Journal for Practice Managers
- All Articles
- Case Studies

How to Write Speech Therapy SOAP Notes (with Examples)
According to the statistics , there are around 13,000 practising SLPs in the UK and around 2.5 million people in the UK have a speech or language difficulty:
- 5% of children enter school with difficulties in speech and language
- 30% of people who have had a stroke have a persisting speech and language disorder.
In terms of the functional duties of a speech therapist, we can single out one very significant duty that should not be overlooked. This is the completion of the necessary documentation in the prescribed form to meet the demands of a huge number of these people. A clinician's ability to manage it is one of the most important indicators of their professionalism.
A therapist devotes a lot of time to writing session notes, conclusions, characteristics, representations, and the design of speech cards. Thus, he should use his working time rationally.
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
When identifying children with peculiarities not only regarding speech development, he makes suggestions for further successful plan of care, or, if necessary, refers them to a specialist (neuropsychiatrist, neuropathologist, otolaryngologist, etc.).
Therefore, in order to save more time on the selection of the necessary phrases, special expressions, and formulations, we have selected a few suggestions for daily notes that simplify filling out the documents, while maintaining their content and accuracy. As a result, they are better able to organize their work and develop their skills in the field of speech-language pathology.
A SOAP note format is one of the most effective ways to fill out a progress note. We are planning to teach you how to use this tool in your private practice. In addition, we are going to give you some lifehacks and tips that will make the client's progress a reality.
SOAP Note Format for Speech Therapy Sessions: What is It?
SOAP notes are widely used by various specialists: mental health professionals , psychologists, caregivers, and speech-language pathologists.
When filling out a document for clients, it is necessary to know the content of regulatory documents related to this issue. It is also necessary to remember the age and individual characteristics of the person based on his diagnostic data, and take into account the results of speech development.
This information is included in the soap note template.
#1. S is for Subjective
The subjective section contains information about the actual state of the patient. Ideally, this part of the notes should be as true to life as possible. What does it mean?
The doctor keeps track of the complaints and speech issues of the patient, as well as other significant information about the patient. He must report only the words of the clients, but not his own thoughts and ideas. It’s not the time for it.
The first priority is to take stock of symptoms and make up a potential and theoretical treatment plan (but not to put it down). Try to use direct speech.
More frequently, the clients of speech pathologists are children, accompanied by their parents. So, sometimes you listen to both of them.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
For example, you can mention:
- Mrs. Smith (Billy’s mother) claims that the child has speech development problems.
- "The child suffered pneumonia at an early age."
- The mother claims that the child prefers to work with his left hand.
- "I find it difficult to come up with a word for a given sound."
- "Billy has been stuttering since he was 3 years old."
- "He is inconsiderate and impulsive."
#2. O is for Objective
The objective section of the notes contains your thoughts, prognoses and conclusions as a professional. The name of the section makes it pretty obvious. Test results, questionnaires, physical examination, fine and gross motor skills, articulation and tempo, speech intelligibility, breathing characteristics, and any other measurable indicators should be included in this section.
You can also provide some additional information (brief – psychological and pedagogical characteristics), if applicable.
The main rule is to avoid value judgments and be completely unbiased.
In the table below you’ll find different aspects to include in the objective part of a treatment note and some examples of possible answers.
#3. A is for Assessment
The assessment section summarizes the achievements of two previous sections. Note-taking at this stage includes analysis of subjective and objective information and interpretation of the whole session.
Now you are finally free to use professional terms and acronyms, as this part of the notes is for professional use only. And if you aren’t able to continue the therapy, a substitute therapist will easily know what to do thanks to your notes from the last session.
Discover more about the essential features of Medesk and claim your free access today!
It should be noted that there is no need to repeat the S and O sections. And also, it’s a bit early to make plans - just wait for the next stage and follow the SOAP structure.
As an example, we give you some assessments of the difficulties of educational material’s assimilation (a child in a primary school):
- Difficulties of adaptation in a school institution;
- Violation of motor skills in the form of insufficient coordination of movements;
- Pedagogical neglect due to unfavorable social conditions of the child;
- Disadvantages of attention, emotional-volitional regulation, self-control;
- Motor disinhibition, hyperactivity;
- Verbal and logical thinking is poorly developed;
- Insufficient development of coherent speech;
- Neurotic and neurosis-like states (fears, tics, mild stuttering, enuresis, etc.)
#4. P is for Planning
The last stage of note-taking is creating future plans for treatment. The plan section contains goals and recommendations for the follow-ups, even some handouts, since the plan is for a client and other healthcare professionals, who will take part in his treatment.
When writing any kind of counseling notes , set goals in the final section and make sure they are realistic and measurable. It's vital for a patient to remain motivated and to believe in recovery. You can easily split the goals into small ones to make a client’s performance and progress more transparent.
Moreover, the plan makes arranging individual sessions easier. Therefore, as a professional who wishes to get the greatest profit for given help, you increase your chances of setting up the next session.
As a bonus, we’ve collected some recommendations you can include in the plan stage:
- Avoid intellectual and psychological stress;
- The child needs an individual approach and constant supervision by adults;
- In order to compensate and equalize the shortcomings of physical, mental and speech development, avoiding overloads, it is recommended to repeat the course of study (or study in a special correctional school);
- It is recommended to consult with specialists...
- Additional rest is recommended;
- Conducting an additional examination in order to determine the child's need for further education, taking into account his level of development;
- The child needs step-by-step guidance and frequent changes in activities;
- Continuation of speech therapy classes according to the schedule 2-3 times a week for 45 minutes;
- Attending a special (correctional) school;
- Classes with parents aimed at developing motor functions, designing, classifying, viewing pictures, reading fairy tales, playing the story; plot-role-playing games; fixing the use of gestures for communication; development of auditory perception (differentiation of sounding toys, sounding pictures in books), onomatopoeia.
Electronic SOAP Note Example
The SOAP format of making notes has proven itself as a convenient, simple, but effective technique.
But do you remember that you should make notes during every session?
Though filling four sections of a note is rather simple, it takes a lot of time and strength to do it manually.
For professionals with a large patient flow (and we are sure, you belong to this category), the use of Electronic Health Records is a must.
The benefits of the software are obvious:
- All necessary stages of your future notes are pre-set for you (with templates ready to be printed)
- You can use an autofill option for the most general data
- The interface is easy and makes it possible to fill out the information right during the session with minimal distractions for the patient.
- It's unreal that the notes have been lost. All data is securely stored.
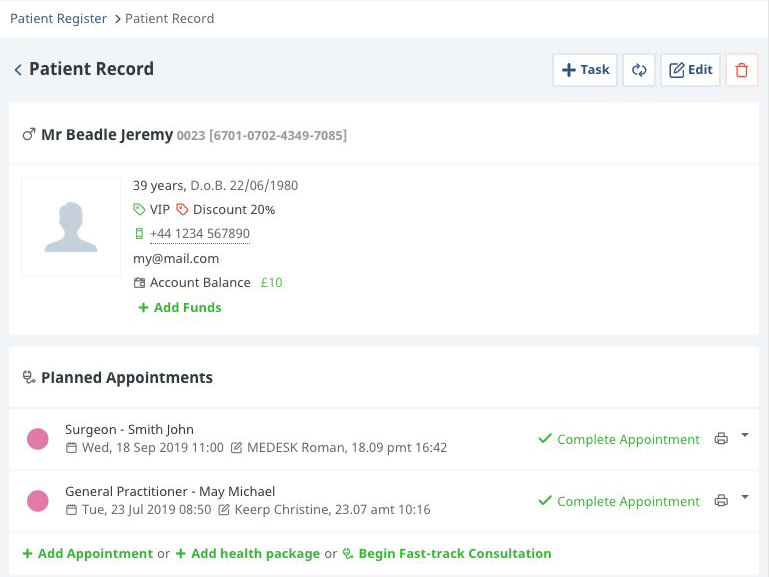
A good SOAP note is the result of the thorough work of a speech specialist. But you can make your practice much easier by implementing EHR in your therapy service.
Join our team of more than ten thousand happy practitioners!
Sign up for free
Get a free account and an on-screen demo from one of our experts.
Should You Charge Your Patient’s a No-Show Fee? Pros & Cons
6 top medical practice management software for your practice in 2024, how to start a physical therapy clinic in 2024 [10 easy steps].
- Online Booking
- Electronic Health Records
- Consultation Form Templates
- Integration
- Task Management
- About Company
social media
Practice Management Blog
Productivity & Mindset
Guide: SOAP Notes for Speech Therapy

As a speech pathologist , it’s important that your SOAP notes are well-structured, accurate, comprehensive, and helpful for both you and your client. This helps ensure that clients receive the best care possible, making your job easier. But when you’re juggling multiple responsibilities, note-taking can suffer. Fortunately, with the right approach, it’s possible to ensure that your SOAP notes are of the highest quality.
What Is a SOAP Note in Speech-Language Pathology?
SOAP notes are widely used for documenting the progress and treatment of clients in various healthcare fields, such as general practice, mental health , and speech therapy. SOAP notes provide a structured format to succinctly document a client’s information , such as reported symptoms and concerns, observations from the clinician, any measurable data, an assessment of the client’s condition, and a plan for treatment moving forward.
Your SOAP notes not only serve as a record of the client’s progress, but they also help to communicate important information to other healthcare team members. Whether you’re a seasoned speech therapist or just starting out, understanding how to write effective SOAP notes is essential to providing top-notch care to your clients.
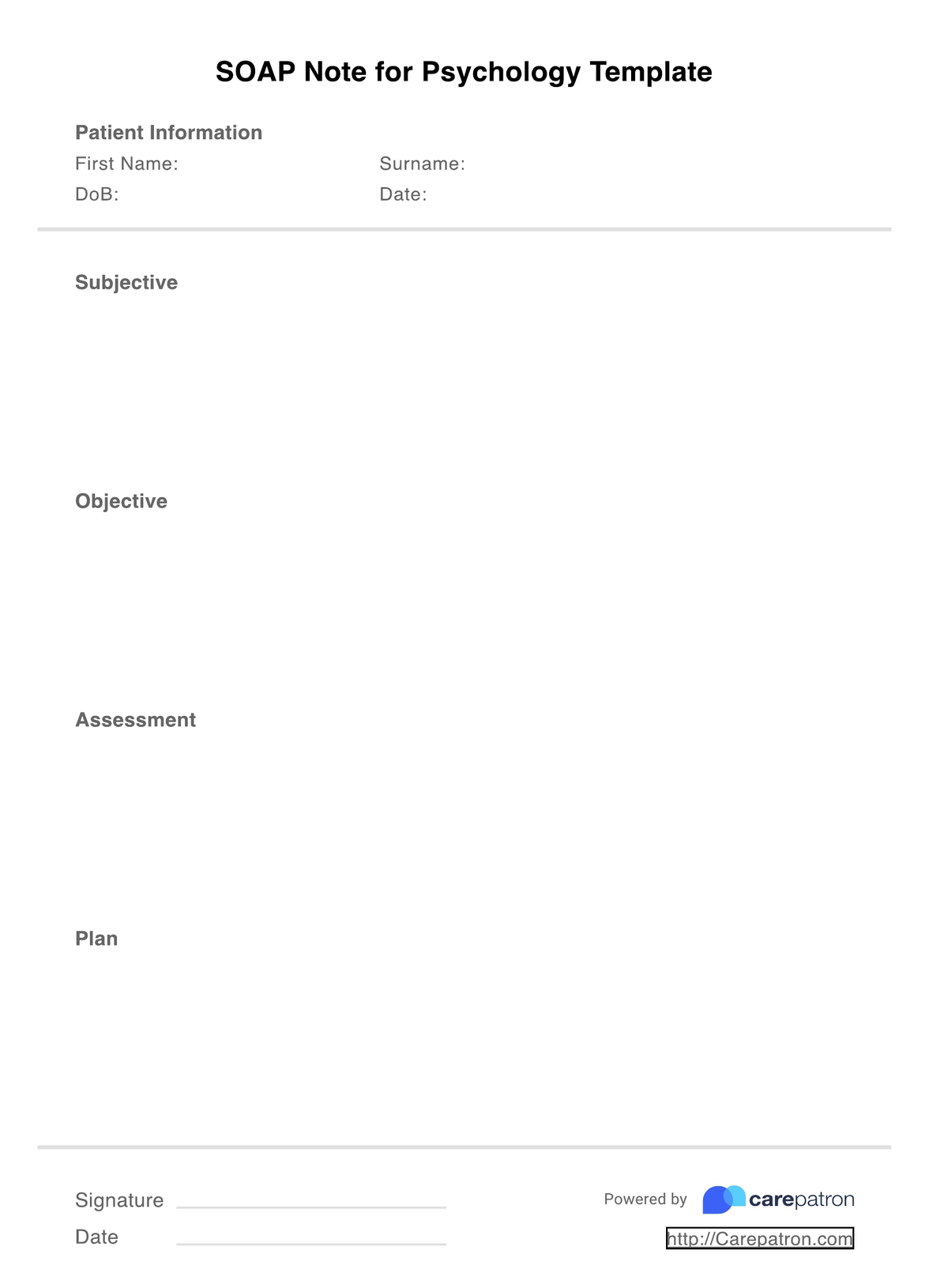
Recommended SOAP Note Format for Speech Therapy Clinics
SOAP stands for S ubjective, O bjective, A ssessment and P lan. These four components of a SOAP note provide a framework for the documentation of speech therapy sessions. In the sections below, we’ll go into more detail about each element.
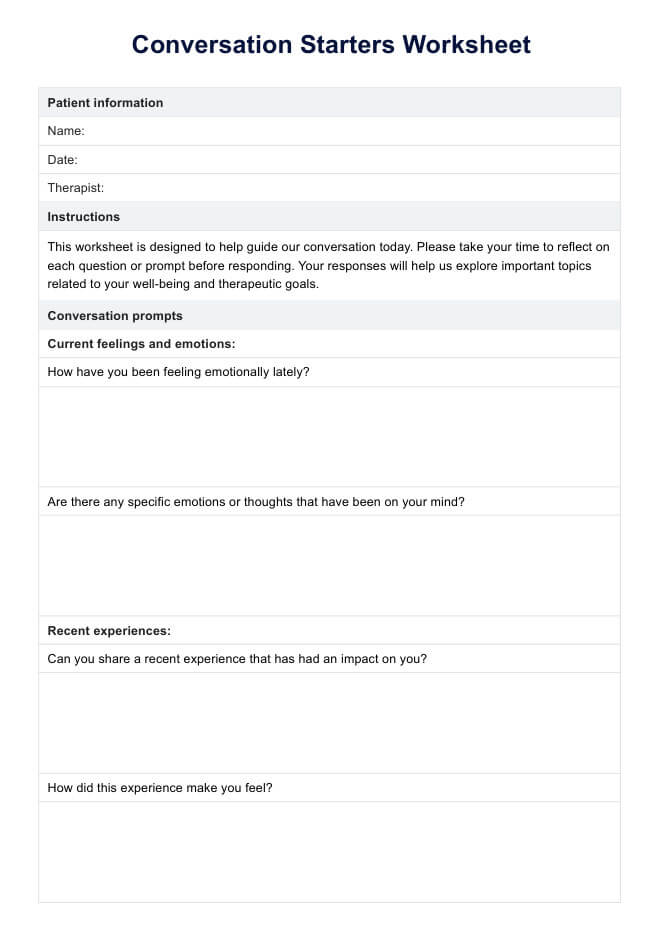
This section is all about what the client is experiencing. It should address client concerns, symptoms, and any other relevant information reported, including the history of treatment, current lifestyle, and any external factors affecting the client.
While this section may contain subjective observations of the client’s mood and demeanor, try to keep things as factual as possible. For example, rather than saying, “The client seemed anxious.” you could say, “The client reported feeling anxious.”. You should also record any medications the client is currently taking.

When writing the objective section of a SOAP note, you should document any measurable or observable information you’ve gathered during your assessment. This includes data such as physical examination findings, vocal range articulation and vocal quality. Record the results here if you perform tests such as a standardized assessment, an audiogram or a hearing test.
This part of your SOAP note should include a summary of your observations and an analysis of the client’s condition. If you come to any conclusions or diagnoses, make sure to include these. This section should be detailed and provide a clear framework for the rest of your note.
Finally, the plan section will include your proposed treatment plan. This could involve regular therapy sessions, advice on lifestyle changes, recommended exercises or any other interventions you deem necessary. Also include how you’ll review the client’s progress, and what goals you have for them to achieve.
How to Write SOAP Notes for Speech Therapy
Here are a few handy tips to help you get started:
Use a SOAP Note Template
Using a template for SOAP notes can help you write clear and consistent notes, saving time by allowing you to fill in the necessary information quickly. By using the same template for all your notes, you can ensure that each note contains the necessary information and is easy to read.
A template also helps to keep your notes cohesive. This provides a consistent structure for all of your SOAP notes, making them easier for other team members to follow and understand.
Be Overly Descriptive
You might be tempted to shorten and quickly sum up your notes to save time – don’t do it! It’s crucial to be detailed and descriptive when writing SOAP notes for speech pathology. It will help you provide a comprehensive overview of the client’s progress.
It’s better to over-explain than to under-explain. Your notes should include any goals set in the session, any interventions used, the date and time of any events, and a detailed record of any observations made during the session.
Write SOAP Notes Immediately Following a Session
It’s strongly recommended that you develop SOAP notes immediately after the speech therapy session. Recalling details is much easier when events are still fresh in your mind. If you wait too long to write up the notes, details may become distorted or forgotten, leading to misunderstandings and inaccurate records.
Make Notes Easy to Understand
Having legible notes ensures that third parties can understand and interpret information. Avoid any kind of shorthand or obscure abbreviations when writing SOAP notes for speech therapy.
Arrange your notes logically and chronologically and separate each section clearly. This improves the readability of your notes and makes it easier for others to understand the information. It’s possible that third parties may need to use your notes for diagnostic purposes or accommodations, so they must be accessible.
Use Direct Quotes
If possible, use direct quotes to illustrate client progress. For example, if the client was able to say a particular word for the first time during their speech therapy session, you could use a direct quote to note this. Doing so provides a more accurate and vivid representation of what occurred during the session. It’s also a useful way of recording client symptoms and progress objectively.
Include Measurable Data
Where possible, include measurable data to give a more accurate report of the client’s progress. For example, if you notice that they’re able to pronounce a certain phrase correctly, note the number of times they could say it in your notes. This provides an objective measure of client progress, which can be used to inform future interventions.
Compare Progress to Previous Sections
Comparing the client’s progress to performance in previous sessions can be illuminating. It allows you to see how they’ve improved over time and any areas that may need additional work or intervention.
By pointing out this information to the client, you can help encourage and motivate them as they strive towards their goals. You can also use this data to adjust the plan of action to better support the client’s needs. It’s a powerful way of demonstrating their progress and provides a sense of accomplishment.
Do a Double-Check
Last, but not least, it’s essential to double-check SOAP notes before submitting them. Some insurance providers may reject reimbursement claims if any sections are missing, so check for gaps or inconsistencies. Even the most experienced clinician can make mistakes (especially when managing a busy caseload), so take the time to review your notes for accuracy and completeness.

Questions to Answer with Your Speech Therapy SOAP Notes
A helpful way of framing your SOAP notes for speech therapy is to ask yourself what information you’d hope to gain by reading someone else’s notes. You can even run through a checklist of questions to ensure you include relevant information.
Here are a few questions to consider when writing SOAP notes:
- What are the client’s goals?
- In what areas is the client progressing?
- In what areas does the client need improvement?
- Is the client ready to finish speech therapy services?
- How was the client’s attitude and behaviour?
- Should any changes be made to their treatment plan?
- What was the outcome of the session?
Asking yourself these questions helps ensure your SOAP notes provide a comprehensive overview of the client’s progress. This also helps to make sure that all relevant information is captured, which can be helpful for third parties that may need to access the notes.
Examples of SOAP Notes for Speech-Language Pathologists
Here are two fictional examples of SOAP notes for speech-language pathologists:
Example 1: Initial Evaluation SOAP Note
Subjective:.
- Client presented with concerns about difficulty speaking clearly and being understood by others.
- Client also mentioned feeling self-conscious about their speech and avoiding social situations because of it.
- Client demonstrated significant difficulty with articulation and phonological processes, including substitutions, omissions and distortions.
- Client also displayed moderate receptive language delays in understanding complex instructions.
Assessment:
- Based on initial evaluation data, the client is presenting with a severe speech disorder impacting their daily communication skills. Further assessment is needed to determine specific areas of need for treatment.
- Refer the client for further assessments, including formal speech and language evaluations.
- Begin therapy sessions to address speech sound disorders, incorporating evidence-based techniques such as motor-based approaches and phonological awareness activities.
- Provide education and resources for family members to support the client’s communication needs at home.
Example 2: Progress Note
- Client reports progress with speech therapy sessions and increased confidence in their verbal communication.
- Client demonstrated improved articulation skills, reducing the number of errors from 60% to 20%.
- Client also displayed improved expressive language abilities, using more complex sentence structures.
- Based on progress data, the client is showing significant improvements in both articulation and expressive language skills. Client’s self-esteem and confidence have also improved.
- Continue therapy sessions focused on speech sound disorders, incorporating activities to further improve articulation accuracy.
- Expand therapy goals to include increasing expressive language abilities and targeting specific communication situations identified by the client as challenging.
- Encourage continued practice of communication strategies in daily life.
- Provide resources for ongoing support and practice at home.
- Schedule a follow-up assessment in 2 months to monitor progress and adjust therapy goals as needed.
Benefits of Using Electronic Speech Therapy Notes
Using an electronic method of recording SOAP notes for speech therapy provides many benefits for busy clinicians:
- Time-efficient : Typing notes into a computer or tablet is much faster than handwriting each note. This can save significant time and energy during a session, allowing clinicians to spend more time engaging with their clients.
- Accurate and easy to read : Computer-generated text is much easier to read than handwriting, especially if multiple clinicians need to access the notes.
- Searchable : Electronic notes can easily be searched using keywords, saving time when revisiting previous notes or looking for certain topics. This makes it easier to access information quickly and efficiently.
By taking advantage of these features, clinicians can spend more time focusing on client progress and goals, and less time worrying about note-taking. Ultimately, this can help to improve the quality of care that clients receive.
Write SOAP Notes for Speech Therapy with Power Diary
Power Diary is a comprehensive client management and appointment booking solution that will help streamline your practice. Our intuitive user interface makes it easy to capture SOAP notes for speech therapy in an efficient and secure way.
Practice Management Software for SLPs
Practice management software transforms the daily grind for Speech-Language Pathologists into a smoother, more efficient process. The software’s ability to store detailed, accessible SOAP notes allows you to document client progress accurately and securely. This not only helps in tracking therapeutic outcomes but also provides a record for future reference, contributing to a more coordinated care approach. It’s like having a digital assistant that organizes schedules, keeps detailed client notes available when needed, and ensures everyone on the team is on the same page.
If you’re interested in learning more about Power Diary and how it can help you write SOAP notes for speech therapy, start a free trial today.
Most Popular
- Best Healthcare Podcasts
- How to Write a Great Referral Feedback Letter
- 5 Ways Your Practice Can Look More Professional
- Balance or Burnout
- The Ultimate Waiting Room Checklist
Power Diary Picks
- 7 Reasons Private Practice Owners Rock
- Is Perfectionism Costing Your Health Practice?
- How to Price Your Health Services
- Ideal Client Profile Blueprint
- Beginner's Guide to SMS Marketing for Your Clinic
- All Articles
- Compliance & Security
- Marketing & Growth
- Power Diary Updates
- Practice Management Tips
- Release Notes
- Reporting & Analytics
Share this on:
Related Articles

Slash Admin Time and Increase Productivity in 4 Moves

Empathetic Distress: Signs & Tips for Prevention

Topics to Discuss with a Therapy Mentor
Update on the Current Change Healthcare Outage
Click here for Therapy Brands FAQs

A Pediatric SOAP Note Example and Helpful Tips for SLPs
We write them every day, but many of us still have questions about how to correctly write a SOAP note. How do you write notes that are simple and also cover all documentation requirements without spending hours for each patient? Here’s your guide to writing SOAP notes quickly and correctly, with examples.
SOAP Note Basics
First, ask yourself why you’re writing this SOAP note- who will see it and what information should it convey? ASHA recommends that clinical notes be comprehensive enough that another SLP could read it and understand your therapy process enough that they could pick up where you left off to continue therapy. Here are examples of each section of a good SOAP note:
S: Subjective
Your impressions of the patient’s level of awareness, mood, and behavior. You can also include direct quotes from the patient. This is a good place to include how a patient feels about their speech improvement or therapy in general.
EXAMPLE: Suzy appeared alert and attentive during the entirety of the session. Her mother reported that Suzy said “I was looking forward to speech all week!”, and that Suzy’s teacher remarked that she has been able to understand Suzy better in the past week.
O: Objective
Measurable information (e.g. data) , including percentages and which goals and objectives were addressed. You can also include the activity that was used to elicit this data.
EXAMPLE: Suzy produced /k/ at the beginning of words with 70% accuracy using a worksheet with 10 /k/ vs /t/ minimal pairs, given 2 verbal reminders (e.g.“Is it Tar or Kar?”) and a mirror for self-correction.
A: Assessment
Your analysis of the session. If possible, compare the patient’s performance across sessions.
EXAMPLE: Suzy’s correct production of /k/ in initial position increased from 60% in imitation and with a visual aid during the last session to 70% during today’s session. Omission of visual aid (picture of mouth producing /l/ sound) did not decrease performance.
Outline the course of treatment and therapy targets for the next session. Include possible activities, plan for reinforcement/cuing, and any changes to objectives, as well as any homework you send home.
EXAMPLE: Suzy continues to improve her production of initial /k/. Continue to fade cues and initial model of the sound for initial /k/ at next session. Sent home 3 minimal pair worksheets from XYZ book and directed Suzy’s mom how to complete them.
Check out this free SOAP note kit that includes a template, checklist, even more SOAP note examples, and 7 Tips to Improve Your Documentation.
Finally, a few more tips for writing better SOAP notes:
Write the notes as soon as you can after the session, or during the last few minutes if allowed. This keeps the information fresh in your mind.
Don’t forget to document any homework you sent home in the Plan section. This will help you know where to start for the next session.
Take advantage of copy-and-paste features if you use an EMR. This allows you to copy the past note and make relevant changes, which is great for therapy that uses similar activities and goals each time.
Fusion Web Clinic makes writing SOAP notes easy with templates, quick phrases, and goal tracking, on the web or on mobile! Check out our documentation page for more information!
About the Author:
Jill Shook, MS, CCC-SLP owns a private practice in Pittsburgh, PA. She created a course for SLPs starting out in private practice, which is available through Northern Speech Services, and blogs about resources for SLPs in private practice at Private Practice SLP . Email her at [email protected]
Free SOAP Note Kit
This kit includes:
- SOAP Note Template
- 7 Tips to Improve Your Pediatric Documentation Handout
- SOAP Note Checklist Handout
- SOAP Note Examples
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
- Skip to footer

The Orange Effect Foundation
Empowering children and young adults with speech disorders
Writing Excellent SOAP Notes for Speech Therapy: 5 Steps
November 11, 2021 By Orange Effect Administrator
Working with children and adults with a speech impairment is a noble endeavor. You can help hundreds of people overcome their speech disabilities if you dedicate your career to the cause. According to the American Speech-Language-Hearing Association , 5-10% of Americans have some form of communication disorder, with nearly 7% experiencing language impairment, aphasia being most commonplace.
To make your treatments as effective as possible, you can adopt the SOAP notes writing approach to your medical reports writing. SOAP is an objective, structured way for medical professionals to organize their thoughts and index them for future reference. What is SOAP all about and how can you use it in speech therapy to help your patients overcome their impairments?
SOAP Notes 101 and the Benefits of Utilizing Them
SOAP is a writing system adopted by numerous doctors and medical practitioners around the globe due to its simplicity and flexibility. It is also a built-in feature in many readily available EMR software applications . SOAP is an acronym that consists of four elements:
- Subjective – What does the patient say about their issue?
- Objective – What does the medical exam say about their issue?
- Assessment – What is your professional opinion on the issue?
- Plan – What is your recommended treatment for the issue?
There are numerous reasons to use SOAP to write your notes in speech therapy . Whether you’re working in a hospital or as a private practitioner, SOAP will make your job easier by helping you organize your findings. You will be able to outline exactly what the patient thinks about their ailment and then write your conclusions to the physical exam after. This helps reduce the length of the examination, makes storing patient data more straightforward, and enables you to recommend the right speech therapy for your patients.
Writing Excellent SOAP Notes for Speech Therapy
- Create a Template to Fill in with Patient Information
Creating a template for your SOAP notes before seeing your speech-impaired patients will make your meetings more productive. With a template consisting of four separate subheadings, you can take quick notes while also talking to them actively. This will allow you to pay more attention to what they’re saying and write down notes between checking their current condition. Your template can be created in a traditional text editor, a cloud writing platform, or an EMR app. For private practitioners, renting EMR software may be pricey so alternatives are also welcome.
- Write Down Keywords and Phrases without Complex Sentences
To speed up the process of taking SOAP notes, you should avoid writing complex sentences with paragraphs of text. There is no need for you to thoroughly explain what happened in the meeting in great detail – you were there. The notes you take are there to help you keep track of your speech impaired patients and no one apart from you will see them. This means you can write notes in whichever style you like, be it by writing keywords down or a short sentence for each SOAP element.
- Take New Notes Whenever You See Patients Again
Given that you are likely to see the same patients more than once, you should take new SOAP notes every time. Your patients’ condition may have changed and you might notice improvements or declines in their speech therapy. Comparing new notes to previous sessions will allow you to map out a better treatment program for each patient. Moreover, it will ensure that you don’t overlook even the most minor detail in your SOAP notes.
- Date, Sign, and Double-Check your Notes After Sessions
To keep things as organized as possible, you should date and sign your SOAP notes whenever you’re done with them. Once your session has finished, go over what you wrote to spot any grammar mistakes or formatting issues. Be especially mindful of the treatment and medicine prescription you’ve assigned (if any) since spelling errors can have consequences. When you’re satisfied with the SOAP notes you took for that session, add your physical or digital signature to the document and file it away.
- Write Down Key Takeaways from the Session in Freehand
It’s always a good idea to outline the key points and takeaways you took from the speech therapy session. In your personal opinion, how well is the patient handling their treatment and how can you help them get closer to their goals? Speech treatment is a highly subjective field where no two patients have the same diagnosis or the extent of it. Think about the SOAP notes you wrote down and write a takeaway for the session before closing the file for now.
SOAP Notes for Speech Therapy Writing Mistakes to Avoid
Now that we’ve seen how SOAP notes can help you in treating speech impairment, it’s important to note several potential mistakes to avoid. While SOAP is extremely effective at helping you organize, you can also find yourself in a position where you automatically, mandatorily fill in blanks.
According to a published medical study , SOAP can often narrow your field of view by requiring you to follow a set path toward treatment. In it, the writers postulated that APSO (Assessment, Plan, Subjective, Objective) may be more practical and that SOAP should be retrofitted on a case-by-case basis. Each entry in your medical reports has to be written meaningfully and with good reasons – which is why you should avoid the following:
- Writing unsourced, anonymous entries into your SOAP notes
- Avoid unclear sentences without conclusions or tangible data
- Don’t repeat yourself in your SOAP notes – only state certain things once
- Write original treatments and recommendations for each patient – don’t copy/paste
- Always proofread, format, and sign your SOAP notes
The purpose of using SOAP for your notes for speech therapy is to ultimately make treating your patients easier. It is a convenient, tried, and tested system for organizing patient findings and writing medical reports.
Today, SOAP is best used via a dedicated EMR app which would make indexing and storing patient data easier than through manual writing. Consider the steps outlined in the previous paragraphs in your practice and see if you can use them to improve your patients’ wellbeing. Even if all it does is help organize your writing, SOAP is still a worthwhile addition to any medical practitioner’s toolset.
Jessica Fender is a researcher and academic content creator. Her job is to facilitate student learning – she creates educational content that aligns with search queries “ write my thesis for me ” and “hire writer.” When Jessica has free time, she enjoys reading, blogging, and hiking.
About Orange Effect Administrator
Meet the Voice Behind the Orange Effect Foundation - your go-to source for valuable insights and resources! The Orange Effect Administrator curates and shares posts tailored for speech therapists, passionate OEF supporters, grant recipients, and parents of children facing speech disorders. Explore our blog to stay informed, inspired, and connected with our vibrant community.

17040 Amber Drive Cleveland, OH 44111 [email protected]
Copyright 2024 orange effect foundation. all rights reserved..
SOAP Notes For Speech Therapy Template
Functional SOAP note template for speech therapy, helping you to streamline your documentation and create compelling and accurate SOAP notes.

By Alex King on Jul 05, 2024.
Fact Checked by RJ Gumban.
What is a speech therapy SOAP notes?
Within the confines of a private practice's therapy room, speech pathologists engage in the art of documenting client progress during speech therapy. After each session, they conscientiously write notes, translating subjective observations into objective data—a crucial aspect for future sessions.
Witnessing patient progress firsthand, therapists find fulfillment in their skilled interventions. The records serve as guideposts, shaping the roadmap for individual sessions and marking tangible strides. This meticulous process measures progress and weaves a growth narrative for the treatment session. It creates a vital bridge connecting the previous session to the promising horizons of the next session.
Speech therapy SOAP notes are a form of clinical documentation that speech therapists use in documenting speech therapy sessions and progress of their clients. As one of the most popular ways to organize progress notes, the SOAP format separates information into four sections: subjective , objective , assessment , and plan . These four sections cover different types of information:
- Subjective : The client's subjective description of their concern, including symptoms and how it affects their day-to-day life. This section often includes direct quotes from the client.
- Objective : Your professional observations about the client's behavior, the interventions you used during the session, and how the client responded. The objective section should also include any tests or assessments that the client completed.
- Assessment : A synthesis of the above sections; your assessment and analysis of the session. This section includes treatment goals and determines progress made by client.
- Plan : The final section outlines the future plan for the client, including any upcoming sessions, goals to be completed, or relevant changes to the treatment plan.
The speech therapy SOAP note template is both intuitive and coherent; it aims to simplify the note-taking process so you can save time without compromising the quality of your documentation. Using a SOAP note template is one of the best ways you can optimize the more administrative aspects of working as a speech therapist. By utilizing this resource, you will be able to save countless hours that can instead be spent treating more clients.
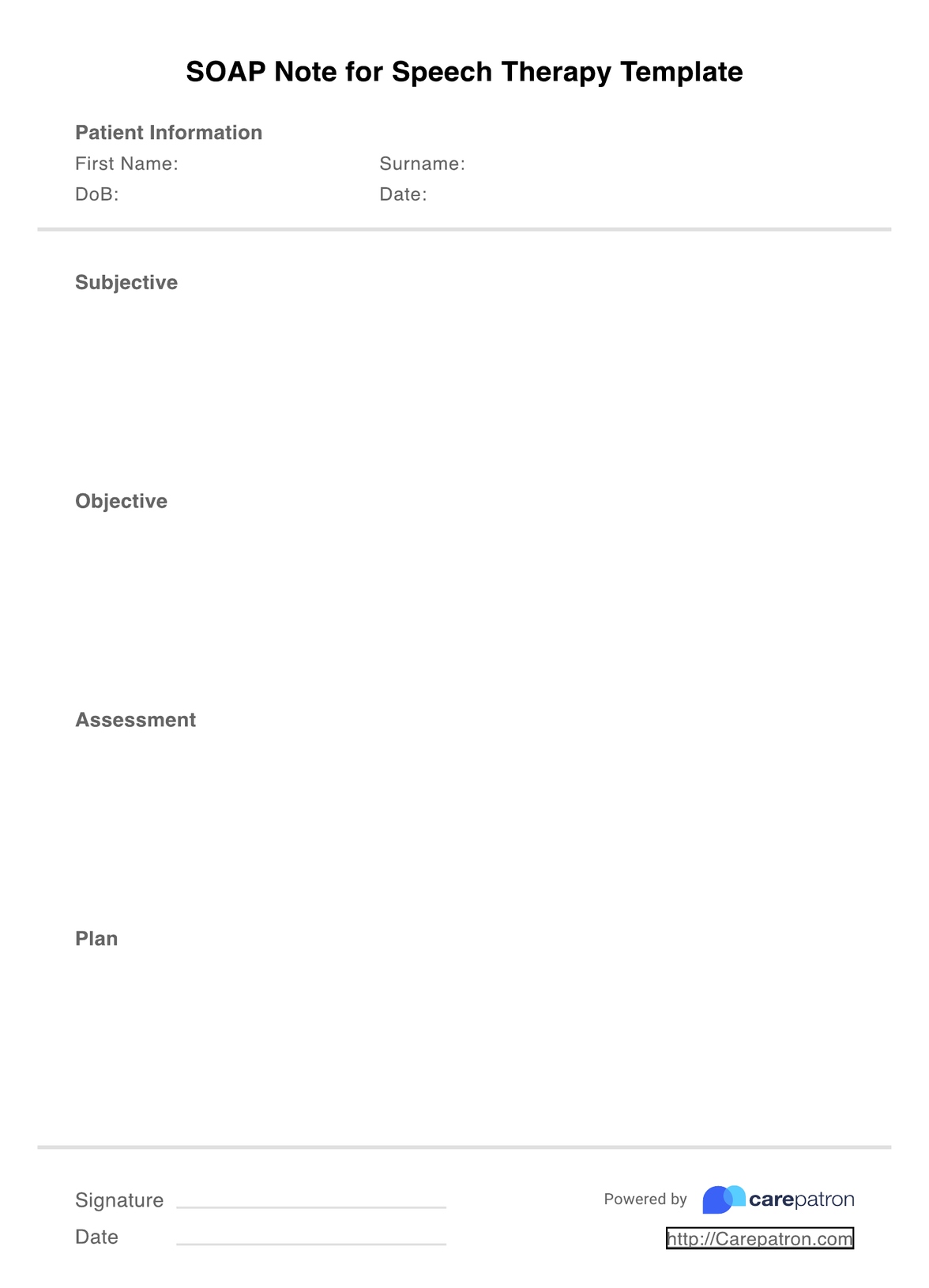
Printable SOAP Notes For Speech Therapy Template
Check out these therapy SOAP note templates to improve your progress notes, productivity, and therapy outcomes for skilled intervention.
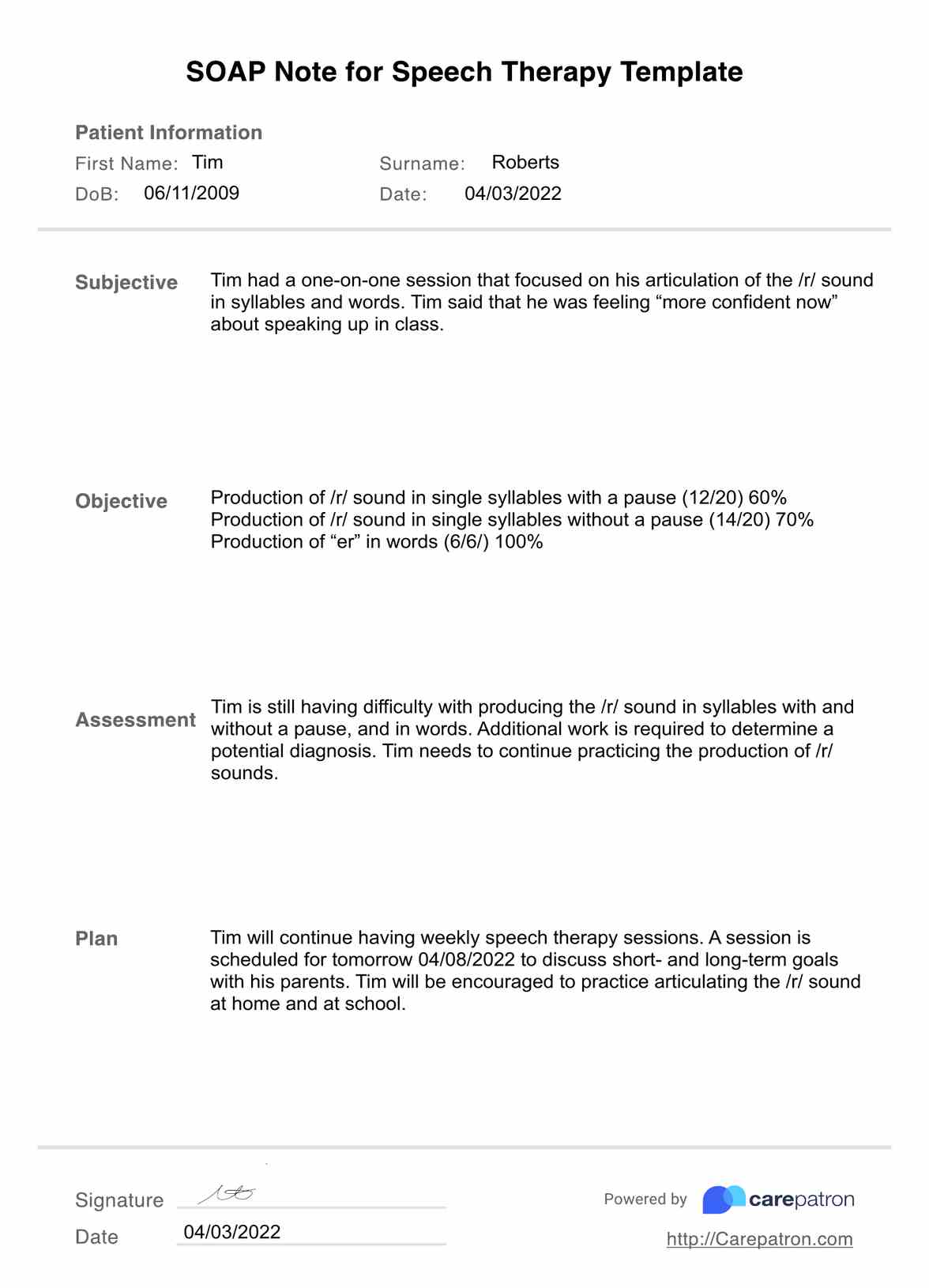
SOAP Notes For Speech Therapy Template Example
How to use this SOAP note template for speech language therapy
Using the speech therapy SOAP note template is very easy. Regardless of whether you are an individual practitioner or work at a speech therapy practice, we have designed this resource with the understanding that most speech therapists lead busy lives and as such, they are on the lookout for simple ways to speed up their documentation. With that in mind, here are four simple steps that can guide your usage of the template:
Step 1: Download the template
The first thing you need to do is click on the link that will take you to the PDF version of the template. From here, you will be able to edit the document where necessary.
Step 2: Fill out the four sections
After you have downloaded the SOAP note template, it's time to fill out the four sections (subjective, objective, assessment, and time). When you are writing your documentation, you want to be as clear and concise as possible, while also including every piece of relevant information based on the patient's response.
Step 3: Don't forget credentials
Every speech therapy SOAP note needs to include certain credentials: your client's name (and ID number where applicable), the date/time of the session, and your own professional credentials. These details are useful when it comes to insurance and billing processes.
Step 4: Store your SOAP note securely
In order to adhere to HIPAA compliance regulations, you need to store your SOAP notes securely. If you store it online, you need to ensure the platform has suitable electronic safeguards so your client's data is protected at all times.
SOAP Notes For Speech Therapy Template example (sample)
We have created the following sample to help you visualize what a completed speech therapy SOAP note might look like. The specific content of each SOAP note will differ depending on your session with each client, but this should give a good overview of the type of information you need to include and where it goes within the template.
Here is an example of what the SOAP note template will look like once it has been properly filled out by a speech therapist:
.png)
Who can use this speech therapy template?
One of the best things about the SOAP note template we have used is how customizable it is to different fields of speech therapy. Essentially, this SOAP note template applies to any kind of speech therapist who has sessions with clients, including those who work as solo practitioners and those who work in group practices.
Additionally, speech therapists often work with a range of clients who may all have different problems, disorders, or assessments, including the following:
- Speech therapy for apraxia
- Speech therapy for aphasia
- Speech therapy for stuttering
- Speech therapy for swallowing difficulty
Further, each of these types of speech therapy is applicable to clients of all ages. The specific methods that speech therapists use to treat these disorders may differ depending on their client's age, but the format for writing SOAP notes will remain the same.
As you can see, the speech therapy SOAP note template is able to be used by pretty much every speech therapist, regardless of where they work or what type of therapy they specialize in!
Why is this template useful for speech therapists?
The most important use of a SOAP note template for speech therapists is how effectively it organizes clinical documentation. Writing accurate notes can be a time-consuming process, but with this template, you can streamline this process without reducing the overall quality of the note. Other uses include:
- Consistency : Writing consistent SOAP notes helps with readability. When you check your previous notes, you can extract relevant information faster if they are consistent, which is much easier if you use a SOAP note template.
- Accuracy : The SOAP note template visually separates the four different sections. Using this template will ensure that you don't accidentally forget to fill out all four sections, helping to improve the overall accuracy of your documentation.
- Suitability : As we mentioned, the SOAP note template has been designed to suit various types of speech therapy. This allows you to access an intuitive SOAP note template and use it for all of your clients, regardless of the differences in their specific speech problems.
.png)
Benefits of using the SOAP Notes For Speech Therapy Template
In addition to having various uses, using the speech therapy SOAP note template has many benefits for your private practice. Some of these advantages include:
Track your client's progress effectively
The biggest reason for writing SOAP notes is, of course, to track your patient's progress. Using a template will assist in making this information consistent, so you can easily compare notes and determine how effectively your treatment plan works.
Communication
Effective communication between care providers is an often overlooked aspect of delivering healthcare. With a SOAP note template, you can ensure that all members of a client's care team have access to the relevant information, helping them to make more informed clinical decisions.
Workflow and productivity
SOAP note templates help to improve the workflow and productivity at speech therapy practices. By streamlining the documentation process, you will be able to save countless hours that can instead be spent completing more important tasks.
SOAP notes can also be shared with insurance companies. If a client's insurance provider is paying for their services, then the provider may reach out looking for certain details. By using a SOAP note template, you can ensure you have an organized system that allows third-parties to access information quickly.
Legal situations
It's important to remember that progress notes are legal documents - this is one of the reasons why you should always prioritize writing accurate and detailed documents. If a legal situation were to arise, having SOAP notes that utilize a template will ensure they are organized and accurate, with a clear description of why certain clinical decisions were made.
Why use Carepatron for SLP SOAP notes?
Carepatron offers an all-in-one practice management software to greatly assist your speech therapy practice when writing SOAP notes. In addition to offering a range of different templates, Carepatron has useful voice-to-text transcription software.
With the recent rise in practice management systems, it can be not easy to find the perfect platform for your business. Nevertheless, we think Carepatron will be the solution you've been looking for. As well as offering clinical documentation tools, Carepatron is integrated with medical billing, coding, appointment scheduling, patient management, and workflow features designed to streamline your administrative processes.
With this all-in-one system, you will be guaranteed to optimize your productivity and save countless hours that can instead be spent doing what you do best: treating clients.
Commonly asked questions
This question doesn’t have a definitive answer, but as a good rule of thumb you should aim for 1-2 pages. You want your SOAP notes to be concise and clear, but without any repetitions.
Yes. SOAP notes are legal documents and every client has the right to access their progress notes. For this reason, it is absolutely essential that the information you include is objective, relevant, and truthful.
Yes, HIPAA has certain regulations that are applicable to SOAP notes. Firstly, HIPAA requires you to keep progress notes for each session with a client. The guidelines also require you to store these notes in a safe and secure way, so confidential information pertaining to your client is protected.
Related Templates
Popular Templates
Join 10,000+ teams using Carepatron to be more productive
| published: | 3 Dec 2020 |
|---|---|
| updated: | 26 Jun 2024 |
- Therapy Tools
Writing SOAP Notes, Step-by-Step: Examples + Templates

Documentation is never the main draw of a helping profession, but progress notes are essential to great patient care. By providing a helpful template for therapists and healthcare providers, SOAP notes can reduce admin time while improving communication between all parties involved in a patient’s care.
In a few sections, we’ll give a clear overview of how therapy SOAP notes are written, along with helpful templates and software you can use to streamline the process even further. If you’re looking for a more efficient, concise way to document your telehealth sessions, this helpful guide will be of value.
How To Write Therapy SOAP Notes
Therapy SOAP notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. [1]
As standardized documentation guidelines, they help practitioners assess, diagnose, and treat clients using information from their observations and interactions.
Importantly, therapy SOAP notes include vital information on a patient’s health status. This information can be shared with other stakeholders involved in their wellbeing for a more informed, collaborative approach to their care, as shown:

It’s critical to remember that digital SOAP notes must be shared securely and privately, using a HIPAA-compliant teletherapy platform . Here, we used Quenza.
The S.O.A.P Acronym
SOAP is an acronym for the 4 sections, or headings, that each progress note contains:
- Subjective: Where a client’s subjective experiences, feelings, or perspectives are recorded. This might include subjective information from a patient’s guardian or someone else involved in their care.
- Objective: For a more complete overview of a client’s health or mental status, Objective information must also be recorded. This section records substantive data, such as facts and details from the therapy session.
- Assessment: Practitioners use their clinical reasoning to record information here about a patient’s diagnosis or health status. A detailed Assessment section should integrate “subjective” and “objective” data in a professional interpretation of all the evidence thus far, and
- Plan: Where future actions are outlined. This section relates to a patient’s treatment plan and any amendments that might be made to it.
A well-completed SOAP note is a useful reference point within a patient’s health record. Like BIRP notes , the SOAP format itself is a useful checklist for clinicians while documenting a patient’s therapeutic progress.[REFERENCE ITEM=”Sando, K. R., Skoy, E., Bradley, C., Frenzel, J., Kirwin, J., & Urteaga, E. (2017). Assessment of SOAP note evaluation tools in colleges and schools of pharmacy. Currents in Pharmacy Teaching and Learning, 9 (4), 576.”]
In the next section, you’ll find an even more in-depth template for SOAP notes that can be used in a wide range of therapeutic sectors.
Therapy SOAP notes include vital information on a client’s health status; this can be shared with other stakeholders for more informed, collaborative patient care.
3 Helpful Templates and Formats
With a solid grasp of the SOAP acronym, you as a practitioner can improve the informative power of your P rogress Notes, as well as the speed with which you write them.
This generally translates into more one-on-one patient time, reduced misunderstandings, and improved health outcomes overall – so the table below should be useful.
SOAP Notes: A Step-By-Step Guide
Podder and colleagues give a great overview of the different subsections that a SOAP progress note can include. Based on their extensive article, we’ve created the following example that you can use as guidance in your work. [1]
| |
|---|---|
| Subjective data from stakeholders and patients create a context for the and sections that follow. Example subsections include: , e.g. their condition, symptoms, or historical diagnoses , often further structured into onset, location, duration, characterization, alleviating and aggravating factors, radiation, temporal factors, and severity (OLDCARTS) , including medical, surgical, family, and social factors , which includes pertinent questions about potentially unmentioned symptoms, and |
| Wherever any tests or factual data are collected, they should be recorded along with subjective information for a more thorough analysis of the client’s condition. |
| An integrated analysis of the combined objective and subjective data to offer a diagnosis. Where an existing condition is a reason for a mental health program, it will relate to changes in status. E.g. Generalized Anxiety Disorder, Repetitive Strain Injury, etc. If applicable, other potential diagnoses are noted along with the practitioner’s rationale for suggesting them. |
| A detailed description of any further actions that need to follow from the therapy, e.g.: |
Occupational Therapy SOAP Notes
In Occupational Therapy , a SOAP Progress Note might include the patient’s injuries and their severity, home exercises, and their effectiveness.
Based on observations and interaction with their client, an OT professional might adjust their treatment program accordingly. [2]
Laid out in the S, O, A, P format on therapy notes software , they might look like this:

Digital SOAP note tools like Quenza, which we’ve used here, will automatically create PDF copies for download, sharing, or HIPAA-compliant storage in a centralized place.

Because SOAP notes are best created while a session is still fresh in their minds, therapists might look for mobile-compatible software. This way, notes can be made on the spot from a tablet or smartphone.
Recommended: How to write Occupational Therapy SOAP Notes (+3 Examples)
Applied Behavior Analysis SOAP Notes
SOAP notes also play a valuable role in Applied Behavior Analysis , by allowing professionals to organize sessions better and communicate with a client’s other medical professionals. Legally, they may also accompany insurance claims to evidence the service being provided. [3]
It is important to remember that ABA SOAP notes , as psychotherapeutic documents, must be stored privately. They may form part of a client’s overall medical file other therapy notes.
| |
|---|---|
| This section details where the session took place, who was present, and their reports of the client’s behavior. |
| Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant frameworks (e.g. Antecedent, Behavior, Consequences). |
| Assessment notes should include evaluations of the current program’s efficacy, describing particular strategies and targets. |
| This section describes any amendments that will be made to the client’s treatment plan |
These illustrative Occupational Therapy SOAP Notes and ABA SOAP Notes also exemplify how versatile SOAP notes can be. [4]
It’s why the framework is a commonly used standard in sectors such as Physical Therapy , Nursing, Rehabilitation, Speech Therapy , and more.
5 Examples of Effective Note-Taking
Many therapy software systems help to speed up the documentation of progress notes through in-built templates and diagnostic codes. At the end of the day, however, clinically valuable notes require careful thought and judgment when it comes to their content.
Effective notes are generally: [5]
- Written immediately following a therapy session. This way, a practitioner’s in-session time is spent focused on patient engagement and care ; writing notes immediately after helps minimize common mistakes such as forgetting details or recall bias.
- Professional. An important part of patient Electronic Health Records , SOAP notes should be legible and make use of professional jargon to serve as a common frame of reference. They should be written in the present tense.
- Concise and specific. Overly wordy progress notes unnecessarily complicate the decision-making process for other practitioners involved in a patient’s care. Brief, but pertinent information helps other providers reach conclusions more efficiently.
- Unbiased: In the Subjective section, particularly, there is little need for practitioners to use weighty statements, overly positive, negative, or otherwise judgmental language. SOAP notes are frequently used both as legal documents and in insurance claims.
- Utilize appropriate details, such as direct quotes: For a more comprehensive document that includes all the salient facts of an encounter.
An effective SOAP note is a useful reference point in a patient’s health record, helping improve patient satisfaction and quality of care.
3 Smart Software Solutions
In this section, we’ve reviewed three of the top practice management software systems offering helpful SOAP note functions.
These include SOAP note templates, discipline-specific codes, and treatment planning features that integrate with therapy progress notes.
|
|
|---|---|
| MyClientsPlus is a mental health practice management solution that runs on the web, Android, and Apple platforms.With a loyal user base and many e-therapy features for telehealth, MCP comes with SOAP note templates that can be easily shared in multi-provider organizations.While it doesn’t offer robust treatment planning features, MyClientsPlus does include sector-specific templates and native support for telehealth sessions. | |
| Name | |
| Price | $24.95+ monthly |
| Good For | Mental Health Coaches, Psychologists, e-Counselors, Therapists, |
| More info |
|
|
|---|---|
| Designed by blended care practitioners, Quenza was developed as an all-in-one solution to address the most common online therapy challenges. Its features include powerful but easy-to-use custom form creation tools for creating SOAP notes, as well as , , progress note templates, psychotherapy notes, and more.Beyond this, however, the app has much more valuable practitioner tools that streamline treatment planning with simple Pathways, create personalized interventions with pre-populated fields, and video therapy or coaching support for interactive, engaging therapeutic materials.Live results tracking gives practitioners insight into real-time client progress, and Quenza is fully HIPAA-compliant for secure storage of SOAP and psychotherapy notes. | |
| Name | |
| Price | $1+ monthly |
| Good For | Mental Health Coaches, Psychologists, e-Counselors, Therapists, Client Engagement, Treatment Planning, |
| More info |
|
|
|---|---|
| e-Counselors, physical therapists, speech therapists, and other practitioners creating SOAP notes will likely find value in ClinicSource SOAP templates.The software allows quick progress notes to be created, and these can then be centralized with a client’s records, alongside their billing history and summaries from each visit.Other features of this therapy notes software include Treatment Progress templates, Patient Evaluation templates, and features for building Care or Treatment Plans. | |
| Name | |
| Price | $59+ monthly |
| Good For | Mental Health Coaches, Psychologists, , Therapists |
| More info |
|
|
|---|---|
| Power Diary has a sizable library of mental health forms that counselors, psychologists, and therapists can use to create treatment plans.SOAP and other session notes can be imported, exported, cloned, or shared to reduce admin time and centralize client records into one handy profile.Despite lacking some of the more robust mental health capabilities, such as e-prescribing, it has a low price tag and is easy for first-time users to navigate. | |
| Name | |
| Price | $5+ monthly |
| Good For | Speech Therapists, Psychologists, e-Counselors, Physical Therapists, Occupational Therapists, Mental Health Coaches |
| More info |
Importance of Accurate and Detailed SOAP Notes
Accurate and detailed SOAP notes are crucial in ensuring effective patient care. They serve as a comprehensive record that provides continuity and clarity in treatment. Detailed notes help in tracking patient progress, identifying patterns, and making informed decisions about future care plans. They also facilitate clear communication among healthcare providers, reducing the risk of errors and misinterpretations.
Moreover, thorough SOAP notes are essential for legal documentation and compliance. They provide a clear, chronological record of patient interactions and clinical decisions, which can be invaluable in case of audits or legal inquiries. Inaccurate or incomplete notes can lead to misunderstandings, compromised patient care, and potential legal repercussions.
Additionally, precise documentation supports better patient outcomes. When healthcare providers have access to accurate and complete information, they can make more effective treatment decisions. This leads to improved patient satisfaction, as patients receive consistent and well-coordinated care. Accurate notes also contribute to research and quality improvement initiatives by providing reliable data for analysis.
Tips for Enhancing SOAP Note Quality
Improving the quality of your SOAP notes can significantly impact patient care and clinical efficiency. Here are some practical tips for enhancing your note-taking:
- Be Clear and Concise: While it’s important to be thorough, avoid unnecessary details that don’t contribute to the patient’s care. Focus on relevant information that supports clinical decision-making.
- Use Standardized Language and Abbreviations: Consistency in terminology and abbreviations helps ensure that all healthcare providers understand the notes. Avoid using uncommon abbreviations that might cause confusion.
- Incorporate Patient Quotes: Including direct quotes from patients can provide valuable context and insight into their condition and concerns. This practice helps capture the patient’s perspective and can aid in more personalized care.
- Regularly Review and Update Notes: Make it a habit to review and update notes regularly to ensure they remain accurate and relevant. This is particularly important for patients with chronic conditions or those undergoing long-term treatment.
By implementing these tips, healthcare providers can create more effective and reliable SOAP notes, ultimately enhancing patient care and clinical outcomes.
Ensuring SOAP Notes are Client-Centered
Client-centered SOAP notes prioritize the unique needs and experiences of the patient, enhancing therapeutic outcomes. Therapists can create a more tailored and effective treatment plan by focusing on individual goals, preferences, and feedback. This approach improves client satisfaction and fosters a collaborative therapeutic relationship, promoting active participation and commitment to the treatment process.
Incorporating Client Feedback: Gathering regular client feedback can provide invaluable insights into their experiences and progress. This can be done through direct questions during sessions or via follow-up questionnaires. By documenting this feedback in the Subjective section, therapists can adjust their strategies to better meet the client’s needs, ensuring that the therapy remains relevant and impactful.
Personalizing Treatment Plans: Each client’s treatment plan should reflect their personal goals and challenges. The Plan section of SOAP notes outlines specific actions tailored to the client’s circumstances. For example, if a client struggles with anxiety in social situations, the plan might include exposure therapy techniques or social skills training designed specifically for their context and preferences.
Building a Collaborative Relationship: A collaborative approach involves the client in decision-making, enhancing their sense of agency and investment in therapy. During the Assessment phase, discuss the client’s perspective on their progress and any concerns they might have. This helps create a more accurate assessment and empowers the client, fostering a more cooperative and effective therapeutic environment.
Tracking Individual Progress: Regularly reviewing and updating SOAP notes ensures that the therapy remains dynamic and responsive to the client’s evolving needs. Documenting specific achievements and challenges in the Objective section helps monitor progress over time, allowing for timely adjustments to the treatment plan. This continual adaptation is crucial for maintaining the therapy’s relevance and effectiveness.
Leveraging Technology for Efficient SOAP Note Management
With the advent of digital tools, managing SOAP notes has become more efficient and secure. Utilizing specialized software can significantly reduce the administrative burden, allowing therapists to focus more on patient care. These technologies offer features such as templates, automatic data entry, and secure storage, which streamline the documentation process and enhance data accuracy.
Digital Templates and Auto-fill Features: Many therapy software solutions provide customizable templates that simplify the process of writing SOAP notes. These templates ensure that all necessary information is captured systematically. Auto-fill features can further expedite note-taking by automatically inserting recurring details, such as client demographics and session dates, thus saving time and reducing the risk of errors.
Secure Storage and Compliance: Ensuring the confidentiality and security of client information is paramount. Digital platforms that comply with HIPAA and other relevant regulations offer encrypted storage solutions, protecting sensitive data from unauthorized access. This secure environment safeguards patient privacy and facilitates easy retrieval and sharing of notes when needed for collaborative care.
Integration with Practice Management Systems: Integrating SOAP note software with broader practice management systems can enhance overall efficiency. Such integration allows for seamless coordination between scheduling, billing, and documentation. For instance, notes from therapy sessions can be directly linked to billing codes, simplifying the administrative workflow and reducing the likelihood of discrepancies.
Real-time Data Access and Updates: Mobile-compatible software lets therapists update SOAP notes in real-time, even during sessions. This immediate documentation ensures that details are accurately recorded while they are still fresh in the therapist’s mind. Moreover, having access to notes on the go allows therapists to review patient history and progress at any time, facilitating more informed and responsive care.
Final Thoughts
With clear, consistent information on a patient’s health status and progress, therapists, psychiatrists, and counselors are much better equipped to manage their well-being. And while note-taking may not be glamorous, harnessing the right software can significantly reduce the time you spend on this vital part of healthcare .
SOAP notes play a pivotal role in streamlined, effective healthcare, and are a daily part of life for many practitioners. If you’ve tried and enjoyed using any particular templates, forms, or therapy notes solutions, let us know in a comment.
We hope this article has helped you streamline your note-taking. To put these tips into practice, don’t forget to try Quenza’s SOAP Notes tools for just $1 a month .
If you want to enhance the wellbeing of your clients more effectively, Quenza will give you everything you need to streamline your therapy notes, so you can focus on delivering the wellness results that matter.
- ^ Podder, V., Lew, V., & Ghassemzadeh, S. (2020). SOAP Notes. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482263/
- ^ Fusion Therapy. (2020). How To Write Therapy SOAP Notes.. Retrieved from: https://blog.fusionwebclinic.com/soap-notes-for-occupational-therapy
- ^ WebABA. (2020). Simple Guidelines for Writing SOAP Notes. Retrieved from https://webaba.com/2020/07/01/aba-practice-daily-simple-guidelines-for-writing-soap-notes/
- ^ Belden, J. L., Koopman, R. J., Patil, S. J., Lowrance, N. J., Petroski, G. F., & Smith, J. B. (2017). Dynamic electronic health record note prototype: seeing more by showing less. The Journal of the American Board of Family Medicine, 30 (6), 691.
- ^ Fusion Therapy. (2020). How To Write Therapy SOAP Notes. Retrieved from: https://blog.fusionwebclinic.com/soap-notes-for-occupational-therapy
thanks for info
Leave a reply Cancel
Your email address will not be published.

Download free guide (PDF)
Discover how to engage your clients on autopilot while radically scaling your coaching practice.
Coach, This Changes Everything (Free PDF)
- (800) 747-9886
How to Write Soap Notes Efficiently for SLPs, OTs, PTs & Therapists
- • ABA , Assessment , Medical Necessity , Mental Health , Practice Management , Tips, Tools, & Tech

What is a SOAP Note?
The Subjective, Objective, Assessment, and Plan (SOAP) Note is an acronym representing a well-known framework for multidisciplinary therapy progress notes. A progress note reflects what was done in a specific session and the uniformity of the SOAP template makes it easier for colleagues and other clinicians to understand your sessions. SOAP notes are also the easiest way to make sure you are including each of your patient’s insurance company’s requirements, as well as advocating for your patient’s medical necessity.
Using the acronym SOAP, the progress note should include subjective, objective, assessment, and plan data. The SOAP note is an efficient way to document in an organized and structured way for:
If your practice offers services such as Occupational Therapy (OT), Physical Therapy (PT), Speech-Language Pathology (SLP), or any additional therapy and wants to increase efficiency and streamline documentation , our SOAP notes tips are a great place to start.
Therapy SOAP Note Definitions
Let’s start with a definition for each section of the therapy SOAP note:
The subjective section of your SOAP notes is dedicated to how the patient describes their symptoms from their point of view. You can get a better description of patient symptoms and experiences by asking open-ended questions like “what do you think is wrong?” or “what’s been going on?”.
The objective section is factual and based on your observations as a therapist or healthcare clinician. This may include results of:
- evidence-based tools
- vital signs
- physical manifestations of symptoms
- any other data relevant to your patient’s case
The assessment section contains all your observations, conclusions, and any diagnosis you have. Make sure to include your reasons with the relevant evidence for these conclusions. In the case of multiple sessions, this section is a place to track the patient’s progress.
The plan refers to your treatment program and your plan for the patient’s next appointment. Include your patient’s feedback and response to your treatment plan, as well as any homework or exercises you have given them to complete before the next session. Be as specific as possible.
Now we’ve defined a SOAP note, let’s go over some best practices that your OT, PT, SLP or ABA therapy practice can implement right now for more efficient SOAP notes.
3 Tips for More Efficient SOAP Notes
Here are 3 tips for SLPs, PTs, OTs & ABA Therapy SOAP Notes:

1. Stick to the Facts
It is important to stick to the facts and provide relevant evidence. Be sure to give a clear picture of what happened during the session and be specific as possible.
Let’s take a look at this Speech Therapy note for example:
Client read “ Good Night Gorilla ” and completed labeling, sequencing, and retelling tasks with 90% accuracy. But he was so tired today. He also produced word-final /k/ on 5/7 trials with visual prompts in single words, and minimal cues. Need to continue using strategies at home and target /k/ and /g/ phonemes.
This is improved from previous sessions, though mild articulation deficits remain and some phonological processes such as final consonant omission and fronting are ongoing. Client benefits from visual cues and is making good progress. Overall expressive language skills improved too.
Implementing the SOAP note framework will help clarify and streamline the data, here is the updated note:
S – Client appeared tired today, reporting waking up several times at night due to night terrors, but was cooperative throughout session.
O – Clinician read “Good Night Gorilla” and client labeled 6/7 animals independently; “armadillo” was challenging. He then organized the animals in the correct order of appearance 7/7 independently and re-told the story correctly. Client pinned the tail on each animal producing the final /k/ sound on 5/7 target words with minimal visual prompts.
A – Client demonstrates improved expressive language, sequencing skills, and articulation overall, though some fronting and final-consonant omissions are ongoing. He benefits from visual cues. Speech intelligibility has improved from prior sessions and client is making good progress toward goals.
P – Continue ST as per plan of care. Target word-final /g/ phoneme and read “ Good Night Moon ” next session.
2. Be Mindful of Colleagues
To help your therapy patients more effectively, it is important to be conscientious about the fact that other clinicians will be reading and reviewing your notes. This includes collaborating with an in-house treatment team and outside sources such as a representative from the patient’s commercial insurance plan.
Be sure not to use shorthand, jargon, or made-up acronyms – instead, utilize common industry terminology and language. This ensures all readers will understand the note and leads to more effective patient care with multidisciplinary collaboration.
3. Implement an EMR (Electronic Medical Records) System
When everyone in your therapy practice uses the same system to access patient data, they have easy access to everything they need without having to dig through paper files or email attachments. This means no more opening multiple tabs on the computer just to find out what services the patient received last week.
With an electronic EMR, EHR , or practice management software, you will have fewer errors on documents like treatment plans, session notes, and insurance claims because the system automatically checks data entry for accuracy before it reaches your patients or payors. This saves time and prevents costly mistakes that can damage your reputation with patients and insurers alike.
Learn more about practice management software for your multidisciplinary therapy practice.
About the Author

Speech-Language Pathologist & Sales Consultant
Olga is a Speech and Language Pathologist with over 12 years of experience in the field, specializing in swallow disorders, accent modification, and speech therapy services for adults working to improve overall personal and professional communication skills. Olga received her Bachelor’s degrees in Psychology and Linguistics from the University of Michigan in 2007 and her Masters in Communication Science and Disorders from Wayne State University in 2010.
She has since worked in several states and healthcare settings, currently residing in Northern VA and providing speech therapy services to clients via teletherapy and in acute care at three local hospitals.
Share with your community
Sign up for our Newsletter
Subscribe to our monthly newsletter on the latest industry updates, Rethink happenings, and resources galore.
Related Resources

Clinical Quality and Financial Health – Must We Choose?

A “Solopreneur” Venture into Health and Fitness

Assessing and Teaching Job-Related Social Skills: Maximizing Success of Neurodiverse Employees
- Our Solutions
- Start-Up ABA
- Scaling Practices
- Enterprise Practices

©2024 Rethink. All rights reserved.
49 W 27th St, 8th floor, New York, NY 10001
- Privacy Notice
- Terms of Use
We Use Cookies
Privacy overview.
| Cookie | Duration | Description |
|---|---|---|
| __hssrc | session | This cookie is set by Hubspot whenever it changes the session cookie. The __hssrc cookie set to 1 indicates that the user has restarted the browser, and if the cookie does not exist, it is assumed to be a new session. |
| elementor | never | This cookie is used by the website's WordPress theme. It allows the website owner to implement or change the website's content in real-time. |
| viewed_cookie_policy | 1 year | The cookie is set by the GDPR Cookie Consent plugin to store whether or not the user has consented to the use of cookies. It does not store any personal data. |
| Cookie | Duration | Description |
|---|---|---|
| __hstc | 5 months 27 days | This is the main cookie set by Hubspot, for tracking visitors. It contains the domain, initial timestamp (first visit), last timestamp (last visit), current timestamp (this visit), and session number (increments for each subsequent session). |
| _ga | 2 years | The _ga cookie, installed by Google Analytics, calculates visitor, session and campaign data and also keeps track of site usage for the site's analytics report. The cookie stores information anonymously and assigns a randomly generated number to recognize unique visitors. |
| _ga_3HH529JMSZ | 2 years | This cookie is installed by Google Analytics. |
| _gcl_au | 3 months | Provided by Google Tag Manager to experiment advertisement efficiency of websites using their services. |
| _gid | 1 day | Installed by Google Analytics, _gid cookie stores information on how visitors use a website, while also creating an analytics report of the website's performance. Some of the data that are collected include the number of visitors, their source, and the pages they visit anonymously. |
| CONSENT | 2 years | YouTube sets this cookie via embedded youtube-videos and registers anonymous statistical data. |
| hubspotutk | 5 months 27 days | HubSpot sets this cookie to keep track of the visitors to the website. This cookie is passed to HubSpot on form submission and used when deduplicating contacts. |
| Cookie | Duration | Description |
|---|---|---|
| test_cookie | 15 minutes | The test_cookie is set by doubleclick.net and is used to determine if the user's browser supports cookies. |
| VISITOR_INFO1_LIVE | 5 months 27 days | A cookie set by YouTube to measure bandwidth that determines whether the user gets the new or old player interface. |
| YSC | session | YSC cookie is set by Youtube and is used to track the views of embedded videos on Youtube pages. |
| Cookie | Duration | Description |
|---|---|---|
| __cf_bm | 30 minutes | This cookie, set by Cloudflare, is used to support Cloudflare Bot Management. |
| __hssc | 30 minutes | HubSpot sets this cookie to keep track of sessions and to determine if HubSpot should increment the session number and timestamps in the __hstc cookie. |
| __lc_cid | 2 years | This is an essential cookie for the website live chat box to function properly. |
| __lc_cst | 2 years | This cookie is used for the website live chat box to function properly. |
| __oauth_redirect_detector | past | This cookie is used to recognize the visitors using live chat at different times inorder to optimize the chat-box functionality. |
How to Write a SOAP Note for Speech Therapy

As a pediatric speech therapist, you know that defensible documentation (i.e., clear and detailed notes) is an essential part of demonstrating your skilled service and getting paid.
Whether you use clinic software or the old pen and paper method, managing your SOAP notes and evaluations can easily become overwhelming when working with multiple patients. But you don’t have to let that affect the quality of your notes.
In this article, I’ll cover some guidelines you can follow to improve your SLP documentation with or without speech therapy documentation software . And remember: better notes mean better therapy and less claim denials.
While every SLP has their own way to document their sessions, these guidelines can help you write notes that include the critical information and present those details in a way that’s easy to digest for caregivers and other therapists. I’ve also included a SOAP note template and some other helpful resources at the bottom of the post.
Feel free to take this information and tailor it to your own note-taking style!
What is the SOAP method?
If you need a refresher on the SOAP method of note taking here’s a reminder:
- S: Subjective. This is a statement about the relevant status or behavior that has been observed in your patient. Example: “Patient’s father said, ‘Her teacher said she can understand her better now.’”
- O: Objective. This section includes quantifiable, measurable, and observable data. “The patient produced /l/ in the final position of words with 70% accuracy.”
- A: Assessment. This is where you interpret what “S” and “O” mean in your report. Example: “The patient’s pronunciation has improved 10% since the last session with visual cues of tongue placement.”
- P: Plan. This is where you look ahead to anticipate the number of sessions needed and what the next session will involve. Example: The patient continues to improve with /I/ in the final position and is reaching goal status of /I/ in the initial position. The next session will focus on /I/ in the medial position.
Whether you’re using our SOAP note template, or you’re creating a template of your own, it will help to keep those details in mind.
How to Write a SOAP Note
The elements of a good SOAP note are largely the same regardless of your discipline.
Your SOAP notes should be no more than 1-2 pages long for each session. A given section will probably have 1-2 paragraphs in all (up to 3 when absolutely necessary).
That’s enough to give a solid overview of what each session involved, how the patient is progressing, and what you anticipate working on in the near future.
Consistency
Keep in mind that length requirements, exact formats, and abbreviations vary from one employer to the next. This is where a template can come in handy.
You should never hesitate to check your employee handbook or ask about the best way for you to handle your SOAP notes so that they are consistent with what your supervisors want to see.
Whenever you’re writing a SOAP note, be sure to keep its purpose in mind. Oftentimes, speech therapists write so many notes that they occasionally lose sight of the real purpose of these notes.
The purpose is to clearly inform caregivers and other therapists about the patient’s current status and progress. They’re also used to document the need for these sessions to an insurance company so that you can be reimbursed.
7 Documentation Guidelines for Better SLP SOAP Notes
Here are seven documentation guidelines that will help improve the quality of your SOAP Notes as a Speech-Language Pathologist.
#1 Use a template
Following a template will be beneficial to your management and organization techniques. You can find plenty of templates online and then adapt them to fit your own unique approach. (In fact, here’s a free SLP SOAP note template !)
You may not always fill out every section of the template for every patient report. If that’s the case, simply leave those sections blank and write in the information that’s important where it belongs.
Following a consistent structure will help you with reference, organization, and comparisons later on. It will improve your level of detailed documentation while also making it easier for you to “fill in the blanks” and finish your notes accurately.
A SOAP note template will also make sure that you are consistently tracking the most important information for each patient.
#2 Write a note for each session
In order to write defensible documentation, you should be creating a unique note for each and every appointment.
The note that you create for each child following every session should describe the patient’s goals and treatment in a way that’s relevant to each individual patient. Different activities and interventions should be clearly justified.
Avoid “cookie cutter” notes that are generic, vague, and/or look the same for all the children you work with. These are a red flag for insurance claims reviewers.
If you’re using EMR software, you should find an option with a wide selection of content that’s able to be customized with unique responses, outcomes, and goals tailored to each child.
#3 Figure out the patient’s goals
When it comes to your SOAP notes, writing goals is crucial. However, setting too many goals can hinder your treatment plan. So be specific to each patient when prioritizing the goals and think about what limitations are the most challenging for them in day-to-day life.
When you create goals, be sure that they are SMART goals . SMART goals are easier for caregivers and other involved parties to digest and support.
A SMART goal is:
- Relevant, and
- Time-Based.
SMART goals break down a goal so that you can look at each aspect and set a date for the goal to be reached.
They also allow you to plan what needs to happen along the way for you to get there.
Make sure each patient’s long-term goals are as functional as possible. You should set short-term goals that help them reach their long-term goals incrementally, keeping them motivated and on the right path.
#4 Don’t put your notes off
The best time to complete your notes is immediately after a session when everything is fresh in your mind. Putting off your notes will increase how long it will take you to be reimbursed for the treatment.
Additionally, the further removed you are from a session, the less you will be able to remember when it comes time to write your notes. This can hinder the treatment plan and lead to you forgetting important details.
#5 Ensure your notes are neat
If you are not using an electronic system and you have opted for pen and paper, be sure that your notes are neat and legible, not only for yourself but for your patients and their caregivers as well. Your notes should be easy to read and structured in a very clear, streamlined way.
One way to keep your notes easy to read is to print out your template and writing directly into the note when it makes sense (even if you don’t use that as your final note).
#6 Include the session’s important points
Documenting each individual session is how you provide evidence about the quality and efficacy of your treatment plan. When you forget or exclude details, caregivers can begin to question the quality of the care you’re providing.
The more details you’re able to write about a given session, the better. These details will help you stay consistent with your treatment methods and replicate your approach where needed.
They can also help you better communicate with other therapists who may be working with your patients to ensure they can pick up where you left off.
#7 Exclude unnecessary information
While you should be detailed with your reports and include all the important and pertinent information, don’t fill your reports with unnecessary information. This makes it harder to read, longer to write, and more difficult for others to process. It will also clutter your note review process.
Focus on writing better, not necessarily more. Know what information is needed in order to tell the story of functional outcomes and medical necessity for your treatment plan.
That’s how you write good notes that will ultimately be reimbursed.
Other Documentation Tips
Here are a few extra tips to help you with your documentation. Like the guidelines above, these tips will help reduce claim denials and improve the effectiveness of your therapy.
Use Speech Therapy Documentation Software
If you have not already begun to use therapy documentation software to keep track of your SOAP notes, there is no better time to start. Nothing beats the versatility, ease of sharing, and security of good speech therapy practice management software .
There are multiple systems out there that you may use to handle your SOAP notes. Your clinic may even already have one in place. If that’s the case, your priority should be learning how to use the system to the fullest.
Oftentimes, even if you know how the basics (like how to create and submit a new note), you may be missing out on some valuable tools that you haven’t yet learned how to access.
On the other hand, if you are still using pen and paper or just a basic Word template for your notes, it’s worth looking into an electronic system that can help you submit your notes more efficiently and be more accurate with your note-taking.
You can find both locally installed software for your work computer and even some cloud-based platforms that can be accessed online whenever you need them.
As times goes by and these systems become more advanced and convenient, it’s likely your clinic will be switching to one in the future anyway. Getting ahead of the curve and learning how to use one of the more popular systems can help you stay relevant in the workforce and may even open up new doors for you at another clinic where such systems are already in place.
Foster Positive Development
Perhaps the absolute best advice you can take as a SLP is getting caregivers actively involved in the speech development of their child. In your SOAP notes, you should be sure to document all home education programs and other activities the child is participating in to help develop their skills.
This is also required by many insurance companies who have requirements for caregiver education and home programs. You should document all education that you are providing to the caregiver including any training you provided about interventions and strategies they can implement at home.
Double-Check Your Notes
In addition to including pertinent information that will help your patient with their development, you also need to double-check all your notes against a template and your clinical guidelines to ensure that you will be reimbursed by the insurance company for your work.
You should also know what services you should be billing for and make sure you are documenting them accurately. Additionally, know when you should bill for the time spent completing your notes as that can be a time-consuming process as well.
Use Action Words
Using action words helps to demonstrate the skilled services that you are providing, which is something insurance companies look for when reviewing claims.
You can find multiple “cheat sheets” online filled with action words tailored for your SLP SOAP notes. These action words can help speed up the note-taking process while also assisting you with documenting the skilled speech therapy services you are providing. accurate, detailed documentation for each session you complete with a patient.
Some key action words include: adapted, addressed, adjusted, clarified, coached, collected, delivered, demonstrated, drilled, established, evaluated, expanded, familiarized, formulated, guided, habituated, identified, initiated, monitored, observed, prompted, reinforced, and so on.
The use of action words can help better illustrate a challenge, progress, or goal that you are attempting to document. Using the right action words can help make your notes clearer and more concise while adding significant value to everything you detail about a given session.
Study Good Examples
The last tip for perfecting your SOAP note-taking method, is to find some great examples to learn from.
Search the web for sample SOAP notes for speech language therapy or ask your colleagues for examples of well done SOAP notes. Then you can model the structure and flow of your notes on them.
- Therapy Brands
- July 18, 2018
Related Posts
Alcohol Awareness Month
The Key to Logik Solutions’ Unparalleled Customer Service
Press Release: Therapy Brands Acquires New Hampshire-Based EchoVantage
Apex EDI Review: 79th Fastest Growing Company
8 Chiropractic Billing Resources
9 Features Every PT, OT, and Speech Therapist Needs in Their EMR
NewCrop is an ONC Certified Health IT Solution
Key to Rehab Facility Efficiency: Revenue Cycle Management
Spotting the Signs of Abuse in Mental Health Clients
The 2024 Physician Fee Schedule: Key Updates for Clinicians
Copied to clipboard!
How to Write SOAP Notes For Speech Therapy: A Step-By-Step Guide (With Examples)
March 16, 2022, share this post.
What are SOAP notes and why are they important for speech therapy?
Subjective .
- Patient's medical history
- Symptoms or complaints related to the reason for speech therapy
- Perception and feelings about the patient's condition and therapy
- Patient's functional abilities and needs in daily life
- Goals or expectations about speech therapy
- Other information that could impact performance or progress in therapy, e.g., poor sleep
Objective
- Results of speech therapy assessments and measurements
- Description of the speech therapy interventions you provide
- Observations about the patient's function
- Observations about the patient's participation in therapy
- Record of what happened during the visit and number of visits provided
Assessment
- Progress toward patient outcomes and goals; whether or not a goal has been met
- Lack of progress toward goals, and reasons why, i.e., complicating factors
- Change in functional level or impairment severity compared to the evaluation or previous treatment sessions
- Inconsistencies between the subjective data and objective data, or differences between what is reported and what is observed during the visit
- When the patient's next visit is scheduled and what will be done to facilitate progress toward goals
- How many visits the patient has remaining before discharge from speech therapy
- Plans to consult with other health providers, e.g., doctor, PT, or OT
- What the patient, family, or caregiver will do to support therapy at home or what they need to do before the next treatment session
- Any resources that need to be prepared before the next visit
- Changes that will be made to the treatment plan, e.g., upgrade goals that were met or discharge ineffective interventions
Putting It All Together

Dana Parker (PTA)
Delete Blog post
Are you sure you want to delete this post? It will be permanently deleted.
Schedule a Demo
Learn more about textexpander from our experts., speech therapy soap note templates and examples.
Speech-language pathologists (SLPs) are vital in assessing and treating communication and swallowing disorders. Accurate documentation in speech therapy, such as SOAP notes, is essential for effective treatment planning and progress tracking. These notes serve as a critical communication tool, ensuring that every nuance of a patient's progress is captured and communicated effectively. Their structured format is designed to streamline the complex data that SLPs work with, making the process of speech therapy more transparent and traceable.
Table of Contents
What is a Speech-Language Pathology (SLP) SOAP Note?
How to write clearly & efficiently with the soap format, benefits of the soap format, soap note template.
- SOAP Note Examples
Type less. Say more.
Leave boring, repetitive copying & pasting in the past. Share text and images wherever you can type--so you can focus on what matters most.
(No credit card required)
A SOAP note is a widely used method of documentation for healthcare providers. For SLPs, it encompasses a patient’s subjective reports, objective data, an assessment of their condition, and a subsequent treatment plan.
Here are the keys to writing notes using the SOAP format for SLPs:
- Subjective: Document the patient’s subjective impressions of their condition. This includes their personal experiences, feelings, and perspectives related to their speech and language issues.
- Objective: Record observable and measurable data collected during the session. This could encompass clinical measurements, test results, and direct observations of the patient’s speech and language abilities.
- Assessment: Evaluate and summarize the patient’s progress and performance within the session. This is where the SLP synthesizes subjective and objective information to form a clinical judgment about the patient’s current status.
- Plan: Develop a strategic approach for ongoing treatment. This includes outlining therapy goals, determining the frequency of sessions, and planning any home exercises or activities.”
Effective SOAP notes are concise and informative. Here are some tips to write clearly and efficiently:
- Be Succinct: Write short, direct sentences. Use bullet points to list symptoms, observations, and actions.
- Prioritize Information: Start with the most critical information that impacts patient care.
- Use Plain Language: Avoid or explain jargon and technical terms. This makes your notes accessible to all healthcare team members.
- Be Specific: Provide enough detail for others to understand the context. For instance, instead of writing “patient showed improvement,” specify “patient’s stuttering decreased by 10% from the last session.”
- Consistency is Key: Use the same format and order each time you write a SOAP note. This predictability makes it easier to find information.
- Reflect on Objectives: Connect the patient’s progress to the treatment objectives. This shows a trajectory of care.
- Review for Clarity: Before finalizing the note, read it to ensure it’s clear and free of ambiguity or errors.
The SOAP format is not just a procedural tool—it is a strategic approach that offers numerous benefits:
- Enhanced Communication: It promotes clear communication between SLPs and other healthcare providers by using a universal structure.
- Focused Documentation: Each section of a SOAP note serves a distinct purpose, ensuring that documentation is comprehensive yet focused.
- Improved Continuity of Care: Standardized notes make it easier for any practitioner to pick up where another left off, providing continuity in multi-provider settings.
- Efficient Review: The format allows for quick scanning of a patient’s history and therapy progress, which is crucial in time-sensitive clinical environments.
- Goal-Oriented Planning: By clearly outlining assessments and plans, SOAP notes help keep the patient’s therapy goals in focus, ensuring that each session contributes to these objectives.
Speech Therapy SOAP Note Template
Here’s a basic template for an SLP SOAP note:
Subjective: – Patient’s reported concerns – Observations about behavior and affect
Objective: – Clinical findings (articulation, fluency, voice, hearing) – Data from the session (error rates, level of assistance needed)
Assessment: – Professional interpretation of objective findings – Progress in comparison to previous sessions
Plan: – Adjustments to therapy objectives – Specific interventions for upcoming sessions – Recommendations for practice at home
Speech Therapy SOAP Note Examples
Using the above template, here are some illustrative examples:
- Subjective: Mr. Thompson, a 58-year-old high school teacher, reports increased difficulty projecting his voice during lectures, causing him to feel fatigued by the end of the day.
- Objective: A voice assessment indicates a 15% reduction in vocal volume and hoarseness post-30 minutes of continuous speaking.
- Assessment: Mr. Thompson demonstrates signs of vocal strain, likely related to voice overuse in a classroom setting, which is exacerbated by inadequate vocal rest and poor hydration.
- Plan: Recommend voice therapy focusing on vocal hygiene and relaxation techniques. Advise a minimum of two therapy sessions per week and regular check-ins with an otolaryngologist. Suggest using a classroom amplifier to reduce strain.
- Subjective: Miss Garcia, a 10-year-old with a repaired cleft palate, expresses frustration with classmates having difficulty understanding her speech, particularly during group activities.
- Objective: Articulation assessment reveals compensatory articulation strategies leading to reduced intelligibility, especially for fricative and affricate sounds.
- Assessment: Despite Miss Garcia’s previous progress, residual articulation challenges continue to affect her speech intelligibility and social interactions at school.
- Plan: Plan to enhance articulation therapy with a focus on fricatives and affricates, utilizing visual aids and tactile feedback. Engage in peer-group activities to improve communicative confidence. Schedule sessions twice a week with additional at-home exercises.
- Subjective: Mr. Jenkins, a 72-year-old retiree with recent left hemisphere stroke, reports frustration with word-finding difficulties and his inability to communicate effectively with his family.
- Objective: During a structured naming task, Mr. Jenkins exhibited a 40% occurrence of anomia, with circumlocution observed during conversation.
- Assessment: Mr. Jenkins’ aphasia impacts his expressive language abilities, contributing to communication deficits that affect his daily interactions and quality of life.
- Plan: Initiate intensive aphasia therapy focusing on naming exercises and functional communication strategies. Incorporate family education sessions for communication partner strategies. Schedule therapy four times per week and provide a list of daily exercises to encourage language retrieval practice.
These examples incorporate specific patient details that provide a clearer picture of individual challenges and tailored therapy plans, demonstrating the personalized nature of speech therapy treatment.
The value of the SOAP note in speech therapy extends far beyond the bounds of routine documentation. The SOAP note is an indispensable tool for SLPs, supporting precise documentation and efficient communication among healthcare providers, thereby ensuring quality patient care.
What is TextExpander
With TextExpander, you can store and quickly expand full email templates, Slack messages, and more anywhere you type. That means no more misspellings, no need to memorize complex instructions, or type the same things over and over again. See for yourself here:
Not able to play the video? Click here to watch the video
Try it for yourself
With TextExpander, you can store and quickly expand full email templates, email addresses, and more anywhere you type. That means you’ll never have to misspell, memorize, or type the same things over and over again.
First, select a snippet you would like to try
Next, type this shortcut below: SOAP SNE1 SNE2 SNE3
Stop typing the same thing over and over again.
With TextExpander, you can easily create custom snippets just like this.
Free for 30 days
Work smarter.
With TextExpander, you can store and quickly expand snippets anywhere you type. That means you'll never have to misspell, memorize, or type the same things over and over, ever again.
Related templates
New patient email templates.
As a medical customer service agent, creating a positive first impression is invaluable. In this article, we present five new patient email templates. These templates will help you communicate effectively with your new patients.
Patient Appointment Email
Effective communication is vital in healthcare and appointment confirmation emails is a key responsibility. In this article are five templates helping streamline communication and enhance patient-provider relationships.
Patient First Billing Email
Providing exceptional customer service is more crucial than ever. In this article, we'll explore the essential elements of crafting compassionate, clear, and effective billing emails that prioritize patient satisfaction.
Less Repetition, More Customer Delight
TextExpander gives your team the power to do what they do best — faster.
Stop repetitive typing
With TextExpander, you can fly through repetitive tasks quickly by expanding the messages your team types regularly w/ just a few keystrokes.
- Create, share, and edit snippets of repetitive text
- Customize and optimize your snippets across teams
- Respond quickly and effectively from any platform
- Reduce burnout, onboard quickly, and ensure team alignment
(No credit card required / Free for 30 days)
- Start Free Trial
- Learning Center
- Getting Started
- Troubleshooting
- Public Groups
- Recruitment
- Customer Support
- Development
- About TextExpander
- Partner with TextExpander
© 2024 TextExpander, Inc. TextExpander is a registered trademark.
Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Tips for Effective SOAP Notes

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
Find the appropriate time to write SOAP notes.
Avoid: Writing SOAP Notes while you are in the session with a patient or client. You should take personal notes for yourself that you can use to help you write SOAP notes.
Avoid: Waiting too long after your session with a client or a patient has ended.
Maintain a professional voice.
Avoid: “The client had a blast during the group therapy session.”
“Had a blast” is informal and not descriptive.
Use instead: “The client smiled and laughed during the group therapy session.”
This statement specifically describes the actions of the client and maintains a formal voice.
Avoid overly wordy phrasing.
Avoid: “Careful consideration and thought have lead this clinician to conclude that the client responds very positively to physical cues.”
This statement is overly wordy and could be simplified to state the main idea in a quicker and more precise manner.
Use instead: “The client shows greater success with activates involving physical cueing.”
This statement quickly draws a conclusion that might be helpful for a future practitioner.
Avoid biased overly positive or negative phrasing.
Avoid: “The client could not even say his own name.”
This statement is judgmental and makes an assumption about the client’s ability without specific evidence to substantiate it.
Use instead: “The client did not verbalize his name after being prompted twice by the clinician, ‘Tell me your name.’”
This statement gives specific information regarding the client’s behavior under specific circumstances without being judgmental.
Be specific and concise.
Avoid: “The client was able to write her name.”
This statement is vague, and it is unnecessary to write “was able to.”
Use instead: “Given a pen, paper, and verbal instructions, the client wrote her name legibly.”
This statement gives specific details regarding the circumstances of the observation and is not overly wordy.
Avoid overly subjective statement without evidence.
Avoid: “Client was very frustrated”
Words like “very” and “a lot” do not help the reader understand behaviors of the client.
Use instead: “Client grimaced and sighed repeatedly during the latter half of the therapy session”
This statement gives the reader a clear description of the client’s behaviors without making assumptions about the client’s internal state that lack specific support.
Avoid pronoun confusion.
Avoid: “The clinician instructed the client to state her name.”
It is unclear whose name the client was asked to say.
Use instead: “The clinician instructed the client to state the client’s first name.“
A commonly used term in some fields that can help to avoid confusion is “this clinician.”
Avoid: “Client stated that his father was in town. He reported that he feels that he frequently
ignores what he says whenever they are together.”
Who is ignoring whom?
Use instead: “Client stated that his father was in town. Client reported that he feels that his
father frequently ignores what the client says whenever they are together.”
Be accurate but nonjudgmental.
While other healthcare professionals are the primary audience of SOAP notes, be sure that the SOAP note is written so that it would not be construed as offensive were a family member to read it.
Avoid: “The client’s mother, obviously mistaken, claimed that Susie said her first word at three months of age.”
The wording “obviously mistaken” is overly judgmental and does not add any important information to the SOAP note.
Use instead: “The client’s mother reported that Susie said her first word at three months of age.”
This statement is accurate and nonjudgmental. A healthcare professional familiar with typical language development would recognize that such an event is implausible.
Home > Blog > What is a SOAP note & How to Write SOAP notes (With Templates)

What is a SOAP note & How to Write SOAP notes (With Templates)
Ehab Youssef

Hate writing progress notes? Join thousands of happy therapists using Mentalyc AI.
Sometimes, one might have nightmares for no reason at all. At other times, your work might be spilling over into your dreams! You are astonished. Aren’t you? Let me explain: you are a mental health provider struggling with hundreds of patient cases.
You scribble down unorganized therapy notes , and you end up crashing with therapeutic standards and regulations, not to mention the huge efforts you wasted trying to remember clients’ information while deciphering useless notes. No worries, we understand how much you are going through; it is for this reason that this blog exists.
In this blog, we tackle one of the most important tools that will arm you with the ability to convey clients’ information accurately, clearly, and succinctly, thereby serving as a key skill you should strive to master: we are talking about SOAP notes in mental health. Writing practical SOAP notes is an essential skill for any mental health professional.
We will also explore the ins and outs of SOAP note templates for anxiety and depression and provide tips and best practices for creating well-organized and informative notes. So, let's dive in!
Let Mentalyc AI Write Your Progress Notes Fast
✅ HIPAA Compliant
✅ Insurance Compliant
✅ SOAP, DAP, EMDR, Intake notes and more
✅ Individual, Couple, Child, Family therapy types
✅ Template Builder
✅ Recording, Dictation, Text & Upload Inputs
SOAP Notes in Mental Health Practice
Although SOAP notes were initially developed for use in medical settings, they have become increasingly popular in mental health practice due to their clear and concise format. Mental health professionals can use SOAP note templates for anxiety and depression for example to ensure they are effectively documenting the essential information needed for effective treatment planning and collaboration with other providers.
There are also other document formats that mental health professionals may encounter or choose to employ, such as DAP (Data, Assessment, Plan) and BIRP (Behavior, Intervention, Response, Plan) notes. Each format has its unique features and benefits, and the choice of which format to use often depends on personal preference and the specific needs of the clinician and their clients. For a more in-depth comparison of these documentation formats, check out our articles on DAP notes and BIRP notes .
What a SOAP note is and how it's used?
A SOAP note is a structured method used for documenting a patient's medical information during a therapy session. The SOAP acronym stands for Subjective, Objective, Assessment, and Plan, which are the four main components of a well-organized note. Developed by Dr. Lawrence Weed in the 1950s, SOAP notes have become the standard method for documenting patient progress and facilitating communication between healthcare providers.
Take your time back! Get your progress notes done automatically.
What is the soap writing method.
The SOAP writing method is a structured approach commonly used in medical and healthcare settings to document patient encounters and organize patient information. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, which represents different sections of the documentation.
The Four Parts of a SOAP Note
1. Subjective
The subjective component of a SOAP note focuses on the patient's personal experiences, feelings, and concerns. This section should include details about the patient's chief complaint, history of present illness, medical and family history, and any relevant social or environmental factors. When writing the subjective portion, it's essential to use the patient's words as much as possible to accurately convey their perspective.
2. Objective
The objective section of a SOAP note records observable data and factual information about the patient. This can include vital signs, physical examination findings, laboratory results, and any additional diagnostic data. In the context of mental health treatment, the objective section may also include details about the patient's appearance, behavior, and speech patterns.
3. Assessment
The assessment portion of a SOAP note is where the healthcare provider evaluates the information gathered during the subjective and objective sections. This section may include a diagnosis, a summary of the patient's progress, and any potential risk factors or complications. In the case of anxiety and depression, the assessment might focus on the severity of symptoms, the effectiveness of current interventions, and any co-occurring conditions.
The plan section outlines the next steps in the patient's treatment, including any changes to their current interventions or the addition of new therapies. For anxiety and depression, this might involve adjustments to medications, the introduction of new coping strategies, or referrals to additional support services.

Increase your practice's revenue and reduce therapist burnout
Are soap notes still used.
Yes, SOAP notes are still widely used in medical and healthcare settings. Despite the emergence of electronic health records (EHRs) and other digital documentation methods, the SOAP format remains a popular and effective way to document patient encounters.
SOAP Note Templates
Anxiety soap note template.
Subjective :
Chief complaint: Patient reports feeling "constantly on edge" and experiencing panic attacks.
History of present illness: Patient describes a 6-month history of increasing anxiety symptoms.
Relevant personal and social history: Recent job loss, family history of anxiety disorders.
Objective :
Appearance: Anxious, fidgety, avoids eye contact.
Behavior: Rapid speech, difficulty sitting still.
Psychiatric symptoms: Reports excessive worry, restlessness, irritability, and sleep disturbances.
Assessment :
Diagnosis: Generalized Anxiety Disorder (GAD).
Progress: Patient has been attending weekly therapy sessions for 2 months with some improvement in symptoms.
Continue weekly therapy sessions focused on cognitive-behavioral techniques.
Consider medication evaluation if symptoms do not continue to improve.
Encourage patient to engage in relaxation exercises and regular physical activity.

Have your progress notes automatically written for you!
Depression soap note template.
Chief complaint: Patient reports feeling "hopeless" and lacking motivation.
History of present illness: Patient describes a 3-month history of depressive symptoms.
Relevant personal and social history: Recent relationship breakup, social isolation, family history of depression.
Appearance: Disheveled, poor eye contact, flat affect.
Behavior: Slow speech, minimal spontaneous movement.
Psychiatric symptoms: Reports persistent sadness, loss of interest in activities, fatigue, and difficulty concentrating.
Diagnosis: Major Depressive Disorder (MDD).
Progress: Patient has been attending bi-weekly therapy sessions for 1 month with minimal improvement in symptoms.
Increase therapy sessions to weekly and incorporate cognitive-behavioral techniques.
Schedule a medication evaluation with a psychiatrist.
Encourage patient to engage in social activities and regular physical activity.
How to Write Effective SOAP Notes
Writing well-organized and informative SOAP notes is crucial for effective treatment planning and communication between healthcare providers. Here are some tips write a soap note of high quality:
1. Be concise and specific : Avoid using vague language or unnecessary details. Instead, focus on providing accurate and relevant information about the patient's condition and treatment plan. 2. Use the patient's words : Whenever possible, use direct quotes from the patient to convey their subjective experiences and feelings accurately. 3. Separate subjective and objective information : Make a clear distinction between the patient's self-reported symptoms (subjective) and the observable data gathered by the healthcare provider (objective). 4. Update the assessment and plan sections regularly : As the patient's condition changes, make sure to update the assessment and plan sections to reflect their current status and treatment goals.
How long should a SOAP note be? (Length and Frequency)
The length of a SOAP therapy note will vary depending on the complexity of the patient's condition and the amount of information that needs to be documented. However, it is essential to keep SOAP notes as concise and clear as possible, including only necessary information.
The frequency of writing SOAP therapy notes depends on the specific requirements of the practice or setting in which you work. However, it is generally recommended to write SOAP notes after each session to ensure timely and accurate documentation.
By writing SOAP notes immediately after a session, you capture the most relevant and accurate information while it is fresh in your mind. This helps to ensure the accuracy of your notes and minimizes the risk of forgetting important details. It also allows you to track the client's progress over time and make informed decisions about their treatment plan.
Writing SOAP notes after each session also promotes consistency in documentation, which is important for effective communication among healthcare professionals involved in the client's care. It provides a standardized format for recording information, making it easier for other professionals to understand the client's history, progress, and treatment goals.
In some cases, there may be exceptions to writing SOAP notes after every session, such as when multiple sessions occur within a short period or when the sessions are part of a continuous treatment plan. In such situations, it may be appropriate to summarize multiple sessions in a single SOAP note, highlighting the key information and progress made during that period.
Ultimately, the frequency of writing SOAP therapy notes should align with the specific needs and requirements of your practice or setting and any legal and regulatory guidelines governing documentation in your jurisdiction.
Organizing and Structuring SOAP Notes
To effectively organize SOAP notes, follow these guidelines:
1. Use a consistent format : Adhering to the standard SOAP format (Subjective, Objective, Assessment, Plan) ensures that your notes are easy to read and understand. 2. Break information into digestible sections : Divide the content into clear sections and use subheadings to further organize the information. 3. Use bullet points and numbered lists: Presenting key points in a visually appealing manner can make your notes easier to read and reference. 4. Update notes regularly : Keep your SOAP notes up-to-date by regularly updating the assessment and plan sections to reflect the patient's current status and treatment goals. 5. Incorporate technology : Consider using practice management software or other digital tools to help you manage and organize your SOAP notes. Many platforms offer built-in SOAP note templates and can automatically organize your notes by client or date, making it easier to access and review your documentation.
What are smart goals in SOAP notes?
SMART goals (Specific, Measurable, Achievable, Relevant, and Time-bound) can be a valuable addition to SOAP therapy notes. They can help healthcare professionals establish clear, objective, and realistic treatment goals for their patients, providing a framework for tracking progress and adjusting treatment plans as needed.
By incorporating SMART goals into SOAP therapy notes, clinicians can effectively measure patient progress, identify areas for improvement, and ensure that the treatment plan aligns with the patient's unique needs and desires.
When writing the Plan section of your SOAP notes, consider using the SMART goal framework to outline specific objectives for your clients' treatment. This can help to clarify expectations, promote accountability, and facilitate communication between you, your clients, and any other professionals involved in their care. Specific: Reduce the frequency and intensity of panic attacks.
Measurable : Decrease the number of panic attacks from 4 per week to 1 per week.
Achievable : Utilize cognitive-behavioral techniques and relaxation exercises to manage anxiety.
Relevant : Addressing panic attacks will improve the patient's overall mental health and quality of life.
Time-bound : Achieve this goal within 3 months of starting treatment.
Are SOAP notes written after every session?
Yes, SOAP notes are typically written after every session or patient encounter to document relevant information about the patient's condition, assessment, and treatment plan.
Pros and Cons of SOAP Notes
While SOAP therapy notes provide an organized and structured approach to documentation, there are some limitations.
1. Standardized format : The structured format of SOAP notes allows healthcare providers to quickly and easily access pertinent information about a patient's condition and treatment plan. 2. Improved communication: SOAP notes facilitate clear and concise communication between healthcare providers, ensuring continuity of care for the patient. 3. Comprehensive documentation : SOAP notes provide a thorough and organized record of a patient's progress, which can be essential for legal and insurance purposes.
1. Time-consuming: Writing detailed and organized SOAP notes can be time-consuming, particularly for busy healthcare professionals. 2. Inconsistent quality : The quality of SOAP notes can vary significantly between providers, which can lead to confusion and miscommunication. 3. Limited focus: Some critics argue that SOAP notes may not adequately capture the complexities of mental health treatment, as they typically focus on a specific problem or diagnosis.
Despite these limitations, SOAP therapy notes remain a valuable tool for healthcare professionals in providing consistent, clear, and organized documentation of patient care.
This video tutorial will teach you how to write effective SOAP notes.
The Bottom Line
SOAP therapy notes are a valuable tool for healthcare professionals in documenting patient care. By adhering to best practices, such as being clear, concise, accurate, and timely, clinicians can optimize the effectiveness of SOAP notes in facilitating communication and continuity of care. Mastering the art of SOAP note writing, utilizing templates, and incorporating best practices will enhance the quality of patient care and improve communication among healthcare providers. Mental health professionals, in particular, can benefit from mastering SOAP therapy notes when working with patients experiencing anxiety and depression. By following the components, templates, and guidelines outlined in this comprehensive guide, healthcare professionals can ensure that their SOAP notes are effective, contributing to the overall quality of care provided to patients.
Last but not least
You are not alone! We are here to transform the note-taking process into growth opportunities. With enough effort and time, you will become proficient in drafting vital psycho-therapeutical documentation. And keep in mind that, as with every skill you need to master in this life, practice makes perfect!
An App for Psychotherapists
Mentalyc is a note-taking tool that uses AI to write notes. With Mentalyc all your note-taking needs are fully automated and your notes are sure to be consistently accurate and well-written. Mentalyc helps you save time, reduce compliance risk, and allow you to focus fully on your client during sessions and not have to scribble notes during your sessions. Mentalyc now offers all kinds of notes. To learn more visit: www.mentalyc.com or Register for a free trial.
Below is an example of a SOAP note written by Mentalyc SOAP Note Generator :
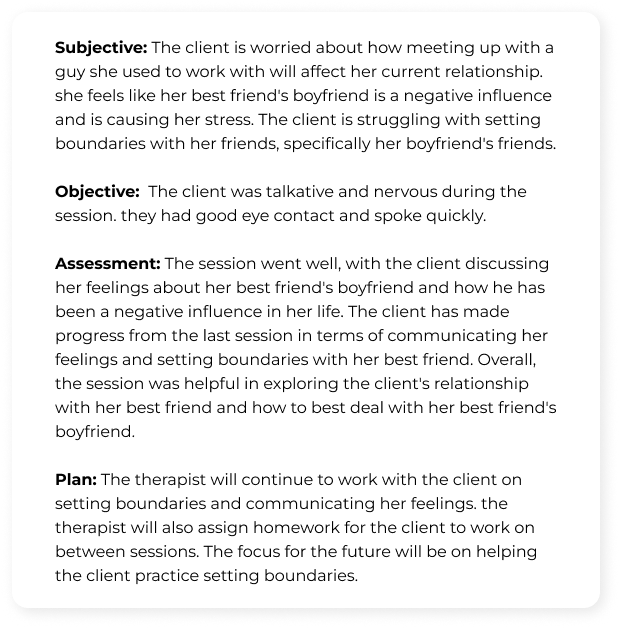
Feel free to reach out to us and give your feedback about this by using the chat function at the bottom right corner of your screen. We would appreciate your feedback.
About the author

Ehab Youssef
Ehab is a licensed psychologist specializing in transformative therapy. With extensive experience and a strong academic background, he utilizes evidence-based techniques to address various mental health concerns. Ehab's therapeutic approach combines process-based cognitive behavioral therapy, psychodynamic therapy, and other modalities to help individuals with depression, anxiety, grief, and personality disorders. As a passionate advocate for mental health, Ehab is dedicated to supporting his clients, supervising therapists, providing corporate counseling, and teaching graduate-level courses.
Learn More About Ehab
All examples of mental health documentation are fictional and for informational purposes only.
See More Posts

Best private practice counseling office decor ideas in 2024

How To Start a Private Practice as an LCSW

Documentation and Private Practice (Free Samples Included!)

Mentalyc Inc.

Copyright © 2021-2024 Mentalyc Inc. All rights reserved.
Meet the team
About our notes
Feature Request
Privacy Policy
Terms of Use
Business Associate Agreement
Contact Support
Affiliate program
Who we serve
Psychotherapists
Group practice owners
Pre-licensed Clinicians
Become a writer
Help articles
Client consent template
How to upload a session recording to Mentalyc
How to record sessions on Windows? (For online sessions)
How to record sessions on MacBook? (For online sessions)
Popular Blogs
Why a progress note is called a progress note
The best note-taking software for therapists
Writing therapy notes for insurance
How to keep psychotherapy notes compliant in a HIPAA-compliant manner
The best Mental health progress note generator - Mentalyc
3 SOAP Note Examples to Help You Write Progress Notes

As a health professional, writing progress notes is a time-consuming part of the job. Using tailored models is key to an efficient writing process and standardized notes.
In this article, we'll delve deeper into an effective way for consistently documenting your client's information: SOAP notes.
We’ll explore each component, provide tips and SOAP note examples for effective documentation.
Whether you're new to using SOAP notes or looking to refresh your knowledge, this guide will help you write clear, concise, and comprehensive SOAP notes.
What is a SOAP note?
SOAP notes are a widely used method of documentation in the healthcare field, particularly in settings where a client's progress needs to be tracked over time.
The SOAP note format was developed by Dr. Lawrence Weed in the 1960's as a way to organize client information in a structured and concise manner. It was initially used in medical records but has since been adopted across various healthcare disciplines, including mental health, occupational therapy, social work, speech therapy, and more.
One of the key strengths of SOAP notes is their effectiveness in documenting progress and conveying relevant information about the client. Whether you're a mental health counsellor documenting a therapy session, an occupational therapist assessing a client's progress, or a speech therapist tracking a client's language development, the SOAP format provides a systematic approach to documentation.
SOAP stands for:
- S Subjective
- O Objective
- A Assessment
SOAP Note Variations
In addition to the traditional SOAP format, there are variations that offer slightly different structures and focuses that may be taken into consideration when choosing a template.
APSO Notes : The APSO format places the Assessment and Plan first, followed by the Subjective and Objective information. APSO notes are often used in settings where the assessment and plan are the primary focus, and require even easier access.
SOAPE Notes : The SOAPE format adds an Education or Evaluation section after the Assessment. This format is particularly useful when documenting an evaluation of the plan or advice transmitted to the client about various aspects of the treatment process is important.
Ultimately, the choice of format should align with the goals of the documentation and the specific needs of the setting. Whether using the traditional SOAP format or one of its variations, the key is to ensure that the note is organized, concise, and effectively communicates the necessary information for continuity of care or evaluation.
Best practices for writing effective SOAP notes
Progress notes are not only a legal requirement for certified mental health professionals, but must also comply with specific standards for both public and private contexts. When writing a progress note, it's essential to consider the following criteria to determine which information to include:
- Relevance: Ensure that the information is pertinent to the client's treatment and progress.
- Organization: Arrange the information in a clear and logical manner.
- Conciseness: Be brief and to the point, avoid unnecessary details.
- Objectivity: Present factual information without personal bias or interpretation.
- Accuracy: Ensure that the information is correct and reflects the client's actual progress.
- Clarity: Use straightforward and easy-to-understand language.
- Legibility: Write in a neat and readable manner.
- Spelling: Check for and correct any spelling errors.
When writing a SOAP note, it’s important to follow the general guidelines for progress notes. The information under each heading should be relevant to the client in question and to the specific consultation context.
Here are some tips for each section:
This section focuses on subjective information that is gathered directly from the client. It should be relevant to the service request and intervention plan. It should not include interpretations and must be verified, with the source clearly identified.
- Client perceptions
- Problem description and its manifestation from the client's perspective
- Social and family context
- Expressed goals, frustrations, complaints, and expectations
- Client’s suggestions for improving their situation
- Assessment of the person’s health (mental, physical) and the intervention plan
- Reported medical and social history, including response to previous treatments and medications
- Information provided by third parties
- Relevant citations
Here, focus on objective observations that can be described clearly as facts. This includes descriptions of behaviours or activities.
- The client's appearance, behaviour or mood
- Manifestations of the client's problem (symptoms)
- Relevant information provided by other professionals
- Results and changes related to the intervention plan
In this section, integrate the subjective and objective information gathered in the previous sections to form your professional opinion.
- Professional understanding guiding the intervention plan or specific actions.
- Clinical understanding of the client’s assessment over time.
- Psychosocial assessment or reassessment.
- Predictions, conclusions, or risk factors.
This section allows you to:
- Identify the problem(s) (diagnosis).
- Justify the intervention plan.
- Identify progress (made or not).
- Understand the client’s understanding and motivation.
- Recognize repeated discrepancies between the client's reports and observations.
- Consider other intervention options or relevant follow-up resources.
- Identify new situations.
In this section, outline the intervention plan and any steps in the client’s treatment, including:
- Follow-up on the intervention plan (objectives, means, etc.)
- Modifications to the intervention plan
- Individualized service plan
- Requests for consultation or referral to other professionals
- Interventions performed or techniques used
- Intervention report
- Follow-up appointments to add to the record
- Date of the next appointment
Download our free PDF template to start using the SOAP notes template in your clinical note-taking.
SOAP Note Examples
Below are examples of SOAP notes in various clinical contexts. Please note that these are for illustrative purposes only and should not be used for actual clinical documentation.
SOAP Note Example for Mental Health Counselling
In mental health counseling, SOAP notes can help document client sessions and track progress, especially with regard to a client's mental health status and treatment plan.
Client reports feeling overwhelmed with work and personal stressors. He describes feeling anxious most of the time and having difficulty sleeping. Client reports increased irritability and difficulty concentrating.
Client's affect is anxious. He appears tense and fidgety during the session. Client's speech is rapid, and he often interrupts himself. Client's body language suggests discomfort.
Client presents with symptoms consistent with generalized anxiety disorder (GAD). Client's symptoms are significantly impacting his daily functioning and well-being. Differential diagnosis includes adjustment disorder with anxiety.
- Continue weekly counselling sessions to address anxiety symptoms and coping strategies.
- Discuss stress management techniques, including mindfulness and relaxation exercises.
- Refer client to doctor for evaluation and possible medication management.
- Schedule follow-up appointment in one week to monitor progress and adjust treatment plan as needed.
SOAP Note Example for Occupational Therapy
SOAP notes offer a structured approach to documenting client assessments, interventions, and outcomes for occupational therapists. They help facilitate effective communication among healthcare professionals and ensure comprehensive client care.
Client reports increased difficulty in performing activities of daily living (ADLs) due to pain and stiffness in the right shoulder. Client states that the pain has been present for the past month and has worsened over time. Pain is rated as 6/10 on the visual analog scale (VAS).
- Observation: Client demonstrates guarding of the right shoulder and limited range of motion during shoulder abduction and flexion.
- Range of motion: Right shoulder abduction limited to 90 degrees, flexion limited to 100 degrees.
- Strength: Weakness noted in the right shoulder, particularly in abduction and flexion.
- Palpation: Tenderness and palpable stiffness noted in the right shoulder joint.
Client presents with symptoms consistent with adhesive capsulitis (frozen shoulder) of the right shoulder. Pain and stiffness are significantly impacting the client's ability to perform ADLs independently.
- Begin treatment with modalities to reduce pain and inflammation, such as ice and ultrasound therapy.
- Initiate a home exercise program focused on improving range of motion and strength in the right shoulder.
- Educate client on activity modification and ergonomic principles to prevent exacerbation of symptoms.
- Schedule weekly occupational therapy sessions to monitor progress and adjust treatment plan as needed.
SOAP Note Example for Social Work
Here is an example demonstrating how social workers can use SOAP notes to document client interactions, interventions, and assess needs. In this context, SOAP notes help track progress, facilitate collaboration with other professionals, and ensure effective care.
Client reports feeling overwhelmed with financial stressors. She recently lost her job and is struggling to make ends meet. Client expresses feelings of shame and embarrassment about her current situation.
- Observation: Client appears anxious and restless during the session. She avoids eye contact and fidgets with her hands.
- Housing: Client is currently living in a shelter and is concerned about finding stable housing.
- Support system: Client reports limited support from family and friends.
Client presents with acute stress related to recent job loss and financial instability. Client's feelings of shame and embarrassment are impacting her self-esteem and ability to seek help.
- Provide crisis intervention to address immediate needs, including connecting client with resources for food, housing, and financial assistance.
- Develop a safety plan with client to address feelings of hopelessness and suicidal ideation.
- Refer client to a support group for individuals experiencing similar challenges.
How to write SOAP notes with Psylio
Psylio is a comprehensive recordkeeping platform designed to streamline note-taking, client appointments, and financial management. With built-in templates, such as the SOAP notes template, using Psylio can help you save time and simplify your workflow.
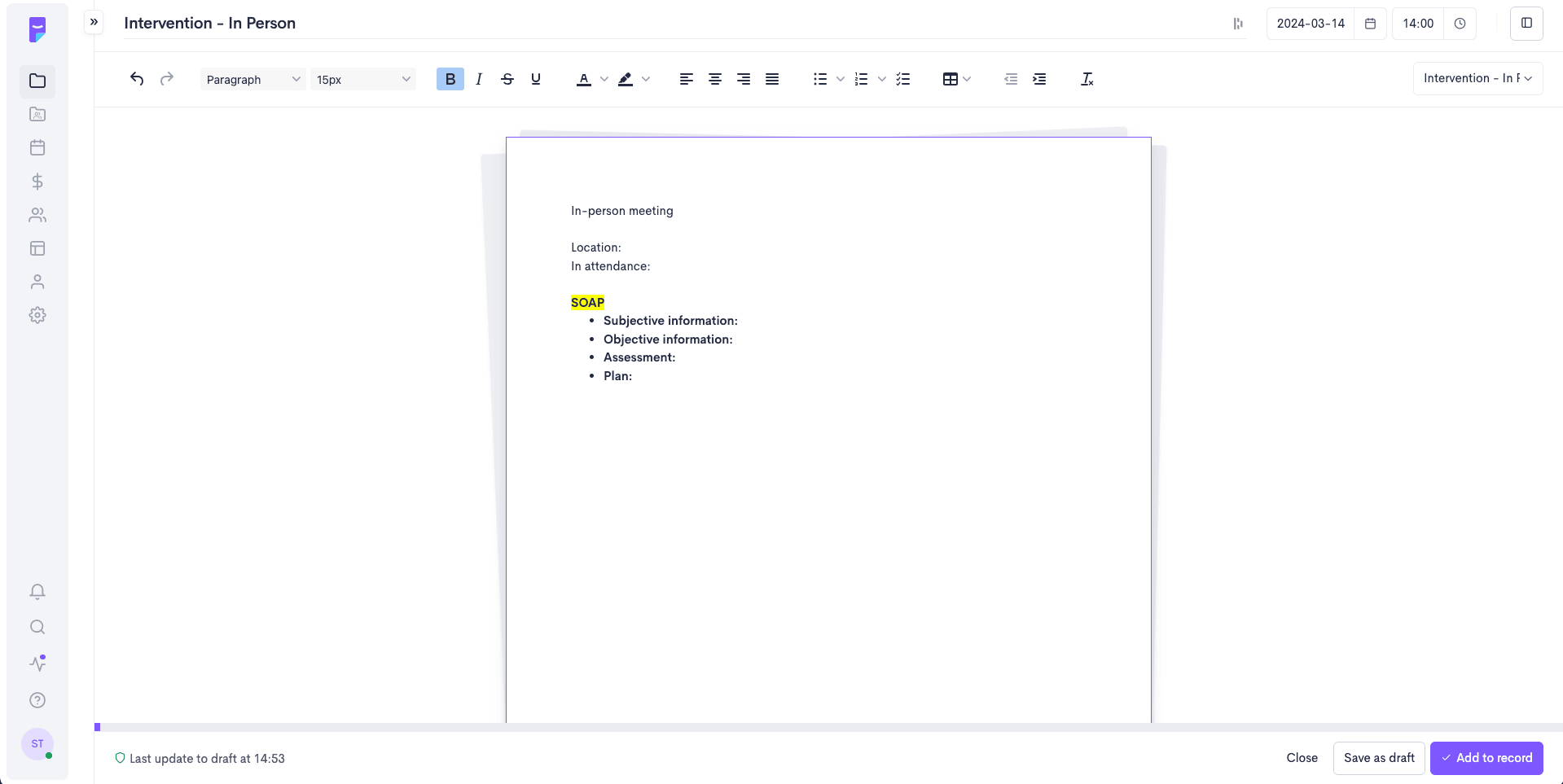
To access the SOAP note template directly integrated into your client progress notes:
A SOAP note is one of several models used in clinical note-taking. And while writing progress notes can be tedious, it's a crucial part of the clinical process.
Using templates based on your preferred models makes progress notes easier to create and ensures standardization across all your notes and among the various professionals in an organization.
Whether you use the templates directly within the Psylio platform or save our free PDF for later use, having access to these tools can free up more time for what matters most - your clients!
About the author
Sophie excels as a French and English content specialist and project coordinator for Optania. With a Bachelor of Arts and a double major in French and English literature, her linguistic expertise brings rigour and excellence to the content produced by the team.
Her experience in coordinating content writing, conducting specialized demonstrations and training, and supporting customer service operations demonstrates her continued commitment. Her passion for language and creating quality content is a constant source of motivation in her work.
Share this post!
Latest stories, patient vs. client: which term should therapists use.
Friday, June 28, 2024
Your Guide to Effective DARP Notes (with PDF Template)
Thursday, May 30, 2024
Wednesday, March 06, 2024

Manage your professional practice effectively with Psylio
Take notes, schedule appointments, manage your finances, and more—all in one place!
Resources & Support
Psylio is not only a recordkeeping platform, it is also a community of highly engaged professionals where sharing and mutual assistance is put forward!
Professional Toolbox
We offer easy and centralized access to various documents, tools and resources for both work and intervention.
A private community to share and help each other
Join a community of passionate and committed professionals. Regardless of your practice environment and clientele, you will undoubtedly benefit from the group’s richness.
Focus on the essentials: your customers

IMAGES
VIDEO
COMMENTS
Check out these examples of SOAP notes for SLPs (speech-language pathologists) for speech therapy disorders like dysphagia, stuttering, etc.
Speech therapy SOAP notes document important data and paint a picture of how the client participated in a session. That's not always easy. A speech-language pathologist's (also known as "SLP") schedule is often filled with back-to-back clients throughout the day. Having a clear understanding of what SLP SOAP notes are, and how to write ...
The SOAP format includes 4 elements for a speech therapy progress note, identified by each letter in the acronym: Subjective. This section usually frames the purpose of the session and the demeanor of the client. It also lists any relevant background information, such as diagnoses, medical history, and current problems and goals.
To Justify Your Skilled Therapy Services. Your note should: Prove that your patient needed skilled speech therapy. Clearly spell out the skilled services you provided and why your patient needed them. Justify any CPT codes you billed for. The interventions you document should match the codes you bill for that session.
The last tip for perfecting your SOAP note-taking method, is to find some great examples to learn from. Search the web for sample SOAP notes for speech language therapy or ask your colleagues for examples of well done SOAP notes. Then you can model the structure and flow of your notes on them. Free SOAP Note Template (And More!) This kit includes:
The main rule is to avoid value judgments and be completely unbiased. In the table below you'll find different aspects to include in the objective part of a treatment note and some examples of possible answers. #3. A is for Assessment. The assessment section summarizes the achievements of two previous sections.
Benefits of Using Electronic Speech Therapy Notes. Using an electronic method of recording SOAP notes for speech therapy provides many benefits for busy clinicians:. Time-efficient: Typing notes into a computer or tablet is much faster than handwriting each note.This can save significant time and energy during a session, allowing clinicians to spend more time engaging with their clients.
Check out this free SOAP note kit that includes a template, checklist, even more SOAP note examples, and 7 Tips to Improve Your Documentation. Finally, a few more tips for writing better SOAP notes: Write the notes as soon as you can after the session, or during the last few minutes if allowed. This keeps the information fresh in your mind.
Writing Excellent SOAP Notes for Speech Therapy. Create a Template to Fill in with Patient Information. Creating a template for your SOAP notes before seeing your speech-impaired patients will make your meetings more productive. With a template consisting of four separate subheadings, you can take quick notes while also talking to them actively.
Learn how to write a SOAP note so you can efficiently track, assess, diagnose, and treat clients. Find free downloadable examples you can use with clients.
Step 3: Don't forget credentials. Every speech therapy SOAP note needs to include certain credentials: your client's name (and ID number where applicable), the date/time of the session, and your own professional credentials. These details are useful when it comes to insurance and billing processes.
How To Write Therapy SOAP Notes. Therapy SOAP notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. ... It's why the framework is a commonly used standard in sectors such as Physical Therapy, Nursing, Rehabilitation, Speech Therapy, and more.
3 Tips for More Efficient SOAP Notes. Here are 3 tips for SLPs, PTs, OTs & ABA Therapy SOAP Notes: 1. Stick to the Facts. It is important to stick to the facts and provide relevant evidence. Be sure to give a clear picture of what happened during the session and be specific as possible. Let's take a look at this Speech Therapy note for example:
They may also help a professional track the progress of a patient and understand the other types of treatment and therapy the patient is receiving. When Writing a SOAP Note: Do. Be concise. Be specific. Write in the past tense. Don't. Make general statements. Use words like "seem" and "appear".
Whenever you're writing a SOAP note, be sure to keep its purpose in mind. Oftentimes, speech therapists write so many notes that they occasionally lose sight of the real purpose of these notes. The purpose is to clearly inform caregivers and other therapists about the patient's current status and progress.
Either way, writing effective SOAP notes is an essential skill in speech therapy. Quality of care and reimbursement depend on it. In this blog post, we'll walk you through the process of writing a great SOAP note for speech therapy, step-by-step, and provide examples of each component.
How to write SOAP notes. As you sit down to write a SOAP note, reflect on your session and allow the four sections of the note template to guide you to document the most important aspects of your client's current state and the progression of your treatment . 1. Subjective. The subjective section is where you document what your client is ...
You will write a SOAP note at the end of every session. The idea of a SOAP note is to be brief, informative, focus on what others need to know (e.g., doctors, nurses, teachers, OT, PT, social worker, another SLP, etc.), and include whatever information an insurance company would need to see to justify your continued involvement with the patient.
Avoid using absolutes such as "always" and "never.". Write legibly. Use language common to the field of mental health and family therapy. Use language that is culturally sensitive. Use correct spelling/grammar. Proofread your notes. Write your note as if you were going to have to defend its contents.
Speech Therapy SOAP Note Examples. Using the above template, here are some illustrative examples: Example 1: Subjective: Mr. Thompson, a 58-year-old high school teacher, reports increased difficulty projecting his voice during lectures, causing him to feel fatigued by the end of the day.
You should take personal notes for yourself that you can use to help you write SOAP notes. Avoid: Waiting too long after your session with a client or a patient has ended. Maintain a professional voice. Avoid: "The client had a blast during the group therapy session.". "Had a blast" is informal and not descriptive.
1. Use a consistent format: Adhering to the standard SOAP format (Subjective, Objective, Assessment, Plan) ensures that your notes are easy to read and understand. 2. Break information into digestible sections: Divide the content into clear sections and use subheadings to further organize the information. 3.
SOAP notes are a widely used method of documentation in the healthcare field, particularly in settings where a client's progress needs to be tracked over time. The SOAP note format was developed by Dr. Lawrence Weed in the 1960's as a way to organize client information in a structured and concise manner. It was initially used in medical records ...