- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
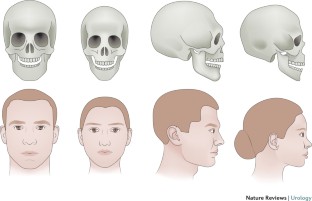
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
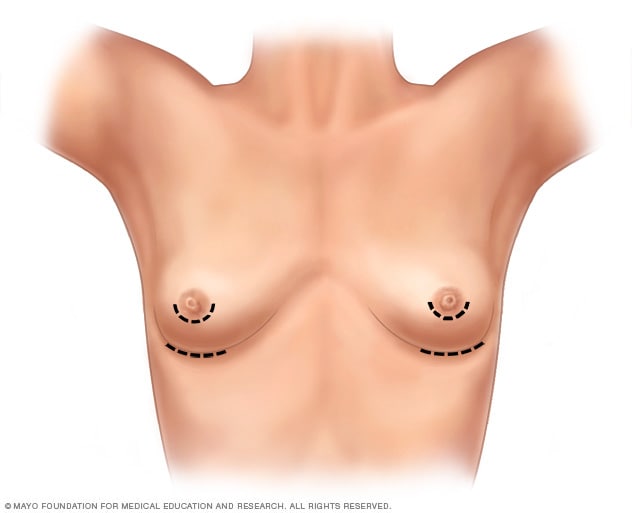
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
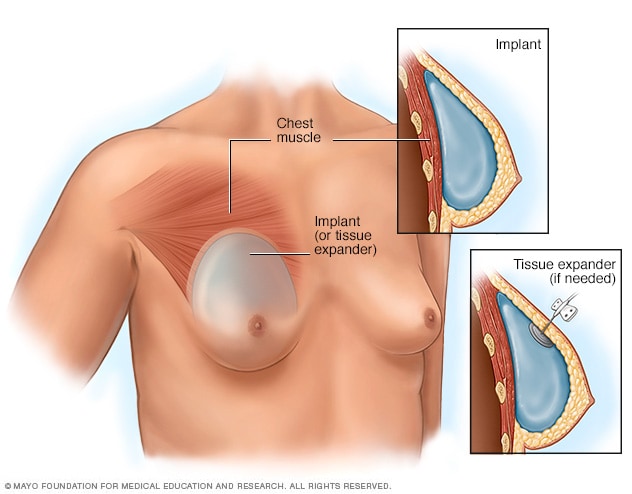
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
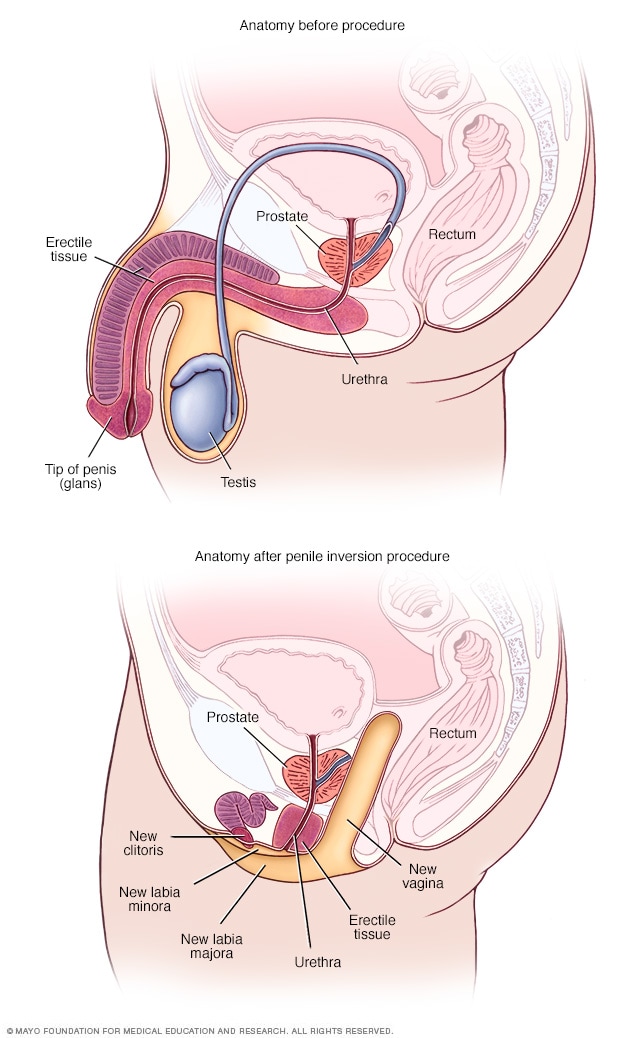
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
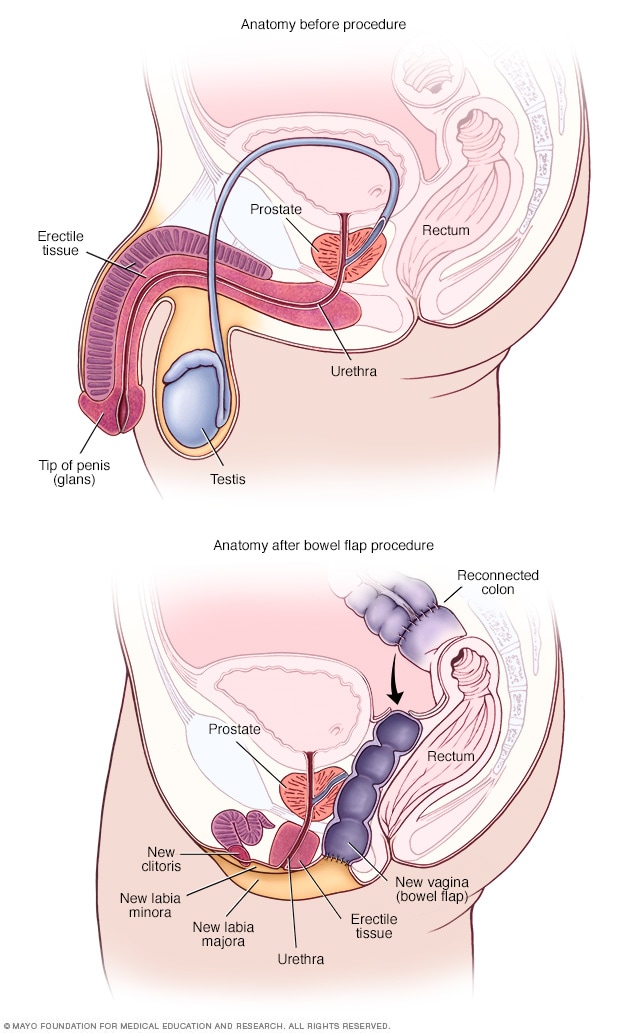
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Female to Male Surgery for Trans Men
As a transgender male, your goal for female to male surgery (FTM) for gender-confirmation can involve top surgery, bottom surgery, or both. You may or may not want facial procedures. It’s up to you.
Female to Male Surgery at UVA
We’re here to offer consultations, second opinions, and information to help you choose and plan. Come to us with your questions and concerns. We’ll explain:
- Procedure options and details
- Recovery and healing
- What to expect of your results
We want you to feel confident about the direction and quality of your care.
Charley's Gender-Confirmation Surgery
From a young age, Charley Burton knew that his body did not match his gender identity – a struggle he kept inside for 50 years. With the help of family nurse practitioner Reagan Thompson, FNP, MSN, RN, and a whole team of caring providers, Charley found a safe place to become his true self. View Charley's story transcript.
FTM Top Surgery
To give you a flatter chest, we’ll have to remove breast tissue. We might also need to move and shrink your areolas.
If you have smaller breasts, we can sometimes use liposuction, which doesn’t involve many incisions.
Larger breasts may require the “double incision” technique. This method saves the pectoralis major muscle, the most defining characteristic of a male chest.
Whatever your breast size, we will use the techniques that optimize the results.
FTM Bottom Surgery
We can give you male genitalia in two different ways:
- Phalloplasty creates a penis and urethra (to stand while urinating). We use tissue from your forearm or thigh. We do this in 2 stages.
- Metoidioplasty takes your existing genital tissue and makes it longer, turning it into a defined phallus. This needs only one surgery.
You may or may not want to also have an operation to remove your internal reproductive organs. A hysterectomy takes out your uterus, fallopian tubes, and ovaries.
Facial Masculinization
Through a combination of procedures, we can sculpt your chin, jaw, and cheeks to appear more masculine. We can also reshape your nose and make your Adam’s apple look bigger. We can use synthetic implants for this work.
Questions? See our transgender surgery FAQs .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 16 May 2017
An overview of female-to-male gender-confirming surgery
- Shane D. Morrison 1 ,
- Mang L. Chen 2 &
- Curtis N. Crane 2
Nature Reviews Urology volume 14 , pages 486–500 ( 2017 ) Cite this article
2676 Accesses
63 Citations
13 Altmetric
Metrics details
- Reconstruction
- Sexual behaviour
Gender-confirming surgery is becoming a more frequently encountered procedure for urologists, plastic surgeons, and gynaecologists
Female-to-male gender-confirming surgery consists of facial masculinization, chest masculinization, body contouring, and genital surgery
Metoidioplasty (hypertrophy with systemic hormones and mobilization of the clitoris with urethroplasty) can produce a sensate microphallus
Phalloplasty can produce an aesthetic and sensate phallus with ability to micturate in a standing position and engage in penetrative sexual intercourse if proper nerve coaptation and prosthetic insertion are performed
Urethral complications following genital surgery in transmen are generally higher than 30% and include urethral fistulas and strictures; revisional urethroplasty can address most urethral complications following genital surgery
Advances in basic sciences, transgender-specific prostheses, and patient-reported outcomes will continue to offer options for improvements in gender-confirming surgery
Gender dysphoria is estimated to occur in approximately 25 million people worldwide, and can have severe psychosocial sequelae. Medical and surgical gender transition can substantially improve quality-of-life outcomes for individuals with gender dysphoria. Individuals seeking to undergo female-to-male (FtM) transition have various surgical options available for gender confirmation, including facial and chest masculinization, body contouring, and genital surgery. The World Professional Association for Transgender Health guidelines should be met before the patient undergoes surgery, to ensure that gender-confirming surgery is appropriate and indicated. Chest masculinization and metoidioplasty or phalloplasty are the most common procedures pursued, and both generally result in high levels of patient satisfaction. Phalloplasty, with a resultant aesthetic and sensate phallus along with implantable prosthetic, can take upwards of a year to accomplish, and is associated with a considerable risk of complications. Urethral complications are most frequent, and can be addressed with revision procedures. A number of scaffolds, implants, and prostheses are now in development to improve outcomes in FtM patients.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Male-to-female gender affirmation surgery: breast reconstruction with Ergonomix round prostheses

Overview on metoidioplasty: variants of the technique

Masculinizing genital gender-affirming surgery: metoidioplasty and urethral lengthening
World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. 7th Version (World Professional Association for Transgender Health, 2011). Standards of care for transgender and gender nonconforming patients to assist all providers caring for patients within this population.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Benjamin, H. The Transsexual Phenomenon (Julian Press, 1966).
Google Scholar
Byne, W. et al . Report of the American Psychiatric Association task force on treatment of gender identity disorder. Arch. Sex. Behav. 41 , 759–796 (2012).
Article PubMed Google Scholar
Dhejne, C. et al . Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS ONE 6 , e16885 (2011).
Article CAS PubMed PubMed Central Google Scholar
Dhejne, C., Oberg, K., Arver, S. & Landen, M. An analysis of all applications for sex reassignment surgery in Sweden, 1960-2010: prevalence, incidence, and regrets. Arch. Sex. Behav. 43 , 1535–1545 (2014).
Lawrence, A. A. Gender assignment dysphoria in the DSM-5. Arch. Sex. Behav. 43 , 1263–1266 (2014).
Leiter, E., Futterweit, W. & Brown, G. R. in Reconstructive Urology Vol. 2 (eds Webster, G., Kirby, R., King, L. & Goldwasser, B.) 921–932 (Blackwell Scientific Publications, 1993).
Winter, S. et al . Transgender people: health at the margins of society. Lancet 388 , 390–400 (2016). Evaluation of the difficulties experienced by transgender patients in seeking healthcare.
Wylie, K. et al . Serving transgender people: clinical care considerations and service delivery models in transgender health. Lancet 388 , 401–411 (2016).
Gooren, L. J. Clinical practice. Care of transsexual persons. N. Engl. J. Med. 364 , 1251–1257 (2011).
Article CAS PubMed Google Scholar
Deutsch, M. B. et al . Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J. Am. Med. Inform. Assoc. 20 , 700–703 (2013).
Article PubMed PubMed Central Google Scholar
Morrison, S. D. The care transition in plastic surgery. Plast. Reconstr. Surg. 136 , 861e–862e (2015).
Morrison, S. D. & Swanson, J. W. Surgical justice. Plast. Reconstr. Surg. 136 , 291e–292e (2015).
De Cuypere, G., Elaut, E. & Heylens, G. Long-term follow-up: psychosocial outcome of Belgian transsexuals after sex reassignment surgery. Sexologies 15 , 126–133 (2006).
Article Google Scholar
De Cuypere, G. et al . Sexual and physical health after sex reassignment surgery. Arch. Sex. Behav. 34 , 679–690 (2005).
Hage, J. J. & Karim, R. B. Ought GIDNOS get nought? Treatment options for nontranssexual gender dysphoria. Plast. Reconstr. Surg. 105 , 1222–1227 (2000).
Lawrence, A. A. Sexuality before and after male-to-female sex reassignment surgery. Arch. Sex. Behav. 34 , 147–166 (2005).
Wierckx, K. et al . Sexual desire in female-to-male transsexual persons: exploration of the role of testosterone administration. Eur. J. Endocrinol. 165 , 331–337 (2011).
Wierckx, K. et al . Sexual desire in trans persons: associations with sex reassignment treatment. J. Sex. Med. 11 , 107–118 (2014). Evaluation of the sexual desires experienced by transgender patients after gender-confirming surgery.
Wierckx, K. et al . Long-term evaluation of cross-sex hormone treatment in transsexual persons. J. Sex. Med. 9 , 2641–2651 (2012).
Wierckx, K. et al . Quality of life and sexual health after sex reassignment surgery in transsexual men. J. Sex. Med. 8 , 3379–3388 (2011).
Zaker-Shahrak, A., Chio, L. W., Isaac, R. & Tescher, J. Economic impact assessment: Gender nondiscrimination in health insurance. (ed. Department of Insurance) (State of California, 2012).
Monstrey, S. et al . Surgical therapy in transsexual patients: a multi-disciplinary approach. Acta Chir. Belg. 101 , 200–209 (2001).
CAS PubMed Google Scholar
Selvaggi, G., Dhejne, C., Landen, M. & Elander, A. The 2011 WPATH standards of care and penile reconstruction in female-to-male transsexual individuals. Adv. Urol. 2012 , 581712 (2012).
Gooren, L. J. Management of female-to-male transgender persons: medical and surgical management, life expectancy. Curr. Opin. Endocrinol. Diabetes Obes. 21 , 233–238 (2014).
Davis, S. R. et al . Testosterone for low libido in postmenopausal women not taking estrogen. N. Engl. J. Med. 359 , 2005–2017 (2008).
Gooren, L. J. & Giltay, E. J. Review of studies of androgen treatment of female-to-male transsexuals: effects and risks of administration of androgens to females. J. Sex. Med. 5 , 765–776 (2008).
Gooren, L. J., Giltay, E. J. & Bunck, M. C. Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience. J. Clin. Endocrinol. Metab. 93 , 19–25 (2008).
Mueller, A. & Gooren, L. Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur. J. Endocrinol. 159 , 197–202 (2008).
Van Caenegem, E. et al . Bone mass, bone geometry, and body composition in female-to-male transsexual persons after long-term cross-sex hormonal therapy. J. Clin. Endocrinol. Metab. 97 , 2503–2511 (2012).
Monstrey, S. J., Ceulemans, P. & Hoebeke, P. Sex reassignment surgery in the female-to-male transsexual. Semin. Plast. Surg. 25 , 229–244 (2011).
Morrison, S. D., Perez, M. G., Carter, C. K. & Crane, C. N. Pre- and post-operative care with associated intra-operative techniques for phalloplasty in female-to-male patients. Urol. Nurs. 35 , 134–138 (2015).
Morrison, S. D., Perez, M. G., Nedelman, M. & Crane, C. N. Current state of female-to-male gender confirming surgery. Curr. Sex. Health Rep. 7 , 38–48 (2015).
Selvaggi, G. & Bellringer, J. Gender reassignment surgery: an overview. Nat. Rev. Urol. 8 , 274–282 (2011).
Morrison, S. D. et al . Educational exposure to transgender patient care in plastic surgery training. Plast. Reconstr. Surg. 138 , 944–953 (2016). Evaluation of resident exposure to transgender patient care in plastic surgery.
Obedin-Maliver, J. et al . Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA 306 , 971–977 (2011).
Dy, G. W. et al . Exposure to and attitudes regarding transgender education among urology residents. J. Sex. Med. 13 , 1466–1472 (2016). Evaluation of resident exposure to transgender patient care in urology.
Morrison, S. D. et al . Facial feminization: systematic review of the literature. Plast. Reconstr. Surg. 137 , 1759–1770 (2016).
Ousterhout, D. K. Dr. Paul Tessier and facial skeletal masculinization. Ann. Plast. Surg. 67 , S10–S15 (2011).
Deschamps-Braly, J. C., Sacher, C. L., Fick, J. & Ousterhout, D. K. First female-to-male facial confirmation surgery with description of a new procedure for masculinization of the thyroid cartilage (Adam's apple). Plast. Reconstr. Surg. 139 , 883e–887e (2017). First report of facial masculinization in transmen.
Monstrey, S. et al . Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast. Reconstr. Surg. 121 , 849–859 (2008). Algorithmic approach to chest wall masculinization.
Richards, C. & Barrett, J. The case for bilateral mastectomy and male chest contouring for the female-to-male transsexual. Ann. R. Coll. Surg. Engl. 95 , 93–95 (2013).
Berry, M. G., Curtis, R. & Davies, D. Female-to-male transgender chest reconstruction: a large consecutive, single-surgeon experience. J. Plast. Reconstr. Aesthet. Surg. 65 , 711–719 (2012).
Colic, M. M. & Colic, M. M. Circumareolar mastectomy in female-to-male transsexuals and large gynecomastias: a personal approach. Aesthetic Plast. Surg. 24 , 450–454 (2000).
Nelson, L., Whallett, E. J. & McGregor, J. C. Transgender patient satisfaction following reduction mammaplasty. J. Plast. Reconstr. Aesthet. Surg. 62 , 331–334 (2009).
Vukadinovic, V., Stojanovic, B., Majstorovic, M. & Milosevic, A. The role of clitoral anatomy in female to male sex reassignment surgery. ScientificWorldJournal 2014 , 437378 (2014).
Weyers, S. et al . Gynaecological aspects of the treatment and follow-up of transsexual men and women. Facts Views Vis. Obgyn. 2 , 35–54 (2010).
CAS PubMed PubMed Central Google Scholar
Ergeneli, M. H., Duran, E. H., Ozcan, G. & Erdogan, M. Vaginectomy and laparoscopically assisted vaginal hysterectomy as adjunctive surgery for female-to-male transsexual reassignment: preliminary report. Eur. J. Obstet. Gynecol. Reprod. Biol. 87 , 35–37 (1999).
Weyers, S., Selvaggi, G. & Monstrey, S. Two-stage versus one-stage sex reassignment surgery in female-to-male transsexual individuals. Gynecol. Surg. 3 , 190–194 (2006).
Morrison, S. D. et al . Phalloplasty: a review of techniques and outcomes. Plast. Reconstr. Surg. 138 , 594–615 (2016). Contemporary evaluation of techniques and outcomes of phalloplasty.
Perrone, A. M. et al . Hysterectomy and bilateral salpingoovariectomy in a transsexual subject without visible scaring. Diagn. Ther. Endosc. 2010 , 845029 (2010).
Chen, Y. J. et al . Single-port compared with conventional laparoscopic-assisted vaginal hysterectomy: a randomized controlled trial. Obstet. Gynecol. 117 , 906–912 (2011).
Bogliolo, S. et al . Robotic single-site surgery for female-to-male transsexuals: preliminary experience. ScientificWorldJournal 2014 , 674579 (2014).
Obedin-Maliver, J., Light, A., Dehaan, G., Steinauer, J. & Jackson, R. Vaginal hysterectomy as a viable option for female-to-male transgender men. Obstet. Gynecol. 123 (Suppl. 1), 126S–127S (2014).
Djordjevic, M. L. et al . Urethral lengthening in metoidioplasty (female-to-male sex reassignment surgery) by combined buccal mucosa graft and labia minora flap. Urology 74 , 349–353 (2009).
Djordjevic, M. L. & Bizic, M. R. Comparison of two different methods for urethral lengthening in female to male (metoidioplasty) surgery. J. Sex. Med. 10 , 1431–1438 (2013). Assessment of outcomes of urethral lengthening following metoidioplasty.
Zhang, Y. F. et al . Is vaginal mucosal graft the excellent substitute material for urethral reconstruction in female-to-male transsexuals? World J. Urol. 33 , 2115–2123 (2015).
Hage, J. J. & Bloem, J. J. Review of the literature on construction of a neourethra in female-to-male transsexuals. Ann. Plast. Surg. 30 , 278–286 (1993).
Hage, J. J., Bouman, F. G. & Bloem, J. J. Construction of the fixed part of the neourethra in female-to-male transsexuals: experience in 53 patients. Plast. Reconstr. Surg. 91 , 904–910 (1993).
Rohrmann, D. & Jakse, G. Urethroplasty in female-to-male transsexuals. Eur. Urol. 44 , 611–614 (2003).
Selvaggi, G. & Elander, A. Penile reconstruction/formation. Curr. Opin. Urol. 18 , 589–597 (2008).
Salgado, C. J., Chim, H., Tang, J. C., Monstrey, S. J. & Mardini, S. Penile reconstruction. Semin. Plast. Surg. 25 , 221–228 (2011).
Hage, J. J. & De Graaf, F. H. Addressing the ideal requirements by free flap phalloplasty: some reflections on refinements of technique. Microsurgery 14 , 592–598 (1993).
Monstrey, S. et al . Penile reconstruction: is the radial forearm flap really the standard technique? Plast. Reconstr. Surg. 124 , 510–518 (2009). Largest evaluation of outcomes of RFFF phalloplasty.
Zhang, W. R., Garrett, G. L., Arron, S. T. & Garcia, M. M. Laser hair removal for genital gender affirming surgery. Transl Androl. Urol. 5 , 381–387 (2016).
Durfee, R. & Rowland, W. in Proceedings of the Second Interdisciplinary Symposium on Gender Dysphoria Syndrome (eds Laub, D. R. & Gandy, P.) 181–183 (Stanford Univ. Press, 1973).
Lebovic, G. S. & Laub, D. R. in Reconstructive and Plastic Surgery of the External Genitalia (eds Ehrlich, R. M. & Alter, G. J.) 355–360 (WB Saunders, 1999).
Hage, J. J. Metaidoioplasty: an alternative phalloplasty technique in transsexuals. Plast. Reconstr. Surg. 97 , 161–167 (1996).
Hage, J. J. & van Turnhout, A. A. Long-term outcome of metaidoioplasty in 70 female-to-male transsexuals. Ann. Plast. Surg. 57 , 312–316 (2006).
Oakley, S. H. et al . Innervation and histology of the clitoral-urethal complex: a cross-sectional cadaver study. J. Sex. Med. 10 , 2211–2218 (2013).
Djordjevic, M. L. et al . Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience. J. Sex. Med. 6 , 1306–1313 (2009).
Perovic, S. V. & Djordjevic, M. L. Metoidioplasty: a variant of phalloplasty in female transsexuals. BJU Int. 92 , 981–985 (2003).
Takamatsu, A. & Harashina, T. Labial ring flap: a new flap for metaidoioplasty in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62 , 318–325 (2009).
Bogoras, N. Über die volle plastische Wiederherstellung eines zum Koitus fähigen Penis (Peniplastica totalis) [German]. Zentralbl. Chir. 63 , 1271–1276 (1936).
Gillies, H. & Millard, R. The Principles and Art of Plastic Surgery Vol. II 369–388 (Little, Brown and Company, 1957).
Kaplan, I. A rapid method for constructing a functional sensitive penis. Br. J. Plast. Surg. 24 , 342–344 (1971).
Puckett, C. L., Reinisch, J. F. & Montie, J. E. Free flap phalloplasty. J. Urol. 128 , 294–297 (1982).
Hu, W. et al . A preliminary report of penile transplantation: part 2. Eur. Urol. 50 , 1115–1116 (2006).
Hu, W. et al . A preliminary report of penile transplantation. Eur. Urol. 50 , 851–853 (2006).
Morrison, S. D. et al . Penile replantation: a retrospective analysis of outcomes and complications. J. Reconstr. Microsurg. 33 , 227–232 (2017).
Monstrey, S. et al . Radial forearm phalloplasty: a review of 81 cases. Eur. J. Plast. Surg. 28 , 206–212 (2005).
Bettocchi, C., Ralph, D. J. & Pryor, J. P. Pedicled pubic phalloplasty in females with gender dysphoria. BJU Int. 95 , 120–124 (2005).
Shaeer, O. & El-Sebaie, A. Construction of neoglans penis: a new sculpturing technique from rectus abdominis myofascial flap. J. Sex. Med. 2 , 259–265 (2005).
Terrier, J. E., Courtois, F., Ruffion, A. & Morel Journel, N. Surgical outcomes and patients' satisfaction with suprapubic phalloplasty. J. Sex. Med. 11 , 288–298 (2014).
Alanis, S. Z. An innovation in total penis reconstruction. Plast. Reconstr. Surg. 43 , 418–422 (1969).
Davies, D. Phalloplasty. S. Afr. Med. J. 31 , 990–991 (1957).
Davies, D. M. & Matti, B. A. A method of phalloplasty using the deep inferior epigastric flap. Br. J. Plast. Surg. 41 , 165–168 (1988).
Dubin, B. J., Sato, R. M. & Laub, D. R. Results of phalloplasty. Plast. Reconstr. Surg. 64 , 163–170 (1979).
Santi, P. et al . Immediate reconstruction of the penis using an inferiorly based rectus abdominis myocutaneous flap. Plast. Reconstr. Surg. 81 , 961–964 (1988).
Zhang, Y., Lu, L., Zhang, W., Jiang, H. & Zhu, X. A simple and effective method for phalloplasty in female-to-male transsexuals. Plast. Reconstr. Surg. 126 , 264e–265e (2010).
Lumen, N., Hoebeke, P. & Oosterlinck, W. Urethroplasty for urethral strictures: quality assessment of an in-home algorithm. Int. J. Urol. 17 , 167–174 (2010).
Krauss, E. M., Tung, T. H. & Moore, A. M. Free functional muscle transfers to restore upper extremity function. Hand Clin. 32 , 243–256 (2016).
Ranno, R. et al . Neo-phalloplasty with re-innervated latissimus dorsi free flap: a functional study of a novel technique. Acta Chir. Plast. 49 , 3–7 (2007).
Ranno, R., Hyza, P., Vesely, J., Dessy, L. A. & Kadanka, Z. An objective evaluation of contraction power of neo-phallus reconstructed with free re-innervated LD in female-to-male transsexuals. Acta Chir. Plast. 49 , 8–12 (2007).
Mori, R. L. & Angermeier, K. W. Staged urethroplasty in the management of complex anterior urethral stricture disease. Transl Androl. Urol. 4 , 29–34 (2015).
PubMed PubMed Central Google Scholar
Djordjevic, M. L., Bumbasirevic, M. Z., Vukovic, P. M., Sansalone, S. & Perovic, S. V. Musculocutaneous latissimus dorsi free transfer flap for total phalloplasty in children. J. Pediatr. Urol. 2 , 333–339 (2006).
Lin, C. T. & Chen, L. W. Using a free thoracodorsal artery perforator flap for phallic reconstruction — a report of surgical technique. J. Plast. Reconstr. Aesthet. Surg. 62 , 402–408 (2009).
Perovic, S. V., Djinovic, R., Bumbasirevic, M., Djordjevic, M. & Vukovic, P. Total phalloplasty using a musculocutaneous latissimus dorsi flap. BJU Int. 100 , 899–905 (2007).
Vesely, J. et al . New technique of total phalloplasty with reinnervated latissimus dorsi myocutaneous free flap in female-to-male transsexuals. Ann. Plast. Surg. 58 , 544–550 (2007).
Kessler, T. M. et al . Long-term results of surgery for urethral stricture: a statistical analysis. J. Urol. 170 , 840–844 (2003).
Mathur, R. K. et al . Single-stage preputial skin flap urethroplasty for long-segment urethral strictures: evaluation and determinants of success. BJU Int. 113 , 120–126 (2014).
Taguchi, H., Saito, K. & Yamada, T. A simple method of total reconstruction of the penis. Case reports. Plast. Reconstr. Surg. 60 , 454–456 (1977).
Hage, J. J., Winters, H. A. & Van Lieshout, J. Fibula free flap phalloplasty: modifications and recommendations. Microsurgery 17 , 358–365 (1996).
Sadove, R. C., Sengezer, M., McRoberts, J. W. & Wells, M. D. One-stage total penile reconstruction with a free sensate osteocutaneous fibula flap. Plast. Reconstr. Surg. 92 , 1314–1323 (1993).
McRoberts, J. W. & Sadove, R. C. Penile reconstruction with a free sensate osteocutaneous fibula flap in the surgical management of the intersex patient. Adv. Exp. Med. Biol. 511 , 283–287 (2002).
Sengezer, M., Ozturk, S., Deveci, M. & Odabasi, Z. Long-term follow-up of total penile reconstruction with sensate osteocutaneous free fibula flap in 18 biological male patients. Plast. Reconstr. Surg. 114 , 439–450 (2004).
Dabernig, J., Chan, L. K. & Schaff, J. Phalloplasty with free (septocutaneous) fibular flap sine fibula. J. Urol. 176 , 2085–2088 (2006).
Papadopulos, N. A., Schaff, J. & Biemer, E. The use of free prelaminated and sensate osteofasciocutaneous fibular flap in phalloplasty. Injury 39 (Suppl. 3), S62–S67 (2008).
Salgado, C. J., Rampazzo, A., Xu, E. & Chen, H. C. Treatment of dyspareunia by creation of a pseudojoint in rigid bone following total penile reconstruction with fibular osteocutaneous flap. J. Sex. Med. 5 , 2947–2950 (2008).
Sun, G. C. & Huang, J. J. One-stage reconstruction of the penis with composite iliac crest and lateral groin skin flap. Ann. Plast. Surg. 15 , 519–528 (1985).
Cutting, C. B. & McCarthy, J. G. Comparison of residual osseous mass between vascularized and nonvascularized onlay bone transfers. Plast. Reconstr. Surg. 72 , 672–675 (1983).
Weiland, A. J., Phillips, T. W. & Randolph, M. A. Bone grafts: a radiologic, histologic, and biomechanical model comparing autografts, allografts, and free vascularized bone grafts. Plast. Reconstr. Surg. 74 , 368–379 (1984).
Zielinski, T. Phalloplasty using a lateral groin flap in female-to-male transsexuals. Acta Chir. Plast. 41 , 15–19 (1999).
Akoz, T., Erdogan, B., Gorgu, M., Kapucu, M. R. & Kargi, E. Penile reconstruction in children using a double vascular pedicle composite groin flap. Scand. J. Urol. Nephrol. 32 , 225–230 (1998).
Akoz, T. & Kargi, E. Phalloplasty in a female-to-male transsexual using a double-pedicle composite groin flap. Ann. Plast. Surg. 48 , 423–427 (2002).
Puckett, C. L. & Montie, J. E. Construction of male genitalia in the transsexual, using a tubed groin flap for the penis and a hydraulic inflation device. Plast. Reconstr. Surg. 61 , 523–530 (1978).
Felici, N. & Felici, A. A new phalloplasty technique: the free anterolateral thigh flap phalloplasty. J. Plast. Reconstr. Aesthet. Surg. 59 , 153–157 (2006).
Lee, G. K., Lim, A. F. & Bird, E. T. A novel single-flap technique for total penile reconstruction: the pedicled anterolateral thigh flap. Plast. Reconstr. Surg. 124 , 163–166 (2009).
Hasegawa, K., Namba, Y. & Kimata, Y. Phalloplasty with an innervated island pedicled anterolateral thigh flap in a female-to-male transsexual. Acta Med. Okayama 67 , 325–331 (2013).
PubMed Google Scholar
Morrison, S. D. et al . Modification of the tube-in-tube pedicled anterolateral thigh flap for total phalloplasty: the mushroom flap. Ann. Plast. Surg. 72 (Suppl. 1), S22–S26 (2014).
Mutaf, M. A new surgical procedure for phallic reconstruction: Istanbul flap. Plast. Reconstr. Surg. 105 , 1361–1370 (2000).
Hoebeke, P. B. et al . Erectile implants in female-to-male transsexuals: our experience in 129 patients. Eur. Urol. 57 , 334–340 (2010).
Lumen, N. et al . Erectile implants in female-to-male transsexuals: our experience in 130 patients [abstract]. Eur. Urol. Suppl. 7 , 117 (2008).
Neuville, P. et al . Surgical outcomes of erectile implants after phalloplasty: retrospective analysis of 95 procedures. J. Sex. Med. 13 , 1758–1764 (2016). Recent evaluation of outcomes of prosthetics in phalloplasty.
Gurjala, A. N., Nazerali, R. S., Salim, A. & Lee, G. K. World's first baby born through natural insemination by father with total phalloplasty reconstruction. Ann. Plast. Surg. 76 (Suppl. 3), S179–S183 (2016).
Sinove, Y. et al . Preoperative planning of a pedicled anterolateral thigh (ALT) flap for penile reconstruction with the multidetector CT scan. Handchir. Mikrochir. Plast. Chir. 45 , 217–222 (2013).
Liu, C. Y., Wei, Z. R., Jiang, H., Zhao, Y. Z. & Zhang, Y. F. Preconstruction of the pars pendulans urethrae for phalloplasty with digestive mucosa using a prefabricated anterolateral thigh flap in a one-arm patient. Plast. Reconstr. Surg. Glob. Open 1 , e53 (2013).
Rubino, C. et al . Innervated island pedicled anterolateral thigh flap for neo-phallic reconstruction in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62 , e45–e49 (2009).
Chang, T. S. & Hwang, W. Y. Forearm flap in one-stage reconstruction of the penis. Plast. Reconstr. Surg. 74 , 251–258 (1984).
Monstrey, S. et al . Radial Forearm Phalloplasty: a Review of 91 Cases. ANIR-ANHP 6 , 193–199 (2004).
Selvaggi, G. et al . Genital sensitivity after sex reassignment surgery in transsexual patients. Ann. Plast. Surg. 58 , 427–433 (2007). Evaluation of genital sensitivity following phalloplasty for transmen.
Fang, R. H., Kao, Y. S., Ma, S. & Lin, J. T. Phalloplasty in female-to-male transsexuals using free radial osteocutaneous flap: a series of 22 cases. Br. J. Plast. Surg. 52 , 217–222 (1999).
Kim, S. K. et al . The etiology and treatment of the softened phallus after the radial forearm osteocutaneous free flap phalloplasty. Arch. Plast. Surg. 39 , 390–396 (2012).
Trost, L., Wanzek, P. & Bailey, G. A practical overview of considerations for penile prosthesis placement. Nat. Rev. Urol. 13 , 33–46 (2016).
Biemer, E. Penile construction by the radial arm flap. Clin. Plast. Surg. 15 , 425–430 (1988).
Doornaert, M. et al . Penile reconstruction with the radial forearm flap: an update. Handchir. Mikrochir. Plast. Chir. 43 , 208–214 (2011).
Matti, B. A., Matthews, R. N. & Davies, D. M. Phalloplasty using the free radial forearm flap. Br. J. Plast. Surg. 41 , 160–164 (1988).
Salgado, C. J. et al . Immediate pedicled gracilis flap in radial forearm flap phalloplasty for transgender male patients to reduce urinary fistula. J. Plast. Reconstr. Aesthet. Surg. 69 , 1551–1557 (2016).
Selvaggi, G. et al . Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast. Reconstr. Surg. 118 , 1171–1177 (2006).
Bardsley, A. F., Soutar, D. S., Elliot, D. & Batchelor, A. G. Reducing morbidity in the radial forearm flap donor site. Plast. Reconstr. Surg. 86 , 287–292 (1990).
Boorman, J. G., Brown, J. A. & Sykes, P. J. Morbidity in the forearm flap donor arm. Br. J. Plast. Surg. 40 , 207–212 (1987).
Richardson, D., Fisher, S. E., Vaughan, E. D. & Brown, J. S. Radial forearm flap donor-site complications and morbidity: a prospective study. Plast. Reconstr. Surg. 99 , 109–115 (1997).
Van Caenegem, E. et al . Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. J. Sex. Med. 10 , 1644–1651 (2013).
Rieger, U. M. et al . Comparative study of the free microvascular groin flap: optimizing the donor site after free radial forearm flap phalloplasty. Urology 95 , 192–196 (2016).
Fang, R. H., Lin, J. T. & Ma, S. Phalloplasty for female transsexuals with sensate free forearm flap. Microsurgery 15 , 349–352 (1994).
Gottlieb, L. J. & Levine, L. A. A new design for the radial forearm free-flap phallic construction. Plast. Reconstr. Surg. 92 , 276–283 (1993).
Hage, J. J., Bouman, F. G., de Graaf, F. H. & Bloem, J. J. Construction of the neophallus in female-to-male transsexuals: the Amsterdam experience. J. Urol. 149 , 1463–1468 (1993).
Kim, S. K., Lee, K. C., Kwon, Y. S. & Cha, B. H. Phalloplasty using radial forearm osteocutaneous free flaps in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62 , 309–317 (2009).
Koshima, I., Tai, T. & Yamasaki, M. One-stage reconstruction of the penis using an innervated radial forearm osteocutaneous flap. J. Reconstr. Microsurg. 3 , 19–26 (1986).
Leriche, A. et al . Long-term outcome of forearm flee-flap phalloplasty in the treatment of transsexualism. BJU Int. 101 , 1297–1300 (2008).
Ma, S., Cheng, K. & Liu, Y. Sensibility following innervated free radial forearm flap for penile reconstruction. Plast. Reconstr. Surg. 127 , 235–241 (2011).
Ma, S., Liu, Y., Chang, T. & Cheng, K. Long-term follow-up of sensation recovery of the penis reconstructed by Cheng's method. Plast. Reconstr. Surg. 127 , 1546–1552 (2011).
Papadopulos, N. A., Schaff, J. & Biemer, E. Usefulness of free sensate osteofasciocutaneous forearm and fibula flaps for neophallus construction. J. Reconstr. Microsurg. 17 , 407–412 (2001).
Sasaki, K., Nozaki, M., Morioka, K. & Huang, T. T. Penile reconstruction: combined use of an innervated forearm osteocutaneous flap and big toe pulp. Plast. Reconstr. Surg. 104 , 1054–1058 (1999).
Song, C., Wong, M., Wong, C. H. & Ong, Y. S. Modifications of the radial forearm flap phalloplasty for female-to-male gender reassignment. J. Reconstr. Microsurg. 27 , 115–120 (2011).
Vriens, J. P., Acosta, R., Soutar, D. S. & Webster, M. H. Recovery of sensation in the radial forearm free flap in oral reconstruction. Plast. Reconstr. Surg. 98 , 649–656 (1996).
Waits, C. A., Toby, E. B., Girod, D. A. & Tsue, T. T. Osteocutaneous radial forearm free flap: long-term radiographic evaluation of donor site morbidity after prophylactic plating of radius. J. Reconstr. Microsurg. 23 , 367–372 (2007).
Ma, S., Cheng, K., Liu, Y. & Chen, F. A new surgical procedure for penile reconstruction by combined free radial forearm flap and dorsalis pedis flap. Urology 97 , 232–237 (2016).
Hoebeke, P., de Cuypere, G., Ceulemans, P. & Monstrey, S. Obtaining rigidity in total phalloplasty: experience with 35 patients. J. Urol. 169 , 221–223 (2003).
Selvaggi, G. et al . Scrotal reconstruction in female-to-male transsexuals: a novel scrotoplasty. Plast. Reconstr. Surg. 123 , 1710–1718 (2009). Presentation of the novel technique for transman scrotoplasty.
Hage, J. J., Bouman, F. G. & Bloem, J. J. Constructing a scrotum in female-to-male transsexuals. Plast. Reconstr. Surg. 91 , 914–921 (1993).
Millard, D. R. Jr. Scrotal construction and reconstruction. Plast. Reconstr. Surg. 38 , 10–15 (1966).
Reid, C. F. & Wright, J. H. Jr. Scrotal reconstruction following an avulsion injury. J. Urol. 133 , 681–682 (1985).
Sengezer, M. & Sadove, R. C. Scrotal construction by expansion of labia majora in biological female transsexuals. Ann. Plast. Surg. 31 , 372–376 (1993).
Still, E. F. II & Goodman, R. C. Total reconstruction of a two-compartment scrotum by tissue expansion. Plast. Reconstr. Surg. 85 , 805–807 (1990).
Lumen, N., Monstrey, S., Goessaert, A. S., Oosterlinck, W. & Hoebeke, P. Urethroplasty for strictures after phallic reconstruction: a single-institution experience. Eur. Urol. 60 , 150–158 (2011). Analysis of outcomes and techniques for urethral fistula and stricture repair in phalloplasty.
Wilson, S. C. et al . Fasciocutaneous flap reinforcement of ventral onlay buccal mucosa grafts enables neophallus revision urethroplasty. Ther. Adv. Urol. 8 , 331–337 (2016).
Dabernig, J., Shelley, O. P., Cuccia, G. & Schaff, J. Urethral reconstruction using the radial forearm free flap: experience in oncologic cases and gender reassignment. Eur. Urol. 52 , 547–553 (2007).
Garaffa, G., Ralph, D. J. & Christopher, N. Total urethral construction with the radial artery-based forearm free flap in the transsexual. BJU Int. 106 , 1206–1210 (2010).
Kim, S. K., Moon, J. B., Heo, J., Kwon, Y. S. & Lee, K. C. A new method of urethroplasty for prevention of fistula in female-to-male gender reassignment surgery. Ann. Plast. Surg. 64 , 759–764 (2010).
Bayramicli, M. & Akdeniz, Z. D. Urethra reconstruction with lateral pectoral flap in female-to-male transsexual patients. J. Plast. Reconstr. Aesthet. Surg. 69 , 1558–1560 (2016).
De Filippo, R. E., Yoo, J. J. & Atala, A. Urethral replacement using cell seeded tubularized collagen matrices. J. Urol. 168 , 1789–1792 (2002).
Chen, K. L., Eberli, D., Yoo, J. J. & Atala, A. Bioengineered corporal tissue for structural and functional restoration of the penis. Proc. Natl Acad. Sci. USA 107 , 3346–3350 (2010).
Joo, K. J. et al . Porcine vesical acellular matrix graft of tunica albuginea for penile reconstruction. Asian J. Androl. 8 , 543–548 (2006).
Kwon, T. G., Yoo, J. J. & Atala, A. Autologous penile corpora cavernosa replacement using tissue engineering techniques. J. Urol. 168 , 1754–1758 (2002).
Kropp, B. P. et al . Use of small intestinal submucosa for corporal body grafting in cases of severe penile curvature. J. Urol. 168 , 1742–1745 (2002).
Raya-Rivera, A. M. et al . Tissue-engineered autologous vaginal organs in patients: a pilot cohort study. Lancet 384 , 329–336 (2014).
Sopko, N. A. et al . Ex vivo model of human penile transplantation and rejection: implications for erectile tissue physiology. Eur. Urol. 71 , 584–593 (2017).
Tuffaha, S. H. et al . Using the dorsal, cavernosal, and external pudendal arteries for penile transplantation: technical considerations and perfusion territories. Plast. Reconstr. Surg. 134 , 111e–119e (2014).
Selvaggi, G., Branemark, R., Elander, A., Liden, M. & Stalfors, J. Titanium-bone-anchored penile epithesis: preoperative planning and immediate postoperative results. J. Plast. Surg. Hand. Surg. 49 , 40–44 (2015).
Selvaggi, G., Elander, A. & Branemark, R. Penile epithesis: preliminary study. Plast. Reconstr. Surg. 126 , 265e–266e (2010).
Massie, J. P., Morrison, S. D., Smith, J. R., Wilson, S. C. & Satterwhite, T. Letter to the editor regarding “Surgical outcome after penile inversion vaginoplasty: a retrospective study of 475 transgender women” by Buncamper et al . Plast. Reconstr. Surg. http://dx.doi.org/10.1097/PRS.0000000000003479 (2017).
Berli, J. U. et al . What surgeons need to know about gender confirmation surgery when providing care for transgender individuals: a review. JAMA Surg. 152 , 394–400 (2017).
Download references
Author information
Authors and affiliations.
Division of Plastic and Reconstructive Surgery, Department of Surgery, University of Washington School of Medicine, 1959 NE Pacific Street, Seattle, 98195, WA, USA
Shane D. Morrison
Brownstein & Crane Surgical Services, 575 Sir Francis Drake Blvd, Ste 1, Greenbrae, 94904, CA, USA
Mang L. Chen & Curtis N. Crane
You can also search for this author in PubMed Google Scholar
Contributions
S.D.M., C.N.C and M.C. researched data for article, made substantial contributions to discussions of content, and reviewed and edited the manuscript before submission. S.D.M. and M.C. wrote the article.
Corresponding author
Correspondence to Curtis N. Crane .
Ethics declarations
Competing interests.
The authors declare no competing financial interests.
PowerPoint slides
Powerpoint slide for fig. 1, powerpoint slide for fig. 2, powerpoint slide for fig. 3, powerpoint slide for fig. 4, powerpoint slide for fig. 5, powerpoint slide for fig. 6, powerpoint slide for fig. 7, powerpoint slide for table 1.
Inherent discordance of a patient's gender expression and their anatomy leading to distress
Tissue forming the nipple and surrounding areola on the breast or chest
A physical examination test to determine the patency of the palmar or plantar arches as a correlate for the dominant inflow vessel to the hand or foot. Most commonly it is used in the hand where the radial and ulnar arteries are both occluded with pressure from the examiners hand and each is released sequentially while maintaining the pressure on the other artery. The perfusion of the hand is monitored to ensure both vessels can perfuse the hand.
A person born as a male and whose gender identity is male.
Urological procedure for urethral strictures, in which the ventral aspect of the phallus is opened through the urethra. The urethra is secured to the skin and urine is diverted. A second stage completed months later is used to repair the urethra with grafted tissue over a catheter.
Flaps containing multiple tissue types (skin, bone, mucosa.) based on a single angiosome used for complex reconstruction.
Local flap used for advancing tissue generally to cover a wound, but can be used in other procedures. An incision shaped like a V is made through the subcutaneous tissue, advanced into its new position relying on subcutaneous perfusion, and closed in a Y pattern.
Closure of a urethral stricture with a longitudinal incision followed by a transverse closure.
A person born with female sexual organs, but whose gender identity is male
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Morrison, S., Chen, M. & Crane, C. An overview of female-to-male gender-confirming surgery. Nat Rev Urol 14 , 486–500 (2017). https://doi.org/10.1038/nrurol.2017.64
Download citation
Published : 16 May 2017
Issue Date : August 2017
DOI : https://doi.org/10.1038/nrurol.2017.64
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Geschlechtsinkongruenz – definition, diagnosestellung und transitionsoptionen.
- Antje Feicke
- Barbara Mijuskovic
Urologie in der Praxis (2023)
(De-)centralized health care delivery, surgical outcome, and psychosocial health of transgender and gender-diverse people undergoing vaginoplasty: results of a retrospective, single-center study
- Andreas Koehler
- Bernhard Strauß
- Timo O. Nieder
World Journal of Urology (2023)
Gender Affirmation Surgery for the Transmasculine Patient
- Michael Callegari
- Gaetan Pettigrew
- Shubham Gupta
Current Obstetrics and Gynecology Reports (2022)
Urethral complications after gender reassignment surgery: a systematic review
- L. R. Doumanian
International Journal of Impotence Research (2021)
Suprapubic phalloplasty in transmen: surgical results and critical review
- Manon Terrier
- Nicolas Morel-Journel
- Paul Neuville
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
How Gender Reassignment Surgery Works (Infographic)
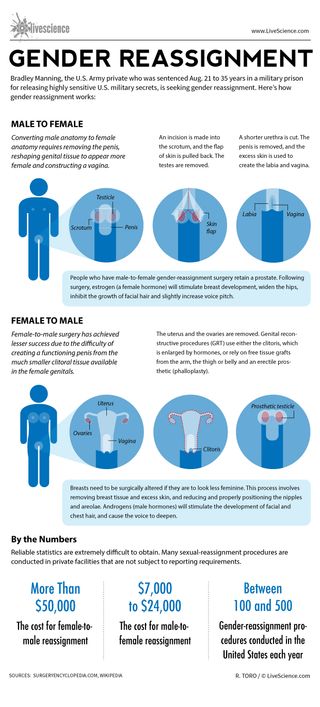
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Scientists made mice with Y chromosomes female by deleting just 6 tiny molecules
Man's years of premature ejaculation had a rare cause
James Webb telescope discovers the 2 earliest galaxies in the known universe — and 1 is shockingly big
Most Popular
- 2 James Webb telescope sees 'birth' of 3 of the universe's earliest galaxies in world-1st observations
- 3 Space photo of the week: NASA sees a 'Platypus' move on Jupiter's moon Europa
- 4 Things are finally looking up for the Voyager 1 interstellar spacecraft
- 5 Double cicada bloom 2024: Google Doodle celebrates once-in-221-year event with band of bugs
- 2 Secrets of radioactive 'promethium' — a rare earth element with mysterious applications — uncovered after 80-year search
- 3 Auroras could paint Earth's skies again in early June. Here are the key nights to watch for.
- 4 Elusive 'octopus squid' with world's largest biological lights attacks camera in striking new video
- 5 Nightmarish 'footballfish' washes up dead on US beach in potential 1st-of-its-kind occurrence
Treatment - Gender dysphoria
Treatment for gender dysphoria aims to help people live the way they want to, in their preferred gender identity or as non-binary.
What this means will vary from person to person, and is different for children, young people and adults. Waiting times for referral and treatment are currently long.
Treatment for children and young people
If your child may have gender dysphoria, they'll usually be referred to one of the NHS Children and Young People's Gender Services .
Your child or teenager will be seen by a multidisciplinary team including a:
- clinical psychologist
- child psychotherapist
- child and adolescent psychiatrist
- family therapist
- social worker
The team will carry out a detailed assessment, usually over 3 to 6 appointments over a period of several months.
Depending on the results of the assessment, options for children and teenagers include:
- family therapy
- individual child psychotherapy
- parental support or counselling
- group work for young people and their parents
- regular reviews to monitor gender identity development
- referral to a local Children and Young People's Mental Health Service (CYPMHS) for more serious emotional issues
Most treatments offered at this stage are psychological rather than medical. This is because in many cases gender variant behaviour or feelings disappear as children reach puberty.
Hormone therapy in children and young people
Some young people with lasting signs of gender dysphoria who meet strict criteria may be referred to a hormone specialist (consultant endocrinologist). This is in addition to psychological support.
Puberty blockers and gender-affirming hormones
Puberty blockers (gonadotrophin-releasing hormone analogues) are not available to children and young people for gender incongruence or gender dysphoria because there is not enough evidence of safety and clinical effectiveness.
From around the age of 16, young people with a diagnosis of gender incongruence or gender dysphoria who meet various clinical criteria may be given gender-affirming hormones alongside psychosocial and psychological support.
These hormones cause some irreversible changes, such as:
- breast development (caused by taking oestrogen)
- breaking or deepening of the voice (caused by taking testosterone)
Long-term gender-affirming hormone treatment may cause temporary or even permanent infertility.
However, as gender-affirming hormones affect people differently, they should not be considered a reliable form of contraception.
There is some uncertainty about the risks of long-term gender-affirming hormone treatment.
Children, young people and their families are strongly discouraged from getting puberty blockers or gender-affirming hormones from unregulated sources or online providers that are not regulated by UK regulatory bodies.
Transition to adult gender identity services
Young people aged 17 or older may be seen in an adult gender identity clinic or be referred to one from a children and young people's gender service.
By this age, a teenager and the clinic team may be more confident about confirming a diagnosis of gender dysphoria. If desired, steps can be taken to more permanent treatments that fit with the chosen gender identity or as non-binary.
Treatment for adults
Adults who think they may have gender dysphoria should be referred to a gender dysphoria clinic (GDC).
Find an NHS gender dysphoria clinic in England .
GDCs have a multidisciplinary team of healthcare professionals, who offer ongoing assessments, treatments, support and advice, including:
- psychological support, such as counselling
- cross-sex hormone therapy
- speech and language therapy (voice therapy) to help you sound more typical of your gender identity
For some people, support and advice from the clinic are all they need to feel comfortable with their gender identity. Others will need more extensive treatment.
Hormone therapy for adults
The aim of hormone therapy is to make you more comfortable with yourself, both in terms of physical appearance and how you feel. The hormones usually need to be taken for the rest of your life, even if you have gender surgery.
It's important to remember that hormone therapy is only one of the treatments for gender dysphoria. Others include voice therapy and psychological support. The decision to have hormone therapy will be taken after a discussion between you and your clinic team.
In general, people wanting masculinisation usually take testosterone and people after feminisation usually take oestrogen.
Both usually have the additional effect of suppressing the release of "unwanted" hormones from the testes or ovaries.
Whatever hormone therapy is used, it can take several months for hormone therapy to be effective, which can be frustrating.
It's also important to remember what it cannot change, such as your height or how wide or narrow your shoulders are.
The effectiveness of hormone therapy is also limited by factors unique to the individual (such as genetic factors) that cannot be overcome simply by adjusting the dose.
Find out how to save money on prescriptions for hormone therapy medicines with a prescription prepayment certificate .
Risks of hormone therapy
There is some uncertainty about the risks of long-term cross-sex hormone treatment. The clinic will discuss these with you and the importance of regular monitoring blood tests with your GP.
The most common risks or side effects include:
- blood clots
- weight gain
- dyslipidaemia (abnormal levels of fat in the blood)
- elevated liver enzymes
- polycythaemia (high concentration of red blood cells)
- hair loss or balding (androgenic alopecia)
There are other risks if you're taking hormones bought over the internet or from unregulated sources. It's strongly recommended you avoid these.
Long-term cross-sex hormone treatment may also lead, eventually, to infertility, even if treatment is stopped.
The GP can help you with advice about gamete storage. This is the harvesting and storing of eggs or sperm for your future use.
Gamete storage is sometimes available on the NHS. It cannot be provided by the gender dysphoria clinic.
Read more about fertility preservation on the HFEA website.
Surgery for adults
Some people may decide to have surgery to permanently alter body parts associated with their biological sex.
Based on the recommendations of doctors at the gender dysphoria clinic, you will be referred to a surgeon outside the clinic who is an expert in this type of surgery.
In addition to you having socially transitioned to your preferred gender identity for at least a year before a referral is made for gender surgery, it is also advisable to:
- lose weight if you are overweight (BMI of 25 or over)
- have taken cross-sex hormones for some surgical procedures
It's also important that any long-term conditions, such as diabetes or high blood pressure, are well controlled.
Surgery for trans men
Common chest procedures for trans men (trans-masculine people) include:
- removal of both breasts (bilateral mastectomy) and associated chest reconstruction
- nipple repositioning
- dermal implant and tattoo
Gender surgery for trans men includes:
- construction of a penis (phalloplasty or metoidioplasty)
- construction of a scrotum (scrotoplasty) and testicular implants
- a penile implant
Removal of the womb (hysterectomy) and the ovaries and fallopian tubes (salpingo-oophorectomy) may also be considered.
Surgery for trans women
Gender surgery for trans women includes:
- removal of the testes (orchidectomy)
- removal of the penis (penectomy)
- construction of a vagina (vaginoplasty)
- construction of a vulva (vulvoplasty)
- construction of a clitoris (clitoroplasty)
Breast implants for trans women (trans-feminine people) are not routinely available on the NHS.
Facial feminisation surgery and hair transplants are not routinely available on the NHS.
As with all surgical procedures there can be complications. Your surgeon should discuss the risks and limitations of surgery with you before you consent to the procedure.
Life after transition
Whether you've had hormone therapy alone or combined with surgery, the aim is that you no longer have gender dysphoria and feel at ease with your identity.
Your health needs are the same as anyone else's with a few exceptions:
- you'll need lifelong monitoring of your hormone levels by your GP
- you'll still need contraception if you are sexually active and have not yet had any gender surgery
- you'll need to let your optician and dentist know if you're on hormone therapy as this may affect your treatment
- you may not be called for screening tests as you've changed your name on medical records – ask your GP to notify you for cervical and breast screening if you're a trans man with a cervix or breast tissue
- trans-feminine people with breast tissue (and registered with a GP as female) are routinely invited for breast screening from the ages of 50 up to 71
Find out more about screening for trans and non-binary people on GOV.UK.
NHS guidelines for gender dysphoria
NHS England has published what are known as service specifications that describe how clinical and medical care is offered to people with gender dysphoria:
- Non-surgical interventions for adults
- Surgical interventions for adults
- Interim service specification for specialist gender incongruence services for children and young people
Review of gender identity services
NHS England has commissioned an independent review of gender identity services for children and young people. The review will advise on any changes needed to the service specifications for children and young people.
Page last reviewed: 28 May 2020 Next review due: 28 May 2023
Healthdirect Free Australian health advice you can count on.
Medical problem? Call 1800 022 222. If you need urgent medical help, call triple zero immediately
healthdirect Australia is a free service where you can talk to a nurse or doctor who can help you know what to do.
Gender affirming surgery
7-minute read
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
What is gender affirming surgery?
Gender affirming surgery refers to a variety of procedures that some trans or gender diverse people may use to affirm their gender.
Surgery is just one option for gender affirming care. All trans and gender diverse people are unique and will choose to affirm their gender in a way that feels right for them.
Gender affirming care might include:
- Social affirmation, such as changing names, pronouns, hair or clothing.
- Legal affirmation, such as changing legal name or gender.
- Medical affirmation, with hormones or surgery.
Read more about gender incongruence, gender dysphoria , and gender affirming care here.
This article talks more about gender affirming surgery.
What happens during gender affirming surgery?
There are many different gender affirming surgeries and procedures. They may include making changes to your face, chest, genitals, or other body parts.
For people assumed male at birth, feminising surgeries may include:
- Breast augmentation with insertion of breast implants.
- Facial feminisation — changing the shape of any or all facial features.
- Vocal surgery — shortening the vocal cords for a higher, more feminine voice.
- Tracheal shave — reducing the size of the ‘Adam’s apple’.
- Fillers or liposuction, to achieve a more typically feminine shape.
- Orchiectomy, or removal of testicles.
- Bottom surgery or ‘genital reconfiguration surgery’, involving changes to the genitals.
Bottom surgery is called ‘genital reconfiguration surgery’. This was previously known as ‘sex reassignment surgery’ or ‘gender confirmation surgery’. The name change shows that your genitals don’t define your sex or gender.
Feminising bottom surgery may involve a combination of the following procedures:
- Removing the testicles (orchiectomy).
- Removing and reshaping tissue from the penis to make a vulva. This includes external labia or lips, and a clitoris. This is known as vulvoplasty.
- Shortening the urethra (tube that you urinate — wee — from).
- Creation of a vaginal canal (vaginoplasty). This is a complicated step which some people choose to skip. After surgery, vaginal dilators will need to be used to maintain the shape of the vaginal canal.
For people assumed female at birth, masculinising surgeries may include:
- Top surgery, with reduction or removal of breast tissue (mastectomy). This creates a flatter or more neutral chest. There are many different techniques used to achieve this.
- Liposuction to achieve a more typically masculine shape.
- Hysterectomy , or removal of the uterus (womb) and ovaries.
- Bottom surgery or genital reconfiguration surgery. This involves changes to the genitals.
Masculinising bottom surgery may involve a combination of the following procedures:
- Hysterectomy, if not already performed.
- Vaginectomy, or removal of the vagina.
- Creation of a penis, which may include metoidioplasty or phalloplasty.
- Metoidioplasty involves making a penis shape wrapping tissue around the clitoris after it is enlarged by testosterone hormone therapy.
- Phalloplasty involves making a larger penis with tissue from the arm, thigh, back, or abdomen. This involves lengthening the urethra to be able to urinate from the tip of the new penis. An inflatable penile implant may be inserted inside the penis to allow an erection.
Is gender affirming surgery right for me?
Choosing to undergo any surgery is a big decision. Everyone affirms their gender in different ways, and that may or may not include surgery.
Surgery is permanent so you need to make sure it’s the right choice for you. Surgery doesn’t make you more or less trans.
Before being able to access gender affirming surgery, you need to meet the criteria below:
- A history of gender incongruence (for 6 months or more).
- The ability to make a fully informed decision.
- Be over the age of 16 for top surgery, or 18 for bottom surgery. Some surgeons will provide surgery to younger people in very specific situations.
- Ensure that any physical or mental health conditions are well managed.
You will need letters of support from a mental health professional before having gender affirming surgery.
For top surgery, one letter is required. For bottom surgery two letters are required. For bottom surgery, you are also required to have ‘lived as your current gender’ for 12 months, meaning you have socially transitioned. The letter needs to state that surgery is appropriate for you and is likely to help affirm your gender and reduce any gender dysphoria that may be present.
If you are taking gender affirming hormones, or want to take hormones in the future, you should do this for 12 months before having surgery. This is to allow any significant body changes to occur before surgery.
Most people who have surgery are happy with their results and feel more comfortable in their bodies. But some people are disappointed with the results, or find that any gender dysphoria that was present is not fully resolved. Make sure you discuss any difficult feelings with your doctor or psychologist.
What questions should I ask before surgery?
It’s important to talk about the pros and cons of surgery in detail with your doctor. It’s a good idea to ask to see pictures of how other people look after surgery.
Questions to ask your surgeon include:
- What different surgical techniques are there?
- What are the pros and cons of each technique for me?
- What results can I expect?
- What are the possible risks and complications?
For help in having the discussion, visit healthdirect’s Question Builder .
What should I expect after surgery?
Surgical recovery can be long and uncomfortable. Your surgeon will be able to give you more information on what can be expected before, during, and after surgery. This might include spending time in hospital afterwards, any special dressings, surgical garments, or follow up care.
Make sure you do everything your doctor tells you and go to all follow-up appointments. This will help you get the best results from your surgery.
Having surgery is a big deal. Even if you’ve been looking forward to it and are happy with the result, it can still be quite confronting. It might take some time to get used to your new body.
Talk to your doctor if you are feeling any distress following surgery.
How much will gender affirming surgery cost me?
Gender affirming surgery can be very expensive. It can cost between $20,000 to more than $100,000, depending on which procedures you need.
Your surgeon will be able to tell you how much surgery will cost. The cost may include specialist visits before and after surgery, surgeon and anaesthetist fees, hospital and theatre costs, and any other products or services necessary.
Some costs may be covered by Medicare, such as specialist consults if you have a referral from your doctor. Unfortunately, most gender affirming surgery in Australia is done privately, meaning there will be large out-of-pocket costs.
You should ask your surgeon what Medicare item numbers they use. You can check the Medicare rebate at MBS Online .
Some private health insurance will also help with gender affirming surgery. If you have health insurance, it’s important to check with your health fund first about your level of cover. There is a range of health insurance comparison sites available online, such as privatehealth.gov.au .
Legal matters
Changing your gender on your passport, licence, Medicare card or birth certificate all require separate processes. These vary between states and territories. In some states and territories, you must have undergone specific types of gender affirmation surgery to change the gender marker on your birth certificate.
You can find out more about the specific processes at TransHub .
You are legally protected by the Sex Discrimination Act from discrimination on the grounds of sexual orientation, gender identity or intersex status. Visit the Australian Government Attorney-General’s Department for more details.
Where can I get more information on gender affirming surgery?
- TransHub has information about gender affirming surgery.
- The Gender Centre (NSW) provides resources and support.
- Transgender Victoria has resources and links to other services.
- The Australian Professional Association for Trans Health (AusPATH) lists some providers.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: June 2022
Search our site for
- Transgender
- Gender Dysphoria
Need more information?
These trusted information partners have more on this topic.
Top results
Understanding Gender Identity | headspace
Gender identity is your sense of whether you are a man, woman, nonbinary, gender fluid or a combination of one or more of these identities. Learn more about gender identity and how you can get help from headspace.
Read more on headspace website


Everything you need to know about gender identity | Gender Identity
If you’ve ever wondered ‘what does gender mean?’, you’re not alone. Gender and identity exists on a diverse spectrum. Learn more about gender in this guide.
Read more on ReachOut.com website

Understanding gender identity and young people | headspace
It's important to understand the ways your young person can express their gender identity. Visit headspace to learn about gender identity in young people.
Gender Identity Examples, Meaning & Definition | Kids Helpline
Gender identity is more than being male or female. Kids Helpline can help you understand what it is and how you can understand your own identity.
Read more on Kids Helpline website

Gender dysphoria & identity: kids & teens | Raising Children Network
Gender identity is feeling male, female, both or neither. Gender dysphoria is when your child is distressed by feeling different from their birth gender.
Read more on raisingchildren.net.au website

Gender dysphoria & diversity: support | Raising Children Network
If your child is gender diverse or experiencing gender dysphoria, support means embracing their gender identity. Your support boosts your child’s wellbeing.
How Emma learnt to accept herself and her gender identity | ReachOut Australia
Emma, a young transgender woman, shares how reaching out for support helped her to accept her gender identity.
Supporting a transgender teenager - ReachOut Parents
Learn how best to support your teen as they embrace their gender identity, with ReachOut Australia and Ross Jacobs from QLife.
Your child’s gender diversity: your family | Raising Children Network
If your child is gender diverse, it’s OK if you and your child’s siblings have mixed feelings about your child’s gender identity. It’s good to seek support.
Gender diversity - a QLife guide for health professionals
Many people assume that gender is binary; that all people are women or men. However, gender can more accurately be thought of as a colour palette, with many possible shades of identity and subtle expressions of gender far beyond only woman or man.
Read more on QLife website

RACGP - LGBTIQA+ Family abuse and violence
Reproduced with permission from The Royal Australian College of General Practitioners
Read more on RACGP - The Royal Australian College of General Practitioners website

RACGP - Care of older LGBTI people
Reproduced with permission from The Royal Australian College of General Practitioners. The historical pathologising of older lesbian, gay, bisexual, transgender and intersex (LGBTI) people’s bodies and relationships continue to adversely affect their health and wellbeing
Bisexuality - a QLife guide for health professionals
Bisexual people are attracted to people of multiple genders and these attractions may be fluid over time.
Young people - QLife guide tip sheet
Social conditions for the acceptance of LGBTI (lesbian, gay, bisexual, transgender and intersex) people have improved dramatically in Australia in recent years.
Coming out, inviting in and disclosure
‘Coming out’ typically refers to acknowledging one’s sexuality or samegender attractions to oneself and disclosing this to others.
Antidepressants in adolescence - Australian Prescriber
Antidepressant drugs are not the first-line treatment for adolescents with mild symptoms of depression.
Read more on Australian Prescriber website

Clinical guidelines – Intersex Human Rights Australia
Are clinical guidelines enough to eliminate human rights violations against intersex people in medical settings? Reviewing the evidence, we believe they are inadequate, and their prerequisites do not exist.
Read more on Intersex Human Rights Australia website

For Health Professionals | Cancer in Aboriginal and Torres Strait Islander People - Our mob and cancer
Culturally appropriate, optimal cancer care for Aboriginal and Torres Strait Islander people Cancer is the third leading cause of burden of disease for Aboriginal and Torres Strait Islander people
Read more on Cancer Australia - Our Mob and Cancer website

The Health and Care of First Nations Australians | Ausmed
First Nations Australians are diverse peoples with a variety of histories, cultures, languages and experiences. In order to deliver appropriate and culturally competent care, it is essential to understand the care needs and health of First Nations peoples.
Read more on Ausmed Education website

Healthdirect Australia is not responsible for the content and advertising on the external website you are now entering.
Healthdirect 24hr 7 days a week hotline
24 hour health advice you can count on
1800 022 222
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
Support for this browser is being discontinued
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Jump to content
Updated visitor policies
Other michigan medicine sites.
- About Michigan Medicine
- UofMHealth.org
- Medical School
- Find a Clinical Trial

Michigan Medicine
Federated search page form block, quick links.
- Patient Portal Login
- For Health Providers
- Maps & Directions
Gender Confirmation Surgery
The University of Michigan Health System offers procedures for surgical gender transition. Working together, the surgical team of the Comprehensive Gender Services Program, which includes specialists in plastic surgery, urology and gynecology, bring expertise, experience and safety to procedures for our transgender patients.
Access to gender-related surgical procedures for patients is made through the University of Michigan Health System Comprehensive Gender Services Program .
The Comprehensive Gender Services Program adheres to the WPATH Standards of Care , including the requirement for a second-opinion prior to genital sex reassignment.
Available surgeries:
Male-to-Female: Tracheal Shave Breast Augmentation Facial Feminization Male-to-Female genital sex reassignment
Female-to-Male: Hysterectomy, oophorectomy, vaginectomy Chest Reconstruction Female-to-male genital sex reassignment
Sex Reassignment Surgeries (SRS)
At the University of Michigan Health System, we are dedicated to offering the safest proven surgical options for sex reassignment (SRS.) Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain specialists and a reconstructive plastic surgeon. A multi-disciplinary team helps to best protect the health of the patient.
For patients receiving mental health and medical services within the University of Michigan Health System, the UMHS-CGSP will coordinate all care including surgical referrals. For patients who have prepared for surgery elsewhere, the UMHS-CGSP will help organize the needed records, meet WPATH standards, and coordinate surgical referrals. Surgical referrals are made through Sara Wiener the Comprehensive Gender Services Program Director.
Male-to-female sex reassignment surgery
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris.
During this procedure, a surgeon makes “like become like,” using parts of the original penis to create a sensate neo-vagina. The testicles are removed, a procedure called orchiectomy. The skin from the scrotum is used to make the labia. The erectile tissue of the penis is used to make the neoclitoris. The urethra is preserved and functional.
This procedure provides for aesthetic and functional female genitalia in one 4-5 hour operation. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation. What to Expect: Vaginoplasty at Michigan Medicine .
Female-to-male sex reassignment
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a female-to-male sex reassignment surgery will be offered a phalloplasty, generally using the radial forearm flap method.
This procedure, which can be done at the same time as a hysterectomy/vaginectomy, creates an aesthetically appropriate phallus and creates a urethera for standing urination. Construction of a scrotum with testicular implants is done as a second stage. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected] . W e will assist you in obtaining what you need to qualify for surgery.
- Quick Links
- Make An Appointment
- Our Services
- Price Estimate
- Price Transparency
- Pay Your Bill
- Patient Experience
- Careers at UH
Schedule an appointment today

Vaginoplasty: Male to Female (MTF) Genital Reconstructive Surgery
What is vaginoplasty.
Vaginoplasty is a surgical procedure during which surgeons remove the penis and testicles and create a functional vagina. This achieves resolution of gender dysphoria and allows for sexual activity with compatible genitalia. The highly sensitive skin and tissues from the penis are preserved and used to construct the vaginal lining and build a clitoris, resulting in genitals with appropriate sensations. Scrotal skin is used to increase the depth of the vaginal canal. Penile, scrotal and groin skin are refashioned to make the labia majora and minora, and the urethral opening is relocated to an appropriate female position. The final result is an anatomically congruent, aesthetically appealing, and functionally intact vagina. Unless there is a medical reason to do so, the prostate gland is not removed.
University Hospitals has the only reconstructive urology program in the region offering MTF vaginoplasty and other genital gender affirmation surgical procedures. Call 216-844-3009 to schedule a consultation.
Penile Inversion Technique for Vaginoplasty
Penile inversion is the most common type of vaginoplasty and is considered the gold standard for male to female genital reconstruction. This type of gender affirmation surgery can last from two to five hours and is performed with the patient under general anesthesia.
The skin is removed from the penis and inverted to form a pouch which is then inserted into the vaginal cavity created between the urethra and rectum. The urethra is partially removed, shortened and repositioned. Labia majora and labia minora (outer and inner lips), and a clitoris are created. After everything has been sutured in place, a catheter is inserted into the urethra and the area is bandaged. The bandages and catheter will typically remain in place for four to five days. For some patients, a shallow depth vaginoplasty is recommended. This allows for a functional vagina but removes the need for vaginal dilation and douching.
Outcomes after vaginoplasty are excellent, and patients can expect to have aesthetic outcomes and sexual functionality similar to that for cis-women (people that were assigned female sex characteristics at birth and identify as female).
Complications after vaginoplasty are rare, but patients are advised to talk to their doctor about postsurgical risks and how to best manage them.
Things to Consider Before Having a Penile Inversion Vaginoplasty
- Given that the skin used to construct the new vaginal lining may have abundant hair follicles, patients are recommended to undergo hair removal (either electrolysis or laser hair removal) prior to the vaginoplasty procedure to eliminate the potential for vaginal hair growth. A full course of hair removal can take several months.
- Patients with fertility concerns should talk to their doctor about ways to save and preserve their sperm before having a vaginoplasty.
- It is always recommended that patients talk with a therapist in the months leading up to surgery to ensure they are mentally prepared for the transition.
- In accordance with the World Professional Association of Transgender Health (WPATH) standards of care, patients are required be on appropriate cross-gender hormone therapy for a year, live in the gender-congruent role for a year, and have 2 mental health letters endorsing their suitability for surgery.
Postoperative Care of Your New Vagina
To ensure that your newly constructed vagina maintains the desired depth and width, your UH surgeon will give you a vaginal dilator to begin using as soon as the bandages are removed. Use the dilator regularly according to your surgeon’s recommendations. This will usually involve inserting the device for ten minutes several times per day for the first three months. After that, once per day for three months followed by two to three times a week until a full year has passed.
Furthermore, regular douching and cleaning of the vagina is recommended. Your surgeon will give you general guidelines for this as well. Approximately 1 out of 10 people who have a vaginoplasty end up requiring a second, minor surgery to correct some of the scarring from the first surgery and improve the function and cosmetic appearance.
Most genital gender affirmation surgeries are covered by insurance. In cases where they are not, your surgeon’s office will guide you through the self-pay options.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Biomed Res Int

Sexuality after Male-to-Female Gender Affirmation Surgery
1 Department of Urology, University Hospital Essen, University Duisburg-Essen, Germany
2 Department of Urology, Kliniken Essen-Mitte, Essen, Germany
3 General Practice van Hal, Essen, Germany
R. Rossi Neto
4 Clinica Urologia, General Hospital Ernesto Simoes Filho, Salvador, Brazil
B. Hadaschik
Male-to-Female (MtF) gender affirmation surgery (GAS) comprises the creation of a functional and aesthetic perineogenital complex. This study aimed to evaluate the effect of GAS on sexuality. We retrospectively surveyed all 254 MtF transsexual patients who had undergone GAS with penile inversion vaginoplasty at the Department of Urology, University Hospital Essen, Germany, between 2004 and 2010. In total, we received 119 completed questionnaires after a median of 5.05 years since surgery. Of the study participants, 33.7% reported a heterosexual, 37.6% a lesbian, and 22.8% a bisexual orientation related to the self-perceived gender. Of those who had sexual intercourse, 55.8% rated their orgasms to be more intensive than before, with 20.8% who felt no difference. Most patients were satisfied with the sensitivity of the neoclitoris (73.9%) and with the depth of the neovaginal canal (67.1%). The self-estimated pleasure of sexual activity correlated significantly with neoclitoral sensitivity but not with neovaginal depth. There was a significant correlation between the ease with which patients were able to become sexually aroused and their ability to achieve orgasms. In conclusion, orgasms after surgery were experienced more intensely than before in the majority of women in our cohort and neoclitoral sensitivity seems to contribute to enjoyment of sexual activity to a greater extent than neovaginal depth.
1. Introduction
Male-to-female (MtF) gender affirmation surgery (GAS) comprises the resection of all clearly defining features of male genitalia. The aim is the formation of a perineogenital complex in appearance and function as feminine as possible [ 1 ] with a sensitive clitoris to enable orgasms. GAS should be performed by a surgeon with specialized competence in genital reconstructive techniques [ 2 ]. The aim is to “create a perineogenital complex as feminine in appearance and function as possible” [ 1 ]. There is a broad agreement that GAS has a positive impact on gender dysphoria [ 3 – 13 ]. The inversion of penile skin is used by most gender surgeons. While some trans ∗ and gender nonconforming people do not require surgical therapy to express their preferred gender role and identity, others see GAS as a pivotal step to relieve their gender dysphoria [ 14 ]. GAS might reduce risk of stigmatization and discrimination in venues like swimming pools and health clubs or when dealing with authorities [ 2 , 15 ]. Without doubt surgery has a positive effect on subjective wellbeing and sexual function [ 16 – 18 ].
Sexual orientation can change after GAS [ 19 ] but little is known about changes of orgasmic experience after GAS. Bartolucci et al. found a positive impact of cross gender hormone replacement therapy on sexual quality of life in transgender who had not undergone GAS yet [ 20 ]. However effects of GAS in this field remain unclear so far. This study aimed to evaluate the effect of GAS on sexuality and satisfaction with sexual life of MtF-transgender patients.
2. Material and Methods
2.1. participants.
Our study cohort comprised all 254 MtF patients who had undergone GAS with penile inversion vaginoplasty at the Department of Urology, University Hospital Essen, Germany, between 2004 and 2010, as has been previously reported [ 6 ]. Transsexualism was diagnosed by two independent mental healthcare professionals competent to work with gender dysphoric adults in accordance with 10th version of the International Classification of Diseases (ICD-10). All patients were contacted by mail using their last known address and asked if they would be willing to answer the questionnaire. In cases of invalid addresses the local residents' registration offices were contacted in order to reconsign a new questionnaire. Patients who had not sent back the questionnaire could not be followed up due to previous anonymization.
2.2. Statistics
Statistical calculation was performed using Statistical Package for the Social Sciences (SPSS 21.0). Fisher's exact test and Chi Square were used to compare categorical and ordinal variables in independent samples. The Mann–Whitney U test was used to compare satisfaction scale distribution of two independent samples. This nonparametric test was used in preference to the t-test because the Shapiro–Wilk test indicated that distribution was not normal. Spearman's correlation analysis was performed.
In total, 119 completed questionnaires were received, all of which were included in the evaluation (response rate 46.9%). Due to anonymization of the questionnaires, it was not possible to obtain information on patients' ages. However, the average age of a comparable cohort of patients at our department between 1995 and 2008 [ 21 ] was 36.7 years (16 to 68 years). Not all patients completed the questionnaire, so for some questions the total number of responses was not 119. The results are given in absolute numbers and percentage in relation to total participants or number of answers. After a median of 5.05 years (standard deviation: 1.6 years; range: 1 to 7 years) since surgery, 67 participants (56.3% of the total cohort) did not encounter sexual intercourse on a regular basis at the time of questioning (which depicts 67.7% of those who answered that question). Twenty of the 119 patients (16.8%) did not answer this question. Of those who answered the question nearly a quarter (n = 24; 24.2%) reported a mean frequency of one to three times per month, seven (7.1%) stated a frequency of one to three times per week, and one woman (1.0%) stated a frequency of over three times per week. Time since GAS did not correlate with the frequency of intercourse and the self-rated intensity of orgasms. There was neither an association of the extent to which women felt female themselves nor with the degree to which they felt considered as women with time since surgery.
In our cohort, 18 (15.1% of all participants) patients refused to answer regarding sexual attraction related to the self-perceived gender. Of those who answered (n = 101), slightly more of the patients (n = 38; 37.6%) indicated a sexual attraction towards women than towards men (n = 34; 33.7%). 23 women (22.8%) were attracted by both men and women and six (5.9%) neither by men nor by women ( Figure 1 ). In total, 38 subjects (41.3%) were highly satisfied, 30 (32.6%) were satisfied, 18 (19.6%) were not satisfied, and six (6.5%) were highly unsatisfied with the sensitivity of the neoclitoris ( Figure 2 ). This question was not answered by 27 individuals (22.7% of all participants). When asked how satisfied the women were with the depth of the neovaginal canal, 19 were very satisfied (20.9%), 42 (46.2%) were satisfied, 23 (25.3%) were unsatisfied, and seven (7.7%) were very unsatisfied, with 28 (23.5% of all participants) not answering the question ( Figure 3 ). We asked our patients whether it was easy to get sexually aroused. In total 91 women responded to this question, and about a quarter (n = 28; 23.5% of all participants) declined to answer. Of these 91 women 22 (24.2%) stated that this was always easy; for 43 (47.3%) it was mostly easy; for 15 (16.5%) it was seldom easy; and for eleven women (12.1%) it was never easy to get sexually aroused. The modality as to how orgasms were achieved is shown in Figure 4(a) (absolute numbers of patients; n = 119) and Figure 4(b) (percentages expressed in relation to total answers; n = 126). The majority of participants achieved an orgasm with masturbation, followed by sexual intercourse and “other” not further specified sexual practices. 29 women (24.4% of all participants) did not answer that question. Of those who answered that question (n = 77), 43 women (55.8%) quoted that orgasms were more intense after GAS compared with those experienced before surgery, 18 (23.4%) women stated that it was less intense than before, and 16 (20.8%) felt no difference. Frequency of achieved orgasms changed in our cohort after GAS. Of all 119 patients 41 (34.5%) refused to answer that question. Of the residual 78 women 41 (52.6%) indicated that orgasms were achieved less frequently, 21 women (26.9%) reported more frequent orgasms, and for 16 women (20.5%), frequency did not change. In order to gather information on patients' general satisfaction with their sex lives, they were asked to place themselves on a Likert scale ranging from 0 (“very dissatisfied”) to 10 (“very satisfied”). Nearly a quarter of participants either selected scores from 0 to 3 (n = 29; 24.4%), from 4 to 6 (n = 30; 25.2%), or from 7 to 10 (n = 29; 24.4%) or refused to answer (n = 31; 26.1%). Figure 5 shows a detailed illustration. We received feedback regarding pleasure of sexual activity from 88 women (73.9%). Of these respondents 31 (35.2%) stated that sexual activity was always pleasurable; 44 (50.0%) said it was sometimes pleasurable and 13 (14.8%) never felt pleasure with sexual activity. In our cohort, there was a significant correlation between the ease of getting sexually aroused and the ability to achieve an orgasm (r s = 0.616, p = 0.01). The better the sexual arousal, the easier it was to achieve an orgasm. The correlation between arousal and sensitivity of the neoclitoris was less distinctive but still significant (r s = 0.506, p = 0.01). The self-estimated pleasure of sexual activity was significantly correlated with the sensitivity of the neoclitoris (r s = 0.508, p = 0.01) but not with the depth of the neovaginal canal (r s = 0.198, p = 0.079); i.e., neoclitoral sensitivity seems to contribute to the enjoyment of sexual activity to a greater extent than the depth of the neovagina.

Sexual orientation related to the self-perceived gender.

Satisfaction with neoclitoral sensitivity.

Satisfaction with neovaginal depth.

Modality as to how orgasms were achieved (multiple answers possible). (a) Absolute number of patients. MB = masturbation; SI = sexual intercourse; OT = other (not further specified); NO = no orgasm; NA = no answer. (b) Modality as percentage of answers.

Patients' general satisfaction with their sex lives. Likert scale ranging from 0 (“very dissatisfied”) to 10 (“very satisfied”).
4. Discussion
Overall, subjective satisfaction rates can be expected to be 80% and higher after GAS [ 22 ]. Löwenberg reported a general satisfaction with the outcome of GAS to be even over 90% [ 10 ]. Studies often stress the emphasis on functional or aesthetic aspects after GAS [ 5 – 7 , 23 – 25 ] or, at best, on sexual quality of life before GAS [ 20 , 26 ]. To our best knowledge, this is the first study placing a particular focus on sexual life after MtF GAS.
In our study, sexual attraction was referred to the self-perceived sexual identity on the basis of self-identification. Accordingly, we used the term “heterosexual” or “homosexual” when participants reported on sexual attraction towards men (natal men as well as transmen) and women, respectively. Due to the existing stigmatization of homosexual and lesbian individuals in a heteronormative community or to patients' wish for social desirability, it is possible that reports on the prevalence of homosexuality (gay and lesbian) are underestimations. A representative study with over 14.000 men and women in Germany reported on a prevalence of 4% of men and 3% of women who self-identified as “gays”. Another 9% of male and 20% of female heterosexual participants felt sexually attracted by the same sex without identifying themselves as gay [ 27 ]. International surveys found a prevalence of homosexuality in up to 3% with regional and age-dependent variations [ 28 – 32 ]. In our study, the percentage of homosexuality (gay and lesbian) related to self-perceived gender was much higher. This could be because the interviewees knew the interrogators well, had generally revealed their sexual orientation beforehand, and had no fear of societal stigmatization. There is also the possibility that the rate of homo- and bisexuality is, in fact, higher in transsexuals compared with nontranssexuals. [ 33 ] Lawrence found a change in predominant sexual attraction in 232 MtF transsexuals before and after genital reassignment [ 19 ]. In her study, 54% and 25% of participants reported a gynephile orientation before and after surgery, respectively. Androphilic orientation changed from 9% preoperatively to 34% postoperatively. Regarding asexuality, we followed the definition of Prause and Graham who found that asexuality is defined to be a lack of sexual interest or desire, rather than a lack of sexual experience [ 34 ]. In our cohort, in total 6% of the women self-identified as asexual. Bogaert reported on approximately 1% asexual individuals of a total sample size of over 18.000 (nontranssexual) British residents, with more women being asexual than men [ 35 ]. He found both biological and psychosocial factors contributing to the development of asexuality. Prause and Graham found significantly lower sexual arousability and lower sexual excitation in asexual individuals with a prevalence of 4% [ 34 ]. A reduced sensitivity of the neoclitoris could therefore be a prognostic factor for asexuality. Our results support this assumption. The sensitivity of the neoclitoris correlated with the ability of sexual arousal and achieving an orgasm, as well as with the self-estimated pleasure of sexual activity. In our cohort, satisfaction with the sensitivity of the neoclitoris was higher than with the depth of the neovaginal canal. This could be due to the time of questioning, which was a median of 5.05 years after GAS. While neoclitoral sensitivity is unlikely to diminish, it is more likely that the neovaginal canal shrinks over time. Of the subjects 6% reported a stenosis of the neovagina and 45% a loss of initial neovaginal depth [ 25 ]. The longer the period after GAS is, the more prevalent the stenosis of the neovaginal canal seems to be [ 36 ]. Ineffective dilatation of the neovaginal canal is obviously a key factor contributing to neovaginal stenosis. Over half of all patients (58%) do not use vaginal dilators appropriately, which is a major reason for this kind of long-term complication [ 36 ].
Postsurgical sexuality plays an important role in overall satisfaction and depends substantially on the functionality of the neovagina [ 5 , 6 ]. Satisfaction with functionality ranges between 56% and 84% [ 7 , 9 , 10 , 37 , 38 ]. Previously, we reported a satisfaction rate with functionality, including satisfaction with depth and breadth of the neovagina and the satisfaction with penetration or intercourse, to be 72% (“very satisfied” and “satisfied”) or 91% (including also “mostly satisfied”) [ 6 ]. The self-reported enjoyment of sexual activity correlated significantly and to a greater extent with neoclitoral sensitivity than with neovaginal dimensions, which was not significant. Though genital dimensions were not surveyed in our study, penile size often exceeds the depth of the vaginal canal in natal women without causing problems with, or pain during, sexual intercourse. However in contrast to a skin derived vaginal canal of transgender women the vagina of natal women is able to expand 2.5 to 3.5 cm in length when sexually stimulated [ 39 ]. Neoclitoral sensitivity is usually assessed by means simply of asking the women and can be biased by the patients' wish for social desirability. In this retrospective study we could not rule this out. However, we previously introduced a measurement tool to assess semiquantitatively the sensitivity with a customary brush and a tuning fork [ 40 ] which could be used for future studies on this topic. Though the rate of women, who were able to achieve an orgasm, was lower in the present study than in an earlier cohort from our department [ 9 ], our data aligns well with comparable studies of a similar size [ 11 , 19 , 41 – 43 ]. Interestingly, Dunn et al. found a similar rate of natal women who were unsure or not able to achieve an orgasm during intercourse (16%) or masturbation (14%) [ 44 ]. In total 55.8% of the women in our study rated their orgasms postoperatively as more intense than before surgery, one in five women (20.8%) felt no difference, and 23.4% reported less intense orgasms after surgery. These results are roughly in line with a study by Buncamper et al. [ 45 ]. Since it is very unlikely that handling of the neurovascular bundle during surgery will make the neoclitoris more sensitive than the glans penis was before, a possible explanation could be that postoperative patients were able to experience orgasm for the first time in a body that matched their perception. Furthermore, a decline in sexual desire after sex reassignment therapy (hormonal and surgical) could contribute to an altered orgasmic experience [ 46 ]. Interestingly, in their systematic review, Guillamon et al. reported on results of three longitudinal studies showing a transformation in the brain morphology of MtF after initiation of cross sex hormonal therapy towards a more female morphology [ 47 ]. Moreover, receiving hormonal treatment was one of the factors related to a better subjective perception of sexual quality of life [ 20 ]. Rolle et al. registered a cerebral modification after sex reassignment in fifteen MtF transsexual individuals towards a more female cognitive response [ 48 ]. It is unclear whether this could explain differences in subjective orgasm experience before and after GAS. Further prospective studies with a larger sample size are needed to validate this preliminary aspect.
5. Limitations
The study was limited by its retrospective character with a response rate below 50%. Suicide is a very unlikely reason for nonparticipation since the suicide rate after successful GAS is not higher than in the general population [ 49 ]. However, contacting trans-female patients for long-term follow-up is generally difficult [ 3 , 37 , 50 – 54 ] particularly in countries like Germany where there is no central registration. Another reason is that patients often move following successful surgery [ 5 ]. Response rates to surveys in retrospective research in this field are between 19% [ 54 ] and 79% [ 55 ]. With 49%, Löwenberg et al. achieved a similar response rate in a follow-up inquiry of a comparable cohort [ 10 ]. Another bias could be that the answers represent patients' wishes for social desirability, rather than the reality of their situation. However, this cannot be verified retrospectively.
6. Conclusion
To our best knowledge, this was the first study to survey sexuality after MtF GAS in a very detailed way. In the majority of women, orgasms after surgery were experienced more intense than before. In our cohort, neoclitoral sensitivity seems to contribute to enjoyment of sexual activity to a greater extent than the depth of the neovaginal canal.
Acknowledgments
The authors acknowledge support by the Open Access Publication Fund of the University of Duisburg-Essen. This study has been conducted without external funding. Expenses have been financed by the Clinic for Urology, University Hospital Essen, University Duisburg-Essen, Germany.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Ethical Approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Parts of the data were presented as an abstract at the 2nd Biennial Conference “Contemporary TransHealth in Europe: Focus on Challenges and Improvements” 2017 in Belgrade, Serbia.
The Christian Post
To enjoy our website, you'll need to enable JavaScript in your web browser. Please click here to learn how.
You are using an outdated browser. Please upgrade your browser to improve your experience.
Recommended

US Air Force promoted drag events on military bases, internal documents show

1 million-member regional body leaves United Methodist Church over gay marriage, clergy

Pastor Mark Driscoll wants Jesus to return before Election Day

Harrison Butker, KC Chiefs visit White House weeks after kicker criticized Biden's abortion stance

'The Chosen' severs ties with Angel Studios, claims breach of contract

Samuel Alito is right — as usual

The antisemitism virus starts in K-12

Why is modern medicine against motherhood?

Does biology need 'queer theory'?

The woke right just proved the Constitution is alive and well (part 2)
Adults who undergo trans surgeries at 12 times higher risk of attempting suicide: report.

Trans-identifying adults who underwent body-mutilating surgeries as part of an effort to look like the opposite sex had an elevated suicide attempt risk, according to a recent study.
The study , titled “Risk of Suicide and Self-Harm Following Gender-Affirmation Surgery,” was published in April in the medical science journal Cureus. Researchers conducted the study by assessing over 90 million adults aged 18 to 60.
According to the study, individuals who underwent “gender-affirming surgery” had a 12-fold higher suicide attempt risk than those who did not. The researchers found that 3.5% of people who had an elective trans surgery were treated for attempting suicide. As the study reported, 0.3% of patients who did not undergo a surgical procedure did not attempt suicide.

Get Our Latest News for FREE
One critic of the study, trans-identified journalist Erin Reed, published an analysis on his Substack page, Erin in The Morning, refuting its findings. The analysis claims that the authors' methodology raises questions about the study's accuracy.
Reed questioned the study’s results, taking issue with the research because, he claimed, it compared people who had trans surgeries to non-trans-identifying individuals to determine if said surgeries increased the risk of suicide.
“To accurately assess whether transgender surgeries increase suicide risk, the correct control group would be transgender people who did not have surgery or, even more accurately, those who were denied surgery,” Reed wrote. “It would be like judging the effectiveness of a new teaching method by comparing college students using the new method to those who never went to college, rather than to college students using the old method.”
Dietrich Jehle, one of the study’s authors, said in a statement to The Christian Post that they “looked at associations with outcomes rather than causation in a large propensity matched retrospective study.” Jehle serves as professor and chair of the Sealy Department of Emergency Medicine at the University of Texas Medical Branch in Galveston, Texas.
“We did not look at the effect of surgery — just the outcomes of the population that had gender affirmation surgery,” Jehle told CP, adding that trans-identifying individuals typically have higher rates of depression.
“[I should emphasize] that we did not use individuals that wanted gender affirmation surgery and were not granted the surgery as a control as patients are required to undergo at least two psychiatric evaluations in order to qualify for surgery (i.e., patients who qualify for surgery are at lower suicide risk than the group who wants surgery but does not qualify regardless of whether the group that qualifies undergoes surgery),” Jehle added.
According to the researcher, the “key point” of the study is that individuals who have undergone a trans surgery “need comprehensive psychiatric care in the years following the surgery.”
“Our conclusion might be better worded: Patients who undergo gender-affirming surgery are associated with significantly elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support,” Jehle said.
He further told CP that researchers used "Z87.890" for the study, which is a code used in medical records to indicate whether someone has a history of undergoing trans procedures.
Regarding the methodology, the study consisted of four separate cohorts. The first Cohort, A, consisted of 1,501 adults aged 18 to 60, who underwent a trans surgery and later sought emergency care for suicidal ideation. Cohort B was intended to serve as the study’s control group, and it consisted of adults aged 18 to 60 who had gone to an emergency room for mental health concerns but had no history of having undergone a sex-change operation.
Another group, Cohort C, served as the study’s second control group, and it consisted of adults aged 18 to 60, who went to the ER and had tubal litigation (surgery performed on women to prevent pregnancy) or a vasectomy but they did not undergo “gender-affirmation surgery.”
“A secondary analysis involving a control group with pharyngitis, referred to as cohort D, was conducted to validate the results from cohort C,” the study stated.
The study concluded, “Gender-affirming surgery is significantly associated with elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support.”
Brandon Showalter, a social commentator for The Christian Post, who has done extensive research on the topic of gender dysphoria and so-called gender-affirming surgeries, noted that there can be a variety of factors that cause a person to feel compelled to end his or her life.
"While I'm not surprised to see these higher numbers in this latest research, the prevailing challenge for critics of these procedures is to make visible the harms of this experimental medicalization and irreversible surgeries, which are numerous aside from any consideration about how those medical practices might contribute to suicide," Showalter stated.
Discussions about the effectiveness of so-called “gender-affirming care” and the potentially negative impact on an individual’s mental health are ongoing.
In October 2019, a study published in the American Journal of Psychiatry initially highlighted the mental health benefits associated with “gender-affirming” surgeries. Researchers analyzed the records of 9.7 million Swedes in the national population registry. Between 2005 and 2015, 1018 of the 2,679 individuals diagnosed with "gender incongruence" underwent surgery to remove their genitals or permanently alter their bodies.
The study authors highlighted a supposed 8% decrease in mood and anxiety disorders for postoperative patients each year after the surgery. The authors later posted a correction after several media outlets reported on the finding, stating their data “demonstrated no advantage of surgery in relation to subsequent mood or anxiety disorder-related health care visits or prescriptions or hospitalizations following suicide attempts.”
A separate extensive long-term study conducted in Sweden by scholars at the Karolinska Institute and Gothenburg University concluded that "after sex reassignment, [trans-identified individuals] have considerably higher risks for mortality, suicidal behavior, and psychiatric morbidity than the general population."
The study analyzed 324 individuals (191 male-to-female, 133 female-to-male) for over 30 years after a sex-change surgery from a period of 1973 to 2003.
Samantha Kamman is a reporter for The Christian Post. She can be reached at: [email protected] . Follow her on Twitter: @Samantha_Kamman
Was this article helpful?
Help keep The Christian Post free for everyone.
By making a recurring donation or a one-time donation of any amount, you're helping to keep CP's articles free and accessible for everyone.
We’re sorry to hear that.
Hope you’ll give us another try and check out some other articles. Return to homepage.
Psychiatry journal issues major correction to study on trans surgeries effect on mental health
44% of trans-identified individuals report ‘serious psychological distress,' one-third experienced homelessness, aclu sues ohio over law banning sex-change surgeries for minors, men in women's sports, appeals court says wva, nc can’t bar medicaid coverage for elective trans surgeries, most popular.

Pastor Mark Driscoll wants Jesus to return before Election Day as civil war chatter abounds

Church finance manager pleads guilty to stealing $775K through complex scheme

More Articles

Group of Brands
- Search Close Search submit
There is still time to register for the ISAPS Congress, in Cartagena or on demand
Procedure: Male to Female Gender Reassignment Surgery (MTF GRS)
Male-to-female gender reassignment surgery (MTF GRS) is a complex and irreversible genital surgery for male transsexual who is diagnosed with gender identity disorder and has a strong desire to live as female. The procedure is to remove all male genital organs including the penis and testes with the construction of female genitalia composed of labia major/minor, clitoris and neovagina simultaneously.
The patient who is fit for this surgery must strictly follow the standard of care set by the World Professional Association of Transgender Healthcare (WPATH) or equivalent criteria; Express desire or live in another gender role (Male gender) long enough, under hormonal replacement therapy, evaluated and approved by a psychiatrist or other qualified professional gender therapist.
Apart from genital surgery, the patient would seek other procedures to allow them to live as female smoothly such as breast aesthetic surgery, facial feminization surgery, body contouring, hair removal, voice change surgery, etc.
Interested in having this procedure?
Useful Information
Ensure you consider all aspects of a procedure. You can speak to your surgeon about these areas of the surgery in more detail during a consultation.
The surgery is quite complicated and only a handful of surgeons are able to perform this procedure. It can be completed in one stage or more stages depending on techniques and surgeons. The average surgical time ranges between 5-8 hours. There are several options of neovaginal construction depending on the type of tissue, single or in combination, such as penile skin, scrotal skin, large intestine, small intestine, or peritoneum.
The procedure is done under general anesthesia and might be combined with spinal anesthesia for faster recovery by reducing the usage of anesthetic gas.
Inpatient/Outpatient
The patient will be hospitalized as an in-patient for between 5-14 days depending on the technique and surgeon. The patient will have a urinary catheter at all times in the hospital.
Additional Information
What is the recovery process.
During hospitalization, the patient must be restricted in bed continuously or intermittently for several days between 3-5 days. After release from the hospital, the patient can return to their normal lives but not have to do physical exercise during the first 2 months after surgery. The patient has to do vaginal dilation continuously for 6 months to maintain the neovagina canal until completely healed and is ready for sexual intimacy.
What are the results?
With the good surgical technique, the result is very satisfying with an improved quality of life. The patient is able to live in a female role completely and happily either on their own or with their male or female partners.
What are the risks?
The most frequent complication of MTF GRS is bleeding, wound infection, skin flap or graft necrosis, urinary stenosis, neovaginal contracture, unsightly scar or deformed genitalia, vaginal fistula, etc. The revision procedures to improve external appearance are composed of secondary labiaplasty/ urethroplasty/ perineoplasty/ and vulvaplasty. The other revision procedure is secondary vaginoplasty to help the patient able to have sexual intimacy with the partner.
- Patient Information
- Global Statistics
- Media Centre
- Global Sponsors
- Privacy Policy
19 Mantua Road, Mount Royal, NJ 08061 United States
Registration number: 0330131
US Office: +1-603-643-2325
UK Office: +44 20 7038 7812
© 2022 International Society of Aesthetic Plastic Surgery. All Rights Reserved.
- Create an account
Log into My ISAPS
Forgot your password? Reset it here
Join the ISAPS Community
All members will continue to receive information relevant to their membership and ISAPS events.
I confirm by clicking below I would like to receive information about:
Welcome to the ISAPS community
By creating an account, you can:.
- Register for events
- Update your personal details
- Gain access to ISAPS publications and video library
- Become a member (explore our memberships here)
ISAPS Members can also:
- Access your member benefits
- Secure discounted member rates for events
- Read the Aesthetic Plastic Surgery Journal
- Gain full access to the video library
- View the Members Directory
- Update your 'Find a Surgeon' profile details
- Renew/Upgrade your Membership
The first step to becoming a part of the community is creating an account, so join us!

COMMENTS
Female-to-male surgery is a type of gender-affirmation or gender-affirming surgery. There are multiple forms of gender-affirming surgery, including altering the genital region, known as "bottom ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning.. Often used to refer to phalloplasty, metoidoplasty, or vaginectomy, sex reassignment surgery can also more broadly refer to many procedures an individual may have ...
Featured Expert: Fan Liang, M.D. Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including: Creating the penis. Lengthening the urethra so you are able to stand to urinate. Creating the tip (glans) of the penis. Creating the scrotum.
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Female-to-male gender reassignment surgery (FTM GRS) is a complex and irreversible genital surgery for female transsexual who is diagnosed with gender identity disorder and has a strong desire to live as male. The procedure is to remove all female genital organs including the uterus, ovaries, and vagina with the construction of male genitalia ...
FTM Bottom Surgery. We can give you male genitalia in two different ways: Phalloplasty creates a penis and urethra (to stand while urinating). We use tissue from your forearm or thigh. We do this in 2 stages. Metoidioplasty takes your existing genital tissue and makes it longer, turning it into a defined phallus.
His confidence in this new approach is the result of nearly three decades of expertise and innovation in SRS and urogenital reconstructive surgery, which includes 600 male-to-female vaginoplasties, 900 female-to-male metoidioplasties, 300 female-to-male phalloplasties, and the co-development of a penile disassembly technique for epispadias repair.
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Gender transition can substantially improve quality-of-life in individuals with gender dysphoria, and various surgical options are available for female-to-male (FtM) transition, including facial ...
The authors provide a state-of-the-art overview of the different gender reassignment surgery procedures that can be performed in a female-to-male transsexual. ... Ceulemans P, et al. Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast Reconstr Surg. 2008; 121 (3):849-859. [Google Scholar] Webster J P ...
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000. Between 100 to 500 gender-reassignment procedures are ...
Treatment Gender dysphoria. Treatment. Treatment for gender dysphoria aims to help people live the way they want to, in their preferred gender identity or as non-binary. What this means will vary from person to person, and is different for children, young people and adults. Waiting times for referral and treatment are currently long.
This was previously known as 'sex reassignment surgery' or 'gender confirmation surgery'. The name change shows that your genitals don't define your sex or gender. ... Gender identity is more than being male or female. Kids Helpline can help you understand what it is and how you can understand your own identity. Read more on Kids ...
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris. During this procedure, a surgeon makes "like become like," using parts of the original penis to create a ...
Your surgeon will give you general guidelines for this as well. Approximately 1 out of 10 people who have a vaginoplasty end up requiring a second, minor surgery to correct some of the scarring from the first surgery and improve the function and cosmetic appearance. Most genital gender affirmation surgeries are covered by insurance.
During this period, 214 patients underwent penile inversion vaginoplasty. Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18-61 years); the average of operative time was 3.3 h (range 2-5 h); the average duration of hormone therapy before surgery was 12 years (range 1-39).
Abstract. Male-to-Female (MtF) gender affirmation surgery (GAS) comprises the creation of a functional and aesthetic perineogenital complex. This study aimed to evaluate the effect of GAS on sexuality. We retrospectively surveyed all 254 MtF transsexual patients who had undergone GAS with penile inversion vaginoplasty at the Department of ...
Most insurance plans cover gender-affirming hormone therapy, which used to be called hormone replacement therapy (HRT). Most plans also cover gender-affirming surgery, which used to be called gender reassignment surgery. That means you can get the care you need to help express your gender identity and more fully be your authentic self.
A hand holds up a small transgender pride flag. The blue and pink stripes represent the colors for a boy and girl, while the white stripe represents self-declared gender identities, such as transitioning, intersex, neutral and undefined gender. | Getty Images Trans-identifying adults who underwent body-mutilating surgeries as part of an effort to look like the opposite sex had an elevated ...
Male-to-female gender reassignment surgery (MTF GRS) is a complex and irreversible genital surgery for male transsexual who is diagnosed with gender identity disorder and has a strong desire to live as female. The procedure is to remove all male genital organs including the penis and testes with the construction of female genitalia composed of ...
(The Center Square) - California female prison guards are required by prison policy to strip search individuals who have transitioned from men to women, according to a report from National Review. "Incarcerated individuals who are transgender, non-binary, or intersex must be searched according to the gender designation of the institution where they are housed or based on the individual's ...