Medical Student Research Journal
Michigan state university college of human medicine.


Growth and Experiences of a Student-Led Patient Navigation Program Serving Individuals Experiencing Homelessness
Please find below the third article featured in our Winter 2024 Issue, enjoy!
http://msrj.chm.msu.edu/wp-content/uploads/2024/04/MSRJ262_final.pdf
Background : Those experiencing homelessness face disproportionately large barriers in access to healthcare. Patient Navigation is a service that provides disadvantaged populations with guidance through healthcare systems. Acting as a patient navigator is found to help enhance learning in the pre-clinical years of medical school. Developed by medical students, the Patient Navigator Program (PNP) pairs medical students trained as patient navigators with individuals experiencing homelessness. The uniqueness of this program lies in its fully student-run format, simultaneously providing individuals experiencing homelessness with longitudinal navigation services toward self-defined goals and medical students with exposure to a disadvantaged and underserved population in their early years of medical school. The purpose of this study is to evaluate the growth and student experiences of PNP from its inception and inform those who aim to develop similar student-run patient navigation programs.
Methods : Participation metrics in the program were extracted from volunteer records, and five 30-min student leader semi-structured interviews were conducted using open-ended questions to investigate the experiences of those who developed the program. Interviews were transcribed, and responses were categorized by themes.
Results : Enduring involvement in PNP over years was demonstrated quantitatively through participation metrics and qualitatively through interviews. Positive aspects of participation in PNP were meeting and working with other students, utilizing their creative vision in developing the program, learning about those experiencing homelessness and the local resources available to them, shaping career goals and academic interests, and learning the soft skills necessary for medical clerkships. Negative experiences primarily revolved around time constraints of the program in addition to their academic responsibilities. Commonly stated advice included identifying an appropriate faculty mentor and building strong relationships with community partners.
Conclusions : Participation in PNP was felt to be beneficial both personally and professionally. Reporting these perspectives and experiences will provide insight to future student-led programs at other institutions.
Uncommon Presentation of Benign Dermatofibroma of Thigh: A Case Report
Here’s the second article featured in our Winter 2024 Issue, enjoy!
http://msrj.chm.msu.edu/wp-content/uploads/2024/04/MSRJ263_final.pdf
Abstract: Dermatofibromas (DF) are small, noncancerous skin lesions typically found in the dermis layer of the skin and are often composed of a variable combination of inflammatory cells, which classically present as a firm, nonpainful, skin-colored nodule on the extremities or trunk. We present a case of a 53-year-old woman with a medical history of psoriasis who had bilateral leg swelling, erythema, and dry skin for which she underwent a punch biopsy of the left thigh. The punch biopsy sample was found to be a dermatofibroma, which was negative for malignancy or atypia. The skin rash and associated symptoms were due to Candida intertrigo, which was treated with broad-spectrum antibiotics and fluconazole. Following this, she was discharged and prescribed a course of fluconazole and linezolid for continued treatment of Candida intertrigo. This case report describes a rare presentation of benign dermatofibroma.
Medical Students’ Perspectives on Pregnant or Parenting Peers: A Cross-Sectional Survey
We’re back after some technical difficulties! Big thanks to everyone for their patience. Please find below the first addition to our Winter 2024 Issue, enjoy!
http://msrj.chm.msu.edu/wp-content/uploads/2024/04/MSRJ257_final.pdf
Purpose: Limited institutional resources exist for pregnant and parenting medical students; however, students’ opinions regarding pregnancy in medical school have not been reported. The authors assessed medical students’ perspectives regarding pregnant or parenting peers and underlying bias or resource gaps.
Methods: An online, cross-sectional survey was distributed in October 2022 to medical students at Michigan State University College of Human Medicine (n = 806) to explore demographics, bias, family planning, and available resources. Descriptive analyses, a two- tailed t-test comparing female and male responses, and a one-way analysis of variance test comparing medical school classes were used.
Results: The survey response rate was 13.2% (n = 106). Few respondents (n = 4, 3.8%) had been pregnant during medical school. The majority (n = 67, 71.3%) indicated family plans influence specialty choice. Furthermore, 78.0% (n = 42) cited career and education as their reason for choosing to delay pregnancy. Other descriptive analyses identified that 80.0% (n = 75) of respondents were not aware of resources available for pregnant or parenting classmates. Also, 13.0% (n = 12) of respondents had witnessed bias toward a pregnant medical student. Differences in opinions between males and females were present regarding bias and support available. Differences between medical student classes also exist regarding opinions indicating pregnancy as a barrier during school. The statements with the strongest overall agreement were: Pregnant medical students are resilient, face additional challenges, and parental leave should be available in medical school.
Conclusion: This study provides new information regarding pregnancy opinions in medical school and highlights pregnant medical students’ challenges and biases. We revealed common delays in pregnancy due to career or educational choices and uncovered the strong consensus among students that parental leave should be an option. Support efforts are warranted to decrease biases and offer parental leave to promote equity and inclusion.
Physiopathology of Extrapulmonary Tuberculosis: A Literature Review
Please enjoy this new addition to our Fall Issue!
http://msrj.chm.msu.edu/wp-content/u ploads/2023/11/MSRJ254_final.pdf
Introduction: Extrapulmonary tuberculosis (EPTB) is an infection by mycobacteria in any part of the body other than the lungs. There is information on tuberculosis infection from more than 3,000 years ago, and despite the knowledge that there is about the disease, nowadays, it is estimated that a quarter of the world population is infected and 15% of the cases are extrapulmonary.
Aims: This literature review aims to present the physiopathology of the most common EPTB, update and summarize the current diagnostic and therapeutic advances for the EPTB reviewed, as well as describe the physiopathological implications of coinfection with human immunodeficiency virus (HIV).
Methods: A literature review was performed for which PubMed, Cochrane Library, and Google Scholar databases were consulted using the following keywords: Tuberculosis, Epidemiology, Physiopathology, Diagnosis, and Therapy. Only articles published from 2016 to 2022, evaluated with a score ≥ 10 based on the Scale for the Assessment of Narrative Review Articles (SANRA) score were included, obtaining a total of 38 bibliographic sources.
Discussion: Depending on the system or organ affected, it is how the physiopathological process is carried through as well as how the clinical features manifest and the diagnostic approach is made. The diagnostic and therapeutic strategies of each type of EPTB have been widely studied; however, although technological innovation has contributed to the development of new diagnostic techniques, the treatment of almost all EPTB has remained the same over time, which consists of the same 6-month regimen of therapy as in pulmonary tuberculosis. Furthermore, tuberculosis treatment has been severely affected by rifampicin resistance and concomitant HIV infection.
Conclusion: The physiopathology of the different EPTBs is well described; nevertheless, a better understanding of how the disease spreads and develops will allow us to create new diagnostic resources and improve therapeutic targets for this disease, which still has a substantial presence worldwide.
Impact of Imposter Phenomenon on Medical Learners and Clinicians: A Scoping Review
http://msrj.chm.msu.edu/wp-content/upl oads/2023/11/MS RJ251_final.pdf
Objective: The imposter phenomenon (IP) is the belief that one does not deserve success. Medical students, residents, and physicians experience IP at significant rates, often due to the stress of mastering the extensive diagnostic information and treatment modalities as well as the competitive nature of medicine. We aimed to identify the main factors of IP in medical students, residents, and physicians in the available literature to increase awareness of IP in medical education.
Methods: In this scoping review, PubMed, PsycINFO, Cochrane Library, Embase, Scopus, Web of Science, Google Scholar, Northern Lights Conference Abstracts, and Dissertations & Theses databases were systematically searched for relevant studies published before June 2020. Articles that examined IP in medical students, residents, and attending physicians were retained. References were hand- searched following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach. Extracted data were tabulated to summarize characteristics and main findings from each study. Content analysis of this table identified major themes in the available literature.
Results: Twenty-four journal articles published between 1978 and 2020 were included. Three main themes were identified, including specific demographic characteristics of IP (n = 14), the professional impact (n = 10), and the psychological impact (n = 17) of IP. For demographic characteristics, IP was higher in older individuals (n = 3), racial and/or ethnic minorities (n = 2), and women (n = 12). Married individuals experienced less IP (n = 2). For professional impact, IP increased during career transitions or professional challenges (n = 8). For psychological impact, IP was associated with reduced self-esteem (n = 7), a negative self-concept (n = 2), increased self-doubt (n = 3), and perfectionism (n = 3). Depression, anxiety (n = 3), and burnout (n = 6) were also heightened with IP.
Conclusion: Results revealed a multitude of factors influencing IP. Increased awareness of the presence, impact, and severity of IP assists medical educators to combat its negative effects. Further research is needed to improve treatments for IP in this population and to better understand the impact of IP on diversity, career trajectory, and career satisfaction in medicine.
Use of telehealth for cancer screening in primary care during COVID-19: an analysis of the Council of Academic Family Medicine Educational Research Alliance Survey 2022
http://msrj.chm.msu.ed u/wp-content/uploads/ 2023/11/MSRJ247_final.pdf
Background: The COVID-19 pandemic caused rapid uptake of telemedicine in primary care settings affecting cancer screening.
Objective: This study aimed to understand provider perception of future cancer incidence and telehealth feasibility in cancer screening.
Methods: Data were gathered and analyzed as part of the 2020 Council of Academic Family Medicine’s (CAFM) Educational Research Alliance (CERA) survey for primary analysis. The 2020 General Member COVID Survey examined demographics, the impact of faculty isolation, E-learning experience, cancer screening during COVID-19, and outpatient prenatal care. Survey participants were practicing family medicine physicians who were members of one of the CAFM organizations, with a response rate of 14.5%. Descriptive statistics were calculated. Analysis of Variance (ANOVA) was used to evaluate the relationship between telehealth sufficiency and provider age or year they earned their highest degree. Logistic regression evaluated the relationship between telehealth sufficiency and institution type.
Results: 54% of respondents believe that there will be an increase in late-stage cancer. Respondents whose practice settings were not affiliated with medical schools were 1.94 times more likely to feel that telehealth would not be sufficient for cancer screenings in the future (odds ratio [OR] = 1.94, 95% confidence interval [CI]: 1.28, 2.93).
Conclusion: While our study shows that in light of the COVID-19 pandemic, primary care physicians believe there will be an increase in later stage cancer; they can also use telehealth to adequately maintain cancer screening practices. This research serves as a starting point to understanding where, in cancer screening, telehealth can be useful and how practitioners can provide high-quality hybrid care.
When Cannabis Use Goes Wrong: An Epidemiologic Study of Cardiopulmonary Symptoms in Patients That Present to Emergency Departments
http://msrj.chm.msu.edu/wp-content/uploads/2023/11/MSRJ242_final.pdf
Background: Increased availability and use of cannabis in Michigan have led to a marked increase in emergency department (ED) visits associated with the drug’s adverse cardiopulmonary effects. However, few people are aware of these potential cardiopulmonary side effects. Recognition of these presenting symptoms is critical for emergency clinicians to provide timely and effective care, make accurate diagnoses, and safeguard the health of patients who may be experiencing toxic effects from cannabis use.
Study objective: To describe the prevalence, clinical features, and disposition of cannabis cardiopulmonary toxicity in a community- based study.
Methods: This was a retrospective cohort analysis of all patients diagnosed with toxicity related to cannabis use. Patients were seen at eight EDs over a 26-month study period (November 2018–December 2020). Affiliated institutions included three university-affiliated hospitals, a children’s tertiary care facility, and four rural medical centers. Data collected included demographics, clinical features, and treatment outcomes in patients presenting to the ED with cardiopulmonary symptoms (CPS) versus those experiencing other forms of cannabis toxicity.
Results: During the study period, 1,174 patients were evaluated for cannabis toxicity. A total of 318 patients (27.1%) had a cardiopulmonary chief complaint (CPS group) and 856 (72.9%) experienced other forms of cannabis toxicity, predominantly symptoms of intoxication, cannabis hyperemesis syndrome, or neuropsychiatric complaints. The CPS group presented with tachycardia (36.5%), dyspnea (34.3%), chest tightness (28.6%), palpitations (17.9%), and hypertension (8.2%). CPS patients were more likely to be older (32.6 vs. 24.3 years, p < 0.001), ingested edible cannabis (36.8% vs. 9.2%, p < 0.001), and have a history of polysubstance abuse (17.6 vs. 12.0%, p = 0.013). These patients also had a longer ED length of stay (4.9 vs. 3.8 h, p < 0.001) and significantly more hospital admissions (10.1% vs. 6.3%, p = 0.027).
Conclusions: Cardiopulmonary toxicity is common after acute or chronic cannabis exposures, occurring in over one-quarter of ED patients in this community-based study. These troublesome findings highlight the risks associated with using cannabis for recreational or therapeutic purposes.
Volume 11: Special Fall 2023
Welcome to our special fall issue! This publication contains the abstract from the Society for Academic Emergency Medicine’s Midwest Regional Meeting held in Grand Rapids, MI on September 14, 2023. Please enjoy!
http://msrj.chm.msu.edu/wp-content/uploads/2023/10/MSRJ_Vol-11-Special-Fall-2023_final.pdf
Volume 10: Spring 2023 Issue
Thank you to our authors, cover artist, peer reviewers, faculty reviewers, and mentors for making this issue possible. We appreciate your support and commitment to promoting the scientific achievement of medical students.
https://msrj.chm.msu.edu/wp-content/uploads/2023/04/MSRJ_Vol-10-Spring-2023.pdf
Do Probiotics Prevent Gestational Diabetes in Obese/Overweight patients? A Systematic Review
The final article to be included in our Spring 2023 issue is linked below. Enjoy!
https://msrj.chm.msu.edu/wp-content/uploads/2023/04/236-ePub-final.pdf
Introduction: While some studies suggest probiotic supplements may prevent Gestational Diabetes Mellitus (GDM), it is unclear if probiotics effectively prevent GDM among overweight and obese patients. This systematic review synthesizes recommendations for clinical practice and future research by evaluating the quality of evidence regarding Lactobacillus and Bifidobacterium containing probiotics to prevent GDM among obese and overweight patients.
Methods: PubMed, Embase, CINAHL, and Web of Science were searched using appropriate MeSH terms. Results were limited to randomized controlled trials published between 2011-2021. Titles and abstracts were screened for relevance after duplicates were removed. Included studies diagnosed GDM according to by International Association of Diabetes and Pregnancy Study Group criteria, suspended probiotic use prior to intervention, excluded participants with altered glucose metabolism, included participants with a BMI ≥25kg/m2, and provided a specified dose of probiotic supplements. Articles without statistical analysis were excluded. Resulting articles were critically appraised using Version 2 of the Cochrane Risk of Bias tool.
Results: This search strategy resulted in 24 articles after duplicates were removed. Five double- blind randomized controlled trials found the incidence of GDM during the third trimester was not significantly different between probiotic and control groups. There was wide variation in the bacterial species, dose and duration of probiotic treatments used. All studies have a high risk of bias due to non-adherence to the treatment.
Discussion: This review used a highly sensitive criteria for GDM diagnosis that may mask a preventative effect of probiotics. Non-compliance may bias results towards the null given insufficient analysis of the effect of adhering to the intervention. No patterns between length of probiotic intervention or probiotic species and improved glucose tolerance were noted.
Conclusions: Current evidence is not sufficient to recommend probiotic supplements to prevent GDM in overweight and obese patients. Future evidence should address the effect of adhering to probiotic interventions and develop consistent probiotic intervention protocols.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to get involved in...
How to get involved in research as a medical student
- Related content
- Peer review
- Anna Kathryn Taylor , final year medical student 1 ,
- Sarah Purdy , professor of primary care and associate dean 1
- 1 Faculty of Health Sciences, University of Bristol, UK
Participating in research gives students great skills and opportunities. Anna Taylor and Sarah Purdy explain how to get started
This article contains:
-How to get involved with research projects
-Questions to ask yourself before starting research
-What can you get published? Research output
-Advice for contacting researchers
-Different types of research explained
-Stages of research projects
Students often go into medicine because of a desire to help others and improve patients’ physical and mental wellbeing. In the early years of medical school, however, it can seem as if you are not making much difference to patient care. Involvement in research can provide exciting opportunities to work as part of a team, improve career prospects, and most importantly add to the evidence base, leading to better outcomes for patients.
Research is usually multidisciplinary, including clinical academics (medical doctors who spend part of their working life doing research), nurses, patients, scientists, and researchers without a medical background. Involvement in such a team can improve your communication skills and expand your understanding of how a multidisciplinary team works.
Participating in research can also help you to develop skills in writing and critical appraisal through the process of publishing your work. You may be able to present your work at conferences—either as a poster or an oral presentation—and this can provide valuable points for job applications at both foundation programme and core training level. This is particularly important if you are considering a career in academia. You will also develop skills in time management, problem solving, and record keeping. You might discover an area of medicine in which you are keen to carry out further work. For some people, getting involved in research as a medical student can be the first step in an academic career.
Kyla Thomas, National Institute for Health Research clinical lecturer in public health at the University of Bristol, says, “my first baby steps into a clinical academic career started with a research project I completed as a medical student. That early involvement in research opened my eyes to a whole new world of opportunities that I never would have considered.
“Importantly, participating in undergraduate research sets students apart from their colleagues. Applying for foundation posts is a competitive process and it is a definite advantage if you have managed to obtain a peer reviewed publication.”
Getting involved with research projects
Although it is possible to do research at medical school, it is important to be realistic about how much free time you have. It might be possible to set up your own research project, but this will require substantial planning in terms of writing research protocols, gaining ethical approval, and learning about new research methodologies. Other opportunities for research that make less demands on your time include:
Intercalated degrees—these often have time set aside for research in a specific area, so it is important to choose your degree according to what you might like to do for your dissertation (for example, laboratory-based work in biochemistry, or qualitative research in global health. Some subjects may have options in both qualitative and quantitative research).
Student selected components or modules can provide a good opportunity to be involved in an ongoing study or research project. If you have a long project period, you might be able to develop your own small project.
Electives and summer holidays can also provide dedicated time for research, either within the United Kingdom or in another country. They can allow you to become established in a research group if you’re there for a few weeks, and can lead to a longstanding relationship with the research group if you continue to work with them over your medical school career.
If you don’t know what to do, contacting the Student Audit and Research in Surgery (STARSurg), 1 the National Student Association of Medical Research (NSAMR), 2 or your medical school’s research society may be a good place to start.
The INSPIRE initative, 3 coordinated by the Academy of Medical Sciences, gives support and grants to help students take part in research. Some UK medical schools have small grants for elective and summer projects, and organise taster days for students to get an idea of different research areas.
You may also be able to access other grants or awards to support your research. Some of the royal colleges, such as the Royal College of General Practitioners and the Royal College of Psychiatrists, offer bursaries to students doing research in their holidays or presenting at conferences. Other national organisations, such as the Medical Women’s Federation, offer bursaries for elective projects.
Box 1: Questions to ask yourself before starting research
What are you interested in? There is no point getting involved in a project area that you find boring.
How much time do you have available? It is crucial to think about this before committing to a project, so that your supervisor can give you an appropriate role.
What do you want to get out of your research experience? Do you want a brief insight into research? Or are you hoping for a publication or presentation?
Do you know any peers or senior medical students who are involved in research? Ask them about their experiences and whether they know of anyone who might be willing to include you in a project.
Box 2: Research output
Publication —This is the “gold standard” of output and usually consists of an article published in a PubMed ID journal. This can lead to your work being cited by another researcher for their paper, and you can get up to two extra points on foundation programme applications if you have published papers with a PubMed ID.
Not all research will get published, but there are other ways to show your work, such as presenting at conferences:
Oral presentation —This involves giving a short talk about your research, describing the background, methods, and results, then talking about the implications of your findings.
Poster presentation —This involves creating a poster, usually A1 or A2 in size, summarising the background, methods, and results of your research. At a conference, presenters stand by their poster and answer questions from other delegates.
Contacting researchers
Most universities have information about their research groups on their websites, so spend some time exploring what studies are being carried out and whether you are interested in one of the research topics.
When contacting a member of the research group, ask if they or someone else within their team would be willing to offer you some research experience. Be honest if you don’t have any prior experience and about the level of involvement you are looking for, but emphasise what it is about their research that interests you and why you want to work with them. It’s important to have a flexible approach to what they offer you—it may not initially sound very exciting, but it will be a necessary part of the research process, and may lead to more interesting research activity later.
Another way to make contact with researchers is at university talks or lectures. It might be intimidating to approach senior academics, but if you talk to them about your interest they will be more likely to remember you if you contact them later on.
Box 3: What can students offer research teams?—Views from researchers
“Medical students come to research with a ‘fresh eyes’ perspective and a questioning mindset regarding the realities of clinical practice which, as a non-medic myself, serves to remind me of the contextual challenges of implementing recommendations from our work.”
Alison Gregory, senior research associate, Centre for Academic Primary Care, University of Bristol, UK.
“Enthusiasm, intelligence, and a willingness to learn new skills to solve challenges—bring those attributes and you’ll be valuable to most research teams.”
Tony Pickering, consultant anaesthetist and Wellcome Trust senior research fellow, University of Bristol, UK.
Box 4: Different types of research
Research aims to achieve new insights into disease, investigations, and treatment, using methodologies such as the ones listed below:
Qualitative research —This can be used to develop a theory and to explain how and why people behave as they do. 4 It usually involves exploring the experience of illness, therapeutic interventions, or relationships, and can be compiled using focus groups, structured interviews, consultation analysis, 5 or ethnography. 6
Quantitative research —This aims to quantify a problem by generating numerical data, and may test a hypothesis. 7 Research projects can use chemicals, drugs, biological matter, or even computer generated models. Quantitative research might also involve using statistics to evaluate or compare interventions, such as in a randomised controlled trial.
Epidemiological research —This is the study of the occurrence and distribution of disease, the determinants influencing health and disease states, and the opportunities for prevention. It often involves the analysis of large datasets. 4
Mixed methods research —This form of research incorporates both quantitative and qualitative methodologies.
Systematic reviews —These provide a summary of the known evidence base around a particular research question. They often create new data by combining other quantitative (meta-analysis) or qualitative (meta-ethnography) studies. They are often used to inform clinical guidelines.
Box 5: Stages of research projects
Project conception—Come up with a hypothesis or an objective for the project and form the main research team.
Write the research protocol—Produce a detailed description of the methodology and gain ethical approval, if needed.
Carry out the methodology by collecting the data.
Analyse the data.
Decide on the best way to disseminate your findings—for example, a conference presentation or a publication—and where you will do this.
Write up your work, including an abstract, in the format required by your chosen journal or conference.
Submit . For conference abstracts, you may hear back swiftly whether you have been offered the chance to present. Publication submissions, however, must be peer reviewed before being accepted and it can take over a year for a paper to appear in print.
Originally published as: Student BMJ 2017;25:i6593
Competing interests: AKT received grant money from INSPIRE in 2013.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ STARSurg. Student Audit and Research in Surgery. 2016. www.starsurg.org .
- ↵ NSAMR. National Student Association of Medical Research. 2016. www.nsamr.org .
- ↵ The Academy of Medical Sciences. About the INSPIRE initiative. 2016. www.acmedsci.ac.uk/careers/mentoring-and-careers/INSPIRE/about-INSPIRE/ .
- ↵ Ben-Shlomo Y, Brookes ST, Hickman M. Lecture Notes: Epidemiology, Evidence-based Medicine and Public Health. 6th ed . Wiley-Blackwell, 2013 .
- ↵ gp-training.net. Consultation Theory. 2016. www.gp-training.net/training/communication_skills/consultation/consultation_theory.htm .
- ↵ Reeves S, Kuper A, Hodges BD. Qualitative research methodologies: ethnography. BMJ 2008 ; 337 : a1020 . doi:10.1136/bmj.a1020 pmid:18687725 . OpenUrl FREE Full Text
- ↵ Porta M. A Dictionary of Epidemiology. 5th ed . Oxford University Press, 2008 .
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Medical Student Research: An Integrated Mixed-Methods Systematic Review and Meta-Analysis
Affiliations Faculty of Medicine, Cairo University, Cairo, Egypt, Okinawa Institute of Science and Technology Graduate University, Okinawa, Japan
Affiliation Okinawa Institute of Science and Technology Graduate University, Okinawa, Japan
Affiliation European Institute of Oncology (IEO), Milano, Italy
* E-mail: [email protected]
Affiliation National Cancer Institute, Cairo University, Cairo, Egypt
- Mohamed Amgad,
- Marco Man Kin Tsui,
- Sarah J. Liptrott,

- Published: June 18, 2015
- https://doi.org/10.1371/journal.pone.0127470
- Reader Comments
Despite the rapidly declining number of physician-investigators, there is no consistent structure within medical education so far for involving medical students in research.
To conduct an integrated mixed-methods systematic review and meta-analysis of published studies about medical students' participation in research, and to evaluate the evidence in order to guide policy decision-making regarding this issue.
Evidence Review
We followed the PRISMA statement guidelines during the preparation of this review and meta-analysis. We searched various databases as well as the bibliographies of the included studies between March 2012 and September 2013. We identified all relevant quantitative and qualitative studies assessing the effect of medical student participation in research, without restrictions regarding study design or publication date. Prespecified outcome-specific quality criteria were used to judge the admission of each quantitative outcome into the meta-analysis. Initial screening of titles and abstracts resulted in the retrieval of 256 articles for full-text assessment. Eventually, 79 articles were included in our study, including eight qualitative studies. An integrated approach was used to combine quantitative and qualitative studies into a single synthesis. Once all included studies were identified, a data-driven thematic analysis was performed.
Findings and Conclusions
Medical student participation in research is associated with improved short- and long- term scientific productivity, more informed career choices and improved knowledge about-, interest in- and attitudes towards research. Financial worries, gender, having a higher degree (MSc or PhD) before matriculation and perceived competitiveness of the residency of choice are among the factors that affect the engagement of medical students in research and/or their scientific productivity. Intercalated BSc degrees, mandatory graduation theses and curricular research components may help in standardizing research education during medical school.
Citation: Amgad M, Man Kin Tsui M, Liptrott SJ, Shash E (2015) Medical Student Research: An Integrated Mixed-Methods Systematic Review and Meta-Analysis. PLoS ONE 10(6): e0127470. https://doi.org/10.1371/journal.pone.0127470
Academic Editor: Emmanuel Manalo, Kyoto University, JAPAN
Received: April 1, 2014; Accepted: April 15, 2015; Published: June 18, 2015
Copyright: © 2015 Amgad et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Data Availability: All data are included within the manuscript
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The education of health professionals has seen two revolutions over the past century. The first revolution-marked by what is known as The Flexner Report in 1910- was the effective integration of basic sciences into health education. The second revolution, initiated by the Welch-Rose report in 1915, introduced the concept of problem-based learning into medical education. In 2010, a special report was published by a global commission, The Commission on Education of Health Professionals for the 21 st Century, aimed at updating the standards of an ideal medical curriculum. The committee strongly recommended a new medical educational model that emphasized flexibility and adaptability of traditionally rigid curricula to local and community needs [ 1 ]. Despite these educational advances, there are certain aspects of medical education that remain unstructured and largely variant between medical schools; among these is medical student participation in research. Moreover, there is an alarming decline in the number of physician-scientists in the US, which threatens the progress of translational medicine in the upcoming era [ 2 – 4 ].
In the U.S., outstanding students willing to enter medical school may apply for the National Institute of Health (NIH) funded Medical Scientist Training Program (MSTP) [ 5 ]. This program offers students the opportunity to get a good feel for what a physician-scientist career entails through a funded MD/PhD. The value of those MD/PhD programs is well established; a 2010 study by Brass et al, investigating the outcomes of half of all NIH-funded MD/PhD programs (24 programs in total) found that these programs were very successful at reaching their goals of training future physician-scientists. In fact, 81% of MD/PhD graduates landed academic positions and 82% of them were actively engaged in research [ 6 ]. Nevertheless, due to limited funding, MD/PhD graduates only constitute 3% of the US medical student population, highlighting the value of alternative pipelines for the creation of research-active physicians [ 7 ]. Moreover, organizational and contextual factors might make the support of costly MD/PhD programs difficult to implement in other countries.
Several other programs have also been devised to offer medical and health sciences students the chance to participate in research [ 8 – 13 ]. One of the common forms of medical student research engagement is Intercalated Bachelor of Science (iBSc) degrees. These are particularly common in the UK, and are characterized by research time-out periods between the basic and clinical years of medical school. Students who take intercalated degrees graduate with an extra BSc beside their medical degree. The value of such short-term research placements should not be underestimated. In fact, the benefits of undergraduate research have been discussed richly in the literature, though there were relatively fewer papers focusing primarily on medical student research [ 14 – 16 ]. Unlike many other degrees, a medical degree is at the interface of science and social service. It is therefore expected that the benefits of, and motivations behind, medical student participation in research are different from those of non-medical students [ 17 ].
A 2005 systematic review of the literature by Straus et al investigated the factors that influence career choice in academic medicine among residents, fellows and staff physicians [ 18 ]. Their review found a positive effect of having dual degrees or fellowships beside the medical degree, and of publishing research conducted during medical school. Further, the review highlighted the role of mentorship and desire to teach. Despite the presence of a large body of evidence investigating the impact of, and factors related to, medical student research, a systematic analysis of this evidence is missing. This makes the data seem conflicting and disorganized, and undermines the apparent overall strength of evidence.
This paper is a mixed-methods systematic review and meta-analysis of published studies investigating various aspects of medical student research, including its impact on the development of research-active physicians, difficulties faced by medical students performing research and potential solutions to overcome these difficulties. Our hope is that this work serves to complement the review by Straus et al, and helps provide a thorough overview of the evidence needed for curricular and educational policy reforms [ 18 ].
We aimed to satisfy the following objectives in this review:
Primary Objectives: (a) To examine the short- and long- term influence of curricular and extracurricular undergraduate medical research on the scientific productivity of medical students, measured by the number of published manuscripts, research awards or attainment of faculty rank. (b) To describe the influence of curricular and extracurricular medical student research on the career choice of medical students.
Secondary Objectives: (a) To explore the current forms in which medical students are engaged in research projects, as well as the prevalence of non-mandatory research exposure among medical students. (b) To identify the factors related to medical student engagement in research projects. (c) To investigate miscellaneous issues of relevance, including the pros and cons of research time-out periods (with a focus on Intercalated Bachelor of Science degrees), differences between countries with developing and developed economies and gender equality in medical student research engagement, perceptions and productivity.
Developing economies were identified according to the International Monetary Fund's World Economic Outlook Report [ 19 ]. We counted as a "medical student" anyone who is enrolled in the core medical school program, regardless of program duration, and whose graduation would guarantee the degree Bachelor of Medicine, Bachelor of Surgery (MBBS) or its equivalent (MD, in the US, for example). It should be noted that in the US model of medical education, admission into medical school is on a graduate-entry basis by default, and the first medical degree earned is called the "MD". In the non-graduate entry model, on the on the other hand, the term "MD" is reserved for higher research degrees (postgraduate degrees) in clinical medical and surgical disciplines. Graduate-entry medical students were included, but not MD/PhD students, residents or postgraduate students. The reasons behind excluding studies focusing on MD/PhD students is that this sub-population is considered to be different from the general student population, especially that their enrollment in the medical program was–by definition- meant to prepare them for physician-scientist careers. It may be argued that graduate-entry medical students who had a higher degree (MSc or PhD) at the time of matriculation also constitute a separate sub-population. Hence, we addressed any reported differences between these sub-populations in our results. "Medical student research" was defined as any activity performed by medical students that is driven by inquiry or hypothesis and that legitimately incorporates basic principles of the scientific method. This includes original research, review articles, case reports etc.
We followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement guidelines in this systematic review and meta-analysis, and the relevant checklist can be found as S1 File [ 20 ]. Between March 2012 and September 2013, periodic searches were performed in the following databases for potentially relevant studies: MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews, Cochrane Methodology Register (CMR), Educational Resources Information Center (ERIC), Center for Reviews and Dissemination (CRD), ISI Web of Science and Google Scholar. Further, we searched the bibliographies of the included studies for other potential publications on the subject. Our search strategy included the following keywords in various combinations: medical student; medical students; undergraduate; medical; research; intercalated; bachelor; BSc; iBSc; theses; thesis; developing. The search strategy used for PubMed was as follows: ((((((medical student research) OR undergraduate research) OR medical thesis) OR intercalated bachelor) OR intercalated BSc) OR iBSc) OR undergraduate research developing.
Inclusion criteria: All study designs, including cross-sectional, prospective, retrospective and interventional studies, randomized controlled trials and qualitative studies.
Exclusion criteria: Studies containing inadequate information about the participants and type of study; studies in languages other than English; studies assessing outcomes unrelated to medical student research; theses or commentaries; studies aimed at postgraduates or undergraduates other than medical students; studies whose main population was MD/PhD students. Graduate-entry medical students, nonetheless, were not excluded from this review.
Two of the authors independently reviewed the studies that met these criteria and any disagreements were resolved by consensus. Basic data extraction tables were then used to extract the main finding and characteristics of each of the included studies. Quantitative studies (reporting odds ratios (OR's), p-values, percentages or other statistical measures) were separated from qualitative studies in order to improve the judgment of cumulative evidence.
Qualitative studies were included in order to help contextualize the quantitative outcomes and to provide insights and entry points for future research. Qualitative studies were defined as those studies which satisfied the following criteria: a) Their aims did not include the extraction of quantitative outcomes and thus did not perform any statistical analysis; b) They present original research with clearly-defined study populations; c) They utilize qualitative research methods, including semi-structured and unstructured interviews, open-ended survey questions, focus groups and examination of records and documents.
An integrated methodology was utilized to assimilate quantitative and qualitative outcomes into a single mixed-methods synthesis [ 21 , 22 ]. After relevant studies have been identified, a thematic analysis was performed. The literature search and article inclusion/exclusion strategy was aimed at retrieving all articles relevant to the subject of medical students' research, without prior conceptions or theories about expected outcomes. Hence, our thematic analysis was data-driven (as opposed to being theory-driven) [ 22 ]. Quantitative and qualitative outcomes were discussed together under relevant thematic subject headings.
Two types of quantitative outcomes were used for meta-analysis: percentages (for explorative outcomes) and odds ratios (for interventional/associative outcomes). Whenever relevant or needed, the corresponding authors (or, if unavailable, other authors) of included studies were contacted to get the raw data needed for meta-analysis. In some cases, other outcomes beside the ones mentioned in the original paper were identified in the raw data and used for the meta-analysis.
Further details about the methodology used in this paper, including outcome-specific quality assessment, statistical methods used and the strategy used to tackle study heterogeneity and potential publication bias can be found in our supporting information ( S2 File ).
Results and Discussion
Our search returned 31,367 records in the various databases. After reviewing the abstracts, 31,111 were excluded because they were either duplicates in various databases or satisfied one or more of the exclusion criteria mentioned earlier. 256 articles met (or were suspected to meet) our inclusion criteria upon reviewing their abstract and were thus retrieved for full-text assessment. Eventually 79 articles were found to match the selection criteria and were included in this review. More details about the article selection process can be seen in Fig 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0127470.g001
Of the 79 articles retrieved, 71 were of quantitative nature, seven were of qualitative nature and one had both quantitative and qualitative components. Fifty-two articles were self-reported questionnaire studies with response rates ranging from 7.9% to 100%. Ten survey-based articles had response rates less than 60%. Twenty-three studies used a more objective research strategy that relied on searching institutional databases and records, two used both questionnaires and objective database searching and two had an unknown/undisclosed methodology. There were 47 cross-sectional studies, 25 retrospective studies, three prospective studies, three intervention studies and one study with an unknown/undisclosed design. Fifty-seven studies were performed in a single institution (including four qualitative study) and 22 studies involved multiple institutions (including four qualitative studies). Further, there were 14 studies that reported the effects of certain research programs or initiatives, whose study population might or might not be affiliated with multiple institutions. Sixteen studies assessed the value of intercalated BSc's (iBSc's) and 14 studies were carried out in developing countries.
After thematic analysis was performed, the resultant themes and sub-themes, outlined in Fig 2 , also served as the scaffold for writing this paper. The data extraction and quality assessment worksheet and the relevant sensitivity plots can also be found in the supporting information files ( S3 and S4 Files , respectively) [ 7 , 8 , 10 , 11 , 23 – 90 ].
https://doi.org/10.1371/journal.pone.0127470.g002
Assessing the current situation
We assessed the current state of medical student research by focusing on two main outcome measures: interest in- and exposure- to research among the medical student population. Both of these outcomes are explorative in nature (rely on proportions rather than odds ratios) and have been quantitatively pooled to yield a weighed estimate value. The results have been summarized in Fig 3 [ 7 , 10 , 26 , 28 , 32 , 47 – 49 , 52 , 54 , 55 , 58 , 63 , 67 – 69 , 71 – 75 , 80 – 82 , 85 , 90 – 92 ] .
Forest Plot symbols: * The axis, not the data, is shown in logit scale for aesthetic purposes. Table symbols: * Mandatory exposure (in the form of curricular components or graduation theses) was excluded from this analysis. Abbreviations used: D, developing countries; H, higher commitment to a research career; I, intercalated Bachelor of Science degree (iBSc). Dates are shown beside studies that may be confused with others referenced in this review having the same similar first-author names.
https://doi.org/10.1371/journal.pone.0127470.g003
Interest in research among medical students.
While the only reliable method for probing interest in medical research is assessing actual voluntary research involvement, survey data (self-reported interest) may provide insights into any discrepancies between interest and actual involvement. To avoid pooling survey data that are too heterogeneous, we made a distinction between survey questions that ask about general interest in research and those specifically asking medical students about their interest in making commitments to research during their future careers.
I1a: Interest in performing research: A pooled weighed estimate of 72% of medical students reported having interest in performing research (0.72, 0.57–0.83). One particularly high estimate was that reported by De Olivera and colleagues, which showed that 90% of its 1004 student sample had interest in performing research [ 74 ]. However, even when this study was excluded from the analysis as a possible exception, the pooled weighed estimate remained fairly high (0.67, 0.53–0.79) ( S4 File ).
I1b: Interest in a career involving research: The single best estimator of career intentions of US medical graduates is probably the Graduation Questionnaire (GQ), developed by The Association of American Medical Colleges (AAMC) in 1978 [ 7 ]. In 2013, 63% of the 13,180 respondents indicated intentions to become somewhat-to-exclusively involved in research during their medical careers, including 17% who planned "significant" or "exclusive" future involvement. This huge sample size approaches a true census, with 81.8% of the US fresh medical graduate population being covered.
Upon quantitative pooling of our included studies, we found that about 31% of medical students (0.31, 0.19–0.46) were interested in a career involving research, and 12% (0.12, 0.07–0.21) showed interest in "significant" (higher) commitment to research during their future careers. One particularly important, high-quality study was that of McManus and colleagues, showing that 6.9% of UK medical students planned to pursue academic careers (or found them to be very appealing) [ 85 ]. When we calculated the pooled outcome excluding MacManus et al or the AAMC data, the pooled proportion was not markedly changed ( S4 File ).
It should be noted that there is considerable variation in the proportions reported in our included studies. This may reflect inherent (true) variability in students' research interests due to diversity of settings and study populations (as has been discussed in S2 File ). We also believe that there are other potential contributors to this variability, most notably the ambiguity of wording of survey questions. For example, many studies did not make a clear distinction between interest in an academic (university faculty) medicine career, and interest in a career involving some research outside of academia.
I2. Medical students’ exposure to research.
Even today there is no consistent way in which undergraduate medical students are incorporated into research. For example, students may be engaged in research through summer research electives [ 9 , 45 ], mandatory curricular study modules [ 90 ], extracurricular research activities [ 93 ], or they might decide to intercalate for one or more years to obtain a BSc beside their medical degree. In Germany, it is mandatory for medical students to submit a thesis outlining the results of a research project in order to graduate with the title "Doctor" [ 30 ]. This requirement has also been reported in Peru, Finland, France and some U.S. universities such as Yale [ 24 , 27 , 76 , 94 ]. The AAMC 2013 Graduation Questionnaire shows that 68.2% of US medical graduates participated in a research project with a faculty member on a mandatory or volunteer basis and 41.7% co-authored a research paper [ 7 ].
If we exclude papers describing medical schools asking for mandatory graduation theses or research modules, we find that a little less than one third of medical students participated in research projects (0.31, 0.22–0.41). The proportion exposed to “prolonged” periods of research (>6 weeks) is even less (0.22, 0.16–0.28).
In the U.S., different medical schools have different research expectations, and the exposure of medical students to non-mandatory research seems to be largely dependent on medical school influence. Duke University, for example, incorporates students into summer-long research projects [ 95 ]. On the other hand, Stanford University, the University of Pittsburg and Warren Alpert Medical Schools incorporate students into longitudinal research projects in parallel with their academic studies [ 95 – 97 ]. This longitudinal approach may help in solving some of the reported problems of time-out research, such as the reluctance of medical students towards detachment from their colleagues and financial worries about spending extra time in college. Indeed, the success of Stanford is particularly evident, with 90% of medical students participating in research projects [ 91 ].
We found that the pooled proportion of medical students reporting some interest in research is higher than that of students who were actually involved in research projects. This may be due to: a) self-reported interest may not necessarily reflect serious willingness to pursue research; or b) lack of opportunities to meet students’ interest due to lack of funding, supervision and encouragement or inflexible curricula that leave little or no time for research ( S5 File ) [ 45 , 47 – 50 , 52 , 55 , 57 , 68 , 74 ].
II. Factors related to- or affecting medical student research
We identified four main factors affecting medical student research: previous research experience, academic success, having a higher degree (MSc or PhD) at the time of matriculation and financial factors. The effects of the first three factors were reported using odds ratios due to the presence of untreated groups ( Fig 4 ) [ 32 , 47 , 52 – 55 , 58 , 62 , 63 , 67 , 79 , 81 , 92 , 98 ], while the fourth factor (financial influence) was pooled using proportions from survey studies ( Fig 5 ) [ 55 , 57 , 59 , 67 , 82 ]. Moreover, we discuss the results of various studies reporting other relevant factors that could not be meta-analyzed, including the role of mentorship and competitive residencies in shaping medical students’ perceptions about- and attitudes towards research.
Forest Plot symbols: * The axis, not the data, is shown in log scale for aesthetic purposes. Abbreviations used: D , developing countries; I , intercalated Bachelor of Science degree (iBSc); M , motivation to perform research; K , research knowledge or skills; C , confidence in research competencies; In , interest in research. For some studies, odds ratios and 95% confidence interval values were reported, but not the raw numbers.
https://doi.org/10.1371/journal.pone.0127470.g004
https://doi.org/10.1371/journal.pone.0127470.g005
II1. Effect of previous research experience.
Students who participated in research projects during medical school were over three times as likely to report interest in research involvement during their future careers (OR = 3.55, 1.84–6.83). Two studies [ 92 , 98 ], which were not included in the pooled weighed estimate, reported paired outcomes, with non-significant differences in research career interests after research exposure. Additionally, we found that medical school research involvement has no significant correlation with attitudes or motivation towards research (OR = 2.05, 0.99–4.24).
It is difficult to conclude that self-reported interest is a direct effect of exposure to research, since reverse causality cannot be excluded. That is, it is logical to assume that a fairly large proportion of students who had pre-existing interest in a career in research decide to participate in research projects. As a matter of fact, students in two of the included studies agreed that research participation strengthened pre-existing interest in a research career [ 90 , 91 ]. These findings also make sense in light of the fact that over half of all medical students reported having some interest in a career involving research ( Fig 3 ). Another possible explanation for the above results is that students who have had prior research experience have better research knowledge and skills, and are therefore more confident about their ability to succeed were they to undertake research projects during their future careers. Indeed, in a series of interviews conducted by Jones et al, students who undertook an intercalated BSc in primary healthcare reported a positive influence of the experience on their appreciation of the research process [ 99 ]. Similarly, a thematic analysis of 905 SSC (Student Selected Component) projects by Murdoch-Eaton et al provided by medical students at six UK medical schools revealed gain of various research-related skills [ 90 ]. These results are also supported by eleven quantitative studies, summarized in S5 File [ 11 , 37 , 39 , 40 , 46 , 47 , 55 , 64 , 82 , 89 , 91 ].
II2. Effect of having a higher degree (MSc or PhD) prior to medical school.
II2a: Having a higher degree is associated with involvement in- (or planned involvement in-) research: Siemens et al report that medical students who had a higher degree prior to enrolment in medical school were almost four times more likely to perform research during medical school (OR = 3.95, 2.22–7.01) [ 52 ]. However, data provided by Cruser et al showed no significant difference between the two groups regarding their planned involvement in future research (OR = 1.01, 0.57–1.79) and Gerrard et al actually reported the reverse trend, with higher degree graduate-entry medical students actually being less likely to pursue an iBSc [ 54 , 81 ]. This is consistent with data we obtained from Mahesan et al, which shows that graduate-entry medical students (having any degree prior to matriculation) were almost ten times less likely to pursue an intercalated degree (OR = 0.01, 0.00–0.13) [ 62 ].
Since career progress (especially the pursuit of competitive residency) is a major motive behind medical student research, it may be argued that medical students with a higher degree view this aspect of their Curriculum Vitae (CV) as being “complete enough” and hence devalue the pursuit of another degree. In fact, to the medical student with a prior degree, an iBSc will almost always result in degree duplication, even if the skills and knowledge base of the iBSc course were completely different from those of the other degree already gained by the student.
II2b: Other advantages of having a higher degree (MSc. or PhD.): There is no significant correlation between having a higher degree prior to medical school enrolment and research interest or motivation. However, as might be expected, higher degree graduate-entry medical students were more knowledgeable about research, showed better research skills and had higher confidence in their research competencies ( Fig 4 ). This is expected, given that almost all higher degrees have a compulsory research component.
II3. Effect of academic success.
II3a: Academic success is associated with attitudes towards basic medical sciences or medical research: The data we obtained from Hren et al shows an association between higher Grade Point Average (GPA) and attitudes towards research (OR = 1.83, 1.42–2.36) [ 79 ]. Cruser et al’s data, on the other hand, shows no significant difference between highest MCAT (Medical College Admission Test) scores and attitude scores [ 54 ]. Perhaps GPA during medical school, but not before admission, is a factor that influences attitudes. However, we believe the evidence in favor or against this hypothesis is weak and further investigation is needed in the future.
II3b: Academic success is associated with involvement in- (or planned involvement in-) research: The weighed pooled odds ratio from four included studies shows no association between academic success and involvement (or planned involvement) in research projects (OR = 1.00, 0.62–1.64). The only study showing a significant correlation was Brancati et al, which asserts that students who were academically successful (top third of their class) were more likely to choose an academic career (OR = 2.11, 1.30–3.42) compared to their less successful peers (lower third) [ 32 ]. However, this study investigates choice of an academic career rather than involvement (or planned involvement) in research during or right after medical school. Hence, it may be argued that this study should be excluded from the analysis as it measures a different outcome, in which case the pooled odds ratio remains non-significant (0.82, 0.59–1.15). We suggest further investigation into this issue using studies with more favorable, preferably prospective, designs.
II4. Financial factors affect the appeal of research to medical students.
About half of medical students who chose not to get involved in research reported being deterred by financial factors (0.50, 0.46–0.54) ( Fig 5 ) [ 55 , 57 , 59 , 67 , 82 ]. Nicholson et al and Stubbs et al both show that about half of medical students who choose not to intercalate do so for financial reasons [ 59 , 82 ]. In addition, Galletly et al also reported that about half (48%) of medical students asserted that perceived lower salaries of academicians was an important factor behind their decision not to pursue an academic career [ 55 ]. The consistency of the findings by the former two studies with the latter one suggests that it's not just the short-term financial burden of pursuing an intercalated degree that deters medical students from getting involved in research, but a general long-term financial concern. Financial worries, particularly the fear of running out of grant money and the financial stress of academic careers, were indeed cited by students interviewed by O'Sullivan et al among the deterrents to academic career pursuit [ 100 ].
Similarly, Yamazaki et al and Kumar et al both showed that a considerable fraction of the general medical student population displayed concerns about the financial stability of a research career (45% and 12%, respectively) [ 57 , 67 ].
II5. Career progression is a main motive behind performing research during medical school.
The result from seven included studies indicate that career progression is a main motive (if not the main motive) behind performing research during medical school. These results indicate that in a large fraction of cases, medical students perform research for purely pragmatic reasons (related to their residencies or further post-graduate education), rather than pursuing research for the value it has in and of itself ( Table 1 ) [ 48 , 49 , 52 , 54 , 55 , 82 , 86 ].
https://doi.org/10.1371/journal.pone.0127470.t001
Four studies mentioned the role competitive residencies play in driving medical students to perform research, and in fact students in three of those studies believed that seeking competitive residency was–explicitly- the main motive to perform research during medical school. The results from a qualitative study by Shapiro et al support this conclusion by showing that the motives behind research participation include (but are not limited to) pragmatic targets such as improving the students' relationship with faculty [ 101 ].
These conclusions are consistent with other results reported here showing that: a) there is a discrepancy between interest in clinical practice and interest in a research career ( S5 File ) [ 45 , 51 , 56 , 57 ] and b) there is a correlation between interest in academia or basic medical sciences and interest in research ( S5 File ) [ 55 – 57 ].
Combined, these findings indicate that any policies aimed at boosting medical students’ engagement in research have to align research involvement with the career progress and success of students. In much the same way that peer-reviewed publications are a key competitive edge in academia and in competitive residency applications, it must become clear that research is more than just an accessory when it comes to ordinary clinical practice.
II6. Other factors related- to or affecting medical student research.
As Reynolds has discussed, it is simply not enough to match students with professors in research projects, as good quality research requires real mentorship [ 102 ]. Research instructors also act as role models to encourage students to pursue careers in academic medicine. Further, finding the right mentor is important to ensure that students provide a working and intellectual input into the research projects, rather than simple assistantship in lab work or data collection ( Table 2 ) [ 48 , 52 , 57 , 58 , 82 ].
https://doi.org/10.1371/journal.pone.0127470.t002
This is not always going to be easy; the results from two qualitative studies show that the complexity of ethical approval procedures (whether in terms of time or paperwork) is a major difficulty facing supervisors and students alike [ 90 , 103 ]. Further, the absence of clear, well-structured research governance may result in some aversion to faculty-mentored student research. This was the case in two qualitative studies, where students cited problems with approachability of faculty members and expressed concerns about being used as "free labor" on research projects [ 90 , 101 ].
In fact, Murdoch-Eaton et al's aforementioned project content analysis, while revealing some gain in useful research skills, also highlighted the failed attainment of a balanced skill-set; the majority of student projects involved information gathering and data processing, while fewer projects involved actual student engagement in research methodology development or critical analysis of data [ 90 ].
It may be presumed that the relatively short duration of the undergraduate research experience could limit its publication or citation potential. Indeed, Dyrbye et al found that graduates with a 17–18 week-long research experience published significantly less papers in which they appeared as first authors than their peers who spent 21-weeks doing research [ 29 ]. Further, Fede et al showed that the annual Undergraduate Medical Congress of ABC foundation (COMUABC) had a smaller proportion of abstracts accepted for publication in peer-reviewed journals in comparison to conferences of practicing physicians [ 70 ]. Conversely, Van Eyk et al. reported that the average number of citations of Dutch medical student publications was actually higher than the average citations for papers in the same field. [ 41 ]
A number of studies investigated factors that prevent medical students from being involved in research. Poor mentorship, lack of role models and perceived lower salaries of academic physicians were among the key factors cited ( S5 File ) . The previous findings were also supported by four qualitative studies ( Table 3 ) [ 17 , 45 , 90 , 99 – 101 , 103 , 104 ] .
https://doi.org/10.1371/journal.pone.0127470.t003
In addition, institutional influence as well as the type and length of available research opportunities were found to be relevant factors in determining whether students choose to engage in research [ 51 , 53 ]. McLean and co-authors provided an excellent set of tips to bolster the involvement of students in academic medicine projects and potentially overcome some the aforementioned limitations [ 105 ].
. The importance of psycho-cognitive factors in determining medical students' motivation towards- and engagement in- research was also highlighted in the qualitative literature. One of the most important motives behind performing research is curiosity. Not only is curiosity a main motive behind pursuing research while in medical school (as has been shown by Shapiro et al [ 101 ]), it is one of the very early psycho-cognitive predictors of persistence into scientific or research disciplines even before enrolment into medical school [ 17 , 104 ]. Conversely, perceived lack of competence may deter medical students from pursuing research-active careers [ 45 ].
III) Assessing the impact and effect of medical student research
We assessed three main outcomes that reflect the short- and long- term impact of medical student research: 1) the proportion of research performed during medical school that culminates in a peer-reviewed journal publication, 2) the effect of medical school research on the career choice and future research involvement of medical students, and 3) the effect of medical student research on long- term success in academia. The first outcome has been summarized in Fig 6 [ 10 , 24 , 25 , 27 , 29 – 31 , 37 , 38 , 41 , 49 , 64 , 75 , 76 , 93 , 106 ] and the latter two are shown in Fig 7 [ 8 , 25 , 26 , 31 , 43 , 44 , 66 , 68 , 81 , 83 , 85 , 90 ].
Since the duration of research exposure will almost always affect the publication outcome, it has been shown too. Forest Plot symbols: * The axis, not the data, is shown in logit scale for aesthetic purposes. Table symbols: * The duration is probably prolonged (possibly months long); ** 20–40 European medical school credits; || For published projects, the average duration was 18 months. D , developing countries; I , intercalated Bachelor of Science degree (iBSc); HQ , relatively high quality publication (indexed in Medline, Scopus or Medic), HF , first-author publication in a relatively high quality journal. Dates are shown beside studies that may be confused with others referenced in this review having the same similar first-author names.
https://doi.org/10.1371/journal.pone.0127470.g006
Forest Plot symbols: * The axis, not the data, is shown in log scale for aesthetic purposes. Table symbols: * at least one first-author publication; ** at least one citation; || more than 20 citations. For some studies, odds ratios and 95% confidence interval values were reported, but not the raw numbers.
https://doi.org/10.1371/journal.pone.0127470.g007
III1. Medical student research results in a publishable product.
Peer-reviewed journal publications are generally considered to be the best indicator of research productivity, and it may be viewed as a major metric (though not the only one) of the “return on investment” in supporting and funding medical student research. An average of 30% (0.30, 0.19–0.44) of research performed by medical students resulted in a peer-reviewed journal publication. When only higher quality publications were included in the analysis (indexed in Medline, Scopus or Medic), the proportion remained more or less the same (0.31, 0.18–0.47). Subgroup analysis of studies investigating the research productivity of graduation theses revealed that 26% (0.26, 0.10–0.52) of graduation theses result in higher quality publications.
As expected, all studies reporting first -authored peer-reviewed publication by medical students described instances of prolonged research exposure. An average of 13% (0.13, 0.06–0.27) of medical student research resulted in a first-authored peer-reviewed publication. The pooled outcome remained the same when only higher quality publications (Medline-, Scopus- or Medic- indexed) were included in the analysis (0.13, 0.05–0.30).
A few initiatives, aimed at propping up medical student publication output, have gained popularity over the last few years. Those initiatives include a number of student-run journals and journal spaces dedicated solely for medical student research publications [ 107 – 110 ]. A subset of these journals is Medline-indexed and some even involve undergraduates in the peer-review process. Similarly, the Yale Journal of Biology and Medicine annually publishes Yale's student thesis abstracts [ 111 ]. These initiatives, we suppose, will help in promoting student participation in research and comfort students about publication issues. To our knowledge, there is no systematic investigation in the literature so far regarding the quality of research published in medical student research journals in comparison to field-specific journals. Hence, we would like to take a conservative stance whenever we see such hierarchical "segmentation" of the scientific enterprise; the stringency of research assessment, in our opinion, should be indiscriminant to the identity of the study authors.
It is important to note that the failure of publication of medical student research may be reflective of other factors beside the success and relative contribution of the student. For example, Weber et al showed that 55% of the papers submitted to a medical specialty conference did not reach the stage of publication five years later [ 112 ]. Similarly, Riveros et al found that half of the clinical trials reporting results in ClinicalTrials.gov had no corresponding journal publication [ 113 ]. Keeping this in mind, the results by Cursiefen et al should not be surprising; showing that medical students were among the authors of 28% of the papers produced by a German medical faculty, even though only 66% of medical student research resulted in a publication [ 30 ].
III2. Research during medical school is associated with later involvement in research projects.
Students who took part in research projects during medical school were more likely to get involved in (or report planned involvement in-) research later in their careers (OR = 3.58, 1.82–7.04). When a subgroup analysis was performed to include only studies that explicitly refer to academic careers (as opposed to brief research encounters), students who performed research during medical school were over six times as likely to pursue academic careers (OR = 6.42, 1.37–29.98) than their “untreated” peers.
With one exception, none of the included studies had a prospective design; hence reverse causality cannot be excluded, and is in fact very likely (students planning academic medicine careers choosing to get involved in research during medical school). Indeed, the only prospective study included (McManus et al [ 85 ]) showed that at the time of application to medical school, students who later chose to take an intercalated degree were already significantly more likely to report definite or highly likely choice of academic medicine careers (OR = 1.37, 1.13–1.66). Just before graduation, however, this likelihood had a substantial increase (OR = 3.45, 2.27–5.24). Together, these results indicate that medical school research strengthens pre-existing interest in an academic career.
A qualitative study by O'sullivan et al emphasized the value of early research exposure in giving medical students the opportunity to entertain the thought of pursuing academic careers [ 114 ]. Such exposure, they concluded, may sometimes even discourage students from pursuing academia, but is necessary nonetheless given the lack of sufficient free time during post-graduation residency to experience research.
III3. Research during medical school is associated with long-term success in academia.
Three studies showed that physicians who performed research during medical school were more likely to attain faculty rank long after graduation [ 8 , 32 , 66 ]. While this has implications on the decision of individual medical students to pursue research, we argue that it has little bearing on policy decision-making, since faculty positions are awarded on a competitive basis. Indeed, Brancati et al showed that this effect was dependent on the publication status of research performed during medical school [ 32 ]. In other words, students who did not publish their research were not significantly more likely to attain higher faculty rank on the long run. Hence, the fact that medical student research is associated with higher likelihood of attaining faculty positions has little implications regarding the systematic incorporation of research into medical curricula.
Students who performed research during medical school were more than twice as likely to author at least one peer-reviewed publication later in their career (OR = 2.31, 1.88–2.83). This remained true after the exclusion of Chusid et al [ 25 ] (which correlates successful publication of graduation theses with long-term publication success) from the analysis (OR = 2.26, 1.83–2.77). They were also twice as likely to acquire first-authorship (OR = 2.21, 1.56–3.13). The total number of publications and ability to secure grants, too, was reported to be significantly higher among students with medical school research experience [ 81 ]. Evered et al, on the other hand, found no significant difference in either of those measures between both groups [ 66 ]. Moreover, students who performed research during medical school were more likely to be cited at least once [ 66 ], had a higher total citation count [ 81 ], were more likely to be cited more than 20 times [ 66 ], and had higher odds of receiving awards [ 8 , 81 ] later in their careers.
While this data provides strong evidence of a correlation between medical school research and long-term success in academia, a causal relationship cannot be established since students who decide to perform research may already have a keen interest in research. Nonetheless, a causal relationship is quite likely since early research experience (especially if it culminates in a first-authored publication) would naturally enhance the career prospects and significantly improve the CV’s of early career medical graduates. Overall, we believe that the long-term impact of medical school research is inadequately assessed, and that further evidence is needed using prospective study designs with proper adjustment for baseline status.
III4. Research during medical school is correlated with career choice of- (or interest in a career in-) the same or related specialty as the research project.
Three of the studies that met the broad inclusion criteria reported results from control or “untreated” groups. Other studies reported results only from treated groups and hence were excluded from the analysis. Overall, students are 2.7 times as likely to be interested in careers in the same (or related) clinical specialty as the research project they got involved in during medical school. As with many other conclusions in this review, a causal relationship cannot be determined from this apparent correlation. This is especially true in the case of competitive residencies (and is particularly relevant to US residencies), where research experience in the same specialty gives recent graduates a competitive edge over their peers without such experience.
The relationship between medical school research and clinical practice was also touched upon in two of the included qualitative studies. Shapiro et al showed that many faculty members mentored student research in family practice in order to attract students to the same specialty [ 101 ]. Indeed, students interviewed by Jones et al believed an iBSc in primary healthcare provided them with deeper insights into patient care and a more thorough understanding of evidence-based clinical practice [ 99 ].
IV) Miscellaneous topics related to medical student research
In the following section of this review we discuss a number of miscellaneous topics relevant to medical student research. Three of these topics were discussed in light of quantitative data, and are summarized in Fig 8 [ 28 , 29 , 47 – 49 , 53 , 54 , 58 , 59 , 62 , 63 , 67 , 71 , 79 , 81 , 83 , 88 , 89 , 92 ] and Fig 9 [ 24 , 27 , 33 , 37 , 38 , 50 , 64 , 70 ]. Though they did not pass our inclusion criteria, four of the citations screened were personal perspectives provided by medical students, and are worth mentioning for enriching the discussion. They discussed the importance of the research experience on their medical career [ 115 , 116 ], the importance of medical students' research in increasing national research output [ 117 ] and the relevance of lab research involving animals to appreciation of human anatomy and physiology [ 118 ].
Forest Plot symbols: * The axis, not the data, is shown in log scale for aesthetic purposes. Abbreviations used: D, developing countries; I, intercalated Bachelor of Science degree (iBSc); FC , studies measuring final year academic performance and controlling for baseline performance. Dates are shown beside studies that may be confused with others referenced in this review having the same similar first-author names. For some studies, odds ratios and 95% confidence interval values were reported, but not the raw numbers.
https://doi.org/10.1371/journal.pone.0127470.g008
https://doi.org/10.1371/journal.pone.0127470.g009
IV1. Effect of prolonged research time-off on subsequent academic performance.
One of the issues discussed in the literature is the effect of prolonged research time-off amid the medical program on subsequent clinical knowledge. This question has been assessed in the context of iBSc degrees in a recent review [ 119 ]. All but one of our included studies investigated the effect of taking an intercalated degree on subsequent academic performance. The results have been conflicting; two studies that either matched groups by previous performance or adjusted for pre-clinical scores found no evidence of improvement in scores [ 88 , 120 ]. All five other studies that met our inclusion criteria reported an improvement in academic performance.
Due to heterogeneity in academic assessment methods and high possibility of confounding, we only pooled the studies for which we could extract odds ratio values that: a) measure final year academic scores and b) control for previous academic performance. Three studies met these two inclusion criteria, all of which reported the effect of iBSc degrees. On average, students who took some time off to perform research were twice as likely to outperform their peers (OR = 1.99, 1.39–2.84), even after adjustment for previous academic performance. It is noteworthy that all pooled studies investigated research time-off that was around one year in duration (iBSc), and that the positive effect of research time-off on subsequent academic performance may actually be reversed if the research delays are prolonged. Dyrbye et al pinned down a critical period of three years, after which medical students start to lose clinical knowledge and skills by the time they return to the core medical program [ 28 ].
IV2. Gender equality in medical student research.
There is no apparent gender difference regarding the following outcomes: Interest in a career in research ; involvement in research during medical school ; attitudes towards research ; interest in- or motivation towards- performing research ; research knowledge or skills. However, on average, males seem to be significantly more likely to publish (or submit for publication) the research they performed during medical school (OR = 1.59, 1.26–2.01). The reasons behind this gender gap in publication are unclear to us, and have been inadequately researched. Since there is no apparent gender difference in research perceptions, attitudes, motivations or knowledge, we suspect that the gender difference in publications is due to factors unrelated to research such as the overall academic environment or psychosocial factors. Indeed, these findings are consistent with a 2006 study by Jagsi et al showing a generalized gender gap in the authorship of academic medical articles in six major medical journals. Whatever the reasons behind gender differences in publication, they underlie a general issue not specific to medical school research [ 121 ].
IV3. Type and field of research performed by medical students.
The majority of medical student research is original in nature (as opposed to literature reviews). We were interested in finding out what percentage of these research projects were in the basic sciences, since this issue is of particular relevance to translational research. We found that the proportion was highly variable between different studies. In four of the five included studies less than half of medical student research was lab-based basic research, and the pooled weighted estimate was 0.32, 0.14–0.49. Given the relevance of research to competitive residency applications, it should not come as a surprise that lab-based projects do not constitute the majority of medical student research. Nonetheless, these results indicate that efforts directed at increasing the number of physician scientists involved in translational research should not only be directed at bolstering research involvement, but also improving the appeal of basic lab-based research to medical students.
IV4. Compulsory vs. elective medical school research.
The question of whether undergraduate medical research should be made compulsory or elective has been discussed in the literature, and is a matter of debate [ 37 , 97 , 122 ]. Arguments in favor of mandatory incorporation revolve around the ever-increasing importance of evidence-based clinical practice, while arguments against it revolve around the importance of focusing on clinical skills education. Diez et al. recommended against Germany's dissertation requirement, due to the steady decline in the number of successful dissertations [ 123 ]. Our results tell a similar story; the fraction of graduation theses resulting in a first-authored higher quality publication was smaller than the overall average (0.07, 0.03–0.14). At first, this may seem counterintuitive, as one may predict that the systematic incorporation of research as a necessary graduation requirement would raise the fraction culminating in a first-authored higher quality publication. However, one needs to bear in mind that since graduation theses are an obligatory requirement, a fraction of those students performing research may not be interested at all in what they are doing. Taking this into consideration, it should not come as a surprise that percentages as high as 34% (Cohen et al [ 38 ]) and 31% (Dyrbye et al [ 29 ]) of voluntary medical student research were reported to result in first-authored Medline-indexed publications. Weihrauch et al and Pabst et al, on the other hand, reported favorable results in terms of the personal and professional value of the German dissertation requirement [ 124 , 125 ].
IV5. The situation in countries with developing economies.
We retrieved studies that were performed in India [ 67 , 72 ], Uganda [ 68 ], China [ 69 ], Brazil [ 70 , 74 ], UAE [ 71 ], Croatia [ 73 , 79 ], Pakistan [ 75 , 77 , 80 , 86 ], Peru [ 76 ], and Turkey [ 78 ].
The number of medical schools and the research budget in developing countries are alarmingly mismatched with their needs [ 1 ]. This disparity, we believe, reflects naturally on the status of medical student research. In fact, medical student research might be even more important in developing countries than in developed countries, due to the pressing need to adapt international standards to local community needs.
Medical students in developing countries arguably face a set of extra challenges and are influenced by a number of different factors in comparison to developed countries [ 126 ]. For example, the high student-to-teacher ratio makes it increasingly difficult for medical students to have mentors and role models. Even research based on statistical analysis of patient records is often difficult to perform in many medical schools, due to suboptimal Information and Communications Technology (ICT) infrastructure in hospitals and in teaching premises in countries with developing economies [ 127 ]. While excellent research may of course be performed in resource-poor countries, it is preferable that any reform in research funding is coupled with a well-developed educational and managerial infrastructure; otherwise the research output may be largely suboptimal [ 128 ]. Worryingly, an essay by Silva et al. reported a decrease in the ratio of Undergraduate Student Research Assistant Programs (USRA's) to the number of undergraduates in Brazil over the past years [ 129 ].
Students’ interest in research was higher in countries with developing economies than in developed countries (0.82, 0.67–0.91 vs. 0.47, 0.26–0.69). One possible explanation for this finding is that the lack of opportunities causes higher eagerness to perform research. Another, possibly more likely, explanation is higher career-related anxiety in lower-income settings, with a resultant boost in research interest. Indeed, students in developing countries were not significantly less exposed to research, a result which may be reflective of the higher interest rates, bolstering research engagement despite inadequacies in resources. These results are supported by the findings of Baig et al, showing that 40% of Pakistani medical students viewed research as a tool to secure competitive residencies in the US [ 86 ].
Conclusions and Future Directions
Overall, our review shows that there’s considerable variability in medical student research exposure, engagement and productivity among different medical schools. A large proportion of the medical student population is interested in research, but is deterred by practical difficulties, including the lack of opportunities and funding. The benefits of research exposure on the short- and long-term scientific productivity is well documented in the literature, and a clear correlation is identified between medical school research engagement and later engagement in research projects (including the choice of an academic career). However, the number of well-controlled, high-quality prospective studies on the topic is limited and it is difficult to exclude reverse-causality. Existing evidence suggests that medical school research does have a positive effect on the choice of an academic career, but it does so through strengthening pre-existing interest. Financial worries, gender, having a higher degree (MSc or PhD) before matriculation and perceived competitiveness of the residency of choice are among the factors that affect the engagement of medical students in research and their scientific productivity.
Another potential limitation of this review is publication bias. It is conceivable that medical schools where students had a positive experience with research rush to publish their results, whereas others with experiences that were not so positive blamed it on the design of the program without publishing their results. It is also clear that there are plenty of successful undergraduate research programs that do not publish their results.
We suggest that more studies are done to assess the different structural and managerial aspects of standardized undergraduate medical research, as well as the differences between compulsory research components, elective research components, intercalated BSc's and extracurricular research in terms of academic, professional and psycho-cognitive effects. Further, we recommend more investigation into the quality and citation potential of published medical student research in comparison to that of established researchers and physicians.
Supporting Information
S1 file. prisma guidelines checklist..
https://doi.org/10.1371/journal.pone.0127470.s001
S2 File. Supplementary methodology file.
https://doi.org/10.1371/journal.pone.0127470.s002
S3 File. Quality assessment and quantitative data extraction sheet.
Abbreviations used: D, developing countries; I, intercalated Bachelor of Science degree (iBSc); X, Cross-sectional; R, Retrospective; I , Interventional; Pro , Prospective; Q, questionnaire; DS , database search; IN, interview.
https://doi.org/10.1371/journal.pone.0127470.s003
S4 File. Sensitivity plots for the pooled effect size values calculated.
https://doi.org/10.1371/journal.pone.0127470.s004
S5 File. Supplementary tables accompanying the main text.
https://doi.org/10.1371/journal.pone.0127470.s005
Acknowledgments
We would like to acknowledge with gratitude the following authors (and their co-authors) for sending us raw numbers to be used in our meta-analysis: Dr Nishanthan Mahesan, Dr des Anges Cruser, Dr Louise Burgoyne, Dr Neel Halder, Dr Cherrie Galletly, Dr Tracy Air, Dr Anna Chur-Hansen, Dr Craig Ziegler, Dr Ruth B. Greenberg, Dr Darko Hren, Dr Robert Siemens and Dr Matko Marusic.
Author Contributions
Conceived and designed the experiments: MA MMKT SJL ES. Performed the experiments: MA MMKT ES. Analyzed the data: MA MMKT SJL ES. Contributed reagents/materials/analysis tools: MA MMKT SJL ES. Wrote the paper: MA MMKT SJL ES.
- View Article
- PubMed/NCBI
- Google Scholar
- 5. National Institute of General Medical Sciences: Medical Scientist Training Program [Internet]. Available: http://www.nigms.nih.gov/Training/InstPredoc/PredocOverview-MSTP.htm . Accessed 14 April 2015.
- 7. Association of American Medical Colleges. Medical School Graduation Questionnaire—2013 all school summary report [Internet]. Available: https://www.aamc.org/download/350998/data/2013gqallschoolssummaryreport.pdf . Accessed 14 April 2015.
- 19. International Monetary Fund. World Economic Outlook Database [Internet]. 2013. Available: http://www.imf.org/external/pubs/ft/weo/2013/01/weodata/index.aspx . Accessed 14 April 2015.
- 22. Dixon-woods M, Agarwal S, Young B, Jones D, Sutton A. Integrative approaches to qualitative and quantitative evidence. Health Development Agency; 2004. Available: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.96.8783&rep=rep1&type=pdf . Accessed 14 April 2015.
- 107. Journal of Young Investigators [Internet]. Available: http://www.jyi.org/site/ . Accessed 14 April 2015.
- 108. Internationl Medical Journal of Students’ Research [Internet]. Available: http://www.imjsr.org/ . Accessed 14 April 2015.
- 109. McGill Journal of Medicine [Internet]. Available: http://www.med.mcgill.ca/mjm/ . Accessed 14 April 2015.
- 110. American Journal of Undergraduate Research [Internet]. Available: http://www.ajur.uni.edu/index.html . Accessed 14 April 2015.
Advertisement
Teaching Medical Research to Medical Students: a Systematic Review
- Published: 08 January 2021
- Volume 31 , pages 945–962, ( 2021 )
Cite this article

- Gabriel Sheng Jie Lee 1 ,
- Yip Han Chin 1 ,
- Aimei Amy Jiang 1 ,
- Cheng Han Mg 1 ,
- Kameswara Rishi Yeshayahu Nistala 1 ,
- Shridhar Ganpathi Iyer 2 , 3 ,
- Shuh Shing Lee 4 ,
- Choon Seng Chong ORCID: orcid.org/0000-0003-0669-7307 1 , 5 &
- Dujeepa D. Samarasekera 4
942 Accesses
15 Citations
14 Altmetric
Explore all metrics
Research literacy remains important for equipping clinicians with the analytical skills to tackle an ever-evolving medical landscape and maintain an evidence-based approach when treating patients. While the role of research in medical education has been justified and established, the nuances involving modes of instruction and relevant outcomes for students have yet to be analyzed. Institutions acknowledge an increasing need to dedicate time and resources towards educating medical undergraduates on research but have individually implemented different pedagogies over differing lengths of time.
While individual studies have evaluated the efficacy of these curricula, the evaluations of educational methods and curriculum design have not been reviewed systematically. This study thereby aims to perform a systematic review of studies incorporating research into the undergraduate medical curriculum, to provide insights on various pedagogies utilized to educate medical students on research.
Studies predominantly described two major components of research curricula—(1) imparting basic research skills and the (2) longitudinal application of research skills. Studies were assessed according to the 4-level Kirkpatrick model for evaluation. Programs that spanned minimally an academic year had the greatest proportion of level 3 outcomes (50%). One study observed a level 4 outcome by assessing the post-intervention effects on participants. Studies primarily highlighted a shortage of time (53%), resulting in inadequate coverage of content.
This study highlighted the value in long-term programs that support students in acquiring research skills, by providing appropriate mentors, resources, and guidance to facilitate their learning. The Dreyfus model of skill acquisition underscored the importance of tailoring educational interventions to allow students with varying experience to develop their skills. There is still room for further investigation of multiple factors such as duration of intervention, student voluntariness, and participants’ prior research experience. Nevertheless, it stands that mentoring is a crucial aspect of curricula that has allowed studies to achieve level 3 Kirkpatrick outcomes and engender enduring changes in students.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
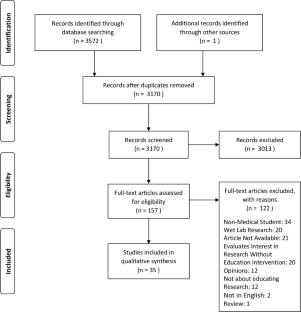
Similar content being viewed by others

Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature

Ethical Issues in Research: Perceptions of Researchers, Research Ethics Board Members and Research Ethics Experts

A Medical Science Educator’s Guide to Selecting a Research Paradigm: Building a Basis for Better Research
John J, Riva RE, Daza J, Toma A, Whyte R, Agarwal G, et al. Medical students’ challenges and suggestions regarding research training: a synthesis of comments from a cross-sectional survey. Can Med Educ J. 2019;10(3):e91–100.
Article Google Scholar
Fernandez A, Chen V, Quan J, Martinez A, Flowers L, Aronson L. Evaluation of a medical student research and career development program to increase diversity in academic medicine. J Assoc Am Med Coll. 2019;94(8):1220–8.
Louise N, Burgoyne SOF, Boylan Geraldine B. Undergraduate medical research: the student perspective. Med Educ Online. 2010;10:15.
Google Scholar
David William Moraes MJ, Menegazzo WR, Menegazzo MS, Veloso S, Machry MC, Costanzi M, et al. Interest in research among medical students: challenges for the undergraduate education. Rev Ass Med Bras. 2016;62:652–8.
Stone C, Dogbey GY, Klenzak S, Van Fossen K, Tan B, Brannan GD. Contemporary global perspectives of medical students on research during undergraduate medical education: a systematic literature review. Taylor Francis. 2018;23(1):1537430.
Amgad M, Tsui MMK, Liptrott SJ, Shash E. Medical student research: an integrated mixed-methods systematic review and meta-analysis. PLoS ONE. 2015;10(6):e0127470.
Yaow CYL, Mok HT, Ng CH, Devi MK, Iyer S, Chong CS. Difficulties faced by general surgery residents. A qualitative systematic review. J Surg Educ. 2020;77(6):1396–406.
Kastner M, Antony J, Soobiah C, Straus SE, Tricco AC. Conceptual recommendations for selecting the most appropriate knowledge synthesis method to answer research questions related to complex evidence. J Clin Epidemiol. 2016;73:43–9.
Shannon H-FHSE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Ng CH, Ong ZH, Koh JWH, Ang RZE, Tan LHS, Tay KT, et al. Enhancing interprofessional communications training in internal medicine. Lessons drawn from a systematic scoping review from 2000 to 2018. J Contin Educ Heal Prof. 2020;40(1):27–35.
Kirkpatrick D. Evaluation of training. New York: McGraw Hill; 1967.
Reed DC, Cook DA, Beckman T, Levine R, Kern D, Wright SM. Association between funding and quality of published medical education research. JAMA. 2007:298. https://doi.org/10.1001/jama.298.9.1002 .
Sideris M, Hanrahan J, Staikoglou N, Pantelidis P, Pidgeon C, Psychalakis N, et al. Optimizing engagement of undergraduate students in medical education research: the eMERG training network. Ann Med Surg. 2018;31:6–10.
Chaturvedi S, Aggarwal OP. Training interns in population-based research: learners’ feedback from 13 consecutive batches from a medical school in India. Med Educ. 2001;35(6):585–9.
Dorrance KA, Denton GD, Proemba J, la Rochelle J, Nasir J, Argyros G, et al. An internal medicine interest group research program can improve scholarly productivity of medical students and foster mentoring relationships with internists. Teach Learn Med. 2008;20(2):163–7.
Knight SE, Van Wyk JM, Mahomed S. Teaching research: a programme to develop research capacity in undergraduate medical students at the University of KwaZulu-Natal, South Africa. BMC Med Educ. 2016;16:61.
Burge SK, Hill JH. The medical student summer research program in family medicine. Fam Med. 2014;46(1):45–8.
Gold IW, Jayne HA. Development and evaluation of a one-month research track in emergency medicine for medical students. Ann Emerg Med. 1987;16(6):686–8.
Gregory SW, Otoole R. Teaching sociological-research methods to medical-students. Teach Sociol. 1987;15(2):128–35.
Ahsin S, Abbas S, Zaidi N, Azad N, Kaleem F. Reciprocal benefit to senior and junior peers: an outcome of a pilot research workshop at medical university. JPMA. 2015;65(8):882–4.
Akman M, Unalan PC, Kalaca S, Kaya CA, Cifcili S, Uzuner A. A three-year mandatory student research program in an undergraduate medical curriculum in Turkey. Kuwait Med J. 2010;42(3):205–10.
Alamodi AA, Abu-Zaid A, Anwer LA, Khan TA, Shareef MA, Shamia AA, et al. Undergraduate research: an innovative student-centered committee from the Kingdom of Saudi Arabia. Med Teacher. 2014;36:S36–42.
Cain L, Kramer G, Ferguson M. The Medical Student Summer Research Program at the University of Texas Medical Branch at Galveston: building research foundations. Med Educ Online. 2019;24(1):1581523.
Cha S, Ross JS, Sacajiu G, Lurie P. Assessment of a research-based health activism curriculum for medical students. J Gen Intern Med. 2006;19:122–122.
Cluver J, Book S, Brady K, Back S, Thornley N. Engaging medical students in research: reaching out to the next generation of physician-scientists. Acad Psychiatry. 2014;38(3):345–9.
Dehaven MJ, Chen L. Teaching medical students research while reaching the underserved. Fam Med. 2005;37(5):315–7.
Dehaven MJ, Gimpel NE, Dallo FJ, Billmeier TM. Reaching the underserved through community-based participatory research and service learning: description and evaluation of a unique medical student training program. J Public Health Manag Pract. 2011;17(4):363–8.
Devi V, Ramnarayan K, Abraham RR, Pallath V, Kamath A, Kodidela S. Short-term outcomes of a program developed to inculcate research essentials in undergraduate medical students. J Postgrad Med. 2015;61(3):163–8.
Dicianno BE, Glick RM, Sowa GA, Boninger ML. Processes and outcomes from a medical student research training program in integrative, complementary, and alternative medicine. Am J Phys Med Rehabil. 2016;95(10):779–86.
Fishleder AJ, Henson LC, Hull AL. Cleveland Clinic Lerner College of Medicine: an innovative approach to medical education and the training of physician investigators. Acad Med. 2007;82(4):390–6.
Gallin EK, Le Blancq SM, Gallin EK, Le Blancq SM. Launching a new fellowship for medical students: the first years of the Doris Duke Clinical Research Fellowship Program. J Invest Med (Decker Publishing). 2015;53(2):73–81.
Gillman J, Pillinger M, Plottel CS, Galeano C, Maddalo S, Hochman JS, et al. Teaching translational research to medical students: the New York University School of Medicine’s Master’s of Science in Clinical Investigation Dual-Degree Program. Clin Transl Sci. 2015;8(6):734–9.
Gonzales AO, Westfall J, Barley GE. Promoting medical student involvement in primary care research. Fam Med. 1998;30(2):113–6.
Kelly L, Rourke J. Research electives in rural health care. Can Fam Physician. 2002;48:1476–80.
Laskowitz DT, Drucker RP, Parsonnet J, Cross PC, Gesundheit N. Engaging students in dedicated research and scholarship during medical school: the long-term experiences at Duke and Stanford. Acad Med. 2010;85(3):419–28.
Marusic A, Marusic M. Teaching students how to read and write science: a mandatory course on scientific research and communication in medicine. Acad Med. 2003;78(12):1235–9.
Mullan JR, Weston KM, Rich WC, McLennan PL. Investigating the impact of a research-based integrated curriculum on self-perceived research experiences of medical students in community placements: a pre- and post-test analysis of three student cohorts. BMC Med Educ. 2014;14:161.
Patra S, Khan AM. Development and implementation of a competency-based module for teaching research methodology to medical undergraduates. J Educ Health Promot. 2019;8:164–164.
Riley SC, Morton J, Ray DC, Swann DG, Davidson DJ. An integrated model for developing research skills in an undergraduate medical curriculum: appraisal of an approach using student selected components. Perspect Med Educ. 2013;2(4):230–47.
Sanford T, Chancer Z, Kiyosaki K. Medical student research at the John A. Burns School of Medicine (JABSOM): the Research Interest Group. Hawaii Med J. 2010;69(7):172–3.
Shapiro J, Coggan P, Rubel A, Morohasi D, Fitzpatrick C, Danque F. The process of faculty-mentored student research in family medicine: motives and lessons. Fam Med. 1994;26(5):283–9.
Zorzi A, Rourke J, Kennard M, Peterson M, Miller K. Combined research and clinical learning make Rural Summer Studentship Program a successful model. Rural Remote Health. 2005;5(4):401.
Black ML, Curran MC, Golshan S, Daly R, Depp C, Kelly C, et al. Summer research training for medical students: impact on research self-efficacy. Clin Transl Sci. 2013;6(6):487–9.
Cruser A, Brown SK, Ingram JR, et al. Learning outcomes from a biomedical research course for second year osteopathic medical students. Osteopath Med Primary Care. 2010;4:7p-7p.
Jawaid M, Ashraf J. Initial experience of eLearning research module in undergraduate medical curriculum of Dow University of Health Sciences: development and students perceptions. Pakistan J Med Sci. 2012;28(4):591–6.
Gallin EK, Le Blancq SM. Launching a new fellowship for medical students: the first years of the Doris Duke Clinical Research Fellowship Program. J Invest Med (Decker Publishing). 2005;53(2):73–81.
Hren D, Lukic IK, Marusic A, Vodopivec I, Vujaklija A, Hrabak M, et al. Teaching research methodology in medical schools: students’ attitudes towards and knowledge about science. Med Educ. 2004;38(1):81–6.
Kumar D, Singh US, Solanki R. Assessment of a group activity based educational method to teach research methodology to undergraduate medical students of a rural medical college in Gujarat India. J Clin Diagn Res. 2015;9(7):LC01–3.
Campbell TA, Campbell DE. Faculty/student mentor program: effects on academic performance and retention. Res High Educ. 1997;38(6):727–42.
Kusurkar RA, Ten Cate TJ, Vos CMP, Westers P, Croiset G. How motivation affects academic performance: a structural equation modelling analysis. Adv Health Sci Educ. 2013;18(1):57–69.
Eva KW, Regehr G. Exploring the divergence between self-assessment and self-monitoring. Adv Health Sci Educ. 2011;16(3):311–29.
Parsonnet J, Gruppuso PA, Kanter SL, Boninger M. Required vs. elective research and in-depth scholarship programs in the medical student curriculum. Acad Med. 2010;85(3):405–8.
Dreyfus SE, Dreyfus HL. A five-stage model of the mental activities involved in directed skill acquisition. 1980.
Book Google Scholar
Hooi SC, Koh DR, Chow VT. The NUS MBBS-PhD programme: nurturing clinician-scientists for tomorrow. Ann Acad Med Singap. 2005;34(6):163c–5c.
Afacan EAÖ. Problems encountered during the scientific research process in graduate education: the Institute of Educational Sciences. High Educ Stud. 2018;8(2):47–57.
Bair M, Enomoto E. Demystifying research: what’s necessary and why administrators need to understand it. NASSP Bull. 2013;97:124–38.
Murdoch-Eaton D, Drewery S, Elton S, Emmerson C, Marshall M, Smith JA, et al. What do medical students understand by research and research skills? Identifying research opportunities within undergraduate projects. Med Teacher. 2010;32(3):e152–60.
Lyon LJ. Development of teaching expertise viewed through the Dreyfus model of skill acquisition. J Scholarsh Teach Learn. 2015;15(1):88–105.
Carraccio CL, Benson BJ, James Nixon L, Derstine PL. From the educational bench to the clinical bedside: translating the Dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83(8):761–7.
Field A. Understanding the Dreyfus model of skill acquisition to improve ultrasound training for obstetrics and gynaecology trainees. Ultrasound. 2014;22:118–22.
McKenna L, French J. A step ahead: teaching undergraduate students to be peer teachers. Nurse Educ Pract. 2011;11(2):141–5.
Stigmar M. Peer-to-peer teaching in higher education: a critical literature review. Mentoring Tutoring. 2016;24(2):124–36.
Collier PJ. Why peer mentoring is an effective approach for promoting college student success. Metropolitan Univ. 2017;28(3):9.
Smith S, Newsome A, Hawkins W, Bland C, Branan T. Teaching research skills to student pharmacists: a multi-campus, multi-semester applied critical care research elective. Curr Pharm Teach Learn. 2020;12:735–40.
Download references
Acknowledgments
The authors would like to thank Ms. Annelissa Chin from Yong Loo Lin School of Medicine, medical library for assisting us with the search strategy.
Author information
Authors and affiliations.
Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Gabriel Sheng Jie Lee, Yip Han Chin, Aimei Amy Jiang, Cheng Han Mg, Kameswara Rishi Yeshayahu Nistala & Choon Seng Chong
Division of Hepatobiliary & Pancreatic Surgery, Department of Surgery, National University Hospital, Singapore, Singapore
Shridhar Ganpathi Iyer
Liver Transplantation, National University Centre for Organ Transplantation, National University Hospital, Singapore, Singapore
Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Shuh Shing Lee & Dujeepa D. Samarasekera
Division of Colorectal Surgery, Department of Surgery, National University Hospital, 1E Kent Ridge Road, Singapore, 119228, Singapore
Choon Seng Chong
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Choon Seng Chong .
Ethics declarations
Conflict of interest.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions.
Reprints and permissions
About this article
Lee, G.S.J., Chin, Y.H., Jiang, A.A. et al. Teaching Medical Research to Medical Students: a Systematic Review. Med.Sci.Educ. 31 , 945–962 (2021). https://doi.org/10.1007/s40670-020-01183-w
Download citation
Accepted : 01 December 2020
Published : 08 January 2021
Issue Date : April 2021
DOI : https://doi.org/10.1007/s40670-020-01183-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dreyfus model
- Medical undergraduates
- Research education
- Skill acquisition
- Find a journal
- Publish with us
- Track your research
Teaching Medical Research to Medical Students: a Systematic Review
Affiliations.
- 1 Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore.
- 2 Division of Hepatobiliary & Pancreatic Surgery, Department of Surgery, National University Hospital, Singapore, Singapore.
- 3 Liver Transplantation, National University Centre for Organ Transplantation, National University Hospital, Singapore, Singapore.
- 4 Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore.
- 5 Division of Colorectal Surgery, Department of Surgery, National University Hospital, 1E Kent Ridge Road, Singapore, 119228 Singapore.
- PMID: 34457935
- PMCID: PMC8368360
- DOI: 10.1007/s40670-020-01183-w
Phenomenon: Research literacy remains important for equipping clinicians with the analytical skills to tackle an ever-evolving medical landscape and maintain an evidence-based approach when treating patients. While the role of research in medical education has been justified and established, the nuances involving modes of instruction and relevant outcomes for students have yet to be analyzed. Institutions acknowledge an increasing need to dedicate time and resources towards educating medical undergraduates on research but have individually implemented different pedagogies over differing lengths of time.
Approach: While individual studies have evaluated the efficacy of these curricula, the evaluations of educational methods and curriculum design have not been reviewed systematically. This study thereby aims to perform a systematic review of studies incorporating research into the undergraduate medical curriculum, to provide insights on various pedagogies utilized to educate medical students on research.
Findings: Studies predominantly described two major components of research curricula-(1) imparting basic research skills and the (2) longitudinal application of research skills. Studies were assessed according to the 4-level Kirkpatrick model for evaluation. Programs that spanned minimally an academic year had the greatest proportion of level 3 outcomes (50%). One study observed a level 4 outcome by assessing the post-intervention effects on participants. Studies primarily highlighted a shortage of time (53%), resulting in inadequate coverage of content.
Insights: This study highlighted the value in long-term programs that support students in acquiring research skills, by providing appropriate mentors, resources, and guidance to facilitate their learning. The Dreyfus model of skill acquisition underscored the importance of tailoring educational interventions to allow students with varying experience to develop their skills. There is still room for further investigation of multiple factors such as duration of intervention, student voluntariness, and participants' prior research experience. Nevertheless, it stands that mentoring is a crucial aspect of curricula that has allowed studies to achieve level 3 Kirkpatrick outcomes and engender enduring changes in students.
Supplementary information: The online version contains supplementary material available at 10.1007/s40670-020-01183-w.
Keywords: Curricula; Dreyfus model; Medical undergraduates; Research education; Skill acquisition.
© International Association of Medical Science Educators 2021.
Publication types
- Open access
- Published: 20 January 2024
From master’s thesis to research publication: a mixed-methods study of medical student publishing and experiences with the publishing process
- Maria Björklund ORCID: orcid.org/0000-0001-8027-1297 1 ,
- Ramin Massoumi ORCID: orcid.org/0000-0001-8875-6440 2 &
- Bodil Ohlsson ORCID: orcid.org/0000-0002-9142-5244 3 , 4
BMC Medical Education volume 24 , Article number: 75 ( 2024 ) Cite this article
1126 Accesses
2 Altmetric
Metrics details
Medical student master’s theses are often carried out as research projects, and some are published as research papers in journals. We investigated the percentage of master’s theses conducted by 5th -year students at the Medical Degree Program at Lund University, Sweden, that subsequently served as the basis for research publications. In addition, we explored both student and supervisor experiences with the publishing process.
A cohort of four semesters of student data covering the period from 2019 to 2020 ( n = 446) was searched in PubMed, Embase and the Web of Science to assess whether they had been published as research papers. Surveys were sent to students ( n = 121) and supervisors ( n = 77) to explore their experiences with the publishing process.
We found that 33% (149 of 446) of the students in the 2019–2020 cohort subsequently published their theses, and 50% of these students were listed as first authors. Most students published original research. Students ( n = 21) and supervisors ( n = 44) reported that the publishing process was time-consuming and that students needed multilevel support from supervisors to achieve successful publication. The publishing process was reported by 79% of the students to have led to additional learning. Most of the papers (126 of 149, 85%) had a clinical or patient-oriented focus.
A high percentage of the student publications in which students are listed as first authors require engagement from both students and supervisors. Supervisors play an essential role in supporting students in a successful publication process. Most of the published papers were either clinical or patient-oriented research.
Peer Review reports
In medical education, reading research papers, knowing research methods, and performing critical appraisals of research are important for following medical developments and understanding the rationale behind treatment strategies [ 1 , 2 ]. The approach to student involvement and its application in research-related learning activities seems to vary in form, content and level across medical degree programs. The development of research skills is encouraged for the benefits it brings to the medical profession; e.g., such research is encouraged by the Association for Medical Education in Europe (AMEE) [ 3 ]. The involvement of faculty as coauthors with students is one means of engaging students in authentic research projects and can be conceptualized as research-based learning. Given that this term has no uniform definition, it can include many activities at different levels, ranging from understanding research content and methods to applying these techniques in the production of research projects or publications [ 4 , 5 ]. Research skills or research activities are other commonly mentioned concepts. These concepts encompass the reviewing of research, methodological competencies, reflection, and communication skills along with content knowledge [ 4 , 6 ]. Research publishing in itself is aimed at reporting and communicating new research findings and the way that an original study was conducted [ 7 ]. In medical education, students are trained in reading, understanding, assessing and synthesizing original research papers. For students, writing and publishing a research paper adds an extra dimension to research engagement, implying an active role as an author in engaging in the process all the way to publication. In this scenario, the students not only act as readers or critics but also learn to conduct research projects. The roles and responsibilities of the authors are defined by the International Committee of Medical Journal Editors (ICMJE), which states that authorship implies responsibility and accountability for published work. Authors make substantial contributions to the research, draft and approve the final version to be published, and agree to accountability for all aspects of the work [ 8 ]. Subsequently, student-active work is needed to fulfill the author criteria for students, which is addressed through collaboration with their supervisor and research team. Transforming a master’s thesis into a research paper can be an extracurricular activity in which students practice the writing workflow, prepare a manuscript to meet a journal’s format requirements, collect feedback from their coauthors for revision of the text, and finally submit the manuscript, all under supervision. This also includes revising the manuscript after comments from reviewers and editors have been collected, as well as preparing a response to reviewers [ 7 ].
The main objective of this study is the investigation of the number of 5th -year medical students in the Medical Degree (MD) program at Lund University that succeeded in publishing their master’s theses as research publications. In addition, we explore the experiences of both students and supervisors regarding the publication process and student learning experiences.
The Faculty of Medicine at Lund University has 2900 full-time students and more than 1000 PhD students [ 9 ]. The MD Program in Sweden recently changed from a 5.5 to a 6-year program, and at Lund University, new students are enrolled every semester. Together with medical and clinical knowledge and skills, a curriculum designed to facilitate progressive student learning of research methods and applications, including assessments, is integrated throughout the MD program [ 10 ].
Master’s thesis course, content and structure, learning objectives and assessment
The learning objectives of the master’s thesis course taken in the 5th year of the program are focused on students’ ability to evaluate research papers and understand ethical, juridical, and methodological aspects of the research. Students should be able to create a project plan, run a project under supervision, independently find relevant research and synthesize it into their project background. To help students fulfill these learning objectives, lectures and workshops on research methodology, information retrieval and academic writing are offered.
Prior to their 5th year, the students need to find a supervisor who is available for consultation throughout the course. Supervisors need to hold a PhD in any field applicable to the science and practice of medicine. The thesis is evaluated by an expert assessor with extensive experience in thesis assessment, who then provides feedback to the student’s written thesis and its oral presentation. The evaluation of the written thesis is similar to the research review process of a scientific peer-reviewed journal.
Data collection
Tracking of published student theses.
The records of 446 students who completed their master’s theses over the course of four semesters during the 2019–2020 timeframe were reviewed to determine whether their thesis projects had been published as a research paper. If so, the journal and its impact factor, together with the type of publication (original paper/systematic review or other), were documented. To track publications, the databases PubMed (National Library of Medicine), Embase (Elsevier) and Web of Science (Clarivate) were used. The journal impact factor (of 2021) was retrieved from Journal Citation Reports (InCites). The databases were chosen because they were considered to cover the most relevant journals likely to publish these students’ work. The family names of students and supervisors were searched in combination since we considered it less likely that students would publish their work as single authors. Spelling variations were tested for names with special characters or double family names. Ambiguities, either where a student was likely to have made a change in project focus or title or unambiguously connecting authors with a publication or several possible publications was difficult, were followed up on by cross-checking theses records.
Surveys to students and supervisors
Surveys were sent to students in the fall 2022 cohort ( n = 102) and to students in the 2019–2020 cohort, when publications were identified and students provided contact addresses ( n = 19). The surveys were also sent to supervisors in the fall 2022 cohort ( n = 77). The survey distributions for the student cohorts and supervisors are described in Table 1 .
The survey was designed to collect respondent experiences of the publishing process in regard to student learning, student use of previously acquired research skills, student knowledge of research methods and the level of independence exhibited in student work. The survey questions were answered anonymously and are available in Appendix 1 . For practical reasons, the surveys were not sent to the same cohorts as the publication tracking cohorts. Medical students in Sweden graduated after 5.5 years and were difficult to reach for follow-up questions. Nevertheless, we managed to trace certain students who had published their work and provided their personal email addresses for contact purposes. Supervisors are often engaged for many years, as some of them may have served as supervisors in the publication tracking cohort, thus making them easier to contact for follow-up questions.

Statistical analysis
The statistical analysis of the survey results was performed in SPSS (version 29, 2022). Fisher’s exact test was used for categorical data, and the Mann‒Whitney U test was used for ordinal data. A P value ≤ 0.05 was considered to indicate statistical significance.
Ethical considerations and approval
Ethical approval.
by the Swedish Ethical Review Authority was waived since the surveys sent to respondents were answered anonymously and the answers could not be traced back to the responders. No sensitive personal data were available for identifying the responders. The responders were informed of the way that how the survey results would be processed and that by answering the survey they were will give informed consent to participate. [Swedish Ethical Review Authority on the Ethical Review act: https://etikprovningsmyndigheten.se/en/what-the-act-says/ ]
Number and type of student publications
The results of our student publication tracking are summarized in Table 2 . In total, we tracked 446 student theses, 149 (33%) of which were published as a research paper. The students were the first authors of 50% of the publications, and the most common publication type was original research papers. We also found a few systematic reviews, one narrative review, conference abstracts, a poster and a preprint. The time span of the publication process and the range of impact factors of the journals are illustrated in Table 2 . Several students collaborated and published their work in conjunction with fellow students as part of a research group. We counted the individual student contributions to publication; if two students in the same cohort had a joint publication, we counted both students as publishers.
Most of the 149 published papers (85%) had a clinical or patient-oriented focus, for instance, diagnostics, screening, clinical management, therapy, follow-up and prognostics, complications, lifestyle, risk factors/risk management in health care, or mental health. Some of the study designs applied included randomized controlled trials, clinical trials, observational studies, multicenter studies, and registry studies.
Survey results of student and supervisor experiences with publishing
Forty-four (57%) supervisors and 21 (17%) students responded to the survey, but not all respondents answered all questions. Of the total number of student respondents, 9 (43%) had published their theses as research publications, while 12 (57%) were in the process of publishing. All the responding supervisors reported that they had worked with students who had or were about to publish. In general, supervisors provided us with extended comments in their responses, which contributed to capturing more in-depth perspectives in regard to their experiences.
Learning from the publishing process
Sixteen (84%) of the 19 students responding on the question indicated that they applied their previous learning of research methodology to their publishing endeavors, whereas 3 (16%) reported that they did not utilize their previous learning in this regard. Two students expressed that their previous curricular activities in research methodology served as a suitable foundation for their thesis. 27 (64%) of the 42 supervisors responding on the question reported that students applied skills and knowledge from previous learning activities and that many took a scientific approach to the work. There were also individual variations in the levels of student preparedness. However, as 15 (36%) of the supervisors noted, the publishing process is new to students, and they often need considerable guidance. Moreover, publishing does not occur without any previous knowledge or experience with research methodology. Most of the students (79%) reported that the publishing process led to additional learning, in contrast to 21% who reported that they did not incur any extra learning. The time and effort required for publishing, including generating more advanced statistics, adapting the thesis to a journal paper format, and responding to peer review and communication skills, were mentioned as specific new learning experiences.
A majority of the supervisors (95%) reported that students who published also gained additional experience from the research methodology in the sense of deepening their knowledge of the medical topic. The difference between the peer-review process and the examination process for theses was reported as another aspect of learning. The supervisors acknowledged the positive learning effects for students who authored published research papers in various aspects of managing the project, preparing for submission, and adhering to deadlines. In contrast, a few supervisors noted that not all students were able to perform these tasks independently and that some required substantial assistance. Supervisors also expressed that some students lacked patience; e.g., some students expressed impatience in working with adaptations of the thesis and responding to reviewer comments.
Support needs in the publishing process
All the students emphasized the significant need for assistance throughout the publishing process, but they provided few detailed comments in their responses. Supervisors expressed a similar need to support the students; see the comparison in Fig. 1 .
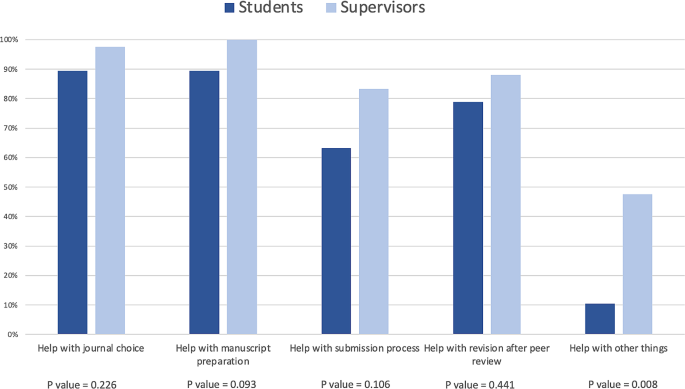
Student support needs in the publishing process: Comparison of student (n = 19) and supervisor (n = 42) experiences. Fisher’s exact test was used. A P value ≤ 0.05 was considered to indicate statistical significance
Supervisors reported that they helped students connect with the other coauthors, which was beneficial for student learning. In the publishing process, students are required to adapt their theses to specific journal requirements and write more concise and clear texts, which, according to some supervisors, took more time than students thought it would. Proofreading and obtaining help in formatting figures and tables were also mentioned as very important factors. Some supervisors reported that additional material or statistical analysis as well as methodological considerations were sometimes needed to succeed in publishing.
The supervisors also commented that the quality levels of theses guided their decision to pursue publication and engage with students as coauthors. Some students also required help with communicating their publication at conferences or meetings, according to supervisors.
Level of student independence in the publishing process
Students generally reported having some or a low level of independence in the publishing process. A few reported higher levels of independence, either in writing the manuscript and/or in data analysis.
Supervisors reported slightly higher levels of independence on the part of students and commented that the level of independence varied across students. A comparison of perceived independence is presented in Fig. 2 .
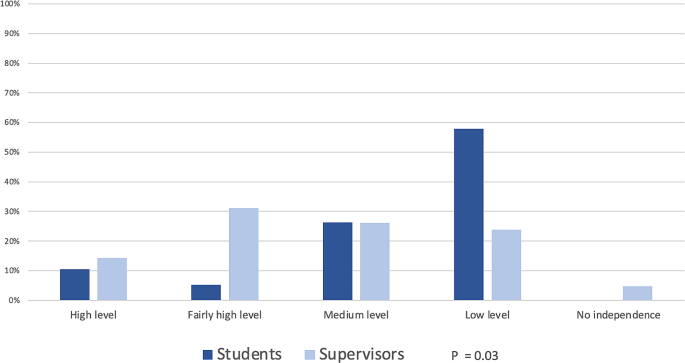
Level of student independence in the publishing process: Comparison of student and supervisor experiences Students ( n = 19) and supervisors ( n = 42) rated the perceived levels of student independence on a five-point scale. Mann‒Whitney U test was used. A P value ≤ 0.05 was considered to indicate statistical significance
In this study, we investigated a cohort of medical degree students over four semesters ranging from 2019 to 2020 to assess whether their master’s theses had been published as research papers. We found that 33% of the articles had been published. Different methods have been applied in previous research on student submissions, publishing rates and student authorship; Skovgard et al. [ 11 ] and Griffin et al. [ 12 ] followed up on student cohorts, while Kan et al. [ 13 ] and Svider et al. [ 14 ] investigated specific journals for student publications. The extent to which and how research activities are integrated into the curriculum may also vary across educational and geographical contexts. Most of the studies were from the United States, followed by the United Kingdom and Australia, as reported by Carberry et al. [ 15 ]. This makes comparisons difficult because of the differences in educational contexts and methods of publication tracking among these contexts. The share of student authorship varies: Skovgard et al. [ 11 ] studied a cohort of Danish students where 52% managed to publish at least one paper, and Griffin et al. [ 12 ] reported a UK student cohort where 14% (72 of 515) of the authors submitted research articles for publication. Kan et al. [ 13 ] and Svider et al. [ 14 ] tracked student publications in journals and revealed student authorship percentages of 12–19% and 19–37%, respectively. Amgad et al. [ 16 ] estimated student publishing rates to be 25–30% in their meta-analysis. Our results of 33%, show a higher rate of student publication than previous studies showed. In this group, 50% of the students were first authors, which is a high proportion in comparison to the findings of previous studies, including those of Amgad et al. [ 16 ], where 13% of the students were first authors, while Kan et al. [ 13 ] and Skovgard et al. [ 11 ] reported 17–25% and 43%, respectively.
The experiences reported by students and researchers showed that the publishing process can be beneficial for student learning. There were differences between student and supervisor experiences regarding student levels of independence, where some students reported their estimated level of independence to be lower than that reported by their supervisor. The reports of the students regarding support needs were similar to those of their supervisors. Supervisors emphasized that students required substantial assistance to a greater extent than the students themselves did, and such assistance seemed to be vital to a successful publication process. This result is also in line with the findings of previous studies in which students described having an engaged supervisor or mentor as the most helpful factor, followed by the support of the research team, course leaders and peers [ 12 , 17 , 18 ]. This heavy reliance of the student on the supervisor was also reported by Althubaiti et al. [ 19 ]. Our results reveal that students valued training in efficiently working with a team, which was also reported as a positive outcome in previous research [ 14 , 20 ]. Maher et al. [ 21 ] described a faculty culture in which the publishing process is regarded as a socialization process leading to academic authorship, team collaboration and competent writing as an important factor affecting student-faculty publishing.
Our results reveal that most of the publications of our student sample seems to be clinically or patient-oriented. In previous research, the focus (such as basic or clinical science) and form (reviews or original papers) of student publications seemed to vary depending on the educational context. Stockfelt et al. [ 6 ] reported that 45% of students perform basic science or laboratory projects, approximately one-third of the students engage in clinical research, and the remaining students pursue a combination of research activities. Wickramasinghe et al. [ 22 ] reported that reviews, followed by original studies, are the most common form of student publication. Amgad et al. [ 16 ] reported that most students publish original research papers, and whether these are in basic or clinical science varies, but the majority of them are on the clinical side, which is well aligned with our results.
Even though many of our students go on to publish, we do not believe that requiring such publication as part of the program would be feasible or result in positive outcomes. Voluntary publishing has also been discussed in previous studies, which have emphasized its importance for student motivation and for developing a sound future research culture [ 15 , 18 , 23 ]. Helping students become motivated to engage in research by progressively working with research competencies that have been integrated into a curriculum that culminates in a master’s thesis is likely a better strategy [ 10 ]. This longitudinal approach can have positive effects on student publishing, as suggested by Mullan et al. [ 24 ], even if such a curriculum has yet to be evaluated.
Limitations
In our data collection, we aimed for a rigorous approach in determining whether a student thesis had been published as a research paper. However, it is possible that some of the student theses were published in journals that were not indexed by the databases chosen for publication tracking. Another limitation is that students in the fall 2020 cohort may still be in the process of publishing and hence may not be captured in our data. With these limitations in mind, we believe our investigation has resulted in a general and fairly accurate overview of the number of theses that are published as research papers.
We sent the survey to a partly different cohort than the one used for publication tracking. As the survey responses were anonymous, it was not possible to distinguish the different cohorts within the survey results. It is possible that students who have already published have had different learning experiences than students who are still in the publishing process. However, the experiences expressed by students, the impact on learning, and the role of supervisors were found to be more closely associated with the publishing process itself than contingent on the specific cohort to which a student or supervisor belonged. The surveys allowed for detailed comments in the responses, and the supervisors used that option more than students. Due to the low response rate of students, the low rate of student comments, and the lack of representativeness of the results, further investigations into student learning experiences during the publishing process are needed.
In this study, we investigated the percentage of medical students in the 2019–2020 cohort who subsequently published their master’s theses as research publications. We found a 33% publication rate, and students were listed as the first author in 50% of the publications. The publishing process demands a significant amount of time, and students need to be aware of the additional time required in addition to their master’s thesis work.
Engaged supervisors were found to be essential for a successful publication process, as they provided students with the necessary support in preparing their manuscripts. Student publishing can constitute an additional learning activity in student research projects, provided that such publishing is voluntary and builds on students’ intrinsic motivation to perform research.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
The Association for Medical Education in Europe
International Committee of Medical Journal Editors
Medical Degree
Albarqouni L, Hoffmann T, Straus S, Olsen NR, Young T, Ilic D, Shaneyfelt T, Haynes RB, Guyatt G, Glasziou P. Core competencies in evidence-based practice for Health professionals: Consensus Statement based on a systematic review and Delphi Survey. JAMA Netw Open. 2018;1(2):e180281.
Article Google Scholar
Cuschieri A, Cuschieri S. Medical students’ perceptions on Research: results from a small European Island State. Med Sci Educ. 2021;31(6):1991–9.
Laidlaw A, Aiton J, Struthers J, Guild S. Developing research skills in medical students: AMEE Guide No. 69. Med Teach. 2012;34(9):e754–771.
Thiem J, Preetz R, Haberstroh S. How research-based learning affects students’ self-rated research competences: evidence from a longitudinal study across disciplines. Stud High Educ 2023:1–13.
Wessels I, Rueß J, Gess C, Deicke W, Ziegler M. Is research-based learning effective? Evidence from a pre–post analysis in the social sciences. Stud High Educ. 2020;46(12):2595–609.
Stockfelt M, Karlsson L, Finizia C. Research interest and activity among medical students in Gothenburg, Sweden, a cross-sectional study. BMC Med Educ. 2016;16(1):226.
Day RA, Gastel B. How to write and publish a scientific paper. Santa Barbara, Calif.: Greenwood; 2011.
Google Scholar
International Committee of Medical Journal Editors. Defining the Role of Authors and Contributors https://www.icmje.org/recommendations/browse/roles-and-responsibilities/defining-the-role-of-authors-and-contributors.html . Accessed 2023 March 22.
Faculty of Medicine. Faculty of Medicine at Lund University https://www.medicine.lu.se/faculty-medicine-lund-university . Accessed 2023 May 5.
Björklund M, Perez MT, Regnér S, Garwicz M. Learning progression from basic scientific scholarship to evidence-based medicine: a multimodal approach [Working paper]. In. Lund: Lund University; 2020:22.
Skovgaard M, Okkels N, Christensen MK, Telinius N, Hauge EM. Publication rate and PhD enrolment following a medical pre-graduate research programme. Dan Med J 2015;62(9).
Griffin MF, Hindocha S. Publication practices of medical students at British medical schools: experience, attitudes and barriers to publish. Med Teach. 2011;33(1):e1–8.
Kan CK, Qureshi MM, Paracha M, Sachs TE, Sarfaty S, Hirsch AE. Effect of Medical Student contributions on Academic Productivity: analysis of Student Authorship over Time. Adv Med Educ Pract. 2021;12:481–9.
Svider PF, Husain Q, Mauro KM, Folbe AJ, Baredes S, Eloy JA. Impact of mentoring medical students on scholarly productivity. Int Forum Allergy Rhinol. 2014;4(2):138–42.
Carberry C, McCombe G, Tobin H, Stokes D, Last J, Bury G, Cullen W. Curriculum initiatives to enhance research skills acquisition by medical students: a scoping review. BMC Med Educ. 2021;21(1):312.
Amgad M, Man Kin Tsui M, Liptrott SJ, Shash E. Medical Student Research: an Integrated mixed-methods systematic review and Meta-analysis. PLoS ONE. 2015;10(6):e0127470.
Syeda M, Woodend J, Liu J, Roy S. Ready to leave the Nest? Education Graduate Students’ voices on Publishing. Int J Teach Learn High Educ. 2020;32(1):107–16.
Weaver AN, McCaw TR, Fifolt M, Hites L, Lorenz RG. Impact of elective versus required medical school research experiences on career outcomes. J Investig Med. 2017;65(5):942–8.
Althubaiti A, Althubaiti SM. Medical research: what to expect in a student-supervisor relationship. BMC Med Educ. 2022;22(1):774.
Rosenkranz SK, Wang S, Hu W. Motivating medical students to do research: a mixed methods study using self-determination theory. BMC Med Educ. 2015;15:95.
Maher MA, Timmerman BC, Feldon DF, Strickland D. Factors affecting the occurrence of Faculty-Doctoral Student Coauthorship. J High Educ. 2016;84(1):121–43.
Wickramasinghe DP, Perera CS, Senarathna S, Samarasekera DN. Patterns and trends of medical student research. BMC Med Educ. 2013;13:175.
Horta H, Li H. Nothing but publishing: the overriding goal of PhD students in mainland China, Hong Kong, and Macau. Stud High Educ. 2022;48(2):263–82.
Mullan JR, Weston KM, Rich WC, McLennan PL. Investigating the impact of a research-based integrated curriculum on self-perceived research experiences of medical students in community placements: a pre- and post-test analysis of three student cohorts. BMC Med Educ. 2014;14:161.
Download references
Acknowledgements
We would like to give special thanks to Kerstin Troein for administrative support with data collection. We also wish to give warm thanks to Håkan Andersson for statistical advice and support and to Martin Garwicz for reviewing and offering valuable feedback regarding the manuscript.
Open access funding provided by Lund University.
Author information
Authors and affiliations.
Library & ICT, Faculty of Medicine, Lund University, Lund, Sweden
Maria Björklund
Translational Cancer Research, Department of Laboratory Medicine, Lund University, Medicon Village, Lund, Sweden
Ramin Massoumi
Department of Clinical Sciences, Lund University, Malmö, Lund, Sweden
Bodil Ohlsson
Department of Internal Medicine, Skåne University Hospital, Malmö, Sweden
You can also search for this author in PubMed Google Scholar
Contributions
MB and BO initiated and designed the study. MB and BO collected the data. MB, BO and RM analyzed and interpreted the results. MB designed the tables and figures. MB wrote the original draft of the manuscript. MB, BO and RM contributed to the writing and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Maria Björklund .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval by the Swedish Ethical Review Authority was waived since the surveys sent to respondents were answered anonymously and the answers could not be traced back to the responders. No sensitive personal data were available for identifying the responders. The responders were informed of the way that how the survey results would be processed and that by answering the survey they were will give informed consent to participate. [Swedish Ethical Review Authority on the Ethical Review act: https://etikprovningsmyndigheten.se/en/what-the-act-says/ ]
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Björklund, M., Massoumi, R. & Ohlsson, B. From master’s thesis to research publication: a mixed-methods study of medical student publishing and experiences with the publishing process. BMC Med Educ 24 , 75 (2024). https://doi.org/10.1186/s12909-024-05060-7
Download citation
Received : 26 September 2023
Accepted : 15 January 2024
Published : 20 January 2024
DOI : https://doi.org/10.1186/s12909-024-05060-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Student publishing
- Supervisors
- Master’s theses
- Research publications
- Publication process
- Student performance
- Learning experience
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
77 interesting medical research topics for 2024
Last updated
25 November 2023
Reviewed by
Brittany Ferri, PhD, OTR/L
Medical research is the gateway to improved patient care and expanding our available treatment options. However, finding a relevant and compelling research topic can be challenging.
Use this article as a jumping-off point to select an interesting medical research topic for your next paper or clinical study.
- How to choose a medical research topic
When choosing a research topic , it’s essential to consider a couple of things. What topics interest you? What unanswered questions do you want to address?
During the decision-making and brainstorming process, here are a few helpful tips to help you pick the right medical research topic:
Focus on a particular field of study
The best medical research is specific to a particular area. Generalized studies are often too broad to produce meaningful results, so we advise picking a specific niche early in the process.
Maybe a certain topic interests you, or your industry knowledge reveals areas of need.
Look into commonly researched topics
Once you’ve chosen your research field, do some preliminary research. What have other academics done in their papers and projects?
From this list, you can focus on specific topics that interest you without accidentally creating a copycat project. This groundwork will also help you uncover any literature gaps—those may be beneficial areas for research.
Get curious and ask questions
Now you can get curious. Ask questions that start with why, how, or what. These questions are the starting point of your project design and will act as your guiding light throughout the process.
For example:
What impact does pollution have on children’s lung function in inner-city neighborhoods?
Why is pollution-based asthma on the rise?
How can we address pollution-induced asthma in young children?
- 77 medical research topics worth exploring in 2023
Need some research inspiration for your upcoming paper or clinical study? We’ve compiled a list of 77 topical and in-demand medical research ideas. Let’s take a look.
- Exciting new medical research topics
If you want to study cutting-edge topics, here are some exciting options:
COVID-19 and long COVID symptoms
Since 2020, COVID-19 has been a hot-button topic in medicine, along with the long-term symptoms in those with a history of COVID-19.
Examples of COVID-19-related research topics worth exploring include:
The long-term impact of COVID-19 on cardiac and respiratory health
COVID-19 vaccination rates
The evolution of COVID-19 symptoms over time
New variants and strains of the COVID-19 virus
Changes in social behavior and public health regulations amid COVID-19
Vaccinations
Finding ways to cure or reduce the disease burden of chronic infectious diseases is a crucial research area. Vaccination is a powerful option and a great topic to research.
Examples of vaccination-related research topics include:
mRNA vaccines for viral infections
Biomaterial vaccination capabilities
Vaccination rates based on location, ethnicity, or age
Public opinion about vaccination safety
Artificial tissues fabrication
With the need for donor organs increasing, finding ways to fabricate artificial bioactive tissues (and possibly organs) is a popular research area.
Examples of artificial tissue-related research topics you can study include:
The viability of artificially printed tissues
Tissue substrate and building block material studies
The ethics and efficacy of artificial tissue creation
- Medical research topics for medical students
For many medical students, research is a big driver for entering healthcare. If you’re a medical student looking for a research topic, here are some great ideas to work from:
Sleep disorders
Poor sleep quality is a growing problem, and it can significantly impact a person’s overall health.
Examples of sleep disorder-related research topics include:
How stress affects sleep quality
The prevalence and impact of insomnia on patients with mental health conditions
Possible triggers for sleep disorder development
The impact of poor sleep quality on psychological and physical health
How melatonin supplements impact sleep quality
Alzheimer’s and dementia
Cognitive conditions like dementia and Alzheimer’s disease are on the rise worldwide. They currently have no cure. As a result, research about these topics is in high demand.
Examples of dementia-related research topics you could explore include:
The prevalence of Alzheimer’s disease in a chosen population
Early onset symptoms of dementia
Possible triggers or causes of cognitive decline with age
Treatment options for dementia-like conditions
The mental and physical burden of caregiving for patients with dementia
- Lifestyle habits and public health
Modern lifestyles have profoundly impacted the average person’s daily habits, and plenty of interesting topics explore its effects.
Examples of lifestyle and public health-related research topics include:
The nutritional intake of college students
The impact of chronic work stress on overall health
The rise of upper back and neck pain from laptop use
Prevalence and cause of repetitive strain injuries (RSI)
- Controversial medical research paper topics
Medical research is a hotbed of controversial topics, content, and areas of study.
If you want to explore a more niche (and attention-grabbing) concept, here are some controversial medical research topics worth looking into:
The benefits and risks of medical cannabis
Depending on where you live, the legalization and use of cannabis for medical conditions is controversial for the general public and healthcare providers.
Examples of medical cannabis-related research topics that might grab your attention include:
The legalization process of medical cannabis
The impact of cannabis use on developmental milestones in youth users
Cannabis and mental health diagnoses
CBD’s impact on chronic pain
Prevalence of cannabis use in young people
The impact of maternal cannabis use on fetal development
Understanding how THC impacts cognitive function
Human genetics
The Human Genome Project identified, mapped, and sequenced all human DNA genes. Its completion in 2003 opened up a world of exciting and controversial studies in human genetics.
Examples of human genetics-related research topics worth delving into include:
Medical genetics and the incidence of genetic-based health disorders
Behavioral genetics differences between identical twins
Genetic risk factors for neurodegenerative disorders
Machine learning technologies for genetic research
Sexual health studies
Human sexuality and sexual health are important (yet often stigmatized) medical topics that need new research and analysis.
As a diverse field ranging from sexual orientation studies to sexual pathophysiology, examples of sexual health-related research topics include:
The incidence of sexually transmitted infections within a chosen population
Mental health conditions within the LGBTQIA+ community
The impact of untreated sexually transmitted infections
Access to safe sex resources (condoms, dental dams, etc.) in rural areas
- Health and wellness research topics
Human wellness and health are trendy topics in modern medicine as more people are interested in finding natural ways to live healthier lifestyles.
If this field of study interests you, here are some big topics in the wellness space:
Gluten sensitivity
Gluten allergies and intolerances have risen over the past few decades. If you’re interested in exploring this topic, your options range in severity from mild gastrointestinal symptoms to full-blown anaphylaxis.
Some examples of gluten sensitivity-related research topics include:
The pathophysiology and incidence of Celiac disease
Early onset symptoms of gluten intolerance
The prevalence of gluten allergies within a set population
Gluten allergies and the incidence of other gastrointestinal health conditions
Pollution and lung health
Living in large urban cities means regular exposure to high levels of pollutants.
As more people become interested in protecting their lung health, examples of impactful lung health and pollution-related research topics include:
The extent of pollution in densely packed urban areas
The prevalence of pollution-based asthma in a set population
Lung capacity and function in young people
The benefits and risks of steroid therapy for asthma
Pollution risks based on geographical location
Plant-based diets
Plant-based diets like vegan and paleo diets are emerging trends in healthcare due to their limited supporting research.
If you’re interested in learning more about the potential benefits or risks of holistic, diet-based medicine, examples of plant-based diet research topics to explore include:
Vegan and plant-based diets as part of disease management
Potential risks and benefits of specific plant-based diets
Plant-based diets and their impact on body mass index
The effect of diet and lifestyle on chronic disease management
Health supplements
Supplements are a multi-billion dollar industry. Many health-conscious people take supplements, including vitamins, minerals, herbal medicine, and more.
Examples of health supplement-related research topics worth investigating include:
Omega-3 fish oil safety and efficacy for cardiac patients
The benefits and risks of regular vitamin D supplementation
Health supplementation regulation and product quality
The impact of social influencer marketing on consumer supplement practices
Analyzing added ingredients in protein powders
- Healthcare research topics
Working within the healthcare industry means you have insider knowledge and opportunity. Maybe you’d like to research the overall system, administration, and inherent biases that disrupt access to quality care.
While these topics are essential to explore, it is important to note that these studies usually require approval and oversight from an Institutional Review Board (IRB). This ensures the study is ethical and does not harm any subjects.
For this reason, the IRB sets protocols that require additional planning, so consider this when mapping out your study’s timeline.
Here are some examples of trending healthcare research areas worth pursuing:
The pros and cons of electronic health records
The rise of electronic healthcare charting and records has forever changed how medical professionals and patients interact with their health data.
Examples of electronic health record-related research topics include:
The number of medication errors reported during a software switch
Nurse sentiment analysis of electronic charting practices
Ethical and legal studies into encrypting and storing personal health data
Inequities within healthcare access
Many barriers inhibit people from accessing the quality medical care they need. These issues result in health disparities and injustices.
Examples of research topics about health inequities include:
The impact of social determinants of health in a set population
Early and late-stage cancer stage diagnosis in urban vs. rural populations
Affordability of life-saving medications
Health insurance limitations and their impact on overall health
Diagnostic and treatment rates across ethnicities
People who belong to an ethnic minority are more likely to experience barriers and restrictions when trying to receive quality medical care. This is due to systemic healthcare racism and bias.
As a result, diagnostic and treatment rates in minority populations are a hot-button field of research. Examples of ethnicity-based research topics include:
Cancer biopsy rates in BIPOC women
The prevalence of diabetes in Indigenous communities
Access inequalities in women’s health preventative screenings
The prevalence of undiagnosed hypertension in Black populations
- Pharmaceutical research topics
Large pharmaceutical companies are incredibly interested in investing in research to learn more about potential cures and treatments for diseases.
If you’re interested in building a career in pharmaceutical research, here are a few examples of in-demand research topics:
Cancer treatment options
Clinical research is in high demand as pharmaceutical companies explore novel cancer treatment options outside of chemotherapy and radiation.
Examples of cancer treatment-related research topics include:
Stem cell therapy for cancer
Oncogenic gene dysregulation and its impact on disease
Cancer-causing viral agents and their risks
Treatment efficacy based on early vs. late-stage cancer diagnosis
Cancer vaccines and targeted therapies
Immunotherapy for cancer
Pain medication alternatives
Historically, opioid medications were the primary treatment for short- and long-term pain. But, with the opioid epidemic getting worse, the need for alternative pain medications has never been more urgent.
Examples of pain medication-related research topics include:
Opioid withdrawal symptoms and risks
Early signs of pain medication misuse
Anti-inflammatory medications for pain control
- Identify trends in your medical research with Dovetail
Are you interested in contributing life-changing research? Today’s medical research is part of the future of clinical patient care.
As your go-to resource for speedy and accurate data analysis , we are proud to partner with healthcare researchers to innovate and improve the future of healthcare.
Editor’s picks
Last updated: 11 January 2024
Last updated: 15 January 2024
Last updated: 25 November 2023
Last updated: 12 May 2023
Last updated: 30 April 2024
Last updated: 18 May 2023
Last updated: 10 April 2023
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next.

Users report unexpectedly high data usage, especially during streaming sessions.

Users find it hard to navigate from the home page to relevant playlists in the app.

It would be great to have a sleep timer feature, especially for bedtime listening.

I need better filters to find the songs or artists I’m looking for.
Log in or sign up
Get started for free
A Realistic Guide to Medical School
Written by UCL students for students
Top 10 Tips: Getting into Research as a Medical Student
Introducing our new series: Top 10 Tips – a simple guide to help you achieve your goals!
In this blog post, Jessica Xie (final year UCL medical student) shares advice on getting into research as a medical student.

Disclaimers:
- Research is not a mandatory for career progression, nor is it required to demonstrate your interest in medicine.
- You can dip into and out of research throughout your medical career. Do not feel that you must continue to take on new projects once you have started; saying “no, thank you” to project opportunities will allow you to focus your energy and time on things in life that you are more passionate about for a more rewarding experience.
- Do not take on more work than you are capable of managing. Studying medicine is already a full-time job! It’s physically and mentally draining. Any research that you get involved with is an extracurricular interest.

I decided to write this post because, as a pre-clinical medical student, I thought that research only involved wet lab work (i.e pipetting substances into test tubes). However, upon undertaking an intercalated Bachelor of Science (iBSc) in Primary Health Care, I discovered that there are so many different types of research! And academic medicine became a whole lot more exciting…
Here are my Top 10 Tips on what to do if you’re a little unsure about what research is and how to get into it:
TIP 1: DO YOUR RESEARCH (before getting into research)
There are three questions that I think you should ask yourself:
- What are my research interests?
Examples include a clinical specialty, medical education, public health, global health, technology… the list is endless. Not sure? That’s okay too! The great thing about research is that it allows deeper exploration of an area of Medicine (or an entirely different field) to allow you to see if it interests you.
2. What type of research project do I want to do?
Research evaluates practice or compares alternative practices to contribute to, lend further support to or fill in a gap in the existing literature.
There are many different types of research – something that I didn’t fully grasp until my iBSc year. There is primary research, which involves data collection, and secondary research, which involves using existing data to conduct further research or draw comparisons between the data (e.g. a meta-analysis of randomised control trials). Studies are either observational (non-interventional) (e.g. case-control, cross-sectional) or interventional (e.g. randomised control trial).
An audit is a way of finding out if current practice is best practice and follows guidelines. It identifies areas of clinical practice could be improved.
Another important thing to consider is: how much time do I have? Developing the skills required to lead a project from writing the study protocol to submitting a manuscript for publication can take months or even years. Whereas, contributing to a pre-planned or existing project by collecting or analysing data is less time-consuming. I’ll explain how you can find such projects below.
3. What do I want to gain from this experience?
Do you want to gain a specific skill? Mentorship? An overview of academic publishing? Or perhaps to build a research network?
After conducting a qualitative interview study for my iBSc project, I applied for an internship because I wanted to gain quantitative research skills. I ended up leading a cross-sectional questionnaire study that combined my two research interests: medical education and nutrition. I sought mentorship from an experienced statistician, who taught me how to use SPSS statistics to analyse and present the data.
Aside from specific research skills, don’t forget that you will develop valuable transferable skills along the way, including time-management, organisation, communication and academic writing!
TIP 2: BE PROACTIVE
Clinicians and lecturers are often very happy for medical students to contribute to their research projects. After a particularly interesting lecture/ tutorial, ward round or clinic, ask the tutor or doctors if they have any projects that you could help them with!
TIP 3: NETWORKING = MAKING YOUR OWN LUCK
Sometimes the key to getting to places is not what you know, but who you know. We can learn a lot from talking to peers and senior colleagues. Attending hospital grand rounds and conferences are a great way to meet people who share common interests with you but different experiences. I once attended a conference in Manchester where I didn’t know anybody. I befriended a GP, who then gave me tips on how to improve my poster presentation. He shared with me his experience of the National institute of Health Research (NIHR) Integrated Academic Training Pathway and motivated me to continue contributing to medical education alongside my studies.
TIP 4: UTILISE SOCIAL MEDIA
Research opportunities, talks and workshops are advertised on social media in abundance. Here are some examples:
Search “medical student research” or “medsoc research” into Facebook and lots of groups and pages will pop up, including UCL MedSoc Research and Academic Medicine (there is a Research Mentoring Scheme Mentee Scheme), NSAMR – National Student Association of Medical Research and International Opportunities for Medical Students .
Search #MedTwitter and #AcademicTwitter to keep up to date with ground-breaking research. The memes are pretty good too.
Opportunities are harder to come by on LinkedIn, since fewer medical professionals use this platform. However, you can look at peoples’ resumes as a source of inspiration. This is useful to understand the experiences that they have had in order to get to where they are today. You could always reach out to people and companies/ organisations for more information and advice.
TIP 5: JOIN A PRE-PLANNED RESEARCH PROJECT
Researchers advertise research opportunities on websites and via societies and organisations such as https://www.remarxs.com and http://acamedics.org/Default.aspx .
TIP 6: JOIN A RESEARCH COLLABORATIVE
Research collaboratives are multiprofessional groups that work towards a common research goal. These projects can result in publications and conference presentations. However, more importantly, this is a chance to establish excellent working relationships with like-minded individuals.
Watch out for opportunities posted on Student Training and Research Collaborative .
Interested in academic surgery? Consider joining StarSurg , BURST Urology , Project Cutting Edge or Academic Surgical Collaborative .
Got a thing for global health? Consider joining Polygeia .
TIP 7: THE iBSc YEAR: A STEPPING STONE INTO RESEARCH
At UCL you will complete an iBSc in third year. This is often students’ first taste of being involved in research and practicing academic writing – it was for me. The first-ever project that I was involved in was coding data for a systematic review. One of the Clinical Teaching Fellows ended the tutorial by asking if any students would be interested in helping with a research project. I didn’t really know much about research at that point and was curious to learn, so I offered to help. Although no outputs were generated from that project, I gained an understanding of how to conduct a systematic review, why the work that I was contributing to was important, and I learnt a thing or two about neonatal conditions.
TIP 8: VENTURE INTO ACADEMIC PUBLISHING
One of the best ways to get a flavour of research is to become involved in academic publishing. There are several ways in which you could do this:
Become a peer reviewer. This role involves reading manuscripts (papers) that have been submitted to journals and providing feedback and constructive criticism. Most journals will provide you with training or a guide to follow when you write your review. This will help you develop skills in critical appraisal and how to write an academic paper or poster. Here are a few journals which you can apply to:
- https://thebsdj.cardiffuniversitypress.org
- Journal of the National Student Association of Medical Researchjournal.nsamr.ac.uk
- https://cambridgemedicine.org/about
- https://www.bmj.com/about-bmj/resources-reviewers
Join a journal editorial board/ committee. This is a great opportunity to gain insight into how a medical journal is run and learn how to get published. The roles available depend on the journal, from Editor-in-Chief to finance and operations and marketing. I am currently undertaking a Social Media Fellowship at BJGP Open, and I came across the opportunity on Twitter! Here are a few examples of positions to apply for:
- Journal of the National Student Association of Medical Researchjournal.nsamr.ac.uk – various positions in journalism, education and website management
- https://nsamr.ac.uk – apply for a position on the executive committee or as a local ambassador
- Student BMJ Clegg Scholarship
- BJGP Open Fellowships
TIP 9: GAIN EXPERIENCE IN QUALITY IMPROVEMENT
UCL Be the Change is a student-led initiative that allows students to lead and contribute to bespoke QIPs. You will develop these skills further when you conduct QIPs as part of your year 6 GP placement and as a foundation year doctor.
TIP 10: CONSIDER BECOMING A STUDENT REPRESENTATIVE
You’ll gain insight into undergraduate medical education as your role will involve gathering students’ feedback on teaching, identifying areas of curriculum that could be improved and working with the faculty and other student representatives to come up with solutions.
It may not seem like there are any research opportunities up for grabs, but that’s where lateral thinking comes into play: the discussions that you have with your peers and staff could be a source of inspiration for a potential medical education research project. For example, I identified that, although we have lectures in nutrition science and public health nutrition, there was limited clinically-relevant nutrition teaching on the curriculum. I then conducted a learning needs assessment and contributed to developing the novel Nutrition in General Practice Day course in year 5.
Thanks for reaching the end of this post! I hope my Top 10 Tips are useful. Remember, research experience isn’t essential to become a great doctor, but rather an opportunity to explore a topic of interest further.
One thought on “Top 10 Tips: Getting into Research as a Medical Student”
This article was extremely helpful! Alothough, I’m only a junior in high school I have a few questions. First, is there anyway to prepare myself mentally for this challenging road to becoming a doctor? check our PACIFIC best medical college in Rajasthan
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Copyright © 2018 UCL
- Freedom of Information
- Accessibility
- Privacy and Cookies
- Slavery statement
- Reflect policy
Please check your email to activate your account.
« Go back Accept

Comprehensive Guide to Research from the Perspective of a Medical Student
- By Dmitry Zavlin, M.D.
- February 9, 2017
- Medical Student , Pre-med
G uest post from Dmitry Zavlin, MD, a research fellow in Houston, Texas. He has been highly productive in his research endeavors and below describes a comprehensive guide to getting involved in research.
Without any doubt whatsoever, high USMLE scores, strong recommendation letters from faculty members, a multitude of away rotations, and an updated and accurate résumé make up the foundation of a strong application for a residency position. Nevertheless, from my personal experience, one topic remains crucial that many medical students either love or hate (or try not to think about it): research . It is an extracurricular activity that enables someone to stand out from the crowd and present oneself as a diverse and multitasking character. These traits are especially favorable when it comes to applying to competitive residency programs with high applicant to position ratios. I encourage every future graduate to look into this topic since – and as astonishing as this may seem – medical school is the ideal opportunity to get your name out there. You don’t need to take a year off from classes or be on an M.D., Ph.D. track. Even those students that do not seek academic careers have a benefit from engaging in scientific duties . It helps you understand the mechanisms of research, the bureaucratic obstacles, the medical challenges, and teaches you communication with peers and faculty. Furthermore, you learn how to read, analyze, and interpret scientific publications of others. And trust me, it’s not all gold that gets printed in journals . On first glance, getting involved in unpaid ventures while you are in class, on rotation, at home studying or just taking some time off for yourself might seem like a bad deal. Yet with a sincere approach towards this subject, you can strengthen your résumé, top off your application, and learn skills that will serve you well into your career as a doctor.
The following lines are intended to display my personal experience that I have made at my medical school and in my interactions with students, residents, fellows, and attendings at my current position.
Choosing your Project
First things first. Naturally, you would want to participate and conduct research in a field of medicine you might see yourself in after graduation. However, as mentioned before, this is not a K.O. criterion. Plenty of personal experiences tell me stories of students who were involved in one area and then switched and matched in a completely different specialty of medicine or completely left the patient-care sector. Therefore, consider your engagement in scientific tasks more of as a symbolization for your work ethic and your ability to perform in a team.
My first tip is to contact the department at your home medical school, introduce yourself, write 1-2 sentences describing your motivations and goals, and ask to sit down with some faculty members or scientific staff to discuss your involvement in any research activities.
Larger departments usually have secretaries or an academic office where your email is less likely to get lost compared to the inbox of a busy professor who receives hundreds of emails per day. Personally, I would aim for junior faculty and potentially senior residents who are experienced enough to conduct research on a high level but are not too far away from the life of a young medical student. Certain departments further have specific full-time research staff that is definitely a great resource for any scientific venture. While it may be helpful to work with the director and senior faculty directly, the sad reality is often that they typically have many academic and administrative duties and activities at their institutions that might not go along well with the schedule of an ambitious student and cause frustration in the long run.
When you meet, make sure to gain and write down as many details as possible:
- What is the topic, what is the goal of this project?
- What type of format is it? (See below)
- What is the current status?
- Who is involved in this research project, what is the team, what are the people to contact?
- What will be my duties?
- Any bureaucratic issues to be aware of (IRB approval, grants, finances)?
- What is the prognosis? Are there any deadlines?
Lastly, ask about the current literature on that topic so you know what your team’s role is going to be in this scientific field. Although one core concept of any research result is reproducibility, it often remains a challenge to publish a project that has already been performed and presented or printed before. Getting involved in an area that is in quick development with high turnaround is subsequently a strong recommendation.
Types of Evidence-Based Research
Now, I would like to talk about the most common options you will encounter when presented with an array of project offers. That way you know their perks and pitfalls before you commit to anything serious and long-lasting and potentially even waste any valuable and limited time of yours.
- Case Reports: These are the most basic and least powerful of scientific contributions to medicine. Give or take, a case report is the summarized hospital or clinic chart of a treated patient who presented with a problem A and was managed with therapy B. A case report that is typically 2-3 pages long with a short intro, a compact case discussion, and perhaps some photos is the closest thing you will get to a patient note you learned to write in early medical school. Their lack of medical value makes them hard to get published in journals and students should not solely rely on these projects as they may not ultimately be accepted by journals. Recommendation: 3/5
- Case Series, Retrospective Study: These layouts are my personal recommendation as they allow quality results within a short period and are not time-consuming or require large long-term commitment as others. Typical examples are an analysis of patients who presented with the same diagnosis or underwent an identical procedure. The difference between a case series and a retrospective study is that for the latter, the patients can be stratified into different subgroups (similar to “case control study”) and statistical calculations can be performed to achieve significant conclusions. Recommendation: 5/5
- Prospective Studies: In these studies, patients are gathered in one or multiple cohorts and are followed-up over long periods of time by lab results, imaging, physical exams etc. These require great time commitment and, from a student perspective, typically only allow a certain amount of participation. These are usually studies for physicians with long relationships with their patients. Recommendation: 3/5
- (Randomized) Clinical Trials : The peak of evidence-based medical research. Similar as prospective studies yet require more planning, IRB approval, and lots of work with industry, grants, protocols, etc. Student involvement is usually marginal. Recommendation: 2/5
- Basic Science, Animal Work: Although these projects require training, approval, and a large amount of preparation, student participation is common in many areas of basic science. The advantage of these laboratory activities is a certain amount of flexibility on when certain tasks and duties can be performed. Within certain limitations, a medical student can get involved in animal or basic science research and assist in specific jobs suitable to his or her personal schedule. Even partial involvement can be enough to get one’s name on a publication. However, lab work can be monotonous and frustrating at times when experiments do not deliver the anticipated results. Sitting in non-stimulation laboratories requires a certain type of character. Recommendation: 4/5
- Descriptions of Innovations: Purely descriptive publications of new surgical techniques, innovative technology, new pharmaceutical drugs, or simply personal statements on evolving subjects, etc. This type of work often demands a given level of expertise and is not typically suitable for graduate research. Recommendation: 2/5
- Reviews, Meta-Analyses: These types of written compositions are based on a literature review. The author’s job is to read through countless, often hundreds of previous publications and create a summary regarding a specific medical topic. Reviews and meta-analysis are particularly useful for issues that are prevalent and have delivered many reports in the past. Whereas a review merely lists the findings of previous research groups, a meta-analysis is able to pool data and conduct statistical analyses. These projects allow great flexibility and can be finished from any location but do not underestimate the time needed to achieve proper results. Recommendation: 4/5
Formats of Publication
What follows is a list of mediums that allow you to get your work to the public. Albeit the concept of most research activities is similar and progresses on akin paths, it is important to agree on a goal early in the research process. Journal articles, for example need to be of highest quality and impeccable when submitted. Presentations must be tailored accordingly depending on what audience you are planning to address. Book chapters need clear guidelines to ensure that your handiwork fits well to the other parts of the volume. Make sure to discuss this topic with your seniors to understand their expectations from you.
- Journal Articles: These are the highest quality format that you can use to submit your research work for the world to see. Upon arrival at the journal’s office, the editorial office first reviews your manuscript and determines its eligibility. Next, it is sent off to a number of anonymous reviewers who judge your documents and suggest if it is worth publication, if it needs changes, or if it should be rejected. Being an author on articles in peer-reviewed journal is the strongest support to improve your application. Recommendation: 5/5
- Podium Presentations: These are typically 5-15min PowerPoint conferences or similar in front of regional, national, and international audiences of students, residents, nurses, scientists, and board-certified physicians. While your work might be less accessible to the world than published articles, it is still recommended to submit your accomplishments to such conventions. Aim for national conferences rather than regional ones. Recommendation: 4/5 for (inter)national, 3/5 for regional conferences
- Poster Presentations: A classic poster session is where you travel to a conference, hang your poster with a summary of your research findings (similar to a short abstract) and are available for others to review your work and ask questions. In some cases, poster sessions are requested by conferences when you apply for podium presentations but your projects are not considered beneficial enough. Recommendation: 3/5
- Book Chapters: Senior physicians, faculty members, or experts on a certain field are sometimes asked to write segments of medical or scientific books that are soon to be brought on sale to the market. In certain cases, students or residents write segments of such book chapters for the senior author. From personal experience, these projects are a long-term process as they go into extreme medical detail. On the upside, publication with your name on it is almost guaranteed. Unfortunately, these types of publications are not of high evidence-based research and should only be considered as a secondary side project Recommendation: 3/5
Basic and Necessary Know-How
After choosing your project you need to learn and understand how the scientific process works once you have your results ready for publication. Conducting the studies, experiments, and the literature reviews is one part of the research job. Presenting your findings is the other side of the coin. Read many publications on the same subject and study what a paper is supposed to look like. Analyze the language the authors use. It has to be straight to the point, factual, objective, leave out unnecessary information yet avoid long soporific segments of repeating details. Your audience will want to hear a hypothesis, the methodology of your venture on how said hypothesis should be tested, your results, and an antiseptic interpretation thereof. Having a senior writer review your work is therefore crucial in the beginnings of a research career.
Next, and this may seem like a no-brainer, learn how to properly and efficiently use today’s available technology to your advantage. Learn the most important features of your word processing software. Get access to a tool that allows to sort and list literature references and full versions of articles, preferably in PDF format. If you share files with others or work simultaneously at different sites, use a cloud service to keep your files in synchronization across all your devices. Any photo, video, or graph-editing software with some artistic skills might come in handy as well. Lastly, learn some basic mathematical and statistical skills and obtain a statistical software. Research is nothing if you cannot back up your story by some hard numbers. Study what a t-test, a type I error, and a type II error are and how they work. Understand when you have to use chi-square and when the Fisher’s exact test . This list goes on and on. You do not need a Ph.D. degree in biometrics or stochastic calculus to be involved in medical research but even basic skills can set you far ahead of others and you will stand out from the crowd. Additionally, all these things I just mentioned facilitate your projects by incredible amounts and allow you to publish your results faster. Capitalize on the technology that is available today!
Finally, learn how to revise current literature and how to look for references to back up your ideas or contrast your data to those of other groups. In the end, research is a competition almost like any other business sector; except that money is not necessarily the number one objective but rather prestige and impact. Pubmed is a valuable search engine, for instance, that allows you to go through the MEDLINE database and find similar publications to your project. UpToDate is a practical tool that is constantly refreshed by countless experts and gives access to the latest guidelines on specific topics. One of my former attendings always said that publishing a paper is like selling a car: you have to know the market and emphasize the upsides of your work to gain interest of others. Have all these files clean and tide on your computer from day 1, so you can keep a good overview of things and track your progress.
Further Aspects to Consider
When you start a new research project, figure out who your team is that you will be working with as this will determine the authors and their order on a potential publication. Make sure your name appears on the final manuscript if you have brought significant effort and input towards the project. As the New England Journal of Medicine, one of the largest and most prestigious journals in the field, states:
“Credit for authorship requires (a) substantial contributions to the conception and design; or the acquisition, analysis, or interpretation of the data, (b) the drafting of the article or critical revision for important intellectual content, (c) final approval of the version to be published, and (d) agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.”
The more work you put in, the further your name should appear up front. The final position of a scientific publication is usually reserved for the senior author (principal investigator) and the head of the team.
The last issue that needs to be mentioned here are finances. Even if you are working on a retrospective study and are just simply scrolling through patient charts to gather data, special software, travel to conferences, fees for journals (author processing charge for open access) can rapidly add up. Basic science ventures may require additional funding. Knowing your resources is crucial for any research. The discussion of money may seem like a sensitive subject and “above your pay grade” yet I recommend approaching this topic with open cards when the right moment comes.
Final Words
Despite the downsides of scientific work, I still believe the majority of students should experience the art of research that has made medicine what it is now. Yes, research is frequently frustrating and consumes many of your physical and mental resources. Yes, a majority of jobs after residency do not include research. Still, I will never forget the great feeling of my first accepted publication and when I immediately continued to strive towards the next challenge. Henceforward, research had something rewarding and appealing about it. In the long run, this highly dynamic profession is probably not suited for all future physicians, yet I can only repeat myself and encourage everyone to give it a try.
Dmitry Zavlin graduated with an M.D. from the Technical University of Munich in 2015.
He currently works as a research fellow in Houston.
To contact the author, please visit www.zavlin.com
Dmitry Zavlin, M.D.

First Day of Medical School – 4 Things to Know
Medical school is a completely different beast from your pre-med years in college. Here are four things you should know and prepare for in order to have the most productive, effective, and happy experience of medical school!
Premed and Medical Student Summer Research Guide
We break down the value of summer research, how to find research positions, and tips to make the most of summer research opportunities.

How to Find an Undergraduate Research Position
Research is a crucial component of any medical school application. Utilize the following tips to streamline the process of finding an ideal research position.
This Post Has One Comment
Awesome summary, really helpful for me as a med student!
Leave a Reply Cancel reply

Join the Insider Newsletter
Receive regular exclusive MSI content, news, and updates! No spam. One-click unsubscribe.
Customer Note Premed Preclinical Med Student Clinical Med Student
You have Successfully Subscribed!

IMAGES
VIDEO
COMMENTS
In particular, medical research equips clinicians with skills to critically analyze the clinical relevance of papers to provide invaluable insights into novel treatments. The integration of research into medical education has been documented to have translated into skills valuable to future clinical practice.
These journals specifically seek submissions from physicians in training and are accessible for newcomers in publishing. The Harvard Medical Student Review - The Harvard Medical Student Review is student-founded, student-managed and student-administered, under the guidance of faculty and staff. Its mission is to provide a platform for students to contribute to important issues facing health ...
Methods: An online, cross-sectional survey was distributed in October 2022 to medical students at Michigan State University College of Human Medicine (n = 806) to explore demographics, bias, family planning, and available resources. Descriptive analyses, a two- tailed t-test comparing female and male responses, and a one-way analysis of ...
Research in Medical Education: A Primer for Medical Students II. Why should I do a MedEd research project? Why are medical students especially qualified to do MedEd research? As medical students, you are front and center of the medical education process! Oftentimes, great ideas about "what works" in education are dashed on the shoals of ...
Participating in research gives students great skills and opportunities. Anna Taylor and Sarah Purdy explain how to get started ### This article contains: Students often go into medicine because of a desire to help others and improve patients' physical and mental wellbeing. In the early years of medical school, however, it can seem as if you are not making much difference to patient care.
This paper is a mixed-methods systematic review and meta-analysis of published studies investigating various aspects of medical student research, including its impact on the development of research-active physicians, difficulties faced by medical students performing research and potential solutions to overcome these difficulties.
The American Medical Student Research Journal: Created by medical students, this journal gives future physician-scientists the opportunity to develop the critical thinking skills needed to succeed in academia and clinical practice. The journal is written, reviewed and edited by medical students working under the guidance of faculty mentors.
Experts possess experience in conducting research and writing research papers and are able to function more intuitively when tackling challenges and solving ... Boninger ML. Processes and outcomes from a medical student research training program in integrative, complementary, and alternative medicine. Am J Phys Med Rehabil. 2016;95(10):779-86
There was an exponential increase in medical student research from 1980-2010. Medical student was the first author in 170 (48.6%) studies and 55 studies were authored by a single medical student. ... The contributions of authors to multiauthored biomedical research papers. JAMA. 1994, 271 (6): 438-442. 10.1001/jama.1994.03510300044036.
These papers can be based on global health experiences, bench work, or library research resulting in a systematic review of existing medical literature. Although SPs can take many forms, all students work with a mentor to develop their paper idea, write a paper proposal, and to complete the SP. The SP is based on the student's research ...
A paper questionnaire was developed, piloted, and administered to medical students at 33 medical schools in China. ... Medical student research engagement is significantly positively associated with medical students' learning outcomes, especially in the Science and Scholarship domain and the Professionalism domain. Besides, men benefit more ...
Phenomenon: Research literacy remains important for equipping clinicians with the analytical skills to tackle an ever-evolving medical landscape and maintain an evidence-based approach when treating patients. While the role of research in medical education has been justified and established, the nuances involving modes of instruction and relevant outcomes for students have yet to be analyzed.
Medical student master's theses are often carried out as research projects, and some are published as research papers in journals. We investigated the percentage of master's theses conducted by 5th -year students at the Medical Degree Program at Lund University, Sweden, that subsequently served as the basis for research publications. In addition, we explored both student and supervisor ...
These issues result in health disparities and injustices. Examples of research topics about health inequities include: The impact of social determinants of health in a set population. Early and late-stage cancer stage diagnosis in urban vs. rural populations. Affordability of life-saving medications.
TIP 4: UTILISE SOCIAL MEDIA. Research opportunities, talks and workshops are advertised on social media in abundance. Here are some examples: Facebook. Search "medical student research" or "medsoc research" into Facebook and lots of groups and pages will pop up, including UCL MedSoc Research and Academic Medicine (there is a Research ...
Ideally, this area of excitement will also align with the focus of your Scholarly Paper. The Office of Medical Student Research is available and eager to help you accomplish this. Please call Ms. Donna Moscato at 718.430.2080 to make an appointment with Dr. Vagish Hemmige. Note that the Office of Medical Student Research is located on the 5th ...
Students have received a paper survey consisting of 38 questions. Questions have covered issues related to interests expressed in high school, motivations for choosing medical studies, research interests and activities at university, and plans for a future career. ... For example, The Medical Student Research Programme in Norway has led to an ...
Comprehensive Guide to Research from the Perspective of a Medical Student. By Dmitry Zavlin, M.D. February 9, 2017. Medical Student, Pre-med. Research. G uest post from Dmitry Zavlin, MD, a research fellow in Houston, Texas. He has been highly productive in his research endeavors and below describes a comprehensive guide to getting involved in ...
Abstract. Background: Footnote # All authors contributed equally to this work. Research training is essential in a modern undergraduate medical curriculum. Our evaluation aimed to (a) gauge students' awareness of research activities, (b) compare students' perceptions of their transferable and research-specific skills competencies, (c) determine students' motivation for research and (d ...
Readers respond to funding academic medical centers, the 'residency research arms race,' and more. By Patrick Skerrett. Reprints. Molly Ferguson for STAT. STAT now publishes selected Letters ...