Find adoption answers, support, training, or professional resources
- Mission and Vision
- Staff and Board
- Internships
- Media & Press Room
- Job Openings for Adoption Professionals
- Social Work CE
- Training for Professionals
- Pre-Adoptive Parents
- Adoptive Parents
- Adopted Persons
- Birth Parents
- Expectant Parents
- Adoption Advocate Publication

Adoption by the Numbers
Profiles in adoption.
- Take Action
- Upcoming Events
- Adoption Hall of Fame
- National Adoption Conference
- Legacy Society
- Families For All Development Fund
- Family Formation Partners
- Annual Report
Adoption Research
We provide accurate, reliable, and up-to-date reports that inform and equip professionals, policymakers, and the public at large to improve and strengthen adoption.
In 2021, we conducted the largest survey ever of adoptive parents. NCFA explored the profile of adoptive parents, their experiences, and what has changed in adoption over time.
In 2022, we surveyed birth parents across the U.S. and conducted focus groups with birth moms to better understand this diverse population, their decision-making and levels of satisfaction, their relationship with their birth children, experiences with stigma and support, and much more.
In 2023, we researched the experiences of adult adoptees through a nationwide survey.
The Importance of Adoption Research
Policymakers and legislators look to research-based facts and statistics to inform their decision-making. Professionals draw from the most recent studies and reports to better understand the needs of the populations they are serving and identify areas for growth in their work. Members of the media, authors, and other content creators look to NCFA's expertise to help them identify the most relevant and accurate information about adoption as they cover current events and raise awareness about stories and issues in adoption.

A comprehensive study of adoption data from 2019 and 2020 across all 50 states.

An ongoing research project to explore the demographic characteristics and personal experiences of adoptive parents, birth parents, and adoptees.

General Adoption Statistics & Data
Quick links to the most recent national statistics
- Trends by type of adoption
- Adoptions from Foster Care
- Intercountry Adoptions
- Nationally Representative Data on Adoption Children in the United States
Start typing & press 'enter'
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Adoption research, practice, and societal trends: Ten years of progress
Affiliation.
- 1 Independent Practice.
- PMID: 29283657
- DOI: 10.1037/amp0000218
Adoption involves the legal transfer of parental rights and responsibilities from a child's birth parents to adults who will raise the child (Reitz & Watson, 1992). Research related to adoption has expanded over the past 10 years and has incorporated more focus on implications for practice and public policy. This expansion has reflected increased awareness of the lived experience of adopted individuals, in addition to that of adoptive families and birth or first parents and families, collectively known as the adoption kinship network (Grotevant & McRoy, 1998). Trends discussed included research and social trends or movements (2007-2017) since the publication of the final article in a series of articles in the psychological literature related to adoption in The Counseling Psychologist (Baden & Wiley, 2007; Lee, 2003; O'Brien & Zamostny, 2003; Wiley & Baden, 2005; Zamostny, O'Brien, Baden, & Wiley, 2003; Zamostny, Wiley, O'Brien, Lee, & Baden, 2003). This article summarizes the social trends and research related to adoption over the last 10 years, including longitudinal and meta-analytic studies, increased research and conceptualization of ethnic and racial identity development, research on microaggressions, and research on diverse adoptive families, including those with gay and lesbian parents. Social trends included increased knowledge related to Internet accessibility, genetic information, continued focus on openness, and viewing adoption through a more critical lens. Implications are discussed for the development of programs that enhance competence of mental health professionals and adoption professionals in adoption-competent practice. (PsycINFO Database Record
(c) 2017 APA, all rights reserved).
PubMed Disclaimer
Similar articles
- Adoptive parenting. Grotevant HD, Lo AY. Grotevant HD, et al. Curr Opin Psychol. 2017 Jun;15:71-75. doi: 10.1016/j.copsyc.2017.02.020. Epub 2017 Feb 22. Curr Opin Psychol. 2017. PMID: 28813273 Review.
- Does parental sexual orientation matter? A longitudinal follow-up of adoptive families with school-age children. Farr RH. Farr RH. Dev Psychol. 2017 Feb;53(2):252-264. doi: 10.1037/dev0000228. Epub 2016 Oct 20. Dev Psychol. 2017. PMID: 27762565
- Parent adjustment over time in gay, lesbian, and heterosexual parent families adopting from foster care. Lavner JA, Waterman J, Peplau LA. Lavner JA, et al. Am J Orthopsychiatry. 2014;84(1):46-53. doi: 10.1037/h0098853. Am J Orthopsychiatry. 2014. PMID: 24826826
- [Homosexual parenthood and child development: present data]. Fond G, Franc N, Purper-Ouakil D. Fond G, et al. Encephale. 2012 Feb;38(1):10-5. doi: 10.1016/j.encep.2011.05.005. Epub 2011 Jul 5. Encephale. 2012. PMID: 22381718 Review. French.
- Family pediatrics: report of the Task Force on the Family. Schor EL; American Academy of Pediatrics Task Force on the Family. Schor EL, et al. Pediatrics. 2003 Jun;111(6 Pt 2):1541-71. Pediatrics. 2003. PMID: 12777595
- Food and Trauma: Anthropologies of Memory and Postmemory. Strand M. Strand M. Cult Med Psychiatry. 2023 Jun;47(2):466-494. doi: 10.1007/s11013-022-09785-2. Epub 2022 Apr 4. Cult Med Psychiatry. 2023. PMID: 35377110 Free PMC article.
- Risk of eating disorders in international adoptees: a cohort study using Swedish national population registers. Strand M, Zhang R, Thornton LM, Birgegård A, D'Onofrio BM, Bulik CM. Strand M, et al. Epidemiol Psychiatr Sci. 2020 May 26;29:e131. doi: 10.1017/S2045796020000451. Epidemiol Psychiatr Sci. 2020. PMID: 32452335 Free PMC article.
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- American Psychological Association
- Ovid Technologies, Inc.
Other Literature Sources
- scite Smart Citations
- Genetic Alliance
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Systematic review
- Open access
- Published: 24 June 2024
A systematic review of experimentally tested implementation strategies across health and human service settings: evidence from 2010-2022
- Laura Ellen Ashcraft ORCID: orcid.org/0000-0001-9957-0617 1 , 2 ,
- David E. Goodrich 3 , 4 , 5 ,
- Joachim Hero 6 ,
- Angela Phares 3 ,
- Rachel L. Bachrach 7 , 8 ,
- Deirdre A. Quinn 3 , 4 ,
- Nabeel Qureshi 6 ,
- Natalie C. Ernecoff 6 ,
- Lisa G. Lederer 5 ,
- Leslie Page Scheunemann 9 , 10 ,
- Shari S. Rogal 3 , 11 na1 &
- Matthew J. Chinman 3 , 4 , 6 na1
Implementation Science volume 19 , Article number: 43 ( 2024 ) Cite this article
1958 Accesses
18 Altmetric
Metrics details
Studies of implementation strategies range in rigor, design, and evaluated outcomes, presenting interpretation challenges for practitioners and researchers. This systematic review aimed to describe the body of research evidence testing implementation strategies across diverse settings and domains, using the Expert Recommendations for Implementing Change (ERIC) taxonomy to classify strategies and the Reach Effectiveness Adoption Implementation and Maintenance (RE-AIM) framework to classify outcomes.
We conducted a systematic review of studies examining implementation strategies from 2010-2022 and registered with PROSPERO (CRD42021235592). We searched databases using terms “implementation strategy”, “intervention”, “bundle”, “support”, and their variants. We also solicited study recommendations from implementation science experts and mined existing systematic reviews. We included studies that quantitatively assessed the impact of at least one implementation strategy to improve health or health care using an outcome that could be mapped to the five evaluation dimensions of RE-AIM. Only studies meeting prespecified methodologic standards were included. We described the characteristics of studies and frequency of implementation strategy use across study arms. We also examined common strategy pairings and cooccurrence with significant outcomes.
Our search resulted in 16,605 studies; 129 met inclusion criteria. Studies tested an average of 6.73 strategies (0-20 range). The most assessed outcomes were Effectiveness ( n =82; 64%) and Implementation ( n =73; 56%). The implementation strategies most frequently occurring in the experimental arm were Distribute Educational Materials ( n =99), Conduct Educational Meetings ( n =96), Audit and Provide Feedback ( n =76), and External Facilitation ( n =59). These strategies were often used in combination. Nineteen implementation strategies were frequently tested and associated with significantly improved outcomes. However, many strategies were not tested sufficiently to draw conclusions.
This review of 129 methodologically rigorous studies built upon prior implementation science data syntheses to identify implementation strategies that had been experimentally tested and summarized their impact on outcomes across diverse outcomes and clinical settings. We present recommendations for improving future similar efforts.
Peer Review reports
Contributions to the literature
While many implementation strategies exist, it has been challenging to compare their effectiveness across a wide range of trial designs and practice settings
This systematic review provides a transdisciplinary evaluation of implementation strategies across population, practice setting, and evidence-based interventions using a standardized taxonomy of strategies and outcomes.
Educational strategies were employed ubiquitously; nineteen other commonly used implementation strategies, including External Facilitation and Audit and Provide Feedback, were associated with positive outcomes in these experimental trials.
This review offers guidance for scholars and practitioners alike in selecting implementation strategies and suggests a roadmap for future evidence generation.
Implementation strategies are “methods or techniques used to enhance the adoption, implementation, and sustainment of evidence-based practices or programs” (EBPs) [ 1 ]. In 2015, the Expert Recommendations for Implementing Change (ERIC) study organized a panel of implementation scientists to compile a standardized set of implementation strategy terms and definitions [ 2 , 3 , 4 ]. These 73 strategies were then organized into nine “clusters” [ 5 ]. The ERIC taxonomy has been widely adopted and further refined [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 ]. However, much of the evidence for individual or groups of ERIC strategies remains narrowly focused. Prior systematic reviews and meta-analyses have assessed strategy effectiveness, but have generally focused on a specific strategy, (e.g., Audit and Provide Feedback) [ 14 , 15 , 16 ], subpopulation, disease (e.g., individuals living with dementia) [ 16 ], outcome [ 15 ], service setting (e.g., primary care clinics) [ 17 , 18 , 19 ] or geography [ 20 ]. Given that these strategies are intended to have broad applicability, there remains a need to understand how well implementation strategies work across EBPs and settings and the extent to which implementation knowledge is generalizable.
There are challenges in assessing the evidence of implementation strategies across many EBPs, populations, and settings. Heterogeneity in population characteristics, study designs, methods, and outcomes have made it difficult to quantitatively compare which strategies work and under which conditions [ 21 ]. Moreover, there remains significant variability in how researchers operationalize, apply, and report strategies (individually or in combination) and outcomes [ 21 , 22 ]. Still, synthesizing data related to using individual strategies would help researchers replicate findings and better understand possible mediating factors including the cost, timing, and delivery by specific types of health providers or key partners [ 23 , 24 , 25 ]. Such an evidence base would also aid practitioners with implementation planning such as when and how to deploy a strategy for optimal impact.
Building upon previous efforts, we therefore conducted a systematic review to evaluate the level of evidence supporting the ERIC implementation strategies across a broad array of health and human service settings and outcomes, as organized by the evaluation framework, RE-AIM (Reach, Effectiveness, Adoption, Implementation, Maintenance) [ 26 , 27 , 28 ]. A secondary aim of this work was to identify patterns in scientific reporting of strategy use that could not only inform reporting standards for strategies but also the methods employed in future. The current study was guided by the following research questions Footnote 1 :
What implementation strategies have been most commonly and rigorously tested in health and human service settings?
Which implementation strategies were commonly paired?
What is the evidence supporting commonly tested implementation strategies?
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA-P) model [ 29 , 30 , 31 ] to develop and report on the methods for this systematic review (Additional File 1). This study was considered to be non-human subjects research by the RAND institutional review board.
Registration
The protocol was registered with PROSPERO (PROSPERO 2021 CRD42021235592).
Eligibility criteria
This review sought to synthesize evidence for implementation strategies from research studies conducted across a wide range of health-related settings and populations. Inclusion criteria required studies to: 1) available in English; 2) published between January 1, 2010 and September 20, 2022; 3) based on experimental research (excluded protocols, commentaries, conference abstracts, or proposed frameworks); 4) set in a health or human service context (described below); 5) tested at least one quantitative outcome that could be mapped to the RE-AIM evaluation framework [ 26 , 27 , 28 ]; and 6) evaluated the impact of an implementation strategy that could be classified using the ERIC taxonomy [ 2 , 32 ]. We defined health and human service setting broadly, including inpatient and outpatient healthcare settings, specialty clinics, mental health treatment centers, long-term care facilities, group homes, correctional facilities, child welfare or youth services, aging services, and schools, and required that the focus be on a health outcome. We excluded hybrid type I trials that primarily focused on establishing EBP effectiveness, qualitative studies, studies that described implementation barriers and facilitators without assessing implementation strategy impact on an outcome, and studies not meeting standardized rigor criteria defined below.
Information sources
Our three-pronged search strategy included searching academic databases (i.e., CINAHL, PubMed, and Web of Science for replicability and transparency), seeking recommendations from expert implementation scientists, and assessing existing, relevant systematic reviews and meta-analyses.
Search strategy
Search terms included “implementation strateg*” OR “implementation intervention*” OR “implementation bundl*” OR “implementation support*.” The search, conducted on September 20, 2022, was limited to English language and publication between 2010 and 2022, similar to other recent implementation science reviews [ 22 ]. This timeframe was selected to coincide with the advent of Implementation Science and when the term “implementation strategy” became conventionally used [ 2 , 4 , 33 ]. A full search strategy can be found in Additional File 2.
Title and abstract screening process
Each study’s title and abstract were read by two reviewers, who dichotomously scored studies on each of the six eligibility criteria described above as yes=1 or no=0, resulting in a score ranging from 1 to 6. Abstracts receiving a six from both reviewers were included in the full text review. Those with only one score of six were adjudicated by a senior member of the team (MJC, SSR, DEG). The study team held weekly meetings to troubleshoot and resolve any ongoing issues noted through the abstract screening process.
Full text screening
During the full text screening process, we reviewed, in pairs, each article that had progressed through abstract screening. Conflicts between reviewers were adjudicated by a senior member of the team for a final inclusion decision (MJC, SSR, DEG).
Review of study rigor
After reviewing published rigor screening tools [ 34 , 35 , 36 ], we developed an assessment of study rigor that was appropriate for the broad range of reviewed implementation studies. Reviewers evaluated studies on the following: 1) presence of a concurrent comparison or control group (=2 for traditional randomized controlled trial or stepped wedge cluster randomized trial and =1 for pseudo-randomized and other studies with concurrent control); 2) EBP standardization by protocol or manual (=1 if present); 3) EBP fidelity tracking (=1 if present); 4) implementation strategy standardization by operational description, standard training, or manual (=1 if present); 5) length of follow-up from full implementation of intervention (=2 for twelve months or longer, =1 for six to eleven months, or =0 for less than six months); and 6) number of sites (=1 for more than one site). Rigor scores ranged from 0 to 8, with 8 indicating the most rigorous. Articles were included if they 1) included a concurrent control group, 2) had an experimental design, and 3) received a score of 7 or 8 from two independent reviewers.
Outside expert consultation
We contacted 37 global implementation science experts who were recognized by our study team as leaders in the field or who were commonly represented among first or senior authors in the included abstracts. We asked each expert for recommendations of publications meeting study inclusion criteria (i.e., quantitatively evaluating the effectiveness of an implementation strategy). Recommendations were recorded and compared to the full abstract list.
Systematic reviews
Eighty-four systematic reviews were identified through the initial search strategy (See Additional File 3). Systematic reviews that examined the effectiveness of implementation strategies were reviewed in pairs for studies that were not found through our initial literature search.
Data abstraction and coding
Data from the full text review were abstracted in pairs, with conflicts resolved by senior team members (DEG, MJC) using a standard Qualtrics abstraction form. The form captured the setting, number of sites and participants studied, evidence-based practice/program of focus, outcomes assessed (based on RE-AIM), strategies used in each study arm, whether the study took place in the U.S. or outside of the U.S., and the findings (i.e., was there significant improvement in the outcome(s)?). We coded implementation strategies used in the Control and Experimental Arms. We defined the Control Arm as receiving the lowest number of strategies (which could mean zero strategies or care as usual) and the Experimental Arm as the most intensive arm (i.e., receiving the highest number of strategies). When studies included multiple Experimental Arms, the Experimental Arm with the least intensive implementation strategy(ies) was classified as “Control” and the Experimental Arm with the most intensive implementation strategy(ies) was classified as the “Experimental” Arm.
Implementation strategies were classified using standard definitions (MJC, SSR, DEG), based on minor modifications to the ERIC taxonomy [ 2 , 3 , 4 ]. Modifications resulted in 70 named strategies and were made to decrease redundancy and improve clarity. These modifications were based on input from experts, cognitive interview data, and team consensus [ 37 ] (See Additional File 4). Outcomes were then coded into RE-AIM outcome domains following best practices as recommended by framework experts [ 26 , 27 , 28 ]. We coded the RE-AIM domain of Effectiveness as either an assessment of the effectiveness of the EBP or the implementation strategy. We did not assess implementation strategy fidelity or effects on health disparities as these are recently adopted reporting standards [ 27 , 28 ] and not yet widely implemented in current publications. Further, we did not include implementation costs as an outcome because reporting guidelines have not been standardized [ 38 , 39 ].
Assessment and minimization of bias
Assessment and minimization of bias is an important component of high-quality systematic reviews. The Cochrane Collaboration guidance for conducting high-quality systematic reviews recommends including a specific assessment of bias for individual studies by assessing the domains of randomization, deviations of intended intervention, missing data, measurement of the outcome, and selection of the reported results (e.g., following a pre-specified analysis plan) [ 40 , 41 ]. One way we addressed bias was by consolidating multiple publications from the same study into a single finding (i.e., N =1), so-as to avoid inflating estimates due to multiple publications on different aspects of a single trial. We also included high-quality studies only, as described above. However, it was not feasible to consistently apply an assessment of bias tool due to implementation science’s broad scope and the heterogeneity of study design, context, outcomes, and variable measurement, etc. For example, most implementation studies reviewed had many outcomes across the RE-AIM framework, with no one outcome designated as primary, precluding assignment of a single score across studies.
We used descriptive statistics to present the distribution of health or healthcare area, settings, outcomes, and the median number of included patients and sites per study, overall and by country (classified as U.S. vs. non-U.S.). Implementation strategies were described individually, using descriptive statistics to summarize the frequency of strategy use “overall” (in any study arm), and the mean number of strategies reported in the Control and Experimental Arms. We additionally described the strategies that were only in the experimental (and not control) arm, defining these as strategies that were “tested” and may have accounted for differences in outcomes between arms.
We described frequencies of pair-wise combinations of implementation strategies in the Experimental Arm. To assess the strength of the evidence supporting implementation strategies that were used in the Experimental Arm, study outcomes were categorized by RE-AIM and coded based on whether the association between use of the strategies resulted in a significantly positive effect (yes=1; no=0). We then created an indicator variable if at least one RE-AIM outcome in the study was significantly positive (yes=1; no=0). We plotted strategies on a graph with quadrants based on the combination of median number of studies in which a strategy appears and the median percent of studies in which a strategy was associated with at least one positive RE-AIM outcome. The upper right quadrant—higher number of studies overall and higher percent of studies with a significant RE-AIM outcome—represents a superior level of evidence. For implementation strategies in the upper right quadrant, we describe each RE-AIM outcome and the proportion of studies which have a significant outcome.
Search results
We identified 14,646 articles through the initial literature search, 17 articles through expert recommendation (three of which were not included in the initial search), and 1,942 articles through reviewing prior systematic reviews (Fig. 1 ). After removing duplicates, 9,399 articles were included in the initial abstract screening. Of those, 48% ( n =4,075) abstracts were reviewed in pairs for inclusion. Articles with a score of five or six were reviewed a second time ( n =2,859). One quarter of abstracts that scored lower than five were reviewed for a second time at random. We screened the full text of 1,426 articles in pairs. Common reasons for exclusion were 1) study rigor, including no clear delineation between the EBP and implementation strategy, 2) not testing an implementation strategy, and 3) article type that did not meet inclusion criteria (e.g., commentary, protocol, etc.). Six hundred seventeen articles were reviewed for study rigor with 385 excluded for reasons related to study design and rigor, and 86 removed for other reasons (e.g., not a research article). Among the three additional expert-recommended articles, one met inclusion criteria and was added to the analysis. The final number of studies abstracted was 129 representing 143 publications.
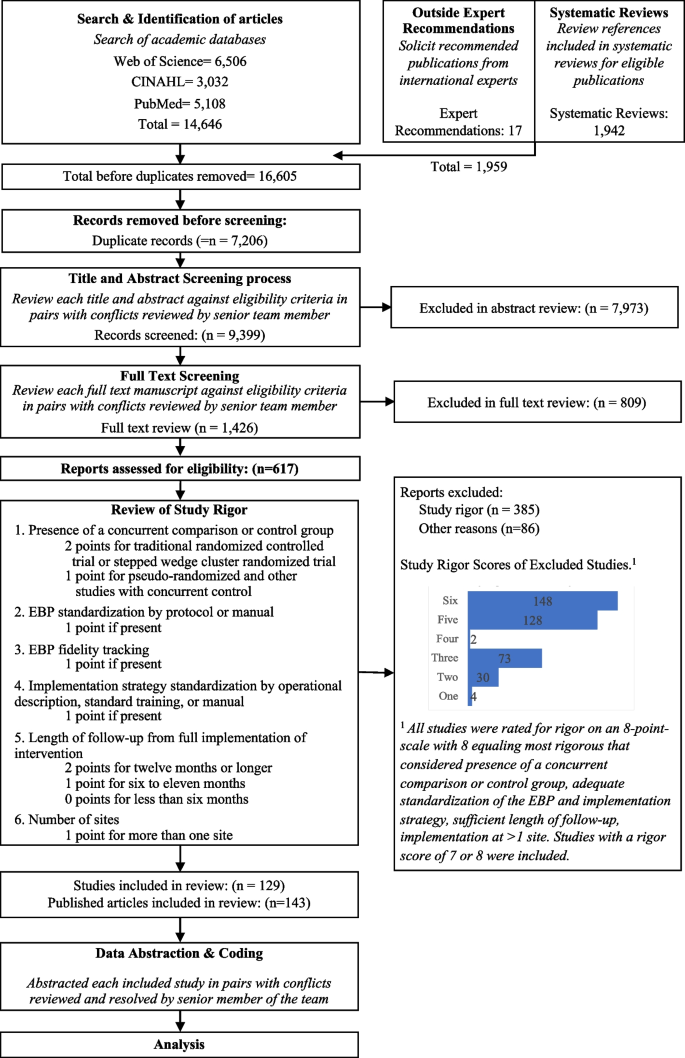
Expanded PRISMA Flow Diagram
The expanded PRISMA flow diagram provides a description of each step in the review and abstraction process for the systematic review
Descriptive results
Of 129 included studies (Table 1 ; see also Additional File 5 for Summary of Included Studies), 103 (79%) were conducted in a healthcare setting. EBP health care setting varied and included primary care ( n =46; 36%), specialty care ( n =27; 21%), mental health ( n =11; 9%), and public health ( n =30; 23%), with 64 studies (50%) occurring in an outpatient health care setting. Studies included a median of 29 sites and 1,419 target population (e.g., patients or students). The number of strategies varied widely across studies, with Control Arms averaging approximately two strategies (Range = 0-20, including studies with no strategy in the comparison group) and Experimental Arms averaging eight strategies (Range = 1-21). Non-US studies ( n =73) included more sites and target population on average, with an overall median of 32 sites and 1,531 patients assessed in each study.
Organized by RE-AIM, the most evaluated outcomes were Effectiveness ( n = 82, 64%) and Implementation ( n = 73, 56%); followed by Maintenance ( n =40; 31%), Adoption ( n =33; 26%), and Reach ( n =31; 24%). Most studies ( n = 98, 76%) reported at least one significantly positive outcome. Adoption and Implementation outcomes showed positive change in three-quarters of studies ( n =78), while Reach ( n =18; 58%), Effectiveness ( n =44; 54%), and Maintenance ( n =23; 58%) outcomes evidenced positive change in approximately half of studies.
The following describes the results for each research question.
Table 2 shows the frequency of studies within which an implementation strategy was used in the Control Arm, Experimental Arm(s), and tested strategies (those used exclusively in the Experimental Arm) grouped by strategy type, as specified by previous ERIC reports [ 2 , 6 ].
Control arm
In about half the studies (53%; n =69), the Control Arms were “active controls” that included at least one strategy, with an average of 1.64 (and up to 20) strategies reported in control arms. The two most common strategies used in Control Arms were: Distribute Educational Materials ( n =52) and Conduct Educational Meetings ( n =30).
Experimental arm
Experimental conditions included an average of 8.33 implementation strategies per study (Range = 1-21). Figure 2 shows a heat map of the strategies that were used in the Experimental Arms in each study. The most common strategies in the Experimental Arm were Distribute Educational Materials ( n =99), Conduct Educational Meetings ( n =96), Audit and Provide Feedback ( n =76), and External Facilitation ( n =59).
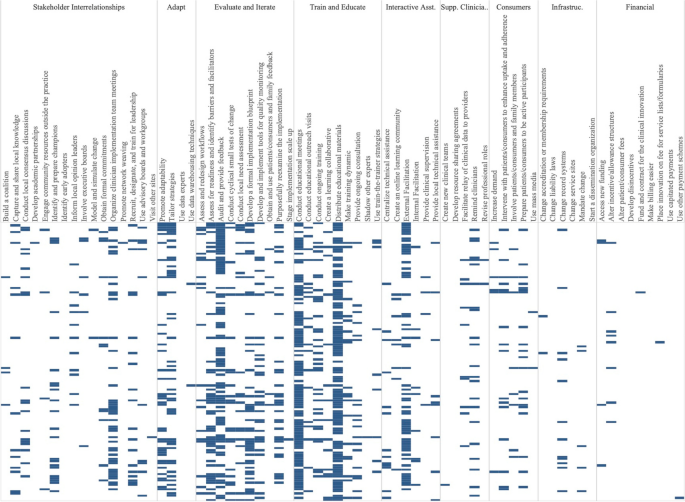
Implementation strategies used in the Experimental Arm of included studies. Explore more here: https://public.tableau.com/views/Figure2_16947070561090/Figure2?:language=en-US&:display_count=n&:origin=viz_share_link
Tested strategies
The average number of implementation strategies that were included in the Experimental Arm only (and not in the Control Arm) was 6.73 (Range = 0-20). Footnote 2 Overall, the top 10% of tested strategies included Conduct Educational Meetings ( n =68), Audit and Provide Feedback ( n =63), External Facilitation ( n =54), Distribute Educational Materials ( n =49), Tailor Strategies ( n =41), Assess for Readiness and Identify Barriers and Facilitators ( n =38) and Organize Clinician Implementation Team Meetings ( n =37). Few studies tested a single strategy ( n =9). These strategies included, Audit and Provide Feedback, Conduct Educational Meetings, Conduct Ongoing Training, Create a Learning Collaborative, External Facilitation ( n =2), Facilitate Relay of Clinical Data To Providers, Prepare Patients/Consumers to be Active Participants, and Use Other Payment Schemes. Three implementation strategies were included in the Control or Experimental Arms but were not Tested including, Use Mass Media, Stage Implementation Scale Up, and Fund and Contract for the Clinical Innovation.
Table 3 shows the five most used strategies in Experimental Arms with their top ten most frequent pairings, excluding Distribute Educational Materials and Conduct Educational Meetings, as these strategies were included in almost all Experimental and half of Control Arms. The five most used strategies in the Experimental Arm included Audit and Provide Feedback ( n =76), External Facilitation ( n =59), Tailor Strategies ( n =43), Assess for Readiness and Identify Barriers and Facilitators ( n =43), and Organize Implementation Teams ( n =42).
Strategies frequently paired with these five strategies included two educational strategies: Distribute Educational Materials and Conduct Educational Meetings. Other commonly paired strategies included Develop a Formal Implementation Blueprint, Promote Adaptability, Conduct Ongoing Training, Purposefully Reexamine the Implementation, and Develop and Implement Tools for Quality Monitoring.
We classified the strength of evidence for each strategy by evaluating both the number of studies in which each strategy appeared in the Experimental Arm and the percentage of times there was at least one significantly positive RE-AIM outcome. Using these factors, Fig. 3 shows the number of studies in which individual strategies were evaluated (on the y axis) compared to the percentage of times that studies including those strategies had at least one positive outcome (on the x axis). Due to the non-normal distribution of both factors, we used the median (rather than the mean) to create four quadrants. Strategies in the lower left quadrant were tested in fewer than the median number of studies (8.5) and were less frequently associated with a significant RE-AIM outcome (75%). The upper right quadrant included strategies that occurred in more than the median number of studies (8.5) and had more than the median percent of studies with a significant RE-AIM outcome (75%); thus those 19 strategies were viewed as having stronger evidence. Of those 19 implementation strategies, Conduct Educational Meetings, Distribute Educational Materials, External Facilitation, and Audit and Provide Feedback continued to occur frequently, appearing in 59-99 studies.
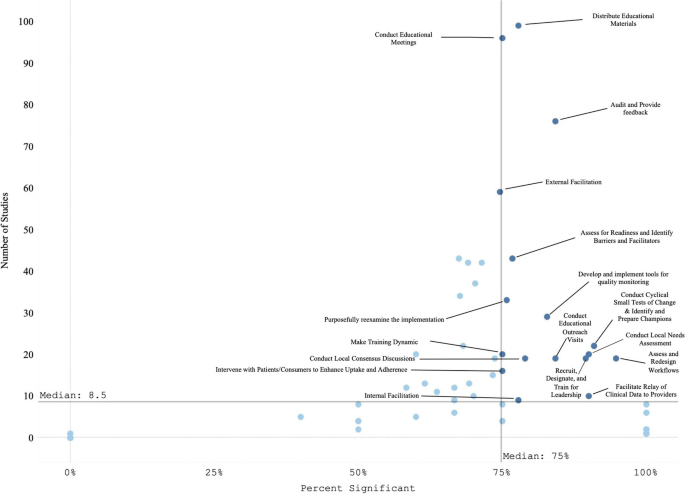
Experimental Arm Implementation Strategies with significant RE-AIM outcome. Explore more here: https://public.tableau.com/views/Figure3_16947017936500/Figure3?:language=en-US&publish=yes&:display_count=n&:origin=viz_share_link
Figure 4 graphically illustrates the proportion of significant outcomes for each RE-AIM outcome for the 19 commonly used and evidence-based implementation strategies in the upper right quadrant. These findings again show the widespread use of Conduct Educational Meetings and Distribute Educational Materials. Implementation and Effectiveness outcomes were assessed most frequently, with Implementation being the mostly commonly reported significantly positive outcome.
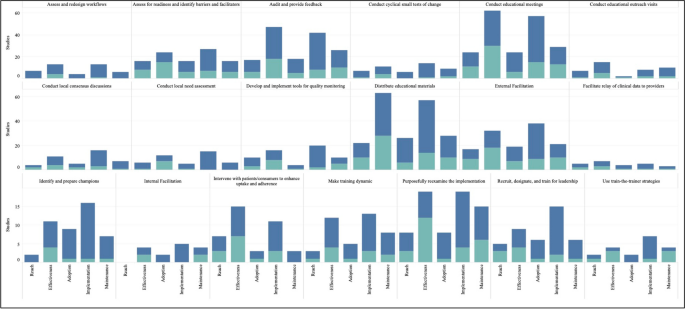
RE-AIM outcomes for the 19 Top-Right Quadrant Implementation Strategies . The y-axis is the number of studies and the x-axis is a stacked bar chart for each RE-AIM outcome with R=Reach, E=Effectiveness, A=Adoption, I=Implementation, M=Maintenance. Blue denotes at least one significant RE-AIM outcome; Light blue denotes studies which used the given implementation strategy and did not have a significant RE-AIM . Explore more here: https://public.tableau.com/views/Figure4_16947017112150/Figure4?:language=en-US&publish=yes&:display_count=n&:origin=viz_share_link
This systematic review identified 129 experimental studies examining the effectiveness of implementation strategies across a broad range of health and human service studies. Overall, we found that evidence is lacking for most ERIC implementation strategies, that most studies employed combinations of strategies, and that implementation outcomes, categorized by RE-AIM dimensions, have not been universally defined or applied. Accordingly, other researchers have described the need for universal outcomes definitions and descriptions across implementation research studies [ 28 , 42 ]. Our findings have important implications not only for the current state of the field but also for creating guidance to help investigators determine which strategies and in what context to examine.
The four most evaluated strategies were Distribute Educational Materials, Conduct Educational Meetings, External Facilitation, and Audit and Provide Feedback. Conducting Educational Meetings and Distributing Educational Materials were surprisingly the most common. This may reflect the fact that education strategies are generally considered to be “necessary but not sufficient” for successful implementation [ 43 , 44 ]. Because education is often embedded in interventions, it is critical to define the boundary between the innovation and the implementation strategies used to support the innovation. Further specification as to when these strategies are EBP core components or implementation strategies (e.g., booster trainings or remediation) is needed [ 45 , 46 ].
We identified 19 implementation strategies that were tested in at least 8 studies (more than the median) and were associated with positive results at least 75% of the time. These strategies can be further categorized as being used in early or pre-implementation versus later in implementation. Preparatory activities or pre-implementation, strategies that had strong evidence included educational activities (Meetings, Materials, Outreach visits, Train for Leadership, Use Train the Trainer Strategies) and site diagnostic activities (Assess for Readiness, Identify Barriers and Facilitators, Conduct Local Needs Assessment, Identify and Prepare Champions, and Assess and Redesign Workflows). Strategies that target the implementation phase include those that provide coaching and support (External and Internal Facilitation), involve additional key partners (Intervene with Patients to Enhance Uptake and Adherence), and engage in quality improvement activities (Audit and Provide Feedback, Facilitate the Relay of Clinical Data to Providers, Purposefully Reexamine the Implementation, Conduct Cyclical Small Tests of Change, Develop and Implement Tools for Quality Monitoring).
There were many ERIC strategies that were not represented in the reviewed studies, specifically the financial and policy strategies. Ten strategies were not used in any studies, including: Alter Patient/Consumer Fees, Change Liability Laws, Change Service Sites, Develop Disincentives, Develop Resource Sharing Agreements, Identify Early Adopters, Make Billing Easier, Start a Dissemination Organization, Use Capitated Payments, and Use Data Experts. One of the limitations of this investigation was that not all individual strategies or combinations were investigated. Reasons for the absence of these strategies in our review may include challenges with testing certain strategies experimentally (e.g., changing liability laws), limitations in our search terms, and the relative paucity of implementation strategy trials compared to clinical trials. Many “untested” strategies require large-scale structural changes with leadership support (see [ 47 ] for policy experiment example). Recent preliminary work has assessed the feasibility of applying policy strategies and described the challenges with doing so [ 48 , 49 , 50 ]. While not impossible in large systems like VA (for example: the randomized evaluation of the VA Stratification Tool for Opioid Risk Management) the large size, structure, and organizational imperative makes these initiatives challenging to experimentally evaluate. Likewise, the absence of these ten strategies may have been the result of our inclusion criteria, which required an experimental design. Thus, creative study designs may be needed to test high-level policy or financial strategies experimentally.
Some strategies that were likely under-represented in our search strategy included electronic medical record reminders and clinical decision support tools and systems. These are often considered “interventions” when used by clinical trialists and may not be indexed as studies involving ‘implementation strategies’ (these tools have been reviewed elsewhere [ 51 , 52 , 53 ]). Thus, strategies that are also considered interventions in the literature (e.g., education interventions) were not sought or captured. Our findings do not imply that these strategies are ineffective, rather that more study is needed. Consistent with prior investigations [ 54 ], few studies meeting inclusion criteria tested financial strategies. Accordingly, there are increasing calls to track and monitor the effects of financial strategies within implementation science to understand their effectiveness in practice [ 55 , 56 ]. However, experts have noted that the study of financial strategies can be a challenge given that they are typically implemented at the system-level and necessitate research designs for studying policy-effects (e.g., quasi-experimental methods, systems-science modeling methods) [ 57 ]. Yet, there have been some recent efforts to use financial strategies to support EBPs that appear promising [ 58 ] and could be a model for the field moving forward.
The relationship between the number of strategies used and improved outcomes has been described inconsistently in the literature. While some studies have found improved outcomes with a bundle of strategies that were uniquely combined or a standardized package of strategies (e.g., Replicating Effective Programs [ 59 , 60 ] and Getting To Outcomes [ 61 , 62 ]), others have found that “more is not always better” [ 63 , 64 , 65 ]. For example, Rogal and colleagues documented that VA hospitals implementing a new evidence-based hepatitis C treatment chose >20 strategies, when multiple years of data linking strategies to outcomes showed that 1-3 specific strategies would have yielded the same outcome [ 39 ]. Considering that most studies employed multiple or multifaceted strategies, it seems that there is a benefit of using a targeted bundle of strategies that are purposefully aligns with site/clinic/population norms, rather than simply adding more strategies [ 66 ].
It is difficult to assess the effectiveness of any one implementation strategy in bundles where multiple strategies are used simultaneously. Even a ‘single’ strategy like External Facilitation is, in actuality, a bundle of narrowly constructed strategies (e.g., Conduct Educational Meetings, Identify and Prepare Champions, and Develop a Formal Implementation Blueprint). Thus, studying External Facilitation does not allow for a test of the individual strategies that comprise it, potentially masking the effectiveness of any individual strategy. While we cannot easily disaggregate the effects of multifaceted strategies, doing so may not yield meaningful results. Because strategies often synergize, disaggregated results could either underestimate the true impact of individual strategies or conversely, actually undermine their effectiveness (i.e., when their effectiveness comes from their combination with other strategies). The complexity of health and human service settings, imperative to improve public health outcomes, and engagement with community partners often requires the use of multiple strategies simultaneously. Therefore, the need to improve real-world implementation may outweigh the theoretical need to identify individual strategy effectiveness. In situations where it would be useful to isolate the impact of single strategies, we suggest that the same methods for documenting and analyzing the critical components (or core functions) of complex interventions [ 67 , 68 , 69 , 70 ] may help to identify core components of multifaceted implementation strategies [ 71 , 72 , 73 , 74 ].
In addition, to truly assess the impacts of strategies on outcomes, it may be necessary to track fidelity to implementation strategies (not just the EBPs they support). While this can be challenging, without some degree of tracking and fidelity checks, one cannot determine whether a strategy’s apparent failure to work was because it 1) was ineffective or 2) was not applied well. To facilitate this tracking there are pragmatic tools to support researchers. For example, the Longitudinal Implementation Strategy Tracking System (LISTS) offers a pragmatic and feasible means to assess fidelity to and adaptations of strategies [ 75 ].
Implications for implementation science: four recommendations
Based on our findings, we offer four recommended “best practices” for implementation studies.
Prespecify strategies using standard nomenclature. This study reaffirmed the need to apply not only a standard naming convention (e.g., ERIC) but also a standard reporting of for implementation strategies. While reporting systems like those by Proctor [ 1 ] or Pinnock [ 75 ] would optimize learning across studies, few manuscripts specify strategies as recommended [ 76 , 77 ]. Pre-specification allows planners and evaluators to assess the feasibility and acceptability of strategies with partners and community members [ 24 , 78 , 79 ] and allows evaluators and implementers to monitor and measure the fidelity, dose, and adaptations to strategies delivered over the course of implementation [ 27 ]. In turn, these data can be used to assess the costs, analyze their effectiveness [ 38 , 80 , 81 ], and ensure more accurate reporting [ 82 , 83 , 84 , 85 ]. This specification should include, among other data, the intensity, stage of implementation, and justification for the selection. Information regarding why strategies were selected for specific settings would further the field and be of great use to practitioners. [ 63 , 65 , 69 , 79 , 86 ].
Ensure that standards for measuring and reporting implementation outcomes are consistently applied and account for the complexity of implementation studies. Part of improving standardized reporting must include clearly defining outcomes and linking each outcome to particular implementation strategies. It was challenging in the present review to disentangle the impact of the intervention(s) (i.e., the EBP) versus the impact of the implementation strategy(ies) for each RE-AIM dimension. For example, often fidelity to the EBP was reported but not for the implementation strategies. Similarly, Reach and Adoption of the intervention would be reported for the Experimental Arm but not for the Control Arm, prohibiting statistical comparisons of strategies on the relative impact of the EBP between study arms. Moreover, there were many studies evaluating numerous outcomes, risking data dredging. Further, the significant heterogeneity in the ways in which implementation outcomes are operationalized and reported is a substantial barrier to conducting large-scale meta-analytic approaches to synthesizing evidence for implementation strategies [ 67 ]. The field could look to others in the social and health sciences for examples in how to test, validate, and promote a common set of outcome measures to aid in bringing consistency across studies and real-world practice (e.g., the NIH-funded Patient-Reported Outcomes Measurement Information System [PROMIS], https://www.healthmeasures.net/explore-measurement-systems/promis ).
Develop infrastructure to learn cross-study lessons in implementation science. Data repositories, like those developed by NCI for rare diseases, U.S. HIV Implementation Science Coordination Initiative [ 87 ], and the Behavior Change Technique Ontology [ 88 ], could allow implementation scientists to report their findings in a more standardized manner, which would promote ease of communication and contextualization of findings across studies. For example, the HIV Implementation Science Coordination Initiative requested all implementation projects use common frameworks, developed user friendly databases to enable practitioners to match strategies to determinants, and developed a dashboard of studies that assessed implementation determinants [ 89 , 90 , 91 , 92 , 93 , 94 ].
Develop and apply methods to rigorously study common strategies and bundles. These findings support prior recommendations for improved empirical rigor in implementation studies [ 46 , 95 ]. Many studies were excluded from our review based on not meeting methodological rigor standards. Understanding the effectiveness of discrete strategies deployed alone or in combination requires reliable and low burden tracking methods to collect information about strategy use and outcomes. For example, frameworks like the Implementation Replication Framework [ 96 ] could help interpret findings across studies using the same strategy bundle. Other tracking approaches may leverage technology (e.g., cell phones, tablets, EMR templates) [ 78 , 97 ] or find novel, pragmatic approaches to collect recommended strategy specifications over time (e.g.., dose, deliverer, and mechanism) [ 1 , 9 , 27 , 98 , 99 ]. Rigorous reporting standards could inform more robust analyses and conclusions (e.g., moving toward the goal of understanding causality, microcosting efforts) [ 24 , 38 , 100 , 101 ]. Such detailed tracking is also required to understand how site-level factors moderate implementation strategy effects [ 102 ]. In some cases, adaptive trial designs like sequential multiple assignment randomized trials (SMARTs) and just-in-time adaptive interventions (JITAIs) can be helpful for planning strategy escalation.
Limitations
Despite the strengths of this review, there were certain notable limitations. For one, we only included experimental studies, omitting many informative observational investigations that cover the range of implementation strategies. Second, our study period was centered on the creation of the journal Implementation Science and not on the standardization and operationalization of implementation strategies in the publication of the ERIC taxonomy (which came later). This, in conjunction with latency in reporting study results and funding cycles, means that the employed taxonomy was not applied in earlier studies. To address this limitation, we retroactively mapped strategies to ERIC, but it is possible that some studies were missed. Additionally, indexing approaches used by academic databases may have missed relevant studies. We addressed this particular concern by reviewing other systematic reviews of implementation strategies and soliciting recommendations from global implementation science experts.
Another potential limitation comes from the ERIC taxonomy itself—i.e., strategy listings like ERIC are only useful when they are widely adopted and used in conjunction with guidelines for specifying and reporting strategies [ 1 ] in protocol and outcome papers. Although the ERIC paper has been widely cited (over three thousand times, accessed about 186 thousand times), it is still not universally applied, making tracking the impact of specific strategies more difficult. However, our experience with this review seemed to suggest that ERIC’s use was increasing over time. Also, some have commented that ERIC strategies can be unclear and are missing key domains. Thus, researchers are making definitions clearer for lay users [ 37 , 103 ], increasing the number of discrete strategies for specific domains like HIV treatment, acknowledging strategies for new functions (e.g., de-implementation [ 104 ], local capacity building), accounting for phases of implementation (dissemination, sustainment [ 13 ], scale-up), addressing settings [ 12 , 20 ], actors roles in the process, and making mechanisms of change to select strategies more user-friendly through searchable databases [ 9 , 10 , 54 , 73 , 104 , 105 , 106 ]. In sum, we found the utility of the ERIC taxonomy to outweigh any of the taxonomy’s current limitations.
As with all reviews, the search terms influenced our findings. As such, the broad terms for implementation strategies (e.g., “evidence-based interventions”[ 7 ] or “behavior change techniques” [ 107 ]) may have led to inadvertent omissions of studies of specific strategies. For example, the search terms may not have captured tests of policies, financial strategies, community health promotion initiatives, or electronic medical record reminders, due to differences in terminology used in corresponding subfields of research (e.g., health economics, business, health information technology, and health policy). To manage this, we asked experts to inform us about any studies that they would include and cross-checked their lists with what was identified through our search terms, which yielded very few additional studies. We included standard coding using the ERIC taxonomy, which was a strength, but future work should consider including the additional strategies that have been recommended to augment ERIC, around sustainment [ 13 , 79 , 106 , 108 ], community and public health research [ 12 , 109 , 110 , 111 ], consumer or service user engagement [ 112 ], de-implementation [ 104 , 113 , 114 , 115 , 116 , 117 ] and related terms [ 118 ].
We were unable to assess the bias of studies due to non-standard reporting across the papers and the heterogeneity of study designs, measurement of implementation strategies and outcomes, and analytic approaches. This could have resulted in over- or underestimating the results of our synthesis. We addressed this limitation by being cautious in our reporting of findings, specifically in identifying “effective” implementation strategies. Further, we were not able to gather primary data to evaluate effect sizes across studies in order to systematically evaluate bias, which would be fruitful for future study.
Conclusions
This novel review of 129 studies summarized the body of evidence supporting the use of ERIC-defined implementation strategies to improve health or healthcare. We identified commonly occurring implementation strategies, frequently used bundles, and the strategies with the highest degree of supportive evidence, while simultaneously identifying gaps in the literature. Additionally, we identified several key areas for future growth and operationalization across the field of implementation science with the goal of improved reporting and assessment of implementation strategies and related outcomes.
Availability and materials
All data for this study are included in this published article and its supplementary information files.
We modestly revised the following research questions from our PROSPERO registration after reading the articles and better understanding the nature of the literature: 1) What is the available evidence regarding the effectiveness of implementation strategies in supporting the uptake and sustainment of evidence intended to improve health and healthcare outcomes? 2) What are the current gaps in the literature (i.e., implementation strategies that do not have sufficient evidence of effectiveness) that require further exploration?
Tested strategies are those which exist in the Experimental Arm but not in the Control Arm. Comparative effectiveness or time staggered trials may not have any unique strategies in the Experimental Arm and therefore in our analysis would have no Tested Strategies.
Abbreviations
Centers for Disease Control
Cumulated Index to Nursing and Allied Health Literature
Dissemination and Implementation
Evidence-based practices or programs
Expert Recommendations for Implementing Change
Multiphase Optimization Strategy
National Cancer Institute
National Institutes of Health
The Pittsburgh Dissemination and Implementation Science Collaborative
Sequential Multiple Assignment Randomized Trial
United States
Department of Veterans Affairs
Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139.
Article PubMed PubMed Central Google Scholar
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21.
Waltz TJ, Powell BJ, Chinman MJ, Smith JL, Matthieu MM, Proctor EK, et al. Expert recommendations for implementing change (ERIC): protocol for a mixed methods study. Implement Sci IS. 2014;9:39.
Article PubMed Google Scholar
Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, et al. A Compilation of Strategies for Implementing Clinical Innovations in Health and Mental Health. Med Care Res Rev. 2012;69:123–57.
Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10:109.
Perry CK, Damschroder LJ, Hemler JR, Woodson TT, Ono SS, Cohen DJ. Specifying and comparing implementation strategies across seven large implementation interventions: a practical application of theory. Implement Sci. 2019;14(1):32.
Community Preventive Services Task Force. Community Preventive Services Task Force: All Active Findings June 2023 [Internet]. 2023 [cited 2023 Aug 7]. Available from: https://www.thecommunityguide.org/media/pdf/CPSTF-All-Findings-508.pdf
Solberg LI, Kuzel A, Parchman ML, Shelley DR, Dickinson WP, Walunas TL, et al. A Taxonomy for External Support for Practice Transformation. J Am Board Fam Med JABFM. 2021;34:32–9.
Leeman J, Birken SA, Powell BJ, Rohweder C, Shea CM. Beyond “implementation strategies”: classifying the full range of strategies used in implementation science and practice. Implement Sci. 2017;12:1–9.
Article Google Scholar
Leeman J, Calancie L, Hartman MA, Escoffery CT, Herrmann AK, Tague LE, et al. What strategies are used to build practitioners’ capacity to implement community-based interventions and are they effective?: a systematic review. Implement Sci. 2015;10:1–15.
Nathan N, Shelton RC, Laur CV, Hailemariam M, Hall A. Editorial: Sustaining the implementation of evidence-based interventions in clinical and community settings. Front Health Serv. 2023;3:1176023.
Balis LE, Houghtaling B, Harden SM. Using implementation strategies in community settings: an introduction to the Expert Recommendations for Implementing Change (ERIC) compilation and future directions. Transl Behav Med. 2022;12:965–78.
Nathan N, Powell BJ, Shelton RC, Laur CV, Wolfenden L, Hailemariam M, et al. Do the Expert Recommendations for Implementing Change (ERIC) strategies adequately address sustainment? Front Health Serv. 2022;2:905909.
Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259.
Google Scholar
Moore L, Guertin JR, Tardif P-A, Ivers NM, Hoch J, Conombo B, et al. Economic evaluations of audit and feedback interventions: a systematic review. BMJ Qual Saf. 2022;31:754–67.
Sykes MJ, McAnuff J, Kolehmainen N. When is audit and feedback effective in dementia care? A systematic review. Int J Nurs Stud. 2018;79:27–35.
Barnes C, McCrabb S, Stacey F, Nathan N, Yoong SL, Grady A, et al. Improving implementation of school-based healthy eating and physical activity policies, practices, and programs: a systematic review. Transl Behav Med. 2021;11:1365–410.
Tomasone JR, Kauffeldt KD, Chaudhary R, Brouwers MC. Effectiveness of guideline dissemination and implementation strategies on health care professionals’ behaviour and patient outcomes in the cancer care context: a systematic review. Implement Sci. 2020;15:1–18.
Seda V, Moles RJ, Carter SR, Schneider CR. Assessing the comparative effectiveness of implementation strategies for professional services to community pharmacy: A systematic review. Res Soc Adm Pharm. 2022;18:3469–83.
Lovero KL, Kemp CG, Wagenaar BH, Giusto A, Greene MC, Powell BJ, et al. Application of the Expert Recommendations for Implementing Change (ERIC) compilation of strategies to health intervention implementation in low- and middle-income countries: a systematic review. Implement Sci. 2023;18:56.
Chapman A, Rankin NM, Jongebloed H, Yoong SL, White V, Livingston PM, et al. Overcoming challenges in conducting systematic reviews in implementation science: a methods commentary. Syst Rev. 2023;12:1–6.
Article CAS Google Scholar
Proctor EK, Bunger AC, Lengnick-Hall R, Gerke DR, Martin JK, Phillips RJ, et al. Ten years of implementation outcomes research: a scoping review. Implement Sci. 2023;18:1–19.
Michaud TL, Pereira E, Porter G, Golden C, Hill J, Kim J, et al. Scoping review of costs of implementation strategies in community, public health and healthcare settings. BMJ Open. 2022;12:e060785.
Sohn H, Tucker A, Ferguson O, Gomes I, Dowdy D. Costing the implementation of public health interventions in resource-limited settings: a conceptual framework. Implement Sci. 2020;15:1–8.
Peek C, Glasgow RE, Stange KC, Klesges LM, Purcell EP, Kessler RS. The 5 R’s: an emerging bold standard for conducting relevant research in a changing world. Ann Fam Med. 2014;12:447–55.
Article CAS PubMed PubMed Central Google Scholar
Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–7.
Shelton RC, Chambers DA, Glasgow RE. An Extension of RE-AIM to Enhance Sustainability: Addressing Dynamic Context and Promoting Health Equity Over Time. Front Public Health. 2020;8:134.
Holtrop JS, Estabrooks PA, Gaglio B, Harden SM, Kessler RS, King DK, et al. Understanding and applying the RE-AIM framework: Clarifications and resources. J Clin Transl Sci. 2021;5:e126.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ [Internet]. 2021;372. Available from: https://www.bmj.com/content/372/bmj.n71
Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A Glossary for Dissemination and Implementation Research in Health. J Public Health Manag Pract. 2008;14:117–23.
Eccles MP, Mittman BS. Welcome to Implementation Science. Implement Sci. 2006;1:1.
Article PubMed Central Google Scholar
Miller WR, Wilbourne PL. Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addict Abingdon Engl. 2002;97:265–77.
Miller WR, Brown JM, Simpson TL, Handmaker NS, Bien TH, Luckie LF, et al. What works? A methodological analysis of the alcohol treatment outcome literature. Handb Alcohol Treat Approaches Eff Altern 2nd Ed. Needham Heights, MA, US: Allyn & Bacon; 1995:12–44.
Wells S, Tamir O, Gray J, Naidoo D, Bekhit M, Goldmann D. Are quality improvement collaboratives effective? A systematic review BMJ Qual Saf. 2018;27:226–40.
Yakovchenko V, Chinman MJ, Lamorte C, Powell BJ, Waltz TJ, Merante M, et al. Refining Expert Recommendations for Implementing Change (ERIC) strategy surveys using cognitive interviews with frontline providers. Implement Sci Commun. 2023;4:1–14.
Wagner TH, Yoon J, Jacobs JC, So A, Kilbourne AM, Yu W, et al. Estimating costs of an implementation intervention. Med Decis Making. 2020;40:959–67.
Gold HT, McDermott C, Hoomans T, Wagner TH. Cost data in implementation science: categories and approaches to costing. Implement Sci. 2022;17:11.
Boutron I, Page MJ, Higgins JP, Altman DG, Lundh A, Hróbjartsson A. Considering bias and conflicts of interest among the included studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. 2019. https://doi.org/10.1002/9781119536604.ch7 .
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne J. Assessing risk of bias in a randomized trial. Cochrane Handb Syst Rev Interv. 2019;6:205–28.
Reilly KL, Kennedy S, Porter G, Estabrooks P. Comparing, Contrasting, and Integrating Dissemination and Implementation Outcomes Included in the RE-AIM and Implementation Outcomes Frameworks. Front Public Health [Internet]. 2020 [cited 2024 Apr 24];8. Available from: https://www.frontiersin.org/journals/public-health/articles/ https://doi.org/10.3389/fpubh.2020.00430/full
Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess Winch Engl. 2004;8:iii–iv 1-72.
CAS Google Scholar
Beidas RS, Kendall PC. Training Therapists in Evidence-Based Practice: A Critical Review of Studies From a Systems-Contextual Perspective. Clin Psychol Publ Div Clin Psychol Am Psychol Assoc. 2010;17:1–30.
Powell BJ, Beidas RS, Lewis CC, Aarons GA, McMillen JC, Proctor EK, et al. Methods to Improve the Selection and Tailoring of Implementation Strategies. J Behav Health Serv Res. 2017;44:177–94.
Powell BJ, Fernandez ME, Williams NJ, Aarons GA, Beidas RS, Lewis CC, et al. Enhancing the Impact of Implementation Strategies in Healthcare: A Research Agenda. Front Public Health [Internet]. 2019 [cited 2021 Mar 31];7. Available from: https://www.frontiersin.org/articles/ https://doi.org/10.3389/fpubh.2019.00003/full
Frakt AB, Prentice JC, Pizer SD, Elwy AR, Garrido MM, Kilbourne AM, et al. Overcoming Challenges to Evidence-Based Policy Development in a Large. Integrated Delivery System Health Serv Res. 2018;53:4789–807.
PubMed Google Scholar
Crable EL, Lengnick-Hall R, Stadnick NA, Moullin JC, Aarons GA. Where is “policy” in dissemination and implementation science? Recommendations to advance theories, models, and frameworks: EPIS as a case example. Implement Sci. 2022;17:80.
Crable EL, Grogan CM, Purtle J, Roesch SC, Aarons GA. Tailoring dissemination strategies to increase evidence-informed policymaking for opioid use disorder treatment: study protocol. Implement Sci Commun. 2023;4:16.
Bond GR. Evidence-based policy strategies: A typology. Clin Psychol Sci Pract. 2018;25:e12267.
Loo TS, Davis RB, Lipsitz LA, Irish J, Bates CK, Agarwal K, et al. Electronic Medical Record Reminders and Panel Management to Improve Primary Care of Elderly Patients. Arch Intern Med. 2011;171:1552–8.
Shojania KG, Jennings A, Mayhew A, Ramsay C, Eccles M, Grimshaw J. Effect of point-of-care computer reminders on physician behaviour: a systematic review. CMAJ Can Med Assoc J. 2010;182:E216-25.
Sequist TD, Gandhi TK, Karson AS, Fiskio JM, Bugbee D, Sperling M, et al. A Randomized Trial of Electronic Clinical Reminders to Improve Quality of Care for Diabetes and Coronary Artery Disease. J Am Med Inform Assoc JAMIA. 2005;12:431–7.
Dopp AR, Kerns SEU, Panattoni L, Ringel JS, Eisenberg D, Powell BJ, et al. Translating economic evaluations into financing strategies for implementing evidence-based practices. Implement Sci. 2021;16:1–12.
Dopp AR, Hunter SB, Godley MD, Pham C, Han B, Smart R, et al. Comparing two federal financing strategies on penetration and sustainment of the adolescent community reinforcement approach for substance use disorders: protocol for a mixed-method study. Implement Sci Commun. 2022;3:51.
Proctor EK, Toker E, Tabak R, McKay VR, Hooley C, Evanoff B. Market viability: a neglected concept in implementation science. Implement Sci. 2021;16:98.
Dopp AR, Narcisse M-R, Mundey P, Silovsky JF, Smith AB, Mandell D, et al. A scoping review of strategies for financing the implementation of evidence-based practices in behavioral health systems: State of the literature and future directions. Implement Res Pract. 2020;1:2633489520939980.
PubMed PubMed Central Google Scholar
Dopp AR, Kerns SEU, Panattoni L, Ringel JS, Eisenberg D, Powell BJ, et al. Translating economic evaluations into financing strategies for implementing evidence-based practices. Implement Sci IS. 2021;16:66.
Kilbourne AM, Neumann MS, Pincus HA, Bauer MS, Stall R. Implementing evidence-based interventions in health care:application of the replicating effective programs framework. Implement Sci. 2007;2:42–51.
Kegeles SM, Rebchook GM, Hays RB, Terry MA, O’Donnell L, Leonard NR, et al. From science to application: the development of an intervention package. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 2000;12:62–74.
Wandersman A, Imm P, Chinman M, Kaftarian S. Getting to outcomes: a results-based approach to accountability. Eval Program Plann. 2000;23:389–95.
Wandersman A, Chien VH, Katz J. Toward an evidence-based system for innovation support for implementing innovations with quality: Tools, training, technical assistance, and quality assurance/quality improvement. Am J Community Psychol. 2012;50:445–59.
Rogal SS, Yakovchenko V, Waltz TJ, Powell BJ, Kirchner JE, Proctor EK, et al. The association between implementation strategy use and the uptake of hepatitis C treatment in a national sample. Implement Sci. 2017;12:1–13.
Smith SN, Almirall D, Prenovost K, Liebrecht C, Kyle J, Eisenberg D, et al. Change in patient outcomes after augmenting a low-level implementation strategy in community practices that are slow to adopt a collaborative chronic care model: a cluster randomized implementation trial. Med Care. 2019;57:503.
Rogal SS, Yakovchenko V, Waltz TJ, Powell BJ, Gonzalez R, Park A, et al. Longitudinal assessment of the association between implementation strategy use and the uptake of hepatitis C treatment: Year 2. Implement Sci. 2019;14:1–12.
Harvey G, Kitson A. Translating evidence into healthcare policy and practice: Single versus multi-faceted implementation strategies – is there a simple answer to a complex question? Int J Health Policy Manag. 2015;4:123–6.
Engell T, Stadnick NA, Aarons GA, Barnett ML. Common Elements Approaches to Implementation Research and Practice: Methods and Integration with Intervention Science. Glob Implement Res Appl. 2023;3:1–15.
Michie S, Fixsen D, Grimshaw JM, Eccles MP. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implement Sci IS. 2009;4:40.
Smith JD, Li DH, Rafferty MR. The Implementation Research Logic Model: a method for planning, executing, reporting, and synthesizing implementation projects. Implement Sci IS. 2020;15:84.
Perez Jolles M, Lengnick-Hall R, Mittman BS. Core Functions and Forms of Complex Health Interventions: a Patient-Centered Medical Home Illustration. JGIM J Gen Intern Med. 2019;34:1032–8.
Schroeck FR, Ould Ismail AA, Haggstrom DA, Sanchez SL, Walker DR, Zubkoff L. Data-driven approach to implementation mapping for the selection of implementation strategies: a case example for risk-aligned bladder cancer surveillance. Implement Sci IS. 2022;17:58.
Frank HE, Kemp J, Benito KG, Freeman JB. Precision Implementation: An Approach to Mechanism Testing in Implementation Research. Adm Policy Ment Health. 2022;49:1084–94.
Lewis CC, Klasnja P, Lyon AR, Powell BJ, Lengnick-Hall R, Buchanan G, et al. The mechanics of implementation strategies and measures: advancing the study of implementation mechanisms. Implement Sci Commun. 2022;3:114.
Geng EH, Baumann AA, Powell BJ. Mechanism mapping to advance research on implementation strategies. PLoS Med. 2022;19:e1003918.
Pinnock H, Barwick M, Carpenter CR, Eldridge S, Grandes G, Griffiths CJ, et al. Standards for Reporting Implementation Studies (StaRI) Statement. BMJ. 2017;356:i6795.
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm Policy Ment Health Ment Health Serv Res. 2011;38:65–76.
Hooley C, Amano T, Markovitz L, Yaeger L, Proctor E. Assessing implementation strategy reporting in the mental health literature: a narrative review. Adm Policy Ment Health Ment Health Serv Res. 2020;47:19–35.
Proctor E, Ramsey AT, Saldana L, Maddox TM, Chambers DA, Brownson RC. FAST: a framework to assess speed of translation of health innovations to practice and policy. Glob Implement Res Appl. 2022;2:107–19.
Cullen L, Hanrahan K, Edmonds SW, Reisinger HS, Wagner M. Iowa Implementation for Sustainability Framework. Implement Sci IS. 2022;17:1.
Saldana L, Ritzwoller DP, Campbell M, Block EP. Using economic evaluations in implementation science to increase transparency in costs and outcomes for organizational decision-makers. Implement Sci Commun. 2022;3:40.
Eisman AB, Kilbourne AM, Dopp AR, Saldana L, Eisenberg D. Economic evaluation in implementation science: making the business case for implementation strategies. Psychiatry Res. 2020;283:112433.
Akiba CF, Powell BJ, Pence BW, Nguyen MX, Golin C, Go V. The case for prioritizing implementation strategy fidelity measurement: benefits and challenges. Transl Behav Med. 2022;12:335–42.
Akiba CF, Powell BJ, Pence BW, Muessig K, Golin CE, Go V. “We start where we are”: a qualitative study of barriers and pragmatic solutions to the assessment and reporting of implementation strategy fidelity. Implement Sci Commun. 2022;3:117.
Rudd BN, Davis M, Doupnik S, Ordorica C, Marcus SC, Beidas RS. Implementation strategies used and reported in brief suicide prevention intervention studies. JAMA Psychiatry. 2022;79:829–31.
Painter JT, Raciborski RA, Matthieu MM, Oliver CM, Adkins DA, Garner KK. Engaging stakeholders to retrospectively discern implementation strategies to support program evaluation: Proposed method and case study. Eval Program Plann. 2024;103:102398.
Bunger AC, Powell BJ, Robertson HA, MacDowell H, Birken SA, Shea C. Tracking implementation strategies: a description of a practical approach and early findings. Health Res Policy Syst. 2017;15:1–12.
Mustanski B, Smith JD, Keiser B, Li DH, Benbow N. Supporting the growth of domestic HIV implementation research in the united states through coordination, consultation, and collaboration: how we got here and where we are headed. JAIDS J Acquir Immune Defic Syndr. 2022;90:S1-8.
Marques MM, Wright AJ, Corker E, Johnston M, West R, Hastings J, et al. The Behaviour Change Technique Ontology: Transforming the Behaviour Change Technique Taxonomy v1. Wellcome Open Res. 2023;8:308.
Merle JL, Li D, Keiser B, Zamantakis A, Queiroz A, Gallo CG, et al. Categorising implementation determinants and strategies within the US HIV implementation literature: a systematic review protocol. BMJ Open. 2023;13:e070216.
Glenshaw MT, Gaist P, Wilson A, Cregg RC, Holtz TH, Goodenow MM. Role of NIH in the Ending the HIV Epidemic in the US Initiative: Research Improving Practice. J Acquir Immune Defic Syndr. 1999;2022(90):S9-16.
Purcell DW, Namkung Lee A, Dempsey A, Gordon C. Enhanced Federal Collaborations in Implementation Science and Research of HIV Prevention and Treatment. J Acquir Immune Defic Syndr. 1999;2022(90):S17-22.
Queiroz A, Mongrella M, Keiser B, Li DH, Benbow N, Mustanski B. Profile of the Portfolio of NIH-Funded HIV Implementation Research Projects to Inform Ending the HIV Epidemic Strategies. J Acquir Immune Defic Syndr. 1999;2022(90):S23-31.
Zamantakis A, Li DH, Benbow N, Smith JD, Mustanski B. Determinants of Pre-exposure Prophylaxis (PrEP) Implementation in Transgender Populations: A Qualitative Scoping Review. AIDS Behav. 2023;27:1600–18.
Li DH, Benbow N, Keiser B, Mongrella M, Ortiz K, Villamar J, et al. Determinants of Implementation for HIV Pre-exposure Prophylaxis Based on an Updated Consolidated Framework for Implementation Research: A Systematic Review. J Acquir Immune Defic Syndr. 1999;2022(90):S235-46.
Chambers DA, Emmons KM. Navigating the field of implementation science towards maturity: challenges and opportunities. Implement Sci. 2024;19:26, s13012-024-01352–0.
Chinman M, Acosta J, Ebener P, Shearer A. “What we have here, is a failure to [replicate]”: Ways to solve a replication crisis in implementation science. Prev Sci. 2022;23:739–50.
Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117.
Lengnick-Hall R, Gerke DR, Proctor EK, Bunger AC, Phillips RJ, Martin JK, et al. Six practical recommendations for improved implementation outcomes reporting. Implement Sci. 2022;17:16.
Miller CJ, Barnett ML, Baumann AA, Gutner CA, Wiltsey-Stirman S. The FRAME-IS: a framework for documenting modifications to implementation strategies in healthcare. Implement Sci IS. 2021;16:36.
Xu X, Lazar CM, Ruger JP. Micro-costing in health and medicine: a critical appraisal. Health Econ Rev. 2021;11:1.
Barnett ML, Dopp AR, Klein C, Ettner SL, Powell BJ, Saldana L. Collaborating with health economists to advance implementation science: a qualitative study. Implement Sci Commun. 2020;1:82.
Lengnick-Hall R, Williams NJ, Ehrhart MG, Willging CE, Bunger AC, Beidas RS, et al. Eight characteristics of rigorous multilevel implementation research: a step-by-step guide. Implement Sci. 2023;18:52.
Riley-Gibson E, Hall A, Shoesmith A, Wolfenden L, Shelton RC, Doherty E, et al. A systematic review to determine the effect of strategies to sustain chronic disease prevention interventions in clinical and community settings: study protocol. Res Sq [Internet]. 2023 [cited 2024 Apr 19]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10312971/
Ingvarsson S, Hasson H, von Thiele Schwarz U, Nilsen P, Powell BJ, Lindberg C, et al. Strategies for de-implementation of low-value care—a scoping review. Implement Sci IS. 2022;17:73.
Lewis CC, Powell BJ, Brewer SK, Nguyen AM, Schriger SH, Vejnoska SF, et al. Advancing mechanisms of implementation to accelerate sustainable evidence-based practice integration: protocol for generating a research agenda. BMJ Open. 2021;11:e053474.
Hailemariam M, Bustos T, Montgomery B, Barajas R, Evans LB, Drahota A. Evidence-based intervention sustainability strategies: a systematic review. Implement Sci. 2019;14:N.PAG-N.PAG.
Michie S, Atkins L, West R. The behaviour change wheel. Guide Des Interv 1st Ed G B Silverback Publ. 2014;1003:1010.
Birken SA, Haines ER, Hwang S, Chambers DA, Bunger AC, Nilsen P. Advancing understanding and identifying strategies for sustaining evidence-based practices: a review of reviews. Implement Sci IS. 2020;15:88.
Metz A, Jensen T, Farley A, Boaz A, Bartley L, Villodas M. Building trusting relationships to support implementation: A proposed theoretical model. Front Health Serv. 2022;2:894599.
Rabin BA, Cain KL, Watson P, Oswald W, Laurent LC, Meadows AR, et al. Scaling and sustaining COVID-19 vaccination through meaningful community engagement and care coordination for underserved communities: hybrid type 3 effectiveness-implementation sequential multiple assignment randomized trial. Implement Sci IS. 2023;18:28.
Gyamfi J, Iwelunmor J, Patel S, Irazola V, Aifah A, Rakhra A, et al. Implementation outcomes and strategies for delivering evidence-based hypertension interventions in lower-middle-income countries: Evidence from a multi-country consortium for hypertension control. PLOS ONE. 2023;18:e0286204.
Woodward EN, Ball IA, Willging C, Singh RS, Scanlon C, Cluck D, et al. Increasing consumer engagement: tools to engage service users in quality improvement or implementation efforts. Front Health Serv. 2023;3:1124290.
Norton WE, Chambers DA. Unpacking the complexities of de-implementing inappropriate health interventions. Implement Sci IS. 2020;15:2.
Norton WE, McCaskill-Stevens W, Chambers DA, Stella PJ, Brawley OW, Kramer BS. DeImplementing Ineffective and Low-Value Clinical Practices: Research and Practice Opportunities in Community Oncology Settings. JNCI Cancer Spectr. 2021;5:pkab020.
McKay VR, Proctor EK, Morshed AB, Brownson RC, Prusaczyk B. Letting Go: Conceptualizing Intervention De-implementation in Public Health and Social Service Settings. Am J Community Psychol. 2018;62:189–202.
Patey AM, Grimshaw JM, Francis JJ. Changing behaviour, ‘more or less’: do implementation and de-implementation interventions include different behaviour change techniques? Implement Sci IS. 2021;16:20.
Rodriguez Weno E, Allen P, Mazzucca S, Farah Saliba L, Padek M, Moreland-Russell S, et al. Approaches for Ending Ineffective Programs: Strategies From State Public Health Practitioners. Front Public Health. 2021;9:727005.
Gnjidic D, Elshaug AG. De-adoption and its 43 related terms: harmonizing low-value care terminology. BMC Med. 2015;13:273.
Download references
Acknowledgements
The authors would like to acknowledge the early contributions of the Pittsburgh Dissemination and Implementation Science Collaborative (Pitt DISC). LEA would like to thank Dr. Billie Davis for analytical support. The authors would like to acknowledge the implementation science experts who recommended articles for our review, including Greg Aarons, Mark Bauer, Rinad Beidas, Geoffrey Curran, Laura Damschroder, Rani Elwy, Amy Kilbourne, JoAnn Kirchner, Jennifer Leeman, Cara Lewis, Dennis Li, Aaron Lyon, Gila Neta, and Borsika Rabin.
Dr. Rogal’s time was funded in part by a University of Pittsburgh K award (K23-DA048182) and by a VA Health Services Research and Development grant (PEC 19-207). Drs. Bachrach and Quinn were supported by VA HSR Career Development Awards (CDA 20-057, PI: Bachrach; CDA 20-224, PI: Quinn). Dr. Scheunemann’s time was funded by the US Agency for Healthcare Research and Quality (K08HS027210). Drs. Hero, Chinman, Goodrich, Ernecoff, and Mr. Qureshi were funded by the Patient-Centered Outcomes Research Institute (PCORI) AOSEPP2 Task Order 12 to conduct a landscape review of US studies on the effectiveness of implementation strategies with results reported here ( https://www.pcori.org/sites/default/files/PCORI-Implementation-Strategies-for-Evidence-Based-Practice-in-Health-and-Health-Care-A-Review-of-the-Evidence-Full-Report.pdf and https://www.pcori.org/sites/default/files/PCORI-Implementation-Strategies-for-Evidence-Based-Practice-in-Health-and-Health-Care-Brief-Report-Summary.pdf ). Dr. Ashcraft and Ms. Phares were funded by the Center for Health Equity Research and Promotion, (CIN 13-405). The funders had no involvement in this study.
Author information
Shari S. Rogal and Matthew J. Chinman are co-senior authors.
Authors and Affiliations
Center for Health Equity Research and Promotion, Corporal Michael Crescenz VA Medical Center, Philadelphia, PA, USA
Laura Ellen Ashcraft
Department of Biostatistics, Epidemiology, and Informatics, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA
Center for Health Equity Research and Promotion, VA Pittsburgh Healthcare System, Pittsburgh, PA, USA
David E. Goodrich, Angela Phares, Deirdre A. Quinn, Shari S. Rogal & Matthew J. Chinman
Division of General Internal Medicine, Department of Medicine, University of Pittsburgh, Pittsburgh, PA, USA
David E. Goodrich, Deirdre A. Quinn & Matthew J. Chinman
Clinical & Translational Science Institute, University of Pittsburgh, Pittsburgh, PA, USA
David E. Goodrich & Lisa G. Lederer
RAND Corporation, Pittsburgh, PA, USA
Joachim Hero, Nabeel Qureshi, Natalie C. Ernecoff & Matthew J. Chinman
Center for Clinical Management Research, VA Ann Arbor Healthcare System, Ann Arbor, Michigan, USA
Rachel L. Bachrach
Department of Psychiatry, University of Michigan Medical School, Ann Arbor, MI, USA
Division of Geriatric Medicine, University of Pittsburgh, Department of Medicine, Pittsburgh, PA, USA
Leslie Page Scheunemann
Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine, University of Pittsburgh, Department of Medicine, Pittsburgh, PA, USA
Departments of Medicine and Surgery, University of Pittsburgh, Pittsburgh, Pennsylvania, USA
Shari S. Rogal
You can also search for this author in PubMed Google Scholar
Contributions
LEA, SSR, and MJC conceptualized the study. LEA, SSR, MJC, and JOH developed the study design. LEA and JOH acquired the data. LEA, DEG, AP, RLB, DAQ, LGL, LPS, SSR, NQ, and MJC conducted the abstract, full text review, and rigor assessment. LEA, DEG, JOH, AP, RLB, DAQ, NQ, NCE, SSR, and MJC conducted the data abstraction. DEG, SSR, and MJC adjudicated conflicts. LEA and SSR analyzed the data. LEA, SSR, JOH, and MJC interpreted the data. LEA, SSR, and MJC drafted the work. All authors substantially revised the work. All authors approved the submitted version and agreed to be personally accountable for their contributions and the integrity of the work.
Corresponding author
Correspondence to Laura Ellen Ashcraft .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
The manuscript does not contain any individual person’s data.
Competing interests
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., supplementary material 4., supplementary material 5., supplementary material 6., supplementary material 7., supplementary material 8., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ashcraft, L.E., Goodrich, D.E., Hero, J. et al. A systematic review of experimentally tested implementation strategies across health and human service settings: evidence from 2010-2022. Implementation Sci 19 , 43 (2024). https://doi.org/10.1186/s13012-024-01369-5
Download citation
Received : 09 November 2023
Accepted : 27 May 2024
Published : 24 June 2024
DOI : https://doi.org/10.1186/s13012-024-01369-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Implementation strategy
- Health-related outcomes
Implementation Science
ISSN: 1748-5908
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
“What does adoption mean to a child?”
Get Free Info
related articles
- Questions from Adoptees
5 Adoption Research Studies That Might Surprise You
Explaining the best adoption studies for adoptees like you.
As an adoptee, you may be curious to learn more about adoption as a whole. It may help you gain a better understanding of your own story and adoption history.
For instance, you might be looking for adoption studies that reveal something new that you may not have known. So, where do you begin your search? That’s where we come in to help.
There are plenty of studies on adoption out there that have led to new, groundbreaking discoveries. But, they’re scattered throughout the internet. To make things easier, we’ve compiled this detailed list of five of the best adoption research studies we could find.
1. Benefits of Early Adoption Closure
You know firsthand that adoption is far from a simple journey, and there are a slew of different adoption outcomes. Research has shown , though, that adoptive parents should aim to tell their children that they were adopted before the child has turned three.
This study comes from Montclair State University, and it was first published in the Journal of Family Issues . In short, this research showed that adults who discovered their adoption after the age of three experienced more difficult emotions and were less satisfied with their lives from a general standpoint. For the most part, the later in life that the adoptee discovered their adoption, the higher the emotional distress often was.
This particular study has contradicted older adoption research studies that recommended adoptive parents to talk to their children about their adoption between the ages of four and 13. American Adoptions educates families on the importance of introducing their child’s adoption story as early as possible, even as an infant through bedtime stories and other children’s books about adoption.
If you would like to read more about this Montclair State University study, then you can check it out here .
2. Breaking the Stigma Against Adoption
Unfortunately, there is a stigma surrounding adoption, and it can lead many birth and adoptive parents to reconsider their options. There is nothing wrong with choosing the best path for you and your child, and some adoption research studies show how we can cultivate a healthier culture by discussing adoption.
For instance, this article from the Institute for Family Studies (IFS) makes several suggestions on how we can help break the stigma toward adoption. One way we can do this is by using positive adoption language . For example, instead of saying “give a baby up for adoption,” people can say “place a baby for adoption” or “create an adoption plan” instead. Words are important because they can shape how we think about certain topics, such as adoption.
If you are interested in reading the full IFS article, then you can do so here .
3. Open Adoption Is More Beneficial for Adoptees than Closed Adoption
You may have heard of terms such as “open adoption” and “closed adoption.”
Open adoption is when you grow up knowing who your birth family is and why you were placed for adoption in the first place. Closed adoption , on the other hand, is when you don’t know who your birth parents are. You also know next to nothing about your adoption story.
Adoption has changed quite a bit within the past few decades. While close adoption used to be the norm, that’s no longer the case. After extensive research about the benefits of open adoption, it has now become the standard for adoptions in the modern age.
The vast majority of adoptions today are open, which in turn means that many more adoptees are satisfied with their adoption experiences.
There are plenty of adoption research studies about open and closed adoption, and this study shows that open adoption is often more beneficial for adoptees than its closed counterpart. To be more specific, adolescents who have regular contact with their birth family are more satisfied with their adoptions than those without contact.
This is because more openness in adoption allows adoptees to have a better understanding of their story and prevents identity issues surrounding their adoption. For more information on this case study, be sure to check it out here .
4. Discussing Adoption with Birth Parents Can Be Beneficial
Speaking of open adoption plans , there are also quite a few adoption case studies about a term known as “communicative openness.”
Similar to how more openness in adoption can be beneficial for adoptees, there are also benefits associated with “communicative openness” for adoptees. In simpler terms, this means that adoptees are free to discuss their adoption and their feelings about it with their birth parents.
So, what are the benefits, exactly?
- Adoptees who discuss their adoption openly with their birth parents often develop a higher sense of self-esteem.
- They also tend to have fewer behavioral issues and trust their birth parents more.
- On top of this, they have fewer feelings of alienation and higher family functioning from a general standpoint.
If you would like to see the full study for yourself, then you can view it here .
5. Most Adoptees Know Why They Were Placed for Adoption
Because of the benefits of “communicative openness” for many adoptees, there are some adoption research studies that observe how many adoptees know about their adoption.
For instance, a study from the U.S. Department of Health and Human Services found that 97% of adoptees know their adoption stories.
The study also discovered that 87% of adoptive families with children five or older felt that their child’s feelings toward adoption were either “positive” or “mostly positive.” If you want to read the comprehensive study for yourself, then you can do that here .
As an adoptee, it can be interesting to read about various adoption research studies. Although these five studies lead to important discoveries, you can always check out more studies on your own by browsing them here .
Disclaimer Information available through these links is the sole property of the companies and organizations listed therein. American Adoptions provides this information as a courtesy and is in no way responsible for its content or accuracy.
- Research article
- Open access
- Published: 05 February 2021
Increasing adoption rates at animal shelters: a two-phase approach to predict length of stay and optimal shelter allocation
- Janae Bradley 1 &
- Suchithra Rajendran ORCID: orcid.org/0000-0002-0817-6292 2 , 3
BMC Veterinary Research volume 17 , Article number: 70 ( 2021 ) Cite this article
41k Accesses
18 Citations
75 Altmetric
Metrics details
Among the 6–8 million animals that enter the rescue shelters every year, nearly 3–4 million (i.e., 50% of the incoming animals) are euthanized, and 10–25% of them are put to death specifically because of shelter overcrowding each year. The overall goal of this study is to increase the adoption rates at animal shelters. This involves predicting the length of stay of each animal at shelters considering key features such as animal type (dog, cat, etc.), age, gender, breed, animal size, and shelter location.
Logistic regression, artificial neural network, gradient boosting, and the random forest algorithms were used to develop models to predict the length of stay. The performance of these models was determined using three performance metrics: precision, recall, and F1 score. The results demonstrated that the gradient boosting algorithm performed the best overall, with the highest precision, recall, and F1 score. Upon further observation of the results, it was found that age for dogs (puppy, super senior), multicolor, and large and small size were important predictor variables.
The findings from this study can be utilized to predict and minimize the animal length of stay in a shelter and euthanization. Future studies involve determining which shelter location will most likely lead to the adoption of that animal. The proposed two-phased tool can be used by rescue shelters to achieve the best compromise solution by making a tradeoff between the adoption speed and relocation cost.
As the problem of overpopulation of domestic animals continues to rise, animal shelters across the nation are faced with the challenge of finding solutions to increase the adoption rates. In the United States, about 6–8 million dogs and cats enter animal shelters every year, and 3–4 million of those animals are euthanized [ 1 ]. In other words, about 50% of the total canines and felines that enter animal shelters are put to death annually. Moreover, 10–25% of the total euthanized population in the United States is explicitly euthanized because of shelter overcrowding each year [ 2 ]. Though animal shelters provide incentives such as reduced adoption fees and sterilizing animals before adoption, only a quarter of total animals living in the shelter are adopted.
Animal adoption from shelters and rescues
There are various places to adopt an animal, and each potential owner must complete the adoption process and paperwork to take their new animal home [ 3 ]. Public and private animal shelters include animal control, city and county animal shelters, and police and health departments. Staff and volunteers run these facilities. Animals may also be adopted from a rescue organization, where pets are fostered in a home or a private boarding facility. These organizations are usually run by volunteers, and animals are viewed during local adoption events that are held at different locations, such as a pet store [ 3 ].
There could be several reasons for the euthanization of animals in a shelter, such as overcrowding, medical issues (ex. sick, disabled), or behavioral issues (ex. too aggressive). The causes for the overpopulation of animals include failure to spay or neuter animals leading to reckless breeding habits and abandonment or surrender of offspring, animal abandonment from owners who are no longer able to take care of or do not want the animal, and individuals still buying from pet stores [ 4 ]. With the finite room capacity for animals that are abandoned or surrendered, overpopulation becomes a key challenge [ 5 ]. Though medical and behavioral issues are harder to solve, the overpopulation of healthy adoptable animals in shelters is a problem that can be addressed through machine learning and predictive analytics.
Literature review
In this section, we describe the research conducted on animal shelters evaluating euthanasia and factors associated with animal adoption. The articles provide insights into factors that influence the length of stay and what characteristics influence adoption.
Studies have been conducted investigating the positive influence of pre-adoption neutering of animals on the probability of pet adoption [ 2 ]. The author investigated the impact of the cooperation of veterinary medical schools in increasing pet adoption by offering free sterilization. Results demonstrated that the collaboration between veterinary hospitals and local animal shelters decreased the euthanization of adoptable pets.
Hennessy et al. [ 6 ] conducted a study to determine the relationship between the behavior and cortisol levels of dogs in animal shelters and examined its effect in predicting behavioral issues after adoption. Shore et al. [ 7 ] analyzed the reasons for returning adopted animals by owners and obtained insights for these failed adoptions to attain more successful future approvals. The researchers found that prior failed adoption had led to longer-lasting future acceptances. They hypothesized that the failed adoptions might lead owners to discover their dog preferences by assessing their living situation and the type of animal that would meet that requirement.
Morris et al. [ 8 ] evaluated the trends in income and outcome data for shelters from 1989 to 2010 in a large U.S. metropolitan area. The results showed a decrease in euthanasia, adoption, and intake for dogs. For cats, a reduction in intake was observed until 1998, a decrease in euthanasia was observed until 2000, and the adoption of cats remained the same. Fantuzzi et al. [ 9 ] explored the factors that are significant for the adoption of cats in the animal shelter. The study investigated the effects of toy allocation, cage location, and cat characteristics (such as age, gender, color, and activity level). Results demonstrated that the more active cats that possessed toys and were viewed at eye level were more likely to impress the potential adopter and be adopted. Brown et al. [ 10 ] conducted a study evaluating the influence of age, breed, color, and coat pattern on the length of stay for cats in a no-kill shelter. The authors concluded that while color did not influence the length of stay for kittens, whereas gender, coat patterning, and breed were significant predictors for both cats and kittens.
Machine learning
Machine learning is one possible tool that can be used to identify risk factors for animal adoption and predict the length of stay for animals in shelters. Machine learning is the ability to program computers to learn and improve all by itself using training experience [ 11 ]. The goal of machine learning is to develop a system to analyze big data, quickly deliver accurate and repeatable results, and to adapt to new data independently. A system can be trained to make accurate predictions by learning from examples of desired input-output data. More specifically, machine learning algorithms are utilized to detect classification and prediction patterns from large data and to develop models to predict future outcomes [ 12 ]. These patterns show the relationship between the attribute variables (input) and target variables (output) [ 13 ].
Widely used data mining tasks include supervised learning, unsupervised learning, and reinforcement learning [ 14 ]. Unsupervised learning involves the use of unlabeled datasets to train a system for finding hidden patterns within the data [ 15 ]. Clustering is an example of unsupervised learning. Reinforcement learning is where a system is trained through direct interaction with the environment by trial and error [ 15 ]. Supervised learning encompasses classification and prediction using labeled datasets [ 15 ]. These classification and regression algorithms are used to classify the output variable with a discrete label or predict the outcome as a continuous or numerical value. Traditional algorithms such as neural networks, decision trees, and logistic regression typically use supervised learning. Figure 1 provides a pictorial of the steps for developing and testing a predictive model.
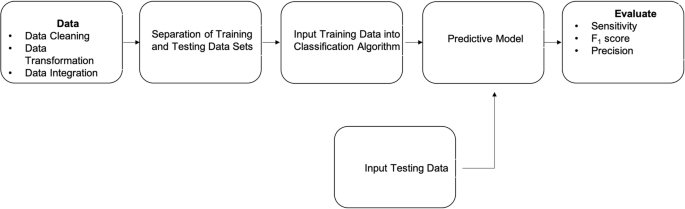
Pictorial Representation of Developing a Predictive Model
Contributions to the literature
Although prior studies have investigated the impact of several factors, such as age and gender, on the length of stay, they focus on a single shelter, rather than multiple organizations, as in this study. The goal of this study is to investigate the length of stay of animals at shelters and the factors influencing the rate of animal adoption. The overall goal is to increase adoption rates of pets in animal shelters by utilizing several factors to predict the length of stay. Machine learning algorithms are used to predict the length of stay of each animal based on numerous factors (such as breed, size, and color). We address several objectives in this study that are listed below.
Identify risk factors associated with adoption rate and length of stay
Utilize the identified risk factors from collected data to develop predictive models
Compare statistical models to determine the best model for length of stay prediction
Exploratory Data results
From Fig. 2 , it is evident that the return of dogs is the highest outcome type at 43.3%, while Fig. 3 shows that the adoption of cats is the highest outcome type at 46.1%. Both figures illustrate that the euthanization of both cats and dogs is still prevalent (~ 20%). The results from Table 1 demonstrate that the longest time spent in the shelter is at 355 days by a male cat that is adopted and a female dog that is euthanized. Observing the results, adoption has the lowest variance among all animal types compared to the other outcome types. Adopted male cats have the lowest variance for days spent in the shelter, followed by female dogs. Female cats that are returned have the highest variance for days spent in the shelter.
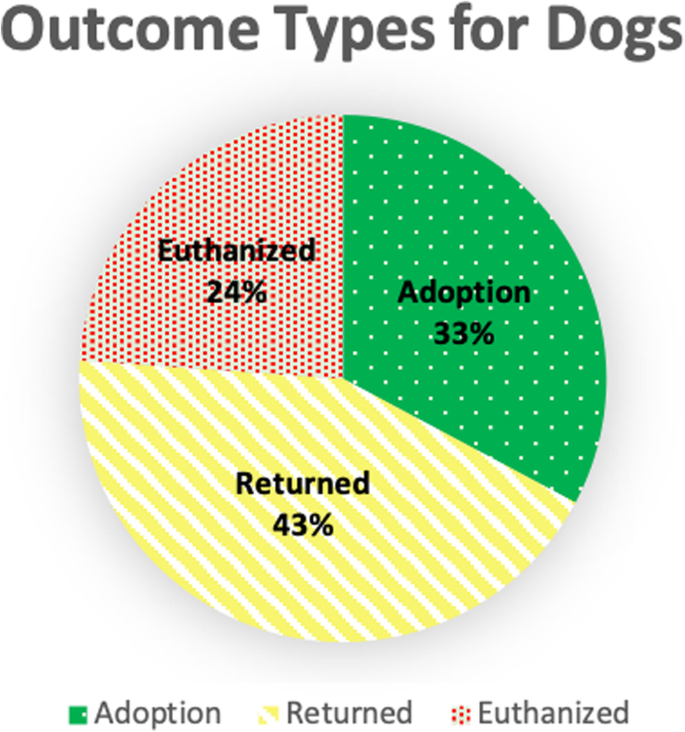
Distribution of Outcome Types for Dogs
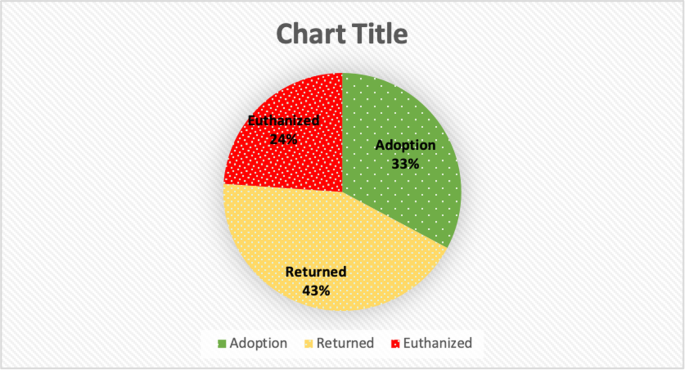
Distribution of Outcome Types for Cats
Figure 4 shows a comparison of cats and dogs for the three different outcome types. It is observed from the data that there are more dogs returned than cats. From Fig. 5 , it is observed that the number of days a dog stays in the shelter decreases as the age increases. This is not expected, as it is predicted that the number of days in a shelter would be lower for younger dogs and puppies. This observation could be due to having more data points for younger dogs.
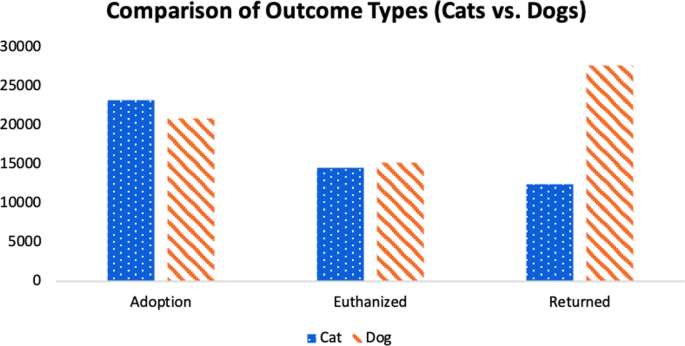
Comparison of Outcome Types for Cats and Dogs
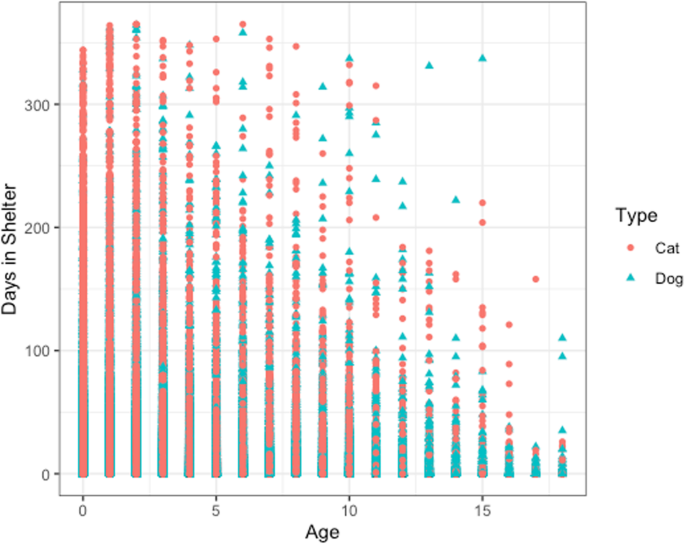
Age vs. Days in Shelter for Cats and Dogs
Machine learning results
Examining Table 2 , it is clear that the most proficient predictive model is developed by the gradient boosting algorithm for this dataset, followed by the random forest algorithm. The logistic regression algorithm appears to perform the worst with low precision, recall, and F1 score performance metrics for all categories of length of stay. For the prediction of low length of stay in a shelter, the random forest algorithm is the best performing model in comparison to the others at around 64–70% performance for precision, recall, and F1 score. The ANN algorithm is found to be the best when evaluating the precision and F1 score for medium length of stay, while the random forest algorithm is better for assessing recall. However, the performance of these models in predicting the medium length of stay for the given dataset is low for all three-performance metrics. The gradient boosting algorithm performs the best when predicting the high length of stay. Finally, the gradient boosting and random forest algorithms perform well when predicting the very high length of stay at around 70–80%.
Results from Table 2 also demonstrate that the model developed from the gradient boosting algorithm has a higher performance when predicting the high length of stay that leads to adoption, and when the outcome is euthanization. Evaluating the average of all three-performance metrics for all algorithms, the gradient boosting is the most proficient model at almost 60%, while logistic regression appears to be the worst. Table 2 also provides the computational time for each machine learning algorithm. For the given dataset, logistic regression runs the fastest at 9.41 s, followed by gradient boosting, artificial neural network, and finally, random forest running the longest. The gap in the performance measure ( pm ) is calculated by \( \frac{p{m}_{best}-p{m}_{worst}}{p{m}_{best}} \) , and is nearly 34, 39, and 32% for precision, recall, and F1 score, respectively.
Table 3 provides information on the top features or factors from each machine learning algorithm. Observing the table, we find that age (senior, super senior, and puppy), size (large and small), and color (multicolor) has a significant impact or influence on the length of stay. Specifically, we observe that older-aged animals (senior and/or super senior) appear as a significant factor for every algorithm. For the artificial neural network, older age is the #2 and #3 predictor, and super senior is the #2 predictor for the gradient boosting algorithm. Large and small-sized animals are also observed to be important features, as both are shown as the #1 predictor in the gradient boosting and ANN algorithms. The results also demonstrate that gender, animal type, other colors besides multicolor, middle age, and medium-sized animals did not significantly impact the length of stay.
Results from our study provided information on what factors are significant in influencing length of stay. Brown et al. [ 10 ] conducted research that found that age, breed designation, coat color, and coat pattern influenced the length of stay for cats in animal shelters. Similar to these studies, observations from our study also suggest that age and color have a significant impact or influence on the length of stay.
Determining which algorithm will develop the best model for the given set of data is critical to predict the length of stay and minimize the chances of euthanization. The goal of predictive analytics is to develop a model that best approximates the true mapping function for the relationship between the input and output variables. To approximate this function, parametric or non-parametric algorithms can be used. Parametric algorithms simplify the unknown function to a known form. Non-parametric algorithms do not make assumptions about the structure of the mapping function, allowing free learning of any functional form. In this study, we utilize both parametric (logistic regression and artificial neural network) and non-parametric (random forest and gradient boosting) algorithms on the given data. Observing the results from Table 2 , the gradient boosting and random forest (non-parametric algorithms) perform the best on the dataset. It is observed from the results that using a non-parametric approach leads to a better approximation of the true mapping function for the given records. These results also support prior studies on parametric versus non-parametric methods. Neely et al. [ 16 ] detailed the theoretical superiority of non-parametric algorithms for detecting pharmacokinetic and pharmacodynamic subgroups in a study population. The author suggests this superiority comes from the lack of assumptions made about the distribution of parameter values in a dataset. Bissantz et al. [ 17 ] discussed a resampling algorithm that evaluates the deviations between parametric and non-parametric methods to be noise or systematic by comparing parametric models to a non-parametric “supermodel”. Results demonstrate the non-parametric model to be significantly better. The use of algorithms that do not approximate the true function of the relationship between input and output provides better performance results for this application as well.
Current literature also supports the use of ensemble methods to increase prediction accuracy and performance. Dietterich [ 18 ] discussed the ongoing research into developing good ensemble methods as well as the discovery that ensemble algorithms are often more accurate than individual algorithms that are used to create them. Pandey, and S, T [ 19 ]. conducted a study to compare the accuracy of ensemble methodology on predicting student academic performance as research has demonstrated better results for composite models over a single model. This study applied ensemble techniques on learning algorithms (AdaBoost, Random Forest, Rotation Forest, and Bagging). For our study with the given records, the results support this claim. Both the gradient boosting and random forest algorithms are ensemble algorithms and performed the best on the animal shelter data.
Results from Table 2 demonstrate the best performance of the gradient boosting and random forest algorithm when the length of stay was classified as very high or the animal was euthanized. This is beneficial as the models can predict long stays where the outcome is euthanasia. This can lead to shelters identifying at-risk animals and implementing methods and solutions to ensure their adoption. These potential methods are the second phase of this research study, which will involve relocating animals to shelters where they will more likely be adopted. This phase is discussed in the future directions section.
Studies have been conducted evaluating euthanasia-related stress on workers (e.g., [ 1 ]). In other words, overpopulation not only leads to euthanasia but can, in turn, cause mental and emotional problems for the workers. For instance, Reeve et al. [ 20 ] evaluated the strain related to euthanasia among animal workers. Results demonstrated that euthanasia related strain was prevalent, and an increase in substance abuse, job stress, work causing family conflict, complaints, and low job satisfaction was observed. Predicting the length of stay for animals will aid in them being more likely to be adopted and will lead to fewer animals being euthanized, adding value not only to animals finding a home but also less stress on the workers.
The approach developed in this paper could be beneficial not only to reduce euthanasia but also to reduce overcrowding in shelters operated in countries where euthanasia of healthy animals is illegal, and all animals must be housed in shelters until adoption (or natural death). It is essential to develop an information system for a collaborative animal shelter network in which the entities can coordinate with each other, exchanging information about the animal inventory. Another benefit of this study is that it investigates applying machine learning to the animal care domain. Previous studies have looked into what factors influence the length of stay; however, this study utilizes these factors in addition to classification algorithms to predict how long an animal will stay in the shelter. Moreover, the use of a prescriptive analytics approach is discussed in this paper, where the predictions made by the machine learning algorithms will be used along with a goal programming model to decide in what shelter is an animal most likely to be adopted.
Limitations of this study include lack of behavioral data, limited sample size, and the use of simple algorithms. The first limitation, lack of behavioral data of the animal during intake and outcome, would be beneficial to develop a more comprehensive model. Though behavioral problems are harder to solve, having data would provide insight into how long these animals with behavioral issues are staying in shelters and what the outcome is. Studies have shown that behavioral problems play a significant role in preventing bonding between owners and their animals and one of the most common reasons cited for animal surrender [ 21 , 22 ]. These behavioral problems can include poor manners, too much energy, aggression, and destruction of the household. Dogs surrendered to shelters because of behavioral issues have also been shown to be less likely to be adopted or rehomed, and the ones that are adopted are more likely to be returned [ 21 ]. Studies have also been conducted to evaluate the effect of the length of time on the behavior of dogs in rescue shelters [ 23 , 24 , 25 ]. Most of them concluded that environmental factors led to changes in the behavior of dogs and that a prolonged period in a shelter may lead to unattractive behavior of dogs to potential owners. Acquiring information on behavioral problems gives more information for the algorithm to learn when developing the predictive model. This allows more in-depth predictions to be made on how long an animal will stay in a shelter, which could also aid in adoption. This approach can be used to shorten the length of stay, which makes sure that healthy animals are not developing behavioral problems in the shelters. It is not only crucial for the animal to be adopted, but also that the adoption is a good fit between owner and pet. Shortening the length of stay would also lessen the chance that the animal will be returned by the adopter because of behavior. Having this information will also allow shelters to find other shelters close by where animals with behavioral issues are more likely to be adopted. To overcome this limitation of the lack of data on behavioral problems, behavioral issues will be used as a factor and will be specifically asked for when acquiring data from shelters.
Another limitation includes collecting more data from animal shelters across the United States, allowing for more representative data to be collected and inputted into these algorithms. However, this presents a challenge due to most shelters being underfunded and low on staff. Though we reached out to shelters, most replied that they lacked the resources and staff to provide the information needed. Future work would include applying for funding to provide a stipend to staff for their assistance in gathering the data from respective shelters. With more data, the algorithm has more information to learn on, which could improve the performance metrics of the predictive models developed. There may also be other factors that show to be significant as more data is collected.
Finally, the last limitation is the use of simpler algorithms. This study considers basic ML algorithms. Nevertheless, in recent years, there has been development in the ML field of more complex networks. For instance, Zhong et al. [ 26 ] proposed a novel reinforcement learning method to select neural blocks and develop deep learning networks. Results demonstrated high efficiency in comparison to most of the previous deep network search approaches. Though only four algorithms were considered, future work would investigate deep learning networks, as well as bagging algorithms. Using more complex algorithms could ensure that if intricate patterns in the data are present, the algorithm can learn them.
Future direction
Phase 2: goal programming approach for making relocation decisions.
Using the information gathered in this study, we can predict the type of animals that are being adopted the most in each region and during each season of the year. To accomplish this, we utilize a two-phase approach. The first phase was leveraging the machine learning algorithms to predict the length of stay of each animal based on numerous factors (such as breed, size, and color). Phase-2 involves determining the best shelter to transport adoptable animals to increase the adoption rates, based on several conflicting criteria. This criterion includes predicted length of stay from phase-1, the distance between where the animal is currently housed and the potential animal shelters, transportation costs, and transportation time. Therefore, our goal is to increase adoption rates of pets in animal shelters by utilizing several factors to predict the length of stay, as well as determine the optimal animal shelter location where the animal will have the least amount stay in a shelter and most likely be adopted.
After predicting the length of stay of an incoming animal that is currently housed in the shelter l ′ using the machine learning algorithms, the next phase is to evaluate the potential relocation options for that animal. This strategic decision is specifically essential if the length of stay of the animal at its current location is high/very high. Nevertheless, while making this relocation decision, it is also necessary to consider the cost of transporting the animal between the shelters. For instance, if a dog is brought into a shelter in Houston, Texas, and is estimated to have a high/very high length of stay. Suppose if the dog is predicted to have a low length of stay at New York City and a medium length of stay at Oklahoma City, then a tradeoff has to be made between the relocation cost and the adoption speed. The objectives, length of stay, and relocation costs are conflicting and have to be minimized. Phase-2 attempts to yield a compromise solution that establishes a trade-off between these two criteria.
Goal programming (GP) is a widely used approach to solve problems involving multiple conflicting criteria. Under this method, each objective function is assigned as a goal, and a target value is specified for the individual criterion [ 27 ]. These target numbers can be fulfilled by the model with certain deviations, while the objective of the GP model is to minimize these deviations. Pertaining to this study, the desired values for the length of stay and relocation cost is pre-specified in the model and can be fulfilled with deviations. The GP model attempts to minimize these deviations. Thus, this technique attempts to produce a solution that is as close as possible to the targets, and the model solutions are referred to as the “most preferred solution” by prior studies (e.g., [ 28 , 29 ]).
As mentioned earlier, the primary task to be completed using this phase-2 goal programming approach is the relocation decisions considering the adoption speed and the cost of transporting the animal from the current location.
Model notations
Sets and Indices: | |
|---|---|
∈ | Set of shelter locations |
Parameters: | |
| Index for shelter location that is currently hosting the incoming animal |
| Size of the animal (small, medium, and large) |
| Type of animal (dog, cat, etc.) |
| Length of stay of the animal at shelter . is categorical and is obtained from the output of Phase-1. |
\( {r}_{l^{\prime },l} \) | Relocation cost if the animal is transported between shelters (that is currently hosting the animal) and |
, , | Remaining housing units available for animal type of size at shelter . Typically shelters are designed such that there is a fixed number of rooms for each animal’s size and type. |
| Upper bound on the length of stay |
| Upper bound on the relocation cost |
Goal Parameters: | |
| Desired value for the preferred length of stay |
| Desired value for the preferred relocation cost |
Variables: | |
|
|
0 otherwise | |
\( {d}_g^{-} \) | Negative deviation variable for goal |
\( {d}_g^{+} \) | Positive deviation variable for goal |
Goal programming model formulation
Goal constraints.
Objective 1: Minimize the overall length of stay of the animal under consideration (Eq. 1 ).
Goal constraint for objective 1: The corresponding goal constraint of objective 2 is given using Equation [ 30 ].
Objective 2: Minimize the overall relocation cost for transporting the animal under consideration (Eq. 3 ).
Goal constraint for objective 2: The corresponding goal constraint of objective 2 is given using Equation [ 18 ].
Hard constraints
Equation [ 9 ] ensures that the animal can be assigned to only one shelter.
The animal can be accommodated in shelter l only if there are a shelter capacity and type for that particular animal size category, and this is guaranteed using constraint [ 31 ]. It is important to note that both y and s are input parameters , whereas l is the set of shelters.
Equation [ 21 ] sets an upper limit on the length of stay category if the shelter l is assigned as the destination location. This prevents relocating animals to a shelter that might potentially have a high or very high length of stay.
Similarly, Equation [ 32 ] sets an upper limit on the relocation cost, if the shelter l is assigned as the destination location. This prevents relocating animals to a very far location. The current shelter location, l ′ , that is hosting the animal is an input parameter.
Objective function
Since the current problem focuses on minimizing the expected length of stay and relocation cost, the objective function of the goal programming approach is to reduce the sum of the weighted positive deviations given in Equations ([ 18 , 30 ], as shown in Equation [ 6 ].
where w g is the weight assigned for each goal g .
It is necessary to scale the deviation (since the objectives have different magnitudes as well as units) to avoid a biased solution.
If the scaling factors are represented by f g for goal g , then the scaled objective function is given in Equation [ 14 ].
Using this goal programming approach, the potential relocation options are evaluated considering the length of stay from phase-1. This phase-2 goal programming approach is useful, especially if the length of stay of the animal at its current location is high/very high, and a trade-off has to be made between relocation cost and length of stay. Phase-2 acts as a recommendation tool for assisting administrators with relocation decisions.
Nearly 3–4 million animals are euthanized out of the 6–8 million animals that enter shelters annually. The overall objective of this study is to increase the adoption rates of animals entering shelters by using key factors found in the literature to predict the length of stay. The second phase determines the best shelter location to transport animals using the goal programming approach to make relocation decisions. To accomplish this objective, first, the data is acquired from online sources as well as from numerous shelters across the United States. Once the data is acquired and cleaned, predictive models are developed using logistic regression, artificial neural network, gradient boosting, and random forest. The performance of these models is determined using three performance metrics: precision, recall, and F1 score.
The results demonstrate that the gradient boosting algorithm performed the best overall, with the highest precision, recall, and F1 score. Followed closely in second is the random forest algorithm, then the artificial neural network, and then finally, the logistic regression algorithm is the worst performer. We also observed from the data that the gradient boosting performed better when predicting the high or very high length of stay. Further observing the results, it is found that age for dogs (e.g., puppy, super senior), multicolor, and large and small size are important predictor variables.
The findings from this study can be utilized to predict how long an animal will stay in a shelter, as well as minimize their length of stay and chance of euthanization by determining which shelter location will most likely lead to the adoption of that animal. For future studies, we will implement phase 2, which will determine the best shelter location to transport animals using the goal programming approach to make relocation decisions.
Data description
A literature review is conducted to determine the factors that might potentially influence the length of stay for animals in shelters. These factors include gender, breed, age, and several other variables that are listed in Table 4 . These features will be treated as input variables for the machine learning algorithms. Overall, there are eight input or predictor variables and one output variable, which is the length of stay.
Animal shelter intake and outcome data are publicly made available by several state/city governments on their website (e.g., [ 33 , 34 ]), specifically in several southern and south-western states. These online sources provide datasets for animal shelters from Kentucky (150,843 data rows), California (334,016), Texas (155,115), and Indiana (4132). Since there is no nationwide database for animal shelters, information is also collected through individual animal shelters that conduct euthanization of animals. We contacted over 100 animal shelters across the United States and inquired for data on the factors mentioned in Table 4 . We received responses from 20 of the animal shelters that were contacted. Most responses received stated there was not enough staff or resources to be able to provide this information. From the responses that were received back, only four shelters were able to provide any information. Of those four, only two of the datasets contained the factors and information needed, which are Colorado (8488 data rows) and Arizona (4, 667 data rows).
The data that is collected from the database and animal shelters included information such as animal type, intake and outcome date, gender, color, breed, and intake and outcome status (behavior of animal entering the shelter and behavior of animal at outcome type). These records also included information on several types of animals, such as dogs, cats, birds, rabbits, and lizards. For this study, the focus is on dogs and cats. After filtering through these records, we found that only California, Kentucky, Colorado, Arizona, and Indiana had all of the factors needed for the study. Upon downloading data from the database and receiving data from the animal shelters, the acquired data underwent data integration, data transformation, and data cleaning (as detailed in Fig. 1 ). After data pre-processing, there are over 113,000 animal records.
Data cleaning methods
Next, data cleaning methods are utilized to detect discrepancies in the data, such as missing values, erroneous data, and inconsistencies. Data cleaning is an essential step for obtaining unbiased results [ 35 , 36 ]. In other words, identifying and cleaning erroneous data must be performed before inputting the data into the algorithm as it can significantly impact the output results.
The following is a list of commonly used data cleaning techniques in the literature [ 11 ]:
Substitution with Median: Missing or incorrect data are replaced with the median value for that predictor variable.
Substitution with a Unique Value: Erroneous data are replaced with a value that does not fall within the range that the input variables can accept (e.g., a negative number)
Discard Variable and Substitute with a Median: When an input variable has a significant number of missing values, these values are removed from the dataset, and the features that remain with missing or erroneous values are replaced with the median.
Discard Variable and Substitute with a Unique Value: Input variables with a significant number of missing values are removed from the dataset, and the features that remain with missing or erroneous values are coded as − 1.
Remove Incomplete Rows Entirely: Incomplete Rows are removed from the dataset.
Data preprocessing
Some animal breeds are listed in multiple formats and are changed to maintain uniformity. An example of this is a Russian Blue cat, which is formatted in several ways such as “Russian”, “Russian Blue”, and “RUSSIAN BLUE”. Animals with multiple breeds such as “Shih Tzu/mix” or “Shih Tzu/Yorkshire Terr” are classified as the first breed listed. Other uncommon breeds are classified as “other” for simplicity. Finally, all animal breeds are summarized into three categories (small, medium, or large) using the American Kennel Clubs’ breed size classification [ 37 ]. Part of the data cleansing process also includes categorizing multiple colors found throughout the sample size into five distinct color categories (brown, black, blue, white, and multicolor). We classified age into five categories for dogs and cats (puppy or kitten, adolescent, adult, senior, super senior). The puppy or kitten category includes data points 0–1 year, adolescence includes data points 2–3 years old, adulthood includes animals 4–7 years of age, and senior animals are 8–10 years of age. Any animal that is older than ten years are categorized as a super senior, based on the recommendations provided in Wapiti Labs [ 38 ].
As mentioned previously, the output variable is the length of stay and is classified as low, medium, high, and very high/euthanization. The length of stay is calculated by taking the difference between the intake date and outcome date. To remove erroneous data entries and special cases, the number of days in the animal shelter is also capped at a year. The “low” category represents animals that are returned (in which case, they are assigned the days in the shelter as 0) or spent less than 8 days before getting adopted. It is important to keep these animals at the shelter so that the owner may find them or they are transferred to their new homes. Animals that stayed in a shelter for 9–42 days and are adopted are categorized as “medium” length of stay. The “high” category is given to animals that stayed in the shelter for 43–365 days. Finally, animals that are euthanized are categorized as “very high”.
After integrating all data points from each animal shelter, the sample size includes 119,691 records. After the evaluation of these data points, 5436 samples are found to have miscellaneous (such as a negative length of stay) or missing values. After applying data cleaning techniques, the final cleaned dataset includes 114,256 data points, with 50,466 cat- and 63,790 dog-records.
Machine learning algorithms to predict the length of stay
The preprocessed records are then separated into training and testing datasets based on the type of classification algorithm used. Studies have demonstrated the need for testing and comparing machine learning algorithms, as the performance of the models depends on the application. While an algorithm may develop a predictive model that performs well in one application, it may not be the best performing model for another. A comparison between the statistical models is conducted to determine the overall best performing model. In this section, we provide a description as well as the advantages of each classification algorithm that is utilized in this study.
Logistic regression
Logistic regression (LR) is a machine learning algorithm that is used to understand the probability of the occurrence of an event [ 39 ]. It is typically used when the model output variable is binary or categorical (see Fig. 6 ), unlike linear regression, where the dependent variable is numeric [ 40 ]. Logistic regression involves the use of a logistic function, referred to as a “sigmoid function” that takes a real-valued number and maps it into a value between 0 and 1 [ 41 ]. The probability that the length of stay of the animal at a specific location will be low, medium, high, or very high, is computed using the input features discussed in Table 4 .
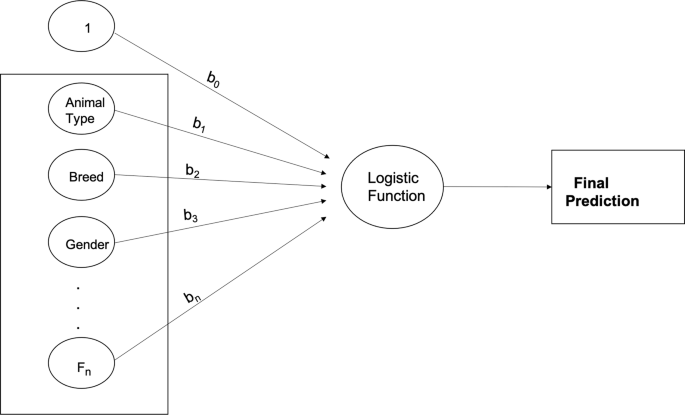
Pictorial Representation of the Logistic Regression Algorithm
The linear predictor function to predict the probability that the animal in record i has a low, medium, high, and very high length of stay categories is given by Equations ( 11 ) –[ 3 ], respectively.
Where β v , l is a set of multinomial logistic regression coefficients for variable v of the length of stay category l , and x v , i is the input feature v corresponding to data observation i .
Artificial neural network
Artificial Neural Network (ANN) algorithms were inspired by the brain’s neuron, which transmits signals to other nerve cells [ 40 , 42 ]. ANN’s were designed to replicate the way humans learn and were developed to imitate the operational sequence in which the body sends signals in the nervous system [ 43 ]. In an ANN, there exists a network structure with directional links connecting multiple nodes or “artificial neurons”. These neurons are information-processing units, and the ties that connect them represent the relationship between each of the connected neurons. Each ANN consists of three layers - the input layer, hidden layer, and the output layer [ 32 , 44 ]. The input layer is where each of the input variables is fed into the artificial neuron. The neuron will first calculate the sum of multiple inputs from the independent variables. Each of the connecting links (synapses) from these inputs has a characterized weight or strength that has a negative or positive value [ 32 ]. When new data is received, the synaptic weight changes, and learning will occur. The hidden layer learns the relationship between the input and output variables, and a threshold value determines whether the artificial neuron will fire or pass the learned information to the output layer, as shown in Fig. 7 . Finally, the output layer is where labels are given to the output value, and backpropagation is used to correct any errors.
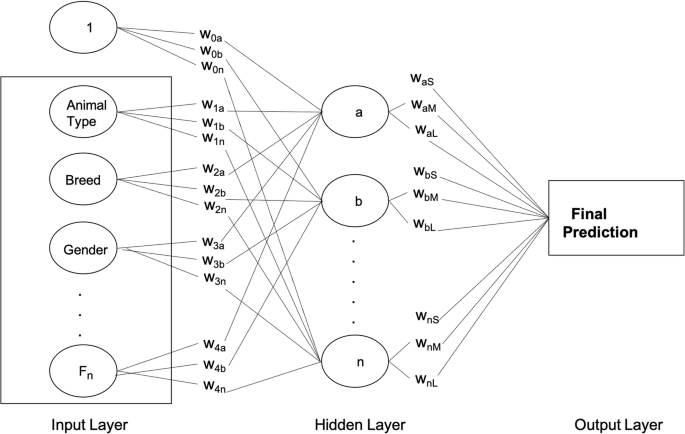
Pictorial Representation of the Artificial Neural Networks
Random Forest
The Random Forest (RF) algorithm is a type of ensemble methodology that combines the results of multiple decision trees to create a new predictive model that is less likely to misclassify new data [ 30 , 45 ]. Decision Trees have a root node at the top of the tree that consists of the attribute that best classifies the training data. The attribute with the highest information gain (given in Eq. 16 ) is used to determine the best attribute at each level/node. The root node will be split into more subnodes, which are categorized as a decision node or leaf node. A decision node can be divided into further subnodes, while a leaf node cannot be split further and will provide the final classification or discrete label. RF algorithm uses mtree and ntry as the two main parameters in developing the multiple parallel decision trees. Mtree specifies how many trees to train in parallel, while ntry defines the number of independent variables or attributes to choose to split each node [ 30 ].. The majority voting from all parallel trees gives the final prediction, as given in Fig. 8 .
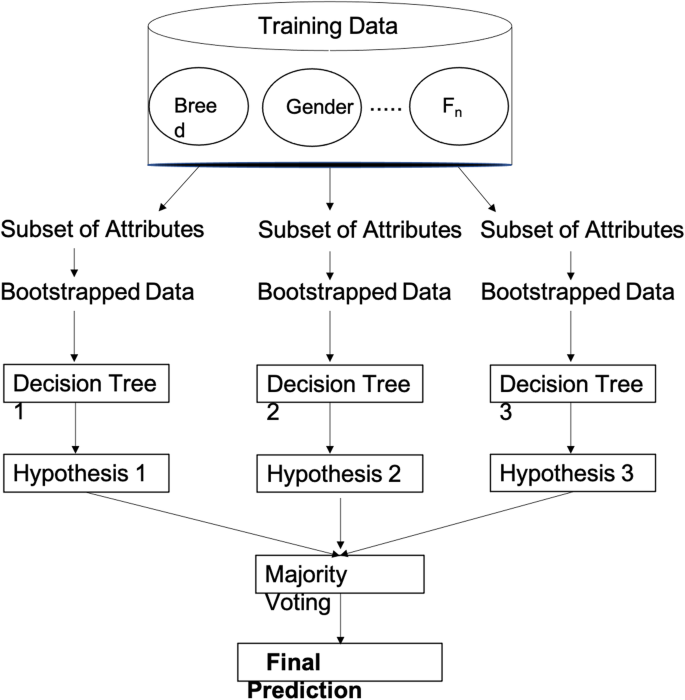
Pictorial Representation of the Random Forest Algorithm
Gradient boosting
Boosting is another type of ensemble method that combines the results from multiple predictive algorithms to develop a new model. While the RF approach is built solely on decision trees, boosting algorithms can use various algorithms such as decision trees, logistic regression, and neural networks. The primary goal of boosting algorithms is to convert weak learners into stronger ones by leveraging weighted averages to identify “weak classifiers” [ 31 ]. Samples are assigned an initial uniformed weight, and when incorrectly labeled by the algorithm, a penalty of an increase in weight is given [ 46 ]. On the other hand, samples that are correctly classified by the algorithm will decrease in weight. This process of re-weighing is done until a weighted vote of weak classifiers is combined into a robust classifier that determines the final labels or classification [ 46 ]. For our study, gradient boosting (GB) will be used on decision trees for the given dataset, as illustrated in Fig. 9 .
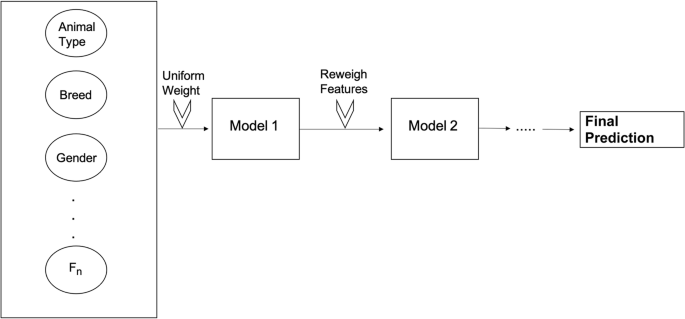
Pictorial Representation of Boosting Algorithm
Machine learning model parameters
The clean animal shelter data is split into two datasets: training and testing data. These records are randomly placed in the two groups to train the algorithms and to test the model developed by the algorithm. 80% of the data is used to train the algorithm, while the other 20% is used to test the predictive model. To avoid overfitting, a tenfold cross-validation procedure is used on the training data. There are no parameters associated with the machine learning of logistic regression algorithms. However, a grid search method is used to tune the parameters of the random forest, gradient boosting, and artificial neural network algorithms. This allows the best parameter in a specific set to be chosen by running an in-depth search by the user during the training period.
The number of trees in the random forest and gradient boosting algorithms is changed from 100 to 1000 in increments of 100. A learning rate of 0.01, 0.05, and 0.10 is used based on the recommendations of previous studies [ 47 ]. The minimum observations for the trees’ terminal node are set to vary from 2 to 10 in increments of one, while the splitting of trees varies from 2 to 10 in increments of two. A feed-forward method is used to develop the predictive model using the artificial neural network algorithm. The feed-forward algorithm consists of three layers (input, hidden, output) as well as backpropagation learning. The independent and dependent variables represent the input and output layers. Since the input and output layers are already known, an optimal point is reached for the number of nodes when between 1 and the number of predictors. This means that for our study, the nodes of the hidden layer vary from 1 to 8. The learning rate values used to train the ANN are 0.01, 0.05, and 0.10.
To find the optimal setting for each machine learning algorithm, a thorough search of their corresponding parameter space is performed.
Performance measures
In this study, we use three performance measures to evaluate the ability of machine learning algorithms in developing the best predictive model for the intended application. The measures considered are precision, F1 score, and sensitivity/recall to determine the best model given the inputted data samples. Table 5 provides a confusion matrix to define the terms used for all possible outcomes.
Precision evaluates the number of correct, true positive predictions by the algorithm while still considering the incorrectly predicted positive when it should have been negative (Eq. 17 ). By having high precision, this means that there is a low rate of false positives or type I error. Sensitivity or recall evaluates the number of true positives that are correctly predicted by the algorithm while considering the incorrectly predicted negative when it should have been positive (Eq. 18 ). Recall is a good tool to use when the focus is on minimizing false negatives (type II error). F1 score (shown in Eq. 19 ) evaluates both type I and type II errors and assesses the ability of the model to resist false positives and false negatives. This performance metric evaluates the robustness (low number of missed classifications), as well as the number of data points that are classified correctly by the model.
Availability of data and materials
Most of the datasets used and/or analyzed during the current study were publicly available online as open source data. The data were available in the website details given below:
https://data.bloomington.in.gov/dataset
https://data.louisvilleky.gov/dataset
https://data.sonomacounty.ca.gov/Government
We also obtained data from Sun Cities 4 Paws Rescue, Inc., and the Rifle Animal Shelter. No administrative permission was required to access the raw data from these shelters.
Abbreviations
Logistic Regression
Artificial Neural Network
Gradient Boosting
Goal Programming
Coefficient of Variation
Anderson KA, Brandt JC, Lord LK, Miles EA. Euthanasia in animal shelters: Management's perspective on staff reactions and support programs. Anthrozoös. 2013;26(4):569–78. https://doi.org/10.2752/175303713X13795775536057 .
Article Google Scholar
Clevenger J, Kass PH. Determinants of adoption and euthanasia of shelter dogs spayed or neutered in the University of California veterinary student surgery program compared to other shelter dogs. J Veterinary Med Educs. 2003;30(4):372–8.
Animal Humane Society. (n.d.). Retrieved November 2019, from https://www.animalhumanesociety.org/ .
Home. (2016, July 15). Retrieved November 2019, from http://www.americanhumane.org/ .
Rogelberg SG, DiGiacomo N, Reeve CL, Spitzmüller C, Clark OL, Teeter L, et al. What shelters can do about euthanasia-related stress: an examination of recommendations from those on the front line. J Appl Anim Welf Sci. 2007;10(4):331–47. https://doi.org/10.1080/10888700701353865 .
Article CAS PubMed Google Scholar
Hennessy MB, Voith VL, Mazzei SJ, Buttram J, Miller DD, Linden F. Behavior and cortisol levels of dogs in a public animal shelter, and an exploration of the ability of these measures to predict problem behavior after adoption. Appl Anim Behav Sci. 2001;73(3):217–33.
Shore ER. Returning a recently adopted companion animal: Adopters' reasons for and reactions to the failed adoption experience. J Appl Anim Welf Sci. 2005;8(3):187–98.
Article CAS Google Scholar
Morris KN, Gies DL. Trends in intake and outcome Data for animal shelters in a large U.S. metropolitan area, 1989 to 2010. J Appl Anim Welf Sci. 2014;17(1):59–72. https://doi.org/10.1080/10888705.2014.856250 .
Fantuzzi JM, Miller KA, Weiss E. Factors relevant to adoption of cats in an animal shelter. J Appl Anim Welf Sci. 2010;13(2):174–9.
Brown WP, Morgan KT. Age, breed designation, coat color, and coat pattern influenced the length of stay of cats at a no-kill shelter. J Appl Anim Welf Sci. 2015;18(2):169–80.
Srinivas, S., & Rajendran, S. (2017). A Data-driven approach for multiobjective loan portfolio optimization using machine-learning algorithms and mathematical programming. In big Data analytics using multiple criteria decision-making models (pp. 175-210): CRC press.
Waller MA, Fawcett SE. Data science, predictive analytics, and big Data: a revolution that will transform supply chain design and management. J Bus Logist. 2013;34(2):77–84.
Kantardzic M. DATA MINING: concepts, models, methods, and algorithms. 2nd ed: IEEE: Wiley; 2019.
Jordan MI, Mitchell TM. Machine learning: trends, perspectives, and prospects. Science. 2015;349(6245):255–60.
Kavakiotis I, Tsave O, Salifoglou A, Maglaveras N, Vlahavas I, Chouvarda I. Machine learning and Data mining methods in diabetes research. Computational Structural Biotechnol J. 2017;15:104–16. https://doi.org/10.1016/j.csbj.2016.12.005 .
Neely MN, van Guilder MG, Yamada WM, Schumitzky A, Jelliffe RW. Accurate detection of outliers and subpopulations with Pmetrics, a nonparametric and parametric pharmacometric modeling and simulation package for R. Ther Drug Monit. 2012;34(4):467–76. https://doi.org/10.1097/FTD.0b013e31825c4ba6 .
Article PubMed PubMed Central Google Scholar
Bissantz N, Munk A, Scholz A. Parametric versus non-parametric modelling? Statistical evidence based on P-value curves. Mon Not R Astron Soc. 2003;340(4):1190–8. https://doi.org/10.1046/j.1365-8711.2003.06377.x .
Dietterich TG. Ensemble methods in machine learning. Berlin: Heidelberg; 2000.
Book Google Scholar
Pandey M, S, T. A comparative study of ensemble methods for students' performance modeling. Int J Computer ApplS. 2014;103:26–32. https://doi.org/10.5120/18095-9151 .
Reeve CL, Rogelberg SG, Spitzmüller C, Digiacomo N. The caring-killing paradox: euthanasia-related strain among animal-shelter Workers1. J Appl Soc Psychol. 2005;35(1):119–43. https://doi.org/10.1111/j.1559-1816.2005.tb02096.x .
Gates MC, Zito S, Thomas J, Dale A. Post-adoption problem Behaviours in adolescent and adult dogs rehomed through a New Zealand animal shelter. Animals : an open access journal from MDPI. 2018;8(6):93. https://doi.org/10.3390/ani8060093 .
Weiss E, Gramann S, Drain N, Dolan E, Slater M. Modification of the feline-Ality™ assessment and the ability to predict adopted Cats' behaviors in their new homes. Animals : an open access journal from MDPI. 2015;5(1):71–88. https://doi.org/10.3390/ani5010071 .
Normando S, Stefanini C, Meers L, Adamelli S, Coultis D, Bono G. Some factors influencing adoption of sheltered dogs. Anthrozoös. 2006;19(3):211–24.
Protopopova A, Mehrkam LR, Boggess MM, Wynne CDL. In-kennel behavior predicts length of stay in shelter dogs. PLoS One. 2014;9(12):e114319.
Wells DL, Graham L, Hepper PG. The influence of length of time in a rescue shelter on the behaviour of Kennelled dogs. Anim Welf. 2002;11(3):317–25.
CAS Google Scholar
Zhong G, Jiao W, Gao W, Huang K. Automatic design of deep networks with neural blocks. Cogn Comput. 2020;12(1):1–12.
Rajendran S, Ravindran AR. Multi-criteria approach for platelet inventory management in hospitals. Int J Operational ResS. 2020;38(1):49–69.
Bastian ND, McMurry P, Fulton LV, Griffin PM, Cui S, Hanson T, Srinivas S. The AMEDD uses goal programming to optimize workforce planning decisions. Interfaces. 2015;45(4):305–24.
Rajendran S, Ansaripour A, Kris Srinivasan M, Chandra MJ. Stochastic goal programming approach to determine the side effects to be labeled on pharmaceutical drugs. IISE Transactions on Healthcare Systems Engineering. 2019;9(1):83–94.
Cutler DR, Edwards TC Jr, Beard KH, Cutler A, Hess KT, Gibson J, Lawler JJ. Random forests for classification in ECOLOGY. Ecology. 2007;88(11):2783–92.
Friedman J, Hastie T, Tibshirani R. Additive logistic regression: a statistical view of boosting (with discussion and a rejoinder by the authors). Ann Stat. 2000;28(2):337–407.
Ge Z, Song Z, Ding SX, Huang B. Data mining and analytics in the process industry: the role of machine learning. IEEE Access. 2017;5:20590–616.
Open Data: City of Austin Texas: Open Data: City of Austin Texas. (n.d.). Retrieved March 2019, from https://data.austintexas.gov//Health-and-Community-Services/Austin-Animal-Center-Outcomes/9t4d-g238 .
County of Sonoma: Open Data: Open Data. (n.d.). Retrieved March 2019, from https://data.sonomacounty.ca.gov/Government/Animal-Shelter-Intake-and-Outcome/924a-vesw .
Kambli A, Sinha AA, Srinivas S. Improving campus dining operations using capacity and queue management: a simulation-based case study. J Hosp Tour Manag. 2020;43:62–70.
Rajendran S, Zack J. Insights on strategic air taxi network infrastructure locations using an iterative constrained clustering approach. Transport Res Part E: Logistics and Transportation Review. 2019;128:470–505.
American Kennel Club. (n.d.). Retrieved November 2019, from http://www.akc.org/ .
Elk Antler Supplements & Chews: Wapiti Labs, Inc. (n.d.). Retrieved November 2019, from https://www.wapitilabsinc.com/ .
Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code for Biol Med. 2008;3(1):17.
Delen D, Walker G, Kadam A. Predicting breast cancer survivability: a comparison of three data mining methods. Artif Intell Med. 2005;34(2):113–27.
Kim A, Song Y, Kim M, Lee K, Cheon JH. Logistic regression model training based on the approximate homomorphic encryption. BMC Med Genet. 2018;11(4):83.
Google Scholar
Srinivas S, Ravindran AR. Optimizing outpatient appointment system using machine learning algorithms and scheduling rules: a prescriptive analytics framework. Expert Syst Appl. 2018;102:245–61. https://doi.org/10.1016/j.eswa.2018.02.022 .
LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521:436.
Shih H, Rajendran S. Comparison of time series methods and machine learning algorithms for forecasting Taiwan blood Services Foundation’s blood supply. Journal of healthcare engineering. 2019;2019.
Srinivas S, Salah H. Consultation length and no-show prediction for improving appointment scheduling efficiency at a cardiology clinic: a data analytics approach. Int J Med Inform. 2020;145:104290.
Rokach L. Ensemble-based classifiers. Artif Intell Rev. 2010;33(1):1–39.
Srinivas S. A machine learning-based approach for predicting patient punctuality in ambulatory care centers. Int J Environ Res Public Health. 2020;17(10):3703.
Download references
Acknowledgments
We would like to thank the Sun Cities 4 Paws Rescue, Inc., and the Rifle Animal Shelter for providing the length of stay reports in order to complete this study.
This research was not funded by any agency/grant.
Author information
Authors and affiliations.
Department of Bioengineering, University of Missouri Columbia, Columbia, MO, 65211, USA
Janae Bradley
Department of Industrial and Manufacturing Systems Engineering, University of Missouri Columbia, Columbia, MO, 65211, USA
Suchithra Rajendran
Department of Marketing, University of Missouri Columbia, Columbia, MO, 65211, USA
You can also search for this author in PubMed Google Scholar
Contributions
JB performed data mining, data cleaning and analyses of the animal shelter data and machine learning algorithms. JB was also a major contributor in writing the manuscript. SR performed data mining, cleaning, and analyses of the machine learning algorithms, as well as the goal programming. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Suchithra Rajendran .
Ethics declarations
Ethics approval and consent to participate.
Most of the datasets used in this study are open source and are publicly available. The remaining data was collected from animal shelters with their consent to use the data for research purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bradley, J., Rajendran, S. Increasing adoption rates at animal shelters: a two-phase approach to predict length of stay and optimal shelter allocation. BMC Vet Res 17 , 70 (2021). https://doi.org/10.1186/s12917-020-02728-2
Download citation
Received : 07 January 2020
Accepted : 22 December 2020
Published : 05 February 2021
DOI : https://doi.org/10.1186/s12917-020-02728-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Animal shelter
- High euthanization rates
- Machine learning algorithms
- Prediction models
- Goal programming approach
- Decision support tool
BMC Veterinary Research
ISSN: 1746-6148
- General enquiries: [email protected]
'Adoption, not abortion?' How the Dobbs decision is affecting adoption in the U.S.

Madelynn Ballenger discovered she was pregnant for the second time at 20 years old. Already a single mother to a young son, she didn’t know whether she could take on a second child physically or financially.
“It was really, really scary,” Ballenger said. “I didn’t have a job. I wasn’t in a good position to be expecting another child.”
It was September 2021, the month Texas’ ban on abortions after six weeks took effect, and Ballenger was five weeks pregnant. That left her little time to decide whether to keep the baby or terminate the pregnancy — if she could even find an available appointment to get an abortion.
“I was already so stressed out, and I was just like, how am I supposed to make this decision in such a short amount of time?” Ballenger said. “How am I supposed to know what’s good for me, what’s good for my whole situation, in just a few days? No woman should be forced to make that kind of decision in less than two weeks. That’s just not humane.”
She opted to carry the baby to term. Then, 48 hours after she gave birth to a healthy boy, Ballenger made the agonizing decision to place him in adoptive care.
“It was the hardest thing I’ve ever done,” she said. “It’s the most difficult thing I’ll ever do.”

For years, anti-abortion activists argued that overturning Roe v. Wade would lead more women with unwanted pregnancies to turn to adoption. “Adoption! Not abortion!” was a common message featured on posters and chanted through megaphones at anti-abortion rallies. But more than a year after the Supreme Court’s Dobbs decision , its impact on the adoption landscape is proving to be multifaceted and complicated to measure.
Some adoption agencies are seeing significant upticks in the number of infants placed in adoptive care, while others say it’s still too early to tell what role Dobbs is playing.
Kristen Hamilton, the director of communications at the nonprofit National Council for Adoption, one of the nation’s largest networks of adoption professionals, said the group has seen “a lot of variances” among adoption agencies in states with strict abortion laws.
“In some cases, they are seeing an uptick in the number of babies that are being placed for adoption, while in other cases, things have remained relatively similar to what they were before the Dobbs decision,” Hamilton said.
Mark Melson, the president and CEO of the Texas-based Gladney Center for Adoption, which facilitates adoptions nationwide, said the center has seen a 30% increase in infant domestic adoptions in the past year. Inquiries from pregnant women who call to learn about their adoption options, meanwhile, are up 55%, he said.

Melson said that the trend may partly be due to a decline in Covid rates and restrictions but that he believes the Dobbs ruling has played a key role.
“In conversations we’ve had with our birth mothers, some have indicated that had they had an ability to get an abortion, they at least would have considered it,” he said.
Robert Lamarche, the director of ACF Adoptions, an agency based in Florida, said that since Dobbs, he has noticed a change in the stage of pregnancy at which women call the agency.
“We used to typically get calls from women in their second trimester,” Lamarche said. “Now we get calls from women when they’re four weeks pregnant, five weeks pregnant, calling to figure out their options.”
But Lamarche said his agency hasn’t seen a significant uptick in adoption placements. He added, though, that if Florida’s Supreme Court allows its ban on abortions after six weeks to go into effect, that may change.
Will more babies with medical challenges be put up for adoption?
A primary challenge in assessing national adoption trends is that states don’t have to report infant domestic adoptions.
“Unlike adoptions from foster care or adoptions that take place through the intercountry adoption system, there is no requirement for infant domestic adoption data to be aggregated and reported out publicly,” Hamilton said.
It’s also hard to estimate the number of women who, facing unwanted pregnancies, choose to parent their children, rather than give them up for adoption. Past research suggests that’s the more common choice: A 2017 study found that women were more likely to parent or have abortions than to place infants for adoption, regardless of their education levels, race, socioeconomic statuses or familial arrangements.
Lamarche said he is concerned the Dobbs decision could still cause more babies with genetic or physical anomalies, including Down syndrome, to be placed in adoptive care.
“A lot of those genetic anomalies are not detected until the second trimester, and these might have been pregnancies people would choose to terminate,” he said.
His agency is able to find homes for all the medically challenged babies placed in its hands, Lamarche added, but he worries that could change.
“If the number goes up 25 to 30%, we’re going to have a problem, because we’re not going to have families for all the children,” he said.
More opportunities for predatory ‘baby brokers’
Kelsey Vander Vliet Ranyard, the director of policy and advocacy at Ethical Family Building, a nonprofit organization focused on making domestic adoptions safer and more transparent, said she worries that the number of vulnerable women pursued by so-called baby brokers could rise.
Such unlicensed agents, Ranyard said, charge fees to would-be adoptive parents. Then, in some cases, women who aren’t fluent English speakers are coerced into signing adoption papers without fully understanding what they are signing. Other times, Ranyard said, pregnant women get duped by slick internet ads that suggest they will be financially compensated for relinquishing their babies.
“I do think there’s a potential for more women to be coerced and forced to make choices they never wanted to make,” she said.
Ranyard, who gave her own newborn up for adoption in 2016, added that more also needs to be done to support birth mothers, including providing better postpartum care and establishing a system to connect birth mothers with therapists or support groups.
“Adoption is not something that is over the day the birth mother signs the adoption papers,” Ranyard said. “That’s a decision she’s going to be thinking about every day, maybe for the rest of her life.”

Cases of postpartum depression traditionally are detected and monitored by pediatricians who check in on new mothers during their newborns’ medical visits. Women who place their babies in adoptive care, though, don’t often get that kind of care — nor are they routinely provided with mental health services. A survey last year by the National Council for Adoption found that only 50% of birth mothers who requested counseling received it.
“There is absolutely a gap between what women need in their healing journey after placement and what they’re actually receiving,” Hamilton said.
Ballenger said she suffered from postpartum depression.
“They say, ‘OK, if you don’t want to do an abortion, just do an adoption.’ But it’s not that simple,” she said, adding: “I still have bad days. I still remember those days [with him] in the hospital. Like they’re burned into my head forever. It’s traumatizing.”
Still, Ballenger said, she is grateful to have entered into an open adoption and selected a couple who has provided a loving home for her son.

“Just seeing him with his adoptive parents has helped me come up with a lot of clarity. Just seeing how happy he is, how taken care of he is, how amazing his life’s going to be,” she said.
Ballenger has since made a series of TikTok videos to help other birth mothers know they’re not alone.
“It’s OK to make this decision. It’s going to be hard,” she said, addressing those women. “There are going to be days where you feel like you can’t go on anymore. But it’s going to be OK.”
Mary Pflum is a national field producer for NBC News, based in New York.
To read this content please select one of the options below:
Please note you do not have access to teaching notes, breathing new life: exploring the cutting edge of technology adoption in the textile industry.
Research Journal of Textile and Apparel
ISSN : 1560-6074
Article publication date: 8 July 2024
This comprehensive review study aims to analyze the current state of technology adoption (TA) within the textile industry, with a particular focus on the economic, environmental, and social dimensions.
Design/methodology/approach
Twenty-four articles from the Scopus database, spanning from January 2015 to March 2024, were meticulously selected for analysis. The review uses a qualitative approach, synthesizing diverse perspectives to provide a holistic understanding of TA in the textile sector.
The review highlights a noticeable lag in the adoption of new technologies, particularly in developing nations like India, within the textile industry. Despite significant technological advancements, there remains a gap between innovation and implementation. Sustainable approaches to mitigate environmental impacts emerge as a key focus, underscoring the need for operational enhancements and policy interventions.
Research limitations/implications
The study’s reliance on articles from the SCOPUS database presents a limitation, potentially overlooking relevant research from other sources.
Practical implications
Practitioners in the textile industry can benefit from the review’s insights by understanding the importance of integrating technological advancements sustainably. By leveraging innovative solutions and collaborating with policymakers, firms can enhance operational efficiency while minimizing environmental impacts, thus ensuring long-term competitiveness.
Social implications
Efforts to advance TA in the textile industry have significant social implications, including job creation, improved working conditions and reduced environmental harm.
Originality/value
Study addressed the insights for policymakers, industry practitioners and researchers seeking to drive technological innovation while addressing socio-economic and environmental challenges.
- Technology adoption
- Textile industry
- Sustainable manufacturing
- Literature review
Acknowledgements
Declaration of interest statement .
Funding: No funding support has been availed from any source for this study.
Conflicts of interest: The authors declare that they have no conflict of interest in connection to this research study.
Availability of data – All the data are provided in the manuscripts themselves. No extra or hidden data is there.
Chourasiya, R. and Pandey, S. (2024), "Breathing new life: exploring the cutting edge of technology adoption in the textile industry", Research Journal of Textile and Apparel , Vol. ahead-of-print No. ahead-of-print. https://doi.org/10.1108/RJTA-03-2024-0043
Emerald Publishing Limited
Copyright © 2024, Emerald Publishing Limited
Related articles
All feedback is valuable.
Please share your general feedback
Report an issue or find answers to frequently asked questions
Contact Customer Support

USask establishes Jarislowsky and BMO Chair in Regenerative Agriculture
Dr. Kate Congreves (PhD) has been appointed the Jarislowsky and BMO Chair in Regenerative Agriculture at the University of Saskatchewan (USask) to lead research supporting the wider-scale adoption of beneficial production and environmental practices necessary for food security.
“As the new chair, Dr. Congreves will strengthen Canada’s agriculture sector by providing leadership in regenerative agriculture, working with producers to identify and evaluate best practices, and creating new teaching and mentoring opportunities for students,” said Dr. Angela Bedard-Haughn (PhD), dean of the College of Agriculture and Bioresources at USask. “This investment in USask research means new potential to maximize environmental benefits of agricultural systems and minimize environmental impacts, all while maintaining and increasing food production.”
The Jarislowsky and BMO Chair in Regenerative Agriculture was established by a $4 million endowment with a donation of $2 million from the Jarislowsky Foundation, $1 million from BMO, and $1M from the USask Greystone Heritage Trust to significantly expand research capacity in regenerative agriculture at USask.
“Building a more sustainable future has been a long-standing priority for the Jarislowsky Foundation,” said Stephen Jarislowsky, founder and president of the foundation. “The research led by Dr. Congreves and her team will make an impact on agriculture, climate, and food production through advancing the science and encouraging the adoption of sustainable farming practices across Canada and beyond.”
The Jarislowsky Foundation supports research chairs to promote excellence in teaching, mentoring and research.
“At BMO, we are long-time supporters of the agricultural sector and proud of our clients, who are among the most innovative producers in the world in regenerative agriculture,” said Allison Hakomaki, head of Agriculture, Public Sector and Emerging Industries, BMO. “We know how vital sustainable practices are to the resilience of our farmers and the future of food in Canada and, driven by our purpose, to Boldly Grow the Good in business and life and our commitment to a sustainable future , we recognize the importance of supporting initiatives like the University of Saskatchewan’s research in this field.”
During the chair’s five-year term, Congreves’ research will inform sustainable nitrogen (N) management for healthy agroecosystems. Nitrogen is simultaneously an essential nutrient for crop production and a major environmental concern. Better understanding of N cycling is necessary and is a timely priority with policymakers interested in developing strategies to better manage N. Congreves will explore interdisciplinary collaborations with agricultural researchers in other areas of expertise such as water, livestock and health, and with social scientists, economists, and philosophers to develop evidence-based recommendations that will be pertinent to Canada’s progress towards a sustainable future.
“Regenerative agriculture is an ecosystem-based approach to crop production—one that embodies reciprocity with the land by improving soil health, enhancing biodiversity, and reducing negative impacts of inputs like N fertilizer. A promising strategy to design regenerative agroecosystems is the diversification of cropping systems,” said Congreves, an associate professor in the College of Agriculture and Bioresources.
Understanding how diversification can tighten the N cycle for sustainable soil management and regenerative agriculture is a major focus. Congreves’ work explores the controls on soil N transformations, plant N uptake, and N losses, and is aimed at better understanding the flow of N and its cycling in diversified agroecosystems.
Congreves joined USask in 2017 and leads an internationally recognized research program focused on sustainable agriculture and horticulture with an emphasis on diversified field crop and vegetable crop production systems. She specializes in soil health measurement and management, nitrogen cycling and use efficiency, and greenhouse gas emissions and mitigation. Congreves is an award-winning researcher and serves USask as a Sustainability Faculty Fellow.
The chair’s research will be supported by the BMO Soil Analytical Lab at USask, recently established to help alleviate a critical bottleneck in digital agriculture research and providing key analytical capabilities for research in regenerative agriculture.
Together, we will undertake the research the world needs. We invite you to join by supporting critical research at USask.
USask receives record $417M in awarded research funding in 2023/24
Usask achieves personal best in qs world university rankings, usask researchers discover swath of previously undocumented polar bear dens, usask researchers part of discovery of three extinct walnuts in arctic.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Factors Associated with Adoption and Adoption Intentions of Nonparental Caregivers
Matthew d. bramlett.
1 National Center for Health Statistics
Laura F. Radel
2 U.S. Department of Health and Human Services’ Office of the Assistant Secretary for Planning and Evaluation
Data from the 2011–2012 National Survey of Children’s Health and the 2013 National Survey of Children in Nonparental Care were used to fit a multinomial logistic model comparing three groups to those who never considered adoption: those who ever considered, but are not currently planning adoption; those planning adoption; and those who adopted. Adoption may be more likely when the caregiver is a nonkin foster parent, a foster care agency was involved, and/or financial assistance is available. Those with plans to adopt but who have not adopted may face adoption barriers such as extreme poverty, lower education and being unmarried.
INTRODUCTION
Thousands of children in America are waiting to be adopted from foster care. The latest Adoption and Foster Care Analysis and Reporting System (AFCARS) report shows that from 2009 to 2013, there were approximately 400,000 children in foster care at any given time, with about the same number (250,000) entering and exiting foster care each year. More than 100,000 children are officially “waiting to be adopted” in each year, but less than 60,000 actually are adopted annually ( US DHHS, 2014a ). The number of children adopted from foster care has consistently been between 50,000 and 57,000 since at least 2002 despite the number waiting to be adopted being consistently twice as high or more ( US DHHS, 2014b ).
Researchers such as Leathers et al. (2012) have observed that, “little research has focused on factors that predict adoption or influence foster parents’ decision to adopt” (p.892). One factor that has been examined often using administrative data on children in foster care is the type of foster caregiver: kin to the child or not. Carnochan, Moore and Austin (2013) discuss numerous studies that found that kinship care is associated with longer stays in foster care. Berrick and colleagues (1994) found that kin foster parents are less likely than nonkin foster parents to adopt, and that a frequent reason was that the kin foster parent felt that the child was “already family” and did not feel a need to adopt to make that relationship more formalized, even though many intended to care for the child throughout childhood anyway ( Berrick, Barth & Needell, 1994 : p.57). Nationally, of adopted children in 2007 who had been adopted from foster care, 23% of adoptions were by relatives ( Malm, Vandivere & McKlindon, 2011 ).
Many other factors have been found to differentiate adoptive foster families from nonadoptive foster families. Those that have been found to predict adoption include: characteristics of the child, such as younger age ( Carnochan et al ., 2013 ; McDonald et al ., 2007 ; Snowden et al ., 2008 ; Connell et al ., 2006 ); characteristics of the birth family, such as whether the parental rights were relinquished ( Carnochan et al ., 2013 ); characteristics of the adoptive family, such as white race ( Carnochan et al ., 2013 ) and being married ( Carnochan et al ., 2013 , McDonald et al ., 2007 ;); and system characteristics such as receipt of Temporary Assistance for Needy Families (TANF) or subsidies ( McDonald et al ., 2007 ).
Factors that have been found to be associated with lower likelihood of adoption include characteristics of the child such as black race ( Carnochan et al ., 2013 ; McDonald et al ., 2007 ; Snowden et al ., 2008 ); characteristics of the birth family, such as whether the child was physically or sexually abused ( Carnochan et al ., 2013 ; McDonald et al ., 2007 ; Connell et al ., 2006 ); and system characteristics such as negative caseworker attitudes ( Carnochan et al ., 2013 ) and higher number of prior placements ( Carnochan et al ., 2013 ; McDonald et al ., 2007 ). Yampolskaya et al., (2014) suggest that older children with a history of being abused have very low odds of being adopted.
Physical and mental disability have shown inconsistent effects in prior research. McDonald and colleagues (2007) found that emotional problems and mental retardation were related to longer waits for adoption, while other diagnosed conditions showed a similar but weaker relationship. Similarly, Connell et al . (2006) found that diagnosed mental conditions were associated with lower likelihood for adoption while disability had no effect. Some research has shown that physical disability is associated with higher odds of adoption while emotional problems are associated with lower odds of adoption ( Snowden et al ., 2008 ). Leathers et al . (2012) showed that externalizing behavior problems such as oppositional or aggressive behavior were negatively associated with adoption while internalizing problems such as depression and anxiety had no effect. Zill and Bramlett (2014) showed that diagnosed ADHD, but not depression/anxiety, behavior/conduct disorder, or receipt of mental health care, was significantly more likely among children adopted from foster care than among children in foster care, but in that kind of comparison it is possible that the ADHD was not diagnosed until after the adoption or developed after the adoption.
While most research examining factors associated with adoption examine children available for adoption who did and did not get adopted, some researchers have approached the issue from the opposite direction by asking adoptive parents what motivated them to adopt. Vandivere, Malm and Radel (2009) report the most frequently cited reason adoptive parents gave for adopting was to provide a permanent home for a child in need, which was a motivating factor for the adoptive parents of 81% of all adopted children ages 0–17 in 2007, and for adoptive parents of 86% of children adopted from foster care. It can be argued that all children in foster care, or even all children living apart from any biological or adoptive parents, are in need of a permanent home. Other reasons given for adopting include: to expand the family (61%), because of infertility (39%), or because they wanted a sibling for a child (24%) ( Malm, Vandivere & McKlindon, 2011 ). Reasons given for specifically choosing to adopt from foster care rather than from another country or through a private domestic adoption include lower cost (60%), faster process (28%), wanting a special needs child (24%), and wanting an older child (14%) ( Malm, Vandivere & McKlindon, 2011 ).
We have chosen here to examine adoption among all children living without a biological or adoptive parent present in the household (i.e., all children in nonparental care). Most of these children are living with grandparents or foster parents, some with other relatives (e.g. aunts, uncles, older siblings), and a few are living with nonrelatives such as godparents, family friends, coaches, or others. We include all children in nonparental care in our analysis because the populations of children in relative care outside the child welfare system and inside the child welfare system are indistinct. That a child is in relative foster care may depend less on the child’s circumstances and need for a permanent family than on state policy choices as well as whether relatives or child welfare authorities were first to step in to address the parent’s unavailability.
The present authors have previously compared the health and well-being of types of children who have and have not been adopted: stepchildren who have and have not been adopted by their step-parent ( Bramlett, 2010 ), children living with relatives who did and did not adopt them ( Radel, Bramlett & Waters, 2010 ), and children in foster care and adopted from foster care ( Zill & Bramlett, 2014 ). Each of these analyses was limited in not being able to distinguish, among caregivers who had not adopted, those who wanted to adopt or were in the process of adopting the children in their care – i.e., those most likely to adopt among the pool of potential adopters. The 2013 National Survey of Children in Nonparental Care ( http://www.cdc.gov/nchs/slaits/nscnc.htm ) includes the necessary data to examine the factors associated with both adoption and adoption intentions for a national sample of children in noninstitutionalized nonparental care (i.e., children in households with no parents present).
McDonald, et al. (2007) partitioned the adoption process into discrete elements of placement and finalization to better predict speed of adoption. We are partitioning the earlier adoption decision into elements of considering, planning, and carrying out the adoption to better predict characteristics associated with different stages of deciding to adopt and adopting. Two national studies have examined the frequency which with those who say they have considered adoption actually do so. Both found that relatively few follow through and take steps to adopt. Jones (2008) using data from the National Survey of Family Growth found that 36 percent of ever married women in 2002 had considered adopting, but only 17 percent had taken steps to adopt and only 1.7 percent had actually adopted a child. Harris Interactive and the Dave Thomas Foundation for Adoption (2007) similarly found in a national opinion survey that many more people reported having seriously considered adoption than had acted to do so.
The present study contributes to the “Finding adoptive families” aspect of this current special issue of Adoption Quarterly by examining characteristics of the child, the caregiver, and the living arrangement that are associated with adoption and the caregiver’s adoption intentions using a large-scale, population-based national survey of children in nonparental care.
Data were drawn from two national surveys conducted by the National Center for Health Statistics (NCHS): the 2011–2012 National Survey of Children’s Health (NSCH), a nationally-representative survey of households with children, and the 2013 National Survey of Children in Nonparental Care (NSCNC), which re-interviewed almost 1,300 households identified as nonparental care households in the NSCH, including foster care, grandparent care, and other households with no parents present. Both surveys were modules of NCHS’ State and Local Area Integrated Telephone Survey (SLAITS). NSCH was sponsored by the Health Resources and Services Administration’s Maternal and Child Health Bureau, while NSCNC was sponsored by the Department of Health and Human Services’ Office of the Assistant Secretary for Planning and Evaluation, with supplemental funding from the Annie E. Casey Foundation.
NSCH was a random-digit-dial landline and cell telephone survey that interviewed 95,677 households with children throughout the 50 states and the District of Columbia. The NSCH sample is nationally representative of children aged 0 to 17 years in households in the United States in 2011–2012. One child in each household with children was randomly selected to be the target of the NSCH interview. Respondents were adults in the household who were knowledgeable about the child’s health, usually the child’s mother.
NSCNC was a follow-back survey 1–2 years after the NSCH for children who had been living in households with no parents present and were ages 0–16 in 2011–2012 (i.e., during the administration of the NSCH). Follow-back interviews were conducted via telephone with a current caregiver of the child, in some cases the parent who had reunited with the child since the NSCH interview. The NSCH had a 51% cooperation rate among eligible households but a 23% overall response rate (partly due to the inclusion of cell-phone sample to maximize coverage of the population), and NSCNC had a 52% completion rate among eligible households 1–2 years later. Weighting adjustments were applied such that the population estimated by the weighted sample of completed NSCNC interviews matched that of the pool of eligible households demographically. This dramatically reduced estimated nonresponse bias such that remaining bias in weighted estimates was smaller than sampling error. More information about NSCH and NSCNC may be found at: http://www.cdc.gov/nchs/slaits.htm or by referring to the associated documentation published by the SLAITS program ( CDC, 2013 ; CDC, 2014 ).
The analysis sample for the current study included those children in the NSCNC who were not living with a biological parent at NSCNC (i.e., had not been reunited with a parent between interviews). This restriction placed 1,160 of the 1,298 NSCNC children in the analysis sample.
Statistical Analysis
Weighted estimates were calculated using SUDAAN to account for the complex sample design of the NSCH ( RTI, 2008 ). A multinomial logistic regression model was fitted that compares 3 levels of adoption intentions and behavior, relative to those who never considered adoption: 1) those who ever considered, but are not currently planning to adopt; 2) those currently planning to adopt; and 3) those who adopted the child in the 1–2 years between the NSCH and NSCNC interviews. Further analysis examined the caregiver-reported reasons that discouraged those without current plans to adopt from adopting.
The dependent variable is derived from multiple questions on the survey. Children whose caregivers responded that they and/or their spouse/partner had adopted the child, or who lived with adoptive parents at NSCNC interview, were coded to “adopted.” Caregivers were asked whether they had ever considered adopting the child and whether they were currently planning to adopt the child and these questions were used to categorize children into the remaining groups.
The multinomial model includes measures from various domains: characteristics of the child, of the household, and of the caregiver; aspects of the nonparental care living arrangement; and indicators of caregivers’ parenting characteristics. Additionally, a continuous variable measuring the number of days between the NSCH and NSCNC interviews was included as a control variable.
In addition to child demographics (age, sex and race/ethnicity), other child characteristics include: overall health (rated excellent or very good versus good/fair/poor); whether the child received mental health care in the 12 months prior to the NSCNC interview; whether the child has Attention-Deficit/Hyperactivity Disorder (ADHD); whether the child has special health care needs (any of five health care consequences resulting from a chronic health condition: (1) ongoing need for prescription medications; (2) ongoing need for specialized therapies; (3) ongoing need for more health care services than most children the same age; (4) treatment for a behavioral, developmental or emotional problem; and/or (5) activity limitation); and eight measures of adverse family experiences (AFEs) the child may have had: whether (1) the household had often found it hard to afford basics and whether the child had ever (2) experienced the death of a parent, (3) experienced the divorce or separation of a parent, (4) experienced the incarceration of a parent, (5) witnessed violence in the home, (6) experienced or witnessed violence in the neighborhood, (7) lived with a mentally ill person, or (8) lived with a substance abuser.
Household socioeconomic characteristics include income relative to Federal Poverty Level (FPL), in four categories (0–50% or “very poor,” 50–100% or “poor,” 100–200% or “near-poor,” and more than 200% or “not-poor”), and education of caregiver respondent and spouse (if present) – whichever is higher – in two categories (less than or equal to high school versus more than high school).
Caregiver characteristics include type of nonparental care (foster kin, foster non-kin, nonfoster grandparent care, other nonfoster nongrandparent); caregiver age; caregiver marital status (married versus never or formerly married); caregiver employment status (indicators that the caregiver or spouse is employed full-time and that the caregiver or spouse is retired); caregiver’s health insurance type (private/employment-based, public or uninsured); whether the caregiver owns the home or not; whether either the caregiver or spouse is not in excellent or very good overall health, whether either the caregiver or spouse is not in excellent or very good mental health, whether the caregiver is depressed, and whether the child is of a different race or ethnicity than the caregiver.
Aspects of the living arrangement include whether Child Protective Services (CPS) or a foster care agency was involved in placing the child in the living arrangement; whether the caregiver received any money for caring for the child; whether the caregiver felt s/he had been very well prepared to care for the child; and whether the caregiver felt that information about adoption and custody issues and legal assistance had been difficult to obtain. Parenting characteristics include whether the caregiver felt that s/he had a good understanding of the child and whether the caregiver usually or always felt at least one form of parenting stress (anger at the child, feeling bothered at the child’s actions, or feeling that the child is harder to care for than normal).
Child sex, race/ethnicity, overall health, ADHD, special health care needs, AFEs, and parenting stress are measures drawn from NSCH (and some values may have changed between surveys). The remaining covariates are drawn from (and measured at) NSCNC. Including all these measures in the model, many with small amounts of missing data, results in a large percentage (25%) of cases being dropped from the model due to nonoverlapping missing data on one or another variable. To counter this, covariates were dropped from the model in descending order of p-value (i.e., least significant effect dropped first), if three conditions were met: 1) the covariate had a nontrivial amount of missing data, 2) the covariate had never been significant in any model permutation examined, and 3) removing the variable did not substantially change other results in the model. The final model that resulted from this process had 12.8% of the sample with missing data for any model covariate. (Dropping ADHD, which is significant in the model but has 5% missing data, would reduce the missing data in the model to 7% of the sample but since dropping this variable had no appreciable effect on the magnitude or direction of the other effects in the model, ADHD was retained). Characteristics included in the final model are shown in Table 1 , while characteristics dropped from the model because of nonsignificance and missing data are shown in Table 2 .
Means and Percentages of Model Covariates by Level of Adoption Intention and Behavior
| Covariate | All children (n=1160) | By Model Dependent Variable | |||
|---|---|---|---|---|---|
| Never considered (n=498) | Ever considered, not planning (n=322) | Current plans to adopt (n=186) | Already adopted (n=154) | ||
| Mean (standard error) | |||||
| Days between interviews | 552.2 (8.24) | 535.2 (13.83) | 563.5 (16.01) | 560.4 (17.69) | 572.6 (13.19) |
| Child Age in years | 11.1 (0.33) | 12.3 (0.46) | 11.3 (0.49) | 9.8 (0.88) | 9.1 (0.63) |
| Caregiver Age in years | 57.1 (0.92) | 58.6 (1.63) | 59.0 (1.41) | 53.1 (1.99) | 57.1 (1.61) |
| Percent (standard error) | |||||
| Child Sex is Male | 47.3 (3.43) | 48.7 (5.47) | 50.1 (5.85) | 42.4 (8.13) | 48.1 (6.73) |
| Child Race/ethnicity is Hispanic | 15.6 (3.07) | 13.1 (4.43) | 10.5 (3.70) | 24.4 (8.69) | 14.1 (4.76) |
| Non-Hispanic (NH) White | 37.4 (3.02) | 36.6 (4.84) | 49.4 (5.75) | 27.7 (6.60) | 38.3 (6.47) |
| NH Black | 36.6 (3.37) | 44.0 (5.78) | 27.9 (5.89) | 33.6 (7.66) | 35.6 (6.51) |
| NH Other | 10.4 (1.92) | 6.3 (1.51) | 12.2 (2.82) | 14.3 (6.13) | 12.0 (3.68) |
| Excellent/very good health | 78.4 (2.68) | 81.7 (3.87) | 80.8 (3.86) | 74.5 (7.08) | 69.4 (6.18) |
| Special health care needs | 40.3 (3.59) | 30.8 (4.74) | 35.9 (5.29) | 59.1 (7.77) | 39.1 (6.52) |
| Has ADHD | 19.7 (2.60) | 14.2 (3.17) | 23.2 (4.94) | 24.4 (6.68) | 22.9 (6.01) |
| Experienced divorce/separation | 45.0 (3.38) | 48.9 (5.45) | 52.5 (5.95) | 33.5 (7.57) | 41.7 (6.58) |
| Ever lived with mentally ill | 26.1 (2.80) | 25.7 (4.30) | 29.0 (4.79) | 24.1 (6.91) | 26.5 (5.64) |
| Ever lived with substance abuser | 46.9 (3.46) | 44.8 (5.55) | 53.3 (5.89) | 44.5 (8.16) | 47.2 (6.77) |
| HH income relative to Federal Poverty Level (FPL) 0–50%(very poor) | 17.2 (3.33) | 11.1 (3.11) | 10.1 (3.94) | 34.3 (9.20) | 12.2 (4.33) |
| FPL 50–100% (poor) | 19.4 (2.74) | 17.6 (4.07) | 21.8 (5.33) | 20.4 (6.37) | 17.8 (5.20) |
| FPL 100–200% (near-poor) | 29.4 (3.03) | 38.9 (5.53) | 29.1 (5.46) | 13.5 (4.02) | 35.4 (6.93) |
| FPL >200% (not poor) | 34.0 (3.40) | 32.5 (5.48) | 39.0 (5.57) | 31.9 (7.59) | 34.5 (6.31) |
| Highest education <=High school | 50.1 (3.57) | 44.6 (5.45) | 43.9 (5.97) | 61.9 (8.09) | 55.9 (6.57) |
| Kin Foster care | 10.7 (2.10) | 12.3 (3.61) | 6.9 (3.25) | 12.6 (4.68) | 8.2 (4.21) |
| Nonkin Foster care | 7.2 (1.93) | 1.5 (0.53) | 7.8 (3.93) | 12.5 (5.81) | 14.9 (5.18) |
| Nonfoster grandparent care | 59.5 (3.70) | 63.4 (6.06) | 65.8 (5.91) | 50.9 (8.54) | 51.1 (6.77) |
| Nonfoster nongrandparent | 22.6 (3.37) | 22.9 (6.19) | 19.4 (4.85) | 23.9 (6.71) | 25.8 (6.33) |
| Caregiver respondent is married | 45.2 (3.55) | 50.4 (5.49) | 45.5 (5.68) | 35.3 (7.82) | 49.7 (6.68) |
| Caregiver owns home | 57.9 (3.57) | 63.4 (5.57) | 64.1 (6.08) | 42.4 (8.31) | 62.6 (6.74) |
| Any fulltime employee in home | 41.1 (3.57) | 42.1 (5.51) | 49.4 (5.95) | 35.0 (7.90) | 33.2 (6.32) |
| Any retiree in home | 23.1 (2.43) | 26.3 (4.23) | 27.3 (4.90) | 11.6 (3.62) | 31.1 (5.66) |
| Caregiver or spouse not in excellent/very good health | 58.3 (3.67) | 59.9 (5.92) | 55.2 (5.93) | 59.4 (8.18) | 56.3 (6.51) |
| CPS/agency helped arrange care | 32.3 (3.18) | 21.7 (4.25) | 27.9 (5.33) | 39.5 (8.32) | 65.8 (6.07) |
| Received payment for care | 57.8 (3.48) | 55.3 (5.46) | 55.4 (5.71) | 56.3 (8.64) | 78.4 (4.60) |
| Caregiver was very well prepared | 57.3 (3.50) | 57.4 (5.48) | 54.3 (5.74) | 59.3 (8.24) | 58.3 (6.98) |
| Difficult to obtain adoption info | 18.8 (2.61) | 6.6 (1.47) | 22.2 (5.09) | 34.1 (7.71) | 18.9 (5.30) |
| Easy to obtain | 48.7 (3.53) | 47.6 (5.57) | 48.7 (5.87) | 40.6 (8.72) | 74.7 (5.96) |
| Not needed/never knew of it | 32.6 (3.65) | 45.8 (5.79) | 29.1 (5.53) | 25.2 (7.70) | 6.4 (3.51) |
| Difficult to obtain legal info | 13.6 (2.28) | 14.3 (3.69) | 8.9 (3.33) | 17.4 (5.51) | 12.2 (4.22) |
| Easy to obtain | 37.7 (3.25) | 33.6 (5.30) | 41.2 (5.81) | 32.8 (7.57) | 59.1 (6.56) |
| Not needed/never knew of it | 48.7 (3.48) | 52.1 (5.65) | 49.9 (5.83) | 49.8 (8.45) | 28.7 (6.21) |
| Good understanding of child | 82.1 (2.54) | 74.4 (4.88) | 83.4 (4.85) | 94.5 (2.07) | 77.5 (5.30) |
| Usually/always feel stressed | 12.9 (2.07) | 11.7 (3.21) | 14.9 (3.85) | 13.2 (4.90) | 12.6 (3.68) |
CPS is Child Protective Services.
Percentages of Additional Preliminary Model Covariates * by Level of Adoption Intention and Behavior
| Covariate | All children (n=1160) | By Model Dependent Variable | |||
|---|---|---|---|---|---|
| Never considered (n=498) | Ever considered, not planning (n=322) | Current plans to adopt (n=186) | Already adopted (n=154) | ||
| Percent (standard error) | |||||
| Often hard to get by on income | 37.6 (3.60) | 36.1 (5.27) | 33.0 (5.54) | 45.3 (8.61) | 34.0 (6.76) |
| Experienced death of guardian | 17.3 (2.24) | 20.8 (3.99) | 17.4 (4.24) | 13.4 (4.06) | 12.9 (4.24) |
| Experienced parent incarceration | 38.8 (3.34) | 35.9 (5.11) | 43.7 (5.71) | 42.4 (8.66) | 29.2 (5.60) |
| Experienced violence in home | 30.1 (3.03) | 24.3 (3.86) | 31.7 (5.13) | 36.2 (8.23) | 33.5 (6.47) |
| Experienced neighbor violence | 23.7 (2.73) | 23.8 (4.25) | 25.5 (4.68) | 23.6 (6.76) | 19.4 (4.88) |
| Transracial/transethnic child | 18.0 (2.61) | 12.6 (2.83) | 16.0 (3.99) | 25.3 (7.57) | 25.0 (6.02) |
| Caregiver or spouse not in | |||||
| excellent/vg mental health | 40.3 (3.54) | 41.8 (5.28) | 36.8 (5.89) | 40.8 (8.93) | 41.0 (6.61) |
| Caregiver is depressed | 10.0 (2.23) | 12.1 (4.06) | 12.0 (5.48) | 4.9 (2.32) | 10.8 (4.36) |
| Child received mental health care | 30.2 (3.26) | 27.7 (4.60) | 26.4 (4.62) | 33.4 (8.38) | 40.1 (6.82) |
| Caregiver insurance type: private | 32.1 (3.43) | 32.8 (5.19) | 38.4 (6.22) | 26.6 (8.02) | 29.6 (6.60) |
| Public | 47.0 (3.82) | 41.1 (5.40) | 46.1 (6.34) | 55.8 (9.29) | 51.7 (7.59) |
| No insurance | 20.9 (4.02) | 26.1 (6.84) | 15.5 (4.39) | 17.6 (8.62) | 18.7 (6.24) |
Overall, of children living in nonparental care at the time of the NSCH interview, 8.8% were living with adoptive parents (i.e., had been adopted) by the time of the NSCNC interview 1 to 2 years later and an additional 23.6% had caregivers with current plans to adopt them. In 20.9% of cases, caregivers had considered adopting but had no current plans to adopt the child and for 36%, caregivers had never considered adoption (the remaining 10.7% were living with biological parents at the time of the NSCNC interview – the above percentages, calculated among those not reunited with biological parents, were 9.9% adopted, 26.4% with caregivers planning to adopt, 23.4% with caregivers who considered adoption but were not planning adoption, and 40.3% with caregivers who had never considered adoption).
Table 1 shows means and percentages for model covariates, for the full analytic sample and by categories of the dependent variable. It is possible to read the four categories of the dependent variable, from left to right in this table, as an ordinal scale with ascending probabilities of adoption (culminating in 100% probability in the “already adopted” column). One model domain stands out (caregiving placement characteristics) because the “already adopted” group significantly differs from all other groups on almost all the variables in that domain. One column also stands out in that those children whose caregivers plan to adopt significantly differ in many ways from the other groups, notably that the children are much more likely to have special health care needs and to live in very poor households and their caregivers are much less likely to own their homes or live in households that include any retired people and are more likely to feel that they have a good understanding of the child.
Table 2 shows percentages, for the full analytic sample and by categories of the dependent variable, for variables that were dropped from the model. Since all were dropped from the model from a combination of both a) missing data and b) high p-value (very low significance), it is not surprising that all of the comparisons in Table 2 are nonsignificant. However, nonsignificant findings can be important, and what Table 2 shows is that certain characteristics are –perhaps surprisingly – not associated with adoption intentions or adoption. Specifically, caregiver insurance type, caregiver and child mental health issues, transracial/transethnic placement, and many adverse family events that may have contributed to the child’s placement in nonparental care do not seem to impact whether a nonparental caregiver considers, plans or carries out the adoption of the child in their care.
Table 3 shows the multinomial logistic regression results comparing each of three subgroups of children to children whose nonparental caregiver never considered adoption: those whose caregivers have considered adoption but are not currently planning to adopt, those whose caregivers are currently planning to adopt, and those whose caregivers adopted the child between the NSCH and NSCNC interviews. Higher odds ratios show the higher likelihood of the outcome relative to the reference group. Ever considered, not currently planning to adopt— Factors associated with higher odds of considering but not planning adoption include ADHD, nonkin foster care status and having experienced difficulty obtaining information about adoption or custody issues. Factors associated with lower odds of considering but not planning adoption include currently married status and having experienced difficulty obtaining legal assistance. The child’s non-Hispanic black race/ethnicity, kin foster care status and either the caregiver or caregiver’s spouse having less than very good overall health were marginally significant (i.e., significant at the p<0.10 level but not at the 0.05 level) with a lower likelihood of a caregiver having considered adopting .
Multinomial Logistic Regression Model of Adoption Intentions & Behavior
| Model Covariates | Ordinal Outcomes relative to “Never Considered Adopting” | ||
|---|---|---|---|
| Ever considered adopting, not currently planning to adopt | Currently planning to adopt | Already adopted since NSCH interview | |
| Odds Ratio (95% Confidence Interval) | |||
| Age at NSCNC interview | 0.97 (0.90–1.04) | 0.81 (0.73–0.91) | 0.85 (0.77–0.95) |
| Sex: Male | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Female | 1.05 (0.60–1.84) | 1.01 (0.49–2.07) | 0.83 (0.36–1.91) |
| Race/Ethnicity: Hispanic | 1.73 (0.57–5.22) | 8.11 (2.12–31.10) | 3.16 (0.80–12.46) |
| Non-Hispanic White | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Non-Hispanic Black | 0.53 (0.25–1.12) | 1.77 (0.63–4.96) | 1.30 (0.40–4.25) |
| Non-Hispanic Other | 1.54 (0.65–3.67) | 1.53 (0.50–4.72) | 2.98 (0.82–10.80) |
| Overall health is excellent/very good | 0.61 (0.29–1.26) | 1.52 (0.54–4.27) | 0.40 (0.16–0.98) |
| Not excellent/very good | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Child has Special Health Care Needs | 0.81 (0.42–1.55) | 5.57 (2.08–14.89) | 1.28 (0.42–3.89) |
| Does not have SHCN | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Currently has ADHD | 2.38 (1.04–5.47) | 1.23 (0.42–3.55) | 1.67 (0.59–4.72) |
| Does not have ADHD | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Experienced parent divorce/separation | 1.20 (0.61–2.34) | 0.46 (0.21–1.04) | 1.48 (0.62–3.52) |
| Did not experience div/sep | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Ever lived with mentally ill | 0.75 (0.38–1.47) | 0.79 (0.30–2.08) | 0.33 (0.12–0.96) |
| Never lived with mentally ill | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Ever lived with substance abuser | 1.16 (0.59–2.31) | 2.39 (1.02–5.62) | 1.41 (0.61–3.25) |
| Never lived with substance abuser | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Income (Federal Poverty Level): 0–50% | 0.55 (0.16–1.90) | 0.50 (0.14–1.84) | 1.02 (0.18–5.83) |
| 50–100% FPL | 0.92 (0.37–2.27) | 0.20 (0.06–0.68) | 0.57 (0.16–2.08) |
| 100–200% FPL | 0.83 (0.40–1.75) | 0.10 (0.03–0.32) | 0.69 (0.21–2.25) |
| >200–400% FPL | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Highest Education in HH: <=High School | 0.70 (0.37–1.30) | 3.66 (1.70–7.87) | 1.33 (0.55–3.21) |
| >High School | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Caregiver type: Kin foster care | 0.34 (0.11–1.07) | 1.48 (0.33–6.63) | 0.03 (0.00–0.19) |
| Nonkin foster care | 13.08 (1.56–109.76) | 11.36 (1.58–81.64) | 2.45 (0.26–23.12) |
| Nonfoster grandparent care | 1.17 (0.54–2.53) | 1.18 (0.44–3.12) | 0.38 (0.12–1.26) |
| Nonfoster nongrandparent | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Caregiver Marital Status: Married | 0.42 (0.22–0.81) | 0.24 (0.10–0.56) | 0.66 (0.25–1.74) |
| Formerly or Never Married | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Caregiver owns home | 0.57 (0.27–1.20) | 0.19 (0.08–0.43) | 0.46 (0.18–1.20) |
| Does not own home | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Caregiver or spouse’s physical health not excellent/very good | 0.54 (0.28–1.03) | 0.30 (0.13–0.67) | 0.29 (0.12–0.69) |
| Physical health is ex/vg | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Caregiver or spouse is retired | 0.77 (0.35–1.67) | 1.02 (0.37–2.83) | 2.77 (0.93–8.20) |
| Neither is retired | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Caregiver or spouse fulltime employed | 1.75 (0.81–3.81) | 0.96 (0.37–2.48) | 0.94 (0.28–3.10) |
| Neither is employed fulltime | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Caregiver Age | 1.01 (0.97–1.06) | 0.96 (0.92–1.00) | 1.01 (0.95–1.08) |
| Agency/CPS involved in placement | 1.04 (0.50–2.17) | 2.29 (0.84–6.26) | 5.75 (2.34–14.16) |
| Agency/CPS not involved | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Received payment for caregiving | 0.68 (0.37–1.26) | 0.71 (0.31–1.60) | 3.12 (1.35–7.21) |
| No payment last 12 months | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Caregiver was very well prepared | 0.95 (0.515–1.77) | 1.63 (0.77–3.46) | 1.79 (0.74–4.33) |
| Not very well prepared | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Difficulty obtaining adoption info | 3.66 (1.36–9.89) | 8.58 (3.02–24.39) | 2.66 (0.93–7.59) |
| No difficulty with adoption info | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Info not needed/never knew of it | 0.46 (0.23–0.92) | 0.59 (0.21–1.66) | 0.17 (0.04–0.74) |
| Difficulty obtaining legal assistance | 0.20 (0.07–0.56) | 1.18 (0.36–3.86) | 0.35 (0.12–1.01) |
| No difficulty w/legal assistance | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Not needed/never knew of it | 1.00 (0.51–1.97) | 1.43 (0.61–3.35) | 0.22 (0.09–0.54) |
| Good understanding of child’s problems | 1.65 (0.69–3.93) | 4.79 (1.61–14.26) | 0.41 (0.14–1.18) |
| Not good understanding | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Usually/always feel parenting stress | 0.93 (0.41–2.13) | 0.51 (0.16–1.59) | 0.65 (0.23–1.87) |
| Don’t usually/always feel stress | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Days between NSCH, NSCNC interviews | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.01) |
Currently planning to adopt (relative to those who never considered adoption)
Factors associated with higher odds of planning adoption include the child being of Hispanic race/ethnicity (relative to non-Hispanic white), having special health care needs, or having lived with a substance abuser; lower household education; nonkin foster care status; having experienced difficulty obtaining information about adoption; and having a good understanding of the child. Factors associated with lower odds of planning adoption include older child age, poor or near-poor household income status (relative to not-poor), currently married status, home ownership, and either the caregiver or caregiver’s spouse having less than very good overall health. Ever having experienced parental separation or divorce and older caregiver age were marginally significant.
Already adopted (relative to those who never considered adoption)
Factors associated with higher odds of adoption include foster care agency or CPS involvement in the child’s placement in the home and receipt of payment for caring for the child. The child’s non-Hispanic other race/ethnicity, either the caregiver or caregiver’s spouse (if present) being retired, and having experienced difficulty obtaining information about adoption were marginally significant. Factors associated with lower odds of adoption include the child’s older age, excellent/very good overall health status, and ever having lived with the mentally ill; kin foster care status; and either the caregiver or caregiver’s spouse having less than very good overall health. Difficulty obtaining legal assistance and having a good understanding of the child were marginally significant.
Some of the strongest effects in table 3 include that children in kin foster care were much less likely to have already been adopted (OR of 0.03) and children in nonkin foster care were more likely to have caretakers who had either once considered adoption (OR 13.08) or had current plans (OR 11.36) to adopt. Additionally, children were much more likely to have been adopted already if the CPS agency had been involved in their placement (OR 5.75) or the caregivers received payment for caring for the child (OR 3.12). Having special health care needs was associated with a much higher likelihood of current adoption plans (OR 5.57) while factors associated with a particularly low likelihood of current adoption plans included low income (OR of 0.20 for poor caregivers and 0.10 for near poor caregivers), married caregivers (OR 0.24), caregivers who were homeowners (OR 0.19) and poor caregiver health (OR 0.30).
Some factors were significantly associated with more than one level of adoption intention or behavior. Older child age was associated with lower odds of both adoption and planning to adopt. Kin foster status was associated with lower odds of adoption or considering adoption while nonkin foster status was associated with higher odds of considering or planning adoption. Being married was associated with lower odds of considering or planning to adopt. Less-than-excellent or very good overall health on the part of the caregiver or caregiver’s spouse (if present) was associated with lower odds for all three outcomes; while having had difficulty with obtaining information about adoption or custody issues was associated with higher odds for all three outcomes.
Factors not associated with adoption intentions or behavior at any level, beyond those dropped from the model and shown in Table 2 , include child sex, caregiver preparation, and parenting stress. The child having experienced parental separation or divorce, caregiver employment and caregiver age each had only one effect that was marginally significant.
Table 4 shows the reasons given for why those not currently planning to adopt were discouraged from adopting the child in their care. The most common reasons given for not planning to adopt were financial concerns and issues related to the birth parents (not relinquishing parental rights, strong parent-child attachment, parental discouragement) while the least common reasons given were child issues such as age, health, transracial status or behavior problems. Two thirds of nonparental caregivers either had another unspecified reason for not adopting (42%) or reported that there were no discouraging factors (27%).
Factors that Discouraged Nonparental Caregivers from Adopting
| Reason for Not Planning to Adopt | Percent (standard error) among Nonparental Caregivers Not Currently Planning to Adopt |
|---|---|
| Parental rights not relinquished by parents or terminated | 11.6 (2.63) |
| Financial concerns | 8.5 (1.59) |
| Child still emotionally attached to biological parents | 6.0 (1.84) |
| Child’s parents discouraged adoption | 4.2 (1.49) |
| Caregiver’s health or age | 2.6 (0.82) |
| Adoption process too complicated or difficult | 2.4 (0.91) |
| Child’s health problems that caregiver can’t handle long-term | 0.4 (0.14) |
| Problems between child and caregiver’s family members | 0.3 (0.13) |
| Child was too old | 1.0 (0.38) |
| Child’s behavior problems/juvenile justice system issues | 0.1 (0.05) |
| Child’s race/ethnicity differs from caregiver’s family | 0.1 (0.11) |
| Other | 41.6 (3.92) |
| No discouraging factors | 26.6 (3.89) |
Previous research on step-parent adoptions, relative care adoptions and adoptions from foster care (in each case comparing children adopted or not adopted) showed that adopting households tend to have comparable or more favorable socioeconomic attributes than nonadopting households. Foster and step adopters had higher household income and education compared to foster and step nonadopters, while relative adopters and nonadopters did not differ in education and income ( Zill & Bramlett, 2014 ; Bramlett, 2010 ; Radel, Bramlett & Waters, 2010 ). As the current sample includes foster care and relative care households but not step-parent households, we expected to see a weak effect of higher education and income among adopters, relative to nonadopters (the foster effect diluted by the relative care non-effect). The results of the multinomial model, at first glance, would seem to show the expected effect for income and the opposite effect for education: adoption plans are less likely among the poor and near-poor than among the not-poor and are more likely among households with lower education than those with any college education, relative to those who never considered adopting.
However, income and education are only significant for predicting adoption plans and are not significant for predicting actual adoption, relative to never having considered adoption, specifically. The comparison group differs, potentially explaining the different income effect from that found in prior studies (that the already-adopted group does not have higher income than the group least likely to adopt). As Table 1 shows, household income and education did not significantly differ between children whose caregivers had never considered adoption and children who had been adopted. But both groups significantly differed from those whose caregivers had current plans to adopt, who had a significantly greater proportion in the “very-poor” income category ( Table 1 ). And this group, with lower income, would have been included in the “had not adopted” group if the comparison had been done as in the prior studies, comparing the adopted to the not adopted. This conclusion highlights a limitation in analyses comparing types of children who have and have not been adopted, without distinguishing between those whose caregivers want to adopt and those whose caregivers have never considered adoption.
This finding also highlights the difference between adoption behavior and adoption intentions. Those children who have been adopted were less likely to live in very poor households; those whose caregivers plan to adopt them, but have not completed it yet, were almost three times as likely to live in very poor households, as seen in Table 1 . This might indicate that some households intend to adopt but are unable to hurdle barriers to adoption that those with more resources are able to hurdle. This seems even more likely given that receipt of payment for caring for the child is associated with adoption ( Table 3 ) and financial concerns was one of the most-endorsed reasons discouraging nonadopters from adopting ( Table 4 ). The NSCNC sample includes many nonfoster caregivers who would not be eligible for subsidies that foster parents can receive, which may contribute to low adoption rates for those not in foster care.
The marital status effect may reflect a similar situation, in that the finding that unmarried caregivers are more likely to consider adoption or have current plans to adopt – but not necessarily to actually adopt – may be the result of barriers to adoption, in this case preferences to place children with married caregivers rather than unmarried caregivers. Although the traditional preference for married adoptive parents is not as strong as it once was and roughly one-third of children adopted from foster care are adopted by single adoptive parents ( US DHHS, 2014a ), some states continue to favor married couples over single persons as adoptive parents ( Wilson & Wilcox, 2006 ; Associated Press, 2011 ). Private adoption agencies are generally not bound by state preferences for children in foster care and can and sometimes do restrict adoption by unmarried caregivers ( Gardino et al ., 2010 ).
There was a somewhat discrepant finding regarding child age, in that the model showed significantly lower likelihoods of adopting or planning to adopt for older children, but child age was also one of the least-endorsed reasons discouraging caregivers from adopting. A potentially lengthy adoption process makes little sense for older children if they are going to be adults or almost adults by the time the adoption is finalized. It is also likely that older children have more established social and emotional ties to their parents that they and their caregivers are not eager to dismiss by terminating parental rights, particularly if the caregiver is a relative. Kin caregivers may also think of this issue as “parental ties” rather than “child’s age” as being the factor discouraging the adoption. To investigate whether the age effect only applies to the oldest children, we estimated the model separately for teenagers (ages 13–17) and preteens (ages 1–12) (results not shown). In the teen model, the age effects were considerably stronger than in the full model (with ORs of 0.24 and 0.52 for currently planning to adopt and adoption instead of 0.81 and 0.85 respectively). In the preteen model, the age effects were weaker than in the full model (ORs of 0.83 and 0.98). Future research could consider modeling the effect of age as a curvilinear relationship to account for this issue.
Caregiver health was one of the few covariates that was significantly associated with all three outcomes, in that considering adoption, planning adoption and adopting are all less likely if either the caregiver or caregiver’s spouse (if present in the household) has less than excellent or very good overall health. The other covariates that were associated with all three outcomes were difficulty obtaining information about adoption and custody issues, and kin/nonkin foster status.
Difficulty obtaining adoption information and legal assistance were included in the model as attributes of the placement process that could have influenced adoption decisions and intentions. The model suggests that those who had difficulty obtaining information about adoption were more likely than those who found such information easily to consider or plan adoption (and to adopt as well, although that effect was not significant at the 0.05 level). This counter-intuitive finding is probably reflecting that those who do not wish to adopt are not actively looking for adoption information. Table 1 shows that among those who adopted, adoption information was much more likely to be easily obtained than difficult to obtain (75% versus 19%, respectively – a much larger difference than among those considering or planning adoption) but that the proportion of adopted children whose caregivers found that information hard to obtain was still three times as high as for those whose caregivers never considered adoption – explaining the model effect – because most of the nonadopters had presumably not tried very hard to obtain it. Thus, this variable should be considered a control variable rather than a predictor.
Kin/nonkin status of foster parents also had consistent effects, although not always significant at the 0.05 level: kin foster parents are less likely to adopt or consider adoption and nonkin foster parents are more likely to consider or plan to adopt. This finding is consistent with prior research ( Carnochan et al ., 2013 ; Berrick, Barth & Needell, 1994 ). Berrick, Barth and Needell (1994) indicated that kin foster parents are older, poorer, in poorer health, and more likely to be single than nonkin foster parents; our model controlled for all those attributes and still found that kin foster parents are less likely to adopt their foster children. Berrick, Barth and Needell (1994) found that the most frequently-cited reason among kin foster parents for not adopting was that they felt they were “already family” (p.57) and thus did not need to formalize that status with adoption. This, if true, may highlight a policy conundrum – there is a preference to place foster children with relatives and a preference to have foster parents adopt the child ( Bussiere, 1998 ), and they may be contradictory goals to some extent. This is a key reason why the title IV-E kinship guardianship assistance program was created by the Fostering Connections to Success and Increasing Adoptions Act of 2008 (P.L. 110-351), to provide another financially supported option for permanency for relatives who planned to care for the child until adulthood but who were not interested in adoption ( Stoltzfus, 2008 ). Future research is needed to determine whether guardianships are equal to adoptions in achieving stable, long-lasting permanency for children.
The relationship between a child’s mental health and his or her odds of being adopted is not clear. Analysis comparing adopted children to nonadopted children found that mental health issues such as learning disability, developmental delay, and emotional or behavioral problems are more prevalent among the population of adopted children ( Bramlett, Radel & Blumberg, 2007 ). Specific to the population of children in relative care, Radel, Bramlett and Waters (2010) showed that developmental delay was more prevalent among children adopted by relatives than among unadopted children in relative care, while mental health care, learning disability and behavior/conduct problems did not differ between the groups. Specific to the foster care population, Zill and Bramlett (2014) showed that ADHD was more prevalent among children adopted from foster care than among children in foster care, while mental health care, depression/anxiety and behavior/conduct problems did not differ between the groups. Others have indicated that mental health diagnoses and emotional or behavioral problems are associated with lower odds of being adopted from foster care ( Connell et al ., 2006 ; Snowden, Leon & Sieracki, 2008 ; Leathers et al., 2012 ). Mental health conditions may operate differently from physical disabilities as some studies have found physical disabilities increase the probability of adoption ( Snowden, Leon & Sieracki, 2008 ; Akin, 2011). This may factor into findings by Malm, Vandivere and McKlindon (2011) who demonstrate that among children adopted from foster care, 24% had foster parents who were motivated to adopt the child specifically because they wanted a special needs child (which could mean children with either physical or mental health conditions, or both).
If analyses of all adopted children ( Bramlett, Radel & Blumberg, 2007 ) or of children adopted from foster care ( Zill & Bramlett, 2014 ) show a higher percent of certain mental health issues than for nonadopted children, while mental health issues also make foster children less adoptable ( Connell et al ., 2006 ; Snowden, Leon & Sieracki, 2008 ; Leathers et al., 2012 ), it suggests that the background and process of being adopted (i.e., the conditions that precipitated the child being available for adoption and the uncertainty associated with changing caregivers, perhaps more than once) contribute to mental health issues (an eminently reasonable conclusion). It is also possible that some children with mental health conditions while in foster care do not get diagnosed with those conditions until after they are adopted. Research has suggested that adoptive parents may compensate for not being the child’s natural parents by seeking the best medical care possible ( Kirk, 1984 ; Case & Paxson, 2001 ; Bramlett, Radel & Blumberg, 2007 ). Further, mental health issues may develop or intensify as children age, so there may be reason for diagnosis after adoption of problems that do not manifest until later. ADHD in particular tends to get diagnosed once children go to school and might not initially be diagnosed in younger children, so depending on age at adoption, the diagnosis might come after the adoption. A recent report from NCHS indicates that only one-third of children with ADHD were diagnosed before age 6 ( Visser et al., 2015 ). We included measures of the child’s ADHD, receipt of mental health care, and whether they had ever lived with someone who was mentally ill as well as indicators of caregiver depression and less than very good caregiver/spouse mental health. We found that most of these did not predict adoption intentions or adoption in our model, while having ever lived with a mentally ill person was associated with lower odds of adoption, and having ADHD was associated with greater odds of considering adoption. Obviously, more research is needed to address this issue.
For those caregivers not planning to adopt, the reasons given why adoption was discouraged tended to focus on issues related to cost or the birth parents, notably the failure to terminate or relinquish parental rights and parental discouragement of the adoption ( McDonald et al. (2007) showed that termination of parental rights can speed the adoption process substantially.) Issues related to the child, such as older age, transracial status, and behavior problems or juvenile justice system involvement, were the least-endorsed reasons. However, the majority of nonadopting caregivers did not endorse any of the reasons assessed in the survey, suggesting that there are many unique reasons why nonparental caregivers do not adopt the children in their care. Some respondents indicated that adoption was not necessary but did not specify why this was the case; others responded with some version of “the parents are still in the child’s life” or with an expectation or hope that the child would be reunited with parents, while a few indicated that the current situation was working and did not need to be “fixed.” This issue warrants exploration in future research.
We found that many of the issues that kin raise as discouraging them from adoption relate to the parents rather than the child. Thus, a key issue for ensuring permanence will be resolving mixed feelings of kin caregivers toward the birth parent(s) and making adoption an acceptable choice that does not feel like they or the child are giving up on or betraying the parent. Merritt (2008) showed that children’s feeling toward adoption by foster parents or kin developed over time, with more expressing an adoption preference as time went on. Treating adoption intentions as a process rather than a point in time choice may be helpful in increasing adoptions among this segment of the child welfare population.
Limitations
Findings from NSCH and NSCNC are based on parents’ experiences and perceptions. Information provided about health status and health care was not verified with health care professionals. Despite weighting adjustments to minimize nonresponse bias and evidence to suggest that remaining estimated biases tend to be smaller than sampling error ( CDC, 2014 ), the low response rate means that bias resulting from nonresponse cannot be completely ruled out.
Largely due to the state-level sample design of the NSCH, which sampled each state and the District of Columbia in approximately equal sample sizes, design effects for national analyses tend to be large and confidence intervals around odds ratios are sometimes quite wide, even when odds ratios are statistically significant. Therefore, comparisons of the magnitudes of effects should include consideration of these confidence interval widths and may not be appropriate.
The most prevalent reasons – other than “other reason” – for not planning to adopt applied to fewer than 12% of children whose caregivers were not planning to adopt, while almost 42% had an “other reason.” Respondents who answered “other reason” were asked to specify, and most provided a reason that did not match existing categories. The verbatim responses included few related to issues with the child being the factor that discouraged adoption. This supports the conclusion based on Table 4 that issues with the birth parents were more prevalent than issues with the child as reasons for not adopting. The large number of unique responses provides a challenge in analyzing reasons for not adopting.
Despite these limitations, the authors know of no other data source than NSCNC that includes a large-scale, population-based national sample of all noninstitutionalized children living in nonparental care – i.e., the pool of adoptable children – and that includes survey content directly relevant to this population, such as adoption intentions and motivations/deterrents.
Nonparental caregivers may be more likely to consider adoption or take action to adopt the children in their care when the caregiver is a nonkin foster parent, a foster care agency or CPS was involved in the placement of the child, and/or financial assistance is available. They may be less likely to adopt if the child is older (especially among teenagers), if the caregiver is in poor health or is married, or if the caregiver type is kin foster care. Those with current plans to adopt but who have not yet adopted may face barriers to adoption such as extreme poverty, lower education and being unmarried. Discouraging reasons given for not considering or planning adoption tend to reflect issues with the birth parents more than issues with the child. However, the majority of nonadopting caregivers did not endorse any of the reasons assessed in the survey, suggesting that there are many unique reasons why nonparental caregivers do not adopt the children in their care.
- Associated Press. [Accessed 4/21/2015]; Married couples get adoption preference. 2011 at http://www.fox10phoenix.com/story/18119923/married-couples-get-adoption-preference .
- Berrick JD, Barth RP, Needell B. A comparison of kinship foster homes and foster family homes: Implications for kinship foster care as family preservation. Children and Youth Services Review. 1994; 16 (1/2):33–63. [ Google Scholar ]
- Bramlett MD. When stepparents adopt: Demographic, health and health care characteristics of adopted children, stepchildren, and adopted stepchildren. Adoption Quarterly. 2010; 13 (3/4):248–267. [ Google Scholar ]
- Bramlett MD, Radel LF, Blumberg SJ. The health and well-being of adopted children. Pediatrics. 2007; 119 (S1):S54–S60. [ PubMed ] [ Google Scholar ]
- Bussiere A. The Development of Adoption Law. Adoption Quarterly. 1998; 1 (3):3–25. [ Google Scholar ]
- Carnochan S, Moore M, Austin MJ. Achieving Timely Adoption. Journal of Evidence-Based Social Work. 2013; 10 :2010–219. [ PubMed ] [ Google Scholar ]
- Case A, Paxson C. Mothers and others: Who invests in children’s health? Journal of Health Economics. 2001; 20 :301–328. [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention (CDC), National Center for Health Statistics, State and Local Area Integrated Telephone Survey. 2011–2012 National Survey of Children’s Health Frequently Asked Questions. 2013 Apr; Available from: http://www.cdc.gov/nchs/slaits/nsch.htm .
- CDC, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. National Survey of Children in Nonparental Care: Frequently Asked Questions and Guidelinesfor Data Users. 2014 Apr; Available from: http://www.cdc.gov/nchs/slaits/nscnc.htm .
- Connell CM, Katz KH, Saunders L, Tebes JK. Leaving foster care – The influence of child and case characteristics on exit rates. Children and Youth Services Review. 2006; 28 :780–798. [ Google Scholar ]
- Gardino SL, Russell AE, Woodruff TK. Adoption After Cancer: Adoption Agency Attitudes and Perspectives on the Potential to Parent Post-Cancer. Cancer Treatment Research. 2010; 156 :153–170. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harris Interactive and the Dave Thomas Foundation for Adoption. National foster care adoption attitudes survey. 2007 Retrieved from www.davethomasfoundation.org/getdoc/9999a5f5-33ed-40fb-aedc-a676adc98546/Harris_DTFA-Report_FINAL_2_29_08 .
- Jones J. Vital and Health Statistics. 27. Vol. 23. Hyattsville, MD: National Center for Health Statistics, U.S. Department of Health and Human Services; 2008. Adoption experiences of women and men and demand for children to adopt by women 18–44 years of age in the United States, 2002. Retrieved from www.cdc.gov/nchs/data/series/sr_23/sr23_027.pdf . [ PubMed ] [ Google Scholar ]
- Kirk HD. Shared Fate: A Theory and Method of Adoptive Relationships. Port-Angeles, WA: Ben-Simon; 1984. [ Google Scholar ]
- Leathers SJ, Spielfogel JE, Gleeson JP, Rolock N. Behavior problems, foster home integration and evidence-based behavioral interventions: What predicts adoption of foster children? Children and Youth Services Review. 2012; 34 :891–899. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Malm K, Vandivere S, McKlindon A. Children Adopted from Foster Care: Child and Family Characteristics, Adoption Motivation, and Well-Being. Washington: U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation; 2011. [ Google Scholar ]
- McDonald T, Press A, Billings P, Moore T. Partitioning of the adoption process to better predict permanency. Child Welfare. 2007; 86 (3):5–32. [ PubMed ] [ Google Scholar ]
- Merritt, Darcey Placement preferences among children living in foster or kinship care: A cluster analysis. Children and Youth Services Review. 2008; 30 :1336–1344. [ Google Scholar ]
- Radel LF, Bramlett MD, Waters A. Legal and informal adoption by relatives in the U.S.: Comparative characteristics and well-being from a nationally representative sample. Adoption Quarterly. 2010; 13 (3/4):268–291. [ Google Scholar ]
- Research Triangle Institute. SUDAAN Language Manual, Release 10.0. Research Triangle Park, NC: Research Triangle Institute; 2008. [ Google Scholar ]
- Snowden J, Leon S, Sieracki J. Predictors of children in foster care being adopted: A classification tree analysis. Children and Youth Services Review. 2008; 30 :1318–1327. [ Google Scholar ]
- Stoltzfus E. Child Welfare: The Fostering Connections to Success and Increasing Adoptions Act of 2008 (CRS Report RL34704) Washington, DC: The Congressional Research Service; 2008. [Accessed 4/21/2015]. at http://assets.opencrs.com/rpts/RL34704_20081009.pdf . [ Google Scholar ]
- U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children's Bureau. [Accessed 4/9/2015]; The AFCARS Report, No. 21: Preliminary Estimates for FY 2013 as of July 2014. 2014a at http://www.acf.hhs.gov/sites/default/files/cb/afcarsreport21.pdf .
- U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children's Bureau. [Accessed 4/9/2015]; Trends in Foster Care and Adoption: FFY 2002-FFY 2013. 2014b at http://www.acf.hhs.gov/sites/default/files/cb/trends_fostercare_adoption2013.pdf .
- Vandivere S, Malm K, Radel L. Adoption USA: A Chartbook Based on the 2007 National Survey of Adoptive Parents. Washington, D.C: The U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation; 2009. [Accessed 4/15/2015]. at http://aspe.hhs.gov/hsp/09/NSAP/chartbook/ [ Google Scholar ]
- Wilson RF, Wilcox WB. Bringing Up Baby: Adoption, Marriage, and the Best Interests of the Child. William & Mary Bill of Rights Journal. 2006; 14 (3):883–908. [ Google Scholar ]
- Visser SN, Zablotsky B, Holbrook JR, Danielson ML, Bitsko RH. National Health Statistics Reports. Vol. 81. Hyattsville, MD: National Center for Health Statistics, U.S. Department of Health and Human Services; 2015. Diagnostic experiences of children with Attention-deficit/Hyperactivity Disorder. Retrieved from http://www.cdc.gov/nchs/data/nhsr/nhsr081.pdf . [ PubMed ] [ Google Scholar ]
- Yampolskaya S, Sharrock P, Armstrong MI, Strozier A, Swanke J. Profiles of children placed in out-of-home care: Association with permanency outcomes. Children and Youth Services Review. 2014; 36 :195–200. [ Google Scholar ]
- Zill N, Bramlett MD. Health and well-being of children in foster care and children adopted from foster care. Children and Youth Services Review. 2014; 40 :29–40. [ Google Scholar ]
- Study protocol
- Open access
- Published: 02 July 2024
Improving medication adherence among persons with cardiovascular disease through m-health and community health worker-led interventions in Kerala; protocol for a type II effectiveness-implementation research-(SHRADDHA-ENDIRA)
- Jaideep C. Menon 1 ,
- Denny John 2 ,
- Aswathy Sreedevi ORCID: orcid.org/0000-0002-6037-9265 3 ,
- Chandrasekhar Janakiram 4 ,
- Akshaya R 3 ,
- Sumithra S 5 ,
- Aravind M S 6 ,
- Mathews Numpeli 7 ,
- Bipin Gopal 8 ,
- Renjini B A 7 ,
- Sajeev P K 9 ,
- Ravivarman Lakshmanaswamy 10 &
- Abhishek Kunwar 11
Trials volume 25 , Article number: 437 ( 2024 ) Cite this article
11 Accesses
7 Altmetric
Metrics details
Cardiovascular disease (CVD) is the leading cause of mortality worldwide, and at present, India has the highest burden of acute coronary syndrome and ST-elevation myocardial infarction (MI). A key reason for poor outcomes is non-adherence to medication.
The intervention is a 2 × 2 factorial design trial applying two interventions individually and in combination with 1:1 allocation ratio: (i) ASHA-led medication adherence initiative comprising of home visits and (ii) m-health intervention using reminders and self-reporting of medication use. This design will lead to four potential experimental conditions: (i) ASHA-led intervention, (ii) m-health intervention, (iii) ASHA and m-health intervention combination, (iv) standard of care. The cluster randomized trial has been chosen as it randomizes communities instead of individuals, avoiding contamination between participants. Subcenters are a natural subset of the health system, and they will be considered as the cluster/unit. The factorial cluster randomized controlled trial (cRCT) will also incorporate a nested health economic evaluation to assess the cost-effectiveness and return on investment (ROI) of the interventions on medication adherence among patients with CVDs. The sample size has been calculated to be 393 individuals per arm with 4–5 subcenters in each arm. A process evaluation to understand the effect of the intervention in terms of acceptability, adoption (uptake), appropriateness, costs, feasibility, fidelity, penetration (integration of a practice within a specific setting), and sustainability will be done.
The effect of different types of intervention alone and in combination will be assessed using a cluster randomized design involving 18 subcenter areas. The trial will explore local knowledge and perceptions and empower people by shifting the onus onto themselves for their medication adherence. The proposal is aligned to the WHO-NCD aims of improving the availability of the affordable basic technologies and essential medicines, training the health workforce and strengthening the capacity of at the primary care level, to address the control of NCDs. The proposal also helps expand the use of digital technologies to increase health service access and efficacy for NCD treatment and may help reduce cost of treatment.
Trial registration
The trial has been registered with the Clinical Trial Registry of India (CTRI), reference number CTRI/2023/10/059095.
Peer Review reports
Administrative information
Note: the numbers in curly brackets in this protocol refer to SPIRIT checklist item numbers. The order of the items has been modified to group similar items (see http://www.equator-network.org/reporting-guidelines/spirit-2013-statement-defining-standard-protocol-items-for-clinical-trials/ ).
Title {1} | SPIRIT guidance: Descriptive title identifying the study design, population, interventions, and, if applicable, trial acronym.
|
Trial registration {2a and 2b}. | SPIRIT guidance: Trial identifier and registry name. If not yet registered, name of intended registry. Item 2b is met if the register used for registration collects all items from the World Health Organization Trial Registration Data Set. |
Protocol version {3} | SPIRIT guidance: Date and version identifier. Version 3. 23 February 2024. |
Funding {4} | SPIRIT guidance: Sources and types of financial, material, and other support. Financial support from WHO, Geneva, Alliance for Health Policy and System research |
Author details {5a} | SPIRIT guidance: Affiliations of protocol contributors. Jaideep C Menon, Professor, Adult Cardiology, AIMS, Kochi Denny John, Adjunct Professor, Ramaiah University of applied Sciences Aswathy S, Professor, Community Medicine Chandrasekhar J, Professor, Public Health Dentistry Akshaya R, Senior Resident, Community Medicine Sumithra S, Senior Lecturer, St John’s research Institute Aravind MS, Research Associate, Public Health, AIMS, Kochi Mathews Numpeli, CHC MO, DHS, Govt of Kerala Bipin Gopal, State nodal Officer- NCDs, Kerala Renjini BA, MO, DHS, Govt of Kerala Sajeev PK, NHM Coordinator, Kalady Ravivarman L, WHO NCD officer, India Country Office Abhishek Kunwar, NPO NCD, WHO India |
Name and contact information for the trial sponsor {5b} | SPIRIT guidance: Name and contact information for the trial sponsor. Dr Sarah Rylance, Medical Officer for Chronic Respiratory Diseases, Focal point for NCD Research and Innovation World Health Organization HQ |
Role of sponsor {5c} | SPIRIT guidance: Role of study sponsor and funders, if any, in study design; collection, management, analysis, and interpretation of data; writing of the report; and the decision to submit the report for publication, including whether they will have ultimate authority over any of these activities. Study sponsor does not have any role in the study design, collection, management, analysis and interpretation of data |
Introduction
Background and rationale {6a}.
Cardiovascular disease (CVD) is the leading cause of mortality worldwide, and at present, India has the highest burden of acute coronary syndrome and ST-elevation myocardial infarction (MI) [ 1 ]. A key reason for poor outcomes is non-adherence to medication. The WHO has reported that non-adherence to drugs in chronic conditions is as high as 50%, and 30% of re-admissions are related to non-compliance to medication. In its 2003 report [ 2 ], WHO states that “increasing the effectiveness of adherence interventions may have a far greater impact on the health of the population than any improvement in specific medical treatment.”
A systematic review published in 2015 on adherence to medication had eleven studies from India reporting adherence rates (using pills taken, prescribed doses taken, changes, etc.) using Morisky Medication Adherence Score (MMAS) in the range of 0–51.2% [ 3 , 4 , 5 , 6 , 7 , 8 ]. The factors associated with non-adherence to medications were forgetfulness, difficulty in remembering, and stopping medication upon feeling better/worse.
Various interventions have been studied to increase medication adherence for cardiovascular disease in India. These include the use of combination therapy or polypill [ 9 , 10 , 11 ], use of community health workers (CHW) for simplified hypertension management with the aid of a smart-phone-based electronic decision support system [ 12 ], “task shifting” interventions to CHWs for CVD risk reduction through behavioral change [ 13 ], improving adherence to drugs, lifestyle changes, and clinical risk markers in patients of acute coronary syndromes [ 14 , 15 ] and use of CHWs and doctors in primary health center (PHC) to assess CVD risk with clinical decision support being provided through an m-health platform by doctors sitting remotely [ 16 ]. Studies have also identified the use of mobile technology by health workers in resource-limited settings for health delivery improvement [ 17 ]. The different studies mentioned have looked at m-health or CHWs alone to improve adherence to medication, lifestyle changes, or as a platform for treatment, with varied results.
We measured adherence in 2064 patients of coronary artery disease (CAD) the ENDIRA cohort using the MMAS-8 in the year 2019. Our results revealed poor adherence to chronic care medications in CAD patients. On an average, only 2.8 of the mandated 4 drugs (beta blocker, ACE Inhibitor /ARB, statin, and anti-platelet) were being taken by patients regularly [ 18 ]. The mean value of MMAS was 4 out of a possible 8, reflecting poor adherence [ 19 ]. A study on the feasibility of an m-health intervention in the same cohort for the prevention and management of CAD revealed that the use and ownership of mobiles was 88% (2015), 92% were willing to receive mobile health advice [ 19 ], 70% preferred voice calls over SMS, 85.9% would send self-recorded blood pressure, weight, and blood glucose to a doctor or community health worker [ 19 ]. Given that the results of our study revealed poor adherence and that use of m-health for CVD was both acceptable and feasible, the obvious next step would be in trying to improve adherence using these resources.
Objectives {7}
Primary objective.
To assess the effectiveness of using m-health and community health worker-led interventions for improving adherence to drugs in patients with cardiovascular disease using m-health and community health worker intervention individually and in combination in comparison to control group.
Secondary objective
To assess the effects of using the interventions (m-health and community health worker-led interventions) for improving adherence to drugs among heart disease patients on implementation outcomes such as acceptability and adoption.
To assess the cardiometabolic risk factors among first degree relatives of patients with heart disease
Trial design {8}
It is a 2 × 2 factorial design trial applying two interventions individually and in combination with a 1:1 allocation ratio. Two interventions are applied individually and in combination: (i) ASHA-led medication adherence initiative comprising of home visits, and (ii) m-health intervention using reminders and self-reporting of medication use. This design will lead to four potential experimental conditions: (i) ASHA-led intervention, (ii) m-health intervention, (iii) ASHA and m-health intervention combination, (iv) standard of care.
Methods: participants, interventions, and outcomes
Study setting {9}.
The study will be implemented in the ENDIRA (Epidemiology of Non-communicable Diseases in Rural Areas) cohort (n-114,064 individuals) which includes 2064 patients with heart disease in whom adherence to drugs for heart disease has already been assessed. The ENDIRA cohort is spread over 5 primary health centers consisting of 18 subcenters where the health details of all individuals have been recorded. In order to avoid contamination in the treatment allocation and its response, at least 10 km of distance among villages will be maintained and they will be clubbed into 4 groups.
The intervention will be implemented in Angamaly block consisting of five local self-government areas namely Mookkannoor, Kalady, Thuravoor, Karukutty, and Manjapra with a population of 18,638, 20,407, 20,475, 26,811, and 14,668 in Ernakulam district [ 20 ] in Kerala state, India, respectively.
Eligibility criteria {10}
The study samples will consist of adult community members with diagnosis of CAD, valvular disease, heart failure, and rhythm disorders in the target areas who provide informed consent.
Eligibility criteria
Diagnosed case of CAD who have received treatment for MI/STEMI/UA or diagnosed using a coronary angiogram or CT coronary angiogram or have undergone revascularization and are on medications.
Other cardiovascular cases such as rhythm disorders, valve disorders, and heart failure identified as pumping disorders by the community will also be a part of the study. Male or female aged 18 years or more will be considered.
Resident of village during the baseline survey.
Has no plans to migrate in next 12 months from the date of initiation of intervention.
Exclusion criteria
Persons who are bedridden and are unable to answer the questions.
Pregnant or lactating mothers
Individuals with cognitive impairment
Who will take informed consent? {26a}
Informed consent will be taken by the accredited social health activist of the area who will be collecting the data. The data collection will be through an application called SHRADDHA (which means care). The participant’s digital signature will be obtained on the tablet.
Additional consent provisions for collection and use of participant data and biological specimens {26b}
Blood samples will be collected to assess random blood sugar and HbA1c among cardiac patients with type 2 DM after obtaining consent. These samples will be tested using point-of-care devices and will not be stored. We will request consent for review of participants’ medical records, and for the collection of blood samples to assess random blood sugar and HbA1c among the cardiac patients with type 2 diabetes. But this trial does not involve collecting biological specimens for storage.
Interventions
Explanation for the choice of comparators {6b}.
Results of our study revealed poor adherence and that use of m-health for CVD was both acceptable and feasible. Various interventions have been studied to increase medication adherence for cardiovascular disease in India such as use of combination therapy or polypill, use of community health workers (CHW) for simplified hypertension management with the aid of a smart phone-based electronic decision support system, so we decided to use factorial study design where study units would be assigned to ASHA and no ASHA group. Following this they would be assigned to m-health and no m-health group. Thus, there are four arms to the study: namely ASHA, ASHA and m-health, m-health, and standard of care.
Intervention description {11a}
The intervention content is prepared after discussion with the stakeholders such as ASHAs, Medical Officers, and patients. Qualitative data would be obtained from unstructured or semi-structured interviews exploring the individual’s understanding of the use of medicines, potential obstacles and incentives to adherence, useful strategies to improve adherence. Interview guide for In-Depth-Interviews and Key-Informant Interviews will be developed after a thorough literature search. In-Depth Interviews will be done with the participants and their relatives to identify individual’s understanding of the use of medicines, potential obstacles and incentives to adherence, useful strategies to improve adherence, and other questions spontaneously raised during the interview. For Key-Informant Interviews, Health care providers such as doctors, the multipurpose health worker, ASHAs, and pharmacists (about 10) will be interviewed till saturation Is reached. Focus group discussions (FGD) will be conducted among adherent CVD patients and nonadherent CVD patients. About 3-4 such FGD will be conducted till data saturation is reached. This will be repeated at endline.
Community health worker directed visits to the house of the patient, where they will explain the use of drugs and the various roles of the different classes of drugs along with taking a pill count and giving health advice and counselling with a PowerPoint on a tablet. The frequency of visits is twice a month for the first 3 months, and once a month for the next 3 (11 visits in all). A schedule of visits with the areas to be highlighted in each visit such as diet, physical activity, tobacco, and alcohol will be prepared and given.
Before the commencement of the intervention training, sessions for community health workers (ASHAs) in the intervention arm will be conducted. This will comprise of three sessions of 6 h each and would include curriculum-based training modules on CVD, HTN, diabetes, dyslipidemia; awareness of the role each of the 4 classes of drugs in AS-CVD plays in secondary prevention; sensitization to the role of adherence in preventing recurrence; sensitization to the side effects of the drugs and counselling skill training. Role of lifestyle changes such as diet, physical activity, tobacco, and alcohol will also be carried out.
The envisaged m-health platform is a two-way system through which messages or jingles (audio clips) could be passed back and forth between the care provider (ASHA, Research assistant, or doctor) and the recipient (patient). Individual patient details gathered and entered on a Tab PC get stored on a central server. The data is anonymized and coded individually, with a 12-digit UID. In clusters where the m-health intervention is planned, individual patients could download and activate an already developed App, which is a free download from the Google play store [Ente app (my app)]. The individual patient would be able to access his personal health record as entered, by way of the App. This App would serve as a two-way channel of communication between the patient and caregiver. In the other clusters, individual patients could download their personal data and the App, with the communication channel remaining blocked.
Bi-monthly reminders via text or audio messages and weekly reminders on taking medicines at the time of a scheduled dose by way of a beep or tune and health advice by way of messages are sent for the first 3 months, followed by monthly reminders of text messages the next 3 and weekly drug reminder tunes.
Community health worker and m-health
Health worker (ASHA)-directed visits to the house of the patient, where they will explain the use of drugs and the various roles of the different classes of drugs along with taking a pill count and giving health advice and counselling. The frequency of visits is twice a month for the first 3 months, and once a month for the next 3. In addition, bi-monthly reminders via text or audio messages and weekly reminders on taking medicines at the time of a scheduled dose by way of a beep or tune and health advice by way of messages are sent for the first 3 months, followed by monthly reminders of text messages the next 3 and weekly drug reminder tunes.
Standard of care (SoC) is patient-initiated physician visit with health advice and treatment as prescribed by the treating doctor.
In all the groups, the patients can visit the doctor in case of any need or emergency.
After completion of baseline survey in all clusters, intervention will be implemented in intervention clusters for 6 months. All the participants in the intervention and control arms will be permitted to use standard treatment for CVD. Community health worker-directed visits to the house of the patient, where they will explain the use of drugs and the various roles of the different classes of drugs along with taking a pill count and giving health advice and counselling. The frequency of visits is twice a month for the first 3 months, and once a month for the next 3 (9 visits in all). Table 1 shows the timepoint for the intervention implementation.
Criteria for discontinuing or modifying allocated interventions {11b}
This is not applicable as the intervention is to improve medication adherence, so there will be no special criteria for discontinuing or modifying allocated intervention.
Strategies to improve adherence to interventions {11c}
The various interventions are for the improvement of adherence as measured by the Morisky Medication Adherence scale [ 21 ].
Relevant concomitant care permitted or prohibited during the trial {11d}
Relevant concomitant care is permitted.
Provisions for post-trial care {30}
This is a non-pharmacological intervention; therefore, there are no specific post trial care provisions.
Outcomes {12}
Primary, secondary, and other outcomes.
The primary outcome is the adherence of patients as measured by Morisky adherence scale [ 21 ] at the beginning of the study, midterm, and at the end. The secondary outcomes include Quality of Life (EuroQOL) [ 22 ], blood pressure, random blood sugar, HbA1c among the cardiac patients with type 2 diabetes, mortality events, and other unintended outcomes will also be recorded. The analysis will include change from baseline. Adherence is chosen as the main outcome as the objective is to study the impact of the various interventions singly and in combination on adherence in comparison to standard of care. Various symptoms, such as dyspnea, fatigue, edema, difficulty sleeping, depression, and chest pain associated with CVD limits activities of daily life [ 23 ]. Therefore, it is important to measure the quality of life before and after the intervention. Metabolic control can result from better adherence to medication and a better awareness of the importance to adhering to medication. Therefore, meeting targets of blood pressure, blood sugar levels, and HbA1c will be considered as secondary outcomes.
Participant timeline {13}
Sample size {14}.
Based on the learnings from the previous study, the rate of missing data due to electronic data collection will be low.
Phases 1 and 2: planning and baseline evaluation
The process of developing the intervention will start with the development of the initial concepts based on the available literature and interaction with healthcare professionals working in the rural areas.
Baseline study
Selection and training of team : The team will deliver the training to the selected project coordinator and the field staff. Field staff (part-time) will be recruited by the investigators on the advice of village head and/or NCD clinic in-charge. He/she should be a member of community preferably the accredited social health activist with an interest in health care and community, willingness to learn, and leadership qualities. A strong commitment to work in the community will be identified as an important criteria for the selection of all the team members. After a sensitization session of the data collectors/field staff, they will be asked to prepare a list of persons with cardiovascular disease including coronary artery disease, valvular disease, arrhythmias, and heart failure. Hands on sessions to download the App and collect data will be provided.
In Phase 2, baseline evaluation will be initiated in the study areas after obtaining the ethics committee approval. Written informed consent will be obtained from the study participants. Participants will receive a participant information sheet (PIS) outlining the rationale for the study, details on interventions, the steps, and protocols to be followed throughout the study, potential side effects and risks, benefits, a confidentiality statement, the option to withdraw from the study at any time, and the investigators’ contact information. The baseline survey performed by ASHAs will be done through a survey app called SHRADDHA. The variables collected would include (1) basic demographic information, including age, income, gender, marital status, religion, and occupation; (2) lifestyle-related factors such as physical activity, tobacco use, and alcohol consumption, dietary factors intake of fruits and vegetables, cooking oil and red meats; (3) disease details including for diabetes, hypertension, dyslipidemia, stroke and CAD, COPD, and surgeries; and (4) current medications. Questions will be explained to each participant to help them get familiar with the contents, instructions for filling them out will be given, and the responses will be recorded. On the home visit, the Field staff/ASHA will also record height and weight, measure sugars with a glucometer, and take a photo of the most recent prescription. All of this will be recorded in the app. Glycosylated hemoglobin will also be measured among the cardiac patients with diabetes using the point of care device called Lumira Dx.
Sample size : Sample size was estimated assuming an improvement of 10% in medication adherence at the end of a 6-month period in either m-health or community health worker-led intervention compared to control group. This 10% improvement will lead to an effect size of 0.4 units in medication adherence through m-health or community health worker-led intervention and an effect size of 0.8 units in combined intervention (m-health and community health worker-led intervention) compared to the control group. The 10% was an assumption considering that large differences are not possible in a community setting and was based on another community-based study which has also used 10% improvement of adherence score [ 24 ].
To observe a difference of 0.4 units in the medication adherence between study groups, with a standard deviation of 1.8, 5% level of significance (adjusted for multiple comparison) and 80% power, the sample size needed will be 238 participants in each of the study groups. After accounting for a design effect (cluster effect) and 10% attrition, the number of participants required per group will be 393, a total of 1572 participants.
Recruitment {15}
Working through the public health system, keeping in mind the proximity of the ASHAs to the community, it is expected that adequate participant enrolment can be achieved. Monitoring and supervision by the project team will assist in timely completion. The time period of recruitment is from February to May, 2024. After the recruitment, the randomization will be done and intervention will be administered for 6 months. Expected to finish by November 2024 and endline assessment in December 2024.
Assignment of interventions: allocation
Sequence generation {16a}.
Allocation of intervention and sequence generation will be as follows. Codes will be randomly assigned to the four interventions (ASHA, m-health, ASHA + m-health, and control groups) namely A, B, C, and D. In the next step, randomization list will be generated using RANDOM ALLOC software. Eighteen subcenters will be randomized into 4 study groups (A, B, C, and D) using different permutations of ABCD. Each subcenter will be allocated random numbers ranging from 1 to 18 using random number generators and random shuffling of this number. Interventions will be allocation to the subcenters in the sequence of random shuffled numbers as per the randomization list.
Concealment mechanism {16b}
It will be an open-label trial as concealment is not possible. However, study site allocation will be done only after completing baseline assessment and agreements with sites to participate.
Implementation {16c}
The allocation sequence will be generated by the Statistician, enrolment will be by the Field coordinator and the Field coordinator will assign subcenter as it is a cluster randomized trial.
Assignment of interventions: blinding
Who will be blinded {17a}.
Data analysts will be blinded. The ASHA workers, patients, and outcome assessors are not blinded.
Procedure for unblinding if needed {17b}
In this study, the ASHA workers, patients, and outcome assessors will not be blinded. Only the data analysts will be blinded. The data analyst will be unblinded if there are any outlier biochemical values which requires immediate action so that the patient can be intimated.
Data collection and management
Plans for assessment and collection of outcomes {18a}.
The primary outcome adherence will be measured by Morisky 8-item adherence questionnaire which has been validated in various countries including India and in various disease conditions. The eight-item Morisky Medication Adherence Scale (MMAS-8) is a structured self-report measure of medication-taking behavior that has been widely used in various cultures [ 25 , 26 , 27 ].It has a maximum score of 8.
The quality of life will be measured by the EuroQol five‐dimensions – 3‐level (EQ5D) which is a versatile quality of life (QOL) instrument with five dimensions (mobility, self‐care, usual activities, pain/discomfort, and anxiety/depression) and a visual analog scale. The questionnaire has also been found to be valid and reliable in various disease conditions including cardiovascular and cancer in India and neighboring countries [ 28 , 29 ].Random blood sugar among the patient and family member will be measured by the ASHA as per standard methods using a glucometer. Blood pressure will also be measured using the electronic Blood pressure will be recorded with the OMRON HEM 7124 automatic blood pressure monitor (Shimogyo-ku, Kyoto, Japan) by measuring upper arm BP. A laboratory technician will measure Glycosylated Haemoglobin using the Lumira Dx point of care device.
Real-time data entry will be monitored, and wherever there are difficulties with using the app, support will be provided by the field coordinator.
Plans to promote participant retention and complete follow-up {18b}
All efforts will be made to retain all participants in the study. As they are also part of the earlier ENDIRA study, there is a good rapport with the study group, local self-government, and frontline health workers. Loss to follow-up may result from migration to their children’s places of living or death or for other reasons. The characteristics of the patients who drop out will be recorded and compared to those who are in the study.
Data management {19}
As the data is collected through the SHRADDHA app, the data will be exported to excel and checked for completion each day. According to the data collected, feedback, and monitoring will be done to ensure correct and complete entries. Duplicate entries will be checked for and removed.
Confidentiality {27}
The data of the patients will be anonymized, and each patient will be assigned a unique id. From the app de-identified anonymized data will be stored in Excel. This will be stored confidentially before, during, and after the trial.
Plans for collection, laboratory evaluation, and storage of biological specimens for genetic or molecular analysis in this trial/future use {33}
In this study, blood samples will be collected to assess random blood sugar and HbA1c. These tests are done using point-of-care devices. The blood samples will not be stored in the current trial.
Statistical methods
Statistical methods for primary and secondary outcomes {20a}.
Several models will be run to test for the main outcomes, implementation outcomes, and related research questions. Mixed linear and logistic effects models as appropriate will be used to identify differences between the groups (ASHA, ASHA and m-health, m-health, control group), where random effects will be used for the clusters and fixed effects will be used for effects of ASHA workers and of m-health. The primary dependent variable in the models will be change in adherence measured by the Morisky scale. Models will also be fitted for the secondary outcomes such as change in blood pressure, random blood sugar, Hba1c levels, and quality of life. Subsequently, covariates such as age, sex, and co-morbidities will be added to the models to adjust for potential confounders.
Interim analyses {21b}
In this study, the intervention is done to improve the medication adherence through health education by ASHA workers, m-health, or both. Since the risk due to the intervention is minimal or none, interim analysis, and stopping guidelines have not been prescribed by the ethical committee and therefore there will not be any stopping guidelines.
Methods for additional analyses (e.g., subgroup analyses) {20b}
Subgroup analysis will not be carried out. However, for the primary and secondary outcome variables, covariates such as age, sex, and co-morbidities will be considered as potential confounders in the mixed effect model analysis.
Methods in analysis to handle protocol non-adherence and any statistical methods to handle missing data {20c}
Nonadherence will be managed by the intention to treat analysis and if there are too many missing data, imputations will be considered. Mixed method analysis will be considered for intention to treat analysis. Also depending on the percentage of data missingness and assumption for data missing in the study variables, appropriate missing data imputation technique will be used.
Plans to give access to the full protocol, participant-level data, and statistical code {31c}
Full protocol can be given. Full dataset can be given with the permission of the Institution, WHO, and Government.
Oversight and monitoring
Composition of the coordinating center and trial steering committee {5d}.
There is only one site for the study; therefore, the coordinating and steering committee will be situated at the site. The coordinating center is the Community Health Centre (CHC). The ASHA’s work is coordinated through the CHC by the National Health mission coordinators. The trial steering committee (TSC) monitors recruitment, communicates, and provides conflict resolution and timely advice. They meet every 6 weeks. Local organization and implementation is taken care of by the NHM coordinators and a responsible person reporting to the Principal Investigator from the Project management group. Trainings and other group meetings are conducted by the project management group. Consent is obtained by the ASHA. Periodic meetings are conducted by the Project management group (investigators) team to monitor progress. The stakeholder groups are apprised of the progress of the trial, role of intervention, and its possible benefit.
Composition of the data monitoring committee, its role and reporting structure {21a}
This study is measuring adherence which is a low-risk intervention; therefore, a data monitoring committee is not required. The project management group meets every 2 weeks. The Trial Steering Group and the independent Data Monitoring and Ethics Committee meet to review conduct throughout the trial period.
Adverse event reporting and harms {22}
As this study is measuring adherence of an intervention, no adverse events or serious adverse events and harms from the intervention are anticipated. But if there are any, they will be reported to relevant regulatory bodies such as Project management group, Trial steering Committee, District Health Authority, and Ethics Committee. Trial deviations will be reported to the ethical committee.
Frequency and plans for auditing trial conduct {23}
The meetings of the Project management group, Trial Steering group, independent data monitoring, and Ethics Committee periodically will also serve to audit the trial.
Plans for communicating important protocol amendments to relevant parties (e.g. trial participants, ethical committees) {25}
Before the start and at the start, there have been some minor modifications which has been updated to the ethical committee and subsequently uploaded in the CTRI.
Dissemination plans {31a}
The results of the study will be published in standard journals. Social media and Stakeholder workshops will be used to disseminate the findings. A lay summary will be shared with all participants.
The present study will promote much needed research and innovation for increasing adherence among patients with cardiovascular disease. The effect of different types of intervention alone and in combination will be assessed using a cluster randomized design involving 18 subcenter areas. This factorial cluster randomized controlled trial will benefit by increasing the drug adherence for NCD using m-health platform and frontline health workers. The trial will explore local knowledge, perceptions and empower people by shifting the onus onto themselves for their medication adherence.
The proposal is aligned to the WHO-NCD aims of improving the availability of affordable basic technologies and essential medicines, improving adherence for non-communicable diseases (NCDs). It also aligns to WHO-NCD aim of training the health workforce and strengthening the capacity of health systems, particularly at the primary care level, to address the control of NCDs. The proposal also helps expand the use of digital technologies to increase health service access and efficacy for NCD treatment and may help reduce the cost of treatment.
The proposal helps implementation of WHO-PEN protocol for Self-Care guidelines including utilizing frontline health workers in improving self-care in patients of heart disease, counselling to improving adherence and self-care, considering patients’ beliefs and concerns about drugs and their effect. The research is also aligned to the WHO-HEARTS package, both by way of A&T of the HEARTS where A- consists of information on CVD medicine and technology procurement, quantification, distribution, management, and handling of supplies at facility level. T- consists of guidance and examples on team-based care and task shifting related to the care of CVD. The research is also aligned with the Sustainable Development Goals (SDG) goal in relation to NCD of reducing by one third premature mortality from non-communicable diseases through prevention and treatment.
There are significant expected implementation challenges to note. First, the trial involves working with the primary clinics providing NCD screening and detection services, and building an effective partnership with the state government of Kerala where the project will be implemented will be crucial for its success. Second, medication nonadherence for patients with chronic diseases is extremely common with 40–50% of patients prescribed medications for management of diabetes and hypertension [ 30 ]. There exist treatment-related barriers, such as treatment complexity, side effects (or fear of side effects), inconvenience, cost, and time, and other barriers such as poor practitioner-patient relationship, aspects of which are beyond the scope of the intervention [ 30 ].
If successful, the medication adherence intervention, using m-health and ASHAs, has the potential to constitute evidence-based practice for improving medication adherence for CVD in India, and in similar developing countries.
Trial status
The current protocol is version 3 dated 23–02-2024. The recruitment began on November 30, 2023 and is expected to be complete by May 30, 2024. The submission has been delayed due to unavoidable circumstances such as elections and heatwave.
Availability of data and materials {29}
The investigators will have access to the final data set. There are no contractual agreements which limit access to investigators. The investigators in the field collect the data and the data is with them. Any data required to support the protocol can be supplied on request.
Abbreviations
Angiotensin-converting enzyme
Angiotensin II receptor blocker
Accredited social health activist
- Coronary artery disease
Community health workers
Chronic obstructive pulmonary disease
Cluster randomized control trial
Computed tomography
Clinical Trials Registry—India
Cardiovascular diseases
Epidemiology of Non-Communicable Diseases in Rural Areas
Hypertension
Low-middle-income countries
Mobile Health
Myocardial infarction
Morisky Medication Adherence Score
Non-communicable diseases
Primary health center
Quality of Life
Return on investment
Sustainable Development Goals
Short Message Service
ST elevation myocardial infarction
Unstable angina
World Health Organization
Sreeniwas Kumar A, Sinha N. Cardiovascular disease in India: A 360 degree overview. Medical Journal Armed Forces India. 2020;76(1):1–3.
Article CAS PubMed PubMed Central Google Scholar
Sabaté E, ed. Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization; 2003.
Baroletti S, Dell’Orfano H. Medication adherence in cardiovascular disease. Circulation. 2010;121:1455–8.
Article PubMed Google Scholar
Prabhakaran D, Jeemon P, Roy A. Cardiovascular disease in India, Current epidemiology and future directions. Circulation. 2016;133:1605–20.
Akeroyd JM, Chan WJ, Kamal AK, Palaniappan L, Virani SS. Adherence to cardiovascular medications in the South Asian population: A systematic review of current evidence and future directions. World J Cardiol. 2015;7(12):938–47.
Article PubMed PubMed Central Google Scholar
Fathima FN, Shanbhag DN, Hegde SKB, Sebastian B, Briguglio S. Cross Sectional Study of Adherence to Prescribed Medications among Individuals Registered at a High Risk Clinic in a Rural Area in Bangalore, India. Indian J Publ Health Research and Development. 2013;4(3):90–4.
Article Google Scholar
Venkatachalam J, Abrahm SB, Singh Z, Stalin P, Sathya GR. Determinants of Patient’s Adherence to Hypertension Medications in a Rural Population of Kancheepuram District inTamilNadu. SouthIndia Indian J Community Med. 2015;40:33–7.
Article CAS Google Scholar
Kumar N, Unnikrishnan B, Thapar R, Mithra P, Kulkarni V, Holla R, Bhagawan D, Mehta I. Factors associated with adherence to antihypertensive treatment among patients attention atertiary care hospital in Mangalore. South India IJCRR. 2014;6:77–85.
Google Scholar
Bahl VK, Jadhav UM, Thacker HP. Management of hypertension with the fixed combination of perindopril and amlodipine in daily clinical practice: results from the STRONG prospective, observational, multicenter study. Am J Cardiovasc Drugs. 2009;9:135–42.
Article CAS PubMed Google Scholar
Soliman EZ, Mendis S, Dissanayake WP, Somasundaram NP, Gunaratne PS, Jayasingne IK, Furberg CD. A Polypill for primary prevention of cardiovascular disease: a feasibility study of the World Health Organization. Trials. 2011;12:3.
Thom S, Poulter N, Field J, Patel A, Prabhakaran D, Stanton A, Grobbee DE, Bots ML, Reddy KS, Cidambi R, et al. Effects of a fixed-dose combination strategy on adherence and risk factors in patients with or at high risk of CVD:theUMPIRE randomized clinical trial. JAMA. 2013;310:918–29.
Ajay VS, Tian M, Chen H, Wu Y, Li X, Dunzhu D, et al. A cluster-randomized controlled trial to evaluate the effects of a simplified cardiovascular management program in Tibet, China and Haryana, India: study design and rationale. BMC Public Health. 2014;14(1):924.
Jeemon P, Narayanan G, Kondal D, et al. Task shifting of frontline community health workers for cardiovascular risk reduction: design and rationale of a cluster randomised controlled trial (DISHAstudy) in India. BMC Public health. 2016;16:264.
Kamath DY, Xavier D, Gupta R, Devereaux PJ, Sigamani A, Hussain T, et al. Rationale and design of a randomized controlled trial evaluating community health worker–based interventions for the secondary prevention of acute coronary syndromes in India (SPREAD). Am Heart J. 2014;168(5):690–7.
Sharma KK, Gupta R, Mathur M, Natani V, Lodha S, Roy S, Xavier D. Non-physician health workers for improving adherence to medications and healthy lifestyle following acute coronary syndrome: 24-month follow-up study. Indian Heart J. 2016;68(6):832–40.
Peiris D, Praveen D, Kishor M, et al. SMART health India: A stepped-wedge, a cluster randomised controlled trial of a community health worker managed mobile health intervention for people assessed at high cardiovascular disease risk in rural India. PLOS One. 2019;14(3):e0213708.
Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med. 2013;10(1): e1001363.
Banerjee A, Menon JC, et al. A learning health system for secondary prevention in cardiovascular disease in Kerala using informatics and non-physician health workers (LHSCVD). Indian Heart J. 2018;70:S2.
Feinberg L, Menon JC, et al. Potential for mobile health (m-Health) prevention of cardiovascular diseases in Kerala: A population-based survey. Indian Heart J. 2017;69:182–99.
Angamaly Municipality City Population Census 2011-2024 | Kerala. [cited 2024 Jun 3]. Available from: https://www.census2011.co.in/data/town/803285-angamaly-kerala.html
Janežič A, Locatelli I, Kos M. Criterion validity of 8-item Morisky Medication Adherence Scale in patients with asthma. PLoS ONE. 2017;12(11):e0187835. https://doi.org/10.1371/journal.pone.0187835.PMID:29190693;PMCID:PMC5708647 .
EQ-5D-3LUserguide-23–07.pdf. [cited 2024 Jun 3]. Available from: https://euroqol.org/wp-content/uploads/2023/11/EQ-5D-3LUserguide-23-07.pdf
Heo S, Lennie TA, Okoli C, Moser DK. Quality of life in patients with heart failure: ask the patients. Heart Lung. 2009;38(2):100–8.
Xavier D, Gupta R, Kamath D, Sigamani A, Devereaux PJ, George N, et al. Community health worker-based intervention for adherence to drugs and lifestyle change after acute coronary syndrome: a multicentre, open, randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(3):244–53.
Surekha A, Fathima FN, Agrawal T, Misquith D. Psychometric Properties of Morisky Medication Adherence Scale (MMAS) in Known Diabetic and Hypertensive Patients in a Rural Population of Kolar District, Karnataka. Indian Journal of Public Health Research & Development. 2016;7(2):250.
Grover A, Oberoi M. Self-reported Morisky eight item medication adherence scale is a reliable and valid measure of compliance to statins in hyperlipidemic patients in India. Indian Heart J. 2020;72(4):319–20.
Okello S, Nasasira B, Muiru ANW, Muyingo A. Validity and Reliability of a Self-Reported Measure of Antihypertensive Medication Adherence in Uganda. PLoS ONE. 2016;11(7):e0158499.
Mahesh PKB, Gunathunga MW, Jayasinghe S, Arnold SM, Senanayake S, Senanayake C, et al. Construct validity and reliability of EQ-5D-3L for stroke survivors in a lower middle-income setting. Ceylon Med J. 2019;64(2):52–8.
Tripathy S, Hansda U, Seth N, Rath S, Rao PB, Mishra TS, et al. Validation of the EuroQol Five-dimensions - Three-Level Quality of Life Instrument in a Classical Indian Language (Odia) and Its Use to Assess Quality of Life and Health Status of Cancer Patients in Eastern India. Indian J Palliat Care. 2015;21(3):282–8.
Kleinsinger F. The Unmet Challenge of Medication Nonadherence. Perm J. 2018;22:18–033. https://doi.org/10.7812/TPP/18-033 .
Download references
Acknowledgements
The authors acknowledge the Accredited Social Health Activists, Dr Naseema Najeeb CHC MO, Dr Sunil Kumar, and Mr Sunny V V.
Funded by WHO NCD Division and NCD Alliance, Geneva.
WHO Reference 2023/1376413–0.
The funding body does not have a role in the design, data collection, analysis, and interpretation of data.
Author information
Authors and affiliations.
Adult Cardiology, AIMS, Amrita Vishwa Vidyapeetham, Kochi, India
Jaideep C. Menon
Ramaiah University of Applied Sciences, Bengaluru, India
Community Medicine, AIMS, Amrita Vishwa Vidyapeetham, Kochi, India
Aswathy Sreedevi & Akshaya R
Public Health Dentistry, Amrita School of Dentistry, Amrita Vishwa Vidyapeetham, Kochi, India
Chandrasekhar Janakiram
StJohn’s Research Institute, Bangalore, India
AIMS, Kochi, India
Aravind M S
MO, DHS, Govt of Kerala, Ernakulam, India
Mathews Numpeli & Renjini B A
NCD, DHS, Govt of Kerala, Kerala, Thiruvananthapuram, India
Bipin Gopal
CHC, Kalady, Kalady, India
India Country Office, New Delhi, India
Ravivarman Lakshmanaswamy
NPO NCD, WHO India, New Delhi, India
Abhishek Kunwar
You can also search for this author in PubMed Google Scholar
Contributions
➙JCM is the Chief investigator, conceived the study, led the proposal and protocol development, Funding Acquisition, Methodology, Writing – Original Draft Preparation, Review & Editing
➙DJ—Conceptualization, Methodology, Writing – Original Draft Preparation, Review & Editing
➙AS—Development of proposal, Funding Acquisition, Methodology, Writing – Original Draft Preparation, Review & Editing
➙CJ—Development of proposal, Funding Acquisition, Methodology, Project Administration, Formal Analysis, Writing – Review & Editing
➙AR—Analysis, Project Administration, Supervision, Writing – Original Draft Preparation, Review & Editing
➙SS—Analysis, Sample calculation, Methodology, Visualization, Writing—Review & Editing
➙AMS—Project Administration, Supervision, Writing – Original Draft Preparation, Review & Editing
➙MN—Methodology, Project Administration, Supervision, Writing – Review & Editing
➙BG—Conceptualization, Methodology, Writing – Review & Editing
➙RBA—Project administration, Methodology, Writing – Review & Editing,
➙RL—Investigation, Methodology, Writing – Review & Editing
➙AK—Investigation, Methodology, Writing – Review & Editing
➙All the authors have read and approved the final manuscript.
Corresponding author
Correspondence to Aswathy Sreedevi .
Ethics declarations
Ethics approval and consent to participate {24}.
Ethical Review Board of Amrita Institute of Medical Sciences had approved the study dated 23–02-2024 number ECASM-AIMS-2024–098. Written, informed consent to participate will be obtained from all participants. Ethical approval has been obtained.
Consent for publication {32}
Informed consent has been obtained and the model consent form can be made available. No identifying images or other personal or clinical details of participants are presented here or will be presented in reports of the trial results.
Competing interests {28}
The authors declare that there are no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Menon, J.C., John, D., Sreedevi, A. et al. Improving medication adherence among persons with cardiovascular disease through m-health and community health worker-led interventions in Kerala; protocol for a type II effectiveness-implementation research-(SHRADDHA-ENDIRA). Trials 25 , 437 (2024). https://doi.org/10.1186/s13063-024-08244-0
Download citation
Received : 09 May 2024
Accepted : 11 June 2024
Published : 02 July 2024
DOI : https://doi.org/10.1186/s13063-024-08244-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Factorial study design
- Valvular disease
- Heart failure
- Implementation Research
- Medication adherence
- Morisky Medication Adherence Scale
ISSN: 1745-6215
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Adoption Research. We provide accurate, reliable, and up-to-date reports that inform and. equip professionals, policymakers, and the public at large to improve. and strengthen adoption. In 2021, we conducted the largest survey ever of adoptive parents. NCFA explored the profile of adoptive parents, their experiences, and what has changed in ...
Abstract. Research with adoptive families offers novel insights into longstanding questions about the significance of attachment across the lifespan. We illustrate this by reviewing adoption research addressing two of attachment theory's central ideas. First, studies of children who were adopted after experiencing severe adversity offer ...
They gradually develop a self-concept (how they see themselves) and self-esteem (how much they like what they see) ( 2 ). Ultimately, they learn to be comfortable with themselves. Adoption may make normal childhood issues of attachment, loss and self-image ( 2) even more complex. Adopted children must come to terms with and integrate both their ...
Throughout the review, we draw from three literatures: research on foster children and foster care; research on domestic adoption; and research on internationally adopted children. It is important to acknowledge that, although these children share similar vulnerabilities, the experiences of foster and domestically adopted children differ from ...
In this integrative review, research pertaining to the physical, cognitive, socioemotional, and psychological effects of adoption on foster children was examined. A systematic review of the ...
The current article provides a review of adoption research since its inception as a field of study. Three historical trends in adoption research are identified: the first focusing on risk in ...
The reference lists of included studies, articles citing included studies and selected journals (Adoption & Fostering, Adoption Quarterly) were searched for relevant papers, and three authors in the field were contacted to supplement the electronic database search. In an effort to reduce publication bias, grey literature sources (Action for ...
This review seeks to summarise the post-adoption variables associated with adopted children's mental health or behavioural difficulties to inform future research and shape interventions. A search for publications that assess associated risk and protective factors using Web of Science, Psychinfo, Medline and Sociological Abstracts identified ...
The current article provides a review of adoption research since its inception as a field of study. Three historical trends in adoption research are identified: the first focusing on risk in adoption and identifying adoptee—nonadoptee differences in adjustment; the second examining the capacity of adopted children to recover from early adversity; and the third focusing on biological ...
This article summarizes the social trends and research related to adoption over the last 10 years, including longitudinal and meta-analytic studies, increased research and conceptualization of ethnic and racial identity development, research on microaggressions, and research on diverse adoptive families, including those with gay and lesbian ...
View PDF View EPUB. This special issue of the Journal of Family Communication highlights the role of communication processes in adoption placements. Six original, peer-reviewed, empirical articles comprise this special issue. Together, these articles represent cutting-edge research on the formative dialogue that sustains adoption kinship networks.
The current article provides a review of adoption research since its inception as a field of study. Three historical trends in adoption research are identified: the first focusing on risk in adoption and identifying adoptee—nonadoptee differences in adjustment; the second examining the capacity of adopted children to recover from early adversity; and the third focusing on biological ...
The authors would like to acknowledge the adoptive parents who generously shared their experiences during the research; Adoption UK for enabling access to them; the Health and Social Care Board (HSCB) who funded this study and for their inspiration, expertise and support. Special thanks to my practice assessor Una Lernihan at the HSCB; the ...
of adoption. From the beginnings of modern adoption research in the late 1960s and 1970s, researchers have found adoption to be an emancipatory institution for children who faced pre-adoption trauma or high-risk future life trajectories (Bohman, 1971; Rutter, Brodzinsky, & Palacios, 2005). However, adoption research also demonstrates that
Implementation strategies are "methods or techniques used to enhance the adoption, implementation, and sustainment of evidence-based practices or programs" (EBPs) [].In 2015, the Expert Recommendations for Implementing Change (ERIC) study organized a panel of implementation scientists to compile a standardized set of implementation strategy terms and definitions [2,3,4].
How and why individuals adopt innovations has motivated a great deal of research. This article examines individuals' computing adoption processes through the lenses of three adoption theories: Rogers's innovation diffusion theory, the Concerns-Based Adoption Model, the Technology Acceptance Model, and the United Theory of Acceptance and Use of Technology.
Adoption.com. Adoption.com is the internet's most-used adoption site. It provides a wide variety of adoption-related services, including Parent Profiles, Reunion Registry, and a Photolisting of waiting children. Adoption.com seeks to promote and support adoption for all members of the triad.
To make things easier, we've compiled this detailed list of five of the best adoption research studies we could find. 1. Benefits of Early Adoption Closure. You know firsthand that adoption is far from a simple journey, and there are a slew of different adoption outcomes. Research has shown, though, that adoptive parents should aim to tell ...
The past several decades have seen a shift in attention in adoption research. While much of the early research was concerned with differences between adopted and nonadopted individuals and the effects of early adversity (e.g. Juffer & van IJzendoorn, 2005; Kumsta et al., 2015), there is currently a growing focus on the individual experiences and circumstances that shape the adjustment of ...
Background Among the 6-8 million animals that enter the rescue shelters every year, nearly 3-4 million (i.e., 50% of the incoming animals) are euthanized, and 10-25% of them are put to death specifically because of shelter overcrowding each year. The overall goal of this study is to increase the adoption rates at animal shelters. This involves predicting the length of stay of each animal ...
Past research suggests that's the more common choice: A 2017 study found that women were more likely to parent or have abortions than to place infants for adoption, regardless of their education ...
This comprehensive review study aims to analyze the current state of technology adoption (TA) within the textile industry, with a particular focus on the economic, environmental, and social dimensions.,Twenty-four articles from the Scopus database, spanning from January 2015 to March 2024, were meticulously selected for analysis.
Abstract. Most adoption agencies today allow a child's biological and adoptive families to know one another and maintain contact. This move toward openness instead of secrecy presents opportunities and challenges. The study reported here explores young adult adoptees' reactions to growing up in open adoptions.
In the past, most researchers attributed greater developmental and mental health risks for adopted individuals primarily to the vulnerabilities and adversities they experienced prior to adoption (e.g., genetics, prenatal complications, neglect, abuse, multiple foster care placements, orphanage life). More recently, the role of post-adoption ...
"The research led by Dr. Congreves and her team will make an impact on agriculture, climate, and food production through advancing the science and encouraging the adoption of sustainable farming practices across Canada and beyond." The Jarislowsky Foundation supports research chairs to promote excellence in teaching, mentoring and research.
The Securities and Exchange Commission today adopted rules to enhance and standardize climate-related disclosures by public companies and in public offerings.
Adoption & Fostering is a quarterly peer reviewed journal which has been at the cutting edge of debate on childcare issues for over 50 years. It is the only UK journal dedicated to adoption and fostering issues, providing an international forum for a wide range of professionals: academics and practitioners in social work, psychology, law, medicine, education...
Researchers such as Leathers et al. have observed that, "little research has focused on factors that predict adoption or influence foster parents' decision to adopt" (p.892). One factor that has been examined often using administrative data on children in foster care is the type of foster caregiver: kin to the child or not.
Cardiovascular disease (CVD) is the leading cause of mortality worldwide, and at present, India has the highest burden of acute coronary syndrome and ST-elevation myocardial infarction (MI). A key reason for poor outcomes is non-adherence to medication. The intervention is a 2 × 2 factorial design trial applying two interventions individually and in combination with 1:1 allocation ratio: (i ...