
The Compass for SBC
Helping you Implement Effective Social and Behavior Change Projects
Project Example
Home > All Project Examples > Learning for Life: Classroom Activities for HIV and AIDS Education

Learning for Life: Classroom Activities for HIV and AIDS Education
This workbook provides activities to help students prevent new HIV infections and gain skills related to coping with all aspects of HIV and AIDS. Gaining this knowledge and these skills can help students live a healthy lifestyle, complete a basic education, and consequently reach their potential to attain their life goals.
The book covers all aspects of HIV and AIDS education, which includes not only basic information about HIV and AIDS and prevention strategies, but also HIV counseling, testing, treatment, and care; gender inequalities; stigma and discrimination; and involvement of people living with or affected by HIV and AIDS. It also contains lessons tailored to students in three different age groups: under age 10, ages 10–14, and ages 15+. The age groups have been determined by the changes that occur in the development of children and adolescents in relation to cognitive ability and psychosocial and sexual growth.
Source: Education Development Center, Education International, World Health Organization
Date of Publication: August 9, 2021
SIMILIAR RESOURCES
- Toolkit for Transition of Care and Other Services for Adolescents Living with HIV
- Positive Connections: Leading Information and Support Groups for Adolescents Living with HIV
- Adolescents Living with HIV (ALHIV) Toolkit
- Engaging Men in HIV and AIDS at the Service Delivery Level
- Orientation Programme on Adolescent Health for Health-Care Providers
- How to Conduct Effective Pretests
- Addressing the Needs of Young People Living with HIV
- Optimizing Entry Into and Retention in HIV Care and ART Adherence for PLWHA
- Interpersonal Communication for Immunization (IPC-I)
- Training Toolkit on MSM Programming for the MENA Region
- Treating Adolescents with HIV: Tools for Building Skills in Cultural Competence, Clinical Care, and Support
- Caring for Those with HIV Learning Package
- BA Zambia Implementation Package: Ni Zii!: A Toolkit for Implementors
- Choose Life: A Guide for Peer Educators and Youth Leaders
- Sexual and Reproductive Health Training Manual for Young People
Primary Audience(s)
Topic areas.
- HIV and AIDS
Share this Article
< Back to my filtered results
Learning for life: classroom activities for HIV and AIDS education
The EFAIDS Programme partners Education International, the Education Development Centre and the World Health Organisation present the most recent EFAIDS resource "Learning for Life: Classroom Activities for HIV and AIDS education" a toolkit destined to support teachers to address themes relating to HIV and AIDS with their students. The kit is composed of worksheets classified according to age groupings; under 10, 10-14 years, 15 and older. Age-appropriate activities and lesson plan templates combine to give teachers a valuable reference around which to conduct lessons with their pupils designed to foster skills to protect themselves from HIV and support those in their schools and communities who are living with HIV. The book adopts a life-skills approach whereby students are empowered to take responsibility for their own decision-making and are provided with the knowledge conducive to safe behaviour. Activities to overcome stigma and discrimination related to HIV and AIDS are included in each age-group section and students are encouraged to adopt inclusive values. The EFAIDS Programme advocates a broad based approach to school health with HIV and AIDS addressed within the wider context of healthy lifestyles. After consultation and testing during 2009 with teacher unions in the Caribbean and sub-Saharan Africa regions the publication is now available to be downloaded online or ordered on CD. EI encourages teacher unions participating in the EFAIDS Programme to tailor the material to the classroom context in their countries. To facilitate its wide use in schools in Africa, Asia and the Caribbean, the toolkit is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Licence, meaning that users are free to copy, distribute and adapt the text as long as the source is attributed as "Learning for Life: Classroom Activities for HIV and AIDS education".
What Are HIV and AIDS?
- How Is HIV Transmitted?
- Who Is at Risk for HIV?
- Symptoms of HIV
- U.S. Statistics
- Impact on Racial and Ethnic Minorities
- Global Statistics
- HIV and AIDS Timeline
- In Memoriam
- Supporting Someone Living with HIV
- Standing Up to Stigma
- Getting Involved
- HIV Treatment as Prevention
- Pre-exposure Prophylaxis (PrEP)
- Post-exposure Prophylaxis (PEP)
- Preventing Sexual Transmission of HIV
- Alcohol and HIV Risk
- Substance Use and HIV Risk
- Preventing Perinatal Transmission of HIV
- HIV Vaccines
- Long-acting HIV Prevention Tools
- Microbicides
- Who Should Get Tested?
- HIV Testing Locations
- HIV Testing Overview
- Understanding Your HIV Test Results
- Living with HIV
- Talking About Your HIV Status
- Locate an HIV Care Provider
- Types of Providers
- Take Charge of Your Care
- What to Expect at Your First HIV Care Visit
- Making Care Work for You
- Seeing Your Health Care Provider
- HIV Lab Tests and Results
- Returning to Care
- HIV Treatment Overview
- Viral Suppression and Undetectable Viral Load
- Taking Your HIV Medicine as Prescribed
- Tips on Taking Your HIV Medication Every Day
- Paying for HIV Care and Treatment
- Other Health Issues of Special Concern for People Living with HIV
- Alcohol and Drug Use
- Coronavirus (COVID-19) and People with HIV
- Hepatitis B & C
- Vaccines and People with HIV
- Flu and People with HIV
- Mental Health
- Mpox and People with HIV
- Opportunistic Infections
- Sexually Transmitted Infections
- Syphilis and People with HIV
- HIV and Women's Health Issues
- Aging with HIV
- Emergencies and Disasters and HIV
- Employment and Health
- Exercise and Physical Activity
- Food Safety and Nutrition
- Housing and Health
- Traveling Outside the U.S.
- Civil Rights
- Workplace Rights
- Limits on Confidentiality
- National HIV/AIDS Strategy (2022-2025)
- Implementing the National HIV/AIDS Strategy
- Prior National HIV/AIDS Strategies (2010-2021)
- Key Strategies
- Priority Jurisdictions
- HHS Agencies Involved
- Learn More About EHE
- Ready, Set, PrEP
- Ready, Set, PrEP Pharmacies
- Ready, Set, PrEP Resources
- AHEAD: America’s HIV Epidemic Analysis Dashboard
- HIV Prevention Activities
- HIV Testing Activities
- HIV Care and Treatment Activities
- HIV Research Activities
- Activities Combating HIV Stigma and Discrimination
- The Affordable Care Act and HIV/AIDS
- HIV Care Continuum
- Syringe Services Programs
- Finding Federal Funding for HIV Programs
- Fund Activities
- The Fund in Action
- About PACHA
- Members & Staff
- Subcommittees
- Prior PACHA Meetings and Recommendations
- I Am a Work of Art Campaign
- Awareness Campaigns
- Global HIV/AIDS Overview
- U.S. Government Global HIV/AIDS Activities
- U.S. Government Global-Domestic Bidirectional HIV Work
- Global HIV/AIDS Organizations
- National Black HIV/AIDS Awareness Day February 7
- HIV Is Not A Crime Awareness Day February 28
- National Women and Girls HIV/AIDS Awareness Day March 10
- National Native HIV/AIDS Awareness Day March 20
- National Youth HIV & AIDS Awareness Day April 10
- HIV Vaccine Awareness Day May 18
- National Asian & Pacific Islander HIV/AIDS Awareness Day May 19
- HIV Long-Term Survivors Awareness Day June 5
- National HIV Testing Day June 27
- Zero HIV Stigma July 21
- Southern HIV/AIDS Awareness Day August 20
- National Faith HIV/AIDS Awareness Day August 27
- National African Immigrants and Refugee HIV/AIDS and Hepatitis Awareness Day September 9
- National HIV/AIDS and Aging Awareness Day September 18
- National Gay Men's HIV/AIDS Awareness Day September 27
- National Latinx AIDS Awareness Day October 15
- World AIDS Day December 1
- Event Planning Guide
- U.S. Conference on HIV/AIDS (USCHA)
- National Ryan White Conference on HIV Care & Treatment
- AIDS 2020 (23rd International AIDS Conference Virtual)
Want to stay abreast of changes in prevention, care, treatment or research or other public health arenas that affect our collective response to the HIV epidemic? Or are you new to this field?
HIV.gov curates learning opportunities for you, and the people you serve and collaborate with.
Stay up to date with the webinars, Twitter chats, conferences and more in this section.
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
What Is HIV?
HIV ( human immunodeficiency virus ) is a virus that attacks cells that help the body fight infection, making a person more vulnerable to other infections and diseases. It is spread by contact with certain bodily fluids of a person with HIV, most commonly during unprotected sex (sex without a condom or HIV medicine to prevent or treat HIV), or through sharing injection drug equipment.
If left untreated, HIV can lead to the disease AIDS ( acquired immunodeficiency syndrome ).
The human body can’t get rid of HIV and no effective HIV cure exists. So, once you have HIV, you have it for life. Luckily, however, effective treatment with HIV medicine (called antiretroviral therapy or ART) is available. If taken as prescribed, HIV medicine can reduce the amount of HIV in the blood (also called the viral load) to a very low level. This is called viral suppression. If a person’s viral load is so low that a standard lab can’t detect it, this is called having an undetectable viral load. People with HIV who take HIV medicine as prescribed and get and keep an undetectable viral load can live long and healthy lives and will not transmit HIV to their HIV-negative partners through sex .
In addition, there are effective methods to prevent getting HIV through sex or drug use, including pre-exposure prophylaxis (PrEP) , medicine people at risk for HIV take to prevent getting HIV from sex or injection drug use, and post-exposure prophylaxis (PEP) , HIV medicine taken within 72 hours after a possible exposure to prevent the virus from taking hold. Learn about other ways to prevent getting or transmitting HIV .
What Is AIDS?
AIDS is the late stage of HIV infection that occurs when the body’s immune system is badly damaged because of the virus.
In the U.S., most people with HIV do not develop AIDS because taking HIV medicine as prescribed stops the progression of the disease.
A person with HIV is considered to have progressed to AIDS when:
- the number of their CD4 cells falls below 200 cells per cubic millimeter of blood (200 cells/mm3). (In someone with a healthy immune system, CD4 counts are between 500 and 1,600 cells/mm3.) OR
- they develop one or more opportunistic infections regardless of their CD4 count.
Without HIV medicine, people with AIDS typically survive about 3 years. Once someone has a dangerous opportunistic illness, life expectancy without treatment falls to about 1 year. HIV medicine can still help people at this stage of HIV infection, and it can even be lifesaving. But people who start HIV medicine soon after they get HIV experience more benefits—that’s why HIV testing is so important.
How Do I Know If I Have HIV?
The only way to know for sure if you have HIV is to get tested . Testing is relatively simple. You can ask your health care provider for an HIV test. Many medical clinics, substance abuse programs, community health centers, and hospitals offer them too. If you test positive, you can be connected to HIV care to start treatment as soon as possible. If you test negative, you have the information you need to take steps to prevent getting HIV in the future.
To find an HIV testing location near you, use the HIV Services Locator .
HIV self-testing is also an option. Self-testing allows people to take an HIV test and find out their result in their own home or other private location. With an HIV self-test, you can get your test results within 20 minutes. You can buy an HIV self-test kit at a pharmacy or online. Some health departments or community-based organizations also provide HIV self-test kits for a reduced cost or for free. You can call your local health department or use the HIV Testing and Care Services Locator to find organizations that offer HIV self-test kits near you. (Contact the organization for eligibility requirements.)
Note: State laws regarding self-testing vary and may limit availability. Check with a health care provider or health department Exit Disclaimer for additional testing options.
Learn more about HIV self-testing and which test might be right for you .
Related HIV.gov Blogs
- HIV Testing Day National HIV Testing Day
- World AIDS Day
- HIVinfo.NIH.gov – HIV and AIDS: The Basics
- CDC – HIV Basics
- NIH – HIV/AIDS
- OWH – HIV and AIDS Basics
- VA – HIV/AIDS Basics
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

HIV/AIDS Awareness and Knowledge among Secondary School Students in China
With a goal of helping design appropriate HIV/AIDS education and prevention programs for adolescents in China, we analyzed data from 995 secondary school students in Nanjing. Our analysis examined the students’ sources of HIV/AIDS information and assessed the overall level, and possible gender and grade (middle school vs. high school) differences, in their HIV/AIDS awareness and knowledge. Data in the current study indicated an overall low and inconsistent level of AIDS knowledge among secondary school students in China. Most of the students could identify models of HIV transmission, but a large proportion held misconceptions regarding symptoms, activities that did not transmit the virus, treatment and preventive measures. The level of using school, family and peers for obtaining information about HIV/AIDS was generally low. There was a discrepancy between the level of utilization and trust of mass media as the main source of HIV/AIDS knowledge. Findings are discussed in terms of implications for HIV/AIDS prevention and education among adolescents in China.
Introduction
While the actual human immunodeficiency virus (HIV) seroprevalence in China remains uncertain, the current official estimate of numbers of persons infected exceeds 740,000 ( China Daily 2009 ). The majority of reported cases are young adults from 20 to 39 years of age ( Chen et al. 2004 ).The steady increase of HIV infection in China underscores the urgent need for education and intervention efforts ( Gill 2006 ; Wu et al. 2007 ). One area of concern for the Chinese government has been the low level of HIV/AIDS awareness and knowledge among the general population ( Gill 2006 ; Wu et al. 2007 ). While still controversial ( Helweg-Larsen and Collins 1997 ; Svenson et al. 1997 ), research in the United States and other Western countries has suggested that sufficient knowledge regarding AIDS is a necessary, albeit inadequate, first step toward effective AIDS prevention and intervention efforts ( DiMatteo 1991 ; Fisher and Fisher 1992 ). Global literature has found that lack of knowledge is often accompanied by initiating or maintaining risky behaviour, limited adoption of preventive measures and negative attitudes toward people living with HIV and AIDS ( Herek et al. 2002 ). The Chinese government has repeatedly emphasized the importance of AIDS knowledge and education (e.g., State Council 1998 ; Wu et al. 2007 ).
While limited data are available about the level of HIV/AIDS awareness and knowledge among adolescents and young adults, existing studies in China suggest an inadequate level of AIDS knowledge and awareness for young adults and other populations. For example, a previous study among 1081 students from eight colleges in two metropolitan areas (Beijing and Nanjing) revealed an inconsistent level of AIDS knowledge among students, with a significant gender and grade difference ( Li et al. 2004 ). While HIV/AIDS knowledge is limited among young adults and in the general population in China, lack of knowledge among adolescents might be even more alarming. This population is at a critical stage of developing sexual intentions and behaviours and forming attitudes toward sexuality and HIV/AIDS-related issues. Because the behaviours and attitudes of a new generation of young people will affect China’s future HIV/AIDS epidemic, education and prevention efforts targeting adolescents have great potential to curtail that epidemic. To develop culturally and developmentally appropriate HIV/AIDS education and prevention programs among adolescents in China, it is necessary to assess their knowledge and awareness of the disease. However, with a few exceptions (e.g., Ip et al. 2001 ), most existing studies of HIV/AIDS knowledge and attitudes among young people were conducted in college populations ( Gao et al. 2001 ; Higgins and Sun 2007 ; Li et al. 2004 ), and limited data are available for secondary school students. Therefore, the current study was designed to assess the overall level of HIV/AIDS awareness and knowledge and to explore possible gender and grade (i.e., middle school vs. high school) differences in AIDS knowledge among secondary school students. The study goal was to help design appropriate HIV/AIDS education and prevention programs for adolescents.
Participants
Data were collected from 10 secondary schools N = 995) in Nanjing, the capital city of Jiangsu province, with a population of 5.3 million. Secondary education in China consists of middle schools (Grades 7 through 9) and high schools (Grades 10 through 12). The local research team members, who were educational researchers in Nanjing and had extensive experience in conducting research in the local schools, were asked to identify schools based on a number of criteria. Participating schools had to serve the general public from a wide range of socio-economic backgrounds and had to be representative of local schools in terms of number of student enrolled and student–teacher ratio. The study protocol was approved by the Institutional Review Boards at West Virginia University in the United States and the Institute of Higher Education Research at Nanjing University in China.
Survey Procedure
School administrators were approached for permission to conduct the survey in their schools. Once the local research team received this permission, they randomly approached classrooms in the schools and recruited students in the classrooms. Approximately 100 students were recruited from each participating school. The research team informed the students that the survey was for research only and that participation was voluntary. Informed consent was obtained before students participated in the survey. A self-administered questionnaire was distributed to the students in attendance in the selected classrooms on the day of survey. Teachers (including those who provided assistance with recruitment) were asked to leave the classrooms during survey administration. Responses were anonymous, and participants were assured of the confidentiality of their response. Each participant was assigned an arbitrary identification number. No identifiable personal information was recorded in the survey or database. Approximately 99% of those approached agreed to complete the questionnaire.
Individual characteristics.
Individual characteristics assessed were gender, age, grade, ethnicity (Han or non-Han, with Han accounting for 92% of the total population nationwide), school performance (4-point scale ranging from “mostly A’s” to “mostly D’s”) and perceived physical health (4-point scale ranging from “excellent” to “poor”). Students were also asked whether they were student leaders or representatives of various groups in the school (e.g., study group, students’ clubs and class- or school-wide organizations). They were also asked whether they received an allowance from parents and whether they were an only child. As well, they were asked if they were dating and whether they had engaged in a number of pre-coital activities (e.g., hugging, kissing and foreplay).
Family characteristics.
Students were asked about their family composition (e.g., living with both birth parents, parents divorced). Paternal and maternal education levels were measured on a 6-point scale ranging from “below elementary school” to “graduate school.” Paternal and maternal occupations were measured using an 11-point response option (e.g., workers, peasants, professionals, administrators, government employees, unemployed). Perceived family economic status was measured using family monthly income on a 6-point scale: below 300 yuan, 300–500, 500–1000, 1000–3000, 3000–5000 and more than 5000 yuan (6.82 Chinese yuan = approximate 1 US dollars).
HIV/AIDS awareness.
Students were asked about their perceived overall AIDS awareness on a 4-point scale: “a lot,” “some,” “little” and “nothing.” Students were also asked whether they knew that AIDS is caused by a virus called “human immunodeficiency virus” (yes/no).
Source of AIDS information.
Students were asked whether they had received AIDS information in the past month from any of 16 sources (e.g., television, radio, magazine, newspaper and billboard). They were asked to select one source they believed could provide the most reliable information. As well, they were asked whom they would turn to if they had a question about AIDS (e.g., doctors, parents, teachers, friends or an AIDS hotline).
AIDS knowledge.
There were three sets of 25 AIDS knowledge questions in different formats. The first consisted of 11 true/false items assessing knowledge of definition and causation. The second contained 12 questions querying modes of HIV transmission on a 5-point scale (very likely, likely, not sure, unlikely and very unlikely). For the purpose of data analysis, the “very likely” and “likely” responses were combined into “likely.” Similarly, “unlikely” and “very unlikely” were combined into “unlikely.” The third set consisted of two questions about AIDS symptoms and preventive measures, with a 4-point scale ranging from “strongly agree” to “strongly disagree.” Responses were combined into two categories, “agree” (strongly agree and agree) and “disagree” (disagree and strongly disagree).
These 25 items were reorganized into five categories of AIDS knowledge: AIDS definition/symptoms (three items), true transmission modes (four items), false transmission modes (ten items), clinical outcomes (three items) and treatment/prevention (five items). The percentage of correct answers was used as a composite score for each of the categories.
First, differences in individual and family characteristics by gender and grade (i.e., middle school vs. high school) were examined using ANOVA (for continuous variables) and the Chi-square test (for categorical variables). Second, the associations between AIDS awareness and selected individual and family characteristics were assessed using ANOVA or the Chi-square test. Third, sources of AIDS knowledge were examined by gender and grade. The “most reliable” ranking was calculated using percentage of endorsement for each of the information resources. Fourth, AIDS knowledge was examined by gender and grade using the Chi-square test. Finally, general linear model (GLM) analysis was performed to assess the effects of gender, grade and their interaction on AIDS knowledge. To control for the potentially confounding effect of family socio-economic status (SES), family income was employed as a proxy of family SES to be included in GLM analysis as a covariate.
Sample Characteristics
The sample consisted of 41% middle school students and 59% high school students, with equal proportions of males and females. The mean age was 15.16 years, with 13.75 for middle school students and 16.10 for high school students. Ninety-six percent of the sample was of Han ethnicity, and 89% lived with both birth parents. As shown in Table 1 , there were some gender and grade differences in demographic characteristics. More female than male students reported being a student/club leader (57% vs. 49%; p < .01), but fewer of them reported excellent/good health (74% vs. 82%; p < .01). More middle school than high school students reported having divorced parents (12% vs. 6%; p < .0001) and receiving top academic performance (e.g., mostly A’s) in school (24% vs. 11%; p < .0001). As well, middle school students reported a higher level of parental education, although only the difference regarding maternal education reached statistical significance ( p < .01). Consistent with their developmental stages, more high school than middle school students reported dating (27% vs. 8%; p < .0001) and engaging in pre-coital activities (23% vs. 13%; p < .0001).
Sample characteristics of 995 secondary students in China
HIV/AIDS Awareness
As shown in Table 2 , 66% of students felt that they knew “a lot or some” about AIDS and 34% knew “little or nothing.” AIDS awareness (or perceived AIDS knowledge) differed significantly by age, as older adolescents (e.g., high school students) perceived themselves knowledgeable about AIDS ( p < .0001). Students’ AIDS awareness level differed significantly according to their parents’ level of education ( p < .01), whether their parents had a professional job ( p < .05) and family monthly income ( p < .0001). Regarding the question of whether they knew about AIDS being caused by HIV, male gender, higher age, being an only child and higher family SES (i.e., higher parental education, professional job and higher family income) were associated with higher levels of awareness. Among students who knew the cause of AIDS, 16% reported they had been dating, compared with 22% of students who said they did not know the cause of AIDS ( p < .05). There was no difference in terms of HIV/AIDS awareness by engagement in pre-coital activities (hugging, kissing and foreplay), although more students engaging in these activities thought that they knew “a lot or some” about AIDS.
HIV/AIDS awareness among secondary students in China
Sources of AIDS Information
Sixty-eight percent of the sample reported having received, in the previous month, information about AIDS from newspapers, 61% from television programs, 60% from the health department/physicians and 48% from magazine articles ( Table 3 ). Forty-five percent reported the source as public information/news boards, 40% as radio programs, 36% as books, 33% as bill posts and 31% as school. Twenty-nine percent reported having received the information from displays in shop windows, 24% from their friends and peers or community organizations, 23% from parents or relatives, 14% from displays in the airport, 13% from the AIDS hotline and 12% from displays on a bus or taxi. While more female students received AIDS information from newspapers (71% vs. 65%; p < .05), more male students received it from other channels (e.g., a bus or taxi display, an airport display, the AIDS hotline). More high school than middle school students received AIDS information from newspapers ( p <.001) and magazine articles ( p <.05), health professionals ( p <.05), radio programs ( p <.01) and public news/information boards ( p <.01).
Sources of HIV/AIDS knowledge among secondary school students in China (%)
Thirty-four percent of the middle and high school students identified television programs as the “most reliable source” of AIDS information, and 32% endorsed health department/physicians (23% middle and 38% high school students; data not shown]). Thirteen percent endorsed AIDS hotlines (16 middle and 12% high school students), followed by books (8%) and newspapers (4%). About 2% of students endorsed radio programs, school and family members. Less than 1% of the sample endorsed community organizations, friends/peers, magazines or various public displays. Endorsements were similar between males and females across all sources.
As shown in the lower section of Table 3 , about half of the youth said they would ask physicians or turn to an AIDS hotline for AIDS-related questions in the future. More high school than middle school students said they would ask physicians (60% vs. 44%, p < .0001). Forty percent of the sample (47% males vs. 34% females, p < .0001) said they would go to local health departments. One quarter (21% male vs. 29% females, p < .01) said they would ask their parents, and about one tenth said they would ask their friends.
AIDS Knowledge
As shown in Table 4 , students responded correctly to 56% of the AIDS knowledge questions. The subcategory with the highest correct response rate was the true transmission mode (87% correct responses), while false transmission mode had the lowest (34% correct responses). Males were more knowledgeable than females in general (57% vs. 54%, p < .01). Males were more knowledgeable about definition/symptoms (61% vs. 54%, p < .0001), false transmission mode (37% vs. 31%, p < .01) and treatment/prevention (68% vs. 64%, p < .01). Females were more knowledgeable about the true transmission mode (89% vs. 85%, p < .01). Overall, high school students were more knowledgeable than middle school students on all categories, although there was no difference between the two groups’ knowledge of definition/symptoms and clinical outcomes.
AIDS knowledge (% of correct answers) among Chinese adolescents by gender and grade
Within all subcategories except true transmission mode, there was substantial variation by item in terms of percentage of correct responses. For example, correct responses ranged from 35% to 83% for definition/symptoms, 20% to 57% for false transmission modes, 48% to 94% for clinical outcomes and 53% to 78% for treatment/prevention.
While students were knowledgeable about the true transmission modes of HIV, there were many misconceptions about false transmission modes. More than two thirds of the sample thought (or were not sure) that a person could contract HIV by “sharing plates, fork or glass,” “using a public toilet,” “being coughed or sneezed on,” “receiving medical care from someone who has the AIDS virus” or “using a public swimming pool.” Only about one fifth did not think they would be likely to get the AIDS virus from being bitten by mosquitoes or other insects.
General linear model (GLM) analysis conducted on mean scores of five categorical scores of AIDS knowledge ( Table 5 ) confirmed the results of bivariate analysis, with significant main effects of gender (Pillai’s F = 8.254, p < .0001) and grade (Pillai’s F = 15.352, p < .0001). All the bivariate differences in various categories of AIDS knowledge by gender and grade remained similar in GLM analysis. In addition, family income was a significant covariate of AIDS knowledge in GLM.
Multivariate analysis (GLM) of AIDS knowledge among adolescents in China
Given the early stage of the HIV/AIDS epidemic in China, awareness and appropriate knowledge may play an important role in preventing further spread of the disease among adolescents and young adults. Data in the current study indicated an overall low and inconsistent level of AIDS knowledge among secondary school students in China. More than one third of students had limited awareness of HIV and AIDS. Consistent with findings from other countries (e.g., Dias et al. 2006 ; Mahat and Scoloveno 2006 ), most could identify true transmission modes, but a large proportion held misconceptions about symptoms, activities that did not transmit the virus, treatment and preventive measures.
Consistent with findings in the United States (e.g., DiClemente et al. 1986 ; Dorman and Rienzo 1988 ) and other countries (e.g., Tavoosi et al. 2004 ; Yoo et al. 2005 ), as well as findings from other populations in China ( Li et al. 2008 , 2009 ), secondary school students in China appear to rely on the mass media (e.g., newspaper, television) as their primary source of AIDS information. Likewise, students ranked television and health department/physicians as the top sources they believed provided the most reliable information about HIV/AIDS. However, only 4% endorsed the newspaper as a reliable source, despite about two thirds of the students having reported getting AIDS/HIV information from newspaper articles.
Data in the current study revealed a significant gender difference in AIDS knowledge among secondary school students, with males being more knowledgeable than females, particularly in the areas concerning HIV/AIDS definition/symptoms, false transmission modes and treatment and prevention. This finding is consistent with studies among college students in China ( Li et al. 2004 ) and other cultures such as Kuwait ( Al-Owaish, et al. 1999 ).
The data suggest that the majority of Chinese secondary school students did not get or did not intend to get HIV/AIDS information from their parents, friends/peers or school teachers. This points to the challenge of discussing sex-related matters or other taboo topics (including HIV/AIDS) with family members, friends and school teachers in Chinese society ( Gao et al. 2001 ; Li 2004 ).
These data may be limited in their representativeness of the general adolescent population in China, since the sample was largely urban, and about 70% of the Chinese population is rural. The data in the current study suggest that AIDS awareness varies among students based on family socio-economic status, with a higher level of awareness in students from wealthier families. This finding is consistent with that from a previous study, which suggested that HIV/AIDS knowledge was much lower in rural than in urban areas in China ( Chen et al. 2004 ). These findings underscore the importance of HIV/AIDS education among adolescents and young adults in rural areas and from socio-economically disadvantaged families and environments.
The findings in the present study, as one of the few efforts in assessing HIV/AIDS knowledge among adolescents in China, have several implications for HIV/AIDS prevention and education among Chinese adolescents and young adults. First, education and wider health promotion and prevention programs targeting adolescents are needed. While these efforts should include both middle and high school students, clearly programs need to begin at an earlier age level (e.g., middle or even elementary schools). HIV/AIDS education and prevention programs need to provide students with accurate information, particularly in dispelling misconceptions about causal contagion of HIV, as these misconceptions may foster negative attitudes in adolescents toward people with HIV/AIDS ( Chen et al. 2004 ).
Second, the students’ low utilization of schools, family and peers in acquiring HIV/AIDS knowledge underscores the great potential of these traditional information channels in HIV/AIDS education and prevention. As current efforts in China in HIV awareness promotion and prevention have largely relied on peer education ( Gao et al. 2001 ) and mass media campaigns ( Wu et al. 2007 ), the mobilization and active involvement of healthcare providers, schools and parents in education and prevention would be critical in fighting the HIV/AIDS epidemic in China.
Third, the knowledge gap between mode of transmission and preventive measures suggests that education and prevention efforts should emphasize the role of condoms and other components of “safer” sex. While a majority (95%) recognized that HIV could be transmitted through sexual intercourse, only about 60% of students agreed that using condoms could prevent HIV. In addition, a substantial global experience supports the observation that mere possession of accurate information does not necessarily lead to behavioural change ( Hays and Hays 1992 ; Mann et al. 1992 ). Other components of effective prevention, including efficacy building, stigma reduction and skill acquisition regarding preventive measures (e.g., condom use) are needed, beyond information dissemination. Finally, the discrepancy between levels of utilization and trust of mass media (e.g., newspapers) among adolescents warrants the attention of educators and policy-makers. The role of mass media in AIDS awareness promotion in China needs to be improved, as mass media serves as one of the main channels for the disseminating AIDS knowledge among adolescents and young adults.
Acknowledgements
This study is in part supported by the World AIDS Foundation [WAF-218 (00-014)]. The authors wish to thank dedicated students and faculty members from Nanjing University for their assistance in field data collection.
- Al-Owaish R, Mossa MAA, Anwar S, Al-Shoumer H and Sharma P. 1999. “ Knowledge, Attitudes, Beliefs, and Practices About HIV/AIDS in Kuwait .” AIDS Education and Prevention 11 ( 2 ): 163–73. [ PubMed ] [ Google Scholar ]
- Chen S, Zhang S and Westley S. 2004. “ HIV/AIDS Awareness Is Improving in China .” Asia-Pacific Population & Policy 69 : 1–4. [ Google Scholar ]
- China Daily. 2009, November 25. “ HIV/AIDS Hits 740,000 Nationwide .” Retrieved March 23, 2010. < http://www.chinadaily.com.cn/china/2009-11/25/content_9040160.htm >.
- Dias SF, Mato MG and GonÇalves AC. 2006. “ AIDS-Related Stigma and Attitudes towards AIDS-Infected People among Adolescents .” AIDS Care 18 ( 3 ): 208–14. [ PubMed ] [ Google Scholar ]
- Dorman SM and Rienzo BA. 1988. “ A Survey of University Students’ AIDS-Related Knowledge and Attitudes .” Journal of the Florida Medical Association 75 ( 7 ): 441–4. [ PubMed ] [ Google Scholar ]
- DiClemente R, Zorn J and Temoshok L. 1986. “ Adolescents and AIDS: Survey of Knowledge, Attitudes and Beliefs about AIDS in San Francisco .” American Journal of Public Health 76 : 1443–5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- DiMatteo MR 1991. The Psychology of Health, Illness, and Medical Care . Pacific Grove, CA: Brooks & Cole. [ Google Scholar ]
- Fisher JD and Fisher WA. 1992. “ Changing AIDS-Risk Behavior .” Psychological Bulletin 111 : 455–74. [ PubMed ] [ Google Scholar ]
- Gao Y, Lu ZZ, Shi R, Sun XY and Cai Y. 2001. “ AIDS and Sex Education for Young People in China .” Reproduction, Fertility and Development 13 : 729–37. [ PubMed ] [ Google Scholar ]
- Gill B 2006. Assessing HIV/AIDS Initiatives in China: Persistent Challenges and Promising Ways Forward (A report of the CSIS task force on HIV/AIDS) . Washington, DC: Center for Strategic and International Studies (CSIS). [ Google Scholar ]
- Hays H, and Hays JR. 1992. “ Students’ Knowledge of AIDS and Sexual Risk Behavior .” Psychological Reports 71 : 649–50. [ PubMed ] [ Google Scholar ]
- Helweg-Larsen M and Collins BE. 1997. “ A Social Psychological Perspective on the Role of Knowledge about AIDS in AIDS Prevention .” Current Directions in Psychological Science 6 ( 2 ): 23–6. [ Google Scholar ]
- Herek GM, Capitanio JP and Widaman KF. 2002. “ HIV-Related Stigma and Knowledge in the United States: Prevalence and Trends, 1991–1999 .” American Journal of Public Health 92 ( 3 ): 371–7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Higgins LT and Sun C. 2007. “ Gender, Social Background and Sexual Attitudes among Chinese Students .” Culture, Health & Sexuality 9 ( 1 ): 31–42. [ PubMed ] [ Google Scholar ]
- Ip W, Chau JPC, Chang AM and Lui MHL. 2001. “ Knowledge of and Attitudes toward Sex among Chinese Adolescents .” Western Journal of Nursing Research 23 ( 2 ): 211–22. [ PubMed ] [ Google Scholar ]
- Li L, Rotheram-Borus MJ, Lu Y, Wu Z, Lin C and Guan J. 2009. “ Mass Media and HIV/AIDS in China .“ Journal of Health Communication 14 ( 5 ): 424–38. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li X, Lin C, Gao Z, Stanton B, Fang X, Yin Q and Wu Y. 2004. “ HIV/STD Knowledge and the Implications for Health Promotion Programs among Chinese College Students: Geographic, Gender and Age Differences .” Health Promotion International 19 ( 3 ): 345–56. [ PubMed ] [ Google Scholar ]
- Li. Y, Scott CS and Li L. 2008. “ Chinese Nursing Students’ HIV/AIDS Knowledge, Attitudes, and Practice Intentions .” Applied Nursing Research 21 ( 3 ): 147–52. [ PubMed ] [ Google Scholar ]
- Mahat G and Scoloveno M. 2006. “ HIV/AIDS Knowledge, Attitudes, and Beliefs among Nepalese Adolescents .” Journal of Advanced Nursing 53 ( 5 ): 583–90. [ PubMed ] [ Google Scholar ]
- Mann JM, Tarantola DJM and Netter TW. 1992. AIDS in the World . Cambridge, MA: Harvard University Press. [ Google Scholar ]
- State Council. 1998. Chinese National Medium- and Long-term Strategic Plan for HIV/AIDS Prevention and Control (1998–2010) . China State Council Document GF (1998)38. Beijing, China: State Council. [ Google Scholar ]
- Svenson L, Carmel S and Varnhagen C. 1997. “ A Review of the Knowledge, Attitudes and Behaviors of University Students Concerning HIV/AIDS .” Health Promotion International 12 : 61–8. [ Google Scholar ]
- Tavoosi A, Zaferani A, Enzevaei A, Tajik P and Ahmadinezhad Z. 2004. “ Knowledge and Attitude towards HIV/AIDS among Iranian Students .“ BMC Public Health 4 : 17. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ and Detels R. 2007. “ Evolution of China’s response to HIV/AIDS .” Lancet 369 ( 9562 ): 621–3. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yoo H, Lee S, Kwon B, Chung S and Kim S. 2005. “ HIV/AIDS Knowledge, Attitudes, Related Behaviors, and Sources of Information among Korean Adolescents .“ The Journal of School Health 75 ( 10 ): 393–9. [ PubMed ] [ Google Scholar ]
Assignment on AIDS
Introduction
Society is like a looking glass. Each and every phenomenon in society is very conspicuous and crystal clear before us. Like many affairs and issues, the vulnerability of HIV/AIDS patient is blatant and flagrant to us. In a complex and complicated social fabrics, AIDS is spreading by leaps and bounds mainly because of unsafe sexual intercourse, coition and copulation. At present, traditional social values and ethos are declining and eroding in full gear. As a result, it is noted that an astronomical and massive change in behavioral, cultural pattern in society. It is straining that the HIV/AIDS patients are deprived and diverted culturally and socially. Most people think that they are the burden of family as well as society. They are dealt with humiliation by the larger segment of society. As a consequence, they do not get enough space and scope to expose themselves to others. For the overall wellbeing of AIDS patients, each and every individual should change his/her behavioral patterns towards them. To this end, all and sundry should come forward with an enriched cultural legacy in the truest sense.
AIDS is a disease that is incurable and intricate in nature. If any body is infected and afflicted with this disease, the aftermath of him/her is sure for death. Because of having this dire nature of the disease, I tried to overhaul the social, behavioral and cultural facets and factors that are intimately associated with this fatal disease. Besides, I postulated to comprehend the anticipated behavior that the infected receive from the remaining social setting in their way of life and livings.
Methodology
In the way of doing this assignment, I went through many medical journals, newspapers and most importantly, I followed lectures of my venerable class teacher. Moreover, I talked to some medical professionals about the service delivery of government and non-government infirmary in case of HIV positive patients. Admittedly, I delve into the social, behavioral and cultural factors that are inexorably coupled and compounded with the very disease, i.e., HIV/AIDS.
Causes, incidence, and risk factors
Important facts about the spread of AIDS include:
- AIDS is the sixth leading cause of death among people ages 25 – 44 in the United States, down from number one in 1995.
- The World Health Organization estimates that more than 25 million people worldwide have died from this infection since the start of the epidemic.
- In 2008, there were approximately 33.4 million people around the world living with HIV/AIDS, including 2.1 million children under age 15.
Human immunodeficiency virus (HIV) causes AIDS. The virus attacks the immune system and leaves the body vulnerable to a variety of life-threatening infections and cancers.
Common bacteria, yeast, parasites, and viruses that usually do not cause serious disease in people with healthy immune systems can cause fatal illnesses in people with AIDS.
HIV has been found in saliva, tears, nervous system tissue and spinal fluid, blood, semen (including pre-seminal fluid, which is the liquid that comes out before ejaculation), vaginal fluid, and breast milk. However, only blood, semen, vaginal secretions, and breast milk have been shown to transmit infection to others.
The virus can be spread (transmitted):
- Through sexual contact — including oral, vaginal, and anal sex
- Through blood — via blood transfusions (now extremely rare in the U.S.) or needle sharing
- From mother to child — a pregnant woman can transmit the virus to her fetus through their shared blood circulation, or a nursing mother can transmit it to her baby in her breast milk
Other methods of spreading the virus are rare and include accidental needle injury, artificial insemination with infected donated semen, and organ transplantation with infected organs.
HIV infection is NOT spread by:
- Casual contact such as hugging
- Participation in sports
- Touching items that were touched by a person infected with the virus
AIDS and blood or organ donation
- AIDS is NOT transmitted to a person who DONATES blood or organs. People who donate organs are never in direct contact with people who receive them. Likewise, a person who donates blood is never in contact with the person receiving it. In all these procedures, sterile needles and instruments are used.
- However, HIV can be transmitted to a person RECEIVING blood or organs from an infected donor. To reduce this risk, blood banks and organ donor programs screen donors, blood, and tissues thoroughly.
People at highest risk for getting HIV include
- Injection drug users who share needles
- Infants born to mothers with HIV who didn’t receive HIV therapy during pregnancy
- People engaging in unprotected sex, especially with people who have other high-risk behaviors, are HIV-positive, or have AIDS
- People who received blood transfusions or clotting products between 1977 and 1985 (before screening for the virus became standard practice)
- Sexual partners of those who participate in high-risk activities (such as injection drug use or anal sex)
AIDS begins with HIV infection. People who are infected with HIV may have no symptoms for 10 years or longer, but they can still transmit the infection to others during this symptom-free period. If the infection is not detected and treated, the immune system gradually weakens and AIDS develops.
Acute HIV infection progresses over time (usually a few weeks to months) to asymptomatic HIV infection (no symptoms) and then to early symptomatic HIV infection. Later, it progresses to AIDS (advanced HIV infection with CD4 T-cell count below 200 cells/mm3 ).
Almost all people infected with HIV, if they are not treated, will develop AIDS. There is a small group of patients who develop AIDS very slowly, or never at all. These patients are called nonprogressors, and many seem to have a genetic difference that prevents the virus from significantly damaging their immune system.
The symptoms of AIDS are mainly the result of infections that do not normally develop in people with a healthy immune system. These are called opportunistic infections.
People with AIDS have had their immune system damaged by HIV and are very susceptible to these opportunistic infections. Common symptoms are:
- Sweats (particularly at night)
- Swollen lymph glands
- Weight loss
Note: At first, infection with HIV may produce no symptoms. Some people, however, do experience flu-like symptoms with fever, rash, sore throat, and swollen lymph nodes, usually 2 – 4 weeks after contracting the virus. Some people with HIV infection stay symptom-free for years between the time when they are exposed to the virus and when they develop AIDS.
Signs and tests
CD4 cells are a type of T cell. T cells are cells of the immune system. They are also called “helper cells.”
The following is a list of AIDS-related infections and cancers that people with AIDS may get as their CD4 count decreases. In the past, having AIDS was defined as having HIV infection and getting one of these other diseases. Today, according to the Centers for Disease Control and Prevention, a person may also be diagnosed with AIDS if they are HIV-positive and have a CD4 cell count below 200 cells/mm3, even if they don’t have an opportunistic infection.
AIDS may also be diagnosed if a person develops one of the opportunistic infections and cancers that occur more commonly in people with HIV infection. These infections are unusual in people with a healthy immune system.
There is no cure for AIDS at this time. However, a variety of treatments are available that can help keep symptoms at bay and improve the quality of life for those who have already developed symptoms.
Antiretroviral therapy suppresses the replication of the HIV virus in the body. A combination of several antiretroviral drugs, called highly active antiretroviral therapy (HAART), has been very effective in reducing the number of HIV particles in the bloodstream. This is measured by the viral load (how much free virus is found in the blood). Preventing the virus from replicating can improve T-cell counts and help the immune system recover from the HIV infection.
HAART is not a cure for HIV, but it has been very effective for the past 12 years. People on HAART with suppressed levels of HIV can still transmit the virus to others through sex or by sharing needles. There is good evidence that if the levels of HIV remain suppressed and the CD4 count remains high (above 200 cells/mm3), life can be significantly prolonged and improved.
However, HIV may become resistant to one combination of HAART, especially in patients who do not take their medications on schedule every day. Genetic tests are now available to determine whether an HIV strain is resistant to a particular drug. This information may be useful in determining the best drug combination for each person, and adjusting the drug regimen if it starts to fail. These tests should be performed any time a treatment strategy begins to fail, and before starting therapy.
When HIV becomes resistant to HAART, other drug combinations must be used to try to suppress the resistant strain of HIV. There are a variety of new drugs on the market for treating drug-resistant HIV.
Treatment with HAART has complications. HAART is a collection of different medications, each with its own side effects. Some common side effects are:
- Collection of fat on the back (“buffalo hump”) and abdomen
- General sick feeling (malaise)
When used for a long time, these medications increase the risk of heart attack, perhaps by increasing the levels of cholesterol and glucose (sugar) in the blood.
Any doctor prescribing HAART should carefully watch the patient for possible side effects. In addition, blood tests measuring CD4 counts and HIV viral load should be taken every 3 months. The goal is to get the CD4 count as close to normal as possible, and to suppress the amount of HIV virus in the blood to a level where it cannot be detected.
Other antiviral medications are being investigated. In addition, growth factors that stimulate cell growth, such as erthythropoetin (Epogen, Procrit, and Recomon) and filgrastim (G-CSF or Neupogen) are sometimes used to treat AIDS-associated anemia and low white blood cell counts.
Medications are also used to prevent opportunistic infections (such as Pneumocystis jiroveci pneumonia) if the CD4 count is low enough. This keeps AIDS patients healthier for longer periods of time. Opportunistic infections are treated when they happen.
Complications
When a person is infected with HIV, the virus slowly begins to destroy that person’s immune system. How fast this occurs differs in each individual. Treatment with HAART can help slow or halt the destruction of the immune system.
Once the immune system is severely damaged, that person has AIDS, and is now susceptible to infections and cancers that most healthy adults would not get. However, antiretroviral treatment can still be very effective, even at that stage of illness.
- Do not use illicit drugs and do not share needles or syringes. Many communities now have needle exchange programs, where you can get rid of used syringes and get new, sterile ones. These programs can also provide referrals for addiction treatment.
- Avoid contact with another person’s blood. You may need to wear protective clothing, masks, and goggles when caring for people who are injured.
- Anyone who tests positive for HIV can pass the disease to others and should not donate blood, plasma, body organs, or sperm. Infected people should tell any sexual partner about their HIV-positive status. They should not exchange body fluids during sexual activity, and should use preventive measures (such as condoms) to reduce the rate of transmission.
- HIV-positive women who wish to become pregnant should seek counseling about the risk to their unborn child, and methods to help prevent their baby from becoming infected. The use of certain medications dramatically reduces the chances that the baby will become infected during pregnancy.
- Safer sex practices, such as latex condoms, are highly effective in preventing HIV transmission. HOWEVER, there is a risk of acquiring the infection even with the use of condoms. Abstinence is the only sure way to prevent sexual transmission of HIV.
The riskiest sexual behavior is receiving unprotected anal intercourse. The least risky sexual behavior is receiving oral sex. There is some risk of HIV transmission when performing oral sex on a man, but this is less risky than unprotected vaginal intercourse. Female-to-male transmission of the virus is much less likely than male-to-female transmission. Performing oral sex on a woman who does not have her period has a low risk of transmission.
HIV-positive patients who are taking antiretroviral medications are less likely to transmit the virus. For example, pregnant women who are on effective treatment at the time of delivery, and who have undetectable viral loads, give HIV to their baby less than 1% of the time, compared with 13% to 40% of the time if medications are not used.
The U.S. blood supply is among the safest in the world. Nearly all people infected with HIV through blood transfusions received those transfusions before 1985, the year HIV testing began for all donated blood.
If you believe you have been exposed to HIV, seek medical attention IMMEDIATELY. There is some evidence that an immediate course of antiviral drugs can reduce the chances that you will be infected. This is called post-exposure prophylaxis (PEP), and it has been used to prevent transmission in health care workers injured by needlesticks.
There is less information available about how effective PEP is for people exposed to HIV through sexual activity or injection drug use, but it appears to be effective. If you believe you have been exposed, discuss the possibility with a knowledgeable specialist (check local AIDS organizations for the latest information) as soon as possible. Anyone who has been sexually assaulted should consider the potential risks and benefits of PEP.
AIDS is a disease caused by the HIV infection, which is basically a weakening of one’s immune system. It can only be spread through blood transfusions, sexual contact and from an infected mother to her unborn child. There are significant misconceptions in the country about the spread and treatment of the HIV/AIDS virus even after so many years of expert knowledge on the subject. Regrettably, even within the medical professions some laid back attitudes exist. This may have been prompted by two factors. Firstly, there are hardly any separate, specialized wards for HIV/AIDS patients. Secondly, medical professionals somehow harbor superstitions about the virus.
Awareness campaigns should be conducted for the greater well being and welfare of the HIV/AIDS patients. The government should immediately ensure adequate access to treatment of the HIV/AIDS victims complete with screening and after care facilities. There should also be separate HIV/AIDS wards in health care facilities and amenities.
- The Daily Star, P-7-8, Date- 1 st December , 2011.
- Del Rio C, Curran JW. Epidemiology and prevention of acquired immunodeficiency syndrome and human immunodeficiency virus infection. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa: Elsevier Churchill Livingstone; 2009:chap 118.
- Piot P. Human immunodeficiency virus infection and acquired immunodeficiency syndrome: A global overview. In: Goldman L, Ausiello D, eds. Cecil Medicine. 23rd ed. Philadlelphia, Pa: Saunders Elsevier; 2007:chap 407.
- Sterling TR, Chaisson RE. General clinical manifestations of human immunodeficiency virus infection (including the acute retroviral syndrome and oral, cutaneous, renal, ocular, metabolic, and cardiac diseases). In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa: Elsevier Churchill Livingstone; 2009:chap 121.
Qualities of Rubber Conveyor Belting Professionals
Finding the right garden polyresin statues, discuss on korean used cars, assignment on solar radiation, effects of deforestation, the alimentary canal, escape velocity in physics, following violent protests, foxconn offers to pay employees to leave the largest iphone factory in the world, this week in apps: ios 15 public beta arrives, android app bundles to replace apks, app consumer spend hits new record, what yuga labs wants to build after raising $450m, latest post, key concepts of electromagnetic induction, electromagnet -working method, climate change impacts the microbial food web in peatlands, ice cores give the earliest proof of fast antarctic ice loss in history, flyback diode, flyback converter.
- Open access
- Published: 22 April 2024
Factors associated with voluntary HIV counseling and testing among young students engaging in casual sexual activity: a cross-sectional study from Eastern China
- Zhongrong Yang 1 na1 ,
- Wanjun Chen 2 na1 ,
- Weiyong Chen 2 ,
- Qiaoqin Ma 2 ,
- Hui Wang 2 ,
- Tingting Jiang 2 ,
- Meihua Jin 1 &
- Xin Zhou 2
BMC Public Health volume 24 , Article number: 1109 ( 2024 ) Cite this article
Metrics details
To investigate the factors associated with voluntary HIV counseling and testing (VCT) among young students engaging in casual sexual activity and to establish a scientific rationale for developing targeted intervention strategies for preventing HIV/AIDS in this population.
Stratified cluster sampling was used to conduct a survey using questionnaires to collect demographic and behavioral information for statistical analysis.
Data from 611 young students, who reported engaging in casual sexual activity, were included in the statistical analysis. Among these, 68 (11.13%) students underwent the VCT. Among young students who engaged in casual sexual activity, those who were non-Zhejiang residents (adjusted odds ratio [ aOR ]: 2.11; 95% Confidence Interval [ CI ]: 1.17–3.80), those who had received AIDS-themed lectures or health education courses from the school in the past year ( aOR = 3.96, 95% CI = 1.49–10.50), those who had received HIV risk self-assessment conducted by the school in the past year ( aOR = 2.31, 95% CI = 1.17–4.59), and those who had engaged in commercial sex activity in the past year ( aOR = 1.98, 95% CI = 1.07–3.66) were more inclined to have undergone VCT. Male students ( aOR = 0.37, 95% CI = 0.18–0.77) and those who used condoms consistently during casual sexual activity ( aOR = 0.45, 95% CI = 0.21–0.97) were less likely to undergo VCT.
Casual sexual activity was relatively prevalent among young students, posing a potential risk for HIV transmission. These findings will be instrumental in the development more effective HIV prevention and control strategies for young students. Additionally, it highlights the necessity of promoting and popularizing VCT among young students without Zhejiang province residency, who are involved in commercial sexual activity, and/or those who lacking HIV education. Moreover, additional research and implementation of refined HIV behavioral interventions specifically tailored to young students are necessary to enhance their awareness and knowledge of HIV prevention.
Peer Review reports
Introduction
Acquired immunodeficiency syndrome (AIDS), caused by the human immunodeficiency virus (HIV), poses a significant threat to public health as an infectious disease and has emerged as a major burden on healthcare systems and is a pressing global public health concern [ 1 , 2 ]. HIV, specifically targets CD4 + T lymphocytes, which play a crucial role in immune function and protecting against attacks on the human immune system. HIV infection results in the widespread destruction of these cells, gradually impairing the immune system and rendering the body susceptible to various other infections. Without treatment, this ultimately leads to systemic organ failure, which often results in death [ 3 ].
Currently, significant progress has been made in global HIV/AIDS prevention and control efforts, leading to a decline in mortality and infection rates [ 4 , 5 ]. The Joint United Nations Programme on HIV and AIDS (i.e., “UNAIDS”) launched an ambitious target of “95-95-95”; 95% of people living with HIV know their infection status, 95% of diagnosed individuals receive sustained antiretroviral therapy, and 95% of treated individuals achieve viral suppression [ 6 ]. The Chinese government places significant emphasis on HIV/AIDS prevention and control, as evidenced by the formulation, implementation, and promotion of a comprehensive range of policies, measures, nation-wide HIV testing and antiretroviral therapy. Simultaneously, China is enhancing the dissemination of knowledge regarding HIV/AIDS prevention and control to raise public awareness for self-protection. Nevertheless, HIV/AIDS prevention and control efforts at both the global and national levels in China encounter several challenges such as insufficient coverage of viral testing, treatment monitoring, and drug resistance. As such, researchers and medical institutions must make additional efforts to implement and enhance prevention and control measures to establish a solid foundation for eventual eradication of HIV/AIDS.
In recent years, there has been growing concern about the increasing severity of the HIV epidemic among young students [ 7 , 8 , 9 ]. The phrase “young people” encompasses individuals between 15 and 24 years of age. Globally, approximately 37.7 million individuals live with HIV/AIDS, approximately 90% of whom are young adults [ 10 ]. In 2017, the number of newly diagnosed cases of HIV infection among Chinese university students was more than ten times higher than in 2006, with 3077 cases reported in 2017 compared to 242 cases in 2006, and the annual growth rate during this period ranged from 30 to 50% [ 9 ]. In recent years, the number of newly reported HIV/AIDS cases among young students in China has remained stable at approximately 3,000 annually [ 11 , 12 ]. Additionally, around 100 new cases of HIV/AIDS have been diagnosed among college students in Zhejiang Province in recent years [ 9 ]. Considering their active sexual behavior, young students who engage in sexual activity may be more vulnerable to sexually transmitted diseases (STDs) including HIV [ 13 , 14 ]. Youth, being the future “pillars of society”, have the potential to contribute to the country’s development by receiving high-quality education and training and becoming professionals in various fields. Therefore, preventing the transmission of HIV among young students is indispensable to their well-being and to society as a whole.
The primary goal of HIV voluntary counseling and testing (VCT) is to encourage and assist individuals in comprehending their HIV infection status and implement appropriate intervention measures through the provision of HIV testing and counseling services [ 15 ]. There are many qualitative reasons for participating in VCT, including individual attention, community mobilization, sexual health services, and awareness of self-protection [ 15 , 16 ]. Research has demonstrated the positive impact of VCT on HIV prevention and control among young students by enhancing their knowledge and awareness of HIV and offering a confidential, reliable, and convenient testing approach, which ultimately increases the chances of early detection, diagnosis, and treatment of individuals who have contracted HIV [ 17 ]. Infected individuals can benefit from VCT through personalized prevention and treatment strategies aimed at reducing the risk for HIV transmission. HIV-negative individuals can enhance their self-protection awareness through counseling, effectively reducing the risk for HIV infection.
To effectively reduce HIV transmission among young students, it is important to implement measures to strengthen health education, promote shifts in social attitudes, and ensure the provision of accessible and affordable VCT services. Currently, there is a limited body of research exploring the factors associated with VCT among young students who engage in casual sexual behavior(s). Casual sexual activities are common among young students, yet there is limited research specifically looking at VCT uptake among this population. Understanding the factors influencing VCT uptake among students engaging in casual sex is crucial for developing targeted interventions to promote HIV testing and reduce transmission. To address this research gap, a cross-sectional survey was conducted in Zhejiang Province, eastern China, to investigate the factors related to VCT uptake among university students engaging in casual sexual activity. This will not only help in strengthening the motivation for our research but also provide a foundation for future studies and public health initiatives aimed at improving HIV testing rates and promoting safer sexual practices among this vulnerable population.

Materials and methods
Sampling method and participants.
The present study used a cross-sectional survey design to investigate factors associated with VCT among college students from 13 universities in 11 districts and municipalities in Zhejiang Province between October and November, 2018. Among these, 3 universities were located in Hangzhou, and each of the remaining 10 cities had 1 university. Universities were selected based on recommendations from local disease control centers. Sample populations were collected using a stratified cluster sampling method. Three departments were randomly selected from each university using a random number table. Subsequently, the selected departments were further divided into four levels based on the students’ academic year (1st to 4th year). Finally, classes were chosen randomly from each level using a random number table. Data collection involved 1241 classes with 31,674 participating students.
Ethical statement
This study protocol was approved by ethics committee of the Zhejiang Provincial Center for Disease Control and Prevention, and this study complied with the declaration of Helsinki and all methods were performed in accordance with the relevant guidelines and regulations of the ethics committee of the Zhejiang Provincial Center for Disease Control and Prevention (No.2018-036). All the participants provided written informed consent.
Questionnaire design
The questionnaire was developed by reviewing the domestic and international literature [ 18 , 19 ], engaging in discussions with the research team, and conducting a preliminary survey of students in a school class. The questionnaire primarily addresses demographic factors, knowledge of HIV prevention and treatment, attitudes toward sex, participation in interventions, and self-confidence in condom usage. Knowledge-based questions in the survey queried statements such as “Whether it can be judged by appearance that a person is infected with HIV” and “Whether it is necessary to actively seek VCT after engaging in high-risk sexual behavior”. Casual sex was defined as the sexual activity that the participant had engaged in with other males or females in the past year, apart from their fixed boyfriend or girlfriend. Commercial sex refers to sexual activity involving monetary transactions.
The effectiveness of measuring condom use involved 3 questions: level of confidence in discussing condom use with sexual partners before engaging in sexual activity; the level of confidence in abstaining from sex or engaging in sexual activity without using a condom, and level of confidence in preparing a condom before engaging in sexual activity. Each question offered respondents 5 options for their confidence levels: very confident, quite confident, confident, not confident, very unconfident, which corresponding scores of 3, 2, 1, 0, and − 1, respectively. The measurement scores were categorized as ≤ 4 or below 5–8, and 9. As per the assessment, the Cronbach’s alpha coefficient for this measurement was determined to be 0.794.
Data collection
This study used a cross-sectional survey design. Students within the school were organized and assembled by teachers, who used their cellphones to scan quick response (i.e., “QR”) codes and completed online electronic surveys. Students not attending the school received a survey link and were instructed to complete it independently based on the instructions provided. Study participants included college students who self-reported engaging in casual sexual activity. There were no statistically significant differences in basic characteristics, such as age, gender, grade, province of household registration, hometown of origin, monthly living expenses, and family relationship, between the excluded population and the participants included in the study. The study participants were categorized into VCT and non-VCT groups.
Household registration system in China
Household registration, known as “hukou,” denotes the officially registered residence documented by the public security authorities and specified in the resident’s household registration booklet and identity card. In line with the chinese household registration regulations and the prevailing household registration management system, newborns must be registered for birth within one month of their arrival by the household head, relatives, or caretakers at the local household registration office where the infant resides. The allocation of urban fundamental public services, encompassing compulsory education, employment assistance, basic pensions, primary healthcare, and housing security, among other services, is determined by the population figures of the hukou region in different areas. Discrepancies may exist across regions, subject to meeting the national minimum guarantee standards. Given potential changes in college students’ hukou due to residential relocations post-enrollment, this study defines the household registration based on the province of registration before university admission.
Quality control
The investigators consisted of professionals from the local disease prevention and control center and counselors from the surveyed classes at various universities. They received standardized training and completed anonymous surveys using a standardized questionnaire. Before the study, the investigators explained the purpose, significance, methods, and privacy protection policy to the research participants, with this information also included in the introduction of the survey questionnaire. The research participants were informed that the investigation aimed to develop strategies for preventing HIV and other STDs among students. Participants were assured of anonymity and that only group data would be analyzed, at the exclusion of any individual identifiable data.
Data analysis
Data analysis was performed using SPSS version 23.0 (IBM Corporation, Armonk, NY, USA). Various variables, including age, sex, grade, province of household registration, source of origin hometown, monthly living expenses, family relationships, sexual attitudes, HIV/AIDS prevention and control knowledge, and sexual behavior characteristics, are expressed as composition ratios or rates. The chi-squared test was used to compare the demographic characteristics of the participants in the VCT. The independent variables included demographic factors, sexual attitudes, knowledge of prevention and control, acceptance of the intervention, and self-efficacy in condom use. Furthermore, a single-factor logistic regression method was used to analyze factors associated with VCT among the participants. Variables with P < 0.2 were incorporated into the model for multivariable logistic regression analysis, ensuring statistical significance. Differences with P < 0.05 were considered to be statically significant.
Demographic characteristics of participants
The study included a sample of university students, consisting of 14,320 males and 17,354 females. In total, 3,771 individuals reported engaging in sexual activity and informed their sexual partners. Among these, 675 (17.90% sexually active students) reported engaging in casual sex. Of these, 64 individuals with missing data were excluded, leaving 611 students who were selected for the analysis, as shown in Fig. 1 . Among the participants who engaged in casual sex, 68 (11.13%) underwent VCT, and had a mean (± SD) age of 20.34 ± 1.98 years. The remaining 543 individuals, comprising 88.87% of the sample, did not undergo VCT, and had an average age of 20.07 ± 1.45 years. Statistically significant differences (i.e., P < 0.05) were observed between the VCT and non-VCT groups regarding sex and grade, whereas no statistically significant differences (i.e., P ≥ 0.05) were found in terms of age, province of household registration, hometown of origin, monthly living expenses, and family relationships (Table 1 ).
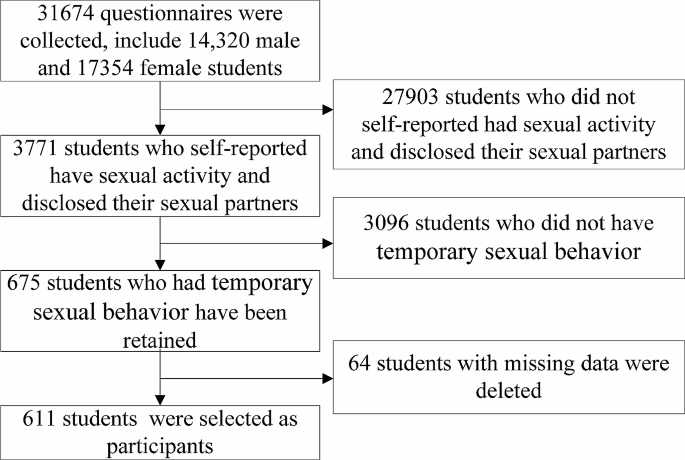
The flowchart for the inclusion and exclusion process
Univariable analysis of factors associated with VCT among the participants
Results of univariable analysis (Table 2 ) revealed that participants who had received AIDS-themed lectures or health education courses from school in the past year (crude odds ratio [ cOR ] 3.75), those who had received HIV risk self-assessment conducted by school in the past year ( cOR = 3.52), those who had engaged in sexual activity with a steady partner in the past year ( cOR = 3.04), and those who had engaged in commercial sex activity in the past year ( cOR = 3.24 ) were more likely to have undergone VCT. Participants who believed that “Whether it can be judged by appearance that a person is infected with HIV” ( cOR = 0.50), and those who used condoms consistently or occasionally during casual sexual activity ( cOR = 0.28 and 0.41, respectively) were less likely to have undergone VCT.
The proportion of participating partners who consistently used condoms was 37.48% (229/611). The rate of consistent condom use was 31.19% (131/420) among the 420 participants who had steady sexual partners in the past year. Participants whose types of steady partners included non-students or students from a different school among the participant ( cOR = 0.47 or 0.49, respectively), and those who used condom consistently during sexual activity with steady partner(s) ( cOR = 0.37) were less likely to have undergone VCT.
Multivariable analysis of factors associated with VCT among the participants
Logistic multivariable regression analysis was performed on variables with P < 0.2 in the univariable analysis, as well as variables including sex, grade, and province of household registration. Analysis revealed (Table 2 ) that, compared with participants in the corresponding control group, the proportion of those with non-Zhejiang household registration undergoing VCT increased by 111% (adjusted OR [ aOR ]: 2.11; 95% Confidence Interval [ CI ]: 1.17–3.80), the proportion of participants who had received AIDS-themed lectures or health education courses from the school in the past year increased by 296% ( aOR : 3.96; 95% CI : 1.49–10.50), the proportion of participants who had received HIV risk self-assessment conducted by the school in the past year increased by 131% ( aOR : 2.31; 95% CI : 1.17–4.59), the proportion of participants who had engaged in commercial sex in the past year increased by 98% ( aOR : 1.98; 95% CI : 1.07–3.66), the proportion of participants who were male participants decreased by 63% ( aOR : 0.37; 95% CI : 0.18–0.77), the proportion of participants who used condom consistently during casual sexual activity decreased by 55% ( aOR : 0.45; 95% CI : 0.21–0.97).
Currently, VCT is a widely acknowledged and effective approach to mitigate the spread of HIV, which enables individuals to be aware of their HIV infection status, choose to undergo HIV testing, and assess the risk for HIV infection, while also developing plans to reduce the risk for HIV infection [ 20 ]. In this study, 68 out of 611 participants (11.13%) had engaged in casual sex underwent VCT, which was lower than that of research in other countries [ 15 , 21 , 22 ]. With advances in social development and globalization, individuals are more open to and proactive in accepting knowledge and information related to AIDS. Nevertheless, the prevention and control of HIV infection still has many challenges, including social discrimination, lack of resources for HIV/AIDS prevention and treatment, and low treatment adherence [ 23 ]. Therefore, there is a need for the continuous promotion of HIV/AIDS awareness and education, strengthening community cooperation, and government support to improve understanding and awareness of HIV/AIDS prevention.
Results of the present study indicated that the proportion of non-Zhejiang residents participating in VCT increased by 111%, which substantiates the expansion and promotion of testing services in Zhejiang Province. This was achieved through various measures, including the establishment of accessible VCT centers, intensified promotion, and educational efforts. The objective was to encourage greater engagement in HIV testing among residents with non-Zhejiang household registration. These measures were part of broader initiatives aimed at increasing VCT uptake among all young students in Zhejiang Province, which promoted the provision of services, making it relatively convenient for university students to access testing services, especially for non-Zhejiang household registration students to participate. Expanded service coverage of VCT and increased efficacy of promotional activities likely contributed to the observed increase in HIV testing rates [ 24 , 25 ]. Nevertheless, it is essential to acknowledge that the 111% increase in VCT participation does not entirely represent the prevalence of HIV infection among residents with non-Zhejiang household registration. Therefore, additional research is required to enhance the promotion and management of HIV/AIDS prevention.
A comprehensive understanding of the transmission routes and preventive measures of AIDS is essential for both individuals and society [ 26 ]. The findings revealed a 296% increase in VCT participation among individuals who engaged in AIDS-themed lectures or school-led health education classes, showcasing the proactive promotion and implementation of AIDS education. Schools’ initiatives in AIDS education primarily encompass professional lectures, training courses, promotional materials, and counseling services [ 21 , 27 ]. This trend demonstrates students’ awareness of AIDS-related matters and validates the efficacy of school-based AIDS education. The notable improvement in these data holds substantial importance in advancing AIDS prevention and control, as well as safeguarding the well-being and safety of students. The active engagement of students in VCT signifies their eagerness to comprehend their health status and promptly undertake the appropriate measures. This positive attitude indicates the effectiveness of AIDS education and establishes a firm groundwork for preventing and controlling the spread of AIDS.
Findings of this study suggest a 131% increase in the proportion of participants who voluntarily sought VCT after undergoing an HIV risk self-assessment in the past year. HIV risk self-assessment increases awareness of the risk for HIV infection and encourages HIV testing [ 28 ]. Active participation in these activities enables students to better identify the potential HIV risks that they may encounter, thereby fostering voluntary engagement in VCT. A prospective controlled study involving healthcare students and teenagers found that peer educators focusing on sexual and reproductive health (SRH) showed a significantly greater improvement in SRH knowledge scores compared to their peers. Furthermore, adolescents engaged in public peer-led health prevention programs demonstrated a more pronounced enhancement in their SRH knowledge scores than their counterparts [ 29 ]. Future efforts should focus on strengthening the promotion of AIDS education and risk self-assessment activities among student groups. By enhancing awareness and knowledge of HIV/AIDS, students will be more inclined to proactively undergo VCT to safeguard their health.
Commercial sexual activity often involves sexual practices among partners for whom infection status is unknown, thereby increasing the risk for STDs [ 30 ]. The study results indicated a 98% increase in the proportion of participants who engaged in commercial sexual activity in the past year and underwent VCT, compared with the group that did not engage in commercial sexual activity. This increase may reflect the participants’ improved understanding of the importance of sexual health and education. Individuals involved in commercial sexual activity may possess better knowledge of sexual health and infectious diseases, as well as the importance of regular sexual health check-ups [ 31 , 32 ]. This heightened awareness will play a crucial role in enhancing sexual health and curbing STD transmission. Failure to take the necessary safety precautions or engage in sexual relationships with partners whose HIV infection status is unknown may increase their susceptibility to infection [ 15 , 27 ]. Hence, an increase in the proportion of individuals engaged in commercial sexual activity who undergo VCT can also be considered a protective measure to detect and manage early HIV infection. This finding underscores the importance of enhancing sexual health education and ensuring accessible VCT services to foster healthier sexual behaviors and control transmission of STDs.
The study findings suggested a 63% decrease in the proportion of male participants in the VCT group compared with the female student group. This increase suggests a heightened focus on self-protection and health among female students. With the growing awareness and understanding of HIV/AIDS, female students are becoming more aware of their own risks and responsibilities, and are actively seeking VCT services to protect their own and others’ health. Numerous non-governmental organizations across various countries advocate and facilitate women’s engagement in VCT services through various measures, including expanding opportunities and resources, and enhancing support and protection for women [ 33 ]. Concurrently, there is a need to augment male students’ involvement in VCT services, which encompasses enhancing education, reinforcing resource allocation, and fostering a more inclusive and supportive environment in social, cultural, and economic terms.
The use of condoms is widely recognized as an effective method for reducing the risk for contracting STDs, and the failure to consistently use condoms during casual sexual encounters increases the risk for transmission of STDs [ 34 ]. Findings from this study revealed that compared to those who never utilized condoms, there was a 55% reduction in the proportion of individuals who consistently used condoms for VCT during casual sexual encounters. Consequently, this reduction in proportion can be interpreted as an indication of behavioral change and a decline in awareness of sexual safety. This could be attributed to either a diminished perception of STD risk among participants or a lack of awareness regarding the significance of the VCT [ 27 ]. Consequently, it is imperative to enhance health education and promote endeavors to augment individuals’ understanding of the significance of practicing safe sex and consistently using condoms during sexual activities.
However, the implementation of VCT activities among young students faces challenges and influencing factors. First, there is a lack of comprehensive sexual education. In many schools and universities, the content and coverage of sex education are very limited, resulting in students engaging in risky sexual activity with inadequate knowledge of the risks and prevention measures for HIV transmission [ 35 ]. Even if VCT services are available within or near school campuses, these students may be unaware of their importance, leading to lower enthusiasm for and participation rates in VCT. Additionally, social and cultural beliefs may have influenced these results. In some societal and cultural environments, discussing sexual behavior and HIV may be regarded as indecent or “taboo”, and could also trigger moral controversies. This discourages students from actively seeking VCT. Some students may choose to remain silent and not seek HIV-related healthcare and counseling services out of fear of discrimination or stigmatization. Additionally, the accessibility of health services cannot be overlooked in terms of their impact on VCT. Some schools and universities lack specialized health facilities, making it difficult for students to access HIV testing and counseling services. If students incur high costs or time undergoing testing, this can reduce their likelihood of participating in VCT activities.
The present study had several limitations, the first of which was its cross-sectional survey design, which precluded the establishment of causal relationships between the factors explored. The potential impact of social desirability bias on self-reported behaviors and attitudes towards VCT and sexual practices would affect the results in this study. Additionally, patients may have experienced recall bias while completing the questionnaires, potentially introducing bias into the results. However, we performed multiple regression analysis to account for confounding variables and minimize systematic errors attributable to individual factors. Moreover, certain variables in the study contained missing values, which may have introduced a degree of bias in the study population. We removed missing variables or classified them separately without changing the results of the multivariate statistical analysis. Given the insignificance of the proportion of missing values in these variables, we excluded them before performing statistical analyses and relevant calculations. However, we did not perform a comparative analysis of awareness of AIDS prevention and control knowledge among students from different majors in this study. For example, students studying medicine or biology may be more aware than study samples in the literature, which may have affected the results. Owing to China’s vast geography and significant differences in socioeconomic levels, and although this survey selected Zhejiang Province as the research region, there may be certain differences when extrapolated to the national level. As such, additional multi-center prospective randomized cohort studies are necessary to validate our findings.
Conclusions
Findings of the present study suggested that college students who engaged in casual sexual activity were more likely to participate in VCT if they were non-Zhejiang residents, attended HIV/AIDS lectures or health education classes within the past year, underwent HIV risk self-assessment, or engaged in commercial sexual activity. Conversely, male students and those who consistently used condoms during casual sexual encounters were less likely to participate in VCT. These findings provide valuable insights for the development of effective HIV prevention and control strategies for young students, highlighting the importance of strengthening VCT promotion and outreach efforts among non-Zhejiang residents, students engaged in commercial sexual activity, and those who have not received HIV/AIDS education. Furthermore, it is crucial to undertake additional research and implement HIV behavioral interventions specifically tailored to young(er) students. This will enhance the awareness of HIV infection and promote safer practices.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
95% confidence interval
Human immunodeficiency virus
Acquired immunodeficiency syndrome
Chinese Yuan
Sexually transmitted diseases
voluntary counseling and testing
Sexual and reproductive health
Li K, Liu B, Ma R, Zhang Q. HIV tissue reservoirs: current advances in Research. AIDS Patient Care STDs. 2023;37(6):284–96.
Article PubMed Google Scholar
Zegeye B, Anyiam FE, Ahinkorah BO, Ameyaw EK, Budu E, Seidu AA, Yaya S. Women’s decision-making capacity and its association with comprehensive knowledge of HIV/AIDS in 23 sub-saharan African countries. Archives Public Health = Archives belges de sante Publique. 2022;80(1):111.
Article Google Scholar
Perkins MV, Joseph SB, Dittmer DP, Mackman N. Cardiovascular Disease and thrombosis in HIV infection. Arterioscler Thromb Vasc Biol. 2023;43(2):175–91.
Article CAS PubMed Google Scholar
Wu Z, Yang C, Ma Y, Wang Y, Zhang Z, Liu Z, Li P, Guo H, Jin Y. The prevalence of HIV-infected patients with virological suppression but a CD4(+) T-cell Count of = 200 Cells/mm(3) after highly active antiretroviral therapy initiation: a Meta-analysis</at. AIDS Rev. 2022;24(1):16–23.
Post WS, Haberlen SA, Witt MD, Zhang L, Jacobson LP, Brown TT, Margolick JB, Kingsley L, Palella FJ Jr., Budoff M. Suboptimal HIV suppression is associated with progression of coronary artery stenosis: the Multicenter AIDS Cohort Study (MACS) longitudinal coronary CT angiography study. Atherosclerosis. 2022;353:33–40.
Article CAS PubMed PubMed Central Google Scholar
Ninnoni JP, Nsatimba F, Agyemang SO, Commey IT, Bennin L, Agyare E, Gyimah L, Senya K, Baddoo NA, Obiri-Yeboah D. An exploratory qualitative study of the psychological effects of HIV diagnosis; the need for early involvement of mental health professionals to improve linkage to care. BMC Public Health. 2023;23(1):2518.
Article PubMed PubMed Central Google Scholar
Mereu A, Liori A, Fadda L, Puddu M, Chessa L, Contu P, Sardu C. What do young people know about HIV? Results of a cross sectional study on 18-24-year-old students. J Prev Med Hyg. 2022;63(4):E541–8.
PubMed PubMed Central Google Scholar
Reeves JM, Zigah EY, Shamrock OW, Aidoo-Frimpong G, Dada D, Batten J, Abu-Ba’are GR, Nelson LE, Djiadeu P. Investigating the impact of stigma, accessibility and confidentiality on STI/STD/HIV self-testing among college students in the USA: protocol for a scoping review. BMJ open. 2023;13(2):e069574.
Chen W, Yang J, Jiang J, He L, Xu Y, Zheng J, Jiang J, Pan X. A spatial analysis of the epidemiology of HIV-infected students in Zhejiang Province, China. BMC Infect Dis. 2021;21(1):430.
Tsegaw M, Kassie A, Alemnew W. Youth friendly reproductive health service utilization and its associated factors among secondary school students, East Belesa district, northwest, Ethiopia, 2022. BMC Health Serv Res. 2023;23(1):184.
Li G, Jiang Y, Zhang L. HIV upsurge in China’s students. Science. 2019;364(6442):711.
Yang Z, Chen W, Ma Q, Chen W, Zhou X, Wang H, Jiang T. Factors associated with the choice of having multiple sexual partners among male college students with casual heterosexual sex in Zhejiang Province, Eastern China. BMC Infect Dis. 2023;23(1):784.
Dai Z, Mi G, Yu F, Chen G, Wang X, He Q. Using a Geosocial networking app to Investigate New HIV infections and related risk factors among Student and Nonstudent men who have sex with men in Chengdu, China: open Cohort Study. J Med Internet Res. 2023;25:e43493.
Mazibuko NE, Saruchera M, Okonji EF. A qualitative exploration of Factors Influencing Non-use of Sexual Reproductive Health Services among University students in South Africa. Int J Environ Res Public Health. 2023;20(3):2418.
Alem AT, Sisay MM, Alemayehu AM. Factors affecting Voluntary HIV/AIDS counseling and testing service utilization among Youth in Gondar City, Northwest Ethiopia. HIV AIDS (Auckl). 2020;12:667–73.
CAS PubMed Google Scholar
Alem AZ, Teshale AB, Liyew AM, Tesema GA, Tesema AK, Yeshaw Y. Determinants of HIV voluntary counseling and testing: a multilevel modelling of the Ethiopian Demographic and Health Survey. BMC Womens Health. 2022;22(1):7.
Teffo ME, Mokgatle MM. Assessing condom use and views on HIV Counselling and Testing among TVET College Students in Limpopo Province, South Africa. Int J Environ Res Public Health. 2023;20(11):6044.
Zhao Y, Wong CK, Miu HY, Yuen WW, Chin WY, Luo T, Wong WC. Translation and validation of a Condom Self-Efficacy Scale (CSES) Chinese Version. AIDS Educ Prevention: Official Publication Int Soc AIDS Educ. 2016;28(6):499–510.
Hanna KM. An adolescent and young adult condom self-efficacy scale. J Pediatr Nurs. 1999;14(1):59–66.
Masrie A, Shawel S, Tamire A, Mandefro M, Gebru T, Seboka Ergiba M, Getachew M. Implementation evaluation of HIV/AIDS Voluntary Counseling and Testing (VCT) Service at Public Health Facilities of Akaki Kality Sub-city, Addis Ababa, Ethiopia. HIV AIDS (Auckl). 2023;15:503–18.
PubMed Google Scholar
Rasweswe MM, Bopape MA, Ntho TA. HIV Voluntary Counselling and Testing Utilisation among School of Healthcare Sciences Undergraduate students at the University of Limpopo. Int J Environ Res Public Health. 2024;21(2):180.
Zango AB, Stutterheim SE, de Vries N, Crutzen R. Determinants of preventive sexual behaviours among first year university students in Beira city, central Mozambique: a cross-sectional study. Reproductive Health. 2024;21(1):3.
Robinson A, Cooney A, Fassbender C, McGovern DP. Examining the Relationship between HIV-Related Stigma and the Health and Wellbeing of children and adolescents living with HIV: a systematic review. AIDS Behav. 2023;27(9):3133–49.
Duflo E, Dupas P, Ginn T, Barasa GM, Baraza M, Pouliquen V, Sharma V. HIV prevention among youth: a randomized controlled trial of voluntary counseling and testing for HIV and male condom distribution in rural Kenya. PLoS ONE. 2019;14(7):e0219535.
Eastment MC, Wanje G, Richardson BA, Nassir F, Mwaringa E, Barnabas RV, Sherr K, Mandaliya K, Jaoko W, McClelland RS. Performance of family planning clinics in conducting recommended HIV counseling and testing in Mombasa County, Kenya: a cross-sectional study. BMC Health Serv Res. 2019;19(1):665.
Wang N, Lan G, Zhu Q, Chen H, Huang J, Meng Q, Shen Z, Liang S, Wu X, Luo L, et al. HIV Epidemiology, Care, and treatment outcomes among Student and Nonstudent youths Living with HIV in Southwest China between 1996 and 2019: historical cohort study. JMIR Public Health Surveillance. 2023;9:e38881.
Cheruiyot C, Magu D, Mburugu P, Sagwe D. Uptake and utilization of institutional voluntary HIV testing and counseling services among students aged 18–24 in Kenya’s public universities. Afr Health Sci. 2019;19(4):3190–9.
Luo Q, Wu Z, Mi G, Xu J, Scott SR. Using HIV Risk Self-Assessment Tools to increase HIV Testing in men who have sex with men in Beijing, China: App-based Randomized Controlled Trial. J Med Internet Res. 2023;25:e45262.
Nuttall A, Mancini J, Lizin C, Hamzaoui S, Mariotti S, Louesdon H, Tardieu S, Viton JM, Delotte J, Bretelle F. Multidisciplinary peer-led sexual and reproductive health education programme in France, a prospective controlled-study. BMC Public Health. 2022;22(1):2239.
Zhou Y, Luo Y, Cheng F, Zeng H, Wu L, Gao L, Xu J. Migration experiences and reported commercial and non-commercial sexual behaviors among newly diagnosed HIV infections in China: a cross-sectional study. BMC Infect Dis. 2023;23(1):370.
Sok S, Hong R, Chhoun P, Chann N, Tuot S, Mun P, Brody C, Yi S. HIV risks and recent HIV testing among transgender women in Cambodia: findings from a national survey. PLoS ONE. 2020;15(9):e0238314.
Fan S, Yang Z, Hou F, Yu M, Luo Z, Liao M, Gong Y, Meng X, Cai Y, Zou H. HIV and Syphilis and sexual risk behaviours among men who have sex with men attending university in China: a systematic review and meta-analysis. Sex Health. 2019;16(6):554–65.
Inambao M, Kilembe W, Canary LA, Czaicki NL, Kakungu-Simpungwe M, Chavuma R, Wall KM, Tichacek A, Pulerwitz J, Thior I, et al. Transitioning couple’s voluntary HIV counseling and testing (CVCT) from stand-alone weekend services into routine antenatal and VCT services in government clinics in Zambia’s two largest cities. PLoS ONE. 2017;12(10):e0185142.
Mitzel LD, Johnson MW, Vanable PA. Delay Discounting and sexual Decision-Making: understanding Condom Use Behavior among U.S. College Students. Arch Sex Behav. 2023;52(6):2605–17.
Ocran B, Talboys S, Shoaf K. Conflicting HIV/AIDS sex education policies and mixed messaging among educators and students in the Lower Manya Krobo Municipality, Ghana. Int J Environ Res Public Health 2022, 19(23):15487.
Download references
Acknowledgements
The authors would like to thank all participants for their valuable contributions to this study.
This study was funded by Huzhou science and technology research plan project (2023GYB28) and Key Laboratory of Emergency Detection for Public Health of Huzhou. The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Author information
Zhongrong Yang and Wanjun Chen contributed equally to this work.
Authors and Affiliations
Huzhou Center for Disease Control and Prevention, Zhejiang province, 313000, Huzhou, China
Zhongrong Yang & Meihua Jin
Department of HIV/STD control and prevention, Zhejiang Provincial Center for Disease Control and Prevention, No.3399, Binsheng Road, 310051, Hangzhou, Zhejiang province, China
Wanjun Chen, Weiyong Chen, Qiaoqin Ma, Hui Wang, Tingting Jiang & Xin Zhou
You can also search for this author in PubMed Google Scholar
Contributions
C.W.Y., M.Q.Q., C.W.J., Z.X., J.M.H. and Y.Z.R. wrote the main manuscript text. C.W.Y., Y.Z.R., W.H. and J.T.T. prepared Table 1, and 2; Fig. 1. All authors reviewed and approved the manuscript.
Corresponding author
Correspondence to Weiyong Chen .
Ethics declarations
Ethics approval and consent to participate.
This study protocol was approved by ethics committee of the Zhejiang Provincial Center for Disease Control and Prevention, and this study complied with the declaration of Helsinki and all methods were performed in accordance with the relevant guidelines and regulations of the ethics committee of the Zhejiang Provincial Center for Disease Control and Prevention (No.2018-036). All participants signed an informed consent form.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yang, Z., Chen, W., Chen, W. et al. Factors associated with voluntary HIV counseling and testing among young students engaging in casual sexual activity: a cross-sectional study from Eastern China. BMC Public Health 24 , 1109 (2024). https://doi.org/10.1186/s12889-024-18562-2
Download citation
Received : 29 December 2023
Accepted : 09 April 2024
Published : 22 April 2024
DOI : https://doi.org/10.1186/s12889-024-18562-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cross-sectional study
- Casual sexual activity
- Associated factors
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Study record managers: refer to the Data Element Definitions if submitting registration or results information.
Search for terms

- Advanced Search
- See Studies by Topic
- See Studies on Map
- How to Search
- How to Use Search Results
- How to Find Results of Studies
- How to Read a Study Record

- Learn About Studies
- Other Sites About Studies
- Glossary of Common Site Terms

- Submit Studies to ClinicalTrials.gov PRS
- Why Should I Register and Submit Results?
- FDAAA 801 and the Final Rule
- How to Apply for a PRS Account
- How to Register Your Study
- How to Edit Your Study Record
- How to Submit Your Results
- Frequently Asked Questions
- Support Materials
- Training Materials

- Selected Publications
- Clinical Alerts and Advisories
- Trends, Charts, and Maps
- Downloading Content for Analysis

- ClinicalTrials.gov Background
- About the Results Database
- History, Policies, and Laws
- ClinicalTrials.gov Modernization
- Media/Press Resources
- Linking to This Site
- Terms and Conditions
- Search Results
- Study Record Detail

Double-blind, Placebo-controlled, Randomized Study of the Tolerability, Safety and Immunogenicity of an Inactivated Whole Virion Concentrated Purified Vaccine (CoviVac) Against Covid-19 of Children at the Age of 12-17 Years Inclusive"
- Study Details
- Tabular View
- No Results Posted

Recruitment of volunteers will be competitive. A maximum of 450 children aged 12 to 17 years inclusive will be screened in the study, of which it is planned to include and randomize 300 children who meet the criteria for inclusion in the study and do not have non-inclusion criteria, data on which will be used for subsequent safety and immunogenicity analysis.
Group 1 - 150 volunteers who will be vaccinated with the Nobivac vaccine twice with an interval of 21 days intramuscularly.
Group 2 - 150 volunteers who will receive a placebo twice with an interval of 21 days intramuscularly.
In case of withdrawal of volunteers from the study, their replacement is not provided.

Inclusion Criteria:
- Volunteers must meet the following inclusion criteria:
Type of participants • Healthy volunteers.
Age at the time of signing the Informed Consent
• from 12 to 17 years inclusive (12 years 0 months 0 days - 17 years 11 months 30 days).
Paul • Male or female.
Reproductive characteristics
- For girls with a history of mensis - a negative pregnancy test and consent to adhere to adequate methods of contraception (use of contraceptives within a month after the second vaccination). Girls should use methods of contraception with a reliability of more than 90% (cervical caps with spermicide, diaphragms with spermicide, condoms, intrauterine spirals).
- For young men capable of conception - consent to adhere to adequate methods of contraception (use of contraceptives within a month after the second vaccination). Young men and their sexual partners should use methods of contraception with a reliability of more than 90% (cervical caps with spermicide, diaphragms with spermicide, condoms, intrauterine spirals).
Research procedures
- Written Informed consent of a volunteer (14 years and older) and one of the parents to participate in a clinical trial.
- Volunteers who are able to fulfill Protocol requirements (i.e. answer phone calls, fill out a Self-observation Diary, come to control visits).
Non-inclusion criteria:
- Volunteers cannot be included in the study if any of the following criteria are present:
SARS-CoV-2 infection
- A case of established COVID-19 disease confirmed by PCR and/or ELISA in the last 6 months.
- History of contacts with confirmed or suspected cases of SARS-CoV-2 infection within 14 days prior to vaccination.
- Positive IgM or IgG to SARS-CoV-2 detected on Screening.
- Positive PCR test for SARS-CoV-2 at Screening / before vaccination.
Diseases or medical conditions
- Serious post-vaccination reaction (temperature above 40 C, hyperemia or edema more than 8 cm in diameter) or complication (collapse or shock-like condition that developed within 48 hours after vaccination; convulsions, accompanied or not accompanied by a feverish state) to any previous vaccination.
- Burdened allergic history (anaphylactic shock, Quincke's edema, polymorphic exudative eczema, serum sickness in the anamnesis, hypersensitivity or allergic reactions to the introduction of any vaccines in the anamnesis, known allergic reactions to vaccine components, etc.).
- Guillain-Barre syndrome (acute polyradiculitis) in the anamnesis.
- The axillary temperature at the time of vaccination is more than 37.0 ° C.
- Positive blood test for HIV, syphilis, hepatitis B/C.
- Acute infectious diseases (recovery earl
Exclusion Criteria:
- • Withdrawal of Informed consent by a volunteer and/or a parent of a volunteer;
- The volunteer was included in violation of the inclusion/non-inclusion criteria of the Protocol;
- Availability of inclusion/non-inclusion criteria before vaccination;
- Any condition of a volunteer that requires, in the reasoned opinion of a medical researcher, the withdrawal of a volunteer from the study;
- The established fact of pregnancy before the second vaccination;
- Taking unauthorized medications (see section 6.2);
- The volunteer's incompetence with the study procedures;
- The volunteer refuses to cooperate or is undisciplined (for example, failure to attend a scheduled visit without warning the researcher and/or loss of communication with the volunteer), or dropped out of observation;
- For administrative reasons (termination of the study by the Sponsor or regulatory authorities), as well as in case of gross violations of the protocol that may affect the results of the study.
- For Patients and Families
- For Researchers
- For Study Record Managers
- Customer Support
- Accessibility
- Viewers and Players
- Freedom of Information Act
- HHS Vulnerability Disclosure
- U.S. National Library of Medicine
- U.S. National Institutes of Health
- U.S. Department of Health and Human Services
- Phone: +90 (212) 875 19 08
- E-Mail: [email protected]
- Company Profile
- Company Policy
- Mission and Vision
- Certificates
- Aluminium Windows
- Aluminium Doors
- Aluminium Sliding Elements
- Aluminium Curtain Walls
- Aluminium Skylight Elements
- Aluminium Frames for Safety and Security
- Aluminium Conservatories
- Metal Panel Sheet Claddings
- Aluminium Entrance Frames
- Glass Structures
- Complementary Items
- Lightweight Steel Structures
- Human Resources OPEN
We are Hiring!
Current job openings, bookkeeper and accounts administrator.
- Organizing the internal accounts, company files and reporting to accountants, company directors,
- Liaising with the suppliers, certificates bodies, external consultants, clients and main office staff ( Fluent in English )
- Assisting Project Managers and Directors with all the paperwork involved during the flow of business,
Preferred Candidate
- Years of Experience: 3-25 years of experience
- Graduated School: Business, Economics, Accounting to similar disciplines
- Level of Education: High School ( Graduate ), Bachelor's ( Graduate )
- Languages: English ( Reading: Advanced, Writing: Advanced, Speaking: Advanced
- Microsoft Office: Excel, Powerpoint, Word ( Advanced )
Position Information
- Company Industry: Aluminium, Building, Architecture
- Job Type: Permanent / Full-time
- Position Level: Staff
- Job Location: United Kingdom, London

IMAGES
VIDEO
COMMENTS
This learning experience about HIV/AIDS for the middle school grades should be delivered by a certified health educator. It should take place during regularly scheduled lessons. Parents will have been notified of the lessons taking place and will be invited to share in the learning via various take-home assignments.
information about STI/HIV. Please see . Community Resources list on our website. 1. Distribute the handout: Health Services Detective. Review it with students. 2. Invite students to complete this assignment at home with a parent or guardian. 3. Be sure to debrief this activity next class.
the support that a person needs when they have HIV or lost their parents to AIDS and how you can provide that support." KEY MESSAGES OF LESSON: 1) People who are living with HIV or AIDS need our support and understanding. 2) People who have had family members die from HIV or AIDS need our support and understanding.
Grade 6: HIV/AIDS. Overview. Students learn about the difference between HIV and AIDS, risk and protective factors for HIV, and that it is safe to be friends with someone who has HIV. Students watch a video and participate in a small group activity to review the fluids that transmit HIV and some true/false statements. Timing.
• Anyone who has unprotected sex is at risk for getting an STI, including HIV. • Not having sex is the only 100% sure way not to get an STI. • STIs do not get passed from casual contact. Lesson Plan - STI Transmission Part I ... HIGH SCHOOL - GRADES 9-12, 2ND EDITION PUBLIC HEALTH - SEATTLE & KING COUNTY, REVISED 2015 www.kingcounty.gov ...
HIV and AIDS These activities will help your student understand how HIV and AIDS affect the body, ... 15 minutes to make the assignment, plus more student time outside class. Activity: Read the TeensHealth.org articles, then using the Internet or resources in your school library, find out: How many people in the United States and worldwide have ...
A person is diagnosed with AIDS when the person has a very low number of T cells (or CD4 cells) or shows signs of a serious infection. Most people in North America get infected by HIV by: Sexual contact Kissing, hugging, or shaking hands Sharing needles or syringes with another person. and c) and b) All of the above.
This workbook provides activities to help students prevent new HIV infections and gain skills related to coping with all aspects of HIV and AIDS. Gaining this knowledge and these skills can help students live a healthy lifestyle, complete a basic education, and consequently reach their potential to attain their life goals. The book covers all ...
This lesson plan is designed for middle school biology or life science classes and introduces human immunodeficiency virus (HIV) infection and (acquired immune deficiency syndrome (AIDS) as a public health problem, including its modes of transmission, treatment, and prevention. Students should have covered lessons in human anatomy and ...
The HIV and AIDS Education Training Module is a training programme for Teachers involved in the delivery of Basic and Higher Education. It consists of 22 similarly structured lessons covering an array of useful topics such as HIV and AIDS: the basics, History and Prevalence of the HIV and AIDS epidemic, HIV and the Immune System, Life Cycle of HIV, How HIV is transmitted, Symptoms of HIV ...
To facilitate its wide use in schools in Africa, Asia and the Caribbean, the toolkit is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Licence, meaning that users are free to copy, distribute and adapt the text as long as the source is attributed as "Learning for Life: Classroom Activities for HIV and AIDS education".
Sequim High School make up assignment for state mandated HIV education: Seniors, In response to the threat of HIV/AIDS in our population, the 1988 Washington State Legislature mandated that a program of prevention education be presented to public school students, beginning in fifth grade. This includes students in the Running Start program.
Review slides 4 and 5 on definitions of HIV and AIDS. 6. If time allows, facilitate discussion about HIV and AIDS myths (slide 7). State 1 or 2 myths and ask participants to describe why it is a myth. 7. Review slides 6-9 about how HIV is and is not transmitted, and stages of HIV/AIDS progression. If time allows ask the class the following:
Human immunodeficiency virus (HIV) is an infection that attacks the body's immune system. Acquired immunodeficiency syndrome (AIDS) is the most advanced stage of the disease. HIV targets the body's white blood cells, weakening the immune system. This makes it easier to get sick with diseases like tuberculosis, infections and some cancers.
AIDS is the late stage of HIV infection that occurs when the body's immune system is badly damaged because of the virus. In the U.S., most people with HIV do not develop AIDS because taking HIV medicine as prescribed stops the progression of the disease. A person with HIV is considered to have progressed to AIDS when: the number of their CD4 ...
Random assignment of participants to intervention: Random selection of participants for assessment: ... Ye X, Shen X, et al. (2010) Evaluation of a school-based HIV/AIDS peer-led prevention programme: the first intervention trial for children of migrant workers in China. Int J STD AIDS 21: 82-86. [Google Scholar]
HIV/AIDS awareness. Students were asked about their perceived overall AIDS awareness on a 4-point scale: "a lot," "some," "little" and "nothing.". Students were also asked whether they knew that AIDS is caused by a virus called "human immunodeficiency virus" (yes/no). Source of AIDS information.
The ten essays in this volume look at the many and complex relationships between HIV/AIDS and education. It is clear that education in an AIDS-infected world cannot be the same as that in an AIDS-free world. It is imperative to adapt educational planning and management principles, curriculum-development goals, and the provision of education itself, in order to take into account this pandemic ...
Assignment on AIDS. Assignment. Introduction. Society is like a looking glass. Each and every phenomenon in society is very conspicuous and crystal clear before us. Like many affairs and issues, the vulnerability of HIV/AIDS patient is blatant and flagrant to us. In a complex and complicated social fabrics, AIDS is spreading by leaps and bounds ...
Peer education is an approach to health promotion in which community members are supported to promote health-enhancing change among their peers. The study assessed the effect of peer health education on HIV/AIDS knowledge amongst in-school adolescents in secondary schools in Imo State. This was an intervention study carried out among 296 and 287 in-school adolescents aged 15 to 19 years ...
Univariable analysis of factors associated with VCT among the participants. Results of univariable analysis (Table 2) revealed that participants who had received AIDS-themed lectures or health education courses from school in the past year (crude odds ratio [cOR] 3.75), those who had received HIV risk self-assessment conducted by school in the past year (cOR = 3.52), those who had engaged in ...
Recruitment of volunteers will be competitive. A maximum of 450 children aged 12 to 17 years inclusive will be screened in the study, of which it is planned to include and randomize 300 children who meet the criteria for inclusion in the study and do not have non-inclusion criteria, data on which will be used for subsequent safety and immunogenicity analysis.
Parents and pupils kept in the dark at blood scandal school Infected blood scandal: Boy, 7, died from Aids after doctor ignored rules In the following years, as the medical trial reached its ...
Find company research, competitor information, contact details & financial data for BETA GIDA, OOO of Elektrostal, Moscow region. Get the latest business insights from Dun & Bradstreet.
Assisting Project Managers and Directors with all the paperwork involved during the flow of business, Preferred Candidate. Years of Experience: 3-25 years of experience. Graduated School: Business, Economics, Accounting to similar disciplines. Level of Education: High School ( Graduate ), Bachelor's ( Graduate )
Many high school essays are written in MLA or APA style. Ask your teacher what format they want you to follow if it's not specified. 3. Provide your own analysis of the evidence you find. Give relevance to the quotes of information you provide in your essay so your reader understands the point you are trying make.... 5 Writing a Perfect ...