How Gender Reassignment Surgery Works (Infographic)
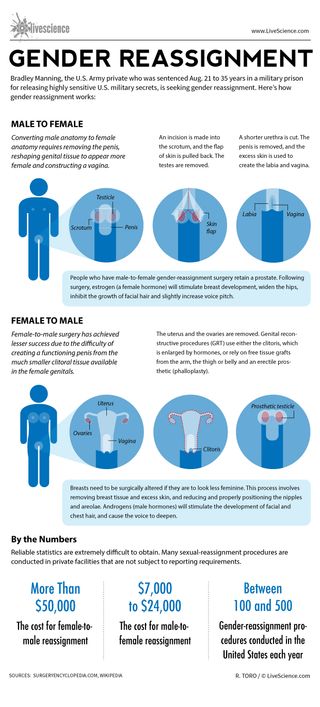
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.

Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Scientists made mice with Y chromosomes female by deleting just 6 tiny molecules
Man's years of premature ejaculation had a rare cause
A telescope on Earth just took an unbelievable photo of Jupiter's moon
Most Popular
- 2 2,000-year-old rock art, including nearly 140-foot-long snake, may mark ancient territories in Colombia, Venezuela
- 3 Early Celtic elites inherited power through maternal lines, ancient DNA reveals
- 4 Viking sword with 'very rare' inscription discovered on family farm in Norway
- 5 100-foot 'walking tree' in New Zealand looks like an Ent from Lord of the Rings — and is the lone survivor of a lost forest
- 2 100-foot 'walking tree' in New Zealand looks like an Ent from Lord of the Rings — and is the lone survivor of a lost forest
- 3 Viking sword with 'very rare' inscription discovered on family farm in Norway
- 4 A 'new star' could appear in the sky any night now. Here's how to see the Blaze Star ignite.
- 5 Black hole 'morsels' could finally prove Stephen Hawking's famous theory right
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health
What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary , to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis)
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
Related Articles
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
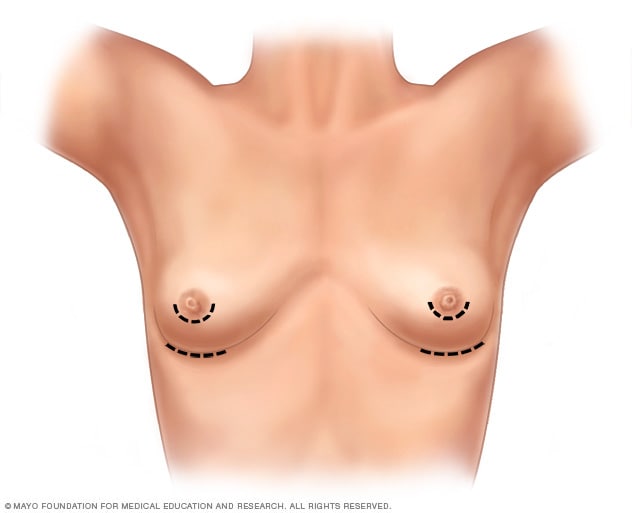
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
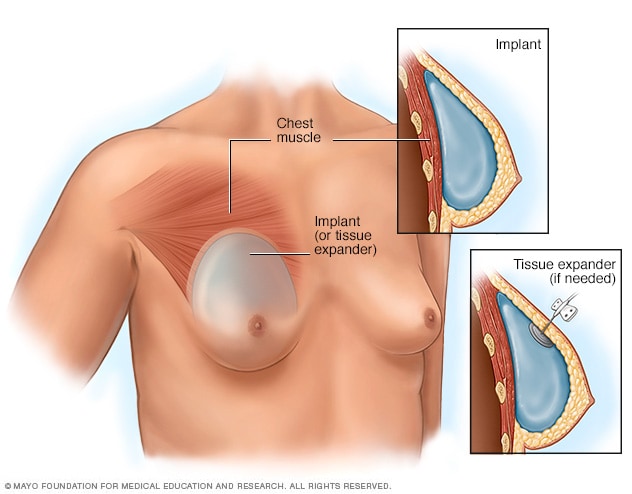
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
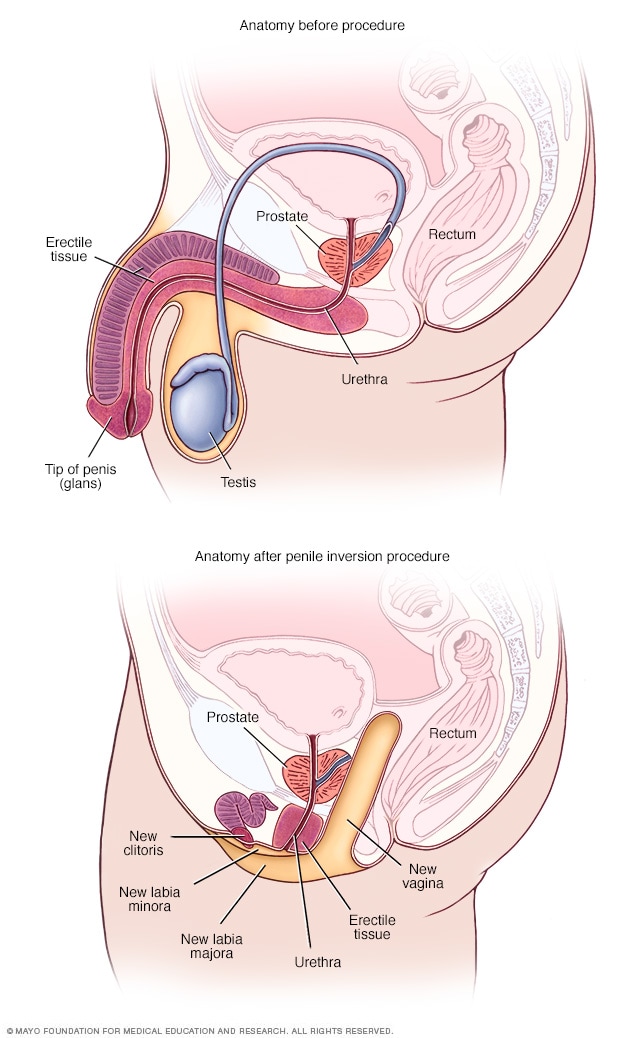
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
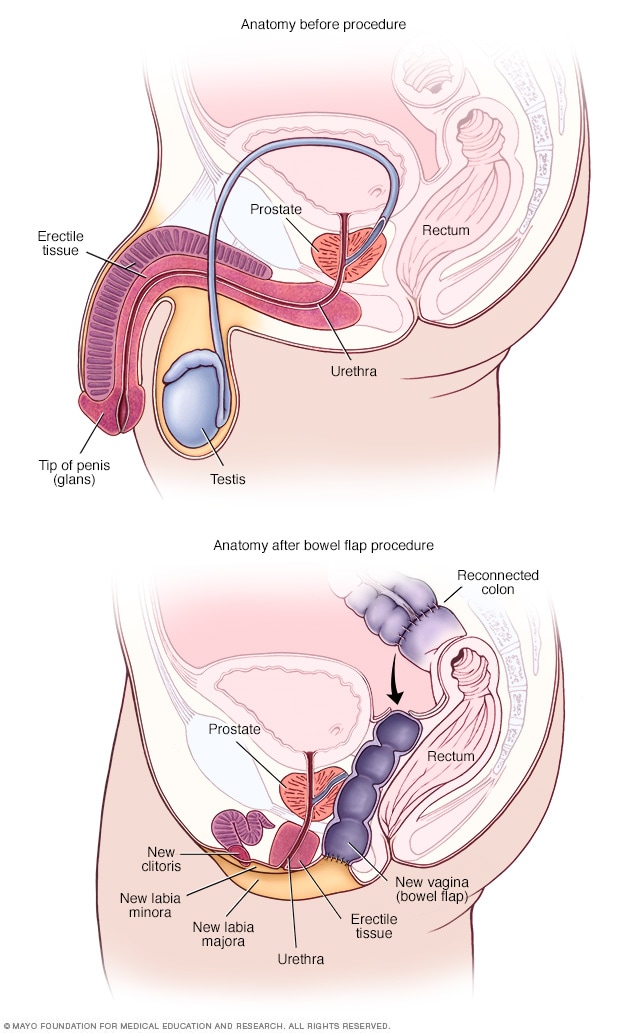
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Jump to content
Updated visitor policies
Other michigan medicine sites.
- About Michigan Medicine
- UofMHealth.org
- Medical School
- Find a Clinical Trial

Michigan Medicine
Federated search page form block, quick links.
- Patient Portal Login
- For Health Providers
- Maps & Directions
Gender Confirmation Surgery
The University of Michigan Health System offers procedures for surgical gender transition. Working together, the surgical team of the Comprehensive Gender Services Program, which includes specialists in plastic surgery, urology and gynecology, bring expertise, experience and safety to procedures for our transgender patients.
Access to gender-related surgical procedures for patients is made through the University of Michigan Health System Comprehensive Gender Services Program .
The Comprehensive Gender Services Program adheres to the WPATH Standards of Care , including the requirement for a second-opinion prior to genital sex reassignment.
Available surgeries:
Male-to-Female: Tracheal Shave Breast Augmentation Facial Feminization Male-to-Female genital sex reassignment
Female-to-Male: Hysterectomy, oophorectomy, vaginectomy Chest Reconstruction Female-to-male genital sex reassignment
Sex Reassignment Surgeries (SRS)
At the University of Michigan Health System, we are dedicated to offering the safest proven surgical options for sex reassignment (SRS.) Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain specialists and a reconstructive plastic surgeon. A multi-disciplinary team helps to best protect the health of the patient.
For patients receiving mental health and medical services within the University of Michigan Health System, the UMHS-CGSP will coordinate all care including surgical referrals. For patients who have prepared for surgery elsewhere, the UMHS-CGSP will help organize the needed records, meet WPATH standards, and coordinate surgical referrals. Surgical referrals are made through Sara Wiener the Comprehensive Gender Services Program Director.
Male-to-female sex reassignment surgery
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris.
During this procedure, a surgeon makes “like become like,” using parts of the original penis to create a sensate neo-vagina. The testicles are removed, a procedure called orchiectomy. The skin from the scrotum is used to make the labia. The erectile tissue of the penis is used to make the neoclitoris. The urethra is preserved and functional.
This procedure provides for aesthetic and functional female genitalia in one 4-5 hour operation. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation. What to Expect: Vaginoplasty at Michigan Medicine .
Female-to-male sex reassignment
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a female-to-male sex reassignment surgery will be offered a phalloplasty, generally using the radial forearm flap method.
This procedure, which can be done at the same time as a hysterectomy/vaginectomy, creates an aesthetically appropriate phallus and creates a urethera for standing urination. Construction of a scrotum with testicular implants is done as a second stage. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected] . W e will assist you in obtaining what you need to qualify for surgery.
May 12, 2022
What the Science on Gender-Affirming Care for Transgender Kids Really Shows
Laws that ban gender-affirming treatment ignore the wealth of research demonstrating its benefits for trans people’s health
By Heather Boerner

As attacks against transgender kids increase in the U.S., Minnesotans hold a rally at the state’s capitol in Saint Paul in March 2022 to support trans kids in Minnesota and Texas and around the country.
Michael Siluk/UCG/Universal Images Group via Getty Images
Editor’s Note (3/30/23): This article from May 2022 is being republished to highlight the ways that ongoing anti-trans legislation is harmful and unscientific.
For the first 40 years of their life, Texas resident Kelly Fleming spent a portion of most years in a deep depression. As an adult, Fleming—who uses they/them pronouns and who asked to use a pseudonym to protect their safety—would shave their face in the shower with the lights off so neither they nor their wife would have to confront the reality of their body.
What Fleming was experiencing, although they did not know it at the time, was gender dysphoria : the acute and chronic distress of living in a body that does not reflect one’s gender and the desire to have bodily characteristics of that gender. While in therapy, Fleming discovered research linking access to gender-affirming hormone therapy with reduced depression in transgender people. They started a very low dose of estradiol, and the depression episodes became shorter, less frequent and less intense. Now they look at their body with joy.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
So when Fleming sees what authorities in Texas , Alabama , Florida and other states are doing to bar transgender teens and children from receiving gender-affirming medical care, it infuriates them. And they are worried for their children, ages 12 and 14, both of whom are agender—a identity on the transgender spectrum that is neither masculine nor feminine.
“I’m just so excited to see them being able to present themselves in a way that makes them happy,” Fleming says. “They are living their best life regardless of what others think, and that’s a privilege that I did not get to have as a younger person.”
Laws Based on “Completely Wrong” Information
Currently more than a dozen state legislatures or administrations are considering—or have already passed—laws banning health care for transgender young people. On April 20 the Florida Department of Health issued guidance to withhold such gender-affirming care. This includes social gender transitioning—acknowledging that a young person is trans, using their correct pronouns and name, and supporting their desire to live publicly as the gender of their experience rather than their sex assigned at birth. This comes nearly two months after Texas Governor Greg Abbott issued an order for the Texas Department of Family and Protective Services to investigate for child abuse parents who allow their transgender preteens and teenagers to receive medical care. Alabama recently passed SB 184 , which would make it a felony to provide gender-affirming medical care to transgender minors. In Alabama, a “minor” is defined as anyone 19 or younger.
If such laws go ahead, 58,200 teens in the U.S. could lose access to or never receive gender-affirming care, according to the Williams Institute at the University of California, Los Angeles. A decade of research shows such treatment reduces depression, suicidality and other devastating consequences of trans preteens and teens being forced to undergo puberty in the sex they were assigned at birth).
The bills are based on “information that’s completely wrong,” says Michelle Forcier, a pediatrician and professor of pediatrics at Brown University. Forcier literally helped write the book on how to provide evidence-based gender care to young people. She is also an assistant dean of admissions at the Warren Alpert Medical School of Brown University. Those laws “are absolutely, absolutely incorrect” about the science of gender-affirming care for young people, she says. “[Inaccurate information] is there to create drama. It’s there to make people take a side.”
The truth is that data from more than a dozen studies of more than 30,000 transgender and gender-diverse young people consistently show that access to gender-affirming care is associated with better mental health outcomes—and that lack of access to such care is associated with higher rates of suicidality, depression and self-harming behavior. (Gender diversity refers to the extent to which a person’s gendered behaviors, appearance and identities are culturally incongruent with the sex they were assigned at birth. Gender-diverse people can identify along the transgender spectrum, but not all do.) Major medical organizations, including the American Academy of Pediatrics (AAP) , the American Academy of Child and Adolescent Psychiatry , the Endocrine Society , the American Medical Association , the American Psychological Association and the American Psychiatric Association , have published policy statements and guidelines on how to provide age-appropriate gender-affirming care. All of those medical societies find such care to be evidence-based and medically necessary.
AAP and Endocrine Society guidelines call for developmentally appropriate care, and that means no puberty blockers or hormones until young people are already undergoing puberty for their sex assigned at birth. For one thing, “there are no hormonal differences among prepubertal children,” says Joshua Safer, executive director of the Mount Sinai Center for Transgender Medicine and Surgery in New York City and co-author of the Endocrine Society’s guidelines. Those guidelines provide the option of gonadotropin-releasing hormone analogues (GnRHas), which block the release of sex hormones, once young people are already into the second of five puberty stages—marked by breast budding and pubic hair. These are offered only if a teen is not ready to make decisions about puberty. Access to gender-affirming hormones and potential access to gender-affirming surgery is available at age 16—and then, in the case of transmasculine youth, only mastectomy, also known as top surgery. The Endocrine Society does not recommend genital surgery for minors.
Before puberty, gender-affirming care is about supporting the process of gender development rather than directing children through a specific course of gender transition or maintenance of cisgender presentation, says Jason Rafferty, co-author of AAP’s policy statement on gender-affirming care and a pediatrician and psychiatrist at Hasbro Children’s Hospital in Rhode Island. “The current research suggests that, rather than predicting or preventing who a child might become, it’s better to value them for who they are now—even at a young age,” Rafferty says.
A Safe Environment to Explore Gender
A 2021 systematic review of 44 peer-reviewed studies found that parent connectedness, measured by a six-question scale asking about such things as how safe young people feel confiding in their guardians or how cared for they feel in the family, is associated with greater resilience among teens and young adults who are transgender or gender-diverse. Rafferty says he sees his role with regard to prepubertal children as offering a safe environment for the child to explore their gender and for parents to ask questions. “The gender-affirming approach is not some railroad of people to hormones and surgery,” Safer says. “It is talking and watching and being conservative.”
Only once children are older, and if the incongruence between the sex assigned to them at birth and their experienced gender has persisted, does discussion of medical transition occur. First a gender therapist has to diagnose the young person with gender dysphoria .
After a gender dysphoria diagnosis—and only if earlier conversations suggest that hormones are indicated—guidelines call for discussion of fertility, puberty suppression and hormones. Puberty-suppressing medications have been used for decades for cisgender children who start puberty early, but they are not meant to be used indefinitely. The Endocrine Society guidelines recommend a maximum of two years on GnRHa therapy to allow more time for children to form their gender identity before undergoing puberty for their sex assigned at birth, the effects of which are irreversible.
“[Puberty blockers] are part of the process of ‘do no harm,’” Forcier says, referencing a popular phrase that describes the Hippocratic Oath, which many physicians recite a version of before they begin to practice.
Hormone blocker treatment may have side effects. A 2015 longitudinal observational cohort study of 34 transgender young people found that, by the time the participants were 22 years old, trans women experienced a decrease in bone mineral density. A 2020 study of puberty suppression in gender-diverse and transgender young people found that those who started puberty blockers in early puberty had lower bone mineral density before the start of treatment than the public at large. This suggests, the authors wrote, that GnRHa use may not be the cause of low bone mineral density for these young people. Instead they found that lack of exercise was a primary factor in low bone-mineral density, especially among transgender girls.
Other side effects of GnRHa therapy include weight gain, hot flashes and mood swings. But studies have found that these side effects—and puberty delay itself—are reversible , Safer says.
Gender-affirming hormone therapy often involves taking an androgen blocker (a chemical that blocks the release of testosterone and other androgenic hormones) and estrogen in transfeminine teens, and testosterone supplementation in transmasculine teens. Such hormones may be associated with some physiological changes for adult transgender people. For instance, transfeminine people taking estrogen see their so-called “good” cholesterol increase. By contrast, transmasculine people taking testosterone see their good cholesterol decrease. Some studies have hinted at effects on bone mineral density, but these are complicated and also depend on personal, family history, exercise, and many other factors in addition to hormones.”
And while some critics point to decade-old study and older studies suggesting very few young people persist in transgender identity into late adolescence and adulthood, Forcier says the data are “misleading and not accurate.” A recent review detailed methodological problems with some of these studies . New research in 17,151 people who had ever socially transitioned found that 86.9 percent persisted in their gender identity. Of the 2,242 people who reported that they reverted to living as the gender associated with the sex they were assigned at birth, just 15.9 percent said they did so because of internal factors such as questioning their experienced gender but also because of fear, mental health issues and suicide attempts. The rest reported the cause was social, economic and familial stigma and discrimination. A third reported that they ceased living openly as a trans person because doing so was “just too hard for me.”
The Harms of Denying Care
Data suggest the effects of denying that care are worse than whatever side effects result from delaying sex-assigned-at-birth puberty. And medical society guidelines conclude that the benefits of gender-affirming care outweigh the risks. Without gender-affirming hormone therapy, cisgender hormones take over, forcing body changes that can be permanent and distressing.
A 2020 study of 300 gender-incongruent young people found that mental distress—including self-harm, suicidal thoughts and depression— increased as the children were made to proceed with puberty according to their assigned sex. By the time 184 older teens (with a median age of 16) reached the stage in which transgender boys began their periods and grew breasts and transgender girls’ voice dropped and facial hair began to appear, 46 percent had been diagnosed with depression, 40 percent had self-harmed, 52 percent had considered suicide, and 17 percent had attempted it—rates significantly higher than those of gender-incongruent children who were a median of 13.9 years old or of cisgender kids their own age.
Conversely, access to gender-affirming hormones in adolescence appears to have a protective effect. In one study, researchers followed 104 teens and young adults for a year and asked them about their depression, anxiety and suicidality at the time they started receiving hormones or puberty blockers and again at the three-month, six-month and one-year mark. At the beginning of the study, which was published in JAMA Network Open in February 2022, more than half of the respondents reported moderate to severe depression, half reported moderate to severe anxiety, and 43.3 percent reported thoughts of self-harm or suicide in the past two weeks.
But when the researchers analyzed the results based on the kind of gender-affirming care the teens had received, they found that those who had access to puberty blockers or gender-affirming hormones were 60 percent less likely to experience moderate to severe depression. And those with access to the medical treatments were 73 percent less likely to contemplate self-harm or suicide.
“Delays in prescribing puberty blockers and hormones may in fact worsen mental health symptoms for trans youth,” says Diana Tordoff, an epidemiology graduate student at the University of Washington and co-author of the study.
That effect may be lifelong. A 2022 study of more than 21,000 transgender adults showed that just 41 percent of adults who wanted hormone therapy received it, and just 2.3 percent had access to it in adolescence. When researchers looked at rates of suicidal thinking over the past year in these same adults, they found that access to hormone therapy in early adolescence was associated with a 60 percent reduction in suicidality in the past year and that access in late adolescence was associated with a 50 percent reduction.
For Fleming’s kids in Texas, gender-affirming hormones are not currently part of the discussion; not all trans people desire hormones or surgery to feel affirmed in their gender. But Fleming is already looking at jobs in other states to protect their children’s access to such care, should they change their mind. “Getting your body closer to the gender [you] identify with—that is what helps the dysphoria,” Fleming says. “And not giving people the opportunity to do that, making it harder for them to do that, is what has made the suicide rate among transgender people so high. We just—trans people are just trying to survive.”
IF YOU NEED HELP If you or someone you know is struggling or having thoughts of suicide, help is available. Call the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK), use the online Lifeline Chat or contact the Crisis Text Line by texting TALK to 741741.
Advertisement
Stages of Gender Reassignment
- Share Content on Facebook
- Share Content on LinkedIn
- Share Content on Flipboard
- Share Content on Reddit
- Share Content via Email

The idea of getting stuck in the wrong body sounds like the premise for a movie in "Freaky Friday," a mother and a daughter swap bodies, and in "Big" and "13 Going on 30," teenagers experience life in an adult's body. These movies derive their humor from the ways in which the person's attitude and thoughts don't match their appearance. A teenager trapped in her mother's body, for example, revels in breaking curfew and playing air guitar, while a teenager trapped in an adult's body is astounded by the trappings of wealth that come with a full-time job. We laugh because the dialogue and actions are so contrary to what we'd expect from someone who is a mother, or from someone who is an employed adult.
But for some people, living as an incongruous gender is anything but a joke. A transgender person is someone who has a different gender identity than their birth sex would indicate. We interchange the words sex, sexuality and gender all the time, but they don't actually refer to the same thing. Sex refers to the parts we were born with; boys, we assume, have a penis, while girls come equipped with a vagina. Sexuality generally refers to sexual orientation , or who we're attracted to in a sexual and/or romantic sense. Gender expression refers to the behavior used to communicate gender in a given culture. Little girls in the U.S., for example, would be expected express their feminine gender by playing with dolls and wearing dresses, and little boys would be assumed to express their masculinity with penchants for roughhousing and monster trucks. Another term is g ender identity, the private sense or feeling of being either a man or woman, some combination of both or neither [source: American Psychological Association ].
Sometimes, a young boy may want to wear dresses and have tea parties, yet it's nothing more than a phase that eventually subsides. Other times, however, there is a longing to identify with another gender or no gender at all that becomes so intense that the person experiencing it can't function anymore. Transgender is an umbrella term for people who identify outside of the gender they were assigned at birth and for some gender reassignment surgeries are crucial to leading a healthy, happy life.

Gender Dysphoria: Diagnosis and Psychotherapy
Real-life experience, hormone replacement therapy, surgical options: transgender women, surgical options: transgender men, gender reassignment: regrets.

Transgender people may begin identifying with a different gender, rather than the one assigned at birth, in early childhood, which means they can't remember a time they didn't feel shame or distress about their bodies. For other people, that dissatisfaction with their biological sex begins later, perhaps around puberty or early adulthood, though it can occur later in life as well.
It's estimated that about 0.3 percent of the U.S. population self-identify as transgender, but not all who are transgender will choose to undergo a gender transition [source: Gates ]. Some may choose to affirm their new gender through physically transforming their bodies from the top down, while others may prefer to make only certain cosmetic changes, such as surgeries to soften facial features or hair removal procedures, for example.
Not all who identify with a gender different than their birth sex suffer from gender dysphoria or go on to seek surgery. Transgender people who do want gender reassignment surgery, however, must follow the standards of care for gender affirmation as defined by the World Professional Association for Transgender Health (WPATH).
In 1980, when gender identity disorder (GID) was first recognized, it was considered a psychiatric disorder. In 2013, though, GID was, in part, reconsidered as biological in nature, and renamed gender dysphoria . It was reclassified as a medical condition in the American Psychological Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-V), a common language and standards protocol manual for the classification of mental disorders. With this classification, transgender people must be diagnosed prior to any treatment [source: International Foundation for Gender Education ].
Gender dysphoria is diagnosed when a person has a persistent desire to become a different gender. The desire may manifest itself as disgust for one's reproductive organs, hatred for the clothing and other outward signs of one's given gender, and/or a desire to act and be recognized as another gender. This desire must be continuously present for six months in order to be recognized as a disorder [source: WPATH].
In addition to receiving the diagnosis from a mental health professional, a person seeking reassignment must also take part in psychotherapy. The point of therapy isn't to ignite a change, begin a conversion or otherwise convince a transgender person that it's wrong to want to be of a different gender (or of no specific gender at all) . Rather, counseling is required to ensure that the person is realistic about the process of gender affirmation and understands the ramifications of not only going through with social and legal changes but with permanent options such as surgery. And because feeling incongruous with your body can be traumatizing and frustrating, the mental health professional will also work to identify any underlying issues such as anxiety, depression, substance abuse or borderline personality disorder.
The mental health professional can also help to guide the person seeking gender reassignment through the next step of the process: real-life experience.

WPATH requires transgender people desiring gender reassignment surgery to live full-time as the gender that they wish to be before pursuing any permanent options as part of their gender transition. This period is a known as real-life experience (RLE) .
It's during the RLE that the transgender person often chooses a new name appropriate for the desired gender, and begins the legal name-change process. That new name often comes with a set of newly appropriate pronouns, too; for example, when Chastity Bono, biologically born as Sonny and Cher's daughter in 1969, began her transition in 2008 she renamed herself as Chaz and instructed people to use "he" rather than "she" [source: Donaldson James ].
In addition to a new name and pronouns, during this time gender-affirming men and women are expected to also adopt the clothing of their desired gender while maintaining their employment, attending school or volunteering in the community. Trans women might begin undergoing cosmetic procedures to rid themselves of body hair; trans men might take voice coaching in attempt to speak in a lower pitch. The goal of real-life experience is to expose social issues that might arise if the individual were to continue gender reassignment. How, for example, will a boss react if a male employee comes to work as a female? What about family? Or your significant other? Sometimes, during RLE people realize that living as the other gender doesn't bring the happiness they thought it would, and they may not continue to transition. Other times, a social transition is enough, and gender reassignment surgery isn't pursued. And sometimes, this test run is the confirmation people need to pursue physical changes in order to fully become another gender.
In addition to the year-long real-life experience requirement before surgical options may be pursued, WPATH recommends hormonal therapy as a critical component to transitioning before surgery. Candidates for hormone therapy may choose to complete a year-long RLE and counseling or complete six months of a RLE or three-months of a RLE/three months of psychotherapy before moving ahead with hormone therapy.
Upon successfully completing a RLE by demonstrating stable mental health and a healthy lifestyle, the transitioning individual becomes eligible for genital reconstructive surgery — but it can't begin until a mental health professional submits a letter (or letters) of recommendation indicating that the individual is ready to move forward [source: WPATH].

Hormone replacement therapy (HRT) , also called cross-sex hormones, is a way for transgender individuals to feel and look more like the gender they identify with, and so it's a major step in gender reassignment. In order to be eligible for hormone therapy, participants must be at least 18 years old (though sometimes, younger adolescents are allowed to take hormone blockers to prohibit their naturally occurring puberty) and demonstrate to a mental health professional that they have realistic expectations of what the hormones will and won't do to their bodies. A letter from that mental health professional is required, per the standards of care established by WPATH.
Hormone therapy is used to balance a person's gender identity with their body's endocrine system. Male-to-female candidates begin by taking testosterone-blocking agents (or anti-androgens ) along with female hormones such as estrogen and progesterone . This combination of hormones is designed to lead to breast growth, softer skin, less body hair and fewer erections. These hormones also change the body by redistributing body fat to areas where women tend to carry extra weight (such as around the hips) and by decreasing upper body strength. Female-to-male candidates begin taking testosterone , which will deepen the voice and may cause some hair loss or baldness. Testosterone will also cause the clitoris to enlarge and the person's sex drive to increase. Breasts may slightly shrink, while upper body strength will increase [source: WPATH].
It usually takes two continuous years of treatment to see the full results of hormone therapy. If a person were to stop taking the hormones, then some of these changes would reverse themselves. Hormone therapy is not without side effects — both men and women may experience an increased risk for cardiovascular disease, and they are also at risk for fertility problems. Some transgender people may choose to bank sperm or eggs if they wish to have children in the future.
Sometimes hormonal therapy is enough to make a person feel he or she belongs to the desired gender, so treatment stops here. Others may pursue surgical means as part of gender reassignment.

Surgical options are usually considered after at least two years of hormonal therapy, and require two letters of approval by therapists or physicians. These surgeries may or may not be covered by health insurance in the U.S. — often only those that are considered medically necessary to treat gender dysphoria are covered, and they can be expensive. Gender reassignment costs vary based on each person's needs and desires; expenses often range between $7,000 and $50,000 (in 2014), although costs may be much greater depending upon the type (gender reconstructive surgeries versus cosmetic procedures) and number of surgeries as well as where in the world they are performed [source: AP ].
Gender affirmation is done with an interdisciplinary team, which includes mental health professionals, endocrinologists, gynecologists, urologists and reconstructive cosmetic surgeons.
One of the first surgeries male-to-female candidates pursue is breast augmentation, if HRT doesn't enlarge their breasts to their satisfaction. Though breast augmentations are a common procedure for cisgender women (those who identify with the gender they were assigned at birth), care must be taken when operating on a biologically male body, as there are structural differences, like body size, that may affect the outcome.
The surgical options to change male genitalia include orchiectomy (removal of the testicles), penile inversion vaginoplasty (creation of a vagina from the penis), clitoroplasty (creation of a clitoris from the glans of the penis) and labiaplasty (creation of labia from the skin of the scrotum) [source: Nguyen ]. The new vagina, clitoris and labia are typically constructed from the existing penile tissue. Essentially, after the testicles and the inner tissue of the penis is removed and the urethra is shortened, the skin of the penis is turned inside out and fashioned into the external labia and the internal vagina. A clitoris is created from excess erectile tissue, while the glans ends up at the opposite end of the vagina; these two sensitive areas usually mean that orgasm is possible once gender reassignment is complete. Male-to-female gender reconstructive surgery typically takes about four or five hours [source: University of Michigan ]. The major complication from this surgery is collapse of the new vaginal cavity, so after surgery, patients may have to use dilating devices.
Trans women may also choose to undergo cosmetic surgeries to further enhance their femininity. Procedures commonly included with feminization are: blepharoplasty (eyelid surgery); cheek augmentation; chin augmentation; facelift; forehead and brow lift with brow bone reduction and hair line advance; liposuction; rhinoplasty; chondrolargynoplasty or tracheal shave (to reduce the appearance of the Adam's apple); and upper lip shortening [source: The Philadelphia Center for Transgender Surgery]. Trans women may pursue these surgeries with any cosmetic plastic surgeon, but as with breast augmentation, a doctor experienced with this unique situation is preferred. One last surgical option is voice modification surgery , which changes the pitch of the voice (alternatively, there is speech therapy and voice training, as well as training DVDs and audio recordings that promise the same thing).

Female-to-male surgeries are pursued less often than male-to-female surgeries, mostly because when compared to male-to-female surgeries, trans men have limited options; and, historically, successful surgical outcomes haven't been considered on par with those of trans women. Still, more than 80 percent of surgically trans men report having sexual intercourse with orgasm [source: Harrison ].
As with male-to-female transition, female-to-male candidates may begin with breast surgery, although for trans men this comes in the form of a mastectomy. This may be the only surgery that trans men undergo in their reassignment, if only because the genital surgeries available are still far from perfect. Forty percent of trans men who undergo genital reconstructive surgeries experience complications including problems with urinary function, infection and fistulas [sources: Harrison , WPATH].
Female-to-male genital reconstructive surgeries include hysterectomy (removal of the uterus) and salpingo-oophorectomy (removal of the fallopian tubes and ovaries). Patients may then elect to have a metoidioplasty , which is a surgical enlargement of the clitoris so that it can serve as a sort of penis, or, more commonly, a phalloplasty . A phalloplasty includes the creation of a neo-phallus, clitoral transposition, glansplasty and scrotoplasty with prosthetic testicles inserted to complete the appearance.
There are three types of penile implants, also called penile prostheses: The most popular is a three-piece inflatable implant, used in about 75 percent of patients. There are also two-piece inflatable penile implants, used only 15 percent of the time; and non-inflatable (including semi-rigid) implants, which are used in fewer than 10 percent of surgeries. Inflatable implants are expected to last about five to 10 years, while semi-rigid options typically have a lifespan of about 20 years (and fewer complications than inflatable types) [source: Crane ].
As with trans women, trans men may elect for cosmetic surgery that will make them appear more masculine, though the options are slightly more limited; liposuction to reduce fat in areas in which cisgender women i tend to carry it is one of the most commonly performed cosmetic procedures.

As surgical techniques improve, complication rates have fallen too. For instance, long-term complication risks for male-to-female reconstructive surgeries have fallen below 1 percent. Despite any complications, though, the overwhelming majority of people who've undergone surgical reconstruction report they're satisfied with the results [source: Jarolím ]. Other researchers have noted that people who complete their transition process show a marked improvement in mental health and a substantial decrease in substance abuse and depression. Compare these results to 2010 survey findings that revealed that 41 percent of transgender people in the U.S. attempted suicide, and you'll see that finally feeling comfortable in one's own skin can be an immensely positive experience [source: Moskowitz ].
It's difficult, though, to paint a complete picture of what life is like after people transition to a new gender, as many people move to a new place for a fresh start after their transition is complete. For that reason, many researchers, doctors and therapists have lost track of former patients. For some people, that fresh start is essential to living their new lives to the fullest, while others have found that staying in the same job, the same marriage or the same city is just as rewarding and fulfilling and vital to their sense of acceptance.
In many ways, the process of gender affirmation is ongoing. Even after the surgeries and therapies are complete, people will still have to deal with these discrimination issues. Transgender people are often at high risk for hate crimes. Regular follow-ups will be necessary to maintain both physical and mental health, and many people continue to struggle with self-acceptance and self-esteem after struggling with themselves for so long. Still, as more people learn about gender reassignment, it seems possible that that these issues of stigma and discrimination won't be so prevalent.
As many as 91 percent Americans are familiar with the term "transgender" and 76 percent can correctly define it; 89 percent agree that transgender people deserve the same rights, privileges and protections as those who are cisgender [source: Public Religion Research Institute ]. But that's not to say that everything becomes completely easy once a person transitions to his or her desired gender.
Depending upon where you live, non-discrimination laws may or may not cover transgender individuals, so it's completely possible to be fired from one's job or lose one's home due to gender expression. Some people have lost custody of their children after divorces and have been unable to get courts to recognize their parental rights. Historically, some marriages were challenged — consider, for example, what happens when a man who is married to a woman decides to become a woman; after the surgery, if the two people decide to remain married, it now appears to be a same-sex marriage, which is now legalized in the U.S. Some organizations and governments refuse to recognize a person's new gender unless genital reconstructive surgery has been performed, despite the fact that some people only pursue hormone therapy or breast surgery [sources: U.S. Office of Personnel Management , Glicksman ].
Lots More Information
Author's note: stages of gender reassignment.
It's interesting how our terminology changes throughout the years, isn't it? (And in some cases for the better.) What we used to call a sex change operation is now gender realignment surgery. Transsexual is now largely replaced with transgender. And with good reason, I think. Knowing that sex, sexuality and gender aren't interchangeable terms, updating "sex change" to "gender reassignment" or "gender affirmation" and "transsexual" to "transgender" moves the focus away from what sounds like something to do with sexual orientation to one that is a more accurate designation.
Related Articles
- How Gender Identity Disorder Works
- Is gender just a matter of choice?
- What is transgender voice therapy?
- How fluid is gender?
- Why do girls wear pink and boys wear blue?
More Great Links
- DSM-5: Gender Dysphoria
- National Center for Transgender Equality
- The Williams Institute
- American Medical Student Association (AMSA). "Transgender Health Resources." 2014. (April 20, 2015) http://www.amsa.org/AMSA/Homepage/About/Committees/GenderandSexuality/TransgenderHealthCare.aspx
- American Psychological Association (APA). "Definition of Terms: Sex, Gender, Gender Identity, Sexual Orientation." 2011. (July 1, 2015) http://www.apa.org/pi/lgbt/resources/sexuality-definitions.pdf
- AP. "Medicare ban on sex reassignment surgery lifted." May 30, 2014. (April 20, 2015) http://www.usatoday.com/story/news/nation/2014/05/30/medicare-sex-reassignment/9789675/
- Belkin, Lisa. "Smoother Transitions." The New York Times. Sept. 4, 2008. (Aug. 1, 2011) http://www.nytimes.com/2008/09/04/fashion/04WORK.html
- Crane, Curtis. "The Total Guide to Penile Implants For Transsexual Men." Transhealth. May 2, 2014. (April 20, 2015) http://www.trans-health.com/2013/penile-implants-guide/
- Donaldson James, Susan. "Trans Chaz Bono Eyes Risky Surgery to Construct Penis." ABC News. Jan. 6, 2012. (April 20, 2015) http://abcnews.go.com/Health/transgender-chaz-bono-seeks-penis-genital-surgery-risky/story?id=15299871Gates, Gary J. "How many people are lesbian, gay, bisexual, and transgender?" April 2011. (July 29, 2015) http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many-People-LGBT-Apr-2011.pdf
- Glicksman, Eve. "Transgender today." Monitor on Psychology. Vol. 44, no. 4. Page 36. April 2013. (April 20, 2015) http://www.apa.org/monitor/2013/04/transgender.aspx
- Harrison, Laird. "Sex-Change Operations Mostly Successful." Medscape Medical News. May 20, 2013. (April 20, 2015) http://www.medscape.com/viewarticle/804432
- HealthResearchFunding.org (HRF). "14 Unique Gender Identity Disorder Statistics." July 28, 2014. (April 20, 2015) http://healthresearchfunding.org/gender-identity-disorder-statistics/
- International Foundation for Gender Education. "APA DSM-5 Sexual and Gender Identity Disorders: 302.85 Gender Identity Disorder in Adolescents or Adults." (April 20, 2015) http://www.ifge.org/302.85_Gender_Identity_Disorder_in_Adolescents_or_Adults
- Moskowitz, Clara. "High Suicide Risk, Prejudice Plague Transgender People." LiveScience. Nov. 18, 2010. (April 20, 2015) http://www.livescience.com/11208-high-suicide-risk-prejudice-plague-transgender-people.html
- Nguyen, Tuan A. "Male-To-Female Procedures." Lake Oswego Plastic Surgery. 2013. (April 20, 2015) http://www.lakeoswegoplasticsurgery.com/grs/grs_procedures_mtf.html
- Public Religion Research Institute. "Survey: Strong Majorities of Americans Favor Rights and Legal Protections for Transgender People." Nov. 3, 2011. (April 20, 2015) http://publicreligion.org/research/2011/11/american-attitudes-towards-transgender-people/#.VSmlgfnF9bw
- Steinmetz, Katy. "Board Rules That Medicare Can Cover Gender Reassignment Surgery." Time. (April 20, 2015) http://time.com/2800307/medicare-gender-reassignment/
- The Philadelphia Center for Transgender Surgery. "Phalloplasty: Frequently Asked Questions." (April 20, 2015) http://www.thetransgendercenter.com/index.php/surgical-procedures/phalloplasty-faqs.html
- U.S. Office of Personnel Management. "Guidance Regarding the Employment of Transgender Individuals in the Federal Workplace." 2015. (April 20, 2015) http://www.opm.gov/diversity/Transgender/Guidance.asp
- University of California, San Francisco - Department of Family and Community Medicine, Center of Excellence for Transgender Health. "Primary Care Protocol for Transgender Patient Care." April 2011. (April 20, 2015) http://transhealth.ucsf.edu/trans?page=protocol-hormones
- University of Miami - Miller School of Medicine, Department of Surgery, Plastic, Aesthetic and Reconstructive Surgery. "Transgender Reassignment." 2015. (April 20, 2015) http://surgery.med.miami.edu/plastic-and-reconstructive/transgender-reassignment-surgery
- University of Michigan Health System. "Gender Affirming Surgery." (April 20, 2015) http://www.uofmhealth.org/medical-services/gender-affirming-surgery
- World Professional Association for Transgender Health (WPATH). "Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People." Version 7. 2012. (April 20, 2015) http://www.wpath.org/uploaded_files/140/files/Standards%20of%20Care,%20V7%20Full%20Book.pdf
- World Professional Association for Transgender Health (WPATH). "WPATH Clarification on Medical Necessity of Treatment, Sex Reassignment, and Insurance Coverage for Transgender and Transsexual People Worldwide." 2015. (April 20, 2015) http://www.wpath.org/site_page.cfm?pk_association_webpage_menu=1352&pk_association_webpage=3947
Please copy/paste the following text to properly cite this HowStuffWorks.com article:


How Gender Confirmation Surgery Actually Works
Over 1,700 male-to-female surgeries were performed in the U.S. in 2016.

Article originally appeared on 04.29.16
Over 1,700 male-to-female gender confirmation surgeries were performed in 2016 in the U.S., according to The American Society of Plastic Surgeons , and around 40,000 post-op transgender people are currently living in the country. It’s an expensive and invasive procedure that allows people who are transgender to have their genitalia altered to match the gender they identify with.
The first medical gender confirmation surgery was in Germany in 1930, and it was performed on Danish artist Lili Elbe, whose story was recently brought to life on screen in the film “The Danish Girl.” The first American to have male-to-female surgery was World War II vet Christine Jorgensen in 1952.
To provide people with a clearer idea of what happens during a male-to-female sexual reassignment surgery, the European Society of Urology released the animated video above. During the surgery, the testes are removed from the scrotum and the tip of the penis is used to create a clitoris. Then the shaft of the penis and scrotum are formed to create the labia and vaginal canal. The surgery is also accompanied by psychotherapy, hormones, and often also a breast augmentation.
Watch the video from the European Society of Urology below:
More on Good.is
Gender In Sports: Leveling The Playing Field - GOOD
Ten Ways to Avoid Gender-Bending Chemicals
What If Gender Roles In Advertising Were Reversed?

Grandfather left in tears after grandson surprises him by restoring his 1954 truck

3 objects found inside the Great Pyramid of Giza keep mysteriously disappearing

25 hilarious live TV moments that still leave us rolling on the floor with laughter

Mysterious iron pillar hasn't rusted despite being out in the open for over 1,600 years

Terrifying clip shows diver recording 'final moments' after being stranded 30 miles off the shore
clock This article was published more than 9 years ago
Here’s how sex reassignment surgery works

In this excellent post , my colleague Steven Petrow advised that if you're wondering whether someone you know is transitioning from one gender to the other, it's best to "check your curiosity and hold your tongue." But we all have questions about a subject that is increasingly mainstream. Aside from the recent coverage of Bruce Jenner 's apparent transition , Laverne Cox last year became the first trans person on the cover of Time magazine, and Amazon debuted “Transparent,” a show about a father who is transitioning.
[UPDATE: Bruce Jenner: ‘Call me Caitlyn’ ]
Here are answers to some of the questions surrounding this issue.
How many people are transgender?
The Williams Institute, a think tank at the UCLA School of Law dedicated to research on sexual orientation law and public policy, estimates that 700,000 Americans are transgender . But a good piece last year on fivethirtyeight.com noted that there are no national surveys. And if there were, there is no agreement on what "trangender" means.
How many people have sex reassignment surgery?
It's very difficult to know. The Encyclopedia of Surgery says that "the number of gender reassignment procedures conducted in the United States each year is estimated at between 100 and 500. The number worldwide is estimated to be two to five times larger." At least one other researcher says there are many more. Marci Bowers, a transgender obstetrician and gynecologist in Burlingame, Calif., who performs the surgeries, said in an interview that she does about 200 per year herself, about three quarters of them male to female.
Fred Ettner, a physician in Evanston, Ill., who works with people going through transition, estimated that only about 25 percent to 30 percent of transgender people have any kind of surgery.
How does one begin the process of changing one's sex?
Under the standards of care adopted by the World Professional Association for Transgender Health (WPATH), the first step usually is meeting with a mental health professional for a diagnosis and psychotherapy. A diagnosis of gender identity disorder or gender dysphoria and a letter of recommendation from the therapist allows a person to begin hormone therapy with a doctor. That is usually followed by a period of living publicly as a member of the opposite sex and, finally, surgery to alter the genitalia and other body parts.
What do hormones do?
Androgens are given to women to help them develop secondary male sex characteristics such as a beard and body hair. Estrogen and anti-androgens are given to men to help change their musculature, skin and fat distribution, all of which will make them appear more feminine. Body hair also diminishes.
But Ettner said the hormones' most important contribution is to reduce the dysphoria transgender people have been struggling with all their lives. After a month or two, their bodies and brains begin aligning.
"It's very obvious to the individuals," Ettner said, adding, "Their brain finally is getting this hormone. They feel differently. They behave differently.
"The first effect is the brain effect," he said.
What is the Real-Life Experience (also known as the Real-Life Test)
Surgeons who follow the WPATH standards of care (which some patients and experts consider too strict) usually require candidates for surgery to live for as long as a year in their preferred gender role. They must work or go to school; do volunteer work; change their first names and prove to the surgeon that people other than their therapists know they are successfully living this way.
What happens during surgery?
Male to female genital surgery is easier, less expensive and generally more successful than female to male surgery. That's one reason why fewer women choose to have surgery on their genitals, Bowers said. (Another is cost.)
In male to female surgery , the testicles and most of the penis are removed and the urethra is cut shorter. Some of the skin is used to fashion a largely functional vagina. A "neoclitoris" that allows sensation can be created from parts of the penis. Men retain their prostates.
In female to male surgery, the breasts, uterus and ovaries are removed (in two separate procedures). A "neophallus" can be constructed using tissue from the forearm or other parts of the body that allows sexual sensation, an expensive procedure. Extending the urethra to allow standing urination has proved to be perhaps the most difficult part of the process, Bowers said.
What other kinds of surgery are performed?
Women wishing to live as men often have mastectomies. Men transitioning to women can have plastic surgery to "feminize" their appearance, including work on their eyes, noses, brows, chins and hairlines. They also can have their Adam's apple shaved down so it is less prominent.
Sounds expensive. Is it covered by insurance?
Bowers and Ettner said a woman who chooses the full range of surgical procedures available would spend $75,000 or more to transition to a male. Switching from male to female might cost in the $40,000 to $50,000 range. Some people have the work done in Thailand, which is well known for the surgery and where the cost is much lower.
Insurance is just beginning to cover some of the costs. Last year, Medicare lifted a 33-year ban on coverage for gender reassignment surgery , and the surgery was performed on 74-year-old Army veteran .
Do many people regret having the surgery?
Anecdotal accounts of regret abound, but overall it appears to be rare. Bowers said that only two of the 1,300 people she has operated on have wanted to go back to their old bodies.
But that doesn't mean that surgery is a miracle cure for the difficulties of gender dysphoria. People who make the transition often lose spouses, families, friends and jobs. They may find themselves completely alone if they relocate to start new lives. Johns Hopkins University, which in the 1960s was one of the first medical institutions to perform sex reassignment surgery, halted the practice when officials concluded that it was not helping the transgendered overall.
A 2o11 study of 324 Swedish transsexuals by the Karolinska Institute showed that "after sex reassignment, [they] have considerably higher risks for mortality, suicidal behaviour, and psychiatric morbidity than the general population. Our findings suggest that sex reassignment, although alleviating gender dysphoria, may not suffice as treatment for transsexualism, and should inspire improved psychiatric and somatic care after sex reassignment for this patient group."
The forgotten history of Bruce Jenner
Transgender etiquette 101
Transgender at 7: Tyler gets a legal name change

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 28 May 2024
Heed lessons from past studies involving transgender people: first, do no harm
- Mathilde Kennis 0 ,
- Robin Staicu 1 ,
- Marieke Dewitte 2 ,
- Guy T’Sjoen 3 ,
- Alexander T. Sack 4 &
- Felix Duecker 5
Mathilde Kennis is a researcher in cognitive neuroscience and clinical psychological science at Maastricht University, the Netherlands.
You can also search for this author in PubMed Google Scholar
Robin Staicu is a neuroscientist and specialist in diversity, equity and inclusion at Maastricht University, the Netherlands.
Marieke Dewitte is a sexologist and assistant professor in clinical psychological science at Maastricht University, the Netherlands.
Guy T’Sjoen is a clinical endocrinologist and professor in endocrinology at Ghent University Hospital, Belgium, the medical coordinator of the Centre for Sexology and Gender at Ghent University Hospital, and one of the founders of the European Professional Association for Transgender Health.
Alexander T. Sack is a professor in cognitive neuroscience at Maastricht University, the Netherlands.
Felix Duecker is an assistant professor in cognitive neuroscience at Maastricht University, the Netherlands.
You have full access to this article via your institution.
Over the past few decades, neuroscientists, endocrinologists, geneticists and social scientists have conducted numerous studies involving transgender people, meaning those whose gender identity does not conform to that typically associated with the sex to which they were assigned at birth. Justifications for doing such research have shifted over the years and, today, investigators are increasingly focused on assessments of transgender people’s mental health or the impact of hormone therapies.
But such work raises challenges. Despite researchers’ best intentions, these studies can perpetuate stigmas and make it even harder for transgender people to access appropriate medical care.
Here we focus on neuroscientific approaches to the study of transgender identity to explore how investigators might navigate these concerns.
Brain scanning
In 1995, neuroscientists at the Netherlands Institute for Brain Research in Amsterdam published findings from a post-mortem study, which included six transgender individuals 1 . They found that the volume of part of the brain’s hypothalamus — called the bed nucleus of the stria terminalis, which tends to be larger in men than in women — corresponded to the gender identity of the transgender individuals, not to their sex assigned at birth. Although the data were only correlative, the researchers suggested that people identify as transgender because of changes in the brain that happen before birth — in other words, that someone can be born with a male-typical body and brain characteristics more typical of a female brain, and vice versa.
Sex and gender in science
Since it was published, the paper has been cited more than 1,000 times, and at least a dozen researchers have probed this theory and related ones using tools such as structural and functional magnetic resonance imaging (MRI).
Although the results of these analyses have been inconsistent, several ideas have nonetheless arisen about a neurobiological basis for gender dysphoria — the distress associated with a person’s gender identity not aligning with the sex they were assigned at birth. These include the ‘own-body perception’ theory 2 , which proposes that a reduced structural and functional connectivity between certain brain networks is responsible. (Previous work has associated these networks with brain regions thought to be involved in people’s ability to link their own body to their sense of self 3 .)
As analytical tools and methods advance, brain research is becoming more sophisticated. The number of neuroscientific studies that include transgender participants has increased considerably since 1991 (see ‘On the rise’).
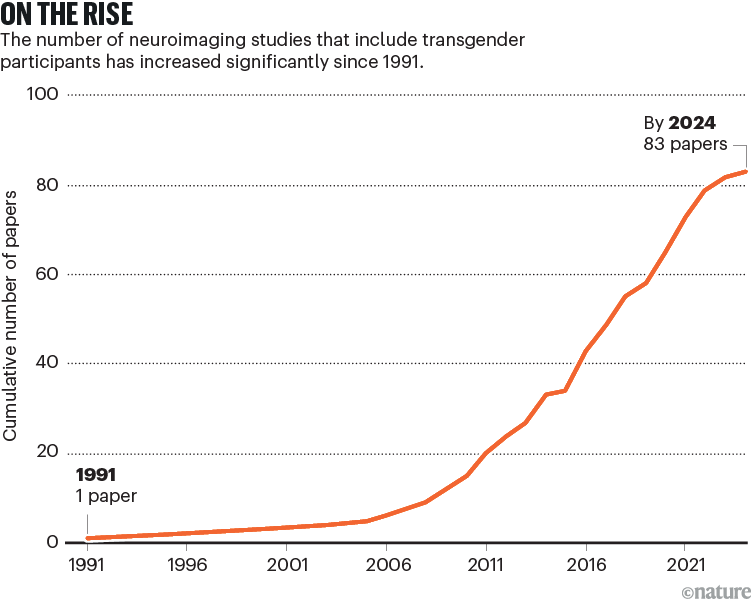
Some neuroscientists are using functional MRI to study the effects of hormone therapy on brain structure 4 and to examine cognitive processes such as face perception 5 . Others are applying machine-learning techniques to establish whether features in brain scans of cis- and transgender people correlate with their gender identity 6 . Researchers are also trying to assess whether particular features identified in brain scans make it more likely that transgender individuals will benefit from gender-affirming hormone therapy 7 . And some are conducting ‘mega-analyses’ — pooling the brain scans of hundreds of participants — to identify brain characteristics that are specific to transgender people 8 .
Help or harm?
One concern arising from such studies is that neuroscientific findings related to transgender identity could make it even harder for some people to access medical treatment that could help them.
In countries or regions where gender-affirming medical treatment is available, individuals often need a diagnosis of ‘gender dysphoria’ or ‘gender incongruence’ to be eligible for hormone therapy or gender-affirming surgery, and to be reimbursed for such treatments. Results from brain scans could be included in the suite of measurements used to assess whether someone is experiencing gender dysphoria or incongruence.
Those in favour of such requirements argue that it is necessary to prevent people taking irreversible steps that they might regret. Hormonal therapy can have adverse effects on fertility, for instance 9 . However, many transgender people argue that whether someone can receive gender-affirming hormone therapy or other treatment shouldn’t depend on a health-care practitioner deciding that they experience ‘enough’ gender dysphoria to be eligible 10 . The current approach, combined with a shortage of specialists qualified to make such diagnoses, has been linked to long waiting lists. In the Netherlands, waiting times can be more than two years .
A second possibility is that neuroscientific findings related to transgender identity will fuel transphobic narratives 11 .
Take the debate on social media and other platforms about gendered public spaces in countries such as the United States , the United Kingdom and Brazil 12 . Some people argue that allowing transgender women to access infrastructure, such as public toilets or women’s prisons, threatens the safety of “real women” . Neuroscientific research is sometimes misused to bolster flawed claims about what ‘real’ means.
Moreover, such studies could exacerbate tensions between scientific and transgender communities.

Scientists are aiming to identify brain characteristics that are specific to transgender people. Credit: Alain Jocard/AFP/Getty
Although cis- and transgender researchers have taken steps to improve people’s understanding, there is a history of tension between the scientific and transgender communities 13 . In the late 1980s, for instance, a sexologist argued that trans women who are mainly attracted to women experience sexual arousal from their own expression of femininity. He described their feelings of gender dysphoria as resulting from paraphilia — a sexual interest in objects, situations or individuals that are atypical 14 . This theory has not held up under broader scientific scrutiny 15 , but it has become notorious in the transgender community and, from our discussions with transgender people and discussions by other groups 16 , it is clear that such studies have reduced transgender people’s trust in science.

How four transgender researchers are improving the health of their communities
In 2021, for example, a neuroimaging study with transgender participants was suspended in the United States after backlash from the transgender community. The study would have involved showing participants images of themselves wearing tight clothes, with the intention of triggering gender dysphoria — an experience that is associated with depression, anxiety, social isolation and an increased risk of suicide. The study’s researchers had acquired ethical approval from their research institute and obtained informed consent from the participants. Yet they had failed to anticipate how the transgender community would perceive their experimental procedure.
In 2022, to learn more about how transgender people view current neuroscientific approaches to the study of transgender identity, we conducted focus-group interviews that lasted for three hours with eight transgender participants — all of whom had differing levels of knowledge about the topic.
The group expressed concern that studies that look for a neurological basis to transgender identities could have a pathologizing effect. “I think questions of aetiology are just inherently wrong,” one participant said. “We don’t ask ‘Why is someone’s favourite colour blue?’. These are questions that come from wanting to pathologize.” Participants also agreed that a biological-determinist approach does not do justice to the complex and layered experience of identifying as transgender.
Decades of work aimed at establishing how science can benefit minority groups 17 suggest that neuroscientists and other scholars could take several steps to ensure they help rather than harm transgender, non-binary and intersex individuals and other people who don’t conform to narrow definitions around sex and gender. Indeed, the four actions that we lay out here are broadly applicable to any studies involving marginalized groups.
Establish an advisory board. Researchers who work with transgender participants should collaborate with an advisory board that ideally consists of transgender people and members of other groups with relevant perspectives, including those who have some understanding of the science in question. Funding agencies should support such initiatives, to help prevent further distrust being sown because of how studies are designed.
Set up multidisciplinary teams. Researchers trained in neuroscience will view phenomena such as transgender identity through a different lens from, say, those trained in psychology. To prevent the outcomes of neuroscientific and other studies being described and published in an overly deterministic and simplistic way 18 , research teams should include social scientists. Ideally, such collaborations would also include transgender researchers or others with diverse gender identities, because their input would help to prevent a cis-normative bias in study design and in the interpretation of results. Indeed, our own group has benefited from this diversity (one of us is transgender).
Prioritize research that is likely to improve people’s lives. Neuroscientists and others engaged in research involving transgender participants, non-binary people or individuals with diverse gender identities should prioritize research questions that are likely to enhance the health of these groups. Although the applications of basic research can be hard to predict, investigations into the neurobiological impacts of hormone treatment on the brain, for instance, could be more directly informative to health-care practitioners and transgender individuals than might investigations into the underlying bases of transgender identity.
Rethink how ethical approval is obtained. Ethical boards at universities typically consist of scientists with diverse backgrounds. But it is unrealistic to expect them to be educated on the sensitivities of every minority group, whether in relation to gender, religion, ethnicity or anything else. One way to address this problem is for ethical boards to require researchers to state what feedback and other information they have gathered through community engagement. A university’s ethical review committee could then evaluate whether the researchers have done enough to understand and address people’s concerns and sensitivities.
Our aim is not to halt scientific enquiry. But when it comes to transgender identity, knowledge cannot be pursued in isolation from the many societal factors that shape how that knowledge is received and acted on.
Nature 629 , 998-1000 (2024)
doi: https://doi.org/10.1038/d41586-024-01521-7
Zhou, J.-N., Hofman, M. A., Gooren, L. J. G. & Swaab, D. F. Nature 378 , 68–70 (1995).
Article PubMed Google Scholar
Manzouri, A., Kosidou, K., & Savic, I. Cereb. Cortex 27 , 998–1010 (2017).
PubMed Google Scholar
Northoff, G. et al. NeuroImage 31 , 440–457 (2006).
Burke, S. M. et al. Cereb. Cortex 28 , 1582–1596 (2018).
Fisher, A. D. et al. J. Clin. Med. 9 , 1731 (2020).
Clemens, B. et al. Cereb. Cortex 30 , 2755–2765 (2020).
Moody, T. D. et al. NeuroImage Clin. 29 , 102517 (2021).
Mueller, S. C. et al. J. Sex. Med. 18 , 1122–1129 (2021).
Nota, N. M., den Heijer, M. & Gooren, L. J. In Endotext (eds Feingold, K. R. et al. ) (MDText, 2000).
Google Scholar
Ashley, F. J. Med. Ethics 45 , 480–482 (2019).
Ching, B. H.-H. & Xu, J. T. Sex Roles 78 , 228–241 (2018).
Article Google Scholar
Pagliarini Bagagli, B., Veriato Chaves, T. & Zoppi Fontana, M. G. Front. Sociol. 6 , 652777 (2021).
Santora, T. Nature Med. 27 , 2074–2077 (2021).
Blanchard, R. J. Nerv . Ment. Dis. 177 , 616–623 (1989).
Serano, J. Sociol. Rev. 68 , 763–778 (2020).
Richards, C., Barker, M., Lenihan, P. & Iantaffi, A. Fem. Psychol. 24 , 248–258 (2014).
Menzies, C. R. Can . J. Native Educ. 25 , 19–36 (2001).
Caselles, E. L. Front. Sociol. 6 , 608328 (2021).
Download references
Reprints and permissions
Competing Interests
The authors declare no competing interests.
Related Articles

Envisioning trans-inclusive and trans-specific cancer care
Let’s talk about (biological) sex
- Neuroscience
- Health care

‘Rainbow’, ‘like a cricket’: every bird in South Africa now has an isiZulu name
News 06 JUN 24
Structure and topography of the synaptic V-ATPase–synaptophysin complex
Article 05 JUN 24

Senescent glia link mitochondrial dysfunction and lipid accumulation

‘I saw that discrimination wasn’t hearsay or rumours — it really did exist’
Career Q&A 05 JUN 24

Is AI misinformation influencing elections in India?
Comment 05 JUN 24

What we do — and don’t — know about how misinformation spreads online
Editorial 05 JUN 24

A dad’s diet affects his sperm — and his sons’ health
News 05 JUN 24

Huge amounts of bird-flu virus found in raw milk of infected cows
Underfunding cannabis research hampers sensible policymaking and boosts the black market
Correspondence 04 JUN 24
Faculty Positions, Aging and Neurodegeneration, Westlake Laboratory of Life Sciences and Biomedicine
Applicants with expertise in aging and neurodegeneration and related areas are particularly encouraged to apply.
Hangzhou, Zhejiang, China
Westlake Laboratory of Life Sciences and Biomedicine (WLLSB)
Faculty Positions in Chemical Biology, Westlake University
We are seeking outstanding scientists to lead vigorous independent research programs focusing on all aspects of chemical biology including...
School of Life Sciences, Westlake University
Postdoctoral Associate- Cancer Epidemiology
Houston, Texas (US)
Baylor College of Medicine (BCM)
Head of Climate Science and Impacts Team (f/m/d)
You will play a pivotal role in shaping the scientific outputs and supporting the organisation's mission and culture. Your department has 20+ staff.
Ritterstraße 3, 10969 Berlin
Climate Analytics gGmbH
Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Warmly Welcomes Talents Abroad
Qiushi Chair Professor; Qiushi Distinguished Scholar; ZJU 100 Young Researcher; Distinguished researcher
No. 3, Qingchun East Road, Hangzhou, Zhejiang (CN)
Sir Run Run Shaw Hospital Affiliated with Zhejiang University School of Medicine
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Follow Puck Worlds online:
- Follow Puck Worlds on Twitter
Site search
Filed under:
- Kontinental Hockey League
Gagarin Cup Preview: Atlant vs. Salavat Yulaev
Share this story.
- Share this on Facebook
- Share this on Twitter
- Share this on Reddit
- Share All sharing options
Share All sharing options for: Gagarin Cup Preview: Atlant vs. Salavat Yulaev
Gagarin cup (khl) finals: atlant moscow oblast vs. salavat yulaev ufa.
Much like the Elitserien Finals, we have a bit of an offense vs. defense match-up in this league Final. While Ufa let their star top line of Alexander Radulov, Patrick Thoresen and Igor Grigorenko loose on the KHL's Western Conference, Mytischi played a more conservative style, relying on veterans such as former NHLers Jan Bulis, Oleg Petrov, and Jaroslav Obsut. Just reaching the Finals is a testament to Atlant's disciplined style of play, as they had to knock off much more high profile teams from Yaroslavl and St. Petersburg to do so. But while they did finish 8th in the league in points, they haven't seen the likes of Ufa, who finished 2nd.
This series will be a challenge for the underdog, because unlike some of the other KHL teams, Ufa's top players are generally younger and in their prime. Only Proshkin amongst regular blueliners is over 30, with the work being shared by Kirill Koltsov (28), Andrei Kuteikin (26), Miroslav Blatak (28), Maxim Kondratiev (28) and Dmitri Kalinin (30). Oleg Tverdovsky hasn't played a lot in the playoffs to date. Up front, while led by a fairly young top line (24-27), Ufa does have a lot of veterans in support roles: Vyacheslav Kozlov , Viktor Kozlov , Vladimir Antipov, Sergei Zinovyev and Petr Schastlivy are all over 30. In fact, the names of all their forwards are familiar to international and NHL fans: Robert Nilsson , Alexander Svitov, Oleg Saprykin and Jakub Klepis round out the group, all former NHL players.
For Atlant, their veteran roster, with only one of their top six D under the age of 30 (and no top forwards under 30, either), this might be their one shot at a championship. The team has never won either a Russian Superleague title or the Gagarin Cup, and for players like former NHLer Oleg Petrov, this is probably the last shot at the KHL's top prize. The team got three extra days rest by winning their Conference Final in six games, and they probably needed to use it. Atlant does have younger regulars on their roster, but they generally only play a few shifts per game, if that.
The low event style of game for Atlant probably suits them well, but I don't know how they can manage to keep up against Ufa's speed, skill, and depth. There is no advantage to be seen in goal, with Erik Ersberg and Konstantin Barulin posting almost identical numbers, and even in terms of recent playoff experience Ufa has them beat. Luckily for Atlant, Ufa isn't that far away from the Moscow region, so travel shouldn't play a major role.
I'm predicting that Ufa, winners of the last Superleague title back in 2008, will become the second team to win the Gagarin Cup, and will prevail in five games. They have a seriously well built team that would honestly compete in the NHL. They represent the potential of the league, while Atlant represents closer to the reality, as a team full of players who played themselves out of the NHL.
- Atlant @ Ufa, Friday Apr 8 (3:00 PM CET/10:00 PM EST)
- Atlant @ Ufa, Sunday Apr 10 (1:00 PM CET/8:00 AM EST)
- Ufa @ Atlant, Tuesday Apr 12 (5:30 PM CET/12:30 PM EST)
- Ufa @ Atlant, Thursday Apr 14 (5:30 PM CET/12:30 PM EST)
Games 5-7 are as yet unscheduled, but every second day is the KHL standard, so expect Game 5 to be on Saturday, like an early start.
Loading comments...
- Yekaterinburg
- Novosibirsk
- Vladivostok

- Tours to Russia
- Practicalities
- Russia in Lists
Rusmania • Deep into Russia
Out of the Centre
Savvino-storozhevsky monastery and museum.

Zvenigorod's most famous sight is the Savvino-Storozhevsky Monastery, which was founded in 1398 by the monk Savva from the Troitse-Sergieva Lavra, at the invitation and with the support of Prince Yury Dmitrievich of Zvenigorod. Savva was later canonised as St Sabbas (Savva) of Storozhev. The monastery late flourished under the reign of Tsar Alexis, who chose the monastery as his family church and often went on pilgrimage there and made lots of donations to it. Most of the monastery’s buildings date from this time. The monastery is heavily fortified with thick walls and six towers, the most impressive of which is the Krasny Tower which also serves as the eastern entrance. The monastery was closed in 1918 and only reopened in 1995. In 1998 Patriarch Alexius II took part in a service to return the relics of St Sabbas to the monastery. Today the monastery has the status of a stauropegic monastery, which is second in status to a lavra. In addition to being a working monastery, it also holds the Zvenigorod Historical, Architectural and Art Museum.
Belfry and Neighbouring Churches

Located near the main entrance is the monastery's belfry which is perhaps the calling card of the monastery due to its uniqueness. It was built in the 1650s and the St Sergius of Radonezh’s Church was opened on the middle tier in the mid-17th century, although it was originally dedicated to the Trinity. The belfry's 35-tonne Great Bladgovestny Bell fell in 1941 and was only restored and returned in 2003. Attached to the belfry is a large refectory and the Transfiguration Church, both of which were built on the orders of Tsar Alexis in the 1650s.

To the left of the belfry is another, smaller, refectory which is attached to the Trinity Gate-Church, which was also constructed in the 1650s on the orders of Tsar Alexis who made it his own family church. The church is elaborately decorated with colourful trims and underneath the archway is a beautiful 19th century fresco.
Nativity of Virgin Mary Cathedral

The Nativity of Virgin Mary Cathedral is the oldest building in the monastery and among the oldest buildings in the Moscow Region. It was built between 1404 and 1405 during the lifetime of St Sabbas and using the funds of Prince Yury of Zvenigorod. The white-stone cathedral is a standard four-pillar design with a single golden dome. After the death of St Sabbas he was interred in the cathedral and a new altar dedicated to him was added.

Under the reign of Tsar Alexis the cathedral was decorated with frescoes by Stepan Ryazanets, some of which remain today. Tsar Alexis also presented the cathedral with a five-tier iconostasis, the top row of icons have been preserved.
Tsaritsa's Chambers

The Nativity of Virgin Mary Cathedral is located between the Tsaritsa's Chambers of the left and the Palace of Tsar Alexis on the right. The Tsaritsa's Chambers were built in the mid-17th century for the wife of Tsar Alexey - Tsaritsa Maria Ilinichna Miloskavskaya. The design of the building is influenced by the ancient Russian architectural style. Is prettier than the Tsar's chambers opposite, being red in colour with elaborately decorated window frames and entrance.

At present the Tsaritsa's Chambers houses the Zvenigorod Historical, Architectural and Art Museum. Among its displays is an accurate recreation of the interior of a noble lady's chambers including furniture, decorations and a decorated tiled oven, and an exhibition on the history of Zvenigorod and the monastery.
Palace of Tsar Alexis

The Palace of Tsar Alexis was built in the 1650s and is now one of the best surviving examples of non-religious architecture of that era. It was built especially for Tsar Alexis who often visited the monastery on religious pilgrimages. Its most striking feature is its pretty row of nine chimney spouts which resemble towers.

Plan your next trip to Russia
Ready-to-book tours.
Your holiday in Russia starts here. Choose and book your tour to Russia.
REQUEST A CUSTOMISED TRIP
Looking for something unique? Create the trip of your dreams with the help of our experts.

- Bahasa Indonesia
- Eastern Europe
- Moscow Oblast
Elektrostal
Elektrostal Localisation : Country Russia , Oblast Moscow Oblast . Available Information : Geographical coordinates , Population, Area, Altitude, Weather and Hotel . Nearby cities and villages : Noginsk , Pavlovsky Posad and Staraya Kupavna .
Information
Find all the information of Elektrostal or click on the section of your choice in the left menu.
- Update data
Elektrostal Demography
Information on the people and the population of Elektrostal.
Elektrostal Geography
Geographic Information regarding City of Elektrostal .
Elektrostal Distance
Distance (in kilometers) between Elektrostal and the biggest cities of Russia.
Elektrostal Map
Locate simply the city of Elektrostal through the card, map and satellite image of the city.
Elektrostal Nearby cities and villages
Elektrostal weather.
Weather forecast for the next coming days and current time of Elektrostal.
Elektrostal Sunrise and sunset
Find below the times of sunrise and sunset calculated 7 days to Elektrostal.
Elektrostal Hotel
Our team has selected for you a list of hotel in Elektrostal classified by value for money. Book your hotel room at the best price.
Elektrostal Nearby
Below is a list of activities and point of interest in Elektrostal and its surroundings.
Elektrostal Page

- Information /Russian-Federation--Moscow-Oblast--Elektrostal#info
- Demography /Russian-Federation--Moscow-Oblast--Elektrostal#demo
- Geography /Russian-Federation--Moscow-Oblast--Elektrostal#geo
- Distance /Russian-Federation--Moscow-Oblast--Elektrostal#dist1
- Map /Russian-Federation--Moscow-Oblast--Elektrostal#map
- Nearby cities and villages /Russian-Federation--Moscow-Oblast--Elektrostal#dist2
- Weather /Russian-Federation--Moscow-Oblast--Elektrostal#weather
- Sunrise and sunset /Russian-Federation--Moscow-Oblast--Elektrostal#sun
- Hotel /Russian-Federation--Moscow-Oblast--Elektrostal#hotel
- Nearby /Russian-Federation--Moscow-Oblast--Elektrostal#around
- Page /Russian-Federation--Moscow-Oblast--Elektrostal#page
- Terms of Use
- Copyright © 2024 DB-City - All rights reserved
- Change Ad Consent Do not sell my data

Serial Killer Quick Reference Guides
#1 Stranglers
- Killer.Cloud
- Serial Killers
- Necrophiliacs
Sergei Ryakhovsky
The balashikha ripper, the hippopotamus, active for 6 years (1988-1993) in russia, confirmed victims, possible victims.
- Serial Killer Profile
- Serial Killer Type
- General Information
- Characteristics
- Cognitive Ability
- Incarceration
- 8 Timeline Events
- Serial Killers Active During Spree
- Boolean Statistical Questions
- 12 Books Written About Sergei Ryakhovsky
- 3 External References
Internal References
Sergei Ryakhovsky (Sergei Vasilyevich Ryakhovsky) a Soviet-Russian serial killer known as the Balashikha Ripper and The Hippopotamus. Ryakhovsky was convicted for the killing of nineteen people in the Moscow area between 1988 and 1993. Ryakhovsky's mainly stabbed or strangulated his victims, he mutilated some bodies, mainly in the genital area. Allegedly Ryakhovsky carried out necrophilic acts on his victims and stole their belongings. Ryakhovsky standing 6’5" tall and weighting 286 pounds, gaining him the nickname, The Hippo. Sergei Ryakhovsky died on January 21st 2005 from untreated tuberculosis while serving his life sentence in prison.
Sergei Ryakhovsky Serial Killer Profile
Serial Killer Sergei Ryakhovsky (aka) the Balashikha Ripper, The Hippopotamus, was active for 6 years between 1988-1993 , known to have ( 19 confirmed / 19 possible ) victims. This serial killer was active in the following countries: Russia
Sergei Ryakhovsky was born on December 29th 1962 in Balashikha, Moscow Oblast, Soviet Union. He had a physically defect. During his education he had academic, social or discipline problems including being teased or picked on.
Sergei Ryakhovsky a necrophile male citizen of Russia.
Prior to his spree he had killed, commited crimes, and served time in jail.
In 1988 (Age 25/26) Sergei Ryakhovsky started his killing spree, during his crimes as a serial killer he was known to rob, commit acts of necrophilia , torture , strangle , rape , mutilate, and murder his victims.
He was arrested on April 13th 1993 (Age 30), sentenced to death by firing squad at a maximum-security penal colony in Solikamsk, Perm Oblast, Russia. He was convicted on charges of murder and other possible charges during his lifetime.
Sergei Ryakhovsky died on January 21st 2005 (Age 42), cause of death: natural causes, untreated tuberculosis at a maximum-security penal colony in Solikamsk, Perm Oblast, Russia.
Profile Completeness: 62%
Sergei Ryakhovsky has been listed on Killer.Cloud since November of 2016 and was last updated 4 years ago.
Sergei Ryakhovsky a known:
( 651 killers ) serial killer.
The unlawful killing of two or more victims by the same offender(s), in separate events. Serial Killer as defined by the FBI at the 2005 symposium.
( 308 killers ) RAPIST
Rape is usually defined as having sexual intercourse with a person who does not want to, or cannot consent.
( 60 killers ) NECROPHILIAC
Necrophilia, also called thanatophilia, is a sexual attraction or sexual act involving corpses. Serial Killer Necrophiliacs have been known to have sex with the body of their victim(s).
( 89 killers ) TORTURER
Torture is when someone puts another person in pain. This pain may be physical or psychological. Tourturers touture their victims.
( 251 killers ) STRANGLER
Strangulation is death by compressing the neck until the supply of oxygen is cut off. Stranglers kill by Strangulation.
Sergei Ryakhovsky Serial Killer Profile:
Updated: 2019-06-30 collected by killer.cloud, 8 timeline events of serial killer sergei ryakhovsky.
The 8 dates listed below represent a timeline of the life and crimes of serial killer Sergei Ryakhovsky. A complete collection of serial killer events can be found on our Serial Killer Timeline .
Back to top Serial Killers Active During
The following serial killers were active during the same time span as Sergei Ryakhovsky (1988-1993).
Jack Harold Jones 2 Victims during 13 Years
Gao chengyong 11 victims during 15 years, michael lee lockhart 3 victims during 2 years, pedro lopez 110 victims during 34 years, serial killers by active year, books that mention sergei ryakhovsky.

Kevin Smith
Serial killer stranglers.
Serial Killer Rapists
Sergey Kuznetsov
Butterfly skin.

Geraldine Fagan
Believing in russia.

Danny Schäfer
Freedom of religion or belief. anti-sect move....
100 of the Most Famous Serial Killers of All...

Stanley M. Burgess
The new international dictionary of pentecost....
External References
- Sergei Ryakhovsky on en.wikipedia.org , Retrieved on Sep 18, 2018 .
- Juan Ignacio Blanco , Sergei Vasilyevich RYAKHOVSKY on murderpedia.org , Retrieved on Sep 18, 2018 .
- Q372816 on www.wikidata.org , Retrieved on Oct 9, 2018 .
Sergei Ryakhovsky is included in the following pages on Killer.Cloud the Serial Killer Database
- #3 of 45[ Page 1 ] of Serial Killers with birthdays in December
- #10 of 60[ Page 1 ] of Serial Killer Necrophiliacs sorted by Confirmed Victims
- #10 of 29[ Page 1 ] of Serial Killers active in Russia
- #10 of 55[ Page 1 ] of Capricorn Serial Killers sorted by Confirmed Victims
- #11 of 89[ Page 1 ] of Serial Killer Torturers sorted by Confirmed Victims
- #27 of 250[ Page 2 ] of Serial Killer Stranglers sorted by Confirmed Victims
- #35 of 307[ Page 3 ] of Serial Killer Rapist sorted by Confirmed Victims
- #63 of 651[ Page 5 ] of serial killers sorted by Confirmed Victims
- #264 of 651[ Page 18 ] of serial killers sorted by Years Active
- #381 of 651[ Page 26 ] of serial killers sorted by Profile Completeness
- #516 of 651[ Page 35 ] of the A-Z List of Serial Killers

IMAGES
VIDEO
COMMENTS
Featured Expert: Fan Liang, M.D. Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including: Creating the penis. Lengthening the urethra so you are able to stand to urinate. Creating the tip (glans) of the penis. Creating the scrotum.
Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too. Studies consistently show that gender affirmation surgery reduces gender dysphoria and related conditions, like anxiety and depression.
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Here's how gender reassignment works: Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina. An incision ...
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to describe people ...
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers ...
Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people. Facial gender surgery: While hormone replacement therapy can help achieve gender affirming changes to the face, surgery may help. Facial gender surgery can include a variety ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected]. We will assist you in obtaining what you need to qualify for surgery. University of Michigan Comprehensive Gender Services Program brings ...
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning.. Often used to refer to phalloplasty, metoidoplasty, or vaginectomy, sex reassignment surgery can also more broadly refer to many procedures an individual may have ...
This article was originally published with the title " What the Science on Gender-Affirming Care for Transgender Kids Really Shows " in SA Health & Medicine Vol. 4 No. 4 (August 2022) doi:10. ...
To achieve the lengthening, the surgeon uses tissues from the cheek, labia minora, or other parts of the vagina. The aim of this is to allow the person to urinate while standing. An advantage of ...
Gender reassignment costs vary based on each person's needs and desires; expenses often range between $7,000 and $50,000 (in 2014), although costs may be much greater depending upon the type (gender reconstructive surgeries versus cosmetic procedures) and number of surgeries as well as where in the world they are performed [source: AP].
Article originally appeared on 04.29.16. Over 1,700 male-to-female gender confirmation surgeries were performed in 2016 in the U.S., according to The American Society of Plastic Surgeons, and ...
Here's how sex reassignment surgery works. By Lenny Bernstein. February 9, 2015 at 7:00 a.m. EST. Bruce Jenner attends the 13th annual Michael Jordan Celebrity Invitational gala in Las Vegas in ...
Summary. Transgender men may choose to have gender-affirming surgery, such as metoidioplasty or phalloplasty. These may provide sensations and functions including erections and urinating standing ...
Over the past few decades, neuroscientists, endocrinologists, geneticists and social scientists have conducted numerous studies involving transgender people, meaning those whose gender identity ...
It really is, like the whole country is hypnotized, and I just think this is a perfect storm of things that are happening all at the same time. ... that didn't work out. She got the money and ...
Much like the Elitserien Finals, we have a bit of an offense vs. defense match-up in this league Final. While Ufa let their star top line of Alexander Radulov, Patrick Thoresen and Igor Grigorenko loose on the KHL's Western Conference, Mytischi played a more conservative style, relying on veterans such as former NHLers Jan Bulis, Oleg Petrov, and Jaroslav Obsut.
Zvenigorod's most famous sight is the Savvino-Storozhevsky Monastery, which was founded in 1398 by the monk Savva from the Troitse-Sergieva Lavra, at the invitation and with the support of Prince Yury Dmitrievich of Zvenigorod. Savva was later canonised as St Sabbas (Savva) of Storozhev. The monastery late flourished under the reign of Tsar ...
Elektrostal Geography. Geographic Information regarding City of Elektrostal. Elektrostal Geographical coordinates. Latitude: 55.8, Longitude: 38.45. 55° 48′ 0″ North, 38° 27′ 0″ East. Elektrostal Area. 4,951 hectares. 49.51 km² (19.12 sq mi) Elektrostal Altitude.
Sergei Ryakhovsky (Sergei Vasilyevich Ryakhovsky) a Soviet-Russian serial killer known as the Balashikha Ripper and The Hippopotamus. Ryakhovsky was convicted for the killing of nineteen people in the Moscow area between 1988 and 1993. Ryakhovsky's mainly stabbed or strangulated his victims, he mutilated some bodies, mainly in the genital area.