- Research article
- Open access
- Published: 01 May 2020

A systematic literature review of existing conceptualisation and measurement of mental health literacy in adolescent research: current challenges and inconsistencies
- Rosie Mansfield ORCID: orcid.org/0000-0002-8703-5606 1 ,
- Praveetha Patalay 2 &
- Neil Humphrey 1
BMC Public Health volume 20 , Article number: 607 ( 2020 ) Cite this article
23k Accesses
49 Citations
19 Altmetric
Metrics details
With an increased political interest in school-based mental health education, the dominant understanding and measurement of mental health literacy (MHL) in adolescent research should be critically appraised. This systematic literature review aimed to investigate the conceptualisation and measurement of MHL in adolescent research and the extent of methodological homogeneity in the field for meta-analyses.
Databases (PsycINFO, EMBASE, MEDLINE, ASSIA and ERIC) and grey literature were searched (1997–2017). Included articles used the term ‘mental health literacy’ and presented self-report data for at least one MHL domain with an adolescent sample (10–19 years). Definitions, methodological and contextual data were extracted and synthesised.
Ninety-one articles were identified. There was evidence of conceptual confusion, methodological inconsistency and a lack of measures developed and psychometrically tested with adolescents. The most commonly assessed domains were mental illness stigma and help-seeking beliefs; however, frequency of assessment varied by definition usage and study design. Recognition and knowledge of mental illnesses were assessed more frequently than help-seeking knowledge. A mental-ill health approach continues to dominate the field, with few articles assessing knowledge of mental health promotion.
Conclusions
MHL research with adolescent samples is increasing. Results suggest that a better understanding of what MHL means for this population is needed in order to develop reliable, valid and feasible adolescent measures, and explore mechanisms for change in improving adolescent mental health. We recommend a move away from ‘mental disorder literacy’ and towards critical ‘mental health literacy’. Future MHL research should apply integrated, culturally sensitive models of health literacy that account for life stage and acknowledge the interaction between individuals’ ability and social and contextual demands.
Peer Review reports
Around 50% of mental health difficulties have their first onset by age 15 [ 1 , 2 ] and are associated with negative outcomes such as lower educational attainment and physical health problems [ 3 ]. Approximately 10–20% of young people are affected worldwide, and many more will experience impairing mental distress at varying degrees across the mental health continuum [ 4 , 5 , 6 , 7 , 8 ]. Adolescence is a critical period of transition, characterised by physical, cognitive, emotional, social and behavioural development [ 9 ]. It has therefore been identified as a particularly important developmental phase for improving ‘mental health literacy’ (MHL) and promoting access to mental health services [ 10 , 11 ]. However, better understanding of the conceptualisation and measurement of MHL in this population is needed.
MHL was first defined as ‘ knowledge and beliefs about mental disorders which aid their recognition, management or prevention’ ( [ 12 ] pp 182) and consisted of six domains: ‘1) the ability to recognise specific disorders or different types of psychological distress; 2) knowledge and beliefs about risk factors and causes; 3) knowledge and beliefs about self-help interventions; 4) knowledge and beliefs about professional help available; 5) attitudes which facilitate recognition and appropriate help-seeking, and 6) knowledge of how to seek mental health information’ ( [ 13 ] pp 396). Domains were later revised to include early recognition, prevention and mental health first aid skills [ 14 ]. The most recent definition comprises four broad domains aligned with current definitions of health literacy: ‘1) understanding how to obtain and maintain positive mental health; 2) understanding mental disorders and their treatments; 3) decreasing stigma related to mental disorders, and 4) enhancing help-seeking efficacy (knowing when and where to seek help and developing competencies designed to improve one’s mental health care and self-management capabilities’ ( [ 15 ] pp 155).
In a review of MHL measurement tools, O’Connor et al. revealed that the most commonly assessed domain was recognition of mental disorders. No studies assessed either knowledge of how to seek information or knowledge of self-help interventions [ 16 ]. The focus on recognition of mental disorders, along with knowledge about risk factors, causes and appropriate treatments, has been criticised for promoting the psychiatric and biogenetic conceptualisation of mental illness [ 17 , 18 ]. Despite being found to reduce blame, biogenetic explanations and attributions can lead to misconceptions about dangerousness and unpredictability and pessimism about recovery [ 19 ]. Early research also suggested that biogenetic causal theories increase a desire for social distance [ 20 , 21 ]. MHL modelled on recognition of psychiatric labels, and diagnostic language such as ‘disorder’, often leads to psychosocial predictors being ignored, and more negative attitudes towards individuals experiencing mental distress [ 22 , 23 ].
These criticisms, in line with broader socio-cultural approaches to literacy [ 24 ] understand MHL as a socio-political practice used to communicate, and make dominant, the psychiatric discourse. This appears to undermine attempts to reduce stigma, the most common outcome of school-based MHL interventions [ 25 ]. In their review of MHL measurement tools, O’Connor et al. excluded all disorder specific scales, claiming that ‘ MHL by definition should encompass knowledge and attitudes relating to a range of mental health disorders and concepts .’ ( [ 16 ] pp 199). Chambers et al. further criticised current MHL definitions for being narrow in focus with a predominantly mental-ill health approach, ignoring the complete mental health state that goes beyond the dichotomy of illness and wellness [ 26 , 27 ]. The difference between literacy about mental disorders and the ability to seek out, comprehend, appraise and apply information relating to the complete mental health state is an emerging point of discussion, and has seen MHL re-defined to include self-acquired knowledge and skills relating to positive psychology [ 28 , 29 ]. This aligns with the World Health Organisation’s (WHO) definition of mental health, which includes subjective wellbeing, optimal functioning and coping, and recognises mental health beyond the absence of disorder [ 30 ].
In response to increasingly inclusive definitions of MHL, Spiker and Hammer presented the argument for MHL as a ‘multi-construct theory, rather than a multi-dimensional construct’ ( [ 31 ] pp 3). The proposal suggested that by stretching the MHL construct, researchers have reduced the consistent use of the definition across studies, resulting in heterogeneous measurement [ 32 ]. Reviews of the psychometric properties of MHL measurement tools support this argument, and conclude that more consistent measurement with valid scales is needed [ 33 , 34 , 35 , 36 ]. Spiker and Hammer also outline problems with construct irrelevant variance [ 31 ], in which measures capture more than they intended to. Furthermore, they note that construct proliferation or the ‘jingle jangle fallacy’ [ 37 ], in which scales may have different labels but measure the same construct, and vice versa, increase problems with discriminant validity. Understanding MHL as a multi-construct theory could help delineate between its broad domains: recognition, knowledge, stigma and help-seeking beliefs, and acknowledge their complexity.
Internationally, there is growing political interest in child and adolescent mental health promotion and education [ 6 , 38 ]. Despite limited evidence, it is suggested that educating the public by improving their ability to recognise mental disorders, and increasing help-seeking knowledge, can promote population mental health [ 39 , 40 ]. Furthermore, a reduction in stigmatising attitudes is consistently reported to improve help-seeking [ 41 , 42 ]. MHL, by definition, includes these interacting domains. However, despite a comprehensive set of reviews that assess the psychometric properties of MHL measurement tools [ 33 , 34 , 35 , 36 ], there is no systematic literature review, to date, that assesses the current conceptualisation and measurement of MHL across adolescent research. Being able to clearly operationalise what is meant by a MHL intervention and meta-analyse their effectiveness, will have implications for the investment in school and population level initiatives. Similarly, being able to conduct time trend analyses that plot possible improvements in adolescents’ MHL against mental health outcomes, will reveal the extent to which population level improvements in MHL promote mental health. First though, we must have a clear picture of the understanding of MHL in adolescent research and how it is currently being measured.
Objectives and research questions
The aim of the current study was therefore to examine the ways in which MHL has been conceptualised and measured in adolescent research to date, and explore the extent of methodological homogeneity in the field for meta-analyses. We set out to answer the following research questions: 1) What are the most common study designs, contexts, and aims? 2) How is MHL conceptualised? 3) What are the most commonly measured domains of MHL, and do these vary by study design and definition usage? 4) To what extent do articles use measures that have evidence of validity for use with adolescent samples? 5) Is there enough methodological homogeneity in the field to conduct meta-analyses?
A protocol was published on PROSPERO in December 2017 (reference: CRD42017082021 ), and was updated periodically to reflect the progress of the review. Relevant PRISMA guidelines for reporting were followed [ 43 ].
Eligibility criteria
Articles were included with adolescent samples aged between 10 and 19 [ 44 ]. Samples with a mean age outside of this range were excluded. If no mean was presented and the age range fell outside of the criterion, articles were only included if results were presented for sub-groups (e.g. 12–17 years from a sample aged 12–25). General MHL and diagnosis-specific literacy research was included. Articles with quantitative study designs and extractable self-report data for at least one time point measurement of any MHL domain were eligible. These criteria ensured that only articles with extractable data from adolescents, who had not yet received any form of intervention were included. At the full text screening phase, articles published before 1997, based on the date of the first MHL definition [ 12 ], and those that did not explicitly use the term ‘mental health literacy’ or a diagnosis-specific equivalent (e.g. ‘depression literacy’) were excluded. By applying this criterion, the current study was able to present the number of articles that measured domains without referring to MHL. Identifying cases where researchers measure the same construct but use different labels is important when considering conceptualisation and meta-analyses.
Only articles available in English were included. Specific populations such as clinical/patient populations and juvenile offenders were excluded, as were university students. In contrast to schools in most countries, universities are not universal, with only a sub-set of young people entering higher education. University samples were therefore not seen as representative and often included participants outside the age criterion. Post-partum and later life neurocognitive disorders (e.g. Alzheimer’s disease) were removed given their limited relevance for this age group. In line with other MHL reviews [ 33 ], articles with a focus on substance abuse were excluded to avoid reviewing a large number of adolescent risk behaviour studies and substance abuse prevention programmes.
Search strategy
The search strategy was developed to include a number of combinations of terms to ensure that literature relating to different domains of MHL were captured. Population terms such as ‘adolescen*’ or ‘young people*’ had to be present and mental health related terms (e.g. ‘mental health’ and ‘mental disorders’) were exploded to capture general MHL and diagnosis-specific studies. Similarly, outcome terms (e.g. ‘health literacy’ and ‘health education’) were exploded, and domain specific terms included (e.g. ‘knowledge’, ‘recogni*’, ‘attitud*’, ‘stigma*’, ‘help-seek*’, ‘prevent*’ or ‘positive*’). See Additional File 1 . for an example search strategy.
Data sources
The following databases were searched from their start date to the search dates (November 2017): PsycINFO, EMBASE, MEDLINE, ASSIA, and ERIC. Key authors were also contacted to identify grey literature. References were harvested from related reviews and all papers identified in the search. Hand searches of key authors’ publication lists were also conducted, and Google Scholar was used to find studies known by the authors but not identified in the database searches.
Article selection
Results from the database searches were saved to Endnote and duplicates were removed. The lead author screened the article titles and abstracts to identify those that met the inclusion criteria. Full texts were then screened and reasons for exclusion were recorded. Any uncertainties were resolved through discussion with other members of the research team. A sub-set of 20 articles were screened at full text stage by the third author, and a strong level of agreement was found (k = .78, p = .001).
Data extraction
Research was assessed on an article level (rather than by study) for the purposes of investigating the conceptualisation of MHL. The fact that authors break MHL down into component parts to write separate articles is support for identifying which domains are more commonly associated with the use of the term. Data on the following methodological factors were extracted from eligible articles using a uniform data extraction form: year of publication, country and setting (community (research conducted outside of the school setting e.g. population level surveys) vs. school-based research), study design (intervention vs. population-based), primary aims, MHL definition and use of the term, general MHL vs. diagnosis-specific literacy, number/types of MHL domains measured, and measurement tools (e.g. vignette, yes/no, Likert scales).
Data analysis
A content analysis was conducted using NVivo 12 to organise articles by their primary aim and understand the conceptualisation of MHL based on the definition presented and use of the term. Frequencies and percentages for each group were calculated and articles coded based on whether they included items related to general MHL or diagnosis-specific literacy. Existing definitions of MHL [ 12 , 13 , 14 , 15 , 28 ] were used to create a coding framework that clearly delineated its broad constituent domains (e.g. recognition, knowledge, stigma and beliefs), the object of these domains (e.g. mental illnesses, mental health prevention and promotion, and help-seeking), and their directionality (e.g. self vs. other) – see Fig. 1 .
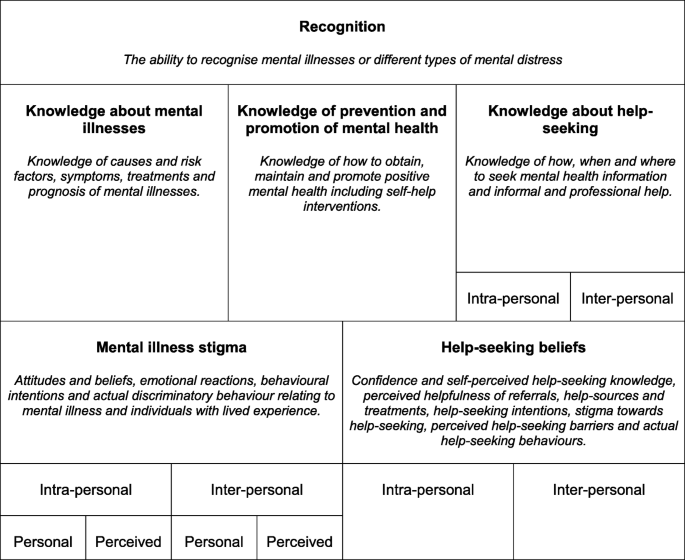
MHL Coding Framework
Mental illness stigma was assessed using existing conceptualisation i.e. personal and perceived stigma relating to self (intra-personal) and others (inter-personal), and broad domains (e.g. attitudes and beliefs, emotional reactions, and social distancing) [ 45 ]. The coding of help-seeking beliefs was informed by the theory of planned behaviour [ 46 ], assessing not only help-seeking intentions but also help-seeking confidence and self-perceived help-seeking knowledge, perceived helpfulness of referrals, help-sources and treatments, help-seeking stigma and perceived help-seeking barriers. A distinction was also made between help-seeking beliefs for self (intra-personal) vs. others (inter-personal). Although not explicitly included in any MHL definition, help-seeking behaviour was also assessed as the term is sometimes confused with help-seeking intentions. Domains were coded at an item level due to many articles presenting this form of data (e.g. % of sample that answered each item correctly as opposed to a scale mean). Frequencies and percentages were produced across all articles and by study design and definition usage.
Assessment of measures
An assessment of all MHL related measurement tools was conducted in order to assess methodological homogeneity across articles, and whether there was evidence that the measures were psychometrically valid for adolescent samples. In order to present instruments with the most comprehensive psychometric assessments, measures were coded based on whether an article existed with the primary aim of establishing its psychometric properties with an adolescent sample.
Article selection and characteristics
In total, 206 articles were identified that presented extractable adolescent data on at least one MHL domain. Of these, 91 articles (44%) used the term ‘mental health literacy’. Those that did not use the term ( N = 115, 56%), were therefore not perceived to have intended to explicitly measure the construct and were not included beyond this point. (see Fig. 2 . for a PRISMA flowchart of articles, Additional File 2 . for the full set of coded articles, and Additional File 3 . for the reference list of included articles).
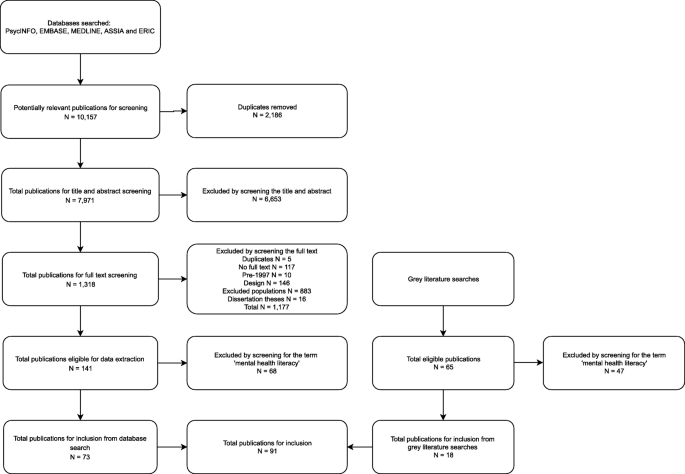
PRISMA Flowchart of Included Studies
Synthesised findings
Design, context and aims.
Figure 3 shows the number of publications by year and country. Australian research dominated the field up until 2013, at which point there was an increase in research being published globally. Australia (34%), USA (15%), Canada (9%), Republic of Ireland (9%) and the UK (8%) have published the majority of research between 2003 and 2017.
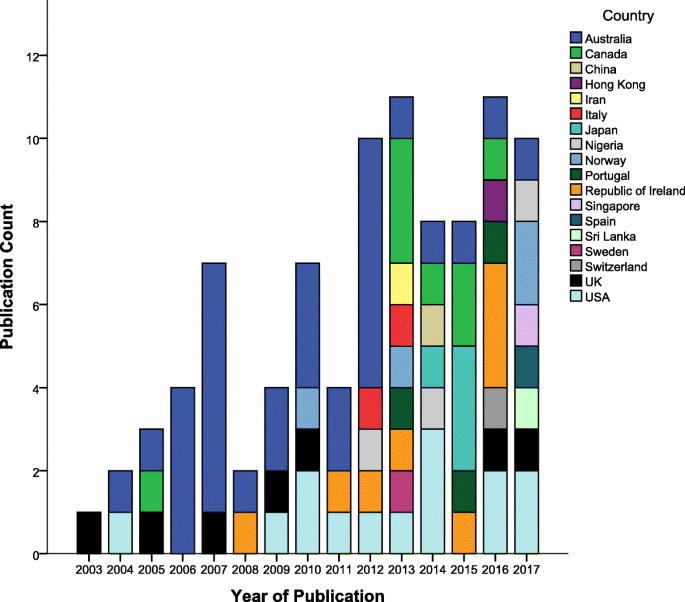
Publication Count by Year and Country
Table 1 presents a summary of articles’ study design, context and primary aim. The majority of articles reported on school-based studies. Articles with the primary aim of describing levels of MHL also included variables such as age, school year, gender, education, socio-economic variables, occupation, urbanicity, mental health status and previous mental health service use.
- Conceptualisation
Of the 91 articles that used the term ‘mental health literacy’, only 41 (45%) defined it. The most common definition, presented by 29 out of 41 (71%) articles, was that coined by Jorm and colleagues [ 12 ]. A further 3 articles (7%) used a simplified or adapted version of this definition [ 47 , 48 , 49 ]. Four articles (10%) defined MHL as related to knowledge only (e.g. ‘knowledge of mental health problems as well as the sources of help available’ ; ( [ 50 ] pp. 485) . The full list of MHL domains presented by Jorm and colleagues [ 13 ], was included in over a third ( N = 14, 34%) of articles that defined the term. However, there was some variation. For example, very few of these articles ( N = 2, 14%) referred to different types of psychological distress as well as mental disorders when presenting the recognition domain. Furthermore, in most cases ( N = 11, 79%), ‘knowledge and beliefs’ was replaced with ‘knowledge’ only, for domains relating to causes and risk factors, self-help strategies and professional help available.
A small number of articles that defined MHL ( N = 5, 12%) presented Jorm’s additional domains relating to mental health first aid skills and advocacy [ 14 ]. Some articles ( N = 4, 10%) provided examples of specific MHL domains, namely recognition of mental disorders and knowledge and beliefs about appropriate help-seeking and treatment, as opposed to presenting a comprehensive list. An emerging group of articles ( N = 5, 12%) either acknowledged mental health promotion as a component of MHL or presented Kutcher and colleagues’ four broad domains including ‘understanding how to obtain and maintain good mental health’ ( [ 15 ] pp 155).
Regardless of whether a definition was provided, approximately one third of identified articles ( N = 31, 34%) referred to MHL as a construct separate to mental illness stigma, with some suggesting that MHL predicts stigma. For example, articles described the measurement of these constructs as separate (e.g. ‘All respondents were then asked a series of questions that assessed sociodemographic characteristics, mental health literacy, stigma …’; ([ 51 ] pp. 941), and referred to or presented a relationship between the two constructs (e.g. ‘Participants with higher MHL displayed more negative attitudes to mental illness’ ; ( [ 52 ] pp. 100) . There were also instances where articles presented MHL as a predictor of help-seeking intentions and attitudes (e.g. ‘Studies indicate that in general, mental health literacy improves help seeking attitudes’ ; [ 53 ] (pp. 2), or used the term MHL to refer only to improved knowledge (e.g. ‘to assess the extent to which the students had learned the curriculum and developed what we called ‘depression literacy’ ; ([ 54 ] pp. 230).
- Measurement
Thirty-nine (43%) articles included items relating to general MHL. The exact terminology varied across studies e.g. mental disorder [ 55 ], mental illness [ 56 ], mental health problem [ 57 ], and mental health issue [ 58 ]. Few articles included items relating to mental health as opposed to mental ill-health. Bjørnsen et al. developed and validated a scale to assess adolescents' knowledge of how to obtain and maintain good mental health [ 28 ]. Kutcher et al. and McLuckie et al. also included an individual knowledge item that assessed an understanding of the complete mental health state (e.g. ‘People who have mental illness can at the same time have mental health’ ) [ 59 , 60 ].
Table 2 . presents the frequency and percentage of articles that assessed different types of diagnosis-specific literacy. In line with this focus, 57 (63%) articles utilized a vignette methodology, basing questions on descriptions, stories and scenarios relating to an individual meeting diagnostic criteria for a given mental disorder. Of these articles, 12 (21%) used comparator vignettes describing individuals with physical health problems (e.g. asthma or diabetes), control characters with good academic attainment, or ‘normal issues’ or mental health problems relating to stressful life events (e.g. the death of an elderly relative or the end of a romantic relationship). Table 3 . presents the frequency and percentage of articles that assessed different domains of MHL.
Measurement tools were too heterogeneous to conduct meta-analyses. As noted in Table 1 , four articles (4%) had the primary aim of validating MHL related measures with adolescent samples [ 28 , 55 , 61 , 62 ]. The scales assessed in Bjørnsen et al. and Pang et al. measured only one broad domain of MHL; knowledge of mental health promotion and mental illness stigma respectively [ 28 , 62 ]. Hart et al. assessed the psychometric properties of a depression knowledge questionnaire and found a one factor general knowledge latent structure to be the best fit to the data [ 61 ]. Campos et al. aimed to provide a more comprehensive assessment of MHL, and by psychometrically assessing a pool of items, developed a 33-item tool with three latent factors: first aid skills and help seeking, knowledge/stereotypes, and self-help strategies [ 55 ]. A further 22 articles (24%), stated that some items or scales had been developed for the purpose of the study.
Thirty-nine articles (43%) stated that they based their items on Jorm and colleagues original MHL survey or later 2006 and 2011 versions [ 12 , 63 ]. Furthermore, two articles (2%) included items from the Mental Health First Aid Questionnaire (MHFAQ) as detailed by Hart et al. [ 64 ]. However, there is no evidence of the validity of these surveys as whole scales, and researchers commonly selected and modified items. The Friend in Need Questionnaire, similar to Jorm and colleagues MHL survey in that it covers multiple MHL domains, was developed by Burns and Rapee to avoid leading multiple-choice answers. Instead, open-ended responses were coded in order to quantify levels of MHL [ 65 ]. Despite finding six articles (7%) that utilised a version of this questionnaire, no published validation paper was found. As part of the Adolescent Depression Awareness Programme (ADAP), an Adolescent Depression Knowledge Questionnaire (ADKQ) was developed and later validated [ 61 ]. Six articles (7%), including the validation paper, presented data using versions of the ADKQ.
Due to the multi-faceted nature of stigma, a range of measurement tools were identified across articles. The Attribution Questionnaire (AQ-27) was originally developed by Corrigan and colleagues [ 66 , 67 ] along with a brief 9-item scale (r-AQ) covering the following emotional reactions: blame, anger, pity, help, dangerousness, fear, avoidance, segregation and coercion. A similar 8-item version (AQ-8-C) was also developed for children [ 68 ]. The r-AQ was adapted by Watson et al. for use with middle school aged adolescents [ 69 ], and a 5-item version was more recently validated by Pinto et al. [ 70 ]. Four articles (4%) identified in this review used variations of the r-AQ.
Link et al. developed the 5-item Social Distance Scale (SDS) [ 71 ], which was later adapted for young people [ 72 ]. This version was more recently validated with a large sample aged 15–25 [ 73 ]. Five articles (5%) cited this version of the SDS. Seven articles (8%) used variations of the World Psychiatric Association’s (WPA) social distance items [ 74 ]; however, no adolescent validation paper was found. This review also found factual and attitudinal WPA scales presented by Pinfold et al. including the Myths and Facts About Schizophrenia Questionnaire. In total, these scales, or modified versions, were used in eight articles (9%), but no validation papers were found. The Reported and Intended Behaviour Scale (RIBS) [ 75 ] was utilised in three articles (3%). This scale has been translated into Japanese and Italian, and there is evidence of its validity with adult and university student samples [ 76 , 77 ]. The evidence of its validity with an adolescent sample was mixed [ 78 ].
The Depression Stigma Scale (DSS) was developed by Griffiths et al. to measure personal and perceived depression stigma [ 79 ]. Yap et al. later validated the DSS and confirmed that personal and perceived stigma were distinct constructs comprised of ‘weak-not-sick’ and ‘dangerous/unpredictable’ factors in a sample aged 15–25 [ 73 ]. Six articles (7%) utilised a version of the DSS, more commonly the items relating to personal stigma. Items from the Opinions about Mental Illness Scale (OMI) were used in two articles (2%). The original scale was cited by both [ 80 ], however, a Chinese version of the OMI has been tested for validity with a sample of secondary school students [ 81 ]. Other validated stigma scales identified included: the Attitudes Toward Serious Mental Illness Scale–Adolescent Version (ATSMI-AV) [ 82 ] ( N = 1, 1%) and the Subjective Social Status Loss Scale [ 83 ] ( N = 1, 1%). Measures of help-seeking attitudes and intentions were often not validated with adolescent samples. Two articles (2%) modified the General Help Seeking Questionnaire (GHSQ), previously validated for use with high school students [ 84 ]. A further two articles (2%) utilised the Self-Stigma of Seeking Help (SSOSH) scale; however, tests of its validity have only been conducted with college students [ 85 ].
The aims of this review were to investigate the conceptualisation and measurement of MHL in adolescent research, and scope the extent of methodological homogeneity for possible meta-analyses. The review clearly shows an increase in school-based MHL research with adolescent samples in recent years. This makes sense given that adolescence is increasingly identified as an important period for improving MHL and access to mental health services [ 6 , 10 , 11 , 38 ]. However, the field is still dominated by research from Western, developed countries and takes a predominantly mental-ill health approach. Furthermore, numerous challenges and inconsistencies have emerged in the field over the past 20 years.
Included articles were required to use the term ‘mental health literacy’ or a diagnosis-specific equivalent. However, by first including all articles that presented data for at least one MHL domain, a large number of articles that measured domains without referring to MHL were revealed. Researchers were measuring the same constructs but providing different labels indicating problems with discriminant validity [ 31 , 37 ]. It must be acknowledged that some of the articles included in the final set may have used the term without intending to measure the whole construct, and some articles were removed that measured multiple domains. For example, 16 intervention studies, previously included in a systematic literature review of the effectiveness of MHL interventions [ 25 ], were excluded from this current review because they did not use the term. Despite the exclusion of some potentially relevant data on a domain level, this criterion was considered most appropriate given one of the aims was to assess the conceptualisation of MHL.
Although under half of the articles identified defined MHL, those that did predominantly used definitions from Jorm and colleagues [ 12 , 13 , 14 ]. However, the various adaptations and interpretations of the original definition has clearly led to a lack of construct travelling in the field, in particular, confusion about the inclusion of beliefs and stigma related constructs as MHL domains. Furthermore, few articles referred to mental health and varying degrees of psychological distress in addition to mental illness, supporting the argument that current MHL definitions take a predominantly mental-ill health approach [ 16 , 26 ].
Although an adolescent specific definition of MHL may not be necessary, definitions frequently adopted by articles in this review were developed for adults. It is important for future research to consider not only cognitive development but also the unique social structures and vulnerabilities of adolescents in the conceptualisation and assessment of MHL. Given that the definition of adolescence in the current study ranges from 10 to 19 years, it is clear that even within this age range, different developmental factors could be considered. Applying integrated models of generic health literacy to MHL that acknowledge the life course and social and environmental determinants should therefore be a future priority [ 86 , 87 ].
Around a third of articles measured recognition of specific mental illnesses, with the majority using open-ended questions such as ‘ What, if anything, do you think is wrong …’, and calculating the % of correct responses. Knowledge of mental illnesses was measured more frequently than knowledge of prevention and promotion, therefore an understanding of the complete mental health state was often neglected [ 27 ]. More research is needed to develop and validate measures that assess the ability to seek out, comprehend, appraise and apply information relating to the complete mental health state as opposed to only assessing literacy of mental disorders. By using measurement tools that predominantly focus on psychiatric labels, there is evidence to suggest that stigma could be increased [ 22 , 23 ]. Given that over three quarters of intervention studies identified in this review included a measure of stigma, future research should consider the way in which mental-ill health approaches to MHL, in terms of intervention content and study measures, may influence stigma related outcomes.
It is perhaps unsurprising that the MHL field continues to be modelled on psychiatric labelling given the influence of Jorm and colleagues early work in Australia that came out of the National Health and Medical Research Council (NHMRC) Social Psychiatry Research Unit [ 12 ]. Kutcher and colleagues MHL definition also has its origins in psychiatry, but more explicitly includes understanding of mental health promotion and stigma reduction [ 15 ]. A growing body of research relating to eating disorders literacy also emphasises the need to distinguish between health promotion, prevention and early intervention initiatives in reducing the population health burden of eating-disordered behaviour and to prioritise mental health promotion programs, including those targeting stigma reduction [ 88 , 89 , 90 ]. This review identified an emerging group of articles that included understanding of how to obtain and maintain good mental health in their conceptualisation of MHL. However, this domain was rarely measured.
Just under half of the articles included items relating to general MHL. However, terminology was varied (e.g. mental illness, mental disorder, mental health problem, mental health issue). Leighton revealed that young people have a lack of conceptual clarity when it comes to these mental health related terms, unsurprising given the lack of consistent definitions in practice [ 91 ]. The range and subjectivity of mental health related terms reduces the meaningfulness of comparisons across MHL studies. Similarly, over half of the articles identified in this review assessed mental illness stigma, but the complexity of the construct caused heterogeneity in measurement. Intentions to seek help were the most commonly measured help-seeking belief; these findings support previous assessments of MHL measurement tools [ 16 ]. Measuring only intentions to seek help, without capturing knowledge of what help is available, will not provide a true picture of actual behaviour change. Findings also suggested that recognition and help-seeking related beliefs may be more directly associated with the MHL construct and, in line with previous literature [ 25 ], mental illness stigma was found to be a common outcome measure in MHL related interventions.
It is worth considering whether the MHL construct should continue to be stretched or whether we should accept that the multiple domains exist in their own right. For example, self-acquired knowledge and skills relating to positive psychology are being investigated, but are only just starting to emerge under the MHL construct [ 28 , 29 ]. Similarly, stigma and help-seeking knowledge and beliefs are assessed as part of, and independently from, the MHL framework. Adopting a multi-construct theory approach to MHL, as suggested by Spiker and Hammer [ 31 ], would see increased focus on developing and validating measures of specific MHL domains in order to better understand the way in which these domains relate to each other.
Developing better MHL theory will help provide clear logic models and theories of change for MHL interventions aiming to improve adolescent mental health, something currently lacking in the field. Although it should be acknowledged that the aims of MHL interventions will vary based on the scope, setting and cultural context, an increased number of validated measures as well as improved MHL theory could inform decisions about the most appropriate domain to measure as the outcome i.e. is the main aim of the intervention to reduce stigma or improve help-seeking. This is particularly important for school-based evaluations of MHL interventions for which respondent burden is often a concern.
We acknowledge that there were some articles in this review that adapted adult measures and tested for face and content validity with child and adolescent mental health professionals, and internal reliability and comprehension with adolescent samples. However, in general there was a lack of psychometric work to assess factor structure of scale-based measures in this age group, with large numbers of articles presenting data on an item level. More research should be conducted like that of Campos et al., working with young people to develop and psychometrically test pools of MHL items to identify latent factors [ 55 ]. This will help to inform future conceptualisation and measurement in this age group.
Even when there was evidence of a measure’s validity for use with adolescents, many articles selected only the items relevant for their study or adapted the scale to fit the cultural context. This may, in part, be an attempt to reduce the number of items and therefore the response burden. However, adaptation to measures based on the cultural discourse around mental health aligns with school-based mental health promotion approaches that account for children’s social, cultural and political contexts [ 92 ]. This raises the important question as to whether we should be trying to test and compare mental health related knowledge across cultures, particularly given the ongoing levels of disagreement amongst mental health professions between and within countries. A previous review of cross-cultural conceptualisations of positive mental health concluded that future definitions should be inclusive and culturally sensitive, and that more work was needed to empirically validate criteria for mental health [ 93 ]. Future research should consider conducting measurement invariance on existing MHL measures across different cultures. A comparison of knowledge items and their pre-defined correct answers, could help understand cultural differences in the discourse around mental health and what it means to be mental health literate across contexts.
Given the increased political interest in mental health promotion and education [ 6 , 38 ], we recommend that MHL research focuses on increasing understanding of ways to promote and maintain positive mental health, including subjective wellbeing, optimal functioning, coping and resilience [ 30 , 94 ]. Examples of knowledge items with true/false responses were identified in the current review and many aligned with a biogenetic conceptualisation of mental illness. Not only could these ‘truths’ cause more negative attitudes towards individuals experiencing mental health difficulties [ 19 ], many mapped directly onto the content of interventions and therefore do not provide any evidence of adolescents’ ability to critically appraise mental health information. To enhance individual and community level critical mental health literacy, the MHL field should apply models of public health literacy that aim to increase empowerment and control over health decisions, and acknowledge the interaction between an individual’s ability and their social and contextual demands [ 86 , 95 , 96 , 97 ]. Given that mental health is a key component of health, it is also worth questioning the usefulness of this separation moving forward; a MHL field that is playing catch up with more developed health literacy approaches could further exaggerate the existing lack of parity of esteem.
MHL research with adolescent populations is on the rise, but this review has highlighted some important areas for future consideration. Increasingly stretched definitions of MHL have led to conceptual confusion and methodological inconsistency, and there is a lack of measures developed and psychometrically tested with adolescents. Furthermore, the field is still dominated by a mental-ill health approach, with limited measures assessing the promotion of positive mental health. We suggest that the MHL field moves away from assessing ‘mental disorder literacy’ and towards critical ‘mental health literacy’. A better understanding of what MHL means for adolescents is needed in order to develop reliable, valid and feasible measures that acknowledge their developmental stage and unique social and contextual demands. In conclusion, by treating MHL as a multi-construct theory, more could be understood about the mechanisms for change in improving adolescent mental health.
Availability of data and materials
Link to PROSPERO review protocol included in the manuscript, example search strategy included as supplementary material.
Abbreviations
- Mental health literacy
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602. https://doi.org/10.1001/archpsyc.62.6.593 .
Article PubMed Google Scholar
Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder. Arch Gen Psychiatry. 2003;60(7):709. https://doi.org/10.1001/archpsyc.60.7.709 .
Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369:1302–13. https://doi.org/10.1016/S0140-6736(07)60368-7 .
Belfer ML. Child and adolescent mental disorders: the magnitude of the problem across the globe. J Child Psychol Psychiatry Allied Discip. 2008;49(3):226–36. https://doi.org/10.1111/j.1469-7610.2007.01855.x .
Article Google Scholar
Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44(10):972–86. https://doi.org/10.1097/01.chi.0000172552.41596.6f .
Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378:1515–25. https://doi.org/10.1016/S0140-6736(11)60827-1 .
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry Allied Discip. 2015;56(3):345–65. https://doi.org/10.1111/jcpp.12381 .
Sadler K, Vizard T, Ford T, Marcheselli F, Pearce N, Mandalia D, et al. Mental health of children and young people in England , 2017. London; 2018. Available from https://files.digital.nhs.uk/A6/EA7D58/MHCYP%202017%20Summary.pdf .
Hagell A, Coleman J, Brooks F. Key data on adolescence 2013. London; 2013. Available from http://www.ayph.org.uk/publications/457_AYPH_KeyData2013_WebVersion.pdf .
Neufeld SAS, Dunn VJ, Jones PB, Croudace TJ, Goodyer IM. Reduction in adolescent depression after contact with mental health services: a longitudinal cohort study in the UK. Lancet Psychiatry. 2017;4(2):120–7. https://doi.org/10.1016/S2215-0366(17)30002-0 .
Article PubMed PubMed Central Google Scholar
O’Connell ME, Boat T, Warner KE. Preventing mental, emotional, and behavioural disorders among young people: progress and possibilities. Washington DC: National Academies Press; 2009. Available from https://www.ncbi.nlm.nih.gov/books/NBK32775/pdf/Bookshelf_NBK32775.pdf .
Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Mental health literacy: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. 1997;166:182–6.
Article CAS PubMed Google Scholar
Jorm AF. Mental health literacy: public knowledge and beliefs about mental disorders. Br J Psychiatry. 2000;177:396–401. https://doi.org/10.1192/bjp.177.5.396 .
Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. 2012;67(3):231–43. https://doi.org/10.1037/a0025957 .
Kutcher S, Wei Y, Coniglio C. Mental health literacy: past, present and future. Can J Psychiatr. 2016;61(3):154–8. https://doi.org/10.1177/0706743715616609 .
O’Connor M, Casey L, Clough B. Measuring mental health literacy: a review of scale-based measures. J Ment Health. 2014;23(4):197–204. https://doi.org/10.3109/09638237.2014.910646 .
Gattuso S, Fullagar S, Young I. Speaking of women’s “nameless misery”: the everyday construction of depression in Australian women’s magazines. Soc Sci Med. 2005;61(8):1640–8. https://doi.org/10.1016/j.socscimed.2005.03.020 .
Read J. Why promoting biological ideology increases prejudice against people labelled “schizophrenic”. Aust Psychol. 2007;42(2):118–28. https://doi.org/10.1080/00050060701280607 .
Kvaale EP, Haslam N, Gottdiener WH. The ‘side effects’ of medicalization: a meta-analytic review of how biogenetic explanations affect stigma. Clin Psychol Rev. 2013;33(6):782–94. https://doi.org/10.1016/j.cpr.2013.06.002 .
Read J, Haslam N, Sayce L, Davies E. Prejudice and schizophrenia: a review of the “mental illness is an illness like any other” approach. Acta Psychiatr Scand. 2006;114(5):303–18. https://doi.org/10.1111/j.1600-0447.2006.00824.x .
Angermeyer MC, Matschinger H. Causal beliefs and attitudes to people with schizophrenia: trend analysis based on data from two population surveys in Germany. Br J Psychiatry. 2005;186:331–4. https://doi.org/10.1192/bjp.186.4.331 .
Kinderman P, Read J, Moncrieff J, Bentall RP. Drop the language of disorder. Evid Based Ment Health. 2013;16(1):2–3. https://doi.org/10.1136/eb-2012-100987 .
Schomerus G, Schwahn C, Holzinger A, Corrigan PW, Grabe HJ, Carta MG, et al. Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand. 2012;125(6):440–52. https://doi.org/10.1111/j.1600-0447.2012.01826.x .
Gee J. Socio-cultural approaches to literacy (literacies). Annu Rev Appl Linguist. 1992;12:31–48.
Wei Y, Hayden JA, Kutcher S, Zygmunt A, McGrath P. The effectiveness of school mental health literacy programs to address knowledge, attitudes and help seeking among youth. Early Interv Psychiatry. 2013;7(2):109–21. https://doi.org/10.1111/eip.12010 .
Chambers D, Murphy F, Keeley HS. All of us? An exploration of the concept of mental health literacy based on young people’s responses to fictional mental health vignettes. Ir J Psychol Med. 2015;32(1):129–36. https://doi.org/10.1017/ipm.2014.82 .
Keyes CLM. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005;73(3):539–48. https://doi.org/10.1037/0022-006X.73.3.539 .
Bjørnsen HN, Eilertsen MB, Ringdal R, Espnes GA, Moksnes UK. Positive mental health literacy: development and validation of a measure among Norwegian adolescents. BMC Public Health. 2017;17(1):717. https://doi.org/10.1186/s12889-017-4733-6 .
Kusan SB. Dialectics of mind, body and place: groundwork for a theory of mental health literacy. SAGE Open. 2013:1–16. https://doi.org/10.1177/2158244013512131 .
World Health Organisation. Mental health: strengthening our response. 2018. Available from: http://www.who.int/mediacentre/factsheets/fs220/en/ .
Spiker DA, Hammer JH. Mental health literacy as theory: current challenges and future directions. J Ment Health. 2018:1–5. https://doi.org/10.1080/09638237.2018.1437613 .
Wacker JG. A theory of formal conceptual definitions: developing theory-building measurement instruments. J Oper Manag. 2004;22(6):629–50. https://doi.org/10.1016/j.jom.2004.08.002 .
Wei Y, McGrath PJ, Hayden J, Kutcher S. Mental health literacy measures evaluating knowledge, attitudes and help-seeking: a scoping review. BMC Psychiatry. 2015;15(1):291. https://doi.org/10.1186/s12888-015-0681-9 .
Wei Y, McGrath PJ, Hayden J, Kutcher S. Measurement properties of tools measuring mental health knowledge: a systematic review. BMC Psychiatry. 2016;16(1):297. https://doi.org/10.1186/s12888-016-1012-5 .
Wei Y, McGrath P, Hayden J, Kutcher S. The quality of mental health literacy measurement tools evaluating the stigma of mental illness: a systematic review. Epidemiol Psychiatr Sci. 2017:1–30. https://doi.org/10.1017/S2045796017000178 .
Wei Y, McGrath PJ, Hayden J, Kutcher S. Measurement properties of mental health literacy tools measuring help-seeking: a systematic review. J Ment Health. 2017:1–13. https://doi.org/10.1080/09638237.2016.1276532 .
Marsh HW. Sport motivation orientations: beware of jingle-jangle fallacies. J Sport Exerc Psychol. 1994;16:365–80.
Department of Health and Education. Transforming children and young people’s mental health provision: a green paper. 2017. Available from https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/664855/Transforming_children_and_young_people_s_mental_health_provision.pdf .
Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust. 2007;187(7):1–5.
Google Scholar
Wright A, Jorm AF, Harris MG, McGorry PD. What’s in a name? Is accurate recognition and labelling of mental disorders by young people associated with better help-seeking and treatment preferences? Soc Psychiatry Psychiatr Epidemiol. 2007;42(3):244–50. https://doi.org/10.1007/s00127-006-0156-x .
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11–27. https://doi.org/10.1017/S0033291714000129 .
Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10. https://doi.org/10.1186/1471-244X-10-113 .
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1 .
World Health Organization. Adolescence: a period needing special attention - age-not-the-whole-story. 2014. Available from http://apps.who.int/adolescent/second-decade/section2/page2/age-not-the-whole-story.html .
Corrigan P. A toolkit for evaluating programs meant to Erase the stigma of mental illness. Illinois Inst Technol. 2012. Available from http://www.scattergoodfoundation.org/sites/default/files/EvaluationToolkit__Corrigan.pdf .
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–221.
Leighton S. Using a vignette-based questionnaire to explore adolescents understanding of mental health issues. Clin Child Psychol Psychiatry. 2010;15(2):231–50. https://doi.org/10.1177/1359104509340234 .
Serra M, Lai A, Buizza C, Pioli R, Preti A, Masala C, et al. Beliefs and attitudes among Italian high school students toward people with severe mental disorders. J Nerv Ment Dis. 2013;201(4):311–8. https://doi.org/10.1097/NMD.0b013e318288e27f .
Ojio Y, Yonehara H, Taneichi S. Effects of school-based mental health literacy education for secondary school students to be delivered by school teachers: a preliminary study. Psychiatry Clin Neurosci. 2015;69:572–9. https://doi.org/10.1111/pcn.12320 .
Swords L, Hennessy E, Heary C. Adolescents’ beliefs about sources of help for ADHD and depression. J Adolesc. 2011;34(3):485–92. https://doi.org/10.1016/j.adolescence.2010.06.002 .
Yap MBH, Reavley N, Jorm AF. Young people’s beliefs about preventive strategies for mental disorders: findings from two Australian national surveys of youth. J Affect Disord. 2012;136(3):940–7. https://doi.org/10.1016/j.jad.2011.09.003 .
O’Keeffe D, Turner N, Foley S, Lawlor E, Kinsella A, O’Callaghan E, et al. The relationship between mental health literacy regarding schizophrenia and psychiatric stigma in the Republic of Ireland. J Ment Health. 2016;25(2):100–8. https://doi.org/10.3109/09638237.2015.1057327 .
Attygalle UR, Perera H, Jayamanne BDW. Mental health literacy in adolescents: ability to recognise problems, helpful interventions and outcomes. Child Adolesc Psychiatry Ment Health. 2017;11(38). https://doi.org/10.1186/s13034-017-0176-1 .
Hess SG, Cox TS, Gonzales LC, Kastelic EA, Mink SP, Rose LE, et al. A survey of adolescents’ knowledge about depression. Arch Psychiatr Nurs. 2004;18(6):228–34. https://doi.org/10.1016/j.apnu.2004.09.005 .
Campos L, Dias P, Palha F, Duarte A, Veiga E. Development and psychometric properties of a new questionnaire for assessing mental health literacy in young people. Univ Psychol. 2016;15(2):61–72. https://doi.org/10.11144/Javeriana.upsy15-2.dppq .
Pinto-Foltz MD, Logsdon M, Myers JA. Feasibility, acceptability, and initial efficacy of a knowledge-contact program to reduce mental illness stigma and improve mental health literacy in adolescents. Soc Sci Med. 2011;72(12):2011–9. https://doi.org/10.1016/j.socscimed.2011.04.006 .
Dogra N, Omigbodun O, Adedokun T, Bella T, Ronzoni P, Adesokan A. Nigerian secondary school children’s knowledge of and attitudes to mental health and illness. Clin Child Psychol Psychiatry. 2012;17(3):336–53. https://doi.org/10.1177/1359104511410804 .
Livingston JD, Tugwell A, Korf-Uzan K, Cianfrone M, Coniglio C. Evaluation of a campaign to improve awareness and attitudes of young people towards mental health issues. Soc Psychiatry Psychiatr Epidemiol. 2013;48(6):965–73. https://doi.org/10.1007/s00127-012-0617-3 .
Kutcher S, Wei Y, Morgan C. Successful application of a Canadian mental health curriculum resource by usual classroom teachers in significantly and sustainably improving student mental health literacy. Can J Psychiatr. 2015;60(12):580–6. https://doi.org/10.1177/070674371506001209 .
Mcluckie A, Kutcher S, Wei Y, Weaver C. Sustained improvements in students’ mental health literacy with use of a mental health curriculum in Canadian schools. BMC Psychiatry. 2014;14(1):379. https://doi.org/10.1186/s12888-014-0379-4 .
Hart SR, Kastelic EA, Wilcox HC, Beth M, Rashelle B, Kathryn JM, et al. Achieving depression literacy: the adolescent depression knowledge questionnaire ( ADKQ ). School Ment Health. 2014;6:213–23. https://doi.org/10.1007/s12310-014-9120-1 .
Pang S, Liu J, Mahesh M, Chua BY, Shahwan S, Lee SP, et al. Stigma among Singaporean youth: a cross-sectional study on adolescent attitudes towards serious mental illness and social tolerance in a multiethnic population. BMJ Open. 2017;7(10):1–12. https://doi.org/10.1136/bmjopen-2017-016432 .
Reavley NJ, Jorm AF. National survey of mental health literacy and stigma. Canberra: Dep Heal Ageing; 2011. Available from https://pdfs.semanticscholar.org/d96a/e351a5b9ecfe6a519c8e4c2dd947873f426e.pdf .
Hart LM, Mason RJ, Kelly CM, Cvetkovski S, Jorm AF. “ teen Mental Health First Aid ”: a description of the program and an initial evaluation. Int J Ment Health Syst 2016;10(3):1–19. doi: https://doi.org/10.1186/s13033-016-0034-1 .
Burns JR, Rapee RM. Adolescent mental health literacy: young people’s knowledge of depression and help seeking. J Adolesc. 2006;29(2):225–39. https://doi.org/10.1016/j.adolescence.2005.05.004 .
Corrigan P, Markowitz FE, Watson A, Rowan D, Corrigan P. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44(2):162–79.
Corrigan PW, Rowan D, Green A, Lundin R, River P, Uphoff-Wasowski K, et al. Challenging two mental illness stigmas: personal responsibility and dangerousness. Schizophr Bull. 2002;28(2):293–309. https://doi.org/10.1093/oxfordjournals.schbul.a006939 .
Corrigan PW, Watson AC, Otey E, Westbrook AL, Gardner AL, Lamb TA, et al. How do children stigmatize people with mental illness? J Appl Soc Psychol. 2007;37(7):1405–17. https://doi.org/10.1177/0020764007078359 .
Watson A, Otey E, Westbrook A, Gardner A, Lamb T, Corrigan P, et al. Changing middle schoolers’ attitudes about mental illness through education. Schizophr Bull. 2004;30(3):563–72. https://doi.org/10.1093/oxfordjournals.schbul.a007100 .
Pinto MD, Hickman R, Logsdon MC, Burant C. Psychometric evaluation of the revised attribution questionnaire (r-AQ) to measure mental illness stigma in adolescents. J Nurs Meas. 2012;20(1):47–58.
Link BG, Bresnahan M, Stueve A, Pescosolido A, Star S. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health. 1999;89(9):1328–33. https://doi.org/10.2105/ajph.89.9.1328 .
Article CAS PubMed PubMed Central Google Scholar
Jorm AF, Wright A. Influences on young people’s stigmatising attitudes towards peers with mental disorders: national survey of young Australians and their parents. Br J Psychiatry. 2008;192(2):144–9. https://doi.org/10.1192/bjp.bp.107.039404 .
Yap MB, Mackinnon A, Reavley N, Jorm AF. The measurement properties of stigmatizing attitudes towards mental disorders: results from two community surveys. Int J Methods Psychiatr Res. 2014;23(1):49–61. https://doi.org/10.1002/mpr.1433 .
Pinfold V, Toulmin H, Thornicroft G, Huxley P, Farmer P, Graham T. Reducing psychiatric stigma and discrimination: evaluation of educational interventions inUK secondary schools. Br J Psychiatry. 2003;182:342–6. https://doi.org/10.1192/bjp.182.4.342 .
Evans-Lacko S, Rose D, Little K, Flach C, Rhydderch D, Henderson C, et al. Development and psychometric properties of the reported and intended behaviour scale (RIBS): a stigma-related behaviour measure. Epidemiol Psychiatr Sci. 2011;20(3):263–71. https://doi.org/10.1017/S2045796011000308 .
Pingani L, Evans-Lacko S, Luciano M, Del Vecchio V, Ferrari S, Sampogna G, et al. Psychometric validation of the Italian version of the reported and intended behaviour scale (RIBS). Epidemiol Psychiatr Sci. 2016;25(5):485–92. https://doi.org/10.1017/S2045796015000633 .
Yamaguchi S, Koike S, Watanabe KI, Ando S. Development of a Japanese version of the reported and intended behaviour scale: reliability and validity. Psychiatry Clin Neurosci. 2014;68(6):448–55. https://doi.org/10.1111/pcn.12151 .
Mansfield R, Humphrey N, Patalay P. Psychometric validation of the reported and intended behavior scale (RIBS) with adolescents. Stigma Heal. 2019. https://doi.org/10.1037/sah0000200 .
Griffiths KM, Christensen H, Jorm AF, Evans K, Groves C. Effect of web-based depression literacy and cognitive behavioural therapy interventions on stigmatising attitudes to depression randomised controlled trial. Br J Psychiatry. 2004;185:342–9. https://doi.org/10.1192/bjp.185.4.342 .
Cohen J, Struening EL. Opinions about mental illness in the personnel of two large mental hospitals. J Abnorm Soc Psychol. 1962;64(5):349–60.
Ng P, Chan KF. Sex differences in opinion towards mental illness of secondary school students in Hong Kong. Int J Soc Psychiatry. 2000;46(2):79–88. https://doi.org/10.1177/002076400004600201 .
Watson AC, Miller FE, Lyons JS. Adolescent attitudes toward serious mental illness. J Nerv Ment Dis. 2005;193(11):769–72. https://doi.org/10.1097/01.nmd.0000185885.04349.99 .
Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, Colditz GA, et al. Adolescents’ perceptions of social status: development and evaluation of a new indicator. Pediatrics. 2001;108(2):1–8. https://doi.org/10.1542/peds.108.2.e31 .
Wilson CJ, Dean FP, Ciarrochi J. Measuring help-seeking intentions: properties of the general help-seeking questionnaire. Can J Couns. 2005;39(1):15.
Vogel DL, Wade NG, Haake S. Measuring the self-stigma associated with seeking psychological help. J Couns Psychol. 2006;53(3):325–37. https://doi.org/10.1037/0022-0167.53.3.325 .
Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80.
Bröder J, Okan O, Bauer U, Bruland D, Schlupp S, Bollweg TM, et al. Health literacy in childhood and youth: a systematic review of definitions and models. BMC Public Health. 2017;17(1):1–25.
Bullivant B, Rhydderch S, Griffiths S, Mitchison D, Mond JM. Eating disorders “mental health literacy”: a scoping review. J Ment Health. 2020:1–14. https://doi.org/10.1080/09638237.2020.1713996 .
Mond JM. Optimizing prevention programs and maximizing public health impact are not the same thing. Eat Disord. 2016;24(1):20–8. https://doi.org/10.1080/10640266.2015.1113824 .
Mond JM. Eating disorders “mental health literacy”: an introduction. J Ment Health. 2014;23(2):51–4. https://doi.org/10.3109/09638237.2014.889286 .
Leighton S. Adolescents’ understanding of mental health problems: conceptual confusion. Jounal Public Ment Heal. 2009;8(2):4–14. https://doi.org/10.1108/17465729200900009 .
O’Toole C. Towards dynamic and interdisciplinary frameworks for school-based mental health promotion. Health Educ. 2017;117(5):452–68. https://doi.org/10.1108/HE-11-2016-0058 .
Vaillant GE. Positive mental health: is there a cross-cultural definition? World Psychiatry. 2012;11(2):93–9. https://doi.org/10.1016/j.wpsyc.2012.05.006 .
Srivastava K. Positive mental health and its relationship with resilience. Ind Psychiatry J. 2011;20(2):75–6. https://doi.org/10.4103/0972-6748.102469 .
Freedman DA, Bess KD, Tucker HA, Boyd DL, Tuchman AM, Wallston KA. Public health literacy defined. Am J Prev Med. 2009;36(5):446–51. https://doi.org/10.1016/j.amepre.2009.02.001 .
Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67(12):2072–8. https://doi.org/10.1016/j.socscimed.2008.09.050 .
Pleasant A, Kuruvilla S. A tale of two health literacies: public health and clinical approaches to health literacy. Health Promot Int. 2008;23(2):152–9. https://doi.org/10.1093/heapro/dan001 .
Download references
Acknowledgements
Not applicable
RM’s PhD is part of the Education for Wellbeing Programme funded by the Department for Education, England (grant number: EOR/SBU/2017/015). The views expressed in this article are those of the author(s) and not necessarily those of the Department for Education, England or its arm’s length bodies, or other Government Departments.
Author information
Authors and affiliations.
Institute of Education, University of Manchester, Ellen Wilkinson Building, M13 9PL, Manchester, UK
Rosie Mansfield & Neil Humphrey
Institute of Education and Faculty of Population Health Sciences, University College London, WC1E 6BT, London, UK
Praveetha Patalay
You can also search for this author in PubMed Google Scholar
Contributions
RM designed the systematic literature review and wrote the protocol published on PROSPERO. RM conducted the initial database search and grey literature search and was responsible for all stages of screening and data extraction. Any uncertainties relating to screening and data extraction were resolved through discussion with NH and PP. A sub-set of articles were screened at full text stage by NH to determine levels of agreement. RM wrote the first draft of the manuscript with input from NH and PP. All authors read and approved the submitted version.
Corresponding author
Correspondence to Rosie Mansfield .
Ethics declarations
Ethics approval and consent to participate.
not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
example search strategy.
Additional file 2.
full set of coded articles.
Additional file 3.
full reference list of included articles.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mansfield, R., Patalay, P. & Humphrey, N. A systematic literature review of existing conceptualisation and measurement of mental health literacy in adolescent research: current challenges and inconsistencies. BMC Public Health 20 , 607 (2020). https://doi.org/10.1186/s12889-020-08734-1
Download citation
Received : 13 December 2019
Accepted : 20 April 2020
Published : 01 May 2020
DOI : https://doi.org/10.1186/s12889-020-08734-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic literature review
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Improving mental health literacy in adolescents: systematic review of supporting intervention studies
Affiliations.
- 1 Sirindhorn College of Public Health, Khon Kaen, Thailand.
- 2 Faculty of Public Health, Mahasarakham University, Mahasarakham, Thailand.
- 3 Boromarajonani College of Nursing, Buddhachinaraj, Phitsanulok, Thailand.
- PMID: 32478983
- DOI: 10.1111/tmi.13449
Abstract in English, French
Objective: Mental health literacy (MHL) in adolescents is an important issue as it can lead to early detection and recognition of mental illness. The aim of this systematic review was to explore the effect of supporting interventions on improving MHL in adolescents.
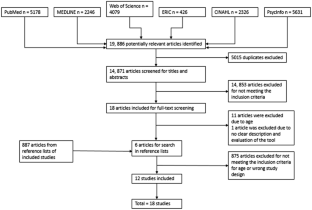
Methods: Systematic literature review by searching the ScienceDirect, Scopus, PubMed, Crochrane and CINAHL databases. Seven of 1107 papers were included in the final review.
Results: Supporting interventions for improving MHL in adolescents could be categorised into school-based and community-based. Both types used an education stand-alone strategy or an education plus contact-based group in their programmes. To provide knowledge of mental illness to adolescents, teaching methods should be interactive and use various media such as group discussion, videos and movies.
Conclusions: School-based and community-based interventions were likely to improve MHL among adolescents. However, further research with objective tool measures is needed to confirm the findings.
Objectif: La littératie sur la santé mentale (LSM) chez les adolescents est un sujet important car elle peut conduire à la détection et à la reconnaissance précoces des maladies mentales. Le but de cette revue systématique était d'explorer l'effet du soutien des interventions sur l'amélioration de la LSM chez les adolescents. MÉTHODES: Analyse systématique de la littérature en recherchant dans les bases de données ScienceDirect, Scopus, PubMed, Crochrane et CINAHL. 7 des 1.107 articles ont été inclus dans l’analyse finale. RÉSULTATS: L’effet des interventions de soutien visant à améliorer la LSM chez les adolescents pourraient être classés en soit du milieu scolaire, soit communautaire. Les deux types ont utilisé une stratégie basée sur l’éducation seule ou sur l'éducation et des contacts dans leurs programmes. Fournir des connaissances de la maladie mentale aux adolescents, les méthodes d'enseignement devraient être interactifs et utiliser divers médias comme la discussion de groupe, des vidéos et des films.
Conclusions: Les interventions en milieu scolaire et communautaires étaient susceptibles d’améliorer la LSM chez les adolescents. Cependant, des recherches supplémentaires avec des mesures d'outils objectives sont nécessaires pour confirmer les résultats.
Keywords: adolescent; community-based intervention; connaissances sur la santé mentale; intervention; intervention communautaire; intervention en milieu scolaire; mental health literacy; revue systématique; school-based intervention; systematic review.
© 2020 John Wiley & Sons Ltd.
PubMed Disclaimer
Similar articles
- Promotion of Mental Health Literacy in Adolescents: A Scoping Review. Nobre J, Oliveira AP, Monteiro F, Sequeira C, Ferré-Grau C. Nobre J, et al. Int J Environ Res Public Health. 2021 Sep 9;18(18):9500. doi: 10.3390/ijerph18189500. Int J Environ Res Public Health. 2021. PMID: 34574427 Free PMC article. Review.
- Exploring MEST: a new universal teaching strategy for school health services to promote positive mental health literacy and mental wellbeing among Norwegian adolescents. Bjørnsen HN, Ringdal R, Espnes GA, Eilertsen MB, Moksnes UK. Bjørnsen HN, et al. BMC Health Serv Res. 2018 Dec 29;18(1):1001. doi: 10.1186/s12913-018-3829-8. BMC Health Serv Res. 2018. PMID: 30594201 Free PMC article.
- "EspaiJove.net"- a school-based intervention programme to promote mental health and eradicate stigma in the adolescent population: study protocol for a cluster randomised controlled trial. Casañas R, Arfuch VM, Castellví P, Gil JJ, Torres M, Pujol A, Castells G, Teixidó M, San-Emeterio MT, Sampietro HM, Caussa A, Alonso J, Lalucat-Jo L. Casañas R, et al. BMC Public Health. 2018 Jul 31;18(1):939. doi: 10.1186/s12889-018-5855-1. BMC Public Health. 2018. PMID: 30064404 Free PMC article.
- Is It Possible to "Find Space for Mental Health" in Young People? Effectiveness of a School-Based Mental Health Literacy Promotion Program. Campos L, Dias P, Duarte A, Veiga E, Dias CC, Palha F. Campos L, et al. Int J Environ Res Public Health. 2018 Jul 6;15(7):1426. doi: 10.3390/ijerph15071426. Int J Environ Res Public Health. 2018. PMID: 29986444 Free PMC article. Clinical Trial.
- Do Web-based Mental Health Literacy Interventions Improve the Mental Health Literacy of Adult Consumers? Results From a Systematic Review. Brijnath B, Protheroe J, Mahtani KR, Antoniades J. Brijnath B, et al. J Med Internet Res. 2016 Jun 20;18(6):e165. doi: 10.2196/jmir.5463. J Med Internet Res. 2016. PMID: 27323907 Free PMC article. Review.
- Adolescents Identify Modifiable Community-Level Barriers to Accessing Mental Health and Addiction Services in a Rural Canadian Town: A Survey Study. Marmura H, Cozzi RRF, Blackburn H, Ortiz-Alvarez O. Marmura H, et al. Pediatr Rep. 2024 May 6;16(2):353-367. doi: 10.3390/pediatric16020031. Pediatr Rep. 2024. PMID: 38804374 Free PMC article.
- Intergenerational Transmission of Mental Health Literacy and Its Mechanism: The Mediating Effect of Parent-Child Relationship and the Moderating Effect of School Mental Health Service. Wang X, Wang S, Song T, Feng K, Li Y. Wang X, et al. Psychol Res Behav Manag. 2024 Mar 14;17:1177-1189. doi: 10.2147/PRBM.S453122. eCollection 2024. Psychol Res Behav Manag. 2024. PMID: 38505347 Free PMC article.
- Assessing the efficacy of the 'Bicho De 7 Cabeças' B-learning school-based program in enhancing mental health literacy and reducing stigma. Meilsmeidth G, Trigueiro MJ, Simões-Silva V, Simões de Almeida R, Portugal P, Gomes PV, de Sousa S, Campos F, Monteiro P, Soutelo AP, Marques A. Meilsmeidth G, et al. BMC Psychol. 2024 Feb 23;12(1):93. doi: 10.1186/s40359-024-01591-2. BMC Psychol. 2024. PMID: 38395937 Free PMC article.
- Mental health literacy and seeking for professional help among secondary school students in Slovakia: a brief report. Sokolová L. Sokolová L. Front Public Health. 2024 Jan 30;12:1333216. doi: 10.3389/fpubh.2024.1333216. eCollection 2024. Front Public Health. 2024. PMID: 38351957 Free PMC article.
- Identifying Mental Health Literacy as a Key Predictor of COVID-19 Vaccination Acceptance among American Indian/Alaska Native/Native American People. Chen X, Winterowd C, Li M, Kreps GL. Chen X, et al. Vaccines (Basel). 2023 Nov 30;11(12):1793. doi: 10.3390/vaccines11121793. Vaccines (Basel). 2023. PMID: 38140196 Free PMC article.
- World Health Organization. Adolescent mental health. 2018. (Available from: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health ).
- Brijnath B, Protheroe J, Mahtani KR et al. Do web-based mental health literacy interventions improve the mental health literacy of adult consumers? Results from a systematic review. J Med Internet Res 2016: 18: e165.
- Jorm A, Korten A, Jacomb P et al. Mental health literacy: A survey of the public’s bility to recognize mental disorders and their beliefs about the effectiveness of treatment. Med J 1997: 166: 182-186.
- Kutcher S, Bagnell A, Wei Y. Mental health literacy in secondary schools: A Canadian approach. Child AdolescPsychiatr Clin N Am 2015: 24: 233-244.
- Bourget Management Consulting for the Canadian Alliance on Mental Illness and Mental Health. Mental health literacy: A review of the literature. (Available from: https://pdfs.semanticscholar.org/5fbd/bb3c7c4968f3ccb37227963568b887873c... .)
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Ovid Technologies, Inc.
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Advertisement
A Systematic Review of Mental Health Literacy Measures for Children and Adolescents
- Systematic Review
- Published: 02 January 2023
- Volume 8 , pages 339–358, ( 2023 )
Cite this article

- Matej Kucera ORCID: orcid.org/0000-0003-3288-232X 1 , 3 , 4 na1 ,
- Hana Tomaskova 1 , 2 ,
- Marek Stodola 5 na1 &
- Anna Kagstrom 1
1954 Accesses
2 Citations
1 Altmetric
Explore all metrics
Mental health literacy is an essential part of preventing mental illnesses. However, the quality of mental health literacy measures remain unknown, as does its universality across various settings and populations. Few studies focus on measures aimed at assessing mental health literacy of children and adolescents that covers knowledge about mental health and mental disorders, strategies to decrease stigma, and enhancement of help-seeking efficacy. The present study aimed to conduct a systematic search to find available measures of mental health literacy of children and adolescents under the age of 19 years. The following databases were searched: Web of Science, PubMed, PsycINFO, MEDLINE, ERIC and CINAHL Plus. COSMIN checklist was applied to assess the methodological quality of each study. Twenty-one mental health literacy measures were identified in 18 studies. The quality of the studies ranged between very good and inadequate. Sixteen measures were universal, implying that they were not diagnostic specific. Two measures scored a full score of four on mental health literacy comprehensiveness. This review revealed that the overall quality of the measurement properties was mixed, that there are limited measures available to evaluate non-diagnostic-specific mental health literacy in universal populations of children and adolescents, and that measures fail to cover key mental health literacy components of knowledge of mental health, illness, stigma, and help-seeking. New measures should be developed to cover this gap in the field of child and adolescent mental health.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies

Evidence-Based Practices for Children, Youth, and Young Adults with Autism: Third Generation Review

Community Interventions to Promote Mental Health and Social Equity
Burns, J. R., & Rapee, R. M. (2006). Adolescent mental health literacy: Young people’s knowledge of depression and help seeking. Journal of adolescence , 29 (2), 225–239.
Article PubMed Google Scholar
Campos, L., Dias, P., Palha, F., Duarte, A., & Veiga, E. (2016). Development and psychometric properties of a new questionnaire for assessing mental health literacy in young people. Universitas Psychologica , 15 (2), 61–72.
Article Google Scholar
Castellvi, P., Casañas, R., Arfuch, V. M., Moreno, G., Torres Torres, J. J., García-Forero, M., & Lalucat-Jo, C., L (2020). Development and validation of the Espaijove. Net mental health literacy (EMHL) test for spanish adolescents. International Journal of Environmental Research and Public Health , 17 (1), 72.
Darraj, H. A., Mahfouz, M. S., Sanosi, A., Badedi, R. M., Sabai, M., Refaei, A. A. A., & Mutawm, H. (2016). Arabic translation and psychometric evaluation of the depression literacy questionnaire among adolescents. Psychiatry Journal . https://doi.org/10.1155/2016/8045262
Article PubMed PubMed Central Google Scholar
Gulliver, A., Griffiths, K. M., & Christensen, H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry , 10 (1), 1–9.
Hart, S. R., Kastelic, E. A., Wilcox, H. C., Beaudry, M. B., Musci, R. J., Heley, K. M., & Swartz, K. L. (2014). Achieving depression literacy: The adolescent depression knowledge questionnaire (ADKQ). School Mental Health , 6 (3), 213–223.
Chaves, C. B., Sequeira, C., Duarte, J. C., Nelas, P. A., Gonçalves, A., & Santos, E. J. R. D. (2021). Mental health literacy: a systematic review of themeasurement instruments . Universidad de Extremadura.
Google Scholar
Jackson, D., & Heatherington, L. (2006). Young Jamaicans’ attitudes toward mental illness: experimental and demographic factors associated with social distance and stigmatizing opinions. Journal of Community Psychology , 34 (5), 563–576.
Jorm, A. F. (2012). Mental health literacy: empowering the community to take action for better mental health. American Psychologist , 67 (3), 231.
Jorm, A. F., Korten, A. E., Jacomb, P. A., Christensen, H., Rodgers, B., & Pollitt, P. (1997). Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Medical Journal of Australia , 166 (4), 182–186.
Kaushik, A., Papachristou, E., Dima, D., Fewings, S., Kostaki, E., Ploubidis, G. B., & Kyriakopoulos, M. (2017). Measuring stigma in children receiving mental health treatment: validation of the paediatric self-stigmatization scale (PaedS). European Psychiatry , 43 , 1–8.
Kellison, I., Bussing, R., Bell, L., & Garvan, C. (2010). Assessment of stigma associated with attention-deficit hyperactivity disorder: psychometric evaluation of the ADHD stigma questionnaire. Psychiatry Research , 178 (2), 363–369.
Kessler, R. C., Foster, C. L., Saunders, W. B., & Stang, P. E. (1995). Social consequences of psychiatric disorders, I: Educational attainment. American Journal of Psychiatry , 152 (7), 1026–1032.
Kieling, C., Baker-Henningham, H., Belfer, M., Conti, G., Ertem, I., Omigbodun, O., & Rahman, A. (2011). Child and adolescent mental health worldwide: evidence for action. The Lancet , 378 (9801), 1515–1525.
Kutcher, S., Bagnell, A., & Wei, Y. (2015). Mental health literacy in secondary schools: a canadian approach. Child and Adolescent Psychiatric Clinics , 24 (2), 233–244.
Kutcher, S., Wei, Y., Costa, S., Gusmão, R., Skokauskas, N., & Sourander, A. (2016). Enhancing mental health literacy in young people (pp. 567–569). Springer.
Kutcher, S., & Wei, Y. (2020). School mental health: a necessary component of youth mental health policy and plans. World Psychiatry , 19 , 174–175.
Mansfield, R., Humphrey, N., & Patalay, P. (2020). Psychometric validation of the reported and intended Behavior Scale (RIBS) with adolescents. Stigma and Health , 5 (3), 284.
McKeague, L., Hennessy, E., O’Driscoll, C., & Heary, C. (2015). Peer mental health stigmatization scale: psychometric properties of a questionnaire for children and adolescents. Child and Adolescent Mental Health , 20 (3), 163–170.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2010). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International Journal Of Surgery , 8 (5), 336–341.
O’Connor, M., Casey, L., & Clough, B. (2014). Measuring mental health literacy–a review of scale-based measures. Journal of Mental Health , 23 (4), 197–204.
Ochoa, S., Martínez-Zambrano, F., Vila-Badia, R., Arenas, O., Casas-Anguera, E., García-Morales, E., & Valduciel, T. (2016). Spanish validation of the social stigma scale: Community attitudes towards mental illness. Revista de Psiquiatría y Salud Mental (English Edition) , 9 (3), 150–157.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., & Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj, 372 , n71. https://doi.org/10.1136/bmj.n71
Pinto, M. D., Hickman, R., Cynthia Logsdon, M., & Burant, C. (2012). Psychometric evaluation of the revised attribution questionnaire (r-AQ) to measure mental illness stigma in adolescents. Journal of Nursing Measurement , 20 (1), 47.
Riebschleger, J., Costello, S., Cavanaugh, D. L., & Grové, C. (2019). Mental health literacy of youth that have a family member with a mental illness: Outcomes from a new program and scale. Frontiers in Psychiatry, 2019 , 2.
Ritchie, H., & Roser, M. (2018). Mental health. Our world in data. Retrieved October, 7 , 2019.
Rosa, A., Loureiro, L., & Sequeira, C. (2016). Literacia em saúde mental sobre abuso de álcool em adolescentes: Desenvolvimento de um instrumento de medida. Revista Portuguesa de Enfermagem de Saúde Mental, 16 , 59–68.
Scott, K. M., Lim, C., Al-Hamzawi, A., Alonso, J., Bruffaerts, R., Caldas-de-Almeida, J. M., & De Jonge, P. (2016). Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry , 73 (2), 150–158.
Serra, M., Lai, A., Buizza, C., Pioli, R., Preti, A., Masala, C., & Petretto, D. R. (2013). Beliefs and attitudes among italian high school students toward people with severe mental disorders. The Journal of Nervous and Mental Disease , 201 (4), 311–318.
Schmeelk-Cone, K., Pisani, A. R., Petrova, M., & Wyman, P. A. (2012). Three scales assessing high school students’ attitudes and perceived norms about seeking adult help for distress and suicide concerns. Suicide and Life‐Threatening Behavior , 42 (2), 157–172.
Skre, I., Friborg, O., Breivik, C., Johnsen, L. I., Arnesen, Y., & Wang, C. E. A. (2013). A school intervention for mental health literacy in adolescents: effects of a non-randomized cluster controlled trial. Bmc Public Health , 13 (1), 1–15.
Terwee, C. B., Mokkink, L. B., Knol, D. L., Ostelo, R. W., Bouter, L. M., & de Vet, H. C. (2012). Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Quality of Life Research , 21 (4), 651–657.
Watson, A. C., Miller, F. E., & Lyons, J. S. (2005). Adolescent attitudes toward serious mental illness. The Journal of Nervous and Mental Disease , 193 (11), 769–772.
Wei, Y., McGrath, P. J., Hayden, J., & Kutcher, S. (2015). Mental health literacy measures evaluating knowledge, attitudes and help-seeking: a scoping review. BMC Psychiatry , 15 (1), 1–20.
Wei, Y., McGrath, P. J., Hayden, J., & Kutcher, S. (2016). Measurement properties of tools measuring mental health knowledge: a systematic review. BMC Psychiatry , 16 (1), 1–16.
Whiteford, H. A., Degenhardt, L., Rehm, J., Baxter, A. J., Ferrari, A. J., Erskine, H. E., & Johns, N. (2013). Global burden of disease attributable to mental and substance use disorders: findings from the global burden of Disease Study 2010. The Lancet , 382 (9904), 1575–1586.
World Health Organization (2021). Helping adolescents thrive toolkit: strategies to promote and protect adolescent mental health and reduce self-harm and other risk behaviours. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF), 2021. Licence: CC BY-NC-SA 3. Geneva PP - Geneva: World Health Organization. Retrieved from http://apps.who.int/iris
Zenas, D., Nielsen, M. G., Fonager, K., Petersen, K. S., Szulevicz, T., & Overgaard, C. (2020). Assessing mental health literacy among danish adolescents-development and validation of a multifaceted assessment tool (the danish MeHLA questionnaire). Psychiatry Research , 293 , 113373.
Download references
This project is supported by EEA and Norway Funds Project: SUPREME Strengthening Universal Prevention, Resources, and Evaluation of Mental Health in Education, funded via the grant “Monitoring a posilování duševního zdraví dětí a adolescent,” grant number ZD-ZDOVA1-025. The funding bodies had no role whatsoever in the design of our program or study, methodology used, data collection, data analysis, data interpretation, or writing of this manuscript.
Author information
Matej Kucera and Hana Tomaskova are first authorship.
Authors and Affiliations
National Institute of Mental Health, Topolová 748, 250 67, Klecany, Czech Republic
Matej Kucera, Hana Tomaskova & Anna Kagstrom
Department of Psychology, Charles University, Prague, Czech Republic
Hana Tomaskova
Second Faculty of Medicine, Charles University, Prague, Czech Republic
Matej Kucera
Faculty of Science, Vrije Universiteit Amsterdam, De Boelelaan 1105, 1081 HV, Amsterdam, The Netherlands
Faculty of Social Sciences, Charles University, Prague, Czech Republic
Marek Stodola
You can also search for this author in PubMed Google Scholar
Contributions
MK participated in the design and study quality assessment, interpretation of the data, and helped draft the manuscript; HT participated in the study design, data management and extraction, and helped draft the manuscript; MS participated in data management and extraction and reviewed the manuscript; AK conceived the study, participated in its design and interpretation of the data, and helped draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Matej Kucera .
Ethics declarations
Conflict of interest.
The authors report no conflict of interests.
Preregistration
This systematic review was registered in International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY), Registration number: INPLASY202290054, DOI number: https://doi.org/10.37766/inplasy2022.9.005 .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Search strategy applied across the databases
Concept 1 (population) < 19) | Concept 2 (assessment tool) | Concept 3 (mental health) | Concept 4 (literacy) | Concept 5 (study type) |
|---|---|---|---|---|
“Child*” OR “adolescen*” OR “youth” | “Assessment*” OR “evaluat*” OR “measur*” OR “test*” OR “scale*” OR “assessment*” OR “psychometrics” OR “questionnaire*” | “Mental health” OR “mental well-being” | “literacy” OR “knowledge” OR “awareness” OR “attitudes” OR “stigma” | Reliability OR effective* OR efficac* OR program evaluation OR validity |
Appendix II
Standards and measurement properties and its taxonomy based on COSMIN
Content validity | |
Box 1. PROM development | |
Box 2. Content validity | The degree to which the content of a PROM is an adequate reflection of the construct to be measured. |
Internal structure | |
Box 3. Structural validity | The degree to which the scores of a PROM are an adequate reflection of the dimensionality of the construct to be measured. |
Box 4. Internal consistency | The degree of the interrelatedness among the items. |
Box 5. Cross-cultural validity\measurement invariance | The degree to which the performance of the items on a translated or culturally adapted PROM are an adequate reflection of the performance of the items of the original version of the PROM |
Remaining measurement properties | |
Box 6. Reliability | The proportion of the total variance in the measurements which is due to ‘true’ differences between patients |
Box 7. Measurement error | The systematic and random error of a patient’s score that is not attributed to true changes in the construct to be measured |
Box 8. Criterion validity | The degree to which the scores of a PROM are an adequate reflection of a ‘gold standard’ |
Box 9. Hypotheses testing for construct validity | Hypotheses testing for construct validity refers to the degree to which the scores of a PROM are consistent with hypotheses based on the assumption that the PROM validly measures the construct to be measured. |
Box 10. Responsiveness | The ability of a PROM to detect change over time in the construct to be measured |
Appendix III
Updated criteria for good measurement properties
Measurement property | Rating | Criteria |
|---|---|---|
Structural validity | + | CTT: CFA: CFI or TLI or comparable measure > 0.95 OR RMSEA < 0.06 OR SRMR < 0.08 IRT/Rasch: No violation of unidimensionality: CFI or TLI or comparable measure > 0.95 OR RMSEA < 0.06 OR SRMR < 0.08 AND no violation of local independence: residual correlations among the items after controlling for the dominant factor < 0.20 OR Q3’s < 0.37 AND no violation of monotonicity: adequate looking graphs OR item scalability > 0.30 AND adequate model fit: IRT: χ2 > 0.01 Rasch: infit and outfit mean squares ≥ 0.5 and ≤ 1.5 OR Z-standardized values > -2 and < 2 |
? | CTT: Not all information for ‘+’ reported IRT/Rasch: Model fit not reported | |
– | Criteria for ‘+’ not met | |
Internal consistency | + | At least low evidence for sufficient structural validity AND Cronbach’s alpha(s) ≥ 0.70 for each unidimensional scale or subscale |
? | Criteria for “At least low evidence for sufficient structural validity” not met | |
– | At least low evidence for sufficient structural validity AND Cronbach’s alpha(s) < 0.70 for each unidimensional scale or subscale | |
Reliability | + | ICC or weighted Kappa ≥ 0.70 |
? | ICC or weighted Kappa not reported | |
– | ICC or weighted Kappa < 0.70 | |
Measurement error | + | SDC or LoA < MIC |
? | MIC not defined | |
– | SDC or LoA > MIC | |
Hypotheses testing for construct validity | + | The result is in accordance with the hypothesis |
? | No hypothesis defined (by the review team) | |
– | The result is not in accordance with the hypothesis | |
Cross-cultural validity/measurement invariance | + | No important differences found between group factors (such as age, gender, language) in multiple group factor analysis OR no important DIF for group factors (McFadden’s R2 < 0.02) |
? | No multiple group factor analysis OR DIF analysis performed | |
– | Important differences between group factors OR DIF was found | |
Criterion validity | + | Correlation with gold standard ≥ 0.70 OR AUC ≥ 0.70 |
? | Not all information for ‘+’ reported | |
– | Correlation with gold standard < 0.70 OR AUC < 0.70 | |
Responsiveness | + | The result is in accordance with the hypothesis7 OR AUC ≥ 0.70 |
? | No hypothesis defined (by the review team) | |
– | The result is not in accordance with the hypothesis OR AUC < 0.70 |
Appendix IV
Methodological quality of each study on a measurement properties
PROM | Tool | Content validity | Internal structure | Remaining measurement properties | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Tool development | Content validity | Structural Validity | Internal Consistency | Cross-cultural validity | Reliability | Measurement error | Criterion validity | Hypotheses testing | Responsiveness | ||
PROM A Riebschleger et al. ( ) | (K-MIR) | D | NR | V | V | NR | NR | NR | NR | NR | NR |
PROM B (Ochoa et al. ( ) | (CAMI - Spanish version) | D | NR | NR | V | NR | V | A | NR | NR | NR |
PROM C McKeague et al. ( ) | Peer mental health stigmatization scale | D | D | NR | D | NR | V | V | NR | V | V |
PROM D Kellison et al. ( ) | (ASQ) | D | D | V | V | NR | V | V | V | V | |
PROM E Pinto et al. ( ) | (r-AQ) | I | NR | V | V | A | NR | NR | NR | NR | |
PROM F Hart et al. ( ) | ADKQ | I | NR | V | V | V | NR | NR | NR | NR | V |
PROM G Burns and Rapee ( ) | Friend in need questionnaire | I | NR | NR | NR | NR | NR | NR | NR | NR | |
PROM H Campos et al. ( ) | (MHLq) | V | V | NR | V | NR | V | V | NR | NR | NR |
PROM I Zenas et al. ( ) | Danish MeHLA questionnaire | V | V | V | V | NR | NR | NR | NR | NR | NR |
PROM J Castellvi et al. ( ) | EspaiJove.net | V | V | NR | V | NR | V | V | NR | V | V |
PROM K Kaushik et al. ( ) | Paediatric (PaedS) | V | V | V | V | NR | NR | NR | NR | V | V |
PROM L Darraj et al. ( ) | (D-lit) | V | V | V | V | NR | A | V | NR | NR | NR |
PROM M Rosa et al. ( ) | MentalHLis-AA | V | V | A | V | NR | NR | NR | NR | NR | NR |
PROM N Serra et al. ( ) | Knowledge of mental disorders | I | NR | V | NR | NR | NR | NR | NR | NR | NR |
PROM O Jackson and Heatherington ( ) | Social contact scale | D | NR | NR | A | NR | NR | NR | NR | NR | NR |
PROM P Jackson and Heatherington ( ) | (OMI) | D | NR | NR | NR | NR | NR | NR | NR | NR | NR |
PROM Q Mansfield et al. ( ) | (RIBS) | D | NR | V | V | NR | NR | NR | NR | V | V |
PROM R Schmeelk-Cone et al. ( ) | (HSA) | D | V | V | V | NR | NR | NR | NR | V | V |
PROM S (Schmeelk-COne et al. ( ) | (RCS) | D | V | V | V | NR | NR | NR | NR | V | V |
PROM T Schmeelk-Cone et al. ( ) | (AHSY) | D | V | V | V | NR | NR | NR | NR | V | V |
PROM U Watson et al. ( ) | (ATSMI-AV) | I | NR | NR | NR | NR | NR | NR | NR | NR | NR |
- V very good, A adequate, D doubtful, I inadequate
Rating of results in each study on measurement properties against the updated criteria for good measurement properties
PROM | Tool | Content validity | Internal structure | Remaining measurement properties | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Relevance rating | Comprehensiveness rating | Comprehensibility rating | Structurl validity | Internal consistency | Cross-cultural validity | Reliability | Measurement error | Criterion validity | Hypotheses testing | Responsiveness | ||
PROM A Riebschleger et al. ( ) | (K-MIR) | NR | NR | NR | + | + | NR | NR | NR | NR | NR | NR |
PROM B Ochoa et al. ( ) | (CAMI - Spanish version) | NR | NR | NR | NR | + | NR | + | ? | NR | NR | NR |
PROM C McKeague et al. ( ) | Peer mental health stigmatization scale | ± | – | – | NR | + | NR | ? | ? | NR | ? | + |
PROM D (Kellison et al., ) | (ASQ) | + | + | + | + | + | NR | + | ? | NR | + | + |
PROM E Pinto et al., ( ) | (r-AQ) | NR | NR | NR | + | + | ? | NR | NR | NR | NR | NR |
PROM F Hart et al. ( ) | (ADKQ) | NR | NR | NR | + | + | ? | NR | NR | NR | NR | ? |
PROM G Burns and Rapee ( ) | Friend in need questionnaire | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
PROM H Campos et al. ( ) | (MHLq) | + | + | + | NR | + | NR | + | ? | NR | NR | NR |
PROM I Zenas et al. ( ) | Danish MeHLA questionnaire | + | + | + | – | + | NR | NR | NR | NR | NR | NR |
PROM J Castellvi et al. ( ) | EspaiJove.net | + | + | + | NR | + | NR | – | ? | NR | ? | ? |
PROM K Kaushik et al. ( ) | Paediatric (PaedS) | + | + | + | + | + | NR | NR | NR | NR | ? | ? |
PROM L Darraj et al. ( ) | (D-lit) | + | + | + | ? | + | NR | ? | ? | NR | NR | NR |
PROM M Rosa et al. ( ) | MentalHLis-AA | + | + | + | ? | – | NR | NR | NR | NR | NR | NR |
PROM N Serra et al. ( ) | Knowledge of mental disorders | NR | NR | NR | ? | NR | NR | NR | NR | NR | NR | NR |
PROM O Jackson and Heatherington ( ) | Social contact scale | NR | NR | NR | NR | + | NR | NR | NR | NR | NR | NR |
PROM P Jackson and Heatherington ( ) | (OMI) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
PROM Q Mansfield et al. ( ) | (RIBS) | NR | NR | NR | + | + | NR | NR | NR | NR | ? | ? |
PROM R Schmeelk-Cone et al. ( ) | (HSA) | + | + | + | ? | + | NR | NR | NR | NR | ? | ? |
PROM S Schmeelk-Cone et al. ( ) | (RCS) | + | + | + | ? | – | NR | NR | NR | NR | ? | ? |
PROM T Schmeelk-Cone et al. ( ) | (AHSY) | + | + | + | ? | – | NR | NR | NR | NR | ? | ? |
PROM U Watson et al. ( ) | (ATSMI-AV) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
- + sufficient, ? indeterminate”, – insufficient, ± inconsistent
Appendix VI
MHL comprehensiveness across the scales
Name of the scales | Authors | MHL 1 | MHL 2 | MHL 3 | MHL 4 |
|---|---|---|---|---|---|
Knowledge of mental illness and recovery scale (K-MIR) | Riebschleger et al. ( ) | 0 | 1 | 1 | 0 |
Community attitudes towards mental illness (CAMI) (Spanish version) | Ochoa et al. ( ) | 0 | 1 | 1 | 0 |
Peer mental health stigmatization scale | McKeague et al. ( ) | 0 | 0 | 1 | 0 |
Revised attribution questionnaire (r-AQ) | Pinto et al. ( ) | 0 | 0 | 1 | 0 |
Friend in need questionnaire | Burns and Rapee ( ) | 0 | 1 | 0 | 1 |
Mental health literacy questionnaire (MHLq) | Campos et al. ( ) | 1 | 1 | 0 | 1 |
Danish MeHLA questionnaire | Zenas et al. ( ) | 1 | 1 | 1 | 1 |
EspaiJove.net | Castellvi et al. ( ) | 1 | 1 | 1 | 1 |
Depression literacy questionnaire (D-lit) | Darraj et al. ( ) | 0 | 1 | 1 | 0 |
Knowledge of mental disorders | Serra et al. ( ) | 0 | 1 | 0 | 0 |
Social contact scale | Jackson and Heatherington ( ) | 0 | 0 | 1 | 0 |
Reported and intended behaviour scale (RIBS) | Mansfield et al. ( ) | 0 | 0 | 1 | 0 |
Help-seeking acceptability (HSA) at school scale | Schmeelk-Cone et al. ( ) | 0 | 0 | 0 | 1 |
Attitudes toward serious mental illness scale - Adolescent version (ATSMI-AV) | Watson et al. ( ) | 0 | 1 | 1 | 0 |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Kucera, M., Tomaskova, H., Stodola, M. et al. A Systematic Review of Mental Health Literacy Measures for Children and Adolescents. Adolescent Res Rev 8 , 339–358 (2023). https://doi.org/10.1007/s40894-022-00202-8
Download citation
Received : 19 October 2022
Accepted : 22 December 2022
Published : 02 January 2023
Issue Date : September 2023
DOI : https://doi.org/10.1007/s40894-022-00202-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health literacy
- Systematic review
- Adolescents
- Mental health
- Find a journal
- Publish with us
- Track your research
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Positive mental health and mental health literacy of informal caregivers: a scoping review.

1. Introduction
2. materials and methods, 3.1. characterization of the studies, 3.2. main results: mental health literacy and positive mental health.
- In the study in which the association between e-health literacy and caregiver burden was examined [ 24 ], a positive association was found between the two (β = 0.14; 95% confidence interval [0.03, 0.27]).
- In the study that aimed to identify the levels of health literacy and explore associations with the quality of life of family caregivers and their perceptions about the role [ 25 ], 78.6% of family caregivers had high levels of health literacy, and in the group of family caregivers with low literacy (21.4%), significant effects were identified in the subjective caregiving burden ( p = 0.041), relationship satisfaction with the patient ( p = 0.028), and caregiving mastery ( p = 0.030), with no difference between the groups regarding quality of life and general mental health.
- In the study examining the association between quality of life (QoL) and family caregivers’ health literacy [ 26 ], the QoL mean score was 180 (of a possible 370); the lowest QoL scores were reported for physical well-being (26.5 ± 7.9), followed by spiritual well-being (35.5 ± 10.7). Cancer health literacy was significantly associated with QoL among participants. While QoL was negatively associated with psychosocial needs (r = −0.55, p < 0.01), QoL was positively correlated with cancer health literacy (r = 0.19, p = 0.04). QoL was significantly correlated (negative) with five of the seven domains of psychosocial needs of family caregivers; the most highly correlated domain was spiritual support (r = −0.30, p < 0. 001), followed by psychological problems (r = −0.24, p < 0.01), information (r = −0.24, p < 0.01), and family/social support (r = −0.19, p = 0.04). Approximately 28% of the variance in quality of life is explained by information practices, psychological problems, and health literacy, with information needs making one of the strongest contributions (2.9%).
- The study that aimed to investigate the characteristics of the caregiving experience according to age at onset of dementia to adapt support programs [ 22 ] shows confidence scores in role performance, namely regarding “Request respite care”, with scores of 51.14 (EOD) and 45.93 (LOD) out of 100; “Cope with behaviors”, with scores of 73.96 (EOD) and 71.15 (LOD); and “Control disturbing thoughts”, with scores of 65.41 (EOD) and 73.28 (LOD). As for the caregiver’s level of distress, the family caregivers presented “Psychological distress”, with scores of 26.17 (EOD) and 23.9 (LOD); “Anxiety”, with scores of 8.79 (EOD) and 7. 74 (LOD); and “Depression”, with scores of 5.89 (EOD) and 5.64 (LOD). The family caregivers showed a positive impact of “caregiving experience” with scores of 27.7 (EOD) and 26.98 (LOD) at the level of caregiver’s esteem and scores of 51.47 (EOD) and 50.3 (LOD) at the level of “Role confidence”. All caregivers were confident in performing their role, reasonably well prepared for future needs, and reported mild depressive and anxious symptoms. However, they lacked informal support, had little confidence in requesting respite care, and reported effects on their health. Comparing the two groups of caregivers, those caring for people with early dementia had more severe perceptions of the cognitive disturbances of people with dementia and reported a better sense of preparation and knowledge of services. Caregivers of spouses with late dementia were more confident in their abilities to control disturbing thoughts. The results also suggest that programs should provide information about support networks to improve the preparedness of caregivers of spouses with early dementia, as well as emphasize positive coping strategies for caregivers to maintain quality relationships with the dependent relative, which influence perceptions of symptoms.
- From the quantitative study [ 28 ] aiming to explore the experiences of family caregivers of people with schizophrenia in outpatient treatment, themes related to family caregivers’ mental health such as emotional burden and anxiety about the future emerge from the thematic analysis.
- The study aimed at measuring the impact of a respite care program on the well-being of family caregivers [ 23 ] revealed improvements at the level of well-being indicators with scores of 3.31 (BR)/2.36 (DR) in terms of stress levels, 2.56 (BR)/1.9 (DR) for general health problem status, 2.02 (BR)/2.88 (DR) in terms of social/recreational activities, 1.83 (BR)/1.46 ± 0.82 (DR) for placing the care recipient in out-of-home care, and 5.24 (BR)/3.06 ± 3.09 (DR) in terms of stress-related health symptoms.
- The study under an intervention program aiming to understand the perceived health literacy and psychosocial health outcomes of family caregivers [ 29 ] shows an increase after intervention; in terms of health literacy, there was an increase in the scores (T0 and T1) at the level of functional health literacy (knowledge) with 3. 7(T0)/4.2 (T1), of interactive health literacy (capability to act) with 3.3 (T0)/3.7 (T1), and of critical health literacy (individual empowerment) with 3.0 (T0)/3. 2 (T1). As for psycho-social health, there is also an increase in scores namely in terms of sense of certainty with 3.0 (T0)/3.2 (T1) and life balance with 2.8 (T0)/2.9 (T1).
4. Discussion
5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- World Health Organization. Mental Health Atlas 2020 ; World Health Organization: Geneve, Switzerland, 2021; ISBN 978-92-4-003670-3. Available online: who.int (accessed on 11 November 2022).
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (accessed on 3 October 2022).
- United Nations in Western Europe. Sustainable Development Guide: 17 Goals to Transform Our World ; United Nations: Brussels, Belgium, 2018. [ Google Scholar ]
- World Health Organization. World Mental Health Report: Transforming Mental Health for All ; World Health Organization: Geneve, Switzerland, 2022. [ Google Scholar ]
- Conselho Nacional de Saúde. Sem Mais Tempo a Perder–Saúde Mental em Portugal: Um Desafio Para a Próxima Década ; Conselho Nacional de Saúde: Lisboa, Portugal, 2019. [ Google Scholar ]
- Lluch, M.T. Evaluación empiríca de un modelo conceptual de salud mental positive. Salud Ment. 2002 , 25 , 42–55. [ Google Scholar ]
- Sequeira, C.; Carvalho, J.; Sampaio, F.; Sá, L.; Lluch-Canut, T.; Roldán-Merino, J. Avaliação das propriedades psicométricas do questionário de saúde mental positiva em estudantes portugueses do ensino superior. Rev. Port. Enferm. Saúde Ment. 2014 , 11 , 45–53. [ Google Scholar ]
- Loureiro, A. Literacia e Saúde Mental Positiva: Tradução e Validação de um Instrumento de Avaliação em Literacia de Saúde mental. Master’s Thesis, Nursing School of Porto, Porto, Portugal, 2018. [ Google Scholar ]
- Galustyan, A.-M. A Literacia em Saúde Mental e o Bem-Estar do Cuidador Informal de Pessoas com Doença Mental. Master’s Thesis, Polytechnic of Porto, Porto, Portugal, 2019. [ Google Scholar ]
- Jorm, A.F.; Korten, A.E.; Jacomb, P.A.; Christensen, H.; Rodgers, B.; Pollitt, P. “Mental Health Literacy”: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med. J. Aust. 1997 , 166 , 182–186. [ Google Scholar ] [ CrossRef ]
- Jorm, A.F. Mental Health Literacy: Public knowledge and beliefs about mental disorders. BJPsych 2000 , 177 , 396–401. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Mehrotra, K.; Nautiyal, S.; Raguram, A. Mental Health Literacy in Family Caregivers: A comparative analysis. Asian J. Psychiatr. 2018 , 31 , 58–62. [ Google Scholar ] [ CrossRef ]
- Abreu-Figueiredo, R.; Sá, L.; Lourenço, T. Death anxiety in palliative care: Validation of the nursing diagnosis. Acta Paul. Enferm. 2019 , 32 , 178–185. [ Google Scholar ] [ CrossRef ]
- Lourenço, T.; Abreu-Figueiredo, R.; Sá, L.O. Clinical validation of the Nanda-I “Caregiver Role Strain” nursing diagnosis in the context of Palliative Care. Texto Context. Enferm. 2021 , 30 . [ Google Scholar ] [ CrossRef ]
- Dixe, M.A.; Querido, A.I. Informal caregiver of dependent person in self-care: Burden-related factors. Referência 2020 , 5 , e20013. [ Google Scholar ] [ CrossRef ]
- Krieger, T.; Researcher, I.H.; Feron, F. Developing a Complex Intervention Programme for Informal Caregivers of Stroke Ssurvivors: The Caregivers’ Guide. Caring. Sci. 2017 , 31 , 146–157. [ Google Scholar ] [ CrossRef ]
- Jung, H.; Sternberg, K.V.; Davis, K. Expanding a Measure of Mental Health Illiteracy: Development and Validation of a Multicomponent Mental Health Literacy Measure. Psychiatry Res. 2016 , 243 , 278–286. [ Google Scholar ] [ CrossRef ]
- Carvalho, D.; Sequeira, C.; Querido, A.; Tomás, C.; Morgado, T.; Valentim, O.; Moutinho, L.; Gomes, J.; Laranjeira, C. Positive Mental Health Literacy: A Concept Analysis. Front. Psychol. 2022 , 13 , 877611. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018 , 18 , 143. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018 , 169 , 467–473. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Grade PRO. Available online: https://www.gradepro.org/resources (accessed on 10 October 2022).
- Wawrziczny, E.; Berna, G.; Ducharme, F.; Kergoat, M.J.; Pasquier, F.; Antoine, P. Characteristics of the spouse caregiving experience: Comparison between early and late-onset dementia. Aging. Ment. Health 2018 , 22 , 1207–1215. [ Google Scholar ] [ CrossRef ]
- Ackerman, L.; Sheaffe, L. Effects of respite care training on respite provider knowledge and confidence, and outcomes for Family Caregivers receiving respite services. Home Health Care Serv. Q. 2018 , 37 , 77–96. [ Google Scholar ] [ CrossRef ]
- Wang, K.; Xiang, G.; Fei, S.; Bishop, N.J. eHealth Literacy and Caregiver Burden Among Chinese Caregivers of Older Adults with Cognitive Impairment: Does Education Matter? J. Appl. Gerontol. 2021 , 40 , 1837–1845. [ Google Scholar ] [ CrossRef ]
- Hahn, E.A.; Boileau, N.R.; Hanks, R.A.; Sander, A.M.; Miner, J.A.; Carlozzi, N.E. Health Literacy, Health Outcomes, and the Caregiver Role in Traumatic Brain Injury. Rehabil. Psychol. 2021 , 65 , 401–408. [ Google Scholar ] [ CrossRef ]
- Gabriel, I.; Creedy, D.; ECoyne, E. Quality of life and associated factors among adults living with cancer and their Family Caregivers. Nurs. Health Sci. 2021 , 23 , 419–429. [ Google Scholar ] [ CrossRef ]
- Wan, K.; Wong, M.M.C. Stress and burden faced by Family Caregivers of people with schizophrenia and early psychosis in Hong Kong. Intern. Med. J. 2019 , 49 , 9–15. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Nuraini, T.; Tumanggor, R.D.; Hungerford, C.; Lees, D.; Cleary, M. Caregiver Burden for People with Schizophrenia in Medan, Indonesia. Issues Ment. Health Nurs. 2020 , 42 , 790–793. [ Google Scholar ] [ CrossRef ]
- Krieger, T.; Feron, F.; Dorant, E. Two-level multi-methodological evaluation of anew complex primary support programme forstroke caregivers in Germany. Ageing Soc. 2020 , 49 , 1–31. [ Google Scholar ] [ CrossRef ]
- Nações Unidas. Available online: https://unric.org/pt/envelhecimento/ (accessed on 13 October 2022).
- Peacock, S.C.; Hammond-Collins, K.; Forbes, D.A. The journey with dementia from the perspective of bereaved Family Caregivers: A qualitative descriptive study. BMC Nurs. 2014 , 13 , 42. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Almeida, A.F.N.; Lopes, L.C.; Machado, C.S.; Santos, N.S. Análise do perfil e da sobrecarga em cuidadores de idosos. Concilium 2022 , 22 , 482–494. [ Google Scholar ] [ CrossRef ]
- Jong, L.; Stahmeyer, J.T.; Eberhard, S.; Zeidler, J.; Damm, K. Willingness and preparedness to provide care: Interviews with individuals of different ages and with different caregiving experiences. BMC Geriatr. 2021 , 21 , 207. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Almeida, K.M.V.; Toye, C.; Silveira, L.V.A.; Slatyer, S.; Hill, K.; Jacinto, A.F. Assessment of functional Health Literacy in Brazilian carers of older people. Dement. Neuropsychol. 2019 , 13 , 180–186. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Hazzan, A.A.; Dauenhauer, J.; Follansbee, P.; Hazzan, J.O.; Allen, K.; Omobepade, I. Family caregiver quality of life and the care provided to older people living with dementia: Qualitative analyses of caregiver interviews. BMC Geriatrics. 2022 , 22 , 86. [ Google Scholar ] [ CrossRef ]
- Melo, H.E.; Severian, P.F.G.; Eid, L.P.; Souza, M.R.; Sequeira, C.A.C.; Souza, M.G.G.; Pompeo, D.A. Impact of anxiety and depression symptoms on perceived self-efficacy in nursing students. Acta Paul. Enferm. 2021 , 34 , eAPE01113. [ Google Scholar ] [ CrossRef ]
- Almeida, K.D.S.; Leite, M.T.; Hildebrandt, L.M. Alzheimer’s family caregivers: Literature review. Rev. Eletr. Enferm. 2009 , 11 . [ Google Scholar ] [ CrossRef ]
- Nunes, T. Estratégias de Comunicação de Organizações do Terceiro Sector: Doença de Alzheimer e Outras Demências em Portugal. Ph.D. Thesis, University Institute of Lisbon (ISCTE), Lisbon, Portugal, 2016. [ Google Scholar ]
- Soong, A.; Au, S.T.; Kyaw, B.M.; Theng, Y.L.; Tudor Car, L. Information needs and information seeking behaviour of people with dementia and their non-professional caregivers: A scoping review. BMC Geriatr. 2020 , 20 , 61. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Yuen, E.Y.N.; Knight, T.; Ricciardelli, L.A.; Burney, S. Health Literacy of caregivers of adult care recipients: A systematic scoping review. Health Soc. Care Comm. 2018 , 26 , e191–e206. [ Google Scholar ] [ CrossRef ]
- Bonaccorsi, G.; Pieralli, F.; Innocenti, M.; Milani, C.; Del Riccio, M.; Donzellini, M.; Baggiani, L.; Lorini, C. Health Literacy among Non-Familial Caregivers of Older Adults: A Study Conducted in Tuscany (Italy). Int. J. Environ. Res. Public Health 2019 , 16 , 3771. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Li, Y.; Hu, L.; Mao, X.; Shen, Y.; Xue, H.; Hou, P.; Liu, Y. Health Literacy, social support, and care ability for caregivers of dementia patients: Structural equation modeling. Geriatr Nurs. 2020 , 41 , 600–607. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yang, Y.; Romine, W.; Oyesanya, T.O.; Park, H.K.; Hendrix, C.C. The Association of Self-esteem with Caregiving Demands, Coping, Burden, and Health Among Caregivers of Breast Cancer Patients: A Structural Equation Modeling Approach. Cancer Nurs. 2022 , 45 , E820–E827. [ Google Scholar ] [ CrossRef ] [ PubMed ]
Click here to enlarge figure
| Study Identification | Sample | ||
|---|---|---|---|
| Authors (Year) Location [Reference] No. | Title | Caregivers | Dependent Person’s Diagnosis |
| Wawrziczny, E.; Berna, G.; Ducharme, F.; Kergoat, M.; Pasquier, F.; Antoine, P. (2018) France [ ] #1 | Characteristics of the spouse caregiving experience: comparison between early- and late-onset dementia | n = 150 Female (31); Mean age = 58.98 | Dementia |
| Ackerman, L.; Sheaffe, L. (2018) USA [ ] #2 | Effects of respite care training on respite provider knowledge and confidence, and outcomes for family caregivers receiving respite services | n = 102 Spouse (21); Children of the person cared for (20) | Not specified |
| Wang, K.; Gao, X.; Sun, F.; Bishop, N. (2021) China [ ] #3 | eHealth literacy and caregiver burden among chinese caregivers of older adults with cognitive impairment: does education matter? | n = 448 300 Female (300); Mean age = 57.82; Spouse (208); Children (77) | Elderly with cognitive impairment |
| Hahn, E.; Boileau, N.; Hanks, R.; Sander, A.; Miner, J.; Carlozzi, N. (2021) USA [ ] #4 | Health literacy, health outcomes, and the caregiver role in traumatic brain injury | n = 131 Female (103); Mean age = 46.2; Spouse (62); Children (11) | Traumatic brain injury |
| Gabriel, I.; Creedy, D.; Coyne, E. (2020) Nigeria [ ] #5 | Quality of life and associated factors among adults living with cancer and their family caregivers | n = 120 Female (85); Mean age = 36.13; Spouses (88) | Cancer |
| Wan, K.; Wong, M. (2019) China [ ] #6 | Stress and burden faced by family caregivers of people with schizophrenia and early psychosis in Hong Kong | 454 Female: 326 Age = 34.8% with more than 46 years | Schizophrenia and psychosis |
| Nuraini, T.; Tumanggor, R.; Hungerford, C.; Lees, D.; Cleary, M. (2021) Indonesia [ ] #7 | Caregiver burden for people with schizophrenia in Medan, Indonesia | n = 10 Female (5); Spouse (6); Children (4) | Schizophrenia |
| Krieger, T.; Feron, F.; Dorant, E. (2020) Germany [ ] #8 | Two-level multi-methodological evaluation of a new complex primary support program for stroke caregivers in Germany | n = 62 | Stroke |
| Reference | Methodological Approach | Results | Study Quality |
|---|---|---|---|
| [ ] #1 | Quantitative Comparative study Questionnaire Revised Scale for Care-giving Self-Efficacy; 14-item Psychological Distress Index; The Caregiver Reaction Assessment; SF-36 Descriptive and inferential statistics | Caregiver’s confidence: request respite care: 51.14 (EOD ), 45.93 (LOD ); cope with behaviors: 73.96 (EOD), 71.15 (LOD); control disturbing thoughts: 65.41 (EOD), 73.28 (LOD); role confidence: 51.47 (EOD), 50.30 (LOD) Caregiver’s level of distress: psychological distress: 26.17 (EOD), 23.90 (LOD); anxiety: 8.79 (EOD), 7.74 (LOD); depression: 5.89 (EOD), 5.64 (LOD); impact of caregiving experience: caregiver’s esteem: 27.70 (EOD), 26.98 (LOD) | Moderate |
| [ ] #2 | Pre- and post-test study (after implementation of Respite Educational and Support Tools REST) Modified version of the instrument developed by the ARCH National Respite Network and Resource Center (NRNRC) ANOVA | Well-being indicators: stress levels: 3.31 ± 1.24 (BR ), 2.36 ± 0.94 (DR ); general health problems status: 2.56 ± 1.19 (BR), 1.9 ± 1.00 (DR); social/recreational activities: 2.02 ± 0.96 (BR), 2.88 ± 0.98 (DR); placing the care recipient in out-of-home care: 1.83 ± 1.12 (BR), 1.46 ± 0.82 (DR); stress-related health symptoms: 5.24 ± 3.70 (BR), 3.06 ± 3.09 (DR) | Moderate |
| [ ] #3 | Quantitative Chinese e-Health Literacy scale (C-eHEals); short version of Zarit Burden Interview Linear regression | Means of caregiver e-health literacy: 2.89 ± 1.23; means of caregiver burden: 2.14 ± 1.10; positive association between e-health literacy and caregiver burden (β = 0.14; 95% confidence interval: [0.03, 0.27]). | Moderate |
| [ ] #4 | Quantitative Caregiver Appraisal Scale TBI-Care Quality of Life (QoL) ; Talking Touchscreen Technology (Health LiTT) ; General Health Status (SF-12) Linear regression | High health literacy: 78.6%; low health literacy: 21.4%; low literacy group significant effects: subjective caregiving burden (p = 0.041), relationship satisfaction with the patient (p = 0.028), caregiving mastery (p = 0.030) | Moderate |
| [ ] #5 | Cross-sectional descriptive design City of Hope Quality of Life (Family Version) Descriptive statistics Linear regression | Mean score QoL: 180.24 ± 22.90 Lowest QoL scores: physical well-being (26.5 ± 7.9); spiritual well-being (35.5 ± 10.7) | High |
| [ ] #6 | Cross-sectional survey Stress Level score scale; Quality of Life level score scale. Correlational and descriptive statistics | Mean stress score = 3.56; mean score for each QoL variable > 3; significative stress and psychosocial overload | High |
| [ ] #7 | Qualitative Unstructured interview Thematic analysis | Emergent themes: lack of knowledge about schizophrenia; emotional overload; anxiety about the future | Low |
| [ ] #8 | Multi-methodological in 2 levels, with 2 connected simultaneous studies and a sequential exploratory draw Pre- and post-test Questionnaire and interview Freebody and Luke’s Health Literacy framework Psycho-social health: 6 items to measure sense of certainty and 4 items for life balance | Health literacy (HL): functional HL (knowledge) [3.7 ± 0.8 (T0), 4.2 ± 0.8 (T1)]; interactive HL (capability to act) [3.3 ± 1.0 (T0), 3.7 ± 0.8 (T1)]; critical HL (individual empowerment) [3.0 ± 0.9 (T0), 3.2 ± 0.8 (T1)] Psycho-social health: sense of certainty [3.0 ± 0.8 (T0), 3.2 ± 0.7 (T1)]; life balance [2.8 ± 0.9 (T0), 2.9 ± 0.9 (T1)] | Moderate |
| MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
Share and Cite
Andrade, C.; Tavares, M.; Soares, H.; Coelho, F.; Tomás, C. Positive Mental Health and Mental Health Literacy of Informal Caregivers: A Scoping Review. Int. J. Environ. Res. Public Health 2022 , 19 , 15276. https://doi.org/10.3390/ijerph192215276
Andrade C, Tavares M, Soares H, Coelho F, Tomás C. Positive Mental Health and Mental Health Literacy of Informal Caregivers: A Scoping Review. International Journal of Environmental Research and Public Health . 2022; 19(22):15276. https://doi.org/10.3390/ijerph192215276
Andrade, Carmen, Márcio Tavares, Hélia Soares, Fábio Coelho, and Catarina Tomás. 2022. "Positive Mental Health and Mental Health Literacy of Informal Caregivers: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 22: 15276. https://doi.org/10.3390/ijerph192215276

Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Study protocol
- Open access
- Published: 27 June 2024
Mental health literacy and academic performance (MHLAP) in high school students: a randomized clinical trial protocol
- Cezar Giosan ORCID: orcid.org/0000-0002-1260-6830 1 ,
- Alexandru Pană 1 ,
- Ana Cosmoiu 1 ,
- Ana-Maria Chira 1 ,
- Ana-Maria Toma 1 ,
- Claudiu-Cristian Papasteri 1 ,
- Cătălin Nedelcea 1 &
- Cătălina Popoviciu 1
Trials volume 25 , Article number: 419 ( 2024 ) Cite this article
57 Accesses
Metrics details
Mental health literacy is a promising avenue of intervention for addressing the development of psychopathology, as well as its associated consequences, such as a decrease in academic performance. The current study aims to test the effectiveness of such an intervention in high school students, focusing on two main formats of delivery: (1) automated and (2) blended.
To achieve this aim, a randomized clinical trial with direct comparisons at three time points between three conditions (automated, blended, and waitlist) was designed. Power analyses yielded a necessary sample size of 264 high school students. The participants will be selected from Romanian high schools.
The current study aims to contribute to the mental health literacy literature by testing the effectiveness of an educational intervention concerning mental health in terms of its benefits for reducing psychopathology and increasing academic performance. The success of such an intervention bears important implications for addressing mental health in the educational system.
Trial registration
Clinicaltrials.gov Identifier: NCT06217744, version 1, 22 January 2024.
Peer Review reports
Mental health literacy and academic performance
Mental disorders represent one of the most important risk factors associated with disability, accounting for more than a quarter of the responsible causes for disability in people between the ages of 15 and 44 [ 1 ]. The worldwide prevalence of any mental disorder in children and adolescents is estimated at 13.4% [ 2 ]. Mental disorders are associated with school absenteeism [ 3 , 4 ], academic-related stress and poorer academic performance, learning capacity, and physical and mental health outcomes [ 5 ].
Even though there are effective mental health interventions for the youth, such as psychotherapy [ 6 ], canine-assisted psychotherapy [ 7 ], or psychiatric medication [ 8 ], to name a few, there are accessibility barriers, ranging from geographical challenges to awareness of such problems in these populations. Some of the main reasons why adolescents avoid seeking mental health help include perceived stigma and shame associated with help-seeking and insufficient mental health-related knowledge [ 9 ]. At the same time, a history of pleasant experiences with mental health services and mental health literacy constitutes some of the most important facilitators for seeking professional help [ 10 ].
This clinical trial aims to address the aforementioned issues by testing the effectiveness of an intervention meant to increase mental health literacy in adolescents through a curriculum available at school level.
Framework and rationale of the present study
Mental health literacy refers to having knowledge of how to recognize, deal with and prevent mental disorders [ 11 ]. Mental health literacy in adolescents can help develop support from parents, friends, or other members in a community, by doing so greatly complementing mental health services [ 12 ].
Unsurprisingly, poorer mental health literacy is associated with increased psychopathology, such as depression [ 13 , 14 ], anxiety, stress, and other mental health outcomes [ 14 ]. There have been efforts to develop mental health literacy interventions, such as The Youth Education and Support (YES) Program, which is geared to grades 5–8 [ 15 ]. Although there is a wide range of mental health literacy interventions [ 16 , 17 , 18 ], most of them are delivered in a classroom format [ 19 , 20 ], even though delivery through the Internet could be a viable option [ 16 ].
Most of the research in this field has been conducted in Australia, and it is unclear to what extent those findings are generalizable to different cultures and economically diverse countries [ 16 ]. The current MHL intervention is informed by "The Mental Health & High School Curriculum Guide" [ 21 ], an evidence-based mental health curriculum initially developed in Canada. Our intervention follows the structure of the aforementioned curriculum (details about the content of the intervention can be found in the “Methods” section of this paper). However, it is not a direct translation. Instead, it incorporates cultural adaptations to suit the Romanian context. Adjustments were made to address specific cultural factors in Romania. This includes adapting the language to reflect local stigmatizing words or expressions, addressing prevalent myths about mental disorders, and incorporating examples and role models relevant to Romanian teenagers. The adaptation process involved input from educational and mental health experts, school focus groups, and educational advocacy groups. The development of the intervention took 6 months. This period included extensive literature reviews, thorough documentation, and group discussions among professionals to ensure comprehensive coverage of key mental health issues relevant to teenagers (e.g., disorders usually starting in adolescence, such as eating disorders, or that might be of particular relevance in academic contexts, such as ADHD), appropriate and engaging language, and relevant examples tailored to their age and interests.
The goal of this study is to test the effectiveness of an intervention designed to promote mental health literacy in adolescents, in the format of a randomized clinical trial.
We aim to (1) determine whether this intervention has an impact on mental health, (2) observe if this intervention has an impact on fostering academic performance, particularly in disadvantaged students (i.e., academic resilience), and (3) examine what type of intervention delivery is more effective: automated versus blended format.
Methods/design
Trial design.
This study is an exploratory randomized clinical trial involving comparisons at three time points (i.e., pre-intervention, post-intervention, 1 month follow-up) between three conditions: (a) automated intervention (consisting of an online, automated delivery of the intervention), (b) blended intervention (online automated delivery of the intervention plus regular contact with facilitators), (c) waitlist, with an allocation ratio of 1:1:1. The contrast between the automated and blended interventions is meant to highlight whether contact with facilitators while receiving psychoeducational materials might have an additive effect.
The design of this study complies with the Consolidated Standards of Reporting Trials (CONSORT) guidelines [ 22 ] and follows the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) Statement 2013 [ 23 ] (see also Additional file 1: SPIRIT checklist and schedule of enrollment, interventions, and assessments).
The current trial is part of a larger project that aims to assess adolescent mental health in Romanian high schools.
General description of the tested application
SCHOLARS is a web-based mental health literacy intervention containing six modules as follows: Module 1: The Stigma of Mental Illness; Module 2: Understanding Mental Health and Mental Illness; Module 3: Information on Specific Mental Illnesses; Module 4: Experiences of Mental Illness; Module 5: Seeking Help and Finding Support; Module 6: The Importance of Well-being. These modules will have both text and videos through which the users will progress. Both the automated and blended interventions are designed to last for three months, with two modules being delivered per month. Participants are encouraged to go through the materials at their own pace and have the option to revisit previous modules as needed. Participants can access the intervention from any location.
The intervention can be accessed through a LimeSurvey link and is compatible with various devices such as computers, tablets, and mobile phones. To ensure that the intervention will be properly delivered through this medium, we initially conducted a brief pilot test on a convenience sample consisting of university students. No issues were encountered during this phase.
Detailed information about the intervention is available on the project's website, which is linked on the initial page of the intervention. This resource allows participants to learn more about the study team responsible for the development of the intervention as well as the associated written and visual materials. Additionally, participants can ask any specific questions by emailing the research team; the email address is provided in the consent form.
Study setting
The data will be collected from several high schools in Romania. They will be both state operated and privately owned. High schools will be enrolled based on their availability and willingness to participate in the study.
Inclusion and exclusion criteria
The current trial will include Romanian high school students, specifically those in grades 9 through 12, aged 14 to 18 years old. Participation in the trial is open to all students within this age and grade range who have access to the internet, regardless of their Internet source. It does not matter where the Internet access comes from, be it from a home connection, school-provided resources, public libraries, or other means. The primary requirement is that these students can reliably access the Internet to participate in the study, ensuring that all eligible participants can engage. Of note is that, in 2021, Romania was ranked on the 5th place in the world in terms of Internet speed and, according to Eurostat, boasts one of the highest Internet penetration rates in Europe [ 24 ]; therefore, access to the Internet of our target population is not problematic.
Study conditions
Experimental—automated intervention.
This intervention will last for 3 months, with two psychoeducational modules delivered per month. The participants will receive a total of 6 modules, which will include both text and video-delivered information, as well as quizzes and practical activities.
Experimental—blended intervention
This intervention will last for 3 months, with two psychoeducational modules delivered per month. The participants will receive a total of 6 modules, which will include the same content as in the educational intervention. In addition, the participants will also have the possibility to engage with a facilitator on a regular basis, either via online live sessions (e.g., via Skype) or on a forum where they can ask questions and receive replies from the team.
Sample size
R version 4.2.2 for Windows (R Foundation for Statistical Computing, Vienna, Austria) was used for the sample size calculation in a linear mixed-effect model (sjstats package). The R statistical computing environment will also be used for future model fitting and evaluation.
We used appropriate methods for two-level-designs [ 25 ] to determine sample size requirements for a cRCT with 3 experimental groups, 4 classrooms per experimental condition, 22 participants per cluster. For our linear mixed-effects model, a sample size of approximately 88 participants per experimental condition for a total sample size of 264 was sufficient to achieve 80% power to detect an effect size of Cohen’s d = 0.4 at an alpha level of 0.05. A medium effect size was assumed based on previous work on digital mental health literacy interventions [ 26 ].
Recruitment
Recruitment will be made from various high schools in Romania.
Assignment to study group
The participants will be randomly assigned to one of the three trial arms (see Fig. 1 ). Randomization will be performed by a research assistant using a simple (unrestricted) randomization sequence that assigns one of three unique numbers (1, 2, or 3) per classroom enrolled in the intervention, signifying the experimental condition. No stratification will be employed. To conceal the allocation mechanism, the same research assistant will use sequentially numbered, opaque, sealed envelopes and will subsequently monitor the assessments and allow access to the application for the participants in the waitlist control group after 6 weeks. Two different research assistants will be responsible with enrolling the participants in the intervention and assigning them to the intervention by maintaining direct contact with student representatives from each classroom that is enrolled in the intervention. Neither the participants nor the psychologists involved in disseminating the intervention to the adolescents will be blinded, as blinding is not feasible given the context of the current trial. The principal investigator and the statisticians curating the dataset and running the data analysis will remain blinded to the study condition until the completion of the study.
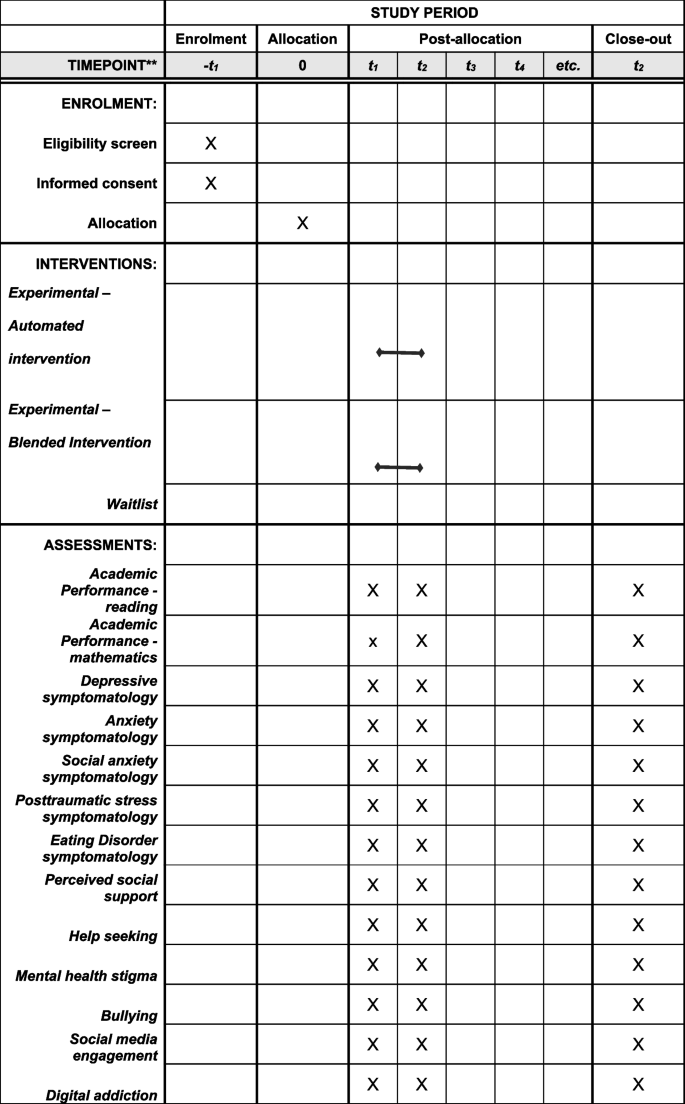
SPIRIT figure highlighting the proposed timeline of the intervention and assessments
Data collection, management, and analysis
Data collection methods.
The primary outcome measures are related to academic performance, well-being, and symptomatology, which will be collected at three time points: pre-intervention, post-intervention, and 1 month follow-up. Academic performance (math and reading comprehension) will be assessed with a sample of items taken from TIMSS (mathematics) and from PIRLS (reading comprehension) [ 27 ].
Measures administered
All the measures included in the current study are self-report questionnaires that have been selected after a careful review of the scientific literature for their appropriateness for being used with adolescents and young people as well as their validity and reliability.
The screening scale contains 26 items and target symptoms not covered by other scales in the instrument [ 28 ]. The first 22 items concern how much or how often participants have been affected by a series of situations in the two weeks before completion. The last four items cover substance use and suicidal thoughts, and participants are instructed to answer “Yes” or “No.”
Attention deficit hyperactivity disorder (ADHD)
To assess ADHD symptomology, the World Health Organization Adult ADHD Self-Report Scale (ASRS) [ 29 ] is used. It consists of six items, and, while it has been developed for adults, it is also suitable for use in adolescents. Participants are asked to indicate how often they have experienced certain situations for the first eight items and to indicate the approximate age when problems with organization, concentration, or impulsivity first occurred, if applicable, at the last item.
Depressive symptomatology
The PHQ-9-A Depression Scale (PHQ-A) [ 30 ] is the adolescent-adapted version of the Patient Health Questionnaire and contains ten items. Participants are instructed to rate on a scale of 0 to 4 how often they felt affected by certain problems and the extent to which these situations (if applicable) affected the respondent professionally, personally, or socially.
The anxiety rating scale [ 31 ] consists of eight items. Participants are asked to indicate on a scale from 0 to 4 how often they felt affected by certain problems and to rate the extent to which these situations (if applicable) affected the respondent professionally, personally, or socially.
Social anxiety
The Severity Measure for Social Anxiety Disorder (SMSAD 11–17) is a ten-item instrument for children and adolescents [ 32 ]. On a Likert-type scale from 0 to 5, participants are asked to indicate how often they experienced various emotions, thoughts, and behaviors in social situations.
Adverse childhood experiences
The Adverse Childhood Experiences Rating Scale employed in this study [ 33 ] is composed of two sections, totaling 19 statements. Participants are instructed to indicate the number of statements that accurately describe their situation growing up.
Posttraumatic stress
The Post Traumatic Symptom scale [ 34 ] consists of 37 items. The first part of the scale presents a series of 17 stressful situations and participants are asked to indicate whether they have been exposed to one or more of these events in their lifetime. The last 20 items refer to the individual's reaction after experiencing a stressful situation.
Bullying will be assessed with the six items used in the World Mental Health Initiative [ 35 ]. The items refer to times when someone is intentionally hurt or scared by a peer in the school setting, on the Internet, and in close relationships.
Eating disorders
The NEDA Eating Disorder Screening Tool [ 36 ] is composed of 14 items. The first 11 items address different aspects of eating behavior and/or self-image. These contain multiple response options, with participants being guided to choose the one that suits them. The last three items refer to information about height, lowest weight in the last year, and current weight.
Social support
The Perceived Social Support Questionnaire [ 37 ] contains six items, measured on a five-point Likert-type scale, where 1 = Does not fit me at all and 5 = Fits me extremely well.
Seeking help
The Attitudes Toward Seeking Professional Psychological Help – Short Form [ 38 ] instrument assesses attitudes towards seeking specialized psychological help. It consists of ten items and participants are asked to express the extent to which they agree with the statements.
Mental health stigma
The Peer Mental Health Stigmatization Scale [ 39 ] assesses stigmatizing attitudes of people experiencing mental health problems. It is composed of 24 items and participants are asked to express the extent to which they agree with the items.
Social media engagement
Social Media engagement will be measured with the Social Media Engagement Questionnaire (SMEQ) [ 40 ]. The questionnaire contains 5 items measured on an 8-point Likert scale (0 = not one day; 7 = every day). Higher scores represent higher engagement with social media.
Digital addiction
Digital Addiction will be measured with the Digital Addiction Scale for Teenagers (DAST) [ 41 ]. This is a 10-item instrument measured on a 7-point Likert scale ranging from never to very often.
Statistical methods
Our study will consist of a multisite cluster randomized trial in which the unit of measurement is at student-level, while randomization takes place at the unit of assignment, at classroom-level. Consequently, it is a low bias cluster-level RCT with potential joiners (i.e., individuals not in intervention clusters at random assignment but who enter later) being excluded and scant possibility of “contamination” or “treatment spillover” to the control classrooms. Analyses will employ linear mixed model with individual-level repeated measures nested within classrooms, nested within schools. Adhering to WWC group design standards [ 42 ], the model will include indicators for each intervention period and interaction terms for assignment to the intervention group and the period associated with the intervention. We will also report on robust standard errors from our fitted models to adequately account for dependence within clusters.
Nevertheless, youth research, and especially youth mental health research, has unique challenges concerning data gathering. First, although we adhere to a strategic research design to reduce missing data, patterns of attrition relating to individual and cluster-level factors will be investigated, including links to social and health variables. Second, challenges in gathering parental consent after classroom-level assignment to experimental condition would yield higher number of leavers, which constitutes individual-level attrition [ 42 ]. If data is missing at random, our analytic choice will yield unbiased estimates of treatment effects [ 43 ]. If data is missing not at random, weighting and multiple imputation would be used. In line with WWC standards [ 42 ] for cluster-level assignment RCTs, we will employ regression imputation, maximum likelihood, or nonresponse weights to address missing values while providing evidence that the approach appropriately adjusts the standard errors for clustering.
The Project Management team will meet monthly to discuss trial implementation or, upon necessity, if any potential difficulties arise. Additionally, the ethics committee is updated 6 months after the start of the trial or in the case that any changes to the trial protocol appear. The monitoring of unintended affects and inadvertent harm (e.g., unexpected, serious increases in symptomatology) will be undergone by team members who are also clinical psychologists and who will make referrals for appropriate interventions (i.e., clinical evaluation or psychotherapy), at which point the intervention will be discontinued immediately. Additionally, any such events will be appropriately and expeditiously reported to the ethics committee at the University of Bucharest.
The team responsible for recruitment and administrative tasks in the trial meets bi-weekly. The group consists of the principal investigator, project leader, and staff responsible for recruitment activities. The project leader, along with a research assistant, will monitor the trial, ensuring the eligibility of potential recruits, checking for the presence of informed consent, documentation of inclusion/exclusion criteria, and randomization for each participant. The project leader and research assistants will maintain constant communication with high schools and other relevant stakeholders.
Ethics and dissemination
This study is approved by the ethics commission at the University of Bucharest. Since the recipients of the intervention are minors, careful consideration has been given to obtaining informed consent from parents or legal guardians, while also properly informing the students about the contents of the intervention that they are enrolled in. Participant data will be confidential and stored on secured servers. Additionally, since we also collect mental health data, special attention will be given to any increase in symptomatology or any participants presenting harm to themselves. If such situations arise, they will be handled by the clinical psychologists in the research team. Any subsequent changes to the protocol will be updated on ClinicalTrials.gov.
Dissemination policy
We plan to publish the trial results in a peer-reviewed journal. Preliminary results will also be presented at international conferences, when appropriate. Additional plans are being made for the publication of the intervention manual. A summary of the results will also be made available for relevant stakeholders (i.e., high schools). Anonymized datasets will be made available upon reasonable request from the corresponding author.
The current trial aims to test the effectiveness of a mental health literacy intervention for high school students, aimed at improving academic performance, as well as increasing well-being and decreasing symptomatology. The intervention will be delivered via two different formats: (1) an educational one, which will be fully automated, and (2) a blended one which will additionally allow contact with facilitators, and it will be contrasted against a waitlist condition. Testing mental health literacy interventions is paramount, as not much is known about their effectiveness on outcomes such as academic performance and symptomatology. Furthermore, since the goal of mental health literacy interventions is to fill in the gaps that other mental health interventions cannot, in terms of their reach and cost-effectiveness, it also becomes highly relevant to test various modes of implementing such interventions, including fully automated ones. Additionally, testing the effectiveness of such interventions in varied cultural and socioeconomic contexts is timely, as this has been previously recognized as a limitation of the literature [ 19 ].
This endeavor, however, is not without its caveats. Firstly, contrasting active interventions against a waitlist control group can artificially inflate effect sizes. However, this approach is more ecological and cost-effective. If results will favor the SCHOLARS intervention, future studies should contrast it against active control conditions or psychological placebos. Secondly, there may be limited adherence to the intervention by the participants (i.e., dropouts). To this end, we aim to monitor and maintain close and constant contact with the enrolled schools, as to minimize drop-out and the risk of non-adherence by participants.
To conclude, the current study has the potential of advancing the field of mental health literacy interventions for adolescents. The success of such interventions might represent an important avenue for preventively addressing the development of mental health concerns and their associated consequences such as decreased academic performance.
Trial status
Trial registration: https://clinicaltrials.gov/study/NCT06217744 , Version 1, 22 January 2024. Recruitment for the trial has begun. Recruitment completion estimated date: November 2024.
Availability of data and materials
The datasets analyzed during the current study and statistical code used to analyze the data will be made available from the corresponding author upon reasonable request.
Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11(1):7–20.
Article PubMed PubMed Central Google Scholar
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345–65.
Article PubMed Google Scholar
Finning K, Ford T, Moore DA, Ukoumunne OC. Emotional disorder and absence from school: findings from the 2004 British child and adolescent mental health survey. Eur Child Adolesc Psychiatry. 2020;29(2):187–98.
Lawrence D, Dawson V, Houghton S, Goodsell B, Sawyer MG. Impact of mental disorders on attendance at school. Aust J Educ. 2019;63(1):5–21.
Article Google Scholar
Pascoe MC, Hetrick SE, Parker AG. The impact of stress on students in secondary school and higher education. Int J Adolesc Youth. 2020;25(1):104–12.
Jeppesen P, Wolf RT, Nielsen SM, Christensen R, Plessen KJ, Bilenberg N, et al. Effectiveness of transdiagnostic cognitive-behavioral psychotherapy compared with management as usual for youth with common mental health problems: a randomized clinical trial. JAMA Psychiat. 2021;78(3):250–60.
Jones MG, Rice SM, Cotton SM. Incorporating animal-assisted therapy in mental health treatments for adolescents: a systematic review of canine assisted psychotherapy. Plos One. 2019;14(1):e0210761.
Article CAS PubMed PubMed Central Google Scholar
Zhou X, Teng T, Zhang Y, Giovane CD, Furukawa TA, Weisz JR, et al. Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: a systematic review and network meta-analysis. Lancet Psychiatry. 2020;7(7):581–601.
Radez J, Reardon T, Creswell C, Lawrence PJ, Evdoka-Burton G, Waite P. Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies. Eur Child Adolesc Psychiatry. 2021;30(2):183–211.
Aguirre Velasco A, Cruz ISS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry. 2020;20(1):293.
Furnham A, Swami V. Mental health literacy: a review of what it is and why it matters. Int Perspect Psychol. 2018;7(4):240–57.
Google Scholar
Jorm AF. Mental health literacy: public knowledge and beliefs about mental disorders. Br J Psychiatry. 2000;177(5):396–401.
Article CAS PubMed Google Scholar
Lam LT. Mental health literacy and mental health status in adolescents: a population-based survey. Child Adolesc Psychiatry Ment Health. 2014;8(1):26.
Tambling RR, D’Aniello C, Russell BS. Mental health literacy: a critical target for narrowing racial disparities in behavioral health. Int J Ment Health Addict. 2021;11:1–15.
Riebschleger J, Costello S, Cavanaugh DL, Grové C. Mental health literacy of youth that have a family member with a mental illness: outcomes from a new program and scale. Front Psychiatry. 2019;10. Available from: https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00002 . Cited 2023 Sep 28
Brijnath B, Protheroe J, Mahtani KR, Antoniades J. Do web-based mental health literacy interventions improve the mental health literacy of adult consumers? Results from a systematic review. J Med Internet Res. 2016;18(6):e5463.
Freţian AM, Graf P, Kirchhoff S, Glinphratum G, Bollweg TM, Sauzet O, et al. The long-term effectiveness of interventions addressing mental health literacy and stigma of mental illness in children and adolescents: systematic review and meta-analysis. Int J Public Health. 2021;66:1604072.
Ren Z, Zhao C, Tian F, Yan Y, Li D, Zhao Z, et al. Meta-analysis of the effect of mental health literacy intervention in Chinese people. Acta Psychol Sin. 2020;52(4):497.
Amado-Rodríguez ID, Casañas R, Mas-Expósito L, Castellví P, Roldan-Merino JF, Casas I, et al. Effectiveness of mental health literacy programs in primary and secondary schools: a systematic review with meta-analysis. Children. 2022;9(4):480.
Liao Y, Ameyaw MA, Liang C, Li W. Research on the effect of evidence-based intervention on improving students’ mental health literacy led by ordinary teachers: a meta-analysis. Int J Environ Res Public Health. 2023;20(2):949.
Kutcher S, Bagnell A, Wei Y. Mental health literacy in secondary schools: a Canadian approach. Child Adolesc Psychiatr Clin N Am. 2015;24(2):233–44.
Lee JS, Ahn S, Lee KH, Kim JH, Schuls KF, Altman DG, CONSORT MD. 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010 Mar 23;340. Available from: https://pubmed.ncbi.nlm.nih.gov/20332509/?dopt=Abstract . Cited 2023 Sep 29
Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–7.
Correspondent CG Bucharest. How Romania built its blazingly fast Internet. EU Reporter. 2023. Available from: https://www.eureporter.co/world/romania/2023/09/09/how-romania-built-its-blazingly-fast-internet/ . Cited 2024 Jun 16
Snijders TAB. Power and sample size in multilevel linear models. In: Encyclopedia of Statistics in Behavioral Science. John Wiley & Sons, Ltd; 2005. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/0470013192.bsa492 . Cited 2023 Nov 17
Yeo G, Reich SM, Liaw NA, Chia EYM. The effect of digital mental health literacy interventions on mental health: systematic review and meta-analysis. J Med Internet Res. 2024;29(26):e51268.
Mullis IVS, Martin MO. TIMSS 2019 Assessment Frameworks. Int Assoc Eval Educ Achiev. 2017; Available from: https://eric.ed.gov/?id=ed596167 . Cited 2023 Nov 12
American Psychiatric Association. DSM-5-TR Self-rated Level 1 Cross-cutting Symptom Measure - Child Age 11-17 [Internet]. 2022. Available from: https://www.psychiatry.org/getmedia/9352851c-d69f-411a-8933-3212e8c29063/APADSM5TR-Level1MeasureChildAge11To17.pdf .
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602.
Johnson JG, Harris ES, Spitzer RL, Williams JBW. The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J Adolesc Health Off Publ Soc Adolesc Med. 2002;30(3):196–204.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. Generalized Anxiety Disorder 7. 2011. Available from: http://doi.apa.org/getdoi.cfm?doi=10.1037/t02591-000 . Cited 2023 Nov 12
Carlton CN, Garcia KM, Richey JA, Ollendick TH. Screening for adolescent social anxiety: psychometric properties of the severity measure for social anxiety disorder. Child Psychiatry Hum Dev. 2022;53(2):237–43.
Finkelhor D, Shattuck A, Turner H, Hamby S. Improving the adverse childhood experiences study scale. JAMA Pediatr. 2013;167(1):70–5.
Nedelcea C, Ciorbea ID, Vasile DL, Ionescu Ș, Papasteri C, Letzner RD, et al. The structure of PTSD. Development of the post traumatic symptom scale from a clinician-based perspective. Eur J Psychotraumatol. 2022;13(1):2066455.
Bond NI, McLafferty M, Lapsley C, Ennis E, Murray E, Heenan D, et al. Familial and bullying victimisation: the impact of early adversity within the home and peer settings on late adolescence and adult psychopathology. J Child Adolesc Trauma. 2023;16(1):43–53.
Fitzsimmons-Craft EE, Balantekin KN, Graham AK, Smolar L, Park D, Mysko C, et al. Results of disseminating an online screen for eating disorders across the U.S.: reach, respondent characteristics, and unmet treatment need. Int J Eat Disord. 2019;52(6):721–9.
Kliem S, Mößle T, Rehbein F, Hellmann DF, Zenger M, Brähler E. A brief form of the perceived social support questionnaire (F-SozU) was developed, validated, and standardized. J Clin Epidemiol. 2015;68(5):551–62.
Fischer EH, Farina A. Attitudes toward seeking professional psychologial help: a shortened form and considerations for research. J Coll Stud Dev. 1995;36(4):368–73.
McKeague L, Hennessy E, O’Driscoll C, Heary C. Peer mental health stigmatization scale: psychometric properties of a questionnaire for children and adolescents. Child Adolesc Ment Health. 2015;20(3):163–70.
Przybylski AK, Murayama K, DeHaan CR, Gladwell V. Motivational, emotional, and behavioral correlates of fear of missing out. Comput Hum Behav. 2013;29(4):1841–8.
Seema R, Heidmets M, Konstabel K, Varik-Maasik E. Development and validation of the digital addiction scale for teenagers (DAST). J Psychoeduc Assess. 2022;40(2):293–304.
What Works Clearinghouse Procedures and Standards Handbook, Version 5.0. U.S. Department of Education, Institute of Education Sciences, National Center for Education Evaluation and Regional Assistance (NCEE); 2022 Jul. Available from: This report is available on the What Works Clearinghouse website at https://ies.ed.gov/ncee/wwc/Handbooks .
Bell ML, Rabe BA. The mixed model for repeated measures for cluster randomized trials: a simulation study investigating bias and type I error with missing continuous data. Trials. 2020;21(1):148.
Download references
Acknowledgements
Not applicable.
Funding for conducting this research has been granted by the Executive Agency for Higher Education, Research, Development and Innovation Funding in Romania (contract number: PN-III-P4-PCE-2021–1528). The funding body was not involved in any way in the design and decision to submit this protocol for publication.
Author information
Authors and affiliations.
University of Bucharest, Bucharest, Romania
Cezar Giosan, Alexandru Pană, Ana Cosmoiu, Ana-Maria Chira, Ana-Maria Toma, Claudiu-Cristian Papasteri, Cătălin Nedelcea & Cătălina Popoviciu
You can also search for this author in PubMed Google Scholar
Contributions
CG is the principal investigator in the current project. CN participated in coordinating the current trial. AP, AC, AMC, AMT, CP, and CP drafted the current manuscript. All authors read and approved the manuscript.
Corresponding author
Correspondence to Cezar Giosan .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval has been granted by the ethics committee of the University of Bucharest.
Consent for publication
Not applicable. No identifying images or other personal or clinical details of participants are presented here or will be presented in reports of the trial results. The participant information materials and informed consent form are available from the corresponding author on request.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Giosan, C., Pană, A., Cosmoiu, A. et al. Mental health literacy and academic performance (MHLAP) in high school students: a randomized clinical trial protocol. Trials 25 , 419 (2024). https://doi.org/10.1186/s13063-024-08270-y
Download citation
Received : 31 March 2024
Accepted : 19 June 2024
Published : 27 June 2024
DOI : https://doi.org/10.1186/s13063-024-08270-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health literacy
- Academic performance
- Mental health
- Randomized clinical trial
ISSN: 1745-6215
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Psychiatry

Mental health literacy measures evaluating knowledge, attitudes and help-seeking: a scoping review
Sun Life Financial Chair in Adolescent Mental Health team, IWK Health Centre, Dalhousie University, 5850 University Ave., P.O Box 9700, Halifax, Nova Scotia B3K 6R8 Canada
Patrick J. McGrath
IWK Health Centre, Nova Scotia Health Authority and Dalhousie University, 5850 University Ave., P.O Box 9700, Halifax, Nova Scotia B3K 6R8 Canada
Jill Hayden
Centre for Clinical Research, Dalhousie University, Room 403, 5790 University Avenue, Halifax, Nova Scotia B3H IV7 Canada
Stan Kutcher
Mental health literacy has received increasing attention as a useful strategy to promote early identification of mental disorders, reduce stigma and enhance help-seeking behaviors. However, despite the abundance of research on mental health literacy interventions, there is the absence of evaluations of current available mental health literacy measures and related psychometrics. We conducted a scoping review to bridge the gap.
We searched PubMed, PsycINFO, Embase, CINAHL, Cochrane Library, and ERIC for relevant studies. We only focused on quantitative studies and English publications, however, we didn’t limit study participants, locations, or publication dates. We excluded non-English studies, and did not check the grey literature (non peer-reviewed publications or documents of any type) and therefore may have missed some eligible measures.
We located 401 studies that include 69 knowledge measures (14 validated), 111 stigma measures (65 validated), and 35 help-seeking related measures (10 validated). Knowledge measures mainly investigated the ability of illness identification, and factual knowledge of mental disorders such as terminology, etiology, diagnosis, prognosis, and consequences. Stigma measures include those focused on stigma against mental illness or the mentally ill; self-stigma ; experienced stigma; and stigma against mental health treatment and help-seeking. Help-seeking measures included those of help-seeking attitudes, intentions to seek help, and actual help-seeking behaviors.
Conclusions
Our review provides a compendium of available mental health literacy measures to facilitate applying existing measures or developing new measures. It also provides a solid database for future research on systematically assessing the quality of the included measures.
Electronic supplementary material
The online version of this article (doi:10.1186/s12888-015-0681-9) contains supplementary material, which is available to authorized users.
Epidemiology of mental illness
Approximately 70 %-75 % of adult mental health problems and mental disorders start to manifest during adolescence or early adulthood (12-25) [ 1 , 2 ]. Globally, mental disorders make up about 1/3 of the burden of illness in adolescence and young adulthood [ 3 ]. Untreated mental health problems and disorders in adolescents and young adults are strong predictors of poor vocational achievements, problematic interpersonal and family functioning, as well as reduced life expectancy due to associated medical conditions, such as diabetes, heart diseases and stroke, respiratory conditions, and suicide [ 4 – 7 ]. However, despite the great burden of illness incurred by these conditions, research shows, worldwide, between 70 %-80 % of young people and adults do not receive the mental health care they need [ 8 – 10 ]. A recent systematic review [ 11 ] of perceived barriers and facilitators for mental health help-seeking indicated that perceived stigma and embarrassment, problems in symptom identification and a preference for self-reliance were the most important intra-personal barriers to mental health help-seeking.
Mental health literacy
Mental health literacy is a significant determinant of mental health and has the potential to improve both individual and population health [ 12 – 14 ]. Evidence shows that improved knowledge about mental health and mental disorders, better awareness of how to seek help and treatment, and reduced stigma against mental illness at individual, community and institutional levels may promote early identification of mental disorders, improve mental health outcomes and increase the use of health services [ 15 – 17 ].
We conceptualize mental health literacy to include 4 domains: 1) understanding how to obtain and maintain good mental health; 2) understanding mental disorders and their treatments; 3) decreasing stigma against mental illness; and 4) enhancing help-seeking efficacy [ 13 , 18 ]. And therefore, mental health literacy addresses 3 inter-related cocepts: knowledge (knowledge of mental illness and positive mental health), attitudes and help-seeking efficacy. This definition is consistent with the current construct of health literacy defined and promoted by the WHO as an empowerment tool for people to participate in their health care [ 19 ].
We located five reviews on the effectiveness of mental health literacy interventions [ 12 , 18 , 20 – 22 ]. In addition there were three literature reviews describing stigma [ 23 – 25 ] and knowledge measures. However, there has been a lack of comprehensive understanding of current available mental health literacy measures. Thus, there exists a need to conduct a study to help better understand strengths and weaknesses of existing measures and to help shape future development of measures. We conducted a scoping review, a systematic approach to map the literature in an area of interest and to accumulate and synthesize evidence available, to bridge the gap. This current scoping review was guided by Arksey and O’Malley’s work (2005) [ 26 ], proposing four purposes: 1. to examine the extent, range and nature of research activity; 2. to determine the value of undertaking a full systematic review; 3. to summarize and disseminate research findings; and 4. to identify research gaps in the existing literature.
We analyzed available mental health literacy measures that focus on four common mental disorders with onset before or during adolescence and young adulthood: Schizophrenia, Depression, Anxiety Disorders, and Attention Deficit Hyperactivity Disorder (ADHD).
We used our definition of mental health literacy [ 13 , 18 ] that is composed of 4 constructs addressing three outcomes: mental health knowledge (including knowledge about positive mental health (construct 1) and knowledge about mental illness and treatments (construct 2)), stigma/attitudes towards mental illness, and help-seeking, to define our search scope.
Search strategy
One of the authors of this review and a health librarian designed the search strategies together. We searched PubMed, PsycINFO, Embase, CINAHL, Cochrane Library, and ERIC between 2013 and 2014, and re-ran the search in 2015. We applied four sets of search terms to identify domains of mental health literacy as outlined in Additional file 1 .
Inclusion criteria
We included quantitative studies that used, developed, or investigated measurement properties of mental health literacy measures evaluating any one, or combinations of the mental health literacy outcomes: knowledge, stigma/attitudes towards mental disorders, and help-seeking. Study designs included any type of quantitative studies: randomized controlled trials (RCTs), cluster RCTs, quasi-experimental studies; cohort studies; cross-sectional/survey studies, and controlled-before-and-after studies (pre/post tests). Only studies published in English were eligible and non-English publications were excluded at the screening stage. Year of publication and study participants, including their age, were not restricted.
Exclusion criteria
Studies were not eligible if they addressed mental health literacy but did not mention or describe the measure applied in the study. Studies of smoking prevention/cessation and other substance use prevention programs were not included. Studies of suicide prevention interventions that did not address related mental disorders, such as Depression were not eligible. Qualitative studies were excluded.
Data extraction and study selection (Charting)
Two reviewers used the search strategy, and independently searched pre-identified databases. We first screened out irrelevant studies which mostly focused on stigma against HIV/AIDS, cognitive behavioral therapies, substance abuse/smoking, resilience scales, and clinical treatment related studies by reviewing titles and abstracts. We then imported the remaining studies, into RefWorks 2.0 database management software (2001) [ 27 ]. Duplicates were removed. We then screened titles and abstracts again and briefly scanned the full text to exclude studies not evaluating target outcomes. All studies that passed this exclusion process were included in the third stage of review for relevance by scanning title, abstracts and the full text for relevancy. At the next stage, we reviewed full-text articles for all the final included studies. Additionally, we added original studies which were referenced in included studies that cited their psychometric properties. We also checked the reference list of included studies for additional studies.
We applied “charting” techniques to conduct data extraction. For scoping reviews, “charting” is a data extraction technique to synthesize and interpret data by “sifting, charting and sorting materials according to key issues and themes” (page 26) [ 26 , 28 ]. The key themes we followed in the “charting” of our data are the three outcome measures: knowledge, attitudes, and help-seeking, which was the base of the data categorization. We also charted data by year of publication, study location, study type, outcome measures, and types of psychometrics examined (e.g., reliability, validity, and responsiveness/sensitivity to change). The detailed charting process for this review is depicted in Fig. 1 .

Charting process (data extraction process)
A data extraction form, developed in advance, was used for data extraction. We categorized studies into four types based on the extent of how psychometric properties were investigated and reported in the study: validation studies with evaluating psychometrics (any type) and/or responsiveness/sensitivity to change as the major purpose of the study (coded as P); studies evaluating effectiveness of interventions or survey studies evaluating psychometrics (any type) and/or responsiveness/sensitivity to change of the outcome measures (coded as I/P or S/P); studies just reporting but not evaluating psychometrics and/or responsiveness/sensitivity to change of the applied tool (coded as I/? or S/?); and studies mentioning the measurement tool applied but not reporting psychometrics (coded as I or S), including studies that quoted psychometrics from other studies, but did not evaluate it in the current study. We then sorted and defined the data by measures on knowledge, attitudes/stigma towards mental illness, and help seeking respectively, listed authors who first applied the tool, and calculated the number of psychometrics studies for each outcome measurement. In addition, we collated all psychometrics studies in separate tables. Figure 1 illustrates this process.
Once this charting process was completed, we reviewed all included studies, developed and populated tables, and created charts and figures according to the above described typology in an Excel spreadsheet. To help ensure consistency in interpretation and validity of the final results, one of the reviewers read and charted all included studies. Then the second reviewer checked all tables and compared and discussed the results with the first reviewer and they came to a consensus on the interpretation of the results. One methodology expert and two content experts were invited to help make the final decision when consensus was not reached between the two reviewers.
Figure 2 presents the flow chart of the screening process and final included studies. A total of 401 studies 1 were identified that met study criteria, including 113 studies containing 69 knowledge measures, 307 studies containing 111 stigma measures, and 91 studies containing 35 help-seeking measures. Measures that modified and applied the concepts of the original ones were not counted as a new measure in our review. Out of the 401 studies, 130 validation studies reported and evaluated psychometrics (reliability, validity and/or the responsiveness/sensitivity to change) of the measures applied (P, I/P, or S/P), including14 knowledge studies (14 measures) (Table 1 ) [ 29 – 42 ], 102 stigma/attitudes studies (65 measures) (Table 2 ) [ 35 , 36 , 39 , 43 – 142 ], and 19 help-seeking studies (10 measures) (Table 3 ) [ 35 , 101 , 143 – 159 ]. These 3 tables summarized characteristics of validated studies, however we only listed authors who developed or first applied the measures although we included and summarized study results from other authors. Of these 130 studies, 5 studies also evaluated and reported responsiveness/sensitivity to change. Total number of studies for each sub-category may not necessarily match the total number of included studies because some studies tested more than one measurement tool in one study.

Search results
Psychometrics of knowledge measures
| Measures | Developer/Author | Reliability | Validity & responsiveness | Content |
|---|---|---|---|---|
| 1.Knowledge about Schizophrenia Questionnaire (KASQ) | Ascher-Svanum, 1999 [ ] | KR-20 = .85, .89 | R; CT | S |
| r it = .46; .51 | ||||
| r = .83 ( < .005) | ||||
| 2. Knowledge About Schizophrenia Test (KAST) | Compton et al., 2007 [ ] | KR-20 = .82 (.45-.78) | CS; CT; CR | S |
| 3. Multiple-Choice Knowledge of Mental Illnesses Test (MC-KOMIT) | Compton et al., 2011 [ ] | α = .68-.75 | R; CS; CT | G |
| r = .79 ( < .001) | ||||
| 4. Mental Health Knowledge Schedule (MAKS); | Evans-Lacko et al., 2010 [ ] | α = .65 | CT | G |
| Lin’s Pc = .71; | ||||
| k = .57-.87 | ||||
| 5. Depression Multiple Choice Question (MCQ) | Gabriel & Violato, 2009 [ ] | α = .68 | CT; CV; FA | D |
| 6. Depression literacy scale (D-Lit) | Kiropoulos et al., 2011 [ ] | α = ..88, .92 | D | |
| r = .78, .80 ( < 0.001) | ||||
| Gulliver et al., 2012 [ ] | α = .70 | |||
| r = .71 ( = .02) | ||||
| 7. Anxiety Literacy Questionnaire (A-Lit) | Gulliver et al., 2012 [ ] | α = .76; | A | |
| r = .83 ( = .003) | ||||
| 8. Test of Knowledge About ADHD (KADD) | Hepperlen et al., 2002 [ ] | α = .81-.82; | FA; CT | ADHD |
| 9. Knowledge about Depression and Mania Inventory (KDMI) | Kronmuller et al., 2008 [ ] | α = .89 (.76-.81); | CC/CR; CT; D; R | D |
| r it = .36-.43 | ||||
| 10. Journey of Hope (JOH) Outcome Survey | Pickett-Schenk et al., 2000 [ ] | α = .75-.83 | CS; FA | G |
| 11. Knowledge of Mental Disorders (KMD) | Serra et al., 2013 [ ] | α = .588 | CS; FA | G |
| 12. Adolescent Depression Knowledge Questionnaire (ADKQ) | Shelley et al., 2014 [ ] | α = .89 | FA | D |
| 13. Mental health disorder recognition questionnaire (MDRQ) | Swami et al., 2011 [ ] | k = .94, .96 | CS; CV | G |
| 14. Mental Health Knowledge Questionnaire (MHKQ) | Wang et al., 2013 [ ] | α = .69 | FA | G |
a internal consistency reliability: Cronbach alpha (α), Kuder-Richardson 20 (KR-20), item to total correlation (r it) ; b test-retest reliability: weighted kappa (k), Pearson correlation coefficient (r), Lin’s Pc; c inter-rater reliability: weighted kappa (k)
CT Content validity, CS Construct validity, CR Criterion validity, CV Convergent validity, CC Concurrent validity, D Discriminant validity, FA Factor analysis, R Responsiveness
G general knowledge, D Depression, S Schizophrenia, ADHD Attention Deficit Hyperactivity Disorder, A Anxiety
Psychometrics of stigma/attitudes measures
| Measures | Developer/Author | Reliability | Validity & responsiveness | Content |
|---|---|---|---|---|
| 1. Social Distance (SD) | Bogardus, 1925 [ ] | |||
| Link Social Distance scale (1987) | Link et al., 1987 [ ] | α = .74; .75; .92 | CS; CR/CV; D; FA | A |
| Bogardus Social Distance Scale (modified) | Angermeyer & Matschinger ., 2003 [ ] | α = .90 | FA | |
| Social distance scale | Link, 1983 [ ] | α = .85, .91; | CS | |
| Reported and Intended Behaviour Scale (RIBS) | Evans-Lacko & Rose et al., 2011 [ ] | α = .85; | ||
| k = .75 | ||||
| RIBS- Japanese (RIBS-J) | Yamaguchi et al., 2014 [ ] | α = .83 | CC; FA | |
| Lin’s Pc = .71 | ||||
| Social Contact Scale | Jackson & Heatherington, 2006 [ ] | α = .55-.75 | FA | |
| The Social Supports Acceptance Scale (SSAS) | Mansouri & Dowell, 1989 [ ] | α = .80-.94 | CS; R | |
| 2. Opinions about Mental Illness (OMI) | Cohen & Struening, 1962 [ ] | CS; FA | A | |
| OMI | Struening & Cohen, 1963 [ ] | α = .299-.80 | FA | |
| OMI in Chinese Community scale (OMICC) | Ng & Chan, 2000 [ ] | α = .87 (.43-.72) | FA | |
| 3. Community Attitudes towards Mental Illness (CAMI) | Taylor & Dear, 1981 [ ] | α = .62-.90 | CS; D; FA | A |
| Fear and Behavioural Intentions (FABI) | Svensson et al., 2011 [ ] | α = .80 | ||
| k = .29-.54 | ||||
| Mental Health Attitude Survey for Police | Clayfield et al., 2011 [ ] | α = .87 | CS; CV; FA | |
| 4. Devaluation-Discrimination tool (DD) | Link 1987 [ ] | α = .73-.83 | CS | A |
| Perceived Discrimination Devaluation (PDD) | Interian et al., 2010 [ ] | α = .80 | CS; CV/CR; FA | |
| Public stigma | Moses, 2009 [ ] | α = .76 | CV; CS; D | |
| K = .79-.90 | ||||
| Stigma-Devaluation Scale (SDS) | Dalky, 2012 [ ] | α = .87 | FA | |
| Depression is a Matter of Will | Aromaa et al., 2010 [ ] | CS; FA | ||
| 5. Depression Stigma scale (DSS) | Griffiths et al., 2004 [ ] | α = .75-.82 | DS; CV; D; FA | A |
| r = .86 ( = .001) | ||||
| 6. Attribution Questionnaire (AQ) | Corrigan et al., 2003 [ ] | α = .70-.96 | CS; FA | A |
| AQ-27 | Brown, 2008 [ ] | α = .60-.93 | CV; FA | |
| ICC = .72-.90 | ||||
| r-AQ | Pinto et al., 2012 [ ] | α = .70 | FA | |
| 7. Internalized Stigma of Mental Illness (ISMI) | Ritsher et al., 2003 [ ] | α = .84-.98 | CS; CC; D; FA; P | C |
| r = .92 (.61-.91) ( < .05) ICC = .78 | ||||
| Parents’ Internalized Stigma of Mental Illness Scale (PISMI) | Zisman-llani et al., 2013 [ ] | α = .61-.78 | FA | |
| ISMI Chinese (ISMIS-C) | Lien et al., 2014 [ ] | α = .90; | CS; FA | |
| ICC = .36-.73 | ||||
| ISMI-10 | Boyd et al., 2014 [ ] | α = .75 | CT; CC; CS | |
| 8. Perceived dangerousness (PD) | Link, et al., 1987 [ ] | α = .85 | CS | A |
| Link Stigma Scale (dangerousness) | Bagley & King, 2005 [ ] | α > .80 | CS; CR; D | |
| Dangerousness Scale (DS) | Penn et al., 1994 [ ] | α = .78 | CS | |
| 9. British Omnibus National Survey (ONS) | Kobau et al., 2010 [ ] | α = .66-.69 | CV; CC; FA | A |
| Changing Mind | Svensson et al., 2011 [ ] | α = .19-.46 | ||
| r :Poor to moderate | ||||
| 10. Self-stigma of Seeking Help (SSOSH) | Vogel et al., 2006 [ ] | α = .88 | CS; P; D; FA | C |
| r = .72 | ||||
| 11. Self-stigma of Mental Illness (SSMIS) | Corrigan et al., 2006 [ ] | α = .64-.91; | CS; D | C |
| r = .62-.82 | ||||
| SSMIS-Short Form | Corrigan et al., 2012 [ ] | α = .22-.87 | CS; D | |
| 12. Attitudes to Mental Illness Questionnaire (AMID) | Luty et al., 2006 [ ] | r = .70; .93 | CC; FA | A |
| 13. Stigma Scale for Receiving Psychological Help (SSRPH) | Komiya et al., 2000 [ ] | α = .72 | CS; CR; FA | D |
| 14. Affective Reaction Scale | Penn et al., 1994 [ ] | α = .86 | CS | A |
| 15. Discrimination and Stigma Scale (DISC) | Brohan et al., 2013 [ ] | α = .78; | CV; DV | B |
| Lin’s Pc = .88, 89 ( < .001) | ||||
| k = 0.45-0.89 | ||||
| K = .62-.97 | ||||
| Questionnaire on Anticipated Discrimination (QUAD) | Gabbidon et al., 2013 [ ] | α = .86; | CV | B |
| Lin’s Pc = .81 | ||||
| k = .41-.80 | ||||
| 16. Mental Illness: Clinician’s Attitudes (MICA) | Kassam et al., 2010 [ ] | α = .79 | CV; DV; FA; R | A |
| Lin’s Pc = .80 ( < .001) | ||||
| MICA-v4 | Gabbidon et al., 2013 [ ] | α = .72; | CV; FA | |
| r it ≥ .2 | ||||
| 17. Day’s Mental Illness Scale (DMISS) | Day et al., 2007 [ ] | α = .71-.86 | CS; FA | A |
| 18. ADHD Stigma Questionnaire (ASQ) | Kellison et al., 2010 [ ] | α = .55-.93; | CS; CV; DV; FA | A |
| ICC = .71(.55-.73) | ||||
| Stigmatization towards Adults ADHD | Fuermaier et al., 2012 [ ] | α = .91 (.61-.87) | CS | |
| 19. Rejection Experiences | Link, 1987 [ ] | α = .73-.85 | CS; CR; CV; D | B |
| K = .79-.90 | ||||
| 20. Generalized Anxiety Stigma Scale (GASS) | Griffiths et al., 2011 [ ] | α = .86-0.91 | CR; CS; CV; D; FA | A |
| r = .55,.58,.91 ( < .0001, .001) | ||||
| 21. Relatives’ opinions toward Schizophrenia | Magliano et al., 1999 [ ] | α = .56-.66; | CS; FA | A |
| K = .36-.84 | ||||
| Questionnaire on the Opinions About Mental Illness (QO) | Magliano et al., 2004 [ ] | α = .42-.72; | FA | A |
| k = .50-1.0 | ||||
| 22. EMIC | Chowdhury et al., 2000 [ ] | α = .66-.76; | A | |
| K = .77-.89 | ||||
| 23. Stigma Concerns about Mental Health Care (SCAMHC) | Interian et al., 2010 [ ] | α = .69 | CS; CV; CR; FA | D |
| 24. Latino Scale for Antidepressant Scale (LSAS) | Interian et al., 2010 [ ] | α = .66 | CS; CV; CT; FA | D |
| 25. Devaluation of Consumer Families Scale | Struening et al., 2001 [ ] | α = .82 | CV; FA | A |
| 26. Devaluation of consumers scale | Struening et al., 2001 [ ] | α = .71-.77 | CV; FA | A |
| 27. Consumer Experiences of Stigma Questionnaire (CESQ) | Bagley & King, 2005 [ ] | α = .79-.82 | CC; CS; CR; D; FA | B |
| 28. Attitudes towards Depression and Its Treatment (ATDT) | Gabriel & Violato, 2010 [ ] | α = .57-.79 | CT; FA | A |
| 29. Stigmatization Scale | Harvey, 2001 [ ] | α = .90, .94 | CS; D; FA; CR | B |
| 30. Psychiatric Skepticism Scale (PSS) | Swami & Furnham, 2011 [ ] | α = .92;.94 | CS; FA | D |
| 31. Emotional Reactions | Angermeyer & Matschinger, 2003 [ ] | CS; FA | A | |
| 32. Labeling of mental illness | Angermeyer & Matschinger, 2003 [ ] | k = 0.85 | A | |
| 33. Personal Attributes | Angermeyer & Matschinger, 2003 [ ] | CS; FA | A | |
| 34. Depression Attitude Questionnaire (DAQ) | Botega et al., 1992 [ ] | FA | A | |
| R-DAQ | Haddad et al., 2015 [ ] | α = .84; | CT; CS; CV; FA | A |
| ICC = .62 | ||||
| 35. Attitudes Toward psychiatry-30 | Burra et al., 1982 [ ] | r it = .10-.64; | CC | D |
| Split-half r = .89, .90; | ||||
| ICC = .51-.87 | ||||
| 36. Opening Minds Scale for Health Care Providers (OMS-HC) | Kassam et al., 2012 [ ] | α = .78; .79; .82 | CS; FA; CT; R | A |
| r it = -.13-.57; | ||||
| ICC = .66 ( < .001) | ||||
| 37. Stigma Scale | King et al., 2007 [ ] | α = .87 (.64-.87); | CS; CC; FA | A |
| k = .41-.71 | ||||
| Chinese Stigma Scale (CSS) | Ho et al., 2015 [ ] | α = .83 (.58-.84) | CC; FA | A |
| 38. Stigma Experiences Scale | Stuart et al., 2005 [ ] | α = .91 | CS | B |
| KR-20 = .83; | ||||
| 39. Attitudes Toward Serious Mental Illness Scale-Adolescent | Watson et al., 2005 [ ] | FA | A | |
| 40. Self reported prejudiced attitudes | Andersson et al., 2010 [ ] | α = .78 | FA | A |
| 41. Self-Stigma of Depression Scale | Barney et al., 2010 [ ] | α = .87 | CS; CV; FA | C |
| ICC = .63 ( = .000) | ||||
| 42. Employer Attitude Questionnaire (EAQ) | Diksa & Rogers, 1996 [ ] | FA | A | |
| 43. 15-Item Stigma Questionnaire | Gibbons et al., 2012 [ ] | α = .85; | CC; CS; CV; CT | B |
| ICC = .75 | ||||
| 44. Attitudes of Nursing Staff towards Co-Workers Returning from Psychiatric and Physical Illnesses | Glozier et al., 2006 [ ] | α = .76-.88 | CS | A |
| 45. Self-Esteem and Stigma Questionnaire (SESQ) | Hayward et al., 2002 [ ] | α = .71-.79; | CS | A |
| r = .63 ( < .0001) | ||||
| 46. Test of Knowledge About ADHD (KADD) | Hepperlen et al., 2002 [ ] | α = .81-.82; | FA | A |
| 47. Beliefs toward Mental Illness (BMI) | Hirai & Clum, 2000 [ ] | α = .91; | CS; CC; FA | A |
| r it = (.22 < r < .72) | ||||
| 48. Depression Self-Stigma Scale (DSSS) | Kanter, 2008 [ ] | α = .79-.95; | CS; CC; FA | C |
| r it = .44-.83 | ||||
| 49. General Attitude Questionnaire | Lam et al., 2005 [ ] | α = .88-.93 | A | |
| r = .72-.94 | ||||
| 50. Secrecy | Link, 1987 [ ] | α = .73-.83 | CS | C |
| 51. Withdrawal | Link, 1987 [ ] | α = .73-.83 | CS | C |
| 52. Attitudes to Severe Mental Illness (ASMI) | Madianos et al., 2012 [ ] | α = .88(.79-.86); | CS; P; FA | A |
| r = .89-.92 ( < .0001) | ||||
| 53. Affiliate Self-Stigma Scale | Mak & Cheung et al., 2008 [ ] | α = .94-.95; | CS; P; FA | C |
| r it = .51-.81 | ||||
| Self-Stigma Scale-Short (SSS-S) | Wu et al., 2015 [ ] | α = .95 | CC; CS; FA | C |
| 54. Knowledge Test of Mental Illness (KT) | Michaels & Corrigan, 2013 [ ] | r = .50-.70 ( < .05; .001) | CC; CS | A |
| 55. Attitudes Toward Social Competence and Integration of People with Mental Illness | Minnebo & Acker et al., 2004 [ ] | α = .77; .79 | FA | A |
| 56. Client Attitude Questionnaire | Morrison & Becker, 1975 [ ] | r = .90; .93 | ? | |
| 57. Libertarian Mental Health Ideology Scale (LMHIS) | Nevid & Morrison, 1980 [ ] | α = .81-.94 | CS; FA | D |
| 58. Personal stigma scale | Schneider et al., 2011 [ ] | α = .62-.92 | FA | A |
| 59. Child stigma scale | Moses, 2009 [ ] | α = .81 | CV; CS; D | C |
| k = .79-.90 | ||||
| 60. Beliefs and attitudes toward people diagnosed with psychosis | Serra et al., 2013 [ ] | α = .69 | FA | A |
| 61. Stigma of Depression Scale | Vega et al., 2010 [ ] | α = .69 | FA | A |
| 62. Perceptions of Stigmatization by Others for Seeking Help (PROSH) | Vogel et al., 2009 [ ] | α = .78-.91 | CS; CC; FA | D |
| r = .82 ( < .001) | ||||
| 63. The Stigma Inventory for Mental Illness | Karidi et al., 2014 [ ] | α = .90 (.75, .85); | CT; CS; CC; FA | C |
| r = .80 ( < .001) | ||||
| 64. Peer Mental Health Stigmatization Scale | McKeague et al., 2015 [ ] | α = .80 (.70, .75); | CT; CS; D; FA | A |
| r = .65, 75 | ||||
| 65. Endorsed and Anticipated Stigma Inventory (EASI) | Vogt et al., 2014 [ ] | r it = .47-.75 | CT; CV; D; FA | A & D |
a Internal consistency reliability: Cronbach alpha (α), Kuder-Richardson 20 (KR-20), item to total correlation (r it), split-half reliability; b test-retest reliability: intraclass correlation coefficient (ICC), weighted kappa (k), Pearson correlation coefficient (r), Lin’s Pc; c inter-rater reliability: weighted kappa (k), Lin’s Pc
CT Content validity, CS Construct validity, CR Criterion validity, CV Convergent validity, CC Concurrent validity, D Discriminant validity, FA Factor analysis, R Responsiveness, DV Divergent validity, P Predictive validity
A Stigma against mental illness or the mentally ill, B Experienced stigma, C self-stigma, D stigma against help-seeking, treatment; mental health institution or psychiatry, ? not reported
Psychometrics of help-seeking measures
| Measures | Author/developer | Reliability | Validity | Content |
|---|---|---|---|---|
| 1. Attitudes towards help-seeking scale (with various modified versions) | Fischer & Turner, 1970 [ ] | α = .83; .86 | FA; CS | A/H |
| r it = -.58 - .56 ( < .0001) | ||||
| r = .73-.89 | ||||
| Attitudes Toward Seeking Professional Psychological Help Scale (ATSPPH) | Fischer & Farina, 1995 [ ] | α = .77-.98;.84;.90 | FA; CS; CR | |
| r it = .54; | ||||
| r = .80 | ||||
| ATSPPH-SF | Elhai, et al., 2008 [ ] | α = .69; .77-.78; .84 | FA; CS | |
| r it > .40 | ||||
| r = .64 ( = .045) | ||||
| 2. Intention of Seeking Counseling Inventory (ISCI) | Cepeda-Benito & Short, 1998 [ ] | α = .89 | FA; CS | I |
| 3. General Help Seeking Questionnaire (GHSQ) | Deane et al., 2001 [ ] | α = .67, .76, .82 | FA | I |
| Gulliver et al., 2012 [ ] | α = .57-.77; | |||
| r = .42-.91 ( < 0.001) | ||||
| Wilson et al., 2005 [ ] | α = .70-.85; | P; CV; DV | ||
| ICC = .86-.92 | ||||
| 4. Jorm Mental health literacy survey (items on attitudes/beliefs towards treatment) | Jorm, Blewitt et al., 2005 [ ] | K = 0.15-1.00 | A/T | |
| Jorm, Mackinnon et al., 2005 [ ] | FA | |||
| Reavley et al., 2014 [ ] | CS | |||
| 5. Help Seeking Intentions | Lee et al., 2014 [ ] | α = .74, .76 | FA | I |
| 6. The New Inventory of Attitudes Towards Seeking Mental Health Services (IASMHS) | Mackenzie et al., 2004 [ ] | α = .87 (.76-.82) | FA; CS | A/H |
| r = .64-.91 ( < 0.01) | ||||
| 7. Help-Seeking Attitude Scale (HSAS) | Nickerson et al., 1994 [ ] | α = .87 | CC | A/H |
| 8. Scale of Attitudes Toward Seeking Psychological Help for Secondary Students (ASPH-S) | Sahin & Uyar, 2011 [ ] | α = .85 (.59-.81) | FA | A/H |
| r it = .41-.57 | ||||
| ICC = .81 | ||||
| 9. Help Seeking Acceptability (HSA) | Schmeelk-Cone et al., 2012 [ ] | α = .84-.88 | FA; CS | A/H |
| r it = .81-.85 | ||||
| 10. Parental Attitudes Toward Psychological Services Inventory (PATPSI) (based on ATSPPH) | Turner, 2012 [ ] | α = .72-.92 | FA; CS | A/H |
| ICC = .66-.90 |
a Internal consistency reliability: Cronbach alpha (α), item to total correlation (r it); b test-retest reliability: intraclass correlation coefficient (ICC), Pearson correlation coefficient (r); c inter-rater reliability: weighted kappa (k)
CT Content validity, CS Construct validity, CR Criterion validity, CV Convergent validity, CC Concurrent validity, D Discriminant validity, FA Factor analysis, DV Divergent validity, P Predictive validity
A/H Beliefs/Attitudes towards help-seeking, I help-seeking intentions, A/T beliefs/attitudes towards treatment
Study characteristics, such as study participants, locations, publication dates, and tool outcomes are reported in Figs. 3 , ,4, 4 , ,5 5 and and6. 6 . Studies were conducted in 32 countries, with the United States of America most commonly, followed by Australia and Canada. Study participants were mainly post-secondary students, especially students in psychology or related professions, followed by the general public, and mental health service users (e.g., patients and their families). Most of the studies (n = 337) were published after the year 2000.

Study participants by study numbers

Study sites by study numbers

Publication dates by study numbers

Measure content in each outcome (knowledge, attitudes and help-seeking) by study numbers
Knowledge measures
The most widely used knowledge measures (by the number of studies in which the measure was applied) include the Mental Health Literacy Questionnaire (MHLQ) by Jorm and colleagues (1997) [ 160 ], Mental Health Knowledge Schedule (MAKS) [ 32 ], the World Psychiatric Association (WPA) “Open the Doors” (WPA-OD) questionnaire [ 161 ], Depression Literacy Scale (DLS) [ 79 ], Knowledge about Schizophrenia Questionnaire (KASQ) [ 29 ], Schizophrenia Knowledge Questionnaire (SKQ) [ 162 ], and In Our Voices (IOV) knowledge measure [ 163 ].
The 69 knowledge measures evaluated general knowledge about mental health, knowledge on specific disorders such as depression, schizophrenia/psychosis, ADHD, and anxiety disorders (Fig. 6 ). They used different approaches to measure knowledge. Some measures, such as those based on the approach by Jorm et al. (1997) [ 160 ] used the recognition of specific mental disorders (e.g., depression or anxiety) from the vignette description of symptoms. Other knowledge measures evaluated factual knowledge about mental illness with the true/false/don’t know approach. This includes fact-based tests on terminology, prevalence, causes, diagnosis, etiology, prognosis, consequences, and course of illness; and knowledge about recognition, support, employment, treatment/help-seeking/controllability, and recovery/coping, etc. (e.g. [ 29 , 32 , 33 , 41 , 79 , 161 – 165 ]). One tool addressed the ability to distinguish mental illness from neurological or somatic illnesses (e.g. [ 39 ]). There were a number of measures combining stigma knowledge and mental health knowledge [ 95 , 166 – 169 ]. Finally, some were self-evaluation measures of extent of knowledge (e.g. [ 170 , 171 ]).
Of the 69 measures, psychometric properties were reported for 26 (38 %). And the rest of the 43 measures (62 %) had no psychometric properties reported. Of 26 measures with reported psychometrics, 14 measures were evaluated for psychometric properties, including 2 measures for responsiveness/sensitivity to change [ 29 , 31 ]. These 14 measures evaluated general mental health knowledge (6 measures), depression (4 measures), schizophrenia (2 measures), ADHD (1 measure), and anxiety disorders (1 measure) (Table 1 ). The rest of the twelve measures only reported but didn’t evaluate psychometrics (internal consistency) and therefore we didn’t include them in Table 1 .
Most knowledge measures applied self-report multiple choice answers (true, false, I don’t know/not sure), or vignettes with open-ended/closed questions (e.g. [ 172 ]), or used Likert-scale statements as self- evaluation formats.
Stigma measures
Of all the stigma measures, the most widely used measures (by the number of studies where the measure was applied) include the Social Distance scale (SD) [ 49 ]; Opinions about Mental Health Illness (OMI) [ 59 ]; Community Attitudes towards Mental Illness (CAMI, a modified version of OMI) [ 134 ]; Devaluation-Discrimination (DD) [ 105 ]; Depression Stigma scale (DSS, also called Personal and Perceived Stigma of Mental Illness) [ 79 ]; Attribution Questionnaire (AQ) [ 61 ]; Internalized Stigma of Mental Illness (ISMI) [ 126 ]; and Perceived Dangerousness (PD) [ 106 ].
The 111 focus of the stigma/attitudes measures included: 1. stigma against mental illness or the mentally ill, such as social distance (the degree to which people are willing to accept the mentally ill in regular social life), personal stigma (participants’ personal attitudes toward people with mental illness) and perceived stigma (participants’ beliefs about others’ attitudes about mental illness); 2. self-stigma; 3. experienced stigma by mental health service users; 4. stigma against mental health treatment, psychiatry, help-seeking, or mental health care facilities. Further, some measures evaluated stigma against specific mental illnesses, such as depression, anxiety, ADHD, and schizophrenia/psychosis. Eleven studies (7 measures) did not report what aspects of stigma were measured (Fig. 6 ).
Social distance measures investigated issues such as a person’s willingness to engage the mentally ill in the workplace and the community (e.g., employment, renting, being neighbors, marriage) [ 46 , 69 , 106 , 108 , 124 , 173 ]. Similarly, measures evaluating stigmatizing experiences by the mentally ill focused on challenges people with mental illness experience in family and social life [ 52 , 75 , 92 , 99 , 126 , 130 ].
Measures evaluating personal and perceived stigma covered areas such as authoritarianism, benevolence, mental hygiene ideology, social restrictions to the mentally ill, and etiology [ 59 , 134 ]. Other measures evaluated components such as stigma related to illness prevalence, consequences, dangerousness/threat, treatment and recovery of mental illness, or the social/family life, social responsibilities, human rights, intelligence [ 36 , 74 , 79 , 81 , 105 , 111 , 116 , 135 ]. In addition, there were personal and perceived stigma measures focusing on emotional/rejection responses, willingness to help, and disclosure concerns [ 44 , 48 , 57 , 61 , 86 , 98 , 124 ].
Self-stigma measures mostly evaluated cognition such as self-esteem, self-confidence, self-satisfaction/concurrence, self-blame; negative emotions such as low pride of oneself, shame, embarrassment, sense of inadequacy, inferiority to others, helpless, pressure; and behaviors such as withdrawal, fear of seeking help, and secrecy [ 47 , 63 , 83 , 92 , 113 , 121 , 136 ].
Measures examining stigma against treatment/help-seeking/mental health care/medical model/psychiatry addressed perspectives and emotions. For example, some measures evaluated stigma towards help seeking (e.g., help-seeking as personal weakness; people seeking help being less likeable, disturbed, posed risks to others, and should hide the fact of seeking help) [ 101 , 137 ]. Other tools [ 55 , 122 , 132 ] investigated stigma toward psychiatry, for example, skepticism towards psychiatry; and stereotypes of psychiatrists, psychiatric hospitals, patients, and psychiatric treatments. Some tools measured emotional responses (e.g., fear, discomfort and embarrassment) to psychological services and mental health care [ 89 , 144 ].
Eighty one (73 %) articles on stigma tools reported on some psychometrics. Sixty five measures had evidence of reliability (e.g., Crobach’s α; item-total correlations; KR-20; test-retest reliability; inter-rater reliability), validity (e.g, construct; concurrent; discriminant; convergent; predicative), or responsiveness/sensitivity to change (Table 2 ). Sixteen measures demonstrated only internal consistency, but none included discussions on how this was measured. Of these 81 measures, 48 evaluated stigma against the mental illness/ the mentally ill in general; 11 were self-stigma measures; 6 evaluated personally experienced stigma; and 12 evaluated stigma against mental health treatment (psychological and pharmacological), psychiatry, help-seeking, or mental health care facilities. One tool did not specify what it measured.
Help-seeking measures
Of the 35 help-seeking related measures, the most widely used are: Attitudes towards Help-Seeking Scale (later modified as Attitudes toward Seeking Professional Psychological Help Scale) (ATSPPH) [ 143 , 147 ]; the mental health literacy questionnaire (MHLQ) that contains items on beliefs towards treatments [ 160 ]; General Help Seeking Questionnaire (GHSQ) [ 145 ]; and Intention of Seeking Counseling Inventory (ISCI) [ 174 ].
These help-seeking measures evaluating help-seeking intentions; beliefs or attitudes towards seeking psychological help for mental health problems or illness; beliefs towards mental health help or treatment in general; actual help-seeking behaviors; help-seeking efficacy (e.g. knowledge about where and how to find help, and who to find help from); self-reported ability to help others; or multiple components such as help-seeking intentions, help-seeking efficacy, and barriers for help-seeking (Fig. 6 ).
Unlike measures of stigma against help-seeking described above, measures evaluating attitudes towards psychological help-seeking mostly addressed: recognition of need for psychological help; interpersonal openness; confidence in and trustworthiness of mental health practitioners [ 143 ]. Measures evaluating beliefs toward treatment mostly evaluated the perceived helpfulness, effectiveness or safety of various interventions [ 150 , 175 ], or the myths of treatment [ 176 ]. One measure [ 177 ] added social norm items on perceived attitudes of others (e.g., friends, employer) on depression intervention.
Measures evaluating help-seeking intentions examined willingness, or preferences to seek help from different sources (e.g., friends, families, professionals, religion, or spiritual healers [ 151 , 172 , 178 - 182 ]. One measure [ 172 ] further evaluated 3 extra dimensions of help-seeking intentions: talking to the listed sources; comfort level of talking to these resources; and helpfulness of these resources. Another tool measured intention levels for various emotional/behavioral challenges among college students [ 144 ]. Two measures didn’t specify how intentions were measured [ 161 , 183 ].
Measures addressing help-seeking behaviors evaluated whether help-seeking was sought, and if so, what type of help was sought (formal vs. informal) for both stressful events and mental illness [ 178 , 181 , 184 , 185 ].
Ten measures had some psychometric evaluation such as internal consistency, reliability, factor analysis, construct validity, and criterion validity [ 143 , 145 , 147 , 149 – 154 , 156 – 159 ]. Details of the psychometrics of these 10 measures are presented in Table 3 . The 10 measures with psychometrics addressed attitudes or beliefs towards help-seeking or treatments, and intentions for help-seeking (Table 3 ). Two measures reported the internal consistency of the tool [ 172 , 181 ], but did not discuss how this were measured, and therefore were not included in the table. No psychometric properties were reported on measures of help-seeking behaviors.
We identified a number of significant issues for consideration. These are: 1) representativeness of study samples; 2) geographic weighting: 3) adequacy of measurement of mental health literacy (knowledge, stigma, and help-seeking).
Representative samples
Almost half of the studies (n = 185) were conducted among adolescents and young adults, particularly with post-secondary students (n = 117) (Fig. 3 ) mostly from health related professions, such as psychology, social work, and nursing. This raises concerns about the generalizability of findings as participants are not representative of the general population.
Even within the context of postsecondary education, much less attention (only 9 studies) has been paid to the mental health literacy of educators, who are important role models and youth influencers in addressing mental health literacy [ 186 ]. Further research into mental health literacy should take these important factors into account.
Geographic weighting
Research on the measurement of mental health literacy started as early as in late 1950’S but did not bloom until after 2000 (n = 336; 84 %) (Fig. 5 ). Most studies (Fig. 4 ) took place in developed countries, especially the United States (n = 170; 42 %). Although there is ethnic diversity in the United States, the United States cannot be seen to represent other cultures. Moreover, different countries have different health systems and this may impact the implementation of mental health literacy approaches. For studies conducted in developing countries, authors either adapted existing measures, or used the conceptual framework from developed countries to create their measures, however, very few discussed the process of translation or the method of cultural adaptation. Therefore, the impact of important contextual factors, such as culture, ethnicity, geographic locations, education and health system, on mental health literacy and its measurement is currently unknown.
Adequacy of measurement
Our analysis suggests that, out of three outcomes of mental health literacy (knowledge, attitudes and help-seeking), most measures evaluated stigma (n = 111), followed by measures that evaluated knowledge (n = 69), and a smaller number of help-seeking (n = 33). Only a relatively small number of measures were validated in any way. Secondly, widely used measures are often not validated. For example, the WPA mental health knowledge questionnaire was applied in 9 studies but no research has been identified to analyze its psychometric properties except for internal consistency.
Given the high proportions of un-validated measures being applied, it was difficult to determine the value of the study results and not possible to conduct cross-study comparisons of different interventions. There is a pressing need to validate these measures before their application.
With the measures that have been validated, there has been no research identified that appraised the quality of psychometric studies, and therefore, we were not able to recommend which measures are better than others. Further, given that the measures included in this review vary in their content, purposes and quality (measurement properties), more advanced research, such as systematic reviews is needed to locate evidence-based measures for use. Consensus-based Standards for the Selection of Health Measurement Instruments (COSMIN) [ 187 ] has been developed to serve this purpose and could be adapted for use in the comparative evaluation of mental health literacy measures.
Further, our review did not identify any measures addressing knowledge of positive/good mental health. Future measures should investigate knowledge on how to obtain and maintain good health as this now is recognized as an important component of mental health literacy.
Our findings indicate that the diagnostic vignette approach is widely used as a measure of mental health knowledge. However, a recent study in which diagnostic vignettes were compared against non-diagnostic vignettes showed an inability of participants to discriminate across “normal” and “ill” categories [ 188 ]. Further study to establish the validity of the diagnostic vignette evaluation approach as a measure of mental health knowledge is needed.
The myths and facts approach to measure knowledge has covered a wide range of aspects of mental health. However, we are unable to determine if there are different and developmentally appropriate knowledge components addressed at different points of the life-span among the current available measures.
The plethora of stigma measures, developed from numerous different ideological models (e.g., labeling theory [ 189 ]; attribution framework model [ 61 ]; cognitive behavioral model [ 190 ]; and social stigma model [ 191 ], has made evaluation of their validity in addressing stigma/attitudes challenging. The challenge has been to both validate each of the specific models and to determine which model may provide a better explanatory prediction for stigma or attitudes in different groups of people.
Further, only a few measures have targeted people’s emotional responses (n = 8) towards mental illness. This is an important area because stigma is associated with self-experience of unpleasant feelings about mental illness and this may influence how people interact with those with mental illness [ 9 ]. Only very recently has research measured the stigma experience of people with mental illness (n = 28 studies). This may provide a more comprehensive picture of how society treats people with mental illness. This may help to provide more concrete and useful information on how stigma interventions should be developed and delivered at both individual and community level.
Despite the challenges discussed above, this review has mapped out how stigma measures were developed and what they intended to measure, and this information may provide researchers and practitioners some guidance on which path to take either in designing their measures, or applying/ adapting existing measures, or developing related interventions or programs in the future.
Help-seeking behaviors are challenging to measure as they are influenced by many factors, such as knowledge about the behaviors, attitudes and beliefs towards the behaviors, social norms, and intentions to perform the given behavior [ 192 ]. Most help-seeking measures in this review have focused on attitudes towards help-seeking/treatment (n = 20) and intentions to seek help (n = 11), and very few measures (n = 4) directly measured actual help-seeking behaviors. Further, all 4 help-seeking behavior measures had no psychometric validation.
As Ajzen and Fishbein [ 191 ] pointed out, behaviors also may be influenced by self-expressed behavioral control which requires a person to have the skills, capacities, resources, and other important capacities needed to perform the behavior. However, we have not identified any measures to address these factors except for one tool measuring help-seeking efficacy (e.g. knowledge about where and how to find help, and who to find help from) [ 178 ].
Limitations
We did not conduct a systematic review of the literature on available mental health literacy measures and therefore we are unable to come to conclusions about the quality of the studies applying the measures. We excluded non-English studies (n = 21 at the title and abstract screening stage) and may have missed important measures in other languages. We did not check the grey literature that includes non peer-reviewed publication or documents/reports produced on all levels of governments and academics, and therefore may have missed some eligible studies. We may also have mistakenly excluded some measures at the first screening stage of reviewing titles and abstracts where measures were not mentioned.
Additionally, although we tried to categorize and interpret measures within the category we attributed them to, some measures may contain items relevant to other categories, however we were unable to distinguish them with available information we have.
Our review provides a compendium of available mental health literacy measurement measures for researchers and practitioners who are interested in applying existing measures or developing new measures that of particular relevance to their work. Because of how we selected eligible studies, our review further automatically forms a comprehensive dataset of current mental health literacy interventions for stakeholders to consider for their use. This review also identifies the many gaps in the field, such as the unbalanced application of knowledge and help-seeking evaluation measures compared to the stigma/attitudes measures, the yet-to-be validated measures in each outcome category, and the lack of measures that measure all components of mental health literacy concurrently. This gap identification could potentially guide future research work in the field. Further, we have conducted a thorough summary and synthesis of the psychometrics properties of included measures, and clarified the need to further investigate the quality of the psychometrics studies. At this stage, most of the measures were created without consultation with the intended participants such as students, teachers, patients or health providers. Future work should focus on joint collaboration across disciplines, between investigators and stakeholders and across more varied demographic and geographic groups.
Acknowledgements
We would like to acknowledge that this study is supported by Yifeng Wei’s Doctoral Research Award - Priority Announcement: Knowledge Translation/Bourse de recherché, issued by the Canadian Institutes of Health Research. Dr. McGrath is supported by a Canada Research Chair. In addition, we would like to express deep appreciation to Ms. Catherine Morgan for her tremendous help with data collection and analysis, and the health librarian, Ms. Robin Parker, who helped with designing the search strategies of this review.
Additional file
Supplementary files contain an example of search strategies in PubMed, and supplementary references of studies that applied mental health literacy measures but did not provide related psychometrics information. (ZIP 97 kb)
1 References of studies that applied mental health literacy measures but did not evaluate the psychometrics of the applied measure were included in the supplementary document unless they were specifically cited in the manuscript.
Competing interests
None of the authors have any competing interests.
Authors’ contributions
YW defined the study scope; developed the study structure; collected and analyzed data; drafted and finalized the manuscript. PM conceived of the study; advised on study scope and structure; reviewed and advised on data analysis; and contributed significantly to manuscript revisions and final writing. JH contributed significantly to the development of research methodology, and participated in the manuscript revision and final writing. SK conceived of the study, participated in the study design and manuscript writing and final revision. All authors read and approved the final manuscript.
Authors’ information
Ms. Yifeng Wei (PhD candidate) is the school mental health lead of the Sun Life Financial Chair in Adolescent Mental Health team at the IWK Health Centre, Halifax, Nova Scotia. Her research interest on school mental health, especially on promoting mental health literacy of students and teachers alike in the secondary school setting, has enabled her to complete this current scoping review.
Dr. Patrick J. McGrath is a clinical psychologist, is Vice President Research, Innovation and Knowledge Translation for the IWK Health Centre and the Nova Scotia Health Authority and Canada Research Chair and Professor of Psychology, Pediatrics, and Psychiatry at Dalhousie University. His research on pain in child health has spanned a wide range of studies on measurement and psychosocial interventions in many different types of pain in infants, children and youth.
Dr. Jill Hayden is the associate professor of Community Health and Epidemiology at Dalhousie University. Her research expertise includes systematic review methods, prognostic research and musculoskeletal health. For many years, she has contributed to the Cochrane Collaboration. Her research is broadly related to improving the quality and use of research evidence for more effective health care decision-making and improved patient outcomes.
Dr. Stan Kutcher is the Sun Life Financial Chair in Adolescent Mental Health at the IWK Health Centre and professor of Psychiatry at Dalhousie University. Dr Kutcher is the leading scientist to develop, promote, and research mental health literacy interventions in Canadian secondary schools.
Contributor Information
Yifeng Wei, Email: [email protected] .
Patrick J. McGrath, Email: [email protected] .
Jill Hayden, Email: ac.lad@nedyahj .
Stan Kutcher, Email: [email protected] .
xReferences

COMMENTS
2. A Paradigm Shift. One of the main criticisms associated with the practice and research of the mental health literacy domain is that studies have mainly focused on mental disorders; however, growing evidence demonstrates that supporting positive mental health has long-term benefits [].In light of this evidence, a new definition of mental health literacy has been proposed; researchers have ...
With an increased political interest in school-based mental health education, the dominant understanding and measurement of mental health literacy (MHL) in adolescent research should be critically appraised. This systematic literature review aimed to investigate the conceptualisation and measurement of MHL in adolescent research and the extent of methodological homogeneity in the field for ...
Literature search (using the Medline and CINAHL databases) and review, covering the last 21 years, followed by concept analysis according to the steps described by Walker and Avant approach. ... Mental health literacy: a review of what it is and why it matters. Int. Perspect. Psychol. 7 240-257. 10.1037/ipp0000094 [Google Scholar] Garmy P ...
Running head: MENT AL HEAL TH LITERACY. Mental health literacy: A review of what it is and why it matters. Abstract. An increasing amount of scholarly work has attempted to understand the reasons ...
1. Introduction. The world is currently facing a very challenging public health problem: the significant prevalence of mental health problems in the general population and adolescents and young people [1,2], as well as their low/moderate levels of mental health literacy [3,4,5].Mental health problems account for 12% of illnesses worldwide, and in developed countries, the figure rises to 23% [].
Mental health literacy (MHL) is a construct that has arisen from the domain of health literacy (HL) and must be understood in that context. ... a systematic review of the literature. J Gen Intern Med. 2004;19(12):1228-1239. Crossref. PubMed. ISI. Google Scholar. 2. Parker RM. Health literacy: a challenge for American patients and their health ...
Abstract Mental health literacy (MHL) has been identified as a factor influencing early help-seeking for mental health problems (MHPs) and stigmatizing attitudes. ... In this way, the present study was conducted with the following objectives: in Phase I, mapping the existing literature through a scoping review; in Phase 2, 28 experts in the ...
Mental health literacy is an essential part of preventing mental illnesses. However, the quality of mental health literacy measures remain unknown, as does its universality across various settings and populations. Few studies focus on measures aimed at assessing mental health literacy of children and adolescents that covers knowledge about mental health and mental disorders, strategies to ...
Background: With an increased political interest in school-based mental health education, the dominant understanding and measurement of mental health literacy (MHL) in adolescent research should be critically appraised. This systematic literature review aimed to investigate the conceptualisation and measurement of MHL in adolescent research and the extent of methodological homogeneity in the ...
Request PDF | Conceptualising and measuring positive mental health literacy: a systematic literature review | Purpose The purpose of this study is to systematically review how positive mental ...
Objective: Mental health literacy (MHL) in adolescents is an important issue as it can lead to early detection and recognition of mental illness. The aim of this systematic review was to explore the effect of supporting interventions on improving MHL in adolescents. Methods: Systematic literature review by searching the ScienceDirect, Scopus, PubMed, Crochrane and CINAHL databases.
Mental health literacy (MHL) is a concept first proposed by Australian researcher Anthony Jorm and colleagues in the late 1990s. Jorm et al. defined MHL as "the knowledge and beliefs about mental disorders that aid their recognition, management or prevention" (Jorm et al., 1997, p. 182).Population-based research on MHL is well advanced (Furnham & Swami, 2018) and has led to the ...
Improving mental health literacy and reducing stigma may facilitate help-seeking and use of mental health services by young people. ... The aim of this systematic literature review was to synthesise and appraise the evidence from RCTs that examine the effectiveness of school-based MH literacy interventions and stigma reduction programmes. The ...
Keywords: Adolescent, Mental health literacy, Systematic literature review, Conceptualisation, Measurement. ... Eating disorders "mental health literacy": a scoping review. J Ment Health. 2020:1-14. 10.1080/09638237.2020.1713996. 89. Mond JM. Optimizing prevention programs and maximizing public health impact are not the same thing.
Despite progress in assessing children and adolescents' men-tal health literacy, reviews of the literature revealed a gap in understanding the efectiveness and psychometric proper-ties of existing measures. This review systematically identi-fied and assessed the psychometric properties of available measures.
An increasing number of scholarly works have attempted to understand the reasons for poor rates of help-seeking for symptoms of mental health disorders all around the world. One particular body of work has focused on "mental health literacy" (MHL), defined as knowledge about mental health disorders that is associated with their recognition, management, and prevention. In this article, we ...
Mental health literacy in non-western countries: A review of the recent literature. Mental Health Review Journal, 19, 84-98. 10.1108/MHRJ-01-2013-0004 First citation in article Crossref, Google Scholar
Mental health literacy significantly and positively influenced help-seeking behavior (t = 2.030, p < 0.05), while perception of community stigma significantly and negatively influenced help ...
Mental health literacy interventions are needed to improve knowledge of mental health, promote help-seeking for mental illness, and reduce stigma and negative attitudes toward mental illness. This review identifies that more good quality research is required of school-based mental health literacy interventions. New research is urgently needed ...
A systematic literature review of existing conceptualisation and measurement of mental health literacy in adolescent research: Current challenges and inconsistencies ... Effectiveness of information and communication technologies interventions to increase mental health literacy: A systematic review. Early Intervention in Psychiatry, 12 (6 ...
Systematic review of existing mental health literacy and related interventions for parents, caregivers and teachers of children aged 5-12 years. ... Humphrey N. A systematic literature review of existing conceptualisation and measurement of mental health literacy in adolescent research: Current challenges and inconsistencies. BMC Public Health.
Positive mental health and mental health literacy are two main concepts to ensure an individual and social state of mental health and well-being. A scoping review of the scientific literature published in the field of health sciences was conducted to identify the relationship between mental health literacy and the positive mental health of family caregivers. A research expression was used to ...
The current study aims to contribute to the mental health literacy literature by testing the effectiveness of an educational intervention concerning mental health in terms of its benefits for reducing psychopathology and increasing academic performance. ... Swami V. Mental health literacy: a review of what it is and why it matters. Int Perspect ...
Egalitarian relationships to improve health and healthcare. Research has shown that the key to a healthy and happy life relies on quality relationships (Gómez et al., Citation 2022; Mineo, Citation 2017).Indeed, there is a wealth of scientific literature on the impact of strong social relationships and friendships on wellbeing and health, both physical and mental (Bosle et al., Citation 2022 ...
Mental health literacy has received increasing attention as a useful strategy to promote early identification of mental disorders, reduce stigma and enhance help-seeking behaviors. ... We did not conduct a systematic review of the literature on available mental health literacy measures and therefore we are unable to come to conclusions about ...