

Reducing Underage Drinking: A Collective Responsibility (2004)
Chapter: executive summary, executive summary.
A lcohol use by young people is dangerous, not only because of the risks associated with acute impairment, but also because of the threat to their long-term development and well-being. Traffic crashes are perhaps the most visible of these dangers, with alcohol being implicated in nearly one-third of youth traffic fatalities. Underage alcohol use is also associated with violence, suicide, educational failure, and other problem behaviors. All of these problems are magnified by early onset of teen drinking: the younger the drinker, the worse the problem. Moreover, frequent heavy drinking by young adolescents can lead to mild brain damage. The social cost of underage drinking has been estimated at $53 billion including $19 billion from traffic crashes and $29 billion from violent crime.
More youth drink than smoke tobacco or use other illegal drugs. Yet federal investments in preventing underage drinking pale in comparison with resources targeted (mostly to youths) at preventing illicit drug use. In fiscal 2000, $71.1 million was targeted at preventing underage alcohol use by the U.S. Departments of Health and Human Services (HHS), Justice, and Transportation. In contrast, the fiscal 2000 federal budget authority for drug abuse prevention (including prevention research) was 25 times higher, $1.8 billion; for tobacco prevention, funding for the Office of Smoking and Health, only one of several HHS agencies involved with smoking prevention, was approximately $100 million, with states spending a great deal more with resources from the states’ Medicaid reimbursement suits against the tobacco companies.
Although it is illegal to sell or give alcohol to youths under age 21, they
do not have a hard time getting it, and they often get it from adults. More than 90 percent of twelfth graders report that alcohol is “very easy” or “fairly easy” to get. And when underage youths drink, they drink more heavily and recklessly than adults. They report that they “usually” drink an average of four and a half drinks, an amount very close to the threshold of five drinks typically used to define heavy drinking (also referred to as binge drinking). In contrast, adult drinkers report usually drinking fewer than three drinks.
In response to a congressional request in the HHS fiscal 2002 appropriations act, the Board on Children, Youth, and Families of the National Research Council and the Institute of Medicine formed the Committee on Developing a Strategy to Reduce and Prevent Underage Drinking. The committee was directed to review a broad range of federal, state, and nongovernmental programs, from environmental interventions to programs focusing directly on youth attitudes and behaviors, and to develop a cost-effective strategy to reduce and prevent underage drinking. In conducting this review, the committee relied on the available scientific literature, including a series of papers written for the committee, public input, and its expertise.
The committee conducted its work within the framework of the current national policy establishing 21 as the minimum legal drinking age in every state. We concentrated more on population-based primary prevention approaches rather than on individually oriented approaches.
STRATEGY OVERVIEW
The committee reached the fundamental conclusion that underage drinking cannot be successfully addressed by focusing on youth alone. Youth drink within the context of a society in which alcohol use is normative behavior and images about alcohol are pervasive. They usually obtain alcohol—either directly or indirectly—from adults. Efforts to reduce underage drinking, therefore, need to focus on adults and must engage the society at large.
The preeminent goal of the recommended strategy is to create and sustain a broad societal commitment to reduce underage drinking. Such a commitment will require participation by multiple individuals and organizations at the national, state, local, and community levels who are in a position to affect youth decisions—including parents and other adults, alcohol producers, wholesalers and retail outlets, restaurants and bars, entertainment media, schools, colleges and universities, the military, landlords, community organizations, and youths themselves. The nation must collectively pursue opportunities to reduce the availability of alcohol to underage
drinkers, the occasions for underage drinking, and the demand for alcohol among young people.
THE STRATEGY
The committee’s proposed strategy for broad societal commitment to reduce underage drinking has ten main components.
National Adult-Oriented Media Campaign
Most adults express concern about youth drinking and support public policy actions to reduce youth access to alcohol. Nonetheless, youth obtain alcohol from adults. Parents tend to dramatically underestimate underage drinking generally and their own children’s drinking in particular. The first component in the strategy calls for the development of a media campaign, including rigorous formative research on effective messages, aimed at increasing specific actions by adults meant to reduce underage drinking and decreasing adult conduct that facilitates underage drinking.
Recommendation 6-1: The federal government should fund and actively support the development of a national media effort, as a major component of an adult-oriented campaign to reduce underage drinking.
Partnership to Prevent Underage Drinking
Despite laws that aim to preclude drinking by those under the age of 21, a significant amount of underage drinking occurs, generating revenues for producers, wholesalers, and retailers of alcoholic beverages, especially beer. The alcohol industry has declared its commitment to reducing underage drinking and has invested in programs with that aim. However, the outcomes of these efforts are not always apparent, and the motives are sometimes questioned. A partnership between the alcohol industry, government, and other private partners would facilitate a coordinated, evidence-based approach to reduce and prevent underage drinking.
Recommendation 7-1: All segments of the alcohol industry that profit from underage drinking, inadvertently or otherwise, should join with other private and public partners to establish and fund an independent nonprofit foundation with the sole mission of reducing and preventing underage drinking.
Alcohol Advertising
A substantial proportion of alcohol advertising reaches an underage audience and is presented in a style that is attractive to youths. For example, television alcohol advertisements routinely appear on programs for which the percentage of underage viewers is greater than the percentage of underage youths in the population. Although a clear causal link between advertising and youth consumption has not been established, youth exposure to advertising and marketing of products with particular appeal to youths should be reduced. Strengthened self-regulation would be in keeping with the industry’s stated commitment to avoid sale to minors and with recommendations by the Federal Trade Commission (FTC) in 1999 regarding industry advertising standards. Only one company has adopted the FTC’s 1999 recommendation that the industry create independent external review boards to address complaints regarding violations of advertising codes. In light of constitutional constraints on direct advertising restrictions, and to enable the industry to be responsive to public concerns about advertising, the most fruitful governmental response would be to facilitate public awareness of advertising practices.
Recommendation 7-2: Alcohol companies, advertising companies, and commercial media should refrain from marketing practices (including product design, advertising, and promotional techniques) that have substantial underage appeal and should take reasonable precautions in the time, place, and manner of placement and promotion to reduce youthful exposure to other alcohol advertising and marketing activity.
Recommendation 7-3: The alcohol industry trade associations, as well as individual companies, should strengthen their advertising codes to preclude placement of commercial messages in venues where a significant proportion of the expected audience is underage, to prohibit the use of commercial messages that have substantial underage appeal, and to establish independent external review boards to investigate complaints and enforce the codes.
Recommendation 7-4: Congress should appropriate the necessary funding for the U.S. Department of Health and Human Services to monitor underage exposure to alcohol advertising on a continuing basis and to report periodically to Congress and the public. The report should include information on the underage percentage of the exposed audience and estimated number of underage viewers of print and broadcasting alcohol advertising in national markets and, for television and radio broadcasting, in a selection of large local or regional markets.
Entertainment Media
Since artistic expression inevitably reflects the culture in which it is embedded, it is hardly surprising that alcohol use and alcohol products are frequently displayed or mentioned in prime-time television, movies, and music. Although the viewing or listening audiences for most of these media products are predominantly adult, some of them are disproportionately underage, and even the predominantly adult audiences inevitably include large numbers of young people. As in the case of commercial alcohol advertising, the entertainment media have a social responsibility to eschew displays or lyrics that portray underage drinking in a favorable light or that glamorize or promote alcohol consumption in products that are targeted toward or likely to be heard or viewed by large underage audiences. Labeling and notice requirements have been voluntarily adopted in analogous contexts. Although the industry restrictions should be undertaken on a voluntary basis, some independent oversight and public awareness of these standards is warranted.
Recommendation 8-1: The entertainment industries should use rating systems and marketing codes to reduce the likelihood that underage audiences will be exposed to movies, recordings, or television programs with unsuitable alcohol content, even if adults are expected to predominate in the viewing or listening audiences
Recommendation 8-2: The film rating board of the Motion Picture Association of America should consider alcohol content in rating films, avoiding G or PG ratings for films with unsuitable alcohol content, and assigning mature ratings for films that portray underage drinking in a favorable light.
Recommendation 8-3: The music recording industry should not market recordings that promote or glamorize alcohol use to young people; should include alcohol content in a comprehensive rating system, similar to those used by the television, film, and video game industries; and should establish an independent body to assign ratings and oversee the industry code.
Recommendation 8-4: Television broadcasters and producers should take appropriate precautions to ensure that programs do not portray underage drinking in a favorable light, and that unsuitable alcohol content is included in the category of mature content for purposes of parental warnings.
Recommendation 8-5: Congress should appropriate the necessary funds to enable the U.S. Department of Health and Human Services to conduct a periodic review of a representative sample of movies, televi -
sion programs, and music recordings and videos that are offered at times or in venues likely to have a significant youth audience (e.g., 15 percent) to ascertain the nature and frequency of lyrics or images pertaining to alcohol. The results of these reviews should be reported to Congress and the public.
Limiting Access
Limiting youth access to alcohol has been shown to be effective in reducing and preventing underage drinking and drinking-related problems. Since 21 became the nationwide legal drinking age, there have been significant decreases in drinking, fatal traffic crashes, alcohol-related crashes, and arrests for “driving under the influence” (DUI) among young people. Given the widespread availability of alcohol and easy access by underage drinkers, minimum drinking age laws must be enforced more effectively, along with social sanctions. The effectiveness of underage drinking laws could be enhanced through such approaches as compliance checks, server training, zero tolerance laws, and graduated driver licensing laws.
Recommendation 9-1: The minimum drinking age laws of each state should prohibit
purchase or attempted purchase, possession, and consumption of alcoholic beverages by persons under 21;
possession of and use of falsified or fraudulent identification to purchase or attempt to purchase alcoholic beverages;
provision of any alcohol to minors by adults, except to their own children in their own residences; and
underage drinking in private clubs and establishments.
Recommendation 9-2: States should strengthen their compliance check programs in retail outlets, using media campaigns and license revocation to increase deterrence.
Communities and states should undertake regular and comprehensive compliance check programs, including notification of retailers concerning the program and follow-up communication to them about the outcome (sale/no sale) for their outlet.
Enforcement agencies should issue citations for violations of underage sales laws, with substantial fines and temporary suspension of license for first offenses and increasingly stronger penalties thereafter, leading to permanent revocation of license after three offenses.
Communities and states should implement media campaigns in conjunction with compliance check programs detailing the program, its purpose, and outcomes.
Recommendation 9-3: The federal government should require states to achieve designated rates of retailer compliance with youth access prohibitions as a condition of receiving relevant block grant funding, similar to the Synar Amendment’s requirements for youth tobacco sales.
Recommendation 9-4: States should require all sellers and servers of alcohol to complete state-approved training as a condition of employment.
Recommendation 9-5: States should enact or strengthen dram shop liability statutes to authorize negligence-based civil actions against commercial providers of alcohol for serving or selling alcohol to a minor who subsequently causes injury to others, while allowing a defense for sellers who have demonstrated compliance with responsible business practices. States should include in their dram shop statutes key portions of the Model Alcoholic Beverage Retail Licensee Liability Act of 1985, including the responsible business practices defense.
Recommendation 9-6: States that allow Internet sales and home delivery of alcohol should regulate these activities to reduce the likelihood of sales to underage purchasers. States should
require all packages for delivery containing alcohol to be clearly labeled as such;
require persons who deliver alcohol to record the recipient’s age identification information from a valid government-issued document (such as a driver’s license or ID card); and
require recipients of home delivery of alcohol to sign a statement verifying receipt of alcohol and attesting that he or she is of legal age to purchase alcohol.
Recommendation 9-7: States and localities should implement enforcement programs to deter adults from purchasing alcohol for minors. States and communities should
routinely undertake shoulder tap or other prevention programs targeting adults who purchase alcohol for minors, using warnings, rather than citations, for the first offense;
enact and enforce laws to hold retailers responsible, as a condition of licensing, for allowing minors to loiter and solicit adults to purchase alcohol for them on outlet property; and
use nuisance and loitering ordinances as a means of discouraging youth from congregating outside of alcohol outlets in order to solicit adults to purchase alcohol.
Recommendation 9-8: States and communities should establish and implement a system requiring registration of beer kegs that records information on the identity of purchasers.
Recommendation 9-9: States should facilitate enforcement of zero tolerance laws in order to increase their deterrent effect. States should
modify existing laws to allow passive breath testing, streamlined administrative procedures, and administrative penalties and
implement media campaigns to increase young peoples’ awareness of reduced blood alcohol content (BAC) limits and of enforcement efforts.
Recommendation 9-10: States should enact and enforce graduated driver licensing laws.
Recommendation 9-11: States and localities should routinely implement sobriety checkpoints.
Recommendation 9-12: Local police, working with community leaders, should adopt and announce policies for detecting and terminating underage drinking parties, including:
routinely responding to complaints from the public about noisy teenage parties and entering the premises when there is probable cause to suspect underage drinking is taking place;
routinely checking, as a part of regular weekend patrols, open areas where teenage drinking parties are known to occur; and
routinely citing underage drinkers and, if possible, the person who supplied the alcohol when underage drinking is observed at parties.
Recommendation 9-13: States should strengthen efforts to prevent and detect use of false identification by minors to make alcohol purchases. States should
prohibit the production, sale, distribution, possession, and use of false identification for attempted alcohol purchase;
issue driver’s licenses and state identification cards that can be electronically scanned;
allow retailers to confiscate apparently false identification for law enforcement inspection; and
implement administrative penalties (e.g., immediate confiscation of a driver’s license and issuance of a citation resulting in a substantial fine) for attempted use of false identification by minors for alcohol purchases.
Recommendation 9-14: States should establish administrative procedures and noncriminal penalties, such as fines or community service, for alcohol infractions by minors.
Youth-Oriented Interventions
Although the proposed strategy focuses mainly on adult attitudes and behavior toward underage drinking and on reducing the availability of alcohol to underage youth, approaches that directly target youth are also needed. A national youth-oriented media campaign to reduce and prevent underage drinking would be premature in the absence of more evidence supporting this approach. However, effective education-oriented approaches in schools and other settings aimed at preventing alcohol use by youths, as well as interventions with youths who have already developed alcohol problems, play a role. Interventions that rely on provision of information alone, or that focus on increasing self-esteem or resisting peer pressure, have not been demonstrated to be effective.
Residential colleges and universities have witnessed serious drinking problems among students under 21. Despite efforts by nearly all campuses to address this problem, heavy drinking has not declined over the past decade. Residential colleges and universities are in a unique position to develop and evaluate comprehensive approaches that address both individual and population-level issues.
Recommendation 10-1: Intensive research and development for a youth-focused national media campaign relating to underage drinking should be initiated. If this work yields promising results, the inclusion of a youth-focused campaign in the strategy should be reconsidered.
Recommendation 10-2: The U.S. Department of Health and Human Services and the U.S. Department of Education should fund only evidence-based education interventions, with priority given both to those that incorporate elements known to be effective and those that are part of comprehensive community programs.
Recommendation 10-3: Residential colleges and universities should adopt comprehensive prevention approaches, including evidence-based screening, brief intervention strategies, consistent policy enforcement, and environmental changes that limit underage access to alcohol. They should use universal education interventions, as well as selective and indicated approaches with relevant populations.
Recommendation 10-4: The National Institute on Alcohol Abuse and Alcoholism and the Substance Abuse and Mental Health Services Administration should continue to fund evaluations of college-based interventions, with a particular emphasis on targeting of interventions to specific college characteristics, and should maintain a list of evidence-based programs.
Recommendation 10-5: The U.S. Department of Health and Human Services and states should expand the availability of effective clinical services for treating alcohol abuse among underage populations and for following up on treatment. The U.S. Department of Education, the U.S. Department of Health and Human Services, and the U.S. Department of Justice should establish policies that facilitate diagnosing and referring underage alcohol abusers and those who are alcohol dependent for clinical treatment.
Community Interventions
Community mobilization can be a powerful vehicle to implement and support interventions, especially those that target community-level policies and practices. Communities can design multipronged comprehensive initiatives that rely on scientifically based strategies and are responsive to the specific problems of their communities. College campuses and local communities have a reciprocal influence on one another in relation to student alcohol use and the need to develop complementary strategies.
Recommendation 11-1: Community leaders should assess the underage drinking problem in their communities and consider effective approaches—such as community organizing, coalition building, and the strategic use of the mass media—to reduce drinking among underage youth.
Recommendation 11-2: Public and private funders should support community mobilization to reduce underage drinking. Federal funding for reducing and preventing underage drinking should be available under a national program dedicated to community-level approaches to reducing underage drinking, similar to the Drug Free Communities Act, which supports communities in addressing substance abuse with targeted, evidence-based prevention strategies.
Government Assistance and Coordination
The ultimate responsibility for preventing and reducing underage drinking lies with the entire national community, not with government alone.
However, the federal and state governments have important responsibilities in addition to enforcing the law. These responsibilities include funding media campaigns, supporting community efforts, monitoring alcohol and entertainment industry portrayals of drinking, monitoring trends in underage drinking and the effectiveness of efforts to reduce it, coordinating multiple agency activities, and supporting continued research and evaluation.
Recommendation 12-1: A federal interagency coordinating committee on prevention of underage drinking should be established, chaired by the secretary of the U.S. Department of Health and Human Services.
Recommendation 12-2: A National Training and Research Center on Underage Drinking should be established in the U.S. Department of Health and Human Services. This body would provide technical assistance, training, and evaluation support and would monitor progress in implementing national goals.
Recommendation 12-3: The secretary of the U.S. Department of Health and Human Services should issue an annual report on underage drinking to Congress summarizing all federal agency activities, progress in reducing underage drinking, and key surveillance data.
Recommendation 12-4: Each state should designate a lead agency to coordinate and spearhead its activities and programs to reduce and prevent underage drinking.
Recommendation 12-5: The annual report of the secretary of the U.S. Department of Health and Human Services on underage drinking should include key indicators of underage drinking.
Recommendation 12-6: The Monitoring the Future Survey and the National Survey on Drug Use and Health should be revised to elicit more precise information on the quantity of alcohol consumed and to ascertain brand preferences of underage drinkers.
Alcohol Excise Taxes
Alcoholic beverages are far cheaper (after adjusting for overall inflation) today than they were in the 1960s and 1970s. While raising excise taxes, and therefore prices, would have some effect on alcohol use by adults, price has been documented to have a differential effect on youth alcohol consumption patterns. Taxes can also be a source of revenue for funding strategies aimed at reducing underage drinking and its associated harms.
Recommendation 12-7: Congress and state legislatures should raise excise taxes to reduce underage consumption and to raise additional revenues for this purpose. Top priority should be given to raising beer taxes, and excise tax rates for all alcoholic beverages should be indexed to the consumer price index so that they keep pace with inflation without the necessity of further legislative action.
Research and Evaluation
Rigorous research and evaluation are needed to assess the effectiveness of specific interventions and to ensure that future refinements of the strategy are grounded in evidence-based approaches. Research related to prototype development for the proposed adult media campaign is a core component of the strategy outlined in this report. In addition, continued research and evaluation are necessary to develop new approaches aimed at reaching all segments of the underage population.
Recommendation 12-8: All interventions, including media messages and education programs, whether funded by public or private sources, should be rigorously evaluated, and a portion of all federal grant funds for alcohol-related programs should be designated for evaluation.
Recommendation 12-9: States and the federal government—particularly the U.S. Department of Health and Human Services and the U.S. Department of Education—should fund the development and evaluation of programs to cover all underage populations.
In sum, our proposed strategy calls for development of a national campaign to engage adults in a concerted effort to stop enabling or ignoring youth drinking. The proposed strategy calls on the alcohol industry to enter a partnership with government and other private funders to implement a coordinated, evidence-based approach to reducing underage drinking. It proposes steps to increase compliance with laws against selling or providing alcohol to minors. It calls for reducing youth exposure to alcohol advertising or music and other entertainment with products and ads that glorify drinking. It recognizes the potential importance of school-based education approaches and the need for residential colleges and universities to implement comprehensive approaches. It calls on local leaders to apply the multiple tools available to address underage drinking within the context of their communities. And it challenges federal and state governments to coordinate their efforts and to raise excise taxes to reduce underage consumption and raise revenues for the proposed strategy. Finally, it recommends ongoing monitoring and continued research and evaluation to facilitate continued refinement of the strategy and its implementation.
Alcohol use by young people is extremely dangerous - both to themselves and society at large. Underage alcohol use is associated with traffic fatalities, violence, unsafe sex, suicide, educational failure, and other problem behaviors that diminish the prospects of future success, as well as health risks – and the earlier teens start drinking, the greater the danger. Despite these serious concerns, the media continues to make drinking look attractive to youth, and it remains possible and even easy for teenagers to get access to alcohol.
Why is this dangerous behavior so pervasive? What can be done to prevent it? What will work and who is responsible for making sure it happens? Reducing Underage Drinking addresses these questions and proposes a new way to combat underage alcohol use. It explores the ways in which may different individuals and groups contribute to the problem and how they can be enlisted to prevent it. Reducing Underage Drinking will serve as both a game plan and a call to arms for anyone with an investment in youth health and safety.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
Reducing the Alcohol Abuse Among the Youth Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Statement of the problem, alternative solutions, the preferred solution, budgetary requirements.
The US government has paid considerable attention to the development of the most favorable environment for the youth. Educational programs are aimed at helping teenagers find their place in American society. Many programs exist to help this population address the most urgent challenges. Too Smart To Start is a program focusing on the prevention of underage alcohol abuse (Substance Abuse and Mental Health Services Administration [SAMHSA], 2017).
The program involves the provision of strategies, as well as resources, to help schools and communities to prevent alcohol abuse among the youth. Davis (2017) notes that initiative groups within communities use this program to address the problem. However, the program can be improved significantly and reach more people. This paper includes a brief discussion of two possible ways to improve the problem and the justification for the use of one of the options.
The level of alcohol abuse among the youth has decreased during the past three decades, but in some cases the changes are insignificant. The most significant improvements are apparent when the use of alcohol within the past 12 months is assessed. For example, almost 80% of 12 – graders, over 70% of 10-graders, and almost 55% of 8-graders reported alcohol use and binge drinking during the past 12 months in 1991 (Patrick & Schulenberg, 2014).
The recent studies show that 70% of 12 th -grade students, 55% of 10 th -grade students, and 30% of 8 th -grade students reported binge drinking and alcohol use during the past 12 months in 2011. The trend is promising, but another assessment shows that the level of alcohol abuse is still rather high and has not changed during the past three decades. Approximately 30% of 12 th -grade students and 20% of 10 th -grade students reported binge drinking or alcohol use within the past 30 days in 1991 (Patrick & Schulenberg, 2014). The figures were almost the same in 2011. It is also important to note that the prevalence of alcohol use is higher in underprivileged communities.
The negative effects of alcohol use on adolescents’ health and academic performance have been explored in detail. Importantly, the levels of alcohol use among adolescents are quite alarming as there is a ban on selling alcohol to people under 21. Researchers stress that teenage alcohol abuse may lead to the persistence of the addiction in adulthood, the development of serious health issues (ulcers, cancer, depression, and so on), poor academic performance (Patrick & Schulenberg, 2014).
As a result, young people can have limited access to higher education and a wide range of employment opportunities, which deteriorates American communities. In simple words, teenagers coming from underprivileged families are at a high risk of alcohol abuse, which results in these populations’ socioeconomic issues. The implementation of effective programs aimed at preventing alcohol abuse among adolescents can break this vicious circle.
Too Smart To Start is one of such programs. It is funded by SAMHSA that is an agency within the USDHHS (United States Department of Health and Human Services). The organization’s budget for the promotion of preventing efforts is $150 million in 2018 (Department of Health and Human Services, 2017). The mission of SAMHSA is to “reduce the impact of substance abuse and mental illness on America’s communities” (SAMHSA, 2017). As has been mentioned above the program in question assists in communities’ struggle against the problem. Organizations, initiative groups, schools, and even individuals can address the program and benefit from the use of resources or assistance in the development of effective strategies to solve issues.
Solution One
Nevertheless, a third of adolescents still use alcohol so more effective solutions should be developed. One of the possible solutions can be the development of a personality-targeted intervention. Conrod et al. (2013) evaluated the effectiveness of a personality-targeted selective program aimed at the prevention of alcohol abuse among adolescents. The researchers claim that such an approach is effective and can be applied in school-based contexts. One of the key factors contributing to the success of the program was the provision of training to the faculty.
To implement this program, it is important to undertake several steps. First, it is important to develop personality-targeted interventions for different personality types. This step will require thorough research and possible collaboration with researchers, mental health professionals, or educators. The next step will be the development of effective training programs for the faculty. It is possible to extend the boundaries of the school-based setting and come up with strategies that can be used by parents or other relatives. Finally, it is important to inform communities about the existence of the new program. The information can be provided through newsletters.
The budgetary requirements for this solution will be comparatively small. The vast majority of the funds will be used to develop the strategies. These resources will be allocated to access databases to search for scholarly resources on the matter, pay to researchers and professionals involved in the process of the development of the programs, etc. It is also necessary to allocate funds to provide the stakeholders with the necessary materials (manuals and other resources). The budget for this program can be up to $100 thousand (with $70,000 for the development of the interventions and $30,000 for the materials and resources).
Solution Two
Another solution can be based on the one mentioned above, but it will require more time and funds. The use of personality-targeted interventions in school-based and family-based settings can be implemented more effectively. The first steps involving the development of the programs will be unchanged. The basis for the new interventions will be the research implemented by Conrod et al. (2013). At that, it is possible to extend the limits of the interventions.
It is necessary to create effective programs that could address the needs of different groups. Apart from focusing on personality types, it is necessary to pay attention to age, ethnicity, culture, socioeconomic status, and academic performance.
The steps associated with communication should also be further developed. Apart from the newsletters, it is essential to develop a far-reaching promotion campaign. Social media can become the primary channel to make communities aware of the new opportunities. To encourage educational establishments and various initiative groups to participate in this program, it is possible to establish a prize. The award can be one of the grants provided by SAMHSA (SAMHSA, 2017).
It can also be effective to send some information directly to the most struggling communities. In many cases, these communities have many issues to address and can simply miss this opportunity. This solution will require a larger investment, but is far-reaching and can improve the situation significantly. The budget requirements will be discussed in detail below (see Table 1).
The second option is the preferred solution as it will reach more people and will be able to address the organization’s mission, which is reducing the effects of substance abuse on American communities. Personality-targeted interventions have proved to be effective and beneficial for the target audience and overall communities (Conrod et al., 2013). Adolescents learn about harms of the alcohol use, about ways to fit in different groups, come to terms with themselves, and feel empowered.
The new program will potentially reduce the number of adolescents who use and abuse alcohol. Specific attention will be paid to underprivileged groups, which will allow them to improve their socioeconomic status in the future. The program can be funded from several resources. SAMHSA can provide the major part of the funds. As for the provision of training to the participants of the program (educators, parents, social workers, etc.), SAMHSA can address state governments as well as local charities or communities to fund the necessary activities.
Although quite substantial investment may be needed, the benefits of the program cannot be overestimated. The necessary funds may reach up to $150,000 depending on the number of participants (see Table 1). 2018 budget of SAMHSA has the necessary funds, but the organization can address other agencies and organizations to help in the implementation of the interventions. One of SAMHSA grants (or several grants if necessary) will be provided to the winners.
Table 1. Budgetary Requirements.
| Activities | US Dollars |
| Research | 30,000 |
| Program Development | 30,000 |
| Staff Training | 10,000 |
| Materials | Over 30,000 |
| Media and Promotion (including materials) | 5,000 |
| Training of the educators or initiative groups | Over 15,000 |
| Award (grant) | 10,000 |
On balance, it is necessary to note that the program that will reduce the level of alcohol use among adolescents will be based on the personality-targeted intervention. The program will address the needs of teenagers who will receive a chance to integrate into society more effectively. The program can become a basis or a starting point for the development of interventions aimed at preventing drug abuse among teenagers. American communities can benefit from such programs if they are implemented properly.
Conrod, P., O’Leary-Barrett, M., Newton, N., Topper, L., Castellanos-Ryan, N., Mackie, C., & Girard, A. (2013). Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse. JAMA Psychiatry, 70 (3), 334-342.
Davis, N. (2017). It takes a community. The Southside Times . Web.
Department of Health and Human Services. (2017). Putting America’s health first . Web.
Patrick, M. E., & Schulenberg, J. E. (2014). Prevalence and predictors of adolescent alcohol use and binge drinking in the United States. Alcohol Research, 35 (2), 193-200.
Substance Abuse and Mental Health Services Administration. (2017). Too smart to start . Web.
- The Psychology of Addiction and Addictive Behaviors
- Crack Cocaine Abuse and Its Social Effects
- Drug and Alcohol Abuse Among Teenagers
- Underage Drinking and Teen Alcohol Abuse
- Drug and Alcohol Abuse
- Illegal Importation of Drugs
- Reflection on Drugs, Narcotics and Treatment Options
- Paul Chabot: Reality Check Concerning Drugs
- Walter Green: Theoretical Orientation of the Practitioner
- Decreasing Overall Alcohol Consumption
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, March 23). Reducing the Alcohol Abuse Among the Youth. https://ivypanda.com/essays/reducing-the-alcohol-abuse-among-the-youth/
"Reducing the Alcohol Abuse Among the Youth." IvyPanda , 23 Mar. 2021, ivypanda.com/essays/reducing-the-alcohol-abuse-among-the-youth/.
IvyPanda . (2021) 'Reducing the Alcohol Abuse Among the Youth'. 23 March.
IvyPanda . 2021. "Reducing the Alcohol Abuse Among the Youth." March 23, 2021. https://ivypanda.com/essays/reducing-the-alcohol-abuse-among-the-youth/.
1. IvyPanda . "Reducing the Alcohol Abuse Among the Youth." March 23, 2021. https://ivypanda.com/essays/reducing-the-alcohol-abuse-among-the-youth/.
Bibliography
IvyPanda . "Reducing the Alcohol Abuse Among the Youth." March 23, 2021. https://ivypanda.com/essays/reducing-the-alcohol-abuse-among-the-youth/.
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .
Our systems are now restored following recent technical disruption, and we’re working hard to catch up on publishing. We apologise for the inconvenience caused. Find out more: https://www.cambridge.org/universitypress/about-us/news-and-blogs/cambridge-university-press-publishing-update-following-technical-disruption
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert

- > Journals
- > Cambridge Prisms: Global Mental Health
- > Global Mental Health
- > Volume 9
- > Alcohol use among adolescents in India: a systematic...

Article contents
Introduction, financial support, conflict of interest, ethical standards, alcohol use among adolescents in india: a systematic review.
Published online by Cambridge University Press: 07 January 2022
- Supplementary materials
Alcohol use is typically established during adolescence and initiation of use at a young age poses risks for short- and long-term health and social outcomes. However, there is limited understanding of the onset, progression and impact of alcohol use among adolescents in India. The aim of this review is to synthesise the evidence about prevalence, patterns and correlates of alcohol use and alcohol use disorders in adolescents from India.
Systematic review was conducted using relevant online databases, grey literature and unpublished data/outcomes from subject experts. Inclusion and exclusion criteria were developed and applied to screening rounds. Titles and abstracts were screened by two independent reviewers for eligibility, and then full texts were assessed for inclusion. Narrative synthesis of the eligible studies was conducted.
Fifty-five peer-reviewed papers and one report were eligible for inclusion in this review. Prevalence of ever or lifetime alcohol consumption ranged from 3.9% to 69.8%; and prevalence of alcohol consumption at least once in the past year ranged from 10.6% to 32.9%. The mean age for initiation of drinking ranged from 14.4 to 18.3 years. Some correlates associated with alcohol consumption included being male, older age, academic difficulties, parental use of alcohol or tobacco, non-contact sexual abuse and perpetuation of violence.
The evidence base for alcohol use among adolescents in India needs a deeper exploration. Despite gaps in the evidence base, this synthesis provides a reasonable understanding of alcohol use among adolescents in India and can provide direction to policymakers.
According to the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019, among adolescents and young adults (aged 10–24 years), alcohol-attributable burden is second highest among all risk factors contributing to disability-adjusted life years in this age group (GBD 2019 Risk Factors Collaborators, 2020 ). The exposure of the adolescent brain to alcohol is shown to result in various cognitive and functional deficits related to verbal learning, attention, and visuospatial and memory tasks, and behavioural inefficiencies such as disinhibition and elevated risk-taking (Spear, Reference Spear 2018 ). Alcohol consumption in adolescents results in a range of adverse outcomes across several domains and includes road traffic accidents and other non-intentional injuries, violence, mental health problems, intentional self-harm and suicide, HIV and other infectious diseases, poor school performance and drop-out, and poor employment opportunities (Hall et al ., Reference Hall, Patton, Stockings, Weier, Lynskey, Morley and Degenhardt 2016 ).
Adolescence is a critical period in which exposure to adversities such as poverty, family conflict and negative life experiences (e.g. violence) can have long-term emotional and socio-economic consequences for adolescents, their families and communities (Knapp et al ., Reference Knapp, Scott and Davies 1999 ; Knapp et al ., Reference Knapp, McCRONE, Fombonne, Beecham and Wostear 2002 ). Substance use, including alcohol, is typically established during adolescence and this period is peak risk for onset and intensification of substance use behaviours that pose risks for short- and long-term health (Anthony and Petronis, Reference Anthony and Petronis 1995 ; DeWit et al ., Reference DeWit, Adlaf, Offord and Ogborne 2000 ; Hallfors et al ., Reference Hallfors, Waller, Bauer, Ford and Halpern 2005 ; Schmid et al ., Reference Schmid, Hohm, Blomeyer, Zimmermann, Schmidt, Esser and Laucht 2007 ; Hadland and Harris, Reference Hadland and Harris 2014 ). As such, early initiation of alcohol use among adolescents can provide a useful indication of the potential future burden among adults including increased risk for academic failure, mental health problems, antisocial behaviour, physical illness, risky sexual behaviours, sexually transmitted diseases, early-onset dementia and the development of alcohol use disorders (AUDs) (Hingson et al ., Reference Hingson, Heeren and Winter 2006 ; King and Chassin, Reference King and Chassin 2007 ; Dawson et al ., Reference Dawson, Goldstein, Patricia Chou, June Ruan and Grant 2008 ; Nordström et al ., Reference Nordström, Nordström, Eriksson, Wahlund and Gustafson 2013 ).
India continues to develop rapidly, and accounts for most of the increase in alcohol consumption per capita for WHO's South-East Asia region (World Health Organization, 2018 ). Although India has a relatively high abstinence rate, many people who do drink are either risky drinkers or have AUDs (Benegal, Reference Benegal 2005 ; Rehm et al ., Reference Rehm, Mathers, Popova, Thavorncharoensap, Teerawattananon and Patra 2009 ). Finally, the existing policies in India have failed to reduce the harm from alcohol because the implementation of alcohol control efforts is fragmented, lacks consensus, is influenced by political considerations, and is driven by narrow economic and not health concerns (Gururaj et al ., Reference Gururaj, Gautham and Arvind 2021 ).
India has the largest population of adolescents globally (253 million people aged 10–19 years), constituting 21% of the population (Government of India, 2011 ; Boumphrey, Reference Boumphrey 2012 ). Additionally, adolescents as young as 13–15 years of age have started consuming alcohol in India (Gururaj et al ., Reference Gururaj, Varghese, Benegal, Rao, Pathak, Singh and Singh 2016 ). Despite this growing public health problem, the official policy response in India remains primarily focused on AUDs, particularly alcohol dependence in adults, with an absolute disregard for the potential of prevention programmes. One potential reason for this is the limited understanding of the onset and progression of alcohol use and AUDs amongst adolescents in India. The aim of this paper is to bridge that knowledge gap by synthesising the evidence about the prevalence and correlates of alcohol use and AUDs in adolescents from India.
The specific objectives are to examine the following in adolescents from India: (a) prevalence of current and lifetime use of alcohol, (b) prevalence of current AUDs, (c) patterns (e.g. frequency, quantity) of alcohol use, (d) sociodemographic, social and clinical correlates of alcohol use and AUDs, and (e) explanatory models of and attitudes towards alcohol use and AUDs, e.g. perceptions of the problem and its causes. This paper synthesises the evidence about alcohol and AUDs using data from a comprehensive review that we conducted of any substance use and substance use disorders amongst adolescents in India.
Systematic review . The review protocol was registered prospectively on Prospero (registration ID CRD 42017080344).
Inclusion and exclusion criteria
There were no limits placed on the year of publication of the paper, gender of the participants and study settings in India. We only included English language publications as academic literature from India is predominantly published in such publications. Adolescents were defined as anyone between 10 and 24 years of age (Sawyer et al ., Reference Sawyer, Azzopardi, Wickremarathne and Patton 2018 ). Studies reporting alcohol use and/or AUDs in a wider age range (including 10–24 years) were included only if data were separately presented for the 10–24-year age group. We included observational studies (surveys, case-control studies, cohort studies), qualitative studies and intervention studies (only if baseline prevalence data were presented). We included studies which examined alcohol use and AUDs defined as per the International Classification of Diseases (ICD)/Diagnostic and Statistical Manual of Mental Disorders (DSM)/clinical criteria or using a standardised screening or diagnostic tool.
We searched the following databases: PsycARTICLES, PsycInfo, Embase, Global Health, CINAHL, Medline and Indmed. The search strategy was organised under the following concepts: substance (e.g. alcohol, drug), misuse/use disorder (e.g. addiction, intoxication), young people (e.g. adolescent, child) and India (e.g. India, names of individual Indian states). The detailed search strategy is listed in Appendix A .
Two reviewers (DG and KW) independently inspected the titles and abstracts of studies identified through the database search. Any conflicts about eligibility between the two reviewers were resolved by AN. If the title and abstract did not offer enough information, the full paper was retrieved to ascertain whether it was eligible for inclusion. Screening of full texts was done by AN, AG and DG; and any conflicts about eligibility were resolved by UB. Screening of the results of the search was done using Covidence ( https://www.covidence.org/ ), an online screening and data extraction tool.
AN searched the following resources to identify relevant grey literature: Open Grey, OAlster, Google, ProQuest, official English language websites of the World Health Organization and World Bank, English language websites of ministries of each state and union territory within India responsible for substance misuse as well as the official websites of the Indian Narcotics Control Bureau and Ministry of Social Justice and Empowerment.
Any grey literature with relevant data published by a recognised non-governmental organisation, state, national or international organisation was included. Studies were included based on the robustness of study design and quality of data. If there were multiple editions of any published piece of grey literature, only the latest published edition of that report was included. Once retrieved, their titles, content pages and summaries were read by AN and if deemed eligible they were added to a list of potentially eligible reports. If the grey literature's summary, content and title did not include enough information, then the full text was examined by AN to determine eligibility for inclusion.
Finally, experts in the field of substance use disorders in India were contacted to explore if they could identify any further useful sources of information and were invited to submit unpublished data and unreported outcomes for possible inclusion into the review. Reference lists of selected studies, grey literature and relevant reviews were inspected for additional potential studies.
A formal data extraction worksheet was designed to extract data relevant to the study aims. The following data were extracted: centre (e.g. name of city), sampling technique, sample (e.g. general population), sample size, age(s), tool used to measure alcohol use and/or AUD, definitions of alcohol use and AUD, prevalence of alcohol use and/or AUD, age of initiation, type of alcohol, quantity and frequency of alcohol use, attitudes towards alcohol use, effect of alcohol on health, social, educational and other domains, and risk factors/correlates of alcohol use and or AUD. Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al ., Reference Moher, Shamseer, Clarke, Ghersi, Liberati and Petticrew 2015 ), a record was made of the number of papers retrieved, the number of papers excluded and the reasons for their exclusion. AT independently performed data extraction, AG checked the data extraction, and AN arbitrated any unresolved issues. The quality of reporting of included studies was examined using the STROBE Statement – checklist of items that should be included in reports of observational studies (Von Elm et al ., Reference Von Elm, Altman, Egger, Pocock, Gøtzsche and Vandenbroucke 2007 ).
A descriptive analysis of the data was conducted, and the results are mainly reported in a narrative format focusing on each of the objectives described above (Popay et al ., Reference Popay, Roberts, Sowden, Petticrew, Arai, Rodgers and Duffy 2006 ).
In total, 6464 references were identified through the search strategies described above. Overall, 251 records were eligible for the wider review, of which 55 were about alcohol use and have been reported in this paper ( Fig. 1 ). Additionally, one report of magnitude of substance use in India which was recommended by an expert was also included (Ambekar et al ., Reference Ambekar, Agrawal, Rao, Mishra, Khandelwal and Chadda 2019 ).
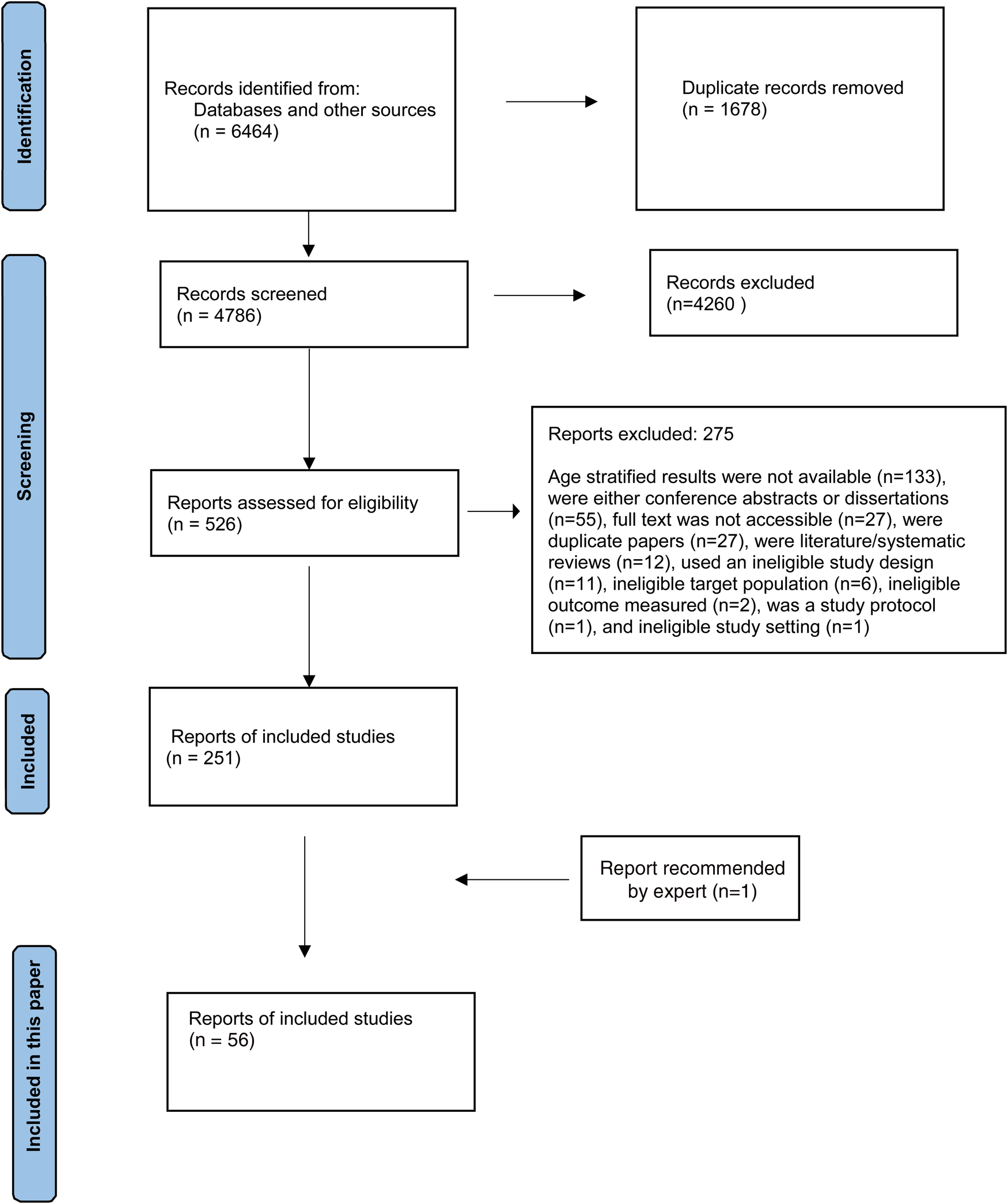
Fig. 1. PRISMA flow diagram.
Study descriptions
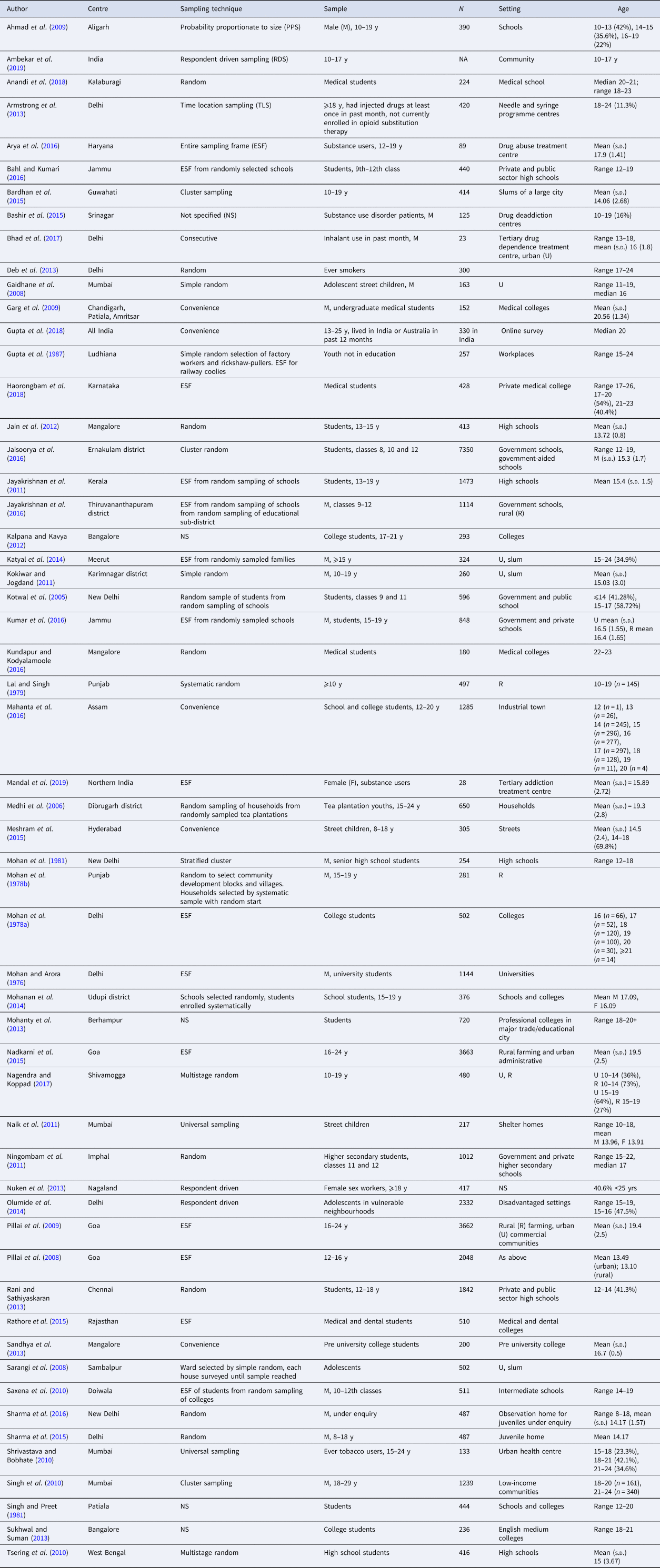
One study was conducted online (Gupta et al ., Reference Gupta, Lam, Pettigrew and Tait 2018 ) and one in a national treatment centre in North India (Mandal et al ., Reference Mandal, Parmar, Ambekar and Dhawan 2019 ), both of which potentially had access to participants from across the country ( Table 1 ). All the rest were conducted at a single or multiple settings in a city, town, district, village or state. The sample size of the studies ranged from 23 (Bhad et al ., Reference Bhad, Jain, Dhawan and Mehta 2017 ) to 7350 (Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ). In studies that reported mean age of the samples, it ranged from 13.10 years (Pillai et al ., Reference Pillai, Patel, Cardozo, Goodman, Weiss and Andrew 2008 ) to 20.56 years (Garg et al ., Reference Garg, Chavan, Singh and Bansal 2009 ).
Table 1 Description of studies included in the review
Prevalence of alcohol use and AUD
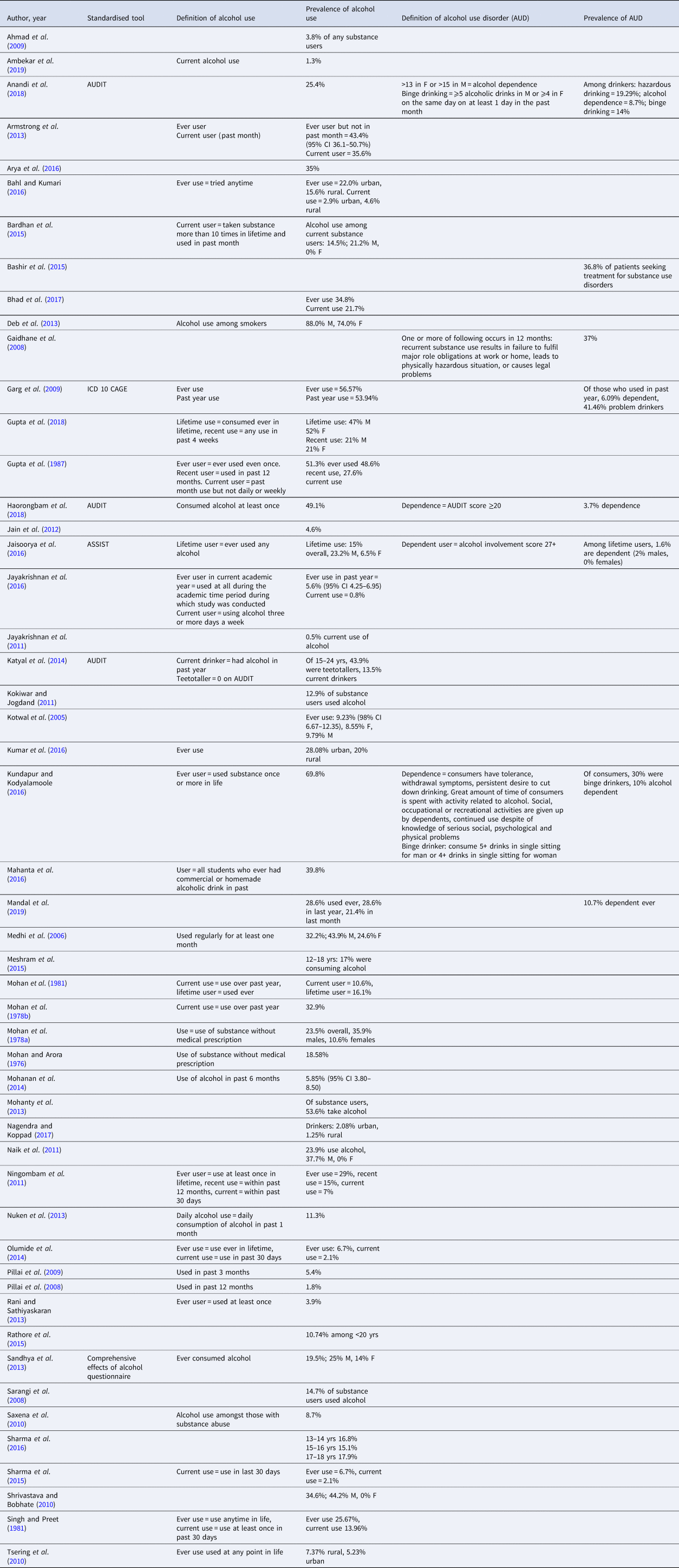
The prevalence of ever use or lifetime use, broadly defined as consumption of alcohol at least once in their lifetime, ranged from 3.9% in school students aged 12–18 years (Rani and Sathiyaskaran, Reference Rani and Sathiyaskaran 2013 ) to 69.8% in 22–23-year-old medical students (Kundapur and Kodyalamoole, Reference Kundapur and Kodyalamoole 2016 ) ( Table 2 ). Ever use in females ranged from 6.5% in students from class 8 to class 12 (age 12–19 years) (Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ) to 52% in an online survey of adolescents aged 13–17 years (Gupta et al ., Reference Gupta, Lam, Pettigrew and Tait 2018 ), and in males it ranged from 9.79% in students from classes 9 and 11 (age up to 17 years) (Kotwal et al ., Reference Kotwal, Thakur and Seth 2005 ) to 47% in an online survey of adolescents aged 13–17 years (Gupta et al ., Reference Gupta, Lam, Pettigrew and Tait 2018 ). The prevalence of ever use in rural areas ranged from 7.37% in high school students (Tsering et al ., Reference Tsering, Pal and Dasgupta 2010 ) to 20% in students aged 15–19 years (Kumar et al ., Reference Kumar, Kumar, Shora, Dewan, Mengi and Razaq 2016 ), and in urban areas it ranged from 5.23% in high school students (Tsering et al ., Reference Tsering, Pal and Dasgupta 2010 ) to 23.08% in students aged 15–19 years (Kumar et al ., Reference Kumar, Kumar, Shora, Dewan, Mengi and Razaq 2016 ).
Table 2 Prevalence of alcohol use and alcohol use disorders
Current use
The definition of current use of alcohol varied across studies. The more commonly used definitions were alcohol consumption at least once in the past year for which the prevalence ranged from 10.6% in senior high school students aged 12–18 years (Mohan et al ., Reference Mohan, Rustagi, Sundaram and Prabhu 1981 ) to 32.9% in 15–19-year-old individuals from rural settings (Mohan et al ., Reference Mohan, Sharma, Darshan, Sundaram and Neki 1978b ); and at least once in the past 30 days (month) for which the prevalence ranged from 2.1% (Sharma et al ., Reference Sharma, Singh, Lal and Goel 2015 ) in 15–19-year olds from disadvantaged urban settings and 35.6% in injectable drug users attending needle and syringe programme centres (Armstrong et al ., Reference Armstrong, Nuken, Samson, Singh, Jorm and Kermode 2013 ). Some studies did not define current use and others used non-standard definition of current use such as ‘who had not used drugs either daily or weekly in the past month’ (27.6%) (Gupta et al ., Reference Gupta, Narang, Verma, Panda, Garg, Munjal and Singh 1987 ), and ‘habit of using alcohol, 3 days or more a week’ (0.8%) (Jayakrishnan et al ., Reference Jayakrishnan, Geetha, Mohanan Nair, Thomas and Sebastian 2016 ). The biggest countrywide survey of substance use in India reported a prevalence of current alcohol use to be 1.3% amongst those aged 10–17 years (Ambekar et al ., Reference Ambekar, Agrawal, Rao, Mishra, Khandelwal and Chadda 2019 ).
Some studies reported the prevalence of AUDs and defined them using standardised tools (Alcohol Use Disorder Identification Test [AUDIT], CAGE questionnaire, Alcohol, Smoking and Substance Involvement Screening Test [ASSIST]), ICD 10 criteria or bespoke definitions. Among medical students (18–23 years) who were drinkers, the prevalence of hazardous drinking was 19.29% (Anandi et al ., Reference Anandi, Halgar, Reddy and Indupalli 2018 ), alcohol dependence was 3.7–10% (Kundapur and Kodyalamoole, Reference Kundapur and Kodyalamoole 2016 ; Haorongbam et al ., Reference Haorongbam, Sathyanarayana and Dhanashree 2018 ), binge drinking 14–30% (Kundapur and Kodyalamoole, Reference Kundapur and Kodyalamoole 2016 ; Anandi et al ., Reference Anandi, Halgar, Reddy and Indupalli 2018 ) and ‘problem drinking’ (not defined) was 41.46% (Garg et al ., Reference Garg, Chavan, Singh and Bansal 2009 ). Among students of classes 8, 10 and 12 (12–19 years), 1.6% (2% males, 0% females) of lifetime users had alcohol dependence (Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ). In adolescent street children (11–19 years), 37% had AUD defined as recurrent substance use resulting in one or more of the following occurring in 12 months: failure to fulfil major role obligations at work or home leads to a physically hazardous situation, or causes legal problems (Gaidhane et al ., Reference Gaidhane, Syed Zahiruddin, Waghmare, Shanbhag, Zodpey and Joharapurkar 2008 ).
Patterns of drinking
Among drinkers, 0.6–10.4% consumed every day (Armstrong et al ., Reference Armstrong, Nuken, Samson, Singh, Jorm and Kermode 2013 ; Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ; Kundapur and Kodyalamoole, Reference Kundapur and Kodyalamoole 2016 ), 19.1–40% consumed at least once a week (Armstrong et al ., Reference Armstrong, Nuken, Samson, Singh, Jorm and Kermode 2013 ; Kundapur and Kodyalamoole, Reference Kundapur and Kodyalamoole 2016 ), 3.8% consumed weekly (Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ), 9.5% consumed less than once a week (Armstrong et al ., Reference Armstrong, Nuken, Samson, Singh, Jorm and Kermode 2013 ) and 10.6% consumed monthly (Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ) ( Table 3 ). Usual median number of drinks consumed among those between 13 and 17 years was 3.5 for both males and females (Gupta et al ., Reference Gupta, Lam, Pettigrew and Tait 2018 ). Among 10–19-year-old males from an urban slum over the past month, 54.2% consumed up to 50 ‘pegs’ of alcohol (Kokiwar and Jogdand, Reference Kokiwar and Jogdand 2011 ). Among males from a low-income community, in those between 18 and 20 years, 88.2% were ‘low drinking’ (low amount/low frequency, low amount/moderate frequency or substantial amount/low frequency), 9.3% were moderate drinking (low amount/high frequency or substantial amount/moderate frequency) and 2.5% were high drinking (substantial amount/high frequency); and in those between 20 and 24 years, 82.6% were low drinking, 13.5% were moderate drinking and 3.8% were high drinking (Singh et al ., Reference Singh, Schensul, Gupta, Maharana, Kremelberg and Berg 2010 ).
Table 3 Initiation of, attitudes towards, patterns of and correlates of drinking
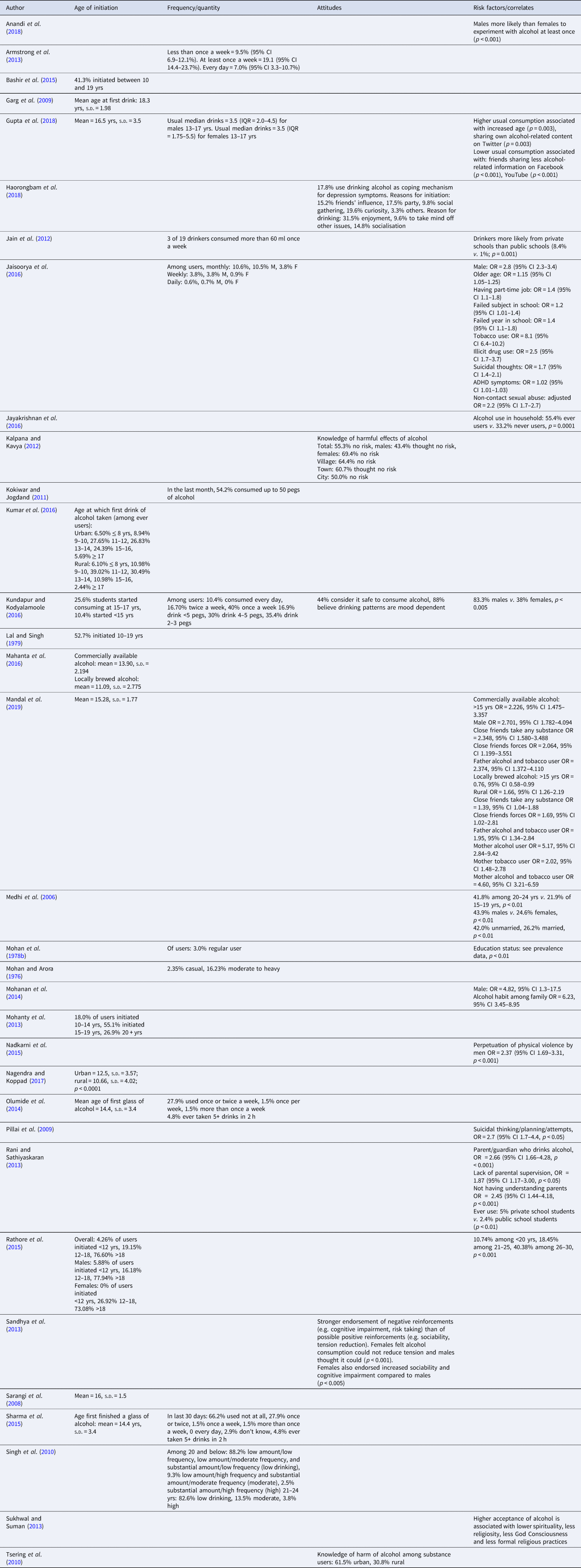
Initiation age
The mean age for initiation of drinking ranged from 14.4 to 18.3 years ( Table 3 ). The mean age of initiation was significantly lower in rural areas compared to urban areas [10.66 ( s.d. 4.02) v . 12.5 ( s.d. 3.57); p < 0.0001] (Nagendra and Koppad, Reference Nagendra and Koppad 2017 ); and locally brewed alcohol [mean ( s.d. ) 11.09 (2.775)] was initiated at a younger age compared to commercially available alcohol in an industrial town [mean ( s.d. ) 13.90 (2.194)] (Mahanta et al ., Reference Mahanta, Mohapatra, Phukan and Mahanta 2016 ).
Among male substance use disorder patients at drug deaddiction centres, 41.3% had initiated alcohol use between 10 and 19 years (Bashir et al ., Reference Bashir, Sheikh, Bilques and Firdosi 2015 ). Among 22–23-year-old medical students, 25.6% had started consuming alcohol between 15 and 17 years, and 10.4% had started consuming alcohol before they were 15 years (Kundapur and Kodyalamoole, Reference Kundapur and Kodyalamoole 2016 ).
In students between 18 and 22 years, 18.0% had initiated drinking between 10 and 14 years, 55.1% had initiated between 15 and 19 years, and 26.9% after 19 years (Mohanty et al ., Reference Mohanty, Tripathy, Palo and Jena 2013 ). Among medical and dental students, 4.26% initiated before 12 years, 19.15% initiated between 12 and 18 years, and 76.60% initiated after 18 years (Rathore et al ., Reference Rathore, Pankaj, Mangal and Saini 2015 ). Comparing males and females, 5.88% males ( v . 0% females) initiated before 12 years, 16.18% ( v . 26.92%) initiated between 12 and 18 years, and 77.94% ( v . 73.08%) initiated after 18 years (Rathore et al ., Reference Rathore, Pankaj, Mangal and Saini 2015 ). Finally, comparing urban and rural drinkers, 6.50% urban drinkers ( v . 6.10% rural) initiated before 8 years, 8.94% ( v . 10.98%) initiated between 9 and 10 years, 27.65% ( v . 39.02%) initiated between 11 and 12 years, 26.83% ( v . 30.49%) initiated between 12 and 14 years, 24.39% ( v . 10.98%) initiated between 15 and 16 years, and 5.69% ( v . 2.44%) initiated after 17 years (Kumar et al ., Reference Kumar, Kumar, Shora, Dewan, Mengi and Razaq 2016 ).
Knowledge and attitudes
Overall, 55.3% of college-going students (17–21 years) believed that there was no risk of harmful effects of alcohol; with more females than males who believed that there was no risk (69.4% v . 43.4%); and a higher proportion from villages (64.4%) thought there was no risk as compared to those from towns (60.7%) or cities (50.0%) (Kalpana and Kavya, Reference Kalpana and Kavya 2012 ) ( Table 3 ). Among medical students (22–23 years), 44% considered it safe to consume alcohol, and 88% believe drinking patterns are mood-dependent (Kundapur and Kodyalamoole, Reference Kundapur and Kodyalamoole 2016 ).
In medical students (17–23 years), reasons for initiation of drinking included curiosity (19.6%), attending a party (17.5%), friends' influence (15.2%) and social gatherings (9.8%); and reasons for continued use included enjoyment (31.5%), as a coping mechanism for depressive symptoms (17.8%), socialisation (14.8%) and to take mind off other issues (9.6%) (Haorongbam et al ., Reference Haorongbam, Sathyanarayana and Dhanashree 2018 ). Among college-going students (mean age 16.7 years; s.d. 0.5) there was a stronger endorsement of negative reinforcements (e.g. cognitive impairment, risk taking) than of possible positive reinforcements (e.g. sociability, tension reduction); and compared to males, significantly more females felt alcohol consumption could not reduce tension and endorsed increased sociability and cognitive impairment (Sandhya et al ., Reference Sandhya, Carol, Kotian and Ganaraja 2013 ). Knowledge of harm of alcohol among substance users was greater in adolescents from urban than rural areas (61.5% v . 30.8%) (Tsering et al ., Reference Tsering, Pal and Dasgupta 2010 ).
Risk factors/correlates
The cross-sectional nature of the studies only allowed the examination of correlates of alcohol use ( Table 3 ). Alcohol consumption was associated with being male (Medhi et al ., Reference Medhi, Hazarika and Mahanta 2006 ; Mohanan et al ., Reference Mohanan, Swain, Sanah, Sharma and Ghosh 2014 ; Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ; Kundapur and Kodyalamoole, Reference Kundapur and Kodyalamoole 2016 ; Anandi et al ., Reference Anandi, Halgar, Reddy and Indupalli 2018 ; Mandal et al ., Reference Mandal, Parmar, Ambekar and Dhawan 2019 ), older age (Medhi et al ., Reference Medhi, Hazarika and Mahanta 2006 ; Rathore et al ., Reference Rathore, Pankaj, Mangal and Saini 2015 ; Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ; Gupta et al ., Reference Gupta, Lam, Pettigrew and Tait 2018 ; Mandal et al ., Reference Mandal, Parmar, Ambekar and Dhawan 2019 ) and going to private rather than public schools (Jain et al ., Reference Jain, Dhanawat, Kotian and Angeline 2012 ; Rani and Sathiyaskaran, Reference Rani and Sathiyaskaran 2013 ). Specifically for locally brewed alcohol, it was associated with younger age and rural residence (Mandal et al ., Reference Mandal, Parmar, Ambekar and Dhawan 2019 ). Alcohol consumption was associated with having a part-time job, and failing a subject or a year in school (Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ).
Alcohol use in adolescents was associated with parental/guardian's use of alcohol or tobacco, lack of parental supervision, and not having ‘understanding’ parents (Rani and Sathiyaskaran, Reference Rani and Sathiyaskaran 2013 ; Mohanan et al ., Reference Mohanan, Swain, Sanah, Sharma and Ghosh 2014 ; Jayakrishnan et al ., Reference Jayakrishnan, Geetha, Mohanan Nair, Thomas and Sebastian 2016 ; Mandal et al ., Reference Mandal, Parmar, Ambekar and Dhawan 2019 ). Alcohol use decreased with a decrease in the frequency of friends sharing alcohol-related information on Facebook and YouTube; and increased frequency of sharing personal alcohol-related content on Twitter was associated with an increase in alcohol use (Gupta et al ., Reference Gupta, Lam, Pettigrew and Tait 2018 ). Alcohol consumption was also associated with close friends using substances (any type) or peer pressure to drink alcohol (Mandal et al ., Reference Mandal, Parmar, Ambekar and Dhawan 2019 ).
Alcohol consumption was associated with tobacco use, illicit drug use, attention deficit hyperactivity disorder (ADHD) symptoms, suicidal thinking, planning and attempts, and non-contact sexual abuse and perpetuation of violence (Nadkarni et al ., Reference Nadkarni, Dean, Weiss and Patel 2015 ; Jaisoorya et al ., Reference Jaisoorya, Beena, Beena, Ellangovan, Jose, Thennarasu and Benegal 2016 ). Finally, higher acceptance of alcohol is associated with lower spirituality, less religiosity, less ‘God Consciousness’ and less formal religious practices (Sukhwal and Suman, Reference Sukhwal and Suman 2013 ).
Quality of reporting studies
In 42 of the 57 studies, there was appropriate reporting of more than 70% of the 22 STROBE criteria ( Appendix B ). Only one study reported on all the 22 criteria (Nadkarni et al ., Reference Nadkarni, Dean, Weiss and Patel 2015 ). For 15 of the 22 criteria, there was appropriate reporting in more than 70% of the studies. The poorest reporting was about study biases, generalisability of the findings, and role of the funder.
The existing evidence base has several limitations which preclude a robust synthesis and any conclusions we draw are, at best, exploratory in nature. Although the information about AUDs is relatively limited, the prevalence among drinkers appears to be high, and the patterns of drinking in a reasonably high proportion were suggestive of risky drinking (heavy drinking that puts the drinker at risk of developing problems), especially considering that this is a young population with a relatively short drinking history.
This is consistent with the steady rise in recorded alcohol consumption in most developing countries, albeit from relatively low base prevalence rates. It also parallels the increases in adult per capita consumption of alcohol and heavy episodic drinking that have been observed in India and other developing economies in east Asia, south Asia and southeast Asia (Shield et al ., Reference Shield, Manthey, Rylett, Probst, Wettlaufer, Parry and Rehm 2020 ). Amongst adolescents, the prevalence of current alcohol use in Sri Lanka was 3.4% (95% CI 2.6–4.3) (Senanayake et al ., Reference Senanayake, Gunawardena, Kumbukage, Wickramasnghe, Gunawardena, Lokubalasooriya and Peiris 2018 ), lifetime alcohol use in males was 45% (26% risky drinking) in Pakistan (Shahzad et al ., Reference Shahzad, Kliewer, Ali and Begum 2020 ), alcohol use was reported by 19% from traditional non-alcohol using ethnic groups and 40% from traditional alcohol using ethnic groups in Nepal (Parajuli et al ., Reference Parajuli, Macdonald and Jimba 2015 ), and 13% in Bhutan (Norbu and Perngparn, Reference Norbu and Perngparn 2014 ).
The data about patterns of drinking observed among adolescents in India are inconclusive but there appears to be some tendency towards heavy drinking. Among adolescents across several countries, there are consistent reports of binge drinking as a social norm among peer groups (Russell-Bennett et al ., Reference Russell-Bennett, Hogan and Perks 2010 ). The prevalence of binge drinking increases from age 15–19 years to the age of 20–24 years, and among drinkers, binge drinking is higher among the 15–19 years age group compared with the total population of drinkers (World Health Organization, 2018 ). This means that 15–24-year-old current drinkers often drink in heavy drinking sessions, and hence, except for the Eastern Mediterranean Region, the prevalence of such drinking among drinkers is high in adolescents (around 45–55%) (World Health Organization, 2018 ).
In India, the age of initiation commonly was mid- to late-teens; and male gender, rural residence and locally brewed alcohol were associated with earlier initiation of drinking. Across most of the world, initiation of alcohol use among adolescents takes place at an early age, usually before the age of 15 years. Among 15-year-olds, there is a high prevalence of alcohol use (50–70%) during the past 30 days in many countries of the Americas, Europe and Western Pacific; and the prevalence is relatively lower in African countries (10–30%) (World Health Organization, 2018 ). However, across the world, there is a huge variation in alcohol use among boys and girls of 15 years of age and vary from 1.2% to 74.0% in boys and 0% to 73.0% in girls (World Health Organization, 2018 ). Finally, with the strategic targeting of adolescents as alcohol consumers by the industry, increasing overall population prevalence and normalisation of drinking alcohol, and the increasing normalisation by virtue of learning more about how adolescents in other countries drink, one could speculate that the age of initiation would reduce and prevalence of alcohol consumption in adolescents in India would rise, in the coming years.
In India, knowledge about alcohol and its potential harms was limited in rural areas. The reasons for starting and continuing drinking were a mix of expected enhancement of positive experiences and dampening of negative affect. This is consistent with findings in Indian adults where alcohol consumption was seen to be mainly associated with expectations about reduction in psychosocial stress and providing pleasure (Nadkarni et al ., Reference Nadkarni, Dabholkar, McCambridge, Bhat, Kumar, Mohanraj and Patel 2013 ). Across the world, adolescents primarily report drinking for social motives or enjoyment – enjoyment (Argentina) (Jerez and Coviello, Reference Jerez and Coviello 1998 ), to make nights out more pleasurable (UK) (Plant et al ., Reference Plant, Bagnall and Foster 1990 ) and being social (Canada) (Kairouz et al ., Reference Kairouz, Gliksman, Demers and Adlaf 2002 ). Coping motives, on the other hand, are less common, but are associated with AUDs later in adulthood (Carpenter and Hasin, Reference Carpenter and Hasin 1999 ). The difference in drinking motives between adolescents from India (a mix of pleasure and coping) and other countries (primarily pleasure), and the similarity between reasons given by Indian adolescents and Indian adults, possibly reflect contextual/cultural differences and will have implications on transferability of interventions from other contexts and wider age-applicability of interventions developed for adults in India.
We can broadly organise our findings about correlates for drinking into socio-demographic characteristics (e.g. age, gender), immediate environment (e.g. parents, friends, digital space) and clinical correlates (e.g. other substance use, suicidal thoughts). Risk and protective factors influencing the use of alcohol in adolescents are both proximal and distal factors and include individual cognitions and peer-influence risk factors (e.g. attitudes favourable to alcohol use and peer drinking), family environment (e.g. parental discipline and family bonding) and school context (e.g. academic commitment and achievement) (Bryant et al ., Reference Bryant, Schulenberg, O'Malley, Bachman and Johnston 2003 ; Fisher et al ., Reference Fisher, Miles, Austin, Camargo and Colditz 2007 ; Patock-Peckham and Morgan-Lopez, Reference Patock-Peckham and Morgan-Lopez 2010 ). Most commonly adolescent males drink more often than adolescent females, but there has been some blurring of the distinction between the genders in developed countries (Currie et al ., Reference Currie, Roberts, Settertobulte, Morgan, Smith and Samdal 2004 ; Hibell et al ., Reference Hibell, Guttormsson, Ahlström, Balakireva, Bjarnason, Kokkevi and Kraus 2009 ). This convergence of drinking patterns is particularly seen in the Nordic countries, Ireland, the UK and the USA, and manifests as almost equal prevalence rates for consumption of spirits and similar frequency of intoxication for both genders (Hibell et al ., Reference Hibell, Guttormsson, Ahlström, Balakireva, Bjarnason, Kokkevi and Kraus 2009 ). Evidence from South Asian countries indicates that male gender, age greater than 14 years, depression, religious beliefs, parental/family members' drinking, reduced parental supervision, peer-drinking/pressure/approval and urban neighbourhood are associated with adolescent drinking (Athauda et al ., Reference Athauda, Peiris-John, Ameratunga, McCool and Wickremasinghe 2020 ).
The most important study finding is that despite several studies over the years, the evidence base has several gaps, notably the limited geographical span, small sample sizes and heterogeneous definitions of alcohol use and AUDs. Of particular importance are the various sample selection strategies, especially for the smaller studies, which limit the generalisability of findings. Another gap is the lack of consistency in the measurement of alcohol use, which is especially critical in a context where ‘standard drink’ does not translate semantically or literally into the vernacular, and there is an immense variability in the types of alcoholic beverages (commercial, licit non-commercial, illicit home-brewed, adulterated alcoholic beverages) and in the type and size of vessels from which alcohol is poured or consumed in. Additionally, there were several gaps in the reporting of many studies which raise questions about their internal validity. In the absence of critical information such as data sources, measurement and statistical methods, it is difficult to draw an inference about the robustness of the studies which had inadequate reporting ( Appendix B ). Finally, although the cross-sectional design of the studies allows us to examine the prevalence of alcohol use and AUDs, it limits the conclusions that we can draw about causal relationships between the various potential risk factors and alcohol use/AUDs.
Although the included studies are not without limitations that are important to consider before drawing conclusions, this synthesis allows us to get a reasonable understanding of alcohol use among adolescents in India and derive preliminary conclusions that the prevalence is high and rising, which brings with it the attendant burden of the associated adverse impacts. Furthermore, despite the gaps in the available data, it carries several implications for policy makers. Because alcohol is an important cause of motor vehicle accidents and suicide, which are the leading causes of death among adolescents in India (Joshi et al ., Reference Joshi, Alim, Maulik and Norton 2017 ), interventions that seek to help adolescents avoid or better manage alcohol consumption are a priority. Examples of such evidence-based interventions include public health engagement campaigns to increase awareness of alcohol-related harms, advocacy through community engagement/mobilisation to promote better enforcement of laws related to drinking, engagement with alcohol outlets to promote responsible beverage service, and engaging adolescents and families including through peer-led classroom curriculum to enhance the resilience of adolescents, improve family socialisation and increase awareness of alcohol-related harms (McLeroy et al ., Reference McLeroy, Norton, Kegler, Burdine and Sumaya 2003 ; Hawkins et al ., Reference Hawkins, Brown, Oesterle, Arthur, Abbott and Catalano 2008 ; Wakefield, Loken, and Hornik, Reference Wakefield, Loken and Hornik 2010 ; Hallgren and Andréasson, Reference Hallgren and Andréasson 2013 ). The most important implication of our review, however, is the need to develop the very nascent literature base through robust studies, especially longitudinal research that can support evidence-based prevention interventions and policy change. Future studies should focus on increasing their geographical span and sample sizes, ensure the use of standard definitions of alcohol use and AUDs which are consistent with global literature, and acknowledge and examine contextual variations in types of alcoholic beverages and type and size of vessels from which alcohol is poured or consumed in. Introducing such measures will enhance the robustness, validity and generalisability of the findings; and allow for better comparisons over time and geography. This would require greater support from the Government through ensuring availability of in-country research funding, prioritisation of the issue and utilisation of the evidence generated to inform its policy on alcohol.
Our review is limited by our inclusion criterion related to language. However, this might not be a major limitation considering that peer-reviewed journals in India are only in English as far as we are aware, and researchers generally disseminate their outputs in English language journals. Our review's major strength lies in its originality (the first such review to comprehensively map the landscape of substance use among adolescents in India), use of robust processes (e.g. double screening) and examination of grey literature to identify any relevant evidence.
To conclude, the evidence base for alcohol use amongst adolescents in India needs further and deeper exploration, but in the meanwhile, the available evidence allows us to get a preliminary understanding of the issue and to make a case for policy action to tackle alcohol consumption in this age group.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/gmh.2021.48
Acknowledgements
We would like to acknowledge Professor Pratima Murthy, Professor Vivek Benegal and Professor Atul Ambekar for helping us identify relevant grey literature.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
There are no real or perceived conflicts of interest in undertaking or publishing this research.
As this is a systematic review, it did not involve any direct data collection from human subjects.
Appendix A: Search strategy
1. abuse.tw
3. misuse.tw
7. disorders.tw
8. disorders/
9. withdraw*.tw
10. withdraw*/
11. withdrawal syndrome.tw
12. withdrawal syndrome/
13. screening.tw
14. screening/
15. overdose.tw
16. overdose/
17. megadose.tw
18. megadose/
19. dependen*.tw
20. dependen*/
21. intoxication.tw
22. intoxication/
23. harm*.tw
25. hazard*.tw
26. hazard*/
27. behavior.tw
28. behavior/
29. Addict*.tw
30. Addict*/
31. alcoholi*.tw
32. alcoholi*/
33. delirium.tw
34. delirium/
35. binge drink*.tw
36. binge drink*/
37. consumption.tw
38. consumption/
39. drink*.tw
40. drink*/
41. sniff*.tw
42. sniff*/
43. snort*.tw
44. snort*/
45. cessation.tw
46. cessation/
47. smok*.tw
49. inject*.tw
50. inject*/
51. OR (1–50)
52. Drug.tw
54. Substance.tw
55. Substance/
56. Alcohol.tw
57. Alcohol/
58. ‘purple drank’.tw
59. ‘purple drank’/
60. 1plsd.tw
62. unclassified drug.tw
63. unclassified drug/
66. chlorobenzoic acid derivative.tw
67. chlorobenzoic acid derivative/
70. Ecstasy.tw
71. Ecstasy/
72. methadone.tw
73. methadone/
74. morphine.tw
75. morphine/
76. buprenorphine.tw
77. buprenorphine/
78. diamorphine.tw
79. diamorphine/
80. amphetamine.tw
81. amphetamine/
82. amphetamine derivative.tw
83. amphetamine derivative/
86. bidi.tw
88. tobacco.tw
89. tobacco/
90. cigarette.tw
91. cigarette/
92. electronic cigarette.tw
93. electronic cigarette/
94. e-cig.tw
96. beedi.tw
98. benzodiazepine derivative.tw
99. benzodiazepine derivative/
100. benzodiazepine.tw
101. benzodiazepine/
102. bhang.tw
103. bhang/
104. Hashish.tw
105. Hashish/
106. cannabi*.tw
107. cannabi*/
108. ‘brown sugar’.tw
109. ‘brown sugar’/
110. medical cannabi*.tw
111. medical cannabi*/
112. tetrahydrocannabinol.tw
113. tetrahydrocannabinol/
114. hash.tw
116. charas.tw
117. charas/
118. cocaine.tw
119. cocaine/
120. cocaine derivative.tw
121. cocaine derivative/
122. smack.tw
123. smack/
124. crack.tw
125. crack/
126. syrup.tw
127. syrup/
128. chlorpheniramine.tw
129. chlorpheniramine/
130. ‘cough syrup’.tw
131. ‘cough syrup’/
132. codeine.tw
133. codeine/
134. dexamphetamine.tw
135. dexamphetamine/
136. dextromethorphan.tw
137. dextromethorphan/
138. 3,4 methylenedioxyamphetamine.tw
139. 3,4 methylenedioxyamphetamine/
140. psychedelic agent.tw
141. psychedelic agent/
142. ganja.tw
143. ganja/
144. 4 aminobutyric acid.tw
145. 4 aminobutyric acid/
146. 4 hydroxybutyric acid.tw
147. 4 hydroxybutyric acid/
148. GHB.tw
150. Ketamine.tw
151. Ketamine/
152. glue.tw
154. heroin.tw
155. heroin/
156. nicotine.tw
157. nicotine/
158. diamorphine.tw
159. diamorphine/
160. inhalant.tw
161. inhalant/
162. kava extract.tw
163. kava extract/
164. kava.tw
166. smokeless tobacco.tw
167. smokeless tobacco/
168. khaini.tw
169. khaini/
170. laughing gas.tw
171. laughing gas/
172. nitrous oxide.tw
173. nitrous oxide/
174. LSD.tw
176. Lysergic acid diethylamide.tw
177. Lysergic acid diethylamide/
178. Acid.tw
180. Lucy.tw
182. magic mushroom.tw
183. magic mushroom/
184. hallucinogenic fungus.tw
185. hallucinogenic fungus/
186. mari#uana.tw
187. marj#uana/
188. MDMA.tw
190. Midomafetamine.tw
191. Midomafetamine/
192. amphetamine.tw
193. amphetamine/
194. methamphetamine.tw
195. Methamphetamine/
196. Crystal meth.tw
197. Crystal meth/
198. Amobarbital.tw
199. Amobarbital/
200. Methylphenidate.tw
201. Methylphenidate/
202. Modafinil.tw
203. Modafinil/
204. Morphine.tw
205. Morphine/
206. Opiod*.tw
207. Opiod*/
208. Opiate*.tw
209. Opiate*/
210. Opium.tw
211. Opium/
212. ‘paint thinner’.tw
213. ‘paint thinner’/
214. promethazine.tw
215. promethazine/
216. psilocybin#.tw
217. psilocybin#/
218. Quaalude.tw
219. Quaalude/
220. Methaqualone.tw
221. Methaqualone/
222. Salvia divinorum.tw
223. Salvia divinorum/
224. Psychotropic agent.tw
225. Psychotropic agent/
226. Snuff.tw
227. Snuff/
228. Chewing tobacco.tw
229. Chewing tobacco/
230. Tramadol.tw
231. Tramadol/
232. Viagra.tw
233. Viagra/
234. Sildenafil.tw
235. Sildenafil/
236. Z-class.tw
237. Z-class/
238. Zdrug.tw
239. Zdrug/
240. Eszopiclone.tw
241. Eszopiclone/
242. Zaleplon.tw
243. Zaleplon/
244. Zoipidem.tw
245. Zoipidem/
246. Zopiclone.tw
247. Zopiclone/
248. Hypnotic agent.tw
249. Hypnotic agent/
250. Prescription durg.tw
251. Prescription drug/
252. Prescription medicine.tw
253. Prescription medicine/
254. Prescription medication.tw
255. Prescription medication/
256. OR (52-255)
257. adolescen*.tw
258. adolescen*/
259. child*.tw
260. child*/
261. youth*.tw
262. youth*/
263. student*.tw
264. student*/
265. girl*.tw
266. girl*/
267. teen*.tw
268. teen*/
269. boy*.tw
271. young adult*.tw
272. young adult*/
273. young*.tw
274. young*/
275. OR (257-274)
276. india.tw
277. India/
278. ‘Indian union’.tw
279. ‘Indian union’/
280. Andaman and Nicobar Island*.tw
281. Andaman and Nicobar Island/
282. Andhra Pradesh.tw
283. Andhra Pradesh/
284. Arunachal Pradesh.tw
285. Arunachal Pradesh/
286. Assam.tw
287. Assam/
288. Bihar.tw
289. Bihar/
290. Dadra and Nagar Haveli.tw
291. Dadra and Nagar Haveli/
292. Chhattisgarh.tw
293. Chhattisgarh/
294. Daman and Diu.tw
295. Daman and Diu/
296. National Capital Territory of New Delhi.tw
297. National Capital Territory of New Delhi/
298. Delhi.tw
299. Delhi/
300. Goa.tw
302. Gujarat.tw
303. Gujarat/
304. Haryana.tw
305. Haryana/
306. Himachal Pradesh.tw
307. Himachal Pradesh/
308. Jammu and Kashmir.tw
309. Janmu and Kashmir/
310. Janmu.tw
311. Janmu/
312. Kashmir.tw
313. Kashmir/
314. Jharkhand.tw
315. Jharkhand/
316. Karnataka.tw
317. Karnataka/
318. Mysore.tw
319. Mysore/
320. Kerala.tw
321. Kerala/
322. Travancore-Cochin.tw
323. Travancore-Cochin/
324. Madhya Pradesh.tw
325. Madhya Pradesh/
326. Madhya Bharat.tw
327. Madhya Bharat/
328. Maharashtra.tw
329. Maharashtra/
330. Manipur.tw
331. Manipur/
332. Meghalaya.tw
333. Meghalaya/
334. Mizoram.tw
335. Mizoram/
336. Nagaland.tw
337. Nagaland/
338. Odisha.tw
339. Odisha/
340. Orissa.tw
341. Orissa/
342. Punjab.tw
343. Punjab/
344. Chandigarh.tw
345. Chandigarh/
346. Rajasthan.tw
347. Rajasthan/
348. Sikkim.tw
349. Sikkim/
350. Tamil Nadu.tw
351. Tamil Nadu/
352. Madras State.tw
353. Madras State/
354. Telangana.tw
355. Telangana/
356. Tripura.tw
357. Tripura/
358. Uttarakhand.tw
359. Uttarakhand/
360. Uttaranchal.tw
361. Uttaranchal/
362. Uttar Pradesh.tw
363. Uttar Pradesh/
364. United Provinces.tw
365. United Provinces/
366. West Bengal.tw
367. West Bengal/
368. Mizoram.tw
369. Mizoram/
370. Nagaland.tw
371. Nagaland/
372. Lakshadweep.tw
373. Lakshadweep/
374. P#d#cherry.tw
375. P#d#cherry/
376. OR (276–375)
377. 51 AND 256 AND
Appendix B: Quality of reporting of peer-reviewed studies included in the review (excluding the report)
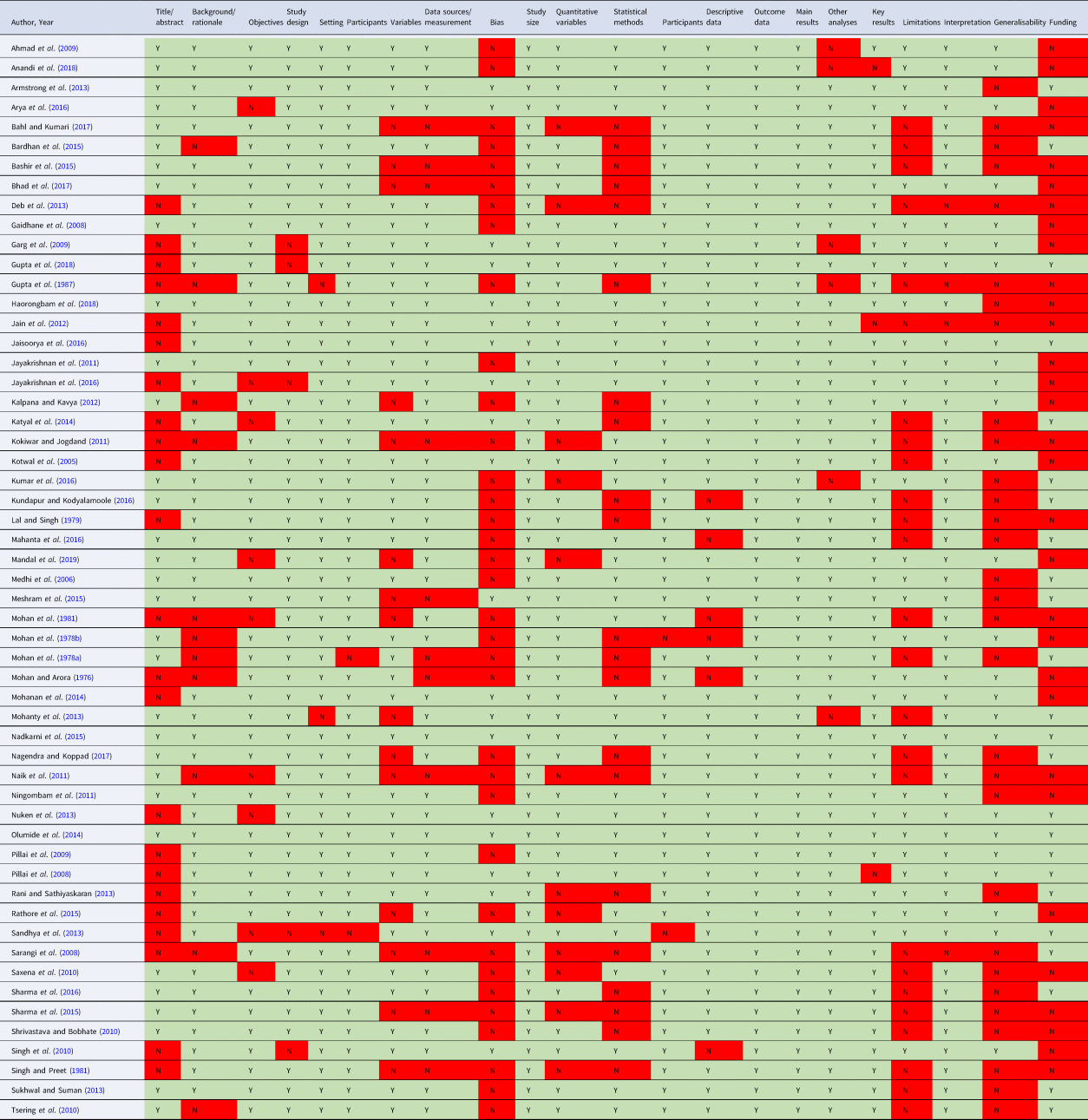
Nadkarni et al. supplementary material

This article has been cited by the following publications. This list is generated based on data provided by Crossref .
- Google Scholar
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Abhijit Nadkarni (a1) (a2) , Allison Tu (a2) (a3) , Ankur Garg (a2) , Devika Gupta (a1) (a2) , Sonal Gupta (a2) , Urvita Bhatia (a2) (a4) , Niharika Tiwari (a2) , Anna Heath (a2) (a5) , Karen Wen (a2) (a6) , Godwin Fernandes (a2) and Richard Velleman (a2) (a7)
- DOI: https://doi.org/10.1017/gmh.2021.48
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.

More teens than ever are overdosing. Psychologists are leading new approaches to combat youth substance misuse
“Just Say No” didn’t work , but experts are employing new holistic programs to help steer kids away—or at least keep them from dying—from illicit substances.
Vol. 55 No. 2 Print version: page 48
- Substance Use, Abuse, and Addiction

For years, students in middle and high schools across the country were urged to “just say no” to drugs and alcohol. But it’s no secret that the Drug Abuse Resistance Education (D.A.R.E.) program, which was typically delivered by police officers who urged total abstinence, didn’t work. A meta-analysis found the program largely ineffective and one study even showed that kids who completed D.A.R.E. were more likely than their peers to take drugs ( Ennett, S. T., et al., American Journal of Public Health , Vol. 84, No. 9, 1994 ; Rosenbaum, D. P., & Hanson, G. S., Journal of Research in Crime and Delinquency , Vol. 35, No. 4, 1998 ).
“We know that the ‘Just Say No’ campaign doesn’t work. It’s based in pure risks, and that doesn’t resonate with teens,” said developmental psychologist Bonnie Halpern-Felsher, PhD, a professor of pediatrics and founder and executive director of several substance use prevention and intervention curriculums at Stanford University. “There are real and perceived benefits to using drugs, as well as risks, such as coping with stress or liking the ‘high.’ If we only talk about the negatives, we lose our credibility.”
Partially because of the lessons learned from D.A.R.E., many communities are taking a different approach to addressing youth substance use. They’re also responding to very real changes in the drug landscape. Aside from vaping, adolescent use of illicit substances has dropped substantially over the past few decades, but more teens are overdosing than ever—largely because of contamination of the drug supply with fentanyl, as well as the availability of stronger substances ( Most reported substance use among adolescents held steady in 2022, National Institute on Drug Abuse ).
“The goal is to impress upon youth that far and away the healthiest choice is not to put these substances in your body, while at the same time acknowledging that some kids are still going to try them,” said Aaron Weiner, PhD, ABPP, a licensed clinical psychologist based in Lake Forest, Illinois, and immediate past-president of APA’s Division 50 (Society of Addiction Psychology). “If that’s the case, we want to help them avoid the worst consequences.”
While that approach, which incorporates principles of harm reduction, is not universally accepted, evidence is growing for its ability to protect youth from accidental overdoses and other consequences of substance use, including addiction, justice involvement, and problems at school. Psychologists have been a key part of the effort to create, test, and administer developmentally appropriate, evidence-based programs that approach prevention in a holistic, nonstigmatizing way.
“Drugs cannot be this taboo thing that young people can’t ask about anymore,” said Nina Christie, PhD, a postdoctoral research fellow in the Center on Alcohol, Substance Use, and Addictions at the University of New Mexico. “That’s just a recipe for young people dying, and we can’t continue to allow that.”

Changes in drug use
In 2022, about 1 in 3 high school seniors, 1 in 5 sophomores, and 1 in 10 eighth graders reported using an illicit substance in the past year, according to the National Institute on Drug Abuse’s (NIDA) annual survey ( Monitoring the Future: National Survey Results on Drug Use, 1975–2022: Secondary School Students , NIDA, 2023 [PDF, 7.78MB] ). Those numbers were down significantly from prepandemic levels and essentially at their lowest point in decades.
Substance use during adolescence is particularly dangerous because psychoactive substances, including nicotine, cannabis, and alcohol, can interfere with healthy brain development ( Winters, K. C., & Arria, A., Prevention Research , Vol. 18, No. 2, 2011 ). Young people who use substances early and frequently also face a higher risk of developing a substance use disorder in adulthood ( McCabe, S. E., et al., JAMA Network Open , Vol. 5, No. 4, 2022 ). Kids who avoid regular substance use are more likely to succeed in school and to avoid problems with the juvenile justice system ( Public policy statement on prevention, American Society of Addiction Medicine, 2023 ).
“The longer we can get kids to go without using substances regularly, the better their chances of having an optimal life trajectory,” Weiner said.
The drugs young people are using—and the way they’re using them—have also changed, and psychologists say this needs to inform educational efforts around substance use. Alcohol and cocaine are less popular than they were in the 1990s; use of cannabis and hallucinogens, which are now more salient and easier to obtain, were higher than ever among young adults in 2021 ( Marijuana and hallucinogen use among young adults reached all-time high in 2021, NIDA ).
“Gen Z is drinking less alcohol than previous generations, but they seem to be increasingly interested in psychedelics and cannabis,” Christie said. “Those substances have kind of replaced alcohol as the cool thing to be doing.”
Young people are also seeing and sharing content about substance use on social media, with a rise in posts and influencers promoting vaping on TikTok and other platforms ( Vassey, J., et al., Nicotine & Tobacco Research , 2023 ). Research suggests that adolescents and young adults who see tobacco or nicotine content on social media are more likely to later start using it ( Donaldson, S. I., et al., JAMA Pediatrics , Vol. 176, No. 9, 2022 ).
A more holistic view
Concern for youth well-being is what drove the well-intentioned, but ultimately ineffective, “mad rush for abstinence,” as Robert Schwebel, PhD, calls it. Though that approach has been unsuccessful in many settings, a large number of communities still employ it, said Schwebel, a clinical psychologist who created the Seven Challenges Program for treating substance use in youth.
But increasingly, those working to prevent and treat youth substance use are taking a different approach—one that aligns with principles Schwebel helped popularize through Seven Challenges.
A key tenet of modern prevention and treatment programs is empowering youth to make their own decisions around substance use in a developmentally appropriate way. Adolescents are exploring their identities (including how they personally relate to drugs), learning how to weigh the consequences of their actions, and preparing for adulthood, which involves making choices about their future. The Seven Challenges Program, for example, uses supportive journaling exercises, combined with counseling, to help young people practice informed decision-making around substance use with those processes in mind.
“You can insist until you’re blue in the face, but that’s not going to make people abstinent. They ultimately have to make their own decisions,” Schwebel said.
Today’s prevention efforts also tend to be more holistic than their predecessors, accounting for the ways drug use relates to other addictive behaviors, such as gaming and gambling, or risky choices, such as fighting, drag racing, and having unprotected sex. Risk factors for substance use—which include trauma, adverse childhood experiences, parental history of substance misuse, and personality factors such as impulsivity and sensation seeking—overlap with many of those behaviors, so it often makes sense to address them collectively.
[ Related: Psychologists are innovating to tackle substance use ]
“We’ve become more sophisticated in understanding the biopsychosocial determinants of alcohol and drug use and moving beyond this idea that it’s a disease and the only solution is medication,” said James Murphy, PhD, a professor of psychology at the University of Memphis who studies addictive behaviors and how to intervene.
Modern prevention programs also acknowledge that young people use substances to serve a purpose—typically either social or emotional in nature—and if adults expect them not to use, they should help teens learn to fulfill those needs in a different way, Weiner said.
“Youth are generally using substances to gain friends, avoid losing them, or to cope with emotional problems that they’re having,” he said. “Effective prevention efforts need to offer healthy alternatives for achieving those goals.”
Just say “know”
At times, the tenets of harm reduction and substance use prevention seem inherently misaligned. Harm reduction, born out of a response to the AIDS crisis, prioritizes bodily autonomy and meeting people where they are without judgment. For some harm reductionists, actively encouraging teens against using drugs could violate the principle of respecting autonomy, Weiner said.
On the other hand, traditional prevention advocates may feel that teaching adolescents how to use fentanyl test strips or encouraging them not to use drugs alone undermines the idea that they can choose not to use substances. But Weiner says both approaches can be part of the solution.
“It doesn’t have to be either prevention or harm reduction, and we lose really important tools when we say it has to be one or the other,” he said.
In adults, harm reduction approaches save lives, prevent disease transmission, and help people connect with substance use treatment ( Harm Reduction, NIDA, 2022 ). Early evidence shows similar interventions can help adolescents improve their knowledge and decision-making around drug use ( Fischer, N. R., Substance Abuse Treatment, Prevention, and Policy , Vol. 17, 2022 ). Teens are enthusiastic about these programs, which experts often call “Just Say Know” to contrast them with the traditional “Just Say No” approach. In one pilot study, 94% of students said a “Just Say Know” program provided helpful information and 92% said it might influence their approach to substance use ( Meredith, L. R., et al., The American Journal of Drug and Alcohol Abuse , Vol. 47, No. 1, 2021 ).
“Obviously, it’s the healthiest thing if we remove substance use from kids’ lives while their brains are developing. At the same time, my preference is that we do something that will have a positive impact on these kids’ health and behaviors,” said Nora Charles, PhD, an associate professor and head of the Youth Substance Use and Risky Behavior Lab at the University of Southern Mississippi. “If the way to do that is to encourage more sensible and careful engagement with illicit substances, that is still better than not addressing the problem.”
One thing not to do is to overly normalize drug use or to imply that it is widespread, Weiner said. Data show that it’s not accurate to say that most teens have used drugs in the past year or that drugs are “just a part of high school life.” In fact, students tend to overestimate how many of their peers use substances ( Dumas, T. M., et al., Addictive Behaviors , Vol. 90, 2019 ; Helms, S. W., et al., Developmental Psychology , Vol. 50, No. 12, 2014 ).
A way to incorporate both harm reduction and traditional prevention is to customize solutions to the needs of various communities. For example, in 2022, five Alabama high school students overdosed on a substance laced with fentanyl, suggesting that harm reduction strategies could save lives in that community. Other schools with less reported substance use might benefit more from a primary prevention-style program.
At Stanford, Halpern-Felsher’s Research and Education to Empower Adolescents and Young Adults to Choose Health (REACH) Lab has developed a series of free, evidence-based programs through community-based participatory research that can help populations with different needs. The REACH Lab offers activity-based prevention, intervention, and cessation programs for elementary, middle, and high school students, including curricula on alcohol, vaping, cannabis, fentanyl, and other drugs ( Current Problems in Pediatric and Adolescent Health Care , Vol. 52, No. 6, 2022 ). They’re also working on custom curricula for high-risk groups, including sexual and gender minorities.
The REACH Lab programs, including the comprehensive Safety First curriculum , incorporate honest discussion about the risks and benefits of using substances. For example: Drugs are one way to cope with stress, but exercise, sleep, and eating well can also help. Because many young people care about the environment, one lesson explores how cannabis and tobacco production causes environmental harm.
The programs also dispel myths about how many adolescents are using substances and help them practice skills, such as how to decline an offer to use drugs in a way that resonates with them. They learn about the developing brain in a positive way—whereas teens were long told they can’t make good decisions, Safety First empowers them to choose to protect their brains and bodies by making healthy choices across the board.
“Teens can make good decisions,” Halpern-Felsher said. “The equation is just different because they care more about certain things—peers, relationships—compared to adults.”
Motivating young people
Because substance use and mental health are so intertwined, some programs can do prevention successfully with very little drug-focused content. In one of the PreVenture Program’s workshops for teens, only half a page in a 35-page workbook explicitly mentions substances.
“That’s what’s fascinating about the evidence base for PreVenture,” said clinical psychologist Patricia Conrod, PhD, a professor of psychiatry at the University of Montreal who developed the program. “You can have quite a dramatic effect on young people’s substance use without even talking about it.”
PreVenture offers a series of 90-minute workshops that apply cognitive behavioral insights upstream (addressing the root causes of a potential issue rather than waiting for symptoms to emerge) to help young people explore their personality traits and develop healthy coping strategies to achieve their long-term goals.
Adolescents high in impulsivity, hopelessness, thrill-seeking, or anxiety sensitivity face higher risks of mental health difficulties and substance use, so the personalized material helps them practice healthy coping based on their personality type. For example, the PreVenture workshop that targets anxiety sensitivity helps young people learn to challenge cognitive distortions that can cause stress, then ties that skill back to their own goals.
The intervention can be customized to the needs of a given community (in one trial, drag racing outstripped substance use as the most problematic thrill-seeking behavior). In several randomized controlled trials of PreVenture, adolescents who completed the program started using substances later than peers who did not receive the intervention and faced fewer alcohol-related harms ( Newton, N. C., et al., JAMA Network Open , Vol. 5, No. 11, 2022 ). The program has also been shown to reduce the likelihood that adolescents will experiment with illicit substances, which relates to the current overdose crisis in North America, Conrod said ( Archives of General Psychiatry , Vol. 67, No. 1, 2010 ).
“People shouldn’t shy away from a targeted approach like this,” Conrod said. “Young people report that having the words and skills to manage their traits is actually helpful, and the research shows that at behavioral level, it really does protect them.”
As young people leave secondary school and enter college or adult life, about 30% will binge drink, 8% will engage in heavy alcohol use, and 20% will use illicit drugs ( Alcohol and Young Adults Ages 18 to 24, National Institute on Alcohol Abuse and Alcoholism, 2023 ; SAMHSA announces national survey on drug use and health (NSDUH) results detailing mental illness and substance use levels in 2021 ). But young people are very unlikely to seek help, even if those activities cause them distress, Murphy said. For that reason, brief interventions that leverage motivational interviewing and can be delivered in a school, work, or medical setting can make a big difference.
In an intervention Murphy and his colleagues are testing, young adults complete a questionnaire about how often they drink or use drugs, how much money they spend on substances, and negative things that have happened as a result of those choices (getting into an argument or having a hangover, for example).
In an hour-long counseling session, they then have a nonjudgmental conversation about their substance use, where the counselor gently amplifies any statements the young person makes about negative outcomes or a desire to change their behavior. Participants also see charts that quantify how much money and time they spend on substances, including recovering from being intoxicated, and how that stacks up against other things they value, such as exercise, family time, and hobbies.
“For many young people, when they look at what they allocate to drinking and drug use, relative to these other things that they view as much more important, it’s often very motivating,” Murphy said.
A meta-analysis of brief alcohol interventions shows that they can reduce the average amount participants drink for at least 6 months ( Mun, E.Y., et al., Prevention Science , Vol. 24, No. 8, 2023 ). Even a small reduction in alcohol use can be life-altering, Murphy said. The fourth or fifth drink on a night out, for example, could be the one that leads to negative consequences—so reducing intake to just three drinks may make a big difference for young people.
Conrod and her colleagues have also adapted the PreVenture Program for university students; they are currently testing its efficacy in a randomized trial across multiple institutions.
Christie is also focused on the young adult population. As a policy intern with Students for Sensible Drug Policy, she created a handbook of evidence-based policies that college campuses can use to reduce harm among students but still remain compliant with federal law. For example, the Drug Free Schools and Communities Act mandates that higher education institutions formally state that illegal drug use is not allowed on campus but does not bar universities from taking an educational or harm reduction-based approach if students violate that policy.
“One low-hanging fruit is for universities to implement a Good Samaritan policy, where students can call for help during a medical emergency and won’t get in trouble, even if illegal substance use is underway,” she said.
Ultimately, taking a step back to keep the larger goals in focus—as well as staying dedicated to prevention and intervention approaches backed by science—is what will help keep young people healthy and safe, Weiner said.
“What everyone can agree on is that we want kids to have the best life they can,” he said. “If we can start there, what tools do we have available to help?”
Further reading
Public Policy Statement on Prevention American Society of Addiction Medicine, 2023
Listen to young people: How to implement harm reduction in the collegiate setting Christie, N. C., 2023
Brief alcohol interventions for young adults: Strengthening effects and disentangling mechanisms to build personalized interventions for widespread uptake Special issue of Psychology of Addictive Behaviors , 2022
Addressing adolescent substance use with a public health prevention framework: The case for harm reduction Winer, J. M., et al., Annals of Medicine , 2022
A breath of knowledge: Overview of current adolescent e-cigarette prevention and cessation programs Liu, J., et al., Current Addiction Reports , 2020
Recommended Reading
Six things psychologists are talking about.
The APA Monitor on Psychology ® sister e-newsletter offers fresh articles on psychology trends, new research, and more.
Welcome! Thank you for subscribing.
Speaking of Psychology
Subscribe to APA’s audio podcast series highlighting some of the most important and relevant psychological research being conducted today.
Subscribe to Speaking of Psychology and download via:

Contact APA
You may also like.

Essay on Alcoholism
Students are often asked to write an essay on Alcoholism in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Alcoholism
Understanding alcoholism.
Alcoholism is a serious issue. It is a disease where a person cannot control their desire to drink alcohol. They keep drinking even when it causes harm.
Alcoholism can be caused by genetics, environment, and mental health. Some people are more prone to it because of their family history. Others might start drinking due to stress or depression.
The Effects
Alcoholism can lead to health problems like liver disease. It can also cause problems at work, school, or with relationships. It’s important to seek help if you or someone you know is struggling.
250 Words Essay on Alcoholism
Introduction.
Alcoholism, also known as alcohol use disorder (AUD), is a chronic disease characterized by an inability to control or abstain from alcohol use despite its negative consequences. It is a pervasive global issue with significant health, social, and economic implications.
Causes and Risk Factors
Impacts and consequences.
The impacts of alcoholism are far-reaching. Physiologically, it can lead to liver disease, cardiovascular problems, and neurological damage. Psychologically, it can result in depression, anxiety, and increased risk of suicide. Socially, it can disrupt relationships, lead to job loss, and contribute to social isolation.
Treatment and Prevention
Treatment for alcoholism typically involves a combination of medication, therapy, and support groups. Prevention strategies include education about the risks of excessive alcohol consumption, early intervention for at-risk individuals, and policies to limit alcohol availability.
Alcoholism is a complex disease with a multitude of contributing factors and consequences. Understanding its causes, impacts, and treatment options is key to addressing this pervasive issue. As future leaders, we must advocate for effective prevention strategies and accessible treatment services to combat alcoholism.
500 Words Essay on Alcoholism
Alcoholism, also known as Alcohol Use Disorder (AUD), is a chronic disease characterized by an inability to control or abstain from alcohol use despite its negative repercussions. It is a multifaceted disease, with complex interactions between genetic, environmental, and psychological factors.
Genetic Underpinnings of Alcoholism
Scientific research has established a strong genetic component to alcoholism. Certain genes can make individuals more susceptible to alcohol addiction, demonstrating that alcoholism is not merely a result of personal weakness or lack of willpower. It is estimated that genetics accounts for about 50% of the risk for AUD. However, having a genetic predisposition does not guarantee the development of alcoholism, indicating the significant role of environmental factors.
Environmental Factors and Alcoholism
The psychological impact of alcoholism.
Alcoholism inflicts significant psychological damage. It can lead to a range of mental health disorders, including depression, anxiety, and increased risk of suicide. Furthermore, alcoholism can negatively impact cognitive functions, impair judgment, and lead to behavioral changes. It is also closely linked to social problems, such as domestic violence, child abuse, and other forms of crime.
Treatment and Recovery
Alcoholism is a treatable disease, with various therapeutic strategies available. These include behavioral treatments, medications, and mutual-support groups. Behavioral treatments aim to change drinking behavior through counseling, while medications can help to manage withdrawal symptoms and prevent relapse. Mutual-support groups like Alcoholics Anonymous provide a supportive community for individuals recovering from alcoholism.
Prevention is Better than Cure
Alcoholism is a complex, multifaceted disease that requires a comprehensive approach for its prevention and treatment. Understanding its genetic, environmental, and psychological dimensions can inform effective strategies to combat this pervasive public health issue. While alcoholism is a serious disease, recovery is possible with the right support and treatment. Therefore, it is essential to foster a supportive environment for those struggling with this disorder, free from stigma and judgment.
That’s it! I hope the essay helped you.
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(11); 2022 Nov

Substance Abuse Amongst Adolescents: An Issue of Public Health Significance
1 School of Epidemiology and Public Health, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Sonali G Choudhari
2 School of Epidemiology and Public Health; Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Sarika U Dakhode
3 Department of Community Medicine, Dr. Panjabrao Deshmukh Memorial Medical College, Amravati, IND
Asmita Rannaware
Abhay m gaidhane.
Adolescence is a crucial time for biological, psychological, and social development. It is also a time when substance addiction and its adverse effects are more likely to occur. Adolescents are particularly susceptible to the negative long-term effects of substance use, including mental health illnesses, sub-par academic performance, substance use disorders, and higher chances of getting addicted to alcohol and marijuana. Over the past few decades, there have been substantial changes in the types of illegal narcotics people consume. The present article deals with the review of substance abuse as a public health problem, its determinants, and implications seen among adolescents. A systematic literature search using databases such as PubMed and Google Scholar was undertaken to search all relevant literature on teenage stimulant use. The findings have been organized into categories to cover essential aspects like epidemiology, neurobiology, prevention, and treatment. The review showed that substance addiction among adolescents between 12 to 19 years is widespread, though national initiatives exist to support young employment and their development. Research on psychological risk factors for teenage substance abuse is vast, wherein conduct disorders, including aggression, impulsivity, and attention deficit hyperactivity disorder, have been mentioned as risk factors for substance use. Parents' attitudes toward drugs, alcohol, academic and peer pressure, stress, and physical outlook are key determinants. Teenage drug usage has a significant negative impact on users, families, and society as a whole. It was found that a lot has been done to provide correct intervention to those in need with the constant development of programs and rehabilitative centers to safeguard the delicate minds of youths and prevent them from using intoxicants. Still, there is much need for stringent policy and program guidelines to curb this societal menace.
Introduction and background
Drug misuse is a widespread issue; in 2016, 5.6% of people aged 15 to 26 reported using drugs at least once [ 1 ]. Because alcohol and illegal drugs represent significant issues for public health and urgent care, children and adolescents frequently visit emergency rooms [ 2 ]. It is well known that younger people take drugs more often than older adults for most drugs. Drug usage is on the rise in many Association of Southeast Asian Nations, particularly among young males between the ages of 15 and 30 years [ 3 ]. According to the 2013 Global Burden of Disease report, drug addiction is a growing problem among teenagers and young people. Early substance use increases the likelihood of future physical, behavioral, social, and health issues [ 4 ]. Furthermore, recreational drug use is a neglected contributor to childhood morbidity and mortality [ 5 ]. One of the adverse outcomes of adolescent substance use is the increased risk of addiction in those who start smoking, drinking, and taking drugs before they are of 18 years. Moreover, most individuals with Substance Use Disorders begin using substances when they are young [ 6 ]. Substance use disorders amongst adolescents have long-term adverse health effects but can be mitigated with efficient treatment [ 7 ].
Childhood abuse is linked to suicidal thoughts and attempts. The particular mental behavior that mediates the link between childhood trauma and adult suicidal ideation and attempts is yet unknown. Recent studies show teens experiencing suicidal thoughts, psychiatric illness symptoms like anxiety, mood, and conduct disorders, and various types of child maltreatment like sexual abuse, corporal punishment, and emotional neglect that further leads to children inclining toward intoxicants [ 8 ]. Although teen substance use has generally decreased over the past five years, prolonged opioid, marijuana, and binge drinking use are still common among adolescents and young adults [ 9 ]. Drug-using students are more prone to commit crimes, including bullying and violent behavior. It has also been connected to various mental conditions, depending on the substance used. On the other hand, it has been linked to social disorder, abnormal behavior, and association with hostile groups [ 10 ]. Adolescent substance users suffer risks and consequences on the psychological, sociocultural, or behavioral levels that may manifest physiologically [ 11 ]. About 3 million deaths worldwide were caused by alcohol consumption alone. The majority of the 273,000 preventable fatalities linked to alcohol consumption are in India [ 12 ], which is the leading contributor. The United Nations Office on Drug and Crime conducted a national survey on the extent, patterns, and trends of drug abuse in India in 2003, which found that there were 2 million opiate users, 8.7 million cannabis users, and 62.5 million alcohol users in India, of whom 17% to 20% are dependent [ 13 ]. According to prevalence studies, 13.1% of drug users in India are under the age of 20 [ 14 ].
In India, alcohol and tobacco are legal drugs frequently abused and pose significant health risks, mainly when the general populace consumes them. States like Punjab and Uttar Pradesh have the highest rates of drug abuse, and the Indian government works hard to provide them with helpful services that educate and mentor them. This increases the burden of non-communicable illnesses too [ 15 ]. In addition, several substances/drugs are Narcotic and Psychotropic and used despite the act named ‘Narcotic Drugs and Psychotropic Substances Act, 1985.
This review article sheds light on ‘substance abuse’ amongst adolescents as an issue of public health significance, its determinants, and its implications on the health and well-being of adolescents.
Methodology
The present article deals with the narrative review of substance abuse as a public health problem, its determinants, and implications seen among adolescents. A systematic literature search using databases such as PubMed and Google Scholar was undertaken to search all relevant literature on teenage stimulant use. The findings have been organized into categories to cover essential aspects like epidemiology, neurobiology, prevention, and treatment. Various keywords used under TiAb of PubMed advanced search were Stimulants, "Drug abuse", "Psychotropic substance", "Substance abuse", addiction, and Adolescents, teenage, children, students, youth, etc., including MeSH terms. Figure Figure1 1 shows the key substances used by youth.

Reasons for abuse
People may initially choose to take drugs for psychological and physical reasons. Psychological issues, including mental illness, traumatic experiences, or even general attitudes and ideas, might contribute to drug usage. Several factors can contribute to emotional and psychosocial stress, compelling one to practice drug abuse. It can be brought on by a loss of a job because of certain reasons, the death of a loved one, a parent's divorce, or financial problems. Even medical diseases and health problems can have a devastating emotional impact. Many take medicines to increase their physical stamina, sharpen their focus, or improve their looks.
Students are particularly prone to get indulged in substance abuse due to various reasons, like academic and peer pressure, the appeal of popularity and identification, readily available pocket money, and relatively easy accessibility of several substances, especially in industrial, urban elite areas, including nicotine (cigarettes) [ 16 , 17 ]. In addition, a relationship breakup, mental illness, environmental factors, self-medication, financial concerns, downtime, constraints of work and school, family obligations, societal pressure, abuse, trauma, boredom, curiosity, experimentation, rebellion, to be in control, enhanced performance, isolation, misinformation, ignorance, instant gratification, wide availability can be one of the reasons why one chooses this path [ 18 ].
The brain grows rapidly during adolescence and continues to do so until early adulthood, as is well documented. According to studies using structural magnetic resonance imaging, changes in cortical grey matter volume and thickness during development include linear and nonlinear transformations and increases in white matter volume and integrity. This delays the maturation of grey and white matter, resulting in poorer sustained attention [ 19 ]. Alcohol drinking excessively increases the likelihood of accidents and other harmful effects by impairing cognitive functions like impulse control and decision-making and motor functions like balance and hand-eye coordination [ 20 ]. Lower-order sensory motor regions of the brain mature first, followed by limbic areas crucial for processing rewards. The development of different brain regions follows different time-varying trajectories. Alcohol exposure has adversely affected various emotional, mental, and social functions in the frontal areas linked to higher-order cognitive functioning that emerge later in adolescence and young adulthood [ 21 ].
Smoking/e-cigarettes
The use of tobacco frequently begins before adulthood. A worryingly high percentage of schoolchildren between 13 and 15 have tried or are currently using tobacco, according to the global youth tobacco survey [ 22 ]. It is more likely that early adolescent cigarette usage will lead to nicotine dependence and adult cigarette use. Teenage smoking has been associated with traumatic stress, anxiety, and mood problems [ 23 ]. Nicotine usage has been associated with a variety of adolescent problems, including sexual risk behaviors, aggressiveness, and the use of alcohol and illegal drugs. High levels of impulsivity have been identified in adolescent smokers.
Additionally, compared to non-smokers, smoking is associated with a higher prevalence of anxiety and mood disorders in teenagers. Smoking is positively associated with suicidal thoughts and attempts [ 24 ]. Peer pressure, attempting something new, and stress management ranked top for current and former smokers [ 25 ]. Most teenagers say that when they start to feel down, they smoke to make themselves feel better and return to their usual, upbeat selves. Smoking may have varying effects on people's moods [ 26 ]. Teenagers who smoke seem more reckless, less able to control their impulses, and less attentive than non-smokers [ 27 ].
Cannabis/Marijuana
Marijuana is among the most often used illegal psychotropic substances in India and internationally. The prevalence of marijuana usage and hospitalizations related to marijuana are rising, especially among young people, according to current trends. Cannabis usage has been connected to learning, working memory, and attention problems. Cannabis has been shown to alleviate stress in small doses, but more significant amounts can cause anxiety, emotional symptoms, and dependence [ 28 ]. Myelination and synaptic pruning are two maturational brain processes that take place during adolescence and the early stages of adulthood. According to reports, these remodeling mechanisms are linked to efficient neural processing. They are assumed to provide the specialized cognitive processing needed for the highest neurocognitive performance. On a prolonged attentional processing test, marijuana usage before age 16 was linked to a shorter reaction time [ 29 ]. Cannabis use alters the endocannabinoid system, impacting executive function, reward function, and affective functions. It is believed that these disturbances are what lead to mental health problems [ 30 ].
MDMA (Ecstasy/Molly)
MDMA (3,4-methylenedioxy-methamphetamine) was a synthetic drug used legally in psychotherapy treatment throughout the 1970s, despite the lack of data demonstrating its efficacy. Molly, or the phrase "molecular," is typically utilized in powder form. Serotonin, dopamine, and norepinephrine are produced more significantly when MDMA is used. In the brain, these neurotransmitters affect mood, sleep, and appetite. Serotonin also causes the release of other hormones that may cause emotions of intimacy and attraction. Because of this, users might be more affectionate than usual and possibly develop ties with total strangers. The effects wear off three to six hours later, while a moderate dose may cause withdrawal symptoms to continue for a week. These symptoms include a decline in sex interest, a drop in appetite, problems sleeping, confusion, impatience, anxiety, sorrow, Impulsivity and violence, issues with memory and concentration, and insomnia are a few of them. Unsettlingly, it is rising in popularity in India, particularly among teenagers [ 31 ].
Opium
In addition to being a top producer of illicit opium, India is a significant drug consumer. In India, opium has a long history. The most common behavioral changes are a lack of motivation, depression, hyperactivity, a lack of interest or concentration, mood swings or abrupt behavior changes, confusion or disorientation, depression, anxiety, distortion of reality perception, social isolation, slurred or slow-moving speech, reduced coordination, a loss of interest in once-enjoyed activities, taking from family members or engaging in other illegal activity [ 32 ]. Except for the chemical produced for medicinal purposes, it is imperative to prohibit both production and usage since if a relatively well-governed nation like India cannot stop the drug from leaking, the problem must be huge in scope [ 33 ].
Cocaine is a highly addictive drug that causes various psychiatric syndromes, illnesses, and symptoms. Some symptoms include agitation, paranoia, hallucinations, delusions, violence, and thoughts of suicide and murder. They may be caused by the substance directly or indirectly through the aggravation of co-occurring psychiatric conditions. More frequent and severe symptoms are frequently linked to the usage of cocaine in "crack" form. Cocaine can potentially worsen numerous mental diseases and cause various psychiatric symptoms.
Table Table1 1 discusses the short- and long-term effects of substance abuse.
| Substance | Mode | Behavioral changes | Short-term physical effects | Long-term physical effects |
| Alcohol | Oral/drinking | Growingly aggressive self-disclosure racy sexual behavior [ ]. | Unsteady speech, Drowsiness, Vomiting, Diarrhea, Uneasy stomach, Headache, Breathing problems, Vision and hearing impairment, Faulty judgment, Diminution of perception and coordination, Unconsciousness, Anemia (loss of red blood cells), Coma, and Blackouts [ ]. | Unintentional injuries such as car crashes, falls, burns, drowning; Intentional injuries such as firearm injuries, sexual assault, and domestic violence; Increased on-the-job injuries and loss of productivity; increased family problems and broken relationships. Alcohol poisoning, High blood pressure, Stroke, and other heart-related diseases; Liver disease, Nerve damage, Sexual problems, Permanent damage to the brain [ ]. Vitamin B deficiency can lead to a disorder characterized by amnesia, apathy, and disorientation. Ulcers, Gastritis (inflammation of stomach walls), Malnutrition, Cancer of the mouth and throat [ ]. |
| Cannabis | Smoked, Vaped, Eaten (mixed in food or brewed as tea) | Hallucinations, emotional swings, forgetfulness, Depersonalization, Paranoia, Delusions Disorientation. Psychosis, Bipolar illness, Schizophrenia [ ]. | Enhanced sensory perception and euphoria followed by drowsiness/relaxation; Slowed reaction time; problems with balance and coordination; Increased heart rate and appetite; problems with learning and memory; anxiety. | Mental health problems, Chronic cough, Frequent respiratory infections. |
| Cocaine (coke/crack) | Snorted, smoked, injected | Violence and hostility, paranoia and hallucinations, and monotonous or stereotyped simple conduct [ ]. Suspiciousness anger\giddiness Irritability, and Impatience [ ]. | Narrowed blood vessels; enlarged pupils; increased body temperature, heart rate, and blood pressure; headache; abdominal pain and nausea; euphoria; increased energy, alertness; insomnia, restlessness; anxiety; erratic and violent behavior, panic attacks, paranoia, psychosis; heart rhythm problems, heart attack; stroke, seizure, coma. | Loss of sense of smell, nosebleeds, nasal damage and trouble swallowing from snorting; Infection and death of bowel tissue from decreased blood flow; Poor nutrition and weight loss; Lung damage from smoking. |
| Heroin | Injected, smoked, snorted | Exaggerated efforts to keep family members out of his or her room or being secretive about where he or she goes with friends; drastic changes in behavior and relationships with family and friends; sudden requests for money without a good reason; sudden disinterest in school activities or work; a drop in grades or work performance; a lack of energy and motivation; and lack of interest in clothes are all examples of these behaviors [ ]. | Euphoria; dry mouth; itching; nausea; vomiting; analgesia; slowed breathing and heart rate. | Collapsed veins; abscesses (swollen tissue with pus); infection of the lining and valves in the heart; constipation and stomach cramps; Liver or kidney disease; pneumonia. |
| MDMA | Swallowed, snorted | A state of exhilarated tranquility or peace greater sensitivity -More vigor both physically and emotionally -Increased intimacy and sociability -Relaxation -Bruxism -Empathy [ ]. | Lowered inhibition; enhanced sensory perception; increased heart rate and blood pressure; muscle tension; nausea; faintness; chills or sweating; sharp rise in body temperature leading to kidney failure or death. | Long-lasting confusion, Depression, problems with attention, memory, and Sleep; Increased anxiety, impulsiveness; Less interest in sex. |
| Cigarettes, Vaping devices, e-cigarettes, Cigars, Bidis, Hookahs, Kreteks | Smoked, snorted, chewed, vaporized | Hyperactivity Inattention [ ]. Anxiety, Tension, enhanced emotions, and focus lower rage and stress, relax muscles, and curbs appetite [ ]. | Increased blood pressure, breathing, and heart rate; Exposes lungs to a variety of chemicals; Vaping also exposes the lungs to metallic vapors created by heating the coils in the device. | Greatly increased risk of cancer, especially lung cancer when smoked and oral cancers when chewed; Chronic bronchitis; Emphysema; Heart disease; Leukemia; Cataracts; Pneumonia [ ]. |
Other cheap substances ( sasta nasha ) used in India
India is notorious for phenomena that defy comprehension. People in need may turn to readily available items like Iodex sandwiches, fevibond, sanitizer, whitener, etc., for comfort due to poverty and other circumstances to stop additional behavioral and other changes in youth discouragement is necessary [ 42 - 44 ].
Curbing drug abuse amongst youth
Seventy-five percent of Indian households contain at least one addict. The majority of them are fathers who act in this way due to boredom, stress from their jobs, emotional discomfort, problems with their families, or problems with their spouses. Due to exposure to such risky behaviors, children may try such intoxicants [ 45 ]. These behaviors need to be discouraged because they may affect the child's academic performance, physical growth, etc. The youngster starts to feel depressed, lonely, agitated and disturbed. Because they primarily revolve around educating students about the dangers and long-term impacts of substance abuse, previous attempts at prevention have all been ineffective. To highlight the risks of drug use and scare viewers into abstaining, some programs stoked terror. The theoretical underpinning of these early attempts was lacking, and they failed to consider the understanding of the developmental, social, and other etiologic factors that affect teenage substance use. These tactics are based on a simple cognitive conceptual paradigm that says that people's decisions to use or abuse substances depend on how well they are aware of the risks involved. More effective contemporary techniques are used over time [ 46 ]. School-based substance abuse prevention is a recent innovation utilized to execute changes, including social resistance skills training, normative education, and competence enhancement skills training.
Peer pressure makes a teenager vulnerable to such intoxicants. Teenagers are often exposed to alcohol, drugs, and smoking either because of pressure from their friends or because of being lonely. Social resistance training skills are used to achieve this. The pupils are instructed in the best ways to steer clear of or manage these harmful situations. The best method to respond to direct pressure to take drugs or alcohol is to know what to say (i.e., the specific content of a refusal message) and how to say it. These skills must be taught as a separate curriculum in every school to lower risk. Standard instructional methods include lessons and exercises to dispel misconceptions regarding drug usage's widespread use.
Teenagers typically exaggerate how common it is to smoke, drink, and use particular substances, which could give off the impression that substance usage is acceptable. We can lessen young people's perceptions of the social acceptability of drug use by educating them that actual rates of drug usage are almost always lower than perceived rates of use. Data from surveys that were conducted in the classroom, school, or local community that demonstrate the prevalence of substance use in the immediate social setting may be used to support this information. If not, this can be taught using statistics from national surveys, which usually show prevalence rates that are far lower than what kids describe.
The role social learning processes have in teen drug use is recognized by competency-improvement programs, and there is awareness about how adolescents who lack interpersonal and social skills are more likely to succumb to peer pressure to use drugs. These young people might also be more inclined to turn to drug usage instead of healthier coping mechanisms. Most competency enhancement strategies include instruction in many of the following life skills: general problem-solving and decision-making skills, general cognitive abilities for fending off peer or media pressure, skills for enhancing self-control, adaptive coping mechanisms for reducing stress and anxiety through the use of cognitive coping mechanisms or be behavioral relaxation techniques, and general social and assertive skills [ 46 ].
Programs formulated to combat the growing risk of substance abuse
The Ministry of Health and Family Welfare developed Rashtriya Kishor Swasthya Karyakram for teenagers aged 10 to 19, with a focus on improving nutrition, sexual and reproductive health, mental health, preventing injuries and violence, and preventing substance abuse. By enabling them to make informed and responsible decisions about their health and well-being and ensuring that they have access to the tools and assistance they need, the program seeks to enable all adolescents in India in realizing their full potential [ 47 ].
For the past six years, ‘Nasha Mukti Kendra’ in India and rehabilitation have worked to improve lives and provide treatment for those who abuse alcohol and other drugs. They provide cost-effective and dedicated therapy programs for all parts of society. Patients come to them from all around the nation. Despite having appropriate programs and therapies that can effectively treat the disorder, they do not employ medication to treat addiction.
Conclusions
Around the world, adolescent drug and alcohol addiction has significantly increased morbidity and mortality. The menace of drugs and alcohol has been woven deep into the fabric of society. As its effects reach our youth, India's current generation is at high stake for the risk associated with the abuse of drugs like cannabis, alcohol, and tobacco. Even though the issue of substance abuse is complicated and pervasive, various stakeholders like healthcare professionals, community leaders, and educational institutions have access to a wealth of evidence-based research that can assist them to adopt interventions that can lower rates of teenage substance misuse. It is realized that while this problem is not specific to any one country or culture, individual remedies might not always be beneficial. Due to the unacceptably high rate of drug abuse that is wreaking havoc on humanity, a strategy for addressing modifiable risk factors is crucial. Because human psychology and mental health influence the choices the youth make related to their indulgence in drug misuse, it is the need of the hour to give serious consideration to measures like generating awareness, counseling, student guidance cells, positive parenting, etc., across the world. It will take time to change this substance misuse behavior, but the more effort we put into it, the greater the reward we will reap.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Alcohol's Effects on Health
Research-based information on drinking and its impact.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Make a difference: talk to your child about alcohol - parents.

Quick Facts
Kids who drink are more likely to be victims of violent crime, to be involved in alcohol-related traffic crashes, and to have serious school-related problems.
You have more influence on your child’s values and decisions about drinking before he or she begins to use alcohol.
Parents can have a major impact on their children’s drinking, especially during the preteen and early teen years.
Introduction
With so many drugs available to young people these days, you may wonder, “Why develop a booklet about helping kids avoid alcohol?” Alcohol is a drug, as surely as cocaine and marijuana are. The National Minimum Legal Drinking Age in the United States is 21. And underage drinking is dangerous. Kids who drink are more likely to:
Be victims of violent crime.
Have serious problems in school.
Be involved in drinking-related traffic crashes.
This guide is geared to parents and guardians of young people ages 10 to 14. Keep in mind that the suggestions on the following pages are just that—suggestions. Trust your instincts. Choose ideas you are comfortable with, and use your own style in carrying out the approaches you find useful. Your child looks to you for guidance and support in making life decisions—including the decision not to use alcohol.
“But my child isn’t drinking yet,” you may think. “Isn’t it a little early to be concerned about drinking?” Not at all. This is the age when some children begin experimenting with alcohol. Even if your child is not yet drinking alcohol, he or she may be receiving pressure to drink. Act now. Keeping quiet about how you feel about your child’s alcohol use may give him or her the impression that alcohol use is OK for kids.
It’s not easy. As children approach adolescence, friends exert a lot of influence. Fitting in is a chief priority for teens, and parents often feel shoved aside. Kids will listen, however. Study after study shows that even during the teen years, parents have enormous influence on their children’s behavior.
The bottom line is that most young teens don’t yet drink. And parents’ disapproval of youthful alcohol use is the key reason children choose not to drink. So make no mistake: You can make a difference.
(Note: This booklet uses a variety of terms to refer to young people ages 10 to 14, including youngsters, children, kids, and young teens.)
Young Teens and Alcohol: The Risks
For young people, alcohol is the drug of choice. In fact, alcohol is used by more young people than tobacco or illicit drugs. Although most children under age 14 have not yet begun to drink, early adolescence is a time of special risk for beginning to experiment with alcohol.
While some parents and guardians may feel relieved that their teen is “only” drinking, it is important to remember that alcohol is a powerful, mood-altering drug. Not only does alcohol affect the mind and body in often unpredictable ways, but teens lack the judgment and coping skills to handle alcohol wisely. As a result:
Alcohol-related traffic crashes are a major cause of death among young people. Alcohol use also is linked with teen deaths by drowning, suicide, and homicide.
Teens who use alcohol are more likely to be sexually active at earlier ages, to have sexual intercourse more often, and to have unprotected sex than teens who do not drink.
Young people who drink are more likely than others to be victims of violent crime, including rape, aggravated assault, and robbery.
Teens who drink are more likely to have problems with school work and school conduct.
The majority of boys and girls who drink tend to binge when they drink.
A person who begins drinking as a young teen is four times more likely to develop alcohol dependence than someone who waits until adulthood to use alcohol.
The message is clear: Alcohol use is unsafe for young people. And the longer children delay alcohol use, the less likely they are to develop any problems associated with it. That’s why it is so important to help your child avoid any alcohol use.
What is binge drinking?
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines binge drinking as a pattern of drinking that brings blood alcohol concentration (BAC) to 0.08 percent—or 0.08 grams of alcohol per deciliter—or higher.* For a typical adult, this pattern corresponds to consuming 4 or more drinks (female), or 5 or more drinks (male), in about 2 hours. Research shows that fewer drinks in the same timeframe result in the same BAC in youth; only 3 drinks for girls, and 3 to 5 drinks for boys, depending on their age and size.
*A BAC of 0.08 percent corresponds to 0.08 grams per deciliter, or 0.08 grams per 100 milliliters.
Your Young Teen's World
Early adolescence is a time of immense and often confusing changes for your son or daughter, which makes it a challenging time for both your youngster and you. Understanding what it’s like to be a teen can help you stay closer to your child and have more influence on the choices he or she makes—including decisions about using alcohol.
Changes in the Brain. Research shows that as a child matures, his or her brain continues to develop too. In fact, the brain’s final, adult wiring may not even be complete until well into the twenties. Furthermore, in some ways, the adolescent brain may be specifically “wired” to help youth navigate adolescence and to take some of the risks necessary to achieve independence from their parents. This may help explain why teens often seek out new and thrilling—sometimes dangerous—situations, including drinking alcohol. It also offers a possible reason for why young teens act so impulsively, often not recognizing that their actions—such as drinking—can lead to serious problems.
Growing Up and Fitting In. As children approach adolescence, “fitting in” becomes extremely important. They begin to feel more self-conscious about their bodies than they did when they were younger and begin to wonder whether they are “good enough”—tall enough, slender enough, attractive enough—compared with others. They look to friends and the media for clues on how they measure up, and they begin to question adults’ values and rules. It’s not surprising that this is the time when parents often experience conflict with their kids. Respecting your child’s growing independence while still providing support and setting limits is a key challenge during this time.
A young teen who feels that he or she doesn’t fit in is more likely to do things to try to please friends, including experimenting with alcohol. During this vulnerable time, it is particularly important to let your children know that in your eyes, they do measure up—and that you care about them deeply.
Did You Know?
That according to a recent national survey, 16 percent of eighth graders reported drinking alcohol within the past month?
That 32 percent of eighth graders reported drinking in the past year?
That 64 percent of eighth graders say that alcohol is easy to get?
That a recent survey shows that more girls than boys ages 12 to 17 reported drinking alcohol?
The Bottom Line: A Strong Parent–Child Relationship
You may wonder why a guide for preventing teen alcohol use is putting so much emphasis on parents’ need to understand and support their children. But the fact is, the best way to influence your child to avoid drinking is to have a strong, trusting relationship with him or her. Research shows that teens are much more likely to delay drinking when they feel they have a close, supportive tie with a parent or guardian. Moreover, if your son or daughter eventually does begin to drink, a good relationship with you will help protect him or her from developing alcohol-related problems.
The opposite also is true: When the relationship between a parent and teen is full of conflict or is very distant, the teen is more likely to use alcohol and to develop drinking-related problems.
This connection between the parent–child relationship and a child’s drinking habits makes a lot of sense when you think about it. First, when children have a strong bond with a parent, they are apt to feel good about themselves and therefore be less likely to give in to peer pressure to use alcohol. Second, a good relationship with you is likely to encourage your children to try to live up to your expectations, because they want to maintain their close tie with you. Here are some ways to build a strong, supportive bond with your child:
Establish open communication. Make it easy for your teen to talk honestly with you. (See box “Tips for Talking With Your Teen.”)
Show you care. Even though young teens may not always show it, they still need to know that they are important to their parents. Make it a point to regularly spend one-on-one time with your child—time when you can give him or her your loving, undivided attention. Some activities to share: a walk, a bike ride, a quiet dinner out, or a cookie-baking session.
Draw the line. Set clear, realistic expectations for your child’s behavior. Establish appropriate consequences for breaking rules and consistently enforce them.
Offer acceptance. Make sure your teen knows that you appreciate his or her efforts as well as accomplishments. Avoid hurtful teasing or criticism.
Understand that your child is growing up. This doesn’t mean a hands-off attitude. But as you guide your child’s behavior, also make an effort to respect his or her growing need for independence and privacy.
Tips For Talking With Your Teen
Developing open, trusting communication between you and your child is essential to helping him or her avoid alcohol use. If your child feels comfortable talking openly with you, you’ll have a greater chance of guiding him or her toward healthy decisionmaking. Some ways to begin:
Encourage conversation. Encourage your child to talk about whatever interests him or her. Listen without interruption and give your child a chance to teach you something new. Your active listening to your child’s enthusiasms paves the way for conversations about topics that concern you.
Ask open-ended questions. Encourage your teen to tell you how he or she thinks and feels about the issue you’re discussing. Avoid questions that have a simple “yes” or “no” answer.
Control your emotions. If you hear something you don’t like, try not to respond with anger. Instead, take a few deep breaths and acknowledge your feelings in a constructive way.
Make every conversation a “win-win” experience. Don’t lecture or try to “score points” on your teen by showing how he or she is wrong. If you show respect for your child’s viewpoint, he or she will be more likely to listen to and respect yours.
Good Reasons For Teens Not To Drink
You want your child to avoid alcohol.
You want your child to maintain self-respect.
The National Minimum Legal Drinking Age is 21.
Drinking at their age can be dangerous.
You may have a family history of alcoholism.
Talking With Your Teen About Alcohol
For many parents, bringing up the subject of alcohol is no easy matter. Your young teen may try to dodge the discussion, and you yourself may feel unsure about how to proceed. To make the most of your conversation, take some time to think about the issues you want to discuss before you talk with your child. Consider too how your child might react and ways you might respond to your youngster’s questions and feelings. Then choose a time to talk when both you and your child have some “down time” and are feeling relaxed.
You don’t need to cover everything at once. In fact, you’re likely to have a greater impact on your child’s decisions about drinking by having a number of talks about alcohol use throughout his or her adolescence. Think of this talk with your child as the first part of an ongoing conversation.
And remember, do make it a conversation, not a lecture! You might begin by finding out what your child thinks about alcohol and drinking.
Your Child’s Views About Alcohol. Ask your young teen what he or she knows about alcohol and what he or she thinks about teen drinking. Ask your child why he or she thinks kids drink. Listen carefully without interrupting. Not only will this approach help your child to feel heard and respected, but it can serve as a natural “lead-in” to discussing alcohol topics.
Important Facts About Alcohol. Although many kids believe that they already know everything about alcohol, myths and misinformation abound. Here are some important facts to share:
Alcohol is a powerful drug that slows down the body and mind. It impairs coordination; slows reaction time; and impairs vision, clear thinking, and judgment.
Beer and wine are not “safer” than distilled spirits (gin, rum, tequila, vodka, whiskey, etc.). A 12-ounce can of beer (about 5 percent alcohol), a 5-ounce glass of wine (about 12 percent alcohol), and 1.5 ounces of 80-proof distilled spirits (40 percent alcohol) all contain the same amount of alcohol and have the same effects on the body and mind.
On average, it takes 2 to 3 hours for a single drink to leave a person’s system. Nothing can speed up this process, including drinking coffee, taking a cold shower, or “walking it off.”
People tend to be very bad at judging how seriously alcohol has affected them. That means many individuals who drive after drinking think they can control a car—but actually cannot.
Anyone can develop a serious alcohol problem, including a teenager.
Good Reasons Not to Drink. In talking with your child about reasons to avoid alcohol, stay away from scare tactics. Most young teens are aware that many people drink without problems, so it is important to discuss the consequences of alcohol use without overstating the case. Some good reasons why teens should not drink:
You want your child to avoid alcohol. Clearly state your own expectations about your child’s drinking. Your values and attitudes count with your child, even though he or she may not always show it.
To maintain self-respect. Teens say the best way to persuade them to avoid alcohol is to appeal to their self-respect—let them know that they are too smart and have too much going for them to need the crutch of alcohol. Teens also are likely to pay attention to examples of how alcohol might lead to embarrassing situations or events—things that might damage their self-respect or alter important relationships.
The National Minimum Legal Drinking Age is 21. Getting caught with alcohol before age 21 may mean trouble with the authorities. Even if getting caught doesn’t lead to police action, the parents of your child’s friends may no longer permit them to associate with your child.
Drinking can be dangerous. One of the leading causes of teen deaths is motor vehicle crashes involving alcohol. Drinking also makes a young person more vulnerable to sexual assault and unprotected sex. And while your teen may believe he or she wouldn’t engage in hazardous activities after drinking, point out that because alcohol impairs judgment, a drinker is very likely to think such activities won’t be dangerous.
You have a family history of alcoholism. If one or more members of your family has suffered from alcoholism, your child may be somewhat more vulnerable to developing a drinking problem.
Alcohol affects young people differently than adults. Drinking while the brain is still maturing may lead to long-lasting intellectual effects and may even increase the likelihood of developing alcohol dependence later in life.
The “Magic Potion” Myth. The media’s glamorous portrayal of alcohol encourages many teens to believe that drinking will make them “cool,” popular, attractive, and happy. Research shows that teens who expect such positive effects are more likely to drink at early ages. However, you can help to combat these dangerous myths by watching TV shows and movies with your child and discussing how alcohol is portrayed in them. For example, television advertisements for beer often show young people having an uproariously good time, as though drinking always puts people in a terrific mood. Watching such a commercial with your child can be an opportunity to discuss the many ways that alcohol can affect people—in some cases bringing on feelings of sadness or anger rather than carefree high spirits.
How to Handle Peer Pressure. It’s not enough to tell your young teen that he or she should avoid alcohol—you also need to help your child figure out how. What can your daughter say when she goes to a party and a friend offers her a beer? (See “Help Your Child Say No.”) Or what should your son do if he finds himself in a home where kids are passing around a bottle of wine and parents are nowhere in sight? What should their response be if they are offered a ride home with an older friend who has been drinking?
Brainstorm with your teen for ways that he or she might handle these and other difficult situations, and make clear how you are willing to support your child. An example: “If you find yourself at a home where kids are drinking, call me and I’ll pick you up—and there will be no scolding or punishment.” The more prepared your child is, the better able he or she will be to handle high-pressure situations that involve drinking.
Mom, Dad, Did You Drink When You Were a Kid?
This is the question many parents dread—yet it is highly likely to come up in any family discussion of alcohol. The reality is that some parents did drink when they were underage. So how can one be honest with a child without sounding like a hypocrite who advises, “Do as I say, not as I did”?
This is a judgment call. If you believe that your drinking or drug use history should not be part of the discussion, you can simply tell your child that you choose not to share it. Another approach is to admit that you did do some drinking as a teenager, but that it was a mistake—and give your teen an example of an embarrassing or painful moment that occurred because of your drinking. This approach may help your child better understand that youthful alcohol use does have negative consequences.
How To Host A Teen Party
Agree on a guest list—and don’t admit party crashers.
Discuss ground rules with your child before the party.
Encourage your teen to plan the party with a responsible friend so that he or she will have support if problems arise.
Brainstorm fun activities for the party.
If a guest brings alcohol into your house, ask him or her to leave.
Serve plenty of snacks and non-alcoholic drinks.
Be visible and available—but don’t join the party!
Taking Action: Prevention Strategies for Parents
While parent–child conversations about not drinking are essential, talking isn’t enough—you also need to take concrete action to help your child resist alcohol. Research strongly shows that active, supportive involvement by parents and guardians can help teens avoid underage drinking and prevent later alcohol misuse.
In a recent national survey, 64 percent of eighth graders said alcohol was “fairly easy” or “very easy” to get and 32 percent reported drinking within the last year. The message is clear: Young teens still need plenty of adult supervision. Some ways to provide it:
Monitor Alcohol Use in Your Home. If you keep alcohol in your home, keep track of the supply. Make it clear to your child that you don’t allow unchaperoned parties or other teen gatherings in your home. If possible, however, encourage him or her to invite friends over when you are at home. The more entertaining your child does in your home, the more you will know about your child’s friends and activities.
Connect With Other Parents. Getting to know other parents and guardians can help you keep closer tabs on your child. Friendly relations can make it easier for you to call the parent of a teen who is having a party to be sure that a responsible adult will be present and that alcohol will not be available. You’re likely to find out that you’re not the only adult who wants to prevent teen alcohol use—many other parents share your concern.
Keep Track of Your Child’s Activities. Be aware of your teen’s plans and whereabouts. Generally, your child will be more open to your supervision if he or she feels you are keeping tabs because you care, not because you distrust him or her.
Develop Family Rules About Youthful Drinking. When parents establish clear “no alcohol” rules and expectations, their children are less likely to begin drinking. Although each family should develop agreements about teen alcohol use that reflect their own beliefs and values, some possible family rules about drinking are:
Kids will not drink alcohol until they are 21.
Older siblings will not encourage younger brothers or sisters to drink and will not give them alcohol.
Kids will not stay at teen parties where alcohol is served.
Kids will not ride in a car with a driver who has been drinking.
Set a Good Example. Parents and guardians are important role models for their children—even children who are fast becoming teenagers. Studies indicate that if a parent uses alcohol, his or her children are more likely to drink as well. But even if you use alcohol, there may be ways to lessen the likelihood that your child will drink. Some suggestions:
Use alcohol in moderation.
Don’t communicate to your child that alcohol is a good way to handle problems. For example, don’t come home from work and say, “I had a rotten day. I need a drink.”
Let your child see that you have other, healthier ways to cope with stress, such as exercise; listening to music; or talking things over with your spouse, partner, or friend.
Don’t tell your kids stories about your own drinking in a way that conveys the message that alcohol use is funny or glamorous.
Never drink and drive or ride in a car with a driver who has been drinking.
When you entertain other adults, serve alcohol-free beverages and plenty of food. If anyone drinks too much at your party, make arrangements for them to get home safely.
Help Your Child Say No
Your child can learn to resist alcohol or anything else he or she may feel pressured into. Let him or her know that the best way to say “no” is to be assertive—that is, say no and mean it.
Resist The Pressure To Drink
Say no and let them know you mean it.
Stand up straight.
Make eye contact.
Say how you feel.
Don’t make excuses.
Stand up for yourself.
Don’t Support Teen Drinking. Your attitudes and behavior toward teen drinking also influence your child. Avoid making jokes about underage drinking or drunkenness, or otherwise showing acceptance of teen alcohol use. Never serve alcohol to your child’s underage friends. Research shows that kids whose parents or friends’ parents provide alcohol for teen get-togethers are more likely to engage in heavier drinking, to drink more often, and to get into traffic crashes. Remember, too, that in almost every State it is illegal to provide alcohol to minors who are not family members.
Help Your Child Build Healthy Friendships. If your child’s friends use alcohol, your child is more likely to drink too. So it makes sense to try to encourage your young teen to develop friendships with kids who do not drink and who are otherwise healthy influences on your child. A good first step is to simply get to know your child’s friends better. You can then invite the kids you feel good about to family get-togethers and outings and find other ways to encourage your child to spend time with those teens. Also, talk directly with your child about the qualities in a friend that really count, such as trustworthiness and kindness, rather than popularity or a “cool” style.
When you disapprove of one of your child’s friends, the situation can be tougher to handle. While it may be tempting to simply forbid your child to see that friend, such a move may make your child even more determined to hang out with him or her. Instead, you might try pointing out your reservations about the friend in a caring, supportive way. You can also limit your child’s time with that friend through your family rules, such as how after-school time can be spent or how late your child can stay out in the evening.
Encourage Healthy Alternatives to Alcohol. One reason kids drink is to beat boredom. So it makes sense to encourage your child to participate in supervised after-school and weekend activities that are challenging and fun. According to a recent survey of preteens, the availability of enjoyable, alcohol-free activities is a big reason for deciding not to use alcohol.
If your community doesn’t offer many supervised activities, consider getting together with other parents and teens to help create some. Start by asking your child and other kids what they want to do, because they will be most likely to participate in activities that truly interest them. Find out whether your church, school, or community organization can help you sponsor a project.
Could My Child Develop a Drinking Problem?
This booklet is primarily concerned with preventing teen alcohol use. We also need to pay attention to the possibility of youthful alcohol abuse. Certain children are more likely than others to drink heavily and encounter alcohol-related difficulties, including health, school, legal, family, and emotional problems. Kids at highest risk for alcohol-related problems are those who:
Begin using alcohol or other drugs before the age of 15.
Have a parent who is a problem drinker or an alcoholic.
Have close friends who use alcohol and/or other drugs.
Have been aggressive, antisocial, or hard to control from an early age.
Have experienced childhood abuse and/or other major traumas.
Have current behavioral problems and/or are failing at school.
Have parents who do not support them, do not communicate openly with them, and do not keep track of their behavior or whereabouts.
Experience ongoing hostility or rejection from parents and/or harsh, inconsistent discipline.
The more of these experiences a child has had, the greater the chances that he or she will develop problems with alcohol. Having one or more risk factors does not mean that your child definitely will develop a drinking problem, but it does suggest that you may need to act now to help protect your youngster from later problems.
Talking with your child is more important now than ever. If your child has serious behavioral problems, you may want to seek help from his or her school counselor, physician, and/or a mental health professional. And if you suspect that your child may be in trouble with drinking, consider getting advice from a health care professional specializing in alcohol problems before talking with your teen (see box “Warning Signs of a Drinking Problem”). To find a professional, contact your family doctor or a local hospital. Other sources of information and guidance may be found in your local Yellow Pages under “Alcoholism” or through one of the resources listed at the end of this booklet.
Warning Signs Of A Drinking Problem
Although the following signs may indicate a problem with alcohol or other drugs, some also reflect normal teenage growing pains. Experts believe that a drinking problem is more likely if you notice several of these signs at the same time, if they occur suddenly, and if some of them are extreme in nature.
Mood changes: flare-ups of temper, irritability, and defensiveness.
School problems: poor attendance, low grades, and/or recent disciplinary action.
Rebelling against family rules.
Switching friends, along with a reluctance to have you get to know the new friends.
A “nothing matters” attitude: sloppy appearance, a lack of involvement in former interests, and general low energy.
Finding alcohol in your child’s room or backpack, or smelling alcohol on his or her breath.
Physical or mental problems: memory lapses, poor concentration, bloodshot eyes, lack of coordination, or slurred speech.
Action Checklist
Establish a loving, trusting relationship with your child.
Make it easy for your teen to talk honestly with you.
Talk with your child about alcohol facts, reasons not to drink, and ways to avoid drinking in difficult situations.
Keep tabs on your young teen’s activities, and join with other parents in making common policies about teen alcohol use.
Develop family rules about teen drinking and establish consequences.
Set a good example regarding your own alcohol use and your response to teen drinking.
Encourage your child to develop healthy friendships and fun alternatives to drinking.
Know whether your child is at high risk for a drinking problem; if so, take steps to lessen that risk.
Know the warning signs of a teen drinking problem and act promptly to get help for your child.
Believe in your own power to help your child avoid alcohol use.
Partnership to End Addiction 485 Lexington Avenue, 3rd Floor New York, NY 10017-6706 212–841–5200 Internet address: https://drugfree.org/
A national resource working to reduce teen substance abuse and to support families impacted by addiction.
National Institute on Alcohol Abuse and Alcoholism Publications Distribution Center P.O. Box 10686 Rockville, MD 20849–0686 301–443–3860 Internet address: http://www.niaaa.nih.gov
Makes available free informational materials on many aspects of alcohol use, alcohol abuse, and alcoholism.
Substance Abuse and Mental Health Services Administration National Drug Information Treatment and Referral Hotline 800–662–HELP (4357) (toll free) Internet address: https://www.samhsa.gov/find-treatment
Provides information, support, treatment options, and referrals to local rehab centers for drug or alcohol problems. Operates 24 hours, 7 days a week.
To download or order, visit https://www.niaaa.nih.gov/publications .
Or write to:
National Institute on Alcohol Abuse and Alcoholism Publications Distribution Center P.O. Box 10686, Rockville, MD 20849–0686
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism

IMAGES
VIDEO
COMMENTS
The short-term effects of underage alcohol misuse involve manslaughter and brutality, suicidal tendencies, sexual misconduct, unintended death and injury related to driving or participating in other dangerous activities after drinking, as well as vandalism and property destruction. Furthermore, research indicates that people who start drinking ...
1. Alcohol is often taken in larger amounts or over a longer period than was intended. 2. There is a persistent desire or unsuccessful efforts to cut down or control alcohol use. 3. A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects. 4.
Adolescence is a critical neurodevelopmental period marked by rising alcohol use. This review summarizes the neural and cognitive effects of alcohol use. Adolescent alcohol use is related to changes in brain structure and function. Heavy alcohol use is associated with poorer cognitive functioning.
In 2022, according to the National Survey on Drug Use and Health (NSDUH), about 19.7% of youth ages 14 to 15 reported having at least 1 drink in their lifetime. 1. In 2022, 5.8 million youth ages 12 to 20 reported drinking alcohol beyond "just a few sips" in the past month. 2.
Alcohol use among adolescents frequently involves binge drinking rather than more frequent consumption of fewer drinks on each occasion. Binge drinking is defined as 4 drinks for women and 5 drinks for men within a 2-hour period. 10 However, this criterion is thought to be too high, particularly for younger adolescents. 11 A detailed clinical report discussing binge drinking was published by ...
Use of alcohol at an early age is associated with future alcohol-related problems. 4,-,6 Data from the National Longitudinal Alcohol Epidemiologic Study 4 substantiated that the prevalence of both lifetime alcohol dependence and alcohol abuse show a striking decrease with increasing age at onset of use. For those aged 12 years or younger at first use, the prevalence of lifetime alcohol ...
Youth use of alcohol remains a pervasive social and public health concern in the United States and a leading cause of disability and mortality during adolescence.1,2 Alcohol use in adolescence has a distinct pattern from adult drinking, whereby adolescents may have fewer drinking occasions but consume relatively high levels per occasion ...
Alcohol use by children, adolescents, and young adults under the legal drinking age of 21 produces human tragedies with alarming regularity.Motor vehicle crashes, homicides, suicides, and other unintentional injuries are the four leading causes of death of 15- to 20-year-olds, and alcohol is a factor in many of these deaths.
Alcohol as a mediator. Inspired by the Actor Network Theory (ANT), we draw attention to how nonhuman objects - in this case alcohol - act on users, engage in practices, and operate in networks (assemblages) (Latour, Citation 2005, p. 68).The actor-network refers to the relations between human and non-human actors (Latour, Citation 1994), and in the context of this study, the relations ...
Alcohol use by young people is dangerous, not only because of the risks associated with acute impairment, but also because of the threat to their long-term development and well-being.Traffic crashes are perhaps the most visible of these dangers, with alcohol being implicated in nearly one-third of youth traffic fatalities.
Background Youth substance use is a public health problem globally, where alcohol is one of the drugs most consumed by children, and youth prevention is the best intervention for drug abuse.
Prospective studies of alcohol or AUD predicting MDD or depressive symptoms. One longitudinal study that focused only on the adolescent years found that higher frequency of alcohol use during early adolescence was associated with MDD during late adolescence 33.Several studies including assessments from adolescence until young adulthood have consistently shown that AUD and sub-threshold AUD ...
Substance abuse during adolescence. The use of substances by youth is described primarily as intermittent or intensive (binge) drinking and characterized by experimentation and expediency (Degenhardt et al., Citation 2016; Morojele & Ramsoomar, Citation 2016; Romo-Avilés et al., Citation 2016).Intermittent or intensive substance use is linked to the adolescent's need for activities that ...
The level of alcohol abuse among the youth has decreased during the past three decades, but in some cases the changes are insignificant. The most significant improvements are apparent when the use of alcohol within the past 12 months is assessed. For example, almost 80% of 12 - graders, over 70% of 10-graders, and almost 55% of 8-graders ...
Alcohol use is typically established during adolescence and initiation of use at a young age poses risks for short- and long-term health and social outcomes. ... Fifty-five peer-reviewed papers and one report were eligible for inclusion in this review. ... Tobacco and alcohol use among the youth of the agricultural tea industry in Assam, India ...
The drugs young people are using—and the way they're using them—have also changed, and psychologists say this needs to inform educational efforts around substance use. Alcohol and cocaine are less popular than they were in the 1990s; use of cannabis and hallucinogens, which are now more salient and easier to obtain, were higher than ever ...
500 Words Essay on Alcoholism Introduction. Alcoholism, also known as Alcohol Use Disorder (AUD), is a chronic disease characterized by an inability to control or abstain from alcohol use despite its negative repercussions. It is a multifaceted disease, with complex interactions between genetic, environmental, and psychological factors.
Introduction and background. Drug misuse is a widespread issue; in 2016, 5.6% of people aged 15 to 26 reported using drugs at least once [].Because alcohol and illegal drugs represent significant issues for public health and urgent care, children and adolescents frequently visit emergency rooms [].It is well known that younger people take drugs more often than older adults for most drugs.
Teens and drinking has continued to progress over the years and the depressant has consumed many lives. Drinking exposure has begun as early as 12 years old, with girls drinking at around the age of 13 and boys at around the age of 11. The inclination to explore the usage of alcohol is caused by many factors such as trying to forget all of one ...
Research shows that fewer drinks in the same timeframe result in the same BAC in youth; only 3 drinks for girls, and 3 to 5 drinks for boys, depending on their age and size. *A BAC of 0.08 percent corresponds to 0.08 grams per deciliter, or 0.08 grams per 100 milliliters. ... Monitor Alcohol Use in Your Home. If you keep alcohol in your home ...
Alcohol is a depressant, which means it slows the function of the central nervous system. Alcohol actually blocks some of the messages trying to get to the brain. This alters a person's perceptions, emotions, movement, vision, and hearing. In very small amounts, alcohol can help a person feel more relaxed or less anxious.
Underage drinking is very common in the United States. Alcohol is the most commonly used and abused drug in the United States, even more so than illicit drugs (Marijuana, Cocaine, etc…) and tobacco. "In 2012 the National Survey on Drug Use and Health reported that 24% of youth aged 12 to 20 years drink alcohol and 15% reported binge drinking.