patient becomes confused, no longer recognising family and friends. Motor neurone disease causes the sufferer to lose mobility in the limbs, having difficulty with speech, swallowing and breathing. Those suffering with Huntington’s Disease develop symptoms of dementia, such as loss of rational thought and poor concentration. Involuntary movements, difficulties with speaking and swallowing, weight loss, depression and anxiety may also occur. Families of individuals suffering with such diseases see their bright, happy relative reduced to a shadow of their former self. Their loved one suffers a slow and painful death. Surely, it is kinder to put a mother, father, brother or sister out of their misery and allow them to die a peaceful death, as is their last wish.
Even if their relatives may be suffering from watching their loved one’s condition detiriorate, they have no right to either decide or put pressure on a person to end their own life because of their own sufffering. Just as it may be the individuals right to die it is also the right of the individuals right to “rage against the dieing of the light” with their support of their family so to speak. While it may be an ‘agony to watch a loved one deteriorate’ many will also want to spend as long as possible with their loved ones, and more than likely a family will be split on the matter meaning that the views of the family would have to have no impact on the matter.
When a person is sick, there a chance that a contagious agent exists within the host. The longer the duration that the individual is kept alive, it may increase the risk of others being affected by the disease if the individual is not handled properly.
isn’t that what a hospital has i mean many people are sick and have diseases which are contagious but they try to get cured that’s why they go to hospitals. This is not a reason for not keeping them alive because what if they actually get cured and got the chance to start a new life. I don’t think that it will REDUCE the spread of diseases becasue there are other people in the hospital that may suffer from different diseases which may be contagious right? so does it stop on terminally ill people that they have a contagious disease that’s why they should be killed??
At the core of a legalized physician assisted suicide (PAS) system is the principal that medical ethics should be governed and regulated by the professionals instead of lawmakers. A PAS system puts the expertise of the doctor and the experience of the patient at the forefront of the issue and views both perspectives rightly as the most credible in a given situation. The law cannot adapt to the specificity and multitude of ethical problems that arise on a situational basis. The law can only take into account circumstances that it foresees and can elaborate on. The highly personal and situational nature of this issue deems it insufficient for legislation, which exists outside the realm of the personal. The foundation of medical ethics relies upon the understanding of the consent (when applicable) of the patient to the procedure and the discretion, judgment, and experience of the medical profession to whom the patient has entrusted their care. The basis of good and ethical health and health systems relies upon the integrity of this. [[http://www.ur.umich.edu/9697/May20_97/artcl10.htm]]
Laws are codifications of what morals exist in a society. Side Opposition wonders how exactly ‘Medical Ethics’ would be defined in the status quo anywhere in the world if these things were not defined through the law. Furthermore, most nations have ways in which the law can in fact be changed, thus giving law the ability to adapt to the specificity and multitude of problems that do exist in regards to health care. Also, without the law then attempts to even test a society with PAS wouldn’t exists anyway. Simply put, the law is what safeguards patients, doctors, and everyone else in the medical field, anywhere. And still, any change in health care can directly affect not just what humans can do, but how humans think about being human (and, therefore, what rights and obligations humans should have). As issues of between medical ethics and the law come into play the importance of prudent use of law to protect health and safety becomes central. Finally, issues of social justice and resource allocation are presented more starkly in the medical care context than in any other context. [[http://academic.udayton.edu/health/syllabi/health/index.htm]]
To ensure that a system maintains the highest ethical standards, numerous safeguards will be implemented. To begin, The patient’s condition must be either a terminal one (meaning incurable) with no hope of recovery and death imminent (Two doctors must overlook the case to verify the diagnosis and prognosis) or suffering irreversible medical conditions that cause them suffering in ways they can no longer tolerate. Secondly, Euthanasia can only be undertaken at the request or with the permission of the patient (Oregon provides a good example by requiring two written requests at least 15 days apart, an oral request and other safeguards to ensure the capability of the patient to make such a serious decision. Also, two doctors must verify the decision-making capability of the patient.) Lastly, Doctors must perform the task of providing means and administering but only if necessary, otherwise the patient will self-administer. [[http://www.oregon.gov/DHS/ph/pas/docs/year1.pdf]]
In the medical profession, there is an unavoidable problem dealing with the prognosis of ‘terminal’ patients. Many problems arise when physicians try to diagnose a disease that will be terminal or try to recognize the terminal phases of an illness. For example, a person who has recently been infected with HIV can be considered to have a condition that will be terminal, yet 10% to 17% of such persons are still without sequelae of immunodeficiency at 20 years. Cardiac disease is the leading cause of death in the United States [34], but persons with atherosclerotic disease are not considered to be terminally ill even though their deaths may occur at any moment. This has much to do with why PAS is very hard to implement. These definitions will differ not just in the US, but in other nations around the world. At the point we recognize this to be true, proposition would be granting the right to PAS for some people, and yet not for others. This is why we look to palliative care, because, at the very least, the standards are clear. [[http://www.annals.org/cgi/content/full/126/2/146]] Furthermore, we say that patients who are terminally ill may have a single disease process (such as a brain tumor) that will, in and of itself, cause death; they may have a disease (such as leukemia) that weakens them to the point where a second condition (such as pneumonia) may overwhelm and kill them; or they may have a combination of diseases, each of which makes the other incurable (for example, severe lung disease and cardiac disease). The prognosis will alter as the patient makes decisions about treatment of the primary disease or intercurrent illnesses. But let’s talk about Oregon: In the first year Oregon voters put PAS into law, 15 patients had undergone PAS. However, only four of the candidates had psychological or psychiatric consultations. Eleven others did not. Since the way in which PAS has been provided in a current system has not been shown to be systematic, it has shown to not be fair either. Surgeons don’t operate without informing a patient of all their options, or doctors do not prescribe prescriptions without allowing for other options, yet PAS physicians have been able to let some patients undergo consulting while others don’t have as much help. Because of this, PAS is inherently unfair on the basis that some patients will have access to more knowledge than others – this is important because all patients are attempting to make the same choice.
Those who have terminal disease that are less common often face more suffering. Without the lobbies and charities behind diseases like lung cancer, brain cancer, etc., palliative care cannot provide the same Quality of Life that other better-funded palliative measures do. [“This study suggests that patients with end stage COPD have significantly impaired quality of life and emotional well being which may not be as well met as those of patients with lung cancer, nor do they receive holistic care appropriate to their needs.” Those in the third world are the most discriminated against in the area of palliative care. They are denied basic analgesics because of their economic situation. “Morphine is a cheap, safe analgesic, yet most patients in developing countries are denied access to this drug.” Palliative care is also weakened in the Third World by “the lack of effective models for…delivery.” The palliative care options are often limited to those available to the family. Though physicians may be available, long-term palliative care is often ineffective as the physicians must respond to a large area of need and the constant support is left up to the family of the patient, who are limited in resources and training. Minority groups are less likely to be given palliative care. Dalits, African Americans, and other minority groups are systemically given poor health care coverage and treatment. The result is that they face more emergency care rather than preventative and more inpatient non-palliative deaths. Without the option for PAS, minority groups often face alienated deaths in the institutions that have alienated them.In the case of the Roma people, both an ethnic and a lifestyle minority are discriminated against without access to PAS. Because of their nomadic way of life, the European healthcare system allows them to fall through the many cracks. When they plead for the right to die, they are denied PAS on “ethical” grounds. The European healthcare system, like many worldwide, is inherently biased to those who have a lifestyle of the majority, i.e. with a permanent residence. [[http://thorax.bmj.com/cgi/content/abstract/55/12/1000]] [[http://www.pubmedcentral.nih.gov/pagerender.fcgi?artid=1295230&pageindex=1]] [[http://www.pubmedcentral.nih.gov/pagerender.fcgi?artid=1295230&pageindex=2#page ]] [[http://www.dalitsolidarity.org/health_overview.php]] [[http://books.google.com/books?id=XKQ-OV72P7YC&lpg=PA153&ots=GyTOY7p0K8&dq=palliative%20care%20blacks&pg=PA153 ]] [[http://www2.warwick.ac.uk/newsandevents/pressreleases/system_frustrates_terminally/ ]]
A inequality in palliative care in places around the world is not enough to justify its circumvention. If anything, the option of PAS not only decreases the growth of the success some palliative care has been able to prevent, but it will prevent it’s growth in the future as well. Legalizing physician-assisted suicide is merely a part of the debate about improving end-of-life care. It cannot be viewed as a quick and easy fix, or a way to protect patients from inadequate care arrangements. Too many people still suffer needlessly, often because doctors and families just do not know how to serve people who are dying. The main problem lies with a lack of knowledge. Many suffer because doctors fail to provide adequate medication for pain. To legalize physician-assisted suicide would make real reform, such as better pain control, less likely. And ultimately hurts the growth of the medical industry. Without the reform of pain medication, patients end up with no prospects to live well while dying. In this scenario, making suicide an option is not offering a genuine choice but instead forcing a decision on the patient who again loses rights under this plan the affirmative have presented. [[http://www.growthhouse.org/mortals/mort2526.html]]
In addition, if there are those whose death is inevitable who would like to be put out of their suffering early, it means that doctors will have a chance to examine their vital organs to see if they can be donated. At later stages of many terminal illnesses, organs are severely weakened and, in some cases, failing – it may not be possible to use them at that point. This will help alleviate the long waiting list there is for organ donations. Thus permitting assisted suicide through euthanasia will not only put the victim out of his/her suffering earlier, but may also help save more lives. More than 102,389 men women and children are waiting for organ transplants in the US alone with only 14,203 eligible donors. PAS is an effective and ethical avenue to decrease this vast and fatal gap. [[http://www.lifelineofohio.org/donation/resources/statistics.aspx]]
Regardless of whether or not a patient decides to under PAS, they have already made the decision to be an organ donor, or not, well before the procedure. There has not been a correlation shown between the number of people willing to be an organ donor if they underwent PAS (From the Oregon studies). We would also say that a push for organs would decrease the amount of care given even with a PAS. Because now the focus is not on the patient but on their organs. In the status quo, people who are registered donors are at times kept on life support against (against their will, something we though, the proposition did not like) to determine the organs sustainability for transplant. Finally, if patients who have been cleared for PAS under the guidelines set out by the proposition, then they are already terminally ill, and thus, have failing organs already, not in good enough condition for transplant. [[http://www.washingtonpost.com/wp-dyn/content/article/2007/04/03/AR2007040302062.html]]
When Michelangelo was asked how he created his masterpiece David, he simply said “I saw David through the stone and I simply chipped away everything that was not David”. Since we on the proposition are on a similar pursuit as Michelangelo in creating a masterpiece, lets first look at what supporting physician-assisted suicide is not: 1) Supporting PAS is not supporting the end of palliative care. The opposition has stated time and time again how palliative care can be a good thing but just needs reform. This offers no direct clash with our plan and our line of argumentation throughout the entire debate. We recognize that palliative care as a viable option for patients, but we also have pointed out some of the pitfalls of palliative care and how PAS can be a benefit to those who have to suffer in these pits in some countries currently. Reform can be achieved in both PAS and palliative care under our plan. Fundamentally, we respect the preference of the patient to choose whichever option. The proposition is on the side of options and a death with dignity for citizens. We denounce the self-proclaiming moral arbiters that would force citizens to die only on the terms that they deem “natural” and “right” in the face of intense suffering and unbearable pain being felt by the patient. 2) Supporting PAS is not supporting the disproportional killing of coerced poor people and stigmatized groups. While this concern is certainly respectable, it is based simply on predicative fears. These fears have been discredited with the empirical evidence that we have provided from countries and states in which PAS is already supported. While we support these groups getting access to PAS, we certainly aren’t forcing them and neither is any outside party, as the data shows. 3) Supporting PAS is not supporting new cultural norms or ideologies that declare some lives are ‘not worth living’. What PAS promotes is that citizen’s are in control of the choice of how they want to end their lives. This idea finds opposition not in the prevailing attitudes of the people, but in the ideologies that someone or something should be in control other than the actual individual, whether it be the government, religion or someone’s definition of nature. It is time to break free from the shackles of these ideals into a world where citizens are individually empowered by supporting the right-to-die. Day by day more and more governments and citizens are recognizing this right and are strongly disavowing the antiquated positions that our opposition has argued for. Now that we have removed what supporting assisted suicide is not, let’s look at what it is: 1) Supporting PAS is supporting a system that addresses the highly personal and situational manner of this issue while enforcing ethical safeguards that protect against any form of abuse to the utmost degree possible. Both sides agree that laws can indeed change, but when should these laws should change is where the debate lies. We refuse to maintain archaic laws in which the consent of the patient and expertise of the doctor is largely ignored. We believe that to support PAS is supporting a flexible and ethical system that can address this complex situation with the patient and doctor in mind and at the forefront. 2) Supporting PAS is supporting the idea that it is the state’s role to create conditions where citizens can make optimal decisions for themselves amongst viable options. We do not support an atmosphere where the state destroys options and makes the decision for its citizens, especially on the most sacred thing a person has, life. 3) Supporting PAS is supporting a system that not only ends lives more humanely, but saves lives as well. We are not advocating a vast increase in quantity but rather a quality increase in organ donation. We have stated that if these terminally ill patients are forced to live prolonged lives, vital organs will become increasingly weaker even if the disease does not directly affect specific organs. The system allows organ donation to be completed more efficiently, effectively and even at all in some cases. The proposition offers quality of life over just mere quantity, choice on how to preserve this quality, and a way to preserve life of many people on organ donation waiting lists. We strongly believe we offer a far better system for these very reasons, masterpiece or not.
Patients that are in comas and have not indicated that they wish to die have the right to continue thier lives until the natural end. Who are we to say that they should die when it is convenient to us? That should be left unto God to decide. This point should be erased. The debate specifically says “Do you agree or disagree with euthanasia or mercy killing?”. What is being advocated is the right of an individual to make a decision, not to have a say or coerce an individual to make the decision to want to die. Although in some cases, involuntary euthanasia has a dark region (grey area).
Coma patients are not ‘living until their natural end’ because modern medicine has developed so we can support them artificially. Perhaps it was God’s will that they die, and we are interefering in this plan by treating them? This point should be erased. The debate specifically says “Do you agree or disagree with euthanasia or mercy killing?”. What is being advocated is the right of an individual to make a decision, not to have a say or coerce an individual to make the decision to want to die. Although in some cases, involuntary euthanasia has a dark region (grey area).
There are strong proponents on both sides of the debate for and against euthanasia. The word euthanasia comes from two Greek words, ôeuö meaning good, and thanatos meaning death. Proponents of euthanasia believe it is everyone’s right to die at a time of their own choosing, and in a manner of their own choosing, when faced with terminal illness rather than suffer through to the bitter end. Opponents argue that euthanasia cannot be a matter of self-determination and personal beliefs, because it is an act that requires two people to make it possible and a complicit society to make it acceptable . They consider euthanasia the equivalent of murder, which is against the law everywhere in civilized society.So, we sould maintain the respect for human life in a secular pluralistic society
The first argument was removed. An appeal to a dictionary or a definition does not make it right or justified in its position. However, it may be speculated or conceived that it is not murder because the premeditated advancement of death by a person of another has been consented to in principle thereby the choice being made is a deliberate one for which one’s right in its very own nature permits the condition to be moral. Secondly for describing euthansia the Germans use the term Sterbehilfe which means “help to die” so while the person and maybe society may be complicit in the “killing of a person” they are accessories and not the actual agents of the killing as they are helping a person to die rather than determining that a person should die, something that would be viewed as murder [[Collins lanugage dictionary]] .
Religious and secular morality decrees that no one has the right to take the life of another human being, A principle stated in the Quaran “[2.28] [Allah] will cause you to die and again bring you to life, then you shall be brought back to Him.” This surah states that if a creator has created an individual than it p.b.u.h will decide whether you live or die and you can not take matters into your own hands.[[ University of Michigan “The Koran” http://quod.lib.umich.edu/cgi/k/koran/koran-idx?type=simple&q1=life&q2=&q3=&amt=0&size=more%5D%5D . This principle must be safeguarded by law, as moral absolutes of this kind are necessary for a functioning legal system.
While religious morality may be precise on who sets decides when a person dies secular values also recognise if a person is suffering unncessarilly they should be helped to eliminate that suffering. Futhermore a person may well be non religious and resent the imposition of religious or secular values on them, values which they may not belive in. [[ Dr Adams “Personal Story- Dignity in Dying” http://www.dignityindying.org.uk/personal-stories/uk/south-west/exeter/dr-adams-story-33.html Accessed 1.06.2009]] Additionally if this arguement is extended, certain individuals pick and choose biblical scripture (not wiping out the land of a certainr ace) or selectively identify parts as something obselete (i.e. agricultural practices). If an individual does this, the individual believes that there is a morality outside of religious morality above the standard for which the biblical or context in which religion takes place and thus it is moot whether the bible says so or not.
The problem that I have always had with euthanasia is that terminally ill patients may choose to die through feelings of guilt. They may feel guilty about the burden that they are putting on their families and choose to die for this reason alone.
Whatever their reasons, a person should be allowed to do as they see fit. It is their life and they have the right to choose how and when it ends.
The prestigious position of doctors could quite easily be abused if euthanasia were to become legalised. A prime example of this would be the late Dr Harold Shipman, who killed between 215 and 260 elderly women[[ Bonnie Malkin et al ” Harold Shipman in dictionary of biography” http://www.telegraph.co.uk/news/uknews/1574271/Harold-Shipman-in-dictionary-of-biography.html Acccessed 01.06.09]] Vulnerable, ill people trust their doctor and if he confidently suggested a course of action, it could be hard to resist. A patient and his family would generally decide in favour of euthanasia according to the details fed to them by their doctor. These details may not even be well founded: diagnoses can be mistaken and new treatment developed which the doctor does not know about. Surely it is wrong to give one or two individuals the right to decide whether a patient should live or die? On the contrary, the majority of doctors would make well-informed, responsible and correct decisions, but for those few like Harold Shipman, they can get away with murder, undetected, for 23 years.[[ Bonnie Malkin et al ” Harold Shipman in dictionary of biography” http://www.telegraph.co.uk/news/uknews/1574271/Harold-Shipman-in-dictionary-of-biography.html Acccessed 01.06.09]]
Harold Shipman committed his crimes when euthanasia was illegal, which illustrates that psychopaths can commit crimes whatever the legal situation. Legalising euthanasia would have no effect on the 0.000001% of society who do this sort of thing. In countries where euthanasia is currently legal, such as Switzerland and the Netherlands, strict legal guidelines are in place to ensure that the process does not include such problems. All patients who request euthanasia require the diagnoses of at least two doctors to verify the terminal nature of their illness, and undergo psychological examination by these doctors and often other experts to examine the reasons for their choice. It is not a situation of “Surely it is wrong to give one or two individuals the right to decide whether a patient should live or die?”; it is one of two medical professionals deciding whether the legal parameters allow them to enact the patient’s wishes. [[ Dutch Ministry of Foreign Affairs”A Guide to the Dutch Termination of life on Request and Assisted Suicide (review procedures) Act – April 2002″ p3 http://www.minbuza.nl/binaries/en-pdf/faq-2008/faq-euthanasie-2008-en.pdf%5D Accessed on 01.06.09]] It is worth noting that, at the moment, doctors can effectively use euthanasia anyway. Firstly, under the “doctrine of double effect”, a doctor is allowed to give a patient, upon their request, a dose of painkilling medication which as a secondary effect speeds up the death of the patient. [[ Alison McIntyre “Doctrine of Double Effect” Stanford Encyclopaedia of Philosophy http://plato.stanford.edu/entries/double-effect/ Accessed 01.06.09 ]]Secondly, all patients have both the right to refuse treatment, and the ability to make a “living will”, which doctors are compelled to consider if the patient is unable to express their wishes during illness. [[ Direct gov “Government, citizens and rights- How to make a living will-http://www.direct.gov.uk/en/Governmentcitizensandrights/Death/Preparation/DG_10029429 01.06.09]]
Ethical safe-guards may not be achieved in the time frame allotted by the affirmative. Oregon physicians, as well as the physicians of Netherland, have been given authority without being in a position to exercise it responsibly. They are expected to inform patients that alternatives are possible without being required to be knowledgeable enough to present those alternatives in a meaningful way, or to consult with someone who is. Meaning that physicians or mental health professionals are advising patients without a complete understanding of end-of-life care available to them, which again goes against the Hippocratic Oath all medical personal must take. They are expected to make decisions about involuntariness without having to see those close to the patient who may be exerting a variety of pressures, from subtle to coercive. They are expected to do all of this without necessarily knowing the patient for longer than 15 days, which is clearly not long enough to fully gain perspective on a person. Since physicians cannot be held responsible for wrongful deaths if they have acted in good faith, substandard medical practice is encouraged, physicians are protected from the con-sequences, and patients are left unprotected while believing they have acquired a new right, and ultimately defeats the purpose of legalizing PAS. [[http://www.psychiatrictimes.com/display/article/10168/54071?pageNumber=5]]
We believe this Argument and the rebuttal for the proposition’s “Ethical Safeguards” argument can be clubbed together, and they have both been responded to together in “Rebuttal: Ethical Safeguards”
The opposition stands with critics of PAS who have found that once assisted suicide is accepted as an available option for competent terminally ill adults, it may be permitted for ever-larger groups of persons, including the non-terminally ill, those whose quality of life is perceived to be diminished by a physical disability, persons whose pain is emotional instead of physical, and so forth. Critics point to the fact that permitting euthanasia and assisted suicide, as is done in the Netherlands, does not prevent violation of procedures (e.g., failure to report) which occurs frequently in the medical profession, or abuse (e.g., involuntary euthanasia). It is further contended by the opposition that adequate safeguards are not possible. For example, requiring written requests to be repeated over a period of time, such as 15 days, and witnessed by two unrelated witnesses while simultaneously involving at least two physicians AND a psychiatrist’s or psychologist’s examination is unrealistic. Persons at the end of their lives typically have neither the energy nor the ability to meet such conditions. In addition, the option of assisted suicide for mentally competent, terminally ill people could give rise to a new cultural norm of an obligation to speed up the dying process and subtly or not-so-subtly influence end-of-life decisions of all sorts. Which ultimately costs the patient one of the three inalienable rights, the pursuit of Life. [[http://www.apa.org/pi/eol/arguments.html]]
1) Many people who choose PAS and are not terminally ill have a physical injury or disease attached to their emotional pain. For instance, Daniel James [[http://www.timesonline.co.uk/tol/news/uk/article4969423.ece]] was paralyzed from a rugby accident and Chantal Sebire [[http://uk.reuters.com/article/idUKL1918252520080319]] whom had a swollen tumor in her sinuses that made her face severely disfigured. These people felt like prisoners to their own existence, their quality of life was in fact diminished not “perceived”. We believe no person or government has a right to keep these people entangled in a web of suffering. We recognize that people can continue their lives even in dire situations, but we believe the government should not force them to continue a life of suffering. 2) The opposition says that a “violation of procedures” can occur, such as a failure to report. Unfortunately we do not live in a world where the medical practice can be absolutely infallible. This is more an argument against any sort of medical procedure, life saving or life ending because these problems are not unique to any medical procedure, whether it be perceived as simple or complex . Involuntary euthanasia is not a problem with our safeguards and able and competent doctors in place. Any doctor that would commit involuntary euthanasia with any form of consent from their patient would do so even without a legal PAS system because they have no regard for ethics. 3) Firstly, it seems the opposition is unclear as to why they object to the conditions that need to be fulfilled; because they are not stringent enough or because they are too stringent to be fulfilled by people who wish to exercise this right? We are not exactly sure how our safeguards can be deemed “not possible” and “unrealistic” when they are the same safeguards put in place in the state of Oregon, which we have already stated in our opening arguments.[[http://www.leg.state.or.us/ors/127.html]] This is not a chimerical proposition as the opposition has dismissed it as but in fact an actual and real life working system that has been around for 11 years. [[http://www.oregonlive.com/opinion/index.ssf/2008/09/washington_states_assistedsuic.html]] This system, under which in fact the right to physician assisted suicide has been exercised by hundreds of patients since the law was passed in Oregon. [[http://www.wrd.state.or.us/DHS/ph/pas/docs/year8.pdf]] 4) Rights do not demand to be exercised. We support the inalienable pursuit of Life but we do not support force-feeding life to citizens whom declare that they no longer want to participate in this pursuit for the ethically justifiable reasons stated in our case. We also grant citizen’s freedom of speech but does that mean they we should ban silence? Where governments allow dissent, it would be ludicrous to demand that all citizens must dissent in order to exercise their right. Instead, any theory of rights must protect the exercising of rights as well as the citizen’s choice to not participate, to not exercise their right. The right to life has to be forfeited at some point, and we support the right for our citizens to choose when they want to forfeit it. We see this in the status quo already – governments have ceased to consider suicide a crime. Why should assisted suicide for terminally ill patients be any different?
A patient may accurately judge their current quality of life to be unacceptable, but adequate care would always increase their quality of life to the point where they would reconsider. In addition, there is also fear that accepting such thoughts as legitimate, rather than simply understandable, could comfort an ideology that considers some lives as being ‘not worth living’, even if the person living this life sees value in it. PAS limits the view of the patient to a mere biological mass. Palliative care providers emphasize compassion, and the will to care for the whole human being. The importance of caring for the whole individual rather than for an organ is underlined, as is the importance of interactions between psychological and physical suffering. For both PAS and palliative care, the worst evil is a poor quality of life. For palliative care providers, however, the worst evil is a poor quality of life that is an obstacle to valuing the time that is left, rather than seeking to destroy the natural life-cycle. [[http://www.psychiatrictimes.com/display/article/10168/54071?pageNumber=5]]
1) Legalizing physician assisted suicide does not mean that it will be forced on all suffering patients. The proposition strongly feels about the freedom of choice, but the opposition would like to eliminate options and funnel suffering people down a path they feel is the right one. 2) The only ideology that this supports is that a citizen’s life and its value is actually in the hands of and defined by citizens instead of some separate entity. We don’t see any sort of logical connection with this slippery slope that they would like us to ride down. 3) We are not advocating an end to palliative care; we believe both systems can co-exist. What we recognize is that there are some huge pitfalls in palliative care (See: “Discrimination in Palliative Care and how PAS can end it” argument) and that PAS can fill these ethically and efficiently. Stating why palliative care may be a good thing doesn’t address why a PAS should not also be a viable option for patients. 4) We don’t believe that anything that is “natural” is always inherently good and anything that is unnatural is inherently bad, as it seems the opposition believes. If we are to agree with this line of argumentation then any sort of medication, treatment and surgery, such as chemotherapy, that can save lives should not be exist either because they also destroy this “natural life-cycle” that our opposition has defined for all of humanity. We don’t believe that they are as omniscient as they seem to think and feel that they are trespassing into very dangerous territory when they attempt to define just how people should die, and force conformation to that definition.
I really like this article as it gives the pros and cons of mercy killing. I will be referencing this article for a school paper I’m writing .
Who is the author?
Yes. Because It can Save Lives & Preserve the Dignified Orderb of International Health Among Others, Especially Our Own Children! My Mother Died of Both TuberCulosis & Liver Cirrhosis In Combination! She Spat Endless Blood & Making a Terrible Mess in My House & Disturbing All Neighbors & Relatives, With All the Expense On My Own Back ALONE! Since I Was Not Yet Married, but Planned To be ….It May Sound Selfish, but I Truly Value the Safety Of Both My Own Health & Of My Own Neighbors! Now Nobody Wants To Catch TB! So I Used An Injection with ****** (I Am Not Allowed to Post This For Security Purposes) To My own Mother, 7 She Then Died A Happy Quiet & Dignified Death! My Neighbors Did Not Like the & Approve the Idea, But I Must Strongly Approve that it Was THe BEST SECURITY MEASUR OF DEFENSE FOR OWN HEALTH`S SAKE! In Order Not to Be CONTAMINATED From the Disease! Since Additionaly * WE LIVED IN A RUARAL PROVINCE & DID NOT HAVE ANY DOCTORS OR HOSPITALS NEARBY AT ALL!
It should be allowed. Everyone has a right to die.
How can we allow a person to suffer immense pain, and agony; to live each bit of his life cursing his fate? Why is it said that they have to suffer it all?????
In this I really disagree because life is one of the best things that God created.He created us to his image and likeness and in this it’s is a wonderful gift from God.We must thank God for this very wonderful and Beutiful Gift that he has given to us…Thank you very much God
you spelt beautiful wrong.
Give me proof that God exists
Ok tell me how can everything can everything come to being without any creator
As we have no right to choose our birth ,so is our death also the matter of obligation?!I believe that depending on the patient’s illness & age, he has the right to choose, life or death?! It’s so personal.Why should he tolerate pain and suffer?! Just to live a few more days or months. So what?!!!
Surely anyone with compassion who has watched the agony of a friend or relative dying in front of them, sometimes over many days or weeks would agree with euthanasia?? After all, it is usually only the difference between a few more mls of morphine!!! We only keep people in a “liveable” state (called palliative care!) with morphine and having watched my own mother trying to die over this past week I have nothing but contempt for people who are insistent it should be God’s will or the person should keep going until the very bitter end. Shame on you! You obviously enjoy watching someone suffer. I would not and never have allow any animal I have owned to suffer this fate.
I take care of my dad who has an end stage type of dementia. He can’t walk. He can’t talk. He can hardly keep his eyes open to see anymore. He might be living with just dementia, bit I’m living in a never-ending nightmare of taking care of someone that doesn’t know who I am. I don’t love this but because someone says euthanasia is illegal, i am living in slavery. Why is it ok for me to end the suffering of a pet bit I have to suffer and let my father suffer. Maybe drugs will ease his pain but is quality of life just living without pain? He can’t do anything meaningful and he doesn’t remember anything he does anyway. This is bullshit, the longer I deal with him, smothering him with a pillow seems more and more tempting. Then you can all complaint about my quality of life as I live rent free with free food in a prison cell that is being paid for with your tax dollars.
My husband and I talked alot about end of life when he was diagbnosed with Frontal Temporal Disease, from a mutation in the gene that resulted in 2 of his syblings dying from ALS. More research indicated that there had been 7 generations of the diease in his family. As we prepared our legal and financial documents and our living wills, he did not want to be kept alive by any means if he could not care for himself and he never wanted to be in a nursing home. He wanted to die quickly. Unfortunately he was healthy and strong but with a brain that was detiorating very quickly to the point where I could not care for him at home alone or with help since I was physically challenged myself. Most of the time his brain was not focused and communications was non existent; however there were occassions where he would plead for his life to be over. As he lost more of his physical abilities and his ability to walk and talk and his body was forgetting how to swallow you could see the pleading in his eyes. I know this is not how he wants his life to end but there are no options but to sit and watch him wadte away. This is just not right for someone who wants the optopn to end their life!
I think mercy killing should be allowed in my country. Having 2 alzheimer’s patients in hands is not easy. The symptoms are getting worse day by day. No medication can cure alzheimer’s nor at least stop it. We have to spend about 1 million per year for medication, and we dont take them to a nursing home. One is bedridden, cannot talk, and needs to be feeded. Another poops on the stairs or in front of the house. In this case, I would consider euthanasia as a good choice. You know, it does not mean we dont love the two of our family, but they will live in this world and can do nothing to make themselves happy. They cannot even remember themselves or what they just did 5 mins ago! Do you see any good on spending 1 million a year on this incurble disease? Or we pay just to keep them with us?
When there is nothing more to live for, physician assisted suicide should be allowed. What is the big deal? It is as simple as that. It is a solution not a problem.
I just think that they or their close family/close friends should have proof as to prevent any killings that were not wanted by the patient and his or her’s family/close friends.
Whether you agree or disagree, it doesn’t matter. People will take their own life with or without help. Let common sense prevail. We should not judge others people’s right to choose. Do we not allow women to choose to abort or not? It is the same thing. A life is a life, we can’t have it both ways and we must be consistent.
We accept mercy killing for animals but we do not care of the suffering and economic disaster of not allowing people to terminate his/her life
let others die in your hands not with your hands
thanks for the details
In Natures Law nothing is good or evil, it is how we interpret the situation. Euthanasia is just another part of natural occurring which happens to all sort of living beings. Just because we humans interpret it differently doesn’t mean such occurring shouldn’t happen.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
UPSC Coaching, Study Materials, and Mock Exams
Enroll in ClearIAS UPSC Coaching Join Now Log In
Call us: +91-9605741000
Euthanasia – Arguments in Favour and Against
Last updated on April 7, 2024 by ClearIAS Team
Euthanasia is the deliberate act of ending a person’s life to relieve them of suffering. It is a complex and ethically sensitive topic that has sparked debates and discussions worldwide. There are different forms of euthanasia, and it is regulated differently in various countries.
Euthanasia (“good death”) is the practice of intentionally ending a life to relieve pain and suffering. It is also known as ‘mercy killing’.
In many countries, there is a divisive public controversy over the moral, ethical, and legal issues of euthanasia. Euthanasia is categorized in different ways, which include voluntary, non-voluntary, or involuntary. Euthanasia is also classified into active and passive Euthanasia.
Table of Contents
Voluntary, Non-Voluntary, and Involuntary Euthanasia
- Voluntary euthanasia: It is conducted with the consent of the patient and is termed voluntary euthanasia. Voluntary euthanasia is legal in some countries. Jurisdictions, where euthanasia is legal, include the Netherlands, Colombia, Belgium, and Luxembourg.
- Non-Voluntary euthanasia: It is conducted where the consent of the patient is unavailable and is termed non-voluntary euthanasia. Non-voluntary euthanasia is illegal in all countries. Examples include child euthanasia, which is illegal worldwide but decriminalized under certain specific circumstances in the Netherlands under the Groningen Protocol.
- Involuntary euthanasia: It is conducted against the will of the patient and is termed involuntary euthanasia. Involuntary euthanasia is usually considered murder.
Passive vs Active euthanasia
Voluntary, non-voluntary, and involuntary euthanasia can all be further divided into passive or active variants.
- Passive euthanasia entails the withholding of common treatments, such as antibiotics, necessary for the continuance of life.
- Active euthanasia entails the use of lethal substances or forces, such as administering a lethal injection, to kill and is the most controversial means.
Euthanasia debate
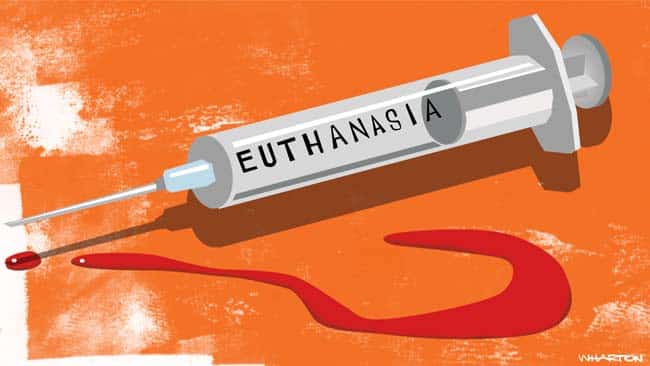
Euthanasia raises profound ethical and moral questions. Supporters argue that it can be a compassionate and dignified way to end suffering, particularly in cases of terminal illness.
Add IAS, IPS, or IFS to Your Name!
Your Effort. Our Expertise.
Join ClearIAS
Opponents argue that it raises significant ethical concerns, including the potential for abuse, coercion, and mistakes in diagnosing terminal conditions.
Arguments in Favor
Historically, the euthanasia debate has tended to focus on several key concerns. According to euthanasia opponent Ezekiel Emanuel, proponents of euthanasia have presented four main arguments:
- that people have a right to self-determination, and thus should be allowed to choose their fate
- assisting a subject to die might be a better choice than requiring that they continue to suffer
- the distinction between passive euthanasia, which is often permitted, and active euthanasia, which is not substantive (or that the underlying principle–the doctrine of double effect–is unreasonable or unsound);
- permitting euthanasia will not necessarily lead to unacceptable consequences. Pro-euthanasia activists often point to countries like the Netherlands and Belgium, and states like Oregon, where euthanasia has been legalized, to argue that it is mostly unproblematic.
- Constitution of India: ‘Right to life’ is a natural right embodied in Article 21 but euthanasia/suicide is an unnatural termination or extinction of life and, therefore, incompatible and inconsistent with the concept of ‘right to life’. The State must protect life and the physician’s duty to provide care and not to harm patients. Supreme Court in Gian Kaur Case 1996 has held that the right to life under Article 21 does not include the right to die.
- Caregiver’s burden: Right-to-die supporters argue that people who have an incurable, degenerative, disabling, or debilitating condition should be allowed to die in dignity. This argument is further defended by those, who have chronic debilitating illness even though it is not terminal such as severe mental illness. The majority of such petitions are filed by the sufferers or family members or their caretakers. The caregiver’s burden is huge and cuts across various financial, emotional, time, physical, mental, and social domains.
- Refusing care: The right to refuse medical treatment is well recognized in law, including medical treatment that sustains or prolongs life. For example, a patient suffering from blood cancer can refuse treatment or deny feeds through a nasogastric tube. Recognition of the right to refuse treatment gives way to passive euthanasia.
- Encouraging organ transplantation: Mercy killing in terminally ill patients provides an opportunity to advocate for organ donation. This, in turn, will help many patients with organ failure waiting for transplantation. Not only does euthanasia give the ‘Right to die‘ for the terminally ill, but also the ‘Right to life‘ for the organ needy patients.
Arguments against
Emanuel argues that there are four major arguments presented by opponents of euthanasia:
- not all deaths are painful;
- alternatives, such as cessation of active treatment, combined with the use of effective pain relief, are available;
- the distinction between active and passive euthanasia is morally significant; and
- legalizing euthanasia will place society on a slippery slope, which will lead to unacceptable consequences
- Euthanasia weakens society’s respect for the sanctity of life.
- Euthanasia might not be in a person’s best interests, for example, getting old-aged parents killed for property will.
- Belief in God’s miracle of curing the terminally ill.
- The prospect of a discovery of a possible cure for the disease shortly.
- Proper palliative care makes euthanasia unnecessary.
- There is no way of properly regulating euthanasia.
- Allowing euthanasia will lead to less good care for the terminally ill.
- Allowing euthanasia undermines the commitment of doctors and nurses to save lives.
- Euthanasia may become a cost-effective way to treat the terminally ill.
- Allowing euthanasia will discourage the search for new cures and treatments for the terminally ill.
- Euthanasia gives too much power to doctors.
Euthanasia in India
Passive euthanasia is legal in India. On 7 March 2011, the Supreme Court of India legalized passive euthanasia using the withdrawal of life support to patients in a permanent vegetative state. The decision was made as part of the verdict in a case involving Aruna Shanbaug, who had been in a Persistent Vegetative State (PVS) for 42 years until she died in 2015.
The Aruna Shanbaug Case
In March 2011, the Supreme Court of India passed a historic judgment permitting Passive Euthanasia in the country. This judgment was passed after Pinki Virani’s plea to the highest court in December 2009 under the Constitutional provision of “Next Friend”. It’s a landmark law which places the power of choice in the hands of the individual, over government, medical or religious control which sees all suffering as “destiny”. The Supreme Court specified two irreversible conditions to permit Passive Euthanasia Law in its 2011 Law:
- The brain-dead for whom the ventilator can be switched off.
- Those in a Persistent Vegetative State (PVS) for whom the feed can be tapered out and pain-managing palliatives be added, according to laid-down international specifications.
The same judgment law also asked for the scrapping of 309 , the code that penalizes those who survive suicide attempts. In December 2014, the Government of India declared its intention.
UPSC Prelims Test Series 2024
Take All-India Mock Exams: Analyse Your Progress!
PIL filed by Common Cause
However, on 25 February 2014, a three-judge bench of the Supreme Court of India termed the judgment in the Aruna Shanbaug case to be ‘inconsistent in itself’ and referred the issue of euthanasia to its five-judge Constitution bench on a PIL filed by Common Cause , which case is the basis of the current debate.
Then, the CJI referred to an earlier Constitution Bench judgment which, in the Gian Kaur case , “did not express any binding view on the subject of euthanasia; rather it reiterated that the legislature would be the appropriate authority to bring change.” Though that judgment said the right to live with dignity under Article 21 was inclusive of the right to die with dignity, it did not conclude the validity of euthanasia, be it active or passive.
“So, the only judgment that holds the field about euthanasia in India is the ruling in the Aruna Shanbaug case, which upholds the validity of passive euthanasia and lays down an elaborate procedure for executing the same on the wrong premise that the Constitution Bench in Gian Kaur had upheld the same,” the CJI said.
Common Cause Case: In 2018, the Supreme Court issued a significant judgment in the Common Cause case. The court recognized the right to die with dignity as a fundamental right and permitted passive euthanasia. It provided guidelines for the process and conditions under which passive euthanasia could be allowed.
Government’s endorsement of Passive Euthanasia
On December 23, 2014, the Government of India endorsed and re-validated the Passive Euthanasia judgment law in a Press Release, after stating in the Rajya Sabha as follows: The Hon’ble Supreme Court of India, while dismissing the plea for mercy killing in a particular case, laid down comprehensive guidelines to process cases relating to passive euthanasia.
Thereafter, the matter of mercy killing was examined in consultation with the Ministry of Law and Justice and it has been decided that since the Hon’ble Supreme Court has already laid down the guidelines, these should be followed and treated as law in such cases. At present, there is no legislation on this subject and the judgment of the Hon’ble Supreme Court is binding on all.
The court rejected active euthanasia using lethal injection. In the absence of a law regulating euthanasia in India, the court stated that its decision becomes the law of the land until the Indian parliament enacts a suitable law. Active euthanasia, including the administration of lethal compounds to end life, is still illegal in India, and in most countries.
As India had no law about euthanasia, the Supreme Court’s guidelines are law until and unless Parliament passes legislation. The following guidelines were laid down:
- A decision has to be taken to discontinue life support either by the parents the spouse or other close relatives, or in the absence of any of them, such a decision can be taken even by a person or a body of persons acting as a next friend. It can also be taken by the doctors attending the patient. However, the decision should be taken bona fide in the best interest of the patient.
- Even if a decision is taken by the near relatives or doctors or next friend to withdraw life support, such a decision requires approval from the High Court concerned.
- When such an application is filled, the Chief Justice of the High Court should forthwith constitute a Bench of at least two Judges who should decide whether to approve or not. A committee of three reputed doctors to be nominated by the Bench, will report the condition of the patient. Before giving the verdict, a notice regarding the report should be given to the close relatives and the State. After hearing the parties, the High Court can give its verdict.
A law commission had proposed legislation on “passive euthanasia”, it said. According to the Centre, the decision to come out with a bill was taken after considering the directives of the apex court, the law commission’s 241st report, and a private member bill introduced in Parliament in 2014.
The Centre said that initially, a meeting was held under the chairmanship of B.P. Sharma, secretary in the Health and Family Welfare Ministry, on May 22, 2015, to examine the draft of The Medical Treatment of Terminally Ill Patients (Protection of Patients and Medical Practitioners) Bill and the draft of The Euthanasia (Regulation) Bill.
This move to introduce a bill is a welcome step to clear the grey areas in the Euthanasia debate. Students can also link to this issue while answering questions on:
- Judicial activism: SC framing laws when the parliament hasn’t. Just like the Visaka case.
- Ethical dilemma in Paper 4 .
In India, euthanasia has no legal aspect , and there is no penal law yet introduced in the IPC that specifically deals with euthanasia.
- However, the Supreme Court of India legalized passive euthanasia in 2018 with some conditions, allowing patients to withdraw medical support if they go into an irreversible coma.
- Passive euthanasia is a matter of ‘living will’, and an adult in their conscious mind is permitted to refuse medical treatment or voluntarily decide not to take medical treatment to embrace death naturally, under certain conditions.
- Individuals are only allowed to draft a living will while in a normal state of health and mind.
- Active euthanasia remains illegal in India.
Read: Living wills
Article by: Jishnu J Raju


Aim IAS, IPS, or IFS?
Prelims cum Mains (PCM) GS Course: Target UPSC CSE 2025 (Online)
₹95000 ₹59000

Prelims cum Mains (PCM) GS Course: Target UPSC CSE 2026 (Online)
₹115000 ₹69000
Prelims cum Mains (PCM) GS Course: Target UPSC CSE 2027 (Online)
₹125000 ₹79000
About ClearIAS Team
ClearIAS is one of the most trusted learning platforms in India for UPSC preparation. Around 1 million aspirants learn from the ClearIAS every month.
Our courses and training methods are different from traditional coaching. We give special emphasis on smart work and personal mentorship. Many UPSC toppers thank ClearIAS for our role in their success.
Download the ClearIAS mobile apps now to supplement your self-study efforts with ClearIAS smart-study training.
Reader Interactions
February 11, 2016 at 3:48 pm
excellent one..
February 24, 2016 at 8:34 pm
Giving passive euthanasia to a patient who is already dead (not literally) is a right choice.Its better than making them as well as others to suffer.
July 20, 2017 at 4:28 pm
so very true.
July 1, 2016 at 10:58 pm
If the patient does not wants to suffer and himself asking for euthanasia then voluntary euthanasia should be made legal because it will be difficult for him to live than to die. But in case of involuntary euthanasia, there should be some specific time limit upto which the patient’s relatives must wait for him to recover but if there is no improvement like in case of coma , after 7-10 years , there is less chances of the patient to recover. In such cases , involuntary euthanasia should be made legal.
March 16, 2017 at 12:37 pm
no it is not possible If the patient tends to recover over a period of time or suddenly he becomes normal then the involuntary euthanasia will become very dangerous
March 16, 2017 at 12:35 pm
Very Very Useful
June 26, 2018 at 8:12 am
Helpful source I can use to rely on research. Thank you so much, clear IAS.
May 17, 2019 at 9:58 pm
Thanku for quality content
May 23, 2020 at 10:27 pm
“Mercy Killing ” is a responsible debate . It mainly depends on persons will on his /her life.
July 2, 2020 at 2:26 pm
Euthanasia should not be accepted as there is always some hope for better.
May 24, 2021 at 11:57 am
If under Article 21 of the constitution, right to live with dignity is inclusive of right to die with dignity, then why should the provisions under the Euthanasia act be restricted to the old and dying patients. There are a lot of people in their 60s and 70s with limited financial resources, who feel neglected / unwanted by the family who would like to die with dignity rather than be dependent on their children or the other members of family. They may be in good health but would still like to self determine to end their life with dignity. In such cases the law should allow for such people to adopt active Euthanasia. Such people could be persuaded to donate their organs which will help save other lives.
August 25, 2021 at 9:40 am
euthanasia cannot be legalised because of its higher probability of misuse. whether it is for property, money or because of any family problem
August 4, 2022 at 12:11 pm
A thought for all: If you do not have a choice to life, i.e. choose to be born then how can choosing your own means of death, be fair or valid? Something you cannot create or re-created is not yours to manage. My say: God is the giver of life and He alone should take it. Our sufferings are a means of learning, loving, understanding and above all our closeness to Almighty God.
June 28, 2023 at 6:36 pm
ur death is already written whether you take it or god does so doesnt matter
September 19, 2022 at 12:47 pm
I can’t put my dog to sleep for I am as old as he; and despite our handicaps he also wants to live like me.
Boghos L. Artinian
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Don’t lose out without playing the right game!
Follow the ClearIAS Prelims cum Mains (PCM) Integrated Approach.
Join ClearIAS PCM Course Now
UPSC Online Preparation
- Union Public Service Commission (UPSC)
- Indian Administrative Service (IAS)
- Indian Police Service (IPS)
- IAS Exam Eligibility
- UPSC Free Study Materials
- UPSC Exam Guidance
- UPSC Prelims Test Series
- UPSC Syllabus
- UPSC Online
- UPSC Prelims
- UPSC Interview
- UPSC Toppers
- UPSC Previous Year Qns
- UPSC Age Calculator
- UPSC Calendar 2024
- About ClearIAS
- ClearIAS Programs
- ClearIAS Fee Structure
- IAS Coaching
- UPSC Coaching
- UPSC Online Coaching
- ClearIAS Blog
- Important Updates
- Announcements
- Book Review
- ClearIAS App
- Work with us
- Advertise with us
- Privacy Policy
- Terms and Conditions
- Talk to Your Mentor
Featured on

and many more...
UPSC Online Coaching: Target CSE 2025
Are you struggling to finish the upsc cse syllabus without proper guidance, take clearias mock exams: analyse your progress.
Analyse Your Performance and Track Your All-India Ranking
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
- Strong Public Support for Right to Die
More Americans Discussing – and Planning – End-of-Life Treatment
Table of contents.
- About this Survey
Summary of Findings
An overwhelming majority of the public supports laws that give patients the right to decide whether they want to be kept alive through medical treatment. And fully 70% say there are circumstances when patients should be allowed to die, while just 22% believe that doctors and nurses should always do everything possible to save a patient.
Public attitudes on these and many other end-of-life issues are unchanged from 1990, despite advances in lifesaving technology, the aging of the population, and the controversy associated with the Terri Schiavo case. Most Americans believe it should be up to individuals not the government or medical professionals to ultimately determine their end-of-life medical decisions.
The Pew Research Center’s survey, conducted Nov. 9-27, 2005 among 1,500 adults, finds that while overall attitudes are largely stable, people are increasingly thinking about and planning for their own medical treatment in the event of a terminal illness or incapacitating medical condition. Public awareness of living wills, already widespread in 1990, is now virtually universal, and the number saying they have a living will has more than doubled from just 12% in 1990 to 29% today.
People also are much more willing to discuss sensitive end-of-life issues with their loved ones than they were a generation ago. Nearly seven-in-ten (69%) of those who are married say they have had a conversation with their husband or wife about their spouse’s wishes for end-of-life medical care; only about half reported doing so in 1990 (51%). Among those with living parents, 57% say they have spoken with their mother and 48% with their father about the parent’s requests for end-of-life treatment.
There is strong sentiment in favor of letting close family members decide whether to continue medical treatment for a terminally ill loved one who is unable to communicate their own wishes. Roughly three-quarters (74%) say a family member should be permitted to make this decision, which is little changed from 1990 (71%).
But Americans make a distinction between allowing a terminally ill person to die and taking action to end someone’s life. The public is deeply divided over legalizing physician-assisted suicide; 46% approve of laws permitting doctors to help patients to end their lives, while about as many are opposed (45%).
Though most Americans say it is sometimes morally acceptable for people with dire medical conditions to take their own lives, acceptance of this practice is highly dependent on circumstances. Six-in-ten feel that people have a moral right to end their lives if they suffer from great pain and have no chance for improvement. But this view changes under less extreme circumstances. For example, just 29% say a person has a moral right to end their life if he or she has become burdensome to family, with 62% saying someone in that situation does not have a moral right to take their life.
The survey finds that in many ways, public attitudes toward death and dying defy easy categorization. A majority believes that it is at least sometimes justifiable for a person to kill their spouse, again in extreme circumstances. Roughly six-in-ten (61%) feel that the ‘mercy killing’ of a spouse is always (6%) or sometimes (55%) justified, if the spouse “was suffering terrible pain from a terminal disease.” About half as many (29%) say such an act is never justified, although that represents a significant increase since 1990 (20%).
People’s views of end-of-life policies and practices do not perfectly mirror their own treatment preferences. While there has been an increase since 1990 in the percentage saying that people generally have a moral right to end their own life if they are facing an incurable illness and great pain (from 55% in 1990 to 60% now), there has also been an increase in the percentage who say they would personally want everything possible done to save their lives in many situations. About a third (34%) now say they would tell their doctor to do “everything possible” to save their life even if faced with a terminal illness and great pain; in 1990, fewer (28%) indicated they wanted everything done to save them in that case.
Other Findings
- People who have helped make end-of-life medical treatment decisions for loved ones are more likely than others to have a living will or to have discussed their wishes for end-of-life care. In addition, more of those who have gone through this experience believe in a moral right to suicide in certain circumstances, and favor ending their own medical treatment in the face of an incurable disease and great pain.
- By a wide margin, the public continues to disapprove of congressional action in 2005 that directed the federal courts to hear the case of Terri Schiavo, the brain-damaged Florida woman who later died after her feeding tube was removed.
- The Democratic Party has a modest advantage with the public in dealing with end-of-life issues. About one-third (34%) say the Democrats could do a better job with such issues, while 22% favor the Republicans.
- There is very little consistency in public attitudes toward what have been characterized as “life” issues abortion, the death penalty, and end-of-life questions. However, abortion opponents, and opponents of the death penalty, are more likely than those who accept these practices to favor doing everything possible to save a life regardless of the circumstances, as well as to oppose physician-assisted suicides.
Right to Die Laws Favored
By more than eight-to-one (84%-10%), the public approves of laws that let terminally ill patients make decisions about whether to be kept alive through medical treatment. This represents a small but significant increase in support for right to die laws since 1990 (79%).
The increase in support has been more pronounced among those over the age of 50 (from 72% to 83% approval), white Catholics (from 80% to 91% approval), and among those who have given a great deal of thought to end-of-life issues (from 79% to 87% approval).
In instances where a terminally ill patient is unable to communicate, the public supports allowing the closest family member to decide whether to continue medical treatment; 74% agree with this approach, while only 15% say that relatives should not be allowed to make such decisions. Here, too, the public is united across political and demographic lines, with approximately three-quarters of Republicans (72%), Democrats (78%), and independents (74%) saying that family members should be able to make treatment decisions for sick relatives.
This strong support for allowing the removal of medical treatment and for allowing family members to make these decisions is reflected in public opinion on the Terri Schiavo controversy. Nearly three-quarters (72%) of the public say that Congress should have stayed out of the Schiavo case, while fewer than one-in-five (17%) say Congress, in its effort to ensure that Schiavo continued to receive medical treatment, did the right thing by requiring federal courts to hear the case. This is essentially unchanged from a July 2005 survey, which found only 20% saying Congress did the right thing.
Large majorities of all social and demographic groups, including Republicans and evangelical Protestants, say that Congress should have stayed out of the Schiavo case. Similarly, even among people who believe that doctors and nurses should make every effort to save a patient’s life, as well as those who think family members should not be able to decide whether to continue medical treatment if a patient’s wishes are not known, solid majorities say that Congress overstepped its bounds in the Schiavo case.
Assisted Suicide: Stark Religious Differences
Though Americans are broadly supportive of allowing patients and their families to decide whether medical treatment should be removed, the public is divided over laws that let doctors prescribe lethal doses of drugs to assist terminally ill patients end their lives. Nearly half (46%) approve of such laws, while about as many (45%) disapprove.
On this issue, Americans are divided along religious and political lines. By two-to-one (61%-30%) white evangelical Protestants oppose physician-assisted suicide laws; by nearly identical margins, white mainline Protestants and seculars approve of such laws. Catholics, on balance, oppose such laws (by 50%-40%).
Small majorities of Democrats (52%) and independents (52%) approve of allowing physician-assisted suicide. Most Republicans oppose these laws (by 55%-34%), and conservative Republicans oppose them by a margin of two-to-one (62%-29%).
Views on assisted suicide are also affected by the amount of thought given to end-of-life issues; 57% of those who have given a great deal of thought to these issues approve of legal assisted suicide, a view shared by only 35% of those who have given little or no thought to these matters.
Politics of End-of-Life Issues
The Democratic Party holds a modest advantage over the GOP as the party seen as better able to handle end-of-life issues. Roughly a third (34%) say the Democrats could do a better job in these matters, compared with 22% who favor the Republicans. Many see neither party as particularly good on the issue (16%) and about a quarter (26%) say they don’t know which party could do a better job.
Predictably, there is a strong partisan component to opinion on this issue, with Republicans favoring the GOP and Democrats favoring the Democratic Party. Independents who choose a side favor Democrats over Republicans (by 27% to 14%), and self-described moderates give the Democrats an even bigger advantage (40% for the Democrats, 16% for the Republicans).
Support for Allowing Patients to Die
The vast majority of Americans 70% say that there are sometimes circumstances in which a patient should be allowed to die; only 22% believe that doctors and nurses should always do everything possible to save the life of a patient. The number of people who think there are times when medical treatment should be ended has changed little since 1990, though the percentage believing that all possible efforts should be made has grown modestly during the period (from 15% in 1990).
Only among African Americans does a majority (51%) think doctors and nurses should always do everything possible to save a patient (40% disagree). In addition, 35% of those ages 18-29 say everything should be done to keep a patient alive; no more than one-in-five in any other age category agrees.
But Fewer Would Halt Treatment for Themselves
While most people support the general idea of stopping medical treatment in some circumstances, fewer would personally ask their doctor to cut off treatment if they faced a terminal or debilitating illness. If facing an incurable illness and suffering a great deal of physical pain, 53% would opt to stop medical treatment, while 34% would tell their doctor to do everything possible to save their life.
Fewer Americans (44%) say they would ask to end care if they had an illness that made them totally dependent on another person for all of their care, while 38% say they would want everything done to save them. There is an almost even division of opinion over ending treatment if a person had no hope of improvement and had difficulty functioning; 42% say they would ask that treatment be halted in that case, while 43% say they would tell their doctor to do everything possible. Since 1990, there has been a modest increase in the numbers who say they want everything done medically under these scenarios.
As with the general question of whether there are circumstances under which care should be stopped, African Americans and younger people are more likely than others to say they would personally want every effort made to save their life. By contrast, older respondents those ages 50 and older are significantly less likely than others to say they would want this type of care. White evangelicals and people who attend religious services at least once per week are also more apt than others to want every effort made on their behalf.
Views of a Parent’s Treatment Wishes
After being asked about their own wishes in response to these situations, respondents who had at least one living parent were asked what their parent would want done in the same circumstances. For the most part, the answers were similar to their own wishes: A small majority says their parent would opt to stop treatment if faced with a terminal illness and great pain, while reactions to the other two scenarios were more divided.
There are no significant differences in opinion about what a person’s mother or father would want done in these circumstances, with one notable exception. In a situation where an illness left the person totally dependent on a family member or another person for care, mothers were thought more apt to choose to have all possible efforts made to save her life (by 47% to 37%), while more respondents thought their fathers would tilt the other way if faced with such a choice (45% stop treatment, 41% do everything possible). For both mothers and fathers in this scenario, there was a significant increase since 1990 in the desire to have all possible efforts at treatment (up nine percentage points for fathers, up 14 points for mothers).
The wishes of respondents were usually, but not always, the same as the wishes of the parent they described. Among respondents who said they would opt to stop treatment if personally faced with a terminal illness and great pain, 71% also said their parent would likely make the same choice; 16% said their parent would probably opt for all available treatment.
More See Doctors as Responsive
A growing number of people believe that doctors and nurses are paying a lot of attention to instructions from patients about whether or not to keep them alive. Three-in-ten think that doctors are paying a lot of attention to patients’ end-of-life wishes, up from 20% in 1990. Overall, nearly seven-in-ten (68%) believe that doctors are paying a lot or some attention to the life-sustaining treatment requests of patients.
People who have played a role in determining the end-of-life treatment of a family member or loved one are more likely than others to believe that doctors and nurses pay close attention to patients’ wishes: 41% say they pay a lot of attention, and 34% say they pay at least some attention. Better educated people are also more likely to think doctors and nursers are paying close attention. Four-in-ten college graduates think doctors are paying a lot of attention to patients about whether or not they want treatment to keep them alive. This is up 16% since 1990 when 24% of college graduates felt this way, the largest increase among any demographic group.
A Moral Right to End One’s Own Life?
A solid majority of Americans (60%) believe a person has a moral right to end their life if they are suffering great pain and have no hope of improvement. Nearly as many (53%) believe a person has a moral right to end their life if suffering from an incurable disease. But far fewer see a right to suicide in other circumstances. Just a third say a person is morally justified in ending their life because living has become a burden. Slightly fewer (29%) favor a right to suicide when a person has become an extremely heavy burden on his or her family.
There are significant gender and racial differences over the moral right to suicide. Men are more likely than women to support a right to end one’s own life in a situation where there is no hope of improvement and great pain (66% for men, 54% for women). A solid majority of whites (62%) say a person has a moral right to end their life under such circumstances, compared with just 43% of African Americans.
Attitudes on this question are also strongly related to the respondent’s religious beliefs, as well as to party and ideology. Fewer than half of white evangelical Protestants (42%) believe that an individual suffering a great deal of pain with no hope of improvement has a moral right to end their life, compared with 73% of white mainline Protestants. Most Catholics (60%) support the moral right to suicide under these circumstances, as do an overwhelming majority of seculars (78%). Similarly wide disparities are seen in terms of church attendance, with frequent attenders less supportive of such a right.
There are wide differences between Republicans and Democrats on this question as well. Fully 83% of liberal Democrats think people have a moral right to end their own lives under these circumstances, while just 41% of conservative Republicans agree. Moderate and liberal Republicans (63%) and conservative and moderate Democrats (62%) fall in between.
Many See ‘Mercy Killing’ as Sometimes Justified
Beyond supporting an individual’s moral right to take their own life under certain circumstances, a majority of the public believes that helping a terminally ill spouse commit suicide or even killing a spouse in this situation can at least be sometimes justified. Despite the stark difference in the framing of these options, the public makes little distinction between justifying the killing of a spouse or helping a spouse to commit suicide.
Most Americans (55%) say that killing a spouse who is terminally ill and suffering from terrible pain is sometimes justified, but far fewer (6%) believe it is always justified. Only 29% say it is never justified, though that is up from 20% when the question was first asked in 1990. White evangelical Protestants are more likely than other religious groups to believe that killing a spouse is never justified, but even among this group only about half (47%) hold this view.
Despite the widespread sentiment that killing a spouse, or helping a spouse commit suicide, is sometimes justified, most people say they cannot imagine actually taking such actions themselves. Only about a third (36%) say they could imagine helping a loved one commit suicide, and even fewer (29%) say they could imagine killing a loved one.
Severely Handicapped Infants
Compared with 15 years ago, more people say that infants born with severe handicaps no matter how severe should receive as much medical treatment as possible. Overall, 60% feel this way, up from 52% in 1990. Just 28% believe that parents have the right to refuse treatment that might save the infant’s life, down from 32% in 1990. African Americans (84%) and younger respondents (70%) are more likely than others to favor providing as much treatment as possible.
Only about half of college graduates (48%) support making every effort medically to save a severely handicapped infant though that is still larger than the percentage saying parents should have the right to refuse treatment (36%).
Support for providing the most treatment possible increases to 65% among people with only a high school diploma and to 73% among those who did not finish high school.
Catholic Priests Raise End-of-Life Issues
Overall, a third of regular churchgoers say that the clergy at their place of worship speak out on end-of-life issues. Roughly half of regular churchgoers say their clergy speak out on abortion (52%) and Iraq (50%). However, only about quarter (27%) say their clergy address the death penalty.
Catholic clergy stand out in their attention to end-of-life issues; half of Catholics who attend church at least monthly say that their clergy speak out on these matters, compared with 28% of evangelical Protestants and 16% of mainline Protestants.
More Catholics than Protestants also report hearing about abortion (71%) and the death penalty (35%) from their clergy.
How Generations Have Changed
This survey made it possible to track opinions and experiences within discrete generations over time most of the key questions were also asked in 1990 and several in 1975 as well. Even though the individuals interviewed in the earlier years were themselves not re-interviewed, the newer polls include age groups that are 15 (or 30) years older and thus represent the same generations interviewed earlier.
One of the most striking changes between 1990 and 2005 is the growth in the number of people who say they have a living will up 17 points, from 12% in 1990 to 29% now. This growth occurred across generations; while the number saying they have living wills increased the most in the oldest cohort (up 38 points), it also grew by at least 20 points in each of the other three cohorts tracked over this time period.
Another notable change since 1975 is the growth in the number of people who see a moral right to suicide for those suffering great pain with no hope of improvement up nearly 20 percentage points compared with three decades ago. However, most of this increase occurred between 1975 and 1990 (from 41% to 55%); since 1990, there has been a more modest rise in the number expressing this view (five points).
Over the past three decades, increased acceptance of a moral right to suicide has been greatest (from 29% to 46%) among the oldest cohort those Americans who were between the ages of 48 and 62 in 1975, and are now ages 78 to 92. But younger generations also are more supportive of a moral right to end one’s life now compared with 1975.
While more people have come to accept a right to suicide over the past 30 years, the trend on so-called “mercy killing” has moved in the opposite direction. The number of people who believe that killing a terminally ill spouse is never justified, while still a minority, has risen nine percentage points since 1990. However, views on this issue have not changed among the middle cohort those people who roughly correspond to the older end of the baby boomer generation (ages 48 to 62).
Abortion, Death Penalty and End-of-Life Issues
Relatively few Americans subscribe to what may be termed as a consistent “ethic of life” opposing both abortion and the death penalty, and favoring the use of all medical means to keep terminally ill patients alive. Abortion opponents and death penalty opponents alike overwhelmingly believe that there are circumstances in which doctors and nurses should let a patient die.
However, abortion opponents stand out for their overwhelming rejection of both physician-assisted suicide and a moral right to end life under extreme circumstances. Two-thirds (66%) of those who oppose abortion in all cases, or make exceptions only for rape, incest, or to save the woman’s life disapprove of legalizing physician-assisted suicide. That compares with 23% of those who believe abortion should be generally available or available under stricter limits. The gap is between these groups is nearly as large in opinions about whether people who are suffering great pain with no hope of improvement have a moral right to end their life.
Attitudes toward the death penalty bear less relationship to views about end-of-life issues. For example, just over half (53%) of death penalty supporters approve of legalizing physician-assisted suicide, compared with 40% of death penalty opponents. Differences on other questions are of similar magnitude.
Death penalty opponents and abortion opponents share common ground and differ with those on the opposite side of both issues in their personal views of when to halt end-of-life medical treatment. Both groups are fairly evenly divided over whether all medical steps should be taken to save their lives, or whether treatment should be halted. By contrast, solid majorities of those who support the death penalty, and those who believe abortion should be generally available, say they would want medical treatment halted if they had a disease with great pain and no hope of improvement.
Recent Experience with a Loved One’s Illness
Over the past five years, more than four-in-ten (42%) Americans have had a relative or close friend suffer from a terminal illness or a coma. For a majority of these people 23% of the general public the issue of withholding life-sustaining treatment for their relative or loved one arose. Both of these findings are on par with the results from a 1991 Kaiser Foundation/Harvard School of Public Health/Boston Globe survey.
Overall, 10% of the public has actually helped in making decisions about how much medical treatment should be given to a terminally ill or comatose friend or relative. Women over age 50 are more likely to report having made these important medical decisions than are people in other age groups; 15% of all women in this age group have made such a medical decision recently. College graduates (14%) and those with higher incomes (15% for those with family income of more than $75,000) are more likely than others to have made such medical decisions.
End-of-Life Planning
Older Americans are much more likely than younger people to have given considerable thought to their end-of-life treatment options. This is reflected as well in the age differences among those who have a living will. While over half of senior citizens (54%) say they have a living will compared with just 25% in 1990 far fewer people in other age groups have living wills.
There also are striking differences in the ways in which people who have recently experienced the terminal illness of a friend or relative and those who have not approach end- of-life issues. Generally, those who have faced such situations are much more likely to have thought about their own end of life treatment and planned accordingly.
And those who have taken on a more significant role on behalf of a gravely ill relative or friend by helping decide on their medical treatment are even more active in thinking about and planning for their own end-of-life treatment.
Fully 64% of those who have recently helped make decisions about the medical treatment of a terminally ill or comatose friend or relative say they have given a great deal of thought to their own preferences in such circumstances. That compares with 45% of those who have had a relative or close friend recently suffer from a terminal illness or coma, but did not participate in treatment decisions; and just 28% of those who have had no recent experience with the serious illness of a close friend or relative.
Similarly, nearly half of those who helped determine medical treatment of a gravely ill loved one (46%) have their own end-of-life wishes written down. That compares with about a third (32%) of those who have experienced the illness of a close friend or relative but did not take part in the decision making, and just 24% among those with no recent experience with a loved one facing death.
Talking About Treatment
Americans for the most part turn to family members when discussing their wishes for end-of-life medical treatment. Nearly four-in-ten (37%) say they have discussed these matters with their spouse, up from 30% in 1990. Among married people, 70% have talked with their spouse about their plans for medical treatment in such circumstances.
While fewer young people than older Americans have discussed their end of life treatment wishes with anyone, they are more likely than other age groups to talk with a parent 30% have done so, the highest percentage in any age group. People ages 65 and older, by contrast, are much more likely than younger people to have discussed their end of life treatment plans with one of their children (40%).
Since 1990, there has been a sizable drop in the percentage of Americans who say, in an open-ended format, that they have discussed their wishes for end-of-life medical treatment with ‘no one.’ Just 19% say that currently, while another 10% say they have given no thought to their end-of-life treatment. That compares with 44% in 1990 who either had talked with no one, or had given no thought to their care.
Talking With Spouses and Parents
Roughly equal numbers of married men (70%) and women (69%) say that they have had a conversation with their spouse about their wishes for end-of-life treatment. But women are much more likely than men to have had a conversation with their mother about her treatment.
Nearly two-thirds of women (65%) say they have had a conversation with their mother about her end-of-life treatment wishes. Only about half of men (48%) have talked with their mothers about such issues. Far fewer women have talked with their fathers about their end-of-life medical decisions. And men are no more likely to have discussed these issues with their fathers than with their mothers (45% father/48% mother).
Views on Aging
A plurality of Americans view the prospect of having more free time as what they look forward to most about getting old, while health concerns are seen as the biggest negative. Among the positives, about a third (35%) say that not having to work or having more free time is what they look forward to most, while 19% mention being able to spend time with their children, grandchildren and other family. Smaller percentages say having good health and being active (10%), travel (4%), and being able to experience changes in the world (2%) are what they most look forward to about old age.
The public expresses a broader array of worries about getting old. Health concerns including worries about cancer and other diseases, mental health, and insurance worries are mentioned most frequently (39%). Roughly one-in-five (19%) worry most about not having enough money in old age and 8% voice concern about losing their ability to care for themselves and being a burden on others. These worries have changed only modestly over the past 15 years.
Nearly a third of those ages 65 and older (31%) say ‘nothing’ when asked what worries them most about getting old. Only about one-in-ten or fewer in other age categories express no worries about getting old. Health concerns are mentioned most frequently by people ages 50-64. Compared with other age groups, those ages 18-29 express a relatively high level of concern over dying. One-in-ten of those under 30 say that their biggest worry about getting old is dying; far fewer people in older age categories, especially those ages 65 and older (2%) express that concern.
Making the Century Mark
Roughly four-in-ten Americans (43%) say they would like to live to be 100 years old, while 47% say they would not like to live to be that old. These findings have not changed much since 1990, when 39% said they would like to live to be 100.
However, there has been an increase since 1990 in the percentages of African Americans, young people and women who say they would like to live to 100. Nearly two-thirds of blacks (65%) say they would like to live to see the century mark, up from 53% in 1990. That compares with just 39% of whites who want to live to 100.
More than half of those under age 30 (55%) say they would like to live to be 100, up from 44% in 1990. By comparison, just 36% of those ages 50 and older want to live that long. More women also express a desire to live to 100 than did so 15 years ago (39% vs. 31%); still, more men than women continue to say they want to live to 100. In addition, people who register the highest levels of personal happiness are more likely than those who are less happy with their lives to want to live to 100 (51% vs. 40%).
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Death & Dying
Highly religious Americans more skeptical of human enhancements such as brain implants, gene editing
5 key themes in americans’ views about ai and human enhancement, ai and human enhancement: americans’ openness is tempered by a range of concerns, biotechnology research viewed with caution globally, but most support gene editing for babies to treat disease, americans are divided by religion on who should get critical care if there is a shortage of ventilators, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
- IAS Preparation
- UPSC Preparation Strategy
- Euthanasia Or Mercy Killing
Euthanasia or Mercy Killing- Moral Dilemma!
Euthanasia refers to the practice of intentionally ending a life in order to relieve pain and suffering. It is categorized as voluntary, non-voluntary and involuntary. Euthanasia can be further classified into active or passive ones. Active euthanasia is an intentional act to deliberately kill a terminally ill patient using various means whereas passive euthanasia happens when medical treatment is removed purposefully resulting in a person’s death to relieve him from unending pain. Until now euthanasia is not legalized in India.
Why in news-
- In 2016 Government proposed a draft bill on passive euthanasia for the first time called “The Medical Treatment of Terminally Ill Patients (Protection of Patients and Medical Practitioners) Bill”.
- Time and again widely debated across the media after the supreme court verdict on the Aruna Shanbaug case.
Aspirants would find this article very helpful while preparing for the UPSC 2022 .
What is Euthanasia?
The phrase “euthanasia” was coined by Sir Francis Bacon. It is also called as ‘mercy killing’ . The term “Euthanasia” has been derived from the two Greek words ‘eu’ and ‘thanotos’, which literally means ‘good death’.
Euthanasia is the practice of intentionally ending a life in order to relieve pain and suffering (provided motive should be good & death must be painless as much as possible) or
“A deliberate intervention was undertaken with the express intention of ending a life, to relieve intractable suffering.” – British House of Lords Select Committee on Medical Ethics.

Broad classification-
- Voluntary Euthanasia (with patients’ consent ) – euthanasia is performed with the patients consent. It is legal in some countries like Belgium, Netherlands, etc.
- Non-voluntary Euthanasia (patient’s consent unavailable) – where a person is unable to give their consent (for example –the patient is in a state of coma or are severely brain-damaged) and another person takes the decision on their behalf, often because the ill person had expressed a wish previously to end their life in such circumstances.
- Involuntary Euthanasia (without asking consent or against the patient’s will) – Euthanasia conducted against the will of the patient is termed involuntary euthanasia. It is also regarded as murder.

All types of euthanasia can be further divided into passive or active types-
a) Active Euthanasia – where a person intentionally intervenes to end someone’s life with the use of lethal substances or forces.
For example- Administering a lethal injection to end life.
b) Passive Euthanasia – where a person causes death by withholding or withdrawing treatment that is essential to maintain life.
For example- stoppage of antibiotics treatment in certain cases where it is necessary for the continuance of life, removal of life support system, etc
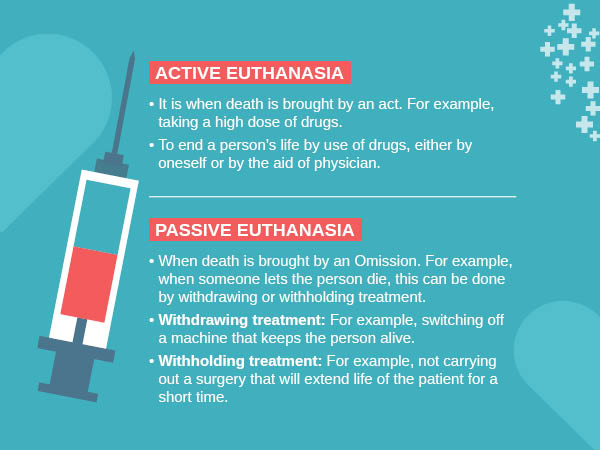
Debate- moral dilemma
Arguments For Euthanasia- According to euthanasia opponent Ezekiel Emanuel , proponents of euthanasia have presented four main arguments:
a) That people have a right to self-determination, and thus should be allowed to choose their own destiny.
b) Assisting a subject to die is a better option than continuing to suffer.
c) The distinction between passive euthanasia( which is frequently allowed) and active euthanasia is not substantive (the underlying principle–the doctrine of double effect is unreasonable) and
d) Allowing euthanasia will not necessarily lead to unacceptable consequences. Pro-euthanasia activists often take examples of countries like the Netherlands, Belgium, Luxembourg, etc. where euthanasia has been legalized to justify that it is mostly trouble-free.
Check the relevant links to prepare for the UPSC exam even better –
Other arguments-
Arguments based on rights
- People got an explicit right to die
- Death is a private subject and if there is no harm done to others then, the state and other people have no right to interfere (libertarian case)
Practical arguments –
- Death is a private subject and if there is no harm done to others then, the state and other people have no right to interfere (libertarian case)
- Allowing people to die may free up scarce health resources (this is a possible argument, but so far no authority has seriously proposed it)
Arguments Against Euthanasia
Similarly, Emanuel argues that there are four major arguments presented by opponents of euthanasia:
- All deaths are not painful.
- Termination of active treatment, combined with the effective use of pain relief are available as alternatives to euthanasia
- The distinction between active and passive euthanasia is morally significant and
- Legalizing euthanasia will put society on a slippery slope, which will lead to unacceptable consequences. (In Oregon 2013, the pain wasn’t one of the top five reasons that people sought euthanasia for. In fact, it was a loss of dignity, and a fear of burdening others).
Ethical arguments
- Euthanasia could weaken society’s respect for the sanctity of life.
- Accepting euthanasia would mean that some lives (those of the sick or disabled) are worth less than others.
- Voluntary euthanasia could start on a slippery slope that may lead to involuntary euthanasia and the killing of people who are thought undesirable.
- Euthanasia might not be in a person’s best interests.
- Euthanasia affects the rights of other people and not just those of the patient
Religious arguments- Religions are opposed to euthanasia for a number of reasons.
a) Euthanasia is against the will and word of God . (God has forbidden it)
- Virtually all religions in their scriptures say ‘you must not kill’. Therefore carrying out any of these would be against God’s command, and would be an attack on the sovereignty of God
b) Euthanasia weakens society’s respect for the sanctity of life .
- Human life is sacred. Human lives are special because God created them. Human beings are made in God’s image. Therefore human life should be protected and preserved, whatever happens
c) law of karma – Suffering may have value (Freedom from worldly life)
- Hinduism and Buddhism see mortal life as part of a continuing cycle in which we take birth, live, die, and are reborn over and over again.
- D uring each cycle of life and death, human beings make progress towards their ultimate aim, which is liberation.
- Thus, shortening life interferes with the law of karma.
d) Voluntary euthanasia could start on a slippery slope that may lead to involuntary euthanasia and the killing of people who are thought undesirable
e) Most religions disapprove of euthanasia. Some absolutely forbid it.
For example, the Roman Catholic church is one of the most active organizations in opposing euthanasia.
f) Virtually all religions state that those who become vulnerable through illness or disability deserve special care and protection, and proper care of life is a much better thing than euthanasia.
g) Non-harm – the principle of ahimsa- Hinduism and Buddhism regard all life as precious. (not just human life). They say that we should try to avoid harming living things and therefore this also rules out killing people, even if they want to die.
Practical arguments
- Proper palliative care could make euthanasia unnecessary.
- Euthanasia cannot be properly regulated
- Permitting euthanasia will lead to less good care for the terminally ill.
- Permitting euthanasia could undermine the commitment of doctors and nurses to save lives.
- Euthanasia may become in the future a cost-effective way to treat the terminally ill.
- Allowing euthanasia could discourage the search for new modes of treatment for the terminally ill.
- Euthanasia could discourage the motivation to provide good care for the dying.
- Euthanasia gives too much authority to doctors.
- Euthanasia exposes vulnerable people to pressure to end their lives.
- Moral pressure on elderly people by selfish families.
- Moral pressure to free up medical resources.
- Patients may feel euthanasia is the only way out when they are abandoned by their families.

Indian scenario
The Medical Treatment of Terminally Ill Patients (Protection of Patients and Medical Practitioners) Bill
- Advance medical directive- also called a living will . It means a directive given by a person that he/she as the case may be shall or shall not be given medical treatment in the future when he/she becomes terminally ill.
- Palliative care –
a) Provision of reasonable medical and nursing procedures for relief of physical pain, suffering, discomfort, or emotional or psychosocial suffering.
b) A reasonable provision for food and water.
- Competent patient – a patient who is not an incompetent patient.
- Incompetent patient- means a minor who is below 16 years of age or of unsound mind or a patient who is unable to-
a) understand information relevant to an informed decision about his/her medical treatment.
b) Retain and use that information to make decisions
c) Not able to make an informed decision due to disturbance in the functioning of the brain/mind.
d) Communicate his /her informed decision by speech, sign, language, or any other mode.
- Informed decision- means the decision as to continuance or withholding or withdrawing medical treatment taken by a patient who is competent and who is or has been informed about-
a) The nature of his/her illness
b) Any alternative form of treatment that is available
c) The consequences of those forms of treatment and
d) Consequences of remaining untreated
- Terminal illness- such illness/injury/degeneration of physical or mental condition which is causing extreme pain and suffering to the patients and according to the medical opinion will inevitably cause the untimely death of the patient concerned
Meaningful existence of life is not possible due to irreversible vegetative condition.
Salient Provisions of the Draft Bill
- Every competent patient, including minors aged above 16 years, has a right to make a decision and express their desire to the medical practitioner attending on her or him on whether to continue further treatment or allow nature to take its own course.
- The Bill provides protection to patients and doctors from any liability for withholding or withdrawing medical treatment and states that palliative care (pain management) can continue.
- When a patient communicates her or his decision to the medical practitioner, such a decision is binding on the medical practitioner. However, it also notes that the medical practitioner must be “satisfied” that the patient is “competent” and that the decision has been taken on free will.
- There will be a panel of medical experts to decide on a case by case basis.
- The medical practitioner has to maintain all details of the patient and ensure he/she takes an informed decision. He is also required to inform the patient whether it would be best to withdraw or continue treatment. If the patient is not in a conscious state, he/she needs to inform family members. In the absence of family members, the medical practitioner needs to inform a person who is a regular visitor.
- The draft also lays down the process for seeking euthanasia, right from the composition of the medical team to move the high court for permission.
- Permission to be obtained from the high court. Any near relative, friend, legal guardian, medical doctor/staff attending the patient, any other person obtaining the leave of the court can apply to the jurisdictional high court. Such an application is treated as an original petition and the chief justice of the high court shall assign the same to the divisional bench without loss of time and the same should be disposed of as far as practical within a month. This bench will nominate and need a report from a committee of three reputed doctors.
- The Bill only portends to legalize what is called “passive euthanasia”, as discussed in the judgement pertaining to Aruna Shaunbaug. Active euthanasia is not being considered “as it is likely to be used by unscrupulous individuals to attain their ulterior motives.”
- Advanced medical directive or living will be void and not binding on any medical practitioner.
- The medical council of India may issue guidelines consistent with the provisions of the bill. It may review and can also modify from time to time
Probable concerns- There have been mixed reactions to the draft bill. Some consider it a “good start”, but others didn’t quite agree. Some of the probable concerns are-
- The draft has disappointed experts who wanted complete clarity on the concept of a living will . While there have been demands for recognizing Advance Medical Directives (also known as a living will) whereby a person declares in advance whether or not treatment should be given if he is terminally-ill and incompetent to take decisions in the future, the government has rightly shot down the proposal.
- Child rights activists opine that in India, signing a contract or marrying before the age of 18 is not permitted, then how can a child decide to live or die.
- concerns for its misuse remain a major issue which ought to be addressed before it becomes a law in our country-
a) Doctors may come under the influence of corruption and fabricate material to prove that it is a terminal case with no chance of recovery.
b) Leaving it solely to the patient’s relatives or to the doctors or next friend to decide whether to withdraw the life support of an incompetent person, there is always a risk that this may be misused by some unscrupulous persons who wish to inherit or otherwise grab the property of the patient.
What is a “living will” and what are debates and arguments in relation to a living will?
In 2014, the Supreme Court had issued notice to all the states seeking their views on whether a terminally ill person can execute a “living will” that his or her life support system be withdrawn if he or she reaches a vegetative state with no hope of revival. The court has also appointed amicus curiae.

A Living Will is a document that sets out a patient’s wishes regarding health care and how they want to be treated if they become seriously ill and unable to make or communicate their own choices . Living wills are also called as active declarations .
Arguments For living will-
- They respect the patient’s human rights, and in particular their right to reject medical treatment.
- Creating them encourages full discussion about end of life decisions.
- Knowing what the patient want means that doctors are more likely to give appropriate treatment.
- They help medical professionals in taking difficult decisions.
- A patient’s family and friends don’t have to take the difficult decisions
Arguments against a living will-
- Writing them may be very depressing.
- It’s difficult for a healthy person adequately to imagine what they would really want in the situations where a living will take effect.
- It may be hard to translate the words of the living will into actual medical action.
- Patients may change their minds but not change their living wills.
- They’re no use if they can’t be found quickly when needed.
In India attempt to commit suicides (Section 309 of the Indian Penal Code ) and abetment of suicide( Section 306 of the IPC) are crimes and both actions are punishable. The problem is that to be able to make a living will, the legislation would need to decriminalize both. Though the court should consider the legitimacy of a will, there are several issues. For example, if the death of the patient is of material value to those are who close to him/her (such as property), the suspicion over the validity of the living can become a legal issue. Thus, there is a need to carefully set up conditions under which a living will be executed.
Summary- There is no point in prolonging the physical agony of a terminally ill person and the mental trauma of their loved ones. Therefore, euthanasia should be made legal in cases where there is no scope of a patient recovering. India however requires a mix of sensitivity and maturity for such an important decision to be taken as it involves ‘right to life’ and ‘right to die with dignity’.
“He who has health has hope, and he who has hope has everything”.-Arabic Proverb
How to approach for the Civil Services Examination
Death is a private matter and if there is no harm to others, the state has no right to interfere.
Human life is sacred. Irrespective of the pain and suffering, human life should be protected and preserved.
GS Paper II- Health-related aspect (public health and safety. Welfare etc)
Practice Questions –
In Prelims-
Which of the following statement is /are correct
- Article 21 of the constitution also deals with the right to die.
- The draft bill legalizes active euthanasia in India.
- According to the draft bill on passive euthanasia, the advanced medical directive shall be void and not binding on any medical practitioner.
- The draft Bill also provides for active euthanasia and physician-assisted suicide in certain cases.
GS paper II-
- Is passive euthanasia finally going to be a reality in India? Discuss?
- Critics of euthanasia claim that Voluntary euthanasia is the start of a slippery slope that leads to involuntary euthanasia and the killing of people who are considered undesirable. Critically discuss?
- Allowing euthanasia undermines the commitment of doctors and nurses to save lives. Critically discuss?
FAQ about Euthanasia or Mercy Killing
Is euthanasia legal in india, what are the different types of euthanasia.
UPSC exam related links are given below for candidates convenience in the preparation.
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Request OTP on Voice Call
Post My Comment
IAS 2024 - Your dream can come true!
Download the ultimate guide to upsc cse preparation.
- Share Share
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.

IMAGES
VIDEO
COMMENTS
Mercy Killing Debate. Euthanasia or physician- assisted suicide, also know as mercy killing, is becoming a prominent public debate. The implications of legalizing assisted suicide are wide-ranging from a medical, legal, political and ethical point of view. The term euthanasia means "good death" in Greek.
Palliative Care. Physician Obligation. Financial Motivations. 1. Legalization. "The right to die should be a matter of personal choice. We are able to choose all kinds of things in life from who we marry to what kind of work we do and I think when one comes to the end of one's life, whether you have a terminal illness or whether you're ...
This highlights the importance of considering why euthanasia should be legal in this essay. ... In Texas, "mercy killing, or euthanasia is not condoned or authorized by Texas law, nor is any act or omission other than to allow the natural process of dying" (Euthanasia Laws). In any other countries like Australia and the United Kingdom ...
Euthanasia: A good death or an act of mercy killing: A global scenario. November 2021. Clinical Ethics 17 (2) DOI: 10.1177/14777509211061844. Authors: Jagadish Rao Padubidri. Kastuba Medical ...
Abstract. With the development in different spheres, including healthcare and legal system, people raised different issues trying to find out which practice is the best one regarding law and ethics that alter with time. Some of them remain unsolved even today and still cause debates. Euthanasia is one of these issues.
Not that there ever was much of a legal or practical question involved. Imagine the precedent set by freeing a killer simply because he killed for love. Othello killed for love, though his passion ...
3.3. Some argue that it's always wrong to intentionally kill someone, so active euthanasia is wrong. In reply, while it's, at least, nearly always wrong to kill people, this is arguably because people usually want to live and do not have lives full of pain. Perhaps killing can be justified when this is not the case.[5]
'Mercy killing' should not lead to 'killing mercy' in the hands of the noble medical professionals. Hence, to keep control over the medical professionals, the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002 discusses euthanasia briefly in Chapter 6, Section 6.7 and it is in accordance with the ...
Euthanasia has been a subject of debate worldwide. It has brought up multiple controversies in different countries and among different societies. Over the years, euthanasia has been an active topic of research in the field of bioethics, owing to its numerous ethical and legal implications.
First, our topic is euthanasia, which is sometimes called "mercy killing.". The word euthanasia relates to the idea of a "good death.". People typically seek euthanasia to avoid a very bad death full of agony, pain, and suffering and all that results from that: for example, people wracked with horrific pain might not be able to ...
A mercy killing is the intentional ending of life of a person who is suffering from a terminal, painful illness. The term-also called "right to die" -is most often used to describe voluntary euthanasia, though it is also used in reference to non-voluntary euthanasia and involuntary euthanasia. Voluntary euthanasia is considered either ...
Mercy killing has been defined as the act of terminating life in a way that alleviates pain and suffering (Brill, 166). Over the years, the ethical nature of mercy killing has been largely debated. Currently, only a few countries have legalized voluntary euthanasia. Although some people argue that mercy killing alleviates pain and is mainly a ...
Euthanasia is against the law in the UK where it is illegal to help anyone kill themselves. Voluntary euthanasia or assisted suicide can lead to imprisonment of up to 14 years. The issue has been ...
In the United States, physician-assisted suicide or aid in dying has always been carefully distinguished from euthanasia. Euthanasia, also called mercy killing, refers to the administration of a lethal medication to an incurably suffering patient. It may be voluntary (the patient requests it) or involuntary. Euthanasia is illegal in the United ...
There is a pressing debate in the United States concerning the implied physicians' obligation to do no harm and the status of legalizing physician-assisted suicide (PAS). Key issues that underpin the debate are important to consider. These include: (1) foundational medical beginnings; (2) euthanasia's historical and legal background context; and (3) the key arguments held by those for and ...
Abstract. Euthanasia often alluded to as mercy killing is a medically assisted slaying in which a doctor is being empowered to induce death in a patient who is potentially in prolonged pain due to ...
The word 'Euthanasia' is derived from Greek, 'Eu' meaning 'good' and 'thanatos' meaning 'death', put together it means 'good death'. Euthanasia is defined as the hastening of death of a patient to prevent further sufferings. Active euthanasia refers to the physician deliberate act, usually the administration of lethal ...
Euthanasia is the deliberate advancement of a person's death for the benefit of that person. In most cases euthanasia is carried out because the person asks to die, but there are cases where a person can't make such a request. A person who undergoes euthanasia is usually terminally ill. Euthanasia can be carried out either by doing ...
Euthanasia ("good death") is the practice of intentionally ending a life to relieve pain and suffering. It is also known as 'mercy killing'. In many countries, there is a divisive public controversy over the moral, ethical, and legal issues of euthanasia. Euthanasia is categorized in different ways, which include voluntary, non ...
And fully 70% say there are circumstances when patients should be allowed to die, while just 22% believe that doctors and nurses should always do everything possible to save a patient. ... Roughly six-in-ten (61%) feel that the 'mercy killing' of a spouse is always (6%) or sometimes (55%) justified, if the spouse "was suffering terrible ...
They are strongly against legalizing mercy killing, emphasizing the holiness of life as a primary criterion by which the countries should start in their considerations. Studying criminal justice systems in the world, the authors concluded that the issue of deprivation of life from compassion is solved on three ways.
It is also called as 'mercy killing'. The term "Euthanasia" has been derived from the two Greek words 'eu' and 'thanotos', which literally means 'good death'. Euthanasia is the practice of intentionally ending a life in order to relieve pain and suffering (provided motive should be good & death must be painless as much as ...
Debates on euthanasia (or mercy killing ) have been a concern in moral, philosophical, legal, theological, cultural and sociological discourse for centuries. The topic of euthanasia inspires a ...