The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.

How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
The nursing process
Cite this chapter.

- Peggy Martin
79 Accesses
The nursing process provides a problem-solving approach to nursing care based on the needs and problems of the individual patient. Whenever possible, the patient and his relatives are encouraged to participate in decisions relating to his care.
‘ Hopefully nurses will soon learn that nursing is a special case of loving. ’ (Jourard, 1971).
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Unable to display preview. Download preview PDF.
References and Further Reading
De La Cuesta, C. (1983), The nursing process: from development to implementation, Journal of Advanced Nursing , 8 , 365–371.
Article Google Scholar
Henderson, V. (1982), The nursing process—is the title right?, Journal of Advanced Nursing , 7 , 103–109.
Jourard, S. M. (1971), The Transparent Self , Van Nostrand Reinhold, New York.
Google Scholar
McGilloway, F. A. (1980), The nursing process: a problem solving approach to patient care, International Journal of Nursing Studies , 17 , 79–90.
Peplau, H. (1952), Interpersonal Relations in Nursing , G. P. Putnam, New York.
Smitherson, C. (1981), Nursing Actions for Health Promotion , F. A. Davis, Philadelphia, Pennsylvania.
Stanton, M., Paul, C., and Reeves, J. S. (1980), An overview of the nursing process. In: The Nursing Theories Conference Group. Nursing Theories: The Base for Professional Nursing Practice , Prentice-Hall, Englewood Cliffs, New Jersey.
Tierney, A. (1983), cited by Ross, T. (1983), Activities of living, Nursing Mirror , 156 , No. 6, 28–29.
Wainwright, P. (1984), Not the nursing process, Nursing Mirror , 158 , No. 21, 22–24.
Further reading
Aggleton, P., and Chalmers, H. (1986), Nursing research, nursing theory and the nursing process, Journal of Advanced Nursing , 11 , 197–202.
Glass, H. (1983), Interventions in nursing: goals or task orientated, International Nursing Review , 30 , No. 2, 52–56.
Johnson, J. (1984), The nursing process and psychiatry, Nursing Mirror, Mental Health Forum , 158 , No. 4, i–ii.
Keane, P. (1981), The nursing process in action 4. The nursing process in a psychiatric context, Nursing Times , 77 , No. 28, 1223–1224.
Martin, L., and Glasper, A. (1986), Core plans: nursing models and the nursing process in action, Nursing Practice , 1 , 268–273.
Miller, A. (1985), Are you using the nursing process?, Nursing Times , 81 , No. 50, 36–39.
Mitchell, J. R. A. (1984), Is nursing any business of doctors? A simple guide to the ‘nursing process’, British Medical Journal , 288 , 21 January, 216–219.
Roe, S., and Farrel, P. (1986), Shaping nursing process, Nursing Practice , 1 , 274–278.
Rowden, R. (1984), Doctors can work with the nursing process: a reply to Professor Mitchell, British Medical Journal , 288 , 21 January, 219–220.
Stockwell, F. (1985), The Nursing Process in Psychiatric Nursing , Croom Helm, London.
Syson Nibbs, L. (1980), Progress through a planned approach, Nursing Mirror , 150 , No. 7, 42–44.
Waters, K. (1985), The nursing process—methodology versus mythology, Nursing Practice , 1 , 92–97.
Further Reading
Bradley, J. C., and Edinberg, M. A. (1982), Communication in the Nursing Context , Appleton Century Crofts, Norwalk, Connecticut.
Collins, M. (1983), Communication in Health Care , C. V. Mosby, St Louis, Missouri.
Spradley, B. W. (1981), Community Health Nursing Concepts and Practice , Little, Brown, Boston, Massachusetts.
Altschul, A. T. (1977), Use of the nursing process in psychiatric care, Nursing Times , 73 , 1412–1413.
Banchik, D. (1983), Psychiatric assessment and case formulation. In: Handbook of Psychiatric Mental Health Nursing (eds Adams, C. G., and Macione, A.), John Wiley, Chichester, West Sussex.
Bermosk, L. S. (1966), Interviewing: a key to therapeutic communication in nursing practice, Nursing Clinics of North America , 1 , No. 2, 205–214.
Bootay, L. S. (1978), Interviewing your patient. In: Nursing Skillbook. Documenting Patient Care Responsibility , Nursing 78 Books, Horsham, Pennsylvania.
Burr, J., and Andrews, J. (1981), Nursing the Psychiatric Patient , 4th edn, Baillière Tindall, London.
Calnan, J. (1983), Talking with Patients , Heinemann Medical, London.
Cooper, J. (1979), Actions really do speak louder than words, American Journal of Nursing , 79 , No. 4, 29–32.
Crow, J. (1979), Assessment. In: The Nursing Process (ed. Kratz, C.), Baillière Tindall, London.
Duberley, J. (1979), Giving nursing care. In: The Nursing Process (ed. Kratz, C.), Bailltère Tindall, London.
Edwards, B. J., and Brilhart, J. K. (1981), Communication in Nursing Practice , C. V. Mosby, St Louis, Missouri.
Eisenman, E. J. P., and Dubbert, P. M. (1977), The mental health assessment interview. In: Psychiatric Mental Health Nursing Contemporary Readings (eds Backer, B. A., Dubbert, P. M., and Eisenman, E. J. P.), Van Nostrand Reinhold, New York.
French, P. (1983), Social Skills for Nursing Practice , Croom Helm, London.
Gillis, L. (1980), Human Behaviour in Illness , 3rd edn, Faber and Faber, London.
Haggerty, V. C. (1971), Listening, Nursing Forum , 10 , No. 4, 382–387.
Hayter, J. (1981), Territoriality as a universal need, Journal of Advanced Nursing , 6 , 79–85.
Hein, E. C. (1980), Communication in Nursing Practice , 2nd edn, Little, Brown, Boston, Massachusetts.
Kron, T. (1981), The Management of Patient Care , W. B. Saunders, Philadelphia, Pennsylvania.
Metz, E. L. (1978), Assessing the older psychiatric patient. In: Mental Health Concepts Applied to Nursing (ed. Dunlap, L. C.), John Wiley, Chichester, West Sussex.
Peplau, H. E. (1952), Interpersonal Relations in Nursing , G. P. Putnam, New York.
Price, B. (1983), Just a few forms to fill in, Nursing Times , 79 , No. 44, 26–29.
Rines, A. R., and Montag, M. L. (1976), Nursing Concepts and Nursing Care , John Wiley, New York.
Snyder, J. C., and Wilson, M. F. (1977), Elements of a psychological assessment, American Journal of Nursing , 77 , No. 2, 235–239.
Ujhely, G. B. (1966), Basic considerations for nurse-patient interaction in the prevention and treatment of emotional disorders, Nursing Clinics of North America , 1 , No. 2, 179–186.
Campbell, C. (1978), Nursing Diagnosis and Intervention in Nursing Practice , John Wiley, New York.
Frijda, N. H. (1982), The meanings of emotional expression. In: Non-verbal Communication Today (ed. Key, M. R.), Mouton, Berlin.
Hill, L. (1981), Don’t stereotype your patient, Journal of Practical Nursing , 31 , No. 8, 34–35.
Joel, L., and Davis, S. (1973), A proposal for baseline data collection for psychiatric care, Perspectives in Psychiatric Care , 11 , No. 2, 48–58.
Maguire, P. (1985), Deficiencies in key interpersonal skills. In: Interpersonal Skills in Nursing Research and Applications (ed. Kagan, C. M.), Croom Helm, London.
O’Brien, M. (1978), Communications and Relationships on Nursing , C. V. Mosby, St Louis, Missouri.
Prange, A. J., and Martin, H. W. (1962), Aids to understanding patients, American Journal of Nursing , 62 , 98–100.
Smitherman, C. (1981), Nursing Actions for Health Promotion , F. A. Davis, Philadelphia, Pennsylvania.
Tissier, J. (1986), The development of a psychiatric nursing assessment form. In: Psychiatric Nursing Research (ed. Brooking, J.), John Wiley, Chichester, West Sussex.
Tremlett, R. (1977), A dangerous practice, Nursing Mirror , 144 , No. 24, 33.
Whyte, L., and Youhill, G. (1984), The nursing process in the care of the mentally ill, Nursing Times , 80 , No. 5, 49–51.
Wilkinson, S. (1981), Factors influencing the relationship between the nurse and the client/patient. In: Process in Clinical Nursing (eds Leonard, B. J., and Redland, A. R.), Prentice-Hall, Englewood Cliffs, New Jersey.
Wilkinson, T. (1979), The problems and the values of objective nursing observations in psychiatric nursing care, Journal of Advanced Nursing , 4 , 151–159.
Bower, F. L. (1982), The Process of Planning Nursing Care , 3rd edn, C. V. Mosby, St Louis, Missouri.
Barnett, D. (1985), Making your plans work, Nursing Times , 81 , No. 2, 24–27.
Castledine, G. (1982), A poor record in writing, Nursing Mirror , 154 , No. 22, 31.
Duberley, J. (1979), Giving nursing care. In: The Nursing Process (ed. Kratz, C.), Baillifere Tindall, London.
Hampshire, G. (1984), Defining goals, Nursing Times , 80 , No. 11, 45–46.
Hunt, J. M., and Marks-Maran, D. J. (1980), Nursing Care Plans. The Nursing Process at Work , H. M. and M. Publishers, Aylesbury, Buckinghamshire.
Matthews, A. (1986), Patient-centred handovers, Nursing Times , 82 , No. 24, 47–48.
Schrock, R. A. (1980), Planning nursing care for the mentally ill, Nursing Times , 76 , No. 16, 704–707.
Vitale, B. A., and Schultz, N. V. (1974), A Problem Solving Approach to Nursing Care Plans: A Program , C. V. Mosby, St Louis, Missouri.
Wright, S. (1985), Real plans for real patients, Nursing Times , 81 , No. 34, 36–38.
Adams, D. M. (1980), Establishing therapeutic relationships. In: Psychiatric Nursing, A Basic Text (ed. Pothier, P. C.), Little, Brown, Boston, Massachusetts.
Anderson, M. L. (1983), Nursing interventions. What did you do that helped? Perspectives in Psychiatric Care , 21 , No. 1, 4–8.
Blondis, M. N., and Jackson, B. E. (1982), Non-verbal Communication with Patients , John Wiley, Chichester, West Sussex.
Brown, M. M., and Fowler, G. R. (1966), Psychodynamic Nursing , W. B. Saunders, Philadelphia, Pennsylvania.
Burgess, A. W., and Lazare, A. (1976), Psychiatric Nursing in the Hospital and the Community , Prentice-Hall, Englewood Cliffs, New Jersey.
Burton, G. (1977), Interpersonal Relations , 4th edn, Tavistock, London.
Butler, R. J., and Rosenthal, G. (1978), Behaviour and Rehabilitation , John Wright, Bristol.
Ellis, J. R., and Nowliss, E. A. (1981), Nursing, A Human Needs Approach , Houghton Mifflin, Boston, Massachusetts.
Grace, H. K., and Camelleri, D. (1981), Mental Health Nursing, A Socio-Psychological Approach , Wm. C. Brown, Dubuque, Iowa.
Marriner, A. (1983), The Nursing Process , C. V. Mosby, St Louis, Missouri.
Murray, R. (1975), Nursing Concepts for Health Promotion , Prentice-Hall, Englewood Cliffs, New Jersey.
Murray, R. B., and Huelskoetter, M. M. W. (1983), Psychiatric Mental Health Nursing: Giving Emotional Care , Prentice-Hall, Englewood Cliffs, New Jersey.
Paterson, J. G., and Zderad, L. T. (1976), Humanistic Nursing , John Wiley, Chichester, West Sussex.
Peplau, H. E. (1986), A celebration of skills, Paper presented at the Third International Congress of Psychiatric Nursing, Imperial College, London.
Robinson, L. (1983), Psychiatric Nursing as a Human Experience , W. B. Saunders, Philadelphia, Pennsylvania.
Travelbee, J. (1971), Interpersonal Aspects of Nursing , 2nd edn, F. A. Davis, Philadelphia, Pennsylvania.
Cooper, S. (1981), What is nursing?, Nursing Times, Occasional Papers , 77 , No. 34, 136.
Dirterle, J. A. (1983), Clinical validation of psychiatric nursing skills, Journal of Nursing Education , 22 , No. 9, 392–394.
Glass, H. (1983), Intervention in nursing: goals or task orientated, International Nursing Review , 30 , No. 2, 52–56.
Henderson, V. (1978), The concept of nursing, Journal of Advanced Nursing , 3 , 75–84.
McMahon, R. A. (1986), Nursing as a therapy, Professional Nurse , 1 , No. 10, 270–272.
Perry, J. (1985), Has the discipline of nursing developed to the stage where nurses do ‘think nursing’?, Journal of Advanced Nursing , 10 , 31–37.
Schoenhofer, S. O. (1984), Support as legitimate nursing action, Nursing Outlook , 32 , No. 4, 218–219.
Bergman, R. (1982), Evaluation of nursing care—could it make a difference?, International Journal of Nursing Studies , 19 , No. 2, 53–60.
Dye, M. C. (1963), Clarifying patient’s communication, American Journal of Nursing , 63 , 56–59.
Lowe, K. (1984), The fourth step of the nursing process evaluation. In: A Systematic Approach to Nursing Care , Open University, Milton Keynes, Buckinghamshire.
Ceccio, J. F., and Ceccio, C. M. (1982), Effective Communication in Nursing: Theory and Practice , John Wiley, New York.
Hargreaves, I. (1975), The nursing process. The key to individualised care, Nursing Times, Occasional Papers , 71 , No. 35, 89–92.
Kron, T. (1981), The Management of Patient Care , W. B. Standard.
Luker, K. (1979), Evaluating nursing care. In: The Nursing Process (ed. Kratz, C.), Bailliere Tindall, London.
Open University (1984), A Systematic Approach to Nursing Care , Open University, Milton Keynes, Buckinghamshire.
Waters, K. (1986), Cause and effect, Nursing Times , 82 , No. 5, 28–30.
Download references
You can also search for this author in PubMed Google Scholar
Editor information
Copyright information.
© 1987 Peggy Martin and the Individual Contributors
About this chapter
Martin, P. (1987). The nursing process. In: Martin, P. (eds) Psychiatric Nursing. Palgrave, London. https://doi.org/10.1007/978-1-349-09408-0_8
Download citation
DOI : https://doi.org/10.1007/978-1-349-09408-0_8
Publisher Name : Palgrave, London
Print ISBN : 978-0-333-43842-8
Online ISBN : 978-1-349-09408-0
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
The Nursing Process: A Comprehensive Guide

In 1958, Ida Jean Orlando began developing the nursing process still evident in nursing care today. According to Orlando’s theory, the patient’s behavior sets the nursing process in motion. Through the nurse’s knowledge to analyze and diagnose the behavior to determine the patient’s needs.
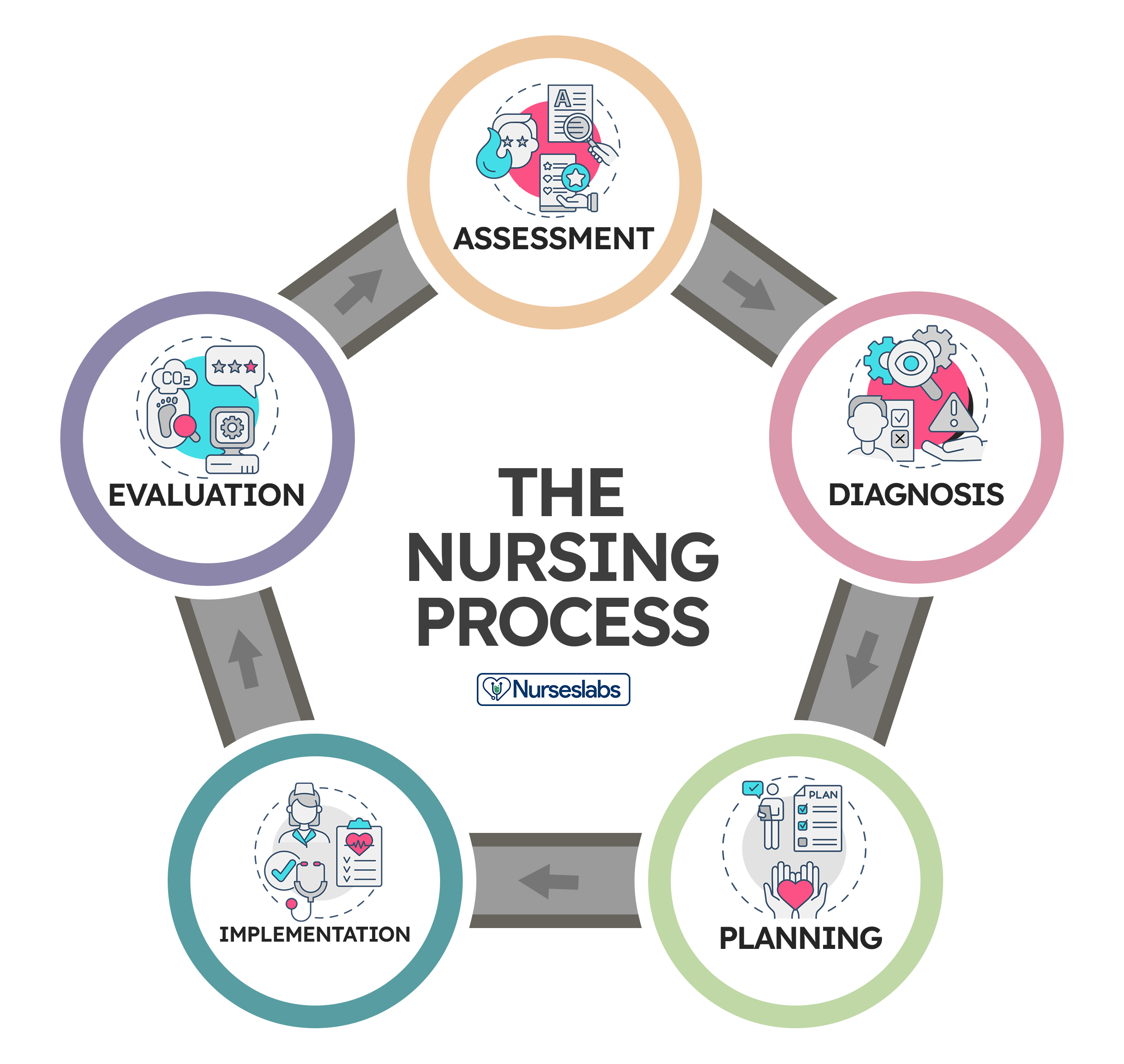
Application of the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EBP) recommendations, and nursing intuition, the nursing process functions as a systematic guide to client-centered care with five subsequent steps. These are assessment , diagnosis, planning, implementation, and evaluation ( ADPIE ).
Table of Contents
What is the nursing process.
- What is the purpose of the nursing process?
Characteristics of the nursing process
Nursing process steps, collecting data, objective data or signs, subjective data or symptoms, verbal data, nonverbal data, primary source, secondary source, tertiary source, health interview, physical examination, observation, validating data, documenting data, 2. diagnosis: “what is the problem” , initial planning, ongoing planning, discharge planning, developing a nursing care plan, behavioral nursing interventions, community nursing interventions, family nursing interventions, health system nursing interventions, physiological nursing interventions, safety nursing interventions, skills used in implementing nursing care, 1. reassessing the client, 2. determining the nurse’s need for assistance, nursing intervention categories, independent nursing interventions, dependent nursing interventions, interdependent nursing interventions, 4. supervising the delegated care, 5. documenting nursing activities, 1. collecting data, 2. comparing data with desired outcomes, 3. analyzing client’s response relating to nursing activities, 4. identifying factors contributing to success or failure, 5. continuing, modifying, or terminating the nursing care plan, 6. discharge planning.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse’s critical thinking to provide the best care possible to the client.
What is the purpose of the nursing process?
The following are the purposes of the nursing process:
- To identify the client’s health status and actual or potential health care problems or needs (through assessment).
- To establish plans to meet the identified needs.
- To deliver specific nursing interventions to meet those needs.
- To apply the best available caregiving evidence and promote human functions and responses to health and illness (ANA, 2010).
- To protect nurses against legal problems related to nursing care when the standards of the nursing process are followed correctly.
- To help the nurse perform in a systematically organized way their practice.
- To establish a database about the client’s health status, health concerns, response to illness, and the ability to manage health care needs.
The following are the unique characteristics of the nursing process:
- Patient-centered . The unique approach of the nursing process requires care respectful of and responsive to the individual patient’s needs, preferences, and values. The nurse functions as a patient advocate by keeping the patient’s right to practice informed decision-making and maintaining patient-centered engagement in the health care setting.
- Interpersonal . The nursing process provides the basis for the therapeutic process in which the nurse and patient respect each other as individuals, both of them learning and growing due to the interaction. It involves the interaction between the nurse and the patient with a common goal.
- Collaborative . The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care.
- Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
- Requires critical thinking . The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation. The acronym ADPIE is an easy way to remember the components of the nursing process. Nurses need to learn how to apply the process step-by-step. However, as critical thinking develops through experience, they learn how to move back and forth among the steps of the nursing process.
The steps of the nursing process are not separate entities but overlapping, continuing subprocesses. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps of the nursing process are detailed below:
1. Assessment: “What data is collected?”
The first phase of the nursing process is assessment . It involves collecting, organizing, validating, and documenting the clients’ health status. This data can be obtained in a variety of ways. Usually, when the nurse first encounters a patient, the nurse is expected to assess to identify the patient’s health problems as well as the physiological, psychological, and emotional state and to establish a database about the client’s response to health concerns or illness and the ability to manage health care needs. Critical thinking skills are essential to the assessment, thus requiring concept-based curriculum changes.
Data collection is the process of gathering information regarding a client’s health status. The process must be systematic and continuous in collecting data to prevent the omission of important information concerning the client.
The best way to collect data is through head-to-toe assessment. Learn more about it at our guide: Head to Toe Assessment: Complete Physical Assessment Guide
Types of Data
Data collected about a client generally falls into objective or subjective categories, but data can also be verbal and nonverbal.
Objective data are overt, measurable, tangible data collected via the senses, such as sight, touch, smell, or hearing, and compared to an accepted standard, such as vital signs, intake and output , height and weight, body temperature, pulse, and respiratory rates, blood pressure, vomiting , distended abdomen, presence of edema , lung sounds, crying, skin color, and presence of diaphoresis.
Subjective data involve covert information, such as feelings, perceptions, thoughts, sensations, or concerns that are shared by the patient and can be verified only by the patient, such as nausea , pain , numbness, pruritus, attitudes, beliefs, values, and perceptions of the health concern and life events.
Verbal data are spoken or written data such as statements made by the client or by a secondary source. Verbal data requires the listening skills of the nurse to assess difficulties such as slurring, tone of voice, assertiveness, anxiety , difficulty in finding the desired word, and flight of ideas.
Nonverbal data are observable behavior transmitting a message without words, such as the patient’s body language, general appearance, facial expressions, gestures, eye contact, proxemics (distance), body language, touch, posture, clothing. Nonverbal data obtained can sometimes be more powerful than verbal data, as the client’s body language may not be congruent with what they really think or feel. Obtaining and analyzing nonverbal data can help reinforce other forms of data and understand what the patient really feels.
Sources of Data
Sources of data can be primary, secondary, and tertiary . The client is the primary source of data, while family members, support persons, records and reports, other health professionals, laboratory and diagnostics fall under secondary sources.
The client is the only primary source of data and the only one who can provide subjective data. Anything the client says or reports to the members of the healthcare team is considered primary.
A source is considered secondary data if it is provided from someone else other than the client but within the client’s frame of reference. Information provided by the client’s family or significant others are considered secondary sources of data if the client cannot speak for themselves, is lacking facts and understanding, or is a child. Additionally, the client’s records and assessment data from other nurses or other members of the healthcare team are considered secondary sources of data.
Sources from outside the client’s frame of reference are considered tertiary sources of data . Examples of tertiary data include information from textbooks, medical and nursing journals, drug handbooks, surveys, and policy and procedural manuals.
Methods of Data Collection
The main methods used to collect data are health interviews, physical examination, and observation.
The most common approach to gathering important information is through an interview. An interview is an intended communication or a conversation with a purpose, for example, to obtain or provide information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. One example of the interview is the nursing health history, which is a part of the nursing admission assessment. Patient interaction is generally the heaviest during the assessment phase of the nursing process so rapport must be established during this step.
Aside from conducting interviews, nurses will perform physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Establishing a good physical assessment would, later on, provide a more accurate diagnosis, planning, and better interventions and evaluation.
Observation is an assessment tool that depends on the use of the five senses (sight, touch, hearing, smell, and taste) to learn information about the client. This information relates to characteristics of the client’s appearance, functioning, primary relationships, and environment. Although nurses observe mainly through sight, most of the senses are engaged during careful observations such as smelling foul odors, hearing or auscultating lung and heart sounds and feeling the pulse rate and other palpable skin deformations.
Validation is the process of verifying the data to ensure that it is accurate and factual. One way to validate observations is through “double-checking,” and it allows the nurse to complete the following tasks:
- Ensures that assessment information is double-checked, verified, and complete. For example, during routine assessment, the nurse obtains a reading of 210/96 mm Hg of a client with no history of hypertension . To validate the data, the nurse should retake the blood pressure and if necessary, use another equipment to confirm the measurement or ask someone else to perform the assessment.
- Ensure that objective and related subjective data are valid and accurate. For example, the client’s perceptions of “feeling hot” need to be compared with the measurement of the body temperature.
- Ensure that the nurse does not come to a conclusion without adequate data to support the conclusion. A nurse assumes tiny purple or bluish-black swollen areas under the tongue of an older adult client to be abnormal until reading about physical changes of aging.
- Ensure that any ambiguous or vague statements are clarified. For example, a 86-year-old female client who is not a native English speaker says that “I am in pain on and off for 4 weeks,” would require verification for clarity from the nurse by asking “Can you describe what your pain is like? What do you mean by on and off?”
- Acquire additional details that may have been overlooked. For example, the nurse is asking a 32-year-old client if he is allergic to any prescription or non-prescription medications. And what would happen if he takes these medications.
- Distinguish between cues and inferences. Cues are subjective or objective data that can be directly observed by the nurse; that is, what the client says or what the nurse can see, hear, feel, smell, or measure. On the other hand, inferences are the nurse’s interpretation or conclusions made based on the cues. For example, the nurse observes the cues that the incision is red, hot, and swollen and makes an inference that the incision is infected.
Once all the information has been collected, data can be recorded and sorted. Excellent record-keeping is fundamental so that all the data gathered is documented and explained in a way that is accessible to the whole health care team and can be referenced during evaluation.
The second step of the nursing process is the nursing diagnosis . The nurse will analyze all the gathered information and diagnose the client’s condition and needs. Diagnosing involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements about a patient’s potential or actual health problem. More than one diagnosis is sometimes made for a single patient. Formulating a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care.
The types, components, processes, examples, and writing nursing diagnosis are discussed more in detail here “ Nursing Diagnosis Guide: All You Need To Know To Master Diagnosing ”
3. Planning: “How to manage the problem?”
Planning is the third step of the nursing process. It provides direction for nursing interventions. When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome.
The planning phase is where goals and outcomes are formulated that directly impact patient care based on evidence-based practice (EBP) guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual’s unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement, and continuity of care across the healthcare continuum.
Types of Planning
Planning starts with the first client contact and resumes until the nurse-client relationship ends, preferably when the client is discharged from the health care facility.
Initial planning is done by the nurse who conducts the admission assessment. Usually, the same nurse would be the one to create the initial comprehensive plan of care.
Ongoing planning is done by all the nurses who work with the client. As a nurse obtain new information and evaluate the client’s responses to care, they can individualize the initial care plan further. An ongoing care plan also occurs at the beginning of a shift. Ongoing planning allows the nurse to:
- determine if the client’s health status has changed
- set priorities for the client during the shift
- decide which problem to focus on during the shift
- coordinate with nurses to ensure that more than one problem can be addressed at each client contact
Discharge planning is the process of anticipating and planning for needs after discharge. To provide continuity of care, nurses need to accomplish the following:
- Start discharge planning for all clients when they are admitted to any health care setting.
- Involve the client and the client’s family or support persons in the planning process.
- Collaborate with other health care professionals as needed to ensure that biopsychosocial, cultural, and spiritual needs are met.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database .
4. Implementation: “Putting the plan into action!”
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect. It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This typically begins with the medical staff conducting any needed medical interventions.
Interventions should be specific to each patient and focus on achievable outcomes. Actions associated with a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks such as medication administration , educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
A taxonomy of nursing interventions referred to as the Nursing Interventions Classification (NIC) taxonomy, was developed by the Iowa Intervention Project. The nurse can look up a client’s nursing diagnosis to see which nursing interventions are recommended.
Nursing Interventions Classification (NIC) System
There are more than 550 nursing intervention labels that nurses can use to provide the proper care to their patients. These interventions are categorized into seven fields or classes of interventions according to the Nursing Interventions Classification system.
These are interventions designed to help a patient change their behavior. With behavioral interventions, in contrast, patient behavior is the key and the goal is to modify it. The following measures are examples of behavioral nursing interventions:
- Encouraging stress and relaxation techniques
- Providing support to quit smoking
- Engaging the patient in some form of physical activity , like walking, to reduce the patient’s anxiety, anger, and hostility
These are interventions that refer to the community-wide approach to health behavior change. Instead of focusing mainly on the individual as a change agent, community interventionists recognize a host of other factors that contribute to an individual’s capacity to achieve optimal health, such as:
- Implementing an education program for first-time mothers
- Promoting diet and physical activities
- Initiating HIV awareness and violence-prevention programs
- Organizing a fun run to raise money for breast cancer research
These are interventions that influence a patient’s entire family.
- Implementing a family-centered approach in reducing the threat of illness spreading when one family member is diagnosed with a communicable disease
- Providing a nursing woman support in breastfeeding her new baby
- Educating family members about caring for the patient
These are interventions that designed to maintain a safe medical facility for all patients and staff, such as:
- Following procedures to reduce the risk of infection for patients during hospital stays.
- Ensuring that the patient’s environment is safe and comfortable, such as repositioning them to avoid pressure ulcers in bed
These are interventions related to a patient’s physical health to make sure that any physical needs are being met and that the patient is in a healthy condition. These nursing interventions are classified into two types: basic and complex.
- Basic. Basic interventions regarding the patient’s physical health include hands-on procedures ranging from feeding to hygiene assistance.
- Complex. Some physiological nursing interventions are more complex, such as the insertion of an IV line to administer fluids to a dehydrated patient.
These are interventions that maintain a patient’s safety and prevent injuries, such as:
- Educating a patient about how to call for assistance if they are not able to safely move around on their own
- Providing instructions for using assistive devices such as walkers or canes, or how to take a shower safely.
When implementing care, nurses need cognitive, interpersonal, and technical skills to perform the care plan successfully.
- Cognitive Skills are also known as Intellectual Skills are skills involve learning and understanding fundamental knowledge including basic sciences, nursing procedures, and their underlying rationale before caring for clients. Cognitive skills also include problem-solving, decision-making, critical thinking, clinical reasoning, and creativity.
- Interpersonal Skills are skills that involve believing, behaving, and relating to others. The effectiveness of a nursing action usually leans mainly on the nurse’s ability to communicate with the patient and the members of the health care team.
- Technical Skills are purposeful “hands-on” skills such as changing a sterile dressing, administering an injection, manipulating equipment, bandaging, moving, lifting, and repositioning clients. All of these activities require safe and competent performance.
Process of Implementing
The process of implementing typically includes the following:
Prior to implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even if an order is written on the care plan, the client’s condition may have changed.
Other nursing tasks or activities may also be performed by non-RN members of the healthcare team. Members of this team may include unlicensed assistive personnel (UAP) and caregivers , as well as other licensed healthcare workers, such as licensed practical nurses/licensed vocational nurses (LPNs/LVNs). The nurse may need assistance when implementing some nursing intervention, such as ambulating an unsteady obese client, repositioning a client, or when a nurse is not familiar with a particular model of traction equipment needs assistance the first time it is applied.
3. Implementing the nursing interventions
Nurses must not only have a substantial knowledge base of the sciences, nursing theory , nursing practice, and legal parameters of nursing interventions but also must have the psychomotor skills to implement procedures safely. It is necessary for nurses to describe, explain, and clarify to the client what interventions will be done, what sensations to anticipate, what the client is expected to do, and what the expected outcome is. When implementing care, nurses perform activities that may be independent, dependent, or interdependent.
Nursing interventions are grouped into three categories according to the role of the healthcare professional involved in the patient’s care:
A registered nurse can perform independent interventions on their own without the help or assistance from other medical personnel, such as:
- routine nursing tasks such as checking vital signs
- educating a patient on the importance of their medication so they can administer it as prescribed
A nurse cannot initiate dependent interventions alone. Some actions require guidance or supervision from a physician or other medical professional, such as:
- prescribing new medication
- inserting and removing a urinary catheter
- providing diet
- Implementing wound or bladder irrigations
A nurse performs as part of collaborative or interdependent interventions that involve team members across disciplines.
- In some cases, such as post- surgery , the patient’s recovery plan may require prescription medication from a physician, feeding assistance from a nurse, and treatment by a physical therapist or occupational therapist.
- The physician may prescribe a specific diet to a patient. The nurse includes diet counseling in the patient care plan. To aid the patient, even more, the nurse enlists the help of the dietician that is available in the facility.
Delegate specific nursing interventions to other members of the nursing team as appropriate. Consider the capabilities and limitations of the members of the nursing team and supervise the performance of the nursing interventions. Deciding whether delegation is indicated is another activity that arises during the nursing process.
The American Nurses Association and the National Council of State Boards of Nursing (2006) define delegation as “the process for a nurse to direct another person to perform nursing tasks and activities.” It generally concerns the appointment of the performance of activities or tasks associated with patient care to unlicensed assistive personnel while retaining accountability for the outcome.
Nevertheless, registered nurses cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to unlicensed assistive personnel include assessment and evaluation of the impact of interventions on care provided to the patient.
Record what has been done as well as the patient’s responses to nursing interventions precisely and concisely.
5. Evaluation: “Did the plan work?”
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened.
Steps in Evaluation
Nursing evaluation includes (1) collecting data, (2) comparing collected data with desired outcomes, (3) analyzing client’s response relating to nursing activities, (4) identifying factors that contributed to the success or failure of the care plan, (5) continuing, modifying, or terminating the nursing care plan, and (6) planning for future nursing care.
The nurse recollects data so that conclusions can be drawn about whether goals have been fulfilled. It is usually vital to collect both objective and subjective data. Data must be documented concisely and accurately to facilitate the next part of the evaluating process.
The documented goals and objectives of the nursing care plan become the standards or criteria by which to measure the client’s progress whether the desired outcome has been met, partially met, or not met.
- The goal was met , when the client response is the same as the desired outcome.
- The goal was partially met , when either a short-term outcome was achieved but the long-term goal was not, or the desired goal was incompletely attained.
- The goal was not met.
It is also very important to determine whether the nursing activities had any relation to the outcomes whether it was successfully accomplished or not.
It is required to collect more data to confirm if the plan was successful or a failure. Different factors may contribute to the achievement of goals. For example, the client’s family may or may not be supportive, or the client may be uncooperative to perform such activities.
The nursing process is dynamic and cyclical. If goals were not sufficed, the nursing process begins again from the first step. Reassessment and modification may continually be needed to keep them current and relevant depending upon general patient condition. The plan of care may be adjusted based on new assessment data. Problems may arise or change accordingly. As clients complete their goals, new goals are set. If goals remain unmet, nurses must evaluate the reasons these goals are not being achieved and recommend revisions to the nursing care plan.
Discharge planning is the process of transitioning a patient from one level of care to the next. Discharge plans are individualized instructions provided as the client is prepared for continued care outside the healthcare facility or for independent living at home. The main purpose of a discharge plan is to improve the client’s quality of life by ensuring continuity of care together with the client’s family or other healthcare workers providing continuing care.
The following are the key elements of IDEAL discharge planning according to the Agency for Healthcare Research and Quality:
- I nclude the patient and family as full partners in the discharge planning process.
- Describe what life at home will be like
- Review medications
- Highlight warning signs and problems
- Explain test results
- Schedule follow-up appointments
- E ducate the patient and family in plain language about the patient’s condition, the discharge process, and next steps throughout the hospital stay.
- A ssess how well doctors and nurses explain the diagnosis, condition, and next steps in the patient’s care to the patient and family and use teach back.
- L isten to and honor the patient’s and family’s goals, preferences, observations, and concerns.
A discharge plan includes specific components of client teaching with documentation such as:
- Equipment needed at home. Coordinate home-based care and special equipment needed.
- Dietary needs or special diet . Discuss what the patient can or cannot eat at home.
- Medications to be taken at home. List the patient’s medications and discuss the purpose of each medicine, how much to take, how to take it, and potential side effects.
- Resources such as contact numbers and addresses of important people. Write down the name and contact information of someone to call if there is a problem.
- Emergency response: Danger signs. Identify and educate patients and families about warning signs or potential problems.
- Home care activities. Educate patient on what activities to do or avoid at home.
- Summary. Discuss with the patient and family about the patient’s condition, the discharge process, and follow-up checkups.
39 thoughts on “The Nursing Process: A Comprehensive Guide”
This article is helpful
So helpful And easy to understand A very good guide for nurses
I’m a clinical instructor teaching Fundamentals this semester. The article will be very helpful to give an in-depth explanation of “The Nursing Process” to students. Thank you.
Very detailed and easy to understand. Thx
Am a student I find it very educative
This is so helpful
Excellent information that is clearly outlined and user friendly.
This is so wonderful thank you
So helpful thank you
this is very helpful thank you
Helpful. So grateful
Is the nursing process the same as “critical thinking”?
Great information! Thanks!
This is very helpful. Thank you
Great explanation, in the understanding of Nursing process
Very Helpful to students, thank you for sharing
Excellent job. A great help to all nursing students. Thank you for sharing. God bless you.
Hi Joycelyn, Thank you so much for your kind words! It’s really rewarding to hear that it’s helping nursing students out there. We’re all about sharing knowledge and making things a bit easier. 😊 If there’s anything else you’d like to see or know, just let me know. And blessings right back at you!
Thank you so much…It’s a very comprehensive reference.
You’re very welcome, A.C! I’m glad you found the nursing process reference comprehensive and useful. Just out of curiosity, is there a particular step in the nursing process you’d like to explore more deeply, or do you have any specific areas where you’d like more detailed information?
I am a nursing student and I see this as a helpful tool, very detailed and easy to understand thanks for sharing
Hi Mawuli, I’m delighted to know that you’re finding our resources helpful! If you have any specific questions or if there’s a particular topic you’d like more information on, please feel free to ask. I’m here to assist you with any nursing-related inquiries you may have. Keep up the great work in your studies! 🩺📚🌟
Keep updating me about Nursing pdfs. You guys are really good at your work!!
Hey Mokete, Thank you so much for the kind words! We’re thrilled to hear that you’re finding our nursing resources helpful. We’ll do our best to keep you updated with more valuable nursing PDFs and information. If there’s anything specific you’d like to see or if you have any questions, feel free to let us know. Keep up the great work in your nursing journey! 👩⚕️📚🌟
Thanks it really helps alot
Glad to be of help! Thank you!
This guideline very useful for Nurses building their competency and practice quality of care of Nursing to use as reference please allow to download free especially to Nurses who live in developing countries since it is not affordable to buy it
You can download the articles by printing them as PDF :) You can use a service called printfriendly (google it) to make PDFs of our webpages.
Excellent work done I’m very happy to see this stuffs
Thank you so much…It’s a very comprehensive reference. God bless you
Hello Theophilus, You’re very welcome, and thank you for the blessings! 😊 I’m glad you found the reference on the nursing process comprehensive. Just out of curiosity, is there a particular part of the nursing process you’re most interested in, or any aspect you’d like to explore more deeply?
God bless you too, and if you have any more questions, feel free to ask!
Very helpful information. Thank you.
Thank you so much, Alisa. If you need more information or help regarding this, let us know.
You’re doing a great job here. Please can you do it in such a way for us to download it as a pdf?
Hi Millicent, Thank you so much for the kind words! 😊 I’m really glad you’re finding the site useful.
Regarding your request to download content as a PDF, a neat trick you can use is the “print” function in your web browser. Here’s how you can do it:
Open the page you want to save as a PDF. -Go to the “File” menu in your browser and select “Print,” or simply press Ctrl+P (Cmd+P on Mac). -In the print window, look for a destination option and select “Save as PDF” or something similar. -Adjust any settings as needed, then click “Save” or “Print,” and choose where you want to save the file on your computer.
This way, you can turn any page into a PDF for your personal use. If you have any more questions or need further assistance, feel free to ask. Always here to help!
Very helpful Thank you
Leave a Comment Cancel reply
The 5 Nursing Process Steps – (Learn Each Step in Detail)

One of the most important tools a nurse can use in practice is the nursing process. Although nursing schools teach first-year students about the nursing process, some nurses fail to grasp the impact its proper use can have on patient care. In this article, I will share information about the nursing process, its history, its purpose, its main characteristics, and the 5 steps involved in carrying out the nursing process. After reading this article, you will be able to answer the question, “what is the nursing process” and understand what is involved in each of the 5 steps of the nursing process. Additionally, throughout this article, after discussing a step of the nursing process, I will share an example of how the nurse would proceed with that step. For this article’s purposes, we will use information about the following patient: Mr. Collie, a fifty-four-year-old white male being admitted to the Medical-Surgical floor for acute congestive heart failure.
What Is The Nursing Process In Simple Words?
When was the nursing process developed, who developed the nursing process, what is the purpose of the nursing process, what are the 7 main characteristics of the nursing process, 1. within the legal scope of practice, 2. based on sound knowledge, 4. client-centered, 5. goal-directed, 6. prioritized, 7. dynamic and cyclical, how many steps are there in the nursing process, what are the 5 steps of the nursing process, step #1: assessment phase, step #2: diagnosis phase, step #3: planning phase, step #4: implementation phase, step #5: evaluation phase, useful resources to gain more information about the nursing process, blogs/websites, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. how is nursing process different from the scientific method, 2. do all nurses use the nursing process, 3. do doctors also use the nursing process, 4. what does adpie stand for, 5. is it always necessary for a nurse to follow all steps of the nursing process, 6. how does critical thinking impact the nursing process, 7. how does a health information system affect the nursing process, 8. how to use maslow hierarchy in the nursing process, 9. which nursing process step includes tasks that can be delegated, 10. which nursing process step includes tasks that cannot be delegated, 11. how does the nursing process apply to pharmacology.

Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Making Decisions and Solving Problems
CHAPTER 6 Making Decisions and Solving Problems Rose Aguilar Welch This chapter describes the key concepts related to problem solving and decision making. The primary steps of the problem-solving and decision-making processes, as well as analytical tools used for these processes, are explored. Moreover, strategies for individual or group problem solving and decision making are presented. Objectives • Apply a decision-making format to list options to solve a problem, identify the pros and cons of each option, rank the options, and select the best option. • Evaluate the effect of faulty information gathering on a decision-making experience. • Analyze the decision-making style of a nurse leader/manager. • Critique resources on the Internet that focus on critical thinking, problem solving, and decision making. Terms to Know autocratic creativity critical thinking decision making democratic optimizing decision participative problem solving satisficing decision The Challenge Vickie Lemmon RN, MSN Director of Clinical Strategies and Operations, WellPoint, Inc., Ventura, California Healthcare managers today are faced with numerous and complex issues that pertain to providing quality services for patients within a resource-scarce environment. Stress levels among staff can escalate when problems are not resolved, leading to a decrease in morale, productivity, and quality service. This was the situation I encountered in my previous job as administrator for California Children Services (CCS). When I began my tenure as the new CCS administrator, staff expressed frustration and dissatisfaction with staffing, workload, and team communications. This was evidenced by high staff turnover, lack of teamwork, customer complaints, unmet deadlines for referral and enrollment cycle times, and poor documentation. The team was in crisis, characterized by in-fighting, blaming, lack of respectful communication, and lack of commitment to program goals and objectives. I had not worked as a case manager in this program. It was hard for me to determine how to address the problems the staff presented to me. I wanted to be fair but thought that I did not have enough information to make immediate changes. My challenge was to lead this team to greater compliance with state-mandated performance measures. What do you think you would do if you were this nurse? Introduction Problem solving and decision making are essential skills for effective nursing practice. Carol Huston (2008) identified “expert decision-making skills” as one of the eight vital leadership competencies for 2020. These processes not only are involved in managing and delivering care but also are essential for engaging in planned change. Myriad technologic, social, political, and economic changes have dramatically affected health care and nursing. Increased patient acuity, shorter hospital stays, shortage of healthcare providers, increased technology, greater emphasis on quality and patient safety, and the continuing shift from inpatient to ambulatory and home health care are some of the changes that require nurses to make rational and valid decisions. Moreover, increased diversity in patient populations, employment settings, and types of healthcare providers demands efficient and effective decision making and problem solving. More emphasis is now placed on involving patients in decision making and problem solving and using multidisciplinary teams to achieve results. Nurses must possess the basic knowledge and skills required for effective problem solving and decision making. These competencies are especially important for nurses with leadership and management responsibilities. Definitions Problem solving and decision making are not synonymous terms. However, the processes for engaging in both processes are similar. Both skills require critical thinking, which is a high-level cognitive process, and both can be improved with practice. Decision making is a purposeful and goal-directed effort that uses a systematic process to choose among options. Not all decision making begins with a problem situation. Instead, the hallmark of decision making is the identification and selection of options or alternatives. Problem solving, which includes a decision-making step, is focused on trying to solve an immediate problem, which can be viewed as a gap between “what is” and “what should be.” Effective problem solving and decision making are predicated on an individual’s ability to think critically. Although critical thinking has been defined in numerous ways, Scriven and Paul (2007) refer to it as “ the intellectually disciplined process of actively and skillfully conceptualizing, applying, analyzing, synthesizing, and/or evaluating information gathered from, or generated by, observation, experience, reflection, reasoning, or communication, as a guide to belief and action.” Effective critical thinkers are self-aware individuals who strive to improve their reasoning abilities by asking “why,” “what,” or “how.” A nurse who questions why a patient is restless is thinking critically. Compare the analytical abilities of a nurse who assumes a patient is restless because of anxiety related to an upcoming procedure with those of a nurse who asks if there could be another explanation and proceeds to investigate possible causes. It is important for nurse leaders and managers to assess staff members’ ability to think critically and enhance their knowledge and skills through staff-development programs, coaching, and role modeling. Establishing a positive and motivating work environment can enhance attitudes and dispositions to think critically. Creativity is essential for the generation of options or solutions. Creative individuals can conceptualize new and innovative approaches to a problem or issue by being more flexible and independent in their thinking. It takes just one person to plant a seed for new ideas to generate . The model depicted in Figure 6-1 demonstrates the relationship among related concepts such as professional judgment, decision making, problem solving, creativity, and critical thinking. Sound clinical judgment requires critical or reflective thinking. Critical thinking is the concept that interweaves and links the others. An individual, through the application of critical-thinking skills, engages in problem solving and decision making in an environment that can promote or inhibit these skills. It is the nurse leader’s and manager’s task to model these skills and promote them in others. FiGURE 6-1 Problem-solving and decision-making model. Decision Making This section presents an overview of concepts related to decision models, decision-making styles, factors affecting decision making, group decision making (advantages and challenges), and strategies and tools. The phases of the decision-making process include defining objectives, generating options, identifying advantages and disadvantages of each option, ranking the options, selecting the option most likely to achieve the predefined objectives, implementing the option, and evaluating the result. Box 6-1 contains a form that can be used to complete these steps. BOX 6-1 Decision-Making Format Objective: _____________________________________ Options Advantages Disadvantages Ranking Add more rows as necessary. Rank priority of options, with “1” being most preferred. Select the best option. Implementation plan: ______________________________________________________________________________ Evaluation plan: __________________________________________________________________________________ A poor-quality decision is likely if the objectives are not clearly identified or if they are inconsistent with the values of the individual or organization. Lewis Carroll illustrates the essential step of defining the goal, purpose, or objectives in the following excerpt from Alice’s Adventures in Wonderland: One day Alice came to a fork in the road and saw a Cheshire Cat in a tree. “Which road do I take?” she asked. His response was a question: “Where do you want to go?” “I don’t know,” Alice answered. “Then,” said the cat, “it doesn’t matter.” Decision Models The decision model that a nurse uses depends on the circumstances. Is the situation routine and predictable or complex and uncertain? Is the goal of the decision to make a decision conservatively that is just good enough or one that is optimal? If the situation is fairly routine, nurse leaders and managers can use a normative or prescriptive approach. Agency policy, standard procedures, and analytical tools can be applied to situations that are structured and in which options are known. If the situation is subjective, non-routine, and unstructured or if outcomes are unknown or unpredictable, the nurse leader and manager may need to take a different approach. In this case, a descriptive or behavioral approach is required. More information will need to be gathered to address the situation effectively. Creativity, experience, and group process are useful in dealing with the unknown. In the business world, Camillus described complex problems that are difficult to describe or resolve as “wicked” (as cited in Huston, 2008 ). This term is apt in describing the issues that nurse leaders face. In these situations, it is especially important for nurse leaders to seek expert opinion and involve key stakeholders. Another strategy is satisficing. In this approach, the decision maker selects the solution that minimally meets the objective or standard for a decision. It allows for quick decisions and may be the most appropriate when time is an issue. Optimizing is a decision style in which the decision maker selects the option that is best, based on an analysis of the pros and cons associated with each option. A better decision is more likely using this approach, although it does take longer to arrive at a decision. For example, a nursing student approaching graduation is contemplating seeking employment in one of three acute care hospitals located within a 40-mile radius of home. The choices are a medium-size, not-for-profit community hospital; a large, corporate-owned hospital; and a county facility. A satisficing decision might result if the student nurse picked the hospital that offered a decent salary and benefit packet or the one closest to home. However, an optimizing decision is more likely to occur if the student nurse lists the pros and cons of each acute care hospital being considered such as salary, benefits, opportunities for advancement, staff development, and mentorship programs. Decision-Making Styles The decision-making style of a nurse manager is similar to the leadership style that the manager is likely to use. A manager who leans toward an autocratic style may choose to make decisions independent of the input or participation of others. This has been referred to as the “decide and announce” approach, an authoritative style. On the other hand, a manager who uses a democratic or participative approach to management involves the appropriate personnel in the decision-making process. It is imperative for managers to involve nursing personnel in making decisions that affect patient care. One mechanism for doing so is by seeking nursing representation on various committees or task forces. Participative management has been shown to increase work performance and productivity, decrease employee turnover, and enhance employee satisfaction. Any decision style can be used appropriately or inappropriately. Like the tenets of situational leadership theory, the situation and circumstances should dictate which decision-making style is most appropriate. A Code Blue is not the time for managers to democratically solicit volunteers for chest compressions! The autocratic method results in more rapid decision making and is appropriate in crisis situations or when groups are likely to accept this type of decision style. However, followers are generally more supportive of consultative and group approaches. Although these approaches take more time, they are more appropriate when conflict is likely to occur, when the problem is unstructured, or when the manager does not have the knowledge or skills to solve the problem. Exercise 6-1 Interview colleagues about their most preferred decision-making model and style. What barriers or obstacles to effective decision making have your colleagues encountered? What strategies are used to increase the effectiveness of the decisions made? Based on your interview, is the style effective? Why or why not? Factors Affecting Decision Making Numerous factors affect individuals and groups in the decision-making process. Tanner (2006) conducted an extensive review of the literature to develop a Clinical Judgment Model. Out of the research, she concluded that five principle factors influence decision making. (See the Literature Perspective below.) Literature Perspective Resource: Tanner, C. A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45 (6), 204-211. Tanner engaged in an extensive review of 200 studies focusing on clinical judgment and clinical decision making to derive a model of clinical judgment that can be used as a framework for instruction. The first review summarized 120 articles and was published in 1998. The 2006 article reviewed an additional 71 studies published since 1998. Based on an analysis of the entire set of articles, Tanner proposed five conclusions which are listed below. The reader is referred to the article for detailed explanation of each of the five conclusions. The author considers clinical judgment as a “problem-solving activity.” She notes that the terms “clinical judgment,” “problem solving,” “decision making,” and “critical thinking” are often used interchangeably. For the purpose of aiding in the development of the model, Tanner defined clinical judgment as actions taken based on the assessment of the patient’s needs. Clinical reasoning is the process by which nurses make their judgments (e.g., the decision-making process of selecting the most appropriate option) ( Tanner, 2006 , p. 204): 1. Clinical judgments are more influenced by what nurses bring to the situation than the objective data about the situation at hand. 2. Sound clinical judgment rests to some degree on knowing the patient and his or her typical pattern of responses, as well as an engagement with the patient and his or her concerns. 3. Clinical judgments are influenced by the context in which the situation occurs and the culture of the nursing care unit. 4. Nurses use a variety of reasoning patterns alone or in combination. 5. Reflection on practice is often triggered by a breakdown in clinical judgment and is critical for the development of clinical knowledge and improvement in clinical reasoning. The Clinical Judgment Model developed through the review of the literature involves four steps that are similar to problem-solving and decision-making steps described in this chapter. The model starts with a phase called “Noticing.” In this phase, the nurse comes to expect certain responses resulting from knowledge gleaned from similar patient situations, experiences, and knowledge. External factors influence nurses in this phase such as the complexity of the environment and values and typical practices within the unit culture. The second phase of the model is “Interpreting,” during which the nurse understands the situation that requires a response. The nurse employs various reasoning patterns to make sense of the issue and to derive an appropriate action plan. The third phase is “Responding,” during which the nurse decides on the best option for handling the situation. This is followed by the fourth phase, “Reflecting,” during which the nurse assesses the patient’s responses to the actions taken. Tanner emphasized that “reflection-in-action” and “reflection-on-action” are major processes required in the model. Reflection-in-action is real-time reflection on the patient’s responses to nursing action with modifications to the plan based on the ongoing assessment. On the other hand, reflection-on-action is a review of the experience, which promotes learning for future similar experiences. Nurse educators and managers can employ this model with new and experienced nurses to aid in understanding thought processes involved in decision making. As Tanner (2006) so eloquently concludes, “If we, as nurse educators, help our students understand and develop as moral agents, advance their clinical knowledge through expert guidance and coaching, and become habitual in reflection-on-practice, they will have learned to think like a nurse” ( p. 210 ). Implications for Practice Nurse educators and managers can employ this model with new and experienced nurses to aid in understanding thought processes involved in decision making. For example, students and practicing nurses can be encouraged to maintain reflective journals to record observations and impressions from clinical experiences. In clinical post-conferences or staff development meetings, the nurse educator and manager can engage them in applying to their lived experiences the five conclusions Tanner proposed. The ultimate goal of analyzing their decisions and decision-making processes is to improve clinical judgment, problem-solving, decision-making, and critical-thinking skills. Internal and external factors can influence how the situation is perceived. Internal factors include variables such as the decision maker’s physical and emotional state, personal philosophy, biases, values, interests, experience, knowledge, attitudes, and risk-seeking or risk-avoiding behaviors. External factors include environmental conditions, time, and resources. Decision-making options are externally limited when time is short or when the environment is characterized by a “we’ve always done it this way” attitude. Values affect all aspects of decision making, from the statement of the problem/issue through the evaluation. Values, determined by one’s cultural, social, and philosophical background, provide the foundation for one’s ethical stance. The steps for engaging in ethical decision making are similar to the steps described earlier; however, alternatives or options identified in the decision-making process are evaluated with the use of ethical resources. Resources that can facilitate ethical decision making include institutional policy; principles such as autonomy, nonmaleficence, beneficence, veracity, paternalism, respect, justice, and fidelity; personal judgment; trusted co-workers; institutional ethics committees; and legal precedent. Certain personality factors, such as self-esteem and self-confidence, affect whether one is willing to take risks in solving problems or making decisions. Keynes (2008) asserts that individuals may be influenced based on social pressures. For example, are you inclined to make decisions to satisfy people to whom you are accountable or from whom you feel social pressure? Characteristics of an effective decision maker include courage, a willingness to take risks, self-awareness, energy, creativity, sensitivity, and flexibility. Ask yourself, “Do I prefer to let others make the decisions? Am I more comfortable in the role of ‘follower’ than leader? If so, why?” Exercise 6-2 Identify a current or past situation that involved resource allocation, end-of-life issues, conflict among healthcare providers or patient/family/significant others, or some other ethical dilemma. Describe how the internal and external factors previously described influenced the decision options, the option selected, and the outcome. Group Decision Making There are two primary criteria for effective decision making. First, the decision must be of a high quality; that is, it achieves the predefined goals, objectives, and outcomes. Second, those who are responsible for its implementation must accept the decision. Higher-quality decisions are more likely to result if groups are involved in the problem-solving and decision-making process. In reality, with the increased focus on quality and safety, decisions cannot be made alone. When individuals are allowed input into the process, they tend to function more productively and the quality of the decision is generally superior. Taking ownership of the process and outcome provides a smoother transition. Multidisciplinary teams should be used in the decision-making process, especially if the issue, options, or outcome involves other disciplines. Research findings suggest that groups are more likely to be effective if members are actively involved, the group is cohesive, communication is encouraged, and members demonstrate some understanding of the group process. In deciding to use the group process for decision making, it is important to consider group size and composition. If the group is too small, a limited number of options will be generated and fewer points of view expressed. Conversely, if the group is too large, it may lack structure, and consensus becomes more difficult. Homogeneous groups may be more compatible; however, heterogeneous groups may be more successful in problem solving. Research has demonstrated that the most productive groups are those that are moderately cohesive. In other words, divergent thinking is useful to create the best decision. For groups to be able to work effectively, the group facilitator or leader should carefully select members on the basis of their knowledge and skills in decision making and problem solving. Individuals who are aggressive, are authoritarian, or manifest self-oriented behaviors tend to decrease the effectiveness of groups. The nurse leader or manager should provide a nonthreatening and positive environment in which group members are encouraged to participate actively. Using tact and diplomacy, the facilitator can control aggressive individuals who tend to monopolize the discussion and can encourage more passive individuals to contribute by asking direct, open-ended questions. Providing positive feedback such as “You raised a good point,” protecting members and their suggestions from attack, and keeping the group focused on the task are strategies that create an environment conducive to problem solving. Advantages of Group Decision Making The advantages of group decision making are numerous. The adage “two heads are better than one” illustrates that when individuals with different knowledge, skills, and resources collaborate to solve a problem or make a decision, the likelihood of a quality outcome is increased. More ideas can be generated by groups than by individuals functioning alone. In addition, when followers are directly involved in this process, they are more apt to accept the decision, because they have an increased sense of ownership or commitment to the decision. Implementing solutions becomes easier when individuals have been actively involved in the decision-making process. Involvement can be enhanced by making information readily available to the appropriate personnel, requesting input, establishing committees and task forces with broad representation, and using group decision-making techniques. The group leader must establish with the participants what decision rule will be followed. Will the group strive to achieve consensus, or will the majority rule? In determining which decision rule to use, the group leader should consider the necessity for quality and acceptance of the decision. Achieving both a high-quality and an acceptable decision is possible, but it requires more involvement and approval from individuals affected by the decision. Groups will be more committed to an idea if it is derived by consensus rather than as an outcome of individual decision making or majority rule. Consensus requires that all participants agree to go along with the decision. Although achieving consensus requires considerable time, it results in both high-quality and high-acceptance decisions and reduces the risk of sabotage. Majority rule can be used to compromise when 100% agreement cannot be achieved. This method saves time, but the solution may only partially achieve the goals of quality and acceptance. In addition, majority rule carries certain risks. First, if the informal group leaders happen to fall in the minority opinion, they may not support the decision of the majority. Certain members may go so far as to build coalitions to gain support for their position and block the majority choice. After all, the majority may represent only 51% of the group. In addition, group members may support the position of the formal leader, although they do not agree with the decision, because they fear reprisal or they wish to obtain the leader’s approval. In general, as the importance of the decision increases, so does the percentage of group members required to approve it. To secure the support of the group, the leader should maintain open communication with those affected by the decision and be honest about the advantages and disadvantages of the decision. The leader should also demonstrate how the advantages outweigh the disadvantages, suggest ways the unwanted outcomes can be minimized, and be available to assist when necessary.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Patient Safety
- Developing the Role of Manager
- Care Delivery Strategies
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

Do problem-solving skills affect success in nursing process applications? An application among Turkish nursing students
Affiliation.
- 1 Department of Nursing, School of Health, Recep Tayyip Erdoğan University, Rize, Turkey.
- PMID: 25098504
- DOI: 10.1111/2047-3095.12043
Purpose: This study aimed to determine the relationship between problem-solving and nursing process application skills of nursing.
Methods: This is a longitudinal and correlational study. The sample included 71 students. An information form, Problem-Solving Inventory, and nursing processes the students presented at the end of clinical courses were used for data collection.
Findings: Although there was no significant relationship between problem-solving skills and nursing process grades, improving problem-solving skills increased successful grades.
Conclusions: Problem-solving skills and nursing process skills can be concomitantly increased.
Clinical revelance: Students were suggested to use critical thinking, practical approaches, and care plans, as well as revising nursing processes in order to improve their problem-solving skills and nursing process application skills.
Keywords: Nursing care plan; nursing process; problem-solving skill.
© 2014 NANDA International, Inc.
- Nursing Process*
- Problem Solving*
- Students, Nursing*
- Research note
- Open access
- Published: 13 March 2018
Implementation of nursing process in clinical settings: the case of three governmental hospitals in Ethiopia, 2017
- Ayele Semachew 1
BMC Research Notes volume 11 , Article number: 173 ( 2018 ) Cite this article
16k Accesses
29 Citations
Metrics details
The purpose of this survey was to evaluate the implementation of the nursing process at three randomly selected governmental hospitals found in Amhara Region North West Ethiopia.
From the total 338 reviewed documents, 264 (78.1%) have a nursing process format attached with the patient’s profile/file, 107 (31.7%) had no nursing diagnosis, 185 (54.7%) of nurses stated their plan of care based on priority, 173 (51.2%) of nurses did not document their interventions based on plan and 179 (53.0%) of nurses did not evaluate their interventions. The overall implementation of nursing process among Felege Hiwot Referal hospital, Debretabor general hospital and Finoteselam general hospitals were 49.12, 68.18, and 69.42% respectively. Nursing professionals shall improve documentation required in implementing the nursing process. Nursing managers (matron, ward heads) shall supervise the overall implementation of nursing process. Hospital nursing services managers (matrons) shall arrange and facilitate case presentations by the nursing staffs which focus on documentation and updates on nursing process. Hospitals need to establish and support nursing process coordinating staff in their institution.

Introduction
Nursing has always been directed to keep people healthy and provide comfort, care, and assurance to the patients. The nursing care, therefore, may involve any number of activities ranging from carrying out complicated technical procedures to something as simple as holding a hand of the patient. The central focus of nursing care is the person receiving care and included the physical, emotional, social and spiritual dimensions of that person. Nursing care, therefore, refers to care of others [ 1 ].
Nurses have many demands on their time as they provide care and document their work in a descriptive manner. In order to better meet the needs of their patients, the nurses developed a care plan with special forms [ 2 ].
Nursing process (NP) is a systematic method which utilizes scientific reasoning, problem-solving and critical thinking to direct nurses in caring for patients effectively [ 3 , 4 ].
The nursing process is a systematic problem-solving approach used to identify, prevent and treat actual or potential health problems and promote wellness. It has five steps; Assessment, Diagnosis, planning, implementation and evaluation [ 5 ].
The nursing process was initially an adapted form of problem-solving technique based on theory used by nurses every day to help patients improve their health and assist doctors in treating patients. Its primary aim is to know the health status and the problems of clients which may be actual or potential. It is made up of a series of stages that are used to achieve the objective—the health improvement of the patient. The use of nursing process can stop at any stage as deemed necessary or can be repeated as needed. This process is inclusive of physical health as well as the emotional aspects of patient health. Nursing knowledge is used throughout the process to formulate changes in approach to the patient’s changing condition [ 6 ].
Many nurse researchers and theorists are in agreement that nursing process is a scientific method for delivering holistic and quality nursing care. Therefore, its effective implementation is critical for improved quality of nursing care. When the quality of nursing care is improved, visibility of nurses’ contribution to patient’s health outcomes becomes distinct. In this way, nurses can justify the claim that nursing is a science and an independent profession [ 7 , 8 ].
Nurses are the largest group of health professionals in all countries. Nursing care quality is closely related to a health care system’s effectiveness. In order to achieve the quality of health care service, quality of nursing care is the key element and to fill this demand application of the nursing process has a significant role, but, in practice, application of the nursing process is not well developed [ 9 ].
The gap between research evidence and clinical practice is one of the most persistent problems in the provision of quality healthcare. Approximately 30–40% of patients do not receive health care according to current scientific evidence and some patients receive unnecessary or harmful care [ 10 ].
Since nurses are the key caregivers in hospitals, they can significantly influence the quality of care provided and, ultimately, treatment and patient outcomes. Despite their knowledge of the nursing process, certain factors limited the ability of nurses to implement it in their daily practice, including lack of time, high patient volume, and high patient turnover. Despite these hurdles, the daily application of the nursing process is characterized by the scientific background of the professionals involved since it requires Knowledge and provides individualized human assistance [ 8 ].
Though application of nursing process is running as a standard of care for many developed countries practically it faces many challenges. Despite there is no strong commitment on the implementation of nursing process in many hospitals in our country the problem is rampant. As we know many studies has been conducted and they identified different factors for the implementation of nursing process. Irrespective of many identified factors that impend nursing process implementation, the purpose of the current survey was to evaluate the implementation of the nursing process at three randomly selected governmental hospitals found in Amhara Region North West Ethiopia.
The study was conducted in three randomly selected governmental hospitals found in Amhara Regional state, North Western Ethiopia, Namely Felege Hiwote Comprehensive Referral Hospital, Debre Tabor General Hospital and Finoteselam General Hospital. The study was conducted from February 30 to March 30/2017.
Study design
Hospital-based descriptive and retrospective study design was used and the nursing process registration in inpatient records was also checked to inquire all pertinent information regarding on the implementation of nursing process.
Source population
All patient documents’ found in the selected hospital’s record unit and in the nursing station room.
Study population
All sampled patient documents’ found in the selected hospital’s record unit and nursing station room having Medical Registration Number (MRN) in the last 6 months.
Inclusion and exclusion criteria
All cases from medical, surgical and orthopedics wards were included whereas cases from the outpatient department were not included.
Sample size determination
Sample size (n) is determined using a single proportion formula using proportion (p) of nursing process implemented 32.7% from a study conducted in Arbaminch General Hospital, South Ethiopia [ 11 ] level of precision (d) 0.05 at 95% confidence interval (Zα/2) that gives 338 cases to be included.
Sampling technique
In order to select a representative sample from each hospital, the total number of inpatients in the last 6 months were obtained and then samples were proportionally allocated for each hospital. Based on this, 160 patient’s documents were seen from Felege Hiwote Comprehensive Referral Hospital, 110 from Debre Tabor General Hospital and 68 were seen from Finote Selam General Hospital. Then systematic random sampling using patients MRN was used to select eligible documents.
Data collection procedures
Instrument for data collection.
Socio-demographic information that includes: age, sex, educational status, marital status, occupation, ethnicity, previous hospitalization, length of hospitalization were included. Nursing process implementation checklist was prepared in English language to assess the documentation which was done by nurse professionals in the three hospitals.
Personnel for data collection
A total of 3 personnel were involved for data collection process and one BSc nurse was assigned to supervise the overall data collection process. All data collectors were oriented for a half day about the instrument and the data collection process.
Data quality control
Before conducting the actual data collection, pretest was done on 5% of the total sample size in Debre Markos Hospital. The collected data were reviewed and checked for completeness and relevance by the supervisor. Incomplete questionnaires were returned to the data collectors on the following day for the correction by revisiting the patient’s document.
Dependent variable
Implementation of nursing process.
Independent variable
Socio-demographic factors
Nursing care provided.
Operational definition and definition of terms
Data procedures and analysis.
The data were edited, coded and entered into Epi-Data version 3.1 and exported to IBM SPSS Statistics Version 20 for analysis. Results of the data analysis were presented in the form of descriptive statistics which included mean, standard deviation and percentages. The results were summarized and presented by tables, charts, and graphs.
Among the reviewed documents 190 (56.2%) were male and 148 (43.8%) were female. Two hundred twenty-four (66.3%) were married whereas 9 (2.7%) were widowed. Three hundred seven (90.8%) were orthodox Christian while 2 (0.6%) were protestant in their religion. Regarding educational status 138 (40.8%) were illiterate were as 45 (13.3%) were completed college and above. Concerning to occupation 75 (22.2%) were housewife whereas 2 (0.6%) were Non-governmental Organizations (NGOs) worker. One hundred eighty-nine (55.9%) were living in the rural part whereas 149 (44.1%) were living in urban areas (Table 1 ). The minimum age of the study participants was 18 and the maximum age was 88, the average hospital stay was almost 8 days.
Overall implementation of nursing process
From the total 338 reviewed documents, 264 (78.1%) have a nursing process attached with the patient’s profile/file, 107 (31.7%) had no nursing diagnosis, 185 (54.7%) of nurses stated their plan of care based on priority, 173 (51.2%) of nurses did not document their interventions based on plan and 179 (53.0%) of nurses did not evaluat e their interventions.
From the total 160 reviewed documents at Felege Hiwote Referral Hospital 100 (62.5%) of patient’s documents had nursing process attached with their file, from 110 reviewed documents at Debretabor General Hospital 99 (90%) of patient’s documents had nursing process attached with their file. Sixty eight documents were reviewed at Finoteselam General Hospital; 65 (95.6%) of patient’s documents had nursing process attached with their file.
Regarding documenting the nursing diagnosis; among the total reviewed 160 documents at Felege Hiwote Referral Hospital 95 (59.4%) had nursing diagnosis whereas from the total 68 reviewed documents at Finoteselam General Hospital 54 (79.4%) had a nursing diagnosis.
Concerning to nursing intervention; 65 (40.6%) of reviewed documents at Felege Hiwote Referral Hospital had a written nursing intervention whereas 63 (57.3%) of reviewed documents at Debretabor General Hospital had a written nursing intervention. Sixty-one (55.5%) documents reviewed at Debretabor General Hospital had evaluated their nursing interventions whereas 66 (41.3%) of reviewed documents at Felege Hiwote Referral Hospital had evaluated their nursing interventions. Overall discrepancies have been found in the implementation of nursing process among the three hospitals (Table 2 ).
The overall implementation of nursing process of the two hospitals namely Debretabor General Hospital and Finoteselam General Hospital had almost similar implementation where as Felege Hiwot Referal Hospital’s performance in implementing the nursing process was low in comparision with the aformentioned two hospitals (Fig. 1 ).
Over-all implementation of nursing process among hospitals in Amhara Region, North West Ethiopia, 2017
The aim of this survey was to evaluate the implementation status of nursing process at three governmental hospitals of Amhara Region, North West Ethiopia. Ethiopia as one of the developing country faced limited resource to implement different health and health-related strategies.
Many studies on the implementation of Nursing Process and associated factors among nurses have been done here in Ethiopia and as well in abroad. But almost all of the study subjects were nurses themselves and as we know these will lead a social anticipated bias that may overestimate the finding. But the current survey may overcome this drawback since we are collecting the data after reviewing patient documents (document review). And the finding of the current survey was low which was 47.0%.
Utilization of the nursing process in many low and middle-income countries has been a challenge [ 7 ]. All of the respondents said that they did not use the nursing process during provision of care to their patients at the time of the study. The majority (75%) of the respondent said that the nurse to patient ratio was not optimal to apply the nursing process [ 9 ]. The main discrepancy here is that before 2015 the implementation of nursing process was not a big deal in many hospitals rather there was a format which was prepared by the federal ministry of health which was different from nursing process. A study was done in Nigeria also revealed that although the trained nurses at the hospital had good theoretical knowledge of the nursing process, they did not apply it in the care of their patients [ 12 ].
Hospital nursing services managers (matrons) shall arrange and facilitate case presentations by the nursing staffs which focus on documentation and updates on nursing process.
The current study is a survey of secondary data from a nursing process implementation and this method does not provide the cause effect relationship.
Abbreviations
- Nursing process
Medical Registration Number
Non-governmental Organizations
Research Ethical Review Committee
Marjorie L, Pearson, Chang B, Lee J, Katherine LLVR. An implicit review method for measuring the quality of in-hospital nursing care of elderly congestive heart failure patients. Monograph Report. Santa Monica California: RAND Corporation; 1997.
Helena M, De Moraes B, Higa R, José M, Tocoginecology M, De Oliveira NR. Evaluation of the nursing process used at a Brazilian teaching hospital. Int J Nurs Terminol Classif. 2010;21(3):8.
Google Scholar
Altamier. Evaluation of implementation of nursing process, among nurses working in Abakaliki metropolis, Abakaliki; 2010.
Carpenito-Moyet. Nursing diagnosis. In: Nursing diagnosis: Application to clinical practic, 10th edition. Philadelphia; 2004.
Aseratie M, Murugan R, Molla M. Assessment of factors affecting implementation of nursing process among nurses in selected governmental hospitals, Addis Ababa, Ethiopia; Cross Sectional Study. J Nurs Care. 2014;3(3):170.
Adeyemo FO. Factors affecting the use of nursing process in health institutions in Ogbomoso Town, Oyo State. Researchgate. 2013; 9. https://www.researchgate.net/publication/235957070 .
Carole M, Wagoro A, Podo C. Mainstreaming Kenya-Nursing Process in clinical settings: the case of Kenya. Int J Africa Nurs Sci. 2015;3:31–9.
Article Google Scholar
Abebe N, Abera H, Ayana M. The implementation of nursing process and associated factors among nurses working in Debremarkos and Finoteselam Hospitals, northwest Ethiopia, 2013. Nurs Care. 2014;3(2):149.
Hagos F, Alemseged F, Balcha F, Berhe S, Aregay A. Application of nursing process and its affecting factors among nurses working in mekelle zone hospitals, Northern Ethiopia. Nurs Res Pract. 2014;2014:675212.
PubMed PubMed Central Google Scholar
Davies B, Edwards N, Ploeg J, Virani T. Insights about the process and impact of implementing nursing guidelines on delivery of care in hospitals and community settings. BMC Health Serv Res. 2008;15:8–29.
Shewangizaw Z, Mersha A. Determinants towards implementation of nursing process. Am J Nurs Sci. 2015;4(3):45–9.
Afolayan JA, Donald B, Baldwin DM, Onasoga O. Evaluation of the utilization of nursing process and patient outcome in psychiatric nursing: case study of psychiatric Hospital Rumuigbo, Port Harcourt. Adv Appl Sci Res. 2013;4(5):34–43.
Download references
Authors’ contributions
AS wrote the proposal, participated in the data collection, analyzed the data, and drafted the paper including the manuscript. The author read and approved the final manuscript.
Acknowledgements
For data collectors and respective hospital administrators.
Competing interests
The author declare no competing interests.
Availability of data and materials
Not applicable.
Consent for publication
Ethics approval and consent to participate.
Ethical clearance was obtained from Research Ethical Review Committee (RERC) of Bahir Dar University College of Medicine and Health Sciences, and permission and supporting letter was secured for each respective hospital administrators before data collection. Written informed consent was also obtained from each ward heads. No names or identifying information were indicated on the checklist, and all confidentiality issues were assured.
No fund was obtained.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Department of Nursing, College of Medicine and Health Sciences, Bahir Dar University, PO Box. 79, Bahir Dar, Ethiopia
Ayele Semachew
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ayele Semachew .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Semachew, A. Implementation of nursing process in clinical settings: the case of three governmental hospitals in Ethiopia, 2017. BMC Res Notes 11 , 173 (2018). https://doi.org/10.1186/s13104-018-3275-z
Download citation
Received : 22 December 2017
Accepted : 05 March 2018
Published : 13 March 2018
DOI : https://doi.org/10.1186/s13104-018-3275-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Implementation
- North West Ethiopia
BMC Research Notes
ISSN: 1756-0500
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 28 April 2024
The effect of perceived organizational justice on workplace deviant behavior of new nurses: the role of emotional labor and psychological capital
- Ran Meng 1 na1 ,
- Zhe Jiang 1 na1 ,
- Guangli Lu 2 &
- Chaoran Chen 1
BMC Nursing volume 23 , Article number: 288 ( 2024 ) Cite this article
142 Accesses
Metrics details
New nurses are prone to workplace deviant behavior in the constrained hospital environment, which will not only directly affect the safety of patients, but also reduce the work efficiency of nurses and bring negative results to the hospital. The purpose of this study was to investigate the relationship between perceived organizational justice, emotional labor, psychological capital, and workplace deviant behavior of new nurses.
A cross-sectional study was used in this study. A survey was conducted in 5 hospitals in Henan Province, Chain from February to April 2023. The sample size was 546. The questionnaire included general information, perceived organizational justice scale, emotional labor scale, psychological capital scale, and workplace deviant behavior scale. SPSS 26.0 and PROCESS Macro were used for data analysis. PROCESS Model 4 and Model 14 were used to verify the model.
This study displays that perceived organizational justice was negatively correlated with emotional labor and workplace deviant behavior, and emotional labor was positively correlated with workplace deviant behavior. Meanwhile, emotional labor plays a partial mediating role between perceived organizational justice and workplace deviant behavior, accounting for 32.7% of the total effect. Moreover, the path of emotional labor on workplace deviant behavior is moderated by psychological capital.
This study further understood the workplace deviant behavior of new nurses, and provided a new perspective for solving this problem. Nurse managers can reduce workplace deviant behavior by enhancing the perceived organizational justice and psychological capital of new nurses and improving emotional labor.
Peer Review reports
Introduction
With the aggravation of the aging population, the demand for high-quality medical care services has intensified [ 1 ]. According to a report by the World Health Organization (WHO), there is still a shortage of more than 5.9 million nurses worldwide [ 2 ]. This means that the number of nurses is far from enough to meet the development of medicine. New nurses are the new human resources of the nursing industry, and their professional competencies directly influence the quality and development of nursing services [ 3 ]. New nurses refer to those who have worked for less than 1 year after graduation [ 4 ]. Faced with the role change from school to hospital and the complex clinical environment, new nurses generally lack confidence in clinical work and have different degrees of workplace maladjustment [ 5 ], resulting in interpersonal sensitivity and anxiety. The challenge extends further as they strive to strike a balance between their professional responsibilities and personal well-being [ 5 ], reducing their enthusiasm for clinical work and causing job burnout [ 6 ]. Moreover, new nurses often experience high-load nursing training before formally starting work, resulting in serious physical and mental load [ 3 ]. At the same time, the working conditions of many nurses and healthcare professionals around the world are also deteriorating due to COVID-19 [ 7 ], further affecting the initiative of nurses and leading to workplace deviant behavior.
Workplace deviant behavior is the voluntary behavior of organization members that violates important organizational norms and threatens the well-being of the organization and its members [ 8 ]. The workplace deviant behavior of nurses includes less harmful behaviors such as absenteeism, idleness, and lying, as well as more harmful behaviors such as spreading rumors, violating medical orders, knowing that medical orders are unreasonable but not followed, and violating nursing practices [ 9 ]. Nurses’ workplace deviant behavior will not only reduce their own work efficiency and work involvement [ 10 , 11 ] but also affect their work performance. In addition, it also increases work pressure and turnover intention of colleagues, weakening job satisfaction, organizational commitment and happiness [ 12 , 13 , 14 ], and affects the stability of the nursing team [ 15 ]. On the other hand, deviant behavior will also affect occupational safety, cause medical safety accidents [ 16 ], and affect doctor-patient relationships. It can be seen that nursing staff’s deviant behavior is relatively common in clinical work, which not only causes negative effects on the team and members but also endangers the safety of patients and affects the process of disease rehabilitation.
Although previous studies have made contributions to the field of workplace deviant behavior, there are still some research gaps. Firstly, previous studies on workplace deviant behavior have mostly focused on inter-enterprise situations [ 17 , 18 ], such as bank employees [ 14 ] and construction workers [ 11 ], while there is still relatively little research on the workplace deviant behavior of new nurses in medical settings. Secondly, there is a lack of research on the mechanisms of workplace deviant behavior. Existing research mostly focuses on the relationship between two variables, and there is insufficient research on the potential mechanisms of multiple variables and workplace deviant behavior, lacking effective theoretical support to guide clinical workers in taking measures. Finally, previous studies have mostly focused on the influence of leadership on workplace deviant behavior of nurses, with little exploration of the significance of nurse own psychological state on workplace deviant behavior, which may be a research gap. Nurses are often subjected to high-pressure work for a long time, and serious mental health problems are inevitable [ 19 ], which are often an important source of behavioral deviation. Therefore, to fill these research gaps, create a safe diagnosis and treatment environment and ensure the stability of the nursing team, it is important to investigate the workplace deviant behavior and mechanism of new nurses.
In previous studies, perceived organizational justice is an important antecedent variable affecting workplace deviant behavior [ 20 , 21 ]. The perception of perceived organizational justice refers to the subjective feeling of organization members on whether the distribution, information and interpersonal relationships of the organization are fair [ 22 ]. A good sense of organizational justice can enhance professional identity [ 23 ], affect the work performance of nurses, and have an important impact on individual work development [ 24 ]. Social cognitive theory is an important theory in organizational behavior. This theory emphasizes that an individual’s behavior is influenced by the situation they are in, and information is integrated through their internal cognition to exhibit corresponding behaviors [ 25 ]. Perceived organizational justice is an important situational factor in an organization, which is an individual’s perception of the organization and can have a significant impact on their behavior. Kakemam [ 26 ] found that perceived organizational justice is negatively correlated with workplace deviant behavior, and significantly negatively predicts workplace deviant behavior, which is consistent with the previous study [ 27 ]. At the same time, study has proved that information justice and work atmosphere can affect workplace deviant behavior [ 28 ]. In order to better understand the perceived organizational justice perception and workplace deviant behavior of new nurses, we proposed the following hypothesis:
The perceived organizational justice of new nurses is negatively correlated with workplace deviant behavior.
Emotional labor has attracted more and more attention among scholars [ 29 , 30 ]. Emotional labor refers to that nurses can reasonably adjust and express their internal and external emotions according to the requirements of their work roles when facing patients [ 31 ]. Appropriate emotional labor can improve nurses’ strain capacity, but a high level of emotional labor will lead to job burnout, depression and other adverse emotions, and also affect patients’ satisfaction with nursing services [ 32 ]. We use conservation of resources theory to reveal the underlying mechanism by which perceived organizational justice affects workplace deviant behavior. The conservation of resources theory includes the spiral principles of resource loss and the spiral principles of resource acquisition [ 33 ]. The former refers to individuals constantly consuming resources when facing pressure, and when they are depleted, they will take action to prevent the continuous loss of resources. The latter is when individuals have more resources, they will choose to acquire more resources to prevent the loss of resources. When nurses experience less sense of justice in the organization, they will adopt emotional labor strategies to cope. Emotional labor, as a new form of labor after physical strength and intelligence [ 30 ], is a source of stress. According to the spiral principle of resource loss in the conservation of resources theory, emotional labor constantly consumes psychological resources and thus produces emotional exhaustion [ 34 ], reduces the happiness of work [ 35 ], and affects work behavior and work state [ 36 ]. In order to compensate for the loss of resources, nurses may adopt negative behaviors, which can lead to workplace deviant behavior. Furthermore, a study of medical personnel showed that emotional labor can positively predict the level of deviant behavior [ 37 ]. Therefore, this study proposes the following hypothesis:
Emotional labor plays a mediating role in the relationship between perceived organizational justice and workplace deviant behavior of new nurses.
Psychological capital is a positive mental state owned by an individual and a potentially available internal resource of an individual, which can help an individual cope with difficulties and setbacks [ 38 ]. It can weaken the adverse effects of negative emotions, and promote the growth and development of an individual [ 38 ]. Studies have pointed out that individual behavior can be influenced by four dimensions of psychological capital (hope, self-efficacy, optimism and resilience) [ 39 ]. Based on the spiral principle of resource acquisition in the conservation of resources theory, people will establish, protect and cultivate their own resource base [ 33 ]. If individuals have enough psychological resources to supplement and cope with resource consumption, the adverse consequences brought by pressure will be effectively alleviated or eliminated [ 40 ]. When emotional labor consumes resources, psychological capital, as a resource supplement, can reduce the level of emotional labor [ 41 ], which can improve the mental health of nurses and alleviate the appearance of workplace deviant behavior. Previous studies have pointed out that emotional labor is correlated with psychological capital [ 42 ]. Kim [ 34 ] found that positive psychological capital and social support of special education teachers can regulate the impact of emotional labor on job burnout, and thus affect career happiness. Other studies have found that psychological capital and psychosocial safety atmosphere can improve the positive service behaviors of service workers towards work and customers [ 43 ], which promotes occupational health and safety. Therefore, the following hypothesis is proposed in this study:
Psychological capital moderates the effect of emotional labor on workplace deviant behavior of new nurses.
Previous studies have shown that perceived organizational justice is related to workplace deviant behavior of nurses, but the effects of emotional labor and psychological capital on perceived organizational justice and workplace deviant behavior have not been deeply explored. Therefore, the purpose of this study is to explore the mediating effect of emotional labor on perceived organizational justice and workplace deviant behavior, as well as the moderating effect of psychological capital, in order to provide a theoretical and practical basis for reducing workplace deviant behavior of new nurses and improving clinical nursing quality. The research framework is shown in Fig. 1 .
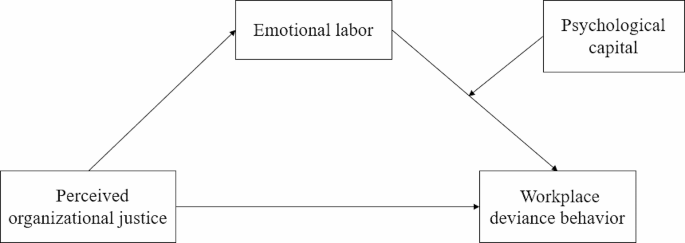
The theoretical framework model of this study
Participants and procedures
In this study, a cross-sectional study was used to investigate 5 hospitals in Henan Province, China from February to April 2023. Inclusion criteria: (1) registered nurses; (2) the working time is less than 1 year; (3) voluntary participation in this study. Exclusion criteria: nurses who go to the hospital for further study. A total of 574 questionnaires were collected for the study. In the process of questionnaire screening, the randomly filled questionnaires and all the questionnaires with the same answers were strictly excluded, and 546 valid questionnaires were obtained in the end.
Demographic characteristics
Demographic information for this study included gender, age, education level, job department, labor relations, working hours per day, and monthly income.
- Emotional labor
The Emotional labor Scale translated by Luo [ 44 ] was adopted to investigate the emotional labor of nurses. It consists of three dimensions: surface acting (7 items), emotional expression (4 items), and deep acting (3 items). One of the items is “In order to serve patients in an appropriate way, I learned to disguise my emotions”. The Cronbach’α of the scale in this study was 0.94.
- Workplace deviant behavior
The workplace deviant behavior scale was developed by Bennett [ 8 ], and Zhang [ 9 ] was translated. There were 21 items in the scale, including behavioral deviation at the interpersonal level (6 items), behavioral deviation at the organizational level (6 items), aggressive behavior toward the service object (2 items), aggressive behavior toward organization members (4 items), and behavior violating labor discipline (3 items). For example, one of the items is “Deliberately concealing some information that others should know”. Cronbach’α of this scale is 0.98.
- Perceived organizational justice
The survey of nurse’s perceived organizational justice was compiled by Colquitt [ 45 ] and translated by Zhang [ 46 ]. The scale consists of 20 items and four dimensions, including distributive justice (4 items), procedural justice (7 items), interpersonal justice (4 items), and information justice (5 items). For example, one of the items is “Leaders respect me”. Cronbach’α of this scale is 0.95.
- Psychological capital
The psychological capital of nurses was measured using the psychological capital questionnaire (PCQ) developed by Luthan [ 47 ]. Luo [ 48 ] was revised according to the characteristics of nursing work in China. The scale consisted of 20 items and was used to test four dimensions of self-efficacy (6 items), hope (6 items), resilience (5 items) and optimism (3 items). For example, one of the items is “I am able to achieve my work goals with full energy.” Cronbach’s α of the questionnaire ranged from 0.72 to 0.92. The Cronbach’s α of this scale in this study was 0.97.
Ethics considerations
The researcher explains the purpose of the scientific study to the hospital manager and obtains permission for the investigation. At the same time, after learning the purpose of the study on the first page of the questionnaire, the respondents voluntarily participated in the study and could withdraw from the survey at any time. The content of the study did not harm the participants’ physical and mental health. Results were used for this study only and non-researchers were not authorized to view the questionnaires collected. This study was approved by the Ethics Committee of Henan University, and the ethics review number is HUSOM2022-375.
Data analysis
SPSS 26.0 and PROCESS Macro were used for data analysis. Confirmatory factor analysis was conducted using AMOS 28. Descriptive statistical methods are used to describe data frequency, mean, standard difference, etc. Pearson correlation analysis was used to verify the correlation among perceived organizational justice, emotional labor, psychological capital and workplace deviant behavior. The influence of demographic data on workplace deviant behavior is analyzed by multiple linear regression. Then, the mediating effect of emotional labor was tested using PROCESS Model 4 developed by Hayes [ 49 ]. Finally, Model 14 was used to verify the moderating effect of psychological capital. We used the 5000 resample bootstrapping method with a 95% CI to test the model. When 95% CI does not include 0, the effect is meaningful. All analyses were two-tailed, and the level of statistical significance was p < 0.05.
Descriptive statistics of population data
The results of the demographic analysis of nurses in this study showed that the majority of nurses were female (72.53%) and had an undergraduate degree (66.85%). 69.78% work in tertiary hospitals. 63.55% are contract workers. New nurses with monthly income below 4000 RMB were more than half (64.28%). The detailed results are shown in Table 1 .
Correlation analysis
The mean value, standard deviation of the study variables and the correlation among variables are shown in Table 2 . The item’s mean scores of perceived organizational justice, emotional labor, psychological capital, and workplace deviant behavior were 3.61 ± 0.75, 3.16 ± 0.90, 4.64 ± 0.83, 1.67 ± 0.98, respectively. Perceived organizational justice and workplace deviant behavior ( r =-0.40, p < 0.01) were negatively correlated, which validates hypothesis 1. Emotional labor was negatively correlated with perceived organizational justice ( r =-0.46, p < 0.01), but positively correlated with workplace deviant behavior ( r = 0.40, p < 0.01).
Confirmatory factor analysis of measurement models
The average variance extracted (AVE) and composite reliability (CR) of the study variables were both higher than the threshold (AVE > 0.5, CR > 0.7) [ 50 ] (Table 2 ), indicating good internal consistency and reliability of the study measurement model. In addition, collinearity diagnosis shows that the variance inflation factor (VIF) is less than 5, indicating that there is no collinearity issue between variables [ 51 ].
To further validate the structural validity of the research variables, we conducted a confirmatory factor analysis using AMOS 28 on perceived organizational justice, emotional labor, psychological capital, and workplace deviant behavior, then compared the hypothesized four factors model with three other possible models (Table 3 ). The results showed that the four factors model had a better fit ( x 2 / df = 2.755, CFI = 0.986, IFI = 0.986, RMSEA = 0.057). This result supports the uniqueness of the model proposed in this study.
Perceived organizational justice and workplace deviant behavior: a moderated mediation test
The results of multiple linear regression analysis of demographic data show that the average monthly income has a significant effect on workplace deviant behavior. Therefore, average monthly income was analyzed as a control variable.
Firstly, Model 4 in the SPSS PROCESS was used to test the mediating effect of emotional labor. The results are shown in Table 4 . Perceived organizational justice had a significant negative predictive effect on workplace deviant behavior (c=-0.52, 95% CI: -0.63 to -0.42). Emotional labor had a significant mediating effect between perceived organizational justice and workplace deviant behavior, and the effect value was − 0.17 (95% CI: -0.23 to -0.12), accounting for 32.7% of the total effect. When perceived organizational justice and emotional labor entered the regression equation together, the predictive effect of perceived organizational justice on workplace deviant behavior was still significant (c’ =-0.35, 95% CI: -0.46 to -0.24). Therefore, emotional labor plays a partial mediating role in the prediction of perceived organizational justice on workplace deviant behavior of new nurses, which validates hypothesis 2.
Secondly, Model 14 in the SPSS PROCESS was used to test the moderating effect of psychological capital, and the test results are shown in Table 5 . Perceived organizational justice significantly negatively predicted workplace deviant behavior ( β = 0.52, p < 0.001). Perceived organizational justice significantly negatively predicted emotional labor ( β =-0.56, p < 0.001). Then, the main effect of emotional labor on workplace deviant behavior was significant ( β = 0.26, p < 0.001), and the interaction terms of perceived organizational justice and emotional labor predicted workplace deviant behavior significantly ( β =-0.23, p < 0.001).
Further simple slope analysis results are shown in Fig. 2 . For new nurses with low psychological capital, emotional labor had a significant positive predictive effect on workplace deviant behavior ( β simple slope = 0.46, 95% CI: 0.34 to 0.58), but for new nurses with high psychological capital, emotional labor had no significant positive predictive effect on workplace deviant behavior ( β simple slope = 0.07, 95% CI: -0.06 to 0.19). The results showed that emotional labor had different predictive effects on the deviation behavior of new nurses under different levels of psychological capital, which validates hypothesis 3. To be specific, emotional labor has a more significant positive predictive effect on workplace deviant behavior when psychological capital is low.
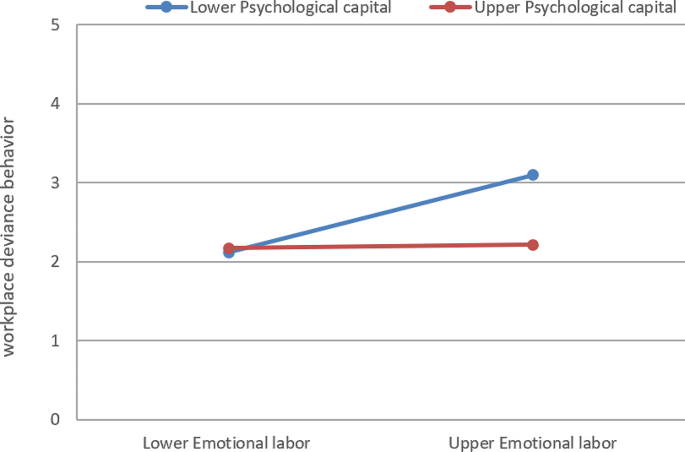
The moderating effect of psychological capital
This study constructed a moderated mediation model to explore the mechanism of the relationship between perceived organizational justice and workplace deviant behavior of new nurses. On the one hand, it illustrates that perceived organizational justice affects the workplace deviant behavior of new nurses through the mediating effect of emotional labor. On the other hand, it explains that psychological capital can regulate the latter half path of intermediary (the influence of emotional labor on workplace deviant behavior). Compared with new nurses with low psychological capital, high psychological capital weakens the influence of emotional labor on workplace deviant behavior. The results of this study provide theoretical and practical significance for the prevention and intervention of work behavior problems of new nurses.
In this study, the perceived organizational justice score is slightly lower than that of Viseu [ 52 ], and the difference in results may be due to the difference in the research objects. In the process of changing from the school environment to the hospital working environment, the complex working environment and interpersonal relationships make the new nurses have a sense of unevenness in the fairness of the hospital organization. The score of emotional labor was similar to that of Yu [ 53 ], indicating that there was a certain level of emotional labor among new nurses. On the one hand, new nurses are still adapting to hospital work, on the other hand, they are faced with an overloaded workload and lack coping skills in dealing with stressful events and negative emotions, so emotional labor may occur. In addition, the level of psychological capital is higher than the previous results of Kim [ 54 ], which may be due to the difference in sample size. Finally, the workplace deviant behavior score was higher than Zhang [ 28 ], indicating that the nursing quality and organizational discipline of new nurses still need to be improved. The reasons may be related to the less experience of new nurses and the lack of predictability and sensitivity to clinical emergencies, which has an impact on the results of work quality.
This study confirmed that perceived organizational justice negatively predicted workplace deviant behavior, indicating that perceived organizational justice was a protective factor for workplace deviant behavior of new nurses, which was consistent with Kakemam’s [ 26 ] research. According to social exchange theory, individuals will evaluate the potential costs and benefits to obtain the best benefit result, and then choose to give back to the organization or help themselves [ 55 ]. Nurses regard their relationship with the organization as a social exchange. When nurses feel fair treatment, they will actively exchange with the hospital, which is reflected in the improvement of work performance [ 23 ]. However, when nurses feel unfair, they will destroy the social exchange and take deviant behaviors to reduce their own losses [ 56 , 57 ]. Therefore, the improvement of organizational justice can reduce deviant behavior. Nursing managers should create a fair organizational environment for new nurses. In the nursing process and the implementation of decision-making control process, managers should pay attention to procedural equity, interpersonal equity, information equity, and distribution equity, so as to make nursing management work more just and transparent, reducing the occurrence of deviant behavior.
This study also found that emotional labor played a mediating role in the relationship between perceived organizational justice and workplace deviant behavior of new nurses. When comparing the new nurses with the surrounding senior nurses and doctors, it is found that there is a big gap in salary and welfare treatment, and nurses feel unfair, which leads them to feel that their labor has not been equally supplemented [ 58 ], resulting in a feeling of injustice. Low perceived organizational justice reduces nurses’ sense of collective belonging, resulting in higher emotional labor [ 59 ]. High emotional labor will lead to emotional exhaustion, job burnout, turnover intention, etc [ 60 , 61 ]., which promote deviant behavior [ 62 ]. At the same time, based on the psychological contract theory [ 63 ], when employees plan to leave the organization, that is, when the turnover intention is high, the employees may not firmly abide by the standard requirements of the organization. A large number of studies have shown that emotional labor will lead to high turnover intention of nurses [ 64 , 65 ], resulting in a series of withdrawal behaviors, work deviation and lower work performance of nurses [ 66 ]. Therefore, nursing managers should reasonably formulate the salary performance appraisal system, reasonably arrange work schedules, pay attention to the emotional changes of new nurses and identify the emotional labor level of nurses as early as possible, and at the same time conduct regular psychological and emotional guidance for new nurses, which is beneficial to reduce the turnover rate of new nurses and improve the quality of work.
This study further found that the path that perceived organizational justice affects the workplace deviant behavior of new nurses through emotional labor is moderated by psychological capital. Specifically, the emotional labor of new nurses with low psychological capital has a stronger predictive effect on workplace deviant behavior, while for new nurses with high psychological capital, the predictive effect is weaker. The research results supported the conservation of resources theory [ 40 ]. In order to alleviate the impact of emotional labor pressure, individuals will mobilize resources to cope. However, for those with poor resources, resource input will not make ends meet, resulting in resource loss, which may lead to deviant behavior [ 67 ]. As an important psychological resource, nurses with high psychological capital have positive psychological qualities such as self-efficacy, hope, resilience and optimism, which provide mental and psychological support for nurses, relieve work pressure [ 68 ], and reduce the harm of resource consumption. At the same time, new nurses with high psychological capital have clear work goals and plans, and they can adapt to the changes of clinical work, quickly integrate into the work environment, and successfully become professional nursing staff [ 69 ], reducing deviant behavior. This suggests that managers should pay attention to the mechanism of psychological capital on workplace deviant behavior. They can create a supportive organizational atmosphere to improve their positive psychological capital, such as providing care and support for medical staff from the organization and carrying out corresponding psychological training courses.
Relevance to clinical practice
New nurses are the young blood of the nursing team and have the potential for career development. However, new nurses have to face many pressures such as work, role and interpersonal relationships after entry. Forced management and restriction will cause a decrease in work efficiency and an increase in the turnover rate of new nurses [ 70 ], resulting in workplace deviant behavior. However, there is a great need for a stable nursing team to provide high-quality nursing services. Therefore, it is very important to reduce the deviation behavior of new nurses. This study provides a theoretical and practical basis for reducing the workplace deviant behavior of new nurses. In order to reduce workplace deviant behavior, first of all, nursing managers should give appropriate authorization at work to build an effective communication platform and opportunities for nurses to participate in decision-making, so that nurses can dare to express their ideas and communicate with managers actively when they feel unfair. At the same time, they should make full use of intelligent stimulation and contingent rewards to improve nurses’ sense of belonging to a team and happiness. Secondly, nursing managers should actively create a united and relaxed working atmosphere to reduce nurse patient conflicts. At the same time, reasonable work schedules should be formulated to reduce work intensity and reduce the emotional labor of new nurses, so that nurses can engage in work with positive emotions and improve the workplace deviant behavior of clinical nurses. Thirdly, nursing managers should pay attention to the psychological capital of new nurses. They can organize collective activities, build a support system, improve the psychological capital of new nurses, and effectively reduce workplace deviant behavior. Finally, the government plays an indispensable role in healthcare. The government can strengthen the supervision of medical institutions, establish clear nursing standards, and optimize the working environment of hospitals. At the same time, the government should attach importance to the psychological education of nurses and offer relevant courses on psychological education, so that newly graduated nurses have good psychological qualities to enter clinical work.
Limitations and future research directions
There are some limitations to this study. First of all, this study was only conducted in Henan Province, which will limit the popularization of the research results. It is suggested that future multi-regional hospital studies should be carried out to make the findings more universal. Secondly, this study was cross-sectional and cannot determine causation. All subsequent studies could conduct longitudinal studies to further explore the links between the variables. Finally, this study used self-reporting to measure variables, and nurses may not fully express their true answers in order to present an ideal social image. Future studies could use more objective measurement methods, such as experimental intervention studies.
In this study, the results showed that emotional labor played a mediating role between perceived organizational justice and workplace deviant behavior of new nurses, and psychological capital moderated the relationship between emotional labor and workplace deviant behavior. Therefore, we suggest that nursing managers on the one hand can guide new nurses to conduct emotional counseling and reasonable management of emotional labor. On the other hand, some support resources can be provided for new nurses, such as reward mechanisms, good doctor-patient relationship maintenance, and nurses can be encouraged to set goals and motivate work to improve the psychological capital level of new nurses. Under the joint action of reducing emotional labor and improving psychological capital, the work behavior of new nurses can be improved to create safe and high-quality nursing services.
Data availability
The data for this study is not publicly available. But it can be obtained from the author on reasonable demand.
Abbreviations
Statistical Product and Service Solutions
Corona Virus Disease 2019
Jang I, Oh D, Kim YS. Factors associated with nursing students’ willingness to care for older adults in Korea and the United States. Int J Nurs Sci. 2019;6(4):426–31. https://doi.org/10.1016/j.ijnss.2019.09.004
Article PubMed PubMed Central Google Scholar
Wan X, Huang H, Zhang Y, Peng Q, Guo X, Wu S, Li Y, Ding Y, Chen C. The effect of prosocial behaviours on Chinese undergraduate nursing students’ subjective well-being: the mediating role of psychological resilience and coping styles. Int J Ment Health Nurs. 2023;32(1):277–89. https://doi.org/10.1111/INM.13081
Article PubMed Google Scholar
Yu C, Jiang J, Zhong M, Zhang H, Duan X. Training load of newly recruited nurses in Grade-A Tertiary hospitals in Shanghai, China: a qualitative study. Bmc Nurs. 2023;22(1). https://doi.org/10.1186/s12912-022-01138-z
Hsiao PR, Lin CC, Han CE, Chen LC, Wang LH, Su CC. Role transition of newly graduated nurses: a qualitative study. Contemp Nurse. 2021;57(6):450–61. https://doi.org/10.1080/10376178.2022.2029519
Labrague LJ. JAA De los Santos 2020 Transition shock and newly graduated nurses’ job outcomes and select patient outcomes: a cross-sectional study. J Nurs Adm Manag 28 5 1070–9 https://doi.org/10.1111/jonm.13033
Article Google Scholar
Xie J, Li J, Wang S, Li L, Wang K, Duan Y, Liu Q, Zhong Z, Ding S, Cheng ASK. Job burnout and its influencing factors among newly graduated nurses: a cross-sectional study. J Clin Nurs. 2021;30(3–4):508–17. https://doi.org/10.1111/jocn.15567
Bourgault AM. The nursing shortage and work expectations are in critical Condition: is anyone listening? Crit Care Nurse. 2022;42(2):8–11. https://doi.org/10.4037/ccn2022909
Bennett RJ, Robinson SL. Development of a measure of workplace deviant. J Appl Psychol. 2000;85(3):349–60. https://doi.org/10.1037/0021-9010.85.3.349
Article CAS PubMed Google Scholar
Zhang H, Liu H, Sheng Y. Development and validation of the evaluation scale of Workplace Deviant Behavior of nurses. J Nurs Sci. 2020;35(18):75–8. https://doi.org/10.3870/j.issn.1001-4152.2020.18.075
Article CAS Google Scholar
Wu M, Wang R, He P, Estay C, Akram Z. Examining how ambidextrous Leadership relates to affective commitment and Workplace Deviant Behavior of employees: the moderating role of Supervisor-Subordinate ExchangeGuanxi. Int J Environ Res Public Health. 2020;17(15). https://doi.org/10.3390/ijerph17155500
Zheng J, Zhang Z, Wu G, Yang Y, Xia N, Liu B. Daily Self-Efficacy, Work Engagement, and deviant behavior among construction professionals and Workers: Cross-level moderating role of Job Control. J Constr Eng Manag. 2021;147(4). https://doi.org/10.1061/(asce)co.1943-7862.0002022
Wang T, Abrantes ACM, Liu Y. Intensive care units nurses’ burnout, organizational commitment, turnover intention and hospital workplace violence: a cross-sectional study. Nurs Open. 2023;10(2):1102–15. https://doi.org/10.1002/nop2.1378
Wang L, Ni X, Li Z, Ma Y, Zhang Y, Zhang Z, Gao L, Liu X, Yan W, Fan L, et al. Mental Health Status of Medical Staff exposed to Hospital Workplace Violence: a prospective cohort study. Front Public Health. 2022;10. https://doi.org/10.3389/fpubh.2022.930118
Nagi AH, Asad M, Khalid Z, Bibi A. The effect of performance appraisal politics on deviant work behavior: the mediating role of job satisfaction. Hum Syst Manage. 2022;41(5):583–96. https://doi.org/10.3233/hsm-211565
Chang S. The influence of employees’withdrawal behaviors on turnover intention and innovative work behavior. Korean J Hum Resour Dev. 2019;22(1):41–64. https://doi.org/10.24991/kjhrd.2019.03.22.1.41
Ma D, Wu J, Wang Y, Yi W. Application of detail management in nursing safety management in operating room. Minerva Med. 2022;113(5). https://doi.org/10.23736/s0026-4806.20.07107-4
Zhang X, Yang Q, Yan Y, Liang S. Family-supportive supervisor behavior and employees’ workplace deviant behavior: Moral disengagement as a mediator. Social Behav Personality. 2022;50(7). https://doi.org/10.2224/sbp.11319
Nair N, Bhatnagar D. Understanding Workplace Deviant Behavior in Nonprofit Organizations toward an integrative conceptual Framework. Nonprofit Manag Leadersh. 2011;21(3):289–309. https://doi.org/10.1002/nml.20026
Xiao Q, Iftikhar Q, Spaeth K, Zhang C, Liang XC, Klarin A, Liu L. The relationship between servant leadership and nurses’ in-role performance: the sequential mediating effects of job autonomy and emotional exhaustion. J Adv Nurs. 2024;80(4):1440–51. https://doi.org/10.1111/jan.15930
Khattak MN, Zolin R, Muhammad N. The combined effect of perceived organizational injustice and perceived politics on deviant behaviors. Int J Confl Manage. 2021;32(1):62–87. https://doi.org/10.1108/ijcma-12-2019-0220
Nasir M, Bashir A. Examining workplace deviant in public sector organizations of Pakistan. Int J Soc Econ. 2012, 39(4).
Chen C, Chen Y, Yang Y, Duan G. Path analysis of the influencing factors of nurses’ organizational justice. Chin J Nurs. 2010;45(10):877–80.
Google Scholar
Yu J-F, Ding Y-M, Jia R-Y, Liang D-D, Wu Z, Lu G-L, Chen C-R. Professional identity and emotional labour affect the relationship between perceived organisational justice and job performance among Chinese hospital nurses. J Nurs Adm Manag. 2022;30(5):1252–62. https://doi.org/10.1111/jonm.13608
Fein EC, Tziner A, Vasiliu C. Perceptions of ethical climate and organizational justice as antecedents to employee performance: the mediating role of employees? Attributions of leader effectiveness. Eur Manag J. 2023;41(1):114–24. https://doi.org/10.1016/j.emj.2021.11.003
Bandura A. Social cognitive theory: an agentic perspective. Ann Rev Psychol. 2001;52:1–26. https://doi.org/10.1146/annurev.psych.52.1.1
Kakemam E, Torkzadeh L, Rouzbahani M, Zahedi H, Chegini Z. The relationship between workplace deviant behaviors and organizational justice among nurses: a cross-sectional survey. Nurs Forum. 2021;56(4):889–96. https://doi.org/10.1111/nuf.12636
Shoaib S, Baruch Y. Deviant behavior in a Moderated-Mediation Framework of incentives, Organizational Justice Perception, and reward expectancy. J Bus Ethics. 2019;157(3):617–33. https://doi.org/10.1007/s10551-017-3651-y
Zhang H, Sheng Y, Li Z, Liu H, Jiang X. Studying on the relationship among nurses’workplace deviant behavior,organizational justice and work stress. J Nurs Sci. 2020;35(16):87–90. http://doi.org/CNKI:SUN:HLXZ.0.2020-16-032 .
Joe SR, eunkyung L. Effects of Emotional Labor and Organizational Justice on Organizational socialization of emergency room nurses. J Korean Acad Nurs Adm. 2017;23(4):397–405. https://doi.org/10.11111/jkana.2017.23.4.397
Iskender MD, Eren H, Caliskan N, Yilmaz E. The relationship between emotional labor level and moral distress. Nurs Ethics. 2023. https://doi.org/10.1177/09697330221140489
Humphrey BEAaRH. Emotional labor in service roles: the influence of identity. Acad Manage Rev. 1993.
Chen Y, Zeng T, Wu M. Effect of nurses’ emotional labor on patient satisfaction from the perspective of resource gain spiral. J Nurs Sci. 2022;37(15):61–5.
Hobfoll SE, Halbesleben J, Neveu J-P, Westman M. Conservation of resources in the Organizational Context: the reality of resources and their consequences. Annual Rev Organizational Psychol Organizational Behav. 2018;10(1):103–28. https://doi.org/10.1038/s41598-020-71501-0
Lee D-g. Influence of Special Education teachers’ emotional labor on their burnout and happiness: the Moderation effects of positive Psychological Capital and Social Support. Special Educ Res. 2019;18(4):5–30.
Riforgiate SE, Howes SS, Simmons MJ. The Impact of Daily Emotional Labor on Health and Well-Being. Manage Communication Q. 2022;36(3):391–417. https://doi.org/10.18541/ser.2019.11.18.4.5
Chang S, Han K, Cho Y. Association of Happiness and Nursing Work Environments with job crafting among Hospital nurses in South Korea. Int J Environ Res Public Health. 2020;17(11). https://doi.org/10.3390/ijerph17114042
Osigwe OC, Ayo AS. Emotional Labour and Deviant Workplace Behaviour among Health workers. Econ Bus. 2021;9(1). https://doi.org/10.2478/AUSEB-2021-0007
Luthans F, Avolio BJ, Avey JB, Norman SM. Positive psychological capital: measurement and relationship with performance and satisfaction. Pers Psychol. 2007;60(3):541–72. https://doi.org/10.1111/j.1744-6570.2007.00083.x
Peterson SJ, Luthans F, Avolio BJ, Walumbwa FO, Zhang Z, PSYCHOLOGICAL CAPITAL AND, EMPLOYEE PERFORMANCE:. A LATENT GROWTH MODELING APPROACH. Pers Psychol. 2011;64(2):427–50. https://doi.org/10.1111/j.1744-6570.2011.01215.x
Halbesleben JRB, Neveu J-P, Paustian-Underdahl SC, Westman M. Getting to the COR: understanding the role of resources in Conservation of resources Theory. J Manag. 2014;40(5):1334–64. https://doi.org/10.1177/0149206314527130
Yin H, Wang W, Huang S, Li H, Psychological, Capital. Emotional labor and exhaustion: examining Mediating and moderating models. Curr Psychol. 2018;37(1):343–56. https://doi.org/10.1007/s12144-016-9518-z
Jun SY. Influences of Burnout, emotional labor, and positive psychological capital on job satisfaction of nurses. J Korean Acad Nurs Adm. 2017;23(2):201–10. https://doi.org/10.11111/jkana.2017.23.2.201
Siami S, Gorji M, Martin A. Psychosocial safety climate and psychological capital for positive customer behavioral intentions in service organizations. Am J Bus. 2023;38(1):1–21. https://doi.org/10.1108/ajb-01-2022-0018
Hong LUO, Qingling SUN, Lihui GU. Effect of emotional labor on professional burnout of nurses. Chin J Nurs. 2008;43(11):969–71. https://doi.org/10.1002/cjoc.200890146
Colquitt JA. On the dimensionality of organizational justice: a construct validation of a measure. J Appl Psychol. 2001;86(3):386–400. https://doi.org/10.1037/0021-9010.86.3.386
Zhang X. Study on the Sense of Organizational Justice of Oil Enterprises’ Staff and Its Influence on Job Satisfaction and Turnover Intention. 2007.
Luthans F, Avey JB, Patera JL. Experimental analysis of a web-based training intervention to develop positive psychological capital. Acad Manage Learn Educ. 2008;7(2):209–21. https://doi.org/10.5465/amle.2008.32712618
Luo H, He Z. The relationships among psychological capital, job burnout and turnover intention in 466 nurses. Chin J Nurs. 2010;45(10):933–5.
Hayes A. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford Press; 2017.
Goretzko D, Siemund K, Sterner P. Evaluating Model Fit of Measurement models in Confirmatory factor analysis. Educ Psychol Meas. 2024;84(1):123–44. https://doi.org/10.1177/00131644231163813
Kock N, Lynn GS. Lateral collinearity and misleading results in Variance-based SEM: an illustration and recommendations. J Association Inform Syst. 2012;13(7):546–80. https://doi.org/10.17705/1jais.00302
Viseu J, Guerreiro S, de Jesus SN, Pinto P. Effect of psychosocial safety climate and organizational justice on affective commitment: a study in the Algarve hotel sector during the COVID-19 pandemic. J Hum Resour Hospitality Tourism. 2022;22(2):320–45. https://doi.org/10.1080/15332845.2023.2154035
Yu M, Lee H. Impact of resilience and job involvement on turnover intention of new graduate nurses using structural equation modeling. Japan J Nurs Sci. 2018;15(4):351–62. https://doi.org/10.1111/jjns.12210
Kim KJ, Yoo MS. The influence of Psychological Capital and Work Engagement on Intention to remain of New Graduate nurses. J Nurs Adm. 2018;48(9):459–65. https://doi.org/10.1097/nna.0000000000000649
Gouldner AW. The norm of reciprocity: a preliminary Statement. Am Sociol Rev. 1960;25(2):161–78.
Cropanzano R, Mitchell MS. Social Exchange Theory: an Interdisciplinary Review. J Manag. 2016;31(6):874–900. https://doi.org/10.1177/0149206305279602
Masterson SS, Lewis K, Goldman BM, Taylor MS. Integrating Justice and Social Exchange: the Differing effects of Fair procedures and Treatment on Work relationships. Acad Manag J. 2000;43(4):738–48. https://doi.org/10.5465/1556364
Zhao J, Xu W, Dong X, Tao S, Liu W, Liang L. Application and prospect of emotional labor in nursing research. Chin Nurs Manage. 2020;20(10):1528–33. https://doi.org/10.3969/j.issn.1672-1756.2020.10.021
Kim H, Leach RB. Mitigating Burnout through Organizational Justice: customer support workers’ experiences of customer injustice and emotional labor. Manage Communication Q. 2021;35(4):497–517. https://doi.org/10.1177/08933189211012040
Jia S, Chengxin F, Qiusha L, Anqi W, Wanchen W, Lifang Z, Haiyuan L, Dongping M, Zhongming C, Wenqiang Y. The status of emotional labour and its influence on job burnout among village doctors during the COVID-19 pandemic in China: a cross-sectional study. BMC Prim Care. 2023;24(1):19. https://doi.org/10.1186/s12875-023-01982-1
Chen C-C, Lan Y-L, Chiou S-L, Lin Y-C. The Effect of Emotional Labor on the Physical and Mental Health of Health professionals: emotional exhaustion has a Mediating Effect. Healthcare. 2023;11(1). https://doi.org/10.3390/healthcare11010104
Lubbadeh T. Job burnout and counterproductive work Behaviour of the Jordanian Bank employees. Organizacija. 2021;54(1):49–62. https://doi.org/10.2478/orga-2021-0004
Li Y, Guo D. Review on psychological contract in organization. Adv Psychol Sci. 2002;10(1):83–90. https://doi.org/10.1109/JQE.2007.897915
Gou L, Ma S, Wang G, Wen X, Zhang Y. Relationship between workplace ostracism and turnover intention among nurses: the sequential mediating effects of emotional labor and nurse-patient relationship. Psychol Health Med. 2022;27(7):1596–601. https://doi.org/10.1080/13548506.2021.1905859
Back C-Y, Hyun ES, Jeung Y, Chang S-J. Mediating effects of Burnout in the Association between Emotional Labor and turnover intention in Korean clinical nurses. Saf Health Work. 2020;11(1):88–96. https://doi.org/10.1016/j.shaw.2020.01.002
Astuti RJ, Maryati T, Harsono M. The Effect of Workplace spirituality on Workplace Deviant Behavior and Employee Performance: the role of job satisfaction. J Asian Finance Econ Bus. 2020;7(12):1017–26. https://doi.org/10.13106/jafeb.2020.vol7.no12.1017
Fei J, Hu Y, Liang L, Meng C, Mei S. Exploring the impact of emotional and cognitive factors on anxiety symptoms of Chinese adolescents: a serial mediation study. Int J Mental Health Addict. 2023. https://doi.org/10.1007/s11469-022-01004-8
Seval EG, Ozcelik BH, Emin A, Hakan K, Ozgur Y. Psychological capital as a moderator in the relationship between job insecurity, job stress, and hotel employees’ turnover intention during the Russia-Ukraine war. Int J Hospitality Manage. 2023;111. https://doi.org/10.1016/J.IJHM.2023.103475
Laschinger HKS, Grau AL. The influence of personal dispositional factors and organizational resources on workplace violence, burnout, and health outcomes in new graduate nurses: a cross-sectional study. Int J Nurs Stud. 2012;49(3):282–91. https://doi.org/10.1016/j.ijnurstu.2011.09.004
Xiao Q, Liang X, Liu L, Klarin A, Zhang C. How do work-life balance programmes influence nurses’ psychological well-being? The role of servant leadership and learning goal orientation. J Adv Nurs. 2023;79(7):2720–31. https://doi.org/10.1111/jan.15654
Download references
Acknowledgements
The authors sincerely thank every nursing worker who participated in this study.
This research was sponsored by the Key Project of Undergraduate Teaching Reform Research and Practice of Henan University (Grant Number: HDXJJG2020-25), and the Research on the Status Quo and Cultivation Mechanism of Social and Emotional Ability of Henan Adolescents (Grant Number: SKL-2022-55).
Author information
Ran Meng and Zhe Jiang contributed equally to this work and should be regarded as co-first authors.
Authors and Affiliations
Institute of Nursing and Health, School of Nursing and Health, Henan University, Kaifeng, China
Ran Meng, Zhe Jiang, Yue Su & Chaoran Chen
Institute of Business Administration, School of Business, Henan University, Kaifeng, China
You can also search for this author in PubMed Google Scholar
Contributions
Ran Meng, Zhe Jiang and Chaoran Chen provided the study design. Ran Meng and Zhe Jiang finished writing the manuscript of the article. Ran Meng, Zhe Jiang, Yue Su conducted data collection and data processing. Chaoran Chen and Guangli Lu proposed key revisions. All authors have read and agreed to the final version of the manuscript.
Corresponding author
Correspondence to Chaoran Chen .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of Henan University, and the ethics review number is HUSOM2022-375. When participants completed the questionnaire and successfully submitted it, it indicated that participants agreed to participate in the study. Therefore, the researchers obtained informed consent from the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Meng, R., Jiang, Z., Su, Y. et al. The effect of perceived organizational justice on workplace deviant behavior of new nurses: the role of emotional labor and psychological capital. BMC Nurs 23 , 288 (2024). https://doi.org/10.1186/s12912-024-01937-6
Download citation
Received : 27 February 2024
Accepted : 15 April 2024
Published : 28 April 2024
DOI : https://doi.org/10.1186/s12912-024-01937-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Nurses can implement the original nursing process to guide patient care for problem solving in nursing. These steps include: Assessment. Use critical thinking skills to brainstorm and gather information. Diagnosis. Identify the problem and any triggers or obstacles. Planning. Collaborate to formulate the desired outcome based on proven methods ...
The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients' well-being and health. This chapter will explain how to use the nursing process as standards of professional nursing practice to provide safe, patient-centered care. ... A lifelong problem-solving approach that integrates ...
Conclusion. The influencing factors of clinical nurses' problem-solving dilemma are diverse. Hospital managers and nursing educators should pay attention to the problem-solving of clinical nurses, carry out a series of training and counselling of nurses by using the method of situational simulation, optimize the nursing management mode, learn to use new media technology to improve the ...
Nursing process (NP) is a systematic method which utilizes scientific reasoning, problem-solving and critical thinking to direct nurses in caring for patients effectively [3, 4]. The nursing process is a systematic problem-solving approach used to identify, prevent and treat actual or potential health problems and promote wellness.
He defines critical thinking as "necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation." ... These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate ...
The nursing process provides a problem-solving approach to nursing care based on the needs and problems of the individual patient. Whenever possible, the patient and his relatives are encouraged to participate in decisions relating to his care.
This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in nurse education curricula Further, it has attracted limited ...
• Discuss 7 steps to problem-solving. Introduction As medicine becomes more and more complex and nursing responsibilities increase, critical thinking—the ability to question and make rational decisions—becomes even more important. Too often, healthcare providers simply follow routines and accept the word of
The nursing process, which is heavily used and frequently described as a problem-solving approach to nursing care, requires a deductive reasoning process which is not the problem-solving process in use during care-giving activities. More knowledge is required on what process is in place as we develop as a profession.
The utilization of nursing process guarantees the provision of professional and effective care. The nursing process provides nurses with the chance to learn problem-solving skills through teamwork, health management, and patient care. Problem-solving is at the heart of nursing process which is why this skill underlies all nursing practices.
To perform a clinical decision‐making process, it is necessary to examine and identify the problem, evaluate the existing solutions, and ultimately select the best option; this process is carried out at the clinic through the nursing process, and in fact, a nursing process is a tool for helping the nurse to make appropriate clinical decision ...
Typical decision theory approaches to the identification of problem solving in nursing have viewed the process as a series of decision formulations that include: decisions about what observations should be made in the patient situation; decisions about deriving meaning from the data observed (clinical inferences); and decisions regarding the ...
The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes. Nursing Process Steps. The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation.
The nursing process is a series of steps nurses take to assess patients, plan for and provide patient care, and evaluate the patient's response to care. It is considered the framework upon which all nursing care is based. ... Critical thinking, problem-solving, and communication skills are necessary to work in this phase. Nurses must also ...
Introduction. Problem solving and decision making are essential skills for effective nursing practice. Carol Huston (2008) identified "expert decision-making skills" as one of the eight vital leadership competencies for 2020. These processes not only are involved in managing and delivering care but also are essential for engaging in planned change.
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
Using a problem-solving approach as a basis for nursing practice requires the use of critical thinking and decision-making. Some experts have referred to that thinking more recently as clinical reasoning. The 2020 NCLEX-RN® Test Plan identifies the nursing process as one of five integrated processes which is defined as "a scientific ...
Abstract. This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills. It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in ...
Purpose: This study aimed to determine the relationship between problem-solving and nursing process application skills of nursing. Methods: This is a longitudinal and correlational study. The sample included 71 students. An information form, Problem-Solving Inventory, and nursing processes the students presented at the end of clinical courses were used for data collection.
Background. Problem solving involves recognizing the difference between the problem solver's current state and the goal state to be reached, and resolving the obstacles that prevent them from achieving the goal [].Acquiring problem-solving ability based on judgment and critical thinking is an important element of nursing education [].Furthermore, the use of effective problem-solving ...
Nursing process (NP) is a systematic method which utilizes scientific reasoning, problem-solving and critical thinking to direct nurses in caring for patients effectively [3, 4]. The nursing process is a systematic problem-solving approach used to identify, prevent and treat actual or potential health problems and promote wellness.
This study further understood the workplace deviant behavior of new nurses, and provided a new perspective for solving this problem. Nurse managers can reduce workplace deviant behavior by enhancing the perceived organizational justice and psychological capital of new nurses and improving emotional labor. ... In the nursing process and the ...
We found clinical nurses' problem-solving ability to have no positive effect on their perception of professionalism. This contrasts with previous studies, which reported that problem-solving ability is helpful for such perception of professionalism . We also found that problem-solving ability does not affect nursing professional perception ...