- Sign In to save searches and organize your favorite content.
- Not registered? Sign up

Recently viewed (0)
- Save Search
- Subscriptions
- Join E-mail List
Patient Case Studies and Panel Discussion: Lymphoma
- Get Citation Alerts
- Download PDF to Print
A heterogeneous group of diseases, lymphomas encompass a range of diagnoses that call for varied treatment approaches. Although some lymphomas require minimal intervention for cure or remission, others can be very difficult to treat and are associated with poor outcomes. At the NCCN 2019 Annual Congress: Hematologic Malignancies, a panel of experts used 3 case studies to develop an evidence-based approach for the treatment of patients with lymphomas. Moderated by Ranjana H. Advani, MD, the session focused on peripheral T-cell lymphoma, primary mediastinal large B-cell lymphoma, follicular lymphoma, and diffuse large B-cell lymphoma.
Lymphomas are a heterogeneous group of diseases with a range of diagnoses that require varied treatment approaches. Although some lymphomas require minimal intervention for cure or remission, others can be difficult to treat and are associated with poor patient outcomes. At the NCCN 2019 Annual Congress: Hematologic Malignancies, a panel of experts identified clinical challenges in managing patients with lymphoma. Moderated by Ranjana H. Advani, MD, Saul A. Rosenberg Professor of Lymphoma, Stanford Cancer Institute, the session focused on 3 case studies, which were used to develop an evidence-based approach for treatment of these patients. Panelists included Jeremy S. Abramson, MD, MMSc, Massachusetts General Hospital Cancer Center; Mrinal Dutia, MD, The Permanente Medical Group; Richard I. Fisher, MD, Fox Chase Cancer Center; and Andrew D. Zelenetz, MD, PhD, Memorial Sloan Kettering Cancer Center.
- Patient Case Study 1: Peripheral T-Cell Lymphoma
In the first case study, a 44-year-old woman presented with a dry, nonproductive cough that she had been experiencing for 2 to 3 months, intermittent bouts of severe shortness of breath, decreased appetite, and a 20-pound weight loss. Chest radiograph revealed mild bilateral pleural effusion and bilateral pulmonary nodules, with the largest nodule measuring 5 cm in the right upper lobe. The patient was admitted for further evaluation, and additional testing was performed (see Figure 1 for results). Bone marrow evaluation revealed no morphologic abnormalities, but complex cytogenetics and the same T-cell clone was found as in the lung biopsy. Therefore, a diagnosis was made of stage IVB peripheral T-cell lymphoma (PTCL) with T-follicular helper (TFH) phenotype most consistent with angioimmunoblastic T-cell lymphoma (AITL).

Patient case study 1: results of further testing.
Abbreviations: NGS, next-generation sequencing; RUL, right upper lobe; SUV, standard uptake value; VATS, video-assisted thoracic surgery.
Citation: Journal of the National Comprehensive Cancer Network J Natl Compr Canc Netw 17, 11.5; 10.6004/jnccn.2019.5028
Dr. Advani explained that this “complicated terminology” comes from recent updates to the WHO classification for PTCL. 1 , 2 Furthermore, she explained that in recent years, advances in molecular biology have helped elucidate the underlying genetic complexity of PTCL and identify mutations and signaling pathways involved in lymphomagenesis. Importantly, many of the same genetic changes observed in AITL are also seen in PTCL not otherwise specified (NOS) that manifest a TFH phenotype. For this designation, the neoplastic cells should express at least 2 or 3 TFH-related antigens, including PD-1, CD10, BCL6, CXCL13, ICOS, SAP, and CCR5.
One potential treatment regimen to use in this patient population is CHOP (cyclophosphamide/doxorubicin/vincristine/prednisone), which is associated with complete response (CR) rates of 50% to 60% in non–anaplastic large cell lymphoma (ALCL) and a 5-year overall survival rate of 40% to 60%. According to Dr. Advani, patients with low International Prognostic Index (IPI) scores perform significantly better; however, relapse is associated with poor patient outcomes. “The ongoing challenge is to achieve higher CR rates and to translate those remissions into long-term survival,” said Dr. Advani.
Another treatment option is the CHOEP regimen, which adds etoposide to CHOP. Retrospective studies suggest that outcomes may be better than historical data with CHOP. 3 – 5 In a prospective trial, the Nordic group evaluated the role of autologous stem cell transplantation after patients achieved a CR/partial response with CHOEP. 6 At a median follow-up of 5 years, the 5-year progression-free survival (PFS) and overall survival (OS) rates for AITL were 49% and 52%, respectively, and 38% and 47% for PTCL-NOS, respectively.
Finally, the phase III ECHELON-2 study was the first prospective trial in PTCL to show an OS benefit over CHOP. 7 Frontline therapy for CD30-positive PTCL comparing brentuximab vedotin + cyclophosphamide/doxorubicin/prednisone (BV-CHP) versus CHOP led to a significant improvement in PFS and OS for patients, with a comparable safety profile. The FDA subsequently approved brentuximab vedotin in combination with CHP for adults with previously untreated systematic ALCL or other CD30-expressing PTCL, including AITL and PTCL-NOS. “Based on these data, currently BV-CHP should be the standard regimen for untreated ALCL and other histologies that are CD30-postive,” said Dr. Advani.
In the current case study, the patient received treatment with CHOEP and growth factor support. However, after 2 cycles, PET/CT scan showed no change in lung lesions with a worsening of right-sided pleural effusion (Deauville score 5). Thoracentesis of the pleural effusion was negative for infection but positive for abnormal T-cell population, with morphologic and immunophenotypic findings consistent with the initial diagnosis of PTCL with TFH phenotype most consistent with AITL. The patient was then started on single-agent brentuximab vedotin every 3 weeks. After 4 cycles, PET/CT scan revealed marked improvement in all lesions (Deauville score 4) and was continued on brentuximab vedotin for an additional 4 doses. PET/CT after 8 cycles revealed the resolution of lung nodules and adenopathy in the right axilla with increased metabolic activity (Deauville score 4).
Currently, 4 agents are FDA-approved for use in relapsed/refractory PTCL: pralatrexate, romidepsin, belinostat, and brentuximab vedotin. Aside from brentuximab vedotin use in ALCL, however, overall response rates are low. Brentuximab vedotin has been evaluated in relapsed/refractory AITL, showing an ORR of 54%. 8 Responses did not correlate with level of CD30 expression.
Although no randomized studies have analyzed the role of consolidative hematopoietic stem cell transplantation, data from the prospective COMPLETE study suggested improved outcomes in patients with PTCL AITL and PTCL-NOS. 9 On the other hand, said Dr. Advani, data from the LYSA study do not support the use of autologous stem cell transplant for upfront consolidation in patients with PTCL-NOS, AITL, or ALK-ALCL who have achieved a complete or partial response after induction. 10
“If patients are young and have achieved remission or even a partial response, most of us tend to transplant because outcomes with relapsed disease are very poor,” Dr. Advani concluded. “None of the approved drugs are home runs. The best chance you get is your first chance.”
- Patient Case Study 2: Primary Mediastinal Large B-Cell Lymphoma
In the second case study, a 21-year-old woman presented with severe cough and weight loss. Physical examination showed dilated veins on the anterior chest wall and no palpable peripheral lymphadenopathy. Chest radiograph revealed right-sided pleural effusion and a large mediastinal mass measuring 10.8 cm. Additional testing was performed. PET/CT scan showed a bulky anterior mediastinal mass with SUV max of 24.1 and subcarinal and right hilar adenopathy. However, no evidence of disease was observed below the diaphragm. Bone marrow biopsy was negative. Mediastinoscopy with a biopsy of the mass showed diffuse lymphoid proliferation of intermediate-size atypical cells positive for CD20, CD79A, PAX5, CD30 (dim), MUM1, BCL2, and BCL6, and negative for CD10, BCL1, and EBER. Florescence in situ hybridization was negative for MYC , BCL2 , and BCL6 rearrangements. The final diagnosis of primary mediastinal large B-cell lymphoma (PMBL) was made.
According to Dr. Advani, current treatment choices for PMBL are CHOP + rituximab (R-CHOP) with radiotherapy versus more intensive regimens, such as dose-adjusted etoposide/prednisone/vincristine/cyclophosphamide/doxorubicin + rituximab (DA-EPOCH-R), without radiotherapy. In one study of DA-EPOCH-R with median follow-up of 8.4 years, PFS and OS were both 90%. 11 Another retrospective multicenter analysis that stratified patients by frontline regimen of either DA-EPOCH-R or R-CHOP showed a higher complete response with DA-EPOCH-R (84% vs 70%; P =.046), but the patients in this arm were also more likely to experience treatment-related toxicities. 12 At 2 years, 89% of patients in the R-CHOP arm and 91% of those in DA-EPOCH-R arm were still alive. Despite these similar outcomes, the consensus among panelists was that DA-EPOCH-R was the preferred option.
The patient in the current case report was started on DA-EPOCH-R, with an initial favorable response: interim imaging showed a reduction in size of the anterior mediastinal mass (5 x 6.3 x 9.6 cm) and resolution of left upper pulmonary nodules. The patient continued on DA-EPOCH-R for 4 additional cycles. PET/CT scans 4 weeks posttreatment revealed a metabolically inactive, irregularly shaped anterior mediastinal mass (5.5 x 4 x 5.2 cm) and a focal area of low metabolic activity within the mass (SUV max 3.5; Deauville score 4). She was asymptomatic, and the decision was made to follow with observation. After 2 months, PET/CT scans showed a stable mediastinal mass with increased metabolic activity (SUV max 6). Biopsy of the mediastinal mass was performed and immunohistochemistry results were consistent with relapsed PMBL; immunohistochemistry showed 30% of large cells were CD20- and CD30-positive.
“With PMBL, most of the cures are from initial therapy,” said Dr. Advani. “Salvage rates in recurrent/refractory disease are quite poor.” Overall response rates in PMBL are 25% versus 48% for diffuse large B-cell lymphoma (DLBCL), and 2-year overall survival is only 15% versus 24%, respectively. 13
Although CD19 CAR T-cell therapy has been approved, said Dr. Advani, there are very limited data on its use in relapsed/refractory PMBL. According to Jeremy S. Abramson, MD, MMSc, Associate Professor of Medicine, Harvard Medical School, and Director of the Lymphoma Center, Massachusetts General Hospital Cancer Center, the limited available data are indeed encouraging in relapsed/refractory PMBL, and are “looking similar” to those for third-line treatment in DLBCL. Currently 3 randomized clinical trials are evaluating CAR T-cells versus autologous stem cell transplant (the current standard of care) as second-line therapy for relapsed/refractory DLBCL, PMBL, and high-grade B-cell lymphomas, and these trials may ultimately change the standard of care in these patients.
Another treatment option for use in patients with relapsed/refractory PMBL is immune checkpoint inhibitors. Pembrolizumab has shown response rates of 40% to 50% and is now approved by the FDA for use in the third-line and beyond. 14 Furthermore, combination brentuximab vedotin + nivolumab showed even more robust activity, with an overall response rate of 73%. 15
The patient in this case study received 5 cycles of pembrolizumab, and PET/CT scans showed a complete metabolic response.
- Patient Case Study 3: From Follicular Lymphoma to DLBCL
In the last case study, a 48-year-old man presented with enlarged lymph nodes in his left neck and right groin measuring up to 2 cm. He was asymptomatic and had no evidence of B symptoms. Laboratory test results were all normal. Excisional biopsy of the left cervical node showed follicular lymphoma (grade 1–2). PET/CT scan revealed left cervical, axillary, and right external iliac and inguinal adenopathy, with the largest node measuring 1.0 x 2.0 cm (SUV max 5.5). There was no splenomegaly or effusions. Bone marrow biopsy showed normal trilineage hematopoiesis. The diagnosis of stage IIIA follicular lymphoma (grade 1–2) was made, with a Follicular Lymphoma International Prognostic Index (FLIPI) score of 1. Panelists agreed that the best approach for this patient was watchful waiting. Therapy was deferred, and the patient was followed with observation.
Two years later, the patient presented with enlarging lymph nodes in his left neck. He was anxious and had mild fatigue. Results of laboratory tests were normal. PET/CT scan showed increased adenopathy above and below the diaphragm, with the largest node (right external iliac node) measuring 3.4 x 2.8 cm (SUV max 8.4). A biopsy of the right external iliac node was performed, with results showing follicular lymphoma (grade 1–2).
Panelists agreed that observation was an acceptable approach for an asymptomatic patients diagnosed with follicular lymphoma with low-volume disease. However, the patient opted for 4 doses of weekly rituximab. Repeat PET/CT (3 months posttreatment with rituximab) showed that most lymph nodes had resolved. Three years later, the patients presented with a new severe pain in the low back radiating down his right leg. MRI of the L-spine showed a T1 hypointense infiltrative mass replacing the L3 vertebral body. A core biopsy of right psoas mass showed that his follicular lymphoma had transformed to DLBCL, germinal center B-cell–like subtype, with double expressors of MYC >40% and BCL2 >50% and MYC translocation–negative, and expression of Ki67 was 90%. IPI score was 4.
Andrew D. Zelenetz, MD, PhD, Professor of Medicine, Memorial Sloan Kettering Cancer Center, explained the unique biology of the “double-expressor” phenotype in DLBCL. “This is the one circumstance where DA-EPOCH-R may have a distinct benefit,” he said. “However, in the absence of MYC translocation, it is not clear that overexpression of MYC, which is biologically driven without the translocation, shows a benefit from this intensive regimen.”
The patient received 6 cycles of DA-EPOCH-R with 4 doses of intrathecal methotrexate. Results of interim and end-of-therapy PET scans showed a metabolic complete response (Deauville score 2).
Double-hit and double-expressor lymphomas tend to have inferior outcomes with R-CHOP therapy, Dr. Advani stated. Several retrospective studies and one prospective trial suggest improved outcomes with intensive chemotherapy for double-hit lymphomas. 16 – 18 “Patients with a very high IPI, advanced-stage disease, or extranodal involvement are the ones that I consider good candidates for DA-EPOCH-R,” she said, and also noted that double-expressor DLBCLs have a higher risk of central nervous system (CNS) relapse independent of CNS-IPI.
The patient in the current case study had a CNS-IPI of 3 and an 11% cumulative incidence of CNS relapse at 2 years. Data support some form of CNS prophylaxis, 19 Dr. Advani concluded, but the jury is still out regarding optimal treatment for double-expressor non-Hodgkin’s lymphoma.
Swerdlow SH , Campo E , Pileri SA , et al. . The 2016 revision of the World Health Organization classification of lymphoid neoplasms . Blood 2016 ; 127 : 2375 – 2390 .
- Search Google Scholar
- Export Citation
Hildyard C , Shiekh S , Browning J , Collins GP . Toward a biology-driven treatment strategy for peripheral T-cell lymphoma . Clin Med Insights Blood Disord 2017 ; 10 :1179545X17705863.
Cederleuf H , Bjerregard Pedersen M , Jerkeman M . The addition of etoposide to CHOP is associated with improved outcome in ALK+ adult anaplastic large cell lymphoma: a Nordic Lymphoma Group study . Br J Haematol 2017 ; 178 : 739 – 746 .
Schmitz N , Trümper L , Ziepert M , et al. . Treatment and prognosis of mature T-cell and NK-cell lymphoma: an analysis of patients with T-cell lymphoma treated in studies of the German High-Grade Non-Hodgkin Lymphoma Study Group . Blood 2010 ; 116 : 3418 – 3425 .
Janikova A , Chloupkova R , Campr V , et al. . First-line therapy for T cell lymphomas: a retrospective population-based analysis of 906 T cell lymphoma patients . Ann Hematol 2019 ; 98 : 1961 – 1972 .
d’Amore F , Relander T , Lauritzsen GF , et al. . Up-front autologous stem-cell transplantation in peripheral T-cell lymphoma: NLG-T-01 . J Clin Oncol 2012 ; 30 : 3093 – 3099 .
Horwitz S , O’Connor OA , Pro B , et al. . Brentuximab vedotin with chemotherapy for CD30-positive peripheral T-cell lymphoma (ECHELON-2): a global, double-blind, randomised, phase 3 trial . Lancet 2019 ; 393 : 229 – 240 .
Horwitz SM , Advani RH , Bartlett NL , et al. . Objective responses in relapsed T-cell lymphomas with single-agent brentuximab vedotin . Blood 2014 ; 123 : 3095 – 3100 .
Park SI , Horwitz SM , Foss FM , et al. . The role of autologous stem cell transplantation in patients with nodal peripheral T-cell lymphomas in first complete remission: Report from COMPLETE, a prospective, multicenter cohort study . Cancer 2019 ; 125 : 1507 – 1517 .
Fossard G , Broussais F , Coelho I , et al. . Role of up-front autologous stem-cell transplantation in peripheral T-cell lymphoma for patients in response after induction: an analysis of patients from LYSA centers . Ann Oncol 2018 ; 29 : 715 – 723 .
Melani C , Advani R , Roschewski M , et al. . End-of-treatment and serial PET imaging in primary mediastinal B-cell lymphoma following dose-adjusted EPOCH-R: a paradigm shift in clinical decision making . Haematologica 2018 ; 103 : 1337 – 1344 .
Shah NN , Szabo , Huntington SF , et al. . R-CHOP versus dose-adjusted R-EPOCH in frontline management of primary mediastinal B-cell lymphoma: a multi-centre analysis . Br J Haematol 2018 ; 180 : 534 – 544 .
Kuruvilla J , Pintilie M , Tsang R , et al. . Salvage chemotherapy and autologous stem cell transplantation are inferior for relapsed or refractory primary mediastinal large B-cell lymphoma compared with diffuse large B-cell lymphoma . Leuk Lymphoma 2008 ; 49 : 1329 – 1336 .
Zinzani PL , Ribrag V , Moskowitz CH , et al. . Safety and tolerability of pembrolizumab in patients with relapsed/refractory primary mediastinal large B-cell lymphoma . Blood 2017 ; 130 : 267 – 270 .
Zinzani PL , Santoro A , Gritt G , et al. . Nivolumab combined with brentuximab vedotin for relapsed/refractory primary mediastinal large B-cell lymphoma: efficacy and safety from the phase II CheckMate 436 study [published online August 9, 2019] . J Clin Oncol . doi: 10.1200/JCO.19.01492
Petrich AM , Gandhi M , Jovanovic B , et al. . Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: a multicenter retrospective analysis . Blood 2014 ; 124 : 2354 – 2361 .
Oki Y , Noorani M , Lin P , et al. . Double hit lymphoma: the MD Anderson Cancer Center clinical experience . Br J Haematol 2014 ; 166 : 891 – 901 .
Dunleavy K , Fanale MA , Abramson JS , et al. . Dose-adjusted EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab) in untreated aggressive diffuse large B-cell lymphoma with MYC rearrangement: a prospective, multicentre, single-arm phase 2 study . Lancet Haematol 2018 ; 5 : e609 – 617 .
Savage KJ , Slack GW , Mottok A , et al. . Impact of dual expression of MYC and BCL2 by immunohistochemistry on the risk of CNS relapse in DLBCL . Blood 2016 ; 127 : 2182 – 2188 .
Disclosures: Dr. Advani has disclosed that she has received grant/research support from Agensys, Inc., Celgene Corporation, Forty Seven, Inc., Janssen Pharmaceutica Products, LP, Kura Oncology, Inc., Merck & Co., Inc., Millennium Pharmaceuticals, Inc., Genentech, Inc./Roche Laboratories, Inc., Pharmacyclics, Regeneron Pharmaceuticals, Inc., Seattle Genetics, Inc.; received consulting fees from AstraZeneca Pharmaceuticals LP, Bayer HealthCare, Gilead Sciences, Inc., Kite Pharma, Kyowa Hakko Kirin Co., Ltd., Cell Medica, Genentech, Inc./Roche Laboratories, Inc., Seattle Genetics, Inc., and Takeda Pharmaceuticals North America, Inc.; and is a scientific advisor for AstraZeneca Pharmaceuticals LP, Bayer HealthCare, Gilead Sciences, Inc., Kite Pharma, Kyowa Hakko Kirin Co., Ltd., Cell Medica, Genentech, Inc./Roche Laboratories, Inc., Seattle Genetics, Inc., and Takeda Pharmaceuticals North America, Inc. Dr. Abramson has disclosed that he receives consulting fees from AbbVie, Inc., Bayer HealthCare, Celgene Corporation, EMD Serono, Genentech, Inc., Janssen Pharmaceutica Products, LP, Karyopharm Therapeutics, Kite Pharma, and Roche Laboratories, Inc. Dr. Dutia has disclosed that she has no interests, arrangements, affiliations, or commercial interests with the manufacturers of any products discussed in this article or their competitors. Dr. Fisher has disclosed that he receives consulting fees from Celgene Corporation and PRIME. Dr. Zelenetz has disclosed that he received consulting fees from AbbVie, Inc., Amgen Inc., AstraZeneca Pharmaceuticals LP, Celgene Corporation, Gilead Sciences, Inc., Janssen Pharmaceutica Products, LP, Novartis Pharmaceuticals Corporation, Adaptive Biotechnologies Corporation, Genentech, Inc./Roche Laboratories, Inc., and Pharmacyclics; is a scientific advisor for AbbVie, Inc., AstraZeneca Pharmaceuticals LP, and MorphoSys AG; and receives grant/research support from BeiGene, Gilead Sciences, Inc., MEI Pharma Inc., and Roche Laboratories, Inc.
Article Sections
- View raw image
- Download Powerpoint Slide
Article Information
- Get Permissions
- Similar articles in PubMed
Google Scholar
Related articles.
- Advertising
- Terms of Use
- Privacy Policy
- Permissions

© 2019-2024 National Comprehensive Cancer Network
Powered by:
- [66.249.64.20|185.194.105.172]
- 185.194.105.172
Character limit 500 /500
- Case report
- Open access
- Published: 15 April 2017
Primary adrenal non-Hodgkin lymphoma: a case report and review of the literature
- Nanik Ram 1 ,
- Owais Rashid 1 ,
- Saad Farooq 2 ,
- Imran Ulhaq 1 &
- Najmul Islam 1
Journal of Medical Case Reports volume 11 , Article number: 108 ( 2017 ) Cite this article
4993 Accesses
16 Citations
1 Altmetric
Metrics details
Lymphomas are cancers that arise from the white blood cells and have been traditionally divided into two large subtypes: Hodgkin and non-Hodgkin lymphoma. B-cell lymphoma is the most common subtype of non-Hodgkin lymphoma; almost 85% of patients with lymphoma have this variant. Lymphomas can potentially arise from any lymphoid tissue located in the body; however, primary adrenal non-Hodgkin lymphoma is extremely rare. We report the history, examination findings, and laboratory results of a 50-year-old man diagnosed with a primary left adrenal diffuse large B-cell lymphoma.
Case presentation
A 50-year-old Pakistani man presented to our hospital with progressively increasing pain and fullness in the left upper quadrant of his abdomen, generalized weakness, easy fatigability, and decreased appetite of 1.5 months’ duration. On examination, he had a blood pressure of 140/80 mmHg with no postural drop, a pulse rate of 106 beats/minute, and no fever. His past medical history was significant for pulmonary tuberculosis 2 years earlier, for which he received antituberculous therapy. Computed tomography revealed a heterogeneous enhancing soft tissue density mass in the left adrenal gland. It measured 7.1 × 5.6 × 9.5 cm. Further laboratory workup revealed the following levels: sodium 135 mEq/L, potassium 4.5 mEq/L, lactate dehydrogenase 905 IU/L, renin 364 IU/ml, aldosterone 5.79 ng/dl, dehydroepiandrosterone sulfate 79.20 μg/dl, urinary vanillylmandelic acid 6.4 mg/24 hours, and a low-dose overnight dexamethasone suppression test result of 3.20 μg/dl. The patient underwent left adrenalectomy. Histopathological test results showed a diffuse large B-cell lymphoma. Immunohistochemical stains were strongly positive for CD20 and negative for CD3, CD5, CD10, and cyclin D1. The patient’s Ki-67 (Mib-1) index was approximately 80%. He received a total of six cycles of cyclophosphamide, doxorubicin, vincristine, and prednisone chemotherapy (rituximab was not given, owing to financial constraints) and was routinely followed pre- and postchemotherapy at our hematology clinic with complete blood count and serum lactate dehydrogenase evaluations. The patient responded to chemotherapy and is currently doing well.
Conclusions
Primary adrenal lymphoma is an extremely rare but rapidly progressive disease. It generally carries a poor prognosis, partly because an optimal treatment protocol has not yet been established. Further studies with larger sample sizes are needed to establish the best treatment option and increase overall survival.
Peer Review reports
The American Cancer Society estimated that more than 70,000 new cases of non-Hodgkin lymphoma (NHL) would be diagnosed in 2016 [ 1 , 2 ]. Although lymphomas arise mainly from lymph nodes, primary extranodal NHL occurs in at least 25% of the cases [ 3 ]. The adrenal gland can be secondarily involved in around 4% of the patients; however, primary adrenal NHL is extremely rare and accounts for less than 1% of all NHL cases [ 4 ]. Primary adrenal lymphoma (PAL) is histologically proven lymphoma of one or both adrenal glands in patients with no prior history of lymphoma. If other organs or lymph nodes besides the adrenal glands are involved, the adrenal lesion must be unequivocally dominant [ 5 ].
PAL occurs predominantly in males in the sixth to seventh decades of life. Most commonly, this lymphoma is a nongerminal center-type diffuse large B-cell lymphoma (DLBCL), which is present in 70% to 80% of the patients [ 6 ]. Patients present with abdominal or lumbar pain; fever; weight loss; and signs of adrenal insufficiency such as hypotension, hyponatremia, fatigue, skin hyperpigmentation, and vomiting [ 7 ]. In occasional instances, it may also be an incidental finding on imaging studies obtained for other purposes, and it is frequently bilateral and bulky at the time of presentation. Several etiological factors, such as Epstein-Barr virus infection, genetic defects in p53 and c-kit, and immune dysregulation, have been implicated in the pathogenesis of this disease [ 5 , 7 ]. Laboratory investigations often show elevated lactate dehydrogenase (LDH), β 2 -microglobulin, C-reactive protein, and ferritinemia, which signify high levels of inflammation associated with PAL [ 6 ].
The prognosis of this condition is generally considered to be poor because PAL is an aggressive disease and progresses rapidly. An average 1-year survival as low as 20% has been reported; however, owing to the rare nature of this disease, prognostic factors are difficult to elucidate [ 5 ].
A 50-year-old Pakistani man known to have had diabetes for 21 years presented to our hospital with progressively increasing pain and fullness in the left upper quadrant of his abdomen, generalized weakness, easy fatigability, and decreased appetite of 1.5 months’ duration. He also complained of nausea and early satiety and had a weight loss of 8 kg over this period. On examination, he was found to have a blood pressure of 140/80 mmHg with no postural drop, a pulse rate of 106 beats/minute, and no fever. His physical examination was otherwise unremarkable. His past medical history was significant for pulmonary tuberculosis 2 years earlier, for which he received antituberculous therapy.
The patient had initially presented at another university hospital 3 weeks earlier. At that time, a laboratory workup and computed tomography (CT) of the abdomen with contrast enhancement were done. Although the results of his complete blood count and renal function test were normal, CT of the abdomen showed a heterogeneous enhancing soft tissue density mass in the left adrenal gland. The mass measured 7.1 × 5.6 cm in transverse and anteroposterior diameter, and the craniocaudal extent of the mass was 9.5 cm. Medially, the mass was abutting the celiac and superior mesenteric arteries, and posteroinferiorly, it was bordering the renal vessels. Paraaortic lymphadenopathy was also present, with the largest one measuring 1.6 cm (Fig. 1 ).
Computed tomography of the patient showing a large left adrenal mass
Further laboratory workup revealed the following levels: sodium 135 mEq/L, potassium 4.5 mEq/L, LDH 905 IU/L, renin 364 IU/ml, aldosterone 5.79 ng/dl, dehydroepiandrosterone sulfate 79.20 μg/dl, urinary vanillylmandelic acid 6.4 mg/24 hours, and a low-dose overnight dexamethasone suppression test result of 3.20 μg/dl. The patient was referred to our urology clinic for surgical removal of his mass. He underwent a left adrenalectomy at the urology clinic on 4 March 2016. Histopathological analysis revealed DLBCL (Figs. 2 and 3 ). The results of immunohistochemical stains were strongly positive for CD20 and negative for CD3, CD5, CD10, and cyclin D1. His Ki-67 (Mib-1) index was approximately 80% (Figs. 4 and 5 ).
Low-power view of the lesion showing diffuse sheets of neoplastic cells (hematoxylin and eosin stain)
High-power view of the lesion showing large-sized neoplastic cells with pleomorphic nuclei, variably prominent nucleoli, and scant cytoplasm. Frequent mitotic figures are also noted (hematoxylin and eosin stain)
CD20 immunohistochemical stain (pan-B) is strongly positive for neoplastic cells
Ki-67 immunohistochemical stain highlights a markedly raised proliferative index in the neoplastic lymphoid population
For further management, the patient was referred to our hematology clinic and was planned for a rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) chemotherapy regimen starting on 18 March 2016. He received a total of six cycles of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP; rituximab was not given, owing to financial constraints) and was routinely followed pre- and postchemotherapy at the hematology clinic with complete blood count and serum LDH evaluations. Positron emission tomography (PET) performed on 24 March 2016 showed metabolically active residual disease over the left adrenal bed. Subcentimetric fluorodeoxyglucose (FDG) deposits were seen in the patient’s L5, L2, and T12 vertebrae, suggestive of marrow infiltration. No evidence of hypermetabolic nodal, hepatic, or splenic involvement was appreciated. However, the patient responded to chemotherapy and is currently doing well. He gained around 8 kg of weight and is following his routine daily activities. A recent PET scan revealed that the previously seen hypermetabolic foci along the left crus, left proximal paraaortic region, and foci of FDG uptake in the lumbar and thoracic vertebrae were not appreciable. The patient’s Deauville 5-point scale score was 0 (complete metabolic response).
To the best of our knowledge, this is the first report describing a case of primary adrenal NHL in Pakistan. Our patient was a man in his fifth decade of life, which, on the basis of published literature, is a relatively young age to have this disease. We treated our patient with a regimen of CHOP; rituximab was not included, owing to financial constraints. Even without rituximab, our patient showed a complete response to therapy. Because primary adrenal NHL is a rare disease, optimal treatment has not yet been established. CHOP or CHOP-like regimens were traditionally used before the introduction of rituximab, with generally dismal results (overall survival between 20% and 50%) [ 7 ]. In the largest study to date on PAL, involving 31 patients given an R-CHOP chemotherapy regimen, complete remission and overall response rates were 54.8% and 87.0%, respectively. Surprisingly, no difference was found in overall survival between unilateral and bilateral NHL of the adrenal gland [ 8 ]. Our patient also underwent adrenalectomy; however, the two largest studies to date showed no survival benefit in patients who underwent adrenalectomy as compared with those who were treated with chemotherapy alone [ 6 , 8 ].
In another study involving 28 patients with PAL, 64% of the patients were treated with a CHOP regimen, 50% with an R-CHOP regimen, and 18% had chemotherapy with doxorubicin, cyclophosphamide, vindesine, bleomycin, and prednisone. The overall survival was 61.6%; however, it was 100% for those who received autologous stem cell transplants, which suggests that this may prolong survival [ 6 ]. The Ki-67 index was high in our patient (80%). Ichikawa et al . reported this index to be greater than 70% in seven patients with primary adrenal DLBCL. They treated all of these patients with rituximab-containing chemotherapy and reported a 2-year survival rate of 57%, although none of the patients died as a result of advancement of lymphoma [ 9 ]. These authors suggested that rituximab-containing chemotherapy with central nervous system (CNS) prophylaxis with methotrexate may be a good treatment option for primary adrenal NHL. Kim et al . reported CNS relapses or progression in four patients, none of whom had received intrathecal prophylaxis [ 8 ].
For our patient, we opted for CT as the initial imaging modality and then confirmed the diagnosis via histology of the resected adrenal gland. Grigg et al . suggested that though magnetic resonance imaging and CT findings can be highly suggestive of NHL, a biopsy should be done for diagnosis. Staging should involve a PET or gallium scan, and in patients with elevated LDH levels, a lumbar puncture should also be done [ 7 ].
According to the International Prognostic Index (IPI), our patient was in the low- to intermediate-risk category, which has an estimated 5-year survival of 51%. However, this scoring system is not specific to PAL; thus, it may be inaccurate in predicting overall survival. Kim et al . found that neither high-risk IPI score nor advanced-stage disease according to the Ann Arbor system had any impact on the overall survival; therefore, they suggested a modified IPI scoring system and a revised staging system, which resulted in significantly improved predictability of overall survival [ 9 ]. The modified scoring and staging criteria may prove beneficial in risk stratification of patients with primary adrenal NHL and also guide treatment.
No protocol for specific treatment in cases of a primary adrenal NHL has yet been established, and multiple authors have used a combination of modalities, including surgery and chemotherapy. Ichikawa et al . argued that perhaps one of the reasons for the poor prognosis is that many patients were previously treated with chemotherapy not containing rituximab and did not receive CNS prophylaxis, which may have decreased overall survival [ 9 ].
PAL is a rare but rapidly progressing disease that should be treated aggressively. Rituximab-containing chemotherapy such as R-CHOP has shown promise by increasing the overall survival of patients with this disease. R-CHOP combined with CNS prophylaxis and autologous stem cell transplant may further increase overall survival, but further studies with larger sample sizes are needed to establish the best treatment option and decide whether surgery and radiation have a role in the management of PAL.
Abbreviations
Cyclophosphamide, doxorubicin, vincristine, and prednisone
Central nervous system
Computed tomography
Diffuse large B-cell lymphoma
Fluorodeoxyglucose
International Prognostic Index
Lactate dehydrogenase
- Non-Hodgkin lymphoma
- Primary adrenal lymphoma
Positron emission tomography
Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone
Vinjamaram S, Estrada-Garcia DA, Hernandez-Ilizaliturri FJ. Non-Hodgkin lymphoma: practice essentials [updated 22 Sep 2016]. http://emedicine.medscape.com/article/203399-overview . Accessed 30 Sep 2016.
American Cancer Society. Cancer facts & figures 2016. Atlanta: American Cancer Society; 2016. https://old.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf . Accessed 6 Jul 2016.
Google Scholar
Kashyap R, Mittal B, Manohar K, Harisankar C, Bhattacharya A, Singh B, et al. Extranodal manifestations of lymphoma on [ 18 F]FDG-PET/CT: a pictorial essay. Cancer Imaging. 2011;11:166–74.
Article PubMed PubMed Central Google Scholar
Metser U, Goor O, Lerman H, Naparstek E, Even-Sapir E. PET-CT of extranodal lymphoma. AJR Am J Roentgenol. 2004;182:1579–86.
Article PubMed Google Scholar
Rashidi A, Fisher SI. Primary adrenal lymphoma: a systematic review. Ann Hematol. 2013;92:1583–93.
Article CAS PubMed Google Scholar
Laurent C, Casasnovas O, Martin L, Chauchet A, Ghesquieres H, Aussedat G, et al. Adrenal lymphoma: presentation, management and prognosis. QJM. 2017;110:103–9.
CAS PubMed Google Scholar
Grigg AP, Connors JM. Primary adrenal lymphoma. Clin Lymphoma. 2003;4:154–60.
Kim YR, Kim JS, Min YH, Hyunyoon D, Shin HJ, Mun YC, et al. Prognostic factors in primary diffuse large B-cell lymphoma of adrenal gland treated with rituximab-CHOP chemotherapy from the Consortium for Improving Survival of Lymphoma (CISL). J Hematol Oncol. 2012;5:49.
Article CAS PubMed PubMed Central Google Scholar
Ichikawa S, Fukuhara N, Inoue A, Katsushima H, Ohba R, Katsuoka Y, et al. Clinicopathological analysis of primary adrenal diffuse large B-cell lymphoma: effectiveness of rituximab-containing chemotherapy including central nervous system prophylaxis. Exp Hematol Oncol. 2013;2:19.
Download references
Acknowledgements
We are grateful to Dr. Sabeeh Siddique for providing the histological figures with explanations.
Availability of data and materials
Data sharing is not applicable to this article, because no datasets were generated or analyzed during the present study.
Authors’ contributions
NR conceived of the study and helped to draft the manuscript. OR and SF were involved in patient care and helped write the case presentation. IU and NI also helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Department of Medicine, Section of Endocrinology, Aga Khan University, Karachi, Pakistan
Nanik Ram, Owais Rashid, Imran Ulhaq & Najmul Islam
Aga Khan University, Stadium Road, Karachi, Pakistan
Saad Farooq
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Owais Rashid .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Ram, N., Rashid, O., Farooq, S. et al. Primary adrenal non-Hodgkin lymphoma: a case report and review of the literature. J Med Case Reports 11 , 108 (2017). https://doi.org/10.1186/s13256-017-1271-x
Download citation
Received : 10 November 2016
Accepted : 21 March 2017
Published : 15 April 2017
DOI : https://doi.org/10.1186/s13256-017-1271-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adrenal mass
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Non-Hodgkin's Lymphoma
- • Broad term for cancers that develop in the lymphocytes, which are white blood cells of the lymphatic system
- • Symptoms include swollen lymph nodes, fever, night sweats, fatigue, unintentional weight loss
- • Treatment includes chemotherapy, radiation therapy, immunotherapy, targeted therapy, active surveillance, surgery, stem cell transplant
- • Involves medical oncology, pediatric hematology and oncology, hematology
- Non-Hodgkin Lymphoma
- Diffuse Large B-Cell Lymphoma
- Hodgkin Lymphoma
- Follicular Lymphoma
What is non-Hodgkin's lymphoma?
What are the types of non-hodgkin's lymphoma, what are the symptoms of non-hodgkin's lymphoma, what are the risk factors for non-hodgkin lymphoma, how is non-hodgkin's lymphoma diagnosed, how is non-hodgkin's lymphoma treated, what is the outlook for people with non-hodgkin's lymphoma, what makes yale medicine unique in its treatment of non-hodgkin's lymphoma.
When a person has painless, enlarged lymph nodes that don’t shrink after a short period of time, doctors may suspect lymphoma, especially if they have had unexplained weight loss or other concerning symptoms, like fever or night sweats.
Doctors classify lymphomas—cancers of the white blood cells known as lymphocytes—into two broad categories: Hodgkin's lymphoma and non-Hodgkin's lymphoma. The conditions have some overlapping symptoms, but doctors (i.e. hematopathologists) tell the difference between the lymphomas by reviewing a biopsy of the affected cells.
More than 81,000 Americans are diagnosed with non-Hodgkin's lymphoma each year, including around 800 children and teenagers. It’s more common among males, older adults, and people with European ancestry.
Non-Hodgkin's lymphoma may occur at any number of places within the body. Some types are slow-spreading—without many symptoms—while others are aggressive, spreading quickly with notable symptoms. Different types of non-Hodgkin's lymphoma respond to treatment differently, and some types have better prognoses than others.
“Since there are more than 60 different subtypes of non-Hodgkin lymphoma, adequate tissue biopsy and review by experienced pathologists is a key first step to managing a new diagnosis of lymphoma,” says Scott Huntington, MD , an Associate Professor of Internal Medicine (Hematology) at Yale Cancer Center.
Non-Hodgkin's lymphoma is an umbrella term for several different types of cancer of the lymphocytes, which are white blood cells found within the lymphatic system, part of the immune system. These non-Hodgkin's cancers don’t contain Reed-Sternberg cells, which are the name for the abnormal cells present in people with Hodgkin's lymphoma.
Within the immune system, different lymphocytes help to keep people healthy in different ways:
- B cells produce antibodies that help people fight infections
- T cells assist B cells, allowing them to create antibodies, which fight infection
- Natural killer (NK) cells fight viruses and cancer cells
All of these specialized white blood cells exist within the lymphatic system, a series of vessels that connect the lymph nodes throughout the body. Within the lymph nodes, these lymphocytes help to filter harmful cells out of the fluid traveling through the lymphatic system.
Other elements of the lymphatic system include the bone marrow, spleen, tonsils, adenoids and thymus, as well as parts of the digestive system and central nervous system.
Someone develops non-Hodgkin's lymphoma when their B-cell, T-cell or NK-cell lymphocytes mutate and multiply uncontrollably. Most commonly, the B cells are affected. (The most common type of non-Hodgkin's lymphoma is diffuse large B-cell lymphoma.)
Non-Hodgkin's lymphoma may develop within the lymph nodes, bone marrow, or any other lymphatic tissue in the body. For example, primary central nervous system (CNS) lymphoma develops in lymph tissue within the brain or spinal cord.
Commonly diagnosed types of non-Hodgkin's lymphoma include:
- Diffuse large B-cell lymphoma
- Follicular lymphoma
- Burkitt lymphoma
- Mantle cell lymphoma
- Anaplastic large cell lymphoma
- Mucosa-associated lymphoid tissue lymphoma
- Extranodal marginal zone lymphoma
- Peripheral T-cell lymphoma
- Small lymphocytic lymphoma or chronic lymphocytic leukemia
Non-Hodgkin's lymphoma may cause a number of symptoms, including:
- Painless, enlarged lymph nodes, often in the neck, armpits, or groin
- Night sweats
- Unintentional weight loss
- Pain in the chest or abdomen
Additionally, some types of non-Hodgkin's lymphoma affect organs outside of the lymphatic system, which may lead to symptoms specific to those organs. If the brain is affected (such as in Central Nervous System [CNS] lymphoma), people may experience neurological symptoms, or if the intestines are involved, people may have gastrointestinal problems.
Doctors don’t know why non-Hodgkin's lymphoma develops, but people who are at greater risk of non-Hodgkin's lymphoma include those who have, or have had:
- An inherited immune disorder
- Epstein-Barr virus (EBV), which may manifest as infectious mononucleosis (mono)
- Human immunodeficiency virus (HIV)
- Hepatitis B or C
- Organ transplants, because of the daily immunosuppressant medication
- Autoimmune diseases, such as Sjögren syndrome, rheumatoid arthritis, Hashimoto’s disease or celiac disease
- History of prior Hodgkin's lymphoma
Additionally, people are at greater risk if they have been exposed to:
- Agricultural chemicals, such as herbicide or insecticide
- Organic solvents, which may be used in paints, glues, dyes and other products
- Radiation therapy
- A high-fat diet
- Ultraviolet radiation Smoking
Doctors confirm non-Hodgkin's lymphoma with a biopsy, but they may suspect the condition after learning about a person’s symptoms, including fever and unexplained weight loss.
During a physical exam, doctors look for enlarged lymph nodes in the neck, chest, and/or groin area. They also ask questions about a patient’s medical history, including HIV status, hepatitis status, whether someone has an autoimmune disease and if they’ve been exposed to certain chemicals at work. Additionally, doctors ask about a family history of non-Hodgkin's lymphoma and other conditions.
When doctors suspect non-Hodgkin's lymphoma, they may ask for additional tests, including a CT scan, a PET scan, blood tests, and a biopsy.
To confirm a suspected diagnosis, doctors surgically remove a lymph node or a section of a lymph node, then biopsy the tissue. They may also biopsy someone’s bone marrow to check for the condition before making a diagnosis, since the bone marrow may be affected.
A variety of treatment approaches may be used for people with non-Hodgkin's lymphoma. Some are appropriate for people with low-grade or slow-spreading disease, while others are recommended for people with aggressive or advanced disease.
Options include:
- An active surveillance approach, which may be right for people with low-grade non-Hodgkin's lymphoma that doesn’t need treatment upon diagnosis
- Chemotherapy, which combines a number of chemotherapy drugs that are designed to target different types of non-Hodgkin's lymphoma
- Targeted therapy, which attacks cancer cells in different ways than chemotherapy drugs
- Immunotherapy, such as monoclonal antibodies or chimeric antigen receptor (CAR) T-cell therapy, which may help the person’s immune system fight the cancer more aggressively
- Radiation therapy, which may be effective when non-Hodgkin's lymphoma is localized and hasn’t moved beyond the lymph nodes; or it may be given to someone after chemotherapy or another treatment regimen. Because possible long-term side effects from radiation therapy can be serious, doctors may avoid using it—or use only low-dose radiation—to treat children.
- Stem cell transplantation with high-dose chemotherapy, which may be given to people who don’t respond well to other treatments or those who relapse
The long-term prognosis for non-Hodgkin's lymphoma varies, depending on the type of disease and whether it’s slow-spreading or aggressive, in addition to other factors, such as a person’s age and overall health. The outlook for most kids and adolescents with non-Hodgkin's lymphoma is good, with survival rates over 90% for those with early-stage disease and between 80% and 90% for more advanced non-Hodgkin lymphoma.
“Diagnostic evaluation and treatments available for non-Hodgkin lymphoma have changed dramatically over the last decade,” says Dr. Huntington. “Yale has expertise across the non-Hodgkin lymphoma care continuum, including pathologists reviewing biopsy specimens, radiologists helping with lymphoma staging, expert clinicians in hematology/oncology, and therapeutic radiation to help optimize treatment outcomes. The multidisciplinary group of physicians, advanced practitioners, nurses, and support staff provide the highest level of care and help facilitate the delivery of several innovative treatment modalities (including stem cell transplantation, and chimeric antigen receptor T cell treatment), which are not available at other Connecticut centers.”
- Patient Care & Health Information
- Diseases & Conditions
- Non-Hodgkin's lymphoma
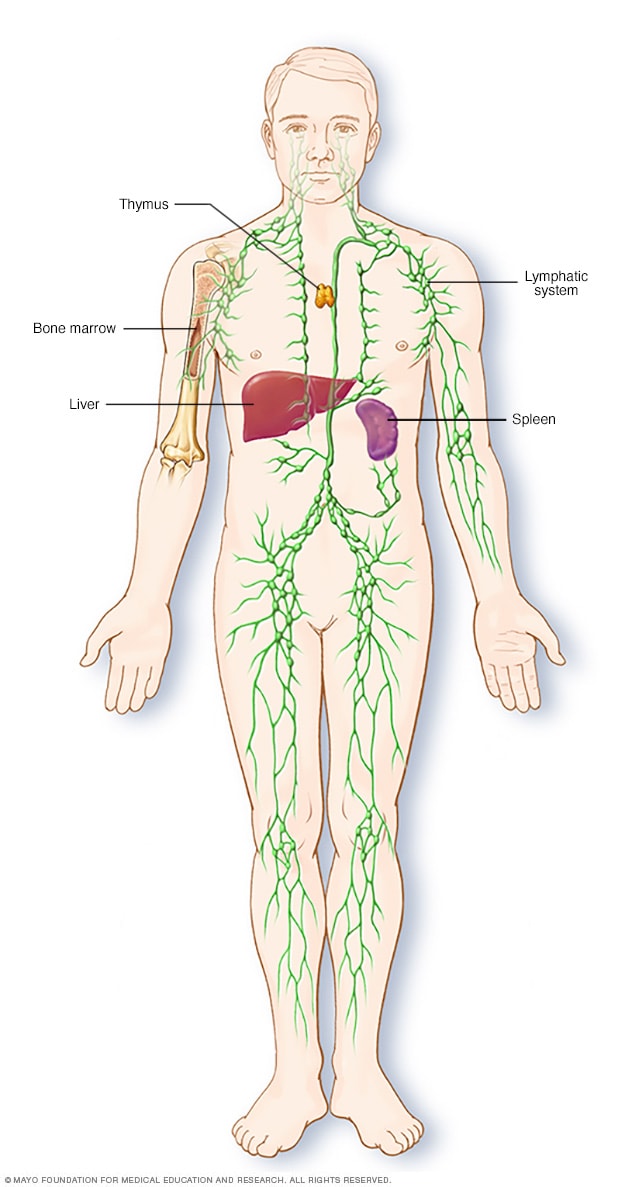
Parts of the immune system
The lymphatic system is part of the body's immune system, which protects against infection and disease. The lymphatic system includes the spleen, thymus, lymph nodes and lymph channels, as well as the tonsils and adenoids.
Non-Hodgkin's lymphoma is a type of cancer that begins in your lymphatic system, which is part of the body's germ-fighting immune system. In non-Hodgkin's lymphoma, white blood cells called lymphocytes grow abnormally and can form growths (tumors) throughout the body.
Non-Hodgkin's lymphoma is a general category of lymphoma. There are many subtypes that fall in this category. Diffuse large B-cell lymphoma and follicular lymphoma are among the most common subtypes. The other general category of lymphoma is Hodgkin's lymphoma.
Advances in diagnosis and treatment of non-Hodgkin's lymphoma have helped improve the prognosis for people with this disease.
Products & Services
- A Book: Living Medicine
- Mayo Clinic Comprehensive Cancer Center
- Chronic lymphocytic leukemia
- Cutaneous B-cell lymphoma
- Cutaneous T-cell lymphoma
- Follicular lymphoma
- Waldenstrom macroglobulinemia
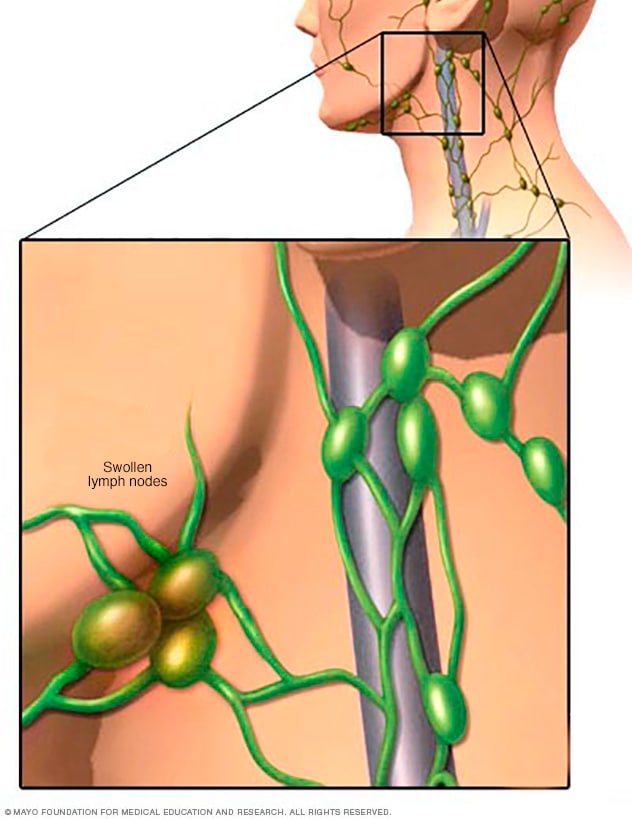
Swollen lymph nodes
One of the most common places to find swollen lymph nodes is in the neck. The inset shows three swollen lymph nodes below the lower jaw.
Signs and symptoms of non-Hodgkin's lymphoma may include:
- Swollen lymph nodes in your neck, armpits or groin
- Abdominal pain or swelling
- Chest pain, coughing or trouble breathing
- Persistent fatigue
- Night sweats
- Unexplained weight loss
When to see a doctor
Make an appointment with your doctor if you have any persistent signs and symptoms that worry you.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get Mayo Clinic cancer expertise delivered to your inbox.
Subscribe for free and receive an in-depth guide to coping with cancer, plus helpful information on how to get a second opinion. You can unsubscribe at any time. Click here for an email preview.
Error Select a topic
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Your in-depth coping with cancer guide will be in your inbox shortly. You will also receive emails from Mayo Clinic on the latest about cancer news, research, and care.
If you don’t receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
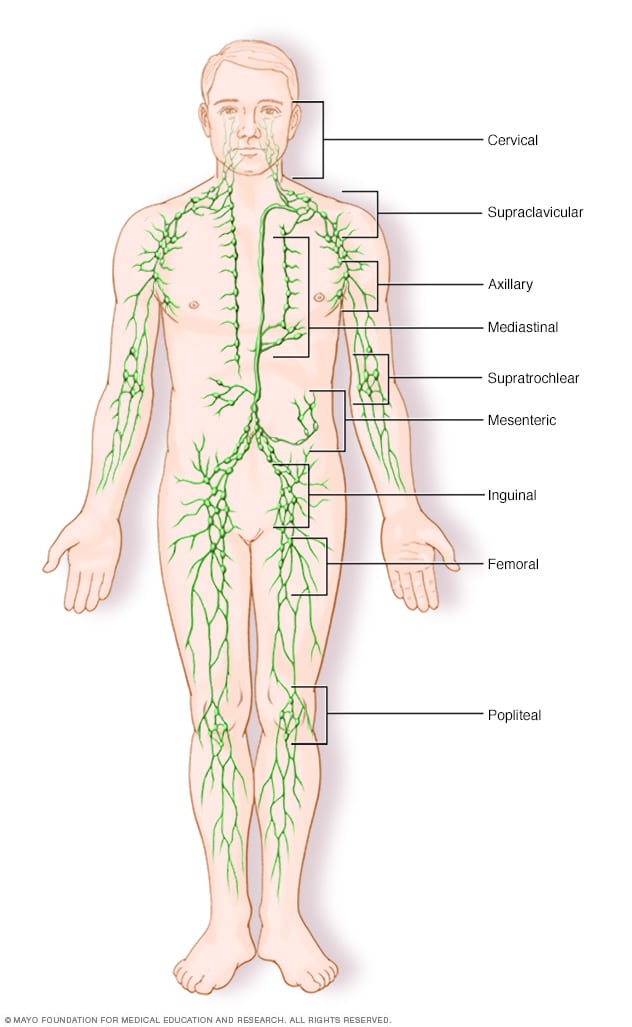
Lymph node clusters
Lymph nodes are bean-sized collections of cells called lymphocytes. Hundreds of these nodes cluster throughout the lymphatic system, for example, near the knee, groin, neck and armpits. The nodes are connected by a network of lymphatic vessels.
In most instances, doctors don't know what causes non-Hodgkin's lymphoma. It begins when your body produces too many abnormal lymphocytes, which are a type of white blood cell.
Normally, lymphocytes go through a predictable life cycle. Old lymphocytes die, and your body creates new ones to replace them. In non-Hodgkin's lymphoma, your lymphocytes don't die, and your body keeps creating new ones. This oversupply of lymphocytes crowds into your lymph nodes, causing them to swell.
B cells and T cells
Non-Hodgkin's lymphoma most often begins in the:
- B cells. B cells are a type of lymphocyte that fights infection by producing antibodies to neutralize foreign invaders. Most non-Hodgkin's lymphoma arises from B cells. Subtypes of non-Hodgkin's lymphoma that involve B cells include diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma and Burkitt lymphoma.
- T cells. T cells are a type of lymphocyte that's involved in killing foreign invaders directly. Non-Hodgkin's lymphoma occurs much less often in T cells. Subtypes of non-Hodgkin's lymphoma that involve T cells include peripheral T-cell lymphoma and cutaneous T-cell lymphoma.
Whether your non-Hodgkin's lymphoma arises from your B cells or T cells helps to determine your treatment options.
Where non-Hodgkin's lymphoma occurs
Non-Hodgkin's lymphoma generally involves the presence of cancerous lymphocytes in your lymph nodes. But the disease can also spread to other parts of your lymphatic system. These include the lymphatic vessels, tonsils, adenoids, spleen, thymus and bone marrow. Occasionally, non-Hodgkin's lymphoma involves organs outside of your lymphatic system.
Risk factors
Most people diagnosed with non-Hodgkin's lymphoma don't have any obvious risk factors. And many people who have risk factors for the disease never develop it.
Some factors that may increase the risk of non-Hodgkin's lymphoma include:
- Medications that suppress your immune system. If you've had an organ transplant and take medicines that control your immune system, you might have an increased risk of non-Hodgkin's lymphoma.
- Infection with certain viruses and bacteria. Certain viral and bacterial infections appear to increase the risk of non-Hodgkin's lymphoma. Viruses linked to this type of cancer include HIV and Epstein-Barr infection. Bacteria linked to non-Hodgkin's lymphoma include the ulcer-causing Helicobacter pylori.
- Chemicals. Certain chemicals, such as those used to kill insects and weeds, may increase your risk of developing non-Hodgkin's lymphoma. More research is needed to understand the possible link between pesticides and the development of non-Hodgkin's lymphoma.
- Older age. Non-Hodgkin's lymphoma can occur at any age, but the risk increases with age. It's most common in people 60 or over.
Non-Hodgkin's lymphoma care at Mayo Clinic
Living with non-hodgkin's lymphoma?
Connect with others like you for support and answers to your questions in the Blood Cancers & Disorders support group on Mayo Clinic Connect, a patient community.
Blood Cancers & Disorders Discussions

374 Replies Sat, May 11, 2024

4 Replies Thu, May 09, 2024

58 Replies Thu, May 09, 2024
- AskMayoExpert. Diffuse large B-cell lymphoma (adult). Mayo Clinic; 2018.
- B-cell lymphomas. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed Feb. 5, 2021.
- T-cell lymphomas. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed Feb. 5, 2021.
- Hoffman R, et al. Diagnosis and treatment of diffuse large B-cell lymphoma and Burkitt lymphoma. In: Hematology: Basic Principles and Practice. 7th ed. Elsevier; 2018. https://www.clinicalkey.com. Accessed Feb. 5, 2021.
- Lymphoma — Non-Hodgkin. Cancer.Net. https://www.cancer.net/cancer-types/41246/view-all. Accessed Feb. 11, 2021.
- Laurent C, et al. Impact of expert pathologic review of lymphoma diagnosis: Study of patients from the French Lymphopath Network. Journal of Clinical Oncology. 2017; doi:10.1200/JCO.2016.71.2083.
- Distress management. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed Feb. 11, 2021.
- Nowakowski GS, et al. Integrating precision medicine through evaluation of cell of origin treatment planning for diffuse large B-cell lymphoma. Blood Cancer Journal. 2019; doi:10.1038/s41408-019-0208-6.
- Lymphoma SPOREs. National Cancer Institute. https://trp.cancer.gov/spores/lymphoma.htm. Accessed Feb. 11, 2021.
- Warner KJ. Allscripts EPSi. Mayo Clinic. Jan. 7, 2021.
- Member institutions. Alliance for Clinical Trials in Oncology. https://www.allianceforclinicaltrialsinoncology.org/main/public/standard.xhtml?path=%2FPublic%2FInstitutions. Accessed Feb. 11, 2021.
- Member institution lists. NRG Oncology. https://www.nrgoncology.org/About-Us/Membership/Member-Institution-Lists. Accessed Feb. 11, 2021.
- Pruthi RK (expert opinion). Mayo Clinic. Feb. 22, 2021.
Associated Procedures
- Bone marrow biopsy
- Bone marrow transplant
- Chemotherapy
- Positron emission tomography scan
- Radiation therapy
News from Mayo Clinic
- All-Star pitcher Liam Hendriks shares how he closed out cancer at Mayo Clinic in Arizona July 21, 2023, 10:08 p.m. CDT
- Mayo Clinic Q and A: What is lymphoma? Nov. 03, 2022, 01:04 p.m. CDT
- Researchers seek to improve success of chimeric antigen receptor-T cell therapy in non-Hodgkin lymphoma May 12, 2022, 07:04 p.m. CDT
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Jacksonville, Florida, and Mayo Clinic in Phoenix/Scottsdale, Arizona, have been recognized among the top Cancer hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Submit Manuscript


Oncology Letters
- International Journal of Oncology
- Molecular and Clinical Oncology
- Experimental and Therapeutic Medicine
- International Journal of Molecular Medicine
- Biomedical Reports
- Oncology Reports
- Molecular Medicine Reports
- World Academy of Sciences Journal
- International Journal of Functional Nutrition
- International Journal of Epigenetics
- Medicine International

- Journal Home
- Current Issue
- Forthcoming Issue
- Open Special Issues
- About Special Issues
- Submit Paper
- Past Two Years
- Past Year 0
- Information
- Online Submission
- Information for Authors
- Language Editing
- Information for Reviewers
- Editorial Policies
- Editorial Board
- Join Editorial Board
- Aims and Scope
- Abstracting and Indexing
- Bibliographic Information
- Information for Librarians
- Information for Advertisers
- Reprints and permissions
- Contact the Editor
- General Information
- About Spandidos
- Conferences
- Job Opportunities
- Terms and Conditions
Non-Hodgkin's lymphoma with uncommon clinical manifestations: A case report
- Yu‑Long Cai
- Xian‑Ze Xiong
- Nan‑Sheng Cheng
View Affiliations
- Corresponding author: Author name
- Published online on: July 15, 2015 https://doi.org/10.3892/ol.2015.3493
- Pages: 1686-1688
This article is mentioned in:
Introduction.
Extranodal lymphoma occurs in ~40% of all patients with lymphoma and has been described in virtually all organs and tissue ( 1 ). Extranodal disease is more common with non-Hodgkin's lymphoma (NHL) ( 2 ), and diffuse large B-cell lymphoma (DLBCL) is the most common histological NHL subtype in adults, accounting for ~25% of all NHL cases ( 3 ). Thus, it is known that gastrointestinal DLBCL is the most frequent form of extranodal lymphoma ( 4 ). However, DLBCL primarily arising in the retroperitoneal region has been rarely reported. The largest series on retroperitoneal DLBCL was published by Pileri et al in 2001 ( 5 ). Moreover, to the best of our knowledge, primary retroperitoneal lymphoma without renal and ureteral involvement affecting the genitourinary system has not been reported until now.
Here, we report the extremely rare case of a young female suffering with primary DLBCL located in the retroperitoneal and gastrointestinal region simultaneously. Unusually, the first symptom of this disease was renal colic. Written informed consent was obtained from the patient for inclusion in the present study.
Case report
Case presentation.
A 33-year-old female presented with a 2-month history of renal colic and abdominal pain, which became aggravated at night. No fever was noted, but there was hematuria when the pain occurred. The patient's weight remained unchanged. Her family history was not contributory. Surgical history included two Caesarean sections 13 and 9 years prior.
Physical examination revealed an ill-defined mass in the right lower hypogastrium and tenderness in the abdomen, but without abdominal distention. There were no enlarged or palpable lymph nodes. The remaining systemic examination was not significant. The peripheral blood count was unremarkable (hemoglobin 109 g/l, red blood cell count 3.81×10 12 /l, white blood cell count 3.05×10 9 /l, and platelet count 230×10 9 /l). The peripheral blood smear revealed no immature cells (66.2% neutrophils, 25.6% lymphocytes, 7.2% monocytes, 1.0% eosinophils and 0.0% basophils). Liver and renal functional tests, bilirubin and electrolytes were normal. Serum tumor markers were negative with the exception of CA-125 values of 63.88 U/ml (normal value, <35 U/ml). The remaining laboratory tests were all within the normal limits.
A normal chest X-ray was obtained. An abdominopelvic contrast-enhanced computed tomography (CT) scan ( Fig. 1 ) revealed: i) A bulky soft-tissue dense mass in the middle of the ascending colon and superior to the ileocecum; heterogeneous enhancement following enhanced scan; thickened anterior of the renal fascia of the right kidney and local parietal peritoneum. ii) Multiple renal cysts in both kidneys. The CT scan did not indicate any bowel involvement, distant metastasis or abdominal lymph node enlargement. The abdominal ultrasound did not reveal any coexisting lesion in the hepato-pancreato-biliary system. Single-photon emission computed tomography (SPECT) renal imaging (99mTc-DTPA) revealed that the glomerular filtration rate was slightly decreased and the upper urinary tract had unobstructed drainage in the two kidneys.
Surgical treatment
Since the tumor had no distant involvement and there was no evidence of worsening symptoms (renal colic and abdominal pain), the patient underwent surgical resection. Intra-operative findings were as follows: no ascites were in the abdominal cavity; no dilation of the small and large bowel; the mass was predominantly located in the right mesocolon and retroperitoneal region, and extended to the distal ileum, ascending colon and the beginning of the transverse colon. Intra-operative biopsy and frozen section study indicated malignancy but did not confirm the tumor type. Complete excision was performed, retaining the right kidney and right ureter due to their lack of involvement. Side-to-side anastomosis of the transverse colon and ileum was used. The patient had an uneventful postoperative recovery. She was discharged from the surgical ward and referred to the hematology clinic for additional evaluation and adjuvant chemotherapy.
Pathological evaluation
The tumor consisted of two masses. The first mass (measuring 9×8×7 cm) was located in the retroperitoneal region, and the second (measuring 2.5×2×2 cm) was located in the mucosa of the ileum, involving the submucosa and muscularis layers as well as the serosa. There was no association between the two masses.
Pathological assessment was performed using immunohistochemistry staining, which revealed positivity for CD20 and Ki67) ( Fig. 2 ). DLBCL was the final confirmed diagnosis.
The patient's general condition remained good and she went on to receive CHOP chemotherapy. After 3 months of follow-up, no postoperative complications were identified.
DLBCL is the most common type of lymphoma worldwide ( 6 ). However, NHL rarely presents with a retroperitoneal or pelvic mass; during post-mortem studies of NHL patients an incident of less than 1% incidence was noted ( 7 ). Due to the uncommon anatomical location, the diagnosis and subsequent management of these patients tend to be difficult. The initial presentation of NHL varies depending on the subtype and involved area, with symptoms including enlarged palpable lymphadenopathy, B-symptoms (fever, weight loss, night sweats), and symptoms secondary to compression of adjacent structures. This is a unique case of retroperitoneal DLBLC, in which the first manifestation was renal colic.
Renal colic mainly occurs in patients with renal or ureteral calculus. Based on the findings of the abdominal CT, abdominal X-ray and SPECT renal imaging, our patient did not suffer with renal or ureteral calculus. Certain studies have reported that the genitourinary system may be affected by retroperitoneal NHL. Domazetovski et al ( 8 ) presented a case of acute renal failure in a patient with DLBLC, and Jaeger et al ( 9 ) reported DLBLC in a male presenting with ureteral stricture. However, the majority of cases have primary renal lymphoma or renal involvement. Renal colic alone without genitourinary involvement, as observed in our patient, is extremely rare, and could only be confirmed by surgery in our case. When the patient initially presented at our hospital, we considered that malignant retroperitoneal tumors account for ~0.1% of all malignancies ( 10 ) and are more common than benign tumors in the retroperitoneal space ( 11 ). As the symptom of renal colic was increasing, it was speculated that there was a high possibility of renal involvement. It is known that the most effective treatment is surgical removal of the tumors, with the exception of chemosensitive tumors, and that a definitive diagnosis can usually be made from the surgical specimens ( 12 ). Thus, considering the patient's wishes, surgery was performed.
Unexpectedly, the tumors were located not only in the retroperitoneal region, but also in the ileum. The latter was relatively small, therefore no signs or symptoms had been noted. According to our pathological evaluation, there was no association between the two masses. Literature regarding this condition is lacking, thus a reasonable explanation may be the variety of extranodal lymphoma. Moreover, surgery indicated that the tumor did not infiltrate the renal or ureteral areas. Thus, renal colic was determined to have been the result of compression.
Although CT is the diagnostic modality of choice ( 13 ), magnetic resonance imaging (MRI) offers superior soft-tissue contrast in comparison with CT. Indeed, a variety of contrast mechanisms have previously been explored for the characterization of lymphoma in the retroperitoneum, including T2-weighted imaging, diffusion-weighted imaging and dynamic contrast-enhanced imaging ( 14 ). The absence of MRI is a limitation in our diagnostic process. In the study of Tambo et al ( 12 ), a clinicopathological review of 46 primary retroperitoneal tumors identified that MRI imaging diagnosis prior to surgery was compatible with the histological diagnosis in only 26 patients (57%), and all six malignant lymphoma patients underwent biopsy or surgical resection. Therefore, if clinical diagnosis cannot be determined by MRI, definitive histological diagnosis by biopsy or tumor resection is required in order to determine the appropriate treatment.
Currently, CHOP therapy is the treatment of choice for DLBLC patients. Since rituximab is a chimeric anti-CD20 IgG1 monoclonal antibody which is a cell surface protein that occurs almost exclusively in mature B-cells, the combination of rituximab and CHOP is likely become the standard for treating patients with DLBLC ( 15 ). The prognosis has improved in recent years owing to the development of various aggressive chemotherapeutic regimens depending on the histological type, stage and age of each patient. Therefore, a definitive histological diagnosis is essential for patients with DLBLC. Our patient did not present with any specific indications for the diagnosis of this rare tumor as the initial manifestation was renal colic. Surgery has a key role in establishing a definitive diagnosis.
Primary retroperitoneal DLBLC has a variable and non-specific presentation and may resemble other neoplastic or inflammatory conditions. Manifestations, laboratory data and imaging alone may initially lead to an incorrect diagnosis. Obtaining a definitive histological diagnosis by surgery and using appropriate chemotherapy played an essential role in the recovery of our patient. This case study indicates the significance of including a differential diagnosis of primary retroperitoneal NHL in patients presenting with a retroperitoneal mass where the first sign of this disease is renal colic.
- Related Articles
September-2015 Volume 10 Issue 3
Print ISSN: 1792-1074 Online ISSN: 1792-1082
Sign up for eToc alerts
Recommend to Library
- Article Options
- Download article ▽ Download PDF Download XML View XML
- View Abstract
- Cite This Article
- Download Citation
- Create Citation Alert
- Remove Citation Alert
- on Spandidos Publications
- Similar Articles
- on Google Scholar
- © Get Permissions
- Journal Metrics
- Impact Factor: 2.9
- Ranked Oncology (total number of cites)
- CiteScore: 6.3
- CiteScore Rank: Q2: #119/366 Oncology
- Source Normalized Impact per Paper (SNIP): 0.725
- SCImago Journal Rank (SJR): 0.639

This site uses cookies
You can change your cookie settings at any time by following the instructions in our Cookie Policy . To find out more, you may read our Privacy Policy . I agree
- Cookie Policy
- Privacy Policy
Advances in Lymphoma Research
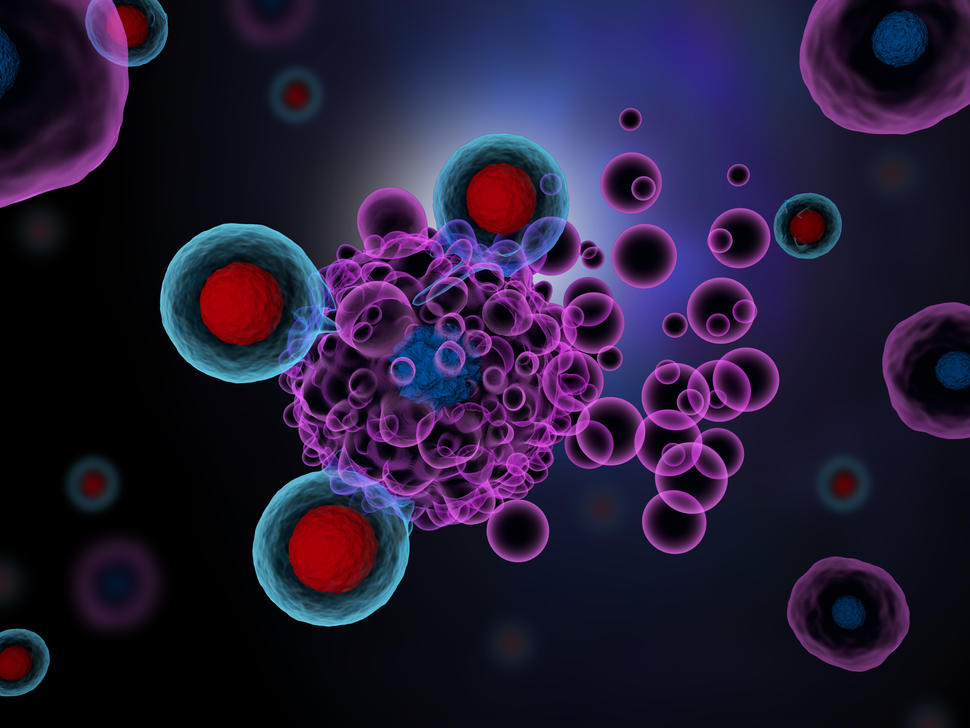
Artist’s rendering of T cells (red and blue spheres) attacking cancer cells. T-cell therapy has been effective in treating certain lymphoma patients.
NCI-funded researchers are working to advance our understanding of how to treat lymphoma . All lymphomas start in the cells of the lymph system , which is part of the body’s immune system. Lymphomas are grouped into two main types: Hodgkin lymphoma and non-Hodgkin lymphoma (sometimes called NHL). But more than 70 different subtypes of the disease exist. Advances in understanding the gene changes that can lead to lymphoma are now helping scientists design more personalized treatments for these subtypes.
This page highlights some of the latest lymphoma research, including clinical advances that may soon translate into improved care and research findings from recent studies.
Treatment of Non-Hodgkin Lymphoma (NHL)
Most people diagnosed with lymphoma have a subtype of non-Hodgkin lymphoma. Non-Hodgkin lymphoma can either be aggressive or indolent .
Aggressive non-Hodgkin lymphoma grows and spreads quickly and usually requires immediate treatment. With modern treatment regimens, almost 70% of people with aggressive non-Hodgkin lymphoma will be considered cured. Research is now largely focused on finding better treatments for the minority of people with aggressive lymphoma who are not cured with initial therapy.
Indolent non-Hodgkin lymphoma grows slowly, and in some cases may not cause symptoms for years. People with indolent disease can often postpone treatment until their symptoms worsen, with no negative effects on survival. But sometimes an indolent lymphoma can turn into aggressive lymphoma, which requires immediate treatment.
Indolent non-Hodgkin lymphoma largely cannot be cured. The past two decades have seen improvements in extending the survival of people who are treated for this type of lymphoma. However, researchers are studying how to improve long-term survival further and working toward potentially curative treatments.
Chemotherapy , radiation therapy , targeted therapy , and immunotherapy are all used in the treatment of non-Hodgkin lymphoma. A stem cell transplant is sometimes used for lymphoma that has recurred, but this procedure has serious side effects. Four CAR T-cell therapies have been approved to treat some types of recurrent lymphoma. However, these newer therapies still can't cure many people with recurrent lymphoma.
Most research on treatment for non-Hodgkin lymphoma is now focused on targeted therapy and immunotherapy. Researchers are also trying to identify gene changes in different types of lymphoma that might be targets for new drug development.
For example, in 2018, a study led by NCI researchers identified genetic subtypes of diffuse large B-cell lymphoma (the most common type of non-Hodgkin lymphoma) that could help explain why some patients with the disease respond to treatment and others don’t. Further studies may lead to more tailored treatments for patients with this type of lymphoma.
New targeted therapies
A signaling pathway is a series of chemical reactions that control one or more cell functions. Many types of non-Hodgkin lymphoma are driven by a signaling pathway called the B-cell receptor signaling pathway. A drug called ibrutinib (Imbruvica) has been developed to shut down that pathway. It is being used and tested in a number of ways:
- In the last several years, the drug has been approved for the treatment of small lymphocytic lymphoma and Waldenstrom macroglobulinemia , both indolent non-Hodgkin lymphomas.
- NCI took part in a randomized clinical trial that tested the addition of ibrutinib to chemotherapy and rituximab (Rituxan) in people newly diagnosed with a certain type of diffuse large B-cell lymphoma . People over the age of 60 had worse outcomes with the addition of ibrutinib. However, patients under the age of 60 who were given ibrutinib had substantially improved survival .
- Other studies have suggested that people whose diffuse large B-cell lymphoma has specific genetic characteristics may especially benefit from treatment with ibrutinib .
- An early-phase NCI-sponsored study tested ibrutinib plus chemotherapy in people with primary central nervous system lymphoma , a very aggressive subtype of non-Hodgkin lymphoma. More than half of the patients in this small study went into complete, long-term remission. A larger study is now underway at the National Institutes of Health (NIH) Clinical Center . That study is also testing this combination in people with lymphoma that began elsewhere in the body but has spread to the central nervous system.
The FDA has approved two other drugs that target the B-cell receptor signaling pathway. Acalabrutinib (Calquence) is approved for relapsed mantle cell lymphoma and small lymphocytic lymphoma . An ongoing study at NCI is testing acalabrutinib, in combination with chemotherapy and rituximab , in people with previously untreated diffuse large B-cell lymphoma.
In 2019, zanubrutinib (Brukinsa) was approved for relapsed mantle cell lymphoma. A fourth drug targeting the B-cell receptor signaling pathway, called pirtobrutinib (Jaypirca) , is now being tested in clinical trials for several different types of non-Hodgkin lymphoma. In 2023, it was approved for the treatment of mantle cell lymphoma that has gotten worse after two or more previous treatments.
Many other targeted therapies are being tested in non-Hodgkin lymphoma. Some that are approved for specific subtypes are listed below.
- Polatuzumab vedotin (Polivy) for the treatment of diffuse large B-cell lymphoma . Clinical trials are testing this drug and related drugs for other types of non-Hodgkin lymphoma.
- Venetoclax (Venclexta) for chronic lymphocytic leukemia and small lymphocytic lymphoma.
- Loncastuximab (Zynlonta) for large B-cell lymphoma that has recurred or did not shrink after other treatments .
- Selinexor (Xpovio) for large B-cell lymphoma that has recurred or did not shrink after other treatments .
- The combination of tafasitamab (Monjuvi) and lenalidomide (Revlimid) for people with large B-cell lymphoma who cannot undergo a stem cell transplant .
- Tazemetostat (Tazverik) for some people with follicular lymphoma that has recurred or did not shrink after other treatments .
However, in lymphoma, resistance to a single agent can occur quickly. Researchers are now testing combinations of targeted therapies to treat non-Hodgkin lymphoma to try to overcome this resistance. For example, ongoing trials led by NCI researchers are testing a five-drug regimen and a six-drug regimen in people with aggressive or indolent B-cell lymphomas whose cancer has relapsed or is resistant to treatment.
Researchers are also trying to make standard treatment regimens less toxic for older patients. In one study, NCI researchers found that the intensity of standard chemotherapy could be reduced in older adults with Burkitt lymphoma , an aggressive type of non-Hodgkin lymphoma, without compromising the potential for a cure.
Immunotherapy
Immunotherapy uses substances to stimulate or suppress the immune system to help the body fight cancer. Several immunotherapies have shown promise in treating different types of lymphoma.
CAR T cells. CAR T cells are a type of immunotherapy in which a patient's T cells, a type of immune cell, are changed in the laboratory so they will better attack cancer cells. Four CAR T-cell therapies have been approved for the treatment of non-Hodgkin lymphoma:
- Axicabtagene ciloleucel (Yescarta) for people with large B-cell lymphoma or follicular lymphoma whose cancer has progressed after receiving one prior treatment regimen.
- Tisagenlecleucel (Kymriah) for adults with one of three types of non-Hodgkin lymphoma .
- Lisocabtagene maraleucel (Breyanzi) for people with some types of B-cell non-Hodgkin lymphoma that has relapsed or has not gotten better after at least two other treatments.
- Brexucabtagene autoleucel (Tecartus) for some people with mantle cell lymphoma that has come back or did not get better with other treatments.
To date, CAR T cells have provided long-term remissions for about one third of adults with aggressive lymphoma who receive them. Large randomized trials have been comparing CAR T-cell therapy to autologous stem cell transplantation at first relapse. In one of these trials, more people who received the CAR T-cell therapy were alive four years after treatment compared with those who received chemotherapy followed by stem cell transplantation. Participants in the other trials are still being followed to see if differences in survival emerge over time.
A phase 2 trial tested CAR T cells as initial therapy in people at very high risk of relapse. In early results, over three-quarters of patients had their cancer go into remission. However, long term results are not yet available and CAR T cells are not FDA approved in this setting.
CAR T cells are also being tested in other lymphoma subtypes, both aggressive and indolent, as well as in patients with lymphoma that has spread to the central nervous system.
Immunomodulating drugs . Immunomodulators are drugs that either stimulate or suppress the immune system. One such drug, lenalidomide (Revlimid) , has been approved in combination with targeted therapies for previously treated follicular lymphoma and marginal zone lymphoma . It is also often used to treat diffuse large B-cell lymphoma.
Novel immunotherapies . Researchers are also testing novel ways to stimulate the immune system to fight lymphoma. In 2018, a small trial showed that combining radiation therapy with the injection of a compound that stimulates the immune system could shrink some indolent B-cell lymphomas. In 2019, a trial that used a vaccine to draw immune cells into tumors in people with indolent non-Hodgkin lymphoma also showed promising results . A phase 2 trial testing this strategy in combination with an immune checkpoint inhibitor is currently underway.
Immunotherapy drugs called bispecific antibodies are also under development. These drugs bind to lymphoma cells and the body’s own immune cells at the same time to bring them together. This allows the immune cells to kill the lymphoma cells. Five bispecific antibodies are in clinical trials for various types of lymphoma, including:
- glofitamab (Columvi), which in a phase 1 trial shrank aggressive lymphoma in people who had received several prior treatments
- epcoritamab (Epkinly), which also shrank previously treated aggressive lymphoma in an early-phase clinical trial
- mosunetuzumab (Mosun), which triggered long-lasting remissions in almost 20% of people with aggressive B-cell non-Hodgkin lymphoma and almost 50% of people with indolent B-cell non-Hodgkin lymphoma in an early-phase clinical trial
Glofitamab and epcoritamab have both received accelerated approval from the FDA for the treatment of some lymphomas that have returned or gotten worse after at least two other treatments.
Hodgkin Lymphoma Treatment
Hodgkin lymphoma is much less common than non-Hodgkin lymphoma. It is mostly seen in early adulthood (age 20–39) and in late adulthood (age 65 and older). More than 75% of all adults newly diagnosed with Hodgkin lymphoma can be cured with standard chemotherapy, radiation therapy, or both. Over the last 5 decades, deaths from Hodgkin lymphoma among adults have fallen more rapidly than deaths from any other cancer type.
Researchers are now focusing on adjusting standard treatment regimens to reduce the long-term side effects and improve quality of life for survivors. They are also testing better ways to treat the minority of patients whose cancer does recur.
Targeted therapies
A protein called CD30 is commonly found on the surface of Hodgkin lymphoma cells. A drug called brentuximab vedotin (Adcetris) that targets this protein has been approved as part of initial treatment for people with advanced Hodgkin lymphoma. Use of this new drug may help older patients avoid what had been the standard treatment with an especially toxic chemotherapy drug.
Clinical trials are now testing brentuximab vedotin combined with other chemotherapy drugs and with immunotherapies. The drug has also been approved by the FDA in combination with chemotherapy for some children and adolescents with Hodgkin lymphoma .
Immune checkpoint inhibitors that help T cells to better kill cancer cells have been effective in some people with recurrent Hodgkin lymphoma. Two such drugs— nivolumab (Opdivo) and pembrolizumab (Keytruda) —have been approved for some patients with Hodgkin lymphoma that has recurred after previous treatments. Researchers are now testing these drugs in combination with other therapies, as well as earlier in treatment for some people with cancer that is likely to recur.
NCI-Supported Research Programs
The Lymphoma Specialized Programs of Research Excellence (Lymphoma SPOREs) are designed to quickly move basic scientific findings into clinical settings. The Lymphoma SPOREs support the development of new immunotherapies, novel targeted therapies, and new methods for determining prognosis for individual patients.
The goal of the International Lymphoma Epidemiology Consortium (InterLymph) is to enhance collaboration among epidemiologists studying lymphoma, provide a forum for the exchange of research ideas, and create a framework for collaborating on analyses that compile data from multiple studies.
The Lymphoma Epidemiology of Outcomes (LEO) Cohort Study was established to address the current and long-term health needs of non-Hodgkin lymphoma patients and survivors. The goal is to support a broad research agenda aimed at identifying novel clinical, epidemiologic, host, genetic, tumor, and treatment factors that significantly influence non-Hodgkin lymphoma prognosis and survivorship.
The Cancer Genome Characterization Initiative (CGCI) is supporting research to identify common gene changes in adult and pediatric cancers. Its results are freely available to the wider cancer research community, to spur the development of new targeted drugs. The HIV+ Tumor Molecular Characterization Project (HTMCP) and Burkitt Lymphoma Genome Sequencing Project (BLGSP) are two active CGCI projects.
Within the Center for Cancer Research , the Lymphoid Malignancies Branch focuses on identifying abnormalities in the immune system and looking at molecular disorders that underlie lymphoid malignancies.
The Clinical Trial Sequencing Project (CTSP) promotes the use of genomics in NCI-sponsored clinical trials. CTSP’s goal is to clarify the molecular basis of response and resistance to therapies studied. Diffuse large B-cell lymphoma is one of the cancer types under study, along with breast and renal cell carcinoma.
Lymphoma Research Results
The following are some of NCI's latest news articles on lymphoma research:
- Cholesterol Drug May Help Protect the Heart during Chemotherapy for Lymphoma
- Three-Drug Regimen Improves Protection against GVHD after Stem Cell Transplant
- Trial Confirms CAR T-Cell Therapy Benefits People with Aggressive Lymphomas
- Brentuximab Approved for High-Risk Hodgkin Lymphoma in Children and Adolescents
- Should CAR T Cells Be Used Earlier in People with Non-Hodgkin Lymphoma?
- Ibrutinib Improves Survival for Younger People with Diffuse Large B-cell Lymphoma
View the full list of Lymphoma Research Results and Study Updates .
- Search Menu
- Advance articles
- Author Guidelines
- Submission Site
- Open Access
- Why Publish with JJCO?
- About Japanese Journal of Clinical Oncology
- Editorial Board
- Reviewer Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, case report.
- < Previous
Two Cases of Non-Hodgkin’s Lymphoma in First Degree Relatives
- Article contents
- Figures & tables
- Supplementary Data
Itsuro Ota, Kenji Shinohara, Kazuhiko Muraki, Naofumi Fukuda, Toru Takahashi, Ryohei Nawata, Yoko Shimohakamada, Two Cases of Non-Hodgkin’s Lymphoma in First Degree Relatives, Japanese Journal of Clinical Oncology , Volume 30, Issue 12, December 2000, Pages 571–573, https://doi.org/10.1093/jjco/hyd143
- Permissions Icon Permissions
Two cases of non-Hodgkin’s lymphoma (NHL) generated within 6 months in first degree relatives, a father and a son, are presented. The NHL was a diffuse large B-cell type in the father and a small cleaved follicular type in the son. Cytogenetic and molecular studies of the lymphoma cells revealed the rearrangement of the immunoglobulin heavy chain (JH) gene in both patients, the mutation of p53 gene in the father and t(14; 18) (q32; q21) in the son. Both patients had low serum immunoglobulin levels. It is not known whether the occurrence of NHL in this family was incidental or pathogenetically related, since there was no clear common molecular abnormality between the father and the son. The pathogenetic mechanism of this familial occurrence of NHL is discussed.
Received July 27, 2000; accepted October 10, 2000.
Hematological malignancy, including malignant lymphoma, acute leukemia, multiple myeloma, chronic lymphocytic leukemia and other myeloproliferative disorders, occurred 3.6 times more frequently in families with hematological malignacy compared with the control study groups of non-neoplastic hematological disorders ( 1 ). Thus it seems that hereditary factors may play an important role in the etiology of hematological malignancy.
There have been few reports of familial occurrences of malignant lymphoma including Hodgkin’s disease (HD) and non-Hodgkin’s lymphoma (NHL) ( 1 – 7 ). Genetic, infectious and environmental factors had been implicated in causing familial malignant lymphoma ( 1 – 7 ). The defective proto-oncogene and inactivation of the tumor suppressor gene, hereditary or acquired immune deficiency, vertical transmission of infectious agents, inability to detoxify carcinogens and exposure to harmful environmental factors may also be involved in the pathogenesis of familial NHL ( 1 – 7 ).
We present two cases of NHL of B-cell origin in first degree relatives, a father and a son, generated within a short period of each other, and discuss the possible common pathogenetic mechanism of the occurrence in these patients.
The pedigree chart is shown in Fig. 1 .
A 73-year-old male, a retired cloth maker, who had been suffering from chronic thyroiditis since September 1998, was admitted to our hospital. He complained of the neck lymph node swelling since March 1999. A thyroid tumor was not observed. Biopsy specimens of the lymph nodes revealed diffuse large cell NHL, and flow cytometric analysis of the lymphoma cells showed CD5 3.0%, CD10 1.1%, CD19 98.1%, CD20 98.3%. A gastroscopic examination of the stomach revealed multiple ulcers and biopsy showed the infiltration of lymphoma cells. HBs antigen and antibodies for HBs, HCV and human T-lymphotropic virus 1 (HTLV1) were negative. Antibodies for Epstein–Barr (EB) virus were not examined. Serum immunoglobulin levels at admission were IgG 400 mg/dl, IgA 98 mg/dl and IgM 17 mg/dl. These levels had not been measured before the onset of NHL. Soluble interleukin (IL)-2 receptor was 1380 u/ml (normal value 220–530 u/ml). Chromosome analysis of lymphoma cells did not reveal any abnormalities. The IgH (JH) gene had been rearranged. The rearrangement of the bcl-2 gene was studied by Southern blotting using a probe of 2.8 kb Eco RI– Hin dIII fragment in exon 3. The bcl-2 gene had not been rearranged. There had been no rearrangement of the chimeric IgH (JH)/ bcl-2 genes. A mutation of the nucleotide of the p53 gene in codon 175 of exon 5 from CAG (Arg) to CAC (His) was observed by Southern blotting and direct sequencing. The EB virus DNA was not observed. The NHL was refractory to repeated courses of chemotherapy consisting of five courses of THP–CVP (pirarubicin, cyclophosphamide, vincristine, prednisolone), three courses of CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) and one course of modified DHAP (dexamethasone, cytosine arabinoside, carboplatin). The patient died in January 2000.
A 43-year-old male, the son of the patient 1, was admitted to our hospital complaining of abdominal fullness in September 1999. The patients had been living together and the son had been working as a tire maker. Physical examination revealed a huge hepatomegaly reaching into the pelvic cavity and generalized lymph node swelling. Biopsy of the lymph nodes revealed small cleaved cell follicular NHL and flow cytometric analysis showed CD5 19.1%, CD10 38.1%, CD19 84.6%, CD20 80.5%. Peripheral blood revealed a WBC of 12 600/µl with 34% atypical lymphocytes. HBs antigen and antibodies for HBs, HCV and HTLV1 were negative. Anti-EB virus early antigen (EA)–DR IgG and viral capsid antigen (VCA) IgM were negative, whereas VCA IgG and Epstein–Barr nuclear antigen (EBNA) were positive. Serum immunoglobulin levels were IgG 674 mg/dl, IgA 85 mg/dl and IgM 9 mg/dl. Soluble IL-2 receptor was 12 800 u/ml. Chromosome analysis of lymphoma cells revealed (A) 46XY, t(14;18) (q32;q21) in 1/10 metaphases and (B) 46, idem add ( 1 ) (q32) in 9/10 metaphases. Rearrangement of the IgH (JH) gene was observed, but there was no change in the bcl-2 gene and the chimeric IgH(JH)/ bcl-2 . Mutation of the p53 gene was not observed. EB virus DNA was not observed. To date, the son’s NHL is responding to chemotherapy consisting of two courses of CHOP and four courses of modified DHAP followed by peripheral blood stem cell transplantation preconditioned with mitoxantrone, cyclophosphamide and etoposide.
The familial risk of NHL is influenced primarily by hematological malignancies rather than other cancers ( 7 ). The risk is associated with a history of lymphoma, the odds ratio being 3.0 in the first degree relatives relative to normal controls, and other hematological malignancies, the odds ratio being 2.0 ( 7 ). In another study, the familial relative risk (FRR) of NHL had been reported as 1.68 in the first degree relatives ( 5 ). Horizontal transmission in HD/HD pairs ( 6 ) and even concordance for HD in identical twins ( 2 ), and vertical transmission in NHL/NHL pairs, have been observed ( 6 ). The median difference in the age of incidence was markedly greater in NHL/NHL pairs than in HD/HD pairs ( 6 ). For NHL/NHL pairs, it was 21 (range 5–32) years, but only 3.5 (range 1–8) years for HD/HD pairs ( 6 ). There was a greater tendency for gender concordancy in NHL/NHL pairs, 75%, than in HD/HD and HD/NHL pairs, 39% ( 6 ). A higher familial risk of NHL for male relatives of male probands had been observed, and FRR was 3.18 for males and 1.09 for females ( 5 ). Our cases were in accordance with these results with the NHL generated in both a father and a son; the difference in the age of disease onset was 30 years, but, they occurred within a short period of 6 months.
Hereditary immune deficiency syndromes such as agammaglobulinemia, Wiskott–Aldrich syndrome and ataxia teleangiectasia ( 3 , 8 ), and acquired immune deficiency such as systemic lupus erythematosus, autoimmune thrombocytopenia or rheumatoid arthritis have frequently been reported in NHL/NHL pairs ( 3 , 6 ). It is also known that B-cell lymphoma frequently develops during immune deficiency after allogeneic bone marrow transplantation ( 9 ). The father in our case suffered from chronic thyroiditis, and chronic antigeneic stimulation in the pathogenesis of autoimmune disorders may cause B-lymphocyte stimulation for proliferation. In addition, both patients had low serum immunoglobulin levels when they were examined at admission. However, those in the father before onset of NHL had not been examined.
A two-hit theory for the pathogenesis of familial NHL has been considered. In the first hit, somatic mutation in proto-oncogene or deletion or inactivation of the tumor suppressor gene occurs, while the second hit might consist of environmental factors ( 1 ).
The bcl-2 gene was originally discovered owing to its involvement in the t(14;18) (q32;q21) translocation. The cytogenetic abnormality causes irregularities in the bcl-2 gene and Bcl-2 protein, and is found in the majority of follicular lymphoma and a variable number of diffuse large cell lymphoma ( 10 , 11 ). In the son, the t(14;18) (q32;q21) was observed,but rearrangements of the bcl-2 gene or chimeric bcl-2 /IgH (JH) genes were not observed. The rearrangements of these genes of B-cell lymphoma including folllicular lymphoma occur less frequently in Japan than in the USA ( 12 , 13 ). Also, the breakpoint of 18q21 in the present case may be differently located from the major breakpoint cluster region ( 13 , 14 ).
A relatively higher mutation of the p53 gene has been observed in B-cell intermediate-grade NHL, as in the father in this study, and in T cell high-grade immunoblastic NHL, in contrast to the relatively low mutation rate in other histopathological subtypes of low-grade NHL such as in follicular mixed or follicular small cleaved NHL ( 14 ). The most frequent genetic alteration that had been observed was a mis-sense mutation that was mainly detected within the region of exons 5–8 ( 14 ). The father in our study exhibited a similar mutation.
The NHL of both patients were pathologically different but they were both of B-cell origin. However, it is considered that most follicular lymphoma will undergo transformation into an aggressive lymphoma, usually exhibiting diffuse large cell histology ( 10 ). Indeed, the majority of hematological malignancy among family members did not belong to the same histological category ( 1 ). The familial link of NHL increased the risk of developing the low-grade follicular type of NHL ( 3 ). The son in our study also had this risk.
The vertical transmission of viruses such as hepatitis B and C, HTLV1 and EB can act as infectious agents for the pathogenesis of NHL ( 3 , 4 ); however, in our cases, the infection by hepatitis B and C virus and HTLV1 was negative, and EB virus DNA in the lymphoma cells was not observed.
Occupational and environmental factors could affect the pathogenesis of NHL ( 3 , 4 ). Farmers have an increased risk of NHL since they may be exposed to oncogenic viruses carried by farm animals and to pesticides ( 3 , 4 ). An increased risk of NHL through work with exposure to solvents, related chemicals and hair dyes has also been reported ( 3 , 4 ). In our study, the environmental and occupational risk factors were unknown; however, since NHL in both patients developed at almost the same time while they were living together, it is possible that environmental factors might have played some part in the development of NHL.
In conclusion, our findings suggest that there may be a possible common pathogenetic mechanism in these two cases of NHL in first degree relatives, although the precise mechanism is unknown. The understanding of gene–environment interactions may provide the answer.
For reprints and all correspondence: Kenji Shinohara, Division of Hematology, Department of Medicine, Yamaguchi Prefecture Central Hospital, Hofu 747-8511, Japan
Abbreviations: NHL, non-Hodgkin’s lymphoma; HD, Hodgkin’s disease; Ig, immunoglobulin; IgH (JH), immunoglobulin heavy chain; IL, interleukin; FRR, familial relative risk
Figure 1. The pedigree chart of the familial occurrence of non-Hodgkin’s lymphoma. The shaded squares indicated by arrows represent a father (I-3) and a son (II-2). The black squares and circles indicate dead persons. The other members are healthy and had not been engaged in special occupations. The age of each family member (years) and cause of death are also shown. Abbreviations: ut ca, uterine cancer; ac, accident.
1 Shpilberg O, Modan M, Modan B, Chetrit A, Fuchs Z, Ramot B. Familial aggregation of hematological neoplasms: a controlled study. Br J Haematol 1994 ; 87 : 75 –80.
2 Mack TM, Cozen W, Shibata DK, Weiss LM, Nathwani BN, Hernandez AM, et al. Concordance for Hodgkin’s disease in identical twins suggesting genetic susceptibility to the young-adult form of the disease. N Engl J Med 1995 ; 332 : 413 –8.
3 Linet MS, Pottern LM. Familial aggregation of hematopoietic malignancies and risk of non-Hodgkin’s lymphoma. Cancer Res 1992 ; 52 (Suppl): 5468 –73.
4 Pearce N, Bethwaite P. Increasing incidence of non-Hodgkin’s lymphoma: occupational and environmental factors. Cancer Res 1992 ; 52 (Suppl): 5496 –500.
5 Goldgar DE, Easton DF, Cannon-Albright LA, Skolnick MH. Systematic population-based assessment of cancer risk in first-degree relatives of cancer probands. J Natl Cancer Inst 1994 ; 86 : 1600 –8.
6 Siebert R, Louie D, Lacher M, Schluger A, Offit K. Familial Hodgkin’s and non-Hodgkin’s lymphoma: different patterns in first-degree relatives. Leukemia Lymphoma 1997 ; 27 : 503 –7.
7 Zhu K, Levine RS, Gu Y, Braun EA, Hall I, Caplan LS, et al. Non-Hodgin’s lymphoma and family history of maligant tumors in a case-controlled study (United States). Cancer Causes Control 1998 ; 9 : 72 –82.
8 Frizzera G, Rosai J, Dehner LP, Spector BD, Kersey JH. Lymphoreticular disorders in primary immunodeficiencies. New findings based on an up-to-date histologic classification of 35 cases. Cancer 1980 ; 46 : 692 –9.
9 Bhatia S, Ramsay NKC, Steinbuch M, Dusenbery KE, Shapiro RS, Weisdorf DJ, et al. Malignant neoplasms following bone marrow transplantation. Blood 1996 ; 87 : 3633 –9.
10 Tsujimoto Y, Cossman J, Jaffe E, Croce CM. Involvement of the bcl-2 gene in human follicular lymphoma. Science 1985 ; 228 : 1440 –3.
11 Gascoyne RD, Adomat SA, Krajewski S, Krajewska M, Horsman DE, Tolcher AW, et al. Prognostic significance of Bcl-2 protein expression and bcl-2 gene rearrangement in diffuse aggressive non-Hodgkin’s lymphoma. Blood 1997 ; 90 : 244 –51.
12 Osada H, Seto M, Ueda R, Emi N, Takagi N, Obata Y, et al. Bcl-2 gene rearrangement analysis in Japanese B-cell lymphoma; novel bcl-2 recombination with immunoglubulinκ chain gene. Jpn J Cancer Res 1989 ; 80 : 711 –5.
13 Matsuyama F, Fukuhara S, Oguma S, Amakawa R, Tanabe S, Kato I, et al. Geographical aspects of bcl-2 gene involvement in Japanese patients with non-Hodgkin’s B-cell lymphomas. Int J Hematol 1992 ; 55 : 71 –9.
14 Osada M, Ishioka C, Ichinohasama R, Kadowaki I, Murakawa Y, Watanabe M, et al. Influence of p53 mutation on pathological grade, but not prognosis of non-Hodgkin’s lymphoma. Anticancer Drug Des 1999 ; 14 : 107 –14.
- b-lymphocytes
- cytogenetics
- immunoglobulin heavy chains
- lymphoma, non-hodgkin
- immunoglobulins
- first degree relative
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1465-3621
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Comprehensive Bridging Radiotherapy for Limited Pre-CART Non-Hodgkin Lymphoma
- 1 Department of Radiation Oncology, Mayo Clinic Jacksonville, Jacksonville, Florida
- 2 Department of Radiation Oncology, Mayo Clinic Rochester, Rochester, Minnesota
- 3 Department of Radiation Oncology, Mayo Clinic Phoenix, Phoenix, Arizona
- 4 Division of Hematology, Mayo Clinic Rochester, Rochester, Minnesota
- 5 Division of Experimental Pathology, Mayo Clinic Rochester, Rochester, Minnesota
- 6 Division of Hematology, Mayo Clinic Phoenix, Phoenix, Arizona
- 7 Division of Hematology, Mayo Clinic Jacksonville, Jacksonville, Florida
Chimeric antigen receptor T-cell therapy (CART) for relapsed/refractory B-cell non-Hodgkin lymphoma (NHL) is associated with 30% durable 5-year complete response rates. 1 Most post-CART relapses have a local component (>80%). 2 , 3 Bridging radiotherapy (BRT) before CART achieves local control rates of more than 80%. 4 This study reported on the role of comprehensive BRT in limited (<5 involved sites) pre-CART disease.
Read More About
Saifi O , Breen WG , Rule WG, et al. Comprehensive Bridging Radiotherapy for Limited Pre-CART Non-Hodgkin Lymphoma. JAMA Oncol. Published online May 09, 2024. doi:10.1001/jamaoncol.2024.1113
Manage citations:
© 2024
Artificial Intelligence Resource Center
Oncology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Watch CBS News
Rowan University graduate inspired to pursue internal medicine after cancer journey
By Ryan Hughes , Alan Wheeler
May 9, 2024 / 7:58 PM EDT / CBS Philadelphia
GLASSBORO, N.J. (CBS) -- The Class of 2024 walked out of Cooper Medical School of Rowan University's commencement ceremony ready to embark on a new journey.
For 28-year-old Keri Cronin, her dream of becoming a doctor is now coming into focus.
"The car ride here my dad was like you've been wanting this since you were 10 years old. So now, 18 years later to see that all come to fruition is a really amazing feeling," said Cronin, as she was surrounded by her family.
Cronin's journey to this moment has not been an easy one. In 2021, in the midst of the pandemic, and during her second year of med school, Cronin was diagnosed with Stage 4 non-Hodgkin's lymphoma. She said the cancer was all over her body and it was eating away at the bone and muscle in her leg.

"I went from reading about it in a textbook, or a case discussion in class, to that being my reality," she said.
Cronin persevered and continued her coursework during the first two cycles of chemotherapy. She spent six months in a wheelchair and took patient interaction exams through a webcam. Then, Cronin's dream was put on hold for a year, as her treatments and cancer battle grew more challenging.
"She went through so much to get here. Very proud of her, she never gave up," said Kim Cronin, Keri's mother.
On Thursday, Cronin walked across the stage, paused for photos, and graduated from med school. Cronin is in remission, and she said her cancer journey inspired her to now study internal medicine and oncology.

"It's amazing I beat cancer. It's amazing that anyone graduates med school, but to do both I feel like is such an amazing feeling and being so close to be able to help families through this journey as well," she said.
Cronin will begin her residency in July at Icahn School of Medicine at Mount Sinai Morningside-West in New York City.
- Rowan University

Ryan Hughes joined CBS News Philadelphia in June 2022. He previously worked at WPTV in West Palm Beach, Florida, where he's covered stories ranging from weeks on the Surfside condo collapse, to the impact of Hurricane Dorian in the Bahamas, and the Super Bowl in Miami.
Featured Local Savings
More from cbs news.

Delaware community remembers 10-year-old boy killed after hit by car walking home from school

NJDOT rejected warnings before 2021 I-295 retaining wall collapse, CBS Philadelphia investigation finds

Cherry Hill community celebrates New Jersey WWII veteran turning 100 at luncheon

New film "Unsung Hero" is a love letter, tribute to mothers, West Philly executive producer says
Sms or Whatsapp only : US: +1(516)494-0538
Case Study: A 65-year-old woman was just been diagnosed with Stage 3 non-Hodgkin’s lymphoma
Education 0
This assignment enables the student to meet the following course outcomes:
- CO 4: Investigate safeguards and decision-making support tools embedded in patient care technologies and information systems to support a safe practice environment for both patients and healthcare workers. (PO 4)
- CO 5: Identify patient care technologies, information systems, and communication devices that support safe nursing practice. (PO 5)
PREPARING THE DISCUSSION
- Demonstrate understanding of concepts for the week
- Integrate outside scholarly sources when required
- Engage in meaningful dialogue with classmates and/or instructor
- Express opinions clearly and logically, in a professional manner
- Use the rubric on this page as you compose your answers.
- Participation early in the week is encouraged to stimulate meaningful discussion among classmates and instructor.
- Enter the discussion often during the week to read and learn from posts.
- Select different classmates for your reply each week
DISCUSSION QUESTION
Case Study: A 65-year-old woman was just been diagnosed with Stage 3 non-Hodgkin’s lymphoma. She was informed of this diagnosis in her primary care physician’s office. She leaves her physician’s office and goes home to review all of her tests and lab results with her family. She goes home and logs into her PHR. She is only able to pull up a portion of her test results. She calls her physician’s office with this concern. The office staff discussed that she had part of her lab work completed at a lab not connected to the organization, part was completed at the emergency room, and part was completed in the lab that is part of the doctor’s office organization.
The above scenario might be a scenario that you have commonly worked with in clinical practice. For many reasons, patients often receive healthcare from multiple organizations that might have different systems.
As you review this scenario, reflect and answer these questions for this discussion.
- What are the pros and cons of the situation in the case study?
- What safeguards are included in patient portals and PHRs to help patients and healthcare professionals ensure safety?
- Do you agree or disagree with the way that a patient obtains Personal Health Records (PHRs)?
- What are challenges for patients that do not have access to all of the PHRs? Remember, only portions of the EHRs are typically included in the PHRs.
Collepals.com Plagiarism Free Papers
Are you looking for custom essay writing service or even dissertation writing services? Just request for our write my paper service, and we'll match you with the best essay writer in your subject! With an exceptional team of professional academic experts in a wide range of subjects, we can guarantee you an unrivaled quality of custom-written papers.
Why Hire Collepals.com writers to do your paper?
Quality- We are experienced and have access to ample research materials.
We write plagiarism Free Content
Confidential- We never share or sell your personal information to third parties.
Support-Chat with us today! We are always waiting to answer all your questions.

Related Posts
Create a recorded video, at least 4 minutes in length, responding to each of prompts below., peptic ulcer disease, solve hw3 with programming problem, solve credit question of both problems and programming(hw1&hw2),and do presentation, leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
All Rights Reserved Terms and Conditions College pals.com Privacy Policy 2010-2018
Study record managers: refer to the Data Element Definitions if submitting registration or results information.
Search for terms

- Advanced Search
- See Studies by Topic
- See Studies on Map
- How to Search
- How to Use Search Results
- How to Find Results of Studies
- How to Read a Study Record

- Learn About Studies
- Other Sites About Studies
- Glossary of Common Site Terms

- Submit Studies to ClinicalTrials.gov PRS
- Why Should I Register and Submit Results?
- FDAAA 801 and the Final Rule
- How to Apply for a PRS Account
- How to Register Your Study
- How to Edit Your Study Record
- How to Submit Your Results
- Frequently Asked Questions
- Support Materials
- Training Materials

- Selected Publications
- Clinical Alerts and Advisories
- Trends, Charts, and Maps
- Downloading Content for Analysis

- ClinicalTrials.gov Background
- About the Results Database
- History, Policies, and Laws
- ClinicalTrials.gov Modernization
- Media/Press Resources
- Linking to This Site
- Terms and Conditions
- Search Results
- Study Record Detail

A Study of ARV-393 in Relapsed/Refractory Non-Hodgkin Lymphoma.
- Study Details
- Tabular View
- No Results Posted

This clinical trial is studying the safety and potential anti-tumor activity of an investigational drug called ARV-393 in patients diagnosed with advanced Relapsed/Refractory non-Hodgkin's lymphoma to determine if ARV-393 may be a possible treatment option.
ARV-393 is thought to work by breaking down a protein present in many types of non-Hodgkins lymphomas, which may prevent, slow or stop tumor growth. This is the first time ARV-393 will be used by people. The investigational drug will be given as an oral tablet.

Inclusion Criteria:
- Eligible participants aged ≥18 years.
- Have relapsed/refractory mature B-cell non-Hodgkin lymphoma (NHL) and ≥2 prior systemic therapies, or histologically confirmed AITL that has recurred or progressed following institutional standard-of-care therapy.
- Participants must also have ≥1 measurable lesion at study entry
- Eastern Cooperative Oncology Group performance status of 0 or 1,
- Freshly biopsied or archival tumor tissue available,
- Participants with adequate organ function,
- Participants must accept and follow pregnancy prevention guidance.
Exclusion Criteria:
- No prior allogeneic stem cell transplant or solid organ transplantation, Autologous stem cell transplant, must not have occurred ≤100 days, previous CAR T-cell therapy ≤60 days, radiotherapy ≤ 2 weeks, systemic anticancer treatment ≤ 5 half-lives or 4 weeks, prior to ARV-393 treatment initiation.
- Participants must not have significant acute or chronic medical illness, including hypereosinophilic syndrome, active interstitial lung disease or pneumonitis, active or uncontrolled infection, or the presence of laboratory abnormalities, that places participants at unacceptable risk if participating in this study.
- Participants with an inability to comply with listed prohibited treatments.
- For Patients and Families
- For Researchers
- For Study Record Managers
- Customer Support
- Accessibility
- Viewers and Players
- Freedom of Information Act
- HHS Vulnerability Disclosure
- U.S. National Library of Medicine
- U.S. National Institutes of Health
- U.S. Department of Health and Human Services
More From Forbes
Fighting cancer: a basic guide to checkpoint inhibitors.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
A woman receiving an IV at the hospital.
This article is part of an ongoing series on novel cancer advances, including immunotherapies such as CAR T therapy and checkpoint inhibitors . Future installments will continue to demystify checkpoint inhibitors and explore the latest research expanding the field.
In March 2011 , a new cancer advance burst into the spotlight. This drug, known as a checkpoint inhibitor , stood out from chemotherapy and other standard cancer treatments. Rather than directly targeting cancer cells, this immunotherapy bolsters the immune system’s innate ability to fight tumors. Initial clinical trials demonstrated that the therapy can improve overall survival and risk of death for patients with one of the deadliest forms of skin cancer, unresectable or metastatic melanoma.
Today, checkpoint inhibitor research branches far beyond melanoma. Scientists are probing to uncover more about the therapy, especially when administered alongside other cancer treatments. Though the journey to understanding checkpoint inhibitors may be overwhelming, this article can guide you through the first steps. Subsequent articles will delve further into specific checkpoint inhibitors and other recent discoveries.
What are Checkpoint Inhibitors?
Checkpoint inhibitors (ICIs) are an antibody-based cancer drug. These infusions contain antibodies that target particular proteins called immune checkpoints.
Typically, the immune system relies on checkpoint proteins to turn off overactive white blood T cells. This mechanism is essential to protecting the body, preventing excitable T cells from harming healthy tissues. However, cancer cells use these checkpoints to their own benefit. By binding to these checkpoints, cancer cells shut off T cells that would otherwise turn against them, leaving them to multiply unrestrained.
Samsung Issues Critical Update For Millions Of Galaxy Users
The best queen mattresses that promote more restful nights, vasiliy lomachenko vs. george kambosos jr: date, time and how to watch.
Inhibitor drugs release the biological restraints on these T cells. Most inhibitors are designed to bind to T cell checkpoint proteins before a cancer cell can; some inhibitors bind to the checkpoint ligand on the cancer cell instead. Either way, these interactions prevent the cancer cell from silencing the T cell. T cells are then free to activate and eliminate the tumors.
What Cancers Do Checkpoint Inhibitors Treat?
Checkpoint inhibitors were first approved for advanced skin cancer. Now, these drugs can treat over 25 types of solid tumors. The list includes:
- Bladder cancer
- Breast cancer
- Colon and rectal cancer
- Kidney cancer
- Liver cancer
- Non-small lung cell cancer
- Pancreatic cancer
Checkpoint inhibitors can also treat Hodgkin and non-Hodgkin lymphoma, two types of blood cancers. However, the FDA has not approved them to treat other blood cancers, such as leukemia or myeloma —although this could change with ongoing research. Another recent immunotherapy, Chimeric Antigen Receptor T Cell Therapy ( CAR T therapy ), has demonstrated more promising results in this arena. Table 1 provides a comprehensive list of cancers treated by specific checkpoint inhibitors.
TABLE 1: List of checkpoint inhibitors currently approved by the FDA. Definitions: Adjuvant, ... [+] treatment before surgery; Unresectable, cancer that cannot be removed entirely with surgery; Metastatic, cancer that has spread.
When to Consider Checkpoint Inhibitors?
Checkpoint inhibitors are increasingly being given as a first treatment, especially for people with advanced melanoma, non-small cell lung cancer (NSCLC), renal cell carcinoma (a type of kidney cancer), or Hodgkin lymphoma who are ineligible for a bone marrow transplant. For other illnesses, including bladder cancer or head and neck cancer, checkpoint inhibitors are considered after other standard treatment options prove ineffective.
Inhibitors can also be administered before surgery or alongside other cancer treatments, such as chemotherapy, radiation and CAR T therapy. Combination treatments synergistically target tumors from distinct angles. For example, chemotherapy and radiation directly damage and kill cancer cells, while the inhibitor encourages immune cells to retaliate. Checkpoint inhibition can allow for less invasive surgery or eliminate the need for surgery in some cases.
Ultimately, the decision to turn to checkpoint inhibitors will depend on each person’s baseline health, what treatment options they have tried, and the projected efficacy of checkpoint inhibitors for their disease.
How Effective Are Checkpoint Inhibitors?
Exactly how effective are checkpoint inhibitors at treating cancer? This can be a difficult question to answer. Checkpoint inhibitors do not cure; rather, they slow or reduce tumor progression to varying degrees. Its efficacy is influenced by several factors, including what treatments a person has already received and the type of cancer at hand. Results can also differ if the infusion is given with other checkpoint inhibitors or cancer treatments.
People with Hodgkin’s lymphoma, melanoma , or solid tumors with specific genetic characteristics (Microsatellite Instability-High, MI-H) tend to respond more readily to checkpoint inhibitor therapy. In one clinical trial, around 87% of participants with Hodgkin’s lymphoma responded to nivolumab, a checkpoint inhibitor by Bristol Myers Squibb. In melanoma, inhibitors can reduce tumor size in around 45-60% of patients with advanced melanoma, a significant improvement over historical response rates of less than 10%. A combination of two inhibitors with different checkpoint targets, CLTA-4 and PD-1 , can further improve outcomes, with five-year overall survival rates exceeding 50% in some studies.
Response rates for other solid tumors range from 15% to 30%. However, it is critical to note that many patients do not respond to checkpoint inhibitor therapy.
TABLE 2: Overall response rates to anti-PD-1/anti-PD-L1 checkpoint inhibitors by cancer type.
What Does the Procedure Look Like?
Checkpoint inhibitors are delivered into the arm through an intravenous (IV) line. The number of infusions needed varies depending on the specific inhibitor drug. They can be administered once or twice a month for up to a year or more.
A blood test is required before each session. These tests establish a baseline and reference point to monitor for any adverse effects during treatment. Other than that, no other pretreatment is needed. The actual session lasts anywhere between 30 and 60 minutes. Afterward, medical staff will monitor the patient for any unwanted reactions.
What Adverse Effects Can Occur?
Checkpoint inhibitors release a surge of immune responses from the body. This mechanism is vital for attacking cancer but can also encourage the immune system to attack normal, healthy cells. As a result, people who take checkpoint inhibitors may experience immune-related adverse effects.
Immune-related symptoms can manifest in several different organs in the body. The skin can develop rashes, itching, or lose patches of color. The colon, lungs and liver can become chronically inflamed. In rarer cases, inflammation can impact the brain. Inhibitor drugs can also trigger the onset of diabetes or a worsening of pre-existing type II diabetes for a minority of patients ( less than 2% ).
Clinicians carefully monitor patients before and after each infusion. They may temporarily suspend treatment and implement corticosteroids or antibiotics to manage symptoms.
Transplant recipients or people with underlying autoimmune conditions should carefully consider whether checkpoint inhibitors are suitable for them. Since these inhibitors stir up the immune system, the treatment could worsen pre-existing conditions. Some studies suggest that symptoms are generally manageable, but each healthcare provider will determine the final call on a case-by-case basis.
Notably, these immune-related reactions are usually less toxic than those caused by chemotherapy and radiation, which target cancer cells directly; hallmarks of chemo or radiation therapy, such as alopecia or lowered blood cell counts, are not typical. However, enhanced toxicity may also occur if checkpoint inhibitors are combined with these other treatments.
Checkpoint inhibitors represent a revolutionary advancement in cancer care, offering a promising alternative to traditional treatments such as chemotherapy and radiation. These medications have shown remarkable efficacy by unleashing the body's immune system to target and destroy cancer cells, particularly in treating advanced melanoma and other solid tumors. However, as with any powerful tool, checkpoint inhibitors possess potential risks and complexities. Furthering this exploration of checkpoint inhibitors, future articles in this series will delve deeper into the intricacies of combining them with other therapies and ongoing research efforts to optimize their effectiveness. Stay tuned for further insights into this evolving frontier of cancer treatment.
- Editorial Standards
- Reprints & Permissions
Join The Conversation
One Community. Many Voices. Create a free account to share your thoughts.
Forbes Community Guidelines
Our community is about connecting people through open and thoughtful conversations. We want our readers to share their views and exchange ideas and facts in a safe space.
In order to do so, please follow the posting rules in our site's Terms of Service. We've summarized some of those key rules below. Simply put, keep it civil.
Your post will be rejected if we notice that it seems to contain:
- False or intentionally out-of-context or misleading information
- Insults, profanity, incoherent, obscene or inflammatory language or threats of any kind
- Attacks on the identity of other commenters or the article's author
- Content that otherwise violates our site's terms.
User accounts will be blocked if we notice or believe that users are engaged in:
- Continuous attempts to re-post comments that have been previously moderated/rejected
- Racist, sexist, homophobic or other discriminatory comments
- Attempts or tactics that put the site security at risk
- Actions that otherwise violate our site's terms.
So, how can you be a power user?
- Stay on topic and share your insights
- Feel free to be clear and thoughtful to get your point across
- ‘Like’ or ‘Dislike’ to show your point of view.
- Protect your community.
- Use the report tool to alert us when someone breaks the rules.
Thanks for reading our community guidelines. Please read the full list of posting rules found in our site's Terms of Service.

IMAGES
VIDEO
COMMENTS
Abstract. Lymphomas are solid tumors of the immune system and include 14% of all head and neck malignancies. Non-Hodgkin lymphomas (NHLs) are a heterogeneous group of lymphoproliferative disorders originating in B-, T-, or natural killer T-cells. They have a wide range of histological appearances and clinical features at presentation, which can ...
The patient in the current case study had a CNS-IPI of 3 and an 11% cumulative incidence of CNS relapse at 2 years. Data support some form of CNS prophylaxis, 19 Dr. Advani concluded, but the jury is still out regarding optimal treatment for double-expressor non-Hodgkin's lymphoma.
The American Cancer Society estimated that more than 70,000 new cases of non-Hodgkin lymphoma (NHL) would be diagnosed in 2016 [1, 2].Although lymphomas arise mainly from lymph nodes, primary extranodal NHL occurs in at least 25% of the cases [].The adrenal gland can be secondarily involved in around 4% of the patients; however, primary adrenal NHL is extremely rare and accounts for less than ...
myeloma, as well as in patients with non-Hodgkin lymphoma (NHL).3-8 Bendamustine has also shown activity in patients with breast cancer and small cell lung cancer.2 Several clinical trials have assessed the efficacy and safety of BR in patients with relapsed mantle cell and indolent B-cell NHL. In a 2005 study by Rummel and col-
2. Case report. 2.1. Case 1. 72 -year-old man was hospitalized in september 2019 with a right lateral cervical mass. He was diagnosed with non -hodgkin's lymphoma mantle cell. He reported to the dental hospital in december 2019 with the complaint of a growth in the left maxillary since one month of the consultation. 2.1.1.
Dr. Olivia C. Smibert: A 48-year-old man with diffuse large B-cell lymphoma was evaluated in the oncology clinic of this hospital because of abdominal pain. The patient had been generally well ...
Learn about non-Hodgkin's lymphoma. ... List your questions from most important to least important in case time runs out. For non-Hodgkin's lymphoma, some basic questions to ask your doctor include: ... Laurent C, et al. Impact of expert pathologic review of lymphoma diagnosis: Study of patients from the French Lymphopath Network. Journal of ...
Non-Hodgkin lymphoma (NHL) can co-exist with autoimmune hemolytic anemia (AIHA), a phenomenon known as AIHA-associated NHL (AIHA/NHL). However, few studies have reported AIHA/NHL incidence or its clinical characteristics. We conducted a retrospective analysis of 20 AIHA/NHL patients treated at our hospital from 2009 to 2018.
Someone develops non-Hodgkin's lymphoma when their B-cell, T-cell or NK-cell lymphocytes mutate and multiply uncontrollably. Most commonly, the B cells are affected. (The most common type of non-Hodgkin's lymphoma is diffuse large B-cell lymphoma.) Non-Hodgkin's lymphoma may develop within the lymph nodes, bone marrow, or any other lymphatic ...
Non-Hodgkin's lymphoma generally involves the presence of cancerous lymphocytes in your lymph nodes. But the disease can also spread to other parts of your lymphatic system. These include the lymphatic vessels, tonsils, adenoids, spleen, thymus and bone marrow. Occasionally, non-Hodgkin's lymphoma involves organs outside of your lymphatic system.
A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. The Non-Hodgkin's Lymphoma Classification Project. Blood 89 (11): 3909-18, 1997. [PUBMED Abstract] Society for Hematopathology Program: Society for Hematopathology Program. Am J Surg Pathol 21 (1): 114-121, 1997.
Extranodal lymphoma occurs in ~40% of all patients with lymphoma and has been described in virtually all organs and tissue ( 1 ). Extranodal disease is more common with non-Hodgkin's lymphoma (NHL) ( 2 ), and diffuse large B-cell lymphoma (DLBCL) is the most common histological NHL subtype in adults, accounting for ~25% of all NHL cases ( 3 ).
NCI-funded researchers are working to advance our understanding of how to treat lymphoma. All lymphomas start in the cells of the lymph system, which is part of the body's immune system. Lymphomas are grouped into two main types: Hodgkin lymphoma and non-Hodgkin lymphoma (sometimes called NHL). But more than 70 different subtypes of the ...
Two cases of non-Hodgkin's lymphoma (NHL) generated within 6 months in first degree relatives, a father and a son, are presented. The NHL was a d ... Caplan LS, et al. Non-Hodgin's lymphoma and family history of maligant tumors in a case-controlled study (United States). Cancer Causes Control. 1998; 9: 72 -82. 8 Frizzera G, Rosai J ...
Chimeric antigen receptor T-cell therapy (CART) for relapsed/refractory B-cell non-Hodgkin lymphoma (NHL) is associated with 30% durable 5-year complete response rates. 1 Most post-CART relapses have a local component (>80%). 2,3 Bridging radiotherapy (BRT) before CART achieves local control rates of more than 80%. 4 This study reported on the role of comprehensive BRT in limited (<5 involved ...
Acute kidney injury (AKI) is a common complication in patients with leukemia and lymphoma. In this single-center non-interventional retrospective study from 2010 to 2022, we aimed to evaluate causes, clinical features, and pathology finding in patients with Hodgkin lymphoma (HL), non-Hodgkin lymphoma/leukemia (NHL/CLL), or lymphoplasmacytic ...
In 2021, in the midst of the pandemic, and during her second year of med school, Cronin was diagnosed with Stage 4 non-Hodgkin's lymphoma. She said the cancer was all over her body and it was ...
Case Study: A 65-year-old woman was just been diagnosed with Stage 3 non-Hodgkin's lymphoma. She was informed of this diagnosis in her primary care physician's office. She leaves her physician's office and goes home to review all of her tests and lab results with her family. She goes home and logs into her PHR.
This is an international, first-in-human, multicenter, open-label Phase 1/2 study to evaluate the safety profile, tolerability of IPH6501, and determine the recommended phase 2 dose (RP2D) for patients with B-Cell non-Hodgkin lymphoma.
A Phase 1 First in Human Study of ARV-393 in Adult Participants With Advanced Non-Hodgkin's Lymphoma: Estimated Study Start Date : April 30, 2024: Estimated Primary Completion Date : December 2025: Estimated Study Completion Date : ... Have relapsed/refractory mature B-cell non-Hodgkin lymphoma (NHL) and ≥2 prior systemic therapies, or ...
The non-Hodgkin's lymphoma of mantle cell type usually consists of atypical small lymphoid cells and has either a nodular or diffuse pattern of growth, or a combination of the two patterns. Nodularity is present, at least focally, in approximately 30% of cases of mantle cell lymphoma at the time of initial diagnosis.
People with Hodgkin's lymphoma, melanoma, or solid tumors with specific genetic characteristics (Microsatellite Instability-High, MI-H) tend to respond more readily to checkpoint inhibitor therapy.