Importance of Daily Oral Care Essay
Introduction, how oral health affects overall health, oral bacteria entering the bloodstream, the mouth is a mirror into person’s health, links between oral health and following diseases, common oral health conditions that may affect the elderly, daily oral hygiene for long-term care residents, daily oral hygiene modifications.
Maintaining oral health is a major issue in the medical field. It is vital in keeping healthy on the whole, along with an imperative effect on the personality of each individual. Keeping good oral health practices may help minimize deadly diseases, and reduce risks of serious illnesses. Oral health involves keeping the mouth, gums, and teeth hygienic, by taking proper care of them and giving them due attention.
Prevention of gums from cavities and diseases is the chief aspect of good oral health. This can be done by regular cleaning, brushing, and flossing of the teeth on a daily basis, which would help prevent bacterial infections and the emergence of plaque. Plaque is caused by constant bacterial action due to a lack of oral hygiene. This bacteria infects the teeth by forming layers upon layers, appearing in the form of tartar.
The bacteria from the mouth, if not removed, can enter the bloodstream, and affect overall health by aggravating pre-existing diseases.
The mouth of a person reflects his personality greatly because it is the main focus while looking at other people during a conversation. It depicts the personal hygiene one possesses and is indicative of the liking for oral hygiene.
Poor oral health has been found linked to many diseases- the relation lies in the fact that the unhygienic conditions of the mouth aggravate any bacterial infections that are present in the body.
Pneumonia is a very common cause of death in elderly nursing home residents. The dental plaque present gives rise to pneumonia-causing bacteria, which get into the respiratory tract through silent aspiration (Jurasek, 2002).

Candidiasis
Candidiasis is a fungal infection that is caused by the yeast Candida Albicans. Denture wearers suffer most from the disease, because of a lack of oral hygiene. It is essential to remove dentures and keep the mouth clean especially after mealtimes (American Dental Association, 2009).
In diabetic patients, oral candidiasis is more prevalent, which can be treated with antifungal medicines. But the most important element is to keep oral hygiene so that such an instance does not initiate. The wounds of diabetic patients take longer to heal, which can affect overall health too.
Heart Disease
The bacteria that affect the gums due to unhygienic conditions of the mouth may enter the bloodstream and also affect the arteries, according to current research. Studies have shown that bacteria infecting the gums can now travel freely throughout the body. The bacteria invade the coronary arteries, causing blockage, and clotting. Another link of oral hygiene to heart disease is the formation of plaque, which causes swelling up of the arteries (American Academy of Periodontology, 2008).
Stroke is also caused due to the same aforementioned reason.
Respiratory Infections
Respiratory infections occur when the bacteria from the gums enter the bloodstream and enter the lungs. Usually, respiratory infections are caused by aspiration or inhaling, but recent studies have shown the bacteria to enter the bloodstream through gum infections. The lower respiratory tract is affected by bacterial invasion.
Bacterial Endocarditis
Bacterial endocarditis is a heart disease in which the valves or inner lining of the heart is affected by germs. Good daily oral hygiene habits may prevent endocarditis, plus, a visit to a dentist every six months, and regular brushing and flossing may also help reduce risks of dental diseases, which may lead to fatal diseases such as the aforementioned (“Infective Endocarditis”, 2009).
Low birth weight and Premature Babies
Premature babies may also result from periodontal disease. When bacteria from the mouth enter the bloodstream, the body produces prostaglandin to fight the bacteria, which causes muscle contraction, resulting in early labor. The bacterium Pgingivalis infects the placenta, which may affect the growth and development of the fetus. Inflammatory chemicals may also be produced in a pregnant woman’s body.
Elderly people may suffer from dry mouth or xerostomia, because of the therapies they are going through. Patients, who are undergoing cancer therapies and the like, develop dry mouth because of the intensity of the medications. They may also be suffering from dry mouth as a result of some other diseases they may be suffering from, like arthritis, bone marrow transplantation, and neurological diseases.
Periodontal Disease
Periodontal diseases occur as a result of bacterial infections, which give rise to root surface caries too.
Root Surface Caries
Root surface caries are seen in these patients because of the long periods they are hospitalized, and are not given the medical attention they may need individually.
Oral Ulcerations
Oral ulcers are additionally a cause of bacterial activity in the inner lining of the mouth, which gives rise to painful blisters and swelling; they are termed oral ulcers.
Brushing Daily
It is essential for every individual to brush teeth regularly, at least once daily, if not twice, to prevent gum diseases. For long-term care residents, because they are being rendered treatment for the disease and may neglect to keep oral hygiene, it is specifically crucial to pay attention to cleanliness. The hospital conditions may also be such that patients are uncomfortable, and may not pay heed to the importance of daily brushing.
Flossing regularly will help remove bacterial films from teeth.
Mouth Rinsing
Mouth rinsing after meal intake is also essential for keeping the gums free of food particles which may enhance bacterial growth.
Sugar-free Chewing gum
The sugars in food tend to stick to the teeth, giving bacteria the chance to act on them, which gradually cause plaque, and eventually, tartar. Thus sugar-free chewing gum would be a good substitute for regular gum, to prohibit infection.
Denture Care
If dentures are worn, they need to be removed regularly for cleaning, and then restored. Dentures need to be washed regularly and the gums need cleaning so that minimal bacterial growths take place to aggravate the disease that already subsists.
OT/PT Consult
Oral hygienic maintenance can be advised by the physician, to the patients. Patients are told the importance of keeping oral hygiene and maintaining it. Consulting always helps, because patients can get convinced verbally, about the importance of keeping the mouth clean, and of brushing teeth. Brushing teeth is the most common and best way to maintain oral health. By tooth brushing, the bacterial film which forms on teeth is removed. This action keeps the buccal cavity protected from any bacterial infections.
One way to improve and make more effective the brushing of teeth is to modify the toothbrush, so as to reach far-reaching areas while cleaning. Duct tape is applied to the handle of the toothbrush, which causes enlargements in the brush. A larger handle helps grasp the toothbrush, which would help in proper cleaning of the teeth (Spratt, et.al, 1997).
Bicycle Handle
The size of the handle of the toothbrush can be increased easily with some household tricks, like the use of a bicycle handle. Floss is helpful in removing plaque from the teeth, and regular flossing is recommended for oral healthcare, even to normal healthy people.
Electric Brush
Electric toothbrushes have also been designed for ease of cleaning the teeth. The electric toothbrush has an oscillating head, due to which it is also called the rotary brush. It has not been found to cleanse better than the ordinary manual brush, however, it is a good modification for the elderly people who would prefer keeping from the trouble of manual brushing.
Another oral hygiene device that may be used is a disposable applicator that attaches to the fingertip of the individual using it. The finger acts like a handle that controls the applicator while it cleanses the gums and oral cavities of the mouth. The gums can be massaged this way too, along with the teeth and interproximal areas. The shape of the applicator is such that it covers the fingertip smoothly, and there is an adhesive at the base, which ensures a good grip. On the top layer, are small bristles that help in the cleaning process.
Simple steps in performing daily oral care in nursing homes may reduce hospital stays and improve the overall quality of living
Simple steps in brushing teeth may help maintain good oral health, which is imperative to the overall health of residents in nursing care. It is apparent that lack of oral hygiene may affect the overall health of individuals, and may worsen the conditions of those who are already suffering from some disease. Daily brushing and mouth cleaning after mealtimes may help reduce risks of disease and may improve the quality of life of individuals who are seeking treatment in the hospital.
Summary of why oral care is imperative to the overall health of residents
Oral care needs to be maintained if good general health is sought because both are interlinked. Residents need to take special care because of their pre-existing illness and have to ensure that their carelessness in oral hygiene will not cause further complications in the disease.
- American Academy of Periodontology (2008).
- Infective Endocarditis (2009) Reference: Wilson W., et al. Prevention of infective endocarditis: Guidelines from the American Heart Association. Circulation, 2007; 115(8). Web.
- Jurasek, G. (2002). Oral Health Affects Pneumonia Riskin the Elderly.
- Spratt, J., Hawley, R. & Hoye, R. (1997). Home Health Care. Principles and Practices. FL 33483, St Lucie Press, 1997, hardback, 388 pp.
- International Marketing Plan in Saudi Arabia
- Health Behaviours Among Adolescents in Saudi Arabia
- Psychology: Chewing Gum' Negative Effects
- Back Pain for the Dentist
- Putting Teeth in Health Care Reform
- Dental Providers Should Be Going Above and Beyond
- COVID-19 Awareness Precautions in King Saud University
- Health Care Providers and Professionals. Nurses and Dentists: A Comparison
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, March 5). Importance of Daily Oral Care. https://ivypanda.com/essays/importance-of-daily-oral-care/
"Importance of Daily Oral Care." IvyPanda , 5 Mar. 2022, ivypanda.com/essays/importance-of-daily-oral-care/.
IvyPanda . (2022) 'Importance of Daily Oral Care'. 5 March.
IvyPanda . 2022. "Importance of Daily Oral Care." March 5, 2022. https://ivypanda.com/essays/importance-of-daily-oral-care/.
1. IvyPanda . "Importance of Daily Oral Care." March 5, 2022. https://ivypanda.com/essays/importance-of-daily-oral-care/.
Bibliography
IvyPanda . "Importance of Daily Oral Care." March 5, 2022. https://ivypanda.com/essays/importance-of-daily-oral-care/.
- Share full article
Advertisement
Supported by
Why Oral Hygiene Is Crucial to Your Overall Health
Gum disease has been associated with a range of health conditions, including diabetes, heart disease, dementia and more. Here’s what experts say you can do to manage the risk.

By Hannah Seo
The inside of your mouth is the perfect place for bacteria to thrive: It’s dark, it’s warm, it’s wet and the foods and drinks you consume provide nutrients for them to eat.
But when the harmful bacteria build up around your teeth and gums, you’re at risk of developing periodontal (or gum) disease , experts say, which is an infection and inflammation in the gums and bone that surround your teeth.
And such conditions in your mouth may influence the rest of your body, said Kimberly Bray, a professor of dental hygiene at the University of Missouri-Kansas City.
A growing yet limited body of research , for instance, has found that periodontal disease is associated with a range of health conditions including diabetes, heart disease, respiratory infections and dementia.
Exactly how oral bacteria affect your overall health is still poorly understood, Dr. Bray said, since the existing research is limited and no studies have established cause-and-effect.
But some conditions are more associated with oral health than others, experts say. Here is what we know.
The health issues linked with oral health
About 47 percent of people aged 30 years and older in the United States have some form of periodontal disease, according to the Centers for Disease Control and Prevention.
In its early stages, called gingivitis, the gums may become swollen, red or tender and may bleed easily. If left untreated, gingivitis may escalate to periodontitis, a more serious form of the disease where gums can recede, bone can be lost, and teeth may become loose or even fall out.
With periodontitis, bacteria and their toxic byproducts can move from the surface of the gums and teeth and into the bloodstream, where they can spread to different organs, said Ananda P. Dasanayake, a professor of epidemiology at the New York University College of Dentistry.
This can happen during a dental cleaning or flossing, or if you have a cut or wound inside your mouth, he said.
If you have inflammation in the mouth that is untreated, some of the proteins responsible for that inflammation can spread throughout the body, Dr. Bray said, and potentially damage other organs.
Of all the associations between oral health and disease, the one with the most evidence is between periodontal disease and diabetes, Dr. Bray said. And the two conditions seem to have a two-way relationship , she added: Periodontal disease seems to increase the risk for diabetes, and vice versa.
Researchers have yet to understand exactly how this might work, but in one review published in 2017 , researchers wrote that the systemic inflammation caused by periodontal disease may worsen the body’s ability to signal for and respond to insulin.
In another study , published in April, scientists found that diabetics who were treated for periodontal disease saw their overall health care costs decrease by 12 to 14 percent.
“You treat periodontal disease, you improve the diabetes,” Dr. Dasanayake said.
If large amounts of bacteria from the mouth are inhaled and settle in the lungs, that can result in bacterial aspiration pneumonia , said Dr. Frank Scannapieco, a professor of oral biology at the University at Buffalo School of Dental Medicine.
This phenomenon has been observed mainly in patients who are hospitalized or older adults in nursing homes, and is a concern for those who can’t floss or brush their teeth on their own, said Dr. Martinna Bertolini, an assistant professor of dental medicine at the University of Pittsburgh School of Dental Medicine.
Preventive dental care such as with professional teeth cleanings, or periodontal treatments like antibiotic therapy, can lower the risk of developing this kind of pneumonia, Dr. Scannapieco said.
Cardiovascular disease
In a report published in 2020 , an international team of experts concluded that there is a significant link between periodontitis and heart attack, stroke, plaque buildup in the arteries, and other cardiovascular conditions.
While researchers haven’t determined how poor oral health might lead to worse heart health, some evidence suggests that periodontal bacteria from the mouth may travel to the arteries in vascular disease patients, potentially playing a role in the development of the disease.
And a 2012 statement from the American Heart Association noted that inflammation in the gums has been associated with higher levels of inflammatory proteins in the blood that have been linked with poor heart health.
Some research also suggests that better oral hygiene practices are linked with lower rates of heart disease.
For example, in a study published in 2019 , researchers reviewed the health records of nearly 250,000 healthy adults living in South Korea and found that over about 10 years, those who regularly brushed their teeth and received regular dental cleanings were less likely to have cardiovascular events than those who had poorer dental hygiene, formed more cavities, experienced tooth loss or developed periodontitis.
Pregnancy complications
A number of studies and reviews have found associations between severe periodontal disease and preterm, low birth weight babies, Dr. Dasanayake said. Though more research is needed to confirm the link.
In a 2019 review , researchers found that treating periodontal disease during pregnancy improved birth weight and reduced the risk of preterm birth and the death of the fetus or newborn.
And in a 2009 study , researchers found that oral bacteria could travel to the placenta — potentially playing a role in chorioamnionitis, a serious infection of the placenta and amniotic fluid that could lead to an early delivery, or even cause life-threatening complications if left untreated.
Research also suggests that bacteria from your mouth may activate immune cells that circulate in the blood, causing inflammation in the womb that could distress the placenta and fetal tissues.
There is longstanding research that periodontitis may induce preterm birth in animals like mice, and that treating these infections can protect against low birth weights and preterm birth.
Researchers have been increasingly interested in the role of oral health in dementia, particularly Alzheimer’s disease, Dr. Scannapieco said.
“Bacteria that are found in the mouth actually have been identified in the brain tissue of patients with Alzheimer’s,” he said, implying a potential role for them in the disease.
In a recent review , scientists noted that oral bacteria — especially those related to periodontitis — could either affect the brain directly via “infection of the central nervous system,” or indirectly by inducing “chronic systemic inflammation” that reaches the brain.
However, there’s no evidence that oral bacteria alone could cause Alzheimer’s, the review authors wrote. Rather, periodontal disease is just one “risk factor” among many for people who are predisposed to Alzheimer’s or other forms of dementia.
Other conditions
Oral bacteria have also been robustly linked with a number of other conditions such as rheumatoid arthritis and osteoporosis , Dr. Bray said. And emerging research is starting to link oral bacteria with kidney and liver disease, as well as colorectal and breast cancers .
But more research is needed to confirm all of these links, the experts said. And we still don’t know if regular dental care and periodontal treatments may help prevent or improve any of the conditions mentioned above, Dr. Scannapieco said.
What you can do
The best way to maintain good oral health is to follow the classic dental care advice , including brushing your teeth twice a day and flossing every day, Dr. Scannapieco said.
“Not all people really appreciate their oral health, and they’re only reminded of it when they have a toothache or some pain,” he added. But it’s important to be just as diligent and proactive about your oral health as you are with exercise or diet or any other aspect of well-being.
Hannah Seo is a reporting fellow for The Times, covering mental and physical health and wellness. More about Hannah Seo
Oral Health

“There is no health without oral health.” You may have heard this statement but what does it mean? The health of our mouth, or oral health, is more important than many of us may realize. It is a key indicator of overall health, which is essential to our well-being and quality of life.
Although preventable to a great extent, untreated tooth decay (or cavities) is the most common health condition worldwide. When we think about the potential consequences of untreated oral diseases including pain, reduced quality of life, lost school days, disruption to family life, and decreased work productivity, making sure our mouths stay healthy is incredibly important. [1]
What is a Healthy Mouth?
The mouth, also called the oral cavity, starts at the lips and ends at the throat. A healthy mouth and well-functioning teeth are important at all stages of life since they support human functions like breathing, speaking, and eating. In a healthy mouth, tissues are moist, odor-free, and pain-free. When we talk about a healthy mouth, we are not just talking about the teeth but also the gingival tissue (or gums) and the supporting bone, known together as the periodontium. The gingiva may vary in color from coral pink to heavily pigmented and vary in pattern and color between different people. Healthy gingiva is firm, not red or swollen, and does not bleed when brushed or flossed. A healthy mouth has no untreated tooth decay and no evidence of lumps, ulcers, or unusual color on or under the tongue, cheeks, or gums. Teeth should not be wiggly but firmly attached to the gingiva and bone. It should not hurt to chew or brush your teeth.
Throughout life, teeth and oral tissues are exposed to many environmental factors that may lead to disease and/or tooth loss. The most common oral diseases are tooth decay and periodontal disease. Good oral hygiene and regular visits to the dentist, combined with a healthy lifestyle and avoiding risks like excess sugar and smoking, help to avoid these two diseases.
Oral Health and Nutrition: What You Eat and Drink Affects Your Teeth
Just like a healthy body, a healthy smile depends on good nutrition. A balanced diet with adequate nutrients is essential for a healthy mouth and in turn, a healthy mouth supports nutritional well-being. Food choices and eating habits are important in preventing tooth decay and gingival disease.
Minerals like calcium and phosphorus contribute to dental health by protecting and rebuilding tooth enamel. [2] Enamel is the hard outer protective layer of the tooth (fun fact: enamel is the hardest substance in the human body). Eating foods high in calcium and other nutrients such as cheese , milk , plain yogurt , calcium-fortified tofu , leafy greens , and almonds may help tooth health. [2] While protein-rich foods like meat, poultry, fish, milk and eggs are great sources of phosphorus.
When it comes to a healthy smile, fruits and vegetables are also good choices since they are high in water and fiber , which balance the sugars they hold and help to clean the teeth. [2] These foods also help stimulate saliva, which helps to wash away acids and food from teeth, both neutralizing acid and protecting teeth from decay. Many fruits and vegetables also have vitamins like vitamin C , which is important for healthy gingiva and healing, and vitamin A, another key nutrient in building tooth enamel.[2]
Water is the clear winner as the best drink for your teeth—particularly fluoridated water. It helps keep your mouth clean and helps fight dry mouth. Fluoride is needed regularly throughout life to protect teeth against tooth decay. [3] Drinking water with fluoride is one of the easiest and most beneficial things you can do to help prevent cavities.

Is carbonated water a healthy choice for my teeth?

How snacking can affect your dental health
Malnutrition and oral health.
Nutrition and oral health are closely related. The World Health Organization defines malnutrition as deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients. This means that malnutrition can be over-nutrition or undernutrition. Dental pain or missing teeth can lead to difficulty chewing or swallowing food which negatively affects nutrition. This may mean eating fewer meals or meals with lower nutritional value due to impaired oral health and increased risk of malnutrition. On the other hand, lack of proper nutrients can also negatively affect the development of the oral cavity, the progression of oral diseases and result in poor healing. [5] In this way, nutrition affects oral health, and oral health affects nutrition.
Nutrition is a major factor in infection and inflammation. [5] Inflammation is part of the body’s process of fighting against things that harm it, like infections and injuries. Although inflammation is a natural part of the body’s immune response to protect and heal the body, it can be harmful if it becomes unbalanced. In this way inflammation is a dominant factor in many chronic diseases. Periodontal diseases and obesity are risk factors involved in the onset and progression of chronic inflammation and its consequences. [6]
Oral Health and General Health
While it may appear that oral diseases only affect the mouth, their consequences can affect the rest of the body as well. There is a proven relationship between oral and general health. Many health conditions may increase the risk of oral diseases, and poor oral health can negatively affect many general health conditions and the management of those conditions. Most oral diseases share common risk factors with chronic diseases like cardiovascular disease , cancers , diabetes , and respiratory diseases. These risk factors include unhealthy diets, particularly those high in added sugar, as well as tobacco and alcohol use. [7]
Infective endocarditis (IE), an infection of the inner lining of the heart muscle, can be caused by bacteria that live on teeth. [8] Gingivitis and periodontitis are inflammatory diseases of the gingiva and supporting structures of the teeth caused by specific bacteria. There is evidence that the surface of inflamed tissue around teeth is the point of entry for the specific bacteria that cause as much as 50% of the IE cases in the U.S. annually. This means that improving oral hygiene may help in reducing the risk of developing IE. In addition, periodontal disease may be associated with heart disease and shares risk factors including tobacco use, poorly controlled diabetes , and stress . [9,10]
Oral health is an important part of prenatal care. Poor oral health during pregnancy can result in poor health outcomes for both mother and baby. For example, studies suggest that pregnant women who have periodontal disease may be more likely to have a baby that is born too early and too small. [7] Hormonal changes during pregnancy, particularly elevated levels of progesterone, increase susceptibility to periodontal disease, which includes gingivitis and periodontitis. For this reason, your dentist may recommend more frequent professional cleanings during your pregnancy.
If you are struggling with morning sickness, the stomach acid from vomiting can erode or wear away tooth enamel. To help prevent the effects of erosion, rinse your mouth with 1 teaspoon of baking soda mixed in a cup of water, then wait 30 minutes before brushing your teeth. [11]
Conditions that impact oral health
Certain conditions may also affect your oral health, including:
- Anxiety and stress. Stress is a normal human reaction that everyone experiences at one point or another. However, stress that is left unchecked can contribute to many health problems including oral health issues. While behavioral changes play a leading role in these poor oral health findings, there are certain physiological effects on the body as well. Stress creates a hormone in the body called cortisol. Spikes in this hormone can weaken the immune system and increase susceptibility to developing periodontal disease. Evidence has shown that stress reduces the flow of saliva which in turn can contribute to dental plaque formation. [12] Certain medications like antidepressants and anti-anxiety medications can also cause dry mouth, increasing risk of tooth decay. Additionally, stress may contribute to teeth grinding (or bruxism), clenching, cold sores, and canker sores.
- Osteoporosis and Paget’s Disease . Medical conditions such as osteoporosis are a fitting example of why it is so important to let your dentist know about all the medications you are taking. Certain medications like antiresorptive agents, a group of drugs that slows bone loss, can influence dental treatment decisions. That is because these medications have been associated with a rare but serious condition called osteonecrosis of the jaw (ONJ), which can damage the jawbone. Bisphosphonates (Fosamax, Actonel, and Boniva) and Denosumab (or Prolia) are examples of antiresorptive agents. Although it can occur spontaneously, ONJ more commonly occurs following surgical dental procedures like extracting a tooth or implant placement. Be sure to tell your dentist if you are taking antiresorptive agents so they can take that into account when developing your treatment plan.

A healthy, pain-free mouth can lead to a better state of mind!
Eating concerns: what to eat if you have….
Depending on the type of orthodontic treatment, your braces may have brackets, bands, and wires. In this case, it is important to avoid eating hard or sticky food. This includes things like nuts, popcorn, hard candy or gum, which could break or displace parts of your orthodontics and potentially delay your treatment. Enjoying pasta, soft veggies, fruits, and dairy products are good choices. Having good oral hygiene is key in making sure tooth decay do not form around the braces. This means making sure the teeth and braces are thoroughly cleaned of food debris so that plaque does not accumulate. Allowing plaque to build-up can cause white spots on the surfaces of the teeth. You can ask your dentist for tips on how to maintain good oral hygiene.
If you have clear trays or aligners that are removable, you should always remove your trays before eating or drinking any liquid other than water. Regardless of whether food is hard or soft, removing your tray before eating helps to ensure effectiveness of your treatment.
If you wear dentures, adjusting to what and how you eat can be a major challenge. When you first get dentures, your mouth and tissue need time to adjust to chewing and biting. Starting with soft foods like soups, smoothies, and applesauce for your first few meals can help make the transition more comfortable. Be mindful of hot dishes and drinks as it can sometimes be difficult to gauge the temperature of your food. After a couple of days, you can move onto more solid foods as your mouth begins to adjust to the dentures. Take care to avoid hard or sticky food and tough meats which could break or damage your dentures. Denture-friendly foods include slow-cooked or ground meats, cooked fish, ripe fruits, and cooked vegetables. A good tip is that if you can cut the food with a fork, chances are the food will not damage your dentures.
Dry mouth or xerostomia can make it difficult to talk, chew, and swallow food. Symptoms of dry mouth may include increased thirst, sore mouth and tongue, difficulty swallowing and talking, and changes in taste. [14] If you are experiencing a dry mouth, it is important to talk to your oral health care provider (as well as primary care provider) to better understand the potential causes and management. Regardless of the cause, you have lots of options for making it easier to eat. First, ensure that you drink plenty of fluids and sip cold water between meals. Chew your food well if you’re having trouble swallowing and only take small bites. Combining solid foods with liquid foods such as yogurt, gravy, sauces, or milk can also help. You want to avoid foods that are acidic, hot, or spicy as these may irritate your mouth further. Good oral care also plays a key role in alleviating dry mouth and preventing tooth decay, which is a common oral complication of dry mouth.
Oral Health Tips
Here are some actions you can take to support good oral health: [15]
- Drink fluoridated water and brush with fluoride toothpaste.
- Practice good oral hygiene. Brush teeth thoroughly twice a day and floss daily between the teeth to remove dental plaque.
- Visit your dentist at least once a year (the average person should go twice a year), even if you have no natural teeth or have dentures.
- Do not use any tobacco products. If you smoke, seek resources to help you quit.
- Limit alcoholic drinks. Some alcoholic beverages can be very acidic, resulting in erosion of tooth enamel, and those with a high alcohol content can lead to dry mouth. Also be mindful of drink mixers, many of which are high in sugar and can increase the risk of tooth decay.
- If you have diabetes , work to support control of the disease. This will decrease the risk for other complications, including gum disease. Treating gum disease may help lower your blood sugar level.
- If your medication causes dry mouth, discuss other medication options with your doctor that may not cause this condition. If dry mouth cannot be avoided, drink plenty of water, chew sugarless gum, and avoid tobacco products and alcohol. Your oral health care provider may be able to recommend over-the-counter or prescription medications to improve your dry mouth as well.
- See your doctor or a dentist if you experience sudden changes in taste and smell.
- When acting as a caregiver, help those who are not able to brush and floss their teeth independently.
- Chew sugar-free xylitol gum between meals and/or when you are unable to brush after a meal.
Bottom Line – There Is No Health Without Oral Health
As growing research and studies reveal the link between oral health and overall health, it becomes more evident that taking care of your teeth isn’t just about having a nice smile and pleasant breath. Studies show that poor oral health is linked to heart disease, diabetes, pregnancy complications, and more, while positive oral health can enhance both mental and overall health. Good oral hygiene and regular visits to the dentist, combined with a healthy lifestyle and avoiding risks like excess sugar and smoking, help to keep your smile and body healthy.
- Oral Cavity (mouth) starts at the lips and ends at the throat including the lips, inside the cheeks and lips, the tongue, gums, under the tongue, and roof of the mouth.
- Enamel is the hard calcified tissue covering the surface of the tooth.
- Gingiva (gums) is the soft tissue covering the necks of the teeth and the jaw bones.
- Periodontium is a group of specialized tissues that surround and support the teeth, including the gingiva and bone.
- Periodontal disease (gum disease) includes gingivitis and periodontitis. Gingivitis is the mildest form, in which the gums become red, swollen, and bleed easily. Gingivitis is reversible with professional treatment and good at-home oral care. If untreated, gingivitis can advance to periodontitis where chronic inflammation causes the tissues and bone that support the teeth to be damaged. Overtime, teeth can become loose and may fall out or need to be removed. [16]
- Check out the Harvard School of Dental Medicine for more information and resources for oral health
- Peres MA, Macpherson LM, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreño CC, Kearns C, Benzian H. Oral diseases: a global public health challenge. The Lancet . 2019 Jul 20;394(10194):249-60.
- American Dental Association. n.d. Nutrition: What you eat affects your teeth . Mouth Healthy.
- Kohn WG, Maas WR, Malvitz DM, Presson SM, Shaddix KK. Recommendations for using fluoride to prevent and control dental caries in the United States. (2001).
- Chi DL, Scott JM. Added sugar and dental caries in children: a scientific update and future steps. Dental Clinics . 2019 Jan 1;63(1):17-33.
- Ehizele AO, Ojehanon PI, Akhionbare O. Nutrition and oral health. Benin Journal of Postgraduate Medicine. 2009;11(1).
- Suvan JE, Finer N, D’Aiuto F. Periodontal complications with obesity. Periodontology 2000 . 2018 Oct;78(1):98-128.
- Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. International journal of health sciences . 2017 Apr;11(2):72.
- Lockhart PB, Brennan MT, Thornhill M, Michalowicz BS, Noll J, Bahrani-Mougeot FK, Sasser HC. Poor oral hygiene as a risk factor for infective endocarditis–related bacteremia. The Journal of the American Dental Association . 2009 Oct 1;140(10):1238-44.
- Borrell LN, Papapanou PN. Analytical epidemiology of periodontitis. Journal of clinical periodontology . 2005 Oct;32:132-58.
- Lockhart PB, Bolger AF, Papapanou PN, Osinbowale O, Trevisan M, Levison ME, Taubert KA, Newburger JW, Gornik HL, Gewitz MH, Wilson WR. Periodontal disease and atherosclerotic vascular disease: does the evidence support an independent association? A scientific statement from the American Heart Association. Circulation . 2012 May 22;125(20):2520-44.
- American Dental Association. (n.d.). Pregnant? 9 Questions You May Have About Your Dental Health
- Reners M, Brecx M. Stress and periodontal disease. International journal of dental hygiene . 2007 Nov;5(4):199-204.
- American Dental Association. (n.d.). Osteoporosis and Oral Health .
- Cancer Treatment Centers of America. (n.d.). Dry mouth .
- Centers for Disease Control and Prevention. 2021. Oral Health Tips .
- The American Academy of Periodontology. (n.d.). Gum Disease Information .
Last reviewed December 2022
Terms of Use
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.
- Research article
- Open access
- Published: 14 July 2020
Incorporating oral health care education in undergraduate nursing curricula - a systematic review
- Vandana Bhagat ORCID: orcid.org/0000-0002-0158-1471 1 ,
- Ha Hoang ORCID: orcid.org/0000-0001-5116-9947 2 ,
- Leonard A. Crocombe ORCID: orcid.org/0000-0002-3916-0058 3 &
- Lynette R. Goldberg ORCID: orcid.org/0000-0002-8217-317X 4
BMC Nursing volume 19 , Article number: 66 ( 2020 ) Cite this article
9114 Accesses
27 Citations
1 Altmetric
Metrics details
The recognised relationship between oral health and general health, the rapidly increasing older population worldwide, and changes in the type of oral health care older people require have raised concerns for policymakers and health professionals. Nurses play a leading role in holistic and interprofessional care that supports health and ageing. It is essential to understand their preparation for providing oral health care.
Objective: To synthesise the evidence on nursing students’ attitudes towards, and knowledge of, oral healthcare, with a view to determining whether oral health education should be incorporated in nursing education.
Data sources : Three electronic databases - PubMed, Scopus, and CINAHL.
Study eligibility criteria, participants and interventions: Original studies addressing the research objective, written in English, published between 2008 and 2019, including students and educators in undergraduate nursing programs as participants, and conducted in Organisation of Economic Co-operation and Development countries.
Study appraisal and synthesis methods: Data extracted from identified studies were thematically analysed, and quality assessment was done using the Mixed Methods Appraisal Tool.
From a pool of 567 articles, 11 met the eligibility criteria. Findings documented five important themes: 1.) nursing students’ limited oral health knowledge; 2.) their varying attitudes towards providing oral health care; 3.) the need for further oral health education in nursing curricula; 4.) available learning resources to promote oral health; and 5.) the value of an interprofessional education approach to promote oral health care in nursing programs.
Limitations: The identified studies recruited small samples, used self-report questionnaires and were conducted primarily in the United States.
Conclusions
The adoption of an interprofessional education approach with a focus on providing effective oral health care, particularly for older people, needs to be integrated into regular nursing education, and practice. This may increase the interest and skills of nursing students in providing oral health care. However, more rigorous studies are required to confirm this. Nursing graduates skilled in providing oral health care and interprofessional practice have the potential to improve the oral and general health of older people.
Peer Review reports
Introduction
Oral health is measured by the absence of orofacial pain, oral infection, periodontal (gum) diseases, tooth decay, tooth loss, and other orofacial diseases and disorders that can affect a person’s overall physical and mental health, and social well-being [ 1 , 2 , 3 ]. This is a particular concern for older people [ 2 , 3 , 4 , 5 ]. The world’s population is ageing rapidly [ 4 ]. Living longer brings challenges when meeting the complex healthcare needs of many older people and ensuring their quality of life. Currently, there is a profound disparity in the oral health of the older population, even in high-income countries [ 5 ].
Worldwide, the oral health of older people, defined as those over 65 years of age, is poor with a high prevalence of dental caries, periodontal diseases, dry mouth problems, and incremental tooth loss [ 5 , 6 ]. Oral health problems often lead to malnutrition, and difficulty with speech and swallowing [ 7 ]. There is increasing evidence of the association of periodontal problems with systemic conditions including type II diabetes, osteoporosis, cardiovascular problems such as myocardial infarction, stroke, coronary heart disease, and aspiration pneumonia that may lead to unplanned hospitalisations [ 8 , 9 , 10 ]. Poor oral health impacts morbidity, mortality, and recovery time after treatment [ 11 , 12 ]. Pain and suffering resulting from oral health problems may influence older people’s mood and behaviour, particularly if they have difficulty in communicating their discomfort [ 13 ]. Poor dental appearance and bad breath can lower self-esteem and exacerbate social isolation [ 14 ]. Thus, oral health problems can have profound physical, psychological, social, and economic consequences.
Most oral health problems experienced by older people are preventable or treatable [ 15 ]. However, they remain underdiagnosed and untreated due to the lack of effective, efficient, and equitable distribution of oral health services [ 15 ]. Reasons for the inadequate delivery of oral health services to older people include limited resources, poor understanding of oral care among nursing staff, lack of interprofessional collaboration, and inadequate policy protocols [ 16 , 17 ]. The lack of time, competing priorities, a high workload, and staffing issues are also significant barriers for providing oral care to older people [ 18 ].
The provision of quality and timely oral health care services to the rapidly increasing older population has become a large challenge for policymakers and health professionals [ 9 , 19 , 20 ]. Many changes have occurred in the oral health care needs of the older population in the twenty-first century due to the preservation of natural teeth, and the placement of complex prostheses such as crowns, bridges, overdentures, and implants. These changes highlight the need for staff trained in providing oral health care to older people [ 21 , 22 ]. With increasing age and ill-health, many people need assistance with their oral and general health care [ 23 , 24 ]. This is particularly true for dependent older adults in residential care communities and hospitals. However, oral health care is a low priority for non-dental health professionals [ 6 , 25 , 26 , 27 ].
Interprofessional education and collaborative practice have been recognised as a valuable approach to alleviate the global health workforce crisis and prepare a health workforce that will better respond to local health needs and ensure safe, holistic practice [ 28 ]. The World Dental Federation (FDI) also supports the need for interprofessional education and collaborative practice to improve access to oral health services [ 29 ]. Involving nurses, primary health care workers, and other allied health professionals in oral health care, will increase the national capacity to reach vulnerable and underserved population groups, including older people [ 6 ]. Nurses account for a large proportion of the health care workforce and are often present at the point of care or supervising direct caregivers [ 30 , 31 ]. Therefore, oral health care education and training are essential for graduating nurses to improve the oral and systemic health of older people [ 32 , 33 , 34 , 35 , 36 ]. Such education and practice provided with an interprofessional approach enables nursing students to contribute, learn and work effectively with other professionals involved in oral health [ 29 ].
Nurses provide care to older people in various settings such as hospitals, residential aged care, rehabilitation units, as well as in the community. Community nurses can educate and empower older people to take an active role in their oral care to prevent oral problems [ 37 ]. Nurses working in residential communities can take a leadership role in ensuring oral health care is integrated into routine nursing care [ 38 ]. Nurses can screen each resident’s oral health upon admission, assess the need for an examination by a dental professional, and prepare and monitor an oral health care plan [ 25 , 39 , 40 ]. Registered nurses can train and supervise personal care assistants in providing support to residents to maintain oral hygiene, monitor adequate nutrition, and identify signs of oral diseases [ 33 ]. Similarly, in hospitals, nurses can promote oral health, screen for any suspicious oral pathology, and make appropriate referrals [ 41 ]. Given interprofessional support, nurses can improve and maintain the oral health of older people when immediate access to an oral health therapist is not available [ 23 ].
To synthesise the evidence on nursing students’ attitudes towards, and knowledge of, oral health care, with a view to determining whether oral health education should be incorporated in nursing education. To our best knowledge, no previous study has summarised the literature on this topic.
Research questions
What do nursing students understand about oral health care?
What are the attitudes of nursing students towards providing oral health care?
Is there evidence of oral health education and training in nursing curricula?
A systematic review was performed following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 42 ].
Eligibility criteria
Original studies addressing the research questions, written in English, published between 2008 and 2019, including students and educators in undergraduate nursing programs as participants, and conducted in Organisation of Economic Co-operation and Development (OECD) countries. The review excluded studies involving students from certificate nursing courses, graduate nursing programs, and midwives. Studies reported in conference proceedings, short communications, thesis, or book chapters were also excluded.
Information sources and search
Three electronic databases were searched: PubMed, Scopus, and CINAHL. Boolean operators with the following keywords and strategy were used: (oral care OR dental health OR oral health OR dental care OR mouth care OR oral hygiene) AND (nursing students OR nurse students OR nurse undergraduates OR nurse educators) AND (curriculum OR curricula OR knowledge OR understanding OR learning OR teaching OR attitudes OR interprofessional education OR interdisciplinary education). A detailed example of the search strategy used for Scopus is outlined (Fig. 1 ). This search strategy was adapted for each of the databases.
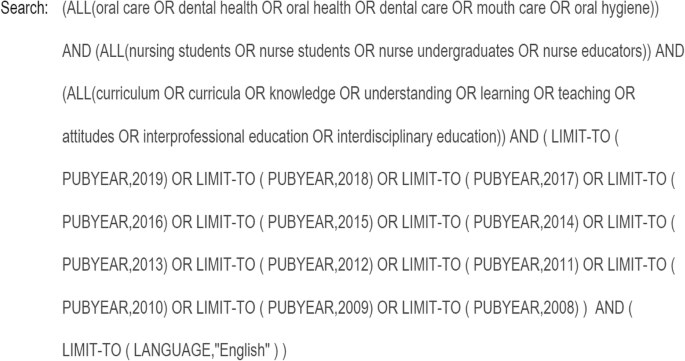
Full electronic search strategy
Study selection
All original studies, including quantitative, qualitative, and mixed-method studies, were selected if they met the eligibility criteria. After an initial search and removing duplicates from the search list, titles and abstracts were independently screened by two authors (VB, HH) and the full texts of identified papers were then sought. Studies not fitting the eligibility criteria were excluded before the full text was reviewed. In cases of disagreement, two additional authors (LC, LG) were consulted to resolve any conflicts. Disagreements were resolved with consensus by referring back to the protocol. Research data were synthesised systematically, and the quality of the included studies was then evaluated.
Data extraction
The data collection form was developed by two authors (VB, HH) referring to previous systematic reviews in the related field; data extraction was then performed independently by VB. The accuracy of the extracted data was verified by the second author (HH). Information collected from the identified articles for this systematic review included: country and setting, details of participants, objectives of the study, research design, description of the main findings related to the three research questions, and the reported limitations of each study (Table 1 ).
Data synthesis
Extracted data were analysed thematically to produce a narrative description of the findings. While thematic synthesis is commonly used for qualitative research outcomes, it can be used for quantitative research outcomes when there is heterogeneity in measurements. Therefore, the process of thematic synthesis was chosen to narrate the findings of this review [ 53 ]. The thematic analysis was conducted according to Braun and Clarke’s guidelines: familiarisation with the data, coding, developing potential themes, reviewing themes, defining themes and reporting data relating to research questions [ 54 ]. The coding process involved segmenting data into similar groups and identifying the relationship between codes. After finishing the coding process, codes were grouped into descriptive themes that captured similarities in the data across identified studies. Finally, selected themes were reviewed, and synthesised data were finalised in relation to the research questions.
A meta-analyses of the identified studies was not possible because of the small number of studies, participants, and heterogeneity.
Quality assessment
The quality assessment of the identified studies was done by two authors (VB, HH) using the Mixed Methods Appraisal Tool (MMAT) [ 55 ]. All studies were screened regarding the clarity of their research questions, and whether collected data addressed the research questions. Studies that passed the screening were then appraised using methodological quality assessment questions relative to the study design. Studies that met all assessment criteria scored 1; studies that met fewer criteria scored less than 1.
From a pool of 567 articles, 11 met the eligibility criteria (Fig. 2 ). A large number of articles were excluded based on the wording of their titles (482), 49 were excluded from reading the abstract, and a further 25 were excluded after reading the full text. Finally, 11 studies were included in this paper. Of the 11 studies, six were conducted in the United States, two in Australia, and one each in Japan, Turkey, and Canada. Studies evaluating nursing students’ oral health knowledge and attitudes of oral health care used cross-sectional survey design; intervention studies assessing the impact of the inclusion of oral health components in nursing curricula used quasi-experimental pre-post survey design, post-survey design, retrospective pre-post survey design, and cross-sectional qualitative design. The study evaluating oral health care resources for older people used a mixed-method design.
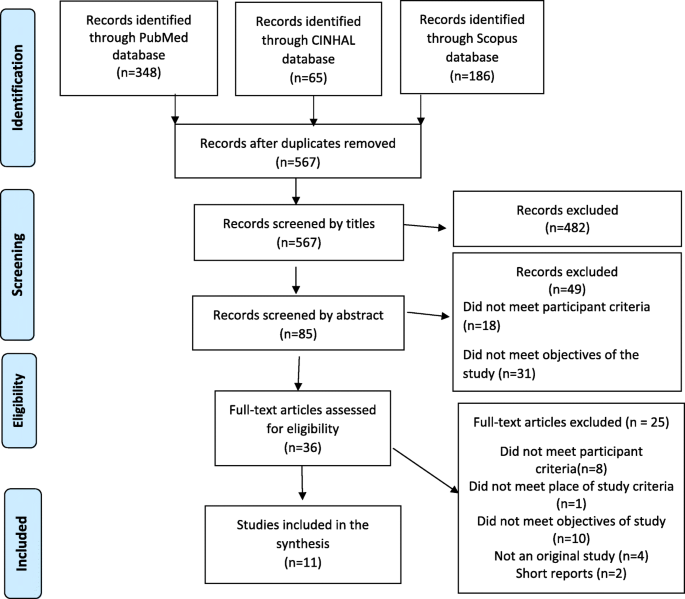
PRISMA flowchart detailing search results and the selection of studies
The main findings of the 11 identified studies were 1.) nursing students’ limited oral health knowledge; 2.) their varying attitudes towards providing oral health care; 3.) the need for further oral health education in nursing curricula; 4.) available learning resources to promote oral health; and 5.) the value of an interprofessional education (IPE) approach to promote oral health care in nursing programs. The results of the quality assessment of the identified papers are shown in Tables 2 , 3 , 4 and 5 .
Synthesis of results: five identified themes
Limited knowledge of oral health care among nursing students.
Only three studies [ 31 , 43 , 45 ] assessed the oral health knowledge of nursing students. Using convenience samples ranging from 30 to163 students, each study used different questionnaires. Data were collected from students belonging to a single university or at different campuses of the same university. Studies conducted in the US and Japan showed students had limited oral health care knowledge and inadequate understanding of the crucial elements of an oral health assessment and promotion of effective oral health practices [ 43 , 45 ]. Only 25% of all participants in the US-based study by Clemmens et al. [ 43 ] were able to recognise the critical components of oral health assessment, despite a majority of students thinking they understood these components. In Japan, Haresaku et al. [ 45 ] found that only half of the nursing students knew that oral health diseases could have an impact on systemic health. An earlier study by Pai et al. [ 31 ] in Australia showed nursing students understood issues related to periodontal diseases; however, the majority of participants were not confident about their understanding and recommended including more detailed oral health content in their nursing curriculum.
Varying attitudes of nursing students towards oral health care
Three studies conducted in the US [ 43 ], Japan [ 45 ], and Turkey [ 44 ] evaluated the attitudes of nursing students towards providing oral health care. Clemmens et al. [ 43 ] found that nursing students felt oral health care to be an essential component for effective nursing practice. A different trend was observed in nursing students from Turkey and Japan. Nursing students from Turkey often avoided going to a dentist until they developed a painful oral condition [ 44 ]. In Japan, the attitudes of nursing students toward oral health appeared negative, with 39.2% of students stating that they were not interested in learning about oral health and practice [ 45 ].
Need for further oral health care education for nursing students
Seven of the 11 studies provided suggestions for including an oral health component in nursing curricula. Six of the seven studies [ 46 , 47 , 48 , 50 , 51 , 52 ] focussed on an interprofessional oral health education model. The remaining study [ 49 ] provided information about resources for older people’s oral health care for nursing curricula.
Available learning resources for nursing students to promote oral health
Lewis et al. [ 49 ] evaluated the relevance of “Building Better Oral Health Communities” (BBOHC) resources for students undertaking a Bachelor of Nursing, Diploma of Nursing, or Certificate III in Aged Care. The BBOHC resources were developed as a part of the Australian government-funded project for aged care workforce training in older people’s oral health care [ 13 ]. The BBOHC consists of five modules: 1) better oral health care, 2) dementia and oral care, 3) understanding the mouth, 4) care for natural teeth, and 5) care for dentures. Participating students were highly satisfied with the content of this resource [ 49 ]. Student learning outcomes showed consistently positive attitudes and substantial enhancements in oral health care knowledge and skills. Educators found the BBOHC content highly relevant in reinforcing a comprehensive approach to older people’s oral health care, which included learning about the consequences of poor health, dry mouth problems, oral health assessment, oral health planning, and timely referral. Educators also found the resources useful in building students’ skills in daily oral hygiene practice by increasing awareness about oral hygiene products, tooth brushing techniques, denture cleaning, and techniques to manage care resistive behaviours [ 49 ].
Value of an Interprofessional education model
An interprofessional education (IPE) model in which nursing students work with, learn from, and contribute to the oral-systemic knowledge of dental and other allied health students has been found effective in improving understanding of nursing students towards their role in oral health care [ 46 , 47 , 48 , 50 , 51 , 52 ]. All the studies focussing on IPE were conducted in the US except the study by Grant et al. [ 46 ], which was conducted in Canada.
As a result of their IPE experiences in lectures and simulation exercises, nursing students showed significant improvement in oral health behaviour, knowledge, and attitudes regarding the importance of oral health care [ 47 , 52 ]. Interprofessional education and practice experiences also increased nursing students’ confidence in conducting oral examinations and providing counselling [ 50 ]. IPE provided the platform for students to explore oral-systemic disease connections in a supportive team culture [ 46 , 48 , 51 ]. IPE helped nursing students to learn oral risk assessments, identify common oral pathologies, engage in oral hygiene activities, use fluoride varnish and work with students from other professions to promote oral health [ 47 ]. IPE clinical experiences focussing on oral-systemic health were valuable in enhancing shared professional skills with hands-on care, facilitating effective communication, and working as a team to develop an integrated plan of care to ensure holistic care [ 50 , 51 ]. Nursing students’ experiences in interprofessional clinical practice were instrumental in understanding how underserved and rural communities could benefit from accessing multiple providers at one place on the same day [ 50 ].
Summary of evidence
This review of 11 identified studies documented limited oral health knowledge and varying attitudes (both favourable and unfavourable) of nursing students towards oral health care. The review identified available learning resources and highlighted the importance of an interprofessional education and practice approach in improving oral health knowledge and attitudes among nursing students.
Growing evidence of the relationship between poor oral health and general systemic health requires urgent attention. The inclusion of oral health care education in nursing curricula, integrated with an interprofessional approach, will strengthen the capability and interest of future nurse practitioners to include evidence-based effective oral health care in routine nursing care. It is important to understand that “oral health care” can be interpreted differently by different health professionals [ 56 ]. For nursing practice, oral health care includes collaboration with dental, medical, and allied health professionals. For nursing students, this entails understanding the factors affecting people’s oral health and oral health-related quality of life, ensuring daily oral care practice, and being able to complete an oral health screening. Such screening includes checking the status and function of oral structures and dentures, swallowing ability, nutritional status, asking each person’s perspective about their oral and general health and whether they have any concerns, and making appropriate referrals. Daily oral care for older people in residential care includes assisting with evidence-based oral hygiene, use of saliva substitutes when appropriate, water hydration, desensitising agents, lip balms, denture cleaning tablets, pastes and adhesive pastes, and fluoride varnishes.
Older people are at particular risk for poor oral health. This review showed a significant gap in the current literature on nursing students’ knowledge of oral health care for older people and how this gap is best addressed through interprofessional education and practice. Interprofessional education and practice is one of the best ways to improve both nursing students’ awareness of the importance of oral health and their role in improving access to and providing oral health services [ 48 , 57 ]. IPE facilitates collaborative work in varying health care settings including educational institutes [ 52 ], dental health clinics [ 47 ], mobile clinics in underserved areas [ 48 ] and hospitals [ 51 ]. While challenges remain in coordinating curricula across disciplines to facilitate students’ involvement in IPE initiatives, providing nursing students with opportunities to include oral health assessments in their assessment of overall body function would significantly improve the health outcomes of older people [ 32 , 58 ]. IPE models have been implemented successfully in many graduate nursing programs in addition to undergraduate nursing programs [ 46 , 59 , 60 , 61 , 62 , 63 ]. The “Smile for Life-National Oral Health Curriculum” has been popular with graduate nursing students [ 17 , 59 , 62 , 63 , 64 ]. This comprehensive oral health curriculum was initially developed in 2005 for primary health workers. It is freely available online and could be readily integrated into IPE activities in nursing curricula ( www.smilesforlifeoralhealth.com ) [ 65 ].
Implementing IPE into nursing curricula requires thought, time, and careful planning to ensure that students from other health-related programs can participate [ 46 , 63 , 66 ]. Organising IPE with students and faculty from different health programs with different health knowledge makes IPE challenging [ 48 ]. Flexibility, willingness, and cooperation among all professionals are needed for effective collaborative and interprofessional learning [ 46 ]. Establishing academic credit for students participating in IPE is an effective way to involve and encourage students in collaborative learning about oral health [ 46 , 66 ].
Effective oral health education must include clinical practice and ideally interprofessional clinical practice. The best way to translate oral health learning to practice is to shift from the traditional physical assessment approach that is Head, Eyes, Ears, Nose, Throat (HEENT) to the Head, Eyes, Ears, Nose, Oral cavity, and Throat (HEENOT) approach for the assessment, diagnosis, and treatment of oral-systemic health [ 17 ]. The HEENOT approach ensures that one does “NOT” leave oral health assessment out of any medical history and physical examination. The success of the HEENOT approach was evidenced by more than 1000 referrals to the Nursing Faculty Practice (NFP) from New York University (NYU) dental clinics between 2008 and 2014. The HEENOT approach resulted in increased care appointments and more than 500 referrals to NYU dental clinics from the NFP [ 17 ]. Another collaborative model provided students in nursing, dental hygiene, and health services management with community-based experience providing affordable oral health services and oral health education [ 67 ]. Nursing students’ involvement in early detection of oral health issues and appropriate, timely referral to a dentist can ensure minimal cost treatment and improve patient-centred care [ 31 ].
This systematic review is a valuable initial step in identifying the current knowledge and attitudes of nursing students towards providing oral health care and recognising factors to reinforce their interest in oral health care, particularly for older people [ 45 ]. Results have several implications for nursing students, nursing educators, nursing education accreditation authorities, and researchers. Nursing students need to understand the importance of oral health, the relationship of poor oral health to systemic disease, the importance of their competency in oral health practices, and their important role in maintaining the health of older people. Oral health education and practical experience occur best in an interprofessional situation to build confidence, motivation, knowledge, and skills. Nursing educators need to understand and implement an interprofessional approach to oral health education and practice in nursing curricula. Nursing education accreditation authorities need to pay attention to develop guidelines to promote oral health care learning and practice among nursing students who are future health professionals. IPE improves workplace practices and productivity, patient health outcomes, staff morale, patient safety, and enables better access to health care [ 28 ]. Ongoing rigorous research is required to understand the extent to which oral health is addressed in nursing curricula in Australia and to evaluate the inclusion and impact of oral health content, delivered through interprofessional education and clinical practice, in undergraduate nursing curricula.
Limitations
Most of the reviewed studies were conducted in the United States and had small sample sizes belonging to a single location; therefore, the results cannot be generalised. Some intervention studies had quasi-experimental designs, and there was a lack of blinding of the intervention leading to questions on the trustworthiness of the study results. Self-report questionnaires were used in the identified studies which may be biased by respondent beliefs. The long-term evaluation results of an integrated oral health learning model are still not available to check the effectiveness of IPE in building nursing students’ capacity in oral healthcare delivery.
This review supports the need to integrate oral health education into nursing curricula, ideally through an IPE approach, to increase nursing students’ knowledge and ability to provide oral care, particularly to maintain the health of older people, and to interest students in providing effective oral care. There is a need to conduct rigorous well-designed studies about how best to achieve this and measure its success. A future nursing workforce with competence in oral health care will help to improve the oral health and quality of life of all people, especially those who are older and dependent on others for care.
Availability of data and materials
All data generated or analysed during this study is included in this article.
Abbreviations
Cumulative Index to Nursing and Allied Health Literature
Organisation of Economic Co-operation and Development
Interprofessional education
Mixed Methods Appraisal Tool
Building Better Oral Health Communities
Head, Eyes, Ears, Nose, Oral cavity, and Throat
New York University
Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Br Dent J. 2016;221(12):792–3.
CAS PubMed Google Scholar
Petersen PE. The World Oral Health report 2003: continuous improvement of oral health in the 21st century - the approach of the WHO global Oral Health Programme. Community Dent Oral Epidemiol. 2003;31(SUPPL. 1):3–24.
PubMed Google Scholar
World Health Organisation. Oral Health. 2020 [cited 17 June 2020]. Available from: https://www.who.int/news-room/fact-sheets/detail/oral-health . Accessed 17 June 2020.
World Health Organisation. Ageing and Health. 2018 [cited 17 June 2020]. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health . Accessed 17 June 2020.
Gil-Montoya JA, Ferreira de Mello AL, Barrios R, Gonzalez-Moles MA, Bravo M. Oral health in the elderly patient and its impact on general well-being: a nonsystematic review. Clin Interventions in Aging. 2015;ume 10:461–7.
Petersen PE, Kandelman D, Arpin S, Ogawa H. Global oral health of older people--call for public health action. Community Dent Health. 2010;27(4 Suppl 2):257–67.
Hopcraft MS. Dental demographics and metrics of oral diseases in the ageing Australian population. Aust Dent J. 2015;60(Suppl 1):2–13.
Gutkowski S. The biggest wound: oral health in long-term care residents. Annals of Long Term Care: Clinical Care and Ageing. 2011;19(7):23–5.
Kandelman D, Petersen PE, Ueda H. Oral health, general health, and quality of life in older people. Special Care Dentistry. 2008;28(6):224–36.
Google Scholar
Seymour GJ, Ford PJ, Cullinan MP, Leishman S, Yamazaki K. Relationship between periodontal infections and systemic disease. Clin Microbiol Infection. 2007;13(S4):3–10.
CAS Google Scholar
Awano S, Ansai T, Soh I, Hamasaki T, Yoshida A, Takehara T, et al. Oral health and mortality risk from pneumonia in the elderly. J Dent Res. 2008;87(4):334–9.
El-Solh AA. Association between pneumonia and Oral Care in Nursing Home Residents. Lung. 2011;189(3):173.
SA Health. Why oral health care is important for older people. 2020 [cited 17 June 2020] Available from: https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/clinical+resources/clinical+programs+and+practice+guidelines/oral+health/oral+health+care+for+older+people/why+oral+health+care+is+important+for+older+people .
Kisely S. No mental Health without Oral Health. Can J Psychiatry. 2016;61(5):277–82.
PubMed PubMed Central Google Scholar
Kossioni AE, Hajto-Bryk J, Maggi S, McKenna G, Petrovic M, Roller-Wirnsberger RE, et al. An Expert Opinion from the European College of Gerodontology and the European Geriatric Medicine Society: European Policy Recommendations on Oral Health in Older Adults 2018:609.
Hearn L, Slack-Smith L. Engaging dental professionals in residential aged-care facilities: staff perspectives regarding access to oral care. Australian J Primary Health. 2016;22(5):445–51.
Haber J, Hartnett E, Allen K, Hallas D, Dorsen C, Lange-Kessler J, et al. Putting the mouth back in the head: HEENT to HEENOT. Am J Public Health. 2015;105(3):437–41.
Hoang H, Barnett T, Maine G, Crocombe L. Aged care staff’s experiences of ‘better Oral Health in residential care training’: a qualitative study. Contemp Nurse. 2018;54(3):268–83.
Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33(2):81–92.
Thomson W, Ma S. An ageing population poses dental challenges. Singap Dent J. 2014;35C:3–8.
Bailey R, Gueldner S, Ledikwe J, Smiciklas-Wright H. The oral health of older adults: an interdisciplinary mandate. J Gerontol Nurs. 2005;31(7):11–7.
Forsell M, Sjögren P, Kullberg E, Johansson O, Wedel P, Herbst B, et al. Attitudes and perceptions towards oral hygiene tasks among geriatric nursing home staff. Int J Dent Hyg. 2011;9(3):199–203.
Gibney JM, Wright FA, D'Souza M, Naganathan V. Improving the oral health of older people in hospital. Australasian J Ageing. 2019;38(1):33–8.
Jablonski RA, Kolanowski A, Therrien B, Mahoney EK, Kassab C, Leslie DL. Reducing care-resistant behaviors during oral hygiene in persons with dementia. BMC Oral Health. 2011;11:30.
Malkin B. The importance of patients’ oral health and nurses’role in assessing and maintaining it. Nurs Times. 2008;105:19–23.
Albrecht M. Oral health educational interventions for nursing home staff and residents. Cochrane Database of Systematic Reviews. (9).
Wårdh I, Hallberg LR, Berggren U, Andersson L, Sörensen S. Oral health care--a low priority in nursing. In-depth interviews with nursing staff. Scand J Caring Sci. 2000;14(2):137–42.
World Health Organisation. Framework for action on interprofessional education and collaborative practice 2010 [cited 17 June 2020]. Available from: https://www.who.int/hrh/resources/framework_action/en/ . Accessed 17 June 2020.
FDI World Dental Federation. Optimal Oral Health through inter-professional education and collaborative practice. 2015 [Available from: https://www.fdiworlddental.org/sites/default/files/media/news/collaborative-practice_digital.pdf ]. Accessed 17 June 2020.
Dolce MC. Integrating oral health into professional nursing practice: an interprofessional faculty tool kit. J Professional Nurs. 2014;30(1):63–71.
Pai M, Ribot B, Tane H, Murray J. A study of periodontal disease awareness amongst third-year nursing students. Contemporary Nurse. 2016;52(6):686–95.
Dolce MC, Haber J, Shelley D. Oral health nursing education and practice program. Nurs Res Pract. 2012;2012:149673.
Rohr. Assessment and care of the mouth: An essential nursing activity, especially for debilitated or dying inpatients. HNE handover for nurses and midwives. 2012;5(1):33–4.
Young LM, Machado CK, Clark SB. Repurposing with purpose: creating a collaborative learning space to support institutional Interprofessional initiatives. Med Reference Services Quarterly. 2015;34(4):441–50.
Hoyles A, Pollard C, Lees S, Glossop D. Nursing students' early exposure to clinical practice: An innovation in curriculum development. Nurse education today. 2000;20:490–8.
Grønkjær LL, Nielsen N, Nielsen M, Smedegaard C. Oral health behaviour, knowledge, and attitude among nursing students. J Nurs Educ Practice. 2017;7(8):1–6.
Daly B, Smith K. Promoting good dental health in older people: role of the community nurse. Brit J Community Nurs. 2015;20(9):431–6.
Hoben M, Kent A, Kobagi N, Huynh KT, Clarke A, Yoon MN. Effective strategies to motivate nursing home residents in oral care and to prevent or reduce responsive behaviors to oral care: a systematic review. PLoS One. 2017;12(6):e0178913.
Tetuan T. The role of the nurse in oral health. Kansas Nurse. 2004;79(10):1–2.
Moore K. Oral health progress in Kansas. Kansas Nurse. 2004;79(10):8–10.
Garry B, Boran S. Promotion of oral health by community nurses. Brit J Community Nurs. 2017;22(10):496–502.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Clemmens D, Rodriguez K, Leef B. Knowledge, attitudes, and practices of baccalaureate nursing students regarding oral health assessment. J Nurs Educ. 2012;51(9):532–5.
Doğan B. Differences in oral health behavior and attitudes between dental and nursing students. J Marmara University Institute of Health Sciences. 2013;3(1):34–40.
Haresaku S, Monji M, Miyoshi M, Kubota K, Kuroki M, Aoki H, et al. Factors associated with a positive willingness to practise oral health care in the future amongst oral healthcare and nursing students. Eur J Dental Educ. 2018;22(3):e634–e43.
Grant L, McKay LK, Rogers LG, Wiesenthal S, Cherney SL, Betts LA. An interprofessional education initiative between students of Dental Hygiene and Bachelor of Science in Nursing. Can J Dent Hyg. 2011;45(1):36–44.
Czarnecki GA, Kloostra SJ, Boynton JR, Inglehart MR. Nursing and dental students' and pediatric dentistry residents' responses to experiences with interprofessional education. J Dent Educ. 2014;78(9):1301–12.
Farokhi MR, Muck A, Lozano-Pineda J, Boone SL, Worabo H. Using Interprofessional education to promote Oral Health literacy in a faculty-student collaborative practice. J Dent Educ. 2018;82(10):1091–7.
Lewis A, Edwards S, Whiting G, Donnelly F. Evaluating student learning outcomes in oral health knowledge and skills. J Clin Nurs. 2018;27(11–12):2438–49.
Nierenberg S, Hughes LP, Warunek M, Gambacorta JE, Dickerson SS, Campbell-Heider N. Nursing and Dental Students' reflections on Interprofessional practice after a service-learning experience in Appalachia. J Dent Educ. 2018;82(5):454–61.
Coan LL, Wijesuriya UA, Seibert SA. Collaboration of Dental hygiene and nursing students on hospital units: an Interprofessional education experience. J Dent Educ. 2019;83(6):654–62.
Dsouza R, Quinonez R, Hubbell S, Brame J. Promoting oral health in nursing education through interprofessional collaborative practice: a quasi-experimental survey study design. Nurse Educ Today. 2019;82:93–8.
Ryan C, Hesselgreaves H, Wu O, Paul J, Dixon-Hughes J, Moss JG. Protocol for a systematic review and thematic synthesis of patient experiences of central venous access devices in anti-cancer treatment. Syst Rev. 2018;7(1):61.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34:285-91.
Koichiro U. Preventing aspiration pneumonia by oral health care. Japan Med Assoc J. 2011;54:39–43.
Goldberg LR, Koontz JS, Rogers N, Brickell J. Considering accreditation in gerontology: the importance of interprofessional collaborative competencies to ensure quality health care for older adults. Gerontol Geriatrics Educ. 2012;33(1):95–110.
Hein C, Schönwetter DJ, Iacopino AM. Inclusion of oral-systemic health in predoctoral/undergraduate curricula of pharmacy, nursing, and medical schools around the world: a preliminary study. J Dent Educ. 2011;75(9):1187–99.
Dolce MC, Parker JL, Marshall C, Riedy CA, Simon LE, Barrow J, et al. Expanding collaborative boundaries in nursing education and practice: the nurse practitioner-dentist model for primary care. J Professional Nurs. 2017;33(6):405–9.
Estes KR, Callanan D, Rai N, Plunkett K, Brunson D, Tiwari T. Evaluation of an Interprofessional Oral Health assessment activity in advanced practice nursing education. J Dent Educ. 2018;82(10):1084–90.
Golinveaux J, Gerbert B, Cheng J, Duderstadt K, Alkon A, Mullen S, et al. Oral health education for pediatric nurse practitioner students. J Dent Educ. 2013;77(5):581–90.
Haber J, Hartnett E, Allen K, Crowe R, Adams J, Bella A, et al. The impact of Oral-systemic Health on advancing Interprofessional education outcomes. J Dent Educ. 2017;81(2):140–8.
Nash WA, Hall LA, Lee Ridner S, Hayden D, Mayfield T, Firriolo J, et al. Evaluation of an interprofessional education program for advanced practice nursing and dental students: the oral-systemic health connection. Nurse Educ Today. 2018;66:25–32.
Kent KA, Clark CA. Open wide and say A-ha: adding Oral Health content to the nurse practitioner curriculum. Nurs Educ Perspect. 2018;39(4):253–4.
Clark MB DA MR, Deutchman M, Gonsalves W, Silk H, Wrightson AS, Quinonez R, Dolce M, Dalal M, Rizzolo D, Sievers K. Smiles for Life: A National Oral Health Curriculum. 2010. Available from: https://www.smilesforlifeoralhealth.com .
Goldberg LR, Brown GR, Mosack VA, Fletcher PA. Student reflections following exposure to a case-based interprofessional learning experience: preliminary findings. J Interprofessional Care. 2015;29(4):380–2.
Duley SI, Fitzpatrick PG, Zornosa X, Barnes WG. A center for oral health promotion: establishing an inter-professional paradigm for dental hygiene, health care management and nursing education. J Dental Hygiene. 2012;86(2):63–70.
Download references
Acknowledgments
We would like to thank all the authors of the studies included in this systematic review. Also, we would like to thank the Centre for Rural Health and the University of Tasmania for providing opportunities for the first author to develop her research skills.
We would also like to thank the reviewers of this manuscript for providing valuable feedback to strengthen the manuscript.
The first author is supported by a Department of Health, Rural Health Multidisciplinary Training Program, and the University of Tasmania Research Scholarship for her doctoral studies.
The funding bodies played no part in the design of the study, collection, analysis and, interpretation of data, nor in writing this manuscript.
Author information
Authors and affiliations.
Centre for Rural Health (CRH), E Block, Newnham Campus, University of Tasmania (UTas), Launceston, Australia
Vandana Bhagat
CRH, E block, Newnham Campus, UTas, Launceston, Australia
CRH, ABC Building, 1 Liverpool Street, Hobart, Hobart CBD Campuses, UTas, Hobart, Australia
Leonard A. Crocombe
Wicking Dementia Research & Education Centre, Room 421C (Level 4), Medical Science 1, UTas, Hobart, Australia
Lynette R. Goldberg
You can also search for this author in PubMed Google Scholar
Contributions
All authors made a substantial contribution to this review. All authors together set the protocols for this review. VB performed the data search and retrieval. Titles and abstracts were independently screened by two authors (VB, HH). VB was involved in data extraction and drafted the manuscript. VB and HH did the methodological quality assessment of all studies. HH, LC, LG revised the subsequent manuscript drafts for content and structure. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Vandana Bhagat .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bhagat, V., Hoang, H., Crocombe, L.A. et al. Incorporating oral health care education in undergraduate nursing curricula - a systematic review. BMC Nurs 19 , 66 (2020). https://doi.org/10.1186/s12912-020-00454-6
Download citation
Received : 15 March 2020
Accepted : 28 June 2020
Published : 14 July 2020
DOI : https://doi.org/10.1186/s12912-020-00454-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Oral health
- Older people
- Understanding
- Interprofessional
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Home — Essay Samples — Nursing & Health — Dentistry — The Importance Of Oral Health
The Importance of Oral Health
- Categories: Dentistry Medicare
About this sample

Words: 1213 |
Published: Nov 26, 2019
Words: 1213 | Pages: 3 | 7 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof Ernest (PhD)
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
3 pages / 1533 words
2 pages / 839 words
1 pages / 673 words
3 pages / 1215 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Dentistry
As a passionate and enthusiastic individual interested in the field of dentistry, I am excited to share my personal statement with you. Throughout this essay, I will provide insight into my educational and professional [...]
Dental hygiene is a crucial aspect of overall health, and as a dental hygienist, you play a vital role in ensuring that patients maintain good oral health. To be successful in this field, it is essential to possess a combination [...]
When asked, “Why do you want to be a dentist?”, one common answer is “they make so much money, and they get to make their own schedules.” Although those are perks that dentists receive, that was not what drew me to dentistry. I [...]
In conclusion, my dream to be a dentist is driven by my passion for oral health, my desire to make a positive impact on people's lives, and my commitment to lifelong learning. Despite the challenges that lie ahead, I am [...]
Periodontium consists of fibrous periodontal ligament which attaches cementum of the tooth to the alveolar bone. The bulk of Periodontal ligament contains neurovascular elements. Cyclic masticatory forces between two mineralized [...]
Time management is crucial ion all the field works. Whoever, it may be a learner, a practitioner, or a renowned doctor, everyone need to manage the time for their best growth. It’s a skill that always leaves a room for better [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Introduction
The etiology and pathogenesis of dental caries, preventive strategies, caries risk assessment, anticipatory guidance, dietary counseling, oral hygiene, other important anticipatory guidance topics, collaboration with dental providers, social determinants of children’s oral health, conclusions, recommendations for pediatricians, lead authors, section on oral health executive committee, 2019–2020, liaisons, 2019–2020, maintaining and improving the oral health of young children.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
David M. Krol , Kaitlin Whelan , THE SECTION ON ORAL HEALTH; Maintaining and Improving the Oral Health of Young Children. Pediatrics January 2023; 151 (1): e2022060417. 10.1542/peds.2022-060417
Download citation file:
- Ris (Zotero)
- Reference Manager
Oral health is an integral part of the overall health of children. Dental caries is a common and chronic disease process with significant short- and long-term consequences. The prevalence of dental caries remains greater than 40% among children 2 to 19 years of age. Although dental visits have increased in all age, race, and geographic categories in the United States, disparities continue to exist, and a significant portion of children have difficulty accessing dental care. As health care professionals responsible for the overall health of children, pediatricians frequently confront morbidity associated with dental caries. Because the youngest children visit the pediatrician more often than they visit the dentist, it is important that pediatricians be knowledgeable about the disease process of dental caries, prevention of disease, interventions to maintain and restore health, and the social determinants of children’s oral health.
Dental caries is the most common chronic disease of childhood, despite increased dental visits. 1 Twenty-three percent of US children 2 to 5 years of age, 52% of children 6 to 8 years of age, and 57% of youth 12 to 19 years of age have caries. 2 Total prevalence of dental caries in youth 2 to 19 years of age in 2015 to 2017 was 45.8%. 3 Significant disparities persist in the receipt of childhood preventive dental care, with young children, uninsured children, children living in poverty, non-Hispanic Black children, children from non–English-speaking households including immigrants and refugees, and children with special health care needs less likely to receive needed preventive oral health care. 2 – 5 American Indian/Alaska Native children have the highest rates of dental caries in the United States. 6 The reasons for these disparities are multifactorial and further explained in the Indian Health Service Data Brief “Oral Health of American Indian and Alaska Native Children Aged 1–4 Years: Results of the 2018–19 IHS Oral Health Survey” and in the American Academy of Pediatrics (AAP) policy statement “Early Childhood Caries in Indigenous Communities,” which focuses on the specific challenges within this population. 6 , 7 There have been slight improvements over time. There has been a 10-percentage point decrease in untreated tooth decay in the primary teeth of children 2 to 5 and 6 to 8 years of age and the permanent teeth of adolescents 12 to 19 years of age when comparing 2011–2016 data with 1999–2004. Mexican American children, children near the poverty line, and children below the poverty line saw improvements in untreated tooth decay; however, disparities continue to persist. 2
A dynamic process takes place at the surface of the tooth that involves constant demineralization and remineralization of the tooth enamel (the caries balance). 8 , 9 Multiple factors affect that dynamic process and can be manipulated in ways that tip the balance toward disease (demineralization) or health (remineralization). These factors include bacteria, sugar, saliva, and fluoride. Because these factors can be manipulated, it is possible for pediatricians and families to prevent, halt, or even reverse the disease process.
Different oral structures and tissues have different and distinct microbial communities (microbiomes). 10 The oral microbiome at the surface of the tooth is referred to as dental plaque. During the disease process of dental caries, bacteria that are aciduric and acidogenic predominate in the dental plaque. Streptococcus mutans is most commonly associated with dental caries, although a larger pathogenic community exists. 11 When environmental factors make it possible to select for these pathogenic bacteria in dental plaque, the disease process begins.
A key environmental factor that allows for selection and proliferation of these pathogenic bacteria is dietary sugar intake. Because these bacteria have the ability to ferment sugars, produce acid, and decrease the pH of the dental plaque, they make possible the selection of other aciduric, acidogenic bacteria that will contribute to disease. As more bacteria produce more acid, the pH at the surface of the tooth decreases. This process causes the demineralization of the tooth enamel. Unimpeded, these long periods of low pH and demineralization will result in cavitation.
Saliva is an important factor in buffering the low pH and bringing these demineralization pressures back to a balance with remineralization. 12 In addition to acting as a buffering agent, saliva also flushes the oral cavity of food particles, provides an environment rich in calcium and phosphate to aid in remineralization, and includes proteins that have antimicrobial activity. When salivary flow is impeded (eg, by disease, iatrogenic), the pH is able to decrease to a lower level, tipping the scales toward demineralization (disease). In addition, the time it takes to buffer back to a normal pH is longer. 12
Another important factor that can affect the balance of demineralization and remineralization is fluoride. More in-depth reviews of fluoride are available elsewhere. 13 – 15 It is important, however, for pediatricians and other child health care providers to understand how fluoride influences the caries balance. Fluoride has 3 key effects on the caries balance: (1) inhibition of demineralization at the tooth surface, (2) enhancement of remineralization, which results in a more acid-resistant tooth surface, and (3) inhibition of bacterial enzymes. 15 The primary effect of fluoride is topical, via fluoridated toothpastes, mouth rinses, varnishes, and silver diamine fluoride, although there is still value in systemic fluoride exposures via fluoridated water and supplements. 15 – 17
Ideally, primary prevention efforts will anticipate and prevent caries before the first sign of disease. Preventive strategies for this multifactorial, chronic disease require a comprehensive and multifocal approach that begins with caries risk assessment. Assessing each child’s risk of caries and tailoring preventive strategies to specific risk factors are necessary for maintaining and improving oral health. There is no single tool that takes into consideration all risk factors and accurately predicts an individual’s susceptibility to caries. However, pediatricians can monitor oral health, both in the office and via telehealth, by focusing on the key risk factors for dental caries associated with diet, bacteria, saliva, and status of the teeth (ie, current and previous caries experience). Consistent with Bright Futures guidelines, pediatricians can perform an oral health screening examination of the mouth at each well-child visit to look for signs of caries. Each visit is an opportunity to assess risk, discuss risk reduction, modify behaviors, and identify goals for improving oral health. The AAP/ Bright Futures Oral Health Risk Assessment Tool, which includes photographs of clinical findings on the examination of the oral cavity, can be found at https://downloads.aap.org/AAP/PDF/oralhealth_RiskAssessmentTool.pdf.18 .
Sugars (but not sugar substitutes) are a critical risk factor in the development of caries. 19 , 20 This does not include sugars that are naturally occurring and present in whole fruit and vegetables or dairy products. The risk of caries is greatest if sugars are consumed at high frequency (and, thus, high amount) and are in a form that remains in the mouth for long periods of time. 19 Examples of key behaviors that place a child at high risk for caries include continual bottle/sippy cup use (with fluids other than water), sleeping with a bottle (with fluids other than water), frequent between-meal snacks of sugars/cooked starch/sugared beverages, sticky foods (raisins, fruit snacks, and gummy vitamins for example), and frequent intake of sugared medications.
The most important and predictive risk factor for caries is previous caries experience. This finding is not surprising, considering the factors that initiated the disease process often continue to exist over time. Early acquisition of S. mutans is also a major risk factor for early childhood caries and future caries experience. 21 Strong evidence demonstrates that mothers are a primary source of S. mutans colonization for their children (eg, utensil sharing, cleaning pacifier with mouth). 22 Thus, an important factor associated with caries risk in young children is the recent or current presence of active dental decay in the primary parent/caregiver. Because it is likely that bacteria will be vertically transmitted, prevention, diagnosis, and treatment of oral diseases in the child’s parent/caregiver are highly beneficial, especially during pregnancy. Dental care and treatment can be provided and is encouraged during pregnancy. There is no additional fetal or maternal risk compared with the risk of not providing dental care. 23
Abnormalities in salivary flow and the structure of the teeth are associated with caries development. Diseases (eg, diabetes mellitus, Sjögren’s syndrome, cystic fibrosis) and medications (eg, antihistamines, anticonvulsants, antidepressants) result in xerostomia (decreased salivary flow). Xerostomia causes reduced availability of saliva to buffer the acid produced by pathogenic bacteria, thus enhancing their ability to damage the tooth enamel. Variations in the anatomic structure of the teeth can also increase the risk of decay. For example, teeth with enamel defects, frequently found in children born preterm, are at increased susceptibility for disease, as are molars with deep pits and fissures. Finally, there is increasing evidence of an association between secondhand smoke exposure and dental caries in children. 24 , 25
Pediatricians can target anticipatory guidance to assist families in preventing dental caries by having a clear understanding of its etiology and the risk factors that lead to and facilitate the spread of this disease. Because the disease of dental caries is multifactorial, anticipatory guidance can also be multifaceted, with a focus on decreasing the risk of disease.
Because intake of sugars is such an important risk factor for dental caries, pediatricians can incorporate anticipatory guidance associated with preventing dental caries into conversations about dietary habits and nutritional intake. Risk of caries may be lower with exclusive breastfeeding for 6 months and continued breastfeeding as complementary foods are introduced for 1 year or longer, as mutually desired by the infant and breastfeeding parent. 26 To decrease the risk of dental caries and increase the chances for the best possible health and developmental outcomes, pediatricians can educate and provide guidance to families on establishing a bedtime routine conducive to optimal oral health (eg, the AAP Brush, Book, Bed program for parents). 27 , 28 Pediatricians can discourage parents/caregivers from putting a child to bed with a bottle to limit sugars on the teeth after brushing and encourage them to wean infants from a bottle by 1 year of age. Parents/caregivers can be counseled on the importance of reducing the frequency of exposure to added sugars in foods and drinks. 29 By limiting the amount and frequency of intake of foods with added sugars, as well as avoiding sugared beverages and juice drinks, caries risk is decreased. Pediatricians can encourage children to drink only water between meals, preferably fluoridated tap water, while discouraging 100% juice intake before 1 year of age, limiting juice to 4 ounces daily for children 1 to 3 years of age and to 4 to 6 ounces daily for children 4 to 6 years of age. 30 Lastly, providers can counsel families to foster eating patterns consistent with guidelines from the US Department of Agriculture. 31
The value of good oral hygiene lies in controlling the levels and activity of disease-causing bacteria in the oral cavity and delivering fluoride to the surface of the tooth. It is important to remember that pathogenic bacteria can be passed from parent/caregiver to child. 22 Thus, anticipatory guidance for both parent/caregiver and child is important. Pediatricians can encourage parents/caregivers to model and maintain good oral hygiene, including regular brushing, flossing, and having a relationship with their own dental provider. Parents/caregivers should be counseled on brushing of a child’s teeth twice a day as soon as the teeth erupt with a grain-of-rice–sized amount of fluoridated toothpaste. After the third birthday, a pea-sized amount can be used. Pediatricians can also encourage parent/caregiver assistance and supervision of brushing children’s teeth until mastery is obtained, usually at around 10 years of age. 32 , 33
The delivery of fluoride to the teeth includes community-based options (water fluoridation), self-administered modalities (fluoride toothpaste, rinses, and supplements), and professional applications (fluoride varnish and silver diamine fluoride). Fluoride is a critically important primary care preventive measure for families, especially those who do not have early and/or consistent ongoing dental care. As part of well-child anticipatory guidance, pediatricians can assess fluoride intake at each preventive visit, including the consumption of fluoridated tap water, and encourage families to protect their child’s teeth with regular delivery of oral and topical fluoride.
Water fluoridation is a community-based intervention that optimizes the level of fluoride in drinking water, resulting in preeruptive and posteruptive protection of the teeth. 34 Water fluoridation is a cost-effective means of preventing dental caries, with the lifetime cost per person equaling less than the cost of 1 dental restoration. 35 , 36 Most bottled waters do not contain an adequate amount of fluoride. Many families at higher risk for dental caries consume primarily bottled water, reducing potential exposure to fluoridated tap water. Fluoride supplements can be prescribed for children 6 months or older whose primary source of drinking water is deficient in fluoride. 16
Fluoride toothpaste is an important way to deliver fluoride to the surface of the tooth. Fluoride toothpaste has been shown to be effective in reducing dental caries in both primary and permanent teeth. 37 , 38 Fluoride mouth rinses are another strategy for topical fluoride application and are associated with reduction in caries in the permanent teeth of children and adolescents, most particularly in a school setting. 39
Fluoride varnish is a professionally applied, sticky resin of highly concentrated fluoride. Application of fluoride varnish 2 to 4 times a year, to either the primary or permanent teeth, is associated with a substantial reduction in dental caries. 40 , 41 In most states, pediatricians can apply fluoride varnish onto the teeth of young children and be paid for the service. The US Preventive Services Task Force recommends that primary care clinicians apply fluoride varnish to the primary teeth of all infants and children starting at the age of primary tooth eruption (B recommendation). 16 More details and recommendations on fluoride can be found in the AAP clinical report “Fluoride Use in Caries Prevention in the Primary Care Setting.” 14
Silver diamine fluoride is a colorless ammonia solution containing silver and fluoride ions that is applied to the tooth. It is used to arrest caries lesions in primary and permanent teeth, including those that have already cavitated to the dentin, and has been shown to be effective in arresting caries in children. 42 When applied to the tooth or any surface, it will stain the surface black. Pediatricians may see more children with such staining and should be aware of its source. Silver diamine fluoride treatment is best used as part of an ongoing caries management plan with the aim of optimizing individualized patient care consistent with the goals of a dental home. A dental home is the ongoing relationship between the dentist and the patient, inclusive of all aspects of oral health care delivered in a comprehensive, continuously accessible, coordinated, and family-centered manner. 43
A frequent topic of discussion with parents/caregivers is nonnutritive oral habits, such as use of pacifiers and thumb/digit sucking. The AAP recommends that parents/caregivers consider offering a pacifier at naptime and bedtime because of a protective effect of pacifiers on the incidence of sudden infant death syndrome after the first month of life. 44 Evaluation by a dentist is indicated for nonnutritive sucking habits that continue beyond 3 years of age. Pacifier suckers are less likely to develop malocclusions (ie, overjet) compared with digit suckers; however, longer duration of pacifier or digit sucking is associated with an increased risk of developing malocclusions. 45 Breastfeeding also decreases the risk of malocclusions. 46
Dental injuries are common. Twenty-five percent of all school-aged children experience some form of dental trauma. 47 Pediatricians can help prevent such trauma by encouraging parents/caregivers to cover sharp corners of household furnishings at the level of walking toddlers, recommend use of car safety seats, and be aware of electrical cord risk for mouth injury. Pediatricians can also encourage mouthguard use during sports activities in which there is a significant risk of orofacial injury (basketball, field hockey, and baseball, for example). 48 , 49 More information on dental trauma is available in the AAP clinical report “Management of Dental Trauma in a Primary Care Setting.” 50
The AAP, the American Academy of Pediatric Dentistry, the American Dental Association, American Dental Hygienists’ Association, and the American Association of Public Health Dentistry all recommend a dental visit for children by 1 year of age. Although pediatricians have the opportunity to provide early assessment of risk for dental caries and anticipatory guidance to prevent disease, it is also important that children establish a dental home.
Depending on where a pediatrician’s practice is located, there are different members of the dental team with whom they may need to coordinate care and may even include as part of their office staff. 51 In addition to dentists, dental hygienists, and dental assistants, some states have expanded scope of practice or even developed new oral health professionals. Such professionals include expanded function dental assistants, dental health aide therapists, dental therapists, advanced dental therapists, independent practice dental hygienists, community dental health coordinators, registered dental hygienists in alternative practice, public health dental hygienists, expanded practice dental hygienists, and others.
There are emerging data regarding pediatric health care providers’ dental referral behaviors and patterns. One study found that children 2 to 5 years of age who received a recommendation from their health care provider to visit the dentist were more likely to have a dental visit. 52 Another study found that children with more preventive well-baby visits between ages 1 and 2 years and ages 2 and 3 years were more likely to have earlier first dental examinations than children with fewer well-baby visits. 53 , 54 However, the number and timing of well-baby visits before 1 year of age were not significantly related to first dental examinations. The US Preventive Services Task Force found no study that evaluated the effects of referral by a primary care clinician to a dentist on caries incidence. 55 Early dental visits have been associated with decreased costs in most 56 – 58 but not all studies. 59
With early referral to a dental provider, there is an opportunity to maintain good oral health, prevent disease, treat disease early, and potentially decrease cost. Establishing such collaborative relationships between physicians and dentists at the community level is essential for increasing access to dental care for all children and improving their oral and overall health.
The determinants of oral health, like oral health itself, are multifaceted. The driving determinants of oral health include genetic and biological factors, health behaviors, access to care, physical environment, and social environment. 60 The focus of this clinical report, to this point, has been focused on biological factors, health behavior, and access to oral health services. The AAP, however, also recommends screening for risk factors related to social determinants of health during all patient encounters. 61 It is important for pediatricians to understand that an approach to children’s oral health must also address social determinants. These social determinants, such as poverty, racism, education, access to healthy foods, culture, and physical environment, as well as access to medical and dental care influence oral health status and oral health inequities in much the same way as they influence overall health and health inequity. Pediatricians can consider and address determinants of oral health at the child, family, and community level. 62 With a robust understanding of how social determinants influence oral health, pediatricians can advocate for policy, system, and environmental changes that create sustainable, comprehensive improvements in children’s oral health and oral health equity. Appropriate payment for screening for social determinants is necessary to facilitate the implementation of screening in pediatric practices.
Oral health is an integral part of the overall health and well-being of children. 63 Pediatricians who are familiar with the science of dental caries, capable of assessing caries risk, comfortable with applying various strategies of prevention and intervention, connected to dental resources, and familiar with the social determinants of children’s health can contribute considerably to the health of their patients. This clinical report, in conjunction with the oral health recommendations of the fourth edition of the AAP Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents , serves as a resource for pediatricians and other pediatric primary care providers to be knowledgeable about addressing dental caries. 64 Because dental caries is such a common and consequential disease process in the pediatric population and such an integral part of the overall health of children, it is essential that pediatricians include oral health in their daily practice of pediatrics.
Assess children’s oral health risks at health maintenance and other relevant visits.
Include anticipatory guidance for oral health as an integral part of comprehensive patient counseling.
Counsel parents/caregivers and patients on ways to reduce the frequency of exposure to sugars in foods and drinks.
Encourage parents/caregivers to maintain their own good oral health and to brush a child’s teeth at least twice a day as soon as teeth erupt with a smear or a grain-of-rice–sized amount of fluoride toothpaste, increasing to a pea-sized amount at 3 years of age.
Advise parents/caregivers to assist in and monitor brushing until 10 years of age.
Refer to the AAP clinical report, “Fluoride Use in Caries Prevention in the Primary Care Setting,” 14 for fluoride administration and supplementation decisions.
Be aware of the dental resources in your community as sources of referral and consultation.
Build and maintain collaborative relationships with local dental providers.
Recommend that every child has a dental home by 1 year of age.
Promote policy, system, and environmental changes that address social determinants of children’s oral health.
Advocate for insurance coverage by all payers for fluoride varnish as a preventive service, as recommended by the US Preventive Services Task Force.
David M. Krol, MD, MPH, FAAP
Kaitlin Whelan, MD, FAAP
Patricia A. Braun, MD, MPH, FAAP, Chairperson
Jeffrey M. Karp, DMDC Eve Kimball, MD, FAAP
Karen Sokal-Gutierrez, MD, MPH, FAAP
Anupama Rao Tate, DMD
John H. Unkel, DDS, MD, MPA, FAAP
Tooka Zokaie, MPH, CLSSGB, American Dental Association
Matt Crespin, MPH, RDH, American Dental Hygienists’ Association
John Fales, DDS, MS, American Academy of Pediatric Dentistry
Ngozi Onyema-Melton, MPH, CHES
Kera Beskin, MPH, MBA
Drs Krol and Whelan conceived and developed the draft clinical report and equally shared in revising the draft; and both authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Clinical reports from the American Academy of Pediatrics benefit from expertise and resources of liaisons and internal (AAP) and external reviewers. However, clinical reports from the American Academy of Pediatrics may not reflect the views of the liaisons or the organizations or government agencies that they represent.
The guidance in this report does not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.
All clinical reports from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.
This document is copyrighted and is property of the American Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication.
FUNDING: No external funding.
FINANCIAL/CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no potential conflicts to disclose.
American Academy of Pediatrics
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Insights into Various Aspects of Oral Health

Oral Health Promotion: Evidences and Strategies
Reviewed: 19 April 2017 Published: 20 September 2017
DOI: 10.5772/intechopen.69330
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Insights into Various Aspects of Oral Health
Edited by Jane Francis Manakil
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
3,515 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Overall attention for this chapters
Oral health promotion is for upliftment of oral health of community rather than an individual and has long‐term impact. Since Ottawa Charter for health promotion is implemented, significant advancements have happened in oral health promotion. Under comprehensive health programs, India has been running oral health promotion programs, and these evidences are shared here. Such examples are apt learning and execution to any part of world having similarities. The chapter put forward the strategic view points to consider further oral health promotion aspects and based on the needs. The authors have gathered various examples from national programs implemented in India. The authors discuss how these programs are linked to the Oral health promotion concept. For example, National tobacco control program which currently running across many states in India, how the banning on tobacco products near school premises helped to reduce the incidence is discussed. The worldwide literature and evidences of oral health promotion strategies are explained. The evidences and strategies mentioned can be significant for another region of world. Unless published, many programs remain hidden and are loss of valuable evidences to oral health science.
- oral health
- oral health promotion
- school health
- dental health
Author Information
Vikram r. niranjan *.
- Queen Mary University of London, UK and S.D. Dental College, Parbhani, India
Vikas Kathuria
- Consultant Dentist, Hadi Hospital, Jabriya, Kuwait
Venkatraman J
- Department of Pathology, Mahatma Gandhi Medical college and Research Institute, Puducherry, India
Arpana Salve
- Senior Registrar, Skin & VD Department, Government Medical College & Hospital, Aurangabad, India
*Address all correspondence to: [email protected]
1. Introduction
The twentieth century was noteworthy in dentistry for many epidemiologic advances that occurred in the study of oral diseases and conditions. These combined efforts of optimum personal, social, biological, behavioral and environmental factors contributed to better oral health. Hence, oral health promotion is a planned effort to build public policies, create supportive environments, strengthen community action, develop personal skills or reorient health services pertaining to influence above factors. Following are enlisted examples of effective oral health promotion:
Promotion of healthy eating
Training of relevant oral hygiene methods
Access to preventive oral health services at the earliest
Promotion of topical fluoride application [ 1 ].
Ottawa Charter principles form a sound base for oral health promotion. This suggest that individuals alone are not at risk but the entire population, which needs to be involved in directing action towards the causes of ill health. Importantly, three principles, that is, partnership, participation and protection, are taken into consideration while planning a public health program or intervention. Empowerment than compelling is the key for successful Oral health promotion while achieving good oral health [ 2 ].
The purpose of this article is threefold. First, it reviews the relevance of need of oral health promotion particularly through the public health surveillance of oral disease burden. Second, it puts forward the evidences from the various examples of oral health promotion programs integrated into general health promotion carried across the India. Finally, the authors briefly discuss the strategies for expanding frame of oral health promotion.
2. Oral health promotion through Ottawa Charter
Health promotion programs achieve success through actions that influence the social, physical, economic and political determinants of health. Health promotion irrefutably acknowledges the broader health determinants and focuses on risk reduction via sensitive policies and actions. Ideally, promotion of health in a day‐to‐day life setting having people live, work, learn and play is credible for efficacious and cost‐effective way of improving oral health and indeed the quality of life. Imperatively, actions that address the determinants of health should not be progressed in isolation. Research evidences suggests that isolated activities can have limited impact, particularly over the long term. For this reason, we suggest using the logic model based on Ottawa Charter to develop a comprehensive oral health promotion program, involving a range of interventions.
The Ottawa Charter was developed by the World Health Organization 1 (WHO) as a framework for constructing health promotion programs that address the wider determinants of health. The charter suggests that programs be built around the following five action areas:
Building healthy public policy
Creating supportive environments
Strengthening community action
Developing personal skills
Reorientating health services [ 2 ].
3. Need for oral health promotion
The remarkable improvements in oral health over the past half century reflect the strong science base for prevention of oral diseases that has been developed and applied in the community, in clinical practice and in the home. Yet, despite the remarkable achievements in recent decades, millions of people worldwide have been excluded from the benefits of socioeconomic development and the scientific advances that have improved health care and quality of life. Social and cultural determinants comprising poverty, lack of education, unsupportive traditions, cultures and beliefs increase the relative risk of oral disease and conditions. For instance, lack of safe water and sanitary facilities are the environmental risk factors for both oral and general health. While, access to high sugar containing foods and unhealthy dietary habits may lead to higher risk of dental caries in certain communities. Improvement in availability, accessibility and feasibility of oral health services can definitely cure and control oral diseases. However, strong evidences suggest that limiting the risks to disease is best possible when health services are primary care and prevention oriented. Clinically, oral health status is measured in terms of causal factors, that is, tobacco, sugar, micro‐flora, which have negative impact on quality of life. Emphasizing the risk behavior modifications, such as curbing use of tobacco and alcohol; restraining sugar intake in terms of quantity, intake frequency and nature; proper oral hygiene practices, is equally important incongruent to social and cultural determinants [ 3 ].
The Global Burden of Disease (GBD) 2010 Study produced comparable estimates of the burden of 291 diseases and injuries in 1990, 2005 and 2010. Pertaining to oral health, dental caries, aggressive periodontitis and tooth loss are considered as global burden, which compared from 1990 to 2010. Criteria used were disability adjusted life‐years (DALYs) and years lived with disability (YLDs) metrics to quantify burden. These oral diseases/conditions encroached 3.9 billion. Among all, prevalence of dental caries in permanent teeth was among the highest prevalent condition evaluated for the entire GBD 2010 study (global prevalence of 35% for all ages combined). Among the top 100 ranking as causes of DALYs, oral diseases also secured a ranking after some serious diseases. Oral diseases altogether affected 15 million DALYs globally with the breakdown as 1.9% of all YLDs; 0.6% of all DALYs. Statistical calculations imply that could be average health loss of 224 years per 100,000 populations. While there was reduction observed for other diseases from 1990 to 2010, DALYs due to oral conditions increased by 20.8%. This was due to population overgrowth and aging. DALYs due to aggressive periodontitis and dental caries increased, however due to extensive tooth loss has decreased. While DALYs differed by age groups and regions, those not by genders. The report revealed the challenging scenario of diversified oral health needs across the globe, with alarming needs in developing countries. Further, the burden of oral diseases has unevenly risen in the past 20 years.
As the noted prevalence of oral diseases is very high and has association with disability, it accounted for a substantial number of DALYs. Dental caries without any treatment was the most prevalent condition among all 291 conditions. Moreover, the disability weight in connection with extensive tooth loss (0.073) was marginally neared to those reported for moderate heart failure (0.068) and moderate consequences of stroke (0.074). Oral diseases received ranking of 31st, 34th and 35th of health outcomes causing YLDs in the category of non‐fatal outcomes. Compared to other non‐communicable diseases/conditions, such as maternal conditions, hypertensive heart disease, schizophrenia, hemoglobinopathies and hemolytic anemias, oral diseases/conditions were ranked higher. While oral conditions scored high index for more YLDs than 25 of 28 categories of cancer, shows its significance in terms of affecting individuals equal to lethal diseases. The other organ cancers, such as stomach, liver and trachea, and bronchus and lung cancers ranked higher than oral diseases [ 4 ].
The global burden of oral conditions is shifting from extensive tooth loss toward aggressive periodontitis and untreated dental caries. Tooth loss is a final common pathway when preventive or conservative treatments to alleviate pain fail or are unavailable. The social, economic, political and cultural determinants of health are significant, and it may be argued that better health can be achieved by reducing poverty. Poverty, poor education and inequality not only result in poor oral health but also affect the way in which people think about their oral health. In spite of excellent oral health care, oral diseases are prevalent. This suggests that improving healthcare services merely will not address the issue, oral health promotion is mandatory. Hence, health policymakers should be made aware of these evidences and directs themselves to restructure the policy framework. Health promotion policy acknowledges complimentary measures such as legislation, fiscal measures, taxation and organizational change altogether. These are best example of a coordinated effort towards creating supportive environments and strengthening community action. Ottawa Charter implementation for health promotion through establishing concrete and effective community actions in setting priorities, making decisions, planning strategies leads to achieve better health. Communities facilitate themselves with self‐help, social support, participation and ownership for development and empowerment. They are the best possible existing human and material resources of community and for community.
Oral health promotion through sensitive health policies and actions which already exist in some parts of world can address the global burden of oral diseases, essentially to improve oral health and quality of life.
4. Evidences: country examples from India
Identifying a significant health issue on the basis of prevalence, incidence, severity, cost, or impact on quality of life is preliminary step to design prevention programs. A combination of community, professional and individual strategies is the cost‐effective and creative methods for oral disease prevention. Incorporating public, practitioners and policymakers into strategic development of oral disease prevention and health promotion intervention is necessary. They should be liable to create a healthy setting, limit risk factors, inform target groups, generate knowledge and thus improve behaviors. This section includes a discussion of knowledge and practices of the public and healthcare providers regarding the oral health promotion. The purpose of this discussion is not to outline specific health promotion strategies to enhance knowledge and practices but to indicate the opportunities and needs for both broad‐based and targeted health promotion programs and activities.
4.1. Oral health promotion in health promoting schools (HPS)
Oral health education has been considered as one of the fundamentals in oral health promotion [ 5 , 6 ]. With education, a child receives training and encouragement especially to stimulate development of skills, aptitude formation and creation of values, which lead to act positively in relation to his oral health and other people’s oral health on a daily basis. High caries risk, change in dentition, ability to change bad habits and facilities to learn make oral health promotion for children a priority. The importance of oral health education programs in schools is significantly reported predominantly in the form of positive learning and behavior in children [ 5 – 11 ].
One‐fifth of the world’s population is adolescent, defined by WHO as a person between 10 and 19 years of age. The oral health promotion programs should primarily focus on this age group who become easy victims of excessive consumption of sweets, sugary beverages, tobacco and alcohol. Commonly, their main association is with home, school and community organizations. These three along with oral health professionals can form an effective alliance to control risks to oral diseases and form oral health promotion programs for young people [ 12 ]. Prevalence of dental caries and gingivitis is high in human populations throughout the world, and over 80% of schoolchildren are affected in some parts of the world. Dental erosion due to excessive carbonated beverages consumption is on rise, which was earlier noticed only among the late adulthood. Enamel defects due to malnourishments, dental trauma due to negligence and safety barriers are some of the increasing evidences in children. Moreover, youth became the easy targets of tobacco‐containing products. Eventually and unknowingly, early start of tobacco consumption manifolds risks of oral precancerous lesions and cancer in life ahead [ 8 , 10 , 13 ].
Strong arguments for oral health promotion through schools include the following:
Personal and social education aimed at developing life skills—Pupils and students can be accessed during their formative years, from childhood to adolescence. Students develop lifelong oral health‐related behavior, as well as beliefs and attitudes are being developed.
Schools can provide a supportive environment for promoting oral health. Access to safe water, for example, may allow for general and oral hygiene programs. Also, provision of mouth guards—accessible and affordable sports protection, a safe physical environment and school policy on bullying and violence between students reduce the risk of dental trauma.
The burden of oral disease in children is significant. Most established oral diseases are irreversible, will last for a lifetime and have an impact on quality of life and general health.
School policies on control of risk behaviors, such as intake of sugary foods and drinks, tobacco use and alcohol consumption.
Schools can provide a platform for the provision of oral health care, that is, preventive and curative services [ 14 – 18 ].
Common risk factor approach‐based oral health promotion policies in schools can lead to improvement in oral health and reduce oral health inequality [ 10 , 16 ].
The need to set up oral health promotion programs in schools is evident, and it can easily be integrated into general health promotion, school curricula and activities. One of the proposed examples has been shown in Figure 1 [ 13 ].

Figure 1.
Integration of oral health in health‐promoting schools: an example from Denmark.
Using the structures and systems already in place as a competent setting for the installation of vital facilities such as safe water and sanitation can instigate oral health promotion in schools. The HPS strategies are effective, leading to potential long‐term cost savings. For instance, Each key components of an HPS, that is, healthy school environment, school health education, school heath services, nutrition and food services, physical exercise and leisure activities, mental health and well‐being, health promotion for staff and community relationships and collaboration , incorporate equal opportunities oral health promotion as well as general health promotion. While oral health issue is specifically addressed, it can be admixed in general health promotion strategy. It is well illustrated in following examples of school health policies as shown in Table 1 [ 13 ].
Table 1.
Examples of oral health‐related school health policies to be promoted in HPS.
There is an association of socio‐economic, geographic factors and type of schools with school based health promoting activities. On an average, students attending private schools belong to more advantaged backgrounds than their counterparts in public schools. Privately managed schools achieve greater efficiency or academic value‐added than publicly‐managed schools [ 18 ]. According to one study, ten out of eleven participated countries (including India) had the large socio‐economic gap between private and public school pupils except Chile [ 19 ]. Moreover, students going to city/town schools generally belonged to more privileged backgrounds than their counterparts in village schools. All the school headmasters in this study reported that primary school student’s absenteeism rate decreased when the students received support in the form of school uniforms, textbooks, meals and various financial assistance schemes. For example, urban schools tend to have greater resources than those in rural. Also, students in private schools had higher levels of positive behavior than those in public schools, and these results were statistically significant for most countries [ 19 ]. Public and private school differ from each other in many ways as better amenities in school, extra‐curricular activities, outdoor and indoor sports, etc. The private school allots more fees from students for such activities/facilities. Consequently, children from upper and high middle socioeconomic status prefer private schools, while children with low socioeconomic strata attend public schools [ 20 ]. Students gain more attention when the student to teacher ratio is higher. Bruneforth et al. [ 19 ] also reported inferior pupil‐teacher ratios in village schools than in city/town schools in India. The children who do not have adult supervision after school are more vulnerable to indulge them into health hazarding habits like smoking, drugs and substance abuse and behavioral problems. The schools providing self care activities after school were found more effective in reducing the prevalence of smoking among ninth‐grade students in Los Angeles and San Diego Counties [ 21 ]. Smoking and chewing tobacco are systematically associated with socioeconomic markers [ 20 ].
4.2. Healthy food at school: Mid Day Meal Scheme of India
The whole school approach with availability of healthy food in school canteen, tuck shops, instructing parents for healthy food and school staff involved in planning for food and curriculum has amplified student’s knowledge. However, it has not led to change in behavior [ 22 , 23 ].
Providing healthy food in schools can meet the nutritional requirement of students and also guide the parents to deal with healthy diet chart for their children. In UK, campaigns like the ones conducted by famous chef, Jamie Oliver, are one example of actions in this area.
In India, Mid Day Meal Scheme in school started in 1925 from a single city, Madras (now Chennai) and now spread to all States. From April 1st, 2008, the program covers all children studying in Government, Local Body and Government‐aided primary and upper primary schools across the country. The Mid Day Meal Scheme is the world’s largest school feeding program reaching out to 0.84 billion primary students and 0.33 billion upper primary Students, in total about 1.2 billion children in over 9.50 ten thousands schools across the country during 2009–2010 [ 24 ].
Unhealthy eating habits and sedentary lifestyles are closely bound not only to various socioeconomic indicators such as the parent’s education levels, financial resources and professional situations, but also to living in economically deprived areas. This suggests significant contributions of gender, age and religion belief to the eating habit. Therefore, Schools should introduce healthy food policy and activity after consulting with school authority, nutrition expert and parents so as to maintain good eating habits among students [ 25 ].
4.3. National tobacco control program of India
Tobacco consumption either in smoke form or smokeless form has deleterious effect general and oral health. Tobacco abuse is the leading preventable cause of death and disease so far. Long list of diseases caused by tobacco abuse includes different cancers – lung cancer, oral cancer, cardiovascular disease, stroke and chronic lung disease. Pertaining to oral health, it causes aggressive periodontitis, tooth loss, wound healing complications and mainly pre‐cancerous or cancerous lesion leading to disfigurement of face. Risk of oral cancer is 10‐fold in smokers than no‐smokers and 11‐fold risk in smokeless tobacco users than non‐users. One can expect a normal life expectancy with early acknowledgement of tobacco health hazards and culminating tobacco use especially below 35 years. Prevention is the prime key factors, and at initial stage, most of the adverse effects of tobacco are reversible. This fact can be used to motivate tobacco using people to curb the use of tobacco [ 26 ].
India is the second largest consumer and producer of tobacco. India accounts for 10% of the world tobacco area and 9% of the production. 30% of cancer deaths, majority of cardiovascular and lung disorders; 40% of tuberculosis and other related diseases are attributed to tobacco consumption. Over 80% of oral cancers are caused due to tobacco use. As per the WHO Global Report on “Tobacco Attributable Mortality” 2012, 7% of all deaths (for ages 30 and over) in India are attributable to tobacco. Ministry of Health and Family Welfare (MoHFW), Government of India inaugurated The National Tobacco Control Program (NTCP) in 2007–2008, as included in 11th five year plan. The program includes objectives as:
Nationwide awareness regarding tobacco use harms and following tobacco control laws.
Necessary actions for strong implementation of the Tobacco Control Laws.
Effective primordial and primary level prevention strategies are planned under the National Tobacco Control Program (NTCP) .
The prime areas under the NTCP as targets are:
Training of trainers, that is, health and social workers, NGOs, school teachers and enforcement officers.
Information, Education and Communication (IEC) activities.
School Programs.
Monitoring tobacco control laws.
Co‐ordination at village level activities.
Medicinal treatment facility for cessation at district level.
Indian government implemented Cigarette and Other Tobacco Products Act (COTPA; addressing tobacco use in public places, tobacco advertising and sale and packaging regulations) since 2003 with comprehensive action in 2005 following the Framework Convention of Tobacco Control (FCTC). Following laws through the lobbying of anti‐tobacco advocates were successfully established by Indian judiciary.
Section 4: Prohibition of smoking in public places.
Section 5: Prohibition of direct and indirect advertisement, promotion and sponsorship of cigarette and other tobacco products.
Section 6a: Prohibition of sale of cigarette and other tobacco products to a person below the age of 18 years.
Section 6b: Prohibition of sale of tobacco products within a radius of 100 yards of educational institutions.
Section 7: Mandatory depiction of statutory warnings (including pictorial warnings) on tobacco packs.)
Section 7(5): Display of tar and nicotine contents on tobacco packs [ 27 ].
The achievements of this national program are examples of apt implementation. Increase in taxation had led to a reduction in self‐reported tobacco sales and consumption at the short‐term end‐point. The GATS data (2009) indicate that 54.7 and 62.9% are aware of health warnings on cigarette and smokeless tobacco packaging, respectively. Trials of school‐based education interventions demonstrated a positive impact on knowledge, advocacy skills and tobacco use. Teaching about the risks of tobacco use for health professional trainees appeared more widespread, but may have reduced slightly post‐FCTC. Community‐based education interventions and education interventions for adult tobacco users appeared beneficial. Moreover, the secondary outcomes of tobacco control programs observed as cleaner streets and air quality, preservation of forests, increased performance at school/work, reduction in fire hazards, healthy mother and infants and indeed a better quality of life. Tobacco‐use outcomes could be improved by school/community‐based and adult education interventions and cessation assistance that are facilitated by training for health professionals and schoolteachers [ 28 ].
4.4. National fluorosis prevention program
Fluoride is an essential mineral for human health. It widely exists in natural water and in foods such as tea, fish and beer. The twentieth century documented association among reduced level of dental caries with communal fluoridated water consumption. Soon, fluoride has become an effective preventive measure for dental caries. Easy incorporation into toothpaste has improved oral health in some parts of world, particularly in developing countries [ 26 ].
However, the other part of world suffers from excessive fluoride in natural environment. Fluorosis, a public health problem, is caused by excess intake of fluoride through drinking water/food products/industrial emission over a long period. Moderate‐level chronic exposure (above 1.5 mg/liter of water–the WHO guideline value for fluoride in water) is more common. Acute high‐level exposure to fluoride is rare and usually due to accidental contamination of drinking‐water or due to fires or explosions. It results in major health disorders like dental fluorosis, skeletal fluorosis and non‐skeletal fluorosis. The late stages of skeletal and dental fluorosis are permanent and irreversible in nature and are detrimental to the health of an individual and the community, which in turn has adverse effects on growth, development & economy of the country. There is no treatment for severe cases of skeletal fluorosis, only efforts can be made towards reducing the disability which has occurred. However, the disease is easily preventable if diagnosed early and steps are taken to prevent intake of excess fluorosis through provision of safe drinking water, promote nutrition and avoid foods with high fluoride content.
Fluorosis is worldwide in distribution and endemic at least in 25 countries. It has been reported from fluoride belts: one that stretches from Syria through Jordan, Egypt, Libya, Algeria, Sudan and Kenya, and another that stretches from Turkey through Iraq, Iran, Afghanistan, India, northern Thailand and China. There are similar belts in the Americas and Japan. In India, fluorosis is mainly due to excessive fluoride in water except in parts of Gujarat and Uttar Pradesh where industrial fluorosis is also seen. The desirable limit of fluoride as per Bureau of Indian Standards (BIS) is 1 ppm (parts per million or 1 mg per liter). High levels of Fluoride were reported in 230 districts of 20 States of India (after bifurcation of Andhra Pradesh in 2014). The population at risk as per population in habitations with high fluoride is 11.7 million as on 1.4.2014. Rajasthan, Gujarat and Andhra Pradesh are worst affected states. Punjab, Haryana, Madhya Pradesh and Maharashtra are moderately affected states, while Tamil Nadu, West Bengal, Uttar Pradesh, Bihar and Assam are mildly affected states.
Understanding the clinical manifestations of fluorosis
Dental fluorosis : It is categorized into mild, moderate and severe dental fluorosis depending on the extent of staining and pitting on the teeth. In severe dental fluorosis, unaesthetic & brittle enamel is found. Vitamins A and D deficiency or a low protein‐energy diet are also linked to enamel defects. Ingestion of fluoride after 6 years of age will not cause dental fluorosis. The teeth could be chalky white and may have white, yellow, brown or black spots or streaks on the enamel surface. Discoloration is away from the gums and bilaterally symmetrical.
Skeletal fluorosis : The early symptoms of skeletal fluorosis include stiffness and pain in the joints. In severe cases, the bone structure may change and ligaments may calcify, with resulting impairment of muscles and pain. Constriction of vertebral canal and intervertebral foramen exerts pressure on nerves, blood vessels leading to paralysis and pain.
Nonskeletal fluorosis/Effects of fluorosis on soft tissues/systems :
Gastrointestinal symptoms: Abdominal pain, excessive saliva, nausea and vomiting are seen after acute high‐level exposure to fluoride.
Neurological manifestation: Nervousness and depression, tingling sensation in fingers and toes, excessive thirst and tendency to urinate.
Muscular manifestations: Muscle weakness and stiffness, pain in the muscle and loss of muscle power, inability to carry out normal routine activities.
Allergic manifestation: Skin rashes, perivascular inflammation—pinkish red or bluish red spot, round or oval shape on the skin that fade and clear up within 7–10 days.
Effects on fetus: Fluoride can also damage a fetus, if the mother consumes water/food with high concentrations of fluoride during pregnancy/breast feeding. Abortions, still births and children with birth defects are common in endemic areas.
Low hemoglobin levels: Fluoride accumulates on the erythrocyte (red blood cells) membrane, which in turn looses calcium content. The membrane which is deficient in calcium content is pliable and is thrown into folds. The shape of erythrocytes is changed. Such RBCs are called echinocytes and found in circulation. The echinocytes undergo phagocytosis (eaten‐up by macrophages) and are eliminated from circulation. This would lead to low hemoglobin levels in patients chronically ill due to fluoride toxicity.
Kidney manifestations: Low volume, dark yellow to red color of urine is seen.
Calcification of ligaments and blood vessel: Forms unique feature of the disease helps in differential diagnosis.
With an aim to prevent and control fluorosis cases, Government of India initiated the National Program for Prevention and Control of Fluorosis (NPPCF) as a new health initiative in 2008–09. During the 11th Plan, 100 districts from 17 States were identified for program implementation. During the 12th 5‐Year Plan period, it is proposed to add another 95 districts for prevention and control of fluorosis. In the 12th Plan, the program has been brought under the Non‐Communicable Disease Flexi‐pool of National Health Mission (NHM).
4.4.1. Goal and objectives
To collect, assess and use the baseline survey data of fluorosis of Ministry of Drinking Water Supply for starting the project.
Comprehensive management of fluorosis in the selected areas.
Capacity building for prevention, diagnosis and management of fluorosis cases.
4.4.2. Strategy
Surveillance of fluorosis in the community and school children.
Capacity building at different level of healthcare delivery system for early detection, management and rehabilitation of fluorosis cases.
Diagnostic facilities in the form of laboratory support and equipment including ion meter to monitor the fluoride content in water and urinary levels at district/hospital/medical college for early detection and confirmation of fluorosis cases.
Health education for prevention and control of fluorosis: (a) Creating awareness about fluorosis disease, drinking water (safe/unsafe), diet editing and diet counseling through interpersonal communication, group discussions, media, posters and wall paintings. (b) Create awareness and skills among the medical as well as paramedical health workers to detect the disease in the community. (c) Provision of safe drinking water, water harvesting (rain water) and other measures in collaboration with Public Health Engineering Department.
Management Efforts are aimed to reduce the fluorosis induced disability and to improve quality of life of affected patients. Medical treatment is mainly supplementation of Vitamins C & D, Calcium, antioxidants and treatment of malnutrition. Treatment of deformity includes physiotherapy, corrective plasters and orthoses (appropriate appliances).
4.4.3. Expected outcome
The expected outcome of the National Program for Prevention & Control of Fluorosis in the districts will be:
Number of fluorosis cases managed and rehabilitated in the program districts.
Capacity for laboratory testing for fluoride in water, urine to be developed.
Trained health sector manpower in Government set up for measuring fluoride in urine and water.
Improve information base for the community and all concerned in the program districts [ 29 ].
Likewise, fluoride is double edge sword, that is, its deficiency and excess both affect the oral health. Hence, science based on effectiveness, safety and benefits should be implemented at different needs at different part of the world.
5. Strategies for oral health promotion
5.1. generation of strategies based on evidences.
WHO aim at building healthy populations involving all communities by combating every possible illness. The organization has recommended strategic framework which focuses and guide on oral health promotion activities/programs.
Reduction in oral disease/condition burden and disability, especially in poor and marginalized populations.
Promoting healthy lifestyles and reducing risk factors to oral health that arise from environmental, economic, social and behavioral causes.
Developing oral health systems that equitably improve oral health outcomes, respond to people’s legitimate demands and are financially fair.
Framing policies in oral health, based on integration of oral health into national and community health programs, and promoting oral health as an effective dimension for development policy of society [ 7 ].
Program goals are broad statements on the overall purpose of a program. For instance, “to eliminate racial disparities in oral cancer survival rates,” “to improve the oral health of nursing home residents” or “ to improve the oral health of country’s children under 5 years. Program objectives are more specific statements of desired endpoints of program.
Objectives of oral health programs should meet SMART criteria:
Specific —they should describe an observable action, behavior or achievement.
Measurable —they are systems, methods or procedures to track to record the action upon which objective is focused.
Achievable —the objective is realistic, based on current environment and resources.
Relevant —the objective is important to the program and is under the control of program.
Time based —there are clearly defined deadlines for achieving the objective [ 3 ].
Designing an oral health promotion program: step by step can be studied as shown in Figure 2 [ 1 ]:
Best practices in oral health promotion and prevention can take various forms, be it education, health promotion, integrating oral health promotion into general health promotion programs, policy changes which promote better oral health, the provision of care services, or programs specifically designed at addressing oral health inequalities. It is interesting to learn how oral health promotion and practices are implemented in through various interventions applying the Ottawa Charter guidelines.

Figure 2.
A step‐by‐step design of an oral health promotion program (based on Ministry of Health, New Zealand, 2006).
5.1.1. Building healthy public policy
Establishing healthy policies is integral in improving oral health. Based on the needs, evidences and situation analysis, National Government, health ministry, local governments, organizations, communities, schools, primary healthcare settings and local stakeholders forms or reforms the healthy policy. Health promotion advocates hold key responsibility to convey appropriate health needs of the population.
Examples of interventions that build healthy public policy
Campaigning to extend the coverage of optimal water fluoridation or water de‐fluoridation based on needs.
Supporting early childhood centers and school boards in developing healthy food and nutrition policies.
Working on policy options that eliminate the advertising of harmful food and beverages to children.
Working with organizations to promote injury prevention policies, for example, mouth‐guards in sport or safe play equipment.
Industrial approach to limit the marketing of carbonated & sugar‐containing drinks to children.
Working to study and develop standards for marketed harmful products to children.
Developing and implementing smoke free environment policies.
5.1.2. Creating supportive environments
Making the healthy choice easy choice is the aim of health promotion. This can be achieved by creating supportive social, physical, biological and cultural environments. These determinants of health directly and indirectly affect the oral health with or without general health consequences. Hence, the needs of local population should be considered in order to design and implementation of health promotion actions. Health promotion practitioners play a lead role in creating supportive environments along with public health units, government agencies, health organizations, NGOs, professional Dental Association, industry organizations and print and digital media.
Interventions that harness creating healthy supportive environments for oral health
Provision of fluoridated toothpastes at subsidized cost that low income group can also avail.
Reforming supermarket’s marketing policies for instance replacing sugary products like chocolates.
Encouragement for usage of smoke‐free environment advertisements and sponsorship for oral health promotion.
Media coverage of healthy food choices which enhance oral health.
Oral health awareness and promotion through social marketing campaigns.
Promoting safe water supply at all the public events.
5.1.3. Strengthening community action
Communities are a powerful force for achieving actions for any health promotion program where the key success factors are: partnership, participation and engagement . Encompassing all the communities for united efforts to understand their own oral health needs and ascertain to improve the oral health outcomes of their community. These health promotion programs may differ with age, society, culture and environment. Among the five actions themes of Ottawa Charter, community action is unique as concentrate on how particular health actions to be carried out. It eventually may turn out to be effective examples to be followed. Important factor for communities to have equitable access to resources to support the control they must have over their own health and development. Hence, strengthening community action is about providing and facilitating access to sufficient and appropriate resources.
Examples of interventions that strengthen community action for oral health
Engaging the community to support water fluoridation/de‐fluoridation and encourage safe water supply.
Engaging communities to participate in school oral health programs through leadership activities.
Empowering communities for healthy eating programs that enhance oral health.
Specific target‐oriented oral health improvement programs based on community cultures.
Community and school collaboration for establishing playgrounds with safe play equipment, barricades for children safety.
5.1.4. Developing personal skills
Personal skills can help individual to take control of his own health. Empowering people with appropriate knowledge and skills to improve and maintain their oral health is essential. Oral health literacy is the way that provides information, education and skills for oral health improvement. Such things help increases the resources available to people to exercise more control over their own health and environments. Health promotion programs needs to be updated that go collateral with changing environment and culture. Hence, continuum for health education, particularly for oral health, throughout life is necessary. Here, comes the role of oral health professionals who forms the bridge between health promotion advocates and health promotion program communities. At community level or at individual level, they create support system to ingress healthy personal skills to improve and maintain oral health. Oral health professionals fulfill this role of trainer by providing information, resources and training.
Interventions that help developing personal skills
Oral health promotion though guided tooth brushing using fluoridated toothpaste as self‐care habits.
Smoking cessation actions under the guidance of Oral health professionals.
Nutritional and dietary education programs which include oral health message.
Encouraging sports authorities for safe environment at sports events such as making sportsmen to put on mouth guards compulsory when required.
5.1.5. Reorientating health services
Health services carry the burden of all diseases by providing three tier cares. With advancing burden of new diseases and population explosion challenges, reorientation of health services is inevitable. The global burden of oral diseases had led to integrate oral health into general health. Indeed, it is giving a new direction for oral health services and recognizing that oral health is not merely a biomedical process. Health services should be reformed such that they not only treat the diseases but also find suitable solutions for health promotion. Strengthening of health services to analyze needs, to understand the socioeconomic determinants of health of the population is required. Such reformation which reduces oral health inequalities and improves oral health‐related quality of life is all about reorienting health services. While prime focus is on primary healthcare services, prevention, allocation, access and cost‐beneficial health services are obligatory to achieve this.
Interventions for reorientating health services
Establishing community‐led oral healthcare providers.
Extensive collaboration with NGOs and social services for oral health promotion, so the curative burden from Government is reduced.
Linking general health services and children oral health care under primary health centers.
Training the trainers, that is, training all health professionals about preventive and social components of oral health promotion.
Facilitating and building knowledge for diagnosing early caries detection programs by primary healthcare professionals.
Health care led healthy policies supporting access to oral health care.
Provision of professional fluoride lack and excess treatment facilities delivered by primary healthcare professionals and community [ 1 ].
Oral health should be an important agenda on the country’s health policy. The above international policy examples envision the challenges and opportunities for better identification, prioritization and integration of oral health services. Collaborative planning and organization may accelerate the process to arrest the global burden of oral diseases and pioneer the oral health promotion. Relevant international developments suggest that some other health promotion frameworks exists that are parallel to Ottawa Charter framework. Although their principles are same, the implementation may differ according to the needs and socio‐cultural environment of the region. One can develop or reform a different model based on above evidences for oral health promotion programs at their region.
5.2. Country examples for oral health promotion program
Investment in simple preventive programs is cost‐effective for prevention of oral diseases and promotion of good oral health which is already proven in Europe. Twenty eight examples of good practice are presented from across Europe as shown in Figure 3 . These cover all areas of oral health promotion across the life course and include programs aimed at pregnant mothers, children and adolescents, the elderly and disadvantaged groups. To solve the problem of poor oral health in other parts of world a thorough evaluation of existing successful policies and programs, identification of evidence‐based interventions can be learned from these programs.

Figure 3.
Examples of good practices in oral health promotion programs existing across the Europe.
These programs outline a number of successful initiatives that can help prevent oral diseases, which reduce the social burden and in turn reduce existing inequalities. This is done with various measures, for instance: prevention programs in communities; limiting social, economic, cultural and environmental risk factors for non‐communicable diseases, oral hygiene promotion, oral health literacy and an appropriate access to oral health care [ 30 ].
6. Conclusion
Gradient shift to rural population to urban area, issues of migrants, urbanization, socio, cultural and environmental changes alienate health promotion. Isolated intervention may not be successful at such circumstances. Oral health promotion actions with different approaches can only improve. Health for all is certainly efficient way than the target specific behaviors. It is evident that an effective and sustainable intervention combines health, society and individual through organization, policy and laws to create healthy living conditions which promotes better quality lifestyle.
WHO is considered as an accountable and reliable organization which provide necessary technical and policy support. Their evidence based guidance enable countries to integrate oral health promotion programs into the general health promotion. The organization has different expertise at Collaboration Centers across globe that is resourceful for oral health promotion guidance. However, most of the developed and developing countries utilize own resources and develop their own action program for health promotion. It is based upon local experiences and strengths, active communities to contribute participation facilitate community empowerment by creating sustainable supporting environment. WHO has given a vision to oral health promotion programs, that is, “think globally—act locally.” To conclude the chapter, an oral health promotion program should focus on following aspects:
Recognition of health determinants, capacity building for designing and implementing interventions to promote oral health.
Community led and based oral health promotion programs, having equal opportunity for marginalized segments of population.
Planning, monitoring and evaluation strategies to be implemented strictly for national oral health promotion activities/programs.
Methods and methodological development to analyze the processes and outcomes of national oral health promotion interventions.
Collaboration with strong of networks and alliances that strengthen local, national and international activities for oral health promotion. Every experience, whether success or failure should be counted and shared to acknowledge the cost‐effective and cost‐beneficial experience that yield to improve oral health quality of life.
Oral health promotion is one practice that involves strategic planning, integrative activities, evidence‐based concepts, evaluation, policy making and other related multifactor. Knowledge generation for oral health promotion through evidence‐based concepts is the goal of this chapter.
Abbreviations
- 1. Ministry of Health. Promoting Oral Health: A Toolkit to Assist the Development, Planning, Implementation and Evaluation of Oral Health Promotion in New Zealand. Wellington: Ministry of Health; 2008
- 2. The World Health Organization. The Ottawa Charter for health promotion. Health Promotion. 1986; 1 :i‐v. Available from: WHO, Geneva: http://www.who.int/hpr/NPH/docs/ottawa_charter_hp.pdf [Accessed: 15 January 2017]
- 3. Rozier G, Pahel B. Patient‐ and population‐reported outcomes in public health dentistry: Oral health related quality of life. In: Oscar A, Chattopadyay A, editors. Dental Clinic of North America: Dental Public Health. 1st ed. India: Sauders; 2008. pp. 333-344. ISBN: 978‐81‐312‐1578‐4
- 4. Marcenes W, Kassebaum NJ, Bernabé E, Flaxman A, Naghavi M, Lopez A, Murray CJ. Global burden of oral conditions in 1990-2010: A systematic analysis. Journal of Dental Research. 2013; 92 :592-597
- 5. The World Health Organization, Oral Health Promotion Through Schools. 1999. Available from: WHO, Geneva: http://who.int/entity/school_youth_health/media/en/89.pdf [Accessed: 24 November 2016]
- 6. Northrop D, Lang C. Local Action Creating Health Promoting Schools. The World Health Organization’s Information Series on School Health. 2000. Available from: WHO, Geneva: http://www.who.int/school_youth_health/media/en/88.pdf [Accessed: 24 November 2016]
- 7. The World Health Organization. Oral Health Promotion: An Essential Element of a Health Promoting School. WHO Information Series on School Health. 2003. Document 11. Available from: WHO, Geneva: http://www.who.int/oral_health/publications/doc11/en/ [Accessed: 24 November 2016]
- 8. Young I. Health promotion in schools – A historical perspective. Promotion & Education. 2005; XII (3-5):112-117
- 9. Gray G, Young I, Barnekow V. Developing a Health‐promoting School. International Union for Health Promotion and Education. 2007. Available from: Schools for Health, Eurore: http://ws10.e‐vision.nl/she_network/upload/pubs/Developingahealthpromotingschool.pdf [Accessed: 24 November 2016]
- 10. Garbin C, Garbin A, Dos Santos K, Lima D. Oral health education in schools: Promoting health agents. International Journal of Dental Hygiene. 2009; 7 (3):212-216
- 11. The World Health Organization. Milestones in Health Promotion: Statements from Global Conferences. Available from: WHO, Geneva, 2009: http://www.who.int/healthpromotion/milestones/en/index.html [Accessed: 24 November 2016]
- 12. Peterson PE. The World Oral Health Report 2003: Continuous Improvement of Oral Health in the 21st Century – The Approach of the WHO Global Oral Health Programme. The World Health Organization. 2003. Available from: WHO, Geneva: http://www.who.int/oral_health/publications/report03/en/print.html/ [Accessed: 15 January 2017]
- 13. Kwan Stella YL, Petersen PE, Pine CM, Borutta A. Health‐promoting schools: An opportunity for oral health promotion. Bulletin of World Health Organization. 2005; 83 (9):677-685
- 14. Tobler N, Stratton H. Effectiveness of school‐based drug education programs: A meta analysis of the research. Journal of Primary Prevention. 1997; 18 (1):71-128
- 15. The World Health Organization. The Health Promoting School – An Investment in Education Health and Democracy. Copenhagen: World Health Organization. 1997
- 16. Sheiham A, Watt RG. The common risk factor approach: A rational basis for promoting oral health. Community Dentistry and Oral Epidemiology. 2000; 28 (6):399-406
- 17. Thomas R, Perera R. School based programming for preventing smoking. Cochrane Database Syst Rev. 2002;(4):CD001293.
- 18. Duraisamy P, James E, Lane J, Tan J. Is there a quantity–quality trade‐off as pupil–teacher ratios increase? Evidence from Tamil Nadu, India. International Journal of Educational Development. 1998; 18 (5):367-383. Available from: http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6VD7‐3V72PXC‐9&_user=125872&_coverDate=09%2F30%2F1998&_rdoc=1&_fmt=high&_orig=search&_sort=d&_docanchor=&view=c&_searchStrId=1434446368&_rerunOrigin=google&_acct=C000010240&_version=1&_urlVersion=0&_userid=125872&md5=13edd3a0f436133a75223cc179317942#b11 [Accessed: 15 January 2017]
- 19. Bruneforth M, Griffin P, Grisay A. Postlethwaite TN, Tran H, Zhang Y. View Inside Primary Schools – A World Education Indicators (WEI) Cross‐national Study. 2008. Available from: UNESCO Institute for Statistics: http://www.unescobkk.org/fileadmin/user_upload/efa/Publications/AViewPrimarySchools_comp.pdf [Accessed: 15 January 2017]
- 20. Gupta M, Gupta BP, Chauhan A, Bhardwaj A. Ocular morbidity prevalence among school children in Shimla, Himachal, North India, Indian Journal of Ophthalmology. 2009; 57 (2):133-138
- 21. Mott JA, Paul AC, Jean RC, Flay B. After‐school supervision and adolescent cigarette smoking: Contributions of the setting and intensity of after‐school self‐care. Journal of Behavioral Medicine. 1999; 22 (1):35-58
- 22. Perry C. Parent Involvement with children’s health promotion: The Minnesota Home Team. American Journal of Public Health. 1988; 78 (9):11156-11160
- 23. St Leger LH, Young I, Blanchard C, Perry M. Promoting Health in Schools: From Evidence to Action. 2010. Available from: International Union for Health Promotion and Education: http://www.iuhpe.org/uploaded/Activities/Scientific_Affairs/CDC/A&E_10June2010.pdf [Accessed: 15 January 2017]
- 24. Mid Day Meal Scheme. Department of School Education and Literacy. Available from: Government of India, Department of Elementary Education and Literacy: http://education.nic.in/Sche.asp [Accessed: 15 January 2017]
- 25. Ayodele AO. Gender, age and religion as determinants of eating habit of youth in Ikenne local government of Ogun state, Nigeria. African Journal Online. 2010. Available from: http://ajol.info/index.php/ejc/article/view/52673/41277 [Accessed: 15 January 2017]
- 26. Public Health England. Delivering Better Oral Health: An Evidence‐based Toolkit for Prevention. London: PHE; 2014
- 27. Centre for Health Informatics (CHI), National Institute of Health and Family Welfare (NIHFW), Ministry of Health and Family Welfare (MoHFW), Government of India. National Tobacco Control Programme (NTCP) [Accessed 15 January 2017]
- 28. McKay AJ, Patel RKK, Majeed A. Strategies for tobacco control in India: A systematic review. Plos One. 2015; 10 (4):e0122610. DOI: 10.1371/journal.pone.0122610
- 29. Centre for Health Informatics (CHI), National Institute of Health and Family Welfare (NIHFW), Ministry of Health and Family Welfare (MoHFW), Government of India. National Programme for Prevention and Control of Fluorosis (NPPCF) [Accessed 15 January 2017]
- 30. Platform for Better Oral Health in Europe. Best Practices in Oral Health Promotion and Prevention from Across Europe. 2015. Available form: www.oralhealthplatform.eu
- WHO = World Health Organization.
© 2017 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Edited by Jane Manakil
Published: 20 September 2017
By Hiroyasu Endo, Terry D. Rees, Hideo Niwa, Kayo Kuy...
1952 downloads
By Ana L. Zamora-Perez, Guillermo M. Zúñiga-González,...
1580 downloads
By Metin Çalisir
1399 downloads
Why good dental care is important to your overall health

A great smile can do so many things. It can light up the room. It can win over new friends. And it can reveal a lot about your health, both inside the mouth and throughout the body. The key to keeping that great smile is taking care of your teeth. That means brushing and flossing, of course — and seeing the dentist at least every 6 months for preventive care.
Otherwise, you could put yourself at risk of dental problems. Dentists now think there’s a link between cavities, tooth decay, gum disease and chronic health problems, including diabetes and heart disease. 1 Learn about the connection and how to help safeguard your health.
3 common dental problems for adults
Many things contribute to dental issues, including your age and your lifestyle habits, including drinking and smoking.2 But so can skipping or putting off dental checkups. 2
Here are some potential problems that may be avoided with routine checkups:
Gum disease
“Initially, your gums will become inflamed, red and swollen, and they’ll bleed while brushing,” says Fatima Khan, D.M.D., a dentist with Altus Dental in Houston. And as the disease progresses, bacteria can get below the gumline and break down the tissue and bone surrounding your teeth, she adds.
With time, the gums can pull away from the tooth. About 42% of adults ages 30 and older have gum disease, also known as periodontitis. 3 And that increases to about 68% in people 65 years and older. 4
As we get older, we may make less saliva, says Dr. Khan. That might not seem like a serious problem. But it can be. We need a healthy amount of saliva to keep our mouths lubricated and to neutralize the acids that can attack the teeth, she adds. Without enough saliva, it’s easier for acid produced by bacteria in the mouth to stick around and cause tooth decay. 5
Tooth decay and cavities
If your teeth have a lot of bacteria, it can combine with food to form a sticky film (known as plaque), which can lead to cavities. 1 A cavity is a small hole in the surface of your tooth. Dentists stop the damage by filling it in.
If your dentist doesn’t fill the hole, the tooth decay starts to spread. That can cause infections throughout your body.1 And if the decay is not addressed, your tooth can become unable to be restored and you could lose it. 6
UnitedHealthcare Medicare Advantage members with dental coverage can download the UnitedHealthcare® app to find dental care, manage plan details and more.
The mouth-body connection
Many dental problems are caused by bacteria. And bacteria can go from your mouth into your bloodstream through bleeding gums or infected or decaying teeth, explains Kami Hoss, D.D.S., the chief executive officer of The Super Dentists, a dental practice in San Diego, and the author of If Your Mouth Could Talk .
Once they’re in the bloodstream, bacteria can go everywhere in the body. That produces infections and inflammation, says Dr. Hoss. And that can trigger serious diseases, including the following:
Heart disease and stroke
Gum disease, missing teeth and even bad brushing habits can increase the risk of high blood pressure and stroke, according to the American Heart Association. 7 The bacteria can trigger infections in the heart valves, especially if a person already has heart valve disease. And they may also contribute to clogged arteries, increasing the chance of a heart attack. 8
9</sup>">Diabetes 9
With diabetes, the sugar levels in your blood are high – that means they’re high in your saliva, too. And that leads to more bacteria, increasing the risk of gum disease. But the relationship goes both ways. Having gum disease can raise your blood sugar levels. And that can up the chances of developing diabetes.
Lung infections and kidney disease
People who already have serious diseases can make things worse if they have gum disease and cavities. If a person has chronic obstructive pulmonary disease, including chronic bronchitis, mouth bacteria can cause more infections in weakened lungs. 10 Periodontal inflammation from gum disease may also make chronic kidney disease worse in patients with the condition, and potentially put those people at risk of kidney failure. 11
Gastrointestinal issues
There are strains of oral bacteria that can affect the health of the GI tract when you swallow, says Dr. Khan. Most of the time, your stomach acid can kill the bacteria. But some strains can get into the intestines. There they can trigger inflammation and an imbalance between good and bad bacteria, she says. And that can lead to inflammatory bowel disease. 12
What helps take care of your teeth
- Find a good dentist and go every 6 months for routine care. That will help keep small cavities from turning into bigger (and more expensive) problems.
- Use a soft or extra-soft toothbrush that won’t damage tooth enamel or irritate gums.
- Ask the dentist to recommend a toothpaste that’s right for you. If you’re more prone to getting cavities, a toothpaste with sodium fluoride may help, recommends Dr. Hoss.
- Look for a mouthwash with prebiotics, such as inulin and xylitol, says Dr. Hoss. Those ingredients kill off bad bacteria and help the beneficial ones thrive.
- Don’t smoke. People who smoke have twice the risk of gum disease as those who don’t. And if you already have gum disease, smoking makes it harder for the gums to heal. 13
Schedule a routine dental cleaning and checkup. Preventing problems may be easier than treating them. It may also be easier to treat a small cavity or the first signs of gum disease than conditions that have progressed. And that’s something to smile about.
Haven’t had a dental visit in a while? It’s never too late to start taking care of your teeth and gums. Already a UnitedHealthcare Medicare Advantage member with dental coverage? Sign in to your plan website to review dental benefits and schedule an appointment.
- Medicare Advantage
- Dual Special Needs Plan

Already a UnitedHealthcare® Medicare Advantage member?
Get more to smile about. Have dental coverage? Review coverage and benefits and schedule routine cleanings and exams with a dentist.
More articles
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Divisions and Offices
- Organization Chart
- Chronic Disease Interventions
- Budget and Funding
- Social Media Resources
- Chronic Disease
Health and Economic Benefits of Oral Disease Interventions
At a glance.
- Oral diseases like cavities and gum disease cause pain and disability for millions of Americans.
- CDC promotes effective interventions, including dental sealants and community water fluoridation, to prevent cavities and save money.

Oral diseases in the United States
Oral diseases —which range from cavities to gum disease to oral cancer—cause pain and disability for millions of Americans. 1 Cavities (also called tooth decay) are one of the most common chronic conditions in the United States. Non-Hispanic Black people, Hispanic people, and American Indian and Alaska Native people generally have the poorest oral health compared to other U.S. racial and ethnic groups. 2
Quick facts
- About 1 in 6 children aged 6 to 11 years have had at least one cavity. More than half of adolescents aged 12 to 19 have had cavities during adolescence, and about 1 in 6 have untreated cavities. 2
- 1 in 4 adults have untreated cavities, and nearly half of those aged 30 or older show signs of gum disease. 2 3 If left untreated, these conditions can lead to tooth loss.
- More than 1 in 6 adults aged 65 or older have lost all their teeth, which can affect nutrition. 2
- People who smoke are 3 times as likely as nonsmokers to lose all of their teeth. 2
The high cost of oral diseases
Annual costs for dental care in the United States is $136 billion. 4 A
- On average, over 34 million school hours are lost each year because of unplanned (emergency) dental care. 5
- Almost $46 billion B is lost in productivity in the United States each year because of untreated oral disease. 6
- In 2017, there were 2.1 million emergency room visits for dental emergencies. Medicaid pays for about 69% of these visits for children and about 40% for adults. 7
- During 1996–2013, $26.5 billion B was spent on dental care for children and adolescents. About 70% of this total was used for preventive services, such as general exams and cleanings, X-rays, and orthodontic treatment (such as braces). 8
- Nearly 18% of working-age adults report that the appearance of their mouth and teeth affects their ability to interview for a job. For people with low incomes, the percentage increases to 29%. 9
Strategies that work
CDC works to improve the nation's oral health by reducing disparities in the rate of cavities and integrating oral health programs into chronic disease prevention and medical care. The agency and its partners promote effective interventions, including dental sealants and community water fluoridation, which are strongly recommended by the U.S. Preventive Services Task Force because they prevent cavities and save money.
- Dental sealants are a quick, easy, and painless way to prevent most of the cavities that children get in their permanent back teeth, where 9 in 10 cavities occur.
- School sealant programs provide dental sealants at no charge to children who are less likely to receive private dental care. Almost 1 million cavities have been prevented in children from low-income households as a result of dental sealants.
- Community water fluoridation is an effective way to deliver fluoride to all community members regardless of age, education, or income. It also saves money for families and the U.S. health care system. 10
- CDC is working to meet the Healthy People 2030 objective of 77.1% of the U.S. population being on community water systems with the recommended amount of fluoride. Currently, 72.7% of the population served by community water systems (more than 209 million people) drink water that contains enough fluoride to protect their teeth. 11
The effectiveness of dental sealants
Benefits of using proven strategies.
- The benefits of school sealant programs are greater than their cost when they serve children at high risk for tooth decay. These programs become cost-saving after 2 years and save more than $11 C for every tooth sealed over 4 years. 12
- Providing sealants to the nearly 7 million children from low-income households who need them could save up to $300 million C in averted dental treatment costs. 13
- One year of providing fluoridated water is estimated to save $6.5 billion D in averted direct and indirect treatment costs. 14
- Communities served by fluoridated water save an average of $32 D per person a year by avoiding treatment for cavities. Communities of 1,000 or more see an average estimated return on investment of $20 for every $1 spent on water fluoridation. 14
- The U.S. health care system could save up to $100 million E a year if dental offices screened patients for diabetes, high blood pressure, and high cholesterol and referred them for treatment. 15
- Costs measured in 2018 U.S. dollars.
- Costs measured in 2015 U.S. dollars. Older cost estimates are likely to be underestimates.
- Costs measured in 2014 U.S. dollars. Older cost estimates are likely to be underestimates.
- Costs measured in 2013 U.S. dollars. Older cost estimates are likely to be underestimates.
- Costs measured in 2011 U.S. dollars. Older cost estimates are likely to be underestimates.
- Oral Health in America: A Report of the Surgeon General . National Institutes of Health, U.S. Dept of Health and Human Services; 2000.
- Centers for Disease Control and Prevention. Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to 2011–2016 . U.S. Dept of Health and Human Services; 2019.
- Eke PI, Dye, BA, Wei L, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol . 2015;86(5):611–622.
- Centers for Medicare & Medicaid Services. 2018 National Health Expenditure Data. NHE Tables: Table 12. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical . Accessed February 18, 2020.
- Naavaal S, Kelekar U. School hours lost due to acute/unplanned dental care. Health Behav Policy Rev . 2018;5(2);66–73.
- Righolt AJ, Jevdjevic M, Marcenes W, Listl S. Global-, regional-, and country-level economic impacts of dental diseases in 2015. J Dent Res . 2018;97(5):501–507.
- Health Policy Institute. Emergency Department Visits for Dental Conditions — A Snapshot . American Dental Association. April 2020. Accessed May 7, 2021. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/community-initiatives/action-for-dental-health/emergency-department-referrals/ed_referral_hpi_infographic.pdf
- Bui AL, Dieleman JL, Hamavid H, et al. Spending on children's personal health care in the United States, 1996-2013. JAMA Pediatr . 2017:171(2):181–189.
- Health Policy Institute. Oral Health and Well-Being in the United States. American Dental Association. Accessed November 22, 2023. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/us-oral-health-well-being.pdf
- Centers for Disease Control and Prevention. Achievements in public health, 1900-1999: fluoridation of drinking watepr to prevent dental caries. MMWR Morbid Mortal Wkly Rep . 1999;48(41):933–940.
- 2020 fluoridation statistics. Centers for Disease Control and Prevention. July 5, 2023. Accessed November 22, 2023. https://www.cdc.gov/fluoridation/php/statistics/2020-water-fluoridation-statistics.html
- Community Preventive Services Task Force. Dental caries (cavities): school-based dental sealant delivery programs. The Community Guide. Accessed November 22, 2023. https://www.thecommunityguide.org/findings/dental-caries-cavities-school-based-dental-sealant-delivery-programs.html
- Vital Signs: dental sealants prevent cavities. Centers for Diseas Control and Prevention. Accessed November 22, 2023. https://archive.cdc.gov/#/details?url=https://www.cdc.gov/vitalsigns/dental-sealants/index.html
- O'Connell JM, Rockwell J, Ouellet J, Tomar SL, Maas W. Costs and savings associated with community water fluoridation in the United States. Health Aff . 2016;35(12):2224–2232.
- Nasseh K, Greenberg B, Vujicic M, Glick M. The effect of chairside chronic disease screenings by oral health professionals on health care dollars. Am J Public Health . 2014;104(4):744–750.
National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP)
CDC's work to prevent chronic diseases across the lifespan and help people manage their chronic diseases to prevent complications.

Take care of your teeth and gums. Oral health can affect your brain.
Poor oral hygiene is associated with an increased risk for myriad health problems, including heart disease, diabetes, cancer, rheumatoid arthritis and early death . The state of our teeth and gums, though, may be vital for our well-being beyond the mouth and body.
Emerging evidence suggests that what goes on in our mouth can affect what goes on in our brain — and may even potentially affect our risk for dementia.
“People should really be aware that oral health is really important,” said Anita Visser , professor in geriatric dentistry at the University of Groningen in the Netherlands.
Severe periodontal disease — chronic inflammation of and damage to the gums and bone that support the teeth — affects about 19 percent of people older than 15 or more than 1 billion people worldwide, according to a 2022 World Health Organization report . More research is needed, but recent observational studies have suggested that oral health may be a modifiable risk factor for Alzheimer’s, the most common type of dementia.
Scientists are still working out whether and how the health of our mouths and minds meld, but they have identified two potential culprits that might explain how gum disease could lead to Alzheimer’s disease: bacteria and inflammation.
Connecting dental and mental health
One of the first studies to document the link between gum disease, tooth loss and Alzheimer’s disease focused on a cohort of aging nuns who were part of a larger study on aging. Researchers tracked 144 of the nuns and found that severe tooth loss was associated with dementia risk up to 6.4 times higher than compared with those who lost fewer teeth.
Other more recent longitudinal studies also found that a higher incidence of tooth loss was associated with cognitive decline. In one small 2016 study of 60 patients with mild to moderate dementia, periodontitis was associated with a sixfold increase in cognitive decline.
Another study, in 2017, of almost 28,000 Taiwanese patients reported that having chronic periodontal disease for 10 or more years corresponded to a 1.7 times increase in the risk for Alzheimer’s disease . A 2022 meta-analysis of 47 longitudinal studies reported that tooth loss and poor oral health are associated with both cognitive decline and dementia.
This research paints an emerging picture of an association between poor oral health and dementia, but there are a number of confounding factors that prevent researchers from drawing definitive conclusions of causation.
The higher rate of dental problems among those with dementia may be a symptom rather than a cause of cognitive decline. People with dementia have a difficult time maintaining their oral health and have an increased risk of developing gum disease , meaning that the association between oral and cognitive health may be bidirectional.
Other known risk factors for dementia, such as smoking and lower educational levels, are also associated with worse oral health . Tooth loss has secondary effects that can affect nutrition and overall health, which can also affect cognition, Mario Dioguardi , a researcher in dental science at the University of Foggia, said in an email.
“It’s really complicated,” said Visser, who wrote a recent review on the association of oral health and Alzheimer’s. “And this is why we cannot say, ‘Oh, if you have periodontitis, you will get Alzheimer’s disease.’ But we know now that if you have severe periodontitis, the chance of getting Alzheimer’s disease is bigger.”
Mouth bacteria may infect the brain
Research has found that bacteria that normally reside in our mouth may also infect the brain and potentially contribute to neurodegeneration in Alzheimer’s disease.
A 2019 study published in Science Advances reported that the DNA of P. gingivalis bacteria, a key pathogen in gum disease, could be found in brain autopsies from Alzheimer's patients. Bacterial DNA was also detected in the cerebrospinal fluid of people living with a probable Alzheimer's disease diagnosis.
Toxic enzymes from the P. gingivalis bacteria were also found in the Alzheimer’s patients’ brains and correlated with the amount of tau protein pathology, a hallmark of the disease.
Orally infecting mice with the bacteria led to the presence of P. gingivalis DNA as well as the accumulation of amyloid β cellular waste — a hallmark of Alzheimer’s — in their brains.
The researchers were able to inhibit the bacterial enzymes in mice infected with P. gingivalis , which reduced amyloid β production and neuroinflammation. (A recent clinical trial targeting those bacterial enzymes fell short, however, and the Food and Drug Administration placed a hold on future trials.)
“The mechanisms through which periodontal bacteria can access the central nervous system remain unknown” but could reach the brain through circulation in the blood or along peripheral nerves, wrote Dioguardi, who was a co-author on a recent review on the role gum disease and oral bacteria play in Alzheimer’s.
Mouth inflammation can affect the brain
If we do not brush our teeth for several days, each tooth develops a thin biofilm called dental plaque that teems with acid-producing bacteria.
“Your body doesn't like these bacteria,” Visser said. “They're on the edge of your teeth and on the edge of your gum.”
With plaque buildup comes inflammation of the gums as our immune system tries to fight off the infection. Gingivitis, the mildest form of periodontal disease, is still reversible; brushing and removing the plaque buildup will allow the gums to heal.
But more severe gum disease, or periodontitis, can follow if the gingivitis is not addressed.
“The whole body is fighting against this bacteria,” Visser said. “ The immune system is really provoked and alert and working really hard against these bacteria.”
This chronic inflammation becomes a vicious cycle: more swelling of the gums enlarges the gap between the teeth and gums, allowing more bacteria to enter, which can lead to inflammation of not only the gums but also the underlying bone. Continued unabated, the body will reject the tooth, causing loosening and eventual loss of the tooth.
This chronic inflammation can spill from the mouth into the rest of the body. Gum disease is linked to an increase in pro-inflammatory molecules in the blood, Dioguardi said.
Chronic inflammation in the body can, in turn, lead to chronic neuroinflammation in the brain, which induces neurodegeneration and plays a key role in Alzheimer’s.
Oral health and dementia
Visser is conducting a longitudinal study collecting oral health data — X-rays of teeth and samples of bacteria — from several hundred patients with cognitive impairment to get more information about how their oral health affects their cognitive risk.
Already, “we saw some really severe cases of oral health problems which are missed by the doctors,” she said.
The challenge of untangling the relationships between our lifestyle, our teeth and our brains remains. “There are so many confounders, lifestyle, smoking, educational level diet,” Visser said. “So it’s really hard to do this research.”
Until more is known, researchers stress that oral hygiene remains one of the simplest and most important ways you can take care of yourself.
“Raising awareness among the population about the increased risk of Alzheimer’s associated with tooth loss and periodontitis can lead to heightened attention towards oral health, ” Dioguardi said in an email.
For better health — and possibly for a healthier brain — keep brushing.
Do you have a question about human behavior or neuroscience? Email [email protected] and we may answer it in a future column.

Distinguishing Health from Wellness: Understanding Key Differences
This essay is about the distinctions between health and wellness, highlighting their unique approaches to well-being. Health is defined as the absence of disease and focuses on physical, mental, and social well-being, often involving reactive measures such as treatments and medical interventions. Wellness, however, is a holistic concept that includes physical, emotional, intellectual, social, spiritual, and environmental well-being. It emphasizes proactive and preventive measures, encouraging individuals to make conscious lifestyle choices that enhance their overall quality of life. The essay underscores that while health and wellness are interconnected, wellness involves a more comprehensive and self-directed approach to achieving a balanced and fulfilling life.
How it works
The notions of well-being and vitality are frequently interchanged, yet they signify distinct facets of our welfare. Grasping the nuances between the two can facilitate a more harmonious and gratifying existence. While both well-being and vitality are pivotal to our overall welfare, they encompass disparate dimensions and methodologies for leading a wholesome life.
Traditionally, vitality is delineated as the nonexistence of ailment or malady. It denotes a condition of physical, psychological, and communal welfare wherein an individual can operate effectively and proficiently.
Vitality is often evaluated through medicinal criteria, encompassing the presence of maladies, hereditary conditions, and corporeal traumas. Medical practitioners usually scrutinize vitality through sundry diagnostics, treatments, and preventative measures aimed at preserving or reinstating an individual’s optimal state of functioning. Consequently, vitality primarily centers on the corporeal and physiological state of a person.
Reflect on how we customarily approach our vitality. When we sense infirmity, we seek out medical practitioners, undergo examinations, and may commence medication. This responsive approach is imperative, particularly when contending with illnesses and conditions that necessitate immediate attention. Vitality, in this context, pertains to certifying our bodies and minds can operate without substantial hindrances. Nonetheless, it does not inherently imply we feel our utmost or are flourishing; it merely signifies we are not afflicted by illness.
Contrariwise, well-being is a broader and more comprehensive notion that transcends mere physical vitality. Well-being embodies an active process of discerning and electing toward a robust and satisfying life. It encompasses myriad dimensions, including physical, emotional, intellectual, communal, spiritual, and environmental welfare. Well-being is not merely the lack of infirmity but entails a proactive approach to existence that underscores personal accountability and a balanced modus vivendi. It is about making conscious decisions to augment overall quality of life and attain one’s full potential.
Envision well-being as a modus vivendi choice, wherein every verdict one makes, from dietary preferences to stress management strategies, constitutes part of a grander scheme to enrich one’s life. It transcends avoiding sickness; it pertains to striving for a condition wherein one feels vibrant, dynamic, and contented. Well-being is proactive. It involves identifying facets of one’s life that could benefit from enhancement and taking strides to effectuate those enhancements. For instance, regular physical exercise, a balanced dietary regimen, sufficient sleep, and stress alleviation are all constituents of well-being that contribute to sustaining good vitality.
One pivotal disparity between vitality and well-being lies in their methodologies to welfare. Vitality frequently encompasses reactive measures, such as managing illnesses and mitigating symptoms subsequent to their occurrence. Conversely, well-being accentuates proactive and preventative measures, encouraging individuals to assume control of their lifestyle preferences and behaviors to avert ailment and foster overall welfare. For instance, someone who embraces well-being does not defer exercising until a medical practitioner counsels it; they integrate physical activity into their diurnal routine because they apprehend it benefits their body and mind in myriad ways.
Another divergence is that vitality is frequently influenced by extrinsic factors such as genetics, milieu, and access to healthcare amenities. Although these factors are also crucial in well-being, the notion of well-being places a greater emphasis on personal accountability and self-preservation. Individuals are urged to take an active stance in their welfare by engaging in practices that enhance their physical, emotional, and spiritual vitality. This self-directed approach empowers individuals to make decisions that harmonize with their principles and aspirations, ultimately culminating in a more fulfilling life.
Additionally, well-being encompasses a broader spectrum of welfare, encompassing mental and emotional vitality, which are often disregarded in conventional vitality paradigms. Emotional well-being, for instance, entails comprehending and managing one’s emotions, cultivating resilience, and nurturing salubrious relationships. Intellectual well-being fosters perpetual learning and mental stimulation, contributing to personal maturation and cognitive acuity. These facets of well-being are indispensable for overall welfare and underscore the holistic essence of the notion.
Social and spiritual well-being are also integral constituents of the well-being framework. Social well-being entails establishing and sustaining salubrious relationships, fostering a sense of camaraderie, and cultivating robust communal networks. It accentuates the significance of affiliation and belongingness in overall welfare. For instance, someone who prioritizes social well-being might routinely convene with friends, partake in communal activities, or volunteer. These pursuits build a support network that can furnish emotional and pragmatic succor when requisite.
Conversely, spiritual well-being entails seeking purpose and significance in life, which can be attained through religious practices, meditation, or alternative forms of introspection. These dimensions of well-being contribute to a sense of equilibrium and contentment that transcends mere physical vitality. For instance, someone might find spiritual well-being through regular supplication, meditation, or communing with nature. These practices can engender a sense of tranquility and purpose that enriches overall welfare.
Environmental well-being is another indispensable facet that considers the repercussions of one’s milieu on overall welfare. This dimension accentuates the importance of inhabiting a salubrious environment, devoid of hazards, and being cognizant of the ecological footprint. It encourages sustainable practices that not only benefit the individual but also the broader community and the planet. For instance, someone fixated on environmental well-being might opt to curtail waste, recycle, and patronize environmentally friendly products and practices.
In summation, while vitality and well-being are interlinked, they epitomize divergent approaches to welfare. Vitality concentrates on the physical state and absence of ailment, often encompassing reactive measures. Conversely, well-being is a holistic and proactive approach that encompasses myriad dimensions of welfare, accentuating personal accountability and balanced living. By comprehending and amalgamating both notions, individuals can achieve a more exhaustive and gratifying state of welfare. Recognizing the disparities between vitality and well-being allows for a more nuanced approach to achieving overall welfare, ultimately culminating in a healthier and more gratifying life.
Attaining well-being is an ongoing process that mandates attentiveness to sundry facets of life. It entails making deliberate decisions and cultivating habits that promote physical, emotional, intellectual, communal, spiritual, and environmental vitality. By adopting a well-being mindset, individuals can proactively manage their vitality, preclude illness, and enhance their quality of life.
For instance, ponder the repercussions of stress on both vitality and well-being. Persistent stress can precipitate a gamut of health issues, including cardiovascular disease, hypertension, and psychological health ailments such as apprehension and despondency. From a vitality perspective, managing stress might encompass medicinal interventions like medication or psychotherapy. From a well-being perspective, managing stress encompasses these medicinal interventions but also comprises lifestyle modifications such as practicing mindfulness, partaking in routine physical activity, nurturing supportive relationships, and engaging in meaningful activities that confer a sense of purpose.
Moreover, well-being exhorts individuals to gaze beyond themselves and contemplate the broader repercussions of their actions. For instance, making ecologically cognizant choices not only contributes to personal welfare but also buttresses the welfare of the planet. This holistic outlook on well-being recognizes that personal vitality is interlinked with the vitality of our communities and environment.
Another exemplar is nutrition. From a vitality standpoint, sound nutrition entails furnishing the body with the requisite nutrients to function optimally and preclude ailment. Nevertheless, from a well-being perspective, nutrition also encompasses relishing the process of eating, comprehending the cultural and communal aspects of cuisine, and making mindful decisions that mirror one’s principles and modus vivendi. This might entail opting for organic sustenance, preparing meals at home with family, or practicing mindful eating to savor the sensory experience of food.
Physical activity is another juncture where vitality and well-being intersect. Vitality guidelines advocate for routine exercise to sustain physical fitness and preclude disease. Conversely, well-being exhorts identifying physical activities that are pleasurable and fulfilling, assimilating movement into diurnal life in a manner that amplifies overall vitality. This might entail exploring diverse forms of exercise to ascertain what one relishes, such as dancing, hiking, or practicing yoga, rather than perceiving exercise as a chore.
Slumber is yet another indispensable constituent. Sound vitality necessitates adequate slumber to afford the body the opportunity to regenerate and rejuvenate. From a well-being perspective, slumber is also about crafting a tranquil environment, instituting a consistent sleep regimen, and acknowledging the importance of repose and relaxation in overall vitality.
Ultimately, the demarcation between vitality and well-being resides in their methodologies and scope. Vitality is a fundamental facet of welfare, ensuring that our bodies and minds are free from maladies and adept at functioning efficaciously. Conversely, well-being is about embracing a holistic and proactive approach to life, recognizing that welfare encompasses much more than merely physical vitality. It is about aspiring for equilibrium, contentment, and a sense of purpose across all dimensions of life.
By assimilating the principles of both vitality and well-being, individuals can craft a comprehensive approach to welfare that bolsters not only their physical vitality but also their emotional, intellectual, communal, spiritual, and environmental vitality. This balanced approach begets a richer, more gratifying life, wherein one not only endures but thrives. Recognizing the disparities and interconnections between vitality and well-being empowers individuals to make discerning decisions that augment their overall quality of life, fostering a state of genuine welfare.
Cite this page
Distinguishing Health from Wellness: Understanding Key Differences. (2024, May 21). Retrieved from https://papersowl.com/examples/distinguishing-health-from-wellness-understanding-key-differences/
"Distinguishing Health from Wellness: Understanding Key Differences." PapersOwl.com , 21 May 2024, https://papersowl.com/examples/distinguishing-health-from-wellness-understanding-key-differences/
PapersOwl.com. (2024). Distinguishing Health from Wellness: Understanding Key Differences . [Online]. Available at: https://papersowl.com/examples/distinguishing-health-from-wellness-understanding-key-differences/ [Accessed: 22 May. 2024]
"Distinguishing Health from Wellness: Understanding Key Differences." PapersOwl.com, May 21, 2024. Accessed May 22, 2024. https://papersowl.com/examples/distinguishing-health-from-wellness-understanding-key-differences/
"Distinguishing Health from Wellness: Understanding Key Differences," PapersOwl.com , 21-May-2024. [Online]. Available: https://papersowl.com/examples/distinguishing-health-from-wellness-understanding-key-differences/. [Accessed: 22-May-2024]
PapersOwl.com. (2024). Distinguishing Health from Wellness: Understanding Key Differences . [Online]. Available at: https://papersowl.com/examples/distinguishing-health-from-wellness-understanding-key-differences/ [Accessed: 22-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers

521 S. Main, Moscow, Idaho 83843 | (208) 882-2669 | [email protected] | 10am - 6pm Mon-Sat, 10am - 4pm Sun

Teeth Aren't Just for Smiling: Oral Care and Its Impact on the Whole Body (Paperback)

- Description
- About the Author
- Reviews & Media
A popular misconception about oral care is that it's primarily about making teeth look as attractive as possible. Advertisements for tooth whiteners and veneers abound, but the fact is that while appearance is important, there's a lot more to oral care than just having a mouth full of straight, pearly white teeth. Dr. Brett Langston has spent his career as a prosthodontist - a dentist who specializes in the restoration of oral health and replacement of missing teeth-solving some of the most challenging dental problems. He feels strongly that most people need to understand that oral health affects general health and wants to encourage people to look beyond appearances and learn to take proper care of their teeth and gums. There's more to it than a quick brush in the morning and evening or choosing a magic toothpaste.
In this book, Dr. Langston will share some of his vast knowledge of proper oral care and reveal that by making a few simple lifestyle changes, people can increase their chances of avoiding pain, tooth loss, and embarrassment. He shares amazing, heartwarming, and sometimes funny stories from his decades of working in the field of prosthodontics. Meet a young man who thought he'd never find love because of the state of his teeth, and a woman who was too embarrassed to sing because of her ill-fitting dentures. Dr. Langston not only changed these people's lives but also taught them how to maintain good oral health for the long haul.
Dr. Langston will also introduce some modern solutions to age-old problems and walk you through your many options when it comes to tooth repair, reconstruction, and maintenance. In language understandable to those outside the field of dentistry, he will show you that progress in the world of oral health has very much kept up with modern technology and will amaze you with what is being done in the field. He believes that there are no hopeless cases when it comes to dental reconstruction.
"This is all very nice" we hear you say. "But I am afraid of the dentist and that's why I don't go." In the book, Dr. Langston will gently encourage you to put aside your fears and make that dental appointment. Pain management has come a long way in the past several decades, and you don't have to be afraid anymore. Once you understand the importance of good oral care to your overall health and what your options are, Dr. Langston and dental professionals like him are waiting to put you at ease and take care of you. Armed with the information you've learned from this book, you can work closely with your dentist to create a care plan that will improve your life and both your oral and general health.
- Dentistry - Prosthodontics
Australian Government Department of Health and Aged Care
Budget 2024–25
Fact sheets and other health, aged care and sport information from the 2024–25 Budget.

Scroll down to access downloads and media.
Ministers' media releases
Budget 2024–25: Cheaper medicines, new Medicare Urgent Care Clinics and more free mental health services in a stronger Medicare
Budget 2024–25: Investing in quality aged care
Portfolio Budget Statements
Budget 2024–25: Health and Aged Care Portfolio Budget Statements
Stakeholder pack
Budget 2024–25: Stakeholder pack
Budget 2024–25: Budget overview
Budget 2024–25: Ensuring all Australians get the health care they need
Fact sheets
Budget 2024–25: Strengthening Medicare
Budget 2024–25: Cheaper medicines
Budget 2024–25: Quality aged care
Budget 2024–25: A fit and healthy Australia
We aim to provide documents in an accessible format. If you're having problems using a document with your accessibility tools, please contact us for help .
- About the department
Is there anything wrong with this page?
Help us improve health.gov.au
If you would like a response please use the enquiries form instead.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Modern Development Problems of Russian Healthcare (Part 1)
V. n. ivanov.
Institute of Economic Forecasting, Russian Academy of Sciences, Moscow, Russia
A. V. Suvorov
Abstract—.
The paper (part 1) analyzes the dynamics of indicators characterizing the state of health of the Russian population. A comparative analysis of the development of healthcare in Russia and other countries is carried out. The conclusion is confirmed that the main problem in the development of Russian healthcare is the insufficient volume of public funding. The drawbacks and limited potential of the adopted funding model are assessed. A possible way to increase public funding is proposed. It is shown that the availability of medical care is reduced as a result of the so-called optimization of healthcare. A possible way to improve the territorial organization of medical services is considered. The effectiveness of the Russian healthcare system in the fight against the coronavirus pandemic is assessed.
The current state of the national healthcare system raises justified concern. The high morbidity and mortality of the population of Russia persist. Sociological studies record a low level of satisfaction of the population with the quality and level of accessibility of medical care. Representatives of the medical community are increasingly criticizing the government’s policy in the field of healthcare, the adopted directions of reforming the industry. At the same time, many of the shortcomings of the implemented strategy for organizing healthcare have been clearly manifested during the epidemic of coronavirus infection COVID-19 and caused significant damage to the socio-economic development of the country.
The state of health of the population. According to official data, in 2018 the total number of registered diseases in the country’s residents amounted to 240 mln, i.e., on average, 1.6 diseases per person. 1 Every fourth person has a disease of the circulatory system; in a population sample of 100 people, 13 were diagnosed with diseases of the musculoskeletal system, 12 had diseases of the genitourinary system, 11 had digestion diseases, 10 had eye diseases, 8 had diseases of the endocrine system, and 5 had neoplasms.
The fastest growing morbidity in the Russian population was observed in the first half of the 1990s during the period of change in the social system, which was characterized by a sharp drop in the level and deterioration of living conditions of the population. An increase in morbidity was observed in relation to almost all classes of diseases, including curable diseases, which were considered almost completely eliminated in the Soviet period. So, for example, in comparison with 1991, the number of patients with a diagnosis of active tuberculosis established for the first time in their life increased by the mid-1990s by more than two times, and the number of patients with a diagnosis of syphilis grew 30 times.
In the 2000s, as compared to the previous decade, the rate of growth in the incidence of diseases of the circulatory system (the number of registered diseases in patients diagnosed for the first time in their lives) increased, while it decreased in many other classes of diseases ( Table 1 ). At the same time, the incidence rate in 2019 was lower than in 1991 only for infectious diseases. Meanwhile, over the past almost thirty years, the number of detected diseases of the endocrine system has increased three and a half times, the number of detected diseases of the circulatory system has grown more than three times, and the number of neoplasms has twice increased. The last two classes of diseases as well as external causes (accidents, traffic injuries, homicides and suicides) are currently the main causes of mortality in the population.
Table 1.
The incidence rate for main classes of diseases (registered diseases in patients with a diagnosis established for the first time in life), thousands
The dynamics of the mortality rate of the population include three time intervals: 1991–1995, 1995–2005, and 2005–2019. In the early 1990s, there was a maximum increase in the overall mortality of the population, which was due, first of all, to a significant deterioration in the socio-economic situation in the country: a deep economic recession, a sharp drop in the standard of living for the majority of the population and an accompanying increase in socio-psychological tension as a result of the inability adapt to new economic conditions [ 1 ]. Moreover, this inability was most characteristic of the younger age cohorts of the population. This is confirmed by the significantly higher growth in mortality at the working age ( Table 2 ).
Table 2.
Mortality from the main death causes (deaths from all causes per 100 000 people)
The increase in mortality in 1991–1995 was noted for all major classes of death causes, while the increase in mortality from external causes was the greatest, which was a direct consequence of the growth of socio-psychological tension. In this regard, it should be noted that social and psychological stress is recognized by WHO experts as main among socioeconomic factors that negatively affect the health of the population and lead to the development of cardiovascular diseases, an increase in mortality from accidents, homicides and suicides; at the same time, this influence is most pronounced in the countries that are carrying out accelerated economic transformations without an adequate social policy [ 2 ].
The degradation of the medical care system also contributed to the growth in mortality in the first half of the 1990s. As radical economic transformations began, funding for Russian healthcare collapsed. The reduction in funding and the deterioration of the material and technical support of the healthcare system resulted in the transition to simplified medical technologies, which in many cases did not provide the previously achieved quality of medical care. This could not but lead to a decrease in its effectiveness.
During the next time interval (1995–2005), the growth rate of total mortality decreased significantly. At the same time, mortality from external causes, primarily in the working age, had a clear tendency to decrease, while mortality from cardiovascular diseases (the main cause of mortality in the population) continued to grow and increased by almost one and a half times compared with 1991. It is due to mortality from diseases of the circulatory system that the increase in the total mortality of the population occurred in the period under review.
It became possible to reverse the growth trend in mortality only in the middle of the 2000s as a result of both an improvement in the socio-economic situation and living conditions of the population and improvement in the medical care system. The latter was facilitated primarily by implementing measures for strengthening the material and technical base of healthcare within the framework of the “Health” national project, which was launched in 2006: large-scale procurement of modern medical equipment, and introduction of modern medical technologies.
Over the past 15 years (2005–2019), the rate of mortality from diseases of the circulatory system and external causes has decreased most significantly. As the socio-economic situation in the country began to improve, mortality from external causes began to decline rapidly and decreased by a third by 2019 compared to 1991. The reduction in mortality from diseases of the circulatory system must be attributed—in contrast to the decrease in mortality from external causes—to achievements of healthcare as a result of the modernization of the system of medical care for patients with cardiovascular diseases: the organization of a network of vascular centers and vascular departments of hospitals, a multiple increase in the number of surgeries on the heart and blood vessels. At the same time, it should be noted that mortality from diseases of the circulatory system in Russia continued to remain at a significantly higher level compared to most economically developed countries [ 3 ]. There is also reason to believe that the rate of mortality from diseases of the circulatory system officially registered in recent years is artificially underestimated. Experts explain this by the fact that the achievement of the target rates of mortality from cardiovascular diseases defined by the 2012 presidential decrees in May is one of the criteria for assessing the performance of regional leaders. As a result, the regions often indicate another concomitant disease of the patient as the cause of death at the suggestion of their leaders [ 4 ]. This is probably the reason for the hard-to-explain increase in mortality from “other diseases” just in elderly patients who usually have several diseases (see Table 2 ).
A generalizing characteristic of the mortality rate and one of the main indicators for assessing the health of the population and the effectiveness of the functioning of the healthcare system is the indicator of average life expectancy (life expectancy at birth). The dynamics of the average life expectancy indicator also include three time intervals ( Table 3 ).
Table 3.
Average life expectancy (years)
In the early 1990s, there was a sharp decline in life expectancy, which was unprecedented in peacetime, primarily for men (see Table 2 ). From the mid-1990s to the mid-2000s, the values of this indicator remained almost unchanged. The observed insignificant increase in the average life expectancy with a simultaneous growth in the total mortality of the population during this period is mainly explained by the decrease in mortality from external causes during this period due to the significantly lower average age of death in comparison with other death causes.
During 2005–2019, the average life expectancy grew, while the difference in the average life expectancy between men and women also decreased due to the higher growth rates for men (see Table 3 ). A significant increase in average life expectancy during this period was primarily due to a decrease in mortality from cardiovascular diseases and mortality from external causes. At the same time, the decrease in mortality from external causes not only made a significant contribution to the growth of average life expectancy, but also largely determined the decrease in the difference in the average life expectancy between women and men due to the lower average age of death from this cause with a fourfold excess of its level in men compared to women. Along with the reduction in mortality from diseases of the circulatory system, a significant decrease in infant mortality must be attributed to the unconditional achievements of domestic healthcare, which contribute to an increase in average life expectancy. The infant mortality rate (the number of children who died under one year of age per 1000 live births) decreased almost three times: from 11.0 in 2005 to 4.1 in 2019.
Despite the observed upward trend in the average life expectancy of the population, Russia is still among the second hundred countries of the world in the WHO ranking for this indicator [ 5 ]. In most developed countries, the average life expectancy of the population is eight to ten years higher than in Russia, and the difference in the life expectancy between women and men is two times less ( Table 4 ). The reasons for Russia’s lag behind other developed countries have a more than half a century history and are explained, first of all, by insufficient financing of the Russian healthcare system.
Table 4.
Life expectancy (in 2019) in Russia and in a number of developed countries, years
Health financing. A global trend is a change in the so-called epidemiological revolutions. By the middle of the 20th century, developed countries almost completed the first epidemiological revolution, which was characterized by significant successes in the fight against diseases that are curable in nature. One of the main results was a significant decrease in mortality, primarily in infant mortality and mortality in working age. As a result, average life expectancy increased by 1960 to about 70 years in most developed countries.
The second epidemiological revolution meant a replacement of the strategy of “treatment up to recovery” with the strategy of prevention and “postponement of fatal complications” of chronic diseases (atherosclerosis, diseases associated with metabolism, etc.), i.e., “moving deaths from these causes to older ages, an increase in the average age of death from them, and, ultimately, a significant increase in life expectancy” [ 6 ].
The implementation of such a strategy requires the development and introduction of new medical technologies, diagnostic and therapeutic equipment, an increase in the number of people employed in healthcare, and the development of pharmaceutical production. All this leads to a significant rise in the cost of medical care and, accordingly, to a significant increase in healthcare costs.
As a result, the dynamics of spending on healthcare have become an indicator of the dynamics of the volume of medical services of the quality required to solve the problems of the second epidemiological revolution. At the same time, it is considered that one of the most adequate indicators of not only the quality, but also the availability of medical care for the population is the value of public expenditures on healthcare and, in particular, the indicator of the share of these expenditures in the gross domestic product (GDP), which allows for cross-country comparisons, including comparison of countries with different levels of economic development. This indicator to the greatest extent reflects the state of health of the population, mortality rate and average life expectancy.
As the analysis shows, there has been a rapid increase in healthcare expenditures since the 1960s in almost all foreign developed countries. At the same time, the growth rates of public healthcare financing significantly exceeded the rates of economic growth of the countries; as a result, the share of these expenditures in GDP increased by no less than 2–3 times by 1990 compared to 1960. Simultaneously, the average life expectancy increased by 5–7 years in most developed countries (see Table 4 ).
In our country, the problems of the first epidemiological revolution were solved quite successfully. As a result, life expectancy increased from 43 years in 1926–1927 (data for the European part of the Russian Soviet Federative Socialist Republic) up to 68.8 years in 1960. The country entered the top twenty countries of the world by this indicator, being only slightly inferior to the leading countries. However, in the next 30 years, the average life expectancy did not increase and in 1990 it was equal to only 69.2 years. At the same time, as calculations show, the amount of public health spending that was calculated as a share of GDP remained almost unchanged. This indicator ( Table 5 ) in 1990 remained at the level of spending in most developed countries in the 1960s.
Table 5.
Public health spending (% of GDP) and average life expectancy (years) in the Soviet Union and other countries in 1960–1990*
* The data for the Russian Soviet Federative Socialist Republic barely differed from the data for the Soviet Union. Data for foreign countries were calculated according to [ 7 , 8 ].
The development of domestic healthcare in the period under review followed the path of building up the network of medical institutions and increasing the training of medical personnel. As a result, the number of hospital beds and the number of doctors in the Russian Soviet Federative Socialist Republic increased more than twice. Given the size of the country’s territory and the nature of the population’s settlement, such an extensive direction of healthcare development seems to be a fully justified way of ensuring universal access to medical care. At the same time, insufficient funding did not make it possible to ensure an improvement in the quality of medical care by the technical and technological re-equipment of domestic healthcare, which was necessary to solve the problems of the second epidemiological revolution. Calculations show, in particular, that the cost of purchasing equipment in total healthcare spending in the period under review was only about 2% [ 9 ].
As a result of insufficient funding, the provision of medical organizations with modern diagnostic and treatment equipment, the use of advanced medical technologies remained at an extremely low level. The provision of modern medicines was also very low. In addition, insufficient funding led to low wages in healthcare. Despite the high educational and professional levels of people employed in this sector, the average salary in healthcare was a quarter lower than the average for the national economy. Our country also lagged significantly behind other developed countries in terms of the ratio of the average wages in healthcare to the this indicator in the economy as a whole.
In the early 1990s, there was a collapse in funding for Russian healthcare. The scale of the fall in public spending is evidenced, first of all, by a sharp decline in wages for people employed in healthcare, which is the main item of expenditure of medical organizations. Calculations show that this indicator decreased in constant prices three times in the first year of radical reforms, and in 1995 it amounted to 47% of the 1991 level. Due to the unreliability of statistics on the values of the deflator of GDP elements in 1992, it is difficult to give an accurate estimate of the magnitude of the fall in total public health spending from 1991 to 1995. According to our calculations with corrections of data for 1992, public health financing decreased about twice over this period.
Table 6 shows the dynamics of the indicator of public health spending for the period from 1995 to 2018 in constant prices, which was calculated on the basis of the deflator of final consumption as an element of the use of GDP.
Table 6.
Public health spending (at constant 1995 prices) and average life expectancy
* In 1995—bln Rubles.
As can be seen from the cited data, public health spending continued to decline in the second half of the 1990s, and the 2000s brought about an increase in financing for healthcare along with the growth of the economy. Given the two-fold drop in funding in the first half of the 1990s, this growth is a recovery growth. The level of funding in 1991 was achieved only in 2010. It is interesting to note that the indicator of average life expectancy in 2010 (68.9 years) became exactly the same as in 1991.
In the second half of the 2000s at a relatively high growth rate of public expenditures (average annual growth was 2.8%), the state of the material and technical base of healthcare improved. The coefficient of renewal of fixed assets increased several times—up to 6% in 2010. At the same time, the share of machinery and equipment in the structure of fixed assets grew (up to 39% in 2010). As noted above, large-scale purchases of modern diagnostic and treatment equipment were carried out during these years within the implementation of the “Health” national project, which made it possible to switch to the use of advanced medical technologies, at least at some medical organizations. First of all, this applies to federal specialized medical centers, the network of which significantly increased, including through the creation of such centers outside Moscow and St. Petersburg.
In general, all this led to an improvement in the quality of medical care and, accordingly, to an increase in its effectiveness. For the first time in Russian history, average life expectancy exceeded the 70‑year threshold in the 2010s and continued to grow until recently. At the same time, the success of the Russian healthcare system significantly lags behind the majority of developed foreign countries. Russia’s lag behind these countries in terms of life expectancy not only has not decreased, but has increased over the past three decades. A similar trend is also observed for the difference in public health expenditures calculated as a share of these expenditures in GDP. As for per capita public spending in comparable prices at purchasing power parity (PPP), the scale of Russia’s lag behind most developed countries is especially large. In terms of per capita financing, Russia lags almost three times behind the average financing for the countries of the Organization for Economic Cooperation and Development (OECD) and 3.5–5 times behind the countries such as Austria, Germany, Canada, Norway, France, and Japan ( Table 7 ).
Table 7.
Public health spending and average life expectancy in the Russian Federation and other countries in 2018*
* Data for the OECD countries are given according to [ 10 ]. ** Per capita spending is calculated using PPP of final consumption in GDP.
Against the background of low public funding in post-Soviet Russia, private spending on healthcare began to grow rapidly: household spending on the purchase of medicines and medical supplies, payments for medical services, and contributions to voluntary medical insurance increased. For the period 1995–2018 in comparable prices, spending for the purchase of medicines and medical goods increased almost 12 times, and spending for payments for medical services grew almost seven times. An advancing growth in private spending was accompanied by an increase in its share in total expenditures on healthcare.
As can be seen from Table 8 , the commercialization of Russian healthcare has become an obvious trend.
Table 8.
Structure of healthcare expenditures and their share in GDP in 1995 and 2018
At the same time, the vector of development was directly opposite to that observed in most developed foreign countries. Historically, the improvement of healthcare systems in these countries followed the path of strengthening the role of the state, the transition from private to public funding. As a result, the current share of private financing in total health spending in developed foreign countries (23% in Belgium and France, 22% in Germany, 21% in Great Britain, 16% in Japan, 15% in Norway [ 10 ]) is significantly lower than in Russia (39%).
As many years of world experience have shown, public funding not only ensures universal access to healthcare, but also allows more efficient use of health resources. In Russia, this experience was ignored, including the conclusions of experts that “private financing of healthcare threatens its values and is ineffective in comparison with public financing” [ 11 ]. In this regard, it should be noted that healthcare is the most costly in the United States, where private funding dominated until recently. Thus, total expenditures on healthcare in the United States in 2018 amounted to 16.9% of GDP, which is almost twice more than the average for OECD countries [ 10 ]. At the same time, the United States occupies one of the last places in terms of average life expectancy (78.6 years) among the countries with a high level of economic development.
The commercialization of Russian healthcare has resulted in the increased inequality in the availability of medical care for the population due to the lack of funds for paid medicine among the majority of the population, especially among its poorest strata. So, for example, according to the data from a sample survey of households cited by Federal State Statistics Service, in 2018 20% of the wealthiest citizens accounted for 70% of paid medical services and 20% of the poorest people accounted for less than 1.5%, or a share almost 50 times less. According to sample studies, every seventh resident of the country and every fifth pensioner could not purchase the medicines necessary for treatment due to a lack of funds.
At the beginning of the period under review, a reform of public health financing took place: in addition to state budget financing, a compulsory health insurance system (CHI) was introduced in 1993, which provides for employers paying insurance premiums for employees to the state federal and territorial CHI funds. It should be emphasized that financing through the CHI, i.e., financing by the introduction of compulsory payments for the working population was originally regarded precisely as an addition to financing from the state budget in the context of a sharp decline in the incomes of the latter. This made it possible to dampen the drop in budget financing to a certain extent.
However, later the CHI system began to be considered as the main model for financing healthcare. A transition was made to a one-channel system of financing, in which the budgets of the constituent entities of the Russian Federation transfer certain amounts (contributions) for the nonworking population to the territorial CHI funds. Territorial funds that also receive employers’ insurance contributions from the federal CHI fund transfer the accumulated funds to private insurance companies that finance the activities of medical organizations. Meanwhile, some types of medical care as well as capital expenditures, including the purchase of expensive equipment, are financed exclusively from the state budget.
The above-described complex and contradictory scheme of healthcare financing (public expenditures are carried out by private insurance companies) is only one of the characteristics of the adopted CHI model. Leaving aside for now the assessment of all the negative consequences of the application of this model, we note two important circumstances. First, as international comparative studies show, the CHI model is more costly compared to the system of financing from the state budget and, moreover, does not provide greater efficiency of medical care, in particular, reduction in the mortality rate of the population (for example, see [ 12 ]).
Second, despite the declared transition to universal compulsory health insurance, the main source of public funding for healthcare is still the state budget rather than personalized insurance premiums for each insured person, as in other countries applying the CHI model. As calculations show, employers’ insurance premiums for employees at a statutory rate amounted in 2018 to just over a third (36%) of public health spending despite the increase in this rate from 3.6% during the introduction of CHI to 5.1% in recent years, and budgetary appropriations accounted for the remaining almost two-thirds (calculations were made according to [ 13 ]).
Proceeding from these two facts, a natural question arises about the expediency of maintaining funding according to the adopted CHI model. Recently, proposals to return to the state budget financing system have been increasingly formulated by many experts (see, for example, [ 14 – 16 ]), including due to the ineffectiveness of the CHI model under the conditions of the coronavirus pandemic. In 2020, the state allocated additional budgetary funding for the development of a network of covid hospitals and additional payments to doctors working with coronavirus patients. At the same time, due to a sharp decrease in the number of patients in polyclinics and noncovid hospitals under the conditions of the pandemic, their financing through compulsory medical insurance decreased, which resulted in large accounts payable of medical organizations to insurance companies that pay for their services under compulsory medical insurance [ 17 ].
Summarizing the above, one cannot but agree with the experts’ conclusion that the fundamental limitation of the financial capabilities of the CHI system is becoming more and more obvious [ 16 ]. Moreover, to restore economic growth, it is necessary to increase consumer demand at the expense of the growth in household incomes. Therefore, it seems reasonable to reduce the insurance burden on the wages of employees. In such a situation, in our opinion, the abandonment of the CHI model and the transition to a system of budgetary financing must be considered fully justified.
Under these conditions, an urgent task is to increase significantly state budget spending on healthcare, which is necessary not only to compensate for falling insurance payments, but also to achieve an acceptable level of financing for healthcare in general. The way to solve this problem is also obvious—the state budget revenues must be increased. Until recently, the revenues of the RF consolidated budget amounted to only 35% of the GDP. This is significantly less than in most developed countries: this figure is 45% on average for the EU countries, and in Belgium, Denmark and Finland it exceeds 50% [ 18 ].
It is currently recognized that one of the main problems of economic development is an increase in the income gap with an increasing concentration of income among one percent of the population. The importance of solving this problem was acknowledged by the President of the Russian Federation in his speech at the last Davos Forum [ 19 ].
In developed foreign countries, a decrease in income concentration is stimulated by high tax rates on incomes of the richest citizens from work and property. As a result, one percent of taxpayers account for most of the collected income tax (in the United States, for example, more than 40% [ 20 ]), which is one of the main items of state budget revenues.
In our opinion, the introduction of a high income tax rate in Russia similarly to developed countries in relation to the incomes of the richest citizens must be considered the first step in solving the problem of increasing the incomes of the consolidated budget of the Russian Federation and, accordingly, increasing public spending on healthcare. The relevance of such a solution is defined as extremely high. According to available estimates, the concentration of income in Russia for one percent of the Russian population corresponds to that in the United States. In both countries, especially in Russia, the authorities are realizing the urgent need to reduce this concentration.
It should be emphasized that we are not talking about the introduction of progressive taxation with a multilevel scale of tax rates in Russia. Objections to the introduction of such a system are to a certain extent justified, given the low income of the vast majority of citizens and the complexity of the administration of such taxation. It is proposed not to go beyond the establishment of an increased tax rate on that part of the income of the richest taxpayers, which exceeds a certain threshold value with maintaining the existing tax rate on all incomes below the established threshold, i.e., incomes of the absolute majority of the population. The amount of the threshold income, above which an increased rate must be applied, as well as the amount of this rate can be determined taking into account the experience of taxation in developed foreign countries: the maximum tax rate they use for that part of an individual’s income that exceeds the established threshold. The corresponding calculations for a number of countries [ 21 – 23 ] are given in Table 9 .
Table 9.
The maximum personal income tax rate and the amount of the annual income above which the maximum rate is applied
* Based on the results of international comparisons for 2017.
1 Here and below, if a specific reservation is not made, the indicators are based on the data of the Federal State Statistics Service published in the “Russian Statistical Yearbook,” statistical collections “Healthcare in Russia,” “Demographic Yearbook of Russia,” “Social Position and Living Standard of the Population of Russia,” and “Regions of Russia.”
Translated by L. Solovyova

IMAGES
VIDEO
COMMENTS
We believe a reform agenda should include strategies for tackling the high costs of, and unequal access to, oral health care. Over the past 20 years, per-person dental care costs have increased by ...
Oral health plays a vital role in the physical, mental, social, and economic well-being of individuals and populations (Peres et al. 2019). The oral cavity and its surrounding structures are essential parts of the human body, integral to its daily functioning and contributing substantially to the overall well-being of individuals. The oral cavity also is the main conduit of human interaction ...
Patients are told the importance of keeping oral hygiene and maintaining it. Consulting always helps, because patients can get convinced verbally, about the importance of keeping the mouth clean, and of brushing teeth. Brushing teeth is the most common and best way to maintain oral health. By tooth brushing, the bacterial film which forms on ...
While the imperative to eliminate disparities in oral health has long been recognized (65, 66, 132), the vital role of access to quality oral health care for people who are low-income, uninsured, and/or members of racial/ethnic minority, immigrant, or rural populations has heretofore received insufficient attention in the public health literature (23, 37, 77, 129).
Oral health is a key indicator of overall health, well-being and quality of life. It encompasses a range of diseases and conditions that include dental caries, Periodontal disease, Tooth loss, Oral cancer, Oral manifestations of HIV infection, Oro-dental trauma, Noma and birth defects such as cleft lip and palate. The Global Burden of Disease Study 2017 estimated that oral diseases affect 3.5 ...
Oral health care professionals are fore frontiers in screening of oral diseases, and in educating patients about oral-systemic health connection. Counseling of patient about optimal oral health is an effective way to make them familiar with oral signs of various systemic diseases. Patients' perception of dental practitioner as a physician is ...
The best way to maintain good oral health is to follow the classic dental care advice, including brushing your teeth twice a day and flossing every day, Dr. Scannapieco said. "Not all people ...
Oral health is an important part of prenatal care. Poor oral health during pregnancy can result in poor health outcomes for both mother and baby. For example, studies suggest that pregnant women who have periodontal disease may be more likely to have a baby that is born too early and too small. [7]
Background: Oral health (OH) has evolved beyond dental concerns to encompass psychosocial dimensions and overall well-being. This study reviews OH strategies within a public health framework to identify key elements for effective OH promotion. Methods: A literature review following PRISMA guidelines identified 42 relevant articles from 62 screened. Five themes emerged: group-level, individual ...
Oral cancer includes cancers of the lip, other parts of the mouth and the oropharynx and combined rank as the 13 th most common cancer worldwide. The global incidence of cancers of the lip and oral cavity is estimated to be 377 713 new cases and 177 757 deaths in 2020. Oral cancer is more common in men and in older people, more deadly in men ...
The importance of oral health is: ⦁ Good oral health means more than having healthy teeth. ⦁ Oral health is integral to general health. ⦁ Safe and effective prevention methods exist to improve oral health for everyone. ⦁ Many hours of school are lost due to dental …show more content…. Purpose of Oral Health Care program Oral health ...
Rationale. Oral health is measured by the absence of orofacial pain, oral infection, periodontal (gum) diseases, tooth decay, tooth loss, and other orofacial diseases and disorders that can affect a person's overall physical and mental health, and social well-being [1,2,3].This is a particular concern for older people [2,3,4,5].The world's population is ageing rapidly [].
Discussion. Oral health is an essential to overall well-being and relates to the quality of life. Childhood dental caries significantly contributes to the burden of pain and is associated with a marked decrease in the quality of life and general health. Keyes and Jordan stated that dental caries involves triad of indispensable factors: bacteria ...
Oral health is an integral part of the overall health of children. Dental caries is a common and chronic disease process with significant short- and long-term consequences. The prevalence of dental caries remains greater than 40% among children 2 to 19 years of age. Although dental visits have increased in all age, race, and geographic categories in the United States, disparities continue to ...
Oral health promotion is for upliftment of oral health of community rather than an individual and has long‐term impact. Since Ottawa Charter for health promotion is implemented, significant advancements have happened in oral health promotion. Under comprehensive health programs, India has been running oral health promotion programs, and these evidences are shared here.
These include inequities in access to dental care, disparities in the prevalence of oral disease, risk behaviors related to oral disease, the relationship between oral health and chronic diseases, and the effect of the COVID-19 pandemic on oral health. Healthy People 2030 is the fifth iteration of national health objectives for the United ...
Why good dental care is important to your overall health. A great smile can do so many things. It can light up the room. It can win over new friends. And it can reveal a lot about your health, both inside the mouth and throughout the body. The key to keeping that great smile is taking care of your teeth. That means brushing and flossing, of ...
Importance Of Dental Health Essay. 704 Words3 Pages. Maintaining good dental health is as important as maintaining our general health, but we usually do not care for our dental health, though it has been proven that poor dental health is linked to other diseases, such as heart disease, diabetes, preterm birth, low birth weight, stomach problems ...
RESULTS. Thirteen studies[3,4,5,6,7,8,9,10,11,12,13,14,15] showed their effectiveness in terms of change in knowledge, the sample size ranged from 42 to 2678 participants.The oral health education group ranged from 14 to 1339. The target population was mainly schools children and care givers of children and the elderly.
The compliance of health professionals, especially dental practitioners, with appropriate oral health measures is relatively high, however, the dental team cannot always assume that the dental patient, who also happens to be a healthcare provider, has meticulous oral habits. Expand. Semantic Scholar extracted view of "Reflections on Clinical ...
The high cost of oral diseases. Annual costs for dental care in the United States is $136 billion. 4 A On average, over 34 million school hours are lost each year because of unplanned (emergency) dental care. 5 Almost $46 billion B is lost in productivity in the United States each year because of untreated oral disease. 6. In 2017, there were 2.1 million emergency room visits for dental ...
Poor oral hygiene is associated with an increased risk for myriad health problems, including heart disease, diabetes, cancer, rheumatoid arthritis and early death. The state of our teeth and gums ...
The essay underscores that while health and wellness are interconnected, wellness involves a more comprehensive and self-directed approach to achieving a balanced and fulfilling life. ... Health Care. Date added: 2024/05/21. Words: 1488. Download: 209. Order Original Essay. ... Dentistry: Fusing Mind, Body, and Oral Wellness. Words: 515. Yoga ...
521 S. Main, Moscow, Idaho 83843 | (208) 882-2669 | [email protected] | 10am - 6pm Mon-Sat, 10am - 4pm Sun
Fact sheet. Budget 2024-25: A fit and healthy Australia. 14 May 2024. Fact sheet. We aim to provide documents in an accessible format. If you're having problems using a document with your accessibility tools, please contact us for help. Publication date: 14 May 2024. Publication type:
All the English-language papers were evaluated based on the inclusion criteria. Publications included original research papers, review articles, and book chapters. ... self-esteem, lack of oral health awareness, and mistrust of dental health care providers. 82 Individuals with mental disorders may be considered a vulnerable group because of ...
Similar to healthcare for the population as a whole, children's healthcare in Russia varies greatly across the regions. Services are far more prevalent in urban areas and big cities, while infrastructure is lacking in many rural parts. Children receive free healthcare in Russia under the OMI system. This includes dental care in Russia. In ...
ESSAYESSAY prize for medicine. The history of tobacco con - trol would have a final chapter on the triumph of harm reduction and the role of innovation. E-cigarettes would have made smoking history. Worst case scenario The story could, however, be very different. Under the worst case scenario global uptake of
A comparative analysis of the development of healthcare in Russia and other countries is carried out. The conclusion is confirmed that the main problem in the development of Russian healthcare is the insufficient volume of public funding. The drawbacks and limited potential of the adopted funding model are assessed.