
- How Do I Become a Clinical Trials Research Nurse?

Steps to Becoming a Clinical Trials Research Nurse - Education & Experience
For the 2023-2024 academic year, we have 112 schools in our MHAOnline.com database and those that advertise with us are labeled “sponsor”. When you click on a sponsoring school or program, or fill out a form to request information from a sponsoring school, we may earn a commission. View our advertising disclosure for more details.
Clinical research is the process of using science to better determine powerful and inventive means of detecting, diagnosing, treating, and preventing diseases and conditions. Clinical trials research nurses help outline trial criteria, write SOPs, evaluate research methods for efficacy, assist MDs or nurse practitioners with live procedures related to their studies, and deepen our collective medical understanding.
The international research community thrives on clinical research nursing. Research nurses are typically responsible for obtaining participants’ consent and recruiting, educating, and monitoring them. Additionally, these professionals report to the lead physician or NP and often coordinate the direct administration and evaluation of those treatments.
Some organizations use the term “clinical trials research nurse,” and others use the abbreviation “CRN.” Due to confusion concerning acronyms, most professional organizations use the former. Regardless of how you identify the position, no one can deny that as the Baby Boomers age, greater resources will be required to study the wide variety of medical problems that this generation faces.
Clinical research nurses maintain the quality, integrity, and honesty of clinical trials in both the public and private sectors, ensuring they comply with local, state, federal, and international regulations. They are often responsible for monitoring and checking in with study participants, completing test procedure paperwork, and structuring follow-up practices. These professionals develop and implement innovative solutions with numerous applications for the betterment of humankind and tackle some of our longest-running questions about human health. As students, prospective clinical trials research nurses study the components of nursing research, nursing theory, and how to evaluate the validity of the research properly.
Keep reading to learn how to become a clinical trials research nurse. Concentrating one’s studies on research nursing means joining the ranks of a small but significant quadrant of the research community.
Step-by-Step Guide to Becoming a Clinical Trials Research Nurse
Step 1 – graduate from high school.
Before graduating from high school, there are many ways that students can prepare for a career as a research nurse in clinical trials. It is recommended that to help prepare for coursework in clinical nursing and research, one should take a wide variety of courses in anatomy, physiology, mathematics, geometry, algebra, chemistry, physics, speech, and psychology. As admission to nursing programs is highly competitive, students are advised to pursue advanced placement coursework and set a goal of maintaining as high a grade point average as possible.
Another way to gain insight into the medical field is to intern at an extended care facility, nursing home, clinic, or teaching hospital. Volunteering, too, can be an excellent way to gain new perspectives on health, care, and nursing theory.
Step 2a – Graduate From an Accredited Nursing Program with an ADN (Two Years, Optional)
An associate’s degree in nursing (ADN) lays a clinical research and theoretical foundation for the work that one will undertake. Introductory coursework in anatomy, physiology, biology, nursing theory, and many more establish a skillset that blends the technical, technological, and medical.
Upon completion of two-year coursework, students will have received one of the following degrees: associate of nursing (AN), an associate of science in nursing (ASN), an associate degree in nursing (ADN), or an associate of applied science in nursing (AASN). Any of these degrees can prepare you to qualify for the NCLEX-RN exam.
Herzing University
The ASN program at Herzing University offers an accelerated, fast-paced course of study for those students wishing to achieve brisk entry into the industry. Students can complete this program in 20 to 24 months, depending on whether they have any transfer credits. General education courses are offered online, while core classes require on-campus attendance.
Made up of 70 to 73 credits, the program includes courses such as fundamentals of nursing; adult nursing systems; therapeutic use of self; pharmacology; nursing process and documentation; nursing management; mental health nursing; family nursing; and medical-surgical nursing.
- Location: Akron, OH; Birmingham, AL; Nashville, TN; Orlando, FL; Tampa, FL
- Accreditation: Higher Learning Commission (HLC)
- Expected Time to Completion: 20 to 24 months
- Estimated Tuition: $695 per credit
Step 2b – Graduate from a Nursing Program With a Bachelor of Science in Nursing (Four Years)
A BSN might be the best path for those interested in diving deeper into clinical trials research nursing. These courses of study build on the basics learned in an associate’s program, focusing on upper-level classes on research theory, nursing practice, and human resource management. At this stage, some aspiring CRNs seek concentrations focusing on clinical trials or research.
Schools such as the University of Michigan and the University of Washington boast top-notch BSN programs.
University of Michigan
The University of Michigan’s bachelor of science program in nursing provides students with a rigorous yet rewarding education filled with unique opportunities that will prepare them to become nurses and thrive as leaders in the field.
Comprising 128 credits, the program includes courses such as the culture of health; pathophysiology; reproductive health; behavioral health; health assessment; human anatomy and physiology; applied statistics; care of the family: infants, children, and adolescents; role transition; and leadership for professional practice.
- Location: Ann Arbor, MI
- Expected Time to Completion: Four years
- Estimated Tuition: Michigan resident ($1,046 to $1,133 per credit); non-resident ($2,654 to $2,815 per credit)
University of Washington
The University of Washington offers a bachelor of science in nursing (BSN) program preparing students for careers as registered nurses. Students in this program will learn from nationally acclaimed faculty members using interactive scenarios. They will learn to practice nursing skills in safe environments before performing them in supervised clinical settings.
Under the guidance of licensed care providers, students in this program will gain more than 1,000 hours of hands-on patient care experience. Students start in this program as college-level juniors after having already completed 60 semester-credits or 90 quarter-credits at the college level or a previous bachelor’s degree in a non-nursing field.
The curriculum includes courses such as foundational skills for professional nurses; foundations of professional nursing practice; foundations in pharmacotherapeutics and pathophysiology; fundamentals of nursing practice for illness care; health equity; healthcare systems and policy; ambulatory care; psychosocial nursing in health and illness; child health; and care coordination and case management.
- Location: Seattle, WA
- Accreditation: Commission on Collegiate Nursing Education (CCNE); Higher Learning Commission (HLC)
- Expected Time to Completion: Two years
- Estimated Tuition: Resident ($4,081 quarterly); non-resident ($13,580 quarterly)
Step 3a – Become Licensed as a Registered Nurse (Timeline Varies)
Each state requires that that state’s respective licensing channels must license those intending to become nurses. This directory collates data on how and where to obtain nursing licensing in all 50 states. Some states require a notarized personal statement or letter of intent with application paperwork.
The NCLEX-RN exam is the American testing standard for all registered nurses. After applying for the exam and offering proof of educational credentials, and meeting all state-specific criteria, nascent nurses must schedule an appointment to take the exam.
Administered by nursing professionals in closed exam rooms on isolated terminals, the exam uses machine learning to adapt its questions to the subject, specialization, and skill set. In some states, all of this work (including the exam) can be completed before a student’s official graduation date. This helps to expedite a nurse’s transition from student to practicing professional. Check state, institution, and employer policies before deciding on this approach.
Additionally, many certificates in clinical research, nursing science, and nursing research can be obtained online and added to one’s credential portfolio. For example, the University of Pittsburgh’s School of Nursing offers a certificate in nursing informatics .
Step 4 – Gain One Year of Clinical Trials Research Experience (One to Two Years, Optional)
Work experience in clinical trials can be critical to obtaining a clinical trials research nurse job. Many employers expect applicants to have already worked in this field. There are numerous ways to gain the necessary work experience, including working in administrative roles in trials, completing an internship, or working as a nursing assistant.
Step 5– Graduate from a Nursing Program with a Master of Science in Nursing (Two to Three Years, Preferred/Optional)
While much less common in customer and public care, advanced degrees in nursing are critical for those who wish to find a place in the leadership of clinical trials and research nursing .
Expanding on the foundations laid in a nursing BS program, an MS with a concentration in clinical research sciences often takes two or three years. Coursework covers clinical research theory, nursing theory, practicums in various healthcare and research environments, research development and coordination, clinical trial management, experiment design, and evidence-based practice, among other subjects. An MS in clinical research nursing positions students to transition into careers as research leads and assistants in pharmaceuticals, consumer products, clinical pathology, virology, oncology, and the study of infectious diseases.
Aside from nursing programs, there are also excellent master’s in clinical research degrees that nurses can complete to gain the necessary education to enter this field.
George Washington University
For example, George Washington University’s online MSHS in clinical and translational research is an excellent option for those looking to continue their education online. For a more traditional pathway, GW also hosts an on-campus clinical and translational research program that has been widely lauded.
The online MSHS program explores clinical administration, biomedical science, health policy, and community health. Graduates learn to develop best practices for bringing the latest medical science findings to the patients. This online program has no residency requirement.
The program’s 36-credit curriculum includes courses such as critical analysis of clinical research; clinical investigation; foundations in clinical and translational research; grantsmanship in translational health science; bioinformatics for genomics; biostatistics for clinical and translational research; and epidemiology translational research, among others.
- Location: Washington, DC
- Accreditation: Middle States Commission on Higher Education (MSCHE)
- Estimated Tuition: $1,315 per credit
Step 6 – Graduate with a Doctoral Degree in Nursing or a Clinical Research Discipline (Four to Seven Years, Optional)
There are two doctoral nursing degrees available, both of which are terminal, meaning that no further paths of education are available to those who hold these degrees. While a doctor of nursing practice (DNP) is a clinical practice degree intended for advanced nurse practitioners, a PhD in clinical research and trials nursing requires pursuing and studying an area of expertise that results in a doctoral dissertation and its defense.
Some advanced nursing programs will accept a BSN as a satisfactory degree when students apply for graduate school. However, the industry standard is to obtain an MSN before entering advanced postgraduate nursing studies. Always remember to contact an institution’s admissions office and check in to their criteria for application.
William Carey University
William Carey University offers a cutting-edge PhD in nursing science. This doctor of philosophy program in nursing education is a terminal degree that prepares DNP graduates to serve as nurse educators and nurse scholars. Except for four weekend meetings per year, this program can be completed entirely online and is a convenient option for full-time working students.
The curriculum includes courses such as role development for the nurse educator; curriculum development and program planning; instructional strategies and evaluation of student learning; creating an online educational environment; advanced curriculum assessment and evaluation; research development; advanced research methodology; and program evaluation.
Applicants to the program must hold a DNP from an accredited school of nursing, a GPA of 3.0, a current unencumbered nursing license, and submit three reference forms, among other requirements.
- Location: Hattiesburg, MS
- Accreditation: Southern Association of Colleges and Schools Commission on Colleges (SACSCOC)
- Estimated Tuition: $610 per trimester hour
Texas Woman’s University
Texas Woman’s University boasts two doctoral nursing programs: one in nursing science and one allowing students who have already obtained a DNP to extend their education and gain a clinical PhD. These programs can be completed either online at the Denton campus or in a hybrid format at the Houston campus.
In the nursing science PhD program, students receive the investigative aptitude, management skills, and advanced nursing knowledge needed to earn a spot at the healthcare leadership table, whether at hospitals, classrooms, or clinical settings. Admission requirements to this program include a current unencumbered U.S. RN license, a bachelor’s or master’s degree in nursing from a nationally accredited program, and a minimum GPA of 3.0.
The PhD in nursing science program requires completion of 60 credits beyond the master’s and includes courses such as philosophy of nursing science; ethical dimensions of nursing; exploring scientific literature; measurement and instrumentation in nursing research; qualitative nursing research; theory for nursing research and practice; quantitative nursing research; and determinants of health.
The DNP-to-PhD bridge program requires the completion of 42 credits. Applicants to this program must have a current unencumbered U.S. RN license, show evidence of graduation from a DNP program offered by a regionally-accredited university with national certification in nursing preferred, and have a minimum GPA of 3.5.
- Location: Denton, TX
- Expected Time to Completion: Two to four years
- Estimated Tuition: $7,140 per semester
University of Central Florida
For those seeking an online degree, the University of Central Florida offers a nursing PhD that has built a web-based curriculum around two on-campus intensives each year. This online PhD prepares graduates for careers at the forefront of nursing science, where they will be contributing to the body of knowledge and leading research in the application of innovative strategies for nursing education and clinical care.
The program requires the completion of 63 credits beyond the master’s degree. Those without an MSN degree should pursue the BSN-to-PhD in nursing program. The BSN-to-PhD program requires the completion of 72 credits beyond a bachelor’s degree.
- Location: Orlando, FL
- Expected Time to Completion: 11 to 15 semesters
- Estimated Tuition: In-state ($288.16 per credit); out-of-state ($1,073.31 per credit)
Step 7 – Obtain Certification Through the Association of Clinical Research Professionals (Timelines Vary, Optional)
Certification through the Association of Clinical Research Professionals (ACRP) demonstrates to employers that the candidate has achieved a high level of competency in clinical research education and training. Clinical trials research nurses can earn two primary certifications: a Certified Clinical Research Associate (CCRA) or a Certified Clinical Research Coordinator (CCRC).
The eligibility requirements for either certificate are the same. Candidates must have 3,000 hours of work experience in the six content areas of clinical research trials. A formal education program may substitute for up to 1,500 hours of work experience.
The content of the exams is similar and includes scientific concepts and research design, ethical and participant safety considerations, product development and regulation, clinical trial operations (GCPSs), study and site management, and data management and informatics. While the exam topics are similar, the CCRC exam is more in-depth and covers more advanced material than the CCRA.
Helpful Resources for Clinical Trials Research Nurses
Many valuable resources are available for prospective research nurses, from non-profits to representative organizations to job boards. Below are some of the most useful resources for those wishing to pursue a career pathway as a clinical trials research nurse:
- Association of Clinical Research Professionals
- Center for Information & Study on Clinical Research Participation
- Clinical Trial Resources (ASCO)
- Council for the Advancement of Nursing Science
- Global Research Nurses
- National Institute of Nursing Research
- NCLEX Registered Nurse Practice Test Questions
- Oncology Nursing Society’s FAQs
- Society of Clinical Research Associates
- Eastern Nursing Research Society (ENRS)
- The Midwest Nursing Research Society (MNRS)
- Southern Nursing Research Society (SNRS)
- The International Association of Clinical Research Nurses (IACRN)
Kimmy Gustafson
With a unique knack for simplifying complex health concepts, Kimmy Gustafson has become a trusted voice in the healthcare realm, especially on MHAOnline.com, where she has contributed insightful and informative content for prospective and current MHA students since 2019. She frequently interviews experts to provide insights on topics such as collaborative skills for healthcare administrators and sexism and gender-related prejudice in healthcare.
Kimmy has been a freelance writer for more than a decade, writing hundreds of articles on a wide variety of topics such as startups, nonprofits, healthcare, kiteboarding, the outdoors, and higher education. She is passionate about seeing the world and has traveled to over 27 countries. She holds a bachelor’s degree in journalism from the University of Oregon. When not working, she can be found outdoors, parenting, kiteboarding, or cooking.
Related Programs
- 1 Online MSN/MBA Dual Degree Programs – Nursing & Business
- 2 Online Master’s Degrees in Food Safety – Regulatory Affairs & Quality Assurance
- 3 Online Master’s in Clinical Nurse Leadership (CNL)
- 4 Online Master’s in Nurse Education (MSN Degree)
- 5 Online Master’s in Nurse Informatics (MSN Degree)
- 6 Online Master’s in Nursing Administration (MSN)
- 7 Online Master’s in Clinical Research Administration Programs
Related FAQs
- 1 Are There Online Nursing Administration Programs That Do Not Require the GRE?
- 2 Clinical Significance vs. Statistical Significance
- 3 How Do I Become a Nurse Administrator?
- 4 How Do You Become a Clinical Research Coordinator (CRC)?
- 5 What Can I Do With a Master’s Degree (MSN) in Nurse Administration?
- 6 What Can You Do with a Degree in Biotechnology?
- 7 What Can You Do with a Degree in Clinical Research Administration?
- 8 What is Clinical Data Management (CDM)?
- 9 What is Nursing Administration?
- 10 What is a Clinical Application Analyst and What Do They Do?
Related Posts
A day in the life of a clinical research associate.
The clinical research associate acts as a liaison between the study's sponsor (e.g., pharmaceutical company) and the clinics where the study takes place. Because results of a clinical trial must be kept entirely transparent and not influenced by the interests of the sponsor, this is a critical role.
Nurse Educator – A Day in the Life
Nurse educators are responsible for helping to train the next generation of nurses. They work in all nursing programs, from associate degrees to doctorates. The two primary places nurse educators work are in educational programs providing instruction and in clinical settings supervising nursing student clinical internships.
How to Get Started with Billing RPM and CCM Codes in a Clinical Practice: Part 1
This article aims to help give practice managers a framework for how to wrap their heads around the RPM/CCM code workflow, so they may better decide if it makes sense to take the next step and run a pilot program of their own.
A Guide to Successful Cancer Registry Virtual Management
Cancer registries are central to a successful organization's cancer program. From quality metrics tracking to regulatory agencies at the highest level, cancer registries perform essential reporting functions and provide crucial data to drive program decisions. As working remotely becomes more of the norm, organizations must be flexible to the needs of cancer registry professionals to work in a virtual environment.
Online MSN in Nursing Administration Programs Ranked by Affordability
Student loan debt has reached epic proportions and the cost of higher education is steadily rising. To help students find affordable programs we’ve outlined the top most affordable online MSN in nursing administration programs in 2021-2022.
- Department of Health and Human Services
- National Institutes of Health
Nursing at the NIH Clinical Center
Clinical research nurse roles.
Health Care Technician The Health Care Technician is a certified nursing assistant in the state of Maryland or has completed the Fundamentals of Nursing course work in a current accredited nursing program. This role supports the activities of the professional nurse by providing patient care functions to assigned patients while maintaining a safe environment.
Patient Care Technician The Patient Care Technician is a certified nursing assistant in the state of Maryland who supports the activities of the professional nurse by independently providing patient care functions to assigned patients while maintaining a safe environment.
Clinical Research Nurse I The Clinical Research Nurse (CRN) I has a nursing degree or diploma from a professional nursing program approved by the legally designated state accrediting agency. The CRN I is a newly graduated registered nurse with 6 months or less of clinical nursing experience. The incumbent functions under the direction of an experienced nurse to provide patient care, while using professional judgment and sound decision making.
Clinical Research Nurse II The CRN II has a nursing degree or diploma from a professional nursing program approved by the legally designated state accrediting agency and has practiced nursing at the NIH Clinical Center for at least 6 months. This nurse independently provides nursing care; identifies and communicates the impact of the research process on patient care; adjusts interventions based on findings; and reports issues/variances promptly to the research team. The CRN II administers research interventions; collects patient data according to protocol specifications; evaluates the patient response to therapy; and integrates evidence-based practice into nursing practice. The CRN II contributes to teams, workgroups and the nursing shared governance process. New skills and knowledge are acquired that are based on self-assessment, feedback from peers and supervisors, and changing clinical practice requirements.
Clinical Research Nurse III The CRN III has a nursing degree or diploma from a professional nursing program approved by the legally designated state accrediting agency at the time the program was completed by the applicant.
The CRN III has practiced nursing at the NIH Clinical Center for at least 1 year. The role spans the professional nursing development from “fully competent” to “expert” nursing practice. The CRN III provides care to acute and complex patient populations, and utilizes appropriate professional judgment and critical decision making in planning and providing care. S/he masters all nursing skills and associated technology for a particular Program of Care and assists in assessing the competency of less experienced nurses. The CRN III participates in the planning of new protocol implementation on the patient care unit; administers research interventions; collects patient data according to protocol specifications; evaluates the patient’ response to therapy; responds to variances in protocol implementation; reports variances to the research team; integrates evidence-based practice into nursing practice; and evaluates patient outcomes. The CRN III assumes the charge nurse and preceptor roles as assigned. Formal and informal feedback is provided by the CRN III to peers and colleagues in support of individual growth and improvement of the work environment.
Senior Clinical Research Nurse The Senior CRN has a nursing degree or diploma from a professional nursing program approved by the legally designated state accrediting agency at the time the program was completed by the applicant.
The Senior CRN serves as a leader in all aspects of nursing practice. S/he demonstrates expertise in the nursing process; professional judgment and decision making; planning and providing nursing care; and knowledge of the biomedical research process. The Senior CRN utilizes basic leadership principles and has an ongoing process of questioning and evaluating nursing practice.
The Senior CRN may have one of three foci:
Specialty Practice- as a clinical expert for a designated patient population or program of care Management- Clinical Manager The Senior CRN-Clinical Manager (CM) is an experienced staff nurse who collaborates with the Nurse Manager and other departmental leadership to assist with operations and management of a patient care area. The CM supervises the delivery of high quality patient care and assures the appropriate use of resources (i.e. staffing, rooms, etc.). The CM interacts with the research teams and support services to promote positive patient care outcomes and maintain protocol integrity. The CM models effective leadership, outstanding communication skills, while promoting a safe, supportive and professional environment. Education- Clinical Educator The Senior CRN-Clinical Educator (CE) is an experienced staff nurse who collaborates with the Nurse Manager and other departmental leadership to oversee educational needs of unit staff. The CE develops/coordinates/evaluates orientation for new unit staff, trains/mentors unit preceptors, serves as a liaison/resource for departmental/Clinical Center/professional educational opportunities, identifies educational needs, coordinates unit in-services, and plans unit educational days. The CE designs, implements and evaluates learning experiences for all staff levels to acquire, maintain, or increase their knowledge and competence. The Clinical Educator teaches at the unit and departmental level.
Nurse Manager The Nurse Manager has 3 to 5 years of recent management experience; advanced preparation (Masters Degree) is preferred. The Nurse Manager has experience in change management, creative leadership and program development; an demonstrates strong communication and collaboration skills to foster an effective partnership with institute personnel.. The Nurse Manager demonstrates a high level of knowledge in a particular specialty practice area and utilizes advanced leadership skills to meet organization goals.
Nurse Educators Nurse Educators play a critical role in preparing staff for an ever-changing clinical research environment. The roles and responsibilities of Nurse Educators are based on the Association for Nursing Professional Development (ANPD) Scope and Standards, and includes: onboarding/orientation, competency management, education, collaborative practice, role development, and inquiry. Nurse Educators function as educators, facilitators, change agents, consultants, researchers, and leaders in the organization.
Clinical Nurse Specialist The Clinical Nurse Specialist (CNS) has a Masters or Doctorate Degree in Nursing from a state-approved school of nursing accredited by either the National League for Nursing Accrediting Commission (NLNAC) or the Commission on Collegiate Nursing Education (CCNE) with a major in the clinical nursing specialty to which the nurse is assigned. The CNS has a minimum of 5 years experience, is certified in a specialty area, and is accountable for a specific patient population within a specialized program of care.
Nurse Consultant The Nurse Consultant serves as an expert advisor and program manager for a specific area of clinical administration or clinical practice management. The incumbent serves as liaison to Clinical Center departments and the ICs for issues related area of expertise and assigned responsibility and to provide communication and consultative services to all credentialed nurses at the Clinical Center.
Nurse Scientist The Nurse Scientist is a nurse with advanced preparation (PhD in nursing or related field) in research principles and methodology, who also has expert content knowledge in a specific clinical area. The primary focus of the role is to (1) provide leadership in the development, coordination and management of clinical research studies; (2) provide mentorship for nurses in research; (3) lead evaluation activities that improve outcomes for patients participating in research studies at the Clinical Center; and (4) contribute to the overall health sciences literature. The incumbent is expected to develop a portfolio of independent research that provides the vehicle for achieving these primary objectives.
Program Director The Program Director serves as the supervisor of a group of expert advisors for a specific area of nursing expertise (education, recruitment and outreach, safety and quality, staffing and workforce planning). The incumbent coordinates, implements, and oversees all the operations of the program they oversee. They serve as the liaison to other Clinical Center departments and the ICs for issues related area of expertise and assigned responsibility and to provide communication and consultative services to all credentialed nurses at the Clinical Center.
NOTE: PDF documents require the free Adobe Reader .
This page last updated on 05/15/2024
You are now leaving the NIH Clinical Center website.
This external link is provided for your convenience to offer additional information. The NIH Clinical Center is not responsible for the availability, content or accuracy of this external site.
The NIH Clinical Center does not endorse, authorize or guarantee the sponsors, information, products or services described or offered at this external site. You will be subject to the destination site’s privacy policy if you follow this link.
More information about the NIH Clinical Center Privacy and Disclaimer policy is available at https://www.cc.nih.gov/disclaimers.html

Home / Nursing Careers & Specialties / Research Nurse
Research Nurse
What does a research nurse do, becoming a research nurse, where do research nurses work, research nurse salary & employment, helpful organizations, societies, and agencies.

What Is a Research Nurse?
Research nurses conduct scientific research into various aspects of health, including illnesses, treatment plans, pharmaceuticals and healthcare methods, with the ultimate goals of improving healthcare services and patient outcomes. Also known as nurse researchers, research nurses design and implement scientific studies, analyze data and report their findings to other nurses, doctors and medical researchers. A career path that requires an advanced degree and additional training in research methodology and tools, research nurses play a critical role in developing new, potentially life-saving medical treatments and practices.
A highly specialized career path, becoming a nurse researcher requires an advanced degree and training in informatics and research methodology and tools. Often, research nurses enter the field as research assistants or clinical research coordinators. The first step for these individuals, or for any aspiring advanced practice nurse, is to earn a Bachelor of Science in Nursing degree and pass the NCLEX-RN exam. Once a nurse has completed their degree and attained an RN license, the next step in becoming a research nurse is to complete a Master's of Science in Nursing program with a focus on research and writing. MSN-level courses best prepare nurses for a career in research, and usually include coursework in statistics, research for evidence-based practice, design and coordination of clinical trials, and advanced research methodology.
A typical job posting for a research nurse position would likely include the following qualifications, among others specific to the type of employer and location:
- MSN degree and valid RN license
- Experience conducting clinical research, including enrolling patients in research studies, implementing research protocol and presenting findings
- Excellent attention to detail required in collecting and analyzing data
- Strong written and verbal communication skills for interacting with patients and reporting research findings
- Experience in grant writing a plus
To search and apply for current nurse researcher positions, visit our job boards .
What Are the Education Requirements for Research Nurses?
The majority of nurse researchers have an advanced nursing degree, usually an MSN and occasionally a PhD in Nursing . In addition to earning an RN license, research nurses need to obtain specialized training in informatics, data collection, scientific research and research equipment as well as experience writing grant proposals, research reports and scholarly articles. Earning a PhD is optional for most positions as a research nurse, but might be required to conduct certain types of research.
Are Any Certifications or Credentials Needed?
Aside from a higher nursing degree, such as an MSN or PhD in Nursing, and an active RN license, additional certifications are often not required for work as a research nurse. However, some nurse researcher positions prefer candidates who have earned the Certified Clinical Research Professional (CCRP) certification offered by the Society for Clinical Research Associates . In order to be eligible for this certification, candidates must have a minimum of two years' experience working in clinical research. The Association of Clinical Research Professionals also offers several certifications in clinical research, including the Clinical Research Associate Certification, the Clinical Research Coordinator Certification and the Association of Clinical Research Professionals – Certified Professional Credential. These certifications have varying eligibility requirements but generally include a number of hours of professional experience in clinical research and an active RN license.
Nurse researchers work in a variety of settings, including:
- Medical research organizations
- Research laboratories
- Universities
- Pharmaceutical companies
A research nurse studies various aspects of the healthcare industry with the ultimate goal of improving patient outcomes. Nurse researchers have specialized knowledge of informatics, scientific research and data collection and analysis, in addition to their standard nursing training and RN license. Nurse researchers often design their own studies, secure funding, implement their research and collect and analyze their findings. They may also assist in the recruitment of study participants and provide direct patient care for participants while conducting their research. Once a research project has been completed, nurse researchers report their findings to other nurses, doctors and medical researchers through written articles, research reports and/or industry speaking opportunities.
What Are the Roles and Duties of a Research Nurse?
- Design and implement research studies
- Observe patient care of treatment or procedures, and collect and analyze data, including managing databases
- Report findings of research, which may include presenting findings at industry conferences, meetings and other speaking engagements
- Write grant applications to secure funding for studies
- Write articles and research reports in nursing or medical professional journals or other publications
- Assist in the recruitment of participants for studies and provide direct patient care for participants
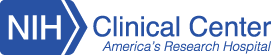
The Society of Clinical Research Associates reported a median salary for research nurses of $72,009 in their SoCRA 2015 Salary Survey , one of the highest-paying nursing specializations in the field. Salary levels for nurse researchers can vary based on the type of employer, geographic location and the nurse's education and experience level. Healthcare research is a growing field, so the career outlook is bright for RNs interested in pursuing an advanced degree and a career in research.
- National Institute of Nursing Research
- Council for the Advancement of Nursing Science
- International Association of Clinical Research Nurses
- Nurse Researcher Magazine
Related Articles
- 4 Short-Length Online and On-Campus BSN Programs to Enroll in for 2024-2025
- 10 Mistakes to Avoid When Selecting an MSN Program
- RN to BSN vs. Direct-Entry BSN: Which is Best For You?
- 10 Short-Length MSN Programs to Enroll in for 2024-2025
- Pros and Cons of the Direct-Entry MSN Program
- Do BSN-Educated Nurses Provide Better Patient Care?
- See all Nursing Articles
- Penn Medicine Biobank (PMBB)
- Center for Human Phenomic Science (CHPS)
- Investigational Drug Service (IDS)
- Biostatistics, Epidemiology and Research Design (BERD)
- Incentive Based Translational Science (IBTS)
- Program in Comparative Animal Biology (PICAB)
- Program in Research Ethics (PRE)
- Center for BioMedical Informatics Core (BMIC)
- Personalized Medicine In Translation (PERMIT)
- Translational Bio-Imaging Center (TBIC)
- Center for Targeted Therapeutics and Translational Nanomedicine (CT 3 N)
- Community Engagement and Research (CEAR)
- Engineered mRNA and Targeted Nanomedicine Core
- Neurobehavior Testing Core
- Study Design and Biostatistics
- Translational Core Laboratories (TCL)
- Research Facilitator
- Funding Opportunities
- Education & Training
- Internal Advisory Committee
- External Advisory Committee
- CTSA Leadership
- Citing the CTSA
- CTSA Oversight
- CTSA Partners
- Hub Response to COVID
- Clinical Research
- Education Overview
- Education & Training Programs
- Clinical Research Professionals
Clinical Research Nursing Certificate

Review the online info session here .
The Institute for Translational Medicine and Therapeutics (ITMAT) Education program offers an online Clinical Research Nursing Certificate. Through a combination of didactic content, highly interactive and engaging learning experiences, and collaboration with other CRNs, the certificate program will prepare nurses to navigate the growing complexities of the clinical research landscape as well as improve the safety, quality, and experience of research participants.
Bridging the gap between clinical care and research operations is an important and timely area of focus for both academic medical centers and study sponsors. The oversight of participants on high risk and early phase research protocols requires expert clinical oversight and coordination of care, and knowledge and experience in research execution. Graduates will have a foundational knowledge of the domains of clinical research nursing including human subjects protection, care coordination and continuity, contribution to science, and study management.
Graduates will:
- Understand care coordination and its application to the research process and the management of research participants
- Utilize quality improvement skills to support participants on clinical research studies
- Integrate new clinical research knowledge and clinical nursing skills
- Apply regulations, processes, and management of human subject research, focusing on the unique nursing contributions to clinical trials of drugs and devices
- Learn skills and tools required to effectively execute clinical research protocols in various patient populations and settings
Applications are currently being accepted to enroll in Fall 2024. The deadline to apply is June 30, 2024.
Contact Amanda Brock, Program Director, with any questions: [email protected]
Program Information
The certificate includes 4 courses and is designed to take 1.5 years.
Clinical Research Nursing Certificate Study Plan
4 Credit Units (CUs)

Please review the Regulatory Affairs Tuition webpage for details.
Applications are currently being accepted for Fall 2024. The deadline to apply is June 30, 2024.
Certificate Eligibility
- Applicants must be licensed nurses with at least 18 months of clinical experience
- An active RN license in any U.S. state
What We're Looking For
- BSN or a bachelor's in any related field preferred
- Existing experience in patient care and clinical expertise
- Strong critical thinking skills and clinical judgment
Application Process
Applicants must submit a full application via the online form in CollegeNET.
Please note, select "Regulatory Affairs Certificate" under Program Information as the program of study in CollegeNet. Based on your personal statement response, we will administratively shift your application to the Clinical Research Nursing Certificate.
Apply Online Now
The application form requires the following documents:
- Upload unofficial undergraduate and graduate, if applicable, transcripts into the application system
- Upon acceptance, candidates will need to provide official transcripts before beginning classes
- What are your short- and long-term professional goals, and how does the Certificate in Clinical Research Nursing help you meet your goals?
- Discuss a challenge, setback, or failure that you have faced in your nursing career. How did it affect you, and what did you learn from the experience?
- Recommender may be faculty or an employer
- The suitability of the Clinical Research Nursing Certificate for the student's stated career goals
- The student's academic ability
- English Language Proficiency (e.g. TOEFL score) for applicants whose bachelor's institution did not conduct courses in English.
The application does not require GRE score submission.
Application Fee: $25
After acceptance, applicants will need to provide proof of RN license and official transcripts.
Application Support
We encourage you to reach out to discuss your interests in the certificate program and answer any questions. Contact Program Director, Amanda Brock, [email protected].
Please review our Student Resources page .
Policies & Disclosures
The University of Pennsylvania values diversity and seeks talented students, faculty and staff from diverse backgrounds. The University of Pennsylvania does not discriminate on the basis of race, color, sex, sexual orientation, gender identity, religion, creed, national or ethnic origin, citizenship status, age, disability, veteran status or any other legally protected class status in the administration of its admissions, financial aid, educational or athletic programs, or other University-administered programs or in its employment practices. Questions or complaints regarding this policy should be directed to the Executive Director of the Office of Affirmative Action and Equal Opportunity Programs, Sansom Place East, 3600 Chestnut Street, Suite 228, Philadelphia, PA 19104-6106; or 215-898-6993 (Voice) or 215-898-7803 (TDD). Specific questions concerning the accommodation of students with disabilities should be directed to the Office of Student Disabilities Services located at the Learning Resources Center, 3820 Locust Walk, Harnwell College House, Suite 110, 215-573-9235 (voice) or 215-746-6320 (TDD).
The federal Jeanne Clery Disclosure of Campus Security Policy and Campus Crime Statistics Act, as amended, requires colleges and universities to provide information related to security policies and procedures and specific statistics for criminal incidents, arrests, and disciplinary referrals to students and employees, and to make the information and statistics available to prospective students and employees upon request. The Campus SaVE Act of 2013 expanded these requirements to include information on and resources related to crimes of interpersonal violence, including dating violence, domestic violence, stalking and sexual assault. Federal law also requires institutions with on-campus housing to share an annual fire report with the campus community.
In addition, the Uniform Crime Reporting Act requires Pennsylvania colleges and universities to provide information related to security policies and procedures to students, employees and applicants; to provide certain crime statistics to students and employees; and to make those statistics available to applicants and prospective employees upon request.
To review the University’s most recent annual report containing this information, please visit the Annual Security and Fire Safety Report or the Penn Almanac Crime Reports .
You may request a paper copy of the report by calling the Office of the Vice President for Public Safety and Superintendent of Penn Police at 215-898-7515 or by emailing [email protected] .
Recognizing the challenges of teaching, learning, and assessing academic performance during the global COVID-19 pandemic, Penn’s admissions committees for graduate and professional programs will take the significant disruptions of the COVID-19 outbreak in 2020 into account when reviewing students’ transcripts and other admissions materials as part of their regular practice of performing individualized, holistic reviews of each applicant. In particular, as we review applications now and in the future, we will respect decisions regarding the adoption of Pass/Fail and other grading options during the period of COVID-19 disruptions. An applicant will not be adversely affected in the admissions process if their academic institution implemented a mandatory pass/fail (or similar) system for the term or if the applicant chose to participate in an optional pass/fail (or similar) system for the term. Penn’s longstanding commitment remains to admit graduate and professional student cohorts composed of outstanding individuals who demonstrate the resilience and aptitude to succeed in their academic pursuits.
Please review the University of Pennsylvania required disclosures .
The University of Pennsylvania is accredited, but there is no separate accreditation for clinical research nursing programs.
The Clinical Research Nursing Certificate program does not currently accept students based outside of the U.S.
Clinical Research Nursing
This Clinical Research Nurse (CRN) program will prepare graduate-level nurses as Clinical Research Nurses, who will improve the conduct of clinical research and ultimately the quality of life for individuals, families, and communities. Research participants’ care and the research process are closely related and balancing these two goals is imperative for high-quality research and nursing care. As the number of clinical trials in the U.S. has increased, the demand for CRNs has also increased.
- Consistent with the American Nurses Association and the International Association of Clinical Research Nurses the scope and standards of practice for clinical research nursing.
- Meets the graduate level scope and standards of Clinical Research Nursing of the ANA and IACRN
- CRNs care for a wide range of participants (healthy to acutely ill) and across settings and specialties.
- Nurses can complete the program in one year full-time or two years part-time
- To provide transdisciplinary education by educating students with other health professionals
- To provide CRNs with high-level clinical skills, critical thinking skills, and, at the same time cognizance of the regulatory, ethical, and scientific issues of the clinical research environment.
- To educate nurses to meet the dual accountabilities of nursing practice and research nursing.
Practicum opportunities
Practicum opportunities are available at major medical centers in the New York City area, such as NYU Langone Health, Memorial Sloan-Kettering Cancer Center, and Rockefeller University.
Program outcomes
- Graduates are prepared to work in teams as research nurses in organizations that conduct clinical research such as universities, academic medical centers, and the pharmaceutical industry.
- Graduates are prepared to administer research interventions, collect patient data according to protocol, evaluate patients’ responses to therapy and integrate evidence-based practice into nursing practice, and evaluate patient outcomes.
- With the increase in clinical research around the world and as the number of clinical trials in the U.S. has increased, there is a strong demand for nurses with these skills.
This program is not a replacement for PhD programs that prepare nurse scientists but provides the foundation for future enrollment in a PhD program.

Clinical Research Training For Nurses: A Guide to Becoming a Clinical Research Nurse
Clinical research training for nurses, guide to becoming a clinical research nurse, what is clinical nursing research.
Nurses are known for providing direct care for patients. However, nurses may take up roles that are completely new to them within the world of clinical research. These roles include clinical research coordinator , educator and manager. They can also take up less traditional role like regulatory specialist, study monitor and IRB (institutional board review) admin.
Regulatory specialist: their activities relate mainly with preparing regulatory documents and communicating with regulatory bodies. Nurses can work as a regulatory affairs specialist, a regulatory operation coordinator, or a regulatory coordinator . They can work within government agencies, pharmaceutical companies, academic medical centers.
Study monitor: they monitor clinical research practices and make sure that it complies with necessary research protocols and regulations. They tend work at government agencies, biotechnology companies, pharmaceutical companies, contract research organizations, device manufacturers etc. Aspiring study monitors can enhance their qualifications with a Pharmacovigilance Certification .
Institutional Review Board (IRB) administrator: they are the professionals in charge of overseeing, administrating, implementing and managing IRB activities, like policies and procedures that relates to protecting human welfare. They can work at all IRBs: local, commercial or central IRB.
Nurses that have developed interest in the field of clinical research can join professional organizations. This provides them with the opportunity to network and continue their education through mediums like conferences, webinars, discussion groups, publications and online resources. These avenues serve as part of their clinical research training .
Certification is often a parameter used to measure professional expertise. This is based on criterion that reflects skill, knowledge, educational preparation, ability, and competence that are developed from experience in that area of specialization. Nurses that developed an interest in clinical research and have taken a clinical research training program have an opportunity to be certified through the:
Society for Clinical Research Professionals, Inc. (Certified Clinical Research Professionals)
Association for Clinical Research Professionals (Certified Clinical Research Associate or Certified Clinical Research Coordinator)
This field of clinical research gives nurses a chance, an opportunity to advance themselves professionally in a field that might not have been explored by them before. The benefits of having a registered nurse cover letter are insurmountable. This also provides a career path that can show family members the benefits of working in the medical field.
Nurses that have gone through the clinical research for nurses , otherwise called research nurse can carry out research on the various aspects of the human health, such as illness, pharmaceutical and health care methods and treatment plans. The main aim of this research is to improve the quality of health care service delivery. Helping patients and their family in a healthcare facility also brings a level of joy that is hard to find in many other career paths.
Roles of Research Nurses
They are responsible for designing and implementing research studies.
They observe procedures for treatment, collect and analyze data.
They report their research results to appropriate quarters.
They write articles and report their research findings in nursing or medical professional publications and journals.
They help in recruiting participants for studies and are involved in providing direct care for the participants.
Clinical research nurse salary can make use of their communication skills as well as their critical thinking skills gotten from their knowledge and experience in healthcare to further their career in this exciting way.
Know that future CRNs can speak to our 24/7 chat and phone advisors to request information on partial scholarships and payment plans for nurses.
2. Clinical Research Nurse Salary
The average pay for a Clinical Research Nurse is $31.28 per hour.
MD Anderson Cancer Center Clinical Research Nurse salaries - $71,503/yr
Northwestern University Clinical Research Nurse salaries - $75,005/yr
NIH Clinical Research Nurse salaries - $77,331/yr
CLINICAL RESEARCH NURSE JOB Description
A clinical research nurse conducts scientific research on different aspects of human health like illnesses, pharmaceuticals, treatment plans and healthcare methods. Their major goal is to improve the quality of healthcare services that are administered to the patients.
Source: Payscale
3. How do I get Clinical Research Nurse Experience?
Experience don’t just jump on you, you have to get it by practice. CCRPS affords you an opportunity to acquire knowledge in clinical research , and not just knowledge but experience as well. Registering for the appropriate course will boost your knowledge base and as well you get experience of clinical research first hand.
As a clinical research nurse, you will be at the forefront of new medical discoveries, and help develop breakthrough cures and medical treatments. The work that you do during your career can help some patients live longer or better quality of life. You may be responsible for studying diseases and disorders, as well as developing new treatment plans. You will also help test new treatments and medications that could possibly change the way a disease or disorder is perceived.
The field of clinical research can be very rewarding and fulfilling. A good research nurse is dedicated to their work and ready to take on everything that the profession throws their way. If you’re looking to pursue a research nursing career, you should have an excellent understanding of the research process as well as the specialty area that you’re studying.
Excellent communication skills are also a must. You must be able to effectively communicate with scientists, physicians, researchers, patients, and corporate executives.
4. What Does a Clinical Research Nurse Do?
The duties of a research nurse will typically depend on their employer and role. Some research nurses may be responsible for studying diseases, while others may help create and improve new medications and other treatments.
clinical research nursing scope and Standards of Practice
Clinical research nurses can take up clinical research jobs in institutions like research organizations, pharmaceutical companies, universities, research laboratories, government agencies and teaching hospitals.
The work that a research nurse does is quite exhaustive and it includes;
They use their knowledge of the basics of clinical research in designing and implementation of research studies.
Observation of the procedures for patient treatment, collection and analyzing of data.
They report their research findings to the relevant authorities. They may also have to present their results at health conferences and publish them in journals.
They write grant applications in order to secure funds to carry out the research.
They render assistance in the process of recruiting study subjects.
They provide direct treatment for research participants.
Research nurses that study diseases and illnesses will often perform a great deal of research, both by studying previous findings and observing patients. They may be required to examine medical journals, for instance, as well as observe, study, and care for patients suffering from a particular disease.
They make decisions based on the observations made as to which patients are the best candidates for certain clinical trials. During clinical trials , the research nurse will administer medications or perform other treatment procedures, During this process, research nurses must closely monitor each patient’s progress. This includes documenting side effects, drug interactions, and the overall efficiency of the medication.
Aside from caring for patients, documenting and recording information during clinical trials are the most important responsibility that a research nurse has. The information and data gathered during the research must be compiled into reports and handed over to senior clinical researchers or specialists.
5. How Do I Become a Research Nurse?
Don’t expect to become a research nurse overnight. It's a lot of work and you are expected to undergo years of training and experience.
The clinical research nurse job is a competitive one and certificates are not just handed out to anybody. The conditions to be eligible to take the certificate exam is that you must be an experienced registered nurse and your experience must include having thousands of hours of experience in the area of clinical research.
How to Become a Registered Nurse (RN) in 2020 that contains everything a person pursuing a nursing job should know - responsibilities, education, salaries and more.
The first step toward becoming a research nurse is to obtain a proper education. You can start with a bachelor’s degree in nursing, although many employers prefer that their research nurses have master’s degrees or even doctoral degrees in their chosen specialty. During your schooling, classes in research and statistics are a must and are courses in your chosen area of expertise.
According to clinical research job websites , many research nurses have a MSN degree and some have a PhD in nursing. Many of them attain these degrees of education in order to give them an edge on getting clinical research positions . While studying, courses in statistics and research are mandatory.
There are two main certifications that clinical research nurses can get from the Association of Clinical Research Professionals (ACRP). You can get certification to become a certified clinical research associate or you can choose to become a certified clinical research coordinator.
Take courses from CCRPS and learn more on how to become a clinical research nurse.
Discover more from Clinical Research Training | Certified Clinical Research Professionals Course
6. Clinical Research Nurse Requirements and Certifications & Nursing Cover Letter
A bachelor's degree in nursing does meet licensure requirements for graduates to become registered nurses (RNs), which qualifies individuals for the specialized certification. Bridge programs, such as an RN-to-Bachelor of Science in Nursing (BSN), require previous nursing education for admission. Nursing students complete traditional classroom courses, laboratory experiences, and a clinical practicum in a medical setting, which includes a hospital, assisted living facility, and long term care center.
For specific education in clinical research , trained RNs enroll in graduate certificate and degree programs. There students are introduced to case studies, ethical research practices, and financial matters affecting the design, implementation, and funding of clinical research trials. In a master's program, studies in research ethics point students towards ethical research practices, including a discussion on human rights, misconduct, and conflicts of interest. Graduate programs will also include quantitative research and a capstone project.
All RN-to-BSN programs will require an RN license to enroll. Master's and graduate certificates will need a bachelor's degree with sufficient prerequisite coursework in the field. In addition, they will need letters of recommendation or reference, a personal statement, and GRE scores.
Becoming a nurse researcher which is a highly specialized career requires an advanced degree and training in informatics and research methodology and tools. The initial step for these individuals, or for any aspiring advanced practice nurse, is to earn a Bachelor of Science in Nursing degree and pass the NCLEX-RN exam. Once a nurse has completed their degree and attained an RN license, the next step is to complete a Master's of Science (MSN) in Nursing program with a focus on research and writing. MSN courses prepare nurses for a career in research and usually include coursework in statistics, research for evidence-based practice, design and coordination of clinical trials , and advanced research methodology.
A TYPICAL JOB POSTING FOR A RESEARCH NURSE POSITION WOULD LIKELY INCLUDE THE FOLLOWING QUALIFICATIONS, AMONG OTHERS SPECIFIC TO THE TYPE OF EMPLOYER AND LOCATION:
MSN degree and valid RN license.
Experience conducting clinical research, including enrolling patients in research studies, Implementing research protocol and presenting findings.
Excellent attention to detail required in collecting and analyzing data.
Strong written and verbal communication skills for interacting with patients and reporting research findings.
For a person to practice nursing legally, acquiring of nursing credentials and certifications is very important. For instance, some nurses who achieve a master's degree (MSN) leave the patient care aspect of nursing, and practice in a more managerial role.
CRA JOB OPPORTUNITIES
If you choose to become a Clinical Research Associate (CRA), you will have a key role in the success of clinical trials. Most CRAs have a nursing background, like yours. You will be the primary contact and support for trial sites, ensuring that the study is conducted according to the protocol, ICH-GCP, regulatory requirements and standard operating procedures (SOPs).
The Clinical Research Associates also offers you the unique opportunity to have an exciting career in the research of drug and medical device development while making a difference in the lives of those around them.
Take courses from CCRPS and learn more on how to become a clinical research professional.
Speak to our 24/7 chat and phone advisors to request information on partial scholarships and payment plans for nurses.

About CCRPS
How much is a clinical research coordinator’s salary.
- About IACRN
- IACRN Board of Directors
- Distinguished CRN Award
- Chapter Governance Committee
- Conference Planning Committee
- Education Committee
- Membership, Marketing & Communications Committee
- IACRN Recommendations on DCT Guidance
- Join a Committee
- IACRN Leadership Program
- Research Projects
- Institutional Membership
- Membership Campaign
- Member Publications
- Publications
- CRN Certification by Portfolio
- 2024 Conference
- Calendar of Events
- 2023 Conference
- 2022 Conference
- Past Events
- Clinical Trials Day
- Post a Position
- Available Positions
Clinical Research Nursing
The specialized practice of professional nursing focused on maintaining equilibrium between care of the research participant and fidelity to the research protocol. This specialty practice incorporates human subject protection; care coordination and continuity; contribution to clinical science; clinical practice; and study management throughout a variety of professional roles, practice settings, and clinical specialties.
Please cite International Association of Clinical Research Nurses. (2012) "Enhancing Clinical Research Quality and Safety Through Specialized Nursing Practice". Scope and Standards of Practice Committee Report.
Clinical Research Nurse
- Madison, Wisconsin
- SCHOOL OF MEDICINE AND PUBLIC HEALTH/CARBONE COMP CANCER CENTER
- Health and Wellness Services
- Partially Remote
- Staff-Full Time
- Staff-Part Time
- Opening at: Apr 26 2024 at 14:25 CDT
- Closing at: May 30 2024 at 23:55 CDT
Job Summary:
The Clinical Research Nurse will join the Clinical Research Central Office (CRCO) at the University of Wisconsin Carbone Cancer Center (UWCCC) to coordinate cancer clinical research within one or more Disease-Oriented Teams. The primary duties of this job involve the management of subjects enrolled in clinical research studies at the UW Carbone Cancer Center. This position will report to the Clinical Team Manager and work under the general direction of the Principal Investigator of each research study. This position has the ability to work remotely 1 day/week and does not include any nights or weekends. Prefer full time FTE, but will consider down to 0.8 FTE for the right candidate. The Clinical Research Nurse must have a high degree of clinical expertise with a specific focus on the treatment of patients with anticancer agents and a specialized nursing competence in the field of Oncology Research.
Responsibilities:
- 10% Secures and schedules logistics for clinical research projects according to the research plan
- 10% Assists in the recruitment and screening of subjects for clinical studies by conducting physical health assessments
- 10% Provides professional nursing care to patients according to established protocols
- 15% Provides appropriate treatment plan direction and information to study participants
- 20% Serves as main point of contact and liaison to project participants, investigators, research sponsors, and the research team delivering study information in accordance with established research project standards and protocols
- 10% Collects, verifies, and enters data into database and analyzes clinical information data
- 15% Serves a primary point of contact for emergent study participant situations related to adverse effects or complications of the study
- 10% May provide expertise, training, and guidance to the community, peers, and/or students
Institutional Statement on Diversity:
Diversity is a source of strength, creativity, and innovation for UW-Madison. We value the contributions of each person and respect the profound ways their identity, culture, background, experience, status, abilities, and opinion enrich the university community. We commit ourselves to the pursuit of excellence in teaching, research, outreach, and diversity as inextricably linked goals. The University of Wisconsin-Madison fulfills its public mission by creating a welcoming and inclusive community for people from every background - people who as students, faculty, and staff serve Wisconsin and the world. For more information on diversity and inclusion on campus, please visit: Diversity and Inclusion
Preferred Bachelor's Degree Nursing
Qualifications:
Minimum one year nursing experience required. Candidates should have exceptional clinical nursing skills and expertise coupled with a strong interest in clinical research. Prior experience working with Oncology patients is preferred. Prior clinical research experience preferred. License/Certification should also include BLS certification required
License/Certification:
Required RN - Registered Nurse - State Licensure And/Or Compact State Licensure Required BCLS - Basic Life Support
Full or Part Time: 80% - 100% This position may require some work to be performed in-person, onsite, at a designated campus work location. Some work may be performed remotely, at an offsite, non-campus work location.
Appointment Type, Duration:
Ongoing/Renewable
Minimum $68,000 ANNUAL (12 months) Depending on Qualifications
Additional Information:
- Work experience should demonstrate dependability, flexibility, and maturity. Candidates must be effective at building interpersonal relationships with constructive interactions, be clear and effective communicators, promote and create collegial environments that value accountability. Employees will also be expected to uphold UWCCC core values as defined below: - Respect: Demonstrate respect for self and others -- behave professionally. - Integrity: Act with integrity and honesty. - Teamwork: Commit to and demonstrate teamwork. - Excellence: Ensure excellence, quality, and high ethical standards in conduct and performance. -TB testing and a Caregiver Background Check will be required at the time of employment. This position has been identified as a position of trust with access to vulnerable populations. The selected candidate will be required to pass an initial Caregiver Check to be eligible for employment under the Wisconsin Caregiver Law and then every four years. - The successful applicant will be responsible for ensuring eligibility for employment in the United States on or before the effective date of the appointment.

How to Apply:
To apply for this position, please click on the "Apply Now" button. You will be asked to upload a resume and cover letter, and provide three professional/supervisor references as a part of the application process. Please ensure that the resume and cover letter address how you meet the minimum/preferred qualifications for the position.
Jennifer Wilkie [email protected] 608-262-8025 Relay Access (WTRS): 7-1-1. See RELAY_SERVICE for further information.
Official Title:
Research Nurse(HS042)
Department(s):
A53-MEDICAL SCHOOL/CARBONE CANC CTR/CANC CTR
Employment Class:
Academic Staff-Renewable
Job Number:
The university of wisconsin-madison is an equal opportunity and affirmative action employer..
You will be redirected to the application to launch your career momentarily. Thank you!
Frequently Asked Questions
Applicant Tutorial
Disability Accommodations
Pay Transparency Policy Statement
Refer a Friend
You've sent this job to a friend!
Website feedback, questions or accessibility issues: [email protected] .
Learn more about accessibility at UW–Madison .
© 2016–2024 Board of Regents of the University of Wisconsin System • Privacy Statement
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Clinical Trials & the Role of the Oncology Clinical Trials Nurse
Elizabeth a. ness.
a Nurse Consultant for Education, Center for Cancer Research, National Cancer Institute
Cheryl Royce
b Chief, Office of Research Nursing, Center for Cancer Research, National Cancer Institute
Clinical trials will continue to be paramount to improving human health. New trial designs and informed consent issues are emerging as a result of genomic profiling and the development of molecularly targeted agents. Many groups and individuals are responsible for ensuring the protection of research participants and the quality of the data produced. The specialty role of the Clinical Trials Nurse (CTN) is critical to the implementation of clinical trials. Oncology CTNs have established competencies that can help guide their practice; yet, not all oncology CTNs are supervised by a nurse. Using the process of engagement, one organization has successfully restructured the oncology CTNs under a nurse-supervised model.
INTRODUCTION
Today’s standard of care was yesterday’s clinical trial. Oncology clinical trials have been and will continue to be the cornerstone for improving outcomes for individuals at risk for and living with cancer. A clinical trial is a type of patient-oriented clinical research study which prospectively assigns a participant, also known as a human subject, to one or more biomedical or behavioral interventions to evaluate health-related outcomes. 1 Discovering these new interventions and developing, implementing, and monitoring a clinical trial involves many groups and individuals ( Box 1 ). Collectively their responsibility is to ensure that the rights and well-being of the research participants are protected and to advance scientific knowledge by ensuring that data generated by the trial is accurate, verifiable, and reproducible. 2 , 3 A key role in successful implementation of a clinical trial is the study coordinator. 4
Key Groups and Individuals Responsible for Ensuring Good Clinical Practice (GCP)
Clinical trials nursing is a specialty practice that includes a variety of roles (e.g., study coordinator, direct care nurse, nurse manager, nurse educator), settings (e.g., academic medical center, private practice, research unit), and clinical specialties (e.g., oncology, cardiology, infectious disease). The clinical trials nurse (CTN) serves as a study coordinator but may have different job titles (e.g., Research Nurse Coordinator, Clinical Research Nurse, Clinical Research Coordinator) and may be supervised by a physician, investigator, or a non-nurse research manager. 5 – 9 The purpose of this article is to provide an overview of clinical trials, highlight the role of the oncology CTN (i.e., the nurse in the role of study coordinator), and share one organization’s process to unite all CTNs under one nursing office.
OVERVIEW OF CLINICAL TRIALS
Good Clinical Practice (GCP) is an international ethical and scientific set of standards for the design and conduct of research involving humans including: protocol design, conduct, performance, monitoring, auditing, recording, analyses, and reporting. It includes both regulations, which are binding, and guidelines or guidances, which are not binding, though recommended to be followed. In response to historical events of the past, regulations and guidelines have been developed ( Box 2 ). 2 – 3
U.S. Regulations Related to Clinical Trials
Several groups with regulatory authority are involved in the conduct of clinical trials in the United States (U.S.). In the Code of Federal Regulations (CFR), the two main titles related to clinical trials are Title 45 (Public Welfare) and Title 21 (Food and Drugs). Guidance documents describe an agency’s interpretation of or policy on a regulatory issue. Title 45 Part 46 is interpreted by the Office for Human Research Protections. The Food and Drug Administration (FDA) interprets Title 21 and its subparts. 11 – 12
There are five types of clinical trials ( Table 1 ). 13 , 14 Treatment clinical trials can further be characterized by phases ( Table 2 ). 14 – 16 Advancements in cancer biology, genomic profiling and the development of molecularly targeted agents (MTAs) have led trialists to re-think traditional trial designs. The emergence of basket, umbrella, and adaptive trials are examples of novel designs now being used in oncology clinical trials ( Table 3 ). 17 – 18
Types of Clinical Trials
Abbreviations: HPV, human papillomavirus; VHL, Von Hippel Lindau (VHL), BRCA1, BReast CAncer genes 1; PET, Positron emission tomography
Phases of Clinical Trials
Trials Designs for Targeted Therapies
MTA, Molecular Target Agent; NCI, National Cancer Institute; MATCH, Molecular Analysis for Therapy Choice; Lung-Map, Lung Cancer Master Protocol; I-SPY 2 Trial, Investigation of Serial Studies to Predict Your Therapeutic Response With Imaging And moLecular Analysis 2
PROTOCOL DEVELOPMENT AND REVIEW PROCESS
A protocol is the written detailed action plan that provides background about the clinical trial, specifies trial objectives, describes the trial’s design and organization, and ensures that trial procedures are carried out consistently, protecting the research participant and providing appropriate data to answer the trial objectives. Box 3 outlines the various sections of a protocol. Protocols undergo various reviews prior to participant enrollment. Some protocols will undergo a scientific review (e.g., NCI-designated cancer centers) and some will need to have additional safety reviews:
Content of a Protocol – Section titles will vary based on the clinical trial sponsor or Institutional Review Board (IRB)
- Radiation safety review if ionizing radiation is used at a frequency greater than standard of care
- Institutional Biosafety Committee (IBC) and Office of Biotechnology Activities (OBA) if human gene transfer is a component of the trial
- Sponsor review if the protocol was written by an investigator and not the sponsor (e.g., NCI sponsored trials). 19
All clinical trial protocols including the informed consent (IC) document undergo an ethical review by an Institutional Review Board (IRB) prior to their implementation. The IRB is a committee charged with the review of human subjects research. Their primary mandate is to protect and safeguard the rights and welfare of human subjects. Internationally, the IRB may be known by other names such as ethical review board or research ethics committee. 19 , 20 It is important to note that a clinical trial cannot begin to enroll participants until it has been approved by the IRB.
INFORMED CONSENT
Informed consent (IC) is a legal and ethical requirement for most health care matters and when conducting clinical research. Informed consent is having the capacity to agree for one’s self to participate in a given situation (e.g., clinical research). Informed consent is an important process in the clinical research. 21 The IC document is a written tool used by the investigator and/or other research team members to guide and reinforce the discussion with a patient about a research study. The IC document includes 8 required and 6 additional elements depending upon the type of study and IRB policy ( Box 4 ). 11 , 22 Each IRB has an IC document template that will need to be used. When working on industry sponsored trials or a trial that is conducted at multiple sites (i.e., multi-site trial), a sample IC document is provided to each investigator for re-formatting per the reviewing IRB’s template.
Elements of an Informed Consent Document( 21 CFR 50 and 45 CRF 46):
An individual’s voluntary agreement to participate in a clinical trial is demonstrated by their signature on the IC document; this is referred to as obtaining consent. However informed consent is an ongoing process of communication and mutual understanding between an individual and investigator. The research participant needs to be provided with additional pertinent new information (e.g., new risks, new procedures) throughout their participation on a clinical trial in order to make a decision to remain on the clinical trial.
The advancements in genomic profiling not only impact trial design, but the IC document and process as well. The National Human Genome Research Institute (NHGRI) recommends that the following be considered when addressing informed consent:
- Broad Versus Specific Consent
- Considerations for Families
- Considerations for Identifiable Populations
- Studies Involving Children
- Studies Involving Participants Who Cannot Give Consent
- Data and Sample Sharing Through Data Repositories and Biobanks
- Return of Results to Participants. 22
THE RESEARCH TEAM
Once the IC document is signed, protocol-specific procedures for eligibility screening will begin. If eligible, the intervention begins, data is collected, monitoring and quality control activities occur, participants are removed from the protocol based on pre-specified criteria, and data is analyzed. The results may published and, if applicable, the results are reported in ClinicalTrials.gov, a registry for publicly and privately supported clinical studies. It is the research team that orchestrates these activities. It is essential for all individuals involved in clinical research to have knowledge and understanding of research-related laws and regulations to ensure GCP. 24 – 26
Every clinical trial has a Principal Investigator (PI) who is accountable for the overall conduct of the trial and will enroll research participants. Other team members may include: sub-investigators, study coordinator (nurse or non-nurse), clinical data manager, and statistician. The types of individuals and responsibilities vary based on the clinical setting. Table 4 outlines the general responsibilities of the PI, study coordinator, and research participant. 24 – 29 It is important to note that U.S. regulations only outline the role of the Investigator, not other research team members.
Responsibilities of the Principal Investigator, Study Coordinator, and Research Participant
ONCOLOGY CLINICAL TRIALS NURSE
In the 1960’s, early chemotherapy clinical trials provided new roles for nurses. The oncology nurse needed to develop new skills and new partnerships with physician investigators while caring for patients on clinical trials. This not only included administering investigational agent(s) but also coordinating the clinical trial. 30 As a nurse, the oncology CTN must adhere to the American Nursing Association Scope and Standards of Practice and Code of Ethics along with their state’s Practice Act. In addition to the responsibilities of the study coordinator listed in Table 4 , the oncology CTN will:
- Provide and coordinate the care of the research participant
- Know the disease(s) being studied
- Understand the basics of genomics and molecularly targeted therapies including implications for participant education and informed consent
- Assess adverse events using the Common Terminology Criteria for Adverse Events (CTCAE)
- Manage toxicities within scope of license and protocol
- Educate research staff and collaborators on an ongoing basis
- Underlying disease process(es)
- Clinical trial (e.g., objectives, schema, adverse events) and their role
- Expectations for cure, control, palliation or no benefit
- Facilitate the ongoing informed consent process
- Advocate for the patient(i.e., research participant) and protocol 26
Based on the wide variation of how the oncology CTN role was implemented across various practice settings and with feedback from the Oncology Nursing Society (ONS) Clinical Trials Nurse Special Interest Group (CTN SIG), the ONS developed competencies for the oncology CTN. A complete set of the competencies can be found at: https://www.ons.org/sites/default/files/ctncompetencies.pdf . 31 Initially published in January 2010, the ONS CTN competencies are undergoing a revision that will:
- Include new functional areas (e.g., data management) incorporating some previous categorizations
- Separate required knowledge from skills and behaviors
- Add recommended resources to aid in knowledge and competency achievement
- Add a more advanced level of competencies for those with more experience or who are functioning at a higher level than the novice CTN.
THE RE-ORGANIZATION OF CTNs: ONE INSTITUTION’S EXPERIENCE
Necessity is the mother of taking chances. - A quote from Roughing It by Mark Twain, American Author and Humorist
The Center for Cancer Research (CCR) is the basic and clinical intramural research program of the National Cancer Institute (NCI). Within the CCR is the Office of the Clinical Director (OCD) which supports CCR’s clinical research program by providing biostatistical expertise, education and training, data management, auditing and monitoring activities, regulatory support and expertise, and informatics for data collection and storage.
The growth of CCR clinical research programs requiring support of the CTN has increased over the years. Historically the management of CTNs fell within the specific programs including CTN recruitment, supervision, training, personnel actions, and performance evaluations. The programs were silos in which the team functioned. By 2011, there were 74 CTNs across 13 programs, supporting 68 Principal Investigators (PIs). As the workload of one program grew there was little to no flexibility to have CTNs cross-cover from another program. The scope and volume of work was discrepant across programs. When programs expanded their research portfolio necessitating more CTN staff, the request was forwarded to the OCD for evaluation and approval. There were no standard performance evaluation metrics. Work practices for leave and attendance and telecommuting were different across programs. Communication practices were not efficient or timely. There were a multitude of reasons that supported the CCR leadership to consider centralizing the CTNs.
In 2011 the CCR leadership recognized that the organization would benefit from an integrated infrastructure for CTNs. The primary purpose was to allow nurses to report to nurses in the hopes of:
- Establishing a career path for CTNs
- Establishing core CTN competencies
- Increasing training
- Developing standard policies for time and attendance
- Allowing for the cross training required to respond to variances in workload
- Establishing an esprit de corps
- Efficiently recruiting and hiring CTNs
- Implementing human resource actions consistently
- Establishing efficient mechanisms for communication
- Ensuring collaboration with the Principal Investigators
OFFICE OF RESEARCH NURSING (ORN)
The new office would be called the Office of Research Nursing (ORN) and would become part of the Office of the Clinical Director. The Deputy Director for the CCR was sensitive to the fact that this was a major cultural shift for CTNs and the PIs. A number of town hall meetings for CTNs and PIs were held in Fall 2012 to present the idea for a new model and to elicit feedback from these stakeholders.
Building the infrastructure for this office took place between September 2012 and March 2013. The ORN was given a budget to include salaries, travel, training and supplies. A Chief needed to be recruited for the office and three team leaders needed to be hired into the ORN. The Chief was an experienced leader in nursing within the CCR with background as a CTN and nurse practitioner. The team leaders selected had a strong background in research nursing, leadership and a strong institutional knowledge. A leadership team formed and an administrative assistant hired with responsibilities for travel, supplies, management of timecards, and facilitation of the recruitment and hiring processes. Performance evaluations were created using the ONS Competencies. The ORN Chief believed that the consolidation of nursing under nursing leadership would have the potential to develop quality CTNs to support clinical research within the organization.
LEADING CHANGE THROUGH ENGAGEMENT
In order for the new model to be successful, the Chief needed to lead change by engaging clinical research staff in a mutually supported vision of the future while being sensitive to the cultural change experienced by the CTNs and the PIs. In Getting Change Right , Seth Kahan shares tips for successful change:
So what’s a change leader to do? Create ways for people to get together and converse. Get them participating, engaged, and involved. This is the road to personal investment, enthusiastic support, and genuine buy-in. This is how you move people across the line from “I have to do this” to “I want to do this.” And that makes all the difference in the world. 32 (p17)
The challenge with the reorganization was getting engagement across the research team.
On the first day in office, the Chief made appointments with each one of the 74 CTNs and interviewed them to understand their background ( Box 5 ), motivations, and career aspirations. CTNs were asked:
Research Nurses Demographics
- How long they had been in their jobs?
- What kept them in their jobs?
- What obstacles did they face preventing them from getting their job done?
- What was on their wish list?
Overwhelmingly, the CTNs said that what kept them in their jobs were the relationships with their colleagues including investigators and other physicians. They felt intellectually challenged by the research protocols and science, autonomous in their positions, and driven to help patients. The overriding impediment related to performing their jobs better was a lack of communication about policies and procedures. They wanted to know best practices and what other nurses were doing that improved their efficiency. Much of the information gained from these interviews was congruent with the reasons for the reorganization of the CTNs. The Chief felt comfortable knowing that the needs of the CCR and the CTNs were in alignment.
Establishing Structure
The ORN leadership team met, developed the ORN draft mission and vision statement that was presented to the CTNs for their input and feedback. This was a key first step to engaging staff in decision making for what was to be a long-term meaningful partnership between leadership and staff.
To provide a unique, cohesive team of superior research nurse specialists to carry out the mission of the CCR through a culture that supports continuing education, mentorship, professional development, and collaboration while balancing comprehensive patient coordination and quality clinical and translational research. - Vision statement for the Office of Research Nursing, 2013
The leadership team participated in a 12 week supervisory course on self-development, program development and leading though change. Training included the legalities of supervision, conflict resolution, leadership development, forming and leading teams, and handling human resource issues. In addition, the Chief and team leads were afforded the opportunity to have three months of individual executive coaching which has proven to be invaluable for the development of the ORN.
The ORN established four teams each with a team lead ( Fig 1 ). The ORN leadership took the following into account:

Organizational Chart for the Office of Research Nursing
- CTN experience
- Existing research team dynamics
- Research team workload (e.g., types of protocols, phases of clinical trials, number of protocols)
- Support staff (e.g., data manager, scheduling support staff, mid-level providers)
The aim was to provide manageable teams for each team leader to supervise while supporting the vision statement of the ORN.
Communication and Transparency
An immediate response to the needs of both the CCR and the CTN was to initiate a communication plan. The ORN developed a monthly newsletter that includes staff recognition, educational opportunities, new policies/procedures, staff departures, staff hires, and regulatory updates. The newsletter is distributed via email and posted on a dedicated website. Informal staff meetings called “Coffee and Chats” began and are held monthly on three different days of the week so that all staff have an opportunity to attend. The purpose of these meetings is for staff to network, share best practices and receive up-to-date information from the leadership team. The CTNs are invited to join the meetings but not required to attend the meetings. Part of the communication plan includes the development of the ORN Wiki page. The site is maintained by the ORN Chief and contains: newsletters, listing of the nurses, their contact information, and procedures for promotion. An email distribution list with all research nurses, ORN leadership, and additional staff from the Office of the Clinical Director (e.g., Deputy Clinical Director, Nurse Educator, Protocol Support Office Director, and Quality Management Coordinator) allows rapid, thorough communication to all CTNs.
Each team leader developed relationships with their CTNs, the teams in which the team leaders worked, and the respective PIs. It was imperative to know what each individual on the research team valued and find ways to help them achieve that as quickly as possible. The team leaders attended research team and data management meetings as well as clinic when needed. The team leaders continue to meet regularly with PIs.
Quickly workgroups began to emerge comprised of staff who identified a need or a problem and developed a team to address solutions. One workgroup emerged to address documentation needs in the electronic medical record. Others workgroups developed including:
- Wellness Committee with a goal of helping CTNs strike work-life balance
- Journal Club to provide CTNs with a forum to discuss peer-reviewed literature related to oncology, nursing or clinical trials
- Model for cross-coverage and what it meant to cover for a CTN who was out of the office.
Making Changes
From its inception the ORN leadership made a strategic decision that changes in practice would be small with a likelihood of being successful and that we would build from there. It was about building trust and respecting staff input. A decision was made that all changes would be presented to the staff with rationale for the change; they would have input; and leadership would listen. The principal investigators and other stakeholders were included in the communications. We would use ‘champions’ to advocate for new ideas and change that needed to be addressed. We would communicate to the staff the final proposal and then roll out the changes and fully communicate to all involved. The first change that was presented was standard operating procedures (SOP) for time, attendance, and telework. This process was successful, as the staff trusted the process allowing for subsequent changes. We established ground rules for conducting business including work schedule options, performance evaluations, and promotion procedures. All changes were approached in the same manner of our change management philosophy.
NOW THAT WE HAVE ENGAGEMENT, TIME TO GET DOWN TO BUSINESS
A priority of the CCR was to improve cross coverage and flexibility to cover workload. There were 4 programs that included only one CTN. We paired these single CTN teams with other CTN(s) to cover workload in times of absences. We also identified the need to have a senior resource CTN who could be deployed to teams for various reasons (e.g., cover for CTN out on extended leave, audit assistance, or coverage due to a temporary increase in workload). This resource CTN was available to precept new staff. Additionally, all team leaders ensured that they had a working knowledge of their team’s protocols so that they could backup a CTN if necessary.
There had been a promotion process in place at the CCR for CTNs who want to be considered for promotion. The process was evaluated by leadership and senior staff who had previously gone through the process. Feedback was elicited from staff and the process was finalized. There are 5 nurses promoted using the new promotion process incorporating a leadership initiative as part of their senior CTN status.
New CTN orientation has been redesigned. Each new CTN is assigned a preceptor. New CTN orientation procedures and standardized checklists have been developed to guide the new CTN and their preceptor. An integral piece of the orientation is the formalized clinical trial training provided by the Nurse Educator.
COMPETENCY ASSESSMENT AND VALIDATION
Once the basic infrastructure of the ORN was created and engagement started, the next initiative was competency assessment and validation. Working with the CCR Nurse Educator, the ORN embarked on developing behavioral indicators for 2 of the 9 ONS competencies (i.e., professional development and documentation) using working groups that included CTNs and leadership. A validation tool was created ( Table 5 ) and the Nurse Educator developed a facilitator’s guide ( Table 6 ) with input from ORN leadership.
Professional Development Competency Validation Sign-off Log
Sample of Professional Development Competency Facilitator’s Guide
The Nurse Educator validated the competency for the ORN Chief and each of the team leaders using the facilitator’s guide. Time was spent discussing how the team leaders would use the guide to validate the research nurses competency. In January 2015 CTNs were notified that competency sign off was to be performed in March. Between January and March 2015 educational sessions were offered to staff and by the end of March all CTNs were signed off on their professional development competency by their team leader. Additional competency validation is ongoing.
ASSESSEMENT OF THE ORN AND FUTURE PLANS
Three years following the inception of the ORN, consolidating the CTNs under one office has been viewed as success by the CTNs and the research teams. This new infrastructure was supported by an organizational commitment to optimize this key resource for the clinical program. Future strategic direction includes completion of competency assessment and validation using the ONS Competencies, development of a workload assessment tool, development of a training and resource manual, and continued commitment to improve communication.
Clinical research is the foundation for improving human health. Clinical trials, a type of clinical research, explore ways to prevent, screen, diagnose, treat and improve quality of life for individuals with a chronic illness. Protecting research participants and ensuring quality data are the responsibility of many individuals and groups. Participant protection includes the ethical review of a protocol and the informed consent of the participant. The protocol serves as a written detailed action plan that supports the scientific rationale for conducting the trial and outlines all trial procedures to be conducted all to ensure the participant’s safety and the quality of the data. A key member of the oncology research team is the oncology CTN who may or may not be supervised by a nurse. Using the process of engagement, one organization has been able to restructure the CTNs into a nurse-supervisor model with direct benefits to the CTN.
- Genomic profiling and the development of molecularly targeted agents (MTAs) have led to novel designs for oncology clinical trials.
- Ensuring human subject protections and quality data are responsibilities for all individuals involved in clinical trials, however the Principal Investigator (PI) is ultimately accountable for the overall conduct of the trial.
- Oncology Clinical Trials Nurses (CTNs) are critical to the implementation of oncology clinical trials.
- Competencies developed by the Oncology Nursing Society help define the specialized role of the oncology Clinical Trials Nurse (CTN).
DISCLOSURES: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
- Open access
- Published: 11 May 2024
Nursing students’ stressors and coping strategies during their first clinical training: a qualitative study in the United Arab Emirates
- Jacqueline Maria Dias 1 ,
- Muhammad Arsyad Subu 1 ,
- Nabeel Al-Yateem 1 ,
- Fatma Refaat Ahmed 1 ,
- Syed Azizur Rahman 1 , 2 ,
- Mini Sara Abraham 1 ,
- Sareh Mirza Forootan 1 ,
- Farzaneh Ahmad Sarkhosh 1 &
- Fatemeh Javanbakh 1
BMC Nursing volume 23 , Article number: 322 ( 2024 ) Cite this article
500 Accesses
Metrics details
Understanding the stressors and coping strategies of nursing students in their first clinical training is important for improving student performance, helping students develop a professional identity and problem-solving skills, and improving the clinical teaching aspects of the curriculum in nursing programmes. While previous research have examined nurses’ sources of stress and coping styles in the Arab region, there is limited understanding of these stressors and coping strategies of nursing students within the UAE context thereby, highlighting the novelty and significance of the study.
A qualitative study was conducted using semi-structured interviews. Overall 30 students who were undergoing their first clinical placement in Year 2 at the University of Sharjah between May and June 2022 were recruited. All interviews were recorded and transcribed verbatim and analyzed for themes.
During their first clinical training, nursing students are exposed to stress from different sources, including the clinical environment, unfriendly clinical tutors, feelings of disconnection, multiple expectations of clinical staff and patients, and gaps between the curriculum of theory classes and labatories skills and students’ clinical experiences. We extracted three main themes that described students’ stress and use of coping strategies during clinical training: (1) managing expectations; (2) theory-practice gap; and (3) learning to cope. Learning to cope, included two subthemes: positive coping strategies and negative coping strategies.
Conclusions
This qualitative study sheds light from the students viewpoint about the intricate interplay between managing expectations, theory practice gap and learning to cope. Therefore, it is imperative for nursing faculty, clinical agencies and curriculum planners to ensure maximum learning in the clinical by recognizing the significance of the stressors encountered and help students develop positive coping strategies to manage the clinical stressors encountered. Further research is required look at the perspective of clinical stressors from clinical tutors who supervise students during their first clinical practicum.
Peer Review reports
Nursing education programmes aim to provide students with high-quality clinical learning experiences to ensure that nurses can provide safe, direct care to patients [ 1 ]. The nursing baccalaureate programme at the University of Sharjah is a four year program with 137 credits. The programmes has both theoretical and clinical components withs nine clinical courses spread over the four years The first clinical practicum which forms the basis of the study takes place in year 2 semester 2.
Clinical practice experience is an indispensable component of nursing education and links what students learn in the classroom and in skills laboratories to real-life clinical settings [ 2 , 3 , 4 ]. However, a gap exists between theory and practice as the curriculum in the classroom differs from nursing students’ experiences in the clinical nursing practicum [ 5 ]. Clinical nursing training places (or practicums, as they are commonly referred to), provide students with the necessary experiences to ensure that they become proficient in the delivery of patient care [ 6 ]. The clinical practicum takes place in an environment that combines numerous structural, psychological, emotional and organizational elements that influence student learning [ 7 ] and may affect the development of professional nursing competencies, such as compassion, communication and professional identity [ 8 ]. While clinical training is a major component of nursing education curricula, stress related to clinical training is common among students [ 9 ]. Furthermore, the nursing literature indicates that the first exposure to clinical learning is one of the most stressful experiences during undergraduate studies [ 8 , 10 ]. Thus, the clinical component of nursing education is considered more stressful than the theoretical component. Students often view clinical learning, where most learning takes place, as an unsupportive environment [ 11 ]. In addition, they note strained relationships between themselves and clinical preceptors and perceive that the negative attitudes of clinical staff produce stress [ 12 ].
The effects of stress on nursing students often involve a sense of uncertainty, uneasiness, or anxiety. The literature is replete with evidence that nursing students experience a variety of stressors during their clinical practicum, beginning with the first clinical rotation. Nursing is a complex profession that requires continuous interaction with a variety of individuals in a high-stress environment. Stress during clinical learning can have multiple negative consequences, including low academic achievement, elevated levels of burnout, and diminished personal well-being [ 13 , 14 ]. In addition, both theoretical and practical research has demonstrated that increased, continual exposure to stress leads to cognitive deficits, inability to concentrate, lack of memory or recall, misinterpretation of speech, and decreased learning capacity [ 15 ]. Furthermore, stress has been identified as a cause of attrition among nursing students [ 16 ].
Most sources of stress have been categorized as academic, clinical or personal. Each person copes with stress differently [ 17 ], and utilizes deliberate, planned, and psychological efforts to manage stressful demands [ 18 ]. Coping mechanisms are commonly termed adaptation strategies or coping skills. Labrague et al. [ 19 ] noted that students used critical coping strategies to handle stress and suggested that problem solving was the most common coping or adaptation mechanism used by nursing students. Nursing students’ coping strategies affect their physical and psychological well-being and the quality of nursing care they offer. Therefore, identifying the coping strategies that students use to manage stressors is important for early intervention [ 20 ].
Studies on nursing students’ coping strategies have been conducted in various countries. For example, Israeli nursing students were found to adopt a range of coping mechanisms, including talking to friends, engaging in sports, avoiding stress and sadness/misery, and consuming alcohol [ 21 ]. Other studies have examined stress levels among medical students in the Arab region. Chaabane et al. [ 15 ], conducted a systematic review of sudies in Arab countries, including Saudi Arabia, Egypt, Jordan, Iraq, Pakistan, Oman, Palestine and Bahrain, and reported that stress during clinical practicums was prevalent, although it could not be determined whether this was limited to the initial clinical course or occurred throughout clinical training. Stressors highlighted during the clinical period in the systematic review included assignments and workload during clinical practice, a feeling that the requirements of clinical practice exceeded students’ physical and emotional endurance and that their involvement in patient care was limited due to lack of experience. Furthermore, stress can have a direct effect on clinical performance, leading to mental disorders. Tung et al. [ 22 ], reported that the prevalence of depression among nursing students in Arab countries is 28%, which is almost six times greater than the rest of the world [ 22 ]. On the other hand, Saifan et al. [ 5 ], explored the theory-practice gap in the United Arab Emirates and found that clinical stressors could be decreased by preparing students better for clinical education with qualified clinical faculty and supportive preceptors.
The purpose of this study was to identify the stressors experienced by undergraduate nursing students in the United Arab Emirates during their first clinical training and the basic adaptation approaches or coping strategies they used. Recognizing or understanding different coping processes can inform the implementation of corrective measures when students experience clinical stress. The findings of this study may provide valuable information for nursing programmes, nurse educators, and clinical administrators to establish adaptive strategies to reduce stress among students going clinical practicums, particularly stressors from their first clinical training in different healthcare settings.
A qualitative approach was adopted to understand clinical stressors and coping strategies from the perspective of nurses’ lived experience. Qualitative content analysis was employed to obtain rich and detailed information from our qualitative data. Qualitative approaches seek to understand the phenomenon under study from the perspectives of individuals with lived experience [ 23 ]. Qualitative content analysis is an interpretive technique that examines the similarities and differences between and within different areas of text while focusing on the subject [ 24 ]. It is used to examine communication patterns in a repeatable and systematic way [ 25 ] and yields rich and detailed information on the topic under investigation [ 23 ]. It is a method of systematically coding and categorizing information and comprises a process of comprehending, interpreting, and conceptualizing the key meanings from qualitative data [ 26 ].
Setting and participants
This study was conducted after the clinical rotations ended in April 2022, between May and June in the nursing programme at the College of Health Sciences, University of Sharjah, in the United Arab Emirates. The study population comprised undergraduate nursing students who were undergoing their first clinical training and were recruited using purposive sampling. The inclusion criteria for this study were second-year nursing students in the first semester of clinical training who could speak English, were willing to participate in this research, and had no previous clinical work experience. The final sample consisted of 30 students.
Research instrument
The research instrument was a semi structured interview guide. The interview questions were based on an in-depth review of related literature. An intensive search included key words in Google Scholar, PubMed like the terms “nursing clinical stressors”, “nursing students”, and “coping mechanisms”. Once the questions were created, they were validated by two other faculty members who had relevant experience in mental health. A pilot test was conducted with five students and based on their feedback the following research questions, which were addressed in the study.
How would you describe your clinical experiences during your first clinical rotations?
In what ways did you find the first clinical rotation to be stressful?
What factors hindered your clinical training?
How did you cope with the stressors you encountered in clinical training?
Which strategies helped you cope with the clinical stressors you encountered?
Data collection
Semi-structured interviews were chosen as the method for data collection. Semi structured interviews are a well-established approach for gathering data in qualitative research and allow participants to discuss their views, experiences, attitudes, and beliefs in a positive environment [ 27 ]. This approach allows for flexibility in questioning thereby ensuring that key topics related to clinical learning stressors and coping strategies would be explored. Participants were given the opportunity to express their views, experiences, attitudes, and beliefs in a positive environment, encouraging open communication. These semi structured interviews were conducted by one member of the research team (MAS) who had a mental health background, and another member of the research team who attended the interviews as an observer (JMD). Neither of these researchers were involved in teaching the students during their clinical practicum, which helped to minimize bias. The interviews took place at the University of Sharjah, specifically in building M23, providing a familiar and comfortable environment for the participant. Before the interviews were all students who agreed to participate were provided with an explanation of the study’s purpose. The time and location of each interview were arranged. Before the interviews were conducted, all students who provided consent to participate received an explanation of the purpose of the study, and the time and place of each interview were arranged to accommodate the participants’ schedules and preferences. The interviews were conducted after the clinical rotation had ended in April, and after the final grades had been submitted to the coordinator. The timings of the interviews included the month of May and June which ensured that participants have completed their practicum experience and could reflect on the stressors more comprehensively. The interviews were audio-recorded with the participants’ consent, and each interview lasted 25–40 min. The data were collected until saturation was reached for 30 students. Memos and field notes were also recorded as part of the data collection process. These additional data allowed for triangulation to improve the credibility of the interpretations of the data [ 28 ]. Memos included the interviewers’ thoughts and interpretations about the interviews, the research process (including questions and gaps), and the analytic progress used for the research. Field notes were used to record the interviewers’ observations and reflections on the data. These additional data collection methods were important to guide the researchers in the interpretation of the data on the participants’ feelings, perspectives, experiences, attitudes, and beliefs. Finally, member checking was performed to ensure conformability.
Data analysis
The study used the content analysis method proposed by Graneheim and Lundman [ 24 ]. According to Graneheim and Lundman [ 24 ], content analysis is an interpretive technique that examines the similarities and differences between distinct parts of a text. This method allows researchers to determine exact theoretical and operational definitions of words, phrases, and symbols by elucidating their constituent properties [ 29 ]. First, we read the interview transcripts several times to reach an overall understanding of the data. All verbatim transcripts were read several times and discussed among all authors. We merged and used line-by-line coding of words, sentences, and paragraphs relevant to each other in terms of both the content and context of stressors and coping mechanisms. Next, we used data reduction to assess the relationships among themes using tables and diagrams to indicate conceptual patterns. Content related to stress encountered by students was extracted from the transcripts. In a separate document, we integrated and categorized all words and sentences that were related to each other in terms of both content and context. We analyzed all codes and units of meaning and compared them for similarities and differences in the context of this study. Furthermore, the emerging findings were discussed with other members of the researcher team. The final abstractions of meaningful subthemes into themes were discussed and agreed upon by the entire research team. This process resulted in the extraction of three main themes in addition to two subthemes related to stress and coping strategies.
Ethical considerations
The University of Sharjah Research Ethics Committee provided approval to conduct this study (Reference Number: REC 19-12-03-01-S). Before each interview, the goal and study procedures were explained to each participant, and written informed consent was obtained. The participants were informed that participation in the study was voluntary and that they could withdraw from the study at any time. In the event they wanted to withdraw from the study, all information related to the participant would be removed. No participant withdrew from the study. Furthermore, they were informed that their clinical practicum grade would not be affected by their participation in this study. We chose interview locations in Building M23that were private and quiet to ensure that the participants felt at ease and confident in verbalizing their opinions. No participant was paid directly for involvement in this study. In addition, participants were assured that their data would remain anonymous and confidential. Confidentiality means that the information provided by participants was kept private with restrictions on how and when data can be shared with others. The participants were informed that their information would not be duplicated or disseminated without their permission. Anonymity refers to the act of keeping people anonymous with respect to their participation in a research endeavor. No personal identifiers were used in this study, and each participant was assigned a random alpha-numeric code (e.g., P1 for participant 1). All digitally recorded interviews were downloaded to a secure computer protected by the principal investigator with a password. The researchers were the only people with access to the interview material (recordings and transcripts). All sensitive information and materials were kept secure in the principal researcher’s office at the University of Sharjah. The data will be maintained for five years after the study is completed, after which the material will be destroyed (the transcripts will be shredded, and the tapes will be demagnetized).
In total, 30 nursing students who were enrolled in the nursing programme at the Department of Nursing, College of Health Sciences, University of Sharjah, and who were undergoing their first clinical practicum participated in the study. Demographically, 80% ( n = 24) were females and 20% ( n = 6) were male participants. The majority (83%) of study participants ranged in age from 18 to 22 years. 20% ( n = 6) were UAE nationals, 53% ( n = 16) were from Gulf Cooperation Council countries, while 20% ( n = 6) hailed from Africa and 7% ( n = 2) were of South Asian descent. 67% of the respondents lived with their families while 33% lived in the hostel. (Table 1 )
Following the content analysis, we identified three main themes: (1) managing expectations, (2) theory-practice gap and 3)learning to cope. Learning to cope had two subthemes: positive coping strategies and negative coping strategies. An account of each theme is presented along with supporting excerpts for the identified themes. The identified themes provide valuable insight into the stressors encountered by students during their first clinical practicum. These themes will lead to targeted interventions and supportive mechanisms that can be built into the clinical training curriculum to support students during clinical practice.
Theme 1: managing expectations
In our examination of the stressors experienced by nursing students during their first clinical practicum and the coping strategies they employed, we identified the first theme as managing expectations.
The students encountered expectations from various parties, such as clinical staff, patients and patients’ relatives which they had to navigate. They attempted to fulfil their expectations as they progressed through training, which presented a source of stress. The students noted that the hospital staff and patients expected them to know how to perform a variety of tasks upon request, which made the students feel stressed and out of place if they did not know how to perform these tasks. Some participants noted that other nurses in the clinical unit did not allow them to participate in nursing procedures, which was considered an enormous impediment to clinical learning, as noted in the excerpt below:
“…Sometimes the nurses… They will not allow us to do some procedures or things during clinical. And sometimes the patients themselves don’t allow us to do procedures” (P5).
Some of the students noted that they felt they did not belong and felt like foreigners in the clinical unit. Excerpts from the students are presented in the following quotes;
“The clinical environment is so stressful. I don’t feel like I belong. There is too little time to build a rapport with hospital staff or the patient” (P22).
“… you ask the hospital staff for some guidance or the location of equipment, and they tell us to ask our clinical tutor …but she is not around … what should I do? It appears like we do not belong, and the sooner the shift is over, the better” (P18).
“The staff are unfriendly and expect too much from us students… I feel like I don’t belong, or I am wasting their (the hospital staff’s) time. I want to ask questions, but they have loads to do” (P26).
Other students were concerned about potential failure when working with patients during clinical training, which impacted their confidence. They were particularly afraid of failure when performing any clinical procedures.
“At the beginning, I was afraid to do procedures. I thought that maybe the patient would be hurt and that I would not be successful in doing it. I have low self-confidence in doing procedures” (P13).
The call bell rings, and I am told to answer Room No. XXX. The patient wants help to go to the toilet, but she has two IV lines. I don’t know how to transport the patient… should I take her on the wheelchair? My eyes glance around the room for a wheelchair. I am so confused …I tell the patient I will inform the sister at the nursing station. The relative in the room glares at me angrily … “you better hurry up”…Oh, I feel like I don’t belong, as I am not able to help the patient… how will I face the same patient again?” (P12).
Another major stressor mentioned in the narratives was related to communication and interactions with patients who spoke another language, so it was difficult to communicate.
“There was a challenge with my communication with the patients. Sometimes I have communication barriers because they (the patients) are of other nationalities. I had an experience with a patient [who was] Indian, and he couldn’t speak my language. I did not understand his language” (P9).
Thus, a variety of expectations from patients, relatives, hospital staff, and preceptors acted as sources of stress for students during their clinical training.
Theme 2: theory-practice gap
Theory-practice gaps have been identified in previous studies. In our study, there was complete dissonance between theory and actual clinical practice. The clinical procedures or practices nursing students were expected to perform differed from the theory they had covered in their university classes and skills lab. This was described as a theory–practice gap and often resulted in stress and confusion.
“For example …the procedures in the hospital are different. They are different from what we learned or from theory on campus. Or… the preceptors have different techniques than what we learned on campus. So, I was stress[ed] and confused about it” (P11).
Furthermore, some students reported that they did not feel that they received adequate briefing before going to clinical training. A related source of stress was overload because of the volume of clinical coursework and assignments in addition to clinical expectations. Additionally, the students reported that a lack of time and time management were major sources of stress in their first clinical training and impacted their ability to complete the required paperwork and assignments:
“…There is not enough time…also, time management at the hospital…for example, we start at seven a.m., and the handover takes 1 hour to finish. They (the nurses at the hospital) are very slow…They start with bed making and morning care like at 9.45 a.m. Then, we must fill [out] our assessment tool and the NCP (nursing care plan) at 10 a.m. So, 15 only minutes before going to our break. We (the students) cannot manage this time. This condition makes me and my friends very stressed out. -I cannot do my paperwork or assignments; no time, right?” (P10).
“Stressful. There is a lot of work to do in clinical. My experiences are not really good with this course. We have a lot of things to do, so many assignments and clinical procedures to complete” (P16).
The participants noted that the amount of required coursework and number of assignments also presented a challenge during their first clinical training and especially affected their opportunity to learn.
“I need to read the file, know about my patient’s condition and pathophysiology and the rationale for the medications the patient is receiving…These are big stressors for my learning. I think about assignments often. Like, we are just focusing on so many assignments and papers. We need to submit assessments and care plans for clinical cases. We focus our time to complete and finish the papers rather than doing the real clinical procedures, so we lose [the] chance to learn” (P25).
Another participant commented in a similar vein that there was not enough time to perform tasks related to clinical requirements during clinical placement.
“…there is a challenge because we do not have enough time. Always no time for us to submit papers, to complete assessment tools, and some nurses, they don’t help us. I think we need more time to get more experiences and do more procedures, reduce the paperwork that we have to submit. These are challenges …” (P14).
There were expectations that the students should be able to carry out their nursing duties without becoming ill or adversely affected. In addition, many students reported that the clinical environment was completely different from the skills laboratory at the college. Exposure to the clinical setting added to the theory-practice gap, and in some instances, the students fell ill.
One student made the following comment:
“I was assisting a doctor with a dressing, and the sight and smell from the oozing wound was too much for me. I was nauseated. As soon as the dressing was done, I ran to the bathroom and threw up. I asked myself… how will I survive the next 3 years of nursing?” (P14).
Theme 3: learning to cope
The study participants indicated that they used coping mechanisms (both positive and negative) to adapt to and manage the stressors in their first clinical practicum. Important strategies that were reportedly used to cope with stress were time management, good preparation for clinical practice, and positive thinking as well as engaging in physical activity and self-motivation.
“Time management. Yes, it is important. I was encouraging myself. I used time management and prepared myself before going to the clinical site. Also, eating good food like cereal…it helps me very much in the clinic” (P28).
“Oh yeah, for sure positive thinking. In the hospital, I always think positively. Then, after coming home, I get [to] rest and think about positive things that I can do. So, I will think something good [about] these things, and then I will be relieved of stress” (P21).
Other strategies commonly reported by the participants were managing their breathing (e.g., taking deep breaths, breathing slowly), taking breaks to relax, and talking with friends about the problems they encountered.
“I prefer to take deep breaths and breathe slowly and to have a cup of coffee and to talk to my friends about the case or the clinical preceptor and what made me sad so I will feel more relaxed” (P16).
“Maybe I will take my break so I feel relaxed and feel better. After clinical training, I go directly home and take a long shower, going over the day. I will not think about anything bad that happened that day. I just try to think about good things so that I forget the stress” (P27).
“Yes, my first clinical training was not easy. It was difficult and made me stressed out…. I felt that it was a very difficult time for me. I thought about leaving nursing” (P7).
I was not able to offer my prayers. For me, this was distressing because as a Muslim, I pray regularly. Now, my prayer time is pushed to the end of the shift” (P11).
“When I feel stress, I talk to my friends about the case and what made me stressed. Then I will feel more relaxed” (P26).
Self-support or self-motivation through positive self-talk was also used by the students to cope with stress.
“Yes, it is difficult in the first clinical training. When I am stress[ed], I go to the bathroom and stand in the front of the mirror; I talk to myself, and I say, “You can do it,” “you are a great student.” I motivate myself: “You can do it”… Then, I just take breaths slowly several times. This is better than shouting or crying because it makes me tired” (P11).
Other participants used physical activity to manage their stress.
“How do I cope with my stress? Actually, when I get stressed, I will go for a walk on campus” (P4).
“At home, I will go to my room and close the door and start doing my exercises. After that, I feel the negative energy goes out, then I start to calm down… and begin my clinical assignments” (P21).
Both positive and negative coping strategies were utilized by the students. Some participants described using negative coping strategies when they encountered stress during their clinical practice. These negative coping strategies included becoming irritable and angry, eating too much food, drinking too much coffee, and smoking cigarettes.
“…Negative adaptation? Maybe coping. If I am stressed, I get so angry easily. I am irritable all day also…It is negative energy, right? Then, at home, I am also angry. After that, it is good to be alone to think about my problems” (P12).
“Yeah, if I…feel stress or depressed, I will eat a lot of food. Yeah, ineffective, like I will be eating a lot, drinking coffee. Like I said, effective, like I will prepare myself and do breathing, ineffective, I will eat a lot of snacks in between my free time. This is the bad side” (P16).
“…During the first clinical practice? Yes, it was a difficult experience for us…not only me. When stressed, during a break at the hospital, I will drink two or three cups of coffee… Also, I smoke cigarettes… A lot. I can drink six cups [of coffee] a day when I am stressed. After drinking coffee, I feel more relaxed, I finish everything (food) in the refrigerator or whatever I have in the pantry, like chocolates, chips, etc” (P23).
These supporting excerpts for each theme and the analysis offers valuable insights into the specific stressors faced by nursing students during their first clinical practicum. These insights will form the basis for the development of targeted interventions and supportive mechanisms within the clinical training curriculum to better support students’ adjustment and well-being during clinical practice.
Our study identified the stressors students encounter in their first clinical practicum and the coping strategies, both positive and negative, that they employed. Although this study emphasizes the importance of clinical training to prepare nursing students to practice as nurses, it also demonstrates the correlation between stressors and coping strategies.The content analysis of the first theme, managing expectations, paves the way for clinical agencies to realize that the students of today will be the nurses of tomorrow. It is important to provide a welcoming environment where students can develop their identities and learn effectively. Additionally, clinical staff should foster an environment of individualized learning while also assisting students in gaining confidence and competence in their repertoire of nursing skills, including critical thinking, problem solving and communication skills [ 8 , 15 , 19 , 30 ]. Another challenge encountered by the students in our study was that they were prevented from participating in clinical procedures by some nurses or patients. This finding is consistent with previous studies reporting that key challenges for students in clinical learning include a lack of clinical support and poor attitudes among clinical staff and instructors [ 31 ]. Clinical staff with positive attitudes have a positive impact on students’ learning in clinical settings [ 32 ]. The presence, supervision, and guidance of clinical instructors and the assistance of clinical staff are essential motivating components in the clinical learning process and offer positive reinforcement [ 30 , 33 , 34 ]. Conversely, an unsupportive learning environment combined with unwelcoming clinical staff and a lack of sense of belonging negatively impact students’ clinical learning [ 35 ].
The sources of stress identified in this study were consistent with common sources of stress in clinical training reported in previous studies, including the attitudes of some staff, students’ status in their clinical placement and educational factors. Nursing students’ inexperience in the clinical setting and lack of social and emotional experience also resulted in stress and psychological difficulties [ 36 ]. Bhurtun et al. [ 33 ] noted that nursing staff are a major source of stress for students because the students feel like they are constantly being watched and evaluated.
We also found that students were concerned about potential failure when working with patients during their clinical training. Their fear of failure when performing clinical procedures may be attributable to low self-confidence. Previous studies have noted that students were concerned about injuring patients, being blamed or chastised, and failing examinations [ 37 , 38 ]. This was described as feeling “powerless” in a previous study [ 7 , 12 ]. In addition, patients’ attitudes towards “rejecting” nursing students or patients’ refusal of their help were sources of stress among the students in our study and affected their self-confidence. Self-confidence and a sense of belonging are important for nurses’ personal and professional identity, and low self-confidence is a problem for nursing students in clinical learning [ 8 , 39 , 40 ]. Our findings are consistent with a previous study that reported that a lack of self-confidence was a primary source of worry and anxiety for nursing students and affected their communication and intention to leave nursing [ 41 ].
In the second theme, our study suggests that students encounter a theory-practice gap in clinical settings, which creates confusion and presents an additional stressors. Theoretical and clinical training are complementary elements of nursing education [ 40 ], and this combination enables students to gain the knowledge, skills, and attitudes necessary to provide nursing care. This is consistent with the findings of a previous study that reported that inconsistencies between theoretical knowledge and practical experience presented a primary obstacle to the learning process in the clinical context [ 42 ], causing students to lose confidence and become anxious [ 43 ]. Additionally, the second theme, the theory-practice gap, authenticates Safian et al.’s [ 5 ] study of the theory-practice gap that exists United Arab Emirates among nursing students as well as the need for more supportive clinical faculty and the extension of clinical hours. The need for better time availability and time management to complete clinical tasks were also reported by the students in the study. Students indicated that they had insufficient time to complete clinical activities because of the volume of coursework and assignments. Our findings support those of Chaabane et al. [ 15 ]. A study conducted in Saudi Arabia [ 44 ] found that assignments and workload were among the greatest sources of stress for students in clinical settings. Effective time management skills have been linked to academic achievement, stress reduction, increased creativity [ 45 ], and student satisfaction [ 46 ]. Our findings are also consistent with previous studies that reported that a common source of stress among first-year students was the increased classroom workload [ 19 , 47 ]. As clinical assignments and workloads are major stressors for nursing students, it is important to promote activities to help them manage these assignments [ 48 ].
Another major challenge reported by the participants was related to communicating and interacting with other nurses and patients. The UAE nursing workforce and population are largely expatriate and diverse and have different cultural and linguistic backgrounds. Therefore, student nurses encounter difficulty in communication [ 49 ]. This cultural diversity that students encounter in communication with patients during clinical training needs to be addressed by curriculum planners through the offering of language courses and courses on cultural diversity [ 50 ].
Regarding the third and final theme, nursing students in clinical training are unable to avoid stressors and must learn to cope with or adapt to them. Previous research has reported a link between stressors and the coping mechanisms used by nursing students [ 51 , 52 , 53 ]. In particular, the inability to manage stress influences nurses’ performance, physical and mental health, attitude, and role satisfaction [ 54 ]. One such study suggested that nursing students commonly use problem-focused (dealing with the problem), emotion-focused (regulating emotion), and dysfunctional (e.g., venting emotions) stress coping mechanisms to alleviate stress during clinical training [ 15 ]. Labrague et al. [ 51 ] highlighted that nursing students use both active and passive coping techniques to manage stress. The pattern of clinical stress has been observed in several countries worldwide. The current study found that first-year students experienced stress during their first clinical training [ 35 , 41 , 55 ]. The stressors they encountered impacted their overall health and disrupted their clinical learning. Chaabane et al. [ 15 ] reported moderate and high stress levels among nursing students in Bahrain, Egypt, Iraq, Jordan, Oman, Pakistan, Palestine, Saudi Arabia, and Sudan. Another study from Bahrain reported that all nursing students experienced moderate to severe stress in their first clinical placement [ 56 ]. Similarly, nursing students in Spain experienced a moderate level of stress, and this stress was significantly correlated with anxiety [ 30 ]. Therefore, it is imperative that pastoral systems at the university address students’ stress and mental health so that it does not affect their clinical performance. Faculty need to utilize evidence-based interventions to support students so that anxiety-producing situations and attrition are minimized.
In our study, students reported a variety of positive and negative coping mechanisms and strategies they used when they experienced stress during their clinical practice. Positive coping strategies included time management, positive thinking, self-support/motivation, breathing, taking breaks, talking with friends, and physical activity. These findings are consistent with those of a previous study in which healthy coping mechanisms used by students included effective time management, social support, positive reappraisal, and participation in leisure activities [ 57 ]. Our study found that relaxing and talking with friends were stress management strategies commonly used by students. Communication with friends to cope with stress may be considered social support. A previous study also reported that people seek social support to cope with stress [ 58 ]. Some students in our study used physical activity to cope with stress, consistent with the findings of previous research. Stretching exercises can be used to counteract the poor posture and positioning associated with stress and to assist in reducing physical tension. Promoting such exercise among nursing students may assist them in coping with stress in their clinical training [ 59 ].
Our study also showed that when students felt stressed, some adopted negative coping strategies, such as showing anger/irritability, engaging in unhealthy eating habits (e.g., consumption of too much food or coffee), or smoking cigarettes. Previous studies have reported that high levels of perceived stress affect eating habits [ 60 ] and are linked to poor diet quality, increased snacking, and low fruit intake [ 61 ]. Stress in clinical settings has also been linked to sleep problems, substance misuse, and high-risk behaviors’ and plays a major role in student’s decision to continue in their programme.
Implications of the study
The implications of the study results can be grouped at multiple levels including; clinical, educational, and organizational level. A comprehensive approach to addressing the stressors encountered by nursing students during their clinical practicum can be overcome by offering some practical strategies to address the stressors faced by nursing students during their clinical practicum. By integrating study findings into curriculum planning, mentorship programs, and organizational support structures, a supportive and nurturing environment that enhances students’ learning, resilience, and overall success can be envisioned.
Clinical level
Introducing simulation in the skills lab with standardized patients and the use of moulage to demonstrate wounds, ostomies, and purulent dressings enhances students’ practical skills and prepares them for real-world clinical scenarios. Organizing orientation days at clinical facilities helps familiarize students with the clinical environment, identify potential stressors, and introduce interventions to enhance professionalism, social skills, and coping abilities Furthermore, creating a WhatsApp group facilitates communication and collaboration among hospital staff, clinical tutors, nursing faculty, and students, enabling immediate support and problem-solving for clinical situations as they arise, Moreover, involving chief nursing officers of clinical facilities in the Nursing Advisory Group at the Department of Nursing promotes collaboration between academia and clinical practice, ensuring alignment between educational objectives and the needs of the clinical setting [ 62 ].
Educational level
Sharing study findings at conferences (we presented the results of this study at Sigma Theta Tau International in July 2023 in Abu Dhabi, UAE) and journal clubs disseminates knowledge and best practices among educators and clinicians, promoting awareness and implementation of measures to improve students’ learning experiences. Additionally we hold mentorship training sessions annually in January and so we shared with the clinical mentors and preceptors the findings of this study so that they proactively they are equipped with strategies to support students’ coping with stressors during clinical placements.
Organizational level
At the organizational we relooked at the available student support structures, including counseling, faculty advising, and career advice, throughout the nursing program emphasizing the importance of holistic support for students’ well-being and academic success as well as retention in the nursing program. Also, offering language courses as electives recognizes the value of communication skills in nursing practice and provides opportunities for personal and professional development.
For first-year nursing students, clinical stressors are inevitable and must be given proper attention. Recognizing nursing students’ perspectives on the challenges and stressors experienced in clinical training is the first step in overcoming these challenges. In nursing schools, providing an optimal clinical environment as well as increasing supervision and evaluation of students’ practices should be emphasized. Our findings demonstrate that first-year nursing students are exposed to a variety of different stressors. Identifying the stressors, pressures, and obstacles that first-year students encounter in the clinical setting can assist nursing educators in resolving these issues and can contribute to students’ professional development and survival to allow them to remain in the profession. To overcome stressors, students frequently employ problem-solving approaches or coping mechanisms. The majority of nursing students report stress at different levels and use a variety of positive and negative coping techniques to manage stress.
The present results may not be generalizable to other nursing institutions because this study used a purposive sample along with a qualitative approach and was limited to one university in the Middle East. Furthermore, the students self-reported their stress and its causes, which may have introduced reporting bias. The students may also have over or underreported stress or coping mechanisms because of fear of repercussions or personal reasons, even though the confidentiality of their data was ensured. Further studies are needed to evaluate student stressors and coping now that measures have been introduced to support students. Time will tell if these strategies are being used effectively by both students and clinical personnel or if they need to be readdressed. Finally, we need to explore the perceptions of clinical faculty towards supervising students in their first clinical practicum so that clinical stressors can be handled effectively.
Data availability
The data sets are available with the corresponding author upon reasonable request.
Almarwani AM. The effect of integrating a nursing licensure examination preparation course into a nursing program curriculum: a quasi-experimental study. Saudi J Health Sci. 2022;11:184–9.
Article Google Scholar
Horntvedt MT, Nordsteien A, Fermann T, Severinsson E. Strategies for teaching evidence-based practice in nursing education: a thematic literature review. BMC Med Educ. 2018;18:172.
Article PubMed PubMed Central Google Scholar
Larsson M, Sundler AJ, Blomberg K, Bisholt B. The clinical learning environment during clinical practice in postgraduate district nursing students’ education: a cross-sectional study. Nurs Open. 2023;10:879–88.
Article PubMed Google Scholar
Sellberg M, Palmgren PJ, Möller R. A cross-sectional study of clinical learning environments across four undergraduate programs using the undergraduate clinical education environment measure. BMC Med Educ. 2021;21:258.
Saifan A, Devadas B, Mekkawi M, Amoor H, Matizha P, James J, et al. Managing the theory-practice gap in nursing education and practice: hearing the voices of nursing students in the United Arab Emirates. J Nurs Manag. 2021;29:1869–79.
Flott EA, Linden L. The clinical learning environment in nursing education: a concept analysis. J Adv Nurs. 2016;72:501–13.
Kalyani MN, Jamshidi N, Molazem Z, Torabizadeh C, Sharif F. How do nursing students experience the clinical learning environment and respond to their experiences? A qualitative study. BMJ Open. 2019;9:e028052.
Mahasneh D, Shoqirat N, Alsaraireh A, Singh C, Thorpe L. From learning on mannequins to practicing on patients: nursing students’ first-time experience of clinical placement in Jordan. SAGE Open Nurs. 2021;7:23779608211004298.
PubMed PubMed Central Google Scholar
Stubin C. Clinical stress among undergraduate nursing students: perceptions of clinical nursing faculty. Int J Nurs Educ Scholarsh. 2020;17:20190111.
Ahmed WAM. Anxiety and related symptoms among critical care nurses in Albaha, Kingdom of Saudi Arabia. AIMS Med Sci. 2015;2:303–9.
Alhassan. Duke Phillips. 2024.
Ekstedt M, Lindblad M, Löfmark A. Nursing students’ perception of the clinical learning environment and supervision in relation to two different supervision models - a comparative cross-sectional study. BMC Nurs. 2019;18:49.
Bradshaw C, Murphy Tighe S, Doody O. Midwifery students’ experiences of their clinical internship: a qualitative descriptive study. Nurse Educ Today. 2018;68:213–7.
McCarthy B, Trace A, O’Donovan M, O’Regan P, Brady-Nevin C, O’Shea M, et al. Coping with stressful events: a pre-post-test of a psycho-educational intervention for undergraduate nursing and midwifery students. Nurse Educ Today. 2018;61:273–80.
Chaabane S, Chaabna K, Bhagat S, Abraham A, Doraiswamy S, Mamtani R, et al. Perceived stress, stressors, and coping strategies among nursing students in the Middle East and North Africa: an overview of systematic reviews. Syst Rev. 2021;10:136.
Pines EW, Rauschhuber ML, Norgan GH, Cook JD, Canchola L, Richardson C, et al. Stress resiliency, psychological empowerment and conflict management styles among baccalaureate nursing students. J Adv Nurs. 2012;68:1482–93.
Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. 1993;55:234–47.
Article CAS PubMed Google Scholar
Boyd MA. Essentials of psychiatric nursing. Philadelphia, PA: Wolters Kluwer; 2017.
Google Scholar
Labrague LJ, McEnroe-Petitte DM, Gloe D, Thomas L, Papathanasiou IV, Tsaras K. A literature review on stress and coping strategies in nursing students. J Ment Health. 2017;26:471–80.
Ni C, Lo D, Liu X, Ma J, Xu S, Li L. Chinese female nursing students’ coping strategies, self-esteem and related factors in different years of school. J Nurs Educ Pract. 2012;2:33–41.
Jan LK, Popescu L. Israel’s nursing students’ stress sources and coping strategies during their first clinical experience in hospital wards-a qualitative research. Soc Work Rev / Rev Asistenta Soc. 2014;13:163–88.
Tung YJ, Lo KKH, Ho RCM, Tam WSW. Prevalence of depression among nursing students: a systematic review and meta-analysis. Nurse Educ Today. 2018;63:119–29.
Speziale HS, Streubert HJ, Carpenter DR. Qualitative research in nursing: advancing the humanistic imperative. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–12.
Bryman A. Integrating quantitative and qualitative research: how is it done? Qual Res. 2006;6:97–113.
Holloway I, Wheeler S. Qualitative research in nursing and healthcare. New York, NY: Wiley; 2013.
Richards L, Morse J. A user’s guide to qualitative methods. London, UK: Sage; 2007.
Lincoln Y, Guba EG. The SAGE handbook of qualitative research. Newbury Park, CA: SAGE Publications Inc; 2017.
Park S, Park KS. Family stigma: a concept analysis. Asian Nurs Res. 2014;8:165–71.
Onieva-Zafra MD, Fernández-Muñoz JJ, Fernández-Martínez E, García-Sánchez FJ, Abreu-Sánchez A, Parra-Fernández ML. Anxiety, perceived stress and coping strategies in nursing students: a cross-sectional, correlational, descriptive study. BMC Med Educ. 2020;20:370.
Albloushi M, Ferguson L, Stamler L, Bassendowski S, Hellsten L, Kent-Wilkinson A. Saudi female nursing students experiences of sense of belonging in the clinical settings: a qualitative study. Nurse Educ Pract. 2019;35:69–74.
Arkan B, Ordin Y, Yılmaz D. Undergraduate nursing students’ experience related to their clinical learning environment and factors affecting to their clinical learning process. Nurse Educ Pract. 2018;29:127–32.
Bhurtun HD, Azimirad M, Saaranen T, Turunen H. Stress and coping among nursing students during clinical training: an integrative review. J Nurs Educ. 2019;58:266–72.
Jamshidi N, Molazem Z, Sharif F, Torabizadeh C, Kalyani MN. The challenges of nursing students in the clinical learning environment: a qualitative study. ScientificWorldJournal. 2016;2016:1846178.
Porter SL. First year nursing students’ perceptions of stress and resilience during their initial clinical placement and the introduction of a stress management app: a mixed methods approach. A thesis submitted in partial fulfilment of the requirements of Edinburgh Napier University, for the award of Doctor of Philosophy. 2019. https://www.napier.ac.uk/~/media/worktribe/output-2086663/first-year-nursing-students-perceptions-of-stress-and-resilience-during-their-initial.pdf
Panda S, Dash M, John J, Rath K, Debata A, Swain D, et al. Challenges faced by student nurses and midwives in clinical learning environment - A systematic review and meta-synthesis. Nurse Educ Today. 2021;101:104875.
Ahmadi G, Shahriari M, Keyvanara M, Kohan S. Midwifery students’ experiences of learning clinical skills in Iran: a qualitative study. Int J Med Educ. 2018;9:64–71.
Harrison-White K, Owens J. Nurse link lecturers’ perceptions of the challenges facing student nurses in clinical learning environments: a qualitative study. Nurse Educ Pract. 2018;32:78–83.
Grobecker PA. A sense of belonging and perceived stress among baccalaureate nursing students in clinical placements. Nurse Educ Today. 2016;36:178–83.
Msiska G, Kamanga M, Chilemba E, Msosa A, Munkhondya TE. Sources of stress among undergraduate nursing students during clinical practice: a Malawian perspective. Open J Nurs. 2019;9:1.
Joolaee S, Amiri SRJ, Farahani MA, Varaei S. Iranian nursing students’ preparedness for clinical training: a qualitative study. Nurse Educ Today. 2015;35:e13–7.
Günay U, Kılınç G. The transfer of theoretical knowledge to clinical practice by nursing students and the difficulties they experience: a qualitative study. Nurse Educ Today. 2018;65:81–6.
Farzi S, Shahriari M, Farzi S. Exploring the challenges of clinical education in nursing and strategies to improve it: a qualitative study. J Educ Health Promot. 2018;7:115.
Hamaideh SH, Al-Omari H, Al-Modallal H. Nursing students’ perceived stress and coping behaviors in clinical training in Saudi Arabia. J Ment Health. 2017;26:197–203.
Yaghoobi A, Mohagheghi H, Zade MY, Ganji K, Olfatii N. The effect of time management training on test anxiety and academic achievement motivation among high school students. J Sch Psychol. 2014;3:131–44.
Kebriaei A, Bidgoli MS, Saeedi A. Relationship between use of time management skills and satisfaction with spending time among students of Zahedan University of Medical Sciences. J Med Educ Dev. 2014;6:79–88.
Chen YW, Hung CH. Predictors of Taiwanese baccalaureate nursing students’ physio-psycho-social responses during clinical practicum. Nurse Educ Today. 2014;34:73–7.
Ab Latif R, Mat Nor MZ. Stressors and coping strategies during clinical practice among diploma nursing students. Malays J Med Sci. 2019;26:88–98.
Al-Yateem N, Almarzouqi A, Dias JM, Saifan A, Timmins F. Nursing in the United Arab Emirates: current challenges and opportunities. J Nurs Manag. 2021;29:109–12.
Baraz-Pordanjani S, Memarian R, Vanaki Z. Damaged professional identity as a barrier to Iranian nursing students’ clinical learning: a qualitative study. J Clin Nurs Midwifery. 2014;3:1–15.
Labrague LJ, McEnroe-Petitte DM, Papathanasiou IV, Edet OB, Tsaras K, Leocadio MC, et al. Stress and coping strategies among nursing students: an international study. J Ment Health. 2018;27:402–8.
Madian AAEM, Abdelaziz MM, Ahmed HAE. Level of stress and coping strategies among nursing students at Damanhour University, Egypt. Am J Nurs Res. 2019;7:684–96.
Wu CS, Rong JR, Huang MZ. Factors associated with perceived stress of clinical practice among associate degree nursing students in Taiwan. BMC Nurs. 2021;20:89.
Zhao FF, Lei XL, He W, Gu YH, Li DW. The study of perceived stress, coping strategy and self-efficacy of Chinese undergraduate nursing students in clinical practice. Int J Nurs Pract. 2015;21:401–9.
Bektaş H, Terkes N, Özer Z. Stress and ways of coping among first year nursing students: a Turkish perspective. J Hum Sci. 2018;15:319–30.
John B, Al-Sawad M. Perceived stress in clinical areas and emotional intelligence among baccalaureate nursing students. J Indian Acad Appl Psychol. 2015;41:76–85.
Mapfumo JS, Chitsiko N, Chireshe R. Teaching practice generated stressors and coping mechanisms among student teachers in Zimbabwe. S Afr J Educ. 2012;32:155–66.
Timmins F, Corroon AM, Byrne G, Mooney B. The challenge of contemporary nurse education programmes. Perceived stressors of nursing students: mental health and related lifestyle issues. J Psychiatr Ment Health Nurs. 2011;18:758–66.
Hegberg NJ, Tone EB. Physical activity and stress resilience: considering those at-risk for developing mental health problems. Ment Health Phys Act. 2015;8:1–7.
Shudifat RM, Al-Husban RY. Perceived sources of stress among first-year nursing students in Jordan. J Psychosoc Nurs Ment Health Serv. 2015;53:37–43.
El Ansari W, Adetunji H, Oskrochi R. Food and mental health: relationship between food and perceived stress and depressive symptoms among university students in the United Kingdom. Cent Eur J Public Health. 2014;22:90–7.
Dias JM, Aderibigbe SA, Abraham MS. Undergraduate nursing students’ mentoring experiences in the clinical practicum: the United Arab Emirates (UAE) perspective. J Nurs Manag. 2022;30:4304–13.
Download references
Acknowledgements
The authors are grateful to all second year nursing students who voluntarily participated in the study.
No funding was received. Not applicable.
Author information
Authors and affiliations.
Department of Nursing, College of Health Sciences, University of Sharjah, POBox, Sharjah, 272272, UAE
Jacqueline Maria Dias, Muhammad Arsyad Subu, Nabeel Al-Yateem, Fatma Refaat Ahmed, Syed Azizur Rahman, Mini Sara Abraham, Sareh Mirza Forootan, Farzaneh Ahmad Sarkhosh & Fatemeh Javanbakh
Health Care Management, College of Health Sciences, University of Sharjah, Sharjah, United Arab Emirates
Syed Azizur Rahman
You can also search for this author in PubMed Google Scholar
Contributions
JMD conceptualized the idea and designed the methodology, formal analysis, writing original draft and project supervision and mentoring. MAS prepared the methodology and conducted the qualitative interviews and analyzed the methodology and writing of original draft and project supervision. NY, FRA, SAR, MSA writing review and revising the draft. SMF, FAS, FJ worked with MAS on the formal analysis and prepared the first draft.All authors reviewed the final manuscipt of the article.
Corresponding author
Correspondence to Jacqueline Maria Dias .
Ethics declarations
Ethics approval and consent to participate.
The Research Ethics Committee (REC) under) the Office of the Vice Chancellor for Research and Graduate Studies UOS approved this study (REC 19-12-03-01-S). Additionally, a written consent was obtained from all participants and the process followed the recommended policies and guidelines of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
Dr Fatma Refaat Ahmed is an editorial board member in BMC Nursing. Other authors do not have any conflict of interest
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dias, J.M., Subu, M.A., Al-Yateem, N. et al. Nursing students’ stressors and coping strategies during their first clinical training: a qualitative study in the United Arab Emirates. BMC Nurs 23 , 322 (2024). https://doi.org/10.1186/s12912-024-01962-5
Download citation
Received : 06 January 2024
Accepted : 22 April 2024
Published : 11 May 2024
DOI : https://doi.org/10.1186/s12912-024-01962-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical practicums
- Coping strategies
- Nursing students
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Infection Prevention and Long-term Care Facility Residents
- Nursing Home Infection Preventionist Training
- PPE in Nursing Homes
- Respiratory Virus Toolkit
- Healthcare-Associated Infections (HAIs)
- The resources on this page can keep you and your loved ones safe.
Long-term care facilities provide many services, both medical and personal care, to people who are unable to live without help.
If you live in a nursing home, assisted living facility or other long-term care facility, you have a higher risk of getting an infection. There are steps you can take to reduce your risk:
- Tell your healthcare provider if you think you have an infection or if your infection is getting worse.
- Take antibiotics exactly as prescribed and tell your healthcare provider if you have any side effects, such as diarrhea.
- Keep your hands clean. Remind staff and visitors to keep their hands clean.
- Get vaccinated against flu and other infections to avoid complications.
Resources for staying safe in long-term care facilities

About C. diff
About Carbapenem-resistant Enterobacterales
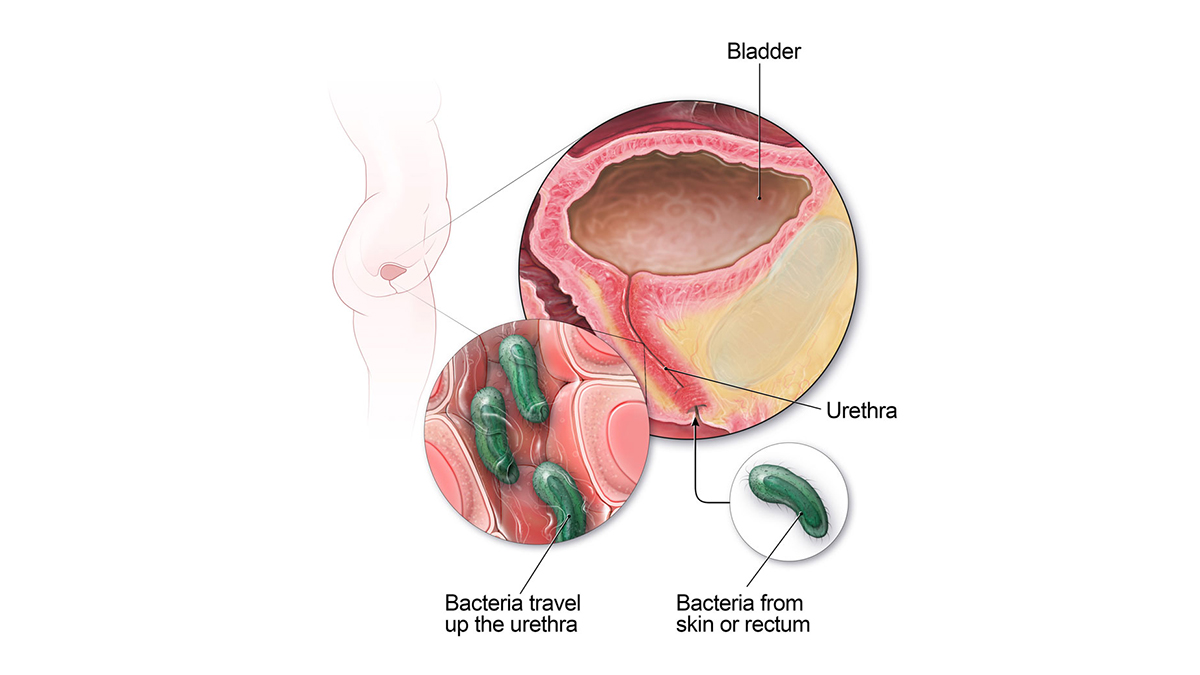
Catheter-associated Urinary Tract Infection Basics
Methicillin-resistant Staphylococcus aureus (MRSA) Basics

Healthy Habits: Antibiotic Do's and Don'ts

About Sepsis

About Norovirus
Resources for family members and caregivers
- Medicare resources for long-term care residents and caregivers.
- Find a nursing home in your area .
This website provides resources for patients, families and caregivers on the prevention of infections in nursing homes and assisted living facilities.
For Everyone
Health care providers.

IMAGES
VIDEO
COMMENTS
Research Nurses, also referred to as Clinical Nurse Researchers or Nurse Researchers, develop and implement studies to investigate and provide information on new medications, vaccinations, and medical procedures. They assist in providing evidence-based research that is essential to safe and quality nursing care. This guide will explain what a Research Nurse does, how much they make, how to ...
Besides patient interactions, a clinical research nurse may be responsible for writing reports or study results, submitting and publishing studies in medical journals, or presenting research findings at a medical conference. What Studies Do Clinical Research Nurses Participate In? Medical research is either quantitative or qualitative.
Clinical research nurses are clinical staff nurses with a central focus on care of research participants. They support study implementation within the context of the care delivery setting and are primarily located in dedicated clinical research settings, such as the NIH Clinical Center and clinical research units located in academic medical ...
A Research Nurse is a professional member of a research team who provides direct patient care for participants in clinical trials. In these studies, volunteers take part in activities related to medical testing and experiments that will help researchers understand more about human health and disease.
Step 1 - Graduate From High School. Before graduating from high school, there are many ways that students can prepare for a career as a research nurse in clinical trials. It is recommended that to help prepare for coursework in clinical nursing and research, one should take a wide variety of courses in anatomy, physiology, mathematics ...
The Nurse Scientist is a nurse with advanced preparation (PhD in nursing or related field) in research principles and methodology, who also has expert content knowledge in a specific clinical area. The primary focus of the role is to (1) provide leadership in the development, coordination and management of clinical research studies; (2) provide ...
During a clinical trial or scientific experiment, a research nurse provides direct treatment and care to all participants. They safeguard the participants' safety, well-being and rights throughout the study. A research nurse specifically studies clinical research methodology, regulatory measures and ethics related to the conduct of clinical ...
The Society of Clinical Research Associates reported a median salary for research nurses of $72,009 in their SoCRA 2015 Salary Survey, one of the highest-paying nursing specializations in the field. Salary levels for nurse researchers can vary based on the type of employer, geographic location and the nurse's education and experience level.
Bridging the gap between clinical care and research operations is an important and timely area of focus for both academic medical centers and study sponsors. The oversight of participants on high risk and early phase research protocols requires expert clinical oversight and coordination of care, and knowledge and experience in research execution.
The role of the clinical research nurse as clinician, advocate, educator, collaborator and leader will be introduced with an emphasis on collaborative practice within clinical and research teams. ... Epidemiology is the study of the distribution and determinants of health and disease in different human populations and the application of methods ...
An estimated 10,000 clinical research nurses (CRNs) are found working across a wide spectrum of roles and settings within the global clinical research enterprise (American Nurses Association and International Association of Clinical Research Nurses, 2016; Wallen and Fisher, 2018).Previous role delineation studies on CRNs have primarily focused on nurses working in acute care, dedicated ...
Clinical Research Nurses' described perceptions and experiences of working to co-ordinate and deliver a range of research as individuals, within their teams, throughout the wider organisation, and beyond. ... Smith V, Yiannakou Y, et al. (2018) Professional identity and the Clinical Research Nurse: A qualitative study exploring issues ...
The work of clinical research nurses can have a wide-ranging impact. Through their involvement, new pharmaceutical interventions can be developed with a clear sense of how those drugs impact patient safety and well-being. Clinical research nurses also assist in the formation of new preventative measures and clinical procedures. Steps to ...
Complete 4,000 practical hours in the clinical research nurse role; Have a complete resume; Provide a 1,000-to-1,500-word clinical research nurse exemplar, which should contain evidence of professional growth and development, practice, team focus and collaboration and quality and safety. The exemplar will comprise 45% of the total score.
Introduction. Nursing is widely considered an art and a science (Jairath et al., 2018), incorporating a systematically organized scientific body of knowledge and evidence-based care (Sten et al., 2021), alongside innovative and thoughtful approaches that ensure safe processes of care delivery.The art and science of the Clinical Research Nurse (CRN) role is found within the weaving of care ...
Contents - Clinical Research Nursing: Scope and Standards of Practice ... Study Management . Roles of the Clinical Research Nurse . Clinician . Manager . Educator . Advocate . Regulatory Specialist . Nurse Scientist . Tenets of Clinical Research Nursing . Principles that Guide Clinical Research Practice .
Clinical Research Nurse Coordinator. Odyssey Systems Consulting Group, Ltd. Hybrid work in Portsmouth, VA 23708. Pay information not provided. Full-time. Assist PI, research team members, and other staff in the preparation of and closeout of clinical research studies. Citizenship: Must be a US citizen.
Know that future CRNs can speak to our 24/7 chat and phone advisors to request information on partial scholarships and payment plans for nurses. 2. Clinical Research Nurse Salary. The average pay for a Clinical Research Nurse is $31.28 per hour. MD Anderson Cancer Center Clinical Research Nurse salaries - $71,503/yr.
The SMART II Study. The purpose of the SMART II study was to evaluate the efficacy of a nurse-delivered intervention aimed to reduce parent distress, and enhance the family environment, resilience, and well-being of AYAs with high-risk cancer and their parents. 13 SMART II was a two-group, randomized controlled, behavioral oncology clinical trial conducted at six sites across the United States.
Clinical Nursing Research (CNR) is a leading international nursing journal, published eight times a year.CNR aims to publish the best available evidence from multidisciplinary teams, with the goal of reporting clinically applicable nursing science and phenomena of interest to nursing. Part of CNR's mission is to bring to light clinically applicable solutions to some of the most complex ...
Responsibilities for clinical research nurse. Assist research investigators in collecting study data and statistics. Assist PI in submitting annual Continuing Review Reports (CRRs) and annual report for the study. Write and review Standard Operating Procedures (SOP) and Study Specific Procedures (SSP) and guidelines.
This specialty practice incorporates human subject protection; care coordination and continuity; contribution to clinical science; clinical practice; and study management throughout a variety of professional roles, practice settings, and clinical specialties. Please cite International Association of Clinical Research Nurses.
The Clinical Nurse Specialist is placed in a decision making position based on expertise, personal and/or delegated authority. Clinical Nurse Specialists interact with members of the nursing Practice Department, physicians, peer groups, other disciplines, State of Utah board of Nursing, members of specialty nursing organizations, faculty at ...
Job Summary: The Clinical Research Nurse will join the Clinical Research Central Office (CRCO) at the University of Wisconsin Carbone Cancer Center (UWCCC) to coordinate cancer clinical research within one or more Disease-Oriented Teams. The primary duties of this job involve the management of subjects enrolled in clinical research studies at the UW Carbone Cancer Center.
The Journal of Clinical Nursing publishes research and developments relevant to all areas of nursing practice- community, ... For example, the pH tests in this study were obtained by nursing staff under typical clinical pressure rather than by specialist nurses conducting a study. The analysis and description of the complications resulting from ...
The clinical trials nurse (CTN) serves as a study coordinator but may have different job titles (e.g., Research Nurse Coordinator, Clinical Research Nurse, Clinical Research Coordinator) and may be supervised by a physician, investigator, or a non-nurse research manager. 5-9 The purpose of this article is to provide an overview of clinical ...
Understanding the stressors and coping strategies of nursing students in their first clinical training is important for improving student performance, helping students develop a professional identity and problem-solving skills, and improving the clinical teaching aspects of the curriculum in nursing programmes. While previous research have examined nurses' sources of stress and coping styles ...
CAR T-cell immunotherapy changes these collected T cells to produce chimeric antigen receptors (or CARs) that adhere to tumors to destroy them. A recent study published in the New England Journal of Medicine, suggests CAR T-cell therapy could become a highly effective treatment for SLE patients who do not respond to current lupus therapeutics ...
As a leading international medical research university with the largest medical faculty in Australia and integration with leading Australian teaching hospitals, we consistently rank in the top 50 universities worldwide for clinical, pre-clinical and health sciences. For more news, visit Medicine, Nursing and Health Sciences or Monash University.
Long-term care facilities provide many services, both medical and personal care, to people who are unable to live without help. If you live in a nursing home, assisted living facility or other long-term care facility, you have a higher risk of getting an infection. There are steps you can take to reduce your risk: