An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

The Obesity Pandemic—Whose Responsibility? No Blame, No Shame, Not More of the Same
“ Imprisoned in every fat man, a thin man is wildly signaling to be let out” Cyril Connolly, rotund British writer, (1903–1974) Can we say this, let alone think it, in 2020?
Introduction
No one doubts the economic costs of obesity, estimated at 5–14% of health expenditure for 2020–2050 ( 1 ), but there is disagreement whether fatness is considered a disease ( 2 ) or a behavioral risk factor, similar to smoking, alcohol and substance abuse that may lead to a disease ( 3 ). Current opinion also emphasizes social determinants and equity, thereby moving away from personal responsibility concepts ( 4 ). Although recent competencies for medical training do recommend chronic disease models and personalized obesity management care plans ( 5 ), there is no mention of topics such as self-management, locus of control or responsibility . It is not clear whether this is because they are considered unimportant or because they are not politically correct—yet, they are critical components for chronic disease management such as diabetes, post-transplant care and obesity ( 6 ). The paradigm chosen has major implications for prevention and treatment strategies.
That the obesity pandemic continues unabated represents a catastrophic failure of government policy, public health, and medicine—but not only of these domains. Table 1 lists different levels of responsibility incorporating the sociotype ecological framework ( 6 ). Levels 1–4 represent context and systems; levels 5–7 society and interpersonal relationships; and levels 8–9 parental and intrapersonal health and psychological make-up. Personal editorial input from a leading obesity journal suggested that “at this point in time, … emphasis on the personal responsibility (rather than the biology), would only add to the stigmatization of obesity in general.” I disagree—and concerning the biology—see the beginning of the discussion section. Without considering aspects of responsibility, obesity management is severely compromised. There are at least two sides to personal responsibility: medicalizing obesity, which reduces it, and parental supervision, which emphasizes it, since fat children are at high risk for adult obesity ( 7 ). Finally, I suggest an integrated nine-level approach that eschews political correctness and hopefully is not more of the same.
The nine multilevel responsibilities and examples of strategies required for tackling obesity.
Why Medicalize Obesity Management?
Insurance regulations may be part of the reason to promote a medical rather than a personal choice paradigm. This has two consequences. First, medicalizing the diagnosis helps ensure continuing insurance coverage for the severely obese. Second, it guarantees long-term reimbursement for the treating physicians. Unfortunately, such medicalization externalizes locus of control ( 8 ), decreases incentives to change lifestyle behaviors and deters self-management necessary to take active responsibility for weight regulation, noting that intelligence has little to do with self-control.
Personal preferences determine what, and how much to eat and to exercise, and how important is body shape (aesthetics) to maintaining a healthy lifestyle. No healthy person chooses to go hungry or be malnourished, but there is an element of choice in becoming obese. These issues are closely linked to socio-economic status, culture, and education. Eating should be enjoyable and potentially controllable, but there are often mitigating factors such as the dependability and affordability of the food supply, peer group and advertising pressures. The price of fast food sometimes makes it irresistible. In the U.S., food security among the disadvantaged is cyclical and highest around the time people get their SNAP (Supplemental Nutrition Assistance Program) food stamp dollars. Intake decreases or switches to higher calorie-per-dollar alternatives as the month progresses, when SNAP purchases run out ( 9 ). Such feast/famine cycles of food assistance may paradoxically contribute to unhealthy eating patterns.
Parental Responsibility for Childhood Obesity?
Parents naturally want to provide for the best growth and development of their children. Parental legal rights are generally overturned to protect a minor if harm is potentially permanent and avoidable (such as refusal of life-sustaining treatment on religious grounds) ( 10 ). Obviously, obesity is serious and can lead to lifelong morbidity. The gap between chronological and biological age widens as obesity increases. Car seats, seat belts, motorcycle helmets, vaccinations, and education are nearly all universally mandated and followed, especially when freely accessible; high-quality food is not. Upstream causes, such as inappropriate overfeeding, food to placate crying, high-calorie, low-nutrient so-called addictive foods, and lack of opportunities to exercise safely in school or in home neighborhoods, all challenge the avoidability criterion.
Holding parents answerable for their child's weight implies that they have the parenting skills (which, universally are not taught) to ensure optimal nutrition quality and quantity and lifestyle for their children. Infant nutrition begins at minus 9 months and breast-feeding protects against obesity. Healthy weight children perform 13% better at school ( 1 ). Throughout childhood, parents are usually well-intentioned and serve, by example, what they eat themselves. Parents have control until the age of about 10, for their children's nutritional choices, exercise and screen time but, by adolescence, the major influencers are peer groups and social media.
Integrated Action Strategies: Not More of the Same
In the final analysis, any change in body weight must follow the first law of thermodynamics. The fact that body fat mass is defended emphasizes, according to the fat cell hypothesis, the importance of early feeding practices, and parental responsibility. Obesity is caused by multifactorial bio-psycho-socio-behavioral influences; it may be inherited but it is not necessarily inevitable. Sometimes, the problem seems genetic because children adopt the eating habits and activity lifestyles of their parents. During evolution Homo sapiens has been programmed to store fat ( 11 ) and to be metabolically efficient. Metabolic efficiency actually increases as a result of weight loss and this is one of the main reasons why weight regain occurs after stopping a diet. Most of our biology as a species has evolved to survive periods of famines (with occasional feasts); but now it is ill equipped to resist the deleterious impact of a sustained surplus of food. Genes have not changed over the past 60 years ( pace epigenetic influences); so the toxic, obesogenic environment is the main culprit for the obesity pandemic. Genes cannot be manipulated from a realistic public health or ethical standpoint. Even if we could attack the biology, say with a drug, this also is not a viable solution. For how long should it be taken—for life? What would be the economic costs? Would the people most in need of it adhere to such treatment? What about the side-effects? Medical management (including bariatric surgery) only helps re-inforce externalizing the “locus of control” without which there can be no long-term chronic disease self-management.
Human history has shown through the sad examples of wars, pestilence and economic deprivations and disparities that obesity cannot occur if food is unavailable. Therefore, we have to attack predominantly the input side of the energy equation through interventions involving the nine levels of responsibility as shown in the Table. The action points listed are not exhaustive, and must be context and time-specific, multi-level and coordinated. They do show, however, the very many options available in tailoring prevention and intervention programs to a particular setting. Preventing obesity is primarily a public health behavior and literacy issue, empowering parental and personal choices. Only when there are health complications should the medical paradigm be appropriate. There are many factors involved, including: cultural issues (norms, values, attitudes) regarding diet (especially the Mediterranean diet) and body shape; lack of knowledge about breast feeding and infant nutrition; lack of physical and economic access to quality food, especially fruits and vegetables (“food deserts,” where neighborhoods lack nearby grocery stores); lack of kitchen facilities (or time) to cook; lack of potable water which leads to over-consumption of sweetened drinks; and lack of protected, well-lit exercise facilities.
To change the environment from obesogenic to leptogenic requires government and municipal policies targeting schools, workplaces, hospitals, and public places. Interventions should be age-appropriate and involve the social media with role models, influencers, sports people, pop stars, and advertising campaigns with the same types of compelling marketing strategies that are used to sell unhealthy, calorie-rich foods. Here, health and politically correct messages are often at odds. Slogans from body-positive activists such as “fat is beautiful” or “proud to be fat” should be replaced by “fat is unhealthy and dangerous.” Smokers do not glorify their habits, neither should the obese; but, no one should be body shamed. Should cultural and identity inappropriateness prevent a thin actor/singer from adding artificial girth to play Falstaff?–of course not. We need to keep a sense of humor and proportion. However, these pressures have become more complicated. When an advertisement or social media post of a well-toned body is portrayed, the ad agency or social media poster is vilified for promoting “unrealistic expectations.” Results from the recent ACTION study ( 12 ), reporting on over 3,000 people with obesity, showed that 82% considered that weight loss was completely their own responsibility while only 5% did not agree. In this paper, “stigma” only appeared once and only in the introduction. However, stigmatization is a worldwide phenomenon with cultural differences ( 13 ). These also apply to underdiagnosed causes of obesity such as binge eating disorders ( 14 ). Addressing and avoiding stigmatization, especially in the media and social networks, are major challenges in managing and dealing with patients with obesity.
Health professionals and society must not be judgmental in treating obesity as an individual moral failing or lack of self-discipline and will power. Instead, we have to recognize that patients with obesity are also products of a society of inequality, yet we must not let society “normalize” obesity and also, at the other extreme, “too thin” models. Mis-placed medical and political correctness that leads to hands-off management of obesity, means abrogation of the physician's responsibility: it should not stop recognizing the health problems and consequences and pressing for treatment. For example, some doctors are now even reluctant to raise the issue of obesity lest they be accused of fat shaming by not accepting their patients' proportions (despite the quote at the head of this opinion piece), and thereby receive poor approval ratings in an atmosphere where popularity is equated with good healthcare.
How much involvement should there be of public health authorities, school personnel or physicians? Should there be mandatory reporting of obesity and eating disorders as for child neglect/abuse or truancy? Much depends on how measurements are made and on what follow-up programs are in place. Lifestyle education and practice should continue throughout schooling, and lunchtimes may serve as educative experiences in manners and food habits, as practiced in Norway, Japan, and elsewhere.
Legislative interventions such as sin taxes and banning soft drink vending machines and junk food advertising to children are all relevant ( 15 ). Regressive taxation may be used to benefit the population for whom it is most oppressive. Such tax revenues may go to providing parks, playgrounds, and education programs for disadvantaged children, all of which improve health outcomes. The food industry, which is part of the problem [high-calorie, nutrient-poor, hyper-palatable products ( 16 )], must also be part of the solution by encouraging reformulations with healthier ingredients, comprehensible front-of-package food labeling and making price reductions for wholesome foods.
Suitable community-valid interventions can be based on Positive Deviant behaviors of the non-obese living in similar disadvantaged situations ( 17 ). There are also Positive Deviant countries such as Japan, Italy, and Switzerland where obesity rates are below 20%.
Obesity is one of the most difficult conditions to manage in healthcare. No-one has found the correct solution because there is no one solution. Comprehensive programs dealing with obesity require coordinated actions at all the nine levels of involvement—national, food system, educational, medical, public health, municipal, societal, parental, and individual. Parental and individual responsibility, choice and self-management clearly have a place near the center of the stage in the obesity tragedy. Otherwise, it is like going to see the play Hamlet and the Prince fails to make an appearance. Individuals are indeed responsible for their health-promoting behaviors but should be held accountable only when they have adequate resources to do so ( 18 ). In conclusion, no one is to be blamed, but everyone has a collective responsibility for working to combat the obesity pandemic—business as usual is no longer an option.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
I thank Professor Janet Fleetwood for very constructive discussions in preparing this opinion piece.

Obesity in America: A Public Health Crisis
Obesity is a public health issue that impacts more than 100 million adults and children in the U.S.
What You Need to Know About Obesity

Getty Images
Obesity has become a public health crisis in the United States. The medical condition, which involves having an excessive amount of body fat, is linked to severe chronic diseases including type 2 diabetes, cardiovascular disease, high blood pressure and cancer. It causes about 1 in 5 deaths in the U.S. each year – nearly as many as smoking, according to a study published in the American Journal of Public Health.
The financial cost of obesity is high as well. According to the U.S. Centers for Disease Control and Prevention , "The estimated annual medical cost of obesity in the United States was $147 billion in 2008 U.S. dollars; the medical cost for people who have obesity was $1,429 higher than those of normal weight."
While researchers say the obesity epidemic began in the U.S. in the 1980s, there has been a sharp increase in obesity rates in the U.S. over the last decade. Nearly 40% of all adults over the age of 20 in the U.S. – about 93.3 million people – are currently obese, according to data published in JAMA in 2018. Every state in the U.S. has more than 20% of adults with obesity, according to the CDC – a significant uptick since 1985, when no state had an obesity rate higher than 15%. Certain states have higher rates than others: there are more obese people living in the South (32.4%) and Midwest (32.3%) than in other parts of the country.
Sugar Taxes and Other Efforts to Reduce Obesity
Federal, state and local governments have moved to address obesity in several ways. On the federal level, several programs – such as the Supplemental Nutrition Assistance Program (SNAP), Women, Infants and Children (WIC) Program, Child and Adult Care Food Program (CACFP) and the Healthy Food FInancing Initiative – as well as the U.S. Departments of Agriculture and Health and Human Services work to make healthier foods affordable and available in underserved communities. To prevent childhood obesity in particular, there are also school and early childhood policies, such as Head Start – a comprehensive early childhood education program – school-based physical education and Safe Routes to School, which promotes walking and biking to and from school and increasing healthy eating and physical activity while reducing the risk of obesity.
In March, the American Academy of Pediatrics and the American Heart Association offered several public policy recommendations , including raising the price of sugary drinks, encouraging federal and state governments to limit the marketing of sugary drinks to kids and teenagers, having vending machines offer water, milk and other healthy beverages, improving nutritional information on labels, restaurant menus and advertisements, and supporting hospitals in establishing policies to discourage the purchase of sugary drinks in their facilities.
Meanwhile, states have implemented laws, largely through early childhood education settings, to improve access to healthy food and increase physical activity in order to promote a healthy weight. These policies stretch from breastfeeding, providing available drinking water and daily physical activity to limited screen time as well as meals and snacks that meet healthy eating standards set by the USDA or CACFP.
City governments have considered, and in some cases implemented, so-called "sin taxes" that aim to make potentially unhealthy food choices less attractive and accessible. Cities including Philadelphia, Boulder, Colorado, and Berkeley, California, levy a tax on sugar-sweetened beverages; The American Public Health Association noted in 2016 that the tax led to a 21% drop in the consumption of sugary drinks in Berkeley alone. (A proposal to expand it to all of California stalled this year .) In Philadelphia , the price of sugary beverages sold in supermarkets, mass merchandisers and pharmacies rose – and sales fell – after the city implemented a tax on those products, but a study found that sales in towns bordering Philadelphia increased.
Some researchers say there's little proof that taxing food or drink choices really changes behavior. In spite of taxes and warnings about the health effects of drinking sugary beverages, eight of every 10 American households buys sodas and other sugary drinks each week, adding up to 2,000 calories per household per week, new research shows .
"Large authoritative systematic reviews of the peer-reviewed scientific literature have failed to illustrate any compelling evidence that economic interventions are effective in promoting any type of dietary behavior change," says Taylor Wallace , principal and CEO of the Think Healthy Group and an adjunct professor in the department of nutrition and food studies at George Mason University.
But others contend that making it more expensive to buy sugary drinks is a step in the right direction.
"We need to ensure that people understand the threat of these products to their health, so they want to reduce their consumption," says Sandra Mullin, senior vice president of policy, advocacy and communication for Vital Strategies, an organization that works to implement health initiatives, and a former public health official in New York City "And [hiking] the price is a prompt for them to do that."
Learn more about obesity:
What is obesity?
Obesity is a chronic disease . It occurs when an excessive amount of body fat affects a person's overall health.
How is obesity diagnosed?
According to the Obesity Action Coalition , a healthcare provider may diagnose a patient with obesity if his or her body mass index, or BMI, is 30 or greater. BMI is a value derived from the weight and height of a person; normal BMI ranges from 20 to 25. There is no lab test, blood screening or other diagnostic used to diagnose obesity.
What is morbid obesity?
Morbid obesity is diagnosed when a person has a BMI of 40 or greater. People can also be diagnosed with morbid obesity if their BMI is 35 if they are also experiencing health complications like high blood pressure or diabetes.
How is being overweight different from being obese?
Obesity has to do with having too much body fat and a Body Mass Index, or BMI, of 30 or more. Being overweight can involve having too much body fat, the Department of Health and Human Services says , but having extra muscle, bone or water can also be a factor.
What causes obesity?
Obesity occurs when a person takes in more calories than he or she burns through normal daily activities and exercise, according to the Mayo Clinic . It is not simply a matter of over-indulgence or a lack of self control, obesity researcher Dr. George Bray said at the first annual U.S. News Combating Childhood Obesity summit , held at Texas Children's Hospital in May.
"Obesity isn't a disease of willpower – it's a biological problem," he said . "Genes load the gun, and environment pulls the trigger."
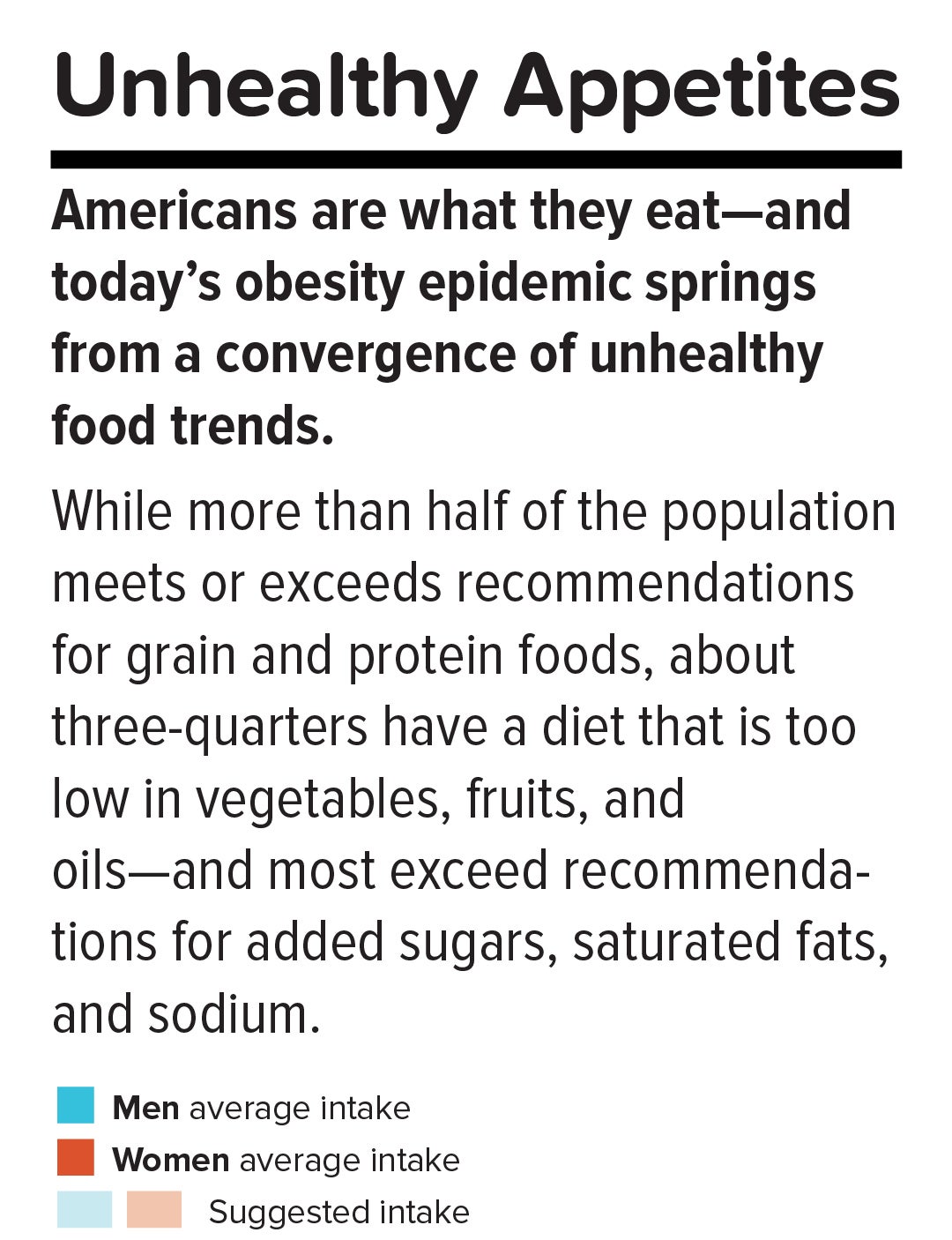
Certain scientific and societal factors – including genetics, the increased consumption of processed foods and sugar-sweetened beverages, and some medications and medical conditions – can increase a person's risk of becoming obese. Age and pregnancy can also trigger weight gain.
The 10 Fattest States in the U.S.

Diet has an important connection to obesity. Studies show the amount of soybean oil Americans consume spiked in the 1960s and 1970s, most likely as highly processed foods became popular, and American adults and children started to weight more around that time, Bray said.
"The fats in our food supply may well be playing a part in our inability to regulate" food intake, Bray said at the obesity summit . Consumption of sugary soft drinks also skyrocketed between 1950 and 2000, he pointed out, as Americans tripled the amount of sweet beverages they drank each year.
Artificial sweeteners have also been linked to obesity . A study presented at the 2018 Experimental Biology meeting suggests artificial sweeteners alter how bodies process fat and obtain energy.
"Despite the addition of these non-caloric artificial sweeteners to our everyday diets, there has still been a drastic rise in obesity and diabetes," one of the study's authors, Brian Hoffmann, assistant professor in the department of biomedical engineering at the Medical College of Wisconsin and Marquette University , said. "In our studies, both sugar and artificial sweeteners seem to exhibit negative effects linked to obesity and diabetes, albeit through very different mechanisms from each other."
What are some of the risk factors for obesity?
Genetic factors include: the amount of body fat a person stores, where it's distributed and how efficiently his or her body metabolizes food into energy.
Medical conditions include: Prader-Willi syndrome, Cushing's syndrome, arthritis and other diseases that can lead to decreased activity. Certain medications – some antidepressants, anti-seizure, diabetes, antipsychotic medications, steroids and beta blockers – can also cause weight gain.
Lifestyle and behavioral factors include: a lack of physical activity that burns calories, smoking, lack of sleep (which can lead to an increased desire to consume calories), eating an unhealthy diet.
Social and economic factors include: not having a safe space to exercise, not having enough money to afford healthier foods, food deserts where grocery stores that carry fresh fruits and vegetables are not available, lack of transportation to access healthy food options.
Can children be obese?
Obesity can be diagnosed at any age. The prevalence of obesity among children and adolescents between ages 2 and 19 was estimated to be 18.5% – more than one in six – between 2015 and 2016, with 13.7 million impacted, according to the CDC's National Center for Health Statistics .
Children who are obese are at risk for developing premature heart disease , the American Heart Association reports. A study of nearly 2.3 million people monitored over the course of 40 years found that the risk of dying from heart disease was two to three times higher if they had been overweight or obese as teens.
Obesity is a problem in other countries as well. A study published in the Lancet in 2017 found that the number of obese 5 to 19 year olds worldwide increased from 11 million in 1975 and to 124 million in 2016. The researchers projected the number of children and adolescents who are obese will surpass those that are moderately or severly underweight by 2022.
How many adult men and women are obese?
U.S. adult obesity prevalence between 2015 and 2016 was nearly 40% – about 93.3 million people, according to the CDC . The highest rate (42.8%) was among adults between the ages of 40 and 59; the prevalence among adults age 20 to 39 years was 35.7%, and 41% among adults age 60 and older. There was no significant difference between men and women overall or by age group, according to the data brief.
What preventable diseases and health issues are associated with obesity?
Mental and physical health problems involving obesity include:
- Type 2 diabetes
- High blood pressure
- Heart disease
- Gallbladder disease
- Cancers (including breast, liver, pancreas, endometrial, colorectal, prostate and kidney)
- High cholesterol
- Osteoarthritis of weight-bearing joints
- Sleep apnea
- Respiratory problems
- Gastroesophageal reflux disease
- Urinary stress incontinence
- Infertility
- Sexual dysfunction
- Physical disability
- Lower work achievement
- Social isolation
What are the financial costs of obesity in the U.S.?
Researchers from the University of Cincinnati in 2008 estimated the cost of medical care to diagnose and treat obesity and its associated health issues to be about $147 billion annually.
The CDC estimates the indirect costs of obesity-related health issues – including absenteeism, premature disability, declines in productiving and earlier mortality – to range from $3 billion and $6.4 billion annually.
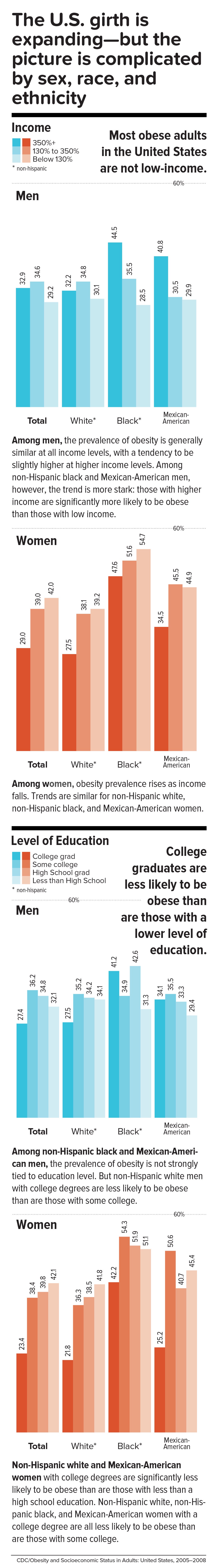
Are certain races more likely to become obese than others?
At 25.8%, Hispanic children and adolescents between the ages of 2 and 19 had the highest prevalence of obesity between 2015 and 2016, according to the National Center for Health Statistics . Meanwhile, obesity prevalence was about 22% among black youths; 14.1% among non-Hispanic whites; and 11% among non-Hispanic Asians. While the report notes that there were no significant differences in the prevalence of obesity between boys and girls by race and Hispanic origin, Hispanic boys in particular had a higher prevalence of obesity than non-Hispanic black boys.
Similarly, non-hispanic black (46.8%) and Hispanic (47%) adults in the U.S. have higher obesity rates than non-Hispanic white (37.9%) and non-Hispanic Asian (12.7%) adults, according to the NCHS. Rates of obesity were especially high among black and Hispanic women, according to the report, surpassing 50%.
How is obesity treated?
Treatment of obesity primarily involves changing a patient's behavior, but surgery to reduce the size of a patient's stomach or alter the digestive tract and medication may also be options for those who have trouble losing weight on their own.
The National Institute of Diabetes and Digestive and Kidney Diseases says common treatments include eating more healthy foods, incorporating more physical activity and changing other habits , such as taking the stairs instead of the elevator. Developing a healthy eating plan with fewer calories, setting realistic and measurable goals, participating in formal weight-management programs and seeking help from family, friends, health professionals and support groups can make it easier to develop healthier habits, though the federal agency warns that setbacks occur and people should be prepared.
Experts say obese patients who lose 5% to 10% of their body weight – about 10 to 20 pounds for a 200-lb person with a BMI indicating obesity, for example – can reduce his or her risk of obesity-related health problems like type 2 diabetes as well as lower blood pressure and cholesterol levels.
Can obesity be prevented?
When it comes to suggestions about how to prevent obesity, common principles stand out across local, state and federal guidelines :
- increase physical activity
- improve nutrition through increased consumption of fruits and vegetables
- encourage breastfeeding
- encourage mobility between work, school and communities.
Some researchers also say that the food industry has a role to play in solving the obesity crisis: Making highly processed and fast food much more expensive could curb consumption and lower the obesity rate in the U.S. over time.
"My former brethren in the soft drink business really fought the issue of obesity early on rather than stepping up and saying, 'OK, we don't wish to be blamed totally for this issue but we still can do something,'" Hank Cardello, a former food company executive who now works as a food policy analyst at the Hudson Institute, a Washington, D.C. think tank, said during the U.S. News Combating Childhood Obesity summit in May. "Larger portions, the whole supersize phenomenon – it's actually proven that that made more money for them" while helping trigger the national obesity epidemic, he explained.
What are the most-obese states in America?
According to the CDC, as of 2017 (the most-recent data available) the most-obese states in America are:
- West Virginia (38.1% of adults)
- Mississippi (37.3%)
- Oklahoma (36.5%)
- Iowa (36.4%)
- Alabama (36.2%)
- Louisiana (36.2%)
- Arkansas (35%)
- Kentucky (34.3%)
- Alaska (34.2%)
- South Carolina (34.1%)
What are the least-obese states in America?
These states have the lowest obesity rates in the U.S., according to the CDC:
- Colorado (22.6% of adults)
- Hawaii (23.8%)
- California (25.1%)
- Utah (25.25%)
- Montana (25.27%)
- New York (25.7%)
- Massachuestts (25.9%)
- Nevada (26.7%)
- Connecticut (26.9%)
- New Jersey (27.3%)
Is obesity a problem in other countries?
The World Health Organization estimates 39% of women and 39% of men ages 18 and older are overweight, with the highest prevalence of obesity on the island of Nauru, at 61%. (The U.S. ranked 12th worldwide, at 36.2%).
Among the 20 most-populous countries worldwide, the United States had the highest level of age-standardized childhood obesity, at 12.7%, while China and India had the highest numbers of obese children in 2015, according to a 2017 University of Washington study . Further, the United States and China had the highest number of obese adults, the study found. That same year, the researchers determined excess body weight to be associated with about 4 million deaths and 120 million disability-adjusted life-years lost.
Rates of adult obesity among the 36 countries in the Organization for Economic Cooperation were highest in the U.S., Mexico, New Zealand and Hungary. They were lowest in Japan and South Korea in 2017, according to an OECD "Obesity Update" report .
Tags: obesity , weight loss , public health
Recommended Articles
National News

Healthiest Communities Health News

Best Countries

Healthiest Communities
- # 1 Los Alamos County, NM
- # 2 Falls Church city, VA
- # 3 Douglas County, CO
- # 4 Morgan County, UT
- # 5 Carver County, MN
You May Also Like
The un says a quarter of the world's children under 5 have severe food poverty. many are in africa.
Associated Press June 6, 2024

EV Sales Boom in Nepal, Helping to Save on Oil Imports, Alleviate Smog

Man in Mexico Died of a Bird Flu Strain That Hadn't Been Confirmed Before in a Human, WHO Says
Associated Press June 5, 2024

FDA Advisers Urge Targeting JN.1 Strain in Recipe for Fall's COVID Vaccines

The Next COVID Vaccine Is Coming
Cecelia Smith-Schoenwalder June 5, 2024


Prevention, prevention, prevention.
Losing weight is hard to do.
In the U.S., only one in six adults who have dropped excess pounds actually keep off at least 10 percent of their original body weight. The reason: a mismatch between biology and environment. Our bodies are evolutionarily programmed to put on fat to ride out famine and preserve the excess by slowing metabolism and, more important, provoking hunger. People who have slimmed down and then regain their weight don’t lack willpower—their bodies are fighting them every inch of the way.
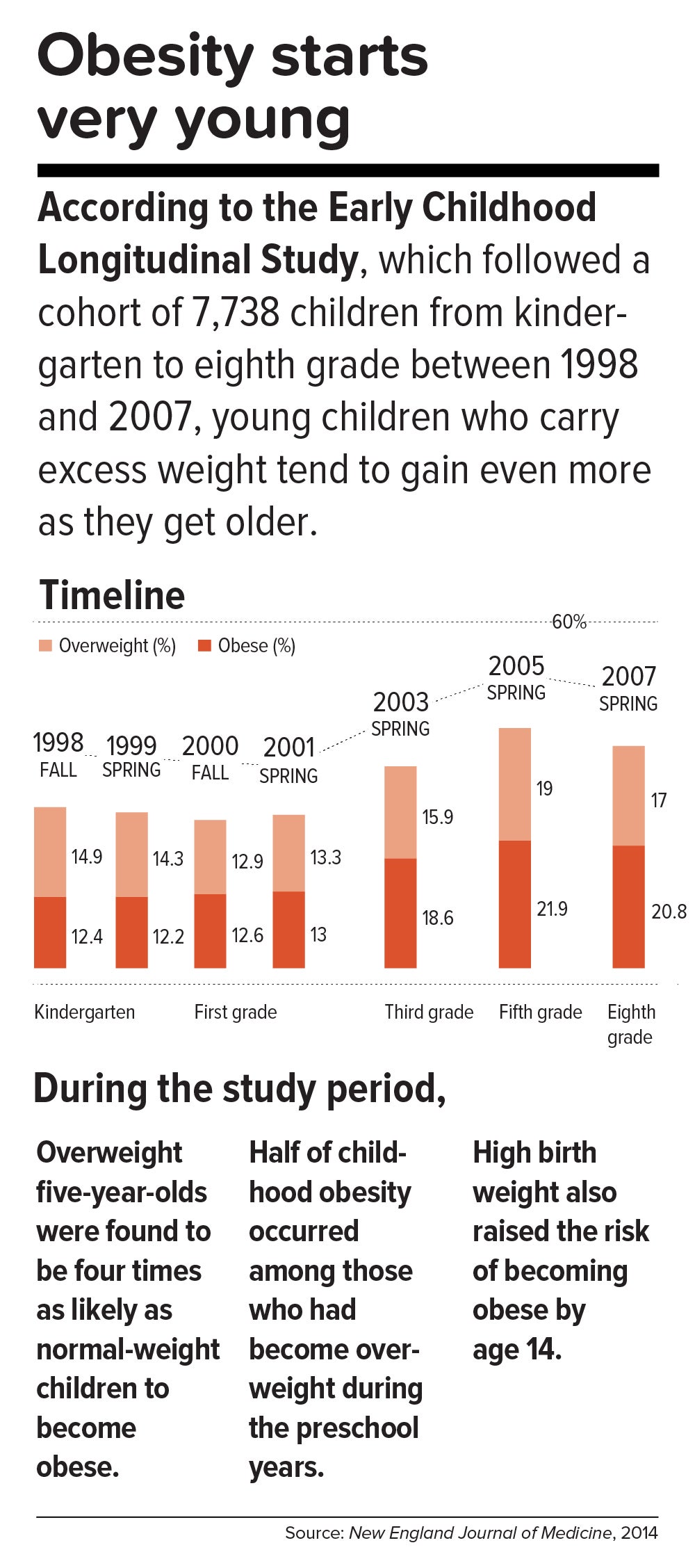
This inborn predisposition to hold on to added weight reverberates down the life course. Few children are born obese, but once they become heavy, they are usually destined to be heavy adolescents and heavy adults. According to a 2016 study in the New England Journal of Medicine , approximately 90 percent of children with severe obesity will become obese adults with a BMI of 35 or higher. Heavy young adults are generally heavy in middle and old age. Obesity also jumps across generations; having a mother who is obese is one of the strongest predictors of obesity in children.
All of which means that preventing child obesity is key to stopping the epidemic. By the time weight piles up in adulthood, it is usually too late. Luckily, preventing obesity in children is easier than in adults, partly because the excess calories they absorb are minimal and can be adjusted by small changes in diet—substituting water, for example, for sugary fruit juices or soda.
Still, the bulk of the obesity problem—literally—is in adults. According to Frank Hu, chair of the Harvard Chan Department of Nutrition, “Most people gain weight during young and middle adulthood. The weight-gain trajectory is less than 1 pound per year, but it creeps up steadily from age 18 to age 55. During this time, people gain fat mass, not muscle mass. When they reach age 55 or so, they begin to lose their existing muscle mass and gain even more fat mass. That’s when all the metabolic problems appear: insulin resistance, high cholesterol, high blood pressure.”
Adds Walter Willett, Frederick John Stare Professor of Epidemiology and Nutrition at Harvard Chan, “The first 5 pounds of weight gain at age 25—that’s the time to be taking action. Because someone is on a trajectory to end up being 30 pounds overweight by the time they’re age 50.”
The most realistic near-term public health goal, therefore, is not to reverse but rather to slow down the trend—and even this will require strong commitment from government at many levels. In May 2017, the Trump administration rolled back recently-enacted standards for school meals, delaying a rule to lower sodium and allowing waivers for regulations requiring cafeterias to serve foods rich in whole grains. If recent expansions in food entitlements and school meals are undermined, “It would be a ‘disaster,’ to use the president’s word,” says Marlene Schwartz, director of the Rudd Center for Obesity & Food Policy at the University of Connecticut. “The federal food programs are incredibly important, not just because of the food and money they provide families, but because supporting better nutrition in child care, schools, and the WIC [Women, Infants, and Children] program has created new social norms. We absolutely cannot undo the progress that we’ve made in helping this generation transition to a healthier diet.”
Get the science right.
It is impossible to prescribe solutions to obesity without reminding ourselves that nutrition scientists botched things decades ago and probably sent the epidemic into overdrive. Beginning in the 1970s, the U.S. government and major professional groups recommended for the first time that people eat a low-fat/high-carbohydrate diet. The advice was codified in 1977 with the first edition of The Dietary Goals for the United States , which aimed to cut diet-related conditions such as heart disease and diabetes. What ensued amounted to arguably the biggest public health experiment in U.S. history, and it backfired.
At the time, saturated fat and dietary cholesterol were believed to be the main factors responsible for cardiovascular disease—an oversimplified theory that ignored the fact that not all fats are created equal. Soon, the public health blitz against saturated fat became a war on all fat. In the American diet, fat calories plummeted and carb calories shot up.
“We can’t blame industry for this. It was a bandwagon effect in the scientific community, despite the lack of evidence—even with evidence to the contrary,” says Willett. “Farmers have known for thousands of years that if you put animals in a pen, don’t let them run around, and load them up with grains, they get fat. That’s basically what has been happening to people: We created the great American feedlot. And we added in sugar, coloring, and seductive promotion for low-fat junk food.”
Scientists now know that whole fruits and vegetables (other than potatoes), whole grains, high-quality proteins (such as from fish, chicken, beans, and nuts), and healthy plant oils (such as olive, peanut, or canola oil) are the foundations of a healthy diet.
But there is also a lot scientists don’t yet know. One unanswered question is why some people with obesity are spared the medical complications of excess weight. Another concerns the major mechanisms by which obesity ushers in disease. Although surplus body weight can itself directly cause problems—such as arthritis due to added load on joints, or breast cancer caused by hormones secreted by fat cells—in general, obesity triggers myriad biological processes. Many of the resulting conditions—such as atherosclerosis, diabetes, and even Alzheimer’s disease—are mediated by inflammation, in which the body’s immune response becomes damagingly self-perpetuating. In this sense, today’s food system is as inflammagenic as it is obesigenic.
Scientists also need to ferret out the nuanced effects of particular foods. For example, do fermented products—such as yogurt, tempeh, or sauerkraut—have beneficial properties? Some studies have found that yogurt protects against weight gain and diabetes, and suggest that healthy live bacteria (known as probiotics) may play a role. Other reports point to fruits being more protective than vegetables in weight control and diabetes prevention, although the types of fruits and vegetables make a difference.
A 2017 article in the American Journal of Clinical Nutrition showed that substituting whole grains for refined grains led to a loss of nearly 100 calories a day—by speeding up metabolism, cutting the number of calories that the body hangs on to, and, more surprisingly, by changing the digestibility of other foods on the plate. That extra energy lost daily—by substituting, say, brown rice for white rice or barley for pita bread—was equivalent to a brisk 30-minute walk. One hundred calories a day, sustained over years, and multiplied by the population is one mathematical equivalent of the obesity epidemic.
A companion study found that adults who ate a whole-grain-rich diet developed healthier gut bacteria and improved immune responses. That particular foods alter the gut microbiome—the dense and vital community of bacteria and other microorganisms that work symbiotically with the body’s own digestive system—is another critical insight. The microbiome helps determine weight by controlling how our bodies extract calories and store fat in the liver, and the microbiomes of obese individuals are startlingly efficient at harvesting calories from food. [To learn more about Harvard Chan research on the gut microbiome, read “ Bugs in the System .”] The hormonal effects of sleep deprivation and stress—two epidemics concurrent and intertwined with the obesity trend—are other promising avenues of research.
And then there are the mystery factors. One recent hypothesis is that an agent known as adenovirus 36 partly accounts for our collective heft. A 2010 article in The Royal Society described a study in which researchers examined samples of more than 20,000 animals from eight species living with or around humans in industrialized nations, a menagerie that included macaques, chimpanzees, vervets, marmosets, lab mice and rats, feral rats, and domestic dogs and cats. Like their Homo sapiens counterparts, all of the study populations had gained weight over the past several decades—wild, domestic, and lab animals alike. The chance that this is a coincidence is, according to the scientists’ estimate, 1 in 10 million. The stumped authors surmise that viruses, gene expression changes, or “as-of-yet unidentified and/or poorly understood factors” are to blame.
Master the art of persuasion.
A 2015 paper in the American Journal of Public Health revealed the philosophical chasm that hampers America’s progress on obesity prevention. It found that 72 to 98 percent of obesity-related media reports emphasize personal responsibility for weight, compared with 40 percent of scientific papers.
A recent study by Drexel University researchers also quantified the political polarization around public health measures. From 1998 through 2013, Democrats voted in line with recommendations from the American Public Health Association 88.3 percent of the time, on average, while Republicans voted for the proposals just 21.3 percent of the time.
Clearly, we can’t count on bipartisan goodwill to stem the obesity crisis. But we can ask what kinds of messages appeal to politically divergent audiences. A stealth strategy may be to avoid even uttering the word “obesity.” On January 1 of this year, Philadelphia’s 1.5-cents-per-ounce excise tax on sugar-sweetened and diet beverages took effect. When Philadelphia Mayor Jim Kenney lobbied voters to approve the tax, his bid centered not on improving health—the unsuccessful pitch of his predecessor—but on raising $91 million annually for prekindergarten programs.
“That’s something lots of people care about and can get behind—it’s a feel-good policy, and it makes sense,” says psychologist Christina Roberto, assistant professor of medical ethics and health policy at the University of Pennsylvania, and a former assistant professor of social and behavioral sciences and nutrition at Harvard Chan. The provision for taxing diet beverages was also shrewd, she adds, because it spread the tax’s pain; since wealthier people are more likely than less-affluent individuals to buy diet drinks, the tax could not be slapped with the label “regressive.”
But Roberto sees a larger lesson in the Philadelphia story. Public health messaging that appeals to values that transcend the individual is less fraught, less stigmatizing, and perhaps more effective. As she puts it, “It’s very different to hear the message, ‘Eat less red meat, help the planet’ versus ‘Eat less red meat, help yourself avoid saturated fat and cardiovascular disease.’”
Supermarket makeovers
Supermarket aisles are other places where public health can shuffle a deck stacked against healthy consumer choices.
With slim profit margins and 50,000-plus products on their shelves, grocery stores depend heavily on food manufacturers’ promotional incentives to make their bottom lines. “Manufacturers pay slotting fees to get their products on the shelf, and they pay promotion allowances: We’ll give you this much off a carton of Coke if you put it on sale for a certain price or if you put it on an end-of-aisle display,” says José Alvarez, former president and chief executive officer of Stop & Shop/Giant-Landover, now senior lecturer of business administration at Harvard Business School. Such promotional payments, Alvarez adds, often exceed retailers’ net profits.
Healthy new products—like flash-frozen dinners prepared with heaps of vegetables and whole grains, and relatively little salt—can’t compete for prized shelf space against boxed mac and cheese or cloying breakfast cereals. One solution, says Alvarez, is for established consumer packaged goods companies to buy out what he calls the “hippie in the basement” firms that have whipped up more nutritious items. The behemoths could apply their production, marketing, and distribution prowess to the new offerings—and indeed, this has started to happen over the last five years.
Another approach is to make nutritious foods more convenient to eat. “We have all of these cooking shows and upscale food magazines, but most people don’t have the time or inclination—or the skills, quite frankly—to cook,” says Alvarez. “Instead, we should focus on creating high-quality, healthy, affordable prepared foods.”
An additional model is suggested by Jeff Dunn, a 20-year veteran of the soft drink industry and former president of Coca-Cola North America, who went on to become an advocate for fresh, healthy food. Dunn served as president and chief executive officer of Bolthouse Farms from 2008 to 2015, where he dramatically increased sales of baby carrots by using marketing techniques common in the junk food business. “We operated on the principles of the three 3 A’s: accessibility, availability, and affordability,” says Dunn. “That, by the way, is Coke’s more-than-70-year-old formula for success.”
Show them the money.
Obesity kills budgets. According to the Campaign to End Obesity, a collaboration of leaders from industry, academia, public health, and policymakers, annual U.S. health costs related to obesity approach $200 billion. In 2010, the nonpartisan Congressional Budget Office reported that nearly 20 percent of the rise in health care spending from 1987 to 2007 was linked to obesity. And the U.S. Centers for Disease Control and Prevention (CDC) found that full-time workers in the U.S. who are overweight or obese and have other chronic health conditions miss an estimated 450 million more days of work each year than do healthy employees—upward of $153 billion in lost productivity annually.
But making the money case for obesity prevention isn’t straightforward. For interventions targeting children and youth, only a small fraction of savings is captured in the first decade, since most serious health complications don’t emerge for many years. Long-term obesity prevention, in other words, doesn’t fit into political timetables for elected officials.
Yet lawmakers are keen to know how “best for the money” obesity-prevention programs can help them in the short run. Over the past two years, Harvard Chan’s Steve Gortmaker and his colleagues have been working with state health departments in Alaska, Mississippi, New Hampshire, Oklahoma, Washington, and West Virginia and with the city of Philadelphia and other locales, building cost-effectiveness models using local data for a wide variety of interventions—from improved early child care to healthy school environments to communitywide campaigns. “We collaborate with health departments and community stakeholders, provide them with the evidence base, help assess how much different options cost, model the results over a decade, and they pick what they want to work on. One constant that we’ve seen—and these are very different political environments—is a strong interest in cost-effectiveness,” he says.
In a 2015 study in Health Affairs , Gortmaker and colleagues outlined three interventions that would more than pay for themselves: an excise tax on sugar-sweetened beverages implemented at the state level; elimination of the tax subsidy for advertising unhealthy food to children; and strong nutrition standards for food and drinks sold in schools outside of school meals. Implemented nationally, these interventions would prevent 576,000, 129,100, and 345,000 cases of childhood obesity, respectively, by 2025. The projected net savings to society in obesity-related health care costs for each dollar invested: $31, $33, and $4.60, respectively.
Gortmaker is one of the leaders of a collaborative modeling effort known as CHOICES—for Childhood Obesity Intervention Cost-Effectiveness Study—an acronym that seems a pointed rebuttal to the reflexive conservative argument that government regulation tramples individual choice. Having grown up not far from Des Plaines, Illinois, site of the first McDonald’s franchise in the country, he emphasizes to policymakers that at this late date, America cannot treat its way out of obesity, given current medical know-how. Only a thoroughgoing investment in prevention will turn the tide. “Clinical interventions produce too small an effect, with too small a population, and at high cost,” Gortmaker says. “The good news is that there are many cost-effective options to choose from.”
While Gortmaker underscores the importance of improving both food choices and options for physical activity, he has shown that upgrading the food environment offers much more benefit for the buck. This is in line with the gathering scientific consensus that what we eat plays a greater role in obesity than does sedentary lifestyle (although exercise protects against many of the metabolic consequences of excess weight). “The easiest way to explain it,” Gortmaker says, “is to talk about a sugary beverage—140 calories. You could quickly change a kid’s risk of excess energy balance by 140 calories a day just by switching from a sugary drink a day to water or sparkling water. But for a 10-year-old boy to burn an extra 140 calories, he’d have to replace an hour-and-a-half of sitting with an hour-and-a-half of walking.”
Small tweaks in adults’ diets can likewise make a big difference in short order. “With adults, health care costs rise rapidly with excess weight gain,” Gortmaker says. “If you can slow the onset of obesity, you slow the onset of diabetes, and potentially not only save health care costs but also boost people’s productivity in the workforce.”
One of Gortmaker’s most intriguing calculations spins off of the food industry’s estimated $633 million spent on television marketing aimed at kids. Currently, federal tax treatment of advertising as an ordinary business expense means that the government, in effect, subsidizes hawking of junk food to children. Gortmaker modeled a national intervention that would eliminate this subsidy of TV ads for nutritionally empty foods and beverages aimed at 2- to 19-year-olds. Drawing on well-delineated relationships between exposure to these advertisements and subsequent weight gain, he found that the intervention would save $260 million in downstream health care costs. Although the effect would probably be small at the individual level, it would be significant at the population level.
Level the playing field through taxes and regulation.
When public health took on cigarette smoking, starting in the 1960s, it did so with robust policies banning television ads and other marketing, raising taxes to increase prices, making public places smoke-free, and offering people treatment such as the nicotine patch. In 1965, the smoking rate for U.S. adults was 42.2 percent; today, it is 16.8 percent.
Similarly, America reduced the rate of deaths caused by motor vehicle accidents—a 90 percent decrease over the 20th century, according to the CDC—with mandatory seat belt laws, safer car designs, stop signs, speed limits, rumble strips, and the stigmatization of drunk driving.
Change the product. Change the environment. Change the culture. That is also the policy recipe for stopping obesity.
Laws that make healthy behaviors easier are often followed by positive changes in those behaviors. And people who are trying to adopt healthy behaviors tend to support policies that make their personal aspirations achievable, which in turn nudges lawmakers to back the proposals.
One debate today revolves around whether recipients of federal Supplemental Nutrition Assistance Program (SNAP) benefits (formerly known as food stamps) should be restricted from buying sodas or junk food. The largest component of the USDA budget, SNAP feeds one in seven Americans. A USDA report, issued last November, found that the number-one purchase by SNAP households was sweetened beverages, a category that included soft drinks, fruit juices, energy drinks, and sweetened teas, accounting for nearly 10 percent of SNAP money spent on food. Is the USDA therefore underwriting the soda industry and planting the seeds for chronic disease that the government will pay to treat years down the line?
Eric Rimm, a professor in the Departments of Epidemiology and Nutrition at the Harvard Chan School, frames the issue differently. In a 2017 study in the American Journal of Preventive Medicine , he and his colleagues asked SNAP participants whether they would prefer the standard benefits package or a “SNAP-plus” that prohibited the purchase of sugary beverages but offered 50 percent more money for buying fruits and vegetables. Sixty-eight percent of the participants chose the healthy SNAP-plus option.
“A lot of work around SNAP policy is done by academics and politicians, without reaching out to the beneficiaries,” says Rimm. “We haven’t asked participants, ‘What’s your say in this? How can we make this program better for you?’” To be sure, SNAP is riddled with nutritional contradictions. Under current rules, for example, participants can use benefits to buy a 12-pack of Pepsi or a Snickers bar or a giant bag of Lay’s potato chips but not real food that happens to be heated, such as a package of rotisserie chicken. “This is the most vulnerable population in the country,” says Rimm. “We’re not listening well enough to our constituency.”
Other innovative fiscal levers to alter behavior could also drive down obesity. In 2014, a trio of strong voices on food industry practices—Dariush Mozaffarian, DrPH ’06, dean of Tufts University’s Friedman School of Nutrition Science and Policy and former associate professor of epidemiology at the Harvard Chan School; Kenneth Rogoff, professor of economics at Harvard; and David Ludwig, professor in the Department of Nutrition at Harvard Chan and a physician at Boston Children’s Hospital—broached the idea of a “meaningful” tax on nearly all packaged retail foods and many chain restaurants, with the proceeds used to pay for minimally processed foods and healthier meals for school kids. In essence, the tax externalizes the social costs of harmful individual behavior.
“We made a straightforward proposal to tax all processed foods and then use the income to subsidize whole foods in a short-term, revenue-neutral way,” explains Ludwig. “The power of this idea is that, since there is so much processed food consumption, even a modest tax—in the 10 to 15 percent range—is not going to greatly inflate the cost of these foods. Their price would increase moderately, but the proceeds would not disappear into government coffers. Instead, the revenue would make healthy foods affordable for virtually the entire population, and the benefits would be immediately evident. Yes, people will pay moderately more for their Coke or for their cinnamon bear claw but a lot less for nourishing, whole foods.”
Another suggestion comes from Sandro Galea, dean of the Boston University School of Public Health, and Abdulrahman M. El-Sayed, a public health physician and epidemiologist. In a 2015 issue of the American Journal of Public Health , they called for “calorie offsets,” similar to the carbon offsets used to mitigate environmental harm caused by the gas and oil industries. A “calorie offset” scheme could hand the food and beverage industries a chance at redemption by inviting them to invest in such undertakings as city farms, cooking classes for parents, healthy school cafeterias, and urban green spaces.
These ambitious proposals face almost impossibly high hurdles. Political battle lines typically pit public health against corporations, with Big Food casting doubt on solid nutrition science, deeming government regulation a threat to free choice, and making self-policing pledges that it has never kept. On the website for the Americans for Food and Beverage Choice, a group spearheaded by the American Beverage Association, is the admonition: “[W]hether it’s at a restaurant or in a grocery store, it’s never the government’s job to decide what you choose to eat and drink.”
Yet surprisingly, many public health professionals are convinced that the only way to stop obesity is to make common cause with the food industry. “This isn’t like tobacco, where it’s a fight to the death. We need the food industry to make healthier food and to make a profit,” says Mozaffarian. “The food industry is much more diverse and heterogeneous than tobacco or even cars. As long as we can help them—through carrots and sticks, tax incentives and disincentives—to move towards healthier products, then they are part of the solution. But we have to be vigilant, because they use a lot of the same tactics that tobacco did.”
Sow what we want to reap.
Americans overeat what our farmers overproduce.
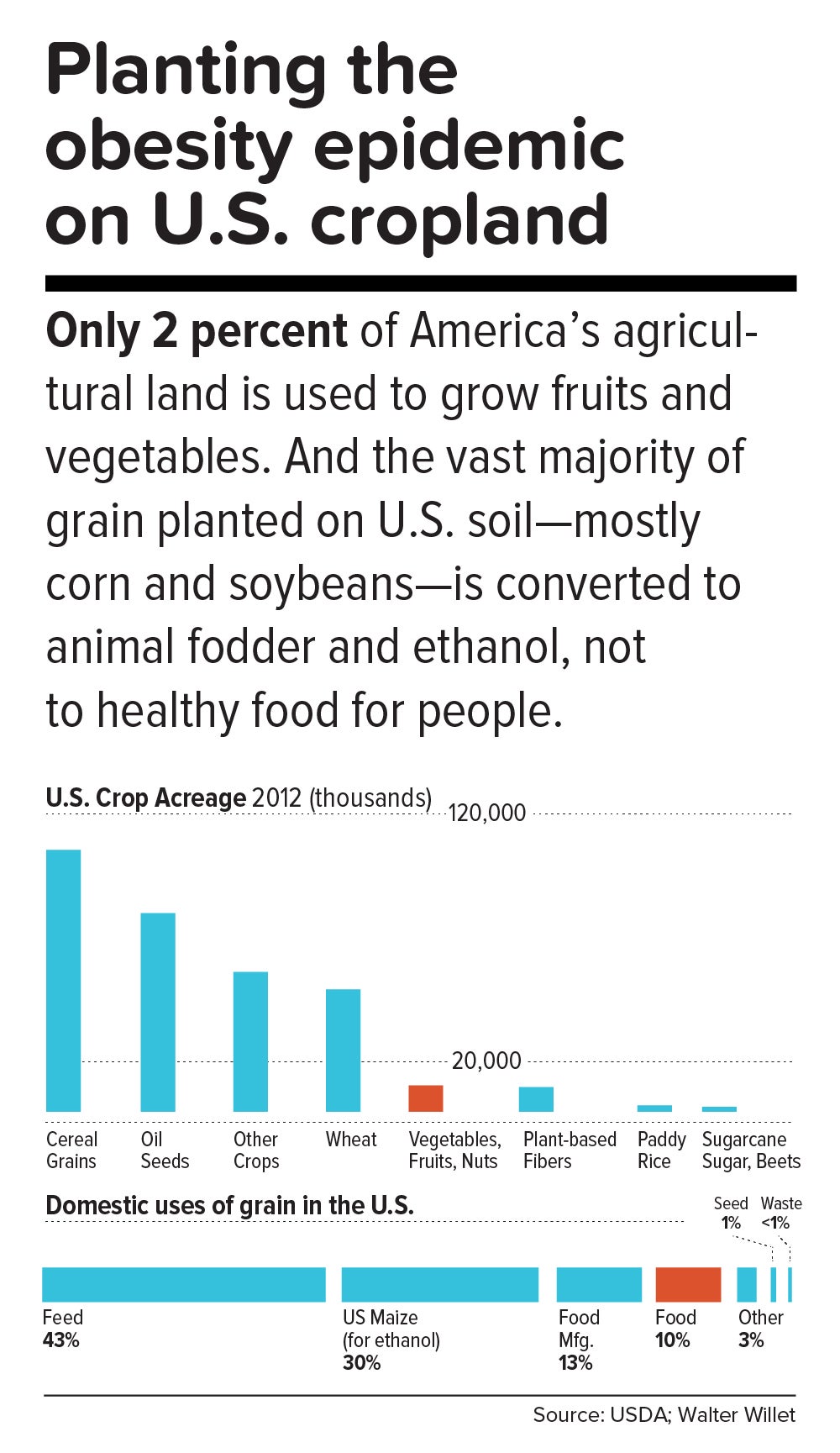
“The U.S. food system is egregiously terrible for human and planetary health,” says Walter Willett. It’s so terrible, Willett made a pie chart of American grain production consumed domestically. It shows that most of the country’s agricultural land goes to the two giant commodity crops: corn and soy. Most of those crops, in turn, go to animal fodder and ethanol, and are also heavily used in processed snack foods. Today, only about 10 percent of grain grown in the U.S. for domestic use is eaten directly by human beings. According to a 2013 report from the Union of Concerned Scientists, only 2 percent of U.S. farmland is used to grow fruits and vegetables, while 59 percent is devoted to commodity crops.
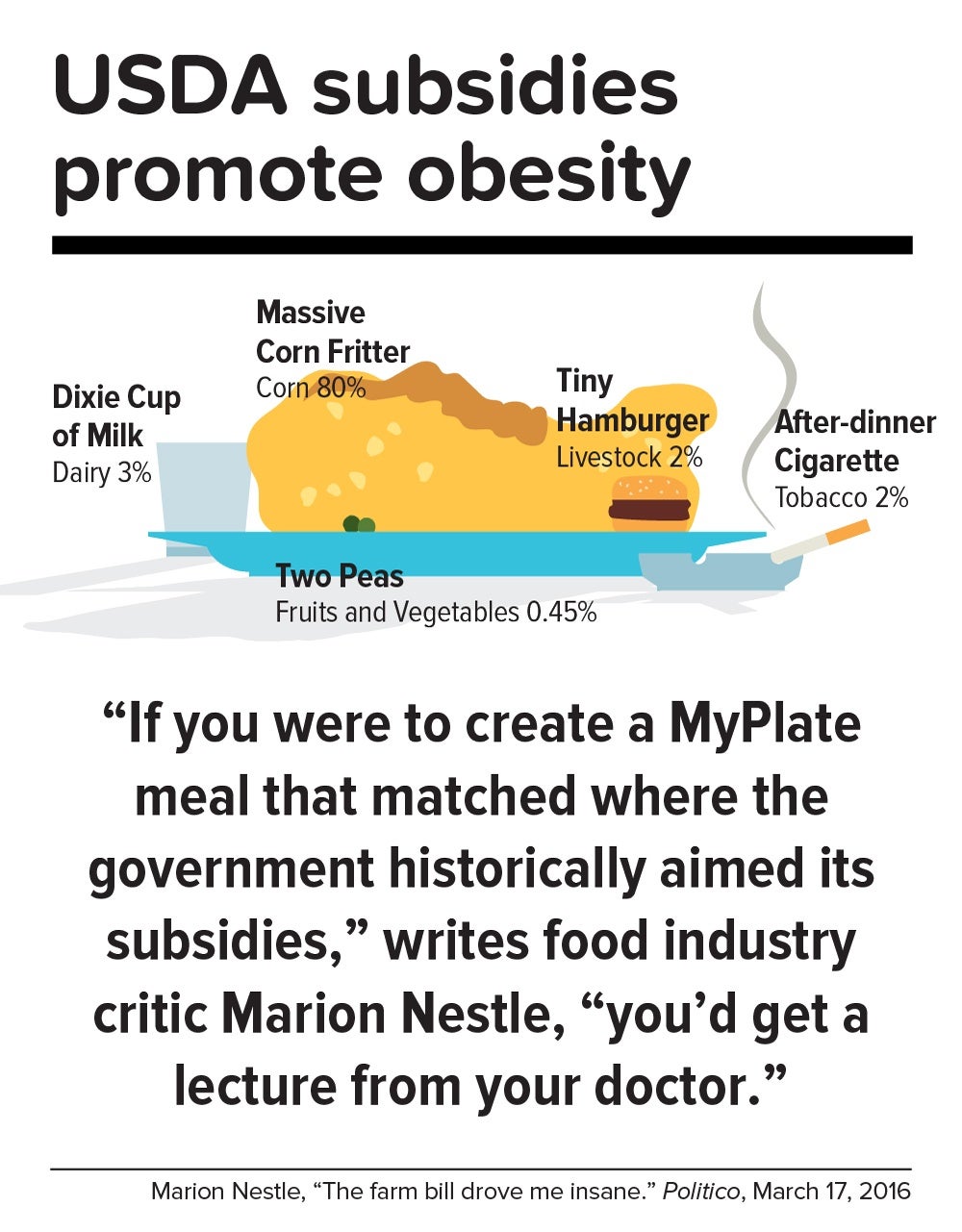
Historically, those skewed proportions made sense. Federal food policies, drafted with the goal of alleviating hunger, preferentially subsidize corn and soy production. And whereas corn or soybeans could be shipped for days on a train, fruits and vegetables had to be grown closer to cities by truck farmers so the produce wouldn’t spoil. But those long-ago constraints don’t explain today’s upside-down agricultural priorities.
In a now-classic 2016 Politico article titled “The farm bill drove me insane,” Marion Nestle illustrated the irrational gap between what the government recommends we eat and what it subsidizes: “If you were to create a MyPlate meal that matched where the government historically aimed its subsidies, you’d get a lecture from your doctor. More than three-quarters of your plate would be taken up by a massive corn fritter (80 percent of benefits go to corn, grains and soy oil). You’d have a Dixie cup of milk (dairy gets 3 percent), a hamburger the size of a half dollar (livestock: 2 percent), two peas (fruits and vegetables: 0.45 percent) and an after-dinner cigarette (tobacco: 2 percent). Oh, and a really big linen napkin (cotton: 13 percent) to dab your lips.”
In this sense, the USDA marginalizes human health. Many of the foods that nutritionists agree are best for us—notably, fruits, vegetables, and tree nuts—fall under the bureaucratic rubric “specialty crops,” a category that also includes “dried fruits, horticulture, and nursery crops (including floriculture).” Farm bills, which get passed every five years or so, fortify the status quo. The 2014 Farm Bill, for example, provided $73 million for the Specialty Crop Block Grant Program in 2017, out of a total of about $25 billion for the USDA’s discretionary budget. (The next Farm Bill, now under debate, will be coming out in 2018.)
By contrast, a truly anti-obesigenic agricultural system would stimulate USDA support for crop diversity—through technical assistance, research, agricultural training programs, and financial aid for farmers who are newly planting or transitioning their land into produce. It would also enable farmers, most of whom survive on razor-thin profit margins, to make a decent living.
In the early 1970s, Finland’s death rate from coronary heart disease was the highest in the world, and in the eastern region of North Karelia—a pristine, sparsely populated frontier landscape of forest and lakes—the rate was 40 percent worse than the national average. Every family saw physically active men, loggers and farmers who were strong and lean, dying in their prime.
Thus was born the North Karelia Project, which became a model worldwide for saving lives by transforming lifestyles. The project was launched in 1972 and officially ended 25 years later. While its initial goal was to reduce smoking and saturated fat in the diet, it later resolved to increase fruit and vegetable consumption.
The North Karelia Project fulfilled all of these ambitions. When it started, for example, 86 percent of men and 82 percent of women smeared butter on their bread; by the early 2000s, only 10 percent of men and 4 percent of women so indulged. Use of vegetable oil for cooking jumped from virtually zero in 1970 to 50 percent in 2009. Fruit and vegetables, once rare visitors to the dinner plate, became regulars. Over the project’s official quarter-century existence, coronary heart disease deaths in working-age North Karelian men fell 82 percent, and life expectancy rose seven years.
The secret of North Karelia’s success was an all-out philosophy. Team members spent innumerable hours meeting with residents and assuring them that they had the power to improve their own health. The volunteers enlisted the assistance of an influential women’s group, farmers’ unions, homemakers’ organizations, hunting clubs, and church congregations. They redesigned food labels and upgraded health services. Towns competed in cholesterol-cutting contests. The national government passed sweeping legislation (including a total ban on tobacco advertising). Dairy subsidies were thrown out. Farmers were given strong incentives to produce low-fat milk, or to get paid for meat and dairy products based not on high-fat but on high-protein content. And the newly established East Finland Berry and Vegetable Project helped locals switch from dairy farming—which had made up more than two-thirds of agriculture in the region—to cultivation of cold-hardy currants, gooseberries, and strawberries, as well as rapeseed for heart-healthy canola oil.
“A mass epidemic calls for mass action,” says the project’s director, Pekka Puska, “and the changing of lifestyles can only succeed through community action. In this case, the people pulled the government—the government didn’t pull the people.”
Could the United States in 2017 learn from North Karelia’s 1970s grand experiment?
“Americans didn’t become an obese nation overnight. It took a long time—several decades, the same timeline as in individuals,” notes Frank Hu. “What were we doing over the past 20 years or 30 years, before we crossed this threshold? We haven’t asked these questions. We haven’t done this kind of soul-searching, as individuals or society as a whole.”
Today, Americans may finally be willing to take a hard look at how food figures in their lives. In a July 2015 Gallup phone poll of Americans 18 and older, 61 percent said they actively try to avoid regular soda (the figure was 41 percent in 2002); 50 percent try to avoid sugar; and 93 percent try to eat vegetables (but only 57.7 percent in 2013 reported they ate five or more servings of fruits and vegetables at least four days of the previous week).
Individual resolve, of course, counts for little in problems as big as the obesity epidemic. Most successes in public health bank on collective action to support personal responsibility while fighting discrimination against an epidemic’s victims. [To learn more about the perils of stigma against people with obesity, read “ The Scarlet F .”]
Yet many of public health’s legendary successes also took what seems like an agonizingly long time to work. Do we have that luxury?
“Right now, healthy eating in America is like swimming upstream. If you are a strong swimmer and in good shape, you can swim for a little while, but eventually you’re going to get tired and start floating back down,” says Margo Wootan, SD ’93, director of nutrition policy for the Center for Science in the Public Interest. “If you’re distracted for a second—your kid tugs on your pant leg, you had a bad day, you’re tired, you’re worried about paying your bills—the default options push you toward eating too much of the wrong kinds of food.”
But Wootan has not lowered her sights. “What we need is mobilization,” she says. “Mobilize the public to address nutrition and obesity as societal problems—recognizing that each of us makes individual choices throughout the day, but that right now the environment is stacked against us. If we don’t change that, stopping obesity will be impossible.”
The passing of power to younger generations may aid the cause. Millennials are more inclined to view food not merely as nutrition but also as narrative—a trend that leaves Duke University’s Kelly Brownell optimistic. “Younger people have been raised to care about the story of their food. Their interest is in where it came from, who grew it, whether it contributes to sustainable agriculture, its carbon footprint, and other factors. The previous generation paid attention to narrower issues, such as hunger or obesity. The Millennials are attuned to the concept of food systems.”
We are at a public health inflection point. Forty years from now, when we gaze at the high-resolution digital color photos from our own era, what will we think? Will we realize that we failed to address the obesity epidemic, or will we know that we acted wisely?
The question brings us back to the 1970s, and to Pekka Puska, the physician who directed the North Karelia Project during its quarter-century existence. Puska, now 71, was all of 27 and burning with big ideas when he signed up to lead the audacious effort. He knows the promise and the perils of idealism. “Changing the world may have been utopic,” he says, “but changing public health was possible.”
News from the School

At Convocation, Harvard Chan School graduates urged to meet climate and public health crises with fresh thinking, collective action

Graduation 2024: Award winners

Once a malaria patient, student now has sights set on stopping the deadly disease

Providing compassionate care to marginalized people
Over one billion obese people globally, health crisis must be reversed - WHO

Facebook Twitter Print Email
On World Obesity Day, marked on Friday, the World Health Organization (WHO) urged countries to do more to reverse what is a preventable health crisis.
According to recent data , more than one billion people worldwide are obese , including 650 million adults, 340 million adolescents and 39 million children. With the numbers still increasing, WHO estimates that by 2025, approximately 167 million people will become less healthy because they are overweight or obese.
Impacts of obesity
Overweight and obesity are defined as abnormal or excessive fat accumulation that may impair health. As a disease that impacts most body systems, obesity affects the heart, liver, kidneys, joints, and reproductive system.
WHO underlined that obesity also leads to a range of noncommunicable diseases (NCDs), such as type 2 diabetes, cardiovascular disease, hypertension and stroke, various forms of cancer, as well as mental health issues.
According to the UN health agency, people with obesity are also three times more likely to be hospitalized for COVID-19 .

Key to prevention: act early
Worldwide obesity has nearly tripled since 1975.
WHO said the key to preventing obesity is to act early. For example, before even considering having a baby, get healthy.
“ Good nutrition in pregnancy, followed by exclusive breastfeeding until the age of 6 months and continued breastfeeding until two years and beyond, is best for all infants and young children,” WHO reiterated.

Global response
At the same time, countries need to work together to create a better food environment so that everyone can access and afford a healthy diet .
To achieve that, steps to be taken include restricting the marketing to children of food and drinks high in fats, sugar, and salt, taxing sugary drinks, and providing better access to affordable, healthy food.
Along with changes in diet , WHO also mentioned the need for exercise.
“Cities and towns need to make space for safe walking, cycling, and recreation, and schools need to help households teach children healthy habits from early on.”
WHO continues to address the global obesity crisis by monitoring global trends and prevalence, developing a broad range of guidance to prevent and treat overweight and obesity, and providing support and guidance for countries.
Action plan to stop obesity
Following a request from Member States, the WHO secretariat is also developing an acceleration action plan to stop obesity, tackle the epidemic in high burden countries and catalyze global action. The plan will be discussed at the 76 World Health Assembly to be held in May.
- food and nutrition
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 02 December 2022
Epidemiology and Population Health
Obesity and the cost of living crisis
- Eric Robinson ORCID: orcid.org/0000-0003-3586-5533 1
International Journal of Obesity volume 47 , pages 93–94 ( 2023 ) Cite this article
10k Accesses
9 Citations
73 Altmetric
Metrics details
- Public health
- Risk factors
2022 has seen the emergence of a global cost of living crisis driven by rapid increases in the cost of energy and food. The result will be a growing number of families experiencing short-term financial turmoil and long-term financial hardship [ 1 ]. Increasing inflation results in households with proportionately less disposable income, and this will invariably impact on food purchasing. One likely impact will be the tipping of many people from lesser economically developed countries into extreme poverty and starvation [ 2 ]. Furthermore, in the context of an already well-established obesity crisis, the cost of living crisis may also create the perfect storm for driving global obesity prevalence further upwards.
Families already have to choose between cheap and readily available energy-dense foods vs. more costly healthier food options, often financially and also in terms of preparation time. As financial hardship hits, choosing the latter will become more difficult. Households with the lowest incomes are less able to place long-term health at the top of their considerations when buying, choosing and cooking food. Recent research suggests that this is one likely reason why lower socioeconomic status is associated with higher BMI [ 3 ]. If left unchecked, the cost of living crisis has the potential to further widen socioeconomic inequalities in obesity by disproportionately affecting disadvantaged families and communities already at risk of obesity.
The stress of financial crises is thought to damage mental health, and the well-being of many of those experiencing financial hardship will be at risk [ 4 ]. Poorer mental health likely decreases motivation in the context of obesity management [ 5 ] and is a risk factor for increased weight gain among the general population, potentially through biopsychological mechanisms such as comfort eating [ 6 ]. Although research is less convincing and comprehensive in humans than in non-human animals, resource deprivation and insecurity may directly impact on biological systems to increase fat deposition and weight gain [ 7 ]. Well before the emergence of the current cost of living crisis, research had documented the concerning number of people worldwide living in food insecurity. Experiencing food insecurity is a risk factor for obesity and other health problems [ 8 ]. The cost of living crisis therefore has potential to move many more into food insecurity and further increase obesity among those already experiencing financial hardship.
Obesity research in the context of the current and future financial crises will have both theoretical and applied value. The COVID-19 pandemic stimulated a large amount of research into understanding how obesity increased risk of death, how those living with obesity were disproportionately affected, and the impact the pandemic has had on obesity prevalence [ 9 ]. The current cost of living crisis provides an (unfortunate) opportunity to study how and why diet, physical activity and obesity are affected in those experiencing acute financial hardship. Furthermore, documenting the impacts that the cost of living crisis has on absolute and relative inequalities in obesity prevalence will be important.
How countries respond to the cost of living crisis will matter, and invariably will differ from one government to another. Although there will be universal efforts to address inflation and financial hardship, in the context of obesity the devil will be in the detail. In recent years the UK government have implemented and proposed the introduction of a range of population-level anti-obesity measures including, among others, banning of price promotions and advertisement of unhealthy food products. However, in response to the cost of living crisis, there are suggestions that government will reverse the introduction of such measures in order to remove constraints on businesses and drive promote economic growth [ 10 ].
If governments deprioritise obesity policy to instead try and spur short-term economic growth, not only will obesity be worsened, but it is likely that there be damaging longer-term economic impacts. The current global burden of obesity is large and will continue to grow if upwards obesity prevalence trends continue. Obesity policy in many countries has historically been fragmented and not been considered in the wider context of other major societal challenges, such as climate change and financial crises. If this continues, then the obesity crisis will be with us for a very long time or even worse, indefinitely.
World Economic Forum. The cost-of-living crisis is having a global impact. Here’s what countries are doing to help. 2022. https://www.weforum.org/agenda/2022/09/cost-of-living-crisis-global-impact/
Ortiz-Juarez E, Molina G, Montoya-Aguire M. United Nations Development Programme, Cost-of-Living Report. 2022. https://www.undp.org/germany/publications/cost-living-report
Robinson E, Jones A, Marty L. The role of health-based food choice motives in explaining the relationship between lower socioeconomic position and higher BMI in UK and US adults. Int J Obes. 2022;46:1818–24.
Frasquilho D, Matos MG, Salonna F, Guerreiro D, Storti CC, Gaspar T, et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health. 2015;16:1–40.
Article Google Scholar
Jones RA, Mueller J, Sharp SJ, Vincent A, Duschinsky R, Griffin SJ, et al. The impact of participant mental health on attendance and engagement in a trial of behavioural weight management programmes: secondary analysis of the WRAP randomised controlled trial. Int J Behav Nutr Phys Activity. 2021;18:1–3.
Konttinen H, Van Strien T, Männistö S, Jousilahti P, Haukkala A. Depression, emotional eating and long-term weight changes: a population-based prospective study. Int J Behav Nutr Phys Activity. 2019;16:1.
Nettle D, Andrews C, Bateson M. Food insecurity as a driver of obesity in humans: the insurance hypothesis. Behav Brain Sci. 2017;40:e105.
Moradi S, Mirzababaei A, Dadfarma A, Rezaei S, Mohammadi H, Jannat B, et al. Food insecurity and adult weight abnormality risk: a systematic review and meta-analysis. Eur J Nutr. 2019;58:45–61.
Jones RA, Christiansen P, Maloney NG, Duckworth JJ, Hugh-Jones S, Ahern AL, et al. Perceived weight-related stigma, loneliness, and mental wellbeing during COVID-19 in people with obesity: a cross-sectional study from ten European countries. Int J Obes. 2022;46:2120–7.
BBC News. Anti-obesity strategy to be reviewed due to cost-of-living crisis. 2022. https://www.bbc.co.uk/news/uk-politics-62900076 .
Download references
ER is funded by a European Research Council starter grant under the European Union’s Horizon 2020 research and innovation programme (Grant reference: PIDS, 803194).
Author information
Authors and affiliations.
Department of Psychology, Eleanor Rathbone Building, University of Liverpool, Liverpool, L69 7ZA, UK
Eric Robinson
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Eric Robinson .
Ethics declarations
Competing interests.
ER has previously received research funding from Unilever and the American Beverage Association for unrelated research projects.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Robinson, E. Obesity and the cost of living crisis. Int J Obes 47 , 93–94 (2023). https://doi.org/10.1038/s41366-022-01242-9
Download citation
Received : 23 September 2022
Revised : 17 November 2022
Accepted : 22 November 2022
Published : 02 December 2022
Issue Date : February 2023
DOI : https://doi.org/10.1038/s41366-022-01242-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The impact of the cost-of-living crisis on population health in the uk: rapid evidence review.
- Jade Meadows
- Miranda Montano
- Gwen Sascha Fernandes
BMC Public Health (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Opinion Addressing the American obesity crisis
Regarding Kate Manne’s Feb. 6 Tuesday Opinion essay, “ A diagnosis for the doctors — fatphobia ”:
We heard echoes of Ms. Manne’s story across the country last summer. During four town hall events held at senior centers and churches, older adults with obesity told the National Council on Aging and National Consumers League : “I feel invisible” when seeking health care.
Every American — regardless of weight or size — deserves to be treated with dignity and have equitable access to quality care. That’s why we developed and launched the nation’s first Obesity Bill of Rights . With obesity now one of the most prevalent and costly chronic diseases in the United States , we must change the national dialogue away from blame and stigma and toward understanding and treatment.
More than 40 organizations have joined our effort to define quality obesity care as the right of all adults and to drive systems change. The Obesity Bill of Rights establishes eight essential rights, so people with obesity will be screened, diagnosed, counseled and treated according to medical guidelines and no longer face widespread weight bias and ageism within the health-care system or face exclusionary coverage policies by insurers and government agencies.
Ms. Manne argued that it is the system that is failing individuals. We agree. The Obesity Bill of Rights is an important step forward. NCL and NCOA are spearheading Right2ObesityCare , a grass-roots movement to engage people with obesity, their caregivers, health professionals, community leaders, employers, and obesity and chronic disease organizations to drive adoption of the Obesity Bill of Rights in clinical settings.
Ramsey Alwin , Arlington
The writer is president and chief executive of the National Council on Aging.
Sally Greenberg , Washington
The writer is chief executive of the National Consumers League.
In her Feb. 6 Tuesday Opinion essay, Kate Manne wrote, “Research has shown that ‘overweight’ people have the lowest risks of premature mortality and that ‘moderately obese’ and ‘normal-weight’ people have similar mortality risks. Yes, being heavier than ‘moderately obese’ is correlated with an increased mortality risk; but so is being very thin (even excluding people who smoked or had preexisting illnesses).”
However, the linked studies paint a different picture. One study concludes : “From a public health perspective, the findings suggest that even moderate levels of overweight may indicate worse health risk profiles than lower body weights, with potentially important implications for chronic disease and health-related quality of life.” Another study Ms. Manne cited concluded that “underweight and obesity, particularly higher levels of obesity, were associated with increased mortality relative to the normal weight category.”
Though there might be some dispute as to the degree to which obesity or overweight represents a health risk, Ms. Manne mischaracterized the current research on the dangers of excess weight.
Raymond Natter , Washington

- Spring 2024
- Tahrir Forum
- Global Forum
- Book Reviews
- Regions and Countries
- Contributors
- eBook: A Global Perspective on the Trump Era
--> .cls-1{fill:#770c1d;}
.cls-1{fill:#770c1d;}.
Support Our Balanced Narrative

The Obesity Crisis
If trends persist, nearly half of the world’s adult population will be overweight or obese by 2030. A comprehensive intervention strategy is required to fight a scourge as damaging to the global economy as war.

Camp for overweight children, Beijing, July 15, 2014. Kevin Frayer/Getty Images
- X (Twitter)
Obesity has become one of our major global economic problems. Many people may be surprised to learn that obesity is jostling with armed conflict and smoking as a human activity with the greatest negative impact on the global economy. It imposes significant costs on healthcare systems; around the world, 2 to 7 percent of all healthcare spending relates to measures to prevent and treat this condition, with up to 20 percent of all healthcare spending attributable to obesity, through related diseases such as type 2 diabetes and heart disease. These healthcare costs place a burden on government finances. Furthermore, overall economic gains and employers are affected by impaired productivity.
The global economic impact of obesity is increasing. The prevalence of obesity is still rising in developed economies, and now, as emerging markets become richer, they, too, are experiencing rising prevalence. The evidence suggests that the economic and societal impact of obesity is deep and lasting. It may entrench social inequalities between generations; obesity in parents appears to increase the risk of obesity in their children through both physiological and behavioral mechanisms.
It is no exaggeration to say that across the globe, obesity and its associated medical conditions have reached crisis proportions. More than 2.1 billion people—nearly 30 percent of the global population—are overweight or obese. That’s nearly two and a half times the number of people who are undernourished. Obesity, which should be preventable, is now responsible for about 5 percent of all deaths worldwide. If its prevalence continues on its current trajectory, almost half of the world’s adult population will be overweight or obese by 2030.
Left unchecked, rising prevalence is very likely to have an even more significant economic impact than it does today—putting pressure on employers and the productivity of their companies and on healthcare systems, and on the public purse. The urgent question is how best to combat it. Tackling obesity requires a comprehensive intervention strategy rolled out at scale.
Complex Causes The root causes of rising obesity are highly complex, spanning evolutionary, biological, psychological, sociological, economic, and institutional factors. A Foresight project of Britain’s Research Councils UK has identified more than a hundred variables that directly or indirectly affect obesity outcomes.
Because of centuries of food insecurity, human beings have evolved with a biological ability to cope with food scarcity rather than abundance. The human body seeks out energy-dense foods and tries to conserve energy as fat. Hormones that regulate hunger and satiety encourage people to seek extra food when food is scarce but do not seem to have the ability to prevent overconsumption or encourage extra calorie burning when food is abundant.
Modern life makes fewer physical demands on many people, who lead less active lifestyles as technology replaces the need for physical labor. With many jobs now sedentary, exercise is a conscious and optional choice. As an illustration of the change, in 1969 about 40 percent of schoolchildren in the United States walked or rode their bicycles to school; by 2001, only 13 percent did so. Over the past fifty years, it has been estimated that a reduction in occupation-related physical activity in the United States has reduced the daily net energy balance by one hundred calories per person, a significant share of the overall change in the energy balance during this period.
Mass urbanization in many regions—the global urban population is growing by sixty-five million a year, the equivalent of adding seven new cities the size of Chicago every twelve months—is boosting incomes but reinforcing a less physical lifestyle. One Chinese study found that urbanization reduces daily energy expenditure by 300 to 400 calories, and traveling to work by car or bus reduces it by a further 200 calories.
Human beings also have a psychological relationship with food that goes beyond a need for basic sustenance. Many of us use food as a reward or to relieve stress, or have a compulsive relationship with certain types of food. There is a correlation between obesity and high rates of some mental health conditions, including depression.
People are highly influenced by social norms and subtle social cues in their eating habits and their attitude toward weight. For instance, if they dine with other people who eat more, they eat more themselves; likewise, those who dine with people who eat less, eat less themselves. One study has shown that 35 percent more calories are consumed when having dinner with a friend than when eating alone, and 96 percent more if dining in a group of seven people. Another study has shown that a person is 57 percent more likely to become obese if a friend has also become obese—evidence of social normalization of the condition.
Food has become much more affordable over the past sixty years. In the United States, the share of average household income spent on food fell from 42 percent in 1900 to 30 percent in 1950 and to 13.5 percent in 2003. This is beneficial in welfare terms, reducing rates of undernutrition and freeing up disposable income.
Many of these factors underline the importance of the environmental context as a driver of obesity prevalence. A helpful lens for examining how the environment affects prevalence is looking at expatriate populations, transplanted from one context to another. For example, British expats who have settled in Abu Dhabi have diabetes prevalence rates of 18 percent, compared with a baseline prevalence of 8 percent in the United Kingdom. Physical environment is one factor, but it is likely that sociocultural variables are also relevant. Various studies suggest a correlation between Hispanic immigrants’ obesity rate and the length of their stay in the United States and the depth of their cultural assimilation; the longer they are in the United States, the more prone they are to obesity as their eating habits change.
The Global Prosperity Factor No country reduced its obesity prevalence between 2000 and 2013. During this period, prevalence grew by 0.5 percentage points or more a year in 130 of the 196 countries for which the Organisation for Economic Co-operation and Development (OECD) documents obesity prevalence data. Prevalence growth has momentum; countries with high prevalence in 2000 have continued to see the highest prevalence growth rates since then. There does not seem to be convergence to a stable obesity prevalence rate internationally. Recent data suggest a plateauing of prevalence in some developed markets, such as Italy, the United Kingdom, and the United States, while Australia, France, Switzerland, and other advanced economies experience continued growth.
Overall obesity prevalence does appear to be correlated with a country’s wealth. It is striking how few countries escape the pattern. Among G-20 nations with per capita GDP exceeding $8,000, only Japan and South Korea have prevalence rates lower than 16 percent. The majority of G-20 countries have rates of more than 20 percent. Looking at children specifically, the prevalence of obesity ranges between 5 and 20 percent.
China, Indonesia, and India currently have lower obesity prevalence rates than advanced economies. However, as rapid industrialization and urbanization boost incomes, the prevalence rates in these fast-growing emerging economies are rising quickly. In India and China, the prevalence of obesity in cities is three to four times the rate in rural areas, reflecting higher incomes in urban areas and therefore higher levels of nutrition and food consumption and often less active labor. The prevalence of obese and overweight people rose at 1.2 percent a year in Chinese adult males between 1985 and 2004 and 1 percent a year in adult females.
This is a pattern we observe across emerging markets. Many of these countries experienced a rise in prevalence of one percentage point a year between 2000 and 2008. Today, many countries have prevalence rates of 20 percent or even 30 percent and now have well-entrenched rising trends. A report from the Overseas Development Institute found that obesity and overweight rates in North Africa, Latin America, and the Middle East were on a par with Europe at 10 to 30 percent obesity in adults and at 30 to 70 percent overweight. Other regions, including South Asia and East Asia, are catching up with advanced economies in obesity prevalence.
All G-20 countries are experiencing year-on-year growth in prevalence of 0.5 to 1.5 percentage points. In the United Kingdom, for instance, more than 80 percent of the population aged 21 to 60 could be obese or overweight by 2030, according to the government’s 2007 Foresight report. Breaking this down by gender, the report estimated that more than 60 percent of men and 50 percent of women would be obese. By 2050, the report estimated, one-quarter of children in the United Kingdom could be obese.
Developed economies have a clear inverse correlation between income levels and the prevalence of obesity, particularly in the case of women and children. Put simply, lower-income groups tend to have higher obesity prevalence. And it seems likely that causation works both ways. Across a range of developed markets, this inverse relationship is most acute for women.
A study conducted by the U.S. Centers for Disease Control and Prevention found that obesity prevalence is generally similar at all income levels for men in the United States (around 30 percent), while for women it was 42 percent at low-income levels versus 29 percent at high-income levels. In Australia the relationship holds across genders, with obesity prevalence ten percentile points higher for adults in the most disadvantaged quintile versus the least disadvantaged one. In several other countries, it has been observed that obesity prevalence for women ranges from 1.6 (United States) to 18.4 (South Korea) times as high at the lower end of the education spectrum as it is for those at the upper end. This relative index of inequality is lower on average for men.
Given that obesity has a higher incidence among disadvantaged households, it also imposes a disproportionate burden on these already disadvantaged households in terms of higher healthcare costs and reduced welfare. This entrenchment of inequalities operates both within countries and at the international level. In emerging economies where public health provision is nascent, these healthcare costs fall directly on households. In addition, there is some evidence that epigenetic factors may disproportionately increase the burden of obesity in emerging markets.
Moreover, it seems that obesity can be passed from generation to generation. There is evidence that obesity risk is tied to parental body mass index (BMI) through both physiological and behavioral mechanisms. Studies find that a mother with a high BMI is a significant predictor of obesity in her children when they grow to adulthood because fetuses develop a compromised metabolism and a resistance to insulin. However, other sociocultural factors and genetic predisposition drive the onset of obesity, too. For instance, eating habits that confound adult eating patterns are typically passed along by parents in early life.
Economic Impact The global economic impact of obesity is roughly $2 trillion, or 2.8 percent of global GDP, according to our analysis, which reflects the fact that obesity places a burden on developed and developing economies alike. This is equivalent to the GDP of Italy or Russia. Obesity today has the same impact on the global economy as armed violence, war, and terrorism, and only a shade less than smoking. These three are far and away the largest global economic impact areas driven by human behavior.
We assessed the current impact to society of fourteen major problems that are caused by humans—that is, those that are the result of human decisions, are amplified by human or societal behavior, or depend on societal, legal, or infrastructural environments created by humans. These ranged from obesity, smoking, and alcoholism to armed violence, climate change, and unsafe sex. This analysis therefore excludes diseases such as malaria but includes the impact of diseases such as heart disease and type 2 diabetes whose prevalence lifestyle choices or other human decisions can drive. Our estimate of the global economic toll of obesity includes the cost of lost economic productivity through a reduction in productive life years, direct costs to healthcare systems, and the investment required to mitigate the impact of obesity.
Of the three sources of cost that we assessed, lost productivity is the most significant in our analysis, accounting for nearly 70 percent of the total global cost of obesity. Some critics may argue that lost productivity should not be included, as it does not generate a direct cost. However, we believe that, while not a direct cost to society, it should be included because it has a negative economic impact. In addition, it should be noted that our estimates are based on the current cost of these burdens. This means that burdens such as climate change and obesity, which result in a higher future cost, are ranked lower than if we had conducted these analyses on a net present value basis.
In most developed economies, obesity ranks among the top three human-generated economic burdens. In the United Kingdom, for instance, obesity has the second-largest impact after smoking, generating an economic loss of more than $70 billion a year in 2012, or 3 percent of GDP. In the United States, armed conflict (and especially spending on the military) has the highest social and economic impact, and obesity is second; obesity generated an impact in the United States of $663 billion a year in 2012, or 4.1 percent of GDP. In both countries, the prevalence and associated cost of obesity are growing, albeit less steeply than in recent decades and in comparison with many emerging markets.
The economic toll of obesity varies more widely in emerging markets. In Mexico, obesity is the largest social impact at 2.5 percent of GDP. We observe comparable burdens in Morocco at 2.8 percent of GDP, in South Africa at 3 percent of GDP, and in Brazil at 2.4 percent of GDP. But in other emerging markets obesity is—as of now—a much less significant economic burden. In Nigeria, for instance, obesity’s impact on the economy is 0.7 percent of GDP, ranking as the thirteenth-largest economic burden; in Indonesia, it has a 1 percent impact, ranking eighth; and in China, the figure is 1.1 percent, ranking ninth.
Health Burdens We assessed the productivity lost due to obesity using the standard measurement of disability-adjusted life years, or DALYs, which measure the number of years that are lost or rendered economically unproductive due to disease. Of the DALYs lost to obesity across the world, around 71 percent are due to premature mortality and 29 percent to disability that has prevented individuals from making their full economic contribution. The number of DALYs lost to obesity today is three times as high in developed economies as it is in emerging markets. However, that gap is narrowing. The rise in the number of DALYs per 100,000 people lost because of obesity slowed in developed economies between 1990 and 2010 but soared by 90 percent in emerging economies.
In Indonesia, for instance, the number of DALYs lost per 100,000 people due to obesity has risen from 184 in 1990 to 885 in 2010, a jump of nearly 400 percent. In South Africa, DALYs lost to obesity totaled 1,577 in 1990 and 2,659 in 2010, an increase of 69 percent. The 29 percent “disability” burden affects employers through lost employee productivity and healthcare costs. Employees with particularly high BMI can be less productive in the workplace due to the range of health problems that obesity can cause, including, for example, arthritis, fatigue, breathlessness, lack of concentration, and depression.
There is also a relationship between obesity and absenteeism from work for health reasons, including frequent medical checkups. In the United Kingdom, for instance, we estimate that the total impact on employers is $7 billion. Of this, $5 billion, or more than two-thirds, comes from decreased productivity in the workplace rather than outright absenteeism. In the United Kingdom, higher health insurance premiums are not a major issue for employers because of the central role of public health through the National Health Service (NHS). By contrast, in the United States higher insurance premiums could contribute as much as $7.7 billion of our $18.9 billion to $21.9 billion overall estimate of the cost of obesity to employers.
McKinsey analysis on healthcare spending in the OECD group of countries has found that, without reform, healthcare spending could grow by 50 to 100 percent between 2007 and 2040. In the United Kingdom alone, the research found that healthcare spending could account for 11 to 14 percent of GDP by 2040. Separately, the World Health Organization estimates that high BMI drives between 2 and 7 percent of global healthcare spending. We observe this correlation clearly in the United Kingdom.
The research found four major drivers of increased spending: an aging population, an explosion of so-called lifestyle diseases, a rise in public expectations, and a lack of value consciousness among healthcare consumers. We cannot address aging populations or rising public expectations of healthcare provision. However, we can tackle a lack of consciousness about value among citizens and a lack of efficiency within healthcare systems, as well as the burden of lifestyle diseases of which obesity is a major driver. Obesity contributes to cardiovascular disease, type 2 diabetes, and some cancers such as kidney, bowel, and breast. Mitigating or reversing the obesity crisis is a critical element of any strategy for achieving sustainable provision of healthcare and managing public budgets.
Today, one in twelve of the global adult population has type 2 diabetes, which is at least partly driven by obesity. In addition, a large number of people suffer from “impaired glucose intolerance,” a pre-diabetes condition that usually leads to the disease unless significant lifestyle changes are made. Type 2 diabetes is both preventable and reversible with lifestyle changes. A U.S. study found that a 7 percent weight loss accompanied by moderate physical activity decreased the number of new diabetes cases by 58 percent among the high-risk population. In the United States, the direct cost of obesity to the healthcare system is estimated to be between $147 billion and $190 billion a year—or about 7 percent of total annual healthcare spending. Per capita medical spending is 24 percent higher for obese individuals than for those who are not obese. Some estimates put the future cost to U.S. healthcare from obesity as high as $344 billion by 2018, or approximately 20 percent of total healthcare spending that year. To put the figure into context, this cost would be greater than the GDP of South Africa today.
In the United Kingdom, the government currently spends about £6 billion ($9.6 billion) a year on the direct medical costs of conditions related to being overweight or obese. That is 5 percent of the entire budget of the NHS. It spends a further £10 billion on diabetes. The cost of obesity and diabetes to the healthcare system is equivalent to the United Kingdom’s combined “protection” budget for the police and fire services, law courts, and prisons; 40 percent of total spending on education; and about 35 percent of the country’s defense budget. The £6 billion cost has increased since 2007, when it was £4 billion to £5 billion. On current projections of rising prevalence of obesity and overweight conditions, the cost to the NHS could increase from between £6 billion and £8 billion in 2015 to between £10 billion and £12 billion in 2030.
Only a small share of the overall cost of obesity comes from investment to mitigate or prevent it, compared with other health- or non-health-related burdens. We estimate that the global investment to prevent obesity is about $5 billion, or only 0.25 percent of the total economic impact of obesity. In comparison, investment in prevention of traffic accidents accounts for about 1.2 percent of the overall cost of such accidents. Instead, obesity spending is weighted toward treatment. For example, the United Kingdom’s largest prevention outlay is £11 million a year through the Change4Life campaign. This is equivalent to only 0.18 percent of what the NHS spends on obesity- and overweight-related conditions. Part of the reason for this is that the effectiveness of preventive approaches is difficult to assess.
Grasping the Nettle Obesity is the result of a multitude of factors, and therefore no single solution is likely to be effective in tackling it. A range of interventions that encourage and empower individuals to make the required behavioral changes will be necessary. These interventions need to be systematic, not only aiming for an immediate impact on the net energy balance but also making sure that change is sustained. A comprehensive portfolio of interventions is also required to target the different needs and responsiveness of various population segments. Governments, healthcare systems, employers, retailers, consumer-goods companies, and consumers themselves all need to play their part.
We set out to develop a comprehensive catalog of interventions that could be used to reduce obesity. Working in conjunction with policy advisors, population-health academics, and individuals from companies, and drawing on an extensive review of research, we have identified seventy-four intervention levers that are being discussed or piloted around the world. The levers fall broadly into eighteen groups, including:
Active Transport Facilitating and encouraging walking, cycling, and public transport, which engender more physical activity.
Healthcare Payors Providing incentives or support to encourage healthy behavior. These can include general financial incentives, such as premium rebates or reward points, or more targeted facilitating incentives such as free gym membership. Payors can also deliver other interventions such as parental and weight-management programs.
Healthy Meals Improving the health quality of meals in controlled settings such as schools and workplaces.
High-Calorie Food and Drink Availability Reducing the ready availability of high-calorie foods to help control impulse consumption, including removing vending machines from schools and workplaces, high-calorie foods from supermarket checkouts, and fast-food retailers from locations outside schools.
Labeling Providing calorie and other nutritional labeling so that consumers can understand the content of their food. Labels can be plain text or “engaging”—an easy-to-interpret assessment of the health of the product (for example, traffic lights).
Media Restrictions Restricting high-calorie food advertising to reduce exposure to marketing that is proven to promote consumption.
Parental Education Empowering and educating parents to promote a healthier lifestyle for their children through regular parental guidance sessions.
Pharmaceuticals Intervening with drugs to reverse obesity rapidly in cases where it is creating immediate health risks.
Portion Control Encouraging appropriate consumption through incremental (for example, 1 to 5 percent) reductions in portion sizes and designing packaging to better delineate portion size to help consumers moderate their consumption.
Price Promotions Restricting promotional activity in high-calorie impulse foods to decrease consumption.
Public Health Campaigns Delivering a public health campaign through multiple media outlets to promote healthy eating and physical activity habits.
Reformulation Incrementally reducing calories in food products to drive subconscious reduction in consumption; introducing new product ranges with improved nutritional profiles.
School Curriculum Introducing additional hours of physical education and healthy nutrition in school curricula to encourage healthier habits.
Subsidies, Taxes, and Prices Changing agricultural policy or regulatory policy to adjust consumer prices and the supply of select food and/or beverage categories.
Surgery Scaling up delivery of bariatric surgery to reduce stomach capacity and deliver immediate change in food consumption.
Urban Environment Making changes to physical spaces and food access to facilitate and encourage healthy habits, such as increasing the walkability of cities and green space, furthering access to community sports facilities, and improving access to grocery stores.
Weight-Management Programs Educating and empowering individuals to change key weight behavior through counseling, physical activity programs, and education.
Workplace Wellness Offering programs and engaging employees to encourage healthy behavior, for example through financial and non-financial incentives, team competitions, and the provision of education and self-management tools such as personal tracking devices.
Based on existing evidence, any single intervention is likely to have only a small overall impact on its own. A systemic, sustained portfolio of initiatives, delivered at scale, is needed to address the health burden. Almost all the identified interventions are cost-effective for society—savings on healthcare costs and higher productivity could outweigh the direct investment required to deliver the intervention when assessed over the full lifetime of target population. In the United Kingdom, such a program could reverse rising obesity, saving about $1.2 billion a year for the NHS.
Education and personal responsibility are critical elements of any program to reduce obesity, but not sufficient on their own. Additional interventions are needed that rely less on conscious choices by individuals and more on changes to the environment and societal norms. Such interventions “reset the defaults” to make healthy behaviors easier. They include reducing default portion sizes, changing marketing practices, and restructuring urban and education environments to facilitate physical activity.
No individual sectors in society—whether they are governments, retailers, consumer-goods companies, restaurants, employers, media organizations, educators, healthcare providers, or individuals—can address obesity on their own. Capturing the full potential impact requires engagement from as many sectors as possible. Successful precedents suggest that a combination of top-down corporate and government interventions with bottom-up community-led ones is required to change public health outcomes. Moreover, some kind of coordination is likely to be required to capture potentially high-impact industry interventions, given that there are market share risks facing any first mover.
Implementing an obesity abatement program at the required scale will not be easy. We see three important elements to consider: 1) deploy as many interventions as possible at scale and delivered effectively by the full range of sectors in society; 2) understand how to align incentives and build cooperation; and 3) do not focus unduly on prioritizing interventions because this can hamper constructive action.
The evidence base on the clinical and behavioral interventions to reduce obesity is far from complete, and ongoing investment in research is imperative. However, in many cases this is proving a barrier to action. It need not be so. We should experiment with solutions and try them out rather than waiting for perfect proof of what works, especially in the many areas where interventions are low risk. We have enough knowledge to be taking more action than we currently are.
A challenge of this magnitude requires an ambitious set of solutions—and the diffuse range of the many sectors of society relevant to this issue makes it even harder to achieve progress. We need to improve our ability to motivate action across such a diverse set of sectors. We believe that research and trial and error in how to deliver a cross-societal response are as important as research in specific intervention areas.
Some experts are questioning whether the net energy balance—that people are eating too much and exercising too little—is the appropriate lens to examine root causes. There is growing interest in the role that different nutrients such as carbohydrates, proteins, and fats play in our metabolism and in hormones that regulate satiety and hunger. Many leading scientists support the view that refined carbohydrates promote weight gain and inhibit weight loss. The science to date on this is inconclusive, and we do not include it in the assessment here without further evidence. However, it is an important area for further research and could refocus the design of obesity interventions. Similarly, there is increasing interest in the role of the microbiome—our intestinal bacteria ecosystem. Scientific evidence from controlled trials suggests that individuals whose bodies contain a greater diversity of bacterial species are less prone to high body BMI and less likely to gain weight. This also is too inconclusive for us to include at this stage. Some commentators take the causal complexity of the problem as a predetermined defeat. They say, “If the causes are so complex, where do we begin?”
We do have a good understanding of the proximate causes, even if the background causes are complex. We know that over the past fifty years, individuals’ daily energy balance equation has changed; physical activity has declined, and energy consumption has increased. Even though there are important outstanding questions about diet composition, gut microbiome, and epigenetics, we are not walking blind with no sense of what to address. However, interventions to increase physical activity, reduce energy consumption, and address diet composition cannot just seek to reverse the historical trends that have left the population where it is today. For example, we cannot, nor would we wish to, reverse the invention of the Internet or the industrialization of agriculture. We need to assess what interventions make sense and are feasible today.
Four Imperatives for Progress As many interventions as possible must be delivered to have significant impact. A holistic approach by the public, private, and third sectors is the best way forward. A program that succeeds in reversing obesity prevalence is likely to require as many interventions as possible to be deployed at scale and with high-quality delivery, our research finds. Deploying a comprehensive set of interventions would need the full set of societal sectors we have identified—local and national government, healthcare payors and providers, schools, employers, food and beverage manufacturers, retailers, restaurants, and food-service providers—to play a role. Coordination will be crucial. Today, government efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, fifteen central government departments; all local authorities with responsibility for health, education, and local planning; sixteen European Union directorates general; and a wide range of non-governmental organizations all have a significant impact on the major intervention areas that we have identified.
Understanding how to align incentives and build cooperation is critical to success. Some attempts to overcome obesity failed because they did not align with the incentives of the required participants. An example of this was the attempt by Michael Bloomberg to ban supersize beverages when he was mayor of New York. This change was blocked in the courts after extensive lobbying and legal action by the soft drink and retail industries. Other initiatives such as EPODE, which originated in France, and the Healthy Weight Commitment Foundation in the United States are leading the way in delivering integrated responses to the issue. If society is to succeed in tackling obesity, it will be necessary to find ways to build on such initiatives, to overcome misaligned incentives, and to coordinate action across a diverse set of societal sectors. The same is true of many of the public health and environmental challenges facing us in the twenty-first century. In the case of regulation to reduce the incidence of smoking, it was not possible to align incentives; in the case of obesity, we believe that it might be possible.
Government, healthcare systems, and private and social-sector organizations and entities should not focus overly on prioritizing interventions because this could hamper constructive action. Only a holistic, broad, and multipronged approach can be successful in reversing the obesity crisis. Interventions in the hands of all relevant societal sectors need to be deployed. Prioritization based on potential impact, cost-effectiveness, and feasibility is always important when making investment decisions. However, in the case of obesity, focusing unduly on priority interventions could be unhelpful given the need for a holistic response. A search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible.
While investment in research should continue, society should also engage in trial and error. Given the scale of the obesity crisis and its economic impact, investment in research, innovation, and experimentation is relatively low. For instance, in total the United Kingdom invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns. To put that in perspective, that is only about 1 percent of the social cost of obesity in the United Kingdom. More investment is required, especially in understanding the effectiveness of intervention measures when they are applied as part of a comprehensive program. But society should also be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions.
This essay is adapted from “Overcoming obesity: An initial economic analysis,” a November 2014 discussion paper by the McKinsey Global Institute
Richard Dobbs is senior partner at McKinsey & Company’s London office and a director of the McKinsey Global Institute, the business and economics research arm of the international consulting firm. He is an Associate Fellow of the Said Business School at Oxford University. He is co-author of Value: The Four Cornerstones of Corporate Finance and, most recently, No Ordinary Disruption: The Four Global Forces Breaking All the Trends . On Twitter: @richard_dobbs.
James Manyika is a senior partner at McKinsey & Company’s San Francisco office and a director of the McKinsey Global Institute, the business and economics research arm of the international consulting firm. He serves as vice chairman on President Obama’s Global Development Council and is a non-resident senior fellow at the Brookings Institution, as well as a member of the Council on Foreign Relations and the Bretton Woods Committee. He is the co-author of No Ordinary Disruption: The Four Global Forces Breaking All the Trends .
Subscribe to Our Newsletter
Related Articles

Sustainable Solutions for an Economic Crisis

“America First” In a World Crisis

Gulf Arab States Review Tax Regimes Amid Economic Crisis

How Will the Coronavirus Crisis Affect Africa’s Developmental Focus?

- Privacy Overview
- Strictly Necessary Cookies
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
Home — Essay Samples — Nursing & Health — Obesity — Essay On Obesity In America
Essay on Obesity in America
- Categories: Obesity
About this sample

Words: 991 |
Published: Mar 5, 2024
Words: 991 | Pages: 2 | 5 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
6 pages / 2684 words
7 pages / 3334 words
1 pages / 445 words
3 pages / 1377 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Obesity
Obesity has become a major public health concern in the United States, with rates steadily increasing over the past few decades. The documentary "Fed Up" explores the role of the food industry, government policies, and societal [...]
According to the World Health Organization, in 2016, more than 1.9 billion adults were overweight, of which around 650 million were obese. In the United States alone, more than 42% of the population is considered obese. This [...]
Obesity has become a major health issue in recent times, with over 39% of adults around the world being overweight and 13% being obese. In the United States, 42.4% of adults are obese, costing the country a staggering $147 [...]
Obesity is a prevalent disease in many countries today, leading to various complications and life-threatening illnesses. While medication intervention is not always necessary, lifestyle changes are often required to treat and [...]
The overweight or obese among the U.S. citizens is inclining at a shocking rate. Currently, it stands at 74.1% which is almost ¾ of our country’s population. It is a frightening truth that needs to be acknowledged by the entire [...]
“What if a war on obesity only makes the problem worse”? argues Author Daniel Engber in his article “Glutton Intolerance”. Discrimination against the obese in our society makes the obesity problem worse. The treatment against [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- About Project
- Testimonials
Business Management Ideas

Essay on Obesity
List of essays on obesity, essay on obesity – short essay (essay 1 – 150 words), essay on obesity (essay 2 – 250 words), essay on obesity – written in english (essay 3 – 300 words), essay on obesity – for school students (class 5, 6, 7, 8, 9, 10, 11 and 12 standard) (essay 4 – 400 words), essay on obesity – for college students (essay 5 – 500 words), essay on obesity – with causes and treatment (essay 6 – 600 words), essay on obesity – for science students (essay 7 – 750 words), essay on obesity – long essay for medical students (essay 8 – 1000 words).
Obesity is a chronic health condition in which the body fat reaches abnormal level. Obesity occurs when we consume much more amount of food than our body really needs on a daily basis. In other words, when the intake of calories is greater than the calories we burn out, it gives rise to obesity.
Audience: The below given essays are exclusively written for school students (Class 5, 6, 7, 8, 9, 10, 11 and 12 Standard), college, science and medical students.
Introduction:
Obesity means being excessively fat. A person would be said to be obese if his or her body mass index is beyond 30. Such a person has a body fat rate that is disproportionate to his body mass.
Obesity and the Body Mass Index:
The body mass index is calculated considering the weight and height of a person. Thus, it is a scientific way of determining the appropriate weight of any person. When the body mass index of a person indicates that he or she is obese, it exposes the person to make health risk.
Stopping Obesity:
There are two major ways to get the body mass index of a person to a moderate rate. The first is to maintain a strict diet. The second is to engage in regular physical exercise. These two approaches are aimed at reducing the amount of fat in the body.
Conclusion:
Obesity can lead to sudden death, heart attack, diabetes and may unwanted illnesses. Stop it by making healthy choices.
Obesity has become a big concern for the youth of today’s generation. Obesity is defined as a medical condition in which an individual gains excessive body fat. When the Body Mass Index (BMI) of a person is over 30, he/ she is termed as obese.
Obesity can be a genetic problem or a disorder that is caused due to unhealthy lifestyle habits of a person. Physical inactivity and the environment in which an individual lives, are also the factors that leads to obesity. It is also seen that when some individuals are in stress or depression, they start cultivating unhealthy eating habits which eventually leads to obesity. Medications like steroids is yet another reason for obesity.
Obesity has several serious health issues associated with it. Some of the impacts of obesity are diabetes, increase of cholesterol level, high blood pressure, etc. Social impacts of obesity includes loss of confidence in an individual, lowering of self-esteem, etc.
The risks of obesity needs to be prevented. This can be done by adopting healthy eating habits, doing some physical exercise regularly, avoiding stress, etc. Individuals should work on weight reduction in order to avoid obesity.
Obesity is indeed a health concern and needs to be prioritized. The management of obesity revolves around healthy eating habits and physical activity. Obesity, if not controlled in its initial stage can cause many severe health issues. So it is wiser to exercise daily and maintain a healthy lifestyle rather than being the victim of obesity.
Obesity can be defined as the clinical condition where accumulation of excessive fat takes place in the adipose tissue leading to worsening of health condition. Usually, the fat is deposited around the trunk and also the waist of the body or even around the periphery.
Obesity is actually a disease that has been spreading far and wide. It is preventable and certain measures are to be taken to curb it to a greater extend. Both in the developing and developed countries, obesity has been growing far and wide affecting the young and the old equally.
The alarming increase in obesity has resulted in stimulated death rate and health issues among the people. There are several methods adopted to lose weight and they include different diet types, physical activity and certain changes in the current lifestyle. Many of the companies are into minting money with the concept of inviting people to fight obesity.
In patients associated with increased risk factor related to obesity, there are certain drug therapies and other procedures adopted to lose weight. There are certain cost effective ways introduced by several companies to enable clinic-based weight loss programs.
Obesity can lead to premature death and even cause Type 2 Diabetes Mellitus. Cardiovascular diseases have also become the part and parcel of obese people. It includes stroke, hypertension, gall bladder disease, coronary heart disease and even cancers like breast cancer, prostate cancer, endometrial cancer and colon cancer. Other less severe arising due to obesity includes osteoarthritis, gastro-esophageal reflux disease and even infertility.
Hence, serious measures are to be taken to fight against this dreadful phenomenon that is spreading its wings far and wide. Giving proper education on benefits of staying fit and mindful eating is as important as curbing this issue. Utmost importance must be given to healthy eating habits right from the small age so that they follow the same until the end of their life.
Obesity is majorly a lifestyle disease attributed to the extra accumulation of fat in the body leading to negative health effects on a person. Ironically, although prevalent at a large scale in many countries, including India, it is one of the most neglect health problems. It is more often ignored even if told by the doctor that the person is obese. Only when people start acquiring other health issues such as heart disease, blood pressure or diabetes, they start taking the problem of obesity seriously.
Obesity Statistics in India:
As per a report, India happens to figure as the third country in the world with the most obese people. This should be a troubling fact for India. However, we are yet to see concrete measures being adopted by the people to remain fit.
Causes of Obesity:
Sedentary lifestyle, alcohol, junk food, medications and some diseases such as hypothyroidism are considered as the factors which lead to obesity. Even children seem to be glued to televisions, laptops and video games which have taken away the urge for physical activities from them. Adding to this, the consumption of junk food has further aggravated the growing problem of obesity in children.
In the case of adults, most of the professions of today make use of computers which again makes people sit for long hours in one place. Also, the hectic lifestyle of today makes it difficult for people to spare time for physical activities and people usually remain stressed most of the times. All this has contributed significantly to the rise of obesity in India.
Obesity and BMI:
Body Mass Index (BMI) is the measure which allows a person to calculate how to fit he or she is. In other words, the BMI tells you if you are obese or not. BMI is calculated by dividing the weight of a person in kg with the square of his / her height in metres. The number thus obtained is called the BMI. A BMI of less than 25 is considered optimal. However, if a person has a BMI over 30 he/she is termed as obese.
What is a matter of concern is that with growing urbanisation there has been a rapid increase of obese people in India? It is of utmost importance to consider this health issue a serious threat to the future of our country as a healthy body is important for a healthy soul. We should all be mindful of what we eat and what effect it has on our body. It is our utmost duty to educate not just ourselves but others as well about this serious health hazard.
Obesity can be defined as a condition (medical) that is the accumulation of body fat to an extent that the excess fat begins to have a lot of negative effects on the health of the individual. Obesity is determined by examining the body mass index (BMI) of the person. The BMI is gotten by dividing the weight of the person in kilogram by the height of the person squared.
When the BMI of a person is more than 30, the person is classified as being obese, when the BMI falls between 25 and 30, the person is said to be overweight. In a few countries in East Asia, lower values for the BMI are used. Obesity has been proven to influence the likelihood and risk of many conditions and disease, most especially diabetes of type 2, cardiovascular diseases, sleeplessness that is obstructive, depression, osteoarthritis and some cancer types.
In most cases, obesity is caused through a combination of genetic susceptibility, a lack of or inadequate physical activity, excessive intake of food. Some cases of obesity are primarily caused by mental disorder, medications, endocrine disorders or genes. There is no medical data to support the fact that people suffering from obesity eat very little but gain a lot of weight because of slower metabolism. It has been discovered that an obese person usually expends much more energy than other people as a result of the required energy that is needed to maintain a body mass that is increased.
It is very possible to prevent obesity with a combination of personal choices and social changes. The major treatments are exercising and a change in diet. We can improve the quality of our diet by reducing our consumption of foods that are energy-dense like those that are high in sugars or fat and by trying to increase our dietary fibre intake.
We can also accompany the appropriate diet with the use of medications to help in reducing appetite and decreasing the absorption of fat. If medication, exercise and diet are not yielding any positive results, surgery or gastric balloon can also be carried out to decrease the volume of the stomach and also reduce the intestines’ length which leads to the feel of the person get full early or a reduction in the ability to get and absorb different nutrients from a food.
Obesity is the leading cause of ill-health and death all over the world that is preventable. The rate of obesity in children and adults has drastically increased. In 2015, a whopping 12 percent of adults which is about 600 million and about 100 million children all around the world were found to be obese.
It has also been discovered that women are more obese than men. A lot of government and private institutions and bodies have stated that obesity is top of the list of the most difficult and serious problems of public health that we have in the world today. In the world we live today, there is a lot of stigmatisation of obese people.
We all know how troubling the problem of obesity truly is. It is mainly a form of a medical condition wherein the body tends to accumulate excessive fat which in turn has negative repercussions on the health of an individual.
Given the current lifestyle and dietary style, it has become more common than ever. More and more people are being diagnosed with obesity. Such is its prevalence that it has been termed as an epidemic in the USA. Those who suffer from obesity are at a much higher risk of diabetes, heart diseases and even cancer.
In order to gain a deeper understanding of obesity, it is important to learn what the key causes of obesity are. In a layman term, if your calorie consumption exceeds what you burn because of daily activities and exercises, it is likely to lead to obesity. It is caused over a prolonged period of time when your calorie intake keeps exceeding the calories burned.
Here are some of the key causes which are known to be the driving factors for obesity.
If your diet tends to be rich in fat and contains massive calorie intake, you are all set to suffer from obesity.
Sedentary Lifestyle:
With most people sticking to their desk jobs and living a sedentary lifestyle, the body tends to get obese easily.
Of course, the genetic framework has a lot to do with obesity. If your parents are obese, the chance of you being obese is quite high.
The weight which women gain during their pregnancy can be very hard to shed and this is often one of the top causes of obesity.
Sleep Cycle:
If you are not getting an adequate amount of sleep, it can have an impact on the hormones which might trigger hunger signals. Overall, these linked events tend to make you obese.
Hormonal Disorder:
There are several hormonal changes which are known to be direct causes of obesity. The imbalance of the thyroid stimulating hormone, for instance, is one of the key factors when it comes to obesity.
Now that we know the key causes, let us look at the possible ways by which you can handle it.
Treatment for Obesity:
As strange as it may sound, the treatment for obesity is really simple. All you need to do is follow the right diet and back it with an adequate amount of exercise. If you can succeed in doing so, it will give you the perfect head-start into your journey of getting in shape and bidding goodbye to obesity.
There are a lot of different kinds and styles of diet plans for obesity which are available. You can choose the one which you deem fit. We recommend not opting for crash dieting as it is known to have several repercussions and can make your body terribly weak.
The key here is to stick to a balanced diet which can help you retain the essential nutrients, minerals, and, vitamins and shed the unwanted fat and carbs.
Just like the diet, there are several workout plans for obesity which are available. It is upon you to find out which of the workout plan seems to be apt for you. Choose cardio exercises and dance routines like Zumba to shed the unwanted body weight. Yoga is yet another method to get rid of obesity.
So, follow a blend of these and you will be able to deal with the trouble of obesity in no time. We believe that following these tips will help you get rid of obesity and stay in shape.
Obesity and overweight is a top health concern in the world due to the impact it has on the lives of individuals. Obesity is defined as a condition in which an individual has excessive body fat and is measured using the body mass index (BMI) such that, when an individual’s BMI is above 30, he or she is termed obese. The BMI is calculated using body weight and height and it is different for all individuals.
Obesity has been determined as a risk factor for many diseases. It results from dietary habits, genetics, and lifestyle habits including physical inactivity. Obesity can be prevented so that individuals do not end up having serious complications and health problems. Chronic illnesses like diabetes, heart diseases and relate to obesity in terms of causes and complications.
Factors Influencing Obesity:
Obesity is not only as a result of lifestyle habits as most people put it. There are other important factors that influence obesity. Genetics is one of those factors. A person could be born with genes that predispose them to obesity and they will also have difficulty in losing weight because it is an inborn factor.
The environment also influences obesity because the diet is similar in certain environs. In certain environments, like school, the food available is fast foods and the chances of getting healthy foods is very low, leading to obesity. Also, physical inactivity is an environmental factor for obesity because some places have no fields or tracks where people can jog or maybe the place is very unsafe and people rarely go out to exercise.
Mental health affects the eating habits of individuals. There is a habit of stress eating when a person is depressed and it could result in overweight or obesity if the person remains unhealthy for long period of time.
The overall health of individuals also matter. If a person is unwell and is prescribed with steroids, they may end up being obese. Steroidal medications enable weight gain as a side effect.
Complications of Obesity:
Obesity is a health concern because its complications are severe. Significant social and health problems are experienced by obese people. Socially, they will be bullied and their self-esteem will be low as they will perceive themselves as unworthy.
Chronic illnesses like diabetes results from obesity. Diabetes type 2 has been directly linked to obesity. This condition involves the increased blood sugars in the body and body cells are not responding to insulin as they should. The insulin in the body could also be inadequate due to decreased production. High blood sugar concentrations result in symptoms like frequent hunger, thirst and urination. The symptoms of complicated stages of diabetes type 2 include loss of vision, renal failure and heart failure and eventually death. The importance of having a normal BMI is the ability of the body to control blood sugars.
Another complication is the heightened blood pressures. Obesity has been defined as excessive body fat. The body fat accumulates in blood vessels making them narrow. Narrow blood vessels cause the blood pressures to rise. Increased blood pressure causes the heart to start failing in its physiological functions. Heart failure is the end result in this condition of increased blood pressures.
There is a significant increase in cholesterol in blood of people who are obese. High blood cholesterol levels causes the deposition of fats in various parts of the body and organs. Deposition of fats in the heart and blood vessels result in heart diseases. There are other conditions that result from hypercholesterolemia.
Other chronic illnesses like cancer can also arise from obesity because inflammation of body cells and tissues occurs in order to store fats in obese people. This could result in abnormal growths and alteration of cell morphology. The abnormal growths could be cancerous.
Management of Obesity:
For the people at risk of developing obesity, prevention methods can be implemented. Prevention included a healthy diet and physical activity. The diet and physical activity patterns should be regular and realizable to avoid strains that could result in complications.
Some risk factors for obesity are non-modifiable for example genetics. When a person in genetically predisposed, the lifestyle modifications may be have help.
For the individuals who are already obese, they can work on weight reduction through healthy diets and physical exercises.
In conclusion, obesity is indeed a major health concern because the health complications are very serious. Factors influencing obesity are both modifiable and non-modifiable. The management of obesity revolves around diet and physical activity and so it is important to remain fit.
In olden days, obesity used to affect only adults. However, in the present time, obesity has become a worldwide problem that hits the kids as well. Let’s find out the most prevalent causes of obesity.
Factors Causing Obesity:
Obesity can be due to genetic factors. If a person’s family has a history of obesity, chances are high that he/ she would also be affected by obesity, sooner or later in life.
The second reason is having a poor lifestyle. Now, there are a variety of factors that fall under the category of poor lifestyle. An excessive diet, i.e., eating more than you need is a definite way to attain the stage of obesity. Needless to say, the extra calories are changed into fat and cause obesity.
Junk foods, fried foods, refined foods with high fats and sugar are also responsible for causing obesity in both adults and kids. Lack of physical activity prevents the burning of extra calories, again, leading us all to the path of obesity.
But sometimes, there may also be some indirect causes of obesity. The secondary reasons could be related to our mental and psychological health. Depression, anxiety, stress, and emotional troubles are well-known factors of obesity.
Physical ailments such as hypothyroidism, ovarian cysts, and diabetes often complicate the physical condition and play a massive role in abnormal weight gain.
Moreover, certain medications, such as steroids, antidepressants, and contraceptive pills, have been seen interfering with the metabolic activities of the body. As a result, the long-term use of such drugs can cause obesity. Adding to that, regular consumption of alcohol and smoking are also connected to the condition of obesity.
Harmful Effects of Obesity:
On the surface, obesity may look like a single problem. But, in reality, it is the mother of several major health issues. Obesity simply means excessive fat depositing into our body including the arteries. The drastic consequence of such high cholesterol levels shows up in the form of heart attacks and other life-threatening cardiac troubles.
The fat deposition also hampers the elasticity of the arteries. That means obesity can cause havoc in our body by altering the blood pressure to an abnormal range. And this is just the tip of the iceberg. Obesity is known to create an endless list of problems.
In extreme cases, this disorder gives birth to acute diseases like diabetes and cancer. The weight gain due to obesity puts a lot of pressure on the bones of the body, especially of the legs. This, in turn, makes our bones weak and disturbs their smooth movement. A person suffering from obesity also has higher chances of developing infertility issues and sleep troubles.
Many obese people are seen to be struggling with breathing problems too. In the chronic form, the condition can grow into asthma. The psychological effects of obesity are another serious topic. You can say that obesity and depression form a loop. The more a person is obese, the worse is his/ her depression stage.
How to Control and Treat Obesity:
The simplest and most effective way, to begin with, is changing our diet. There are two factors to consider in the diet plan. First is what and what not to eat. Second is how much to eat.
If you really want to get rid of obesity, include more and more green vegetables in your diet. Spinach, beans, kale, broccoli, cauliflower, asparagus, etc., have enough vitamins and minerals and quite low calories. Other healthier options are mushrooms, pumpkin, beetroots, and sweet potatoes, etc.
Opt for fresh fruits, especially citrus fruits, and berries. Oranges, grapes, pomegranate, pineapple, cherries, strawberries, lime, and cranberries are good for the body. They have low sugar content and are also helpful in strengthening our immune system. Eating the whole fruits is a more preferable way in comparison to gulping the fruit juices. Fruits, when eaten whole, have more fibers and less sugar.
Consuming a big bowl of salad is also great for dealing with the obesity problem. A salad that includes fibrous foods such as carrots, radish, lettuce, tomatoes, works better at satiating the hunger pangs without the risk of weight gain.
A high protein diet of eggs, fish, lean meats, etc., is an excellent choice to get rid of obesity. Take enough of omega fatty acids. Remember to drink plenty of water. Keeping yourself hydrated is a smart way to avoid overeating. Water also helps in removing the toxins and excess fat from the body.
As much as possible, avoid fats, sugars, refined flours, and oily foods to keep the weight in control. Control your portion size. Replace the three heavy meals with small and frequent meals during the day. Snacking on sugarless smoothies, dry fruits, etc., is much recommended.
Regular exercise plays an indispensable role in tackling the obesity problem. Whenever possible, walk to the market, take stairs instead of a lift. Physical activity can be in any other form. It could be a favorite hobby like swimming, cycling, lawn tennis, or light jogging.
Meditation and yoga are quite powerful practices to drive away the stress, depression and thus, obesity. But in more serious cases, meeting a physician is the most appropriate strategy. Sometimes, the right medicines and surgical procedures are necessary to control the health condition.
Obesity is spreading like an epidemic, haunting both the adults and the kids. Although genetic factors and other physical ailments play a role, the problem is mostly caused by a reckless lifestyle.
By changing our way of living, we can surely take control of our health. In other words, it would be possible to eliminate the condition of obesity from our lives completely by leading a healthy lifestyle.
Health , Obesity
Get FREE Work-at-Home Job Leads Delivered Weekly!

Join more than 50,000 subscribers receiving regular updates! Plus, get a FREE copy of How to Make Money Blogging!
Message from Sophia!
Like this post? Don’t forget to share it!
Here are a few recommended articles for you to read next:
- Essay on Cleanliness
- Essay on Cancer
- Essay on AIDS
- Essay on Health and Fitness
No comments yet.
Leave a reply click here to cancel reply..
You must be logged in to post a comment.
Billionaires
- Donald Trump
- Warren Buffett
- Email Address
- Free Stock Photos
- Keyword Research Tools
- URL Shortener Tools
- WordPress Theme
Book Summaries
- How To Win Friends
- Rich Dad Poor Dad
- The Code of the Extraordinary Mind
- The Luck Factor
- The Millionaire Fastlane
- The ONE Thing
- Think and Grow Rich
- 100 Million Dollar Business
- Business Ideas
Digital Marketing
- Mobile Addiction
- Social Media Addiction
- Computer Addiction
- Drug Addiction
- Internet Addiction
- TV Addiction
- Healthy Habits
- Morning Rituals
- Wake up Early
- Cholesterol
- Reducing Cholesterol
- Fat Loss Diet Plan
- Reducing Hair Fall
- Sleep Apnea
- Weight Loss
Internet Marketing
- Email Marketing
Law of Attraction
- Subconscious Mind
- Vision Board
- Visualization
Law of Vibration
- Professional Life
Motivational Speakers
- Bob Proctor
- Robert Kiyosaki
- Vivek Bindra
- Inner Peace
Productivity
- Not To-do List
- Project Management Software
- Negative Energies
Relationship
- Getting Back Your Ex
Self-help 21 and 14 Days Course
Self-improvement.
- Body Language
- Complainers
- Emotional Intelligence
- Personality
Social Media
- Project Management
- Anik Singal
- Baba Ramdev
- Dwayne Johnson
- Jackie Chan
- Leonardo DiCaprio
- Narendra Modi
- Nikola Tesla
- Sachin Tendulkar
- Sandeep Maheshwari
- Shaqir Hussyin
Website Development
Wisdom post, worlds most.
- Expensive Cars
Our Portals: Gulf Canada USA Italy Gulf UK
Privacy Overview
A generation at risk: Is early puberty the new public health crisis?
- Published: Jun. 06, 2024, 11:10 a.m.

Kids are getting their period younger than ever, what does that mean for them in the long-term? Klaus Vedfelt, Annabel Rocha
- Annabel Rocha | [email protected]
A necessary read for the girls, gays and theys and our allies as we navigate a rapidly changing, culturally fraught, complicated country where our bodies are constantly being legislated. Sign up for Honey today!
Today’s young people are hitting puberty earlier and starting menstruation younger. New research reveals that girls in the U.S. started their periods earlier over the last five decades and experienced delays in regulating their cycle.
The number of girls who got their period before age 9 doubled, according to the study published in JAMA Network Open on May 29, with Black, Hispanic, Asian, mixed race and low income youth are more likely to experience early menstruation.
For participants born from 1950 to 1969, the average age of menarche , or their first period, was 12.5 years, with only 9.2% experiencing early or very early menarche, before age 9. Comparatively, participants born between 2000 and 2005 on average hit menarche at 11.9 years, with 16.9% experiencing early or very menarche.
“This is important because early menarche and irregular periods can signal physical and psychosocial problems later in life,” said Zifan Wang , a postdoctoral research fellow at Harvard University TH Chan School of Public Health and lead author of the study.
Periods are major indicators of a person’s health, and the age of puberty is used to measure population health by researchers and entities like the World Health Organization . Generally, countries with a mean menarche age older than 12 face nutrition issues and higher infectious disease rates, while countries whose mean menarche age is younger than 12 face overnutrition and higher risk of chronic diseases, says Lauren Houghton , assistant professor of epidemiology at Columbia University .
“The US is an example of the latter, and the decreasing age of menarche points to possible increases in chronic diseases, including mental health, cardiovascular disease, and breast cancer,” Houghton wrote in commentary accompanying the study . “Just as clinicians regularly check blood pressure, they should also inquire about menstrual health, including last menstrual period, cycle length and regularity, and associated symptoms that occur around menstruation. Menstrual cycle characteristics outside clinical norms or changes over time for an individual may be a warning sign of underlying risk and pathology.”
Obesity, stress and cancer?
Evidence shows early menstruation points to lifelong health issues , and the health concerns researchers believe may be driving younger onset puberty, may also indicate problems in adulthood. One indicator researchers suggest could cause children to get their periods younger and lead to other health issues later in life is high BMI.
“Childhood obesity might be a key factor. Our exploratory analysis suggests BMI at menarche accounts for 46% of the trend toward earlier menarche,” Wang posted on Twitter/X in a thread about the study.
Childhood obesity is a known risk factor of early puberty, according to the National Institutes of Health (NIU), with the rate of childhood obesity tripling since the 1970s . In April, the Centers for Disease Control and Prevention reported that 1 in 5 U.S. children and adolescents were obese , with higher prevalence in Black and Latino youth.
While weight loss can reduce the risks associated with childhood obesity, Most obese children remain obese in adulthood, according to Georgetown University’s Health Policy Institute , increasing their chances of being diagnosed with four of the leading causes of the death in the U.S., heart disease, type II diabetes, stroke and cancer.
In her commentary, Houghton suggested the pandemic stay-at-home mandates required less physical activity in children and was linked to stress, which could be another driver causing earlier puberty.
“It is very likely that BMI and stress interact to accelerate age at menarche and prolong cycle regularity. My working hypothesis is that more stress increases the pool of [sex hormones] androgens and more adipose tissue [body fat] converts the abundance of androgens into estrogens, leading to earlier puberty,” wrote Houghton. “Despite the biology, there is little research that simultaneously investigates mental and physical drivers of menarche and menstrual cycle regularity.”
In March, Stat reported that girls who experience early puberty are more likely to be bullied and have higher rates of depression and other mental health affects that are carried into adulthood . Aviva Sopher, a professor of pediatrics at Columbia University told Stat News that getting your first period at a young age could cause future stress itself.
“With more girls going through puberty earlier, it might make it more comfortable for those experiencing it,” Sopher said . “But on the other hand, in general, girls who go through puberty earlier are at increased risk of sexual abuse because they look very mature, but they’re immature.”
Wang said that the key to unlocking answers as to what’s causing early menstruation, and what this means for women and girls in the future is funding.
“To address these health concerns—which our findings suggest may begin to impact more people, with disproportionate impact on already disadvantaged populations—we need much more investment in menstrual health research,” said Wang.
If you purchase a product or register for an account through a link on our site, we may receive compensation. By using this site, you consent to our User Agreement and agree that your clicks, interactions, and personal information may be collected, recorded, and/or stored by us and social media and other third-party partners in accordance with our Privacy Policy.

Russia's obesity crisis worsens: One-third of population affected
N early 2.5 million people in Russia suffer from obesity, though the actual number may be significantly higher. This issue also significantly affects younger Russians, reports the Moscow Times. The Russian Ministry of Health believes that diseases like obesity harm the economy.
Overweight and obesity are considered lifestyle diseases and represent a global problem. Excess body weight is already ranked as the sixth leading risk factor responsible for deaths worldwide.
Every third resident in Russia suffers from obesity, but official statistics show that this only affects 2% of the population, said Deputy Health Minister of the Russian Federation Yevgeny Kamkin, as quoted by the independent Russian portal Moscow Times.
According to 2023 data, the number of obese people is already nearly 2.5 million, which is 2 percent of the population. "These are official statistics, but the actual number is much higher—perhaps reaching even one-third of the entire population," said the Russian Deputy Health Minister.
Even children in Russia have problems
According to Yevgeny Kamkin, authorities face the task of identifying obese citizens and "properly redirecting them." This disease causes severe economic damage in Russia.
Among children up to the age of 14, obesity was found in 108,000 individuals. Furthermore, over 40,000 adolescents aged 15 to 18 were diagnosed with being overweight.
In October 2023, Health Minister Mikhail Murashko said that 11% of Russians are obese. The Chief Independent Dietitian of the Ministry of Health Viktor Tutelyan stated that every second adult Russian is overweight or obese, and among children, this diagnosis may apply to 20-25%, reports the Moscow Times.
Russian media also reported that in 2022, 13 million Russians suffered from endocrine system diseases, eating disorders, and metabolic disorders. Among them, diabetes was diagnosed in 5.27 million people and obesity in 2.17 million.
It stops cancer cells. Protects against one of the most dangerous tumors
Facing egg crisis, Russians resort to "shell-fie": Social media trend mirrors economic distress
For five years, he stayed confined to his house. One of Russia's heaviest men has passed away


IMAGES
VIDEO
COMMENTS
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
In both children and adults, major consequences of obesity include the development of serious chronic disorders that further reduce quality of life and life span, such as type 2 diabetes, dyslipidemias, hypertension, and cardio‐ and cerebrovascular disease and their consequences in ischemic injuries. 7, 8 Furthermore, in 2020, the SARS‐CoV ...
Introduction. No one doubts the economic costs of obesity, estimated at 5-14% of health expenditure for 2020-2050 (), but there is disagreement whether fatness is considered a disease or a behavioral risk factor, similar to smoking, alcohol and substance abuse that may lead to a disease ().Current opinion also emphasizes social determinants and equity, thereby moving away from personal ...
Obesity has become a public health crisis in the United States. The medical condition, which involves having an excessive amount of body fat, is linked to severe chronic diseases including type 2 ...
At the other end of the malnutrition scale, obesity is one of today's most blatantly visible - yet most neglected - public health problems. Paradoxically coexisting with undernutrition, an escalating global epidemic of overweight and obesity - "globesity" - is taking over many parts of the world. If immediate action is not taken, millions will suffer from an array of serious ...
The other crisis was an unprecedented obesity epidemic that has never reversed course. It was incited not by a sudden wave of individual gluttony (even toddlers are afflicted) but by a radical and toxic change in our food environment. ... compared with 40 percent of scientific papers. A recent study by Drexel University researchers also ...
On World Obesity Day, marked on Friday, the World Health Organization (WHO) urged countries to do more to reverse what is a preventable health crisis. According to recent data, more than one billion people worldwide are obese, including 650 million adults, 340 million adolescents and 39 million children. With the numbers still increasing, WHO ...
International Journal of Obesity 47 , 93-94 ( 2023) Cite this article. 2022 has seen the emergence of a global cost of living crisis driven by rapid increases in the cost of energy and food. The ...
Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity. ... One of the most concerning is the prevalence of obesity as a public health crisis. Another is that obesity increases the risks of individuals for other primary lifestyle diseases, which include ...
Addressing the American obesity crisis. Regarding Kate Manne's Feb. 6 Tuesday Opinion essay, " A diagnosis for the doctors — fatphobia ": We heard echoes of Ms. Manne's story across the ...
Obesity now rivals smoking in terms of health care costs and adverse effects on health and well-being, and the rapid rise in the prevalence of obesity over the past 2 decades shows no signs of leveling off. The current and future consequences of the obesity epidemic for national health make Food Fight a very timely book. Brownell and Horgen challenge the reader to reexamine the toxic ...
Given the scale of the obesity crisis and its economic impact, investment in research, innovation, and experimentation is relatively low. For instance, in total the United Kingdom invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns. ... This essay is adapted from ...
Hook Examples for Obesity Essays "The Silent Epidemic Among Us" Hook "Obesity silently creeps into our lives, affecting millions. Explore the hidden health crisis, its causes, and its far-reaching consequences on individuals and society." ... "Obesity is a public health crisis with wide-ranging effects. Investigate the strain on healthcare ...
Published: Mar 5, 2024. Obesity has become a major public health crisis in the United States, with over 42% of the population considered to be clinically obese. This issue has far-reaching consequences for individuals, families, and the healthcare system, making it a topic of great concern and interest. The obesity epidemic is not just a matter ...
XML. A number of economic, cultural, and contextual factors aredriving urban America's obesity crisis, which can create chronichealth conditions for those least...
Essay on obesity! Find high quality essays on 'Obesity' especially written for school, college, science and medical students. These essays will also guide you to learn about the causes, factors, treatment, management and complications related to obesity. Obesity is a chronic health condition in which the body fat reaches abnormal level.
In the EU, the obesity rate was 16.8 per cent in men while it was slightly lower in women (16.3 per cent). ADVERTISEMENT The highest proportion of obese men (30.6 per cent and women (26.7 per cent ...
The prospect of mammoth profits from selling obesity drugs in high-income markets has sparked a global research rush into the field in the past two years, with more than 200 new weight loss drug ...
Obesity is defined as the most serious reversible health problem similar with smoking in the world. It has been suggested that government programmes are necessary to tackle the obesity problem. This essay will illustrate that such government actions are essential to prevent the obesity crisis and will focus on government programmes in Singapore ...
With the goal of developing a community-informed obesity prevention intervention for rural preschool-aged children, the purpose of this descriptive study was to identify: (1) community settings and intervention strategies to prioritize for an intervention; (2) potential implementation challenges and solutions; and (3) immediate interventions ...
Childhood obesity is a known risk factor of early puberty, according to the National Institutes of Health (NIU), with the rate of childhood obesity tripling since the 1970s. In April, the Centers ...
Obesity is the second-biggest preventable cause of cancer. People over the weight threshold are more than 2.5 times more likely to develop high blood pressure and five times more likely to develop ...
Among children up to the age of 14, obesity was found in 108,000 individuals. Furthermore, over 40,000 adolescents aged 15 to 18 were diagnosed with being overweight.
Obesity among children aged 2 to 19 is projected to rise from 20.6% in 2020 to 33.0% in 2050. ... Please use one of the following formats to cite this article in your essay, paper or report ...
A nationwide strike in Nigeria brought air travel to a standstill and plunged the country into darkness on Monday as union workers forcibly removed operators at the national grid, the nation's ...
Haiti: human rights safeguards and transparency must guide security mission deployment. In a public statement issued today, Amnesty International is raising concerns about the lack of transparency regarding the establishment of human rights safeguards for the Multinational Security Support (MSS) Mission in Haiti, that is expected to be deployed in the coming months.