
Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps

Advancing Cardiovascular Health in India Roundtable: Outcomes Report
Acc news story.
Given the size of both the country and the population, and the fact that roughly 10% of the population lives below the international poverty line, it’s not surprising that the burden of noncommunicable diseases (NCDs), including cardiovascular diseases, is high in India. In fact, mortality from NCDs accounted for 65% of total deaths in India in 2019, of which more than 25% could be attributed to cardiovascular diseases and related risk factors like diabetes.
More recently, updated findings from the Global Burden of Diseases Collaboration, published in the Journal of the American College of Cardiology , showed age-standardized mortality rates from cardiovascular diseases in South Asia, including India, on the rise and ranging from 248.6 to 350.9 per 100,000-persons in 2021. Among all risks for cardiovascular diseases, high systolic blood pressure accounted for the largest proportion of disability-adjusted life years, while air pollution and dietary risks were the leading environmental and behavioral risks, respectively.
These challenges led the ACC to convene a roundtable earlier this year made up of leading cardiovascular clinicians from the ACC and the ACC India Chapter, as well as stakeholders from local nonprofits, government agencies and industry related to cardiovascular disease in India. The goal: to identify potential collaborative solutions to some of the specific cardiovascular challenges in India, ranging from patient access to prevention and screening services and chronic disease management.
“There is an urgency to manage the burden of cardiovascular disease in India,” says ACC President B. Hadley Wilson, MD, FACC . “We need to realize the urgency of this public health crisis and develop a roadmap that will allow us to manage the multiple challenges effectively.”
Roundtable participants highlighted the lack of awareness and education around cardiovascular disease and related risk factors as one of the biggest challenges facing the health care community when it comes to tackling these trends. Discussions centered around potential solutions involving increased accessed to screening and public health campaigns among others. Additionally, participants stressed that new innovations ranging from telemedicine to digital devices that allow for remote monitoring and screening are potential game-changers for managing cardiovascular disease and improving heart health throughout the country. Read the full report .
Clinical Topics: Cardiovascular Care Team
Keywords: Noncommunicable Diseases, ACC International
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
- Search Menu
- Supplements
- Cohort Profiles
- Education Corner
- Author Guidelines
- Submission Site
- Open Access
- About the International Journal of Epidemiology
- About the International Epidemiological Association
- Editorial Team
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Contact the IEA
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- < Previous
Physical activity and risk of coronary heart disease in India
- Article contents
- Figures & tables
- Supplementary Data
Tanuja Rastogi, Mario Vaz, Donna Spiegelman, K Srinath Reddy, AV Bharathi, Meir J Stampfer, Walter C Willett, Alberto Ascherio, Physical activity and risk of coronary heart disease in India, International Journal of Epidemiology , Volume 33, Issue 4, August 2004, Pages 759–767, https://doi.org/10.1093/ije/dyh042
- Permissions Icon Permissions
Background Physical exercise has been inversely associated with coronary heart disease (CHD) risk in Western populations; however, the association has not been examined in India where physical inactivity levels in urban areas are now comparable with the West.
Methods We conducted a hospital-based case-control study and collected data from 350 cases of acute myocardial infarction and 700 controls matched on age, gender, and hospital in New Delhi and Bangalore. We used conditional logistic regression to control for the matching and other risk factors.
Results Of the controls, 48% participated in some form of leisure-time exercise compared with 38% of cases. In age- and sex-adjusted analyses, people in the highest level of leisure-time exercise (>145 metabolic equivalents [MET]-minutes per day, equivalent to 36 minutes of brisk walking per day) had a relative risk of 0.45 (95% CI: 0.31, 0.66) compared with non-exercisers. Multivariate adjustment for other risk factors did not substantially alter the association. We observed a positive association between non-work sedentary activity and CHD risk; people with >3.6 hours per day of sedentary activity (for example, television viewing) had an elevated risk of 1.88 (95% CI: 1.09, 3.20) compared with <70 minutes per day in multivariate analysis.
Conclusion Leisure-time exercise, including as much as 35–40 minutes per day of brisk walking, was protective for CHD risk and sedentary lifestyles were positively associated with risk of CHD. Given limited resources for care of CHD in India and the important role of physical exercise in disease risk in urban India, improvements in physical activity should be promoted.
Cardiovascular disease (CVD) is the leading cause of death in India, 1 and its contribution to mortality is rising; deaths due to CVD are expected to double between 1985–2015. 2 –4 Regular physical activity reduces the risk of obesity, blood lipid abnormalities, hypertension, and non-insulin dependent diabetes mellitus, 5, 6 and has been shown to reduce substantially the risk of coronary heart disease (CHD). Conversely, measures of sedentary lifestyles or physical inactivity have been associated with a 1.5- to 2.4-fold elevation in CHD risk. 5 It is estimated that US$24 billion or 2.4% of the US health care expenditure is directly related to a lack of physical activity. 7
As a result of economic changes and increased mechanization, the prevalence of physical inactivity is increasing in India, particularly in urban areas, to levels comparable with the West. 6, 8, 9 However, the association between leisure-time exercise, sedentary lifestyles, and risk of CHD has not been assessed within India. We conducted a hospital-based case-control study of acute myocardial infarction (AMI) in two major cities in India to address the relation between leisure-time exercise and sedentary activity and risk of CHD. To our knowledge, this is one of the first investigations to date, if not the first, into the relation between physical activity and CHD risk in India.
Study participants
Eligible cases were all patients 21–74 years of age hospitalized with a diagnosis of incident AMI in one of eight urban hospitals in New Delhi and Bangalore between January 1999 and January 2000. The initial three participating hospitals were also part of an investigation of the Indian Council of Medical Research (ICMR), so case subjects were selected according to ICMR study criteria. Definite diagnosis of AMI was based on clinical examination, electrocardiogram (ECG), and cardiac enzymes. 10 Research assistants identified cases by visiting participating hospitals on a daily or biweekly basis and by consulting physicians on duty. Patients were excluded if they had any previous history of myocardial infarction or CHD (including bypass surgery, angina, or stroke) because such prior diagnoses may have altered their exposure history. We also excluded patients if they were pregnant, had a history of cancer, or had a chronic disease of the kidney, liver, gastrointestinal tract, or thyroid. Individuals who suffered an acute viral infection in the 4 weeks prior to admission were also excluded, as were those who failed to provide informed consent. Patients were interviewed approximately 2–5 days after admission. Eligibility criteria were met by 419 cases, and 350 were included in the study. Reasons for exclusions were death (n = 25) or discharge (n = 23) before the interviews could be completed, being too sick to be interviewed (n = 13), or no consent to participate (n = 8).
For each case, two controls matched by age (within 5 years), gender, and hospital were obtained from non-cardiac outpatient clinics or inpatient wards. The same exclusion criteria utilized for cases were applied for control selection. We identified approximately 707 eligible control subjects, of whom 7 declined to be interviewed. Controls were relatively healthy individuals with minor ailments or conditions and were obtained from the following wards and clinics (% of total controls): eye (37%), ear, nose, and throat (21%), dermatology (14%), orthopaedic (10%), surgery (7%), general medicine (7%), gynaecology (3%), other (<1%).
Controls were selected using one of two methods depending on the hospital. In the first method, research assistants were assigned to accompany a particular physician during an outpatient clinic, following a weekly schedule of clinics and wards. At the end of each consultation, the physician or the physician's assistant invited the patient to speak with the research assistants about their lifestyle and diet. Patients that were eligible according to study criteria were then informed of the study and asked to participate. In these situations, participation was 100%. In the second method, research assistants independently identified control patients from clinics and wards. Assistants attempted to approach all individuals present during a particular outpatient clinic or in a specified ward. In large clinics, patients were screened for eligibility and invited to participate according to their queue number (highest number first). This method was used to prevent arbitrariness in the selection of controls. Basic demographic information was collected from all those approached. If an individual was eligible, assistants briefly explained the study and asked if they were willing to participate. Among those approached, only seven individuals who were eligible refused to participate.
Data collection
The study was approved by the relevant institutional review boards. Interviews were conducted in hospital wards or clinics by one of four research assistants and lasted approximately 25 minutes. Research assistants collected data on socioeconomic status, smoking history, history of hypertension, diabetes, hypercholesterolaemia, family history of CVD (including CHD, angina, myocardial infarction, hypertension, diabetes, stroke, sudden death, bypass surgery), dietary intake, types of fat or oils used in cooking, nutritional supplement use, and physical activity. Next, anthropometric measures (height, weight, hip and waist circumferences) were obtained and body mass index (BMI) (weight (kg)/height (m 2 )) and waist to hip ratio (WHR) were calculated. Waist and hip measures were assessed using a standardized tape measure with waist measures taken at the midpoint between the costal margin and iliac crest and hip measures taken at the widest circumference. Study questionnaires were coded and double entered.
Physical activity questionnaire
Physical activity levels were assessed using a validated physical activity questionnaire specific for the Indian population that focused on occupational and other non-leisure time activities, in addition to leisure-time exercise. 11 It was validated by comparing energy expenditure (determined by the questionnaire) with energy intake as measured by 24-hour dietary recalls. A significant positive correlation was reported (r = 0.33, P = 0.02) which was comparable with other validation studies where energy expenditure was assessed using a physical activity questionnaire. 11 –13 Subjects were asked to report the average time spent at work and average frequency of activities related to leisure or recreation, household chores, as well as sedentary and daily activities over the last month. The intensity or metabolic equivalents (MET) of the reported activities were obtained from the Compendium of Physical Activities. 14 For those activities not listed in the Compendium, the MET of a similar activity was assigned. The questionnaire provided an estimate of overall energy expenditure per day and the energy expenditure of specific categories of activities (work, leisure-time exercise, hobbies, chores, and sedentary activities). Metabolic equivalent-minutes (MET-min), a measure of both intensity and duration of specific activities, were also derived to assess levels of leisure-time exercise.
Statistical analysis
To assess the potential for confounding, mean values of CHD risk factors were examined across levels of leisure-time exercise (assessed in met-minutes), sedentary activity (minutes), and work-related activities (minutes) among controls. Continuous covariates were categorized to avoid assumptions of linear associations with the outcome and to minimize the effect of outlying values. Participants were grouped into quartiles (sedentary activity), or into tertiles (leisure time exercise), or two categories depending on the distribution of each variable and the number of subjects within each category. To evaluate the relation between leisure-time exercise and risk of CHD, we used conditional logistic regression, first controlling only for the matching factors (age, sex, hospital), and then, in addition, other potential risk factors. Analysis of leisure-time exercise compared risk associated with different levels of exercise to non-exercisers. Similar analyses were performed for sedentary (non-work) and work-related activities. For work-related activities, total time spent at work, and average time spent sitting, standing, walking, and in strenuous activities at work were assessed. We also examined whether the associations observed with leisure-time exercise and sedentary activity and CHD risk were modified by: age, gender, cigarette and bidi smoking, BMI, WHR, alcohol intake, education, or income. All analyses were conducted in Statistical Analysis Software (version 8).
We enrolled 350 cases and 700 controls, equally recruited from New Delhi and Bangalore. The mean age was 52 years (standard deviation, 11) and 12% were women.
The mean 24-hour energy expenditure among control subjects was 10 536 kJ (standard deviation 2939). Men had higher energy expenditure than women (10 844 compared with 8356 kJ/day). On average, the relative contributions of major type activities to total energy expenditure among controls were 32.2% for work-related activity, 7.7% for sedentary activity, and 4.3% for leisure-time exercise. Approximately, 48% of all controls were participating in some form of leisure-time exercise. This included walking, jogging, yoga, gardening, as well as sports and games such as badminton, swimming or those recreational activities that had MET ranging from 3 to 8. On the other hand, cases spent more time in sedentary activities or behaviours such as watching television, listening to music, reading and writing, or other activities with MET of ≤2. The majority of sedentary time was spent watching television (47%).
The mean values of CHD risk factors across levels of leisure-time physical activity, sedentary, and work-related activity are presented in Table 1 . People in the highest level of leisure-time exercise were older, more educated, consumed fewer cigarettes, and had less family history of CHD, and lower BMI and WHR than non-exercisers. The higher prevalence of history of hypertension and diabetes among exercisers may reflect doctors' recommendations to hypertensives and diabetics to improve physical activity. People with the most sedentary lifestyles were older, had higher socioeconomic status and increased BMI, and consumed more cigarettes yet less bidis (small unfiltered cigarettes) and were less likely to be involved in manual labour than the least sedentary. They also spent less time in work-related activity, and had higher prevalences of hypertension, diabetes, and family history of CHD than the least sedentary. People in the highest level of work activity were usually younger, more educated men who smoked more and were involved in less sedentary activity, but also in less leisure-time exercise than those who had no work-related activity.
Distribution of coronary heart disease (CHD) risk factors according to leisure-time physical activity, sedentary activity and work (occupational) activity status (lowest and highest levels) among control subjects in New Delhi and Bangalore (n = 655)
Age- and sex-adjusted as well as multivariate-adjusted relative risks (RR) for CHD risk factors are presented in Table 2 . Cigarette and bidi smoking, history of high cholesterol, family history of CHD, history of hypertension, and both higher WHR and BMI levels were significant determinants of CHD in this population. 15
Relative risk (RR) of acute myocardial infarction according to potential risk factors
Also adjusted for hospital.
Covariates that were controlled for in multivariate model include: the matching factors: age, sex, hospital; and cigarette smoking (never, past, current: ≥2 cigarettes per day, >2–6, >6–12.5, >12.5), bidi smoking (never, past, current: ≤5.5 bidis per day, >5.5–10, >10–20, >20), body mass index (<21 kg/m 2 , ≥21–23, ≥23–26, ≥26), waist to hip ratio (≤0.91, >0.91–0.95, >0.95–0.98, >0.98), history of hypertension (no, yes), history of diabetes (no, yes), history of high cholesterol (no, yes), family history of coronary heart disease (no, yes), alcohol intake (no intake, any intake), education (none, primary school, middle, secondary, higher secondary, college, graduate/professional), household income (<3000 rupees per month, 3000–6000, 6000–10 000, >10 000), and being Hindu (no, yes).
Coronary heart disease.
In age- and sex-adjusted analyses of leisure-time exercise ( Table 3A ), people in the highest level (>145 MET-min of exercise per day or an equivalent of 36 minutes of brisk walking per day) had a 55% lower risk compared with those who did not exercise (RR = 0.45; 95% CI: 0.31, 0.66; P -value for trend <0.0001). The association remained similar in multivariate analysis ( Figure 1 ). Further adjustment for duration at work and in sedentary activity did not alter the association. We found that the association with leisure-time exercise was significantly modified by cigarette smoking status ( P = 0.03). While both cigarette smokers and non-cigarette smokers were at reduced risk with increased leisure-time exercise, the apparent protective effect was greater among non-smokers.
Relative risk of acute myocardial infarction by level of leisure-time physical exercise a
a Covariates that were controlled for in multivariate model include: the matching factors: age, sex, hospital; and cigarette smoking (never, past, current: ≥2 cigarettes per day, >2–6, >6–12.5, >12.5), bidi smoking (never, past, current: ≤5.5 bidis per day, >5.5–10, >10–20, >20), body mass index (<21 kg/m 2 , ≥21–23, ≥23–26, ≥26), waist to hip ratio (≤0.91, >0.91–0.95, >0.95–0.98, >0.98), history of hypertension (no, yes), history of diabetes (no, yes), history of high cholesterol (no, yes), family history of coronary heart disease (no, yes), alcohol intake (no intake, any intake), education (none, primary school, middle, secondary, higher secondary, college, graduate/professional), household income (<3000 rupees per month, 3000–6000, 6000–10 000, >10 000), and being Hindu (no, yes).
Relative risk (RR) of acute myocardial infarction by leisure-time exercise and sedentary activity
In age- and sex-adjusted analysis of sedentary activity ( Table 3A ), people in the highest level (≥3.6 hours per day of sedentary activity such as sitting or television viewing) had an RR of 1.58 (95% CI: 1.05, 2.36; P -value for trend = 0.02) compared with those in the lowest level (<70 minutes per day of sedentary activity). The association strengthened in multivariate analysis, with those leading the most sedentary lifestyles having an 88% greater risk compared with the least sedentary individuals (RR = 1.88; 95% CI: 1.05, 3.07; P -value for trend = 0.02). Control for leisure-time exercise and duration at work slightly strengthened this association. In further analysis limited specifically to television viewing, people watching a median of 3 hours per day of television were at a marginal, yet not significant, elevation in risk compared with those who did not watch television (RR = 1.22, 95% CI: 0.62, 2.41; P -value for trend = 0.1).
Leisure-time exercise and sedentary activity variables were not highly correlated in our study population (r = 0.09 among controls and r = 0.16 among cases), we therefore were able to examine their joint effect. We conducted this analysis using a multivariate model that included indicator variables for each combination of leisure-time exercise and sedentary activity. Figure 2 illustrates the relation of leisure-time exercise to CHD risk across levels of sedentary activity: people in our study population with the highest amount of leisure-time exercise and the least amount of sedentary activity had over a 70% reduction in risk in multivariate analysis compared with people who were the most sedentary with the least amount of leisure-time exercise. This finding was not altered after further control for work-related activity.
Relative risk of acute myocardial infarction by categories of leisure-time physical exercise across sedentary activity levels a,b
a Reference group consists of people in the lowest category of leisure-time physical exercise who were the most sedentary.
b Multivariate adjusted for the matching factors: age, sex, hospital; and cigarette smoking (never, past, current: ≥2 cigarettes per day, >2–6, >6–12.5, >12.5), bidi smoking (never, past, current: ≤5.5 bidis per day, >5.5–10, >10–20, >20), body mass index (<21 kg/m 2 , ≥21–23, ≥23–26, ≥26), waist to hip ratio (≤0.91, >0.91–0.95, >0.95–0.98, >0.98), history of hypertension (no, yes), history of diabetes (no, yes), history of high cholesterol (no, yes), family history of coronary heart disease (no, yes), alcohol intake (no intake, any intake), education (none, primary school, middle, secondary, higher secondary, college, graduate/professional), household income (<3000 rupees per month, 3000–6000, 6000–10 000, >10 000), and being Hindu (no, yes).
Duration of work per day was associated with an elevation in risk although it was not significant ( Table 3B ). People spending a median of 10 hours per day at work had an RR of 1.9 (95% CI: 1.01, 3.56; P -value for trend = 0.1) compared with those not working. Further adjustment for leisure-time exercise and sedentary activities did not alter the association. The time at work spent sitting (MET = 1.5), standing (MET = 2.0), walking (MET = 3.5), and in strenuous activities (MET = 4.5) were assessed separately ( Tables 3B ). People spending an average of ≥2 hours per day standing had an 85% elevation in risk (RR = 1.85; 95% CI: 1.00, 3.12; P -value for trend = 0.05) compared with those who did not spend any time standing at work. No association with total 24-hour energy expenditure or other categories of activities including household chores was observed.
Relative risk (RR) of acute myocardial infarction by work-related activities
In this urban population of Indian men and women, we observed a strong and dose-dependent inverse association between leisure-time exercise and non-fatal CHD. Risk for CHD decreased across levels of leisure-time exercise, with people exercising the equivalent of 36 minutes of brisk walking per day having less than half the risk of non-exercisers. We also found an association between increased sedentary activity and CHD risk, the equivalent of 3.6 hours per day of sedentary activities such as television viewing was associated with nearly a 90% increase in risk. As well, we observed that increased duration of standing at work was associated with an elevation in risk.
Potential sources of bias in our investigation include the selection of controls and a differential recall among cases compared with control subjects. While the use of population-based controls would be ideal, we addressed selection bias that may arise with use of hospital-based controls by obtaining control subjects from seven different outpatient clinics and inpatient wards in hospitals. Therefore, if an association exists between the exposure of interest and the disease status of one control group, the bias that may result would be diluted. 16 Additionally, we used a systematic method of control selection that would avoid arbitrary selection of controls within wards and clinics. To the extent that physical activity is also protective for these conditions, such bias would attenuate the association observed between physical activity and CHD risk in our study. Selection bias among case subjects, where only cases who survived long enough to be interviewed were included, would also be minimized as only 25 cases did not survive to be included in the study. Although health conscious individuals may have been more likely to give consent for the study, overall participation was high, and bias from this source is likely to be modest. Controls in our population were slightly more educated and had lower incomes than cases, but controlling for socioeconomic factors did not alter our findings. Differential recall of physical activity is also a potential concern; however, research assistants asked case subjects to specifically report on their level of activity and exercise prior to their myocardial infarction. While the potential for recall bias may exist, awareness of heart disease prevention and health consciousness may not be as high among our study population in India as its is in Western countries; hence the likelihood of recall bias may be lower. We also excluded all those with any prior heart disease from the study. As well, while we cannot exclude the possibility that not all activities were reported, interviewers were trained to conduct thorough interviews on all activities done during the day including leisure-time and activities of daily living. While future prospective research within India will adequately address these biases, the case-control design had the advantage of being cost, resource, and time efficient.
The apparent protective effect we observe with moderate-intensity exercises such as brisk walking at a frequency of 35–40 minutes per day is consistent with US recommendations stating that individuals ‘accumulate at least 30 minutes or more of moderate-intensity physical activity on most, or preferably all, days of the week’. 5, 6, 9 As well, findings from a large prospective study of US women indicate that approximately ≥3 hours per week of brisk walking was associated with a 30–40% reduction in CHD risk, 17 and in a cohort of US men, individuals expending the equivalent of 30 minutes in moderate-intensity activities had a 20% lower risk for CHD. 18 Moreover, recent findings from a cohort of post-menopausal US women indicate that the reduction in CVD risk that is associated with vigorous exercise is similar for walking. 19 The elevation in risk observed with increased sedentary activity independent of leisure-time exercise is consistent with research that has described physical activity and physical inactivity (such as television viewing) as different risks. 20, 21 While reduced levels of physical activity lead to lower energy expenditure and lower lean body mass, physical inactivity or sedentary activities may be related to obesity and risk for chronic disease through increase in energy intake and not just lower energy expenditure. Research on work-related activity has generally not shown an association with risk. Data from the Israeli Ischemic Heart Disease Study indicated that among middle-age men leisure-time exercise, but not work-related activity, was associated with a significant reduction in risk for CHD and all-cause mortality. 22 Work-related activity was also associated with a slightly higher all-cause mortality risk among a cohort of Swedish men, but the association did not remain after further control for smoking, occupational class, and alcohol abuse. 23
Several biological mechanisms could explain the beneficial effects of physical activity on CVD risk, including lowering of blood pressure, elevation in high density lipoprotein levels, increased insulin sensitivity, improved endothelial function, and reduced atherogenic cytokine production. 5, 6, 24 –34
Our findings are the first to highlight the adverse health consequences of physical inactivity and the importance of leisure-time exercise in the prevention of CHD risk among Indians. Given limited resources for the care of CHD and the potential benefit of exercise in urban India where physical inactivity levels are now comparable with the West, population-based health strategies should focus on promoting regular physical exercise.
Physical inactivity levels in urban India, where cardiovascular diseases have become the leading cause of death, are now comparable with levels observed in the West.
Approximately 145 metabolic equivalents (MET)-minutes per day of leisure-time exercise, equivalent to 35–40 minutes per day of brisk walking was associated with over a 50% reduction in risk for coronary heart disease (CHD) in this study.
Sedentary lifestyles were associated with an increase in risk; approximately 3.5 hours of, for example, television viewing per day being associated with an 88% elevation in CHD risk.
The protective effect of leisure-time exercise was most beneficial among those who also had the least sedentary lifestyle.
The study findings were consistent with US recommendations stating that individuals ‘accumulate at least 30 minutes or more of moderate-intensity physical activity on most, or preferably all, days of the week’.
We thank Dr Anura Kurpad, Division of Nutrition, St John's Medical College (SJMC) in Bangalore and Dr D Prabhakaran, Department of Cardiology, All India Institute of Medical Sciences (AIIMS) in New Delhi for their support. We are also indebted to the participating hospitals in this multi-center investigation: Dr Prem Pais (SJMC), Dr Subash Chandra (Manipal Heart Foundation), Dr Dinesh K Dhanwal (Lok Nayak JP Hospital), Dr Sushum Sharma (Railways Hospital), Dr Sr Teresita, (St Martha's Hospital), Dr Nagaraj Desai, (Ramaiah Medical College), Dr BP Singh (Mata Chanan Devi Hospital). We thank research assistants, Nisha Punni, Savita Dhatwalia, Smitha JT and AM Anamika; and appreciate the assistance provided by staff at AIIMS (Arti Kohli, Monika Arora, Dr Lakshmi) and SJMC (Sumithra Muthayya, Dr Shobana). This project was supported in part by the Unilever Corporation.
Mukherjee AK. India's health—today and tomorrow. J Indian Med Assoc 1995 ; 93 (8) .
Reddy KS. Cardiovascular disease in India. World Health Stat Q 1993 ; 46 : 101 –07.
Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation 1998 ; 97 : 596 –601.
Bulatao RAO, Stephens PW. Demographic estimates and projections, by region, 1970–2015. In: Jamison DT, Mosley WH (eds). Disease control priorities in developing countries. ( Health Sector Priorities Review No. 13 ) Washington: World Bank, 1990 .
Pate RR, Prat M, Blair SN et al . Physical activity and public health: A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 1995 ; 273 : 402 –07.
DHHS (Department of Health and Human Service). Physical Activity and Health: A Report of the Surgeon General . Atlanta: National Center for Chronic Disease Prevention and Health Promotion, 1996 .
Colditz GA. Economic costs of obesity and inactivity. Med Sci Sports Exerc 1999 ; 31 : S663 –67.
Vaz M, Bharathi AV. Practices and perceptions of physical activity in urban, employed, middle-class Indians. Indian Heart J 2000 ; 52 : 301 –06.
National Institutes of Health. Consensus Development Panel on Physical Activity and Cardiovascular Health. Physical activity and cardiovascular health. JAMA 1996 ; 276 : 241 –46.
Indian Council of Medical Research. Instruction Manual for the National Multicentric Case-Control Study to Identify Risk Factors in Acute Myocardial Infarction . New Delhi: ICMR, 1999 .
Bharathi AV, Sandhya N, Vaz M. The development and characteristics of a physical activity questionnaire for epidemiologic studies in urban middle class Indians. Indian J Med Res 2000 ; 111 : 95 –102.
Albanes D, Conway JM, Taylor PR, Moe PW, Judd J. Validation and comparison of eight physical activity questionnaires. Epidemiology 1990 ; 1 : 65 –71.
Arroll B, Jackson R, Beaglehole R. Validation of a three-month physical activity questionnaire with a seven-day food intake and physical activity diary. Epidemiology 1991 ; 2 : 296 –99.
Ainsworth BE, Haskell WL, Leon AS et al . Compendium of Physical Activities: Classification of energy costs of human physical activities. Med Sci Sports Exerc 1993 ; 25 : 71 –80.
Rastogi T, Reddy KS, Spiegelman D et al . Cigarette and bidi smoking and risk of coronary heart disease among Indians (Abstract). Presented at the International Conference on Preventive Cardiology . Osaka, Japan, 2001 .
Rothman K, Greenland S. Modern Epidemiology. 2nd Edn. Ch. 7 . Philadelphia: Lippincott-Raven, 1998 .
Manson JE, Hu FB, Rich-Edwards JW et al . A prospective study of walking as compared with vigorous exercise in the prevention of coronary heart disease in women. New Engl J Med 1999 ; 341 : 650 –58.
Sesso HD, Paffenbarger RS, Lee I. Physical activity and coronary heart disease in men: The Harvard Alumni Health Study. Circulation 2000 ; 102 : 975 –80.
Manson JE, Greenland P, LaCroix AZ et al . Walking compared with vigorous exercise for the prevention of cardiovascular events in women. New Engl J Med 2002 ; 347 : 716 –25.
Hernandez B, Gortmaker SL, Colditz GA, Peterson KE, Laird NM, Parra-Cabrera S. Association of obesity with physical activity, television programs and other forms of video viewing among children in Mexico City. Int J Obesity 1999 ; 23 : 845 –54.
Gortmaker S, Dietz W, Cheung L. Inactivity, diet and the fattening of America. J Am Diet Assoc 1990 ; 90 : 1247 –55.
Eaton CB, Medalie JH, Flocke SA, Zyzanski SJ, Yaari S, Goldbourt U. Self-reported physical activity predicts long-term coronary heart disease and all-cause mortalities: 21 years of follow-up of the Israeli Ischemic Heart Disease Study. Arch Family Med 1995 ; 4 : 323 –29.
Rosengren A, Wilhelmsen L. Physical activity protects against coronary death and deaths from all causes in middle-aged men. Evidence from a 20-year follow-up of the primary prevention study in Goteberg. Ann Epidemiol 1997 ; 7 : 69 –75.
Paffenbarger RS, Jung DL, Leung RW, Hyde RT. Physical activity and hypertension: an epidemiological view. Ann Med 1991 ; 23 : 319 –27.
Folsom AR, Prineas RJ, Kaye SA, Munger RG. Incidence of hypertension and stroke in relation to body fat distribution and other risk factors in older women. Stroke 1990 ; 21 : 701 –06.
Fagard RH. Exercise characteristics and the blood pressure response to dynamic physical training. Med Sci Sports Exerc 2001 ; 33 (Suppl.): S484 –92.
Durstine JL, Grandgean PW, Davis PG, Ferguson MA, Alderson NL, DuBose KD. Blood lipids and lipoprotein adaptations to exercise: a quantitative analysis. [Review]. Sports Med 2001 ; 31 : 1033 –62.
Durstine JL, Haskell WL. Effects of exercise training on plasma lipids and lipoproteins. Exerc Sport Sci Rev 1994 ; 22 : 477 –521.
Leon AS, Sanchez OA. Response of blood lipids to exercise training alone or combined with dietary intervention. Med Sci Sports Exerc 2001 ; 33 (Suppl.): S502 –15.
Haskell WL. The influence of exercise training on plasma lipids and lipoproteins in health and disease. Acta Med Scand 1986 ; 711 (Suppl.): 25 –37.
Mayer-Davis E, D'Agostino R, Karter AJ et al ., IRAS Investigators. Intensity and amount of physical activity in relation to insulin sensitivity: The insulin resistance atherosclerosis study. JAMA 1998 ; 279 : 669 –74.
Smith SJ, Dykes R, Douglas JE, Krishnaswamy G, Berk S. Long-term exercise and atherogenic activity of blood mononuclear cells in persons at risk of developing ischemic heart disease. JAMA 1999 ; 281 : 1722 –27.
Hambrecht R, Wolf A, Gielen S et al . Effect of exercise on coronary endothelial function in patients with coronary artery disease. New Engl J Med 2000 ; 342 : 454 –60.
Wannamethee SG, Shaper AG, Alberti KG. Physical activity, metabolic factors, and the incidence of coronary heart disease and type 2 diabetes. Arch Int Med 2000 ; 160 : 210 –16.
- myocardial infarction, acute
- physical activity
- lack of exercise
- coronary heart disease
- coronary heart disease risk
Email alerts
Citing articles via, looking for your next opportunity.
- About International Journal of Epidemiology
- Recommend to your Library
Affiliations
- Online ISSN 1464-3685
- Copyright © 2024 International Epidemiological Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Challenge to research...
Challenge to research on heart disease patterns in India sparks controversy
- Related content
- Peer review
- Ganapati Mudur
A research review has sought a fresh assessment of cardiovascular disease patterns in India, claiming that doctors have argued that coronary heart disease and its risk factors disproportionately affect poor people in India without sufficient evidence.
The review has claimed that many studies looking at the distribution of cardiovascular disease and its risk factors across different socioeconomic sections of the population have drawn inferences that are “often discordant with their own results.” 1
The evidence suggests that deaths from coronary heart disease occur disproportionately among economically advantaged groups, according to the review, which examined 53 studies, including 49 conducted since 1989. The review said that except for high rates of smoking and poor intake of fruits, the other risk factors such as obesity, elevated lipids, and hypertension are more prevalent among the higher socioeconomic groups than among the lower groups.
Subu Subramanian, a professor of population health at the Harvard School of Public Health and the review’s corresponding author, stated: “I think there has been an eagerness to declare a shift in the burden of heart disease in India from the rich to the poor.”
A study of industrial workers from 10 sites in India six years ago had, for example, mentioned a growing vulnerability of the lower socioeconomic groups to coronary heart disease. 2 But, the review said, this study had observed a positive association between socioeconomic status and body mass index, obesity, cholesterol, and triglycerides among men and a negative socioeconomic gradient for smoking, hypertension, and diabetes among women.
Daniel Corsi, a research fellow at the Harvard School of Public Health and a coauthor of the review paper, said: “Many of the Indian studies capture special populations that may not represent all of India, especially the very poor.”
Doctors who led these studies have asserted that India is indeed experiencing a reversal of the cardiovascular burden. Dorairaj Prabhakaran, professor of chronic disease epidemiology at the Public Health Foundation of India in New Delhi, said: “Everything doesn’t change all at once—tobacco use is the first risk factor to reverse—and we’re already seeing this. Hypertension follows, then diabetes, hyperlipidaemia, and obesity reverse last.”
But Subramanian said that there is not enough evidence to support such a sequence of reversal.
The review has expressed concern that the “haste” to suggest that cardiovascular diseases disproportionately burden poor people could increase inequity in healthcare by “unwittingly shifting limited resources from the health concerns of the poor to health concerns of the rich in India.”
It has called on India to invest in a rigorous surveillance programme for cardiovascular diseases, citing how India had to revise downward predicted estimates of HIV infections six years ago after improving mechanisms of HIV surveillance. 3
Many doctors said that they believed a controversy over cardiovascular disease burden in India is unwarranted, given its large population, whether rich or poor.
Sanjay Kinra, a senior lecturer in non-communicable disease epidemiology at the London School of Hygiene and Tropical Medicine said: “There is really no need for any controversy. India has multiple shades of poverty, and what you see depends on where you look—it’s something like the blind men touching an elephant.”
Prashant Joshi, a professor of medicine at the Indira Gandhi Government Medical College in Nagpur, said: “The truth is that coronary heart disease and its risk factors remain undetected, untreated, or poorly managed in huge numbers of poor people because of lack of access to healthcare services.”
Doctors also pointed out that the presentation of cardiovascular diseases could differ across different sections of the population. Yogesh Jain, a paediatrician with Jan Swasthya Sahyog (people’s health support group), a non-government organisation that runs healthcare services for rural populations in the eastern state of Chhattisgarh, said: “We do see heart disease among the poor, but many among them have rheumatic heart disease. It is a large burden.”
Cite this as: BMJ 2013;346:f3155
- ↵ Subramanian SV, Corsi DJ, Subramanyam MA, Smith GD. Jumping the gun: the problematic discourse on socioeconomic status and cardiovascular health in India. Int J Epidemiol 2013 ;1-17, doi: 10.1093/ije/dyt017 .
- ↵ Reddy KS, Prabhakaran D, Jeemon P, Thankappan KR, Joshi P, Chaturvedi V, et al. Educational status and cardiovascular risk profile in Indians. Proc Natl Acad Sci U S A 2007 ; 104 : 16263 -8. OpenUrl Abstract / FREE Full Text
- ↵ Mudur G. India reduces estimated count of people living with HIV. BMJ 2007 ; 335 : 67 . OpenUrl FREE Full Text
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Cardiovascular Disease in India
Ischemic heart disease deaths are rising in India, particularly in rural areas and among young adults, while deaths from stroke have dropped in most parts of the country, according to a study in The Lancet Global Health .
The international team of researchers used verbal autopsies collected from 2001 to 2013 among 2.4 million households to derive mortality rates and trends in ischemic heart disease and stroke by sex and birth cohort throughout the country.
Read More About
Friedrich M. Cardiovascular Disease in India. JAMA. 2018;320(11):1097. doi:10.1001/jama.2018.13373
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Login to your account
If you don't remember your password, you can reset it by entering your email address and clicking the Reset Password button. You will then receive an email that contains a secure link for resetting your password
If the address matches a valid account an email will be sent to __email__ with instructions for resetting your password
Access provided by
Download started.
- PDF [433 KB] PDF [433 KB]
- Add To Online Library Powered By Mendeley
- Add To My Reading List
- Export Citation
- Create Citation Alert
Cardiovascular disease (CVD) and its associated risk factors among older adults in India: Evidence from LASI Wave 1
- Jhumki Kundu Jhumki Kundu Contact Affiliations International Institute for Population Sciences, Deonar, Mumbai, 400088, India Search for articles by this author
- Risk factors
- Older adults
1. Introduction
- Google Scholar
World Health Organization (2021). Noncommunicable Diseases. Retrieved September 2, 2021, from WHO website: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases .
- Mensah G.A.
- Johnson C.O.
- Miranda J.J.
- Barrientos-Gutiérrez T.
- Corvalan C.
- Devereaux P.J.
- Prabhakaran D.
- Rangarajan S.
- Varghese C.
- Ramadoss A.
- World Health Organization
- Global Burden Of Diseases
- Gaziano T.A.
- Ahluwalia N.S.
- Curtis A.B.
- Sharma U.C.
- Sinclair D.A.
- Mulvagh S.L.
- BaireyMerz C.N.
- Buring J.E.
- Manson J.E.
- Halter J.B.
- Crandall J.P.
- Goldberg A.
- Harkless L.
- Toedebusch R.
- Belenchia A.
Sarwar, N., Gao, P., KondapallySeshasai, S. R., Gobin, R., Kaptoge, S., & Di Angelantonio, E. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet [Internet]. 2.
- Farzadfar F.
- O'donnell M.J.
- Rao-Melacini P.
- Lloyd-Jones D.M.
- D'AgostinoSr R.B.
2. Data & methods
2.1 variable description, 2.2 statistical methods.
- Open table in a new tab
4. Discussion
- Giardina E.G.
- Turner M.B.
- Appelman Y.E.
- Morrish N.J.
- Stevens L.K.
- Fuller J.H.
- Bijnen F.C.
- Caspersen C.J.
- Mosterd W.L.
5. Conclusion
Availability of data and material, ethics approval & consent to participate, consent for publication, credit authorship contribution statement, declaration of competing interest, acknowledgements.
- National Centers for Disease Control and Prevention
- World health organization
- INTERHEART Study Investigators
Article info
Publication history, identification.
DOI: https://doi.org/10.1016/j.cegh.2021.100937
User license

For non-commercial purposes:
- Read, print & download
- Redistribute or republish the final article
- Text & data mine
- Translate the article (private use only, not for distribution)
- Reuse portions or extracts from the article in other works
Not Permitted
- Sell or re-use for commercial purposes
- Distribute translations or adaptations of the article
ScienceDirect
- View Large Image
- Download Hi-res image
- Download .PPT
Related Articles
- Access for Developing Countries
- Articles & Issues
- Articles In Press
- Current Issue
- Past Issues
- For Authors
- Author Information
- Researcher Academy
- Submit a Manuscript
- Journal Info
- About the Journal
- Contact Information
- Editorial Board
- New Content Alerts
The content on this site is intended for healthcare professionals.
- Privacy Policy
- Terms and Conditions
- Accessibility
- Help & Contact

- Research article
- Open access
- Published: 02 July 2021
Cardiovascular disease (CVD): assessment, prediction and policy implications
- Shazia Rehman 1 , 2 , 3 ,
- Erum Rehman 4 ,
- Muhammad Ikram 5 &
- Zhang Jianglin 1 , 2
BMC Public Health volume 21 , Article number: 1299 ( 2021 ) Cite this article
8695 Accesses
22 Citations
1 Altmetric
Metrics details
A Correction to this article was published on 12 July 2021
This article has been updated
The study aims to predict and assess cardiovascular disease (CVD) patterns in highly affected countries such as Pakistan, India, China, Kenya, the USA, and Sweden. The data for CVD deaths was gathered from 2005 to 2019.
We utilized non-homogenous discrete grey model (NDGM) to predict growth of cardiovascular deaths in selected countries. We take this process a step further by utilizing novel Synthetic Relative Growth Rate (RGR) and Synthetic Doubling Time (Dt) model to assess how many years it takes to reduce the cardiovascular deaths double in numbers.
The results reveal that the USA and China may lead in terms of raising its number of deaths caused by CVDs till 2027. However, doubling time model suggests that USA may require 2.3 years in reducing the cardiovascular deaths.
Conclusions
This study is significant for the policymakers and health practitioners to ensure the execution of CVD prevention measures to overcome the growing burden of CVD deaths.
Peer Review reports
Introduction
The upsurge of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection in early 2020 caused a disease pandemic known as COVID-19 [ 1 , 2 ]. There is practically no country in the world which is not influenced by COVID-19 and the health services worldwide have never operated under this tremendous burden. Everything begun in Wuhan [ 3 ], China, but it has expanded exponentially all over the world. The core of the pandemic then moved to Europe and the US [ 4 ]. Studies also shown that patients with Cardiovascular Disease (CVD) are especially at great risk of COVID-19 mortality owing to their frailty and vulnerability [ 5 , 6 ]. Patients with pre-existent CV risk factors and CVDs are among the most vulnerable with significantly greater risk of developing SARS-CoV-2 infection, acquiring CV complications associated with COVID-19, and having undesirable consequences [ 7 ].
Since the number of deaths has been increasing globally due to different reasons, CVD is one of the world’s most significant causes of mortality and morbidity. During the past decade, the number of deaths from CVD has increased by 12.5% globally [ 8 , 9 ]. There are various reasons behind this progressive number of cardiovascular deaths. In 2016, the primarily cause of total global burden of CVD was ischemic heart disease (IHD) contributed to 49% of total burden of CVD, followed by stroke with 33% of total CVD burden. In comparison, other CVD causes account for a significantly lower percentage of the global disease burden [ 10 ].
CVDs have affected all the income level countries, especially low- and middle-income countries (LMIC) contribute the greatest portion to the overall CVD burden, specifically in terms of deaths at younger ages than in high-income countries, because of scarce human and financial resources [ 11 , 12 , 13 ]. Whereas, several of the largest LMIC had an increase in the overall burden of CVD; in decreasing pattern of percent burden increase, those included: India (15.4%), Bangladesh (27.4%), Indonesia (8.8%), China (6.6%), the Philippine (25.3%), and Mexico (19.7%) [ 14 ]. However, the CVD burden remains the most significant per capita in Eastern Europe and Central Asia. While, East Asia and South Asia are roots to the increased CVD burden, because of their growing and aging of the populations [ 15 ]. The 2016 Global Burden of Diseased Disease (GBD) report reveals that non-communicable diseases (NCDs) comprise 40% of the total age standardized global disease burden for women and about 50% of the global standardized men ‘s overall age burden. CVD alone accounted for 20% of women ‘s total burden and 24% of men ‘s total burden [ 16 ]. The frequency of steady or growing CVD Disability Adjusted Life-Year (DALY) epidemiological drivers vary across different countries. In countries such as Japan, a reduced CVD mortality rate has been offset by accelerated population aging. A slight rise of the CVD rate is associated with population ageing and limited resources in South Asian countries such as Pakistan, India, and Bangladesh [ 17 ].
Several epidemiological studies have forecast future trends in the occurrence of CVD and mortality rates for all age groups in various countries of the world [ 18 , 19 , 20 ], yet little is known about the absolute burden of deaths. To prepare for future cardiovascular care needs with certainty, the purpose of this study is to forecast the number of deaths caused by CVD from 2020 to 2027 of six higly effected countries which include Pakistan, India, China, Keyna, the USA and Sweden. We employed advanced mathematical modeling, namely Non-Homogenous Discrete Grey Model (NDGM) to predict the cardiovascular deaths of selected countries. The grey forecasting models, especially, the NDGM model, can be superior to other forecasting models in the context of small samples and poor information [ 21 ]. Hence, we have utilized NDGM model in the current paper to predict the future trends of CVD of top six countries globally. Further, a novel Synthetic Relative Growth Rate (RGR) and Synthetic Doubling Time ( D t ) models employed to undertake a comparative analysis of CVD relative growth rate among six countries. Moreover, Mean Absolute Percentage Error (MAPE) % criterion was used to measure the accuracy of NDGM model. Hence, present research is a pioneer study to forecast relative growth and required time to reduce the number of deaths double in number caused by CVD among six countries. The study is principally significant for the policymakers to convey, empower and stimulate the execution of CVD prevention approaches to end this growing burden of CVD during the ongoing COVID-19 pandemic and time ahead.
The rest of paper follow as: Section 2 represent the research methodology. Whereas the result and discussion section are presented in section 3. Finally, conclusion, policy implications along with study limitations presented in last section is study.
Research methodology
This section provides steps involved in development of NDGM model. Additionally, synthetic RGR and synthetic D t models have been discussed to analyze the growth and time of CVD deaths for selected countries. Finally, the performance evaluation of NDGM model through MAPE is also elaborated in this section.
Data source and study population
The CVD number of deaths data was abstracted from the official website of Our World in Data for the period 2005–2019. The top six countries which are Pakistan, India, China, Kenya, USA and Sweden with highly affected from cardiovascular deaths were selected, globally. The source of the data available at Our World in Data was the global burden of disease (GBD) collaborative network (2016), World Health Organization (WHO) and Institute for health metrics and evaluation (IHME) 2017. Grey system software (v8.0) has been used to forecast cardiovascular deaths for the period of 2020 to 2027 by NDGM. However, MATLAB and MS EXCEL were also used to solve NDGM. The current analysis and modeling methodology were employed for the first time in the study of forecasting CVD related deaths. The structure of forecasting the CVD deaths is operationalized in this study presented in Fig. 1 .
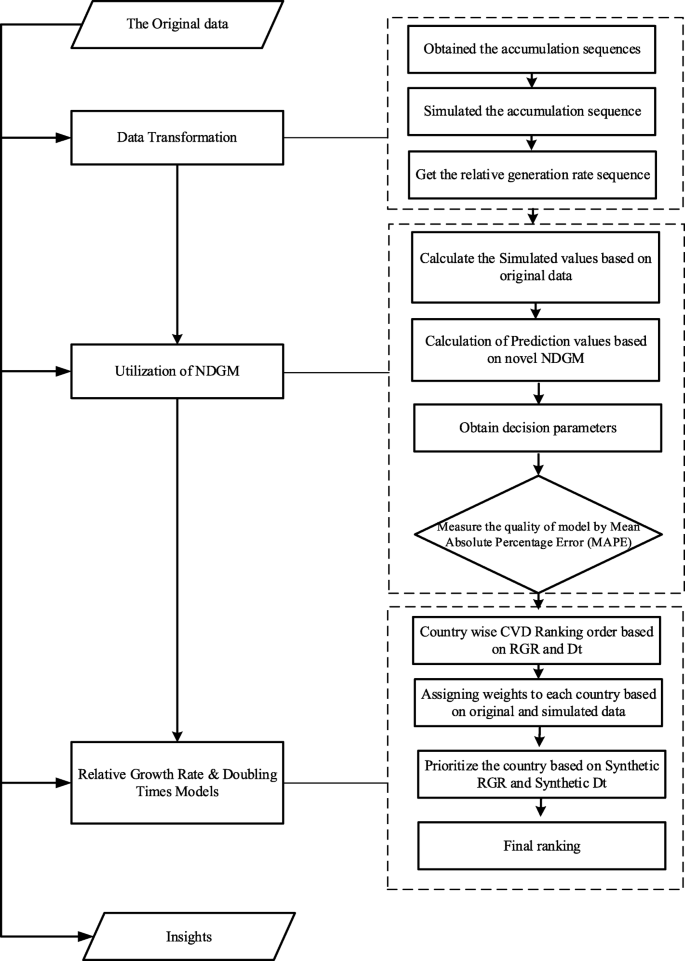
Framework operationalized in this study
Grey forecasting model
In 1982 Deng Julong originally introduced the concept of a Grey Systems Theory (GST) as a scientific theory for predicting uncertain system, which involves limited and inadequate information. Ultimately, theoretical forecasts based on the grey framework surpassed the standards of statistical and mathematical methods [ 22 ]. Theory of grey systems has been applied successfully in several fields so far [ 23 , 24 , 25 ] and grey prediction theory is a significant branch of the theory of grey systems. There are five major types of grey prediction, such as time series forecasts, calamity forecasts, seasonal calamity forecasts, topological forecasts, and systemic forecasts. Till date, GS theory has introduced a variety of theories and techniques like grey mathematics, grey modeling, grey forecasting, grey clustering, grey decision making, grey programming, grey relational analysis, and grey control, which has been effectively implemented in various fields and has shown satisfactory results [ 26 , 27 ]. The key benefit of grey theory is that it can manage both with limited and uncertain information with great precision. It functions as an analytical tool particularly in situations where data is inadequate.
Nonhomogeneous discrete grey model (NDGM)
In order to predict data, there are different types of grey models, we will analyze NDGM to predict future cardiovascular deaths. The NDGM system is designed on the basis of law of approximation non-homogenous exponential growth in accordance with assumptions of a sequence of real data [ 24 ] [ 28 ];. Xie et al. [ 25 ] recommended that the actual data sequence is a concurrence with a homogenous pattern like GM (1, 1). The accuracy level of NDGM model is considerably improved over other grey models so far as mean sequence value and value set of intervals [ 29 ]. NDGM model has been utilized in various fields, for example, in a study the electricity consumption of Turkey was predicted and analyzed the NDGM as best fit and more accurate prediction model over other grey forecasting models [ 30 ]. Whereas, Duan et al. forecast the crude oil consumption in China and investigated that NDGM showed superior performance [ 31 ].
x (0) , represent the original data sequence and x (1) follows the accumulated data sequence in NDGM model so, we can write as follows:
Where, \( {\hat{x}}^{(1)} \) (L), is the forecasting value of x (1) along with parameters β 1, β 2, β 3 and β 4. So, we can write the above equation in matrix form as this: if L = 1, 2, and 3 …. n-1
The input data shows constant sequence in single case in order to satifsy NDGM parameters β1, β2, β3, and β4 by applying the following relation:
The following formula to be used to calculate β4 for minimizing the sum of square error:
For further knowledge about NDGM model, its parameter and properties, Liu et. al. (2010) is referred [ 25 ].
Performance evaluation approach of NDGM
We employed mean absolute percentage error (MAPE) to evaluate the accuracy of NDGM model. The formula to calculate MAPE % is as follows:
Where y (0) ( k ) represents the original sequence of data and \( {\hat{y}}^{(0)}(k) \) denotes the forecasting sequence data values.
Relative growth rate (RGR) and doubling time (D t ) analysis
To best of our knowledge, there is no model available to check the growth rate for cardiovascular deaths. In this manner, RGR model was used to analyze the relative growth of cardiovascular deaths for selected countries [ 32 ]. Two parameters ( D t and RGR) were employed in order to forecast the number of deaths caused by CVD of selected countries by utilizing NDGM model. The equation of RGR is given by,
Where L 2 denotes the cumulative number of cardiovascular deaths in year t 2 & L 1 represent the cumulative number of cardiovascular deaths in year t 1 ,as in our case, the equation can be reduced to
The D t is the time required for publications to reduce the number of cardiovascular deaths for a given RGR is represented as:
In our case, it can be written as:
Synthetic RGR and synthetic doubling time model
In any case, if the RGR and D t make an alternate pattern, when compared with that of actual data pattern create issue, in this regard synthetic Relative Growth Rate (RGR syn ) and Synthetic Doubling Time (D syn ) models have been introduced [ 33 ]. The equation for Synthetic Relative Growth Rate (RGR syn ) model can be written as follows:
Whereas RGR original denotes the Relative Growth Rate of original data and RGR forecast explains the Relative Growth Rate of predicted values. However, θ indicate relative weights coefficient and its value can be taken as 0.5 in general.
The Synthetic Doubling Time (D syn ) model is presented as:
Here, D original demonstrates the Doubling Time obtained from original data values, whereas RGR forecast indicate Relative Growth Rate based on forecasting data values.
We employed NDGM to forecast the relative growth of cardiovascular deaths among six participated countries. The calculated simulated values for the data 2005–2019 are shown in Tables 1 , 2 , 3 , 4 , 5 , and 6 . Table 1 shows the forecasts results for Pakistan. The values obtained from MAPE % demonstrate the effectiveness level of 97.05% which shows NDGM as a best-fit grey model to forecast number of deaths caused by CVD. The simulated values based on NDGM showed an increasing trend for future. Figure 1 has been shown to better understand the comparison between actual data and the simulated NDGM data from 2005 to 2027 against the increasing deaths pattern for CVD in Pakistan.
With the turn of the century, CVDs became the leading cause of mortality in India. Table-2 represents the results from India with the MAPE accuracy level of 98.35%. The NDGM based simulated values also showed an inclined pattern in progressive number of cardiovascular deaths in future.
Table 3 represents the results for china. The forecast values based on NDGM simulated data showed an anticipated trend until 2027. The MAPE accuracy level turned out to be 96.88%. The NDGM model findings are found consistent with a range of other cardiovascular disease predictions in China, as the burden of CVD was increasing and primary and secondary prevention is likely to be core health policy priorities in the immediate future [ 34 , 35 ].
Likewise, Tables 4 , 5 and 6 represents the results for Kenya, USA and Sweden with MAPE accuracy level of 97.77, 96.8 and 97.74% respectively (Table 8 ). These findings are similar with some prior findings in which increasing trends have been reported [ 36 ]. According to a study in USA if projected trends in ischemic stroke mortality continue, increase in US stroke deaths will outpace overall population growth, with a doubling in deaths by the year 2032 [ 37 ]. For an easy and clear comparison of cardiovascular raising trends, Fig. 2 a-f can be seen. All participated countries showed an increasing trend in raising their number of cardiovascular deaths, except for Sweden. A study has reported decline in mortality and incidence of cardiovascular related diseases since 1980s in Sweden. Changes in lifestyle have helped to break the increasing trend in CVD [ 38 ]. The outcomes reveal that the MAPE accuracy level for NDGM in case of India is found slightly higher than the rest of the five countries whereas Pakistan, Kenya and Sweden showed almost same MAPE accuracy level. The average MAPE accuracy level for NDGM showed a value of 97.44% (Table 8 ). The anticipated future trends in cardiovascular deaths for the participated countries compel to focus on the importance of increased investment in prevention and treatment of CVD.
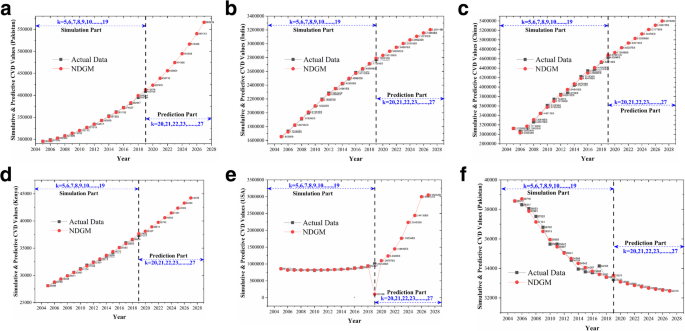
a Simulative and Predictive values of NDGM for Pakistan. b Simulative and Predictive values of NDGM for India. c Simulative and Predictive values of NDGM for China. d Simulative and Predictive values of NDGM for Kenya. e Simulative and Predictive values of NDGM for USA. f Simulative and Predictive values of NDGM for Sweden
CV death growth and doubling time model based on NDGM
The relative growth rates and doubling time model have been employed to calculate the relative growth of cardiovascular deaths and an expected time to reduce the deaths in selected countries. Table 7 represents the ranking order of six countries for an estimated RGR and doubling time (Dt) as per original and simulated data. The RGR equation of original data showed a ranking order given below:
To calculate the required time for cardiovascular death reduction among six countries based on original data, the following sequence was observed as per doubling time (D t ) model:
The above-mentioned findings demonstrate that the relative growth of cardiovascular deaths in China as an upper middle-income country and USA as a high-income country rank higher followed by India, Pakistan, Kenya and Sweden based on original data. On the contrary, the doubling time model suggest that developed countries like USA and Sweden require an additional time and endeavors to reduce cardiovascular deaths double in number than in developing countries (India, Pakistan, China, Kenya). Therefore, the relative growth rate can be a source of competitive edge among developing and developed countries.
Likewise, we utilized NDGM-based simulated data to find out the status of deaths due to CVD for the period from 2020 to 2027. As indicated by RGR sequence, the following results was acquired:
Approximately same sequence was observed based on the simulated data. For the period 2020–2027, USA and China may endure progressively number of deaths due to CVD in terms of RGR i.e. (3.29%) and (2.75%) respectively followed-by Pakistan, Kenya, India and Sweden.
As per doubling time (D t ) model, the following pattern of results is obtained:
Our findings also revealed that USA and Sweden need relatively additional timespan to double reduce the number of cardiovascular deaths, followed by Kenya, India, Pakistan and China.
By using NDGM (based on actual and simulated data), we forecast the number of cardiovascular deaths for the period from 2020 to 2027.
Synthetic RGR and synthetic DTM for cardiovascular deaths
Presently a query arises here eventually as which country may endure maximum number of deaths by CVD in the long run. Therefore, to respond the query synthetic indices by original and forecasting values have been calculated.
By using synthetic indices, the sequence obtained for RGR is as follows:
As per synthetic doubling time model D t, we obtained a sequence as follows:
Both sequences are found almost similar to the sequences obtained against the actual data thus the results are aligned with the actual data and the feasibility of the synthetic models has also been tested successfully.
In spite of significant reductions in incidence and mortality, CVDs are still the greatest reason for death globally, both in terms of health and economic cost. We built up a forecasting framework to estimate the expected number of cardiovascular deaths in Pakistan, India, China, Kenya, the USA and Sweden by utilizing the most accurate methodology of the grey forecasting framework. Results depicted that grey prediction model was effectively applied to forecast the number of deaths caused by CVD for the period from 2020 to 2027. In addition, this study also suggests an expected time to reduce the number of deaths double in numbers using doubling time (D t ) formula. All six countries showed an increasing trend in forecasting number of deaths due to CVD for the period 2020–2027, except for Sweden. However, the results indicated that USA and China are more likely to suffer from cardiovascular deaths in future followed by Pakistan, Kenya, India and Sweden. Though China found prone to suffer maximum deaths in future, the doubling time (D t ) suggests less time expected to control and prevent from cardiovascular deaths double in number.
The results confirm that developed countries need relatively more time to reduce the deaths double in numbers whereas, developing countries require less time to do so. Whereas the USA and China may lead in terms of raising its cardiovascular mortality in future. While in case of lower middle-income countries, India and Pakistan are more likely to suffer from cardiovascular deaths in future followed by Kenya and Sweden. Figuratively speaking, a sword of Damocles hangs over the people of the USA and China, indeed most of the entire world, for the near future. Through CVD prevention and the implementation of workable approaches, we are foreseeing a future wherein the CVD epidemic is being tamed.
Statistics from various parts of the world show a large percentage of cerebrovascular and CV associated diseases in patients with COVID-19, which posed several questions about the higher sensitivity of patients with any of these comorbidities to the novel coronavirus, and also the function of CVD in progression and COVID-19 patient prognosis. Patients with Cardiovascular diseases should be monitored by their healthcare professionals with special preventive procedures for COVID-19 infection. The level of severity of both the primary respiratory syndrome and risk of adverse events is elevated in patients associated with COVID-19 and also with pre-existing cardiovascular diseases. Hospitals and health care networks must embrace a comprehensive approach to provide all patients with the best quality treatment, irrespective of their COVID-19 status. This is especially significant for the cardiology community, considering patients with prior symptoms of CVD and risk factors are potentially more likely to experience COVID-19 and encounter undesirable consequences. As the rate of infection rises, several cardiac patients may seek immediate treatment for either COVID-19 associated diseases or common cardiac complications. Most of these patients would need a cardiac intervention while at the same time getting SARS-CoV-2 infection.
COVID-19, triggered by SARS-CoV-2, is a worldwide pandemic emerging in real time. Cardiovascular and associated comorbidities are very common in COVID-19 patients and those are at greater risk of morbidity and mortality. COVID-19 raised an additional constraint on pre-existing CVDs. Findings from COVID-19 infection with a significant number of patients showed that fatality rate was of 10.5% for CVD among 72,314 COVID-19 cases [ 39 ]. Studies have revealed that there is a greater risk of mortality among patients hospitalized with COVID-19 due to CVD. Given the growing number of COVID-19 patients other than regular clinical presentations of illness, CVD in COVID-19 infected patients appear to be alarming [ 40 , 41 ]. CVDs have played an important role in patient outcomes infected from the virus. Thus, careful review and monitoring of CVD in COVID-19 patients are required, from diagnosis to bedside.
CV associated complications have been identified in prior respiratory infections with related etiology and their occurrence affects the severity of the illness, so even pneumonia related hospitalization is found related with long-term and short-term risk of CVD [ 42 ]. Infection from viruses lead to an imbalance in cardiac supply and demand, as well as an increase in systemic inflammation. Consequently, patients with pre-existing CVD are more likely to experience acute cardiac complications, and thrombosis, and lead to severe infections. An investigation from a meta-analysis analyzed pooled prevalence of CVD in COVID-19 infected patients in various countries. The following are the findings of the meta-analysis: the US (24%), Brazil (50%), Netherlands (44%), Germany (46%), Iran (4%), Italy (25%), China (8%), South Korea (11%), Spain (17%), Switzerland (71%), United Kingdome (15%), and France (48%) Fig. 3 a. The prevalence of CV complications in infected patients was shown to be substantially correlated with ICU admissions and mortality in that meta-analysis Fig. 3 b [ 44 ].
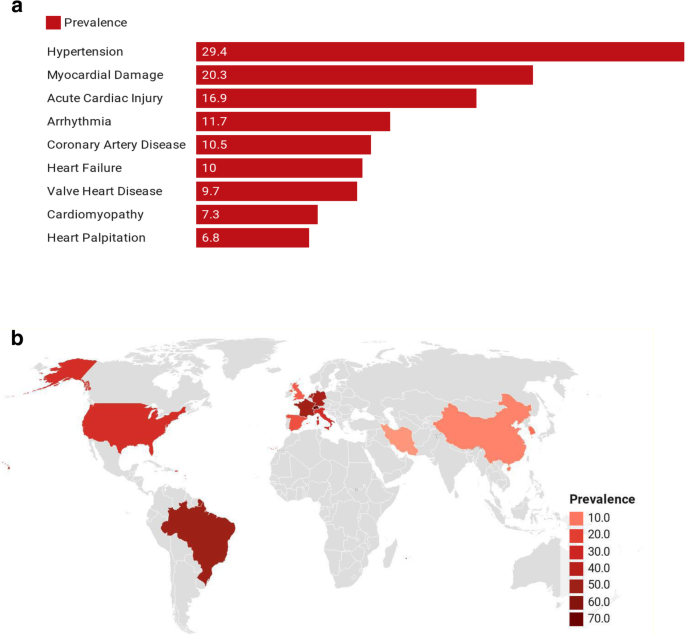
a Prevalence of Cardiovascular Complications Among COVID-19 Patients ( Source [ 44 ];). b Cardiovascular Disease Burden among COVID-19 Patients in different countries ( Source [ 44 ];)
However, valid information to assess the exact burden of CVD is inadequate in many parts of the world, which compels the foundation of nationwide prevention and management policies. It is clear that while many advances have been introduced in our comprehension of worldwide CVD epidemiology, there is wide variation present in data, mainly in MICs and LICs such as Pakistan and India. In these regions, there is a requirement for significantly advanced frameworks for the supervision of risk factors and disease and for strategies that can diminish CVD’s morbidity and mortality at a low cost in ways that are practical and sustainable. The former can be achieved with large but simple health surveys that gather reliable data on health behaviors, CVD associated risk factors, incidence, and mortality, and access to health care in every region of the world.
Though these predictions are sober, they do not need to become true, as CVD is potentially preventable. Improving risk factors at population level in the past obviously had a decisive effect on the reduction in death rates for CVD worldwide. Several studies have shown that there is a considerable decrease in CVD mortality rates among individuals with favorable levels of significant CVD risks [ 45 ] [ 8 , 46 ]. Likewise, people who practice a healthy lifestyle face a comparatively lower risk of suffering from cardiovascular related diseases. A greater emphasis on prevention may therefore alter these anticipated trends in the future and eventually may overcome the growing pandemic of COVID-19.
Limitations
The present study has several limitations. The data from Our World in Data, however comprehensive and easily accessible to almost all countries and regions, is based on regularly available data from those countries and regions. Variations may occur in the robustness of the data selection and processing and reliability of the cause of the death. Secondly, these predictions are made for developed and developing countries data together, and their generalizability to other countries should be considered with caution. It should be acknowledged that there are many differences between developed and developing countries when comparing health-care systems and how diseases are dealt. We believe that this has kept our analysis conservative. Another limitation of the study is the application of single grey prediction model which is NDGM. The further research can be carried out by employing other grey prediction models and should consider the other regions of the world for more insight information.
In conclusion, CVD plays a key role in disease burden and mortality in COVID-19 patients. Since CVD complications in COVID-19 patients could be fatal, they must be carefully monitored and managed in the case of an acute illness. It is yet not clear whether the prevalence of cardiovascular comorbidities poses independent risk or if this is affected by other factors such as age etc. The results from the forecasting model against all selected countries showed an increasing trend in terms of raising its number of deaths due to CVD till 2027, except for Sweden. However, the growth rate for the USA (RGR: 2.71%) and China (RGR: 2.55%) was found relatively higher than the rest of the three countries. The findings also revealed that USA (2.3 years) and Sweden (2.2 years) may require relatively additional timespan to double reduce the number of cardiovascular deaths when compared with China (2.1 years). The findings of this study can aid policymakers, doctors, and front-line healthcare workers in making evidence-based decisions and reducing the mortality and morbidity associated with this 21st-century pandemic.
Availability of data and materials
The data used in the current study is available publicly at www.ourworldindata.com .
Change history
12 july 2021.
A Correction to this paper has been published: https://doi.org/10.1186/s12889-021-11450-z
Abbreviations
- Cardiovascular disease
Non-homogeneous discrete grey model
Even Grey Model
Discrete Grey Model
Severe acute respiratory syndrome coronavirus 2
Relative Growth Rate
Doubling Time
Grey Systems Theory
Ischemic Heart Disease
Low- and middle-income Countries
Global Burden of Disease
Non-communicable diseases
Disability adjusted life-years
Mean Absolute Percentage Error
World Health Organization
Institute of health metrics and evaluation
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. https://doi.org/10.1016/S0140-6736(20)30566-3 .
Article CAS PubMed PubMed Central Google Scholar
Siddiqi HK, Neilan TG. COVID-19, Immuno-oncology and cardiovascular disease: viewpoint from the intersection. J Cardiovasc Transl Res. 2020;13(3):347–8. https://doi.org/10.1007/s12265-020-10013-8 .
Article PubMed PubMed Central Google Scholar
Liu Z, Magal P, Seydi O, Webb G. Understanding unreported cases in the COVID-19 epidemic outbreak in Wuhan, China, and the importance of major public health interventions. Biology. 2020;9:50.
Article CAS PubMed Central Google Scholar
Tadic M, Cuspidi C, Mancia G, Dell’Oro R, Grassi G. COVID-19, hypertension and cardiovascular diseases: Should we change the therapy? Pharmacol Res. 2020;13:104906.
Article Google Scholar
Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Syndr Clin Res Rev. 2020;14(3):247–50. https://doi.org/10.1016/j.dsx.2020.03.013 .
Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, et al. COVID-19 and cardiovascular disease. Circulation. 2020;141(20):1648–55. https://doi.org/10.1161/CIRCULATIONAHA.120.046941 .
Article CAS PubMed Google Scholar
Ganatra S, Dani SS, Shah S, Asnani A, Neilan TG, Lenihan D, et al. Management of cardiovascular disease during coronavirus disease (COVID-19) pandemic. Trends Cardiovasc Med. 2020;30(6):315–25. https://doi.org/10.1016/j.tcm.2020.05.004 .
Joseph P, Leong D, McKee M, Anand SS, Schwalm JD, Teo K, et al. Reducing the global burden of cardiovascular disease, part 1: the epidemiology and risk factors. Circ Res. 2017;121(6):677–94. https://doi.org/10.1161/CIRCRESAHA.117.308903 .
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25.
Watkins DA, Beaton AZ, Carapetis JR, Karthikeyan G, Mayosi BM, Wyber R, et al. Rheumatic heart disease worldwide: jacc scientific expert panel. J Am College Cardiol. 2018;72:1397–416.
Bowry ADK, Lewey J, Dugani SB, Choudhry NK. The burden of cardiovascular disease in low-and middle-income countries: epidemiology and management. Can J Cardiol. 2015;31(9):1151–9. https://doi.org/10.1016/j.cjca.2015.06.028 .
Article PubMed Google Scholar
Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P. The economic burden of cardiovascular disease and hypertension in low-and middle-income countries: a systematic review. BMC Public Health. 2018;18(1):975. https://doi.org/10.1186/s12889-018-5806-x .
Rehman S, Li X, Wang C, Ikram M, Rehman E, Liu M. Quality of care for patients with acute myocardial infarction (AMI) in Pakistan: a retrospective study. Int J Environ Res Public Health. 2019;16(20):3890. https://doi.org/10.3390/ijerph16203890 .
Article PubMed Central Google Scholar
Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371(9):818–27. https://doi.org/10.1056/NEJMoa1311890 .
Ohira T, Iso H. Cardiovascular disease epidemiology in Asia. Circ J. 2013;2013:CJ-13.
Google Scholar
Benziger CP, Roth GA, Moran AE. The global burden of disease study and the preventable burden of NCD. Glob Heart. 2016;11(4):393–7. https://doi.org/10.1016/j.gheart.2016.10.024 .
Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333–41.
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–44. https://doi.org/10.1161/CIR.0b013e31820a55f5 .
Chernova IV, Sumin SA, Bobyr MV, Seregin SP. Forecasting and diagnosing cardiovascular disease based on inverse fuzzy models. Biomed Eng. 2016;49:263–7.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2018;137(12):e67–492. https://doi.org/10.1161/CIR.0000000000000558 .
Ikram M, Sroufe R, Zhang Q, Ferasso M. Assessment and prediction of environmental sustainability: novel grey models comparative analysis of China vs. the USA. Environ Sci Pollut Res. 2021;28(14):17891–912. https://doi.org/10.1007/s11356-020-11418-3 .
Article CAS Google Scholar
Chiang JS, Wu PL, Chiang SD, Chang TJ, Chang ST, Wen KL. Introduction to Grey system theory. J Grey Syst. 1998;1:1–24.
Rehman E, Ikram M, Feng MT, Rehman S. Sectoral-based CO2 emissions of Pakistan: a novel Grey relation analysis (GRA) approach. Environ Sci Pollut Res. 2020;27(23):29118–29. https://doi.org/10.1007/s11356-020-09237-7 .
Javed SA, Liu S. Predicting the research output/growth of selected countries: application of even GM (1, 1) and NDGM models. Scientometrics. 2018;115(1):395–413. https://doi.org/10.1007/s11192-017-2586-5 .
Xie N-M, Liu S-F, Yang Y-J, Yuan C-Q. On novel grey forecasting model based on non-homogeneous index sequence. Appl Math Model. 2013;37(7):5059–68. https://doi.org/10.1016/j.apm.2012.10.037 .
Wu L-F, Liu S-F, Cui W, Liu D-L, Yao T-X. Non-homogenous discrete grey model with fractional-order accumulation. Neural Comput Appl. 2014;25(5):1215–21. https://doi.org/10.1007/s00521-014-1605-1 .
Ikram M, Zhang Q, Sroufe R. Developing integrated management systems using an AHP-fuzzy VIKOR approach. Bus Strateg Environ. 2020;29(6):2265–83. https://doi.org/10.1002/bse.2501 .
Liu S, Forrest JYL. Grey systems: theory and applications: Springer; 2010. https://doi.org/10.1007/978-3-642-13938-3 .
Ikram M, Mahmoudi A, Shah SZA, Mohsin M. Forecasting number of ISO 14001 certifications of selected countries: application of even GM (1,1), DGM, and NDGM models. Environ Sci Pollut Res. 2019;26(12):12505–21. https://doi.org/10.1007/s11356-019-04534-2 .
Kusakci AO, Ayvaz B. Electrical energy consumption forecasting for Turkey using grey forecasting technics with rolling mechanism. In: Conference Proceedings of 2015 2nd international conference on knowledge-based engineering and innovation: KBEI 2015. Tehran: Iran University of Science and Technology; 2016.
Duan H, Lei GR, Shao K. Forecasting crude oil consumption in China using a grey prediction model with an optimal fractional-order accumulating operator. Complexity. 2018;2018:1–12. https://doi.org/10.1155/2018/3869619 .
Bajwa RS, Yaldram K, Rafique S. A scientometric assessment of research output in nanoscience and nanotechnology: Pakistan perspective. Scientometrics. 2013;94(1):333–42. https://doi.org/10.1007/s11192-012-0699-4 .
Liu S, Yang Y, Forrest J. Grey data analysis. Singapore: Springer; 2017.
Shen C, Ge J. Epidemic of cardiovascular disease in China: current perspective and prospects for the future. Circulation. 2018;138(4):342–4. https://doi.org/10.1161/CIRCULATIONAHA.118.033484 .
Stevens W, Peneva D, Li JZ, Liu LZ, Liu G, Gao R, et al. Estimating the future burden of cardiovascular disease and the value of lipid and blood pressure control therapies in China. BMC Health Serv Res. 2016;16:1–10.
Pearson-Stuttard J, Guzman-Castillo M, Penalvo JL, Rehm CD, Afshin A, Danaei G, et al. Modeling future cardiovascular disease mortality in the United States: national trends and racial and ethnic disparities. Circulation. 2016;133(10):967–78. https://doi.org/10.1161/CIRCULATIONAHA.115.019904 .
Elkins JS, Johnston SC. Thirty-year projections for deaths from ischemic stroke in the United States. Stroke. 2003;34(9):2109–12. https://doi.org/10.1161/01.STR.0000085829.60324.DE .
Bengtsson T, Keilman N. Old and new perspectives on mortality forecasting. Cham: Springer Nature; 2019.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42. https://doi.org/10.1001/jama.2020.2648 .
Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811–8. https://doi.org/10.1001/jamacardio.2020.1017 .
Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system. JAMA Cardiol. 2020;5(7):831–40. https://doi.org/10.1001/jamacardio.2020.1286 .
Violi F, Cangemi R, Calvieri C. Hospitalization for pneumonia and risk of cardiovascular disease. JAMA. 2015;313(17):1753. https://doi.org/10.1001/jama.2015.3130 .
Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116(10):1666–87. https://doi.org/10.1093/cvr/cvaa106 .
Hessami A, Shamshirian A, Heydari K, Pourali F, Alizadeh-Navaei R, Moosazadeh M, et al. Cardiovascular diseases burden in COVID-19: Systematic review and meta-analysis: medRxiv; 2020. https://doi.org/10.1016/j.ajem.2020.10.022 .
Barber RM, Fullman N, Sorensen RJD, Bollyky T, McKee M, Nolte E, et al. Healthcare access and quality index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the global burden of disease study 2015. Lancet. 2017;390(10091):231–66. https://doi.org/10.1016/S0140-6736(17)30818-8 .
Fuster V, Kelly BB, Vedanthan R. Promoting global cardiovascular health: moving forward. Circulation. 2011;123(15):1671–8. https://doi.org/10.1161/CIRCULATIONAHA.110.009522 .
Download references
Acknowledgments
Not applicable.
This work is supported by the Union Program of Science and Health of Hunan Province, China (2019JJ80011). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Dermatology, Shenzhen People’s Hospital, The Second Clinical Medical College, Jinan University, The first Affiliated Hospital, Southern University of Science and Technology, Shenzhen, 518020, Guangdong, China
Shazia Rehman & Zhang Jianglin
Candidate Branch of National Clinical Research Center for Skin Diseases, Shenzhen, 518020, Guangdong, China
Department of Biostatistics, School of Public Health, Harbin Medical University, Harbin, China
Shazia Rehman
Department of Mathematics& Statistics, School of Statistics, Southwestern University of Finance and Economics, Chengdu, China
Erum Rehman
College of Management, Research Institute of Business Analytics and Supply Chain, Management, Shenzhen University, Shenzhen, China
Muhammad Ikram
You can also search for this author in PubMed Google Scholar
Contributions
SR wrote the first draft of the article and conceptualized the overall study. SR and MI are involved in the data analysis. SR, ER and MI wrote the final manuscript. ZJL is responsible for project administration and supervision of the overall manuscript. All authors contributed to a second and third iteration of the manuscript, and everyone read and approved the final manuscript.
Corresponding author
Correspondence to Zhang Jianglin .
Ethics declarations
Ethics approval and consent to participate.
This study used secondary data and did not involve human subjects directly, informed consent was not obtained from the patients.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised as it erroneously contained red text in the equations under the section Relative growth rate (RGR) and doubling time (Dt) analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Rehman, S., Rehman, E., Ikram, M. et al. Cardiovascular disease (CVD): assessment, prediction and policy implications. BMC Public Health 21 , 1299 (2021). https://doi.org/10.1186/s12889-021-11334-2
Download citation
Received : 16 September 2020
Accepted : 21 June 2021
Published : 02 July 2021
DOI : https://doi.org/10.1186/s12889-021-11334-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Relative growth rate
- Doubling time model, assessment, forecast
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Indian Diet for Gestational Diabetes, What to eat, what to avoid
Early Signs of Heart Disease in India Everything You Need To Know
Last updated on January 10, 2022
Content By: Dr. Nikita Toshi BDS, Assistant Manager (Medical Review), Dr. Ritu Budania MBBS, MD (Pharmacology) Head, Medical Affairs &

In this article
Any medical condition that affects the regular functioning of the heart might be the reason for early signs of heart disease or what we also know as cardiovascular diseases. Common heart conditions include rheumatic heart disease, congenital heart disease, arrhythmia (or irregular heartbeat) diseases of heart valves and blockage, commonly known as coronary artery disease.
So how healthy is your heart? Read on to understand what heart disease is, the early signs of heart disease in Indian adults and its underlying causes and risk factors. Also, learn about the diagnosis and treatment methods for heart diseases in India recommended by expert cardiologists to keep your heart healthy at all times.

Dr. Nikita Toshi
BDS, Assistant Manager (Medical Review)

Reviewed by
Dr. Ritu Budania
MBBS, MD (Pharmacology) Head, Medical Affairs
Understanding Heart Disease: How it Occurs in Indian Patients
What is Heart Disease?
The term heart disease is a blanket term for various heart-related diseases . It is important to detect the early signs of heart disease in adults to prevent any fatality. Heart diseases are a major cause of sudden death in the United States. Coronary heart disease, which affects the coronary circulation of the heart , is the most common heart disease affecting adults worldwide.
Is Heart Disease a common condition in India?
According to the World Health Organization, around 35,40,000 deaths occur in India due to cardiovascular disease (CVD), with it being more prevalent among the younger population. It is found that Indians have the highest rate of coronary artery disease (CAD). According to studies, India’s age-standardized CVD death rate is higher than the global average rate. In India, Tamil Nadu, Punjab and Kerala have the highest CVD rates.
Research has shown that cardiovascular disease is known to be the leading global cause of death due to non-communicable disease, accounting for more than 17.3 million deaths per year . In 2019, 17.9 million alone died of CVD . Out of these deaths, 85% were caused by heart attack and stroke. These statistical data emphasize the need for people to be aware of the early signs of heart disease and the ways it can be prevented to avoid a fatal outcome.
Types of Heart Diseases
Now that we know what heart disease is, let us have a look at some of the different types of heart diseases:
Rheumatic heart disease – A rheumatic heart disease is a form of chronic heart disease that is often caused by rheumatic fever and affects the connective tissues of the body including joints and valves of the heart. This type of heart ailment predominantly affects children but can occur at any age. The rheumatic cardiovascular disease symptoms include – chest pain, excess fatigue, irregular heart rate and weakness. Fever, rashes and pain in joints may also be present.
Valvular heart disease – This particular disease affects one or more of the four valves of the heart – aortic, mitral, pulmonary and tricuspid valves. People who are older are most susceptible to valvular heart diseases. Valvular heart disease affects the normal functioning of the heart valves by hardening and thinning the valves, which in turn, affects the blood flow and circulation in the body. The valvular cardiovascular disease symptoms include frequent fainting, severe fatigue, swelling on ankles, feet or abdomen and palpitations.
Hypertensive heart disease – One of the most common heart diseases, hypertensive heart disease causes include high blood pressure, which is responsible for damaging the blood vessels.
Cerebrovascular disease – Heart diseases may affect the blood flow to the brain and one of the most common causes of this disease is atherosclerosis (hardening or thickening of artery walls caused by the buildup of fat deposits). The signs of heart problems in this type of heart disease include severe thickening and accumulation of fat in the arteries. Cerebrovascular diseases can be identified by a blood clot in an artery of the brain, a blood clot in a vein of the brain or a deranged lipid profile. The common cerebrovascular heart disease prevention methods include bringing about lifestyle changes like eating a healthy diet and exercising regularly.
Conditions that occur due to the abnormal rhythm of the heart – Arrhythmia is one such condition. It simply refers to an irregular heartbeat. The heart might beat too fast (tachycardia) or it might beat too slowly (bradycardia). Arrhythmia based conditions can be an emergency but sometimes it could be harmless too. Nevertheless, it is recommended to consult a doctor the moment you experience these symptoms to avoid further complications – chest pain, palpitations, dizziness and shortness of breath.
Conditions associated with heart wall defects – Many types of congenital heart diseases fall under this category. In patients suffering from these conditions, the walls existing between the left and right chambers of the heart might not have been formed properly. As a result of which, the blood flows back into the other chambers of the heart, putting more pressure on the heart. Congenital heart diseases can be identified by low birth weight, breathlessness, delayed growth and so on.
Inflammatory heart disease – This heart ailment is caused due to inflammation of the pericardium (the membrane that surrounds the heart), radiation therapy, fungal and bacterial infection, myocarditis (inflammation of the heart muscle) and cancer. The symptoms include left side heart pain, dry cough, anxiety, fatigue and difficulty breathing.
Coronary Artery Disease – Also referred to as ischemic heart disease, this heart disease is caused by the buildup of plaque in the walls of coronary arteries which supply blood to the heart. The plaque buildup narrows the arteries, resulting in reduced blood flow to the heart, which in turn can cause chest pain, shortness of breath or even heart attack in case of an entire blockage of the arteries. High cholesterol levels, high blood pressure levels, diabetes and obesity are the major risks for coronary artery disease.
In a Nutshell
- The term heart disease is a blanket term for various heart-related diseases.
- Common heart conditions include rheumatic heart disease, congenital heart disease, Arrhythmia and coronary artery disease.
- Hypertensive heart disease is one of the most common types of heart disease in Indian patients and is associated with high blood pressure that invariably damages the blood vessels.

What are the causes and risk factors of heart diseases? Understanding the basics
Heart diseases have the ability to significantly affect one’s quality of life. In order to prevent heart diseases and lower your risk, it is important to know how it occurs. Some of the major causes and risk factors of heart diseases include:
High blood pressure – According to medical studies, hypertensive heart disease is considered a leading cause of death in patients with high blood pressure. This condition includes different types of heart diseases, including heart failure, left ventricular hypertrophy and ischemic heart disease. Untreated high blood pressure can also lead to left ventricular hypertrophy, a condition where the heart muscles thicken, which increases the pressure on the heart. This condition affects the heart’s working and makes it tough for the heart to pump enough blood, decreasing the oxygen supply to various organs.
High cholesterol and triglycerides – High levels of cholesterol in your body can lead to early signs of heart problems . Hypertension and thickening of artery walls affect the coronary circulation of the heart and serve as risk factors for different types of heart problems . High LDL cholesterol levels and low HDL cholesterol levels can lead to clogged arteries causing further complications. Since our body requires oxygen to function, a decreased supply of oxygen can affect the normal functioning of the heart. As per medical experts, by the time patients realize that their recommended and normal cholesterol levels are deranged, they are already at risk of developing various types of heart problems . In such a case, the only preventive step a person can take is to get regular cardiac tests done and find ways to lower their cholesterol levels by altering their diet and lifestyle.
Smoking – Smoking is one of the leading causes of heart diseases in India. Smoking can increase triglycerides in the blood and make the blood sticky and thick, making it more likely to clot. This increases the risks of left side heart pain . Other harmful health effects of smoking include – increasing plaque, fat, cholesterol and calcium buildup.
Excessive alcohol consumption – Regular and excessive alcohol consumption causes about 95,000 deaths in a single year in the US. Furthermore, deaths due to drinking account for at least 1 in 10 working-age adult deaths . Harmless as it may seem, excessive drinking can, over time, lead to the development of various types of heart problems . It can lead to severe heart conditions , such as cardiomyopathy and an irregular heartbeat.
Being overweight and obese – Being overweight is one of the major cardiovascular disease risk factors in children and adults. Obesity indicates high cholesterol levels in your body. It puts patients at a greater risk of developing health complications due to clogged arteries . Additionally, obesity can also lead to diabetes, high blood pressure and this, in turn, can lead to heart congestion .
Relationship between diabetes and heart disease – Uncontrolled diabetes is one of the major causes of several heart conditions . According to the American Heart Association, the risk of developing CVD in people with diabetes is more than double that in the general population. Also, as per medical research, death due to CVD is 70% higher in adults with diabetes.
A family history of heart disease – According to medical studies, patients who have one or more cases of heart disease in their family are at an increased risk of developing the condition at a more severe stage. Their family history makes them “genetically vulnerable” to also developing heart diseases. Additionally, this also makes one more vulnerable to developing diabetes, abnormally high cholesterol levels, obesity, hypertension or high blood pressure, all of which are proven potential risk factors of heart disease.
Poor dietary choices – It has been proven across several medical research studies that unhealthy eating habits can lead to Indian adults developing high cholesterol levels, ultimately leading to various heart ailments including blockage and heart congestion . There is no denying that cholesterol is crucial for the body’s normal functioning and cell membranes. However, high levels of triglycerides and low-density lipoprotein or LDL are responsible for causing heart-related trouble in patients. High-density lipoprotein or HDL helps reduce LDL levels in the body and thereby also brings down occurrences of cardiovascular disease risk factors .
Age – It has been observed and studied that people over the age of 65 are at a higher risk of developing several heart conditions . With age, the buildup of fatty deposits on the walls of arteries also increases, thus putting older people at an increased risk of developing symptoms of heart disease .
Lack of physical activity – Not performing enough physical movement or activities can increase the chances of developing the symptoms of a blocked artery and other metabolic disorders . It has been observed that people who are less active and less inclined towards performing physical exercises are at a greater risk of developing hypertension, diabetes and heart diseases in the future .
Sleep apnea – Research indicates a direct relationship between sleep apnea and heart problem symptoms in females and males. Thus, seeking treatment for sleep apnea is bound to improve the overall health and can help minimize the chances of a heart attack. Obstructive sleep apnea causes the oxygen levels in the blood to fall suddenly, leading to excessive production and release of adrenaline or epinephrine in the body. This increases blood pressure and stress on the heart. Moreover, obstructive sleep apnea can also cause atrial fibrillation, a form of irregular heartbeat.
High stress and anxiety levels – Individuals who go through regular anxiety or panic attacks are more likely to develop heart-related disorders that may present as left side heart pain which affects their cardiovascular health . Depression also reduces blood flow to the heart and increases the production of cortisol – a stress hormone in the body. This may not cause any heart trouble initially. However, with time, it can cause an increase in cardiovascular disease risk factors .
Leaky heart valves – As we all know, there are four valves in the heart, namely – the tricuspid, the mitral, the pulmonary and the aortic. They have flaps that allow the blood to flow in the correct direction. A leaky valve can lead to backflow of blood which in turn causes overworking of the heart. This increases the risk of other complications.
Due to some infections, autoimmune conditions, congenital malformations or cancers – As per experts, infections, medical conditions, such as Alzheimer’s, genetic defects and disorders all contribute towards heart problems in women and men.
- The most common causes associated with heart diseases include high blood pressure, high cholesterol, diabetes, obesity, high alcohol consumption, smoking, etc.
- Due to some infections, autoimmune conditions, congenital disabilities or cancers, risk factors for heart diseases may increase.
Warning Signs of Heart Disease In Indian Men: What to watch out for
In India, the occurrence of sudden cardiac death is found to be higher in men than in women. The heart diseases which are most common among men are heart attacks, heart failures, coronary artery disease, angina and arrhythmias. Despite the severity of the risks, the awareness regarding early signs of a heart attack in women and men is considered poor.
Did you know?
Out of one crore annual deaths in India, cardiovascular disease is responsible for 20.3% of deaths in men .
It is reported that 50% of the heart attacks in Indian men occur under 50 years of age and 25% of the heart attacks in Indian men occur under 40 years of age.
Over the past few years, it has been observed that half the men who die of a sudden heart attack had no symptoms of any heart disease or signs of blockage in the heart. This chilling revelation only increases the importance of getting regular heart-related tests from time to time.
What are the most common heart diseases that affect men?
Some of the most common heart diseases that affect men include irregular heartbeat or arrhythmia, coronary heart disease, heart attacks, heart valve disease, poor coronary circulation of heart , congenital heart disease, cardiomyopathy (affecting the heart muscles), pericardial disease, the Marfan syndrome, aorta disease, blood vessel or vascular disease.
What are the risk factors for heart disease in men?
As per reports, men are at a higher risk of developing heart diseases than women. Men develop heart diseases 10 years earlier than most women do. Erectile dysfunction: it’s time to address this health issue as it is a significant risk factor for heart disease in men. Studies show that 57% of men who had undergone bypass surgery and 64% of men who had experienced a heart attack had, at least at one point, had erectile dysfunction. Similarly, having low testosterone levels also indicate certain heart problems affecting the coronary circulation of the heart in men. Additionally, increased levels of stress, anxiety, depression, sedentary lifestyle, habits like smoking and alcohol intake can also lead to cardiovascular diseases and problems. Stress can increase blood pressure in the body and is considered one of the main causes of heart palpitations in men.
What are some of the heart disease symptoms that men experience?
The common symptoms of heart diseases in men are as follows:
What are some of the signs of a heart attack in men ?
The following are the signs of a heart attack in males. However, not all men will experience these signs. However, even at the slightest onset, it is advised to consult a doctor to confirm your diagnosis and avoid an unpleasant complication or outcome.
What are the signs of stroke in men?
The following are some of the common symptoms and signs of stroke in males:
How to provide aid during a heart emergency?
The patient’s recovery depends on how quickly care and medical services are delivered. To prevent yourself from suffering a sudden cardiac arrest, make sure you get regular heart-related tests done by a health professional from time to time.
How to care for a male heart patient?
Diet – Consult a doctor to know the right diet for the male patient and encourage them to follow it religiously.
Exercise – As a caretaker, encourage the patient to stay active and do exercises that will help strengthen his cardiovascular system.
Lifestyle modifications – Following a good routine to eat, sleep and exercise on time every day can be very helpful. Practising self-care and relaxation techniques for being emotionally fit is also recommended. Encourage them to quit smoking and alcohol for good health.
Regular checkup – Schedule heart-related tests periodically and follow up regularly with their doctor on their treatment plans and medications to limit the risk of complications.
Stay informed – Learn about the causes of heart palpitation and other heart abnormalities that can occur in male patients in order to offer the most effective care.
Quit unhealthy habits – Smoking and excessive alcohol intake can be very harmful to your heart. Encourage them to stay away from these harmful habits.
- Out of one crore deaths in India, cardiovascular disease is responsible for 20.3% of deaths in men.
- Most of the signs of heart diseases in men include pressure and feeling of tightness in the chest, discomfort in the arm, back, especially on the left side, pain in the chest, sweating, weakness and nausea.
- To prevent yourself from suffering from sudden cardiac arrest, make sure you follow a healthy diet and lifestyle and get regular heart-related tests done by a health professional.
Common Signs of Heart Disease in Indian Women What you should know
When one talks of heart diseases, one often pictures a man. However, heart disease is one of the leading causes of death in women (keeping aside the change in stats during the period of Pandemic). The early signs of a heart attack in women and their risk factors are different from those of men, thus leaving most women confused. However, knowing the common symptoms of heart trouble can help women improve their overall heart health. In addition to this, women, just like men, must also get regular heart-related tests performed at professional clinics and hospitals.
Nearly 8.6 million women die due to cardiovascular disease each year. This is more than the percentage of men dying due to stroke each year.
Out of one crore annual deaths in India, cardiovascular disease is responsible for 16.9% of deaths in women.
What are the signs and symptoms of heart diseases in women?
It is possible for women to not exhibit any symptoms of heart disease before suffering from a sudden cardiac arrest. Specific risk factors like diabetes in women, gestational diabetes, PCOS, breast cancer itself or therapy for breast cancer may also increase the chances of developing heart disease. This makes it very important for women to visit a cardiologist to get regular heart-related tests done. Getting these heart-related tests at regular intervals will help keep track of the overall health of the female. The following are the unique symptoms seen on women:
What are the signs of a heart attack in women?
Some of the most common signs of a heart attack in women include :
What are the signs of stroke in women?
These are the most common signs of a stroke are:
How to care for a female heart patient?
If you notice any heart problem symptoms in females, consult a doctor without delay.
Consult a dietician.
Encourage them to reduce their salt intake.
Ensure that they do not consume processed or packaged food and limit the intake of sugary foods.
Help with stress management.
Motivate them to opt for a healthy lifestyle – eating, sleeping and exercising on time.
Some time for self-care and hobbies.
Make sure they take all their medications timely.
Do not ignore prolonged female chest pains and consult a medical professional to know more and protect yourself from common heart problem symptoms in females .
- Nearly 8.6 million women die due to cardiovascular disease each year.
- The common heart attack signs in women include – tightness in the chest; pain in the arm, shoulders, jaw, neck, back, especially on one side of the body; shortness of breath; cold sweats; dizziness; fatigue; headache, etc.
- Getting the heart-related diagnosis and tests at regular intervals will help keep track of the overall health of the females.
Diagnosis of heart diseases: Detecting it early for an easier recovery
While heart conditions have the potential to cause a lot of bodily harm, the worst thing you can do when you experience heart-related symptoms is to ignore them. Experiencing symptoms like dizziness, chest pain, nausea and vomiting can easily be confused with other conditions and thus increases the importance of an early diagnosis.
There are several tests used to diagnose heart disease in India. They include:
Electrocardiogram (ECG or EKG) – This test records the electrical signals in the heart, which can be used to detect any underlying signs of a heart attack in women and men. This test can be easily performed in any doctor’s clinic or hospital and is most commonly done to know the signs of any heart trouble in patients.
Holter monitoring – Also known as ambulatory Electrocardiograms or ECG, this test helps diagnose early signs of heart trouble, early signs of a heart attack in women and can help prevent chances of a heart attack.
Echocardiogram – This diagnostic test uses ultrasound waves to examine the heart valves and chambers and evaluate how well the heart is functioning. This helps to identify signs of heart disease like weak heart muscle, blood clots inside the heart and to spot abnormalities in the heart. Thus it helps prevent early signs of a heart attack in women and men.
Stress test – Stress tests help diagnose heart problems, coronary artery diseases and other heart disorders.
Angiogram/Cardiac catheterization – This is a common type of cardiac catheterization procedure that helps diagnose heart problems in women.
Cardiac computerized tomography (CT) scan – Computed Tomography or CT scan captures multiple images of different layers of the heart to diagnose the cause of heart blockage in females and males.
Cardiac magnetic resonance imaging (MRI) – This method is the most used method to diagnose any underlying symptoms of heart blockage in males and females.
Cardiac markers – Cardiac biomarkers of cardiac enzymes are useful for detecting damages in the heart valves and muscles and therefore diagnose symptoms of heart disease in women and men.
How much can one benefit from an early diagnosis?
The simple answer is a lot! Cardiovascular disease has emerged as one of the most potent chronic illnesses affecting both males and females. Therefore, an early diagnosis of any heart problems in wome n and men can help prevent the chance of a heart attack and other complications.
- There are several diagnostic tests for heart diseases, some of which include an Electrocardiogram, Holter monitoring, CT scan, Blood tests and so on.
- An early diagnosis of any heart problems can help prevent the chance of a heart attack.
Treatment for heart diseases in India: Surgical and non-surgical options for easy management
Medications to manage heart diseases.
A few of the medications for heart diseases include:
Anticoagulants or blood thinners – They help reduce the clotting ability of the blood.
Antiplatelet agents – They help prevent blood clots in people who have had a heart attack.
ACE Inhibitors, beta-blockers and diuretics – They have also been used widely for treating cardiovascular diseases.
However, it is recommended that you consult your doctor before taking any of these medications.
Types of medical procedures or surgeries performed depending on the heart condition
Some common heart surgeries and treatments for managing heart problems in women, men and children are as follows:
Angioplasty – Angioplasty is a procedure used to open clogged coronary arteries which are blood vessels that supply blood to the heart. It involves inserting a balloon or catheter in a blocked coronary artery to widen it, thereby improving blood flow to your heart.
Stent Implantation – Angioplasty is mostly followed by placing a device which is a small wire mesh tube called a stent, inside a coronary artery to prevent the artery from narrowing again. This surgical procedure is termed stent placement.
Thrombolytic therapy – Thrombolytic therapy, also known as, thrombolysis, is an emergency treatment to dissolve blood clots forming in arteries, which are the main cause of heart attacks and stroke. It involves the administration of clot-busting drugs through an IV or a long catheter.
CABG – Commonly known as bypass surgery, coronary artery bypass graft (CABG) is a procedure that redirects blood around blocked or partially blocked coronary arteries to facilitate better flow of blood to the heart. It can help provide relief from symptoms like chest pain and shortness of breath and also reduce the risk of dying of heart disease.
Pacemaker surgery – This surgery involves the implantation of a pacemaker, otherwise called a cardiac pacing device, a small electronic device that is usually placed in the chest that can help regulate your heartbeat. It significantly prevents your heartbeat from slowing to a dangerously low rate.
Home remedies and lifestyle changes to help manage heart conditions in Indian men and women:
There are several home remedies and lifestyle changes that can help to reduce the chances of heart diseases in men and women. Try to:
- The medicines that are helpful in treating heart attacks will be prescribed by your cardiologist and should be taken regularly. Some common heart surgeries are – Stent Implantation, Angioplasty, Bypass Surgery, Pacemaker Implantation and more.
- Home remedies like diet and lifestyle changes can help to reduce the chances of a heart attack.
Prevention of heart diseases: Staying heart healthy in a fast-paced culture
Some of the preventive measures of heart diseases include:
Exercise regularly – Staying physically active can help in controlling your weight, strengthening your heart and improving your blood circulation.
Maintain a healthy weight – Losing extra weight can go a long way in managing risk factors of heart diseases such as type 2 diabetes, high blood pressure and high cholesterol.
Quit smoking and limit alcohol – Men should limit their alcohol intake to 2 drinks per day and women should not have more than one drink in a day to reduce the risk of developing heart disease. It is best if you do not smoke and consume alcohol at all.
8 incredible foods that are good for your heart – Consume a lot of fruits, vegetables and whole grains, legumes and lean meat and try to avoid processed carbohydrates, saturated fats and minimize your intake of salt and sugar.
Keep diabetes under control – Monitor your blood sugar levels regularly and adopt dietary and lifestyle changes to keep them under control.
Check your blood pressure – Since high blood pressure is a major risk factor, it is important to be screened at least once a year and take medications to maintain your blood pressure within normal limits.
Monitor your cholesterol and triglyceride – It is recommended to check your cholesterol and triglyceride levels once every 4 – 6 months. If you have high cholesterol, medications, lifestyle and dietary changes can significantly help in minimizing the risk of heart disease.
Conclusion and Outlook
You can easily prevent many heart diseases by introducing the above-mentioned lifestyle changes. Additionally, you must consult a doctor if you experience any of the symptoms of a heart attack. After all, prevention is always better than cure!
- Some of the preventive measures of heart diseases include maintaining a healthy weight, exercising regularly, quitting smoking and limiting alcohol, eating a heart-healthy diet, managing stress, keeping diabetes under control, etc.
- You must consult a doctor if you experience any of the symptoms of a heart attack.
Frequently Asked Questions on Early Signs of Heart Disease in Indian Adults
What are the warning signs of clogged arteries.
The common warning signs of clogged arteries include chest pain, difficulty breathing, extreme fatigue and weakness.
What does heart blockage feel like?
A heart blockage may provide a feeling of tightness and severe pain around the chest. It is always better to consult your doctor in case of any slight pain around the chest.
What are the signs of a silent heart attack?
Silent heart attack signs include pain in the arms, jaws, chest, anxiety, shortness of breath, sweating and dizziness.
What is the best test to check for heart problems?
The best tests to check for heart problems are ECG, Echo and blood tests. However, you must consult your doctor to know more about the different types of tests and the ones you must get done depending upon your symptoms.
What's a bad heart rate?
A bad heart rate is when your heartbeat is above 100 beats per minute or below 60 heartbeats per minute.
Will a chest x-ray show heart blockage?
Yes, a chest X-ray can indicate heart blockage, enlargement and also detect the calcium deposits in the blood vessels. But you will require more tests prescribed by your doctor for a confirmatory diagnosis.
When should I get my heart checked?
An individual after the age of 30 must get regular heart-health tests every year. The frequency of the tests may increase in the case of heart patients or if the person experiences any signs of heart disease. Also, anyone who has recovered from a COVID infection should get a cardiac check-up after 3 months or as advised by the doctor.
How can I test my heart health at home?
You can check your heart health by monitoring your pulse rate and checking your blood pressure. You can book blood tests like HbA1c, lipid profile and cardiac markers online for home sample collection.
Doctor's Section
Leave a comment.
- India Today
- Business Today
- Reader’s Digest
- Harper's Bazaar
- Brides Today
- Cosmopolitan
- Aaj Tak Campus
- India Today Hindi
Study reveals high blood pressure could start in childhood
A new study suggested that children and teenagers who are obese are more likely to have high blood pressure as adults (aged 50-64 years). .
Listen to Story

- Children and teenagers who are obese are more likely to have high blood pressure as adults
- Over 1.28 billion adults aged 30-79 years are living with hypertension around the world
- High blood pressure is having a systolic blood pressure at or above 140mmHg or diastolic blood pressure at or above 90mmHg
High blood pressure or hypertension has become one of the leading markers of heart disease, the leading cause of death worldwide. Since this condition is often associated with adults, a new study has found that hypertension can, in fact, originate in childhood.
High blood pressure is defined as a systolic blood pressure (SBP) at or above 140mmHg or diastolic blood pressure (DBP) at or above 90mmHg.
The study suggested that children and teenagers who are obese are more likely to have high blood pressure as adults (aged 50-64 years).
The researchers said that this information can help parents prevent obesity in children during their development years as it could reduce the chances of heart diseases arising from high blood pressure later in life.
The new research to be presented at this year's European Congress on Obesity (ECO) in Venice, Italy (12-15 May) was a result of a Swedish-based population study.
It showed that high blood pressure in adult men increased from high childhood BMI (body mass index at age 8 years) and greater BMI change during puberty (BMI at 20 years minus childhood BMI), independent of each other.
In women, blood pressure in middle age increased in linear association with greater pubertal BMI change, but not childhood BMI .
“Our results suggest that preventing overweight and obesity beginning in childhood matters when it comes to achieving a healthy blood pressure in later life”, said lead author Dr Lina Lilja from the University of Gothenburg in Sweden.

The authors note that the results are from observational findings, so more studies are needed to understand whether there are specific ages in childhood and/or adolescence when BMI is particularly important to blood pressure in adulthood.
There are limitations to the study. Blood pressure was measured at a single point in time, the analyses didn't include risk factors such as diet and physical activity which could have influenced the results.
Since most of the study participants were white, the results may not be the same as people from other racial or ethnic groups. Published By: Daphne Clarance Published On: Apr 1, 2024 ALSO READ | Curing cancer: An Indian scientist's quest to find the antidote
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Med J Armed Forces India
- v.77(3); 2021 Jul
Machine learning–based heart disease prediction system for Indian population: An exploratory study done in South India
a Research Scholar (Computer Science & Engineering), Dayananda Sagar University, Bengaluru, India
Bondu Venkateswarlu
b Associate Professor (Computer Science & Engineering), Dayananda Sagar University, Bengaluru, India
Baljeet Maini
c Professor Pediatrics, Teerthanker Mahaveer Medical College & Research Centre, Moradabad, India
Dheeraj Marwaha
d Senior Software Engineer, Microsoft India, Hyderabad, India
In India, huge mortality occurs due to cardiovascular diseases (CVDs) as these diseases are not diagnosed in early stages. Machine learning (ML) algorithms can be used to build efficient and economical prediction system for early diagnosis of CVDs in India.
A total of 1670 anonymized medical records were collected from a tertiary hospital in South India. Seventy percent of the collected data were used to train the prediction system. Five state-of-the-art ML algorithms (k-Nearest Neighbours, Naïve Bayes, Logistic Regression, AdaBoost and Random Forest [RF]) were applied using Python programming language to develop the prediction system. The performance was evaluated over remaining 30% of data. The prediction system was later deployed in the cloud for easy accessibility via Internet.
ML effectively predicted the risk of heart disease. The best performing (RF) prediction system correctly classified 470 out of 501 medical records thus attaining a diagnostic accuracy of 93.8%. Sensitivity and specificity were observed to be 92.8% and 94.6%, respectively. The prediction system attained positive predictive value of 94% and negative predictive value of 93.6%. The prediction model developed in this study can be accessed at http://das.southeastasia.cloudapp.azure.com/predict/
Conclusions
ML-based prediction system developed in this study performs well in early diagnosis of CVDs and can be accessed via Internet. This study offers promising results suggesting potential use of ML-based heart disease prediction system as a screening tool to diagnose heart diseases in primary healthcare centres in India, which would otherwise get undetected.
Introduction
Cardiovascular diseases (CVDs) are the foremost reason of disease burden and mortality all over the world. Approximately 30% of total deaths (17.9 million) occurred due to CVDs globally in 2016. 1 The situation is critically serious in low- and middle-income countries like India. During the past three decades, the number of deaths due to CVDs has increased significantly from 15.2% to 28.1% in India. 2 Prevalence of CVDs was observed to be as high as 54.5 million cases in 2016. 3 CVDs are often detected in advanced stages amongst the underprivileged patients. Due to various reasons, Indian public healthcare system is still not capable in effectively preventing non-communicable diseases like CVDs. Efficient healthcare in terms of affordability, accessibility and quality is still far from being within reach of many. 4 Shortage of facilities in rural areas hampers medical diagnostic and therapeutic help in the initial stage of disease. Despite the government initiatives of health insurance (which are mainly for therapeutic care only) for poor people, the major section of Indian population does not have preventive health check-up benefits. 5 All these reasons lead to delayed treatment and increase in morbidity and mortality. 6
Amalgamation of ML-based prediction system in primary healthcare centres can potentially aid hugely in the prevention of CVDs in India. Recent advancements in the field of computer science have proved that machine learning (ML) algorithms can generate huge meaningful information from the immense data generated by the healthcare sector. 7 This information can be used for the diagnosis of diseases at initial stage, which can thus aid in the prevention of diseases. ML-based tools for efficient healthcare are fetching a huge attention globally. As an example, ML-based tools have recently been successfully implemented in the fields of ophthalmology and oncology in the United States. 8 , 9 Available literature reveals the development of highly accurate prediction systems for CVDs. 10 , 11 , 12 , 13 All the research studies done for early detection of CVDs as reported in the literature so far are based on the freely available online data set provided by ML repository of University of California, Irvine. 14 This data set provides information about 76 medical attributes of 303 medical records gathered from hospitals of Western countries. Information obtained from diagnostic tests like electrocardiogram, treadmill test, fluoroscopy test etc. is available in the above-mentioned data set. However, these medical tests are neither accessible nor affordable to a major section of Indian population. 15 Thus, the prediction systems developed so far are not suitable for Indian population. Moreover, some of the primary risk factors responsible for heart diseases in India, like, obesity, lack of physical activity, physiological stress, smoking and alcohol consumption etc. have not been considered in the ML-based studies so far.
As the importance of early detection of CVD is increasingly being realized, there is a definite need of developing ML-based prediction system for CVDs specifically suitable for Indian scenario.
This study was carried out with the following objectives: a) Development of a high-performance and cost-effective ML-based heart disease prediction system using routine clinical data specifically suited for Indian population and b) Deployment of the prediction system in public cloud to ensure easy accessibility via Internet particularly beneficial for rural areas in India.
Materials and methods
Study setting.
This study is an interdisciplinary research work carried out by collaboration of data scientists and specialist doctors. The study was approved by institutional ethical committee. Members of ethical committee deemed that data privacy is ensured by using anonymized medical records of existing/retrospective cohort.
Data collection
By a random selection after applying the exclusion criteria, anonymized medical records of heart patients as well as of healthy persons were collected from a tertiary hospital in South India. Anonymization ensured data privacy as the personal details of the patients were not collected for the study.
Exclusion criteria: 1) Medical data sets corresponding to pregnant females, 2) patients reporting chronic kidney disease, severe mental illness, atrial fibrillation, 3) patients who reported the prolonged use of anti-depressants, antibiotics and medicines for asthma, tuberculosis and cancer, 4) patients who are prescribed oral corticosteroids, antipsychotic drugs and immunosuppressants and 5) patients younger than 20 years or older than 100 years.
After applying these exclusion criteria, the final data set comprised of 1670 medical records belonging to people between the age 30–79 years. Study population included 881 males and 789 females. Ethnicity of all records in this study was observed to be Asian. Eight-hundred and seventy-four records did not have hypertension, while rest 796 reported hypertension. Of 1670 records, 928 reported to consume alcohol. Eight-hundred and twenty-eight records belonged to smokers. Nine-hundred and twenty records complained of stress and anxiety in life. Of 1670 records, 893 records (53.47%) were diagnosed with CVDs and remaining 777 records (46.53%) were of healthy persons with no CVDs. The persons who visited the hospital for routine check-ups and were not diagnosed with any heart disease are referred to as healthy persons (CVD risk: low) in this study.
Risk factor attributes
People living in rural parts of the country are usually unaware of the potential risk factors of heart diseases. They usually neglect the early signs of heart disease. Since the study has been carried out especially for rural areas, the clinical attributes already known to be the potential risk factors of CVDs along with lifestyle attributes associated with heart disease were chosen for this study. These attributes include age, gender, weight, height, total cholesterol levels, smoking habits, alcohol, diabetes, hypertension, family history of CVDs, intake of healthy diet, physical activity/exercise habits and stress/anxiety in life. Body mass index (BMI) was calculated internally by the software. Table 1 represents the details of risk factors considered in this study.
Description of attributes used in the study.
Diagnostic procedures like treadmill test and fluoroscopy (used extensively in similar studies done so far) were not considered relevant for this study to ensure cost-effectiveness. Tests for triglycerides, serum creatinine, C-reactive protein, serum fibrinogen, gamma glutamyl transferase, lipoprotein, apolipoprotein B, homocysteine, insulin test etc. although associated with the risk of heart diseases, were also not considered in this study as these medical tests are not feasible/affordable for rural population for which the research is aimed for.
Study population characteristics
Out of 1670 records, 893 were positive cases of CVD while remaining 777 records were negative cases of CVD ensuring that the data set is balanced and is not skewed in favour of any class. In the data set, mean age of patients with heart disease is 66.2 years while mean age of healthy people was 57.3 years. Mean total cholesterol for healthy people was 188 mg/dL while the mean total cholesterol for heart patients was high at 237.7 mg/dL. Mean weight of heart patients was observed to be 85.4 kg while the mean weight of healthy people was 69.4 kg. It was observed that only 27.3% of heart patients were females. Nearly 95% of healthy people reported that they used to exercise regularly. Chi-square test of independence and t -test were carried out in the study subjects on ‘prior basis’ to determine the statistical significance of categorical and numeric input attributes, respectively, in determining heart disease. 16 These tests were used to ensure the validity of data of study variables, since the performance of AI algorithms is affected by the data of variables used to train the algorithms. Descriptive characteristics of these study population variables have been represented in Table 2 .
Study Population Descriptive Characteristics.
∗p-value < 0.05 is statistically significant.
Methodology
Python 3.7 programming language was used for building ML-based heart disease prediction system. Powerful software libraries supported by Python namely NumPy, Pandas, Seaborn, Statsmodels.api, SciPy and Sklearn etc. were used for exploratory analysis of data 17 and implementing five ML algorithms namely k-Nearest Neighbours (k-NN), Naïve Bayes (NB), Logistic Regression (LR), AdaBoost (AB) and Random Forest (RF). This study also has typical binary classification where 13 input attributes are observed to determine if there is a high risk of heart disease in a patient (risk of CVD = high) or not (risk of CVD = low). Fig. 1 shows the workflow diagram of complete project.

Workflow diagram of the study. This figure depicts the complete workflow of the study. The medical data set of 1670 records were gathered (in random fashion). Seventy percent data samples used to train the models. Test subset comprised the rest 30% of medical records. Five machine learning algorithms are applied to train the training subset. The prediction system was hosted on the public cloud for easy accessibility.
Data pre-processing
It was observed that there were no missing values or outliers in the data.
Since the ML algorithms can process only numerical data, the categorical attributes were label encoded. Gender female was encoded as 1 while male as 0. For all the other categorical variables like diabetes, stress, exercise etc., the presence (yes) was encoded as 1 while absence (no) was encoded as 0. High risk of CVD was encoded as 1 while low risk of CVD was encoded as 0.
Building the model
Using the train_test_split function supported by scikit learn library, the complete medical data set was randomly split into two portions in the ratio 70:30 referred as training and test/validation subset, respectively. Out of total 1670 records, training subset had 1169 records while test subset had 501 records. Detailed information about the training and test subsets is provided in Table 3 . The total number of records in the training data set were 1169, of which 656 records correspond to CVDs while 513 records belonged to healthy people not diagnosed with CVDs.
Details of training and test subsets.
ML algorithms with well demonstrated performance for classification namely NB, LR and k-NN were applied to build the prediction model.
Applying ensembling algorithms for better performance
Research has proved that the performance of a ML-based prediction system can be improvised using ensembling techniques. 18 Ensembling is a union of individual classifying algorithms. Bagging ensemble algorithms namely RF and boosting ensemble algorithms namely adaptive boosting AB were also implemented for enhanced performance.
Testing the performance of the model
The performance of prediction models developed using k-NN, NB and LR algorithms was analysed using the validation subset of 501 records as shown in Table 4 . Of these records, 237 were confirmed cases of CVDs while remaining 264 records correspond to healthy people not diagnosed with CVDs. Prevalence of disease in validation subset was 237/501 = 47.3%
Performance of machine learning algorithms on validation set of 501 records.
Analysis of confusion matrix is a standard way to check the performance of ML-based prediction system. Confusion matrix has four components namely true positives (TPs), true negatives (TNs), false positives (FPs) and false negatives (FNs).
TPs: Heart patients who are predicted correctly to have heart diseases.
TNs: Healthy persons who are predicted correctly to be healthy.
FPs: Healthy persons predicted incorrectly to have heart diseases (Type 1 error).
FNs: Heart patient predicted incorrectly to be healthy (Type 2 error).
These values are used to calculate accuracy, specificity, sensitivity, positive predictive value (PPV) and negative predictive value (NPV). PPV and NPV depend on the prevalence of disease.
A brief description of these parameters is given below.
- i. Classification accuracy: This parameter represents that part of total predictions that were correct. Accuracy = (TN + TP)/(TN + FN + FP + TP)
- ii. Sensitivity: This parameter reflects the ratio of cases that were accurately predicted with heart disease to the total number of actual cases of heart disease. Mathematically, sensitivity = TP/TP + FN
- iii. Specificity: This parameter calculates the ratio of cases that are correctly predicted with no heart disease to the entire count of actual cases with no heart disease. Mathematically, Specificity = TN/FP + TN
- iv. PPV: This parameter reflects the ratio of cases that are correctly predicted with heart diseases to the total count of cases predicted to have heart disease. Mathematically, PPV = TP/TP + FP
- v. NPV: This parameter reflects the ratio of cases correctly predicted to be healthy to the total count of cases predicted to be healthy. Mathematically, NPV = TN/TN + FN
Fine tuning of hyperparameters
Grid Search for cross-validation was used to identify the best hyperparameters for the learning algorithms. Grid Search CV class from sklearn library was used for this purpose.
Deployment on the public cloud
The best performance prediction system built using RF model was deployed in Microsoft Azure cloud for better accessibility. 19 ‘ Pickle ’ and ‘ Flask ’ software libraries of Python programming language were used for this purpose. 20 Hosting the prediction system on cloud enables it to be easily accessed from anywhere in the world via Internet. This is highly useful feature for healthcare sector of India, which faces the major issue of shortage of medical facilities especially in rural areas. Accessing this prediction system is as easy as accessing an e-mail via Internet.
CVD prediction system was developed by applying five well-established ML algorithms on the training data set. The performance was tested on the validation test set of 501 records. Prevalence of disease in validation subset was 237/501 = 47.3% Performance metrics namely accuracy, sensitivity, specificity, PPV and NPV were calculated for each algorithm. The performance results of all classifiers are given in Table 4 .
The best hyperparameters for k-NN (n_neighbors = 12) resulted in a performance of sensitivity 89%, specificity 87.1%, PPV 86.1%, NPV 89.8%. The performance of NB was found to better than k-NN. Sensitivity 88.6%, specificity 87.8%, PPV 86.7%, NPV 89.5% were achieved by NB.
LR with hyperparameters (C = 1, penalty = l2) performed well in classifying people with low risk or high risk of CVDs. LR correctly classified 455 out of 501 records, thus attaining a classification accuracy of 90.8%. Sensitivity 90.7% and specificity were 90.7% and 90.9%, respectively. PPV was observed to be 89.9% while NPV was 91.6%.
Models built using ensemble techniques (RF and AB) performed better than LR. AB model was trained with Stage-wise Adaptive Modelling using a Multi-class Exponential loss function (n_estimators = 30) while RF based on ‘gini index’ with n_estimators = 150 resulted in the best performance. Sensitivity and specificity of AB model was 91.9% and 93.1%, respectively, while RF reported 92.8% sensitivity and 94.6% specificity. PPV 94% and NPV 93.6% were achieved by RF–based prediction model.
Interpretation of ML-based models is not easy, and these are usually considered as ‘black boxes. However, logistic regression–based models are quite interpretable. Logistic regression was implemented using the Logit function (Binomial family) based on maximum likelihood estimation method to predict CVD risk using statsmodels.api library of Python. Fig. 2 shows the summary of results obtained.

Study population characteristics mean (standard deviation) of numerical attributes along with p-values of t -test to indicate the statistical significance for two groups: high risk/low risk of cardiovascular disease (CVDs). Count (%) of categorical attributes in two groups: high risk/low risk of CVDs.
Male gender, diabetes, hypertension, high cholesterol level, smoking and alcohol were significantly associated with CVD. Lack of exercise and stress were observed to be more prevalent in CVD group (p value < 0.05).
Estimate column in the summary reflects the natural logarithm of odds ratio of getting diagnosed with high risk of heart disease keeping all other features constant. Due to negative values of log (odds ratio) it is inferred that females had a low risk of CVDs compared with males. Regular exercise and intake of healthy diet were observed to be associated with low risk of CVDs; on the other hand, diabetes, hypertension, stress, smoking and family history tend to result in high risk of CVDs.
The odds ratio column in the summary suggests how the odds ratio of being detected with high risk of CVD change if all other attributes are kept constant. Hypertension tends to increase the odds ratio of high risk of CVDs by 1.573 while the odds ratio drops significantly to 0.328 with regular physical exercise. Odds ratio of high risk of CVD for females is 0.788 compared with males.
Ensemble algorithms (RF and AB) are based on decision trees and attribute importance is graded according to selection occurrence frequency of an attribute as a decision node decided based on information gain and entropy. Variable importance for boosting algorithm was decided based on the impurity-based scores using feature_importances_ from sklearn library of Python. Attributes exercise, weight, total cholesterol, hypertension and age were the top five important attributes for AB algorithm. In case of RF prediction system, variable importance scores for attributes weight, exercise, total cholesterol, hypertension, and gender were found to be maximum for predicting CVDs. Variable importance for AB algorithms and RF is represented graphically in Fig. 3 (a) and (b), respectively.

Variable importance. (a) Variable importance for AdaBoost-based prediction model. (b) Variable importance for Random Forest–based prediction model.
RF-based CVD prediction model (trained on 1169 records and tested on 501 records) is hosted on cloud and can be easily accessed at das.southeastasia.cloudapp.azure.com/predict/
The input attributes of the patient are entered into the system. The system predicts if the patient has low risk of CVDs or high risk. Sample screenshots of the result obtained using the prediction system are shown in Fig. 4 .

Using cardiovascular disease (CVD) prediction model to test the risk of CVDs. The medical practitioner enters the patient's clinical parameters as well as attributes related to his lifestyle to predict the risk of CVD.
In the recent years, substantial research studies have been carried out to build methods for diagnosing heart diseases in early stages. Various feature selection techniques were applied in the research carried out by Takci. 21 (2018), and the resulting prediction system attained an accuracy of 84.81%. Similar study was carried out by Kausar et al. and an accuracy of 88.41% was obtained. 22 Prediction system developed by Khalid Raza using ensembling technique (2019) attained an accuracy of 88.88%. 23 A similar accuracy level of 89% was achieved by the prediction system developed by Haq et al. in 2019. 24 Using artificial neural network to design a prediction system Alic et al. achieved an accuracy of 91% in their research study. 25 But importantly, the prediction system developed in all of these studies do not work effectively well for Indian population as these models are based on data collected from Western countries and do not take into consideration lifestyle-related risk factors responsible for CVDs (lack of physical activity, family history, alcohol etc.). Moreover, these systems rely on the results of medical tests like ECG, treadmill test, fluoroscopy tests etc., which are not feasible in Indian primary health centres in the existing scenario.
The accuracy attained in the present study is 93.8%. The prediction system developed in this research uses 13 clinical parameters and identifies the risk of a person to have heart disease. Compared with the studies done so far, this study has been carried out on Indian population, and the potential risk factors like high body weight, lack of exercise, psychological stress, family history, smoking and alcohol consumption habits have been considered in this study (unlike the studies quoted previously). It is worth noting that the system developed in this study is highly cost-effective compared with earlier studies as expensive tests like fluoroscopy and treadmill tests have not been taken into consideration. Easy accessibility of the prediction system via Internet is also an added remarkable feature of this study, which was not reported by earlier studies. It is worth mentioning here that prediction model developed in this pilot study predicts output depending on the study population attribute trends it was trained on. Once the ML models are trained and tested on voluminous data sets, it can be used as a screening tool in rural India and can help in the prevention of CVDs.
Cost-effectiveness, excellent performance and easy accessibility of the prediction system via Internet defend the use of ML-based prediction system as a screening tool for CVD detection in India.
To the best of our knowledge, this study was first of its kind in Indian context. Developed countries like the United Kingdom and the United States are investing their resources to carry to research for developing ML-based prediction models for diagnosing heart diseases in primary healthcare centres. 26 , 27 It is recommended that similar studies should be promoted in India. The current national health policy (2017) of our government, laying stress on preventive health will be more meaningful and fruitful if advancement in this field is made as early as possible. 28 We propose larger studies of multicentric nature for development of AI prediction systems for CVD screening in our country, which is facing ever increasing load of morbidity and mortality due to CVD being detected in late advanced stages. Premier institutes of medicine and technology can collaborate in this regard to diagnose other lifestyle diseases and non-communicable diseases like malignancies. Cardiological Society of India (CSI) can help in this regard. Other modern techniques like artificial neural networks can be applied to further improve the performance of the system.
Limitations of the study
This study used a data set of 1670 patients reporting to a tertiary care private setup in a south Indian metropolitan city where largely the higher income group seeks the medical care. This potentially may seem biased in reader's mind, but this study was aimed only to detect the robustness of a prediction model based on ML. The results obtained from the prediction system developed in this study are based on the attribute trends of the study population on which the model is trained on. In future the model needs to be trained on huge data sets collected from diverse regions before using it as a screening tool.
The study portrays the capability of ML algorithms to predict CVDs in Indian population. Issues of affordability and accessibility in healthcare sector of India can be addressed using ML-based models, which can be easily accessed via Internet even in the rural parts of the country. It is proposed to build and test the performance of similar systems using voluminous cardiac data sets belonging to all economic sections of the society collected from various regions of India. We recommend similar studies of multicentric nature across entire country. To achieve the sustainable development goals laid down by World Health Organization, it is high time, we as a country do take timely advantage of ML-based prediction systems in improving preventive care aspect of public healthcare system. 29
What is already known?
ML-based tools have shown remarkable performance in diagnosing various serious diseases in initial stages in healthcare centres of developed countries.
What does this study add?
An indigenous high-performance ML-based CVD prediction system easily accessible via Internet is proposed for existing Indian healthcare system. Healthcare in India can be made more affordable and accessible using ML-based prediction systems.
Disclosure of competing interest
The authors have none to declare.
Acknowledgements
The authors express their heartfelt gratitude to Sagar Hospitals, Jayanagar, Bengaluru, for providing anonymized information of patients' health parameters for carrying out this study. No funding was received for this project.

IMAGES
VIDEO
COMMENTS
Hypertensive heart disease, among other CVDs, is a significant problem in India, with 261 694 deaths in 2013; this is an increase of 138% in comparison with the number of deaths in 1990. 12 Rheumatic heart disease also continues to be a problem in several parts of India, with an estimated 88 674 deaths (7 per 100 000 population) in the year ...
Another significant problem in India, among other CVD's, is that of hypertensive heart disease, with 261,694 deaths in 2013 (an increase of 138% in comparison with 1990). Rheumatic heart disease remains in epidemic proportions in India with an estimated prevalence of 1.5-2 per 1000 individuals.
Cardiovascular diseases (CVD) are the leading cause of death and disability in India. The CVD epidemic in Indians is characterized by a higher relative risk burden, an earlier age of onset, higher case fatality and higher premature deaths. For decades, researchers have been trying to understand the reason for this increased burden and propensity of CVD among Indians. It can partly be explained ...
The burden from the leading cardiovascular diseases in India—ischaemic heart disease and stroke—varies widely between the states. Their increasing prevalence and that of several major risk factors in every part of India, especially the highest increase in the prevalence of ischaemic heart disease in the less developed low ETL states, indicates the need for urgent policy and health system ...
Just over a fifth (21.1%) have hypertension which can increase risk of heart attack, heart failure, kidney disease or stroke Taking action… In line with WHO's Global action plan for the prevention and control of NCDs 2013-2020, in 2015 India became the first country to develop specific national targets and
Morbidity and mortality trends. CVDs remain the leading cause of death globally, including in India and the United States. In 2016, there were an estimated 62.5 and 12.7 million years of life lost prematurely due to CVD in India and the United States, respectively .Ischemic heart disease and stroke were estimated to account for approximately 15% to 20% and 6% to 9% of all deaths in these regions .
In 2016, the estimated prevalence of CVDs in India was estimated to be 54.5 million. 1 One in 4 deaths in India are now because of CVDs with ischemic heart disease and stroke responsible for >80% of this burden. 1 These diseases tend to affect patients in the most productive years of their lives and result in catastrophic social and economic ...
Of the 1209 patients who were enrolled in the registry, 834 (69%) were male. Most common etiology of heart failure was ischemic heart disease (72%), followed by dilated cardiomyopathy (13%) and rheumatic heart disease (8%). Mean duration of hospital stay was 6 days (IQR 4-9 days), and nearly all patients (94%) received diuretics.
Cardiovascular diseases (CVDs) have now become the leading cause of mortality in India. A quarter of all mortality is attributable to CVD. Ischemic heart disease and stroke are the predominant causes and are responsible for >80% of CVD deaths. The Global Burden of Disease study estimate of age-standardized CVD death rate of 272 per 100 000 ...
The goal: to identify potential collaborative solutions to some of the specific cardiovascular challenges in India, ranging from patient access to prevention and screening services and chronic disease management. "There is an urgency to manage the burden of cardiovascular disease in India," says ACC President B. Hadley Wilson, MD, FACC ...
Heart rate recovery in normal and obese males with and without parental history of cardiovascular disease Journal of Family Medicine and Primary Care , 10.4103/jfmpc.jfmpc_132_20 , 9 (5) : 2379 , .
In 2016, there were an estimated 62.5 and 12.7 million years of life lost prematurely due to CVD in India and the United States, respectively (4). Ischemic heart disease and stroke were estimated to account for approximately 15% to 20% and 6% to 9% of all deaths in these regions (5). Table 1 displays trends in age-standardized CVD prevalence ...
Cardiovascular disease (CVD) is the leading cause of death in India, 1 and its contribution to mortality is rising; deaths due to CVD are expected to double between 1985-2015. 2 -4 Regular physical activity reduces the risk of obesity, blood lipid abnormalities, hypertension, and non-insulin dependent diabetes mellitus, 5, 6 and has been shown to reduce substantially the risk of coronary ...
A research review has sought a fresh assessment of cardiovascular disease patterns in India, claiming that doctors have argued that coronary heart disease and its risk factors disproportionately affect poor people in India without sufficient evidence. The review has claimed that many studies looking at the distribution of cardiovascular disease and its risk factors across different ...
Ischemic heart disease deaths are rising in India, particularly in rural areas and among young adults, while deaths from stroke have dropped in most parts of th ... autopsies collected from 2001 to 2013 among 2.4 million households to derive mortality rates and trends in ischemic heart disease and stroke by sex and birth cohort throughout the ...
According to the World Health Report of 2002, deaths due to CHD in India rose from 1.17 million in 1991 to 1.59 million in 2000 and 2.03 million in 2010. 32 A total of nearly 64 million cases of CVD are likely in the year 2015, of which nearly 61 million would be CHD cases (the remaining would include stroke, rheumatic heart disease and ...
The study indicated that the overall self-reported prevalence of diagnosed CVDs was 29.4% for older adults age 45 and above in India. Age was associated with increased risk of CVD Female older adults were more likely to have CVDs than male.The place of residence also had a stronger association with CVDs.In addition, high cholesterol, diabetes and physical inactivity were key risk factors for ...
The study aims to predict and assess cardiovascular disease (CVD) patterns in highly affected countries such as Pakistan, India, China, Kenya, the USA, and Sweden. The data for CVD deaths was gathered from 2005 to 2019. We utilized non-homogenous discrete grey model (NDGM) to predict growth of cardiovascular deaths in selected countries. We take this process a step further by utilizing novel ...
Cardiovascular diseases (CVDs) are the leading cause of death globally, taking an estimated 17.9 million lives each year. CVDs are a group of disorders of the heart and blood vessels and include coronary heart disease, cerebrovascular disease, rheumatic heart disease and other conditions. More than four out of five CVD deaths are due to heart attacks and strokes, and one third of these deaths ...
As a consequence, cardiovascular disease (CVD) has emerged as the leading cause of death all over India, with coronary heart disease (CHD) affecting Indians at least 5-6 years earlier than their western counterparts 1, 2. Current estimates from disparate cross-sectional studies indicate the prevalence of CHD to be between 7-13 per cent in urban ...
In a Nutshell. Out of one crore deaths in India, cardiovascular disease is responsible for 20.3% of deaths in men. Most of the signs of heart diseases in men include pressure and feeling of tightness in the chest, discomfort in the arm, back, especially on the left side, pain in the chest, sweating, weakness and nausea.
The researchers said that this information can help parents prevent obesity in children during their development years as it could reduce the chances of heart diseases arising from high blood pressure later in life.. The new research to be presented at this year's European Congress on Obesity (ECO) in Venice, Italy (12-15 May) was a result of a Swedish-based population study.
Introduction. Cardiovascular diseases (CVDs) are the foremost reason of disease burden and mortality all over the world. Approximately 30% of total deaths (17.9 million) occurred due to CVDs globally in 2016. 1 The situation is critically serious in low- and middle-income countries like India. During the past three decades, the number of deaths due to CVDs has increased significantly from 15.2 ...