Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- How to Write a Literature Review | Guide, Examples, & Templates

How to Write a Literature Review | Guide, Examples, & Templates
Published on January 2, 2023 by Shona McCombes . Revised on September 11, 2023.
What is a literature review? A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research that you can later apply to your paper, thesis, or dissertation topic .
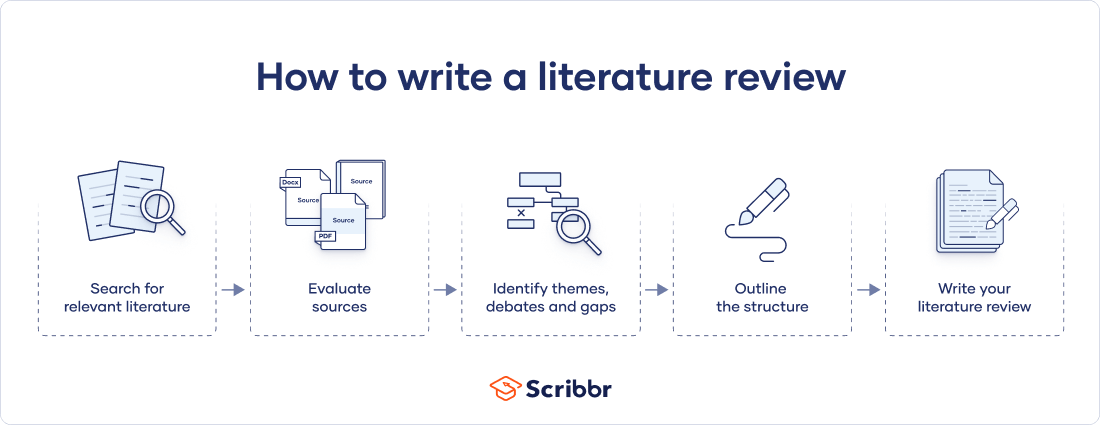
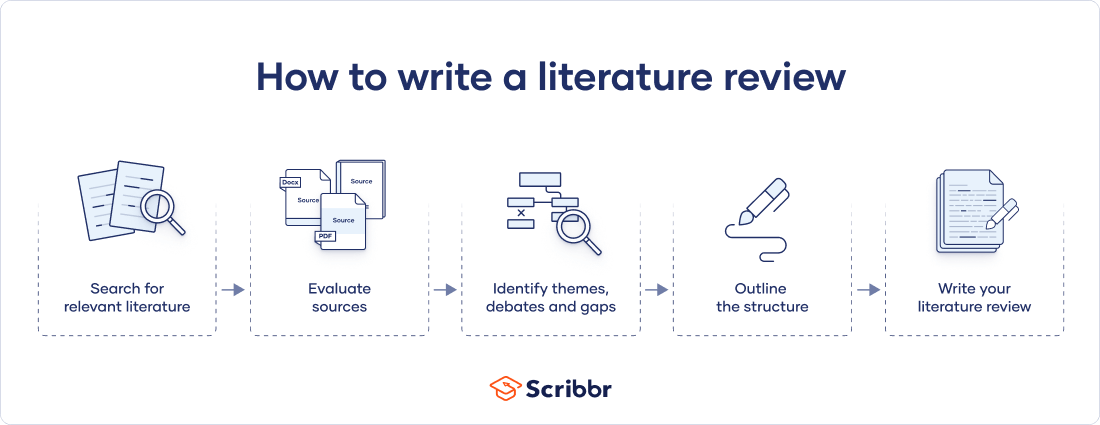
There are five key steps to writing a literature review:
- Search for relevant literature
- Evaluate sources
- Identify themes, debates, and gaps
- Outline the structure
- Write your literature review
A good literature review doesn’t just summarize sources—it analyzes, synthesizes , and critically evaluates to give a clear picture of the state of knowledge on the subject.
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes

Table of contents
What is the purpose of a literature review, examples of literature reviews, step 1 – search for relevant literature, step 2 – evaluate and select sources, step 3 – identify themes, debates, and gaps, step 4 – outline your literature review’s structure, step 5 – write your literature review, free lecture slides, other interesting articles, frequently asked questions, introduction.
- Quick Run-through
- Step 1 & 2
When you write a thesis , dissertation , or research paper , you will likely have to conduct a literature review to situate your research within existing knowledge. The literature review gives you a chance to:
- Demonstrate your familiarity with the topic and its scholarly context
- Develop a theoretical framework and methodology for your research
- Position your work in relation to other researchers and theorists
- Show how your research addresses a gap or contributes to a debate
- Evaluate the current state of research and demonstrate your knowledge of the scholarly debates around your topic.
Writing literature reviews is a particularly important skill if you want to apply for graduate school or pursue a career in research. We’ve written a step-by-step guide that you can follow below.
Don't submit your assignments before you do this
The academic proofreading tool has been trained on 1000s of academic texts. Making it the most accurate and reliable proofreading tool for students. Free citation check included.

Try for free
Writing literature reviews can be quite challenging! A good starting point could be to look at some examples, depending on what kind of literature review you’d like to write.
- Example literature review #1: “Why Do People Migrate? A Review of the Theoretical Literature” ( Theoretical literature review about the development of economic migration theory from the 1950s to today.)
- Example literature review #2: “Literature review as a research methodology: An overview and guidelines” ( Methodological literature review about interdisciplinary knowledge acquisition and production.)
- Example literature review #3: “The Use of Technology in English Language Learning: A Literature Review” ( Thematic literature review about the effects of technology on language acquisition.)
- Example literature review #4: “Learners’ Listening Comprehension Difficulties in English Language Learning: A Literature Review” ( Chronological literature review about how the concept of listening skills has changed over time.)
You can also check out our templates with literature review examples and sample outlines at the links below.
Download Word doc Download Google doc
Before you begin searching for literature, you need a clearly defined topic .
If you are writing the literature review section of a dissertation or research paper, you will search for literature related to your research problem and questions .
Make a list of keywords
Start by creating a list of keywords related to your research question. Include each of the key concepts or variables you’re interested in, and list any synonyms and related terms. You can add to this list as you discover new keywords in the process of your literature search.
- Social media, Facebook, Instagram, Twitter, Snapchat, TikTok
- Body image, self-perception, self-esteem, mental health
- Generation Z, teenagers, adolescents, youth
Search for relevant sources
Use your keywords to begin searching for sources. Some useful databases to search for journals and articles include:
- Your university’s library catalogue
- Google Scholar
- Project Muse (humanities and social sciences)
- Medline (life sciences and biomedicine)
- EconLit (economics)
- Inspec (physics, engineering and computer science)
You can also use boolean operators to help narrow down your search.
Make sure to read the abstract to find out whether an article is relevant to your question. When you find a useful book or article, you can check the bibliography to find other relevant sources.
You likely won’t be able to read absolutely everything that has been written on your topic, so it will be necessary to evaluate which sources are most relevant to your research question.
For each publication, ask yourself:
- What question or problem is the author addressing?
- What are the key concepts and how are they defined?
- What are the key theories, models, and methods?
- Does the research use established frameworks or take an innovative approach?
- What are the results and conclusions of the study?
- How does the publication relate to other literature in the field? Does it confirm, add to, or challenge established knowledge?
- What are the strengths and weaknesses of the research?
Make sure the sources you use are credible , and make sure you read any landmark studies and major theories in your field of research.
You can use our template to summarize and evaluate sources you’re thinking about using. Click on either button below to download.
Take notes and cite your sources
As you read, you should also begin the writing process. Take notes that you can later incorporate into the text of your literature review.
It is important to keep track of your sources with citations to avoid plagiarism . It can be helpful to make an annotated bibliography , where you compile full citation information and write a paragraph of summary and analysis for each source. This helps you remember what you read and saves time later in the process.
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
To begin organizing your literature review’s argument and structure, be sure you understand the connections and relationships between the sources you’ve read. Based on your reading and notes, you can look for:
- Trends and patterns (in theory, method or results): do certain approaches become more or less popular over time?
- Themes: what questions or concepts recur across the literature?
- Debates, conflicts and contradictions: where do sources disagree?
- Pivotal publications: are there any influential theories or studies that changed the direction of the field?
- Gaps: what is missing from the literature? Are there weaknesses that need to be addressed?
This step will help you work out the structure of your literature review and (if applicable) show how your own research will contribute to existing knowledge.
- Most research has focused on young women.
- There is an increasing interest in the visual aspects of social media.
- But there is still a lack of robust research on highly visual platforms like Instagram and Snapchat—this is a gap that you could address in your own research.
There are various approaches to organizing the body of a literature review. Depending on the length of your literature review, you can combine several of these strategies (for example, your overall structure might be thematic, but each theme is discussed chronologically).
Chronological
The simplest approach is to trace the development of the topic over time. However, if you choose this strategy, be careful to avoid simply listing and summarizing sources in order.
Try to analyze patterns, turning points and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred.
If you have found some recurring central themes, you can organize your literature review into subsections that address different aspects of the topic.
For example, if you are reviewing literature about inequalities in migrant health outcomes, key themes might include healthcare policy, language barriers, cultural attitudes, legal status, and economic access.
Methodological
If you draw your sources from different disciplines or fields that use a variety of research methods , you might want to compare the results and conclusions that emerge from different approaches. For example:
- Look at what results have emerged in qualitative versus quantitative research
- Discuss how the topic has been approached by empirical versus theoretical scholarship
- Divide the literature into sociological, historical, and cultural sources
Theoretical
A literature review is often the foundation for a theoretical framework . You can use it to discuss various theories, models, and definitions of key concepts.
You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research.
Like any other academic text , your literature review should have an introduction , a main body, and a conclusion . What you include in each depends on the objective of your literature review.
The introduction should clearly establish the focus and purpose of the literature review.
Depending on the length of your literature review, you might want to divide the body into subsections. You can use a subheading for each theme, time period, or methodological approach.
As you write, you can follow these tips:
- Summarize and synthesize: give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: don’t just paraphrase other researchers — add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically evaluate: mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: use transition words and topic sentences to draw connections, comparisons and contrasts
In the conclusion, you should summarize the key findings you have taken from the literature and emphasize their significance.
When you’ve finished writing and revising your literature review, don’t forget to proofread thoroughly before submitting. Not a language expert? Check out Scribbr’s professional proofreading services !
This article has been adapted into lecture slides that you can use to teach your students about writing a literature review.
Scribbr slides are free to use, customize, and distribute for educational purposes.
Open Google Slides Download PowerPoint
If you want to know more about the research process , methodology , research bias , or statistics , make sure to check out some of our other articles with explanations and examples.
- Sampling methods
- Simple random sampling
- Stratified sampling
- Cluster sampling
- Likert scales
- Reproducibility
Statistics
- Null hypothesis
- Statistical power
- Probability distribution
- Effect size
- Poisson distribution
Research bias
- Optimism bias
- Cognitive bias
- Implicit bias
- Hawthorne effect
- Anchoring bias
- Explicit bias
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a thesis, dissertation , or research paper , in order to situate your work in relation to existing knowledge.
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarize yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
The literature review usually comes near the beginning of your thesis or dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
A literature review is a survey of credible sources on a topic, often used in dissertations , theses, and research papers . Literature reviews give an overview of knowledge on a subject, helping you identify relevant theories and methods, as well as gaps in existing research. Literature reviews are set up similarly to other academic texts , with an introduction , a main body, and a conclusion .
An annotated bibliography is a list of source references that has a short description (called an annotation ) for each of the sources. It is often assigned as part of the research process for a paper .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, September 11). How to Write a Literature Review | Guide, Examples, & Templates. Scribbr. Retrieved June 11, 2024, from https://www.scribbr.com/dissertation/literature-review/
Is this article helpful?
Shona McCombes
Other students also liked, what is a theoretical framework | guide to organizing, what is a research methodology | steps & tips, how to write a research proposal | examples & templates, get unlimited documents corrected.
✔ Free APA citation check included ✔ Unlimited document corrections ✔ Specialized in correcting academic texts

Get science-backed answers as you write with Paperpal's Research feature
What is a Literature Review? How to Write It (with Examples)
A literature review is a critical analysis and synthesis of existing research on a particular topic. It provides an overview of the current state of knowledge, identifies gaps, and highlights key findings in the literature. 1 The purpose of a literature review is to situate your own research within the context of existing scholarship, demonstrating your understanding of the topic and showing how your work contributes to the ongoing conversation in the field. Learning how to write a literature review is a critical tool for successful research. Your ability to summarize and synthesize prior research pertaining to a certain topic demonstrates your grasp on the topic of study, and assists in the learning process.
Table of Contents
- What is the purpose of literature review?
- a. Habitat Loss and Species Extinction:
- b. Range Shifts and Phenological Changes:
- c. Ocean Acidification and Coral Reefs:
- d. Adaptive Strategies and Conservation Efforts:
How to write a good literature review
- Choose a Topic and Define the Research Question:
- Decide on the Scope of Your Review:
- Select Databases for Searches:
- Conduct Searches and Keep Track:
- Review the Literature:
- Organize and Write Your Literature Review:
- How to write a literature review faster with Paperpal?
- Frequently asked questions
What is a literature review?
A well-conducted literature review demonstrates the researcher’s familiarity with the existing literature, establishes the context for their own research, and contributes to scholarly conversations on the topic. One of the purposes of a literature review is also to help researchers avoid duplicating previous work and ensure that their research is informed by and builds upon the existing body of knowledge.

What is the purpose of literature review?
A literature review serves several important purposes within academic and research contexts. Here are some key objectives and functions of a literature review: 2
1. Contextualizing the Research Problem: The literature review provides a background and context for the research problem under investigation. It helps to situate the study within the existing body of knowledge.
2. Identifying Gaps in Knowledge: By identifying gaps, contradictions, or areas requiring further research, the researcher can shape the research question and justify the significance of the study. This is crucial for ensuring that the new research contributes something novel to the field.
Find academic papers related to your research topic faster. Try Research on Paperpal
3. Understanding Theoretical and Conceptual Frameworks: Literature reviews help researchers gain an understanding of the theoretical and conceptual frameworks used in previous studies. This aids in the development of a theoretical framework for the current research.
4. Providing Methodological Insights: Another purpose of literature reviews is that it allows researchers to learn about the methodologies employed in previous studies. This can help in choosing appropriate research methods for the current study and avoiding pitfalls that others may have encountered.
5. Establishing Credibility: A well-conducted literature review demonstrates the researcher’s familiarity with existing scholarship, establishing their credibility and expertise in the field. It also helps in building a solid foundation for the new research.
6. Informing Hypotheses or Research Questions: The literature review guides the formulation of hypotheses or research questions by highlighting relevant findings and areas of uncertainty in existing literature.
Literature review example
Let’s delve deeper with a literature review example: Let’s say your literature review is about the impact of climate change on biodiversity. You might format your literature review into sections such as the effects of climate change on habitat loss and species extinction, phenological changes, and marine biodiversity. Each section would then summarize and analyze relevant studies in those areas, highlighting key findings and identifying gaps in the research. The review would conclude by emphasizing the need for further research on specific aspects of the relationship between climate change and biodiversity. The following literature review template provides a glimpse into the recommended literature review structure and content, demonstrating how research findings are organized around specific themes within a broader topic.
Literature Review on Climate Change Impacts on Biodiversity:
Climate change is a global phenomenon with far-reaching consequences, including significant impacts on biodiversity. This literature review synthesizes key findings from various studies:
a. Habitat Loss and Species Extinction:
Climate change-induced alterations in temperature and precipitation patterns contribute to habitat loss, affecting numerous species (Thomas et al., 2004). The review discusses how these changes increase the risk of extinction, particularly for species with specific habitat requirements.
b. Range Shifts and Phenological Changes:
Observations of range shifts and changes in the timing of biological events (phenology) are documented in response to changing climatic conditions (Parmesan & Yohe, 2003). These shifts affect ecosystems and may lead to mismatches between species and their resources.
c. Ocean Acidification and Coral Reefs:
The review explores the impact of climate change on marine biodiversity, emphasizing ocean acidification’s threat to coral reefs (Hoegh-Guldberg et al., 2007). Changes in pH levels negatively affect coral calcification, disrupting the delicate balance of marine ecosystems.
d. Adaptive Strategies and Conservation Efforts:
Recognizing the urgency of the situation, the literature review discusses various adaptive strategies adopted by species and conservation efforts aimed at mitigating the impacts of climate change on biodiversity (Hannah et al., 2007). It emphasizes the importance of interdisciplinary approaches for effective conservation planning.
Strengthen your literature review with factual insights. Try Research on Paperpal for free!
Writing a literature review involves summarizing and synthesizing existing research on a particular topic. A good literature review format should include the following elements.
Introduction: The introduction sets the stage for your literature review, providing context and introducing the main focus of your review.
- Opening Statement: Begin with a general statement about the broader topic and its significance in the field.
- Scope and Purpose: Clearly define the scope of your literature review. Explain the specific research question or objective you aim to address.
- Organizational Framework: Briefly outline the structure of your literature review, indicating how you will categorize and discuss the existing research.
- Significance of the Study: Highlight why your literature review is important and how it contributes to the understanding of the chosen topic.
- Thesis Statement: Conclude the introduction with a concise thesis statement that outlines the main argument or perspective you will develop in the body of the literature review.
Body: The body of the literature review is where you provide a comprehensive analysis of existing literature, grouping studies based on themes, methodologies, or other relevant criteria.
- Organize by Theme or Concept: Group studies that share common themes, concepts, or methodologies. Discuss each theme or concept in detail, summarizing key findings and identifying gaps or areas of disagreement.
- Critical Analysis: Evaluate the strengths and weaknesses of each study. Discuss the methodologies used, the quality of evidence, and the overall contribution of each work to the understanding of the topic.
- Synthesis of Findings: Synthesize the information from different studies to highlight trends, patterns, or areas of consensus in the literature.
- Identification of Gaps: Discuss any gaps or limitations in the existing research and explain how your review contributes to filling these gaps.
- Transition between Sections: Provide smooth transitions between different themes or concepts to maintain the flow of your literature review.
Write and Cite as you go with Paperpal Research. Start now for free.
Conclusion: The conclusion of your literature review should summarize the main findings, highlight the contributions of the review, and suggest avenues for future research.
- Summary of Key Findings: Recap the main findings from the literature and restate how they contribute to your research question or objective.
- Contributions to the Field: Discuss the overall contribution of your literature review to the existing knowledge in the field.
- Implications and Applications: Explore the practical implications of the findings and suggest how they might impact future research or practice.
- Recommendations for Future Research: Identify areas that require further investigation and propose potential directions for future research in the field.
- Final Thoughts: Conclude with a final reflection on the importance of your literature review and its relevance to the broader academic community.
Conducting a literature review
Conducting a literature review is an essential step in research that involves reviewing and analyzing existing literature on a specific topic. It’s important to know how to do a literature review effectively, so here are the steps to follow: 1
Choose a Topic and Define the Research Question:
- Select a topic that is relevant to your field of study.
- Clearly define your research question or objective. Determine what specific aspect of the topic do you want to explore?
Decide on the Scope of Your Review:
- Determine the timeframe for your literature review. Are you focusing on recent developments, or do you want a historical overview?
- Consider the geographical scope. Is your review global, or are you focusing on a specific region?
- Define the inclusion and exclusion criteria. What types of sources will you include? Are there specific types of studies or publications you will exclude?
Select Databases for Searches:
- Identify relevant databases for your field. Examples include PubMed, IEEE Xplore, Scopus, Web of Science, and Google Scholar.
- Consider searching in library catalogs, institutional repositories, and specialized databases related to your topic.
Conduct Searches and Keep Track:
- Develop a systematic search strategy using keywords, Boolean operators (AND, OR, NOT), and other search techniques.
- Record and document your search strategy for transparency and replicability.
- Keep track of the articles, including publication details, abstracts, and links. Use citation management tools like EndNote, Zotero, or Mendeley to organize your references.
Review the Literature:
- Evaluate the relevance and quality of each source. Consider the methodology, sample size, and results of studies.
- Organize the literature by themes or key concepts. Identify patterns, trends, and gaps in the existing research.
- Summarize key findings and arguments from each source. Compare and contrast different perspectives.
- Identify areas where there is a consensus in the literature and where there are conflicting opinions.
- Provide critical analysis and synthesis of the literature. What are the strengths and weaknesses of existing research?
Organize and Write Your Literature Review:
- Literature review outline should be based on themes, chronological order, or methodological approaches.
- Write a clear and coherent narrative that synthesizes the information gathered.
- Use proper citations for each source and ensure consistency in your citation style (APA, MLA, Chicago, etc.).
- Conclude your literature review by summarizing key findings, identifying gaps, and suggesting areas for future research.
Whether you’re exploring a new research field or finding new angles to develop an existing topic, sifting through hundreds of papers can take more time than you have to spare. But what if you could find science-backed insights with verified citations in seconds? That’s the power of Paperpal’s new Research feature!
How to write a literature review faster with Paperpal?
Paperpal, an AI writing assistant, integrates powerful academic search capabilities within its writing platform. With the Research feature, you get 100% factual insights, with citations backed by 250M+ verified research articles, directly within your writing interface with the option to save relevant references in your Citation Library. By eliminating the need to switch tabs to find answers to all your research questions, Paperpal saves time and helps you stay focused on your writing.
Here’s how to use the Research feature:
- Ask a question: Get started with a new document on paperpal.com. Click on the “Research” feature and type your question in plain English. Paperpal will scour over 250 million research articles, including conference papers and preprints, to provide you with accurate insights and citations.
- Review and Save: Paperpal summarizes the information, while citing sources and listing relevant reads. You can quickly scan the results to identify relevant references and save these directly to your built-in citations library for later access.
- Cite with Confidence: Paperpal makes it easy to incorporate relevant citations and references into your writing, ensuring your arguments are well-supported by credible sources. This translates to a polished, well-researched literature review.
The literature review sample and detailed advice on writing and conducting a review will help you produce a well-structured report. But remember that a good literature review is an ongoing process, and it may be necessary to revisit and update it as your research progresses. By combining effortless research with an easy citation process, Paperpal Research streamlines the literature review process and empowers you to write faster and with more confidence. Try Paperpal Research now and see for yourself.
Frequently asked questions
A literature review is a critical and comprehensive analysis of existing literature (published and unpublished works) on a specific topic or research question and provides a synthesis of the current state of knowledge in a particular field. A well-conducted literature review is crucial for researchers to build upon existing knowledge, avoid duplication of efforts, and contribute to the advancement of their field. It also helps researchers situate their work within a broader context and facilitates the development of a sound theoretical and conceptual framework for their studies.
Literature review is a crucial component of research writing, providing a solid background for a research paper’s investigation. The aim is to keep professionals up to date by providing an understanding of ongoing developments within a specific field, including research methods, and experimental techniques used in that field, and present that knowledge in the form of a written report. Also, the depth and breadth of the literature review emphasizes the credibility of the scholar in his or her field.
Before writing a literature review, it’s essential to undertake several preparatory steps to ensure that your review is well-researched, organized, and focused. This includes choosing a topic of general interest to you and doing exploratory research on that topic, writing an annotated bibliography, and noting major points, especially those that relate to the position you have taken on the topic.
Literature reviews and academic research papers are essential components of scholarly work but serve different purposes within the academic realm. 3 A literature review aims to provide a foundation for understanding the current state of research on a particular topic, identify gaps or controversies, and lay the groundwork for future research. Therefore, it draws heavily from existing academic sources, including books, journal articles, and other scholarly publications. In contrast, an academic research paper aims to present new knowledge, contribute to the academic discourse, and advance the understanding of a specific research question. Therefore, it involves a mix of existing literature (in the introduction and literature review sections) and original data or findings obtained through research methods.
Literature reviews are essential components of academic and research papers, and various strategies can be employed to conduct them effectively. If you want to know how to write a literature review for a research paper, here are four common approaches that are often used by researchers. Chronological Review: This strategy involves organizing the literature based on the chronological order of publication. It helps to trace the development of a topic over time, showing how ideas, theories, and research have evolved. Thematic Review: Thematic reviews focus on identifying and analyzing themes or topics that cut across different studies. Instead of organizing the literature chronologically, it is grouped by key themes or concepts, allowing for a comprehensive exploration of various aspects of the topic. Methodological Review: This strategy involves organizing the literature based on the research methods employed in different studies. It helps to highlight the strengths and weaknesses of various methodologies and allows the reader to evaluate the reliability and validity of the research findings. Theoretical Review: A theoretical review examines the literature based on the theoretical frameworks used in different studies. This approach helps to identify the key theories that have been applied to the topic and assess their contributions to the understanding of the subject. It’s important to note that these strategies are not mutually exclusive, and a literature review may combine elements of more than one approach. The choice of strategy depends on the research question, the nature of the literature available, and the goals of the review. Additionally, other strategies, such as integrative reviews or systematic reviews, may be employed depending on the specific requirements of the research.
The literature review format can vary depending on the specific publication guidelines. However, there are some common elements and structures that are often followed. Here is a general guideline for the format of a literature review: Introduction: Provide an overview of the topic. Define the scope and purpose of the literature review. State the research question or objective. Body: Organize the literature by themes, concepts, or chronology. Critically analyze and evaluate each source. Discuss the strengths and weaknesses of the studies. Highlight any methodological limitations or biases. Identify patterns, connections, or contradictions in the existing research. Conclusion: Summarize the key points discussed in the literature review. Highlight the research gap. Address the research question or objective stated in the introduction. Highlight the contributions of the review and suggest directions for future research.
Both annotated bibliographies and literature reviews involve the examination of scholarly sources. While annotated bibliographies focus on individual sources with brief annotations, literature reviews provide a more in-depth, integrated, and comprehensive analysis of existing literature on a specific topic. The key differences are as follows:
| Annotated Bibliography | Literature Review | |
| Purpose | List of citations of books, articles, and other sources with a brief description (annotation) of each source. | Comprehensive and critical analysis of existing literature on a specific topic. |
| Focus | Summary and evaluation of each source, including its relevance, methodology, and key findings. | Provides an overview of the current state of knowledge on a particular subject and identifies gaps, trends, and patterns in existing literature. |
| Structure | Each citation is followed by a concise paragraph (annotation) that describes the source’s content, methodology, and its contribution to the topic. | The literature review is organized thematically or chronologically and involves a synthesis of the findings from different sources to build a narrative or argument. |
| Length | Typically 100-200 words | Length of literature review ranges from a few pages to several chapters |
| Independence | Each source is treated separately, with less emphasis on synthesizing the information across sources. | The writer synthesizes information from multiple sources to present a cohesive overview of the topic. |
References
- Denney, A. S., & Tewksbury, R. (2013). How to write a literature review. Journal of criminal justice education , 24 (2), 218-234.
- Pan, M. L. (2016). Preparing literature reviews: Qualitative and quantitative approaches . Taylor & Francis.
- Cantero, C. (2019). How to write a literature review. San José State University Writing Center .
Paperpal is an AI writing assistant that help academics write better, faster with real-time suggestions for in-depth language and grammar correction. Trained on millions of research manuscripts enhanced by professional academic editors, Paperpal delivers human precision at machine speed.
Try it for free or upgrade to Paperpal Prime , which unlocks unlimited access to premium features like academic translation, paraphrasing, contextual synonyms, consistency checks and more. It’s like always having a professional academic editor by your side! Go beyond limitations and experience the future of academic writing. Get Paperpal Prime now at just US$19 a month!
Related Reads:
- Empirical Research: A Comprehensive Guide for Academics
- How to Write a Scientific Paper in 10 Steps
- How Long Should a Chapter Be?
- How to Use Paperpal to Generate Emails & Cover Letters?
6 Tips for Post-Doc Researchers to Take Their Career to the Next Level
Self-plagiarism in research: what it is and how to avoid it, you may also like, addressing peer review feedback and mastering manuscript revisions..., how paperpal can boost comprehension and foster interdisciplinary..., what is the importance of a concept paper..., how to write the first draft of a..., mla works cited page: format, template & examples, how to ace grant writing for research funding..., powerful academic phrases to improve your essay writing , how to write a high-quality conference paper, how paperpal’s research feature helps you develop and..., how paperpal is enhancing academic productivity and accelerating....
Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Writing a Literature Review

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays). When we say “literature review” or refer to “the literature,” we are talking about the research ( scholarship ) in a given field. You will often see the terms “the research,” “the scholarship,” and “the literature” used mostly interchangeably.
Where, when, and why would I write a lit review?
There are a number of different situations where you might write a literature review, each with slightly different expectations; different disciplines, too, have field-specific expectations for what a literature review is and does. For instance, in the humanities, authors might include more overt argumentation and interpretation of source material in their literature reviews, whereas in the sciences, authors are more likely to report study designs and results in their literature reviews; these differences reflect these disciplines’ purposes and conventions in scholarship. You should always look at examples from your own discipline and talk to professors or mentors in your field to be sure you understand your discipline’s conventions, for literature reviews as well as for any other genre.
A literature review can be a part of a research paper or scholarly article, usually falling after the introduction and before the research methods sections. In these cases, the lit review just needs to cover scholarship that is important to the issue you are writing about; sometimes it will also cover key sources that informed your research methodology.
Lit reviews can also be standalone pieces, either as assignments in a class or as publications. In a class, a lit review may be assigned to help students familiarize themselves with a topic and with scholarship in their field, get an idea of the other researchers working on the topic they’re interested in, find gaps in existing research in order to propose new projects, and/or develop a theoretical framework and methodology for later research. As a publication, a lit review usually is meant to help make other scholars’ lives easier by collecting and summarizing, synthesizing, and analyzing existing research on a topic. This can be especially helpful for students or scholars getting into a new research area, or for directing an entire community of scholars toward questions that have not yet been answered.
What are the parts of a lit review?
Most lit reviews use a basic introduction-body-conclusion structure; if your lit review is part of a larger paper, the introduction and conclusion pieces may be just a few sentences while you focus most of your attention on the body. If your lit review is a standalone piece, the introduction and conclusion take up more space and give you a place to discuss your goals, research methods, and conclusions separately from where you discuss the literature itself.
Introduction:
- An introductory paragraph that explains what your working topic and thesis is
- A forecast of key topics or texts that will appear in the review
- Potentially, a description of how you found sources and how you analyzed them for inclusion and discussion in the review (more often found in published, standalone literature reviews than in lit review sections in an article or research paper)
- Summarize and synthesize: Give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: Don’t just paraphrase other researchers – add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically Evaluate: Mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: Use transition words and topic sentence to draw connections, comparisons, and contrasts.
Conclusion:
- Summarize the key findings you have taken from the literature and emphasize their significance
- Connect it back to your primary research question
How should I organize my lit review?
Lit reviews can take many different organizational patterns depending on what you are trying to accomplish with the review. Here are some examples:
- Chronological : The simplest approach is to trace the development of the topic over time, which helps familiarize the audience with the topic (for instance if you are introducing something that is not commonly known in your field). If you choose this strategy, be careful to avoid simply listing and summarizing sources in order. Try to analyze the patterns, turning points, and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred (as mentioned previously, this may not be appropriate in your discipline — check with a teacher or mentor if you’re unsure).
- Thematic : If you have found some recurring central themes that you will continue working with throughout your piece, you can organize your literature review into subsections that address different aspects of the topic. For example, if you are reviewing literature about women and religion, key themes can include the role of women in churches and the religious attitude towards women.
- Qualitative versus quantitative research
- Empirical versus theoretical scholarship
- Divide the research by sociological, historical, or cultural sources
- Theoretical : In many humanities articles, the literature review is the foundation for the theoretical framework. You can use it to discuss various theories, models, and definitions of key concepts. You can argue for the relevance of a specific theoretical approach or combine various theorical concepts to create a framework for your research.
What are some strategies or tips I can use while writing my lit review?
Any lit review is only as good as the research it discusses; make sure your sources are well-chosen and your research is thorough. Don’t be afraid to do more research if you discover a new thread as you’re writing. More info on the research process is available in our "Conducting Research" resources .
As you’re doing your research, create an annotated bibliography ( see our page on the this type of document ). Much of the information used in an annotated bibliography can be used also in a literature review, so you’ll be not only partially drafting your lit review as you research, but also developing your sense of the larger conversation going on among scholars, professionals, and any other stakeholders in your topic.
Usually you will need to synthesize research rather than just summarizing it. This means drawing connections between sources to create a picture of the scholarly conversation on a topic over time. Many student writers struggle to synthesize because they feel they don’t have anything to add to the scholars they are citing; here are some strategies to help you:
- It often helps to remember that the point of these kinds of syntheses is to show your readers how you understand your research, to help them read the rest of your paper.
- Writing teachers often say synthesis is like hosting a dinner party: imagine all your sources are together in a room, discussing your topic. What are they saying to each other?
- Look at the in-text citations in each paragraph. Are you citing just one source for each paragraph? This usually indicates summary only. When you have multiple sources cited in a paragraph, you are more likely to be synthesizing them (not always, but often
- Read more about synthesis here.
The most interesting literature reviews are often written as arguments (again, as mentioned at the beginning of the page, this is discipline-specific and doesn’t work for all situations). Often, the literature review is where you can establish your research as filling a particular gap or as relevant in a particular way. You have some chance to do this in your introduction in an article, but the literature review section gives a more extended opportunity to establish the conversation in the way you would like your readers to see it. You can choose the intellectual lineage you would like to be part of and whose definitions matter most to your thinking (mostly humanities-specific, but this goes for sciences as well). In addressing these points, you argue for your place in the conversation, which tends to make the lit review more compelling than a simple reporting of other sources.
The Sheridan Libraries
- Write a Literature Review
- Sheridan Libraries
- Find This link opens in a new window
- Evaluate This link opens in a new window
What Will You Do Differently?
Please help your librarians by filling out this two-minute survey of today's class session..
Professor, this one's for you .
Introduction
Literature reviews take time. here is some general information to know before you start. .
- VIDEO -- This video is a great overview of the entire process. (2020; North Carolina State University Libraries) --The transcript is included --This is for everyone; ignore the mention of "graduate students" --9.5 minutes, and every second is important
- OVERVIEW -- Read this page from Purdue's OWL. It's not long, and gives some tips to fill in what you just learned from the video.
- NOT A RESEARCH ARTICLE -- A literature review follows a different style, format, and structure from a research article.
| Reports on the work of others. | Reports on original research. | |
| To examine and evaluate previous literature. | To test a hypothesis and/or make an argument. May include a short literature review to introduce the subject. |
Steps to Completing a Literature Review

- Next: Find >>
- Last Updated: Sep 26, 2023 10:25 AM
- URL: https://guides.library.jhu.edu/lit-review
How to Write a Literature Review
What is a literature review.
- What Is the Literature
- Writing the Review
A literature review is much more than an annotated bibliography or a list of separate reviews of articles and books. It is a critical, analytical summary and synthesis of the current knowledge of a topic. Thus it should compare and relate different theories, findings, etc, rather than just summarize them individually. In addition, it should have a particular focus or theme to organize the review. It does not have to be an exhaustive account of everything published on the topic, but it should discuss all the significant academic literature and other relevant sources important for that focus.
This is meant to be a general guide to writing a literature review: ways to structure one, what to include, how it supplements other research. For more specific help on writing a review, and especially for help on finding the literature to review, sign up for a Personal Research Session .
The specific organization of a literature review depends on the type and purpose of the review, as well as on the specific field or topic being reviewed. But in general, it is a relatively brief but thorough exploration of past and current work on a topic. Rather than a chronological listing of previous work, though, literature reviews are usually organized thematically, such as different theoretical approaches, methodologies, or specific issues or concepts involved in the topic. A thematic organization makes it much easier to examine contrasting perspectives, theoretical approaches, methodologies, findings, etc, and to analyze the strengths and weaknesses of, and point out any gaps in, previous research. And this is the heart of what a literature review is about. A literature review may offer new interpretations, theoretical approaches, or other ideas; if it is part of a research proposal or report it should demonstrate the relationship of the proposed or reported research to others' work; but whatever else it does, it must provide a critical overview of the current state of research efforts.
Literature reviews are common and very important in the sciences and social sciences. They are less common and have a less important role in the humanities, but they do have a place, especially stand-alone reviews.
Types of Literature Reviews
There are different types of literature reviews, and different purposes for writing a review, but the most common are:
- Stand-alone literature review articles . These provide an overview and analysis of the current state of research on a topic or question. The goal is to evaluate and compare previous research on a topic to provide an analysis of what is currently known, and also to reveal controversies, weaknesses, and gaps in current work, thus pointing to directions for future research. You can find examples published in any number of academic journals, but there is a series of Annual Reviews of *Subject* which are specifically devoted to literature review articles. Writing a stand-alone review is often an effective way to get a good handle on a topic and to develop ideas for your own research program. For example, contrasting theoretical approaches or conflicting interpretations of findings can be the basis of your research project: can you find evidence supporting one interpretation against another, or can you propose an alternative interpretation that overcomes their limitations?
- Part of a research proposal . This could be a proposal for a PhD dissertation, a senior thesis, or a class project. It could also be a submission for a grant. The literature review, by pointing out the current issues and questions concerning a topic, is a crucial part of demonstrating how your proposed research will contribute to the field, and thus of convincing your thesis committee to allow you to pursue the topic of your interest or a funding agency to pay for your research efforts.
- Part of a research report . When you finish your research and write your thesis or paper to present your findings, it should include a literature review to provide the context to which your work is a contribution. Your report, in addition to detailing the methods, results, etc. of your research, should show how your work relates to others' work.
A literature review for a research report is often a revision of the review for a research proposal, which can be a revision of a stand-alone review. Each revision should be a fairly extensive revision. With the increased knowledge of and experience in the topic as you proceed, your understanding of the topic will increase. Thus, you will be in a better position to analyze and critique the literature. In addition, your focus will change as you proceed in your research. Some areas of the literature you initially reviewed will be marginal or irrelevant for your eventual research, and you will need to explore other areas more thoroughly.
Examples of Literature Reviews
See the series of Annual Reviews of *Subject* which are specifically devoted to literature review articles to find many examples of stand-alone literature reviews in the biomedical, physical, and social sciences.
Research report articles vary in how they are organized, but a common general structure is to have sections such as:
- Abstract - Brief summary of the contents of the article
- Introduction - A explanation of the purpose of the study, a statement of the research question(s) the study intends to address
- Literature review - A critical assessment of the work done so far on this topic, to show how the current study relates to what has already been done
- Methods - How the study was carried out (e.g. instruments or equipment, procedures, methods to gather and analyze data)
- Results - What was found in the course of the study
- Discussion - What do the results mean
- Conclusion - State the conclusions and implications of the results, and discuss how it relates to the work reviewed in the literature review; also, point to directions for further work in the area
Here are some articles that illustrate variations on this theme. There is no need to read the entire articles (unless the contents interest you); just quickly browse through to see the sections, and see how each section is introduced and what is contained in them.
The Determinants of Undergraduate Grade Point Average: The Relative Importance of Family Background, High School Resources, and Peer Group Effects , in The Journal of Human Resources , v. 34 no. 2 (Spring 1999), p. 268-293.
This article has a standard breakdown of sections:
- Introduction
- Literature Review
- Some discussion sections
First Encounters of the Bureaucratic Kind: Early Freshman Experiences with a Campus Bureaucracy , in The Journal of Higher Education , v. 67 no. 6 (Nov-Dec 1996), p. 660-691.
This one does not have a section specifically labeled as a "literature review" or "review of the literature," but the first few sections cite a long list of other sources discussing previous research in the area before the authors present their own study they are reporting.
- Next: What Is the Literature >>
- Last Updated: Jan 11, 2024 9:48 AM
- URL: https://libguides.wesleyan.edu/litreview
- UConn Library
- Literature Review: The What, Why and How-to Guide
- Introduction
Literature Review: The What, Why and How-to Guide — Introduction
- Getting Started
- How to Pick a Topic
- Strategies to Find Sources
- Evaluating Sources & Lit. Reviews
- Tips for Writing Literature Reviews
- Writing Literature Review: Useful Sites
- Citation Resources
- Other Academic Writings
What are Literature Reviews?
So, what is a literature review? "A literature review is an account of what has been published on a topic by accredited scholars and researchers. In writing the literature review, your purpose is to convey to your reader what knowledge and ideas have been established on a topic, and what their strengths and weaknesses are. As a piece of writing, the literature review must be defined by a guiding concept (e.g., your research objective, the problem or issue you are discussing, or your argumentative thesis). It is not just a descriptive list of the material available, or a set of summaries." Taylor, D. The literature review: A few tips on conducting it . University of Toronto Health Sciences Writing Centre.
Goals of Literature Reviews
What are the goals of creating a Literature Review? A literature could be written to accomplish different aims:
- To develop a theory or evaluate an existing theory
- To summarize the historical or existing state of a research topic
- Identify a problem in a field of research
Baumeister, R. F., & Leary, M. R. (1997). Writing narrative literature reviews . Review of General Psychology , 1 (3), 311-320.
What kinds of sources require a Literature Review?
- A research paper assigned in a course
- A thesis or dissertation
- A grant proposal
- An article intended for publication in a journal
All these instances require you to collect what has been written about your research topic so that you can demonstrate how your own research sheds new light on the topic.
Types of Literature Reviews
What kinds of literature reviews are written?
Narrative review: The purpose of this type of review is to describe the current state of the research on a specific topic/research and to offer a critical analysis of the literature reviewed. Studies are grouped by research/theoretical categories, and themes and trends, strengths and weakness, and gaps are identified. The review ends with a conclusion section which summarizes the findings regarding the state of the research of the specific study, the gaps identify and if applicable, explains how the author's research will address gaps identify in the review and expand the knowledge on the topic reviewed.
- Example : Predictors and Outcomes of U.S. Quality Maternity Leave: A Review and Conceptual Framework: 10.1177/08948453211037398
Systematic review : "The authors of a systematic review use a specific procedure to search the research literature, select the studies to include in their review, and critically evaluate the studies they find." (p. 139). Nelson, L. K. (2013). Research in Communication Sciences and Disorders . Plural Publishing.
- Example : The effect of leave policies on increasing fertility: a systematic review: 10.1057/s41599-022-01270-w
Meta-analysis : "Meta-analysis is a method of reviewing research findings in a quantitative fashion by transforming the data from individual studies into what is called an effect size and then pooling and analyzing this information. The basic goal in meta-analysis is to explain why different outcomes have occurred in different studies." (p. 197). Roberts, M. C., & Ilardi, S. S. (2003). Handbook of Research Methods in Clinical Psychology . Blackwell Publishing.
- Example : Employment Instability and Fertility in Europe: A Meta-Analysis: 10.1215/00703370-9164737
Meta-synthesis : "Qualitative meta-synthesis is a type of qualitative study that uses as data the findings from other qualitative studies linked by the same or related topic." (p.312). Zimmer, L. (2006). Qualitative meta-synthesis: A question of dialoguing with texts . Journal of Advanced Nursing , 53 (3), 311-318.
- Example : Women’s perspectives on career successes and barriers: A qualitative meta-synthesis: 10.1177/05390184221113735
Literature Reviews in the Health Sciences
- UConn Health subject guide on systematic reviews Explanation of the different review types used in health sciences literature as well as tools to help you find the right review type
- << Previous: Getting Started
- Next: How to Pick a Topic >>
- Last Updated: Sep 21, 2022 2:16 PM
- URL: https://guides.lib.uconn.edu/literaturereview
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Dissertation
- What is a Literature Review? | Guide, Template, & Examples
What is a Literature Review? | Guide, Template, & Examples
Published on 22 February 2022 by Shona McCombes . Revised on 7 June 2022.
What is a literature review? A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research.
There are five key steps to writing a literature review:
- Search for relevant literature
- Evaluate sources
- Identify themes, debates and gaps
- Outline the structure
- Write your literature review
A good literature review doesn’t just summarise sources – it analyses, synthesises, and critically evaluates to give a clear picture of the state of knowledge on the subject.
Instantly correct all language mistakes in your text
Be assured that you'll submit flawless writing. Upload your document to correct all your mistakes.

Table of contents
Why write a literature review, examples of literature reviews, step 1: search for relevant literature, step 2: evaluate and select sources, step 3: identify themes, debates and gaps, step 4: outline your literature review’s structure, step 5: write your literature review, frequently asked questions about literature reviews, introduction.
- Quick Run-through
- Step 1 & 2
When you write a dissertation or thesis, you will have to conduct a literature review to situate your research within existing knowledge. The literature review gives you a chance to:
- Demonstrate your familiarity with the topic and scholarly context
- Develop a theoretical framework and methodology for your research
- Position yourself in relation to other researchers and theorists
- Show how your dissertation addresses a gap or contributes to a debate
You might also have to write a literature review as a stand-alone assignment. In this case, the purpose is to evaluate the current state of research and demonstrate your knowledge of scholarly debates around a topic.
The content will look slightly different in each case, but the process of conducting a literature review follows the same steps. We’ve written a step-by-step guide that you can follow below.
The only proofreading tool specialized in correcting academic writing
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Correct my document today
Writing literature reviews can be quite challenging! A good starting point could be to look at some examples, depending on what kind of literature review you’d like to write.
- Example literature review #1: “Why Do People Migrate? A Review of the Theoretical Literature” ( Theoretical literature review about the development of economic migration theory from the 1950s to today.)
- Example literature review #2: “Literature review as a research methodology: An overview and guidelines” ( Methodological literature review about interdisciplinary knowledge acquisition and production.)
- Example literature review #3: “The Use of Technology in English Language Learning: A Literature Review” ( Thematic literature review about the effects of technology on language acquisition.)
- Example literature review #4: “Learners’ Listening Comprehension Difficulties in English Language Learning: A Literature Review” ( Chronological literature review about how the concept of listening skills has changed over time.)
You can also check out our templates with literature review examples and sample outlines at the links below.
Download Word doc Download Google doc
Before you begin searching for literature, you need a clearly defined topic .
If you are writing the literature review section of a dissertation or research paper, you will search for literature related to your research objectives and questions .
If you are writing a literature review as a stand-alone assignment, you will have to choose a focus and develop a central question to direct your search. Unlike a dissertation research question, this question has to be answerable without collecting original data. You should be able to answer it based only on a review of existing publications.
Make a list of keywords
Start by creating a list of keywords related to your research topic. Include each of the key concepts or variables you’re interested in, and list any synonyms and related terms. You can add to this list if you discover new keywords in the process of your literature search.
- Social media, Facebook, Instagram, Twitter, Snapchat, TikTok
- Body image, self-perception, self-esteem, mental health
- Generation Z, teenagers, adolescents, youth
Search for relevant sources
Use your keywords to begin searching for sources. Some databases to search for journals and articles include:
- Your university’s library catalogue
- Google Scholar
- Project Muse (humanities and social sciences)
- Medline (life sciences and biomedicine)
- EconLit (economics)
- Inspec (physics, engineering and computer science)
You can use boolean operators to help narrow down your search:
Read the abstract to find out whether an article is relevant to your question. When you find a useful book or article, you can check the bibliography to find other relevant sources.
To identify the most important publications on your topic, take note of recurring citations. If the same authors, books or articles keep appearing in your reading, make sure to seek them out.
You probably won’t be able to read absolutely everything that has been written on the topic – you’ll have to evaluate which sources are most relevant to your questions.
For each publication, ask yourself:
- What question or problem is the author addressing?
- What are the key concepts and how are they defined?
- What are the key theories, models and methods? Does the research use established frameworks or take an innovative approach?
- What are the results and conclusions of the study?
- How does the publication relate to other literature in the field? Does it confirm, add to, or challenge established knowledge?
- How does the publication contribute to your understanding of the topic? What are its key insights and arguments?
- What are the strengths and weaknesses of the research?
Make sure the sources you use are credible, and make sure you read any landmark studies and major theories in your field of research.
You can find out how many times an article has been cited on Google Scholar – a high citation count means the article has been influential in the field, and should certainly be included in your literature review.
The scope of your review will depend on your topic and discipline: in the sciences you usually only review recent literature, but in the humanities you might take a long historical perspective (for example, to trace how a concept has changed in meaning over time).
Remember that you can use our template to summarise and evaluate sources you’re thinking about using!
Take notes and cite your sources
As you read, you should also begin the writing process. Take notes that you can later incorporate into the text of your literature review.
It’s important to keep track of your sources with references to avoid plagiarism . It can be helpful to make an annotated bibliography, where you compile full reference information and write a paragraph of summary and analysis for each source. This helps you remember what you read and saves time later in the process.
You can use our free APA Reference Generator for quick, correct, consistent citations.
To begin organising your literature review’s argument and structure, you need to understand the connections and relationships between the sources you’ve read. Based on your reading and notes, you can look for:
- Trends and patterns (in theory, method or results): do certain approaches become more or less popular over time?
- Themes: what questions or concepts recur across the literature?
- Debates, conflicts and contradictions: where do sources disagree?
- Pivotal publications: are there any influential theories or studies that changed the direction of the field?
- Gaps: what is missing from the literature? Are there weaknesses that need to be addressed?
This step will help you work out the structure of your literature review and (if applicable) show how your own research will contribute to existing knowledge.
- Most research has focused on young women.
- There is an increasing interest in the visual aspects of social media.
- But there is still a lack of robust research on highly-visual platforms like Instagram and Snapchat – this is a gap that you could address in your own research.
There are various approaches to organising the body of a literature review. You should have a rough idea of your strategy before you start writing.
Depending on the length of your literature review, you can combine several of these strategies (for example, your overall structure might be thematic, but each theme is discussed chronologically).
Chronological
The simplest approach is to trace the development of the topic over time. However, if you choose this strategy, be careful to avoid simply listing and summarising sources in order.
Try to analyse patterns, turning points and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred.
If you have found some recurring central themes, you can organise your literature review into subsections that address different aspects of the topic.
For example, if you are reviewing literature about inequalities in migrant health outcomes, key themes might include healthcare policy, language barriers, cultural attitudes, legal status, and economic access.
Methodological
If you draw your sources from different disciplines or fields that use a variety of research methods , you might want to compare the results and conclusions that emerge from different approaches. For example:
- Look at what results have emerged in qualitative versus quantitative research
- Discuss how the topic has been approached by empirical versus theoretical scholarship
- Divide the literature into sociological, historical, and cultural sources
Theoretical
A literature review is often the foundation for a theoretical framework . You can use it to discuss various theories, models, and definitions of key concepts.
You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research.
Like any other academic text, your literature review should have an introduction , a main body, and a conclusion . What you include in each depends on the objective of your literature review.
The introduction should clearly establish the focus and purpose of the literature review.
If you are writing the literature review as part of your dissertation or thesis, reiterate your central problem or research question and give a brief summary of the scholarly context. You can emphasise the timeliness of the topic (“many recent studies have focused on the problem of x”) or highlight a gap in the literature (“while there has been much research on x, few researchers have taken y into consideration”).
Depending on the length of your literature review, you might want to divide the body into subsections. You can use a subheading for each theme, time period, or methodological approach.
As you write, make sure to follow these tips:
- Summarise and synthesise: give an overview of the main points of each source and combine them into a coherent whole.
- Analyse and interpret: don’t just paraphrase other researchers – add your own interpretations, discussing the significance of findings in relation to the literature as a whole.
- Critically evaluate: mention the strengths and weaknesses of your sources.
- Write in well-structured paragraphs: use transitions and topic sentences to draw connections, comparisons and contrasts.
In the conclusion, you should summarise the key findings you have taken from the literature and emphasise their significance.
If the literature review is part of your dissertation or thesis, reiterate how your research addresses gaps and contributes new knowledge, or discuss how you have drawn on existing theories and methods to build a framework for your research. This can lead directly into your methodology section.
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a dissertation , thesis, research paper , or proposal .
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarise yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
The literature review usually comes near the beginning of your dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
McCombes, S. (2022, June 07). What is a Literature Review? | Guide, Template, & Examples. Scribbr. Retrieved 11 June 2024, from https://www.scribbr.co.uk/thesis-dissertation/literature-review/
Is this article helpful?
Shona McCombes
Other students also liked, how to write a dissertation proposal | a step-by-step guide, what is a theoretical framework | a step-by-step guide, what is a research methodology | steps & tips.
- Resources Home 🏠
- Try SciSpace Copilot
- Search research papers
- Add Copilot Extension
- Try AI Detector
- Try Paraphraser
- Try Citation Generator
- April Papers
- June Papers
- July Papers

How To Write A Literature Review - A Complete Guide

Table of Contents
A literature review is much more than just another section in your research paper. It forms the very foundation of your research. It is a formal piece of writing where you analyze the existing theoretical framework, principles, and assumptions and use that as a base to shape your approach to the research question.
Curating and drafting a solid literature review section not only lends more credibility to your research paper but also makes your research tighter and better focused. But, writing literature reviews is a difficult task. It requires extensive reading, plus you have to consider market trends and technological and political changes, which tend to change in the blink of an eye.
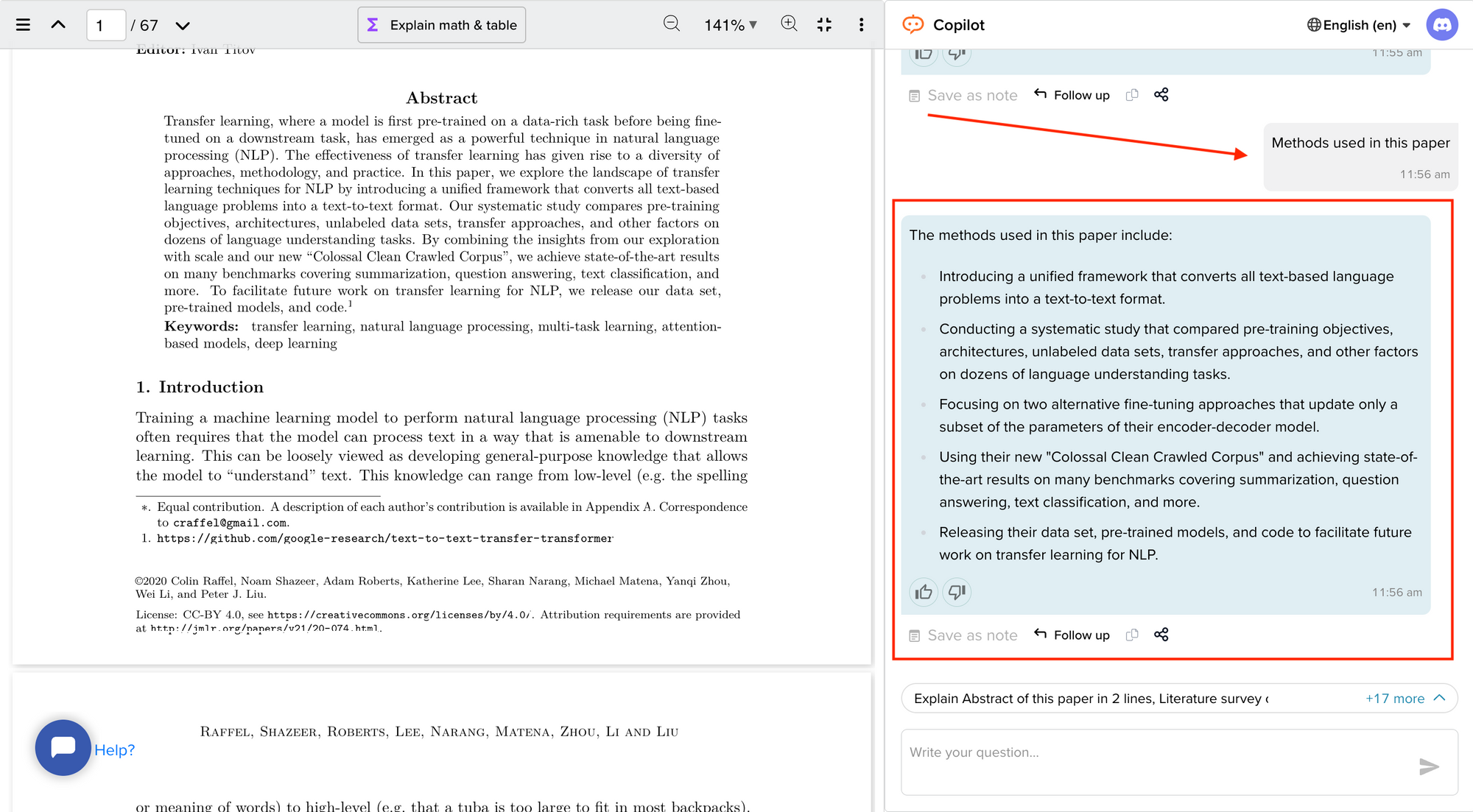
Now streamline your literature review process with the help of SciSpace Copilot. With this AI research assistant, you can efficiently synthesize and analyze a vast amount of information, identify key themes and trends, and uncover gaps in the existing research. Get real-time explanations, summaries, and answers to your questions for the paper you're reviewing, making navigating and understanding the complex literature landscape easier.
In this comprehensive guide, we will explore everything from the definition of a literature review, its appropriate length, various types of literature reviews, and how to write one.
What is a literature review?
A literature review is a collation of survey, research, critical evaluation, and assessment of the existing literature in a preferred domain.
Eminent researcher and academic Arlene Fink, in her book Conducting Research Literature Reviews , defines it as the following:
“A literature review surveys books, scholarly articles, and any other sources relevant to a particular issue, area of research, or theory, and by so doing, provides a description, summary, and critical evaluation of these works in relation to the research problem being investigated.
Literature reviews are designed to provide an overview of sources you have explored while researching a particular topic, and to demonstrate to your readers how your research fits within a larger field of study.”
Simply put, a literature review can be defined as a critical discussion of relevant pre-existing research around your research question and carving out a definitive place for your study in the existing body of knowledge. Literature reviews can be presented in multiple ways: a section of an article, the whole research paper itself, or a chapter of your thesis.
A literature review does function as a summary of sources, but it also allows you to analyze further, interpret, and examine the stated theories, methods, viewpoints, and, of course, the gaps in the existing content.
As an author, you can discuss and interpret the research question and its various aspects and debate your adopted methods to support the claim.
What is the purpose of a literature review?
A literature review is meant to help your readers understand the relevance of your research question and where it fits within the existing body of knowledge. As a researcher, you should use it to set the context, build your argument, and establish the need for your study.
What is the importance of a literature review?
The literature review is a critical part of research papers because it helps you:
- Gain an in-depth understanding of your research question and the surrounding area
- Convey that you have a thorough understanding of your research area and are up-to-date with the latest changes and advancements
- Establish how your research is connected or builds on the existing body of knowledge and how it could contribute to further research
- Elaborate on the validity and suitability of your theoretical framework and research methodology
- Identify and highlight gaps and shortcomings in the existing body of knowledge and how things need to change
- Convey to readers how your study is different or how it contributes to the research area
How long should a literature review be?
Ideally, the literature review should take up 15%-40% of the total length of your manuscript. So, if you have a 10,000-word research paper, the minimum word count could be 1500.
Your literature review format depends heavily on the kind of manuscript you are writing — an entire chapter in case of doctoral theses, a part of the introductory section in a research article, to a full-fledged review article that examines the previously published research on a topic.
Another determining factor is the type of research you are doing. The literature review section tends to be longer for secondary research projects than primary research projects.
What are the different types of literature reviews?
All literature reviews are not the same. There are a variety of possible approaches that you can take. It all depends on the type of research you are pursuing.
Here are the different types of literature reviews:
Argumentative review
It is called an argumentative review when you carefully present literature that only supports or counters a specific argument or premise to establish a viewpoint.
Integrative review
It is a type of literature review focused on building a comprehensive understanding of a topic by combining available theoretical frameworks and empirical evidence.
Methodological review
This approach delves into the ''how'' and the ''what" of the research question — you cannot look at the outcome in isolation; you should also review the methodology used.
Systematic review
This form consists of an overview of existing evidence pertinent to a clearly formulated research question, which uses pre-specified and standardized methods to identify and critically appraise relevant research and collect, report, and analyze data from the studies included in the review.
Meta-analysis review
Meta-analysis uses statistical methods to summarize the results of independent studies. By combining information from all relevant studies, meta-analysis can provide more precise estimates of the effects than those derived from the individual studies included within a review.
Historical review
Historical literature reviews focus on examining research throughout a period, often starting with the first time an issue, concept, theory, or phenomenon emerged in the literature, then tracing its evolution within the scholarship of a discipline. The purpose is to place research in a historical context to show familiarity with state-of-the-art developments and identify future research's likely directions.
Theoretical Review
This form aims to examine the corpus of theory accumulated regarding an issue, concept, theory, and phenomenon. The theoretical literature review helps to establish what theories exist, the relationships between them, the degree the existing approaches have been investigated, and to develop new hypotheses to be tested.
Scoping Review
The Scoping Review is often used at the beginning of an article, dissertation, or research proposal. It is conducted before the research to highlight gaps in the existing body of knowledge and explains why the project should be greenlit.
State-of-the-Art Review
The State-of-the-Art review is conducted periodically, focusing on the most recent research. It describes what is currently known, understood, or agreed upon regarding the research topic and highlights where there are still disagreements.
Can you use the first person in a literature review?
When writing literature reviews, you should avoid the usage of first-person pronouns. It means that instead of "I argue that" or "we argue that," the appropriate expression would be "this research paper argues that."
Do you need an abstract for a literature review?
Ideally, yes. It is always good to have a condensed summary that is self-contained and independent of the rest of your review. As for how to draft one, you can follow the same fundamental idea when preparing an abstract for a literature review. It should also include:
- The research topic and your motivation behind selecting it
- A one-sentence thesis statement
- An explanation of the kinds of literature featured in the review
- Summary of what you've learned
- Conclusions you drew from the literature you reviewed
- Potential implications and future scope for research
Here's an example of the abstract of a literature review
Is a literature review written in the past tense?
Yes, the literature review should ideally be written in the past tense. You should not use the present or future tense when writing one. The exceptions are when you have statements describing events that happened earlier than the literature you are reviewing or events that are currently occurring; then, you can use the past perfect or present perfect tenses.
How many sources for a literature review?
There are multiple approaches to deciding how many sources to include in a literature review section. The first approach would be to look level you are at as a researcher. For instance, a doctoral thesis might need 60+ sources. In contrast, you might only need to refer to 5-15 sources at the undergraduate level.
The second approach is based on the kind of literature review you are doing — whether it is merely a chapter of your paper or if it is a self-contained paper in itself. When it is just a chapter, sources should equal the total number of pages in your article's body. In the second scenario, you need at least three times as many sources as there are pages in your work.
Quick tips on how to write a literature review
To know how to write a literature review, you must clearly understand its impact and role in establishing your work as substantive research material.
You need to follow the below-mentioned steps, to write a literature review:
- Outline the purpose behind the literature review
- Search relevant literature
- Examine and assess the relevant resources
- Discover connections by drawing deep insights from the resources
- Structure planning to write a good literature review
1. Outline and identify the purpose of a literature review
As a first step on how to write a literature review, you must know what the research question or topic is and what shape you want your literature review to take. Ensure you understand the research topic inside out, or else seek clarifications. You must be able to the answer below questions before you start:
- How many sources do I need to include?
- What kind of sources should I analyze?
- How much should I critically evaluate each source?
- Should I summarize, synthesize or offer a critique of the sources?
- Do I need to include any background information or definitions?
Additionally, you should know that the narrower your research topic is, the swifter it will be for you to restrict the number of sources to be analyzed.
2. Search relevant literature
Dig deeper into search engines to discover what has already been published around your chosen topic. Make sure you thoroughly go through appropriate reference sources like books, reports, journal articles, government docs, and web-based resources.
You must prepare a list of keywords and their different variations. You can start your search from any library’s catalog, provided you are an active member of that institution. The exact keywords can be extended to widen your research over other databases and academic search engines like:
- Google Scholar
- Microsoft Academic
- Science.gov
Besides, it is not advisable to go through every resource word by word. Alternatively, what you can do is you can start by reading the abstract and then decide whether that source is relevant to your research or not.
Additionally, you must spend surplus time assessing the quality and relevance of resources. It would help if you tried preparing a list of citations to ensure that there lies no repetition of authors, publications, or articles in the literature review.
3. Examine and assess the sources
It is nearly impossible for you to go through every detail in the research article. So rather than trying to fetch every detail, you have to analyze and decide which research sources resemble closest and appear relevant to your chosen domain.
While analyzing the sources, you should look to find out answers to questions like:
- What question or problem has the author been describing and debating?
- What is the definition of critical aspects?
- How well the theories, approach, and methodology have been explained?
- Whether the research theory used some conventional or new innovative approach?
- How relevant are the key findings of the work?
- In what ways does it relate to other sources on the same topic?
- What challenges does this research paper pose to the existing theory
- What are the possible contributions or benefits it adds to the subject domain?
Be always mindful that you refer only to credible and authentic resources. It would be best if you always take references from different publications to validate your theory.
Always keep track of important information or data you can present in your literature review right from the beginning. It will help steer your path from any threats of plagiarism and also make it easier to curate an annotated bibliography or reference section.
4. Discover connections
At this stage, you must start deciding on the argument and structure of your literature review. To accomplish this, you must discover and identify the relations and connections between various resources while drafting your abstract.
A few aspects that you should be aware of while writing a literature review include:
- Rise to prominence: Theories and methods that have gained reputation and supporters over time.
- Constant scrutiny: Concepts or theories that repeatedly went under examination.
- Contradictions and conflicts: Theories, both the supporting and the contradictory ones, for the research topic.
- Knowledge gaps: What exactly does it fail to address, and how to bridge them with further research?
- Influential resources: Significant research projects available that have been upheld as milestones or perhaps, something that can modify the current trends
Once you join the dots between various past research works, it will be easier for you to draw a conclusion and identify your contribution to the existing knowledge base.
5. Structure planning to write a good literature review
There exist different ways towards planning and executing the structure of a literature review. The format of a literature review varies and depends upon the length of the research.
Like any other research paper, the literature review format must contain three sections: introduction, body, and conclusion. The goals and objectives of the research question determine what goes inside these three sections.
Nevertheless, a good literature review can be structured according to the chronological, thematic, methodological, or theoretical framework approach.
Literature review samples
1. Standalone
2. As a section of a research paper
How SciSpace Discover makes literature review a breeze?
SciSpace Discover is a one-stop solution to do an effective literature search and get barrier-free access to scientific knowledge. It is an excellent repository where you can find millions of only peer-reviewed articles and full-text PDF files. Here’s more on how you can use it:
Find the right information
Find what you want quickly and easily with comprehensive search filters that let you narrow down papers according to PDF availability, year of publishing, document type, and affiliated institution. Moreover, you can sort the results based on the publishing date, citation count, and relevance.
Assess credibility of papers quickly
When doing the literature review, it is critical to establish the quality of your sources. They form the foundation of your research. SciSpace Discover helps you assess the quality of a source by providing an overview of its references, citations, and performance metrics.
Get the complete picture in no time
SciSpace Discover’s personalized suggestion engine helps you stay on course and get the complete picture of the topic from one place. Every time you visit an article page, it provides you links to related papers. Besides that, it helps you understand what’s trending, who are the top authors, and who are the leading publishers on a topic.
Make referring sources super easy
To ensure you don't lose track of your sources, you must start noting down your references when doing the literature review. SciSpace Discover makes this step effortless. Click the 'cite' button on an article page, and you will receive preloaded citation text in multiple styles — all you've to do is copy-paste it into your manuscript.
Final tips on how to write a literature review
A massive chunk of time and effort is required to write a good literature review. But, if you go about it systematically, you'll be able to save a ton of time and build a solid foundation for your research.
We hope this guide has helped you answer several key questions you have about writing literature reviews.
Would you like to explore SciSpace Discover and kick off your literature search right away? You can get started here .
Frequently Asked Questions (FAQs)
1. how to start a literature review.
• What questions do you want to answer?
• What sources do you need to answer these questions?
• What information do these sources contain?
• How can you use this information to answer your questions?
2. What to include in a literature review?
• A brief background of the problem or issue
• What has previously been done to address the problem or issue
• A description of what you will do in your project
• How this study will contribute to research on the subject
3. Why literature review is important?
The literature review is an important part of any research project because it allows the writer to look at previous studies on a topic and determine existing gaps in the literature, as well as what has already been done. It will also help them to choose the most appropriate method for their own study.
4. How to cite a literature review in APA format?
To cite a literature review in APA style, you need to provide the author's name, the title of the article, and the year of publication. For example: Patel, A. B., & Stokes, G. S. (2012). The relationship between personality and intelligence: A meta-analysis of longitudinal research. Personality and Individual Differences, 53(1), 16-21
5. What are the components of a literature review?
• A brief introduction to the topic, including its background and context. The introduction should also include a rationale for why the study is being conducted and what it will accomplish.
• A description of the methodologies used in the study. This can include information about data collection methods, sample size, and statistical analyses.
• A presentation of the findings in an organized format that helps readers follow along with the author's conclusions.
6. What are common errors in writing literature review?
• Not spending enough time to critically evaluate the relevance of resources, observations and conclusions.
• Totally relying on secondary data while ignoring primary data.
• Letting your personal bias seep into your interpretation of existing literature.
• No detailed explanation of the procedure to discover and identify an appropriate literature review.
7. What are the 5 C's of writing literature review?
• Cite - the sources you utilized and referenced in your research.
• Compare - existing arguments, hypotheses, methodologies, and conclusions found in the knowledge base.
• Contrast - the arguments, topics, methodologies, approaches, and disputes that may be found in the literature.
• Critique - the literature and describe the ideas and opinions you find more convincing and why.
• Connect - the various studies you reviewed in your research.
8. How many sources should a literature review have?
When it is just a chapter, sources should equal the total number of pages in your article's body. if it is a self-contained paper in itself, you need at least three times as many sources as there are pages in your work.
9. Can literature review have diagrams?
• To represent an abstract idea or concept
• To explain the steps of a process or procedure
• To help readers understand the relationships between different concepts
10. How old should sources be in a literature review?
Sources for a literature review should be as current as possible or not older than ten years. The only exception to this rule is if you are reviewing a historical topic and need to use older sources.
11. What are the types of literature review?
• Argumentative review
• Integrative review
• Methodological review
• Systematic review
• Meta-analysis review
• Historical review
• Theoretical review
• Scoping review
• State-of-the-Art review
12. Is a literature review mandatory?
Yes. Literature review is a mandatory part of any research project. It is a critical step in the process that allows you to establish the scope of your research, and provide a background for the rest of your work.
But before you go,
- Six Online Tools for Easy Literature Review
- Evaluating literature review: systematic vs. scoping reviews
- Systematic Approaches to a Successful Literature Review
- Writing Integrative Literature Reviews: Guidelines and Examples
You might also like

Consensus GPT vs. SciSpace GPT: Choose the Best GPT for Research

Literature Review and Theoretical Framework: Understanding the Differences

Types of Essays in Academic Writing - Quick Guide (2024)

How to Write a Literature Review: Six Steps to Get You from Start to Finish
Writing-a-literature-review-six-steps-to-get-you-from-start-to-finish.
Tanya Golash-Boza, Associate Professor of Sociology, University of California
February 03, 2022
Writing a literature review is often the most daunting part of writing an article, book, thesis, or dissertation. “The literature” seems (and often is) massive. I have found it helpful to be as systematic as possible when completing this gargantuan task.
Sonja Foss and William Walters* describe an efficient and effective way of writing a literature review. Their system provides an excellent guide for getting through the massive amounts of literature for any purpose: in a dissertation, an M.A. thesis, or preparing a research article for publication in any field of study. Below is a summary of the steps they outline as well as a step-by-step method for writing a literature review.
How to Write a Literature Review
Step One: Decide on your areas of research:
Before you begin to search for articles or books, decide beforehand what areas you are going to research. Make sure that you only get articles and books in those areas, even if you come across fascinating books in other areas. A literature review I am currently working on, for example, explores barriers to higher education for undocumented students.
Step Two: Search for the literature:
Conduct a comprehensive bibliographic search of books and articles in your area. Read the abstracts online and download and/or print those articles that pertain to your area of research. Find books in the library that are relevant and check them out. Set a specific time frame for how long you will search. It should not take more than two or three dedicated sessions.
Step Three: Find relevant excerpts in your books and articles:
Skim the contents of each book and article and look specifically for these five things:
1. Claims, conclusions, and findings about the constructs you are investigating
2. Definitions of terms
3. Calls for follow-up studies relevant to your project
4. Gaps you notice in the literature
5. Disagreement about the constructs you are investigating
When you find any of these five things, type the relevant excerpt directly into a Word document. Don’t summarize, as summarizing takes longer than simply typing the excerpt. Make sure to note the name of the author and the page number following each excerpt. Do this for each article and book that you have in your stack of literature. When you are done, print out your excerpts.
Step Four: Code the literature:
Get out a pair of scissors and cut each excerpt out. Now, sort the pieces of paper into similar topics. Figure out what the main themes are. Place each excerpt into a themed pile. Make sure each note goes into a pile. If there are excerpts that you can’t figure out where they belong, separate those and go over them again at the end to see if you need new categories. When you finish, place each stack of notes into an envelope labeled with the name of the theme.
Step Five: Create Your Conceptual Schema:
Type, in large font, the name of each of your coded themes. Print this out, and cut the titles into individual slips of paper. Take the slips of paper to a table or large workspace and figure out the best way to organize them. Are there ideas that go together or that are in dialogue with each other? Are there ideas that contradict each other? Move around the slips of paper until you come up with a way of organizing the codes that makes sense. Write the conceptual schema down before you forget or someone cleans up your slips of paper.
Step Six: Begin to Write Your Literature Review:
Choose any section of your conceptual schema to begin with. You can begin anywhere, because you already know the order. Find the envelope with the excerpts in them and lay them on the table in front of you. Figure out a mini-conceptual schema based on that theme by grouping together those excerpts that say the same thing. Use that mini-conceptual schema to write up your literature review based on the excerpts that you have in front of you. Don’t forget to include the citations as you write, so as not to lose track of who said what. Repeat this for each section of your literature review.
Once you complete these six steps, you will have a complete draft of your literature review. The great thing about this process is that it breaks down into manageable steps something that seems enormous: writing a literature review.
I think that Foss and Walter’s system for writing the literature review is ideal for a dissertation, because a Ph.D. candidate has already read widely in his or her field through graduate seminars and comprehensive exams.
It may be more challenging for M.A. students, unless you are already familiar with the literature. It is always hard to figure out how much you need to read for deep meaning, and how much you just need to know what others have said. That balance will depend on how much you already know.
For people writing literature reviews for articles or books, this system also could work, especially when you are writing in a field with which you are already familiar. The mere fact of having a system can make the literature review seem much less daunting, so I recommend this system for anyone who feels overwhelmed by the prospect of writing a literature review.
*Destination Dissertation: A Traveler's Guide to a Done Dissertation
Image Credit/Source: Goldmund Lukic/Getty Images

Watch our Webinar to help you get published
Please enter your Email Address
Please enter valid email address
Please Enter your First Name
Please enter your Last Name
Please enter your Questions or Comments.
Please enter the Privacy
Please enter the Terms & Conditions

How research content supports academic integrity

Finding time to publish as a medical student: 6 tips for Success

Software to Improve Reliability of Research Image Data: Wiley, Lumina, and Researchers at Harvard Medical School Work Together on Solutions

Driving Research Outcomes: Wiley Partners with CiteAb

ISBN, ISSN, DOI: what they are and how to find them

Image Collections for Medical Practitioners with TDS Health

How do you Discover Content?

Writing for Publication for Nurses (Mandarin Edition)

Get Published - Your How to Webinar

Finding time to publish as a medical student: 6 tips for success
Related articles.
Learn how Wiley partners with plagiarism detection services to support academic integrity around the world
Medical student Nicole Foley shares her top tips for writing and getting your work published.
Wiley and Lumina are working together to support the efforts of researchers at Harvard Medical School to develop and test new machine learning tools and artificial intelligence (AI) software that can
Learn more about our relationship with a company that helps scientists identify the right products to use in their research
What is ISBN? ISSN? DOI? Learn about some of the unique identifiers for book and journal content.
Learn how medical practitioners can easily access and search visual assets from our article portfolio
Explore free-to-use services that can help you discover new content
Watch this webinar to help you learn how to get published.

How to Easily Access the Most Relevant Research: A Q&A With the Creator of Scitrus
Atypon launches Scitrus, a personalized web app that allows users to create a customized feed of the latest research.

Effectively and Efficiently Creating your Paper
FOR INDIVIDUALS
FOR INSTITUTIONS & BUSINESSES
WILEY NETWORK
ABOUT WILEY
Corporate Responsibility
Corporate Governance
Leadership Team
Cookie Preferences
Copyright @ 2000-2024 by John Wiley & Sons, Inc., or related companies. All rights reserved, including rights for text and data mining and training of artificial technologies or similar technologies.
Rights & Permissions
Privacy Policy
Terms of Use
Reference management. Clean and simple.
What is a literature review? [with examples]
What is a literature review?
The purpose of a literature review, how to write a literature review, the format of a literature review, general formatting rules, the length of a literature review, literature review examples, frequently asked questions about literature reviews, related articles.
A literature review is an assessment of the sources in a chosen topic of research.
In a literature review, you’re expected to report on the existing scholarly conversation, without adding new contributions.
If you are currently writing one, you've come to the right place. In the following paragraphs, we will explain:
- the objective of a literature review
- how to write a literature review
- the basic format of a literature review
Tip: It’s not always mandatory to add a literature review in a paper. Theses and dissertations often include them, whereas research papers may not. Make sure to consult with your instructor for exact requirements.
The four main objectives of a literature review are:
- Studying the references of your research area
- Summarizing the main arguments
- Identifying current gaps, stances, and issues
- Presenting all of the above in a text
Ultimately, the main goal of a literature review is to provide the researcher with sufficient knowledge about the topic in question so that they can eventually make an intervention.
The format of a literature review is fairly standard. It includes an:
- introduction that briefly introduces the main topic
- body that includes the main discussion of the key arguments
- conclusion that highlights the gaps and issues of the literature
➡️ Take a look at our guide on how to write a literature review to learn more about how to structure a literature review.
First of all, a literature review should have its own labeled section. You should indicate clearly in the table of contents where the literature can be found, and you should label this section as “Literature Review.”
➡️ For more information on writing a thesis, visit our guide on how to structure a thesis .
There is no set amount of words for a literature review, so the length depends on the research. If you are working with a large amount of sources, it will be long. If your paper does not depend entirely on references, it will be short.
Take a look at these three theses featuring great literature reviews:
- School-Based Speech-Language Pathologist's Perceptions of Sensory Food Aversions in Children [ PDF , see page 20]
- Who's Writing What We Read: Authorship in Criminological Research [ PDF , see page 4]
- A Phenomenological Study of the Lived Experience of Online Instructors of Theological Reflection at Christian Institutions Accredited by the Association of Theological Schools [ PDF , see page 56]
Literature reviews are most commonly found in theses and dissertations. However, you find them in research papers as well.
There is no set amount of words for a literature review, so the length depends on the research. If you are working with a large amount of sources, then it will be long. If your paper does not depend entirely on references, then it will be short.
No. A literature review should have its own independent section. You should indicate clearly in the table of contents where the literature review can be found, and label this section as “Literature Review.”
The main goal of a literature review is to provide the researcher with sufficient knowledge about the topic in question so that they can eventually make an intervention.
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 5. The Literature Review
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
A literature review surveys prior research published in books, scholarly articles, and any other sources relevant to a particular issue, area of research, or theory, and by so doing, provides a description, summary, and critical evaluation of these works in relation to the research problem being investigated. Literature reviews are designed to provide an overview of sources you have used in researching a particular topic and to demonstrate to your readers how your research fits within existing scholarship about the topic.
Fink, Arlene. Conducting Research Literature Reviews: From the Internet to Paper . Fourth edition. Thousand Oaks, CA: SAGE, 2014.
Importance of a Good Literature Review
A literature review may consist of simply a summary of key sources, but in the social sciences, a literature review usually has an organizational pattern and combines both summary and synthesis, often within specific conceptual categories . A summary is a recap of the important information of the source, but a synthesis is a re-organization, or a reshuffling, of that information in a way that informs how you are planning to investigate a research problem. The analytical features of a literature review might:
- Give a new interpretation of old material or combine new with old interpretations,
- Trace the intellectual progression of the field, including major debates,
- Depending on the situation, evaluate the sources and advise the reader on the most pertinent or relevant research, or
- Usually in the conclusion of a literature review, identify where gaps exist in how a problem has been researched to date.
Given this, the purpose of a literature review is to:
- Place each work in the context of its contribution to understanding the research problem being studied.
- Describe the relationship of each work to the others under consideration.
- Identify new ways to interpret prior research.
- Reveal any gaps that exist in the literature.
- Resolve conflicts amongst seemingly contradictory previous studies.
- Identify areas of prior scholarship to prevent duplication of effort.
- Point the way in fulfilling a need for additional research.
- Locate your own research within the context of existing literature [very important].
Fink, Arlene. Conducting Research Literature Reviews: From the Internet to Paper. 2nd ed. Thousand Oaks, CA: Sage, 2005; Hart, Chris. Doing a Literature Review: Releasing the Social Science Research Imagination . Thousand Oaks, CA: Sage Publications, 1998; Jesson, Jill. Doing Your Literature Review: Traditional and Systematic Techniques . Los Angeles, CA: SAGE, 2011; Knopf, Jeffrey W. "Doing a Literature Review." PS: Political Science and Politics 39 (January 2006): 127-132; Ridley, Diana. The Literature Review: A Step-by-Step Guide for Students . 2nd ed. Los Angeles, CA: SAGE, 2012.
Types of Literature Reviews
It is important to think of knowledge in a given field as consisting of three layers. First, there are the primary studies that researchers conduct and publish. Second are the reviews of those studies that summarize and offer new interpretations built from and often extending beyond the primary studies. Third, there are the perceptions, conclusions, opinion, and interpretations that are shared informally among scholars that become part of the body of epistemological traditions within the field.
In composing a literature review, it is important to note that it is often this third layer of knowledge that is cited as "true" even though it often has only a loose relationship to the primary studies and secondary literature reviews. Given this, while literature reviews are designed to provide an overview and synthesis of pertinent sources you have explored, there are a number of approaches you could adopt depending upon the type of analysis underpinning your study.
Argumentative Review This form examines literature selectively in order to support or refute an argument, deeply embedded assumption, or philosophical problem already established in the literature. The purpose is to develop a body of literature that establishes a contrarian viewpoint. Given the value-laden nature of some social science research [e.g., educational reform; immigration control], argumentative approaches to analyzing the literature can be a legitimate and important form of discourse. However, note that they can also introduce problems of bias when they are used to make summary claims of the sort found in systematic reviews [see below].
Integrative Review Considered a form of research that reviews, critiques, and synthesizes representative literature on a topic in an integrated way such that new frameworks and perspectives on the topic are generated. The body of literature includes all studies that address related or identical hypotheses or research problems. A well-done integrative review meets the same standards as primary research in regard to clarity, rigor, and replication. This is the most common form of review in the social sciences.
Historical Review Few things rest in isolation from historical precedent. Historical literature reviews focus on examining research throughout a period of time, often starting with the first time an issue, concept, theory, phenomena emerged in the literature, then tracing its evolution within the scholarship of a discipline. The purpose is to place research in a historical context to show familiarity with state-of-the-art developments and to identify the likely directions for future research.
Methodological Review A review does not always focus on what someone said [findings], but how they came about saying what they say [method of analysis]. Reviewing methods of analysis provides a framework of understanding at different levels [i.e. those of theory, substantive fields, research approaches, and data collection and analysis techniques], how researchers draw upon a wide variety of knowledge ranging from the conceptual level to practical documents for use in fieldwork in the areas of ontological and epistemological consideration, quantitative and qualitative integration, sampling, interviewing, data collection, and data analysis. This approach helps highlight ethical issues which you should be aware of and consider as you go through your own study.
Systematic Review This form consists of an overview of existing evidence pertinent to a clearly formulated research question, which uses pre-specified and standardized methods to identify and critically appraise relevant research, and to collect, report, and analyze data from the studies that are included in the review. The goal is to deliberately document, critically evaluate, and summarize scientifically all of the research about a clearly defined research problem . Typically it focuses on a very specific empirical question, often posed in a cause-and-effect form, such as "To what extent does A contribute to B?" This type of literature review is primarily applied to examining prior research studies in clinical medicine and allied health fields, but it is increasingly being used in the social sciences.
Theoretical Review The purpose of this form is to examine the corpus of theory that has accumulated in regard to an issue, concept, theory, phenomena. The theoretical literature review helps to establish what theories already exist, the relationships between them, to what degree the existing theories have been investigated, and to develop new hypotheses to be tested. Often this form is used to help establish a lack of appropriate theories or reveal that current theories are inadequate for explaining new or emerging research problems. The unit of analysis can focus on a theoretical concept or a whole theory or framework.
NOTE: Most often the literature review will incorporate some combination of types. For example, a review that examines literature supporting or refuting an argument, assumption, or philosophical problem related to the research problem will also need to include writing supported by sources that establish the history of these arguments in the literature.
Baumeister, Roy F. and Mark R. Leary. "Writing Narrative Literature Reviews." Review of General Psychology 1 (September 1997): 311-320; Mark R. Fink, Arlene. Conducting Research Literature Reviews: From the Internet to Paper . 2nd ed. Thousand Oaks, CA: Sage, 2005; Hart, Chris. Doing a Literature Review: Releasing the Social Science Research Imagination . Thousand Oaks, CA: Sage Publications, 1998; Kennedy, Mary M. "Defining a Literature." Educational Researcher 36 (April 2007): 139-147; Petticrew, Mark and Helen Roberts. Systematic Reviews in the Social Sciences: A Practical Guide . Malden, MA: Blackwell Publishers, 2006; Torracro, Richard. "Writing Integrative Literature Reviews: Guidelines and Examples." Human Resource Development Review 4 (September 2005): 356-367; Rocco, Tonette S. and Maria S. Plakhotnik. "Literature Reviews, Conceptual Frameworks, and Theoretical Frameworks: Terms, Functions, and Distinctions." Human Ressource Development Review 8 (March 2008): 120-130; Sutton, Anthea. Systematic Approaches to a Successful Literature Review . Los Angeles, CA: Sage Publications, 2016.
Structure and Writing Style
I. Thinking About Your Literature Review
The structure of a literature review should include the following in support of understanding the research problem :
- An overview of the subject, issue, or theory under consideration, along with the objectives of the literature review,
- Division of works under review into themes or categories [e.g. works that support a particular position, those against, and those offering alternative approaches entirely],
- An explanation of how each work is similar to and how it varies from the others,
- Conclusions as to which pieces are best considered in their argument, are most convincing of their opinions, and make the greatest contribution to the understanding and development of their area of research.
The critical evaluation of each work should consider :
- Provenance -- what are the author's credentials? Are the author's arguments supported by evidence [e.g. primary historical material, case studies, narratives, statistics, recent scientific findings]?
- Methodology -- were the techniques used to identify, gather, and analyze the data appropriate to addressing the research problem? Was the sample size appropriate? Were the results effectively interpreted and reported?
- Objectivity -- is the author's perspective even-handed or prejudicial? Is contrary data considered or is certain pertinent information ignored to prove the author's point?
- Persuasiveness -- which of the author's theses are most convincing or least convincing?
- Validity -- are the author's arguments and conclusions convincing? Does the work ultimately contribute in any significant way to an understanding of the subject?
II. Development of the Literature Review
Four Basic Stages of Writing 1. Problem formulation -- which topic or field is being examined and what are its component issues? 2. Literature search -- finding materials relevant to the subject being explored. 3. Data evaluation -- determining which literature makes a significant contribution to the understanding of the topic. 4. Analysis and interpretation -- discussing the findings and conclusions of pertinent literature.
Consider the following issues before writing the literature review: Clarify If your assignment is not specific about what form your literature review should take, seek clarification from your professor by asking these questions: 1. Roughly how many sources would be appropriate to include? 2. What types of sources should I review (books, journal articles, websites; scholarly versus popular sources)? 3. Should I summarize, synthesize, or critique sources by discussing a common theme or issue? 4. Should I evaluate the sources in any way beyond evaluating how they relate to understanding the research problem? 5. Should I provide subheadings and other background information, such as definitions and/or a history? Find Models Use the exercise of reviewing the literature to examine how authors in your discipline or area of interest have composed their literature review sections. Read them to get a sense of the types of themes you might want to look for in your own research or to identify ways to organize your final review. The bibliography or reference section of sources you've already read, such as required readings in the course syllabus, are also excellent entry points into your own research. Narrow the Topic The narrower your topic, the easier it will be to limit the number of sources you need to read in order to obtain a good survey of relevant resources. Your professor will probably not expect you to read everything that's available about the topic, but you'll make the act of reviewing easier if you first limit scope of the research problem. A good strategy is to begin by searching the USC Libraries Catalog for recent books about the topic and review the table of contents for chapters that focuses on specific issues. You can also review the indexes of books to find references to specific issues that can serve as the focus of your research. For example, a book surveying the history of the Israeli-Palestinian conflict may include a chapter on the role Egypt has played in mediating the conflict, or look in the index for the pages where Egypt is mentioned in the text. Consider Whether Your Sources are Current Some disciplines require that you use information that is as current as possible. This is particularly true in disciplines in medicine and the sciences where research conducted becomes obsolete very quickly as new discoveries are made. However, when writing a review in the social sciences, a survey of the history of the literature may be required. In other words, a complete understanding the research problem requires you to deliberately examine how knowledge and perspectives have changed over time. Sort through other current bibliographies or literature reviews in the field to get a sense of what your discipline expects. You can also use this method to explore what is considered by scholars to be a "hot topic" and what is not.
III. Ways to Organize Your Literature Review
Chronology of Events If your review follows the chronological method, you could write about the materials according to when they were published. This approach should only be followed if a clear path of research building on previous research can be identified and that these trends follow a clear chronological order of development. For example, a literature review that focuses on continuing research about the emergence of German economic power after the fall of the Soviet Union. By Publication Order your sources by publication chronology, then, only if the order demonstrates a more important trend. For instance, you could order a review of literature on environmental studies of brown fields if the progression revealed, for example, a change in the soil collection practices of the researchers who wrote and/or conducted the studies. Thematic [“conceptual categories”] A thematic literature review is the most common approach to summarizing prior research in the social and behavioral sciences. Thematic reviews are organized around a topic or issue, rather than the progression of time, although the progression of time may still be incorporated into a thematic review. For example, a review of the Internet’s impact on American presidential politics could focus on the development of online political satire. While the study focuses on one topic, the Internet’s impact on American presidential politics, it would still be organized chronologically reflecting technological developments in media. The difference in this example between a "chronological" and a "thematic" approach is what is emphasized the most: themes related to the role of the Internet in presidential politics. Note that more authentic thematic reviews tend to break away from chronological order. A review organized in this manner would shift between time periods within each section according to the point being made. Methodological A methodological approach focuses on the methods utilized by the researcher. For the Internet in American presidential politics project, one methodological approach would be to look at cultural differences between the portrayal of American presidents on American, British, and French websites. Or the review might focus on the fundraising impact of the Internet on a particular political party. A methodological scope will influence either the types of documents in the review or the way in which these documents are discussed.
Other Sections of Your Literature Review Once you've decided on the organizational method for your literature review, the sections you need to include in the paper should be easy to figure out because they arise from your organizational strategy. In other words, a chronological review would have subsections for each vital time period; a thematic review would have subtopics based upon factors that relate to the theme or issue. However, sometimes you may need to add additional sections that are necessary for your study, but do not fit in the organizational strategy of the body. What other sections you include in the body is up to you. However, only include what is necessary for the reader to locate your study within the larger scholarship about the research problem.
Here are examples of other sections, usually in the form of a single paragraph, you may need to include depending on the type of review you write:
- Current Situation : Information necessary to understand the current topic or focus of the literature review.
- Sources Used : Describes the methods and resources [e.g., databases] you used to identify the literature you reviewed.
- History : The chronological progression of the field, the research literature, or an idea that is necessary to understand the literature review, if the body of the literature review is not already a chronology.
- Selection Methods : Criteria you used to select (and perhaps exclude) sources in your literature review. For instance, you might explain that your review includes only peer-reviewed [i.e., scholarly] sources.
- Standards : Description of the way in which you present your information.
- Questions for Further Research : What questions about the field has the review sparked? How will you further your research as a result of the review?
IV. Writing Your Literature Review
Once you've settled on how to organize your literature review, you're ready to write each section. When writing your review, keep in mind these issues.
Use Evidence A literature review section is, in this sense, just like any other academic research paper. Your interpretation of the available sources must be backed up with evidence [citations] that demonstrates that what you are saying is valid. Be Selective Select only the most important points in each source to highlight in the review. The type of information you choose to mention should relate directly to the research problem, whether it is thematic, methodological, or chronological. Related items that provide additional information, but that are not key to understanding the research problem, can be included in a list of further readings . Use Quotes Sparingly Some short quotes are appropriate if you want to emphasize a point, or if what an author stated cannot be easily paraphrased. Sometimes you may need to quote certain terminology that was coined by the author, is not common knowledge, or taken directly from the study. Do not use extensive quotes as a substitute for using your own words in reviewing the literature. Summarize and Synthesize Remember to summarize and synthesize your sources within each thematic paragraph as well as throughout the review. Recapitulate important features of a research study, but then synthesize it by rephrasing the study's significance and relating it to your own work and the work of others. Keep Your Own Voice While the literature review presents others' ideas, your voice [the writer's] should remain front and center. For example, weave references to other sources into what you are writing but maintain your own voice by starting and ending the paragraph with your own ideas and wording. Use Caution When Paraphrasing When paraphrasing a source that is not your own, be sure to represent the author's information or opinions accurately and in your own words. Even when paraphrasing an author’s work, you still must provide a citation to that work.
V. Common Mistakes to Avoid
These are the most common mistakes made in reviewing social science research literature.
- Sources in your literature review do not clearly relate to the research problem;
- You do not take sufficient time to define and identify the most relevant sources to use in the literature review related to the research problem;
- Relies exclusively on secondary analytical sources rather than including relevant primary research studies or data;
- Uncritically accepts another researcher's findings and interpretations as valid, rather than examining critically all aspects of the research design and analysis;
- Does not describe the search procedures that were used in identifying the literature to review;
- Reports isolated statistical results rather than synthesizing them in chi-squared or meta-analytic methods; and,
- Only includes research that validates assumptions and does not consider contrary findings and alternative interpretations found in the literature.
Cook, Kathleen E. and Elise Murowchick. “Do Literature Review Skills Transfer from One Course to Another?” Psychology Learning and Teaching 13 (March 2014): 3-11; Fink, Arlene. Conducting Research Literature Reviews: From the Internet to Paper . 2nd ed. Thousand Oaks, CA: Sage, 2005; Hart, Chris. Doing a Literature Review: Releasing the Social Science Research Imagination . Thousand Oaks, CA: Sage Publications, 1998; Jesson, Jill. Doing Your Literature Review: Traditional and Systematic Techniques . London: SAGE, 2011; Literature Review Handout. Online Writing Center. Liberty University; Literature Reviews. The Writing Center. University of North Carolina; Onwuegbuzie, Anthony J. and Rebecca Frels. Seven Steps to a Comprehensive Literature Review: A Multimodal and Cultural Approach . Los Angeles, CA: SAGE, 2016; Ridley, Diana. The Literature Review: A Step-by-Step Guide for Students . 2nd ed. Los Angeles, CA: SAGE, 2012; Randolph, Justus J. “A Guide to Writing the Dissertation Literature Review." Practical Assessment, Research, and Evaluation. vol. 14, June 2009; Sutton, Anthea. Systematic Approaches to a Successful Literature Review . Los Angeles, CA: Sage Publications, 2016; Taylor, Dena. The Literature Review: A Few Tips On Conducting It. University College Writing Centre. University of Toronto; Writing a Literature Review. Academic Skills Centre. University of Canberra.
Writing Tip
Break Out of Your Disciplinary Box!
Thinking interdisciplinarily about a research problem can be a rewarding exercise in applying new ideas, theories, or concepts to an old problem. For example, what might cultural anthropologists say about the continuing conflict in the Middle East? In what ways might geographers view the need for better distribution of social service agencies in large cities than how social workers might study the issue? You don’t want to substitute a thorough review of core research literature in your discipline for studies conducted in other fields of study. However, particularly in the social sciences, thinking about research problems from multiple vectors is a key strategy for finding new solutions to a problem or gaining a new perspective. Consult with a librarian about identifying research databases in other disciplines; almost every field of study has at least one comprehensive database devoted to indexing its research literature.
Frodeman, Robert. The Oxford Handbook of Interdisciplinarity . New York: Oxford University Press, 2010.
Another Writing Tip
Don't Just Review for Content!
While conducting a review of the literature, maximize the time you devote to writing this part of your paper by thinking broadly about what you should be looking for and evaluating. Review not just what scholars are saying, but how are they saying it. Some questions to ask:
- How are they organizing their ideas?
- What methods have they used to study the problem?
- What theories have been used to explain, predict, or understand their research problem?
- What sources have they cited to support their conclusions?
- How have they used non-textual elements [e.g., charts, graphs, figures, etc.] to illustrate key points?
When you begin to write your literature review section, you'll be glad you dug deeper into how the research was designed and constructed because it establishes a means for developing more substantial analysis and interpretation of the research problem.
Hart, Chris. Doing a Literature Review: Releasing the Social Science Research Imagination . Thousand Oaks, CA: Sage Publications, 1 998.
Yet Another Writing Tip
When Do I Know I Can Stop Looking and Move On?
Here are several strategies you can utilize to assess whether you've thoroughly reviewed the literature:
- Look for repeating patterns in the research findings . If the same thing is being said, just by different people, then this likely demonstrates that the research problem has hit a conceptual dead end. At this point consider: Does your study extend current research? Does it forge a new path? Or, does is merely add more of the same thing being said?
- Look at sources the authors cite to in their work . If you begin to see the same researchers cited again and again, then this is often an indication that no new ideas have been generated to address the research problem.
- Search Google Scholar to identify who has subsequently cited leading scholars already identified in your literature review [see next sub-tab]. This is called citation tracking and there are a number of sources that can help you identify who has cited whom, particularly scholars from outside of your discipline. Here again, if the same authors are being cited again and again, this may indicate no new literature has been written on the topic.
Onwuegbuzie, Anthony J. and Rebecca Frels. Seven Steps to a Comprehensive Literature Review: A Multimodal and Cultural Approach . Los Angeles, CA: Sage, 2016; Sutton, Anthea. Systematic Approaches to a Successful Literature Review . Los Angeles, CA: Sage Publications, 2016.
- << Previous: Theoretical Framework
- Next: Citation Tracking >>
- Last Updated: Jun 11, 2024 1:40 PM
- URL: https://libguides.usc.edu/writingguide
Harvey Cushing/John Hay Whitney Medical Library
- Collections
- Research Help
YSN Doctoral Programs: Steps in Conducting a Literature Review
- Biomedical Databases
- Global (Public Health) Databases
- Soc. Sci., History, and Law Databases
- Grey Literature
- Trials Registers
- Data and Statistics
- Public Policy
- Google Tips
- Recommended Books
- Steps in Conducting a Literature Review
What is a literature review?
A literature review is an integrated analysis -- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question. That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
A literature review may be a stand alone work or the introduction to a larger research paper, depending on the assignment. Rely heavily on the guidelines your instructor has given you.
Why is it important?
A literature review is important because it:
- Explains the background of research on a topic.
- Demonstrates why a topic is significant to a subject area.
- Discovers relationships between research studies/ideas.
- Identifies major themes, concepts, and researchers on a topic.
- Identifies critical gaps and points of disagreement.
- Discusses further research questions that logically come out of the previous studies.
APA7 Style resources
APA Style Blog - for those harder to find answers
1. Choose a topic. Define your research question.
Your literature review should be guided by your central research question. The literature represents background and research developments related to a specific research question, interpreted and analyzed by you in a synthesized way.
- Make sure your research question is not too broad or too narrow. Is it manageable?
- Begin writing down terms that are related to your question. These will be useful for searches later.
- If you have the opportunity, discuss your topic with your professor and your class mates.
2. Decide on the scope of your review
How many studies do you need to look at? How comprehensive should it be? How many years should it cover?
- This may depend on your assignment. How many sources does the assignment require?
3. Select the databases you will use to conduct your searches.
Make a list of the databases you will search.
Where to find databases:
- use the tabs on this guide
- Find other databases in the Nursing Information Resources web page
- More on the Medical Library web page
- ... and more on the Yale University Library web page
4. Conduct your searches to find the evidence. Keep track of your searches.
- Use the key words in your question, as well as synonyms for those words, as terms in your search. Use the database tutorials for help.
- Save the searches in the databases. This saves time when you want to redo, or modify, the searches. It is also helpful to use as a guide is the searches are not finding any useful results.
- Review the abstracts of research studies carefully. This will save you time.
- Use the bibliographies and references of research studies you find to locate others.
- Check with your professor, or a subject expert in the field, if you are missing any key works in the field.
- Ask your librarian for help at any time.
- Use a citation manager, such as EndNote as the repository for your citations. See the EndNote tutorials for help.
Review the literature
Some questions to help you analyze the research:
- What was the research question of the study you are reviewing? What were the authors trying to discover?
- Was the research funded by a source that could influence the findings?
- What were the research methodologies? Analyze its literature review, the samples and variables used, the results, and the conclusions.
- Does the research seem to be complete? Could it have been conducted more soundly? What further questions does it raise?
- If there are conflicting studies, why do you think that is?
- How are the authors viewed in the field? Has this study been cited? If so, how has it been analyzed?
Tips:
- Review the abstracts carefully.
- Keep careful notes so that you may track your thought processes during the research process.
- Create a matrix of the studies for easy analysis, and synthesis, across all of the studies.
- << Previous: Recommended Books
- Last Updated: Jan 4, 2024 10:52 AM
- URL: https://guides.library.yale.edu/YSNDoctoral
- University of Texas Libraries
Literature Reviews
- What is a literature review?
- Steps in the Literature Review Process
- Define your research question
- Determine inclusion and exclusion criteria
- Choose databases and search
- Review Results
- Synthesize Results
- Analyze Results
- Librarian Support
What is a Literature Review?
A literature or narrative review is a comprehensive review and analysis of the published literature on a specific topic or research question. The literature that is reviewed contains: books, articles, academic articles, conference proceedings, association papers, and dissertations. It contains the most pertinent studies and points to important past and current research and practices. It provides background and context, and shows how your research will contribute to the field.
A literature review should:
- Provide a comprehensive and updated review of the literature;
- Explain why this review has taken place;
- Articulate a position or hypothesis;
- Acknowledge and account for conflicting and corroborating points of view
From S age Research Methods
Purpose of a Literature Review
A literature review can be written as an introduction to a study to:
- Demonstrate how a study fills a gap in research
- Compare a study with other research that's been done
Or it can be a separate work (a research article on its own) which:
- Organizes or describes a topic
- Describes variables within a particular issue/problem
Limitations of a Literature Review
Some of the limitations of a literature review are:
- It's a snapshot in time. Unlike other reviews, this one has beginning, a middle and an end. There may be future developments that could make your work less relevant.
- It may be too focused. Some niche studies may miss the bigger picture.
- It can be difficult to be comprehensive. There is no way to make sure all the literature on a topic was considered.
- It is easy to be biased if you stick to top tier journals. There may be other places where people are publishing exemplary research. Look to open access publications and conferences to reflect a more inclusive collection. Also, make sure to include opposing views (and not just supporting evidence).
Source: Grant, Maria J., and Andrew Booth. “A Typology of Reviews: An Analysis of 14 Review Types and Associated Methodologies.” Health Information & Libraries Journal, vol. 26, no. 2, June 2009, pp. 91–108. Wiley Online Library, doi:10.1111/j.1471-1842.2009.00848.x.
Meryl Brodsky : Communication and Information Studies
Hannah Chapman Tripp : Biology, Neuroscience
Carolyn Cunningham : Human Development & Family Sciences, Psychology, Sociology
Larayne Dallas : Engineering
Janelle Hedstrom : Special Education, Curriculum & Instruction, Ed Leadership & Policy
Susan Macicak : Linguistics
Imelda Vetter : Dell Medical School
For help in other subject areas, please see the guide to library specialists by subject .
Periodically, UT Libraries runs a workshop covering the basics and library support for literature reviews. While we try to offer these once per academic year, we find providing the recording to be helpful to community members who have missed the session. Following is the most recent recording of the workshop, Conducting a Literature Review. To view the recording, a UT login is required.
- October 26, 2022 recording
- Last Updated: Oct 26, 2022 2:49 PM
- URL: https://guides.lib.utexas.edu/literaturereviews

Libraries | Research Guides
Literature reviews, what is a literature review, learning more about how to do a literature review.
- Planning the Review
- The Research Question
- Choosing Where to Search
- Organizing the Review
- Writing the Review
A literature review is a review and synthesis of existing research on a topic or research question. A literature review is meant to analyze the scholarly literature, make connections across writings and identify strengths, weaknesses, trends, and missing conversations. A literature review should address different aspects of a topic as it relates to your research question. A literature review goes beyond a description or summary of the literature you have read.
- Sage Research Methods Core Collection This link opens in a new window SAGE Research Methods supports research at all levels by providing material to guide users through every step of the research process. SAGE Research Methods is the ultimate methods library with more than 1000 books, reference works, journal articles, and instructional videos by world-leading academics from across the social sciences, including the largest collection of qualitative methods books available online from any scholarly publisher. – Publisher
- Next: Planning the Review >>
- Last Updated: May 2, 2024 10:39 AM
- URL: https://libguides.northwestern.edu/literaturereviews
What Is A Literature Review?
A plain-language explainer (with examples).
By: Derek Jansen (MBA) & Kerryn Warren (PhD) | June 2020 (Updated May 2023)
If you’re faced with writing a dissertation or thesis, chances are you’ve encountered the term “literature review” . If you’re on this page, you’re probably not 100% what the literature review is all about. The good news is that you’ve come to the right place.
Literature Review 101
- What (exactly) is a literature review
- What’s the purpose of the literature review chapter
- How to find high-quality resources
- How to structure your literature review chapter
- Example of an actual literature review
What is a literature review?
The word “literature review” can refer to two related things that are part of the broader literature review process. The first is the task of reviewing the literature – i.e. sourcing and reading through the existing research relating to your research topic. The second is the actual chapter that you write up in your dissertation, thesis or research project. Let’s look at each of them:
Reviewing the literature
The first step of any literature review is to hunt down and read through the existing research that’s relevant to your research topic. To do this, you’ll use a combination of tools (we’ll discuss some of these later) to find journal articles, books, ebooks, research reports, dissertations, theses and any other credible sources of information that relate to your topic. You’ll then summarise and catalogue these for easy reference when you write up your literature review chapter.
The literature review chapter
The second step of the literature review is to write the actual literature review chapter (this is usually the second chapter in a typical dissertation or thesis structure ). At the simplest level, the literature review chapter is an overview of the key literature that’s relevant to your research topic. This chapter should provide a smooth-flowing discussion of what research has already been done, what is known, what is unknown and what is contested in relation to your research topic. So, you can think of it as an integrated review of the state of knowledge around your research topic.

What’s the purpose of a literature review?
The literature review chapter has a few important functions within your dissertation, thesis or research project. Let’s take a look at these:
Purpose #1 – Demonstrate your topic knowledge
The first function of the literature review chapter is, quite simply, to show the reader (or marker) that you know what you’re talking about . In other words, a good literature review chapter demonstrates that you’ve read the relevant existing research and understand what’s going on – who’s said what, what’s agreed upon, disagreed upon and so on. This needs to be more than just a summary of who said what – it needs to integrate the existing research to show how it all fits together and what’s missing (which leads us to purpose #2, next).
Purpose #2 – Reveal the research gap that you’ll fill
The second function of the literature review chapter is to show what’s currently missing from the existing research, to lay the foundation for your own research topic. In other words, your literature review chapter needs to show that there are currently “missing pieces” in terms of the bigger puzzle, and that your study will fill one of those research gaps . By doing this, you are showing that your research topic is original and will help contribute to the body of knowledge. In other words, the literature review helps justify your research topic.
Purpose #3 – Lay the foundation for your conceptual framework
The third function of the literature review is to form the basis for a conceptual framework . Not every research topic will necessarily have a conceptual framework, but if your topic does require one, it needs to be rooted in your literature review.
For example, let’s say your research aims to identify the drivers of a certain outcome – the factors which contribute to burnout in office workers. In this case, you’d likely develop a conceptual framework which details the potential factors (e.g. long hours, excessive stress, etc), as well as the outcome (burnout). Those factors would need to emerge from the literature review chapter – they can’t just come from your gut!
So, in this case, the literature review chapter would uncover each of the potential factors (based on previous studies about burnout), which would then be modelled into a framework.
Purpose #4 – To inform your methodology
The fourth function of the literature review is to inform the choice of methodology for your own research. As we’ve discussed on the Grad Coach blog , your choice of methodology will be heavily influenced by your research aims, objectives and questions . Given that you’ll be reviewing studies covering a topic close to yours, it makes sense that you could learn a lot from their (well-considered) methodologies.
So, when you’re reviewing the literature, you’ll need to pay close attention to the research design , methodology and methods used in similar studies, and use these to inform your methodology. Quite often, you’ll be able to “borrow” from previous studies . This is especially true for quantitative studies , as you can use previously tried and tested measures and scales.

How do I find articles for my literature review?
Finding quality journal articles is essential to crafting a rock-solid literature review. As you probably already know, not all research is created equally, and so you need to make sure that your literature review is built on credible research .
We could write an entire post on how to find quality literature (actually, we have ), but a good starting point is Google Scholar . Google Scholar is essentially the academic equivalent of Google, using Google’s powerful search capabilities to find relevant journal articles and reports. It certainly doesn’t cover every possible resource, but it’s a very useful way to get started on your literature review journey, as it will very quickly give you a good indication of what the most popular pieces of research are in your field.
One downside of Google Scholar is that it’s merely a search engine – that is, it lists the articles, but oftentimes it doesn’t host the articles . So you’ll often hit a paywall when clicking through to journal websites.
Thankfully, your university should provide you with access to their library, so you can find the article titles using Google Scholar and then search for them by name in your university’s online library. Your university may also provide you with access to ResearchGate , which is another great source for existing research.
Remember, the correct search keywords will be super important to get the right information from the start. So, pay close attention to the keywords used in the journal articles you read and use those keywords to search for more articles. If you can’t find a spoon in the kitchen, you haven’t looked in the right drawer.
Need a helping hand?
How should I structure my literature review?
Unfortunately, there’s no generic universal answer for this one. The structure of your literature review will depend largely on your topic area and your research aims and objectives.
You could potentially structure your literature review chapter according to theme, group, variables , chronologically or per concepts in your field of research. We explain the main approaches to structuring your literature review here . You can also download a copy of our free literature review template to help you establish an initial structure.
In general, it’s also a good idea to start wide (i.e. the big-picture-level) and then narrow down, ending your literature review close to your research questions . However, there’s no universal one “right way” to structure your literature review. The most important thing is not to discuss your sources one after the other like a list – as we touched on earlier, your literature review needs to synthesise the research , not summarise it .
Ultimately, you need to craft your literature review so that it conveys the most important information effectively – it needs to tell a logical story in a digestible way. It’s no use starting off with highly technical terms and then only explaining what these terms mean later. Always assume your reader is not a subject matter expert and hold their hand through a journe y of the literature while keeping the functions of the literature review chapter (which we discussed earlier) front of mind.
Example of a literature review
In the video below, we walk you through a high-quality literature review from a dissertation that earned full distinction. This will give you a clearer view of what a strong literature review looks like in practice and hopefully provide some inspiration for your own.
Wrapping Up
In this post, we’ve (hopefully) answered the question, “ what is a literature review? “. We’ve also considered the purpose and functions of the literature review, as well as how to find literature and how to structure the literature review chapter. If you’re keen to learn more, check out the literature review section of the Grad Coach blog , as well as our detailed video post covering how to write a literature review .

Psst… there’s more!
This post is an extract from our bestselling short course, Literature Review Bootcamp . If you want to work smart, you don't want to miss this .
You Might Also Like:

16 Comments
Thanks for this review. It narrates what’s not been taught as tutors are always in a early to finish their classes.
Thanks for the kind words, Becky. Good luck with your literature review 🙂
This website is amazing, it really helps break everything down. Thank you, I would have been lost without it.
This is review is amazing. I benefited from it a lot and hope others visiting this website will benefit too.
Timothy T. Chol [email protected]
Thank you very much for the guiding in literature review I learn and benefited a lot this make my journey smooth I’ll recommend this site to my friends
This was so useful. Thank you so much.
Hi, Concept was explained nicely by both of you. Thanks a lot for sharing it. It will surely help research scholars to start their Research Journey.
The review is really helpful to me especially during this period of covid-19 pandemic when most universities in my country only offer online classes. Great stuff
Great Brief Explanation, thanks
So helpful to me as a student
GradCoach is a fantastic site with brilliant and modern minds behind it.. I spent weeks decoding the substantial academic Jargon and grounding my initial steps on the research process, which could be shortened to a couple of days through the Gradcoach. Thanks again!
This is an amazing talk. I paved way for myself as a researcher. Thank you GradCoach!
Well-presented overview of the literature!
This was brilliant. So clear. Thank you
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Literature Reviews
What this handout is about.
This handout will explain what literature reviews are and offer insights into the form and construction of literature reviews in the humanities, social sciences, and sciences.
Introduction
OK. You’ve got to write a literature review. You dust off a novel and a book of poetry, settle down in your chair, and get ready to issue a “thumbs up” or “thumbs down” as you leaf through the pages. “Literature review” done. Right?
Wrong! The “literature” of a literature review refers to any collection of materials on a topic, not necessarily the great literary texts of the world. “Literature” could be anything from a set of government pamphlets on British colonial methods in Africa to scholarly articles on the treatment of a torn ACL. And a review does not necessarily mean that your reader wants you to give your personal opinion on whether or not you liked these sources.
What is a literature review, then?
A literature review discusses published information in a particular subject area, and sometimes information in a particular subject area within a certain time period.
A literature review can be just a simple summary of the sources, but it usually has an organizational pattern and combines both summary and synthesis. A summary is a recap of the important information of the source, but a synthesis is a re-organization, or a reshuffling, of that information. It might give a new interpretation of old material or combine new with old interpretations. Or it might trace the intellectual progression of the field, including major debates. And depending on the situation, the literature review may evaluate the sources and advise the reader on the most pertinent or relevant.
But how is a literature review different from an academic research paper?
The main focus of an academic research paper is to develop a new argument, and a research paper is likely to contain a literature review as one of its parts. In a research paper, you use the literature as a foundation and as support for a new insight that you contribute. The focus of a literature review, however, is to summarize and synthesize the arguments and ideas of others without adding new contributions.
Why do we write literature reviews?
Literature reviews provide you with a handy guide to a particular topic. If you have limited time to conduct research, literature reviews can give you an overview or act as a stepping stone. For professionals, they are useful reports that keep them up to date with what is current in the field. For scholars, the depth and breadth of the literature review emphasizes the credibility of the writer in his or her field. Literature reviews also provide a solid background for a research paper’s investigation. Comprehensive knowledge of the literature of the field is essential to most research papers.
Who writes these things, anyway?
Literature reviews are written occasionally in the humanities, but mostly in the sciences and social sciences; in experiment and lab reports, they constitute a section of the paper. Sometimes a literature review is written as a paper in itself.
Let’s get to it! What should I do before writing the literature review?
If your assignment is not very specific, seek clarification from your instructor:
- Roughly how many sources should you include?
- What types of sources (books, journal articles, websites)?
- Should you summarize, synthesize, or critique your sources by discussing a common theme or issue?
- Should you evaluate your sources?
- Should you provide subheadings and other background information, such as definitions and/or a history?
Find models
Look for other literature reviews in your area of interest or in the discipline and read them to get a sense of the types of themes you might want to look for in your own research or ways to organize your final review. You can simply put the word “review” in your search engine along with your other topic terms to find articles of this type on the Internet or in an electronic database. The bibliography or reference section of sources you’ve already read are also excellent entry points into your own research.
Narrow your topic
There are hundreds or even thousands of articles and books on most areas of study. The narrower your topic, the easier it will be to limit the number of sources you need to read in order to get a good survey of the material. Your instructor will probably not expect you to read everything that’s out there on the topic, but you’ll make your job easier if you first limit your scope.
Keep in mind that UNC Libraries have research guides and to databases relevant to many fields of study. You can reach out to the subject librarian for a consultation: https://library.unc.edu/support/consultations/ .
And don’t forget to tap into your professor’s (or other professors’) knowledge in the field. Ask your professor questions such as: “If you had to read only one book from the 90’s on topic X, what would it be?” Questions such as this help you to find and determine quickly the most seminal pieces in the field.
Consider whether your sources are current
Some disciplines require that you use information that is as current as possible. In the sciences, for instance, treatments for medical problems are constantly changing according to the latest studies. Information even two years old could be obsolete. However, if you are writing a review in the humanities, history, or social sciences, a survey of the history of the literature may be what is needed, because what is important is how perspectives have changed through the years or within a certain time period. Try sorting through some other current bibliographies or literature reviews in the field to get a sense of what your discipline expects. You can also use this method to consider what is currently of interest to scholars in this field and what is not.
Strategies for writing the literature review
Find a focus.
A literature review, like a term paper, is usually organized around ideas, not the sources themselves as an annotated bibliography would be organized. This means that you will not just simply list your sources and go into detail about each one of them, one at a time. No. As you read widely but selectively in your topic area, consider instead what themes or issues connect your sources together. Do they present one or different solutions? Is there an aspect of the field that is missing? How well do they present the material and do they portray it according to an appropriate theory? Do they reveal a trend in the field? A raging debate? Pick one of these themes to focus the organization of your review.
Convey it to your reader
A literature review may not have a traditional thesis statement (one that makes an argument), but you do need to tell readers what to expect. Try writing a simple statement that lets the reader know what is your main organizing principle. Here are a couple of examples:
The current trend in treatment for congestive heart failure combines surgery and medicine. More and more cultural studies scholars are accepting popular media as a subject worthy of academic consideration.
Consider organization
You’ve got a focus, and you’ve stated it clearly and directly. Now what is the most effective way of presenting the information? What are the most important topics, subtopics, etc., that your review needs to include? And in what order should you present them? Develop an organization for your review at both a global and local level:
First, cover the basic categories
Just like most academic papers, literature reviews also must contain at least three basic elements: an introduction or background information section; the body of the review containing the discussion of sources; and, finally, a conclusion and/or recommendations section to end the paper. The following provides a brief description of the content of each:
- Introduction: Gives a quick idea of the topic of the literature review, such as the central theme or organizational pattern.
- Body: Contains your discussion of sources and is organized either chronologically, thematically, or methodologically (see below for more information on each).
- Conclusions/Recommendations: Discuss what you have drawn from reviewing literature so far. Where might the discussion proceed?
Organizing the body
Once you have the basic categories in place, then you must consider how you will present the sources themselves within the body of your paper. Create an organizational method to focus this section even further.
To help you come up with an overall organizational framework for your review, consider the following scenario:
You’ve decided to focus your literature review on materials dealing with sperm whales. This is because you’ve just finished reading Moby Dick, and you wonder if that whale’s portrayal is really real. You start with some articles about the physiology of sperm whales in biology journals written in the 1980’s. But these articles refer to some British biological studies performed on whales in the early 18th century. So you check those out. Then you look up a book written in 1968 with information on how sperm whales have been portrayed in other forms of art, such as in Alaskan poetry, in French painting, or on whale bone, as the whale hunters in the late 19th century used to do. This makes you wonder about American whaling methods during the time portrayed in Moby Dick, so you find some academic articles published in the last five years on how accurately Herman Melville portrayed the whaling scene in his novel.
Now consider some typical ways of organizing the sources into a review:
- Chronological: If your review follows the chronological method, you could write about the materials above according to when they were published. For instance, first you would talk about the British biological studies of the 18th century, then about Moby Dick, published in 1851, then the book on sperm whales in other art (1968), and finally the biology articles (1980s) and the recent articles on American whaling of the 19th century. But there is relatively no continuity among subjects here. And notice that even though the sources on sperm whales in other art and on American whaling are written recently, they are about other subjects/objects that were created much earlier. Thus, the review loses its chronological focus.
- By publication: Order your sources by publication chronology, then, only if the order demonstrates a more important trend. For instance, you could order a review of literature on biological studies of sperm whales if the progression revealed a change in dissection practices of the researchers who wrote and/or conducted the studies.
- By trend: A better way to organize the above sources chronologically is to examine the sources under another trend, such as the history of whaling. Then your review would have subsections according to eras within this period. For instance, the review might examine whaling from pre-1600-1699, 1700-1799, and 1800-1899. Under this method, you would combine the recent studies on American whaling in the 19th century with Moby Dick itself in the 1800-1899 category, even though the authors wrote a century apart.
- Thematic: Thematic reviews of literature are organized around a topic or issue, rather than the progression of time. However, progression of time may still be an important factor in a thematic review. For instance, the sperm whale review could focus on the development of the harpoon for whale hunting. While the study focuses on one topic, harpoon technology, it will still be organized chronologically. The only difference here between a “chronological” and a “thematic” approach is what is emphasized the most: the development of the harpoon or the harpoon technology.But more authentic thematic reviews tend to break away from chronological order. For instance, a thematic review of material on sperm whales might examine how they are portrayed as “evil” in cultural documents. The subsections might include how they are personified, how their proportions are exaggerated, and their behaviors misunderstood. A review organized in this manner would shift between time periods within each section according to the point made.
- Methodological: A methodological approach differs from the two above in that the focusing factor usually does not have to do with the content of the material. Instead, it focuses on the “methods” of the researcher or writer. For the sperm whale project, one methodological approach would be to look at cultural differences between the portrayal of whales in American, British, and French art work. Or the review might focus on the economic impact of whaling on a community. A methodological scope will influence either the types of documents in the review or the way in which these documents are discussed. Once you’ve decided on the organizational method for the body of the review, the sections you need to include in the paper should be easy to figure out. They should arise out of your organizational strategy. In other words, a chronological review would have subsections for each vital time period. A thematic review would have subtopics based upon factors that relate to the theme or issue.
Sometimes, though, you might need to add additional sections that are necessary for your study, but do not fit in the organizational strategy of the body. What other sections you include in the body is up to you. Put in only what is necessary. Here are a few other sections you might want to consider:
- Current Situation: Information necessary to understand the topic or focus of the literature review.
- History: The chronological progression of the field, the literature, or an idea that is necessary to understand the literature review, if the body of the literature review is not already a chronology.
- Methods and/or Standards: The criteria you used to select the sources in your literature review or the way in which you present your information. For instance, you might explain that your review includes only peer-reviewed articles and journals.
Questions for Further Research: What questions about the field has the review sparked? How will you further your research as a result of the review?
Begin composing
Once you’ve settled on a general pattern of organization, you’re ready to write each section. There are a few guidelines you should follow during the writing stage as well. Here is a sample paragraph from a literature review about sexism and language to illuminate the following discussion:
However, other studies have shown that even gender-neutral antecedents are more likely to produce masculine images than feminine ones (Gastil, 1990). Hamilton (1988) asked students to complete sentences that required them to fill in pronouns that agreed with gender-neutral antecedents such as “writer,” “pedestrian,” and “persons.” The students were asked to describe any image they had when writing the sentence. Hamilton found that people imagined 3.3 men to each woman in the masculine “generic” condition and 1.5 men per woman in the unbiased condition. Thus, while ambient sexism accounted for some of the masculine bias, sexist language amplified the effect. (Source: Erika Falk and Jordan Mills, “Why Sexist Language Affects Persuasion: The Role of Homophily, Intended Audience, and Offense,” Women and Language19:2).
Use evidence
In the example above, the writers refer to several other sources when making their point. A literature review in this sense is just like any other academic research paper. Your interpretation of the available sources must be backed up with evidence to show that what you are saying is valid.
Be selective
Select only the most important points in each source to highlight in the review. The type of information you choose to mention should relate directly to the review’s focus, whether it is thematic, methodological, or chronological.
Use quotes sparingly
Falk and Mills do not use any direct quotes. That is because the survey nature of the literature review does not allow for in-depth discussion or detailed quotes from the text. Some short quotes here and there are okay, though, if you want to emphasize a point, or if what the author said just cannot be rewritten in your own words. Notice that Falk and Mills do quote certain terms that were coined by the author, not common knowledge, or taken directly from the study. But if you find yourself wanting to put in more quotes, check with your instructor.
Summarize and synthesize
Remember to summarize and synthesize your sources within each paragraph as well as throughout the review. The authors here recapitulate important features of Hamilton’s study, but then synthesize it by rephrasing the study’s significance and relating it to their own work.
Keep your own voice
While the literature review presents others’ ideas, your voice (the writer’s) should remain front and center. Notice that Falk and Mills weave references to other sources into their own text, but they still maintain their own voice by starting and ending the paragraph with their own ideas and their own words. The sources support what Falk and Mills are saying.
Use caution when paraphrasing
When paraphrasing a source that is not your own, be sure to represent the author’s information or opinions accurately and in your own words. In the preceding example, Falk and Mills either directly refer in the text to the author of their source, such as Hamilton, or they provide ample notation in the text when the ideas they are mentioning are not their own, for example, Gastil’s. For more information, please see our handout on plagiarism .
Revise, revise, revise
Draft in hand? Now you’re ready to revise. Spending a lot of time revising is a wise idea, because your main objective is to present the material, not the argument. So check over your review again to make sure it follows the assignment and/or your outline. Then, just as you would for most other academic forms of writing, rewrite or rework the language of your review so that you’ve presented your information in the most concise manner possible. Be sure to use terminology familiar to your audience; get rid of unnecessary jargon or slang. Finally, double check that you’ve documented your sources and formatted the review appropriately for your discipline. For tips on the revising and editing process, see our handout on revising drafts .
Works consulted
We consulted these works while writing this handout. This is not a comprehensive list of resources on the handout’s topic, and we encourage you to do your own research to find additional publications. Please do not use this list as a model for the format of your own reference list, as it may not match the citation style you are using. For guidance on formatting citations, please see the UNC Libraries citation tutorial . We revise these tips periodically and welcome feedback.
Anson, Chris M., and Robert A. Schwegler. 2010. The Longman Handbook for Writers and Readers , 6th ed. New York: Longman.
Jones, Robert, Patrick Bizzaro, and Cynthia Selfe. 1997. The Harcourt Brace Guide to Writing in the Disciplines . New York: Harcourt Brace.
Lamb, Sandra E. 1998. How to Write It: A Complete Guide to Everything You’ll Ever Write . Berkeley: Ten Speed Press.
Rosen, Leonard J., and Laurence Behrens. 2003. The Allyn & Bacon Handbook , 5th ed. New York: Longman.
Troyka, Lynn Quittman, and Doug Hesse. 2016. Simon and Schuster Handbook for Writers , 11th ed. London: Pearson.
You may reproduce it for non-commercial use if you use the entire handout and attribute the source: The Writing Center, University of North Carolina at Chapel Hill
Make a Gift
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PLoS Comput Biol
- v.9(7); 2013 Jul

Ten Simple Rules for Writing a Literature Review
Marco pautasso.
1 Centre for Functional and Evolutionary Ecology (CEFE), CNRS, Montpellier, France
2 Centre for Biodiversity Synthesis and Analysis (CESAB), FRB, Aix-en-Provence, France
Literature reviews are in great demand in most scientific fields. Their need stems from the ever-increasing output of scientific publications [1] . For example, compared to 1991, in 2008 three, eight, and forty times more papers were indexed in Web of Science on malaria, obesity, and biodiversity, respectively [2] . Given such mountains of papers, scientists cannot be expected to examine in detail every single new paper relevant to their interests [3] . Thus, it is both advantageous and necessary to rely on regular summaries of the recent literature. Although recognition for scientists mainly comes from primary research, timely literature reviews can lead to new synthetic insights and are often widely read [4] . For such summaries to be useful, however, they need to be compiled in a professional way [5] .
When starting from scratch, reviewing the literature can require a titanic amount of work. That is why researchers who have spent their career working on a certain research issue are in a perfect position to review that literature. Some graduate schools are now offering courses in reviewing the literature, given that most research students start their project by producing an overview of what has already been done on their research issue [6] . However, it is likely that most scientists have not thought in detail about how to approach and carry out a literature review.
Reviewing the literature requires the ability to juggle multiple tasks, from finding and evaluating relevant material to synthesising information from various sources, from critical thinking to paraphrasing, evaluating, and citation skills [7] . In this contribution, I share ten simple rules I learned working on about 25 literature reviews as a PhD and postdoctoral student. Ideas and insights also come from discussions with coauthors and colleagues, as well as feedback from reviewers and editors.
Rule 1: Define a Topic and Audience
How to choose which topic to review? There are so many issues in contemporary science that you could spend a lifetime of attending conferences and reading the literature just pondering what to review. On the one hand, if you take several years to choose, several other people may have had the same idea in the meantime. On the other hand, only a well-considered topic is likely to lead to a brilliant literature review [8] . The topic must at least be:
- interesting to you (ideally, you should have come across a series of recent papers related to your line of work that call for a critical summary),
- an important aspect of the field (so that many readers will be interested in the review and there will be enough material to write it), and
- a well-defined issue (otherwise you could potentially include thousands of publications, which would make the review unhelpful).
Ideas for potential reviews may come from papers providing lists of key research questions to be answered [9] , but also from serendipitous moments during desultory reading and discussions. In addition to choosing your topic, you should also select a target audience. In many cases, the topic (e.g., web services in computational biology) will automatically define an audience (e.g., computational biologists), but that same topic may also be of interest to neighbouring fields (e.g., computer science, biology, etc.).
Rule 2: Search and Re-search the Literature
After having chosen your topic and audience, start by checking the literature and downloading relevant papers. Five pieces of advice here:
- keep track of the search items you use (so that your search can be replicated [10] ),
- keep a list of papers whose pdfs you cannot access immediately (so as to retrieve them later with alternative strategies),
- use a paper management system (e.g., Mendeley, Papers, Qiqqa, Sente),
- define early in the process some criteria for exclusion of irrelevant papers (these criteria can then be described in the review to help define its scope), and
- do not just look for research papers in the area you wish to review, but also seek previous reviews.
The chances are high that someone will already have published a literature review ( Figure 1 ), if not exactly on the issue you are planning to tackle, at least on a related topic. If there are already a few or several reviews of the literature on your issue, my advice is not to give up, but to carry on with your own literature review,

The bottom-right situation (many literature reviews but few research papers) is not just a theoretical situation; it applies, for example, to the study of the impacts of climate change on plant diseases, where there appear to be more literature reviews than research studies [33] .
- discussing in your review the approaches, limitations, and conclusions of past reviews,
- trying to find a new angle that has not been covered adequately in the previous reviews, and
- incorporating new material that has inevitably accumulated since their appearance.
When searching the literature for pertinent papers and reviews, the usual rules apply:
- be thorough,
- use different keywords and database sources (e.g., DBLP, Google Scholar, ISI Proceedings, JSTOR Search, Medline, Scopus, Web of Science), and
- look at who has cited past relevant papers and book chapters.
Rule 3: Take Notes While Reading
If you read the papers first, and only afterwards start writing the review, you will need a very good memory to remember who wrote what, and what your impressions and associations were while reading each single paper. My advice is, while reading, to start writing down interesting pieces of information, insights about how to organize the review, and thoughts on what to write. This way, by the time you have read the literature you selected, you will already have a rough draft of the review.
Of course, this draft will still need much rewriting, restructuring, and rethinking to obtain a text with a coherent argument [11] , but you will have avoided the danger posed by staring at a blank document. Be careful when taking notes to use quotation marks if you are provisionally copying verbatim from the literature. It is advisable then to reformulate such quotes with your own words in the final draft. It is important to be careful in noting the references already at this stage, so as to avoid misattributions. Using referencing software from the very beginning of your endeavour will save you time.
Rule 4: Choose the Type of Review You Wish to Write
After having taken notes while reading the literature, you will have a rough idea of the amount of material available for the review. This is probably a good time to decide whether to go for a mini- or a full review. Some journals are now favouring the publication of rather short reviews focusing on the last few years, with a limit on the number of words and citations. A mini-review is not necessarily a minor review: it may well attract more attention from busy readers, although it will inevitably simplify some issues and leave out some relevant material due to space limitations. A full review will have the advantage of more freedom to cover in detail the complexities of a particular scientific development, but may then be left in the pile of the very important papers “to be read” by readers with little time to spare for major monographs.
There is probably a continuum between mini- and full reviews. The same point applies to the dichotomy of descriptive vs. integrative reviews. While descriptive reviews focus on the methodology, findings, and interpretation of each reviewed study, integrative reviews attempt to find common ideas and concepts from the reviewed material [12] . A similar distinction exists between narrative and systematic reviews: while narrative reviews are qualitative, systematic reviews attempt to test a hypothesis based on the published evidence, which is gathered using a predefined protocol to reduce bias [13] , [14] . When systematic reviews analyse quantitative results in a quantitative way, they become meta-analyses. The choice between different review types will have to be made on a case-by-case basis, depending not just on the nature of the material found and the preferences of the target journal(s), but also on the time available to write the review and the number of coauthors [15] .
Rule 5: Keep the Review Focused, but Make It of Broad Interest
Whether your plan is to write a mini- or a full review, it is good advice to keep it focused 16 , 17 . Including material just for the sake of it can easily lead to reviews that are trying to do too many things at once. The need to keep a review focused can be problematic for interdisciplinary reviews, where the aim is to bridge the gap between fields [18] . If you are writing a review on, for example, how epidemiological approaches are used in modelling the spread of ideas, you may be inclined to include material from both parent fields, epidemiology and the study of cultural diffusion. This may be necessary to some extent, but in this case a focused review would only deal in detail with those studies at the interface between epidemiology and the spread of ideas.
While focus is an important feature of a successful review, this requirement has to be balanced with the need to make the review relevant to a broad audience. This square may be circled by discussing the wider implications of the reviewed topic for other disciplines.
Rule 6: Be Critical and Consistent
Reviewing the literature is not stamp collecting. A good review does not just summarize the literature, but discusses it critically, identifies methodological problems, and points out research gaps [19] . After having read a review of the literature, a reader should have a rough idea of:
- the major achievements in the reviewed field,
- the main areas of debate, and
- the outstanding research questions.
It is challenging to achieve a successful review on all these fronts. A solution can be to involve a set of complementary coauthors: some people are excellent at mapping what has been achieved, some others are very good at identifying dark clouds on the horizon, and some have instead a knack at predicting where solutions are going to come from. If your journal club has exactly this sort of team, then you should definitely write a review of the literature! In addition to critical thinking, a literature review needs consistency, for example in the choice of passive vs. active voice and present vs. past tense.
Rule 7: Find a Logical Structure
Like a well-baked cake, a good review has a number of telling features: it is worth the reader's time, timely, systematic, well written, focused, and critical. It also needs a good structure. With reviews, the usual subdivision of research papers into introduction, methods, results, and discussion does not work or is rarely used. However, a general introduction of the context and, toward the end, a recapitulation of the main points covered and take-home messages make sense also in the case of reviews. For systematic reviews, there is a trend towards including information about how the literature was searched (database, keywords, time limits) [20] .
How can you organize the flow of the main body of the review so that the reader will be drawn into and guided through it? It is generally helpful to draw a conceptual scheme of the review, e.g., with mind-mapping techniques. Such diagrams can help recognize a logical way to order and link the various sections of a review [21] . This is the case not just at the writing stage, but also for readers if the diagram is included in the review as a figure. A careful selection of diagrams and figures relevant to the reviewed topic can be very helpful to structure the text too [22] .
Rule 8: Make Use of Feedback
Reviews of the literature are normally peer-reviewed in the same way as research papers, and rightly so [23] . As a rule, incorporating feedback from reviewers greatly helps improve a review draft. Having read the review with a fresh mind, reviewers may spot inaccuracies, inconsistencies, and ambiguities that had not been noticed by the writers due to rereading the typescript too many times. It is however advisable to reread the draft one more time before submission, as a last-minute correction of typos, leaps, and muddled sentences may enable the reviewers to focus on providing advice on the content rather than the form.
Feedback is vital to writing a good review, and should be sought from a variety of colleagues, so as to obtain a diversity of views on the draft. This may lead in some cases to conflicting views on the merits of the paper, and on how to improve it, but such a situation is better than the absence of feedback. A diversity of feedback perspectives on a literature review can help identify where the consensus view stands in the landscape of the current scientific understanding of an issue [24] .
Rule 9: Include Your Own Relevant Research, but Be Objective
In many cases, reviewers of the literature will have published studies relevant to the review they are writing. This could create a conflict of interest: how can reviewers report objectively on their own work [25] ? Some scientists may be overly enthusiastic about what they have published, and thus risk giving too much importance to their own findings in the review. However, bias could also occur in the other direction: some scientists may be unduly dismissive of their own achievements, so that they will tend to downplay their contribution (if any) to a field when reviewing it.
In general, a review of the literature should neither be a public relations brochure nor an exercise in competitive self-denial. If a reviewer is up to the job of producing a well-organized and methodical review, which flows well and provides a service to the readership, then it should be possible to be objective in reviewing one's own relevant findings. In reviews written by multiple authors, this may be achieved by assigning the review of the results of a coauthor to different coauthors.
Rule 10: Be Up-to-Date, but Do Not Forget Older Studies
Given the progressive acceleration in the publication of scientific papers, today's reviews of the literature need awareness not just of the overall direction and achievements of a field of inquiry, but also of the latest studies, so as not to become out-of-date before they have been published. Ideally, a literature review should not identify as a major research gap an issue that has just been addressed in a series of papers in press (the same applies, of course, to older, overlooked studies (“sleeping beauties” [26] )). This implies that literature reviewers would do well to keep an eye on electronic lists of papers in press, given that it can take months before these appear in scientific databases. Some reviews declare that they have scanned the literature up to a certain point in time, but given that peer review can be a rather lengthy process, a full search for newly appeared literature at the revision stage may be worthwhile. Assessing the contribution of papers that have just appeared is particularly challenging, because there is little perspective with which to gauge their significance and impact on further research and society.
Inevitably, new papers on the reviewed topic (including independently written literature reviews) will appear from all quarters after the review has been published, so that there may soon be the need for an updated review. But this is the nature of science [27] – [32] . I wish everybody good luck with writing a review of the literature.
Acknowledgments
Many thanks to M. Barbosa, K. Dehnen-Schmutz, T. Döring, D. Fontaneto, M. Garbelotto, O. Holdenrieder, M. Jeger, D. Lonsdale, A. MacLeod, P. Mills, M. Moslonka-Lefebvre, G. Stancanelli, P. Weisberg, and X. Xu for insights and discussions, and to P. Bourne, T. Matoni, and D. Smith for helpful comments on a previous draft.
Funding Statement
This work was funded by the French Foundation for Research on Biodiversity (FRB) through its Centre for Synthesis and Analysis of Biodiversity data (CESAB), as part of the NETSEED research project. The funders had no role in the preparation of the manuscript.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 03 June 2024
The effectiveness of digital twins in promoting precision health across the entire population: a systematic review
- Mei-di Shen 1 ,
- Si-bing Chen 2 &
- Xiang-dong Ding ORCID: orcid.org/0009-0001-1925-0654 2
npj Digital Medicine volume 7 , Article number: 145 ( 2024 ) Cite this article
638 Accesses
3 Altmetric
Metrics details
- Public health
- Risk factors
- Signs and symptoms
Digital twins represent a promising technology within the domain of precision healthcare, offering significant prospects for individualized medical interventions. Existing systematic reviews, however, mainly focus on the technological dimensions of digital twins, with a limited exploration of their impact on health-related outcomes. Therefore, this systematic review aims to explore the efficacy of digital twins in improving precision healthcare at the population level. The literature search for this study encompassed PubMed, Embase, Web of Science, Cochrane Library, CINAHL, SinoMed, CNKI, and Wanfang Database to retrieve potentially relevant records. Patient health-related outcomes were synthesized employing quantitative content analysis, whereas the Joanna Briggs Institute (JBI) scales were used to evaluate the quality and potential bias inherent in each selected study. Following established inclusion and exclusion criteria, 12 studies were screened from an initial 1321 records for further analysis. These studies included patients with various conditions, including cancers, type 2 diabetes, multiple sclerosis, heart failure, qi deficiency, post-hepatectomy liver failure, and dental issues. The review coded three types of interventions: personalized health management, precision individual therapy effects, and predicting individual risk, leading to a total of 45 outcomes being measured. The collective effectiveness of these outcomes at the population level was calculated at 80% (36 out of 45). No studies exhibited unacceptable differences in quality. Overall, employing digital twins in precision health demonstrates practical advantages, warranting its expanded use to facilitate the transition from the development phase to broad application.
PROSPERO registry: CRD42024507256.
Similar content being viewed by others
Digital twins for health: a scoping review


Digital twins in medicine
The health digital twin to tackle cardiovascular disease—a review of an emerging interdisciplinary field
Introduction.
Precision health represents a paradigm shift from the conventional “one size fits all” medical approach, focusing on specific diagnosis, treatment, and health management by incorporating individualized factors such as omics data, clinical information, and health outcomes 1 , 2 . This approach significantly impacts various diseases, potentially improving overall health while reducing healthcare costs 3 , 4 . Within this context, digital twins emerged as a promising technology 5 , creating digital replicas of the human body through two key steps: building mappings and enabling dynamic evolution 6 . Unlike traditional data mining methods, digital twins consider individual variability, providing continuous, dynamic recommendations for clinical practice 7 . This approach has gained significant attention among researchers, highlighting its potential applications in advancing precision health.
Several systematic reviews have explored the advancement of digital twins within the healthcare sector. One rapid review 8 identified four core functionalities of digital twins in healthcare management: safety management, information management, health management/well-being promotion, and operational control. Another systematic review 9 , through an analysis of 22 selected publications, summarized the diverse application scenarios of digital twins in healthcare, confirming their potential in continuous monitoring, personalized therapy, and hospital management. Furthermore, a quantitative review 10 assessed 94 high-quality articles published from 2018 to 2022, revealing a primary focus on technological advancements (such as artificial intelligence and the Internet of Things) and application scenarios (including personalized, precise, and real-time healthcare solutions), thus highlighting the pivotal role of digital twins technology in the field of precision health. Another systematic review 11 , incorporating 18 framework papers or reviews, underscored the need for ongoing research into digital twins’ healthcare applications, especially during the COVID-19 pandemic. Moreover, a systematic review 12 on the application of digital twins in cardiovascular diseases presented proof-of-concept and data-driven approaches, offering valuable insights for implementing digital twins in this specific medical area.
While the existing literature offers valuable insights into the technological aspects of digital twins in healthcare, these systematic reviews failed to thoroughly examine the actual impacts on population health. Despite the increasing interest and expanding body of research on digital twins in healthcare, the direct effects on patient health-related outcomes remain unclear. This knowledge gap highlights the need to investigate how digital twins promote and restore patient health, which is vital for advancing precision health technologies. Therefore, the objective of our systematic review is to assess the effectiveness of digital twins in improving health-related outcomes at the population level, providing a clearer understanding of their practical benefits in the context of precision health.
Search results
The selection process for the systematic review is outlined in the PRISMA flow chart (Fig. 1 ). Initially, 1321 records were identified. Of these, 446 duplicates (446/1321, 33.76%) were removed, leaving 875 records (875/1321, 66.24%) for title and abstract screening. Applying the pre-defined inclusion and exclusion criteria led to the exclusion of 858 records (858/875, 98.06%), leaving 17 records (17/875, 1.94%) for full-text review. Further scrutiny resulted in the exclusion of one study (1/17, 5.88%) lacking health-related outcomes and four studies (4/17, 23.53%) with overlapping data. Ultimately, 12 (12/17, 70.59%) original studies 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 were included in the systematic review. Supplementary Table 1 provides a summary of the reasons for exclusion at the full-text reading phase.
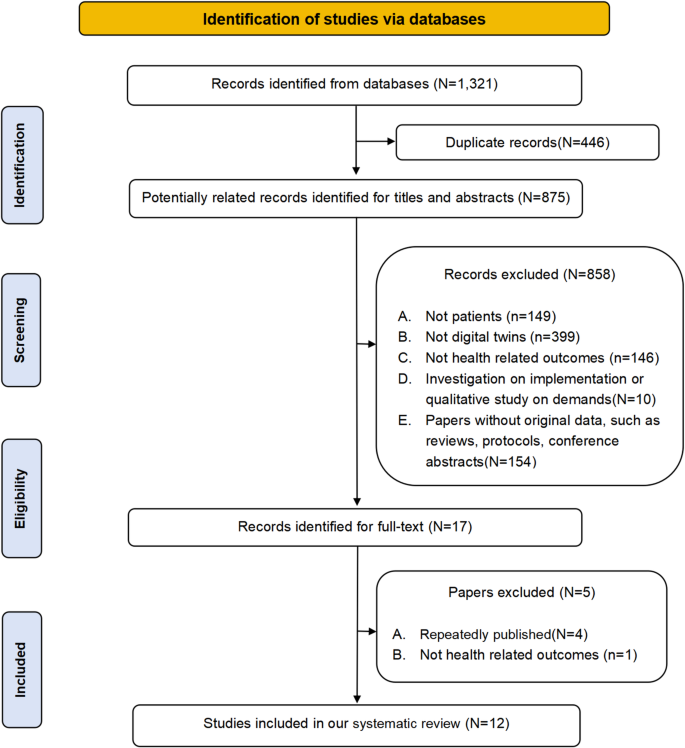
Flow chart of included studies in the systematic review.
Study characteristics
The studies included in this systematic review were published between 2021 (2/12, 16.67%) 23 , 24 and 2023 (8/12, 66.67%) 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 . Originating from diverse regions, 4/12 studies (33.33%) were from Asia 13 , 14 , 21 , 24 , 5/12 (41.67%) from America 15 , 17 , 19 , 20 , 22 , and 3/12 (25.00%) from Europe 16 , 18 , 23 . The review encompassed various study designs, including randomized controlled trials (1/12, 8.33%) 14 , quasi-experiments (6/12, 50.00%) 13 , 15 , 16 , 18 , 19 , 21 , and cohort studies (5/12, 41.67%) 17 , 20 , 22 , 23 , 24 . The sample sizes ranged from 15 13 to 3500 patients 19 . Five studies assessed the impact of digital twins on virtual patients 15 , 16 , 18 , 19 , 20 , while seven examined their effect on real-world patients 13 , 14 , 17 , 21 , 22 , 23 , 24 . These patients included had various diseases, including cancer (4/12, 33.33%) 15 , 16 , 19 , 22 , type 2 diabetes (2/12, 16.66%) 13 , 14 , multiple sclerosis (2/12, 16.66%) 17 , 18 , qi deficiency (1/12, 8.33%) 21 , heart failure (1/12, 8.33%) 20 , post-hepatectomy liver failure (1/12, 8.33%) 23 , and dental issues (1/12, 8.33%) 24 . This review coded interventions into three types: personalized health management (3/12, 25.00%) 13 , 14 , 21 , precision individual therapy effects (3/12, 25.00%) 15 , 16 , 18 , 19 , 20 , 22 , and predicting individual risk (3/12, 25.00%) 17 , 23 , 24 , with a total of 45 measured outcomes. Characteristics of the included studies are detailed in Table 1 .
Risk of bias assessment
The risk of bias for the studies included in this review is summarized in Fig. 2 . In the single RCT 14 assessed, 10 out of 13 items received positive responses. Limitations were observed due to incomplete reporting of baseline characteristics and issues with blinding. Among the six quasi-experimental studies evaluated, five (83.33%) 13 , 15 , 16 , 18 , 21 achieved at least six positive responses, indicating an acceptable quality, while one study (16.67%) 19 fell slightly below this threshold with five positive responses. The primary challenges in these quasi-experimental studies were due to the lack of control groups, inadequate baseline comparisons, and limited follow-up reporting. Four out of five (80.00%) 17 , 20 , 22 , 23 of the cohort studies met or exceeded the criterion with at least eight positive responses, demonstrating their acceptable quality. However, one study (20.00%) 24 had a lower score due to incomplete data regarding loss to follow-up and the specifics of the interventions applied. Table 1 elaborates on the specific reasons for these assessments. Despite these concerns, the overall quality of the included studies is considered a generally acceptable risk of bias.
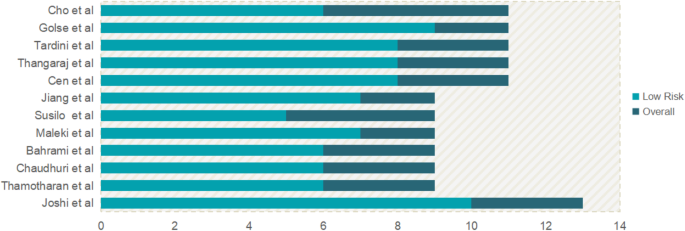
The summary of bias risk via the Joanna Briggs Institute assessment tools.
The impact of digital twins on health-related outcomes among patients
This review includes 12 studies that collectively assessed 45 outcomes, achieving an overall effectiveness rate of 80% (36 out of 45 outcomes), as depicted in Fig. 3a . The digital twins analyzed were coded into three functional categories: personalized health management, precision individual therapy effects, and predicting individual risks. A comprehensive analysis of the effectiveness of digital twins across these categories is provided, detailing the impact and outcomes associated with each function.
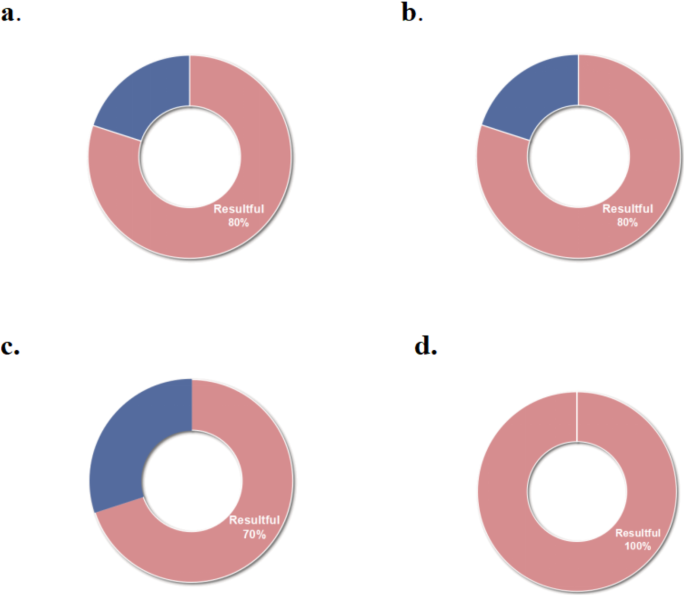
a The overall effectiveness of digital twins; b The effectiveness of personalized health management driven by digital twins; c The effectiveness of precision individualized therapy effects driven by digital twins; d The effectiveness of prediction of individual risk driven by digital twins.
The effectiveness of digital twins in personalized health management
In this review, three studies 13 , 14 , 21 employing digital twins for personalized health management reported an effectiveness of 80% (24 out of 30 outcomes), as shown in Fig. 3b . A self-control study 13 involving 15 elderly patients with diabetes, used virtual patient representations based on health information to guide individualized insulin infusion. Over 14 days, this approach improved the time in range (TIR) from 3–75% to 86–97%, decreased hypoglycemia duration from 0–22% to 0–9%, and reduced hyperglycemia time from 0–98% to 0–12%. A 1-year randomized controlled trial 14 with 319 type 2 diabetes patients, implemented personalized digital twins interventions based on nutrition, activity, and sleep. This trial demonstrated significant improvements in Hemoglobin A1c (HbA1C), Homeostatic Model Assessment 2 of Insulin Resistance (HOMA2-IR), Nonalcoholic Fatty Liver Disease Liver Fat Score (NAFLD-LFS), and Nonalcoholic Fatty Liver Disease Fibrosis Score (NAFLD-NFS), and other primary outcomes (all, P < 0.001; Table 2 ). However, no significant changes were observed in weight, Alanine Aminotransferase (ALT), Fibrosis-4 Score (FIB4), and AST to Platelet Ratio Index (APRI) (all, P > 0.05). A non-randomized controlled trial 21 introduced a digital twin-based Traditional Chinese Medicine (TCM) health management platform for patients with qi deficiency. It was found to significantly improve blood pressure, main and secondary TCM symptoms, total TCM symptom scores, and quality of life (all, P < 0.05). Nonetheless, no significant improvements were observed in heart rate and BMI (all, P > 0.05; Table 2 ).
The effectiveness of digital twins in precision individual therapy effects
Six studies 15 , 16 , 18 , 19 , 20 , 22 focused on the precision of individual therapy effects using digital twins, demonstrating a 70% effectiveness rate (7 out of 10 outcomes), as detailed in Fig. 3c . In a self-control study 15 , a data-driven approach was employed to create digital twins, generating 100 virtual patients to predict the potential tumor biology outcomes of radiotherapy regimens with varying contents and doses. This study showed that personalized radiotherapy plans derived from digital twins could extend the median tumor progression time by approximately six days and reduce radiation doses by 16.7%. Bahrami et al. 16 created 3000 virtual patients experiencing cancer pain to administer precision dosing of fentanyl transdermal patch therapy. The intervention led to a 16% decrease in average pain intensity and an additional median pain-free duration of 23 hours, extending from 72 hours in cancer patients. Another quasi-experimental study 18 created 3000 virtual patients with multiple sclerosis to assess the impact of Ocrelizumab. Findings indicated Ocrelizumab can resulted in a reduction in relapses (0.191 [0.143, 0.239]) and lymphopenic adverse events (83.73% vs . 19.9%) compared to a placebo. American researchers 19 developed a quantitative systems pharmacology model using digital twins to identify the optimal dosing for aggressive non-Hodgkin lymphoma patients. This approach resulted in at least a 50% tumor size reduction by day 42 among 3500 virtual patients. A cohort study 20 assessed the 5-year composite cardiovascular outcomes in 2173 virtual patients who were treated with spironolactone or left untreated and indicated no statistically significant inter-group differences (0.85, [0.69–1.04]). Tardini et al. 22 employed digital twins to optimize multi-step treatment for oropharyngeal squamous cell carcinoma in 134 patients. The optimized treatment selection through digital twins predicted increased survival rates by 3.73 (−0.75, 8.96) and dysphagia rates by 0.75 (−4.48, 6.72) compared to clinician decisions, with no statistical significance.
The effectiveness of digital twins in predicting individual risk
Three studies 17 , 23 , 24 employing digital twins to predict individual patient risks demonstrated a 100% effectiveness rate (5 out of 5 outcomes), as shown in Fig. 3d . A cohort study 17 used digital twins to forecast the onset age for disease-specific brain atrophy in patients with multiple sclerosis. Findings indicated that the onset of progressive brain tissue loss, on average, preceded clinical symptoms by 5-6 years among the 519 patients ( P < 0.01). Another study 23 focused on predicting postoperative liver failure in 47 patients undergoing major hepatectomy through mathematical models of blood circulation. The study highlighted that elevated Postoperative Portal Vein pressure (PPV) and Portocaval Gradient (PCG) values above 17.5 mmHg and 13.5 mmHg, respectively, correlated with the measured values (all, P < 0.0001; Table 2 ). These indicators were effective in predicting post-hepatectomy liver failure, accurately identifying three out of four patients who experienced this complication. Cho et al. 24 created digital twins for 50 adult female patients using facial scans and cone-beam computed tomography images to evaluate the anteroposterior position of the maxillary central incisors and forehead inclination. The analysis demonstrated significant differences in the position of the maxillary central incisors ( P = 0.04) and forehead inclination ( P = 0.02) between the two groups.
This systematic review outlines the effectiveness of digital twins in improving health-related outcomes across various diseases, including cancers, type 2 diabetes, multiple sclerosis, qi deficiency, heart failure, post-hepatectomy liver failure, and dental issues, at the population level. Distinct from prior reviews that focused on the technological dimensions of digital twins, our analysis shows the practical applications of digital twins in healthcare. The applications have been categorized into three main areas: personalized health management, precision individual therapy effects, and predicting individual risks, encompassing a total of 45 outcomes. An overall effectiveness of 80% was observed across these outcomes. This review offers valuable insights into the application of digital twins in precision health and supports the transition of digital twins from construction to population-wide implementation.
Digital twins play a crucial role in achieving precision health 25 . They serve as virtual models of human organs, tissues, cells, or microenvironments, dynamically updating based on real-time data to offer feedback for interventions on their real counterparts 26 , 27 . Digital twins can solve complex problems in personalized health management 28 , 29 and enable comprehensive, proactive, and precise healthcare 30 . In the studies reviewed, researchers implemented digital twins by creating virtual patients based on personal health data and using simulations to generate personalized recommendations and predictions. It is worth noting that while certain indicators have not experienced significant improvement in personalized health management for patients with type 2 diabetes and Qi deficiency, it does not undermine the effectiveness of digital twins. Firstly, these studies have demonstrated significant improvements in primary outcome measures. Secondly, improving health-related outcomes in chronic diseases is an ongoing, complex process heavily influenced by changes in health behaviors 31 , 32 . While digital twins can provide personalized health guidance based on individual health data, their impact on actual behaviors warrants further investigation.
The dual nature of medications, providing benefits yet potentially leading to severe clinical outcomes like morbidity or mortality, must be carefully considered. The impact of therapy is subject to various factors, including the drug attributes and the specific disease characteristics 33 . Achieving accurate medication administration remains a significant challenge for healthcare providers 34 , underscoring the need for innovative methodologies like computational precise drug delivery 35 , 36 , a example highlighted in our review of digital twins. Regarding the prediction of individual therapy effects for conditions such as cancer, multiple sclerosis, and heart failure, six studies within this review have reported partly significant improvements in patient health-related outcomes. These advancements facilitate the tailored selection and dosing of therapy, underscoring the ability of digital twins to optimize patient-specific treatment plans effectively.
Furthermore, digital twins can enhance clinical understanding and personalize disease risk prediction 37 . It enables a quantitative understanding and prediction of individuals by continuously predicting and evaluating patient data in a virtual environment 38 . In patients with multiple sclerosis, digital twins have facilitated predictions regarding the onset of disease-specific brain atrophy, allowing for early intervention strategies. Similarly, digital twins assessed the risk of liver failure after liver resection, aiding healthcare professionals in making timely decisions. Moreover, the application of digital twins in the three-dimensional analysis of patients with dental problems has demonstrated highly effective clinical significance, underscoring its potential across various medical specialties. In summary, the adoption of digital twins has significantly contributed to advancing precision health and restoring patient well-being by creating virtual patients based on personal health data and using simulations to generate personalized recommendations and predictions.
Recent studies have introduced various digital twin systems, covering areas such as hospital management 8 , remote monitoring 9 , and diagnosing and treating various conditions 39 , 40 . Nevertheless, these systems were not included in this review due to the lack of detailed descriptions at the population health level, which constrains the broader application of this emerging technology. Our analysis underscores the reported effectiveness of digital twins, providing unique opportunities for dynamic prevention and precise intervention across different diseases. Multiple research methodologies and outcome measures poses a challenge for quantitative publication detection. This systematic review employed a comprehensive retrieval strategy across various databases for screening articles on the effectiveness of digital twins, to reduce the omission of negative results. And four repeated publications were excluded based on authors, affiliation, population, and other criteria to mitigate the bias of overestimating the digital twins effect due to repeated publication.
However, there are still limitations. Firstly, the limited published research on digital twins’ application at the population level hinders the ability to perform a quantitative meta-analysis, possibly limiting our findings’ interpretability. We encourage reporting additional high-quality randomized controlled trials on the applicability of digital twins to facilitate quantitative analysis of their effectiveness in precision health at the population level. Secondly, this review assessed the effectiveness of digital twins primarily through statistical significance ( P -value or 95% confidence interval). However, there are four quasi-experimental studies did not report statistical significance. One of the limitations of this study is the use of significant changes in author self-reports as a criterion in these four quasi-experimental studies for identifying effectiveness. In clinical practice, the author’s self-reported clinical significance can also provide the effectiveness of digital twins. Thirdly, by focusing solely on studies published in Chinese and English, this review may have omitted relevant research available in other languages, potentially limiting the scope of the analyzed literature. Lastly, our review primarily emphasized reporting statistical differences between groups. Future work should incorporate more application feedback from real patients to expose digital twins to the nuances of actual patient populations.
The application of digital twins is currently limited and primarily focused on precision health for individual patients. Expanding digital twins’ application from individual to group precision health is recommended to signify a more extensive integration in healthcare settings. This expansion involves sharing real-time data and integrating medical information across diverse medical institutions within a region, signifying the development of group precision health. Investigating both personalized medical care and collective health management has significant implications for improving medical diagnosis and treatment approaches, predicting disease risks, optimizing health management strategies, and reducing societal healthcare costs 41 .
Digital twins intervention encompasses various aspects such as health management, decision-making, and prediction, among others 9 . It represents a technological and conceptual innovation in traditional population health intervention. However, the current content design of the digital twins intervention is insufficient and suggests that it should be improved by incorporating more effective content strategies tailored to the characteristics of the target population. Findings from this study indicate that interventions did not differ significantly in our study is from digital twins driven by personalized health management, which means that compared with the other two function-driven digital twins, personalized health management needs to receive more attention to enhance its effect in population-level. For example, within the sphere of chronic disease management, integrating effective behavioral change strategies into digital twins is advisable to positively influence health-related indicators, such as weight and BMI. The effectiveness of such digital behavior change strategies has been reported in previous studies 42 , 43 . The consensus among researchers on the importance of combining effective content strategies with digital intervention technologies underscores the potential for this approach to improve patient health-related outcomes significantly.
The applications of digital twins in precision health are mainly focused on model establishment and prediction description, with limited implementation in multi-center settings. A more robust and detailed data foundation is recommended to improve clinical decision-making and reduce the likelihood of imprecise treatments. This requires continuous updating and capturing of dynamic information by digital twins in the future, as well as the improvement of the data platform that facilitates mapping, interaction, and iterative optimization. Integrating digital twins effectively into clinical workflows can support clinical interventions, assist physicians in making informed decisions, and increase the standard of patient care 6 .
The accessibility of health data is a significant challenge for the clinical implementation of digital twins. Although the internet and information technology have significantly enhanced health data availability, health data, including information systems and electronic health records, remain heterogeneous and are difficult to share 44 . Health data often contains confidential patient information, as well as unreliable information, posing challenges for implementing digital twins in healthcare settings. The primary technology utilized in digital twins, artificial intelligence algorithms, demands high-performance hardware devices and software platforms for data analysis 45 , necessitating healthcare organizations to allocate increased investment and budget for computing infrastructure supporting digital twins’ application. Therefore, future research should be focused on the technical aspects of digital twins to resolve these challenges. The automated processing of health data using a large language model and the rapid conversion of complex natural language texts into comprehensive knowledge texts are encouraged. The development of high-performance computing technology is essential for cost-effective computing requirements, which can facilitate the application of digital twins in clinical practice 46 .
Overall, this systematic review offers a comprehensive overview of digital twins in precision health, examining their impact at the population level. The findings indicate a significant overall effectiveness rate of 80% for the measured outcomes, highlighting digital twins’ pivotal role in advancing precision health. Future research should broaden the application of digital twins across various populations, integrate proven content strategies, and implement these approaches in various healthcare settings. Such efforts will maximize the benefits of digital technologies in healthcare, promoting more precise and efficacious strategies, thereby elevating patient outcomes and improving overall healthcare experiences. While digital twins offer great promise for precision health, their broad adoption and practical implementation are still in the early stages. Development, and application are essential to unlock the full potential of digital twins in revolutionizing healthcare delivery.
This systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines 47 . The protocol for this systematic review was prospectively registered on PROSPERO, which can be accessed via the following link: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42024507256 . The registered protocol underwent an update, which included polishing the title of the article, modifying the limitation of the control group and language in the inclusion/exclusion criteria, and refining the process of data synthesis and analysis to enhance that clarity and readability of this systematic review. These modifications were updated in the revision notes section of the PROSPERO.
Literature search strategy
Literature searches were conducted in PubMed, Embase, Web of Science, Cochrane Library, CINAHL, SinoMed, CNKI, and Wanfang Database, covering publications up to December 24, 2023. A comprehensive search strategy was developed using a combination of Medical Subject Headings terms and free-text terms, as detailed in Supplementary Table 2 . Furthermore, reference lists of articles and reviews meeting the inclusion criteria were reviewed for additional relevant studies.
Inclusion and exclusion criteria
The inclusion criteria for this systematic review included: 1) Population: Patients diagnosed with any diseases or symptoms; 2) Intervention: Any interventions involving digital twins; 3) Controls: Non-digital twin groups, such as standard care or conventional therapy, as well as no control group; 4) Outcomes: Health-related outcomes as the primary outcomes of interest; 5) Study design: All study designs that measured patient health-related outcomes after digital twins were included, including intervention studies and predictive cohort studies.
Initially, duplicates were removed. Exclusion criteria included: 1) Papers lacking original data, such as reviews, protocols, and conference abstracts; 2) Studies not in English or Chinese; 3) Surveys focusing on implementation and qualitative studies related to requirements. In cases of data duplication, the most comprehensive data report was included.
Study selection and Data extraction
Following the automatic removal of duplicates, two independent reviewers (MD.SHEN and SB.CHEN) conducted initial screenings of titles and abstracts against the predefined inclusion and exclusion criteria to identify potentially relevant studies. Afterward, the same reviewers examined the full texts of these shortlisted articles to confirm their suitability for inclusion. This process also involved checking the reference lists of these articles for any additional studies that might meet the criteria. Data from the included studies were systematically extracted using a pre-designed extraction form. Recorded information included the first author’s name, publication year, country of origin, type of study, sample size, study population, intervention, controls, measurements, and an appraisal of each study. Disagreements between the reviewers were resolved by consultation with a third senior reviewer (XD.DING), ensuring consensus.
Quality appraisal
The Joanna Briggs Institute (JBI) scales 48 were used to assess the quality and potential bias of each study included in the review, employing specific tools tailored to the type of study under evaluation. These tools feature response options of “yes,” “no,” “unclear,” or “not applicable” for each assessment item. For randomized controlled trials (RCTs), the JBI scale includes 13 items, with answering “yes” to at least six items indicating a high-quality study. Quasi-experimental studies were evaluated using a nine-item checklist, where five or more positive responses qualify the research as high quality. Cohort studies underwent evaluation through an 11-item checklist, with six or more affirmative responses indicating high quality. The assessment was independently carried out by two reviewers (MD.SHEN and SB.CHEN), and any disagreements were resolved through consultation with a third senior reviewer (XD.DING), ensuring the integrity and accuracy of the quality assessment.
Data synthesis and analysis
Given the heterogeneity in type of study and outcome measures, a meta-analysis was deemed unfeasible. Instead, a quantitative content analysis was employed to analyze all the selected studies 49 , 50 . Key information was extracted using a pre-designed standardized form, including the first author’s name, patient characteristics, intervention functional characteristics, measurements, results, effectiveness, and adverse events. Two reviewers (MD.SHEN and SB.CHEN) independently coded digital twin technology into three categories for descriptive analysis: personalized health management, precision individual therapy effects, and predicting individual risk, based on its functional characteristics. The Kappa statistic was applied to evaluate the inter-rater reliability during the coding process, yielding a value of 0.871, which signifies good agreement between the researchers 51 , 52 . The assessment of digital twins effectiveness was based on statistical significance ( P -value or 95% confidence interval). Outcomes with statistical significance were labeled as “resultful,” whereas those lacking statistical significance were deemed “resultless.” For quasi-experimental studies, significant changes in the authors’ self-reports were used to determine the effectiveness in the absence of reporting of statistical significance. The proportion of effectiveness was calculated as the number of “resultful” indicators divided by the total number of outcomes within each category.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Code availability
Code sharing is not applicable to this article as no codes were generated or analyzed during the current study.
Fu, M. R. et al. Precision health: A nursing perspective. Int. J. Nurs. Sci. 7 , 5–12 (2020).
PubMed Google Scholar
Naithani, N., Sinha, S., Misra, P., Vasudevan, B. & Sahu, R. Precision medicine: Concept and tools. Med. J., Armed Forces India 77 , 249–257 (2021).
Article PubMed Google Scholar
Payne, K. & Gavan, S. P. Economics and precision medicine. Handb. Exp. Pharmacol. 280 , 263–281 (2023).
Ielapi, N. et al. Precision medicine and precision nursing: the era of biomarkers and precision health. Int. J. Gen. Med. 13 , 1705–1711 (2020).
Article PubMed PubMed Central Google Scholar
Corral-Acero, J. et al. The ‘Digital Twin’ to enable the vision of precision cardiology. Eur. Heart J. 41 , 4556–4564 (2020).
Ferdousi, R., Laamarti, F., Hossain, M. A., Yang, C. S. & Saddik, A. E. Digital twins for well-being: an overview. Digital Twin 1 , 2022 (2022).
Article Google Scholar
Vallée, A. Digital twin for healthcare systems. Front. Digital health 5 , 1253050 (2023).
Elkefi, S. & Asan, O. Digital twins for managing health care systems: rapid literature review. J. Med. Internet Res. 24 , e37641 (2022).
Sun, T., He, X. & Li, Z. Digital twin in healthcare: Recent updates and challenges. Digital Health 9 , 20552076221149651 (2023).
Sheng, B. et al. Detecting latent topics and trends of digital twins in healthcare: A structural topic model-based systematic review. Digital Health 9 , 20552076231203672 (2023).
Khan, A. et al. A scoping review of digital twins in the context of the Covid-19 pandemic. Biomed. Eng. Comput. Biol. 13 , 11795972221102115 (2022).
Coorey, G. et al. The health digital twin to tackle cardiovascular disease-a review of an emerging interdisciplinary field. NPJ Digital Med. 5 , 126 (2022).
Thamotharan, P. et al. Human Digital Twin for Personalized Elderly Type 2 Diabetes Management. J. Clin. Med. 12 , https://doi.org/10.3390/jcm12062094 (2023).
Joshi, S. et al. Digital twin-enabled personalized nutrition improves metabolic dysfunction-associated fatty liver disease in type 2 diabetes: results of a 1-year randomized controlled study. Endocr. Pract. : Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinologists 29 , 960–970 (2023).
Chaudhuri, A. et al. Predictive digital twin for optimizing patient-specific radiotherapy regimens under uncertainty in high-grade gliomas. Front. Artif. Intell. 6 , 1222612–1222612 (2023).
Bahrami, F., Rossi, R. M., De Nys, K. & Defraeye, T. An individualized digital twin of a patient for transdermal fentanyl therapy for chronic pain management. Drug Deliv. Transl. Res. 13 , 2272–2285 (2023).
Article CAS PubMed PubMed Central Google Scholar
Cen, S., Gebregziabher, M., Moazami, S., Azevedo, C. J. & Pelletier, D. Toward precision medicine using a “digital twin” approach: modeling the onset of disease-specific brain atrophy in individuals with multiple sclerosis. Sci. Rep. 13 , 16279 (2023).
Maleki, A. et al. Moving forward through the in silico modeling of multiple sclerosis: Treatment layer implementation and validation. Comput. Struct. Biotechnol. J. 21 , 3081–3090 (2023).
Susilo, M. E. et al. Systems-based digital twins to help characterize clinical dose–response and propose predictive biomarkers in a Phase I study of bispecific antibody, mosunetuzumab, in NHL. Clin. Transl. Sci. 16 , 1134–1148 (2023).
Thangaraj, P. M., Vasisht Shankar, S., Oikonomou, E. K. & Khera, R. RCT-Twin-GAN Generates Digital Twins of Randomized Control Trials Adapted to Real-world Patients to Enhance their Inference and Application. medRxiv : the preprint server for health sciences , https://doi.org/10.1101/2023.12.06.23299464 (2023).
Jiang, J., Li, Q. & Yang, F. TCM Physical Health Management Training and Nursing Effect Evaluation Based on Digital Twin. Sci. Progr. 2022 , https://doi.org/10.1155/2022/3907481 (2022).
Tardini, E. et al. Optimal treatment selection in sequential systemic and locoregional therapy of oropharyngeal squamous carcinomas: deep Q-learning with a patient-physician digital twin dyad. J. Med. Int. Res. 24 , e29455 (2022).
Google Scholar
Golse, N. et al. Predicting the risk of post-hepatectomy portal hypertension using a digital twin: A clinical proof of concept. J. Hepatol. 74 , 661–669 (2021).
Cho, S.-W. et al. Sagittal relationship between the maxillary central incisors and the forehead in digital twins of korean adult females. J. Personal. Med. 11 , https://doi.org/10.3390/jpm11030203 (2021).
Imoto, S., Hasegawa, T. & Yamaguchi, R. Data science and precision health care. Nutr. Rev. 78 , 53–57 (2020).
Drummond, D. & Coulet, A. Technical, ethical, legal, and societal challenges with digital twin systems for the management of chronic diseases in children and young people. J. Med. Internet Res. 24 , e39698 (2022).
Bertezene, S. The digital twin in health: Organizational contributions and epistemological limits in a context of health crisis. Med. Sci. M/S 38 , 663–668 (2022).
Johnson, K. B. et al. Precision Medicine, AI, and the Future of Personalized Health Care. Clin. Transl. Sci. 14 , 86–93 (2021).
Powell, J. & Li, X. Integrated, data-driven health management: A step closer to personalized and predictive healthcare. Cell Syst. 13 , 201–203 (2022).
Article CAS PubMed Google Scholar
Delpierre, C. & Lefèvre, T. Precision and personalized medicine: What their current definition says and silences about the model of health they promote. Implication for the development of personalized health. Front. Sociol. 8 , 1112159 (2023).
Raiff, B. R., Burrows, C. & Dwyer, M. Behavior-analytic approaches to the management of diabetes mellitus: current status and future directions. Behav. Anal. Pract. 14 , 240–252 (2021).
Ahern, D. K. et al. Behavior-based diabetes management: impact on care, hospitalizations, and costs. Am. J. Managed care 27 , 96–102 (2021).
Tyson, R. J. et al. Precision dosing priority criteria: drug, disease, and patient population variables. Front. Pharmacol. 11 , 420 (2020).
Walton, R., Dovey, S., Harvey, E. & Freemantle, N. Computer support for determining drug dose: systematic review and meta-analysis. BMJ (Clin. Res.) 318 , 984–990 (1999).
Article CAS Google Scholar
Friedrichs, M. & Shoshi, A. History and future of KALIS: Towards computer-assisted decision making in prescriptive medicine. J. Integr. Bioinform. 16 , https://doi.org/10.1515/jib-2019-0011 (2019).
Zhao, H. et al. Identifying the serious clinical outcomes of adverse reactions to drugs by a multi-task deep learning framework. Commun. Biol. 6 , 870 (2023).
Thiong’o, G. M. & Rutka, J. T. Digital twin technology: the future of predicting neurological complications of pediatric cancers and their treatment. Front. Oncol. 11 , 781499 (2021).
Sun, T., He, X., Song, X., Shu, L. & Li, Z. The digital twin in medicine: a key to the future of healthcare? Front. Med. 9 , 907066 (2022).
Sarp, S., Kuzlu, M., Zhao, Y. & Gueler, O. Digital twin in healthcare: a study for chronic wound management. IEEE J. Biomed. health Inform. 27 , 5634–5643 (2023).
Chu, Y., Li, S., Tang, J. & Wu, H. The potential of the Medical Digital Twin in diabetes management: a review. Front. Med. 10 , 1178912 (2023).
Barricelli, B. R., Casiraghi, E. & Fogli, D. A survey on digital twin: definitions, characteristics, applications, and design implications. IEEE Access 7 , 167653–167671 (2019).
Keller, R. et al. Digital behavior change interventions for the prevention and management of type 2 diabetes: systematic market analysis. J. Med. Internet Res. 24 , e33348 (2022).
Priesterroth, L., Grammes, J., Holtz, K., Reinwarth, A. & Kubiak, T. Gamification and behavior change techniques in diabetes self-management apps. J. diabetes Sci. Technol. 13 , 954–958 (2019).
Venkatesh, K. P., Raza, M. M. & Kvedar, J. C. Health digital twins as tools for precision medicine: Considerations for computation, implementation, and regulation. NPJ digital Med. 5 , 150 (2022).
Venkatesh, K. P., Brito, G. & Kamel Boulos, M. N. Health digital twins in life science and health care innovation. Annu. Rev. Pharmacol. Toxicol. 64 , 159–170 (2024).
Katsoulakis, E. et al. Digital twins for health: a scoping review. NPJ Digital Med. 7 , 77 (2024).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clin. Res. ed.) 372 , n71 (2021).
Barker, T. H. et al. Revising the JBI quantitative critical appraisal tools to improve their applicability: an overview of methods and the development process. JBI Evid. Synth. 21 , 478–493 (2023).
Manganello, J. & Blake, N. A study of quantitative content analysis of health messages in U.S. media from 1985 to 2005. Health Commun. 25 , 387–396 (2010).
Giannantonio, C. M. Content Analysis: An Introduction to Its Methodology, 2nd edition. Organ. Res. Methods 13 , 392–394 (2010).
Rigby, A. S. Statistical methods in epidemiology. v. Towards an understanding of the kappa coefficient. Disabil. Rehabilitation 22 , 339–344 (2000).
Lantz, C. A. & Nebenzahl, E. Behavior and interpretation of the kappa statistic: resolution of the two paradoxes. J. Clin. Epidemiol. 49 , 431–434 (1996).
Download references
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and affiliations.
School of Nursing, Peking University, Beijing, China
Mei-di Shen
Department of Plastic and Reconstructive Microsurgery, China-Japan Union Hospital, Jilin University, Changchun, Jilin, China
Si-bing Chen & Xiang-dong Ding
You can also search for this author in PubMed Google Scholar
Contributions
MD.SHEN contributed to the data collection, analysis and the manuscript writing. SB.CHEN contributed to the data collection and analysis. XD.DING contributed to the critical revision of the manuscript as well as the initial study conception. All authors read and approved the final manuscript, and jointly take responsibility for the decision to submit this work for publication.
Corresponding author
Correspondence to Xiang-dong Ding .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary file, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Shen, Md., Chen, Sb. & Ding, Xd. The effectiveness of digital twins in promoting precision health across the entire population: a systematic review. npj Digit. Med. 7 , 145 (2024). https://doi.org/10.1038/s41746-024-01146-0
Download citation
Received : 29 January 2024
Accepted : 22 May 2024
Published : 03 June 2024
DOI : https://doi.org/10.1038/s41746-024-01146-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 26 September 2023
The impact of community engagement as a public health intervention to support the mental well-being of single mothers and children living under housing insecure conditions – a rapid literature review
- Natasha Joseph 1 ,
- Anne-Marie Burn 2 &
- Joanna Anderson 2
BMC Public Health volume 23 , Article number: 1866 ( 2023 ) Cite this article
2657 Accesses
5 Altmetric
Metrics details
In the UK, the population of homelessness and housing insecurity is increasing among families headed by mothers. The unique stressors of housing insecurity and living in accommodations ill-suited to long-term dwellings increase mental distress for mothers and children. Community engagement interventions present a public health opportunity to alleviate adverse outcomes for vulnerable families.
To synthesise and evaluate evidence of the impact of community engagement interventions in supporting the mental well-being of mothers and children living under housing insecure conditions. To synthesise the components of community engagement interventions as a public health intervention in alleviating mental well-being and non-health outcomes of mothers and children living under housing insecurity.
A systematic search of five online bibliographic databases (MEDLINE, EMBASE, PsychINFO, Global Health and Child Development & Adolescent Studies) and grey literature (Carrot2) was conducted in May 2022. Primary studies with community engagement components and housing-insecure single-mother families were included. Intervention data was extracted using the TIDieR checklist and a community engagement keywording tool. The studies’ quality was critically appraised using the MetaQAT framework.
Ten studies meeting inclusion criteria were identified, across two countries (USA & UK). Data from the studies reported positive significant effects for health and personal maternal outcomes in addition to higher positive effects for child health outcomes (e.g., decrease in depression symptoms). Interventions targeting social support and self-efficacy demonstrated potential to improve maternal and child outcomes via the maternal-child relationship. Community engagement at the design, delivery and evaluation intervention stages increased the level of community engagement, however there were tentative links to directly improving mental well-being outcomes.
There is evidence to suggest that community engagement may be applied as an effective intervention in supporting the mental well-being of mothers and children living under housing insecurity. Proposed intervention effectiveness may be achieved via psychosocial pathways such as improved maternal self-efficacy and social support. However, more embedded long-term process evaluations of these interventions are needed to establish maintenance of these observed benefits and to understand to what extent the findings apply to the UK context.
Peer Review reports
Housing is a recognised social determinant of health [ 1 ]. Chronic shortages of affordable housing, high housing costs and stagnating wages contribute to the UK housing crisis and increase the risk of homelessness for families on low incomes [ 2 ]. Housing insecurity is related to household expenditure where severe insecurity increases the risk of evictions, the prevalence of temporary accommodation and homelessness [ 2 , 3 , 4 ]. Temporary accommodation is offered to at-risk families who seek help from their local authority and are granted by recognising their ‘statutory homeless’ status [ 5 ]. In 2021, 1.2 million households were reported to be on the English local authority housing waiting list due to housing insecurity [ 6 ] and 96,060 households were living in temporary accommodation in England, including 121,680 dependent children [ 7 ]. Current policies are focused on demand-level interventions to address the shortfall in housing, with minimal investment in increasing the housing supply [ 8 ]. In 2012, the combination of housing availability and welfare cuts led to a 19% increase in councils providing temporary accommodation to vulnerable households [ 2 ]. To meet the rising housing demand, local council spending increased in the private rented sector, reducing the standard of accommodation. Experiences of overcrowding and poor housing conditions increased as hostels, office conversions and bed-and-breakfast hotels are utilised as temporary accommodations [ 9 ]. However, the term ‘temporary’ acts as a misnomer as families can live in dwellings for months extending into years as they await to be rehoused in suitable long-term accommodation [ 9 , 10 ]. The UK charity Shelter, identified 61% of households have spent a year or more living in temporary accommodation, increasing to more than two thirds (68%) of families [ 11 , 12 , 13 ]. Further data from 2014 identified over 2000 families with children who have spent between five to ten years living in temporary accommodation in London, an area which has the highest proportion of families living in temporary accommodation in the UK [ 14 ]. In 2023, 83,473 children were currently living in temporary accommodation in London which equates to at least one child in every London classroom is homeless on average [ 15 ].
- Community engagement
Prolonged exposure to housing ill-suited for a long-term dwelling has a well-established link to adverse mental well-being and poor child development [ 16 ]. Parents living in temporary accommodation have poorer mental health outcomes such as depression and anxiety compared to housing-secure parents [ 17 ]. In addition, the parental-child relationship model elucidates the translation of poor parental mental well-being to adverse childhood experiences as shown in poor educational attainment, mental health and behavioural outcomes [ 3 , 18 ]. Families headed by single mothers form the majority of families living in temporary accommodation in the UK [ 19 ]. Given the chronic stressors and mental well-being disparities, therein lies the need to adapt public health interventions for single mothers experiencing chronic housing insecurity.
NICE guidelines recognise public health interventions such as area-based initiatives and urban regeneration programmes to reduce health inequalities [ 20 ]. The intention is to tackle the socioeconomic determinants of health through investments that reduce deprivation such as funding education, income, housing, and employment initiatives. However, such macro-level interventions encounter pitfalls such as poor assessment criteria for measuring individual impacts such as health outcomes [ 21 , 22 ]. Furthermore, area-based initiatives may fail to equitably incorporate dialogue between marginalised communities and decision-makers in institutions owing to asymmetric power structures, cultural differences, and poor relationships with statutory organisations [ 20 ]. Consequently, the barriers culminate to prevent the development of contextually suitable interventions for the local population [ 23 , 24 ].
Community engagement is an umbrella term that describes a ‘range of approaches aimed to maximise the involvement of local communities in local initiatives to improve their health and well-being and reduce health inequalities’ ([ 20 ] p 11–12). The operationalisation of community engagement into practice can take multiple forms of activities with varying levels of member involvement: information-giving, consultation, joint decision-making, collaboration and supporting independent community interest through empowerment [ 25 ]. This paper will utilise the conceptual framework put forth by O’Mara-Eves et al. (2013) where community engagement is conceptualised within health interventions through a dynamic framework that incorporates the processes involved with community engagement and omits unidirectional forms of engagement such as information-giving in favour of bidirectional engagement [ 26 ].
A rapid review was carried out to synthesise and evaluate evidence of community engagement programmes in supporting the mental well-being of children and mothers living under housing insecurity. In addition, the review aimed to evaluate the effectiveness of interventions and the components of the intervention involved in alleviating poor mental well-being outcomes for single families.
Search strategy
The report followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 27 ]. A comprehensive search of both peer- and non-peer-reviewed articles from online bibliographic databases and grey literature search using relevant MeSH words or subheadings of keywords was conducted in May 2022.
Studies of community engagement as a health intervention for the support of mental well-being among children and mothers experiencing housing insecurity were identified from five bibliographic databases (MEDLINE, EMBASE, PsychINFO, Global Health and Child Development & Adolescent Studies).
Grey literature searches for empirical primary data were conducted using a hand-search reference list of included studies and relevant reviews. To maintain robustness, the majority of grey literature searches were conducted on Carrot2 Clustering Engine ( https://search.carrot2.org/ ). The search engine was the preferred domain due to the higher reproducibility of the search strategy in comparison to Google [ 28 ].
The search strategy related to the population, outcome, and intervention (Table 1 ). Full-search strategies are available in Appendix Tables 1 – 5 . The search strategy aimed to capture the broad spectrum of terms that fall under umbrella phrases such as community engagement and mental wellbeing by using synonyms and proximity searching.
Housing insecurity has no clear definition but is characterised as a spectrum ranging from no access to housing of reasonable quality to complete access to housing of reasonable quality in absence of threats (e.g. financial precarity) [ 29 ]. Housing insecure inclusion ranges from homeless shelters, bed-and-breakfast, sofa surfing, temporary accommodation, and characteristics such as overcrowding.
Community engagement is defined as ‘involving communities in decision-making and the planning, design, governance and/or delivery of services’ ([ 30 ] p. 11). Approaches include but are not limited to healthcare forums, service user networks, peer-led interventions or volunteering [ 26 ].
Inclusion and exclusion criteria
The inclusion criteria are outlined in Table 2 . Studies were selected based on the PICO framework (population, intervention, comparator and outcomes) [ 31 ]. Only studies published in English language were included and there was no limit placed on the publication date. Focusing on papers written in English enabled the review to identify countries with similar definitions of homelessness to aid interpretation [ 32 ]. Non-peer-reviewed literature was searched to include interventions conducted in non-academic institutions such as charity websites.
Screening and selection
All retrieved titles and abstracts were reviewed by one reviewer (NJ) with a second reviewer independently screening 12% of eligible studies based on the inclusion and exclusion criteria (JA). The interrater reliability was deemed to be in fair agreement (Cohen’s Kappa = 0.31) for the title and abstract screenings [ 33 ]. The third reviewer (A-MB) independently resolved conflicts with planned discussions. Full texts of all eligible articles were retrieved and screened by one reviewer (NJ) using the eligibility criteria and excluded with reason.
Data extraction
Data were extracted based on study characteristics (study aims, sample, methods, outcomes). The intervention characteristics (e.g., study context, intervention reason, intervention details, location of intervention, intervention deliverer) were extracted using the TIDieR checklist to standardise the reporting of the intervention [ 34 , 35 ] (Appendix Table 10 ). Outcomes for mothers and children are extracted from O’Mara-Eves et al. (2013) keywording tool ([ 26 ] p. 181–189) which categorises the type of intervention based on health, community, personal and process outcomes with identification of positive, non-significant and negative findings from outcomes (Appendix Table 13 ). Data on the community engagement components were extracted using the tool developed by O’Mara-Eves et al. (2013) Keywording tool ([ 26 ] p. 181–189). Data was analysed by one reviewer (NJ) and verified by a second reviewer (JA).
Data analysis
Due to the heterogeneity of the papers, subgroup analysis was used to explore the impact of interventions across mothers and children respectively. Post-extraction, the reported outcomes were analysed with descriptive statistics. In addition, the heterogeneity of the populations across the papers was organised using the O’Mara-Eves et al. (2013) Keywording tool ([ 26 ] p. 181–189) to capture population characteristics such as ethnicity, social economic position, place of residence, education, employment status, gender, marital status and age (Appendix Table 14 ).
Critical appraisal
The critical appraisal of the papers was evaluated using the Public Health Ontario Meta-tool for Quality Appraisal (MetaQAT) [ 36 ]. MetaQAT framework includes four domains: reliability, relevancy, validity, and applicability in addition to the study-specific appraisal tool (Appendix Tables 6 – 8 ). MetaQAT was deemed the most appropriate tool as it provides a systematic and rigorous approach to assessing the broad spectrum of research designs. Furthermore, the tool is contextually relevant to the public health field and overcomes the limitations of critical appraisal tools designed for clinical medicine [ 37 ].
The electronic bibliographic database search resulted in 3277 articles following the removal of 1168 duplicates. The screening phase consisted of title and abstract screening where 3277 studies were screened, and 56 studies were screened at the full-text level. The grey literature search resulted in 121 records and after the screening, one paper contributed to the total number of included studies ( n = 10). Non-published grey literature was not identified from the search. Figure 1 illustrates the study selection process using the PRISMA guidelines.

PRISMA Flow diagram of the study selection process
Of the 10 studies included in the review, eight were conducted in the United States, and two in the United Kingdom. The studies used various study designs, including observational case–control ( n = 4), randomised control trial ( n = 3) and quasi-experimental ( n = 3). The characteristics of included studies are summarised in Table 3 . Two studies had no comparator groups based on the quasi-experimental study designs. Eight studies contained a comparator such as service/treatment/case as usual ( n = 5) or alternative comparable group ( n = 3). The comparable sample group were used to compare populations to identify significant differences in health needs (e.g., between low-income families and families in shelters) or whether the intervention required greater adaptation to suit the target population.
Sample sizes were relatively small varying from 15 to 267 participants, with four studies focusing on mothers experiencing housing insecurity, one focusing on children experiencing housing insecurity, and five focusing on both mothers and children. All studies with children as participants addressed health outcomes such as child behaviour and mental health service use ( n = 5). All studies with mothers as participants included three types of outcomes: health outcomes such as maternal mental well-being ( n = 7), personal outcomes such as self-efficacy ( n = 4) or community outcomes such as social support / social capital ( n = 2). The categorisation of outcomes was based on the O’Mara-Eves et al., (2013) data extraction tool ([ 26 ] p. 191–195).
Quality of studies
The critical appraisal of included studies is summarised in Table 4 and provided in detail in Appendix Tables 6 – 8 . The MetaQAT tool identified the quality of included studies based on relevancy, reliability, validity, and applicability to the public health context [ 36 ]. The majority of papers had a high quality of relevancy ( n = 9) and validity ( n = 9). Five studies had the highest level of reliability which included the reporting of consent and ethical approval from a university board. The distinction between moderate to high reliability was the presence of board ethical approval in addition to participant consent.
Components of community engagement characteristics
Community engagement health interventions contain multiple and complex components to adapt to the needs of the target population. The components focus on the level of community engagement and contextual factors of community engagement interventions. Table 5 outlines the labels of community engagement based on O’Mara-Eves et al., (2013) extraction tool and identified community organisation label as the most frequent strategy followed by peer strategy. A full break down of community engagement strategy label by study can be found in Appendix Table 15 .
Level of community engagement
The extraction of community engagement characteristics aims to identify the level of community involvement within stages of the intervention such as the design and planning of the intervention, the delivery, and the intervention evaluation (Table 6 ). Categorising involvement was based on O’Mara-Eves et al., (2013) extraction tool which identified six levels of involvement: leading, collaborating, consulted, informed, and not involved (or not clear). Two studies maintained high levels of community engagement at each stage of the intervention [ 39 , 40 ]. The majority of studies relied on informing-based delivery of community engagement. Low levels of community engagement are involved in the designing and planning phase of the intervention with only two UK studies providing evidence of community engagement at preliminary stages [ 39 , 40 ].
Contextual components of community engagement
Various types of deliverers were involved in implementing the intervention such as health professionals, community workers, counsellors, social workers, and peers such as mothers experiencing housing insecurity (Table 7 ). Interventions were conducted in a range of settings such as shelters, churches, clinics, and community centres. Two study interventions took place in housing agencies which are supportive sites with a range of services to support families experiencing housing insecurity and act as an intermediary between temporary accommodation and permanent housing (Table 7 ). The studies adopted various intervention strategies to improve maternal and child outcomes. The most frequent intervention strategy included providing social support (20%), education (12%) and access to services (12%) (Table 8 ). Four studies provided training, three to participants [ 39 , 40 , 42 ] and one to interventionists [ 46 ]. Volunteers were described in the context of providing childcare so that mothers could fully participate in the intervention. The intervention duration ranged from 1 to 30 months (Appendix Table 9 ).
Process evaluation of intervention
Eight out of the 10 studies contained a process evaluation of the intervention. Table 9 summarises the process evaluation across the included studies. The process evaluation identifies the nature of delivery and adherence to the intervention to understand the effectiveness of the intervention for the target population. Four studies analysed the participants’ fidelity to the intervention. Four studies analysed the acceptability and satisfaction of the intervention. Bradley et al. (2020) adopted a mixture of questionnaires and qualitative interviews to determine the acceptability and feasibility of the intervention. Three studies identified training provided to interventionists (care managers and primary care physicians). No study provided an evaluation of cost-effectiveness. Seven studies provided information about the sources of funding from charities ( n = 1) and research/state grants ( n = 6).
Nabors et al. (2004) evaluated acceptability and accessibility process variables using questionnaires given to children and teachers respectively [ 44 ]. Gewirtz et al. (2015) identified fidelity to intervention using attrition analysis of the participant follow-ups and identified no significant differences between the intervention group and control [ 41 ]. Fidelity to community, counselling or medical services was identified using a structured review in Lee et al. (2010) [ 42 ]. Brown et al. (2020) reported high satisfaction rates with the implementation and planning of an intervention, but lower ratings were given for participant involvement in the intervention planning [ 40 ]. Bradley et al. (2020) provided the perspectives of mothers living in hostels on the appropriateness of the adapted intervention content and feasibility within the environment [ 39 ].
Effectiveness of community engagement intervention
The analysis of the 10 studies identified two broad intervention categories: community-based models ( n = 6) and peer-led models ( n = 4). The community-based models are characterised by a trained professional as the lead, where the intervention pathway is facilitated through the relationship between a trained professional and the mother and/or child (Table 10 ). The peer-based models focus on the relationship between different mothers and/or children experiencing housing insecurity but are not solely led by professionals or facilitated through the professional-mother/child relationship (Table 11 ). Improvements to social support were observed across the intervention groups under community-based studies [ 38 , 43 ]. Improvements in attendance to appointments with a health professional were observed [ 44 , 46 , 47 ]. In addition, reductions in mental distress conditions such as depression were observed in two studies, however the reduction could not be attributed to the community-based interventions as no difference was identified upon control-intervention group comparison [ 45 , 46 ]. Studies under the peer-based models observed social support outcomes being impacted by the level of housing insecurity where no change was observed [ 39 , 40 ]. Bradley et al. (2020) operationalised social support into seven domains and two total network analysis in a pre-post study design [ 39 ]. Domains affected by resource availability and physical environment such as material aid, socialising, tangible assistance identified no changes from baseline and 6-month follow-up [ 39 ]. However, the intervention identified positive changes in domains relating to social need such as network size for advice/information, network for pregnancy/childcare support, total network satisfaction and intimate interaction [ 39 ].
Maternal outcomes
Nine studies investigated maternal outcomes for mothers experiencing housing insecurity ( n = 4 maternal outcomes only, n = 5 both maternal and child outcomes). One of the nine studies addressed maternal outcomes by providing targeted interventions and compared mothers experiencing housing insecurity (living in the hostel) with mothers living in low-income community-based stable housing [ 44 ]. The purpose was to identify whether specific needs differ among the population groups. The nine remaining studies targeted and delivered the intervention to the same housing-insecure population either without a comparator group [ 39 , 40 ] or had a service/treatment/ care-as-usual comparator group [ 38 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. Appendix Tables 11 and 12 outlines the comparison between comparator groups and interventions in the included studies. The effectiveness of studies is based on the impact of outcomes (health, personal and community).
Thirty maternal indicators were isolated across the 10 studies and were categorised using the O’Mara-Eves et al., (2013) extraction tool ([ 26 ] p. 191–195) which included 15 health outcomes, nine personal outcomes and six community outcomes. Maternal health outcomes indicators included parental stress, mental well-being, parenting scale (reactivity, hostility), mental health service use, depression, and anxiety (Tables 10 and 11 ). Nine maternal indicators from the 10 studies identified significant findings related to health outcomes for mothers experiencing housing insecurity following an intervention. Four maternal indicators identified no significant changes to health outcomes and two maternal indicators identified a negative finding post-intervention. The two negative findings were identified by Lee et al. (2010) who compared mothers living in housing insecurity to low-income mothers living in a community-based setting. The study identified mothers under housing insecurity had worse scores on parenting confidence, and relational frustration within the parent–child relationship and also experienced worse psychological distress compared to mothers in the community intervention group [ 42 ].
Personal outcomes
Maternal indicators for personal outcomes included self-efficacy, financial stress, transitioning out of homeless shelters, and health literacy. Eight positive findings were identified out of ten personal outcomes across the included studies (self-efficacy, financial stress, communication, family unity and transitioning out of homeless shelter and health literacy for sub-group analysis) (Table 12 ). Studies included overall findings which identified outcome changes when combining both the intervention and comparator groups. Brown et al., (2020) identified an overall non-significant finding for health literacy post-intervention however upon sub-group analysis, the health literacy among mothers that had low health literacy at baseline had significant improvement in health literacy at follow-up ( p = 0.003) [ 40 ].
Community outcomes
Three studies captured community outcomes for maternal indicators which included social support, family variables such as family conflict and bonding, and social capital (Table 13 ). McWhirter (2006) identified no significant changes to family variables such as a decrease in the family conflict in both group and overall analysis however, whole group analysis of social support demonstrated improved social support [ 43 ]. Brown et al. (2020) reported improvement in social support among specific categories such as the network size for advice/information ( p = 0.001), pregnancy/childcare support ( p = 0.049), intimate interaction ( p = 0.019), and for total satisfaction with a social network ( p = 0.04) [ 40 ]. Abell et al. (2009) identified improved social support in the intervention group compared to the control group [ 38 ].
Child outcomes
Six out of the ten studies included outcomes for children experiencing housing insecurity. One study included child outcomes only [ 44 ] and five studies included both child and maternal outcomes [ 38 , 39 , 41 , 42 , 47 ]. One of the six studies addressed child outcomes by providing targeted interventions and comparing children experiencing housing insecurity (shelter) and children from low-income backgrounds at high risk of poor behavioural outcomes and academic attainment [ 44 ]. The five remaining studies addressed child outcomes by providing interventions to the housing-insecure population with a comparator group (service/treatment/care-as-usual). The summary of child health outcomes is described in Table 14 . One study used statistical modelling to analyse the influence of parenting practices and outcomes on child outcomes in the controlled study design. Gewirtz et al. (2015) conducted a hierarchical linear growth model which indicated that more effective observed parenting practices predicted high reported child strengths (ѱ = 1.58, p < 0.1) where for every one unit in observed parenting there where 1.58 unit increase on the interpersonal strength scale [ 41 ]. In addition, parenting self-efficacy predicated increased in child strengths (ѱ = 0.20, p < 0.01) [ 41 ]. Furthermore, children in the intervention group had greater reductions in depressive symptoms relative to the sample group (ѱ= −2.13, p < 0.01) [ 41 ].
The 4567 papers were identified, and post-screening 10 included studies were extracted. The majority of papers were undertaken in the UK and US after 2010 and the most common study design were observational (case–control) studies [ 42 , 43 , 44 , 47 ]. The study quality of the papers from the UK was of high quality across all assessment components (relevancy, reliability, validity, and applicability) [ 39 , 40 ]. Greater variation in the reliability of studies owing to the reporting of participant consent and ethical approval from a university board. Two papers identified moderate to high levels of fidelity to interventions with multiple sessions indicating better participant engagement [ 40 , 41 ]. A large majority of papers with interventions that targeted maternal health outcomes, such as parental mental health, parenting practices and mental health service use, presented positive results ( n = 9/16) [ 39 , 40 , 45 , 46 , 48 ]. Social support is captured as both an outcome and an intervention strategy. This reflects the dual meaning of community engagement as both a method and an end goal to facilitate improved health outcomes ([ 26 ] p. 45). Within the review, social support was the most frequent intervention strategy among the 10 papers. Social support is cited within the literature as a resource that can alleviate the stressors of homelessness experienced by mothers [ 49 ]. Non-health indicators such as social support, may provide a potential pathway for addressing maternal mental well-being. For example, the community outcomes of social support and the social network had positive results ( n = 2) which led to an increase in network size and quality of social relationships [ 38 , 40 , 43 ]. Further research corroborates the review finding, where it is indicated that social support can act as a protective factor against maternal depression [ 50 , 51 ]. In the context of housing insecurity, peer relationships and social support can buffer against unique stressors and address the disparity in mental health outcomes compared to the general population [ 49 , 52 ].
The review demonstrated the high level of community engagement as an opportunity to increase access to statutory services by acting as a point of first entry [ 40 ]. From an institutional perspective, local authorities describe the profile of individuals experiencing housing insecurity as “hard to reach” or “hidden populations” due to their underrepresentation in the census and low engagement with local services [ 53 , 54 ]. The majority of papers ( n = 9) within the review reported a high proportion (defined as 60% or more of the sample) of non-white minority ethnic groups in the sample population of mothers and children who experience housing insecurity [ 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ] (Appendix Table 14 ). Minority groups are also institutionally categorised as ‘hard-to-reach’ [ 53 ]; three papers within the review cited African American and Black African ethnic groups as the majority of the sample population. Broader research cites factors that contribute to being ‘hard to reach’ as a lack of awareness of available statutory services, organisational obstacles to access services (such as language barriers) and lack of cultural suitability [ 53 , 55 ]. However, the review and further research support the use of peers, counsellors and community health workers as deliverers to the intervention to create relationships with marginalised communities, increase engagement and enable improvements in health outcomes [ 56 ]. The high engagement demonstrated by community engagement interventions renders the term “hard to reach” obsolete and highlights the institutional tendencies of adopting a “one size fits all” approach to health promotion [ 57 , 58 ]. For instance, recent research suggests women in African communities locate mental health problems as a social issue than solely a clinical problem [ 40 , 59 , 60 ]. Subsequently, the review conceptualises community engagement as a cultural adaptation mechanism to improve intervention implementation by understanding contextual sensitivities of marginalised and housing insecure experiences. In addition, the incorporation of process evaluations within five identified studies provided a feedback mechanism that captured the needs of the community in order to adapt to the housing insecure context [ 18 , 26 ]. For instance, the review identified an intervention that adapted an evidence-based programme to support mothers and children living in a hostel and observed improved child behaviour and parenting practice outcomes [ 39 ]. However, the participant evaluation identified concerns about privacy within hostel setting and inappropriate parenting techniques that were suggested such as 'time-out' due to the lack of space to carry out the technique in the small temporary accommodation [ 39 ]. In doing so, the review aims to operationalise a grassroots perspective that shifts the blame of being ‘hard to reach’ away from marginalised communities and allow public health practitioners to recognise the iterative process of adapting interventions to support communities in need. Furthermore, the review embraces the heterogeneity of community engagement interventions by isolating the various components, locations, and theoretical approaches. This allows policy makers and practitioners to identify potential touchpoints when engaging housing-insecure mothers, as well as highlighting the need for innovation and in-depth contextual knowledge of the population’s needs when developing interventions.
Strengths and limitations
To the best of our knowledge, this is the first rapid review which looks at the impact of community engagement for single mothers and children experiencing housing insecurity. Consequently, the review provides insight for primary research to integrate community engagement within health interventions to better support vulnerable mothers and children. The combination of the O’Mara-Eves et al. (2013) conceptual framework, social-ecological model and maternal-child relationship provides the theoretical tools to disentangle the multivariate influences and illuminate intervention pathways for health outcomes. The basis of the rapid review captured a broad spectrum of studies from various settings such as social services, school-based environments, non-clinical health centres and shelters. The different settings reflect the potential service entry points that single mothers facing housing insecurity may encounter [ 61 , 62 ].
The review aimed to rigorously search for relevant papers from extensive sources. However, there is a possibility that relevant titles may be unintentionally missed due to publication bias and the ambiguous and varied terminology surrounding community engagement. In addition, the team capacity, funding and time frame to conduct the search and screening is shorter than 12 months in comparison to other community engagement systematic review studies which may contribute to further omission and potential selection bias [ 63 , 64 ]. Furthermore, due to the nature of the rapid review there is a risk of unintentional omission during screening.
Most papers were conducted in the USA and only two were in the UK. Consequently, the generalisability of results from the review is limited, especially concerning the power dynamics between institutions, governmental bodies and communities, funding structures and available resources. Therefore, public health practitioners and policymakers should interpret the results with caution by considering the contextual sensitivities in areas they aim to support.
In summary, there is promising descriptive evidence of community engagement as an effective intervention towards improving the mental well-being of mothers and children living under housing insecure conditions. The review identified tentative evidence to support psychosocial maternal outcomes (self-efficacy and social support) as a potential pathway to improve maternal mental health and child outcomes; more research is needed to determine the direction and evidence of mediation pathways. In the absence of meta-analytical data, the review cannot evaluate the magnitude of the effectiveness nor make claims of causation but provides insight into modes of targeting vulnerable marginalised populations. The evidence identifies the relationship between adapted community-specific components of community engagement and greater support for maternal-child health outcomes. The review highlights the importance of process evaluations within community engagement to enable the iterative intervention adaptations to facilitate a better fit for the community rather than assuming a ‘one size fits all approach’ [ 26 ]. Consequently, the paper aims to reify the importance of understanding local knowledge for public health practitioners, policymakers, and academics within the field. Institutions working with vulnerable populations can avoid transplanting interventions from one context into another but aim to centre high levels of community engagement within the stages of public health intervention development.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Marmot M. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post-2010 – the Marmot Review. In: Fair Society, Healthy Lives. Eyal N, Hurst SA, Norheim OF, Wikler D, editors. 2010. https://doi.org/10.1093/acprof:oso/9780199931392.003.0019 .
Fetzer T, Sen S, Souza P. Housing insecurity, homelessness and populism: Evidence from the UK. Warwick: NBER Work Pap Ser; 2019.
Google Scholar
Bess KD, Miller AL, Mehdipanah R. The effects of housing insecurity on children’s health: a scoping review. Health Promot Int. 2022. https://doi.org/10.1093/heapro/daac006 .
Stuckler D, Reeves A, Loopstra R, Karanikolos M, McKee M. Austerity and health: the impact in the UK and Europe. Eur J Public Health. 2017;27 suppl_4:18–21. https://doi.org/10.1093/eurpub/ckx167 .
Article Google Scholar
Fitzpatrick S, Pleace N. The statutory homelessness system in England: a fair and effective rights-based model? Hous Stud. 2012;27:232–51. https://doi.org/10.1080/02673037.2012.632622 .
Department for Levelling Up, Housing and Communities. National statistics - Social housing lettings in England, tenants: April 2021 to March 2022. 2023. https://www.gov.uk/government/statistics/social-housing-lettings-in-england-april-2021-to-march-2022/social-housing-lettings-in-england-tenants-april-2021-to-march-2022 . Accessed 6 Sep 2023.
Wilson W, Barton C. Households in temporary accommodation (England). UK: House of Commons Library; 2022.
Jacobs K, Pawson H. Introduction to the special edition: ‘the politics of housing policy.’ Hous Stud. 2015;30:651–5. https://doi.org/10.1080/02673037.2015.1082273 .
Edwards R. Making temporary accommodation permanent: the cost for homeless families. Crit Soc Policy. 1995;15:60–75. https://doi.org/10.1177/026101839501504305 .
Children’s Comissoner. Bleak Housing: Tackling the Crisis of Family Homelessness. England: Children’s Comissioner for England; 2019.
Keilloh H. The ticking time bomb of temporary accommodation on a generation of children’s mental health. Chartered Institute of Housing. 2023. https://www.cih.org/blogs-and-articles/the-ticking-time-bomb-of-temporary-accommodation-on-a-generation-of-children-s-mental-health . Accessed 29 May 2023.
Pennington J. Not-so-temporary accommodation. Shelter. 2022. https://blog.shelter.org.uk/2022/12/not-so-temporary-accommodation/ . Accessed 29 May 2023.
Shelter. Shelter - still living in limbo: why the use of temporary accommodation must end | Trust for London. Trust for London. 2023. https://trustforlondon.org.uk/research/shelter-still-living-in-limbo-why-the-use-of-temporary-accommodation-must-end/ . Accessed 6 Jul 2023.
Halpin Z. Temporary accommodation in London: research findings and policy recommendations. London: Shelter; 2014.
London Councils. One in 50 Londoners homeless as ‘housing disaster unfolds in capital’. London Councils. 2023. https://beta.londoncouncils.gov.uk/news/2023/one-50-londoners-homeless-housing-disaster-unfolds-capital . Accessed 2 Aug 2023.
Croft LA, Marossy A, Wilson T, Atabong A. A building concern? The health needs of families in temporary accommodation. J Public Health. 2021;43:581–6. https://doi.org/10.1093/pubmed/fdaa056 .
Rosenthal DM, Hayward A, Ucci M, Teakle A, O’Toole S, Whitaker L, et al. 576 Parental mental health and associations between living in temporary accommodation and socio-political determinants during the COVID-19 pandemic. In: British Association for Community Child Health. BMJ Publishing Group Ltd and Royal College of Paediatrics and Child Health; 2022. A71–2. https://doi.org/10.1136/archdischild-2022-rcpch.117 .
Bassuk EL, Beardslee WR. Depression in homeless mothers: addressing an unrecognized public health issue. Am J Orthopsychiatry. 2014;84:73–81. https://doi.org/10.1037/h0098949 .
Article PubMed Google Scholar
Department for Levelling Up, Housing and Communities. Statutory Homelessness Live Tables | Statutory Homelessness in England (Table TA2). https://www.gov.uk/government/statistical-data-sets/live-tables-on-homelessness#statutory-homelessness-live-tables . Accessed 29 May 2023.
NICE. Community engagement: improving health and wellbeing and reducing health inequalities | NICE Guideline. London: National Institute for Health and Care Excellence; 2016.
Thomson H, Atkinson R, Petticrew M, Kearns A. Do urban regeneration programmes improve public health and reduce health inequalities? A synthesis of the evidence from UK policy and practice (1980–2004). J Epidemiol Community Health. 2006;60:108–15. https://doi.org/10.1136/jech.2005.038885 .
Article PubMed PubMed Central Google Scholar
Thomson H. A dose of realism for healthy urban policy: lessons from area-based initiatives in the UK. J Epidemiol Community Health. 2008;62:932–6. https://doi.org/10.1136/jech.2007.068775 .
Article CAS PubMed Google Scholar
Strobl J. Achieving wider participation in strategic health planning: experience from the consultation phase of Liverpool’s City Health Plan’. Health Promot Int. 2000;15:215–25. https://doi.org/10.1093/heapro/15.3.215 .
World Health Organisation. Community participation in local health and sustainable development: approaches and techniques. Geneve: World Health Organization. Regional Office for Europe; 2002.
Wilcox D. Community participation and empowerment: putting theory into practice. RRA Notes. 1994;21:78–83.
O’Mara-Eves A, Brunton G, McDaid D, Oliver S, Kavanagh J, Jamal F, et al. Community engagement to reduce inequalities in health: a systematic review, meta-analysis and economic analysis. Southampton (UK): NIHR Journals Library; 2013.
Page, McKenzie, Bossuyt, Boutron, Hoffmann, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
Philips V. Searching the deep web and grey literature. 2022.
Frederick TJ, Chwalek M, Hughes J, Karabanow J, Kidd S. How stable is stable? defining and measuring housing stability. J Community Psychol. 2014;42:964–79. https://doi.org/10.1002/jcop.21665 .
Swainston K, Summerbell C. The effectiveness of community engagement approaches and methods for health promotion interventions. Teeside: University of Teeside; 2008.
Higgins JPT, Thomas J. Cochrane Handbook for Systematic Reviews of Interventions (Wiley Cochrane Series). 2nd edition. Wiley-Blackwell. 2019.
Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384:1529–40. https://doi.org/10.1016/S0140-6736(14)61132-6 .
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22:276–82. https://doi.org/10.11613/BM.2012.031 .
Cotterill S, Knowles S, Martindale A-M, Elvey R, Howard S, Coupe N, et al. Getting messier with TIDieR: embracing context and complexity in intervention reporting. BMC Med Res Methodol. 2018;18:12. https://doi.org/10.1186/s12874-017-0461-y .
Campbell M, Katikireddi SV, Hoffmann T, Armstrong R, Waters E, Craig P. TIDieR-PHP: a reporting guideline for population health and policy interventions. BMJ. 2018;361:k1079. https://doi.org/10.1136/bmj.k1079 .
Rosella LC, Pach B, Morgan S, Bowman C, Ontario Agency for Health Protection and Promotion (Public Health Ontario). Meta-tool for quality appraisal of public health evidence: PHO MetaQAT. Toronto, ON: Queen’s Printer for Ontario; 2015.
Rosella L, Bowman C, Pach B, Morgan S, Fitzpatrick T, Goel V. The development and validation of a meta-tool for quality appraisal of public health evidence: Meta Quality Appraisal Tool (MetaQAT). Public Health. 2016;136:57–65. https://doi.org/10.1016/j.puhe.2015.10.027 .
Abell ML, Davey TL, Clark P, Perkins NH. Community case management intervention for hard-to-place homeless families leaving emergency shelter. J Soc Distress Homeless. 2009;19:121–47. https://doi.org/10.1179/105307809805365109 .
Bradley C, Day C, Penney C, Michelson D. “Every day is hard, being outside, but you have to do it for your child”: Mixed-methods formative evaluation of a peer-led parenting intervention for homeless families. Clin Child Psychol Psychiatry. 2020;25:860–76. https://doi.org/10.1177/1359104520926247 .
Brown J, Luderowski A, Namusisi-Riley J, Moore-Shelley I, Bolton M, Bolton D. Can a Community-Led Intervention Offering Social Support and Health Education Improve Maternal Health? A Repeated Measures Evaluation of the PACT Project Run in a Socially Deprived London Borough. Int J Environ Res Public Health. 2020;17. https://doi.org/10.3390/ijerph17082795 .
Gewirtz AH, DeGarmo DS, Lee S, Morrell N, August G. Two-year outcomes of the Early Risers prevention trial with formerly homeless families residing in supportive housing. J Fam Psychol. 2015;29:242–52. https://doi.org/10.1037/fam0000066 .
Lee SS, August GJ, Gewirtz AH, Klimes-Dougan B, Bloomquist ML, Realmuto GM. Identifying unmet mental health needs in children of formerly homeless mothers living in a supportive housing community sector of care. J Abnorm Child Psychol. 2010;38:421–32. https://doi.org/10.1007/s10802-009-9378-1 .
McWhirter PT. Community therapeutic intervention for women healing from trauma. The Journal for Specialists in Group Work. 2006;31:339–51. https://doi.org/10.1080/01933920600918857 .
Nabors LA, Weist MD, Shugarman R, Woeste MJ, Mullet E, Rosner L. Assessment, prevention, and intervention activities in a school-based program for children experiencing homelessness. Behav Modif. 2004;28:565–78. https://doi.org/10.1177/0145445503259517 .
Samuels J, Fowler PJ, Ault-Brutus A, Tang D-I, Marcal K. Time-limited case management for homeless mothers with mental health problems: effects on maternal mental health. J Soc Social Work Res. 2015;6:515–39. https://doi.org/10.1086/684122 .
Weinreb L, Upshur CC, Fletcher-Blake D, Reed G, Frisard C. Managing depression among homeless mothers: pilot testing an adapted collaborative care intervention. Prim Care Companion CNS Disord. 2016;18. https://doi.org/10.4088/PCC.15m01907 .
Zhang AL, Limaye N, Means RH. Social determinants of health for pregnant housing-insecure women through an integrated, innovative care delivery model. J Gen Intern Med. 2021;36(Suppl 1):S381. https://doi.org/10.1007/s11606-021-06830-5 .
Zhang J, Lee S-K, Piehler TF, Gewirtz AH, August GJ. Bidirectional relations between parenting practices and child externalizing behaviors in formerly homeless families: a random-intercept cross-lagged panel analysis. Parent Sci Pract. 2020;20:177–99. https://doi.org/10.1080/15295192.2019.1694833 .
Tischler V, Rademeyer A, Vostanis P. Mothers experiencing homelessness: mental health, support and social care needs. Health Soc Care Community. 2007;15:246–53. https://doi.org/10.1111/j.1365-2524.2006.00678.x .
Lefkovics E, Rigó J, Kovács I, Talabér J, Szita B, Kecskeméti A, et al. Effect of maternal depression and anxiety on mother’s perception of child and the protective role of social support. J Reprod Infant Psychol. 2018;36:434–48. https://doi.org/10.1080/02646838.2018.1475726 .
McManus BM, Poehlmann J. Maternal depression and perceived social support as predictors of cognitive function trajectories during the first 3 years of life for preterm infants in Wisconsin. Child Care Health Dev. 2012;38:425–34. https://doi.org/10.1111/j.1365-2214.2011.01253.x .
Vostanis P, Tischler V, Cumella S, Bellerby T. Mental health problems and social supports among homeless mothers and children victims of domestic and community violence. Int J Soc Psychiatry. 2001;47:30–40. https://doi.org/10.1177/002076400104700403 .
Boag-Munroe G, Evangelou M. From hard to reach to how to reach: a systematic review of the literature on hard-to-reach families. Res Pap Educ. 2012;27:209–39. https://doi.org/10.1080/02671522.2010.509515 .
Bristow K, Edwards S, Funnel E, Fisher L, Gask L, Dowrick C, et al. Help seeking and access to primary care for people from “Hard-to-Reach” groups with common mental health problems. Int J Family Med. 2011;2011:490634. https://doi.org/10.1155/2011/490634 .
Article CAS PubMed PubMed Central Google Scholar
Kovandžić M, Chew-Graham C, Reeve J, Edwards S, Peters S, Edge D, et al. Access to primary mental health care for hard-to-reach groups: from “silent suffering” to “making it work.” Soc Sci Med. 2011;72:763–72. https://doi.org/10.1016/j.socscimed.2010.11.027 .
Cyril S, Smith BJ, Possamai-Inesedy A, Renzaho AMN. Exploring the role of community engagement in improving the health of disadvantaged populations: a systematic review. Glob Health Action. 2015;8:29842. https://doi.org/10.3402/gha.v8.29842 .
Wise J. NICE chief criticises “one size fits all” approach to health promotion. BMJ. 2009;338 Jun10 1:b2326–b2326. https://doi.org/10.1136/bmj.b2326 .
Hui A, Latif A, Hinsliff-Smith K, Chen T. Exploring the impacts of organisational structure, policy and practice on the health inequalities of marginalised communities: Illustrative cases from the UK healthcare system. Health Policy. 2020;124:298–302. https://doi.org/10.1016/j.healthpol.2020.01.003 .
Brown JSL, Casey SJ, Bishop AJ, Prytys M, Whittinger N, Weinman J. How black African and white British women perceive depression and help-seeking: a pilot vignette study. Int J Soc Psychiatry. 2011;57:362–74. https://doi.org/10.1177/0020764009357400 .
Elias L, Singh A, Burgess RA. In search of “community”: a critical review of community mental health services for women in African settings. Health Policy Plan. 2021. https://doi.org/10.1093/heapol/czaa140 .
Rabiah-Mohammed F, Oudshoorn A, Forchuk C. Gender and experiences of family homelessness. J Soc Distress Homelessness. 2020;29:151–60. https://doi.org/10.1080/10530789.2019.1679420 .
Portwood SG, Shears JK, Nelson EB, Thomas ML. Examining the impact of family services on homeless children. Child Fam Soc Work. 2015;20:480–93. https://doi.org/10.1111/cfs.12097 .
Waffenschmidt S, Knelangen M, Sieben W, Bühn S, Pieper D. Single screening versus conventional double screening for study selection in systematic reviews: a methodological systematic review. BMC Med Res Methodol. 2019;19:132. https://doi.org/10.1186/s12874-019-0782-0 .
Shemilt I, Khan N, Park S, Thomas J. Use of cost-effectiveness analysis to compare the efficiency of study identification methods in systematic reviews. Syst Rev. 2016;5:140. https://doi.org/10.1186/s13643-016-0315-4 .
Download references
Acknowledgements
Not applicable.
This review was not supported by any external funding.
Author information
Authors and affiliations.
Department of Public Health and Primary Care, University of Cambridge, Cambridge, CB2 0SR, UK
Natasha Joseph
Department of Psychiatry, University of Cambridge, Cambridge, CB2 0SZ, UK, Herchel Smith Building for Brain and Mind Sciences, Forvie Site, Robinson Way
Anne-Marie Burn & Joanna Anderson
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the conceptualisation and design of the study. Literature searches were conducted by N.J. and J.K.A. All authors took part in the study selection and data extraction. N.J. conducted the data analysis and interpretation. N.J. prepared the first draft of the manuscript. All authors contributed to and approved the final manuscript.
Corresponding author
Correspondence to Anne-Marie Burn .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Search Strategy.
Additional file 2:
Quality of included studies (Critical appraisal).
Additional file 3:
Intervention characteristics.
Additional file 4:
Sample characteristics.
Additional file 5:
Community Engagement Study Outcomes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Joseph, N., Burn, AM. & Anderson, J. The impact of community engagement as a public health intervention to support the mental well-being of single mothers and children living under housing insecure conditions – a rapid literature review. BMC Public Health 23 , 1866 (2023). https://doi.org/10.1186/s12889-023-16668-7
Download citation
Received : 16 December 2022
Accepted : 31 August 2023
Published : 26 September 2023
DOI : https://doi.org/10.1186/s12889-023-16668-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Housing insecurity
- Homelessness
- Public health interventions
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Open access
- Published: 24 May 2024
Vertebral hemangiomas: a review on diagnosis and management
- Kyle Kato 1 ,
- Nahom Teferi 2 ,
- Meron Challa 1 ,
- Kathryn Eschbacher 3 &
- Satoshi Yamaguchi 2
Journal of Orthopaedic Surgery and Research volume 19 , Article number: 310 ( 2024 ) Cite this article
476 Accesses
2 Altmetric
Metrics details
Vertebral hemangiomas (VHs) are the most common benign tumors of the spinal column and are often encountered incidentally during routine spinal imaging.
A retrospective review of the inpatient and outpatient hospital records at our institution was performed for the diagnosis of VHs from January 2005 to September 2023. Search filters included “vertebral hemangioma,” "back pain,” “weakness,” “radiculopathy,” and “focal neurological deficits.” Radiographic evaluation of these patients included plain X-rays, CT, and MRI. Following confirmation of a diagnosis of VH, these images were used to generate the figures used in this manuscript. Moreover, an extensive literature search was conducted using PubMed for the literature review portion of the manuscript.
VHs are benign vascular proliferations that cause remodeling of bony trabeculae in the vertebral body of the spinal column. Horizontal trabeculae deteriorate leading to thickening of vertical trabeculae which causes a striated appearance on sagittal magnetic resonance imaging (MRI) and computed tomography (CT), “Corduroy sign,” and a punctuated appearance on axial imaging, “Polka dot sign.” These findings are seen in “typical vertebral hemangiomas” due to a low vascular-to-fat ratio of the lesion. Contrarily, atypical vertebral hemangiomas may or may not demonstrate the “Corduroy” or “Polka-dot” signs due to lower amounts of fat and a higher vascular component. Atypical vertebral hemangiomas often mimic other neoplastic pathologies, making diagnosis challenging. Although most VHs are asymptomatic, aggressive vertebral hemangiomas can present with neurologic sequelae such as myelopathy and radiculopathy due to nerve root and/or spinal cord compression. Asymptomatic vertebral hemangiomas do not require therapy, and there are many treatment options for vertebral hemangiomas causing pain, radiculopathy, and/or myelopathy. Surgery (corpectomy, laminectomy), percutaneous techniques (vertebroplasty, sclerotherapy, embolization), and radiotherapy can be used in combination or isolation as appropriate. Specific treatment options depend on the lesion's size/location and the extent of neural element compression. There is no consensus on the optimal treatment plan for symptomatic vertebral hemangioma patients, although management algorithms have been proposed.
While typical vertebral hemangioma diagnosis is relatively straightforward, the differential diagnosis is broad for atypical and aggressive lesions. There is an ongoing debate as to the best approach for managing symptomatic cases, however, surgical resection is often considered first line treatment for patients with neurologic deficit.
Introduction
Vertebral hemangiomas (VHs) are benign vascular lesions formed from vascular proliferation in bone marrow spaces that are limited by bony trabeculae [ 1 ]. VHs are quite common and are often incidental findings on spinal computed tomography (CT) and magnetic resonance imaging (MRI) of patients presenting with back or neck pain [ 2 , 3 ]. Previous, large autopsy series such as Schmorl (1926) and Junghanns (1932) found a VH prevalence of 11% in adult specimens [ 1 , 4 ]. However, the prevalence is believed to be higher as modern imaging techniques allow for better detection of small VHs that may not be easily diagnosed on autopsy specimens [ 5 ]. They can occur at any age but are most often seen in individuals in their 5th decade of life with a slight female preponderance [ 2 , 6 , 7 ]. Most VHs are found in the thoracic or lumbar spinal column and often involve the vertebral body, though they can extend to the pedicle, lamina, or spinous process, and may span multiple spinal segments [ 5 ].
The vast majority of VHs are asymptomatic, quiescent lesions [ 3 ]. Prior studies have stated less than 5% of VHs are symptomatic [ 8 , 9 ], although the 2023 study by Teferi et. al. demonstrated 35% of their 75 VH patients presented with symptoms including localized pain, numbness, and/or paresthesia [ 1 ]. 85% of symptomatic cases in this series were found to have VHs localized in the thoracic spine [ 1 ].
Among symptomatic VHs, up to 20–45% of cases may exhibit aggressive features including damage to surrounding bone and soft tissue or demonstrate rapid growth that extends beyond the vertebral body and invades the paravertebral and/or epidural space [ 1 , 5 , 10 , 11 ]. When “aggressive”, VHs may compress the spinal cord and nerve roots causing severe symptoms [ 1 , 5 ]. 45% of symptomatic VH patients present with neurologic deficits secondary to compressive lesions, bony expansion, disrupted blood flow, or vertebral body collapse while the remaining 55% present solely with back pain [ 8 , 12 , 13 , 14 , 15 ].
VHs are primarily diagnosed with radiographs, CT, and MRI, although other studies such as angiography, nuclear medicine studies, and positron emission—computed tomography (PET-CT) have been previously utilized to a lesser extent [ 1 , 15 , 16 , 17 , 18 , 19 ]. Radiologically, these lesions can be grouped into Typical, Atypical, and Aggressive subtypes (see radiological features). Histologically, VHs are composed of varying proportions of adipocytes, blood vessels, and interstitial edema which leads to thickening of vertical trabeculae in the affected vertebra [ 5 ]. This histopathology leads to the characteristic “polka-dot” sign on axial CT/MRI and “corduroy” sign on coronal and sagittal CT/MRI [ 5 , 20 ].
In terms of management, conservative treatment with observation and pain control are the mainstay of treatment for asymptomatic VH patients and those with mild-to-moderate pain respectively [ 21 ]. Surgical decompression is indicated for patients with neurologic deficits including compressive myelopathy or radiculopathy [ 22 ]. Other symptomatic patients have a wide variety of treatment options available including sclerotherapy, embolization, radiotherapy, and/or vertebroplasty [ 1 , 5 , 23 ]. The best approach in managing an individual patient with a symptomatic VH has not been elucidated and there have been different management algorithms suggested based on varying institutional experiences [ 1 , 5 , 24 , 25 ].
This article will review what is currently known regarding VHs. Diagnostic techniques and challenges will be highlighted as well as current treatment recommendations from the literature.
A retrospective review of the inpatient and outpatient hospital records at our institution was performed for the diagnosis of VHs from January 2005 to September 2023. Search filters included “vertebral hemangioma” "back pain,” “weakness,” “radiculopathy,” and “focal neurological deficits.” Radiographic evaluation of these patients included plain X-rays, CT, and MRI. Following confirmation of a diagnosis of VH, these images were used to generate the figures used in this manuscript. Moreover, an extensive literature search was conducted using PubMed for the literature review portion of the manuscript.
68 Articles were selected from our PubMed search. This article will review what is currently known about VHs. Diagnostic techniques and challenges will be highlighted as well as current treatment recommendations from the literature.
Histopathological features
VHs are benign tumors composed of various sized blood vessels, adipocytes, smooth muscle, fibrous tissue, hemosiderin, interstitial edema, and remodeled bone [ 5 , 7 , 26 , 27 ]. Macroscopically, they appear as soft, well-demarcated, dark red masses with intralesional, sclerotic boney trabeculae and scattered blood-filled cavities lending to a honeycomb appearance [ 5 , 6 , 7 ].
Microscopically, there are four subtypes of hemangiomas based on vascular composition: capillary, cavernous, arteriovenous (AV), and venous hemangiomas [ 28 ] (Fig. 1 ). Capillary hemangiomas are composed of small, capillary-sized blood vessels while cavernous hemangiomas present with collections of larger, dilated blood vessels [ 1 ]. AV hemangiomas are composed of interconnected arterial and venous networks while an abnormal collection of veins comprises venous hemangiomas [ 1 ]. VHs are predominately capillary and cavernous subtypes with thin-walled blood vessels surrounded by edematous stroma and boney trabeculae that permeate the bone marrow space [ 1 , 7 , 27 ]. In a sample of 64 surgically treated VHs cases, Pastushyn et al. reported 50% were capillary subtype, 28% were cavernous subtype, and 22% were mixed [ 29 ]. Occasionally, secondary reactive phenomena such as fibrous and/or adipose involution of bone marrow and remodeling of bone trabeculae may be seen [ 7 , 26 ]. Symptomatic VHs can be caused by all hemangioma subtypes, and there are no distinguishing features between subtypes on imaging [ 1 ]. However, cavernous and capillary subtypes are associated with favorable postsurgical outcomes [ 29 ].
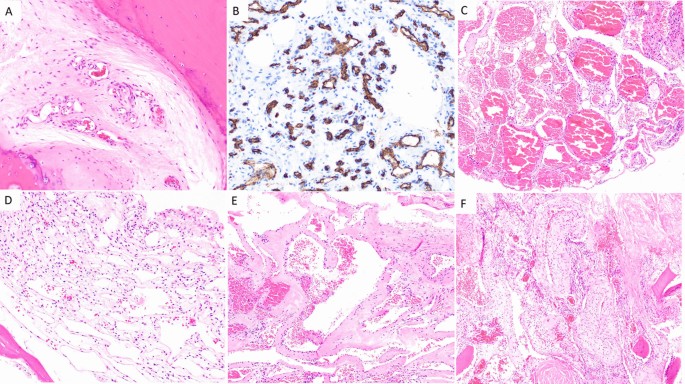
Capillary hemangioma ( A and B ): A H&E 200× magnification showing proliferation of small caliber vessels within a fibrous stroma with surrounding bone, B CD34 immunohistochemical stain, 200× magnification highlighting small caliber vascular spaces. Cavernous hemangioma ( C and D ): C H&E 100× magnification showing proliferation of thin-walled, dilated, blood filled vascular channels, D H&E 200× magnification: Thin-walled, dilated vascular channels within a loose stroma with adjacent mature bone. Venous hemangioma ( E and F ): E H&E 100 × magnification showing abnormal proliferation of thick-walled vessels with dilated lumens. F H&E 100× magnification reveals tightly packed, thick-walled vessels with adjacent fragments of mature bone
Radiographic features
The histopathology of VHs gives rise to imaging features used to classify VHs as typical, atypical, or aggressive [ 13 ]. Typical and atypical MRI findings are correlated with the intralesional ratio of fat to vascular components [ 20 ]. Lesions with a high fat content are more likely to demonstrate features of typical VHs while those with a high vascular content (atypical VHs) tend to present without these findings [ 5 , 30 , 31 ]. Aggressive VHs have features including destruction of the cortex, invasion of the epidural and paravertebral spaces, and lesions extending beyond the vertebral body [ 13 , 15 , 20 ].
Laredo et al. demonstrated that VHs with a higher fatty content are generally quiescent lesions, while those with a higher vascular content are more likely to display “active” behavior and potentially evolve into compressive lesions [ 20 ]. Therefore, asymptomatic VHs can display both typical or atypical imaging findings while symptomatic lesions are more likely to present with atypical or aggressive findings [ 1 ]. Despite radiographically typical VHs being relatively easy to diagnose, atypical and aggressive VHs are much more challenging to recognize as they do not present with classic imaging findings and often mimic other pathologies such as multiple myeloma, metastatic bone lesions, and inflammatory conditions [ 5 , 30 , 31 ]. Compressive VHs often have coinciding radiologic and clinical classifications due to the correlation between aggressive behavior and compressive symptoms [ 5 ].
While MRI, CT, and radiographs are the primary imaging modalities used in the workup of VHs, other studies have also been used. Angiography will occasionally be performed to identify feeding/draining vessels and evaluate the blood supply to the spinal cord [ 5 ]. Multiphase technetium 99-methyl diphosphonate ( 99 Tc-MDP) bone scintigraphy may show increased tracer uptake in all phases (perfusion, blood pool, and delayed) due to technetium 99-labeled red blood cell accumulation in the tumors, which occurs in all hemangiomas [ 16 ]. PET-CT has been used to classify VHs as “hot” or “cold” lesions based on the degree of 18-FDG and 68-Ga DOTATATE uptake [ 17 , 18 , 19 ]. Although angiography is useful in clarifying the vascular network of aggressive VHs primarily, nuclear medicine studies offer a much more limited contribution to diagnosis when compared to CT and MRI [ 5 ].
Typical VHs
The collection of thin-walled, blood-filled spaces that comprise VHs cause resorption of horizontal trabeculae and reinforcement of vertical trabeculae, leading to a pattern of thickened vertical trabeculae interspersed with lower density bone of the nonexpanding vertebral body [ 15 , 31 , 32 ]. This composition is responsible for the “corduroy cloth” appearance seen in typical VHs on radiographic images [ 31 ].
On unenhanced axial CT images, typical VHs are characterized by a “polka dot” appearance, termed polka-dot sign. This is caused by small, punctate areas of high attenuation from hyperdense trabeculae surrounded by hypodense stroma [ 20 , 33 ] (Fig. 2 ). Like radiographs, sagittal and coronal CT images display the “corduroy” sign caused by thickened trabeculae in a field of hypodense bone (Fig. 2 ). There is no extraosseous extension of the hemangioma in typical VHs [ 5 ].

Sagittal ( A ) and axial ( B ) CT scans of a typical VH in an asymptomatic 50-year-old male demonstrating the “Corduroy” and “Polka-dot” signs respectively. Sagittal ( C ) and axial ( D ) T1-weighted MRIs of typical VHs are predominately hyperintense with areas of hypo-intensity due to thickening of vertical trabeculae. Sagittal ( E ) and axial ( F ) T2-weighted MRIs of typical VHs also appear as hyperintense lesions with areas of hypo-intensity that may demonstrate the “Corduroy” and “Polka-dot” signs as seen in CT images of typical VHs
Typical VHs tend to appear as hyperintense lesions on T1- and T2-weighted MRI sequences due to predominately fatty overgrowth with penetrating blood vessels [ 31 ] (Fig. 2 ). There are punctate areas of slight hypointensity within the lesion on axial T1-weighted MRI due to thickened vertical trabeculae which resembles the “polka-dot" sign [ 5 ] (Fig. 2 ). These trabeculae appear as linear striations on sagittal/coronal T1- and T2-weighted MRI [ 5 ] (Fig. 2 ). Fluid-sensitive sequences (i.e. short-tau inversion recovery or fat-saturated T2-weighted MRI) appear slightly hyperintense due to the vascular components of the lesion, and T1-weighted MRI with contrast demonstrates heterogenous enhancement of the lesion [ 3 ] (Fig. 3 ).
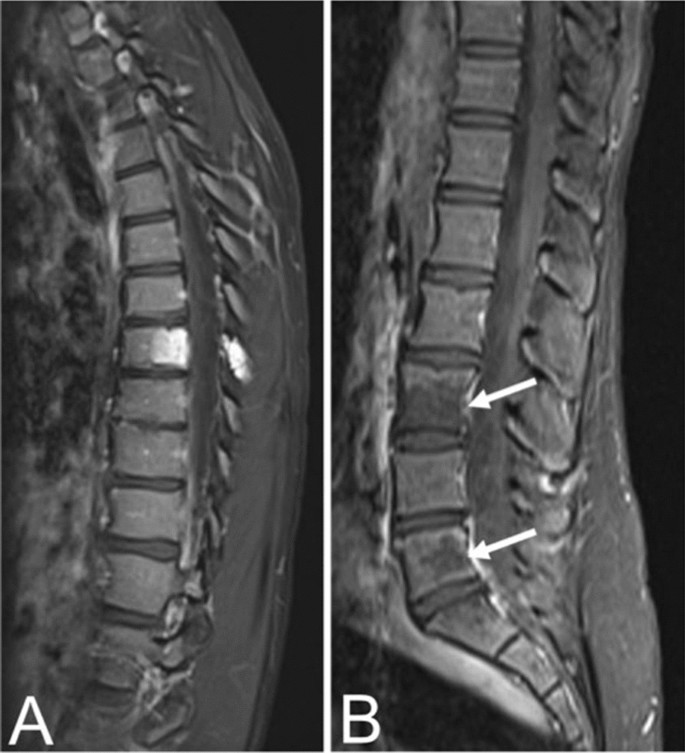
Contrast-enhanced T1 MRIs of a T8 VH in an asymptomatic fourteen-year-old female ( A ) and L3, L5 VHs in a thirty-one-year-old female with back pain ( B ), illustrating the heterogenous presentation of hemangiomas on post-contrast MRI
Atypical VHs
In contrast to typical VHs, atypical VHs tend to have a higher vascular component-to-fat ratio and may not demonstrate the classical imaging findings such as the “corduroy” and “polka-dot” signs [ 5 ]. This composition gives the lesion an iso- to hypointense appearance on T1-weighted MRI as well as a very high intensity appearance on T2-weighted and fluid-sensitive MRI [ 20 , 31 ] (Fig. 4 ). Atypical VHs often mimic primary bony malignancies or metastases and are more likely to demonstrate aggressive features, often making them difficult to diagnose [ 12 , 13 , 14 , 15 ].
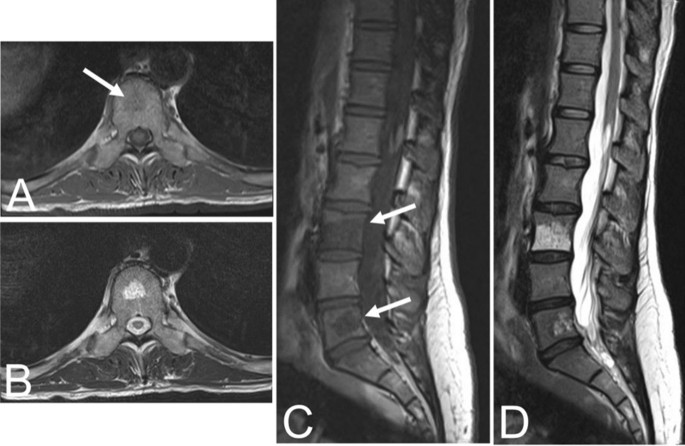
Asymptomatic fifty-six-year-old male with a T9 atypical vertebral hemangioma that appears iso- to hypointense on axial T1 MRI ( A ) and hyperintense on axial T2 MRI ( B ). Atypical vertebral hemangiomas of the L3 and L5 vertebral bodies in a thirty-one-year-old female who presented with backpain. Sagittal T1 ( C ) and T2 ( D ) demonstrate hypo- and hyperintense lesions respectively
Aggressive VHs
Aggressive VHs routinely have atypical features on any imaging modality [ 1 , 5 ]. They may appear radiographically normal or show nonspecific findings such as osteoporosis, pedicle erosion, cortex expansion, vertebral collapse, or irregular vertical trabeculae associated with lytic areas of varying size [ 13 , 15 ] (Fig. 5 ).

Fifty-five-year-old female with an aggressive vertebral hemangioma of the L4 vertebral body with extension into the spinal canal. A Sagittal T1 MRI shows hypo-intensity of the entire vertebral body, although vertebral height is maintained. B Sagittal T2 MRI redemonstrates the lesion but appears hyperintense due to the vascularity of the hemangioma. Axial T1 ( C ) and T2 ( D ) MRI show involvement of the pedicles bilaterally and extension of the lesion into the anterior epidural space
CT findings are often nonspecific, including features such as extraosseous soft tissue expansion, cortical ballooning, or cortical lysis [ 34 , 35 ]. As with atypical VHs, the “corduroy” and “polka-dot” signs may not be readily visualized in aggressive or destructive lesions due to the higher vascular-to-fat ratio common in these hemangiomas [ 5 ]. However, it is important to be mindful of these signs because they can guide to the correct diagnosis. Other CT features that may assist in the diagnosis of inconspicuous VHs include extension of the lesion into the neural arch, involvement of the entire vertebral body, or an irregular honeycomb pattern due to serpentine vascular channels and fatty proliferation within the network of reorganizing bony trabeculae [ 20 ]. Vertebral fractures are rare due to the reinforcement of vertical trabeculae [ 1 ].
The composition of aggressive VHs, with a hypervascular stroma and less fat, results in a hypointense lesion on T1-weighted MRI [ 20 , 31 ] (Fig. 5 ). Again, this may conceal the “corduroy” and “polka-dot” signs which remain amongst the most useful imaging findings in the diagnosis of VHs, particularly in cases where other findings are nonspecific [ 5 ]. These non-specific findings may include hyperintensity on T2-weighted MRI due to the vascular components of the lesion (Fig. 5 ), which is also seen in most neoplastic and inflammatory lesions [ 31 ]. Areas of hyperintensity on fluid-sensitive MRI and the presence of lipid-dense content within the lesion may be seen as well [ 31 , 36 ]. Other features suggestive of an aggressive VH include a maintained vertebral body height, a sharp margin with normal marrow, an intact cortex adjacent to a paraspinal mass, or enlarged paraspinal vessels, however these findings are also nonspecific and relatively uncommon [ 5 , 13 ]. Although highly unusual, there have been cases of aggressive VHs with extensive intraosseous fatty stroma and simultaneous extraosseous extension of the lesion, permitting a straightforward diagnosis [ 36 ].
Even though some aggressive VHs may be diagnosed on CT and MRI, challenging cases may warrant the use of more advanced imaging techniques for accurate diagnosis. Higher fluid content relative to cellular soft tissue gives hemangiomas a bright appearance on diffusion weighted imaging (DWI) with elevated apparent diffusion coefficient (ADC) values, distinguishing them from metastases [ 37 ]. Volume transfer constant (K trans ) and plasma volume, which reflect capillary permeability and vessel density respectively, are quantitative measures derived from dynamic contrast enhanced magnetic resonance imaging (DCE MRI) perfusion imaging that can also be used to differentiate VHs and metastases [ 38 ]. K trans and plasma volume are both low in VHs and elevated in metastatic lesions [ 38 ]. Furthermore, aggressive VHs may show a signal drop when comparing non-contrast T1-weighted MRI with and without fat suppression, as well as microscopic lipid content on chemical shift imaging [ 39 ]. Finally, characteristic findings of aggressive VHs in angiography include vertebral body arteriole dilation, multiple capillary phase blood pools, and complete vertebral body opacification [ 15 ].
Laredo et al. [ 15 ] proposed a six-point scoring system to assist in the diagnosis of aggressive VHs based on the more common features observed in radiographs and CT. One point was given for each of the following findings: a soft tissue mass, thoracic location between T3–T9, involvement of the entire vertebral body, an irregular honeycomb appearance, cortical expansion, and extension into the neural arch [ 15 ]. The authors suggest that aggressive VHs should be suspected when a patient presents with nerve root pain in association with three or more of these features [ 15 ]. However, additional studies are needed to determine the utility of this scoring system as the predictive power has not been determined [ 5 ].
Some VHs are difficult to diagnose because they can have nonspecific findings on radiographs, CT, and MRI, making characteristic findings such as the “corduroy” and “polka-dot” signs, when present, important diagnostic features. VHs may also coexist with other vertebral lesions, further complicating the diagnosis. In these cases, angiography can differentiate a VH from a nonvascular lesion [ 40 ]. Ultimately, a biopsy may be required for accurate diagnosis, especially when there is potential for a malignant lesion such as angiosarcoma or epithelioid hemangioendothelioma.
Clinical features
VHs are often noted incidentally on spinal imaging and are often observed in patients in their fifth to sixth decade of life. Studies have shown that vertebral hemangiomas exhibit a slight female preponderance, with a male-to-female ratio of 1:1.5. [ 6 ]. Clinically, most VHs are asymptomatic and quiescent lesions, which rarely demonstrate active behavior and become symptomatic [ 41 ]. VHs occur most frequently in the thoracic spine [ 42 ], followed by the lumbar spine and cervical spine; sacral involvement is very rare [ 43 ].
When symptomatic, VHs can present with localized back pain or result in neurologic symptoms that are attributable to spinal cord compression, nerve root compression, or both, leading to myelopathy and/or radiculopathy [ 1 ]. At least 4 mechanisms of spinal cord and nerve root compression have been suggested: (1) hypertrophy or ballooning of the posterior cortex of the vertebral body caused by the angioma, (2) extension of the angioma through the cortex into the epidural space, (3) compression fracture of the involved vertebra, and (4) epidural hematoma [ 44 ]. When aggressive and symptomatic with spinal cord compression, VHs tend to occur in the thoracic spine [ 42 ].
Boriani et al. classified VHs into 4 groups based on the presence of symptoms and radiographic findings [ 45 ]. These include: Type I—latent, mild bony destruction with no symptoms; Type II—active, bony destruction with pain; Type III—aggressive, asymptomatic lesion with epidural and/or soft-tissue extension; and Type IV—aggressive, neurologic deficit with epidural and/or soft tissue extension.
Management options
Most VHs are asymptomatic and do not require treatment [ 1 , 21 ]. Treatment is indicated in cases with back pain or neurological symptoms, including myelopathy and/or radiculopathy, often caused by neuronal compression or vertebral fracture [ 1 ]. Previously, surgery was the primary treatment option offered to these patients, which was associated with an increased risk of complications, particularly intraoperative bleeding [ 1 ]. New modalities such as vertebroplasty have since gained traction as adjuncts or alternatives to surgery [ 1 ]. Today, there are several management options available for the treatment of symptomatic VHs, including conservative medical therapy, surgery, percutaneous techniques, radiotherapy, or a combination of these modalities [ 1 , 46 ].
There is no consensus on the best treatment strategy, however recently Teferi et. al. proposed a treatment algorithm for VHs based on their institutional experience and literature review (Fig. 6 ) [ 1 ]. They recommend conservative management for typical, asymptomatic VHs, CT-guided biopsy and metastatic workup with PET-CT for radiographically atypical VHs, surgical intervention with or without adjuvant therapy in cases with epidural spinal cord compression or vertebral compression fracture, and radiotherapy for recurrent, asymptomatic VHs following surgery.
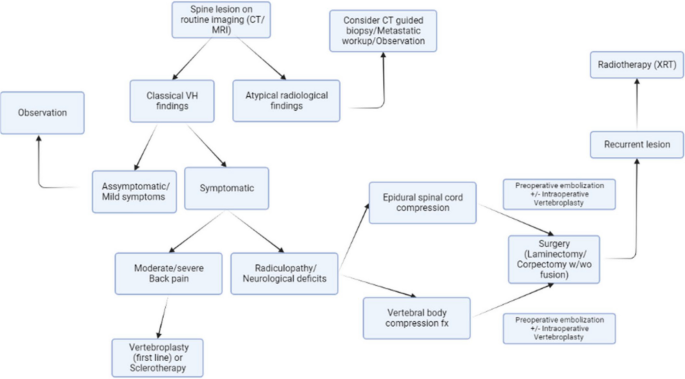
Algorithm for diagnosis and management of VHs proposed by Teferi et al. [ 1 ]
Surgical treatment of VHs is recommended in cases with rapid or progressive neurologic symptoms including compressive myelopathy or radiculopathy [ 47 ]. Baily et al. documented the first case of surgical management for VHs after they successfully resolved a patient’s paraplegia secondary to an aggressive VH [ 48 ]. Prior to the 1960s, the average neurological recovery rate was 73% (range, 43–85%) with a mortality rate of 11.7% [ 49 ]. This is consistent with a series published by Ghormley et al. in 1941 where 5 symptomatic VH patients were treated with decompressive laminectomy and postoperative radiotherapy. Although three patients achieved partial or complete resolution of neurologic deficits, the procedure resulted in the death of the remaining two patients secondary to significant blood loss [ 50 ]. There were very few cases of symptomatic VHs documented prior to the 1960s, with one literature review reporting only 64 instances of VHs with neurologic dysfunction [ 49 ]. More recent studies demonstrate improvement in surgical outcomes with neurological recovery reaching 100% and mortality as low as 0% [ 42 ].
The goal of surgery is to decompress neural elements and stabilize the spine [ 1 ]. Potential options include corpectomy, involving resection of a portion of the vertebral body containing the hemangioma, followed by anterior column reconstruction and/or laminectomy, which offers indirect decompression [ 1 ]. The selected approach depends on the size of the hemangioma and the extent of vertebral body and/or neural arch involvement due to potential weaknesses in the anterior column and the location of the epidural intrusion into the spinal canal [ 1 ]. For example, corpectomy and reconstruction could be performed in cases with ventral spinal cord compression while cases with dorsal compression could be treated with laminectomy [ 1 ].
Corpectomy has an increased risk of substantial intraoperative blood loss, up to 5 L in some cases, due to the hypervascular nature of VHs [ 1 , 51 ]. Acosta et al. reported an average blood loss of 2.1 L in their series of 10 aggressive VHs treated with corpectomy [ 51 ]. Conversely, laminectomy has a lower surgical burden and reduced risk of significant intraoperative blood loss [ 1 ]. Laminectomy blood loss can be further reduced by nearly 50% by performing vertebroplasty before laminectomy [ 8 ]. Preoperative embolization of VHs should also be considered to minimize intraoperative blood loss and reduce mortality [ 1 , 22 ].
Goldstein et al. demonstrated that en bloc resection may not be necessary, as intralesional resection produced equivalent long-term survival and prevention of recurrence in their series of 65 patients [ 47 ]. However, there have not been any large-scale studies comparing outcomes and recurrence rates of indirect decompression versus corpectomy [ 1 ].
The treatment algorithm proposed by Teferi et al. suggests dividing symptomatic VH patients with radiculopathy or neurological deficit into cohorts of epidural spinal cord compression (ESCC) versus vertebral body compression fracture to determine appropriate surgical intervention (Fig. 6 ) [ 1 ]. Patients with ESCC are encouraged to undergo preoperative embolization followed by laminectomy with or without fusion depending on spinal stability, or preoperative embolization followed by corpectomy and fusion if ESCC is accompanied by extensive anterior column compromise [ 1 ]. Conversely, the recommended treatment for symptomatic VHs secondary to vertebral body compression fracture is posterior laminectomy with decompression and fusion [ 1 ].
Whether through corpectomy or laminectomy, surgical management of VHs has a low recurrence rate [ 1 ]. Piper et al. reported complete remission in 84% of VHs treated surgically in their 2020 meta-analysis [ 52 ]. They also reported a severe complication rate, including pathological fracture, significant intraoperative blood loss, wound infection, and cerebrospinal fluid leak, of 3.5% [ 1 , 52 ].
Percutaneous techniques
Percutaneous techniques include vertebroplasty, sclerotherapy, and embolization which have been rising in popularity as treatment options for VHs in isolation or in combination with surgery [ 1 ].
Vertebroplasty is a minimally invasive procedure that improves the structural integrity of a vertebra by injecting an acrylic compound, such as polymethyl methacrylate (PMMA), into a lesion [ 1 ]. It was first utilized in the treatment of VHs by Galibert et al. in 1987 [ 53 ]. PMMA causes thrombosis and irreversible sclerosis of the hemangiomatous venous pool, shrinking the lesion and consolidating trabecular microfractures [ 1 ]. It allows for rapid recovery of mobility, enhances anterior column support, and provides vertebral stabilization, but does not induce new bone formation due to poor biological activity and absorbability [ 54 , 55 ]. Vertebroplasty is particularly effective in alleviating back pain in VH patients with intravertebral fractures by providing an immediate analgesic effect and has previously been recommended as stand-alone first line therapy for VHs with moderate to severe back pain without neurologic compromise [ 1 , 54 ]. It can also be used in combination with surgery to reduce intraoperative blood loss when given as a preoperative adjunct therapy [ 8 ]. The most common complication of vertebroplasty is extravasation of injected compound outside the vertebral body with rates of 20–35% [ 55 , 56 ]. However, some researchers suggest small amounts of extravasation should be considered a stopping point rather than a complication as the vast majority of cases are asymptomatic [ 55 , 56 ]. In a series of 673 vertebroplasty cases, Layton et al. reported extravasation in 25% of patients with only 1% developing clinical symptoms of new onset radiculopathy (5 patients) or symptomatic pulmonary embolism (1 patient) [ 56 ]. Their second most common complication was rib fracture related to lying prone on the fluoroscopy table during the procedure which occurred in 1% of cases (7 patients) [ 56 ].
Alternatively, sclerotherapy involves direct intralesional injection of ethanol under percutaneous CT-guidance which causes thrombosis and destruction of endothelium, resulting in devascularization, shrinkage of the lesion, and, consequently, decompression of the neural elements [ 46 ]. It was first described as a treatment for VHs in 1994 by Heiss et al. and is less common in the treatment of VHs [ 57 ]. CT angiography is a prerequisite to target the most hypervascular subsection of the lesion and ensure patients are candidates for the procedure without leakage of contrast media, which occurred in 25% of patients in a series of 18 cases [ 58 ]. There are reports of intraoperative sclerotherapy as an adjunct to surgery, but the sample sizes are similarly limited [ 59 , 60 ]. Complications of direct ethanol injection include neurologic deterioration (including Brown- Sequard syndrome), pathologic fractures, and VH recurrence [ 46 , 61 ].
The last option for percutaneous intervention is trans-arterial embolization of feeding vessels using particulate agents [ 1 ]. It has been used as a preoperative adjunct therapy with surgery to reduce blood loss as well as a primary treatment for VHs alone or in conjunction with vertebroplasty [ 41 , 62 , 63 , 64 ]. In a series of 26 patients, Premat et al. demonstrated embolization combined with vertebroplasty was safe and effective in treating pain associated with aggressive VHs but was less effective in resolving motor deficits [ 65 ]. The primary role for embolization in the treatment of compressive VHs is preoperative adjunct therapy to reduce the risk of procedural bleeding [ 62 ].
- Radiotherapy
Radiotherapy (XRT) is a noninvasive approach that can obliterate hemangiomas and relieve pain through vascular necrosis and/or anti-inflammatory effects [ 1 ]. It is a suitable option for VH patients with back pain and no neurologic deficits, or as postoperative adjunct therapy after suboptimal surgical decompression. Patients with neural element compromise often require prompt decompression to prevent irreversible injury that is more appropriately managed with surgery rather than the delayed response offered by XRT [ 1 , 21 , 66 ]. Neurological deficits may, in fact, be aggravated by XRT, as demonstrated in 20% of patients with aggressive VHs from a series of 29 cases by Jiang et al. [ 8 ]. Multiple studies have proclaimed a 60–80% success rate in eliminating symptoms from VHs using XRT, which increases to over 90% when including partial symptom relief [ 8 , 67 , 68 ]. This does include neurological deficits in some cases, but the response of these symptoms to XRT continues to vary [ 52 ]. A radiation dose of at least 34 Gy was recommended by Heyd et al. after their multicenter study identified significantly greater symptom relief and recurrence control compared to lower doses [ 67 ].
XRT is gaining popularity as a postoperative adjunct therapy intended to reduce local recurrence, especially in subtotal resections [ 8 , 52 , 67 ]. There is a 50% recurrence rate in partial resections without adjunct XRT [ 8 , 11 ]. The extent to which XRT can reduce recurrence has not been fully elucidated and has been suggested for future study [ 52 ]. However, these potential benefits must be weighed against the known adverse effects including nausea, fatigue, anorexia, ileus, radionecrosis, and specifically in spinal XRT, radiation myelitis [ 1 , 8 , 52 ].
VHs are often asymptomatic, incidental findings on routine spinal imaging that do not require treatment or follow-up imaging unless they become symptomatic. Most can be diagnosed with characteristic CT and MRI findings while atypical lesions may be difficult to differentiate from alternative diagnoses. Some authors suggest the utilization of emerging imaging techniques such as DWI or DCE MRI to differentiate atypical lesions from malignancies, which is a promising solution that requires further research. Other authors suggest observation with regular follow-up may be the best course of management for asymptomatic, atypical lesions while others still recommend biopsy for definitive diagnosis of atypical lesions. Regardless, there is a consensus that symptomatic lesions should be treated. Most authors recommend surgical decompression for treatment in patients with neurological deficits, but there is ongoing debate as to the optimal treatment for back pain alone. There are several treatment options which should be considered case-by-case given the properties of various lesions. Management algorithms have been suggested but additional research is required to identify the optimal treatment for the many different classifications of VHs.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- Vertebral hemangioma
Computed tomography
Magnetic resonance imaging
Arteriovenous
Positron emission-computed tomography
Technetium 99-methyl diphosphonate
Diffusion weighted imaging
Apparent diffusion coefficient
Volume transfer constant
Dynamic contrast enhanced magnetic resonance imaging
Epidural spinal cord compression
Polymethyl methacrylate
Teferi N, Chowdhury AJ, Mehdi Z, Challa M, Eschbacher K, Bathla G, Hitchon P. Surgical management of symptomatic vertebral hemangiomas: a single institution experience and literature review. Spine J. 2023;23(9):1243–54.
Article PubMed Google Scholar
Rodallec MH, Feydy A, Larousserie F, Anract P, Campagna R, Babinet A, Zins M, Drapé JL. Diagnostic imaging of solitary tumors of the spine: what to do and say. Radiographics. 2008;28(4):1019–41.
Baudrez V, Galant C, Vande Berg BC. Benign vertebral hemangioma: MR-histological correlation. Skelet Radiol. 2001;30:442–6.
Article CAS Google Scholar
Huvos AG. Hemangioma, lymphangioma, angiomatosis/lymphangiomatosis, glomus tumor. Bone tumors: diagnosis, treatment, and prognosis. 2nd ed. Philadelphia: Saunders. 1991;553–78.
Gaudino S, Martucci M, Colantonio R, Lozupone E, Visconti E, Leone A, Colosimo C. A systematic approach to vertebral hemangioma. Skelet Radiol. 2015;44:25–36.
Article Google Scholar
Campanacci M. Hemangioma. In: Campanacci M, editors. Bone and soft tissue tumors: clinical features, imaging, pathology and treatment. Padova: Piccin Nuova Libraria & Wien: Springer; 1999. p. 599–618.
Hameed M, Wold LE. Hemangioma. In: Fletcher CDM, Bridge JA, Hogendoorn P, Mertens F, editors. WHO classification of tumors of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. p. 332.
Google Scholar
Jiang L, Liu XG, Yuan HS, Yang SM, Li J, Wei F, Liu C, Dang L, Liu ZJ. Diagnosis and treatment of vertebral hemangiomas with neurologic deficit: a report of 29 cases and literature review. Spine J. 2014;14(6):944–54.
Unni KK, Inwards CY. Dahlin's bone tumors: general aspects and data on 10,165 cases. Lippincott Williams & Wilkins; 2010.
Corniola MV, Schonauer C, Bernava G, Machi P, Yilmaz H, Lemée JM, Tessitore E. Thoracic aggressive vertebral hemangiomas: multidisciplinary management in a hybrid room. Eur Spine J. 2020;29:3179–86.
Fox MW, Onofrio BM. The natural history and management of symptomatic and asymptomatic vertebral hemangiomas. J Neurosurg. 1993;78(1):36–45.
Article CAS PubMed Google Scholar
Murphey MD, Fairbairn KJ, Parman LM, Baxter KG, Parsa MB, Smith WS. From the archives of the AFIP. Musculoskeletal angiomatous lesions: radiologic-pathologic correlation. Radiographics. 1995;15(4):893–917.
Cross JJ, Antoun NM, Laing RJ, Xuereb J. Imaging of compressive vertebral haemangiomas. Eur Radiol. 2000;10:997–1002.
Alexander J, Meir A, Vrodos N, Yau YH. Vertebral hemangioma: an important differential in the evaluation of locally aggressive spinal lesions. Spine. 2010;35(18):E917–20.
Laredo JD, Reizine D, Bard M, Merland JJ. Vertebral hemangiomas: radiologic evaluation. Radiology. 1986;161(1):183–9.
Elgazzar AH. Musculoskeletal system. In: Synopsis of pathophysiology in nuclear medicine. New York: Springer; 2014. p. 90–2.
Choi YY, Kim JY, Yang SO. PET/CT in benign and malignant musculoskeletal tumors and tumor-like conditions. In: Editors. Seminars in musculoskeletal radiology. Thieme Medical Publishers; 2014. pp. 133–48
Brogsitter C, Hofmockel T, Kotzerke J. 68Ga DOTATATE uptake in vertebral hemangioma. Clin Nucl Med. 2014;39(5):462–3.
Basu S, Nair N. “Cold” vertebrae on F-18 FDG PET: causes and characteristics. Clin Nucl Med. 2006;31(8):445–50.
Laredo JD, Assouline E, Gelbert F, Wybier M, Merland JJ, Tubiana JM. Vertebral hemangiomas: fat content as a sign of aggressiveness. Radiology. 1990;177(2):467–72.
Dang L, Liu C, Yang SM, Jiang L, Liu ZJ, Liu XG, Yuan HS, Wei F, Yu M. Aggressive vertebral hemangioma of the thoracic spine without typical radiological appearance. Eur Spine J. 2012;21:1994–9.
Article PubMed PubMed Central Google Scholar
Kato S, Kawahara N, Murakami H, Demura S, Yoshioka K, Okayama T, Fujita T, Tomita K. Surgical management of aggressive vertebral hemangiomas causing spinal cord compression: long-term clinical follow-up of five cases. J Orthop Sci. 2010;15:350–6.
Klekamp J, Samii M. Epidermal Tumors. In: Surgery of spinal tumors. Springer; 2007. p. 321–522.
Blecher R, Smorgick Y, Anekstein Y, Peer A, Mirovsky Y. Management of symptomatic vertebral hemangioma: follow-up of 6 patients. Clin Spine Surg. 2011;24(3):196–201.
Subramaniam MH, Moirangthem V, Venkatesan M. Management of aggressive vertebral haemangioma and assessment of differentiating pointers between aggressive vertebral haemangioma and metastases—a systematic review. Global Spine J. 2023;13(4):1120–33.
Hart JL, Edgar MA, Gardner JM. Vascular tumors of bone. In: Seminars in diagnostic pathology. WB Saunders; 2014. p. 30–8.
Dorfman HD, Czerniak B. Vascular lesions. In: Dorfman HD, Czerniak B, editors. Bone tumors. St. Louis: Mosby; 1998. p. 729–814.
Rudnick J, Stern M. Symptomatic thoracic vertebral hemangioma: a case report and literature review. Arch Phys Med Rehabil. 2004;85(9):1544–7.
Pastushyn AI, Slin’ko EI, Mirzoyeva GM. Vertebral hemangiomas: diagnosis, management, natural history and clinicopathological correlates in 86 patients. Surg Neurol. 1998;50(6):535–47.
Blankstein A, Spiegelmann R, Shacked I, Schinder E, Chechick A. Hemangioma of the thoracic spine involving multiple adjacent levels: case report. Spinal Cord. 1988;26(3):186–91.
Hanrahan CJ, Christensen CR, Crim JR. Current concepts in the evaluation of multiple myeloma with MR imaging and FDG PET/CT. Radiographics. 2010;30(1):127–42.
Ross JS, Masaryk TJ, Modic MT, Carter JR, Mapstone T, Dengel FH. Vertebral hemangiomas: MR imaging. Radiology. 1987;165(1):165–9.
Persaud T. The polka-dot sign. Radiology. 2008;246(3):980–1.
Nguyen JP, Djindjian M, Gaston A, Gherardi R, Benhaiem N, Caron JP, Poirier J. Vertebral hemangiomas presenting with neurologic symptoms. Surg Neurol. 1987;27(4):391–7.
Gaston A, Nguyen JP, Djindjian M, Le Bras F, Gherardi R, Benhaiem N, Marsault C. Vertebral haemangioma: CT and arteriographic features in three cases. J Neuroradiol. 1985;12(1):21–33.
CAS PubMed Google Scholar
Friedman DP. Symptomatic vertebral hemangiomas: MR findings. AJR Am J Roentgenol. 1996;167(2):359–64.
Winfield JM, Poillucci G, Blackledge MD, Collins DJ, Shah V, Tunariu N, Kaiser MF, Messiou C. Apparent diffusion coefficient of vertebral haemangiomas allows differentiation from malignant focal deposits in whole-body diffusion-weighted MRI. Eur Radiol. 2018;28:1687–91.
Morales KA, Arevalo-Perez J, Peck KK, Holodny AI, Lis E, Karimi S. Differentiating atypical hemangiomas and metastatic vertebral lesions: the role of T1-weighted dynamic contrast-enhanced MRI. Am J Neuroradiol. 2018;39(5):968–73.
Article CAS PubMed PubMed Central Google Scholar
Shi YJ, Li XT, Zhang XY, Liu YL, Tang L, Sun YS. Differential diagnosis of hemangiomas from spinal osteolytic metastases using 3.0 T MRI: comparison of T1-weighted imaging, chemical-shift imaging, diffusion-weighted and contrast-enhanced imaging. Oncotarget. 2017;8(41):71095–104.
McEvoy SH, Farrell M, Brett F, Looby S. Haemangioma, an uncommon cause of an extradural or intradural extramedullary mass: case series with radiological pathological correlation. Insights Imaging. 2016;7(1):87–98.
Teferi N, Abukhiran I, Noeller J, Helland LC, Bathla G, Ryan EC, Nourski KV, Hitchon PW. Vertebral hemangiomas: diagnosis and management. A single center experience. Clin Neurol Neurosurg. 2020;190:105745.
Acosta FL Jr, Sanai N, Chi JH, Dowd CF, Chin C, Tihan T, Chou D, Weinstein PR, Ames CP. Comprehensive management of symptomatic and aggressive vertebral hemangiomas. Neurosurg Clin N Am. 2008;19(1):17–29.
Wang B, Zhang L, Yang S, Han S, Jiang L, Wei F, Yuan H, Liu X, Liu Z. Atypical radiographic features of aggressive vertebral hemangiomas. JBJS. 2019;101(11):979–86.
Jayakumar PN, Vasudev MK, Srikanth SG. Symptomatic vertebral haemangioma: endovascular treatment of 12 patients. Spinal cord. 1997;35(9):624–8.
Boriani S, Weinstein JN, Biagini R. Primary bone tumors of the spine: terminology and surgical staging. Spine. 1997;22(9):1036–44.
Doppman JL, Oldfield EH, Heiss JD. Symptomatic vertebral hemangiomas: treatment by means of direct intralesional injection of ethanol. Radiology. 2000;214(2):341–8.
Goldstein CL, Varga PP, Gokaslan ZL, Boriani S, Luzzati A, Rhines L, Fisher CG, Chou D, Williams RP, Dekutoski MB, Quraishi NA. Spinal hemangiomas: results of surgical management for local recurrence and mortality in a multicenter study. Spine. 2015;40(9):656–64.
Bailey P, Bucy PC. Cavernous hemangioma of the vertebrae. J Am Med Assoc. 1929;92(21):1748–51.
Krueger EG, Sobel GL, Weinstein C. Vertebral hemangioma with compression of spinal cord. J Neurosurg. 1961;18(3):331–8.
Ghormley RK, Adson AW. Hemangioma of vertebrae. JBJS. 1941;23(4):887–95.
Acosta FL Jr, Sanai N, Cloyd J, Deviren V, Chou D, Ames CP. Treatment of Enneking stage 3 aggressive vertebral hemangiomas with intralesional spondylectomy: report of 10 cases and review of the literature. Clin Spine Surg. 2011;24(4):268–75.
Piper K, Zou L, Li D, Underberg D, Towner J, Chowdhry AK, Li YM. Surgical management and adjuvant therapy for patients with neurological deficits from vertebral hemangiomas: a meta-analysis. Spine. 2020;45(2):E99-110.
Galibert P, Deramond H, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987;33(2):166–8.
Guarnieri G, Ambrosanio G, Vassallo P, Pezzullo MG, Galasso R, Lavanga A, Izzo R, Muto M. Vertebroplasty as treatment of aggressive and symptomatic vertebral hemangiomas: up to 4 years of follow-up. Neuroradiology. 2009;51:471–6.
Kim BS, Hum B, Park JC, Choi IS. Retrospective review of procedural parameters and outcomes of percutaneous vertebroplasty in 673 patients. Interv Neuroradiol. 2014;20(5):564–75.
Layton KF, Thielen KR, Koch CA, Luetmer PH, Lane JI, Wald JT, Kallmes DF. Vertebroplasty, first 1000 levels of a single center: evaluation of the outcomes and complications. Am J Neuroradiol. 2007;28(4):683–9.
CAS PubMed PubMed Central Google Scholar
Heiss JD, Doppman JL, Oldfield EH. Relief of spinal cord compression from vertebral hemangioma by intralesional injection of absolute ethanol. N Engl J Med. 1994;331(8):508–11.
Bas T, Aparisi F, Bas JL. Efficacy and safety of ethanol injections in 18 cases of vertebral hemangioma: a mean follow-up of 2 years. Spine. 2001;26(14):1577–81.
Murugan L, Samson RS, Chandy MJ. Management of symptomatic vertebral hemangiomas: review of 13 patients. Neurol India. 2002;50(3):300.
Singh P, Mishra NK, Dash HH, Thyalling RK, Sharma BS, Sarkar C, Chandra PS. Treatment of vertebral hemangiomas with absolute alcohol (ethanol) embolization, cord decompression, and single level instrumentation: a pilot study. Neurosurgery. 2011;68(1):78–84.
Niemeyer T, McClellan J, Webb J, Jaspan T, Ramli N. Brown-Sequard syndrome after management of vertebral hemangioma with intralesional alcohol: a case report. Spine. 1999;24(17):1845.
Singh PK, Chandra PS, Vaghani G, Savarkar DP, Garg K, Kumar R, Kale SS, Sharma BS. Management of pediatric single-level vertebral hemangiomas presenting with myelopathy by three-pronged approach (ethanol embolization, laminectomy, and instrumentation): a single-institute experience. Childs Nerv Syst. 2016;32:307–14.
Yao KC, Malek AM. Transpedicular N-butyl cyanoacrylate-mediated percutaneous embolization of symptomatic vertebral hemangiomas. J Neurosurg Spine. 2013;18(5):450–5.
Kawahara N, Tomita K, Murakami H, Demura S, Yoshioka K, Kato S. Total en bloc spondylectomy of the lower lumbar spine: a surgical techniques of combined posterior-anterior approach. Spine. 2011;36(1):74–82.
Premat K, Clarençon F, Cormier É, Mahtout J, Bonaccorsi R, Degos V, Chiras J. Long-term outcome of percutaneous alcohol embolization combined with percutaneous vertebroplasty in aggressive vertebral hemangiomas with epidural extension. Eur Radiol. 2017;27:2860–7.
Yang ZY, Zhang LJ, Chen ZX, Hu HY. Hemangioma of the vertebral column: a report on twenty-three patients with special reference to functional recovery after radiation therapy. Acta Radiol Oncol. 1985;24(2):129–32.
Heyd R, Seegenschmiedt MH, Rades D, Winkler C, Eich HT, Bruns F, Gosheger G, Willich N, Micke O, German Cooperative Group on Radiotherapy for Benign Diseases. Radiotherapy for symptomatic vertebral hemangiomas: results of a multicenter study and literature review. Int J Radiat Oncol* Biol* Phys. 2010;77(1):217–25.
Asthana AK, Tandon SC, Pant GC, Srivastava A, Pradhan S. Radiation therapy for symptomatic vertebral haemangioma. Clin Oncol. 1990;2(3):159–62.
Download references
Acknowledgements
Not applicable.
The University of Iowa Hospitals and Clinics provided funding for this research.
Author information
Authors and affiliations.
University of Iowa Carver, College of Medicine, Iowa City, IA, USA
Kyle Kato & Meron Challa
Department of Neurosurgery, University of Iowa Carver, College of Medicine, Iowa City, IA, USA
Nahom Teferi & Satoshi Yamaguchi
Department of Pathology, University of Iowa Carver, College of Medicine,, Iowa City, IA, USA
Kathryn Eschbacher
You can also search for this author in PubMed Google Scholar
Contributions
KK performed a portion of the literature review and was a major contributor in writing the manuscript/generating figures. NT performed most of the literature review and was a major contributor in reviewing the manuscript. MC contributed to writing the manuscript. KE provided histological images for figures. SY was a major contributor in reviewing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Kyle Kato .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Consent was obtained to publish Fig. 6 from Teferi et al. [ 1 ].
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kato, K., Teferi, N., Challa, M. et al. Vertebral hemangiomas: a review on diagnosis and management. J Orthop Surg Res 19 , 310 (2024). https://doi.org/10.1186/s13018-024-04799-5
Download citation
Received : 02 April 2024
Accepted : 18 May 2024
Published : 24 May 2024
DOI : https://doi.org/10.1186/s13018-024-04799-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Laminectomy
- Sclerotherapy
- Vertebroplasty
Journal of Orthopaedic Surgery and Research
ISSN: 1749-799X
- Submission enquiries: [email protected]
- Open access
- Published: 29 September 2021
Defining ethical challenge(s) in healthcare research: a rapid review
- Guy Schofield ORCID: orcid.org/0000-0002-9055-292X 1 , 3 ,
- Mariana Dittborn ORCID: orcid.org/0000-0003-2903-6480 2 ,
- Lucy Ellen Selman ORCID: orcid.org/0000-0001-5747-2699 3 &
- Richard Huxtable ORCID: orcid.org/0000-0002-5802-1870 1
BMC Medical Ethics volume 22 , Article number: 135 ( 2021 ) Cite this article
21k Accesses
15 Citations
11 Altmetric
Metrics details
Despite its ubiquity in academic research, the phrase ‘ethical challenge(s)’ appears to lack an agreed definition. A lack of a definition risks introducing confusion or avoidable bias. Conceptual clarity is a key component of research, both theoretical and empirical. Using a rapid review methodology, we sought to review definitions of ‘ethical challenge(s)’ and closely related terms as used in current healthcare research literature.
Rapid review to identify peer-reviewed reports examining ‘ethical challenge(s)’ in any context, extracting data on definitions of ‘ethical challenge(s)’ in use, and synonymous use of closely related terms in the general manuscript text. Data were analysed using content analysis. Four databases (MEDLINE, Philosopher’s Index, EMBASE, CINAHL) were searched from April 2016 to April 2021.
393 records were screened, with 72 studies eligible and included: 53 empirical studies, 17 structured reviews and 2 review protocols. 12/72 (17%) contained an explicit definition of ‘ethical challenge(s), two of which were shared, resulting in 11 unique definitions. Within these 11 definitions, four approaches were identified: definition through concepts; reference to moral conflict, moral uncertainty or difficult choices; definition by participants; and challenges linked to emotional or moral distress. Each definition contained one or more of these approaches, but none contained all four. 68/72 (94%) included studies used terms closely related to synonymously refer to ‘ethical challenge(s)’ within their manuscript text, with 32 different terms identified and between one and eight different terms mentioned per study.
Conclusions
Only 12/72 studies contained an explicit definition of ‘ethical challenge(s)’, with significant variety in scope and complexity. This variation risks confusion and biasing data analysis and results, reducing confidence in research findings. Further work on establishing acceptable definitional content is needed to inform future bioethics research.
Peer Review reports
Methodological rigour within research is a cornerstone in the production of high-quality findings and recommendations. Across the range of empirical methodologies, a broad collection of protocol development tools, methodology guidelines, and reporting guidelines have been developed and evidence of their use is increasingly required by journals [ 1 , 2 , 3 , 4 , 5 , 6 ]. Within both empirical bioethics and descriptive ethics, there has been an accompanying increase in the acknowledgment of the importance of methodological rigour in the empirical elements, including within the recent consensus statement on quality standards in empirical bioethics research by Ives et al. [ 7 , 8 , 9 ]. Aligned with this aim for rigour, definitional clarity of key terms used within a research project is a component of research quality [ 10 , 11 ]. Improving the quality of empirical bioethics is also itself an ethical imperative [ 9 ].
We recently conducted a systematic review examining ‘ethical challenges’ as reported by specialist palliative care practitioners [ 12 ]. Our review, alongside our initial scoping search findings and reading of the literature, suggested that, although many authors use the term ‘ethical challenge(s)’ in empirical ethics research, there appeared to be no commonly described or accepted definition. Furthermore, papers retrieved rarely defined ‘ethical challenge(s)’ explicitly , which has also been noted by other researchers examining other topic areas [ 13 , 14 , 15 ]. Our review further suggested that authors frequently use terms closely related to ‘ethical challenge(s)’—such as ‘moral dilemmas’ or ‘ethical issues’—interchangeably with ‘ethical challenge(s)’ throughout manuscripts, rather than staying with the original term. Research shows that non-philosophers may understand these related terms in heterogeneous ways which may additionally affect understanding of texts across different readerships [ 16 , 17 ].
Without a clear definition of an ethical challenge, each researcher must use individual judgement to ascertain whether they have identified an instance of one within their dataset. This potentially generates an unnecessary source of bias, particularly if multiple researchers are involved in data collection, extraction, or analysis. This risks generating misleading ethical analyses, evaluations, or recommendations. Additionally, and more broadly, if primary studies do not define the term, then work based on these—such as systematic reviews of individual studies or those undertaking secondary data analysis—may unknowingly compare different phenomena without a mechanism for mitigating the effects this introduces.
In the hope of prompting a debate on this topic, we therefore undertook a rapid review, which aimed to explore existing definitions of “ethical challenge(s)” and the use of other closely related terms within recent empirical healthcare ethics literature.
We conducted a rapid review examining the usage of the term ‘ethical challenge(s)’ over the last 5 years in published research articles, in order to identify and summarise if, and how, the term was defined. As a secondary aim, we examined authors’ uses of closely related alternative terms within the included article texts separate to their use within any explicit definitions that may be present.
Rapid reviews use abridged systematic review methodology to understand the evidence base on a particular topic in a time and resource efficient manner [ 18 , 19 , 20 , 21 , 22 ]. Comparative reviews of topics in which both a rapid review and a systematic review had been undertaken demonstrated that the overall conclusions were similar, although rapid reviews were less likely to contain social and economic data, and systematic reviews contained more detailed recommendations [ 18 , 19 , 20 , 23 , 24 ]. The Cochrane Rapid Review Methods Group has recently released interim methodological guidelines for undertaking rapid reviews [ 6 ], advising authors to describe where their protocol deviates from a systematic review and detail any biases that these deviations may introduce [ 18 , 19 , 21 ]. We have followed the Cochrane recommended methodology [ 6 ]. A rapid review reporting guideline is currently under development [ 25 ] and this review is therefore reported based on the PRISMA 2020 statement for systematic reviews, with justifications provided where our approach deviated [ 26 ].
Prospective review protocol registration on the PROSPERO database is the current gold standard, but, at the time of writing, PROSPERO does not accept records for rapid reviews [ 27 ]. The protocol was therefore not published in advance.
Eligibility criteria
The inclusion and exclusion criteria are summarised in Table 1 . We used Strech et al.’s Methodology, Issues, Participants (MIP) structure for our eligibility criteria, which is recommended for systematic reviews in ‘empirical bioethics’ [ 28 ]. The criteria reflect three assumptions. First, that the inclusion of ‘ethical challenge(s)’ in the title would increase the likelihood that this was the authors’ preferred term for the concept under investigation, and therefore increase the probability of a definition being provided. Second, that studies aiming to describe empirical data and identify ethical challenges in real-world contexts are most likely to contain a definition to guide researchers in identifying these challenges as they collect and analyse data. Third, that structured reviews of studies of ethical challenges are likely to include a definition to allow researchers to reliably recognise an ethical challenge in retrieved records. We used a 5-year timeframe as a date restriction. This reflected a balance between adequately covering recent use of the term and time and resource restrictions of the rapid review.
Information sources
The search strategy was as follows:
‘ethical challenge’.ti OR ‘ethical challenges’.ti.
We searched Medline (Ovid interface), Philosopher’s Index (OVID interface), EMBASE (OVID interface), and CINAHL (Cumulative Index to Nursing and Allied Health Literature, EBSCO interface) for studies indexed over a five-year period between April 2016 and April 2021. These resources cover the breadth of healthcare research. Including Philosopher’s Index increased coverage of the bioethics literature. We did not search the grey literature [ 6 ]. The search strategy was tested by successfully retrieving three sentinel studies known to the research team.
Study selection
Retrieved studies were imported into Endnote X9.2 [ 29 ]. Records unavailable through institutional subscriptions were requested from corresponding authors. If unavailable 14 days after the request, the record was excluded. A random sample of 20% of records were dual screened at the title/abstract level by GS/MD. After discussion, the remainder were screened by GS. At full-text screening, a further 20% were dual screened by GS/MD and, again after discussion, the remaining studies were screened by GS.
Data extraction and analysis
Data extraction was undertaken using a pre-piloted form, with the first 5 records dually extracted by GS and MD. Data from the remaining included studies was then extracted by GS, with correctness and completeness checked by MD. We collected data on date of publication, authors, journal, country (for primary studies), methodology, definition of ‘ethical challenge(s)’ (present (yes/no)) and (where offered) the definition provided, and any closely related terms used, with counts of all terms used in each article. For closely related terms, data was extracted from the authors’ text, but not from direct quotations from qualitative research. Where definitions of ‘ethical challenge(s)’ were offered and/or related terms were identified, these were categorised and counted following the principles of summative content analysis [ 30 ]. Summative content analysis combines both the quantitative counting of specific content or words/terms with latent content analysis to identify and categorise their meanings. We identified keywords (‘ethical challenge(s)’ and closely related terms) deployed by the authors of the included papers, both prior to and during data analysis, and analysed the retrieved definitions. This approach allowed for exploration of both the content of definitions and development of insights into the use of related terms.
Risk of bias assessment
The focus of the rapid review was the definition of the term ‘ethical challenge(s)’ within retrieved records. We therefore did not undertake quality assessment for the included studies and reviews.
831 records were retrieved, reduced to 393 after de-duplication. 238 records were excluded after reviewing the title and/or abstract. 157 records were identified for full text screening, with 3 unavailable [ 31 , 32 , 33 ]. 82 records were excluded at full text stage and 72 records were included for analysis. See Fig. 1 for the PRISMA flowchart.
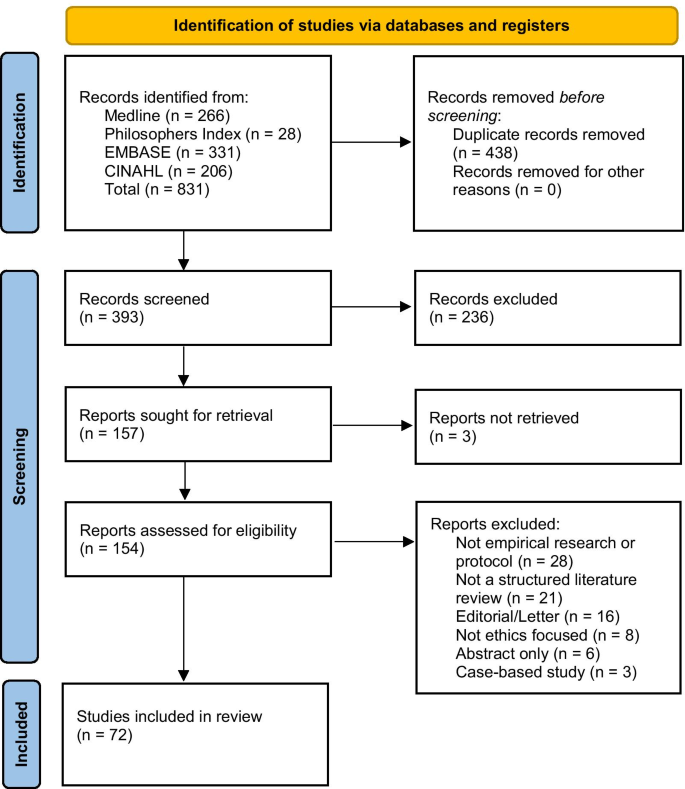
PRISMA flow diagram of record identification
Record characteristics
Of the 72 included records, 53 were empirical studies [ 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 ], 10 non-systematic reviews [ 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 ], 7 systematic reviews [ 12 , 13 , 14 , 97 , 98 , 99 , 100 ], 1 systematic review protocol [ 101 ], and 1 non-systematic review protocol [ 102 ]. Of the 53 empirical studies, 42 (79%) were qualitative studies [ 34 , 35 , 36 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 47 , 48 , 50 , 51 , 52 , 54 , 55 , 56 , 57 , 58 , 60 , 62 , 63 , 64 , 65 , 66 , 67 , 69 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 79 , 80 , 81 , 83 , 84 , 85 , 86 ], 6 (12%) used a mixed methods approach [ 45 , 46 , 53 , 59 , 61 , 68 ], and 5 (10%) were quantitative [ 37 , 49 , 70 , 78 , 82 ]. 7/56 empirical studies, all qualitative interview studies, recruited participants internationally with no specific location stated [ 40 , 54 , 55 , 58 , 60 , 63 , 73 ]. Of the remaining studies, all but one were single-country studies: Botswana [ 75 ], Canada [ 41 , 65 ], China [ 57 ], Denmark [ 39 , 43 ], Dominican Republic [ 44 ], Germany [ 51 , 84 ], India [ 61 ], Iran [ 38 , 46 , 49 , 68 , 70 , 71 , 72 , 78 , 82 , 98 ], Italy [ 45 ], Mexico [ 87 ], the Netherlands [ 76 ], New Zealand [ 47 ], Norway [ 42 , 52 , 56 , 64 , 80 , 81 , 83 ], Saudi Arabia [ 34 , 35 , 36 , 37 ], Tanzania [ 69 , 74 ], Uganda [ 67 ], UK [ 86 ], and USA [ 50 , 53 , 59 , 62 , 66 , 77 , 79 , 85 , 85 ]. The remaining study was undertaken in both Sierra Leone and the UK [ 48 ]. See Table 2 for a summary.
12/72 (17%) of retrieved studies offered an explicit definition for ‘ethical challenge(s)’ [ 12 , 13 , 14 , 48 , 50 , 56 , 57 , 66 , 69 , 81 , 98 , 101 ]. Definitions were more likely to be found in more recent publications, with 4/12 included studies published in 2016–2018 [ 14 , 48 , 56 , 81 ], and 8/12 published in 2019–2021 [ 12 , 13 , 50 , 57 , 66 , 69 , 98 , 101 ]. The included study locations were evenly distributed, matching the overall pattern of retrieved studies, with studies from high- [ 48 , 50 , 56 , 66 , 81 ], middle- [ 57 , 98 ], and low-income settings [ 48 , 69 ]. The identified studies included eight qualitative studies [ 48 , 50 , 56 , 57 , 66 , 69 , 81 , 98 ], 3 systematic reviews [ 12 , 13 , 14 ], and 1 systematic review protocol [ 101 ]. Two of these records were the systematic review protocol and the report from our group, which accordingly contained the same definition [ 12 , 101 ], leaving 11 unique definitions. Definitions of ‘ethical challenge(s)’ identified in included studies are provided in Table 3 . Additionally, 68/72 (94%) reports used closely related terms synonymously in place of ‘ethical challenge(s)’ throughout their manuscript text, with between 1 and 8 different terms used within each report, and 32 different terms were identified. This occurred in both those reports that contained a definition and those that did not. See Table 4 for terms and frequencies.
Those records that offered explicit definitions used four approaches: (1) definition through concepts [ 12 , 57 , 66 ]; (2) reference to moral conflict, moral uncertainty or difficult choices [ 13 , 14 , 48 , 57 , 69 , 98 ]; (3) definition by study participants [ 12 , 48 , 50 , 56 ]; or (4) challenges as linked to their ability to generate emotional or moral distress within healthcare practitioners [ 14 , 14 , 66 , 81 ]. Each definition was associated with one or more of the identified elements, although none covered all four approaches. We describe these approaches below.
Approach 1: definition through concepts
This approach involves primarily defining ‘ethical challenge(s)’ in terms of related concepts. All three definitions using this approach defined ‘ethical challenge(s)’ as a summative collection of related concepts, including ‘ethical dilemmas’, ‘moral dilemmas’, ‘moral challenges’, ‘ethical issues’, and ‘ethical conflicts’ [ 12 , 57 , 66 ], for example:
‘The expression “ethical challenges” mainly refers to ethical dilemmas and ethical conflicts as well as other scenarios where difficult choices have to be made’ [ 57 ] p34
Only one went on to define the other concepts they utilised, ‘ethical dilemmas’ and ‘ethical conflicts’:
‘Ethical dilemmas are described as situations that cannot be solved; decisions made between two options may be morally plausible but are equally problematic due to the circumstances. Ethical conflicts, on the contrary, arise when one is aware of the necessity of proper actions but he or she may have trouble exercising these actions because of certain internal or external factors.’ [ 57 ] p34
Approach 2: moral conflict, moral uncertainty or difficult choices
This approach anchors an ethical challenge to the requirement for an agent to make a (difficult) choice in a situation where moral principles conflict, or there is moral uncertainty as to the ‘right’ way forward.
‘In this context, ethical challenge refers to the situation whereby every alternative is morally wrong and still one has to make a choice’ [ 69 ] p676 ‘An ethical challenge occurs when one does not know how to behave and act in the best way…’ [ 14 ] p93
Approach 3: definition by study participants
Four of the definitions involved research participants themselves defining something as an ‘ethical challenge’ [ 12 , 48 , 50 , 56 ], with three studies explicitly stating that participants would lead this definitional work [ 48 , 50 , 56 ]. Draper & Jenkins offer a starting definition, adopted from Schwartz et al. [ 103 ] with which to prime participants, while Forbes and Phillips [ 50 ] and Jakobsen and Sørlie [ 56 ] left the definition fully with their participants (Table 3 ). Finally, Schofield et al. proposed a very broad definition (Table 3 ), alongside the specific statement that either participants or researchers could nominate something as an ‘ethical challenge’ [ 12 ].
Approach 4: emotional or moral distress
This final approach was to tie ethical challenges to situations where participants feel ‘discomfort’, emotional distress or more specifically moral distress or moral residue [ 14 , 66 , 81 ]. Larkin et al. are clear that this distress must be tied to moral causes, but Hem et al. and Storaker et al. also refer more broadly to ‘discomfort’ [ 14 ] and ‘emotional stress’ [ 81 ] respectively. For example:
‘In this article, ethical challenges refer to values that entail emotional and moral stress in healthcare personnel.’ [ 81 ] p557
To the authors’ knowledge, this is the first rapid review to examine the use of the term ‘ethical challenge(s)’ in empirical healthcare research literature. Notably, only 12/72 (17%) of included studies published in the last 5 years contained a definition for ‘ethical challenge(s)’, despite this being the focus of the research being reported. The definitions identified were found in qualitative studies and systematic reviews and were evenly distributed geographically across high-, middle- and low-income settings. Definitions contained one or more of the identified approaches, although none contained elements from all four. Taken together, these findings suggest that a clear definition of ‘ethical challenge(s)’, and consistent use thereof, is currently lacking.
The four approaches indicate the diverse approaches to understanding ‘ethical challenge(s)’. Approaches 1 and 2 explore the concept from opposite viewpoints, with approach 1 looking from the conceptual perspective, through terms such as ‘dilemmas’ and ‘conflict’, and approach 2 from a participant perspective, specifically in those situations in which someone is trying to make a decision in circumstances where the preferred option is not possible or when they perceive there to be clash in values they feel are important. Within the concept-led definitions (approach 1), the use of a plurality of terms highlights a potential risk of bias, as different readers may interpret these differently. For example, some terms, such as ‘moral dilemma’, have relatively well understood specific meanings for some readers, particularly those with philosophical training [ 104 , 105 , 106 ]. The presence in the literature of specific and multiple meanings for some related terms highlights the importance of empirical studies providing a definition of these additional terms alongside their primary definition for ‘ethical challenge(s)’. This is more likely to be relevant where an a priori definition is used, but may be relevant to any prompting text for studies using a participant-led process, as in the study by Draper and Jenkins [ 48 ]. This clarity is important for both readers and future researchers who may undertake a secondary analysis of the data.
Approach 3 involves facilitating participants to nominate something as an ethical challenge [ 12 , 48 , 50 , 56 ]. This speaks to an important question about who, in a research context, is permitted to define or describe the object of interest, in this case ‘ethical challenge(s)’. Restricting the identification of ‘ethical challenge(s)’ to researchers alone may introduce bias by excluding input from those without bioethical ‘expertise’, but with important lived experience of the context under investigation. There is evidence that although clinicians can be sensitive to major ethical dilemmas, they can be less sensitive to small everyday ethical elements in clinical practice, and that ethical awareness varies between individuals [ 107 , 108 ]. Additionally, there is evidence in healthcare ethics research that patients and carers identify ethical challenges in situations that healthcare workers do not [ 109 ]. Therefore, relying entirely on a particular stakeholders’ perspectives (such as clinicians’) may risk missing important ethical challenges present in a scenario (assuming, of course, that we can settle what counts as an ‘ethical challenge(s)’).
In Approach 4, ethical challenges were linked to situations in which participants felt discomfort [ 14 ], emotional stress [ 81 ], moral distress or moral residue [ 66 ]. These concepts are themselves defined in quite varied ways (see, for example, definitions of ‘moral distress’ in a systematic review by Morley et al. [ 110 ]), potentially leading to additional conceptual confusion. Identifying triggers for moral distress is important, as high levels of moral distress are known to have negative impacts on work environments and lead to increased levels of compassion fatigue, increased staff turnover rates and poorer patient outcomes [ 110 , 111 , 112 ]. However, it is also possible that the requirement that, to be identified as an ethical challenge, the situation must invoke stress or distress might result in the under-identification of ethical challenges. We anticipate that many practitioners will daily manage multiple low-level ethical challenges, many of which will not generate moral distress or leave a moral residue. As such, the presence of moral distress may not be sufficient or even necessary in order to label a moral event an ‘ethical challenge’. However, the relationship between ‘ethical challenge(s)’ and moral distress is complex, and some might argue that the latter has an important relationship to the former. For example, moral distress, as conceived by Jameton and others [ 110 , 113 , 114 ], is linked to the after-effects of having to handle ethical challenge(s), so some researchers might view the generation of moral distress as relevant to identifying ethical challenges.
Although our review revealed these four approaches, the wider literature indicates there may be alternative approaches available. For example, other potential approaches would define ethical challenges as events that interact with moral principles, such as autonomy, beneficence, non-maleficence or justice, as proposed by Beauchamp and Childress [ 115 ], or as events in which those principles clash, for example as used by Klingler et al. in their research focusing on ethical issues in health surveillance [ 116 ]. However, these approaches were not seen amongst our included papers.
Returning to our included papers, the high rates of use of closely related terms within included manuscript texts may add to difficulties in understanding the exact object of interest if these terms are being used as synonyms for ‘ethical challenge(s)’. This may be particularly the case if terms used include those such as ‘moral dilemma’, which (as shown above) will have specific meanings for some readers. Interchangeable, undefined usage of these terms by study authors within study texts risks further exacerbating the problems caused by a lack of definitional clarity.
Strengths and limitations
This rapid review is the first systematic attempt to describe the definitions of ‘ethical challenge(s)’ available within the recent published literature.
There are, however, five limitations to note. First, the review only includes results from the past 5 years, which inevitably means that older publications, which may have contained further definitions of ‘ethical challenge(s)’, were excluded. The focus on the previous 5 years does, however, allow for an assessment of the term’s use(s) within a reasonable period of time and was felt to be appropriate given the aims and resources available to this project.
Second, our three assumptions listed in the methodology section may have excluded some records that contained a relevant definition. However, these assumptions, and the resulting focus on two search terms, allowed for a balance between retrieved record numbers and team resources.
Third, the four databases searched were chosen for their focus on the healthcare ethics literature; we may therefore may have missed relevant usage in other fields or disciplines. Similarly, we did not search the grey literature, which might have excluded relevant research.
Fourth, for resource reasons, the assessment as to whether a related term was being used interchangeably in the text was undertaken by a single researcher (GS). This subjective assessment risks miscalculating both the number of interchangeable terms identified and the frequency counts.
Finally, we did not review the theoretical literature for conceptual definitions of ‘ethical challenge(s)’, hence the definitions we identified might not match completely conceptual understandings of the term. However, our review shows how the term is currently being used in the research literature. Indeed, if there are strong conceptual definitions within the theoretical literature, then it is clear that they are currently not reaching the researchers whose work was identified by our review.
This review is the first, to our knowledge, to identify and describe definitions (and uses) of the widely-utilised concept of ‘ethical challenge(s)’ within healthcare research. Only 17% (12/72) of retrieved papers presented an explicit definition of ‘ethical challenge(s)’ before beginning to investigate this concept in context. The definitions found contained one or more of four identified approaches, with significant cross-reference to related terms and concepts which themselves have variation in their accepted meanings. We recommend that researchers define the phenomenon of interest—in this case, ‘ethical challenge(s)’—to help ensure clarity. This should either be a priori, or, if using an approach that includes participant participation in the generation of the definition, reporting their final working definition a posteriori. The choice of definition should be justified, including the decision as to whether to include participants in this process. Additionally, if a definition references other conceptual terms, then consideration should be given to defining these as well.
The results of this rapid review suggest that a common conceptual understanding of the term ‘ethical challenge(s)’ is lacking within empirical bioethical research and that there is a need for researchers in this area to consider what conceptual formulations might be most useful. Again, failure to use definitions of crucial research concepts within empirical bioethics research potentially generates confusion and avoidable bias within research outputs, risking misleading ethical analyses, evaluations, and resulting recommendations. We therefore hope this review will help stimulate debate amongst empirical bioethics researchers on possible definitional content for such a commonly used term and prompt further discussion and research. Additionally, given the central role of patient and public partnership and involvement in research, further thought should be given to who should be involved in nominating something as a challenge worthy of study.
Following on from this work, there would be value in conducting an empirical bioethical project combining a full systematic review of definitions of ‘ethical challenge(s)’ (and related terms) integrated with an exploration of the conceptual literature to generate recommendations for approaches towards the content of potential definitions, perhaps related to the identified approaches above. Such a project could also ask authors who currently use the term ‘ethical challenge(s)’ in their research how they conceptualise this. Furthermore, work to better understand the benefits of including study participants in the definition process is also important. Finally, whilst researchers should justify whatever approach they choose to take, there may be merit in examining whether anything is lost if studies lack a robust or agreed definition, or whether doing so affords a flexibility and openness that allows for a broader range of ethical challenges to be identified.
Availability of data and materials
All data is presented in this manuscript.
Critical Appraisal Skills Programme. CASP Qualitative Checklist. 2018. https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist.pdf . Accessed 16 Aug 2018.
Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups | The EQUATOR Network. https://www.equator-network.org/reporting-guidelines/coreq/ . Accessed 2 Apr 2020.
Standards for reporting qualitative research: a synthesis of recommendations | The EQUATOR Network. https://www.equator-network.org/reporting-guidelines/srqr/ . Accessed 2 Apr 2020.
Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 2018;13:2.
Article Google Scholar
The EQUATOR Network | Enhancing the QUAlity and Transparency of Health Research. https://www.equator-network.org/ . Accessed 2 Apr 2020.
Garritty C, Gartlehner G, Nussbaumer-Streit B, King VJ, Hamel C, Kamel C, et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol. 2021;130:13–22.
Singh I. Evidence, epistemology and empirical bioethics. In: Cribb A, Ives J, Dunn M, editors. Empirical bioethics: theoretical and practical perspectives. Cambridge: Cambridge University Press; 2016. p. 67–83. https://doi.org/10.1017/9781139939829.006 .
Chapter Google Scholar
Ives J, Dunn M, Molewijk B, Schildmann J, Bærøe K, Frith L, et al. Standards of practice in empirical bioethics research: towards a consensus. BMC Med Ethics. 2018;19:68.
Mertz M, Inthorn J, Renz G, Rothenberger LG, Salloch S, Schildmann J, et al. Research across the disciplines: a road map for quality criteria in empirical ethics research. BMC Med Ethics. 2014;15:17.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Cronin P, Ryan F, Coughlan M. Concept analysis in healthcare research. Int J Ther Rehabil. 2010;17:62–8.
Schofield G, Dittborn M, Huxtable R, Brangan E, Selman LE. Real-world ethics in palliative care: a systematic review of the ethical challenges reported by specialist palliative care practitioners in their clinical practice. Palliat Med. 2021;35:315–34.
Heggestad AKT, Magelssen M, Pedersen R, Gjerberg E. Ethical challenges in home-based care: a systematic literature review. Nurs Ethics. 2020;28:628–44.
Hem MH, Gjerberg E, Husum TL, Pedersen R. Ethical challenges when using coercion in mental healthcare: a systematic literature review. Nurs Ethics. 2018;25:92–110.
Lillemoen L, Pedersen R. Ethical challenges and how to develop ethics support in primary health care. Nurs Ethics. 2013;20:96–108.
Saarni SI, Halila R, Palmu P, Vänskä J. Ethically problematic treatment decisions in different medical specialties. J Med Ethics. 2008;34:262–7.
Self D, Skeel J, Jecker N. A comparison of the moral reasoning of physicians and clinical medical ethicists. Acad Med. 1993;68:852–5.
Ganann R, Ciliska D, Thomas H. Expediting systematic reviews: methods and implications of rapid reviews. Implement Sci IS. 2010;5:56.
Cameron A. Rapid versus full systematic reviews: an inventory of current mathods and practice in health technology assessment. Stepney: Royal Australasian College of Dental Surgeons; 2007.
Google Scholar
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. 2015;13:224.
Haby MM, Chapman E, Clark R, Barreto J, Reveiz L, Lavis JN. What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice: a rapid review. Health Res Policy Syst. 2016;14:83.
Gough D, Thomas J, Oliver S. Clarifying differences between review designs and methods. Syst Rev. 2012;1:28.
Watt A, Cameron A, Sturm L, Lathlean T, Babidge W, Blamey S, et al. Rapid reviews versus full systematic reviews: an inventory of current methods and practice in health technology assessment. Int J Technol Assess Health Care. 2008;24:133–9.
Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D. Evidence summaries: the evolution of a rapid review approach. Syst Rev. 2012;1:10.
Stevens A, Garritty C, Hersi M, Moher D. Developing PRISMA-RR, a reporting guideline for rapid reviews of primary studies (Protocol). 2018. https://www.equator-network.org/wp-content/uploads/2018/02/PRISMA-RRprotocol.pdf . Accessed 6 Oct 2019.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
PROSPERO: International prospective register of systematic reviews. https://www.crd.york.ac.uk/prospero/ . Accessed 10 June 2021.
Strech D, Synofzik M, Marckmann G. Systematic reviews of empirical bioethics. J Med Ethics. 2008;34:472–7.
The Endnote Team. Endnote X9.2. Philadelphia, PA: Clarivate Analysis; 2013.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88.
Khalili M. Iranian nurses’ ethical challenges in controlling children’s fever. Int J Pharm Res. 2018;10:337–40.
Rezaee N. Ethical challenges in cancer care: a qualitative analysis of nurses’ perceptions. Res Theory Nurs Pract. 2019;33:169–82.
Bartnik E. Ethical challenges in genetics. J Med Liban. 2019;67:138–40.
Alahmad G, Aljohani S, Najjar MF. Ethical challenges regarding the use of stem cells: interviews with researchers from Saudi Arabia. BMC Med Ethics. 2020;21:1–7.
Alahmad G, Al-Kamli H, Alzahrani H. Ethical challenges of pediatric cancer care: interviews with nurses in Saudi Arabia. Cancer Control. 2020;27:1073274820917210.
Alahmad G, Richi H, BaniMustafa A, Almutairi AF. Ethical challenges related to the novel coronavirus (COVID-19) outbreak: interviews with professionals from Saudi Arabia. Front Med. 2021. https://doi.org/10.3389/fmed.2021.620444 .
Alahmad G, AlSaqabi M, Alkamli H, Aleidan M. Ethical challenges in consent procedures involving pediatric cancer patients in Saudi Arabia: an exploratory survey. Dev World Bioeth. 2021. https://doi.org/10.1111/dewb.12308 .
Bijani M, Mohammadi F. Ethical challenges of caring for burn patients: a qualitative study. BMC Med Ethics. 2021;22:1–10.
Bladt T, Vorup-Jensen T, Sædder E, Ebbesen M. Empirical investigation of ethical challenges related to the use of biological therapies. J Law Med Ethics. 2020;48:567–78.
Boulanger RF, Komparic A, Dawson A, Upshur REG, Silva DS. Developing and implementing new TB technologies: key informants’ perspectives on the ethical challenges. J Bioeth Inq. 2020;17:65–73.
Bourbonnais A, Rousseau J, Lalonde M-H, Meunier J, Lapierre N, Gagnon M-P. Conditions and ethical challenges that could influence the implementation of technologies in nursing homes: a qualitative study. Int J Older People Nurs. 2019;14:e12266.
Brodtkorb K, Skisland AV-S, Slettebø Å, Skaar R. Preserving dignity in end-of-life nursing home care: some ethical challenges. Nord J Nurs Res. 2017;37:78–84.
Bruun H, Lystbaek SG, Stenager E, Huniche L, Pedersen R. Ethical challenges assessed in the clinical ethics Committee of Psychiatry in the region of Southern Denmark in 2010–2015: a qualitative content analyses. BMC Med Ethics. 2018;19:62.
Canario Guzmán JA, Espinal R, Báez J, Melgen RE, Rosario PAP, Mendoza ER. Ethical challenges for international collaborative research partnerships in the context of the Zika outbreak in the Dominican Republic: a qualitative case study. Health Res Policy Syst. 2017;15:82.
Carnevale F, Delogu B, Bagnasco A, Sasso L. Correctional nursing in Liguria, Italy: examining the ethical challenges. J Prev Med Hyg. 2018;59:E315.
Delpasand K, Nazari Tavakkoli S, Kiani M, Abbasi M, Afshar L. Ethical challenges in the relationship between the pharmacist and patient in Iran. Int J Hum Rights Healthc. 2020;13:317–23.
Donnelly S, Walker S. Enabling first and second year doctors to negotiate ethical challenges in end-of-life care: a qualitative study. BMJ Support Palliat Care. 2021. https://doi.org/10.1136/bmjspcare-2020-002672 .
Draper H, Jenkins S. Ethical challenges experienced by UK military medical personnel deployed to Sierra Leone (operation GRITROCK) during the 2014–2015 Ebola outbreak: a qualitative study. BMC Med Ethics. 2017;18:77.
Ebrahimi A, Ebrahimi S. Pediatric residents’ and attending physicians’ perspectives on the ethical challenges of end of life care in children. J Med Ethics Hist Med. 2018;11:16.
Forbes S, Phillips C. Ethical challenges encountered by clinical trials nurses: a grounded theory study. Oncol Nurs Forum. 2020;47:428–35.
Gágyor I, Heßling A, Heim S, Frewer A, Nauck F, Himmel W. Ethical challenges in primary care: a focus group study with general practitioners, nurses and informal caregivers. Fam Pract. 2019;36:225–30.
Haugom W, Ruud E, Hynnekleiv T. Ethical challenges of seclusion in psychiatric inpatient wards: a qualitative study of the experiences of Norwegian mental health professionals. BMC Health Serv Res. 2019;19:879.
Hawking M, Kim J, Jih M, Hu C, Yoon JD. “Can virtue be taught?”: a content analysis of medical students’ opinions of the professional and ethical challenges to their professional identity formation. BMC Med Educ. 2020;20:380.
Hyder A, Krubiner C. Ethical challenges in designing and implementing health systems research: experiences from the field. AJOB Empir Bioeth. 2016;7:209–17.
Jackson C, Gardy JL, Shadiloo HC, Silva DS. Trust and the ethical challenges in the use of whole genome sequencing for tuberculosis surveillance: a qualitative study of stakeholder perspectives. BMC Med Ethics. 2019;20:43.
Jakobsen R, Sørlie V. Ethical challenges: trust and leadership in dementia care. Nurs Ethics. 2016;23:636–45.
Jia Y, Chen O, Xiao Z, Xiao J, Bian J, Jia H. Nurses’ ethical challenges caring for people with COVID-19: a qualitative study. Nurs Ethics. 2021;28:33–45.
Kalkman S, van Thiel GJMW, Grobbee DE, Meinecke A-K, Zuidgeest MGP, van Delden JJM, et al. Stakeholders’ views on the ethical challenges of pragmatic trials investigating pharmaceutical drugs. Trials. 2016;17:419.
Kasper J, Mulye A, Doobay-Persaud A, Seymour B, Nelson BD. Perspectives and solutions from clinical trainees and mentors regarding ethical challenges during global health experiences. Ann Glob Health. 2020;86:34.
Kelley MC, Brazg T, Wilfond BS, Lengua LJ, Rivin BE, Martin-Herz SP, et al. Ethical challenges in research with orphans and vulnerable children: a qualitative study of researcher experiences. Int Health. 2016;8:187–96.
Kemparaj VM, Panchmal GS, Kadalur UG. The top 10 ethical challenges in dental practice in indian scenario: dentist perspective. Contemp Clin Dent. 2018;9:97.
Klitzman R. Unconventional combinations of prospective parents: ethical challenges faced by IVF providers. BMC Med Ethics. 2017;18:18.
Komparic A, Dawson A, Boulanger RF, Upshur REG, Silva DS. A failure in solidarity: ethical challenges in the development and implementation of new tuberculosis technologies. Bioethics. 2019;33:557–67.
Laholt H, McLeod K, Guillemin M, Beddari E, Lorem G. Ethical challenges experienced by public health nurses related to adolescents’ use of visual technologies. Nurs Ethics. 2019;26:1822–33.
Laliberté M, Williams-Jones B, Feldman DE, Hunt M. Ethical challenges for patient access to physical therapy: views of staff members from three publicly-funded outpatient physical therapy departments. Narrat Inq Bioeth. 2017;7:157–69.
Larkin ME, Beardslee B, Cagliero E, Griffith CA, Milaszewski K, Mugford MT, et al. Ethical challenges experienced by clinical research nurses: a qualitative study. Nurs Ethics. 2019;26:172–84.
Mbalinda SN, Bakeera-Kitaka S, Amooti DL, Magongo EN, Musoke P, Kaye DK. Ethical challenges of the healthcare transition to adult antiretroviral therapy (ART) clinics for adolescents and young people with HIV in Uganda. BMC Med Ethics. 2021;22:1–14.
Mehdipour Rabori R, Dehghan M, Nematollahi M. Nursing students’ ethical challenges in the clinical settings: a mixed-methods study. Nurs Ethics. 2019;26:1983–91.
Mlughu TS, Anaeli A, Joseph R, Sirili N. Voluntary HIV counseling and testing among commercial motorcyclist youths: an exploration of ethical challenges and coping mechanisms in Dar es Salaam. HIVAIDS - Res Palliat Care. 2020;12:675–85.
Moeini S, Shahriari M, Shamali M. Ethical challenges of obtaining informed consent from surgical patients. Nurs Ethics. 2020;27:527–36.
Naseri-Salahshour V, Sajadi M. Ethical challenges of novice nurses in clinical practice: Iranian perspective. Int Nurs Rev. 2020;67:76–83.
Naseri-Salahshour V, Sajadi M. From suffering to indifference: reaction of novice nurses to ethical challenges in first year of clinical practice. Iran J Nurs Midwifery Res. 2019;24:251.
Nicholls SG, Carroll K, Zwarenstein M, Brehaut JC, Weijer C, Hey SP, et al. The ethical challenges raised in the design and conduct of pragmatic trials: an interview study with key stakeholders. Trials. 2019;20:765.
Pancras G, Shayo J, Anaeli A. Non-medical facilitators and barriers towards accessing haemodialysis services: an exploration of ethical challenges. BMC Nephrol. 2018;19:342.
Sabone M, Mazonde P, Cainelli F, Maitshoko M, Joseph R, Shayo J, et al. Everyday ethical challenges of nurse-physician collaboration. Nurs Ethics. 2020;27:206–20.
Seekles W, Widdershoven G, Robben P, van Dalfsen G, Molewijk B. Inspectors’ ethical challenges in health care regulation: a pilot study. Med Health Care Philos. 2017;20:311–20.
Segal AG, Frasso R, Sisti DA. County jail or psychiatric hospital? Ethical challenges in correctional mental health care. Qual Health Res. 2018;28:963–76.
Shayestefar S, Hamooleh MM, Kouhnavard M, Kadivar M. Ethical challenges in pediatrics from the viewpoints of Iranian pediatric residents. J Compr Pediatr. 2018. https://doi.org/10.5812/compreped.62747 .
Sinow C, Burgart A, Char DS. How anesthesiologists experience and negotiate ethical challenges from drug shortages. AJOB Empir Bioeth. 2020;12:84–91.
Slettebø Å, Skaar R, Brodtkorb K, Skisland A. Conflicting rationales: leader’s experienced ethical challenges in community health care for older people. Scand J Caring Sci. 2018;32:645–53.
Storaker A, Nåden D, Sæteren B. From painful busyness to emotional immunization: nurses’ experiences of ethical challenges. Nurs Ethics. 2017;24:556–68.
Taebi M, Bahrami R, Bagheri-Lankarani N, Shahriari M. Ethical challenges of embryo donation in embryo donors and recipients. Iran J Nurs Midwifery Res. 2018;23:36.
Tønnessen S, Solvoll B-A, Brinchmann BS. Ethical challenges related to next of kin - nursing staffs’ perspective. Nurs Ethics. 2016;23:804–14.
Ullrich A, Theochari M, Bergelt C, Marx G, Woellert K, Bokemeyer C, et al. Ethical challenges in family caregivers of patients with advanced cancer—a qualitative study. BMC Palliat Care. 2020;19:1–13.
Verma A, Smith AK, Harrison KL, Chodos AH. Ethical challenges in caring for unrepresented adults: a qualitative study of key stakeholders. J Am Geriatr Soc. 2019;67:1724–9.
Morley G, Ives J, Bradbury-Jones C. Moral distress and austerity: an avoidable ethical challenge in healthcare. Health Care Anal. 2019;27:185–201.
Ayala-Yáñez R, Ruíz-López R, McCullough LB, Chervenak FA. Violence against trainees: urgent ethical challenges for medical educators and academic leaders in perinatal medicine. J Perinat Med. 2020;48:728–32.
Binns C, Lee M, Kagawa M. Ethical challenges in infant feeding research. Nutrients. 2017;9:59.
Čartolovni A, Habek D. Guidelines for the management of the social and ethical challenges in brain death during pregnancy. Int J Gynecol Obstet. 2019;146:149–56.
Hofmann B. Informing about mammographic screening: ethical challenges and suggested solutions. Bioethics. 2020;34:483–92.
Hunt M, Pal NE, Schwartz L, O’Mathúna D. Ethical challenges in the provision of mental health services for children and families during disasters. Curr Psychiatry Rep. 2018;20:60.
Johnson S, Parker M. Ethical challenges in pathogen sequencing: a systematic scoping review. Wellcome Open Res. 2020;5:119.
MacDonald S, Shemie S. Ethical challenges and the donation physician specialist: a scoping review. Transplantation. 2017. https://doi.org/10.1097/TP.0000000000001697 .
Saigle V, Racine E. Ethical challenges faced by healthcare professionals who care for suicidal patients: a scoping review. Monash Bioeth Rev. 2018;35:50–79.
Saigle V, Séguin M, Racine E. Identifying gaps in suicide research: a scoping review of ethical challenges and proposed recommendations. IRB Ethics Hum Res. 2017;39:1–9.
Wilson E, Kenny A, Dickson-Swift V. Ethical challenges in community-based participatory research: a scoping review. Qual Health Res. 2018;28:189–99.
Martins Pereira S, Hernández-Marrero P. Ethical challenges of outcome measurement in palliative care clinical practice: a systematic review of systematic reviews. Ann Palliat Med. 2018;7:S207–18.
Saghafi A, Bahramnezhad F, Poormollamirza A, Dadgari A, Navab E. Examining the ethical challenges in managing elder abuse: a systematic review. J Med Ethics Hist Med. 2019. https://doi.org/10.18502/jmehm.v12i7.1115 .
West E, Stuckelberger A, Pautex S, Staaks J, Gysels M. Operationalising ethical challenges in dementia research—a systematic review of current evidence. Age Ageing. 2017;46:678–87.
Ewuoso C, Hall S, Dierickx K. How do healthcare professionals respond to ethical challenges regarding information management? A review of empirical studies. Glob Bioeth. 2021;32:67–84.
Schofield G, Brangan E, Dittborn M, Huxtable R, Selman L. Real-world ethics in palliative care: protocol for a systematic review of the ethical challenges reported by specialist palliative care practitioners in their clinical practice. BMJ Open. 2019;9:e028480.
Sun W, Wilson MG, Schreiber D, Wang RH. Ethical challenges related to assistive product access for older adults and adults living with a disability: a scoping review protocol. Syst Rev. 2017;6:24.
Schwartz L, Sinding C, Hunt M, Elit L, Redwood-Campbell L, Adelson N, et al. Ethics in humanitarian aid work: learning from the narratives of humanitarian health workers. AJOB Prim Res. 2010;1:45–54.
McConnell T. Moral Dilemmas. In: Zalta EN, editor. The Stanford Encyclopedia of Philosophy. Fall 2018. Metaphysics Research Lab, Stanford University; 2018. https://plato.stanford.edu/archives/fall2018/entries/moral-dilemmas/ . Accessed 30 Oct 2019.
Tessman L. Moral failure: on the impossible demands of morality. New York, NY: Oxford University Press; 2014. http://search.ebscohost.com/login.aspx?direct=true&scope=site&db=nlebk&db=nlabk&AN=859724 . Accessed 5 Nov 2019.
Ejder Apay S, Gürol A, Gür EY, Church S. Midwifery students’ reactions to ethical dilemmas encountered in outpatient clinics. Nurs Ethics. 2020;27:1542–55.
Milliken A, Ludlow L, DeSanto-Madeya S, Grace P. The development and psychometric validation of the Ethical Awareness Scale. J Adv Nurs. 2018;74:2005–16.
Truog RD, Brown SD, Browning D, Hundert EM, Rider EA, Bell SK, et al. Microethics: the ethics of everyday clinical practice. Hastings Cent Rep. 2015;45:11–7.
Woods S, Beaver K, Luker K. User’s views of palliative care services: ethical implications. Nurs Ethics Int J Health Care Prof. 2000;7:314–26.
Morley G, Ives J, Bradbury-Jones C, Irvine F. What is ‘moral distress’? A narrative synthesis of the literature. Nurs Ethics. 2017;26:646–62.
Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. 2009;20:330–42.
Mason VM, Leslie G, Clark K, Lyons P, Walke E, Butler C, et al. Compassion fatigue, moral distress, and work engagement in surgical intensive care unit trauma nurses: a pilot study. Dimens Crit Care Nurs DCCN. 2014;33:215–25.
Jameton A. Nursing practice: the ethical issues. Englewood Cliffs: Prentice-Hall; 1984.
Tigard DW. The positive value of moral distress. Bioethics. 2019;33:601–8.
Beauchamp TL, Childress JF. Principles of biomedical ethics. New York: Oxford University Press; 1979.
Klingler C, Silva DS, Schuermann C, Reis AA, Saxena A, Strech D. Ethical issues in public health surveillance: a systematic qualitative review. BMC Public Health. 2017;17:295.
Solvoll B-A, Hall EO, Brinchmann BS. Ethical challenges in everyday work with adults with learning disabilities. Nurs Ethics. 2015;22:417–27.
Download references
Acknowledgements
Not applicable.
GS is supported by a Wellcome Trust Research Award for Health Professionals (208129/Z/17/Z). LES is funded by a Career Development Fellowship from the National Institute for Health Research. RH is part-funded by the Wellcome Trust (209841/Z/17/Z) and the NIHR Biomedical Research Centre at University Hospitals Bristol NHS Foundation Trust and the University of Bristol. He serves on various local, regional, and national ethics committees and related groups. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health, or any of the other organisations with and for whom the authors work.
Author information
Authors and affiliations.
Centre for Ethics in Medicine, Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, BS8 2PS, UK
Guy Schofield & Richard Huxtable
Paediatric Bioethics Centre, Great Ormond Street Hospital, London, WC1N 3JH, UK
Mariana Dittborn
Palliative and End of Life Care Research Group, Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, BS8 2PS, UK
Guy Schofield & Lucy Ellen Selman
You can also search for this author in PubMed Google Scholar
Contributions
GS, MD and RH conceived of the idea for the review; LES, GS, MD and RH designed the review protocol; GS and MD conducted the literature searching, screening, data extraction and led on data interpretation but all authors were involved; GS led on drafting the manuscript; all authors critically revised the manuscript for content and approved the version to be published. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Guy Schofield .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that there are no conflicts of interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schofield, G., Dittborn, M., Selman, L.E. et al. Defining ethical challenge(s) in healthcare research: a rapid review. BMC Med Ethics 22 , 135 (2021). https://doi.org/10.1186/s12910-021-00700-9
Download citation
Received : 10 June 2021
Accepted : 03 September 2021
Published : 29 September 2021
DOI : https://doi.org/10.1186/s12910-021-00700-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ethical challenges
- Rapid review
- Empirical bioethics
- Moral dilemmas
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]
- Research article
- Open access
- Published: 13 July 2022
Goal setting with young people for anxiety and depression: What works for whom in therapeutic relationships? A literature review and insight analysis
- Jenna Jacob ORCID: orcid.org/0000-0003-1006-1547 1 ,
- Milos Stankovic 2 ,
- Inga Spuerck 2 &
- Farhad Shokraneh 3
BMC Psychology volume 10 , Article number: 171 ( 2022 ) Cite this article
15k Accesses
7 Citations
21 Altmetric
Metrics details
Goal setting and goal-focused work is widely used in young people’s mental health settings. However, little is known about how, why or for whom this is helpful. This study aims to explore the mechanisms of collaborative goal setting as part of therapeutic relationships: is it helpful for young people experiencing anxiety and/or depression, how and why/not, for whom, and under what circumstances?
Online database searches generated 10,907 records. Seven unique studies are included, combined with insight analysis from directed discussions with international advisors with lived experience of anxiety and/or depression and therapy (N = 8; mean age = 20.8), and mental health academics/clinicians (N = 6).
Findings are presented as a narrative synthesis and suggest that goal setting is helpful to young people experiencing anxiety and/or depression because it helps build good therapeutic relationships through open communication and building trust. Goal setting helps make things more manageable, enabling young people to feel supported and have ownership of their care. Individual preferences, or high levels of distress, trauma, low confidence, hopelessness, negative past experiences of goal setting, perfectionism, and rumination are considered limiting factors to goal setting. Additionally, contextual factors including country and long-term therapy are explored.
Whilst the resultant sample is small, emphasis on the voices of young people in the research is both prominent and of paramount importance. Several key literature gaps are identified, including evidenced links to the reduction in symptoms. Priority must be given to researching unhelpful mechanisms of goal setting for young people experiencing anxiety and/or depression, to avoid any potential iatrogenic effects.
Peer Review reports
Collaborative goal setting within therapeutic mental health settings refers to agreements made between young people and practitioners about specific therapy areas of focus: topics of personalised and meaningful outcome. Goals are concrete representations of intended endpoints, which fill the perceived gap between the current and desired end state [ 1 ]. Goals are usually formulated at the start of therapeutic interventions through a series of discussions. These differ from academic, physical rehabilitation, or general life goals, although there could be overlap. Progress towards these agreed goals may then be tracked over time, often through ratings on numerical scales, and there are tools available to support this. For example, the Goal Based Outcome tool (GBO; [ 2 ]) which comprises setting up to three goals and scoring progress between 0 and 10, is widely used to track progress against goal setting in youth mental health settings. Whilst goal tracking may lead to a shift in practitioners’ work to be goal focused [ 3 ], goals may also sit alongside usual clinical work, to track progress [ 4 ]. Goals set in therapy tend to be focused and specific, e.g., to deal with something in the immediacy, like a phobia [ 5 ], but it is important that these goals attain to more global goals [ 6 ], or are viewed as a “means to an end”.
Goals may take time to set, and can change and become more specific during the therapeutic process, for example, at the beginning of contact with a practitioner, a young person might have a general goal like “to feel less depressed”, but over time the young person, along with the practitioner, may learn more about the mechanisms behind the depression and may define more precise goals like “being able to stop negative thinking” or “being able to cope with flashbacks”. The types of phrases used by practitioners to help young people define goals may include: “what do you want to be different?”, “what will you get off your back?”, “where do you want to get to?”, and “how do you want things to change?” [ 4 , 6 ].
Goal setting and tracking in therapeutic settings is grounded in motivation theory [ 7 , 8 , 9 ] such that working towards goals is a continuous feedback loop which builds on self-efficacy, self-determination and motivation to continue to strive towards goals, acting as a self-regulation strategy [ 10 , 11 ]. Goal setting may be more feasible or acceptable to individuals with particular personality traits e.g., individuals who attribute successes and failures to external factors are less likely to find meaning in striving towards goals than those who attribute successes and failures to their own actions [ 12 ].
Further, young people have described recovery from depression as nested within relationships (e.g., [ 13 ]), portraying recovery as an intentional process, contingent on shared goals and joint action in relationships [ 14 ]. Good therapeutic relationships are considered a key element of effective therapy [ 15 , 16 , 17 , 18 ]. Also known as working relationships, or working/therapeutic alliance, this refers to the connection, bond or partnership between the young person and practitioner. Three key elements of therapeutic alliance have been identified in the literature: bond, tasks, and goals [ 19 ]. In a recent review of the effects of cognitive behavioural therapy (CBT) for young people experiencing anxiety and/or depression, three studies reported small-to-medium effect sizes for the correlational relationship between therapeutic alliance and symptom reduction [ 20 ]. This provides limited evidence linking goal collaboration to reduced anxiety/depression symptoms for young people, despite fair evidence supporting links between goal collaboration and positive adult anxiety and depression outcomes [ 21 ]. It is argued that goal agreement is a fundamental element missing from much work with young people, and it has been referred to as a “social contract” [ 22 ]. This emphasis on relationships is particularly important when working with young people with acute, or multifarious difficulties, where relationships are complex, difficult to develop and maintain (e.g., [ 23 ]).
Existing evidence suggests that there are certain elements of mental health support for young people that are effective, but there is a lack of identification and knowledge about mechanisms to refine and improve this support [ 24 ]. Specifically, there is a paucity of research exploring the mechanisms underpinning why goal setting may be helpful for some young people, and not others. There are likely to be confounding variables which interplay the effectiveness of goals, depression and/or anxiety, cognition, and motivation, yet there is little research that has explored this in clinical settings with young people.
The aim of this study is to summarise existing literature, supplemented by discussions with international advisors to contextualise and aid interpretation of the findings. The research question is:
“Is collaborative goal setting helpful or unhelpful to young people experiencing anxiety and/or depression, as an element of therapeutic relationships? a. Why/why not and how? b. For whom? c. Under what circumstances?”
A mixed methodological approach combined reviews of peer-reviewed, grey literature and additional sources (e.g., websites), with consultation with experts by experience. The risk of expert view biasing the findings was mitigated via the validating steps outlined below. The study was designed by the lead researcher, and other researchers in the team, in collaboration with the peer researchers.
Whilst it is acknowledged that there are important outcome areas such as quality of life and existential factors, aside from symptom reduction, the focus of this study was to specifically explore the research questions in relation to potential anxiety and depression symptom reduction. Anxiety and depression were focused on as the most common mental health difficulties worldwide. This focus on medicalised symptomology differs from quality of life, which is a multi-dimensional construct comprised of several domains, such as psychological, physical, and social wellbeing. Anxiety, depression, therapeutic relationships, and goal progress are routinely measured using self- and proxy-reported outcome measures, with numerical rating scales. It was anticipated that the research question would not be adequately explored through findings from outcome measures alone. Based on some initial scoping work, we determined that there would be more evidence on the effectiveness of goal setting and tracking via qualitative enquiry, including narratives. The exploration of the nuances identified in the research question was key to the study, and so it was important to give precedence to young people’s voices through existing research and youth advisors, combined with findings from any relevant supporting measures. Such explorations would not be possible through quantitative enquiry of outcome measure data.
Goal setting alongside usual clinical work and goals work (goal focused interventions) were differentiated from implicit goal-oriented practice, non-directive approaches and paternalistic approaches to support in this study. This meant that to be included in the literature synthesis, goals needed to be explicitly identified as an approach to progress tracking, and/or informing the work. This study also focused on individual settings, and whilst these relationships may include parents/carers in a triad, the primary focus was on the relationship built between the practitioner and the young person. This was due to the complexities and potential dilution of agreeing goals and developing therapeutic relationships in group work and with parents/carers in addition. Ethical approval was not required because this study did not involve collection nor analysis of primary data, and youth advisors were consulted on in the capacity of being part of the advisory group, rather than within the capacity of research participants [ 25 ].
Literature review
First, search terms and inclusion and exclusion criteria were agreed in collaboration with the academic/clinical and youth advisors (See Additional file 1 : Appendix 1 Inclusion and exclusion criteria and Search Strategies). The project was registered with PROSPERO (number: CRD42021259611).
Second, searches of ten online databases were conducted (PsycINFO (OVID), MEDLINE (OVID), EMBASE (OVID), Web of Science core collection, current contents connect, SciELOCitation Index, Cochrane Library of Systematic Reviews, CINAHL (EBSCO), ERIC (EBSCO), and child and adolescent studies (EBSCO)). The search strategy developed for each database comprised three concepts: anxiety and/or depression (condition), goals (intervention) and therapeutic alliance or general views on goal setting, e.g., perspective, view, narrative (intervention/outcome). Searches were restricted to the past 20 years (2000-present). Citation tracking of included papers was performed. Retrieved hits were exported to EndNote 20 [ 26 ], Rayyan [ 27 ] and Excel for title/abstract screening.
Third, two researchers (FS, JJ) independently screened titles and abstracts. Where one researcher (JJ) was an author in retrieved studies, screening was conducted by the other researcher (FS), to ensure unbiased screening. Fourth, two researchers (JJ, IS) explored resultant literature main texts, extracting and synthesising relevant information. Key literature identified by researchers and advisors was added. The quality of the studies was assessed using criteria for qualitative studies ([ 28 ]; See Additional file 1 : Appendix 2 Core Criteria for Quality Assessment of Qualitative Studies).
Grey literature search
Google and Google Scholar title search, Google Books, PsycEXTRA, PsyArXiv, and ProQuest Dissertations and Theses were used. Google's Site Search was used to search American Psychological Association, British Psychological Society, Australian Psychological Society, European Federation of Psychologists' Associations, International Association of Applied Psychology, Association for Psychological Science, International Union of Psychological Science, Canadian Psychological Association, and UN-affiliated websites (.int domains). To identify more relevant literature, ResearchRabbit.ai was used to track the citations to the included studies. As a result of Google title search, websites were identified and browsed. The searches were restricted to those: (1) written in English, (2) published from January 2000 to August 2021, (3) focused on goal setting with young people experiencing mental health difficulties. Two researchers (FS, JJ) independently screened titles and abstracts of the resultant sources for relevance.
Insight analysis
An advisory group was formed at the study’s outset, comprising: (1) young people with lived experience of anxiety and/or depression and therapy (N = 8; age range 15–26 years; mean age = 20.8; female (includes transgender) N = 5; and male (includes transgender) N = 3; located in Brazil, Pakistan, Spain, Turkey, and UK); and (2) academics and clinicians (N = 6; female N = 1, male N = 5; located in Norway and UK). Criteria for youth advisors to take part where that they were around the age of interest (14–24 years) and had lived experience of anxiety and/or depression and had previously -or currently-experienced receiving a mental health intervention. Youth advisors’ experience of anxiety and/or depression was balanced across advisors. Youth advisors were recruited via adverts circulated by a European network of peer advisors with international reach, and signed an agreement at the outset of the project, by way of consent to participate, which included specific duties and responsibilities of what would be expected of them, as well as hours and reimbursement details. For those under 18 years old, parent/carer consent and agreements were gained. One-to-one meetings between each youth advisor and the participation lead for the study were conducted before and after the study took place. A written agreement was made between the lead research organisation, and the participation organisation which facilitates the network of peer advisors.
Academic/clinical advisors were experienced and specialised in goals work and were recruited via existing networks. Criteria for academic/clinical advisors were that they had research and/or clinical experience in the field of mental health goal setting with young people (academic N = 6; clinical N = 4; categories not mutually exclusive). Written agreements were made between the lead research organisation, and each academic/clinical advisor.
Directed discussions were held at six advisory group meetings (two academic/clinical and four youth) facilitated by two researchers (JJ, MS) and conducted in English. All advisors spoke English, but time was given in the meetings to check understanding, as English was not a native language for many. The academic/clinical and youth advisors met separately, enabling the youth advisors to share openly with their peers. These discussions focused on the research question and drawing inferences about resultant findings, as well as appraising the evidence to identify key literature gaps. The summary of findings from the literature review was presented via PowerPoint to the advisors. The questions asked were broadly: is setting goals an important part of the relationship with the therapist and why/not; do these findings align with your experiences; is there anything you can think of that has not been considered; are there any elements of these findings that do not make sense in your experience; how do you interpret and understand these findings within the context of your own experience? Youth advisors were asked additional questions about the nature of language, for example, what do you think about the term “goal”? Is it the word you use, is it understandable, how does it translate to your national languages?. Field notes were taken, alongside notes in advisors’ own words on the JamBoard interactive workspace, allowing for anonymous contributions. Analysis comprised four stages. First, one researcher (MS) organised field notes and comments into a narrative summary. Second, one researcher (JJ) used the nuanced elements of the research question to organise the summary. Third, feedback was sought from advisors to evaluate and assess whether it was a true reflection of the discussions. Fourth, one researcher (JJ) refined and renamed the themes.
Online searches generated 10,907 records. Ten potentially eligible studies were identified. Upon screening full texts, seven unique studies met the selection criteria (See Fig. 1 and Table 1 ).
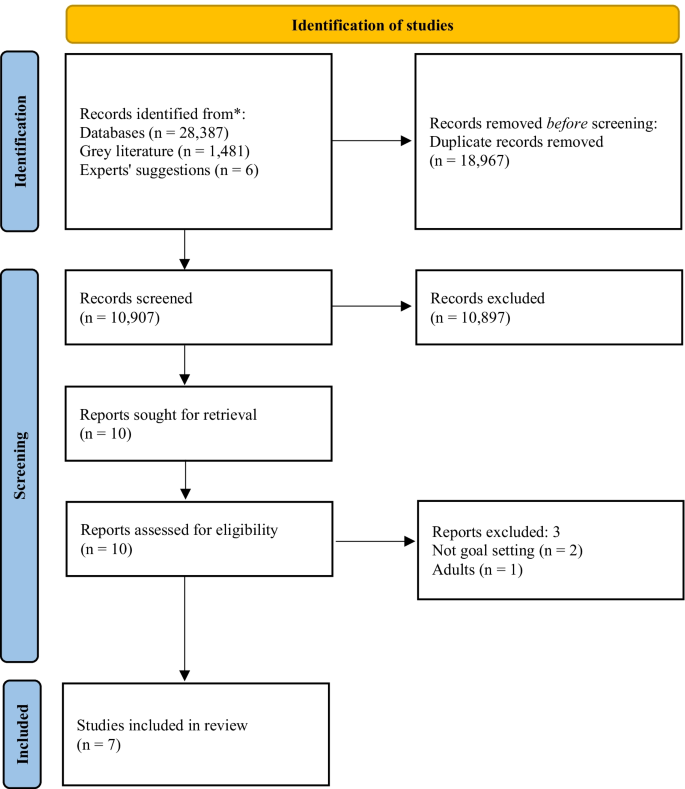
PRISMA flow chart of the study selection process. From: Page, M.J., McKenzie, J.E., Bossuyt, P.M., Boutron, I., Hoffmann, T.C., Mulrow, C.D. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(n71)
Included studies comprised three narrative case studies [ 29 , 30 , 31 ] a randomised control trial [ 32 ]; a narrative review [ 33 ] a practitioners’ guidance document [ 34 ]; and a naturalistic study [ 35 ]. Critical appraisal of the evidence (Table 1 ) demonstrates that caution must be exercised when considering the findings. The main strength of the included studies is the voice of young people through verbatim quotes, and for some, strong consideration of the researchers’ impact. However, less strength is attributed to the dependability or generalisability of the findings, mainly due to the high proportion of small-and-homogenous samples. The advisors’ discussion summaries were organised into themes within the nuances of the research question: Why/why not and how? For whom? Under what circumstances?”, and presented as a narrative synthesis.
Why/why not and how (mechanisms)
A conduit for open communication.
Six studies described collaborative goal setting as a conduit for communication [ 29 , 30 , 31 , 33 , 34 , 35 ]. Specifically, agreement on goals leads to open communication, a shared understanding of difficulties and ways forward [ 29 , 31 , 35 ]. Formulating goals was described as key to helping young people to feeling understood, valued and that practitioners are listening to them [ 33 , 34 , 35 ]. Collaborative goal setting enables young people and practitioners to make genuine disclosures, not necessarily otherwise possible [ 30 ] and facilitates mutual support [ 31 ].
Both academic/clinical and youth advisors said that open communication and trust were key, broadly agreeing that goal setting could be helpful to support building trusting relationships. It was agreed that collaboratively agreeing goals may take time and should not happen immediately. Rather, practitioners should work flexibly, aiming to understand what is comfortable for young people experiencing anxiety and/or depression. Some youth advisors said that relationships need to be built first, with trust established prior to goal setting, particularly when goal setting feels complicated. It was agreed by youth and academic/clinical advisors that goal setting should be led by young people and guided by practitioners, sharing responsibility. Youth advisors considered open communication the most crucial factor in therapy, with a sense that much therapeutic work cannot take place without it.
Feel supported and involved
Young people value receiving support to split actions into smaller manageable steps, with encouragement from practitioners stimulating validation that their goals are achievable ([ 35 ], and youth advisors). Being given choice about goal content and how this translates into the options for care was identified as an important part of the process in the literature [ 35 ]. Evidence suggests that this leads to a sense of autonomy and control over what happens to young people and enables them to feel involved in the process and increases engagement [ 30 , 33 , 35 ]. This was not directly addressed by the academic/clinical advisors in their discussions.
Nature of difficulties
All seven studies, and youth and academic/clinical advisors, suggested that goal setting was a helpful element of therapeutic relationships for young people experiencing anxiety and/or depression, and more broadly with other undefined presenting difficulties. Both academic/clinical and youth advisors agreed that there was no need to separate specific attributes of anxiety or depression, due in part, to high proportions of comorbidity.
Age, and previous experiences
Three studies described difficulties for young people engaging in goal setting [ 32 , 33 , 34 ]. These were: age-appropriate quests for independence interfering with establishing collaborative relationships with adults [ 32 ]; significant and repeated traumas impacting development, relationships and challenges ordering thoughts, particularly within the context of long-term therapy [ 34 ]; low confidence or feelings of hopelessness; and poor previous experiences of goal setting [ 33 ]. Youth advisors agreed that previous life experiences were important, e.g., views of goal setting in therapeutic settings were impacted by how successful they had been in achieving past goals, regardless of goal type. Academic/clinical advisors agreed that personal factors such as previous experiences and factors surrounding—or leading to—difficulties, may lead to challenges setting goals in the first instance.
Levels of distress, personality traits and preferences
Youth and academic/clinical advisors suggested that specific unhelpful elements may depend on the young person, and sometimes levels of distress, rather than the nature of difficulties. Some youth advisors expressed preferences for practitioner-directed work, particularly in times of high distress, e.g.,: “If I’m going through something very bad, I can be very frustrated/sad so I can’t think clear” (youth advisor) . It was also agreed that goals may exacerbate anxiety, particularly at times of overwhelm, whilst for others this could be a helpful anxiety reduction approach, e.g., in exposure therapy. Youth advisors said that ensuring goals are achievable is key to building good therapeutic relationships, and the impact on anxiety/depression; the individual’s capacity to set goals should be considered, e.g., someone struggling with day-to-day tasks may find even small goals too challenging. Youth advisors considered perfectionism to be important, where some people may feel pressure to achieve goals. A sense of hopelessness, or procrastination, and rumination also, where delaying tasks may result in delaying work on goals. For some youth advisors, goal setting felt especially important, whilst for others it was not, rather a supportive relationship was identified as most important, and they could not see how that would be developed through goal setting. Academic/clinical advisors said that young people’s preferences to work on goals, or not, was in itself of key importance to the therapeutic relationship. There was no evidence from the included literature to support/oppose these points.
Language and power dynamics
Linked to preferences, youth advisors said that young people tend not to like the term “goal” because they attribute it to work and formal settings, whereas “therapeutic goals” are personal with deeper meaning. Academic/clinical advisors discussed using alternative language for goal setting and goal directed work, and the importance of being led by the young person. Posing questions such as “What do you want to change?” is suggested as an alternative in the literature ([ 33 ]; p.47). Youth advisors said that whilst some young people may feel able to say they do not want to set goals, others may not, due to the young person-practitioner power imbalance, which has implications for relationships, and therapeutic work. There was no further evidence from the included literature to support/oppose these points.
Under what circumstances (contextual factors)
Broadly helpful.
All seven studies suggested that goal setting was a helpful element of therapeutic relationships for young people within the research contexts. This included year-long narrative therapy with interpersonal therapy and CBT techniques in alliance with the family [ 29 ]; multimodal family therapy [ 31 ]; Gestalt therapy [ 30 ]; either CBT, short-term psychoanalytic psychotherapy or brief psychosocial intervention [ 32 ]; UK child and adolescent mental health services [ 33 , 34 ] and UK inpatient settings [ 35 ]. All studies were based in Western high-income countries. Academic/clinical and youth advisors agreed with this assessment.
Review points and referral routes
Reviewing progress towards goals too frequently could give the impression that practitioners are more interested in gauging their own success, rather than in the young person as a whole person, and rating could end up being done by rote, making goals increasingly meaningless [ 34 ] . Academic/clinical and youth advisors agreed with this, discussing the need to work with goals in a flexible manner. Additionally, young people may not recognise the symptoms identified, particularly when referred for treatment by another party (e.g., parents/carers), which is crucial to enable collaborative goal setting [ 32 ]. Challenges associated with thinking of goals in this way was addressed by the academic/clinical and youth advisors in wider discussions elsewhere (see therapy contexts).
Culture and therapy contexts
Youth and academic/clinical advisors located in Western high-income countries agreed that it may depend on types of interventions offered and practitioner’s preferred working style, but young people largely have agency to set goals. However, it was recognised by the youth and academic/clinical advisors that some young people in some countries do not have agency to set goals. There, decisions are made by families, in collaboration with practitioners, and so less consideration is given to young people’s perspectives. It was suggested that, in some countries, there is no concept of setting goals (e.g., a youth advisor discussed their experience in Pakistan), and ongoing stigma associated with mental health difficulties, which may lead to distrust, scepticism in, and a disconnect with practitioners. Youth advisors said that this may also be true in other countries not represented. A youth advisor suggested that young people in Brazil were relaxed towards goal setting and would not mind if goals were not achieved; directed therapy was considered more helpful.
Youth and academic/clinical advisors discussed goals in long-term therapy as potentially feeling restrictive, with challenges associated with thinking of what goals might be. Both long-and short-term goal setting within this context may feel meaningless, which if then pressed by the practitioner, has a negative impact on relationships. Academic/clinical advisors said that the feasibility of goal setting in the first instance is likely to be attributable to the factors young people who might be offered long-term therapy might have, rather than the work itself leading to these challenges. Youth and academic/clinical advisors also said that where there are multiple needs and risks, goals need to be simpler to feel manageable. Youth advisors said that sometimes there were concerns about the achievement of goals equating to treatment ending, which felt unsettling. There was no evidence from the included literature to support/oppose these points.
This study aimed to provide a synthesis of existing literature, identifying knowledge gaps. Whilst much may be drawn from related research, caution must be exercised when translating findings into other contexts [ 11 ], and whilst promising, generalising adult findings to youth must be exercised with an abundance of caution. Evidence suggests that adults and children think differently; as children grow, their cognitive processes develop, and their contexts and perspectives change, impacting on understandings of the self and the world around them. Further, models of recovery from depression are notably different between adults and young people [ 14 ]. As such, we have focused on evidence from the youth field in our discussion, and further highlight the paucity of research with young people in this area.
The included evidence originates from Western high-income and largely specialist settings; further research in majority world countries is urgently required. Many studies identified in initial searches only partially met inclusion criteria. This evidence paucity may suggest goal setting is not embedded in service standards or practice in most countries, or other limiting factors such as the general underfunding of youth mental health research. Some examples were derived from the insight analysis, highlighting the advisors’ value, who helped contextualise and interpret evidence, grounded in lived experience. However, whilst the research question pertained to the effectiveness of goal setting as part of therapeutic relationships, the findings were related to the feasibility, or acceptability of goal setting itself. Links between effective goal setting, good therapeutic relationships and positive outcomes are inferred based on evidence that partially supports the research question, and the discussions with the advisory group, but no evidence relating to anxiety or depression outcomes was found in this study. Future research should consider in depth explorations of mechanisms of goal setting within therapeutic relationships, for young people experiencing anxiety and/or depression.
For many young people, goal setting is a helpful tool for building good therapeutic relationships via open communication. These findings support previous research which partially address the research question: young people find goal setting to be helpful to therapeutic relationships through the development of a shared language and understanding [ 3 ]. It has been suggested that goals are a mechanism of change via a means for “common ground” to be established [ 3 ]. Finding common ground and a shared understanding are particularly pertinent in youth mental health settings, where there are multiple stakeholders involved [ 36 , 37 , 38 ], which can be a balancing act [ 39 ]. Establishing this mutuality of situations is considered the key facilitator of engagement when referred for therapy by others [ 40 ]. Further, ownership of goals located with young people is important [ 41 ], which in turn gives young people ownership of their care, which can be motivational [ 42 , 43 ]. Young people experiencing anxiety may find goal setting an effective strategy due to links with avoidance motivation; such that they have reported pursuing approach goals to avoid negative emotional consequences of not doing so [ 44 ]. The ability of young people to maintain focus on the pursuit of personal goals has also been demonstrated as a moderator of depression and suicide [ 45 ].
One included study explicitly discussed parents/carers within collaborative goals and therapeutic relationships, as a foundation for mutual support [ 31 ]. Stronger relationships between both young people, parents/carers and practitioners and/or involving both young people and parents/carers in decision-making have been demonstrated to predict more positive outcomes [ 39 , 46 ]. Young people are often referred by their parents/carers, which must be considered, particularly where literature highlights challenges of setting goals when young people do not agree with the referral or recognise the difficulties [ 22 , 32 ]. Prior research has demonstrated that young people from minoritized ethnic groups are more likely to be referred for mental health support via social care and the youth justice system compared to their White British counterparts, who are commonly referred via primary care in the UK [ 47 ]. Further, evidence suggests that increases in emotional autonomy result in a shift from dependence on adults in adolescence, to reliance upon peers for support [ 48 ] particularly amongst girls [ 49 ], which may align with the developmental interference with building relationships outside of goal setting found by Cirasola and colleagues [ 32 ]. It has been argued that for young people who have difficulties building and maintaining relationships, the therapeutic relationship is particularly important (e.g., [ 23 ]). It is also noteworthy that young people in some countries may not have agency to set goals, a significant limiting factor. There are cultural and service level factors which were not explored. In some cultures, advice is sought from family and religious leaders over mental health professionals (e.g., [ 50 ]). Organisational level factors have also been found to hinder and influence therapeutic processes [ 40 ]. Further research is needed into referral routes, and intersections between systems, practice, and young people’s preferences.
Several elements of goal setting were identified as unhelpful for young people experiencing anxiety and/or depression, supporting previous literature. These discussions centred on the feasibility/acceptability of goals, rather than goal setting being detrimental to therapeutic relationships per se. Nevertheless, it is suggested that these factors were primarily related to the person, and that “personal” factors may be driven by underlying difficulties. For example, low confidence, hopelessness, levels of distress, perfectionism, and rumination (e.g., [ 51 , 52 , 53 , 54 , 55 ], may all be elements of anxiety and/or depression. Academic/clinical and youth advisors agreed that goals may become clearer over time, particularly for young people experiencing depression and purposeless, and through collaboration, goals could be formulated. The importance of considering specific challenges of goal setting during long-term therapy was highlighted. Academic/clinical and youth advisors discussed challenges associated with identifying priority areas for work, and that goals continue to flex and change, with the potential for goals work to feel too restrictive. This is in support of previous research suggesting that it is important that goals are worked on flexibly [ 3 ] with space for them to change; specifically in relation to depression. Compared to those with low levels of depression, young people with high levels of depression are more able to disengage with unhelpful goals over time and to set new goals, which in turn may predict lower levels of depressive symptoms over a year later [ 56 ]. This sense of goals flexing, feeling unique and changeable has been mirrored in descriptions of therapeutic relationships themselves [ 23 ]. There was a clear steer from youth advisors that the relationship independent of goal setting was key to good outcomes, and that this was a priority; that without the trusting relationship, there is no facilitator for goal setting. This is an important contradiction to the literature, warranting further exploration. One suggestion is that the initial goals for long-term therapy should be on relationship building, but reviewed, so the therapeutic relationship itself does not remain the primary goal [ 34 ]. Another key finding is that goals take time to establish, and pressure to set goals may render them meaningless, which also supports previous research [ 51 ]. Young people often do not know what their goals are [ 57 ], which impacts trust building, relationships and thus, therapeutic work. In support of prior research which defines recovery as contingent on shared goals and joint action in relationships [ 14 ], links found between goals, trust building and therapeutic relationships in the present study align with research on trauma informed care, and emotional and relational safety (see, [ 58 ]). Further consideration should be given to this area, particularly clinical implications, and interactions with levels of distress.
Whilst support approaches that incorporate structured goal setting are often characterised by a greater emphasis on client-centredness, the links between personally meaningful outcomes and the specific behaviour change techniques required to progress towards goals are not clear. Further, the person-centred focus is hypothesised as a conduit to positive ratings of self-efficacy, quality of life and service satisfaction, but evidence is lacking [ 11 ]. Whilst previous literature from within the youth mental health field suggests that working on goals is motivating and increases self-efficacy [ 34 , 42 ], evidence is still limited. Goal setting may be useful to young people because, whilst not necessarily synonymous, it has been demonstrated as a facilitative element of shared decision-making [ 59 , 60 ]. This collaborative way of working through shared understanding and the development of good therapeutic relationships [ 61 ] may be especially helpful to young people experiencing depression as it enables them to exercise control over their own feelings and behaviour [ 43 ] at a time when they may be experiencing feelings of hopelessness and purposeless. Whilst educated links are made to shared decision-making, further research should explore whether there is an embedded link to goals and therapeutic relationships.
Strengths and limitations
The mixed-methodological approach was a particular strength, with literature findings bolstered by lived experience. However, whilst advisors were from diverse demographic groups, not all groups were represented.
Whilst every attempt was made to include as many goal setting search terms as possible, the language is broad and fluid, meaning certain terms may have been missed. Still, the high number of results returned from literature searches suggests the strategy may need refinement. Nevertheless, we chose to ensure a large return given the subject’s broad nature. At the screening stage, the focus on explicitly identified goal setting and goal work made the identification of included studies less ambiguous, but meant that studies focused on implicit goals work would not have been included, reducing the number of studies included in the final synthesis.
Prior assumptions and knowledge of this topic will have influenced the researchers’ interpretation of the findings, even subconsciously. This includes the decision to use the nuanced elements of the research question to organise the findings. The researchers were located in Belgium, Germany, and the UK at the time of the study, which risks the perpetuation of the status quo of Western high-income-originating dominated research. Further, the findings were contextualised and linked to prior theory primarily by a researcher outside the age range of interest (JJ). The impact of both issues was mitigated via advisors, particularly those within majority world countries and the age range of interest, and the peer researchers entrenched in the research team (MS, IS), who provided contextual depth and understanding to the findings.
Literature focused on goal setting as helpful for young people with anxiety and/or depression is overwhelmingly supportive, but this leaves research gaps regarding in which ways, for whom and under what circumstances goal setting might be unhelpful. Priority must be given to researching unhelpful mechanisms of goal setting, to avoid potential iatrogenic effects. Accessibility could be improved through exploration of the intersections between systems/contexts (e.g., country), therapeutic practice (e.g., practitioner’s training/preferences) and young people’s preferences. Further research is also needed to explore mechanisms by which goal setting may help to reduce anxiety and/or depression symptoms, as well as other important areas of outcome, such as quality of life, using e.g., mediation analysis.
Scaling up in countries with well-developed systems could mean embedding goals in guidelines for anxiety and/or depression; in service specifications, including monitoring and reporting change mechanisms; staff training in consistency; and some interagency forums to align goal processes. For majority world countries with less developed systems, largely relying on non-specialist services e.g., NGOs, goals may be paradoxically more important for maximising limited resources. Despite nothing suggesting goal setting could not practically be scaled-up globally, cultural considerations may be a limiting factor in some places.
Preferences to not work on goals may be driven by the limiting factors identified, such as hopelessness or high distress. Practitioners should work through this first, reviewing the option to work on goals over time, respecting young people’s preferences. Flexibility is important, and ownership of goals located with young people is essential, particularly to those experiencing depression, enabling them to exercise control over their feelings and behaviour when they may be feeling hopeless and/or purposeless. Finally, there may be a unique opportunity for goals to facilitate work with young people experiencing high distress levels or who have experienced trauma, due to links to emotional and relational safety and building trusting relationships.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available to protect the confidentiality of the small number of advisors, but may be available from the corresponding author’s organisation, on reasonable request.
Abbreviations
Cognitive behavioural therapy
Goal based outcomes tool
United Kingdom
Austin JT, Vancouver JB. Goal constructs in psychology: structure, process, and content. Psychol Bull. 1996;122(3):338–75.
Article Google Scholar
Law D. Goals and goal based outcomes (GBOs): some useful information. London: Internal CORC Publication; 2011.
Google Scholar
Di Malta G, Oddli HW, Cooper M. From intention to action: a mixed methods study of clients’ experiences of goal-oriented practices. J Clin Psychol. 2019;75(20):1770–89.
Article PubMed Google Scholar
Law D, Jacob J. Goals and goal based outcomes: some useful information. 3rd ed. London: CAMHS Press; 2015.
Grosse M, Grawe HK. Bern inventory of treatment goals: part 1. Development and first application of a taxonomy of treatment goal themes. Psychother Res. 2002;12:79–99.
Law D. The goal-based outcome (GBO) tool. Guidance notes. [Internet]. Goals in Therapy. 2019. Available from: https://goalsintherapycom.files.wordpress.com/2019/02/gbo-version-2.0-guide-final-1st-feb-2019.pdf .
Bandura A. Self-regulation of motivation and action through goal systems. In: Bandura A, editor. Cognitive perspectives on emotion and motivation. Dordrecht: Springer; 1988. p. 37–61.
Chapter Google Scholar
Manderlink G, Harackiewicz JM. Proximal versus distal goal setting and intrinsic motivation. J Personal Soc Psychol. 1984;47:918–28.
Maslow AH. A theory of human motivation. Psychol Rev. 1943;50:370–96.
Harkin B, Webb TL, Chang BP, Prestwich A, Conner M, Kellar I, Benn Y, Sheeran P. Does monitoring goal progress promote goal attainment? A meta-analysis of the experimental evidence. Psychol Bull. 2016;142(2):198–229.
Levack WM, Weatherall M, Hay-Smith EC, Dean SG, McPherson K, Siegert RJ. Goal setting and strategies to enhance goal pursuit for adults with acquired disability participating in rehabilitation. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD009727.pub2 .
Article PubMed PubMed Central Google Scholar
Mellat N, Lavasani MG. The role of epistemological beliefs, motivational constructs and Information processing strategies in regulation of learning. Procedia Soc Behav Sci. 2011;30(1):1761–9.
Leavey JE. Youth experiences of living with mental health problems: emergence, loss, adaptation and recovery (ELAR). Can J Community Ment Health. 2009;24(2):109–26.
Simonds LM, Pons RA, Stone NJ, Warren F, John M. Adolescents with anxiety and depression: Is social recovery relevant? Clin Psychol Psychother. 2014;21(4):289–98.
Castonguay LG. Predicting the effect of cognitive therapy for depression: a study of unique and common factors. J Consult Clin Psychol. 1996;64:497–504.
Duncan BL. The heart and soul of change second edition: delivering what works in therapy. Washington: American Psychological Association; 2010.
Book Google Scholar
Messer SB. Let’s face facts: common factors are more potent than specific therapy ingredients. Clin Psychol Sci Pract. 2002;9:21–5.
Kazdin AE, Siegel TC, Bass D. Drawing on clinical practice to inform research on child and adolescent psychotherapy: survey of practitioners. Prof Psychol Res Pract. 1990;21(3):189–98.
Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychother Theory Res Pract. 1979;16(3):252–60.
Luong HK, Drummond SPA, Norton PJ. Elements of the therapeutic relationship in CBT for anxiety disorders: a systematic review. J Anxiety Disord. 2020;76:102322. https://doi.org/10.1016/j.janxdis.2020.102322 .
Shick Tryon G, Birch SE, Verkuilen J. Meta-analyses of the relation of goal consensus and collaboration to psychotherapy outcome. Psychotherapy. 2018;55(4):372–83.
DiGiuseppe R, Linscott J, Jilton R. Developing the therapeutic alliance in child-adolescent psychotherapy. Appl Prev Psychol. 1996;5(2):85–100.
Hartley S, Redmond T, Berry K. Therapeutic relationships within child and adolescent mental health inpatient services: a qualitative exploration of the experiences of young people, family members and nursing staff Short. PsyArXiv. 2021. https://doi.org/10.31234/osf.io/w2nct .
Wolpert M, Pote I, Sebastian C. Identifying and integrating active ingredients for mental health. Lancet Psychiatry. 2021;8(9):741–3.
INVOLVE. Briefing note for researchers: Public involvement in NHS, public health and social care research [Internet]. 2012. Available from: https://www.invo.org.uk/wp-content/uploads/2012/04/INVOLVEBriefingNotesApr2012.pdf .
Gotschall T. EndNote 20 desktop version. J Med Libr Assoc JMLA. 2021;109(3):520.
PubMed Google Scholar
Ouzzani M, Hammady H, Fedorowicz ZEA. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):1–10.
Hannes K. Chapter 4: Critical appraisal of qualitative research. In: Njbahkhahjlsl C, editor. Supplementary guidance for inclusion of qualitative research in cochrane systematic reviews of interventions version 1. London: Cochrane Collaboration Qualitative Methods Group; 2011. p. 4.
Bennett LR. Adolescent depression: meeting therapeutic challenges through an integrated narrative approach. J Child Adolesc Psychiatr Nurs. 2012;25(4):184–94.
Berdondini L, Elliott R, Shearer J. Collaboration in experiential therapy. J Clin Psychol. 2012;68(2):159–67.
Diamond GM, Diamond GS, Liddle HA. The therapist–parent alliance in family-based therapy for adolescents. J Clin Psychol. 2000;56(8):1037–50.
Cirasola A, Midgley N, Fonagy P, Martin P, MGoodyer I, Reynolds S, et al. The factor structure of the working alliance inventory short-form in youth psychotherapy: an empirical investigation. Psychother Res. 2021;31(4):535–47. https://doi.org/10.1080/10503307.2020.1765041 .
Feltham A, Martin K, Walker L. Using goals in therapy: the perspective of people with lived experience. In: Cooper M, Law D, editors. Working with goals in psychotherapy and counselling. Oxford: Oxford University Press; 2018. p. 73–85.
Law D, Wolpert M. Guide to using outcomes and feedback tools with children, young people and families. Formally known as the COOP document. London: CAMHS Press; 2014.
Martin K. A critical realist study of shared decision-making in young people’s mental health inpatient units. Bristol: Bristol University Press; 2019.
Hawks JM. Exploring the therapeutic alliance with adolescents and their caregivers: A qualitative approach. Diss Abstr Int Sect A Humanit Soc Sci. 2016;77(4-A(E)):No-Specified. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc13&NEWS=N&AN=2016-37856-098 .
Marks D. Fostering parental growth and enhancing the therapeutic alliance: key tasks for the child psychotherapist. J Child Psychother. 2020;46(1):20–34. https://doi.org/10.1080/0075417X.2020.1743736 .
Shpigel MS, Diamond GM. Good versus poor therapeutic alliances with non-accepting parents of same-sex oriented adolescents and young adults: a qualitative study. Psychother Res. 2014;24(3):376–91. https://doi.org/10.1080/10503307.2013.856043 .
Paul M. Decision-making about children’s health care. Adv Psychiatr Treat. 2004;10:301–11.
Stige SH, Eik I, Oddli HW, Moltu C. Negotiating system requirements to secure client engagement—therapist strategies in adolescent psychotherapy initiated by others. Front Psychol. 2021. https://doi.org/10.3389/fpsyg.2021.704136 .
Marshall SL, Oades LG, Crowe TP. Australian mental health consumers’ contributions to the evaluation and improvement of recovery oriented service provision. Isr J Psychiatry Relat Sci. 2010;47(3):198–205.
Cairns A, Kavanagh D, Dark F, McPhail SM. Setting measurable goals with young people: qualitative feedback from the goal attainment scale in youth mental health. Br J Occup Ther. 2015;78(4):253–9.
Grossoehme DH, Gerbetz L. Adolescent perceptions of meaningfulness of psychiatric hospitalization. Clin Child Psychol Psychiatry. 2004;9(4):589–96.
Dickson JM, Moberly NJ. Goal internalization and outcome expectancy in adolescent anxiety. J Abnorm Child Psychol. 2013;41(3):389–97.
Abrera AM. Depression and suicide risk among adolescents: exploring the moderating role of benevolence and goal-orientation. In: The 6 th ASEAN regional union psychological society (ARUPS) congress “driving mental revolution in the psychological century: enhancing psychological services for a better future. Bali; 2018. p. 56.
Edbrooke-Childs J, Jacob J, Argent R, Patalay P, Deighton JWM. The relationship between child-and parent-reported shared decision making and child-, parent-, and clinician-reported treatment outcome in routinely collected child mental health services data. Clin Child Psychol Psychiatry. 2016;21(2):324–38.
Edbrooke-Childs J, Patalay P. Ethnic differences in referral routes to youth mental health services. J Am Acad Child Adolesc Psychiatry. 2019;58(3):368–75.
Steinberg L, Silverberg SB. The vicissitudes of autonomy in early adolescence. Child Dev. 1986;57:841–51.
Slavin LA, Rainer KL. Gender differences in emotional support and depressive symptoms among adolescents: a prospective analysis. Am J Community Psychol. 1990;18(3):407–21.
Ciftci A, Jones N, Corrigan PW. Mental health stigma in the muslim community. J Muslim Ment Health. 2013;7(1):17–32.
Bromley C, Westwood S. Young people’s participation: views from young people on using goals. Child Fam Clin Psychol Rev. 2013;1:29–40.
Clarke SP, Oades LG, Crowe TP, Caputi P, Deane FP. The role of symptom distress and goal attainment in promoting aspects of psychological recovery for consumers with enduring mental illness. J Ment Health. 2009;18(5):389–97.
Trent ES, Viana AG, Raines EM, Woodward EC, Zvolensky MJCA. Exposure to parental threatening behaviors and internalizing psychopathology in a trauma-exposed inpatient adolescent sample: the role of difficulties with goal-directed behaviors. J Nerv Ment Dis. 2019;207(11):969–76.
Moberly NJ, Watkins ER. Negative affect and ruminative self-focus during everyday goal pursuit. Cogn Emot. 2010;24(4):729–39.
Steen A, Berghuis H, Braam AW. Lack of meaning, purpose and direction in life in personality disorder: a comparative quantitative approach using Livesley’s general assessment of personality disorder. Personal Ment Health. 2019;13(3):144–54.
Wrosch C, Miller GE. Depressive symptoms can be useful: self-regulatory and emotional benefits of dysphoric mood in adolescence. J Pers Soc Psychol. 2009;96(6):1181–90.
Troupp C. Distinguishing patient-generated outcome measures in CAMHS from a bespoke sandwich. Child Fam Clin Psychol Rev. 2013;1(1):19–28.
Taylor J, Shostak L, Rogers A, Mitchell P. Rethinking mental health provision in the secure estate for children and young people: a framework for integrated care (SECURE STAIRS). Safer Communities. 2018;17(4):193–201.
Cheng H, Hayes D, Edbrooke-Childs J, Martin K, Chapman L, Wolpert M. What approaches for promoting shared decision making are used in child mental health? A scoping review. Helen MIR mHealth uHealth. 2017;7(6):77.
Langer DA, Jensen-Doss A. Shared decision-making in youth mental health care: using the evidence to plan treatments collaboratively. J Clin Child Adolesc Psychol. 2018;47(5):821–31.
Coulter A, Edwards A, Elwyn G, Thomson R. Implementing shared decision making in the UK. Z Evid Fortbild Qual Gesundhwes. 2011;105(4):300–4.
Download references
Acknowledgements
The authors would like to thank the advisors, for their invaluable contribution from start to finish, including useful comments an early draft: Duncan Law, Elmas Aybike Yılmaz, Hanne Oddli, Isabella Valério, Jacob People, Josh D., Julian Edbrooke-Childs, Katya Proctor, Laura Calomarde Juárez, Mick Cooper, Nick Morgan, Panos Vostanis, Syeda Zeenat R., and Theo Jackson. Thank you to Bernice Appiah, Shade Davies and Shadia Robertson for helpful discussions about the findings, and assistance with evidence synthesis, and to Inês Pote from the Wellcome Active Ingredients team, and Jasmine Harju-Seppanen, for useful comments on a previous draft. The authors also wish to thank Zoe Thomas for incredibly useful advice and guidance regarding literature searches.
This work was funded by a Wellcome Trust Mental Health Priority Area “Active Ingredients” 2021 commission awarded to JJ at the Anna Freud Centre. It was a requirement of the funding team that the research design comprised a literature review, and that the involved and worked collaboratively with young people with lived experience of anxiety and/or depression throughout the course of the project. Members of the funding team provided feedback on an early draft of this manuscript.
Author information
Authors and affiliations.
Child Outcomes Research Consortium, Anna Freud Centre, 4-8 Rodney Street, London, N1 9JH, UK
Jenna Jacob
Euro Youth Mental Health, The Block, 35 Churchgate, Hitchin, SG5 1DN, UK
Milos Stankovic & Inga Spuerck
Systematic Review Consultants, 9 Sandfield Road, Nottingham, NG7 1QR, UK
Farhad Shokraneh
You can also search for this author in PubMed Google Scholar
Contributions
JJ conceptualised the study, prepared the first draft protocol and search strategy, refining this with the study authors and advisors. JJ undertook the library database searches for published literature, partially screened the titles and abstracts of literature, screened all full texts, led communication with study authors and advisors, led four advisory group meetings, maintained the databases which were used to extract and manage study data, prepared, and revised the manuscript. MS contributed to the first draft protocol and search strategy, led communication with youth advisors, led two advisory group meetings, created the narrative summaries, and contributed to the manuscript. IS contributed to the first draft protocol and search strategy, supported communication with youth advisors, screened full texts for further relevant literature, and contributed to the manuscript. FS conducted the grey literature searches, screened all potential title and abstracts from all searches (published and unpublished literature), maintained the databases which were used to extract and manage study data, and contributed to the manuscript. All study advisors were invited to comment on the protocol and initial search terms, and were invited to comment on earlier drafts of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jenna Jacob .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this research was not required because it does not involve collection nor analysis of primary data, and youth advisors were consulted on in the capacity of being part of the advisory group, to discuss their interpretation of the findings, rather than within the capacity of research participants.
Consent for publication
Not applicable.
Competing interests
JJ works on the Child Outcomes Research Consortium (CORC) project at the Anna Freud National Centre for Children and Families, which encourages the use of outcome measures in youth mental health settings amongst its members. No other authors report any competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. appendix 1..
Inclusion and exclusion criteria and Search Strategies. Appendix 2 Core Criteria for Quality Assessment of Qualitative Studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jacob, J., Stankovic, M., Spuerck, I. et al. Goal setting with young people for anxiety and depression: What works for whom in therapeutic relationships? A literature review and insight analysis. BMC Psychol 10 , 171 (2022). https://doi.org/10.1186/s40359-022-00879-5
Download citation
Received : 16 March 2022
Accepted : 30 June 2022
Published : 13 July 2022
DOI : https://doi.org/10.1186/s40359-022-00879-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Youth mental health
- Goal setting
- Therapeutic alliance
- Outcome measurement
- Active ingredients
- Goal based outcomes
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Systematic Review
- Open access
- Published: 30 May 2024
Patient experiences: a qualitative systematic review of chemotherapy adherence
- Amineh Rashidi 1 ,
- Susma Thapa 1 ,
- Wasana Sandamali Kahawaththa Palliya Guruge 1 &
- Shubhpreet Kaur 1
BMC Cancer volume 24 , Article number: 658 ( 2024 ) Cite this article
263 Accesses
Metrics details
Adherence to chemotherapy treatment is recognized as a crucial health concern, especially in managing cancer patients. Chemotherapy presents challenges for patients, as it can lead to potential side effects that may adversely affect their mobility and overall function. Patients may sometimes neglect to communicate these side effects to health professionals, which can impact treatment management and leave their unresolved needs unaddressed. However, there is limited understanding of how patients’ experiences contribute to improving adherence to chemotherapy treatment and the provision of appropriate support. Therefore, gaining insights into patients’ experiences is crucial for enhancing the accompaniment and support provided during chemotherapy.
This review synthesizes qualitative literature on chemotherapy adherence within the context of patients’ experiences. Data were collected from Medline, Web of Science, CINAHL, PsychINFO, Embase, Scopus, and the Cochrane Library, systematically searched from 2006 to 2023. Keywords and MeSH terms were utilized to identify relevant research published in English. Thirteen articles were included in this review. Five key themes were synthesized from the findings, including positive outlook, receiving support, side effects, concerns about efficacy, and unmet information needs. The review underscores the importance for healthcare providers, particularly nurses, to focus on providing comprehensive information about chemotherapy treatment to patients. Adopting recommended strategies may assist patients in clinical practice settings in enhancing adherence to chemotherapy treatment and improving health outcomes for individuals living with cancer.
Peer Review reports
Introduction
Cancer can affect anyone and is recognized as a chronic disease characterized by abnormal cell multiplication in the body [ 1 ]. While cancer is prevalent worldwide, approximately 70% of cancer-related deaths occur in low- to middle-income nations [ 1 ]. Disparities in cancer outcomes are primarily attributed to variations in the accessibility of comprehensive diagnosis and treatment among countries [ 1 , 2 ]. Cancer treatment comes in various forms; however, chemotherapy is the most widely used approach [ 3 ]. Patients undergoing chemotherapy experience both disease-related and treatment-related adverse effects, significantly impacting their quality of life [ 4 ]. Despite these challenges, many cancer patients adhere to treatment in the hope of survival [ 5 ]. However, some studies have shown that concerns about treatment efficacy may hinder treatment adherence [ 6 ]. Adherence is defined as “the extent to which a person’s behaviour aligns with the recommendations of healthcare providers“ [ 7 ]. Additionally, treatment adherence is influenced by the information provided by healthcare professionals following a cancer diagnosis [ 8 ]. Patient experiences suggest that the decision to adhere to treatment is often influenced by personal factors, with family support playing a crucial role [ 8 ]. Furthermore, providing adequate information about chemotherapy, including its benefits and consequences, can help individuals living with cancer gain a better understanding of the advantages associated with adhering to chemotherapy treatment [ 9 ].
Recognizing the importance of adhering to chemotherapy treatment and understanding the impact of individual experiences of chemotherapy adherence would aid in identifying determinants of adherence and non-adherence that are modifiable through effective interventions [ 10 ]. Recently, systematic reviews have focused on experiences and adherence in breast cancer [ 11 ], self-management of chemotherapy in cancer patients [ 12 ], and the influence of medication side effects on adherence [ 13 ]. However, these reviews were narrow in scope, and to date, no review has integrated the findings of qualitative studies designed to explore both positive and negative experiences regarding chemotherapy treatment adherence. This review aims to synthesize the qualitative literature on chemotherapy adherence within the context of patients’ experiences.
This review was conducted in accordance with the Joanna Briggs Institute [ 14 ] guidelines for systemic review involving meta-aggregation. This review was registered in PROSPERO (CRD42021270459).
Search methods
The searches for peer reviewed publications in English from January 2006-September 2023 were conducted by using keywords, medical subject headings (MeSH) terms and Boolean operators ‘AND’ and ‘OR’, which are presented in the table in Appendix 1 . The searches were performed in a systematic manner in core databases such including Embase, Medline, PsycINFO, CINAHL, Web of Science, Cochrane Library, Scopus and the Joanna Briggs Institute (JBI). The search strategy was developed from keywords and medical subject headings (MeSH) terms. Librarian’s support and advice were sought in forming of the search strategies.
Study selection and inclusion criteria
The systematic search was conducted on each database and all articles were exported to Endnote and duplicates records were removed. Then, title and abstract of the full text was screened by two independent reviewers against the inclusion criteria. For this review, populations were patients aged 18 and over with cancer, the phenomenon of interest was experiences on chemotherapy adherence and context was considered as hospitals, communities, rehabilitation centres, outpatient clinics, and residential aged care. All peer-reviewed qualitative study design were also considered for inclusion. Studies included in this review were classified as primary research, published in English since 2006, some intervention implemented to improve adherence to treatment. This review excluded any studies that related to with cancer and mental health condition, animal studies and grey literature.
Quality appraisal and data extraction
The JBI Qualitative Assessment and Review Instrument for qualitative studies was used to assess the methodological quality of the included studies, which was conducted by the primary and second reviewers independently. There was no disagreement between the reviews. The qualitative data on objectives, study population, context, study methods, and the phenomena of interest and findings form the included studies were extracted.
Data synthesis
The meta-aggregation approach was used to combine the results with similar meaning. The primary and secondary reviewers created categories based on the meanings and concept. These categories were supported by direct quotations from participants. The findings were assess based on three levels of evidence, including unequivocal, credible, and unsupported [ 15 , 16 ]. Findings with no quotation were not considered for synthesis in this review. The categories and findings were also discussed by the third and fourth reviewers until a consensus was reached. The review was approved by the Edith Cowan University Human Research Ethics Committee (2021–02896).
Study inclusion
A total of 4145 records were identified through a systematic search. Duplicates ( n = 647) were excluded. Two independent reviewers conducted screening process. The remaining articles ( n = 3498) were examined for title and abstract screening. Then, the full text screening conducted, yielded 13 articles to be included in the final synthesis see Appendix 2 .
Methodological quality of included studies
All included qualitative studies scored between 7 and 9, which is displayed in Appendix 3 . The congruity between the research methodology and the research question or objectives, followed by applying appropriate data collection and data analysis were observed in all included studies. Only one study [ 17 ] indicated the researcher’s statement regarding cultural or theoretical perspectives. Three studies [ 18 , 19 , 20 ] identified the influence of the researcher on the research and vice-versa.
Characteristics of included studies
Most of studies conducted semi-structured and in-depth interviews, one study used narrative stories [ 19 ], one study used focus group discussion [ 21 ], and one study combined focus group and interview [ 22 ] to collect data. All studies conducted outpatient’s clinic, community, or hospital settings [ 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 ]. The study characteristics presented in Appendix 4 .
Review findings
Eighteen findings were extracted and synthesised into five categories: positive outlook, support, side effects, concern about efficacy and unmet information needs.
Positive outlook
Five studies discussed the link between positivity and hope and chemotherapy adherence [ 19 , 20 , 23 , 27 , 28 ]. Five studies commented that feeling positive and avoid the negativity and worry could encourage people to adhere in their mindset chemotherapy: “ I think the main thing for me was just keeping a positive attitude and not worrying, not letting myself worry about it ” [ 20 ]. Participants also considered the positive thoughts as a coping mechanism, that would help them to adhere and complete chemotherapy: “ I’m just real positive on how everything is going. I’m confident in the chemo, and I’m hoping to get out of her soon ” [ 23 ]. Viewing chemotherapy as part of their treatment regimen and having awareness of negative consequences of non-adherence to chemotherapy encouraged them to adhere chemotherapy: “ If I do not take medicine, I do not think I will be able to live ” [ 28 ]. Adhering chemotherapy was described as a survivor tool which helped people to control cancer-related symptoms: “ it is what is going to restore me. If it wasn’t this treatment, maybe I wasn’t here talking to you. So, I have to focus in what he is going to give me, life !” [ 27 ]. Similarly, people accepted the medical facts and prevent their life from worsening; “ without the treatment, it goes the wrong way. It is hard, but I have accepted it from the beginning, yes. This is how it is. I cannot do anything about it. Just have to accept it ” [ 19 ].
Finding from six studies contributed to this category [ 20 , 21 , 23 , 24 , 25 , 29 ]. Providing support from families and friends most important to the people. Receiving support from family members enhanced a sense responsibility towards their families, as they believed to survive for their family even if suffered: “ yes, I just thought that if something comes back again and I say no, then I have to look my family and friends in the eye and say I could have prevented it, perhaps. Now, if something comes back again, I can say I did everything I could. Cancer is bad enough without someone saying: It’s your own fault!!” [ 29 ]. Also, emotional support from family was described as important in helping and meeting their needs, and through facilitation helped people to adhere chemotherapy: “ people who genuinely mean the support that they’re giving […] just the pure joy on my daughter’s face for helping me. she was there day and night for me if I needed it, and that I think is the main thing not to have someone begrudgingly looking after you ” [ 20 ]. Another study discussed the role family, friends and social media as the best source of support during their treatment to adhere and continue “ I have tons of friends on Facebook, believe it or not, and it’s amazing how many people are supportive in that way, you know, just sending get-well wishes. I can’t imagine going through this like 10 years ago whenever stuff like that wasn’t around ” [ 23 ]. Receiving support from social workers was particularly helpful during chemotherapy in encouraging adherence to the chemotherapy: “ the social worker told me that love is courage. That was a huge encouragement, and I began to encourage myself ” [ 25 ].
Side effects
Findings from five studies informed this category [ 17 , 21 , 22 , 25 , 26 ]. Physical side effects were described by some as the most unpleasure experience: “ the side effects were very uncomfortable. I felt pain, fatigue, nausea, and dizziness that limited my daily activities. Sometimes, I was thinking about not keeping to my chemotherapy schedule due to those side effect ” [ 17 ]. The impact of side effects affected peoples’ ability to maintain their independence and self-care: “ I couldn’t walk because I didn’t have the energy, but I wouldn’t have dared to go out because the diarrhoea was so bad. Sometimes I couldn’t even get to the toilet; that’s very embarrassing because you feel like you’re a baby ” [ 26 ]. Some perceived that this resulted in being unable to perform independently: “ I was incredibly weak and then you still have to do things and you can’t manage it ” [ 22 ]. These side effect also decreased their quality of life “ I felt nauseated whenever I smelled food. I simply had no appetite when food was placed in front of me. I lost my sense of taste. Food had no taste anymore ” [ 25 ]. Although, the side effects impacted on patients´ leisure and free-time activities, they continued to undertake treatment: “ I had to give up doing the things I liked the most, such as going for walks or going to the beach. Routines, daily life in general were affected ” [ 21 ].
Concern about efficacy
Findings form four studies informed this category [ 17 , 18 , 24 , 28 ]. Although being concerned about the efficacy of the chemotherapy and whether or not chemotherapy treatment would be successful, one participant who undertook treatment described: “the efficacy is not so great. It is said to expect about 10% improvement, but I assume that it declines over time ” [ 28 ]. People were worried that such treatment could not cure their cancer and that their body suffered more due to the disease: “ I was really worried about my treatment effectiveness, and I will die shortly ” [ 17 ]. There were doubts expressed about remaining the cancer in the body after chemotherapy: “ there’s always sort of hidden worries in there that whilst they’re not actually taking the tumour away, then you’re wondering whether it’s getting bigger or what’s happening to it, whether it’s spreading or whatever, you know ” [ 24 ]. Uncertainty around the outcome of such treatment, or whether recovering from cancer or not was described as: “it makes you feel confused. You don’t know whether you are going to get better or else whether the illness is going to drag along further” [ 18 ].
Unmet information needs
Five studies contributed to this category [ 17 , 21 , 22 , 23 , 26 ]. The need for adequate information to assimilate information and provide more clarity when discussing complex information were described. Providing information from clinicians was described as minimal: “they explain everything to you and show you the statistics, then you’re supposed to take it all on-board. You could probably go a little bit slower with the different kinds of chemo and grappling with these statistics” [ 26 ]. People also used the internet search to gain information about their cancer or treatments, “I’ve done it (consult google), but I stopped right away because there’s so much information and you don’t know whether it’s true or not ” [ 21 ]. The need to receive from their clinicians to obtain clearer information was described as” I look a lot of stuff up online because it is not explained to me by the team here at the hospital ” [ 23 ]. Feeling overwhelmed with the volume of information could inhibit people to gain a better understanding of chemotherapy treatment and its relevant information: “ you don’t absorb everything that’s being said and an awful lot of information is given to you ” [ 22 ]. People stated that the need to know more information about their cancer, as they were never dared to ask from their clinicians: “ I am a low educated person and come from a rural area; I just follow the doctor’s advice for my health, and I do not dare to ask anything” [ 17 ].
The purpose of this review was to explore patient’s experiences about the chemotherapy adherence. After finalizing the searches, thirteen papers were included in this review that met the inclusion criteria.
The findings of the present review suggest that social support is a crucial element in people’s positive experiences of adhering to chemotherapy. Such support can lead to positive outcomes by providing consistent and timely assistance from family members or healthcare professionals, who play vital roles in maintaining chemotherapy adherence [ 30 ]. Consistent with our study, previous research has highlighted the significant role of family members in offering emotional and physical support, which helps individuals cope better with chemotherapy treatment [ 31 , 32 ]. However, while receiving support from family members reinforces individuals’ sense of responsibility in managing their treatment and their family, it also instils a desire to survive cancer and undergo chemotherapy. One study found that assuming self-responsibility empowers patients undergoing chemotherapy, as they feel a sense of control over their therapy and are less dependent on family members or healthcare professionals [ 33 ]. A qualitative systematic review reported that support from family members enables patients to become more proactive and effective in adhering to their treatment plan [ 34 ]. This review highlights the importance of maintaining a positive outlook and rational beliefs as essential components of chemotherapy adherence. Positive thinking helps individuals recognize their role in chemotherapy treatment and cope more effectively with their illness by accepting it as part of their treatment regimen and viewing it as a tool for survival. This finding is supported by previous studies indicating that positivity and positive affirmations play critical roles in helping individuals adapt to their reality and construct attitudes conducive to chemotherapy adherence [ 35 , 36 ]. Similarly, maintaining a positive mindset can foster more favourable thoughts regarding chemotherapy adherence, ultimately enhancing adherence and overall well-being [ 37 ].
This review identified side effects as a significant negative aspect of the chemotherapy experience, with individuals expressing concerns about how these side effects affected their ability to perform personal self-care tasks and maintain independent living in their daily lives. Previous studies have shown that participants with a history of chemotherapy drug side effects were less likely to adhere to their treatment regimen due to worsening symptoms, which increased the burden of medication side effects [ 38 , 39 ]. For instance, cancer patients who experienced minimal side effects from chemotherapy were at least 3.5 times more likely to adhere to their treatment plan compared to those who experienced side effects [ 40 ]. Despite experiencing side effects, patients were generally willing to accept and adhere to their treatment program, although one study in this review indicated that side effects made some patients unable to maintain treatment adherence. Side effects also decreased quality of life and imposed restrictions on lifestyle, as seen in another study where adverse effects limited individuals in fulfilling daily commitments and returning to normal levels of functioning [ 41 ]. Additionally, unmet needs regarding information on patients’ needs and expectations were common. Healthcare professionals were considered the most important source of information, followed by consultation with the internet. Providing information from healthcare professionals, particularly nurses, can support patients effectively and reinforce treatment adherence [ 42 , 43 ]. Chemotherapy patients often preferred to base their decisions on the recommendations of their care providers and required adequate information retention. Related studies have highlighted that unmet needs among cancer patients are known factors associated with chemotherapy adherence, emphasizing the importance of providing precise information and delivering it by healthcare professionals to improve adherence [ 44 , 45 ]. Doubts about the efficacy of chemotherapy treatment, as the disease may remain latent, were considered negative experiences. Despite these doubts, patients continued their treatment, echoing findings from a study where doubts regarding efficacy were identified as a main concern for chemotherapy adherence. Further research is needed to understand how doubts about treatment efficacy can still encourage patients to adhere to chemotherapy treatment.
Strengths and limitation
The strength of this review lies in its comprehensive search strategy across databases to select appropriate articles. Additionally, the use of JBI guidelines provided a comprehensive and rigorous methodological approach in conducting this review. However, the exclusion of non-English studies, quantitative studies, and studies involving adolescents and children may limit the generalizability of the findings. Furthermore, this review focuses solely on chemotherapy treatment and does not encompass other types of cancer treatment.
Conclusion and practical implications
Based on the discussion of the findings, it is evident that maintaining a positive mentality and receiving social support can enhance chemotherapy adherence. Conversely, experiencing treatment side effects, concerns about efficacy, and unmet information needs may lead to lower adherence. These findings present an opportunity for healthcare professionals, particularly nurses, to develop standardized approaches aimed at facilitating chemotherapy treatment adherence, with a focus on providing comprehensive information. By assessing patients’ needs, healthcare professionals can tailor approaches to promote chemotherapy adherence and improve the survival rates of people living with cancer. Raising awareness and providing education about cancer and chemotherapy treatment can enhance patients’ understanding of the disease and its treatment options. Utilizing videos and reading materials in outpatient clinics and pharmacy settings can broaden the reach of educational efforts. Policy makers and healthcare providers can collaborate to develop sustainable patient education models to optimize patient outcomes in the context of cancer care. A deeper understanding of individual processes related to chemotherapy adherence is necessary to plan the implementation of interventions effectively. Further research examining the experiences of both adherent and non-adherent patients is essential to gain a comprehensive understanding of this topic.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request. on our submission system as well.
World Health Organization. Cancer 2021 [ https://www.who.int/news-room/fact-sheets/detail/cancer .
Klapheke A, Yap SA, Pan K, Cress RDDHSDCA. Sociodemographic disparities in chemotherapy treatment and impact on survival among patients with metastatic bladder cancer. Urologic Oncology: Seminars Original Investigations. 2018;36(6):19–308.
Article Google Scholar
Moth EB, Kiely BE, Naganathan V, Martin A, Blinman P. How do oncologists make decisions about chemotherapy for their older patients with cancer? A survey of Australian oncologists. Support Care Cancer. 2018;26(2):451–60.
Article CAS PubMed Google Scholar
Khamboon T, Pakanta I. Intervention for symptom cluster management of fatigue, loss of appetite, and anxiety among patients with lung cancer undergoing chemotherapy. Asia-Pacific J Oncol Nurs. 2021;8(3):267–75.
Garcia ACM, Camargos Junior JB, Sarto KK, Silva Marcelo CAd, Paiva EMC, Nogueira DA, Mills J. Quality of life, self-compassion and mindfulness in cancer patients undergoing chemotherapy: a cross-sectional study. Eur J Oncol Nurs. 2021;51:N.PAG-N.PAG.
Horne R, Chapman SCE, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about Medicines prescribed for long-term conditions: a Meta-Analytic Review of the necessity-concerns Framework. PLoS ONE. 2013;8(12):e80633.
Article PubMed PubMed Central Google Scholar
WHO. Adherence to long-term therapies: evidence for action. Geneva, Switzerland: World Health Organisation; 2003.
Google Scholar
Warby A, Dhillon HM, Kao S, Vardy JL. A survey of patient and caregiver experience with malignant pleural mesothelioma. Support Care Cancer. 2019;27(12):4675–86.
Article PubMed Google Scholar
Arunachalam SS, Shetty AP, Panniyadi N, Meena C, Kumari J, Rani B, et al. Study on knowledge of chemotherapy’s adverse effects and their self-care ability to manage - the cancer survivors impact. Clin Epidemiol Global Health. 2021;11:100765.
Article CAS Google Scholar
Nizet P, Touchefeu Y, Pecout S, Cauchin E, Beaudouin E, Mayol S, et al. Exploring the factors influencing adherence to oral anticancer drugs in patients with digestive cancer: a qualitative study. Support Care Cancer. 2022;30(3):2591–604.
Clancy C, Lynch J, Oconnor P, Dowling M. Breast cancer patients’ experiences of adherence and persistence to oral endocrine therapy: a qualitative evidence synthesis. Eur J Oncol Nurs. 2020;44.
Magalhães B, Fernandes C, Lima L, Martinez-Galiano JM, Santos C. Cancer patients’ experiences on self-management of chemotherapy treatment-related symptoms: A systematic review and thematic synthesis. Eur J Oncol Nurs. 2020;49.
Peddie N, Agnew S, Crawford M, Dixon D, MacPherson I, Fleming L. The impact of medication side effects on adherence and persistence to hormone therapy in breast cancer survivors: a qualitative systematic review and thematic synthesis. Breast. 2021;58:147–59.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ: Br Med J. 2009;339(7716):332–6.
Joanna Briggs Institute. The Joanna Briggs Institute critical appraisal tools for use in JBI systematic reviews. Checklist for qualitative research. 2017.
Zachary M, Kylie P, Craig L, Edoardo A, Alan P. Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol [Internet]. 2014;14(1):108.
Iskandarsyah A, de Klerk C, Suardi DR, Soemitro MP, Sadarjoen SS, Passchier J. Psychosocial and cultural reasons for Delay in seeking help and Nonadherence to treatment in Indonesian women with breast Cancer: a qualitative study. Health Psychol. 2014;33(3):214–21.
Chircop D, Scerri J. The lived experience of patients with Non-hodgkin’s lymphoma undergoing chemotherapy. Eur J Oncol Nurs. 2018;35:117–21.
Kvåle K, Synnes O. Living with life-prolonging chemotherapy—control and meaning‐making in the tension between life and death. Eur J Cancer Care. 2018;27(1):1.
Staneva AA, Beesley VL, Niranjan N, Gibson AF, Rowlands I, Webb PM. I wasn’t gonna let it stop me: exploring women’s experiences of getting through chemotherapy for ovarian cancer. Cancer Nurs. 2019;42(2):E31–8.
Talens A, Guilabert M, Lumbreras B, Aznar MT, López-Pintor E. Medication Experience and Adherence to Oral Chemotherapy: A Qualitative Study of Patients’ and Health Professionals’ Perspectives. Int J Environ Res Public Health. 2021;18(8).
Dumas L, Lidington E, Appadu L, Jupp P, Husson O, Banerjee S, et al. Exploring older women’s attitudes to and experience of treatment for advanced ovarian cancer: a qualitative phenomenological study. Cancers. 2021;13(6):1207.
Albrecht TA, Keim-Malpass J, Boyiadzis M, Rosenzweig M. Psychosocial experiences of young adults diagnosed with acute leukemia during hospitalization for induction chemotherapy treatment. J Hospice Palliat Nurs. 2019;21(2):167–73.
Beaver K, Williamson S, Briggs J. Exploring patient experiences of neo-adjuvant chemotherapy for breast cancer. Eur J Oncol Nurs. 2016;20:77–86.
Chou J-F, Lu YY. Intraperitoneal chemotherapy: the lived experiences of Taiwanese patients with ovarian cancer. Clin J Oncol Nurs. 2019;23(6):E100–6.
Farrell C, Heaven C. Understanding the impact of chemotherapy on dignity for older people and their partners. Eur J Oncol Nurs. 2018;36:82–8.
Wakiuchi J, Silva Marcon S, de Oliveira DC, Aparecida Sales C. Rebuilding subjectivity from the experience of cancer and its treatment. Revista Brasileira De Enfermagem. 2019;72(1):125–33.
Yagasaki K, Komatsu H, Takahashi T. Inner conflict in patients receiving oral anticancer agents: a qualitative study. BMJ Open [Internet]. 2015; 5(4).
Gassmann C, Kolbe N, Brenner A. Experiences and coping strategies of oncology patients undergoing oral chemotherapy: first steps of a grounded theory study. Eur J Oncol Nurs. 2016;23:106–14.
Tang GX, Yan PP, Yan CL, Fu B, Zhu SJ, Zhou LQ, et al. Determinants of suicidal ideation in gynecological cancer patients. Psycho-oncology. 2016;25(1):97–103.
Oven Ustaalioglu B, Acar E, Caliskan M. The predictive factors for perceived social support among cancer patients and caregiver burden of their family caregivers in Turkish population. Int J Psychiatry Clin Pract. 2018;22(1):63–9.
Levkovich I, Cohen M, Karkabi K. The experience of fatigue in breast Cancer patients 1–12 Month Post-chemotherapy: a qualitative study. Behav Med. 2019;45(1):7–18.
Simchowitz B, Shiman L, Spencer J, Brouillard D, Gross A, Connor M, Weingart SN. Perceptions and experiences of patients receiving oral chemotherapy. Clin J Oncol Nurs. 2010;14(4):447–53.
Rashidi A, Kaistha P, Whitehead L, Robinson S. Factors that influence adherence to treatment plans amongst people living with cardiovascular disease: a review of published qualitative research studies. Int J Nurs Stud 2020;110(103727).
Aydogan U, Doganer YC, Komurcu S, Ozturk B, Ozet A, Saglam K. Coping attitudes of cancer patients and their caregivers and quality of life of caregivers. Indian J Palliat Care. 2016;22(2):150–6.
Langford DJ, Morgan S, Cooper B, Paul S, Kober K, Wright F, et al. Association of personality profiles with coping and adjustment to cancer among patients undergoing chemotherapy. Psycho-oncology. 2020;29(6):1060–7.
Jamie MJ, Pensak NA, Sporn NJ, MacDonald JJ, Lennes IT, Safren SA et al. Treatment satisfaction and adherence to oral chemotherapy in patients with Cancer. J Oncol Pract. 2017;13(2).
Tsai Y-F, Huang W-C, Cho S-F, Hsiao H-H, Liu Y-C, Lin S-F, et al. Side effects and medication adherence of tyrosine kinase inhibitors for patients with chronic myeloid leukemia in Taiwan. Medicine. 2018;97(26):415.
D S, M P, G R, S H. Importance of medication adherence and factors affecting it. IP Int J Compr Adv Pharmacolog. 2020;3(2):69–77.
Bekalu YE, Wudu MA, Gashu AW. Adherence to Chemotherapy and Associated factors among patients with Cancer in Amhara Region, Northeastern Ethiopia, 2022. A cross-sectional study. Cancer Control. 2023;30.
Hsu H-C, Liou W-S, Chiang A-J, Tsai S-Y, Jeang S-R, Wu S-L, et al. Longitudinal perceptions of the side effects of chemotherapy in patients with gynecological cancer. Support Care Cancer. 2017;25(11):3457–64.
Gow K, Rashidi A, Whithead L. Factors influencing medication adherence among adults living with diabetes and comorbidities: a qualitative systematic review. Curr Diab Rep. 2023:1–7.
Rashidi A, Whitehead L, Kaistha P. Nurses’ perceptions of factors influencing treatment engagement among patients with cardiovascular diseases: a systematic review. BMC Nurs. 2021;20(1):251.
Zebrack BJ, Block R, Hayes-Lattin B, Embry L, Aguilar C, Meeske KA, et al. Psychosocial service use and unmet need among recently diagnosed adolescent and young adult cancer patients. Cancer. 2013;119(1):201–14.
Timmers L, Boons CCLM, van den Verbrugghe M, Van Hecke A, Hugtenburg JG. Supporting adherence to oral anticancer agents: clinical practice and clues to improve care provided by physicians, nurse practitioners, nurses and pharmacists. BMC Cancer. 2017;17(1).
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
School of Nursing and Midwifery, Edith Cowan University, 270 Joondalup Drive, Joondalup, Perth, WA, 6027, Australia
Amineh Rashidi, Susma Thapa, Wasana Sandamali Kahawaththa Palliya Guruge & Shubhpreet Kaur
You can also search for this author in PubMed Google Scholar
Contributions
First author (AR) and second author (ST) conceived the review and the second author oversight for all stages of the review provided by the second author. All authors (AR), (ST), (WG) and (SK) undertook the literature search. Data extraction, screening the included papers and quality appraisal were undertaken by all authors (AR), (ST), (WG) and (SK). First and second authors (AR) and (ST) analysed the data and wrote the first draft of the manuscript and revised the manuscript and all authors (AR), (ST), (WG) and (SK) approved the final version of the manuscript.
Corresponding author
Correspondence to Amineh Rashidi .
Ethics declarations
Ethics approval and consent to participate.
The review was approved by the Edith Cowan University Human Research Ethics Committee (2021–02896). A proposal for the systematic review was assessed by the Edith Cowan University Human Research Ethics Committee and deemed not appropriate for full ethical review. However, a Data Management Plan (2021-02896-RASHIDI) was approved and monitored as part of this procedure. Raw data was extracted from the published manuscripts and authors could not identify individual participants during or after this process.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, supplementary material 5, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Rashidi, A., Thapa, S., Kahawaththa Palliya Guruge, W. et al. Patient experiences: a qualitative systematic review of chemotherapy adherence. BMC Cancer 24 , 658 (2024). https://doi.org/10.1186/s12885-024-12353-z
Download citation
Received : 17 November 2023
Accepted : 07 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1186/s12885-024-12353-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chemotherapy treatment
- Medication adherence
- Qualitative research
- Patients experiences
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 07 June 2024
The association between empathy and burnout in medical students: a systematic review and meta-analysis
- P. Cairns 1 ,
- A. E. Isham 2 &
- R. Zachariae 1 , 3
BMC Medical Education volume 24 , Article number: 640 ( 2024 ) Cite this article
101 Accesses
Metrics details
Burnout levels in medical students are higher than in other student groups. Empathy is an increasingly desired outcome of medical schools. Empathy is negatively associated with burnout in physicians. Our objective was to quantitatively review the available literature on associations between empathy and burnout in medical students, and to explore associations between specific empathy aspects (cognitive and affective) and burnout sub-dimensions (emotional exhaustion, depersonalization and personal accomplishment).
A comprehensive search of the literature published up until January 2024 was undertaken in the PubMed, EMBASE, CINAHL, The Cochrane Library, and PsycINFO databases. Two independent reviewers screened 498 records and quality-rated and extracted data from eligible studies. The effect size correlations (ESr) were pooled using a random-effects model and between-study variation explored with meta-regression. The review was preregistered with PROSPERO (#CRD42023467670) and reported following the PRISMA guidelines.
Twenty-one studies including a total of 27,129 medical students published between 2010 and 2023 were included. Overall, empathy and burnout were negatively and statistically significantly associated (ESr: -0.15, 95%CI [-0.21; -0.10], p < .001). When analyzing sub-dimensions, cognitive empathy was negatively associated with emotional exhaustion (ESr: -0.10, 95%CI [-0.17; -0.03], p = .006) and depersonalization (ESr: -0.15, 95%CI [-0.24; 0.05], p = .003), and positively associated with personal accomplishment (ESr: 0.21, 95%CI [0.12; 0.30], p < .001). Affective empathy was not statistically significantly associated with emotional exhaustion, depersonalization or personal accomplishment. Supplementary Bayesian analysis indicated the strongest evidence for the positive association between cognitive empathy and personal accomplishment. Response rate and gender moderated the relationship so that higher response rates and more male respondents strengthen the negative association between empathy and burnout.
Greater empathy, in particular cognitive empathy, is associated with lower burnout levels in medical students. This appears to be primarily driven by cognitive empathy's positive association with personal accomplishment.
Protocol registration
#CRD42023467670
Peer Review reports
The purpose of this systematic review and meta-analysis was to examine the relationship between empathy and burnout in medical students. Burnout, defined as a state of emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment [ 1 ], has become a pervasive issue within the medical field. One systematic review and meta-analysis of 4,664 international medical residents reported an overall burnout prevalence rate of 35.7% [ 2 ]. In US physicians, reports indicate a prevalence of burnout of 37.9%, compared to 27.8% in the general population [ 3 ]. Research indicates that burnout prevalence rates in medical students range from 7 to 75.2%, depending on the country in which the study was carried out, the instruments used and the cutoff-criteria for burnout symptomatology [ 4 ], with an overall suggested prevalence rate of 37.23% [ 5 ]. One US study found that 49.6% of medical students may experience burnout, compared to 35.7% of U.S. college graduates aged 22 to 32 [ 6 ]. Prospective studies suggest that burnout may increase from the first year of medical school to the final year [ 7 , 8 ].
Burnout among medical students has been found to be associated with poorer academic performance, increased rates of substance abuse, and impaired mental health, which could impact future physicians' ability to provide high quality, compassionate patient care [ 9 ]. Individual studies suggest that burnout may also be negatively associated with medical student empathy [ 10 ] .
Although multiple definitions of empathy have been suggested [ 11 ], it is generally considered to have three dimensions: cognitive empathy in which physicians use their cognitive abilities to take the perspective of their patient, an affective component in which physicians feel the emotions they believe their patient is experiencing, and a behavioral component in which the physicians communicate their understanding [ 12 ]. A consensus has grown around the definition of therapeutic empathy in recent years, defined as ' a physician's ability to understand the patient, communicate that understanding and act upon it in a therapeutic way. ' [ 13 ]. This definition prioritizes the cognitive understanding of the patient over the affective feeling of their emotions [ 14 ].
Medical students are increasingly expected to use and develop empathy as part of their medical education, as shown in curriculums specifically highlighting communication skills and empathy [ 15 , 16 ]. This is important given that empathetic healthcare consultations are associated with increased physician-patient trust [ 17 ], improved psychological and physical patient outcomes [ 18 , 19 ], and an increase in patient satisfaction by lowering patient anxiety and distress [ 19 , 20 ].
Therapeutic empathy may have benefits for physicians as well as patients. One systematic review of healthcare workers found negative associations between empathy and subdimensions of burnout: emotional exhaustion, depersonalization and reduced personal accomplishment [ 21 ]. Specifically, the authors found a negative association between perspective-taking (cognitive empathy) and depersonalization, and a positive association between perspective-taking and personal accomplishment. Similarly, they found a negative association between empathic concern (affective empathy) and depersonalization and a positive association between empathic concern and personal accomplishment. Emotional exhaustion was not related to either perspective-taking or empathic concern. Potential moderators were not explored in this systematic review, but a number of individual studies have suggested that gender [ 22 ] and age [ 23 ], amongst other variables, are also associated with empathy and burnout with the possibility of acting as moderators. Empathic concern (affective empathy) is higher in women compared to men, and perspective-taking (cognitive empathy) is higher in women and younger people compared to men and older people [ 23 ].
Despite having similarly high burnout levels to physicians, no systematic review and meta-analysis has explored the possible association between empathy and burnout in medical students. Given the high levels of burnout in medical students and an increasing focus on empathic skills in medical education, the aim of this systematic review and meta-analysis was to explore the possible association between empathy and burnout in medical students. This knowledge could be important for developing preventive strategies to avoid burnout, maintaining the mental health of medical students, promoting medical career sustainability and ensuring quality of care for present and future patients.
Purpose of the study
This systematic review and meta-analysis aimed to provide a quantitative synthesis of the existing literature on the relationship between empathy and burnout in medical students. We addressed the following research questions:
What is the overall association between empathy and burnout in medical students?
Are specific dimensions of empathy (cognitive, emotional, behavioral) differentially related to specific burnout dimensions (emotional exhaustion, depersonalization, reduced personal accomplishment)?
What moderating factors may influence the relationship between empathy and burnout in medical students (e.g. gender, age, study level, region)?
The protocol for the present study was preregistered in the International Prospective Register of Systematic Reviews (PROSPERO) (#CRD42023467670) [ 24 ]. The present study deviates from the protocol in the following ways: a) due to an existing systematic review on healthcare workers, physicians were no longer included as a population of interest, and b) due to a lack of studies, compassion fatigue was not included as a focus of this review. The review was conducted in accordance with the guidelines for Meta-Analysis Of Observational Studies in Epidemiology (MOOSE) [ 25 ] and is reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 26 ].
Search strategy and selection criteria
A comprehensive literature search was conducted on September 22, 2023 as per protocol, with an updated search conducted on January 10, 2024. The updated search only included medical students because physicians were no longer a population of interest. No publication date restrictions were applied. The electronic databases searched were: PubMed, EMBASE, CINAHL, The Cochrane Library, and PsycINFO. Where possible, relevant MeSH (Medical Subject Headings) terms or MeSH term equivalents were included in each database search. The specific search terms were: medical student* AND empathy AND burnout.
The study inclusion criteria were guided by the PICO (Population, Intervention/Exposure, Comparator, Outcome) approach [ 27 ]. Population: Medical students; Exposure: Medical school; Comparator: N/A; Outcome: Empathy and burnout assessed with a standardized, validated measurement scale. The study exclusion criteria were Population: Non-medical students; Exposure: Non-medical school; Comparator: N/A; Outcome: Non-empathy and burnout measures. Empathy and burnout assessed with non-standardized, unvalidated measurement scales.
We included correlational studies, including cross-sectional and longitudinal, prospective survey-based studies. Furthermore, only English-language papers published in peer-reviewed journals were considered eligible. We chose not to include non-English papers, as this might introduce biases related to language, publication bias, methodological heterogeneity, and challenges in access and quality assessment. While inclusivity is important, the potential for bias introduced by non-English papers outweighs the benefits of attempting a more comprehensive review. We excluded randomized controlled trials (RCTs), qualitative studies, case studies, open trials, uncontrolled trials, reviews and study protocols. The reason for this was that they were not designed to collect correlational data and test correlational hypotheses, or that they do not provide quantitative data. Additionally, including data from trials, e.g., baseline or control group data, may provide less generalizable data due to often highly selected study samples and that data are likely to be influenced by the experimental setup of such trials. Grey literature, for example, conference abstracts, trial registrations, dissertations and studies with N<10 was also not considered eligible.
The literature search and data extraction were conducted using the Covidence systematic review software [ 28 ]. In the first round of screening, PC and AEI independently screened the title and abstract of all identified references and excluded ineligible studies. In the second round of screening, the full text of the remaining studies were evaluated independently by PC and AEI and reasons for exclusion were registered. After each screening, the two authors discussed discrepancies, and reached a negotiated decision. Uncertainties and disagreements were discussed with the last author (RZ).
Quality assessment
A methodological quality assessment was undertaken independently by two authors (PC and AEI) for all included studies, using the National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [ 29 ]. The quality terms included whether the studies had a clearly defined research question and study population, whether the participation rate of eligible participants was at least 50%, whether the subjects were recruited from the same or similar populations, whether inclusion and exclusion criteria were used for all participants, whether a sample size justification such as a power description was provided, and if key confounding variables were measured and adjusted for statistically, among other questions.
Data extraction
Data extraction was performed independently by two authors (PC and AEI) and included authors, publication year, empathy aspect (cognitive, affective or behavioral), burnout dimension (emotional exhaustion, depersonalization or personal accomplishment), correlation statistic (Pearson's r , Spearman's ρ , or standardized β values), sample size, effect direction, whether the correlation was adjusted for other covariates (yes or no), number of covariates, study design (cross-sectional or longitudinal), response rate (as percentage), whether the relationship between empathy and burnout in medical students was the primary focus of the study (yes or no), sampling method (convenience, random), sample mean age, gender of participants (percent women), country, region (e.g., North America, Middle East, Europe, Asia), study level (early, late, or mixed), empathy scale, empathy subscale, burnout scale and burnout subscale. A meta-analysis was conducted when a minimum of three studies assessing an association between an empathy and a burnout dimension were available.
Categorization of empathy and burnout data
Empathy in the context of medical education is a multidimensional construct that encompasses cognitive, emotional, and behavioral components [ 12 ]. Cognitive empathy refers to the ability to understand the thoughts and perspectives of others, emotional empathy involves feeling and sharing the emotions of others, and behavioral empathy entails demonstrating empathetic behaviors, such as active listening and providing emotional support [ 30 ]. In the caring professions, 11 empathy measurement tools are available [ 31 ]. In order to make a meta-analysis possible and reduce the complexity of the findings, all empathy questionnaires were categorized as measuring either cognitive, affective or behavioral empathy. The study characteristics table (Table 1 ) provides the measurement tool used in each study and the empathy aspect categorized by the authors.
Burnout among medical students is usually conceptualized within the framework of the Maslach Burnout Inventory (MBI), which identifies three key dimensions: emotional exhaustion, depersonalization, and reduced personal accomplishment [ 1 ]. Emotional exhaustion refers to feelings of fatigue and emotional depletion, depersonalization involves cynicism and detachment from patients, and reduced personal accomplishment reflects a diminished sense of personal achievement and competence [ 1 ]. However, at least four other measurement tools for occupational burnout exist [ 51 ] with various dimensions, broadly aligning with the three dimensions of the MBI. All burnout questionnaires were categorized as measuring either emotional exhaustion, depersonalization or personal accomplishment. The study characteristics table (Table 1 ) provides the measurement tool used in each study and the burnout dimensions it was categorized as covering.
The three dimensions of burnout have different directions. For emotional exhaustion and depersonalization, greater scores signify greater burnout. For personal accomplishment, higher scores indicate less burnout. Therefore, when examining the association between global empathy and global burnout, correlations between empathy and personal accomplishment were reverse scored. When calculating the associations between the specific aspects of empathy and the various dimensions of burnout, personal accomplishment was not reverse scored.
Meta-analytic strategy
The effect size correlation (ESr) was used as the standardized effect size for the association between empathy and burnout. If correlations were not reported directly, ESr was converted from other data, for example, differences between means and standard deviations, regression coefficients, numbers or rates of study participants in relevant groups, χ 2 , F , or t statistics using various formulas. The calculations were conducted independently by two authors (PC and AEI) and checked by a third author (RZ) in case of disagreement. In case of missing data from the published report, the data was requested from the authors.
Effect sizes were calculated for both the unadjusted bivariate associations and the associations found in multivariate analyses adjusted for other covariates. Correlations between global empathy and global burnout were operationalized as the averaged correlations across the various individual dimensions for each study. The ESr was also used as a standardized effect size for the association between the different aspects of empathy (cognitive, affective and behavioural) and the dimensions of burnout (emotional exhaustion, depersonalization and personal accomplishment). The pooled effect size (ESr) and its 95% confidence interval was calculated using a random effects model. Heterogeneity was explored by calculating the I 2 statistic. The I 2 statistic is an estimate of the variance in a pooled ES that is accounted for by heterogeneity, i.e., true differences between effect sizes rather than sampling error [ 52 ]. We also calculated Tau ( T ), which represents the standard deviation of the true effect sizes, and the 95% prediction interval. The prediction interval takes both the random error and the systematic variance into consideration and quantifies the distribution of the ESs, indicating the range that 95% of results of future studies (from the same family of studies) are expected to fall within [ 53 ].
Publication bias, i.e., the tendency for statistically significant findings in the hypothesized direction to be more likely to be published, is a widespread problem in meta-analyses [ 54 ]. Although publication bias may be less likely in correlational than effect studies, we explored the possibility of using funnel plots and Egger's tests [ 55 ], but only when K > 10 (K = number of studies) [ 54 ]. If the results were suggestive of possible publication bias, we planned a sensitivity analysis adjusting the effect sizes using the Duval and Tweedie trim-and-fill method [ 56 ].
Possible sources of heterogeneity were explored with moderator analyses. When data were available for 10 independent samples or more, the possible influence of both continuous moderators (i.e., mean sample age, percent of women in the sample, response rate) and dichotomous moderators (i.e., student study level (late vs. early) and study quality (good or fair vs. poor)) were analyzed with meta-regression (computational model: maximum likelihood). For dichotomous moderators, the variable had to show sufficient variability, i.e. K > 3 in the smallest category. The R 2 equivalent was calculated for moderators reaching statistical significance.
All analyses were conducted using Comprehensive Meta-Analysis v4 [ 57 ] and various formulas in Microsoft Excel.
Supplementary Bayesian analyses
To aid the interpretation of the results, a Bayesian Model-Averaged meta-analysis [ 58 ] was conducted. The procedure examines the results of four models: a) Fixed-effect null hypothesis (fH 0 ), b) fixed-effect alternative hypothesis (fH 1 ), c) random-effects null hypothesis (rH 0 ), and d) random effects alternative hypothesis (rH 1 ). Bayesian Model-Averaged analysis thus avoids selecting either a fixed- or random-effects model and addresses two questions considering the observed data: What is the plausibility that the overall effect is non-zero and the ES are heterogeneous? An uninformed prior probability was chosen, i.e., 25%, of each of the four models, and 2000 iterations were used. With regard to parameter distributions, previously recommended defaults were chosen [ 58 ]. Thus, a zero-centered Cauchy prior with a scale of 0.707 for the ES was used. For the between-study variation, an empirically informed prior distribution on non-zero between-study deviation estimates based on standardized mean difference ESs from 705 meta-analyses published in Psychological Bulletin between 1990 and 2013 was used [ 59 ]. This distribution has been approximated by an Inverse-Gamma (1, 0.15) prior on the standard deviation (Tau) [ 58 ]. For each analysis, we calculated the Bayes Factor (BF) [ 60 ], which represents the posterior probability of the alternative hypothesis (H 1 ) relative to the probability of the null hypothesis. Based on the BF, the strength of the evidence was then categorized as "weak", “moderate”, “strong”, “very strong”, and “decisive” [ 61 ]. The Bayesian analyses were conducted with the computer software JASP (Version 0.17.1) [ 62 ].
Search results
A total of 498 articles were identified through digital database searches. After removal of duplicates, a total of 311 records were eligible for title and abstract screening. A total of 265 records were excluded after screening, leaving 46 articles eligible for full text screening. 25 articles were then excluded primarily due to “not responding to request for additional data” (68%), leaving 21 papers that were included in the systematic review. Ninety percent agreement was achieved by reviewers during the abstract review process and 95% agreement during full-text screening. All disagreements were resolved through negotiation. This negotiation involved the two reviewers PC and AEI providing the reason for their decision to include or exclude the relevant study. These reasons were then double-checked by both PC and AEI reviewing the individual study collaboratively. This led to agreement on whether to include or exclude the study in question. The study selection process is visualized in Fig. 1 . Authors of 25 studies were contacted and asked to provide additional data. Seven authors replied and provided the requested data.
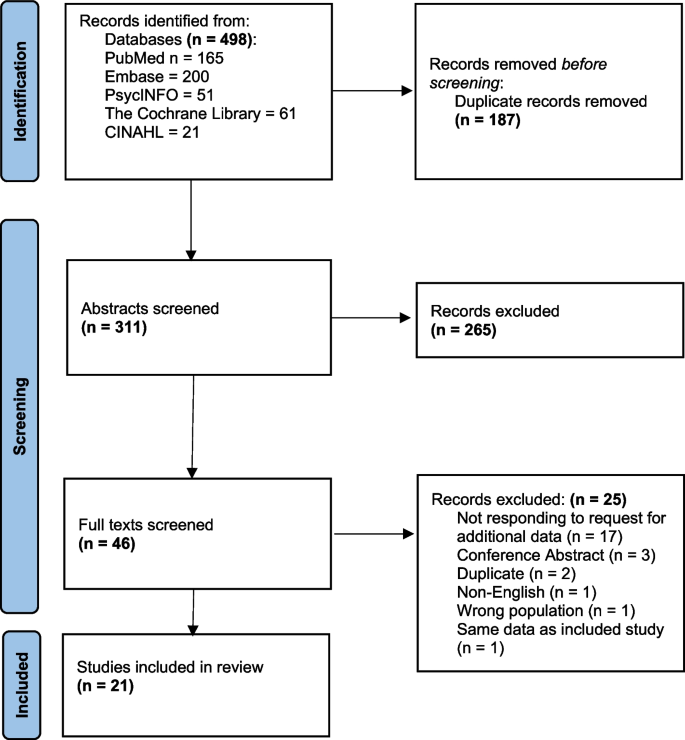
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram
Study characteristics
The participant characteristics, the empathy and burnout dimensions examined, the measurement tools used, and other characteristics of the included studies are summarized in Table 1 . The identified studies reported on 21 independent samples including a total of 27,129 medical students, with sample sizes ranging from 76 [ 47 ] to 14,126 [ 41 ]. The included articles were published between 2010 and 2023. The studies were broadly geographically distributed, with 7 studies conducted in North America, 4 in Asia, 4 in Europe, 3 in South America, 2 in Oceania, and 1 in the Middle East. Mean sample ages ranged from 19.9 [ 50 ] to 27.7 [ 41 ] years, with an overall weighted mean sample age of 25.2 years. The majority (90.4%) of the studies ( K = 19) used a cross-sectional design, and 9.6% ( K = 2) used a longitudinal design. As the majority of studies employed cross-sectional surveys across multiple study years, it was not possible to construct a continuous study year variable. We, therefore, categorized the study year as either early (years 1-3), late (years 4-6+), or mixed (1-6+).
Quality rating
See supplementary table S1 for an overview of the quality ratings of each study. Two studies were assessed to be of good quality (>9 criteria met), and 19 studies to be of fair quality (5 to 9 criteria met). Studies received high ratings when they presented a clear definition of the research question and study population, when there was a sufficient timeframe between longitudinal measurements, and when a sample size justification, i.e., statistical power calculation, was reported.
Overall association between empathy and burnout
The most commonly used scale to assess empathy was the Jefferson Scale of Empathy - Student version (K = 8), followed by the Interpersonal Reactivity Index (K = 7). The most commonly used scale to assess burnout was the Maslach Burnout Inventory – Student version (K = 5) and the Oldenburg Burnout Inventory (K = 5), followed by the Maslach Burnout Inventory – General Survey (K = 4) and the Maslach Burnout Inventory – Human Services Scale (K = 4). As mentioned above, empathy was characterized as having cognitive, affective, and behavioral components. Due to a lack of studies (K = 1), the behavioral aspect of empathy was not explored in this meta-analysis.
As shown in Table 2 and Fig. 2 , global empathy was negatively associated with global burnout in medical students, with the pooled correlation corresponding to a small effect size [ 63 ]. The supplementary Bayesian analysis indicated that, based on the available evidence, the alternative hypothesis, i.e., that the association between global empathy and global burnout is non-zero, was approximately 35 times more likely than the null hypothesis, corresponding to “very strong evidence” [ 61 ].
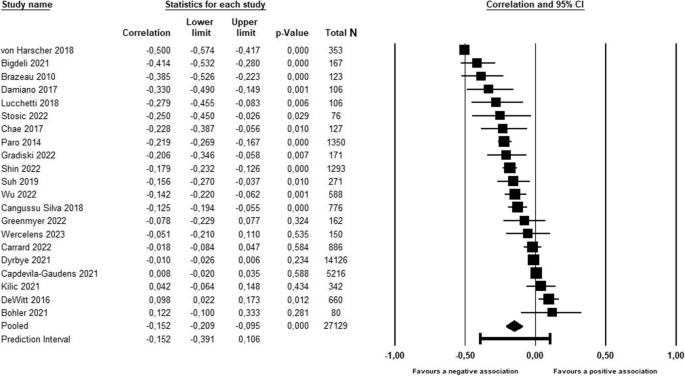
Forest plot of the association between empathy global and burnout global
As seen in Table 2 , the associations between global empathy and the three subcomponents of burnout all reached statistical significance. Again, the correlations were of small magnitude (ESr -0.19 to 0.20) and in the expected directions, with negative associations between global empathy and emotional exhaustion and depersonalization, and a positive association between global empathy and personal accomplishment. While there was “very strong evidence” for depersonalization and personal accomplishment, the results of the Bayesian analysis favored the null hypothesis for emotional exhaustion, albeit only with moderate level of evidence.
Associations between sub-dimensions of empathy and burnout
As shown in Table 2 , the associations between cognitive empathy and the three sub-dimensions of burnout all reached statistical significance. Again, the correlations were of small magnitude (ESr -0.10 to 0.21) and in the expected directions, with negative associations between cognitive empathy and emotional exhaustion and depersonalization, and a positive association between cognitive empathy and personal accomplishment. While there was “decisive evidence” for personal accomplishment and “weak evidence” for depersonalization, the results of the Bayesian analysis favored the null hypothesis for emotional exhaustion, albeit only with weak level of evidence.
As seen in Table 2 , the associations between affective empathy and the three sub-dimensions of burnout did not reach statistical significance. The results of the Bayesian analysis favored the null hypothesis with “strong evidence” for emotional exhaustion, “moderate evidence” for depersonalization, and “weak evidence” for personal accomplishment.
Publication bias
When examining the overall results, i.e., the association between global empathy and global burnout, we found no clear indications of possible publication bias. When inspecting the funnel plot (See supplementary materials, Figure S1), it did not appear particularly skewed, and neither Egger’s regression test ( p = 0.311) nor the rank correlation tests for Funnel plot asymmetry ( p = 0.740) reached statistical significance.
Heterogeneity
As shown in Table 2 , the results were characterized by considerable heterogeneity, with I 2 values ranging from 91.9% to 95.9%. This suggests that very high proportions of the variation in the correlations between empathy and burnout are explained by systematic, i.e., non-random, between-study differences. Based on the variation of the true values, the prediction intervals, i.e., the range of values that the results of 95% of future similar studies are expected to fall within, were wide for most association estimates.
Moderating variables
As seen in Table 3 , when exploring the potential sources of heterogeneity, the percentage of women in the sample and the response rate were the most consistent statistically significant moderators of the associations between empathy and burnout, explaining between 25% and 73% of the variation. The positive slopes found for the percentage of women and the associations between global empathy and global burnout and depersonalization, and the negative slope found for the association between global empathy and personal accomplishment, indicates that stronger negative associations between empathy and burnout were found in samples with fewer women, i.e., more men. The slopes found for response rates indicated that stronger associations in the expected direction between global empathy and two of the burnout dimensions were found in studies with higher response rates. The results for the remaining moderators, i.e., sample mean age, student study level (early vs. late), and study quality (good or fair vs. poor) did either not reach statistical significance or could not be analyzed due to insufficient data.
The purpose of this systematic review and meta-analysis was to examine the relationship between empathy and burnout in medical students. We found a negative, statistically significant association between empathy and burnout in medical students, with a small effect size. This relationship appeared to be primarily driven by cognitive empathy, which was negatively associated with emotional exhaustion and depersonalization and positively associated with personal accomplishment. Affective empathy was not statistically significant with any of the burnout sub-dimensions. Gender moderated the relationship between empathy and burnout such that the negative relationship between empathy and burnout was stronger in samples with more men. Finally, the response rates of included studies also moderated the relationship between empathy and burnout such that stronger, negative association between empathy and depersonalization and a stronger, positive association between empathy and personal accomplishment were found in studies with higher response rates. Sample mean age, student study level, and study quality either did not reach statistical significance or could not be analyzed due to insufficient data.
These results have some shared findings with that of a systematic review and meta-analysis examining empathy and burnout in healthcare workers, specifically doctors and nurses [ 21 ]. In this population, shared findings with our results included a negative association between perspective taking (cognitive empathy) and depersonalization, and a positive association with personal accomplishment. Furthermore, they also found no association between empathic concern (affective empathy) and emotional exhaustion. Some results from this population differed to ours. They did not find a significant association between perspective taking (cognitive empathy) and emotional exhaustion, which we did albeit with a Bayes Factor below 1 indicating weak support for the null hypothesis (no association between cognitive empathy and emotional exhaustion). Furthermore, empathic concern (affective empathy) was significantly negatively associated with depersonalization and significantly positively associated with personal accomplishment in their sample, whereas our sample showed no association between affective empathy and any burnout subscale.
The lack of associations or small effect size correlations between emotional exhaustion and cognitive and affective empathy which both we and the review including doctors and nurses [ 21 ] present, suggest that emotional exhaustion may not be influenced so much by empathy-related factors, but perhaps things such as high workloads and lack of sleep [ 64 ]. Possible explanations for differences between our findings could be that there are differences between how medical students’ and healthcare workers’ affective empathy and burnout interact, or that our use of multiple affective empathy scales compared to their use of the IRI only impacted the results.
Given that empathy involves other-orientated processes, including considering the other person’s perspective and feeling the emotions that the other may be experiencing, the negative association between empathy and depersonalization is less surprising.
Given that cognitive empathy involves taking the other person’s perspective, one could have expected that the main driver of the negative association between cognitive empathy and burnout was a negative association with depersonalization (viewing people as objects rather than human beings). Although this negative association was statistically significant, the main driver of cognitive empathy’s negative association with burnout was clearly a positive association with personal accomplishment. One explanation for this could be that by using cognitive empathy, medical students may be able to give the patients they encounter more personalized care plans that suit the patient’s life situation and values, as well as creating rapport and a sense of trust [ 65 ]. Medical students may perceive this as clinical competence, especially if they pass communication-based assessments such as OSCEs [ 66 ] as a result of this, and feel a sense of personal accomplishment. This greater sense of personal accomplishment may contribute to feeling less burnt out.
The finding that gender moderated the relationship between empathy and burnout such that the negative relationship between empathy and burnout was stronger in samples with more men, is a novel finding. Evidence suggests that both burnout and empathy levels are higher in women, yet the authors of the present study did not note any ceiling effect in women’s empathy or burnout scores in the eligible studies, or greater variability in men’s empathy or burnout scores which could explain gender’s moderating effect. One possible explanation is that women’s empathy is more robust so that that they can maintain higher empathy even whilst experiencing higher burnout, but further research is warranted.
The non-significant findings of this meta-analysis are also of interest. Affective empathy was not statistically significantly related to any of the burnout sub-dimensions. The lack of association between affective empathy and emotional exhaustion provided the strongest support for the null hypothesis of any association analyzed in this meta-analysis, as shown by a Bayes Factor approaching zero. These results do not support the idea that higher affective empathy is associated with higher emotional exhaustion or lower emotional exhaustion. Affective empathy was primarily measured using the Empathic Concern component of the Interpersonal Reactivity Index, which assesses an individual’s ‘ feeling for ’ another individual [ 67 ]. Other questionnaires assessing affective empathy included the Toronto Empathy Questionnaire, and subscales of the Empathy Quotient, the Questionnaire of Cognitive and Affective Empathy, and the Basic Empathy Questionnaire. These questionnaires generally assess an individual’s ‘ feeling with ’ another individual [ 31 ]. The results related to affective empathy did not appear to depend on the questionnaire used or the conceptualization of affective empathy as ‘ feeling for’ or ‘ feeling with ’ another. However, the affective empathy questionnaires used in the included studies do not have the highest reliability and validity [ 31 ] and these associations had the highest heterogeneity scores. This provides some doubts in interpreting these results, and further research is warranted.
Clinical implications
Although the results of this review do not provide evidence of direct causal links between empathy and burnout, they do indicate that in situations where medical student empathy is high, burnout is highly likely to be low, and vice versa. Given that medical student burnout is associated with poorer academic performance, increased rates of substance abuse, and impaired mental health [ 9 ], and higher medical student empathy is associated with higher personal accomplishment and clinical competence [ 68 ], medical educators are advised to create learning environments which foster empathy and reduce burnout. By creating preventative strategies to avoid burnout, maintaining the mental health of medical students, incorporating empathy-enhancing curriculums and promoting medical career sustainability, they can ensure quality of care for present and future patients.
Recommendations for future research
The vast majority of studies present in the literature and available for analysis used self-reported empathy measures. Although these scales are helpful ways to measure internal empathic attitudes among medical students, patient-rated empathy scales can provide useful information on patients’ ability to detect these attitudes. Future studies could examine the associations between patient-rated empathy and burnout in medical students. It is also well-known that self-efficacy, i.e., the confidence in one’s ability to exert a certain behavior, is a reliable predictor of the actual behavior [ 69 ], and future studies could explore the possible associations between medical student empathy and their self-efficacy in exhibiting patient-centered behaviors in the interaction with patients [ 70 ].
The behavioral component of empathy was not analyzed due to a lack of studies measuring it (K = 1) but could provide useful information on the expression of medical student internal empathic attitudes. Future studies could examine the associations between behavioral empathy and burnout in medical students. It was also not possible to examine study year as a moderating variable as studies did not report results from single year groups. Given that empathy may decline as medical students progress through medical school and burnout may increase [ 7 , 8 ], it may of use to observe the correlation between these two variables year-by-year.
Study limitations
Some study limitations should be noted. First, the high I 2 values suggest that a large proportion of the variation in results stems from underlying systematic differences between the available studies, rather than random error. While we identified two possible sources of the between-study variation, i.e., gender and response rates, the remaining included moderators either failed to explain a significant proportion of the variation or the data were not sufficient to conduct an analysis. Second, the included studies had assessed empathy and burnout with a range of different scales, diminishing across-study comparability and increasing between-study variability. Despite the fact that the most valid, standardized empathy measurement scales were used, the validity and reliability of these scales are still the topic of debate [ 31 ]. Thirdly, the majority of the studies included in this meta-analysis were cross-sectional in their study design and used bivariate correlations. Finally, burnout can be conceptualized in different ways, and it is possible that our merging of different concepts into one of the three MBI sub-dimensions: emotional exhaustion, depersonalization and personal accomplishment, may have reduced their explanatory power. For example, we combined the OBLI’s ‘disengagement’ sub-dimension with the MBI’s ‘depersonalization’. However, when rerunning the analysis separately for disengagement and depersonalization, it did not affect the results.
Due to only one study measuring behavioral empathy, we were not able to analyze its association with burnout. Further studies which categorize behaviors such as active listening and addressing patient emotions as behavioral empathy and analyze the association between these behaviors and burnout are required.
Our study is the first systematic review and meta-analysis to examine the association between empathy and burnout in medical students. Our results confirm an overall negative relationship between empathy and burnout in medical students. Furthermore, cognitive empathy appears to be negatively associated with the burnout sub-dimensions of emotional exhaustion and depersonalization and most robustly positively associated with personal accomplishment. Affective empathy was not consistently associated with any of the burnout sub-dimensions. Future research should examine which modifiable parts of the medical learning environment could be altered to lower burnout and foster empathy.
Availability of data and materials
Data is provided within the manuscript or supplementary information files. For extraction sheets, please contact the author Patrick Cairns [email protected]
Abbreviations
Effects size correlations
The International Prospective Register of Systematic Reviews
The guidelines for Meta-Analysis Of Observational Studies in Epidemiology
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Medical Subject Headings
Population, Intervention/Exposure, Comparator, Outcome
Maslach Burnout Inventory
Bayes Factor
Objective, structured, clinical examination
Maslach C, Schaufeli WB, Leiter MP. Job burnout. Ann Rev Psychol. 2001;52(1):397–422.
Article Google Scholar
Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, Souza T, Gonçalves AK. Burnout syndrome among medical residents: A systematic review and meta-analysis. PloS One. 2018;13(11):e0206840.
Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, West CP, Sloan J, Oreskovich MR. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–85.
Erschens R, Keifenheim KE, Herrmann-Werner A, Loda T, Schwille-Kiuntke J, Bugaj TJ, Nikendei C, Huhn D, Zipfel S, Junne F. Professional burnout among medical students: systematic literature review and meta-analysis. Med Teach. 2019;41(2):172–83.
Almutairi H, Alsubaiei A, Abduljawad S, Alshatti A, Fekih-Romdhane F, Husni M, Jahrami H. Prevalence of burnout in medical students: A systematic review and meta-analysis. Int J Soc Psychiatry. 2022;68(6):1157–70.
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med. 2014;89(3):443–51.
Ranasinghe PD, Owusu JT, Bertram A, Michtalik H, Yeh HC, Cofrancesco J Jr, Levine D, Miller ER III, Marinopoulos S. Depressive symptoms and burnout among medical students: a prospective study. J Gen Intern Med. 2022;37(1):64–9.
Ofei-Dodoo S, Moser SE, Kellerman R, Wipperman J, Paolo A. Burnout and other types of emotional distress among medical students. Med Sci Educ. 2019;29:1061–9.
IsHak W, Nikravesh R, Lederer S, Perry R, Ogunyemi D, Bernstein C. Burnout in medical students: a systematic review. Clin Teach. 2013;10(4):242–5.
Paro HB, Silveira PS, Perotta B, Gannam S, Enns SC, Giaxa RR, Bonito RF, Martins MA, Tempski PZ. Empathy among medical students: is there a relation with quality of life and burnout? PloS One. 2014;9(4):e94133.
Cuff BM, Brown SJ, Taylor L, Howat DJ. Empathy: a review of the concept. Emot Rev. 2016;8(2):144–53.
Nembhard IM, David G, Ezzeddine I, Betts D, Radin J. A systematic review of research on empathy in health care. Health Serv Res. 2023;58(2):250–63.
Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002;52(Suppl):S9-12.
Google Scholar
Howick J, Bizzari V, Dambha-Miller H. Therapeutic empathy: what it is and what it isn’t. J Royal Soc Med. 2018;111(7):233–6.
Venktaramana V, Loh EK, Wong CJ, Yeo JW, Teo AY, Chiam CS, Foo DJ, Teo F, Liang J, Raveendran V, Chng LC. A systematic scoping review of communication skills training in medical schools between 2000 and 2020. Med Teach. 2022;44(9):997–1006.
Winter R, Ward A, Norman RI, Howick J. A survey of clinical empathy training at UK medical schools. BMC Med Educ. 2023;23(1):1–3.
Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237–51.
Howick J, Moscrop A, Mebius A, Fanshawe TR, Lewith G, Bishop FL, Mistiaen P, Roberts NW, Dieninytė E, Hu XY, Aveyard P. Effects of empathic and positive communication in healthcare consultations: a systematic review and meta-analysis. J Royal Soc Med. 2018;111(7):240–52.
Mistiaen P, Van Osch M, Van Vliet L, Howick J, Bishop FL, Di Blasi Z, Bensing J, Van Dulmen S. The effect of patient–practitioner communication on pain: a systematic review. Eur J Pain. 2016;20(5):675–88.
Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76-84.
Delgado N, Delgado J, Betancort M, Bonache H, Harris LT. What is the link between different components of empathy and burnout in healthcare professionals? A systematic review and meta-analysis. Psychol Res Behav Manag. 2023;31:447–63.
Suh WW, Cho SH, Yoo JY, Kim HS, Song HR, Kim WJ, Lee SM, Hong M. Relationship between psychological correlates and empathy in medical students: a cross-sectional study. Psychiatry Investig. 2019;16(10):766.
Sommerlad A, Huntley J, Livingston G, Rankin KP, Fancourt D. Empathy and its associations with age and sociodemographic characteristics in a large UK population sample. PloS One. 2021;16(9):e0257557.
Booth A, Clarke M, Dooley G, Ghersi D, Moher D, Petticrew M, Stewart L. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev. 2012;1(1):1–9.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. J Am Med Assoc. 2000;283(15):2008–12.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;1(88):105906.
Sackett DL. Evidence-based medicine. InSeminars in perinatology. 1997 (Vol. 21, No. 1, p. 3–5). Philadelphia: WB Saunders.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. 2024
National Heart, Lung, and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. National Institutes of Health; 2014. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools .
Hojat M, Spandorfer J, Louis DZ, Gonnella JS. Empathic and sympathetic orientations toward patient care: conceptualization, measurement, and psychometrics. Acad Med. 2011;86(8):989–95.
Hong H, Han A. A systematic review on empathy measurement tools for care professionals. Educ Gerontol. 2020;46(2):72–83.
Bigdeli S, Arabshahi SK, Zazoly AZ, Norouzi A, Yazd NA, Hosseini AF. Empathy, quality of life and occupational burnout among medical students. Res Dev Med Educ. 2021;10(1):21.
Bohler TE, Brown RF, Dunn S. Relationship between affective state and empathy in medical and psychology students. Aust Psychol. 2021;56(4):311–23.
Brazeau CM, Schroeder R, Rovi S, Boyd L. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(10):S33-6.
Cangussu Silva A, Ezequiel OD, Damiano RF, Granero Lucchetti AL, DiLalla LF, Dorsey JK, Lucchetti G. Translation, transcultural adaptation, and validation of the empathy, spirituality, and wellness in medicine scale to the Brazilian Portuguese Language. Teach Learn Med. 2018;30(4):404–14.
Capdevila-Gaudens P, García-Abajo JM, Flores-Funes D, García-Barbero M, García-Estañ J. Depression, anxiety, burnout and empathy among Spanish medical students. PloS One. 2021;16(12):e0260359.
Carrard V, Bourquin C, Berney S, Schlegel K, Gaume J, Bart PA, Preisig M, Schmid Mast M, Berney A. The relationship between medical students’ empathy, mental health, and burnout: a cross-sectional study. Med Teach. 2022;44(12):1392–9.
Chae SJ, Jeong SM, Chung YS. The mediating effect of calling on the relationship between medical school students’ academic burnout and empathy. Korean J Med Educ. 2017;29(3):165.
Damiano RF, DiLalla LF, Lucchetti G, Dorsey JK. Empathy in medical students is moderated by openness to spirituality. Teach Learn Med. 2017;29(2):188–95.
DeWitt D, Canny BJ, Nitzberg M, Choudri J, Porter S. Medical student satisfaction, coping and burnout in direct-entry versus graduate-entry programmes. Med Educ. 2016;50(6):637–45.
Dyrbye LN, Satele D, West CP. Association of characteristics of the learning environment and US medical student burnout, empathy, and career regret. JAMA Netw Open. 2021;4(8):e2119110.
Gradiski IP, Borovecki A, Ćurković M, San-Martín M, Delgado Bolton RC, Vivanco L. Burnout in international medical students: characterization of professionalism and loneliness as predictive factors of burnout. Int J Environ Res Public Health. 2022;19(3):1385.
Greenmyer JR, Montgomery M, Hosford C, Burd M, Miller V, Storandt MH, Lakpa KL, Tiongson C. Guilt and burnout in medical students. Teach Learn Med. 2022;34(1):69–77.
Kilic R, Nasello JA, Melchior V, Triffaux JM. Academic burnout among medical students: respective importance of risk and protective factors. Public Health. 2021;1(198):187–95.
Lucchetti G, Damiano RF, DiLalla LF, Lucchetti AL, Moutinho IL, da Silva Ezequiel O, Kevin Dorsey J. Cross-cultural differences in mental health, quality of life, empathy, and burnout between US and Brazilian medical students. Acad Psychiatry. 2018;42:62–7.
Shin HS, Park H, Lee YM. The relationship between medical students’ empathy and burnout levels by gender and study years. Patient Educ Counsel. 2022;105(2):432–9.
Stosic MD, Blanch-Hartigan D, Aleksanyan T, Duenas J, Ruben MA. Empathy, friend or foe? Untangling the relationship between empathy and Burnout in helping professions. J Soc Psychol. 2022;162(1):89–108.
von Harscher H, Desmarais N, Dollinger R, Grossman S, Aldana S. The impact of empathy on burnout in medical students: new findings. Psychol Health Med. 2018;23(3):295–303.
Wercelens VO, Bueno ML, Bueno JL, Abrahim RP, Ydy JG, Zanetti HR, Montayre J, Maximiano-Barreto MA. Empathy and psychological concerns among medical students in Brazil during the COVID-19 pandemic. Int J Psychiatry Med. 2023;23:00912174231179069.
Wu W, Ma X, Liu Y, Qi Q, Guo Z, Li S, Yu L, Long Q, Chen Y, Teng Z, Li X. Empathy alleviates the learning burnout of medical college students through enhancing resilience. BMC Med Educ. 2022;22(1):1–1.
Shoman Y, Marca SC, Bianchi R, Godderis L, Van der Molen HF, Canu IG. Psychometric properties of burnout measures: a systematic review. Epidemiol Psychiatr Sci. 2021;30:e8.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003;327(7414):557–60.
IntHout J, Ioannidis JP, Rovers M, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6(7):e010247.
Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002.
Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63.
Borenstein, M., et al., Comprehensive Meta-Analysis Version 4. 2022, Englewood: Biostat.
Gronau QF, van Erp S, Heck DW, Cesario J, Jonas KJ, Wagenmakers E-J. A Bayesian model-averaged meta-analysis of the power pose effect with informed and default priors: the case of felt power. Comprehensive Results Soc Psychol. 2017;2:123–38.
van Erp S, Verhagen AJ, Grasman RPPP, Wagenmakers E-J. Estimates of between-study heterogeneity for 705 meta-analyses reported in Psychological Bulletin from 1990–2013. J Open Psychol Data. 2017;5:4.
Goodman SN. Toward evidence-based medical statistics. 2: The Bayes factor. Ann Intern Med. 1999;130(12):1005–13.
Jeffreys H. The theory of probability. 3rd ed. Oxford, UK: Oxford University Press; 1961.
JASP_Team. JASP (Version 0.17. 1)[Computer Software]. 2023.
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Erlbaum Associates; 1988.
Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38:438–44.
Wu Q, Jin Z, Wang P. The relationship between the physician-patient relationship, physician empathy, and patient trust. J Gen Internal Med. 2022;37(6):1388–93.
Harden RM. What is an OSCE? Med Teach. 1988;10(1):19–22.
Davis MH. Measuring individual differences in empathy: Evidence for a multidimensional approach. J Personal Soc Psychol. 1983;44(1):113.
Casas RS, Xuan Z, Jackson AH, Stanfield LE, Harvey NC, Chen DC. Associations of medical student empathy with clinical competence. Patient Educ Counsel. 2017;100(4):742–7.
Bandura A. Self-efficacy - The exercise of control. New York: Freeman and Company; 1997.
Zachariae R, O’Connor M, Lassesen B, Olesen M, Kjaer LB, Thygesen M, et al. The self-efficacy in patient-centeredness questionnaire - a new measure of medical student and physician confidence in exhibiting patient-centered behaviors. BMC Med Educ. 2015;15:150.
Download references
Patrick Cairns was funded by a PhD Fellowship from Aarhus University School of Business and Social Sciences. No other funding sources were used.
Author information
Authors and affiliations.
Unit for Psycho-Oncology & Health Psychology, Department of Psychology and Behavioural Sciences, Aarhus University, Aarhus, Denmark
P. Cairns & R. Zachariae
Research and Development Department, Division of Mental Health Services, Akershus University Hospital, Sykehusveien 25, 1478, Nordbyhagen, Norway
A. E. Isham
Department of Oncology, Aarhus University Hospital, Aarhus, Denmark
R. Zachariae
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the protocol of this systematic review and meta-analysis. The literature search and data export were performed by PC. Titles and abstracts were screened by PC and AEI. PC and AEI performed full text review, validated by RZ. Data extraction and quality ratings were performed by PC and AEI and validated by RZ. RZ and PC were responsible for the analyses. PC and RZ wrote the first draft manuscript, and all authors critically revised the manuscript and approved the final version.
Corresponding author
Correspondence to P. Cairns .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1. , supplementary material 2. , rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Cairns, P., Isham, A.E. & Zachariae, R. The association between empathy and burnout in medical students: a systematic review and meta-analysis. BMC Med Educ 24 , 640 (2024). https://doi.org/10.1186/s12909-024-05625-6
Download citation
Received : 19 January 2024
Accepted : 03 June 2024
Published : 07 June 2024
DOI : https://doi.org/10.1186/s12909-024-05625-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical students
- Systematic review
- Meta-analysis
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Step 5 - Write your literature review. Like any other academic text, your literature review should have an introduction, a main body, and a conclusion. What you include in each depends on the objective of your literature review. Introduction. The introduction should clearly establish the focus and purpose of the literature review.
A literature review is a critical analysis and synthesis of existing research on a particular topic. It provides an overview of the current state of knowledge, identifies gaps, and highlights key findings in the literature. 1 The purpose of a literature review is to situate your own research within the context of existing scholarship ...
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays).
Steps to Completing a Literature Review. Find. Conduct searches for relevant information. Evaluate. Critically review your sources. Summarize. Determine the most important and relevant information from each source, theories, findings, etc. Synthesize. Create a synthesis matrix to find connections between resources, and ensure your sources ...
Your report, in addition to detailing the methods, results, etc. of your research, should show how your work relates to others' work. A literature review for a research report is often a revision of the review for a research proposal, which can be a revision of a stand-alone review. Each revision should be a fairly extensive revision.
3. Evaluate and select literature. 4. Analyze the literature. 5. Plan the structure of your literature review. 6. Write your literature review. Other resources to help you write a successful literature review.
Example: Predictors and Outcomes of U.S. Quality Maternity Leave: A Review and Conceptual Framework: 10.1177/08948453211037398 ; Systematic review: "The authors of a systematic review use a specific procedure to search the research literature, select the studies to include in their review, and critically evaluate the studies they find." (p. 139).
A literature review is often the foundation for a theoretical framework. You can use it to discuss various theories, models, and definitions of key concepts. You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research. Step 5: Write your literature review
How to write a literature review in 6 steps. How do you write a good literature review? This step-by-step guide on how to write an excellent literature review covers all aspects of planning and writing literature reviews for academic papers and theses.
The best proposals are timely and clearly explain why readers should pay attention to the proposed topic. It is not enough for a review to be a summary of the latest growth in the literature: the ...
As mentioned above, writing your literature review is a process, which I'll break down into three steps: Finding the most suitable literature. Understanding, distilling and organising the literature. Planning and writing up your literature review chapter. Importantly, you must complete steps one and two before you start writing up your chapter.
Structure planning to write a good literature review; 1. Outline and identify the purpose of a literature review. As a first step on how to write a literature review, you must know what the research question or topic is and what shape you want your literature review to take. Ensure you understand the research topic inside out, or else seek ...
Step One: Decide on your areas of research: Before you begin to search for articles or books, decide beforehand what areas you are going to research. Make sure that you only get articles and books in those areas, even if you come across fascinating books in other areas. A literature review I am currently working on, for example, explores ...
The purpose of a literature review. The four main objectives of a literature review are:. Studying the references of your research area; Summarizing the main arguments; Identifying current gaps, stances, and issues; Presenting all of the above in a text; Ultimately, the main goal of a literature review is to provide the researcher with sufficient knowledge about the topic in question so that ...
A literature review may consist of simply a summary of key sources, but in the social sciences, a literature review usually has an organizational pattern and combines both summary and synthesis, often within specific conceptual categories.A summary is a recap of the important information of the source, but a synthesis is a re-organization, or a reshuffling, of that information in a way that ...
A literature review is an integrated analysis-- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question.That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
A literature or narrative review is a comprehensive review and analysis of the published literature on a specific topic or research question. The literature that is reviewed contains: books, articles, academic articles, conference proceedings, association papers, and dissertations. It contains the most pertinent studies and points to important ...
Writing a literature review requires a range of skills to gather, sort, evaluate and summarise peer-reviewed published data into a relevant and informative unbiased narrative. Digital access to research papers, academic texts, review articles, reference databases and public data sets are all sources of information that are available to enrich ...
A literature review is a review and synthesis of existing research on a topic or research question. A literature review is meant to analyze the scholarly literature, make connections across writings and identify strengths, weaknesses, trends, and missing conversations. A literature review should address different aspects of a topic as it ...
Demonstrate your knowledge of the research topic. Identify the gaps in the literature and show how your research links to these. Provide the foundation for your conceptual framework (if you have one) Inform your own methodology and research design. To achieve this, your literature review needs a well-thought-out structure.
The word "literature review" can refer to two related things that are part of the broader literature review process. The first is the task of reviewing the literature - i.e. sourcing and reading through the existing research relating to your research topic. The second is the actual chapter that you write up in your dissertation, thesis or ...
A literature review discusses published information in a particular subject area, and sometimes information in a particular subject area within a certain time period. A literature review can be just a simple summary of the sources, but it usually has an organizational pattern and combines both summary and synthesis.
Literature reviews are in great demand in most scientific fields. Their need stems from the ever-increasing output of scientific publications .For example, compared to 1991, in 2008 three, eight, and forty times more papers were indexed in Web of Science on malaria, obesity, and biodiversity, respectively .Given such mountains of papers, scientists cannot be expected to examine in detail every ...
The inclusion criteria for this systematic review included: 1) Population: Patients diagnosed with any diseases or symptoms; 2) Intervention: Any interventions involving digital twins; 3) Controls ...
Of the 10 studies included in the review, eight were conducted in the United States, and two in the United Kingdom. The studies used various study designs, including observational case-control (n = 4), randomised control trial (n = 3) and quasi-experimental (n = 3). The characteristics of included studies are summarised in Table 3. Two ...
Radiographic evaluation of these patients included plain X-rays, CT, and MRI. Following confirmation of a diagnosis of VH, these images were used to generate the figures used in this manuscript. Moreover, an extensive literature search was conducted using PubMed for the literature review portion of the manuscript.
Despite its ubiquity in academic research, the phrase 'ethical challenge(s)' appears to lack an agreed definition. A lack of a definition risks introducing confusion or avoidable bias. Conceptual clarity is a key component of research, both theoretical and empirical. Using a rapid review methodology, we sought to review definitions of 'ethical challenge(s)' and closely related terms as ...
Included studies comprised three narrative case studies [29,30,31] a randomised control trial []; a narrative review [] a practitioners' guidance document []; and a naturalistic study [].Critical appraisal of the evidence (Table 1) demonstrates that caution must be exercised when considering the findings.The main strength of the included studies is the voice of young people through verbatim ...
Studies included in this review were classified as primary research, published in English since 2006, some intervention implemented to improve adherence to treatment. This review excluded any studies that related to with cancer and mental health condition, animal studies and grey literature. Quality appraisal and data extraction
The protocol for the present study was preregistered in the International Prospective Register of Systematic Reviews (PROSPERO) (#CRD42023467670) [].The present study deviates from the protocol in the following ways: a) due to an existing systematic review on healthcare workers, physicians were no longer included as a population of interest, and b) due to a lack of studies, compassion fatigue ...