- Case Report
- Open access
- Published: 17 July 2023

Unforeseen complications: a case of dengue shock syndrome presenting with multi-organ dysfunction in a subtropical region
- Syed Muhammad Owais 1 ,
- Farrukh Ansar ORCID: orcid.org/0000-0002-9056-5245 2 ,
- Muhammad Saqib ORCID: orcid.org/0000-0003-3645-6416 3 ,
- Khatira Wahid 1 ,
- Khalid Rashid ORCID: orcid.org/0000-0002-4771-6896 4 , 5 &
- Hassan Mumtaz ORCID: orcid.org/0000-0003-2881-2556 6 , 7
Tropical Medicine and Health volume 51 , Article number: 39 ( 2023 ) Cite this article
3557 Accesses
1 Citations
1 Altmetric
Metrics details
Dengue fever, a viral illness transmitted by the Aedes mosquito, is capable of causing a range of serious complications, including fulminant hepatic failure, renal dysfunction, encephalitis, encephalopathy, neuromuscular and ophthalmic disorders, seizures, and cardiomyopathy.
Case description
This report details the case of a 30-year-old lactating woman with no notable medical history who presented to the emergency department with symptoms of high-grade fever, altered mental status, and seizures. Upon imaging, bilateral infarcts in the thalami and cerebellar hemispheres were observed, consistent with cerebellitis and dengue encephalitis.
Patient treatment and outcome
The patient was admitted to the intensive care unit and received appropriate treatment. Following a critical phase and successful patient stabilization, she was transferred to a high dependency unit for a week before being discharged with recommendations for follow-up care.
This case illustrates the broad spectrum of complications that can arise as a result of dengue infection and the importance of timely diagnosis and management in improving patient outcomes. Further investigation is required to better understand the mechanisms underlying these complications and to formulate specific guidelines for the prevention and treatment of dengue shock syndrome.
Introduction
Dengue fever is a viral infection transmitted by the Aedes mosquito. It is caused by one of four serotypes of the dengue virus (DENV 1–4). The dengue virus belongs to the Flaviviridae family of ribonucleic acid (RNA) viruses [ 1 ]. Dengue is an endemic disease in tropical and subtropical countries, putting almost four billion people worldwide at risk. The prevalence of dengue has rapidly increased in the Southeast Asian region in recent years. It is important for people living in or traveling to areas where dengue is prevalent to take precautions to protect themselves from mosquito bites and to seek medical attention if they develop symptoms of dengue fever [ 2 ]. Dengue shock syndrome (DSS) is the most severe manifestation of dengue infection and can have a mortality rate of up to 20% if not treated appropriately. DSS is characterized by a rapid drop in blood pressure, leading to shock and organ failure. Early diagnosis and management of DSS is crucial for improving patient outcomes. It is important for healthcare providers to be aware of the signs and symptoms of DSS and to initiate prompt treatment in order to prevent complications and reduce mortality [ 1 ]. It has been suggested that there are over 350 million reported cases of dengue and 22,000 related deaths worldwide each year [ 3 ]. Generally, dengue infection is characterized by a high-grade fever accompanied by rigors, chills, body aches, and a transient macular rash. However, in rare cases, complicated dengue infection can lead to severe complications such as fulminant hepatic failure, renal dysfunction, encephalitis, encephalopathy, neuromuscular and ophthalmic disorders, seizures, and cardiomyopathy [ 4 ]. Severe hepatic involvement associated with dengue infection is very rare. According to a large retrospective cohort study from the Hospital for Tropical Disease in Thailand, the incidence of acute liver failure in symptomatic dengue patients was less than 0.5%, but it had a significant mortality rate of 66%. This highlights the importance of early diagnosis and management of dengue infection in order to prevent complications and reduce mortality [ 5 ].
Case presentation
A 30-year-old lactating mother in subtropical South Asia with no significant past medical or surgical history presented to the emergency room with chief complaints of high-grade fever, altered mental status, and seizure. High grade and intermittent fever had been present since five days prior to admission, accompanied by rigors and chills. The patient’s mental status altered gradually starting with a loss of orientation and progressing to complete obtundation. The patient also experienced abrupt localized seizure in her lower limbs every half to one hour, without generalized tonic–clonic seizures or tongue bites. The patient did not have any bowel or bladder incontinence.
Physical examination revealed body temperature of 101 ºF, blood pressure of 99/64 mmHg, pulse of 144/min, oxygen saturation of 94% on room air, a respiratory rate of 36/min and a Glasgow Coma Scale score of 5/15 with a fixed constricted pupil. A malar rash on the face, palmar erythema, left lower extremity focal seizures, prolonged capillary refill, cold, clammy, and mottled skin were observed. The rest of the physical examination was unremarkable. The patient's random blood glucose was 180 mg/dl, and there were no signs of meningismus. Blood test revealed a hemoglobin level of 12.7 g/dL, a platelet count of 105 × 10 9 /L, and neutrophils of 27.5 × 10 9 /L. The alanine transaminase was 1394 U/L, C-reactive protein was 19.2 mg/dL, creatinine was 1.79 mg/dL, activated partial thromboplastin time was 61.7 s, procalcitonin was 0.00835 mg/dl, and Troponin I was raised at 0.00012168 mg/dl.
An echocardiography report showed an ejection fraction of 35–39% with mild pulmonary hypertension and moderate left ventricular systolic dysfunction. A brain computed tomography (CT) scan showed hypodensity in both the thalami and cerebellar hemispheres, suggesting bilateral thalamic and cerebellar infarcts and a possibility of cerebellitis and encephalitis. Grey–white matter differentiation appeared intact, and there was no evidence of a focal mass, midline shift, or hematoma. A brain magnetic resonance imaging (MRI) showed bilateral, almost symmetrical, high signals on T2-weighted and fluid-attenuated inversion recovery images in the thalami cerebellar hemispheres and bilateral cerebral cortices, which indicated the possibility of encephalitis or postictal ischemic changes. An enhanced CT scan of the chest and abdomen showed bilateral basal atelectasis, hepatomegaly, a distended gallbladder and enlarged bilateral iliacus muscles with internal hyperdense and hypodense areas suggesting the possibility of bilateral iliacus hematomas with some liquefaction.
The patient was diagnosed as sepsis, metabolic acidosis (evident from serum bicarbonate levels of 18 mEq/L, arterial pCO2 of 29 mmHg and a pH of 7.23), respiratory distress, acute kidney injury, heart failure due to myocarditis, acute liver injury and possible brain edema. Sudden onset of high-grade fever, systemic symptoms with multiple organ failure and local endemic situation arose the possibility of dengue shock syndrome although normal platelet count and absence of petechial rashes on the body were not compatible.
Further investigation revealed positive dengue non-specific antigen 1 (Dengue NS1 Ag) and positive dengue immunoglobulin M antibody (Dengue IgM Ab)done using qualitative Wondfo© One Step Dengue NS1 Antigen kits. A graphical summary of the case as well as the table of investigations can be seen in Fig. 1 .
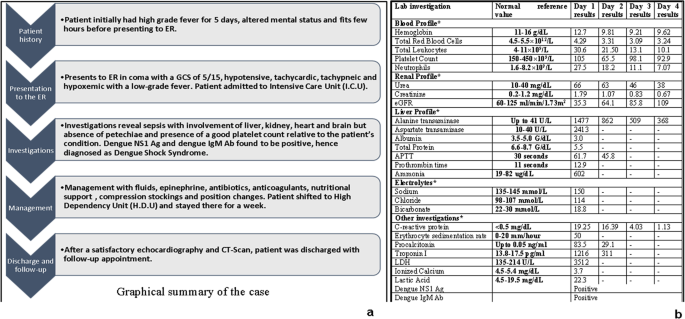
Summary of the case ( a ) and table of investigations ( b ). *Only the deranged values have been reported; Dengue NS1 Ag: dengue non-specific antigen 1; Dengue IgM Ab: dengue immunoglobulin M antibody
The patient was admitted to the intensive care unit and intravenous fluids were started (3% normal saline, 100 ml/h) with 0.10 μg/kg/min of norepinephrine. Mechanical ventilation was initiated due to the patient's deteriorating respiratory status, suspected secondary bacterial infection and herpes encephalitis, intravenous antibiotics (ceftriaxone 1 g/12 h and azithromycin 500 mg/day) and acyclovir (400 mg/8 h). In addition, the patient received intravenous insulin (0.1 units/kg/h) to maintain normal blood sugar levels and intravenous vasopressin (0.01 units/min) to maintain optimal blood pressure (above 120 mmHg systolic and above 80 mmHg diastolic) on the first day of admission. The patient soon started responding to treatment with gradual improvement in consciousness and laboratory findings.
The patient's renal function was monitored closely, and hemodialysis was initiated on the first day of admission. The patient's liver function was also monitored, and she received intravenous N -acetylcysteine and a low-fat diet. N-acetylcysteine (NAC) was administered in a specific dosing regimen. Initially, a bolus dose of 150 mg/kg body weight was administered, followed by a maintenance dosage of 12.5 mg/kg/h over a duration of 4 h. Subsequently, the maintenance dosage was adjusted to 6.25 mg/kg/h and continued for up to 72 h.
The patient's condition improved gradually over the next few days, and the mechanical ventilation was discontinued on the fourth day of admission. The patient was transferred to the high dependency unit for further management and stayed there for a week. After satisfactory echocardiography (revealing ejection fraction of 59% with a cardiac output 6.0 L per minute and a heart rate of 80 beats per minute, indicating a normal cardiac profile) and CT scan results (resolution of thalamic and cerebellar involvement seen on previous CT scans), the patient was discharged and advised to follow-up. CT scan and MRI images taken before recovery are shown in Figs. 2 and 3 , respectively. CT scan of the brain, revealed bilateral thalamic and cerebellar infarcts, suggesting brain involvement. Additionally, a magnetic resonance imaging (MRI) of the brain showed abnormal signals in the thalami, cerebellar hemispheres, and bilateral cerebral cortices, indicating the presence of dengue encephalitis or postictal ischemic changes. These imaging findings support the diagnosis of neurological involvement in the patient.
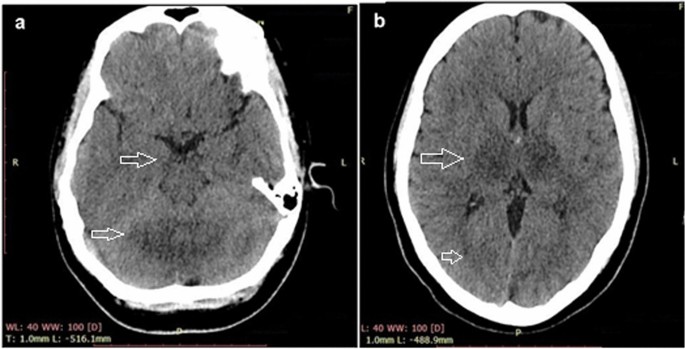
CT scan showing bilateral thalamic and cerebellar hypodensities ( a , b ); patient details are hidden to protect patient privacy
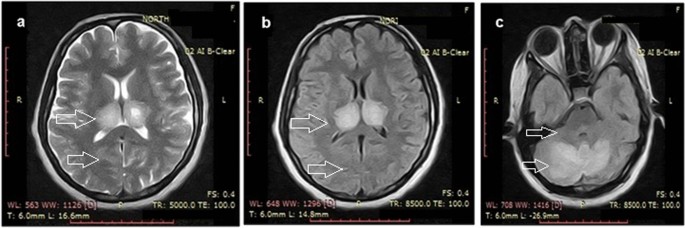
MRI scan showing bilateral thalamic and cerebellar infarcts ( a – c ); patient details are hidden to protect patient privacy
The patient was conscious towards the end of day 1 and slowly improved function. There was a mild residual muscle weakness in the proximal thigh muscles which improved in the subsequent days. This could be due to the lower limb seizures that were observed in the initial phase of admission. There were no signs of muscle paralysis observed in the patient. A recovery CT scan done on day 4 showed resolution of brain findings seen on CT previously as shown in Fig. 4 .

CT scan of the brain after recovery showing resolution of all findings seen on previous CT scan; patient details are hidden to protect patient privacy
The relationship between dengue fever and neurological manifestations was first described in 1976, and multiple studies since then have shown that dengue fever can be associated with neurological complications [ 6 , 7 ]. Neurological manifestations of dengue fever can include headaches, irritability, alteration of consciousness, insomnia, and focal neurological deficits. These manifestations may be associated with encephalitis and seizures [ 6 ]. Dengue fever presents various neurological manifestations that can be classified into three distinct categories. The first category involves direct neurotropism, leading to conditions such as encephalitis, meningitis, myelitis, and myositis. The second category encompasses systemic complications, which include encephalopathy, stroke, and hypokalemic paralysis. Lastly, there are post-infectious or immune-mediated manifestations, such as acute disseminated encephalomyelitis (ADEM), Guillain–Barré syndrome (GBS), and optic neuritis [ 8 ].
In our case, the patient belonged to a subtropical region of South Asia and presented with altered mental status, seizure, and low Glasgow Coma Scale score, which were indicative of neurological involvement. This was supported by a CT scan showing bilateral thalamic and cerebellar infarcts due to possible brain edema, possibly indicating cerebellitis and dengue encephalitis. Myocarditis and cardiac dysfunction are rare but recognized complications of dengue fever. Earlier studies have reported on these complications, but did not specify which serotype was most commonly associated with them. More recent studies, however, have suggested that dengue virus serotype 2 (DENV-2) may be particularly implicated in causing myocardial dysfunction in children. Cardiac complications of dengue fever tend to manifest early in the disease course, and common electrocardiographic changes include T-wave inversion. These findings have been described in the literature previously [ 9 ]. In the current case, our patient was suspected to have myocarditis, which was later confirmed by the presence of a raised Troponin I level and a low ejection fraction on echocardiography. Acute kidney injury (AKI) is a significant complication that can occur in patients with dengue fever, particularly in those who are hospitalized for extended periods of time. The etiology of AKI in dengue fever is not fully understood, but proposed mechanisms include rhabdomyolysis, hemodynamic instability, acute glomerular injury, and hemolysis, all of which can lead to tubular necrosis, thrombotic microangiopathy, and acute glomerulopathy. Unfortunately, patients with dengue fever who develop renal complications such as AKI have a higher mortality rate. There are currently no specific recommendations for the treatment of AKI in dengue patients, and treatment typically involves conventional renal replacement therapy [ 10 ]. Dengue fever can affect the liver, which is the most commonly affected organ in patients with this infection. Liver involvement can range from mild elevation of hepatic transaminases to severe acute liver failure. The mechanisms behind liver injury in dengue fever are not fully understood, but may include hypoxic liver injury due to shock, direct virological attack on hepatocytes, and immunological damage to the liver. The management of acute liver injury in dengue fever can be challenging, as there are few guidelines available on the best approach. In the past, some studies have suggested that the use of NAC as an antidote for acetaminophen toxicity may be beneficial in the management of acute liver failure in dengue fever, as it has been associated with reduced mortality and high transplant-free survival, particularly when used in the early stages of the disease [ 11 ]. In our case, the administration of NAC was based on evidence from a recent meta-analysis conducted by Walayat et al. [ 12 ], which highlighted the significant improvement in overall survival associated with NAC, even in cases of non-acetaminophen-related acute liver failure [ 12 ]. The underlying pathophysiology of dengue fever involves a complex interplay between the virus and host-specific factors. The dengue virus replicates inside host cells, triggering the release of immune-mediated destruction and cytokines. While there is increased vascular permeability, plasma leakage is typically confined to the pleural and peritoneal cavities and does not result in generalized edema. The development of hemorrhagic diathesis is thought to be caused by liver damage that leads to decreased secretion of coagulative factors and albumin. The virus also replicates in the adrenal gland, contributing to sodium loss and hypotension. The presence of petechiae, which are small red or purple spots on the skin, is likely due to capillary fragility, thrombocytopenia, and cytokines that disrupt vascular integrity [ 13 , 14 ]. In dengue infection, both thrombosis and brain edema are potential mechanisms underlying the vascular involvement observed in cerebellitis and dengue encephalitis. Thrombosis can occur due to endothelial dysfunction and increased vascular permeability, leading to impaired blood flow and infarction in cerebral blood vessels. Meanwhile, the inflammatory response triggered by dengue fever can cause brain edema through the release of cytokines and immune mediators, resulting in increased blood–brain barrier permeability and fluid accumulation in the brain tissue. Brain edema can subsequently compress surrounding vessels and compromise blood flow, potentially leading to ischemic events and infarction [ 15 ]. It is evident from the CT images that the patient in our case most probably had ischemic changes due to brain edema that resolved in the subsequent days as evident in follow-up recovery brain CT scan which shows no residual findings.
Our patient presented to the emergency department with encephalopathy leading to coma, a neurological complication of dengue fever. There is a difference between encephalopathy and encephalitis in dengue virus infection which can be seen in Table 1 .
Upon examination, the patient was found to be in shock, as indicated by tachycardia, tachypnea, hypotension, cold, clammy, and mottled skin, and prolonged capillary refill. The presence of palmar erythema and malar rash may have been due to the physiological effects of pregnancy. Initially, the absence of petechiae and a good platelet count led us to suspect a case of non-dengue viral sepsis. However, dengue antigenic testing eventually revealed a positive result. This case is unique in that it involved multiple organ involvement mimicking viral sepsis, but without evidence of petechiae and a relatively good platelet count given the patient's condition. The diagnosis of dengue infection was ultimately reached through extensive testing and an astute clinical approach.
The patient was suffering from acute liver injury, acute kidney injury (AKI), heart failure (myocarditis), hypernatremia, and possible brain edema. While previous reports have described similar complications of dengue fever, this case is unusual in that it involved all of these complications simultaneously [ 16 , 17 , 18 ]. Our treatment regimen was in accordance with the guidelines provided by the Centers for Disease Control and Prevention [ 19 ]. Our treatment approach was also informed by based on the findings of multiple randomized controlled trials studied by Kalayanarooj et al. [ 20 ]. In the management of our patient, we focused on restoring and maintaining intravascular volume for sufficient end-organ perfusion. To this end, we administered intravenous fluids and norepinephrine to improve hemodynamics and normalize blood pressure, as well as antibiotics to control sepsis. We did not use beta blockers to lower the patient's heart rate, but closely monitored it instead. Other treatments included oral proton pump inhibitors to prevent stress ulcers, whole-nutrition in the form of Ensure®, compression stockings to prevent deep vein thrombosis, and any other necessary medications. There are many reasons why our case is unique. First, the case presents a unique and rare combination of serious complications of dengue fever, including dengue encephalitis, suspected myocarditis, acute kidney injury, and acute liver failure. This is an unusual presentation of dengue fever that has not been widely reported in the literature and would be of interest to healthcare professionals and researchers studying this disease. Second, the case report provides a detailed account of the patient's clinical presentation, diagnostic workup, and management, including the specific treatment strategies employed to address each of the complications. This information would be valuable to other healthcare professionals caring for patients with dengue fever and could inform future clinical practice. Finally, the successful management of the patient's multiple serious complications and the patient's eventual recovery make this an informative and inspiring case report that would be of interest to a wide audience. More interdisciplinary and evidence-based studies are required to make guidelines and decide on diagnosis and optimum fluid management in dengue infections complicated by encephalopathy in lactating women with dengue infection complicated by multiple complications. The guidelines are essential to facilitate management and prevent any adverse outcomes.
CARE checklist
In conclusion, dengue fever presented in our case with a wide range of complications involving various organs, such as the brain, kidneys, liver, and myocardium. These complications ranged from encephalitis and seizures to acute kidney injury and myocarditis. It is important for healthcare professionals to be aware of the potential complications of dengue fever and to promptly diagnose and manage them in order to improve patient outcomes.
Patient’s own perspective
The patient reported “As a young, healthy mother, I never expected to wind up in the intensive care unit struggling for my life. But that's exactly what happened when I contracted dengue fever. It all started with a high fever came on suddenly. I figured I had just caught a bug and would be feeling better soon, but my condition only seemed to get worse. Before long, I was experiencing changes in my mental status. When I arrived at the hospital, I was rushed to the emergency department for evaluation. The doctors told me that I had dengue fever and that it had caused complications, including brain inflammation. They immediately started me on treatment and transferred me to the intensive care unit. The next few days were a blur. I remember being hooked up to a lot of machines and feeling very weak and tired. My family was by my side, and the doctors and nurses were all very kind and compassionate, but I was in a lot of pain and was barely able to communicate. Eventually, I started to improve. I was transferred to a high dependency unit and was able to receive more targeted care. After a week, I was finally stable enough to be discharged from the hospital. Looking back, I am grateful to have survived this terrifying experience. But I also hope that others can learn from my story and take the necessary precautions to protect themselves from dengue fever. If you're traveling to an area where dengue is prevalent, be sure to use insect repellent and take other precautions to avoid mosquito bites. And if you do start to feel sick, don't wait to seek medical attention. Early diagnosis and treatment can make all the difference.”
Availability of data and materials
The data collected and analyzed during this case report are available upon request, subject to ethical and legal considerations. All data will be de-identified to protect the privacy of the patient.
Khetarpal N, Khanna I. Dengue fever: causes, complications, and vaccine strategies. J Immunol Res. 2016;2016:6803098. https://doi.org/10.1155/2016/6803098 . ( Epub 2016/08/16 ).
Article CAS PubMed PubMed Central Google Scholar
Brady OJ, Gething PW, Bhatt S, Messina JP, Brownstein JS, Hoen AG, et al. Refining the global spatial limits of dengue virus transmission by evidence-based consensus. PLoS Negl Tropic Dis. 2012;6(8):e1760. https://doi.org/10.1371/journal.pntd.0001760 . ( Epub 2012/08/11 ).
Article Google Scholar
Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, et al. The global distribution and burden of dengue. Nature. 2013;496(7446):504–7. https://doi.org/10.1038/nature12060 . ( Epub 2013/04/09 ).
Carod-Artal FJ, Wichmann O, Farrar J, Gascón J. Neurological complications of dengue virus infection. Lancet Neurol. 2013;12(9):906–19. https://doi.org/10.1016/s1474-4422(13)70150-9 . ( Epub 2013/08/21 ).
Article PubMed Google Scholar
Kye Mon K, Nontprasert A, Kittitrakul C, Tangkijvanich P, Leowattana W, Poovorawan K. Incidence and clinical outcome of acute liver failure caused by dengue in a hospital for tropical diseases, Thailand. Am J Trop Med Hygiene. 2016;95(6):1338–44. https://doi.org/10.4269/ajtmh.16-0374 . ( Epub 2016/12/09 ).
Peter S, Malhotra N, Peter P, Sood R. Isolated Bell’s palsy - an unusual presentation of dengue infection. Asian Pac J Trop Med. 2013;6(1):82–4. https://doi.org/10.1016/s1995-7645(12)60207-7 . ( Epub 2013/01/16 ).
Article CAS PubMed Google Scholar
Solomon T, Dung NM, Vaughn DW, Kneen R, Thao LT, Raengsakulrach B, et al. Neurological manifestations of dengue infection. Lancet. 2000;355(9209):1053–9. https://doi.org/10.1016/s0140-6736(00)02036-5 . ( Epub 2000/04/01 ).
Kulkarni R, Pujari S, Gupta D. Neurological manifestations of dengue fever. Ann Indian Acad Neurol. 2021;24(5):693–702. https://doi.org/10.4103/aian.AIAN_157_21 .
Article PubMed PubMed Central Google Scholar
Kularatne SA, Pathirage MM, Medagama UA, Gunasena S, Gunasekara MB. Myocarditis in three patients with dengue virus type DEN 3 infection. Ceylon Med J. 2006;51(2):75–6. https://doi.org/10.4038/cmj.v51i2.1362 . ( Epub 2006/12/22 ).
Oliveira JF, Burdmann EA. Dengue-associated acute kidney injury. Clin Kidney J. 2015;8(6):681–5. https://doi.org/10.1093/ckj/sfv106 . ( Epub 2015/11/28 ).
Suganthan N, Sakthilingham G, Kumanan T. Dengue fever complicated with acute liver failure: a case report of expanded dengue syndrome and literature review. SAGE Open Med Case Rep. 2020. https://doi.org/10.1177/2050313x20913428 .
Walayat S, Shoaib H, Asghar M, Kim M, Dhillon S. Role of N-acetylcysteine in non-acetaminophen-related acute liver failure: an updated meta-analysis and systematic review. Ann Gastroenterol. 2021;34(2):235–40. https://doi.org/10.20524/aog.2021.0571 .
Martina BE, Koraka P, Osterhaus AD. Dengue virus pathogenesis: an integrated view. Clin Microbiol Rev. 2009;22(4):564–81. https://doi.org/10.1128/cmr.00035-09 . ( Epub 2009/10/14 ).
Sellahewa KH. Pathogenesis of dengue haemorrhagic fever and its impact on case management. ISRN Infect Dis. 2013;2013:571646. https://doi.org/10.5402/2013/571646 .
Adane T, Getawa S. Coagulation abnormalities in Dengue fever infection: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2021;15(8):e0009666. https://doi.org/10.1371/journal.pntd.0009666 .
Arora S, Nathaniel SD, Paul JC, Hansdak SG. Acute liver failure in dengue haemorrhagic fever. BMJ Case Rep. 2015. https://doi.org/10.1136/bcr-2015-209443 . ( Epub 2015/05/27 ).
Lee I-K, Lee W-H, Liu J-W, Yang KD. Acute myocarditis in dengue hemorrhagic fever: a case report and review of cardiac complications in dengue-affected patients. Int J Infect Dis. 2010;14(10):e919–22. https://doi.org/10.1016/j.ijid.2010.06.011 .
Vachvanichsanong P, Thisyakorn U, Thisyakorn C. Dengue hemorrhagic fever and the kidney. Arch Virol. 2016;161(4):771–8. https://doi.org/10.1007/s00705-015-2727-1 . ( Epub 2015/12/25 ).
Dengue clinician guide. Centers for Disease Control and Prevention; 2023. https://www.cdc.gov/dengue/resources/dengue-clinician-guide_508.pdf . Accessed 8 Jan 2023.
Kalayanarooj S, Rothman AL, Srikiatkhachorn A. Case management of dengue: lessons learned. J Infect Dis. 2017;215(suppl_2):S79–88. https://doi.org/10.1093/infdis/jiw609 .
Hendarto SK, Hadinegoro SR. Dengue encephalopathy. Acta Paediatr Jpn. 1992;34(3):350–7. https://doi.org/10.1111/j.1442-200x.1992.tb00971.x .
Borawake K, Prayag P, Wagh A, Dole S. Dengue encephalitis. Indian J Crit Care Med. 2011;15(3):190–3. https://doi.org/10.4103/0972-5229.84896 .
Angibaud G, Luaute J, Laille M, Gaultier C. Brain involvement in Dengue fever. J Clin Neurosci. 2001;8(1):63–5. https://doi.org/10.1054/jocn.2000.0735 .
Download references
Acknowledgements
Author information, authors and affiliations.
Northwest General Hospital & Research Centre, Peshawar, Pakistan
Syed Muhammad Owais & Khatira Wahid
Quaid e Azam International Hospital, Rawalpindi, Pakistan
Farrukh Ansar
Khyber Medical College, Peshawar, Pakistan
Muhammad Saqib
James Cook University Hospital, Middlesbrough, UK
Khalid Rashid
University of Sunderland, Sunderland, England, UK
Maroof International Hospital, Islamabad, Pakistan
Hassan Mumtaz
Health Services Academy, Islamabad, Pakistan
You can also search for this author in PubMed Google Scholar
Contributions
SMO, FA and MS were lead authors and wrote the majority of the paper. FA conceived the study and contributed significantly to the design and planning of the study as well. MS was involved in the data collection and analysis, and contributed to the interpretation of the results as well. SMO, KR, KW and HM provided critical review and feedback on the manuscript. All authors contributed to the writing and editing of the final manuscript and approved the submitted version.
Corresponding author
Correspondence to Muhammad Saqib .
Ethics declarations
Ethics approval and consent to participate.
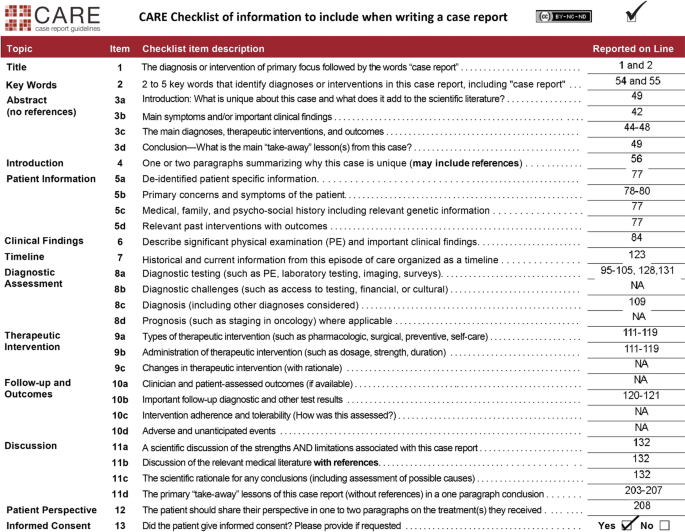
The care of patient described in this case report was conducted in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from the patient before any clinical procedures were performed. All personal and identifying information has been de-identified to protect the privacy of the patient. A CARE checklist is provided in Fig. 5 .
Consent for publication
Informed consent was obtained for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Owais, S.M., Ansar, F., Saqib, M. et al. Unforeseen complications: a case of dengue shock syndrome presenting with multi-organ dysfunction in a subtropical region. Trop Med Health 51 , 39 (2023). https://doi.org/10.1186/s41182-023-00530-y
Download citation
Received : 08 May 2023
Accepted : 11 July 2023
Published : 17 July 2023
DOI : https://doi.org/10.1186/s41182-023-00530-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Severe dengue
- Tropical climates
- Breast feeding
- Postpartum sepsis
- Neurological manifestations
- Myocarditis
- Acute renal failure
- Acute liver failure
- Case reports
Tropical Medicine and Health
ISSN: 1349-4147
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
University of Nevada, Reno

- ScholarWorks | University of Nevada, Reno
- Theses and Dissertations
- Electronic Theses and Dissertations
Dengue Fever: An Examination and Case Study

Ravikumar, Visesh 2016 Dengue Fever - An Examination and Case Study.pdf
View/ download.
Degree Level
Degree name.
Citations in Web of Science©
Permanent link
Additional information, collections.
- Electronic Theses and Dissertations [5214]
Information
- Case report
- Open access
- Published: 08 August 2018
Lessons learnt from managing a case of dengue hemorrhagic fever complicated with acute liver failure and acute kidney injury: a case report
- Chamara Dalugama 1 &
- Indika Bandara Gawarammana 1
Journal of Medical Case Reports volume 12 , Article number: 215 ( 2018 ) Cite this article
4656 Accesses
15 Citations
6 Altmetric
Metrics details
Dengue is a common arboviral infection with a diverse spectrum of clinical manifestations. Dengue hemorrhagic fever is a more severe form of infection characterized by plasma leak and hemoconcentration. Although hepatic dysfunction is common in dengue illness, massive liver necrosis is rarely reported. Lactic acidosis is a poor prognostic marker in liver failure related to dengue. Management of acute renal injury in dengue hemorrhagic fever due to prolonged shock is challenging as the fluid reabsorption during the recovery phase expands the intravascular volume and precipitates heart failure and pulmonary edema.
Case presentation
We report the case of a 43-year-old Sri Lankan Sinhalese woman with serologically confirmed dengue fever presenting with evidence of plasma leakage developing acute liver failure evidenced by deranged liver functions, coagulopathy, and altered sensorium and acute kidney injury with anuria. She had elevated serum lactate levels. In addition to the “standard care,” she was managed with intravenously administered N-acetyl cysteine and blood transfusions, even in the absence of bleeding or dropping packed cell volume, targeting a higher packed cell volume anticipating a better oxygenation at tissue level. Continuous veno-venous hemodialysis was employed and continued for 138 hours removing the fluids reabsorbed during the recovery phase to prevent her from developing heart failure and pulmonary edema. She made full recovery with no sequelae.
Conclusions
N-acetyl cysteine and packed cell transfusion aiming at a higher packed cell volume to maintain adequate tissue perfusion during shock may be beneficial in acute liver failure due to dengue virus. The use of a continuous form of renal replacement such as continuous veno-venous hemodialysis is of paramount importance in managing fluid states in the recovery phase of dengue hemorrhagic fever in those with renal impairment. Interesting observations made in the fluid dynamics during the reabsorption phase need further studies preferably with an animal model.
Peer Review reports
Dengue fever (DF) is a common arboviral disease that is endemic in Southeast Asia; DF has four distinct serotypes [ 1 ]. Dengue illness has a diverse clinical spectrum ranging from asymptomatic subclinical infection to severe multiorgan involvement and death [ 2 ]. Dengue illness encompasses changeable unusual manifestations [ 3 , 4 , 5 ]. Hepatic dysfunction is well reported both in DF and dengue hemorrhagic fever (DHF). Liver involvement can be varied ranging from mild to moderate elevation of serum transaminases to fulminant liver failure [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 ]. Various mechanisms are postulated to explain the hepatic dysfunction seen in dengue illness including direct viral damage, immunological injury, and hypoxic injury due to reduced hepatic perfusion during shock [ 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 ]. The role of N-acetyl cysteine (NAC) in liver injury is debated [ 22 , 23 , 24 ]. Lactic acidosis is a poor prognostic marker in DHF [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 ]. Acute oliguric renal failure is known to occur in patients presenting with prolonged shock. Renal impairment with oliguria raises concerns because the reabsorption of fluid during the recovery phase of DHF can lead to fluid overload and pulmonary edema. We report a case of a late presentation of DHF complicated with liver necrosis, lactic acidosis, and acute renal failure managed successfully. The use of NAC, the use of serum lactate levels to monitor improvement, the role of pack cell transfusion to improve tissue level oxygenation, and prophylactic employment of continuous veno-venous hemodialysis (CVVHD) anticipating the fluid overload during recovery in the background of renal impairment are discussed as important management strategies. Interesting observations on fluid dynamics were made during the fluid reabsorption in the recovery phase.
We report a case of a 43-year-old Sri Lankan Sinhalese woman who presented to our Teaching Hospital, Peradeniya, in the morning with a history of fever, arthralgia, myalgia, and headache of 4 days’ duration. She had been previously diagnosed as having type 2 diabetes mellitus and dyslipidemia for which she received treatment with satisfactory control of the medical conditions and she had normal renal functions.
She had experienced postural dizziness since the afternoon of the previous day and she had had nausea, vomiting, and abdominal pain since the morning of the previous day. Soon after admission she collapsed in our emergency care unit. She was severely dehydrated with cold clammy peripheries. Her pulse rate was 130 beats per minute with an unrecordable blood pressure. She had reduced breath sounds in the base of her right lung and marked tenderness over the right hypochondrium with flank dullness with shifting. She was drowsy, but arousable.
Her complete blood count showed hemoglobin of 15.3 g/dL, platelet count of 74 × 10 3 /microL, and white cell count of 3.22 × 10 6 /microL. Her serum creatinine was 277 micromole/L with potassium of 5.8 mmol/L. Alanine transaminase (ALT) was 6542 U/L with aspartate transaminase (AST) of 30,617 U/L. Her serum albumin value was 24 g/L. A bedside ultrasound scan demonstrated bilateral pleural effusions (more in the right) with free fluid in her abdomen. A diagnosis of DHF with decompensated shock complicated with acute liver failure and acute kidney injury was made. DF was confirmed by positive non-structural protein 1 (NS1) antigen and serotype was identified as dengue virus type 2 (DEN-2). Both dengue immunoglobulin M (IgM) and immunoglobulin G (IgG) were positive suggesting a secondary infection with dengue virus (DENV). She was screened for alternative causes for liver necrosis including hepatitis A immunoglobulin A, hepatitis B surface antigen, hepatitis C IgM, leptospirosis serology, and rickettsial serology, which were negative. Her baseline transaminase levels and serum creatinine done 1 month earlier at a medical clinic were within the normal range. She denied taking supra-therapeutic dose of paracetamol or other native medical preparations for her fever. She had been treated with metformin and atorvastatin until the previous night.
She was assumed to be at the peak of the critical phase of DF (that is, 24 hours in the plasma leakage) on admission. On admission her packed cell volume (PCV) was 44%. (Her baseline PCV was 33% for hemoglobin of 10.5 g/dL in her clinic book.) She was given a 10 ml/kg crystalloid bolus (500 ml) over 15 minutes followed by 10 ml/kg bolus over 1 hour. She was given a 10 ml/kg dextran 40% bolus in the next hour. She had heavy per vaginal bleeding and one episode of melena. Her PCV dropped from 44 to 33% without clinical improvement and she had low urine output (< 0.5 ml/kg). She was administered packed cells to maintain the PCV around 40% to a total volume of 1200 ml.
During the latter 24 hours of the critical phase of DF, she had severe metabolic acidosis with lactic acidosis: PH of 7.2, bicarbonate 8 mmol/L, and partial pressure of carbon dioxide 16 mmHg with a lactate level of 12 mmol/L, which was corrected medically with 8.4% sodium bicarbonate 200 ml in divided boluses. Her ionized calcium was persistently low and corrected with multiple boluses of intravenously administered calcium gluconate. Her blood sugar was checked every 2 hours and corrected accordingly.
At the end of presumed critical phase, we gave her 5500 ml of fluid including normal saline, dextran, and packed cells. She was conscious, rational, but drowsy. She had a spiking high temperature. She was icteric but not pale. She was breathless at rest with oxygen saturation of 85% on room air, which increased to 95% with 60% oxygen via mask. Her pulse rate was 120 beats per minute with blood pressure of 140/100 mmHg. She had bilateral pleural effusions up to mid zone. Her liver was 5 cm below the costal margin with normal upper border and markedly tender. She had gross ascites in a horseshoe-shaped distribution. Her serum creatinine was raised to 345 micromol/L with serum potassium of 5.8 mmol/L and during the last 6 hours of the critical phase she was anuric. Her ALT was 8010 U/L and AST 41546 U/L. Her prothrombin time was 22.1 seconds (control 12 seconds) and activated partial thromboplastin time (APTT) was 42 seconds (control 26 seconds). C-reactive protein (CRP) was 240 U/L. Her blood sugars were elevated toward the end of presumed leaking phase of DHF.
At the end of the presumed leaking phase of DHF our patient had: massive liver necrosis; acute kidney injury with acidosis, hyperkalemia, and anuria; deranged clotting with bleeding; and symptomatic volume overload with large plural effusions and gross ascites. Many concerns rose at this point regarding management:
The fluid in the third space mainly in the pleural and peritoneal cavities would get reabsorbed and as she probably had an established acute kidney injury with anuria, the reabsorbed fluid would accumulate in her intravascular compartment leading to expansion of intravascular volume and massive volume overload with pulmonary edema and heart failure.
Massive liver necrosis with deranged synthetic function would worsen the lactic acidosis which in turn would have a negative effect on the inotropic effect of her heart, clotting derangements might aggravate the bleeding risk, and ongoing hypoxia of the liver might further damage her liver.
Sepsis with high fever and elevated inflammatory markers. What is the focus?
Management of uncontrolled blood sugar. Is it due to her existing type of diabetes or pancreatitis?
She was started on continuous renal replacement therapy (CRRT) with CVVHD. We decided to keep CVVHD running and titrate the ultrafiltrate according to the volume state. Observations on central venous pressure (CVP) and blood pressure were made hourly. Intermittent measurements of her inferior vena cava (IVC) diameter and internal jugular vein (IJV) diameter were noted. We assumed that reabsorption of the fluid in the third space would increase the CVP, distend the IJV and IVC, and would increase mainly the diastolic pressure. Depending on the above assumptions, observations were made and ultrafiltrate was gradually increased. Surprisingly, fluid reabsorption occurred in an exponential pattern over a period of 5–6 days and came to a halt abruptly (Figs. 1 and 2 ). Maximum ultrafiltrate was 280 ml/hour. Heparin was not used in CVVHD due to high risk of bleeding.
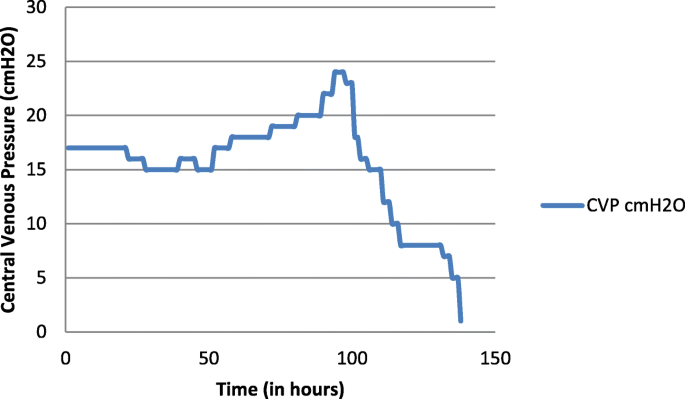
Change in the central venous pressure of the patient over time. CVP central venous pressure
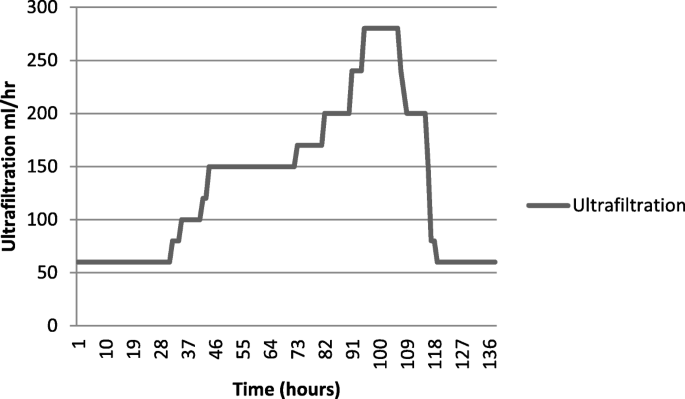
The ultrafiltration removed by continuous veno-venous hemodialysis per hour plotted against time
She was started on intravenous NAC 100 mg/hour infusion which was continued for 5 days. She was given orally administered metronidazole 400 mg 8 hourly and syrup lactulose to maintain bowel motion 2–3 times per day. She was started on an intravenous infusion of proton pump inhibitors, intravenously administered tranexamic acid, and orally administered norethisterone. She was given intravenously administered vitamin K 10 mg daily for 3 days. She was given 4 units of fresh frozen plasma and 10 units of cryoprecipitate, and 6 units of platelets to correct the coagulopathy. She was transfused with packed cells to maintain PCV around 40% in order to maintain adequate oxygenation of hepatocytes. CVVHD was continued and her lactate level was noted to decline gradually.
She had spiking high fevers on day 3 of hospital stay with high CRP. Septic screening was done with blood culture and urine culture and intravenously administered ceftriaxone was changed over to renal-adjusted dose of intravenously administered meropenem and teicoplanin. Later cultures were negative after 72 hours of incubation. However, gradually her fever settled by lysis of fever over the days.
Although during the presumed critical phase her blood sugar was rather low, her blood sugar started to rise over the days. She was a type 2 diabetic with good control with metformin. Her blood sugar was checked hourly and insulin infusion was continued and titrated according to her blood sugar. Her amylase was 450 U/L (normal range 1–37 U/L).
Over a period of 6 days she was closely monitored. Gradually her transaminases declined, her lactate level normalized, and serum creatinine reduced and normalized (Table 1 ). Her urine output gradually increased. CVVHD was terminated after 138 hours of dialysis. She was discharged on ninth day of admission after restoring her full physiology. She was discharged on Mixtard insulin (biphasic isophane insulin injection) for diabetic control. She was reviewed in the ward after 3 days, 7 days, and at 1 month after discharge. Her renal functions and liver functions were within the normal range. She was started again on metformin and atorvastatin 1 week after discharge and insulin was discontinued.
DF is a common mosquito-borne viral disease among humans seen mainly in the Asia-Pacific region [ 1 ]. It can present with a diverse clinical spectrum ranging from asymptomatic infection or simple undifferentiated fever to DHF with multiorgan failure. Four distinct dengue viral serotypes (DEN-1 to DEN-4) are known to cause illness. Infection with one serotype confers protection from reinfection with the same serotype, while reinfection with different serotypes confers no long-term protection and may even predispose plasma leak and worse clinical outcome [ 2 ]. No specific antiviral therapy is available for DF. Dengue infection can present with various unusual manifestations. Most of these manifestations of DF are under-reported, under-recognized, or not casually linked to DF including hepatitis and liver failure [ 3 ], myositis [ 4 ], and encephalitis and other neurological manifestations [ 5 ].
We report a case of a middle-age woman with diabetes and dyslipidemia who presented late to our hospital while peaking in the leaking phase of DHF. Her DHF was complicated with massive liver necrosis, acute renal failure with anuria and gross volume overload, and secondary sepsis. After an extensive literature search we believe that this case is the first who survived this sort of complicated DF. We would like to discuss the management principles that we employed in this success story.
Liver dysfunction is a well-recognized feature in both DF and DHF. Liver involvement in dengue infection could be suspected in patients with DF complaining of abdominal pain, nausea, vomiting, and anorexia [ 6 ]. Hepatomegaly is present in both DF and DHF but more common in DF [ 7 ]. Clinical jaundice has been detected in 1.7–17% of cases in various series [ 7 , 8 ]. A mild to moderate increase in the transaminases is common in DF and DHF, and AST was higher than ALT [ 9 , 10 , 11 ]. The AST released from damaged striated muscle, cardiac muscle, and erythrocytes could explain the levels of AST that are higher than those of ALT in patients with DF at an earlier stage [ 12 , 13 ]. Therefore, a rise in AST might not be a true reflection of hepatic involvement. The pathogenesis of liver injury in dengue infection is yet to be fully elucidated. Possible hypotheses include direct effects of the virus or host immune response on liver cells, circulatory compromise, and metabolic acidosis and/or hypoxia caused by hypotension or localized vascular leakage inside the liver [ 14 ]. Studies have shown that DENV readily infects the liver cells in mouse models [ 15 ]. High levels of cytokines particularly interleukin-22 (IL-22) and interleukin-17 (IL-17) were found in mouse models which may be responsible for the cytokine-induced liver damage [ 16 ]. Sung et al. observed the infiltration of hepatocytes with natural killer cells followed by T cells and this was found to be associated with the apoptosis of hepatocytes [ 17 ].
Histopathological studies of postmortem specimens of patients who had a fatal outcome have shown that the liver is congested with liver cell necrosis and apoptosis, predominantly in midzonal and centrilobular areas, macrovascular steatosis, and Councilman bodies. Many postmortem reports show little or no inflammation [ 18 , 19 ]. It is interesting that similar centrilobular necrosis is a typical finding in hypoxic hepatitis [ 20 ]. Considering the fact that a severe form of liver necrosis is seen among the patients with DHF who present late with prolonged shock, we can postulate the fact that hypoxic injury due to reduced hepatic perfusion is probably an important contributor to the causation of liver damage. By contrast, few cases of fulminant liver failure have been reported in the absence of shock [ 3 ]. Khongphatthanayothin et al. reported an interesting case of liver failure from DENV infection with reversal of portal venous blood flow [ 21 ]. They postulated that hepatic sinusoidal obstruction coupled with shock might have been the underlying mechanism of liver failure in this disease [ 21 ].
Our patient presented at the peak of the leaking phase and collapsed on admission with cold and clammy peripheries. She had very high transaminases with deranged clotting and venous blood gas showing elevated lactate levels. Her liver involvement could be multifactorial including direct viral damage, immunological damage, hypoxia due to dehydration, and intravascular volume depletion due to leaking. It was further exacerbated by ongoing gastrointestinal and per vaginal bleeding. We aggressively resuscitated with crystalloids followed up by colloids. We considered transfusion of packed cells to maintain PCV around 40% to maintain adequate oxygenation to her liver.
She was started on intravenous NAC infusion at a rate of 100 mg/hour. NAC scavenges free radicals, improves antioxidant defense, and acts as a vasodilator to improve oxygen delivery and consumption [ 22 ]. However, limited data are available in the literature regarding the efficacy of NAC in DF-related liver dysfunction. A retrospective analysis on NAC in dengue-associated liver failure by Kumarasena et al . showed that five patients who survived out of eight were in early (coma grade 1, 11) liver failure stage at the time when NAC was started [ 23 ]. Habaragamuwa and Dissanayaka reported another case of hepatitis following dengue treated with NAC with success [ 24 ]. Large randomized trials should be carried out to establish its efficacy along with appropriate dosage, timing, and duration of treatment. We decided to continue NAC until our patient’s liver enzymes were less than 500 U/L.
Lactic acidosis resulting from excess accumulation of lactate and protons is associated with increased mortality and poor clinical outcome [ 25 ]. Hyperlactatemia occurs when lactate production exceeds lactate consumption. In tissue hypoxia lactate is overproduced as a result of decreased mitochondrial oxidation [ 26 ] that could be either due to generalized hypoxia or microcirculatory dysfunction [ 27 , 28 ]. Coexisting acidosis might further reduce the renal excretion of lactate. At the hyperdynamic stage of sepsis or shock, epinephrine-dependent stimulation of the β 2 -adrenoceptor augments the glycolytic flux both directly and through enhancement of the sarcolemmal Na + , K + -ATPase which lead to overproduction of lactate [ 29 ]. The liver accounts for up to 70% of whole-body lactate clearance [ 30 ]. Hyperlactatemia is common in acute fulminant liver disease, reflecting both reduced clearance and increased production of lactate by the liver [ 31 ]. Metformin interferes with oxidative phosphorylation and suppresses hepatic gluconeogenesis which can lead to hyperlactatemia in rare cases [ 32 ].
The lactic acidosis that developed in our patient could be multifactorial. She had poorly controlled diabetes and was on the maximum dose of metformin, she presented in severe shock due to plasma leakage and dehydration, and developed acute liver failure and renal failure. All these events could have contributed to her hyperlactatemia. High lactate levels will further suppress myocardial contractility and worsen the acidosis which will act as a vicious cycle deteriorating physiology.
The management strategies employed in this patient were:
Aggressive resuscitation with fluids during the initial shock including crystalloids and colloids.
Use of packed cells to maintain PCV around 40% to improve oxygen carrying capacity.
Supplementary oxygen to the patient during shock.
Use of CVVHD employed as a form of renal replacement therapy to remove lactate from the body and correct the acidosis.
Patients with DHF develop selective plasma leakage manifested as accumulation of fluid in pleural and abdominal cavities and hemoconcentration. The leakage is assumed to last approximately 48 hours and is followed by a spontaneous and rapid resolution but has wide individual variations [ 33 ]. Increased vascular permeability is mediated by an interplay between DENV, immune cells and endothelial cells with adhesion molecules, enzymes and cytokines according to the current evidence [ 33 ]. Very limited information is available in the literature regarding the rate and duration of plasma leak and about reabsorption of fluid in the pleura and peritoneal cavities during recovery. Understanding the trends in fluid leakage and reabsorption of dengue has been hampered by a lack of animal models.
During recovery from DHF, extravasated fluid will be reabsorbed and a functioning kidney would filter the extra volumes of fluid and the patient will be polyuric. Our patient’s clinical course was complicated by acute renal failure, which was probably the result of acute tubular necrosis due to her late presentation with prolonged shock. She was anuric in the initial days of recovery. She was given 5500 ml of fluid during the presumed leaking phase of DHF and she had bilateral moderate to severe pleural effusions and gross ascites. We hypothesized that if she reabsorbed this excess fluid in the third space into the intravascular compartment with non-functioning renal tissue to filter it out, she would soon be intravascularly expanded which would lead to acute left ventricular failure and pulmonary edema. So we decided to have a renal replacement method prophylactically anticipating the reabsorption of fluid in the cavities. CVVHD was selected as the method of renal replacement therapy as it can be used continuously for a longer period, with less effect on the hemodynamics as opposed to intermittent hemodialysis.
What is the guide to assess the rate and volume of fluid reabsorption into the intravascular compartment?
We decided to make serial measurements of
IVC diameter and collapsibility
IJV diameter and collapsibility
Diastolic blood pressure (DBP)
CVP and DBP were considered as hard measurements, whereas IJV and ICV diameters and collapsibility had intra-operator and inter-operator variability. Ultrafiltration of the CVVHD was titrated according to the above measurements. Interesting observations were made during this period.
Our patient’s CVP gradually increased reflecting reabsorption of fluid into the vascular compartment and we gradually increased the ultrafiltration starting from a figure of 60 ml/hour. CVP peaked in the 95th hour of CVVHD and ultrafiltration was increased in an exponential manner up to 280 ml/hour. CVP was maintained at the peak for 4 hours and a dramatic decline was noted in the central pressures indicating termination of fluid reabsorption. Over the next 24 hours CVP dropped from 24 cm H 2 O to 1 cm H 2 O and ultrafiltration was brought down to zero rapidly and CVVHD terminated. During the period of dialysis she was maintained on orally administered fluids at 50 ml per hour and she was anuric on initial 3 days of CVVHD and gradually improved over time. Total ultrafiltration removed 18.5 L over a period of 138 hours. She would not have survived the exponential rise in intravascular volume during reabsorption with poor renal function. The key for survival was the timely arrangement of renal replacement therapy.
Fluid dynamics during reabsorption has never been described before in DHF. In the index patient reabsorption took a longer period than is described in a timeframe of 48 hours in the literature and it occurred in an exponential pattern, plateaued, and abruptly ceased.
Management of a patient with DHF complicated with acute liver failure, lactic acidosis, and acute kidney injury is challenging. Although conclusions cannot be drawn from a single case report we emphasize importance of the following management strategies.
Use of NAC in hepatic dysfunction in dengue illness.
Increasing PCV by transfusing blood to increase the oxygen-carrying capacity even in the absence of a compelling indication for a transfusion in the “standard care.”
Lactate level to be used as a prognostic marker and as a tool to guide treatment.
Use of CVVHD in those with acute renal impairment and DHF during the recovery phase to maintain intravascular volume without leading to heart failure and pulmonary edema.
Large randomized trials should be carried out to establish the efficacy of these treatment strategies to support the above observations and change current practice.
We believe that the fluid dynamics we have observed in the index case need to be tested in a proposed animal model and it will open up new research areas and will generate new knowledge in the management of DF.
Halstead SB. Dengue. Curr Opin Infect Dis. 2002;15(5):471–6.
Article PubMed Google Scholar
Wilder-Smith A, Schwartz E. Dengue in travelers. N Engl J Med. 2005;353:924–32.
Article PubMed CAS Google Scholar
Trung DT, Thao LTT, Hien TT, et al . Liver involvement associated with dengue infection in adults in Vietnam. Am J Tropical Med Hyg. 2010;83(4):774–80. https://doi.org/10.4269/ajtmh.2010.10-0090 .
Article Google Scholar
Dalugama C, Ralapanawa U, Jayalath T. Dengue myositis and review of literature. Clin Cas Repo Rese Trials. 2017;2:16–8.
Google Scholar
Koley TK, Jain S, Sharma H, et al . Dengue encephalitis. J Assoc Physicians India. 2003;51:422–3.
PubMed CAS Google Scholar
Karoli R, Fatima J, Siddiqi Z, Kazmi KI, Sultania AR. Clinical profile of dengue infection at a teaching hospital in North India. J Infect Dev Ctries. 2012;6:551–4.
Saha AK, Maitra S, Hazra SC. Spectrum of hepatic dysfunction in 2012 dengue epidemic in Kolkata, West Bengal. Indian J Gastroenterol. 2013;32:400–3.
Trung DT, Thao le TT, Hien TT, Hung NT, Vinh NN, Hien PT, Chinh NT, Simmons C, Wills B. Liver involvement associated with dengue infection in adults in Vietnam. Am J Trop Med Hyg. 2010;83:774–80.
Article PubMed PubMed Central Google Scholar
Souza LJ, Alves JG, Nogueira RM, Gicovate Neto C, Bastos DA, Siqueira EW, Souto Filho JT, Cezario Tde A, Soares CE, Carneiro Rda C. Aminotransferase changes and acute hepatitis in patients with dengue fever: analysis of 1,585 cases. Braz J Infect Dis. 2004;8:156–63.
Kuo CH, Tai DI, Chang-Chien CS, Lan CK, Chiou SS, Liaw YF. Liver biochemical tests and dengue fever. Am J Trop Med Hyg. 1992;47:265–70. [PubMed]
Nguyen TL, Nguyen TH, Tieu NT. The impact of dengue haemorrhagic fever on liver function. Res Virol. 1997;148:273–7.
Nath P, Agrawal DK, Mehrotra RM. Ultrastructural changes in skeletal muscles in dengue virus-infected mice. J Pathol. 1982;136:301–5.
Lee LK, Gan VC, Lee VJ, Tan AS, Leo YS, Lye DC. Clinical relevance and discriminatory value of elevated liver aminotransferase levels for dengue severity. PLoS Negl Trop Dis. 2012;6:e1676.
Article PubMed PubMed Central CAS Google Scholar
Itha S, Kashyap R, Krishnani N, Saraswat VA, Choudhuri G, Aggarwal R. Profile of liver involvement in dengue virus infection. Natl Med J India. 2005;18:127–30.
PubMed Google Scholar
Cabrera-Hernandez A, Thepparit C, Suksanpaisan L, Smith DR. Dengue virus entry into liver (HepG2) cells is independent of hsp90 and hsp70. J Med Virol. 2007;79(4):386–92.
Guabiraba R, Besnard AG, Marques RE, Maillet I, Fagundes CT, Conceicao TM, Rust NM, Charreau S, Paris I, Lecron JC. IL-22 modulates IL-17A production and controls inflammation and tissue damage in experimental dengue infection. Eur J Immunol. 2013;43(6):1529–44.
Sung JM, Lee CK, Wu-Hsieh BA. Intrahepatic infiltrating NK and CD8 T cells cause liver cell death in different phases of dengue virus infection. PLoS One. 2012;7(9):e46292.
Martina BE, Koraka P, Osterhaus AD. Dengue virus pathogenesis: an integrated view. Clin Microbiol Rev. 2009;22(4):564–81.
Aye KS, Charngkaew K, Win N, Wai KZ, Moe K, Punyadee N, Thiemmeca S, Suttitheptumrong A, Sukpanichnant S, Prida M. Pathologic highlights of dengue hemorrhagic fever in 13 autopsy cases from Myanmar. Hum Pathol. 2014;45(6):1221–33.
Henrion J. Hypoxic hepatitis. Liver Int. 2012;32(7):1039–52.
Khongphatthanayothin A, Mahayosnond A, Poovorawan Y. Possible cause of liver failure in patient with dengue shock syndrome. Emerg Infect Dis. 2013;19(7):1161–3. https://doi.org/10.3201/eid1907.121820 .
Sklar GE, Subramaniam M. Acetylcysteine treatment for non-acetaminophen-induced acute liver failure. Ann Pharmacother. 2004;38:498–500.
Kumarasena RS, Mananjala Senanayake S, Sivaraman K, de Silva AP, Dassanayake AS, Premaratna R, et al . Intravenous N-acetylcysteine in dengue-associated acute liver failure. Hepatol Int. 2010;4:533–4.
Habaragamuwa BWP, Dissanayaka P. N-acetylcystein in dengue associated severe hepatitis. Indian J Crit Care Med. 2014;18(3):181–2. https://doi.org/10.4103/0972-5229.128712.
Nichol AD, Egi M, Pettila V, et al . Relative hyperlactatemia and hospital mortality in critically ill patients: a retrospective multi-Centre study. Crit Care. 2010;14:R25.
Madias NE. Lactic acidosis. Kidney Int. 1986;29:752–74.
Ince C. The microcirculation is the motor of sepsis. Crit Care. 2005;9(Suppl 4):S13–9.
Nimmannitya S, Thisyakorn U, Hemsrichart V. Dengue haemorrhagic fever with unusual manifestations. Southeast Asian J Trop Med Public Health. 1987;18:398–406.
Levy B, Desebbe O, Montemont C, Gibot S. Increased aerobic glycolysis through beta2 stimulation is a common mechanism involved in lactate formation during shock states. Shock. 2008;30:417–21.
Jeppesen JB, Mortensen C, Bendtsen F, Møller S. Lactate metabolism in chronic liver disease. Scand J Clin Lab Invest. 2013;73:293–9.
Murphy ND, Kodakat SK, Wendon JA, et al . Liver and intestinal lactate metabolism in patients with acute hepatic failure undergoing liver transplantation. Crit Care Med. 2001;29:2111–8.
Silvestre J, Carvalho S, Mendes V, et al . Metformin-induced lactic acidosis: a case series. J Med Case Rep. 2007;1:126. https://doi.org/10.1186/1752-1947-1-126 .
Srikiatkhachorn A. Plasma leakage in dengue hemorrhagic fever. Thromb Haemost. 2009;102(6):1042–9. https://doi.org/10.1160/TH09-03-0208 .
Download references
Acknowledgements
We acknowledge Prof. Vasanthi Pinto and the medical staff of Teaching Hospital, Peradeniya for the support given to us during the management of the patient.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and affiliations.
Department of Medicine, University of Peradeniya, Peradeniya, Sri Lanka
Chamara Dalugama & Indika Bandara Gawarammana
You can also search for this author in PubMed Google Scholar
Contributions
CD and IBG examined, assessed, and were involved in the management of the patient. Both authors collected data and analyzed. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Chamara Dalugama .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was not obtained for the publication of this case report as this does not involve sharing of the personal details of the patient.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Dalugama, C., Gawarammana, I.B. Lessons learnt from managing a case of dengue hemorrhagic fever complicated with acute liver failure and acute kidney injury: a case report. J Med Case Reports 12 , 215 (2018). https://doi.org/10.1186/s13256-018-1766-0
Download citation
Received : 08 November 2017
Accepted : 07 July 2018
Published : 08 August 2018
DOI : https://doi.org/10.1186/s13256-018-1766-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dengue hemorrhagic fever
- Liver failure
- Acute kidney injury
- N-acetyl cysteine
- Packed cell transfusion
- Continuous veno-venous hemodialysis (CVVHD)
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Case report
- Open access
- Published: 26 August 2020
A case report of dengue hemorrhagic fever complicated with diabetic ketoacidosis in a child: challenges in clinical management
- V. Thadchanamoorthy 1 &
- Kavinda Dayasiri 2
BMC Pediatrics volume 20 , Article number: 403 ( 2020 ) Cite this article
3470 Accesses
4 Citations
Metrics details
Diabetic ketoacidosis (DKA) is a common presentation of type 1 diabetes mellitus (T1DM) precipitated by various bacterial and viral infections. Dengue infection is no exception for this and can be a precipitating factor for DKA. The presentation of DKA with dengue haemorrhagic fever (DHF) has been reported in adults. However, it is very rarely observed in children.
Case presentation
We present the case of a paediatric patient who was previously healthy and subsequently, developed polyuria (above 3 ml/kg/hour), irritability and high blood glucose (724 mg/dl) during the critical phase of DHF. DKA was diagnosed with DHF and managed successfully with insulin and intravenous fluids. He recovered without complications and discharged home with follow up being arranged at the endocrinology clinic.
Conclusions
When both DHF and DKA present together in a patient, meticulous monitoring of glycaemic control as well as fluid management is required to reduce the potential risk for severe complications of both conditions. Since there are no similar paediatric case reported in the literature, this case report might inspire paediatricians to anticipate the possibility of DKA in children with DHF.
Peer Review reports
Dengue has a wide spectrum of clinical manifestations which may be mild to severe and can be severe enough to cause death due to dengue shock syndrome. Worldwide estimates suggest that annual incidence of dengue fever and DHF has been 100 million and 500,000 respectively. Ninety percent of DHF cases are children under 15 years old [ 1 , 2 ]. Dengue fever similar to other viral infections is known to precipitate diabetic ketoacidosis in patients with diabetes. Both insulin dependent and independent diabetes can increase the release of pro-inflammatory cytokines and intensify the risk of plasma leakage in dengue fever. Acute pancreatitis is a rare complication of severe dengue infection, which could be a contributory factor for diabetic ketoacidosis. The clear understanding of the comorbidity and mortality between the two diseases is vital in patient management during acute illness.
There is only limited research evidence with regard to actual fluid requirement during critical phase of dengue haemorrhagic fever as plasma leakage is dynamic and can occur at different rates across the critical phase [ 3 ]. Therefore, current practice of fluid management in DHF depends, to a greater extent, on expertise of the managing clinicians and a number of assumptions regarding evolution of plasma leakage. Urine output is considered as a reliable indicator of haemodynamic stability in patients with DHF and maintaining urine output between 0.5–1 ml/kg/hour is considered appropriate to prevent both shock and fluid overload that carry high risk of mortality. However, it is crucial that clinicians are mindful of potential confounding factors such as hyperglycemia. As a patient with dengue fever presents with hyperglycemia, urine output becomes an unreliable indicator of haemodynamic status and patient might have polyuria even during shock [ 4 ]. We report a child who was initially admitted for dengue fever and subsequently developed DHF associated with polyuria and irritability needing more fluids to maintain vital signs during the critical period of DHF. He was ultimately diagnosed as having type − 1 diabetes mellitus associated diabetic ketoacidosis with DHF. The report enlightens the importance of consideration of differential causes for surprisingly high urine output in patients with DHF associated shock and clinical decision making based on meticulous overall haemodynamic assessments. Management of this patient would be a thought-provoking and challenging task for clinicians and their teams.
A 13-year-old previously healthy boy was admitted with fever, generalized body ache, headache, cough and mild diarrhea for 4 days and abdominal pain and vomiting for 2 days. His urine output was satisfactory. Dengue NSI antigen done on day 3 febrile illness was positive. He had no history of thirst, weight loss, and increased frequency of urination. On examination he was febrile (99.5F), ill looking, and flushed but was rational and heamodyanamically stable. Blood pressure had been 100/70 mmHg with pulse pressure of 30 mmHg. Pulse was of good volume and rate had been 155 / minute. His Complete Blood Count showed leukopenia (WBC- 1.5 × 10 3 / cumm), and thrombocytopenia (platelet count - 100 × 10 3 /cumm). Haemoglobin was 13 g/dL, and haematocrit was 38. Random blood glucose on admission was 104 mg/dl. Abdominal examination showed 3 cm hepatomegaly and there was no clinical evidence of pleural effusion. He was provisionally diagnosed as having DHF and haemodynamic monitoring was commenced while he was on oral rehydration fluids at rate of 75 ml per hour. The child tolerated oral rehydration fluids well and did not need intravenous fluids including dextrose solutions.
On day five, he started to deteriorate with low volume pulse, tachycardia (rate of more than 180/min), cold clammy extremities and narrow pulse pressures whilst on intravenous 0.9% saline (4 ml/kg/hour) and oral fluids (1 ml/kg/hour). Clinical examination of lungs showed slight reduction of air entry on right side with vesicular breathing and no added sounds were heard. However, his urine output remained surprisingly satisfactory (more than1.5 mL/kg/hour). In addition, he became more irritable, thirsty, tachypnoic and had severe generalized abdominal tenderness whilst on two units of 0.9% saline 10 mL/kg boluses followed by 5 mL/kg/hour infusions. He continuously had disproportionately increased urine output (more than 2 mL/kg/hour) and pulse pressure varied between 15 to 20 mmHg. His Complete Blood Count showed WBC - 4.5 × 10 3 (N − 60 %, L-34%), haemoglobin - 16 g/dL, platelets - 60x10 3 mm/l, and haematocrit - 48. C-reactive protein (CRP) was elevated (12 mg/dl). Renal functions (Na- 140 mmol/L, K-4.3 mmol/L, serum creatinine 0.9 mg/dl) were normal apart from raised blood urea (60 mg/dL). Liver functions were deranged (Alanine transaminase − 240 IU/L, Aspartate transaminase-546 IU/L). Serum amylase was normal (44 U/L) Chest X-ray was normal apart from mild haziness all over the lungs. Ultrasound revealed mild ascites and bilateral pleural effusions. Capillary blood glucose was 724 mg/dl. He was transferred from local hospital to intensive care unit (ICU), in the tertiary care hospital for further management of diabetic ketoacidosis co-occurring with DHF. As he had high fever with unstable haemodynamic parameters and CRP was elevated, he was commenced broad spectrum empirical intravenous antibiotics. However, antibiotics were stopped following negative blood cultures.
In ICU, he had moderate to severe metabolic acidosis with arterial blood gas showing pH -7.17, pCO2-23 mmHg, pO2- 75 mmHg, HCO3- 12mmo/l and base excess-(− 14). Urine ketone bodies were positive. Blood ketones were not performed due to unavailability of this investigation in the hospital. He was resuscitated with dextran 40 with the dose of 10 ml/ kg once. Then he was started 0.9% saline with soluble insulin infusion at 0.1 u/kg/hour and blood glucose was monitored hourly until glucose levels dropped between 200 and 328 mg/dl. Intravenous fluid (0.9%saline) was adjusted between 5 and 7 ml/kg/h depending on the vital signs. We did not administer intravenous dextrose as it might have worsened hypovolaemia by the ongoing plasma leakage, producing more hydrostatic pressure and also producing osmotic diuresis. Instead child was advised to take foods which contained complex carbohydrate. Fluids were adjusted hourly according to pulse pressure which was more than minimum 20 mmHg and capillary refilling time was maintained below 2 s. The management was not guided both by urine output which had been more than expected and pulse rate due to presence of high fever. In addition, potassium was added to fluids as serum electrolyte revealed Na-140 mmol/L, and K-3.0 mmol/L while on insulin. As he improved after 24 h of critical period, his fluids and insulin were reduced to half. He was not commenced intravenous bicarbonate as repeat arterial blood gas showed improved findings (pH 7.32, PCO2-30 mmHg, PO2-80 mmHg, HCO2–18, Base excess (− 8)) following correction of dehydration and glucose with insulin. The lowest platelet count was 12x10 3 and renal function had been within normal range on the day 6 of illness. Intravenous Insulin was changed to subcutaneous insulin after 48 h of critical period and urine ketone bodies were noted to be negative.
After 72 h of ICU care, he was transferred to medical ward where he was continued on subcutaneously insulin and food according to dietician’s advice. Blood glucose, urine ketone body, renal functions, liver functions and hematological parameters were repeated until they were normalized. His HbA1C was 5.1% and Glutamic acid decarboxylase autoantibody had been positive (22 IU/L). Other type 1 diabetes related autoantibodies could not be performed due to limited financial resources in patient’s family. Both IgM and IgG dengue antibodies were positive on day 7 and dengue infection was notified to infection control team of the local hospital. Intravenous antibiotic was discontinued after 5 days with normal CRP. He was discharged after 2 weeks of hospital stay with the postprandial blood sugar being 146 mg/dl and fasting blood sugar being 100 mg/dl. Follow up was arranged at the endocrinology clinic. He was reviewed after 6 months and 1 year in the paediatric clinic and found to have been in good health and HbA1C was within normal range (5.3–5.5%). He is currently on insulin pump therapy under the care of paediatrician, paediatric endocrinologist and dietician. His growth and school performance had been within normal limits at one-year follow up.
Discussion and conclusions
We report the case of this young boy who was initially admitted with dengue fever but subsequently developed DKA during the critical period of DHF. The rarity of this co-incidence in the paediatric age group and unexpected challenges in management of this child might inspire paediatricians. Altered haemostasis and plasma leakage have been two important pathophysiological mechanisms in DHF. Vascular leakage is caused by a transient increase in vascular permeability due to endothelial dysfunction and subsequent occurrence of haemoconcentration. The elevation of hematocrit greater than 20% is typically used as a cut-off to define the presence of leakage in dengue [ 5 ]. In patients with vascular leakage, excess intravenous fluid therapy can aggravate fluid accumulation and precipitates respiratory distress while substandard fluid treatment can cause shock. The osmotic diuresis in DKA results in large volume depletion. Typical total body water deficit among patients with DKA is 100 mL/kg of body weight, and the deficit becomes even higher with fluid loss in the phase of fluid leakage in DHF. Therefore, continuous monitoring and careful use of intravenous fluids are crucial in the management of patients with both DHF and DKA. The initial fluid therapy would be isotonic solutions to maintain satisfactory tissue perfusion and urine output should be at least 0.5 mL/kg/hour whilst insulin infusion is running. Intravenous fluids can be reduced gradually when plasma leakage decreases towards the end of the critical period which is usually signposted by an increase in urine output or decrease in hematocrit [ 6 ]. The reported child developed DKA during the critical period of DHF. We followed combined national and international guidelines for management of DKA and DHF. We managed the child with isotonic fluids and dextran 40 to restore the hypovolaemia. In addition, we were also guided by previous reports of dengue presenting with diabetes in adults [ 4 , 7 ] as we could not find any reported cases in children. Literature reported in adults had been mainly dengue infection diagnosed in patients with insulin independent diabetes mellitus (type 2).
DHF was considered as a trigger factor for DKA in this patient who had previously undiagnosed diabetes mellitus. There were few case reports of dengue triggering diabetic ketoacidosis [ 4 , 7 , 8 ]. Supradish et al. reported the case of a 16-year-old Thai girl who presented in dengue shock showing signs of severe dehydration and ascites [ 7 ] and one other review article reported that those who had diabetes were two and half times as likely to have dengue hemorrhagic fever [ 9 ] The physiopathology of dengue hemorrhagic fever leads to amplification of the immune response following presence of heterotypic antibodies against a serotype of the dengue virus at the time of new infection [ 10 ]. Thus Type 1 diabetes mellitus is commonly associated with autoimmunity and the immune system may be persistently activated with signs of inflammation in tissues and capillaries, and is more likely to lead to inflammation and liberation of pro-inflammatory cytokines in tissues, particularly in the endothelium, explaining the higher risk of plasma leak in dengue fever [ 11 ].
Although ideal total body water deficit is 100 mL/kg in children with severe DKA, the actual deficit increases more than ideal deficit in the presence of fluid leakage. Both DHF related shock and fluid deficit due to DKA were managed in this patient with 0.9% saline with frequent monitoring of blood glucose, blood gases and haemodynamic parameters including pulse rate, and pulse pressure. Fluid intake was adjusted to keep urine output at least 0.5 mL/kg/hour and pulse pressure at least 20 mmHg. Early recognition of DKA and DHF are crucial in preventing complications related to both conditions.
The reported patient had hypovolaemia with surprisingly high urine output during the critical phase of DHF due to concurrent DKA. This situation in critical phase of DHF made fluid management more difficult even with central venous pressure monitoring. Fluids were adjusted every hour with insulin dose until the child reached recovery phase with meticulous blood glucose monitoring. As the reported child tolerated food well, cooperated with the management and was conscious throughout the critical period, he made a rapid and complete recovery of both complications without needing invasive monitoring. Meticulous non-invasive monitoring in the intensive care needed more human resources and added more mental stress to clinicians and their team who treated this child.
We further could not use any invasive monitoring to adjust the fluid management as his platelet had been low although invasive monitoring was available in the tertiary care hospital. This was another challenge the clinicians faced during fluid management as he had a high chance of internal bleeding while inserting the central cannulas. Fortunately, the child did not have bleeding at any time of illness and non-invasive monitoring sufficed. As this patient was admitted to local hospital where patient had been managed with limited facilities including human resources, timely diagnosis of coexisting diabetic mellitus was a challenge in the management of this child and possibly contributed for a delay in transfer to the intensive care unit. However, the diagnosis of diabetic ketoacidosis was made without much delay, and the child improved without developing any unacceptable complications. The authors recommend that urine output should be carefully reviewed in all patients with DHF on individual basis and differential causes for discordant urine output should be identified and managed without delay to prevent complications.
Dengue can rarely present with various atypical endocrinological manifestations in children. Every clinician must anticipate DKA in children with disproportionately high urine output during dengue infection even though it is rare in children. Scrupulous and frequent monitoring is an important step in identifying co-morbidities and treating these children. We were channeled with contradicting findings of urine output and vital parameters to make the diagnosis successfully.
Availability of data and materials
The data that support the findings of this case report are available from Medical Records Department, Batticaloa Teaching Hospital, but restrictions apply to the availability of these data, which were used under license for the current report and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of Medical Records Department, Batticaloa Teaching Hospital, Sri Lanka.
Abbreviations
Dengue haemorrhagic fever
Diabetic ketoacidosis
Alanine transaminase
Aspartate transaminase
Haemoglobin A 1C
Intensive Care Unit
Malavige GN, Fernando S, Fernando DJ, Seneviratne SL. Review Dengue viral infections. Postgrad Med J. 2004;80:588–601. https://doi.org/10.1136/pgmj.2004.019638 .
Article CAS PubMed PubMed Central Google Scholar
Kularatne SA. Dengue fever. BMJ. 2015;351:h4661. https://doi.org/10.1136/bmj.h4661 .
Article CAS PubMed Google Scholar
Kularatne SA, Weerakoon KG, Munasinghe R, Ralapanawa UK, Pathirage M. Trends of fluid requirement in dengue fever and dengue haemorrhagic fever: a single centre experience in Sri Lanka. BMC Res Notes. 2015;8:130. Published 2015 Apr 8. https://doi.org/10.1186/s13104-015-1085-0 .
Article PubMed PubMed Central Google Scholar
Dalugama C, Gawarammana IB. Dengue hemorrhagic fever complicated with transient diabetic ketoacidosis: a case report. J Med Case Rep. 2017;11(1):302. Published 2017 Oct 28. https://doi.org/10.1186/s13256-017-1476-z .
Srikiatkhachorn A, Spiropoulou CF. Vascular events in viral hemorrhagic fevers: a comparative study of dengue and hantaviruses. Cell Tissue Res. 2014;355:621–33. https://doi.org/10.1007/s00441-014-1841-9 .
World Health Organization. WHO Guidelines Approved by the Guidelines Review Committee. In: Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control: New Edition. Geneva: WHO Press; 2009. p. 1–144.
Google Scholar
Supradish PO, Rienmanee N, Fuengfoo A, Kalayanarooj S. Dengue hemorrhagic fever grade III with diabetic ketoacidosis: a case report. J Med Assoc Thail. 2011;94:0–40.
Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crises in adult patients with diabetes. A consensus statement from the American Diabetes Association. Diabetes Care. 2006;29:2739–48. https://doi.org/10.2337/dc06-9916 .
Figueiredo MA, Rodrigues LC, Barreto ML, et al. Allergies and diabetes as risk factors for dengue hemorrhagic fever: results of a case control study. PLoS Negl Trop Dis. 2010;4(6):e699. Published 2010 Jun 1. https://doi.org/10.1371/journal.pntd.0000699 .
Halstead SB. The pathogenesis of dengue: molecular epidemiology in infections disease. Am J Epidemiol. 1981;114(5):632–48. https://doi.org/10.1093/oxfordjournals.aje.a113235 .
Brown JM, Wilson TM, Metcalfe DD. The mast cell and allergic diseases: role in pathogenesis and implications for therapy. Clin Exp Allergy. 2008;38(1):4–18. https://doi.org/10.1111/j.1365-2222.1997.tb00665.x .
Download references
Acknowledgements
We would like to thank Dr. K. Dharshini, Consultant Endocrinologist, and Dr. N. Yogananth, Consultant Anaesthetist.
No funding was received.
Author information
Authors and affiliations.
Faculty of Health Care Sciences, Eastern University, Batticaloa, Sri Lanka
V. Thadchanamoorthy
Base Hospital, Mahaoya, Sri Lanka
Kavinda Dayasiri
You can also search for this author in PubMed Google Scholar
Contributions
VT led clinical management of the patient and wrote manuscript. KD performed literature survey, wrote and edited the manuscript. Both authors read and approved final version of the manuscript.
Corresponding author
Correspondence to Kavinda Dayasiri .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Written informed consent was obtained from patient’s legal guardian for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Thadchanamoorthy, V., Dayasiri, K. A case report of dengue hemorrhagic fever complicated with diabetic ketoacidosis in a child: challenges in clinical management. BMC Pediatr 20 , 403 (2020). https://doi.org/10.1186/s12887-020-02300-9
Download citation
Received : 28 April 2020
Accepted : 17 August 2020
Published : 26 August 2020
DOI : https://doi.org/10.1186/s12887-020-02300-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Fluid therapy
BMC Pediatrics
ISSN: 1471-2431
- Submission enquiries: [email protected]
- General enquiries: [email protected]


Clinical Presentation
- Dengue can range from asymptomatic infection or mild illness to severe disease.
- An estimated 1 in 4 dengue virus infections are symptomatic. Symptomatic dengue virus infection most commonly presents as a mild to moderate, nonspecific, acute febrile illness.
- Infection with one of the four dengue viruses will induce long-lived immunity for that specific virus.
- Because there are four dengue viruses, people can be infected with DENV multiple times in their life.
- The second infection with DENV is a risk factor for severe dengue.
- Early clinical findings are nonspecific but require a high index of suspicion because recognizing early signs of shock and promptly initiating intensive supportive therapy can reduce risk of death among patients with severe dengue to <0.5%.
- See Box 3-01 for information regarding the World Health Organization (WHO) guidelines for classifying dengue.
In November 2009, WHO issued a new guideline that classifies symptomatic cases as dengue or severe dengue.
Dengue is defined by a combination of ≥2 clinical findings in a febrile person who traveled to or lives in a dengue-endemic area. Clinical findings include nausea, vomiting, rash, aches and pains, a positive tourniquet test, leukopenia, and the following warning signs: abdominal pain or tenderness, persistent vomiting, clinical fluid accumulation, mucosal bleeding, lethargy, restlessness, and liver enlargement. The presence of a warning sign may predict severe dengue in a patient.
Severe dengue is defined by dengue with any of the following symptoms: severe plasma leakage leading to shock or fluid accumulation with respiratory distress; severe bleeding; or severe organ impairment such as elevated transaminases ≥1,000 IU/L, impaired consciousness, or heart impairment.
From 1975 through 2009, symptomatic dengue virus infections were classified according to the WHO guidelines as dengue fever, dengue hemorrhagic fever (DHF), and dengue shock syndrome (the most severe form of DHF). The case definition was changed to the 2009 clinical classification after reports that the case definition of DHF was both too difficult to apply in resource-limited settings and too specific, as it failed to identify a substantial proportion of severe dengue cases, including cases of hepatic failure and encephalitis. The 2009 clinical classification has been criticized for being overly inclusive, as it allows several different ways to qualify for severe dengue, and nonspecific warning signs are used as diagnostic criteria for dengue. Lastly, the new guidelines have been criticized because they do not define the clinical criteria for establishing severe dengue (with the exception of providing laboratory cutoff values for transaminase levels), thereby leaving severity determination up to individual clinical judgment.
Dengue begins abruptly after a typical incubation period of 5–7 days, and the course follows 3 phases: febrile, critical, and convalescent.
Febrile Phase
- Fever typically lasts 2–7 days and can be biphasic.
- Other signs and symptoms may include severe headache; retro-orbital eye pain; muscle, joint, and bone pain; macular or maculopapular rash; and minor hemorrhagic manifestations including petechia, ecchymosis, purpura, epistaxis, bleeding gums, hematuria, or a positive tourniquet test result.
- Some patients have injected oropharynx and facial erythema in the first 24–48 hours after onset.

Warning Signs
Warning signs of progression to severe dengue occur in the late febrile phase around the time of defervescence, and include persistent vomiting, severe abdominal pain, fluid accumulation, mucosal bleeding, difficulty breathing, lethargy/restlessness, postural hypotension, liver enlargement, and progressive increase in hematocrit (i.e., hemoconcentration).
Critical Phase
- The critical phase of dengue begins at defervescence and typically lasts 24–48 hours.
- Most patients clinically improve during this phase, but those with substantial plasma leakage can, within a few hours, develop severe dengue as a result of a marked increase in vascular permeability.
- Initially, physiologic compensatory mechanisms maintain adequate circulation, which narrows pulse pressure as diastolic blood pressure increases.
- Patients with severe plasma leakage may have pleural effusions, ascites, hypoproteinemia, or hemoconcentration.
- Patients may appear to be well despite early signs of shock. However, once hypotension develops, systolic blood pressure rapidly declines, and irreversible shock and death may ensue despite resuscitation.
- Patients can also develop severe hemorrhagic manifestations, including hematemesis, bloody stool, or menorrhagia, especially if they have been in prolonged shock. Uncommon manifestations include hepatitis, myocarditis, pancreatitis, and encephalitis.
Convalescent Phase
- As plasma leakage subsides, the patient enters the convalescent phase and begins to reabsorb extravasated intravenous fluids and pleural and abdominal effusions.
- As a patient’s well-being improves, hemodynamic status stabilizes (although he or she may manifest bradycardia), and diuresis ensues. The patient’s hematocrit stabilizes or may fall because of the dilutional effect of the reabsorbed fluid, and the white cell count usually starts to rise, followed by a recovery of platelet count.
- The convalescent-phase rash may desquamate and be pruritic.
Laboratory findings commonly include leukopenia, thrombocytopenia, hyponatremia, elevated aspartate aminotransferase and alanine aminotransferase, and a normal erythrocyte sedimentation rate.
Dengue During Pregnancy
- Data are limited on health outcomes of dengue in pregnancy and effects of maternal infection on the developing fetus.
- Perinatal transmission can occur, and peripartum maternal infection may increase the likelihood of symptomatic infection in the newborn.
- Of 41 perinatal transmission cases described in the literature, all developed thrombocytopenia, most had evidence of plasma leakage evidenced by ascites or pleural effusions, and fever was absent in only two cases. Nearly 40% had a hemorrhagic manifestation, and 1 in 4 had hypotension.
- Perinatally infected neonates typically become ill during the first week of life.
- Placental transfer of maternal IgG against dengue virus (from a previous maternal infection) may increase risk for severe dengue among infants infected at 6–12 months of age, when the protective effect of these antibodies wanes.
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Research article
- Open access
- Published: 20 September 2021
A study on knowledge, attitudes and practices regarding dengue fever, its prevention and management among dengue patients presenting to a tertiary care hospital in Sri Lanka
- K. P. Jayawickreme ORCID: orcid.org/0000-0001-9503-2854 1 ,
- D. K. Jayaweera 1 ,
- S. Weerasinghe 1 ,
- D. Warapitiya 1 &
- S. Subasinghe 1
BMC Infectious Diseases volume 21 , Article number: 981 ( 2021 ) Cite this article
17k Accesses
6 Citations
1 Altmetric
Metrics details
The World Health Organization (WHO) has ranked dengue as one of the top ten threats to Global health in 2019. Sri Lanka faced a massive dengue epidemic in 2017, the largest outbreak in the country during the last three decades, consisting of 186,101 reported cases, and over 320 deaths. The epidemic was controlled by intense measures taken by the health sector. However, the reported dengue cases and dengue deaths in 2019 were significantly higher than that of 2018. Deaths were mostly due to delay in hospitalization of severe dengue patients. The mortality of dengue hemorrhagic fever is 2–5% if detected early and treated promptly, but is high as 20% if left untreated.
A descriptive cross-sectional study was done among patients with dengue fever presenting to the Sri Jayawardenepura General Hospital during October 2019. Data was collected using a questionnaire comprising 20 questions based on knowledge, attitudes and practices on dengue, which were categorized into questions on awareness of mortality and severity of dengue burden, prevention of dengue vector mosquito breeding and acquiring the infection, patient’s role in dengue management, and warning signs requiring prompt hospitalization.
The mean KAP score on all questions was 55%, while a majority of 65.2% patients scored moderate KAP scores (50–75%) on all questions, and only 7.6% had high KAP scores (> 75%). The highest categorical mean score of 62% was on awareness of dengue prevention, followed by 54% on awareness of dengue burden, and only 51% on dengue management. Only 5.3% patients scored high scores on awareness of dengue management, followed by 28.5%, and 40.9% patients scoring high scores on awareness of dengue burden, and awareness of prevention of dengue respectively. The mean KAP scores on all questions increased with increasing age category.
The population relatively has a better awareness of dengue prevention, as compared to awareness of dengue mortality and dengue management. The identified weak point is patient awareness of the patients’ role in dengue management, and identifying warning signs requiring prompt hospitalization. This results in delay in treatment, which is a major cause for increased mortality. There was a correlation between those who had good knowledge on dengue burden and those who were aware of patients’ role in dengue management. An action plan should be implemented to improve public awareness through education programs on the role of the public and patients in dengue management to drive a better outcome.
Peer Review reports
The World Health Organization (WHO) has ranked dengue as one of the top ten threats to Global health in 2019 [ 1 ]. Brady et al. estimates a 3.9 billion prevalence of people, accounting to 40%-50% of the world’s population being at risk of infection. 128 countries worldwide are at risk of dengue infection, of which 70% of the global burden being in Asia [ 2 , 3 ]. The reported dengue cases to WHO increased from < 0.5 million in 2000 to > 3.34 million in 2016, characterized by a worldwide outbreak [ 4 ]. Although the world-wide numbers declined in 2017, there was a significant rise again in 2019 with 4.3 million cases worldwide. The highest number of dengue cases worldwide in 2019 in descending order were reported in Brazil, Philippines, Vietnam, Mexico, Nicaragua, Malaysia and India respectively, with Sri Lanka being placed in the 8th place worldwide, and in the 5th place in Asia [ 5 ]. Following a steady rise in annual dengue cases, Sri Lanka faced a massive dengue epidemic in 2017, which was the largest outbreak in the country during the last three decades, consisting of 186,101 reported cases, and over 320 deaths. The epidemic was controlled by intense measures taken by the health sector. However, the reported dengue cases rose again in 2019 reaching 102,746, being twice the number of reported cases of 51,659 in 2018, indicating re-emergence of an outbreak in 2019. A majority of cases being in the western province, with 20% in the Colombo district [ 6 ]. The dengue deaths in 2019 were 90; higher than the total dengue deaths in 2018 being 58, albeit with reduced mortality rate per overall cases [ 6 , 7 ]. The mortality of dengue fever is < 1%, and that of dengue hemorrhagic fever is 2–5% if detected early and treated promptly, but is high as 20% if dengue hemorrhagic fever is left untreated [ 8 ].
Dengue virus is a flavivirus transmitted by mosquito vectors, such as Aedes aegypti and Aedes albopictus. Dengue fever was first serologically confirmed in Sri Lanka in 1962 [ 9 ]. All four serotypes of dengue virus, DENV-1 to DENV-4 have been circulating in the country, and each serotype has many genotypes [ 9 ]. The most common cause for occurrence of new epidemics is the shift of the circulating serotype and genotype of the dengue virus, which is predisposed by increased foreign travel introducing new strains [ 9 ]. The dengue outbreak in 2003 was predominantly due to DENV-3 and DENV-4. The outbreaks in 2006, 2009 and 2010 was predominantly due to DENV-1 [ 9 ]. The predominant serotype in the 2017 epidemic was DENV-2 which was infrequent since 2009 [ 10 ]. The outbreak in 2019 was predominantly due to previously latent serotype DENV-3 [ 11 ].
The WHO published and implemented a “Global Strategy for Dengue Prevention And Control” targeting the years from 2012 to 2020, with the goals of improving dengue mortality, and morbidity by the year 2020, and estimating the true disease burden. The main elements of the global strategy were diagnosis and case management, integrated surveillance and outbreak preparedness, sustainable vector control, future vaccine implementation, basic operational and implementation research [ 12 ].This global strategy follows 10 priority areas for planning dengue emergency response, adapted from Rigau-Pérez and Clark in 2005, which also includes Engaging the community and relevant professional groups about dengue control as well as their participation in dengue prevention and control [ 13 ].
A recent study in Malaysia, showed that the population had only an average knowledge, and poor attitudes and practices on dengue prevention. They identified that a significant percentage had erroneous beliefs, such as fogging being the mainstay of dengue vector control. It had led them to a false sense of security, while evading actual measures that should be taken. They also identified that a proportion of people believed they had no responsibility in preventing dengue breeding, which needed urgent attention. They highlighted that it was impossible to reduce dengue prevalence without community participation, and concluded that measures were urgently required to educate the public to change their attitudes. The Communications for behavioral changes program on dengue prevention were subsequently implemented by Health departments of Malaysia to improve dengue awareness and prevention [ 14 ].
Although there had been a few studies on public awareness on dengue prevention, there was limited evidence focused on public awareness on their role in dengue prevention and management. It is therefore very important to take active measures to reduce the incidence and mortality of dengue, for which the responsibility lies not only with health professionals, but also with the general public. The purpose of this study is to identify the level of awareness in patients on preventing and managing dengue infection, and awareness of the patient’s role and responsibility in the above. Our goals were to identify areas in dengue control and management that need improvement, to implement policies that raise patient participation to deliver a better outcome of dengue infection, its complications and its management.
Study design
This is a descriptive cross-sectional study assessing the knowledge, attitudes, and practices on dengue fever, its prevention and the patient’s role in management, among the dengue patients presenting to a tertiary care hospital in Sri Lanka during the month of October 2019.
Study setting
The study was done among a random sample of 132 patients with dengue fever or dengue hemorrhagic fever who were admitted to adult medical wards for treatment at the Sri Jayawardenepura General Hospital during October 2019. These patients comprised people from draining areas of the western province of Sri Lanka.
Sample size
The number of patients who presented to the Sri Jayawardenepura General hospital in the month of October 2019 was 200. A sample size of 132 was calculated with a confidence interval of 95%, to match the population to assess a statistically significant result.
Participants
The study population was randomly selected among adult patients older than 13 years of age admitted with dengue infection to the medical wards of the Sri Jayawardenepura General Hospital during the month of October 2019.
Participants were not selected from the same family who would likely to be influenced by similar knowledge, to avoid bias of pseudo-replication.
Data collection
Data collection was commenced after obtaining the approval from the institutional Ethical Review committee of the Sri Jayawardenepura General Hospital and Postgraduate Training Centre (SJGH/20/ERC/017). Data was collected using a self-administered validated questionnaire regarding Knowledge, Attitudes, and Practices (KAP) on dengue in languages English, Sinhala, and Tamil which were translated and extensively reviewed for validation (Additional file 1 : Appendix S1, Additional file 2 : Appendix S2, Additional file 3 : Appendix S3).
Data was collected from randomly selected participants, only after informed written consent was obtained. The questionnaires were filled by the participants themselves using the validated questionnaire of the language convenient to them. The study investigators were with them while filling the questionnaire in case the participants needed to clarify any questions in order to ensure quality. The data was collected anonymously, while strict confidentiality of the responses and the results was maintained.
The questionnaire consisted of 20 questions which, comprised 5 questions on knowledge, 6 questions on attitudes, and 9 questions on practices on dengue fever and haemorrhagic fever, its prevention and patient’s role in management. Prior to analysis they were then re-categorized into questions on awareness of:
mortality and severity of dengue burden—5 questions
prevention of dengue vector mosquito breeding and acquiring the infection—5 questions
patient’s role in dengue management, and warning signs requiring prompt hospitalization—10 questions
The responses to each question was analyzed with percentage estimated of correct responses. The total marks scored by each participant to the whole questionnaire was estimated as a percentage, which has been defined as the “KAP score”. KAP score is an abbreviation used for the total score of the questions based on K nowledge, A ttitudes, and P ractices regarding dengue burden, dengue prevention and management in this study. The total results were categorized as “low” when KAP were < 50%, “moderate” when KAP scores were 50–75%, and “high” when KAP scores were > 75%.
Statistical methods
Data was analyzed using the SPSS (Statistical Package for the Social Sciences) software. All the questionnaire sheets were filled completely and none of the sheets were excluded. The mean of the KAP score of each category was calculated. The percentage of the population who scored low, moderate and high KAP scores was calculated separately. The responses to each of the 20 questions were analyzed separately to infer the areas which needed further improvement in awareness of the general public on dengue.
The study population comprised 61% males, and 39% females with a male: female ratio of 3:2. When categorizing by age, 42% of the study population was less than 30 years old, 36% were between 30 and 50 years old, and 22% were more than 50 years old. Of those who were between 30 and 50 years, 35% were graduates or diploma holders. Of those who were more than 50 years old, 21% were graduates or diploma holders. When categorizing by level of education, 10% of the population was currently schooling, 8% were adults educated up to less than ordinary level (O/L) at school who were not graduates or diploma holders, 18% were adults educated up to O/L at school who were not graduates or diploma holders, 34% were adults educated up to advanced level (A/L) at school who were not graduates or diploma holders, 24% were adults who had completed school education and were undergraduates, 6% were adults who had completed school education and were graduates or diploma holders (Table 1 ).
The mean KAP score of the sample population from the questionnaire was 55.04%. When categorizing the KAP scores as low (< 50%), moderate (50–75%), and high (> 75%), a majority of 65.2% of the population had moderate KAP scores. 27.3% had low KAP scores, and only 7.6% had high KAP scores (Fig. 1 ).
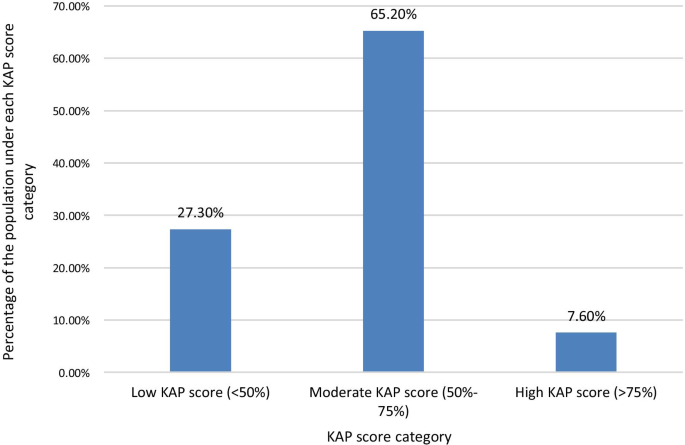
Percentage of the study population who scored under each KAP score level Category. When categorizing the KAP scores as low (< 50%), moderate (50–75%), and high (> 75%) scores, a majority of 65.2% of the population had moderate KAP scores. 27.3% had low KAP scores, and only 7.6% had high KAP scores
The KAP score achieved was higher with increasing age. The highest mean total KAP score of 57.86% was among those > 50 years of age, with those aged < 30 years having a mean KAP score of 53.48% and those aged 30–50 years having a mean KAP score of 55.21% (Fig. 2 ). The mean KAP score on awareness of dengue mortality and burden among the age categories < 30 years, 30–50 years, and > 50 years was 49.29, 56.88, and 58.57% respectively. The mean KAP score on awareness on prevention of dengue vector breeding and acquiring the infection among the age categories < 30 years, 30–50 years, and > 50 years was 63.57, 59.38, and 63.57% respectively. The mean KAP score on awareness of patients’ role in dengue management and warning signs requiring prompt hospital admission among the age categories < 30 years, 30–50 years, and > 50 years was 49.82, 52.08, and 51.79% respectively (Fig. 3 ).
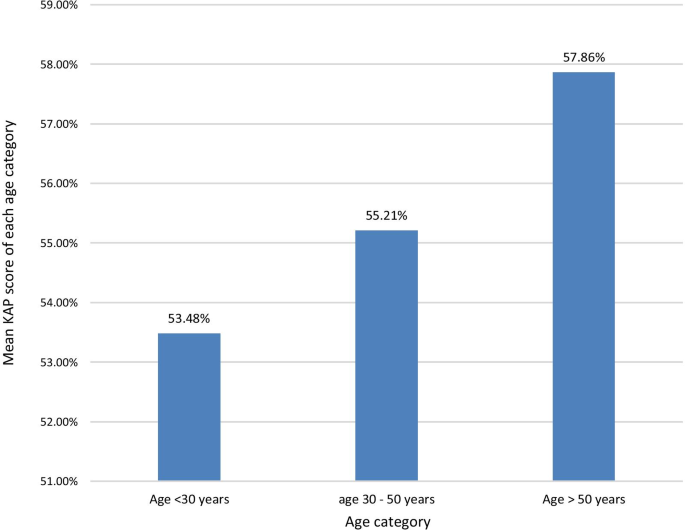
The mean KAP score of each age category. The KAP score achieved was higher with increasing age. The highest mean KAP score of 57.86% was among those > 50 years of age, with those aged < 30 years having a mean KAP score of 53.48% and those aged 30–50 years having a mean KAP score of 55.21%
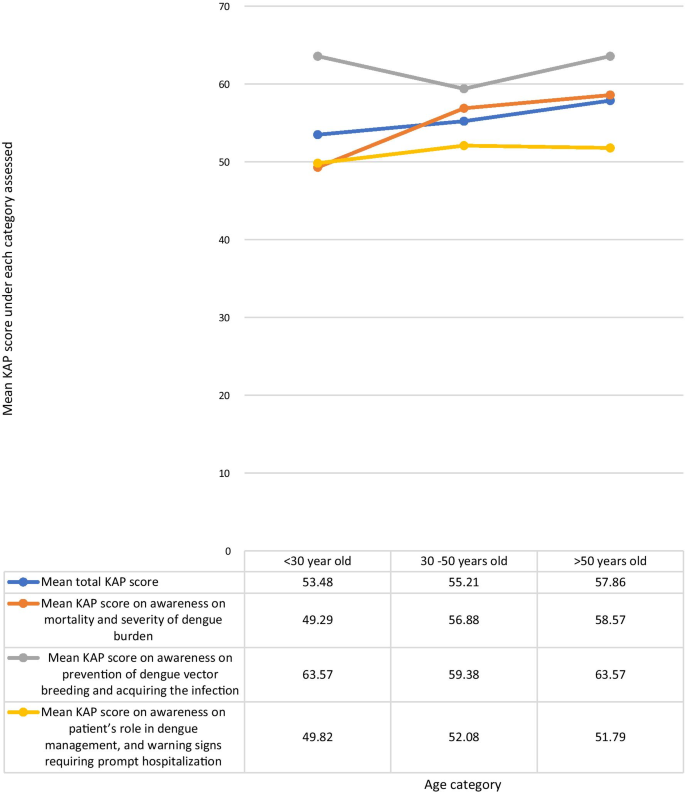
Comparison of the total KAP score, awareness on mortality and severity ofdengue burden, awareness on prevention of dengue vector breeding and acquiring the infection, and awareness on patient’s role in dengue management, and warning signs requiring prompt hospitalization under each age category
The mean KAP score was higher among those with higher educational qualification levels. The highest mean KAP score of 58.13% was among graduates and professional diploma holders of any field, and the lowest score of 49% was among adults educated in school up to below O/L. The mean total KAP score among those currently schooling was 54.62%. Adults who were not undergraduates, graduates, or diploma holders, who were out of school, but were educated at school up to O/L and those who had completed schooling after A/L had mean total KAP scores of 53.96 and 54.67% respectively. The mean KAP score on awareness of dengue mortality and severity of dengue burden among each of the age categories; schooling, adults educated less than O/L, adults educated up to O/L, adults educated up to A/L, under graduates, graduates or diploma holders were 50.77, 42, 60.83, 50.44, 58.75, and 55% respectively. The mean KAP scores on awareness on prevention of dengue vector breeding and acquiring the infection among each of the educational categories in above order were 60, 60, 60, 64, 60.94, 67.5% respectively. The mean KAP scores on awareness of the patient’s role in dengue management and warning signs requiring prompt hospital admission among each of the educational categories in above order were 53.85, 45, 44.58, 51.56, 55, 55% respectively (Fig. 4 ). The mean KAP score among females was 55.48%. and that of males was 54.75%.
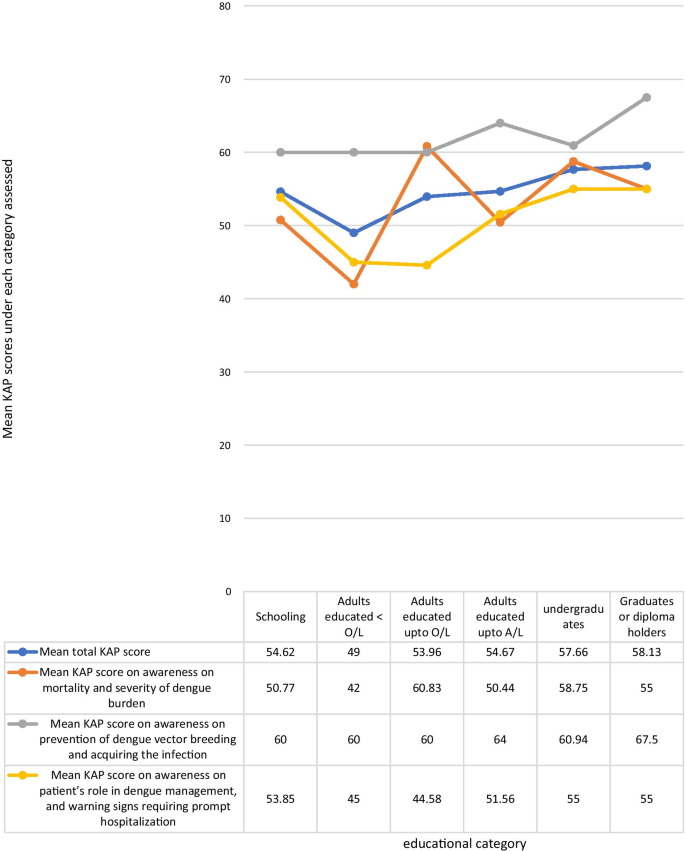
Comparison of the total KAP score, awareness on mortality and severity of dengue burden, awareness on prevention of dengue vector breeding and acquiring the infection, and awareness on patient’s role in dengue management, and warning signs requiring prompt hospitalization under each educational category
When analyzing data by categorizing the questions by the awareness on the area assessed, the highest mean KAP score of 62.05% was on questions on awareness of prevention of dengue vector breeding and acquiring the infection, while the lowest mean KAP score of 51.06% was on questions on awareness of patient’s role in dengue management, and warning signs requiring prompt hospitalization. The mean KAP score on awareness of dengue mortality and severity of burden was 54.02% (Fig. 5 ). On analysis of questions related to awareness of dengue mortality and severity of burden, only 28.8% had high KAP scores, 40.9% had low KAP scores, and 30.3% had moderate KAP scores. On the analysis of questions related to awareness on dengue prevention, an equal percentage of 40.9% had low and high KAP scores respectively, and 18.2% had moderate KAP scores. Analysis of questions related to awareness on patient’s role in dengue management and warning signs prompting hospitalization showed, only 5.3% had high KAP scores, 62.9% had moderate KAP scores, and 31.8% had low KAP scores (Fig. 6 ).
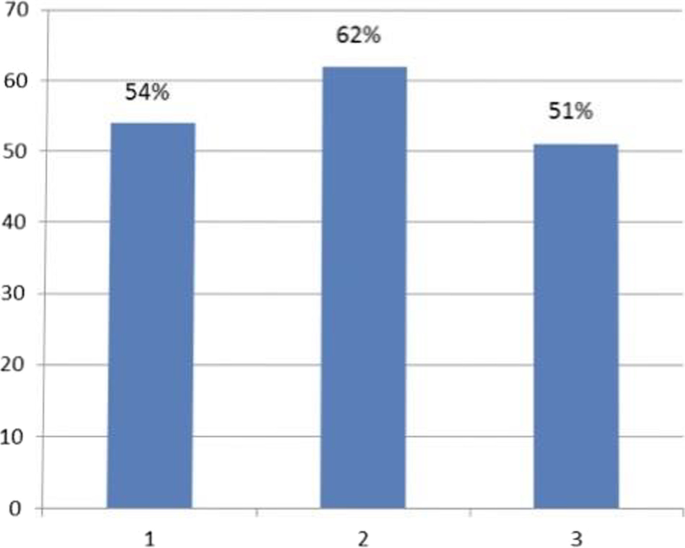
Mean KAP score of each area assessed. 1. Mean KAP score on awareness of mortality and severity of dengue burden- 54%. 2. Mean KAP score on awareness of prevention of dengue breeding and acquiring the infection—62%. 3. Mean KAP score on awareness of patient’s role in dengue management, and warning signs requiring prompt hospitalization—51%
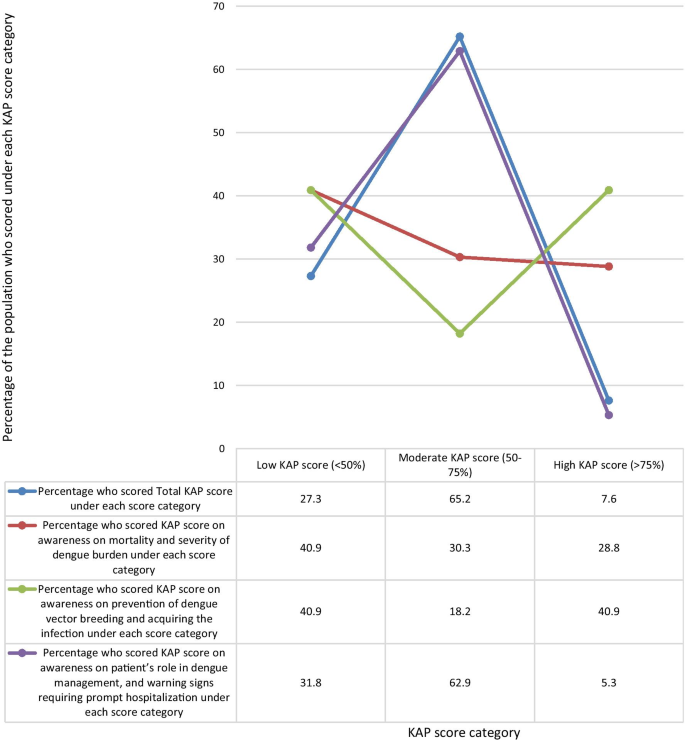
Comparison of percentage of the population who scored low (< 50%), moderate (50%-75%), and high (> 75%) KAP scores under each area assessed
There is no statistically significant correlation between the mean KAP scores on awareness of dengue mortality and severity of dengue burden, and the mean KAP scores on awareness on prevention of dengue vector breeding and acquiring infection according to the spearman’s test (p = 0.084). Although there is a statistically significant correlation between the mean KAP scores on awareness of dengue mortality and severity of dengue burden, and the mean KAP scores on awareness of patient’s role in dengue management and warning signs requiring prompt hospital admission according to the spearman’s test (p = 0.015).
The populations response to each individual question is shown in Table 2 . The percentage of the population who knew the correct answer for the questions on awareness of dengue burden and mortality were as follows: The number of reported dengue cases in Sri Lanka for the year during the outbreak in 2017 was close to 200,000 (42%), The number of reported dengue cases in the year 2019 is higher than that of 2018 (52%), Of 100 persons who get dengue fever only 1 or less persons would die per year when detected early and proper access to medical care (The mortality of dengue fever is < 1%) (60%), The mortality rate of dengue hemorrhagic fever is 2–5%, but is high as 20% if left untreated (60%), The WHO has ranked dengue as one of the top ten threats to Global health in 2019 (56%).
The percentage of the population who knew the correct answer for the questions on awareness of dengue prevention were as follows: all persons with dengue fever do not need to be notified to the Public Health Inspector (PHI) (39%), dengue vector mosquitoes breed in muddy water (52%), The peak biting times of the dengue mosquito is morning and evening (80%), If a person gets dengue fever once in their life, they will be immune to it and will not get dengue fever again (44%), discarded tires, coconut shells, and plastic containers collecting rain water in the garden should be destroyed to prevent dengue vector breeding (96%).
The percentage of the population who knew the correct answer to the questions on awareness of dengue management and warning signs which require prompt hospitalization were as follows: There is a special drug available to treat dengue fever (43%), papaya leaf juice increases the platelet count and thus helps treat dengue fever (33%), dengue patients with a platelet count < 150,000/mm 3 with a rapid drop are recommended to be admitted to hospital (85%), abdominal pain in a dengue patient is not an indication for hospital admission (32%), all pregnant mothers with dengue fever are recommended to be admitted in hospital irrespective of the platelet count (83%), NS1 antigen can be tested on any day since the onset of fever to diagnose dengue fever (23%), a negative report of dengue IgM antibody done on the second day since onset of fever means the patient does not have dengue fever (17%), When a dengue patient has a platelet count > 150,000/mm3 and does not meet criteria which require hospital admission, they should drink 2500 ml of oral fluids per day at home (40%), When a dengue patient has a platelet count > 150,000/mm3 and does not meet criteria which require hospital admission, they should check their Full blood count daily to assess the drop in platelet count (65%), dengue patients should avoid having red or brown drinks (89%).
Dengue virus has four serotypes. Acquisition of dengue infection due to one serotype does not give immunity against a subsequent infection with another serotype, though there is about a two years period of cross-protection [ 15 ]. All four serotypes share only 60–75% identity at amino acid level, and are thus considered as different viruses [ 14 ]. Infection from one serotype gives life-long immunity against that particular serotype [ 10 , 15 ]. Once the cross protection wanes off, secondary dengue infection is more severe than primary dengue infection [ 10 , 15 ]. However only 44% of the study population were aware that occurrence of dengue infection once, does not prevent occurrence of the disease again.
Dengue transmission increases during the rainy season in Sri Lanka, mostly in July, due to increasing dengue vector mosquito breeding places. Other causes for increase in the number of dengue cases is urbanization, climate change, and poor vector control and prevention of disease [ 10 ]. 96% of our cohort were aware of the need to destroy and clean water collecting areas, to prevent breeding of the dengue vector, while 84% of the cohort of a similar study done in the central province of Sri Lanka was aware of this same fact. This is probably because the latter study was done in 2015, prior to the dengue epidemic in 2017 [ 16 ]. Intense measures were taken in the country by which the epidemic in 2017 was controlled. This included clean-up campaigns, awareness programs, National dengue prevention and control, National Strategic framework (2016–2020) to align their action with the WHO Global strategy for dengue prevention and control (2012–2020), The Presidential Task Force on Dengue (PTF) and National dengue control unit of the Ministry of Health launched a rapid inter-sectoral program for prevention and control of dengue [ 7 ]. Awareness programs were held in rural and urban community gatherings, taught in school and institutions, shared on social media, television and radio [ 7 ]. However, data regarding the targeted population for these awareness programs was sparse. Dengue is ranked the third commonest notifiable disease in Sri Lanka, by which means the health sector can implement active vector control measures in the identified areas [ 17 ]. Only 39% of the study population was aware that all persons with dengue fever should be notified to the PHI. The low number of people who were aware of the importance of notifying dengue cases to the PHI, was probably due to the general public being unaware of the PHI’s role in dengue prevention, and lack of awareness of their responsibility in notifying cases, and it’s importance in vector control. Lack of notification of disease hinders action taken for vector control, which gives a falsely lower number of reported cases than the actual number. People should be educated on this to improve notification and vector control. Notification to the PHI of dengue patients managed at home or in the hospital should be made mandatory to avoid negligence in notification. This study population had a relatively good awareness about dengue breeding sites and biting times, probably due to awareness programs during the 2017 epidemic. Literature has shown the importance of improving knowledge on dengue prevention to control dengue outbreaks [ 18 ].
A study in Vietnam during the dengue epidemic in 2017 showed that 91% of the study population considered dengue to be dangerous to very dangerous [ 19 ]. Our study evaluated patients already being admitted for treatment of dengue at the Sri Jayawardenepura general hospital, comprising of patients from the western province, which has the highest dengue burden in the country. A similar study was done in the central province of Sri Lanka by Jayalath et al . among out patients visiting the Peradeniya hospital for reasons other than dengue. Jayalath et al. showed that 95% of their study population knew dengue was a severe disease [ 16 ]. 75% of the cohort of a similar study done among patients being admitted for treatment of dengue fever, in the northern province of Sri Lanka in 2017, knew that dengue was a severe disease [ 20 ]. Our study population had a moderate mean KAP score (54%) on questions on awareness on dengue severity and burden. 40.9% of the population had low awareness on severity and burden of dengue, and only 28.8% had high awareness on its severity and burden. This difference in evidence regarding awareness of severity of dengue in the above studies, could be because the questions by which awareness was evaluated was different in the three studies, and because our study, and the study in the northern province evaluated patients who had already acquired dengue fever and were admitted for treatment at that time. It could also be speculated that these populations acquired dengue infection due to their lack of awareness in prevention of disease.
This lack of awareness on the severity of dengue and it’s burden is probably due to most dengue patients uneventfully recovering from uncomplicated dengue fever, and due to successful dengue management by the healthcare system in the country. This study identified that those who had good awareness on the mortality and severity of the burden of dengue, also had a good awareness about their role in managing dengue, as well as warning signs requiring prompt hospital admission. It can be concluded that there is a strong correlation between those who have an appreciation of the gravity of the symptoms caused by dengue, and the likelihood of them educating themselves on dengue management and their active participation in it. Rozita et al. showed that people who were infected by dengue, or had a family member infected by the disease had better knowledge, attitudes and practices about dengue compared to those who did not [ 21 ]. A study in Singapore in 2017 after the country’s largest dengue epidemic showed that attitudes and practices regarding dengue among primary care physicians significantly improved after experiencing the epidemic [ 22 ]. Chanthalay S et al . showed that those who had better knowledge and attitudes regarding dengue are more likely to take precautions to prevent the disease [ 23 ]. Those who have good awareness will have a good understanding of the gravity and impact of the disease, will know the importance of preventing it, and will be aware of necessary preventive measures.
The mortality of dengue fever is < 1%, and that of dengue hemorrhagic fever is 2–5% if detected early and treated promptly, but is high as 20% if dengue hemorrhagic fever is left untreated [ 8 ]. In 2015 Malhi et al. reported that the presence of comorbidities like diabetes mellitus, hypertension, chronic kidney disease, allergies, asthma, ischemic heart disease and hepatic anomalies, as well as delay in identification and treatment were linked to increased mortality from dengue [ 24 ]. However, in 2017 a study by the same authors showed that 50% of dengue deaths were of previously healthy individuals with no comorbidities [ 25 ]. Therefore, the leading cause for dengue related complications and deaths is delayed identification and treatment of disease. This can be due to delays by the patient or health staff, mostly due to delayed patient presentation to the hospital [ 26 ].Studies have shown that late presentation of dengue fever to the hospital leads to increased development of dengue haemorrhagic fever, dengue shock syndrome, multi-organ involvement like acute kidney injury, and increased mortality [ 26 , 27 , 28 ]. According to the study findings, by identifying areas where the public has misconceptions and misunderstandings about dengue fever, its prevention and management, we can implement steps to improve those loop holes. By following correct practices, avoiding malpractices, and timely hospital admission, his will reduce dengue fatality, improve the outcome, and will also reduce the burden on the healthcare system.
The national Guidelines on dengue management indicates the need for hospital admission in a dengue patient if the platelet count is < 100,000, or platelet count between 100,000- 150,000 with a rapid drop in platelets, fever for three days with any warning signs such as abdominal pain, persistent vomiting, mucosal bleeding, lethargy and restlessness [ 29 ]. Irrespective of the above criteria, admission is required in dengue patients who are pregnant, elderly, obese, with comorbidities, or with adverse social circumstances [ 29 ]. In this study, 85 and 83% patients respectively were aware of the indication for admission as per the platelet count or if pregnant, but only 32% patients knew admission was indicated with warning signs like abdominal pain. Therefore, people need to be educated about warning signs of severe dengue infection. People who do not require admission must be educated about cautious self-management at home until they require admission [ 29 ]. By doing so there will be less likelihood to miss warning signs, will have improved outcome, and there will be less burden to hospital staff. Only 40% of patients knew about fluid management at home, but 89% knew to avoid red drinks.
Serological testing is important to confirm the diagnosis of dengue fever when the presentation is atypical or when unsure of the diagnosis. NS1 antigen is tested in the patient’s blood on the first few days of the disease and has a sensitivity of 60–90%. Dengue IgM antibody will be positive in the patient’s blood only after the 5th day of illness [ 29 ]. Therefore, patients should be educated about the ideal time to do each test to avoid false negatives being reported by doing the test at the wrong time of the illness. However, dengue infection cannot be excluded by a negative serological lab report. Few patients knew about the timing of testing, with only 23% and 17% being aware of the timing of testing, and sensitivity of NS1 antigen and dengue IgM respectively. It is important that health care professionals guide patients on the correct timing to do the serological tests. It would be prudent to do such serological tests only on request by a physician, to avoid patients testing at the wrong time, and getting a report which cannot be interpreted at that time of the illness. False negatives of serological testing can further be avoided by laboratory staff rechecking the patients’ day of the illness, and the physicians request form prior to drawing blood.
This study shows that people had misconceptions about dengue management. Only 43% knew there was no special drug to treat dengue fever. There is no particular drug to treat dengue, but is managed by careful monitoring and fluid tailoring resuscitation [ 29 ]. A tetravalent live attenuated dengue vaccine has been registered for use in several countries [ 15 ]. In sero-negative individuals it is believed that the vaccine mimics a silent natural infection, giving temporary cross-protection against all serotypes, and subsequently causing severe dengue infection when primarily infected [ 15 ]. However, its efficacy varies in different countries and is not currently recommended for use in Sri Lanka [ 15 ]. The use of papaya leaf juice in dengue management had recently gained interest, leading to many people consuming the juice assuming improvement of dengue infection. Research has shown papaya leaf juice to improve platelet counts, but has not shown to prevent or reduce fluid leaking in dengue hemorrhagic fever [ 30 ]. This can adversely cause early rise in platelet count masking the onset of fluid leaking, which can be detrimental in managing dengue hemorrhagic fever. 33% of our cohort believed papaya leaf juice helped treat dengue fever, while 13.4% of the cohort in a study done in Sri Lanka in 2015 believed the same to be true. This is probably because the concept of the effect of papaya leaf juice on platelet count came in to light only later on [ 16 ].
This study demonstrated an increasing trend in awareness on all categories, such as among people with a higher level of education, and maturity by age, indicating that education and maturity are important factors for improved awareness. Kumanan et al. showed a significant association between educational level and knowledge regarding dengue fever, and no significant association between educational level and preventive practices [ 20 ]. The trend in our study demonstrated on Fig. 3 suggests that responses in the awareness on dengue mortality and severity of dengue burden steadily increased with age, and strongly influence the mean total KAP scores. The highest awareness in all age categories was on dengue prevention and the lowest awareness in all categories was on patients’ role in dengue management and warning signs requiring prompt hospitalization (Fig. 3 ).
There was inadequate awareness among adults who dropped out of school prior to completion of the full school education up to advanced level even when they are older. This may demonstrate a population with lower level of understanding of the information given, and those who were not regularly educated at school regarding dengue infection as they dropped out. Those who drop out of school are also those who usually have a poor social background, and they may also have inadequate access to social media and electronic media to receive updates about dengue mortality, prevention and management. This highlights the need for any information to reach the people of all social backgrounds when implementing strategies to improve public awareness on dengue infection. Dissemination of information should be done in various ways targeting different populations of different levels of understanding. People with lower education levels should be the main target group requiring more advice and education regarding the patient’s role in dengue management.
This population has a relatively a better awareness on dengue prevention as compared to awareness of dengue mortality and dengue management. This is possibly due to prior media education of the public on prevention during the previous epidemic in 2017. The identified weak point is patient awareness on the patient’s role in dengue management, as well as identifying warning signs requiring prompt hospitalization. It causes delay in treatment, which is a major cause for increased mortality. The trend demonstrated on Fig. 5 suggests that responses in the dengue management and warning signs prompt hospitalization area strongly influence the total KAP scores. This indicates that patient awareness on the role of the public and patients on dengue management is critical in the outcome of dengue infection. An action plan should be implemented targeting improving public awareness by education programs on the role of the public and patients in dengue management, to improve outcome.
The general public play a major role in prevention and management of dengue fever, and influence the outcome. Jayalath et al. showed that 30% of their population believed the responsibility of dengue prevention lay with the public, while 66% believed both the public and the government were responsible [ 16 ]. In order to improve involvement of patients and the public in dengue prevention, control and management, attention should be paid on educating the public and patients on the disease.
Limitations and recommendations for future research
This study focused on 132 patients from one hospital. Therefore, the conclusions can be relevant only to draining areas in the vicinity of this hospital, and may not represent the knowledge, attitudes and practices in other parts of Sri Lanka. However, since majority of the dengue cases in the country are concentrated in the western province, of which a significant number of patients present to the Sri Jayawardenepura General Hospital, the findings of this study may represent the most dengue dense area in the country. Large scale future research from all parts of the country may be beneficial to infer the knowledge, attitudes, and practices of the country as whole.
The general public was educated about Dengue infection by various means, including messages on social media, electronic media, awareness programs at schools, and village meetings, posters and distribution of leaflets, during the dengue epidemic in 2017. This study did not extensively evaluate whether the study participants had been exposed to these prior teaching about Dengue infection, and if they did, by what means they were educated. However almost all the study participants had access to electronic and social media. This may not be the same when inferring on the population in some rural parts of Sri Lanka who may not have similar access to such media education. Awareness programs and active participation of the general public in dengue prevention and management should be implemented. We suggest future follow up research of the awareness on dengue infection among the public, before and after implementing formal dengue awareness strategies to assess the effectiveness of it. In addition to follow up research before and after implementing disease awareness steps, we also suggest future research to assess an association and comparison of dengue mortality and outcome before and after implementing practices to further educate the public, in order to identify its impact on dengue management and outcome.
The population has relatively a better awareness on dengue prevention, as compared to awareness of dengue mortality and dengue management. The identified weak point is patient awareness on the patient’s role in dengue management, and identifying warning signs requiring prompt hospitalization causing delay in treatment, which is a major cause for increased mortality. There was a correlation between those who had good knowledge on dengue burden and those who were aware of the patients’ role in dengue management. There is also an increasing trend in awareness on all categories, especially among people with a higher level of education, and maturity by age, indicating that education and maturity are important factors for improved awareness. An action plan should be implemented targeting improving public awareness on the role of the public and patients in dengue management to improve outcome.
Availability of data and materials
The raw data sets analyzed during the current study are available on reasonable request from the corresponding author.
Abbreviations
Dengue virus
Knowledge attitudes and practices
Ordinary level at school
Advanced level at school
Ten threats to global health in 2019. World Health Organization. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 . Accessed 4 Jan 2020.
Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, et al. The global distribution and burden of dengue. Nature. 2013;496(7446):504–7.
Article CAS Google Scholar
Brady OJ, Gething PW, Bhatt S, Messina JP, Brownstein JS, Hoen AG, et al. Refining the global spatial limits of dengue virus transmission by evidence-based consensus. PLoS Negl Trop Dis. 2012;6(8):e1760.
Article Google Scholar
Dengue and severe dengue. World health organization.4th November 2019. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue . Accessed 4 Nov 2019.
Dengue worldwide overview 2019. European Centre for Disease Prevention and Control. https://www.ecdc.europa.eu/en/dengue-monthly . Accessed 4 Jan 2020.
Epidemiology unit, Ministry of Health Sri Lanka. Dengue, disease surveillance trends. http://www.epid.gov.lk . Accessed 4 Jan 2020.
Dengue DREF final report 2017. Dengue Sri Lanka. International federation of red cross and red crescent societies. https://www.chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/viewer.html?pdfurl=https%3A%2F%2Freliefweb.int%2Fsites%2Freliefweb.int%2Ffiles%2Fresources%2FMDRLK007dfr.pdf&clen=1774569&chunk=true . Accessed 4 Jan 2020.
Lahiri M, Fisher D, Tambyah PA. Dengue mortality: reassessing the risks in transition countries. Trans R Soc Trop Med Hyg. 2008;102(10):1011–6.
Sirisena PDNN, Noordeen F. Evolution of dengue in Sri Lanka—changes in the virus, vector, and climate. Int J Infect Dis. 2014;19:6–12.
Jayarajah U, Faizer S, de Zoysa I, Senevirathne SL. A large Dengue epidemic affects Sri Lanka in 2017. IJPSAT. 2017;6(1):84–6.
Google Scholar
National Dengue control unit. Ministry of Health, Nutrition, and Indigenous Medicine. http://www.dengue.health.gov.lk . Accessed 4 Jan 2020.
World Health Organization. Global strategy for dengue prevention and control 2012–2020. Geneva: World Health Organization
Rigau-Pérez JG, Clark GG. Còmo responder a una epidemia de dengue: vision global y experiencia en Puerto Rico [How to respond to a dengue outbreak: global vision and experience in Puerto Rico]. Pan Am J Public Health. 2005;17:282–93.
Selvarajoo S, Liew JWK, Tan W, et al. Knowledge, attitude and practice on dengue prevention and dengue seroprevalence in a dengue hotspot in Malaysia: a cross-sectional study. Sci Rep. 2020;10(1):9534. https://doi.org/10.1038/s41598-020-66212-5 .
Article CAS PubMed PubMed Central Google Scholar
Applicability of dengue vaccines. Weekly epidemiological report. Apublication of the Epidemiological unit, Ministry of Health, nutrition and indigenous medicine, Sri Lanka. 18th - 24th March 2017. Volume 44. no. 12. https://www.chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/viewer.html?pdfurl=http%3A%2F%2Fwww.epid.gov.lk%2Fweb%2Fimages%2Fpdf%2Fwer%2F2017%2Fvol_44_no_12-english.pdf&clen=1799202&chunk=true . Accessed 6 Jan 2020.
Jayalath T, Ralapanawa U, Karunaratne S, Dassanayake UKA, Pathirage M, et al. Knowledge and attitude regarding dengue fever among the outdoor patients of the teaching hospital Peradeniya, Sri Lanka. Int J Med Res Health Sci. 2018;7(1):77–84.
Annual health bulletin of Sri Lanka. Department of Health Services, Colombo, Sri Lanka (2002)
Al-Zurfi BM, Fuad MD, Abdelqaderm MA, Baobaidm MF, Elnajehm M, Ghazim HF, Ibrahim MH, Abdullah MR. Knowledge, attitude and practice of dengue fever and health education programme among students of Alam shah science school, Cheras Malaysia Malays. J Public Health Med. 2006;6:62–7.
Nguye HV, Than PQT, Nguyen TH, Vu GT, et al. Knowledge, attitude and practice about dengue fever among patients experiencing the 2017 Outbreak in Vietnam. Int J Environ Res Public Health. 2017;2019(16):976.
Kumanan T, Logeswaran D. A study on knowledge, attitude and practices regarding dengue among hospitalized patients from Northern Sri Lanka. Sri Lankan J Infect Dis. 2018;8(2):127–32. https://doi.org/10.4038/sljid.v8i2.8220 .
Wan Rozita WM, Yap BW, Veronica S, Muhammad AK, Lim KH, Sumarni MG. Knowledge, attitude and practice (KAP) survey on dengue fever in an urban malay residential area in Kuala Lumpur. Malays J Public Health Med. 2006;6:62–7.
Junxiong P, ZoeJane-Lara H, Tun LH, Jing Y, Yee SL. Assessing changes in knowledge, attitude and practices of dengue diagnosis and management among primary care physicians after the largest dengue epidemic in Singapore. BMC Infect Dis. 2017;17:428.
Chanthalay S, Jiraporn C, Somsak W, Cheerwith R. Knowledge, attitudes and preventive behaviours related to dengue vector breeding control measures among adults in communities of Vientiane, capital of Lao PDR. J Infect Public Health. 2015;8:466–73.
Mallhi TH, Khan AH, Adnan AS, et al. Clinico-laboratory spectrum of dengue viral infection and risk factors associated with dengue hemorrhagic fever: a retrospective study. BMC Infect Dis. 2015. https://doi.org/10.1186/s12879-015-1141-3 .
Article PubMed PubMed Central Google Scholar
Mallhi TH, Khan AH, Sarriff A, Adnan AS, Khan YH. Determinants of mortality and prolonged hospital stay among dengue patients attending tertiary care hospital: a cross-sectional retrospective analysis. BMJ Open. 2017;7(7):e016805.
Mallhi TH, Adnan AS, Khan AH, Habib Y, et al. Patients related diagnostic delay in dengue: an important cause of morbidity and mortality. Clin Epidemiol Glob Health. 2016;4(4):200–1.
Yatra IM. Disease history and delayed diagnosis of dengue infection as risk factors for dengue shock syndrome in Wangaya Hospital Denpasar. Public Health Prev Med Arch. 2015. https://doi.org/10.15562/phpma.v3i2.108 .
Nguyen Thi KT, Nguyen Ngoc AT, Khau MT, Nguyen TT, Luong CQ. Epidemiology analysis of deaths associated with dengue hemorrhagic fever in Southern Viet Nam in 1999–2000. Dengue Bull. 2001;25:28–32.
Guidelines on the management of dengue fever and dengue haemorrhagic fever in adults. National Guidelines 2012. Ministry of Health, Sri Lanka.
Rajapakse S, de Silva NL, Weeratunga P, et al. Carica papaya extract in dengue: a systematic review and meta-analysis. BMC Complement Altern Med. 2019;19:265. https://doi.org/10.1186/s12906-019-2678-2 .
Download references
Acknowledgements
We all express our gratitude to all participants who consented to take part in this study.
Authors’ information
SS is a Consultant Physician [MBBS, MD, FRACP] Medical unit, Sri Jayawardenepura General Hospital. KPJ [MBBS], DKJ [MBBS] and DW [MBBS] are Registrars in Internal medicine, and SW is a Senior Registrar in Medicine at the Sri Jayawardenepura General Hospital.
No funding was obtained for this study.
Author information
Authors and affiliations.
Sri Jayewardenepura General Hospital, Kotte, Sri Lanka
K. P. Jayawickreme, D. K. Jayaweera, S. Weerasinghe, D. Warapitiya & S. Subasinghe
You can also search for this author in PubMed Google Scholar
Contributions
Data collection was done by KPJ, DKJ and DW. Analysis, interpretation of data, literature review and writing of the report was done by KPJ. SS and SW guided the study and corrected the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to K. P. Jayawickreme .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was taken from the institutional Ethical Review committee of the Sri Jayawardenepura General Hospital and Postgraduate Training Centre to conduct this study (SJGH/20/ERC/017). Informed written consent was taken from all the participants. All the participants were above the age of 13 years. In the very few participants aged between 13 and 16, informed written consent was obtained from both the participant and the parent or guardian.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix s1..
Questionnaire in English.
Additional file 2: Appendix S2.
Questionnaire in Sinhala.
Additional file 3: Appendix S3.
Questionnaire in Tamil.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jayawickreme, K.P., Jayaweera, D.K., Weerasinghe, S. et al. A study on knowledge, attitudes and practices regarding dengue fever, its prevention and management among dengue patients presenting to a tertiary care hospital in Sri Lanka. BMC Infect Dis 21 , 981 (2021). https://doi.org/10.1186/s12879-021-06685-5
Download citation
Received : 03 April 2020
Accepted : 13 September 2021
Published : 20 September 2021
DOI : https://doi.org/10.1186/s12879-021-06685-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dengue fever
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

41 templates

el salvador
32 templates
49 templates

21 templates
16 templates

28 templates
Dengue Fever Case Report
Dengue fever case report presentation, premium google slides theme and powerpoint template.
This template is specifically crafted to assist medical professionals in presenting their dengue fever case studies with precision and clarity. With its customizability and visually appealing slides, you can effectively highlight the key aspects of the case, including symptoms, diagnosis, treatment, and outcomes. Impress your colleagues and stakeholders with informative charts, diagrams, and customizable sections. Save time and present your dengue fever case study with confidence using this expertly designed Google Slides and PowerPoint template!
Features of this template
- 100% editable and easy to modify
- 21 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
What are the benefits of having a Premium account?
What Premium plans do you have?
What can I do to have unlimited downloads?
Don’t want to attribute Slidesgo?
Gain access to over 22400 templates & presentations with premium from 1.67€/month.
Are you already Premium? Log in
Related posts on our blog

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.9(2); 2020 Feb
Clinical profile and atypical manifestation of dengue fever cases between 2011 and 2018 in Chennai, India
Kamalraj mohan.
1 Department of Microbiology, Sri Muthukumaran Medical College Hospital and Research Institute, Affiliated to the Tamil Nadu Dr. M.G.R. Medical University, Chikkarayapuram, Chennai, Tamil Nadu, India
Jeevan Malaiyan
Sowmya nasimuddin, ravin sathyaseelan devasir.
2 Department of General Medicine, Sri Muthukumaran Medical College Hospital and Research Institute, Affiliated to the Tamil Nadu Dr. M.G.R. Medical University, Chikkarayapuram, Chennai, Tamil Nadu, India
PradeepRaj Meenakshi-Sundaram
Santhiya selvaraj, bharathi krishnasamy.
3 Institute of Microbiology, Madurai Medical College, Affiliated to the Tamil Nadu Dr. M.G.R. Medical University, Madurai, Tamil Nadu, India
Sumathi Gnanadesikan
Muthulakshmi karthikeyan.
4 Department of Microbiology, Meenakshi Medical College Hospital and Research Institute, Meenakshi Academy of Higher Education and Research, Kancheepuram, Tamil Nadu, India
Mohanakrishnan Kandasamy
Nithyalakshmi jayakumar, dhevahi elumalai, gokul g. ra, introduction:.
Dengue fever is a common mosquito-borne viral disease which has reached alarming size in the past few years. It is endemic in more than 100 countries and significant differences were found in clinical profile and atypical manifestation.
Aim of the Study:
A retrospective observational study of clinical profile and atypical manifestations in patients with dengue fever.
Materials and Methods:
Serum samples were collected from clinically suspected cases of dengue fever and it was confirmed by NS1 antigen, IgM, and IgG antibody by ELISA. Clinical details and atypical manifestations were recorded.
Observation:
During the study period, a total of 2502 patients were suspected to have dengue infection, of which 464 (18.5%) samples were found to be positive for dengue viral infection. A majority of the cases were males [268 (57%)] when compared with females [196 (42%)]. Fever was the most common clinical presentation seen in all the patients, followed by headache (78.4%), myalgia (61%), body pain (49.3%), vomiting (40%), joint pain (31.5%), dry cough (19%), nausea (14%), abdominal pain (8%), diarrhea (5.6%), retro-orbital pain (04%), burning micturition (2.4%), and rashes (0.6%). Among atypical manifestations, hepatomegaly [32 (7%)] was the most common, followed by splenomegaly [23 (5%)], bradycardia [18 (4%)], meningitis [6 (1.2%)], hemoptysis [5 (1%)], acalculous cholecystitis [4 (0.8%)], and acute pancreatitis [2 (0.4%)]. The study of hematological parameters showed thrombocytopenia was present in 179 (38.5%) patients, followed by leukopenia [77 (17%)] and raised hematocrit [29 (6.2%)].
Conclusion:
During ongoing epidemics, the clinical profile and atypical manifestations in clinically suspected dengue patients should be investigated early so that severe forms can be treated promptly.
Introduction
Dengue, a common mosquito-borne viral disease, occurs in tropical and subtropical countries especially South and Southeast Asia countries, the Caribbean, Central, and South America, and Africa. Dengue virus (DENV) infection is the most rapidly spreading disease in the world with a 30-fold increase in incidence in the past 50 years.[ 1 ] The first dengue fever in India was reported in 1956 from Vellore and the first dengue hemorrhagic fever occurred in Calcutta in 1963.[ 2 ] Dengue is caused by one of the four serotypes of DEVN (DENV-1–DENV-4) belonging to the family Flaviviridae .[ 3 ] All the four serotypes of the virus have been in circulation and documented in Tamil Nadu.[ 4 ] Dengue fever is an acute febrile illness with frontal headache, retro-ocular pain, muscle pain, joint pain, and rash, even though other signs and symptoms could also be present (such as lymphadenopathy, petechiale, nausea, hepatomegaly, and different types of hemorrhagic manifestations).[ 5 ] Atypical manifestations are rare and include encephalopathy, encephalitis, seizures, hepatocellular damage, acalculous cholecystitis, myocarditis, pericardial effusion, and severe gastrointestinal hemorrhage.[ 6 , 7 ] The clinical presentation in dengue depends on the virus strain, as well as the age and immune status of the host.[ 3 ] This study aims to elucidate the salient clinical feature and laboratory findings of serologically confirmed cases of dengue fever. The elucidation of clinical profile is very important for primary care, management, and thus crucial for saving life.
Aim of the Study
This study aims to study the clinical profile and atypical manifestations in patients with dengue fever.
Materials and Methods
This retrospective observational study was conducted during the period from July 2011 to December 2018 at Sri Muthukumaran Medical College, Hospital and Research Institute, Chennai, India. Informed consent was taken from each patient and the study was approved by Institutional Ethical Committee (obtained on 23.12.2016 (46/IECs)). Serum samples were collected from clinically suspected cases of dengue and were confirmed by NS1 antigen, IgM, and IgG antibody by ELISA (J. Mitra and Co. Pvt. Ltd.). A detailed history was taken and careful clinical examination was performed on all the positive cases. Hematological parameters such as platelet count, hemoglobin, hematocrit (HCT) levels, complete blood count (CBC), and white blood cell count (WBC) were also recorded.
Observation
During the study period, a total of 2502 patients were suspected to have dengue fever, out of which 464 (18.5%) samples were found to be positive. In our study population, the highest numbers of dengue-positive cases were screened in the year 2017 (74.8%), followed by 2013 (27.7%) and 2016 (18.8%) as shown in [ Table 1 ]. A majority of the cases were males 268 (57.7%) and females were 196 (42.2%). About 45% of positive cases belonged to adult age groups (18–44 years) followed by younger age group <18 years (30%) [ Table 2 ]. Fever was the most common clinical presentation which was found among all the patients, followed by headache (78.4%), myalgia (61.2%), body pain (49.3%), vomiting (40%), joint pain (31%), dry cough (19%), nausea (13.5%), abdominal pain (8%), diarrhea (5.6%), retro-orbital pain (4%), burning micturition (2.5%), and rashes (0.6%) [ Table 3 ]. In this study, 90 (19.3%) patients had atypical manifestations. Hepatomegaly [32 (7%)] was the most common manifestation, followed by splenomegaly [23 (5%)], bradycardia [18 (4%)], meningitis [6 (1.2%)], hemoptysis [5 (1%)], acalculous cholecystitis [4 (0.8%)], and acute pancreatitis [2 (0.4%)] [ Table 4 ]. The majority of the patients were positive for NS 1 Ag 290 (62.5%) followed by IgG 80 (17.2%), IgM 53 (11.4%), and IgM + IgG 41 (9%) as shown in [ Table 5 ]. Raised HCT was found in 29 (6.2%) and leukopenia (<4000/mm 3 ) was found in 77 (16.5%) patients. Thrombocytopenia was observed in 179 (38.5%) cases [ Table 6 ].
Year-wise distribution of dengue cases during the study period
Age and sex-wise distribution of dengue cases ( n =464)
Clinical features of dengue -positive cases ( n =464)
Atypical clinical manifestations in dengue patients ( n =90)
Serological marker distribution of dengue cases
Hematological parameters of dengue-positive cases ( n =464)
Dengue is emerging as a major health problem and regular outbreaks of dengue infection have been occurring throughout India.[ 8 , 9 ] The provision of adequate care to patients with suspected dengue in primary care settings requires effective clinical evaluation, laboratory testing, and qualified professionals who know how to recognize warning signs and give appropriate guidance to prevent expended dengue.[ 10 ] Rapid urbanization, globalization, increasing population, poor solid waste, and water management have given rise to new habitats for mosquito breeding thereby increasing the number of cases and deaths.[ 1 , 11 ] The identification of dengue cases is possible by distinct clinical features. Studies describe that atypical manifestations in dengue fever are multisystemic and multifaceted with organ involvement, such as liver, brain, heart, kidney, and central nervous system.[ 12 ] In this study, we investigated the different clinical profile and atypical manifestations.
Incidences of dengue positivity were increasing for the past few years. In our study, we found that the highest number of dengue-positive cases was reported in the year 2017 (74.8%), 2013 (27.7%), and 2016 (18.8%), which were similar to that of previous studies reported.[ 13 , 14 ] Studies revealed that the majority of the cases were in the age group of 15–44 years, followed by other groups. In this study, males [268 (57.7%)] were predominant than females [196 (42.2%)]. These findings well correlate with previous studies.[ 15 ] Fever was the most common clinical presentation which was found among all the presenting patients (100%). Headache (78%) and myalgia (61%) were seen in the majority of cases, followed by joint pain (31%), dry cough (19%), abdominal pain (8%), diarrhea (5.6%), vomiting (32%), and nausea (14%) which is concordant with the study by Hasan SR et al .[ 16 ]
Atypical symptoms have been observed in this study, which is low compared with previous study done by Nagarajan N et al .[ 17 ] Retro-orbital pain as a cardinal feature of dengue fever was seen in few (4%), of our patients, while Denys EF et al . had reported 16.1%.[ 18 ] Burning micturition (8%), hemoptysis (2%), and rashes (0.2%) were not frequent in our study when compared with other studies.[ 19 ] Hepatomegaly is highly specific for the development of both dengue hemorrhagic fever and dengue shock syndrome. In our study, 31 (7%) patients had hepatomegaly which correlates with a previous study done by Row EK et al .[ 20 ] In our study, splenomegaly was 5% which is concordant with a previous study reported by Anurag Prasad et al .[ 21 ] Other less common atypical manifestations were bradycardia [18 (4%)], meningitis [6 (1.2%)], hemoptysis [5 (1%)], acalculous cholecystitis [4 (0.8%)], and acute [pancreatitis 2 (0.4%)]. This differs from other studies where bradycardia, meningitis, hemoptysis, and acalculous cholecystitis were detected in higher percentage of confirmed dengue fever.[ 22 , 23 , 24 , 25 ]
Out of 2038 samples of clinically suspected dengue cases, 464 (23%) were found to be positive by ELISA. The majority of the samples were found positive for NS1 antigen 290 (63%), which indicates high sensitivity of the test for early diagnosis of disease, followed by IgG and IgM antibodies, which is similar to a study conducted by Anand et al .[ 26 ] In our study, thrombocytopenia was present in 179 (39%) patients <150,000/mm 3 , which is slightly less than the study conducted by Ahmed NH et al . Recent studies have established HCT > 40% as a prognostic factor for severe dengue.[ 26 , 27 , 28 , 29 ] In our study, we have found raised HCT in 29 (6.2%) patients. Low leucocyte count may be due to virus-induced inhibition of myeloid progenitor cells or due to destruction.[ 30 ] We found that 11% had leucocyte count <5000, almost similar to a study by Chaloemwong J et al .[ 31 ] An understanding of the course of disease progression, risk factors, recognition of the warning signs, and look out for clinical problems during the different phases of the disease will enable primary care physicians to manage dengue fever in an appropriate and timely manner to reduce morbidity and mortality.[ 32 ] Primary care physician should impart health education about dengue fever to the rural community regularly, through health camps or interpersonal communication based on health awareness programs.[ 33 ] Thus, atypical presentations should prompt us to investigate for dengue especially during ongoing epidemics so that primary care and management is very important in preventing expanded dengue syndrome.
To conclude, the clinical profile of the dengue fever cases is changing in different epidemics, even in the same regions and with the period of time. Primary care physician should have a high index of suspicion to detect and timely manage the atypical manifestations of dengue fever as they are no more a rare entity and will continue to rise so long as they are looked for carefully in dengue patients. This study thus indicates the need for a continuous seroepidemiological surveillance for the early and definite identification of the clinical features and atypical manifestations of dengue infection.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Acknowledgement
The authors sincerely thank the physicians, staff nurse, and technicians of Sri Muthukumaran Medical College Hospital and Research Institute, Chennai, India, for providing their help in identifying the patient, collection of clinical data, and obtaining serum samples.

IMAGES
VIDEO
COMMENTS
Illness course. Day 6: Increased redness of hands and arms; hands mildly swollen. Fevers down. Overall feels better. Day 7: On call physician by patient because of widely fluctuating heart rate and pulse ox (he has a home monitor) with associated LH and SOB. Advised to urgently go to ED for evaluation, however patient did not go.
Dengue (den-gee) Fever (DF) is a mosquito-borne disease caused by the dengue virus. The virus belongs to the family Flaviviridae and genus flavivirus.1 Like other flaviviruses, such. as yellow fever virus and West Nile virus, the dengue virus utilizes single stranded RNA as its. genetic content.1 The disease is found primarily in tropical and ...
Abstract. Dengue is the major cause of arthropod-borne viral disease in the world. It presents with high fever, headache, rash, myalgia, and arthralgia and it is a self-limiting illness. Severe dengue can occur in some cases resulting in dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS). We present a case of a 32-year-old male ...
Presentation of Case. Dr. Hayden S. Andrews ... Dengue fever usually develops in patients within a few days after a mosquito bite and can manifest as a nonspecific febrile illness with headache ...
Dengue fever is one of the commonest infections affecting a large population of people in Sri Lanka. During the 5 years from 2012 to 2016, nearly 800 Dengue cases were reported per week . The Dengue fever outbreak in 2017 in Sri Lanka was caused by DENV-2 virus. It is assumed that the 2018 cases were also caused by the same . Dengue has a wide ...
Abstract. Dengue fever is an arboviral infection spread by the Aedes mosquito with a wide spectrum of presentations encompassing simple flu-like illness to hemorrhagic manifestations. Hemorrhagic complications range from simple petechiae and purpura to gastrointestinal bleeding, hematuria, and severe central nervous system (CNS) bleeds.
Dengue is the major cause of arthropod-borne viral disease in the world. It presents with high fever, headache, rash, myalgia, and arthralgia and it is a self-limiting illness. Severe dengue can occur in some cases resulting in dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS). We present a case of a 32-year-old male patient of high-grade fever, bilateral subconjunctival ...
The classification denotes two clinical spectrums- dengue fever (DF) and dengue haemorragic fever (DHF). Most cases are stereotype and amenable to fluid resuscitation. However, unusual manifestations cause fatalities and often overlooked. This study describes 10 such dengue cases to fill the knowledge gaps. Case presentation
Dengue fever, a viral illness transmitted by the Aedes mosquito, is capable of causing a range of serious complications, including fulminant hepatic failure, renal dysfunction, encephalitis, encephalopathy, neuromuscular and ophthalmic disorders, seizures, and cardiomyopathy. This report details the case of a 30-year-old lactating woman with no notable medical history who presented to the ...
Background Dengue fever and dengue hemorrhagic fever incidence is increasing in Sri Lanka, especially among the young population. Uncommon presentations of this common illness make diagnostic dilemmas and can delay standard treatment which leads to unfavorable outcomes. Case presentation An 18-year-old Sri Lankan Sinhalese boy presented with a history of 1 day of fever and an episode of ...
Dengue Fever is a mosquito-borne disease found primarily in tropical regions of the Earth. Although not prevalent in much of the western world, dengue appears to be an emerging virus, which prompts a need for further understanding. The purpose of this study is to provide a general overview of the virus, followed by a closer examination of one ...
Case presentation. We report the case of a 43-year-old Sri Lankan Sinhalese woman with serologically confirmed dengue fever presenting with evidence of plasma leakage developing acute liver failure evidenced by deranged liver functions, coagulopathy, and altered sensorium and acute kidney injury with anuria. She had elevated serum lactate levels.
Background Diabetic ketoacidosis (DKA) is a common presentation of type 1 diabetes mellitus (T1DM) precipitated by various bacterial and viral infections. Dengue infection is no exception for this and can be a precipitating factor for DKA. The presentation of DKA with dengue haemorrhagic fever (DHF) has been reported in adults. However, it is very rarely observed in children. Case presentation ...
A case-control study including 150 cases and 150 controls was conducted in Chattogram district of Bangladesh. Cases were confirmed dengue patients admitted in Chattogram medical college hospital and Bangladesh institute of tropical and infectious diseases during August and September 2019. On the other hand, controls were non-dengue patients ...
Dengue fever is an arboviral infection spread by the Aedes mosquito with a wide spectrum of presentations encompassing simple flu-like illness to hemorrhagic manifestations. Hemorrhagic complications range from simple petechiae and purpura to gastrointestinal bleeding, hematuria, and severe central nervous system (CNS) bleeds. Herein we present a case of a 38-year-old male with dengue fever ...
In November 2009, WHO issued a new guideline that classifies symptomatic cases as dengue or severe dengue. Dengue is defined by a combination of ≥2 clinical findings in a febrile person who traveled to or lives in a dengue-endemic area. Clinical findings include nausea, vomiting, rash, aches and pains, a positive tourniquet test, leukopenia, and the following warning signs: abdominal pain or ...
Background The World Health Organization (WHO) has ranked dengue as one of the top ten threats to Global health in 2019. Sri Lanka faced a massive dengue epidemic in 2017, the largest outbreak in the country during the last three decades, consisting of 186,101 reported cases, and over 320 deaths. The epidemic was controlled by intense measures taken by the health sector. However, the reported ...
Premium Google Slides theme and PowerPoint template. This template is specifically crafted to assist medical professionals in presenting their dengue fever case studies with precision and clarity. With its customizability and visually appealing slides, you can effectively highlight the key aspects of the case, including symptoms, diagnosis ...
Case Studies in Pediatric Critical Care - June 2009. To save this book to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account.
The Case 8 describe presentation of dengue predominantly with diarrhea that might mislead the clinician as bacillary dysentery. ... Futrakul P, Sangkawibha N, Ahandrik S. Hemostatic and platelet kinetic studies in dengue hemorrhagic fever. Am J Trop Med Hyg. 1977; 26 (5):975-984. doi: 10.4269/ajtmh.1977.26.975. [Google Scholar ] 20. Funahara ...
Dengue Case Management Dengue is the fastest-growing arborvirus infection with a rapidly evolving epidemiology. During the past 50 years, the worldwide incidence of dengue has risen 30-fold. The World Health Organization estimates that 50 100 million dengue infections occur each year in
The first dengue fever in India was reported in 1956 from Vellore and the first dengue hemorrhagic fever occurred in Calcutta in 1963. Dengue is caused by one of the four serotypes of DEVN (DENV-1-DENV-4) belonging to the family Flaviviridae. All the four serotypes of the virus have been in circulation and documented in Tamil Nadu.