- ConscienHealth
- Advocacy Organizations
- Affiliates & Advocates
- Service Partners
- Publications
- LATEST NEWS


Discipline and the Obesity That No One Wants to See
Discipline – or the lack of it – is something that is sometimes offered up as an explanation for obesity. Public health professionals, employers, and physicians gathered at a medical forum in Baltimore last week to discuss obesity and how health plans can address this growing health concern. One physician who is medical director for a large health insurer asked at the end of a presentation on the physiology of obesity:
This is all very interesting, but isn’t obesity simply a matter of self-discipline? I mean the food might be available, but does that mean that you have to eat it all? Why do we pretend obesity is a medical issue?
As a matter of fact, complex physiology regulates how our bodies energy absorb, use, and store energy as fat. In obesity, that physiology causes the body to store fat in an unhealthy way. Obesity is no more a failure of discipline than high blood pressure is. It is a failure of physiology. It requires care, not blame.
Stereotypical thinking assumes that people with obesity are undisciplined or suffering from a number of other character flaws. It is well documented in studies of weight bias and stigma that many healthcare professionals harbour such attitudes. Such thinking is often used as an excuse for ignoring obesity and for neglecting the medical needs of people who have it.
A new editorial by Daniele Di Pauli in Eating and Weight Disorders points out that weight bias should not be overlooked:
As health professionals, and scientific societies, we cannot allow the stigma toward obesity to go unnoticed like happens to Icarus, in the painting by Pieter Bruegel the Elder, in which no one seems to notice the son of Daedalus fallen from the sky into the sea.
Unfortunately, bias against people living with obesity has been quietly overlooked for far too long. Health professionals who are inclined to blame people for their illness should reflect upon the purpose of their chosen profession.
Click here for the editorial by Di Pauli.
Order, photograph © A Not Very Creative Mind / flickr
Subscribe by email to follow the accumulating evidence and observations that shape our view of health, obesity, and policy.
Your email:
June 12, 2016
12 Responses to “Discipline and the Obesity That No One Wants to See”
June 12, 2016 at 8:45 am, M said:
I suspect part of the issue is that doctors are being told “You have to address obesity with your patients!” There’s two parts here, I think. One is the bizarre idea that fat people don’t know they’re fat. (I suspect they’re confusing people who say “I am perfectly healthy otherwise. Who cares what I weigh?” with fat people thinking they’re skinny.) The other is the too common belief that “address” means bully and shame into restrictive dieting, instead of making sure the patient is eating well and regularly exercising – just as they should be doing for their thin patients, as well.
Studies show that doctors often think that fat people are non-compliant, likely from a belief that “If they cannot control what they eat how can we expect them to follow treatment?” The frightening truth of the “death by obesity” statistic is that doctors may have a role in those deaths.
June 12, 2016 at 4:33 pm, Ted said:
Unfortunately, much of what you say has been shown to be true in research on weight bias. This is a case where the “cure” is worse than the problem. It certainly makes the problem worse.
June 12, 2016 at 9:51 am, Stephen Phillips said:
The concept of obesity resulting from willful misconduct is as old as ignorance.
Stephen Phillips American Association of Bariatric Counselors
June 12, 2016 at 10:10 am, Beth Bianca said:
Thank you for being an advocate for our community. Discipline is great if you have to lose 20 pounds. However, those of us who have tried using discipline over and over our entire lives and end up heavier are obviously dealing with something different.
I wrote an article last month that was published in the Huffington Post. It addressed the judgement against weight-loss surgery and how people do not think discipline is required for the results. Therefore, people looked at weight-loss surgery results as “not counting” as much as using “diet and exercise alone. Absolutely absurd.
June 12, 2016 at 4:30 pm, Ted said:
You are right, Beth. Thanks for speaking up!
June 13, 2016 at 5:30 am, Mary-Jo Overwater said:
I firmly believe in the importance of discipline in life. Exercising discipline to stay on task when one is distracted or wants to give up or to reign in impulsive behaviors can be character-building and really help one enjoy feelings of accomplishment and strength. People who are hard-wired to be naturally slim or self-regulators, but who have put on 10-25 lbs with age or change of lifestyle circumstances have better success when they exercise discipline because their bodies respond more efficiently to treatments and to any lifestyle changes to eat more healthfully/ balanced again and/or to exercise. Discipline is rewarded in these cases and affirms the argument for discipline.
But, when it comes to weight management in obesity, it is naïve and ignorant to assert it has a key role to solving the struggle with obesity. Most of my obese clients who struggle with their weight are, in fact, often MORE disciplined than people who don’t have the (patho)physiology of obesity. The amount and focus of self-control and dedication exhibited for long periods of time in keeping dietary intake either restricted or certainly much less than their bodies are hard-wired to ‘require’ and to sustain exercise regimes often much longer and more intense than non-obese individuals, takes incredible discipline Then, after all that effort, to see little or no change on the scale or in your clothes size, or even in your biomarkers — well, it’s soul-crushing.
So, people with obesity and people who treat obesity need the facts before any true assessments and/or decisions about courses of action can be made. In my case, as a person who is BOTH — I work with people who struggle with weight and I, myself, struggle with my weight. I know the reality that growing up obese and being obese for a good part of my early adulthood has set my body up to fight tremendous odds to get me at a certain ‘ideal’ weight. I exert tremendous discipline in pushing myself to exercise at least 5 times a week and in stopping eating when I know I’ve had enough. I am not hard-wired to stop. I do believe that discipline has kept me from being 50, maybe 100 lbs more than I am now.
But, believe me, it IS at times, soul-destroying. What makes it even worse is when other fellow-dietitians or anyone else, for that matter, make presumptive judgements. The reality of weight bias is extremely destructive. I could go for a bypass or pursue medical treatment and I may do so at some point. Right now, my labs and biomarkers are all good and I feel healthy and vital, despite being 40-50 lbs more than I have been at my lowest weight before my second pregnancy. Exercising discipline is important for me, but having a clear understanding of the limitations of discipline has been extremely uplifting and actually keeps me even more motivated to keep up with my healthier choices. 🙂
June 13, 2016 at 5:36 am, Ted said:
Beautifully well said, Mary-Jo. Thank you!
June 13, 2016 at 12:24 pm, Katherine Rivard said:
In even high-level corporate Health Coaching Companies, where boss women are heavy and at the top, the idea of a skinny subordinate is reason to limit their advancement.
So the flip side of “I am working on it” shows up in the numbers reflecting that weight is actually not managed because it is a human reason to suggest that people of managed weight don’t sit down enough to get their work done and are less devoted to the female boss. I have seen this unspoken and not addressed until the research came back showing that weight is least likely to change in the workplace neighborhood.
June 13, 2016 at 10:24 pm, ejh said:
Ted —
I find others have well described the personal dynamic of issues surrounding obesity — so I am grateful and feel no need to further discuss it.
HOWEVER — I would like to know what the response was to the physicians question about lack of discipline and blame the fat person mentality…. Did he listen? Do you think he LEARNED anything? Scares me that someone in his position would remain so ignorant. Ten years ago maybe I could see it…. so I am curious…
As always, thanks for your column.
June 14, 2016 at 4:44 am, Ted said:
Thanks for asking, Jean. The presenter responded that obesity has many causes and an undisciplined personality is not one of them. The presenter went on to describe the physiology of obesity, but my assessment was that the questioner was not listening. He left the room several times. At lunch, he tried to persuade another HCP, who was a bariatric surgery patient, that her problems with obesity since early childhood were due to emotional problems. He was not doing a lot of listening.
June 14, 2016 at 8:09 pm, John said:
The blog is a breath of fresh air. It’s so hard to find folk that understand this complex chronic disease. Yet the facts about the physiology are clear. We somehow allow this disorder of regulation to be treated differently to others like blood pressure, diabetes and cancer. It’s interesting diabetes and hypertension generate complications – obesity generates co-morbidities!
Come how this is different? Why?
But this blog is the exception. Other blogs that follow a little touch of the truth are condemned for their clear error in that “we all know it’s all about bad choices”!
But, we are not winning. Can you imagine the outcry if we just treated 1% of those with type 2 diabetes with effective care beyond lifestyle advice. I think the word is negligence.
June 15, 2016 at 5:44 am, Ted said:
Thanks, John. You make some excellent points. In particular, the comparison to the failure of regulating glucose, blood pressure, lipids, and cell growth will stick with me. Thanks!
Search this blog
- access to care
- anti-obesity medicines
- bariatric surgery
- childhood obesity
- evidence based medicine
- food industry
- food policy
- health disparities
- health economics
- health insurance
- health outcomes
- health reporting
- Obesity Action Coalition
- obesity care
- obesity causes
- obesity prevention
- obesity statistics
- obesity treatment
- physical activity
- public health
- scientific integrity
- scientific rigor
- semaglutide
- The Obesity Society
- weight bias
- weight discrimination
- weight loss
- weight stigma
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- February 2012
- January 2012
- October 2011
- February 2011
- January 2011
- December 2010
- October 2010
- September 2010
- October 2009
- August 2009
- Consumer Trends
- Food & Nutrition
- Food Industry
- Health & Obesity
- Health Policy
- Scientific Meetings & Publications

outstanding advocacy
Recognized by The Obesity Society & Obesity Action Coalition
©2009-2013 ConscienHealth. All rights reserved. | Website Design by Mariela Antunes | Hosting by DTS

Self-Control
Research suggests that we assume overweight people lack self-control, research examines the effects of body size and weight on person perception..
Posted September 21, 2021 | Reviewed by Abigail Fagan
- What Is Self-Control?
- Find a therapist to help with self-control
- People judge each other based on a variety of factors, including body size and weight.
- Thinner individuals, compared to heavier people, are judged as more competent, perhaps because they are assumed to have greater self-control.
- Heavier people are seen as warmer, and thinner people as more emotionally constricted, perhaps because size signals emotional expressiveness.

Do you have an anti-fat bias?
Suppose you are shown a picture of two new coworkers, one thin and one overweight or obese: What judgments might you make about these two coworkers based on their body weight and body size? For instance, would they appear to you equally competent (i.e. dominant, skillful, intelligent, efficient) and warm (i.e. friendly, trustworthy, kind, helpful, sincere)?
Think about these questions as I describe the findings of three studies by Bryksina et al., published in the August 2021 issue of Social Psychological and Personality Science . The paper concludes body size (i.e. being thin vs. overweight or obese) influences judgments of warmth and competence.
Investigating body size and judgments of competence and warmth
The sample comprised 482 participants (44% female, average age of 36 years) from Mechanical Turk, randomly assigned to one of six conditions: target’s gender (male or female) X target’s body size (below vs. average vs. above).
Participants read a scenario regarding a person (“target”) and rated the target’s various attributes: warmth (“warm, kind, nurturing, and a nice person”), competence (“independent, organized, respected by others, and high in social status”), self-control , emotional expressiveness, and attractiveness (being “attractive, good-looking, sexy, and beautiful”).
Analysis of data showed heavier targets were seen as warmer and more emotionally expressive but less attractive, less competent, and possessing less self-control.
This was a conceptual replication of the first investigation, though the body size manipulation was presented visually instead of verbally (i.e. no written scenarios).
The sample consisted of 349 people (47% female, average age of 35 years). There were four conditions: target’s gender (male/female) X body size (heavy vs. thin).
Pictures of targets were manipulated using Photoshop. Participants were presented with a picture of a target and rated the person’s warmth (being warm, good-natured, caring, nurturing), competence (being competent, capable, intelligent, confident), self-control, and emotional expressiveness.
The results agreed with those of the above investigation.
Here, the researchers manipulated perceptions of self-control and emotional expressiveness to determine if these traits can explain the observed inferences of warmth and competence in relation to body weight and size.
Sample: 481 individuals; 45% female; mean age of 34 years. Six conditions were used: target’s gender X target descriptions (low expressiveness and low self-control vs. high expressiveness and low self-control vs. low expressiveness and high self-control).
For example, the target with low emotional expressiveness and low self-control was characterized as not very emotional, nor good at resisting temptation or working toward long-term goals , etc.
After reading three target descriptions, participants viewed a photo of the target (who was of average weight) and evaluated him or her in terms of competence (being competent, capable, effective, skillful), and warmth (being warm, generous, kind, nurturing).
Analysis of data suggested the high expressiveness condition was associated with higher warmth ratings, while the high self-control condition was associated with higher competence ratings.
In short, when a target of average weight was described as more emotionally expressive, he or she was perceived as warmer; when the target was described as having higher self-control, he or she was perceived as more competent.
Overweight and warm vs. thin and competent?
In summary, though body weight and size have been previously linked with judgments of beauty and attractiveness , the present findings suggest body size also influences judgments of warmth and competence:
- Thinner individuals (compared to heavier) are judged as more competent. Why? Perhaps because being thin signals a greater ability to exercise self-control.
- Heavier individuals are perceived as warmer, while thinner ones are perceived as emotionally constricted, possibly because body size signals emotional expressiveness.

These findings agree with previous research. For instance—as discussed in an article on the influence of body shapes (e.g., classically feminine, rectangular) on first impressions—people typically assume thinner individuals are more cautious and disciplined, while heavier ones are more careless, lazy, and disorganized. Of course, in the present investigations, heavier people were seen as warmer and more capable of showing emotions; nevertheless, they were also seen as lacking competence and self-control.

Not judging by appearances
Severely overweight or obese people are painfully familiar with fatphobia and obesity stigma (e.g., fat shaming )—with various assumptions linking greater weight with qualities like gluttony, poor hygiene, laziness, lack of willpower, and especially, low competence. Though a minority of fat stereotypes are “positive” (e.g., happy, fun, jolly, warm), all stereotypes are fixed or oversimplified beliefs; they ignore differences and reduce human beings to caricatures.
What the research by Bryksina and colleagues found is that weight stereotypes and stigma may occur even if a person is only moderately overweight. Or underweight. This suggests obesity stigma and anti-fat bias but also anti-thin bias are more prevalent than assumed.
Here's the takeaway:
It is important to keep in mind your own weight biases when judging a stranger’s self-control, competence, warmth, or emotional expressiveness.
Be it evaluating a political candidate, a new student, a job applicant, or a romantic date, weight biases can be highly consequential. Of course, the same applies to evaluating yourself . Yes, I am referring to self-stigma . Indeed, obese people “often endorse the same negative stereotypes of obese individuals as do those who are thinner; they also display high levels of explicit and implicit anti-fat prejudice ”
One way to try to reduce and overcome obesity stigma and anti-fat bias, and more generally, any weight bias, is to remind ourselves of coworkers, friends, neighbors, or acquaintances who do not fit these stereotypes. For example, we might recall a very loving relative who happens to be thin or a very competent classmate on the heavier side. Doing so could guard against premature judgments based solely on appearances, allowing us to move past stereotypes and really get to know others. And, importantly, to get to know ourselves.

Arash Emamzadeh attended the University of British Columbia in Canada, where he studied genetics and psychology. He has also done graduate work in clinical psychology and neuropsychology in U.S.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Newsletters
- Account Activating this button will toggle the display of additional content Account Sign out
Fat Lies Revisited
Obesity, self-discipline, and stigma..
Last week, I wrote about obesity as a failure of self-discipline . A lot of you wrote back to let me have it. In the Fray , blogs , and e-mail, you told me I was wrongheaded and just plain mean. Some of this is miscommunication, but it’s my fault. I was trying to explain something important, and I botched it. Let me try again.
The topic was a study published in the New England Journal of Medicine . It documented weight trends in a social network originating in Framingham, Mass. What the study illustrated, according to its authors, was “psychosocial mechanisms of the spread of obesity” through “a change in [one’s] perception of the social norms regarding the acceptability of obesity.” As your friends get fat, you start to think their degree of fatness is OK for you, too.
That’s the important point. Now let’s talk about what it means—and doesn’t.
1. It doesn’t mean you should ditch your fat friends. The study’s implication, as I described it, is that “if you find yourself caught in a fattening social network, you have three options. You can resist the fattening norm. You can try to reverse it. Or you can ditch your fat friends.” The authors discouraged the ditching option on the grounds that friendship is good for your health. Instead, they suggested, you should spend more time “forming ties with underweight or normal weight friends.”
Ugh. This is a classic case of scientists inventing the kind of argument they’re comfortable with—a scientific one—for what’s really a moral point. The invented argument is well-intended but bogus. If you spend more time with “underweight or normal weight friends,” you’re spending less time with overweight friends. That’s a mathematical and social fact, just like more time at the office means less at home. Nor does the healthiness of friendship require you to keep your fat friends. By trading them in for thinner friends, you’d end up with just as many friends as you had before. So, I made those points, because I don’t like deceptions.
Then I did something stupid: I ended the piece. I neglected to spell out what I assumed: You shouldn’t ditch your fat friends anyway —not for health reasons but because the point of friendship is that you don’t go around ditching your friends every time that might be “in your interest.” Your friend may develop an addiction, fall on hard times, or get a disease. Standing by him could become inconvenient in lots of ways. Do it anyway, because a person is more than his wealth or his disease and because friendship is more than convenience. If your friend develops something harmful and remediable, such as an addiction, you should help him fight it. That’s what I was clumsily trying to say.
2. It doesn’t mean all fat is acquired through lack of discipline. Some fat, as I explained last week, is genetically or environmentally induced. But I added that
such factors can’t account for the spread pattern documented in this study. Genetics can’t explain it, since having a fat friend was more likely to predict a person’s obesity than having a fat sibling was. Environmental constraints can’t explain it, since faraway friends made a difference, while next-door neighbors didn’t. Availability of food can’t explain it, since friends had a bigger effect than spouses did.
I was trying to distinguish two categories of fat: the kind some people acquire despite their best efforts and the “psychosocial” kind nearly all of us can get from slacking off. Some people came into the Framingham study carrying the first kind. As the study went on, others developed the latter kind. I was too sloppy about maintaining this distinction. For example, I wrote, “Obesity spreads culturally.” No. Some obesity spreads culturally.
3. Stigma is dangerous. What most infuriated readers was my conclusion that “responsibility and stigma are part of the solution.” To the extent that fat is acquired through lack of discipline and loss of concern about proper weight, that’s true. But I’m having second thoughts about stigma, because its nature is more sentimental than rational. Sentiments are crude, probably too crude to distinguish one kind of fat from another. You can’t tell from looking at a chubby guy whether he’s cursed with bad metabolism or just watches too much television. So, stigma could do more harm than good. Somehow, we need to reinforce norms against “psychosocial” weight gain without blaming people who have been dealt a bad hand.
Also, I should have distinguished two different ways in which “social norms regarding the acceptability of obesity” can change. One is that people stop caring about being fat. The other way is that they still care, but their definition of fat slides. The Framingham study doesn’t clarify which process was going on. If what’s sliding is the standard of obesity, rather than concern about being fat in general, then people may not need a forceful cultural message against obesity. They may just need clarification of where the line is.
Many of you argued that there’s already plenty of stigma against fat. If we’re talking about people constrained by factors beyond their control, I agree, since in their case, any stigma is too much. But if we’re talking about controlling the psychosocial spread of obesity among the larger population, then no, the current level of stigma isn’t doing the job. Obesity is spreading worldwide , and sliding norms are a big part of it.
Exhibit A : Last year, nutritionists presented data from a study of middle-aged Americans. Participants were asked to classify themselves as underweight, normal weight, overweight, or obese. Then they were weighed. Only 15 percent of obese people, compared with more than 70 percent of normal and overweight people, classified themselves correctly.
Exhibit B : In a 1985 survey by the NPD group, 55 percent of U.S. adults agreed that “[a] person who is not overweight is a lot more attractive.” By 2005, only 24 percent agreed. The firm concluded, “Perhaps Americans have found that the easiest way to deal with their weight is to change their attitude.”
What these data suggest, together with the Framingham study, is a cultural erosion of norms against fat. We need to confront it. As somebody who preaches self-discipline to others, I’m sorry that my carelessness got in the way of making the point.
- Research article
- Open access
- Published: 16 April 2015
Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators
- Pedro J Teixeira 1 ,
- Eliana V Carraça 1 ,
- Marta M Marques 1 ,
- Harry Rutter 2 ,
- Jean-Michel Oppert 3 , 4 ,
- Ilse De Bourdeaudhuij 5 ,
- Jeroen Lakerveld 6 &
- Johannes Brug 7
BMC Medicine volume 13 , Article number: 84 ( 2015 ) Cite this article
66k Accesses
376 Citations
335 Altmetric
Metrics details
Relapse is high in lifestyle obesity interventions involving behavior and weight change. Identifying mediators of successful outcomes in these interventions is critical to improve effectiveness and to guide approaches to obesity treatment, including resource allocation. This article reviews the most consistent self-regulation mediators of medium- and long-term weight control, physical activity, and dietary intake in clinical and community behavior change interventions targeting overweight/obese adults.
A comprehensive search of peer-reviewed articles, published since 2000, was conducted on electronic databases (for example, MEDLINE) and journal reference lists. Experimental studies were eligible if they reported intervention effects on hypothesized mediators (self-regulatory and psychological mechanisms) and the association between these and the outcomes of interest (weight change, physical activity, and dietary intake). Quality and content of selected studies were analyzed and findings summarized. Studies with formal mediation analyses were reported separately.
Thirty-five studies were included testing 42 putative mediators. Ten studies used formal mediation analyses. Twenty-eight studies were randomized controlled trials, mainly aiming at weight loss or maintenance (n = 21). Targeted participants were obese (n = 26) or overweight individuals, aged between 25 to 44 years (n = 23), and 13 studies targeted women only. In terms of study quality, 13 trials were rated as “strong”, 15 as “moderate”, and 7 studies as “weak”. In addition, methodological quality of formal mediation analyses was “medium”. Identified mediators for medium-/long-term weight control were higher levels of autonomous motivation, self-efficacy/barriers, self-regulation skills (such as self-monitoring), flexible eating restraint, and positive body image. For physical activity, significant putative mediators were high autonomous motivation, self-efficacy, and use of self-regulation skills. For dietary intake, the evidence was much less clear, and no consistent mediators were identified.
Conclusions
This is the first systematic review of mediational psychological mechanisms of successful outcomes in obesity-related lifestyle change interventions. Despite limited evidence, higher autonomous motivation, self-efficacy, and self-regulation skills emerged as the best predictors of beneficial weight and physical activity outcomes; for weight control, positive body image and flexible eating restraint may additionally improve outcomes. These variables represent possible targets for future lifestyle interventions in overweight/obese populations.
Peer Review reports
Lifestyle treatment interventions for obesity typically target changes in diet and physical activity through strategies like setting adequate goals and enhancing patients’ motivation, changing their beliefs and expectations, and providing guidance in the use of a variety of self-regulation skills (such as self-monitoring), all of which are thought to influence behavior change and maintenance [ 1 - 4 ]. A wide variety of health behavior change theories has been employed to provide conceptual organization of these determinants, including social cognitive theories such as the theory of planned behavior [ 5 ], theories of motivation such as self-determination theory [ 6 ], theories distinguishing between motivational and post-motivational or volitional phases [ 7 ] such as the health action process approach (HAPA) [ 8 ], and self-regulation models such as control theory [ 9 ]. Since all these theories address the regulation of a person’s behavior in the service of some goal or desired outcome, through intrapersonal factors, in this paper we broadly refer to intervening variables in this process as self-regulation factors .
Behavior modification in general, and “comprehensive lifestyle interventions” in particular [ 10 ] are currently the first recommended step in obesity management. However, so far, randomized controlled trials evaluating the effectiveness of programs that target lifestyle behavior have shown mixed effects and, if effective, they have generally resulted in only small changes in target behaviors [ 11 - 15 ]. In addition, the evidence shows that relatively little if any weight loss accomplished in treatment programs is maintained over the long term [ 16 ]. Furthermore, few studies have analyzed why, or by which mechanisms, interventions are successful for some individuals and not for others. Clearly, there is a need for research that identifies causal predictors of long-term weight control, including successful weight loss and maintenance [ 17 ].
Despite the limited success of available interventions in reversing the current trends in obesity prevalence, approaches focusing on individual behavior change remain an important topic of interest in obesity research. Several reasons justify this assertion. First, these interventions typically focus on behaviors (for example, diet and physical activity), which have widespread consequences for health, with or without weight loss. Second, if and when individuals are able to successfully self-regulate their behaviors, these effects tend to be sustainable, which is essential for having a lasting impact on health; moreover, this successful self-regulation may also “transfer” to, and help change, other health behaviors [ 18 ]. Third, although some interventions targeting individuals may be ineffective on their own, they might be able to contribute to the effectiveness of strategies that integrate multiple levels (that is, strategies that include individual-level and environmental-level approaches) [ 19 ]. Finally, the potential for dissemination of individual-level intervention approaches is considerable, given that a sizable number of overweight and obese persons will seek professional help at some point in their lives. Consequently, improving the efficacy of such interventions has substantial clinical as well as public health relevance.
One recent development in studies testing lifestyle interventions for obesity is their ability to identify the mechanisms or processes by which interventions induce meaningful and lasting change in their (most successful) participants. These mechanisms can generally be named predictors (or determinants ) of success, and some studies have gone one step further to evaluate the extent to which they may be causal mediators of intervention effects. Testing of mediation, using appropriate methods, is a critical step in this field; it provides the strongest possible inference for the identification of elements in interventions which are causally “responsible” for achieving desired outcomes [ 20 ].
Success and failure in the self-regulation of health behaviors involve multiple psychological and behavioral aspects. The aim of this review was to identify and summarize psychological self-regulation mediators of successful weight change, or change in energy balance-related behavior (physical activity and diet), in clinical and community behavior change obesity interventions. Because eventual weight regain is frequent after behavior and/or weight change interventions, particular attention was given to studies reporting long-term outcomes, that is, one year or more after the beginning of the intervention.
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [ 21 ].
Eligibility criteria
Studies were included in this review if they were intervention studies published since 2000 in the English language, used experimental designs, and referred to clinical or community behavior change interventions with overweight/obese adults (≥18 years old) aiming to reduce overweight/obesity. This review was limited to “lifestyle interventions” defined as interventions that promote change in energy balance-related behaviors (such as diet and physical activity, as the outcomes) and self-regulatory factors (such as motivation and self-monitoring, as the potential mediators) relevant for overweight/obesity treatment, typically in settings involving personal contact between interventionists and participants. There were no restrictions with respect to the format and duration of the intervention. To be eligible, studies should also report outcomes assessed at least 6 months after the start of the intervention; include a quantitative assessment of change in weight/BMI, physical activity (for example, self-reported or accelerometer-derived minutes of moderate and vigorous physical activity, daily pedometer steps, attendance to PA sessions), or dietary intake (for example, energy intake, fat intake, fruit and vegetable intake) as well as a quantitative assessment of potential mediators of successful behavior change. We decided not to distinguish predictors of weight loss and predictors of weight loss maintenance, choosing instead to divide the studies according to the length of measurement periods (shorter versus longer than 12 months). While it is possible that predictors of those two processes differ, to appropriately evaluate predictors of weight loss maintenance, we would have to rely on studies of successful weight losers, and preferably including psychological measures before and after the maintenance period. Only one intervention study fit both criteria.
An a priori list of mediators was used for study inclusion/exclusion, based on previous work in this area (for example, [ 2 , 22 ]). Only mediators representing individual-level self-regulatory processes were considered (that is, those related to skills, motivation, competence , coping mechanisms, beliefs, physical self-perceptions, and eating regulation factors such as disinhibition, restraint, and perceived hunger). Mediators associated with personality factors, social support, and health-related outcomes (such as psychological distress, quality of life, and well-being) were excluded. Finally, eligible studies were required to report the effect of the intervention on hypothesized mediator(s) and the association of the putative mediator with the outcomes of interest.
Search strategy and study selection
A comprehensive search of peer-reviewed articles published between January 2000 and February 2014 (including online ahead of print publication) was conducted in six electronic databases (Pubmed, MEDLINE, PsycINFO, the Cochrane Library, Web of Knowledge, and SPORTDiscus). The decision to restrict the selection to studies published since 2000 is based on the fact that recent development in studies testing the effectiveness of lifestyle interventions for obesity makes older studies less externally valid. For instance, in 1995, Friedman and Brownell [ 23 ] alerted for the need of a “third generation” of obesity treatment studies analyzing causal mechanisms between psychosocial variables and weight change. Despite this, one decade later, it has been observed that very few studies had investigated such mechanisms, and even fewer looked into long-term changes [ 2 ].
Searches included various combinations of four sets of terms: i) terms concerning the health condition or population of interest (overweight/obesity); ii) terms concerning the intervention(s)/exposure(s) evaluated (for example, behavior change/lifestyle obesity interventions); iii) terms respecting the outcomes of interest (weight change, physical activity, and dietary intake); iv) terms concerning the predictors/mediators of interest (psychological, self-regulation); and v) terms concerning the type of analyses of relevance (for example, mediation, correlates, predictors). (See Additional file 1 for a search example; complete search strategies can be obtained from the authors). Other sources included manual cross-referencing of bibliographies cited in previous reviews [ 2 , 22 , 24 - 26 ] and included studies, as well as manual searches of the content of key scientific journals ( Obesity Reviews; International Journal of Obesity; Obesity (Silver Spring); International Journal of Behavioral Nutrition and Physical Activity; Journal of the American Dietetic Association; Psychology of Sports and Exercise; Health Psychology; Journal of Behavioral Medicine; Preventive Medicine ).
Titles, abstracts, and references of potential articles were reviewed by two authors (EVC, MM) to identify studies that met the eligibility criteria. Duplicate entries were manually removed. Relevant articles were then retrieved for a full read. The same two authors reviewed the full text of potential studies, and decisions to include or exclude studies in the review were made by consensus.
Data coding and extraction
A data extraction form was developed, informed by the PRISMA statement for reporting systematic reviews [ 21 ] and the Cochrane Collaboration’s tool for assessing risk of bias [ 27 ]. Data extraction included information about study details (authors, year, country of publication, affiliations, and funding), participants (characteristics, recruitment, setting, attrition, compliance, and blinding), study design and setting, outcomes of interest, mediators/predictors (in/out list), intervention length and characteristics, psychosocial instruments, and statistical analysis, including mediation techniques (a complete coding form can be obtained from the authors). Authors of included studies were contacted when necessary to retrieve missing data in published reports.
Considering that the main focus of this review was the identification of mediators, data extraction was performed separately, starting with the studies formally testing mediation (see Additional file 2 ), followed by those that reported both the effect of the intervention on hypothesized mediators ( path a ) and the association of the putative mediator with the outcomes of interest ( path b ), but did not test mediation (see Additional file 3 ). Regarding mediation and specifically in studies with formal mediation tests, researchers could use Baron and Kenny’s approach [ 28 ] and check whether the main effects were reduced in the presence of the mediator, or employ more sophisticated techniques to directly test the significance of the indirect effect through the mediator (for instance, by following MacKinnon’s approach [ 29 ], and using Preacher and Hayes mediation procedures or structural equation modeling). Additional file 4 presents a detailed description of the mediation analyses procedures and estimates for each study. In the latter (that is, predictor studies), we generally looked at a) whether significant intervention-control differences existed for a given variable (or pre-post change in non-controlled designs); b) whether there was an association between these changes (in intervention group only) and changes in the outcome (weight/PA/diet) in this group. If both were present, results were deemed consistent with mediation.
Quality assessment
The quality of included studies was assessed using an adapted version of the Quality Assessment Tool for Quantitative Studies, developed by the Effective Public Health Practice Project [ 30 ], and recommended for use by the Cochrane Public Health Review Group [ 27 ]. The current adaptation was based on recommendations from several authors [ 31 , 32 ], and has been used in a previous systematic review conducted as part of the SPOTLIGHT project [ 33 ]. This tool was adapted to allow the evaluation of both experimental and observational studies and contains 19 items, guiding the assessment of eight key methodological domains – 1) study design, 2) blinding, 3) representativeness (selection bias), 4) representativeness (withdrawals/dropouts), 5) confounders, 6) data collection, 7) data analysis, and 8) reporting. Each domain is classified as Strong (low risk of bias/high methodological quality), Moderate , or Low (high risk of bias/low methodological quality) methodological quality. A global rating is determined based on the scores of each component (see Additional file 5 for a full description of the Assessment Tool components and scoring system). Two researchers independently rated each of the eight domains and overall quality (EVC, MM). Discrepancies were resolved by consensus.
For studies employing formal tests of mediation, assessment of methodological quality was complemented with a checklist tool developed specifically for mediation analysis by Lubans, Foster, and Biddle [ 34 ], and subsequently adapted by Rhodes and Pfaeffli [ 35 ]. This tool includes 11 questions answered with a yes (1) or no (0) format, whose scores are added to generate a global score. High quality is represented by scores between 9 and 11, moderate quality ranges between 5 and 8, and low quality is considered when scores are below 5 (see Additional file 5 for a full description of the Checklist components and scoring system). Methodological quality of the mediation analyses was also rated by two authors (EVC, MM), with conflicting judgments discussed to reach agreement. Inter-rater agreement was good (Cohen’s kappa = 0.78).
Data synthesis
This review analyzed psychological and self-regulation mediators and predictors of change in body weight or BMI (primary outcome), physical activity, and dietary intake, separately (Note: we will use the term predictors when studies did not test for formal mediation, and mediators when they did). Intervention effects on the outcomes of interest were included in Additional files 2 and 3 . Results were divided according to the length of assessment of the outcomes, into short-term (<12 months from the start of the intervention) and long-term (≥12 months), so that those variables mediating/predicting more sustainable outcomes (the main focus of this review) could be more easily identified. Twelve months has been indicated by an expert panel on obesity as an appropriate threshold between weight loss and the maintenance of the weight lost [ 10 ]. In the synthesis of data derived from studies formally testing mediation, only controlled trials were included, to further strengthen inference regarding intervention effects on mediators and outcomes. In the case of prediction studies (not formally testing mediation), we included both controlled and uncontrolled trials, to capitalize on the (relatively) larger number of studies available, which would otherwise be excluded using the more stringent criteria. Table 1 describes the 35 included studies. In Tables 2 , 3 , 4 , 5 , 6 , and 7 , mediation-specific results are discriminated from the general results, provided that the main goal of this review was the identification of self-regulation mediators in behavior change obesity interventions. The overall results (considering multivariate, bivariate/correlational, and mediation analyses) are also presented in each table (Tables 2 , 3 , 4 , 5 , 6 , and 7 ). A total of 42 mediators/predictors were identified across outcomes. To facilitate data interpretation, considering the very large number of individual variables, these were grouped together by similarity into categories. Categorization was done through the extraction of information from primary studies on the definition and operationalization of the constructs. The following 12 categories were formed: Self-regulatory skills use, Processes of change, Coping mechanisms, Self-efficacy/barriers, Autonomous motivation, Controlled motivation, Decisional balance, Outcomes expectations/beliefs, Body image/physical self-worth, Cognitive restraint, Eating disinhibition, Perceived hunger. Please refer to Additional file 6 for full details regarding the mediators/predictors identified per outcome.
Finally, Tables 2 , 3 , 4 , 5 , 6 , and 7 show, separately for each mediator/predictor, the number of studies that have analyzed it, the number of times it was tested (some of them within the same study), and the number of times a significant effect was found. Results are presented for mediation-specific results and for the overall results.
Study selection
The literature search yielded a total of 1,394 potentially relevant records. Eight additional articles that were identified through manual searches and cross-referencing were added, bringing the total number of potential articles to 1,404. Of these, 770 abstracts were assessed for eligibility (634 duplicates removed). After the initial screening of titles and abstracts, 692 articles were excluded (Figure 1 ). Some articles were excluded for multiple reasons. Thirty-five articles describing 32 unique lifestyle interventions met the eligibility criteria and were therefore included [ 36 - 70 ]. Papers reporting on the same intervention are identified in Additional files 2 and 3 .
Flow diagram of studies.
Study characteristics
The characteristics of included studies are summarized in Table 1 (for further details, see Additional files 2 and 3 ). Most studies (n = 28) were randomized controlled trials, mainly aiming at weight loss or weight loss maintenance (n = 21). Most interventions took place in university (n = 15) or fitness club settings (n = 12), and most lasted more than 6 months (n = 29). However, only 11 trials included a follow-up assessment period and, of these, more than half were shorter than 12 months. Most studies were based on, or at least informed by, one or more theories of behavior change; the most frequent being social cognitive theory (n = 23), the transtheoretical model (n = 5), and self-determination theory (n = 3). Eight interventions were grounded in other theories, including group dynamics theory, problem solving model, theory of planned behavior, health belief model, and self-regulation theory. Four studies did not report using any theoretical framework. Samples were mostly composed of obese individuals (n = 26), aged between 25 to 44 years old (n = 23), and 13 studies targeted women only.
Twenty-six studies evaluated mediators/predictors of weight change, of which 17 reported medium/long-term outcomes; 19 studies evaluated mediators/predictors of physical activity, with 8 of them reporting medium/long-term outcomes; finally, 11 studies investigated dietary intake as the outcome measure, 4 of them in the medium/long-term. Weight-related measurements were performed with calibrated digital scales, and weight changes were expressed in weight change percent from baseline (n = 9), in kilograms (n = 10), as residualized scores regressed on the baseline scores (n = 6), or as BMI changes (n = 3). Regarding physical activity, objective measures were employed in 4 studies (for example, accelerometry, pedometry) and self-reported instruments in 17 studies; of these, 6 used the Seven-Day Physical Activity Recall [ 71 ] and 6 studies used the Godin Leisure-Time Exercise Questionnaire [ 72 ]. Dietary and caloric intake, indirectly assessed through the number of servings, was collected with the Food Intake Questionnaire in most studies (n = 5), followed by the Three-Day Food Records in most of the studies (n = 3), and the Block Food-Frequency Questionnaire (n = 1).
The overall results of the quality assessment can be found in Table 1 and the total quality score for each study in Additional files 2 and 3 (for a detailed classification of each item and study see Additional file 7 ). Regarding the overall methodological quality of the studies, 13 studies were rated as ”strong”, 15 were classified as ”moderate”, and 7 were rated as ”weak”. All included studies scored strong on the Study design , as they were experimental. Thirteen studies were rated as weak regarding Blinding of participants (during recruitment) and outcome assessors, 13 were rated as moderate, 8 as strong, and 1 did not receive a rating, as it was a non-randomized trial. All studies except two (one scored weak and the other scored strong) scored moderate regarding Representativeness (selection bias). Regarding reporting of Withdrawals and dropouts , 5 studies were rated as weak, 16 as moderate, and 14 as strong. Four studies scored weak in the adjustment of analysis for Confounders , 10 scored moderate, and 21 strong. In terms of Data collection tools, 4 studies were rated as weak as they did not provide information on the validity or reliability of the measures used, 11 were classified as moderate, and 17 as strong. Three studies were not rated as they used a larger dataset for which information on psychometric properties of the measures is already provided. All studies scored strong in the use of Appropriate statistical analyses . In terms of Reporting, 30 studies were rated as strong, and 5 studies as moderate.
In addition, studies including formal tests of mediation (n = 10) were classified as of moderate (n = 10) quality on the mediation analysis checklist. None of the studies reported conducting pilot studies to test mediation, and in all except two studies, there was no specific information regarding the power of the analysis to detect mediation. In only six studies were the outcomes controlled for baseline values.
Mediators/predictors tested in studies with weak methodological quality are identified in Tables 2 , 3 , 4 , 5 , 6 , and 7 . Overall, there appeared to be no association between the methodological quality of the studies and the results of the mediation analyses. Only 2 out of the 7 studies with a global weak score reported significant results for all mediator/predictors.
Mediators/predictors of weight control
Of the total number of studies investigating mediators/predictors of weight control (n = 26), 9 looked into short-term outcomes (<12 months) [ 47 - 49 , 51 , 52 , 54 , 57 , 62 , 70 ]. Twenty-one variables, grouped into nine categories, were tested as mediators/predictors of short-term weight control (Table 2 ). None of the studies performed formal tests of mediation. In the overall analyses (in this case, all were multivariate), self-regulation skill use emerged as the most consistent predictor of short-term weight control (consistent with mediation in 92% of the times it was tested [12 times in 6 studies]). Other variables that appear promising as mediators of short-term weight control were higher self-efficacy (and/or lower perceived barriers) and more positive body image, both consistent with mediation in 67% of the times they were tested (a total of 9 and 6 times, respectively). In the case of self-efficacy, 2 (out of 6) studies presented with low methodological quality. Although lower eating disinhibition also appears to find empirical support in non-formal mediation analyses, these results come from a single, weak quality study, and are correlational in nature. There were no other consistent mediators/predictors of short-term weight control.
Seventeen studies investigated potential mediators/predictors of long-term (≥12 months) weight outcomes, the main focus of the review [ 36 , 39 , 40 , 43 - 45 , 55 , 56 , 58 , 59 , 63 - 66 ]. Of these, six were RCTs that included formal tests of mediation [ 36 , 39 , 40 , 43 - 45 ]. Thirty variables, grouped in 12 categories, were tested as potential mediators/predictors (Table 3 ). The variables with stronger empirical support in formal mediation studies were body image, which was significant in all the times it was tested (3 times), and self-regulation skills, which was identified as a mediator in 67% of the times it was tested (2 times out of 3 studies). Self-efficacy was a significant mediator in 2 of the 3 times it was tested. For autonomous motivation and flexible eating restraint, results appear promising but derive from a single study in each case. Results observed in non-mediation analyses were consistent with the most stringent analyses, especially those concerning self-regulation skill use, autonomous motivation, and self-efficacy. For self-regulation skill use, significant effects were found in 83% of the 6 times it was tested, and every time in multivariate analyses. For autonomous motivation, results were consistent with mediation in all cases, but they originate from only two studies. On the other hand, empirical support from non-mediation analyses for other variables like body image and self-efficacy appears comparatively weaker and correlation-based; yet, the number of times each of these variables was tested is substantially higher (34 and 28 times, respectively). Eating disinhibition, which appeared to be an additional predictor in the short-term, does not seem to be consistent in the long-term provided that it was significant only in 38% of the 16 times it was tested. There were no other consistent mediators/predictors of long-term weight control.
Mediators/predictors of physical activity
Of the total number of studies investigating mediators/predictors of physical activity (n = 19), 11 looked into short-term outcomes (less than 6 months beyond the start of the intervention) [ 37 , 46 , 51 - 53 , 60 , 61 , 67 - 70 ]. Of these, only one formally tested mediation [ 37 ]. Fourteen variables, grouped in seven categories, were tested as mediators/predictors of short-term weight control (Table 4 ). Regarding mediation-specific results, body image emerged as a significant mediator only in one of the two times it was tested. In non-mediation studies, stronger empirical support was found for self-regulation skill use, which was significant in 11 of the 13 times it was tested (corresponding to 7 different studies). Body image and self-efficacy appear to be promising as mediators of short-term physical activity, showing significant results in 4 (out of 6) and 10 (out of 15) times they were tested, respectively. No other consistent mediators/predictors of short-term physical activity were identified.
Eight studies analyzed mediators/predictors of long-term physical activity [ 36 , 38 , 41 - 43 , 50 , 64 , 65 ], of which five used formal tests of mediation [ 36 , 38 , 41 - 43 ]. Twenty-three variables, grouped in nine categories, were tested as predictors (Table 5 ). The main predictors of long-term physical activity were autonomous motivation and self-efficacy, considering both mediation-specific analyses and the overall analyses. For autonomous motivation, results from two studies showed that mediation analyses were significant in 83% of the times and overall analyses showed consistency with mediation in 93% of the times (out of 14). For self-efficacy, results originated from 6 different studies. Mediation analyses were significant in 67% of the times self-efficacy was tested (6 times); and in the overall analyses, results were consistent with mediation in 75% of the times (out of 12). Controlled motivation was also consistently unrelated with physical activity outcomes, independent of the type of analyses performed. Finally, self-regulation skill use appears to mediate long-term physical activity in one out of two (formal mediation) and two out of the three (all analyses) times tested, but these results derive from two studies with low methodological quality.
Mediators/predictors of dietary intake
Of the total number of studies (n = 11) investigating mediators/predictors of dietary intake, seven looked into short-term outcomes [ 46 , 53 , 61 , 67 - 70 ] and four into long-term outcomes [ 41 , 50 , 64 , 65 ]. Only one study formally tested mediation [ 41 ]. Seven variables (grouped in three categories) were tested as mediators/predictors of short-term dietary intake, while 12 variables (grouped in seven categories) were tested in the long-term (Tables 6 and 7 ). Self-efficacy/barriers and self-regulation skill use appear promising as mediators of dietary intake in the short-term, both showing results consistent with mediation in 75% of the times they were tested (12 times out of 6 studies for self-efficacy, and 12 times out of 5 studies for self-regulation skills). No consistent mediators/predictors were identified in the longer time frame. Yet, self-efficacy was consistently unrelated with long-term dietary intake, looking less promising as a mediator (results were consistent with mediation only in 2 of the 8 times it was tested).
This review sought to identify the most consistent individual-level mediators of weight change, physical activity, and obesity-related dietary variables, in the context of lifestyle obesity interventions aimed at overweight and obese adults. These mediators or predictors of intervention effects were assessed by self-report, and are thought to represent psychological mechanisms or processes by which interventions affect body weight, through changes in energy-balance related behaviors. Note that this review did not focus on the efficacy of the interventions’ main effects per se. However, mediation mechanisms can be evaluated even in the absence of main significant effects of interventions, particularly in controlled trials [ 20 ].
Special emphasis was given to variables tested as formal mediators of changes in the outcomes of interest, as this provides the best possible inferences regarding causal determinants of behavior change [ 73 ]; to the extent a consistent mediator is identified, it can more confidently be targeted in future interventions of comparable characteristics. Moreover, because it is unlikely that any single factor (self-regulatory or otherwise) by itself will explain a large share of variance of change in complex behaviors such as physical activity and diet (as a result of an intervention), the identification of groups of significant predictors, which can be then discussed in the context of current theories of behavior change, can additionally contribute to understanding the role of theory in health behavior change [ 74 , 75 ].
As in many systematic reviews of behavior change interventions, the diversity of studies available - reflected on a similarly diverse set of independent (and dependent) variables, study designs, measurement methods, populations represented, and so forth - is a substantial limitation. In the present review, the large number of predictors per study, combined with substantial heterogeneity in study length, type and format of interventions (for example, web-based, face to face, group-based), and assessments employed for each variable made the task at hand especially difficult. In this scenario, the fact that several variables were identified as predictors or, in some cases, actual mediators of intervention-related change in weight control and physical activity is encouraging. Specifically, the present review shows that positive changes in body image, in autonomous motivation for physical activity, in self-efficacy (and fewer perceived barriers), and in the use of self-regulation skills (such as self-monitoring) are promising aspects that may explain the variability of results in current lifestyle obesity treatment interventions. Increases in flexible restraint could also be in this group with respect to weight outcomes, but with lower inference. Therefore, these are currently the best evidence-based candidates to target in future individual-level, real-world interventions in this domain.
Some qualifications to the previous conclusions are of note. First, for short-term results, formal tests of mediation were only reported for one of the outcomes of interest (physical activity) and taking into account only two mediators (body image/self-worth and self-efficacy/barriers). Second, there are currently too few studies using dietary variables as outcomes to allow us to draw meaningful conclusions, and only one study tested formal mediation for both time frames. Third, the external validity of some of the reported findings, such as regarding self-regulation skills and autonomous motivation, may be limited, because these findings were derived from few studies conducted by a small number of research groups, using similar study designs.
Body image appeared important as a mechanism leading to change in body weight in several studies. Body image is a multidimensional concept [ 76 ] that depicts attitudes, perceptions, and in some cases behaviors associated with mental representations of one’s body (or some of its parts) [ 77 , 78 ]. Poor body image often reflects a high level of concern with body weight or shape, what is known as dysfunctional investment in body image, when body esteem occupies an excessive role as a determinant of overall self-esteem [ 79 ]. Previous reviews [ 2 , 22 ] have identified poor body image as a predictor of less success at body weight loss (or, conversely, better body image as a positive factor in obesity treatment interventions). Potential reasons for this association range from excessive psychological pressure leading to more rigid and inconsistent eating regulation [ 80 - 82 ] - poor body image being associated with a history of failed attempts and thus being a marker for other physiological, psychological, or socio-environmental risk factors for weight gain/regain [ 83 , 84 ] - to motivational factors in which external pressures and goals predominate but tend not to produce behavior change in consistent or healthy ways (for example, wanting to be thin for reasons related to social comparison and perceived desirability) [ 85 - 87 ].
Autonomous motivation, a concept derived from self-determination theory (SDT, [ 88 ]), generally indicates the degree to which individuals self-endorse, feel that they have a choice about, and attribute deeply reflected value to a certain behavior. In contrast with the most common quantitative view of motivation (how much?), the level of autonomy represents a qualitative analysis of people’s psychological energy to act, which is perceived as internal (reflecting a sense of “ownership” over the behavior). Autonomous motivation is often associated with goals such as pursuing positive personal challenges, attaining/preserving health and well-being, social affiliation, personal development, and self-expression [ 89 ]. Additionally, because self-determined, well-internalized behaviors are associated with the satisfaction of the needs for autonomy, competence, and relatedness - and with the feelings of internal coherence and well-being that are thought to emerge from those experiences - this provides an explanation for the behavior to be pursued consistently [ 89 ]. A recent meta-analysis [ 90 ] and other reviews provide empirical support for both the SDT motivation model and the association of autonomous motivation with health behavior change in different areas [ 91 ].
Self-efficacy and perceived barriers are common variables in several theoretical frameworks concerned with health behaviors [ 92 , 93 ]. Self-efficacy measures one’s confidence to successfully implement a course of action by successfully organizing internal and external resources [ 94 ]. Although efficacy can be assessed towards other aspects of behavior regulation, it is commonly conceptualized and assessed as “barriers efficacy” or confidence to overcome internal or external obstacles that may stand in the way of one’s actions. Indeed, the correlation between self-efficacy and perceived barriers is usually high [ 56 ] (which explains our decision to group these variables in the same category). Although conceptual differences exist, self-efficacy is often equated to the concept of perceived behavior control (from the theory of planned behavior) or perceived competence (as used in self-determination theory). In practical and simple terms, enhancing confidence and competence about a given health behavior appears to be helpful in overcoming barriers - namely in initial stages of adoption - and is often a first step to increase and improve motivation for change.
Flexible eating restraint involves regulating one’s food intake so that no particular behavior is forbidden and thus subject to rigid control and scrutiny [ 95 ]. Flexible restraint is generally associated with less internal pressure to diet and a more gradual understanding of the diet’s impact on energy balance. It stands in opposition to rigid restraint [ 96 ]. Although, in the past, cognitive restraint was measured as a unified concept, its separation into flexible and rigid dimensions is increasingly frequent in obesity studies and has proven useful in understanding diet and weight regulation, particularly in the long-term. For example, we found that flexible, but not rigid or total restraint, mediated 24-month weight loss in overweight women [ 39 ] and, in the present review, results for the total restraint scale and the flexible scale also differed, as in other studies [ 97 ]. More broadly, psychological flexibility appears to predict health and psychological well-being [ 97 ], is thought to reflect more committed, values-based goal pursuit [ 98 , 99 ] and is considered a hallmark of self-determination [ 89 ], factors which may help explain successful health behavior self-regulation.
Finally, the use of certain self-regulation skills, for instance, monitoring weight, diet, and activity, as well as employing goal setting and planning techniques, was also identified as a relatively consistent predictor of successful outcomes, most especially in the shorter-term analyses. In brief, some of these skills may be important for people to ultimately act on their positive intentions. Sometimes associated with self-regulation theories ( cf . [ 100 ]) these variables are more skill-based (in some cases, they are discrete behaviors in themselves) and somewhat different than the previous set of predictors, more intrapsychic. Notably, recent behavior change models focusing on the “intention-behavior gap” (see, for example, [ 7 , 101 , 102 ]) make the distinction between motivational and implementation phases (sometimes referred to as “volitional” or “post-motivational”), with self-regulation skills reviewed in the present study falling in the latter phase [ 103 ]. Results from the present review suggest that some combination of motivational and implementation factors is important. Although this needs confirmation, there is some indication that the latter may be especially useful in early stages of behavioral adoption, whereas motivational factors may be operative along the entire continuum from adoption to maintenance, as highlighted recently in a separate study [ 104 ].
In looking at the collective findings from the present analysis, the temptation to interpret them in an integrative way is unavoidable. In principle, there should be “a logic” as to why this set of predictors emerged and not a different one, even considering the intrinsic limitations of the available data (see below). In this exercise, we are informed by our own research, for instance, linking improved eating regulation, including flexible eating, with improved body image [ 105 ] and with exercise autonomous motivation [ 18 ] and also by other studies. For example, recently, in a large dataset of women in New Zealand, autonomous motivation for eating was associated with less binge eating and slower speed of eating (and a much healthier diet), indicative of improved eating self-regulation [ 106 ]. The literature looking at relations between body image and eating behavior is also fertile in suggesting a close association between improved body image, improved eating regulation, and better weight control (see, for example, [ 55 , 87 ]). In this respect, an attempt was recently made to provide an integrative view of eating regulation and weight maintenance, which also includes an explanation for the etiology and role of body image concerns and disordered eating, while considering motivational and self-regulatory aspects [ 80 ]. It links goals (such as appearance versus health focus) and the predominant approach to eating regulation (such as rigid versus flexible restraint; focus on quality versus quantity) with the satisfaction of the needs for competence, autonomy, and relatedness, resulting in more or less adaptive diet and weight regulation (see Figures one and two in [ 80 ] for more details). The evidence from other recent systematic reviews and meta-analyses, showing that more autonomous forms of health behavior regulation, in physical activity [ 91 ], weight control [ 2 ], and in health more generally [ 90 ] are predictive of better adherence and improved outcomes, is also consistent with the relationships found in the present study.
While some limitations of the present work have been presented above, others need to be considered when interpreting the findings of this review. The large heterogeneity in the study-specific mediation methods and estimates reported in the primary studies prevented us from deriving a single comparable estimate for each variable and reporting on the pooled magnitude of mediation effects. This variability, as well as the limited number of studies for each mediator, did not recommend the use of meta-analytical techniques to pool data across studies. In this review, we used a narrative synthesis approach including vote counting of the number of significant mediation effects for a given variable in relation to all tests of mediation available for that variable. Although this method is not as robust as other quantitative approaches to synthesize data, it provides a reasonably good indication of whether that variable can be identified as a formal mediator (or a variable consistent with mediation) of each intervention, for each specific outcome. It should also be considered that in the primary studies included in this review, statistical significance of the mediation effects was typically the parameter used to infer that a given variable mediated the intervention effect.
Some studies were characterized by poor methodological quality, and none of the studies employing formal mediation analysis presented strong methodological quality. Nonetheless, for most mediators we did not find an association between the methodological quality of the studies and the direction/strength of the effects reported. As exceptions, we did find that in the analyses in which eating disinhibition had consistent significant effects, this was tested mostly in studies of poor quality. A similar result was found for self-regulation skills for the long-term effects in physical activity and dietary intake. Future reviews would benefit from sensitivity analyses. The diversity of outcome measures, especially for physical activity, is also a limitation, as different types of physical activity may be predicted by different factors. The fact that the coding of study characteristics was based on the description provided in the articles is also limiting, given that in many cases these descriptions did not provide enough information regarding mediation analysis, which measures were used, or the content of the interventions. Future studies should provide more detail on the content of the interventions and self-regulation factors addressed to facilitate data interpretation and inference. The choice of the year 2000 to start our search was largely arbitrary and could be seen as a limitation. Finally, the inclusion of non-controlled trials in some of the analyses could be viewed as a limiting factor; on balance, we found this an acceptable compromise (for non-mediation studies only) against the prospect of altogether excluding several studies from this review.
These limitations notwithstanding, this study identified a small number of intervention-related aspects with supporting evidence for an important role played in the difficult path of successful weight control. Since all evidence was derived from intervention studies and independent variables were analyzed as to their mediating position in the behavioral causal chain (although with variable levels of inference), we believe this is a first step leading to their formal inclusion in recommendations for lifestyle programs aiming at weight control. In practical terms, this could mean that strategies or “behavior change techniques” [ 107 ] identified as the most effective to specifically change these variables (for example, self-efficacy [ 108 ] or autonomous motivation [ 109 ]) would be integrated into future interventions in a widespread fashion, and that health professionals would be appropriately trained on how to target them regularly in their practices. It could also mean that bedside instruments (such as brief questionnaires or interview items) would be made available for professionals to quickly assess their patients for these variables (for example, to assess their body image or level of self-regulation skill use [ 1 , 110 ]) and tailor interventions to the most relevant targets for each person. In the area of motivation enhancement, the techniques and instruments used in motivational interviewing [ 111 , 112 ] are a good example of such potential application in medicine and health care.
In conclusion, based on the scientific literature to date, autonomous motivation, self-efficacy, and self-regulation skill use emerge as the most promising individual-level mediators of positive weight outcomes and increased physical activity. For long-term weight control, promoting a positive body image and flexible eating control may also be important. These aspects represent potential entry points for future lifestyle obesity interventions in adults.
Sniehotta FF, Scholz U, Schwarzer R. Bridging the intention-behaviour gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol Health. 2005;20:143–60.
Google Scholar
Teixeira PJ, Going SB, Sardinha LB, Lohman TG. A review of psychosocial pre-treatment predictors of weight control. Obes Rev. 2005;6:43–65.
CAS PubMed Google Scholar
Maes S, Karoly P. Self-regulation assessment and intervention in physical health and illness: a review. Appl Psychol Int Rev. 2005;54:267–99.
Bandura A. The primacy of self-regulation in health promotion. Appl Psychol Health Well Being. 2005;54:245–54.
Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action control. Berlin Heidelberg: Springer; 1985. p. 11–39.
Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. New York: Plenum; 1985. p. 113–48.
Heckhausen H, Gollwitzer P. Thought contents and cognitive functioning in motivational versus volitional states of mind. Motiv Emot. 1987;11:101–20.
Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol Health Well Being. 2008;57:1–29.
Carver CS, Scheier MF. On the self-regulation of behavior. New York: University Press; 1998.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129:S139–40.
Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the diabetes prevention program into the community. The DEPLOY Pilot Study Am J Prev Med. 2008;35:357–63.
PubMed Google Scholar
Eriksson MK, Franks PW, Eliasson M. A 3-year randomized trial of lifestyle intervention for cardiovascular risk reduction in the primary care setting: the Swedish Björknäs study. PLoS One. 2009;4:e5195.
PubMed PubMed Central Google Scholar
Kinmonth AL, Wareham NJ, Hardeman W, Sutton S, Prevost AT, Fanshawe T, et al. Efficacy of a theory-based behavioural intervention to increase physical activity in an at-risk group in primary care (ProActive UK): a randomised trial. Lancet. 2008;371:41–8.
van Sluijs EMF, van Poppel MNM, van Mechelen W. Stage-based lifestyle interventions in primary care: are they effective? Am J Prev Med. 2004;26:330–43.
Lakerveld J, Bot SD, Chinapaw MJ, van Tulder MW, Kostense PJ, Dekker JM, et al. Motivational interviewing and problem solving treatment to reduce type 2 diabetes and cardiovascular disease risk in real life: a randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:47.
Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–41.
Rossner S, Hammarstrand M, Hemmingsson E, Neovius M, Johansson K. Long-term weight loss and weight-loss maintenance strategies. Obes Rev. 2008;9:624–30.
Mata J, Silva MN, Vieira PN, Carraça EV, Andrade AM, Coutinho SR, et al. Motivational “spill-over” during weight control: increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol. 2009;28:709–16.
Lakerveld J, Brug J, Bot S, Teixeira P, Rutter H, Woodward E, et al. Sustainable prevention of obesity through integrated strategies: the SPOTLIGHT project’s conceptual framework and design. BMC Public Health. 2012;12:1471–2458.
Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–83.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6:67–85.
Friedman MA, Brownell KD. Psychological correlates of obesity: moving to the next research generation. Psychol Bull. 1995;117:3–20.
Barte J, ter Bogt NC, Bogers RP, Teixeira PJ, Blissmer B, Mori TA, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev. 2010;11:899–906.
Franz MJ, Van Wormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight loss outcomes: a systematic review and meta-analysis of weight loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–67.
Curioni CC, Lourenco PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes (Lond). 2005;29:1168–74.
CAS Google Scholar
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Br Med J. 2011;343:d5928.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82.
MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614.
Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1:176–84.
Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al. Evaluating non-randomised intervention studies. Health Technol Assess. 2003;7:iii–x.1–173.
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet. 1999;354:1896–900.
Mackenbach JD, Rutter H, Compernolle S, Glonti K, Oppert JM, Charreire H, et al. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health. 2014;14:233.
Lubans DR, Foster C, Biddle S. A review of mediators of behavior in interventions to promote physical activity among children and adolescents. Prev Med. 2008;47:463–70.
Rhodes RE, Pfaeffli LA. Mediators of physical activity behaviour change among adult non-clinical populations: a review update. Int J Behav Nutr Phys Act. 2010;7:37–48.
Silva MN, Markland D, Carraça EV, Vieira PN, Coutinho SR, Minderico CS, et al. Exercise autonomous motivation predicts 3-year weight loss in women. Med Sci Sports Exerc. 2011;43:728–37.
Annesi JJ, Unruh JL, Marti CN, Gorjala S, Tennant G. Effects of the coach approach intervention on adherence to exercise in obese women: assessing mediation of social cognitive theory factors. Res Q Exerc Sport. 2011;82:99–108.
Roesch SC, Norman GJ, Villodas F, Sallis JF, Patrick K. Intervention-mediated effects for adult physical activity: a latent growth curve analysis. Soc Sci Med. 2010;71:494–501.
Teixeira PJ, Silva MN, Coutinho SR, Palmeira AL, Mata J, Vieira PN, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity (Silver Spring). 2010;18:725–35.
Perri MG, Limacher MC, Durning PE, Janicke DM, Lutes LD, Bobroff LB, et al. Extended-care programs for weight management in rural communities: the treatment of obesity in underserved rural settings (TOURS) randomized trial. Arch Intern Med. 2008;168:2347–54.
Burke V, Beilin LB, Cutt HE, Mansour J, Mori TA. Moderators and mediators of behaviour change in a lifestyle program for treated hypertensives: a randomized controlled trial (ADAPT). Health Educ Res. 2008;23:583–91.
Silva MN, Markland DM, Vieira PN, Coutinho SR, Carraça EV, Palmeira AL, et al. Helping overweight women become more active: need support and motivational regulations for different forms of physical activity. Psychol Sports Exerc. 2010;11:591–601.
Anderson-Bill ES, Winett RA, Wojcik JR, Williams DM. Aging and the social cognitive determinants of physical activity behavior and behavior change: evidence from the Guide to Health trial. J Aging Res. 2011. doi:10.4061/2011/505928.
Palmeira AL, Markland DA, Silva MN, Branco TL, Martins SC, Minderico CS, et al. Reciprocal effects among changes in weight, body image, and other psychological factors during behavioral obesity treatment: a mediation analysis. Int J Behav Nutr Phys Act. 2009;6:9.
Coughlin JW, Gullion CM, Brantley PJ, Stevens VJ, Bauck A, Champagne CM, et al. Behavioral mediators of treatment effects in the weight loss maintenance trial. Ann Behav Med. 2013;46:369–81.
CAS PubMed PubMed Central Google Scholar
Lee RE, O’Connor DP, Smith-Ray R, Mama SK, Medina AV, Reese-Smith JY, et al. Mediating effects of group cohesion on physical activity and diet in women of color: health is power. Am J Health Promot. 2012;26:e116–25.
Annesi JJ, Vaughn LL. Relationship of exercise volume with change in depression and its association with self-efficacy to control emotional eating in severely obese women. Adv Prev Med. 2011. doi:104061/2011/514271.
Annesi JJ, Gorjala S. Relationship of exercise program participation with weight loss in adults with severe obesity: assessing psychologically based mediators. South Med J. 2010;103:1119–23.
Linde JA, Rothman AJ, Baldwin AS, Jeffery RW. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychol. 2006;25:282–91.
Riebe D, Blissmer B, Greene G, Caldwell M, Ruggiero L, Stillwell KM, et al. Long-term maintenance of exercise and healthy eating behaviors in overweight adults. Prev Med. 2005;40:769–78.
Gallagher KI, Jakicic JM, Napolitano MA, Marcus BH. Psychosocial factors related to physical activity and weight loss in overweight women. Med Sci Sports Exerc. 2006;38:971–80.
Annesi JJ, Marti CN. Path analysis of exercise treatment-induced changes in psychological factors leading to weight loss. Psychol Health. 2011;26:1081–98.
Annesi JJ. Self-regulatory skills usage strengthens the relations of self-efficacy for improved eating, exercise, and weight in the severely obese: toward an explanatory model. Behav Med. 2011;37:71–6.
Annesi JJ. Behaviorally supported exercise predicts weight loss in obese adults through improvements in mood, self-efficacy, and self-regulation, rather than by caloric expenditure. Pers J. 2011;15:23–7.
Palmeira AL, Branco TL, Martins SC, Minderico CS, Silva MN, Vieira PN, et al. Change in body image and psychological well-being during behavioral obesity treatment: Associations with weight loss and maintenance. Body Image. 2010;7:187–93.
Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Metcalfe LL, Blew RM, et al. Exercise motivation, eating, and body image variables as predictors of weight control. Med Sci Sports Exerc. 2006;38:179–88.
Annesi JJ. Relations of changes in physical self-appraisal and perceived energy with weight change in obese women beginning a supported exercise and nutrition information program. Soc Behav Personal Int J. 2007;35:295–300.
Moore SD, King AC, Kiernan M, Gardner CD. Outcome expectations and realizations as predictors of weight regain among dieters. Eat Behav. 2011;12:60–3.
Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: a 1 year effectiveness study. Public Health Nutr. 2009;12:2382–91.
Annesi JJ, Whitaker AC. Weight loss and psychologic gain in obese women - participants in a supported exercise intervention. The Permanente Journal. 2008;12:36–45.
Annesi JJ. Supported exercise improves controlled eating and weight through its effects on psychosocial factors: extending a systematic research program toward treatment development. Pers J. 2012;16:7–18.
Karhunen L, Lyly M, Lapveteläinen A, Kolehmainen M, Laaksonen DE, Lähteenmäki L, Poutanen K. Psychobehavioural factors are more strongly associated with successful weight management than predetermined satiety effect or other characteristics of diet. J Obes. 2012. doi:10.1155/2012/274068.
Wing RR, Papandonatos G, Fava JL, Gorin AA, Phelan S, McCaffery J, et al. Maintaining large weight losses: the role of behavioral and psychological factors. J Consult Clin Psychol. 2008;76:1015–21.
McGuire MT, Jeffery RW, French SA, Hannan PJ. The relationship between restraint and weight and weight-related behaviors among individuals in a community weight gain prevention trial. Int J Obes Relat Metab Disord. 2001;25:574–80.
Burke V, Mansour J, Mori TA, Beilin LB, Cutt HE, Wilson A. Changes in cognitive measures associated with a lifestyle program for treated hypertensives: a randomized controlled trial (ADAPT). Health Educ Res. 2008;23:202–17.
Warziski MT, Sereika SM, Styn MA, Music E, Burke LE. Changes in self-efficacy and dietary adherence: the impact on weight loss in the PREFER study. J Behav Med. 2008;31:81–92.
Annesi JJ, Mareno N. Temporal aspects of psychosocial predictors of increased fruit and vegetable intake in adults with severe obesity: mediation by physical activity. J Community Health. 2014;39:454–63.
Annesi J. Effects of treatment differences on psychosocial predictors of exercise and improved eating in obese, middle-age adults. J Phys Act Health. 2013;10:1024–31.
Annesi JJ, Porter KJ. Reciprocal effects of treatment-induced increases in exercise and improved eating, and their psychosocial correlates, in obese adults seeking weight loss: a field-based trial. Int J Behav Nutr Phys Act. 2013;10:133.
Fitzpatrick SL, Bandeen-Roche K, Stevens VJ, Coughlin JW, Rubin RR, Brantley PJ, et al. Examining the behavioral processes through which lifestyle interventions promote weight loss: results from the PREMIER Trial. Obesity (Silver Spring). 2014;22:1002–7.
Blair SN, Haskell WL, Ho P, Paffenbager Jr RS, Vranizan KM, Farquhar JW, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122:794–804.
Godin G, Shephard RJ. Godin leisure-time exercise questionnaire. Med Sci Sports Exerc. 1997;29:S36–8.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. NY: Guilford Press; 2013.
Hagger MS. Theoretical integration in health psychology: unifying ideas and complementary explanations. Br J Health Psychol. 2009;14:189–94.
Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26:1479–98.
Cash TF. Cognitive-behavioral perspectives on body image. In: Cash TF, Pruzinsky T, editors. Body image: a handbook of theory, research, and clinical practice. New York: Guilford Press; 2002. p. 38–46.
Cash TF. A ‘negative body image’. In: Cash TF, Pruzinsky T, editors. Body image: a handbook of theory, research, and clinical practice. New York: Guilford Press; 2002. p. 269–76.
Avalos L, Tylka TL, Wood-Barcalow N. The body appreciation scale: development and psychometric evaluation. Body Image. 2005;2:285–97.
Cash TF, Melnyk SE, Hrabosky JI. The assessment of body image investment: an extensive revision of the appearance schemas inventory. Int J Eat Disord. 2004;35:305–16.
Verstuyf J, Patrick H, Vansteenkiste M, Teixeira PJ. Motivational dynamics of eating regulation: a self-determination theory perspective. Int J Behav Nutr Phys Act. 2012. 9:21. doi:10.1186/1479-5868-9-21.
Pelletier LG, Dion SC. An examination of general and specific motivational mechanisms for the relations between body dissatisfaction and eating behaviors. J Soc Clin Psychol. 2007;26:303–33.
Boone L, Soenens B, Braet C. Perfectionism, body dissatisfaction, and bulimic symptoms: the intervening role of perceived pressure to be thin and thin ideal internalization. J Soc Clin Psychol. 2011;30:1043–68.
Fabricatore A, Wadden T. Psychological functioning of obese individuals. Diabetes Spectrum. 2003;16:245–52.
Schwartz MB, Brownell KD. Obesity and body image. Body Image. 2004;1:43–56.
Verstuyf J, Vansteenkiste M, Soenens B. Eating regulation and bulimic symptoms: the differential correlates of health-focused and appearance-focused eating regulation. Body Image. 2012;9:108–17.
Thogersen-Ntoumani C, Ntoumanis N, Nikitaras N. Unhealthy weight control behaviours in adolescent girls: a process model based on self-determination theory. Psychol Health. 2010;25:535–50.
Pelletier LG, Dion SC, D’Angelo MS, Reid RD. Why do you regulate what you eat? Relationships between forms of regulation, eating behaviors, sustained dietary behavior change, and psychological adjustment. Motiv Emot. 2004;28:245–77.
Ryan RM, Deci EL. Self-regulation and the problem of human autonomy: does psychology need choice, self-determination, and will? J Pers. 2006;74:1557–85.
Deci EL, Ryan RM. The ‘what’ and ‘why’ of goal pursuits: human needs and the self-determination of behavior. Psychoanal Inq. 2000;11:227–68.
Ng JYY, Ntoumanis N, Thøgersen-Ntoumani C, Deci EL, Ryan RM, Duda JL, et al. Self-determination theory applied to health contexts: a meta-analysis. Perspect Psychol Sci. 2012;7:325–40.
Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. 2012;9:78.
Armitage CJ, Conner M. Social cognition models and health behaviour: a structured review. Psychol Health. 2000;15:173–89.
Williams SL, French DP. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour - and are they the same? Health Educ Res. 2011;26:308–22.
Bandura A. Self-efficacy: the exercise of control. New York: W.H. Freeman and Company; 1997.
Westenhoefer J. Dietary restraint and disinhibition: is restraint a homogeneous construct? Appetite. 1991;16:45–55.
Bryant EJ, King NA, Blundell JE. Disinhibition: its effects on appetite and weight regulation. Obes Rev. 2008;9:409–19.
Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clin Psychol Rev. 2010;30:865–78.
McCracken LM. Committed action: an application of the psychological flexibility model to activity patterns in chronic pain. J Pain. 2013;14:828–35.
Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44:1–25.
Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28:690–701.
Hagger MS, Luszczynska A. Implementation intention and action planning interventions in health contexts: state of the research and proposals for the way forward. Appl Psychol Health Well Being. 2014;6:1–47.
Sniehotta FF. Towards a theory of intentional behaviour change: plans, planning, and self-regulation. Br J Health Psychol. 2009;14:261–73.
Hagger M, Chatzisarantis N. An integrated behavior change model for physical activity. Exerc Sport Sci Rev. 2014;42:62–9.
D’Angelo ME, Pelletier LG, Reid RD, Huta V. The roles of self-efficacy and motivation in the prediction of short- and long-term adherence to exercise among patients with coronary heart disease. Health Psychol. 2014;33:1344–53.
Carraça EV, Silva MN, Markland D, Vieira PN, Minderico CS, Sardinha LB, et al. Body image change and improved eating self-regulation in a weight management intervention in women. Int J Behav Nutr Phys Act. 2011;8:75–85.
Leong SL, Madden C, Gray A, Horwath C. Self-determined, autonomous regulation of eating behavior is related to lower body mass index in a nationwide survey of middle-aged women. J Acad Nutr Diet. 2012;112:1337–46.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95.
Olander EK, Fletcher H, Williams S, Lou A, Turner A, French DP. What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2013;10:29.
Su Y-L, Reeve J. A meta-analysis of the effectiveness of intervention programs designed to support autonomy. Educ Psychol Rev. 2011;23:159–88.
Janssen V, Gucht V, Exel H, Maes S. A self-regulation lifestyle program for post-cardiac rehabilitation patients has long-term effects on exercise adherence. J Behav Med. 2014;37:308–21.
Miller W, Rollnick S. Motivational interviewing: helping people change. 3rd ed. NY: The Guilford Press; 2012.
Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat. 2005;28:19–26.
Download references
Acknowledgements
This work is part of the SPOTLIGHT project and is funded by the Seventh Framework Program (CORDIS FP7) of the European Commission, HEALTH (FP7-HEALTH-2011-two-stage), Grant agreement no. 278186. The content of this article reflects only the authors’ views, and the European Commission is not liable for any use that may be made of the information contained therein.
Other information
This systematic review is reported in accordance with the PRISMA statement for reporting systematic reviews [ 21 ].
Author information
Authors and affiliations.
Interdisciplinary Centre for the Study of Human Performance (CIPER), Faculty of Human Kinetics, University of Lisbon, Lisbon, Portugal
Pedro J Teixeira, Eliana V Carraça & Marta M Marques
European Centre on Health of Societies in Transition, London School of Hygiene and Tropical Medicine, London, UK
Harry Rutter
Department of Nutrition Pitié-Salpetrière (AP-HP), Université Pierre et Marie Curie-Paris 6, Paris, France
Jean-Michel Oppert
UREN (Nutritional Epidemiology Research Unit), Université Paris 13, Sorbonne Paris Cité, Inserm (U557), Inra (U1125), Cnam, F-93017, Bobigny, France
Department of Movement and Sport Sciences, Ghent University, Ghent, Belgium
Ilse De Bourdeaudhuij
Department of General Practice and Elderly Care, The EMGO Institute for Health and Care Research, VU University Medical Center, Amsterdam, the Netherlands
Jeroen Lakerveld
Department of Epidemiology and Biostatistics, The EMGO Institute for Health and Care Research, VU University Medical Center, Amsterdam, the Netherlands
Johannes Brug
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Pedro J Teixeira .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
PJT, JB, JL, JMO, HR, and IB conceived the study, and PJT and EVC developed a systematic review protocol. EVC and MM conducted the literature search and selected the studies based on the title and the abstract. EVC and MM extracted and coded the data from all studies. Study outcomes were summarized by PJT, EVC, and MM. They wrote the initial draft of the manuscript, and JB, JL, JMO, HR, and IB made significant revisions and contributions. All authors read and approved the final manuscript.
Additional files
Additional file 1:.
An Example of the Conducted Search (Medline).
Additional file 2:
Characteristics of Included Studies With Formal Mediation Analyses.
Additional file 3:
Characteristics of Included Studies Without Formal Mediation Analyses.
Additional file 4:
Indirect effects’ estimates in studies with formal mediation analysis.
Additional file 5:
EPHPP Quality Assessment Tool (adapted by the SPOTLIGHT Consortium).
Additional file 6:
Complete results for weight change, physical activity and dietary behaviors.
Additional file 7:
Consensus Ratings of Methodological Study Quality.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/4.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Teixeira, P.J., Carraça, E.V., Marques, M.M. et al. Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med 13 , 84 (2015). https://doi.org/10.1186/s12916-015-0323-6
Download citation
Received : 12 November 2014
Accepted : 11 March 2015
Published : 16 April 2015
DOI : https://doi.org/10.1186/s12916-015-0323-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lifestyle interventions
- Self-regulation
- Weight control
- Physical activity
- Dietary intake
- Maintenance
- Behavior change
- Mediation analysis
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Consensus Statement
- Open access
- Published: 04 March 2020
Joint international consensus statement for ending stigma of obesity
- Francesco Rubino 1 , 2 ,
- Rebecca M. Puhl 3 na1 ,
- David E. Cummings 4 , 5 na1 ,
- Robert H. Eckel 6 , 7 ,
- Donna H. Ryan 8 ,
- Jeffrey I. Mechanick 9 , 10 ,
- Joe Nadglowski 11 ,
- Ximena Ramos Salas 12 , 13 ,
- Phillip R. Schauer 8 ,
- Douglas Twenefour 14 ,
- Caroline M. Apovian 15 , 16 ,
- Louis J. Aronne 17 ,
- Rachel L. Batterham 18 , 19 , 20 ,
- Hans-Rudolph Berthoud 21 ,
- Camilo Boza 22 ,
- Luca Busetto 23 ,
- Dror Dicker 24 , 25 ,
- Mary De Groot 26 ,
- Daniel Eisenberg 27 ,
- Stuart W. Flint 28 , 29 ,
- Terry T. Huang 30 , 31 ,
- Lee M. Kaplan 32 ,
- John P. Kirwan 33 ,
- Judith Korner 34 ,
- Ted K. Kyle 35 ,
- Blandine Laferrère 36 ,
- Carel W. le Roux ORCID: orcid.org/0000-0001-5521-5445 37 ,
- LaShawn McIver 38 ,
- Geltrude Mingrone 1 , 39 , 40 ,
- Patricia Nece 11 ,
- Tirissa J. Reid 41 ,
- Ann M. Rogers 42 ,
- Michael Rosenbaum 43 ,
- Randy J. Seeley 44 ,
- Antonio J. Torres 45 &
- John B. Dixon 46
Nature Medicine volume 26 , pages 485–497 ( 2020 ) Cite this article
107k Accesses
445 Citations
1959 Altmetric
Metrics details
- Metabolic syndrome
People with obesity commonly face a pervasive, resilient form of social stigma. They are often subject to discrimination in the workplace as well as in educational and healthcare settings. Research indicates that weight stigma can cause physical and psychological harm, and that affected individuals are less likely to receive adequate care. For these reasons, weight stigma damages health, undermines human and social rights, and is unacceptable in modern societies. To inform healthcare professionals, policymakers, and the public about this issue, a multidisciplinary group of international experts, including representatives of scientific organizations, reviewed available evidence on the causes and harms of weight stigma and, using a modified Delphi process, developed a joint consensus statement with recommendations to eliminate weight bias. Academic institutions, professional organizations, media, public-health authorities, and governments should encourage education about weight stigma to facilitate a new public narrative about obesity, coherent with modern scientific knowledge.
Similar content being viewed by others

A systematic review and multivariate meta-analysis of the physical and mental health benefits of touch interventions
Julian Packheiser, Helena Hartmann, … Frédéric Michon

Worldwide divergence of values
Joshua Conrad Jackson & Danila Medvedev
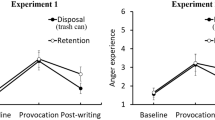
Anger is eliminated with the disposal of a paper written because of provocation
Yuta Kanaya & Nobuyuki Kawai
Individuals with obesity face not only increased risk of serious medical complications but also a pervasive, resilient form of social stigma. Often perceived (without evidence) as lazy, gluttonous, lacking will power and self-discipline, individuals with overweight or obesity are vulnerable to stigma and discrimination in the workplace, education, healthcare settings, and society in general. Weight stigma can cause considerable harm to affected individuals, including physical and psychological consequences. The damaging impact of weight stigma, however, extends beyond harm to individuals. The prevailing view that obesity is a choice and that it can be entirely reversed by voluntary decisions to eat less and exercise more can exert negative influences on public health policies, access to treatments, and research 1 , 2 , 3 .
Although raising awareness of the negative consequences of weight stigma is important, awareness alone is not sufficient to eliminate the issue. Challenging and changing widespread, deep-rooted beliefs, longstanding preconceptions, and prevailing mindsets requires a new public narrative of obesity that is coherent with modern scientific knowledge. Given the pervasiveness of societal weight bias, this goal can only be achieved through the concerted efforts of a broad group of stakeholders, including healthcare providers (HCPs), researchers, the media, policymakers, and patients.
To best inform HCPs, policymakers, and the public about stigma associated with obesity, a multi-disciplinary group of international experts, including representatives of ten scientific organizations (Table 1 ), reviewed available evidence on the causes and harms of weight stigma, developing a joint consensus statement with recommendations to eliminate weight bias.
A specific goal—representing novelty from previous related initiatives—was to address the gap between stigmatizing narratives around obesity and current scientific knowledge regarding mechanisms of body-weight regulation. The overarching objective was to gather a broad group of experts and scientific organizations to recognize the problem and, to our knowledge for the first time, ‘speak with one voice’ about this important issue.
Here we report the conclusions of this exercise and resulting joint consensus statements, with a call to action for all stakeholders to take a pledge (Box 1 ) to end weight stigma and discrimination.
Box 1 Pledge to eliminate weight bias and stigma of obesity
We recognize that
Individuals affected by overweight and obesity face a pervasive form of social stigma based on the typically unproven assumption that their body weight derives primarily from a lack self-discipline and personal responsibility.
Such portrayal is inconsistent with current scientific evidence demonstrating that body-weight regulation is not entirely under volitional control, and that biological, genetic, and environmental factors critically contribute to obesity.
Weight bias and stigma can result in discrimination, and undermine human rights, social rights, and the health of afflicted individuals.
Weight stigma and discrimination cannot be tolerated in modern societies.
The use of stigmatizing language, images, attitudes, policies, and weight-based discrimination, wherever they occur.
To treat individuals with overweight and obesity with dignity and respect.
To refrain from using stereotypical language, images, and narratives that unfairly and inaccurately depict individuals with overweight and obesity as lazy, gluttonous, and lacking willpower or self-discipline.
To encourage and support educational initiatives aimed at eradicating weight bias through dissemination of current knowledge of obesity and body-weight regulation.
To encourage and support initiatives aimed at preventing weight discrimination in the workplace, education, and healthcare settings.
Methodology
Partner organizations and selection of voting delegates.
The consensus-development conference was convened by F.R. (conference director), jointly with the following partner organizations: American Association of Clinical Endocrinologists, American Association for Metabolic and Bariatric Surgery, American Diabetes Association, Diabetes UK, European Association for the Study of Obesity, International Federation for the Surgery of Obesity and Metabolic Disorders, Obesity Action Coalition, Obesity Canada, The Obesity Society, and World Obesity Federation.
The conference director (F.R.), co-chairs (D.E.C., D.H.R., and J.B.D.), and the partner organizations appointed a multidisciplinary expert panel (Table 1 ) of 36 internationally recognized academics representing multiple scientific disciplines, including endocrinology, nutrition, internal medicine, surgery, psychology, molecular biology, cardiology, gastroenterology, primary care, public health, and health policy. The expert panel also included patient-advocacy experts, plus an individual with obesity to speak on behalf of patients. Given that the main aim of this consensus conference was not to define weight stigma or assess it from an ethical perspective, we did not include ethicists in the expert panel.
The 36 members of the expert panel, who constituted voting delegates for the entire consensus-development process, were selected primarily from academics with documented expertise about the topics of the conference and relevant publication records. Each of the ten partner societies used their own criteria to choose their representatives for the expert panel. Criteria included, expertise in weight stigma, obesity, and/or previous participation in relevant committees or initiatives related to weight stigma. One independent, non-voting moderator (O.B.C.) with previous experience in Delphi methodology administered questionnaires for the modified Delphi process and chaired the face-to-face meeting of voting delegates.
Review of evidence
A subgroup of expert panel members (F.R., D.E.C., and J.B.D.) contributed to a review of scientific publications in Medline on a broad set of topics related to weight bias, stigma, and discrimination. Specific, preset research questions for the review of evidence included: (i) prevalence of weight bias and stigma (in the media, healthcare, education, and workplace); (ii) psychologically and physically harmful effects on individuals; (iii) impact on access to care and research, and evidence of workplace weight discrimination; (iv) biological mechanisms of weight regulation in physiology and disease; (v) clinical evidence of uptake and barriers to access of available treatments; and (vi) mechanisms of body-weight regulation and energy homeostasis. We also searched broader data sources for references to weight discrimination in current legislation.
Members of the expert panel with specific expertise (R.M.P., C.A., L.J.A., D.H.R., T.J.R., and S.W.F.) were also tasked to independently conduct a short narrative review of current knowledge on one of the above research questions, according to their specific expertise.
Given the objectives of the consensus conference, the diversity of the subjects under consideration, and the variance in quality of evidence across disciplines, we considered a broad evidence base, including previously published systematic reviews, and various types of observational studies, experimental medicine, and translational studies in animals (weight-regulation mechanisms). For evidence about media portrayal of obesity, we used a 2010 review based on PsycINFO database searches using weight bias and stigmatization-related terms and phrases to identify journal articles published in English between 1994 and 2009 (ref. 4 ). We also identified papers related to these subjects in Medline published between 2011 and 2019. To assess beliefs about obesity, type 2 diabetes, and related treatment options, we used research surveys and pools of opinion conducted among HCPs and/or the general public, and reported in Medline.
A document with the results of this review was circulated among the rest of the group in preparation for the modified Delphi process, seeking further input.
Delphi-like consensus-development process
Based on results of the review of evidence, a subgroup of expert panel members with special expertise in specific subtopics developed questionnaires, including a set of statements and recommendations that were believed to summarize and reflect available evidence. These questionnaires were then circulated among the expert panel. An online Delphi-like method was used to measure the degree of consensus for the statements and recommendations by a web-based survey tool (SurveyMonkey; https://www.surveymonkey.co.uk ). We adapted the original Delphi method 5 to the scopes and nature of this exercise. Unlike other Delphi studies, in which the first round consists mainly of open-ended questions, we used agree/disagree questions designed by a subgroup of members of the expert panel (F.R., S.W.F., D.E.C., and J.B.D.) for the first round.
Approximately three weeks before the survey was first administered, we informed potential participants of the objectives of the study, provided information about the Delphi process, and invited them to contribute. Participants were assured that responses were confidential, with individual responses known only to the impartial, non-voting survey moderator.
The moderator administered the questionnaires through two rounds of Delphi-like process. Delegates who did not agree with the proposed statements were asked to state their reasons and propose amendments. A further (third) round of Delphi was administered after the in-person meeting. All questions also contained a box for individual, non-compulsory comments.
Each survey round was conducted over two weeks: one week for response acquisition (including e-mail reminders before the closing date), and one week for data analysis and preparation of the subsequent round. A personalized email message was sent to each respondent with a URL link to the survey.
Response rate for both of the first two Delphi rounds was 34/36 expert panel members, and all 36 members responded in the third Delphi round.
In-person consensus meeting
Supporting evidence and draft conclusions generated through the Delphi process were presented at the 4th World Congress on Interventional Therapies for Type 2 Diabetes 2019 (WCITD2019, New York, 10 April, 2019). Proceedings were open to public comment by other experts in the field (WCITD2019 faculty members) and by the entire audience through opinion polls, using real-time electronic voting (Turning Technology software). On 10 April 10, 2019, voting delegates met face-to-face to review, amend, and vote on each consensus statement.
Final steps
After the meeting in New York, the document with conclusions reached by the experts underwent a final review and approval through a third round of Delphi process.
The final consensus document, including the ‘Pledge to Eliminate Weight Bias and Stigma of Obesity’ (Box 1 ), was then submitted to the scientific committees and executive boards of partner organizations and other stakeholders for review and endorsement. A subgroup of the expert panel (F.R., R.M.P., D.E.C., R.H.E., D.H.R., J.I.M., J.N., X.R.S., P.R.S., D.T., and J.B.D.) generated the first draft of the report. The draft report was then circulated among all other members of the expert panel for further input and approval before submission for publication.
All members of the expert panel, all partner organizations, and additional organizations listed in Box 2 have formally endorsed the statement and taken the pledge to eliminate weight stigma.
Box 2 Organizations that have endorsed the statement and/or accepted to take the pledge to eliminate weight stigma as of 26 February 2020
Partner organizations
American Association of Clinical Endocrinologists (AACE)
American Association for Metabolic and Bariatric Surgery (ASMBS)
American Diabetes Association (ADA)
Diabetes UK
European Association for the Study of Obesity (EASO)
International Federation for the Surgery of Obesity and metabolic Disorders (IFSO)
Obesity Action Coalition (OAC)
Obesity Canada
The Obesity Society (TOS), USA
World Obesity Federation (WOF)
Other scientific and patient societies
American Academy of Sleep Medicine (AASM)
American Society for Nutrition (ASN)
Association of British Clinical Diabetologists (ABCD)
The Australian National Association of Clinical Obesity Services (NACOS)
Australian and New Zealand Metabolic and Obesity Surgery Society (ANZMOSS)
Austrian Society for Obesity and Metabolic Surgery
Brazilian Society for Bariatric and Metabolic Surgery (SBCBM)
British Obesity and Metabolic Surgery Society (BOMSS)
Canadian Association of Cardiovascular Prevention and Rehabilitation (CACPR)
Canadian Association of Occupational Therapists (Association Canadienne des ergothérapeutes)
The Canadian Society of Endocrinology and Metabolism (CSEM)
CIHR-SPOR Chair in Innovative, Patient-Oriented, Behavioural Clinical Trials
Chilean Society for Bariatric and Metabolic Surgery
Colegio Mexicano de Cirurgia Para la Obesidad y Enfermedades Metabolicas
Croatian Society of Obesity
Dietitians of Canada
Dutch Society for Metabolic and Bariatric Surgery (DSMBS)
The Endocrine Society (USA)
European Coalition for People Living with Obesity (ECPO)
French Clinical Research Network in Obesity (FORCE)
French Society for Research and Care of Obesity (AFERO)
French Society of Bariatric and Metabolic Surgery (SOFFCO-MM)
Hellenic Medical Association for Obesity (HMAO)
Hellenic Society for Bariatric and Metabolic Surgery
Hellenic Society for the Study of Obesity, Metabolism and Eating Disorders
Hong Kong Association for the Study of Obesity
Hong Kong Obesity Society
Hong Kong Society for Metabolic and Bariatric Surgery
Hungarian Society for the Study of Obesity
International Behavioural Trials Network (IBTN)
International Society for the Perioperative Care of the Obese Patient (ISPCOP)
Irish Society for Clinical Nutrition and Metabolism (IrSPEN)
The Israeli Association for the Study of Obesity
Italian Obesity Society (SIO)
Korean Society for the Study of Obesity (KSSO)
Latin American Federation of Obesity (FLASO)
The Lithuanian Society of Bariatric Surgery
Mexican Society of Obesity
National Lipid Association (USA)
Norwegian Society for the Surgery of Obesity
Obesity Australia
Obesity Care Advocacy Network (OCAN)
Obesity Collective
Obesity Medicine Association (USA)
Obesity Society of Nigeria
The Obesity Surgery Society India (OSSI)
Romanian Federation of Diabetes, Nutrition, Metabolic diseases
The Royal College of Physicians -RCP- (UK)
Russian Society of Bariatric Surgeons
Sociedad Argentina de Cirugia de la Obesidad Enfermedad Metabolica y Otras Relacionados con la Obesidad
Sociedad Argentina de Obesidad y Trastornos Alimentarios
Sociedad Española de Cirugía de la Obesidad y Enfermedades Metabólicas (SECO)
Society of American Gastrointestinal and Endoscopic Surgeons (SAGES)
Society of Behavioral Medicine (SBM)
The Society for Surgery of the Alimentary Tract (SSAT)
South African Society for Surgery Obesity and Metabolism
UK Association for the Study of Obesity
Scientific and medical journals
The Annals of Surgery
Cell Metabolism (Cell Press)
Cell Reports Medicine (Cell Press)
Clinical Obesity
The Lancet Diabetes & Endocrinology
Med (Cell Press)
Nature Research (all journals)
Obesity Reviews
Obesity Science and Practice
Obesity Surgery
Pediatric Obesity
Surgery for Obesity and Related Diseases (SOARD)
Trends in Endocrinology and Metabolism (Cell Press)
Trends in Molecular Medicine (Cell Press)
Academic institutions and hospitals
Baker Heart and Diabetes Institute. Melbourne, Australia
The Charles Perkins Institute, University of Sydney (Australia)
Geisinger Obesity Institute, Geisinger Health System, Danville, PA (USA)
King’s College Hospital NHS Foundation Trust (UK)
King’s College London (UK)
London Bridge Hospital, London (UK)
Pennington Biomedical Research Center (USA)
Specialized Centers for Obesity Management (GCC-CSO) (France)
St Vincent Private Hospital, Dublin (Ireland)
Summer M. Redstone Center, Milken Institute School of Public Health, George Washington University (USA)
Technische Universität Dresden; Faculty of Medicine Carl Gustav Carus (Germany)
Transcampus of Technische Universität Dresden; Faculty of Medicine Carl Gustav Carus (Germany) and King’s College London
University College London Hospitals NHS Foundation Trust (UK)
University of Connecticut Rudd Center for Food Policy & Obesity (USA)
The Veneto Obesity Network (Italy)
Parliamentary groups
The All-Party Parliamentary Group on Obesity (APPG): a group of cross-party members of the House of Commons and House of Lords campaigning for improved prevention and treatment of obesity (UK)
Descriptors of grade of consensus
A supermajority rule was used to define consensus. Consensus was considered to have been reached when > 67% of the experts agreed on a given topic. However, language was iteratively modified to maximize agreement, and the degree of consensus for each statement was graded according to the following scale: grade U was 100% agreement (unanimous); grade A was 90–99% agreement; grade B was 78–89% agreement; and grade C was 67–77% agreement. This grading scale is meant to indicate statements that reflect unanimous or near-unanimous opinions (grades U and A), strong agreement with little variance (grade B), or a consensus statement that reflects an averaging of more and possibly extremely diverse opinions (grade C). All statements included in this consensus document achieved either grades U or A, which we report for each statement.
The first questionnaire asked 58 questions, including six on expert panel demographic information. During the three Delphi-like rounds and the in-person voting session, the expert panel eliminated five consensus questions that were deemed to be duplicative or redundant. Our iterative changes throughout the process yielded 47 final statements (Tables 2 and 3 ), all with > 89% consensus (grades A and U), as summarized in Box 3 .
In this document, we use the terms ‘weight stigma’, ‘weight-based stereotypes’, or ‘weight bias’ to refer to biases against individuals with overweight and obesity, not underweight. We provide definitions in Box 4 .
Box 3 Executive summary
(Grade of consensus (GoC): U is unanimous; A is >90% consensus)
Weight stigma is reinforced by misconceived ideas about body-weight regulation and lack of awareness of current scientific evidence. Weight stigma is unacceptable in modern societies, as it undermines human rights, social rights, and the health of afflicted individuals (GoC: A).
Research indicates that weight stigma can cause significant harm to affected individuals. Individuals who experience it suffer from both physical and psychological consequences, and are less likely to seek and receive adequate care (GoC: U).
Despite scientific evidence to the contrary, the prevailing view in society is that obesity is a choice that can be reversed by voluntary decisions to eat less and exercise more. These assumptions mislead public health policies, confuse messages in popular media, undermine access to evidence-based treatments, and compromise advances in research (GoC: A).
For the reasons above, weight stigma represents a major obstacle in efforts to effectively prevent and treat obesity and type 2 diabetes. Tackling stigma is not only a matter of human rights and social justice, but also a way to advance prevention and treatment of these diseases (GoC: A).
Academic institutions, professional organizations, media, public health authorities, and government should encourage education about weight stigma and facilitate a new public narrative of obesity, coherent with modern scientific knowledge (GoC: U).
Box 4 Definitions
Weight stigma refers to social devaluation and denigration of individuals because of their excess body weight, and can lead to negative attitudes, stereotypes, prejudice, and discrimination.
Weight-based stereotypes include generalizations that individuals with overweight or obesity are lazy, gluttonous, lacking in willpower and self-discipline, incompetent, unmotivated to improve their health, non-compliant with medical treatment, and are personally to blame for their higher body weight.
Weight discrimination refers to overt forms of weight-based prejudice and unfair treatment (biased behaviors) toward individuals with overweight or obesity.
Weight bias internalization occurs when individuals engage in self-blame and self-directed weight stigma because of their weight. Internalization includes agreement with stereotypes and application of these stereotypes to oneself and self-devaluation 6 .
Explicit weight bias refers to overt, consciously held negative attitudes that can be measured by self-report.
Implicit weight bias consists of automatic, negative attributions and stereotypes existing outside of conscious awareness.
Summary of evidence
Prevalence of weight bias, stigma, and discrimination.
Substantial research has demonstrated that weight stigma and discrimination are pervasive, global issues 7 , 8 . Weight stigma has been documented in multiple societal domains, including the workplace, education, healthcare settings, and within families 9 , 10 . Stigma has persisted despite the markedly increased prevalence of obesity in recent decades. Among adults with obesity, the prevalence of weight discrimination is 19–42%, with higher rates among those with higher body-mass index (BMI), and among women compared with men 11 , 12 , 13 .
Estimates from a 2018 study suggest that approximately 40–50% of US adults with overweight and obesity experience internalized weight bias, and about 20% of US adults experience this at high levels 14 . Internalized weight bias is present in individuals across diverse body-weight categories, but especially among individuals with higher BMI who are trying to lose weight 14 .
Evidence suggests that the media is a pervasive source of weight bias and can reinforce stigma through the use of inaccurate framing of obesity and inappropriate images, language, and terminology that attribute obesity entirely to personal responsibility 15 . It has been estimated that over two thirds of images accompanying US media reports of obesity contain weight stigma, and experimental studies show that viewing these types of images leads to increased weight bias 16 .
Weight bias has been reported among HCPs in the United States and around the world, including among primary care providers, endocrinologists, cardiologists, nurses, dietitians, mental health professionals, medical trainees, and professionals engaged in research and clinical management of obesity 17 , 18 .
Physical and mental health consequences of weight stigma
Children with overweight and obesity are frequently subject to weight-based teasing and bullying at school. Compared with students of lower body weight, adolescents with overweight or obesity are significantly more likely to experience social isolation 19 , 20 , 21 and are at increased risk for relational, verbal, cyber, and physical victimization 22 . They are also more susceptible to developing mental health disorders, especially anxiety and depression, in addition to obesity, type 2 diabetes, and cardiovascular disease in later life 23 .
Weight stigma, rather than obesity itself, may be particularly harmful to mental health and is associated with depressive symptoms, higher anxiety levels, lower self-esteem, social isolation, perceived stress, substance use 24 , 25 , 26 , unhealthy eating and weight-control behaviors, such as binge eating and emotional overeating 27 . Experimental studies also show, paradoxically, that exposing individuals to weight stigma can lead to increased food intake, regardless of BMI 3 , 28 . Correlative and randomized-controlled studies also show that experience of weight stigma is linked with lower levels of physical activity, higher exercise avoidance 29 , 30 , 31 , consumption of unhealthy diets, and increased sedentary behaviors 1 , 2 , 3 , as well as increased obesity and weight gain over time 32 , and increased risk of transitioning from overweight to obesity in both adults and adolescents 33 , 34 , 35 .
Individuals with overweight and obesity who experience weight discrimination show higher levels of circulating C-reactive protein 36 , cortisol 37 , long-term cardio-metabolic risk 38 , and increased mortality 39 compared with those who do not experienced weight discrimination.
Quality of care and health care utilization
Evidence suggests that physicians spend less time in appointments and provide less education about health to patients with obesity compared with thinner patients 17 , and patients who report having experienced weight bias in the healthcare setting have poor treatment outcomes 40 and might be more likely to avoid future care 41 . Obesity also adversely impacts age-appropriate cancer screening, which can lead to delays in breast, gynecological, and colorectal cancer detection 42 .
A thematic analysis of 21 studies examined the perceptions of weight bias and its impact on engagement with primary health care services 43 . Negative influences on engagement with primary care were evaluated and ten themes were identified: contemptuous, patronizing, and disrespectful treatment, lack of training, ambivalence, attribution of all health issues to excess weight, assumptions about weight gain, barriers to health care utilization, expectation of differential health care treatment, low trust and poor communication, avoidance or delay of health services, and seeking medical advice from multiple HCPs.
The widespread, but unproven, assumption that body weight is entirely controllable by lifestyle choices and that self-directed efforts can reverse even severe forms of obesity or type 2 diabetes 44 could explain the low level of public support for coverage of anti-obesity interventions beyond diet and exercise 45 , regardless of their evidence base. For example, many public and private health insurers either do not provide coverage or have substantive limitations in the coverage of metabolic surgery, including fulfilment of a number of criteria for which there is limited or no clinical evidence 46 , 47 . These attitudes are in stark contrast with coverage of treatment for other chronic diseases (for example, cancer, heart disease, and osteoarthritis) that are not conditional to similar restrictions, and for which use of similarly arbitrary coverage criteria would be socially indefensible and ethically objectionable.
Stigmatization of surgical treatment for obesity
Metabolic surgery (also known as bariatric surgery) provides a compelling example of how weight stigma can also extend to treatments for obesity. Compared with individuals who lose weight using diet and exercise alone, those who lose weight through metabolic surgery can be at risk of stronger stigma because they are stereotyped as being lazy and being less responsible for their weight loss 48 , 49 . It is not surprising that many hide their surgical status 49 .
Despite evidence of efficacy and cost-effectiveness 50 , 51 of surgical interventions for obesity, only 0.1–2% of surgical candidates who qualify worldwide currently undergo such surgery 52 . A research survey in the United States showed that only 19.2% of responders supported insurance coverage of metabolic operations 45 .
Weight stigma and public health policies
Historical examples of illnesses whose social construction incorporated moral judgments about the role of individuals’ actions in contracting the disease (for example, plague, cholera, syphilis, HIV/AIDS), demonstrate that stigma can interfere with public heath efforts to control epidemics 53 . These examples also highlight the importance of initiatives aimed at combatting stigma and social exclusion (for example, United Nations General Assembly Special Session on HIV/AIDS and 2002–2003 World AIDS Campaign) 54 .
Public health efforts to date have typically neglected stigma as a barrier in efforts to address obesity. By contrast, some public health strategies openly embrace stigmatization of individuals with obesity, based on the assumption that shame will motivate them to change behavior and achieve weight loss through a self-directed diet and increased physical exercise 55 . Both observational and randomized-controlled studies show that these strategies can result in the opposite effect, and may instead induce exercise avoidance, consumption of unhealthy diets, and increased sedentary behaviors 1 , 2 , 3 , leading to poor metabolic health, increased weight gain 56 , 57 , and reduced quality of life 57 .
Some public health messages and government-supported anti-obesity campaigns also characterize the merits of prevention of obesity as a preferable alternative to treatments for established obesity, such as pharmacotherapy or surgery, which are often considered more expensive. This is a misconception, as it frames prevention and treatment as being mutually exclusive, whereas these approaches should generally be directed toward two distinct populations, with different needs.
Discrimination in employment
Workplace discrimination against individuals with overweight and obesity is common in high-income countries 58 . Individuals with obesity have reported receiving lower starting salaries, can be ranked as less qualified, and can work longer hours than do thinner employees 59 . Persons with obesity can be perceived to be less suitable for employment and are less likely to be invited for an interview 60 , or, if employed, are perceived to be less successful compared with thinner peers 61 . Women with obesity are the especially unlikely to be hired 62 .
A UK study of 119,669 individuals aged 37−73 years found a strong association between higher BMI and lower socioeconomic status, especially in women 63 . Similarly, a US study reported that overweight women are more likely to work in lower-paying jobs and make less money compared with average-size women and all men 64 .
For the vast majority of individuals with obesity who experience discrimination in recruitment or the workplace, there is generally no protection under current legislations 62 . Although some US states have recently introduced a legislation that protects against height and weight discrimination 65 , the Civil Rights Act of 1964 does not identify weight as a protected characteristic, and only in some instances a condition of very high BMI can meet the definition of disability under a 2008 amendment of the Americans with Disabilities Act legislation 66 . This amendment, however, does not cover individuals who are not disabled, even though they can also be victims of weight discrimination.
Similarly, in 2014 the European Court of Justice ruled that being severely overweight could be considered a disability if this condition disrupts an employee’s ability to work. However, obesity per se is generally not specified as a disabling condition in current EU employment law; hence, most anti-discrimination laws require interpretation of whether a person with obesity has a disability. The UK Equality Act (2010) 67 specifically prohibits discrimination on the grounds of age, disability, gender reassignment, marriage and civil partnership, pregnancy, maternity, race, ethnicity, religion or belief, sex, and sexual orientation—but not for obesity.
Weight bias and research
Research into obesity and diabetes is underfunded compared with other diseases, relative to their burden and costs on society. For example, the US National Institutes of Health’s projected budgets for cancer, HIV/AIDS, and digestive diseases are 5–10 times greater than the budget for obesity, despite that the latter affecting substantially more Americans.
Among the 5,623 participants in a recent multi-national research survey (the ASK study), higher weight stigma was associated with lower prioritization of spending on obesity research 44 . There are also several ways in which stigma can hinder support of research and scientific advances. For instance, oversimplified notion that obesity is caused by eating too much and exercising too little, implies that the causes of obesity and its epidemic are well-understood, and not complex. In this context, research designed to elucidate etiologic mechanisms of obesity may not be perceived as a priority. Furthermore, funding could be skewed toward projects that are anticipated to be effective (that is, implementation of behavior and lifestyle interventions), reducing support for investigation of novel methods of prevention and treatment or implementation of available evidence-based therapies (that is, pharmaceutical or surgical approaches).
Causes and contributors for weight stigma
Evidence from several countries 68 , 69 , 70 , 71 shows that when individuals attribute the causes of obesity primarily to internal, controllable factors or personal choices, they exhibit higher weight bias, whereas acknowledging the complex causes of obesity (including elements such as genetics, biology, and environmental factors) is associated with lower levels of weight bias and less blame. These findings suggest that the prevailing narrative of obesity in news coverage, public health campaigns, and political discourse—centered heavily on notions of personal responsibility 72 , 73 —can play an important part in the expression of weight stigma and reinforce weight-based stereotypes 74 .
The absence of national laws that prohibit weight discrimination can also contribute to expression of weight stigma, as it communicates a societal message that weight stigma is acceptable and tolerable. However, evidence in North America, Europe, Australia, and Iceland suggests that there might be substantial public support to enact and pass legislation to prohibit weight discrimination 75 , 76 .
The gap between scientific evidence and misconceptions in the public narrative
The notion that the causes of overweight and obesity depend on individuals’ faults, such as laziness and gluttony, stems from the assumption that body weight is entirely under volitional control. This assumption and many of its corollaries are now at odds with a definitive body of biological and clinical evidence developed over the last few decades.
1. Body weight = calories in – calories out
This equation is often oversimplified in the public narrative of obesity, and even by HCPs, as if the two variables (calories in and calories out) were dependent only on two factors, amount of food consumed and exercise performed, therefore implying that body weight is completely controllable by voluntary decisions to eat less and exercise more.
However, both variables of the equation depend on factors additional to just eating and exercising. For instance, energy intake depends on the amount of food consumed, but also on the amount of food-derived energy absorbed through the gastrointestinal tract, which in turn is influenced by multiple factors, such as digestive enzymes, bile acids, microbiota, gut hormones, and neural signals, none of which are under voluntary control. Similarly, energy output is not entirely accounted for by physical activity, which only contributes to ~30% of total daily energy expenditure. Metabolic rate accounts for 60–80% of total daily energy expenditure, with the thermic effect of feeding constituting approximately 10% 77 . Thus, even when individuals expend energy via exercise, except for elite athletes the overall contribution to energy expenditure is relatively small 78 .
The existence of a powerful, precise homeostatic system that maintains body weight within a relatively narrow, individualized range is supported by scientific evidence. This regulatory system can counteract voluntary efforts to reduce body weight by activating potent compensatory biologic responses (for example, increased appetite and decreased metabolic rate) that promote weight regain. Clinical evidence shows that a 10% weight loss elicits compensatory changes in energy expenditure 79 , and modifications of appetite signals that increase hunger and reduce satiety. These metabolic and biologic adaptations can persist long-term after losing weight and continue even after partial weight regain 80 .
2. Obesity is primarily caused by voluntary overeating and a sedentary lifestyle
Although this concept might appear to be a straightforward conclusion, given common personal experiences of the fluctuations of body weight during periods of excess energy intake or sedentary lifestyle, the evidence supports a more nuanced situation. For example, in a Canadian study that used accelerometers to measure physical activity, girls with obesity took more steps per day than girls within the normal weight range 81 . Similar findings have been observed for adults 82 . Despite substantially higher levels of physical activity, total daily energy expenditure among hunter-gatherers in Africa’s savannahs today is largely similar to that of adults living in modern European or US cities, where obesity prevalence is high 83 . These findings contrast with conventional views that primarily attribute the cause of obesity to sedentary lifestyles and suggest that compensatory metabolic adaptations maintain total energy expenditure relatively constant among human populations and across various levels of physical activities.
Additional evidence is now also available indicating other possible causes and contributors to obesity, including genetic 84 and epigenetic factors 85 , foodborne factors 86 , sleep deprivation and circadian dysrhythmia 87 , psychological stress, endocrine disruptors, medications, and intrauterine and intergenerational effects. These factors do not require overeating or physical inactivity to explain excess weight 88 , 89 , 90 . A dominant role of genetic factors in obesity pathogenesis has also been demonstrated in studies comparing the concordance of body weight among fraternal versus identical twins 91 , for example, as well as studies of adults adopted as infants compared with their biological and adoptive parents 77 , 92 . Hence, overeating and reduced physical activity, when present, might be symptoms rather than the root causes of obesity 93 . Finally, the frequent failure of therapeutic and public-health strategies focused on the recommendation to ‘eat less and move more’ should call into question a causal role of voluntary overeating and sedentary lifestyle as primary causes of obesity.
3. Obesity is a lifestyle choice
Persons with obesity typically recognize obesity as a serious health problem, rather than a conscious choice. More than two thirds of 3,008 individuals with obesity surveyed in the ACTION Study considered obesity to be as or more serious than other health conditions, including high blood pressure, diabetes, and depression 94 . Given the negative effects of obesity on quality of life, the well-known risks of serious complications and reduced life expectancy associated with it, it is a misconception to define obesity as a choice.
4. Obesity is a condition, not a disease
Labeling obesity as a disease, risk factor, or condition has implications for treatment and policy development and can contribute to promoting or mitigating stigmatizing views toward affected individuals. An argument often used against labeling obesity a disease is that doing so communicates a societal message that individual responsibility is not relevant in obesity, thus reducing adherence to healthier lifestyles. Defining obesity as a disease, or not, however, should be based on objective medical and biological evidence, not sociologic implications.
The criteria generally used for recognition of disease status are clearly fulfilled in many individuals with obesity as commonly defined, albeit not all. These criteria include specific signs or symptoms (such as increased adiposity), reduced quality of life, and/or increased risk of further illness, complications, and deviation from normal physiology—or well-characterized pathophysiology (for example, inflammation, insulin resistance, and alterations of hormonal signals regulating satiety and appetite).
As reviewed in a statement from the World Obesity Federation 95 , many medical societies as well as the World Health Organization, the US Food and Drug Association, the US National Institutes of Health, and the Nagoya Declaration have now defined obesity as a disease or disease process.
Admittedly, however, defining obesity as a disease, but measuring it only by BMI thresholds (as in contemporary medical practice), risks labeling as ill some individuals who, despite possibly being at risk of future illness, have no current evidence of disease—for example, in cases where high BMI results from being particularly muscular or having short stature. This potential risk of misdiagnosis underscores the inadequacy of current diagnostic criteria for obesity, and the need to identify more meaningful clinical and biological criteria than just BMI to diagnose the disease.
5. Severe obesity is usually reversible by voluntarily eating less and exercising more
This assumption is also not supported by evidence. First, body weight and fat mass are known to be regulated by numerous physiological mechanisms, beyond voluntary food intake and physical exercise. A large body of clinical evidence has shown that voluntary attempts to eat less and exercise more render only modest effects on body weight in most individuals with severe obesity 96 , 97 . When fat mass decreases, the body responds with reduced resting energy expenditure 79 , 80 and changes in signals that increase hunger and reduce satiety 93 (for example, leptin, ghrelin) 98 . These compensatory metabolic and biologic adaptations promote weight regain and persist for as long as persons are in the reduced-energy state, even if they gain some weight back 98 .
Metabolic surgery is often referred to as an easy way out, based on assumptions that these interventions mechanically restrict food intake in a manner that individuals are not sufficiently disciplined to achieve on their own. However, evidence demonstrates that surgical interventions elicit numerous metabolic effects opposite to the compensatory physiologic responses normally triggered by diet-induced weight reduction, thereby promoting major, long-term weight loss 99 . Such mechanisms include a paradoxical decrease in appetite and increase in metabolic rate, which change adaptively in the opposite directions to those following most non-surgical weight loss 77 . There are also favorable post-operative alterations in gastrointestinal hormones, bile-acid signaling, gut microbiota, absorption and utilization of glucose by the gut, modulations of gastrointestinal nutrient signaling that influence insulin sensitivity, and others 100 .
In this initiative, we sought to inform HCPs, policymakers, and the public about the prevalence, causes, and harmful consequences of weight stigma. A novel, specific goal not formulated in prior related initiatives was to address the gap between popular, stigmatizing narratives around obesity and current scientific knowledge regarding mechanisms of body-weight regulation. We found ample evidence of pervasive weight bias and stigma in many diverse domains of society, causing serious mental and physical harm to individuals with obesity. We met our primary objective of gathering a broad group of experts and scientific organizations to appraise the problem and, to our knowledge for the first time, speak with one voice against this important issue, pledging to do what we can to end it (pledge in Box 1 , executive summary in Box 3 , and recommendations in Table 3 ).
There are several limitations to our work. For example, largely owing to the nature of relevant publications, we did not perform a formal systematic review with stringent criteria for levels of evidence. Our method of literature study was closer to a structured rapid review, performed over approximately 6 months, and it only included English-language papers. Also, although our expert panel comprised representatives from ten nations spanning five continents, it was heavily weighted toward individuals from the United States and other high-income countries. Much of the evidence base is also derived from these regions. It is important to note, however, that our final report has been formally endorsed by over 100 organizations at the time of publication (Box 2 ), including some from low-income and middle-income countries—attesting to the global relevance of the problem and our statements. A strength of our work is that we engaged a diverse group of panelists including academics from disparate disciplines, representatives of patient-advocacy organizations and patients. The broad endorsement of this statement and pledge by a diverse group of organizations, including scientific societies, patient-advocacy groups, academic and medical centers, scientific journals, and a parliamentary group provides an unprecedented opportunity for a concerted effort of all stakeholders to effectively tackle this important problem for medicine and society.
Conclusions
Weight stigma and discrimination are pervasive and cause significant harm to affected individuals. The widespread narrative of obesity in the media, in public health campaigns, in political discourse, and even in the scientific literature attributing the cause of obesity primarily to personal responsibility has an important role in the expression of societal weight stigma, and reinforces weight-based stereotypes. Weight stigma can mislead clinical decisions, and public health messages, and could promote unproductive allocation of limited research resources. Weight bias and stigma can result in discrimination, and undermine human rights, social rights, and the health of afflicted individuals. Explaining the gap between scientific evidence, and a conventional narrative of obesity built around unproven assumptions and misconceptions might help to reduce weight bias, and its harmful effects. A concerted effort of all stakeholders is required to promote educational, regulatory, and legal initiatives designed to prevent weight stigma and discrimination.
Bauer, C. & Rosemeier, A. A handicap for life - overweight and obesity in pre-school children in Karlsruhe. Gesundheitswesen 66 , 246–250 (2004).
CAS PubMed Google Scholar
Hayden-Wade, H. A. et al. Prevalence, characteristics, and correlates of teasing experiences among overweight children vs. non-overweight peers. Obes. Res. 13 , 1381–1392 (2005).
PubMed Google Scholar
Schvey, N. A., Puhl, R. M. & Brownell, K. D. The impact of weight stigma on caloric consumption. Obesity 19 , 1957–1962 (2011).
Ata, R. N. & Thompson, J. K. Weight bias in the media: a review of recent research. Obes. Facts 3 , 41–46 (2010).
PubMed PubMed Central Google Scholar
Gordon, T. J. The Delphi method. Futur. Res. Methodol. 4 , 2–15 (1994).
Google Scholar
Corrigan, P. W., Watson, A. C. & Barr, L. The self-stigma of mental illness: Implications for self-esteem and self-efficacy. J. Soc. Clin. Psychol. 25 , 875–884 (2006).
Brewis, A., SturtzSreetharan, C. & Wutich, A. Obesity stigma as a globalizing health challenge. Global. Health 14 , 20 (2018).
Flint, S. W., Hudson, J. & Lavallee, D. UK adults’ implicit and explicit attitudes towards obesity: a cross-sectional study. BMC Obes. 2 , 31 (2015).
Pearl, R. L. Weight bias and stigma: public health implications and structural solutions. Soc. Issues Policy Rev. 12 , 146–182 (2018).
Lydecker, J. A., O’Brien, E. & Grilo, C. M. Parents have both implicit and explicit biases against children with obesity. J. Behav. Med. 41 , 784–791 (2018).
Puhl, R. M., Andreyeva, T. & Brownell, K. D. Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int. J. Obes. 32 , 992–1000 (2008).
CAS Google Scholar
Spahlholz, J., Baer, N., König, H. H., Riedel-Heller, S. G. & Luck-Sikorski, C. Obesity and discrimination—a systematic review and meta-analysis of observational studies. Obes. Rev. 17 , 43–55 (2016).
Andreyeva, T., Puhl, R. M. & Brownell, K. D. Changes in perceived weight discrimination among Americans, 1995-1996 through 2004-2006. Obesity 16 , 1129–1134 (2008).
Puhl, R. M., Himmelstein, M. S. & Quinn, D. M. Internalizing weight stigma: prevalence and sociodemographic considerations in US adults. Obesity 26 , 167–175 (2018).
Heuer, C. A., McClure, K. J. & Puhl, R. M. Obesity stigma in online news: a visual content analysis. J. Health Commun. 16 , 976–987 (2011).
Puhl, R. M., Luedicke, J. & Heuer, C. A. The stigmatizing effect of visual media portrayals of obese persons on public attitudes: does race or gender matter? J. Health Commun. 18 , 805–826 (2013).
Phelan, S. M. et al. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes. Rev. 16 , 319–326 (2015).
CAS PubMed PubMed Central Google Scholar
Sabin, J. A., Marini, M. & Nosek, B. A. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS One 7 , e48448 (2012).
Pont, S. J., Puhl, R., Cook, S. R. & Slusser, W. Stigma experienced by children and adolescents with obesity. Pediatrics 140 , e20173034 (2017).
Mannan, M., Mamun, A., Doi, S. & Clavarino, A. Prospective associations between depression and obesity for adolescent males and females—a systematic review and meta-analysis of longitudinal studies. PLoS One 11 , e0157240 (2016).
Puhl, R. M. & King, K. M. Weight discrimination and bullying. Best Pract. Res. Clin. Endocrinol. Metab. 27 , 117–127 (2013).
Waasdorp, T. E., Mehari, K. & Bradshaw, C. P. Obese and overweight youth: risk for experiencing bullying victimization and internalizing symptoms. Am. J. Orthopsychiatry 88 , 483–491 (2018).
Takizawa, R., Danese, A., Maughan, B. & Arseneault, L. Bullying victimization in childhood predicts inflammation and obesity at mid-life: a five-decade birth cohort study. Psychol. Med. 45 , 2705–2715 (2015).
Wu, Y. K. & Berry, D. C. Impact of weight stigma on physiological and psychological health outcomes for overweight and obese adults: A systematic review. J. Adv. Nurs. 74 , 1030–1042 (2018).
Papadopoulos, S. & Brennan, L. Correlates of weight stigma in adults with overweight and obesity: a systematic literature review. Obesity 23 , 1743–1760 (2015).
Jackson, S. E., Steptoe, A., Beeken, R. J., Croker, H. & Wardle, J. Perceived weight discrimination in England: a population-based study of adults aged >50 years. Int. J. Obes. 39 , 858–864 (2015).
Vartanian, L. R. & Porter, A. M. Weight stigma and eating behavior: a review of the literature. Appetite 102 , 3–14 (2016).
Major, B., Hunger, J. M., Bunyan, D. P. & Miller, C. T. The ironic effects of weight stigma. J. Exp. Soc. Psychol. 51 , 74–80 (2014).
Han, S., Agostini, G., Brewis, A. A. & Wutich, A. Avoiding exercise mediates the effects of internalized and experienced weight stigma on physical activity in the years following bariatric surgery. BMC Obes. 5 , 18 (2018).
Sattler, K. M., Deane, F. P., Tapsell, L. & Kelly, P. J. Gender differences in the relationship of weight-based stigmatisation with motivation to exercise and physical activity in overweight individuals. Health Psychol. Open 5 , 2055102918759691 (2018).
Jackson, S. E. & Steptoe, A. Association between perceived weight discrimination and physical activity: a population-based study among English middle-aged and older adults. BMJ Open 7 , e014592 (2017).
Sutin, A. R. & Terracciano, A. Perceived weight discrimination and obesity. PLoS One 8 , e70048 (2013).
Hunger, J. M. & Tomiyama, A. J. Weight labeling and obesity: a longitudinal study of girls aged 10 to 19 years. JAMA Pediatr. 168 , 579–580 (2014).
Quick, V., Wall, M., Larson, N., Haines, J. & Neumark-Sztainer, D. Personal, behavioral and socio-environmental predictors of overweight incidence in young adults: 10-yr longitudinal findings. Int. J. Behav. Nutr. Phys. Act. 10 , 37 (2013).
Puhl, R. M. et al. Experiences of weight teasing in adolescence and weight-related outcomes in adulthood: A 15-year longitudinal study. Prev. Med. 100 , 173–179 (2017).
Sutin, A. R., Stephan, Y., Luchetti, M. & Terracciano, A. Perceived weight discrimination and C-reactive protein. Obesity 22 , 1959–1961 (2014).
Jackson, S. E., Kirschbaum, C. & Steptoe, A. Perceived weight discrimination and chronic biochemical stress: a population-based study using cortisol in scalp hair. Obesity 24 , 2515–2521 (2016).
Vadiveloo, M. & Mattei, J. Perceived weight discrimination and 10-year risk of allostatic load among US adults. Ann. Behav. Med. 51 , 94–104 (2017).
Sutin, A. R., Stephan, Y. & Terracciano, A. Weight discrimination and risk of mortality. Psychol. Sci. 26 , 1803–1811 (2015).
Gudzune, K. A., Bennett, W. L., Cooper, L. A. & Bleich, S. N. Patients who feel judged about their weight have lower trust in their primary care providers. Patient Educ. Couns. 97 , 128–131 (2014).
Puhl, R., Peterson, J. L. & Luedicke, J. Motivating or stigmatizing? Public perceptions of weight-related language used by health providers. Int. J. Obes. 37 , 612–619 (2013).
Aldrich, T. & Hackley, B. The impact of obesity on gynecologic cancer screening: an integrative literature review. J. Midwifery Womens Health 55 , 344–356 (2010).
lberga, A., Edache, I., Forhan, M. & Russell-Mayhew, S. Weight bias and health care utilization: A scoping review. Prim. Health Care Res. Dev. 20 , E116 (2019).
O’Keeffe, M., Flint, S.W., Watts, K. & Rubino, F. Knowledge gaps and weight stigma shape attitudes toward obesity: insights from the ASK study. Lancet Diabetes Endocrinol. https://doi.org/10.1016/S2213-8587(20)30073-5 (2020).
Dolan, P. et al. Assessment of public attitudes toward weight loss surgery in the United States. JAMA Surg. 154 , 264–266 (2019).
Kim, J. J. Evidence base for optimal preoperative preparation for bariatric surgery: does mandatory weight loss make a difference? Curr. Obes. Rep. 6 , 238–245 (2017).
Keith, C. J. Jr., Goss, L. E., Blackledge, C. D., Stahl, R. D. & Grams, J. Insurance-mandated preoperative diet and outcomes after bariatric surgery. Surg. Obes. Relat. Dis. 14 , 631–636 (2018).
Vartanian, L. R. & Fardouly, J. The stigma of obesity surgery: negative evaluations based on weight loss history. Obes. Surg. 23 , 1545–1550 (2013).
Hansen, B. B. & Dye, M. H. Damned if you do, damned if you don’t: the stigma of weight loss surgery. Deviant Behav. 39 , 137–147 (2018).
Rubino, F. et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care 39 , 861–877 (2016).
Sjostrom, L. Review of the key results from the Swedish Obese Subjects (SOS) trial: a prospective controlled intervention study of bariatric surgery. J. Intern. Med. 273 , 219–234 (2013).
Dixon, J. B. Regional differences in the coverage and uptake of bariatric-metabolic surgery: A focus on type 2 diabetes. Surg. Obes. Relat. Dis. 12 , 1171–1177 (2016).
Gruskin, S., Mann, J. & Tarantola, D. Past, present, and future: AIDS and human rights. Health Hum. Rights 2 , 1–3 (1998).
Parker, R. & Aggleton, P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc. Sci. Med. 57 , 13–24 (2003).
Callahan, D. Obesity: chasing an elusive epidemic. Hastings Cent. Rep. 43 , 34–40 (2013).
Puhl, R. M. & Heuer, C. A. The stigma of obesity: a review and update. Obesity 17 , 941–964 (2009).
Puhl, R. & Suh, Y. Health consequences of weight stigma: implications for obesity prevention and treatment. Curr. Obes. Rep. 4 , 182–190 (2015).
Rudolph, C. W., Wells, C. L., Weller, M. D. & Baltes, B. B. A meta‐analysis of empirical studies of weight‐based bias in the workplace. J. Vocat. Behav. 74 , 1–10 (2009).
Schulte, P. A. et al. Work, obesity, and occupational safety and health. Am. J. Public Health 97 , 428–436 (2007).
Agerström, J. & Rooth, D. O. The role of automatic obesity stereotypes in real hiring discrimination. J. Appl. Psychol. 96 , 790–805 (2011).
Flint, S. W. & Snook, J. Obesity and discrimination: the next ‘big issue’? International J. Discrimination Law 14 , 183–193 (2014).
Flint, S. W. et al. Obesity discrimination in the recruitment process: “You’re not hired!”. Front. Psychol. 7 , 647 (2016).
Tyrrell, J. et al. Height, body mass index, and socioeconomic status: mendelian randomisation study in UK Biobank. Br. Med. J. 352 , i582 (2016).
Shinall, J. B. Occupational characteristics and the obesity wage penalty. Vanderbilt Law and Economics Research Paper No. 16–12; Vanderbilt Public Law Research Paper No. 16–23, https://ssrn.com/abstract=2379575 (7 October 2015).
Rushing, B. et al. An Act making discrimination on the basis of height and weight unlawful. Commonwealth of Massachusetts Bill H.952, https://malegislature.gov/Bills/190/H952 (18 January 2017).
Pomeranz, J. L. & Puhl, R. M. New developments in the law for obesity discrimination protection. Obesity 21 , 469–471 (2013).
Equality and Human Rights Commission. Equality Act 2010. http://www.legislation.gov.uk/ukpga/2010/15/contents (2010).
Persky, S. & Eccleston, C. P. Impact of genetic causal information on medical students’ clinical encounters with an obese virtual patient: health promotion and social stigma. Ann. Behav. Med. 41 , 363–372 (2011).
Hilbert, A. et al. Causal attributions of obese men and women in genetic testing: implications of genetic/biological attributions. Psychol. Health 24 , 749–761 (2009).
Teachman, B. A., Gapinski, K. D., Brownell, K. D., Rawlins, M. & Jeyaram, S. Demonstrations of implicit anti-fat bias: the impact of providing causal information and evoking empathy. Health Psychol. 22 , 68–78 (2003).
Puhl, R. M. et al. A multinational examination of weight bias: predictors of anti-fat attitudes across four countries. Int. J. Obes. 39 , 1166–1173 (2015).
Barry, C. L., Jarlenski, M., Grob, R., Schlesinger, M. & Gollust, S. E. News media framing of childhood obesity in the United States from 2000 to 2009. Pediatrics 128 , 132–145 (2011).
Kim, S. H. & Willis, L. A. Talking about obesity: news framing of who is responsible for causing and fixing the problem. J. Health Commun. 12 , 359–376 (2007).
Blaine, B. & McElroy, J. Selling stereotypes: weight loss infomercials, sexism, and weightism. Sex Roles 46 , 351–357 (2002).
Puhl, R. M. et al. Potential policies and laws to prohibit weight discrimination: public views from 4 countries. Milbank Q. 93 , 691–731 (2015).
Hilbert, A. et al. Public support for weight-related antidiscrimination laws and policies. Obes. Facts 10 , 101–111 (2017).
Morton, G. J., Cummings, D. E., Baskin, D. G., Barsh, G. S. & Schwartz, M. W. Central nervous system control of food intake and body weight. Nature 443 , 289–295 (2006).
Hall, K. D. et al. Energy balance and its components: implications for body weight regulation. Am. J. Clin. Nutr. 95 , 989–994 (2012).
Leibel, R. L., Rosenbaum, M. & Hirsch, J. Changes in energy expenditure resulting from altered body weight. N. Engl. J. Med. 332 , 621–628 (1995).
Hall, K. D., Kerns, J. C., Brychta, R. & Knuth, N. D. Response to “Overstated metabolic adaptation after ‘The Biggest Loser’ intervention”. Obesity 24 , 2026 (2016).
Colley, R. C. et al. Physical activity of Canadian children and youth: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 22 , 15–23 (2011).
Colley, R. C. et al. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 22 , 7–14 (2011).
Pontzer, H. et al. Hunter-gatherer energetics and human obesity. PLoS One 7 , e40503 (2012).
Maes, H. H., Neale, M. C. & Eaves, L. J. Genetic and environmental factors in relative body weight and human adiposity. Behav. Genet. 27 , 325–351 (1997).
Heindel, J. J., Newbold, R. & Schug, T. T. Endocrine disruptors and obesity. Nat. Rev. Endocrinol. 11 , 653–661 (2015).
Chassaing, B. et al. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature 519 , 92–96 (2015).
Arble, D. M., Bass, J., Laposky, A. D., Vitaterna, M. H. & Turek, F. W. Circadian timing of food intake contributes to weight gain. Obesity 17 , 2100–2102 (2009).
Tremblay, A. & Chaput, J. P. About unsuspected potential determinants of obesity. Appl. Physiol. Nutr. Metab. 33 , 791–796 (2008).
Keith, S. W. et al. Putative contributors to the secular increase in obesity: exploring the roads less traveled. Int. J. Obes. 30 , 1585–1594 (2006).
McAllister, E. J. et al. Ten putative contributors to the obesity epidemic. Crit. Rev. Food Sci. Nutr. 49 , 868–913 (2009).
Börjeson, M. The aetiology of obesity in children. A study of 101 twin pairs. Acta Paediatr. Scand. 65 , 279–287 (1976).
Stunkard, A. J. et al. An adoption study of human obesity. N. Engl. J. Med. 314 , 193–198 (1986).
Sharma, A. M. & Padwal, R. Obesity is a sign - over-eating is a symptom: an aetiological framework for the assessment and management of obesity. Obes. Rev. 11 , 362–370 (2010).
Kaplan, L. M. et al. Perceptions of barriers to effective obesity care: results from the national ACTION study. Obesity 26 , 61–69 (2018).
Bray, G. A., Kim, K. K. & Wilding, J. P. H., World Obesity, F. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes. Rev. 18 , 715–723 (2017).
Franz, M. J. et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J. Am. Diet. Assoc. 107 , 1755–1767 (2007).
Wadden, T. A. et al. A two-year randomized trial of obesity treatment in primary care practice. N. Engl. J. Med. 365 , 1969–1979 (2011).
Sumithran, P. et al. Long-term persistence of hormonal adaptations to weight loss. N. Engl. J. Med. 365 , 1597–1604 (2011).
Cummings, D. E. & Rubino, F. Metabolic surgery for the treatment of type 2 diabetes in obese individuals. Diabetologia 61 , 257–264 (2018).
Batterham, R. L. & Cummings, D. E. Mechanisms of Diabetes Improvement Following Bariatric/Metabolic Surgery. Diabetes Care 39 , 893–901 (2016).
Download references
Acknowledgements
We thank O. Barata Cavalcanti from the World Obesity Federation (WOF) for her critical role in this consensus conference as moderator of the Delphi process, and E. Papada, D. Qanaq, G. Chamseddine, S. Cremona, and M.F. Russo from King’s College London for their assistance with formatting of tables. We acknowledge contributions of W. Cefalu, who participated as a member of the expert panel in his role of Chief Scientific, Medical and Mission Officer of the American Diabetes Association. The face-to-face meeting of the expert panel was hosted by the WCITD2019, which supported travel expenses. WCITD2019 was managed by Kenes Group and was supported by Medtronic (major sponsor), Ethicon (major sponsor), Novo Nordisk, Fractyl Laboratories, GI Dynamics, Cairn Diagnostics, Keyron, and Aventic Group. These sponsors played no role in the selection of voting delegates, the Delphi process, the WCITD2019 program, or the writing of this paper.
Author information
These authors contributed equally: Rebecca M. Puhl, David E. Cummings.
Authors and Affiliations
King’s College London, Department of Diabetes, School of Life Course Science, London, UK
Francesco Rubino & Geltrude Mingrone
King’s College Hospital, Bariatric and Metabolic Surgery, London, UK
Francesco Rubino
Rudd Center for Food Policy & Obesity, University of Connecticut, Hartford, CT, USA
Rebecca M. Puhl
UW Medicine Diabetes Institute, University of Washington, Seattle, WA, USA
David E. Cummings
Weight Management Program, Virginia Puget Sound Health Care System, University of Washington, Seattle, WA, USA
Division of Endocrinology, Metabolism & Diabetes, University of Colorado Anschutz Medical Campus, Aurora, CO, USA
Robert H. Eckel
Division of Cardiology, University of Colorado Anschutz Medical Campus, Aurora, CO, USA
Pennington Biomedical Research Center, Louisiana State University, Baton Rouge, LA, USA
Donna H. Ryan & Phillip R. Schauer
The Marie-Josee and Henry R. Kravis Center for Clinical Cardiovascular Health at Mount Sinai Heart, New York, NY, USA
Jeffrey I. Mechanick
Divisions of Cardiology and Endocrinology, Diabetes and Bone Disease, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Obesity Action Coalition, Tampa, FL, USA
Joe Nadglowski & Patricia Nece
Obesity Canada, Edmonton, Canada
Ximena Ramos Salas
European Association for the Study of Obesity, Teddington, UK
Diabetes UK, London, UK
Douglas Twenefour
Boston University School of Medicine, Boston, MA, USA
Caroline M. Apovian
Center for Nutrition and Weight Management, Boston Medical Center, Boston, MA, USA
Comprehensive Weight Control Center, Division of Endocrinology, Diabetes and Metabolism, Weill Cornell Medicine, New York, NY, USA
Louis J. Aronne
National Institute of Health Research, University College London Hospitals Biomedical Research Centre, London, UK
Rachel L. Batterham
University College London Hospital Foundation Trust, London, UK
Centre for Obesity Research, Department of Medicine, University College London, London, UK
Neurobiology of Nutrition and Metabolism Department, Pennington Biomedical Research Centre, Louisiana State University System, Baton Rouge, LA, USA
Hans-Rudolph Berthoud
Centro de Innovación Clinica Las Condes Universidad Adolfo Ibañez, Santiago, Chile
Camilo Boza
Department of Internal Medicine, University of Padova, Padua, Italy
Luca Busetto
Hasharon Hospital-Rabin Medical Center, Sackler School of Medicine, Tel-Aviv University, Tel-Aviv, Israel
Dror Dicker
Obesity Management Task Force, European Association for the Study of Obesity, Teddington, UK
Department of Medicine, Indiana University School of Medicine, Indianapolis, IN, USA
Mary De Groot
Department of Surgery, Stanford School of Medicine and Palo Alto Virginia Health Care System, Stanford, CA, USA
Daniel Eisenberg
School of Psychology, University of Leeds, Leeds, UK
Stuart W. Flint
Scaled Insights, Nexus, University of Leeds, Leeds, UK
Department of Health Policy & Management, Center for Systems & Community Design, New York, NY, USA
Terry T. Huang
NYU-CUNY Prevention Research Center, Graduate School of Public Health & Health Policy, City University of New York, New York, NY, USA
Obesity, Metabolism and Nutrition Institute, Massachusetts General Hospital, Boston, MA, USA
Lee M. Kaplan
Integrated Physiology and Molecular Medicine, Pennington Biomedical Research Center, Baton Rouge, LA, USA
John P. Kirwan
Department of Medicine, Columbia University Irving Medical Center, New York, NY, USA
Judith Korner
ConscienHealth, Pittsburgh, PA, USA
Ted K. Kyle
Division of Endocrinology, Columbia University, New York, NY, USA
Blandine Laferrère
Diabetes Complications Research Centre, University College Dublin, Dublin, Ireland
Carel W. le Roux
Government Affairs & Advocacy, American Diabetes Association, Arlington, VA, USA
LaShawn McIver
Fondazione Policlinico Universitario A. Gemelli, IRCCS, Rome, Italy
Geltrude Mingrone
Catholic University, Rome, Italy
Division of Endocrinology, Diabetes & Metabolism, Columbia University College of Physicians and Surgeons, New York, NY, USA
Tirissa J. Reid
Pennsylvania State Hershey Medical Center, Hershey, PA, USA
Ann M. Rogers
Columbia University Irving Medical Center, New York, NY, USA
Michael Rosenbaum
Department of Surgery, University of Michigan, Ann Arbor, MI, USA
Randy J. Seeley
Hospital Clinico San Carlos. Universidad Complutense de Madrid, Madrid, Spain
Antonio J. Torres
Baker IDI Heart and Diabetes Institute, Melbourne, Australia
John B. Dixon
You can also search for this author in PubMed Google Scholar
Contributions
F.R. conceived the idea of an international consensus conference on the stigma of obesity and was the main organizer and director of WCITD2019. F.R., D.H.R., D.E.C., and J.B.D. co-chaired the expert panel. F.R., D.E.C., R.M.P., R.H.E., D.H.R., J.I.M., J.N., X.R.S., P.R.S., D.T., and J.B.D. served as members of the Writing Committee, which prepared the first draft of this report and participated in subsequent development. All co-authors of this report served as voting delegates in the expert panel, participated in the appraisal of evidence and in the Delphi process to craft the consensus statements, and reviewed and approved this report.
Corresponding author
Correspondence to Francesco Rubino .
Ethics declarations
Competing interests.
None of the members of the organizing committee (F.R., D.E.C., D.H.R. and J.B.D.) and none of the voting members of the expert panel received payment for their participation. Travel expenses for the face-to-face meeting of the expert panel were supported by Medtronic, Ethicon, Novo Nordisk, Fractyl Laboratories, GI Dynamics, Cairn Diagnostics, Keyron, and Aventic Group. C.M.A. has participated on advisory boards for Nutrisystem, Zafgen, Sanofi-Aventis, Orexigen, EnteroMedics, GI Dynamics, Gelesis, Novo Nordisk, Bariatrix, Xeno Biosciences, Rhythm Pharmaceuticals, Eisai, and Scientific Intake; has received research funding from Aspire Bariatrics, GI Dynamics, Takeda, the Vela Foundation, Gelesis, Energesis, Coherence Lab, and Novo Nordisk; and owns stock in Science-Smart LLC. L.J.A. has received consulting fees from and serves on advisory boards for Jamieson Laboratories, Pfizer, Novo Nordisk, Eisai, Real Appeal, Janssen, and Gelesis; has also received research funding from Aspire Bariatrics, Allurion, Eisai, AstraZeneca, Gelesis, Janssen, Eli Lily, and Novo Nordisk; serves on the board of directors for Intellihealth/BMIQ, MYOS, and Jamieson Laboratories; and has equity in Intellihealth/BMIQ, ERX, Zafgen, Gelesis, MYOS, and Jamieson Laboratories. R.L.B. is a principle investigator for clinical trials funded by Novo Nordisk and Fractyl (all funds go directly to the institution); and has consultancy agreements with Novo Nordisk, Pfizer, GSK, and International Medical Press. C.B. is a principal investigator on a study of metabolic surgery funded by Prodigies; and has received fees from Ethicon Endosurgery. B.L. is on the Scientific Advisory Board of Novo Nordisk; has received speaker fees from Bruno Farmaceutici; and has a research grant from Enzymmanagemen. D.E.C. is on the Scientific Advisory Boards of G.I. Dynamics, DyaMx, Magnamosis, and Metavention. J.B.D. has consultancies with Bariatric Advantage, iNova, and Reshape; is on advisor boards for Novo Nordisk and Nestlé Health Science; and receives research support from NHMRC. M.deG. has received funds from Lifescan Diabetes Institute, Inc., and the Kenner Family Foundation. R.H.E. has received funds from Amgen, Kowa, Sanofi, and Novo Nordisk. S.W.F. has received from Novo Nordisk for travel; and support for working with media. L.M.K. has received funds from Boehringer Ingelheim, Ethicon, Gelesis, GI Dynamics, Johnson & Johnson, Pfizer, Novo Nordisk, and Rhythm Pharmaceuticals. J.P.K. has received grants and research support from the National Institutes of Health, Ethicon, Covidien, Metagenics, Alliance for Potato Research and Education, CrossFit, Nestlé Research, General Mills, and Robard Corporation; is on advisory panels for Bristol-Myers Squibb, AstraZeneca, Novo Nordisk, and Cereal Partners; and receives speaker fees from Elli Lilly, Pfizer, and ILSI. J.K. is on the scientific advisory board of Digma Medical, GI Dynamics, and Applied Biosciences; and consults for Esquagama. T.K.K. has received consulting fees from Tivity Health, Novo Nordisk, and Gelesis. C.W.leR. is on the advisory boards and speaker bureaus for NovoNordisk, GI Dynamics, Keyron, Herbalife, Sanofi, Johnson & Johnson, Medtronic, and Boehringer Ingelheim; and owns shares in Keyron. J.I.M. has received honoraria for lectures and program development from Abbott Nutrition. G.M. has received fees for consultations from Novo Nordisk, Johnson & Johnson, and Fractyl Inc. J.N. is an employee of the Obesity Action Coalition. R.M.P. has received research grant support from the Rudd Foundation, and WW, Inc. F.R. is on advisory boards for GI Dynamics, Keyron, and NovoNordisk; has received consulting fees from Ethicon Endosurgery and Medtronic; and has received research funding from Ethicon Endosurgery and Medtronic. D.H.R. has an equity interest in start-up companies engaged in various aspects of weight management (Gila Therapeutics, Scientific Intake, Xeno Biosciences, Epitomee, and Calibrate); is on the Speaker’s Bureau of Novo Nordisk and Bausch Health; has served as an advisor or consultant to Alyvent, Amgen, Bausch Health, Boehringer Ingelheim, Epitomee, Gila Therapeutics, IFA Celtic, Janssen, Kensai Therapeutics, Novo Nordisk, Phenomix, Real Appeal (United Health), ReDesign Health (Calibrate), Sanofi, and Scientific Intake; and serves on the steering committee for the SELECT cardiovascular outcome trial for Novo Nordisk’s investigational product semaglutide. P.R.S. is a Board Member and Advisory Panel member for GI Dynamics; has consulted for Ethicon, Medtronic, WL Gore, and BD Surgical; has received research support from Ethicon, NIH, Medtronic, and Pacira; and has equity in SEHQC and LLC. R.J.S. receives research support from Novo Nordisk, Pfizer, Kintai, Ionis, Zafgen, and Astra Zeneca; has received consulting fees from Novo Nordisk, Kintai, Ionis, Sanofi, and Scohia; and has equity in ReDesign Health and Zafgen. T.D. is an employee of Diabetes UK.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Rubino, F., Puhl, R.M., Cummings, D.E. et al. Joint international consensus statement for ending stigma of obesity. Nat Med 26 , 485–497 (2020). https://doi.org/10.1038/s41591-020-0803-x
Download citation
Received : 07 February 2020
Accepted : 14 February 2020
Published : 04 March 2020
Issue Date : April 2020
DOI : https://doi.org/10.1038/s41591-020-0803-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Weight stigma in healthcare settings: the experience of arab and jewish bariatric surgery candidates in israel.
- Yara Zahra-Zeitoun
- Roni Elran-Barak
- Yael Latzer
Israel Journal of Health Policy Research (2024)
Raising awareness of anti-fat stigma in healthcare through lived experience education: a continuing professional development pilot study
- Christine Heidebrecht
- Dianne Fierheller
BMC Medical Education (2024)
Reducing greenhouse gas emissions in a bariatric surgical unit is a complex but feasible project
- Jerome Dargent
Scientific Reports (2024)
Fat phobia scale-short form and beliefs about obese persons scale: cross-cultural adaptation to Brazilian Portuguese
- Gabriela Cristina Arces de Souza
- Maria Fernanda Laus
- Camila Cremonezi Japur
Discover Psychology (2024)
Obesity Bias and Stigma, Attitudes, and Beliefs Among Intern Doctors: a Cross-sectional Study from Türkiye
- Servet Aker
- Mustafa Kürşat Şahin
Obesity Surgery (2024)

Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Physical activity motives, barriers, and preferences in people with obesity: A systematic review
Roles Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft
* E-mail: [email protected]
Affiliations Department of Nursing, University of Québec en Outaouais, Gatineau, QC, Canada, Institut du savoir Montfort-Recherche, Ottawa, ON, Canada, Centre de recherche du Centre Intégré de Santé et Services Sociaux de l’Outaouais, Gatineau, QC, Canada
Roles Data curation, Formal analysis, Investigation, Validation, Writing – review & editing
Affiliation Institut du savoir Montfort-Recherche, Ottawa, ON, Canada
Affiliation Department of Nursing, State University of Northern Paraná, Bandeirantes, PR, Brazil
Roles Data curation, Validation, Visualization, Writing – review & editing
Affiliation Faculty of Health Sciences, School of Human Kinetics, University of Ottawa, Ottawa, ON, Canada
Roles Data curation, Investigation, Writing – review & editing
Affiliations Faculty of Physical Activity Sciences, University of Sherbrooke and Research Center on Aging, CIUSSS de l’Estrie–CHUS, Sherbrooke, QC, Canada, Institut des Sciences et Industries du vivant et de l’environnement, AgroParisTech, Paris, France
Roles Data curation, Formal analysis, Validation, Writing – review & editing
Affiliation Department of Nursing, University of Québec en Outaouais, Gatineau, QC, Canada
Roles Conceptualization, Formal analysis, Writing – review & editing
Affiliation Faculty of Physical Activity Sciences, University of Sherbrooke and Research Center on Aging, CIUSSS de l’Estrie–CHUS, Sherbrooke, QC, Canada
Roles Validation, Writing – review & editing
Affiliation Department of Psychiatry and Human Behavior, Weight Control and Diabetes Research Center, The Miriam Hospital/Brown Alpert Medical School, Providence, RI, United States of America
Roles Conceptualization, Formal analysis, Methodology, Validation, Writing – review & editing
Affiliations Faculty of Medicine, School of Kinesiology and Physical Activity Sciences, Université de Montréal, Montréal, QC, Canada, Centre de Recherche de l’Institut Universitaire en Santé Mentale de Montréal, Montréal, QC, Canada
- Aurélie Baillot,
- Stéphanie Chenail,
- Naiara Barros Polita,
- Mylène Simoneau,
- Mathilde Libourel,
- Evy Nazon,
- Eléonor Riesco,
- Dale S. Bond,
- Ahmed J. Romain

- Published: June 23, 2021
- https://doi.org/10.1371/journal.pone.0253114
- Reader Comments
Although the benefits of physical activity (PA) are well known, physical inactivity is highly prevalent among people with obesity. The objective of this systematic review was to i) appraise knowledge on PA motives, barriers, and preferences in individuals with obesity, and ii) quantify the most frequently reported PA motives, barriers and preferences in this population.
Six databases (Pubmed, CINAHL, Psyarticle, SportDiscus, Web of science and Proquest) were searched by independent reviewers to identify relevant quantitative or qualitative articles reporting PA motives, barriers or preferences in adults with body mass index ≥ 30 kg/m 2 (last searched in June 2020). Risk of bias for each study was assessed by two independent reviewers with the Mixed Methods Appraisal Tool (MMAT).
From 5,899 papers identified, a total of 27 studies, 14 quantitative, 10 qualitative and 3 mixed studies were included. About 30% of studies have a MMAT score below 50% (k = 8). The three most reported PA motives in people with obesity were weight management, energy/physical fitness, and social support. The three most common PA barriers were lack of self-discipline/motivation, pain or physical discomfort, and lack of time. Based on the only 4 studies available, walking seems to be the preferred mode of PA in people with obesity.
Conclusions
Weight management, lack of motivation and pain are key PA motives and barriers in people with obesity, and should be addressed in future interventions to facilitate PA initiation and maintenance. Further research is needed to investigate the PA preferences of people with obesity.
Citation: Baillot A, Chenail S, Barros Polita N, Simoneau M, Libourel M, Nazon E, et al. (2021) Physical activity motives, barriers, and preferences in people with obesity: A systematic review. PLoS ONE 16(6): e0253114. https://doi.org/10.1371/journal.pone.0253114
Editor: Saravana Kumar, University of South Australia, AUSTRALIA
Received: June 29, 2020; Accepted: May 30, 2021; Published: June 23, 2021
Copyright: © 2021 Baillot et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: Canadian Health Research Institute NRF 155266. AB is the recipient of salary awards from the Fonds de recherche du Québec-Santé (FRQ-S). The funders have no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Obesity is a major public health issue in North America affecting more than 25% of adults in Canada, and 40% of adults in the United States [ 1 , 2 ]. Obesity contributes to impaired physical and mental health-related quality of life, and increased morbidity and mortality [ 3 , 4 ]. Physical activity (PA) is a cornerstone of interdisciplinary obesity management [ 5 , 6 ]. Indeed, the benefits of regular PA on weight management, body composition, physical fitness, and cardiometabolic health in people with obesity are well documented [ 7 – 10 ]. However, more than half of Canadians and Americans living with obesity report to be insufficiently active [ 11 , 12 ]. Furthermore, adherence to structured PA interventions is poor and drop-out rates ranged from 20% to 80% [ 13 ].
In the context of PA intervention, a mismatch between patients’ preferences or motives, and the PA intervention planned could negatively impact PA engagement [ 14 ]. Integrating preferences into interventions has been considered as a patient-oriented strategy to improve participation and adherence as patients feel included in their decisions [ 14 – 17 ]. Moreover, from a PA perspective, previous research highlights that when people with obesity were offered to self-select their PA intensity, they accumulated more PA over time [ 18 , 19 ]. Along with PA preferences among individuals with obesity, it is important to understand PA motives and barriers to inform clinicians, and health stakeholders on the development of strategies to better improve PA behavior in this population [ 20 – 23 ].
Past systematic reviews on PA motives, barriers and preferences have been performed in various clinical populations (e.g., type 2 diabetes) [ 24 – 27 ]. Although several qualitative and quantitative studies are available on this topic in people with obesity, to our knowledge, none have systematically summarized this information. Only one systematic review of qualitative studies has been carried out on PA motives and barriers in people with severe obesity [ 28 ], and reported that weight loss was the main reason for exercising, followed by other motives, such as the risk of diseases, and skills improvement. Moreover, physical (e.g., health problems, weight, and pain), and psychosocial barriers (e.g., embarrassment, self-blame, lack of safety, and time) were also reported in this study [ 28 ].
Therefore, the objectives of the present systematic review were to i) appraise current qualitative and quantitative knowledge on PA motives, barriers and preferences in people with obesity, and ii) quantify which PA motives, barriers and preferences were more common in this population.
Materials and methods
Protocol and registration.
The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines were used to perform this review [ 29 ]. The protocol was pre-registered in PROSPERO (CRD42020141447).
Eligibility criteria
Quantitative and qualitative studies were included in this review if they met the following inclusion criteria: i) constituted primary research published in peer-reviewed journals with full-text available in English or French; ii) focused on adults (≥ 18 years old) with a body mass index (BMI) ≥ 30 kg/m 2 (or more than 75% of the sample with BMI ≥ 30 kg∕m 2 if the study did not exclusively include people with obesity or did not perform sub analysis in people with obesity); iii) reported motives, barriers or preferences to PA.
To define PA, the standard definition of Caspersen et al. (1985) and endorsed by the World Health Organization “any bodily movement produced by skeletal muscles that results in energy expenditure” was used in the present systematic review [ 30 ]. Motives were defined as any perceived reasons to increase and maintain PA, and barriers as any challenges reported by participants reducing PA initiation and maintenance [ 25 ]. Preferences were considered as patient-reported favourite choices concerning PA modalities, context, type, and supervision.
During the full-text papers selection, authors (AB, AJR, ER) decided by consensus to exclude studies that focused more on specific sub-populations with obesity, given that it would have not been possible to clearly distinguish whether PA motives, barriers, and preferences should be attributed to obesity or the coexistent condition/circumstance. These specific subpopulations included: pregnant women [ 31 – 33 ], cancers survivors [ 34 – 37 ], people with intellectual disabilities [ 38 ], veterans living with schizophrenia [ 39 ], and bariatric surgery patients [ 40 – 51 ].
Information sources and search
A systematic search of eligible studies was conducted in six different databases (Pubmed, CINAHL, PsycArticles, SportDiscus, Web of science and Proquest). Reference lists from eligible studies, the 10 first pages of Google Scholar and Open Grey database, as well as personal records were checked to identify other potentially relevant studies (AB, AJR, DB).”
The search was performed on July 23, 2019 without date restriction, using research equation including keywords and Medical Subject Headings (Mesh) terms developed with a university librarian. For example, the PubMed search strategy was the following: "Exercise"[Mesh] AND "Obesity"[Mesh] AND ("Motivation"[Mesh] OR "Patient Preference "[Mesh] OR "preference*"[All Fields] OR "barrier*"[All Fields] OR "facilitator*"[All Fields]) OR "obstacle*"[All Fields]) AND "humans"[MeSH Terms] AND (English[lang] OR French[lang]) AND "adult"[MeSH Terms]. The search strategy was modified for each database, considering their specificities. An updated search was performed on June 04 (2020) to retrieve any potential studies published since the initial search. See supplemental material S1 File for detailed search strategies for each database. The search in Grey literature was performed on April 26, 2021.
Study selection
All retrieved citations were imported into EndNote software (Version X9), and duplicate records were removed by one reviewer (ML). Two independent students’ reviewers (ML and MS) paired with senior reviewers (AB and AJR) screened records using a data extraction form against inclusion and exclusion criteria, first according to titles and abstracts, and then to the full-text papers of the selected abstracts. Disagreements were resolved by a third party (AB or AJR). If necessary, authors were contacted in case of missing or incomplete data for the study selection step.
Data collection process
The following data were extracted by one review author (SC) using a data extraction form developed for the present review, and double-verified by two others (NBP, MS): authors; publication year; study setting; country; study design; sample size; participants’ characteristics (age, sex, BMI and comorbidities); methods to appraise PA motives, barriers and preferences; and results: survey/questionnaire items with the score or frequency associated for quantitative studies, and first and second constructs with adjectives reflecting the importance of the outcomes (many, several, etc.) for qualitative studies. To be extracted, PA motives and barriers should have been reported in the results section. Disagreements were resolved by having a fourth review author (AB) returning to the full text(s) to check the accuracy of extracted data.
Data synthesis process
A thematic synthesis of the data extracted from qualitative studies was used following the steps proposed by Thomas and Harden [ 52 ]. First, line-by-line coding driven by the objectives was performed by one reviewer (NBP). Then, similar codes were grouped into descriptive themes, including first and second order constructs, which were verified by a second reviewer (SC). Analytical themes were generated by the interpretation of descriptive themes and validated by two authors (SC, AB). Finally, themes were compared and integrated to quantitative categories. Results on PA motives and barriers extracted from qualitative and quantitative studies were classified in three main categories: physical, psychological and socio-ecological by two reviewers (SC and NBP) [ 25 ], and then reviewer authors (AB, AJR, SC, NBP) created subcategories by consensus to merge similar items and constructs.
Regarding the statistical part, though a meta-analysis of proportion was planned to further rank each PA motives, barriers and preferences individually, this option was not found to be feasible given the small number of included studies per section and the high heterogeneity between included studies. Alternatively, based on the scale from Clifford et al. [ 24 ], we created a score of importance for each PA motive and barrier subcategory. Briefly, a score of importance ranging from 0 to 3 was assigned to each PA motive and barrier subcategory in each study (see Table 1 for details) by two independent reviewers (AB, SC). Disagreements were resolved during discussion with a third reviewer (AJR). For example, a score of 3 was assigned to pain as a PA barrier in studies reporting 50% or more of participants checked the item pain as a PA barrier. To then obtain a rank for each PA motive and barrier, a global score was calculated by summing each PA motive and barrier score across all the studies (maximal score of 33 for PA motives; 11 studies × 3, and 69 for PA barriers; 23 studies × 3).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0253114.t001
For PA preferences, a narrative synthesis was favoured given the small number of studies (k = 4) and the high heterogeneity between studies.
Risk of bias in individual studies
Risk of bias for each of the included studies was assessed by two independent reviewers (AB, SC) for quantitative studies, two other independent reviewers for qualitative studies (NBP, EN), and two independent reviewers for mixed studies (NR, AB) with the Mixed Methods Appraisal Tool (MMAT-Version11), adapted for this review. Any discrepancies were mediated by a third reviewer (AJR). Given the descriptive nature of our research objectives, the following criteria were used for quantitative studies: 1) Is the sampling strategy relevant to address the research question? 2) Is the sample representative of the target population? 3) Are the measurements appropriate? 4) Is the risk of nonresponse bias low? The 5 criteria for qualitative and mixed methods studies were those reported in the MMAT (respectively: 1. Is the qualitative approach appropriate to answer the research question? 2. Are the qualitative data collection methods adequate to address the research question? 3. Are the findings adequately derived from the data? 4. Is the interpretation of results sufficiently substantiated by data? 5. Is there coherence between qualitative data sources, collection, analysis and interpretation? / 1. Is there an adequate rationale for using a mixed method design to address the research question? 2. Are the qualitative data collection methods adequate to address the research question? 3. Are the outputs of the integration of qualitative and quantitative components adequately interpreted? 4. Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? 5. Do the different components of the study adhere to the quality criteria of each tradition of the methods involved?) [ 53 , 54 ]. Each criterion was assessed as being fulfilled (1 point) or not fulfilled/insufficient information for adequate assessment (0 point), leading to a global score of 4 for quantitative studies, and 5 for qualitative and mixed studies. Scores were then converted to percentage to facilitate between-studies comparison.
The electronic searches generated 5,899 studies; which was reduced to 4,189 after removing duplicates. Following this step, 3,857 records were excluded based on title and abstract, with 52% of them because they did not present the outcomes of interest. Twenty-seven studies in total were included in this review ( Fig 1 ).
https://doi.org/10.1371/journal.pone.0253114.g001
Study characteristics
Table 2 describes studies and participants’ characteristics. Briefly, 14 quantitative studies (51.9%) [ 55 – 68 ], 10 qualitative studies (37.0%) [ 69 – 78 ], and 3 mixed studies (11.1%) [ 79 – 81 ] were included. Among quantitative studies, 11 studies were observational [ 55 – 59 , 63 – 68 ], and 3 were interventional studies [ 60 – 62 ]. However, all interventional studies reported information about barriers and/or motives to habitual PA, not about PA intervention. Almost half of the studies were performed in the United States (k = 13) [ 56 , 58 , 59 , 61 – 63 , 65 , 69 , 70 , 74 , 79 – 81 ], and 37.0% published in the last five years (2015–2020; k = 10) [ 55 , 56 , 65 , 68 – 71 , 74 , 75 , 79 ]. A total of 8,065 participants with obesity were assessed within the included studies (k = 27), with a median age of 46 years old (range 37.8–62.0) (k = 10 because information is missing for people with obesity in 17 studies). More than half of the studies included over 70% of women in their sample (51.9%; k = 14) [ 56 , 58 , 59 , 61 – 63 , 65 , 69 , 72 , 74 , 77 , 79 – 81 ], 37.0% included only women (k = 10) [ 56 , 58 , 61 – 63 , 69 , 74 , 77 , 79 , 81 ], and 7.4% included only men (k = 2) [ 55 , 78 ].
https://doi.org/10.1371/journal.pone.0253114.t002
Regarding the outcomes of interest, PA barriers were assessed in 24 studies (88.9%) [11 quantitative, 10 qualitative, and 3 mixed studies] [ 55 – 63 , 65 , 68 – 81 ], motives in 11 studies (40.7%) [2 quantitative, 8 qualitative, and 1 mixed studies] [ 55 , 64 , 69 , 71 – 75 , 77 , 78 , 81 ], and preferences in 4 studies (14.8%) [3 quantitative and 1 qualitative studies] [ 60 , 66 , 67 , 74 ].
Risk of bias
More than half of the quantitative studies have a MMAT score below 50% (57.1%, k = 8) [ 55 – 57 , 60 – 62 , 64 , 65 , 68 ], and all qualitative and mixed studies had a score above 50% (see Table 2 and supplemental S1 Table ). The scores of the quantitative studies below 50% are explained by the fact that non-probability sampling was performed in these studies, impacting the representativeness of the sample and our ability to know the nonresponse rate.
Findings for physical activity motives
The 12 PA motives identified were classified in different categories of motives: 6 psychosocial (50.0%), 3 socio-ecological (25.0%) and 3 physical motives (25.0%) ( Fig 2 and supplemental data S2 Table ). More than half (k = 7/12, 58.3%) of PA motives comes from both quantitative and qualitative studies, 33.3% (k = 4/12) from qualitative studies only, and 8.3% (k = 1/12) from quantitative study ( Fig 2 ). In the different included studies, the three most reported PA motives among studies were weight management (k = 8/11, 72.7%), energy/physical fitness (k = 6/11, 54.5%), and social support (k = 6/11, 54.5%) ( Fig 2 ). Regarding PA motives in terms of ranking, the three with the highest scores of importance were also weight management (score = 20), energy/physical fitness (score = 13) and social support (score = 12) ( Fig 3 ).
https://doi.org/10.1371/journal.pone.0253114.g002
https://doi.org/10.1371/journal.pone.0253114.g003
Findings for physical activity barriers
Barriers were classified in three categories being socio-ecological barriers (k = 9; 39.1%), psychological barriers (k = 8; 34.8%), and physical barriers (k = 6; 26.1%) ( Fig 4 and supplemental data S3 Table ). Except for stigma (only qualitative studies), each PA barrier was studied in both quantitative and qualitative studies, and the most reported PA barriers among studies being lack of self-discipline/motivation (k = 15/24, 62.5%), pain/ physical discomfort (k = 13/24, 54.2%), lack of time (k = 13/24, 54.2%), lack of social support (k = 13/24, 54.2%) and lack of access to equipment, facilities or professionals (k = 13/24, 54.2%) ( Fig 4 ).
https://doi.org/10.1371/journal.pone.0253114.g004
The top three physical barriers to PA with the highest score of importance were pain/physical discomfort (score = 31.5), fatigue/lack of energy (score = 23.5) and poor health (score = 20) ( Fig 5 ). Regarding psychological barriers to PA, lack of self-discipline/motivation (score = 34.5), lack of interest/enjoyment (score = 17.7), and lack of skills/confidence (score = 17.0) were the most frequently reported ( Fig 5 ). For socio-ecological barriers to PA, lack of time (score = 28.3), lack of social support (score = 24.0) and cost (score = 22.0) were the three barriers with the highest score of importance ( Fig 5 ).
https://doi.org/10.1371/journal.pone.0253114.g005
Findings for physical activity preferences
Among the four studies reporting results on PA preferences in people with obesity, two provided information on PA preferences (50%) [ 60 , 74 ], one on preferred PA context (25%) [ 66 ], and one on preferred PA delivery mode for intervention (25%) [ 67 ].
Only, Labrunée et al. (2012) and Joseph et al. (2017) provided data on PA type preferences in people with obesity (n = 23 and 25, respectively). Labrunée et al. (2012) asked to classify PA by order of preference the type of physical activity, while Joseph et al. (2017) asked the following open question: “What type of physical activity or exercise do you enjoy doing?”. Among people with obesity walking was the most preferred/enjoyed activity for both men and women [ 60 , 74 ]. Otherwise, the other preferred PA were cycling, swimming and rowing in the Labrunée et al. (2012) study [ 60 ], and dance or Zumba, cycling, water activities, and martial arts in the Joseph et al. (2017) study which was performed among women with obesity [ 74 ]. Resistance training was less often identified as a preferred type of PA [ 74 ].
Regarding the preferred PA context, Burton et al. (2012) examined it among 1781 middle-aged adults with obesity [ 66 ] by asking them to indicate their agreement, neutrality (no preference) or disagreement with a preference for each PA context. Results showed that 78% of participants preferred low-cost or no-cost PA, 61% preferred PA interventions that are not just about exercise, and 50% opted for PA with a format/routine set. Moreover, 26%, 15%, and 16% of participants, respectively, preferred supervised, team-based and competitive PA. Nearly a quarter (23%) of participants reported a preference toward PA requiring skills and practice, and less than half of participants preferred vigorous PA (30%) done at a fixed schedule time (43%). In terms of location, 86% of participants reported a preference for PA that can be done close to home, and 59% preferred outdoor activities. Regarding social settings, 73% of individuals indicated a preference towards activities that can be performed alone, 49% preferred activities with people around their age and 28% with individuals with same sex.
Short et al. (2014) analyzed the preferred PA intervention delivery mode, and provided the prevalence of people with obesity in four groups of people according to their most preferred mode of delivery (n = 1137 with 341 people with obesity): face-to-face program with an instructor (36% of survey responders including 35% of people with obesity), group-based program (44% of survey responders including 27% of people with obesity), program that can be done on their own using mailed and printed materials (11% of survey responders including 26% of people with obesity), programs that can be done on their own using internet (9% of survey responders including 24% of people with obesity) [ 67 ].
Comparison between BMI classes
Among the currently available studies (k = 27), only a few have investigated whether PA motives (k = 2), barriers (k = 6) and preferences (k = 2) differed among individuals with and without obesity. As shown in Table 3 , weight management (k = 2/2), was the only motive that differed across BMI classes [ 55 , 64 ]. Studies reported that weight management was a more prevalent PA motivator in adults with obesity compared to adults without obesity [ 55 , 64 ]. Regarding PA barriers, though no difference between BMI classes were noted in socio-ecological barriers, weight (k = 3/3; [ 61 , 79 , 81 ]), lack of self-discipline/motivation (k = 4/5; [ 59 , 61 , 68 , 79 , 80 ]) and self-consciousness (k = 3/3; [ 59 , 61 , 81 ] were more frequently reported by individuals with obesity than those without obesity.
https://doi.org/10.1371/journal.pone.0253114.t003
Based on the two studies that have investigated associations between BMI or obesity with PA preferences [ 66 , 67 ], social context seems particularly important among individuals with obesity. In fact, supervised [ 66 ], face-to-face [ 67 ] intervention was preferred to group-based intervention. However, in a context of group-based intervention, Burton et al. (2011) reported that homogeneous groups in terms of age and sex were preferred for individuals with a BMI greater than 30 kg/m 2 [ 66 ].
The objective of the present study was to investigate PA motives, barriers and preferences in people with obesity. To our knowledge, the present review is the first to systematically address these questions in this population. From the studies (i.e. 14 quantitative, 10 qualitative, and 3 mixed methods) included in this review, 48.2% were performed in the United States with a clear predominance of women participants. Barriers to PA were most frequently investigated (k = 24) followed by PA motives (k = 11), and preferences to PA (k = 4).
The three most common PA motives reported by people with obesity, based on the scale of Clifford et al. [ 24 ], were weight management, energy/physical fitness and social support.
Unsurprisingly, weight management was the most frequently reported motive for PA in people with obesity, in accordance with previous qualitative review in people with severe obesity [ 28 ]. In addition, weight management is the only motive in individuals with obesity, which differs significantly from adults without obesity according to our literature review [ 55 , 64 , 81 ] ( Table 3 ). This motive is an important factor for health professionals to consider when developing and implementing PA interventions. Indeed, previous studies showed that PA alone produces only modest weight loss [ 7 ], and could therefore lead to PA discontinuation. So, to facilitate PA over time, people should be informed that in a weight management context, PA has a more important role in terms of weight loss maintenance or waist circumference reduction, [ 6 , 7 ].
The second most frequently reported PA motive in people with obesity was physical fitness improvement . This motive is relevant given that an improvement of physical fitness can be achieved through PA interventions in people with obesity [ 6 ]. In addition, previous studies support the importance of physical fitness by showing that physically fit people with obesity have a reduced rate of all-cause mortality compared to unfit people with and without obesity [ 82 ]. However, weight and low physical fitness are also PA barriers in people with obesity, as shown in our results (Figs 4 and 5 ). Consequently, these barriers should be addressed and previous studies showed that PA counseling, and intervention tailored to physical fitness and weight could improve them [ 83 , 84 ].
According to our literature review, key PA barriers were lack of motivation/self-discipline, pain/physical discomfort, and lack of time in people with obesity.
Low motivation and lack of time are non-weight related PA barriers prominent in non-clinical and clinical populations [ 24 , 48 , 85 , 86 ]. However, studies included in our review seem to indicate that lack of self-discipline/motivation is more often reported in people with obesity ( Table 3 ). Behavioral interventions including motivational interviewing are effective options to address lack of motivation, given its efficacy to improve PA adherence [ 87 ]. Regarding lack of time to exercise, though often underlined, several time-use studies highlighted that this PA barrier is more likely to reflect a low priority attributed to PA compared to other activities [ 86 , 88 ]. Moreover, people who have free time are not more active, thus simply helping them to find time for PA in their day might not improve PA in people with obesity [ 86 ]. It could be beneficial to implement behavioural interventions in people with obesity to support them to find motivation to change PA habits in this context. Several time-efficient solutions can be proposed like PA during transportation, PA during work break, reducing TV viewing, [ 86 , 87 ]. As a response to lack of time, it may be tempting to recommend high-intensity interval training to overcome time barriers, given the assumption that with higher intensity, exercise duration can be reduced, and seems equally effective to reduce fat mass and more effective to increase physical fitness in people with obesity compared with moderate-intensity continuous training [ 89 – 91 ]. Nevertheless, there is a debate regarding the relevance of high- compared to moderate-intensity exercise in adults living with obesity to increase long-term PA levels [ 92 ]. Indeed, knowing that adults living with obesity 1) avoid vigorous-intensity PA [ 93 , 94 ], and 2) are willing to accept longer exercise durations if the intensity remains low [ 95 ] emphasizing high intensity could be counter productive.
Regarding pain , the second most frequently reported PA barriers, people with obesity are more likely to suffer from pain [ 96 , 97 ], explaining why it is an important barrier to PA in this population, consistently put forward in other studies [ 98 ], and also compared to other BMI classes [ 61 ]. Previous studies hypothesized a bidirectional association between pain and PA in people with obesity. Musculoskeletal pain, the main source of pain described in qualitative studies can act as a functional limitation to engage and maintain PA [ 97 ]. At the same time, regular PA can reduce chronic musculoskeletal pain in people with obesity, due to its potential positive impacts on inflammation, psychological outcomes (e.g., mood, pain catastrophizing, etc.), muscle strength and coordination [ 97 ]. Nevertheless, PA for pain management in people with obesity requires support to tailor its practice, safety and efficacy [ 97 ]. The adjustment of PA volume (duration, intensity, frequency), joint range of motion during exercise, as well as the type of PA (non-impact PA) are valuable strategies that can be used for the pain management in order to increase PA adherence [ 97 ].
Weigh t is also a major physical obstacle to PA in people with obesity compared to people without obesity [ 61 , 79 , 81 ]. Interestingly, qualitative data from a study included in this review [ 81 ] revealed that women tend to perform more exercise when they lose weight because doing so gets easier. However, weight loss cannot be considered as facilitator per se given previous studies underlined that even after a massive weight loss, people remain physically inactive [ 98 , 99 ].
No conclusion on PA preferences can be drawn due to the small number of studies, and the different assessment of preferences (context vs. mode of delivery). However, walking seems to be preferred by people with obesity, as in the general North American population [ 100 , 101 ], probably because walking does not require any specific skill, equipment or place, and can be integrated easily into everyday life [ 102 ]. In addition, walking interventions are feasible and effective to improve the health among people with obesity [ 103 ]. Hence, regular walking can be proposed by health professionals as an option in the management of obesity and inactivity.
Considering the comparison between BMI classes, unfortunately, the paucity of data regarding how obesity classes affect PA preferences strongly limits generalization [ 66 , 67 ]. Nevertheless, some reflections emerged from this review and may be considered when PA recommendations are provided. Indeed, it appears that supervised [ 66 ] and individual [ 67 ] PA is preferred among individuals with obesity compared to their counterparts without obesity.
Finally, while there is still inconsistency about the interest in group-based PA [ 66 , 67 ], it seems that exercising with people of the same age and sex may be of importance for adults living with obesity. This suggests that feeling emotionally secure and socially accepted should not be underestimated [ 104 ]. This is consistent with the fact that self-consciousness, a psychological barrier related to self-image and embarrassment during exercise, is a major PA barrier in adults living with obesity compared to other BMI classes ( Table 3 ).
In addition, people with obesity declared that socialization, group belonging, family, professional or peer support motive them to engage, perform and maintain PA practice ( S2 Table ). This result is in accordance with several previous studies showing positive associations between social support with PA attendance and adherence [ 105 , 106 ]. Nevertheless, additional studies are necessary in people with obesity, due to inverse results (no or negative association) to better understand the complex relationship between PA and social support [ 105 , 106 ]. Indeed, social support can be perceived as a PA barrier or motive according to people or context of practice, resulting in PA avoidance and isolation or PA adherence and socialization [ 28 ]. Hence, it may be relevant to work on public health messages to successfully promote PA and favour a lower obesity stigmatization by providing a better training to health professionals [ 107 ].
The main strength of the present review is the systematic inclusion of both qualitative and quantitative literature, allowing a larger integration of PA barriers, motives, and preferences of people with obesity. However, some limitations should be considered to better interpret data. First, only English and French full texts have been included. A second limitation is the characteristics of the included studies as half of studies comes from the United States, and all from occidental countries, and men with obesity are underrepresented. In addition, socioeconomic data of people with obesity are often missing in the included studies, not reported or only reported in all the sample, including people with and without obesity. However, it should be considered that ethnic diversity within the included studies is quite present, with 5 (19.2%) studies performed in ethnic minority groups (Urban Latinas, and African American) [ 56 , 58 , 59 , 62 , 70 ]. Third, the use of a scale to quantify the importance of each barrier and motive is not the most accurate method compared to meta-analysis, but allowed in this context the integration of quantitative and qualitative studies, as well as to compare quantitative results with different kinds of questions (score vs. prevalence, Likert scale vs. yes/no answers). In addition, especially for PA motives, the relevance of this score is limited due to the high number of missing data (score 2 was attributed to more than 60% of the PA motives). Fourth, the change of exclusion criteria during the full-text selection could have introduced bias. However, this choice was made to avoid the capture of barriers, motives and preferences reflecting more the specific condition/circumstance than obesity. Finally, publication bias could also affect our findings.
Based on identified gaps in the literature, future research should focus on more representative sample of people with obesity. To date, most of the studies were conducted with women in occidental countries, and several included quantitative studies have selection bias. A strong need to determine PA preferences in people with obesity has been also identified, given only four studies are currently available. In addition, the use of a common unit (e.g., percentage rather than score) or the development of validated questionnaire in people with obesity could be useful to harmonize results and obtain better idea of the importance of each PA motives, barriers and preferences. Otherwise, self-consciousness, an important barrier in people with obesity ( Table 3 ), as well as stigmatization which was considered only in qualitative study according to our findings ( Fig 4 ) should be systematically considered in future studies. Finally, there is also a need to consider PA motives, barriers, and preferences differences according to gender, age, socioeconomic status, health status, PA level to better address diversity and specific needs. Indeed, differences between sexes have been already shown in people with overweight, with women reported more often being too fat, embarrassed, and with not good enough health as a PA barrier compared to men [ 108 ].
To conclude, weight management, lack of motivation and pain are important PA motives and barriers in people with obesity. PA motives and barriers are both weight and non-weight related in people with obesity. For this reason, weight loss cannot be the only solution to remove PA barriers, and these should be addressed in PA interventions with the support of health professionals to facilitate PA initiation and maintenance. Further research is needed to investigate the PA preferences of people with obesity. Although, one size intervention does not fit all, the improvement of knowledge on PA barriers, motives and preferences would help health professionals to better address them, and develop intervention to reach the larger number of people with obesity in order to decrease physical inactivity in this population.
Supporting information
S1 checklist. prisma 2009 checklist..
https://doi.org/10.1371/journal.pone.0253114.s001
S1 File. Search equation.
https://doi.org/10.1371/journal.pone.0253114.s002
S1 Table. Risk of bias assessed with the Mixed Methods Appraisal Tool.
https://doi.org/10.1371/journal.pone.0253114.s003
S2 Table. Data extraction and classification details for physical activity motives.
https://doi.org/10.1371/journal.pone.0253114.s004
S3 Table. Data extraction and classification details for physical activity barriers.
https://doi.org/10.1371/journal.pone.0253114.s005
Acknowledgments
We would like to thank Simon Bouisset, librarian at University of Québec en Outaouais, Gatineau (Canada) for her contribution to the identification of information sources and database search.
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Statistics Canada. Overweight and obese adults, 2018. Health Fact Sheets. 2019;Catalogue no.82-625-X.
- Reference Manager
- Simple TEXT file
People also looked at
Opinion article, the obesity pandemic—whose responsibility no blame, no shame, not more of the same.

- Braun School of Public Health, Hebrew University-Hadassah Medical School, Jerusalem, Israel
“ Imprisoned in every fat man, a thin man is wildly signaling to be let out”
Cyril Connolly, rotund British writer, (1903–1974)
Can we say this, let alone think it, in 2020?
Introduction
No one doubts the economic costs of obesity, estimated at 5–14% of health expenditure for 2020–2050 ( 1 ), but there is disagreement whether fatness is considered a disease ( 2 ) or a behavioral risk factor, similar to smoking, alcohol and substance abuse that may lead to a disease ( 3 ). Current opinion also emphasizes social determinants and equity, thereby moving away from personal responsibility concepts ( 4 ). Although recent competencies for medical training do recommend chronic disease models and personalized obesity management care plans ( 5 ), there is no mention of topics such as self-management, locus of control or responsibility . It is not clear whether this is because they are considered unimportant or because they are not politically correct—yet, they are critical components for chronic disease management such as diabetes, post-transplant care and obesity ( 6 ). The paradigm chosen has major implications for prevention and treatment strategies.
That the obesity pandemic continues unabated represents a catastrophic failure of government policy, public health, and medicine—but not only of these domains. Table 1 lists different levels of responsibility incorporating the sociotype ecological framework ( 6 ). Levels 1–4 represent context and systems; levels 5–7 society and interpersonal relationships; and levels 8–9 parental and intrapersonal health and psychological make-up. Personal editorial input from a leading obesity journal suggested that “at this point in time, … emphasis on the personal responsibility (rather than the biology), would only add to the stigmatization of obesity in general.” I disagree—and concerning the biology—see the beginning of the discussion section. Without considering aspects of responsibility, obesity management is severely compromised. There are at least two sides to personal responsibility: medicalizing obesity, which reduces it, and parental supervision, which emphasizes it, since fat children are at high risk for adult obesity ( 7 ). Finally, I suggest an integrated nine-level approach that eschews political correctness and hopefully is not more of the same.
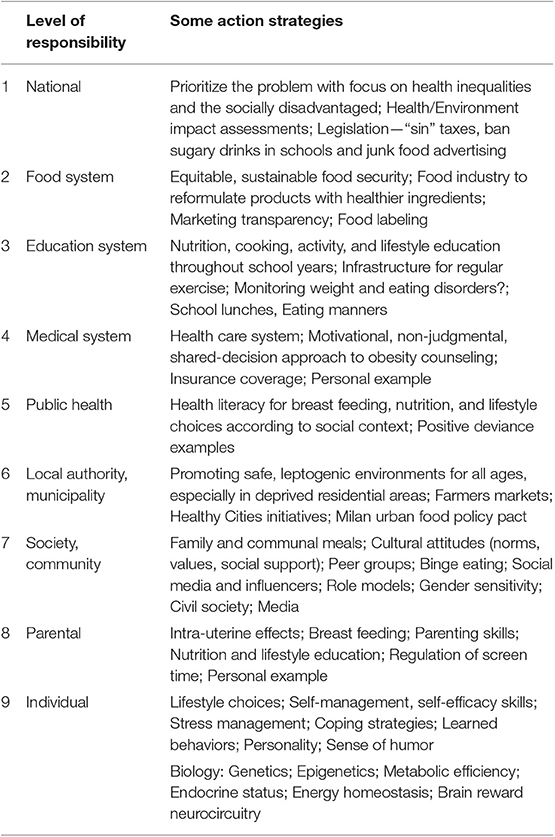
Table 1 . The nine multilevel responsibilities and examples of strategies required for tackling obesity.
Why Medicalize Obesity Management?
Insurance regulations may be part of the reason to promote a medical rather than a personal choice paradigm. This has two consequences. First, medicalizing the diagnosis helps ensure continuing insurance coverage for the severely obese. Second, it guarantees long-term reimbursement for the treating physicians. Unfortunately, such medicalization externalizes locus of control ( 8 ), decreases incentives to change lifestyle behaviors and deters self-management necessary to take active responsibility for weight regulation, noting that intelligence has little to do with self-control.
Personal preferences determine what, and how much to eat and to exercise, and how important is body shape (aesthetics) to maintaining a healthy lifestyle. No healthy person chooses to go hungry or be malnourished, but there is an element of choice in becoming obese. These issues are closely linked to socio-economic status, culture, and education. Eating should be enjoyable and potentially controllable, but there are often mitigating factors such as the dependability and affordability of the food supply, peer group and advertising pressures. The price of fast food sometimes makes it irresistible. In the U.S., food security among the disadvantaged is cyclical and highest around the time people get their SNAP (Supplemental Nutrition Assistance Program) food stamp dollars. Intake decreases or switches to higher calorie-per-dollar alternatives as the month progresses, when SNAP purchases run out ( 9 ). Such feast/famine cycles of food assistance may paradoxically contribute to unhealthy eating patterns.
Parental Responsibility for Childhood Obesity?
Parents naturally want to provide for the best growth and development of their children. Parental legal rights are generally overturned to protect a minor if harm is potentially permanent and avoidable (such as refusal of life-sustaining treatment on religious grounds) ( 10 ). Obviously, obesity is serious and can lead to lifelong morbidity. The gap between chronological and biological age widens as obesity increases. Car seats, seat belts, motorcycle helmets, vaccinations, and education are nearly all universally mandated and followed, especially when freely accessible; high-quality food is not. Upstream causes, such as inappropriate overfeeding, food to placate crying, high-calorie, low-nutrient so-called addictive foods, and lack of opportunities to exercise safely in school or in home neighborhoods, all challenge the avoidability criterion.
Holding parents answerable for their child's weight implies that they have the parenting skills (which, universally are not taught) to ensure optimal nutrition quality and quantity and lifestyle for their children. Infant nutrition begins at minus 9 months and breast-feeding protects against obesity. Healthy weight children perform 13% better at school ( 1 ). Throughout childhood, parents are usually well-intentioned and serve, by example, what they eat themselves. Parents have control until the age of about 10, for their children's nutritional choices, exercise and screen time but, by adolescence, the major influencers are peer groups and social media.
Integrated Action Strategies: Not More of the Same
In the final analysis, any change in body weight must follow the first law of thermodynamics. The fact that body fat mass is defended emphasizes, according to the fat cell hypothesis, the importance of early feeding practices, and parental responsibility. Obesity is caused by multifactorial bio-psycho-socio-behavioral influences; it may be inherited but it is not necessarily inevitable. Sometimes, the problem seems genetic because children adopt the eating habits and activity lifestyles of their parents. During evolution Homo sapiens has been programmed to store fat ( 11 ) and to be metabolically efficient. Metabolic efficiency actually increases as a result of weight loss and this is one of the main reasons why weight regain occurs after stopping a diet. Most of our biology as a species has evolved to survive periods of famines (with occasional feasts); but now it is ill equipped to resist the deleterious impact of a sustained surplus of food. Genes have not changed over the past 60 years ( pace epigenetic influences); so the toxic, obesogenic environment is the main culprit for the obesity pandemic. Genes cannot be manipulated from a realistic public health or ethical standpoint. Even if we could attack the biology, say with a drug, this also is not a viable solution. For how long should it be taken—for life? What would be the economic costs? Would the people most in need of it adhere to such treatment? What about the side-effects? Medical management (including bariatric surgery) only helps re-inforce externalizing the “locus of control” without which there can be no long-term chronic disease self-management.
Human history has shown through the sad examples of wars, pestilence and economic deprivations and disparities that obesity cannot occur if food is unavailable. Therefore, we have to attack predominantly the input side of the energy equation through interventions involving the nine levels of responsibility as shown in the Table. The action points listed are not exhaustive, and must be context and time-specific, multi-level and coordinated. They do show, however, the very many options available in tailoring prevention and intervention programs to a particular setting. Preventing obesity is primarily a public health behavior and literacy issue, empowering parental and personal choices. Only when there are health complications should the medical paradigm be appropriate. There are many factors involved, including: cultural issues (norms, values, attitudes) regarding diet (especially the Mediterranean diet) and body shape; lack of knowledge about breast feeding and infant nutrition; lack of physical and economic access to quality food, especially fruits and vegetables (“food deserts,” where neighborhoods lack nearby grocery stores); lack of kitchen facilities (or time) to cook; lack of potable water which leads to over-consumption of sweetened drinks; and lack of protected, well-lit exercise facilities.
To change the environment from obesogenic to leptogenic requires government and municipal policies targeting schools, workplaces, hospitals, and public places. Interventions should be age-appropriate and involve the social media with role models, influencers, sports people, pop stars, and advertising campaigns with the same types of compelling marketing strategies that are used to sell unhealthy, calorie-rich foods. Here, health and politically correct messages are often at odds. Slogans from body-positive activists such as “fat is beautiful” or “proud to be fat” should be replaced by “fat is unhealthy and dangerous.” Smokers do not glorify their habits, neither should the obese; but, no one should be body shamed. Should cultural and identity inappropriateness prevent a thin actor/singer from adding artificial girth to play Falstaff?–of course not. We need to keep a sense of humor and proportion. However, these pressures have become more complicated. When an advertisement or social media post of a well-toned body is portrayed, the ad agency or social media poster is vilified for promoting “unrealistic expectations.” Results from the recent ACTION study ( 12 ), reporting on over 3,000 people with obesity, showed that 82% considered that weight loss was completely their own responsibility while only 5% did not agree. In this paper, “stigma” only appeared once and only in the introduction. However, stigmatization is a worldwide phenomenon with cultural differences ( 13 ). These also apply to underdiagnosed causes of obesity such as binge eating disorders ( 14 ). Addressing and avoiding stigmatization, especially in the media and social networks, are major challenges in managing and dealing with patients with obesity.
Health professionals and society must not be judgmental in treating obesity as an individual moral failing or lack of self-discipline and will power. Instead, we have to recognize that patients with obesity are also products of a society of inequality, yet we must not let society “normalize” obesity and also, at the other extreme, “too thin” models. Mis-placed medical and political correctness that leads to hands-off management of obesity, means abrogation of the physician's responsibility: it should not stop recognizing the health problems and consequences and pressing for treatment. For example, some doctors are now even reluctant to raise the issue of obesity lest they be accused of fat shaming by not accepting their patients' proportions (despite the quote at the head of this opinion piece), and thereby receive poor approval ratings in an atmosphere where popularity is equated with good healthcare.
How much involvement should there be of public health authorities, school personnel or physicians? Should there be mandatory reporting of obesity and eating disorders as for child neglect/abuse or truancy? Much depends on how measurements are made and on what follow-up programs are in place. Lifestyle education and practice should continue throughout schooling, and lunchtimes may serve as educative experiences in manners and food habits, as practiced in Norway, Japan, and elsewhere.
Legislative interventions such as sin taxes and banning soft drink vending machines and junk food advertising to children are all relevant ( 15 ). Regressive taxation may be used to benefit the population for whom it is most oppressive. Such tax revenues may go to providing parks, playgrounds, and education programs for disadvantaged children, all of which improve health outcomes. The food industry, which is part of the problem [high-calorie, nutrient-poor, hyper-palatable products ( 16 )], must also be part of the solution by encouraging reformulations with healthier ingredients, comprehensible front-of-package food labeling and making price reductions for wholesome foods.
Suitable community-valid interventions can be based on Positive Deviant behaviors of the non-obese living in similar disadvantaged situations ( 17 ). There are also Positive Deviant countries such as Japan, Italy, and Switzerland where obesity rates are below 20%.
Obesity is one of the most difficult conditions to manage in healthcare. No-one has found the correct solution because there is no one solution. Comprehensive programs dealing with obesity require coordinated actions at all the nine levels of involvement—national, food system, educational, medical, public health, municipal, societal, parental, and individual. Parental and individual responsibility, choice and self-management clearly have a place near the center of the stage in the obesity tragedy. Otherwise, it is like going to see the play Hamlet and the Prince fails to make an appearance. Individuals are indeed responsible for their health-promoting behaviors but should be held accountable only when they have adequate resources to do so ( 18 ). In conclusion, no one is to be blamed, but everyone has a collective responsibility for working to combat the obesity pandemic—business as usual is no longer an option.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
I thank Professor Janet Fleetwood for very constructive discussions in preparing this opinion piece.
1. OECD. The Heavy Burden of Obesity: The Economics of Prevention. Paris: OECD Health Policy Studies; OECD Publishing (2019).
Google Scholar
2. Jastreboff AM, Kotz CM, Kahan S, Kelly AS, Heymsfield SB. Obesity as a disease: the obesity society 2018 position statement. Obesity (Silver Spring) . (2019) 27:7–9. doi: 10.1002/oby.22378
PubMed Abstract | CrossRef Full Text | Google Scholar
3. British Psychological Society. Psychological Perspectives on Obesity: Addressing Policy, Practice and Research Priorities. Leicester: The British Psychological Society (2019).
4. Kumanyika SK. A framework for increasing equity impact in obesity prevention. Am J Public Health . (2019) 109:1350–7. doi: 10.2105/AJPH.2019.305221
5. Kushner RF, Horn DB, Scott Butsch W, Brown JD, Duncan K, Fugate CS, et al. Development of obesity competencies for medical education: a report from the obesity medicine education collaborative. Obesity . (2019) 27:1063–7. doi: 10.1002/oby.22471
6. Berry EM, De Geest S. Tell me what you eat and I will tell you your sociotype: coping with diabesity. Rambam Maimonides Med J . (2012) 3:e0010. doi: 10.5041/RMMJ.10077
7. Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med. (2017) 377:2145–53. doi: 10.1056/NEJMoa1703860
8. Anastasiou CA, Fappa E, Karfopoulou E, Gkza A, Yannakoulia M. Weight loss maintenance in relation to locus of control: the medweight study. Behav Res Ther . (2015) 71:40–4. doi: 10.1016/j.brat.2015.05.010
9. Hamrick KS, Andrews M. SNAP participants' eating patterns over the benefit month: a time use perspective. PLoS ONE . (2016) 11:e0158422. doi: 10.1371/journal.pone.0158422
10. Varness T, Allen DB, Carrel AL, Fost N. Childhood obesity and medical neglect. Pediatrics . (2009) 123:399–406. doi: 10.1542/peds.2008-0712
11. Prentice AM, Henning BJ, Fulford AJ. Evolutionary origins of the obesity epidemic: natural selection of thrifty genes or genetic drift following predation release? Int J Obes. (2008) 32:1607–10. doi: 10.1038/ijo.2008.147
12. Kaplan LM, Golden A, Jinnett K, Kolotkin RL, Kyle TK, Look M, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity . (2018) 26:61–9. doi: 10.1002/oby.22054
13. Brewis A, SturtzSreetharan C, Wutich A. Obesity stigma as a globalizing health challenge. Global Health. (2018) 14:20. doi: 10.1186/s12992-018-0337-x
14. Brownley KA, Berkman ND, Peat CM, Lohr KN, Cullen KE, Bann CM, et al. Binge-eating disorder in adults: a systematic review and meta-analysis. Ann Intern Med. (2016) 165:409–20. doi: 10.7326/M15-2455
15. Eisenberg M, Atallah R, Grandi SM, Windle SB, Berry EM. Legislative approaches to tackling the obesity epidemic in Canada. CMAJ . (2011) 183:1496–500. doi: 10.1503/cmaj.101522
CrossRef Full Text | Google Scholar
16. Fazzino TL, Rohde K, Sullivan DK. Hyper-palatable foods: development of a quantitative definition and application to the US food system database. Obesity. (2019) 27:1761–8. doi: 10.1002/oby.22639
17. BanerjeeES, Herring SJ, Hurley K, Puskarz K, Yebernetsky K, LaNoue M. Determinants of successful weight loss in low-income African American women: a positive deviance analysis. J Prim Care Community Health . (2018) 9:2150132718792136. doi: 10.1177/2150132718792136
18. Adler NE, Stewart J. Reducing obesity: motivating action while not blaming the victim. Millbank Q . (2009) 87:49–70. doi: 10.1111/j.1468-0009.2009.00547.x
Keywords: obesity, prevention and self-management, parental and individual responsibility, political correctness, sociotype, nine-level action plans, public health and medicine
Citation: Berry EM (2020) The Obesity Pandemic—Whose Responsibility? No Blame, No Shame, Not More of the Same. Front. Nutr. 7:2. doi: 10.3389/fnut.2020.00002
Received: 01 December 2019; Accepted: 10 January 2020; Published: 31 January 2020.
Reviewed by:
Copyright © 2020 Berry. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elliot M. Berry, elliotb@ekmd.huji.ac.il
- Get Connected
- Find a Provider
- Why the OAC Exists
- OAC Mission, Vision and Goals
- Our Beliefs and Demands
- Board of Directors
- Annual Reports
- Financial Reports
- OAC Newsroom
- Media Guidelines
- Learn about Obesity
- Learn about Childhood/Adolescent Obesity
- Treatment for Obesity
- Support Tools
- Order Resources
- OAC Image Gallery
- Helpful Links
- Your Weight Matters Convention
- OAC Resource Library
- Access to Care
- Weight Bias
- International Obesity Collborative
- Public Policy Comments
- Getting Started with Advocacy
- Advocacy Resources
- OAC Action Center
- How to Make an Impact
- Join the OAC’s Community
- Share Your Story
- Take Action
- Premium Access Membership
- Awareness Campaigns
- Chairman’s Council
- Other Ways to Support
- Planned Giving
- Make a Donation
- How Your Support Helps
- Monthly Giving Program
- Partners in Action

Self Esteem, Insecurity and Obesity
by Sean G. Connolly, PhD
The comment in the support group captured a common sentiment, “After failure, failure and failure of diets and weight-loss efforts, there is always that little voice in the back of your mind that says, ‘Maybe you are going to be one of the failures at this.’”
The voice of self-doubt and insecurity can be loud, persistent, discouraging and even destructive to our efforts. We can all resonate with poisonous self-talk that invades different areas of our lives. The importance of self esteem in achieving life goals, including weight-loss, is immeasurable. It is a factor in all our human endeavors. Understanding how our self esteem has been shaped and influenced in our lives can help us gain the essential awareness for change.
It Begins at Birth
The feedback and comments start immediately following birth, such as “Oh, what a beautiful baby!” “What a big baby!” Of course, the infant is oblivious to it all. But, before long in life, the child becomes very aware of the value of the feedback from the world around them. Praise and criticism are absorbed deep inside our psyche, not forgotten easily, especially if the comments are negative.
Self esteem is born within us, and we become aware of how important it is to begin to meet the expectations of others. We begin to seek out from others clues to our worth, acceptability and our own self. Sometimes we can hide the real self inside and put a lot of energy into pleasing others. Our self esteem is developed from feedback from the world around us and our interpretation of it. People make comments about others on personality, appearance, weight, looks or talent, be them complimentary or uncomplimentary.
Psychological Cravings
Human beings have two psychological cravings. The first is for love, affection, warmth and caring. Kids want desperately to be loved. That is what gives a child, and an adult, a sense of security. Kids feel there is one sure place where they are loved, in their “home.” Most parents make an effort to feed this hunger daily. That craving is always with us, into adulthood, although not as “needy.”
The second craving humans have is for approval, recognition or affirmation. Kids are not shy about it, “Mom, look what I got in school today;” “Dad, are you coming to my soccer game?” This is what molds and shapes our self-esteem. This hunger for approval is carried from the family into society. As we grow older, the cravings never disappear, but are nourished in different ways. And sometimes, as adults we have to nourish these cravings ourselves. Compliments are never too plentiful or trustworthy, in society, especially the work environment.
As the child grows up and goes to daycare, begins school, visits relatives and friends, develops relationships, attends church, joins clubs, participates in sports and later in life finds a job and works on a career, the feedback and comments come and are often uninvited. It is this feedback that shapes and influences our self-esteem.
Awareness of Feedback
We become more aware of the feedback, such as the looks, the reactions, the comments, the avoidance, the engagement in conversation, the occasion of being ignored, not being picked for the squad, winning and losing competitions, doing well or poorly in school, evaluations at work, assessment of career goals and interactions with neighbors and friends. We all hope for positive feedback.
However, we all know from experience there will be that negative feedback: that one comment a teacher, parent or relative made and can still echo in our mind, such as a friend’s unexplainable rejection, a coach who put a label on us, a peer who was blatant in his or her dislike, comments on our weight or size, etc.
The more positive feedback we receive and internalize, the more secure in ourselves we feel. The more negative the feedback, the more insecure we can feel. We can begin to build a wall around ourselves, to protect ourselves from excessive criticism, put-downs, labeling or any adult scripting failure for our lives.
A useful reflective activity is to journey back into our developmental history of our self esteem and ask ourselves what feedback did people, especially significant others, give us about our personality, intelligence, friendliness, attractiveness, looks, potential in life, talent, lack of talent, behavior and our body.
Dealing with Comments
We cannot control the comments of others, often uninvited, but we can control how we deal with them. We are all aware of society’s negative reactions to obesity, and when it is personalized, it can really hurt. Many patients have reported throughout the years the teasing, criticisms, looks, accusations, rejections, exclusions and words. And no matter how well-defended we might be, it can be painful.
The pain can be hidden, subdued, pushed aside, but always there undermining our sense of security. We can even have, consciously or unconsciously, agreed with the negative feedback, and accepted it as part of who we are.
Suggestions to Help
- Give yourself the right to feel good about yourself and feel more secure: say out loud, when no one is around, “I have the right to feel good about myself.” It is important to hear yourself say these words out loud for it to be effective. You may have to say it numerous times to match the feelings to the words. The more you say the words, the sooner they will be programmed into your mind.
- You may have to give yourself “permission” to feel good about yourself, if you have been brainwashed growing up that you had no right to do that: “I choose to give myself permission to feel good about myself.” Repeat it until you believe it.
- Select some affirmation statements to program in positive thinking. These are statements that empower you to change negative thinking about yourself in areas that are important to us. For example, “I affirm my intelligence.” “I affirm my ability to be successful at what I chose to do.” For a selection of affirmation statements related to self-esteem and weight-loss surgery success, see our Web site www.thealgosgroup.com .
- Take a few affirmation statements that fit particularly for you and put them on your mirror and repeat them out loud every morning and during the day until they become part of you.
- Counseling and life coaching can help you along in promoting self-perceptions that have an impact on our self-esteem.
With a secure and confident “self” we can be more successful in achieving any behavioral goal. As children, we could not “fight back.” As adults, we can affirm ourselves, program positive thoughts in our mind, silence the negative “voices” in our head, choose not to be affected by the comments, filter the feedback and promote self-confidence.
You can repair a damaged and insecure self esteem. The task is to re-program negative thoughts in your mind and replace them with positive thoughts, with time, as it is not an immediate change. Let me reassure you that you can develop a positive self esteem throughout time and utilize it effectively to achieve weight-loss goals.
About the Author: Seán G. Connolly, PhD, is a licensed psychologist, specializing in health and rehabilitation psychology, and consults with several bariatric surgeons in San Antonio. His main focus in the area of obesity is coaching weight-loss surgery patients to achieve their weight-loss goals.
Related Resources
Weight And Health
Help the OAC to raise awareness, advocate for improved access, provide evidence-based education, fight to eliminate weight bias and discrimination and elevate the conversation of weight and its impact on health.

Mental Health Corner: The Impact of Family Weight Bias on Health
by Robyn Pashby, PhD Winter 2024 “No one is ever going to date you if you don’t…

Dealing with Spousal Support and Sabotage
by Leslie M. Golden, MD, MPH, ABOM Diplomate Winter 2024 The journey to overcoming obesity is a…

OAC Health Talks: Using Music for Self Care
Did you know that stress can have an impact on weight? Many people increase their food intake…
Registration for Your Weight Matters Virtual is NOW OPEN! Experience the latest science-based education on weight and health. May 18-19
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How to Prevent Obesity
Daniel Llao Calvet / Getty Images
- Early Prevention
- Stress Reduction
- Improving Sleep
- Next in Obesity Guide Obesity Facts and Statistics: What You Need to Know
Preventing obesity involves making healthy lifestyle choices every day. To prevent obesity, you need to stay active, follow a healthy diet, and get adequate sleep. Obesity prevention also involves saying no to certain preferences, like soft drinks, or driving short distances when you could walk instead.
Obesity is generally defined as a chronic disease characterized by excessive body fat. More than 42% of adults and 19% of children and adolescents in the U.S. have obesity, and those numbers are rising. Obesity is often caused by a combination of risk factors, including genetics , poor diet, sedentary behaviors , medical conditions, and lack of access to healthy foods.
While obesity prevention should start in childhood, it is never too late to start making healthier choices. This article discusses how to prevent obesity starting in childhood and later in life. It includes diet, exercise, and lifestyle strategies, along with how these strategies can reduce your obesity risk.
Preventing Obesity in Childhood
Obesity often begins in childhood . Research shows that if a person has obesity at age 5, they are more likely to have obesity as an adult. Conversely, if a child does not have obesity at age 5, their lifetime risk of obesity is significantly lower.
Obesity results from a combination of genetic, environmental, and lifestyle factors. Although families cannot change their genes, they can model healthy lifestyle patterns for children to start preventing obesity from a young age.
To prevent obesity in childhood, families can:
- Promote healthy eating: Families can try swapping out processed snacks like potato chips for healthier snacks like baked cinnamon apple crisps. Saying no to soft drinks is another great starting point.
- Get active together: Parents and children can both benefit from engaging in physical activity together. Make a tradition of physical activity, like playing frisbee or riding bikes together after school. Children ages 6 to 17 should get 60 minutes of physical activity per day.
- Ensure consistent sleep: Children who don't get enough sleep have a greater risk of developing obesity, type 2 diabetes, and other health conditions. The amount of uninterrupted sleep your child needs depends on their age group, but the key is a consistent bedtime—even on weekends.
- Minimize screen time: Too much screen time in childhood increases the risk of obesity, poor sleep, unhealthy eating, and more. Whenever possible, it's important to replace screen time with family time or physical activity. At a minimum, screens should be turned off at least one hour before bed.
If you are concerned about your child's weight, reach out to a healthcare provider. Your provider may be able to help you identify lifestyle factors that are contributing to your child's weight gain. They can also assess any health risks your child may have based on their weight or your family history.
Diet to Prevent Obesity
Obesity can be prevented by following basic principles of healthy eating . Here are simple changes you can make to your eating habits that will help you lose weight and prevent obesity.
Eat More Fruits and Vegetables
Eating a diet rich in fruits and vegetables decreases the risk of obesity. Fruits and vegetables contain a variety of beneficial nutrients and are associated with a lower risk for diabetes and insulin resistance . They are also high in fiber, which keeps you feeling full with fewer calories and ensures your digestive system stays regulated.
Focus on filling your plate with whole vegetables and fruits at every meal. Aim for lots of natural colors—carrots, sweet potatoes, broccoli, bananas, eggplant—the more color, the merrier.
Go easy (or eliminate) protein sources that are heavy in saturated fats, such as red meat and dairy. If you choose to cut out meat entirely, consult with a healthcare provider to ensure you are not at risk for nutritional deficiencies.
Does a Plant-Based Diet Prevent Obesity?
Eating more plant foods and less animal foods lowers insulin resistance and contributes to a healthier body mass index (BMI, an imperfect but commonly used metric). Following a plant-based diet will not increase the risk of obesity. However, more research is needed to evaluate the benefits of plant-based diets for reducing obesity long-term.
Avoid Processed Foods
Highly processed foods , like white bread and many boxed snack foods, are a common source of empty calories, which tend to add up quickly. A 2019 study found that people who were offered a highly processed diet consumed more calories and gained weight, while those offered a minimally processed diet ate less and lost weight.
There are many healthy alternatives to processed snacks that can be just as satisfying, such as:
- Unsalted almonds, cashews, walnuts, and pistachios
- Roasted chickpeas
- Crispy lettuce wraps
- Frozen yogurt-covered blueberries
- Baked banana chips
While it may take a little more time and creativity, planning and preparing healthy snacks can be an enjoyable and rewarding experience.
Limit Sugar and Artificial Sweeteners
It is important to keep your intake of added sugars low. According to current dietary guidelines, most adult women should have no more than 24 grams of sugar per day, while most adult men should have no more than 36.
Major sources of added sugar to avoid include:
- Sugary beverages, including sodas and energy or sports drinks
- Grain desserts like pies, cookies, and cakes
- Fruit drinks (which are seldom 100% fruit juice)
- Dairy desserts like ice cream
Artificial sweeteners have been linked to obesity and diabetes , too. While some natural sweeteners like agave do not raise glucose as fast as table sugar, they still raise blood sugar and should also be used in moderation.
Reduce Saturated Fats
Numerous studies show that eating foods high in saturated fat contributes to obesity. Foods that are high in saturated fats include:
- Whole and reduced-fat milk
- Butter and dairy desserts
- Meat products, such as sausage, bacon, beef, hamburgers
- Cookies and other grain-based desserts
- Many fast-food dishes
Focus instead on sources of healthy fats (monounsaturated and polyunsaturated fats) like:
- Olive oil and canola oils
- Pumpkin and sesame seeds
Although these fats are healthier for you, they should still be limited to about 20% to 35% of daily calories. People with elevated cholesterol or vascular disease may need an even lower level.
Pay Attention to Beverages
A single, 12-ounce can of Coca-Cola contains 39 grams of sugar. That means one can of Coke alone exceeds the recommended daily intake of sugar.
Sugar and calories in soft drinks, energy drinks, sports drinks, and juices quickly add up and may contribute to weight gain. But drinks marketed as "sugar-free" and "low-calorie" aren't much better. Artificially sweetened drinks also carry a risk of numerous health problems, including obesity.
Rather than focusing on which artificial sweetener is best, it's better to avoid sweeteners in general. Make water or unsweetened drinks and your go-to instead.
Cook at Home
People who prepare meals at home are less likely to gain weight or develop type 2 diabetes, studies show.
One such study found that people who ate home-cooked meals more than five times per week were 28% less likely to have an overweight BMI than people who ate home-cooked meals less than three times per week. Eating more home-cooked meals was also associated with having less body fat.
BMI is a dated, flawed measure. It does not take into account factors such as body composition , ethnicity, sex, race, and age. Even though it is a biased measure, BMI is still widely used in the medical community because it’s an inexpensive and quick way to analyze a person’s potential health status and outcomes.
Exercising to Prevent Obesity
Most national and international guidelines recommend that the average adult get at least 150 minutes of moderate-intensity physical activity per week. That means at least 30 minutes per day, five days per week.
Researchers have also found that people who walk at a brisk or fast pace are more likely to have a lower weight, lower BMI, and lower waist circumference compared to individuals doing other activities.
In addition, experts recommend keeping active throughout the day, whether by using a standing desk, taking frequent stretch breaks, or finding ways to work in walking meetings throughout your day.
Reducing Stress to Prevent Obesity
Chronic stress raises levels of the stress hormone cortisol and leads to weight gain. It can also result in poor dietary choices, as cortisol and other stress hormones can increase “carb cravings” and make it difficult to exercise good judgment and willpower.
Look into the many healthy ways to beat stress, and find what works best for you. This might include:
- Going for a daily walk
- Engaging in regular yoga or tai chi
- Listening to music you love
- Getting together with friends
Studies show having a pet can lower blood pressure. Additionally, pets, especially dogs, can increase your level of physical activity and help you stave off weight gain.
Improving Sleep to Prevent Obesity
The role of sleep in overall well-being cannot be overstated. This extends to the goal of preventing obesity, too. The Centers for Disease Control and Prevention recommends seven or more hours of sleep for adults 18 and over and even more sleep for younger people.
Studies have linked later bedtimes to weight gain over time. One of these studies included 137,000 people from 26 countries. It showed that, compared to people who go to bed before 10 p.m., people who go to bed after 10 have a 20% greater risk of general and abdominal obesity. Meanwhile, the risk is up to 38% higher in people who go to bed after 2 a.m.
If you are having trouble falling asleep earlier, it may help to:
- Set a consistent bedtime.
- Make sure your bedroom is quiet, dark, and a comfortable temperature.
- Keep phones, computers, and televisions out of the bedroom.
- Cut off screen time within one hour of going to bed.
- Avoid large meals and caffeine before bedtime.
- Increase physical exercise to help your body relax better at night.
There are several possible contributors to obesity. The fact that the two biggest ones—diet and activity—are ones you can influence is good news. A healthy lifestyle that puts exercise and eating at its center can also bring myriad other health benefits. Getting good sleep and finding ways to reduce stress is important, too.
If you have made significant lifestyle changes and are still gaining weight or unable to lose weight, see a healthcare professional to rule out other possible causes of weight gain.
National Institute of Diabetes and Digestive and Kidney Diseases. Overweight and obesity statistics .
Eunice Kennedy Shriver National Institute of Child Health and Human Development. Obesity begins early .
Centers for Disease Control and Prevention. Preventing childhood obesity: 5 things families can do .
Centers for Disease Control and Prevention. Defining adult overweight & obesity .
World Health Organization. Obesity and overweight .
Martins F, Conde S. Impact of diet composition on insulin resistance . Nutrients . 2022 Sep;14(18):3716. doi:10.3390/nu14183716
Hall KD, Ayuketah A, Brychta R, et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake . Cell Metab . 2019;30(1):67–77.e3. doi:10.1016/j.cmet.2019.05.008
Harvard T.H. Chan. Added sugar .
Daoust L. Artificial sweeteners and type 2 diabetes . Nat Food . 2023;4(1):739. doi:10.1038/s43016-023-00846-2
University of Illinois Urbana-Champaign. Is agave nectar a healthier alternative to sugar? .
Harvard T.H. Chan. Types of fat .
PennState Extension. Fat facts, the right amount for a healthy diet .
Debras C, Chazelas E, Sellem L, et al. Artificial sweeteners and risk of cardiovascular diseases: Results from the prospective NutriNet-Santé cohort . BMJ . 2022 Sep;378(1):e071204. doi:10.1136/bmj-2022-071204
Mills S, Brown H, Wrieden W, White M, Adams J. Frequency of eating home cooked meals and potential benefits for diet and health: Cross-sectional analysis of a population-based cohort study . Int J Behav Nutr Phys Act . 2017 Aug;14(1):109. doi:10.1186/s12966-017-0567-y
Department of Health and Human Services. Physical activity guidelines for Americans . 2nd ed. Department of Health and Human Services.
Lordan G, Pakrashi D. Do all activities “weigh” equally? How different physical activities differ as predictors of weight . Risk Anal . 2015;35(11):2069-2086. doi:10.1111/risa.12417
Chao A, Jastreboff A, White M, Grilo C, Sinha R. Stress, cortisol, and other appetite-related hormones: Prospective prediction of 6-month changes in food cravings and weight . Obesity (Silver Spring) . 2017 Apr;25(4):713-720. doi:10.1002/oby.21790
Surma S, Oparil S, Narkiewicz K. Pet ownership and the risk of arterial hypertension and cardiovascular disease . Curr Hypertens Rep . 2022;24(8):295–302. doi:10.1007/s11906-022-01191-8
Miyake K, Kito K, Kotemori A, et al. Association between pet ownership and obesity: A systematic review and meta-analysis . Int J Environ Res Pub Health . 2020 May;17(10):3498. doi:10.3390/ijerph17103498
Centers for Disease Control and Prevention. How much sleep do I need?
Tse L, Wang C, Rangarajan S, et al. Timing and length of nocturnal sleep and daytime napping and associations with obesity types in high-, middle-, and low-income countries . JAMA Netw Open . 2021;4(6):e2113775. doi:10.1001/jamanetworkopen.2021.13775
Centers for Disease Control and Prevention. Tips for better sleep .
Asarnow LD, McGlinchey E, Harvey AG. Evidence for a possible link between bedtime and change in body mass index . Sleep . 2015;38(10):1523-1527. doi:10.5665/sleep.5038
Flint E, Cummins S, Sacker A. Associations between active commuting, body fat, and body mass index: population based, cross sectional study in the United Kingdom [correction published in BMJ. 2015;350:h2056]. BMJ . 2014;349:g4887. doi:10.1136/bmj.g4887
World Health Organization. Promoting fruit and vegetable consumption around the world .
By Yasmine S. Ali, MD, MSCI Yasmine Ali, MD, is board-certified in cardiology. She is an assistant clinical professor of medicine at Vanderbilt University School of Medicine and an award-winning physician writer.
Home — Essay Samples — Nursing & Health — Obesity — Conclusion For Obesity
Conclusion for Obesity
- Categories: Obesity
About this sample

Words: 644 |
Published: Mar 19, 2024
Words: 644 | Page: 1 | 4 min read
Table of contents
Introduction:, the health consequences:, the societal implications:, root causes:, prevention and treatment:, the role of policy:, the power of community:, conclusion:.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof Ernest (PhD)
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 746 words
1 pages / 619 words
3 pages / 1587 words
2 pages / 866 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Obesity
Obesity is a medical condition characterized by excessive body fat accumulation that poses a risk to health. It is a global problem that affects both developed and developing countries. The prevalence of obesity has increased [...]
In recent years, the issue of obesity has become a global epidemic. Obesity is a condition where a person has an excessive amount of fat, which can lead to numerous health problems. According to the World Health Organization [...]
According to recent studies, obesity has become a global epidemic, affecting millions of people worldwide. Obesity is not only a personal health issue but also a societal concern. It is linked to various health problems and has [...]
According to the World Health Organization, in 2016, more than 1.9 billion adults were overweight, of which around 650 million were obese. In the United States alone, more than 42% of the population is considered obese. This [...]
The overweight or obese among the U.S. citizens is inclining at a shocking rate. Currently, it stands at 74.1% which is almost ¾ of our country’s population. It is a frightening truth that needs to be acknowledged by the entire [...]
Obesity has become a major public health crisis in the United States, with over 42% of the population considered to be clinically obese. This issue has far-reaching consequences for individuals, families, and the healthcare [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Mol Cell Biol
- v.13(7); 2021 Jul

Obesity: causes, consequences, treatments, and challenges
Obesity has become a global epidemic and is one of today’s most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer ( Bluher, 2019 ).
Obesity is mainly caused by imbalanced energy intake and expenditure due to a sedentary lifestyle coupled with overnutrition. Excess nutrients are stored in adipose tissue (AT) in the form of triglycerides, which will be utilized as nutrients by other tissues through lipolysis under nutrient deficit conditions. There are two major types of AT, white AT (WAT) and brown AT, the latter is a specialized form of fat depot that participates in non-shivering thermogenesis through lipid oxidation-mediated heat generation. While WAT has been historically considered merely an energy reservoir, this fat depot is now well known to function as an endocrine organ that produces and secretes various hormones, cytokines, and metabolites (termed as adipokines) to control systemic energy balance. Studies over the past decade also show that WAT, especially subcutaneous WAT, could undergo ‘beiging’ remodeling in response to environmental or hormonal perturbation. In the first paper of this special issue, Cheong and Xu (2021) systematically review the recent progress on the factors, pathways, and mechanisms that regulate the intercellular and inter-organ crosstalks in the beiging of WAT. A critical but still not fully addressed issue in the adipose research field is the origin of the beige cells. Although beige adipocytes are known to have distinct cellular origins from brown and while adipocytes, it remains unclear on whether the cells are from pre-existing mature white adipocytes through a transdifferentiation process or from de novo differentiation of precursor cells. AT is a heterogeneous tissue composed of not only adipocytes but also nonadipocyte cell populations, including fibroblasts, as well as endothelial, blood, stromal, and adipocyte precursor cells ( Ruan, 2020 ). The authors examined evidence to show that heterogeneity contributes to different browning capacities among fat depots and even within the same depot. The local microenvironment in WAT, which is dynamically and coordinately controlled by inputs from the heterogeneous cell types, plays a critical role in the beige adipogenesis process. The authors also examined key regulators of the AT microenvironment, including vascularization, the sympathetic nerve system, immune cells, peptide hormones, exosomes, and gut microbiota-derived metabolites. Given that increasing beige fat function enhances energy expenditure and consequently reduces body weight gain, identification and characterization of novel regulators and understanding their mechanisms of action in the beiging process has a therapeutic potential to combat obesity and its associated diseases. However, as noticed by the authors, most of the current pre-clinical research on ‘beiging’ are done in rodent models, which may not represent the exact phenomenon in humans ( Cheong and Xu, 2021 ). Thus, further investigations will be needed to translate the findings from bench to clinic.
While both social–environmental factors and genetic preposition have been recognized to play important roles in obesity epidemic, Gao et al. (2021) present evidence showing that epigenetic changes may be a key factor to explain interindividual differences in obesity. The authors examined data on the function of DNA methylation in regulating the expression of key genes involved in metabolism. They also summarize the roles of histone modifications as well as various RNAs such as microRNAs, long noncoding RNAs, and circular RNAs in regulating metabolic gene expression in metabolic organs in response to environmental cues. Lastly, the authors discuss the effect of lifestyle modification and therapeutic agents on epigenetic regulation of energy homeostasis. Understanding the mechanisms by which lifestyles such as diet and exercise modulate the expression and function of epigenetic factors in metabolism should be essential for developing novel strategies for the prevention and treatment of obesity and its associated metabolic diseases.
A major consequence of obesity is type 2 diabetes, a chronic disease that occurs when body cannot use and produce insulin effectively. Diabetes profoundly and adversely affects the vasculature, leading to various cardiovascular-related diseases such as atherosclerosis, arteriosclerotic, and microvascular diseases, which have been recognized as the most common causes of death in people with diabetes ( Cho et al., 2018 ). Love et al. (2021) systematically review the roles and regulation of endothelial insulin resistance in diabetes complications, focusing mainly on vascular dysfunction. The authors review the vasoprotective functions and the mechanisms of action of endothelial insulin and insulin-like growth factor 1 signaling pathways. They also examined the contribution and impart of endothelial insulin resistance to diabetes complications from both biochemical and physiological perspectives and evaluated the beneficial roles of many of the medications currently used for T2D treatment in vascular management, including metformin, thiazolidinediones, glucagon-like receptor agonists, dipeptidyl peptidase-4 inhibitors, sodium-glucose cotransporter inhibitors, as well as exercise. The authors present evidence to suggest that sex differences and racial/ethnic disparities contribute significantly to vascular dysfunction in the setting of diabetes. Lastly, the authors raise a number of very important questions with regard to the role and connection of endothelial insulin resistance to metabolic dysfunction in other major metabolic organs/tissues and suggest several insightful directions in this area for future investigation.
Following on from the theme of obesity-induced metabolic dysfunction, Xia et al. (2021) review the latest progresses on the role of membrane-type I matrix metalloproteinase (MT1-MMP), a zinc-dependent endopeptidase that proteolytically cleaves extracellular matrix components and non-matrix proteins, in lipid metabolism. The authors examined data on the transcriptional and post-translational modification regulation of MT1-MMP gene expression and function. They also present evidence showing that the functions of MT1-MMP in lipid metabolism are cell specific as it may either promote or suppress inflammation and atherosclerosis depending on its presence in distinct cells. MT1-MMP appears to exert a complex role in obesity for that the molecule delays the progression of early obesity but exacerbates obesity at the advanced stage. Because inhibition of MT1-MMP can potentially lower the circulating low-density lipoprotein cholesterol levels and reduce the risk of cancer metastasis and atherosclerosis, the protein has been viewed as a very promising therapeutic target. However, challenges remain in developing MT1-MMP-based therapies due to the tissue-specific roles of MT1-MMP and the lack of specific inhibitors for this molecule. Further investigations are needed to address these questions and to develop MT1-MMP-based therapeutic interventions.
Lastly, Huang et al. (2021) present new findings on a critical role of puromycin-sensitive aminopeptidase (PSA), an integral non-transmembrane enzyme that catalyzes the cleavage of amino acids near the N-terminus of polypeptides, in NAFLD. NAFLD, ranging from simple nonalcoholic fatty liver to the more aggressive subtype nonalcoholic steatohepatitis, has now become the leading chronic liver disease worldwide ( Loomba et al., 2021 ). At present, no effective drugs are available for NAFLD management in the clinic mainly due to the lack of a complete understanding of the mechanisms underlying the disease progress, reinforcing the urgent need to identify and validate novel targets and to elucidate their mechanisms of action in NAFLD development and pathogenesis. Huang et al. (2021) found that PSA expression levels were greatly reduced in the livers of obese mouse models and that the decreased PSA expression correlated with the progression of NAFLD in humans. They also found that PSA levels were negatively correlated with triglyceride accumulation in cultured hepatocytes and in the liver of ob/ob mice. Moreover, PSA suppresses steatosis by promoting lipogenesis and attenuating fatty acid β-oxidation in hepatocytes and protects oxidative stress and lipid overload in the liver by activating the nuclear factor erythroid 2-related factor 2, the master regulator of antioxidant response. These studies identify PSA as a pivotal regulator of hepatic lipid metabolism and suggest that PSA may be a potential biomarker and therapeutic target for treating NAFLD.
In summary, papers in this issue review our current knowledge on the causes, consequences, and interventions of obesity and its associated diseases such as type 2 diabetes, NAFLD, and cardiovascular disease ( Cheong and Xu, 2021 ; Gao et al., 2021 ; Love et al., 2021 ). Potential targets for the treatment of dyslipidemia and NAFLD are also discussed, as exemplified by MT1-MMP and PSA ( Huang et al., 2021 ; Xia et al., 2021 ). It is noted that despite enormous effect, few pharmacological interventions are currently available in the clinic to effectively treat obesity. In addition, while enhancing energy expenditure by browning/beiging of WAT has been demonstrated as a promising alternative approach to alleviate obesity in rodent models, it remains to be determined on whether such WAT reprogramming is effective in combating obesity in humans ( Cheong and Xu, 2021 ). Better understanding the mechanisms by which obesity induces various medical consequences and identification and characterization of novel anti-obesity secreted factors/soluble molecules would be helpful for developing effective therapeutic treatments for obesity and its associated medical complications.
- Bluher M. (2019). Obesity: global epidemiology and pathogenesis . Nat. Rev. Endocrinol . 15 , 288–298. [ PubMed ] [ Google Scholar ]
- Cheong L.Y., Xu A. (2021). Intercellular and inter-organ crosstalk in browning of white adipose tissue: molecular mechanism and therapeutic complications . J. Mol. Cell Biol . 13 , 466–479. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cho N.H., Shaw J.E., Karuranga S., et al. (2018). IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045 . Diabetes Res. Clin. Pract . 138 , 271–281. [ PubMed ] [ Google Scholar ]
- Gao W., Liu J.-L., Lu X., et al. (2021). Epigenetic regulation of energy metabolism in obesity . J. Mol. Cell Biol . 13 , 480–499. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Huang B., Xiong X., Zhang L., et al. (2021). PSA controls hepatic lipid metabolism by regulating the NRF2 signaling pathway . J. Mol. Cell Biol . 13 , 527–539. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Loomba R., Friedman S.L., Shulman G.I. (2021). Mechanisms and disease consequences of nonalcoholic fatty liver disease . Cell 184 , 2537–2564. [ PubMed ] [ Google Scholar ]
- Love K.M., Barrett E.J., Malin S.K., et al. (2021). Diabetes pathogenesis and management: the endothelium comes of age . J. Mol. Cell Biol . 13 , 500–512. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ruan H.-B. (2020). Developmental and functional heterogeneity of thermogenic adipose tissue . J. Mol. Cell Biol . 12 , 775–784. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Xia X.-D., Alabi A., Wang M., et al. (2021). Membrane-type I matrix metalloproteinase (MT1-MMP), lipid metabolism, and therapeutic implications . J. Mol. Cell Biol . 13 , 513–526. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Essay on Self Discipline for Students and Children
500+ words essay on self discipline.
Self-discipline means self-control, which gives you inner strength and a way to control yourself, actions, and reactions. It is one of the most important and useful skills to achieve success and everyone should possess this quality. Self-discipline comes naturally to some people. And some people can achieve it with some effort. The effort made is worth it as it changes life for the better. It just means exercising self- control. A person who stays in control has the ability to take charge of his/her actions and reactions.

Tips to Achieve Self-discipline
- Set your goals: – The first step towards leading a disciplined life is to set goals. Goals give you a clear idea about what needs to be achieved. One must always set a timeline for your goals. This serves as a driving force and motivates you to work hard. It is a good idea to set both short term and long term goals and create a well thought out plan to achieve them.
- Do meditation:- Meditation is one of the best ways to channel our energy in the right direction. It helps maintain focus, acquaints us with our inner self and furthers better self- control. It is the stepping stone for a disciplined life. Meditating for half an hour every day can help in inculcating self-discipline.
- Set a Routine:- Those who set a routine and follow it daily lead a more disciplined life. It is suggested to list all the tasks that you require accomplishing in a given day. Write them in the order of their priority, set a timeline for each and act accordingly. This is a good way to lead an organized and disciplined life.
- Stay away from distractions :- In this technology-driven world, there are numerous things that can distract us and take charge of our lives. Our mobile phones, television, and chatting apps are some of the new age things that are a big hindrance in practicing self-discipline. No matter how determined we are to study, work or sleep on time, we tend to get distracted at the beep of our phone. Social media platforms, chatting apps and web series are extremely addictive and hamper work. In order to practice self-discipline, it is important to stay away from these distractions. Put your phone on silent or keep it at a distance when you sit to study or work. Similarly, just put your phone away at bedtime and instead pick a book to read.
- Reward yourself :- Reward yourself for every goal you achieve. This will motivate you to work harder to achieve more. This is a good way to trick your brain to inculcate self-discipline.
- Take proper sleep :- You can inculcate self-discipline only when you are well-rested. So, it is essential to sleep for eight hours each night. Maintaining a good sleep cycle is also essential. This means that you should try sleeping and waking up at the same time each day. A power nap during the afternoon can help further.
- Stay Positive : – Many people want to inculcate self-discipline but are unable to because they somehow believe that it is difficult to achieve. They feel that it is too much to ask for and that they shall not be able to practice it. This is the wrong approach. You can achieve anything in life if you stay positive and believe in yourself. So, you should stay positive. It is a pre-requisite for inculcating self-discipline.
Get the huge list of more than 500 Essay Topics and Ideas
Self Discipline Benefits and Importance
Self-discipline helps you to overcome the bad habits by meditating regularly. It gives you the ability not to give up after failure and setbacks, develop self-control, provide the ability to resist distractions, helps you to motivate yourself until you accomplish your goals.
Achieving self-discipline may be difficult but in order to lead a healthy personal and professional life, it is very important. A self-disciplined person makes optimum use of the time. Hence, he can achieve more and do more work as compared to a person who is not self-disciplined. We should, therefore, make some efforts to achieve it.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App


Essay on Self Discipline
Students are often asked to write an essay on Self Discipline in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Self Discipline
Introduction.
Self-discipline is the ability to control one’s feelings and overcome weaknesses. It’s about making choices that lead to healthy, productive behaviors.
Importance of Self-Discipline
Self-discipline is crucial for success. It helps us focus on our goals, resist temptations, and persist in the face of adversity.
Building Self-Discipline
Building self-discipline requires practice. Start small, create routines, and gradually take on bigger challenges.
Benefits of Self-Discipline
Self-discipline leads to improved focus, better health, and achievement of goals. It also fosters resilience and self-confidence.
In conclusion, self-discipline is a vital skill that everyone should cultivate for a successful and fulfilling life.
Also check:
- 10 Lines on Self Discipline
- Paragraph on Self Discipline
- Speech on Self Discipline
250 Words Essay on Self Discipline
Self-discipline, an essential attribute for personal and professional success, refers to the ability to control one’s emotions, behavior, and desires, aligning them with set goals. It is a skill that enables individuals to overcome impulses, procrastinate less, and stay focused on their objectives.
The Importance of Self-Discipline
Self-discipline is a cornerstone of personal development and self-improvement. It fosters resilience, enabling individuals to endure hardships and persevere in the face of challenges. Furthermore, it promotes time management, allowing for the prioritization of tasks according to their importance and urgency. This leads to increased productivity and efficiency.
Self-Discipline and Success
The correlation between self-discipline and success is well-established. Those with high self-discipline tend to perform better academically and professionally. They are also more likely to maintain a healthy lifestyle, manage stress effectively, and demonstrate higher levels of happiness.
Developing Self-Discipline
Developing self-discipline requires consistent effort and practice. It starts with setting clear, achievable goals, followed by creating a plan to reach them. Regular self-reflection is crucial to assess progress and make necessary adjustments. Moreover, cultivating a positive mindset can significantly enhance one’s self-discipline.
In conclusion, self-discipline is a vital skill that significantly impacts personal and professional life. It is a key determinant of success and can be cultivated through consistent effort, goal setting, and self-reflection. Thus, it is imperative for college students to understand its importance and work towards enhancing their self-discipline.
500 Words Essay on Self Discipline
Introduction to self-discipline.
Self-discipline, an essential characteristic for personal and professional success, is the ability to control one’s feelings and overcome weaknesses. It involves acting according to what you think instead of how you feel in the moment. It’s a sign of inner strength and control of oneself and one’s actions.
Self-discipline is of paramount importance for achieving goals. It is the backbone of successful people who manage to excel in their fields. It is the driving force that compels individuals to resist negative impulses and distractions. Self-discipline is the key to consistency and continuity in any endeavor, be it academic, personal, or professional. It helps in maintaining focus, thus enabling individuals to make constructive decisions that lead to positive outcomes.
Self-Discipline and Time Management
Time management and self-discipline are intertwined. Effective time management necessitates self-discipline, and conversely, self-discipline aids in the efficient use of time. When one practices self-discipline, they can better allocate their time, prioritizing tasks based on their importance and deadlines. This results in improved productivity and efficiency.
Self-Discipline and Emotional Control
Self-discipline also plays a crucial role in emotional control. It helps individuals manage their emotions, preventing them from taking impulsive actions that could have negative consequences. By practicing self-discipline, individuals can make rational decisions rather than emotional ones, leading to better outcomes in both personal and professional life.
Building self-discipline is a gradual process that requires patience and perseverance. It begins with setting clear goals and establishing a plan to achieve them. It requires consistent practice and the willingness to step out of one’s comfort zone. Regular exercise, a healthy diet, and adequate sleep are also integral in fostering self-discipline as they enhance mental strength and focus.
Challenges and Solutions
The path to self-discipline is fraught with challenges. Procrastination, lack of motivation, and distractions are common obstacles. However, these can be overcome by developing a strong will, maintaining a positive mindset, and implementing effective strategies like time-blocking, goal-setting, and mindfulness.
In conclusion, self-discipline is a vital skill that significantly contributes to success in various life aspects. It enhances focus, aids in time management, and helps control emotions. Despite the challenges encountered in its cultivation, with determination and the right strategies, one can successfully develop and strengthen their self-discipline.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Value of Discipline
- Essay on Cyber Crime
- Essay on Christmas Celebration in School
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

IMAGES
VIDEO
COMMENTS
Discipline - or the lack of it - is something that is sometimes offered up as an explanation for obesity. Public health professionals, employers, and physicians gathered at a medical forum in Baltimore last week to discuss obesity and how health plans can address this growing health concern. One physician who is medical director for a large ...
1. INTRODUCTION. In the last 30 years, most of the developed world has witnessed mass population‐level weight gain. 1 For example, the majority of adults in the United States and England are now considered medically to have overweight (a body mass index [BMI] of 25-29.9 kg/m 2) or obesity (a BMI of 30 kg/m 2 and above). 2 , 3 Living with obesity is thought to reduce life expectancy by as ...
Introduction. Obesity is defined by The World Health Organisation as "abnormal or excessive fat accumulation that may impair health" [].The prevalence of obesity has risen exponentially over the last 50 years and is now so widespread that many have announced a state of obesity pandemic [2, 3].In 2016, WHO estimated that globally, over 1.9 billion adults were overweight, including more than ...
This highlights the need for people with overweight and obesity to enhance self-regulation skills and not merely gaining self-regulation knowledge in overcoming self-regulation barriers. Notably, participants attributed large amounts of weight gain to the COVID-19 measure of working from home, where they had easy access to food without being ...
Not judging by appearances. Severely overweight or obese people are painfully familiar with fatphobia and obesity stigma (e.g., fat shaming)—with various assumptions linking greater weight with ...
No. Some obesity spreads culturally. 3. Stigma is dangerous. What most infuriated readers was my conclusion that "responsibility and stigma are part of the solution.". To the extent that fat ...
Relapse is high in lifestyle obesity interventions involving behavior and weight change. Identifying mediators of successful outcomes in these interventions is critical to improve effectiveness and to guide approaches to obesity treatment, including resource allocation. This article reviews the most consistent self-regulation mediators of medium- and long-term weight control, physical activity ...
Table 3 Consensus statements on the stigma of obesity: recommendations. Full size table. In this document, we use the terms 'weight stigma', 'weight-based stereotypes', or 'weight bias ...
Introduction. Obesity is a major public health issue in North America affecting more than 25% of adults in Canada, and 40% of adults in the United States [1,2].Obesity contributes to impaired physical and mental health-related quality of life, and increased morbidity and mortality [3,4].Physical activity (PA) is a cornerstone of interdisciplinary obesity management [5,6].
The results showed that after adding the mediating variable self-other overlap, the direct path from PT to positive obesity stereotypes (β = 0.13, p < 0.01) and the indirect path from PT to self-other overlap (β = 0.26, p < 0.001) and from self-other overlap to positive obesity stereotypes (β = 0.10, p < 0.05) were all significant.
No one doubts the economic costs of obesity, estimated at 5-14% of health expenditure for 2020-2050 [1], but there is disagreement whether fatness is considered a disease [2] or a behavioral risk factor, similar to smoking, alcohol and substance abuse that may lead to a disease [3]. Current opinion also emphasizes social determinants, thereby moving away from personal responsibility concepts ...
People with obesity experience discrimination from an early age that often stems from the stigma associated with the disease. The belief held that people with obesity are lazy, overindulgent, and lack self-control is incorrect and has the potential to negatively impact many aspects of a patient's life. Therefore, the healthcare team and the larger medical community need to acknowledge the ...
American Psychologist, Vol. 75, No. 2, 2020. Clinical Practice Guideline for the Treatment of Obesity and Overweight in Children and Adolescents APA, 2018. Even mild obesity can put people at risk for serious COVID-19 complications. New research and interventions from psychologists could help people who want to lose the weight.
1 INTRODUCTION. Overweight and obesity account for 4 million annual deaths globally 1 and are estimated to reduce gross domestic product by 3.3% in Organisation for Economic Co-operation and Development countries. 2 Overweight prevalence is on a steep rise in Europe while having stabilized at an all-time high of 73.1% among US adults. 2, 3 Individuals with obesity have an approximately two ...
Self Esteem, Insecurity and Obesity. by Sean G. Connolly, PhD. Fall 2010. The comment in the support group captured a common sentiment, "After failure, failure and failure of diets and weight-loss efforts, there is always that little voice in the back of your mind that says, 'Maybe you are going to be one of the failures at this.'".
To prevent obesity, you need to stay active, follow a healthy diet, and get adequate sleep. Obesity prevention also involves saying no to certain preferences, like soft drinks, or driving short distances when you could walk instead. Obesity is generally defined as a chronic disease characterized by excessive body fat.
Conclusion: In conclusion, the consequences of obesity are far-reaching and demand urgent attention. From the individual health implications to the societal and economic burdens, the impact of this epidemic cannot be ignored. However, by understanding the root causes, implementing prevention strategies, and advocating for policy changes, we can ...
Discipline, a term often associated with stringent rules and limitations, is in essenc, a potent force that fosters self-regulation, purposeful living, and personal growth. It forms the foundation for success across all life's spheres, including personal development, academic achievement, and societal harmony.
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
Importance of Self Discipline Essay: Self-Discipline means having control over oneself; it provides self-control overreactions, actions, and oneself and boosts a person's inner strength. Self- Discipline is the most important skill a person should possess. One of the main attributes of Self-Discipline is its ability to abdicate immediate pleasure and gratification. Self-Discipline does not ...
Self Discipline Benefits and Importance. Self-discipline helps you to overcome the bad habits by meditating regularly. It gives you the ability not to give up after failure and setbacks, develop self-control, provide the ability to resist distractions, helps you to motivate yourself until you accomplish your goals. Conclusion.
500 Words Essay on Self Discipline ... However, these can be overcome by developing a strong will, maintaining a positive mindset, and implementing effective strategies like time-blocking, goal-setting, and mindfulness. Conclusion. In conclusion, self-discipline is a vital skill that significantly contributes to success in various life aspects ...