Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 27 December 2018

Prevalence and phenomenology of violent ideation and behavior among 200 young people at clinical high-risk for psychosis: an emerging model of violence and psychotic illness
- Gary Brucato 1 ,
- Paul S. Appelbaum 1 ,
- Michael D. Masucci 1 ,
- Stephanie Rolin 1 ,
- Melanie M. Wall 1 ,
- Mark Levin 1 ,
- Rebecca Altschuler 1 ,
- Michael B. First 1 ,
- Jeffrey A. Lieberman 1 &
- Ragy R. Girgis 1
Neuropsychopharmacology volume 44 , pages 907–914 ( 2019 ) Cite this article
1935 Accesses
16 Citations
6 Altmetric
Metrics details
- Risk factors
- Signs and symptoms
In a previously reported longitudinal study of violent ideation (VI) and violent behavior (VB) among 200 youths at clinical high-risk (CHR) for psychosis, we found that VI, hitherto underinvestigated, strongly predicted transition to first-episode psychosis (FEP) and VB, in close temporal proximity. Here, we present participants’ baseline characteristics, examining clinical and demographic correlates of VI and VB. These participants, aged 13–30, were examined at Columbia University Medical Center’s Center of Prevention and Evaluation, using clinical interviews and the structured interview for psychosis-risk syndromes (SIPS). At the onset of our longitudinal study, we gathered demographics, signs and symptoms, and descriptions of VI and VB. One-third of participants reported VI ( n = 65, 32.5%) at baseline, experienced as intrusive and ego-dystonic, and associated with higher suspiciousness and overall positive symptoms. Less than one-tenth reported VB within 6 months of baseline ( n = 17, 8.5%), which was unrelated to SIPS-positive symptoms, any DSM diagnosis or other clinical characteristic. The period from conversion through post-FEP stabilization may be characterized by heightened risk of behavioral disinhibition and violence. We provide a preliminary model of how violence risk may peak at various points in the course of psychotic illness.
You have full access to this article via your institution.
Similar content being viewed by others

Suicidal behavior across a broad range of psychiatric disorders
Self-harm behaviour and externally-directed aggression in psychiatric outpatients: a multicentre, prospective study (viormed-2 study)
Borderline personality disorder: associations with psychiatric disorders, somatic illnesses, trauma, and adverse behaviors
Introduction.
Schizophrenia and other psychotic disorders are generally preceded by an attenuated or clinical high-risk (CHR) phase, characterized by delusional ideas, perceptual disturbances, and disorganization of thought, with lower levels of conviction, intensity, frequency, and behavioral impact than seen in full-blown psychosis [ 1 ]. Such subthreshold positive symptoms are evaluated using the structured interview for psychosis-risk syndromes (SIPS) [ 2 ], a measure that delineates an attenuated positive symptom syndrome (APSS). This construct served as the basis for the attenuated psychosis syndrome (APS), included in the current edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as a condition warranting further research [ 3 ]. Both the APS and APSS are highly heterogeneous, with regard to diagnosis, encompassing individuals with possible features of a number of other DSM categories, but who display a specific constellation of symptoms suggestive of potential emergent psychosis. Such persons are uncommon, with an estimated prevalence in the general population as low as 0.3% and an estimated annual incidence of 1/10,000 [ 4 ]. Furthermore, relatively few CHR individuals, generally not more than 30–35% in the most robust samples, actually progress to full-blown psychotic illness [ 1 ].
A newly emerging line of inquiry suggests that the CHR state may constitute a period of increased risk for violence, a topic of considerable current interest. Although most individuals with mental illness are not dangerous and the majority of violence is committed by people without mental disorders, there is some evidence that positive symptoms of full-blown schizophrenia and other psychoses [ 5 , 6 , 7 , 8 , 9 ], such as delusions and hallucinations, are related to VB [ 10 , 11 , 12 , 13 , 14 , 15 ]. Nonadherence to medications [ 16 , 17 ] and poor insight [ 18 ] have been shown to mediate this. Nielssen and Large [ 19 ], examining the prevalence of homicide in psychosis, reported that approximately 1 in 9000 persons with psychosis who have received treatment commit homicide each year, while 1 homicide occurs for every 629 presentations of first-episode psychosis. Other research suggests that alcohol [ 20 , 21 ] or drug abuse [ 22 , 23 , 24 , 25 ] are the key mediating factors, and may account for more of the risk than psychosis [ 26 , 27 , 28 , 29 , 30 ]. Langeveld et al. [ 31 ] prospectively examined violence, as well as multiple clinical characteristics, including substance use, among 178 first-episode participants for 10 years. A decade postbaseline, 20% of participants had been arrested or incarcerated, though most of these events occurred before baseline. At the 10-year follow-up, 15% had exposed others to threats or violence in the prior year. Illegal drug use at baseline and the 5-year mark was predictive of violence in the year preceding endpoint evaluation.
Other possible mediating factors have been identified. A report from the UK National EDEN study [ 32 ] suggested that there may be multiple pathways to violence in first-episode psychosis and that lifelong antisocial traits should be considered alongside psychotic symptomatology. A meta-regression analysis of 100 studies by Witt et al. [ 33 ] found criminal history, substance, or alcohol use, nonadherence with psychotherapy and medication, poor impulse control, and prior hostile behavior to be associated with violence. Coid et al. [ 34 ] particularly implicate paranoid ideation as the link between violence and psychosis.
Violence risk in the CHR phase of psychotic illness has been far less frequently examined. Marshall et al. [ 35 ] reported that 24% of 442 CHR individuals described violent content during SIPS interviews, with 12% reporting multiple types of violent content. Such content was associated with more severe positive symptoms, anxiety, negative beliefs about oneself, and being the target of bullying prior to age 16. Notably, violent content was defined to include thoughts of harm to the self by others—that is to say, suspicious concerns with violent content—which constituted the most common subtype. Content surrounding hurting others (11.54%) and perceptual disturbances related to interpersonal violence (3.17%) were less common. Violent content in relation to actual violent behaviors was not investigated.
Recently, we presented results of a longitudinal study of 200 CHR youth, ages 13–30. Each was examined for up to 2 years for VI and VB using the SIPS and clinical interview [ 36 ]. Violent content was rated according to categories drawn from the MacArthur Community Violence Interview [ 29 ]. VB within the 6 months preceding initial assessment and VI at baseline both very strongly predicted transition to first-episode psychosis (FEP), as well as VB within an average of 1 week (SD = 35 days) following conversion. This promising finding was independent of more than 40 clinical and demographic variables. Moreover, the targets of the participants’ baseline VI were found to be entirely different than those ultimately attacked, perhaps suggesting impulsivity, and loss of executive control with the transition to frank psychosis.
The hypothesis that violence risk may increase as CHR individuals approach conversion to frank psychosis has some independent empirical support. More prominent psychotic symptoms and less insight have been found to increase the risk of violent acts [ 18 , 24 , 37 ]. Moreover, the aforementioned meta-analysis by Nielssen and Large [ 19 ] found that 38.5% of homicides committed by individuals with psychotic illness occur during the FEP, prior to first receiving treatment. We know of no reports of a higher prevalence of homicide in the psychosis-risk state. A prior meta-analysis by Fazel et al. [ 38 ] also reported that schizophrenia and other psychoses are associated with violence, particularly homicide, and that the relationship between violence (excluding homicide) and psychosis may be largely related to comorbid substance use. However, individual studies considering the temporal relationship between violence and first onset of psychotic symptoms were not examined.
In the present report, we examine the baseline demographic and clinical characteristics of a comparatively large cohort of CHR individuals. Our specific aim was to describe clinical correlates of VI and VB in the 6 months prior to baseline, considering associations with specific signs and symptoms assessed by the SIPS.
Data were collected at the Center of Prevention and Evaluation (COPE), an outpatient research program for the evaluation and treatment of attenuated positive symptoms at the New York State Psychiatric Institute (NYSPI)/Columbia University Medical Center (CUMC) in New York City. The NYSPI Institutional Review Board approved the research. All adults provided written informed consent, while minors provided written assent, with written informed consent obtained from a parent.
Participants
Potential participants were referred to COPE between 2003 and 2016 by a network of academic centers, private practitioners, clinics, and hospitals, or were self-referred after reviewing the center’s web site, for evaluation of possible emergent psychotic symptoms. Participants were between the ages of 13 and 30 and were required to have symptoms that meet criteria for at least one of the psychosis-risk syndromes delineated in the SIPS (see Supplementary Material for specific definitions). These include the aforementioned APSS, the genetic risk and functional decline syndrome and the brief intermittent psychosis syndrome (BIPS). However, it should be noted that all 200 participants met APSS criteria and none met BIPS criteria. Exclusion criteria included lack of proficiency in English; a current or lifetime DSM psychotic disorder, including affective psychoses; a DSM disorder better accounting for the clinical presentation; I.Q. < 70; medical conditions affecting the central nervous system; marked risk of harm to self or others; unwillingness to participate in research; geographic distance; or a DSM diagnosis of current substance or alcohol abuse or dependence. Use of antipsychotic medication was not exclusionary, provided that there was clear evidence that positive symptoms of an attenuated, but never fully psychoticlevel syndrome were present at medication onset. The study sample is described in Table 1 .
The data presented here were collected at baseline. In addition to a general clinical interview, each participant was also evaluated with either the Diagnostic Interview for Genetic Studies [ 39 ] or Structured Clinical Interview for DSM-IV-I Disorders, Patient Edition (SCID-I/P); [ 40 ]. Those under age 16 completed the Kiddie Schedule for Affective Disorders and Schizophrenia, Present and Lifetime Version (K-SADS-PL) [ 41 ].
The SIPS [ 42 ], with which all participants were examined, involves a semistructured interview that probes for past and current signs and symptoms of attenuated versus threshold psychotic illness. It defines criteria for psychosis-risk states, as well as threshold psychosis. The measure contains 19 subscales, divided into positive, negative, disorganization, and general symptom components. The critical items for determining attenuated versus full-blown psychosis, are the five positive symptoms: P.1.: unusual thought content/delusional ideas, P.2.: suspiciousness/persecutory ideas, P.3.: grandiose ideas, P.4.: perceptual abnormalities/hallucinations, and P.5.: disorganized communication. These are scored 0–6 according to specific anchors provided for each symptom that distinguish among degrees of frequency, conviction, and behavioral impact: 0, absent; 1, questionably present; 2, mild; 3, moderate; 4, moderately severe; 5, severe, but not psychotic; and 6, psychotic, delusional conviction, at least intermittently. Negative, disorganization, and general signs and symptoms are rated from 0 (absent) to 6 (extreme) (see Supplementary Material for specific subscales).
APSS criteria, satisfied by all participants described here, require that one or more of the 5 positive symptoms occurs at a score of 3–5 and is new or has worsened by 1 or more points in the past 12 months, and no score of 6 on a positive symptom has ever been achieved. SIPS administrators were certified and established scoring consensus.
Frank psychosis is defined by the SIPS as having met criteria for a score of 6 on one or more positive symptoms in one’s lifetime for at least 1 h per day at an average frequency of 4 days per week over one month, and/or serious danger or disorganization as the result of the positive symptom(s).
VI and VB were coded as “present” or “not present.” Information about VB in the 6 months prior to baseline was amassed via the SIPS, the clinical interview, and collateral information from prior records, family members and referral sources. It was defined as any violent or aggressive act, including those with a deadly weapon, any assault producing injury, threat with a deadly weapon in hand, sexual assault, assault producing no injury (e.g., pushing or slapping), or use of a weapon without threats or injury. These were defined based on the categories for violence and other aggressive acts established in the MacArthur Community Violence Interview [ 29 ]. In accord with this framework, assault with no injury was categorized as Other Aggressive Acts (OAA). VI encompassed any violent or aggressive fantasies or thoughts directed toward others, intrusive or nonintrusive, which we categorized by adapting the MacArthur interview framework to score VI at baseline in the same manner as VB and OAA.
Statistical analyses
All statistical analyses were performed using SPSS version 22 [ 43 ]. Categorical variables were analyzed using the chi-square test of associations and continuous variables with t-tests. The dependent variables were the presences of either VI or VB. A Fisher’s exact p value was calculated for chi-square analyses with small expected cell counts. For tests failing Levene’s test for equality of variance, a corrected test statistic was calculated.
Violent ideation
Approximately, one-third of the sample presented with VI ( n = 65, 32.5%; see Table 2 ), almost uniformly experienced as ego-dystonic and intrusive in nature. To better understand this, ideational content was divided into the subcategories of “severe” violence and ideation related to OAA. Severe VI was defined as thought content involving serious harm to another person, with or without a weapon. Within this category, 20 respondents reported thoughts or mental images of causing serious harm to another with their fists, feet or other body parts. Eighteen described VI of harming another person with a weapon (including guns, knives, saws, and razors), six reported VI that was sexual in nature (rape and sexual assault), and two described VI involving killing others with bombs. In three cases, VI involved causing the death of another person in an unspecified manner. Four respondents described VI in which they caused both serious injury with a weapon and sexual harm. Two endorsed thoughts and mental images of causing serious harm with a weapon and with fire, and one had thoughts of causing serious sexual harm, as well as harm without a weapon.
Ideation related to OAA involves violence toward another that might not result in serious harm. This group ( n = 9) included 8 individuals with VI of shoving, slapping, throwing people a short distance, and/or nonserious hitting. One individual reported minor VI of an unspecified nature.
There were no sex or ethnic (i.e., Hispanic vs. non-Hispanic) differences between individuals with and without VI. Interestingly, individuals identifying as Caucasian reported less VI than other racial groups. Those with VI were more likely to have symptoms that met criteria for schizotypal personality disorder (SPD; χ 2 (1) = 5.88; p = 0.015), comorbid with the SIPS APSS category, and to report histories of nonsexual trauma ( χ 2 (1) = 4.93; p = 0.026). Medication status; suicidality, including both suicidal ideation and suicidal behavior; and history of sexual trauma did not distinguish between those with and without VI. Comorbid DSM diagnoses did not significantly differ between those with and without VI.
Individuals with VI reported higher degrees of suspiciousness, as well as total overall positive symptoms than those without (see Table 3 ). A statistical association between VI and SIPS symptom P.1.: unusual thought content/delusional ideas was observed, though this is undoubtedly due to the fact that VI was frequently reported by participants when responding to P.1. inquiries probing for intrusive ideas and a sense of one’s thoughts being out of one’s control.
There was no significant difference in negative symptoms among those with and without VI. Individuals with VI exhibited higher scores for unusual behavior and appearance; more bizarre ideas (e.g., ideas which are not scientifically plausible and are difficult to understand); and higher total disorganization scores. Individuals with VI were also noted to experience more severely dysphoric mood states. Other SIPS symptom subscales were comparable between those with and without VI.
Violent behavior
Evidence and/or self-report of VB in the 6 months preceding baseline were found in less than one-tenth of the sample ( n = 17, 8.5%). When present, VB was unrelated to sex, ethnicity, or race. There were no differences in terms of sexual or nonsexual trauma histories, suicidal ideation, suicidal behavior, medication status, or comorbid DSM diagnoses between individuals with and without prebaseline VB. There were no differences between individuals with and without VB with regard to any individual SIPS subscale, or in terms of positive, negative, disorganization, or general symptoms.
The present study describes violent behaviors and thoughts reported by 200 young people at clinical high-risk of psychotic illness at the onset of a 2-year longitudinal study. The prospective aspects of the study have been previously described [ 36 ]. Here, we explore relationships between violent thoughts at baseline, violent actions in the 6-month period preceding research participation, and psychiatric diagnoses and SIPS interview subscales, advancing our understanding of how psychosis and violence risk may coexist or develop in tandem in certain individuals.
Analyses revealed that thoughts and mental images with violent content, generally experienced as intrusive and ego-dystonic, were common in our sample, occurring in one-third of participants. The content of this ideation was found typically to be severe in nature, involving physical harm to others using one’s body or a weapon. Sexual content was uncommon. Violent thoughts appear to be relatively common in attenuated psychosis. Thus, violent thoughts of this nature may constitute part of the phenomenology of attenuated psychosis, analogous to suicidal thoughts in a significant number of depressed persons. However, actual suicide attempts in depression and violence in the CHR state are far less common. The frequency of VI in our CHR cohort is potentially important: as noted in our previous report, VI was an extremely good predictor in our cohort of both conversion to threshold psychosis and, within an average of seven days (SD = 35 days) postpsychosis onset, violent actions toward others. However, given the potential stigmatization of the already marginalized CHR population, we should emphasize that most individuals in our cohort who described VI never actually progressed to VB. Furthermore, it should be noted that violence among CHR persons may be multidetermined, or entirely unrelated to VI or psychotic symptoms.
Results also indicated that violent thoughts are generally related to overall positive symptoms, and particularly to suspiciousness. A review by Darrell-Berry et al. [ 44 ] of 15 studies examining the relationship between paranoia and violence found that, in the most rigorous investigations, a positive association emerged between these factors. It is intriguing, however, that, in our research, VI was virtually never elicited by questions inquiring about suspicious ideas on the SIPS [ 36 ]. It is unclear whether this may relate to the wording of suspiciousness inquiries in the SIPS. However, rather than suggest that CHR persons with some degree of paranoia are more likely to harbor violent thoughts, it may be that both suspiciousness and VI are commonly co-occurring, but not necessarily related, manifestations of a nascent psychotic illness in some individuals. The finding that a history of non-sexual trauma is associated with VI has some support in Marshall et al.'s [ 35 ] finding that violent content on the SIPS was linked with more incidents of bullying prior to age 16. The findings that, in our cohort, VI was statistically associated with non-Caucasian race and comorbid SPD have no precedent in the CHR literature. Additional research is needed before meaningful interpretations can be ventured.
By contrast, violent actions in the 6-month period preceding baseline were remarkably uncommon, occurring in less than one-tenth of the cohort. Given that information regarding prebaseline violence was dependent on self-report by participants, as well as collateral information from family members and referrers, it is unclear to what degree information about prebaseline violent acts may be underrepresented, although there are reasons to believe that self and collateral report offer more complete data than official records [ 29 ].
These results demonstrating relationships between VI and positive symptoms are consistent with Marshall et al.’s [ 35 ] finding regarding the frequency of violent content in an independent CHR sample, as well as VB in syndromal psychosis [ 45 ]. The collective data reveal that individuals with psychotic illness may be at the highest risk for violence around the time of conversion to psychosis through the remission of the FEP. Moreover, some data suggest that periods of intensification of symptoms (e.g., the perihospitalization period) during the chronic state of psychotic illness also represent periods of slightly increased risk for violence, though the risk may not be as high as during the FEP period [ 29 ]. Thus, the overall picture, which we have incorporated into a preliminary model (see Fig. 1 ), suggests that, in the phase of attenuated positive symptoms that generally precedes full-blown psychosis, violent thoughts and mental images are commonly experienced, but are either not acted upon or dismissed as inconsistent with individuals’ actual thoughts and desires. However, such thoughts are strongly associated with later progression to threshold psychosis and subsequent aggression, such that they may constitute critical aspects of assessments of conversion status and violence risk, if independently validated, in future research. Moreover, it is with the conversion to FEP that one is most likely to act out aggressively.
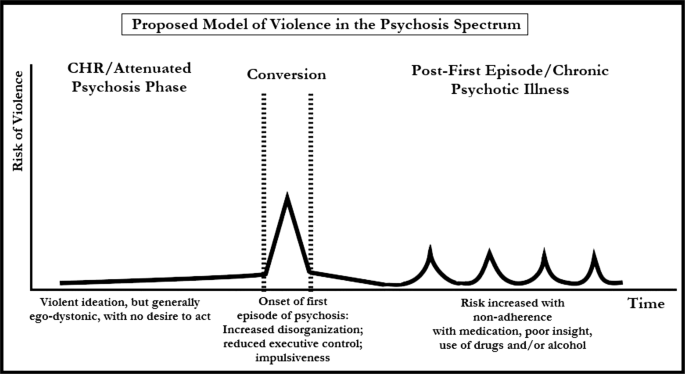
Proposed model of violence in the psychosis spectrum
The literature and our research, on balance, suggest that this window of increased risk closes only after the FEP has stabilized, perhaps following a period of treatment. Furthermore, our previously described data tell us that this postconversion aggression is generally unfocused and impulsive in nature, affecting targets other than those initially envisioned by participants in thoughts and mental images [ 36 ]. This point is intriguing in light of our finding here that a SIPS index of unusual behavior and appearance was associated with VI in our cohort. The facts may collectively indicate that violence risk is associated with gradual deterioration of executive behavioral controls as one transitions to psychosis. What is unclear is whether the reduced risk after the first episode is related to medications, psychotherapy, the natural progression of the condition, or some other compensatory factor, which warrants further research.
Among the limitations of our research is that it was conducted at a single site, reducing the generalizability of our findings, pending attempts at replication. Generalizability may have also been impacted by the elimination of persons with certain clinical features from our CHR sample; specifically, those whose presentations meet criteria for current substance or alcohol abuse or dependence [ 26 , 33 ] or who were deemed too clinically acute to participate in research (i.e., at imminent risk of violence and requiring evaluation in the emergency room). These exclusions may have significantly affected reports of both past and current violent thoughts and behaviors. Moreover, excluding individuals with histories of substance or alcohol abuse and/or risk of imminent serious aggression may have reduced the number of participants with symptoms associated with comorbid conduct disorder in childhood or antisocial personality disorder in adulthood, which may also have affected the degree of violence in our population. There is some literature to suggest that a history of delinquent behaviors may increase the likelihood of violence in psychotic illness [ 32 , 45 ]. Additionally, a very small number of individuals did not complete baseline screening beyond the SIPS, such that we have some missing data. It also unclear to what degree social bias may have led to minimization of reporting of VI and VB. Finally, all participants were voluntarily presenting for treatment, which may distinguish this sample from nonhelp-seeking CHR persons.
However, our sample size of 200 participants is comparatively large, as individuals whose symptoms meet criteria for attenuated psychotic illness are decidedly uncommon. Another strength of the study lies in the inclusion of VI, and not solely VB, in the variables we examined. We believe that our collective findings regarding the frequency of VI in the CHR state and its predictive nature may, with time and additional study, offer a promising new window for research and clinical intervention.
Funding and disclosure
This work was supported by the National Institutes of Health: Center for Research Resources and the National Center for Advancing Translational Sciences (grant numbers UL1TR000040, 2KL2RR024157, K23MH066279, R21MH086125, R01P50MH086385, R01MH093398-01, K23MH106746). This project was supported by the Brain and Behavior Research Foundation; Lieber Center for Schizophrenia Research; and the New York State Office of Mental Health Research Foundation for Mental Hygiene.
Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Richer-Rossler A, Schultze-Lutter F, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–20.
Article Google Scholar
Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–15.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5 edn. Washington, DC: American Psychiatric Association; 2013.
Book Google Scholar
Addington J, Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, et al. North American Prodromal Longitudinal Study: a collaborative multisite approach to prodromal schizophrenia research. Schizophr Bull. 2007;33:665–72.
Douglas KS, Guy LS, Hart SD. Psychosis as a risk factor for violence to others: a meta-analysis. Psychol Bull. 2009;135:679–706.
Hodgins S, Mednick SA, Brennan PA, Schulsinger F, Engberg M. Mental disorder and crime. Evidence from a Danish birth cohort. Arch Gen Psychiatry. 1996;53:489–96.
Article CAS Google Scholar
Lindqvist P, Allebeck P. Schizophrenia and crime. A longitudinal follow-up of 644 schizophrenics in Stockholm. Br J Psychiatry. 1990;157:345–50.
Swanson JW, Swartz MS, Essock SM, Osher FC, Wagner HR, Goodman LA, et al. The social-environmental context of violent behavior in persons treated for severe mental illness. Am J Public Health. 2002;92:1523–31.
Taylor PJ, Bragado-Jimenez MD. Women, psychosis and violence. Int J Law Psychiatry. 2009;32:56–64.
Coid JW, Ullrich S, Kallis C, Keers R, Barker D, Cowden F, et al. The relationship between delusions and violence: findings from the East London first episode psychosis study. JAMA Psychiatry. 2013;70:465–71.
Keers R, Ullrich S, Destavola BL, Coid JW. Association of violence with emergence of persecutory delusions in untreated schizophrenia. Am J Psychiatry. 2014;171:332–9.
McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatr Serv. 2000;51:1288–92.
Taylor PJ, Leese M, Williams D, Butwell M, Daly R, Larkin E. Mental disorder and violence. A special (high security) hospital study. Br J Psychiatry. 1998;172:218–26.
Ullrich S, Keers R, Coid JW. Delusions, anger, and serious violence: new findings from the MacArthur Violence Risk Assessment Study. Schizophr Bull. 2014;40:1174–81.
Bartels SJ, Drake RE, Wallach MA, Freeman DH. Characteristic hostility in schizophrenic outpatients. Schizophr Bull. 1991;17:163–71.
Elbogen EB, Van Dorn RA, Swanson JW, Swartz MS, Monahan J. Treatment engagement and violence risk in mental disorders. Br J Psychiatry. 2006;189:354–60.
Yesavage JA. Inpatient violence and the schizophrenic patient: an inverse correlation between danger-related events and neuroleptic levels. Biol Psychiatry. 1982;17:1331–7.
CAS PubMed Google Scholar
Buckley PF, Hrouda DR, Friedman L, Noffsinger SG, Resnick PJ, Camlin-Shingler K. Insight and its relationship to violent behavior in patients with schizophrenia. Am J Psychiatry. 2004;161:1712–4.
Nielssen O, Large M. Rates of homicide during the first episode of psychosis and after treatment: a systematic review and meta-analysis. Schizophr Bull. 2010;36:702–12.
Eronen M, Tiihonen J, Hakola P. Schizophrenia and homicidal behavior. Schizophr Bull. 1996;22:83–89.
Rasanen P, Tiihonen J, Isohanni M, Rantakallio P, Lehtonen J, Moring J. Schizophrenia, alcohol abuse, and violent behavior: a 26-year followup study of an unselected birth cohort. Schizophr Bull. 1998;24:437–41.
Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2009;66:152–61.
Rolin SA, Marino LA, Pope LG, Compton MT, Lee RJ, Rosenfeld B, et al. (2018). Recent violence and legal involvement among young adults with early psychosis enrolled in Coordinated Specialty Care. Early Interv Psychiatry 1–9. E-pub ahead May 9, 2018, https://doi.org/10.1111/eip.12675 .
Swartz MS, Swanson JW, Hiday VA, Borum R, Wagner HR, Burns BJ. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry. 1998;155:226–31.
Arseneault L, Moffitt TE, Caspi A, Taylor PJ, Silva PA. Mental disorders and violence in a total birth cohort: results from the Dunedin Study. Arch Gen Psychiatry. 2000;57:979–86.
Fazel S, Langstrom N, Hjern A, Grann M, Lichtenstein P. Schizophrenia, substance abuse, and violent crime. J Am Med Assoc. 2009b;301:2016–23.
Foley SR, Kelly BD, Clarke M, McTigue O, Gervin M, Kamali M, et al. Incidence and clinical correlates of aggression and violence at presentation in patients with first episode psychosis. Schizophr Res. 2005;72:161–8.
Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: data from the MacArthur Violence Risk Assessment Study. Am J Psychiatry. 2000;157:566–72.
Steadman HJ, Mulvey EP, Monahan J, Robbins PC, Appelbaum PS, Grisso T, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55:393–401.
Chang WC, Chan SS, Hui CL, Chan SK, Lee EH, Chen EY. Prevalence and risk factors for violent behavior in young people presenting with first-episode psychosis in Hong Kong: a 3-year follow-up study. Aust N Z J Psychiatry. 2015;49:914–22.
Langeveld J, Bjørkly S, Auestad B, Barder H, Evensen J, Ten Velden Hegelstad W, et al. Treatment and violent behavior in persons with first episode psychosis during a 10-year prospective follow-up study. Schizophr Res. 2014;156:272–6.
Winsper C, Singh SP, Marwaha S, Amos T, Lester H, Everard L, et al. Pathways to violent behavior during first-episode psychosis: a report from the UK National EDEN Study. JAMA Psychiatry. 2013;70:1287–93.
Witt K, van Dorn R, Fazel S. Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies. PloS ONE. 2013;8:e55942.
Coid JW, Ullrich S, Bebbington P, Fazel S, Keers R. Paranoid ideation and violence: meta-analysis of individual subject data of 7 population surveys. Schizophr Bull. 2016;42:907–15.
Marshall C, Deighton S, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, et al. The violent content in attenuated psychotic symptoms. Psychiatry Res. 2016;242:61–66.
Brucato G, Appelbaum PS, Lieberman JA, Wall MM, Feng T, Masucci MD, et al. A longitudinal study of violent behavior in a psychosis-risk cohort. Neuropsychopharmacology. 2018;43:264–71.
Arango C, Barba AC, Gonzalez-Salvador T, Ordoriez AC. Violence in inpatients with schizophrenia: a prospective study. Schizophr Bull. 1999;25:493–503.
Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med. 2009a;6:e1000120.
Nurnberger JI Jr, Blejar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, et al. Diagnostic interview for genetic studies. Rationale, unique features, and training. Arch General Psychiatry. 1994;51:849–59.
First MB, Spitzer RL, Gibbon M, Williams JBW (2002). Structured clinical interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). New York: Biometrics Research, NYSPI.
Kaufman JB, Birmaher D, Brent D, Rao U, Ryan N. Kiddie-Sads-Present and Lifetime Version (K-SADS-PL). Pittsburgh, PA: University of Pittsburgh Department of Psychiatry; 1996.
Google Scholar
McGlashan TH, Miller TJ, Woods SW, Hoffman RE, Davidson LA. A scale for the assessment of prodromal symptoms and states. In: Miller TJ, Mednick SA, McGlashan TH, Liberger J, Johannessen JO, (editors). Early Intervention in Psychotic Disorders. Dordrecht, The Netherlands: Kluwer Academic Publishers; 2001. p. 135–49.
Chapter Google Scholar
IBM Corporation. IBM SPSS Statistics for Windows. 22.0 edn. Armonk, NY: IBM Corporation; 2013.
Darrell-Berry H, Berry K, Bucci S. The relationship between paranoia and aggression in psychosis: a systematic review. Schizophr Res. 2016;172:169–76.
Swanson JW, Swartz MS, Van Dorn RA, Elbogen EB, Wagner HR, Rosenheck RA, et al. A national study of violent behavior in persons with schizophrenia. Arch Gen Psychiatry. 2006;63:490–9.
Download references
Acknowledgments
We acknowledge the individuals who participated in this study.
Author information
Authors and affiliations.
The New York State Psychiatric Institute/Columbia, University Medical Center, New York, NY, USA
Gary Brucato, Paul S. Appelbaum, Michael D. Masucci, Stephanie Rolin, Melanie M. Wall, Mark Levin, Rebecca Altschuler, Michael B. First, Jeffrey A. Lieberman & Ragy R. Girgis
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Gary Brucato .
Ethics declarations
Competing interests.
R.G. acknowledges receiving research support from Otsuka, Allergan/Forest, BioAvantex, and Genentech. J.L. has received support administered through his institution in the form of funding or medication supplies for investigator initiated research from Lilly, Denovo, Biomarin, Novartis, Taisho, Teva, Alkermes, and Boehringer Ingelheim, and is a member of the advisory board of Intracellular Therapies and Pierre Fabre. He neither accepts nor receives any personal financial remuneration for consulting, advisory board or research activities. He holds a patent from Repligen and receives royalty payments from “SHRINKS: The Untold Story of Psychiatry.” The remaining authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary material, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Brucato, G., Appelbaum, P.S., Masucci, M.D. et al. Prevalence and phenomenology of violent ideation and behavior among 200 young people at clinical high-risk for psychosis: an emerging model of violence and psychotic illness. Neuropsychopharmacol. 44 , 907–914 (2019). https://doi.org/10.1038/s41386-018-0304-5
Download citation
Received : 19 September 2018
Revised : 14 December 2018
Accepted : 16 December 2018
Published : 27 December 2018
Issue Date : April 2019
DOI : https://doi.org/10.1038/s41386-018-0304-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Psychometric properties of an arabic translation of the long (12 items) and short (7 items) forms of the violent ideations scale (vis) in a non-clinical sample of adolescents.
- Feten Fekih-Romdhane
- Diana Malaeb
- Souheil Hallit
BMC Psychiatry (2024)
Feasibility and Utility of Different Approaches to Violence Risk Assessment for Young Adults Receiving Treatment for Early Psychosis
- Stephanie A. Rolin
- Jennifer Scodes
- Paul S. Appelbaum
Community Mental Health Journal (2022)
Bullying in clinical high risk for psychosis participants from the NAPLS-3 cohort
- Jean Addington
Social Psychiatry and Psychiatric Epidemiology (2022)
The Impact of Increasing Community-Directed State Mental Health Agency Expenditures on Violent Crime
- John S. Palatucci
- Alan C. Monheit
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Research article
- Open access
- Published: 23 January 2017
Mental illness and violent behavior: the role of dissociation
- Aliya R. Webermann 1 &
- Bethany L. Brand 2
Borderline Personality Disorder and Emotion Dysregulation volume 4 , Article number: 2 ( 2017 ) Cite this article
43k Accesses
12 Citations
67 Altmetric
Metrics details
The role of mental illness in violent crime is elusive, and there are harmful stereotypes that mentally ill people are frequently violent criminals. Studies find greater psychopathology among violent offenders, especially convicted homicide offenders, and higher rates of violence perpetration and victimization among those with mental illness. Emotion dysregulation may be one way in which mental illness contributes to violent and/or criminal behavior. Although there are many stereotyped portrayals of individuals with dissociative disorders (DDs) being violent, the link between DDs and crime is rarely researched.
We reviewed the extant literature on DDs and violence and found it is limited to case study reviews. The present study addresses this gap through assessing 6-month criminal justice involvement among 173 individuals with DDs currently in treatment. We investigated whether their criminal behavior is predicted by patient self-reported dissociative, posttraumatic stress disorder and emotion dysregulation symptoms, as well as clinician-reprted depressive disorders and substance use disorder.
Past 6 month criminal justice involvement was notably low: 13% of the patients reported general police contact and 5% reported involvement in a court case, although either of these could have involved the DD individual as a witness, victim or criminal. Only 3.6% were recent criminal witnesses, 3% reported having been charged with an offense, 1.8% were fined, and 0.6% were incarcerated in the past 6 months. No convictions or probations in the prior 6 months were reported. None of the symptoms reliably predicted recent criminal behavior.
Conclusions
In a representative sample of individuals with DDs, recent criminal justice involvement was low, and symptomatology did not predict criminality. We discuss the implications of these findings and future directions for research.
Stereotypes abound in the media regarding violent behavior and crimes among those with mental illness. One need not look further than popular crime television shows, the latest blockbuster film or news stories on perpetrators of atrocities such as school shootings or terrorist attacks. Researchers have worked to unpack the complex question of what role mental illness plays in violence, if any, especially in light of mass shootings in the United States at Sandy Hook Elementary, Virginia Tech University and Pulse Nightclub, among others. Researchers generally agree that there is some relationship between mental illness and the risk for violence, such that mental illness increases the risk for violence perpetration as well as victimization, but there is less consensus on the specific psychopathology and symptoms that contribute to violence.
A brief literature review on mental illness and violent behavior
Stereotypes about mental illness and violence are common among the general public. Link, Phelan, Bresnahan, Stueve and Pescosolido [ 1 ] presented a large sample ( N = 1444) with vignettes of people with mental illness, in which no violent behavior or thoughts were described, and inquired how likely it was that the “patient” would be violent. Many participants believed it likely that the hypothetical mentally ill individual would perpetrate violence: 17% of respondents endorsed violence as likely among those with minor interpersonal problems, and 33% and 61% thought violence was likely among people with major depression or schizophrenia, respectively. Individuals with mental illness are frequently aware of others’ negative perceptions of them, which can worsen isolation, negative affect and treatment adherence [ 2 , 3 ].
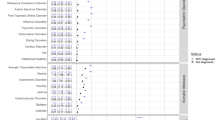
Individuals with psychological disorders that are highly stigmatized and misunderstood, such as schizophrenia, borderline personality disorder (BPD) and dissociative identity disorder (DID), often face harmful and inaccurate stereotypes which portray them as dangerous and untreatable menaces who require psychiatric or forensic institutionalization. However, as we will review in this study, it is a myth that individuals with DID are the most likely patients in the mental health system to be violent. Various methodologies have been used to study the link between mental illness and violence including: reporting on the prevalence of mental illness among convicted violent offenders, typically homicide defendants; examining violent behavior and crime among clinical populations; and assessing prevalence of violent behavior and crime among those with mental illness in the general population (see Tables 1 , 2 , 3 , 4 and 5 below for the results of studies utilizing each of these methodologies). Many studies examine only violence perpetration, but some examine victimization as well [ 4 – 6 ] (Table 1 ).
In research on the prevalence of mental illness among violent offenders, multiple studies have found the highest rates of violence among individuals with substance use disorders, rather than schizophrenia, BPD and other psychotic disorders [ 7 – 11 ] (Tables 2 and 3 ). Rates of substance use disorders (including alcohol use disorders and illicit substance use disorders) among self-reported violent offenders range from 20 to 42% [ 7 , 11 , 12 ] (Table 2 ). Rates of substance use disorders among convicted homicide offenders are lower but still noteworthy, ranging from 1 to 20% [ 8 , 9 , 13 , 14 ] (Table 3 ).
Other studies have approached the question of how mental illness intersects with violence through examining rates of violent behavior among clinical populations. These studies tend to focus on severe/serious mental illness (SMI), that is, disorders which cause or are associated with serious functional impairment or limitations on major life activities [ 15 ]. The majority of studies on violent behavior among SMI patients focus on schizophrenia, although some also include other SMIs such as bipolar disorder and antisocial personality disorder (Table 4 ). Studies on violent behavior and homicide among individuals with schizophrenia indicate these individuals are at increased risk for both violence perpetration and victimization, but that violence is often predicted by comorbid substance use, medication noncompliance and a recent history of being assaulted [ 16 – 18 ]. Studies on violent behavior among individuals with BPD indicate that emotion dysregulation is a longitudinal mediator of violent behavior and may be a primary mechanism that increases risk for violence in this population [ 19 , 20 ]. The complex DDs, including DID, have been conceptualized as disorders of emotional dysregulation and are often highly comorbid with BPD [ 21 ]. The association of emotion dysregulation with violence in DDs should be further examined.
Dissociative disorders and violent behavior
Notably missing from almost all studies on the intersection of mental illness and violent crime are individuals with dissociative disorders (DDs), including DID and DD not otherwise specified (DDNOS in DSM-IV)/other specified DD (OSDD in DSM-5). This is true of mixed clinical population studies [ 22 – 25 ], studies on violence and mental illness in the general population [ 7 , 11 , 12 , 26 ], as well as forensic studies of convicted violent offenders [ 8 , 9 , 13 , 14 , 27 ]. Although DID is missing from almost all the research on mental illness and violence, it gets an inordinate amount of focus in films about mental illness, particularly those in the horror and thriller genres such as Split , Psycho, Fight Club or Secret Window which portray people with dissociative self-states as prone to violence including homicide, or within comedies that poke fun at the “outlandishness” of dissociative self-states, such as Me, Myself and Irene. Given the paucity of research on violent behavior among individuals with DDs, coupled with the saturation of stereotypic portrayals of DDs in the media, misunderstanding abounds regarding what role dissociation plays in violent behavior, if any.
A few studies have examined dissociative symptoms, rather than DDs, as a predictor of violent interpersonal behavior within mixed clinical populations (Table 4 ). They typically focus on trait dissociation, that is, chronic and enduring dissociative experiences across multiple contexts [ 28 ], compared to state dissociation, e.g., transient, not enduring and time-limited dissociative experiences [ 29 ], the latter of which are often anecdotally reported by violent offenders, such as amnesia for a violent episode and violence-related dissociative episodes [ 30 ]. Quimby and Putnam [ 31 ] found that among adult psychiatric inpatients, trait dissociation was positively correlated with patient sexual aggression via staff reports. Kaplan and colleagues [ 32 ] found a positive correlation between trait dissociation and patient-reported general aggression among psychiatric outpatients. Dissociation has also been posited to play a role in the intergenerational transmission of domestic violence: grouping young mothers who were survivors of childhood maltreatment based on whether or not they abused their own children, Egeland and Susman-Stillman [ 33 ] found significantly greater trait dissociation among mothers who were abusive as compared to those who were not.
A number of case study reviews, conducted nearly three decades ago, reported high rates of violent behavior among patients with DID, according to reports by their treating clinicians [ 34 – 38 ] (Table 5 ). These studies were typically conducted with small samples derived from the authoring clinician’s case load, relied on clinician reports rather than patient self-report, utilized adult lifetime reporting timeframes rather than specified time frames (the latter is more typical of current studies on violence and mental illness), and did not attempt to objectively verify violent behavior through criminal records or other official documentation. Many studies inquired about DID patients’ violent and/or homicidal dissociative self-states. Footnote 1 Therapists reported that between 33 and 70% of DID patients had violent self-states [ 34 – 37 ]. At times, aggressive self-states within individuals with DID threaten other self-states, which some patients perceive to be internalized homicidal ideation and/or threats, but if carried out, would result in suicide and not homicide. Some of the studies reviewed above did not distinguish violent self-states who were violent towards the individual themselves versus those who were externally violent toward others [ 34 – 36 ]. Putnam and colleagues [ 37 ] make the distinction that while 70% of those with DID had violent or homicidal self-states, 53% of the aggressive self-states were “internally homicidal,” that is, with homicidal ideation toward another self-state. Some DID patients may misperceive these internally aggressive self-states as external violent people, rather than the patient being self-destructive or suicidal [ 39 ]. Putnam and colleagues [ 37 ] describe internalized homicidal behavior as occurring among 53% of their 100 DID patient sample. Some DID patients may also experience flashbacks of past violence perpetrated by another person against them and mistakenly believe they are perpetrating violence against someone else when in fact they are experiencing an intrusive recollection of the past [ 39 ].
Within these aforementioned case studies, clinicians reported that 38–55% of their DID patients had a history of any violent behavior [ 34 , 36 – 38 ]. Ross and Norton [ 38 ] reported that of 236 DID patients, 29% of the males and 10% of females reported being convicted of a crime, and the same percentage reported a history of incarceration. While the type of conviction and reason for incarceration were not specified, Ross and Norton [ 38 ] describe more antisocial behavior among men than women. Loewenstein and Putnam [ 36 ] and Putnam and colleagues [ 37 ] report high rates of sexual assault perpetration among their DID patient samples. Among an all-male sample, Loewenstein and Putnam [ 36 ] reported 13% of patients reported having perpetrated a sexual assault, while in a predominately female sample, Putnam and colleagues [ 37 ] reported 20% of patients reported having perpetrated sexual assault. Lewis, Yeager, Swica, Pincus and Lewis [ 40 ] reported severe childhood maltreatment and adult psychopathology among 12 DID inmates who were incarcerated for homicide. Two studies found 19% of DID patients had completed homicide [ 36 , 37 ]. Loewenstein and Putnam [ 36 ] attribute this extremely high rate of violent behavior to the childhood maltreatment these patients experienced which increases their risk for aggression and violence, as well as their reliance on an all-male sample, who have higher rates of violence. Alternatively, Putnam and colleagues [ 37 ] describe confusion about “personified intraphysic conflicts” among the patients leading to misperceptions about the degree of actual violence among DID patients, as described above.
These numbers are concerning, but they are not consistent with more recent studies of DD patients and clinicians that utilize different sampling techniques and designs. Within the international prospective Treatment of Patients with DD (TOP DD) Network Study, only 2% of clinicians and 4–7% of patients report that DD (including both DID and DDNOS/OSDD) patients perpetrated sexual coercion or sexual assault toward a partner in their adult lifetime [ 41 ]. Additionally, rates of perpetration of intimate partner violence were low among DD patients, according to therapists: only 3.5% of DD patients were reported by their TOP DD therapists as having perpetrated physical or sexual abuse toward a partner in their adult lifetime [ 6 ].
To date, no studies have examined the variables that might contribute to violence and/or criminal behavior among individuals with DDs. Given the important role that emotion dysregulation has had in predicting violence among individuals with BPD, emotion dysregulation should be examined as a possible contributing factor among individuals with DDs. Dissociative and PTSD symptoms may also be associated with violence or criminal behavior due to the possibility that when highly symptomatic, individuals with DDs may be overwhelmed and unable to manage their symptoms such that they become vulnerable to dyscontrol. Lastly, potential psychological comordities to DDs related to violent behavior within the literature, such as mood and substance use disorders, should be examined as potential explanatorty variables for recent criminal justice involvement.
The present study
Many questions remain regarding what role mental illness plays in violence. Are mentally ill individuals more likely to perpetrate violence compared to people who do not have mental illness? What psychiatric diagnoses are most highly associated with violent behavior and crime? Are individuals with DDs particularly likely to engage in violent and/or criminal behavior? The present study attempts to provide evidence on violent behavior and crime among individuals with DDs engaged in outpatient treatment.
The purpose of our study was threefold; first, to provide a review of the extant literature on DDs and violent behavior; second, to describe the prevalence of recent criminal justice involvement among a sample of treatment-engaged individuals with DDs; and third, to assess symptomatic predictors of violent behavior and crime among individuals with DDs, including dissociative, emotion dysregulation, posttraumatic stress disorder (PTSD) and depressive symptoms, as well as problematic substance use. We hypothesized that crime rates would be low in our sample of individuals with DDs, with the majority of patients reporting no recent criminal history or involvement with the criminal justice system, unless their involvement was as victims of crime. Additionally, we hypothesized that the aforementioned symptoms (dissociation, emotion dysregulation, PTSD, depression and substance use) would not be significantly associated with recent criminal behavior and justice system involvement.
Overview and recruitment
Clinician and patient participants were recruited through the Treatment of Patients with Dissociative Disorders (TOP DD) Network study. The TOP DD Network study is a longitudinal educational intervention study of patients with DDs who are diagnosed with either DID or DDNOS/OSDD. Over the course of 1 year, patients and clinicians watched weekly 7–15 min psychoeducational and skills training videos and completed written reflection and behavioral exercises. Additionally, therapist and patient participants completed surveys every 6 months (at baseline, 6, 12, 18 and 24 months) that provided additional clinical and behavioral data.
Clinicians were recruited through listservs for mental health professionals, professional trauma conferences and emails to participated in the first TOP DD study [ 42 , 43 ]. Clinicians were asked to enroll as a dyad with one DD patient from their caseload. All clinician and patient participants completed a voluntary consent process, and the study was approved by the Towson University Institutional Review Board. Eligibility requirements for patients in the TOP DD Network study included a DD diagnosis (DID, DDNOS or OSDD); being in treatment with their current clinician for at least 3 months prior to starting the study; reading English at an 8 th grade level; being willing to continue in individual therapy and complete approximately 2 ½ hours weekly of study activities; and being able to tolerate references to trauma, dissociation and safety struggles.
Participants
The total TOP DD Network study included 242 patients who completed baseline measures, presented after the screening measures which verified study eligibility. TOP DD Network study patient participants were majority female (88.6%), Caucasian (82.1%), middle-aged ( Median = 41), highly-educated (50.9% had at least a college diploma), and primarily resided in the United States (42.3%), although the study recruited internationally with a sizeable portion derived from Norway (27.5%) as well as other countries (30.2%). About half of participants (55.2%) were either in a dating or married relationship. Patients were primarily diagnosed by their therapists as having DID (63.4%). Clinician participants were primarily female (80%) and Caucasian (91.3%). Most reported years of experience as therapists ( Median = 15), as well as in treating trauma ( Median = 13), and dissociation ( Median = 8). Clinicians primarily worked in private practice (81.1%) or in an outpatient clinic or hospital (41.6%).
Patient measures
Criminal justice involvement.
DD patients were asked about involvement with the criminal justice system in the last 6 months including contact with the police, charges, convictions, court cases, fines, incarceration, probation, referral to mental health through the criminal justice system, and serving as a criminal witness. Participants could respond yes or no to these questions. Clinicians were not asked about their patients’ recent criminal justice involvement.
Trait dissociation
Trait dissociation was measured at baseline by the Dissociative Experiences Scale-II (DES) [ 28 ]. DES is a 28-item, 10-point scale (ranging from 0 to 100% of the time) where the participant indicates what percentage of the time a particular dissociative experience occurred within the past month. A meta-analysis by van Ijzendoorn and Schuengel [ 44 ] demonstrated test-retest reliability of .78–.93, α = .93, and convergent validity of r = .67. The measure was scored by adding the item frequency values and dividing by the total number of items, yielding an average summary score for each participant.
- Emotion dysregulation
Emotional dysregulation was measured at baseline by the Difficulties with Emotion Regulation Scale (DERS) [ 45 ]. DERS is a 36-item, 5-point scale (ranging from almost never [0–10% of the time] to almost always [91–100% of the time]) where the participant indicates what percentage of the time a particular difficulty with emotion regulation applies to them. The DERS has six subscales encompassing difficulties with accepting emotions, goal-directed behavior, impulse control, as well as lack of emotional awareness, emotional clarity and emotion regulation strategies. Gratz and Roemer [ 45 ] reported α > .80 for the six DERS subscales, while Mitsopoulou, Kafetsios, Karademas, Papastefanakis & Simos [ 46 ] demonstrated a test-retest reliability ranging from .63 to 81 for the six DERS subscales. The measure was scored by summing the item frequency values.
Posttraumatic stress disorder
PTSD symptomatology and severity was measured with PTSD Checklist-Civilian (PCL-C) [ 47 ]. The PCL-C is a 17-item, 5-point scale (ranging from not at all to extremely) where a participant indicates how often they have experienced a particular PTSD symptom within the past month. A total score of 50 points is the typical cutoff indicating a possible PTSD diagnosis [ 48 ]. Weathers and colleagues [ 47 ] reported a test–retest reliability of .96 with a retest interval of 2 to 3 days [ 47 ]. The measure was scored by summing all items together.
Depressive disorders were assessed by having clinicians report whether their patient currently had a diagnosis of either dysthymia or major depression (yielding answers of yes or no). Major depressive disorder and persistent depressive disorder (e.g., dysthymia) were assessed as potential predictors of criminal behavior.
Substance use
Substance use disorders were assessed by having clinicians report whether their patient currently had a diagnosis of a substance use disorder (differentiated from a substance/medication-induced mental disorder; answers were yes or no.)
Binary logistic regression was utilized to assess symptomatic predictors of recent criminal justice involvement in individuals with DDs. Logistic regression was chosen because it predicts membership for a dichotomous dependent variable (i.e., criminal justice involvement) from multiple independent variables, and is appropriate in cases of unequal group sample sizes. We ran eight separate logistic regressions to assess symptomatic predictors of each of the eight criminal justice involvement variables. We report Nagelkerke R squared effect sizes on the significant omnibus models. We adjusted alpha levels to account for multiple hypothesis testing, and the critical p -value = 0.0062. The sample size for the logistic regression models was N = 125, as variables were used from both clinician and patient surveys, and both pre-baseline screening and baseline surveys, which each contained slightly different sample sizes.
Prevalence of recent criminal justice involvement
Among 173 DD patients, 12.7% reported contact with the police within the last 6 months; the reasons for this contact were not queried. The patients reported low rates of recent criminal behavior in the last 6 months (Table 6 ): 4.8% reported involvement in a court case, although it is unknown what role the patient played in the court proceedings (e.g., witness, victim, alleged criminal); 3.6% were witnesses in a criminal case; 3% reported a legal charge; 1.8% reported a fine (s); 1.2% reported a criminal justice mental health referral; and 0.6% reported having been incarcerated. None of the 173 DD patients reported convictions or probation during the most recent 6 months.
Regarding the nature of criminal justice involvement, patients had the option of explaining criminal justice involvement they labeled as “other.” Eight individuals elected to complete the “other” open text box, indicating the following: calling the non-emergency police due to loud neighbors; reporting a substance abusing child to the police; reporting criminal offenses; participating in divorce court and domestic violence orders; receiving a traffic ticket; “[meeting] with secret service;” reporting a suspicious vehicle; and being admitted to the hospital with police involvement.
Symptomatic predictors of criminal justice involvement
Within binary logistic regressions assessing symptomatic predictors of eight types of recent criminal justice involvement, symptomatology significantly predicted recent contact with police, χ 2 (6) = 13.28, p < .05, Nagelkerke R 2 = 0.17. Post-hoc tests indicated that only PTSD symptoms (via the PCL-C) significantly predicted recent contact with police, p < .01. However, after applying the critical p -value = 0.0062, neither the omnibus model nor the post-hoc tests remained significant.
Symptomatology also significantly predicted recent contact with the court system, χ 2 (6) = 26.18, p < .001, Nagelkerke R 2 = 0.59. Post-hoc tests indicated that PTSD symptoms (via the PCL-C) significantly predicted recent contact with the court system, p < 01, as well as a substance use disorder diagnosis (via clinician report), p < .01. However, after applying the critical p -value = 0.0062, the post-hoc tests did not remain significant.
The present study had three aims: first, to provide a review of the extant literature on DDs and violent behavior; second, to describe the prevalence of recent criminal justice involvement among a sample of treatment-engaged individuals with DDs; and third, to assess symptomatic predictors of recent criminal justice involvement within the DD sample.
As we hypothesized, criminal justice involvement among individuals with DDs within the prior 6 months was low, according to patient self-reports. Specifically, patients reported the following in the prior 6 months: 4.8% were involved in a court proceeding, 3.6% were witnesses in a criminal case, 3% had a legal charge, 1.8% received a fine (s), 1.2% received a criminal justice mental health referral, and only 0.6% had been incarcerated. None of the DD patients reported convictions or probation during the past 6 months. This contrasts with prior case study reviews of DID patients in which clinicians reported a history of violent behavior among 29–55% of DID patients, and severely violent crime (e.g., homicide and sexual assault) among upwards of 20% of patients [ 34 , 36 – 38 ]. While the prior studies assess lifetime rates, as compared to the present study’s 6-month time frame, and relied on clinician reports rather than patient self-reports, the inconsistencies are instructive. The contrasting results may mean that as sampling and assessment techniques develop, research on individuals with DDs will increasingly suggest they are not as prone to violence or crime as initially thought, as violence towards self may have been conflated with violence towards others. Individuals with DD seem to pose a greater threat to themselves then to anyone else, as reflected in their very high rates of self-injurious behavior and frequent suicide attempts [ 42 , 43 , 49 ].
Additionally, our hypothesis that symptoms of emotion dysregulation, dissociation, PTSD, depression (major depressive disorder and persistent depressive disorder), and substance use disorder were not associated with criminal justice involvement in our sample was supported. Out of eight different types of recent criminal justice involvement, symptoms were able to significantly predict only DD patients’ recent contact with police, as well as recent court involvement, but the former omnibus model did not remain significant after applying the critical alpha which adjusted for Type I error due to multiple hypothesis testing. Regarding recent court involvement, PTSD symptoms and substsance use disorder symptoms significantly predicted recent court involvement, but again, these post-hoc tests did not remain significant after applying the critical alpha. Thus, no symptoms reliably predicted criminal behavior among those with DDs. More importantly, dissociative symptoms did not significantly predict any type of criminal justice involvement among our sample of DD patients. This counters the notion that dissociative symptoms increase risk for criminal and violent behavior. It is also possible that given the high level of dissociation and PTSD among our sample, the strength of the relationships could have been attenuated due to a ceiling effect.
Our study’s major limitations concern selection bias and the nature of data available on patients’ criminal justice involvement. First, our participants are in psychotherapeutic treatment and thus may not be representative of those with DDs who do not present to treatment, nor of those in the criminal justice system who have DDs and dissociation. Additionally, by definition, our sample experience severe and chronic trait dissociation, but some criminal behavior may be more related to state dissociation [ 29 , 30 ]. Second, our data on patients’ criminal justice system involvement was limited: we did not collect clinician reports of patients’ recent criminal justice involvement, details regarding the nature of patients’ recent criminal justice involvement (i.e., our data on police contact and court cases are ambiguous as to whether they indicate possible criminal behavior or being involved as a witness or victim), nor data on lifetime criminal justice involvement. Many studies on mental illness and violent behavior use lifetime rates, and thus this would facilitate comparisons across studies.
Using patient self-reports of criminal justice involvement in the present study may have provided more accurate responses than only using clinician reports, as it is possible that patients would not report criminal behavior to their clinicians due to social desirability concerns and taboos around criminality, although clinician reports would have been a useful adjunct to patient self-reports. Future studies should review criminal justice records for this population because lifetime memories can be difficult to accurately solicit due to amnesia, and due to the confusion some patients may experience between past and present as well as internal versus external events [ 39 ]. Future studies should assess both lifetime and recent criminal justice involvement, utilizing clinician reports and criminal justice records in addition to patient self-reports.
Studies on psychopathology and violent behavior should include DD individuals in their samples. Small forensic studies have assessed DDs in violent offenders [ 40 ] but larger epidemiological studies of violent offenders have not included DDs, despite assessing a range of psychopathology among offenders [ 7 – 9 , 11 – 14 , 26 , 27 ].
In summary, recent criminal justice involvement among our DD clinical sample is low, according to patient self-reports and is not predicted by dissociative, PTSD or emotion dysregulation symptoms, nor by clinician reported substance abuse disorders or mood disorders. This provides compelling evidence contradicting public and media misconceptions and stereotypes of those with DDs as highly prone to criminality and violence. Public awareness about DDs needs to improve through thoughtful and accurate portrayals of DD, as well as all mental illnesses, in media and literature so that stereotypes and stigma are replaced with understanding and scientifically based knowledge. Enduring stigmas portraying those with mental illness as violent may have considerable negative impacts on their treatment engagement, ability to seek out social support, and overall quality of life [ 2 , 3 ]. Reductions in stereotypes and stigma will allow those with mental illness to live more comfortably and safely and allow the general public to also be less fearful and more compassionate towards those with DDs and all forms of mental illness.
Sometimes referred to as personalities, identities or parts.
Abbreviations
Borderline personality disorder
- Dissociative disorders
Dissociative disorder not otherwise specified
Difficulties with Emotion Regulation Scale
Dissociative Experiences Scale
Dissociative identity disorder
Diagnostic and Statistical Manual of Mental Disorders
Other specified dissociative disorder
PTSD Checklist-Civilian
Severe mental illness
Treatment of Patients with Dissociative Disorders Network Study
Link BG, Phelan JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: Labels, causes, dangerousness, and social distance. Am J Public Health. 1999;89(9):1328–33.
Article CAS PubMed PubMed Central Google Scholar
Gonzales L, Davidoff KC, Nadal KL, Yanos PT. Microaggressions experienced by persons with mental illnesses: An exploratory study. Psychiatr Rehabil J. 2015;38(3):234–41.
Article PubMed Google Scholar
Stuart H. Media portrayal of mental illness and its treatments: What effect does it have on people with mental illness? CNS Drugs. 2006;20(2):99–106.
Crisanti AS, Frueh BC, Archambeau O, Steffen JJ, Wolff N. Prevalence and correlates of criminal victimization among new admissions to outpatient mental health services in Hawaii. Community Ment Health J. 2014;50(3):296–304.
Teplin LA, McClelland GM, Abram KM, Weiner DA. Crime victimization in adults with severe mental Illness: Comparison with the National Crime Victimization Survey. Arch Gen Psychiatry. 2005;62(8):911–21.
Article PubMed PubMed Central Google Scholar
Webermann AR, Brand BL, Chasson GS. Childhood maltreatment and intimate partner violence in dissociative disorder patients. Eur J Psychotraumatol. 2014;5:1–8.
Article Google Scholar
Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2009;66(2):152–61.
Fazel S, Grann M. Psychiatric morbidity among homicide offenders: A Swedish population study. Am J Psychiatry. 2004;161(11):2129–31.
Flynn S, Abel KM, While D, Mehta H, Shaw J. Mental illness, gender and homicide: A population-based descriptive study. Psychiatry Res. 2011;185(3):368–75.
González RA, Igoumenou A, Kallis C, Coid JW. Borderline personality disorder and violence in the UK population: Categorical and dimensional trait assessment. BMC Psychiatry. 2016;16:1–10.
Swanson JW, Holzer CE, Ganju VK, Jono RT. Violence and psychiatric disorder in the community: Evidence from the Epidemiologic Catchment Area surveys. Hosp Community Psychiatry. 1990;41(7):761–70.
CAS PubMed Google Scholar
Coker KL, Smith PH, Westphal A, Zonana HV, McKee SA. Crime and psychiatric disorders among youth in the US population: An analysis of the national comorbidity survey–adolescent supplement. J Am Acad Child Adolesc Psychiatry. 2014;53(8):888–98.
Rodway C, Flynn S, While D, Rahman MS, Kapur N, Appleby L, Shaw J. Patients with mental illness as victims of homicide: A national consecutive case series. Lancet Psychiatry. 2014;1(2):129–34.
Simpson AF, McKenna B, Moskowitz A, Skipworth J, Barry-Walsh J. Homicide and mental illness in New Zealand, 1970–2000. British J Psychiatry. 2004;185(5):394–8.
Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15–4927, NSDUH Series H-50). Center for Behavioral Health Statistics and Quality. 2015. https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf . Retrieved 3 Aug 2016.
Gourion D. Schizophrenia and violence: A common developmental pathway? In: Verrity PM, editor. Violence and aggression around the globe. Hauppauge: Nova; 2007. p. 29–44.
Google Scholar
Swanson JW, Borum R, Swartz MS, Monahan J. Psychotic symptoms and disorders and the risk of violent behaviour in the community. Crim Behav Ment Health. 1996;6(4):309–29.
Walsh E, Gilvarry C, Samele C, Harvey K, Manley C, Tattan T, Tyrer P, Creed F, Murray R, Fahy T. Predicting violence in schizophrenia: A prospective study. Schizophr Res. 2004;67(2–3):247–52.
Newhill CE, Eack S, Mulvey EP. A growth curve analysis of emotion dysregulation as a mediator for violence in individuals with and without borderline personality disorder. J Pers Disord. 2012;26(3):452–67.
Scott LN, Stepp SD, Pilkonis PA. Prospective associations between features of borderline personality disorder, emotion dysregulation, and aggression. Pers Disord. 2014;5(3):278–88.
Brand BL, Lanius RA. Chronic complex dissociative disorders and borderline personality disorder: Disorders of emotion dysregulation? Borderline Personal Disord Emot Dysregul. 2014;1:13.
Bruce M, Cobb D, Clisby H, Ndegwa D, Hodgins S. Violence and crime among male inpatients with severe mental illness: Attempting to explain ethnic differences. Soc Psychiatry Psychiatr Epidemiol. 2014;49(4):549–58.
Hodgins S, Alderton J, Cree A, Aboud A, Mak T. Aggressive behaviour, victimisation and crime among severely mentally ill patients requiring hospitalisation. British J Psychiatry. 2007;191(4):343–50.
Matejkowski JC, Cullen SW, Solomon PL. Characteristics of persons with severe mental illness who have been incarcerated for murder. J Am Acad Psychiatry Law. 2008;36(1):74–86.
PubMed Google Scholar
Jordan B, Schlenger WE, Fairbank JA, Caddell JM. Prevalence of psychiatric disorders among incarcerated women: Convicted felons entering prison. Arch Gen Psychiatry. 1996;53(6):513–9.
Article CAS PubMed Google Scholar
Crime in the United States, 2014. United States Department of Justice, Federal Bureau of Investigation.2015. https://ucr.fbi.gov/crime-in-the-u.s/2014/crime-in-the-u.s.-2014/cius-home . Retrieved 3 Aug 2016.
Wilcox DE. The relationship of mental illness to homicide. Am J Forensic Psychiatry. 1985;6(1):3–15.
Carlson EB, Putnam FW. An update on the Dissociative Experiences Scale. Dissociation. 1993;6(1):16–27.
Kruger C, Mace CJ. Psychometric validation of the State Scale of Dissociation (SSD). Psychol Psychother Theory Res Pract. 2002;75:33–51.
Moskowitz A. Dissociation and violence: A review of the literature. Trauma Violence Abuse. 2004;5(1):21–46.
Quimby LG, Putnam FW. Dissociative symptoms and aggression in a state mental hospital. Diss. 1991;4(1):21–4.
Kaplan ML, Erensaft M, Sanderson WC, Wetzler S, Foote B, Asnis GM. Dissociative symptomatology and aggressive behavior. Compr Psychiatry. 1998;39(5):271–6.
Egeland B, Susman-Stillman A. Dissociation as a mediator of child abuse across generations. Child Abuse Negl. 1996;20(11):1123–32.
Dell PF, Eisenhower JW. Adolescent multiple personality disorder: A preliminary study of eleven cases. J Am Acad Child Adolesc Psychiatry. 1990;29(3):359–66.
Kluft RP. The parental fitness of mothers with multiple personality disorder: A preliminary study. Child Abuse Negl. 1987;11(2):273–80.
Loewenstein RJ, Putnam FW. The clinical phenomenology of males with MPD: A report of 21 cases. Dissociation. 1990;3(3):135–43.
Putnam FW, Guroff JJ, Silberman EK, Barban L, Post RM. Clinical phenomenology of multiple personality disorder: review of 100 recent cases. J Clin Psychiatry. 1986;47(6):285–93.
Ross CA, Norton GR. Differences between men and women with multiple personality disorder. Hosp Community Psychiatry. 1989;40(2):186–8.
International Society for the Study of Trauma and Dissociation. Guidelines for treating dissociative identity disorder in adults, third revision. J Trauma Dissociation. 2011;12(2):115–87.
Lewis D, Yeager CA, Swica Y, Pincus JH, Lewis M. Objective documentation of child abuse and dissociation in 12 murderers with dissociative identity disorder. Am J Psychiatry. 1997;154(12):1703–10.
Webermann AR, Brand BL. The sitting duck syndrome: What contributes to dissociative patients’ being victims and perpetrators of violence? Symposium to be presented to the 33rd Annual International Society for the Study of Trauma and Dissociation (ISSTD) Conference. 2016.
Brand BL, Classen C, Lanius R, Loewenstein R, McNary S, Pain C, Putnam FW. A naturalistic study of dissociative identity disorder and dissociative disorder not otherwise specified patients treated by community clinicians. Psychol Trauma. 2009;1(2):153–71.
Brand BL, McNary SW, Myrick AC, Classen CC, Lanius R, Loewenstein RJ, Pain C, Putnam FW. A longitudinal naturalistic study of patients with dissociative disorders treated by community clinicians. Psychol Trauma. 2013;5(4):301–8.
van Ijzendoorn MH, Schuengel C. The measurement of dissociation in normal and clinical populations: Meta-analytic validation of the Dissociative Experiences Scale (DES). Clin Psychol Rev. 1996;16(5):365–82.
Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26(1):41–54.
Mitsopoulou E, Kafetsios K, Karademas E, Papastefanakis E, Simos PG. The Greek version of the Difficulties in Emotion Regulation Scale: Testing the factor structure, reliability and validity in an adult community sample. J Psychopathol Behav Assess. 2013;35(1):123–31.
Weathers FW, Litz BT, Huska JA, Keane TM. The PTSD Checklist—Civilian Version (PCL-C). Boston: National Center for PTSD; 1994.
Weathers FW, Ford J. Psychometric review of PTSD Checklist. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville: Sidran Press; 1996. p. 250–1.
Webermann AR, Myrick AC, Taylor CL, Chasson GS, Brand BL. Dissociative, depressive, and PTSD severity as correlates of non-suicidal self-injury and suicidality in dissociative disorder patients. J Trauma Dissociation. 2016;17(1):67–80.
Download references
Acknowledgements
The authors warmly thank the patients and therapists who generously donated their time to participate in the TOP DD Network study.
The authors declare that this research was funded by foundations (i.e., ANS Research, Constantinidas Family Foundation), private donations (including from Anne Bartello and family, Brad Foote, M.D. and gifts made to Sheppard Pratt Health System’s Trauma Disorders Research Program and Towson University’s Foundation), and grants from Towson University.
Availability of data and materials
Please contact corresponding author for data requests.
Authors’ contributions
ARW conducted the literature review, analyzed the data and drafted the manuscript. BLB is the Principal Investigator for the study from which the data is derived (the TOP DD Network Study), developed the methods and assisted in manuscript writing. Both authors read and approved the final manuscript.
Authors’ information
Aliya R. Webermann, M.A., is a clinical/community doctoral student at University of Maryland, Baltimore County (UMBC), USA and a graduate of the clinical psychology master’s program at Towson University. Ms. Webermann’s research primarily concerns the links between intimate partner violence, complex trauma and trauma and dissociative disorders. Bethany L. Brand, Ph.D., is the Martha A. Mitten Professor of Psychology at Towson University and maintains an independent practice in clinical psychology on Towson, Maryland, USA. She serves as an expert witness in criminal, civil, disability and employment matters. Dr. Brand conducts research on the assessment and treatment of trauma disorders, including the assessment of feigned dissociative disorders.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The TOP DD Network Study received approval from the Towson University Institutional Review Board in 2014, IRB number IRB00002844. All particpants completed an informed consent process before participating in the study.
Author information
Authors and affiliations.
University of Maryland Baltimore County, 1000 Hilltop Circle, Math/Psychology Building Rm. 312, Baltimore County, Baltimore, MD, 21250, USA
Aliya R. Webermann
Department of Psychology, Towson University, Towson, 21252, MD, USA
Bethany L. Brand
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Aliya R. Webermann .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Webermann, A.R., Brand, B.L. Mental illness and violent behavior: the role of dissociation. bord personal disord emot dysregul 4 , 2 (2017). https://doi.org/10.1186/s40479-017-0053-9
Download citation
Received : 30 October 2016
Accepted : 13 January 2017
Published : 23 January 2017
DOI : https://doi.org/10.1186/s40479-017-0053-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Criminal behavior
- Dissociation
- Violent crime
Borderline Personality Disorder and Emotion Dysregulation
ISSN: 2051-6673
- General enquiries: [email protected]
- Open access
- Published: 09 August 2019
The psychological subtype of intimate partner violence and its effect on mental health: protocol for a systematic review and meta-analysis
- Sarah Dokkedahl ORCID: orcid.org/0000-0003-3090-4660 1 ,
- Robin Niels Kok 2 , 3 ,
- Siobhan Murphy 1 ,
- Trine Rønde Kristensen 4 ,
- Ditte Bech-Hansen 1 &
- Ask Elklit 1
Systematic Reviews volume 8 , Article number: 198 ( 2019 ) Cite this article
65k Accesses
50 Citations
48 Altmetric
Metrics details
Background/aim
Psychological violence is estimated to be the most common form of intimate partner violence (IPV). Despite this, research on the independent effect of psychological violence on mental health is scarce. Moreover, the lack of a clear and consistent definition of psychological violence has made results difficult to compare. The present study therefore aims to consolidate knowledge on psychological violence by conducting a systematic review and random-effects meta-analysis on the association between psychological violence and mental health problems, when controlling for other types of violence (e.g. physical and sexual) and taking into account severity, frequency, and duration of psychological violence.
The present study is registered in the International Prospective Register for Systematic Reviews (PROSPERO; #CRD42018116026) and the study design follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Additional file 1 ). A dual search will be conducted in the electronic databases PsycINFO, PubMed, EMBASE, and Web of Science. Data will be extracted using Endnote and Covidence and a meta-analysis will be conducted using Metafor-package in the programming language R. The Quality Assessment Tool for Quantitative Studies developed by the Effective Public Health Practice Project will be used to assess the quality of the included studies (i.e. weak, moderate and strong).
Results and discussion
The present review will help consolidate knowledge on psychological violence by evaluating whether frequency, severity or actual “type” of psychological violence produces the most harm. A thorough quality assessment will help overcome potential limitations regarding expected variations in terminology and assessment of psychological violence.
Systematic review registration
PROSPERO CRD42018116026 .
Peer Review reports
Intimate partner violence (IPV) is a global health problem characterized as any behaviour within an intimate relationship that causes physical, psychological or sexual harm [ 1 ]. At present, it is well-documented that IPV can cause extensive mental health consequences among its victims [ 2 , 3 , 4 , 5 ]. IPV can be characterized as an interpersonal trauma, and symptoms of posttraumatic stress disorder (PTSD) have been identified in 31–84.4% of women exposed to IPV [ 2 ]; along with other comorbid symptoms such as depression, anxiety, suicidality, substance abuse and sleep disturbances [ 2 , 5 , 6 ].
The subtype of psychological violence (compared to physical and sexual violence) is estimated to be the most common form of IPV in both the USA [ 7 ] and Europe [ 8 ], affecting between 35 and 49% of men and women. This has led legislators in some European countries to criminalize psychological violence as an independent offence, making it equally punishable as physical violence (e.g. Norway [ 9 ] and England [ 10 ]). Although some researchers have argued that psychological violence in itself cannot be classified as a trauma, as it does not meet the first criterion of diagnosing PTSD (i.e. threat to life or physical integrity [ 11 , 12 ]), a more recent review on IPV and mental health argues that psychological violence can independently cause PTSD, depression and anxiety [ 13 ].
Despite both legal recognition of psychological violence and documentation of its effect on mental health, the conceptualization of the phenomenon is ambiguous in both research and clinical practice. Acts of psychological violence are distributed along a continuum starting from what is commonly termed psychological aggression (e.g. yelling and insults) and ending with more severe abuse, often labelled coercion (e.g. threats and isolation). How we interpret psychological aggression and how we distinguish it from more severe abuse depends, among other things, on the context in which it occurs, when it occurred in a sequence, how it was interpreted and whether it was perceived as abusive [ 11 ].
Another challenge is that psychological violence is often characterized in different ways. For example, the conceptualization of “coercive control” can generally be understood in two ways: firstly, as an overall attempt to control one’s partner, in which IPV is a way of achieving control; secondly, as a subtype of IPV which is similar to—or a part of—the concept of psychological violence. The former is described in a structural perspective as more severe and gender-asymmetrical and is generally understood to be a representation of gender inequality [ 14 , 15 , 16 , 17 , 18 ]. The latter reflects a continuum of IPV from psychological aggression to more controlling behaviours constituting an assault [ 11 ]. Moreover, these are theoretical distinctions that have proven difficult for researchers and practitioners to conceptualize and apply.
The distinction between psychological violence and coercion is evident from the WHO, who define psychological violence (i.e. emotional or psychological abuse) such as “insults, belittling, constant humiliation, intimidation (e.g. destroying things), threats of harm, threats to take away children”, while controlling behaviour is defined as “isolating a person from family and friends; monitoring their movements; and restricting access to financial resources, employment, education or medical care” [ 1 ] (p. 1). The specific acts of violence separate these two definitions, while the overall psychological harm combines them. Likewise, the European Institute of Gender Equality (EIGE) states an overall definition of psychological violence, which can be understood from the perspective of caused harm: “Any act or behaviour which causes psychological harm to the partner or former partner. Psychological violence can take the form of, among others, coercion, defamation, a verbal insult or harassment” 19 (p. 45).
These variations in terminology are inevitably reflected in the psychometric instruments developed to assess psychological violence (Table 1 ; identified by the Centers for Disease Control and Prevention and the National Unit [ 20 ] against IPV in Denmark, LUV [ 21 ]). Indeed, the varying use of subscales (e.g. #7 and #9) and differing definitions of psychological violence make the findings from these studies difficult to compare and stresses the need to evaluate how the effect on mental health is influenced by such variations. For example, some instruments assess psychological aggression (e.g. #10), while others measure more severe controlling behaviours (e.g. #4). Furthermore, other instruments focus less on the act of violence and more on the effect on the victim (e.g. #12). When measuring the effect of psychological violence on mental health, the difference between acts and effects can be crucial. Evidence demonstrates that some acts defined as psychologically violent (i.e. threats to kill/harm) have been found to significantly load on a physical violence factor, most likely due to the aspect of physical threat, which makes the psychological and physical aspect hard to differentiate [ 11 ]. Furthermore, a majority of these assessment tools make use of frequency scores that do not differentiate between the severity of items. As such, items of psychological aggression (i.e. being called “ugly” and “worthless”) are equated to severe controlling behaviour and threats (i.e. threats to kill or take away children). This exemplifies how important these distinctions are if we wish to understand the independent effect of psychological violence on mental health. Examining mental health while evaluating the instruments used to measure the phenomenon will help us understand whether severity, frequency or actual “type” of psychological violence produces the most harm on the victim’s mental health [ 11 ].
In addition to problems with the conceptualization, a number of methodological challenges further characterize the field, e.g. sampling, design, scoring and gender bias [ 11 ]. Focusing on psychological aggression in lesbian, gay and bisexual individuals, Mason et al. [ 22 ] highlight the need for future research to clearly and consistently define psychological violence and separate it from other types of violence seeing that a more consistent definition will facilitate better comparisons across studies. The research group further stresses that scoring methods (e.g. frequency vs. dichotomous scoring) influence the magnitude of the effect size, which makes results difficult to compare. This challenge is further complicated by the use of self-administered questionnaires that may lack systematic development [ 22 ]. Moreover, Follingstad [ 11 ] emphasizes the need to differentiate between samples (i.e. dating relationships and marital or long-term cohabiting relationships), seeing that dating relationships are characterized by quantitatively and qualitatively less psychological violence. Finally, the majority of assessment tools are developed to specifically measure female victimization of psychological violence, despite male victimization being reported at equally high rates in some studies [ 7 ]. Although fewer studies have focused on the effects on mental health among male victims of psychological violence, studies indicate that they too present symptoms of anxiety, depression and sleep disturbances [ 13 , 23 ].
The aim of the present systematic review is to build on existing knowledge [ 13 ] concerning the effect of psychological violence on mental health, while evaluating the psychometric instruments used to assess psychological violence about how they conceptualize the phenomenon. To this day, most studies on IPV and mental health have pooled scores of physical, psychological and sexual IPV in their reporting [ 2 , 4 ], making a distinction of the individual effect of psychological violence difficult. When directly examining the effect of psychological violence, the lack of a clear and consistent definition of psychological violence has made results difficult to compare [ 13 , 22 ]. Consequently, important information is lost. The present study therefore aims to consolidate knowledge on psychological violence by evaluating whether frequency, severity or actual “type” of psychological aggression is associated with the most harm on mental health [ 11 ]. Methodological challenges will be considered by conducting quality assessments of all included studies, and results will control for the presence of physical and sexual violence (i.e. severity, duration and frequency). When possible, mediating and moderating factors will be evaluated, as well as potential gender differences. Based on the results, a discussion on assessment tools and methodological challenges will provide the grounds for recommendations concerning future research.
To sum up, the aim of this systematic review and meta-analysis is fourfold: (1) to estimate the individual effect of psychological violence on mental health (e.g. PTSD, depression and anxiety); (2) to estimate whether frequency, severity or actual “type” of violence is associated with the most harm; (3) to investigate gender, sampling and cultural differences through moderation analyses; and (4) to discuss the somewhat vague terminology and methodological challenges.
Methods and design
Methods of review.
The present protocol has been written in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines and is presented in accordance with the PRISMA-P checklist (Additional file 1 ). The protocol has further been registered in PROSPERO (#CRD42018116026).
The systematic review will be conducted as an individual and dual process by two researchers (SD + DBH) in regard to screening, eligibility and inclusion. Screening will be done on a title basis, followed by an abstract and full-text basis. A third researcher (RK) from the team will be consulted to resolve issues regarding disagreement of eligibility and inclusion on a full-text basis. If sufficient data can be extracted, a random-effects meta-analysis will be conducted on the extracted data.
It is expected that not all studies report the recorded data on psychological violence, but rather cluster subtypes of IPV (i.e. physical, sexual and psychological violence). In such cases, the corresponding authors will be contacted and invited to share the raw data.
Key definitions of the systematic review
Intimate partner violence.
As proposed in a statistical definition by EIGE, IPV is defined as “any act of physical, sexual, psychological or economic violence that occurs between former or current spouses or partners, whether or not the perpetrator shares or has shared the same residence with the victim” [ 19 ] (p. 44). This definition has been proposed to aid the EU member states to collect and compare administrative data on violence against women in a standardized manner [ 19 ].
- Psychological violence
A broad terminology for psychological violence is used in both scientific literature and in clinical practice (e.g. psychological violence, emotional abuse, coercion, psychological aggression). For clarity, this review will use the term psychological violence seeing that this definition links it directly to other types of IPV (e.g. physical or sexual violence), while emphasizing a core psychological aspect of harm in both the act of perpetration as well as the effect of victimization. The variation in terminology will shortly be addressed in the discussion.
In the current protocol, psychological violence will be defined by an overall definition combining that of both the WHO [ 1 ] (i.e. both emotional/psychological abuse and controlling behaviours) and the European Institute of Gender Equality [ 19 ]: “Any act or behaviour which causes psychological harm to the partner or former partner. Psychological violence can take the form of, among others, coercion, defamation, a verbal insult or harassment” [ 19 ] (p. 45), including belittling, constant humiliation, intimidation (e.g. destroying things), threats of harm, threats to take away children and/or isolating a person from family and friends; monitoring their movements; and restricting access to financial resources, employment, education or medical care [ 1 ] (p. 1). A broad definition will allow for studies using varying definitions to be included and will be assessed through subgroup analyses. The different definitions will be evaluated and discussed based on their effect on mental health.

Mental health in this context
As mentioned above, it has previously been argued that psychological violence alone cannot be characterized as a trauma [ 11 ]. However, recent studies have identified an association between psychological violence and PTSD [ 13 ]. Based on these findings, the authors consider psychological violence a potential traumatic event and wish to further examine the relationship between psychological violence and PTSD. Other mental health consequences identified are based on the National Institute for Health and Care Excellence (NICE) guidelines and comorbid mental health problems of PTSD [ 24 ], i.e. depression, anxiety, alcohol or drug abuse, suicidality, sexual problems, sleep problems, problems with concentration, somatization and functional problems (e.g. social, educational, or occupational) as well as feelings of shame and guilt.
Search method
A dual search will be conducted in the electronic databases PsycINFO, PubMed, EMBASE and Web of Science. Other methods used for identifying relevant research include reference checking and hand-searching of grey literature. Furthermore, the following scientific journals will be hand-searched: Journal of Interpersonal Violence and Journal of Violence and Victims .
Criteria for including studies
The review will include studies of psychological violence on mental health when controlling for other types of partner abuse. Hence, studies including an adult (≥ 18 years) population of victims of IPV (dating samples, national samples, clinical settings, etc.) that report on psychological violence specifically. Many studies are expected to include groups of comparison (e.g. non-abused or other types of abuse); however, comparisons are not required.
Furthermore, the review will only include peer-reviewed articles in English, German, Dutch or Scandinavian languages (i.e. Norwegian, Swedish or Danish).
Criteria for excluding studies
The review will exclude case studies, reviews, commentaries, editorials, letters to editorials, book chapters and other non-primary research articles.
Search string
See Table 2 for the PsycINFO search string.
Main outcome of interest
To investigate the independent effect of psychological violence on mental health. A meta-analysis will be performed to estimate the effect of psychological violence on PTSD, depression and anxiety. A narrative summary will present all related mental health problems as defined by the NICE guidelines [ 24 ].
Secondary outcomes of interest include the following:
How does “type” of psychological violence affect mental health?
How does frequency and severity affect mental health outcomes? (e.g. high frequency and/or low severity or low frequency and/or high severity).
Are there potential gender differences in mental health consequences with regard to psychological violence?
Will controlling for previous trauma affect the association between psychological violence and mental health?
Does sample population differ in mental health consequences? (e.g. dating samples vs. treatment samples)
Finally, the systematic review aims to evaluate included psychometric tools measuring psychological violence and how potential variations in the conceptualization of psychological violence affects results.
Data extraction
Data will be extracted with help from Endnote and Covidence. Meta-analyses will be conducted using the programming language R. The authors will design a data extraction form. The form will include authors, year, sample size, population, country, age, gender, design, IPV assessment tool(s), mental health assessment, primary outcome (effect size), secondary outcome(s), timeframe of assessment (lifetime or specified), scoring method(s), previous trauma and previous mental health problems. Data will be extracted by one reviewer (SD), and independently cross-checked by another reviewer (DBH). Inconsistencies in data extraction will be resolved between the reviewers by referring to the source study until a consensus is reached.
Quality assessment
The “Quality Assessment Tool for Quantitative Studies” developed by the Effective Public Health Practice Project [ 25 ] will be used to assess the quality of the included studies. This is in line with previous research evaluating IPV psychometric tools [ 26 ]. Assessment will be based on six components: (1) selection bias, (2) study design, (3) confounders, (4) blinding, (5) data collection methods and (6) withdrawals and dropouts [ 24 , 25 ]. Two researchers (SD and DBH) will classify studies on three levels: weak, moderate and strong. If classifications are inconsistent a third researcher (RK) will be involved and classification will be discussed until consensus is reached. If possible, moderation analyses will compare studies of strong vs. weak quality.
Plan for data synthesis
As demonstrated above, studies on psychological violence are quite heterogeneous in regard to conceptualization, psychometrics, sampling, design, scoring, and so forth. Therefore, we will perform a random-effects meta-analysis, because we expect high heterogeneity in the included studies. The random-effects meta-analysis assumes variance in effect across studies due to real differences in effect as well as by chance. The meta-analysis will help estimate the common effect of psychological violence on mental health (i.e. PTSD, depression and anxiety) by synthesizing individual results. If possible, moderation analyses will compare studies according to quality assessment and varying samples. The I 2 statistic will be used to test for heterogeneity, and as suggested, an I 2 statistic above 75% implies considerable heterogeneity, while an I 2 statistic below 40% is not considered to be a concern [ 27 ].
The included studies are expected to report effect sizes of varying types (i.e. correlation, regression, mean differences and association of categorical variables, e.g. odds ratio). For data synthesis, the reported effect sizes will be recoded into the same type of effect size using the programming language R. For this meta-analysis, we expect to perform a stepwise analysis according to the outcome of interest. For the main outcome of interest, as well as subgroup analyses, the meta-analysis will be conducted with effect sizes based on correlations. Additionally, the impact of the duration and frequency of psychological violence will be estimated by using meta-regression. The Metafor-package for the programming language R will be applied to conduct the meta-analysis [ 28 ].
The present review will build on existing knowledge by statistically synthesizing results on the effect of psychological violence on mental health. The review will help consolidate knowledge on psychological violence by evaluating whether frequency, severity or actual “type” of psychological violence produces the most harm. This will strengthen our knowledge on psychological violence, and how best to assess and conceptualize the phenomenon.
While conducting the systematic review, we expect to encounter several limitations. The varying terminology and definitions of psychological violence will make results difficult to compare, just as the many and varying psychometrics tools will (Table 1 ). This is further complicated by the fact that many studies are likely to not even use validated instruments but instead base their results on a few self-constructed items. The review will aim to overcome these limitations by thorough quality assessment of the included studies with help from the Quality Assessment Tool for Quantitative Studies [ 25 ] and by performing relevant subgroup analyses. This does not only apply to psychological violence, but also mental health definitions and the psychometric instruments used to assess symptomatology. By critically examining the applied definitions and terminology as well as methodological challenges (e.g. sampling, design, scoring and gender bias) the review will serve as a status quo of the field and make grounds for future recommendations.
Finally, the systematic review is expected to have several clinical implications. We expect the meta-analysis to deepen our understanding of the different subtypes of psychological violence and how they independently interact with mental health outcomes. Likewise, we expect to give clarity on psychological violence and whether it should be understood as a traumatic event equal to other types of abuse (e.g. physical or sexual violence). Developing both preventive efforts and treatment programmes such information is important if we wish to directly target the needs of those affected by psychological violence and raise awareness to encourage both victims and perpetrators to seek help.
In research, this systematic review is expected to inspire researchers to clearly and consistently define psychological violence while carefully considering the psychometrics used to measure the phenomenon, as well as other methodological challenges. Moreover, we expect to get clarity on any potential gender bias.
On a final note, this work will hopefully inspire others to conduct similar research on children who grow up as either witnesses or victims of psychological violence.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
World Health Organization. Understanding and addressing violence against women: 2012. Retrieved from: http://apps.who.int/iris/bitstream/handle/10665/77432/WHO_RHR_12.36_eng.pdf?sequence=1 .
Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. J Fam Violence. 1999;14(2):99–132.
Article Google Scholar
Dutton MA, Green BL, Kaltman SI, Roesch DM, Zeffiro TA, Krause ED. Intimate partner violence, PTSD, and adverse health outcomes. J Interpers Violence. 2006;21(7):955–68.
Johnson DM, Zlotnick C, Perez S. The relative contribution of abuse severity and PTSD severity on the psychiatric and social morbidity of battered women in shelters. Behavior Therapy. 2008;39:232–41.
Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, et al. Intimate partner violence and incident depressive symptoms and suicide attempts: A systematic review of longitudinal studies. PLOS Med. 2013;10(5):e1001439.
Pigeon WR, Cerulli CJD, Richards HMS, He H, Perlis M, Caine E. Sleep disturbances and their association with mental health among women exposed to intimate partner violence. J Women’s Health. 2011;20(12):1923–9.
Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and. Prevention. 2011; Retrieved from: https://www.cdc.gov/violenceprevention/pdf/nisvs_report2010-a.pdf .
European Union Agency for Fundamental Rights (EUAFR). Violence against women, an EU-wide survey: Main results. Vienna: European Union Agency for Fundamental Rights; 2014. Retrieved from https://fra.europa.eu/en/publication/2014/violence-against-women-eu-wide-survey-main-results-report .
Aas G, Andersen T. Mishandlingsbestemmelsen – En evaluering av loven mot mishandling I nære relasjoner jf. Strl. § 219 (§ 282/283). Politihøgskolen, Oslo; 2017. Retrieved from: https://phs.brage.unit.no/phs-xmlui/handle/11250/2427624 .
Home Office. Controlling or coercive behaviour in an intimate or family relationship – statutory guidance. framework. December, 2015; Retrieved from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/482528/Controlling_or_coercive_behaviour_-_statutory_guidance.pdf .
Follingstad DR. The impact of psychological aggression on women’s mental health and behavior – the status of the field. Trauma, Violence, Abuse. 2009;10(3):271–89.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM - IV - TR . Washington, DC: American Psychiatric Association; 2000.
Google Scholar
Lagdon S, Armour C. Stringer. Adult experiences of mental health outcomes as a result of intimate partner violence victimization: A systematic review. Eur J Psychotraumatol. 2014;5:24794.
Stark E. Coercive control. New York: Oxford University Press; 2007.
Stark E. Do violent acts equal abuse? Sex roles. 2010;62:201–11.
Johnson MP. Patriarchal terrorism and common couple violence. J Marriage Fam. 1995;57(2):283–94.
Johnson MP. A typology of domestic violence. Boston, MA: Northeastern University Press; 2008.
Walby S, Towers J. Untangling the concept of coercive control: Theorizing domestic violent crime. Criminology Criminal Justice. 2018;18(1):7–28.
EIGE. Glossary of definitions of rape, femicide, and intimate partner violence; 2017. Retrieved from: https://eige.europa.eu/rdc/eige-publications/glossary-definitions-rape-femicide-and-intimate-partner-violence
Thompson MP, Basile KC, Hertz MF, Sitterle D. Measuring intimate violence victimization and perpetration: A compendium of assessment tools. Atlanta (GA): Centers for Disease Control and Prevention, National Center Injury. Prev Control. 2006.
Oldrup, H., Andersen, S., Kjær. S., Nielsen, NH., von Rosen, CB. Psykiske, fysiske og sociale konsekvenser af psykisk vold i parforhold – kortlægning af forskning. Lev Uden Vold. København; 2018. Retrieved from: https://levudenvold.dk/wp-content/uploads/2018/08/rapport-konsekvenser-af-psykisk-vold-web.pdf
Mason TB, Lewis RJ, Milletich RJ, Kelley ML, Minifie JB, Derlega VJ. Psychological aggression in lesbian, gay, and bisexual individuals’ intimate relationships: A review of prevalence, correlates, and measurement issues. Aggress Violent Behav. 2014;19:219–34.
Próspero M. The effect of coercion in aggression and mental health among reciprocally violent couples. J Fam Violence. 2008;23:195–202.
National Collaborating Centre for Mental Health. Post-traumatic stress disorder – the management of ptsd in adults and children in primary and secondary care. National Clinical Practice Guidelines Number 26. The Royal College of Psychiatrists & The British Psychological Society. Gaskell and the British Psychological Society. Cromwell Press Limited, Trowbridge, Wiltshire; 2005. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK56494/pdf/Bookshelf_NBK56494.pd .
National Collaborating Centre for Methods of and Tools. Qualitative assessment tool for quantitative studies. Hamilton, ON: McMaster University; 2008. (Updated 03 October, 2017). Retrieved from: https://www.nccmt.ca/knowledge-repositories/search/14 .
Arkins B, Begley C, Higgins A. Measures for screening intimate partner violence: A systematic review. J Psychiatr Ment Health Nurs. 2016;23:217–35.
Article CAS Google Scholar
Cooper H. Research synthesis and meta-analysis. 5 th Ed. Duke University: Sage Publications, Inc.; 2017.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:3:1–48.
Shepard MF, Campbell JA. The Abusive Behavior Inventory: A measure of psychological and physical abuse. J Interpers Violence. 1992; 7 :291–305.
Hegarty K, Sheehan M, Schonfeld C. A multidimensional definition of partner abuse: Development and preliminary validation of the Composite Abuse Scale. J Fam Violence. 1999;14:399–415.
Hegarty K, Bush R, Sheehan M. The Composite Abuse Scale: Further development and assessment of reliability and validity of a multidimensional partner abuse measure in clinical settings. Violence Victims. 2005;20:529–47.
Sullivan CM, Bybee DI. Reducing violence using community-based advocacy for women with abusive partners. J Consult Clin Psychol. 1999;67:43–53.
Sullivan CM, Parisian JA, Davidson WS. Index of psychological abuse: Development of a measure. Poster presentation at the annual conference of the American Psychological Association. San Francisco (CA; 1991.
O’Leary KD. Psychological abuse: A variable deserving critical attention in domestic violence. Violence Victims. 1999;14:3–23.
Rodenburg FA, Fantuzzo JW. The Measure of Wife Abuse: Steps toward the development of a comprehensive assessment technique. J Fam Violence. 1993;8:203–28.
Murphy CM, Hoover SA. Measuring emotional abuse in dating relationships as a multifactorial construct. Violence Victims. 1999;14:39–53.
Murphy C, Hoover S, Taft C. The Multidimensional Measure of Emotional Abuse: Factor structure and subscale validity. Toronto: Association for the Advancement of Behavior Therapy; 1999.
Hudson WW. The WALMYR assessment scales scoring manual. Tallahassee (FL): WALMYR Publishing Company; 1997.
Sackett LA, Saunders DG. The impact of different forms of psychological abuse on battered women. Violence and Victims. 1999;14:105–77.
Tolman RM. The development of a measure of psychological maltreatment of women by their male partners. Violence Victims. 1989;4:159–77.
Tolman RM. The validation of the Psychological Maltreatment of Women Inventory. Violence Victims. 1999;14:25–37.
Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scale (CTS2): development and preliminary psychometric data. J Fam Iss. 1996;17:283–316.
Straus MA, Hamby SL, Warren WL. The Conflict Tactics Scale handbook . Los Angeles (CA: Western Psychological Services; 2003.
Foshee VA, Linder GF, Bauman KE, et al. The Safe Dates project: Theoretical basis, evaluation design, and selected baseline findings. Am J of Prev Med. 1996;12:39–47.
Foshee VA, Bauman KE, Arriaga XB, Helms RW, Koch GG, Linder GF. An evaluation of Safe Dates, an adolescent dating violence program. Am J Public Health. 1998;88:45–50.
Smith PH, Earp JL, DeVellis R. Measuring battering: Development of the Women’s Experiences with Battering (WEB) Scale. Women’s. Womens Health. 1995;(1):273–88.
Smith PH, Smith JB, Earp JL. Beyond the measurement trap: A reconstructed conceptualized and measurement of woman battering. Psychology of Women Quarterly. 1999;23:177–93.
Smith PH, Thornton GE, DeVellis R, Earp J, Coker AL. A population-based study of the prevalence and distinctiveness of battering, physical assault, and sexual assault in intimate relationships. Violence Against Women. 2002;8:1208–32.
Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil AHITS. A short domestic violence screening tool for use in a family practice setting. Fam Med. 1999;30(7):508–12.
Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil A. HITS: a short domestic violence screening tool for use in a family practice setting. Fam Med. 1998;30(7):508-12.
Swahnberg IMK, Wijma B. The NorVold Abuse Abuse Questionnaire (NorAQ) – a validation of new measures of emotional, physical, and sexual abuse, and abuse in the health care system among women. Eur J Public Health. 2003;13:361–6.
Graham-Kevan N, Archer J. Physical aggression and control in heterosexual relationships: The effect of sampling. Violence Victims. 2003;18(2):181–96.
Follingstad DR, Coyne S, Gambone L. A representative measure of psychological aggression and its severity. Violence Victims. 2005;20(1):25–38.
Dutton, MA., Goodman, L., Schmidt, RJ. Development and validation of coercive control measure for intimate partner violence – final technical report. COSMOS Corporation: Bethesda, Maryland; 2005. Retrieved from: https://www.ncjrs.gov/pdffiles1/nij/grants/214438.pdf
Follingstad DR. A measure of psychological abuse normed on a nationally representative sample of adults. J Interpers Violence. 2010;26(6):1–21.
Rogers JM, Follingstad DR. Women’s experience to psychological abuse: Does that experience predict mental health outcomes? J Fam Violence. 2014;29(6):595–611.
Campbell DW, Campbell J, King C, Parker B, Ryan J. Violence Victims. 1994;9(3):259–74.
Campbell JC, Webster DW, Glass N. The danger assessment – validation of a lethality risk assessment instrument for intimate partner femicide. J Interpers Violence. 2009;24(4):653–74.
Download references
Acknowledgements
Not applicable.
These materials have received financial support from The Danish Victims Fund. The execution, content, and results of the materials are the sole responsibly of the authors. The analysis and viewpoints that have been made evident from the materials belong to the authors and do not necessarily reflect the views of The Council of The Danish Victims Fund. Funding was granted to Sarah Dokkedahl.
Author information
Authors and affiliations.
National Centre of Psychotraumatology, Department of Psychology at the University of Southern Denmark, 5230, Odense M, Denmark
Sarah Dokkedahl, Siobhan Murphy, Ditte Bech-Hansen & Ask Elklit
Department of Psychology at the University of Southern Denmark, Odense, Denmark
Robin Niels Kok
Centre for Innovative Medical Technology, Odense University Hospital, Odense, Denmark
Centre for persons subjected to violence, Frederiksberg Hospital, Frederiksberg, Denmark
Trine Rønde Kristensen
You can also search for this author in PubMed Google Scholar
Contributions
The present protocol has been prepared and written by the corresponding author Sarah Dokkedahl, with contributions from all the co-authors. All authors have contributed to the development of the search string and Robin Kok contributed in the development of the plan for data synthesis. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Sarah Dokkedahl .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
PRISMA-P 2015 Checklist (DOCX 30 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Dokkedahl, S., Kok, R.N., Murphy, S. et al. The psychological subtype of intimate partner violence and its effect on mental health: protocol for a systematic review and meta-analysis. Syst Rev 8 , 198 (2019). https://doi.org/10.1186/s13643-019-1118-1
Download citation
Received : 06 December 2018
Accepted : 26 July 2019
Published : 09 August 2019
DOI : https://doi.org/10.1186/s13643-019-1118-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emotional abuse, Intimate partner violence
- Mental health
- Psychometrics
- Abbreviations
- DSM Diagnostic and statistical manual of mental disorders
- EIGE European Institute of Gender Equality
- ICD International Classification of Diseases
- IPV Intimate Partner Violence
- NICE National Institute for Health and Care Excellence
- PMWI Psychological Maltreatment of Women Inventory
- PTSD Posttraumatic Stress Disorder
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Advisory Board
- Publications
- Data & Tools
- News & Analysis
- Stepping Up
- Justice Reinvestment
- Reentry 2030
- Justice & Mental Health Collaboration Program (JMHCP)
- More Projects
- Career Opportunities
- Partner With Us
- Stay Connected

Addressing Misconceptions about Mental Health and Violence
Despite public perception that there is a direct connection between mental health and violence, research shows that this relationship is complex and that the presence of a mental illness doesn’t automatically predispose a person to violent behavior. As criminal justice professionals work to protect public safety, it’s important that their policies and practices reflect accurate information, not common misperceptions. This brief addresses these misconceptions, presents important information about risk factors for violence, and offers ways that criminal justice professionals can help mitigate such risks.
Project Credits
About the author.
When incidents of violence occur, the public is sometimes quick to assume that the person (or people) involved has a mental illness. This can be for numerous reasons, but largely, it is that misconceptions about mental health and violence are often perpetuated in media and public discourse. In fact, despite prevailing beliefs about a direct connection between the two, research shows that the relationship between violence and mental illness is complex, and the presence of a mental illness does not automatically predispose a person to violent behavior. 1
As criminal justice professionals work to protect public safety, it is important that their policies and practices reflect accurate information, not common misperceptions. Additionally, they need to understand the real risk factors and warning signs of violence to minimize the risk of violence among the people they supervise or encounter. This brief addresses common misconceptions about the relationship between mental illness and violence, presents important information about risk factors for violence, and offers ways that criminal justice professionals can help mitigate these risks.
Dispelling Misconceptions
Many people are not familiar with the signs, symptoms, and effects of various mental illnesses, and therefore sometimes use mental illness as an explanation when seeking reasons for seemingly senseless acts of violence. The public also often does not understand the complex nature of the relationship between mental illness and violence. Below are three important facts people should know.
1. People with mental illnesses are not more likely to be violent than the general public.
The perception that people with mental illnesses are more prone to violence is based on the stigma surrounding mental illnesses and the ways in which researchers study this relationship. For example, most research on mental illness is conducted in inpatient treatment settings, but evidence indicates that people receiving inpatient treatment have a higher risk of violence than people in outpatient settings. 2
The National Council for Mental Wellbeing says that having a diagnosed mental illness is not, in the absence of other factors, a sufficient risk to warrant fear of mass violence. 3
2. People with mental illnesses are more likely to cause self-harm or be victims of violence than to inflict harm on others. 4
Serious mental illnesses (SMI) such as depression, bipolar disorder, and borderline personality disorder may at times increase the risk of danger to oneself. 5
This can include suicidal ideation, parasuicidal behaviors, 6 and self-harm. However, there are no accurate data to support the belief that people with mental illnesses are more likely to be violent toward others. Indeed, research shows the opposite—people with mental illnesses account for only about 4 percent of violent crime in the United States. 7 When there is a direct relationship between people with SMI and violence, factors such as substance use 8 and environmental stressors, such as poverty and housing instability are associated with the connection. 9
3. Clinical assessments are not the most effective way to determine a person’s risk of violence.
Although clinical behavioral health practitioners have often been asked to determine the risk of violence a person with mental illness poses, research shows that clinicians’ judgment regarding risk is no better than chance. 10 Instead, the use of actuarial violence risk assessment tools are more accurate, and tools have been developed to determine risk for specific types of violence including sexual violence 11 and workplace violence. 12 It is also important to keep in mind that clinicians and violence risk assessment tools , like most people and tools used in the criminal justice system, have inherent biases, even when there are good intentions. Criminal justice professionals should receive implicit bias training even when using violence risk assessment tools to mitigate some of these concerns.
Risk factors for violence
While people with mental illnesses are not predisposed to violent behavior, criminal justice professionals should still understand key risk factors for violence. These factors include:
Prior history of violent behavior
Previous acts of violence can be a risk factor for future violence, especially if other risk factors were and are present.13
Times of crisis
During times of crisis, anyone can be at an increased risk for acting out violently because they may have a lower tolerance for frustrations when stressed. For some people, this tolerance can drop so low that they are less able to control their behaviors. It is important to distinguish between a diagnosable mental illness and someone with mental health needs, however.14 For example, if someone is experiencing a time of stress, trauma, or crisis, such as being fired from a job, the breakdown of a relationship, or the loss of a loved one, it can be a risk factor for violence regardless of whether they have been diagnosed with a mental illness.15
Command auditory hallucinations
When someone is experiencing auditory hallucinations telling them to act in violence, this is considered a risk because they may follow the command.16 This may be especially true if the person has a history of acting on these types of commands. Increased stress may make this risk even more acute.
Substance use
Substance use can be a stand-alone risk factor or increase other risk factors for violence, especially co-occurring substance use and mental illness.17 Intoxication by some substances can increase the risk for violence, especially stimulants.18 Agitation, due to withdrawal or intoxication, is a sign someone should be assessed for risk of violence.
Mitigating Risks of Violence: Practical Steps
1. understand the research. .
Becoming familiar with the research and data on the relationship between mental illness and violence—as well as the general causes and risk factors for violent behavior—can help criminal justice professionals recognize warning signs and avoid misconceptions and biases. Understanding the research can also help agencies choose the most appropriate actuarial violence risk assessment tool, as well as help focus resources on people at highest risk for becoming violent based on the chosen assessment instrument.
2. Provide ongoing training.
Staff who may encounter people at risk of committing violence should be trained on recognizing risk factors and intervention methods, like de-escalation techniques. They should also receive implicit bias training and education on stereotypes so that they do not assume a person is dangerous simply because of a mental illness. This is especially important for Black, Indigenous, and People of Color (BIPOC) with mental illnesses, who can be seen as intimidating to some staff due to premature judgments, limited personal experiences, or prejudices.
3. Leverage community resources and their clinical expertise.
Criminal justice professionals should partner with local behavioral health treatment providers and access resources that can help them recognize people who are at risk to act violently. This can also help facilitate referrals when people are experiencing a mental health crisis. As partners, clinicians may be able to provide trainings to criminal justice staff on ways to identify signs and symptoms of risk. This partnership can also help make criminal justice staff aware of all the mental health resources that exist in their community, such as diversion programs, Assertive Community Treatment (ACT) Teams, or as a last resort, civil commitment .
The Council of State Governments Justice Center offers free in-depth subject matter expertise and can connect you to jurisdictions that are supporting people with serious mental illness to help them avoid violent behavior. Visit the Center for Justice and Mental Health Partnerships to learn more.
Additional Resources
Mass Violence in America: Causes, Impacts, and Solutions by National Council for Mental Wellbeing
Understanding and Managing Risks for People with Behavioral Health Needs by The Council of State Governments Justice Center
1 Seena Fazel et al., “Schizophrenia and Violence: Systematic Review and Meta-Analysis,” PLOS Medicine 6, no. 8 (2009).
2 Solveig Osborg Ose et al., “Risk of Violence Among Patients in Psychiatric Treatment: Results from a National Census,” Nordic Journal of Psychiatry 71, no. 8 (2017): 551.
3 Note that the National Council for Mental Wellbeing defines an act of mass violence as an event in which four or more people are killed. See National Council for Mental Wellbeing, Mass Violence in America Executive Summary (Washington, DC: National Council for Mental Wellbeing, 2019), v.
4 Jeanne Y Choe et al., “Perpetration of Violence, Violent Victimization, and Severe Mental Illness: Balancing Public Health Concerns,” Psychiatric Services 59, no. 2 (2008): 153–64; Kimberlie Dean et al., “Risk of Being Subjected to Crime, Including Violent Crime, After Onset of Mental Illness: A Danish National Registry Study Using Police Data,” JAMA Psychiatry 75, no. 7 (2018): 689–696.
5 “Mental Illness and Suicide,” Suicide Awareness Voices of Education, accessed August 18, 2021 .
6 Virpi Leppanen et al., “Association of Parasuicidal Behavior to Early Maladaptive Schemas and Schema Modes in Patients with BPD: The Oulu BPD Study,” Personality and Mental Health 10 (2016): 61.
7 “This means that even if all of the association between mental illness and violence could somehow be eliminated, we would still have to confront 96 percent of the violence in the United States.” See John S. Rozel and Edward P. Mulvey, “The Link Between Mental Illness and Firearm Violence: Implications for Social Policy and Clinical Practice,” Annual Review of Clinical Psychology 13, (2017): 445–69.
8 Seena Fazel et al., “Schizophrenia and Violence: Systematic Review and Meta-Analysis,” PLOS Medicine 6, no. 8 (2009); Because substance use disorder is a criminogenic risk factor, which increases the likelihood someone will commit another crime, a high criminogenic risk level may increase the risk of violent crime. See also Fred Osher et al., Adults with Behavioral Health Needs Under Correctional Supervision: A Shared Framework for Reducing Recidivism and Promoting Recovery (New York: The Council of State Governments Justice Center, 2012) .
9 Eric B. Elbogen and Sally C. Johnson, “The Intricate Link Between Violence and Mental Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions,” Arch Gen Psychiatry 66, no. 2 (2009): 152–161.
10 Claudia C. Hurducas et al., “Violence Risk Assessment Tools: A Systematic Review of Surveys,” International Journal of Forensic Mental Health 13, no. 3 (2014): 182 ; J. Monahan, The Clinical Prediction of Violent Behavior: An Assessment of Clinical Techniques (Lanham, MD: Jason Aronson, 1981).
12 Dr. J. Reid Meloy, Dr. Stephen G. White, and Dr. Stephen Hart, “Workplace Assessment of Targeted Violence Risk: The Development and Reliability of the WAVR-21,” Journal of Forensic Sciences 58, no. 5 (2013): 1353.
13 Mairead Dolan and Regine Blattner, “The Utility of the Historical Clinical Risk-20 Scale as a Predictor of Outcomes in Decisions to Transfer Patients from High to Lower Levels of Security –A UK Perspective,” BMC Psychiatry 10, no. 76 .
14 In times of transition or stress, many people may experience some mental health needs that don’t rise to the level of a diagnosable mental illness. They may benefit from behavioral health supports like talk therapy or skill-building exercises to strengthen coping skills. See American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (Arlington, VA: American Psychiatric Association, 2013).
15 In one study of 28 acts of violence, every person who committed the act had recent stressors reported. See National Council for Mental Wellbeing, Mass Violence in America Executive Summary (Washington, DC: National Council for Mental Wellbeing, 2019), 11.
16 R. Upthegrove et al., “Understanding Auditory Verbal Hallucinations: A Systematic Review of Current Evidence,” Acta Pschiatrica Scandanavica 188 (2016): 355.
17 Elbogen and Johnson, “The Intricate Link Between Violence and Mental Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions.”
18 Rebecca McKetin et al., “Does Methamphetamine Use Increase Violent Behavior? Evidence From a Prospective Longitudinal Study,” Addiction 109 (2014): 901.7. “This means that even if all of the association between mental illness and violence could somehow be eliminated, we would still have to confront 96 percent of the violence in the United States.” See John S. Rozel and Edward P. Mulvey, “The Link Between Mental Illness and Firearm Violence: Implications for Social Policy and Clinical Practice,” Annual Review of Clinical Psychology 13, (2017): 445–69.
Writing: Deirdra Assey, CSG Justice Center
Research : Deirdra Assey, CSG Justice Center
Advising: Julia Kessler and Demetrius Thomas, CSG Justice Center
Editing: Darby Baham and Emily Morgan, CSG Justice Center
Design: Michael Bierman
Public Affairs: Ruvi Lopez, CSG Justice Center
Web Development : Andrew Currier
This project was supported by Grant No. 2019-MO-BX-K001 awarded by the Bureau of Justice Assistance. The Bureau of Justice Assistance is a component of the Department of Justice’s Office of Justice Programs, which also includes the Bureau of Justice Statistics, the National Institute of Justice, the Office of Juvenile Justice and Delinquency Prevention, the Office for Victims of Crime, and the SMART Office. Points of view or opinions in this document are those of the author and do not necessarily represent the official position or policies of the U.S. Department of Justice.

********This application deadline has passed******** With support from the U.S. Department of Justice’s Office of…

Unlike drug courts, which have been informed by national standards for 10 years, mental health courts (MHCs)…

With support from the U.S. Department of Justice’s Office of Justice Programs’ Bureau of Justice Assistance, The Council…
With support from the U.S. Department of Justice’s Office of Justice Programs’…
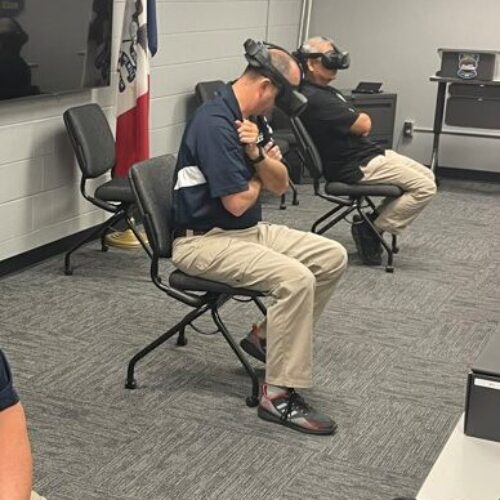
On March 9, 2024, President Joe Biden signed a $460 billion spending…

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Psychiatry Neurosci
- v.43(4); 2018 Jul
Are people with psychiatric disorders violent?
“Guns don’t kill people, the mentally ill do.” Ann Coulter, social and political commentator, Jan. 16, 2013 1
“Mental health is often a big problem underlying these tragedies.” Paul Ryan, Speaker of the US House of Representatives, Feb. 15, 2018 2
“…sicko came to a school with bad intentions.” Donald Trump, US President, Feb. 22, 2018 3
Are people with psychiatric disorders violent? The relevant data are influenced by reporting biases (e.g., changing willingness to report assaults) and the varying likelihood of being caught, convicted, and diagnosed, but there is compelling evidence that those with mental health problems are more likely than others to commit violent crimes. Analyses of the population-wide Swedish National Crime Register suggest that, compared to the general population, violent crime rates are doubled for patients with schizophrenia and bipolar mood disorders and tripled for those with unipolar depression. 4 – 6 These are nontrivial differences triggering attention-grabbing headlines and fears of people with mental illness. 7 , 8
The converse question is worth asking also: Are violent individuals more likely to have psychiatric disorders? Here again, the data are influenced by multiple factors, but most evidence suggests that they have elevated rates of psychopathology, with mood and psychotic disorders occurring in prison populations at up to 4 times that seen in community samples. 9 , 10
It is informative to consider these figures in context. For example, homicide rates in Manitoba are double the Canadian average. Homicide rates in the United States are triple those in Canada. 11 , 12 Despite this, few would take seriously headlines fearfully declaring “American Tourists Swarming Our Town!” Indeed, people with mental illnesses are 10–20 times more likely to commit suicide than homicide, and they are more likely than most to be victims of crime. 13 These numbers provide yet more reasons to deliver adequate care to those with mental health problems. They also indicate that fears of the mentally ill are no better founded than fears of Manitobans.
What about personality disorders?
Almost by definition, people with antisocial and related personality disorders commonly exhibit socially objectionable behaviours. 14 Despite this, personality disorder diagnoses provide poor predictive value for violent behaviour. The two best predictors are actuarial strategies, 15 which focus on diverse demographic and behavioural histories, and use of the HCR-20 (Historical, Clinical, Risk Management), a 20-item checklist designed to estimate the probability of future violence. 16 In common practice the HCR-20 is administered by clinicians and given in conjunction with the Psychopathy Checklist (PCL). Perhaps surprising to some, the predictive value of the HCR-20 is not diminished when it is administered without item H7 (personality disorder) and the PCL. 16
Can levels of violence be lowered by treating more psychiatric patients?
Recent mass shootings in schools have prompted calls to increase mental health care funding as a strategy to decrease violence. If the money becomes available, much good might be accomplished. However, no more than 3%–5% of interpersonal violence is attributable to serious mental disorders. 17 – 19 Paranoid, depressive and grandiose personality features are seen in some mass murderers, but these events are rare, accounting for less than 1% of homicides; there is no compelling evidence that the perpetrators display elevated levels of more serious pathology. 8 In the absence of these associations there are better reasons for improving mental health care, including those that do not stigmatize patients. * There are also better strategies for reducing violence.
How can violence levels be lowered?
As a start, it might help to remind ourselves that homicide rates (the most reliable of violence figures) are at historic lows — lower than two decades ago, lower than two centuries ago, lower than five centuries ago. 11 , 12 , 20 To decrease interpersonal violence further, greater access to mental health care can be one component, but it should not be the only one. Other factors that at least covary with high homicide rates (and, often, mental illness) include low average age of the community, high levels of unemployment, high income inequality gaps, low proportions of immigrants, poor living conditions, and cultural norms that valorize violence as a response to frustration. 8 , 21 – 24 Effective strategies are challenging to identify, but include adequate neighbourhood policing accompanied by fast and fair sentencing, early childhood education programs, more equitable access to socioeconomic opportunities, and greater support for both victims and perpetrators. 25 – 28
The role of clinicians is challenging too. The ability to predict violent behaviour is poor, and policies that putatively promote public health can harm individual patients. † This noted, some things help. Accidental shootings and suicide rates can be decreased by gun safety practices (e.g., safe storage), 19 , 29 and clinicians working in communities with high gun ownership levels might find themselves in a position to advise. In the rare case when a patient expresses violent intent toward a specific person, clinicians in the United States have a legal obligation to report it. 30 In Canada, reporting is required by many professional organizations, though not by the criminal code. 31
Gun control laws have a role to play too, and they receive much public support. Unfortunately, many have been poorly designed and implemented, sufficiently so that their efficacy is less than might be supposed, particularly when compared to what could have been accomplished if the expended money and effort had been directed elsewhere. This noted, there is modest evidence that some laws can help. This includes high-quality background checks that focus on risk (e.g., history of impulsive angry behaviour) rather than mental illness, temporary restrictions of gun access during periods of crisis (e.g., family member–initiated, court-mandated gun-violence restraining orders), and banning firearms in settings where the possibility of violence is elevated (e.g., bars, demonstrations, holidays, weekends). 19 , 23 , 32 – 34 “Stand your ground” laws, in comparison, can increase the risk of homicide. 34 Each of these contributing factors is aggravated by substance use, 35 , 36 though in at least some populations, this association might be driven by pre-existing behavioural tendencies. 37
Violent behaviour reflects the confluence of many, often intricately interacting, factors. Despite this complexity, the steady decrease in homicide rates provides optimism that progress can be made. Many of the contributing factors are within the domain of psychiatry. This includes obtaining a better understanding of biological, psychological, legal and other sociocultural factors that influence problematic behaviours, and using this information when making decisions about patients and policy. Our communities will be best served, it is proposed, if we focus on these features while avoiding the temptation to use fears of the mentally ill to obtain more funding.
Acknowledgements
The author thanks Dr. Anne Crocker, director of research and academics, Institut Philippe-Pinel de Montréal; and professor, Department of Psychiatry, Université de Montréal, for feedback on an earlier version of this editorial.
The views expressed in this editorial are those of the author(s) and do not necessarily reflect the position of the Canadian Medical Association or its subsidiaries, the journal’s editorial board or the Canadian College of Neuropsychopharmacology.
* Stigmatization fosters self-loathing, increases symptoms, and decreases treatment-seeking, worsening long-term outcomes. For readers of JPN , these consequences need not be belaboured.
† Some well-intentioned public policies can be harmful to individual patients. For example, confiscating firearms from people with a history of mental health problems irrespective of their behaviour not only stigmatizes them further, but also erodes a sense of personal autonomy and client–clinician trust.
Competing interests: None declared.

Is Mental Illness the Cause or the Result of Violence?
Research calls for us to know the difference..
Posted August 25, 2022 | Reviewed by Lybi Ma
By David Spiegel, M.D., with Sarah Sherwood, M.A.
The recent horrific shootings in Philadelphia, Buffalo, and at Robb Elementary School in Uvalde, Texas, perfectly illustrate some of the reasons that many children and their parents are experiencing troubling mental health issues. They're living in a very frightening world that feels out of control. We watch as Russia invades its neighbor Ukraine. Sars-Co-V-2 infects, kills, and mutates around the world. Wildfires spread as the globe heats. And for parents, who want to model the right response for their kids, the levels of fear and anxiety are also higher than ever recorded.
Earlier this Spring, the U.S. Department of Health and Human Services (HHS) published a study in the American Medical Association’s journal JAMA Pediatrics that reports significant increases in the number of children diagnosed with mental health conditions. The study, conducted by the Health Resources and Services Administration (HRSA), finds that between 2016 and 2020, the number of children ages 3-17 years diagnosed with anxiety grew by 29 percent and those with depression by 27 percent. According to the American Psychological Association (APA), adults and parents are experiencing anxiety as well. 1 In a mental health study we conducted early in the pandemic, we found that young people and women were the most profoundly affected. 1
Mental Illness Vs. Just Plain Violent
Our country pays a high price for each act of mass violence. Not only the immediate victims, survivors, their families and friends, but our communities, children, and families suffer. How do we explain the violence that the perpetrator inflicted? It has become popular to assert that mental illness is the cause. But is it?
The APA asserts that diagnosis alone cannot determine who may commit violence. 2 In fact, the vast majority of violent offenders are not mentally ill, as years of research have proven. According to research published by the APA, of all crimes committed by people with serious mental disorders, only 7.5 percent were directly related to symptoms of mental illness. 3 Furthermore, in the study, there was no relationship between mental illness symptoms and the crime . Yet, we continue to associate mental illness and criminality, often with intense debate. 4
In fact, more often than not, we are blaming the victims. We know that people with mental illness are actually more likely to be a victim of violent crime than a perpetrator of a crime. 5 Many of the symptoms of psychiatric conditions are behaviors considered antisocial or criminal. 6 As a result, we have the false perception of a causal relationship between psychiatric illness and criminality.
People naturally want to feel safer, and they have turned to owning guns themselves as a solution, attempting to calm their stress and anxiety over the increase in violence in the country. In a Stanford study of 26.3 million California residents published in the New England Journal of Medicine (NEJM), among those who had acquired handguns, the risk of suicide by firearm was 7.8 times higher for men and 35 times higher for women compared with non-handgun owners. 2 Suicide rates by other means were not any higher among handgun owners. This study confirmed a previous case-control study also published in the New England Journal of Medicine , that showed that in homes containing firearms, the odds of dying by suicide are three to five times greater than among non-gun owners. 7
In a more recent study, the Stanford team addressed the question of whether possession of firearms at home provides protection against homicide. 3 In this study of 17.6 million California residents, the researchers found that the rates of death by homicide were more than twice as high among those who lived in homes with guns, and the risk of being killed by a spouse or intimate partner was seven-fold higher; 84 percent of these victims were women. Thus, the presence of a firearm in the home provided risk, not protection.
This is especially important because one in three homes in the U.S. contain at least one firearm, and the evidence from ecological and case-controlled research suggests that gun access has the opposite effect. It is clear that gun violence is a cause of mental illness, not the product of it. Easy access to guns increases the risk of suicide, homicide, and serious injury. The threat of such tragedies and their occurrence causes substantial mental stress, and prevention is always preferable. Direct and indirect exposure to such dangers has deleterious effects on our mental health.
How We Can Respond to the Stress of Violence in Our Society
Still, those who witness violence can be greatly affected by what they see, even on the evening news. All of us need, at the very least, remedies for our fear and anxiety, ones that really work. These solutions should involve a plan of daily mental health maintenance. Having a daily practice of de-compressing after watching the news or whenever one is stressed by societal troubles is paramount. It is wise to limit the daily amount of traumatic input from social and other media. Verbal and physical conflict is now a constant reality in our culture, with cult-like characters who shock us, almost daily. We must make sure we take good care of ourselves.

As a researcher and psychiatrist, I have spent my career talking about stress and the benefits of hypnosis and self-hypnosis to relieve stress. Because of years of close examination and study, we know that hypnosis, the oldest known therapy , helps with the stress and anxiety we’ve been experiencing. Think of hypnosis as a natural anesthesia for stress. Proven by years of science, it provides deep relaxation and the state of flow we need to reset our busy, worried brains. Like meditation practice, many people are capable of doing hypnosis on their own.
Other therapeutic tools that may help, when used regularly, are:
- Self-hypnosis via technology can be more convenient and private than a hypnosis session
- Calming music can create a hypnotic state as well
- Cognitive therapy or talking through what you feel
- Talking with a close friend you feel you can confide in
- Meaningful volunteer work
We need this reset because stress and anxiety have become all too common. You can set up a healthy, daily practice of reversing stress that is proven by science. Better yet, you want to have a household that is more stress and anxiety resistant for years to come.
Co-author Sarah Sherwood is a science writer and social scientist based in San Mateo, California.
1.Adamson MM, Phillips A, Seenivasan S, Martinez J, Grewal H, Kang X, Coetzee J, Luttenbacher I, Jester A, Harris OA, Spiegel D. International Prevalence and Correlates of Psychological Stress during the Global COVID-19 Pandemic. International journal of environmental research and public health. 2020;17(24). Epub 2020/12/17. PubMed PMID: 33321950; PMCID: PMC7763004.
2.Studdert DM, Zhang Y, Swanson SA, Prince L, Rodden JA, Holsinger EE, Spittal MJ, Wintemute GJ, Miller M. Handgun Ownership and Suicide in California . N Engl J Med. 2020;382(23):2220-9. PubMed PMID: 32492303.
3.Studdert DM, Zhang Y, Holsinger EE, Prince L, Holsinger AF, Rodden JA, Wintemute GJ, Miller M. Homicide Deaths Among Adult Cohabitants of Handgun Owners in California , 2004 to 2016: A Cohort Study. Annals of internal medicine. 2022;175(6):804-11. Epub 20220405. PubMed PMID: 35377715.

David Spiegel, M.D. , is Willson Professor and Associate Chair of Psychiatry and Behavioral Sciences at Stanford University School of Medicine, and a co-founder of stress reduction app, Reveri.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Opportunities & Announcements
- Funding Strategy for Grants
- Grant Writing & Approval Process
- Managing Grants
- Clinical Research
- Small Business Research
Research on the Mental Health Consequences of Violence and Trauma
Program Announcement
The National Institute of Mental Health (NIMH) encourages investigator-initiated research to enhance scientific understanding about the etiology of psychopathology related to violence and trauma, as well as studies to develop and test effective treatments, services, and prevention strategies in this area. The NIMH mission encompasses the conduct and support of biomedical and behavioral research, and the translation of scientifically generated information into clinical applications and interventions implemented in the community.
The populations and phenomenon of concern include children, youth, adults, and the elderly, males and females, and all racial and ethnic groups. Studies of interest can focus on victims/survivors of interpersonal violence and crime, such as child abuse and neglect, rape, sexual assault, family violence, community violence and victims/survivors of major traumatic events, such as combat and war, mass shootings, terrorism, natural and technological disaster, refugee trauma and relocation, and torture.
Because the consequences of violence and traumatic stress typically involve several factors, the portfolio of NIMH research is multidisciplinary in nature. For example, the portfolio encompasses animal studies of the biological and behavioral effects of unpredictable and uncontrollable stress, mechanistic and descriptive studies of behavioral and biological dysregulation in humans, and clinical studies examining how the severity of post traumatic symptoms is linked to neural functioning, processing of memories, and interpretations of trauma. It also encompasses research to develop, test, and disseminate effective interventions addressing the sequelae of violence and trauma. NIMH encourages research that incorporates genetic, environmental, and neurobiological parameters as they relate to adjustment and psychopathology throughout life, as well as studies of implementation of proven treatments at the individual, clinic, organizational, and systems levels.
Areas of interest include:
- Studies of interactions among psychosocial and biological risk factors that increase or decrease risk for and course (escalation, persistence, and cessation) of psychopathology.
- Studies of the type and incidence of mental disorders resulting from exposure to violence and traumatic events, including studies of psychological or biological changes; also studies of the diagnosis, assessment, and course of PTSD and other trauma-related disorders and the appropriate threshold for clinical significance.
- Studies of psychosocial and psychobiological risk factors associated with differential risk of negative effects in different victim subgroups, as well as studies of psychosocial and psychobiological mechanisms by which interventions work and for whom.
- Research on the contributions of sleep patterns and pathophysiological indicators of stress and anxiety, including the failure to extinguish negative imagery, on risk and resilience.
- Development of assessment and screening instruments to guide treatment planning and management plans for victims of violence and traumatic events.
- Intervention studies testing the efficacy and refinement of individual, family, and/or community-level models and methods of prevention, treatment and services.
- Studies of system level effects of post-disaster service delivery.
- Studies of the effectiveness of interventions for victimization in various social and community settings, and the influence of social, institution, and community settings on the availability of interventions, program participation, and outcomes; use of different conceptual and intervention models with various social and cultural groups.
- Development of innovative, effective, and ethical methods of obtaining and maintaining the participation in research of victims of violence and traumatic events.
Potential applicants are encouraged to consult with program contacts regarding relevant research announcements and grant types.
Farris Tuma, Sc.D. Division of Adult Translational Research and Treatment Development National Institute of Mental Health 6001 Executive Boulevard, Room 5197, MSC 9589 Bethesda, MD 20892-9589 Telephone: 301-443-5944 Fax: 301-480-4415 Email: [email protected]
Steven J. Zalcman, M.D. Division of Adult Translational Research and Treatment Development National Institute of Mental Health 6001 Executive Boulevard, Room 7177 MSC 9639 Bethesda, MD 20892-9639 301-443-1692 Fax: 301-402-4740 Email: [email protected]
Denise Juliano-Bult, MSW Division of Services and Intervention Research National Institute of Mental Health 6001 Executive Boulevard, Room 7146 MSC 963 Bethesda, MD 20892-9639 Phone: 301-443-1638 Fax: 301-443-4045 Email: [email protected]
Advertisement
Sexual Violence and Psychological Distress: The Roles of Coping Self-Efficacy, Self-Blame, Shame, Activism, and Feminism
- Original Article
- Published: 11 October 2022
- Volume 87 , pages 419–434, ( 2022 )
Cite this article

- Charlotte Strauss Swanson ORCID: orcid.org/0000-0002-7444-7513 1 &
- Dawn M. Szymanski 1
1753 Accesses
3 Citations
Explore all metrics
In the current study, we investigated potential direct and indirect effects of exposure to sexual violence on posttraumatic stress disorder (PTSD) symptom severity and depression, and anti-sexual activism and feminist identification as moderators of these effects, among a sample of 440 United States women who had experienced sexual assault in adulthood. We found that sexual violence exposure was both directly and indirectly related to PTSD symptom severity via less trauma coping self-efficacy, greater behavioral and characterological self-blame, and more shame. Sexual violence exposure was also indirectly related to depression via the same explanatory variables, except for behavioral self-blame. Contrary to our hypotheses, results indicated that involvement in anti-sexual activism and feminist identification did not buffer the direct and indirect links between exposure to sexual violence and PTSD symptom severity and depression. However, we found that involvement in anti-sexual assault activism was associated with greater coping self-efficacy and higher depression, and feminist identification was associated with less self-blame and shame. Results from this study may inform clinical interventions for survivors of sexual violence and improve overall care for this population.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

Anti-Sexual Assault Activism and Positive Psychological Functioning among Survivors
Anxiety and depressive symptoms among people living with hiv and childhood sexual abuse: the role of shame and posttraumatic growth.

Sexual Victimization and Mental Health Among LGBQ + College Students: Examining Social Support and Trauma-Related Drinking as Mediators
Availability of data and material.
The data and materials can be obtained by emailing the first author.
Aiken, L. S., & West, S. G. (1991). Multiple regression: Testing and interpreting interactions . Sage.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5 th ed.). American Psychiatric Association.
Andrews, B., Qian, M., & Valentine, J. D. (2002). Predicting depressive symptoms with a new measure of shame: The Experience of Shame Scale. British Journal of Clinical Psychology, 41 , 29–42. https://doi.org/10.1348/014466502163778
Article PubMed Google Scholar
Ayres, M. M., Friedman, C. K., & Leaper, C. (2009). Individual and situational factors related to young women’s likelihood of confronting sexism in their everyday lives. Sex Roles, 61 , 449–460. https://doi.org/10.1007/s11199-009-9635-3
Article PubMed PubMed Central Google Scholar
Babcock, J. C., Roseman, A., Green, C. E., & Ross, J. M. (2008). Intimate partner abuse and PTSD symptomatology: Examining mediators and moderators of the abuse-trauma link. Journal of Family Psychology, 22 (6), 809–818. https://doi.org/10.1037/a0013808
Beck, J. G., McNiff, J., Clapp, J. D., Olsen, S. A., Avery, M. L., & Hagewood, J. H. (2011). Exploring negative emotion in women experiencing intimate partner violence: Shame, guilt, and PTSD. Behavior Therapy, 42 , 740–750. https://doi.org/10.1016/j.beth.2011.04.001
Benight, C. C., & Bandura, A. (2004). Social cognitive theory of posttraumatic recovery: The role of perceived self-efficacy. Behaviour Research and Therapy, 42 (10), 1129–1148. https://doi.org/10.1016/j.brat.2003.08.008
Benight, C. C., Harding-Taylor, A. S., Midboe, A. M., & Durham, R. L. (2004). Development and psychometric validation of a domestic violence coping self-efficacy measure (DV-CSE). Journal of Traumatic Stress, 17 , 505–508. https://doi.org/10.1007/s10960-004-5799-3
Benight, C. C., Shoji, K., James, L. E., Waldrep, E. E., Delahanty, D. L., & Cieslak, R. (2015). Trauma coping self-efficacy: A context-specific self-efficacy measure for traumatic stress. Psychological Trauma: Theory, Research, Practice, and Policy, 7 (6), 591–599. https://doi.org/10.1037/tra0000045
Article Google Scholar
Bhuptani, P. H., Kaufman, J. S., Messman-Moore, T. L., Gratz, K. L., & DiLillo, D. (2019). Rape disclosure and depression among community women: The mediating roles of shame and experiential avoidance. Violence against Women, 25 (10), 1226–1242. https://doi.org/10.1177/1077801218811683
Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM−5 (PCL−5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28 , 489–498. https://doi.org/10.1002/jts.22059
Bovin, M. J., Marx, B. P., Weathers, F. W., Gallagher, M. W., Rodriguez, P., Schnurr, P. P., & Keane, T. M. (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychological Assessment, 28 (11), 1379–1391. https://doi.org/10.1037/pas0000254
Breitenbecher, K. H. (2006). The relationships among self-blame, psychological distress, and sexual victimization. Journal of Interpersonal Violence, 21 (5), 597–611. https://doi.org/10.1177/0886260506286842
Brown, L. (2006). Still subversive after all these years: The relevance of feminist therapy in the age of evidence-based practice. Psychology of Women Quarterly, 30 , 15–24. https://doi.org/10.1111/j.1471-6402.2006.00258.x
Budden, A. (2009). The role of shame in posttraumatic stress disorder: A proposal for a socio-emotional model for DSM–5. Social Science & Medicine, 69 , 1032–1039. https://doi.org/10.1016/j.socscimed.2009.07.032
Campbell, R., Dworkin, E., & Cabral, G. (2009). An ecological model of the impact of sexual assault on women’s mental health. Trauma, Violence, & Abuse, 10 , 225–246. https://doi.org/10.1177/1524838009334456
Carlson, E. B., Smith, S. R., Palmieri, P. A., Dalenberg, C., Ruzek, J. I., Kimerling, R., Burling, T. A., & Spain, D. A. (2011). Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment, 23 , 463–477. https://doi.org/10.1037/a0022294
Carretta, R. F., & Szymanski, D. M. (2020). Stranger harassment and PTSD symptoms: Roles of self-blame, shame, fear, feminine norms, and feminism. Sex Roles, 82 , 525–540. https://doi.org/10.1007/s11199-019-01073-5
Cieslak, R., Benight, C. C., & Caden Lehman, V. (2008). Coping self-efficacy mediates the effects of negative cognitions on posttraumatic distress. Behaviour Research and Therapy, 46 (7), 788–798. https://doi.org/10.1016/j.brat.2008.03.007
Conlin, S. (2017). Feminist therapy: A brief integrative review of theory, empirical support, and call for new directions. Women’s Studies International Forum, 62 , 78–82. https://doi.org/10.1016/j.wsif.2017.04.002
Conlin, S. E., Douglass, R. P., Moradi, B., & Ouch, S. (2020). Examining feminist and critical consciousness conceptualizations of women’s subjective well-being. The Counseling Psychologist . https://doi.org/10.1177/0011000020957992
Cortina, L. M., & Kubiak, S. P. (2006). Gender and posttraumatic stress: Sexual violence as an explanation for women’s increased risk. Journal of Abnormal Psychology, 115 (4), 753–759. https://doi.org/10.1037/0021-843X.115.4.753
Davis, K. C., Gilmore, A. K., Stappenbeck, C. A., Balsan, M. J., George, W. H., & Norris, J. (2014). How to score the Sexual Experiences Survey? A comparison of nine methods. Psychology of Violence, 4 (4), 445–461. https://doi.org/10.1037/a0037494
DeBlaere, C., Brewster, M., Bertsch, K., Decarlo, A., Kegel, K., & Presseau, C. (2014). The protective power of collective action for sexual minority women of color: An investigation of multiple discrimination experiences and psychological distress. Psychology of Women Quarterly, 38 , 20–32. https://doi.org/10.1177/0361684313493252
DeCou, C. R., Cole, T. T., Lynch, S. M., Wong, M. M., & Matthews, K. C. (2017). Assault-related shame mediates the association between negative social reactions to disclosure of sexual assault and psychological distress. Psychological Trauma: Theory, Research, Practice, and Policy, 9 , 166–172. https://doi.org/10.1037/tra0000186
DeCou, C. R., Mahoney, C. T., Kaplan, S. P., & Lynch, S. M. (2019). Coping self-efficacy and trauma-related shame mediate the association between negative social reactions to sexual assault and PTSD symptoms. Psychological Trauma: Theory, Research, Practice and Policy, 11 (1), 51–54. https://doi.org/10.1037/tra0000379
Draucker, C. B., Martsolf, D. S., Ross, R., Cook, C. B., Stidham, A. W., & Mweemba, P. (2009). The essence of healing from sexual violence: A qualitative metasynthesis. Research in Nursing and Health, 32 , 366–378. https://doi.org/10.1002/nur.20333
Eisele, H., & Stake, J. (2008). The differential relationship of feminist attitudes and feminist identity to self-efficacy. Psychology of Women Quarterly, 32 (3), 233–244. https://doi.org/10.1111/j.1471-6402.2008.00432.x
Elliot, D. M., Mok, D. S., & Briere, J. (2005). Adult sexual assault: Prevalence, symptomatology, and sex differences in the general population. Journal of Traumatic Stress, 17 (3), 203–211. https://doi.org/10.1023/B:JOTS.0000029263.11104.23
Feiring, C., & Taska, L. S. (2005). The persistence of shame following sexual abuse: A longitudinal look at risk and recovery. Child Maltreatment, 10 , 337–349. https://doi.org/10.1177/1077559505276686
Field, A. (2013). Discovering statistics using IBM SPSS statistics . Sage.
Google Scholar
Fischer, A. R., & Good, G. E. (1994). Gender, self, and others: Perceptions of the campus environment. Journal of Counseling Psychology, 41 (3), 343–355. https://doi.org/10.1037/0022-0167.41.3.343
Ford, J., Stockton, P., Kaltman, S., & Green, B. (2006). Disorders of extreme stress (DESNOS) symptoms are associated with type and severity of interpersonal trauma exposure in a sample of healthy young women. Journal of Interpersonal Violence , 21 , 1399–1416. https://doi-org.proxy.lib.utk.edu/10.1177/0886260506292992
Foster, M. D. (2000). Positive and negative responses to personal discrimination: Does coping make a difference? The Journal of Social Psychology, 140 , 93–106. https://doi.org/10.1080/00224540009600448
Frazier, P. A. (2000). The role of attributions and perceived control in recovery from rape. Journal of Personal & Interpersonal Loss, 5 , 203–225. https://doi.org/10.1080/10811440008409753
Frazier, P. (2002). Rape Attribution Questionnaire . [Unpublished manuscript]. Department of Psychology, University of Minnesota.
Frazier, P. A. (2003). Perceived control and distress following sexual assault: A longitudinal test of a new model. Journal of Personality and Social Psychology, 84 , 1257–1269. https://doi.org/10.1037/0022-3514.84.6.1257
Fritz, M. S., & MacKinnon, D. P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18 (3), 233–239. https://doi.org/10.1111/j.1467-9280.2007.01882.x
Gefter, J. R., Bankoff, S. M., Valentine, S. E., Rood, B. A., & Pantalone, D. W. (2013). Feminist beliefs associated with young women’s recovery from male-perpetrated abuse. Women & Therapy, 36 , 332–355. https://doi.org/10.1080/02703149.2013.799987
Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2 nd Ed.). Guildford.
James, S. E., Herman, J. L., Rankin, S., Keisling, M., Mottet, L., & Anafi, M. (2016). The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality.
Janoff-Bulman, R. (1979). Characterological versus behavioral self-blame: Inquiries into depression and rape. Journal of Personality and Social Psychology, 37 , 1798–1809. https://doi.org/10.1037/0022-3514.37.10.1798
Kennedy, A. C., & Prock, K. A. (2016). I still feel like I am not normal: A review of the role of stigma and stigmatization among female survivors of child sexual abuse, sexual assault, and intimate partner violence. Trauma, Violence & Abuse, 19 (5), 512–527. https://doi.org/10.1177/1524838016673601
Klar, M., & Kasser, T. (2009). Some benefits of being an activist: Measuring activism and its role in psychological well-being. Political Psychology, 30 , 755–777. https://doi.org/10.1111/j.1467-9221.2009.00724.x
Koss, M. P., Abbey, A., Campbell, R., Cook, S., Norris, J., Testa, C., Ullman, S., West, C., & White, J. (2007). Revising the SES: A collaborative process to improve assessment of sexual aggression and victimization. Psychology of Women Quarterly, 31 , 357–370. https://doi.org/10.1111/j.1471-6402.2007.00385.x
Koss, M. P., Figueredo, A. J., & Prince, R. J. (2002). Cognitive mediation of rape’s mental, physical and social health impact: Tests of four models in cross-sectional data. Journal of Consulting and Clinical Psychology, 70 , 926–941. https://doi.org/10.1037/0022-006X.70.4.926
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16 , 606–613. https://doi.org/10.1016/j.jad.2008.06.026
Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B. W., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114 , 163–173. https://doi.org/10.1016/j.jad.2008.06.026
Kucharska, J. (2018). Feminist identity styles, sexual and non-sexual traumatic events, and psychological well-being in a sample of polish women. Journal of Interpersonal Violence, 33 (1), 117–136. https://doi.org/10.1177/0886260515600163
La Bash, H., & Papa, A. (2014). Shame and PTSD symptoms. Psychological Trauma: Theory, Research, Practice, and Policy, 6 , 159–166. https://doi.org/10.1037/a0032637
Landrine, H., & Klonoff, E. A. (1997). Discrimination against women: Prevalence, consequences, remedies . Sage.
Leaper, C., & Arias, D. M. (2011). College women’s feminist identity: A multidimensional analysis with implications for coping with sexism. Sex Roles, 64 , 475–490. https://doi.org/10.1007/s11199-011-9936-1
Leavy, R. L., & Adams, E. M. (1986). Feminism as a correlate of self-esteem, self-acceptance, and social support among lesbians. Psychology of Women Quarterly, 10 , 321–326. https://doi.org/10.1111/j.1471-6402.1986.tb00757.x
López-Castro, T., Saraiya, T., Zumberg-Smith, K., & Dambreville, N. (2019). Association between shame and posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 32 (4), 484–495. https://doi.org/10.1002/jts.22411
Luszczynska, A., Benight, C., & Cieslak, R. (2009). Self-efficacy and health-related outcomes of collective trauma: A systematic review. European Psychologist, 14 , 51–62. https://doi.org/10.1027/1016-9040.14.1.51
Mahoney, C. T., Lynch, S. M., & Benight, C. C. (2021). The indirect effect of coping self-efficacy on the relation between sexual violence and PTSD symptoms. Journal of Interpersonal Violence, 36 (21–22), 9996–10012. https://doi.org/10.1177/0886260519881525
Miller, A. K., Handley, I. M., Markman, K. D., & Miller, J. H. (2010). Deconstructing self-blame following sexual assault: The critical roles of cognitive content and process. Violence against Women, 16 (10), 1120–1137. https://doi.org/10.1177/1077801210382874
Moor, A., & Farchi, M. (2011). Is rape-related self-blame distinct from other post traumatic attributions of blame? A comparison of severity and implications for treatment. Women & Therapy, 34 (4), 447–460. https://doi.org/10.1080/02703149.2011.591671
Nishith, P., Mechanic, M. B., & Resick, P. A. (2000). Prior interpersonal trauma: The contribution to current PTSD symptoms in female rape victims. Journal of Abnormal Psychology, 109 , 20–25. https://doi.org/10.1037/0021-843X.109.1.20
Peter-Hagene, L. C., & Ullman, S. E. (2018). Longitudinal effects of sexual assault victims’ drinking and self-blame on posttraumatic stress disorder. Journal of Interpersonal Violence, 33 (1), 83–93. https://doi.org/10.1177/0886260516636394
Peterson, C., Schwartz, S. M., & Seligman, M. E. (1981). Self-blame and depressive symptoms. Journal of Personality and Social Psychology, 41 (2), 253–259. https://doi.org/10.1037/0022-3514.41.2.253
Scarpa, A., Haden, S. C., & Hurley, J. (2006). Community violence victimization and symptoms of posttraumatic stress disorder: The moderating effects of coping and social support. Journal of Interpersonal Violence, 21 (4), 446–469. https://doi.org/10.1177/0886260505285726
Sigurvinsdottir, R., Ullman, S. E., & Canetto, S. S. (2020). Self-blame, psychological distress, and suicidality among African American female sexual assault survivors. Traumatology, 26 (1), 1–10. https://doi.org/10.1037/trm0000195
Smith, S. G., Chen, J., Basile, K. C., Gilbert, L. K., Merrick, M. T., Patel, N., Walling, M., & Jain, A. (2017). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010–2012 State Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/pdf/nisvs-statereportbook.pdf
Strauss Swanson, C., & Szymanski, D. M. (2020). From pain to power: An exploration of activism, the #MeToo Movement, and healing from sexual assault trauma. Journal of Counseling Psychology, 67 , 653–668. https://doi.org/10.1037/cou0000429
Strauss Swanson, C., & Szymanski, D. M. (2021). Anti-sexual assault activism and positive psychological functioning among survivors. Sex Roles, 85 (1–2), 25–38. https://doi.org/10.1007/s11199-020-01202-5
Szymanski, D. M. (2004). Relations among dimensions of feminism and internalized heterosexism in lesbians and bisexual women. Sex Roles, 51 (3/4), 145–159. https://doi.org/10.1023/B:SERS.0000037759.33014.55
Szymanski, D. M., & Owens, G. P. (2009). Group-level coping as a moderator between heterosexism and sexism and psychological distress in sexual minority women. Psychology of Women Quarterly, 33 , 197–205. https://doi.org/10.1111/j.1471-6402.2009.01489.x
Ullman, S. E., & Filipas, H. H. (2001). Predictors of PTSD symptom severity and social reactions in sexual assault victims. Journal of Traumatic Stress, 14 , 369–389. https://doi.org/10.1023/A:1011125220522
Ullman, S. E., Filipas, H. H., Townsend, S. M., & Starzynski, L. L. (2007). Psychosocial correlates of PTSD symptom severity in sexual assault survivors. Journal of Traumatic Stress, 20 , 821–831. https://doi.org/10.1002/jts.20290
Ullman, S. E., & Peter-Hagene, L. (2014). Social reactions to sexual assault disclosure, coping, perceived control and PTSD symptoms in sexual assault victims. Journal of Community Psychology, 42 (4), 495–508. https://doi.org/10.1002/jcop.21624
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5) . U.S. Department of Veteran Affairs. http://www.ptsd.va.gov
Weiss, K. G. (2010). Too ashamed to report: Deconstructing the shame of sexual victimization. Feminist Criminology, 5 , 286–310. https://doi.org/10.1177/1557085110376343
Weston, R., & Gore, P. A. (2006). A brief guide to structural equation modeling. The Counseling Psychologist, 34 , 719–751. https://doi.org/10.1177/0011000006286345
Wilson, J. P., Drozdek, B., & Turkovic, S. (2006). Posttraumatic shame and guilt. Trauma, Violence & Abuse, 7 (2), 122–141. https://doi.org/10.1177/1524838005285914
Zinzow, H. M., Resnick, H. S., McCauley, J. L., Amstadter, A. B., Ruggiero, K. J., & Kilpatrick, D. G. (2012). Prevalence and risk of psychiatric disorders as a function of variant rape histories: Results from a national survey of women. Social Psychiatry and Psychiatric Epidemiology, 47 (6), 893–902. https://doi.org/10.1007/s00127-011-0397-1
Download references
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and affiliations.
Department of Psychology, University of Tennessee, 311 Austin Peay, Knoxville, TN, 37996-0900, USA
Charlotte Strauss Swanson & Dawn M. Szymanski
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Charlotte Strauss Swanson .
Ethics declarations
Ethics approval.
The research involved human participants and included an informed consent that was approved by our university’s Institutional Review Board.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Strauss Swanson, C., Szymanski, D.M. Sexual Violence and Psychological Distress: The Roles of Coping Self-Efficacy, Self-Blame, Shame, Activism, and Feminism. Sex Roles 87 , 419–434 (2022). https://doi.org/10.1007/s11199-022-01314-0
Download citation
Accepted : 18 July 2022
Published : 11 October 2022
Issue Date : October 2022
DOI : https://doi.org/10.1007/s11199-022-01314-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sexual violence
- Self-efficacy
- Sexual assault survivors
- Find a journal
- Publish with us
- Track your research

COMMENTS
In this Review, we summarise evidence on the association between different mental disorders and violence, with emphasis on high quality designs and replicated findings. Relative risks are typically increased for all violent outcomes in most diagnosed psychiatric disorders compared with people without psychiatric disorders, with increased odds in the range of 2-4 after adjustment for familial ...
A growing body of research is helping to tease apart why some people with serious mental illness are prone to violence while others are not, and how clinicians and others can help through improved treatment and informed myth-busting. DeAngelis, T. (2022, July 11). Mental illness and violence: Debunking myths, addressing realities.
Abstract. The debate about addressing mental illness and violence often ignores key facts. Many people experience mental illnesses, so having had a diagnosed illness is not a very specific predictor of violent behavior. This means that many proposed policy approaches, from expanded screening to more institutionalization, are unlikely to be ...
People with mental illness are generally considered to be more likely to perpetrate violence than the general population; 2 however, evidence of significant levels of physical victimization is increasingly recognized. 3 Although violence towards people diagnosed with mental illness is common, there is little evidence that it is decreasing: A ...
Our results indicate that people with alcohol dependence, depressive disorder, panic disorder, social phobia or GAD are at risk of psychological victimisation after adjustment for childhood trauma. ... Elbogen EB and Johnson SC (2009) The intricate link between violence and mental disorder: results from the national epidemiologic survey on ...
The relationship between mental health and violence is complex and often misunderstood, with a number of misperceptions around risk of violence and victimization. Speakers discussed the stigma and discrimination that people with mental illness experience, particularly in the media. They also discussed the need for additional research on the intersection of mental health and violence, noting ...
Introduction. For decades, a key concern in the mental health field has been whether psychiatric disorders increase the risk of violence. Although associations between serious mental illness and violence have long been identified, the precise nature of these associations has been the topic of considerable research, public health, and policy debate.
considerable research, public health, and policy debate. The importance of the associations between mental illness and violence is underscored by the inclusion of violence risk as a key criterion for hospital detention in mental health laws, and from public surveys suggesting that the perception of violence in people with psychiatric
Violence and abuse are endemic worldwide and are frequently experienced by people with mental health problems. However, although violence and abuse are recognised as important in understanding how mental health problems develop, there has been little research focused on the commonest form of abuse—domestic abuse—or sexual abuse in adulthood and their relationship with mental health.
Although most individuals with mental illness are not dangerous and the majority of violence is committed by people without mental disorders, there is some evidence that positive symptoms of full ...
This paper offers a criminologically informed framework to guide research on the relationship between mental disorder and violence. Criminological theories examined include social learning, social stress, social control, rational choice, and social disorganization. In addition, the "criminal careers" and "local life circumstance" methodologies are reviewed. It is argued that adopting a ...
In research on the prevalence of mental illness among violent offenders, multiple studies have found the highest rates of violence among individuals with substance use disorders, rather than schizophrenia, BPD and other psychotic disorders [7-11] (Tables 2 and 3).Rates of substance use disorders (including alcohol use disorders and illicit substance use disorders) among self-reported violent ...
Intimate partner violence (IPV) is a global health problem characterized as any behaviour within an intimate relationship that causes physical, psychological or sexual harm [].At present, it is well-documented that IPV can cause extensive mental health consequences among its victims [2,3,4,5].IPV can be characterized as an interpersonal trauma, and symptoms of posttraumatic stress disorder ...
Throughout history and in all known societies, people have believed that mental disorder and violence were somehow related. The consensus of modern scholarly opinion, however, has been that no such relationship exists. Recent epidemiological studies cast doubt on this no-relationship position. Evidence now indicates that mental disorder may be a consistent, albeit modest, risk factor for the ...
Mitigating Risks of Violence: Practical Steps. 1. Understand the research. Becoming familiar with the research and data on the relationship between mental illness and violence—as well as the general causes and risk factors for violent behavior—can help criminal justice professionals recognize warning signs and avoid misconceptions and biases.
Donald Trump, US President, Feb. 22, 2018 3. Are people with psychiatric disorders violent? The relevant data are influenced by reporting biases (e.g., changing willingness to report assaults) and the varying likelihood of being caught, convicted, and diagnosed, but there is compelling evidence that those with mental health problems are more ...
Research investigating the link between mental health, crime and violence often rely on populations that are at a high-risk of violent and criminal behaviour, such as prison inmates and psychiatric patients. As a result of this selection bias, the relationship between mental health, criminal and violent behaviour is significantly over-estimated ...
Some of the neurobiological mechanisms of violent behavior are similar or identical to those that operate in suicidal behavior. 3. Substance use, personality disorders, major mental disorders, head injuries, and other diagnosable disorders contribute to the level of community violence. However, recent evidence points to neurobiological ...
People with mental illness are much more often the victims of violence rather than the perpetrators. However, people with some types of mental disorder are more likely to be violent than others in the general population, a fact that is uncomfortable for many in the mental health sector. While there is little evidence to suggest that people with mental illness in general (usually those with ...
According to research published by the APA, of all crimes committed by people with serious mental disorders, only 7.5 percent were directly related to symptoms of mental illness. 3 Furthermore, in ...
The National Institute of Mental Health (NIMH) encourages investigator-initiated research to enhance scientific understanding about the etiology of psychopathology related to violence and trauma, as well as studies to develop and test effective treatments, services, and prevention strategies in this area.
In the current study, we investigated potential direct and indirect effects of exposure to sexual violence on posttraumatic stress disorder (PTSD) symptom severity and depression, and anti-sexual activism and feminist identification as moderators of these effects, among a sample of 440 United States women who had experienced sexual assault in adulthood. We found that sexual violence exposure ...
b. Those with psychological disorders are much more prone to random violent crime than others. c. Studies have found that those with psychological disorders are more likely than those without a psychological disorder to be a victim of crime. d. Focusing gun restrictions only on mentally ill people will likely reduce gun violence.