- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health

What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis)
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
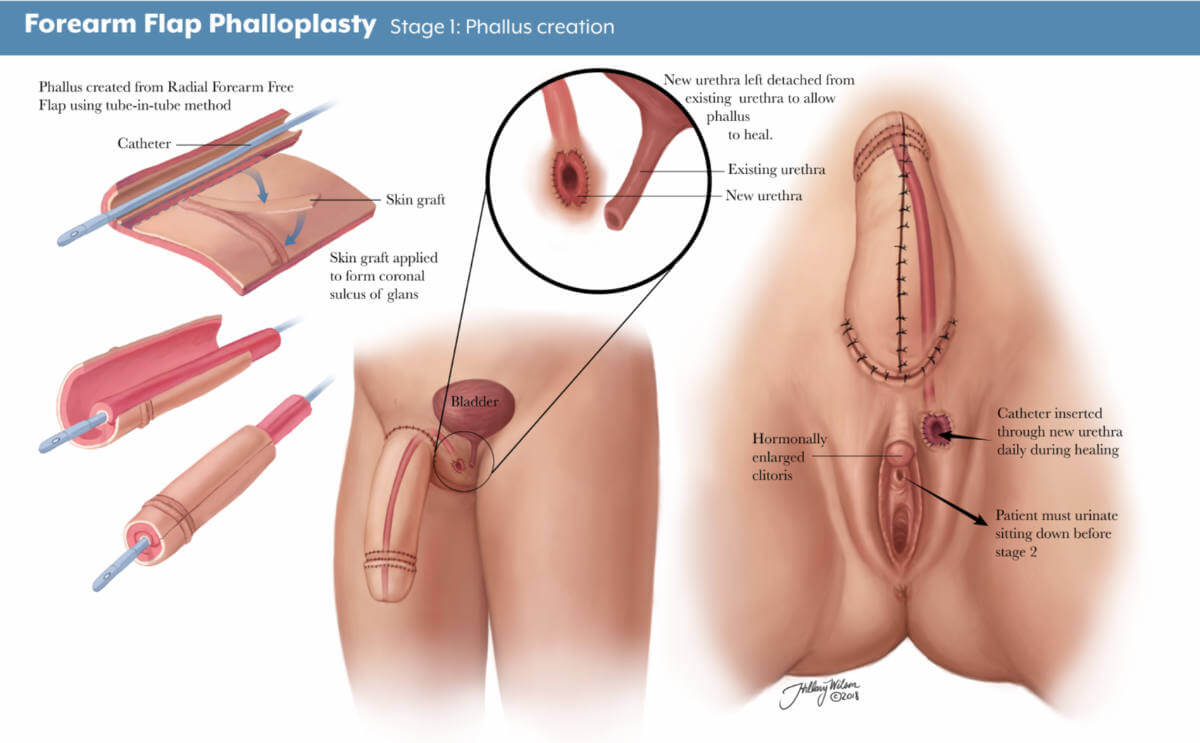
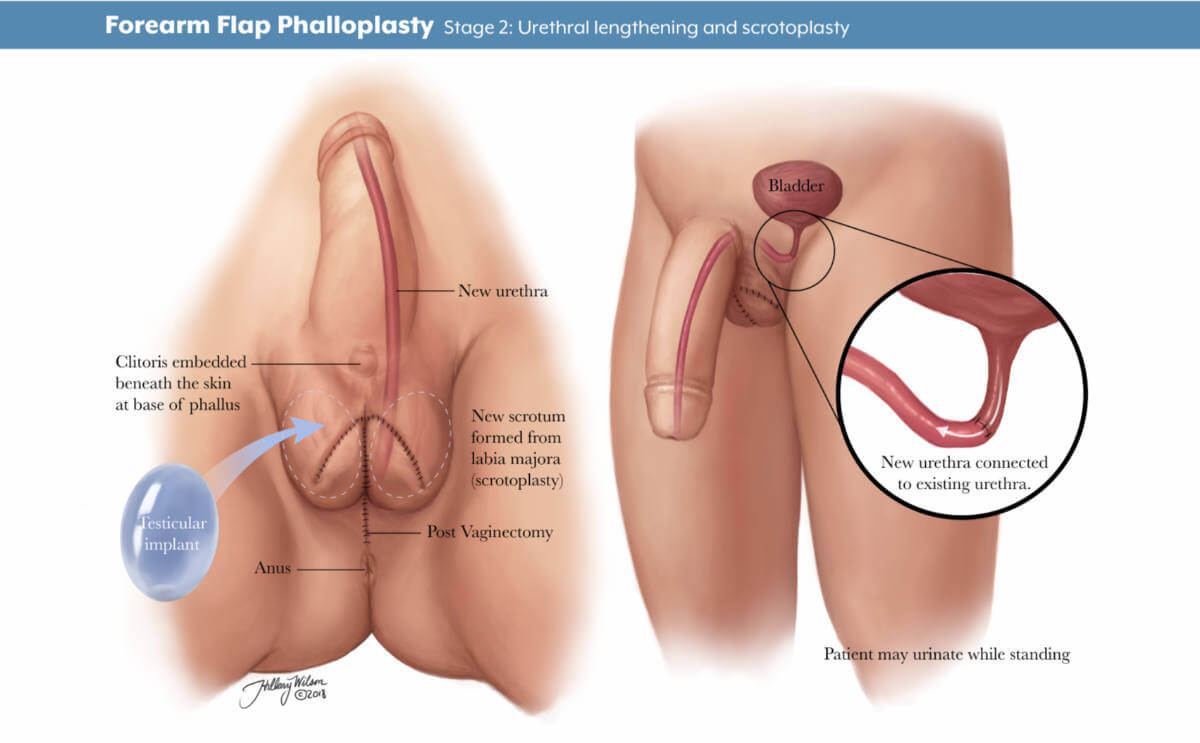
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
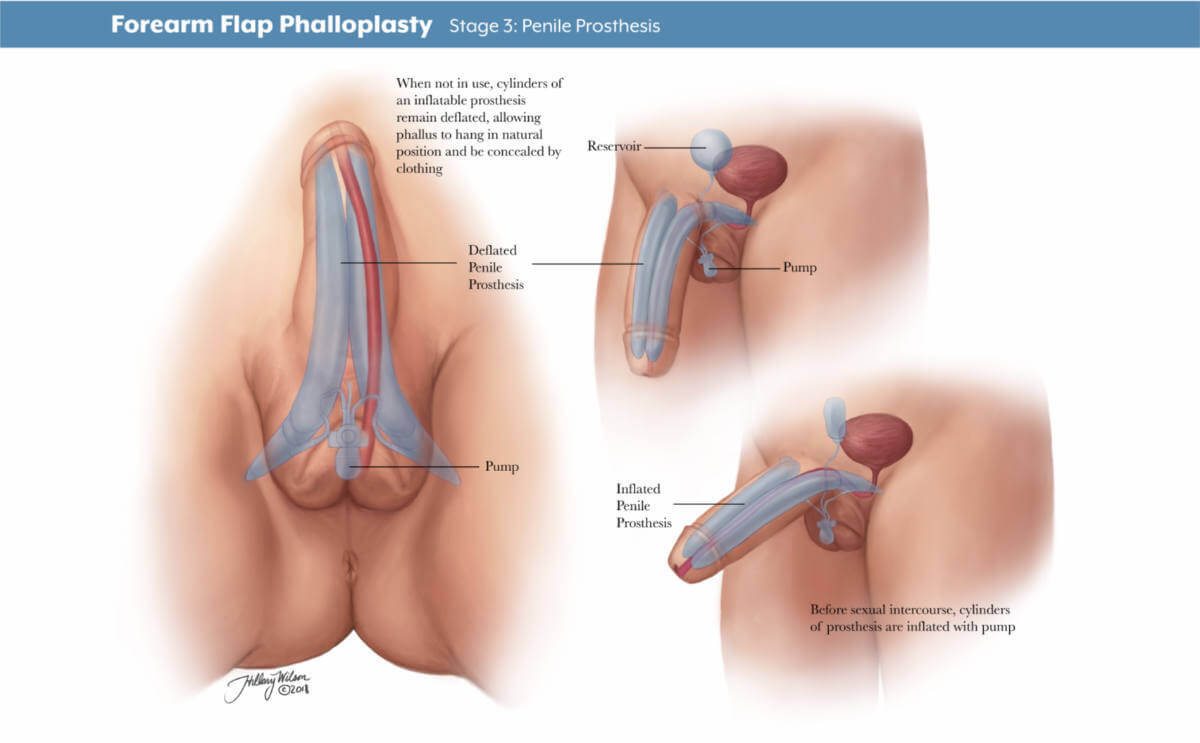
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
Related Articles
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Phalloplasty for Gender Affirmation
Featured Expert:

Fan Liang, M.D.
Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including:
- Creating the penis
- Lengthening the urethra so you are able to stand to urinate
- Creating the tip (glans) of the penis
- Creating the scrotum
- Removing the vagina, uterus and ovaries
- Placing erectile and testicular implants
- Skin grafting from the donor tissue site
Gender affirmation surgery is customized to each individual. Your surgical plan may include more or fewer of these steps and procedures. Fan Liang, M.D. , medical director of the Center for Transgender and Gender Expansive Health at Johns Hopkins, explains what you should know.
Are there different types of phalloplasty?
Phalloplasty involves using skin flaps, which are areas of skin moved from one area of the body to another. The skin flap is then reshaped, contoured and reattached to the groin to create the penis. There are three approaches the surgeon may use to construct the penis, using skin from the arm (radial forearm free flap), leg (anterolateral thigh flap) or side (latissimus dorsi flap).
There are pros and cons to each approach. Factors for choosing skin flap locations include the patient’s health and fat distribution, nerve function, blood flow and desired surgical outcomes.
What is a radial forearm free flap?
A radial forearm free flap (RFFF) involves taking the skin, fat, nerves, arteries and veins from your wrist to about halfway up your forearm to create the penis. Typically, the surgeon will use your nondominant hand so it is easier for you to recover and return to your day-to-day activities.
During your surgical consultation, the doctor will check the blood flow to your arm and hand noninvasively. This involves temporarily putting pressure on arteries then releasing the pressure to test blood distribution in the arm and hand.
There are three stages to this procedure.
- Stage 1: The first stage of an RFFF approach is creating the penis using tissue from the forearm. The area where the forearm tissue is taken will require a skin graft. This may occur at the time of the initial phalloplasty surgery, or it may occur three to five weeks afterward. If it occurs later, patients will have a temporary skin covering over the forearm to help it heal.
- Stage 2: The second stage, scheduled about five to six months later, may include lengthening the urethra to allow for urination out of the tip of the penis, creating the scrotum and removing the vagina, and other procedures depending on the patient’s individualized plan.
- Stage 3: The third stage of surgery involves putting in place testicle implants and an erectile device to help the patient achieve an erection. The third stage typically takes place 12 months after the second.
Will I have a say in how the phalloplasty is staged and the surgical plan?
Your gender affirmation surgery is highly personalized. Depending on what is most important to you, your surgery team will work with you on a customized plan beforehand. You and your surgeon will discuss your priorities and decide which procedures are right for you. Each stage will be scheduled to ensure your health and safety and provide the best chance of good results.
How long will I be in the hospital?
After your stage 1 surgery, you will stay as an inpatient for four to five days. Your surgical team will frequently monitor the blood supply to the tissue that has been used to create your new penis and ensure you are able to use the bathroom and walk around after surgery. Procedures for stages 2 and 3 do not require a hospital stay.
Will I need a catheter?
During your inpatient stay for stage 1 surgery, you will have a suprapubic tube that goes directly into your bladder and another catheter in your native urethra for at least five days. It is typically removed in the hospital before you go home.
If you decide not to have urethral lengthening as part of stage 2, you will have a Foley catheter placed in the operating room and removed before you leave the hospital. If you decide to have urethral lengthening, you will go home with a Foley catheter in the new urethra and a suprapubic tube. A clamp ensures that the urethra does not leak urine.
What is a suprapubic tube?
A suprapubic tube (SPT) allows urine to drain from your bladder. It is placed in the lower part of your abdomen, below the belly button. The SPT stays in for four to five weeks, depending on your healing and recovery.
When will my SPT be removed?
Before the SPT is removed, around four weeks after surgery, a urologist will perform a retrograde urethrogram. This involves putting dye into the bladder through the new urethra. An X-ray tracks the dye to see if the new urethra is open and ready for urination. If so, the doctor will clamp the SPT and you will be allowed to urinate from your new urethra. If everything looks good after a few days, the SPT is removed.
Forearm Flap Phalloplasty
Stage 1: phallus creation. Enlarged image .
Stage 2: urethral lengthening and scrotoplasty. Enlarged image .
Stage 3: penile prosthesis. Enlarged image .
Other Skin Flaps Used in Phalloplasty
What is an anterolateral thigh flap.
An anterolateral thigh flap (ALT) uses skin, fat, nerves, arteries and veins from the leg to create a penis. A special vascular CT scan can help the surgeon examine the blood supply of each leg to determine which leg will be better for creating the skin flap.
The stage of the ALT phalloplasty are similar to the RFFF. The area where the thigh tissue is taken will also require a skin graft. The resulting scar on the thigh can be covered with shorts.
What is a musculocutaneous latissimus dorsi flap?
A musculocutaneous latissimus dorsi skin flap (MLD) involves the skin, fat, nerves, arteries and veins from the side of your back to create a penis. The surgeon may order a special CT scan to look at the blood flow throughout the donor site area.
The stages of the MLD phalloplasty are similar to the RFFF and ALT. However, the area from which the back tissue is taken usually does not require a skin graft and can be closed in a straight line. The scar can be covered with a shirt. Patients may experience some initial weakness raising their arm, but this improves with time.
How is penis size determined?
Penis size depends on patient preferences and the skin flap harvested from your body. Thinner patients with less fat on the skin flap will have a penis with less girth. Alternatively, patients with a greater amount of fat will have a thicker penis.
The length of the penis depends on the patient’s donor site, but typically it is about 5–6 inches. After the first stage, the penis may decrease in size as postoperative swelling decreases and the tissue settles into its new location.
What determines scrotum size?
Scrotum size is specific to the patient and depends on the amount of skin that is present in the genital area before phalloplasty. The more genital tissue there is, the larger the scrotum and the testicular implants can be.
There are different ways to create the scrotum, including a procedure called V-Y scrotoplasty, a technique that creates a pouch to hold testicular implants. AART silicone round carving blocks have been approved by the FDA to be used as implants.
Procedures to Discuss with Your Physician Before Phalloplasty
Each individual undergoing gender confirmation surgery is different. Your surgeon will work with you to discuss which procedures, and their timing, are best for you and your goals.
Should I have a hysterectomy before phalloplasty surgery?
For those interested in this procedure, hysterectomies are typically done before phalloplasty and do not require a vaginectomy.
Urethral Lengthening Before Phalloplasty
If you choose to have urethral lengthening, this procedure involves lengthening your existing urethra so that you are able to urinate out of the tip of the penis. It involves connecting your current urethra to the new urethra created in the shaft of the penis.
Not all patients choose to have urethral lengthening; however, this will be a necessary step if you want to stand when you urinate. It is also important to know that if you decide not to have urethral lengthening in stage 1 of your phalloplasty, it will not be possible to have the lengthening procedure later.
Complications of Urethral Lengthening
The most common complications for urethral lengthening include urethral strictures (narrowed areas of the urethra), fistula (creation of a passageway between the urethra and another location) and diverticula (formation of a pouch in the urethra). This may require an additional surgical procedure to fix.
What is a metoidioplasty?
A metoidioplasty is a surgical procedure to achieve masculine-appearing genitalia with fewer steps than a phalloplasty. The skin of the labia and around the clitoris is lengthened to achieve the appearance of a penis. Some people prefer to undergo a metoidioplasty if they do not want to use tissue from their arms or legs to create a penis or if they prefer a shorter, more straightforward surgery.
A metoidioplasty procedure has a quicker recovery and fewer complications. Surgeons can discuss metoidioplasty with patients and help them decide if this option is right for them.
Will I need to have hair removal?
Yes, before surgery, after you consult with the surgical team and choose a skin flap site, you will get a template for hair removal that you can give to your hair removal professional.
What if I have a tattoo on my preferred donor site?
As long as there is good blood flow and nerve function, donor sites — even those with a tattoo — can be used.
Penile Function and Sensation After Phalloplasty
What can i do with a reconstructed penis.
Penis function is determined by what you and your surgery team agree on for your surgical plan. If it is important for you to urinate out of the tip of your penis, then urethral lengthening may be a good choice for you. If sensation is most important, your team will focus on a donor site with good nerve innervation. If penetrative sex is most important, and you would like to maintain an erection, then implanting an erectile prosthetic can be part of your surgery plan.
Can I get an erection after phalloplasty?
In stage 3 phalloplasty, a urologist can place a prosthetic erectile device which will allow you to maintain an erection. As of September 2022, no implantable prosthetic devices have been FDA-approved for phalloplasty. Instead, the surgeon can use a device intended for patients with erectile dysfunction to allow transmasculine patients to achieve an erection. There is a risk of infection and implant rejection with an erectile implant . If this happens, it may take six months before another device can be placed into the penis.
What kind of sensation and feeling can I expect?
Sensation recovery varies by patient. Nerve regeneration can begin as early as three weeks after surgery, but it can take longer in some patients. Sometimes sensation can take up to a year or longer. Return of nerve sensation is not guaranteed. As nerves regenerate and strengthen connections, you might experience shooting pain, tingling or electrical sensations. As time goes on, the tingling feeling begins to subside.
What is nerve hookup during phalloplasty?
Nerve hookup involves taking existing nerves from the donor site, such as the arm, and connecting them to nerves located in the pelvis. This allows you to have sensation in the reconstructed penis.
What is clitoral burying during phalloplasty surgery?
Clitoral burying involves moving the clitoris into the base of the penis to increase sensation. This is typically done at stage 2.
Is orgasm possible after phalloplasty?
Orgasm is possible after phalloplasty, especially if your surgery plan emphasizes preserving sensation. It is important to note that your penis will not ejaculate with semen at the time of orgasm.
Find a Doctor
Specializing In:
- Gender Affirmation Surgery
- Transgender Health
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
- Plastic and Reconstructive Surgery
Find Additional Treatment Centers at:

Request an Appointment

Vaginoplasty for Gender Affirmation

Top Surgery

Facial Feminization Surgery (FFS)
Related Topics
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
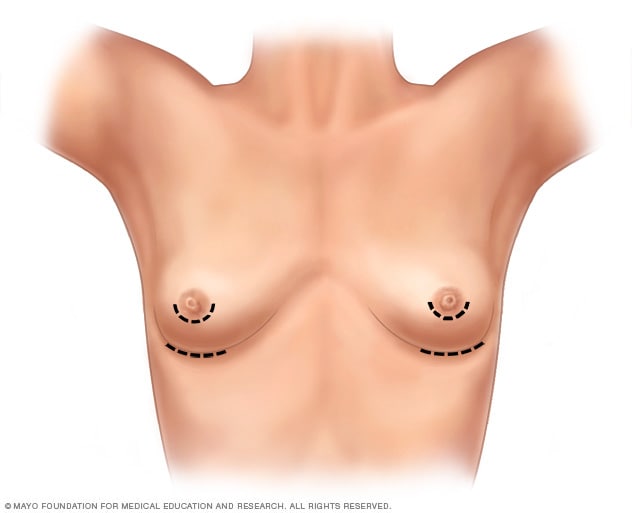
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
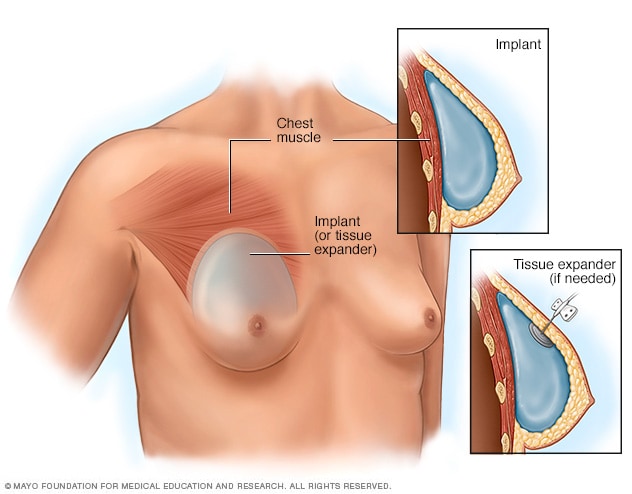
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
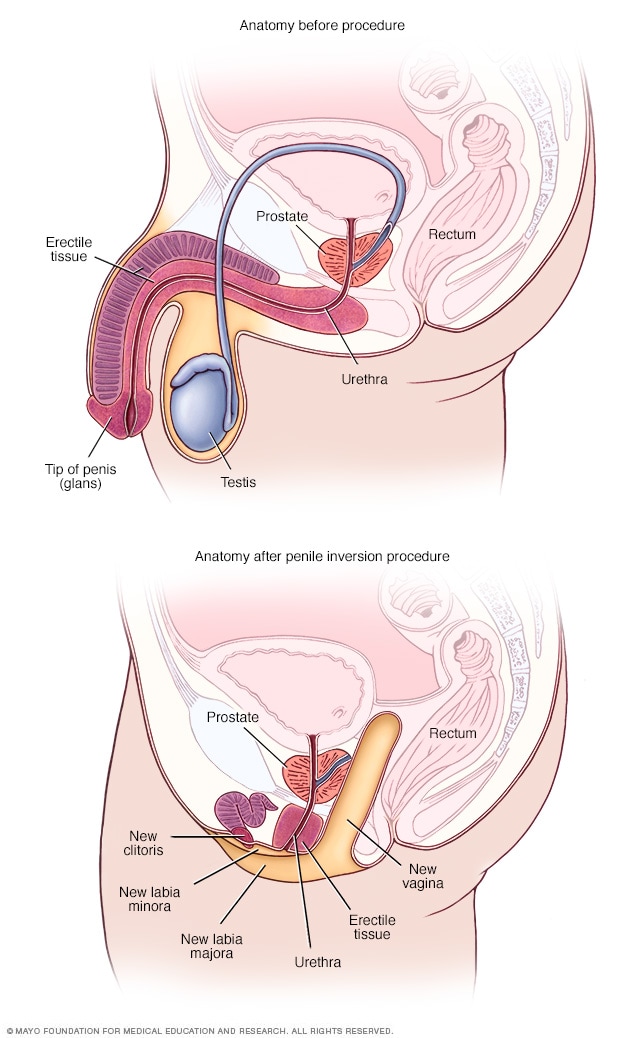
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
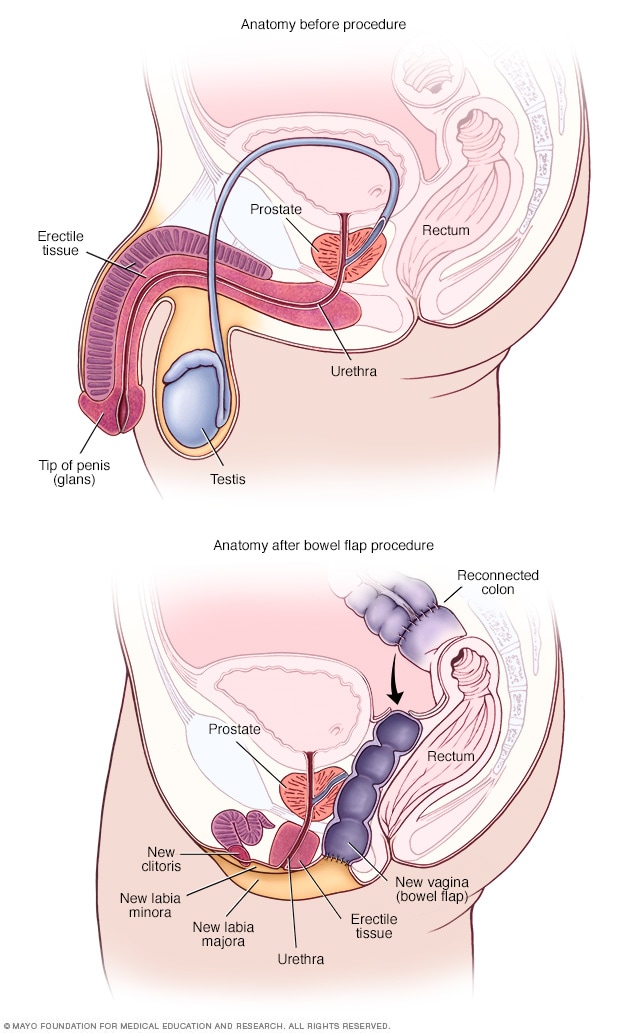
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
The Go-To Guide to Gender Surgeons
Find a qualified surgeon for gender-affirming care.
Start Your Search
Find a Surgeon
Search by U.S. State, Procedure and Insurance Search by Country and Procedure Browse the Global Surgeon Maps
The Go-To Guide To Gender Surgeons

- Health Conditions
- Health Products
What to know about female-to-male surgery

Female-to-male surgery is a type of gender-affirmation or gender-affirming surgery. There are multiple forms of gender-affirming surgery, including altering the genital region, known as “bottom” surgery.
There are multiple forms of gender-affirming surgery, including the removal of breasts — a mastectomy — and the altering of the genital region, known as “bottom” surgery.
Examples of bottom surgery include:
- removal of the uterus called a hysterectomy
- removal of the vagina, known as a vaginectomy
- construction of a penis through metoidioplasty or phalloplasty
This article describes female-to-male gender-affirming surgeries. It also discusses recovery and what to expect from a transgender penis.

Before having female-to-male gender-affirming surgery, a person will often receive testosterone replacement therapy (TRT) .
They may then undergo one or more of the following types of procedures.
Chest restructuring or top surgery
A person in transition may wish to have a subcutaneous mastectomy to remove breast tissue. The surgeon will also make alterations to the appearance and position of the nipples. Many people refer to these procedures as “top surgery.”
Meanwhile, TRT will stimulate the growth of chest hair. A 2022 study notes that complications from gender-affirming mastectomy procedures are low, and satisfaction rates are incredibly high.
Removal of the uterus, ovaries, and fallopian tubes
A person may wish to undergo this type of surgery if they are uncomfortable having a uterus, ovaries, or fallopian tubes or if hormone therapy does not stop menstruation.
In a partial hysterectomy, a surgeon will remove only the uterus. In a total hysterectomy, they will also remove the cervix.
A bilateral salpingo-oophorectomy involves the removal of the right and left fallopian tubes and ovaries.
Metoidioplasty
A metoidioplasty is a method of constructing a new penis, or neopenis. Research from 2021 shows this procedure has a low risk of complication and a high satisfaction level. A metoidioplasty has positive cosmetic and functional outcomes.
This procedure involves changing the clitoris into a penis. A person will receive hormone therapy before the surgery to enlarge the clitoris for this purpose. During the procedure, the surgeon also removes the vagina in a vaginectomy.
In addition, they lengthen the urethra and position it through the neopenis. To achieve the lengthening, the surgeon uses tissues from the cheek, labia minora, or other parts of the vagina. The aim of this is to allow the person to urinate while standing.
An advantage of metoidioplasty is that the neopenis may become erect due to the erectile abilities of clitoral tissue.
Phalloplasty
A phalloplasty uses grafted skin — usually from the arm, thigh, back, or abdomen — to form a neopenis. Compared with a metoidioplasty, a phalloplasty results in a larger penis. However, this neopenis cannot become erect on its own.
After a period of recovery, a person can have a penile implant. This can allow them to get and maintain erections and have penetrative sex.
Disadvantages of a phalloplasty include the number of surgical visits and revisions that may be necessary, as well as the cost, which is typically higher than that of a metoidioplasty.
Scrotoplasty
A person may decide to have a scrotoplasty — creating a scrotum — alongside a metoidioplasty or phalloplasty.
In a scrotoplasty, a surgeon hollows out and repositions the labia majora to form a scrotum and inserts silicone testicular implants.
The recovery time from female-to-male surgery varies, depending on the type of procedure and factors such as the person’s overall health and lifestyle choices. For example, smoking slows down recovery and increases the risk of complications following surgery.
Following gender-affirming surgery, most people need to stay in the hospital for at least a couple of days.
After leaving the hospital, the person must rest and limit strenuous activity.
Complications
As with any surgery, all gender-affirming surgeries carry a risk of:
- reactions to anesthesia
Some complications of a metoidioplasty or phalloplasty include :
- Urethral fistula: A tunneled connection that forms between the urethra and another part of the body.
- Urethral stricture: A narrowing that causes a blockage of urine flow within the urethra.
A person who has had a phalloplasty may experience scarring in the area where the surgeon has taken the graft or a skin graft failure.
What to expect
A person who undergoes a metoidioplasty may have erections and enjoy more sensation in their neopenis. However, the penis will be relatively small in size. A neopenis that results from a phalloplasty is usually larger, though it may be less sensitive. To have erections, a person will need a penile implant.
These procedures can improve a person’s quality of life, and most people report high levels of satisfaction.
A 2018 study found that 94–100% of participants who had undergone gender-affirming surgery reported satisfaction with the surgical results, with the variance depending on the type of procedure.
The 6% of people who reported dissatisfaction or regret did so due to preoperative psychological symptoms or complications following the procedures.
The outlook for female-to-male surgery depends on the type of surgery, the person’s health, and other factors. Most people report satisfaction following the procedure.
It is important to work closely with a qualified plastic surgeon, urologist, gynecologist , and mental health professional to ensure the best outcome.
It is also essential to follow recovery guidelines and attend all follow-up appointments.
There are several types of gender-affirming surgeries that a person can help a person during a transition.
These procedures broadly fall into top or bottom surgery. Top surgery is a colloquial term for chest restructuring procedures, while bottom surgery refers to operations changing genitalia. There are multiple forms of both surgeries and can include the removal of breast tissue and the creation of a penis.
Last medically reviewed on July 12, 2023
- Cosmetic Medicine / Plastic Surgery
- Sexual Health / STDs
How we reviewed this article:
- Bordas N, et al. (2021). Metoidioplasty: Surgical options and outcomes in 813 cases. https://www.frontiersin.org/articles/10.3389/fendo.2021.760284/full
- Carbonnel M, et al. (2021). The uterus in transgender men. https://www.sciencedirect.com/science/article/pii/S0015028221005811
- General surgery — possible complications. (n.d.). https://stanfordhealthcare.org/medical-treatments/g/general-surgery/complications.html
- Purohit RS, et al. (2022). Penile prosthesis in transgender men after phalloplasty. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9398527/
- Tang A, et al. (2022). Gender-affirming mastectomy trends and surgical outcomes in adolescents. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9555285/
- van de Grift TC, et al. (2018). Surgical satisfaction, quality of life, and their association after gender-affirming surgery: A follow-up study. https://www.ncbi.nlm.nih.gov/pubmed/28471328
- World Health Organization. (2020). Smoking greatly increases risk of complications after surgery [Press release]. https://www.who.int/news/item/20-01-2020-smoking-greatly-increases-risk-of-complications-after-surgery
Share this article
Latest news
- Western diet could impact gut inflammation, leading to chronic conditions
- Immunotherapy before and after surgery may improve lung cancer survival rates
- Obstructive sleep apnea during REM stage linked to memory decline
- Unique brain circuits may be linked to eating habits, weight loss
- Counting steps or logging minutes? What is the best way to measure exercise?
Related Coverage
Medicare pays for gender reassignment surgeries and hormone replacement therapy, when the surgery is deemed medically necessary. There may be several…
It is important to know about sexual health. Learn more about sexual health for transgender men here.
Transgender men face a number of mental health concerns. Working past personal and societal stigmas may help them access care and find the support…
If a person has itchy stitches during healing, they can use antihistamine medication or cold compresses for relief. Learn more.
Transplant rejection occurs when the recipient's immune system attacks the transplanted organ. Learn more about early signs and how to prevent…
Transgender Health Program
Gender-affirming surgery.
OHSU surgeons are leaders in gender-diverse care. We provide specialized services tailored to the needs and goals of each patient. We offer:
- Specialists who do hundreds of surgeries a year.
- Plastic surgeons, urologists and other specialists who are leading experts in bottom surgery, top surgery and other gender-affirming options.
- Vocal surgery with a highly trained ear, nose and throat doctor.
- Peer volunteers who can provide support during visits.
- Welcoming care for every patient, every gender and every journey.

Our surgical services
We offer many gender-affirming surgery options for transgender and nonbinary patients, including options within the following types. We also welcome you to request a procedure that isn’t listed on our pages.
Top surgery:
- Gender-affirming mastectomy
- Gender-affirming breast augmentation
Bottom surgery:
- Phalloplasty and metoidioplasty , including vagina-preserving options
- Vaginoplasty and vulvoplasty , including penile-preserving options
Hysterectomy
Nullification surgery, oophorectomy, orchiectomy.
Bottom surgery options also include:
- Scrotectomy
- Scrotoplasty
- Urethroplasty
- Vaginectomy
Additional gender-affirming options:
- Adam’s apple surgery
Vocal surgery
Face and body surgery, preparing for surgery.
Please see our patient guide page to learn about:
- Steps to surgery
- WPATH standards of care
- The letter of support needed for some surgeries
For patients
Request services.
Please fill out an online form:
- I am seeking services for myself.
- I am seeking services for someone else.
Other questions and concerns
Contact us at:
- 503-494-7970
- [email protected]
Refer a patient
- Please complete our Request for Transgender Health Services referral form and fax with relevant medical records to 503-346-6854 .
- Learn more on our For Health Care Professionals page.
At OHSU, our gynecologic surgeon, Dr. Lishiana Shaffer, specializes in hysterectomies (uterus and cervix removal; often combined with oophorectomy, or ovary removal) for gender-diverse patients. She does more than 150 a year.
We also offer a Transgender Gynecology Clinic with a gender-neutral space. Services include surgery. Referrals and appointments are made through the OHSU Center for Women's Health, though the space is not in the center. Call 503-418-4500 to request an appointment.
Some patients choose hysterectomy to:
- More closely align their bodies with their gender identity.
- With ovary removal, to remove a main source of the hormone estrogen.
- To end pain caused by testosterone therapy that shrinks the uterus.
- To end the need for some gynecologic exams, such Pap smears.
Preparation: We usually recommend a year of hormone therapy first, to shrink the uterus. We don’t require a year of social transition.
How hysterectomy is done
Most often, we use a minimally invasive laparoscope and small incisions in the belly. We usually recommend removing fallopian tubes as well, to greatly reduce the risk of ovarian cancer.
Most patients spend one night in the hospital. Recovery typically takes about two weeks. You’re encouraged to walk during that time but to avoid heavy lifting or strenuous exercise.
Considerations and risks
Hysterectomy is usually safe, and we have a low rate of complications. Risks can include blood clots, infection and scar tissue. Because of a possible link between hysterectomy and higher risk of cardiovascular disease, your doctors may recommend regular tests.
Removing the uterus also ends the ability to carry a child. OHSU fertility experts offer options such as egg freezing before treatment, and connecting patients with a surrogacy service.
OHSU offers nullification surgery to create a gender-neutral look in the groin area.
Nullification surgery may include:
- Removing the penis (penectomy)
- Removing the testicles (orchiectomy)
- Reducing or removing the scrotum (scrotectomy)
- Shortening the urethra
- Removing the uterus (hysterectomy)
- Removing the vagina (vaginectomy)
The procedure takes several hours. Patients can expect to spend one to two nights in the hospital. Recovery typically takes six to eight weeks. Patients are asked to limit walking and to stick to light to moderate activity for four weeks. They should wait three months before bicycling or strenuous activity.
Nullification surgery cannot be reversed. Risks can include:
- Changes in sensation
- Dissatisfaction with the final look
- Healing problems
Removing the penis and testicles or the uterus also affects the ability to conceive a child. OHSU fertility experts offer options such as freezing eggs and connecting patients with a surrogacy service.
Having a gynecologic surgeon remove one or both ovaries is often done at the same time as a hysterectomy. We do nearly all these surgeries with a minimally invasive laparoscope and small incisions in the belly.
Most patients spend one night in the hospital and return to their regular routine in about two weeks.
The ovaries produce estrogen, which helps prevent bone loss and the thickening of arteries. After removal, a patient should be monitored long-term for the risk of osteoporosis and cardiovascular disease.
We encourage patients to keep at least one ovary to preserve fertility without egg freezing. This also preserves some hormone production, which can avoid early menopause.
At OHSU, expert urologists do orchiectomies (testicle removal). Patients may choose this option:
- To remove the body’s source of testosterone
- As part of a vaginoplasty or vulvoplasty (surgeries that create a vagina and/or vulva)
- To relieve dysphoria (some patients choose only this surgery)
Removing the testicles usually means a patient can stop taking a testosterone blocker. Patients may also be able to lower estrogen therapy.
How orchiectomy is done
The surgeon makes an incision in the scrotum. The testicles and the spermatic cord, which supplies blood, are removed. Scrotal skin is removed only if the patient specifically requests it. The skin is used if the patient plans a vaginoplasty or vulvoplasty.
You will probably go home the same day. Patients can typically resume normal activities in a week or two.
Reducing testosterone production may increase the risk of bone loss and cardiovascular disease, so we recommend regular tests. Without prior fertility treatment, orchiectomy also ends the ability to produce children. Serious risks are uncommon but include bleeding, infection, nerve damage and scarring.
Adam’s apple reduction (laryngochrondoplasty)
Dr. Joshua Schindler, an ear, nose and throat doctor who does Adam’s apple and vocal surgeries, completed his training at Johns Hopkins University.
Laryngochrondoplasty is also known as Adam’s apple reduction or a tracheal shave (though the trachea, or windpipe, is not affected).
A surgeon removes thyroid cartilage at the front of the throat to give your neck a smoother appearance. This procedure can often be combined with facial surgery.
Thin incision: At OHSU, this procedure can be done by an ear, nose and throat doctor (otolaryngologist) with detailed knowledge of the neck’s anatomy. The surgeon uses a thin incision, tucked into a neck line or fold. It can also be done by one of our plastic surgeons, typically with other facial surgery.
In an office or an operating room: Our team can do a laryngochrondoplasty in either setting, which may limit a patient’s out-of-pocket expenses.
OHSU also offers Adams’ apple enhancement surgery.
Many patients find that hormone therapy and speech therapy help them achieve a voice that reflects their identity. For others, vocal surgery can be added to raise the voice’s pitch.
Voice therapy: Patients have voice and communication therapy before we consider vocal surgery. Your surgeon and your speech therapist will assess your voice with tests such as videostroboscopy (allowing us to see how your vocal cords work) and acoustic voice analysis.
Effective surgery: We use a surgery called a Wendler glottoplasty. It’s done through the mouth under general anesthesia. The surgeon creates a small controlled scar between the two vocal cords, shortening them to increase tension and raise pitch. Unlike techniques that can lose effectiveness over time, this surgery offers permanent results.
Hormone therapy can bring out desired traits, but it can’t change the underlying structure or remove hair follicles. Our highly trained surgeons and other specialists offer options. Patients usually go home the same day or spend one night in a private room.
Face options:
- Browlift (done with the forehead)
- Cheek augmentation
- Chin surgery (genioplasty), including reductive, implants or bone-cut options
- Eyelid surgery
- Face-lift, neck lift
- Forehead lengthening
- Forehead reduction, including Type 3 sinus setback and orbital remodeling
- Hairline advancement (done with the forehead)
- Jawline contouring
- Lip lift and/or augmentation
- Lipofilling (transferring fat using liposuction and filling)
- Nose job (rhinoplasty)
Body options:
Hormone treatment may not result in fat distribution consistent with your gender. We offer liposuction and fat grafting to reshape areas of the body.
How Gender Reassignment Surgery Works (Infographic)
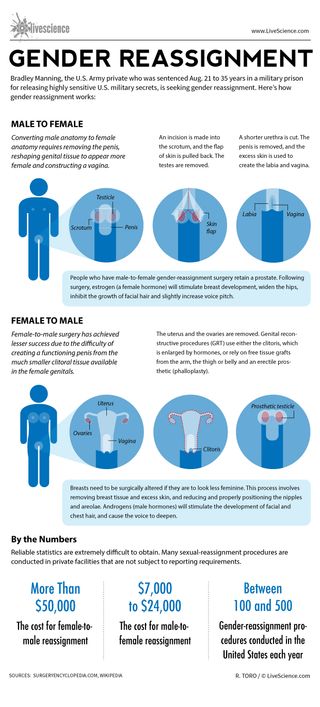
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Man's years of premature ejaculation had a rare cause
Viagra alternatives? Study of mouse erections hints at new ways to treat erectile dysfunction
Scientists grow diamonds from scratch in 15 minutes thanks to groundbreaking new process
Most Popular
- 2 James Webb telescope confirms there is something seriously wrong with our understanding of the universe
- 3 Massive study of 8,000 cats reveals which breeds live longest
- 4 Some of the oldest stars in the universe found hiding near the Milky Way's edge — and they may not be alone
- 5 Newfound 'glitch' in Einstein's relativity could rewrite the rules of the universe, study suggests
- 2 Creepy Deep-Sea Anglerfish Captured in Rare Video
- 3 Can a commercial airplane do a barrel roll?
- 4 Mysterious L-shaped structure found near Egyptian pyramids of Giza baffles scientists
- 5 In a 1st, HIV vaccine triggers rare and elusive antibodies in human patients
Do I need a referral to see a specialist? Learn more here . Explore the Department Directory Learn more about Telehealth Appointments Protect Yourself from West Nile Virus
How to schedule your APPOINTMENT at Denver Health: CURRENT PATIENTS: Login to MyChart to schedule appointments or call 303-436-4949 . NEW PATIENTS: Schedule an appointment online or call 303-436-4949 . NEED CARE? Schedule a Virtual Urgent Care appointment or click here to find an Urgent Care clinic .
MyChart Login
Login to MyChart
MyChart for Mobile
Download the MyChart mobile app for access to your healthcare information. Managing your healthcare has never been more simple. Download for iPhone and Android .
MyChart Sign Up
Learn about MyChart features , and sign up for an account .
Virtual Urgent Care Now Available for Denver Health MyChart Users
Denver Health MyChart users can now have a virtual urgent care visit with one of our expert providers. It’s easy and convenient to get the urgent care you need from the comfort of your home, using your smartphone, tablet or computer.
Click here for more details

- Departments & Services
- Conditions & Treatments
- Our Locations
- Find a Provider
- Pharmacy / Prescriptions
- Pay my bill
- Main Campus (303) 436-6000
- Appointments (303) 436-4949
- Lean Academy 855-888-5326
- Nurseline (303) 739-1211
- Pharmacy (303) 389-1390
- Telehealth (303) 436-4949
Make an Appointment
Hours of operation, gender affirming surgery (sex reassignment surgery).
Thank you for your interest in gender affirming surgery at Denver Health. There is no one-size-fits-all approach for the gender affirmation process and we are here to support you in your journey. We are proud to offer surgeries with a truly talented multi-disciplinary team of surgeons. Our services are growing as the unique needs of each individual evolve. Currently we offer the following gender affirming surgeries: MTF Top Surgery , FTM Top Surgery , Orchiectomy , FTM Hysterectomy , and Vaginoplasty surgeries.
What is Gender Affirming Surgery?
Gender affirming surgery, also known as sex reassignment surgery (SRS) or confirmation surgery, is the surgical procedure(s) by which a transgender or non-binary person’s physical appearance and functional abilities are changed to align with the gender they know themselves to be.
Complete Our Surgical Interest Form
If you are interested in a gender affirmation surgery at Denver Health, please complete one of the following forms.
Top Surgery and Hysterectomy
For vaginoplasty, breast augmentation and orchiectomy, our approach to surgical assessment.
Denver Health adheres to the guidelines for surgical assessment as described in the World Professional Association for Transgender Health Standards of Care, 8th Version . The standards were created by international agreement using the latest scientific research on transgender health so that doctors can best meet the unique health care needs of transgender and gender-nonconforming people. Most insurance companies also adhere to these guidelines.
Patients may provide referral letters from their own outside mental health providers, or the assessment process via our Behavioral Health team. Patients seeking to undergo the assessment at Denver Health should make an appointment with our Behavioral Health Team .
Read more about common frequently asked general surgery questions:
How long will my hospital stay be.
Hospital stays will vary based on specific patient response.
MTF top surgery, FTM chest surgery, FTM Hysterectomy, and orchiectomy surgery patients are usually released from the hospital the same day of surgery. Vaginoplasty patients typically spend 3 days in the hospital during recovery.
What medications will I be prescribed after surgery?
You will likely receive painkillers and antibiotics to reduce the chance of infection.
- 0 && newsLoaded" class="" data-id="{044698B9-FA04-4636-994D-47662155601F}" ref="news"> News
- 0 && blogLoaded" class="" data-id="{9AB9C6CB-06BD-4D71-867F-FAB69D88F93C}" ref="blog"> Blog Articles
- 0 && storiesLoaded" class="" data-id="{71E64EA2-1956-4F7C-A67D-579E0BB54378}" ref="stories"> Patient Stories
- May 22 Labor and Delivery Tour for Expectant Families
- May 29 Labor and Delivery Tour for Expectant Families
- Jun 5 Labor and Delivery Tour for Expectant Families
- Jun 8 Boot Camp for New Dads ®
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, male-to-female gender-affirming surgery: 20-year review of technique and surgical results.

- 1 Serviço de Urologia, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 2 Serviço de Psiquiatria, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 3 Serviço de Psiquiatria, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current study, a retrospective cohort, we report the 20-years outcomes of the gender-affirming surgery performed at a single Brazilian university center, examining demographic data, intra and postoperative complications. During this period, 214 patients underwent penile inversion vaginoplasty.
Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18–61 years); the average of operative time was 3.3 h (range 2–5 h); the average duration of hormone therapy before surgery was 12 years (range 1–39). The most commons minor postoperative complications were granulation tissue (20.5 percent) and introital stricture of the neovagina (15.4 percent) and the major complications included urethral meatus stenosis (20.5 percent) and hematoma/excessive bleeding (8.9 percent). A total of 36 patients (16.8 percent) underwent some form of reoperation. One hundred eighty-one (85 percent) patients in our series were able to have regular sexual intercourse, and no individual regretted having undergone GAS.
Conclusions: Findings confirm that it is a safety procedure, with a low incidence of serious complications. Otherwise, in our series, there were a high level of functionality of the neovagina, as well as subjective personal satisfaction.
Introduction
Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ( 1 ). The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ( 1 ). Gender identity-affirming care, for those who desire, can include hormone therapy and affirming surgeries, as well as other procedures such as hair removal or speech therapy ( 1 ).
Since 1998, the Gender Identity Program (PROTIG) of the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul, Brazil has provided public assistance to transsexual people, is the first one in Brazil and one of the pioneers in South America. Our program offers psychosocial support, health care, and guidance to families, and refers individuals for gender-affirming surgery (GAS) when indicated. To be eligible for this surgery, transsexual individuals must have been adherent to multidisciplinary follow-up for at least 2 years, have a minimum age of 21 years (required for surgical procedures of this nature), have a positive psychiatric or psychological report, and have a diagnosis of GD.
Gender-affirming surgery (GAS) is increasingly recognized as a therapeutic intervention and a medical necessity, with growing societal acceptance ( 2 ). At our institution, we perform the classic penile inversion vaginoplasty (PIV), with an inverted penis skin flap used as the lining for the neovagina. Studies have demonstrated that GAS for the management of GD can promote improvements in mental health and social relationships for these patients ( 2 – 5 ). It is therefore imperative to understand and establish best practice techniques for this patient population ( 2 ). Although there are several studies reporting the safety and efficacy of gender-affirming surgery by penile inversion vaginoplasty, we present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
Patients and Methods
Subjects and study setup.
This is a retrospective cohort study of Brazilian transgender women who underwent penile inversion vaginoplasty between January of 2000 and March of 2020 at the Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil. The study was approved by our institutional medical and research ethics committee.
At our institution, gender-affirming surgery is indicated for transgender women who are under assistance by our program for transsexual individuals. All transsexual women included in this study had at least 2 years of experience as a woman and met WPATH standards for GAS ( 1 ). Patients were submitted to biweekly group meetings and monthly individual therapy.
Between January of 2000 and March of 2020, a total of 214 patients underwent penile inversion vaginoplasty. The surgical procedures were performed by two separate staff members, mostly assisted by residents. A retrospective chart review was conducted recording patient demographics, intraoperative and postoperative complications, reoperations, and secondary surgical procedures. Informed consent was obtained from all individual participants included in the study.
Hormonal Therapy
The goal of feminizing hormone therapy is the development of female secondary sex characteristics, and suppression/minimization of male secondary sex characteristics.
Our general therapy approach is to combine an estrogen with an androgen blocker. The usual estrogen is the oral preparation of estradiol (17-beta estradiol), starting at a dose of 2 mg/day until the maximum dosage of 8 mg/day. The preferred androgen blocker is spironolactone at a dose of 200 mg twice a day.
Operative Technique
At our institution, we perform the classic penile inversion vaginoplasty, with an inverted penis skin flap used as the lining for the neovagina. For more details, we have previously published our technique with a step-by-step procedure video ( 6 ). All individuals underwent intestinal cleansing the evening before the surgery. A first-generation cephalosporin was used as preoperative prophylaxis. The procedure was performed with the patient in a dorsal lithotomy position. A Foley catheter was placed for bladder catheterization. A inverted-V incision was made 4 cm above the anus and a flap was created. A neovaginal cavity was created between the prostate and the rectum with blunt dissection, in the Denonvilliers space, until the peritoneal fold, usually measuring 12 cm in extension and 6 cm in width. The incision was then extended vertically to expose the testicles and the spermatic cords, which were removed at the level of the external inguinal rings. A circumferential subcoronal incision was made ( Figure 1 ), the penis was de-gloved and a skin flap was created, with the de-gloved penis being passed through the scrotal opening ( Figure 2 ). The dorsal part of the glans and its neurovascular bundle were bluntly dissected away from the penile shaft ( Figure 3 ) as well as the urethra, which included a portion of the bulbospongious muscle ( Figure 4 ). The corpora cavernosa was excised up to their attachments at the symphysis pubis and ligated. The neoclitoris was shaped and positioned in the midline at the level of the symphysis pubis and sutured using interrupted 5-0 absorbable suture. The corpus spongiosum was reduced and the urethra was shortened, spatulated, and placed 1 cm below the neoclitoris in the midline and sutured using interrupted 4-0 absorbable suture. The penile skin flap was inverted and pulled into the neovaginal cavity to become its walls ( Figure 5 ). The excess of skin was then removed, and the subcutaneous tissue and the skin were closed using continuous 3-0 non-absorbable suture ( Figure 6 ). A neo mons pubis was created using a 0 absorbable suture between the skin and the pubic bone. The skin flap was fixed to the pubic bone using a 0 absorbable suture. A gauze impregnated with Vaseline and antibiotic ointment was left inside the neovagina, and a customized compressive bandage was applied ( Figure 7 —shows the final appearance after the completion of the procedures).

Figure 1 . The initial circumferential subcoronal incision.

Figure 2 . The de-gloved penis being passed through the scrotal opening.

Figure 3 . The dorsal part of the glans and its neurovascular bundle dissected away from the penile shaft.
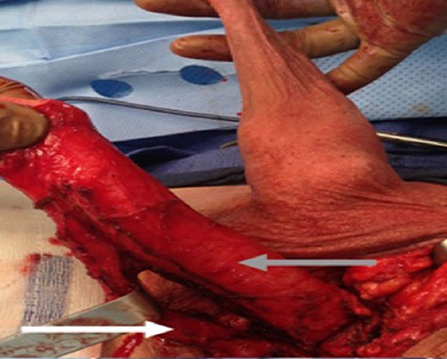
Figure 4 . The urethra dissected including a portion of the bulbospongious muscle. The grey arrow shows the penile shaft and the white arrow shows the dissected urethra.

Figure 5 . The inverted penile skin flap.
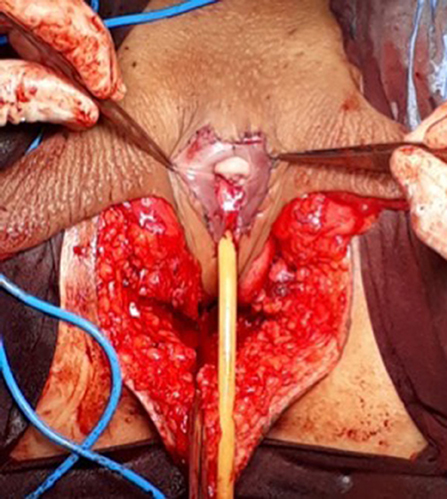
Figure 6 . The neoclitoris and the urethra sutured in the midline and the neovaginal cavity.
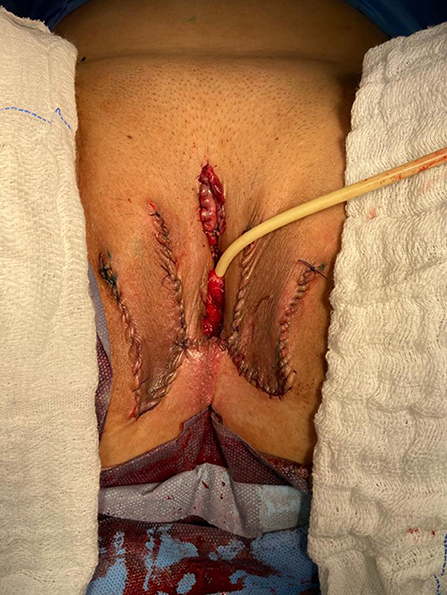
Figure 7 . The final appearance after the completion of the procedures.
Postoperative Care and Follow-Up
The patients were usually discharged within 2 days after surgery with the Foley catheter and vaginal gauze packing in place, which were removed after 7 days in an ambulatorial attendance.
Our vaginal dilation protocol starts seven days after surgery: a kit of 6 silicone dilators with progressive diameter (1.1–4 cm) and length (6.5–14.5 cm) is used; dilation is done progressively from the smallest dilator; each size should be kept in place for 5 min until the largest possible size, which is kept for 3 h during the day and during the night (sleep), if possible. The process is performed daily for the first 3 months and continued until the patient has regular sexual intercourse.
The follow-up visits were performed 7 days, 1, 2, 3, 6, and 12 months after surgery ( Figure 8 ), and included physical examination and a quality-of-life questionnaire.

Figure 8 . Appearance after 1 month of the procedure.
Statistical Analysis
The statistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Outcome measures were intra-operative and postoperative complications, re-operations. Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented as continuous variables. Frequencies and percentages are reported for dichotomous and ordinal variables.
Patient Demographics
During the period of the study, 214 patients underwent penile inversion vaginoplasty, performed by two staff surgeons, mostly assisted by residents ( Table 1 ). The average age at the time of surgery was 32.2 years (range 18–61 years). There was no significant increase or decrease in the ages of patients who underwent SRS over the study period (Fisher's exact test: P = 0.065; chi-square test: X 2 = 5.15; GL = 6; P = 0.525). The average of operative time was 3.3 h (range 2–5 h). The average duration of hormone therapy before surgery was 12 years (range 1–39). The majority of patients were white (88.3 percent). The most prevalent patient comorbidities were history of tobacco use (15 percent), human immunodeficiency virus infection (13 percent) and hypertension (10.7 percent). Other comorbidities are listed in Table 1 .
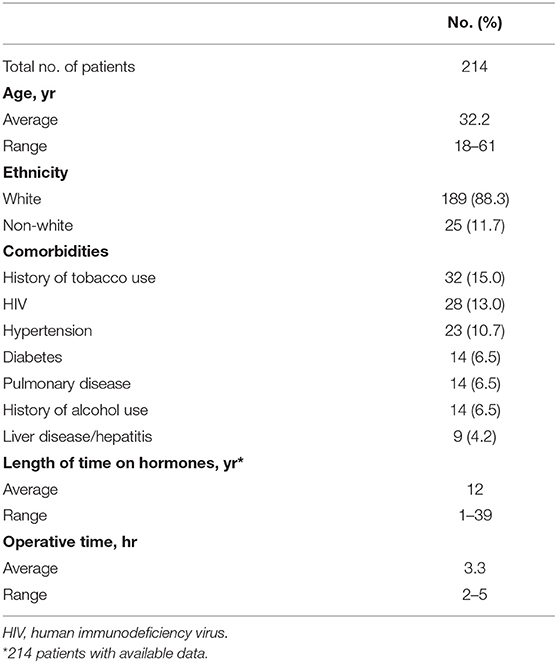
Table 1 . Patient demographics.
Multidisciplinary follow-up was comprised of 93.45% of patients following up with a urologist and 59.06% of patients continuing psychiatric follow-up, median follow-up time of 16 and 9.3 months after surgery, respectively.
Postoperative Results
The complications were classified according to the Clavien-Dindo score ( Table 2 ). The most common minor postoperative complications (Grade I) were granulation tissue (20.5 percent), introital stricture of the neovagina (15.4 percent) and wound dehiscence (12.6 percent). The major complications (Grade III-IV) included urethral stenosis (20.5 percent), urethral fistula (1.9 percent), intraoperative rectal injury (1.9 percent), necrosis (primarily along the wound edges) (1.4 percent), and rectovaginal fistula (0.9 percent). A total of 17 patients required blood transfusion (7.9 percent).
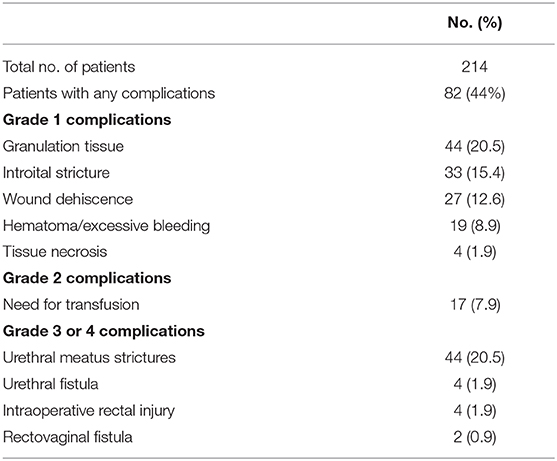
Table 2 . Complications after penile inversion vaginoplasty.
A total of 36 patients (16.8 percent) underwent some form of reoperation.
One hundred eighty-one (85 percent) patients in our series were able to have regular sexual vaginal intercourse, and no individual regretted having undergone GAS.
Penile inversion vaginoplasty is the gold-standard in gender-affirming surgery. It has good functional outcomes, and studies have demonstrated adequate vaginal depths ( 3 ). It is recognized not only as a cosmetic procedure, but as a therapeutic intervention and a medical necessity ( 2 ). We present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
The mean age of transsexual women who underwent GAS in our study was 32.2 years (range 18–61 years), which is lower than the mean age of patients in studies found in the literature. Two studies indicated that the mean ages of patients at time of GAS were 36.7 years and 41 years, respectively ( 4 , 5 ). Another study reported a mean age at time of GAS of 36 years and found there was a significant decrease in age at the time of GAS from 41 years in 1994 to 35 years in 2015 ( 7 ). According to the authors, this decrease in age is associated with greater tolerance and societal approval regarding individuals with GD ( 7 ).
There was no grade IV or grade V complications. Excessive bleeding noticed postoperatively occurred in 19 patients (8.9 percent) and blood transfusion was required in 17 cases (7.9 percent); all patients who required blood transfusions were operated until July 2011, and the reason for this rate of blood transfusion was not identified.
The most common intraoperative complication was rectal injury, occurring in 4 patients (1.9 percent); in all patients the lesion was promptly identified and corrected in 2 layers absorbable sutures. In 2 of these patients, a rectovaginal fistula became evident, requiring fistulectomy and colonic transit deviation. This is consistent with current literature, in which rectal injury is reported in 0.4–4.5 percent of patients ( 4 , 5 , 8 – 13 ). Goddard et al. suggested carefully checking for enterotomy after prostate and bladder mobilization by digital rectal examination ( 4 ). Gaither et al. ( 14 ) commented that careful dissection that closely follows the urethra along its track from the central tendon of the perineum up through the lower pole of the prostate is critical and only blunt dissection is encouraged after Denonvilliers' fascia is reached. Alternatively, a robotic-assisted approach to penile inversion vaginoplasty may aid in minimizing these complications. The proposed advantages of a robotic-assisted vaginoplasty include safer dissection to minimize the risk of rectal injury and better proximal vaginal fixation. Dy et al. ( 15 ) has had no rectal injuries or fistulae to date in his series of 15 patients, with a mean follow-up of 12 months.
In our series, we observed 44 cases (20.5 percent) of urethral meatus strictures. We credit this complication to the technique used in the initial 5 years of our experience, in which the urethra was shortened and sutured in a circular fashion without spatulation. All cases were treated with meatal dilatation and 11 patients required surgical correction, being performed a Y-V plastic reconstruction of the urethral meatus. In the literature, meatal strictures are relatively rare in male-to-female (MtF) GAS due to the spatulation of the urethra and a simple anastomosis to the external genitalia. Recent systematic reviews show an incidence of five percent in this complication ( 16 , 17 ). Other studies report a wide incidence of meatal stenosis ranging from 1.1 to 39.8 percent ( 4 , 8 , 11 ).
Neovagina introital stricture was observed in 33 patients (15.4 percent) in our study and impedes the possibility of neovaginal penetration and/or adversely affects sexual life quality. In the literature, the reported incidence of introital stenosis range from 6.7 to 14.5 percent ( 4 , 5 , 8 , 9 , 11 – 13 ). According to Hadj-Moussa et al. ( 18 ) a regimen of postoperative prophylactic dilation is crucial to minimize the development of this outcome. At our institution, our protocol for vaginal dilation started seven days after surgery and was performed three to four times a day during the first 3 months and was continued until the individual had regular sexual intercourse. We treated stenosis initially with dilation. In case of no response, we propose a surgical revision with diamond-shaped introitoplasty with relaxing incisions. In recalcitrant cases, we proposed to the patient a secondary vaginoplasty using a full-thickness skin graft of the lower abdomen.
One hundred eighty-one (85 percent) patients were classified as having a “functional vagina,” characterized as the capacity to maintain satisfactory sexual vaginal intercourse, since the mean neovaginal depth was not measured. In a review article, the mean neovaginal depth ranged from 10 to 13.5 cm, with the shallowest neovagina depth at 2.5 cm and the deepest at 18 cm ( 17 ). According to Salim et al. ( 19 ), in terms of postoperative functional outcomes after penile inversion vaginoplasty, a mean percentage of 75 percent (range from 33 to 87 percent) patients were having vaginal intercourse. Hess et al. found that 91.4% of patients who responded to a questionnaire were very satisfied (34.4%), satisfied (37.6%), or mostly satisfied (19.4%) with their sexual function after penile inversion vaginoplasty ( 20 ).
Poor cosmetic appearance of the vulva is common. Amend et al. reported that the most common reason for reoperation was cosmetic correction in the form of mons pubis and mucosa reduction in 50% of patients ( 16 ). We had no patient regrets about performing GAS, although 36 patients (16.8 percent) were reoperated due to cosmetic issues. Gaither et al. propose in order to minimize scarring to use a one-stage surgical approach and the lateralization of surgical scars to the groin ( 14 ). Frequently, cosmetic issues outcomes are often patient driven and preoperative patient education is necessary ( 14 ).
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) ( 21 ). The authors found that GAS promotes the improvement of psychological aspects and social relations. However, even 1 year after GAS, MtF persons continue to report problems in physical and difficulty in recovering their independence. In a systematic review and meta-analysis of QOL and psychosocial outcomes in transsexual people, researchers verified that sex reassignment with hormonal interventions more likely corrects gender dysphoria, psychological functioning and comorbidities, sexual function, and overall QOL compared with sex reassignment without hormonal interventions, although there is a low level of evidence for this ( 22 ). Recently, Castellano et al. assessed QOL in 60 Italian transsexuals (46 transwomen and 14 transmen) at least 2 years after SRS using the WHOQOL-100 (general QOL score and quality of sexual life and quality of body image scores) to focus on the effects of hormonal therapy. Overall satisfaction improved after SRS, and QOL was similar to the controls ( 23 ). Bartolucci et al. evaluated the perception of quality of sexual life using four questions evaluating the sexual facet in individuals with gender dysphoria before SRS and the possible factors associated with this perception. The study showed that approximately half the subjects with gender dysphoria perceived their sexual life as “poor/dissatisfied” or “very poor/very dissatisfied” before SRS ( 24 ).
Our study has some limitations. The total number of operated patients is restricted within the long follow-up period. This is due to a limitation in our health system, which allows only 1 sexual reassignment surgery to be performed per month at our institution. Neovagin depth measurement was not performed routinely in the follow-up of operated patients.
Conclusions
The definitive treatment for patients with gender dysphoria is gender-affirming surgery. Our series demonstrates that GAS is a feasible surgery with low rates of serious complications. We emphasize the high level of functionality of the vagina after the procedure, as well as subjective personal satisfaction. Complications, especially minor ones, are probably underestimated due to the nature of the study, and since this is a surgical population, the results may not be generalizable for all transgender MTF individuals.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Hospital de Clínicas de Porto Alegre. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM: conception and design, data acquisition, data analysis, interpretation, drafting the manuscript, review of the literature, critical revision of the manuscript and factual content, and statistical analysis. ML and TR: conception and design, data interpretation, drafting the manuscript, critical revision of the manuscript and factual content, and statistical analysis. DS, KS, AF, AC, PT, AG, and RC: conception and design, data acquisition and data analysis, interpretation, drafting the manuscript, and review of the literature. All authors contributed to the article and approved the submitted version.
This study was supported by the Fundo de Incentivo à Pesquisa e Eventos (FIPE - Fundo de Incentivo à Pesquisa e Eventos) of Hospital de Clínicas de Porto Alegre.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-non-conforming people, version 7. Int J Transgend. (2012) 13:165–232. doi: 10.1080/15532739.2011.700873
CrossRef Full Text | Google Scholar
2. Massie JP, Morrison SD, Maasdam JV, Satterwhite T. Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plast Reconstruct Surg. (2018) 141:911–921. doi: 10.1097/PRS.0000000000004427
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Pan S, Honig SC. Gender-affirming surgery: current concepts. Curr Urol Rep . (2018) 19:62. doi: 10.1007/s11934-018-0809-9
4. Goddard JC, Vickery RM, Qureshi A, Summerton DJ, Khoosal D, Terry TR. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int . (2007) 100:607–13. doi: 10.1111/j.1464-410X.2007.07017.x
5. Rossi NR, Hintz F, Krege S, Rübben H, Vom DF, Hess J. Gender reassignment surgery – a 13 year review of surgical outcomes. Eur Urol Suppl . (2013) 12:e559. doi: 10.1016/S1569-9056(13)61042-8
6. Silva RUM, Abreu FJS, Silva GMV, Santos JVQV, Batezini NSS, Silva Neto B, et al. Step by step male to female transsexual surgery. Int Braz J Urol. (2018) 44:407–8. doi: 10.1590/s1677-5538.ibju.2017.0044
7. Aydin D, Buk LJ, Partoft S, Bonde C, Thomsen MV, Tos T. Transgender surgery in Denmark from 1994 to 2015: 20-year follow-up study. J Sex Med. (2016) 13:720–5. doi: 10.1016/j.jsxm.2016.01.012
8. Perovic SV, Stanojevic DS, Djordjevic MLJ. Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. (2001) 86:843–50. doi: 10.1046/j.1464-410x.2000.00934.x
9. Krege S, Bex A, Lümmen G, Rübben H. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. (2001) 88:396–402. doi: 10.1046/j.1464-410X.2001.02323.x
10. Wagner S, Greco F, Hoda MR, Inferrera A, Lupo A, Hamza A, et al. Male-to-female transsexualism: technique, results and 3-year follow-up in 50 patients. Urol International. (2010) 84:330–3. doi: 10.1159/000288238
11. Reed H. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin PlasticSurg. (2011) 25:163–74. doi: 10.1055/s-0031-1281486
12. Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. (2015) 12:1837–45. doi: 10.1111/jsm.12936
13. Sigurjonsson H, Rinder J, Möllermark C, Farnebo F, Lundgren TK. Male to female gender reassignment surgery: surgical outcomes of consecutive patients during 14 years. JPRAS Open. (2015) 6:69–73. doi: 10.1016/j.jpra.2015.09.003
14. Gaither TW, Awad MA, Osterberg EC, Murphy GP, Romero A, Bowers ML, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. (2018) 199:760–5. doi: 10.1016/j.juro.2017.10.013
15. Dy GW, Sun J, Granieri MA, Zhao LC. Reconstructive management pearls for the transgender patient. Curr. Urol. Rep. (2018) 19:36. doi: 10.1007/s11934-018-0795-y
16. Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. (2013) 64:141–9. doi: 10.1016/j.eururo.2012.12.030
17. Horbach SER, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med . (2015) 12:1499–512. doi: 10.1111/jsm.12868
18. Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. (2018) 6:457–68.e2. doi: 10.1016/j.sxmr.2017.11.005
19. Salim A, Poh M. Gender-affirming penile inversion vaginoplasty. Clin Plast Surg. (2018) 45:343–50. doi: 10.1016/j.cps.2018.04.001
20. Hess J, Rossi NR, Panic L, Rubben H, Senf W. Satisfaction with male-to-female gender reassignment surgery. DtschArztebl Int. (2014) 111:795–801. doi: 10.3238/arztebl.2014.0795
21. Silva DC, Schwarz K, Fontanari AMV, Costa AB, Massuda R, Henriques AA, et al. WHOQOL-100 before and after sex reassignment surgery in brazilian male-to-female transsexual individuals. J Sex Med. (2016) 13:988–93. doi: 10.1016/j.jsxm.2016.03.370
22. Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol . (2010) 72:214–31. doi: 10.1111/j.1365-2265.2009.03625.x
23. Castellano E, Crespi C, Dell'Aquila C, Rosato R, Catalano C, Mineccia V, et al. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest . (2015) 38:1373–81. doi: 10.1007/s40618-015-0398-0
24. Bartolucci C, Gómez-Gil E, Salamero M, Esteva I, Guillamón A, Zubiaurre L, et al. Sexual quality of life in gender-dysphoric adults before genital sex reassignment surgery. J Sex Med . (2015) 12:180–8. doi: 10.1111/jsm.12758
Keywords: transsexualism, gender dysphoria, gender-affirming genital surgery, penile inversion vaginoplasty, surgical outcome
Citation: Moisés da Silva GV, Lobato MIR, Silva DC, Schwarz K, Fontanari AMV, Costa AB, Tavares PM, Gorgen ARH, Cabral RD and Rosito TE (2021) Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Front. Surg. 8:639430. doi: 10.3389/fsurg.2021.639430
Received: 17 December 2020; Accepted: 22 March 2021; Published: 05 May 2021.
Reviewed by:
Copyright © 2021 Moisés da Silva, Lobato, Silva, Schwarz, Fontanari, Costa, Tavares, Gorgen, Cabral and Rosito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriel Veber Moisés da Silva, veber.gabriel@gmail.com
This article is part of the Research Topic
Gender Dysphoria: Diagnostic Issues, Clinical Aspects and Health Promotion
Jump to content
Updated visitor policies
Other michigan medicine sites.
- About Michigan Medicine
- UofMHealth.org
- Medical School
- Find a Clinical Trial

Michigan Medicine
Federated search page form block, quick links.
- Patient Portal Login
- For Health Providers
- Maps & Directions
Gender Confirmation Surgery
The University of Michigan Health System offers procedures for surgical gender transition. Working together, the surgical team of the Comprehensive Gender Services Program, which includes specialists in plastic surgery, urology and gynecology, bring expertise, experience and safety to procedures for our transgender patients.
Access to gender-related surgical procedures for patients is made through the University of Michigan Health System Comprehensive Gender Services Program .
The Comprehensive Gender Services Program adheres to the WPATH Standards of Care , including the requirement for a second-opinion prior to genital sex reassignment.
Available surgeries:
Male-to-Female: Tracheal Shave Breast Augmentation Facial Feminization Male-to-Female genital sex reassignment
Female-to-Male: Hysterectomy, oophorectomy, vaginectomy Chest Reconstruction Female-to-male genital sex reassignment
Sex Reassignment Surgeries (SRS)
At the University of Michigan Health System, we are dedicated to offering the safest proven surgical options for sex reassignment (SRS.) Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain specialists and a reconstructive plastic surgeon. A multi-disciplinary team helps to best protect the health of the patient.
For patients receiving mental health and medical services within the University of Michigan Health System, the UMHS-CGSP will coordinate all care including surgical referrals. For patients who have prepared for surgery elsewhere, the UMHS-CGSP will help organize the needed records, meet WPATH standards, and coordinate surgical referrals. Surgical referrals are made through Sara Wiener the Comprehensive Gender Services Program Director.
Male-to-female sex reassignment surgery
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris.
During this procedure, a surgeon makes “like become like,” using parts of the original penis to create a sensate neo-vagina. The testicles are removed, a procedure called orchiectomy. The skin from the scrotum is used to make the labia. The erectile tissue of the penis is used to make the neoclitoris. The urethra is preserved and functional.
This procedure provides for aesthetic and functional female genitalia in one 4-5 hour operation. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation. What to Expect: Vaginoplasty at Michigan Medicine .
Female-to-male sex reassignment
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a female-to-male sex reassignment surgery will be offered a phalloplasty, generally using the radial forearm flap method.
This procedure, which can be done at the same time as a hysterectomy/vaginectomy, creates an aesthetically appropriate phallus and creates a urethera for standing urination. Construction of a scrotum with testicular implants is done as a second stage. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected] . W e will assist you in obtaining what you need to qualify for surgery.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.16(4); 2024 Apr
- PMC11063965

Risk of Suicide and Self-Harm Following Gender-Affirmation Surgery
John j straub.
1 Department of Emergency Medicine, University of Texas Medical Branch at Galveston, Galveston, USA
Krishna K Paul
Lauren g bothwell, sterling j deshazo, georgiy golovko.
2 Department of Pharmacology, University of Texas Medical Branch at Galveston, Galveston, USA
Michael S Miller
3 Department of Psychiatry and Behavioral Services, University of Texas Medical Branch at Galveston, Galveston, USA
Dietrich V Jehle
Introduction.
With the growing acceptance of transgender individuals, the number of gender affirmation surgeries has increased. Transgender individuals face elevated depression rates, leading to an increase in suicide ideation and attempts. This study evaluates the risk of suicide or self-harm associated with gender affirmation procedures.
This retrospective study utilized de-identified patient data from the TriNetX (TriNetX, LLC, Cambridge, MA) database, involving 56 United States healthcare organizations and over 90 million patients. The study involved four cohorts: cohort A, adults aged 18-60 who had gender-affirming surgery and an emergency visit (N = 1,501); cohort B, control group of adults with emergency visits but no gender-affirming surgery (N = 15,608,363); and cohort C, control group of adults with emergency visits, tubal ligation or vasectomy, but no gender-affirming surgery (N = 142,093). Propensity matching was applied to cohorts A and C. Data from February 4, 2003, to February 4, 2023, were analyzed to examine suicide attempts, death, self-harm, and post-traumatic stress disorder (PTSD) within five years of the index event. A secondary analysis involving a control group with pharyngitis, referred to as cohort D, was conducted to validate the results from cohort C.
Individuals who underwent gender-affirming surgery had a 12.12-fold higher suicide attempt risk than those who did not (3.47% vs. 0.29%, RR 95% CI 9.20-15.96, p < 0.0001). Compared to the tubal ligation/vasectomy controls, the risk was 5.03-fold higher before propensity matching and remained significant at 4.71-fold after matching (3.50% vs. 0.74%, RR 95% CI 2.46-9.024, p < 0.0001) for the gender affirmation patients with similar results with the pharyngitis controls.
Gender-affirming surgery is significantly associated with elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support.
The prevalence of transgender individuals in the United States is approximately 0.3% to 0.6% of the adult population based on self-reporting studies [ 1 ]. Investigations that only include individuals with transgender diagnostic codes, hormone therapy, or gender-affirming surgery report a much lower rate of approximately 0.008% of the population [ 2 ]. People who identify as transgender are shown to have a higher risk of suicide in the United States and across many other countries [ 3 - 6 ].
In 2021, the Centers for Disease Control reported that 48,183 people died by suicide in the United States. Depression, substance abuse, other mental illness, legal/financial problems, harmful relationships, community risk factors, and easy access to lethal means are contributing factors to successful suicide. Transgender individuals have a higher prevalence of depression across several age groups, often due to life experiences that include discrimination, harassment, violence, misgendering, and enacted stigma that may generate poor mental health outcomes and harmful behaviors [ 4 , 7 , 8 ]. It is widely accepted that depression puts an individual at higher risk for suicidal ideation and suicide attempts [ 9 ]. Individuals at higher risk for suicide and post-traumatic stress disorder (PTSD) should have comprehensive psychiatric interventions and care throughout their lifetime. A better understanding of the relationship between suicide and gender affirmation remains particularly important.
There is ongoing controversy surrounding the benefits of gender-affirmation surgery on mental health [ 10 - 20 ]. This controversy reflects diverse perspectives within the medical and research communities, emphasizing the need for a more comprehensive understanding of the psychological outcomes of gender-affirming procedures. Despite the increasing acceptance of transgender individuals, questions persist about the psychological outcomes of gender-affirming procedures. Responses to the discussion surrounding the benefits of gender-affirmation surgery have been diverse, as evidenced by studies conducted by Branstrom and colleagues [ 11 ], Almazan et al. [ 13 ], and others [ 10 , 14 - 20 ].
The purpose of this study is to assess the risk of adverse outcomes, specifically suicide, death, self-harm, and PTSD in the five years following gender-affirmation surgery. Suicide risk over time among patients who received gender-affirmation surgery is compared to individuals in several control groups. The TriNetX (TriNetX, LLC, Cambridge, MA) database will be utilized to better understand the relationship between sex change and these outcomes.
This article was previously presented virtually as a meeting abstract at the 2023 Texas College of Emergency Physicians (TCEP) Research Forum on April 07, 2023.
Materials and methods
TriNetX is a global health research network providing access to de-identified retrospective electronic medical records. The database consists of over 90 million patients from 56 healthcare organizations (HCOs) within the United States. This study utilized TriNetX to identify patients who had a “personal history of sex reassignment” and evaluate their relative risk for suicide attempt, death, suicide/self-harm, and PTSD. The term “sex reassignment” was based on the International Classification of Diseases, 10th Revision (ICD-10) code in the database but will be referred to as the current term “gender-affirmation surgery” for the remaining article. All outcomes were evaluated during the five years after gender-affirmation surgery.
Patients who have undergone gender-affirmation surgery of all sexes, races, and ethnicities were identified by using the ICD-10 code, ICD10CM:Z87.890. Sex, race, and ethnicity were derived from the electronic medical record. Patients who have undergone gender-affirmation surgery are identified by their affirmed gender. A total of four cohorts were identified for this study. Cohort A consisted of patients ages 18 to 60 who had both gender-affirmation surgery and an emergency visit. Cohort B was the study control group that consisted of patients ages 18 to 60 who had no history of gender-affirmation surgery but had an emergency visit. In this database, propensity matching is not possible for very large cohorts, more than 8.3 million patients with 12 covariates.
Additional control groups were chosen to perform propensity matching, which controls for confounders. Cohort C was the study's second control group and consisted of adult patients (18-60 years) who had no history of gender-affirmation surgery, had an emergency visit, and had a tubal ligation or vasectomy. Patients who had undergone tubal ligation were identified through the ICD-10 code, ICD10CM:Z98.51, while the vasectomy procedure was identified by Current Procedural Terminology (CPT), CPT:55250. A secondary sub-group analysis, cohort D, was performed utilizing acute pharyngitis (ICD10CM:J02) as a control group for patients aged 18-60 that was run on June 2, 2023. This was performed to ensure that the vasectomy or bilateral tubal ligation (BTL) group acted as an appropriate control. The relative risk for suicide attempt, death, suicide/self-harm, and PTSD was evaluated during the five years following gender-affirmation surgery in comparison to those without gender-affirmation surgery with the diagnosis of pharyngitis. Cohort A was used again and compared with cohort D, which included patients presenting to the emergency room after diagnosis of acute pharyngitis.
The outcome analysis between the three cohorts was performed for four events: suicide attempt (ICD10CM:T14.91), death (vital status: deceased), suicide/self-harm (ICD10CM:T14.91 or ICD10CM:X71-X83), and PTSD (ICD10CM:F43.1). An analysis was performed utilizing the measures contained in the TriNetX platform, which compared the individual outcomes between cohorts A and B and also cohorts A and C within the designated time frame. Patients who had the outcome before the time window were excluded from the analysis. The final TriNetX data reported RR, 95% CI, ORs, and a risk comparison expressed as a p-value. To control potentially confounding risk factors for the measured outcomes, the propensity matching tool in TriNetX was utilized. Factors involved in the data propensity matching are based on age at index, race, ethnicity, and sex. Propensity matching was only performed between the comparison of cohorts A and C, but not cohort B, due to the large sample size limitation.
Propensity score matching (PSM) is often used in observational studies to reduce confounding biases. It has been investigated and well-documented regarding its properties for statistical inference. PSM is a quasi-experimental method in which the researcher uses statistical techniques to construct an artificial control group by matching the affected group with a non-affected group of similar characteristics. Using these matches, the researcher can estimate the difference between both groups without the confounding variables’ influence [ 21 ]. To justify our use of propensity matching for age, race, sex, and ethnicity, we considered established risk factors for suicide such as older age, male gender identity, and racial or ethnic minority status [ 3 , 4 ].
The cohort was analyzed descriptively using univariate and bivariate frequencies with chi-square and t-testing to assess differences. All eligible persons in the cohort were analyzed using both binary event estimation with RRs, 95% CIs, and probability values. Using the TriNetX database, a 1:1 propensity match using linear and logistic regression for age, sex, race, and ethnicity was employed for maximum generalization of the United States population. Greedy nearest-neighbor matching was used with a tolerance of 0.1 and a difference between propensity scores less than or equal to 0.1. Comparisons were made between cohorts before and after propensity matching. Statistical significance was set at a two-sided alpha <0.05. TriNetX provides data that have been de-identified, and as a result, an Institutional Review Board (IRB) review is not required for this study [ 22 ]. Three comparison reports were generated on February 4, 2023. Data gathered from HCOs was from February 4, 2003, to February 4, 2023.
We identified 15,609,864 adult patients from TriNetX who were adults and had a visit to an emergency department within the United States Collaborative Network. Cohort A consisted of 1,501 adult patients who had a visit to the emergency department and a history of gender-affirmation surgery. Cohort B consisted of 15,608,363 patients who had an emergency visit but no history of gender-affirmation surgery. Cohort C consisted of 142,093 adult patients who had a visit to the emergency department and no history of gender-affirmation surgery but had a vasectomy or BTL.
Without propensity matching between cohorts A and B, patients with a history of gender-affirmation surgery exhibited a significantly higher risk for each possible outcome compared to patients without a history of gender-affirmation surgery (Table (Table1). 1 ). Patients who had a history of gender-affirmation surgery had a 12.12 times greater risk of suicide attempts (3.47% vs. 0.29%, RR 95% CI 9.20-15.96, p < 0.0001) vs. patients who had no history of gender-affirmation surgery. In patients with a history of gender-affirmation surgery, there was a 3.35 times greater risk of being deceased (4.9% vs. 1.5%, RR 95% CI 2.673-4.194, p < 0.0001). Patients with a history of gender-affirmation surgery had a 9.88 times higher risk of self-harm or suicide (4.5% vs. 0.5%, RR 95% CI 7.746-12.603, p < 0.0001). Lastly, patients who had a history of gender-affirmation surgery had a 7.76 times higher risk of PTSD (9.2% vs. 1.2%, RR 95% CI 6.514-9.244, p < 0.0001).
PTSD, post-traumatic stress disorder
Before the propensity matching of cohorts A and C, there was a significantly higher risk for each outcome when considering patients with a history of gender-affirmation surgery compared to those without a history of gender-affirmation surgery but with a prior vasectomy or BTL (Table (Table2). 2 ). Patients with a history of gender-affirmation surgery had a 5.03 times higher risk of suicide attempts (3.5% vs. 0.7%, RR 95% CI 3.795-6.676, p < 0.0001), a 2.37 times higher risk of being deceased (4.9% vs. 2.1%, RR 95% CI 1.889-2.982, p < 0.0001), a 5.44 times higher risk of suicide or self-harm (4.5% vs. 0.8%, RR 95% CI 4.233-6.981, p < 0.0001), and a 3.74 times higher risk of PTSD (9.2% vs. 2.5%, RR 95% CI 3.125-4.463, p < 0.0001) compared to patients without a history of gender-affirmation surgery but with a prior vasectomy or BTL.
After propensity matching of cohorts A and C, each cohort had 1,489 patients of similar age at index, race, and ethnicity (Tables (Tables3 3 - -4). 4 ). Patients who had a history of gender-affirmation surgery compared to patients without a gender-affirmation surgery history but had a vasectomy or BTL showed significantly higher risks for each outcome (Table (Table3). 3 ). The adjusted suicide attempt risk for patients with gender-affirmation surgery compared to no history of gender-affirmation surgery but with a prior BTL or vasectomy was adjusted to a 4.71 times greater risk (3.50% vs. 0.74%, RR 95% CI 2.46-9.024, p < 0.0001). The risk of being deceased was 4.26 times greater in patients with a history of gender-affirmation surgery vs. patients with no history of gender-affirmation surgery but vasectomy or BTL (4.9% vs. 1.1%, RR 95% CI 2.520-7.191, p < 0.0001). Patients with a history of gender-affirmation surgery showed a 5.10 times higher risk of suicide or self-harm compared to patients with no history of gender-affirmation surgery but vasectomy or BTL (4.5% vs. 0.9%, RR 95% CI 2.816-9.227, p < 0.0001). Lastly, patients with a history of gender-affirmation surgery showed a 3.23 times higher risk for PTSD compared to patients with no history of gender-affirmation surgery but vasectomy or BTL (9.2% vs. 2.8%, RR 95% CI 2.278-4.580, p < 0.0001).
Cohort A: Adult patients who had a visit to the emergency department and a history of sexual reassignment.
Cohort C: Adult patients who had a visit to the emergency department and no history of sexual reassignment but had a vasectomy or bilateral tubal ligation.
The secondary sub-group analysis utilizing pharyngitis (N = 1,390,880) as a control revealed that patients presenting to the emergency department with a history of gender-affirmation surgery had a 7.95 times greater risk of suicide attempt than patients with pharyngitis (1.5% vs. 0.2%, RR CI 5.379-11.755, p < 0.0001), a 3.65 times greater risk of death (4.6% vs. 1.3%, RR CI 2.921-4.563, p < 0.0001), a 7.33 times greater risk of suicide or self-harm (2.7% vs. 0.4%, RR CI 5.448-9.850, p < 0.0001), and a 4.61 times greater risk of PTSD (9.2% vs. 2.0%, RR CI 3.901-5.438, p < 0.0001) compared to patients who were sent to the emergency department following acute pharyngitis. After propensity matching, mortality was 3.59 times greater in patients with a history of gender-affirmation surgery (4.6% vs. 1.3%, RR CI 2.224-5.806, p < 0.0001), and PTSD was 5.49 times greater (9.2% vs. 1.7%, RR CI 3.648-8.267, p < 0.0001) compared to patients with acute pharyngitis. There were too few suicides or self-harm outcomes to report results from the propensity-matched pharyngitis group. These results were similar to the results with cohort C.
The purpose of this study was to explore the relationship between gender-affirmation surgery and the risk of suicide outcomes compared to two control groups with data from 2003 to 2023. The significance of this investigation lies not only in its scale but also in its methodology, as it relies on real-world data rather than meta-analyses and self-reported surveys.
The first controlled group was a large number of patients who had emergency department visits but had not had gender-affirmation surgery. Propensity matching is not possible in the TriNetX database for large groups with millions of patients like the first control group. The second control group consisted of individuals who had not had gender-affirmation surgery but had either a vasectomy or BTL. This control group was selected to allow for propensity matching. Propensity matching was done for this comparison to control for the confounding influence of age, sex, and race/ethnicity. This is particularly important since the rate of successful suicide is much higher in men. At the start of this study, the hypothesis that was proposed predicted individuals who had undergone gender-affirmation surgery would have a greater risk of suicide, death, and self-harm compared to the two controls. This was confirmed by comparing the two control groups. In the second analysis, it was determined that patients who had undergone gender affirmation had a statistically significant increase in suicide attempts, death, self-harm, and PTSD after completion of gender affirmation in comparison with those who had undergone BTL or vasectomy and had not undergone gender-affirmation before propensity matching. After propensity matching our cohorts for age at index, race, and ethnicity, we also found a statistically significant increased risk of suicide attempts, death, self-harm/suicide, and PTSD. These outcomes confirmed the hypothesis. The secondary sub-group analysis utilizing pharyngitis as a control showed results that were comparable to the BTL/vasectomy control group, validating cohort C as an appropriate control group for propensity matching.
These data are supported by previous studies from multiple geographic regions of the globe, including Lebanon [ 3 ], Turkey [ 3 ], Pakistan [ 4 ], China [ 5 ], and Canada [ 6 ], as well as data from within the United States [ 3 - 4 , 6 ]. The large size of our study is an asset to our findings, which will help further our understanding of the relationship between sex change and suicide. To our knowledge, a study of this size has not been described in the literature. Using two control groups, a) those who had not experienced gender-affirmation surgery and had presented to the emergency department and b) a group that had not experienced gender-affirmation surgery, had visited the emergency department, and had a vasectomy or BTL, also helped effectively control for confounding variables utilizing propensity matching. Over the last 20 years, this study demonstrated a 12.12 times greater risk of suicide utilizing the first control group and a 4.71 to 5.03 times increased risk with the other control groups.
Transgender individuals, encompassing both those seeking gender-affirming surgery and those who have undergone it, demonstrate a significantly elevated risk of developing PTSD compared to the general population [ 10 , 23 ]. Among those who seek access to gender-affirming surgery, the commonality of discrimination, interpersonal assault, and a lack of social support have been identified as influential factors in the development of PTSD within this group [ 23 ]. Financial stress and insufficient insurance coverage prove to be significant obstacles for those trying to access gender-affirming surgery. Additionally, the limited availability of medical professionals with expertise in gender-affirming procedures, particularly in areas of lower socioeconomic status, further exacerbates the challenges faced by individuals seeking such care [ 10 ]. However, it is important to consider PTSD development in those who have undergone gender-affirming procedures. The emergence of PTSD following surgery often stems from the pre-operative challenges (such as harassment, limited social support, etc.) in conjunction with suboptimal surgical outcomes and insufficient psychiatric assistance.
This study has revealed a significantly elevated prevalence of PTSD in post-operative transgender individuals, with a 7.76-fold increase in comparison to cohort B and a 3.74-fold increased risk compared to cohort C after propensity matching. These findings were consistent with other studies investigated previously. A study conducted by Livingston et al. in 2022 used probabilistic and rule-based modeling on Veterans Health Administration (VHA) records from 1999 to 2021 to assess the differences in PTSD prevalence among 9,995 transgender and 29,985 cisgender veterans (1:3 ratio). They concluded that transgender veterans experienced PTSD at 1.5-1.8 times the rate of veterans identifying as cisgender, especially higher in recent users of VHA services [ 24 ]. There have proven to be many obstacles when comparing our findings to other studies assessing general population PTSD risk in those who have undergone gender-affirmation surgery. A 2018 systematic review conducted by Valentine et al. showed that many studies used assessment tools not particularly appropriate for evaluating mental health in transgender or gender non-conforming individuals [ 25 ]. The poor psychometric framework has led to many studies not acknowledging confounding and contextual variables, such as exposure to discrimination or minority identity when assessing PTSD in this demographic [ 10 , 25 ]. To avoid the repeated shortcomings of prior research, future studies should employ rigorous and reliable assessment tools such as cross-sectional studies or the collection of prospective data [ 25 ]. Improving transgender representation in emerging PTSD treatment trials is another step in improving the understanding and management of PTSD in transgender individuals [ 10 ].
In light of the examination of the relationship between gender-affirmation surgery and mental health outcomes discussed in this study, it is imperative to acknowledge the broader landscape of research on this topic. Our investigation contributes broad insight, examining real-world data over two decades and encompassing a diverse cohort. However, to further expand upon the contextual significance, it is essential to compare findings from other studies that explore multifaceted aspects of mental health post-gender-affirmation surgery. A study published in the American Journal of Psychiatry by Branstrom et al. in October 2019 drew strong conclusions regarding the positive impact of gender-affirmation surgery on mental health [ 11 ]. However, the study faced criticism of its methodology, leading to a correction/retraction by the journal's editors that stated, "the results demonstrated no advantage of surgery about subsequent mood or anxiety disorder-related health care visits or prescriptions or hospitalizations following suicide attempts” [ 12 ]. In a subsequent study conducted in 2021, Almazan et al. compared the mental health outcomes of a group of patients who were not approved for gender-affirmation surgery with a group that had undergone the surgery [ 13 ].
Their findings suggested better mental health outcomes for those who underwent surgery, but notable limitations warrant careful interpretation. First, the study conducted a comparison between two groups: one that had not been approved for surgery, a process requiring two mental health screenings as per the World Professional Association for Transgender Health's standard of care recommendations, and another group that had already undergone surgery. Therefore, it is plausible that the surgery group could inherently have been healthier, irrespective of the surgery. Second, when the analysis was broadened to include lifetime outcomes, the positive association with the surgery became insignificant [ 14 ].
Although our study has revealed a statistically significant increase in suicide risk among those who have undergone gender-affirming surgery, it remains vital to recognize and support the positive impacts that these surgical interventions can have on the lives of transgender individuals. The results of a study by Park et al., published in October 2022 in the Annals of Plastic Surgery, provide a different perspective on the enduring effectiveness and consequences of gender-affirmation surgery [ 20 ]. While our research specifically examined the risk of suicide, death, self-harm, and PTSD in the five years following surgery, Park et al. surveyed the outcomes of 15 gender-affirming surgeries over a more extended period. Their results reveal an improvement in patient well-being, with high satisfaction levels, reduced dysphoria, and persistent mental health benefits even decades after surgery. Notably, the study highlights the durability of these positive outcomes and significantly reduced suicidal ideation following gender-affirmation surgery.
The number of non-gender-conforming individuals continues to increase globally. It is likely, therefore, that a growing number of medical professionals will care for an individual who has undergone gender-affirmation at some point in their career. Apart from additional assistance in surgical recovery, the most common aftercare needs for patients following gender-affirmation surgery is consultation with a mental health professional [ 26 ]. To properly address the mental health needs of transgender individuals, Lapinski et al. emphasize the significance of cultural competency, a patient-focused approach, and collaborative efforts involving psychiatric professionals [ 27 - 30 ]. Transgender individuals tend to see mental health care providers and face discrimination in clinical settings at a far higher rate than the cis-gendered population [ 27 , 28 , 30 ]. Competent medical care following gender-affirming surgery is vital in effectively managing PTSD and its respective mental health challenges for this population [ 27 ].
It is important to note that this study has several limitations. The retrospective cohort design can only demonstrate associations but not causality. However, the larger size of this study, in conjunction with propensity matching, gives this investigation a greater power to identify differences between groups. Additionally, with the extensive timeline of data collection, the findings are relevant and contemporary to modern situations. A limitation of the study design could include the fact that only adult data was analyzed, so the research cannot be generalized to those under the age of 18. The data were also only extracted from a population of residents from the United States. Patients who have undergone gender-affirmation surgery and our control groups may have refrained from disclosing their suicidal ideations or other psychiatric symptoms to their medical providers, potentially influenced by societal pressures or other factors such as perceived attitudes toward those with psychiatric complaints. It may be worth examining if groups considering gender-affirmation surgery who have not yet received the surgery share the same increased risk levels for suicidal actions and ideations. However, given the standard practice of undergoing psychiatric testing before being approved for gender-affirmation surgery, individuals contemplating the procedure may potentially pose a greater suicide risk compared to those who have been approved for surgery.
Conclusions
The results of this study show that gender-affirmation surgery is associated with a significantly higher risk of suicide, death, suicide/self-harm, and PTSD compared to control groups in this real-world database. With suicide being one of the most common causes of death for adolescent and middle-aged individuals, it is clear that we must work to prevent these unfortunate outcomes. This further reinforces the need for comprehensive psychiatric care in the years that follow gender-affirmation surgery.
Greedy nearest-neighbor matching
The most common implementation of propensity matching is pair-matching, in which pairs of treated and control participants are formed. There are several common implementations of pair-matching. The most commonly used is greedy nearest-neighbor matching (NNM), which we used, in which a treated participant is selected at random and then matched to the control participant whose propensity score is closest to that of the treated participant. The process is described as greedy because, at each stage, the control is selected who is closest to the currently considered treated participant, even if that untreated participant would serve better as a control for a subsequently treated participant. This process is then repeated until a matched control participant has been selected for each treated participant. This process generally uses matching without replacement so that once a control participant is matched to a treated participant, that control participant is no longer available to match to a subsequently treated participant. A refinement to NNM is NNM with a caliper restriction. Using this approach, a control participant is an acceptable match for a treated participant only if the difference in their propensity scores is less than a maximum amount (the caliper width or distance). For technical reasons, one typically matches the logit of the propensity score and uses a caliper width that is defined as a proportion of the (0.1-0.2) SD of the logit of the propensity score. A crucial step in any study that uses PSM is to assess the degree to which matching the propensity score resulted in the formation of a matched sample in which the distribution of baseline characteristics is similar between treated and control participants. This assessment is critical as it allows both the researcher and readers to assess whether matching the estimated propensity score has removed systematic baseline differences between treatments. The use of the standardized difference, which is the difference in means in units of SD, is often used for assessing the similarity of matched treated and control participants. Some authors have suggested that a threshold of 0.10 (or 10%) be used to denote acceptable balance after matching. Once an acceptable balance has been achieved, analysts can unblind themselves to the outcome and compare outcomes between treated and control participants in the matched sample. The analyses conducted in the propensity score-matched sample can be similar to those that would be done in an RCT with a similar outcome.
Funding Statement
This study was conducted with the support of the Institute for Translational Sciences at the University of Texas Medical Branch, supported in part by a Clinical and Translational Science Award (UL1 TR001439) from the National Center for Advancing Translational Sciences, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors have declared that no competing interests exist.
Author Contributions
Acquisition, analysis, or interpretation of data: Krishna K. Paul, John J. Straub, Lauren G. Bothwell, Sterling J. Deshazo, Georgiy Golovko, Michael S. Miller, Dietrich V. Jehle
Drafting of the manuscript: Krishna K. Paul, John J. Straub, Lauren G. Bothwell, Sterling J. Deshazo, Dietrich V. Jehle
Critical review of the manuscript for important intellectual content: Krishna K. Paul, John J. Straub, Lauren G. Bothwell, Sterling J. Deshazo, Georgiy Golovko, Michael S. Miller, Dietrich V. Jehle
Supervision: Krishna K. Paul, Dietrich V. Jehle
Concept and design: Georgiy Golovko, Dietrich V. Jehle
Human Ethics
Consent was obtained or waived by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Risk of Suicide and Self-Harm Following Gender-Affirmation Surgery
Affiliations.
- 1 Department of Emergency Medicine, University of Texas Medical Branch at Galveston, Galveston, USA.
- 2 Department of Pharmacology, University of Texas Medical Branch at Galveston, Galveston, USA.
- 3 Department of Psychiatry and Behavioral Services, University of Texas Medical Branch at Galveston, Galveston, USA.
- PMID: 38699117
- PMCID: PMC11063965
- DOI: 10.7759/cureus.57472
Introduction With the growing acceptance of transgender individuals, the number of gender affirmation surgeries has increased. Transgender individuals face elevated depression rates, leading to an increase in suicide ideation and attempts. This study evaluates the risk of suicide or self-harm associated with gender affirmation procedures. Methods This retrospective study utilized de-identified patient data from the TriNetX (TriNetX, LLC, Cambridge, MA) database, involving 56 United States healthcare organizations and over 90 million patients. The study involved four cohorts: cohort A, adults aged 18-60 who had gender-affirming surgery and an emergency visit (N = 1,501); cohort B, control group of adults with emergency visits but no gender-affirming surgery (N = 15,608,363); and cohort C, control group of adults with emergency visits, tubal ligation or vasectomy, but no gender-affirming surgery (N = 142,093). Propensity matching was applied to cohorts A and C. Data from February 4, 2003, to February 4, 2023, were analyzed to examine suicide attempts, death, self-harm, and post-traumatic stress disorder (PTSD) within five years of the index event. A secondary analysis involving a control group with pharyngitis, referred to as cohort D, was conducted to validate the results from cohort C. Results Individuals who underwent gender-affirming surgery had a 12.12-fold higher suicide attempt risk than those who did not (3.47% vs. 0.29%, RR 95% CI 9.20-15.96, p < 0.0001). Compared to the tubal ligation/vasectomy controls, the risk was 5.03-fold higher before propensity matching and remained significant at 4.71-fold after matching (3.50% vs. 0.74%, RR 95% CI 2.46-9.024, p < 0.0001) for the gender affirmation patients with similar results with the pharyngitis controls. Conclusion Gender-affirming surgery is significantly associated with elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support.
Keywords: gender affirmation; post traumatic stress disorder (ptsd); self-harm; suicide; transgender.
Copyright © 2024, Straub et al.
Grants and funding
Bias of InfoWars
- Balanced News
- Story of the Week
- News Curation Principles
- Newsletters
- Balanced Search
People Who Undergo Gender-Reassignment Surgery Have a 12x Increased Risk of Suicide

People who undergo gender-reassignment surgery have a 12x increased risk of attempting to commit suicide, according to a new study, as well as suffering other mental-health problems like PTSD and self-harm. The study, published in the journal Cureus, clearly shows that undergoing gender-reassignment, where the patient’s genitals are surgically rearranged and they also embark on a regimen of hormonal therapy, carries significant, potentially deadly, risks. The researchers note, “There is ongoing controversy surrounding the benefits of gender-affirmation surgery on mental health.” Their aim was to explore the risk of “adverse...
Related Coverage

AllSides Picks

May 21st, 2024

Divided We Fall (author)

More News about General News from the Left , Center and Right
From the left, from the center, from the right.

Call for better access to gender-affirming surgery after Kiwi teen attempts to remove own breasts at home
Paddy Gower interviewed New Zealand's own genital gender-affirmation surgeon in 2023 on Paddy Gower Has Issues Credits: Image: Getty, Video: Newshub
Warning: this article contains an image of the attempted surgery
An attempt by a New Zealand teenager to remove their own breasts following YouTube instructions has prompted calls for better access to gender affirming surgery.
The 18-year-old, referred to as Patient Z, arrived at a hospital emergency department after a botched attempt to complete a left mastectomy at home.
Details of the case were published in the New Zealand medical journal on Friday in an article written by three Wellington surgeons.
The teenager was awaiting female-to-male gender affirmation surgery at the time.
More from Newshub
The article said he decided to attempt the surgery himself due to the wait times for a referral in the public system, an inability to afford private surgery and the "significant psychological stress of having breasts at an upcoming pool party."
"He had demonstrated premeditation by watching a ‘how to’ video on YouTube," said the doctors who wrote the case study.
Patient Z had also prepared 'appropriate equipment', marked the incision and considered how to numb the pain and stop the bleeding.
After spending several hours trying to remove his left breast, he became worried he would damage a nerve and went to hospital.
Surgeons then performed a double mastectomy.
"After discussing the risks, including irreversibility, poor cosmetic outcome/asymmetry and loss of both nipples, he proceeded to have a completion left mastectomy and symmetrising right mastectomy," the article said.
"He was reviewed by the acute mental health team and was deemed to have capacity to consent, with no active mood disorder, psychosis or suicidality."
Dr Rita Yang, the only surgeon who performs genital gender affirmation operations in New Zealand , told Newshub it was “extremely distressing” to hear about the case.
"It could have easily ended with this person dying," she said.
“All surgeries come with life-threatening risks even when performed by surgeons. I implore anyone who needs gender affirming surgery to never even consider this for the sake of their own life.”
Dr Yang said top surgery - the reshaping of the breasts to be more masculine – is complex and can take a specialist surgeon up to four hours to complete.
“It involves highly trained operating room staff, anaesthetists, nurses, and hospital-level wraparound care. There are few reconstructive surgeons in New Zealand qualified to perform this surgery and even then there are serious risks that must be mitigated," Yang told Newshub.
The patient Z case study was written by Wellington Hospital surgeons Dr Mairarangi Haimona, Dr Sue Hui Ong and Dr Scott Diamond. In the article, they call for better access to gender reassignment surgery.
"In Aotearoa New Zealand, there is an overwhelming unmet need for masculinising chest reconstruction for transgender men."
"A lack of access to gender-affirming surgery led to this act of desperation," they wrote.
A 2019 report from the 'Counting Ourselves' survey found only 13 percent of trans men who had chest reconstruction surgery had access through the public system
"This is a significant under-service and likely an under-representation of the unmet need due to poor documentation and lack of information of how to access services," said the doctors.
The lengthy assesment process for patients to qualify for gender affirmation surgery is highlighted as an issue in the medical journal article.
Some are left waiting as long as a decade for surgery, and many don't end up having it due to the cost.
"With increasing demand and associated psychological and possible physical harm it is crucial for public services to be more accessible to an under-served population, " the doctors said.
Patient Z "healed well" following the hospital surgery.
"He reported improvement in self-esteem and self-confidence and his ability to complete school work, and was looking forward to enrolling at university."


‘Butchers were murderously wrong’: New study finds risk of suicide jumps 12-fold AFTER gender surgery
A new study has found that people who’ve undergone transgender surgery boast a much higher risk of committing suicide.
Published last month in Cureus, a medical science journal, the study specifically found that “[g]ender-affirming surgery is significantly associated with elevated suicide attempt risks.”
The researchers reached this conclusion by analyzing the healthcare data of 90 million adults aged 18 to 60. They specifically looked at emergency room treatment data for those who’d undergone transgender surgery.
The patients were divided into four groups — one containing people who’d undergone transgender surgery and an E.R. visit, and one containing people who’d undergone no transgender surgery but who had partaken in an E.R. visit.
The third group included “adults with emergency visits, tubal ligation or vasectomy, but no gender-affirming surgery,” and the fourth group included patients with pharyngitis.
https://t.co/XttOf6tqDP As usual, #Democrats have taken a word and twisted its meaning. I don’t see from the results how mutilation and toxic chemicals affirm anything. It appears to make things worse. pic.twitter.com/KnfHcGRTxz — Mimzy Borogroves No DM’s (@MBorogroves) May 5, 2024
What the researchers found is that “[i]ndividuals who underwent gender-affirming surgery had a 12.12-fold higher suicide attempt risk than those who did not.”
Of the patients who’d transitioned, a whopping 3.5 percent were later treated for suicide attempts. Conversely, only a paltry 0.3 percent of non-transitioned parents reported a suicide attempt.
The study’s findings sharply contrast the Biden administration’s claim that transgender surgery prevents suicide versus promoting it.
“Research demonstrates that gender-affirming care improves the mental health and overall well-being of gender diverse children and adolescents,” a handout from the Biden HHS reads.
“Because gender-affirming care encompasses many facets of healthcare needs and support, it has been shown to increase positive outcomes for transgender and nonbinary children and adolescents,” it continues.”
But this clearly isn’t true.
Responding to the latest study, DailyWire+ host Dr. Jordan B. Peterson slammed President Joe Biden and also Canadian Prime Minister Justin Trudeau for promoting transgender surgery.
“12x the suicide rate post ‘gender affirming’ surgery,” he wrote in a tweet. “The butchers and liars were murderously wrong.”
“The Cass report indicated this. Canada and the US are still enabling this. That’s you @POTUS and @JustinTrudeau and it is utterly barbarous and inexcusable. Putting children to the knife. ‘Follow the science,’ gentlemen,” he added.
12x the suicide rate post “gender affirming” surgery The butchers and liars were murderously wrong The Cass report indicated this Canada and the US are still enabling this That’s you @POTUS and @JustinTrudeau and it is utterly barbarous and inexcusable Putting children to the… — Dr Jordan B Peterson (@jordanbpeterson) May 16, 2024
Responding to Peterson’s tweet, many expressed agreement.
Psychiatric patients need treatment not surgery, it not the 1940’s. — 3percenter (@David61780271) May 16, 2024
The people who pushed this ideology onto others – especially children – need to be behind bars. — Richard (@RedWallPleb) May 16, 2024
30 years from now after the dust settles it will be impossible to find a supporter of this. People are keeping receipts. There will be no amnesty. — Furious_George (@furious15074) May 16, 2024
Anyone involved in the manipulation, mutilation and sterilization of children should be arrested and prosecuted to the fullest extent of the law! To prey on children when they are at their most vulnerable is beyond contemptible! Why?? — Judy (@Judy1732243) May 17, 2024
The gender identity gang lie. They lie about everything. It is a lie to claim a person can change their sex. It is a lie that puberty blockers are reversible. It is a lie that surgery can transition a person. Lie after lie after lie. — Kirralie Smith (@KirralieS) May 16, 2024
The release of the study last month came around the same time that Dr. Hilary Cass, one of England’s top pediatricians, released her own damning report about transgender surgery.
“Her final report, published last month, concluded that the evidence supporting the use of puberty-blocking drugs and other hormonal medications in adolescents was ‘remarkably weak,'” according to The New York Times.
On her recommendation, the U.K.’s National Health Service stopped prescribing puberty blockers outside of clinical trials. Cass also recommended that testosterone and estrogen only be prescribed with “extreme caution.”
Meanwhile, last year a study out of Denmark reportedly found that people who identify as transgender boast a suicide death rate 3.5 times higher than those who don’t.
Transgender people in Denmark have a significantly higher risk of suicide than other groups, an analysis of nearly seven million people over the last four decades found. The study is the first in the world to analyze national suicide data for this group. https://t.co/VH0FTrmT4z pic.twitter.com/KKIhDHJfQk — Alix (@AlixG_2) June 28, 2023
DONATE TO BIZPAC REVIEW
Please help us! If you are fed up with letting radical big tech execs, phony fact-checkers, tyrannical liberals and a lying mainstream media have unprecedented power over your news please consider making a donation to BPR to help us fight them. Now is the time. Truth has never been more critical!
- Recent Posts
- Chicago mom told ‘no units to send’ after calling 911 over home invasion, advised to call alderman - May 19, 2024
- Maryland ‘first’ in nation to answer Biden’s call to ‘end gun violence’ - May 19, 2024
- ‘Butchers were murderously wrong’: New study finds risk of suicide jumps 12-fold AFTER gender surgery - May 19, 2024
We have no tolerance for comments containing violence, racism, profanity, vulgarity, doxing, or discourteous behavior. If a comment is spam, instead of replying to it please click the ∨ icon below and to the right of that comment. Thank you for partnering with us to maintain fruitful conversation.
BPR INSIDER COMMENTS
Scroll down for non-member comments or join our insider conversations by becoming a member . We'd love to have you!
Leave a Reply Cancel reply
You must be logged in to post a comment.
Latest Articles

- job opportunities
- privacy policy
- DUMPSTER FIRE NEWS
- * NEW * WE THE PEOPLE WINE
- * NEW * WE THE PEOPLE STORE
International Analysis

How Taiwan’s New President May Change His Country’s Tense Relationship With China
Politics News

Georgia’s Democratic Voters Render Their Verdict on Fani Willis
Society Commentary

What Ted Cruz, Katie Britt Get Wrong About IVF
Society News

Several Homeless Encampments Cleared in DC
Security News

Congress Seeks Answers to ‘Unprecedented Surge’ of Chinese Nationals Arriving at Border
Law News

Why Biden’s Border Crisis Challenges Police in Every State
Security Commentary

Unprecedented Surge in Chinese Illegal Immigration Raises Security Concerns: The BorderLine
Society Commentary

SOCIETAL ROT, Part 3: How Blue Cities’ Flouting of Federal Immigration Laws Has Proved Fatal
Society Commentary

Who Benefits From Destabilization of America?
Energy Commentary

Forget Tariffs: Biden Should Look to Domestic Mining to Thwart Chinese EVs
Security News

Senate Will Try Again to Pass Border Bill, Schumer Says
Economy Commentary

These 2 Bipartisan Proposals Would Hold Presidents Accountable for ‘Improper’ Payments

Biden Invokes Privilege, a Taxpayer-Funded ‘Catch and Kill’ Operation, to Block Release of Special Counsel Interview
Politics News

EXCLUSIVE: HHS Chief Routinely Checked Progress of Biden Election-Meddling Directive, Records Show

‘A Travesty of Justice’: House Speaker Dissects the Left’s ‘Lawfare’ Campaign Against Trump

Biden Education Department Shared Activists’ Memo on Mobilizing Dem-Leaning Voters
Politics Commentary

Will Democrats Pay a Price for Their Crumbling Lawfare Strategy Against Trump?
Politics Analysis

EXCLUSIVE: Ted Cruz Sets the Record Straight After SPLC Claims He Spread ‘Antisemitic Trope’
Society Analysis

EXCLUSIVE: Federal Farm Credit Agency Plows Ahead With DEI, ‘Queer’ Farming

EXCLUSIVE: DOJ’s Kristen Clarke Testified She Was Never Arrested. Court Records and Text Messages Indicate She Was.

EXCLUSIVE: She Survived a Death Camp. Facing Biden DOJ Charges, She Is Prepared to Die in Prison
Education Commentary

Universities Are Morally and Intellectually Destructive
International Analysis

Iran’s President Is Dead. What Happens Now?
International Commentary

US Must Oppose International Criminal Court Bid to Prosecute Israeli Prime Minister, Defense Chief

Her Daughter Was Harassed By a Boy on the Girls’ Team. Now, She’s Speaking Out to Save Title IX
Education Analysis

Parents Are Winning Education Revolution With School Choice, Corey DeAngelis Says
Study finds gender-transition surgeries drastically increase suicide risk.
S.A. McCarthy / @pipesmoknpapist / May 21, 2024
A new study shows gender-transition surgeries increase the risk of patient suicide, a finding consistent with previous research. Pictured: Adm. Rachel L. Levine, center, assistant secretary for health in the U.S. Department of Health and Human Services, is flanked onstage Oct. 21 by Jesse Ehrenfeld, president of the American Medical Association, and Charlotte Clymer, a transgender activist and military veteran, during PFLAG's national convention in Washington. (Photo: Paul Morigi/Getty Images)

Get your FREE digital copy of The Heritage Foundation’s Founders’ Almanac.
While some in the U.S. health community continue to claim that gender-transition procedures save lives, a new study shows that these surgeries increase the risk of suicide.
A study published last month entitled “Risk of Suicide and Self-Harm Following Gender-Affirmation Surgery” evaluated patient data from nearly 60 U.S. health care organizations, comprising millions of patients.
Over 1,500 patients, called “Cohort A,” were described as “adults aged 18-60 who had gender-affirming surgery and an emergency visit”; nearly 16 million patients, called “Cohort B,” who were a “control group of adults with emergency visits but no gender-affirming surgery.”
Almost 150,000 patients, “Cohort C,” were described as “adults with emergency visits, tubal ligation or vasectomy, but no gender-affirming surgery.” A fourth group, “Cohort D,” was examined to “validate the results from Cohort C.”
Data analyzed covered 20 years, from Feb. 4, 2003, to Feb. 4, 2023. The study concluded: “Individuals who underwent gender-affirming surgery had a 12.12-fold higher suicide attempt risk than those who did not.”
Those who had undergone gender-transition surgeries were nearly five times more likely to attempt suicide than those who had undergone tubal ligations or vasectomies, the study found. It warned: “Gender-affirming surgery is significantly associated with elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support.”
The findings are in line with the conclusions of numerous other studies. For example, research published in the journal BMJ Mental Health earlier this year found that gender-transition procedures such as hormone drugs and surgeries have “not been shown to reduce even suicidal ideation, and suicidal ideation is not equal to actual suicide risk.”
And in Sweden, an extensive 30-year-long study concluded that suicide rates increase after gender-transition surgeries, rising to at least 20 times the suicide rate of the general population.
A report from the U.K. last year found that over a third of children who were prescribed puberty blockers and hormone drugs suffered worsened mental health. And a study from Finland discovered that those who identify as transgender typically manifest “many more common psychiatric needs” than the general population, but that gender-transition procedures don’t alleviate or cure those mental health issues.
Countless other studies have shown that gender-transition procedures are harmful, especially to children. A study published in March suggested that puberty blockers have numerous harmful effects on children, including an increased risk of cancer in boys.
As it turns out, transgenderism activists have been aware of the “debilitating” effects of gender-transition procedures for years. Leaked internal files from the World Professional Association for Transgender Health, or WPATH, demonstrated that members of the organization were acutely aware of the “debilitating” and “potentially fatal” effects of gender-transition procedures, which they also implied they didn’t “fully understand.”
This was further confirmed earlier this year with publication of a series of video presentations from WPATH’s 2022 Global Education Institute .
In those videos, WPATH “experts” discussed how they know little about the long-term effects of hormone drugs, other than the permanent damage done to fertility.
The organization’s experts also discussed how puberty blockers are irreversible and may have devastating impacts on both future fertility and current brain development; how gender-transition procedures don’t alleviate mental health issues and may make them worse; and the dangers associated with surgical interventions, including high complication rates, severe damage to healthy tissue, and potential side effects such as healing delays or necrosis.
Lately, experts outside the U.S. have sounded the alarm over the potential and largely unstudied dangers of gender-transition procedures, especially for children.
Both England and Scotland have halted the prescription of puberty blockers and hormone drugs to minors, with England’s National Health Service warning that “there is not enough evidence of safety and clinical effectiveness” to support their use.
Some leading clinical psychologists publicly apologized for their profession’s role in promoting “gender-affirming care” and called for a thorough review and possible reform of the psychological and psychiatric profession’s standards. And the NHS revised its official constitution to declare sex a “biological” reality, instead of giving preference to “gender identity.”
The U.K. is 1 of 5 European countries that have put the brakes on gender-transition procedures for minors. France, Sweden, Finland, and Norway all also warned that there is insufficient evidence to support puberty blockers, hormone drugs, and surgeries for children; the U.S. has become an “outlier” by continuing to endorse the practice.
Last year, Assistant Health and Human Services Secretary Rachel Levine, a man who identifies as a woman, declared : “We often say that gender-affirming care is health care, gender-affirming care is mental health care, and gender-affirming care is literally suicide prevention care.”
However, when pressed to provide evidence supporting the claim, Levine could produce only a single, two-page PDF document citing one study conducted by an LGBTQ activist group.
Originally published by The Washington Stand
Join the millions of people who benefit from The Daily Signal’s fair, accurate, trustworthy reporting with direct access to:
- Intelligence from inside Washington
- Deep policy understanding from over 100 experts
Don’t have time to read the Washington Post or New York Times? Then get The Morning Bell, an early morning edition of the day’s most important political news, conservative commentary and original reporting from a team committed to following the truth no matter where it leads.
Ever feel like the only difference between the New York Times and Washington Post is the name? We do. Try the Morning Bell and get the day’s most important news and commentary from a team committed to the truth in formats that respect your time…and your intelligence.
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Appeals court upholds ruling requiring Georgia county to pay for a transgender deputy’s surgery
Anna Lange, a sheriff’s sergeant in Houston County, Ga., poses for a picture, Nov. 14, 2023. A federal appeals court has upheld a lower court’s ruling that a Georgia county illegally discriminated against the sheriff’s deputy by failing to pay for her gender-affirming surgery. In its ruling Monday, May 13, 2024 the 11th U.S. Circuit Court of Appeals said it was tasked with determining whether a health insurance provider can be held liable under the Civil Rights Act of 1964 for denying coverage for a procedure because an employee is transgender. (AP Photo/Jeff Amy, file)
- Copy Link copied
ATLANTA (AP) — A federal appeals court has upheld a lower court’s ruling that a Georgia county illegally discriminated against a sheriff’s deputy by failing to pay for her gender-affirming surgery.
In its ruling Monday, the 11th U.S. Circuit Court of Appeals said it was tasked with determining whether a health insurance provider can be held liable under the Civil Rights Act of 1964 for denying coverage for a procedure because an employee is transgender. The three-judge panel decided in a 2-1 vote that it can and that the lower court had ruled correctly.
Houston County Sgt. Anna Lange, an investigator for the Houston County sheriff’s office, had sued Sheriff Cullen Talton and the county in 2019 after she was denied coverage.
“I have proudly served my community for decades and it has been deeply painful to have the county fight tooth and nail, redirecting valuable resources toward denying me basic health care – health care that the courts and a jury of my peers have already agreed I deserve,” Lange said in a news release from the Transgender Legal Defense and Education Fund, which represented her.
A woman who answered the phone at the sheriff’s office Tuesday said she would pass along a message seeking comment.
U.S. District Court Judge Marc Treadwell ruled in 2022 that the county’s refusal to cover Lange’s prescribed gender-affirmation surgery amounted to illegal sex discrimination under the Civil Rights Act of 1964. Treadwell’s order cited the U.S. Supreme Court’s 2020 decision finding that a Michigan funeral home could not fire an employee for being transgender.
The judge ordered the county’s insurance plan to pay for the surgery and Lange eventually underwent the procedure. A jury awarded Lange $60,000 in damages in 2022.
The county sought to undo Treadwell’s order and the damage award.
Title VII of the Civil Rights Act of 1964 says an employer cannot “discriminate against any individual with respect to his (or her) compensation, terms, conditions, or privileges of employment, because of such individual’s race, color, religion, sex, or national origin.”
The 11th Circuit opinion says the Supreme Court clarified in another Georgia case that discrimination based on the fact that someone is transgender “necessarily entails discrimination based on sex.”

Emilia Pérez: A musical film about drug cartels and gender reassignment? So bonkers it works
C annes needs big flexes from its trusted auteurs, not just films where they play it safe and stay in their lanes. Few flexes come bigger, love it or hate it, than Emilia Pérez .
Whatever lane we’ve tried to stick the French director Jacques Audiard in before now – he of the Palme d’Or-winning Dheepan (2015) and Bafta-winning prison drama A Prophet (2009) – he chicanes here across about five at once, with a reckless disregard for oncoming traffic.
This is a musical with around a dozen choreographed song-and-dance numbers – not a semi-musical like Barbie , but a full-scale one. It’s mostly set in Mexico City yet was mainly shot in Paris. Oh, and it’s all about cartel violence and gender reassignment.
Sicario with songs? Selena Gomez veering from karaoke to kidnapping? Almost any two of its elements feel like an unpromisingly eccentric combo. Audiard’s trick is to make the overblown mélange into something amazingly confident – it’s clever, earnest, ridiculous, knowing, forceful and absolutely bonkers. It’s hard to believe he pulls it off, but he does.
Before we get to the musical number in a clinic with the chorus “Rhinoplasty! Vaginoplasty!”, there’s a first act to explain everything. Zoë Saldana plays Rita, a paralegal full of self-loathing – but with a lot of great dance moves – who’s sick of the corrupt system she’s part of: she helps murderers get acquitted and feels she’s wasting her life.
Then she gets abducted by a cartel boss named Manitas (Karla Sofía Gascón), who wants to pay her $2 million to relocate him and his family well away from the hell he’s helped create. More to the point, he wants to become a woman, having faked his own death, and to pose as a distant cousin: not even his tough cookie of a wife (a spunky Gomez) is in on the plan.
Gascón, a Spanish transgender actress, plays the character with beguiling panache both pre- and post-surgery. An especially brilliant notion is that Manitas, with gold grills, tattoos and an aggressive presence, is a man who got ahead by faking his outsized masculinity. “Born in a pigsty”, as we learn in one ballad, he had to be the biggest bastard in the criminal ecosystem to survive. He wants to live more purely, which he thinks a gender reset is going to make possible.
“Emilia Pérez” steps in, then, with Manitas supposedly dead, and only Rita knows the score. Emilia, though, remains tethered inescapably to her past – by the children who find her smell poignantly familiar, and also a conscience haunted by the many deaths on her hands. She doesn’t want to be “dead-named”, but it would be a form of moral cowardice to deny her previous identity altogether, which complicates the film’s stance – controversially, no doubt – on whether “he” can be fully erased by the “she”.
Gomez gets maybe three-and-a-half songs – the strongest is her last – in a role they might have beefed up more: her fling with a pimp played by Édgar Ramirez is purely functional. Still, it’s not as if Audiard doesn’t have enough to cram in, as the film hurtles towards a gun-toting, explosive finale that will be as polarising as everything else. This wild ride could easily be his threat for a second Palme. We all know that Greta Gerwig , chairing the jury, loves her musicals – but she’s certainly never seen one like this before.
130 min, cert TBC. Screening at Cannes Film Festival; UK release date TBC
Play The Telegraph’s brilliant range of Puzzles - and feel brighter every day. Train your brain and boost your mood with PlusWord, the Mini Crossword, the fearsome Killer Sudoku and even the classic Cryptic Crossword.


IMAGES
VIDEO
COMMENTS
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria. Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX ...
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. To help provide guidance for those considering gender affirmation surgery, two experts from the Johns Hopkins Center for Transgender Health answer questions about what to expect before and after your surgery.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to describe people ...
Featured Expert: Fan Liang, M.D. Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including: Creating the penis. Lengthening the urethra so you are able to stand to urinate. Creating the tip (glans) of the penis. Creating the scrotum.
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning. Often used to refer to phalloplasty, metoidoplasty, or vaginectomy, sex reassignment surgery can also more broadly ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Transgender women may experience a decrease in sex drive after gender-affirming surgery. According to a 2020 article, people can stop taking anti- testosterone medication and may experience a ...
The Crane Center for Transgender Surgery has announced the launch of a gender-affirming hormone clinic at their transgender wellness center in Austin, Texas. The new clinic offers hormone replacement therapy for transgender and non-binary adults through an informed consent model. Both in-office and telemedicine appointments are available.
Female-to-male surgery is a type of gender-affirmation or gender-affirming surgery. There are multiple forms of gender-affirming surgery, including altering the genital region, known as "bottom ...
She does more than 150 a year. We also offer a Transgender Gynecology Clinic with a gender-neutral space. Services include surgery. Referrals and appointments are made through the OHSU Center for Women's Health, though the space is not in the center. Call 503-418-4500 to request an appointment.
Here's how gender reassignment works: Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina. An incision ...
Gender affirming surgery, also known as sex reassignment surgery (SRS) or confirmation surgery, is the surgical procedure (s) by which a transgender or non-binary person's physical appearance and functional abilities are changed to align with the gender they know themselves to be.
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current ...
Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain ...
Gender-affirming surgery is significantly associated with elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support. ... The term "sex reassignment" was based on the International Classification of Diseases, 10th Revision (ICD-10) code in the database but will be referred to as the ...
Abstract. Introduction With the growing acceptance of transgender individuals, the number of gender affirmation surgeries has increased. Transgender individuals face elevated depression rates, leading to an increase in suicide ideation and attempts. This study evaluates the risk of suicide or self-harm associated with gender affirmation procedures.
Ariana Marini. |. June 27, 2018. Gender-affirming surgery is the only medically necessary intervention specifically denied to US armed services veterans. Gender dysphoria, the distress a person ...
From The Right. People who undergo gender-reassignment surgery have a 12x increased risk of attempting to commit suicide, according to a new study, as well as suffering other mental-health problems like PTSD and self-harm. The study, published in the journal Cureus, clearly shows that undergoing gender-reassignment, where the patient's ...
In the article, they call for better access to gender reassignment surgery. "In Aotearoa New Zealand, there is an overwhelming unmet need for masculinising chest reconstruction for transgender men."
12x the suicide rate post "gender affirming" surgery. The butchers and liars were murderously wrong. The Cass report indicated this Canada and the US are still enabling this.
Data analyzed covered 20 years, from Feb. 4, 2003, to Feb. 4, 2023. The study concluded: "Individuals who underwent gender-affirming surgery had a 12.12-fold higher suicide attempt risk than ...
H.4624, the Help Not Harm bill, applies to physicians and mental health providers and codifies several definitions, such as gender transition procedures and genital gender reassignment surgery.It ...
ATLANTA (AP) — A federal appeals court has upheld a lower court's ruling that a Georgia county illegally discriminated against a sheriff's deputy by failing to pay for her gender-affirming surgery.. In its ruling Monday, the 11th U.S. Circuit Court of Appeals said it was tasked with determining whether a health insurance provider can be held liable under the Civil Rights Act of 1964 for ...
Oh, and it's all about cartel violence and gender reassignment. ... plays the character with beguiling panache both pre- and post-surgery. An especially brilliant notion is that Manitas, with ...