
Transforming the understanding and treatment of mental illnesses.
Información en español

Celebrating 75 Years! Learn More >>
Research funded by nimh, research conducted at nimh (intramural research program), priority research areas.
- Research Resources
The National Institute of Mental Health (NIMH), part of the National Institutes of Health (NIH), is the lead federal agency for research on mental disorders, supporting research that aims to transform the understanding and treatment of mental illnesses through basic and clinical research. Learn more about NIMH-funded research areas, policies, resources, initiatives, and research conducted by NIMH.
Notify the NIMH Press Team about NIMH-funded research that has been submitted to a journal for publication, and we may be able to promote the findings.

NIMH Strategic Plan
The NIMH Strategic Plan for Research outlines the Institute's research goals and priorities over the next five years. Learn more about the Strategic Plan.
NIMH supports research at universities, medical centers, and other institutions via grants, contracts, and cooperative agreements. Learn more about NIMH research areas, policies, resources, and initiatives:
- Research Domain Criteria (RDoC)
- Policies and Procedures
- Inside NIMH - Funding and Research News
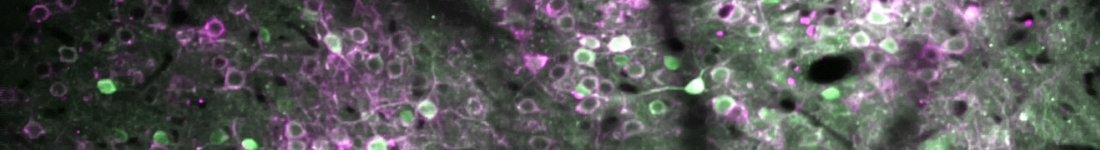
The Division of Intramural Research Programs (IRP) is the internal research division of the NIMH. Over 40 research groups conduct basic neuroscience research and clinical investigations of mental illnesses, brain function, and behavior at the NIH campus in Bethesda, Maryland. Learn more about research conducted at NIMH:
- Intramural Investigators
- Intramural Research Groups
- Fellowships and Training
- Office of the Scientific Director
- Collaborations and Partnerships
- Join a Study
- IRP News and Events

- Research Areas
- NIMH Priority Research Areas
- Highlighted Research Initiatives
- Women Leading Mental Health Research
Resources for Researchers
- Psychosocial Research at NIMH: A Primer
- Genomics Research Guidance for Grant Applicants
NIMH Women Leading Mental Health Research
Diversity in the scientific workforce enhances excellence, creativity, and innovation. NIMH and the National Institutes of Health (NIH) are committed to increasing diversity in the scientific workforce. Learn more about early-career women scientists whose NIMH-funded research is playing a role in advancing our mission of transforming the understanding and treatment of mental illnesses.
- Frontiers in Psychology
- Health Psychology
- Research Topics
Mental Health of Healthcare Professionals
Total Downloads
Total Views and Downloads
About this Research Topic
Mental health issues (including anxiety, depression, stress, burnout, suicidality, tobacco and alcohol use) in various healthcare professionals, such as physicians of different specialties, nurses working in various settings, psychologists, have become increasing concerns in many countries. Studies suggested ...
Keywords : Mental health, Healthcare professionals, Psychological resilience and well-being, Correlates, Effective interventions
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
- Signs of Addiction
Health care Professionals and Mental Health
Butler center for research - december 2021.

- Addiction Resources
- Addiction Journals and Abstracts
- Addiction Research Library
- About the Butler Center for Research
Download the Health Care Professionals and Mental Health Research Update.
Introduction
Every day, health care professionals (HCPs) are tasked with performing lifesaving actions and guarding the well-being of our communities. HCPs carry a tremendous weight of responsibility to perform at a high level, which can come with repercussions regarding their own mental health. Research shows that HCPs suffer from mental illnesses such as depression, anxiety, stress and substance abuse at a greater rate than that of the general population. 1, 2, 3, 4, 5 With HCPs working tirelessly to provide care to victims of the COVID-19 pandemic, on top of the demanding needs of their own specialties, it is even more evident that HCPs are in great need of mental health support. As one article remarks, HCPs "will be the heroes of the day, but we will need them for tomorrow." 6
Poor Mental Health in HCPs vs. the General Population
Recent research has documented the prevalence of poor mental health trends in HCPs. It is evident that they suffer from stress, anxiety, depression, PTSD and substance abuse at a higher rate than the general population of the United States. 7 A number of studies have found:
- In a survey of U.S. physicians, 87% of respondents report they are severely burned out or stressed. 7
- In comparison to the 3.1% of the U.S. population who report experiencing anxiety, 52% of emergency medical professionals have varying degrees of anxiety. 2, 8
- The average prevalence of depression among physicians is estimated to be 28.8%, ranging from 20.9% to 43.2%, depending on specialty and field. 3 This can be compared to the estimated 7.1% of all U.S. adults who suffer from depressive symptoms. 9
- The prevalence of PTSD in U.S. adults is estimated to be 3.8%. PTSD among emergency physicians was found to be 15.8%. 4
Lastly, while the rates of substance abuse for HCPs and the general population were fairly similar, it should be noted that prevalence of substance abuse among HCPs is particularly disturbing as they are the caregivers responsible for the health and wellbeing of the general population. 5 Therefore, while substance abuse severely affects any individual, the repercussions of substance abuse among HCPs have the potential to cause much more harm.
How Is COVID-19 Affecting This Trend?
While the pandemic has proved to be challenging for everyone, it should be noted that HCPs are particularly vulnerable to emotional distress in the current pandemic due to their close proximity to the disease and the high demand for their services. 10 HCPs may experience a range of stressors during this time such as uncertain prognoses, shortages of protective resources, conflicting messages from authorities, the anxiety around the risk of contagion, and concern about infecting and caring for their loved ones. 10, 11 Perhaps overlooked may be the psychological stress related to the ambiguity of COVID-19. As one study remarks, HCPs are neither prepared nor trained to let people die whom they could save under normal circumstances.10 The great volume of traffic in hospitals—combined with shortage of materials and overworking—prevents HCPs from performing at their highest quality. These factors may lead to incidences of moral injury, or the psychological distress that results from actions, or the lack of them, that violate a provider's moral or ethical code. 6
While COVID-19 is a new and not yet fully understood disease, it is not our first pandemic. A study that tracked the mental health of HCPs after the SARS outbreak found that hospital workers, particularly doctors and nurses, were more susceptible to psychological disorders after participating in the treatment of SARS patients over a decade ago. This suggests that their participation in fighting a pandemic may have weakened and worsened their mental health in the long run. 12 A similar study showed that HCPs who worked in SARS units and hospitals during the outbreak also reported depression, anxiety, fear and frustration as a result of the stressful environment they were working in. 13 This research indicates that the effects of the current pandemic are likely to continue affecting HCPs long after the pandemic has slowed. Based on experience from past viral epidemics, the development and implementation of mental health assessment, support, treatment and services are crucial and pressing goals for the health response to the COVID-19 outbreak. 13
What Is Causing Poor Mental Health in HCPs?
Occupational factors central to any career in the health care field present obstacles to positive mental health in HCPs. The very characteristics that make an HCP successful in their role—such as conscientiousness, obsessiveness and perfectionism—may also increase their risk of developing mental health problems and increase their inability to unwind and replenish their inner resources. 14 Furthermore, the lifestyle of an HCP itself may be a source of poor mental health.
Several studies suggest that poor mental health in HCPs is exacerbated by: 15, 16
- Extensive workload and long hours
- Over-demanding patients
- Scanty resources
- Ethical and legal issues
- Constant exposure to stressful situations and the need for critical decision-making
- Fear of failure
These stressors not only appear once an HCP is steadily employed in a hospital or specialty; rather it has been found that the root of such tensions often originates in medical school. A study of medical students in Ethiopia found that one in two students struggle with depression, one in three reported anxiety and one in five reported comorbid depression and anxiety. 17 These statistics indicate that medical school represents the beginning of poor mental health trends for HCPs. The study hypothesized that a new environment, new friends and being apart from family could be central to the higher rates of anxiety in medical students. 17
What Are the Consequences of Poor Mental Health for HCPs?
The personal and professional repercussions of poor mental health on HCPs are well documented in research. A study of burnout in physicians in the U.S. found emotional exhaustion, depersonalization and a sense of reduced accomplishment to be highly prevalent across specialties. 18 Furthermore, a survey of nearly 5,000 U.S. physicians showed that 43.9% reported at least one symptom of burnout, which is emotional exhaustion due to constant exposure to stressful situations in the workplace. This study indicated that burnout in HCPs manifests personally and professionally. 19
In terms of professional consequences, burnout may cause: 18
- Increased medical errors
- Risk of malpractice
- Reduced patient satisfaction
- Failure of interpersonal relationships
- The untimely departure of physicians from their jobs
With regard to personal consequences, burnout may lead to: 18
- Increased incidence of stress
- Increased odds of substance abuse and dependence
- Increased risk of depression
- An increase in suicidality and suicidal ideation
A study of the professional consequences of poor mental health in HCPs found that in a population of 7,905 surgeons, 8% committed major medical errors due to lapses in judgment, and both burnout and depression were independent risk factors for major medical errors. 20 Research evaluating occupational stress among physicians identified that the majority of physicians in their study admitted that patient care is affected negatively by their stress at work. 21 Thus it is clear that HCPs will not be able to deliver the highest quality of care they can if they are struggling with poor mental health. This indicates that while HCPs would benefit greatly from mental health support and resources, so would patients.
Support for HCPs through Programs and Interventions
Some hospital administrators have implemented programs to target stress reduction among their HCPs. A research review of interventions designed to improve the well-being of general practitioners found that cognitive, behavioral and mindfulness-based interventions significantly reduced stress in doctors when implemented by hospital staff. 22 This study concluded that, after the implementation of a 10-week mindfulness-based intervention, a significant reduction in stress and anxiety was reported in general practitioners and persisted at a six-month follow-up. 22
Other researchers have pointed to resources outside of work as being crucial to positive mental health in HCPs. For example, one study found that the family environment is an important protective factor against the development of depressive disorders, and therefore, seeking support at home could halt the growth of poor mental health trends. 16 Another study found that prevention of burnout and stress disorders requires rest and disconnection. 10 While these relaxation and disconnection opportunities could be provided by the hospital or organization, they could also be explored outside the workplace with family or friends. 10
In a recent research review, six studies exploring mental health interventions mainly focused on individual approaches, most often requiring health care workers to initiate contact. Proactive organizational approaches could be less stigmatizing and more effective; more research providing evidence on the efficacy of interventions/strategies is needed. 23 While many health organizations have committed resources to the well-being of HCPs, only a few have published their protocols of intervention. The majority opted for helpline services, usually applicable and effective for urgent social and psychological problems. 24
The scientific community has pointed out that there is a need to develop tailored mental health interventions for HCPs. 25 Yet current findings of emotional distress among health care workers might indicate that the health care system is not able to effectively help the helpers. 23 Understanding the risks and mental health impact(s) that health care workers experience and identifying possible interventions to address adverse effects are invaluable. 23
HCPs carry immense responsibility in their day-to-day work, which may have detrimental effects on their mental health. Excellent professional performance as an HCP is often synonymous with managing the taxing aspects of the job such as long work hours, constant exposure to stressful situations and the pressure to make split-second decisions with an individual's life weighing in the balance. Because of these factors, HCPs face mental illness at a higher rate than the general population; however, few resources are made readily available to them. While this dilemma was present before the current pandemic, COVID-19 has only exacerbated the stress and pressure on HCPs, and it threatens to have long-term effects on frontline workers. Programs have been implemented to improve the mental health of HCPs and have shown success in reducing stress, anxiety and depression. However, the research community has pointed out that there is a need to develop more mental health interventions tailored to health care professionals.
HCPs face mental illness at a higher rate than the general population; however, few resources are made readily available to them
The hazelden betty ford foundation experience.
Hazelden Betty Ford Foundation offers comprehensive addiction treatment programs designed specifically for health care professionals (HCP). These programs follow evidence-based best practices for addressing the unique problems faced by HCPs as patients and recovering addicts. The programs also offer help with issues related to professional licensure, employment and medical reputation.
How To Use This Information
For health care professionals: The health care field is demanding, and stressors are inevitable. Sometimes it can become routine to ignore the effects of stress and trauma, and miss the signs that you need support. It is important to check in with yourself frequently. Reach out for support if you are experiencing warning signs that may include feeling irritable or angry, anxious, depressed, lonely or constantly sad; isolating yourself and having a lack of trust in others; struggling to sleep or oversleeping; pursuing new or increased substance use; or experiencing physical issues that impact you in unexpected ways. Taking care of yourself is essential.
For health care administrators: Know your staff by watching for changes in work habits, attendance patterns and interactions with others. Be sure to show support, provide resources and encourage self-care.
- Rotenstein, L. S., Ramos, M. A., Torre, M., Segal, J. B., Peluso, M. J., Guille, C., Sen, S., & Mata, D. A. (2016). Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. Journal of the American Medical Association, 316(21), 2214–2236. doi:10.1001/jama.2016.17324
- Alharthy, N., Alrajeh, O. A., Almutairi, M., & Alhajri, A. (2017). Assessment of anxiety level of emergency health-care workers by generalized anxiety disorder-7 tool. International Journal of Applied & Basic Medical Research, 7(3), 150–154. doi.org/10.4103/2229-516x.212963
- Mata, D. A., Ramos, M. A., Bansal, N., Khan, R., Guille, C., Di Angelantonio, E., & Sen, S. (2015). Prevalence of depression and depressive symptoms among resident physicians: A systematic review and meta-analysis. Journal of the American Medical Association, 314(22), 2373–2383. doi:10.1001/jama.2015.15845
- DeLucia, J. A., Bitter, C., Fitzgerald, J., Greenberg, M., Dalwari, P., & Buchanan, P. (2019). Prevalence of post-traumatic stress disorder in emergency physicians in the United States. Western Journal of Emergency Medicine, 20(5), 740–746. doi:10.5811/westjem.2019.7.42671
- Baldisseri, M. R. (2007) Impaired healthcare professional. Critical Care Medicine, 35(2 Suppl), S106–S116. doi:10.1097/01.CCM.0000252918.87746.96
- Greenberg, N., Docherty, M., Gnanapragasam, S., & Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ, 368, Article m1211. doi.org/10.1136/bmj.m1211
- Rosenstein, A. H. (2012). Physician stress and burnout: Prevalence, cause, and effect. American Academy of Orthopaedic Surgeons Now, 6(8), 31–34. physiciandisruptivebehavior.com/admin/articles/31.pdf
- Anxiety and Depression Association of America. (n.d.). Generalized anxiety disorder (GAD). Retrieved July 26, 2021 from adaa.org/understanding-anxiety/generalized-anxiety-disorder-gad
- National Institute of Mental Health. (2019). Major depression. Retrieved July 26, 2021, from nimh.nih.gov/health/statistics/major-depression.shtml
- Vieta, E., Pérez, V., & Arango, C. (2020). Psychiatry in the aftermath of COVID-19. Revista de Psiquiatría y Salud Mental, 13(2), 105–110. doi.org/10.1016/j.rpsm.2020.04.004
- Pfefferbaum, B., & North, C. S. (2020). Mental health and the COVID-19 pandemic. The New England Journal of Medicine, 383(6), 510–512. doi:10.1056/NEJMp2008017
- Lu, W., Wang, H., Lin, Y., & Li, L. (2020). Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Research, 288, Article 112936. doi.org/10.1016/j.psychres.2020.112936
- Xiang, Y-T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., & Ng, C. H. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry, 7(3), 228–229. doi.org/10.1016/S2215-0366(20)30046-8
- Outhoff, K. (2019). Depression in doctors: A bitter pill to swallow. South African Family Practice, 61(1), 13–16. doi.org/10.4102/safp.v61i1.5046
- Atif, K., Khan, H. U., Zia-Ullah, M. A., Shah, F. S., & Latif, A. (2016). Prevalence of anxiety and depression among doctors: The unscreened and undiagnosed clientele in Lahore, Pakistan. Pakistan Journal of Medical Sciences, 32(2), 294–298. dx.doi.org/10.12669/pjms.322.8731
- Tabalipa, F. O., de Souza, M. F., Pfützenreuter, G., Lima, V. C., Traebert, E., & Traebert, J. (2015). Prevalence of anxiety and depression among medical students. Revista Brasileira de Educação Médica, 39(3), 388–394. dx.doi.org/10.1590/1981-52712015v39n3e02662014
- Kebede, M. A., Anbessie, B., & Ayano, G. (2019). Prevalence and predictors of depression and anxiety among medical students in Addis Ababa, Ethiopia. International Journal of Mental Health Systems, 13, Article 30. doi.org/10.1186/s13033-019-0287-6
- Patel, R. S., Bachu, R., Adikey, A., Malik, M., & Shah, M. (2018). Factors related to physician burnout and its consequences: A review. Behavioral Sciences, 8(11), Article 98. doi.org/10.3390/bs8110098
- Shanafelt, T. D., West, C. P., Sinsky, C., Trockel, M., Tutty, M., Satele, D. V., Carlasare, L. E., & Dyrbye, L. N. (2019). Changes in burnout and satisfaction with work-life integration in physicians and the general U.S. working population between 2011 and 2017. Mayo Clinical Proceedings, 94(9), 1681–1694. doi.org/10.1016/j.mayocp.2018.10.023
- Garrouste-Orgeas, M., Perrin, M., Soufir, L., Vesin, A., Blot, F., Maxime, V., Beuret, P., Troché, G., Klouche, K., Argaud, L., Azoulay, E., & Timsit, J-F. (2015). The Iatroref study: Medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensive Care Medicine, 41(2), 273–284. doi.org/10.1007/s00134-014-3601-4
- Tür, F. Ç, Toker, I., Şaşmaz, C. T., Hacar, S., & Türe, B. (2016). Occupational stress experienced by residents and faculty physicians on night shifts. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 24, Article 34. doi.org/10.1186/s13049-016-0225-4
- Murray, M., Murray, L., & Donnelly, M. (2016). Systematic review of interventions to improve the psychological well-being of general practitioners. BMC Family Practice, 17, Article 36. doi.org/10.1186/s12875-016-0431-1
- Muller, A. E., Hafstad, E. V., Himmels, J. P. W., Smedslund, G., Flottorp, S., Stensland, S. Ø., Stroobants, S., Van de Velde, S., & Vist, G. E. (2020). The mental health impact of the COVID-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Research, 293, Article 11344. doi.org/10.1016/j.psychres.2020.113441
- Buselli, R., Corsi, M., Veltri, A., Baldanzi, S., Chiumiento, M., Del Lupo, E., Marino, R., Necciari, G., Caldi, F., Foddis, R., Guglielmi, G., & Cristaudo, A. (2021). Mental health of health care workers (HCWs): A review of organizational interventions put in place by local institutions to cope with new psychosocial challenges resulting from COVID-19. Psychiatry Research, 299, Article 113847. doi.org/10.1016/j.psychres.2021.113847
- Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., Ballard, C., Christensen, H., Cohen Silver, R., Everall, I., Ford, T., John, A., Kabir, T., King, K., Madan, I., Michie, S., Przybylski A. K., Shafran, R., Sweeney A., … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. doi.org/10.1016/S2215-0366(20)30168-1
Harnessing science, love and the wisdom of lived experience, we are a force of healing and hope for individuals, families and communities affected by substance use and mental health conditions.
- Warning Signs and Symptoms
- Mental Health Conditions
- Common with Mental Illness
- Mental Health By the Numbers
- Individuals with Mental Illness
- Family Members and Caregivers
- Kids, Teens and Young Adults
- Maternal & New Parent Mental Health
- Veterans & Active Duty
- Identity and Cultural Dimensions
- Frontline Professionals
- Mental Health Education
- Support Groups
- NAMI HelpLine
- Publications & Reports
- Podcasts and Webinars
- Video Resource Library
- Justice Library
- Find Your Local NAMI
- Find a NAMIWalks
- Attend the NAMI National Convention
- Fundraise Your Way
- Create a Memorial Fundraiser
- Pledge to Be StigmaFree
- Awareness Events
- Share Your Story
- Partner with Us
- Advocate for Change
- Policy Priorities
- NAMI Advocacy Actions
- Policy Platform
- Crisis Intervention
- State Fact Sheets
- Public Policy Reports
- About Mental Illness
Types of Mental Health Professionals
Many types of mental health care professionals can help you achieve your recovery goals. These professionals work in inpatient facilities, such as general hospitals and psychiatric facilities, and outpatient facilities, such as community mental health clinics, schools and private practices.
Health care professional job titles and specialties can vary by state. The descriptions below give an overview of what to look for and what credentials to expect from a mental health professional. Finding the right professional is easier when you understand the different areas of expertise and training.
The NAMI HelpLine can provide information on how to find various mental health professionals and resources in your area. Please note that we are unable to provide specific recommendations to individual providers as we are unable to speak to the quality of their care.
Assessment And Therapy
Therapists can help someone better understand and cope with thoughts, feelings and behaviors. They can also offer guidance and help improve a person’s ability to achieve life goals. These mental health professionals may also help assess and diagnosis mental health conditions.
Psychologists
Psychologists hold a doctoral degree in clinical psychology or another specialty such as counseling or education. They are trained to evaluate a person’s mental health using clinical interviews, psychological evaluations and testing. They can make diagnoses and provide individual and group therapy. Some may have training in specific forms of therapy like cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT) and other behavioral therapy interventions.
Degree requirements: Doctor of Philosophy (Ph.D.) in a field of psychology or Doctor of Psychology (Psy.D.). Licensure & credentials: Psychologists are licensed by licensure boards in each state.
Counselors, Clinicians, Therapists
These masters-level health care professionals are trained to evaluate a person’s mental health and use therapeutic techniques based on specific training programs. They operate under a variety of job titles—including counselor, clinician, therapist or something else—based on the treatment setting. Working with one of these mental health professionals can lead not only to symptom reduction but to better ways of thinking, feeling and living.
Degree requirements: master’s degree (M.S. or M.A.) in a mental health-related field such as psychology, counseling psychology, marriage or family therapy, among others. Licensure & Certification: Varies by specialty and state. Examples of licensure include:
- LPC, Licensed Professional Counselor
- LMFT, Licensed Marriage and Family Therapist
- LCADAC, Licensed Clinical Alcohol & Drug Abuse Counselor
Clinical Social Workers
Clinical social workers are trained to evaluate a person’s mental health and use therapeutic techniques based on specific training programs. They are also trained in case management and advocacy services.
Degree requirements: master’s degree in social work (MSW). Licensure & credentials: Examples of licensure include:
- LICSW, Licensed Independent Social Workers
- LCSW, Licensed Clinical Social Workers
- ACSW, Academy of Certified Social Workers
Prescribe And Monitor Medication
The following health care professionals can prescribe medication . They may also offer assessments, diagnoses and therapy.
Psychiatrists
Psychiatrists are licensed medical doctors who have completed psychiatric training. They can diagnose mental health conditions, prescribe and monitor medications and provide therapy. Some have completed additional training in child and adolescent mental health, substance use disorders or geriatric psychiatry.
Degree requirements: Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO), plus completion of residency training in psychiatry. Licensure & credentials: Licensed physician in the state where they are practicing; may also be designated as a Board Certified Psychiatrist by the Board of Neurology and Psychiatry.
Psychiatric Or Mental Health Nurse Practitioners
Psychiatric or mental health nurse practitioners can provide assessment, diagnosis and therapy for mental health conditions or substance use disorders. In some states, they are also qualified to prescribe and monitor medications. Requirements also vary by state as to the degree of supervision necessary by a licensed psychiatrist.
Degree requirements: Master of Science (MS) or Doctor of Philosophy (Ph.D.) in nursing with specialized focus on psychiatry. Licensure & credentials: Licensed nurse in the state where they are practicing. Examples of credentials include, but are not limited to:
- NCLEX, National Council Licensure Examination
- PMHNP-BC, Board Certification in psychiatric nursing through the American Academy of Nurses Credentialing Center
Primary Care Physicians
Primary care physicians and pediatricians can prescribe medication, but you might consider visiting someone who specializes in mental health care. Primary care and mental health professionals should work together to determine an individual’s best treatment plan.
Degree requirements: Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (DO). Licensure & credentials: Licensed physician in the state where they are practicing.
Family Nurse Practitioners
Family nurse practitioners (FNP) can provide general medical services like those of a primary care physician, based on each state’s laws. Like primary care physicians, they can prescribe medication, but you might consider visiting someone who specializes in mental health care. Family nurse practitioners and mental health professionals should work together to determine an individual’s best treatment plan.
Degree requirements: Master of Science (M.S.) or Doctor of Philosophy (Ph.D.) in nursing. Licensure & credentials: Licensed nurse in the state where they are practicing. Examples of credentials include:
- FNP-BC, Family Nurse Practitioner Board Certified
Psychiatric Pharmacists
Psychiatrist pharmacists are advanced-practice pharmacists who specialize in mental health care. They can prescribe or recommend appropriate medications if allowed in their state and practice setting. They are skilled at medication management—meaning they evaluate responses and modify treatment, manage medication reactions and drug interactions, and provide education about medications. Many have completed additional training in child/adolescent psychiatry, substance use disorders or geriatric psychiatry.
Degree requirements: Doctor of Pharmacy (PharmD). Completion of residency training in psychiatric pharmacy is not required, but is common. Licensure & credentials: Licensed pharmacist in the state where they practice; may also be designated a Board Certified Psychiatric Pharmacist by the Board of Pharmacy Specialties.
Other Professionals You May Encounter
Certified peer specialists.
These specialists have lived experience with a mental health condition or substance use disorder. They are often trained, certified and prepared to assist with recovery by helping a person set goals and develop strengths. They provide support, mentoring and guidance.
Social Workers
Social workers (B.A. or B.S.) provide case management, inpatient discharge planning services, placement services and other services to support healthy living.
Pastoral Counselors
Pastoral counselors are clergy members with training in clinical pastoral education. They are trained to diagnose and provide counseling. Pastoral counselors can have equivalents to a doctorate in counseling.
Updated April 2020

Know the warning signs of mental illness

Learn more about common mental health conditions
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264 , text “helpline” to 62640 , or chat online. In a crisis, call or text 988 (24/7).
Why the reliance on data? Findings and statistics from research studies can impact us emotionally, add credibility to an article, and ground us in the real world. However, the importance of research findings reaches far beyond providing knowledge to the general population. Research and evaluation studies — those studies that assess a program’s impact — are integral to promoting mental health and reducing the burden of mental illness in different populations.
Mental health research identifies biopsychosocial factors — how biological, psychological and social functioning are interacting — detecting trends and social determinants in population health. That data greatly informs the current state of mental health in the U.S. and around the world. Findings from such studies also influence fields such as public health, health care and education. For example, mental health research and evaluation can impact public health policies by assisting public health professionals in strategizing policies to improve population mental health.
Research helps us understand how to best promote mental health in different populations. From its definition to how it discussed, mental health is seen differently in every community. Thus, mental health research and evaluation not only reveals mental health trends but also informs us about how to best promote mental health in different racial and ethnic populations. What does mental health look like in this community? Is there stigma associated with mental health challenges? How do individuals in the community view those with mental illness? These are the types of questions mental health research can answer.
Data aids us in understanding whether the mental health services and resources that are available meet mental health needs. Many times the communities where needs are the greatest are the ones where there are limited services and resources available. Mental health research and evaluation informs public health professionals and other relevant stakeholders of the gaps that currently exist so they can prioritize policies and strategies for communities where gaps are the greatest.
Research establishes evidence for the effectiveness of public health policies and programs. Mental health research and evaluation help develop evidence for the effectiveness of healthcare policies and strategies as well as mental health promotion programs. This evidence is crucial for showcasing the value and return on investment for programs and policies, which can justify local, state and federal expenditures. For example, mental health research studies evaluating the impact of Mental Health First Aid (MHFA) have revealed that individuals taking the course show increases in knowledge about mental health, greater confidence to assist others in distress, and improvements in their own mental wellbeing. They have been fundamental in assisting organizations and instructors in securing grant funding to bring MHFA to their communities.
The findings from mental health research and evaluation studies provide crucial information about the specific needs within communities and the impacts of public education programs like MHFA. These studies provide guidance on how best to improve mental health in different contexts and ensure financial investments go towards programs proven to improve population mental health and reduce the burden of mental illness in the U.S.
In 2021, in a reaffirmation of its dedication and commitment to mental health and substance use research and community impact, Mental Health First Aid USA introduced MHFA Research Advisors. The group advises and assists Mental Health First Aid USA on ongoing research and future opportunities related to individual MHFA programs, including Youth MHFA, teen MHFA and MHFA at Work.
Through this advisory group and evaluation efforts at large, Mental Health First Aid USA will #BeTheDifference for mental health research and evaluation across communities in the US.
Learn more about MHFA Research Advisors and how you can share your research with us.
Get the latest MHFA blogs, news and updates delivered directly to your inbox so you never miss a post.
Share and help spread the word.
Related stories.
No related posts.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español

You are here
Nih research matters.
April 23, 2024
Research in Context: Treating depression
Finding better approaches.
While effective treatments for major depression are available, there is still room for improvement. This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs.

Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness, anxiety, hopelessness, frustration, or guilt. You may not enjoy the activities you usually do. These feelings tend to be only temporary. Once circumstances change, and the source of stress goes away, your mood usually improves. But sometimes, these feelings don’t go away. When these feelings stick around for at least two weeks and interfere with your daily activities, it’s called major depression, or clinical depression.
In 2021, 8.3% of U.S. adults experienced major depression. That’s about 21 million people. Among adolescents, the prevalence was much greater—more than 20%. Major depression can bring decreased energy, difficulty thinking straight, sleep problems, loss of appetite, and even physical pain. People with major depression may become unable to meet their responsibilities at work or home. Depression can also lead people to use alcohol or drugs or engage in high-risk activities. In the most extreme cases, depression can drive people to self-harm or even suicide.
The good news is that effective treatments are available. But current treatments have limitations. That’s why NIH-funded researchers have been working to develop more effective ways to treat depression. These include finding ways to predict whether certain treatments will help a given patient. They're also trying to develop more effective drugs or, in some cases, find new uses for existing drugs.
Finding the right treatments
The most common treatments for depression include psychotherapy, medications, or a combination. Mild depression may be treated with psychotherapy. Moderate to severe depression often requires the addition of medication.
Several types of psychotherapy have been shown to help relieve depression symptoms. For example, cognitive behavioral therapy helps people to recognize harmful ways of thinking and teaches them how to change these. Some researchers are working to develop new therapies to enhance people’s positive emotions. But good psychotherapy can be hard to access due to the cost, scheduling difficulties, or lack of available providers. The recent growth of telehealth services for mental health has improved access in some cases.
There are many antidepressant drugs on the market. Different drugs will work best on different patients. But it can be challenging to predict which drugs will work for a given patient. And it can take anywhere from 6 to 12 weeks to know whether a drug is working. Finding an effective drug can involve a long period of trial and error, with no guarantee of results.
If depression doesn’t improve with psychotherapy or medications, brain stimulation therapies could be used. Electroconvulsive therapy, or ECT, uses electrodes to send electric current into the brain. A newer technique, transcranial magnetic stimulation (TMS), stimulates the brain using magnetic fields. These treatments must be administered by specially trained health professionals.
“A lot of patients, they kind of muddle along, treatment after treatment, with little idea whether something’s going to work,” says psychiatric researcher Dr. Amit Etkin.
One reason it’s difficult to know which antidepressant medications will work is that there are likely different biological mechanisms that can cause depression. Two people with similar symptoms may both be diagnosed with depression, but the causes of their symptoms could be different. As NIH depression researcher Dr. Carlos Zarate explains, “we believe that there’s not one depression, but hundreds of depressions.”
Depression may be due to many factors. Genetics can put certain people at risk for depression. Stressful situations, physical health conditions, and medications may contribute. And depression can also be part of a more complicated mental disorder, such as bipolar disorder. All of these can affect which treatment would be best to use.
Etkin has been developing methods to distinguish patients with different types of depression based on measurable biological features, or biomarkers. The idea is that different types of patients would respond differently to various treatments. Etkin calls this approach “precision psychiatry.”
One such type of biomarker is electrical activity in the brain. A technique called electroencephalography, or EEG, measures electrical activity using electrodes placed on the scalp. When Etkin was at Stanford University, he led a research team that developed a machine-learning algorithm to predict treatment response based on EEG signals. The team applied the algorithm to data from a clinical trial of the antidepressant sertraline (Zoloft) involving more than 300 people.

EEG data for the participants were collected at the outset. Participants were then randomly assigned to take either sertraline or an inactive placebo for eight weeks. The team found a specific set of signals that predicted the participants’ responses to sertraline. The same neural “signature” also predicted which patients with depression responded to medication in a separate group.
Etkin’s team also examined this neural signature in a set of patients who were treated with TMS and psychotherapy. People who were predicted to respond less to sertraline had a greater response to the TMS/psychotherapy combination.
Etkin continues to develop methods for personalized depression treatment through his company, Alto Neuroscience. He notes that EEG has the advantage of being low-cost and accessible; data can even be collected in a patient’s home. That’s important for being able to get personalized treatments to the large number of people they could help. He’s also working on developing antidepressant drugs targeted to specific EEG profiles. Candidate drugs are in clinical trials now.
“It’s not like a pie-in-the-sky future thing, 20-30 years from now,” Etkin explains. “This is something that could be in people's hands within the next five years.”
New tricks for old drugs
While some researchers focus on matching patients with their optimal treatments, others aim to find treatments that can work for many different patients. It turns out that some drugs we’ve known about for decades might be very effective antidepressants, but we didn’t recognize their antidepressant properties until recently.
One such drug is ketamine. Ketamine has been used as an anesthetic for more than 50 years. Around the turn of this century, researchers started to discover its potential as an antidepressant. Zarate and others have found that, unlike traditional antidepressants that can take weeks to take effect, ketamine can improve depression in as little as one day. And a single dose can have an effect for a week or more. In 2019, the FDA approved a form of ketamine for treating depression that is resistant to other treatments.
But ketamine has drawbacks of its own. It’s a dissociative drug, meaning that it can make people feel disconnected from their body and environment. It also has the potential for addiction and misuse. For these reasons, it’s a controlled substance and can only be administered in a doctor’s office or clinic.
Another class of drugs being studied as possible antidepressants are psychedelics. These include lysergic acid diethylamide (LSD) and psilocybin, the active ingredient in magic mushrooms. These drugs can temporarily alter a person’s mood, thoughts, and perceptions of reality. Some have historically been used for religious rituals, but they are also used recreationally.
In clinical studies, psychedelics are typically administered in combination with psychotherapy. This includes several preparatory sessions with a therapist in the weeks before getting the drug, and several sessions in the weeks following to help people process their experiences. The drugs are administered in a controlled setting.
Dr. Stephen Ross, co-director of the New York University Langone Health Center for Psychedelic Medicine, describes a typical session: “It takes place in a living room-like setting. The person is prepared, and they state their intention. They take the drug, they lie supine, they put on eye shades and preselected music, and two therapists monitor them.” Sessions last for as long as the acute effects of the drug last, which is typically several hours. This is a healthcare-intensive intervention given the time and personnel needed.
In 2016, Ross led a clinical trial examining whether psilocybin-assisted therapy could reduce depression and anxiety in people with cancer. According to Ross, as many as 40% of people with cancer have clinically significant anxiety and depression. The study showed that a single psilocybin session led to substantial reductions in anxiety and depression compared with a placebo. These reductions were evident as soon as one day after psilocybin administration. Six months later, 60-80% of participants still had reduced depression and anxiety.
Psychedelic drugs frequently trigger mystical experiences in the people who take them. “People can feel a sense…that their consciousness is part of a greater consciousness or that all energy is one,” Ross explains. “People can have an experience that for them feels more ‘real’ than regular reality. They can feel transported to a different dimension of reality.”
About three out of four participants in Ross’s study said it was among the most meaningful experiences of their lives. And the degree of mystical experience correlated with the drug’s therapeutic effect. A long-term follow-up study found that the effects of the treatment continued more than four years later.
If these results seem too good to be true, Ross is quick to point out that it was a small study, with only 29 participants, although similar studies from other groups have yielded similar results. Psychedelics haven’t yet been shown to be effective in a large, controlled clinical trial. Ross is now conducting a trial with 200 people to see if the results of his earlier study pan out in this larger group. For now, though, psychedelics remain experimental drugs—approved for testing, but not for routine medical use.
Unlike ketamine, psychedelics aren’t considered addictive. But they, too, carry risks, which certain conditions may increase. Psychedelics can cause cardiovascular complications. They can cause psychosis in people who are predisposed to it. In uncontrolled settings, they have the risk of causing anxiety, confusion, and paranoia—a so-called “bad trip”—that can lead the person taking the drug to harm themself or others. This is why psychedelic-assisted therapy takes place in such tightly controlled settings. That increases the cost and complexity of the therapy, which may prevent many people from having access to it.
Better, safer drugs
Despite the promise of ketamine or psychedelics, their drawbacks have led some researchers to look for drugs that work like them but with fewer side effects.
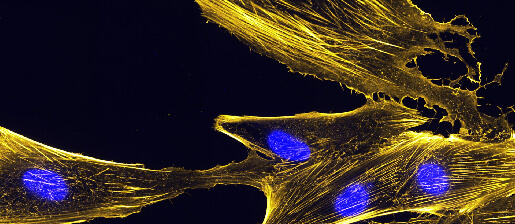
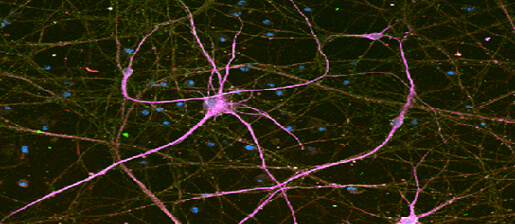
Depression is thought to be caused by the loss of connections between nerve cells, or neurons, in certain regions of the brain. Ketamine and psychedelics both promote the brain’s ability to repair these connections, a quality called plasticity. If we could understand how these drugs encourage plasticity, we might be able to design drugs that can do so without the side effects.

Dr. David Olson at the University of California, Davis studies how psychedelics work at the cellular and molecular levels. The drugs appear to promote plasticity by binding to a receptor in cells called the 5-hydroxytryptamine 2A receptor (5-HT2AR). But many other compounds also bind 5-HT2AR without promoting plasticity. In a recent NIH-funded study, Olson showed that 5-HT2AR can be found both inside and on the surface of the cell. Only compounds that bound to the receptor inside the cells promoted plasticity. This suggests that a drug has to be able to get into the cell to promote plasticity.
Moreover, not all drugs that bind 5-HT2AR have psychedelic effects. Olson’s team has developed a molecular sensor, called psychLight, that can identify which compounds that bind 5-HT2AR have psychedelic effects. Using psychLight, they identified compounds that are not psychedelic but still have rapid and long-lasting antidepressant effects in animal models. He’s founded a company, Delix Therapeutics, to further develop drugs that promote plasticity.
Meanwhile, Zarate and his colleagues have been investigating a compound related to ketamine called hydroxynorketamine (HNK). Ketamine is converted to HNK in the body, and this process appears to be required for ketamine’s antidepressant effects. Administering HNK directly produced antidepressant-like effects in mice. At the same time, it did not cause the dissociative side effects and addiction caused by ketamine. Zarate’s team has already completed phase I trials of HNK in people showing that it’s safe. Phase II trials to find out whether it’s effective are scheduled to begin soon.
“What [ketamine and psychedelics] are doing for the field is they’re helping us realize that it is possible to move toward a repair model versus a symptom mitigation model,” Olson says. Unlike existing antidepressants, which just relieve the symptoms of depression, these drugs appear to fix the underlying causes. That’s likely why they work faster and produce longer-lasting effects. This research is bringing us closer to having safer antidepressants that only need to be taken once in a while, instead of every day.
—by Brian Doctrow, Ph.D.
Related Links
- How Psychedelic Drugs May Help with Depression
- Biosensor Advances Drug Discovery
- Neural Signature Predicts Antidepressant Response
- How Ketamine Relieves Symptoms of Depression
- Protein Structure Reveals How LSD Affects the Brain
- Predicting The Usefulness of Antidepressants
- Depression Screening and Treatment in Adults
- Serotonin Transporter Structure Revealed
- Placebo Effect in Depression Treatment
- When Sadness Lingers: Understanding and Treating Depression
- Psychedelic and Dissociative Drugs
References: An electroencephalographic signature predicts antidepressant response in major depression. Wu W, Zhang Y, Jiang J, Lucas MV, Fonzo GA, Rolle CE, Cooper C, Chin-Fatt C, Krepel N, Cornelssen CA, Wright R, Toll RT, Trivedi HM, Monuszko K, Caudle TL, Sarhadi K, Jha MK, Trombello JM, Deckersbach T, Adams P, McGrath PJ, Weissman MM, Fava M, Pizzagalli DA, Arns M, Trivedi MH, Etkin A. Nat Biotechnol. 2020 Feb 10. doi: 10.1038/s41587-019-0397-3. Epub 2020 Feb 10. PMID: 32042166. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. J Psychopharmacol . 2016 Dec;30(12):1165-1180. doi: 10.1177/0269881116675512. PMID: 27909164. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. Agin-Liebes GI, Malone T, Yalch MM, Mennenga SE, Ponté KL, Guss J, Bossis AP, Grigsby J, Fischer S, Ross S. J Psychopharmacol . 2020 Feb;34(2):155-166. doi: 10.1177/0269881119897615. Epub 2020 Jan 9. PMID: 31916890. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Vargas MV, Dunlap LE, Dong C, Carter SJ, Tombari RJ, Jami SA, Cameron LP, Patel SD, Hennessey JJ, Saeger HN, McCorvy JD, Gray JA, Tian L, Olson DE. Science . 2023 Feb 17;379(6633):700-706. doi: 10.1126/science.adf0435. Epub 2023 Feb 16. PMID: 36795823. Psychedelic-inspired drug discovery using an engineered biosensor. Dong C, Ly C, Dunlap LE, Vargas MV, Sun J, Hwang IW, Azinfar A, Oh WC, Wetsel WC, Olson DE, Tian L. Cell . 2021 Apr 8: S0092-8674(21)00374-3. doi: 10.1016/j.cell.2021.03.043. Epub 2021 Apr 28. PMID: 33915107. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. Nature . 2016 May 26;533(7604):481-6. doi: 10.1038/nature17998. Epub 2016 May 4. PMID: 27144355.
Connect with Us
- More Social Media from NIH

Latest Issue
Psychiatry’s new frontiers
Hope amid crisis
Recent Issues
- AI explodes Taking the pulse of artificial intelligence in medicine
- Health on a planet in crisis
- Real-world health How social factors make or break us
- Molecules of life Understanding the world within us
- The most mysterious organ Unlocking the secrets of the brain
- All Articles
- The spice sellers’ secret
- ‘And yet, you try’
- Making sense of smell
- Before I go
- My favorite molecule
- View all Editors’ Picks
- Diversity, Equity & Inclusion
- Infectious Diseases
- View All Articles
Reasons for hope
Solutions for the mental health crisis emerge through innovative research, diagnostics and treatments
By Nina Bai
Illustration by Jules Julien
Photography by Leslie Williamson

It’s the spring of hope for mental health, astir with novel discoveries, life-changing therapies and more openness than ever before — yet, for many, it feels like the winter of despair. The pandemic years, that crucible of stress, isolation and uncertainty, fueled and exposed mental health problems. In 2022, nearly 1 in 4 American adults (about 59 million people) said they experienced a mental illness in the previous year, but only half of those afflicted reported receiving any mental health treatment.
Among children and adolescents, the prevalence of mental illness, which had been steadily creeping upward, jumped during the pandemic, according to the U.S. Substance Abuse and Mental Health Services Administration. In 2019, 15.7% of American adolescents aged 12-17 reported experiencing a major depressive episode in the past year. In 2022, that number was 19.5%. That same year, 13.4% of adolescents — just over 1 in 8 — seriously thought about killing themselves.
And even as the pandemic has stoked demand for mental health care, it also has worn down the mental health workforce, already short-handed, with early retirements and widespread burnout. Access to affordable, effective interventions remains a daunting barrier. People face long waiting lists and lack of insurance coverage. Many treatable conditions remain undiagnosed because people lack a way to obtain assessments.
Yet, below this perfect storm of mental health crisis, there is a strong undercurrent of hope that begins in the lab. Research is leading the way toward treatments that are more effective, more personalized and more accessible.
“The manner in which we know the brain now, compared with what we knew in previous decades, is incredibly different,” said Victor Carrión , MD, the John A. Turner, MD, Endowed Professor for Child and Adolescent Psychiatry and vice chair of the department of psychiatry and behavioral sciences.

Direct impact on patients
New imaging technologies allow researchers to see the neural circuitry that goes awry in neuropsychiatric disorders, lab-grown clumps of brain tissue — known as organoids — can simulate the impact of genetics in autism, and artificial intelligence can surmise signals that predict the onset of depression and anxiety.
Moreover, these discoveries, rather than moving slowly through specialist silos, can now rapidly inform new treatments. “Collaboration is vital for translation, and our departmental awards and programs promote and emphasize synergy between research and clinical practice,” said Laura Roberts , MD, the Katharine Dexter McCormick and Stanley McCormick Memorial Professor and chair of the department of psychiatry and behavioral sciences.
“Our bench scientists doing tremendous research also work alongside our clinicians to make sure that new knowledge translates to the clinical setting and has a direct impact on patient care,” she said.
Researchers developing transcranial magnetic stimulation, for example, work with clinicians who treat patients with severe depression to design clinical trials, and their techniques are informed by teams inventing new ways to measure the flow of brain signals and those building virtual reality models of the brain.
A clearer understanding of the biology of mental health disorders not only leads to breakthrough treatments — but just as powerfully, helps dissipate stigma.
“There’s been a large shift in stigma in the past 25 years,” said Heather Gotham , PhD, clinical professor of psychiatry and behavioral sciences, who leads the coordination of a nationwide network of centers dedicated to implementing evidence-based mental health care.
The Mental Health Technology Transfer Center Network, funded by the Substance Abuse and Mental Health Services Administration, offers training in preventing school violence, substance use in the workplace, adolescent depression and more, and it offers support for mental health providers seeing refugees and asylum seekers.
“Collaboration is vital for translation, and our departmental awards and programs promote and emphasize synergy between research and clinical practice.” Laura Roberts, the Katharine Dexter McCormick and Stanley McCormick Memorial Professor and chair of the department of psychiatry and behavioral sciences
“One thing that’s made a difference is the greater understanding that mental health disorders and substance use disorders are chronic, relapsing disorders of the body, just like diabetes and heart disease,” Gotham said.
With this new awareness, more people want to be mental health literate. In the past few years, Gotham has seen a surge of interest, from a broader community, in the network’s online courses — from teachers, for example, who want to be more responsive to the needs of students and reduce stigma in the classroom.
Less stigma also means more money for research and mental health services. Funding for mental health has become a rare bipartisan issue. In 2022, Congress passed the Bipartisan Safer Communities Act, which has provided $245 million to fund mental health services like training for school personnel, first responders and law enforcement and expanding the 988 suicide and crisis lifeline.
Stanford Medicine researchers know that to make the most impact with their discoveries they must reach those who need help the most — through online symptom screenings, virtual therapy, group therapy, inclusive clinical trials and community interventions.
They are training mental health professionals locally and globally in new evidence-based techniques. Providers in more than 38 countries, for example, have been trained in cue-centered therapy, a 15-week treatment program developed at Stanford Medicine to help children and teens recover from chronic trauma. Recently, pro bono training in cue-centered therapy was provided to clinicians in Ukraine.
What gives Roberts hope is that a more open conversation on mental health is drawing together experts from different fields with a shared purpose. “It used to be that clinicians would stay in their clinical practice and refer to journals for new research, and researchers would stay in the lab and never see a patient — and we don’t have that now,” she said. “I see more openness and more flexibility from the current generation of researchers and clinicians.”
Read on in this issue of Stanford Medicine to learn about some of the ways Stanford Medicine researchers and clinicians are advancing the understanding of mental health and sharing that knowledge.
Nina Bai is a science writer in the Stanford Medicine Office of Communications.
Email the author
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Research: More People Use Mental Health Benefits When They Hear That Colleagues Use Them Too
- Laura M. Giurge,
- Lauren C. Howe,
- Zsofia Belovai,
- Guusje Lindemann,
- Sharon O’Connor

A study of 2,400 Novartis employees around the world found that simply hearing about others’ struggles can normalize accessing support at work.
Novartis has trained more than 1,000 employees as Mental Health First Aiders to offer peer-to-peer support for their colleagues. While employees were eager for the training, uptake of the program remains low. To understand why, a team of researchers conducted a randomized controlled trial with 2,400 Novartis employees who worked in the UK, Ireland, India, and Malaysia. Employees were shown one of six framings that were designed to overcome two key barriers: privacy concerns and usage concerns. They found that employees who read a story about their colleague using the service were more likely to sign up to learn more about the program, and that emphasizing the anonymity of the program did not seem to have an impact. Their findings suggest that one way to encourage employees to make use of existing mental health resources is by creating a supportive culture that embraces sharing about mental health challenges at work.
“I almost scheduled an appointment about a dozen times. But no, in the end I never went. I just wasn’t sure if my problems were big enough to warrant help and I didn’t want to take up someone else’s time unnecessarily.”
- Laura M. Giurge is an assistant professor at the London School of Economics, and a faculty affiliate at London Business School. Her research focuses on time and boundaries in organizations, workplace well-being, and the future of work. She is also passionate about translating research to the broader public through interactive and creative keynote talks, workshops, and coaching. Follow her on LinkedIn here .
- Lauren C. Howe is an assistant professor in management at the University of Zurich. As head of research at the Center for Leadership in the Future of Work , she focuses on how human aspects, such as mindsets, socioemotional skills, and leadership, play a role in the changing world of work.
- Zsofia Belovai is a behavioral science lead for the organizational performance research practice at MoreThanNow, focusing on exploring how employee welfare can drive KPIs.
- Guusje Lindemann is a senior behavioral scientist at MoreThanNow, in the social impact and organizational performance practices, working on making the workplace better for all.
- Sharon O’Connor is the global employee wellbeing lead at Novartis. She is a founding member of the Wellbeing Executives Council of The Conference Board, and a guest lecturer on the Workplace Wellness postgraduate certificate at Trinity College Dublin.
Partner Center

The Well-Rested Educator: 7 Tips for Sounder Slumber

Alyssa Provencio
Experts constantly emphasize the fundamental importance of adequate sleep for maintaining optimal health and well-being.
As educators, we likely even promote healthy sleep habits for our students, recognizing that well-rested learners are more engaged and alert during class.
But do we give that same attention to our own sleep habits?
Quality of sleep can affect so many aspects of our daily functioning including our ability to focus, energy levels, mental health, and mood.
You have likely heard about the number of hours you should sleep, the position you should sleep in, or the pillow you should buy. While some of this advice can be useful, you may be looking for something to make a longer-lasting change in your sleep quality.
Sleep hygiene is a set of practices that can be incorporated into your daily routine to improve quality of sleep. Therapists will often talk with clients about strategies for sleep hygiene, and we will cover a few of these here.
- Get regular sleep . Going to bed and waking up at a consistent time, even on your day off, can help you maintain a healthy circadian rhythm . Try using a sleep diary like this one to track your sleep pattern for a couple of weeks.
- Avoid caffeine later in the day . Caffeine (i.e. coffee, tea, chocolate, etc.) acts as a stimulant and can stay in your system for 6-10 hours, making it more difficult to fall asleep.
- Avoid naps . Napping can disrupt your circadian rhythm. If naps are difficult to avoid, try napping before 3 pm and for no longer than an hour.
- Use your bed for sleep . Try to use your bed for sleeping rather than a place you also use for working, eating, watching TV, etc. This will help your body associate your bed with sleep rather than activity or even stress.
- Don’t just lay awake . If you are having a hard time falling asleep after 20 minutes, get out of bed and do something calming or boring. Try meditating, doodling, or even reading the dictionary. Avoid bright lights or stimulating activities and when you feel tired, return to bed.
- Make your bedroom comfortable . Setting up your bedroom to create comfort is important for associating your bedroom with sleep. A dark, quiet, cool room is best for quality sleep – an eye mask, earplugs, and/or a fan can be useful tools.
- Develop a sleep ritual . Having a short, 15-minute nightly practice to help your body feel ready to sleep can help you fall asleep. This can look like taking a warm bath, a meditation or relaxation practice ( try this audio-guided box breathing activity !), or reading a book.
It is important to consider that sleep difficulties related to medical conditions, such as insomnia, may require medical treatment and sleep hygiene can be a supplemental practice. If you have concerns with your sleep, it may be a good idea to talk with your medical doctor. Additionally, some strategies might work better for you than others – take what fits with your culture and lifestyle! Sweet dreams 😊
Alyssa Provencio is currently a student clinician at the Scanlan Center for School Mental Health and is a student in the University of Iowa College of Education’s Counseling Psychology Doctoral Program .
Business Roundtable announces new mental health initiative for employee well-being

Good morning.
Mental health is both a personal and a professional issue for leaders . In addition to doing what they can to operate at the top of their mental game, leaders have to create conditions for employees to thrive.
In 2022, Gallup estimated that workers’ mental health issues cost the U.S. economy $47.6 billion annually in lost productivity alone, and four in 10 U.S. workers said their jobs had a somewhat negative or extremely negative impact on their mental health. That’s, in part, why the Business Roundtable today launched its Mental Health Initiative aimed at identifying the best practices for companies to promote mental well-being in the workplace. The initiative also includes resources, training programs, peer forums, and tools for managers.
The issue isn’t that effective strategies don’t exist. It’s that leaders need to create a culture and practices that encourage the awareness and adoption of mental health benefits and remove the stigma around discussing mental well-being at work.
Business Roundtable member and Cigna CEO David Cordani sees the initiative “as an opportunity to supercharge, through a variety of means, the curation of best practices.” One is finding opportunities to connect. “You can see higher levels of vitality and mental well-being for individuals who are physically at a worksite versus those who are not,” Cordani says.
Cordani, for one, has learned what matters for his mental health.
“I essentially get about an hour of exercise in every day to start my day. I find that I get centered when I do that,” he says. Volunteerism (“givers get”) and managing his calendar to take an active role in his children’s lives are also key. So as a leader, he tries to make it possible for his employees to do the same.
Meanwhile, CEOs have been sharing with us what Fortune means to them. Today, I want to share what Sen. Mark Warner (D-Va.) wrote:
“While I’m not a business leader, I was in business before I was in politics, and I’ve always trusted the CEO Daily to give me a good snapshot of the state of business. I’ve always appreciated (its) objective view of how leaders can steer businesses that create value for shareholders, but also for employees and their communities.”
That’s a value proposition we intend to now build upon. Let me know how we’re doing .
More news below.
Diane Brady @dianebrady [email protected]
Who will be HSBC’s next CEO?
Since Noel Quinn’s shock exit from HSBC, the biggest question remains: Who will replace the chief executive officer at Europe’s largest bank? Both internal and external candidates will be considered, the bank said in a statement. With nearly two decades at HSBC under his belt, chief financial officer Georges Elheder is a clear front-runner for the prized gig. Who else could be in the running? Bloomberg
Dividends payments soar
Dividend payments to shareholders over the past three years grew 14 times faster than workers’ pay across 31 major economies, an Oxfam report has revealed. In 2023, the richest 1% pocketed an average of $9,000 in dividends — equivalent to eight months’ wages for the average worker, the report said . “You have to think about what kind of world we want to live in,” Alex Maitland, health and inequality policy advisor at Oxfam International, told Fortune .
Tesla’s supercharger team sacked
In the latest round of layoffs at Tesla, Elon Musk has sacked two senior executives and several hundreds of employees, including the entire supercharger team. Among those let go is Rebecca Tinucci, the company’s top female manager. Tesla’s supercharger system is among the largest charging networks in the world, so the move raises questions over the future of the charging business. Financial Times
AROUND THE WATERCOOLER
An $850 million retail giant is giving candidates their questions before a job interview because ‘nerves can seriously impact performance’ by Orianna Rosa Royle
Amazon’s generative AI business has hit a multibillion-dollar run rate that’s reaccelerated cloud growth by Jason Del Rey
Berkshire Hathaway prepares for its first annual meeting in decades without Charlie Munger by Chris Morris
Coca-Cola only sold 1% more drinks last quarter, but it raised prices 13%. Its CEO said it has ‘the right strategies’ for sustained success by Sasha Rogelberg
Binance founder Changpeng ‘CZ’ Zhao sentenced to 4 months, will enter prison as country’s richest inmate by Leo Schwartz
Exclusive: Ikea is rolling out its third round of price cuts in a year across thousands of products as it eases shoppers’ inflation pain by Prarthana Prakash
T his edition of CEO Daily was curated by Orianna Rosa Royle.
Latest in Newsletters

You’ll probably need to learn a new acronym to keep up with the latest AI trend

You don’t need an AI assistant in a box like the new Rabbit R1—unless it’s your smartphone

Binance founder’s cooperation got him a light sentence. So what did he tell the feds?

Most people are lonely at work. Women get lonelier as they climb the ladder

The father of the 401(k) on the downsides of his most famous creation

What current CFOs can learn from a pair of ‘qualitatively different’ accounting scandals
Most popular.

Furious Mexican farmers are ripping out water pumps for avocado orchards and berry fields, risking cartel reprisal

Move over, American dream: The goal of many Gen Z and millennial women is now to be a DINK—with dual income and no kids

Starbucks flags unusual phenomenon for ‘disappointing’ sales: It’s too popular with morning commuters

Tesla slashes its summer internship program to cut costs, as Elon Musk fights to save his $45 billion pay plan

Peloton, the fallen fitness unicorn, faces a harsh truth despite its shiny new deal with Hyatt hotels: ‘I don’t think they thought [about] what was going to happen post-pandemic’

Novo Nordisk’s market value of $570 billion is now bigger than the entire Danish economy—creating a ‘Nokia risk’ for Denmark
NSF graduate research fellowships go to 16 Tar Heels
The prestigious National Science Foundation award supports education, professional development and research.

This year, 12 graduate students and four undergraduates at UNC-Chapel Hill received fellowships from the National Science Foundation Graduate Research Fellowship Program . Their research covers several STEM-related fields, including biology, sociology, genetics and anthropology.
Begun in 1952, this fellowship is the oldest of its kind directly supporting graduate students in STEM. Its purpose is not only to ensure the quality and vitality in U.S. scientific and engineering workforces but also to broaden and diversify the talent in STEM-related professions. Federal funding through a three-year stipend provides educational support, professional development and international research opportunities for recipients.
Beth Mayer-Davis, dean of The Graduate School, noted that the recipients of this year’s awards are making fundamental strides in overcoming obstacles that affect the lives of people and the environment not just in North Carolina but around the globe.
“The excellent work of these students highlights the depth of knowledge being generated through graduate education at UNC-Chapel Hill,” Mayer-Davis said. “It is this kind of impactful research that sets Carolina students apart as our next generation of leaders.”
The UNC-Chapel Hill chapter of the Materials Research Society partnered with The Graduate School to help students develop key skills and provide opportunities to network with scientific professionals. One such opportunity is the NSF GRFP peer-review workshop. This annual peer-review workshop provides senior undergraduates and first- and second-year graduate students an environment to meet one-on-one with NSF GRFP fellows.
These UNC-Chapel Hill graduate students received NSF fellowships:
- Andrew Boyle , College of Arts and Sciences’ physics and astronomy department.
- Henry Dieckhaus , UNC Eshelman School of Pharmacy.
- Abigail Foes , UNC Gillings School of Global Public Health.
- Georgina Gemayel , College of Arts and Sciences’ geography and environment department.
- Camryn Gloor , College of Arts and Sciences’ chemistry department.
- Lauren Hutchinson , College of Arts and Sciences’ chemistry department.
- Micah Hysong , College of Arts and Sciences’ and UNC School of Medicine’s genetics and molecular biology curriculum.
- Athena Owirodu , College of Arts and Sciences’ sociology department.
- Ryan Salcido , College of Arts and Sciences’ and UNC School of Medicine’s genetics and molecular biology curriculum.
- Gates Schneider , UNC School of Medicine’s biological and biomedical sciences program.
- Samuel Weaver , College of Arts and Sciences’ chemistry department.
- Adriana Wisniewski , College of Arts and Sciences’ anthropology department.
These UNC-Chapel Hill undergraduate students received NSF fellowships:
- Stephanie Caddell , College of Arts and Sciences’ earth, marine and environmental sciences department.
- Xinyi Li , College of Arts and Sciences’ and North Carolina State University’s biomedical engineering joint department.
- Christine Mendoza , College of Arts and Sciences’ computer science department.
- Dain Ruiz , College of Arts and Sciences’ biology department.
Read the 2024 awardee list.
John Wood Sweet is documenting the life of Venture Smith, who wrote an account of his enslavement and freedom.

Coxswain steers toward career in sustainability
Senior Karen Jordan pursues a future in the food industry while also guiding rowers on a club crew team.

2024 Massey Awards recognize employees’ service to Carolina
The recipients include two housekeepers, two administrators, two academic staff members and one executive assistant.

Nursing alumnus trains with NASA
Over eight days at sea, Joey Biddix worked with astronauts and Navy specialists to prepare for a water recovery mission.

Nature is good for kids
A new study from FPG researchers suggests preschoolers living near green space have better mental health.

Washington Week introduces students to alumni diplomats
Tar Heels networked about foreign affairs careers through this UNC Global Affairs program.

Lifelong learner finds personal renaissance
After years of working in the business world, Jennifer Wu earns a doctorate in art history from Carolina.
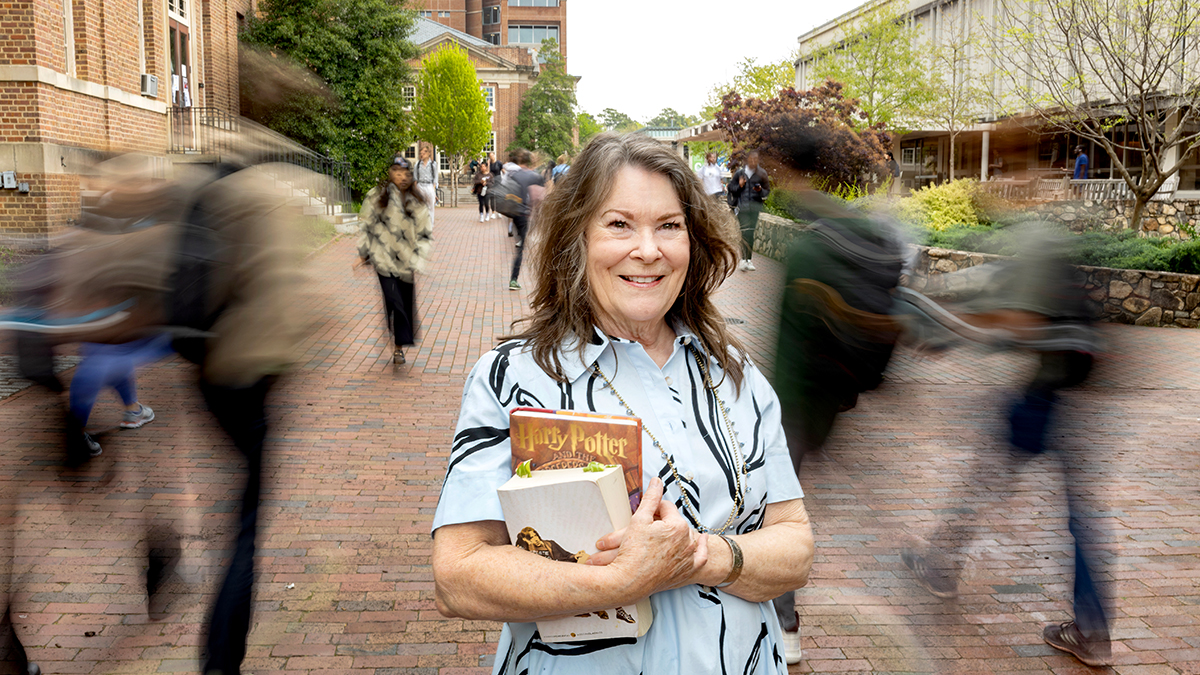
After a 54-year break, she’s graduating
Janet Hoffmann Vitolo, who left Carolina after her junior year in 1970, just completed her bachelor’s degree.
Share on Mastodon

COMMENTS
Background. Digital mental health may be understood as the use of digital technologies to support and improve mental health conditions and provide mental health care, including screening, health promotion, prevention, early intervention, treatment, and relapse prevention [1-3].It encompasses a wide range of modalities, including internet research [], monitoring and assessment ...
Despite the role of healthcare professionals in understanding mental health stigma and its impact on recovery, a look into current literature reveals a pattern of investigating stigma and recovery from the standpoint of service-users and the general public, with a scarcity of research done to address the perspectives of healthcare professionals ...
Mental Health of Healthcare Workers in Times of Pandemics and Crisis. During the COVID-19 pandemic, which has been the cause of more than 2.85 million deaths worldwide to date (5th April, 2021) and rising, many healthcare workers, both within medical care and the mental health sector, have been experiencing challenges in adapting quickly to changes in patient volume, mounting demands, clinical ...
Scope of Mental Health Promotion and Prevention in the Current Situation. Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses (18, 36-42).There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe ...
While mental health professionals may not espouse stigmatised views towards their patients' struggles, they may do so towards those of their colleagues (Zerubavl & O'Dougherty-Wright, 2012). Moreover, research indicates that mental health professionals are resistant to stigma reduction (Harris et al., 2016). This may be, ...
Occupational wellbeing of mental health professionals. Research suggests that mental health professionals report high levels of poor occupational wellbeing such as burnout or compassion fatigue (McCormack, MacIntyre, O'shea, Herring, & Campbell, Citation 2018; O'connor, Muller Neff, & Pitman, Citation 2018; Singh et al., Citation 2020, Singh & Hassard, 2021).
Research around mental health professionals with lived experience often focusses on the negative aspects. Zamir et al. identified that researchers generally did not specifically look for positive experiences of sharing lived experience. Therefore, there is a risk that stigma in the literature may be perpetuated due to researcher bias.
According to the World Health Organization, mental health is defined as a state of mental wellbeing that enables individuals to cope with stresses, realize their abilities, work well, learn well, and contribute to society (World Health Organization., 2003).Compared to the general population, healthcare professionals are more likely to encounter mental health problems, and these symptoms not ...
Implications and Directions for Future Research. Implicit biases of mental health service providers can con-tribute to the misinterpretation of emotional expressions and high health care costs associated with improper treat-ment. These effects can perpetuate mental health disparities throughout the care continuum.
In 20,947 healthcare workers in 42 organizations across the United States between May 28, 2020 and October 1, 2020, we found higher levels of stress and burnout in both clinical and non-clinical staff, including nursing assistants, medical assistants, housekeeping, and social workers.
The National Institute of Mental Health (NIMH) is the Nation's leader in research on mental disorders, supporting research to transform the understanding and treatment of mental illnesses. Below you can learn more about NIMH funded research areas, policies, resources, initiatives, and research conducted by NIMH on the NIH campus.
Mental health issues (including anxiety, depression, stress, burnout, suicidality, tobacco and alcohol use) in various healthcare professionals, such as physicians of different specialties, nurses working in various settings, psychologists, have become increasing concerns in many countries. Studies suggested that the situation has worsened during the COVID-19 pandemic era, due to many ...
"Mental health professionals" are increasingly speaking out about their own experiences of using mental health services. However, research suggests that they face identity-related dilemmas because social conventions tend to assume two distinct identities: "professionals" as relatively socially powerful and "patients" as comparatively powerless.
Recent research has documented the prevalence of poor mental health trends in HCPs. It is evident that they suffer from stress, anxiety, depression, PTSD and substance abuse at a higher rate than the general population of the United States. 7 A number of studies have found: The prevalence of PTSD in U.S. adults is estimated to be 3.8%. PTSD ...
Colonisation and related discourse remain evident in mental health research (Dudgeon et al., 2014a; Kennedy et al., 2022), and for the knowledge generated in any research project to be meaningful to Aboriginal and Torres Strait Islander communities, the process of the research needs to be culturally safe (Lindeman et al., 2011; Lindeman and ...
The use of mental health apps continues to skyrocket. Certain apps, such as digital therapeutics, can cost between $300 and $1,500 per year and are typically not covered by insurance. Psychologists are advocating at the state and federal level for health insurance organizations to cover the fees. Even though digital therapeutics have ...
When a patient with psychiatric illness commits suicide, it may impact the mental well-being of mental health professionals dealing with the patient.[14 31 32] Studies conducted on the impact of clinical supervision on levels of burnout among psychiatric nurses found that adequate and effective clinical supervision of psychiatric nurses during ...
Research suggests that in addition to the general population, mental health professionals also stigmatize mental illness, and this has implications for public health and policy [1, 3, 5, 6, 12]. Provider-based stigma occurs when occupational groups endorse the stigmatization of the people they are meant to help and is related to negative ...
Psychiatrists are specialized doctors who diagnose, treat, and prevent mental, emotional, and behavioral disorders using a combination of psychiatric medicine, physical exams, and lab tests. They ...
Many types of mental health care professionals can help you achieve your recovery goals. These professionals work in inpatient facilities, such as general hospitals and psychiatric facilities, and outpatient facilities, such as community mental health clinics, schools and private practices. Health care professional job titles and specialties can vary by state. The descriptions below give […]
Mental health research and evaluation informs public health professionals and other relevant stakeholders of the gaps that currently exist so they can prioritize policies and strategies for communities where gaps are the greatest. Research establishes evidence for the effectiveness of public health policies and programs.
This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs. ... due to the cost, scheduling difficulties, or lack of available providers. The recent growth of telehealth services for mental health has improved access in some ...
In 2021, there were 708,100 social workers, according to the BLS. This includes 113,810 social workers who specifically worked in mental health and substance abuse in 2021. Overall, this ...
Less stigma also means more money for research and mental health services. Funding for mental health has become a rare bipartisan issue. In 2022, Congress passed the Bipartisan Safer Communities Act, which has provided $245 million to fund mental health services like training for school personnel, first responders and law enforcement and ...
Novartis has trained more than 1,000 employees as Mental Health First Aiders to offer peer-to-peer support for their colleagues. While employees were eager for the training, uptake of the program ...
This study is part of the research project entitled 'Mental health professionals' attitudes toward mental healthcare: associations with work satisfaction indices' funded by Small Scale Project of the Special Account for Research, University of Crete, Greece. Reference number: 10635.
As director of The Pew Charitable Trusts' behavioral health programs, Dr. Brandee Izquierdo oversees the organization's projects on substance use treatment and prevention and suicide risk reduction. This interview about her professional, academic, and lived expertise has been edited for length and clarity.
The state of Iowa's hub for school mental health research, professional development, and clinical services. Learn 7 expert tips for better sleep hygiene as an educator. Improve your sleep quality with strategies like keeping a consistent sleep schedule, avoiding late caffeine, using your bed only for sleep, and developing a calming bedtime routine.
Poor mental health costs the U.S. economy $47.6 billion annually, according to Gallup. Good morning. Mental health is both a personal and a professional issue for leaders. In addition to doing ...
Federal funding through a three-year stipend provides educational support, professional development and international research opportunities for recipients. Beth Mayer-Davis, dean of The Graduate School, noted that the recipients of this year's awards are making fundamental strides in overcoming obstacles that affect the lives of people and ...