

Essay on Breastfeeding
Students are often asked to write an essay on Breastfeeding in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Breastfeeding
What is breastfeeding.
Breastfeeding is a natural way of feeding a baby. It involves a mother giving her milk to her baby directly from her breasts. This milk is produced in the mother’s body and is rich in nutrients that are perfect for the baby’s growth and development.
Benefits of Breastfeeding
Breastfeeding has many benefits. It helps the baby grow strong and healthy. It also helps the mother and baby bond. The mother’s milk has antibodies that protect the baby from illnesses. It’s also free and always available, making it convenient.
Challenges in Breastfeeding
Some mothers may face challenges in breastfeeding. These can include pain, difficulty in the baby latching on, or not producing enough milk. It’s important to seek help from a doctor or a lactation consultant if these problems occur.
Support for Breastfeeding
Support for breastfeeding mothers is very important. Family members, friends, and healthcare providers can provide this support. They can help by offering encouragement, providing comfortable spaces for breastfeeding, and giving helpful advice.
Breastfeeding is a natural and beneficial way of feeding a baby. While it can present challenges, with the right support, these can be overcome. It’s a beautiful way to bond with the baby and provide the best nutrition.
250 Words Essay on Breastfeeding
Breastfeeding is the process of feeding a baby with milk directly from the mother’s breast. It is a natural act that has been practiced since the beginning of human existence. Breast milk is the best food source for newborns and infants.
The Importance of Breastfeeding
Breastfeeding is very important for both the baby and the mother. For the baby, breast milk provides all the necessary nutrients. It is easy to digest and helps protect the baby from illnesses. For the mother, breastfeeding can help her body recover faster after giving birth. It also creates a strong bond between the mother and the baby.
The Benefits of Breastfeeding
Breastfeeding offers many benefits. It helps the baby grow and develop properly. It also reduces the risk of the baby getting sick. For mothers, breastfeeding can help them lose weight after pregnancy. It can also lower their risk of certain health problems like breast cancer.
Breastfeeding Challenges
Even though breastfeeding is natural, it can be challenging for some mothers. Some common problems include pain, difficulty getting the baby to latch, and concerns about producing enough milk. But with support and practice, most of these challenges can be overcome.
There are many resources available to support breastfeeding mothers. These include lactation consultants, breastfeeding classes, and support groups. Remember, it’s okay to ask for help if you’re having trouble with breastfeeding.
In conclusion, breastfeeding is a beneficial and natural process that provides numerous health benefits for both the mother and the baby. Despite the challenges, with the right support, most mothers can successfully breastfeed their babies.
500 Words Essay on Breastfeeding
Understanding breastfeeding.
Breastfeeding is a natural process where a mother feeds her baby with milk produced from her breasts. It’s the first food a baby eats after they are born. This milk is rich in nutrients, which helps the baby grow strong and healthy. It’s the best food for newborns and infants.
Benefits of Breastfeeding for Babies
Breastfeeding offers many benefits to babies. First, breast milk has all the necessary nutrients that a baby needs for the first six months of life. It has proteins, fats, vitamins, and minerals in the right amounts. It also has antibodies, which are like soldiers in our bodies. They fight off harmful germs and keep the baby healthy.
Breast milk is also easy for the baby to digest. It helps the baby gain weight and grow at a healthy pace. Besides, it lowers the baby’s risk of getting allergies, asthma, and infections. It even makes the baby smarter as it boosts brain development.
Benefits of Breastfeeding for Mothers
Not only babies, but mothers also gain from breastfeeding. It helps the mother’s body recover from childbirth more quickly. It can also help the mother lose the weight she gained during pregnancy.
Breastfeeding can also lower the mother’s risk of getting certain diseases later in life. These include breast cancer, ovarian cancer, and type 2 diabetes. Besides health benefits, breastfeeding also helps to build a strong emotional bond between the mother and the baby.
Challenges of Breastfeeding
While breastfeeding is beneficial, it can sometimes be challenging. Some mothers may have difficulty producing enough milk. Others may find it painful or uncomfortable. Babies may also have trouble latching on to the breast correctly.
But don’t worry, help is available. Doctors, nurses, and lactation consultants can provide support and advice to make breastfeeding easier. They can teach mothers how to position the baby correctly and how to handle common breastfeeding problems.
In conclusion, breastfeeding is a wonderful gift that mothers can give to their babies. It provides the best nutrition for the baby and offers many health benefits for both the mother and the baby. Despite the challenges, with the right support and guidance, most mothers can successfully breastfeed their babies. Remember, every drop of breast milk counts, and every breastfeeding journey is unique and special.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Education For Development
- Essay on Education As A Human Right
- Essay on Education And Success
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

- Open access
- Published: 26 November 2021
Women’s Perceptions and Experiences of Breastfeeding: a scoping review of the literature
- Bridget Beggs 1 ,
- Liza Koshy 1 &
- Elena Neiterman 1
BMC Public Health volume 21 , Article number: 2169 ( 2021 ) Cite this article
12k Accesses
23 Citations
4 Altmetric
Metrics details
Despite public health efforts to promote breastfeeding, global rates of breastfeeding continue to trail behind the goals identified by the World Health Organization. While the literature exploring breastfeeding beliefs and practices is growing, it offers various and sometimes conflicting explanations regarding women’s attitudes towards and experiences of breastfeeding. This research explores existing empirical literature regarding women’s perceptions about and experiences with breastfeeding. The overall goal of this research is to identify what barriers mothers face when attempting to breastfeed and what supports they need to guide their breastfeeding choices.
This paper uses a scoping review methodology developed by Arksey and O’Malley. PubMed, CINAHL, Sociological Abstracts, and PsychInfo databases were searched utilizing a predetermined string of keywords. After removing duplicates, papers published in 2010–2020 in English were screened for eligibility. A literature extraction tool and thematic analysis were used to code and analyze the data.
In total, 59 papers were included in the review. Thematic analysis showed that mothers tend to assume that breastfeeding will be easy and find it difficult to cope with breastfeeding challenges. A lack of partner support and social networks, as well as advice from health care professionals, play critical roles in women’s decision to breastfeed.
While breastfeeding mothers are generally aware of the benefits of breastfeeding, they experience barriers at individual, interpersonal, and organizational levels. It is important to acknowledge that breastfeeding is associated with challenges and provide adequate supports for mothers so that their experiences can be improved, and breastfeeding rates can reach those identified by the World Health Organization.
Peer Review reports
Public health efforts to educate parents about the importance of breastfeeding can be dated back to the early twentieth century [ 1 ]. The World Health Organization is aiming to have at least half of all the mothers worldwide exclusively breastfeeding their infants in the first 6 months of life by the year 2025 [ 2 ], but it is unlikely that this goal will be achieved. Only 38% of the global infant population is exclusively breastfed between 0 and 6 months of life [ 2 ], even though breastfeeding initiation rates have shown steady growth globally [ 3 ]. The literature suggests that while many mothers intend to breastfeed and even make an attempt at initiation, they do not always maintain exclusive breastfeeding for the first 6 months of life [ 4 , 5 ]. The literature identifies various barriers, including return to paid employment [ 6 , 7 ], lack of support from health care providers and significant others [ 8 , 9 ], and physical challenges [ 9 ] as potential factors that can explain premature cessation of breastfeeding.
From a public health perspective, the health benefits of breastfeeding are paramount for both mother and infant [ 10 , 11 ]. Globally, new mothers following breastfeeding recommendations could prevent 974,956 cases of childhood obesity, 27,069 cases of mortality from breast cancer, and 13,644 deaths from ovarian cancer per year [ 11 ]. Global economic loss due to cognitive deficiencies resulting from cessation of breastfeeding has been calculated to be approximately USD $285.39 billion dollars annually [ 11 ]. Evidently, increasing exclusive breastfeeding rates is an important task for improving population health outcomes. While public health campaigns targeting pregnant women and new mothers have been successful in promoting breastfeeding, they also have been perceived as too aggressive [ 12 ] and failing to consider various structural and personal barriers that may impact women’s ability to breastfeed [ 1 ]. In some cases, public health messaging itself has been identified as a barrier due to its rigid nature and its lack of flexibility in guidelines [ 13 ]. Hence, while the literature on women’s perceptions regarding breastfeeding and their experiences with breastfeeding has been growing [ 14 , 15 , 16 ], it offers various, and sometimes contradictory, explanations on how and why women initiate and maintain breastfeeding and what role public health messaging plays in women’s decision to breastfeed.
The complex array of the barriers shaping women’s experiences of breastfeeding can be broadly categorized utilizing the socioecological model, which suggests that individuals’ health is a result of the interplay between micro (individual), meso (institutional), and macro (social) factors [ 17 ]. Although previous studies have explored barriers and supports to breastfeeding, the majority of articles focus on specific geographic areas (e.g. United States or United Kingdom), workplaces, or communities. In addition, very few articles focus on the analysis of the interplay between various micro, meso, and macro-level factors in shaping women’s experiences of breastfeeding. Synthesizing the growing literature on the experiences of breastfeeding and the factors shaping these experiences, offers researchers and public health professionals an opportunity to examine how various personal and institutional factors shape mothers’ breastfeeding decision-making. This knowledge is needed to identify what can be done to improve breastfeeding rates and make breastfeeding a more positive and meaningful experience for new mothers.
The aim of this scoping review is to synthesize evidence gathered from empirical literature on women’s perceptions about and experiences of breastfeeding. Specifically, the following questions are examined:
What does empirical literature report on women’s perceptions on breastfeeding?
What barriers do women face when they attempt to initiate or maintain breastfeeding?
What supports do women need in order to initiate and/or maintain breastfeeding?
Focusing on women’s experiences, this paper aims to contribute to our understanding of women’s decision-making and behaviours pertaining to breastfeeding. The overarching aim of this review is to translate these findings into actionable strategies that can streamline public health messaging and improve breastfeeding education and supports offered by health care providers working with new mothers.
This research utilized Arksey & O’Malley’s [ 18 ] framework to guide the scoping review process. The scoping review methodology was chosen to explore a breadth of literature on women’s perceptions about and experiences of breastfeeding. A broad research question, “What does empirical literature tell us about women’s experiences of breastfeeding?” was set to guide the literature search process.
Search methods
The review was undertaken in five steps: (1) identifying the research question, (2) identifying relevant literature, (3) iterative selection of data, (4) charting data, and (5) collating, summarizing, and reporting results. The inclusion criteria were set to empirical articles published between 2010 and 2020 in peer-reviewed journals with a specific focus on women’s self-reported experiences of breastfeeding, as well as how others see women’s experiences of breastfeeding. The focus on women’s perceptions of breastfeeding was used to capture the papers that specifically addressed their experiences and the barriers that they may encounter while breastfeeding. Only articles written in English were included in the review. The keywords utilized in the search strategy were developed in collaboration with a librarian (Table 1 ). PubMed, CINAHL, Sociological Abstracts, and PsychInfo databases were searched for the empirical literature, yielding a total of 2885 results.
Search outcome
The articles deemed to fit the inclusion criteria ( n = 213) were imported into RefWorks, an online reference manager tool and further screened for eligibility (Fig. 1 ). After the removal of 61 duplicates and title/abstract screening, 152 articles were kept for full-text review. Two independent reviewers assessed the papers to evaluate if they met the inclusion criteria of having an explicit analytic focus on women’s experiences of breastfeeding.
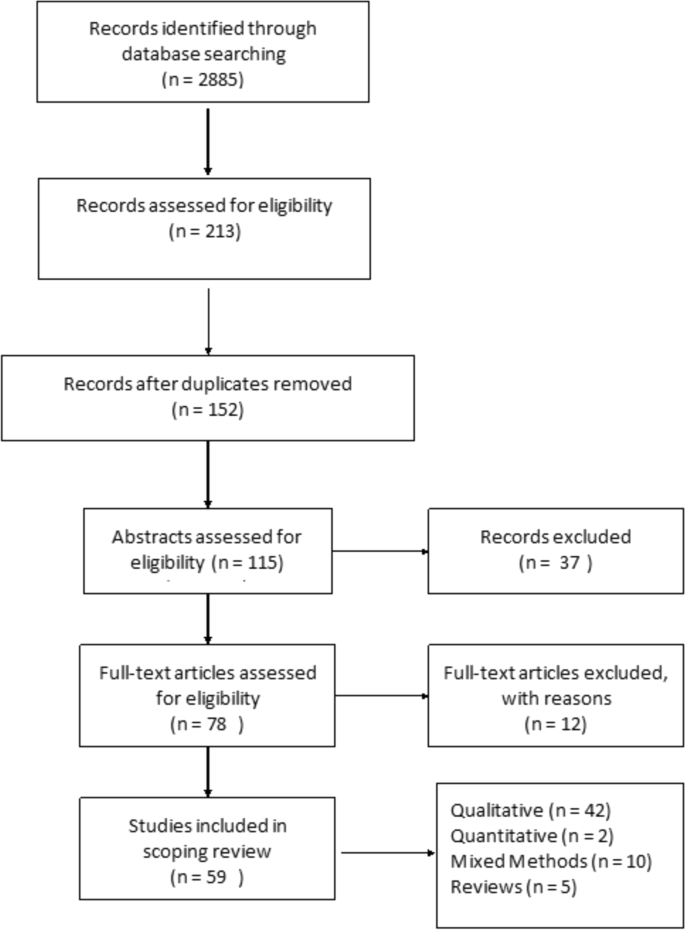
Prisma Flow Diagram
Quality appraisal
Consistent with scoping review methodology [ 18 ], the quality of the papers included in the review was not assessed.
Data abstraction
A literature extraction tool was created in MS Excel 2016. The data extracted from each paper included: (a) authors names, (b) title of the paper, (c) year of publication, (d) study objectives, (e) method used, (f) participant demographics, (g) country where the study was conducted, and (h) key findings from the paper.
Thematic analysis was utilized to identify key topics covered by the literature. Two reviewers independently read five papers to inductively generate key themes. This process was repeated until the two reviewers reached a consensus on the coding scheme, which was subsequently applied to the remainder of the articles. Key themes were added to the literature extraction tool and each paper was assigned a key theme and sub-themes, if relevant. The themes derived from the analysis were reviewed once again by all three authors when all the papers were coded. In the results section below, the synthesized literature is summarized alongside the key themes identified during the analysis.
In total, 59 peer-reviewed articles were included in the review. Since the review focused on women’s experiences of breastfeeding, as would be expected based on the search criteria, the majority of articles ( n = 42) included in the sample were qualitative studies, with ten utilizing a mixed method approach (Fig. 2 ). Figure 3 summarizes the distribution of articles by year of publication and Fig. 4 summarizes the geographic location of the study.
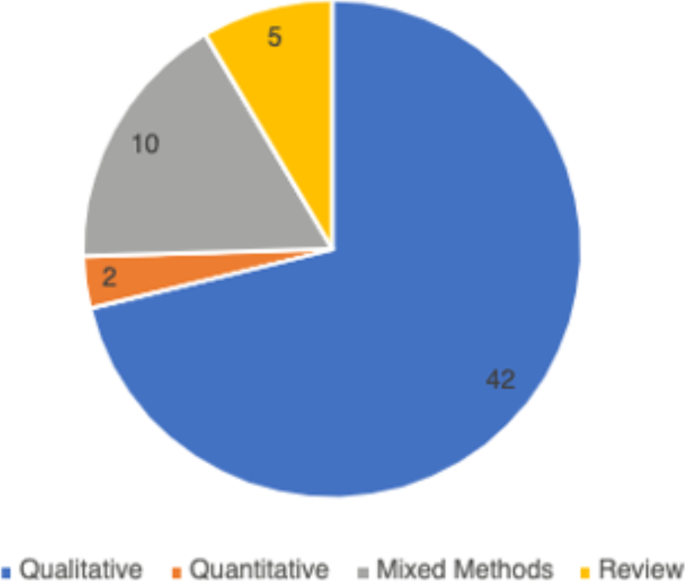
Types of Articles

Years of Publication
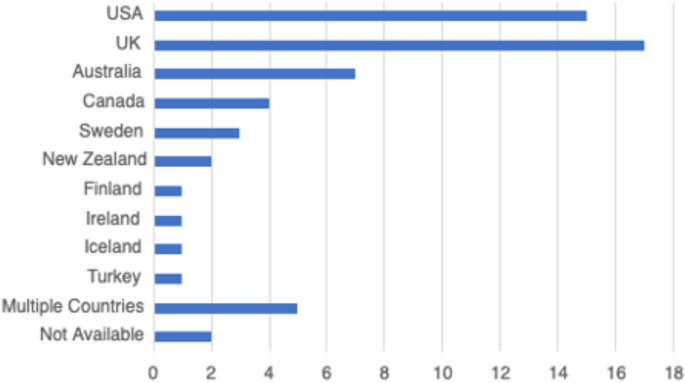
Countries of Focus Examined in Literature Review
Perceptions about breastfeeding
Women’s perceptions about breastfeeding were covered in 83% ( n = 49) of the papers. Most articles ( n = 31) suggested that women perceived breastfeeding as a positive experience and believed that breastfeeding had many benefits [ 19 , 20 ]. The phrases “breast is best” and “breastmilk is best” were repeatedly used by the participants of studies included in the reviewed literature [ 21 ]. Breastfeeding was seen as improving the emotional bond between the mother and the child [ 20 , 22 , 23 ], strengthening the child’s immune system [ 24 , 25 ], and providing a booster to the mother’s sense of self [ 1 , 26 ]. Convenience of breastfeeding (e.g., its availability and low cost) [ 19 , 27 ] and the role of breastfeeding in weight loss during the postpartum period were mentioned in the literature as other factors that positively shape mothers’ perceptions about breastfeeding [ 28 , 29 ].
The literature suggested that women’s perceptions of breastfeeding and feeding choices were also shaped by the advice of healthcare providers [ 30 , 31 ]. Paradoxically, messages about the importance and relative simplicity of breastfeeding may also contribute to misalignment between women’s expectations and the actual experiences of breastfeeding [ 32 ]. For instance, studies published in Canada and Sweden reported that women expected breastfeeding to occur “naturally”, to be easy and enjoyable [ 23 ]. Consequently, some women felt unprepared for the challenges associated with initiation or maintenance of breastfeeding [ 31 , 33 ]. The literature pointed out that mothers may feel overwhelmed by the frequency of infant feedings [ 26 ] and the amount as well as intensity of physical difficulties associated with breastfeeding initiation [ 33 ]. Researchers suggested that since many women see breastfeeding as a sign of being a “good” mother, their inability to breastfeed may trigger feelings of personal failure [ 22 , 34 ].
Women’s personal experiences with and perceptions about breastfeeding were also influenced by the cultural pressure to breastfeed. Welsh mothers interviewed in the UK, for instance, revealed that they were faced with judgement and disapproval when people around them discovered they opted out of breastfeeding [ 35 ]. Women recalled the experiences of being questioned by others, including strangers, when they were bottle feeding their infants [ 9 , 35 , 36 ].
Barriers to breastfeeding
The vast majority ( n = 50) of the reviewed literature identified various barriers for successful breastfeeding. A sizeable proportion of literature (41%, n = 24) explored women’s experiences with the physical aspects of breastfeeding [ 23 , 33 ]. In particular, problems with latching and the pain associated with breastfeeding were commonly cited as barriers for women to initiate breastfeeding [ 23 , 28 , 37 ]. Inadequate milk supply, both actual and perceived, was mentioned as another barrier for initiation and maintenance of breastfeeding [ 33 , 37 ]. Breastfeeding mothers were sometimes unable to determine how much milk their infants consumed (as opposed to seeing how much milk the infant had when bottle feeding), which caused them to feel anxious and uncertain about scheduling infant feedings [ 28 , 37 ]. Women’s inability to overcome these barriers was linked by some researchers to low self-efficacy among mothers, as well as feeling overwhelmed or suffering from postpartum depression [ 38 , 39 ].
In addition to personal and physical challenges experienced by mothers who were planning to breastfeed, the literature also highlighted the importance of social environment as a potential barrier to breastfeeding. Mothers’ personal networks were identified as a key factor in shaping their breastfeeding behaviours in 43 (73%) articles included in this review. In a study published in the UK, lack of role models – mothers, other female relatives, and friends who breastfeed – was cited as one of the potential barriers for breastfeeding [ 36 ]. Some family members and friends also actively discouraged breastfeeding, while openly questioning the benefits of this practice over bottle feeding [ 1 , 17 , 40 ]. Breastfeeding during family gatherings or in the presence of others was also reported as a challenge for some women from ethnic minority groups in the United Kingdom and for Black women in the United States [ 41 , 42 ].
The literature reported occasional instances where breastfeeding-related decisions created conflict in women’s relationships with significant others [ 26 ]. Some women noted they were pressured by their loved one to cease breastfeeding [ 22 ], especially when women continued to breastfeed 6 months postpartum [ 43 ]. Overall, the literature suggested that partners play a central role in women’s breastfeeding practices [ 8 ], although there was no consistency in the reviewed papers regarding the partners’ expressed level of support for breastfeeding.
Knowledge, especially practical knowledge about breastfeeding, was mentioned as a barrier in 17% ( n = 10) of the papers included in this review. While health care providers were perceived as a primary source of information on breastfeeding, some studies reported that mothers felt the information provided was not useful and occasionally contained conflicting advice [ 1 , 17 ]. This finding was reported across various jurisdictions, including the United States, Sweden, the United Kingdom and Netherlands, where mothers reported they had no support at all from their health care providers which made it challenging to address breastfeeding problems [ 26 , 38 , 44 ].
Breastfeeding in public emerged as a key barrier from the reviewed literature and was cited in 56% ( n = 33) of the papers. Examining the experiences of breastfeeding mothers in the United States, Spencer, Wambach, & Domain [ 45 ] suggested that some participants reported feeling “erased” from conversations while breastfeeding in public, rendering their bodies symbolically invisible. Lack of designated public spaces for breastfeeding forced many women to alter their feeding in public and to retreat to a private or a more secluded space, such as one’s personal car [ 25 ]. The oversexualization of women’s breasts was repeatedly noted as a core reason for the United States women’s negative experiences and feelings of self-consciousness about breastfeeding in front of others [ 45 ]. Studies reported women’s accounts of feeling the disapproval or disgust of others when breastfeeding in public [ 46 , 47 ], and some reported that women opted out of breastfeeding in public because they did not want to make those around them feel uncomfortable [ 25 , 40 , 48 ].
Finally, return to paid employment was noted in the literature as a significant challenge for continuation of breastfeeding [ 48 ]. Lack of supportive workplace environments [ 39 ] or inability to express milk were cited by women as barriers for continuing breastfeeding in the United States and New Zealand [ 39 , 49 ].
Supports needed to maintain breastfeeding
Due to the central role family members played in women’s experiences of breastfeeding, support from partners as well as female relatives was cited in the literature as key factors shaping women’s breastfeeding decisions [ 1 , 9 , 48 ]. In the articles published in Canada, Australia, and the United Kingdom, supportive family members allowed women to share the responsibility of feeding and other childcare activities, which reduced the pressures associated with being a new mother [ 19 , 20 ]. Similarly, encouragement, breastfeeding advice, and validation from healthcare professionals were identified as positively impacting women’s experiences with breastfeeding [ 1 , 22 , 28 ].
Community resources, such as peer support groups, helplines, and in-home breastfeeding support provided mothers with the opportunity to access help when they need it, and hence were reported to be facilitators for breastfeeding [ 19 , 22 , 33 , 44 ]. An increase in the usage of social media platforms, such as Facebook, among breastfeeding mothers for peer support were reported in some studies [ 47 ]. Public health breastfeeding clinics, lactation specialists, antenatal and prenatal classes, as well as education groups for mothers were identified as central support structures for the initiation and maintenance of breastfeeding [ 23 , 24 , 28 , 33 , 39 , 50 ]. Based on the analysis of the reviewed literature, however, access to these services varied greatly geographically and by socio-economic status [ 33 , 51 ]. It is also important to note that local and cultural context played a significant role in shaping women’s perceptions of breastfeeding. For example, a study that explored women’s breastfeeding experiences in Iceland highlighted the importance of breastfeeding in Icelandic society [ 52 ]. Women are expected to breastfeed and the decision to forgo breastfeeding is met with disproval [ 52 ]. Cultural beliefs regarding breastfeeding were also deemed important in the study of Szafrankska and Gallagher (2016), who noted that Polish women living in Ireland had a much higher rate of initiating breastfeeding compared to Irish women [ 53 ]. They attributed these differences to familial and societal expectations regarding breastfeeding in Poland [ 53 ].
Overall, the reviewed literature suggested that women faced socio-cultural pressure to breastfeed their infants [ 36 , 40 , 54 ]. Women reported initiating breastfeeding due to recognition of the many benefits it brings to the health of the child, even when they were reluctant to do it for personal reasons [ 8 ]. This hints at the success of public health education campaigns on the benefits of breastfeeding, which situates breastfeeding as a new cultural norm [ 24 ].
This scoping review examined the existing empirical literature on women’s perceptions about and experiences of breastfeeding to identify how public health messaging can be tailored to improve breastfeeding rates. The literature suggests that, overall, mothers are aware of the positive impacts of breastfeeding and have strong motivation to breastfeed [ 37 ]. However, women who chose to breastfeed also experience many barriers related to their social interactions with significant others and their unique socio-cultural contexts [ 25 ]. These different factors, summarized in Fig. 5 , should be considered in developing public health activities that promote breastfeeding. Breastfeeding experiences for women were very similar across the United Kingdom, United States, Canada, and Australia based on the studies included in this review. Likewise, barriers and supports to breastfeeding identified by women across the countries situated in the global north were quite similar. However, local policy context also impacted women’s experiences of breastfeeding. For example, maintaining breastfeeding while returning to paid employment has been identified as a challenge for mothers in the United States [ 39 , 45 ], a country with relatively short paid parental leave. Still, challenges with balancing breastfeeding while returning to paid employment were also noticed among women in New Zealand, despite a more generous maternity leave [ 49 ]. This suggests that while local and institutional policies might shape women’s experiences of breastfeeding, interpersonal and personal factors can also play a central role in how long they breastfeed their infants. Evidently, the importance of significant others, such as family members or friends, in providing support to breastfeeding mothers was cited as a key facilitator for breastfeeding across multiple geographic locations [ 29 , 34 , 48 ]. In addition, cultural beliefs and practices were also cited as an important component in either promoting breastfeeding or deterring women’s desire to initiate or maintain breastfeeding [ 15 , 29 , 37 ]. Societal support for breastfeeding and cultural practices can therefore partly explain the variation in breastfeeding rates across different countries [ 15 , 21 ]. Figure 5 summarizes the key barriers identified in the literature that inhibit women’s ability to breastfeed.
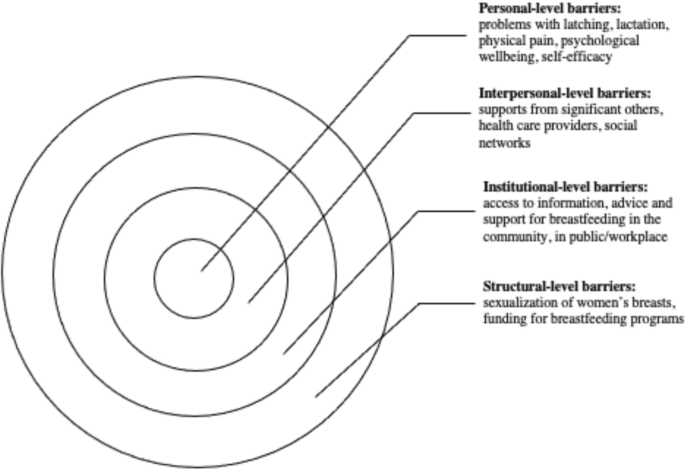
Barriers to Breastfeeding
At the individual level, women might experience challenges with breastfeeding stemming from various physiological and psychological problems, such as issues with latching, perceived or actual lack of breastmilk, and physical pain associated with breastfeeding. The onset of postpartum depression or other psychological problems may also impact women’s ability to breastfeed [ 54 ]. Given that many women assume that breastfeeding will happen “naturally” [ 15 , 40 ] these challenges can deter women from initiating or continuing breastfeeding. In light of these personal challenges, it is important to consider the potential challenges associated with breastfeeding that are conveyed to new mothers through the simplified message “breast is best” [ 21 ]. While breastfeeding may come easy to some women, most papers included in this review pointed to various challenges associated with initiating or maintaining breastfeeding [ 19 , 33 ]. By modifying public health messaging regarding breastfeeding to acknowledge that breastfeeding may pose a challenge and offering supports to new mothers, it might be possible to alleviate some of the guilt mothers experience when they are unable to breastfeed.
Barriers that can be experienced at the interpersonal level concern women’s communication with others regarding their breastfeeding choices and practices. The reviewed literature shows a strong impact of women’s social networks on their decision to breastfeed [ 24 , 33 ]. In particular, significant others – partners, mothers, siblings and close friends – seem to have a considerable influence over mothers’ decision to breastfeed [ 42 , 53 , 55 ]. Hence, public health messaging should target not only mothers, but also their significant others in developing breastfeeding campaigns. Social media may also be a potential medium for sharing supports and information regarding breastfeeding with new mothers and their significant others.
There is also a strong need for breastfeeding supports at the institutional and community levels. Access to lactation consultants, sound and practical advice from health care providers, and availability of physical spaces in the community and (for women who return to paid employment) in the workplace can provide more opportunities for mothers who want to breastfeed [ 18 , 33 , 44 ]. The findings from this review show, however, that access to these supports and resources vary greatly, and often the women who need them the most lack access to them [ 56 ].
While women make decisions about breastfeeding in light of their own personal circumstances, it is important to note that these circumstances are shaped by larger structural, social, and cultural factors. For instance, mothers may feel reluctant to breastfeed in public, which may stem from their familiarity with dominant cultural perspectives that label breasts as objects for sexualized pleasure [ 48 ]. The reviewed literature also showed that, despite the initial support, mothers who continue to breastfeed past the first year may be judged and scrutinized by others [ 47 ]. Tailoring public health care messaging to local communities with their own unique breastfeeding-related beliefs might help to create a larger social change in sociocultural norms regarding breastfeeding practices.
The literature included in this scoping review identified the importance of support from community services and health care providers in facilitating women’s breastfeeding behaviours [ 22 , 24 ]. Unfortunately, some mothers felt that the support and information they received was inadequate, impractical, or infused with conflicting messaging [ 28 , 44 ]. To make breastfeeding support more accessible to women across different social positions and geographic locations, it is important to acknowledge the need for the development of formal infrastructure that promotes breastfeeding. This includes training health care providers to help women struggling with breastfeeding and allocating sufficient funding for such initiatives.
Overall, this scoping review revealed the need for healthcare professionals to provide practical breastfeeding advice and realistic solutions to women encountering difficulties with breastfeeding. Public health messaging surrounding breastfeeding must re-invent breastfeeding as a “family practice” that requires collaboration between the breastfeeding mother, their partner, as well as extended family to ensure that women are supported as they breastfeed [ 8 ]. The literature also highlighted the issue of healthcare professionals easily giving up on women who encounter problems with breastfeeding and automatically recommending the initiation of formula use without further consideration towards solutions for breastfeeding difficulties [ 19 ]. While some challenges associated with breastfeeding are informed by local culture or health care policies, most of the barriers experienced by breastfeeding women are remarkably universal. Women often struggle with initiation of breastfeeding, lack of support from their significant others, and lack of appropriate places and spaces to breastfeed [ 25 , 26 , 33 , 39 ]. A change in public health messaging to a more flexible messaging that recognizes the challenges of breastfeeding is needed to help women overcome negative feelings associated with failure to breastfeed. Offering more personalized advice and support to breastfeeding mothers can improve women’s experiences and increase the rates of breastfeeding while also boosting mothers’ sense of self-efficacy.
Limitations
This scoping review has several limitations. First, the focus on “women’s experiences” rendered broad search criteria but may have resulted in the over or underrepresentation of specific findings in this review. Also, the exclusion of empirical work published in languages other than English rendered this review reliant on the papers published predominantly in English-speaking countries. Finally, consistent with Arksey and O’Malley’s [ 18 ] scoping review methodology, we did not appraise the quality of the reviewed literature. Notwithstanding these limitations, this review provides important insights into women’s experiences of breastfeeding and offers practical strategies for improving dominant public health messaging on the importance of breastfeeding.
Women who breastfeed encounter many difficulties when they initiate breastfeeding, and most women are unsuccessful in adhering to current public health breastfeeding guidelines. This scoping review highlighted the need for reconfiguring public health messaging to acknowledge the challenges many women experience with breastfeeding and include women’s social networks as a target audience for such messaging. This review also shows that breastfeeding supports and counselling are needed by all women, but there is also a need to tailor public health messaging to local social norms and culture. The role social institutions and cultural discourses have on women’s experiences of breastfeeding must also be acknowledged and leveraged by health care professionals promoting breastfeeding.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Wolf JH. Low breastfeeding rates and public health in the United States. Am J Public Health. 2003;93(12):2000–2010. [cited 2021 Apr 21] Available from: http://ajph.aphapublications.org/doi/ https://doi.org/10.2105/AJPH.93.12.2000
World Health Organization, UNICEF. Global nutrition targets 2015: Breastfeeding policy brief 2014.
United Nations International Children’s Emergency Fund (UNICEF). Breastfeeding in the UK. 2019 [cited 2021 Apr 21]. Available from: https://www.unicef.org.uk/babyfriendly/about/breastfeeding-in-the-uk/
Semenic S, Loiselle C, Gottlieb L. Predictors of the duration of exclusive breastfeeding among first-time mothers. Res Nurs Health. 2008;31(5):428–441. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1002/nur.20275
Hauck YL, Bradfield Z, Kuliukas L. Women’s experiences with breastfeeding in public: an integrative review. Women Birth. 2020;34:e217–27.
Hendaus MA, Alhammadi AH, Khan S, Osman S, Hamad A. Breastfeeding rates and barriers: a report from the state of Qatar. Int. J Women's Health. 2018;10:467–75 [cited 2021 Apr 20] Available from: /pmc/articles/PMC6110662/.
Google Scholar
Ogbo FA, Ezeh OK, Khanlari S, Naz S, Senanayake P, Ahmed KY, et al. Determinants of exclusive breastfeeding cessation in the early postnatal period among culturally and linguistically diverse (CALD) Australian mothers. Nutrients. 2019;11(7):1611 [cited 2021 Apr 21] Available from: https://www.mdpi.com/2072-6643/11/7/1611 .
Article Google Scholar
Ayton JE, Tesch L, Hansen E. Women’s experiences of ceasing to breastfeed: Australian qualitative study. BMJ Open. 2019;9(5):26234 [cited 2021 Apr 20] Available from: http://bmjopen.bmj.com/ .
Brown CRL, Dodds L, Legge A, Bryanton J, Semenic S. Factors influencing the reasons why mothers stop breastfeeding. Can J Public Heal. 2014;105(3):e179–e185. [cited 2021 Apr 20] Available from: https://link.springer.com/article/ https://doi.org/10.17269/cjph.105.4244
Sharma AJ, Dee DL, Harden SM. Adherence to breastfeeding guidelines and maternal weight 6 years after delivery. Pediatrics. 2014;134(Supplement 1):S42–S49. [cited 2021 Apr 21] Available from: www.pediatrics.org/cgi/doi/ https://doi.org/10.1542/peds.2014-0646H
Walters DD, Phan LTH, Mathisen R. The cost of not breastfeeding: Global results from a new tool. Health Policy Plan. 2019;34(6):407–17 [cited 2021 Apr 21] Available from: https://academic.oup.com/heapol/article/34/6/407/5522499 .
Friedman M. For whom is breast best? Thoughts on breastfeeding, feminism and ambivalence. J Mother Initiat Res Community Involv. 2009;11(1):26–35 [cited 2021 Apr 20] Available from: https://jarm.journals.yorku.ca/index.php/jarm/article/viewFile/22506/20986 .
Blixt I, Johansson M, Hildingsson I, Papoutsi Z, Rubertsson C. Women’s advice to healthcare professionals regarding breastfeeding: “offer sensitive individualized breastfeeding support” - an interview study. Int Breastfeed J 2019;14(1):51. [cited 2021 Apr 20] Available from: https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-019-0247-4
Obeng C, Dickinson S, Golzarri-Arroyo L. Women’s perceptions about breastfeeding: a preliminary study. Children. 2020;7(6):61 [cited 2021 Apr 21] Available from: https://www.mdpi.com/2227-9067/7/6/61 .
Choudhry K, Wallace LM. ‘Breast is not always best’: South Asian women’s experiences of infant feeding in the UK within an acculturation framework. Matern Child Nutr. 2012;8(1):72–87. [cited 2021 Apr 20] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1740-8709.2010.00253.x
Da Silva TD, Bick D, Chang YS. Breastfeeding experiences and perspectives among women with postnatal depression: a qualitative evidence synthesis. Women Birth. 2020;33(3):231–9.
Kilanowski JF. Breadth of the socio-ecological model. J Agromedicine. 2017;22(4):295–7 [cited 2021 Apr 20] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=wagr20 .
Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8(1):19–32 [cited 2021 Apr 20] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=tsrm20 .
Brown A, Lee M. An exploration of the attitudes and experiences of mothers in the United Kingdom who chose to breastfeed exclusively for 6 months postpartum. Breastfeed Med. 2011;6(4):197–204. [cited 2021 Apr 20] Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2010.0097
Morns MA, Steel AE, Burns E, McIntyre E. Women who experience feelings of aversion while breastfeeding: a meta-ethnographic review. Women Birth. 2021;34:128–35.
Jackson KT, Mantler T, O’Keefe-McCarthy S. Women’s experiences of breastfeeding-related pain. MCN Am J Matern Nurs. 2019;44(2):66–72 [cited 2021 Apr 20] Available from: https://journals.lww.com/00005721-201903000-00002 .
Burns E, Schmied V, Sheehan A, Fenwick J. A meta-ethnographic synthesis of women’s experience of breastfeeding. Matern Child Nutr. 2009;6(3):201–219. [cited 2021 Apr 20] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1740-8709.2009.00209.x
Claesson IM, Larsson L, Steen L, Alehagen S. “You just need to leave the room when you breastfeed” Breastfeeding experiences among obese women in Sweden - A qualitative study. BMC Pregnancy Childbirth. 2018;18(1):1–10. [cited 2021 Apr 20] Available from: https://link.springer.com/articles/ https://doi.org/10.1186/s12884-017-1656-2
Asiodu IV, Waters CM, Dailey DE, Lyndon • Audrey. Infant feeding decision-making and the influences of social support persons among first-time African American mothers. Matern Child Health J. 2017;21:863–72.
Forster DA, McLachlan HL. Women’s views and experiences of breast feeding: positive, negative or just good for the baby? Midwifery. 2010;26(1):116–25.
Demirci J, Caplan E, Murray N, Cohen S. “I just want to do everything right:” Primiparous Women’s accounts of early breastfeeding via an app-based diary. J Pediatr Heal Care. 2018;32(2):163–72.
Furman LM, Banks EC, North AB. Breastfeeding among high-risk Inner-City African-American mothers: a risky choice? Breastfeed Med. 2013;8(1):58–67. [cited 2021 Apr 20]Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2012.0012
Cottrell BH, Detman LA. Breastfeeding concerns and experiences of african american mothers. MCN Am J Matern Nurs. 2013;38(5):297–304 [cited 2021 Apr 20] Available from: https://journals.lww.com/00005721-201309000-00009 .
Wambach K, Domian EW, Page-Goertz S, Wurtz H, Hoffman K. Exclusive breastfeeding experiences among mexican american women. J Hum Lact. 2016;32(1):103–111. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0890334415599400
Regan P, Ball E. Breastfeeding mothers’ experiences: The ghost in the machine. Qual Health Res. 2013;23(5):679–688. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732313481641
Hinsliff-Smith K, Spencer R, Walsh D. Realities, difficulties, and outcomes for mothers choosing to breastfeed: Primigravid mothers experiences in the early postpartum period (6-8 weeks). Midwifery. 2014;30(1):e14–9.
Palmér L. Previous breastfeeding difficulties: an existential breastfeeding trauma with two intertwined pathways for future breastfeeding—fear and longing. Int J Qual Stud Health Well-being. 2019;14(1) [cited 2021 Apr 21] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=zqhw20 .
Francis J, Mildon A, Stewart S, Underhill B, Tarasuk V, Di Ruggiero E, et al. Vulnerable mothers’ experiences breastfeeding with an enhanced community lactation support program. Matern Child Nutr 2020;16(3):16. [cited 2021 Apr 20] Available from: https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/mcn.12957
Palmér L, Carlsson G, Mollberg M, Nyström M. Breastfeeding: An existential challenge - Women’s lived experiences of initiating breastfeeding within the context of early home discharge in Sweden. Int J Qual Stud Health Well-being 2010;5(3). [cited 2021 Apr 21] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=zqhw20https://doi.org/ https://doi.org/10.3402/qhw.v5i3.5397
Grant A, Mannay D, Marzella R. ‘People try and police your behaviour’: the impact of surveillance on mothers and grandmothers’ perceptions and experiences of infant feeding. Fam Relationships Soc. 2018;7(3):431–47.
Thomson G, Ebisch-Burton K, Flacking R. Shame if you do - shame if you don’t: women’s experiences of infant feeding. Matern Child Nutr. 2015;11(1):33–46. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/mcn.12148
Dietrich Leurer M, Misskey E. The psychosocial and emotional experience of breastfeeding: reflections of mothers. Glob Qual. Nurs Res. 2015;2:2333393615611654 [cited 2021 Apr 20] Available from: http://www.ncbi.nlm.nih.gov/pubmed/28462320 .
Fahlquist JN. Experience of non-breastfeeding mothers: Norms and ethically responsible risk communication. Nurs Ethics. 2016;23(2):231–241. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0969733014561913
Gross TT, Davis M, Anderson AK, Hall J, Hilyard K. Long-term breastfeeding in African American mothers: a positive deviance inquiry of WIC participants. J Hum Lact. 2017;33(1):128–139. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0890334416680180
Spencer RL, Greatrex-White S, Fraser DM. ‘I thought it would keep them all quiet’. Women’s experiences of breastfeeding as illusions of compliance: an interpretive phenomenological study. J Adv Nurs. 2015;71(5):1076–1086. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/jan.12592
Twamley K, Puthussery S, Harding S, Baron M, Macfarlane A. UK-born ethnic minority women and their experiences of feeding their newborn infant. Midwifery. 2011;27(5):595–602.
PubMed Google Scholar
Lutenbacher M, Karp SM, Moore ER. Reflections of Black women who choose to breastfeed: influences, challenges, and supports. Matern Child Health J. 2016;20(2):231–9.
Dowling S, Brown A. An exploration of the experiences of mothers who breastfeed long-term: what are the issues and why does it matter? Breastfeed Med. 2013;8(1):45–52. [cited 2021 Apr 20] Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2012.0057
Fox R, McMullen S, Newburn M. UK women’s experiences of breastfeeding and additional breastfeeding support: a qualitative study of baby Café services. BMC Pregnancy Childbirth 2015;15(1):147. [cited 2021 Apr 20] Available from: http://bmcpregnancychildbirth.biomedcentral.com/articles/ https://doi.org/10.1186/s12884-015-0581-5
Spencer B, Wambach K, Domain EW. African American women’s breastfeeding experiences: cultural, personal, and political voices. Qual Health Res. 2015;25(7):974–987. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732314554097
McBride-Henry K. The influence of the They: An interpretation of breastfeeding culture in New Zealand. Qual Health Res. 2010;20(6):768–777. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732310364220
Newman KL, Williamson IR. Why aren’t you stopping now?!’ Exploring accounts of white women breastfeeding beyond six months in the east of England. Appetite. 2018 Oct;1(129):228–35.
Dowling S, Pontin D. Using liminality to understand mothers’ experiences of long-term breastfeeding: ‘Betwixt and between’, and ‘matter out of place.’ Heal (United Kingdom). 2017;21(1):57–75. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1363459315595846
Payne D, Nicholls DA. Managing breastfeeding and work: a Foucauldian secondary analysis. J Adv Nurs. 2010;66(8):1810–1818. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1365-2648.2009.05156.x
Keely A, Lawton J, Swanson V, Denison FC. Barriers to breast-feeding in obese women: a qualitative exploration. Midwifery. 2015;31(5):532–9.
Afoakwah G, Smyth R, Lavender DT. Women’s experiences of breastfeeding: A narrative review of qualitative studies. Afr J Midwifery Womens Health. 2013 ;7(2):71–77. [cited 2021 Apr 21] Available from: https://www.magonlinelibrary.com/doi/abs/ https://doi.org/10.12968/ajmw.2013.7.2.71
Símonardóttir S. Getting the green light: experiences of Icelandic mothers struggling with breastfeeding. Sociol Res Online. 2016;21(4):1.
Szafranska M, Gallagher DL. Polish women’s experiences of breastfeeding in Ireland. Pract Midwife. 2016;19(1):30–2 [cited 2021 Apr 21] Available from: https://europepmc.org/article/med/26975131 .
Pratt BA, Longo J, Gordon SC, Jones NA. Perceptions of breastfeeding for women with perinatal depression: a descriptive phenomenological study. Issues Ment Health Nurs. 2020;41(7):637–644. [cited 2021 Apr 21] Available from: https://www.tandfonline.com/doi/abs/ https://doi.org/10.1080/01612840.2019.1691690
Durmazoğlu G, Yenal K, Okumuş H. Maternal emotions and experiences of mothers who had breastfeeding problems: a qualitative study. Res Theory Nurs Pract. 2020;34(1):3–20. [cited 2021 Apr 20] Available from: http://connect.springerpub.com/lookup/doi/ https://doi.org/10.1891/1541-6577.34.1.3
Burns E, Triandafilidis Z. Taking the path of least resistance: a qualitative analysis of return to work or study while breastfeeding. Int Breastfeed J. 2019;14(1):1–13.
Download references
Acknowledgements
The authors would like to acknowledge the assistance of Jackie Stapleton, the University of Waterloo librarian, for her assistance with developing the search strategy used in this review.
Not applicable.
Author information
Authors and affiliations.
School of Public Health Sciences, University of Waterloo, 200 University Ave West, Waterloo, ON, N2L 3G1, Canada
Bridget Beggs, Liza Koshy & Elena Neiterman
You can also search for this author in PubMed Google Scholar
Contributions
BB was responsible for the formal analysis and organization of the review. LK was responsible for data curation, visualization and writing the original draft. EN was responsible for initial conceptualization and writing the original draft. BB and LK were responsible for reviewing and editing the manuscript. All authors read and approved the final manuscript.
Authors’ information
BB is completing her Bachelor of Science (BSc) degree at the School of Public Health Sciences at the University of Waterloo.
LK is completing her Bachelor of Public Health (BPH) degree at the School of Public Health Sciences at the University of Waterloo.
EN (PhD), is a continuing lecturer at the School of Public Health Sciences at the University of Waterloo. Her areas of expertise are in women’s reproductive health and sociology of health, illness, and healthcare.
Corresponding author
Correspondence to Bridget Beggs .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Beggs, B., Koshy, L. & Neiterman, E. Women’s Perceptions and Experiences of Breastfeeding: a scoping review of the literature. BMC Public Health 21 , 2169 (2021). https://doi.org/10.1186/s12889-021-12216-3
Download citation
Received : 23 June 2021
Accepted : 10 November 2021
Published : 26 November 2021
DOI : https://doi.org/10.1186/s12889-021-12216-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding
- Experiences
- Public health
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
The Radical Joy of Breastfeeding My 3-Year-Old

I’m not supposed to say that I breastfeed my 3-year-old because I like it. I’m supposed to say he needs it, he won’t quit. That I’m surrendering my body and time on the altar of attentive, attached motherhood. He enjoys it too, of course. He usually asks. I rarely offer. We do it a couple of times a day. More on weekends or when he’s hurt, sick, or just wants to. It also feels good. To me. It eases my anxiety. It is sentimental, sensory, and sensual. It fills me with love.
My son is large—in the 99th percentile for weight and height—so when he sits in my lap, his legs extend off the furniture, though he tries to curl them to become the smaller baby he once was. He squeals, then smushes my breast to his face with both hands, sometimes sucking and looking at me, sometimes drinking while driving a Matchbox car along my collarbone.
Years earlier, back in college, I sat beside a mother on an airplane who asked if I minded as she nursed her toddler. I said no, of course not. She schooled me on benefits for babies and the politics of nursing in public. I nodded, tried not to look. I remember feeling a blend of sympathy and discomfort as I tried on a mother identity in my mind—imagined whether I would ever breastfeed in that way, in public, a kid old enough to run, to feed himself, to speak multiclause sentences. It was my first exposure to a person nursing in front of me. I would barely experience that again until my own baby was at my breast.
More from TIME
Read More: I Thought I Had to Breastfeed My Babies. Then I Lost My Breasts
Breastfeeding is necessary and magical, yet American society stymies it from go. Babies need near constant access to their mothers’ bodies and uninterrupted time to figure out feeding, all but impossible in a country that sends a quarter of moms back to work two weeks after birth, denies postpartum support and paid leave, and assaults women’s autonomy. Any modicum of breastfeeding tolerance is for infants doing it, “breast is best” and all. It’s taboo to practice extended breastfeed (i.e., to breastfeed full-on kids). Calling it “extended” makes it an oddity—past what is expected, normal, or reasonable. Beyond its purpose to supply a product that can be extracted in private, fed to your kid by anyone. A pediatrician and an obstetrician separately told me that breastfeeding beyond six months is “just for the mom.” It’s almost certainly not. But so what if it is? It’s curious that when the act tips from benefiting babies to benefiting mothers, the censure flares.
The bulk of research devoted to understanding breastfeeding is on the nutritive benefits during the first six months to the first year of an infant’s life.While bodies like the WHO recommend breastfeeding babies for up to two years or beyond , we know practically nothing about breastfeeding beyond year one because we don’t study it. Still, we do know that breastfeeding’s rewards for mom–at least for the period that’s been the focus of research–are manifold and significant. It has been linked to a reduction in breast and ovarian cancer, and thanks to the oxytocin hit you get when you do it, you may experience a reduction in postpartum depression, stress, and anxiety. It can feel good in your head, in your body. It can create a closeness with your kid. Yet, by the time breastfeeding moves beyond necessity, beyond engorgement, spraying milk everywhere and soaking clothes, you’re urged to quit. Because doing it “for the mom” is wrong.
No one should feel shame about their feeding choices—everyone should make decisions that suit their body and family. I really appreciate that my kid comes to nurse for comfort, to regroup, as a pick-me-up or expression of love, rather than for a meal. Most women won’t experience this. The majority of people giving birth want to breastfeed, but only a quarter of moms exclusively breastfeed for their infant’s first six months as the CDC recommends .
We’re told infant feeding is individual choice. But the hurdles are institutional. “Women not meeting breastfeeding goals is presented as individual failure. That is such a lie. It’s such a fiction,” says Katie Hinde, a lactation researcher and professor of evolutionary biology at Arizona State University. We should receive far more support—from caregivers, health providers, work, family, the government, society. We all deserve the possibility of breastfeeding our kids for as long as we want, if we want to at all, but it’s a choice far too few people get to make.
Read More: Allyson Felix on How Motherhood Made Her an Activist
Even for those who manage to overcome the societal stigma and dearth of support to breastfeed babies in the early months, extended breastfeeding remains largely elusive, because stopping is what’s expected, or demanded. What feels like a natural conclusion to breastfeeding is actually a confluence of forces masquerading as care. As concern for mom, even—her body, space, money, and time. Breastfeeding your kid takes away your productivity and time with other people, so the pump and the bottle are presented as paths to freedom. Instead, they are the beginning of the end.
I think about this now, as I look forward to returning home at the end of the day to nurse my kid who is almost 4. It’s when my shoulders lower, I exhale deeply, snuggle him close, look in his eyes, and get a shot of oxytocin. To nurse is to be flooded with love. Sometimes I wonder why we must find verbal substitutes for what our bodies know and can communicate.
We are a universe away from the existential chaos of infant feeding—stressing that he isn’t getting enough ounces, trying to soothe cracked nipples, and being milked by my partner to unclog my ducts. Breastfeeding now feels gratifying, pleasurable, and anxiety reducing. The longer I do it and enjoy it, the more radical it feels. I’m saying I can do with my body what I want.
This article has been adapted from Birth Control: The Insidious Power of Men Over Motherhood, by Allison Yarrow. Copyright © 2023. Available from Seal Press, an imprint of Perseus Books, LLC, a subsidiary of Hachette Book Group, Inc.
More Must-Reads from TIME
- How Selena Gomez Is Revolutionizing the Celebrity Beauty Business
- TIME100 Most Influential Companies 2024
- Javier Milei’s Radical Plan to Transform Argentina
- How Private Donors Shape Birth-Control Choices
- The Deadly Digital Frontiers at the Border
- What's the Best Measure of Fitness?
- The 31 Most Anticipated Movies of Summer 2024
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
Home — Essay Samples — Nursing & Health — Breastfeeding — Persuasive Speech On Breastfeeding
Persuasive Speech on Breastfeeding
- Categories: Breastfeeding
About this sample

Words: 581 |
Published: Mar 14, 2024
Words: 581 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 866 words
3 pages / 1486 words
1 pages / 536 words
2 pages / 910 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Breastfeeding
In conclusion, breastfeeding is a natural and beneficial method of feeding infants. It provides numerous health benefits for both mother and child, including improved immune function, cognitive development, and reduced risk of [...]
In the research article, a qualitative data analysis method has been used in order to verify the main research question. The four reasons can be provided in support of the claim that it was a qualitative research method. Seven [...]
Breastfeeding in connection with intelligence has long been a study of scientists in psychological professions in the years succeeding a 1929 study on the subject. Argumentation has gone back and forth, with some arguing that [...]
The United States is one of the highest birth rate for teens. If more teens were to take Birth control we would have less abortion rates and less teen pregnancies in the United States. There are many types and the [...]
The healthcare sector substantially has developed over the years thanks to the convenience brought by the current technologies advancements. Nevertheless, there are still many difficulties that the industry has to deal with, [...]
In 2013, Venka Child aged 16 from Bristol worked with Fixers to create a short video about challenges teen mothers go through. In some part of the video, a teen mother is shown opening a fridge which is almost empty. The teen [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Benefits of Breastfeeding Versus Formula-Feeding Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
History of breastfeeding, advantages of breastfeeding over bottle-feeding, advantages of bottle-feeding over breastfeeding, importance of research.
Nowadays, one of the most challenging tasks many young mothers have to face is the necessity of choosing between breastfeeding and formula/bottle-feeding. It is easy to surf the web and find several correlational, cohort, or experimental studies where different authors defend their positions on the chosen topic. On the one hand, breastfeeding is deemed preferable due to its perfect balance of nutrients, protection against allergies and diseases, and easy digestion for babies.
On the other hand, formula-feeding is characterized by certain merits, such as the possibility for another person to feed a baby anytime, a mother’s freedom to be involved in different activities or even start working, and no dependence on the mother-child diet. Although some mothers might still choose to bottle-feed their infants with formula due to practical concerns, research shows that breastfeeding is preferable due to its impact on maternal and child health.
The history of breastfeeding is as long as the existence of life on the planet. In ancient cultures and in modern times women continued to breastfeed children to nourish them. However, some cultures did not focus on breastfeeding as an intimate link between the mother and the child. For example, while most ancient civilizations had mothers feed their children, more structurally segregated Western European countries created the role of a wet nurse – a woman whose job was to breastfeed children of royal and noblewomen.
Various cultures assigned different meanings to the process of breastfeeding and followed their sets of rules to determine how, when, and where to feed children. In ancient times, Egyptian and Greek civilizations did not treat breastfeeding as a job fit only for common folk and allowed women of all social statuses to feed their children. Nevertheless, wet nurses still had a place in the culture and were respected for their work. In Japan, breastfeeding was common but declined in popularity in the 20th century due to the interest of mothers in modern medicine and artificial feeding options. However, with a well-thought-out campaign, the government was able to elevate breastfeeding to be the primary choice of mothers in the country.
Western countries faced similar challenges earlier, during the middle ages, and then again at the beginning of the 19th century. Here, the history of breastfeeding was firmly connected to the cultural aspects of these civilizations. Countries with a rigid societal structure viewed breastfeeding as a job for lower classes and the process became plagued with many preconceptions. The combination of men’s opinions on breastfeeding and their lack of medical knowledge pressured women into declining breastfeeding. Later efforts in raising the popularity of breastfeeding emphasized health benefits for mothers and children and an establishment of an emotional connection between the parent and the child.
The breastfeeding vs. formula-feeding dilemma appears as soon as women find out that they are pregnant. They have to evaluate all the pros and cons of their pregnancy outcomes, understand if they want to take sick leave, and recognize the relationship between baby feeding and health. All circumstances have to be taken into consideration to make the best decision. Both methods, breastfeeding and bottle-feeding, have their advantages and disadvantages.
Sometimes, it is hard to make a choice, and extensive research is required. This dilemma may be considered through the prism of health, social factors, emotional stability, and personal convenience. In this paper, special attention to the works by Belfort et al. (2013), Boué et al. (2018), Fallon, Komninou, Bennett, Halford, and Harrold (2017), Horta and Victoria (2013) will be made to clarify if the benefits of breastfeeding prevail over the benefits of bottle-feeding in terms of health.
The first months after a baby is born may be defined as the period when it is necessary to choose to breastfeed over bottle-feeding and establish a strong mother-child contact. There are many short- and long-term health benefits for both participants of a process that may be enhanced through its exclusivity and duration (Fallon et al., 2017). The representatives of the World Health Organization admit that exclusive breastfeeding during the first six months can decrease morbidity from allergies and gastrointestinal diseases due to the presence of nutritional benefits in human milk (Horta & Victoria, 2013).
For example, the nutrient n-3 fatty acid docosahexaenoic acid (DHA) found in breast milk aims at improving the functions of the brain (Belfort et al., 2013). Therefore, when the advantages of breastfeeding have to be identified, this point plays an important role.
In addition to nutrients, breastfeeding is a method in terms of which infants can control their condition and take as much amount of milk as they may need. They do not take more or less, just the portion they need at that moment. Mothers should take responsibility for the quality of milk they offer to their children and follow simple hygiene rules and schedules.
Another important aspect that underlines the necessity of breastfeeding is the protection of children against diseases and other health threats. Probiotics and prebiotics, also known as important live microorganisms, protect the body and establish a gut microbiota that promotes positive health outcomes through the creation of barriers to pathogens, improvement of metabolic function, and energy salvation (Boué et al., 2018). Stomach viruses and other conditions that may cause discomfort are also significantly reduced with breastfeeding.
Allergies pose another serious threat to infants. It is hard for a mother to comprehend what product is safe for a child and what ingredients should be avoided. Breast milk is characterized by appropriate natural filters and the possibility to avoid ingesting real food until the body is properly developed. It helps babies digest food and uses the enzymes in a mother’s milk to speed up digestion and avoid complications.
Finally, breastfeeding is preferable because of the promotion of the bond between a mother and a child, and its price. This process of feeding is a unique chance for mothers to be relieved from anxiety and develop an emotional attachment to their children. Sometimes, it is not enough for mothers to talk to their children, observe their smile, and touch them. Breastfeeding is an exclusive type of contact that is not available to other people, including even the closest family members. This relationship is priceless. Indeed, when talking about the price, it is also necessary to admit that compared to bottle-feeding, which requires buying special ingredients, bottles, and hygienic goods, breastfeeding is a cheap process with no additional products except a mother and a child being present in it.
However, despite all the benefits of breastfeeding, it is wrong to believe that formula-feeding is solely negative or does not have important characteristics that breast-feeding cannot offer. Many significant aspects should be considered by mothers who still have some doubts about their choice. For example, some mothers may be challenged by poor health or inappropriate health status for breastfeeding.
Mothers may suffer from the inability to breastfeed as they are unable to produce milk or the milk is of poor quality. In these cases, mothers still want to find new ways to be close to their children and support them and formula-feeding is one option that they can rely on on under any condition. No connection between the health problems of a mother and a child is observed. Bottle-feeding creates several good opportunities for mothers to stabilize their personal and professional lives. Fallon et al. (2017) admit that the choice of the formula is usually explained by breastfeeding management, not biological issues. Therefore, the advantages of bottle-feeding over breastfeeding in terms of health care are based on the emotional aspects and mental health of mothers.
An understanding of the differences between breastfeeding and formula-feeding should be based on thorough research. For example, a study developed by Horta and Victoria (2013) asserts that formula-fed children may have serious hormonal and insulin responses to feeding and an increased number of adipocytes compared to breast-fed children. Bottles have to be cleaned and properly stored to avoid the growth of bacteria that may harm a child (Boué et al., 2018). Finally, the study by Fallon et al. (2017) shows that mothers may feel guilt and stigma in case they choose formula as the main method of feeding. All these studies prove that research is a crucial step to comprehend the benefits of breastfeeding nowadays.
In general, it is hard to neglect the existing dilemma of breastfeeding vs. bottle-feeding. Mothers have to weigh all the pros and cons of both processes and understand what method is more appropriate to them. Regarding the chosen cohort and experimental studies and past research, it is concluded that despite several positive socio-cultural and emotional outcomes of formula-feeding, breastfeeding remains the preferred method due to its effects on health, the establishment of mother-child relations, and the promotion of the cognitive development of children.
Belfort, M. B., Rifas-Shiman, S. L., Kleinman, K. P., Guthrie, L. B., Bellinger, D. C., Taveras, E. M.,… Oken, E. (2013). Infant feeding and childhood cognition at ages 3 and 7 years: Effects of breastfeeding duration and exclusivity. JAMA Pediatrics, 167 (9), 836-844.
Boué, G., Cummins, E., Guillou, S., Antignac, J. P., Le Bizec, B., & Membré, J. M. (2018). Public health risks and benefits associated with breast milk and infant formula consumption. Critical Reviews in Food Science and Nutrition, 58 (1), 126-145.
Fallon, V., Komninou, S., Bennett, K. M., Halford, J. C., & Harrold, J. A. (2017). The emotional and practical experiences of formula‐feeding mothers. Maternal & Child Nutrition, 13 (4), 1-14.
Horta, B. L., & Victoria, C. G. (2013). Long-term effects of breastfeeding: A systematic review . Geneva, Switzerland: WHO Press.
- Breastfeeding and Bottle Feeding: Pros and Cons
- Breastfeeding Health Teaching Project
- Transportation and Public Health Issues
- Breastfeeding and Children Immunity
- Angelman Syndrome, Communication and Behavior
- At-Risk Children's Healthcare Programs
- Premature Infants and Their Challenges
- Pediatric Health Care and Insurance in the USA
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, October 23). Benefits of Breastfeeding Versus Formula-Feeding. https://ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/
"Benefits of Breastfeeding Versus Formula-Feeding." IvyPanda , 23 Oct. 2020, ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/.
IvyPanda . (2020) 'Benefits of Breastfeeding Versus Formula-Feeding'. 23 October.
IvyPanda . 2020. "Benefits of Breastfeeding Versus Formula-Feeding." October 23, 2020. https://ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/.
1. IvyPanda . "Benefits of Breastfeeding Versus Formula-Feeding." October 23, 2020. https://ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/.
Bibliography
IvyPanda . "Benefits of Breastfeeding Versus Formula-Feeding." October 23, 2020. https://ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/.
- Open access
- Published: 20 February 2018
Breastfeeding knowledge and attitudes of health professional students: a systematic review
- Shu-Fei Yang ORCID: orcid.org/0000-0001-7056-2613 1 , 3 ,
- Yenna Salamonson 1 , 2 ,
- Elaine Burns 1 &
- Virginia Schmied 1
International Breastfeeding Journal volume 13 , Article number: 8 ( 2018 ) Cite this article
31k Accesses
59 Citations
55 Altmetric
Metrics details
Breastfeeding support from health professionals can be effective in influencing a mother’s decision to initiate and maintain breastfeeding. However, health professionals, including nursing students, do not always receive adequate breastfeeding education during their foundational education programme to effectively help mothers. In this paper, we report on a systematic review of the literature that aimed to describe nursing and other health professional students’ knowledge and attitudes towards breastfeeding, and examine educational interventions designed to increase breastfeeding knowledge and attitudes amongst health professional students.
A systematic review of peer reviewed literature was performed. The search for literature was conducted utilising six electronic databases, CINAHL, MEDLINE, ProQuest, PubMed, Scopus, and Cochrane, for studies published in English from January 2000 to March 2017. Studies focused on nursing students’ or other health professional students’ knowledge, attitudes or experiences related to breastfeeding. Intervention studies to improve knowledge and attitudes, were also included. All papers were reviewed using the relevant Critical Appraisal Skills Programme (CASP) checklist.
Fourteen studies were included in the review. This review indicates that in some settings, health professional students demonstrated mid-range scores on breastfeeding attitudes, and their knowledge of breastfeeding was limited, particularly in relation to breastfeeding assessment and management. All of the studies that tested a specialised breastfeeding education programme, appeared to increase nursing students’ knowledge overall or aspects of their knowledge related to breastfeeding. Several factors were found to influence breastfeeding knowledge and attitudes, including timing of maternal and child health curriculum component, previous personal breastfeeding experience, gender, cultural practices and government legislation.
Conclusions
Based on this review, it appears that nursing curriculum, or specialised programmes that emphasise the importance of breastfeeding initiation, can improve breastfeeding knowledge and attitudes and students’ confidence in helping and guiding breastfeeding mothers.
To achieve the health and optimal growth of infants, the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) recommends that all infants should be exclusively breastfed for the first 6 months and continue to receive breast milk until 2 years of age to supplement other foods [ 1 ]. In addition, the policy statement of American Academy of Paediatrics cites breastfeeding as the ideal form of infant nutrition, providing health benefits for both mothers and infants [ 2 ].
There are a range of factors known to influence a mother’s decision to initiate and maintain breastfeeding including the practical, emotional support, and encouragement from health professionals [ 3 ]. A Cochrane Review reported that breastfeeding support from health professionals can be effective in extending the duration of breastfeeding [ 4 ]. It is therefore important that nursing students and other students in other health professions, acquire knowledge about breastfeeding, and develop skills to support and provide appropriate care to pregnant women, and to mothers with infants, in order to support mothers to breastfeed [ 5 ]. However, health professionals, including nursing students, do not always receive adequate breastfeeding education during their foundational education programme to effectively help mothers [ 6 , 7 ]. There have been two reviews of breastfeeding educational interventions to build capacity in health professionals [ 8 , 9 ]. Spiby et al. [ 8 ] identified a range of educational interventions for healthcare professionals aiming to increase knowledge and support breastfeeding, however due to methodological limitations, they were not able to support any specific approach. Watkins and Dodgson [ 9 ] found that educational interventions that mostly focused on increasing women’s knowledge about breastfeeding, and how to best support breastfeeding, may be effective in modifying maternal behaviour and healthcare providers’ understanding. To date there have been no reviews of interventions to increase the capacity of nursing or other health professional students to support breastfeeding mothers.
In this paper, we report on a systematic review of the literature that aimed to: 1. describe nursing and other health professional students’ knowledge and attitudes towards breastfeeding, and report their confidence in supporting women to breastfeed and 2. examine educational interventions designed to increase breastfeeding knowledge and attitudes amongst health professional students. The review addressed two questions: 1. What is the knowledge, attitudes and confidence of nursing students and other health professional students related to breastfeeding? and 2. Do educational interventions in addition to the standard curriculum, better prepare nursing students and other health professional students to support breastfeeding?
Search strategies
The search for literature was conducted utilising six electronic databases, CINAHL, MEDLINE, ProQuest, PubMed, Scopus, and Cochrane, for studies published in English from January 2000 to March 2017. As nursing curricula change over time, and to select recent publications, the year 2000 was chosen as the start date for the search. The following Medical Subject Headings (MESH) were used in combination: breastfeeding, nursing students, student nurses, medical students and health professional students. Only papers that had examined nursing students’ or other health professional students’ knowledge, attitudes or experiences related to breastfeeding were included. Intervention studies to improve knowledge and attitudes were also included.
Two frameworks were used in determining the inclusion criteria for this review. For non-intervention studies, the PEO (Person; Exposure; Outcome) framework was used: the person was defined as nursing and health professional students; the exposure was the current undergraduate educational programmes related to breastfeeding; the outcomes were defined as knowledge, attitudes or confidence towards breastfeeding. The PICO (Person; Intervention; Control; Outcome) framework was used for intervention studies [ 10 ]. Here the nursing and health professional students were the person, the intervention was the ‘add-on’ or specialised breastfeeding educational programme, the control sought to include other nursing and health professional students, and the outcome was breastfeeding knowledge, attitudes or confidence.
Selection process
A total of 297 papers were exported to the EndNote database, of these 109 were duplicates leaving 188 papers. The titles and abstracts were screened for relevance and a further 64 were removed. 45 papers were read in full and 31 were excluded because: the population was not health professional students; the intervention assessed in the study focused on outcomes for mothers and was not related to health professional student education; or breastfeeding attitudes or knowledge were not reported. One quasi-experimental study reported the findings for nursing students, but the results for the nursing students could not be distinguished from other participants and this paper was therefore excluded. One of the studies focused on midwifery students, it was determined that midwifery students spend extensive periods of time in clinical placement where they can learn about breastfeeding in contrast to nursing, and other health professional students, therefore this study was ultimately excluded. The selection process of the included papers is displayed in Fig. 1 .
PRISMA flow diagram of study selection
Quality appraisal of studies
Fourteen papers met the inclusion criteria and were critiqued using the Critical Appraisal Skills Programme (CASP) tools to evaluate the quality of each study. Two CASP checklists were used, the qualitative research checklist consisted of 10 questions and the cohort study checklist consisted of 12 questions. Qualitative papers may achieve a total score of 10 points [ 11 ]. There were 12 questions in the cohort study checklist, with two questions scoring up to 2 points for a total of 14 points when all criteria were met [ 12 ]. Two authors read each paper and all authors discussed the scores assigned to each paper. We noted a number of study limitations including sample size and methodological issues and these are discussed in the limitations section. No studies were excluded on quality appraisal. The results of CASP scores can be found in Table 1 .
Characteristics of the included studies
Studies included in this review were conducted in seven countries: United States of America (USA), Australia, Hong Kong, Sweden, India, Egypt and Saudi Arabia. The studies included nursing students, medical students and general practice registrars. See Table 1 for summary of the characteristics of the included studies.
Study designs varied: seven were cross-sectional surveys and one was a mixed-methods study that assessed nursing students’ knowledge and or attitudes towards breastfeeding [ 13 ]. Two were qualitative studies that explored nursing students’ attitudes and beliefs about breastfeeding [ 14 , 15 ] and their perspectives on promoting successful breastfeeding [ 15 ]. Three studies reported the validity and reliability of the instruments used [ 16 , 17 , 18 ]. Some of these studies collected data before and/or after standard theory and laboratory based learning in maternal and child health curriculum and or clinical placement [ 6 , 13 , 16 , 17 , 19 , 20 ]. However these studies were not designed to evaluate the standard curriculum.
In addition, four papers reported quasi-experimental studies that tested a specific breastfeeding educational intervention designed to improve knowledge and attitudes, three were in the USA [ 21 , 22 , 23 ] and one in Hong Kong [ 24 ]. Two used a simple pretest and post-test method to measure nursing students’ knowledge related to breastfeeding [ 21 , 22 ], and two had recruited comparison groups to compare the breastfeeding knowledge and attitudes of nursing students in both the intervention and comparison groups [ 23 , 24 ]. The study by Dodgson and Tarrant [ 24 ] assessed nursing students’ breastfeeding knowledge and attitudes after they received the educational intervention, but without a baseline or pretest situation.

Measuring breastfeeding knowledge and attitudes
Several measures including subscales of larger tools were used to measure the breastfeeding knowledge and attitudes of health professional students or other participants. These were the Australian Breastfeeding Knowledge and Attitude Questionnaire [ 6 , 13 , 16 , 18 , 23 ] and the Iowa Infant Feeding Attitude Scale [ 6 , 13 , 17 , 25 ].
Several studies assessed nursing students’ knowledge related to breastfeeding by using modified survey tools with true/false, or don’t know, or multiple-choice questions [ 17 , 19 , 20 , 21 , 22 , 24 ]. Two studies measured the participants’ beliefs about the outcomes of, and attitudes towards, breastfeeding and formula-feeding using a modified version of the Minnesota Infant Feeding Questionnaires [ 26 ] using a 12-item scales with a 7-point response format [ 24 , 27 ].
Breastfeeding education received by students
Standard curriculum.
Some studies described the current undergraduate curriculum indicating that breastfeeding was addressed during the maternal and child health subject. If described, these standard curriculum primarily consisted of classroom and clinical components, discussing topics such as the properties of breast milk, benefits of breastfeeding for both mother and infant, assessment parameters for effective breastfeeding, maternal support, and achievement of proper latch in a didactic instructional manner [ 6 , 16 , 19 , 20 ]. In addition, practical experience was offered through clinical placement at a hospital based maternity unit where nursing students had opportunities to observe and interact with lactation consultants and nurses as they provided breastfeeding support for new mothers [ 6 , 13 , 16 , 19 ].
Specific breastfeeding education interventions
The format and length of the specialised breastfeeding education programmes in the four studies included in this review varied. Two of the education programmes were based on the Baby Friendly Hospital Initiative (BFHI) 20-h breastfeeding curriculum [ 22 , 24 ], one adapted this content in five online modules requiring 16 h to complete [ 22 ], and the other provided the theoretical content in 10 h of face-to-face instruction, and 8 weeks of clinical placement [ 24 ]. Learning content in the four studies consisted of evidence based breastfeeding information [ 21 , 22 , 23 , 24 ].
Health professional students’ knowledge about breastfeeding
Overall, the cross-sectional, descriptive studies found that nursing students, medical students and general practice registrars lacked knowledge about breastfeeding even after completing their maternal and child health unit of study, particularly in relation to how best to support mothers and infants and to intervene if necessary [ 6 , 16 , 17 , 18 , 19 , 20 ]. Two studies, one in Egypt [ 16 ] and one in the USA [ 6 ] reported that nursing students had higher knowledge about the benefits of breastfeeding for the baby and the cost benefits for families and society of breastfeeding but their knowledge of breastfeeding physiology and management was low, even following theoretical and laboratory based clinical education in their course in maternal and child nursing. Amin et al. found the breastfeeding knowledge scores were low irrespective of the educational disciplines of the students [ 17 ]. The responses of medical students and students from College of Education reflected the prevalence of many misconceptions regarding the timely initiation, duration and exclusivity of breastfeeding [ 17 ]. The study by Kakrani et al. explored the knowledge of senior medical and nursing students about the 10 steps of the BFHI in India, and found there was an average level of awareness among nursing and medical students about the ten steps [ 20 ]. They also found that female students were more aware of these BFHI steps than males after the breastfeeding education [ 20 ].
Three studies compared junior and senior nursing students on their knowledge of breastfeeding [ 13 , 19 , 24 ] including benefits, physiology and management. In one study both the junior and senior nursing students were aware of the benefits and physiology of breastfeeding at the two points in time, but knowledge of the management of breastfeeding was significantly higher in the group of graduating students [ 13 ]. In one qualitative study, the researcher assessed nursing students’ knowledge of breastfeeding with their written responses to one question: “What do you consider success factors that promote breastfeeding in Sweden?” [ 15 ]. Most nursing students reported that promoting breastfeeding was important for infant health, and most students demonstrated knowledge about the advantages of breastfeeding, such as “breast milk provides stronger immune protection for the child than formula milk” [ 15 ].
Of the four studies that examined a breastfeeding education programme, each reported a significant positive difference between pre and post-test breastfeeding knowledge scores [ 21 , 22 , 23 , 24 ]. In one study the breastfeeding educational programme was effective in increasing nursing students’ knowledge of the benefits and nutritional value of breastfeeding and management of lactation problems [ 21 ]. Moreover, the 16-h online breastfeeding training increased nursing students’ level of knowledge related to breastfeeding and the majority believed that they were fully able to perform skills to support breastfeeding [ 22 ].
Health professional students’ attitudes towards breastfeeding
Cricco-Lizza used a qualitative approach to investigate the breastfeeding attitudes, beliefs, and personal experiences of nursing students ( n = 12) at the beginning of their formal course work in maternal and child nursing, and the researcher suggested that nursing students’ positive attitudes towards breastfeeding were crucial for promoting breastfeeding initiation [ 14 ]. In Egypt, Ahmed and El Guindy [ 16 ] reported midrange scores on breastfeeding attitudes amongst nursing students and Vandewark [ 13 ] found similar mid-range scores for nursing students in the USA with no differences between the mean breastfeeding attitudes scores of junior and senior nursing students.
One study in the USA found that over one third of nursing students believed that women should not breastfeed in public [ 19 ] and another reported that all students held this belief [ 14 ]. Two intervention studies compared the breastfeeding attitudes of nursing students in both the intervention and comparison groups [ 23 , 24 ] and found the educational intervention did not change students’ attitudes towards breastfeeding but it did alter attitudes towards formula feeding, with students being less favourable toward this practice [ 24 ]. Studies also reported a positive correlation between attitudes towards breastfeeding and breastfeeding knowledge [ 13 , 14 , 16 , 19 ]. Ahmed and El Guindy found that despite Egyptian nursing students having low knowledge scores and not holding strongly positive attitudes towards breastfeeding, more than 70% of the students indicated they were confident or very confident about their ability to support breastfeeding [ 16 ].
Factors influencing breastfeeding knowledge and attitudes
In these studies, several factors were found to influence the level of breastfeeding knowledge and attitudes towards breastfeeding, including stage of student enrolment (for example first year versus final year students), previous personal breastfeeding experience, gender, cultural practices and government legislation.
In the Australian study of GP registrars, Brodribb et al. found that more than 52 weeks personal breastfeeding experience was associated with higher mean breastfeeding knowledge scores, and GP registrars who had personal experience of breastfeeding were more confident in supporting women [ 18 ]. For nursing students, important factors for a positive attitude to breastfeeding included: coming from a predominantly breastfeeding family [ 14 ], or being married, or originating from a rural area [ 17 ]. The study by Pajalic showed that nursing students’ beliefs about the benefits of breastfeeding were influenced by traditions and cultural acceptance of the practice, and government restrictions on infant formula [ 15 ].
This review has synthesised the findings of 14 studies that assessed nursing and other health professional students’ knowledge and attitudes towards breastfeeding and included four studies that specifically tested an educational intervention to improve breastfeeding knowledge.
The findings indicate that in some settings health professional students’ knowledge of breastfeeding was limited, particularly in relation to breastfeeding assessment and management, and did not necessarily improve following the completion of a standard curriculum. Exposure to breastfeeding, either through the course, or personally, was associated with more positive attitudes towards breastfeeding amongst health professional students. Only two studies assessed health professional students’ confidence to support breastfeeding women and Egyptian nursing students appeared highly confident despite low levels of breastfeeding knowledge [ 16 ].
The four studies that examined a specialised breastfeeding educational program appeared to increase nursing students’ knowledge overall or aspects of their knowledge related to breastfeeding, as did the standard curriculum in some of the studies [ 13 , 19 , 23 , 24 ]. In contrast, attitude towards breastfeeding did not appear to be altered by the educational interventions however one study reported that nursing students held less positive attitudes about infant formula after the intervention [ 24 ].
The second step of the Ten Steps to Successful Breastfeeding states that all healthcare staff should be trained in skills necessary to implement this policy [ 28 , 29 ]. The included studies emphasised the importance of health professional students receiving education on breastfeeding and the skills to support new mothers to breastfeed. Despite this, there is variability in the quality of breastfeeding support provided by health professionals, particularly in-hospital postpartum care, and many women are dissatisfied with breastfeeding support and information they receive [ 3 , 30 ]. This implies a gap, both in current undergraduate education, or ongoing education post registration, and in practice. Both nursing and medical students are educated about a wide variety of health concerns and conditions and breastfeeding education may not be prioritised [ 31 ]. If students receive no, or limited, education before their clinical placement, this may compromise the information and support women are offered. Furthermore, nursing students in the USA, Egypt, China, Taiwan, and elsewhere, provide care to women in postpartum units, under supervision [ 6 , 16 , 32 ] and if the supervising health professionals have not had adequate ongoing education they may not appropriately support and mentor the students.
This review highlights the need to determine how breastfeeding knowledge and skills are best facilitated in undergraduate curricula to help students relate theoretical breastfeeding knowledge to practice. Commentators emphasise the need for standardised breastfeeding education curricula to ensure that all undergraduate nursing students are taught similar core breastfeeding concepts regardless of the nursing programme attended [ 33 ].
Implementation guidelines for the Ten Steps to Successful Breastfeeding state that all healthcare staff should receive breastfeeding education including both the knowledge and skills to support women to breastfeed [ 28 , 29 ]. For facility personnel whose role may involve educating, advising or assisting women in relation to breastfeeding, they must have a minimum of 20 h of breastfeeding education, consisting of at least 8 hours theoretical education and at least 3 hours relevant supervised clinical experience on breastfeeding [ 28 , 29 ]. The education program may include various delivery options such as workshops, face-to-face or online education [ 29 ]. Two intervention studies were based on the BFHI 20 h module but both adapted this by either reducing the content to 16 h online [ 22 ] or reducing to 10 h with a significant clinical component of 8 weeks [ 24 ]. Both had positive effects on nursing students’ breastfeeding knowledge.
However, given the constraints of generalist nursing curricula and other courses, time does not necessarily permit a 20 h module on breastfeeding. As a consequence, curricula across the globe vary in the time devoted, and content provided. For example, in the review of educational support for health professionals, Watkins and Dodgson [ 9 ] comment that the length of breastfeeding education varied considerably from 1.5 h to 24 h of face-to-face content ranging from one to eight sessions. In this present review the specialised breastfeeding programmes for nursing students varied from as little as 2 h to 16 h of didactic lecture style as well as simulation role-play or online computer based learning modules with varying impact on nursing students’ breastfeeding knowledge and attitudes.
A range of formats and educational strategies were used in the intervention. These included didactic lecture style as well as simulation and clinical placement. Strategies such as evidence based seminar updates [ 33 ] with case studies [ 34 ] have been identified as useful approaches, in conjunction with, or perhaps replacing, didactic classroom lectures. Providing students with opportunities to practise breastfeeding management skills before actually caring for clients in a clinical setting may increase confidence [ 16 ]. Increasingly online education is used in undergraduate curriculum. Recently, researchers found that the additional online module improved undergraduate nursing students’ learning as well as their confidence in the clinical setting [ 35 ]. Researchers suggest a variety of forms of educational programmes, including workshops, seminars and more traditional teaching programmes are required [ 20 , 33 , 34 ].
Healthcare professionals who are experienced with breastfeeding management play a crucial role in helping nursing students practise basic breastfeeding assessment skills learnt in the classroom and laboratory [ 6 , 32 ]. However, this may be problematic if the healthcare professionals lack knowledge and skill or are inappropriate in the approach they take to providing breastfeeding support. The review by Watkins and Dodgson [ 9 ] and Spiby et al. [ 8 ] indicate that not all health professionals are adequately prepared, and found that many do not feel confident and knowledgeable in managing breastfeeding problems.
Influence of socio-cultural context on breastfeeding attitudes
It was evident in the study by Pajalic from Sweden that the nursing students overall held a positive attitude towards breastfeeding [ 15 ]. Scandinavian countries are well-known for their strong public health policies supporting breastfeeding, and their experience of high levels of breastfeeding initiation and maintenance for the first 6 months after birth [ 36 , 37 ]. In contrast in the USA, breastfeeding rates and the mean breastfeeding attitude scores are lower than those of many other countries [ 13 , 38 ]. Participants in one study were hesitant to continue breastfeeding because feeding the baby themselves challenged their independence, and they had concerns about intimacy with breastfeeding [ 14 ].
In the Middle Eastern countries and countries like Egypt where Islam is the dominant religion, the community and women are guided by the Qur’an which supports breastfeeding [ 39 ]. It was therefore surprising that the nursing students’ attitudes towards breastfeeding, in Egypt, were neutral with low breastfeeding knowledge scores [ 16 ]. It may be that when these Middle Eastern students were surveyed they had not completed their education and lacked the clinical experience that would potentially enhance their breastfeeding knowledge and skills [ 16 ].
Limitations
This review may be limited by the commencement date of year 2000. Other relevant papers published before this date e.g. Freed and colleagues [ 40 ] have informed our discussion. The review is also limited by the quality of some of the included studies. Most included studies had a small response rate [ 13 , 18 , 20 , 27 ], small sample sizes [ 13 , 16 , 19 , 21 , 22 ] and participants were not randomised in the intervention studies [ 21 , 22 , 24 ]. Reliability or validity of the measures used to assess nursing students’ breastfeeding knowledge and attitudes were not presented in all studies. In a number of the included papers we could not determine whether the study sample was representative of the population. Some participants completed the maternal and child health course 1 year prior to the survey and therefore capacity for recall may have affected their ability to answer the questions accurately [ 13 , 19 ]. Some papers do not indicate whether or not the participants had received any breastfeeding content prior to the survey [ 15 , 27 ].
Implications for education of health professionals
These studies emphasise that healthcare professionals, including nurses and doctors should participate in ongoing breastfeeding education [ 6 , 40 ]. Particularly important is the need to challenge nurses’ attitudes and cultural norms related to breastfeeding, in addition to more traditional items such as the treatment methods for mastitis, to fully prepare nursing students to provide care for new mothers [ 19 , 41 ].
It is interesting that no recent studies of nursing students’ breastfeeding knowledge and attitudes were conducted in the United Kingdom (UK) and Australia. This may be because midwives primarily provide breastfeeding support to women. There have been recent studies of both registered midwives’ breastfeeding knowledge and attitudes in Australia [ 42 ] and student midwives in UK [ 43 ]. It is however important that nursing and other health professional students also have the basic knowledge and skills to support breastfeeding women when they are on a postpartum unit, and that they have appropriate supervision and support from qualified health professionals [ 9 ]. It is important that nursing students in countries like UK and Australia, also receive some education related to breastfeeding because they may encounter breastfeeding women in general practices [ 44 ], paediatric wards and also in emergency departments [ 45 ].
While the findings of this review highlight the need for improvements in breastfeeding education in the baccalaureate nursing curriculum, this review provides little guidance as to what content is needed, how long the theoretical and clinical experiences should be and what is the best mode of delivery to increase knowledge and skill. The question remains whether nursing and other health professional students require 20 h of education at undergraduate level including how to manage breastfeeding problems, in order to provide the best support [ 46 ].
It is essential that health professional students have a positive attitude towards breastfeeding, and are able to provide breastfeeding women with the basic information they require. From the studies reviewed, baccalaureate students are considered novices who lack basic breastfeeding knowledge. Not all health professionals are adequately prepared and feel confident and knowledgeable in managing breastfeeding problems. In conclusion, it appears that nursing students can benefit from targeted programes to increase breastfeeding knowledge and attitudes, and their confidence in helping and guiding breastfeeding mothers. To ensure that future health professionals are well prepared to support breastfeeding. It is important that the curriculum is evidence based and culturally appropriate.
Abbreviations
Critical Appraisal Skills Programme
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
United Nations Children’s Fund
World Health Organization
World Health Organization, UNICEF. Global strategy for infant and young child feeding. Geneva: World Health Organization; 2003.
Google Scholar
Gartner LM, Morton J, Lawrence RA, Naylor AJ, O'Hare D, Schanler RJ, Eidelman AI. Breastfeeding and the use of human milk. Pediatrics. 2005;115(2):496–506.
Article PubMed Google Scholar
Schmied V, Beake S, Sheehan A, McCourt C, Dykes F. Women’s perceptions and experiences of breastfeeding support: a metasynthesis. Birth. 2011;38(1):49–60.
McFadden A, Gavine A, Renfrew MJ, Wade A, Buchanan P, Taylor JL, Veitch E, Rennie AM, Crowther SA, Neiman S, MacGillivray S. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev. 2017;2:CD001141.
Lewin LO, O'Connor ME. BreastfeedingBasics: web-based education that meets current knowledge competencies. J Hum Lact. 2012;28(3):407–13.
Ahmed A, Bantz D, Richardson C. Breastfeeding knowledge of university nursing students. Am J Maternal Child Nur. 2011;36(6):361–7.
Article Google Scholar
Wang SF, Chen JY, Chen CH. The current status of breastfeeding education for professionals in Taiwan: a triangulation study. Tzu Chi . Nur J. 2007;6(6):96–102.
Spiby H, McCormick F, Wallace L, Renfrew MJ, D’Souza L, Dyson LA. Systematic review of education and evidence-based practice interventions with health professionals and breast feeding counsellors on duration of breast feeding. Midwifery. 2009;25(1):50–61.
Watkins AL, Dodgson JE. Breastfeeding educational interventions for health professionals: a synthesis of intervention studies. J Spec Ped Nur. 2010;15(3):223–32.
Richardson WS, Wilson MC, Nishikawa J, Hayward RSA. The well-built clinical question: a key to evidence-based decisions. ACP J Club. 1995;123:A12–3.
CAS PubMed Google Scholar
Critical Appraisal Skills Programme International Network. CASP checklists: 10 questions to help you make sense of qualitative study . 2016. http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf . Assessed 21 June 2016.
Critical Appraisal Skills Programme International Network . CASP checklists: 12 questions to help you make sense of cohort study . 2016. http://media.wix.com/ugd/dded87_e37a4ab637fe46a0869f9f977dacf134.pdf . Assessed 21 June 2016.
Vandewark AC. Breastfeeding attitudes and knowledge in bachelor of science in nursing candidates. J Perinat Educ. 2014;23(3):135–41.
Article PubMed PubMed Central Google Scholar
Cricco-Lizza R. Student nurses' attitudes and beliefs about breast-feeding. J Prof Nurs. 2006;22(5):314–21.
Pajalic Z. Nursing students' views on promoting successful breastfeeding in Sweden. Global J Health Sci. 2014;6(5):63–9.
Ahmed A, El Guindy SR. Breastfeeding knowledge and attitudes among Egyptian baccalaureate students. Int Nurs Rev. 2011;58(3):372–8.
Article CAS PubMed Google Scholar
Amin TT, Abdulrahman AG, Al Muhaidib NS, Al OA. Breastfeeding attitudes and knowledge among future female physicians and teachers in Saudi Arabia. Health Sci J. 2014;8(1):102–15.
Brodribb W, Fallon A, Jackson C, Hegney D. Breastfeeding and Australian GP registrars - their knowledge and attitudes. J Hum Lact. 2008;24(4):422–30.
Spear HJ. Baccalaureate nursing students' breastfeeding knowledge: a descriptive survey. Nurse Educ Today. 2006;26(4):332–7.
Kakrani VA, Rathod Waghela HK, Mammulwar MS, Bhawalkar JS. Awareness about "ten steps for successful breastfeeding" among medical and nursing students. Int J Prev Med. 2015;6:40.
Bozzette M, Posner T. Increasing student nurses' knowledge of breastfeeding in baccalaureate education. Nurse Educ Pract. 2013;13(3):228–33.
Cianelli R, Villegas N, Azaiza K, Henderson S, Hooshmand M, Peragallo N. Developing and testing an online breastfeeding training among undergraduate nursing students. Clinical Nursing . Studies. 2014;3(1):82–8.
Davis A, Sherrod RA. Effects of an educational intervention on baccalaureate nursing students' knowledge and attitude in providing breastfeeding support to mothers. Int J Childbirth Educ. 2015;30(4):8–12.
Dodgson JE, Tarrant M. Outcomes of a breastfeeding educational intervention for baccalaureate nursing students. Nurse Educ Today. 2007;27(8):856–67.
Mora Adl RDW, Dungy CI, Losch M, Dusdieker L. The Iowa infant feeding attitude scale: analysis of reliability and validity. J Appl Soc Psychol. 1999;29(11):2362–80.
Duckett L, Henly S, Avery M, Potter S, Hills-Bonczyk S, Hulden R, Savik KA. Theory of planned behavior-based structural model for breast-feeding. Nurs Res. 1998;47(6):325–36.
Dodgson JE, Bloomfield M, Choi M. Are health science students' beliefs about infant nutrition evidence-based? Nurse Educ Today. 2014;34(1):92–9.
World Health Organization, UNICEF. Baby friendly hospital initiative: revised, updated and expanded for integrated care. 2009. http://www.who.int/nutrition/publications/infantfeeding/bfhi_trainingcourse/en/ . Assessed 27 June 2017.
Australian College of Midwives. BFHI handbook for maternity facilities. Canberra: ACM; 2016.
Redshaw M, Henderson J. Learning the hard way : expectations and experiences of infant feeding support. Birth. 2012;39(1):21–9.
Blackman I, Sweet L, Byrne J. Using Rasch analysis to identify midwifery students' learning about providing breastfeeding support. Women and Birth. 2015;28(3):228–35.
Chen CH, Shu HQ, Chi CS. Breastfeeding knowledge and attitudes of health professionals and students. Acta Paediatr Taiwan. 2001;42(4):207–11.
Spatz DL, Pugh LC. The American Academy of Nursing expert panel on breastfeeding. The integration of the use of human milk and breastfeeding in baccalaureate nursing curricula. Nurs Outlook. 2007;55(5):257–63.
Spatz DL. The breastfeeding case study: a model for educating nursing students. J Nurs Educ. 2005;44(9):432–4.
PubMed Google Scholar
Deloian BJ, Lewin LO, O'Connor ME. Use of a web-based education program improves nurses' knowledge of breastfeeding. J Obstet Gynecol Neonatal Nurs. 2015;44(1):77–86.
Lande B, Andersen LF, Bærug A, Trygg KU, Lund-Larsen K, Veierød MB, Aa BG-E. Infant feeding practices and associated factors in the first six months of life: the Norwegian infant nutrition survey. Acta Paediatr. 2003;92:152–61.
Sjöström K, Welander S, Haines H, Andersson E, Hildingsson I. Comparison of breastfeeding in rural areas of Sweden and Australia – a cohort study. Women and Birth. 2013;26(4):229–34.
U.S. Department of Health and Human Services. The surgeon general’s call to action to support breastfeeding. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General; 2011.
El-Zanaty F, Way A. Egypt demographic and health survey 2008. Cairo: Ministry of Health, El-Zanaty and Associates, and Macro International; 2009.
Freed GL, Clark SJ, Harris BG, Methods LDL. Outcomes of breastfeeding instruction for nursing students. J Hum Lact. 1996;12(2):105–10.
Bernaix LW, Beaman ML, Schmidt CA, Harris JK, Miller LM. Success of an educational intervention on maternal/newborn nurses' breastfeeding knowledge and attitudes. J Obstet Gynecol Neonatal Nurs. 2010;39(6):658–66.
Cantrill RM, Creedy DK, Cooke M. How midwives learn about breastfeeding. Australian Midwifery. 2003;16(2):11–6.
Darwent KL, Kempenaar LE. A comparison of breastfeeding women's, peer supporters' and student midwives' breastfeeding knowledge and attitudes. Nurse Educ Pract. 2014;14(3):319–25.
Jeyendra A, Rajadurai J, Chanmugam J, Trieu A, Nair S, Baskaran R, Schmied V. Australian general practitioners’ perspectives on their role in well-child health care. BMC Fam Pract. 2013;14:2.
McLaughlin M, Fraser J, Young J, Keogh S. Paediatric nurses' knowledge and attitudes related to breastfeeding and the hospitalised infant. Breastfeeding Rev. 2011;19(3):13–24.
Shealy KR, Li R, Benton-Davis S, Grummer-Strawn LM. The CDC guide to breastfeeding interventions. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2005.
Download references
Acknowledgements
We would like to acknowledge the authors who conducted and published the original studies.
No funding was sought or received for this study.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Author information
Authors and affiliations.
School of Nursing and Midwifery, Western Sydney University, Penrith, NSW, Australia
Shu-Fei Yang, Yenna Salamonson, Elaine Burns & Virginia Schmied
Centre for Applied Nursing Research (CANR), Ingham Institute for Applied Medical Research, Liverpool, NSW, Australia
Yenna Salamonson
Department of Nursing, Chung Hwa University of Medical Technology, Tainan, Taiwan
Shu-Fei Yang
You can also search for this author in PubMed Google Scholar
Contributions
SFY carried out the literature search and initial screening. SFY, VS, YS and EB then reviewed each of the identified papers and worked in pairs to undertake the quality review. SFY, VS, YS and EB were responsible for the design of the search strategy, data analysis, critical appraisal, and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Shu-Fei Yang .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Yang, SF., Salamonson, Y., Burns, E. et al. Breastfeeding knowledge and attitudes of health professional students: a systematic review. Int Breastfeed J 13 , 8 (2018). https://doi.org/10.1186/s13006-018-0153-1
Download citation
Received : 05 August 2017
Accepted : 14 February 2018
Published : 20 February 2018
DOI : https://doi.org/10.1186/s13006-018-0153-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding
- Breastfeeding knowledge
- Breastfeeding attitudes
- Nursing students
- Health professional students
- Literature review
International Breastfeeding Journal
ISSN: 1746-4358
- General enquiries: [email protected]
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Institute of Medicine (US) Committee on Nutritional Status During Pregnancy and Lactation. Nutrition During Lactation. Washington (DC): National Academies Press (US); 1991.

Nutrition During Lactation.
- Hardcopy Version at National Academies Press
1 Summary, Conclusions, and Recommendations
During the past decade, the benefits of breastfeeding have been emphasized by many authorities and organizations in the United States. Federal agencies have set specific objectives to increase the incidence and duration of breastfeeding (DHHS, 1980, 1990), and the Surgeon General has held workshops on breastfeeding and human lactation (DHHS, 1984, 1985). At the federal and state levels, the Special Supplemental Food Program for Women, Infants, and Children (WIC) has produced materials designed to promote breastfeeding (e.g., Malone, 1980; USDA, 1988). Furthermore, the Office of Maternal and Child Health has sponsored breastfeeding projects (e.g., The Steering Committee to Promote Breastfeeding in New York City, 1986), as have state health departments and others. However, less attention has been given to two general topics: (1) the effects of breastfeeding on the nutritional status and long-term health of the mother and (2) the effects of the mother's nutritional status on the volume and composition of her milk and on the potential subsequent effects of those changes on infant health. The present report was designed to address these topics.
This summary briefly describes the origin of this effort and the process; provides key definitions; reviews what was learned about who is breastfeeding in the United States and if those women are well nourished; discusses nutritional influences on milk volume or composition; and describes how breastfeeding may affect infant growth, nutrition, and health, as well as maternal health. It then presents major conclusions, clinical recommendations, and the research recommendations most directly related to the nutrition of lactating women in the United States.
- Origin Of This Study
This study was undertaken at the request of the Maternal and Child Health Program (Title V, Social Security Act) of the Health Resources and Services Administration, U.S. Department of Health and Human Services. In response to that request, the Food and Nutrition Board's Committee on Nutritional Status During Pregnancy and Lactation and its Subcommittee on Nutrition During Lactation were asked to evaluate current scientific evidence and formulate recommendations pertaining to the nutritional needs of lactating women, giving special attention to the needs of lactating adolescents; women over age 35; and women of black, Hispanic, or Southeast Asian origin. Part of this task included consideration of the effects of maternal dietary intake and nutritional status on the volume and composition of human milk, the appropriateness of various anthropometric methods for assessing nutritional status during lactation, and the effects of lactation both on maternal and infant health and on the nutritional status of both the mother and the infant.
- Approach To The Study
The study was limited to consideration of healthy U.S. women and their healthy, full-term infants. The Subcommittee on Nutrition During Lactation conducted an extensive literature review, consulted with a variety of experts, and met as a group seven times to discuss the data and draw conclusions from them. The Committee on Nutritional Status During Pregnancy and Lactation (the advisory committee) reviewed and commented on the work of the subcommittee and helped establish appropriate linkages between this report and the reports on weight gain and nutrient supplements during pregnancy contained in Nutrition During Pregnancy —a report prepared by two other subcommittees of this advisory committee (IOM, 1990). Compared with earlier reports from the National Research Council, Nutrition During Pregnancy recommended a higher range of weight gain (11.5 to 16 kg, or 25 to 35 lb, for women of normal prepregnancy weight for height). In addition, it advised routine low-dose iron supplementation during pregnancy, but supplements of other vitamins or minerals were recommended only under special circumstances.
In examining the nutritional needs of lactating women, priority was given to energy and to those nutrients believed to be consumed in amounts lower than Recommended Dietary Allowances (RDAs) by many women in the United States. These nutrients include calcium, magnesium, iron, zinc, folate, and vitamin B 6 . Careful attention was given to the effects of lactation on various indicators of nutritional status, such as measurements of levels of biochemical compounds; functions related to specific nutrients; nutrient levels in specific body compartments; and height, weight, or other indicators of body size or adiposity. The subcommittee took into consideration that weight gain recommendations for pregnant women have been raised (see Nutrition During Pregnancy [IOM, 1990]) and that average weight gains of U.S. women during pregnancy have risen over the past two decades.
When possible, a distinction was made between exclusive breastfeeding, defined as the consumption of human milk as the sole source of energy, and partial breastfeeding, defined as the consumption of human milk in combination with formula or other foods, or both.
The nutritional demands imposed by lactation were estimated from data on volume and composition of milk produced by healthy, successfully lactating women, as done in Recommended Dietary Allowances (NRC, 1989). When it was feasible, evidence relating to possible depletion of maternal stores or to a decrease in the specific nutrient content of milk resulting from low maternal intake of the nutrient was also addressed. Because of the complex relationships between the nutrition of the mother and infant, the subcommittee examined the nutrition and growth of the breastfed infant.
The terms maternal health and infant health were interpreted in a broad sense. Consideration was given to both beneficial and adverse consequences for the health of the mother and her offspring, both during lactation and long after breastfeeding has been discontinued. For the mother, there was a search for evidence of differences in outcome related to whether or not she had breastfed. For the infant, evidence was sought for differences in outcome related to the method of feeding (breast compared with bottle). The possible influences of breastfeeding on prevention or promotion of chronic disease were addressed.
To the extent possible, this report includes detailed coverage of published evidence linking maternal nutrition, breastfeeding, and maternal and infant health. Because breastfeeding is encouraged primarily as a method for promoting the health of infants, considerable attention is also directed toward infant health even when there is no established relationship to maternal nutritional status. Recognizing the serious gaps in knowledge of nutrition during lactation, the subcommittee gave much thought to establishing directions for research.
The members of the subcommittee realized that nutrition is not the sole determinant of successful breastfeeding. A network of overlapping social factors including access to maternal leave, instructions concerning breastfeeding, availability of prenatal care, the length of hospital stay following delivery, infant care in the workplace, and the public attitudes toward breastfeeding are important. Given the goals of this report, the subcommittee did not specifically address those factors, but it recognizes that they should be considered in depth by public health groups that are attempting to improve rates of breastfeeding in this and other countries.
- What Was Learned
Who Is Breastfeeding
The incidence and duration of breastfeeding changed markedly during the twentieth century—first declining, then rising, and, from the early 1980s, declining once again. Currently, women who choose to breastfeed tend to be well educated, older, and white. Data on the incidence and duration of breastfeeding in the United States are especially limited for mothers who are economically disadvantaged and for those who are members of ethnic minority groups. The best data for any minority groups are for black women. Their rates of breastfeeding are substantially lower than those for white women, but factors that distinguish breastfeeding from nonbreastfeeding women tend to be similar among black and white women. Social, cultural, economic, and psychological factors that influence infant feeding choices by adolescent mothers are not well understood. In the United States, where few employers provide paid maternity leave, return to work outside the home is associated with a shorter duration of breastfeeding, but little else is known about when mothers discontinue either exclusive or partial breastfeeding. Such data are needed to estimate the total nutrient demands of lactation.
How Can It Be Determined Whether Lactating Women Are Well Nourished
The few lactating women who have been studied in the United States have been characterized as well nourished, but this observation cannot be generalized since these subjects were principally white women with some college education. Women from less advantaged, less well studied populations may be at higher risk of nutritional problems but tend not to breastfeed.
To determine whether women are adequately nourished, investigators use biochemical or anthropometric methods, or both. For lactating women, however, there are serious gaps and limitations in the data collected with these methods. Consequently, there is no scientific basis for determining whether poor nutritional status is a problem among certain groups of these women. To identify the nutrients likely to be consumed in inadequate amounts by lactating women, the subcommittee used an approach involving nutrient densities (nutrient intakes per 1,000 kcal) calculated from typical diets of nonlactating U.S. women. That is, they made the assumption that the average nutrient densities of the diets of lactating women would be the same as those of nonlactating women but that lactating women would have higher total energy intake (and therefore higher nutrient intake). Using this approach, the nutrients most likely to be consumed in amounts lower than the RDAs for lactating women are calcium, zinc, magnesium, vitamin B 6 , and folate.
Data for U.S. women indicate that successful lactation occurs regardless of whether a woman is thin, of normal weight, or obese. Anthropometric measurements (such as weight, weight for height, and skinfold thickness) have not been useful for predicting the success of lactation among the few U.S. women who have been studied. The predictive ability is not known for anthropometric measurements that fall outside the ranges observed in these limited samples.
Lactating women eating self-selected diets typically lose weight at the rate of 0.5 to 1.0 kg (˜1 to 2 lb) per month in the first 4 to 6 months of lactation. Such weight loss is probably physiologic. During the same period, values for subscapular and suprailiac skinfold thickness also decrease; triceps skinfold thickness does not. Not all women lose weight during lactation; studies suggest that approximately 20% may maintain or gain weight.
Biochemical data for lactating women have been obtained only from small, select samples. Such data are of limited use in the clinical situation because there are no norms for lactating women, and the norms for nonpregnant, nonlactating women may not be applicable to breastfeeding women. For example, there appear to be changes in plasma volume post partum, and there are changes in blood nutrient values over the course of lactation that are unrelated to changes in plasma volume.
Does Maternal Nutritional Status or Dietary Intake Influence Milk Volume
The mean volume of milk secreted by healthy U.S. women whose infants are exclusively breastfed during the first 4 to 6 months is approximately 750 to 800 ml/day, but there is considerable variability from woman to woman and in the same woman at different times. The standard deviation of daily milk intake by infants is about 165 ml; thus, 5% of women secrete less than 550 ml or more than 1,200 ml on a given day. The major determinant of milk production is the infant's demand for milk, which in turn may be influenced by the size, age, health, and other characteristics of the infant as well as by his or her intake of supplemental foods. The potential for milk production may be considerably higher than that actually produced, as evidenced by findings that the milk volumes produced by women nursing twins or triplets are much higher than those produced by women nursing a single infant.
Studies of healthy women in industrialized countries demonstrate that milk volume is not related to maternal weight or height or indices of fatness. In developing countries, there is conflicting evidence about whether thin women produce less milk than do women with higher weight for height.
Increased maternal energy intake has not been linked with increased milk production, at least among well-nourished women in industrialized countries. Nutritional supplementation of lactating women in developing countries where undernutrition may be a problem has generally been reported to have little or no impact on milk volume, but most studies have been too small to test the hypothesis adequately and lacked the design needed for causal inference. Studies of animals indicate that there may be a threshold below which energy intake is insufficient to support normal milk production, but it is likely that most studies in humans have been conducted on women with intakes well above this postulated threshold.
The weight loss ordinarily experienced by lactating women has no apparent deleterious effects on milk production. Although lactating women typically lose 0.5 to 1 kg (˜1 to 2 lb) per month, some women lose as much as 2 kg (˜4 lb) per month and successfully maintain milk volume. Regular exercise appears to be compatible with production of an adequate volume of milk.
The influence of maternal intake of specific nutrients on milk volume has not been investigated satisfactorily. Early studies in developing countries suggest a positive association of protein intake with milk volume, but those studies remain inconclusive. Fluids consumed in excess of thirst do not increase milk volume.
Does Maternal Nutritional Status Influence Milk Composition
The composition of human milk is distinct from the milk of other mammals and from infant formulas ordinarily derived from them. Human milk is unique in its physical structure, types and concentrations of macronutrients (protein, fat, and carbohydrate), micronutrients (vitamins and minerals), enzymes, hormones, growth factors, host resistance factors, inducers/modulators of the immune system, and anti-inflammatory agents.
A number of generalizations can be made about the effects of maternal nutrition on the composition of milk (see also Table 1-1 ):
Possible Influences of Maternal Intake on the Nutrient Composition of Human Milk and Nutrients for Which Clinical Deficiency Is Recognizable in Infants.
- Even if the usual dietary intake of a macronutrient is less than that recommended in Recommended Dietary Allowances (NRC, 1989), there will be little or no effect on the total amount of that nutrient in the milk. However, the proportions of the different fatty acids in human milk vary with maternal dietary intake.
- The concentrations of major minerals (calcium, phosphorus, magnesium, sodium, and potassium) in human milk are not affected by the diet. Maternal intakes of selenium and iodine are positively related to their concentrations in human milk, but there is no convincing evidence that the concentrations of other trace elements in human milk are affected by maternal diet.
- The vitamin content of human milk is dependent upon the mother's current vitamin intake and her vitamin stores, but the strength of the relationships varies with the vitamin. Chronically low maternal intake of vitamins may result in milk that contains low amounts of these essential nutrients.
- The content of at least some nutrients in human milk may be maintained at a satisfactory level at the expense of maternal stores. This applies particularly to folate and calcium.
- Increasing the mother's intake of a nutrient to levels above the RDA ordinarily does not result in unusually high levels of the nutrient in her milk; vitamins B 6 and D, iodine, and selenium are exceptions. Studies have not been conducted to evaluate the possibility that high levels of nutrients in milk are toxic to the infant.
- Some studies suggest that poor maternal nutrition is associated with decreased concentrations of certain host resistance factors in human milk, whereas other studies do not suggest this association.
In What Ways May Breastfeeding Affect Infant Growth and Health
Infant nutrition.
Several factors influence the nutritional status of the breastfed infant: the infant's nutrient stores (which are largely determined by the length of gestation and maternal nutrition during pregnancy), the total amount of nutrients supplied by human milk (which is influenced by the extent and duration of breastfeeding), and certain genetic and environmental factors that affect the way nutrients are absorbed and used.
Human milk is ordinarily a complete source of nutrients for the exclusively breastfed infant. However, if the infant or mother is not exposed regularly to sunlight or if the mother's intake of vitamin D is low, breastfed infants may be at risk of vitamin D deficiency. Breastfed infants are susceptible to deficiency of vitamin B 12 if the mother is a complete vegetarian—even when the mother has no symptoms of that vitamin deficiency.
The risk of hemorrhagic disease of the newborn is relatively low. Nonetheless, all infants (regardless of feeding mode or of maternal nutritional status) are at some risk for this serious disease unless they are supplemented with a single dose of vitamin K at birth.
Full-term, exclusively breastfed infants ordinarily maintain a normal iron status for their first 6 months of life, regardless of maternal iron intake. Providing solid foods may reduce the percentage of iron absorbed by the partially breastfed infant, making it important in such cases to ensure that adequate iron is provided in the diet.
Growth and Development
Breastfed infants gain weight at about the same rate as formula-fed infants during the first 2 to 3 months post partum, although breastfed infants usually ingest less milk and thus have a lower energy intake. After the first few months post partum, healthy breastfed infants gain weight more slowly than those who are formula fed. In general, this pattern is not altered by the introduction of solid foods. Differences in linear growth between breastfed and formula-fed infants are small if statistical techniques are used to control differences in size at birth.
Infant Morbidity and Mortality
Several types of health problems occur less often or appear to have less serious consequences in breastfed than in formula-fed infants. These include certain infectious diseases (especially ones involving the intestinal and respiratory tracts), food allergies, and, perhaps, certain chronic diseases. There is suggestive evidence that severe maternal malnutrition might reduce the degree of immune protection afforded by human milk, but further studies will be required to address that issue.
Few infectious agents are commonly transmitted to the infant via human milk. The most prominent ones are cytomegalovirus in all populations that have been studied and human T lymphocytotropic virus type 1 (HTLV-1) in certain Asian populations. The transmission of cytomegalovirus by breastfeeding does not result in disease; the consequences of the transmission of HTLV-1 by breastfeeding are unknown. There are some case reports that indicate that human immunodeficiency virus (HIV) can be transmitted by breastfeeding as a result of the transfusion of HIV-contaminated blood during the immediate postpartum period. The likelihood of transmitting HIV via breastfeeding by women who tested seropositive for the agent during pregnancy has not been determined. Public policy on this issue has ranged from the Centers for Disease Control's recommendation not to breastfeed under these circumstances to the World Health Organization's encouragement to breastfeed, especially among women in developing countries.
In developing countries, mortality rates are lower among breastfed infants than among those who are formula fed. It is not known whether this advantage also holds in industrialized countries, in which death rates are lower in general. It is reasonable to believe that breastfeeding will lead to lower mortality among disadvantaged groups in industrialized countries if they have higher than usual infant and child mortality rates, but this issue has not been studied.
Medications, Drugs, and Environmental Contaminants
The few prescription drugs that are contraindicated during lactation because of potential harm to the infant can usually be avoided and replaced with safer acceptable ones. For example, there are a number of safe and effective substitutes for the antibiotic chloramphenicol, which is contraindicated for lactating women. If treatment with antimetabolites or radiotherapeutics is required by the mother, breastfeeding is contraindicated.
Cigarette smoking and alcohol consumption by lactating women in excess of 0.5 g/kg of maternal weight may be harmful to the infant, partly because of potential reduction in milk volume. Furthermore, a single report (Little et al., 1989) associates heavy alcohol use by the mother with retarded psychomotor development of the infant at 1 year of age. Infrequent cigarette smoking, occasional consumption of small amounts of alcohol, and moderate ingestion of caffeine-containing products are not considered to be contraindicated during breastfeeding. Use of illicit drugs is contraindicated because of the potential for drug transfer through the milk as well as hazards to the mother. Since the limited information on the impact of these habits upon the nutrition of women in the childbearing years is reviewed in Nutrition During Pregnancy (IOM, 1990), they were not considered further by this subcommittee.
In the uncommon situation of a high risk of exposure to such environmental contaminants as organochlorinated compounds (such as dichlorodiphenyl-trichloroethane [DDT] or polychlorinated biphenyls [PCBs]) or toxic metals (such as mercury), risks must be weighed against the benefits of breastfeeding for both mother and infant on a case-by-case basis. In areas of unusually high exposure, levels of the contaminant should be measured in the mother's blood and milk.
How Does Breastfeeding Affect Maternal Nutrition and Health
Breastfeeding substantially increases the mother's requirements for most nutrients. The magnitude of the total increase is most strongly affected by the extent and duration of lactation. Adequacy of intakes of calcium, magnesium, zinc, folate, and vitamin B 6 merits special attention since average intakes may be below those recommended. The net long-term effect of lactation on bone mass is uncertain. Some data associate lactation with short-term bone loss, whereas most recent studies suggest a protective long-term effect. Those data are provocative but of such preliminary nature that no definitive conclusions may be drawn from them.
Although most lactating women lose weight gradually during lactation, some do not. The influence of lactation on long-term postpartum weight retention and maternal risk of adult-onset obesity has not been determined.
A well-documented effect of lactation is delayed return to ovulation. In addition, some recent epidemiologic evidence indicates that breastfeeding may lessen the risk that the mother will develop breast cancer, but the data are not consistent across all studies.
- Conclusions And Recommendations
The major conclusions of the report are as follows.
Women living under a wide variety of circumstances in the United States and elsewhere are capable of fully nourishing their infants by breastfeeding them. Throughout its deliberations, the subcommittee was impressed by evidence that mothers are able to produce milk of sufficient quantity and quality to support growth and promote the health of infants—even when the mother's supply of nutrients and energy is limited. With few exceptions (identified later in the summary under "Infant Growth and Nutrition"), the full-term exclusively breastfed infant will be well nourished during the first 4 to 6 months after birth.
In contrast, the lactating woman is vulnerable to depletion of nutrient stores through her milk. Measures should be taken to promote food intake during lactation that will prevent net maternal losses of nutrients, especially of calcium, magnesium, zinc, folate, and vitamin B 6 .
Breastfeeding is recommended for all infants in the United States under ordinary circumstances. Exclusive breastfeeding is the preferred method of feeding for normal full-term infants from birth to age 4 to 6 months. Breastfeeding complemented by the appropriate introduction of other foods is recommended for the remainder of the first year, or longer if desired. The subcommittee and advisory committee recognize that it is difficult for some women to follow these recommendations for social or occupational reasons. In these situations, appropriate formula feeding is an acceptable alternative.
Data are lacking for use in developing strategies to identify lactating women who are at risk of depleting their own nutrient stores. Although nutrient intake appears adequate for the small number of lactating women who have been studied in the United States, evidence from U.S. surveys of nonpregnant, nonlactating women suggests that usual dietary intake of certain nutrients by disadvantaged women is likely to be somewhat lower than that by women of higher socioeconomic status. Thus, if breastfeeding rates increase among less advantaged women as a result of efforts to promote breastfeeding, it will be important to examine more completely the nutrient intake of these women during lactation.
If lactating women follow eating patterns similar to those of the average U.S. woman in sufficient quantity to meet their energy requirements, they are likely to meet the recommended intakes of all nutrients except perhaps calcium and zinc. However, if they curb their energy intakes, their intakes of several nutrients are likely to be less than the RDA.
Recommendations for Women Who Wish To Breastfeed and for Their Care Providers
Because of serious gaps in information about nutrition assessment and nutrient requirements during lactation and about effects of maternal nutrition on the wide array of components in the milk, the following recommendations should be considered preliminary. Although they reflect the best judgment of the subcommittee and advisory committee, these recommendations are open to reconsideration as the knowledge base grows.
Diet and Vitamin-Mineral Supplementation
Lactating women should be encouraged to obtain their nutrients from a well-balanced, varied diet rather than from vitamin-mineral supplements.
- Provide women who plan to breastfeed or who are already doing so with nutrition information that is culturally appropriate (that is, information that is sensitive to the foodways, eating practices, and health beliefs and attitudes of the cultural group). To facilitate the acquisition of this information, health care providers are encouraged to make effective use of teaching opportunities during prenatal visits, hospitalization following delivery, and routine postpartum visits for maternal or pediatric care.
- Encourage lactating women to follow dietary guidelines that promote a generous intake of nutrients from fruits and vegetables, whole-grain breads and cereals, calcium-rich dairy products, and protein-rich foods such as meats, fish, and legumes. Such a diet would ordinarily supply a sufficient quantity of essential nutrients. The individual recommendations should be compatible with the woman's economic situation and food preferences. The evidence does not warrant routine vitamin-mineral supplementation of lactating women.
- If dietary evaluation suggests that the diet does not provide the recommended amounts of one or more nutrients, encourage the woman to select and consume foods that are rich in those nutrients.
- For women whose eating patterns lead to a very low intake of one or more nutrients, provide individualized diet counseling (preferred) or recommend nutrient supplementation (as described in Table 1-2 ).
- Encourage sufficient intake of fluids—especially water, juice, and milk—to alleviate natural thirst. It is not necessary to encourage fluid intakes above this level.
- The elimination of major nutrient sources (e.g., all dairy products) from the maternal diet to treat allergy or colic in the breastfed infant is not recommended unless there is evidence from oral elimination-challenge studies to determine whether the mother is sensitive or intolerant to the food or that the breastfed infant reacts to the foods ingested by the mother. If a key nutrient source is eliminated from the maternal diet, the mother should be counseled on how to achieve adequate nutrient intake by substituting other foods.
Suggested Measures for Improving Nutrient Intake of Women with Restrictive Eating Patterns.
A Defined Health Care Plan for Lactating Women
There should be a well-defined plan for the health care of the lactating woman that includes screening for nutritional problems and providing dietary guidance. Since preparation for lactation should begin during the prenatal period, the physician, midwife, nutritionist, or other member of the obstetric team should introduce general information about nutrition during lactation and should screen for possible problems related to nutrition. Ideally, more extensive evaluation and counseling should take place during hospitalization for childbirth. If that is precluded by the brevity of the hospital stay, an early visit to an appropriate health care professional by the mother or a visit to the mother's home is advisable.
To implement routine screening economically and practically, the subcommittee considers it sufficient to continue the practice of weighing women (using standard procedures as described in Nutrition During Pregnancy [IOM, 1990]) at scheduled visits and to ask a few simple questions to determine the following:
- Are calcium-rich foods eaten regularly?
- Does the diet include vitamin D-fortified milk or cereal or is there adequate exposure to ultraviolet light?
- Are fruits and vegetables eaten regularly?
- Is the mother a complete vegetarian?
- Is the mother restricting her food intake severely in an attempt to lose weight or to treat certain medical conditions?
- Are there life circumstances (e.g., poverty, or abuse of drugs or alcohol) that might interfere with an adequate diet?
It is not necessary to obtain measurements of skinfold thickness or to conduct laboratory tests as a part of the routine assessment of the nutritional status of lactating women.
The subcommittee recognizes that establishing standard health care procedures for lactating women requires expanded training of health care providers. Activities to achieve this expanded training are being initiated by the Surgeon General's workshop committee comprising representatives from the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Academy of Family Physicians, and other professional organizations.
Breastfeeding Practices
Efforts to support lactation must consider breastfeeding practices.
- Because the early management of lactation has a strong influence on the establishment of an adequate milk supply, breastfeeding guidance should be provided prenatally and continued in the hospital after delivery and during the early postpartum period.
- All hospitals providing obstetric care should provide knowledgeable staff in the immediate postpartum period who have responsibility for providing support and guidance in initiating breastfeeding and measures to promote establishment of an ample supply of milk.
- Breastfeeding practices that are responsive to the infant's natural appetite should be promoted. In the first few weeks, infants should nurse at least 8 times per day, and some may nurse as often as 15 or more times per day. After the first month, infants fed on demand usually nurse 5 to 12 times per day.
Maternal Weight
Women who plan to breastfeed or who are breastfeeding should be given realistic, health-promoting advice about weight change during lactation.
- Advise women that it is normal to lose weight during the first 6 months of lactation. The average rate of weight loss is 0.5 to 1.0 kg (˜ 1 to 2 lb)/month after the first month post partum. However, not all women who breastfeed lose weight; some women gain weight post partum, whether or not they breastfeed. If a lactating woman is overweight, a weight loss of up to 2 kg (˜4.5 lb) per month is unlikely to adversely affect milk volume, but such women should be alert for any indications that the infant's appetite is not being satisfied. Rapid weight loss (>2 kg/month after the first month post partum) is not advisable for breastfeeding women.
- Advise women who choose to curb their energy intake to pay special attention to eating a balanced, varied diet and to including foods rich in calcium, zinc, magnesium, vitamin B 6 , and folate. Encourage energy intake of at least 1,800 kcal/day. Calcium, multivitamin-mineral supplements, or both may be advised when dietary sources are marginal and it is unlikely that appropriate dietary practices will or can be followed. Intakes below 1,500 kcal/day are not recommended at any time during lactation, although fasts lasting less than 1 day have not been shown to decrease milk volume. Liquid diets and weight loss medications are not recommended. Since the impact of curtailing maternal energy intake during the first 2 to 3 weeks post partum is unknown, dieting during this period is not recommended.
Maternal Substance Use and Abuse
The use of illicit drugs should be actively discouraged, and affected women (regardless of their mode of feeding) should be assisted to enter a rehabilitative program that makes provision for the infant. The use of certain legal substances by lactating women is also of concern, including the potential for alcohol abuse.
- There is no scientific evidence that consumption of alcoholic beverages has a beneficial impact on any aspect of lactation performance. If alcohol is used, advise the lactating woman to limit her intake to no more than 0.5 g of alcohol per kg of maternal body weight per day. Intake over this level may impair the milk ejection reflex. For a 60-kg (132-lb) woman, 0.5 g of alcohol per kg of body weight corresponds to approximately 2 to 2.5 oz of liquor, 8 oz of table wine, or 2 cans of beer.
- Actively discourage smoking among lactating women, not only because it may reduce milk volume but because of its other harmful effects on the mother and her infant.
- Discourage intake of large quantities of coffee, other caffeine-containing beverages and medications, and decaffeinated coffee. The equivalent of 1 to 2 cups of regular coffee daily is unlikely to have a deleterious effect on the nursling, although preliminary evidence suggests that maternal coffee intake may adversely influence the iron content of milk and the iron status of the infant.
Infant Growth and Nutrition
The subcommittee recommends that health care providers be informed about the differences in growth between healthy breastfed and formula-fed infants. On average, breastfed infants gain weight more slowly than those fed formula after the first 2 to 3 months. Slower weight gain, by itself, does not justify the use of supplemental formula. When in doubt, clinicians should evaluate adequacy of growth according to the guidelines described by Lawrence (1989).
Regardless of what the mother eats, the following steps should be taken to ensure adequate nutrition of breastfed infants.
- All newborns should receive a 0.5- to 1.0-mg injection or a 1.0-to 2.0-mg oral dose of vitamin K immediately after birth regardless of the type of feeding that will be offered the infant.
- If the infant's exposure to sunlight appears to be inadequate, the infant should be given a 5- to 7.5-µg supplement of vitamin D per day.
- Fluoride supplements should be provided to breastfed infants if the fluoride content of the household drinking-water supply is low (<0.3 ppm)
- When breastfeeding is complemented by other foods, and by 6 months of age in any case, the infant should be given food rich in bioavailable iron or a daily low-dose oral iron supplement.
Infant Health
Health care providers should recognize that breastfeeding is recommended to reduce the incidence and severity of certain infectious gastrointestinal and respiratory diseases and other disorders in infancy. Breastfeeding ordinarily confers health benefits to the infant, but in certain rare cases it may pose some health risks, as indicated below.
- For mothers requiring medication and desiring to breastfeed, the clinician should select the medication least likely to pass into the milk and to the infant.
- Although medications rarely pose a problem during lactation, breastfeeding is contraindicated in the case of a few. Such drugs include antineoplastic agents, therapeutic radiopharmaceuticals, some but not all antithyroid agents, and antiprotozoan agents.
- In those rare cases when there is heavy exposure to pesticides, heavy metals, or other contaminants that may pass into the milk, breastfeeding is not recommended if maternal levels are high.
Recommendations for Nutrition Monitoring
The committee recommends that the U.S. government provide a mechanism for periodically monitoring trends in lactation and developing normative indicators of nutritional status during lactation.
- Monitoring of trends . Data are needed on the incidence and duration of breastfeeding among the population as a whole, and among some particularly vulnerable subpopulations. Exclusive, partial, and minimal breastfeeding should be distinguished; and data should be collected at several ages during infancy. Current or planned surveys by such agencies as the National Center for Health Statistics or the Nutrition Monitoring Division of the U.S. Department of Agriculture could be modified to serve these goals.
- Developing normative indicators of nutritional status . There is a need for data on dietary intakes by, and nutritional status among, lactating women and their relationship to lactation performance. Identification of groups of lactating women who are at nutritional risk is a problem of public health importance.
Research Recommendations
In its deliberations, the subcommittee was well aware that many factors (such as hospital practices, social attitudes, governmental policies, and exposure to infectious agents) may have a great influence on breastfeeding rates and lactation performance and that there is a need for studies to examine approaches that hold the most promise for improving both of these. Similarly, the subcommittee recognized the great need for studies to examine the short- and long-term benefits of breastfeeding in the United States among mothers and infants in all segments of the population, but especially among disadvantaged groups, which currently have the lowest rates of breastfeeding. Research recommendations concerning several of these issues (infant mortality, growth charts for breastfed infants, possible transmission of HIV, indicators of infant nutritional status) are contained in Chapter 10 . They have been excluded from this summary, not because they are unimportant, but rather because they relate only indirectly to the nutrition of healthy U.S. women during lactation.
- Research is needed to develop indicators of nutritional status for lactating women. First, the identification of normative values for nutritional status should be based on observations of representative, healthy, lactating women in the United States. In addition, indicators are needed of both (1) risks of adverse outcomes related to the mother's dietary intake and (2) the potential of the mother or her nursing infant to benefit from interventions designed to improve their nutritional status or health.
- Research is needed to identify groups of lactating women in the United States who are at nutritional risk or who could benefit from nutrition intervention programs. In general, it has been difficult to identify groups of mothers and infants in the United States with nutritional deficits that are severe enough to have measurable functional consequences. Priority should be given to the study of lactating women in subpopulations believed to be at risk of inadequate intake of certain nutrients, such as calcium by blacks and vitamin A by low-income women. The potential influence of culture-specific food beliefs on nutrient intake of lactating women should be included in any such investigations.
- Intervention studies of improved design and technical sophistication are needed to investigate the effects of maternal diet and nutritional status on milk volume; milk composition; infant nutritional status, growth, and health; and maternal health. The nursing dyad (the mother and her infant) has seldom been the focus of studies. Thus, a key aspect of this recommendation is concurrent examination of the mother, the volume and composition of the milk, and the infant. The design of such research needs to be adequate for causal inference; thus, if possible, it should include random assignment of lactating subjects to treatment groups. Appropriate sampling and handling of milk for the valid assessment of energy density, nutrient concentration, and total milk volume are essential, as is accurate measurement of nutrient concentrations.
With regard to the energy balance of lactating women, the threshold below which energy intake is insufficient to support adequate milk production has not yet been identified. Resolution of this question will probably require supplementation studies of women in developing countries whose diets are chronically energy deficient. Although such deficient diets are not common in the United States, identification of the level of energy intake that is too low to support lactation will be useful in establishing guidelines for women who want to breastfeed but who also want to restrict their energy intake to lose weight. Although chronically low energy intakes by women in disadvantaged populations may not be completely analogous to acute energy restriction among otherwise well-nourished women, ethical considerations limit the kinds of investigations that could directly address the influence of energy restriction. In supplementation studies, measurements should be made of lactation performance and of any impact on the mother's nutritional status and health, including the period of lactation amenorrhea.
With regard to specific nutrients, the impact of relatively low intakes of folate, vitamin B 6 , calcium, zinc, and magnesium during lactation on the mother's nutritional status and health needs to be assessed in more detail. As a part of this assessment, studies of the absorption of calcium, zinc, and magnesium during lactation will be useful. There is also a need to identify a reliable indicator of vitamin B 6 status of infants and to document the relationships between this indicator, maternal vitamin B 6 intake, and vitamin B 6 content in milk. Finally, resolution of the conflicting findings concerning the impact of maternal protein intake on milk volume would be desirable.
- DHHS (Department of Health and Human Services). 1980. Promoting Health/Preventing Disease: Objectives for the Nation . Public Health Service, U.S. Department of Health and Human Services, U.S. Government Printing Office, Washington, D.C. 102 pp.
- DHHS (Department of Health and Human Services). 1984. Report of the Surgeon General's Workshop on Breastfeeding and Human Lactation . DHHS Publ. No. HRS-D-MC 84-2. Health Resources and Services Administration, Public Health Service, U.S. Department of Health and Human Services, Rockville, Md. 93 pp.
- DHHS (Department of Health and Human Services). 1985. Followup Report: The Surgeon General's Workshop on Breastfeeding & Human Lactation . DHHS Publ. No. HRS-D-MC 85-2. Health Resources and Services Administration, Public Health Service, U.S. Department of Health and Human Services, Rockville, Md. 46 pp.
- DHHS (Department of Health and Human Services). 1990. Healthy People 2000: National Health Promotion and Disease Prevention Objectives. Conference Edition . U.S. Department of Health and Human Services, Public Health Service, Office of the Assistant Secretary of Health, Washington, D.C. 672 pp.
- IOM (Institute of Medicine). 1990. Nutrition During Pregnancy: Weight Gain and Nutrient Supplements . Report of the Subcommittee on Nutritional Status and Weight Gain During Pregnancy, Subcommittee on Dietary Intake and Nutrient Supplements During Pregnancy, Committee on Nutritional Status During Pregnancy and Lactation, Food and Nutrition Board. National Academy Press, Washington, D.C. 468 pp.
- Lawrence, R.A. 1989. Breastfeeding: A Guide for the Medical Profession , 3rd ed. C.V. Mosby, St. Louis. 652 pp.
- Little, R.E., K.W. Anderson, C.H. Ervin, B. Worthington-Roberts, and S.K. Clarren. 1989. Maternal alcohol use during breastfeeding and infant mental and motor development at one year . N. Engl. J. Med. 321:425-430. [ PubMed : 2761576 ]
- Malone, C. 1980. Breast-Feeding. Cumberland County WIC Program, People's Regional Opportunity Program, Portland, Maine . 13 pp.
- NRC (National Research Council). 1989. Recommended Dietary Allowances , 10 th ed. Report of the Subcommittee on the Tenth Edition of the RDAs, Food and Nutrition Board, Commission on Life Sciences. National Academy Press, Washington, D.C. 284 pp.
- The Steering Committee to Promote Breastfeeding in New York City. 1986. The Art and Science of Breastfeeding . Division of Maternal and Child Health, Bureau of Health Care Delivery and Assistance, Health Resources and Services Administration, U.S. Department of Health and Human Services, Washington, D.C. 74 pp.
- USDA (U.S. Department of Agriculture). 1988. Promoting Breastfeeding in WIC: A Compendium of Practical Approaches . FNS-256. Food and Nutrition Service, U.S. Department of Agriculture, Alexandria, Va. 171 pp.
- Cite this Page Institute of Medicine (US) Committee on Nutritional Status During Pregnancy and Lactation. Nutrition During Lactation. Washington (DC): National Academies Press (US); 1991. 1, Summary, Conclusions, and Recommendations.
- PDF version of this title (3.5M)
- Disable Glossary Links
In this Page
Related information.
- PubMed Links to PubMed
Recent Activity
- Summary, Conclusions, and Recommendations - Nutrition During Lactation Summary, Conclusions, and Recommendations - Nutrition During Lactation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Breastfeeding and Formula Feeding
New mothers have to make critical decisions regarding whether to breastfeed their babies or not. This personal choice will present the cons and pros to both the child and the mother. While many people support the benefits associated with breastfeeding, some might be against it due to various reasons. The purpose of this argumentative paper is to support the assertion that breastfeeding is better than formula feeding in many cases. In the first section, the discussion will present the strongest argument and defense for the subject. The next part will offer the opposing argument and the most appropriate premises. The third section will give a detailed analysis of the reasoning. Biases that might influence both sides will also be presented. The final part will be the conclusion.
Supporting Argument
Best nutritional choice for babies.
For all women, breastfeeding is the best choice for their children since it provides the required nutrients. Newborn babies are usually delicate and require instant vitamins and proteins that are available in breast milk. Such a practice equips these young individuals with germ-fighting antibodies, thereby strengthening their immunities. Some of the leading conditions breastfeeding prevents include asthma, meningitis, obesity, allergy, and diabetes (Brahm & Valdés, 2017).
The formula might be a better alternative to breastfeeding when some mothers are unable to breastfeed. However, its nutritional value or content does not compare with that of breastfeeding. This is true since the available contents might not be balanced, thereby exposing babies to different illnesses. Some of them might include obesity and allergy. This means that formula is not the best nutritional choice for newborn babies. To conclude, the convenience associated with breastfeeding makes it a good choice for mothers.
Defense for First Argument
In most of the cases, companies produce baby formula by mimicking the nutrients contained in breastfeeding. Unfortunately, this product is not comparable with breast milk since it might not provide all the vitamins, carbohydrates, and proteins babies require immediately after birth (Brahm & Valdés, 2017). Breastfeeding ensures that newborns have access to diverse nutrients.
New studies have indicated that breastfeeding is essential for mothers. For example, Brahm and Valdés (2017) indicate that the process helps women burn calories, thereby recording positive health outcomes. They will also reduce their chances of developing various conditions, such as hypertension, breast cancer, diabetes, and cardiovascular disease. The uterus will also shrink within the shortest possible while at the same time meeting the nutritional demands of the baby. The naturalness of breast milk also explains why it is good for babies. This is true since the child will digest it with ease. This means that cases of indigestion and diarrhea will reduce significantly.
Personally, I believe that most of the nutrients associated with formula feeding do not match with the ones obtained from breast milk. Children who breastfed for more than six months after birth will record positive health outcomes (Brahm & Valdés, 2017). They will also not be at risk of these conditions: allergy, diabetes, obesity, and ear infections. Babies who rely on formula feeding have higher chances of developing these illnesses. Mothers can, therefore, breastfeed conveniently and with ease wherever they are since it is the best option for them.
Opposing Argument
Breastfeeding changes every mother’s diet.
Although breastfeeding is a natural practice aimed at meeting the nutritional demands of newborn babies, mothers who select it must be worried about what they drink or eat. This is the case since different products can find their way into breast milk and affect children’s health outcomes, including caffeine, nicotine, and alcohol. Those who decide to feed their babies using baby formula will not have to worry about such issues.
This is one of the main reasons why many parents decide not to breastfeed their babies. Mothers should also consider the importance of eating healthy foods in order to meet their children’s dietary needs (Zhang et al., 2015). This is necessary since the food the mother consumes will dictate most of the nutrients available to the baby. With many diets containing poisonous materials and compounds, parents who consider formula feeding will not have to worry about their babies’ health outcomes.
Since breastfeeding is natural, mothers should be aware of different concerns that have the potential to affect their babies’ health outcomes. Mothers who are breastfeeding or planning to do so should have a clear understanding of what they drink and eat (Zhang et al., 2015). The reasoning behind this argument is that some compounds or chemicals consumed by an individual can be passed through breast milk to the child. This is something that worries many women since they can eat foods containing high levels of mercury and other dangerous chemicals.
Similarly, mothers who drink alcohol are at risk of passing it to their babies. Zhang et al. (2015) suggest that those who have taken beer should not breastfeed before two hours have passed. The same concern emerges when mothers take coffee. These compounds have the potential to trigger different problems in babies, such as irritability and restlessness. These issues can eventually have negative effects on the affected children and disorient their growth and developmental patterns.
The baby formula appears to address most of the problems associated with breast milk. For instance, parents who have small babies will not have to monitor the foods they consume. Using a bottle, caregivers and mothers can feed their babies whenever they are. Individuals who consume alcohol and other harmful products will not have to worry about the health or wellbeing of their children (Rigo et al., 2017). These insights explain why formula feeding can be better than breastfeeding in most of the cases.
Analysis of the Reasoning
The above arguments present key premises that many people in support or against breastfeeding take seriously. The ideas presented in the first section seek to explain why breastfeeding remains the best option in comparison with baby feeding. Some of the key premises include the provision of the required nutrients, convenience, the ability to minimize the risks of diseases, and the promotion of the baby’s health outcomes. Mothers who breastfeed continuously for at least six months after birth will reduce their chances of developing these conditions: breast cancer, hypertension, and obesity. The formula does not provide similar benefits to the baby or the mother (Rigo et al., 2017). These insights are meaningful, true, and acceptable. The conclusion presented in the section supports such premises.
The second section analyzes the issue of formula feeding from an evidence-based perspective. This means that the alternative addresses the unique challenges associated with breastfeeding. The consulted articles and theorists argue that formula feeding minimizes parents’ desire to monitor the foods they consume. The fallacy committed is that caretakers and working women will find excuses to support formula feeding (Zhang et al., 2015).
Individuals who are uncomfortable with breastfeeding will also remain biased and consider the importance of formula. Those who want to provide high-quality milk to their children should consume healthy foods. Such evidence-based premises can empower people who prefer formula feeding.
These opposing arguments present superior ideas that can guide people to make appropriate decisions regarding breastfeeding and baby formula. Personally, I believe that the first section makes a stronger case since breast milk is a good option for all newborns. Mothers should focus on every unique benefit associated with breastfeeding. Such a practice will benefit both the parent and the baby. Formula feeding will minimize most of the benefits associated with breastfeeding (Rigo et al., 2017).
In the second part, evidence-based insights are presented to identify the importance of baby feeding. Those who drink alcohol can benefit from it. This is also the same case for people who are not ready to monitor their diets. Such arguments explain why mothers should consider every opposing idea and make the most appropriate choices.
The above argumentative paper has presented several premises to support the power of breastfeeding over formula feeding. Mothers who provide breast milk to their children will record positive health outcomes and allow their babies to develop much faster. Formula feeding is also identified as useful practice for mothers who are unable to breastfeed due to their personal reasons. From such ideas, it would be appropriate for all researchers and critical thinkers to encourage more mothers to breastfeed for at least six months after birth. They should also guide those who drink coffee or alcohol to create adequate time for their children.
Educational opportunities will also equip more people with new ideas about breastfeeding and formula feeding, thereby empowering them to make superior decisions that can eventually empower their babies. Such a practice will ensure that all women and babies record positive health outcomes and eventually achieve their potential.
Brahm, P., & Valdés, V. (2017). Benefits of breastfeeding and risks associated with not breastfeeding. Revista Chilena de Pediatría, 88 (1), 15-21.
Rigo, J., Hascoët, J., Billeaud, C., Picaud, J., Mosca, F., Rubio, A., … Spalinger, J. (2017). Growth and nutritional biomarkers of preterm infants fed a new powdered human milk fortifier: A randomized trial. Journal of Pediatric Gastroenterology and Nutrition, 65 (4), e83-e93. Web.
Zhang, K., Tang, L., Wang, H., Qiu, L., Binns, C. W., & Lee, A. H. (2015). Why do mothers of young infants choose to formula feed in China? Perceptions of mothers and hospital staff. International Journal f Environmental Research and Public Health, vol. 12 (5), 4520-4532. Web.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2021, June 11). Breastfeeding and Formula Feeding. https://studycorgi.com/breastfeeding-and-formula-feeding/
"Breastfeeding and Formula Feeding." StudyCorgi , 11 June 2021, studycorgi.com/breastfeeding-and-formula-feeding/.
StudyCorgi . (2021) 'Breastfeeding and Formula Feeding'. 11 June.
1. StudyCorgi . "Breastfeeding and Formula Feeding." June 11, 2021. https://studycorgi.com/breastfeeding-and-formula-feeding/.
Bibliography
StudyCorgi . "Breastfeeding and Formula Feeding." June 11, 2021. https://studycorgi.com/breastfeeding-and-formula-feeding/.
StudyCorgi . 2021. "Breastfeeding and Formula Feeding." June 11, 2021. https://studycorgi.com/breastfeeding-and-formula-feeding/.
This paper, “Breastfeeding and Formula Feeding”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: June 11, 2021 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
The Essence of Professionalism in Modern Work Environments
This essay is about the essence of professionalism in modern work environments. It explains that professionalism involves competence, accountability, ethical behavior, effective communication, proper appearance, adaptability, and teamwork. Professionals are dedicated to continuous improvement, maintaining high standards in their work and interactions. They take responsibility for their actions, communicate clearly, and collaborate effectively with others. Professionalism also extends to representing their organizations positively in external settings. By embodying these principles, individuals enhance their careers and contribute to the success and reputation of their organizations.
How it works
Professionalism, an enigmatic entity pervasive within our laborious existence, often eludes precise delineation. At its essence, professionalism encapsulates a spectrum of dispositions, conducts, and benchmarks delineating the comportment of individuals ensconced within professional environs. It transcends mere sartorial conformity or adherence to workplace protocols, epitomizing the ethos of accountability, rectitude, and prowess in one’s vocation.
Competence stands as a cornerstone of professionalism, denoting the possession of requisite aptitudes, erudition, and credentials indispensable for efficacious job execution. Competence is a dynamic facet, necessitating perpetual erudition and acclimation to remain abreast of industry vicissitudes and technological evolutions.
A professional embodies an unwavering dedication to personal and vocational maturation, perennially endeavoring to augment expertise and furnish superlative workmanship.
Accountability constitutes another pivotal tenet of professionalism. Professionals assume onus for their deeds and decisions, cognizant of the reverberations of their endeavors not solely upon themselves, but also upon their cohorts, clientele, and the overarching establishment. Accountability entails reliability, punctuality, and fidelity to commitments. It further encompasses the acknowledgment of fallibility and the imbibition of wisdom from miscues, eschewing the proclivity to deflect culpability onto others.
Ethical rectitude also constitutes a sine qua non of professionalism, encompassing probity, integrity, and allegiance to moral rectitude even amid adversity. Professionals espouse ethical precepts and codes of comportment germane to their sphere, ensuring equitable and translucent conduct. They cultivate trust amongst peers and clients through unwavering adherence to integrity and deference. This ethical bedrock is pivotal for the sustenance of a favorable reputation and the cultivation of a trustworthy workplace milieu.
Communication emerges as another pivotal facet of professionalism. Effective communication transcends mere elucidation of data, entailing active and empathetic listening. Professionals apprehend the import of cogent, courteous, and timely discourse in fostering robust interpersonal bonds and ensuring seamless operationality of their teams. They adeptly modulate their communication paradigm to align with diverse audiences and contexts, be they peers, superiors, or clientele.
Professionalism equally extends to personal presentation within the workplace precincts. It encompasses adherence to stipulated vestiary norms, preservation of an uncluttered and methodical workspace, and manifestation of decorum and reverence for others. Adherence to professional demeanor and comportment contributes to a salubrious workplace ambiance and signifies an individual’s fealty to their charge and organization.
Adaptability increasingly garners recognition as a pivotal facet of professionalism within contemporary, frenetic, and flux-laden labor environs. Professionals must adeptly navigate novel exigencies, embrace metamorphosis, and retain suppleness in their modus operandi. This demands a proactive mindset and facility for critical and inventive cogitation to surmount quandaries. Adaptability further implicates receptiveness to critique and willingness to implement requisite adjustments for ameliorating performance.
Collaboration and teamwork represent quintessential components of professionalism. Professionals discern the import of efficacious collaboration in attaining collective objectives. They posit constructive contributions within their teams, disseminate knowledge, and proffer support to their cohorts. A collaborative ethos engenders communal spirit and facilitates an efficacious and harmonious workplace milieu. Professionals cognize that triumph often burgeons from communal endeavor, and that mutual deference and collaboration are pivotal to its fruition.
Professionalism transcends workplace interactions to encompass external representations of organizational ethos. Whether interfacing at conventions, networking venues, or clienteles, professionals serve as conduits for their enterprises. They extol the values and benchmarks of their organizations, thus fostering a sanguine and professional external persona.
Moreover, professionalism bespeaks a commitment to perpetual amelioration. Professionals assiduously seek avenues for vocational advancement, be it through formal pedagogy, training regimens, or autodidacticism. They remain abreast of industry currents and exemplars, ensuring that their skillsets and erudition remain germane and contemporaneous. This dedication to evolution augments individual efficacy and concomitantly fortifies organizational ascendancy.
In summation, professionalism constitutes a variegated concept encompassing competence, accountability, ethical comportment, communication, presentation, adaptability, teamwork, and perpetual advancement. It transcends mere adherence to statutes; it embodies the ethos and values catalyzing a salutary, dignified, and constructive workplace ambiance. Professionals espouse an unwavering commitment to vocation excellence, comporting themselves with integrity, and incessantly endeavoring to burgeon and refine. Through the embracement of these traits, individuals not only aggrandize their professional trajectories but also engender the ascendancy and renown of their organizations.
Cite this page
The Essence of Professionalism in Modern Work Environments. (2024, Jun 01). Retrieved from https://papersowl.com/examples/the-essence-of-professionalism-in-modern-work-environments/
"The Essence of Professionalism in Modern Work Environments." PapersOwl.com , 1 Jun 2024, https://papersowl.com/examples/the-essence-of-professionalism-in-modern-work-environments/
PapersOwl.com. (2024). The Essence of Professionalism in Modern Work Environments . [Online]. Available at: https://papersowl.com/examples/the-essence-of-professionalism-in-modern-work-environments/ [Accessed: 2 Jun. 2024]
"The Essence of Professionalism in Modern Work Environments." PapersOwl.com, Jun 01, 2024. Accessed June 2, 2024. https://papersowl.com/examples/the-essence-of-professionalism-in-modern-work-environments/
"The Essence of Professionalism in Modern Work Environments," PapersOwl.com , 01-Jun-2024. [Online]. Available: https://papersowl.com/examples/the-essence-of-professionalism-in-modern-work-environments/. [Accessed: 2-Jun-2024]
PapersOwl.com. (2024). The Essence of Professionalism in Modern Work Environments . [Online]. Available at: https://papersowl.com/examples/the-essence-of-professionalism-in-modern-work-environments/ [Accessed: 2-Jun-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
- Mission, Facts and Figures
- Deans, Chairs and Staff
- Leadership Council
- Dean in the News
- Get Involved
- DEIB Mission
- Message from DEIB Associate Dean
- News and Media
- Reading Lists
- The Yale and Slavery Research Project
- Photo Gallery
- Winslow Medal
- Coat of Arms & Mace
- $50 Million Challenge
- For Pandemic Prevention and Global Health
- For Understanding the Health Impacts of Climate Change
- For Health Equity and Justice
- For Powering Health Solutions through Data Science
- For Future Leaders
- For Faculty Leaders
- For Transformational Efforts
- Data, Leadership, and Collaboration at the School of Public Health
- An abiding love for Yale turns into a lasting gift – in 15 minutes
- Endowed Professorship Created at Critical Time for Yale School of Public Health
- Brotherly encouragement spurs gift to support students
- Prestipino creates opportunities for YSPH students, now and later
- Alumna gives back to the school that “opened doors” in male-dominated field
- For Public Health, a Broad Mission and a Way to Amplify Impact
- Couple Endows Scholarship to Put Dreams in Reach for YSPH Students
- A Match Made at YSPH
- A HAPPY Meeting of Public Health and the Arts
- Generous Gift Bolsters Diversity & Inclusion
- Alumni Donations Aid Record Number of YSPH Students
- YSPH’s Rapid Response Fund Needs Donations – Rapidly
- Podiatric Medicine and Orthopedics as Public Health Prevention
- Investing in Future Public Health Leaders
- Support for Veterans and Midcareer Students
- Donor Eases Burden for Policy Students
- A Personal Inspiration for Support of Cancer Research
- Reducing the Burden of Student Debt
- Learning About Global Health Through Global Travel
- A Meeting in Dubai, and a Donation to the School
- Rapid Response Fund
- Planned Giving
- Testimonials
- Faculty, Postdoc Jobs
- For the Media
- Issues List
- PDF Issues for Download
- Editorial Style Guide
- Social Media
- Shared Humanity Podcast
- Health & Veritas Podcast
- Accreditation
- Faculty Directory by Name
- Career Achievement Awards
- Annual Research Awards
- Teaching Spotlights
- Biostatistics
- Chronic Disease Epidemiology
- Climate Change and Health Concentration
- Environmental Health Sciences
- Epidemiology of Microbial Diseases
- Global Health
- Health Policy and Management
- Maternal and Child Health Promotion Track
- Public Health Modeling Concentration
- Regulatory Affairs Track
- Social & Behavioral Sciences
- U.S. Health Justice Concentration
- Why Public Health at Yale
- Events and Contact
- What Does it Take to be a Successful YSPH Student?
- How to Apply and FAQs
- Incoming Student Gateway
- Traveling to Yale
- Meet Students and Alumni
- Past Internship Spotlights
- Student-run Organizations
- MS and PhD Student Leaders
- Staff Spotlights
- Life in New Haven
- Libraries at Yale
- The MPH Internship Experience
- Practicum Course Offerings
- Summer Funding and Fellowships
- Downs Fellowship Committee
- Stolwijk Fellowship
- Climate Change and Health
- Career Management Center
- What You Can Do with a Yale MPH
- MPH Career Outcomes
- MS Career Outcomes
- PhD Career Outcomes
- Employer Recruiting
- Tuition and Expenses
- External Funding and Scholarships
- External Fellowships for PhD Candidates
- Alumni Spotlights
- Bulldog Perks
- Stay Involved
- Board of Directors
- Emerging Majority Affairs Committee
- Award Nomination Form
- Board Nomination Form
- Alumni Engagement Plus
- Mentorship Program
- The Mentoring Process
- For Mentors
- For Students
- Recent Graduate Program
- Transcript and Verification Requests
- Applied Practice and Student Research
- Competencies and Career Paths
- Applied Practice and Internships
- Student Research
- Seminar and Events
- Competencies and Career paths
- Why the YSPH Executive MPH
- Message from the Program Director
- Two-year Hybrid MPH Schedule
- The Faculty
- Student Profiles
- Newsletter Articles
- Approved Electives
- Physicians Associates Program
- Joint Degrees with International Partners
- MS in Biostatistics Standard Pathway
- MS Implementation and Prevention Science Methods Pathway
- MS Data Sciences Pathway
- Internships and Student Research
- Competencies
- Degree Requirements - Quantitative Specialization
- Degree Requirements - Clinical Specialization
- Degree Requirements- PhD Biostatistics Standard Pathway
- Degree Requirements- PhD Biostatistics Implementation and Prevention Science Methods Pathway
- Meet PhD Students in Biostatistics
- Meet PhD Students in CDE
- Degree Requirements and Timeline
- Meet PhD Students in EHS
- Meet PhD Students in EMD
- Meet PhD Students in HPM
- Degree Requirements - PhD in Social and Behavioral Sciences
- Degree Requirements - PhD SBS Program Maternal and Child Health Promotion
- Meet PhD Students in SBS
- Differences between MPH and MS degrees
- Academic Calendar
- Translational Alcohol Research Program
- Molecular Virology/Epidemiology Training Program (MoVE-Kaz)
- For Public Health Practitioners and Workforce Development
- Course Description
- Instructors
- Registration
- Coursera Offerings
- Non-degree Students
- International Initiatives & Partnerships
- NIH-funded Summer Research Experience in Environmental Health (SREEH)
- Summer International Program in Environmental Health Sciences (SIPEHS)
- 2022 Student Awards
- APHA Annual Meeting & Expo
- National Public Health Week (NPHW)
- Leaders in Public Health
- YSPH Dean's Lectures
- The Role of Data in Public Health Equity & Innovation Conference
- Innovating for the Public Good
- Practice- and community-based research and initiatives
- Practice and community-based research and initiatives
- Activist in Residence Program
- Publications
- Health Care Systems and Policy
- Heart Disease and Stroke
- Panels, Seminars and Workshops (Recordings)
- Rapid Response Fund Projects
- SalivaDirect™
- Emerging Infections Program - COVID-NET
- Public Health Modeling Unit Projects
- HIV-AIDS-TB
- The Lancet 2023 Series on Breastfeeding
- 'Omics
- News in Biostatistics
- Biostatistics Overview
- Seminars and Events
- Seminar Recordings
- Statistical Genetics/Genomics, Spatial Statistics and Modeling
- Causal Inference, Observational Studies and Implementation Science Methodology
- Health Informatics, Data Science and Reproducibility
- Clinical Trials and Outcomes
- Machine Learning and High Dimensional Data Analysis
- News in CDE
- Nutrition, Diabetes, Obesity
- Maternal and Child Health
- Outcomes Research
- Health Disparities
- Women's Health
- News in EHS
- EHS Seminar Recordings
- Climate change and energy impacts on health
- Developmental origins of health and disease
- Environmental justice and health disparities
- Enviromental related health outcomes
- Green chemistry solutions
- Novel approaches to assess environmental exposures and early markers of effect
- 1,4 Dioxane
- Reproducibility
- Tissue Imaging Mass Spectrometry
- Alcohol and Cancer
- Olive Oil and Health
- Lightning Talks
- News in EMD
- Antimicrobial Resistance
- Applied Public Health and Implementation Science
- Emerging Infections and Climate Change
- Global Health/Tropical Diseases
- HIV and Sexually Transmitted Infections
- Marginalized Population Health & Equity
- Pathogen Genomics, Diagnostics, and Molecular Epidemiology
- Vector-borne and Zoonotic Diseases
- Disease Areas
- EMD Research Day
- News in HPM
- Health Systems Reform
- Quality, Efficiency and Equity of Healthcare
- Substance Abuse and Mental Health
- Modeling: Policy, Operations and Disease
- Pharmaceuticals, Vaccines and Medical Devices
- Health and Wellbeing
- News in SBS
- Aging Health
- Community Engagement
- Health Equity
- Mental Health
- Reproductive Health
- Sexuality and Health
- Nutrition, Exercise
- Stigma Prevention
- Community Partners
- For Public Health Practitioners
- Reports and Publications
- Fellows Stipend Application
- Agency Application
- Past Fellows
- PHFP in the News
- Frequently Asked Questions
- International Activity
- Research Publications
- Grant Listings
- Modeling Analyses
- 3 Essential Questions Series
INFORMATION FOR
- Prospective Students
- Incoming Students
- myYSPH Members
Student News - EMPH Newsletter, Spring 2024
Commencement 2024.
Photo credit: Harold Shapiro
Congratulations to Ashley Nicole Reynolds Marshall who received the 2024 Student Award for Outstanding Contributions to Advancing Belonging, Equity, and Justice. The awards recognize student scholarship, leadership, innovation, and commitment to public health. As Deputy City Manager for Social Equity for Charlottesville, Virginia, Ashley oversees a robust portfolio that includes the city’s Downtown Job Center and Home to Hope program focused on welcoming formerly incarcerated persons back into the community. Ashley also serves as the city’s Chief Justice, Equity, Diversity, and Inclusion Officer and LGBTQIA+ Liaison.
A new study by Marney White, PhD, MS , and Dr. Jeffrey Cohen, MD , found a significant association between eczema (atopic dermatitis) and eating disorders , highlighting the intricate relationship between dermatological conditions and mental health. White and Cohen discovered their mutual research interests when Cohen enrolled in the EMPH program, in which White is a member of the teaching faculty. The chance encounter laid the foundation for the published study and its multidisciplinary investigative approach.
Jolene Bressi collaborated on a paper in eClinical Medicine . The article is titled, “Prescribing and deprescribing guidance for benzodiazepine and benzodiazepine receptor agonist use in adults with depression, anxiety, and insomnia: an international scoping review.”
Domna Antoniadis was a guest speaker at Yale Law School in March, in a seminar led by Emily Rock, the interim executive director at the Solomon Center for Health Law and Policy, and James Bhandary-Alexander, legal director of the Medical Legal Partnership at the Solomon Center. Domna (shown in the photo at left), talked about her work at a medical legal partnership, and the challenges and opportunities of public health.
Nathan Carroll co-authored an essay for Psychiatric News on the rare emergence of overlapping 13- and 17-year cicada broods . The essay discussed how people who are sensitive to sounds can protect themselves from the constant noise the insects make after they emerge from their underground burrows.
Janna Jansen presented her capstone on food insecurity at the White House to support The White House Challenge to End Hunger and Build Healthy Communities . “Presenting to the Second Gentleman, secretaries of Agriculture, and Health and Human Services, President Biden's domestic policy advisor, and others is certainly something I will never forget,” she said.
Jay Oh was appointed a Certified in Public Health Ambassador for the National Board of Public Health Examiners (NBPHE). He will play a crucial role in advancing public health initiatives by representing NBPHE at professional events, participating in focus groups on marketing activities, and sharing information on NBPHE’s social media platform, among other duties.
Daniel Fitzgerald has developed two software tools, including a tool that assists with analyzing research papers, and a discharge planner that addresses health care shortages, which he created for his capstone. Says Daniel, who presented a poster at the Yale in AI in Medicine Symposium, “there is real potential for AI to replace some of the lost health care jobs, or to support existing staff.”
Kimberly Daviscourt and Jay Oh were teaching fellows for the EMPH course, Foundations of Behavior Change. Jay Oh was a teaching fellow for the fall semester course on ethics.
Charles Leonard recently was awarded a 5-year R01 grant from the National Institute on Aging (NIA). The $2.8 million grant will allow him to continue his epidemiologic research on the population health effects of drug interactions among persons with mental health disorders. His project is titled, “ Drug interactions involving psychoactive drugs .” Charles is an assistant professor of epidemiology at the Perelman School of Medicine at the University of Pennsylvania.
Leah Werner has accepted a position as the Oregon Health & Science University (OHSU) Health Services Associate Medical Director. The position is designed to lead health care transformation at OHSU and help integrate a large hospital system OHSU recently acquired. Also, Leah was invited to submit a full proposal for a data access grant to the Robert Wood Johnson Foundation.

COMMENTS
One of the main benefits of breastfeeding is the provision of essential nutrients. This is due to the fact that the mother's milk contains all the necessary components that ensure the complete and correct development of the baby (1, 6). In addition, they help to reduce the possibility of problems with the digestive system, such as colic (3).
Breastfeeding, initiated within the first hour of birth, provided exclusively for six months, and continued up to two years or beyond with the provision of safe and appropriate complementary foods, is one of the most powerful practices for promoting child survival and wellbeing. Improving breastfeeding rates
The vast majority ( n = 50) of the reviewed literature identified various barriers for successful breastfeeding. A sizeable proportion of literature (41%, n = 24) explored women's experiences with the physical aspects of breastfeeding [ 23, 33 ]. In particular, problems with latching and the pain associated with breastfeeding were commonly ...
Conclusion. In conclusion, breastfeeding is a natural and beneficial method of feeding infants. It provides numerous health benefits for both mother and child, including improved immune function, cognitive development, and reduced risk of diseases.
Breastfeeding the Latch Scoring System. PAGES 2 WORDS 810. For the newborn, birth weight, gestational age, and 1-minute and 5-minute Apgar scores were recorded. Post-discharge phone calls were made on day four and at week six. Each participant was asked if she was still breastfeeding at the time of the phone call.
It helps the mother's body recover from childbirth more quickly. It can also help the mother lose the weight she gained during pregnancy. Breastfeeding can also lower the mother's risk of getting certain diseases later in life. These include breast cancer, ovarian cancer, and type 2 diabetes. Besides health benefits, breastfeeding also ...
Perceptions about breastfeeding. Women's perceptions about breastfeeding were covered in 83% (n = 49) of the papers.Most articles (n = 31) suggested that women perceived breastfeeding as a positive experience and believed that breastfeeding had many benefits [19, 20].The phrases "breast is best" and "breastmilk is best" were repeatedly used by the participants of studies included in ...
9 essay samples found. Breastfeeding refers to the practice of feeding an infant with milk from a woman's breast. Essays on breastfeeding might discuss its health benefits for both infants and mothers, the societal attitudes towards breastfeeding, or the challenges mothers face in breastfeeding, especially in public or work settings.
Breastfeeding Anthropology. Breastfeeding is an action that is bio cultural and biosocial in nature. Breastfeeding is a biological process that involves a woman providing milk for an infant. Culturally speaking, breastfeeding is not always an action by the biological mother. In some cases, the mother needs to return to work not long after birth.
The bulk of research devoted to understanding breastfeeding is on the nutritive benefits during the first six months to the first year of an infant's life.While bodies like the WHO recommend ...
Breastfeeding is a topic that often sparks strong opinions and debates among parents, healthcare professionals, and society as a whole.From the benefits of breast milk for infants to the social stigma surrounding nursing in public, there are numerous aspects to consider when discussing this important issue.
Place an order. Most importantly, breastfeeding promotes a secure attachment between a mother and their infant because this kind of skin to skin contact gives the baby an explicit sense of assurance that he or she is deeply cared for and loved (Brooks, 2013). I learned more about this concept in The Process of Parenting by Jane Brooks because ...
Advantages of bottle-feeding over breastfeeding. Finally, breastfeeding is preferable because of the promotion of the bond between a mother and a child, and its price. This process of feeding is a unique chance for mothers to be relieved from anxiety and develop an emotional attachment to their children. Sometimes, it is not enough for mothers ...
Cognitive benefits. In addition to the nutritional and immunological benefits of breast milk, breastfeeding may help preemies get ahead intellectually. Breast milk is associated with increases in child cognitive ability and educational achievements. Cognitive development of social and psychomotor skills gains increases with the consumption and ...
View our collection of breastfeeding essays. Find inspiration for topics, titles, outlines, & craft impactful breastfeeding papers. Read our breastfeeding papers today!
Cognitive benefits. In addition to the nutritional and immunological benefits of breast milk, breastfeeding may help preemies get ahead intellectually. Breast milk is associated with increases in child cognitive ability and educational achievements. Cognitive development of social and psychomotor skills gains increases with the consumption and ...
Breastfeeding vs. Bottle Feeding Essay. Better Essays. 2468 Words. 10 Pages. 7 Works Cited. Open Document. Very few experts disagree with the fact that breastfeeding is the optimal choice for the infant. However, decreasing breastfeeding rates raise many questions as to why mothers are not choosing the best nutritional choice for their children.
Breastfeeding support from health professionals can be effective in influencing a mother's decision to initiate and maintain breastfeeding. However, health professionals, including nursing students, do not always receive adequate breastfeeding education during their foundational education programme to effectively help mothers. In this paper, we report on a systematic review of the literature ...
During the past decade, the benefits of breastfeeding have been emphasized by many authorities and organizations in the United States. Federal agencies have set specific objectives to increase the incidence and duration of breastfeeding (DHHS, 1980, 1990), and the Surgeon General has held workshops on breastfeeding and human lactation (DHHS, 1984, 1985). At the federal and state levels, the ...
Some studies estimate that a woman who breastfeeds her infant exclusively uses 400 - 600 extra calories a day in producing milk. The composition of breast milk depends on how long the baby nurses. "Research shows that the milk and energy content of breast milk actually decreases after the first year.
New studies have indicated that breastfeeding is essential for mothers. For example, Brahm and Valdés (2017) indicate that the process helps women burn calories, thereby recording positive health outcomes. They will also reduce their chances of developing various conditions, such as hypertension, breast cancer, diabetes, and cardiovascular ...
The main reason claimed by mothers for the introduction of milk and milk products were mainly as a source of calcium for the child. Other reasons include strength of bones and teeth, proper growth and development of the child. Eggs were given to children as a source of vitamin D, protein and to test for allergies.
The components of human milk contain, "proteins, carbohydrates and fats are synthesized in the breasts' alveolar glands. Proteins account for approximately 6% of the calories in human milk and are easier to digest than protein prepared in formula. Carbohydrates account for approximately 42% of the calories in human milk with lactose as the ...
Background: Breastfeeding is the optimal nourishment for infants and it is recommended that children commence breastfeeding within the first hour of birth and be exclusively breastfed for the initial 6 months of life. Our objective was to determine which factors related to mothers could influence the degree of exclusive breastfeeding during hospitalization, as well as to assess breastfeeding ...
Essay Example: Professionalism, an enigmatic entity pervasive within our laborious existence, often eludes precise delineation. At its essence, professionalism encapsulates a spectrum of dispositions, conducts, and benchmarks delineating the comportment of individuals ensconced within professional
Commencement 2024. Congratulations to Ashley Nicole Reynolds Marshall who received the 2024 Student Award for Outstanding Contributions to Advancing Belonging, Equity, and Justice. The awards recognize student scholarship, leadership, innovation, and commitment to public health. As Deputy City Manager for Social Equity for Charlottesville ...