An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health


Factors Influencing Abortion Decision-Making Processes among Young Women
Mónica frederico.
1 International Centre for Reproductive Health (ICRH), Ghent University, 9000 Gent, Belgium; [email protected]
2 Centro de Estudos Africanos, Universidade Eduardo Mondlane, C. P. 1993, Maputo, Mozambique; [email protected]
Kristien Michielsen
Carlos arnaldo, peter decat.
3 Department of Family Medicine and primary health care, Ghent University, 9000 Gent, Belgium; [email protected]
Background: Decision-making about if and how to terminate a pregnancy is a dilemma for young women experiencing an unwanted pregnancy. Those women are subject to sociocultural and economic barriers that limit their autonomy and make them vulnerable to pressures that influence or force decisions about abortion. Objective : The objective of this study was to explore the individual, interpersonal and environmental factors behind the abortion decision-making process among young Mozambican women. Methods : A qualitative study was conducted in Maputo and Quelimane. Participants were identified during a cross-sectional survey with women in the reproductive age (15–49). In total, 14 women aged 15 to 24 who had had an abortion participated in in-depth interviews. A thematic analysis was used. Results : The study found determinants at different levels, including the low degree of autonomy for women, the limited availability of health facilities providing abortion services and a lack of patient-centeredness of health services. Conclusions : Based on the results of the study, the authors suggest strategies to increase knowledge of abortion rights and services and to improve the quality and accessibility of abortion services in Mozambique.
1. Introduction
Abortion among adolescents and youth is a major public health issue, especially in developing countries. Estimates indicate that 2.2 million unplanned pregnancies and 25% (2.5 million) unsafe abortions occur each year, in sub-Saharan Africa, among adolescents [ 1 ]. In 2008, of the 43.8 million induced abortions, 21.6 million were estimated to be unsafe, and nearly all of them (98%) took place in developing countries, with 41% (8.7 million) being performed on women aged 15 to 24 [ 2 ].
The consequences of abortion, especially unsafe abortion, are well documented and include physical complications (e.g., sepsis, hemorrhage, genital trauma), and even death [ 3 , 4 , 5 , 6 ]. The physical complications are more severe among adolescents than older women and increase the risk of morbidity and mortality [ 6 , 7 ]. However, the detrimental effects of unsafe abortion are not limited to the individual but also affect the entire healthcare system, with the treatment of complications consuming a significant share of resources (e.g., including hospital beds, blood supply, drugs) [ 5 , 8 ].
The decision if and how to terminate a pregnancy is influenced by a variety of factors at different levels [ 9 ]. At the individual level these factors include: their marital status, whether they were the victim of rape or incest [ 10 , 11 ], their economic independence and their education level [ 10 , 12 ]. Interpersonally factors include support from one’s partner and parental support [ 12 ]. Societal determinants include social norms, religion [ 9 , 13 ], the stigma of premarital and extra-marital sex [ 14 ], adolescents’ status, and autonomy within society [ 12 ]. At the organizational level, the existence of sex education [ 10 , 14 ], the health care system, and abortion laws influence the decisions if and where to have an abortion.
Those factors are related to power and (gender) inequalities. They limit young women’s autonomy and make them vulnerable to pressure. Additionally, the situation is exacerbated when there is a lack of clarity and information on abortion status, despite the existence of a progressive law in this regard.
For example, Mozambican law has allowed abortion if the woman’s health is at risk since the 1980s [ 15 , 16 , 17 , 18 ]. In 2014, a new abortion law was established that broadened the scope of the original law: women are now also allowed to terminate their pregnancy: (1) if they requested it and it is performed during the first 12 weeks; (2) in the first 16 weeks if it was the result of rape or incest, or (3) in the first 24 weeks if the mother’s physical or mental health was in danger or in cases of fetus disease or anomaly. Women younger than 16 or psychically incapable of deciding need parental consent [ 19 , 20 ].
Notwithstanding the progressive abortion laws in Mozambique, hospital-based studies report that unsafe abortion remains one of the main causes of maternal death in Mozambique [ 3 ]. However, hospital cases are only a small share of unsafe abortions in the country. Many women undergo an abortion in illegal and unsafe circumstances for a variety of reasons [ 3 ], such as legal restrictions, the fear of stigma [ 21 , 22 , 23 ], and a lack of knowledge of the availability of abortion services [ 3 , 9 , 23 ].
According to the 2011 Mozambican Demographic Health Survey (DHS), at least 4.5% of all adolescents reported having terminated a pregnancy [ 24 ]. Unpublished data from the records of Mozambican Association for Family Development (AMODEFA) which has a clinic that offers sexual and reproductive health services, including safe abortion, indicate that from 2010 to 2016 a total of 70,895 women had an induced abortion in this clinic, of which 43% were aged 15 to 24. Of the 1500 women that had an induced abortion in the AMODEFA clinic in the first three months of 2017, 27.9% were also in this age group [ 25 ]. These data show the high demand for (safe) abortion among young women.
For all this described above, Mozambique is an interesting place to study this decision-making process; given the changing legal framework, women may have to navigate gray areas in terms of legality, safety, and access when seeking abortion, which is stigmatized but necessary for the health, well-being, and social position of many young women.
The objective of this study is to explore the individual, interpersonal and environmental factors behind the abortion decision-making process. This entails both the decision to have an abortion and the decision on how to have the abortion. By examining fourteen stories of young women with an episode of induced abortion, we contribute to the documentation of the circumstances around the abortion decision making, and also to inform the policymakers on complexity of this issue for, which in turn can contribute to improve the strategies designed to reduce the cases of maternal morbidity and mortality in Mozambique.
2. Materials and Methods
This is an exploratory study using in-depth interview to explore factors related to abortion decision-making in a changing context. As research on this topic is limited, we opted for a qualitative research framework that aims to identify factors influencing this decision-making process.
2.1. Location of the Study
The study was conducted in two Mozambican cities, Maputo and Quelimane. These cities were selected because they registered more abortions than other cities in the same region. According to the 2014 data from the Direcção Nacional de Planificação, 629 and 698 women, respectively, were admitted to the hospital due to induced abortion complications in Maputo and Quelimane [ 26 ]. Furthermore, the two differ radically in terms of culture, with Maputo in the South being patrilineal and Quelimane in the Central Region matrilineal, which could influence the abortion decision-making process. The fieldwork took place between July–August 2016 and January–February 2017.
2.2. Data Collection
The data were collected through in-depth interviews, asking participants about their experiences with induced abortion and what motivated them to get an abortion. To approach and recruit participants ( Figure 1 ), we used the information collected during a cross-sectional survey with women in the reproductive age (15–49), These women were selected randomly applying multistage cluster based on household registers. The survey was designed to understand women’s sexual and reproductive health and included filter questions that allowed us to identify participants who had undergone an abortion. The information sheet and informed consent form for this household survey included information about a possible follow-up study.

The process of recruitment of the participants.
Participants who were within the age-range 15–24 years and who reported having had an abortion were contacted by phone. In this contact, the researcher (MF) introduced herself, reminded the participant of the study she took part in, explained the follow-up study and asked whether she was willing to participate in this. If she did, an appointment was made at a convenient location. Before each interview, we explained to each participant why she was invited to the second interview. Participants were also informed of interview procedures, confidentiality and anonymity in the management of the data, and the possibility to withdraw from the interview at any time. In total 14, young women (15–24) agreed to participate: nine in Maputo and five in Quelimane. Six of them were interviewed twice to explore further aspects that remained unclear after the first interview. The interviews were conducted in Portuguese.
To start the interview, the participant was invited to tell her life history from puberty until the moment when the abortion occurred. During the conversation, we used probing questions to elicit more details. Gradually, we added questions related to the abortion and factors that influenced the decision process. The main questions were related to the pregnancy history, abortion decision-making, and help-seeking behaviour. The guideline was adapted from WHO tools [ 27 , 28 ]. Before the implementation of the guideline, it was discussed first with another Mozambican researcher to see how they fell regarding the question. After those questions were revised or removed from the guideline.
2.3. Data Analysis
The analysis consisted of three steps: transcription, reading, and codification with NVivo version 11(QSR International Pty Ltd., Doncaster, Australia). After an initial reading, one of the authors (MF) developed a coding tree on factors determining the decision-making. A structured thematic analysis was used to make inferences and elicit key emerging themes from the text-based data [ 29 , 30 ]. The coding tree was based on the ecological model, which is a comprehensive framework that emphasizes the interaction between, and interdependence of factors within and across all levels of a health problem since it considers that the behaviour affects and is affected by multiple levels of influence [ 31 , 32 ].
Next, the codes and the classification were discussed among the researchers (Mónica Frederico, Kristien Michielsen, Carlos Arnaldo and Peter Decat). Finally, the data was interpreted, and conclusions were drawn [ 33 ].
2.4. Ethical Consideration
Before the implementation of this research, we obtained ethical approval from the Institutional Committee of the Faculty of Medicine and Nacional Bioethical Committee for Health (IRB00002657). We also asked for the institutional approval of the Minister of Health and authorities at the provincial and community levels. The participants gave their informed consent after the objectives and interview procedures had been explained to them. The participants were informed that they might be contacted and invited, within six months, to participate in another interview.
2.5. Concepts
The providers are the people who carried out the abortion procedure. These may be categorized into skilled and unskilled providers: the former refers to a professional (i.e., nurse or doctor) offering abortion services to a client, while the latter is someone without any medical training. Another concept that requires further explanation is the legal procedure. This corresponds to a set of steps to be followed to comply with the law [ 19 , 20 ]. Specifically, this means that a committee should authorize the induced abortion and an identification document should be available, as well as an informed consent form from the pregnant woman. If the woman is a minor, consent is given by her legal guardian. An ultrasound exam is required to determine the gestational age.
3.1. Characteristics of the Participants
The characteristics of the interviewees are summarized in Table 1 . The 14 participants were aged 17 to 24 years. Eight had completed secondary school, four had achieved the second level of primary school, and two were university students. Almost all (13) were Christian. Five participants were studying, eight were unemployed, and one was working. The median age of their first sexual intercourse was 15.5 years. Participants reported living with one or both parents (12), with their uncle (1) or alone (1). They lived in suburban areas of Maputo and Quelimane, which are slums with poor living conditions. In these areas, most households earn their income through small businesses that also involve child labour (e.g., selling food or drinks).
Socio-demographic characteristics and abortion procedure.
| Characteristics of Respondents | Categories | Median/Number |
|---|---|---|
| Age (median, range) | - | 21 (min: 17; max: 24) |
| Age at sexual activity onset (median, range) | - | 15.5 (min: 14; max: 18) |
| Education attainment (number) | Primary school | 4 |
| Secondary School | 8 | |
| University | 2 | |
| Religion (number) | Catholic + Evangelic | 13 |
| Muslim | 1 | |
| Occupation (number) | Studying | 5 |
| Without occupation | 8 | |
| Vendor | 1 | |
| Abortion procedure | ||
| Provider characteristics | Skilled | 12 |
| Unskilled | 2 | |
| Location of abortion | Health facility | 7 |
| Outside of health facility | 7 | |
| Treatment for abortion | Pills | 5 |
| Aspiration/curettage | 8 | |
| Traditional medicine | 1 | |
| Followed legal procedure | Yes | 0 |
| No | 14 |
Among the participants, five reported more than one pregnancy. One interviewee first had a stillbirth and then two abortions. Another woman gave birth to a girl and afterward terminated two pregnancies. Two interviewees reported two pregnancies, the first of which was brought to full term and the second one terminated. One woman first had an abortion and afterward gave birth to a child. In short, 14 interviewees in total reported on the experiences and decision-making of 16 abortions. One participant stated that the pregnancy was the consequence of rape. Of the 16 reported abortions, seven were performed after the new law came into force at the end of 2014, and nine were carried out before this time.
3.2. Abortions Stories
In this study, 12 abortions were done by skilled providers and two by unskilled providers. The unskilled providers were a mother and a husband, respectively. None of the cases, whose abortion was done by a skilled provider, included in this study followed the legal procedure.
In the analysis of the interviews, we studied the personal, interpersonal and environmental factors that influenced six different types of abortion stories, see Table 2 : (1) an abortion was performed because the pregnancy was unwanted; (2) an abortion was carried out although the pregnancy was wanted; (3) the abortion was done by an unskilled provider at home; (4) an abortion was carried out by a skilled provider outside the hospital; (5) a particular abortion procedure (medical or chirurgical) was chosen, and (6) the legal procedure was not followed in the hospital. Factors influencing the choice for a particular technical procedure were also examined.
Summary of induced abortion stories. (We changed the table format, please confirm.)
| Abortion Stories | Personal | Interpersonal | Environmental |
|---|---|---|---|
| Unwanted pregnancy (5 + 1 *) | Unable to be a mother | Lack of support | The result of rape |
| Had a bad past experience | |||
| Has another child | |||
| Wanted to study | |||
| Financial problems | |||
| Felt depressed | |||
| Abortion although pregnancy is wanted (7) | Partner did not recognize the child | ||
| Convinced by sister | |||
| Afraid of being sent away | |||
| Convinced/forced by mother | |||
| Partner did not want the child | |||
| Partner’s behaviour changed | |||
| Partner was married | |||
| Unskilled provider (2) | Carried out by partner Carried out by mother | ||
| Abortion outside hospital (8) | Unaware of legal obligations | Provider told us to go to his home | Abortion services are not available in the local healthcare settings |
| Lack of money | Fear of signing a document | ||
| Abortion at home (2) | Mother said that they would kill me at hospital | ||
| Decided by partner | |||
| Technical procedure | Decided by provider (aspiration, curettage **, pills ***) | ||
| Husband gave traditional medicine (1) | |||
| Why the legal procedure is not followed in the hospital (6) | Provider did not inform us about it | Information about legal procedures was not available |
* The result of rape; ** Seven participants; *** six participants.
3.3. Abortion Following an Unwanted Pregnancy
In the stories about unwanted pregnancies, mostly personal factors were mentioned as reasons, with some interviewees stating that they felt unable to be a mother at the time of the pregnancy: “ (It) was at the time that I was taking pills that I got pregnant, and I induced abortion because I was not prepared (for motherhood). ” (24 years)
Some had had a bad experience in the past: “ Maybe I would be abandoned and it would be the same. (Sigh)... I learned with my first pregnancy. ” (23 years)
Also, the existence of another child was mentioned as a reason to have an abortion: “ I got pregnant when I was 20, and I had a baby. When I became pregnant again, my daughter was a child, and I could not have another child. ” (23 years)
For other participants, studies were the main reason why the pregnancy was not wanted: “ He was informed about it, and he said that I should keep it. However, as I wanted to continue my studies, I told him no, no (I) do not. ” (17 years)
At the interpersonal level, a lack of support from the partner was often mentioned as a reason for not wanting the baby: “ He said that he recognizes the paternity, but it is not to keep that pregnancy. ” (22 years)
Women frequently mentioned environmental circumstances related to their poor socio-economic situation: “ I am staying at Mom's house; it is not okay to still be having babies there.” (23 years)
“ At home, we do not have any resources to take care of this child! ” (20 years)
3.4. Abortion Following a Wanted Pregnancy
In these cases, the decision to abort the pregnancy was not made by the woman herself but imposed by others or by the circumstances.
Some participants reported that their parents/family had decided what had to be done: “ They decided while I was at school. If (it) was my decision I would keep it because I wanted it. ” (18 years).
Other young women indicated the refusal of paternity as a reason to terminate the pregnancy.
“ Because my son’s father did not accept the (second) pregnancy. There was a time, we argued with each other, and we terminated the relationship. Later, we started dating again, and I got pregnant. He said it was not possible. ” (21 years)
“ (he) impregnated me and after that, he dumped me, (smiles)… I went to him, and I said that I was pregnant. He said eee: I do not know, that is not my child. ” (20 years).
Some women told the interviewers that they were convinced by their boyfriend to have an abortion: “ I talked to him, and he said okay we are going to have an abortion and I accepted. ” (22 years)
Others mentioned their partner’s indecision and changing attitude as a reason to get an abortion, even though they did want the baby:
“ I told him I was pregnant. First, he said to keep it. (Next) He was different. Sometimes he was calling me, and other times not. I understood that he did not want me. ” (20 years)
The fear of being excluded from their family due to their pregnancy was another reason reported by participants: “ So I went to talk with my older sister, and she said eee, you must abort because daddy will kick you out of our home. ” (20 years)
“ As I am an orphan, and I live with my uncle, they were going to kick me out. No one would assist me. ” (20 years)
3.5. Location of the Abortion: Home-Based Versus Hospital-Based
Two young women reported having had the abortion at home by an unskilled provider. It seems that these unskilled providers than the women (i.e. family members, partner) made the decisions.
“ It was mammy and my sister (who provided the induced abortion services). My sister knows these things. ” (18 years)
“ He (the father of the child) came to my house and took me back to his house. It was that moment when I aborted. ” (21 years)
Of the 16 abortions, seven were performed through health services, by a skilled provider. For some of them, the choice for a health service was influenced by the fact of knowing someone at the health facility.
“ I went to talk to her (friend), and she said that “I have an aunt who works at the hospital, she can help you. Just take money”. ” (20 years)
“ I Already knew who could induce it (abortion). No, I knew that person. I went to the hospital, and I talked to her, (and) she helped me. ” (22 years)
Other participants went to the health facility, but due to the lack of money to pay for an abortion at the facilities they sought help out of the health facility: “ They charged us money that we did not have. The ladies did not want to negotiate anything. I think they wanted 1200 mt (17.1 euros) if I am not wrong. He had a job, but he (boyfriend) did not have that amount of money. ” (22 years)
Some participants reported that they had an abortion outside regular facilities because the health provider recommended going to his house: “ She (mother) was the one who accompanied me. She is the one who knows the doctor. We went to the central hospital, but he (the doctor) was very busy, and he told us to go to his house. ” (17 years)
Others reported the fear of signing a document as a reason to seek help outside of official channels: “ I heard that to induce abortion at the hospital it is necessary for an adult to sign a consent form. I was afraid because I did not know who could accompany me. Because at that time I only wanted to hide it from others. ” (22 years).
3.6. Abortion Procedure
The women were not able to explain why a particular abortion procedure (i.e., pills or aspiration, curettage) was used. It appears that they were not given the opportunity to choose and that they submitted themselves to the procedure proposed by the provider.
“ The abortion was done here at home. They just went to the pharmacy, bought pills and gave them to me. ” (18 years)
3.7. Legal Procedure
None of those treated at the hospital stated that legal procedures were followed. They also mentioned that they had to pay without receiving any official receipt.
“ First we got there and talked to a servant (a helper of the hospital). The servant asked for money for a refreshment so he could talk to a doctor. After we spoke (with servant), he went to the doctor, and the doctor came, and we arranged everything with him. ” (22 years)
“ We went to the health center, and we talked to those doctors or nurses I mean, they said that they could provide that service. It was 1200 mt (17.1 euros), and they were going to deal with everything. They did not give us the chance to sign a document and follow those procedures. ” (20 years)
4. Discussion
The objective of this study was to describe abortion procedures and to explore factors influencing the abortion decision-making process among young women in Maputo and Quelimane.
The study pointed out determinants at the personal, interpersonal and environmental level. Analysing the results, we were confronted with four recurring factors that negatively impacted on the decision-making process: (1) women’s lack of autonomy to make their own decisions regarding the termination of the pregnancy, (2) their general lack of knowledge, (3) the poor availability of local abortion services, and (4) the overpowering influence of providers on the decisions made.
The first factor involves women’s lack of autonomy. In our study, most women indicate that decisions regarding the termination of a pregnancy are mostly taken by others, sometimes against their will. Parents, family members, partners, and providers decide what should happen. As shown in the literature, this lack of autonomy in abortion decision-making is linked to power and gender inequality [ 34 , 35 , 36 , 37 , 38 ]. On the one hand, power reflects the degree to which individuals or groups can impose their will on others, with or without the consent of those others [ 34 , 37 , 38 ]. In this case, the power of the parent/family is observed when they, directly or indirectly, influence their daughters to induce an abortion, for instance by threatening to kick them out of their home. On the other hand, gender inequality is also a factor. This refers to the power imbalance between men and women and is reflected by cases in which the partner makes the decision to terminate the pregnancy [ 38 ]. Besides this, the contextual environment of male chauvinism in Mozambique also makes it more socially acceptable for men to reject responsibility for a pregnancy [ 34 , 35 , 37 , 39 , 40 ]. Finally, women’s economic dependence makes them more vulnerable, dependent and subordinated. For economic reasons, women, have no other choice but to obey and follow the family or partner’s decisions. Closely linked with women’s lack of autonomy is their lack of knowledge. Interviewees report that they do not know where abortion services are provided. They are not acquainted with the legal procedures and do not know their sexual rights. This lack of knowledge among women contributes to the high prevalence of pregnancy termination outside of health facilities and not in accordance with legal procedures.
Our participants often report that abortion services are absent at a local level, as has also been pointed out by Ngwena [ 41 ]. This is a particular problem in Mozambique. Not all tertiary or quaternary health facilities are authorized to perform abortions. The fact that only some tertiary and quaternary facilities are allowed to do so creates a shortage of abortion centres to cover the demand. In fact, only people with a certain level of education and a sufficiently large social network have access to legal and proper abortion procedures.
Finally, our study shows that providers mostly decide on the location, the methods used and the legality of abortion procedures. Patients are highly dependent on the health providers’ commitment, professionality and accuracy and the selected procedures are not mutually decided by the provider and the patient. Providers often do not refer the client to the reference health facility or do not inform them of the legal procedures, creating a gap between law and practice that stimulates illegal and unsafe procedures. The reasons for this are unclear. It might be due to a lack of knowledge among health providers too, and, perhaps, provider saw here an opportunity to supplement the low salary [ 42 ]. Participants who seek help at the health facility they do so contacting the provider in particular, as indication given by someone.
This corroborates with studies conducted by Ngwena [ 41 , 43 ], Doran et al. [ 44 ], Pickles [ 45 ], Mantshi [ 46 ], and Ngwena [ 47 ], which pointed out the obstacles related to the availability of services and providers’ attitudes towards safe abortion, although the law grants the population this right [ 41 , 43 , 44 , 45 , 46 , 47 ]. As Ngwena [ 41 , 43 ] argues, the liberalization of abortion laws is not always put into practice and abortion rights merely exist on paper. Braam’ study [ 48 ] therefore highlights the necessity of clarifying and informing women and providers of the current legislation and ensuring that abortion services are available in all circumstances described in the law.
Finally, despite cultural differences between Maputo and Quelimane, the result did not suggest differences between two areas studied regarding factors influencing the decision to terminate and how the abortion is done. However, the Figure 1 suggests that there was trend to have more participants from Maputo reporting abortion episode in her life than Quelimane. This difference maybe be because Maputo is much more multicultural and the people of this city have more access to information that gives them the opportunity to learn about matter of reproductive health including abortion, than Quelimane. So, due to this there is trend decrease the taboo relation to abortion in Maputo than in Quelimane.
These abortion stories illustrate the lack of autonomy in decision-making process given the power and gender inequalities between adults and young women, and also between man and women . They also show the lack of knowledge not only on the availability of abortion services at some health facilities, as well as, on the new law on abortion. All these lacks that women have are reinforced by poor availability of abortion services and the fact that the providers we not taking their role to help those women, as it is exposed in the next sections.
This study interviewed young women who had an induced abortion at some point in their lives (15 years up to their age at interview date). As such, it does not provide any information on the factors behind the decisions of those who did not terminate their pregnancy.
The results presented in this paper only reflect the perceptions of the young women who had an induced abortion, not those of their parents or partners. The paper is based on qualitative data that provides insights into factors influencing abortion decision-making. Since the sample included in the study is not representative for the population of young women in Mozambique, the results cannot be generalized.
5. Conclusions
Based on the results of the study, we recommend the following measures to improve the abortion decision-making process among young women:
First, strategies should be implemented to increase women's autonomy in decision-making: The study highlighted that gender and power inequalities obstructed young women to make their decision with autonomy. We reiterate the Chandra-Mouli and colleges [ 49 ] message. There is a need to address gender and power inequalities. Addressing gender inequality, and promotion of more equitable power relations leads to improved health outcomes. The interventions to promote gender-equitable and power relationships, as well as human rights, need to be central to all future programming and policies [ 49 ].
Second, patients and the whole population should be better informed about national abortion laws, the recommended and legal procedures and the location of abortion services, since, despite the decision to terminate pregnancy resulted to the imposition, if they were well informed on that, maybe they could be decide on safe and legal abortion, avoiding double autonomy deprivation. At the same time, providers must be informed about the status of national abortion laws. Additionally, they should be trained in communication skills to promote shared decision-making and patient orientation in abortion counseling.
Third, the number of health facilities providing abortions services should be increased, particularly in remote areas.
Finally, health providers should be trained in communication skills to promote shared decision-making and patient orientation in abortion counseling.
The abortion decision-making by young women is an important topic because it refers the decision made during the transitional period from childhood to adulthood. The decision may have life-long consequences, compromising the individual health, career, psychological well-being, and social acceptance. This paper, on abortion decision-making, calls attention to some attitudes that lead to the illegality of abortion despite it was done at a health facility.
Acknowledgments
Authors gratefully acknowledge the support, contribution, and comments from all those who collaborated direct or indirectly, especially Olivier Degomme, Eunice Remane Jethá, Emilia Gonçalves, Cátia Taibo, Beatriz Chongo, Hélio Maúngue and Rehana Capruchand.
Author Contributions
All authors contributed significantly to the manuscript. Mónica Frederico collected data and developed the first analysis. The themes were intensively discussed with Kristien Michielsen, Carlos Arnaldo and Peter Decat. The subsequent versions of the article were written with the active participation of all authors.
Conflicts of Interest
The authors declare no conflicts of interest.
- Open access
- Published: 28 June 2021
Impact of abortion law reforms on women’s health services and outcomes: a systematic review protocol
- Foluso Ishola ORCID: orcid.org/0000-0002-8644-0570 1 ,
- U. Vivian Ukah 1 &
- Arijit Nandi 1
Systematic Reviews volume 10 , Article number: 192 ( 2021 ) Cite this article
21k Accesses
3 Citations
3 Altmetric
Metrics details
A country’s abortion law is a key component in determining the enabling environment for safe abortion. While restrictive abortion laws still prevail in most low- and middle-income countries (LMICs), many countries have reformed their abortion laws, with the majority of them moving away from an absolute ban. However, the implications of these reforms on women’s access to and use of health services, as well as their health outcomes, is uncertain. First, there are methodological challenges to the evaluation of abortion laws, since these changes are not exogenous. Second, extant evaluations may be limited in terms of their generalizability, given variation in reforms across the abortion legality spectrum and differences in levels of implementation and enforcement cross-nationally. This systematic review aims to address this gap. Our aim is to systematically collect, evaluate, and synthesize empirical research evidence concerning the impact of abortion law reforms on women’s health services and outcomes in LMICs.
We will conduct a systematic review of the peer-reviewed literature on changes in abortion laws and women’s health services and outcomes in LMICs. We will search Medline, Embase, CINAHL, and Web of Science databases, as well as grey literature and reference lists of included studies for further relevant literature. As our goal is to draw inference on the impact of abortion law reforms, we will include quasi-experimental studies examining the impact of change in abortion laws on at least one of our outcomes of interest. We will assess the methodological quality of studies using the quasi-experimental study designs series checklist. Due to anticipated heterogeneity in policy changes, outcomes, and study designs, we will synthesize results through a narrative description.
This review will systematically appraise and synthesize the research evidence on the impact of abortion law reforms on women’s health services and outcomes in LMICs. We will examine the effect of legislative reforms and investigate the conditions that might contribute to heterogeneous effects, including whether specific groups of women are differentially affected by abortion law reforms. We will discuss gaps and future directions for research. Findings from this review could provide evidence on emerging strategies to influence policy reforms, implement abortion services and scale up accessibility.
Systematic review registration
PROSPERO CRD42019126927
Peer Review reports
An estimated 25·1 million unsafe abortions occur each year, with 97% of these in developing countries [ 1 , 2 , 3 ]. Despite its frequency, unsafe abortion remains a major global public health challenge [ 4 , 5 ]. According to the World health Organization (WHO), nearly 8% of maternal deaths were attributed to unsafe abortion, with the majority of these occurring in developing countries [ 5 , 6 ]. Approximately 7 million women are admitted to hospitals every year due to complications from unsafe abortion such as hemorrhage, infections, septic shock, uterine and intestinal perforation, and peritonitis [ 7 , 8 , 9 ]. These often result in long-term effects such as infertility and chronic reproductive tract infections. The annual cost of treating major complications from unsafe abortion is estimated at US$ 232 million each year in developing countries [ 10 , 11 ]. The negative consequences on children’s health, well-being, and development have also been documented. Unsafe abortion increases risk of poor birth outcomes, neonatal and infant mortality [ 12 , 13 ]. Additionally, women who lack access to safe and legal abortion are often forced to continue with unwanted pregnancies, and may not seek prenatal care [ 14 ], which might increase risks of child morbidity and mortality.
Access to safe abortion services is often limited due to a wide range of barriers. Collectively, these barriers contribute to the staggering number of deaths and disabilities seen annually as a result of unsafe abortion, which are disproportionately felt in developing countries [ 15 , 16 , 17 ]. A recent systematic review on the barriers to abortion access in low- and middle-income countries (LMICs) implicated the following factors: restrictive abortion laws, lack of knowledge about abortion law or locations that provide abortion, high cost of services, judgmental provider attitudes, scarcity of facilities and medical equipment, poor training and shortage of staff, stigma on social and religious grounds, and lack of decision making power [ 17 ].
An important factor regulating access to abortion is abortion law [ 17 , 18 , 19 ]. Although abortion is a medical procedure, its legal status in many countries has been incorporated in penal codes which specify grounds in which abortion is permitted. These include prohibition in all circumstances, to save the woman’s life, to preserve the woman’s health, in cases of rape, incest, fetal impairment, for economic or social reasons, and on request with no requirement for justification [ 18 , 19 , 20 ].
Although abortion laws in different countries are usually compared based on the grounds under which legal abortions are allowed, these comparisons rarely take into account components of the legal framework that may have strongly restrictive implications, such as regulation of facilities that are authorized to provide abortions, mandatory waiting periods, reporting requirements in cases of rape, limited choice in terms of the method of abortion, and requirements for third-party authorizations [ 19 , 21 , 22 ]. For example, the Zambian Termination of Pregnancy Act permits abortion on socio-economic grounds. It is considered liberal, as it permits legal abortions for more indications than most countries in Sub-Saharan Africa; however, abortions must only be provided in registered hospitals, and three medical doctors—one of whom must be a specialist—must provide signatures to allow the procedure to take place [ 22 ]. Given the critical shortage of doctors in Zambia [ 23 ], this is in fact a major restriction that is only captured by a thorough analysis of the conditions under which abortion services are provided.
Additionally, abortion laws may exist outside the penal codes in some countries, where they are supplemented by health legislation and regulations such as public health statutes, reproductive health acts, court decisions, medical ethic codes, practice guidelines, and general health acts [ 18 , 19 , 24 ]. The diversity of regulatory documents may lead to conflicting directives about the grounds under which abortion is lawful [ 19 ]. For example, in Kenya and Uganda, standards and guidelines on the reduction of morbidity and mortality due to unsafe abortion supported by the constitution was contradictory to the penal code, leaving room for an ambiguous interpretation of the legal environment [ 25 ].
Regulations restricting the range of abortion methods from which women can choose, including medication abortion in particular, may also affect abortion access [ 26 , 27 ]. A literature review contextualizing medication abortion in seven African countries reported that incidence of medication abortion is low despite being a safe, effective, and low-cost abortion method, likely due to legal restrictions on access to the medications [ 27 ].
Over the past two decades, many LMICs have reformed their abortion laws [ 3 , 28 ]. Most have expanded the grounds on which abortion may be performed legally, while very few have restricted access. Countries like Uruguay, South Africa, and Portugal have amended their laws to allow abortion on request in the first trimester of pregnancy [ 29 , 30 ]. Conversely, in Nicaragua, a law to ban all abortion without any exception was introduced in 2006 [ 31 ].
Progressive reforms are expected to lead to improvements in women’s access to safe abortion and health outcomes, including reductions in the death and disabilities that accompany unsafe abortion, and reductions in stigma over the longer term [ 17 , 29 , 32 ]. However, abortion law reforms may yield different outcomes even in countries that experience similar reforms, as the legislative processes that are associated with changing abortion laws take place in highly distinct political, economic, religious, and social contexts [ 28 , 33 ]. This variation may contribute to abortion law reforms having different effects with respect to the health services and outcomes that they are hypothesized to influence [ 17 , 29 ].
Extant empirical literature has examined changes in abortion-related morbidity and mortality, contraceptive usage, fertility, and other health-related outcomes following reforms to abortion laws [ 34 , 35 , 36 , 37 ]. For example, a study in Mexico reported that a policy that decriminalized and subsidized early-term elective abortion led to substantial reductions in maternal morbidity and that this was particularly strong among vulnerable populations such as young and socioeconomically disadvantaged women [ 38 ].
To the best of our knowledge, however, the growing literature on the impact of abortion law reforms on women’s health services and outcomes has not been systematically reviewed. A study by Benson et al. evaluated evidence on the impact of abortion policy reforms on maternal death in three countries, Romania, South Africa, and Bangladesh, where reforms were immediately followed by strategies to implement abortion services, scale up accessibility, and establish complementary reproductive and maternal health services [ 39 ]. The three countries highlighted in this paper provided unique insights into implementation and practical application following law reforms, in spite of limited resources. However, the review focused only on a selection of countries that have enacted similar reforms and it is unclear if its conclusions are more widely generalizable.
Accordingly, the primary objective of this review is to summarize studies that have estimated the causal effect of a change in abortion law on women’s health services and outcomes. Additionally, we aim to examine heterogeneity in the impacts of abortion reforms, including variation across specific population sub-groups and contexts (e.g., due to variations in the intensity of enforcement and service delivery). Through this review, we aim to offer a higher-level view of the impact of abortion law reforms in LMICs, beyond what can be gained from any individual study, and to thereby highlight patterns in the evidence across studies, gaps in current research, and to identify promising programs and strategies that could be adapted and applied more broadly to increase access to safe abortion services.
The review protocol has been reported using Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) guidelines [ 40 ] (Additional file 1 ). It was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database CRD42019126927.
Eligibility criteria
Types of studies.
This review will consider quasi-experimental studies which aim to estimate the causal effect of a change in a specific law or reform and an outcome, but in which participants (in this case jurisdictions, whether countries, states/provinces, or smaller units) are not randomly assigned to treatment conditions [ 41 ]. Eligible designs include the following:
Pretest-posttest designs where the outcome is compared before and after the reform, as well as nonequivalent groups designs, such as pretest-posttest design that includes a comparison group, also known as a controlled before and after (CBA) designs.
Interrupted time series (ITS) designs where the trend of an outcome after an abortion law reform is compared to a counterfactual (i.e., trends in the outcome in the post-intervention period had the jurisdiction not enacted the reform) based on the pre-intervention trends and/or a control group [ 42 , 43 ].
Differences-in-differences (DD) designs, which compare the before vs. after change in an outcome in jurisdictions that experienced an abortion law reform to the corresponding change in the places that did not experience such a change, under the assumption of parallel trends [ 44 , 45 ].
Synthetic controls (SC) approaches, which use a weighted combination of control units that did not experience the intervention, selected to match the treated unit in its pre-intervention outcome trend, to proxy the counterfactual scenario [ 46 , 47 ].
Regression discontinuity (RD) designs, which in the case of eligibility for abortion services being determined by the value of a continuous random variable, such as age or income, would compare the distributions of post-intervention outcomes for those just above and below the threshold [ 48 ].
There is heterogeneity in the terminology and definitions used to describe quasi-experimental designs, but we will do our best to categorize studies into the above groups based on their designs, identification strategies, and assumptions.
Our focus is on quasi-experimental research because we are interested in studies evaluating the effect of population-level interventions (i.e., abortion law reform) with a design that permits inference regarding the causal effect of abortion legislation, which is not possible from other types of observational designs such as cross-sectional studies, cohort studies or case-control studies that lack an identification strategy for addressing sources of unmeasured confounding (e.g., secular trends in outcomes). We are not excluding randomized studies such as randomized controlled trials, cluster randomized trials, or stepped-wedge cluster-randomized trials; however, we do not expect to identify any relevant randomized studies given that abortion policy is unlikely to be randomly assigned. Since our objective is to provide a summary of empirical studies reporting primary research, reviews/meta-analyses, qualitative studies, editorials, letters, book reviews, correspondence, and case reports/studies will also be excluded.
Our population of interest includes women of reproductive age (15–49 years) residing in LMICs, as the policy exposure of interest applies primarily to women who have a demand for sexual and reproductive health services including abortion.
Intervention
The intervention in this study refers to a change in abortion law or policy, either from a restrictive policy to a non-restrictive or less restrictive one, or vice versa. This can, for example, include a change from abortion prohibition in all circumstances to abortion permissible in other circumstances, such as to save the woman’s life, to preserve the woman’s health, in cases of rape, incest, fetal impairment, for economic or social reasons, or on request with no requirement for justification. It can also include the abolition of existing abortion policies or the introduction of new policies including those occurring outside the penal code, which also have legal standing, such as:
National constitutions;
Supreme court decisions, as well as higher court decisions;
Customary or religious law, such as interpretations of Muslim law;
Medical ethical codes; and
Regulatory standards and guidelines governing the provision of abortion.
We will also consider national and sub-national reforms, although we anticipate that most reforms will operate at the national level.
The comparison group represents the counterfactual scenario, specifically the level and/or trend of a particular post-intervention outcome in the treated jurisdiction that experienced an abortion law reform had it, counter to the fact, not experienced this specific intervention. Comparison groups will vary depending on the type of quasi-experimental design. These may include outcome trends after abortion reform in the same country, as in the case of an interrupted time series design without a control group, or corresponding trends in countries that did not experience a change in abortion law, as in the case of the difference-in-differences design.
Outcome measures
Primary outcomes.
Access to abortion services: There is no consensus on how to measure access but we will use the following indicators, based on the relevant literature [ 49 ]: [ 1 ] the availability of trained staff to provide care, [ 2 ] facilities are geographically accessible such as distance to providers, [ 3 ] essential equipment, supplies and medications, [ 4 ] services provided regardless of woman’s ability to pay, [ 5 ] all aspects of abortion care are explained to women, [ 6 ] whether staff offer respectful care, [ 7 ] if staff work to ensure privacy, [ 8 ] if high-quality, supportive counseling is provided, [ 9 ] if services are offered in a timely manner, and [ 10 ] if women have the opportunity to express concerns, ask questions, and receive answers.
Use of abortion services refers to induced pregnancy termination, including medication abortion and number of women treated for abortion-related complications.
Secondary outcomes
Current use of any method of contraception refers to women of reproductive age currently using any method contraceptive method.
Future use of contraception refers to women of reproductive age who are not currently using contraception but intend to do so in the future.
Demand for family planning refers to women of reproductive age who are currently using, or whose sexual partner is currently using, at least one contraceptive method.
Unmet need for family planning refers to women of reproductive age who want to stop or delay childbearing but are not using any method of contraception.
Fertility rate refers to the average number of children born to women of childbearing age.
Neonatal morbidity and mortality refer to disability or death of newborn babies within the first 28 days of life.
Maternal morbidity and mortality refer to disability or death due to complications from pregnancy or childbirth.
There will be no language, date, or year restrictions on studies included in this systematic review.
Studies have to be conducted in a low- and middle-income country. We will use the country classification specified in the World Bank Data Catalogue to identify LMICs (Additional file 2 ).
Search methods
We will perform searches for eligible peer-reviewed studies in the following electronic databases.
Ovid MEDLINE(R) (from 1946 to present)
Embase Classic+Embase on OvidSP (from 1947 to present)
CINAHL (1973 to present); and
Web of Science (1900 to present)
The reference list of included studies will be hand searched for additional potentially relevant citations. Additionally, a grey literature search for reports or working papers will be done with the help of Google and Social Science Research Network (SSRN).
Search strategy
A search strategy, based on the eligibility criteria and combining subject indexing terms (i.e., MeSH) and free-text search terms in the title and abstract fields, will be developed for each electronic database. The search strategy will combine terms related to the interventions of interest (i.e., abortion law/policy), etiology (i.e., impact/effect), and context (i.e., LMICs) and will be developed with the help of a subject matter librarian. We opted not to specify outcomes in the search strategy in order to maximize the sensitivity of our search. See Additional file 3 for a draft of our search strategy.
Data collection and analysis
Data management.
Search results from all databases will be imported into Endnote reference manager software (Version X9, Clarivate Analytics) where duplicate records will be identified and excluded using a systematic, rigorous, and reproducible method that utilizes a sequential combination of fields including author, year, title, journal, and pages. Rayyan systematic review software will be used to manage records throughout the review [ 50 ].
Selection process
Two review authors will screen titles and abstracts and apply the eligibility criteria to select studies for full-text review. Reference lists of any relevant articles identified will be screened to ensure no primary research studies are missed. Studies in a language different from English will be translated by collaborators who are fluent in the particular language. If no such expertise is identified, we will use Google Translate [ 51 ]. Full text versions of potentially relevant articles will be retrieved and assessed for inclusion based on study eligibility criteria. Discrepancies will be resolved by consensus or will involve a third reviewer as an arbitrator. The selection of studies, as well as reasons for exclusions of potentially eligible studies, will be described using a PRISMA flow chart.
Data extraction
Data extraction will be independently undertaken by two authors. At the conclusion of data extraction, these two authors will meet with the third author to resolve any discrepancies. A piloted standardized extraction form will be used to extract the following information: authors, date of publication, country of study, aim of study, policy reform year, type of policy reform, data source (surveys, medical records), years compared (before and after the reform), comparators (over time or between groups), participant characteristics (age, socioeconomic status), primary and secondary outcomes, evaluation design, methods used for statistical analysis (regression), estimates reported (means, rates, proportion), information to assess risk of bias (sensitivity analyses), sources of funding, and any potential conflicts of interest.
Risk of bias and quality assessment
Two independent reviewers with content and methodological expertise in methods for policy evaluation will assess the methodological quality of included studies using the quasi-experimental study designs series risk of bias checklist [ 52 ]. This checklist provides a list of criteria for grading the quality of quasi-experimental studies that relate directly to the intrinsic strength of the studies in inferring causality. These include [ 1 ] relevant comparison, [ 2 ] number of times outcome assessments were available, [ 3 ] intervention effect estimated by changes over time for the same or different groups, [ 4 ] control of confounding, [ 5 ] how groups of individuals or clusters were formed (time or location differences), and [ 6 ] assessment of outcome variables. Each of the following domains will be assigned a “yes,” “no,” or “possibly” bias classification. Any discrepancies will be resolved by consensus or a third reviewer with expertise in review methodology if required.
Confidence in cumulative evidence
The strength of the body of evidence will be assessed using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) system [ 53 ].
Data synthesis
We anticipate that risk of bias and heterogeneity in the studies included may preclude the use of meta-analyses to describe pooled effects. This may necessitate the presentation of our main findings through a narrative description. We will synthesize the findings from the included articles according to the following key headings:
Information on the differential aspects of the abortion policy reforms.
Information on the types of study design used to assess the impact of policy reforms.
Information on main effects of abortion law reforms on primary and secondary outcomes of interest.
Information on heterogeneity in the results that might be due to differences in study designs, individual-level characteristics, and contextual factors.
Potential meta-analysis
If outcomes are reported consistently across studies, we will construct forest plots and synthesize effect estimates using meta-analysis. Statistical heterogeneity will be assessed using the I 2 test where I 2 values over 50% indicate moderate to high heterogeneity [ 54 ]. If studies are sufficiently homogenous, we will use fixed effects. However, if there is evidence of heterogeneity, a random effects model will be adopted. Summary measures, including risk ratios or differences or prevalence ratios or differences will be calculated, along with 95% confidence intervals (CI).
Analysis of subgroups
If there are sufficient numbers of included studies, we will perform sub-group analyses according to type of policy reform, geographical location and type of participant characteristics such as age groups, socioeconomic status, urban/rural status, education, or marital status to examine the evidence for heterogeneous effects of abortion laws.
Sensitivity analysis
Sensitivity analyses will be conducted if there are major differences in quality of the included articles to explore the influence of risk of bias on effect estimates.
Meta-biases
If available, studies will be compared to protocols and registers to identify potential reporting bias within studies. If appropriate and there are a sufficient number of studies included, funnel plots will be generated to determine potential publication bias.
This systematic review will synthesize current evidence on the impact of abortion law reforms on women’s health. It aims to identify which legislative reforms are effective, for which population sub-groups, and under which conditions.
Potential limitations may include the low quality of included studies as a result of suboptimal study design, invalid assumptions, lack of sensitivity analysis, imprecision of estimates, variability in results, missing data, and poor outcome measurements. Our review may also include a limited number of articles because we opted to focus on evidence from quasi-experimental study design due to the causal nature of the research question under review. Nonetheless, we will synthesize the literature, provide a critical evaluation of the quality of the evidence and discuss the potential effects of any limitations to our overall conclusions. Protocol amendments will be recorded and dated using the registration for this review on PROSPERO. We will also describe any amendments in our final manuscript.
Synthesizing available evidence on the impact of abortion law reforms represents an important step towards building our knowledge base regarding how abortion law reforms affect women’s health services and health outcomes; we will provide evidence on emerging strategies to influence policy reforms, implement abortion services, and scale up accessibility. This review will be of interest to service providers, policy makers and researchers seeking to improve women’s access to safe abortion around the world.
Abbreviations
Cumulative index to nursing and allied health literature
Excerpta medica database
Low- and middle-income countries
Preferred reporting items for systematic review and meta-analysis protocols
International prospective register of systematic reviews
Ganatra B, Gerdts C, Rossier C, Johnson BR, Tuncalp O, Assifi A, et al. Global, regional, and subregional classification of abortions by safety, 2010-14: estimates from a Bayesian hierarchical model. Lancet. 2017;390(10110):2372–81. https://doi.org/10.1016/S0140-6736(17)31794-4 .
Article PubMed PubMed Central Google Scholar
Guttmacher Institute. Induced Abortion Worldwide; Global Incidence and Trends 2018. https://www.guttmacher.org/fact-sheet/induced-abortion-worldwide . Accessed 15 Dec 2019.
Singh S, Remez L, Sedgh G, Kwok L, Onda T. Abortion worldwide 2017: uneven progress and unequal access. NewYork: Guttmacher Institute; 2018.
Book Google Scholar
Fusco CLB. Unsafe abortion: a serious public health issue in a poverty stricken population. Reprod Clim. 2013;2(8):2–9.
Google Scholar
Rehnstrom Loi U, Gemzell-Danielsson K, Faxelid E, Klingberg-Allvin M. Health care providers’ perceptions of and attitudes towards induced abortions in sub-Saharan Africa and Southeast Asia: a systematic literature review of qualitative and quantitative data. BMC Public Health. 2015;15(1):139. https://doi.org/10.1186/s12889-015-1502-2 .
Say L, Chou D, Gemmill A, Tuncalp O, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):E323–E33. https://doi.org/10.1016/S2214-109X(14)70227-X .
Article PubMed Google Scholar
Benson J, Nicholson LA, Gaffikin L, Kinoti SN. Complications of unsafe abortion in sub-Saharan Africa: a review. Health Policy Plan. 1996;11(2):117–31. https://doi.org/10.1093/heapol/11.2.117 .
Abiodun OM, Balogun OR, Adeleke NA, Farinloye EO. Complications of unsafe abortion in South West Nigeria: a review of 96 cases. Afr J Med Med Sci. 2013;42(1):111–5.
CAS PubMed Google Scholar
Singh S, Maddow-Zimet I. Facility-based treatment for medical complications resulting from unsafe pregnancy termination in the developing world, 2012: a review of evidence from 26 countries. BJOG. 2016;123(9):1489–98. https://doi.org/10.1111/1471-0528.13552 .
Article CAS PubMed Google Scholar
Vlassoff M, Walker D, Shearer J, Newlands D, Singh S. Estimates of health care system costs of unsafe abortion in Africa and Latin America. Int Perspect Sex Reprod Health. 2009;35(3):114–21. https://doi.org/10.1363/3511409 .
Singh S, Darroch JE. Adding it up: costs and benefits of contraceptive services. Estimates for 2012. New York: Guttmacher Institute and United Nations Population Fund; 2012.
Auger N, Bilodeau-Bertrand M, Sauve R. Abortion and infant mortality on the first day of life. Neonatology. 2016;109(2):147–53. https://doi.org/10.1159/000442279 .
Krieger N, Gruskin S, Singh N, Kiang MV, Chen JT, Waterman PD, et al. Reproductive justice & preventable deaths: state funding, family planning, abortion, and infant mortality, US 1980-2010. SSM Popul Health. 2016;2:277–93. https://doi.org/10.1016/j.ssmph.2016.03.007 .
Banaem LM, Majlessi F. A comparative study of low 5-minute Apgar scores (< 8) in newborns of wanted versus unwanted pregnancies in southern Tehran, Iran (2006-2007). J Matern Fetal Neonatal Med. 2008;21(12):898–901. https://doi.org/10.1080/14767050802372390 .
Bhandari A. Barriers in access to safe abortion services: perspectives of potential clients from a hilly district of Nepal. Trop Med Int Health. 2007;12:87.
Seid A, Yeneneh H, Sende B, Belete S, Eshete H, Fantahun M, et al. Barriers to access safe abortion services in East Shoa and Arsi Zones of Oromia Regional State, Ethiopia. J Health Dev. 2015;29(1):13–21.
Arroyave FAB, Moreno PA. A systematic bibliographical review: barriers and facilitators for access to legal abortion in low and middle income countries. Open J Prev Med. 2018;8(5):147–68. https://doi.org/10.4236/ojpm.2018.85015 .
Article Google Scholar
Boland R, Katzive L. Developments in laws on induced abortion: 1998-2007. Int Fam Plan Perspect. 2008;34(3):110–20. https://doi.org/10.1363/3411008 .
Lavelanet AF, Schlitt S, Johnson BR Jr, Ganatra B. Global Abortion Policies Database: a descriptive analysis of the legal categories of lawful abortion. BMC Int Health Hum Rights. 2018;18(1):44. https://doi.org/10.1186/s12914-018-0183-1 .
United Nations Population Division. Abortion policies: A global review. Major dimensions of abortion policies. 2002 [Available from: https://www.un.org/en/development/desa/population/publications/abortion/abortion-policies-2002.asp .
Johnson BR, Lavelanet AF, Schlitt S. Global abortion policies database: a new approach to strengthening knowledge on laws, policies, and human rights standards. Bmc Int Health Hum Rights. 2018;18(1):35. https://doi.org/10.1186/s12914-018-0174-2 .
Haaland MES, Haukanes H, Zulu JM, Moland KM, Michelo C, Munakampe MN, et al. Shaping the abortion policy - competing discourses on the Zambian termination of pregnancy act. Int J Equity Health. 2019;18(1):20. https://doi.org/10.1186/s12939-018-0908-8 .
Schatz JJ. Zambia’s health-worker crisis. Lancet. 2008;371(9613):638–9. https://doi.org/10.1016/S0140-6736(08)60287-1 .
Erdman JN, Johnson BR. Access to knowledge and the Global Abortion Policies Database. Int J Gynecol Obstet. 2018;142(1):120–4. https://doi.org/10.1002/ijgo.12509 .
Cleeve A, Oguttu M, Ganatra B, Atuhairwe S, Larsson EC, Makenzius M, et al. Time to act-comprehensive abortion care in east Africa. Lancet Glob Health. 2016;4(9):E601–E2. https://doi.org/10.1016/S2214-109X(16)30136-X .
Berer M, Hoggart L. Medical abortion pills have the potential to change everything about abortion. Contraception. 2018;97(2):79–81. https://doi.org/10.1016/j.contraception.2017.12.006 .
Moseson H, Shaw J, Chandrasekaran S, Kimani E, Maina J, Malisau P, et al. Contextualizing medication abortion in seven African nations: A literature review. Health Care Women Int. 2019;40(7-9):950–80. https://doi.org/10.1080/07399332.2019.1608207 .
Blystad A, Moland KM. Comparative cases of abortion laws and access to safe abortion services in sub-Saharan Africa. Trop Med Int Health. 2017;22:351.
Berer M. Abortion law and policy around the world: in search of decriminalization. Health Hum Rights. 2017;19(1):13–27.
PubMed PubMed Central Google Scholar
Johnson BR, Mishra V, Lavelanet AF, Khosla R, Ganatra B. A global database of abortion laws, policies, health standards and guidelines. B World Health Organ. 2017;95(7):542–4. https://doi.org/10.2471/BLT.17.197442 .
Replogle J. Nicaragua tightens up abortion laws. Lancet. 2007;369(9555):15–6. https://doi.org/10.1016/S0140-6736(07)60011-7 .
Keogh LA, Newton D, Bayly C, McNamee K, Hardiman A, Webster A, et al. Intended and unintended consequences of abortion law reform: perspectives of abortion experts in Victoria, Australia. J Fam Plann Reprod Health Care. 2017;43(1):18–24. https://doi.org/10.1136/jfprhc-2016-101541 .
Levels M, Sluiter R, Need A. A review of abortion laws in Western-European countries. A cross-national comparison of legal developments between 1960 and 2010. Health Policy. 2014;118(1):95–104. https://doi.org/10.1016/j.healthpol.2014.06.008 .
Serbanescu F, Morris L, Stupp P, Stanescu A. The impact of recent policy changes on fertility, abortion, and contraceptive use in Romania. Stud Fam Plann. 1995;26(2):76–87. https://doi.org/10.2307/2137933 .
Henderson JT, Puri M, Blum M, Harper CC, Rana A, Gurung G, et al. Effects of Abortion Legalization in Nepal, 2001-2010. PLoS ONE. 2013;8(5):e64775. https://doi.org/10.1371/journal.pone.0064775 .
Goncalves-Pinho M, Santos JV, Costa A, Costa-Pereira A, Freitas A. The impact of a liberalisation law on legally induced abortion hospitalisations. Eur J Obstet Gynecol Reprod Biol. 2016;203:142–6. https://doi.org/10.1016/j.ejogrb.2016.05.037 .
Latt SM, Milner A, Kavanagh A. Abortion laws reform may reduce maternal mortality: an ecological study in 162 countries. BMC Women’s Health. 2019;19(1). https://doi.org/10.1186/s12905-018-0705-y .
Clarke D, Muhlrad H. Abortion laws and women’s health. IZA discussion papers 11890. Bonn: IZA Institute of Labor Economics; 2018.
Benson J, Andersen K, Samandari G. Reductions in abortion-related mortality following policy reform: evidence from Romania, South Africa and Bangladesh. Reprod Health. 2011;8(39). https://doi.org/10.1186/1742-4755-8-39 .
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj-Brit Med J. 2015;349.
William R. Shadish, Thomas D. Cook, Donald T. Campbell. Experimental and quasi-experimental designs for generalized causal inference. Boston, New York; 2002.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–55. https://doi.org/10.1093/ije/dyw098 .
Bernal JL, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol. 2018;47(6):2082–93. https://doi.org/10.1093/ije/dyy135 .
Meyer BD. Natural and quasi-experiments in economics. J Bus Econ Stat. 1995;13(2):151–61.
Strumpf EC, Harper S, Kaufman JS. Fixed effects and difference in differences. In: Methods in Social Epidemiology ed. San Francisco CA: Jossey-Bass; 2017.
Abadie A, Diamond A, Hainmueller J. Synthetic control methods for comparative case studies: estimating the effect of California’s Tobacco Control Program. J Am Stat Assoc. 2010;105(490):493–505. https://doi.org/10.1198/jasa.2009.ap08746 .
Article CAS Google Scholar
Abadie A, Diamond A, Hainmueller J. Comparative politics and the synthetic control method. Am J Polit Sci. 2015;59(2):495–510. https://doi.org/10.1111/ajps.12116 .
Moscoe E, Bor J, Barnighausen T. Regression discontinuity designs are underutilized in medicine, epidemiology, and public health: a review of current and best practice. Journal of Clinical Epidemiology. 2015;68(2):132–43. https://doi.org/10.1016/j.jclinepi.2014.06.021 .
Dennis A, Blanchard K, Bessenaar T. Identifying indicators for quality abortion care: a systematic literature review. J Fam Plan Reprod H. 2017;43(1):7–15. https://doi.org/10.1136/jfprhc-2015-101427 .
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4 .
Jackson JL, Kuriyama A, Anton A, Choi A, Fournier JP, Geier AK, et al. The accuracy of Google Translate for abstracting data from non-English-language trials for systematic reviews. Ann Intern Med. 2019.
Reeves BC, Wells GA, Waddington H. Quasi-experimental study designs series-paper 5: a checklist for classifying studies evaluating the effects on health interventions-a taxonomy without labels. J Clin Epidemiol. 2017;89:30–42. https://doi.org/10.1016/j.jclinepi.2017.02.016 .
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. https://doi.org/10.1136/bmj.39489.470347.AD .
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. https://doi.org/10.1002/sim.1186 .
Download references
Acknowledgements
We thank Genevieve Gore, Liaison Librarian at McGill University, for her assistance with refining the research question, keywords, and Mesh terms for the preliminary search strategy.
The authors acknowledge funding from the Fonds de recherche du Quebec – Santé (FRQS) PhD doctoral awards and Canadian Institutes of Health Research (CIHR) Operating Grant, “Examining the impact of social policies on health equity” (ROH-115209).
Author information
Authors and affiliations.
Department of Epidemiology, Biostatistics and Occupational Health, Faculty of Medicine, McGill University, Purvis Hall 1020 Pine Avenue West, Montreal, Quebec, H3A 1A2, Canada
Foluso Ishola, U. Vivian Ukah & Arijit Nandi
You can also search for this author in PubMed Google Scholar
Contributions
FI and AN conceived and designed the protocol. FI drafted the manuscript. FI, UVU, and AN revised the manuscript and approved its final version.
Corresponding author
Correspondence to Foluso Ishola .
Ethics declarations
Ethics approval and consent to participate.
Not applicable
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
PRISMA-P 2015 Checklist. This checklist has been adapted for use with systematic review protocol submissions to BioMed Central journals from Table 3 in Moher D et al: Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews 2015 4:1
Additional File 2:.
LMICs according to World Bank Data Catalogue. Country classification specified in the World Bank Data Catalogue to identify low- and middle-income countries
Additional File 3: Table 1
. Search strategy in Embase. Detailed search terms and filters applied to generate our search in Embase
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ishola, F., Ukah, U.V. & Nandi, A. Impact of abortion law reforms on women’s health services and outcomes: a systematic review protocol. Syst Rev 10 , 192 (2021). https://doi.org/10.1186/s13643-021-01739-w
Download citation
Received : 02 January 2020
Accepted : 08 June 2021
Published : 28 June 2021
DOI : https://doi.org/10.1186/s13643-021-01739-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Abortion law/policies; Impact
- Unsafe abortion
- Contraception
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 03 October 2018
Decision-making preceding induced abortion: a qualitative study of women’s experiences in Kisumu, Kenya
- Ulrika Rehnström Loi ORCID: orcid.org/0000-0002-3455-8606 1 ,
- Matilda Lindgren 1 ,
- Elisabeth Faxelid 1 ,
- Monica Oguttu 2 , 3 &
- Marie Klingberg-Allvin 4 , 5
Reproductive Health volume 15 , Article number: 166 ( 2018 ) Cite this article
37k Accesses
41 Citations
1 Altmetric
Metrics details
Unwanted pregnancies and unsafe abortions are prevalent in regions where women and adolescent girls have unmet contraceptive needs. Globally, about 25 million unsafe abortions take place every year. In countries with restrictive abortion laws, safe abortion care is not always accessible. In Kenya, the high unwanted pregnancy rate resulting in unsafe abortions is a serious public health issue. Gaps exist in knowledge regarding women’s decision-making processes in relation to induced abortions in Kenya. Decision-making is a fundamental factor for consideration when planning and implementing contraceptive services. This study explored decision-making processes preceding induced abortion among women with unwanted pregnancy in Kisumu, Kenya.
Individual face-to-face in-depth interviews were conducted with nine women aged 19–32 years old. Women who had experienced induced abortion were recruited after receiving post-abortion care at the Jaramogi Oginga Odinga Teaching and Referral Hospital (JOOTRH) or Kisumu East District Hospital (KDH) in Kisumu, Kenya. In total, 15 in-depth interviews using open-ended questions were conducted. All interviews were tape-recorded, transcribed and coded manually using inductive content analysis.
Respondents described their own experiences regarding decision-making preceding induced abortion. This study shows that the main reasons for induced abortion were socio-economic stress and a lack of support from the male partner. In addition, deviance from family expectations and gender-based norms highly influenced the decision to have an abortion among the interviewed women. The principal decision maker was often the male partner who pressed for the termination of the pregnancy indirectly by declining his financial or social responsibilities or directly by demanding termination. In some cases, the male partner controlled decision-making by arranging an unsafe abortion without the woman’s consent. Strategic choices regarding whom to confide in were employed as protection against abortion stigma. This contributed to a culture of silence around abortion and unwanted pregnancy, a factor that made women more vulnerable to complications.
Conclusions
The findings suggest that financial, social and gender-based dependencies influence women’s agency and perceived options in decision-making regarding abortion.
Peer Review reports
Plain English summary
Unwanted pregnancies and pregnancy termination are common in countries where women who want to prevent or delay childbearing have limited access to contraceptives. Around 25 million unsafe abortions take place worldwide each year. Recent evidence shows that nearly half a million induced abortions take place in Kenya every year. In this study, we used in-depth interviews to explore the decision-making processes preceding induced abortion among women with unwanted pregnancies in Kisumu, Kenya.
This study shows that the interviewed women decided to terminate their pregnancies for the following reasons: poverty, poor timing of the pregnancy and absence of support from male partners. The main decision maker was usually the male partner who pressed for the termination of the pregnancy indirectly by declining his financial or social responsibilities or directly by forcing his partner to terminate the pregnancy. In some cases, the male partner arranged an unsafe abortion without the woman’s knowledge or consent. Participants were affected by social stigma and carefully selected whom to talk to about the abortion. This strategy was used as protection against humiliation and shame. This contributed to a culture of silence around abortion and unwanted pregnancy, a factor that made women vulnerable to complications.
Where women and adolescent girls have unmet contraceptive needs, unwanted pregnancies and unsafe abortions are common. About 25 million unsafe abortions (45% of all induced abortions) occur globally, most of them (97%) in low resource settings [ 1 ]. Despite the availability of safe and effective interventions, unsafe abortions still contribute to maternal morbidity and mortality [ 2 ]. The majority of maternal deaths due to unsafe abortions occur in low-income settings where women experience low social status combined with legal and social restrictions to sexual and reproductive rights [ 3 ]. Women tend to opt for unsafe abortions where safe abortion services are not acceptable, accessible or affordable [ 4 ]. The number of unsafe abortions tends to be higher among poor women because women with strong social or economic resources are more likely to access safe abortions, regardless of the legal context [ 5 ].
The World Health Organization (WHO) defines unsafe abortion as “ the termination of an unwanted pregnancy by persons lacking the necessary skills, or in an environment lacking minimal medical standards, or both” [ 6 ], while also emphasising the impact of the social and legal context on abortion safety [ 7 ]. A recent study showed the disparity in abortion safety between low- and high-resource settings, indicating that in high-resource settings almost all abortions were safe, while only one in four abortions in Africa were safe [ 1 ].
The 2030 Agenda for Sustainable Development renewed the commitments by 193 Member States of the United Nations to reduce global maternal mortality through universal access to sexual and reproductive health (SRH) services, education and information. Moreover, sexual and reproductive health and rights (SRHR), ensuring the ability to make decisions about one’s contraceptive and own health, is core to the post-2015 goals because of its remarkable potential to contribute to sustainable development [ 8 ].
Contraceptives allow women/couples to decide if and when to become pregnant. Modern contraceptives play an important role in reducing maternal deaths by preventing unwanted pregnancies and prolonging birth intervals [ 9 ]. Contraceptives are, however, underutilised in many low-resource settings [ 10 , 11 ], largely as a result of limited availability of a range of contraceptive methods, including to modern long-acting reversible contraceptive methods [ 11 ], and social stigma surrounding young women’s contraceptive use [ 12 ].
Women’s decision-making preceding an induced abortion is influenced by factors at different levels [ 13 , 14 ]. Individual-level factors include marital status, education level, economic independency and whether the woman was a victim of rape or incest [ 15 ]. Interpersonal factors such as parental and partner support have also been found to influence decision-making [ 15 ], as have societal determinants like religion and social stigma and norms [ 13 ]. Relevant organisational factors include access to sexuality education [ 15 ] and the availability of facilities providing abortion services [ 14 ].
The Kenyan context
The majority of the population in Kenya is Christian (83%), with 48% identifying as Protestant and 24% as Roman Catholic [ 16 ]. Kenyan women are economically dependent on men, and Kenyan cultures are largely patriarchal [ 17 ]. Marriage occurs comparatively early; among women aged 25–49 the median age at first marriage was 20.2 years. About 53% of married women of reproductive age use a modern contraceptive method. Among married women aged 15–49 years, 18% have unmet contraceptive need, which contributes to a high total fertility rate (3.9 births per woman) [ 18 ].
A recent national study estimated that about 464,000 induced abortions occur in Kenya annually, with a national abortion rate of 48 abortions per 1000 women of reproductive age (15–49 years) [ 19 ]. This figure is above the rate for all of sub-Saharan Africa (SSA), which is 31 abortions per 1000 women of reproductive age [ 20 ]. It is estimated that the induced abortion rate in Kenya is highest in the Rift Valley region and the combined Nyanza and Western regions [ 19 ].
Until 2010, abortion was only legally allowed to save the life of a pregnant woman. However, in 2010 a revised constitution was adopted permiting abortion when “ in the opinion of a trained health professional, there is need for emergency treatment, or the life or health of the mother is in danger, or if permitted by any other written law ” [ 21 ]. Thus far, the implementation of the constitution has been slow, and both knowledge and practice may differ throughout the country. A lack of transparency and clarity with regard to the circumstances in which abortion is legal contributes to Kenya’s high maternal mortality ratio (MMR) [ 22 ]. The MMR in Kenya has remained almost constant since 1990. According to the 2014 Kenya Demographic Health Survey, the MMR is 362 maternal deaths per 100,000 live births, and unsafe abortion is a major contributor [ 18 ]. Due to restrictive abortion legislation in Kenya [ 21 ], limited access to quality healthcare and stigma, most abortions occur outside authorised health care facilities and are classified as therefore considered unsafe [ 23 ].
Kenya is an important location to study women’s decision-making preceding induced abortion given its high MMR, changing legal framework, social stigma surrounding unplanned pregnancies and the socioeconomic status of the majority of women in the country.
Nyanza province, in which Kisumu is the principal city, has one of the highest MMRs in Kenya [ 24 ], and the total fertility rate for this province is 4.3 children per woman, the fourth highest in the country [ 18 ].
Aim of the study
The aim of this study was to explore decision-making preceding induced abortion among women with unwanted pregnancies in Kisumu, western Kenya.

Study setting
The study was conducted at the Jaramogi Oginga Odinga Teaching and Referral Hospital (JOOTRH) and Kisumu East District Hospital (KDH) in Kisumu, western Kenya. Kisumu Medical and Education Trust (KMET), a non-governmental organisation, supported the collaboration with these two public hospitals in Kisumu. At the time of the study, the two facilities treated approximately 80 women per month for abortion-related complications.
Research team and reflexivity
The authors recognise the significance of reflexivity and transparency regarding researcher subjectivity in qualitative research. The research team consisted of five female researchers. The first author (URL) had prior relevant experience from an MSc in Public Health and as a PhD student in the researched subject. The second author (ML) is a social scientist (MSc student) with an interest in women’s SRH. The third author (EF) is a professor in Reproductive and Perinatal Health Care with broad experience conducting quantitative and qualitative research in Kenya and other low-income countries. The fourth author (MO) is the Executive Director of KMET with vast SRH experience in the region. The final author (MKA) is a professor with a PhD in International Health who has extensive experience conducting research in low-resource settings using both quantitative and qualitative methods.
Conducting and transcribing the interviews was physically and emotionally exhausting. During data collection and interview transcription the researchers (ML and URL) had daily contact and discussed their personal experiences. The deep emotional experience of conducting these interviews allowed them to empathise with participants and was used during analysis.
Study design, sample selection and data collection
In total, 15 individual, in-depth interviews (IDIs) were conducted with nine women aged 19–32 years old. Follow-up interviews were conducted with six of the women. Purposive sampling was used to select women seeking care for abortion-related complications. The following inclusion criteria were used: 1) women over 18 years of age 2) who experienced an induced abortion, 3) received post-abortion care (PAC) at JOOTRH or KDH and 4) were willing to be interviewed.
Midwives at the two public hospitals in Kisumu identified possible interviewees between 1 January 2014 to 31 May 2014 by asking PAC-seeking women if they had tried to induce the abortion. All women who met the inclusion criteria and were asked to participate agreed to be interviewed. The respondents were informed about the study’s aim and were assured of their confidentiality. Seven respondents were recruited from JOOTRH and two from KDH. Six women were interviewed face-to-face 7–10 days after receiving PAC, two were interviewed at the time of a three-month follow-up and one woman was approached while she was still admitted at the ward. In addition, a repeated interview was offered to all respondents approximately 2–5 weeks after the initial interview. Five of the respondents were interviewed face-to-face a second time, while one respondent was interviewed over the phone due to distance. Three respondents declined the request for a repeat interview. The reason for conducting follow-up interviews was to further enhance understanding and enrich the material as trust and affinity were built between researcher and informant.
The women were interviewed between February and April 2014 at JOOTRH and KDH by one of the authors (ML) who has a master’s degree in Gender Studies and conducted previous studies in Cultural Anthropology. She was trained in qualitative methodologies and at the time of the study was a postgraduate student in Global Health. The fact that the interviewer was not a clinician and a non-Kenyan might have encouraged respondents to speak to her more openly about a sensitive subject. During one interview the researcher used an interpreter to translate from Lou to English. The translator was an assistant from KMET. During the other interviews, the researcher was the only person in the room with the respondent. The interviews lasted on average 45 min.
A semi-structured interview schedule, using open-ended questions and suggestions for probing, was developed by the research team. The schedule was pilot tested and modified prior to initial data collection. The questions were framed to study women’s decision-making preceding induced abortion, including the role played by their social networks.
Field notes were written directly after each interview to reflect on initial thoughts and reactions. With the written consent of the respondents, all interviews were tape-recorded and transcribed verbatim, including notations for nonverbal expressions, for analysis by the first and second authors (URL and ML) on an ongoing basis as data collection progressed. The interview with a translator was also transcribed in English. The research team met regularly to review progress and discuss interview techniques. Data collection continued until data saturation was reached [ 25 ]. Table 1 presents the characteristics of the respondents.
Data analysis
The data were analysed by the first and second authors (URL and ML) using inductive content analysis, including open coding, category development and abstraction [ 25 , 26 ].
Inductive content analysis is a qualitative approach used to unconditionally analysing the data [ 27 ]. While analysis had already begun during interview transcription, open coding was conducted during the first reading of the transcripts. Thereafter, the transcripts were read through several times and coded manually. Meaning units were identified and transferred to Excel for classification into subcategories, generic categories and main categories. The process of analysis is presented in Fig. 1 . Meaning units and categories were discussed and compared amongst all members of the research team in order to further improve the analysis and to maximise rigour [ 26 ].
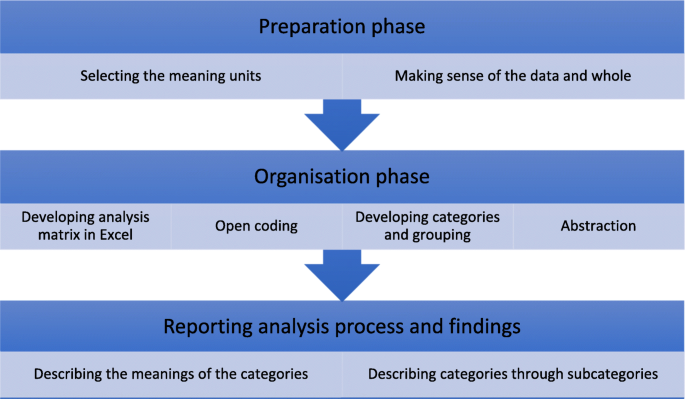
Inductive content analysis process [ 27 ]
Inductive content analysis resulted in three main categories: 1) Reasons for induced abortion , 2) A culture of silence and 3) Choosing abortion despite risks and limited information. The results are presented according to these main categories together with their generic categories and citations from the interviews to clarify the findings. The abstraction process is illustrated in Fig. 2 .
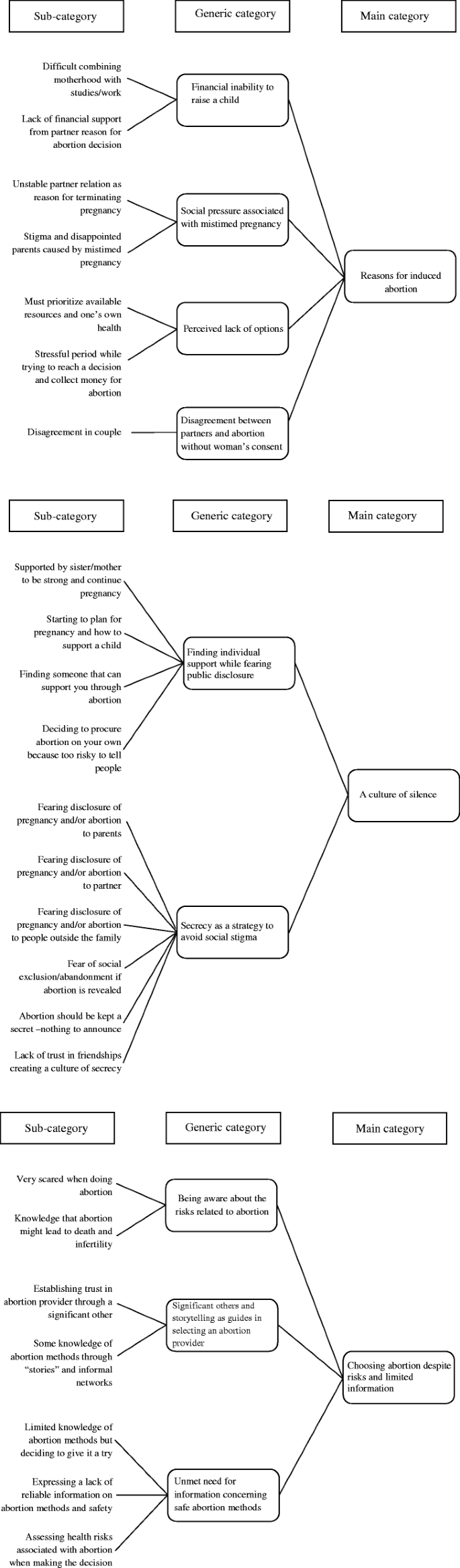
Coding tree describing the abstraction process
Reasons for induced abortion
The first main category, Reasons for induced abortion , is described through four generic categories: 1) Financial inability to raise a child , 2) Social pressure associated with mistimed pregnancy , 3) Perceived lack of options and 4) Disagreement between partners and abortion without the woman’s consent.
Financial inability to raise a child
All women described their pregnancies as mistimed, unplanned or unwanted at the time of conception. A lack of financial stability or support were described by most women as driving factors for the decision to terminate the pregnancy.
“I was financially unstable to sustain those children.” (Respondent 8)
In some cases, the woman was the main provider of the household, and the pregnancy jeopardised the stability of her income. The pregnancy might diminish her employment opportunities, as an employer could decide to let a woman go once it was evident she was pregnant. Therefore, pregnancy termination provided the respondents with the potential for continued employment and secured economic independence.
“When [the pregnancy] is visible, you will be sacked. And when you are [alone] at home, who will support you? I have to work.” (Respondent 6)
Women who were still students and living with their parents indicated that their parents would not financially support their costs of living and studies as well as the costs of raising an additional child.
The married respondents stressed that they had to prioritise resources and take care of the children they already had. All women with children mentioned the importance of providing an education for them. High school fees were frequently cited. The respondents stated they could not afford to educate an additional child. Several women specifically articulated their partner’s unwillingness to financially support a child as the reason for terminating the pregnancy.
Furthermore, financial constraints were perceived as a barrier to safe abortion. Women frequently cited not being able to afford to pay a professional to perform the abortion.
Social pressure associated with mistimed pregnancy
The unmarried respondents were concerned about the risk of negative views from family and community members if they continued the pregnancy at that particular time. Although engaged and employed, some women expected to be criticised and “talked about” by people in the community due to the mistimed pregnancy.
“Because [---] okay, people usually talk; in Kenya people will talk. Where you are staying, there are some people, those people like to gossip, people will definitely talk. [---] They’ll say you are still in your mother’s house [---] They won’t be able to understand…and some will even criticise your relationship.” (Respondent 5)
Others explained that having a child would end a harmonious relationship with their parents. Several young women living with their parents mentioned that they would not be welcome in their parents’ house if they were pregnant.
“[---] she [mother] took me to the training [in hotel management and hospitality], she spend some money there,and then I didn’t tell her [about the pregnancy] because she won’t be happy because maybe she will then think that she had taken me to the training and spent money there, and then I will not be able to go and just sit at home [---] She would kick me out of the house, and maybe she would stop the training [---].” (Respondent 7)
The need for a supportive social network, including a stable partnership, emerged as fundamental to avoid severe conflicts in the decision-making process. Social networks could include actors providing either financial or couched support. Male partners had a significant direct or indirect influence on participants’ decisions to opt for induced abortions. Several women expressed unstable partner relationships as a reason why they had chosen to have an abortion.
“I already have two children, I am everything for these children… I am the mother and the father for these two children, so a third one would be too much problem. I just decided. I have to because that man never convinced me; I was not convinced at all that that man would provide anything.” (Respondent 6)
Single women were afraid to raise a child alone.
“So, I just thought that I have another kid and the father is not contributing with the school fees. Even my mother denied helping me. Yeah, for my kid and me also; so that’s why I decided to do away with the abortion.” (Respondent 7)
The social network was emphasised as central for single mothers. An additional child became an added burden, which could not be placed on family or friends.
Perceived lack of options
Some women expressed guilt and distress about lying to their partners and family about the pregnancy. Additionally, women expressed feelings such as heightened shame and self-blame because abortion was perceived as immoral and improper.
“I felt bad because it was like murdering someone, but [---] I felt part of killing the kid because [---] I felt miserable for like a week [---] two weeks.” (Respondent 2)
However, due to their economic, social or health circumstances, the termination of the pregnancy was considered the only available option.
“I didn’t have any option because I just knew that the situation I was in [HIV positive]; I was not able to [---] take care of this baby [---] according to the situation [HIV positive] now I was in.” (Respondent 7)
While some women said that they decided on an abortion immediately upon realising they were pregnant, several respondents described experiencing a lot of stress and ambivalence in trying to decide what to do.
“I was still deciding what to do; I was still doubting. So many things run into my mind until I come with the decision to do [---] to [---] to [---] end the pregnancy. At that time [---] [I] even think I lost [---] [weight] cause [because of the] stress I have [---] having so many stress [---] losing weight cause of the stress.” (Respondent 3)
Disagreement between partners and abortion without the woman’s consent
Almost all women expressed some kind of disagreement with their partner in relation to the pregnancy. Some women articulated that they terminated the pregnancy without notifying their partner, fearing the possible consequences of anger, violence and divorce. On the other hand, a few women expressed their intention to abort and were discouraged and warned not to proceed by the partner. Participants articulated that their partners believed abortion was wrong and could cause complications and death. All single respondents decided not to reveal the pregnancy to their ex-partners. Although some of the respondents decided to terminate the pregnancy, others expressed that they were forced or even misled to terminate the pregnancy by their partners. When women were misled, their respective partners attempted to convince them to opt for an abortion. Although the women insisted on keeping the pregnancy, clandestine abortion providers supported the partners to induce abortion without the women’s consent.
“He suggested for the abortion to be done, I told him no. [---] So he insisted, and he insisted. When he saw I’m not participating, he used a trick and told me that if you don’t want then I want to advice you on how to be when you are pregnant and what drugs [to] use. [---] He injected me through a vein and told me it’s to improve the appetite… [---] After injecting that drug I became unconscious. When I returned from my unconsciousness I found myself naked and I was bleeding.” (Respondent 1)
This reveals that unsafe abortion in Kenya sometimes happens without the woman’s consent. During the interview Respondent 1 disclosed she had reported her ex-partner to the police. While the women explained their partners’ motives were based on social embarrassment and financial obligations, how the partners themselves would describe the situation and justify their actions is beyond the scope of this research.
A culture of silence
The main category A culture of silence is described through two generic categories: 1) Finding individual support while fearing public disclosure and 2) Secrecy as a strategy to avoid social stigma .
Finding individual support while fearing public disclosure
As seen under the first main category, several respondents described the time after they discovered they were pregnant as very stressful. While all of them feared public disclosure to some extent, they also expressed the need to tell someone about their condition. In many cases this person was a sister or a friend who had also been through an induced abortion. Most respondents were reluctant to tell their partners because they feared disagreement or abandonment. Among the women who informed their partners about the pregnancy, this confession commonly entailed asking for financial support. A majority of the non-married respondents also acknowledge that they were reluctant to tell their parents and preferred that their partner did not know about the pregnancy.
Respondents tended to keep the pregnancy to themselves for several weeks due to their fear of possible reactions. If the secret was shared, it had to be with a trustworthy person, usually a sister, as a tactic to avoid public disclosure. Furthermore, women feared receiving opposing advice, which could indicate that they had already made the decision to terminate the pregnancy and only sought affirmation.
“I was doubting what to do and on the other hand afraid of sharing with anybody. I believed if I share it with so many people some people will give me other advice, some will give me this; that’s why I ended up sharing with my sister that I’m staying with because I trusted her.” (Respondent 4)
Not infrequently, respondents indicated that they had chosen to state that the pregnancy had ended in a miscarriage instead of an induced abortion. Women made strategic choices regarding whom they confided in. While some women had the support of a sister or a female friend, others assessed the risk of telling someone to be so profound that they decided to keep the secret to themselves, which meant they had no one who could support them.
“I did not ask someone for advice because if you ask one they will start talking about it and everybody will know about it, so I was afraid to talk about it to someone [---] and maybe it will go back to my partner, and I didn’t want that to happen. [---].” (Respondent 8)
Fear of negative consequences and death as a result of the abortion led some women to share their intention to terminate the pregnancy. Women expressed the desire to inform at least one person about the abortion; if there were negative consequences, someone would know where to look for the woman if she were not to return home.
Secrecy as a strategy to avoid social stigma
The majority of women expressed fear of rumours, social isolation and judgment if the abortion were revealed. Respondents believed that people in the community would perceive them as “killers”. Additionally, they believed their peers would exclude them and avoid interacting with them. Social stigma and discrimination were expressed as segregation, as well as being perceived as a prostitute, labelled as a murderer, accused of being unfaithful and believed to be a poor candidate for marriage.
“ In campus if you get pregnant and your boyfriend says I cannot take care of the baby, I’m not the father and stuff, they will start saying you are just like the others [---] maybe you have sex for money? Maybe you don’t know the father of the kid? [---] So, they start calling you names like whore, slut [---] Someone says you are just a whore like anyone else, and after that everyone starts to isolate you [---]” (Respondent 2)
Fear of judgment and losing social respect created a culture of silence, where the harmful nature of rumours and negative responses fostered secrecy and silence surrounding abortion and a mistimed pregnancy. Women became afraid to share their decision to terminate the pregnancy with others, including friends, family and healthcare professionals due to a lack of trust and fear that their confidentiality would not be maintained. Induced abortions were secrets kept to avoid negative reactions.
Religious values and beliefs were apparent in all the interviews. Almost all women mentioned that abortion was a sin and not accepted by their church. Therefore, it was critical that other church members were not aware of the decision to terminate the pregnancy. A few respondents elaborated on this during follow-up interviews, clarifying the guilt, anxiety and angst they felt when attending church. They accused themselves of being sinners and struggled to ask for forgiveness from God.
“You see as a married women [---] you see [---] it seems like the woman is not even ready for the marriage [---] so something is wrong with her that cannot be explained, so they [the husbands] don’t like it so easy, they see it as a sin, so there is no way I can tell about the abortion to him as I know the consequences can be bitter for me [---] when you do such thing [abortion] since you are giving away God’s blood, then you are trying to be like the Father. God gave you the child, and now you are removing it so it’s a sin because you are competing with God.” (Respondent 9)
Choosing abortion despite risks and limited information
The main category Choosing abortion despite being aware of the risks is explained through three generic categories: 1) Being aware of the risks related to abortion , 2) Significant others and storytelling as guides for selecting an abortion provider and 3) Unmet need for information concerning safe abortion methods.
Being aware of the risks related to abortion
The respondents generally described abortion as risky. All of them said they were aware of the health risks of having an abortion. Death, infertility, long-time infection, weakness and loss of body weight were commonly mentioned. Death was the most emphasised consequence and was frequently repeated. Women described having an induced abortion as gambling with life and death.
“I was [very] scared [---] because I know how dangerous it is. But I was like, okay – let it be, and if I’m going to die, so be it, that is how, that is my destiny now. [---] I had now decided; it’s either death or survival. I was ready for anything.” (Respondent 5)
All women highlighted abortion as an unsafe procedure in Kenya. The respondents were fully aware of the severity of abortion complications, and their decisions were framed with this knowledge in mind. Women considered the risk of giving birth to a child to be similarly high. Going through a pregnancy was also associated with health risks (including sickness during and after pregnancy), but abortion was framed as the preferred risk. However, some respondents were anxious about the future and did not want to be blamed for their decision to terminate the pregnancy.
Significant others and storytelling as guides in selecting an abortion provider
Evidence-based information regarding induced abortion was limited. Common information sources about induced abortion methods and procedures were informal social networks at high school and friends who had experience of abortion. Only a few respondents had consulted professional healthcare providers. Some women stated they knew about Marie Stopes, a reliable abortion provider; however, due to high transportation fees they opted for medical abortions using Misoprostol, which was provided by chemists.
“When I was in high school we used to have some cases [of abortion] so I had that knowledge from school, so I just decided to do it on my own. [---] I also knew about other methods, but I was afraid to use the others because I had not tried to do it before.” (Respondent 9)
Unmet need for information concerning safe abortion methods
Respondent knowledge about safe abortion methods was low. Almost all women described induced abortions as very risky, even with the possible consequence of death. The general consensus was that no abortion is safe. Women tended to ask the local chemist about abortion drugs (Misoprostol) or quinine instead of reaching out to safe professional abortion providers due to a lack of accurate understanding of abortion legislation and safe abortion methods in Kenya.
“[Abortion is] when you take drugs [---] traditional herbals also terminate the pregnancy. Some people take juice, highly concentrated juice [---] only those once [are the abortion methods I know of].” (Respondent 6)
“I didn’t know anything. I have a friend who went through it before [---], but she passed away two weeks after the abortion [---].” (Respondent 2)
Similar to previous studies, this study reveals that the main reasons for induced abortion are socio-economic stresses and a lack of support from partners [ 28 , 29 , 30 , 31 ]. In cases where women informed their partners about the pregnancy, the principal decision maker was often the male partner who pressed for pregnancy termination indirectly by declining his financial or social responsibilities or directly by demanding the woman terminate the pregnancy. In some cases, the male partner misled the woman, overruling her decision to continue the pregnancy by arranging an unsafe abortion without her consent. A lack of financial security seemed to diminish participants’ perceptions of available options. Furthermore, as mentioned above, gender-based power relations hindered women from actualising their decisions. Previous studies from Uganda and Ghana have disclosed similar findings where women’s decision-making power regarding abortion was restricted by gender norms and power imbalances [ 30 , 31 , 32 ].
Similar to earlier studies, female friends or sisters were commonly referred to as important sources of information and moral support when undergoing an induced abortion. While sisters were believed to be trusted to keep knowledge about the abortion within the family, important knowledge-sharing also took place via female friends who had themselves been through an abortion. Together with sisters, these friends were regarded as trustworthy.
Regardless of relationship status, all respondents expressed concern about publicly disclosing the abortion, fearing negative remarks, the loss of social respect, isolation and divorce. Similar findings have been shown in Ethiopia, Sri Lanka and Kenya [ 33 , 34 , 35 ] and in further conceptualisations of abortion stigma, which entails shaming and discriminating against women and their families [ 36 , 37 ]. Kumar et al. argue that abortion stigma builds on injustices and discrimination in society by depending on and appropriating existing power axes [ 36 ]. This study showed perceived stigma, referring to the perception that pregnancy termination will result in a woman being seen as inferior, to be very present in the participants’ accounts [ 36 ]. Similar to Shellenberg et al.’s arguments, the fear of judgment effectively curtailed participants’ willingness to disclose their abortion intention or experience [ 37 ]. Women handled these risks by making strategic choices regarding whom they confided in. A lack of trust and the fear of rumours confirm that other people’s opinions are highly important to sustaining a positive social life. In many cases, lying, hiding and planning to escape were preferable to telling the truth.
A direct consequence of this secrecy is that it creates a culture of silence around mistimed pregnancies and abortion. Although it may protect women from social shame, hiding one’s pregnancy and abortion makes women reluctant or scared to seek professional reproductive health information and care, which in turn makes them more vulnerable to complications, morbidities and mortality. This aligns with findings from a similar context showing that fear of stigma related to unintended pregnancy among young women, including the shame it brings to the family, as well as negative social sanctions, is a great driving force for unsafe abortion [ 33 , 38 ]. The study also shows that fear of stigma delays care-seeking and consequently increases the risk of morbidity and mortality.
This study reveals that women encounter challenges in obtaining safe abortion information and services, regardless of the legal status of abortion in the country. A previous study from Kenya has similar findings [ 39 ].
Abortion-related social stigma preventing women’s access to comprehensive SRH
Essential elements regarding abortion-related stigma found in this study should be reflected in the planning and implementation of SRH services in Kenya. Women who participated in this study repeatedly noted significant social stigma around induced abortion, which affected their decision-making regarding pregnancy termination. The abortion-related social stigma revealed in this study delayed and prevented the seeking of professional and safe PAC. Similarly, an earlier facility-based study from Kenya confirms the correlation between stigma and abortion-seeking behaviours among women seeking abortion care [ 40 ]. Young unmarried women faced both the stigma of pregnancy outside of marriage and abortion-related stigma. Previous research has shown comparable findings [ 41 ].
A recent systematic literature review critically analysed abortion stigma among healthcare providers in sub-Saharan Africa and Southeast Asia [ 42 ]. The findings demonstrate that healthcare providers have moral, social and gender-based reservations related to induced abortion. Furthermore, the study reveals that nurses and midwives often have pejorative attitudes towards women seeking abortion care and commonly reported an unwillingness to provide abortion care. As a consequence, nurses and midwives overlooked their responsibilities as caregivers and acknowledged that due to negative rapport between abortion provider and client, women seeking abortion care received inadequate care [ 42 ]. Because stigma is transmissible, it also deters healthcare providers who are prepared to provide abortion care from delivering these services. This stigmatisation enforces negative labels for the caregiver and may result in harmful professional consequences [ 43 ].
Abortion stigma is deep-rooted in government and political landscapes, organisations, communities and personal relationships [ 36 ]. The constant denial of a woman’s right to freely decide on the number and spacing of her children directly influences maternal mortality [ 44 ]. Abortion-related stigma is a barrier to safe and accessible abortion care [ 43 , 45 ]. Hence, decreasing social and cultural stigma around abortion among abortion providers would potentially strengthen women’s access to quality reproductive healthcare and improve women’s health by preventing future unintended pregnancies, as well as induced abortions and related complications.
Strengths and limitations
Despite the high prevalence of induced abortions in Kenya [ 19 , 46 ], there is a shortage of qualitative research that analyses women’s reasons for obtaining induced abortions in the country.
Studies on abortion in Kenya have primarily focused on incidence, clinical outcomes and stigma [ 19 , 39 , 47 , 48 ]. The strengths of the present study are, first, that it focusses on women who terminated their pregnancies in the recent past and thus have fresh memories of the abortion experience. Second, the interviewer was nonclinical, from outside the Kenyan healthcare system and ensured participants’ confidentiality. Third, the interviewer established a rapport with the participants, which facilitated insightful responses. Finally, six respondents agreed to a repeated interview, which provided a unique opportunity to ask follow-up questions, probe for additional information and circle back to key questions to generate richer material.
A limitation of this study is that partners and other significant family members were not included as study subjects. Partners might have given different accounts of the decision-making process. The methodological challenges in gaining access to both partners’ and parents’ accounts first and foremost relate to privacy, as partners and parents were not necessarily informed of the pregnancy and/or abortion. Ethical concerns prevented the recruitment of partners via the participants as this would require the women’s consent, which, in turn, could influence the sample. Similarly, ethical concerns prevented the inclusion of women under 18 years of age in the study and by coincidence there were no women over the age of 32 years interviewed. It could be argued that adolescent women and older women would have responded differently about decision-making preceding induced abortion. Even though research among underage women is difficult to conduct, young women are by far the most affected by severe complications due to unsafe abortions [ 47 ]. More research is therefore needed to understand underlying social attitudes towards young women who have undergone induced abortions.
Furthermore, contraceptive failure and change of pregnancy intention during pregnancy were not included in this study, which could be perceived as a limitation.
The impact of HIV status on decision-making in relation to induced abortion has been demonstrated in other studies [ 49 , 50 ]. This sample included two women who reported themselves as HIV positive, which also influenced their decisions to have induced abortions (along with financial reasons). However, analysis of this relationship should be based on a larger sample.
The results from this qualitative study are the reports of PAC-seeking women in Kenya during in-depth interviews.
A lack of financial independence, a lack of social support, deviance from family expectations and gender-based norms influenced abortion decision-making among women with unwanted pregnancies. Strategic choices regarding whom to confide in were employed as protection against abortion stigma. This, however, contributed to a culture of silence around abortion and mistimed pregnancy. Silence and stigma act as driving forces for unsafe abortions and put women in situations where an unsafe abortion can occur without their consent. Unwanted pregnancies can also be stressful for men, and interventions targeting unsafe abortions must take both sexes into consideration and address the problem of forced abortions as a reproductive health issue.
Abbreviations
Human Immunodeficiency Virus
In-depth interview
Jaramogi Oginga Odinga Teaching and Referral Hospital
Kisumu East District Hospital
Kisumu Medical and Education Trust
Maternal mortality ratio
Post-abortion care
Sexual and reproductive health
Sexual and reproductive health and rights
Sub-Saharan Africa
World Health Organization
Ganatra B, Gerdts C, Rossier C, Johnson BR, Jr., Tuncalp O, Assifi A, et al. Global, regional, and subregional classification of abortions by safety, 2010-14: estimates from a Bayesian hierarchical model. Lancet 2017;390(10110):2372–2381.
Article Google Scholar
Darroch J, Audam S, Biddlecom A, Kopplin G, Riley T, Singh S, et al. Adding it up: investing in contraception and maternal and newborn health. 2017. https://www.guttmacher.org/fact-sheet/adding-it-up-contraception-mnh-2017 . Accessed 16 June 2018.
Google Scholar
World Health Organization. Packages of interventions for family planning, safe abortion care, maternal, newborn and child health. Geneva: World Health Organization; 2010.
World Health Organization. Safe abortion: technical and policy guidance for health systems. Geneva: World Health Organization; 2012.
Singh S, Wulf D, Hussain R, Bankole A, Sedgh G. Abortion worldwide: a decade of uneven progress. New York: Guttmacher Institute; 2009.
World Health Organization. World Health Organization information sheet in unsafe abortion incidence and mortality global and regional levels in 2008 and trends during 1990–2008. Geneva: World Health Organization; 2012.
Ganatra B, Tunçalp Ö, Johnston HB, Johnson BR, Gülmezoglu AM, Temmerman M. From concept to measurement: operationalizing WHO’s definition of unsafe abortion. Bull World Health Organ. 2014;92(3):155.
United Nations. Global Sustainable Development Report. New York: Department of Economic and Social Affairs; 2016. p. 2016.
Petruney T, Wilson LC, Stanback J, Cates W Jr. Family planning and the post-2015 development agenda. Bull World Health Organ. 2014;92(8):548–548A.
Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32:152–74.
Sedgh G, Hussain R. Reasons for contraceptive nonuse among women having unmet need for contraception in developing countries. Stud Fam Plann. 2014;45(2):151-69.
Hakansson M, Oguttu M, Gemzell-Danielsson K, Makenzius M. Human rights versus societal norms: a mixed methods study among healthcare providers on social stigma related to adolescent abortion and contraceptive use in Kisumu. Kenya BMJ Glob Health. 2018;3(2):e000608.
Alhassan AY, Abdul-Rahim A, Akaabre PB. Knowledge, awareness and perceptions of females on clandestine abortion in Kintampo north municipality. Eur Sci J. 2016:95–112.
Frederico M, Michielsen K, Arnaldo C, Decat P. Factors influencing abortion decision-making processes among young women. Int J Environ Res Public Health. 2018;15(2).
Gbagbo FY, Amo-Adjei J, Laar A. Decision-making for induced abortion in the Accra metropolis. Ghana Afr J Reprod Health. 2015;19(2):34–42.
PubMed Google Scholar
Kenya National Bureau of Statistics (KNBS). The 2009 Kenya population and housing census. Kenya National Bureau of statistics (KNBS). https://www.knbs.or.ke/category/census-2009-summary-of-results/ . Accessed 15 June 2018.
Mutongu ZB, Women’s Participation in Community-Based Organizations’ Development as a Strategy for Poverty Reduction in Kenya. https://www.cbeinternational.org/sites/default/files/Women%27s_Muntongu.pdf . Accessed 18 June 2018.
Kenya National Bureau of Statistics. Kenya Demographic and Health Survey 2014. Rockville, MD, USA: Kenya National Bureau of Statistics. https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf . Accessed 18 June 2018.
Mohamed SF, Izugbara C, Moore AM, Mutua M, Kimani-Murage EW, Ziraba AK, et al. The estimated incidence of induced abortion in Kenya: a cross-sectional study. BMC Pregnancy Childbirth. 2015;15:185.
Sedgh G, Singh S, Shah IH, Ahman E, Henshaw SK, Bankole A. Induced abortion: incidence and trends worldwide from 1995 to 2008. Lancet. 2012;379(9816):625–32.
Government of Kenya. The Constitution of Kenya. Revised Edition. Nairobi, Kenya: National Council for Law Reporting (NCLR). 2010. http://www.wipo.int/edocs/lexdocs/laws/en/ke/ke019en.pdf . Accessed 18 June 2018.
Hussain. R. In: Brief: unintended pregnancy and abortion in Kenya. New York: Guttmacher Institute. p. 2012.
Ziraba AK, Izugbara C, Levandowski BA, Gebreselassie H, Mutua M, Mohamed SF, et al. Unsafe abortion in Kenya: a cross-sectional study of abortion complication severity and associated factors. BMC Pregnancy Childbirth. 2015;15:34.
National Council for Population and Development (NCPD) and UNFPA Kenya Country Office. Kenya Population Situation Analysis. Nairobi: NCPD and UNFPA; 2013.
Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. Tenth edition. Philadelphia: Wolters Kluwer Health; 2017.
Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405.
Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Arambepola C, Rajapaksa LC. Decision making on unsafe abortions in Sri Lanka: a case-control study. Reprod Health. 2014;11:91.
Maina BW, Mutua MM, Sidze EM. Factors associated with repeat induced abortion in Kenya. BMC Public Health. 2015;15:1048.
Schwandt HM, Creanga AA, Adanu RM, Danso KA, Agbenyega T, Hindin MJ. Pathways to unsafe abortion in Ghana: the role of male partners, women and health care providers. Contraception. 2013;88(4):509–17.
Chae S, Desai S, Crowell M, Sedgh G. Reasons why women have induced abortions: a synthesis of findings from 14 countries. Contraception. 2017;96(4):233–41.
Cleeve A, Faxelid E, Nalwadda G, Klingberg-Allvin M. Abortion as agentive action: reproductive agency among young women seeking post-abortion care in Uganda. Cult Health Sex. 2017;19(11):1286–300.
Osur J, Orago A, Mwanzo I, Bukusi E. Social networks and decision making for clandestine unsafe abortions: evidence from Kenya. Afr J Reprod Health. 2015;19(1):34–43.
Kebede MT, Hilden PK, Middelthon AL. The tale of the hearts: deciding on abortion in Ethiopia. Cult Health Sex. 2012;14(4):393–405.
Olsson P, Wijewardena K. Unmarried women's decisions on pregnancy termination: qualitative interviews in Colombo, Sri Lanka. Sex Reprod Healthc. 2010;1(4):135–41.
Marlow HM, Wamugi S, Yegon E, Fetters T, Wanaswa L, Msipa-Ndebele S. Women's perceptions about abortion in their communities: perspectives from western Kenya. Reprod Health Matters. 2014;22(43):149–58.
Kumar A, Hessini L, Mitchell EM. Conceptualising abortion stigma. Cult Health Sex. 2009;11(6):625–39.
Shellenberg KM, Moore AM, Bankole A, Juarez F, Omideyi AK, Palomino N, et al. Social stigma and disclosure about induced abortion: results from an exploratory study. Glob Public Health. 2011;6(Suppl 1):S111–25.
Rossier C. Abortion: an open secret? Abortion and social network involvement in Burkina Faso. Reprod Health Matters. 2007;15(30):230–8.
Yegon EK, Kabanya PM, Echoka E, Osur J. Understanding abortion-related stigma and incidence of unsafe abortion: experiences from community members in Machakos and trans Nzoia counties Kenya. Pan Afr Med J. 2016;24:258.
Yegon E, Mwaniki P, Echoka E, Osur J. Correlates of individual-level stigma and unsafe abortions among women seeking abortion care in trans Nzoia and Machakos counties, Kenya. Annals of Tropical Medicine and Public Health. 2016;9(4):226–34.
Gipson JD, Hirz AE, Avila JL. Perceptions and practices of illegal abortion among urban young adults in the Philippines: a qualitative study. Stud Fam Plan. 2011;42(4):261–72.
Rehnstrom Loi U, Gemzell-Danielsson K, Faxelid E, Klingberg-Allvin M. Health care providers' perceptions of and attitudes towards induced abortions in sub-Saharan Africa and Southeast Asia: a systematic literature review of qualitative and quantitative data. BMC Public Health. 2015;15:139.
Hessini L. A learning agenda for abortion stigma: recommendations from the Bellagio expert group meeting. Women Health. 2014;54(7):617–21.
Dunn JT, Lesyna K, Zaret A. The role of human rights litigation in improving access to reproductive health care and achieving reductions in maternal mortality. BMC Pregnancy Childbirth. 2017;17(Suppl 2):367.
World Health Organization. Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. In: Sixth edition; 2011.
Ministry of Health Kenya. Incidence and complications of unsafe abortion in Kenya: Key findings of a national study. 2013. https://www.guttmacher.org/sites/default/files/report_pdf/abortion-in-kenya.pdf . Accessed 18 June 2018.
Mutua MM, Maina BW, Achia TO, Izugbara CO. Factors associated with delays in seeking post abortion care among women in Kenya. BMC Pregnancy Childbirth. 2015;15:241.
Orner P, de Bruyn M, Cooper D. "it hurts, but I don't have a choice, I'm not working and I'm sick": decisions and experiences regarding abortion of women living with HIV in Cape Town, South Africa. Cult Health Sex. 2011;13(7):781–95.
Chi BK, Hanh NT, Rasch V, Gammeltoft T. Induced abortion among HIV-positive women in northern Vietnam: exploring reproductive dilemmas. Cult Health Sex. 2010;12(Suppl 1):S41–54.
Download references
Acknowledgements
The authors wish to express their sincere appreciation to the women who took part in this study and to the directors of JOOTRH and KDH for granting permission to collect data. In addition, special recognition goes to the staff of KMET for their assistance during data collection in Kisumu. This article represents the opinions of the named authors and not the necessarily the views of their institutions or organisations.
The Swedish International Development Agency (Sida) funded the study by providing a Minor Field Study grant to ML. The Doctoral School in Health Care Sciences at Karolinska Institutet provided a PhD grant to URL. The funders had no role in the study planning, implementation or analysis, the decision to publish or the preparation of the manuscript.
Availability of data and materials
The datasets generated and analysed as part of this study are not publicly available in order to maintain the confidentiality of the respondents. However, all transcripts are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Department of Public Health Sciences/IHCAR, Karolinska Institutet, SE-171 77, Stockholm, Sweden
Ulrika Rehnström Loi, Matilda Lindgren & Elisabeth Faxelid
College of Health Sciences, School of Nursing Sciences, University of Nairobi, Nairobi, Kenya
Monica Oguttu
Kisumu Medical Education Trust (KMET), Kisumu, Kenya
Department of Women’s and Children’s Health, Karolinska Institutet, SE-171 77, Stockholm, Sweden
Marie Klingberg-Allvin
School of Education, Health and Social Studies, Dalarna University, Högskolegatan 2, 791 31, Falun, Sweden
You can also search for this author in PubMed Google Scholar
Contributions
MKA and EF conceived the presented study and developed the study design with contributions from URL. ML conducted all face-to-face interviews with support from URL. URL and ML led the content analysis with input from all authors. All authors discussed the results. URL wrote the first draft of the article. All authors commented on and approved the final manuscript. The research team included MO, a Kenyan and senior professional as co-author as she was involved in the study’s planning, supported data collection and also contributed to the improvement of the manuscript.
Corresponding author
Correspondence to Ulrika Rehnström Loi .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was granted by the Regional Ethics Appeals Board in Stockholm (Reference number 2013/902–31/1) and the JOOTRH Ethics and Review Committee in Kisumu (Reference number ERC 42/13). Verbal and written consent were sought and received from all respondents. Information about the confidentiality and safe storage of the data was provided both orally and in writing. The participants were informed that they could withdraw their participation at any time without consequence. Confidentiality was protected as the interviews were conducted in a private room where conversations could not be overheard, and only researchers involved in the study had access to the interview material. Participants were given small financial compensation to cover transportation costs and the potential loss of income; the amount was low enough to not jeopardise the voluntary nature of participation. The study area was not included in the presentation of sociodemographic information to protect the anonymity of the respondents. After conducting the first two interviews, the research team perceived that some women may require professional support. Therefore, the author who conducted the interviews (ML) arranged for such care by KMET.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Rehnström Loi, U., Lindgren, M., Faxelid, E. et al. Decision-making preceding induced abortion: a qualitative study of women’s experiences in Kisumu, Kenya. Reprod Health 15 , 166 (2018). https://doi.org/10.1186/s12978-018-0612-6
Download citation
Received : 31 January 2018
Accepted : 25 September 2018
Published : 03 October 2018
DOI : https://doi.org/10.1186/s12978-018-0612-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decision-making
- Qualitative methodology
- In-depth interviews
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Abortion attitudes, religious and moral beliefs, and pastoral care among Protestant religious leaders in Georgia
Affiliations.
- 1 Department of Population, Family and Reproductive Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, United States of America.
- 2 The Center for Reproductive Health Research in the Southeast, Rollins School of Public Health, Emory University, Atlanta, Georgia, United States of America.
- 3 Hubert Department of Global Health, Rollins School of Public Health, Emory University, Atlanta, Georgia, United States of America.
- 4 Department of Behavioral, Social and Health Education Sciences, Rollins School of Public Health, Emory University, Atlanta, Georgia, United States of America.
- 5 Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia, United States of America.
- 6 Graduate Division of Religion, Laney Graduate School of Arts and Sciences, Emory University, Atlanta, Georgia, United States of America.
- 7 Reproductive Justice Activist and Movement Chaplain, Atlanta, Georgia, United States of America.
- 8 All Souls Church Unitarian, Washington, D.C., United States of America.
- 9 Heilbrunn Department of Population & Family Health, Mailman School of Public Health, Columbia University, New York, NY, United States of America.
- PMID: 32678861
- PMCID: PMC7367465
- DOI: 10.1371/journal.pone.0235971
Objective: The purpose of this study is to explore Protestant religious leaders' attitudes towards abortion and their strategies for pastoral care in Georgia, USA. Religious leaders may play an important role in providing sexual and reproductive health pastoral care given a long history of supporting healing and health promotion.
Methods: We conducted 20 in-depth interviews with Mainline and Black Protestant religious leaders on their attitudes toward abortion and how they provide pastoral care for abortion. The study was conducted in a county with relatively higher rates of abortion, lower access to sexual and reproductive health services, higher religiosity, and greater denominational diversity compared to other counties in the state. Interviews were audio-recorded, transcribed verbatim, and analyzed by thematic analysis.
Results: Religious leaders' attitudes towards abortion fell on a spectrum from "pro-life" to "pro-choice". However, most participants expressed attitudes in the middle of this spectrum and described more nuanced, complex, and sometimes contradictory views. Differences in abortion attitudes stemmed from varying beliefs on when life begins and circumstances in which abortion may be morally acceptable. Religious leaders described their pastoral care on abortion as "journeying with" congregants by advising them to make well-informed decisions irrespective of the religious leader's own attitudes. However, many religious leaders described a lack of preparation and training to have these conversations. Leaders emphasized not condoning abortion, yet being willing to emotionally support women because spiritual leaders are compelled to love and provide pastoral care. Paradoxically, all leaders emphasized the importance of empathy and compassion for people who have unplanned pregnancies, yet only leaders whose attitudes were "pro-choice" or in the middle of the spectrum expressed an obligation to confront stigmatizing attitudes and behaviors towards people who experience abortion. Additionally, many leaders offer misinformation about abortion when offering pastoral care.
Conclusion: These findings contribute to limited empirical evidence on pastoral care for abortion. We found religious leaders hold diverse attitudes and beliefs about abortion, rooted in Christian scripture and doctrine that inform advice and recommendations to congregants. While religious leaders may have formal training on pastoral care in general or theological education on the ethical issues related to abortion, they struggle to integrate their knowledge and training across these two areas. Still, leaders could be potentially important resources for empathy, compassion, and affirmation of agency in abortion decision-making, particularly in the Southern United States.
PubMed Disclaimer
Conflict of interest statement
The authors have declared that no competing interests exist.
Similar articles
- Women leaders perceived barriers and consequences of safe abortion in Rwanda: a qualitative study. Rugema L, Uwase MA, Rukundo A, Nizeyimana V, Mporanyi T, Kagaba A. Rugema L, et al. BMC Womens Health. 2023 Apr 28;23(1):205. doi: 10.1186/s12905-023-02366-4. BMC Womens Health. 2023. PMID: 37118784 Free PMC article.
- Religious leaders' perceptions of advance care planning: a secondary analysis of interviews with Buddhist, Christian, Hindu, Islamic, Jewish, Sikh and Bahá'í leaders. Pereira-Salgado A, Mader P, O'Callaghan C, Boyd L, Staples M. Pereira-Salgado A, et al. BMC Palliat Care. 2017 Dec 28;16(1):79. doi: 10.1186/s12904-017-0239-3. BMC Palliat Care. 2017. PMID: 29282112 Free PMC article.
- [FROM PASTORAL CARE TO SPIRITUAL CARE - TRANSFORMING THE CONCEPTION OF THE ROLE OF THE SPIRITUAL CARE PROVIDER]. Schultz M, Bentur N, Rei Koren Z, Bar Sela G. Schultz M, et al. Harefuah. 2017 Nov;156(11):735-739. Harefuah. 2017. PMID: 29198094 Review. Hebrew.
- Response of religious groups to HIV/AIDS as a sexually transmitted infection in Trinidad. Genrich GL, Brathwaite BA. Genrich GL, et al. BMC Public Health. 2005 Nov 16;5:121. doi: 10.1186/1471-2458-5-121. BMC Public Health. 2005. PMID: 16288659 Free PMC article.
- Women's reproductive health: monotheistic religious perspectives. Schenker JG. Schenker JG. Int J Gynaecol Obstet. 2000 Jul;70(1):77-86. doi: 10.1016/s0020-7292(00)00225-3. Int J Gynaecol Obstet. 2000. PMID: 10884536 Review.
- (Re)-Emerging Challenges in Christian Bioethics: Leading Voices in Christian Bioethics. Iltis A. Iltis A. Christ Bioeth. 2022 Mar 18;28(1):1-10. doi: 10.1093/cb/cbab017. eCollection 2022 Apr. Christ Bioeth. 2022. PMID: 35992505 Free PMC article.
- Jones RK, Jerman J. Population Group Abortion Rates and Lifetime Incidence of Abortion: United States, 2008–2014. Am J Public Health. 2017;107(12):1904–9. 10.2105/AJPH.2017.304042 - DOI - PMC - PubMed
- Jones RK, Witwer E, Jerman J. Abortion Incidence and Service Availability in the United States, 2017. New York: Guttmacher Institute; 2019.
- Kumar A, Hessini L, Mitchell EM. Conceptualising abortion stigma. Cult Health Sex. 2009;11(6):625–39. 10.1080/13691050902842741 - DOI - PubMed
- Cockrill K, Upadhyay UD, Turan J, Greene Foster D. The stigma of having an abortion: development of a scale and characteristics of women experiencing abortion stigma. Perspect Sex Reprod Health. 2013;45(2):79–88. 10.1363/4507913 - DOI - PubMed
- Shellenberg KM, Moore AM, Bankole A, Juarez F, Omideyi AK, Palomino N, et al. Social stigma and disclosure about induced abortion: results from an exploratory study. Glob Public Health. 2011;6 Suppl 1:S111–25. - PubMed
Publication types
- Search in MeSH
Grants and funding
- T32 HD007545/HD/NICHD NIH HHS/United States
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- PubMed Central
- Public Library of Science
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 10 May 2022
The impact of ‘grounds’ on abortion-related outcomes: a synthesis of legal and health evidence
- Fiona de Londras 1 ,
- Amanda Cleeve 2 , 3 ,
- Maria I. Rodriguez 4 &
- Antonella F. Lavelanet 3
BMC Public Health volume 22 , Article number: 936 ( 2022 ) Cite this article
5033 Accesses
8 Citations
21 Altmetric
Metrics details
Where abortion is legal, it is often regulated through a grounds-based approach. A grounds-based approach to abortion provision occurs when law and policy provide that lawful abortion may be provided only where a person who wishes to have an abortion satisfies stipulated ‘grounds’, sometimes described as ‘exceptions’ or ‘exceptional grounds’. Grounds-based approaches to abortion are, prima facie, restrictive as they limit access to abortion based on factors extraneous to the preferences of the pregnant person. International human rights law specifies that abortion must be available (and not ‘merely’ lawful) where the life or health of the pregnant woman or girl is at risk, or where carrying a pregnancy to term would cause her substantial pain or suffering, including but not limited to situations where the pregnancy is the result of rape or incest or the pregnancy is not viable. However, international human rights law does not specify a grounds-based approach as the way to give effect to this requirement. The aim of this review is to address knowledge gaps related to the health and non-health outcomes plausibly related to the effects of a grounds-based approach to abortion regulation. The evidence from this review shows that grounds have negative implications for access to quality abortion and for the human rights of pregnant people. Further, it shows that grounds-based approaches are insufficient to meet states’ human rights obligations. The evidence presented in this review thus suggests that enabling access to abortion on request would be more rights-enhancing than grounds-based approaches to abortion regulation.
Peer Review reports
Where abortion is at least partially legal, it is commonly regulated through a grounds-based approach [ 1 ]. A grounds-based approach occurs when law and policy provides that lawful abortion may be availed of only where a person who wishes to have an abortion satisfies stipulated ‘grounds’, sometimes described as ‘exceptions’ or ‘exceptional grounds’. Grounds are defined as ‘circumstances under which abortion is lawful, that is, allowed or not contrary to law, or explicitly permitted or specified by law’ [ 2 ].
Typical ‘grounds’ include risk to the life or health of the pregnant woman, if the pregnancy results from rape, incest or sexual violence, severe or fatal fetal anomaly, or socio-economic grounds. However, grounds can be expressed in legal texts in ‘vague and confusing’ ways, making them even more difficult to implement [ 2 ]. In many cases these grounds-based approaches exist alongside and interact with other regulatory interventions such as gestational limits, third party authorization requirements, and criminalization to form a complex law and policy framework for abortion provision.
Grounds based approaches to abortion are, prima facie, restrictive as they limit access to abortion based on factors extraneous to the preferences of the pregnant woman. International human rights law (IHRL) specifies that abortion must be available (and not ‘merely’ lawful) where the life and health of the pregnant woman or girl is at risk, or where carrying a pregnancy to term would cause her substantial pain or suffering, including but not limited to situations where the pregnancy is the result of rape or incest or the pregnancy is not viable ([ 3 ], para 4). However, even though IHRL says abortion must be available in these circumstancs this does not mean that grounds-based approaches to abortion regulation are either mandated by or sufficient to satisfy IHRL. Rather, in ensuring that abortion is available in at least these circumstances states must be cognizant of, and must comply with, their broader IHRL obligations. These include obligations to take steps to ensure women do not have to undergo unsafe abortion ([ 4 ], para 6), to reduce maternal morbidity and mortality [ 3 , 5 ], to effectively protect women and girls from the physical and mental risks associated with unsafe abortion [ 3 , 5 ], to ensure that women’s and girls’ right to privacy and confidentiality in sexual and reproductive healthcare is protected, and to respect, protect and fulfil the broader right to the highest attainable standard of physical and mental health, including sexual and reproductive health.
The aim of this review is to address knowledge gaps related to the health and non-health outcomes that, while not directly linked through simple linear causal pathways, are plausibly related to the effects of a grounds-based approach to abortion regulation. The review followed a methodology for integrating human rights in guideline development that has been described elsewhere [ 6 ]. This methodology is well-suited to interventions that are complex, may have multiple interacting components, may be non-linear in their effects, and are often context dependent [ 7 ]. Such complex interventions often interact with one another, such that outcomes related to one individual or community may be dependent on others, and may be impacted positively or negatively by the people, institutions and resources that are arranged together within the larger system in which they are implemented [ 8 ]. This review was conducted as part of the evidence base for the World Health Organization (WHO)‘s recently-published Abortion Care Guideline [ 9 ]. It is one of seven reviews of evidence undertaken by the research team following the same methodological approach.
Throughout this review, and consistent with the approach in the Abortion Care Guideline ([ 9 ], p. xxii), we use the terms women, girls, pregnant women [and girls], pregnant people, and people interchangeably to include all those with the capacity to become pregnant.
Identification of studies and data extraction
This review examined the impact of the intervention of grounds-based approaches on two populations (i) people seeking abortion, and (ii) health professionals. Our study outcomes and search strategy were developed together with experts working in the fields of reproductive health, law, policy, and human rights. Our outcomes of interest included both health and non-health outcomes that, based on a preliminary assessment of the literature [ 10 ], could be linked to the effects of the ‘grounds’ intervention. Outcomes linked to those seeking abortion included delayed abortion, continuation of pregnancy, opportunity costs, reproductive coercion, and disproportionate impact. Outcomes linked to medical professionals included stigmatization, workload implications, referral of patients, and system costs.
We searched the databases PubMed, HeinOnline, and JStor and the search engine Google Scholar. The WHO’s Safe Abortion: technical and policy guidance for health systems (2nd edition) [ 11 ] included data up until 2012, thus, we limited our search to papers published in English after 2010 to the end of November 2020. We did not restrict on study design. We included only manuscripts that undertook original data collection or analysis i.e., quantitative studies (comparative and non-comparative), qualitative and mixed-methods studies, reports, PhD theses, and economic or legal analyses.
The full review team was comprised of four members (AC, FdL, MR and AL). FdL and AL developed the PICO question (People/Population/Patient; Intervention; Comparison (if applicable); Outcomes of Interest). Two reviewers (AC and FdL) conducted an initial screening of the literature. Titles and abstracts were first screened for eligibility using the Covidence® tool; full texts were then reviewed. A third reviewer (AL) confirmed that these studies met inclusion criteria. Two reviewers (FdL and AC) extracted data. Any discrepancies were reviewed and discussed with two additional reviewers (AL and MR). The review team resolved any discrepancies through consensus.
In order to fully understand the implications of the findings for abortion law and policy, we applied human rights standards to the data extracted from these manuscripts. The applicable standards were drawn from a review of the corpus of IHRL in accordance with the methodological approach applied [ 6 ]. They thus exclude regional and national human rights laws. The applicable standards were considered together with the evidence from the included manuscripts in order to identify, (a) which international human rights standards are engaged by grounds, (b) whether the evidence suggests that grounds have positive or negative effects on the enjoyment of rights, and (c) where no data are identified from the manuscripts against outcomes of interest, whether IHRL provides evidence that can further elucidate the impacts and effects of grounds. This is summarized in Tables 2 and 3 below.
Data from included studies were matched to the outcomes and presented in Evidence tables. In these tables the impact of each finding on the outcome was presented, as well as an overall conclusion of the identified findings across outcomes of interest. To summarize the effect of the intervention, across all study designs, we utilized a previously developed approach and incorporated a visual representation of effect direction. The direction of the evidence was illustrated by a symbol which indicated whether, in relation to that particular outcome, the evidence extracted from a study suggested an increase (▲), decrease ( ⊽ ), or no change in the outcome ( ○ ). The symbol did not indicate the magnitude of the effect [ 6 , 8 ].
The initial search generated 5123 citations after duplicates were removed. We screened the titles and abstracts and conducted a full text screening of 130 manuscripts. After applying our exclusion criteria, 19 manuscripts were included in the final analysis (Fig. 1 . Prisma flow diagram).
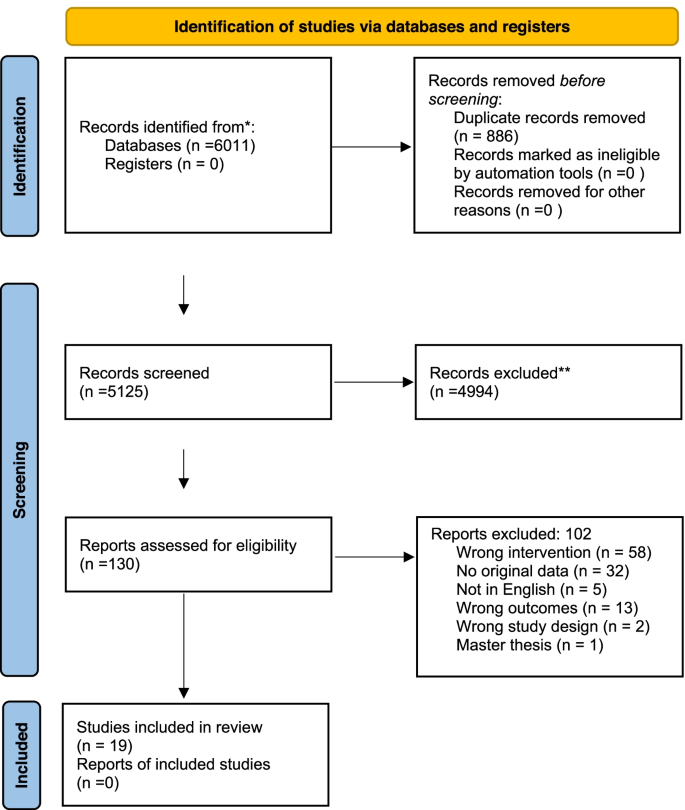
Prisma Flow diagram [ 12 ]
Manuscripts described data from the following settings: Argentina [ 13 ], Australia [ 14 , 15 , 16 , 17 , 18 ], Chile [ 19 , 20 ], Colombia [ 21 , 22 , 23 ], Ethiopia [ 24 ], Ghana [ 25 ], Ireland [ 26 , 27 ], Mexico [ 23 , 28 ], Rwanda [ 29 , 30 ], Thailand [ 31 ], United Kingdom/Great Britain [ 23 , 32 ], and Uruguay [ 33 ]. The characteristics of included manuscripts are presented in Table 1 . For the impact on people seeking abortion we included studies containing information relevant for the outcomes: delayed abortion [ 14 , 20 , 21 , 27 , 30 ] continuation of pregnancy [ 28 , 33 ], opportunity costs [ 13 , 14 , 15 , 16 , 20 , 21 , 22 , 23 , 24 , 26 , 29 , 30 , 31 , 32 ], self-managed abortion [ 26 , 32 ], unlawful abortion [ 25 , 26 , 32 ], reproductive coercion [ 18 , 24 ] and disproportionate impact [ 16 , 18 , 19 , 23 , 31 ]. For the impact on health professionals we included studies containing information relevant to workload implications [ 13 , 18 , 19 , 24 , 25 ], referral to another provider [ 14 ], imposition on conscience or ethics [ 19 , 24 ], stigmatization [ 17 ], and system costs [ 18 , 19 , 27 , 28 , 33 ]. No evidence was identified linking the intervention to the outcomes: family disharmony, exposure to violence or exploitation, or impact on the provider-patient relationship.
Impact of grounds on abortion seekers
A summary of the impacts of grounds-based approaches on abortion seekers and the application to human rights are presented in Table 2 . Evidence identified per study and outcome are presented in Supplementary Tables 1 and 2 .
The evidence from six studies [ 14 , 20 , 21 , 26 , 27 , 30 ] suggests that grounds-based approaches contribute to delays in accessing abortion. This includes delays resulting from inconsistencies in interpretation and application of grounds [ 21 ], questioning or ‘verification’ of women’s claims relating to grounds [ 14 , 21 ], disagreement between medical professionals about whether a ground is satisfied [ 20 ], and health professionals delaying abortion until the pregnant person’s health condition is severe enough that the woman’s condition is deemed life threatening (and thus that a ‘risk to life’ ground is fulfilled) [ 20 , 25 ]. The human rights standards reviewed make it clear that states must take steps to reduce maternal mortality and morbidity ([ 3 , 5 ], paras [8, 10, 24, 30-33]), and to ensure that lawful abortion is safe and accessible [ 3 ]. The evidence from the reviewed studies suggests that grounds are associated with delay in a way that indicates incompatibility with these human rights obligations.
Evidence from two studies suggests that grounds-based laws may indirectly contribute to continuation of pregnancy [ 28 , 33 ]. When grounds-based laws are removed, and first trimester abortion is allowed on request, these studies demonstrated a decrease in fertility, possibly due to a reduction in unplanned births [ 28 , 33 ]. If, as these studies suggest might be the case, grounds are associated with unwanted continuation of pregnancy, they have clear implications for the right to decide on the number and spacing of children, as well as the right to privacy and to the highest attainable standard of physical and mental health. This is reinforced by the findings from two studies, which suggest that grounds-based laws may contribute to reproductive coercion through the denial of an abortion [ 18 , 24 ]. This includes people who seek abortion in circumstances where IHRL requires it to be available, namely where the life and health of the pregnant woman or girl is at risk, or where carrying a pregnancy to term would cause her substantial pain or suffering [ 3 ]. Denial of abortion in such circumstances has been found to amount to torture, cruel, unusual, and degrading treatment or punishment, including where abortion on the grounds of fatal fetal impairment was unlawful [ 34 , 35 ].
States have a long-standing obligation in IHRL to ensure that their regulatory choices—in this case grounds-based approaches to abortion—do not force women to resort to unsafe abortion and, if necessary, to review, reform and liberalize laws to ensure this ([ 3 , 36 ], para 28). Three studies indicate that grounds-based approaches are associated with people availing of unlawful abortion per se [ 25 , 26 , 27 ], while two indicate an association with self-managed abortion [ 26 , 32 ]. Self-managed abortion is not necessarily ‘unsafe’, but when availed of outside of the formal legal system and without the availability of appropriate and high-qualify information, medicines (including for pain management), and, where it is desired, support from trained health workers within the health system it can be understood as less safe [ 37 ]. Thus, grounds-based approaches engage states’ obligation to review, reform and liberalize their laws to reduce recourse to unsafe abortion ([ 36 ], para 28).
Evidence from 15 studies shows that grounds-based approaches contribute to opportunity costs [ 13 , 14 , 15 , 16 , 17 , 20 , 21 , 22 , 23 , 24 , 26 , 29 , 30 , 31 , 32 ]. These costs are varied and include the need to travel for an abortion [ 26 , 27 ], increased financial costs, emotional stress and trauma [ 26 , 27 ] fear or experience of judgement and stigma [ 15 ], bureaucratic and costly protracted legal processes [ 14 , 21 , 29 , 30 ], increased morbidity, being subjected to ‘nterrogations’ and having one’s rape claim questioned [ 16 ], unsafe abortions, and having to carry an unwanted pregnancy or a pregnancy with severe malformations to term [ 18 ].
The findings from some of these studies point to an inconsistency in how grounds are interpreted and applied, which sometimes leads to unpredictability and inequity in terms of abortion access and healthcare quality for the abortion seeker [ 13 , 20 , 23 , 31 ] and requirements to provide legally-unnecessary documentation or ‘proof’ of fulfilling a ground [ 13 , 17 , 19 ]. One study shows that women who could obtain legal support and advice considered it vital to their ability to navigate the system of abortion provision [ 22 ]. In some cases, women who sought abortion based on a recognized ground reported verbal abuse and denial of services [ 21 ], and women who had to travel to access abortion sometimes reported reluctance to seek post-abortion care in cases of complications later [ 32 ]. The findings from other studies indicate that certain grounds, such as health and rape grounds, are consistently interpreted very restrictively, leading to the denial of abortion [ 16 , 17 , 21 , 22 , 23 , 24 , 29 , 30 ]. These studies indicate that a grounds-based approach is not sufficient to ensure that the state’s obligation to ensure abortion is lawful and available when continuing with pregnancy would cause substantial pain and suffering is fulfilled ([ 3 ], para 4).
five studies suggests that grounds-based approaches have a disproportionate impact on some groups of women [ 16 , 18 , 19 , 23 , 31 ] and thus undermine the right to equality and non-discrimination which is fundamental to the right to the highest attainable standard of physical and mental health. These studies suggest that in a grounds-based system of abortion law those with fewer resources [ 19 ], rural women, and women with lower education [ 18 ], as well as those seeking abortion due to rape [ 16 ] and on health grounds [ 23 ] are relatively less able to access abortion than other women.
Impact of grounds on health professionals
A summary of the findings of grounds-based approaches on health professionals and the application of human rights are presented in Table 3 . Evidence identified per study and outcome are presented in Supplementary Tables 1 and 2 .
Evidence from five studies suggests that grounds have workload implications for health professionals [ 13 , 18 , 19 , 24 , 25 ] including difficulties in interpreting and applying the law [ 24 ], preparing detailed files for court reviews [ 18 ], stress and fear of legal repercussions [ 25 ], and frustration with the system when a diagnosis of a non-lethal fetal malformation has been made but abortion is not permitted [ 18 , 19 ]. Findings from one study suggest that, in order to circumvent obstacles posed by or emanating from grounds-based approaches, referrals may be made to another provider operating in a setting where the ground in question does not preclude access to abortion [ 14 ]. One study suggests that where grounds do not permit abortion in situations of diagnosed fetal impairment, health professionals experience this as an imposition on their conscience or ethics [ 19 ]. Indeed, in another study the evidence showed that providers perceive grounds-based approaches as an imposition on their conscience or ethics to the extent that they question whether or not they should provide a legal abortion [ 24 ]. Findings from one study indicate that grounds-based laws may contribute to stigmatization of abortion provision and healthcare professionals ultimately choosing not to involve themselves in abortion care for this reason [ 17 ]. Evidence from five studies suggests that grounds-based laws may contribute to system costs. Indirect contributions to system costs are indicated by continuation of pregnancy and maternal mortality [ 19 , 29 , 33 ]. Direct contributions to system costs include the imposition of costs on court systems, increased workloads forhealthcare professionals [ 18 ], and delays to care for pregnant women with severe health conditions [ 27 ].
Evidence of the impact of grounds on health professionals points not only to their conditions of work but also to the implications of grounds for the health system and, thus, for the right to the highest attainable standard of physical and mental health. That right obliges states to ensure that health-care facilities, goods, and services are available, accessible, acceptable and of good quality ([ 38 ], paras 4, 12).
Overall, the evidence from these studies suggests that grounds-based approaches to abortion regulation undermine the right to health by impacting on health workers and the health system so as to make sexual and reproductive healthcare less available, accessible, and acceptable and to lower its quality.
Making abortion available based on grounds, sometimes after a limited period during which it is available without restriction as to reason, is a common approach to law and policy on abortion. To illustrate, as of February 2019 there were only 16 jurisdictions that prohibited abortion in all circumstances, and seven more where laws prohibited unlawful abortion but failed to specify expressly the grounds for lawful abortion [ 1 ]. States that have recently transitioned from near-total bans on abortion to some or wide legal availability have tended to adopt a grounds-based approach [ 39 , 40 , 41 ]. In addition, several constitutional and other courts have recently intervened to determine the constitutionality of abortion law in specified circumstances [ 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ]. It is clear that using grounds as a mode of designing abortion provision is persistent. However, the evidence presented in this review suggests that this approach is suboptimal from a rights-based perspective. While modes of providing abortion care may vary as a pregnancy develops, whether and if so how abortion is provided should not be determined by legally prescribed grounds but by the preferences of the pregnant person and evidence-based clinical and service delivery protocols [ 9 ].
The evidence from this review shows that grounds-based approaches implicate states’ obligation to ensure that abortion is lawfully available where carrying a pregnancy to term would cause a pregnant woman substantial pain or suffering, where there is a risk to life or health, where pregnancy is a result of rape or incest, or where the pregnancy is not viable ([ 3 ], para 4). This is because grounds-based approaches to abortion provision are per se restrictive and are commonly subject to narrow interpretation, limitation and burdensome procedures so that ‘qualification’ for abortion under such grounds is very difficult to establish. As this can lead to women having recourse to less safe or unsafe abortions, grounds-based approaches engage states’ obligation to take steps, including revising their laws, to ensure women do not have to undergo unsafe abortion ([ 3 , 4 ], para 6), to reduce maternal morbidity and mortality, and to effectively protect women and girls from the physical and mental risks associated with unsafe abortions. The evidence in this review points towards allowing abortion on request as the most effective approach to ensuring that abortion is available in the circumstances required by IHRL. In addition to being an effective mode of satisfying pregnant people’s rights, this would also mean that women are not required—and do not feel obliged—to provide reasons or justifications for their decision to end their pregnancies. Instead of defining only certain circumstances where abortion is permitted and thus, implicitly, justifiable, and the person seeking it deserving of abortion care, the provision of abortion without restriction as to reason would center the pregnant person’s reproductive autonomy and support her in giving effect to her assessment of what is right for her, regardless of circumstances. This is consistent with established frameworks for quality of care as well as with IHRL. Indeed, the WHO has now recommended against grounds-based approaches and recommended that abortion be made available on the request of the pregnant person [ 9 ].
Limitations
This review has limitations. While the studies relate to 13 settings, this is nevertheless limited when compared to the number of jurisdictions that take a grounds-based approach to abortion [ 1 ]. This review also only contains manuscripts published in English. Further research on the impact of grounds in a wider range of settings would be valuable.
The realization of human rights applicable to abortion-related interventions is not a research area that readily lends itself to randomized controlled trials or comparative observational studies; rather, studies are often conducted without comparisons. While this may be considered a limitation from a standard methodological perspective for systematic reviews, it does not limit the ability to identify the human rights law implications of grounds-based approaches. Thus, while standard tools for assessing risk of bias or quality, including GRADE [ 50 ], were unsuitable, given the objective of fully integrating human rights implications into our understanding of the effects of grounds as a regulatory intervention, it was appropriate to engage with a wide variety of sources. Finally, and consistent with the methodological approach pursued [ 6 ], this review applies international, rather than regional or domestic, human rights law to develop a general understanding of the rights-related implications of grounds. The applicability of any individual human rights standard in a specific setting will depend on factors including the state’s ratification of relevant human rights instruments and their status in domestic law ([ 9 ], p. 7).
Conclusions
The evidence from this review shows that grounds-based approaches to abortion limit access to abortion both because they exclude some women due to non-satisfaction of grounds and because they can operate in a way that makes availability and accessibility narrower in practice due to the chilling effects of continued criminalization, the burdens on providers, and the space they leave for conservative and limiting interpretation. Combining the evidence from the review of studies with evidence of applicable human rights standards indicates that grounds-based approaches result in violations of human rights. This points to the regulatory and human rights value of ensuring access to abortion on request of the pregnant person as a rights compliant, autonomy-based, and effective step in putting in place a supportive law and policy framework to support an enabling environment for quality abortion care.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files .
Abbreviations
International Human Rights Law
World Health Organization
Lavelanet A, Johnson BR, Ganatra B. Global abortion policies database: a descriptive analysis of the regulatory and policy environment related to abortion. Best Pract Res Clin Obstet Gynaecol. 2020;62:25–35.
Article Google Scholar
Lavelanet A, Schlitt S, Jonson B, Ganatra B. Global abortion policies database: a descriptive analysis of the legal categories of lawful abortion. BMC Int Health Hum Rights. 2018;18(44):1–10. https://doi.org/10.1186/s12914-018-0183-1 .
Human Rights Committee, General comment no.36; article 6 right to life. 2018 (UN Doc CCPR/C/GC/36).
Google Scholar
Human Rights Committee, General comment no. 28: Equality of rights between men and women) (article 3) (2000) (UN Doc. CCPR/C/21/Rev.1/Add.10).
Committee on the Rights of the Child, General comment no. 4: Adolescent health and development in the context of the Convention on the Rights of the Child. 2003) (UN Doc. CRC/GC/2003/4).
de Londras F, Cleeve A, Rodriguez M, Lavelanet A. Integrating rights and evidence: a technical advance in abortion guideline development. BMJ Glob Health. 2021;6:e004141.
Petticrew M, Knai C, Thomas J, et al. Implications of a complexity perspective for systematic reviews and guideline development in health decision making. BMJ Glob Health. 2019;4:e000899. https://doi.org/10.1136/bmjgh-2018-000899 .
Article PubMed PubMed Central Google Scholar
Thomson HJ, Thomas S. The effect direction plot: visual display of non-standardised effects across multiple outcome domains. Res Synth Methods. 2013;4(95):101. https://doi.org/10.1002/jrsm.1060pmid .
World Health Organization, Abortion care guideline. 2022.
Burris S, Ghorashi A, Foster Cloud L, Rebouché R, Skuster P, Lavelanet A. Identifying data for the empirical assessment of law (IDEAL): a realist approach to research gaps on the health effects of abortion law. BMJ Glob Health. 2021;6:e005120. https://doi.org/10.1136/bmjgh-2021-005120 .
World Health Organization. Safe abortion: technical and policy guidance for health systems. 2nd ed; 2012.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71 . For more information, visit: http://www.prismastatement.org/ .
Ramos S, Romero M, Ramón MA. Health care providers’ opinions on abortion: a study for the implementation of the legal abortion public policy in the province of Santa Fe, Argentina. Reprod Health. 2014;11:72.
Black KI, Douglas H, de Costa C. Women’s access to abortion after 20 weeks’ gestation for fetal chromosomal abnormalities: views and experiences of doctors in New South Wales and Queensland. Austr N Z J Obstet Gynaecol. 2015;55:144.
LaRoche KJ, Wynn LL, Foster AM. We have to make sure you meet certain criteria’: exploring patient experiences of the criminalisation of abortion in Australia. Public Health Res Pract. 2021;31(3):30342011. https://doi.org/10.17061/phrp30342011 .
Article PubMed Google Scholar
Diniz D, Madeiro A, Rosas C. Conscientious objection, barriers, and abortion in the case of rape: a study among physicians in Brazil. Reprod Health Matters. 2014;22(43):141–8.
Madeiro AP, Diniz D. Legal abortion in Brazil—a national study. Cien Saude Colet. 2016;21(2):563–72. https://doi.org/10.1590/1413-81232015212.10352015 .
Mirlesse V, Ville I. The uses of ultrasonography in relation to foetal malformations in Rio de Janeiro, Brazil. Soc Sci Med. 2013;87:168–75.
Casas L, Vivaldi L. Pregnancies and fetal anomalies incompatible with life in Chile: arguments and experiences in advocating for legal reform. Health Hum Rights J. 2017;19(1):95–108.
Maira G, Casas L, Vivaldi L. Abortion in Chile: the long road to legalization and its slow implementation. Health Hum Rights J. 2019;21(2):121–32.
Amado ED, Calderón García MC, Cristancho KR, et al. Obstacles and challenges following the partial decriminalisation of abortion in Colombia. Reprod Health Matters. 2010;18(36):118–26.
DePiñeres T, Raifman S, Mora M, et al. ‘I felt the world crash down on me’: Women’s experiences of being denied legal abortion in Colombia. Reprod Health. 2017;14:133.
Küng SA, Darney BG, Saavedra-Avendaño B, et al. Access to abortion under the health exception: a comparative analysis in three countries. Reprod Health. 2018;15:107.
McLean E, Desalegn DN, Blystad A, Miljeteig I. When the law makes doors slightly open: ethical dilemmas among abortion service providers in Addis Ababa, Ethiopia. BMC Med Ethics. 2019;20:60.
Payne CM, Precourt Debbink M, Steele EA, et al. Why women are dying from unsafe abortion: narratives of Ghanaian abortion providers. Afr J Reprod Health. 2013;17(2):118–28.
PubMed Google Scholar
Aiken ARA, Johnson DM, Broussard K, Padron E. Experiences of women in Ireland who accessed abortion by travelling abroad or by using abortion medication at home: a qualitative study. BMJ Sex Reprod Health. 2018;44:181–6.
Aitken K, Patek P, Murphy ME. The opinions and experiences of Irish obstetric and gynaecology trainee doctors in relation to abortion services in Ireland. J Med Ethics. 2017;43:778–83.
Clarke D and Mühlrad H, “The impact of abortion legalization on fertility and maternal mortality: New Evidence from Mexico” (2016) CINCH series #2016/02.
Påfs J, Rulisa S, Klingberg-Allvin M, et al. Implementing the liberalized abortion law in Kigali, Rwanda: ambiguities of rights and responsibiltiies among health care providers. Midwifery. 2020;80:102568.
Sahin Hodoglugil NN, Ngabo F, Ortego J, et al. Making abortion safer in Rwanda. Afr J Reprod Health. 2017;21(1):82–92.
Arnott G, Sheehy G, Chinthakanan O, Foster A. Exploring legal restrictions, regulatory reform, and geographic disparities in abortion access in Thailand. Health Hum Rights J. 2017;19(1):187–95.
Aiken ARA, Padron E, Broussard K, Johnson D. The impact of Northern Ireland’s abortion laws on women’s abortion decision-making and experiences. BMJ Sex Reprod Health. 2019;45:3–9.
Antón J-I, Ferre Z, Triunfo P. The impact of the legalisation of abortion on birth outcomes in Uruguay. Health Econ. 2018;27:1103–19.
HRC, Amanda Mellet v Ireland. 2013. UN Doc. CCPR/C/116/D/2324/2013.
HRC, Siobhan Whelan v Ireland. 2014. UN Doc CCPR/C/119/D/2425/201.
CESCR. General comment no. 22 on the right to sexual and reproductive health (article 12 of the international covenant on economic, Social and Cultural Rights). 2016. UN Doc. E/C/12/GC/22.
Ganatra B, et al. Global, regional and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model. Lancet. 2017;390(10110):2372–81.
Committee on Economic, Social and Cultural Rights, General comment no. 14: The right to the highest attainable standard of health (article 12 of the International Covenant on Economic, Social and Cultural Rights). 2000. UN Doc. E/C.12/2000/4.
Health (Regulation of Termination of Pregnancy) Act 2018 (Ireland).
Crimes (Amendment) Act 2019 (Gibraltar).
Proclamation No. 414/2004 (2005) (Ethiopia).
National Supreme Court of Justice of Argentina. Corte Suprema de Justicia de la Nación, F, A. L. s/Medida Autosatisfactiva, Expediente Letra “F”, N° 259, Libro XLVI. 2012.
Sentencia C-355/06, Part VI, Constitutional Court of Colombia. 2006.
STC Rol N° 3729(3751)-17 CPT, Constitutional Court of Chile. 2017.
Claim of noncompliance with fundamental Precept no.54. Judge-rapporteur: justice Marco Aurélio. Vote: justice Rosa Weber. Brasília: Supreme Court of Brazil, 2013.
The matter of an application by the Northern Ireland human rights Commission for Judicial Review (Northern Ireland). 2018, UKSC 27.
R (On the application of A and B) v SoS for Health [2017] UKSC 41.
Maneula and family v El Salvador, Inter-American Court of Human Rights, Case 13.069. 2018.
Constitutional Tribunal of Poland, decision K 1/20, 2020.
Alonso-Coello P, Schünemann HJ, Moberg J, et al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1. Introduction. BMJ. 2016;353:i2016.
Download references
Acknowledgements
We record thanks to Alana Farrell for assistance in final preparation of the manuscript.
This work was supported by the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored programme executed by the World Health Organization (WHO). Professor de Londras also acknowledges the support of the Leverhulme Trust through the Philip Leverhulme Prize.
Author information
Authors and affiliations.
Birmingham Law School, University of Birmingham, Birmingham, B15 2TT, UK
Fiona de Londras
Women’s and Children’s Health, Karolinska Institute, Stockholm, Sweden
Amanda Cleeve
Development and Research Training in Human Reproduction (HRP), Department of Sexual and Reproductive Health and Research, UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, World Health Organization, Geneva, Switzerland
Amanda Cleeve & Antonella F. Lavelanet
Department of Obstetrics and Gynecology, Oregon Health and Science University, Portland, Oregon, USA
Maria I. Rodriguez
You can also search for this author in PubMed Google Scholar
Contributions
AL and FdL developed the PICOs and search strategies. AC and FdL did the initial searches. AL, AC, MR and FdL reviewed and finalised data extraction and quality. FdL did the initial manuscript draft. AL prepared the tables and figures. All authors reviewed, finalised and approved the submitted text.
Corresponding author
Correspondence to Fiona de Londras .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: suppl table 1..
Evidence table: Impact on the intervention on abortion seekers. Supple Table 2. Evidence Table: The impact of the intervention on health professionals.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
de Londras, F., Cleeve, A., Rodriguez, M.I. et al. The impact of ‘grounds’ on abortion-related outcomes: a synthesis of legal and health evidence. BMC Public Health 22 , 936 (2022). https://doi.org/10.1186/s12889-022-13247-0
Download citation
Received : 26 November 2021
Accepted : 14 April 2022
Published : 10 May 2022
DOI : https://doi.org/10.1186/s12889-022-13247-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Human rights
- Abortion: grounds
- Abortion: exceptional grounds
- Abortion regulation
- Abortion law
- Abortion on request
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]

IMAGES
COMMENTS
This article presents a research study on abortion from a theoretical and empirical point of view. The theoretical part is based on the method of social documents analysis, and presents a complex perspective on abortion, highlighting items of medical, ethical, moral, religious, social, economic and legal elements.
Standardized outcomes in abortion research could decrease heterogeneity among trials and improve the quality of systematic reviews and clinical guidelines. Researchers should select, collect, and report these core outcomes in future abortion trials.
This is an exploratory study using in-depth interview to explore factors related to abortion decision-making in a changing context. As research on this topic is limited, we opted for a qualitative research framework that aims to identify factors influencing this decision-making process.
Abstract. Background. A country’s abortion law is a key component in determining the enabling environment for safe abortion. While restrictive abortion laws still prevail in most low- and middle-income countries (LMICs), many countries have reformed their abortion laws, with the majority of them moving away from an absolute ban.
Research shows that abortion is a routine medical procedure, and restricting legal access. only results in an increase in unsafe/illegal procedures. Coercing women to continue an unintended. pregnancy to term by limiting abortion access results in a negative impact on their lives, and a high cost.
Abortion is a common medical or surgical intervention used to terminate pregnancy. Although a controversial and widely debated topic, approximately 73 million induced abortions occur worldwide each year, with 29% of all pregnancies and over 60% of unintended pregnancies ending in abortion.
This article provides a critical review of empirical research on attitudes toward abortion among mass publics in the United States, with a view toward suggesting promising avenues for future research. We identify three such themes: Accounting for pro-life movement among mass attitudes in recent years, when the composition.
Research. Open access. Published: 03 October 2018. Decision-making preceding induced abortion: a qualitative study of women’s experiences in Kisumu, Kenya. Ulrika Rehnström Loi, Matilda Lindgren, Elisabeth Faxelid, Monica Oguttu & Marie Klingberg-Allvin. Reproductive Health 15, Article number: 166 ( 2018 ) Cite this article. 37k Accesses.
PMID: 32678861. PMCID: PMC7367465. DOI: 10.1371/journal.pone.0235971. Abstract. Objective: The purpose of this study is to explore Protestant religious leaders' attitudes towards abortion and their strategies for pastoral care in Georgia, USA.
International human rights law specifies that abortion must be available (and not ‘merely’ lawful) where the life or health of the pregnant woman or girl is at risk, or where carrying a pregnancy to term would cause her substantial pain or suffering, including but not limited to situations where the pregnancy is the result of rape or incest or t...