77 interesting medical research topics for 2024
Last updated
25 November 2023
Reviewed by
Brittany Ferri, PhD, OTR/L
Medical research is the gateway to improved patient care and expanding our available treatment options. However, finding a relevant and compelling research topic can be challenging.
Use this article as a jumping-off point to select an interesting medical research topic for your next paper or clinical study.
- How to choose a medical research topic
When choosing a research topic , it’s essential to consider a couple of things. What topics interest you? What unanswered questions do you want to address?
During the decision-making and brainstorming process, here are a few helpful tips to help you pick the right medical research topic:

Focus on a particular field of study
The best medical research is specific to a particular area. Generalized studies are often too broad to produce meaningful results, so we advise picking a specific niche early in the process.
Maybe a certain topic interests you, or your industry knowledge reveals areas of need.
Look into commonly researched topics
Once you’ve chosen your research field, do some preliminary research. What have other academics done in their papers and projects?
From this list, you can focus on specific topics that interest you without accidentally creating a copycat project. This groundwork will also help you uncover any literature gaps—those may be beneficial areas for research.
Get curious and ask questions
Now you can get curious. Ask questions that start with why, how, or what. These questions are the starting point of your project design and will act as your guiding light throughout the process.
For example:
What impact does pollution have on children’s lung function in inner-city neighborhoods?
Why is pollution-based asthma on the rise?
How can we address pollution-induced asthma in young children?
- 77 medical research topics worth exploring in 2023
Need some research inspiration for your upcoming paper or clinical study? We’ve compiled a list of 77 topical and in-demand medical research ideas. Let’s take a look.
- Exciting new medical research topics
If you want to study cutting-edge topics, here are some exciting options:
COVID-19 and long COVID symptoms
Since 2020, COVID-19 has been a hot-button topic in medicine, along with the long-term symptoms in those with a history of COVID-19.
Examples of COVID-19-related research topics worth exploring include:
The long-term impact of COVID-19 on cardiac and respiratory health
COVID-19 vaccination rates
The evolution of COVID-19 symptoms over time
New variants and strains of the COVID-19 virus
Changes in social behavior and public health regulations amid COVID-19
Vaccinations
Finding ways to cure or reduce the disease burden of chronic infectious diseases is a crucial research area. Vaccination is a powerful option and a great topic to research.
Examples of vaccination-related research topics include:
mRNA vaccines for viral infections
Biomaterial vaccination capabilities
Vaccination rates based on location, ethnicity, or age
Public opinion about vaccination safety
Artificial tissues fabrication
With the need for donor organs increasing, finding ways to fabricate artificial bioactive tissues (and possibly organs) is a popular research area.
Examples of artificial tissue-related research topics you can study include:
The viability of artificially printed tissues
Tissue substrate and building block material studies
The ethics and efficacy of artificial tissue creation
- Medical research topics for medical students
For many medical students, research is a big driver for entering healthcare. If you’re a medical student looking for a research topic, here are some great ideas to work from:
Sleep disorders
Poor sleep quality is a growing problem, and it can significantly impact a person’s overall health.
Examples of sleep disorder-related research topics include:
How stress affects sleep quality
The prevalence and impact of insomnia on patients with mental health conditions
Possible triggers for sleep disorder development
The impact of poor sleep quality on psychological and physical health
How melatonin supplements impact sleep quality
Alzheimer’s and dementia
Cognitive conditions like dementia and Alzheimer’s disease are on the rise worldwide. They currently have no cure. As a result, research about these topics is in high demand.
Examples of dementia-related research topics you could explore include:
The prevalence of Alzheimer’s disease in a chosen population
Early onset symptoms of dementia
Possible triggers or causes of cognitive decline with age
Treatment options for dementia-like conditions
The mental and physical burden of caregiving for patients with dementia
- Lifestyle habits and public health
Modern lifestyles have profoundly impacted the average person’s daily habits, and plenty of interesting topics explore its effects.
Examples of lifestyle and public health-related research topics include:
The nutritional intake of college students
The impact of chronic work stress on overall health
The rise of upper back and neck pain from laptop use
Prevalence and cause of repetitive strain injuries (RSI)
- Controversial medical research paper topics
Medical research is a hotbed of controversial topics, content, and areas of study.
If you want to explore a more niche (and attention-grabbing) concept, here are some controversial medical research topics worth looking into:
The benefits and risks of medical cannabis
Depending on where you live, the legalization and use of cannabis for medical conditions is controversial for the general public and healthcare providers.
Examples of medical cannabis-related research topics that might grab your attention include:
The legalization process of medical cannabis
The impact of cannabis use on developmental milestones in youth users
Cannabis and mental health diagnoses
CBD’s impact on chronic pain
Prevalence of cannabis use in young people
The impact of maternal cannabis use on fetal development
Understanding how THC impacts cognitive function
Human genetics
The Human Genome Project identified, mapped, and sequenced all human DNA genes. Its completion in 2003 opened up a world of exciting and controversial studies in human genetics.
Examples of human genetics-related research topics worth delving into include:
Medical genetics and the incidence of genetic-based health disorders
Behavioral genetics differences between identical twins
Genetic risk factors for neurodegenerative disorders
Machine learning technologies for genetic research
Sexual health studies
Human sexuality and sexual health are important (yet often stigmatized) medical topics that need new research and analysis.
As a diverse field ranging from sexual orientation studies to sexual pathophysiology, examples of sexual health-related research topics include:
The incidence of sexually transmitted infections within a chosen population
Mental health conditions within the LGBTQIA+ community
The impact of untreated sexually transmitted infections
Access to safe sex resources (condoms, dental dams, etc.) in rural areas
- Health and wellness research topics
Human wellness and health are trendy topics in modern medicine as more people are interested in finding natural ways to live healthier lifestyles.
If this field of study interests you, here are some big topics in the wellness space:
Gluten sensitivity
Gluten allergies and intolerances have risen over the past few decades. If you’re interested in exploring this topic, your options range in severity from mild gastrointestinal symptoms to full-blown anaphylaxis.
Some examples of gluten sensitivity-related research topics include:
The pathophysiology and incidence of Celiac disease
Early onset symptoms of gluten intolerance
The prevalence of gluten allergies within a set population
Gluten allergies and the incidence of other gastrointestinal health conditions
Pollution and lung health
Living in large urban cities means regular exposure to high levels of pollutants.
As more people become interested in protecting their lung health, examples of impactful lung health and pollution-related research topics include:
The extent of pollution in densely packed urban areas
The prevalence of pollution-based asthma in a set population
Lung capacity and function in young people
The benefits and risks of steroid therapy for asthma
Pollution risks based on geographical location
Plant-based diets
Plant-based diets like vegan and paleo diets are emerging trends in healthcare due to their limited supporting research.
If you’re interested in learning more about the potential benefits or risks of holistic, diet-based medicine, examples of plant-based diet research topics to explore include:
Vegan and plant-based diets as part of disease management
Potential risks and benefits of specific plant-based diets
Plant-based diets and their impact on body mass index
The effect of diet and lifestyle on chronic disease management
Health supplements
Supplements are a multi-billion dollar industry. Many health-conscious people take supplements, including vitamins, minerals, herbal medicine, and more.
Examples of health supplement-related research topics worth investigating include:
Omega-3 fish oil safety and efficacy for cardiac patients
The benefits and risks of regular vitamin D supplementation
Health supplementation regulation and product quality
The impact of social influencer marketing on consumer supplement practices
Analyzing added ingredients in protein powders
- Healthcare research topics
Working within the healthcare industry means you have insider knowledge and opportunity. Maybe you’d like to research the overall system, administration, and inherent biases that disrupt access to quality care.
While these topics are essential to explore, it is important to note that these studies usually require approval and oversight from an Institutional Review Board (IRB). This ensures the study is ethical and does not harm any subjects.
For this reason, the IRB sets protocols that require additional planning, so consider this when mapping out your study’s timeline.
Here are some examples of trending healthcare research areas worth pursuing:
The pros and cons of electronic health records
The rise of electronic healthcare charting and records has forever changed how medical professionals and patients interact with their health data.
Examples of electronic health record-related research topics include:
The number of medication errors reported during a software switch
Nurse sentiment analysis of electronic charting practices
Ethical and legal studies into encrypting and storing personal health data
Inequities within healthcare access
Many barriers inhibit people from accessing the quality medical care they need. These issues result in health disparities and injustices.
Examples of research topics about health inequities include:
The impact of social determinants of health in a set population
Early and late-stage cancer stage diagnosis in urban vs. rural populations
Affordability of life-saving medications
Health insurance limitations and their impact on overall health
Diagnostic and treatment rates across ethnicities
People who belong to an ethnic minority are more likely to experience barriers and restrictions when trying to receive quality medical care. This is due to systemic healthcare racism and bias.
As a result, diagnostic and treatment rates in minority populations are a hot-button field of research. Examples of ethnicity-based research topics include:
Cancer biopsy rates in BIPOC women
The prevalence of diabetes in Indigenous communities
Access inequalities in women’s health preventative screenings
The prevalence of undiagnosed hypertension in Black populations
- Pharmaceutical research topics
Large pharmaceutical companies are incredibly interested in investing in research to learn more about potential cures and treatments for diseases.
If you’re interested in building a career in pharmaceutical research, here are a few examples of in-demand research topics:
Cancer treatment options
Clinical research is in high demand as pharmaceutical companies explore novel cancer treatment options outside of chemotherapy and radiation.
Examples of cancer treatment-related research topics include:
Stem cell therapy for cancer
Oncogenic gene dysregulation and its impact on disease
Cancer-causing viral agents and their risks
Treatment efficacy based on early vs. late-stage cancer diagnosis
Cancer vaccines and targeted therapies
Immunotherapy for cancer
Pain medication alternatives
Historically, opioid medications were the primary treatment for short- and long-term pain. But, with the opioid epidemic getting worse, the need for alternative pain medications has never been more urgent.
Examples of pain medication-related research topics include:
Opioid withdrawal symptoms and risks
Early signs of pain medication misuse
Anti-inflammatory medications for pain control
- Identify trends in your medical research with Dovetail
Are you interested in contributing life-changing research? Today’s medical research is part of the future of clinical patient care.
As your go-to resource for speedy and accurate data analysis , we are proud to partner with healthcare researchers to innovate and improve the future of healthcare.
Get started today
Go from raw data to valuable insights with a flexible research platform
Editor’s picks
Last updated: 21 December 2023
Last updated: 16 December 2023
Last updated: 6 October 2023
Last updated: 25 November 2023
Last updated: 12 May 2023
Last updated: 15 February 2024
Last updated: 11 March 2024
Last updated: 12 December 2023
Last updated: 18 May 2023
Last updated: 6 March 2024
Last updated: 10 April 2023
Last updated: 20 December 2023
Latest articles
Related topics, log in or sign up.
Get started for free

MARK H. EBELL, MD, MS, AND ROLAND GRAD, MD, MSc
June 8, 2020 Editor's Note: The hypertension study (reference 5) is under investigation by the editor of the journal in which it was published due to inconsistencies in the data noted by others. Caution is warranted regarding applying these findings to clinical care.
Am Fam Physician. 2020;101(10):608-617
Author disclosure: Dr. Ebell is cofounder and editor-in-chief of Essential Evidence Plus. See Editor's Note . Dr. Grad has no relevant financial affiliations.
In 2019, regular surveillance of 110 English-language research journals identified 254 studies that met the criteria to become POEMs (patient-oriented evidence that matters). Physician members of the Canadian Medical Association rated these POEMs for their relevance to patients in their practices. This article summarizes the clinical questions and bottom-line answers from the top 20 POEMs of 2019. Taking blood pressure medications at night results in a large mortality reduction over six years compared with morning dosing. Automated devices are the best way to measure blood pressure. Nonfasting lipid profiles are preferred over fasting lipid profiles, and nonfasting and fasting lipid profiles are equally effective at predicting risk. The benefit of statins for primary prevention in people 75 years and older is uncertain at best. Aspirin has no net benefit for primary prevention of cardiovascular disease and has no effect on cancer outcomes. An Italian study found fecal immunochemical testing over five biennial screening cycles has a similar colorectal cancer yield as screening colonoscopy, whereas a meta-analysis found that taking aspirin, an anticoagulant, or a nonsteroidal anti-inflammatory drug has no impact on the positive predictive value of fecal immunochemical testing. Regarding infections, a meta-analysis showed that patients presenting with symptoms of acute respiratory tract infection are unlikely to have pneumonia if vital signs and the lung examination findings are normal. For streptococcal pharyngitis (strep throat), penicillin V at a dosage of 800 mg four times a day for five days is at least as effective as a dosage of 1,000 mg three times a day for 10 days. A primary care study in the United Kingdom reinforced that clinicians should counsel parents of children with lower respiratory tract symptoms to be patient, because these infections can take three weeks or more to fully resolve. Among direct oral anticoagulants, apixaban has the lowest bleeding risk, and cotreating with a proton pump inhibitor significantly reduces bleeding risk. Single ibuprofen doses from 400 to 800 mg significantly reduce acute pain to a similar degree. The two-dose recombinant zoster vaccine is much more effective than the single-dose live, attenuated vaccine but with a greater risk of injection site pain. Exercise helps reduce the risk of falls in older adults. Practice guidelines from 2019 on antithrombotics for atrial fibrillation, the management of type 2 diabetes mellitus, and screening for breast cancer were judged to be especially relevant.
Every year for the past 21 years, a team of experts in evidence-based medicine have systematically reviewed more than 110 English-language research journals to identify the original research most likely to change and improve primary care practice. The team includes experts in family medicine, pharmacology, hospital medicine, and women's health. 1 , 2
The goal of this process is to identify POEMs (patient-oriented evidence that matters). A POEM must report at least one patient-oriented outcome, such as improvement in symptoms, morbidity, or mortality. It should also be free of important methodologic bias, making the results valid and trustworthy. Finally, if applied in practice, the results would change what some family physicians do in patient care by prompting them to adopt a beneficial new practice or discontinue one that is ineffective or harmful. This should improve patient outcomes. Of more than 20,000 research studies published in 2019 in the journals reviewed by the POEMs team, 254 met criteria for validity, relevance, and practice change.
The Canadian Medical Association (CMA) purchases a subscription to POEMs for its members, many of whom receive the daily POEM by email. When members read a POEM, they can rate it with a validated questionnaire called the Information Assessment Method. POEM ratings address the domains of clinical relevance, cognitive impact, use in practice, and expected health benefits if that POEM were to be applied in patient care. 3 , 4 In 2019, each of the 254 POEMs were rated by an average of 1,530 physicians.
In this article, we present the 20 POEMs rated highest for clinical relevance by CMA members in 2019. This installment of our annual series ( https://www.aafp.org/afp/toppoems ) summarizes the clinical question and bottom-line answer for each research study identified as a top 20 POEM, organized by topic and followed by a brief discussion. We also present the three most relevant practice guidelines identified by CMA members. The full text of the POEMs in this article are available at https://www.aafp.org/journals/afp/content/top-poems/2019.html .
Hypertension
Hypertension is among the most common conditions managed by primary care physicians and is the topic of the two POEMs rated most relevant to readers in 2019 ( Table 1 ) . 5 , 6 Researchers randomized 19,168 adults with hypertension to take their antihypertensive medications at bedtime or first thing in the morning. 5 Patients were prescribed an antihypertensive from an approved list of the most common therapies. Patients taking their medications at bedtime had a lower likelihood of the composite outcome of myocardial infarction (MI), coronary revascularization, heart failure, stroke, or cardiovascular death (hazard ratio = 0.55; 95% CI, 0.50 to 0.61; number needed to treat to prevent one event over 6.3 years = 20). All-cause mortality was reduced to a similar extent. This is a large effect for a six-year study, and a practice-changer for many patients and physicians. Best of all, it costs nothing to make this change. See Editor's Note
How we measure blood pressure continues to be a subject of research. The next POEM was a meta-analysis of 31 studies, which included a total of 9,279 patients and compared automated in-office blood pressure readings with in-office manual measurements or ambulatory automated recordings during waking hours (the reference standard). 6 Automated in-office measurements were performed without anyone present to activate the machine and used three to five readings separated by one- to two-minutes. Ambulatory automated measurements were 13.4/5.9 mm Hg lower than the manual in-office measurements and were similar to the in-office automated measurements. To avoid starting or intensifying antihypertensive medication unnecessarily, it is critical to measure blood pressure using an automated device. Patients should also bring in their home device so that it can be calibrated with the office device.
Behavioral Medicine
Behavioral medicine POEMs are summarized in Table 2 . 7 – 9 The first POEM in this group was a well-executed network meta-analysis of medical therapy for generalized anxiety disorder. 7 A network meta-analysis includes studies comparing drugs with each other and with placebo, allowing for direct and indirect comparisons. The meta-analysis included 89 studies involving 25,000 patients and 22 different drugs; none of the studies were longer than 26 weeks. After excluding drugs that were poorly tolerated such as quetiapine (Seroquel), paroxetine (Paxil), and benzodiazepines, the most effective commercially available drugs overall were, in order of effectiveness, bupropion (Wellbutrin), duloxetine (Cymbalta), mirtazapine (Remeron), hydroxyzine, sertraline (Zoloft), pregabalin (Lyrica), venlafaxine, escitalopram (Lexapro), fluoxetine (Prozac), buspirone (Buspar), and citalopram (Celexa). Drugs that did not significantly decrease anxiety scores included imipramine, maprotiline, opipramol (not available in the United States), tiagabine (Gabitril), vilazodone (Viibryd), and vortioxetine (Trintellix). The drugs with the best combination of effectiveness and tolerability were duloxetine, pregabalin, venlafaxine, and escitalopram.
The next POEM included videotaped encounters between 252 patients and 15 English primary care physicians. 8 Patients were asked about the main reason for their visit beforehand, and this reason was almost always addressed during the visit. However, of the 139 patients who identified at least one symptom in the previsit interview, 43 failed to disclose a total of 67 symptoms during the visit, most often stress, worries or sadness; tiredness or sleep problems; problems passing urine; headache; and intimate or other personal problems. Although physicians cannot ask every patient about all of their problems during a visit, it is important to know that patients may not fully disclose symptoms. Physicians should make patients feel as safe as possible while looking for cues to undisclosed symptoms, and routinely asking, “Is there anything else I can help you with?”
The last POEM in the behavioral medicine group was an individual patient data meta-analysis of how early treatment response impacts later outcomes in patients with depression. 9 The researchers combined the individual patient data from 30 randomized trials, with 2,184 patients receiving placebo and 6,058 receiving active therapy. After six weeks of treatment, about 50% of patients in the active treatment group responded to treatment, with 32% achieving remission of symptoms. Response was defined as at least a 50% reduction in the Hamilton Rating Scale for Depression score, and remission was defined as a score of 7 points or less. By 12 weeks, the response rate was 68% in the active treatment group, with 49% achieving remission. Patients with improvement at two weeks were more likely to respond by six weeks, whereas among patients without early improvement, 33% responded by six weeks and 43% by 12 weeks. The absence of an early response does not preclude later response; therefore, physicians should not be too quick to change antidepressant medications.
Cardiovascular
Cardiovascular medicine POEMs are summarized in Table 3 . 10 – 14 The first two POEMs in this group address statin use. Many physicians and laboratory staff continue to insist that patients be fasting for lipid profile testing. The first POEM compared fasting and nonfasting lipid profiles in the same patients four weeks apart. 10 There was little difference between fasting and nonfasting measurements of low-density and high-density lipoprotein cholesterol levels and only a small increase in triglyceride levels (25 mg per dL [0.28 mmol per L]) with nonfasting measurements. Most importantly, the association between lipid levels and subsequent cardiovascular events was identical for fasting and nonfasting lipid measurements. Guidelines support nonfasting lipid measurements. 15 , 16 It is time to simplify our patients' lives and educate local laboratory staff, who often turn away patients who disclose that they are not fasting.
In the next POEM, data were pooled from 28 randomized trials of statins with more than 186,000 total patients. 11 This report focused on the 14,000 patients who were 75 years or older; the median follow-up was five years. There was only a small reduction in the composite outcome of MI and cardiovascular death among all patients (2.6% with statins vs. 3.0% with placebo; number needed to treat = 250 per year); the benefit was significant only in patients with preexisting cardiovascular disease. Statins had no effect on revascularization, stroke, cancer incidence, or cancer mortality.
This was a big year for aspirin studies. The next three POEMs, from two separate trials, examine the benefits and harms of aspirin therapy for primary prevention in contemporary populations. Prior studies that found a net benefit of aspirin for the primary prevention of cardiovascular disease and cancer (mostly colorectal) all recruited patients before 2002. In more recent years, fewer patients smoke or have uncontrolled hypertension, more are taking a statin, and we have widespread colorectal cancer screening. In this context, does aspirin still have a role?
Two aspirin POEMs were from the ASPREE (Aspirin in Reducing Events in the Elderly) trial, which included 19,114 adults 70 years and older in the United States and Australia (65 and older if black or Hispanic). Patients without known cardiovascular disease were randomized to aspirin, 100 mg, or placebo and were followed for a median of 4.7 years. The first POEM found no significant reduction in the likelihood of cardiovascular disease with aspirin, including fatal cardiovascular disease, fatal or nonfatal MI, and fatal or nonfatal ischemic stroke. However, they found a significant increase in major hemorrhages with aspirin. 12 The second POEM from the ASPREE trial found no difference between groups for disability-free survival, defined as a composite of death, dementia, or persistent physical disability. 13 A separate report from the ASPREE investigators (not one of the top 20 POEMs) found an increase in all-cause mortality with aspirin, primarily due to a significant increase in cancer-specific mortality (3.1% vs. 2.3%).
The third aspirin POEM was from the ASCEND (A Study of Cardiovascular Events in Diabetes) trial and included 15,480 adults 40 years and older with diabetes mellitus but no known cardiovascular disease. The patients were randomized to aspirin, 100 mg, or placebo and were followed for a median of 7.4 years. 14 There was a reduction in the composite of nonfatal MI, nonfatal stroke, or cardiovascular death with aspirin, but a corresponding increase in major hemorrhage with no effect on cardiovascular or all-cause mortality.
What do we tell our patients? A recent meta-analysis compared trials of aspirin therapy that recruited patients from 1978 to 2002 with four large trials that recruited patients since 2005. 17 The newer studies showed fewer cardiovascular benefits and no reduction in cancer incidence or mortality with aspirin as primary prevention. Based on a meta-analysis of the four most recent studies with a total of 61,604 patients, for every 1,200 patients taking aspirin instead of placebo for five years, there would be four fewer major cardiovascular events and three fewer ischemic strokes but eight more major hemorrhages, including three more intracranial hemorrhages. This study agrees with recent European guidelines that no longer recommend aspirin for primary prevention. 18 The 2016 U.S. Preventive Services Task Force (USPSTF) and 2019 American College of Cardiology guidelines recommend consideration of aspirin for primary prevention only in selected patients at high cardiovascular risk and low bleeding risk. 19 , 20 The USPSTF recommendation is currently being updated. 21
Cancer Screening
The three POEMs on cancer screening ( Table 4 ) address colorectal cancer. 22 – 24 Fecal immunochemical testing (FIT) is the recommended method for colorectal cancer screening in most countries that have screening programs and is the subject of the first two POEMs in this group. The first POEM is an Italian study that reported the diagnostic yield of five rounds of biennial FIT in persons 50 to 69 years of age submitting a single specimen. 22 The highest rates of detection occurred in the first round, as prevalent cancers were detected, and declined and then stabilized in later rounds. Over the 10-year study, about 25% of men and 18% of women had a positive test result requiring a follow-up colonoscopy. The cumulative rate was 6% for advanced adenoma and 0.85% for colorectal cancer, which are similar to findings in studies of colonoscopy in Italy and the United States. 25 , 26 These results mean we can have confidence in FIT as a screening test while we wait for the results of ongoing randomized trials of FIT vs. colonoscopy-based screening.
The second POEM about FIT was a meta-analysis evaluating the impact of aspirin, nonsteroidal anti-inflammatory drugs, and anticoagulants on the positive predictive value of the test. 23 It could theoretically go in either direction, increasing false positives by making noncancerous lesions more likely to bleed or increasing true positives by making cancers and adenomas more likely to bleed. The researchers found that the use of any of these medications had almost no effect on the positive predictive value, which was approximately 6% for colorectal cancer and 40% for advanced neoplasia. FIT requires only a single specimen and no dietary preparation, and now we know that patients undergoing FIT can continue to take medications that increase bleeding risk.
Finally, a study used a Swedish cancer registry with 173,796 patients to determine the impact of family history on the risk of colorectal cancer. 24 The relative risk of colorectal cancer using no affected relatives as the reference was 1.2 for a single second-degree relative with a history of colorectal cancer, 1.6 for a single first-degree relative or two second-degree relatives, 2.3 for one first-degree relative and one second-degree relative, 2.5 for two first-degree relatives, and 5.4 for one first-degree and two second-degree relatives. However, a previous study found that this family history–related risk is attenuated once patients reach 55 years of age. 27
POEMs on managing infections are summarized in Table 5 . 28 – 30 The first POEM is a meta-analysis of studies that recruited outpatients with acute respiratory tract infections who received chest radiography. 28 The goal was to identify the best sign, symptom, or combination that allows clinicians to rule out community-acquired pneumonia (CAP). The researchers found that for patients with the combination of normal vital signs and normal lung examination findings, the likelihood of CAP is low at 0.4%. This could help reduce unnecessary chest radiography if applied consistently.
The second POEM in this group was selected as one of the top three research studies out of more than 400 presented at the 2019 North American Primary Care Research Group meeting. 29 This Swedish study included 422 adults and children presenting to a primary care physician with moderately severe streptococcal pharyngitis (strep throat). Patients were randomized to penicillin V at a dosage of 800 mg four times a day for five days or 1,000 mg three times a day for 10 days. Those receiving the higher dose over a shorter course of treatment had similar cure rates as those receiving longer-duration therapy, with quicker symptom resolution and no increase in recurrence. Many other studies have found similar results with antibiotics for a range of infections.
An accurate prognosis can potentially help patients avoid unnecessary antibiotic use and return visits. The third POEM in this group recruited 485 healthy children in the United Kingdom, and parents were instructed to contact the researchers every time the child had a respiratory tract infection. 30 One-half of the children had at least one infection, with a median duration of nine days; 90% recovered by day 23. Lower respiratory tract infections were associated with a longer duration of symptoms and ear infections were associated with a shorter duration. This reinforces that clinicians should counsel parents of children with lower respiratory tract symptoms to be patient.
Miscellaneous
Four additional POEMs are summarized in Table 6 . 31 – 34 The first is a cohort study of more than 1.6 million Medicare beneficiaries who started an anticoagulant between 2011 and 2015. 31 Bleeding rates were compared, adjusting for available covariates using propensity score matching (i.e., matching patients who were similar other than choice of anticoagulant). The adjusted incidence of hospitalization for upper gastrointestinal tract bleeding was significantly higher in those who received rivaroxaban (Xarelto) compared with those who received dabigatran (Pradaxa), warfarin (Coumadin), or apixaban (Eliquis); 144 per 10,000 person-years vs. 120, 113, and 73, respectively). For all agents combined, adding a proton pump inhibitor significantly reduced bleeding risk (76 out of 10,000 per year vs. 115 out of 10,000 per year; number needed to treat = 256), although rivaroxaban still had the highest bleeding rate.
The next POEM identified 225 adults presenting to the emergency department with acute pain (mostly musculoskeletal); the average pain score was 6 to 7 out of 10. 32 They were then randomized to a single dose of 400-mg, 600-mg, or 800-mg ibuprofen. An hour after taking the medication, there was no difference between groups, which all had pain scores between 4.4 and 4.5.
The third POEM in this group is a meta-analysis of studies comparing two doses of the recombinant zoster vaccine (Shingrix) with one dose of the live, attenuated vaccine (Zostavax) for the prevention of shingles. 33 Shingrix was more effective but caused more systemic adverse events, although mild, and more injection site pain.
Finally, a systematic review identified 46 studies of the impact of exercise on fall risk in patients 59 years or older. 34 Most of the programs used moderate-intensity exercise, with about one hour of exercise three times per week. The researchers found that exercise significantly decreased the overall risk of falls and resulting injuries but did not affect the risk of multiple falls, hospitalization, or mortality. Fractures were less likely in the exercise group but not significantly.
Practice Guidelines
POEMs sometimes summarize high-impact practice guidelines from important organizations. Key messages from the three highest-rated guidelines are summarized in Table 7 . 35 – 37
The American College of Chest Physicians recommends initiating direct oral anticoagulant therapy in patients with newly diagnosed atrial fibrillation, avoiding aspirin or aspirin plus clopidogrel (Plavix) to prevent thromboembolism, using risk scores for stroke and bleeding, and avoiding cotreatment with aspirin and an anticoagulant if possible. 35
The American Diabetes Association/European Association for the Study of Diabetes guideline for type 2 diabetes mellitus continues to recommend educating patients about diabetes self-management and providing support as the cornerstone of therapy, and metformin as the preferred initial therapy. 36 If a second agent is needed, there are many options, although glucagon-like peptide 1 receptor antagonists or sodium-glucose cotransporter 2 inhibitors are recommended for patients with established heart disease; sodium-glucose cotransporter 2 inhibitors are preferred for patients with heart failure or chronic kidney disease.
The American College of Physicians recommendations for breast cancer screening generally parallel those of the USPSTF, which are supported by the American Academy of Family Physicians. Recommendations include shared decision-making in women 40 to 49 years of age, biennial mammography from 50 to 74 years of age or until the woman's life expectancy is less than 10 years, and eliminating the clinical breast examination as a screening test for women who undergo regular mammography. 37 – 39
The full text of the POEMs discussed in this article is available at https://www.aafp.org/journals/afp/content/top-poems/2019.html .
A list of top POEMs from previous years is available at https://www.aafp.org/afp/toppoems .
Editor's Note: This article was cowritten by Dr. Mark Ebell, who is deputy editor for evidence-based medicine for AFP and cofounder and editor-in-chief of Essential Evidence Plus, published by Wiley-Blackwell, Inc. Because of Dr. Ebell's dual roles and ties to Essential Evidence Plus, the concept for this article was independently reviewed and approved by a group of AFP 's medical editors. In addition, the article underwent peer review and editing by three of AFP 's medical editors. Dr. Ebell was not involved in the editorial decision-making process.—Sumi Sexton, MD, Editor-in-Chief.
The authors thank Wiley-Blackwell, Inc., for giving permission to excerpt the POEMs; Drs. Allen Shaughnessy, Henry Barry, David Slawson, Nita Kulkarni, and Linda Speer for their work in selecting and writing the original POEMs; the academic family medicine fellows and faculty of the University of Missouri–Columbia for their work as peer reviewers; Pierre Pluye, PhD, for his work in codeveloping the Information Assessment Method; and Maria Vlasak for her assistance with copyediting the POEMs for the past 26 years.
Shaughnessy AF, Slawson DC, Bennett JH. Becoming an information master: a guidebook to the medical information jungle. J Fam Pract. 1994;39(5):489-499.
Ebell MH, Barry HC, Slawson DC, et al. Finding POEMs in the medical literature. J Fam Pract. 1999;48(5):350-355.
Grad RM, Pluye P, Mercer J, et al. Impact of research-based synopses delivered as daily e-mail: a prospective observational study. J Am Med Inform Assoc. 2008;15(2):240-245.
Pluye P, Grad RM, Johnson-Lafleur J, et al. Evaluation of email alerts in practice: Part 2. Validation of the information assessment method. J Eval Clin Pract. 2010;16(6):1236-1243.
- Hermida RC, Crespo JJ, Domínguez-Sardiña M, et al. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial [published online October 22, 2019]. Eur Heart J . 2019. Accessed March 10, 2020. https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehz754/5602478
Roerecke M, Kaczorowski J, Myers MG. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension. A systematic review and meta-analysis. JAMA Intern Med. 2019;179(3):351-362.
Slee A, Nazareth I, Bondaronek P, et al. Pharmacological treatments for generalised anxiety disorder [published correction appears in Lancet . 2019;393(10182):1698]. Lancet. 2019;393(10173):768-777.
Paskins Z, Sanders T, Croft PR, et al. Non-disclosure of symptoms in primary care: an observational study. Fam Pract. 2018;35(6):706-711.
de Vries YA, Roest AM, Bos EH, et al. Predicting antidepressant response by monitoring early improvement of individual symptoms of depression: individual patient data meta-analysis. Br J Psychiatry. 2019;214(1):4-10.
Mora S, Chang CL, Moorthy MV, et al. Association of nonfasting vs fasting lipid levels with risk of major coronary events in the Anglo-Scandinavian Cardiac Outcomes Trial–lipid lowering arm. JAMA Intern Med. 2019;179(7):898-905.
Cholesterol Treatment Trialists' Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407-415.
McNeil JJ, Wolfe R, Woods RL, et al.; ASPREE Investigator Group. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018;379(16):1509-1518.
McNeil JJ, Woods RL, Nelson MR, et al.; ASPREE Investigator Group. Effect of aspirin on disability-free survival in the healthy elderly. N Engl J Med. 2018;379(16):1499-1508.
Bowman L, Mafham M, Wallendszus K, et al.; ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379(16):1529-1539.
Nordestgaard BG, Langsted A, Mora S, et al. Fasting is not routinely required for determination of a lipid profile—a joint consensus statement from the European Atherosclerosis Society and European Federation of Clinical Chemistry and Laboratory Medicine. Eur Heart J. 2016;37(25):1944-1958.
Grundy SM, Stone NJ. 2018 cholesterol clinical practice guidelines: Synopsis of the 2018 American Heart Association/American College of Cardiology/Multisociety cholesterol guideline. Ann Intern Med. 2019;170(11):779-783.
Moriarty F, Ebell MH. A comparison of contemporary versus older studies of aspirin for primary prevention [published online November 21, 2019]. Fam Pract . 2019. Accessed March 10, 2020. https://academic.oup.com/fampra/advance-article/doi/10.1093/fampra/cmz080/5637484
Piepoli MF, Hoes AW, Agewall S, et al.; The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37(29):2315-2381.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in J Am Coll Cardiol . 2019;74(10):1429–1430]. J Am Coll Cardiol. 2019;74(10):e177-e232.
Bibbins-Domingo K. Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016;164(12):836-845.
U.S. Preventive Services Task Force. Aspirin use to prevent cardiovascular disease and colorectal cancer: preventive medication. April 2016. Accessed February 14, 2010. https://bit.ly/343LnT6
Zorzi M, Hassan C, Capodaglio G, et al. Long-term performance of colorectal cancer screening programmes based on the faecal immunochemical test. Gut. 2018;67(12):2124-2130.
Nieuwenburg SAV, Vuik FER, Kruip MJHA, et al. Effect of anticoagulants and NSAIDs on accuracy of faecal immunochemical tests (FITs) in colorectal cancer screening: a systematic review and meta-analysis. Gut. 2019;68(5):866-872.
Tian Y, Kharazmi E, Sundquist K, et al. Familial colorectal cancer risk in half siblings and siblings: nationwide cohort study. BMJ. 2019;364:l803.
Imperiale TF, Ransohoff DF, Itzkowitz SH, et al. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med. 2014;370(14):1287-1297.
Segnan N, Senore C, Andreoni B, et al. Comparing attendance and detection rate of colonoscopy with sigmoidoscopy and FIT for colorectal cancer screening. Gastroenterology. 2007;132(7):2304-2312.
Schoen RE, Razzak A, Yu KJ, et al. Incidence and mortality of colorectal cancer in individuals with a family history of colorectal cancer. Gastroenterology. 2015;149(6):1438-1445.e1.
Marchello CS, Ebell MH, Dale AP, et al. Signs and symptoms that rule out community-acquired pneumonia in outpatient adults: a systematic review and meta-analysis. J Am Board Fam Med. 2019;32(2):234-247.
Skoog Ståhlgren G, Tyrstrup M, Edlund C, et al. Penicillin V four times daily for five days versus three times daily for 10 days in patients with pharyngotonsillitis caused by group A streptococci: randomised controlled, open label, non-inferiority study. BMJ. 2019;367:l5337.
Hay AD, Anderson E, Ingle S, et al. Respiratory tract infections in children in the community: prospective online inception cohort study. Ann Fam Med. 2019;17(1):14-22.
Ray WA, Chung CP, Murray KT, et al. Association of oral anticoagulants and proton pump inhibitor cotherapy with hospitalization for upper gastrointestinal tract bleeding. JAMA. 2018;320(21):2221-2230.
Motov S, Masoudi A, Drapkin J, et al. Comparison of oral ibuprofen at three single-dose regimens for treating acute pain in the emergency department: a randomized controlled trial. Ann Emerg Med. 2019;74(4):530-537.
Tricco AC, Zarin W, Cardoso R, et al. Efficacy, effectiveness, and safety of herpes zoster vaccines in adults aged 50 and older: systematic review and network meta-analysis. BMJ. 2018;363:k4029.
de Souto Barreto P, Rolland Y, Vellas B, et al. Association of long-term exercise training with risk of falls, fractures, hospitalizations, and mortality in older adults. A systematic review and meta-analysis. JAMA Intern Med. 2019;179(3):394-405.
Lip GYH, Banerjee A, Boriani G, et al. Antithrombotic therapy for atrial fibrillation: CHEST guideline and expert panel report. Chest. 2018;154(5):1121-1201.
Davies MJ, D'Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669-2701.
Qaseem A, Lin JS, Mustafa RA, et al. Screening for breast cancer in average-risk women: a guidance statement from the American College of Physicians. Ann Intern Med. 2019;170(8):547-560.
U.S. Preventive Services Task Force. Breast cancer: screening. January 2016. Accessed February 14, 2020. https://bit.ly/2ykUZwU
American Academy of Family Physicians. Clinical preventive service recommendation. Breast cancer. Accessed February 14, 2020. https://www.aafp.org/patient-care/clinical-recommendations/all/breast-cancer.html
Continue Reading

More in AFP
More in pubmed.
Copyright © 2020 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Research Topics & Ideas: Nursing
50+ Nursing Research Topic Ideas To Fast-Track Your Project
Finding and choosing a strong research topic is the critical first step when it comes to crafting a high-quality dissertation, thesis or research project. If you’ve landed on this post, chances are you’re looking for a nursing-related research topic , but aren’t sure where to start. Here, we’ll explore a variety of nursing-related research ideas and topic thought-starters, including general nursing, medical-surgical nursing, pediatric nursing, obstetrics and gynaecological nursing, ICU and mental health nursing.
NB – This is just the start…
The topic ideation and evaluation process has multiple steps . In this post, we’ll kickstart the process by sharing some research topic ideas within the nursing domain. This is the starting point, but to develop a well-defined research topic, you’ll need to identify a clear and convincing research gap , along with a well-justified plan of action to fill that gap.
If you’re new to the oftentimes perplexing world of research, or if this is your first time undertaking a formal academic research project, be sure to check out our free dissertation mini-course. In it, we cover the process of writing a dissertation or thesis from start to end. Be sure to also sign up for our free webinar that explores how to find a high-quality research topic.
Overview: Nursing Research Topics
- General nursing-related topics
- Medical-surgical nursing
- Pediatric nursing
- Obstetrics and gynaecological nursing
- ICU nursing
- Mental health nursing
General Nursing Research Topics & Ideas
- The impact of cultural competence on patient care in the UK
- The importance of evidence-based practice in nursing for patients with HIV/AIDS
- The effects of workplace stress on nurse well-being and performance
- The role of nurse-patient communication for patients transitioning from adolescent to adult care
- The impact of technology on nursing practice and patient outcomes
- The importance of interdisciplinary collaboration in healthcare for the rehabilitation of patients post-surgery
- The effects of fatigue on nurse performance in the emergency room
- The impact of nurse staffing levels on patient outcomes in rural areas
- The effectiveness of nurse-led interventions in managing chronic conditions: a case study of diabetes
- The impact of patient-centred care on health outcomes for the elderly
- The importance of patient safety in nursing: bedside nurse vigilance
- The effects of empathy and compassion in critical care nursing
- The role of nursing in disaster preparedness and response: a case study of the Haiti earthquake of 2021
- The impact of the level of nursing education on patient outcomes
- The importance of ethical considerations in frail care nursing practice
Topics & Ideas: Medical-Surgical Nursing
- The impact of bedside care on patient outcomes in medical-surgical units
- The role of the nurse in managing post-operative patient pain
- The effects of nurse-patient ratios on patient outcomes in medical-surgical units
- A systematic review of different approaches to patient education in medical-surgical units
- The relationship between nurse-patient communication and patient satisfaction in medical-surgical units: perspectives and recommendations to improving patient satisfaction
Topics & Ideas: Pediatrics Nursing
- The impact of family-centered care on pediatric patient outcomes with sickle cell anemia
- The role of nursing interventions in promoting developmental and behavioral health in pediatric patients
- The effects of play therapy on anxiety and pain in pediatric patients during hospitilisation
- A systematic review of different approaches to pain management in pediatric cancer patients
- The relationship between parent involvement and post-operative patient outcomes in pediatric units
Ideas: Obstetrics and Gynecological Nursing
- The impact of nurse-led prenatal care on maternal and fetal outcomes in African American communities
- The role of the nurse in promoting sexual and reproductive health for women in the UK
- The effects of midwifery care on maternal satisfaction of primiparous women and birth outcomes
- A comparative study of different approaches to childbirth education for expectant mothers and partners: perceptions of control
- The relationship between lactation support and breastfeeding success of primiparous women
Topics & Ideas: ICU Nursing
- The impact of nursing interventions on patient outcomes in intensive care units in a developing country
- The role of the nurse in managing palliative and end-of-life care in the ICU
- The effects of family presence on patient outcomes and satisfaction in the ICU: A systematic review of the literature
- A comparative study of different approaches to pain management for trauma patients in the ICU
- The relationship between nurse-patient communication and geriatric patient outcomes in ICU
Topics & Ideas: Mental Health Nursing
- The impact of nurse-led therapy on adolescent patient outcomes in mental health settings
- The role of the nurse in promoting recovery and resiliency in mental health patients through group interventions
- The effects of mindfulness-based interventions on stress and anxiety in mental health patients: A systematic literature review
- A comparative study of the role of nurses in applying different approaches to patient education in mental health settings
- The association between nurse-patient therapeutic alliance and patient outcomes in mental health settings
Nursing Dissertation & Theses
While the ideas we’ve presented above are a decent starting point for finding a nursing-related research topic, they are fairly generic and non-specific. So, it helps to look at actual dissertations and theses to see how this all comes together.
Below, we’ve included a selection of research projects from various nursing-related degree programs to help refine your thinking. These are actual dissertations and theses, written as part of Master’s and PhD-level programs, so they can provide some useful insight as to what a research topic looks like in practice.
- Nursing Workload and Interventions of Licensed Nurses in Nursing Homes: An Observational Time and Motion Study (Kang, 2021)
- Missed Nursing Care: Accounting for Education, Experience, and Job Satisfaction in Registered Nurses (Bechard, 2021)
- Examining Predictors of Attitudes and Knowledge of Registered Nurses and Nursing Students in Tennessee toward Pregnant and Perinatal Women with a Substance Use Disorder (Patrylo, 2021)
- A Program Evaluation of the Organizational Readiness for Pathway to Excellence at Two Community Hospitals (Behling, 2021)
- The Impact of Covid-19 Pandemic Policy Decisions on the Wellbeing of Nursing Home Residents in Missouri (White, 2022)
- Battling A Parallel Pandemic: An Evaluation of Sustainable System-Level Nursing Support in Response To COVID-19 (Gifford, 2022)
- Holistic Nursing Process Maps: a Tool for Student Nurses to Operationalize the Nursing Process to Increase Clinical Reasoning (Reyes, 2022)
- Satisfaction and Work-Life Balance in Undergraduate Nursing Faculty: A Mixed-Methods Study (Crawford, 2021)
- The Effect of Mindfulness Meditation on the Stress, Anxiety, Mindfulness, and Self-Compassion Levels of Nursing Students (Heinrich, 2022)
- Effectiveness of Simulation-Based Case Studies in Undergraduate Nursing Students (Becnel, 2022)
- A Telehealth Simulation Experiment: Exploring Prebriefing (Owen, 2022)
- Perceptions of Lateral Violence Among Vocational Nursing Students, Associate Degree Nursing Students, and Bachelor’s Degree Nursing Students (Martha, 2022)
- Nurse Educators’ Description of Ethics from a Disciplinary Perspective: A Qualitative Descriptive Research Study (Cuchetti, 2022)
- A Literature Review of the Relationship Between Oral Health and Pneumonia Risk in the Geriatric Nursing Home Population (Swift, 2021)
Looking at these titles, you can probably pick up that the research topics here are quite specific and narrowly-focused , compared to the generic ones presented earlier. This is an important thing to keep in mind as you develop your own research topic. That is to say, to create a top-notch research topic, you must be precise and target a specific context with specific variables of interest . In other words, you need to identify a clear, well-justified research gap.
Get 1-On-1 Help
If you’re still feeling a bit unsure about how to find a research topic for your nursing dissertation, thesis or research project, check out our private coaching services below.

You Might Also Like:

To learn from the GRAD Coach is a lofty goal for me. I am unable to express my gratitude for your teaching style. I need assistance with my thesis as a master’s in nursing candidate. Please assist me.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Research at Mayo Clinic

Characteristics of physicians as patients.

Weight loss surgery increases kidney transplant rates.

Unraveling Pick’s disease, a rare form of early-onset dementia.

Explore options to join a clinical trial.
Mayo Clinic researchers' new tool links Alzheimer'... Tuesday, April 30, 2024

Research highlights
- Collaboration is vital to shedding light on SCAD in the Spontaneous Coronary Artery Dissection Research Program .
- Visionary leadership in the Van Cleve Cardiac Regenerative Medicine Program is advancing solutions for chronic and complex conditions .
- The Mayo Clinic Pirnie Translational Polycystic Kidney Disease Center is forging new ground in research on PKD and ADPKD .
Areas of Research
Discover research activities, initiatives and projects.
- Laboratories
- Core Resources
- Centers and Programs
- Departments and Divisions
Clinical Trials
Clinical trials testing the effects and safety of new drugs, devices and therapies.
Researchers
About research.
See how Mayo Clinic research advances the science of medicine and improves patient care.
Research Centers
- Cancer Center
- Center for Biomedical Discovery
- Center for Individualized Medicine
- Center for Regenerative Biotherapeutics
- Center for the Science of Health Care Delivery
- All research centers
Publications
See how our academic publishing disseminates the latest in innovative patient care and biomedical research in a variety of venues.
Research in Florida

Research in Arizona

Research in Minnesota

Explore research positions and career opportunities.
- Training grant positions - Careers Training grant positions
- Postdoctoral research opportunities - Careers Postdoctoral research opportunities
- Jobs at Mayo Clinic - Careers Jobs at Mayo Clinic
Institutional Review Board
Protecting the rights, privacy and welfare of research participants.
Research facts & funding
Learn about the vast resources that fuel discovery science at Mayo Clinic.
Philanthropy at Mayo Clinic
Your support accelerates powerful innovations in patient care, research and education.
- Give now - Philanthropy at Mayo Clinic Give now
- Giving to Mayo Clinic - Philanthropy at Mayo Clinic Giving to Mayo Clinic
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
- Open access
- Published: 03 September 2021
A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward
- Abukari Kwame 1 &
- Pammla M. Petrucka 2
BMC Nursing volume 20 , Article number: 158 ( 2021 ) Cite this article
353k Accesses
154 Citations
97 Altmetric
Metrics details
Providing healthcare services that respect and meet patients’ and caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns, beliefs, and contextual variables. Achieving patient-centered care and communication in nurse-patient clinical interactions is complex as there are always institutional, communication, environmental, and personal/behavioural related barriers. To promote patient-centered care, healthcare professionals must identify these barriers and facitators of both patient-centered care and communication, given their interconnections in clinical interactions. A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice.
Peer Review reports
Providing healthcare services that respect and meet patients’ and their caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thus constituting patient-centered care. Care is “a feeling of concern for, or an interest in, a person or object which necessitates looking after them/it” [ 1 ]. The Institute of Medicine (IOM) noted that to provide patient-centered care means respecting and responding to individual patient’s care needs, preferences, and values in all clinical decisions [ 2 ]. In nursing care, patient-centered care or person-centered care must acknowledge patients’ experiences, stories, and knowledge and provide care that focuses on and respects patients’ values, preferences, and needs by engaging the patient more in the care process [ 3 ]. Healthcare providers and professionals are thus required to fully engage patients and their families in the care process in meaningful ways. The IOM, in its 2003 report on Health Professions Education , recognized the values of patient-centered care and emphasized that providing patient-centered care is the first core competency that health professionals’ education must focus on [ 4 ]. This emphasis underscored the value of delivering healthcare services according to patients’ needs and preferences.
Research has shown that effective communication between patients and healthcare providers is essential for the provision of patient care and recovery [ 5 , 6 , 7 , 8 ]. Madula et al. [ 6 ], in a study on maternal care in Malawi, noted that patients reported being happy when the nurses and midwives communicated well and treated them with warmth, empathy, and respect. However, other patients said poor communication by nurses and midwives, including verbal abuse, disrespect, or denial from asking questions, affected their perceptions of the services offered [ 6 ]. Similarly, Joolaee et al. [ 9 ] explored patients’ experiences of caring relationships in an Iranian hospital where they found that good communication between nurses and patients was regarded as “more significant than physical care” among patients.
According to Boykins [ 10 ], effective communication is a two-way dialogue between patients and care providers. In that dialogue, both parties speak and are listened to without interrupting; they ask questions for clarity, express their opinions, exchange information, and grasp entirely and understand what the others mean. Also, Henly [ 11 ] argued that effective communication is imperative in clinical interactions. He observed that health and illness affect the quality of life, thereby making health communication critical and that the “intimate and sometimes overwhelming nature of health concerns can make communicating with nurses and other healthcare providers very challenging” [ 11 ]. Furthermore, Henly [ 11 ] added that patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns. Given the prevalence of face-to-face and device-mediated communications and interactions in healthcare settings, we must explore and clarify who, what, where, when, why, and how interactions with individuals, families, and communities are receiving care and health services [ 11 ].
The value of effective communication in nurse-patient clinical interactions cannot be overemphasized, as “research has shown that communication processes are essential to more accurate patient reporting and disclosure” [ 12 ]. Respectful communication between nurses and patients can reduce uncertainty, enhance greater patient engagement in decision making, improve patient adherence to medication and treatment plans, increase social support, safety, and patient satisfaction in care [ 12 , 13 ]. Thus, effective nurse-patient clinical communication is essential to enhancing patient-centered care and positive care outcomes.
Patient-centered communication, also known as person-centered communication or client-centered communication, is defined as a process that invites and encourages patients and their families to actively participate and negotiate in decision-making about their care needs, as cited in [ 7 ]. Patient-centered communication is crucial in promoting patient-centered care and requires that patients and their caregivers engage in the care process. As McLean [ 14 ] observed, patient-centered care can be enhanced through patient-centered communication by valuing patients’ dignity and rights. Through open communication and collaboration, where information and care plans are shared among care providers, patients, and their families, care provision becomes patient-centered [ 14 ].
Given the interconnected nature of patient-centered care and communication, we must identify the barriers and enablers of patient-centered care and communication and proposed efficient ways to enhance that because patient-centered communication is essential in achieving patient-centered care. Our aim in this paper is to identify the barriers and facilitators of patient-centered care and communication and propose and present a patient-centered care and communication continuum (PC4) Model to explain how patient-centered care can be enhanced in nurse-patient clinical interactions. As Grant and Booth argued, critical reviews are often used to present, analyse, and synthesized research evidence from diverse sources, the outcome of which is a hypothesis or a model as an interpretation of existing data to enhance evidence-based practice [ 15 ]. Thus, this critical literature review study explores the questions: what are the barriers and facilitators of patient-centered care and how can patient-centered care be enhanced through effective clinical communication?
An earlier version of this study was submitted as part of author AK’s doctoral comprehensive exams in February 2021. An interdisciplinary doctoral committee recommended many of the included literature and the questions explored in this study based on the current discourse of patient-centered care advocated for in many healthcare facilities and in recognition of the universal healthcare access objective of the health sustainable development goal. Additional searches for literature were conducted between September and November 2020 using keywords such as barriers and facilitators of nurse-patient interaction, patient-centered care, patient-centered communication , and nurse-patient communication . Databases searched included CINAHL, PubMed, Medline, and Google Scholar. Included studies in this critical review were empirical research on nurse-patient interactions in different care settings published in English and open access. All relevant articles were read, and their main findings relevant to our review questions were identified and organized into themes and subthemes discussed in this paper. Other published studies were read, and together with those that addressed the review question, a model was developed regarding how to enhance patient-centered care through effective communication.
Barriers to Patient-Centered Care and Communication
Nurses constitute a significant workforce of care providers whose practices can severely impact care outcomes (both positive and negative). Nurses spend much time with patients and their caregivers. As a result, positive nurse-patient and caregiver relationships are therapeutic and constitute a core component of care [ 9 , 13 ]. In many instances, nurses serve as translators or patients’ advocates, in addition to performing their primary care duties. Although good nurse-patient relationships positively impact nurse-patient communication and interaction, studies have shown that several factors impede these relationships with significant consequences on care outcomes and quality [ 6 , 16 , 17 ]. Thus, these barriers limit nurses’ and other care providers’ efforts to provide healthcare that meets patients’ and caregivers’ needs. We categorize the barriers to patient-centered care and communication into four kinds: institutional and healthcare system-related, communication-related, environment-related, and personal and behaviour-related barriers. Although these barriers are discussed in separate subheadings, they are interlinked in complex ways during clinical practice.
Institutional and Healthcare System Related Barriers
Many barriers to providing patient-centered care and communication during nurse-patient interactions emanate from healthcare institutional practices or the healthcare system itself. Some of these factors are implicated in healthcare policy or through management styles and strategies.
Shortage of nursing staff, high workload, burnout, and limited-time constituted one complex institutional and healthcare system-level barrier to effective care delivery [ 18 , 19 ]. For instance, Loghmani et al. [ 20 ] found that staffing shortages prevented nurses from having adequate time with patients and their caregivers in an Iranian intensive care unit. Limitations in nursing staff, coupled with a high workload, led to fewer interactions between nurses, patients, and caregivers. Similarly, Anoosheh et al. [ 16 ] found that heavy nursing workload was ranked highest as a limiting factor to therapeutic communication in nurse-patient interactions in Iran.
In a study on communication barriers in two hospitals affiliated with Alborz University of Medical Sciences, Norouzinia et al. [ 21 ] found that shortage of nurses, work overload, and insufficient time to interact with patients were significant barriers to effective nurse-patient interactions. Similar factors are identified as barriers to nurse-patient communication and interactions in other studies [ 13 , 16 , 18 ]. For instance, Amoah et al. [ 16 ] reported that nursing staff shortage and high workload were barriers to patient-centered care and therapeutic communication among Ghanaian nurses and patients. Amoah and colleagues reported a patient’s statement that:
[B]ecause there are few nurses at the ward, sometimes you would want a nurse to attend to you, but he or she might be working on another patient, so in such case, the nurse cannot divide him or herself into two to attend to you both [ 16 ].
Nurses and patients and their caregivers have noted that limited time affects nurse-patient interactions, communication, and care quality. Besides, Yoo et al. [ 22 ] reported that limited visiting hours affected communications between caregivers and nurses in a tertiary hospital in Seoul, Korea. Since the caregivers had limited time to spend with patients, they had little knowledge about the intensive care unit and distrusted the nurses.
Although nursing staff shortage is a significant barrier to patient-centered care and communication that healthcare institutions and managers must know, some healthcare scholars have critique nurses’ complaints of time limitation. For instance, McCabe [ 7 ] argued that the quality of nurse-patient interactions is what matters and not the quantity of time spent with patients and their caregivers. McCabe maintained that “spending long periods with patients does not always result in positive nurse-patient relationships” [ 7 ]. He argued that implementing patient-centered care does not require additional time; hence, nurses’ perceptions of being too busy cannot excuse poor therapeutic communication during clinical interactions. Instead, nurses are encouraged to develop self-awareness, self-reflection, and a commitment to ensuring that patients receive the needed care.
Another institution-related barrier to patient-centered care and communication is the healthcare system’s emphasis on task-centered care. Care providers are more focused on completing care procedures than satisfying patients’ and caregivers’ needs and preferences. This barrier to patient-centered care and communication is acknowledged in several studies [ 7 , 14 , 20 , 22 , 23 ]. For example, McLean [ 14 ] studied dementia care in nursing homes in the United States. She found that patient-centered care and communication in one nursing home (Snow I) were severely affected when nurses, physicians, and care managers focused on completing tasks or observing care and institutional routines to the detriment of satisfying patients’ care needs. However, in the other care home (Snow II), patient-centered care was enhanced as nurses, physicians, and the care home managers focused on addressing patients’ needs and values rather than completing care routines and tasks.
Similarly, Yoo and colleagues [ 22 ] observed that nurse-patient communication was affected when the ICU nurses placed urgency on completing tasks linked directly to patients’ health (e.g., stabilizing vital signs) than communicating to addressed patients’ specific needs. This evidence shows that when nurses are more task-focused, patients and caregivers are treated as bodies and objects, on which medical and care practices must be performed to restore health. Research has shown that when nurses focus on task-oriented care, it becomes hard to provide holistic care to patients or teach and communicate with patients even when nurses are less busy [ 20 ].
Nursing managers and their management styles can affect patient-centered care and communication. Studies have revealed that the management styles that nursing managers implement can either facilitate or impede patient-centered care [ 14 , 22 ]. When nurse managers orient their nursing staff towards task-centered care practices, it affects nurse-patient interaction and communication. Moreover, when nurse managers fail to address their staff’s mental health needs and personal challenges, it influences how nurses attend to patients’ care needs. For example, nurses have indicated that nurse-patient communication is affected when nurse managers are unsupportive or unresponsive to their needs [ 20 ].
In a study exploring nursing and midwifery managers’ perspectives on obstacles to compassion giving and therapeutic care across 17 countries, Papadopoulos et al. [ 24 ] discovered that nurses and midwifery managers’ characteristics and experiences could facilitate or impede compassion and therapeutic interactions in nursing care. Negative personal attitudes, including selfishness, arrogance, self-centeredness, rudeness, lack of leadership skills, the desire for power, and feelings of superiority among nurses and midwifery managers, were obstacles to compassion building. The study further showed that managers who emphasize rules, tasks, and results do not prioritize relationship-building and see their staff as workers rather than team members [ 24 ]. Therefore, nurse managers and care administrators must monitor nurse-patient interaction and communication to address nurses’ concerns and support them, especially in resource-constrained and high patient turnover contexts [ 25 , 26 ].
Communication-Related Barriers
Effective communication is essential to providing patient-centered care. Studies have shown that poor communication between care providers and patients and their caregivers affects care outcomes and perceptions of care quality [ 7 , 16 , 27 , 28 ]. A consistent communication-related barrier in nurse-patient interaction is miscommunication, which often leads to misunderstandings between nurses, patients, and their families [ 20 ]. Other communication-related barriers include language differences between patients and healthcare providers [ 6 , 16 , 27 ], poor communication skills, and patients’ inability to communicate due to their health state, especially in ICU, dementia, or end-of-life care contexts [ 13 , 22 ]. For instance, in their maternity care study, Madula et al. [ 6 ] noted that language barriers significantly affected effective communication between nurses/midwives and expectant mothers. A patient in their study indicated that although many nurses were polite and communicated well, some nurses had challenges communicating with patients in the Chitumbuka language, which affected those nurses’ ability to interact effectively with patients [ 6 ].
Furthermore, Norouzinia et al. [ 21 ] asserted that effective communication could not be established when nurses and patients have a language difference. Moreover, the meanings of certain non-verbal communication acts (e.g., head nodding, eye gaze, touch) can invoke different interpretations across different cultures, which could impede the interactions between patients and nurses. Even in healthcare contexts where nurses and patients speak the same language, “differences in vocabulary, rate of speaking, age, background, familiarity with medical technology, education, physical capability, and experience can create a huge cultural and communication chasm” between nurses and patients [ 12 ]. In ICU and other similar care settings, nurses find it difficult to effectively communicate with patients because the mechanical ventilators made it hard for patients to talk [ 22 ].
To overcome the communication-related barriers, healthcare institutions must make it a responsibility to engage translators and interpreters to facilitate nurse-patient interactions where a language barrier exists. Moreover, nurses working in ICU and other similar settings should learn and employ alternative forms of communication to interact with patients.
Environment-Related Barriers
The environment of the care setting can impact nurse-patient communication and the resulting care. Thus, “good health care experiences start with a welcoming environment” [ 29 ]. Mastors believed that even though good medicine and the hands working to provide care and healing to the sick and wounded are essential, we must not “forget the small things: a warm smile, an ice chip, a warm blanket, a cool washcloth. A pillow flipped to the other side and a boost in bed” [ 29 ]. The environment-related barriers are obstacles within the care setting that inhibit nurse-patient interaction and communication and may include a noisy surrounding, unkept wards, and beds, difficulties in locating places, and navigating care services. Noisy surroundings, lack of privacy, improper ventilation, heating, cooling, and lighting in specific healthcare units can affect nurse-patient communication. These can prevent patients from genuinely expressing their healthcare needs to nurses, which can subsequently affect patient disclosure or make nursing diagnoses less accurate [ 13 , 18 , 21 ]. For instance, Amoah et al. [ 16 ] revealed that an unconducive care environment, including noisy surroundings and poor ward conditions, affected patients’ psychological states, impeding nurse-patient relationships and communication. Moreover, when care services are not well-coordinated, new patients and their caregivers find it hard to navigate the care system (e.g., locating offices for medical tests and consultations), which can constrain patient-centered care and communication.
Reducing the environment-related barriers will require making the care setting tidy/clean, less noisy, and coordinating care services in ways that make it easy for patients and caregivers to access. Coordinating and integrating care services, making care services accessible, and promoting physical comfort are crucial in promoting patient-centered care, according to Picker’s Eight Principles of Patient-Centered Care [ 30 ].
Personal and Behaviour Related Barriers
The kind of nurse-patient relationships established between nurses and patients and their caregivers will affect how they communicate. Since nurses and patients may have different demographic characteristics, cultural and linguistic backgrounds, beliefs, and worldviews about health and illnesses, nurses’, patients’, and caregivers’ attitudes can affect nurse-patient communication and care outcomes. For instance, differences in nurses’ and patients’ cultural backgrounds and belief systems have been identified as barriers to therapeutic communication and care [ 12 , 13 , 21 ]. Research shows that patients’ beliefs and cultural backgrounds affected their communication with nurses in Ghana [ 16 ]. These scholars found that some patients refused a blood transfusion, and Muslim patients refused female nurses to attend to them because of their religious beliefs [ 16 ]. Further, when nurses, patients, or their caregivers have misconceptions about one another due to past experiences, dissatisfaction about the care provided, or patients’ relatives and caregivers unduly interfere in the care process, nurse-patient communication and patient-centered care were affected [ 16 , 21 ].
Similarly, nurse-patient communication was affected when patients or caregivers failed to observe nurses’ recommendations or abuse nurses due to misunderstanding [ 20 ], while patients’ bad attitudes or disrespectful behaviours towards nurses can inhibit nurses’ ability to provide person-centered care [ 31 ]. The above-reviewed studies provided evidence on how patients’ and caregivers’ behaviours can affect nurses’ ability to communicate and deliver patient-centered care.
On the other hand, nurses’ behaviours can also profoundly affect communication and care outcomes in the nurse-patient dyad. When nurses disrespect, verbally abuse (e.g., shouting at or scolding), and discriminate against patients based on their social status, it affects nurse-patient communication, care outcomes, and patient disclosure [ 6 , 32 ]. For instance, Al-Kalaldeh et al. [ 18 ] believe that nurse-patient communication is challenged when nurses become reluctant to hear patients’ feelings and expressions of anxiety. When nurses ignore patients’ rights to share ideas and participate in their care planning, such denials may induce stress, discomfort, lack of trust in nurses, thereby leading to less satisfaction of care [ 18 ].
Furthermore, when nurses fail to listen to patients’ and caregivers’ concerns, coerce patients to obey their rules and instructions [ 16 , 17 , 20 ], or fail to provide patients with the needed information, nurse-patient communication and patient-centered care practices suffer. To illustrate, in Ddumba-Nyanzia et al.‘s study on communication between HIV care providers and patients, a patient remarked that: “I realized no matter how much I talked to the counselor, she was not listening. She was only hearing her point of view and nothing else, [and] I was very upset” [ 17 ]. This quote indicates how care provider attitudes can constrain care outcomes. Due to high workload, limited time, poor remunerations, and shortage of personnel, some nurses can develop feelings of despair, emotional detachment, and apathy towards their job, which can lead to low self-esteem or poor self-image, with negative consequences on nurse-patient interactions [ 13 , 18 ].
Given the significance of effective communication on care, overcoming the above personal and behaviour related barriers to patient-centered care and communication is crucial. Nurses, patients, and caregivers need to reflect on the consequences of their behaviours on the care process. Thus, overcoming these barriers begins with embracing the facilitators of patient-centered care and communication, which we turn to in the next section.
Facilitators of patient-centered care and communication
Patient-centered care and communication can be facilitated in several ways, including building solid nurse-patient relationships.
First, an essential facilitator of patient-centered care and communication is overcoming practical communication barriers in the nurse-patient dyad. Given the importance of communication in healthcare delivery, nurses, patients, caregivers, nursing managers, and healthcare administrators need to ensure that effective therapeutic communication is realized in the care process and becomes part of the care itself. Studies have shown that active listening among care providers is essential to addressing many barriers to patient-centered care and communication [ 7 , 13 ]. Although handling medical tasks promptly in the care process is crucial, the power of active listening is critical, meaningful, and therapeutic [ 22 ]. By listening to patients’ concerns, nurses can identify patients’ care needs and preferences and address their fears and frustrations.
Another facilitator of patient-centered care is by understanding patients and their unique needs [ 25 ], showing empathy and attending attitudes [ 7 , 13 ], expressing warmth and respect [ 22 ], and treating patients and caregivers with dignity and compassion as humans. For instance, McCabe [ 7 ] noted that attending, which obligates nurses to demonstrate that they are accessible and ready to listen to patients, is a patient-centered care process; a fundamental requirement for nurses to show genuineness and empathy, despite the high workload. Showing empathy, active listening, respect, and treating patients with dignity are core to nursing and care, and recognized in the Code of Ethics for Nurses [ 33 ], and further emphasized in the ongoing revision of the Code of Ethics for nurses [ 34 ].
Besides, engaging patients and caregivers in the care process through sharing information, inviting their opinion, and collaborating with them constitutes another facilitator of patient-centered care and communication. When patients and caregivers are engaged in the care process, misunderstandings and misconceptions are minimized. When information is shared, patients and caregivers learn more about their health conditions and the care needed. As McLean [ 14 ] argued, ensuring open communication between care providers and patients and their families is essential to enhancing patient-centered care. Conflicts ensue when patients or their families are denied information or involvement in the care process. As a result, the Harvard Medical School [ 30 ] identified patient engagement, information sharing, and nurse-patient collaboration during care as essential patient-centered care principles.
Finally, health policy must be oriented towards healthcare practices and management to facilitate patient-centered care and communication. These policies, at a minimum, can involve changes in management styles within healthcare institutions, where nurse managers and healthcare administrators reflect on nursing and care practices to ensure that the Code of Ethics of Nurses and patients’ rights are fully implemented. Resource constraints, staff shortages, and ethical dilemmas mainly affect care practices and decision-making. Nonetheless, if patients are placed at the center of care and treated with dignity and respect, most of the challenges and barriers of patient-centered care will diminish. Empowering practicing nurses, equipping them with interpersonal communication skills through regular in-service training, supporting them to overcome their emotional challenges, and setting boundaries during nurse-patient interactions will enhance patient-centered care practices.
In line with the above discussion, Camara et al. [ 25 ] identify three core dimensions that nurses, patients, and caregivers must observe to enhance patient-centered care: treating the patient as a person and seeing the care provider as a person and a confidant. Regarding the first dimension, care providers must welcome patients, listen to them, share information with them, seek their consent, and show them respect when providing care. The second dimension requires that the healthcare provider be seen and respected as a person, and negative perceptions about care providers must be demystified. According to Camara et al. [ 25 ], care providers must not overemphasize their identities as experts but rather establish good relationships with patients to understand patients’ personal needs and problems. Lastly, patients and caregivers must regard care providers as confidants who build and maintain patients’ trust and encourage patients’ participation in care conversations. With this dimension, patients and caregivers must know that nurses and other care providers have the patient at heart and work to meet their care needs and recovery process.
Camara et al.‘s [ 25 ] three dimensions are essential and position patients, their caregivers, and nurses as partners who must engage in dialogic communication to promote patient-centered care. As a result, effective communication, education, and increased health literacy among patients and caregivers will be crucial in that direction.
Enhancing Patient-Centered Care and Communication: A Proposed Model
Nursing care practices that promote patient-centered communication will directly enhance patient-centered care, as patients and their caregivers will actively engage in the care process. To enhance patient-centered communication, we propose person-centered care and communication continuum (PC4) as a guiding model to understand patient-centered communication, its pathways, and what communication and care practices healthcare professionals must implement to achieve person-centered care. In this PC4 Model, we emphasize the person instead of the patient because they are a person before becoming a patient. Moreover, the PC4 Model is supposed to apply to all persons associated with patient care; thus, respect for the dignity of their personhood is crucial.
Although much is written about patient-centered communication in the healthcare literature, there is a gap regarding its trajectory and what communication content enhances patient-centered communication. Also, little is known about how different clinical discourse spaces influence communication and its content during nurse-patient clinical interactions. Using evidence from Johnsson et al. [ 3 ], Murira et al. [ 23 ], and Liu et al. [ 35 ], among other studies, we outline the components of the PC4 Model and how different discourse spaces in the clinical setting and the content of communication impact patient-centered care and communication.
The proposed PC4 Model in this paper has three unbounded components based on the purpose of and how communication is performed among care providers, patients, and their caregivers. Figure 1 illustrates the PC4 Model, its features, and trajectory.
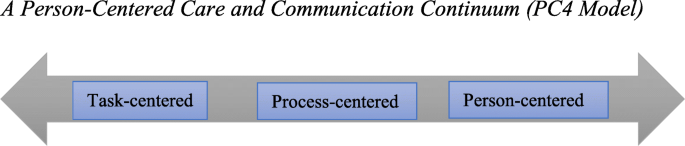
A Person-Centered Care and Communication Continuum (PC4 Model)
Task-Centered Communication
At the lowest end of the PC4 Model is task-centered communication. Here, the care provider’s role is to complete medical tasks as fast as possible with little or no communication with the patient and their caregivers. Patients and caregivers are treated as bodies or objects whose disease symptoms need to be studied, identified, recorded, treated, or cured. As Johnsson et al. [ 3 ] observed, communication content at this stage is mainly biomedically oriented, where nurses and other healthcare professionals focus on the precise medical information (e.g., history taking, medical examination, test results, medication, etc.) about the patient. With a task-centered orientation, nurses make journal entries about their patients’ disease state and ensure that treatment plans, diagnostic tests, and medical prescriptions are completed. Communication at this stage is often impersonal or rigid (see [ 23 ] for details). Care providers may address patients and their caregivers by using informal attributes (e.g., bed 12, the woman in the red shirt, card 8, etc.), thereby ignoring patients’ and caregivers’ personal and unique identities. Patients’ and caregivers’ nonverbal communication signs are mostly overlooked.
Motivations for task-centered communication can be attributed to time limitation, high workload, and staff shortage, thereby pushing nurses and other care providers to reach as many patients as possible. Moreover, the healthcare system’s orientation towards and preference for biomedically-focused care seems to favour task-centered communication [ 7 , 14 ].
Depending on the clinical discourse space under which patient-provider interactions occur, different forms of communication are employed. Clinical discourse spaces can be public (e.g., in the ward, patient bedside), private (e.g., consulting rooms, medical test labs, nurse staff station, etc.), or semi-private (e.g., along the corridor) [ 35 ]. In these clinical discourse spaces, nurse-patient communication can be uninformed (patients or caregivers are not informed about patients’ care conditions or why specific data and routines are performed). It can be non-private (others can hear what the nurse and patient are talking about) or authoritative (care providers demonstrate power and control and position themselves as experts) [ 23 ]. Finally, in task-centered communication, healthcare providers often use medical jargon or terminologies [ 3 ] since the goal of communication is not to engage the patient in the process. Usually, patients or their caregivers are not allowed to ask questions, or their questions get ignored or receive superficial, incomprehensible responses.

Process-Centered Communication
Process-centered communication is an intermediate stage on the continuum, which could slip back into the task-centered or leap forward into person-centered communication. Through process-centered communication, care providers make an effort to know patients and their caregivers as they perform care routines. Care providers ask patients or their caregivers questions to understand the care conditions but may not encourage patients or caregivers to express their thoughts about their care needs. Patients and caregivers are recognized as persons with uniques care needs but may not have the agency to influence the care process. Care providers may chit-chat with patients or their caregivers to pass the time as they record patients’ medical records or provide care. Unlike task-centered communication, there is informative and less authoritative communication between nurses and patients and their caregivers. The goal of process-centered communication could be a mixture of instrumental and relational, with less display of power and control by nurses.
Person-Centered Communication
This is the highest point of the PC4 Model, where patient-centered care is actualized. At this stage of the communication continuum, patients and caregivers are treated as unique persons with specific care needs and are seen as collaborators in the care process. As McLean [ 14 ] observed, caregiving becomes a transactional relationship between the care provider and receiver at the person-centered stage of the continuum. The care itself becomes intersubjective, a mutual relational practice, and an ongoing negotiation for care providers and receivers [ 14 ].
The content of communication at this stage of the continuum is both “personal” and “explanatory” [ 3 ]. Nurses and other healthcare providers create meaningful relationships with patients and their caregivers, understand patients’ concerns, needs, and problems, use open-ended questions to encourage patients or caregivers to express their thoughts and feelings about the care situation. Nurses and other healthcare professionals explain care routines, patients’ health conditions, and management plans in lay language to patients and caregivers through person-centered communication. Accomplishing this level includes employing alternative forms of communication to meet the needs of intensive care unit patients, deaf patients, and ventilated and intubated patients. For instance, it has been shown that “deaf people […] frequently do not have access to clear and efficient communication in the healthcare system, which deprives them of critical health information and qualified health care” [ 36 ]. Empathetic communication practices, including active listening, showing genuine interest in patients’ care, and respect and warmth, become a significant part of nursing care [ 3 , 7 , 14 , 22 ].
Different communication strategies are employed based on the care situation and context. Chit-chatting, as a form of personal communication [ 3 ], use of humor as a communication strategy [ 7 , 8 ], and even maintaining silence [ 28 ] are essential in enhancing person-centered care and communication. Both care providers and patients or their caregivers use relationship-building and -protecting humor (see [ 28 ] for details) to address difficult situations in the care process.
Implications of the PC4 Model for Nursing Practice
Given the values of effective communication in nurse-patient interactions and care outcomes, nurses and other healthcare providers must ensure that they develop therapeutic relationships with patients, their families, and caregivers to promote person-centered care and communication. Achieving that begins with knowing and reflecting on the barriers of therapeutic communication and ways to minimize them. The PC4 Model draws nurses and all healthcare providers’ attention to patient-centered care pathways and how effective communication is necessary. Healthcare professionals, including nurses, must be aware of how their communication orientation–––either oriented toward completing tasks, following care processes or toward addressing patients’ and their caregivers’ needs––can impact patient-centered care. Healthcare providers must observe the care context, patients’ unique situations, their non-verbal language and action, and whether they belong to historically marginalized groups or cultures.
Mastors [ 29 ] has offered healthcare providers some guidance to reflect on as they communicate and interact with patients and caregivers. Thus, (a) instead of asking patients, “What’s the matter?“ care providers must consider asking them, “What’s important to you?“ With this question, the patient is given a voice and empowered to contribute to their own care needs. Care providers should (b) check with patients in the waiting room to update patients whose waiting time has been longer than usual, based on the care context. They should also (c) try to remember their conversations with patients to build on them during subsequent interactions. This continuity can be enhanced by nurse managers reexamining how they deploy care providers to patients. The same nurse can be assigned to the same patients for the duration of the patient’s stay to help patients feel valued and visible [ 29 ].
Knowledge of cultural competence, sensitivity, humility, and interpersonal communication skills will help achieve and implement the PC4 Model. As Cuellar [ 37 ] argues, “[h]umility is about understanding and caring for all people [and] being empathetic.“ Cultural competence is a “dynamic process of acquiring the ability to provide effective, safe, and quality care to the patients through considering their different cultural aspects” [ 38 ]. The concept of cultural competence entails “cultural openness, awareness, desire, knowledge and sensitivity” during care [ 39 ]. It demands that care providers respect and tailor care to align with patients’ and caregivers’ values, needs, practices, and expectations, based on care and moral ethics and understanding [ 39 ]. Active listening and showing compassion as therapeutic relationship-building skills are essential, and continuous education and mentorship will be crucial to developing these skills among healthcare providers.
We invite qualitative and quantitative studies, especially on language use and communication strategies, to explore and evaluate the PC4 Model. Providing in-depth and experiential data on ways to increase its effectiveness as a tool to guide healthcare providers is highly desired. More knowledge can support healthcare providers in offering evidence-based patient-centered care in different healthcare settings and units.
Conclusions
Effective communication is an essential factor in nurse-patient interactions and a core component of nursing care. When communication in the nurse-patient dyad is patient-centered, it becomes therapeutic. It allows for trust and mutual respect in the care process, thereby promoting care practices that address patients’ and caregivers’ needs, concerns, and preferences. We have identified the barriers and facilitators of patient-centered care and communication and proposed a person-centered care and communication continuum (PC4 Model) to demonstrate how patient-centered communication intersects with patient-centered care.
Availability of data and materials
Not applicable.
Abbreviations
Intensive Care Unit
Institution of Medicine
Person-Centered Care and Communication Continuum
Etheredge HR. “Hey sister! Where’s my kidney?“ Exploring ethics and communication in organ transplantation in Gauteng, South Africa, Ph.D. dissertation, Johannesburg. University of the Witwatersrand; 2015.
Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. National Academy Press; 2001.
Johnsson A, Wagman P, Boman A, Pennbrant S. What are they talking about? Content of the communication exchanges between nurses, patients and relatives in a department of medicine for older people: An ethnographic study. J Clin Nurs. 2018 Apr;27(7–9):e1651-9. doi: https://doi.org/10.1111/jocn.14315 .
Long KA. The Institute of Medicine report on health professions education: A bridge to quality. Policy Polit Nurs Pract. 2003 Nov;4(4):259–62. doi: https://doi.org/10.1177/1527154403258304 .
Crawford T, Candlin S, Roger P. (2017). New perspectives on understanding cultural diversity in nurse-patient communication. Collegian, 2017 Feb 1;24(1):63 – 9. https://doi.org/10.1016/j.colegn.2015.09.001 .
Madula P, Kalembo WF, Yu H, Kaminga CA. Healthcare provider-patient communication: A qualitative study of women’s perceptions during childbirth. Reprod Health. 2018 Dec;15(135):1–10. https://doi.org/10.1186/s12978-018-0580-x .
McCabe C. Nurse-patient communication: An exploration of patients’ experiences. J Clin Nurs. 2004 Jan;13(1):41–9.
Schöpf AC, Martin GS, Keating MA. Humor as a communication strategy in provider-patient communication in a chronic care setting. Qual Health Res. 2017 Feb;27(3):374–90. doi: https://doi.org/10.1177/1049732315620773 .
Joolaee S, Joolaei A, Tschudin V, Bahrani N, Nikbakht NA. Caring relationship: the core component of patients’ rights practice as experienced by patients and their companions. J Med Ethics Hist Med. 2010;3(4):1–7.
Google Scholar
Boykins AD. Core communication competences in patient-centered care. The ABNF J. 2014 Apr 1;25(2):40 – 5.
Henly SJ. Health communication research for nursing science and practice. Nurs Res [Editorial] 2016:257–8. doi: https://doi.org/10.1097/NNR.0000000000000171 .
Ruben BD. Communication theory and health communication practice: The more things change, the more they stay the same. Health Commun. 2016 Jan 2;31(1):1–11. doi: https://doi.org/10.1080/10410236.2014.923086 .
Bello P. Effective communication in nursing practice: A literature review. BSc Nursing Thesis. Arcada; 2017. Available at https://core.ac.uk/download/pdf/84798372.pdf Accessed 20 Jan 2021.
McLean A. The person in dementia: A study of nursing home care in the US. Toronto, University of Toronto Press; 2007.
Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libraries J. 2009;26:91–108. Doi: https://doi.org/10.1111/j.1471-1842.2009.00848.x .
Article Google Scholar
Amoah KMV, Anokye R, Boakye SD, Acheampong E, Budu-Ainooson A, Okyere E, Kumi-Boateng G, Yeboah C, Afriyie OJ. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nurs. 2019 Dec;18(4)1–8. https://doi.org/10.1186/s12912-019-0328-0 .
Ddumba-Nyanzia I, Kaawa-Mafigiria D, Johannessen H. Barriers to communication between HIV care providers (HCPs) and women living with HIV about childbearing: A qualitative study. Patient Educ Couns. 2016 May 1:99(5):754–9. https://doi.org/10.1016/j.pec.2015.11.023 .
Al-Kalaldeh M, Amro N, Qtait M. Barriers to effective nurse-patient communication in the emergency department. Emerg Nurse. 2021 Mar 2;29(2). doi: https://doi.org/10.7748/en.2020.e1969 .
Sethi D, Rani MK. Communication barrier in health care setting as perceived by nurses and patient. Int J Nurs Educ 2017 Oct. 2016;9(4):30. doi: https://doi.org/10.5958/j.2320-8651.2.1.001 .
Loghmani L, Borhani F, Abbaszadeh A. Factors affecting the nurse-patients’ family communication in intensive care unit of Kerman: A qualitative study. J Caring Sci. 2014 Mar;3(1):67–2. doi: https://doi.org/10.5681/jcs.2014.008 .
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2016 Jun;8(6):65–4. https://doi.org/10.5539/gjhs.v8n6p65 .
Yoo HJ, Lim OB, Shim JL. Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study. PLoS One. 2020 Jul 9;15(7):e0235694. https://doi.org/10.1371/journal.pone.0235694 .
Murira N, Lützen K, Lindmark G, Christensson K. Communication patterns between healthcare providers and their clients at an antenatal clinic in Zimbabwe. Health Care Women Int. 2003 Feb 1;24(2):83 – 2. https://doi.org/10.1080/07399330390170060 .
Papadopoulos I, Lazzarino R, Koulouglioti C, Aagard M, Akman O, Alpers L-M, Apostolara P, Araneda Bernal J, Biglete-Pangilinan S, Eldar-Regev O, Gonzalez-Gil MT, Kouta C, Zorba A. Obstacles to compassion-giving among nursing and midwifery managers: An international study. Int Nurs Rev. 2020 Aug;11:1–13.
Camara BS, Belaid L, Manet H, Kolie D, Guilard E, Bigirimana T, Delamou A. What do we know about patient-provider interactions in sub-Saharan Africa? A scoping review. Pan Afr Med J. 2020;88(88):1–13. doi: https://doi.org/10.11604/pamj.2020.37.88.24009 .
Kwame A, Petrucka PM. Communication in nurse-patient interaction in healthcare settings in sub-Saharan Africa: A scoping review. Int J Afr Nurs Sci. 2020 Jan 1;12:100198. https://doi.org/10.1016/j.ijans.2020.100198 .
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009 Jun;56(2):243–9.
Vuković M, Gvozdenović BS, Stamatović-Gajić B, Ilić M, Gajić T. Development and evaluation of the nurse quality of communication with patient questionnaire. Srp Arh Celok Lek. 2010;138(1–2):79–4. doi: https://doi.org/10.2298/SARH1002079V .
Article PubMed Google Scholar
Mastors P. (2018). What do patients want, need, and have the right to expect? Nurs Adm Q. 2018 Jul 1;42(3):192-8. doi: https://doi.org/10.1097/NAQ.0000000000000297 .
Harvard Medical School. The Eight Principles of Patient Centered Care; 2015 Nov 18. Available from OneView: https://www.oneviewhealthcare.com/the-eight-principles-of-patient-centered-care/ Accessed 28 Dec 2020.
White J, Phakoe M, Rispel LC. ‘Practice what you preach’: Nurses’ perspectives on the Code of Ethics and Service Pledge in five South African hospitals. Glob Health Action. 2015 Dec 1;8(1):26341. https://doi.org/10.3402/gha.v8.26341 .
Kruger L-M, Schoombee C. The other side of caring: abuse in a South African maternity ward. J Reprod Infant Psychol. 2010 Feb 1;28(1):84–101. doi: https://doi.org/10.1080/02646830903294979 .
International Council of Nurses. ICN Code of Ethics for Nurses; 2012. Available from www.icn.ch/images/stories/documents/about/icncode_english.pdf . Accessed 20 Dec 2020.
Stievano A, Tschudin V. The ICN code of ethics for nurses: A time for revision. Nurs Health Policy Perspect. 2019 Jun;66(2):154–6.
Liu W, Manias E, Gerdtz M. Medication communication during ward rounds on medical wards: Power relations and spatial practices. Health 2012 Mar. 2012;17(2):113–34. doi: https://doi.org/10.1177/1363459312447257 .
Hoglind TA. Healthcare language barriers affect deaf people, too. 2018 Oct 11. Retrieved from Boston University [BU] School of Public Health: Available from https://www.bu.edu/sph/news/articles/2018/healthcare-language-barriers-affect-deaf-people-too/ Accessed 15 Jan 2021.
Cuellar NG. Humility. A concept in cultural sensitivity. JTranscult Nurs [Editorial]. 2018 Apr 26; 29(4):317. https://doi.org/10.1177/1043659618772384 .
Sharifi N, Adib-Hajbaghery M, Najafi M. Cultural competence in nursing: A concept analysis. Int J Nurs Stud. 2019 Nov 1;99(103386):1–8. https://doi.org/10.1016/j.ijnurstu.2019.103386 .
Henderson S, Horne M, Hills R, Kendall E. Cultural competence in healthcare in the community: A concept analysis. Health Soc Care Community. 2018 Jul;26(4):590–603. doi: https://doi.org/10.1111/hsc.12556 .
Download references
Acknowledgments
We express our gratitude to the first author’s doctoral committee members for their valuable comments, suggestions, and critique of an earlier version of this paper. We are also grateful to the anonymous reviewers for the insightful comments and suggestions that have helped us improve the study’s quality.
Authors' information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan, interested in patients' rights in nurse-patient clinical communications and interactions in the hospital setting. He holds two Master of Philosophy degrees in Indigenous Studies and English Linguistics. Abukari's research interests include language use in social interaction, health communication, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is a professor in Nursing and has international research experience with many of her graduate students from Africa, Asia, and the Caribbean. Pammla has published extensively in the field of nursing. Her research interests are vast, including child and maternal health, Indigenous peoples' health, global health, and vulnerable populations, with extensive experiences in qualitative research and indigenous research methodologies. Pammla is co-editor of the BMC Nursing journal and a reviewer for many other academic journals.
The authors have not received any funding for the conduct, preparation, and publication of this paper.
Author information
Authors and affiliations.
College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Abukari Kwame
College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Pammla M. Petrucka
You can also search for this author in PubMed Google Scholar
Contributions
Both authors conceived the topic. PMP recommended the literature, AK searched and added more sources, and drafted the paper. PMP reviewed the paper for intellectual content. Both AK and PMP read and approved the final version.
Corresponding author
Correspondence to Abukari Kwame .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kwame, A., Petrucka, P.M. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs 20 , 158 (2021). https://doi.org/10.1186/s12912-021-00684-2
Download citation
Received : 05 May 2021
Accepted : 18 August 2021
Published : 03 September 2021
DOI : https://doi.org/10.1186/s12912-021-00684-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient-centered care
- Therapeutic communication
- Nurse-patient interactions
- Clinical discourse space
- Patient-centered care and communication continuum
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Top Nursing Research Topics for Students and Professionals
This article was written in collaboration with Christine T. and ChatGPT, our little helper developed by OpenAI.
Nursing research is an essential component of the nursing profession. Its primary purpose is to enhance patient outcomes, elevate the quality of care, and advance nursing as a whole. For nursing students and practitioners, selecting an appropriate research topic is crucial for academic and professional success. This article highlights some current and interesting topics in nursing research that students and professionals can explore.
Nursing Workforce
One of the major topics in nursing research is the challenges that nurses face in their workplace, and how to address them. This is particularly relevant in light of the current shortage of nurses and the healthcare industry’s growing demands.
List of Nursing Research Topics: Nursing Workforce
- The impact of nurse staffing levels on patient outcomes in acute care settings
- The effectiveness of nurse retention strategies on improving nurse job satisfaction
- The role of nursing leadership in creating a positive work environment
- The relationship between nurse staffing ratios and nurse burnout
- The impact of nurse-to-patient ratios on nursing care quality in long-term care settings
- The effectiveness of nurse residency programs in improving new nurse retention rates
- The impact of nursing unit culture on nurse job satisfaction and retention
- The impact of nurse-patient ratios on patient outcomes
- Strategies for retaining experienced nurses in the workforce
- Analyzing the role of advanced practice nurses in healthcare teams
- The challenges and benefits of international nursing recruitment
- Addressing generational differences in the nursing workforce
- The relationship between nurse work schedules and nurse burnout
- The impact of nurse staffing levels on medication errors in hospital settings
- The role of interprofessional collaboration in reducing nursing workload and improving patient outcomes
- The impact of nursing education level on nursing practice and patient outcomes
- The relationship between nurse staffing levels and patient falls in acute care settings
- The impact of nurse workload on patient satisfaction with nursing care
- The role of nursing leadership in promoting staff well-being and reducing burnout
- The relationship between nurse staffing levels and patient mortality rates in critical care settings
- The effectiveness of nurse-led care models in improving patient outcomes and reducing healthcare costs
- The impact of nurse staffing levels on patient readmission rates in acute care settings
- The role of nursing autonomy in improving nursing practice and patient outcomes
- The relationship between nurse job satisfaction and patient outcomes in long-term care settings
- The impact of nursing staff turnover on patient safety and quality of care
- Healthcare management: career paths and requirements
- The role of technology in improving nursing efficiency and reducing workload
- The relationship between nurse staffing levels and patient satisfaction with nursing care
- The impact of nurse staffing levels on nurse job stress and burnout in pediatric settings
- The effectiveness of nurse-led interventions in improving patient outcomes for chronic conditions
- The role of nursing leadership in promoting a culture of safety and reducing patient harm
- The relationship between nurse staffing levels and patient outcomes in psychiatric settings
- The impact of nurse staffing levels on nurse job satisfaction and burnout in emergency departments
- The effectiveness of nursing education programs in improving nurse practice and patient outcomes
- The role of nurse practitioners in improving access to healthcare in underserved communities
- The relationship between nurse staffing levels and patient outcomes in rehabilitation settings
- The impact of nurse staffing levels on nurse retention rates in rural healthcare facilities
- The effectiveness of nurse-led discharge planning in reducing hospital readmissions
- The role of nursing leadership in promoting interprofessional collaboration and teamwork
- The relationship between nurse staffing levels and patient outcomes in outpatient care settings
- The impact of nursing workloads on patient safety in intensive care units
- The role of nursing research in improving nursing practice and patient outcomes
- The relationship between nurse staffing levels and nurse job satisfaction in surgical settings
- The impact of nurse staffing levels on patient satisfaction with pain management in acute care settings
- The effectiveness of nursing education programs in improving nursing knowledge and skills
- The role of nursing advocacy in promoting patient-centered care and improving healthcare outcomes
Medical Studies Overwhelming?
Delegate Your Nursing Papers to the Pros!
Get 15% Discount
+ Plagiarism Report for FREE
Patient Safety
Another crucial area of nursing research is patient safety. Studying ways to enhance patient safety, reduce adverse events, and improve the quality of care in hospitals and other healthcare settings can help prevent patient harm and improve patient outcomes.
List of Nursing Research Topics: Patient Safety
- Exploring the impact of workplace stress on nurses’ job satisfaction and performance
- Investigating the factors that influence nurse turnover and retention rates
- Assessing the role of nurse staffing levels in patient outcomes and quality of care
- Examining the relationship between nurse burnout and patient safety incidents
- Investigating the effectiveness of nursing leadership in creating a positive work environment
- The influence of nursing handovers on patient safety
- Strategies to reduce medication errors in hospital settings
- The role of electronic health records in enhancing patient safety
- Impact of nurse-to-patient ratios on patient safety outcomes
- Evaluating the effectiveness of patient safety training programs for nurses
- Exploring the experiences of nurses from diverse backgrounds in the workplace
- Assessing the impact of shift work on nurses’ physical and mental health
- Investigating the relationship between nurse-patient ratios and patient outcomes
- Examining the role of interprofessional collaboration in improving the nursing work environment
- Exploring the use of technology to improve nursing workflow and productivity
- Mitigating the economic and social costs of heart diseases among the aging population in the US
- Investigating the effectiveness of nursing mentorship programs in retaining new nurses
- Assessing the role of organizational culture in promoting nurse well-being and job satisfaction
- Examining the impact of nursing education on nursing workforce preparedness
- Exploring the factors that contribute to job satisfaction among nurses
- Combating health care-associated infections: a community-based approach
- Investigating the impact of nurse-led care on patient outcomes and satisfaction
- Assessing the effectiveness of nursing support programs for nurses with mental health issues
- Examining the role of nursing unions in advocating for the nursing workforce
- Exploring the experiences of male nurses in the nursing workforce
- Investigating the effectiveness of nurse-led clinics in reducing emergency department visits
- Assessing the impact of nursing teamwork on patient outcomes and quality of care
- Examining the role of nursing informatics in improving nursing workflow and patient care
- Exploring the impact of nursing shortages on patient outcomes and quality of care
- Investigating the effectiveness of nurse-led interventions for reducing hospital readmissions
- Assessing the impact of nursing certification on nursing workforce competence and confidence
- Examining the role of nursing education in promoting cultural competence in the nursing workforce
- Exploring the experiences of nurses working in rural healthcare settings
- Investigating the effectiveness of nursing delegation in improving patient outcomes and quality of care
- Assessing the impact of nursing shortages on nurse job satisfaction and burnout
- Examining the role of nursing research in informing nursing workforce policies and practices
- Exploring the impact of nurse-led quality improvement initiatives on patient outcomes and satisfaction
- Investigating the role of nursing leaders in promoting nursing workforce diversity and inclusion
- Assessing the impact of nursing autonomy on nurse job satisfaction and performance
- Examining the effectiveness of nursing residency programs in preparing new nurses for the workforce
- Exploring the experiences of nurses working in correctional healthcare settings
- Investigating the impact of nurse staffing levels on patient falls and injuries
- Assessing the role of nursing education in promoting evidence-based practice in the nursing workforce
- Examining the effectiveness of nursing preceptorship programs in improving nurse job satisfaction and retention
- Exploring the role of nursing education in preparing nurses for leadership roles in the nursing workforce
- Investigating the effectiveness of nursing empowerment interventions in improving nursing job satisfaction and performance
- Assessing the impact of nursing shortages on the quality of nursing care provided to older adults in long-term care facilities.
Chronic Illness Management
Managing chronic diseases, such as diabetes, cancer, and heart disease, is a significant challenge for healthcare providers. Exploring different strategies for chronic disease management can help improve patient outcomes and enhance the quality of care.
List of Nursing Research Topics: Chronic Illness Management
- The Role of Nurses in Managing Chronic Heart Disease
- Impact of Nurse-led Interventions in Managing Chronic Obstructive Pulmonary Disease (COPD)
- The Effectiveness of Self-management Education in Patients with Type 2 Diabetes
- Nursing Strategies for Chronic Pain Management
- Chronic Kidney Disease Management: A Nursing Perspective
- Palliative Care in Chronic Illness Management
- Community Nursing and Chronic Illness: A Study on Patient Outcomes
- The Role of Nurses in Managing Chronic Pediatric Asthma
- Telehealth and Chronic Disease Management: The Future of Nursing Practice?
- Evaluating the role of nursing in diabetes self-management
- Strategies for improving patient adherence to chronic illness treatment plans
- The impact of nurse-led interventions on chronic obstructive pulmonary disease (COPD) management
- Exploring the role of telehealth in chronic illness follow-up and monitoring
- The effectiveness of nurse-led educational programs for patients with cardiovascular diseases
- The Importance of Nurse-led Clinics in Chronic Illness Management
- The Role of Nursing in Depression Management among Chronically Ill Patients
- Empowering the vulnerable: enhancing health and social care for individuals with specific needs
- Advanced Practice Nurses and Chronic Illness Management: A Systematic Review
- The Impact of Holistic Nursing Care on Chronic Disease Management
- The Effect of Nurse-led Health Education on Compliance in Chronic Disease Patients
- The Role of Family Nurses in the Management of Chronic Illness in Home Settings
- Nursing and the Management of Chronic Illness in Geriatric Populations
- The Influence of Nursing Interventions on Quality of Life in Patients with Chronic Illness
- Challenges Faced by Nurses in Managing Chronic Illness in Low-resource Settings
- Cancer Pain: Assessment, Management, and Patient Empowerment
- Evaluating the Role of School Nurses in Managing Chronic Illnesses in Children
- Developing a Chronic Disease Management Model: The Crucial Role of Nursing
- Nursing Intervention in Lifestyle Modification for Chronic Illness Patients
- The Impact of Patient-Nurse Communication in Chronic Illness Management
- The Role of Nursing in Medication Management for Chronic Illness Patients
- The Effects of Nursing Care Coordination on Chronic Illness Outcomes
- Mental Health and Chronic Illness: The Importance of Psychiatric Nursing
- The Role of Nursing in the Self-Management of Chronic Illness: A Meta-Analysis
- Nursing Interventions for Chronic Illness Management in Rural Areas
- Nurses’ Role in Reducing Hospital Readmissions for Chronic Illness Patients
- Digital healthcare and organizational learning: enhancing patient care through technology and knowledge management
- The Impact of Nursing on Patient Empowerment in Chronic Illness Management
- Cultural Competence in Nursing and Its Effect on Chronic Disease Management
- The Role of Nursing Informatics in Chronic Illness Management
- Evaluating the Role of Community Health Nurses in Chronic Illness Prevention
- The Impact of Home Nursing on Chronic Illness Management in Aging Populations
- The ongoing risk of HIV/AIDS among men who have sex with men
- The Role of Oncology Nurses in the Management of Chronic Cancer Pain
- The Effects of Nursing-led Cognitive Behavioral Therapy in Chronic Illness Management
- The Impact of Advanced Nursing Practice on Health Outcomes in Chronic Disease Management
- The Use of Digital Health Technologies in Chronic Disease Management: A Nursing Perspective
Mental Health
Promoting mental health and well-being in vulnerable patient populations is another important area of nursing research. Nurses can investigate various interventions and programs that can help prevent mental health problems and improve patients’ overall well-being.
List of Nursing Research Topics: Mental Health
- The impact of COVID-19 on mental health in healthcare workers
- The effectiveness of telehealth for delivering mental health services
- The role of social support in promoting mental health and wellbeing
- Investigating the effectiveness of mindfulness-based interventions for mental health
- Examining the use of virtual reality in treating mental health disorders
- The impact of sleep on mental health outcomes
- The role of exercise in promoting mental health and wellbeing
- The effectiveness of psychotherapy in treating depression
- Exploring the relationship between mental health and chronic pain
- Investigating the impact of workplace stress on mental health in nurses
- The effectiveness of nurse-led interventions for patients with depression
- Exploring the impact of nurse-patient relationships on mental health outcomes
- Strategies for improving mental health literacy among nursing professionals
- Evaluating the role of nurses in suicide prevention and intervention
- The challenges and strategies in nursing care for patients with dual diagnoses (co-existing mental health and substance use disorders)
- Examining the use of music therapy for mental health promotion
- The effectiveness of cognitive-behavioral therapy for anxiety disorders
- The relationship between mental health and nutrition
- The impact of trauma on mental health outcomes
- Investigating the use of art therapy in promoting mental health and wellbeing
- The role of spirituality in mental health and coping
- The effectiveness of group therapy for mental health disorders
- The impact of stigma on mental health outcomes
- Examining the effectiveness of psychopharmacology in treating mental health disorders
- The role of family support in promoting mental health and wellbeing
- Investigating the relationship between mental health and substance abuse
- The effectiveness of animal-assisted therapy in promoting mental health and wellbeing
- The impact of social media on mental health outcomes
- Examining the use of humor in promoting mental health and wellbeing
- The effectiveness of cognitive training for improving mental health outcomes
- Investigating the impact of gender and cultural factors on mental health outcomes
- The role of occupational therapy in promoting mental health and wellbeing
- Examining the effectiveness of acceptance and commitment therapy for mental health disorders
- The relationship between mental health and physical activity
- Investigating the use of peer support for mental health promotion
- The effectiveness of mindfulness-based stress reduction for mental health
- The impact of technology on mental health outcomes
- The role of nutrition in treating mental health disorders
- Examining the use of hypnotherapy in promoting mental health and wellbeing
- The effectiveness of psychotherapy for PTSD
- Investigating the relationship between mental health and social determinants of health
- The impact of social isolation on mental health outcomes
- Examining the use of dance therapy in promoting mental health and wellbeing
- The effectiveness of cognitive processing therapy for mental health disorders
- The role of self-care in promoting mental health and wellbeing in nurses
Health Promotion
Research into health promotion strategies using technology, social media, and other digital tools is a rapidly growing area of nursing research. Such research can help identify innovative and effective ways to promote health and well-being in communities and patient populations.
List of Nursing Research Topics: Health Promotion
- The effectiveness of community-based interventions in promoting physical activity and healthy eating habits
- Investigating the impact of social media on health behavior and lifestyle changes
- The role of nursing in promoting healthy behaviors and preventing chronic diseases
- Identifying effective strategies for improving health literacy among underserved populations
- Exploring the use of wearable technology in promoting physical activity and healthy lifestyles
- Evaluating the effectiveness of nurse-led health promotion campaigns on community health outcomes
- The role of nurses in promoting vaccinations in various populations
- Strategies for nurses to address health literacy and its impact on patient outcomes
- The influence of cultural competence in health promotion and disease prevention
- Assessing the role of nurses in promoting physical activity and healthy lifestyles in at-risk populations
- Investigating the role of family support in promoting healthy behaviors among children and adolescents
- Examining the effectiveness of peer-led interventions in promoting healthy lifestyles
- Investigating the impact of workplace wellness programs on employee health and productivity
- The impact of milk consumption on children’s growth
- The role of nursing in promoting smoking cessation and reducing tobacco use
- Exploring the use of motivational interviewing in promoting behavior change and improving health outcomes
- Investigating the effectiveness of mindfulness-based interventions in promoting mental and physical health
- The role of social support in promoting healthy behaviors and preventing chronic diseases
- Examining the effectiveness of school-based interventions in promoting healthy behaviors among children and adolescents
- Exploring the use of technology in promoting health education and behavior change
- Investigating the role of culture and ethnicity in promoting healthy behaviors and preventing chronic diseases
- Nursing: a beautiful blend of art and science
- Examining the effectiveness of community health worker programs in promoting healthy lifestyles
- The role of nursing in promoting healthy aging and preventing age-related diseases
- Investigating the impact of environmental factors on health behavior and lifestyle changes
- Exploring the use of incentives in promoting behavior change and improving health outcomes
- Investigating the effectiveness of group-based interventions in promoting healthy lifestyles
- Examining the impact of policy interventions on health behavior and lifestyle changes
- The effects of sleep deprivation on students’ cognitive functions and emotional state
- The role of nursing in promoting healthy sleep habits and reducing sleep disorders
- Investigating the effectiveness of mobile health interventions in promoting behavior change and improving health outcomes
- Exploring the use of positive psychology interventions in promoting mental and physical health
- Investigating the role of healthcare providers in promoting healthy behaviors and preventing chronic diseases
- Examining the effectiveness of workplace policies in promoting healthy lifestyles
- The role of nursing in promoting healthy sexual behaviors and preventing sexually transmitted infections
- Investigating the impact of stress on health behavior and lifestyle changes
- Exploring the use of community-based participatory research in promoting healthy behaviors and preventing chronic diseases
- The delicate dance: balancing art and science in the nursing profession
- Investigating the role of nutrition in promoting healthy behaviors and preventing chronic diseases
- Examining the effectiveness of self-management interventions in promoting healthy lifestyles
- The role of nursing in promoting healthy pregnancy and preventing maternal and child health problems
- Investigating the impact of socioeconomic status on health behavior and lifestyle changes
- Exploring the use of health coaching in promoting behavior change and improving health outcomes
- Investigating the role of spirituality in promoting mental and physical health
- Examining the effectiveness of school-based policies in promoting healthy lifestyles
- The role of nursing in promoting healthy relationships and preventing intimate partner violence
- Investigating the impact of social determinants of health on health behavior and lifestyle changes
- Exploring the use of mobile applications in promoting healthy behaviors and preventing chronic diseases
- Investigating the role of health literacy in promoting healthy behaviors and preventing chronic diseases
Palliative Care
Improving the quality of life of seriously ill patients and their families during end-of-life care is another critical area of nursing research. Nurses can explore different interventions and support programs that can enhance the palliative care experience.
List of Nursing Research Topics: Palliative Care
- The effectiveness of palliative care on improving quality of life for cancer patients
- Understanding the needs and experiences of family caregivers in palliative care
- Palliative care and end-of-life decision-making: exploring patient and family preferences
- Optimizing the clarifying diagnosis of stomach cancer
- Improving access to palliative care for patients in rural areas
- The role of spirituality in palliative care for terminally ill patients
- Investigating the impact of music therapy on patients receiving palliative care
- Developing effective communication strategies for discussing end-of-life care with patients and families
- Exploring the experiences and needs of patients with non-cancer diagnoses in palliative care
- The impact of nurse-led interventions in improving the quality of life for patients in palliative care
- Evaluating the training needs of nurses in delivering end-of-life care
- The role of nursing in managing symptoms and side effects in palliative care patients
- Strategies for improving communication between nurses and families during end-of-life care
- Assessing the ethical considerations and challenges faced by nurses in palliative care settings
- Evaluating the effectiveness of home-based palliative care programs
- Palliative care for pediatric patients: understanding unique challenges and opportunities
- The impact of cultural and ethnic differences on palliative care provision
- Investigating the role of social support in palliative care for older adults
- The effectiveness of advance care planning in improving end-of-life care
- Understanding the experiences and needs of patients with neurological diseases in palliative care
- Exploring the impact of palliative care on reducing healthcare costs
- Investigating the role of complementary therapies in palliative care
- Improving symptom management in palliative care through medication optimization
- Palliative care and spiritual care: exploring the intersection of these two domains
- The impact of palliative care on reducing hospital readmissions
- Investigating the role of occupational therapy in palliative care
- Developing effective pain management strategies for patients receiving palliative care
- Understanding the experiences and needs of patients with heart failure in palliative care
- The role of pet therapy in improving quality of life for patients in palliative care
- Investigating the impact of palliative care on reducing caregiver burden
- Understanding the experiences and needs of patients with lung disease in palliative care
- Exploring the impact of palliative care on reducing healthcare utilization
- Investigating the role of nutrition in palliative care for patients with cancer
- Understanding the experiences and needs of patients with kidney disease in palliative care
- Improving palliative care for patients with dementia: exploring unique challenges and opportunities
- The role of art therapy in improving quality of life for patients in palliative care
- Investigating the impact of palliative care on reducing emergency department visits
- Developing effective communication strategies for discussing end-of-life care with patients with cognitive impairment
- Understanding the experiences and needs of patients with liver disease in palliative care
- Palliative care for patients with substance use disorders: unique challenges and opportunities
- Investigating the role of physiotherapy in palliative care
- The effectiveness of psychotherapy in improving mental health outcomes for patients in palliative care
- Understanding the experiences and needs of patients with multiple chronic conditions in palliative care
- Improving symptom management in palliative care through non-pharmacological interventions
- Investigating the impact of palliative care on reducing healthcare disparities
- Palliative care and medical aid in dying: exploring ethical and legal considerations
Healthcare Disparities
Studying the factors that contribute to healthcare disparities between different populations and identifying strategies to address these disparities is an important area of nursing research. Nurses can examine the role of social determinants of health in healthcare disparities and propose solutions to improve access and equity in healthcare.
List of Nursing Research Topics: Healthcare Disparities
- Examining the relationship between socioeconomic status and healthcare disparities
- Investigating the impact of implicit bias on healthcare disparities
- Analyzing the impact of racial and ethnic disparities on health outcomes
- Identifying disparities in access to preventative care among different populations
- Exploring the impact of language barriers on healthcare disparities
- Investigating the impact of discrimination on healthcare outcomes
- Identifying disparities in health insurance coverage and access to healthcare services
- Exploring the importance of national health insurance for socioeconomic growth
- Analyzing the impact of geographic location on healthcare disparities
- Evaluating the role of nursing in addressing healthcare disparities in underserved communities
- The impact of socioeconomic factors on patient outcomes and nursing interventions
- Strategies for nurses to promote health equity in diverse patient populations
- Assessing the influence of cultural competence on reducing healthcare disparities
- The role of nursing advocacy in shaping policies to reduce health inequities
- Examining disparities in mental health care access and utilization
- Investigating disparities in maternal and child health outcomes
- Exploring the relationship between healthcare disparities and chronic disease outcomes
- Identifying disparities in end-of-life care and hospice utilization
- Analyzing the impact of cultural differences on healthcare outcomes
- Investigating disparities in healthcare provider communication and patient engagement
- Examining the impact of healthcare policy on healthcare disparities
- Global health learning in nursing and health care disparities
- Identifying disparities in healthcare access and utilization among the LGBTQ+ community
- Exploring the impact of environmental factors on healthcare disparities
- Analyzing the impact of social determinants of health on healthcare disparities
- Investigating disparities in healthcare access and utilization among rural populations
- Examining disparities in healthcare access and utilization among urban populations
- Identifying disparities in healthcare access and utilization among immigrants and refugees
- Analyzing the impact of education level on healthcare disparities
- Investigating disparities in healthcare access and utilization among older adults
- Examining disparities in dental health access and utilization
- Identifying disparities in mental health treatment and access to services
- Analyzing the impact of stigma on healthcare outcomes for marginalized populations
- Investigating disparities in healthcare access and utilization among incarcerated populations
- Exploring disparities in healthcare access and utilization among individuals with disabilities
- Analyzing the impact of institutional racism on healthcare disparities
- Investigating disparities in healthcare access and utilization among low-income populations
- Examining disparities in cancer screening and early detection
- Identifying disparities in access to clinical trials and experimental treatments
- Analyzing the impact of the digital divide on healthcare disparities
- Investigating disparities in healthcare access and utilization among veterans
- Exploring the impact of healthcare worker bias on healthcare disparities
- Examining the relationship between healthcare disparities and infant mortality rates
- Identifying disparities in healthcare access and utilization among people with limited English proficiency
- Analyzing the impact of gender on healthcare disparities
- Investigating disparities in healthcare access and utilization among individuals experiencing homelessness
- Exploring the impact of COVID-19 on healthcare disparities among different populations
Patient-Centered Care
Enhancing patient-centered care, including patient feedback, patient-centered communication, and patient education, is another vital area of nursing research. Nurses can investigate the impact of patient-centered care on patient outcomes and identify ways to incorporate patient preferences and values in the care process.
List of Nursing Research Topics: Patient-Centered Care
- The importance of patient-centered care in improving health outcomes
- Exploring the effectiveness of patient-centered communication in clinical practice
- Assessing patient satisfaction with patient-centered care
- The impact of nursing staffing on patient-centered care
- The role of family and caregiver involvement in patient-centered care
- The use of technology to enhance patient-centered care
- Patient education and empowerment in promoting patient-centered care
- The role of nurses in facilitating shared decision-making in patient care
- Evaluating the impact of personalized care plans on patient outcomes and satisfaction
- Strategies for nurses to engage patients in their care across diverse cultural backgrounds
- The influence of effective communication strategies on the delivery of patient-centered care
- Assessing the barriers and facilitators to implementing patient-centered care in various healthcare settings
- The impact of culture on patient-centered care
- Measuring the quality of patient-centered care in healthcare settings
- The benefits of interdisciplinary collaboration in patient-centered care
- Understanding home dialysis: benefits, barriers, and impacts on elderly patients and the healthcare system
- Addressing language barriers in patient-centered care
- Exploring the challenges of implementing patient-centered care in healthcare organizations
- The role of patient-centered care in reducing healthcare costs
- The impact of patient-centered care on patient safety
- The importance of patient-centered care for vulnerable populations
- The role of leadership in promoting patient-centered care
- Evaluating the impact of patient-centered care on healthcare outcomes
- Examining the effectiveness of patient-centered care in chronic disease management
- The impact of patient-centered care on patient adherence to treatment
- The importance of patient-centered care in pediatric healthcare settings
- The use of patient feedback to improve patient-centered care
- Pediatric oncology: working towards better treatment through evidence-based research
- The role of patient-centered care in addressing health disparities
- Patient-centered care in end-of-life and palliative care settings
- The role of healthcare professionals in promoting patient-centered care
- The impact of patient-centered care on healthcare provider job satisfaction
- The importance of patient-centered care in emergency and critical care settings
- The use of simulation-based training to enhance patient-centered care
- The impact of patient-centered care on patient experience and engagement
- The role of healthcare policy in promoting patient-centered care
- Addressing the needs of patients with complex medical needs in patient-centered care
- The role of the nursing profession in promoting patient-centered care
- Patient-centered care in mental health and psychiatric settings
- The impact of patient-centered care on healthcare provider burnout
- The role of patient-centered care in promoting shared decision-making
- Examining the effectiveness of patient-centered care in rural healthcare settings
- The impact of patient-centered care on patient quality of life
- The use of patient-centered care in managing acute and chronic pain
- Addressing the needs of elderly patients in patient-centered care
- The impact of patient-centered care on healthcare system performance
- Promoting patient-centered care through the use of standardized patient education materials
Nursing Education
Exploring innovative approaches to nursing education and training, such as simulation-based learning and online learning, is a growing area of nursing research. Such research can help identify effective ways to prepare nursing students for their future roles in the healthcare system.
List of Nursing Research Topics: Nursing Education
- The impact of simulation-based training on nursing education outcomes
- The effectiveness of online learning in nursing education
- Innovative approaches to clinical teaching in nursing education
- The role of technology in nursing education
- Student perceptions of nursing education and their impact on learning outcomes
- The impact of cultural competence training on nursing students’ attitudes and behaviors
- The effectiveness of peer-led teaching in nursing education
- Best practices for incorporating interprofessional education into nursing curricula
- The role of reflective practice in nursing education
- The effectiveness of flipped classroom models in nursing education
- The impact of virtual reality and augmented reality tools in nursing education
- Evaluating the effectiveness of online vs. traditional classroom nursing education
- Strategies for enhancing interprofessional education in nursing curricula
- The role of continuous professional development in enhancing nursing competencies
- Assessing the influence of mentorship programs on nursing student success and retention
- Transforming advanced nursing practice: embracing IOM recommendations and higher education
- The impact of mentorship on nursing students’ learning and professional development
- The use of team-based learning in nursing education
- The effectiveness of hands-on skills training in nursing education
- Student perceptions of clinical experiences in nursing education
- The impact of service learning on nursing students’ attitudes and behaviors
- The role of cultural humility in nursing education
- The effectiveness of blended learning in nursing education
- Best practices for incorporating patient-centered care into nursing curricula
- The impact of standardized patient encounters on nursing education outcomes
- Importance and application of patient education technology in healthcare
- The use of case-based learning in nursing education
- The role of faculty development in improving nursing education outcomes
- The effectiveness of clinical reasoning strategies in nursing education
- The impact of nursing education on patient outcomes
- The role of simulation in teaching critical thinking in nursing education
- Best practices for incorporating evidence-based practice into nursing curricula
- The use of gamification in nursing education
- The effectiveness of problem-based learning in nursing education
- The impact of nursing education on student stress and burnout
- The role of intercultural competence in nursing education
- The effectiveness of collaborative learning in nursing education
- The impact of teaching communication skills in nursing education
- Best practices for incorporating patient safety into nursing curricula
- The role of interprofessional collaboration in nursing education
- The effectiveness of clinical coaching in nursing education
- The impact of teaching teamwork skills in nursing education
- The use of high-fidelity simulation in nursing education
- The role of experiential learning in nursing education
- Best practices for incorporating leadership development into nursing curricula
- The impact of nursing education on student retention and graduation rates
- The effectiveness of self-directed learning in nursing education
Healthcare Policy
Studying the impact of healthcare policy on the nursing profession and patient outcomes, including the role of nursing in healthcare reform efforts, is a crucial area of nursing research. Nurses can examine the policy’s effect on healthcare access, quality, and affordability and propose solutions to address policy gaps and challenges.
List of Nursing Research Topics: Healthcare Policy
- The impact of the affordable care act on the nursing profession
- Exploring healthcare informatics: evolution, challenges, and solutions
- The role of nursing in healthcare reform efforts
- The impact of medicare and Medicaid on nursing practice
- The impact of private insurance on nursing practice
- The impact of healthcare policies on nursing workforce development
- Combating workplace violence in nursing: the impact of policies, legislation, and organizational culture
- The role of nursing in healthcare policy decision-making
- The impact of healthcare policies on patient outcomes
- The role of nurses in implementing healthcare policies
- The implications of universal healthcare policies on nursing roles and responsibilities
- Evaluating the impact of health insurance reforms on nursing care delivery
- Strategies for nurses to influence healthcare policy decisions at the national and state levels
- The role of nursing in shaping policies related to patient rights and autonomy
- Assessing the influence of healthcare policy on nursing education and licensure requirements
- Evaluating the impact of nurse advocacy on shaping health policies at local and national levels
- Strategies for nurses to stay updated on changing healthcare policies and their implications
- The role of nursing in shaping policies related to electronic health records and patient privacy
- Assessing the implications of global health policies on nursing practices and education
- The influence of healthcare policies on the scope of practice for advanced practice nurses
- The impact of healthcare policies on nursing education and training
- The impact of healthcare policies on nurse staffing ratios
- The impact of healthcare policies on patient satisfaction
- Understanding the impact of the American Healthcare System Regulatory Acts
- The impact of healthcare policies on healthcare costs
- The impact of healthcare policies on healthcare disparities
- The role of nursing in advocating for healthcare policy changes
- The impact of healthcare policies on patient safety
- The impact of healthcare policies on nursing job satisfaction
- Understanding the US. Health Care Reform: necessity, challenges, and implementation
- The impact of healthcare policies on nursing burnout
- The impact of healthcare policies on nursing retention rates
- The impact of healthcare policies on nursing leadership
- The role of nursing in shaping healthcare policies
- The impact of healthcare policies on healthcare quality
- Workplace violence in healthcare: causes, regulations, and prevention strategies
- The impact of healthcare policies on nursing productivity
- The impact of healthcare policies on healthcare access
- The impact of healthcare policies on nursing workload
- The impact of healthcare policies on nursing autonomy
- The impact of healthcare policies on nursing scope of practice
- The impact of healthcare policies on nursing professional development
- The impact of healthcare policies on nursing research
- The role of nursing in developing healthcare policies
- Massachusetts Health Reform Act: striving for universal coverage and controlled costs
- The impact of healthcare policies on nursing career advancement
- The impact of healthcare policies on nursing licensure and certification
- The impact of healthcare policies on nursing accreditation
- The impact of healthcare policies on nursing ethics
- The impact of healthcare policies on nursing professionalism
- The role of nursing in healthcare policy implementation and evaluation
- The impact of healthcare policies on nursing informatics
- The impact of healthcare policies on nursing diversity and inclusion
- The impact of healthcare policies on nursing practice in rural areas
- The impact of healthcare policies on nursing practice in underserved communities
- The impact of healthcare policies on international nursing practice
The Importance of Research in Nursing
Research is the bedrock of nursing practice. It provides evidence-based knowledge that informs clinical decision-making, enhances patient outcomes, and advances the nursing profession. For nursing students, engaging in research activities offers several benefits:
- Enhanced Clinical Practice
Evidence-based research provides nurses with the latest knowledge and techniques to deliver optimal patient care. It bridges the gap between theoretical learning and practical application, ensuring that patients receive the most current and effective treatments.
- Professional Development
Engaging in research sharpens critical thinking and analytical skills. It fosters a culture of continuous learning, allowing nurses to stay updated with the ever-evolving medical field.
- Contribution to the Field
By conducting research, nurses contribute to the larger body of knowledge in healthcare. Their findings can lead to improvements in patient care, the development of new interventions, or changes in healthcare policies.
- Enhanced Patient Outcomes
Research equips nurses with the knowledge to educate patients, advocate for their needs, and make informed decisions. This ensures better health outcomes and improved patient satisfaction.
- Career Advancement
For those looking to advance in their careers, research can open doors to academic positions, leadership roles, or specialized fields within nursing.
Tips for Selecting a Suitable Research Topic
- Align with Interests
Choose a topic that genuinely interests you. This will keep you motivated throughout the research process.
- Relevance to Current Trends
Consider current trends and challenges in healthcare. Addressing contemporary issues can make your research more impactful.
- Feasibility
Ensure that you have access to the necessary resources and tools to conduct your research. This includes access to participants, equipment, and relevant literature.
It’s essential to choose a topic that’s neither too broad nor too narrow. A well-defined research question will guide your study and ensure it’s manageable.
- Seek Guidance
Don’t hesitate to seek advice from mentors, professors, or professionals in the field. Their insights can help refine your topic and provide valuable direction.
In conclusion, research is a vital component of the nursing profession, driving innovation and ensuring the best patient outcomes. For nursing students and professionals, engaging in research is not only a pathway to academic and career success but also a means to contribute meaningfully to the betterment of patient care.
📎 Related Articles
1. Key EBP Nursing Topics: Enhancing Patient Results through Evidence-Based Practice 2. Nursing Debate Topics: The Importance of Discussing and Debating Nursing Issues 3. Mental Health Nursing Research Topics: Inspiring Ideas for Students 4. Top Nursing Argumentative Essay Topics: Engage in Thought-Provoking Debates 5. Top Nursing Topics for Discussion: Engaging Conversations for Healthcare Professionals 6. Interesting Nursing Research Topics To Choose 7. Examples of Research Questions 8. Exploring Controversial Issues in Nursing: Key Topics and Examples 9. Pediatric Nursing Research Topics for Students: A Comprehensive Guide
Table of content
Crafted with Care:
Nursing Essays!
Precision, Passion, & Professionalism in Every Page.
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
How AI improves physician and nurse collaboration
A new artificial intelligence model helps physicians and nurses work together at Stanford Hospital to boost patient care.
April 15, 2024 - By Hanae Armitage

An artificial intelligence model in use at Stanford Hospital helps physicians and nurses know when a patient may be in decline, so they can act quickly to keep them out of the intensive care unit. vachcameraman - stock.adobe.com
With large language models that take notes during patient visits and algorithms that identify disease, artificial intelligence has begun to prove its worth as an assistant for physicians. But a new study from Stanford Medicine shows the potential of AI as a facilitator — one that helps doctors and nurses connect to achieve more efficient, effective patient care.
The study , which published in JAMA Internal Medicine last month, describes an AI-based model in use at Stanford Hospital that predicts when a patient is declining and flags the patient’s physicians and nurses. Ron Li , MD, a clinical associate professor of medicine and medical informatics director for digital health who is the senior author on the study, said the alert system helps clinicians connect more efficiently and effectively as well as intervene to prevent patients from deteriorating and landing in the intensive care unit.
Li, who worked with informatics postdoctoral scholar and lead author Robert Gallo , MD, on the evaluation, discussed their team’s approach to harnessing the algorithm and how it fosters clinician connection in a ceaselessly buzzing hospital environment. Lisa Shieh , MD, PhD, clinical professor of medicine; Margaret Smith , executive director of the Healthcare AI Applied Research Team , operations for primary care and population health; and Jerri Westphal, nursing informatics manager, also helped lead the study and the implementation of the AI system.

What is a deterioration model and how does AI fit in?
The algorithm is a prediction model that pulls data — such as vital signs, information from electronic health records and lab results — in near-real time to predict whether a patient in the hospital is about to suffer a health decline. Physicians aren’t able to monitor all of these data points for every patient all of the time, so the model runs in the background, looking at these values about every 15 minutes. It then uses artificial intelligence to calculate a risk score on the probability the patient is going to deteriorate, and if the patient seems like they might be declining, the model sends an alert to the care team.
What’s the benefit of having such a model run in a hospital?
The big question I want to answer is, “How do we use AI to build a more resilient health system in high-stakes situations?” There are many ways to do that, but one core characteristic for a resilient system is strong communication channels. This model is powered by AI, but the action it triggers, the intervention, is basically a conversation that otherwise may not have happened.
Nurses and physicians have conversations and handoffs when they change shifts, but it’s difficult to standardize these communication channels due to busy schedules and other hospital dynamics. The algorithm can help standardize it and draw clinicians’ attention to a patient who may need additional care. Once the alert comes into the nurse and physician simultaneously, it initiates a conversation about what the patient needs to ensure they don’t decline to the point of requiring a transfer to the ICU.
Tell me about how your team implemented and evaluated the model.
We integrated this model, which we did not create, into our workflow, but with a few tweaks. Originally, it sent an alert when the patient was already deteriorating, which we didn’t find very helpful. We adjusted the model to focus on predicting ICU transfers and other indicators of health decline.
We wanted to ensure the nursing team was heavily involved and felt empowered to initiate conversations with physicians about adjusting a patient’s care. When we evaluated the tool, which we had running for almost 10,000 patients, we saw a significant improvement in clinical outcomes — a 10.4% decrease in deterioration events, which we defined as transfers to the ICU, rapid response team events, or codes — among a subset of 963 patients with risk scores within a “regression discontinuity window,” which basically means they’re at the cusp of being high risk. These are patients whose clinical trajectory may not be as obvious to the medical team. For that group of patients, this model was especially helpful for encouraging physicians and nurses to collaborate to determine which patients need extra tending.
How have nurses and physicians responded to the integration of this new model?
The model is far from perfect. The reactions have overall been positive, but there is concern about alert fatigue, since not all alerts are flagging a real decline. When the model was validated on data from patients prior to implementation, we calculated that about 20% of patients flagged by the model did end up experiencing a deterioration event within six to 18 hours. At this point, even though it’s not a completely accurate model, it’s accurate enough to warrant a conversation. It shows that the algorithm doesn’t have to be perfect for it to be effective.
With that said, we want to improve the accuracy; you need to do that to improve trust. That’s what we’re working on now.
For more news about responsible AI in health and medicine, sign up for the RAISE Health newsletter.
Register for the RAISE Health Symposium on May 14.

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Hope amid crisis
Psychiatry’s new frontiers

When Patients Do Their Own Research
At its best, medicine will be a process of shared decision making, and doctors need to be prepared.
Listen to this article
Produced by ElevenLabs and News Over Audio (NOA) using AI narration.
Miscarriage early in pregnancy is very common—roughly one-fifth of detected pregnancies are thought to end in miscarriage, mostly in the first trimester. After a single miscarriage, patients are typically told that no further testing is needed; most women go on to have healthy pregnancies.
But after multiple miscarriages, doctors and patients begin a process of figuring out what is going on. In these situations, a lot of patients will take information gathering into their own hands. They’ll compile ideas from Google, WebMD, chat boards, support groups, friends, and friends of friends. Patients may arrive at their doctor’s office with file folders of information, a cobbled-together idea of their possibilities. Meanwhile, doctors have clinical knowledge, but they may struggle—especially given their limited time—to engage with their patients’ ideas and guide them.
Medicine wasn’t always this sort of shared process. Not long ago, medical decision making was largely left to doctors. Patients were a passive bunch, arriving at the doctor with their concerns and symptoms, and departing with their doctor’s orders. But today patients have incredible access to information online and elsewhere, and this has prompted a shift to what is sometimes called “shared decision making”: patients and doctors, together, sharing the burden of making consequential health choices.
Emily Oster: Thinking about pregnancy like an economist
This approach sounds great in principle. Shouldn’t patients be involved in decision making about their own health? In the area of obstetrics, the alternative brings to mind deliveries of the 1950s—white-coated doctors smoking cigarettes in their office while women labor in “twilight sleep,” even, in many cases, strapped to the bed. Surely if women had been involved, they would have opted for something a bit more comfortable.
In practice, though, shared decision making can be a source of frustration and confusion, for both sides. From the patient side, it can feel like doctors are either expecting too much engagement— Isn’t it your job to know what to do?— or not listening and not taking the patient’s ideas and preferences seriously. Sometimes it feels like all of this at once. From the medical side, frustration also comes in several forms—with patients who do not want to engage with the decision, and with those who do but are unwilling to listen to expert advice. Why won’t they listen to me? A patient who arrives with her own research can give the impression that she believes her Google search makes her an expert in medicine.
We, the authors of this article, come at this from both angles—one of us is a doctor, and one of us is an expert in statistics who has made a career of helping millions of pregnant people sort through data to make their own best decisions. We both believe that shared decision making in medicine can work, but many doctor-patient interactions today are not working. In our new book, The Unexpected , we try to provide a road map for improving this interaction, focusing on pregnancy. Our idea is simple. Two things are missing from this conversation: some common knowledge, and a script.
First, patients cannot engage with shared decision making if they do not understand the basics of their condition. To return to the example of miscarriage: A very large share of first-trimester miscarriages are a result of chromosomal abnormalities. If a patient does not know how chromosomes work in conception and what might influence them, discussing miscarriage prevention will be difficult. A patient doesn’t possess a doctor’s understanding of their condition—this would be unrealistic—but acquiring basic knowledge will allow patients to most effectively hear and process what is being said.
In particular, patients may benefit from getting a handle on the fundamental medical terminology associated with whatever symptoms they are presenting. Unfamiliar jargon can spark fear far beyond what one would feel if she knew what was being said. “Antiphospholipid antibody syndrome” sounds terrifying if you don’t know that, for many, it’s a treatable condition. When patients do not understand, many will shut down, unable to ask the questions they have or engage with the choices they need to make.
As a result, before doctors ask people to engage with decisions about their health, they need to prepare them. Our book tries to do this for people facing complicated pregnancy conditions. In other cases—cancer treatment, diabetes, other chronic illnesses—different resources exist. Patients should do some homework before they go to the doctor’s office.
The second thing these conversations need is a script. If patients and their doctor had limitless time to talk, then maybe it would be okay to enter the conversation with only a vague idea of the purpose. But time is limited, and that means a script is key, prioritizing questions where the answers matter for decisions.
To return to the miscarriage example, a script might start with the details of what happened. Knowing exactly when in pregnancy a loss occurred, what kind of testing followed it, and how many times it has happened will shape next steps. A second question is whether there are clues as to why it happened, which will inform whether it will happen again. A script might end by talking about what can be done to decrease risk, if anything.
Read: When evidence says no, but doctors say yes
In the best form of this conversation, the doctor brings a deep understanding of what might be going on medically with the patient, the range of possible tests, and what those tests might reveal to the patient. The patient brings a knowledge of their own preferences and their own emotional state. How much information do they want to know? Would they be willing to use more complex medical treatments if they were recommended? Are they even ready to engage emotionally with thinking about trying for pregnancy again?
The central recognition here is that shared decision making isn’t about both sides bringing the same thing to the table and deliberating about it. It’s about two different types of expertise—expertise in medicine on the part of the doctor, and expertise in herself on the part of the patient. Seeing this, in turn, can help the doctors and the patient both recognize when one decision maker should be paramount, or when a decision requires input from both.
An emergency situation—when, say, a person has been in a bike accident, his blood pressure is low, and he is bleeding from his head—isn’t the time for shared decision making. This is when the medical side takes over. No patient needs to be asked whether they think it’s a good idea to scan their head for a skull fracture. At the other end of the spectrum are decisions such as prenatal genetic screening and testing, which are in many cases almost exclusively about patient values and preferences.
Most decisions fall somewhere in between, requiring medical input but with room for patients’ preferences to play a role. Attempting a vaginal birth after a C-section is an example here—both a repeat Cesarean and an attempted vaginal birth have their risks and benefits. The medical expertise comes in explaining these risks and benefits, but the decision for many women here should come down to their own preferences.
With better understanding, clear scripts, and a sense of when different decision makers should dominate, we believe there is space for some decision making to be truly shared. But one more crucial element should be present: trust. Sometimes the desire by patients to play a role in their medical care can seem like a lack of trust in their doctors. And on the flip side, when patients do not feel like their concerns, ideas, or preferences are being listened to, they can lose trust in their provider to find what is best for them . Good decisions require the trust to recognize that we are all rowing in the same direction, and the willingness to engage so we can get there.
When you buy a book using a link on this page, we receive a commission. Thank you for supporting The Atlantic.
21 Healthcare Topics Patients Cared Most About in 2021 (And How to Plan for 2022)

Solv creates powerful solutions for providers to offer an engaging patient experience, and grow their practice. For patients, we have an app where 9 million healthcare consumers search for care every month. With many consumers turning to Solv for their everyday healthcare needs, we have a team dedicated to making the healthcare system easier for our users to navigate.
For providers, understanding the topics that patients are reading about online can unlock new perspectives. There are a few illuminating takeaways in this data about what patients are missing from their healthcare experience.
Our blog for healthcare consumers was viewed over 1.5 million times in 2021. We compiled all of the trending topics patients cared the most about this year to help you understand what they were concerned about. Here are the top topics (and blogs!) healthcare consumers were reading in 2021.

The majority of patients were reading up on everyday healthcare concerns
From creative ways to remove a splinter to how to fight the flu , healthcare consumers spent the majority of their time online reading up on everyday health concerns. 68% of the readership of our top blogs covered everyday obstacles patients face in seeking care.
What’s the takeaway?
We know that 72% of consumers search for a healthcare provider online , and a whopping 89% of the U.S. population Google their symptoms before they reach out to their doctor. More than ever, patients are taking their health-related questions online.
And you can see the value in patients finding answers online, especially when patient volume is high . Patients can look up simple things—like which foods are healthy—that don’t require a provider.
How to take action
Take advantage of this surging website traffic by building up your own website with blog content. This is a long-term strategy that will inevitably boost your online bookings .
Start a blog on your website, and answer commonly asked questions for your patients online. You can even email or post on social media when these topics are timely—like tips to avoid the flu during respiratory season—to serve as a reminder for your patients.
- 6 Creative Ways to Remove a Splinter | #1 viewed blog in 2021 | 12:55 average minutes spent reading
- Antibiotics: Everything You Need to Know | 7:10 average minutes spent reading
- Can You Get an STD Test at an Urgent Care? | 8:07 average minutes spent reading
- 10 Flu (& COVID-19) Fighters for Your Family | 5:48 average minutes spent reading
- What to Do if You Get a Urinary Tract Infection (UTI) | 19:04 average minutes spent reading
- 4 "Healthy" Foods That Can Kill You | 12:05 average minutes spent reading
- Breast Self-Exams: Do You Need Them? Everything You Need to Know | 21 average minutes spent reading
Patients are investing time in understanding how their healthcare experience should be
Patients are curious about their health. We’ve seen this rising trend in patient behavior since 2017, and it continues 5 years later.
Consumers are becoming active participants in their healthcare. Patients research on Google before they seek care, they want to be prepared for conversations with providers, and they expect to know the cost of the care they are paying for up front.
Patients spent an average of 7.7 minutes reading each of these blogs (and if you’re familiar with marketing and website data, this is extremely high!) This hints to us that healthcare consumers are really invested in the topic.
Patients want to understand and be able to participate in their healthcare experiences.
Get clear on how important your office’s role in your patients’ healthcare experience actually is. Great patient care doesn’t stop at patient experience. Are you being transparent with your pricing and enabling your patients to make the best financial decisions when it comes to their care? Are you helping patients understand how to navigate the healthcare system when they need it? Are you educating patients about when it’s appropriate to seek ambulatory care?
Healthcare is confusing for everyone—but it shouldn’t be. Everyone deserves to be free from the stress of everyday healthcare.
Use these topics as a starting point for what information your own patients might be missing. Create a plan to help patients navigate the confusing healthcare system better, and will improve their experience with your brand.
- What You Need to Know About Going to Urgent Care During Pregnancy
- What is a Nurse Practitioner? Doctors vs. Nurse Practitioners
- Guide to Navigating an Urgent Care Visit Without Insurance
- Reduce Your Urgent Care Wait Time by Booking Your Visit Online
- 5 Mistakes To Avoid When Going to Urgent Care
- What Services Do Urgent Care Centers Provide?
- How Much Does Urgent Care Cost?
COVID topics were focused on getting back to “normal”
Of course, patients were also spending time researching topics related to the COVID-19 pandemic this year. Compared to the information patients wanted about COVID in 2020, most of the top-read articles this year were about getting back to normal. Well, the new normal.
Patients spent 2021 learning to adapt to life with COVID-19. In 2021, they were reading up on vaccination, how to protect themselves and their families, and how to handle un-vaxxed family members during the holidays.
Keep educating your patients on vaccines, their efficacy, and the impact widespread vaccination can have on our population. But keep in mind that your patients are human, and they care most about how the virus affects them and their families. Vaccination means getting back to ‘normal,’ being able to travel again, and feeling safe doing everyday activities.
- COVID Vaccine Booster Shots: What You Need to Know
- Delta Got You Down? Facts About the Variant and Tips To Protect Yourself
- Fully Vaccinated? Here’s What You Can Start Doing Again Safely
- 10 Tips to Help You Find a COVID Vaccine Appointment
- Etiquette Expert: Host a Joyous Thanksgiving and Avoid Covid Conflict
- Solv It! Keeping Kids Healthy in the Face of COVID and the Delta Variant
- Going Back to School During COVID
Understanding the topics that your patients are reading about can unlock powerful information for providers. Use these takeaways and action items to build your 2022 strategies around the office. Are you going to do more education on how your clinic works? Are you going to introduce new information on common healthcare concerns? Revamp your COVID education?
*all reporting based on data from 1/1/21–12/5/21.
Related Articles

Staff Experience and Patient Experience: A Beneficial Circle
One of the most significant challenges facing the healthcare system is staffing shortages. COVID-19 has...

3 Keys to Patient Loyalty In Urgent Care
Healthcare providers enter the field to help people, and urgent care providers are on the front lines of local...

5 ways to increase patient bookings with more online reviews
Patients are savvy and know that they have choices when it comes to their care. With so many options, they look...
This site uses cookies to provide you with a great user experience. By using Solv, you accept our use of cookies.

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Technology as a Tool for Improving Patient Safety
Introduction .
In the past several decades, technological advances have opened new possibilities for improving patient safety. Using technology to digitize healthcare processes has the potential to increase standardization and efficiency of clinical workflows and to reduce errors and cost across all healthcare settings. 1 However, if technological approaches are designed or implemented poorly, the burden on clinicians can increase. For example, overburdened clinicians can experience alert fatigue and fail to respond to notifications. This can lead to more medical errors. As a testament to the significance of this topic in recent years, several government agencies [(e.g. the Agency for Healthcare Research and Quality (AHRQ) and the Centers for Medicare and Medicaid services (CMS)] have developed resources to help healthcare organizations integrate technology, such as the Safety Assurance Factors for EHR Resilience (SAFER) guides developed by the Office of the National Coordinator for Health Information Technology (ONC). 2,3,4 However, there is some evidence that these resources have not been widely used.5 Recently, the Centers for Medicare & Medicaid Services (CMS) started requiring hospitals to use the SAFER guides as part of the FY 2022 Hospital Inpatient Prospective Payment Systems (IPPS), which should raise awareness and uptake of the guides. 6
During 2022, research into technological approaches was a major theme of articles on PSNet. Researchers reviewed all relevant articles on PSNet and consulted with Dr. A Jay Holmgren, PhD, and Dr. Susan McBride, PhD, subject matter experts in health IT and its role in patient safety. Key topics and themes are highlighted below.
Clinical Decision Support
The most prominent focus in the 2022 research on technology, based on the number of articles published on PSNet, was related to clinical decision support (CDS) tools. CDS provides clinicians, patients, and other individuals with relevant data (e.g. patient-specific information), purposefully filtered and delivered through a variety of formats and channels, to improve and enhance care. 7
Computerized Patient Order Entry
One of the main applications of CDS is in computerized patient order entry (CPOE), which is the process used by clinicians to enter and send treatment instructions via a computer application. 8 While the change from paper to electronic order entry itself can reduce errors (e.g., due to unclear handwriting or manual copy errors), research in 2022 showed that there is room for improvement in order entry systems, as well as some promising novel approaches.
Two studies looked at the frequency of and reasons for medication errors in the absence of CDS and CPOE and demonstrated that there was a clear patient safety need. One study found that most medication errors occurred during the ordering or prescribing stage, and both this study and the other study found that the most common medication error was incorrect dose. Ongoing research, such as the AHRQ Medication Safety Measure Development project, aims to develop and validate measure specifications for wrong-patient, wrong-dose, wrong-medication, wrong-route, and wrong-frequency medication orders within EHR systems, in order to better understand and capture health IT safety events.9 Errors of this type could be avoided or at least reduced through the use of effective CPOE and CDS systems. However, even when CPOE and CDS are in place, errors can still occur and even be caused by the systems themselves. One study reviewed duplicate medication orders and found that 20% of duplicate orders resulted from technological issues, including alerts being overridden, alerts not firing, and automation issues (e.g., prefilled fields). A case study last year Illustrated one of the technological issues, in this case a manual keystroke error, that can lead to a safety event. A pharmacist mistakenly set the start date for a medication to the following year rather than the following day , which the CPOE system failed to flag. The authors recommended various alerts and coding changes in the system to prevent this particular error in the future.
There were also studies in 2022 that showed successful outcomes of well-implemented CPOE systems. One in-depth pre-post, mixed-methods study showed that a fully implemented CPOE system significantly reduced specific serious and commonly occurring prescribing and procedural errors. The authors also presented evidence that it was cost-effective and detailed implementation lessons learned drawn from the qualitative data collected for the study. A specific CPOE function that demonstrated statistically significant improvement in 2022 was automatic deprescribing of medication orders and communication of the relevant information to pharmacies. Deprescribing is the planned and supervised process of dose reduction or stopping of a medication that is no longer beneficial or could be causing harm. That study showed an immediate and sustained 78% increase in successful discontinuations after implementation of the software. A second study on the same functionality determined that currently only one third to one half of medications are e-prescribed, and the study proposed that e-prescribing should be expanded to increase the impact of the deprescribing software. It should be noted, however, that the systems were not perfect and that a small percentage of medications were unintentionally cancelled. Finally, an algorithm to detect patients in need of follow-up after test results was developed and implemented in another study . The algorithm showed some process improvements, but outcome measures were not reported.
Usability
Usability of CDS systems was a large focus of research in 2022. Poorly designed systems that do not fit into existing workflows lead to frustrated users and increase the potential for errors. For example, if users are required to enter data in multiple places or prompted to enter data that are not available to them, they could find ways to work around the system or even cease to use it, increasing the potential for patient safety errors. The documentation burden is already very high on U.S. clinicians, 10 so it is important that novel technological approaches do not add to this burden but, if possible, alleviate it by offering a high level of usability and interoperability.
One study used human-factored design in creating a CDS to diagnose pulmonary embolism in the Emergency Department and then surveyed clinician users about their experiences using the tool. Despite respondents giving the tool high usability ratings and reporting that the CDS was valuable, actual use of the tool was low. Based on the feedback from users, the authors proposed some changes to increase uptake, but both users and authors mentioned the challenges that arise when trying to change the existing workflow of clinicians without increasing their burden. Another study gathered qualitative feedback from clinicians on a theoretical CDS system for diagnosing neurological issues in the Emergency Department. In this study too, many clinicians saw the potential value in the CDS tool but had concerns about workflow integration and whether it would impact their ability to make clinical decisions. Finally, one study developed a dashboard to display various risk factors for multiple hospital-acquired infections and gathered feedback from users. The users generally found the dashboard useful and easy to learn, and they also provided valuable feedback on color scales, location, and types of data displayed. All of these studies show that attention to end user needs and preferences is necessary for successful implementation of CDS. However, the recent market consolidation in Electronic Health Record vendors may have an impact on the amount of user feedback gathered and integrated into CDS systems. Larger vendors may have more resources to devote to improving the usability and design of CDS, or their near monopolies in the market may not provide an incentive to innovate further. 11 More research is needed as this trend continues.
Alerts and Alarms
Alerts and alarms are an important part of most CDS systems, as they can prompt clinicians with important and timely information during the treatment process. However, these alerts and alarms must be accurate and useful to elicit an appropriate response. The tradeoff between increased safety due to alerts and clinician alert fatigue is an important balance to strike. 12
Many studies in 2022 looked at clinician responses to medication-related alerts, including override and modification rates. Several of the studies found a high alert override rate but questioned the validity of using override rates alone as a marker of CDS effectiveness and usability. For example, one study looked at drug allergy alerts and found that although 44.8% of alerts were overridden, only 9.3% of those were inappropriately overridden, and very few overrides led to an adverse allergic reaction. A study on “do not give” alerts found that clinicians modified their orders to comply with alert recommendations after 78% of alerts but only cancelled orders after 26% of alerts. A scoping review looked at drug-drug interaction alerts and found similar results, including high override rates and the need for more data on why alerts are overridden. These findings are supported by another study that found that the underlying drug value sets triggering drug-drug interaction alerts are often inconsistent, leading to many inappropriate alerts that are then appropriately overridden by clinicians. These studies suggest that while a certain number of overrides should be expected, the underlying criteria for alert systems should be designed and regularly reviewed with specificity and sensitivity in mind. This will increase the frequency of appropriate alerts that foster indicated clinical action and reduce alert fatigue.
There also seems to be variability in the effectiveness of alert systems across sites. One study looked at an alert to add an item to the problem list if a clinician placed an order for a medication that was not indicated based on the patient’s chart. The study found about 90% accuracy in alerts across two sites but a wide difference in the frequency of appropriate action between the sites (83% and 47%). This suggests that contextual factors at each site, such as culture and organizational processes, may impact success as much as the technology itself.
A different study looked at the psychology of dismissing alerts using log data and found that dismissing alerts becomes habitual and that the habit is self-reinforcing over time. Furthermore, nearly three quarters of alerts were dismissed within 3 seconds. This indicates how challenging it can be to change or disrupt alert habits once they are formed.
Artificial Intelligence and Machine Learning
In recent years, one of the largest areas of burgeoning technology in healthcare has been artificial intelligence (AI) and machine learning. AI and machine learning use algorithms to absorb large amounts of historical and real-time data and then predict outcomes and recommend treatment options as new data are entered by clinicians. Research in 2022 showed that these techniques are starting to be integrated into EHR and CDS systems, but challenges remain. A full discussion of this topic is beyond the scope of this review. Here we limit the discussion to several patient-safety-focused resources posted on PSNet in 2022.
One of the promising aspects of AI is its ability to improve CDS processes and clinician workflow overall. For example, one study last year looked at using machine learning to improve and filter CDS alerts. They found that the software could reduce alert volume by 54% while maintaining high precision. Reducing alert volume has the potential to alleviate alert fatigue and habitual overriding. Another topic explored in a scoping review was the use of AI to reduce adverse drug events. While only a few studies reviewed implementation in a clinical setting (most evaluated algorithm technical performance), several promising uses were found for AI systems that predict risk of an adverse drug event, which would facilitate early detection and mitigate negative effects.
Despite enthusiasm for and promising applications of AI, implementation is slow. One of the challenges facing implementation is the variable quality of the systems. For example, a commonly used sepsis detection model was recently found to have very low sensitivity. 13 Algorithms also drift over time as new data are integrated, and this can affect performance, particularly during and after large disturbances like the COVID-19 pandemic. 14 There is also emerging research about the impact of AI algorithms on racial and ethnic biases in healthcare; at the time of publication of this essay, an AHRQ EPC was conducting a review of evidence on the topic. 15 These examples highlight the fact that AI is not a “set it and forget it” application; it requires monitoring and customization from a dedicated resource to ensure that the algorithms perform well over time. A related challenge is the lack of a strong business case for using high-quality AI. Because of this, many health systems choose to use out-of-the-box AI algorithms, which may be of poor quality overall (or are unsuited to particular settings) and may also be “black box” algorithms (i.e., not customizable by the health system because the vendor will not allow access to the underlying code). 16 The variable quality and the lack of transparency may cause mistrust by clinicians and overall aversion to AI interventions.
In an attempt to address these concerns, one article in 2022 detailed best practices for AI implementation in health systems, focusing on the business case. Best practices include using AI to address a priority problem for the health system rather than treating it as an end itself. Additionally, testing the AI using the health system’s patients and data to demonstrate applicability and accuracy for that setting, confirming that the AI can provide a return on investment, and ensuring that the AI can be implemented easily and efficiently are also important. Another white paper described a human-factors and ergonomics framework for developing AI in order to improve the implementation within healthcare systems, teams, and workflows. The federal government and international organizations have also published AI guidelines, focusing on increasing trustworthiness (National Artificial Intelligence Initiative) 17 and ensuring ethical governance (World Health Organization). 18
Conclusion and Next Steps
As highlighted in this review, the scope and complexity of technology and its application in healthcare can be intimidating for healthcare systems to approach and implement. Researchers last year thus created a framework that health systems can use to assess their digital maturity and guide their plans for further integration.
The field would benefit from more research in several areas in upcoming years. First and foremost, high-quality prospective outcome studies are needed to validate the effectiveness of the new technologies. Second, more work is needed on system usability, how the systems are integrated into workflows, and how they affect the documentation burden placed on clinicians. For CDS specifically, more focus is needed on patient-centered CDS (PC CDS), which supports patient-centered care by helping clinicians and patients make the best decisions given each individual’s circumstances and preferences. 19 AHRQ is already leading efforts in this field with their CDS Innovation Collaborative project. 20 Finally, as it becomes more common to incorporate EHR scribes to ease the documentation burden, research on their impact on patient safety will be needed, especially in relation to new technological approaches. For example, when a scribe encounters a CDS alert, do they alert the clinician in all cases?
In addition to the approaches mentioned in this article, other emerging technologies in early stages of development hold theoretical promise for improving patient safety. One prominent example is “computer vision,” which uses cameras and AI to gather and process data on what physically happens in healthcare settings beyond what is captured in EHR data, 21 including being able to detect immediately that a patient fell in their room. 22
As technology continues to expand and improve, researchers, clinicians, and health systems must be mindful of potential stumbling blocks that could impede progress and threaten patient safety. However, technology presents a wide array of opportunities to make healthcare more integrated, efficient, and safe.
- Cohen CC, Powell K, Dick AW, et al. The Association Between Nursing Home Information Technology Maturity and Urinary Tract Infection Among Long-Term Residents . J Appl Gerontol . 2022;41(7):1695-1701. doi: 10.1177/07334648221082024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9232878/
- https://www.healthit.gov/topic/safety/safer-guides
- https://cds.ahrq.gov/cdsconnect/repository
- https://www.cms.gov/about-cms/obrhi
- McBride S, Makar E, Ross A, et al. Determining awareness of the SAFER guides among nurse informaticists. J Inform Nurs. 2021;6(4). https://library.ania.org/ania/articles/713/view
- Sittig DF, Sengstack P, Singh H. Guidelines for US hospitals and clinicians on assessment of electronic health record safety using SAFER guides. J ama . 2022;327:719-720.
- https://library.ahima.org/doc?oid=300027#.Y-6RhXbMKHt
- https://www.healthit.gov/faq/what-computerized-provider-order-entry#:~:text=Computerized%20provider%20order%20entry%20(CPOE,paper%2C%20fax%2C%20or%20telephone
- https://digital.ahrq.gov/2018-year-review/research-spotlights/leveragin…
- Holmgren AJ, Downing NL, Bates DW, et al. Assessment of electronic health record use between US and non-US health systems. JAMA Intern Med. 2021;181:251-259. https://doi.org/10.1001/jamainternmed.2020.7071
- Holmgren AJ, Apathy NC. Trends in US hospital electronic health record vendor market concentration, 2012–2021. J Gen Intern Med. 2022. https://link.springer.com/article/10.1007/s11606-022-07917-3#citeas
- Co Z, Holmgren AJ, Classen DC, et al. The tradeoffs between safety and alert fatigue: data from a national evaluation of hospital medication-related clinical decision support. J Am Med Inform Assoc. 2020;27:1252-1258. https://pubmed.ncbi.nlm.nih.gov/32620948/
- Wong A, Otles E, Donnelly JP, et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med. 2021;181:1065-1070. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2781307
- Parikh RB, Zhang Y, Kolla L, et al. Performance drift in a mortality prediction algorithm among patients with cancer during the SARS-CoV-2 pandemic. J Am Med Inform Assoc. 2022;30:348-354. https://academic.oup.com/jamia/advance-article/doi/10.1093/jamia/ocac221/6835770?login=false
- https://effectivehealthcare.ahrq.gov/products/racial-disparities-health…
- https://www.statnews.com/2022/05/24/market-failure-preventing-efficient-diffusion-health-care-ai-software/
- https://www.ai.gov/strategic-pillars/advancing-trustworthy-ai/
- Ethics and governance of artificial intelligence for health (WHO guidance). Geneva: World Health Organization; 2021. https://www.who.int/publications/i/item/9789240029200
- Dullabh P, Sandberg SF, Heaney-Huls K, et al. Challenges and opportunities for advancing patient-centered clinical decision support: findings from a horizon scan. J Am Med Inform Assoc. 2022: 29(7):1233-1243. doi: 10.1093/jamia/ocac059. PMID: 35534996; PMCID: PMC9196686.
- https://cds.ahrq.gov/cdsic
- Yeung S, Downing NL, Fei-Fei L, et al. Bedside computer vision: moving artificial intelligence from driver assistance to patient safety. N Engl J Med. 2018;387:1271-1273. https://www.nejm.org/doi/10.1056/NEJMp1716891
- Espinosa R, Ponce H, Gutiérrez S, et al. A vision-based approach for fall detection using multiple cameras and convolutional neural networks: a case study using the UP-Fall detection dataset. Comput Biol Med. 2019;115:103520. https://doi.org/10.1016/j.compbiomed.2019.103520
This project was funded under contract number 75Q80119C00004 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services. The authors are solely responsible for this report’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of the U.S. Department of Health and Human Services. None of the authors has any affiliation or financial involvement that conflicts with the material presented in this report. View AHRQ Disclaimers
Perspective
Perspectives on Safety
Annual Perspective
Patient Safety Innovations
Suicide Prevention in an Emergency Department Population: ED-SAFE
WebM&M Cases
The Retrievals. August 9, 2023
Agent of change. August 1, 2018
Amid lack of accountability for bias in maternity care, a California family seeks justice. August 16, 2023
Mirror, Mirror on the Wall: An Update on the Quality of American Health Care Through the Patient's Lens. April 12, 2006
Improving patient safety by shifting power from health professionals to patients. October 25, 2023
Patient Safety Primers
Discharge Planning and Transitions of Care
Medicines-related harm in the elderly post-hospital discharge. March 27, 2019
Emergency department crowding: the canary in the health care system. November 3, 2021
Advancing Patient Safety: Reviews From the Agency for Healthcare Research and Quality's Making Healthcare Safer III Report. September 2, 2020
Exploring Alternatives To Malpractice Litigation. January 15, 2014
Making Healthcare Safer III. March 18, 2020
Special Section: Patient Safety. May 24, 2006
The Science of Simulation in Healthcare: Defining and Developing Clinical Expertise. November 19, 2008
Compendium of Strategies to Prevent HAIs in Acute Care Hospitals 2014. September 1, 2014
Quality, Safety, and Noninterpretive Skills. November 11, 2015
Patient Safety. November 21, 2018
Ambulatory Safety Nets to Reduce Missed and Delayed Diagnoses of Cancer
Remote response team and customized alert settings help improve management of sepsis.
Using sociotechnical theory to understand medication safety work in primary care and prescribers' use of clinical decision support: a qualitative study. May 24, 2023
Human factors and safety analysis methods used in the design and redesign of electronic medication management systems: a systematic review. May 17, 2023
Journal Article
Reducing hospital harm: establishing a command centre to foster situational awareness.
The potential for leveraging machine learning to filter medication alerts. May 4, 2022
Improving the specificity of drug-drug interaction alerts: can it be done? April 6, 2022
A qualitative study of prescribing errors among multi-professional prescribers within an e-prescribing system. December 23, 2020
The tradeoffs between safety and alert fatigue: data from a national evaluation of hospital medication-related clinical decision support. July 29, 2020
Assessment of health information technology-related outpatient diagnostic delays in the US Veterans Affairs health care system: a qualitative study of aggregated root cause analysis data. July 22, 2020
Reducing drug prescription errors and adverse drug events by application of a probabilistic, machine-learning based clinical decision support system in an inpatient setting. August 21, 2019
Improving medication-related clinical decision support. March 7, 2018
The frequency of inappropriate nonformulary medication alert overrides in the inpatient setting. April 6, 2016
The effect of provider characteristics on the responses to medication-related decision support alerts. July 15, 2015
Best practices: an electronic drug alert program to improve safety in an accountable care environment. July 1, 2015
Impact of computerized physician order entry alerts on prescribing in older patients. March 25, 2015
Differences of reasons for alert overrides on contraindicated co-prescriptions by admitting department. December 17, 2014

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
- Share full article
Advertisement
Supported by
In Reversal, Expert Panel Recommends Breast Cancer Screening at 40
Some researchers said the advice did not go far enough. The panel also declined to recommend extra scans for women with dense breast tissue.

By Roni Caryn Rabin
Citing rising breast cancer rates in young women, an expert panel on Tuesday recommended starting regular mammography screening at age 40, reversing longstanding and controversial guidance that most women wait until 50.
The panel, the U.S. Preventive Services Task Force, finalized a draft recommendation made public last year . The group issues influential advice on preventive health, and its recommendations usually are widely adopted in the United States.
In 2009, the task force raised the age for starting routine mammograms to 50 from 40, sparking wide controversy. At the time, researchers were concerned that earlier screening would do more harm than good, leading to unnecessary treatment in younger women, including alarming findings that lead to anxiety-producing procedures that are invasive but ultimately unnecessary.
But now breast cancer rates among women in their 40s are on the rise, increasing by 2 percent a year between 2015 and 2019, said Dr. John Wong, vice chair of the task force. The panel continues to recommend screening every two years for women at average risk of breast cancer, though many patients and providers prefer annual screening.
“There is clear evidence that starting screening every other year at age 40 provides sufficient benefit that we should recommend it for all women in this country to help them live longer and have a better quality of life,” said Dr. Wong, a primary care clinician at Tufts Medical Center who is the director of comparative effectiveness research for the Tufts Clinical Translational Science Institute.
The recommendations have come under harsh criticism from some women’s health advocates, including Representative Rosa DeLauro, Democrat of Connecticut, and Representative Debbie Wasserman Schultz, Democrat of Florida, who say the advice does not go far enough.
In a letter to the task force in June , they said that the guidance continued to “fall short of the science, create coverage gaps, generate uncertainty for women and their providers, and exacerbate health disparities.”
Weighing in again on a hotly debated topic, the task force also said there was not enough evidence to endorse extra scans, such as ultrasounds or magnetic resonance imaging, for women with dense breast tissue.
That means that insurers do not have to provide full coverage of additional screening for these women, whose cancers can be missed by mammograms alone and who are at higher risk for breast cancer to begin with. About half of all women aged 40 and older fall into this category.
In recent years, more mammography providers have been required by law to inform women when they have dense breast tissue and to tell them that mammography may be an insufficient screening tool for them.
Beginning in September, all mammography centers in the United States will be required to give patients that information.
Doctors often prescribe additional or “supplementary” scans for these patients. But these patients frequently find they have to pay all or some of the charges themselves, even when the additional tests are performed as part of preventive care, which under law should be offered without cost.
Medicare, the government health plan for older Americans, does not cover the additional scans. In the private insurance market, coverage is scattershot, depending on state laws, the type of plan and the plan’s design, among other factors.
The task force sets the standards for what preventive care services must be covered by law by health insurers at no cost to patients.
The panel’s decision not to endorse the extra scans has significant implications for patients, said Robert Traynham, a spokesman for AHIP, the association that represents health insurance companies.
“What that means for coverage is that there is no mandate to cover these specific screenings for women with dense breasts at zero-dollar cost-sharing,” he said.
While some employers may choose to have their health insurance plans do so, it is not required by law, Mr. Traynham said.
Kathleen Costello, a retiree in Southern California who was diagnosed with breast cancer in 2017 when she was 59, said she was convinced that mammograms missed her cancer for many years.
She underwent screening annually, and every year she received a letter saying that she was cancer-free. The letters also told her that she had dense breast tissue and that additional screening was available but not covered by insurance.
Six months after an all-clear mammogram in 2016, she told her doctor that her right breast felt stiff. The doctor ordered a mammogram and an ultrasound.
“In 30 seconds, the ultrasound found the cancer,” Ms. Costello said in an interview, adding that she knew because “the technician blanched and left the room.”
The mass was four centimeters in size, Ms. Costello added: “It’s hard for me to accept that it grew in six months from undetectable to four centimeters.”
But Dr. Wong, of the task force, said there was no scientific evidence to prove that supplemental imaging, by either M.R.I. or ultrasound, reduces breast cancer progression and extends life for women with dense breast tissue.
There is ample evidence, on the other hand, that supplemental screenings may lead to frequent false-positive findings and to biopsies, contributing to stress and unnecessary invasive procedures.
“It’s tragic,” Dr. Wong said. “We are as frustrated as women are. They deserve to know whether supplemental screenings would be helpful.”
But medical organizations like the American College of Radiology endorse supplemental screening for women with dense breast tissue. There is research showing that ultrasound in conjunction with mammography does detect additional cancers in patients with dense tissue, said Dr. Stamatia Destounis, chair of the college’s breast imaging commission.
For women with dense breasts who are at average risk of breast cancer, recent research indicates that M.R.I. is the best supplemental scan, Dr. Destounis said, “with far better cancer detection and more favorable positive predictive values.”
The college also recommends annual screening for women at average cancer risk, rather than screening every two years as recommended by the panel. The radiologists group is pressing for a recommendation that all women should be assessed for breast cancer risk before age 25, so that women at high risk can start screening even before they turn 40.
Growing evidence shows that Black, Jewish and other minority women develop breast cancer and die from it before age 50 more frequently than do other women, Dr. Destounis noted.
Trans men who have not had mastectomies must continue to be screened for breast cancer, she added, and trans women, whose hormone use puts them at greater risk for breast cancer than the average man, should discuss screening with their doctor.
While the panel’s advice to start screening at age 40 is “an improvement,” Dr. Destounis said, the final recommendations “do not go far enough to save women’s lives.”
Roni Caryn Rabin is a Times health reporter focused on maternal and child health, racial and economic disparities in health care, and the influence of money on medicine. More about Roni Caryn Rabin
The Fight Against Breast Cancer
Citing rising breast cancer rates in young women, the U.S. Preventive Services Task Force recommended starting regular mammography screening at age 40 , reversing longstanding guidance that most women wait until 50.
Clinics around the United States are starting to offer patients a new service: having their mammograms read not just by a radiologist, but also by an A.I. model .
Risk calculators can offer a more personalized picture of an individual patient’s breast cancer risk. But experts warn that the results need to be interpreted with the help of a doctor.
We asked doctors to weigh in on the new mammograms guidelines and how younger women can understand and mitigate their breast cancer risk .
Scientists have long known that dense breast tissue is linked to an increased risk of breast cancer. A recent study adds a new twist .
Women are less likely to die when treated by female doctors, study suggests
Hospitalized women are less likely to die or be readmitted to the hospital if they are treated by female doctors, a study published Monday in the Annals of Internal Medicine found.
In the study of people ages 65 and older, 8.15% of women treated by female physicians died within 30 days, compared with 8.38% of women treated by male physicians.
Although the difference between the two groups seems small, the researchers say erasing the gap could save 5,000 women’s lives each year.
The study included nearly 800,000 male and female patients hospitalized from 2016 through 2019. All patients were covered by Medicare. For male hospitalized patients, the gender of the doctor didn’t appear to have an effect on risk of death or hospital readmission.
The data alone doesn’t explain why women fare better when treated by other women. But other studies suggest that women are less likely to experience “miscommunication, misunderstanding and bias” when treated by female doctors, said lead study author Dr. Atsushi Miyawaki, a senior assistant professor of health services research at the University of Tokyo Graduate School of Medicine.
The new research is part of a growing field of study examining why women and minorities tend to receive worse medical care than men and white patients. For example, women and minority patients are up to 30% more likely to be misdiagnosed than white men.
“Our pain and our symptoms are often dismissed,” said Dr. Megan Ranney, dean of the Yale School of Public Health. “It may be that women physicians are more aware of that and are more empathetic.”
Research shows that women are less likely than men to receive intensive care but more likely to report having negative experiences with health care, having their concerns dismissed, and having their heart or pain symptoms ignored, the authors wrote in the new study. Male physicians are also more likely than female doctors to underestimate women’s risk of stroke .
Part of the problem, Miyawaki said, is that medical students get “limited training in women’s health issues.”
Dr. Ronald Wyatt, who is Black, said his 27-year-old daughter recently had trouble getting an accurate diagnosis for her shortness of breath. An emergency room physician told her the problem was caused by asthma. It took two more trips to the emergency room for his daughter to learn that she actually had a blood clot in her lungs, a potentially life-threatening situation.
“There is a tendency for doctors to harbor sexist stereotypes about women, regardless of age, such as the notion that women’s symptoms are more emotional or their pain is less severe or more psychological in origin,” said Wyatt, former chief science and chief medical officer at the Society to Improve Diagnosis in Medicine, a nonprofit research and advocacy group.
Women seem to experience fewer of these problems when treated by other women.
For example, a study published JAMA Surgery in 2021 found that women patients developed fewer complications if their surgeon was female. Another JAMA Surgery study published in 2023 found all patients had fewer complications and shorter hospital stays if they were operated on by female surgeons, who worked more slowly than their male counterparts.
Women primary care doctors also tend to spend more time with their patients , Ranney said. Although that extra attention is great for patients, it also means that women see fewer patients per day and earn less, on average, than male doctors.
Dr. Ashish Jha, dean of the Brown University School of Public Health, said several studies suggest that female doctors follow medical evidence and guidelines , and that their patients have better outcomes.
“There’s lots of variation between women and men physicians,” said Jha, who was not involved in the new study. Women “tend to be better at communication, listening to patients, speaking openly. Patients report that communication is better. You put these things together, and you can understand why there are small but important differences.”
The authors of the study said it’s also possible that women are more forthcoming about sensitive issues with female physicians, allowing them to make more informed diagnoses.
That doesn’t mean that women should switch doctors, said Dr. Preeti Malani, a professor of medicine at the University of Michigan. For an individual patient, the differences in mortality and readmission rates seen in the new study are tiny.
“It would be a mistake to suggest that people need to find physicians of the same gender or race as themselves,” Jha said. “The bigger issue is that we need to understand why these differences exist.”
Malani said she’s curious about what women doctors are doing to prevent patients from needing to be readmitted soon after discharge. “How much care and thought is going into that discharge plan?” Malani asked. “Is that where women are succeeding? What can we learn about cultural humility and asking the right questions?”
Others aren’t convinced that the new study proves a physician’s gender makes a big difference.
Few hospitalized patients are treated by a single doctor, said Dr. Hardeep Singh, a professor at Baylor College of Medicine in Houston and a patient safety researcher at the Michael E. DeBakey VA Medical Center.
Hospital patients are treated by teams of physicians, especially if they need specialist care, in addition to nurses and other professionals, Singh said.
“How often do you see the same doc every day in the hospital?” Singh asked. “The point is that it’s not a one-man or one-woman show. Outcomes are unlikely to depend on one individual, but rather on a clinical team and the local context of care. … One name may appear on your bill, but the care is team-based.”
However, Singh said his research on misdiagnoses shows that doctors in general need to do a better job listening to patients.
Jha said he’d like the health system to learn what women doctors are doing right when they treat other women, then teach all physicians to practice that way.
“We should train everyone to be better at generating trust and being worthy of trust,” Jha said.
Wyatt said the country needs to take several steps to better care for women patients, including “de-biasing training” to teach doctors to overcome stereotypes. The health care system also needs to increase the number of women physicians in leadership, recruit more female doctors and do a better job at retaining them. All physicians also need more understanding of how adverse childhood experiences affect patient health, particularly for women, he said.
“More than once I’ve had white female patients tell me they came to be because I listened and they trusted me,” Wyatt said.
Liz Szabo is an independent health and science journalist. Her work has won multiple national awards. One of her investigations led to a new state law in Virginia.

IMAGES
VIDEO
COMMENTS
Medical research is the gateway to improved patient care and expanding our available treatment options. However, finding a relevant and compelling research topic can be challenging. Use this article as a jumping-off point to select an interesting medical research topic for your next paper or clinical study.
Here, we'll explore a variety of healthcare-related research ideas and topic thought-starters across a range of healthcare fields, including allopathic and alternative medicine, dentistry, physical therapy, optometry, pharmacology and public health. NB - This is just the start….
2. Research in Prehospital Care: State of the Art. Prehospital care is a rapidly evolving field, with ongoing research aiming to improve patient outcomes and optimize emergency medical services [].Current clinical research studies in prehospital care are investigating a range of topics, including airway management, hemorrhage control, pain management, and stroke care [24,25].
Engaged patients can improve health outcomes and transform health care. Patients have several expectations of the health system in regard to value, responsibility ... PE is a relatively new concept and lack of prior research studies on the topic is noted. Second, we have only included papers written in English language and conducted the search ...
This article summarizes the top 20 research studies of 2022 identified as POEMs (patient-oriented evidence that matters), excluding COVID-19. Statins for primary prevention of cardiovascular ...
This should improve patient outcomes. Of more than 20,000 research studies published in 2019 in the journals reviewed by the POEMs team, 254 met criteria for validity, relevance, and practice ...
Patient-centered care was the subject of the 2017 Health System Leadership Conference sponsored by Israel's National Institute for Health Policy Research and held at the Dead Sea. The recent IJHPR articles noted above are clearly a step in the right direction of improving patient-centered care.
General Nursing Research Topics & Ideas. The impact of cultural competence on patient care in the UK. The importance of evidence-based practice in nursing for patients with HIV/AIDS. The effects of workplace stress on nurse well-being and performance. The role of nurse-patient communication for patients transitioning from adolescent to adult care.
Research highlights. The Digital Innovation Lab promotes advances in machine learning and artificial intelligence through cloud-based computing technologies. The Women's Health Research Center supports projects to understand sex differences and how unique processes of the female body affect health. The Collaborative Lupus Initiative for New ...
In this research, we use the term 'patient-centred care' to also cover person-centred care. Patient-centred care is associated with positive outcomes such as patient satisfaction, engagement in care and increased quality of life [12, 13]. However, PCC is poorly understood and implemented .
TOPICS. AI in Medicine; ... because the admission was canceled or the patient was admitted for research purposes). Table 1. ... Patient-care events (57 of 147 events [38.8%]) and adverse drug ...
Providing healthcare services that respect and meet patients' and caregivers' needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient ...
Between January 2022 (Volume 31, Issue 1) and the current May 2023 journal issue (Volume 32, Issue 3), AJCC published 71 reports of original research. These recent papers addressed a wide range of research topics, including bedside patient care, palliative and end-of-life care, intensive care unit (ICU) survivorship, measurement and prediction of patient problems, family concerns ...
Care Management. Care management is a set of activities to improve patient care, reduce unnecessary need for additional medical care, avoid duplication of care, and help patients and their caregivers more effectively manage their health conditions. AHRQ provides data, resources, and research to improve care management of patients with chronic ...
Improving Patient Experience with Hospital Care. Research on Improving Patient Experience. Content last reviewed March 2024. Agency for Healthcare Research and Quality, Rockville, MD. This page summarizes current and recent research funding AHRQ's CAHPS grants related to Improving patient experience with ambulatory and hospital care.
These topics often have the potential to generate innovative and effective research. Consider ethical issues. Consider topics related to ethical issues in nursing practice. For example, bereavement care, , and patient privacy are all ethical issues that can be explored in an EBP project.
List of Nursing Research Topics: Nursing Workforce. The impact of nurse staffing levels on patient outcomes in acute care settings. The effectiveness of nurse retention strategies on improving nurse job satisfaction. The role of nursing leadership in creating a positive work environment.
Guides for key topics in patient safety through context, epidemiology, and relevant AHRQ PSNet content. ... Mental Health Care (Psychiatry and Clinical Psychology) Go to this topic. Neurology. Go to this topic. Obstetrics. ... Agency for Healthcare Research and Quality. 5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364. Careers ...
Nowadays, the topic is extremely relevant, rendering organizational change an urgency. The work is structured on a double level of analysis. In the beginning, the paper collects the overall literature on the topic of organisational change in order to identify, on the basis of the citation network, the main existing theoretical approaches.
The algorithm can help standardize it and draw clinicians' attention to a patient who may need additional care. Once the alert comes into the nurse and physician simultaneously, it initiates a conversation about what the patient needs to ensure they don't decline to the point of requiring a transfer to the ICU.
A patient doesn't possess a doctor's understanding of their condition—this would be unrealistic—but acquiring basic knowledge will allow patients to most effectively hear and process what ...
For providers, understanding the topics that patients are reading about online can unlock new perspectives. There are a few illuminating takeaways in this data about what patients are missing from their healthcare experience. Our blog for healthcare consumers was viewed over 1.5 million times in 2021. We compiled all of the trending topics patients cared the most about this year to help you ...
During 2022, research into technological approaches was a major theme of articles on PSNet. Researchers reviewed all relevant articles on PSNet and consulted with Dr. A Jay Holmgren, PhD, and Dr. Susan McBride, PhD, subject matter experts in health IT and its role in patient safety. Key topics and themes are highlighted below.
About UCSF Health: UCSF Health is recognized worldwide for its innovative patient care, reflecting the latest medical knowledge, advanced technologies and pioneering research. It includes the flagship UCSF Medical Center, which is a top-ranked specialty hospital, as well as UCSF Benioff Children's Hospitals, with campuses in San Francisco and Oakland; Langley Porter Psychiatric Hospital and ...
AMA Update covers a range of health care topics affecting the lives of physicians, residents, medical students and patients. From private practice and health system leaders to scientists and public health officials, hear from the experts in medicine on COVID-19, medical education, advocacy issues, burnout, vaccines and more.
Each vehicle will serve six to eight patients per day. "Additional benefits to patients receiving care at home include reduced risk of serious falls or catching infections in the hospital, as well as other improved outcomes," added Kelly P. Owen, professor of emergency medicine. "The ED to Home program is the next frontier of emergency ...
Breast cancer rates among women in their 40s are on the rise, increasing by 2 percent a year between 2015 and 2019. Credit... Michael Hanschke/picture alliance, via Getty Images
Although the difference between the two groups seems small, the researchers say erasing the gap could save 5,000 women's lives each year. The study included nearly 800,000 male and female ...
Patient and public involvement (PPI) in every aspect of research will add valuable insights from patients' experiences, help to explore barriers and facilitators to their compliance/adherence to assessment and treatment methods, bring meaningful outcomes that could meet their expectations, needs and preferences, reduce health care costs, and improve dissemination of research findings.
(SACRAMENTO) The Food and Drug Administration announced Tuesday that samples of pasteurized milk taken from grocery store shelves had tested positive for bird flu, also known as Highly Pathogenic Avian Influenza (HPAI) or H5N1.On Thursday, the agency announced that one in five milk samples nationwide showed genetic traces of the virus. Milk samples from areas with infected herds were more ...