Advertisement

Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications
- Open access
- Published: 13 February 2021
- Volume 37 , pages 863–880, ( 2021 )
Cite this article
You have full access to this open access article

- Zezhi Li 1 , 2 ,
- Meihua Ruan 3 ,
- Jun Chen 1 , 5 &
- Yiru Fang ORCID: orcid.org/0000-0002-8748-9085 1 , 4 , 5
47k Accesses
112 Citations
16 Altmetric
Explore all metrics
A Correction to this article was published on 17 May 2021
This article has been updated
Major depressive disorder (MDD), also referred to as depression, is one of the most common psychiatric disorders with a high economic burden. The etiology of depression is still not clear, but it is generally believed that MDD is a multifactorial disease caused by the interaction of social, psychological, and biological aspects. Therefore, there is no exact pathological theory that can independently explain its pathogenesis, involving genetics, neurobiology, and neuroimaging. At present, there are many treatment measures for patients with depression, including drug therapy, psychotherapy, and neuromodulation technology. In recent years, great progress has been made in the development of new antidepressants, some of which have been applied in the clinic. This article mainly reviews the research progress, pathogenesis, and treatment of MDD.
Similar content being viewed by others

Molecular Mechanisms of Psilocybin and Implications for the Treatment of Depression

Lavender oil preparation Silexan is effective in mild-to-moderate major depression: a randomized, placebo- and reference-controlled trial
Psilocybin with psychological support for treatment-resistant depression: six-month follow-up.
Avoid common mistakes on your manuscript.
Major depressive disorder (MDD) also referred to as depression, is one of the most severe and common psychiatric disorders across the world. It is characterized by persistent sadness, loss of interest or pleasure, low energy, worse appetite and sleep, and even suicide, disrupting daily activities and psychosocial functions. Depression has an extreme global economic burden and has been listed as the third largest cause of disease burden by the World Health Organization since 2008, and is expected to rank the first by 2030 [ 1 , 2 ]. In 2016, the Global Burden of Diseases, Injuries, and Risk Factors Study demonstrated that depression caused 34.1 million of the total years lived with disability (YLDs), ranking as the fifth largest cause of YLD [ 3 ]. Therefore, the research progress and the clinical application of new discoveries or new technologies are imminent. In this review, we mainly discuss the current situation of research, developments in pathogenesis, and the management of depression.
Current Situation of Research on Depression
Analysis of published papers.
In the past decade, the total number of papers on depression published worldwide has increased year by year as shown in Fig. 1 A. Searching the Web of Science database, we found a total of 43,863 papers published in the field of depression from 2009 to 2019 (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009 – 2019), Articles). The top 10 countries that published papers on the topic of depression are shown in Fig. 1 B. Among them, researchers in the USA published the most papers, followed by China. Compared with the USA, the gap in the total number of papers published in China is gradually narrowing (Fig. 1 C), but the quality gap reflected by the index (the total number of citations and the number of citations per paper) is still large, and is lower than the global average (Fig. 1 D). As shown in Fig. 1 E, the hot research topics in depression are as follows: depression management in primary care, interventions to prevent depression, the pathogenesis of depression, comorbidity of depression and other diseases, the risks of depression, neuroimaging studies of depression, and antidepressant treatment.
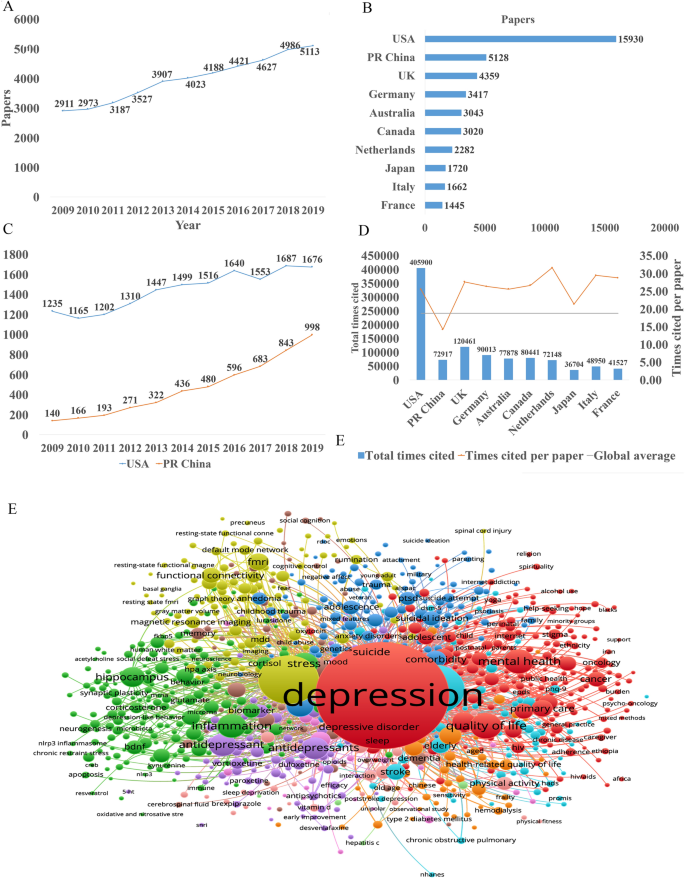
Analysis of published papers around the world from 2009 to 2019 in depressive disorder. A The total number of papers [from a search of the Web of Science database (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009 – 2019), Articles)]. B The top 10 countries publishing on the topic. C Comparison of papers in China and the USA. D Citations for the top 10 countries and comparison with the global average. E Hot topics.
Analysis of Patented Technology Application
There were 16,228 patent applications in the field of depression between 2009 and 2019, according to the Derwent Innovation Patent database. The annual number and trend of these patents are shown in Fig. 2 A. The top 10 countries applying for patents related to depression are shown in Fig. 2 B. The USA ranks first in the number of depression-related patent applications, followed by China. The largest number of patents related to depression is the development of antidepressants, and drugs for neurodegenerative diseases such as dementia comorbid with depression. The top 10 technological areas of patents related to depression are shown in Fig. 2 C, and the trend in these areas have been stable over the past decade (Fig. 2 D).
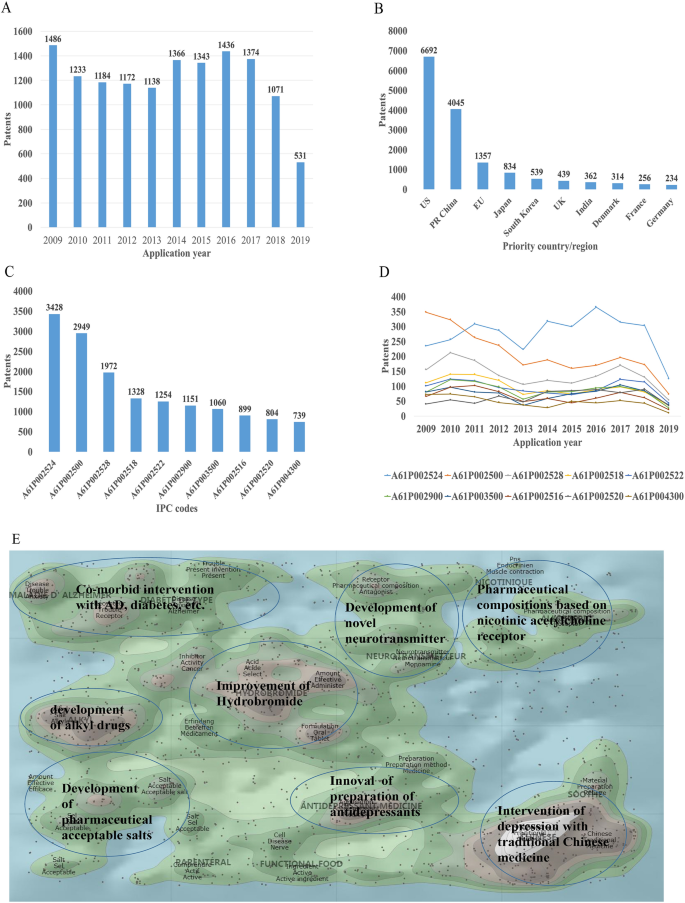
Analysis of patented technology applications from 2009 to 2019 in the field of depressive disorder. A Annual numbers and trends of patents (the Derwent Innovation patent database). B The top 10 countries/regions applying for patents. C The top 10 technological areas of patents. D The trend of patent assignees. E Global hot topic areas of patents.
Analysis of technical hotspots based on keyword clustering was conducted from the Derwent Innovation database using the "ThemeScape" tool. This demonstrated that the hot topic areas are as follows (Fig. 2 E): (1) improvement for formulation and the efficiency of hydrobromide, as well as optimization of the dosage; intervention for depression comorbid with AD, diabetes, and others; (3) development of alkyl drugs; (4) development of pharmaceutical acceptable salts as antidepressants; (5) innovation of the preparation of antidepressants; (6) development of novel antidepressants based on neurotransmitters; (7) development of compositions based on nicotinic acetylcholine receptors; and (8) intervention for depression with traditional Chinese medicine.
Analysis of Clinical Trial
There are 6,516 clinical trials in the field of depression in the ClinicalTrials.gov database, and among them, 1,737 valid trials include the ongoing recruitment of subjects, upcoming recruitment of subjects, and ongoing clinical trials. These clinical trials are mainly distributed in the USA (802 trials), Canada (155), China (114), France (93), Germany (66), UK (62), Spain (58), Denmark (41), Sweden (39), and Switzerland (23). The indications for clinical trials include various types of depression, such as minor depression, depression, severe depression, perinatal depression, postpartum depression, and depression comorbid with other psychiatric disorders or physical diseases, such as schizophrenia, epilepsy, stroke, cancer, diabetes, cardiovascular disease, and Parkinson's disease.
Based on the database of the Chinese Clinical Trial Registry website, a total of 143 clinical trials for depression have been carried out in China. According to the type of research, they are mainly interventional and observational studies, as well as a small number of related factor studies, epidemiological studies, and diagnostic trials. The research content involves postpartum, perinatal, senile, and other age groups with clinical diagnosis (imaging diagnosis) and intervention studies (drugs, acupuncture, electrical stimulation, transcranial magnetic stimulation). It also includes intervention studies on depression comorbid with coronary heart disease, diabetes, and heart failure.
New Medicine Development
According to the Cortellis database, 828 antidepressants were under development by the end of 2019, but only 292 of these are effective and active (Fig. 3 A). Large number of them have been discontinued or made no progress, indicating that the development of new drugs in the field of depression is extremely urgent.
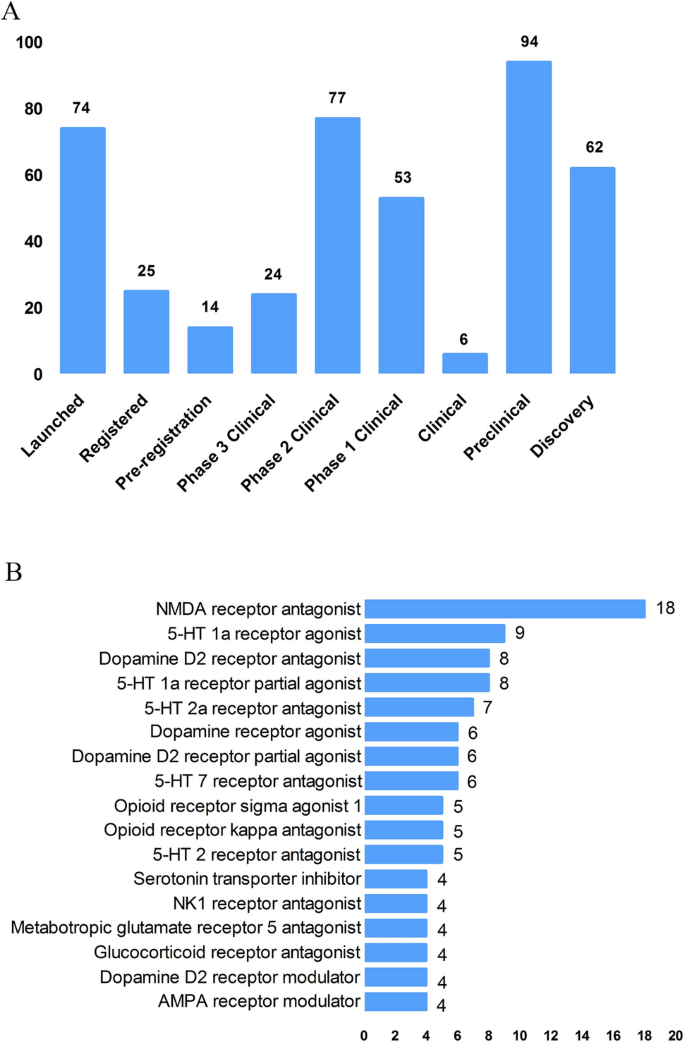
New medicine development from 2009 to 2019 in depressive disorder. A Development status of new candidate drugs. B Top target-based actions.
From the perspective of target-based actions, the most common new drugs are NMDA receptor antagonists, followed by 5-HT targets, as well as dopamine receptor agonists, opioid receptor antagonists and agonists, AMPA receptor modulators, glucocorticoid receptor antagonists, NK1 receptor antagonists, and serotonin transporter inhibitors (Fig. 3 B).
Epidemiology of Depression
The prevalence of depression varies greatly across cultures and countries. Previous surveys have demonstrated that the 12-month prevalence of depression was 0.3% in the Czech Republic, 10% in the USA, 4.5% in Mexico, and 5.2% in West Germany, and the lifetime prevalence of depression was 1.0% in the Czech Republic, 16.9% in the USA, 8.3% in Canada, and 9.0% in Chile [ 4 , 5 ]. A recent meta-analysis including 30 Countries showed that lifetime and 12-month prevalence depression were 10.8% and 7.2%, respectively [ 6 ]. In China, the lifetime prevalence of depression ranged from 1.6% to 5.5% [ 7 , 8 , 9 ]. An epidemiological study demonstrated that depression was the most common mood disorder with a life prevalence of 3.4% and a 12-month prevalence of 2.1% in China [ 10 ].
Some studies have also reported the prevalence in specific populations. The National Comorbidity Survey-Adolescent Supplement (NCS-A) survey in the USA showed that the lifetime and 12-month prevalence of depression in adolescents aged 13 to 18 were 11.0% and 7.5%, respectively [ 11 ]. A recent meta-analysis demonstrated that lifetime prevalence and 12-month prevalence were 2.8% and 2.3%, respectively, among the elderly population in China [ 12 ].
Neurobiological Pathogenesis of Depressive Disorder
The early hypothesis of monoamines in the pathophysiology of depression has been accepted by the scientific community. The evidence that monoamine oxidase inhibitors and tricyclic antidepressants promote monoamine neurotransmission supports this theory of depression [ 13 ]. So far, selective serotonin reuptake inhibitors and norepinephrine reuptake inhibitors are still the first-line antidepressants. However, there remain 1/3 to 2/3 of depressed patients who do not respond satisfactorily to initial antidepressant treatment, and even as many as 15%–40% do not respond to several pharmacological medicines [ 14 , 15 ]. Therefore, the underlying pathogenesis of depression is far beyond the simple monoamine mechanism.
Other hypotheses of depression have gradually received increasing attention because of biomarkers for depression and the effects pharmacological treatments, such as the stress-responsive hypothalamic pituitary adrenal (HPA) axis, neuroendocrine systems, the neurotrophic family of growth factors, and neuroinflammation.
Stress-Responsive HPA Axis
Stress is causative or a contributing factor to depression. Particularly, long-term or chronic stress can lead to dysfunction of the HPA axis and promote the secretion of hormones, including cortisol, adrenocorticotropic hormone, corticotropin-releasing hormone, arginine vasopressin, and vasopressin. About 40%–60% of patients with depression display a disturbed HPA axis, including hypercortisolemia, decreased rhythmicity, and elevated cortisol levels [ 16 , 17 ]. Mounting evidence has shown that stress-induced abnormality of the HPA axis is associated with depression and cognitive impairment, which is due to the increased secretion of cortisol and the insufficient inhibition of glucocorticoid receptor regulatory feedback [ 18 , 19 ]. In addition, it has been reported that the increase in cortisol levels is related to the severity of depression, especially in melancholic depression [ 20 , 21 ]. Further, patients with depression whose HPA axis was not normalized after treatment had a worse clinical response and prognosis [ 22 , 23 ]. Despite the above promising insights, unfortunately previous studies have shown that treatments regulating the HPA axis, such as glucocorticoid receptor antagonists, do not attenuate the symptoms of depressed patients [ 24 , 25 ].
Glutamate Signaling Pathway
Glutamate is the main excitatory neurotransmitter released by synapses in the brain; it is involved in synaptic plasticity, cognitive processes, and reward and emotional processes. Stress can induce presynaptic glutamate secretion by neurons and glutamate strongly binds to ionotropic glutamate receptors (iGluRs) including N-methyl-D-aspartate receptors (NMDARs) and α-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid receptors (AMPARs) [ 26 ] on the postsynaptic membrane to activate downstream signal pathways [ 27 ]. Accumulating evidence has suggested that the glutamate system is associated with the incidence of depression. Early studies have shown increased levels of glutamate in the peripheral blood, cerebrospinal fluid, and brain of depressed patients [ 28 , 29 ], as well as NMDAR subunit disturbance in the brain [ 30 , 31 ]. Blocking the function of NMDARs has an antidepressant effect and protects hippocampal neurons from morphological abnormalities induced by stress, while antidepressants reduce glutamate secretion and NMDARs [ 32 ]. Most importantly, NMDAR antagonists such as ketamine have been reported to have profound and rapid antidepressant effects on both animal models and the core symptoms of depressive patients [ 33 ]. On the other hand, ketamine can also increase the AMPAR pathway in hippocampal neurons by up-regulating the AMPA glutamate receptor 1 subunit [ 34 ]. Further, the AMPAR pathway may be involved in the mechanism of antidepressant effects. For example, preclinical studies have indicated that AMPAR antagonists might attenuate lithium-induced depressive behavior by increasing the levels of glutamate receptors 1 and 2 in the mouse hippocampus [ 35 ].
Gamma-Aminobutyric Acid (GABA)
Contrary to glutamate, GABA is the main inhibitory neurotransmitter. Although GABA neurons account for only a small proportion compared to glutamate, inhibitory neurotransmission is essential for brain function by balancing excitatory transmission [ 36 ]. Number of studies have shown that patients with depression have neurotransmission or functional defects of GABA [ 37 , 38 ]. Schür et al ., conducted a meta-analysis of magnetic resonance spectroscopy studies, which showed that the brain GABA level in depressive patients was lower than that in healthy controls, but no difference was found in depressive patients in remission [ 39 ]. Several postmortem studies have shown decreased levels of the GABA synthase glutamic acid decarboxylase in the prefrontal cortex of patients with depression [ 40 , 41 ]. It has been suggested that a functional imbalance of the GABA and glutamate systems contributes to the pathophysiology of depression, and activation of the GABA system might induce antidepressant activity, by which GABA A receptor mediators α2/α3 are considered potential antidepressant candidates [ 42 , 43 ]. Genetic mouse models, such as the GABA A receptor mutant mouse and conditional the Gad1-knockout mouse (GABA in hippocampus and cerebral cortex decreased by 50%) and optogenetic methods have verified that depression-like behavior is induced by changing the level of GABA [ 44 , 45 ].
Neurotrophin Family
The neurotrophin family plays a key role in neuroplasticity and neurogenesis. The neurotrophic hypothesis of depression postulates that a deficit of neurotrophic support leads to neuronal atrophy, the reduction of neurogenesis, and the destruction of glia support, while antidepressants attenuate or reverse these pathophysiological processes [ 46 ]. Among them, the most widely accepted hypothesis involves brain-derived neurotrophic factor (BDNF). This was initially triggered by evidence that stress reduces the BDNF levels in the animal brain, while antidepressants rescue or attenuate this reduction [ 47 , 48 ], and agents involved in the BDNF system have been reported to exert antidepressant-like effects [ 49 , 50 ]. In addition, mounting studies have reported that the BDNF level is decreased in the peripheral blood and at post-mortem in depressive patients, and some have reported that antidepressant treatment normalizes it [ 51 , 52 ]. Furthermore, some evidence also showed that the interaction of BDNF and its receptor gene is associated with treatment-resistant depression [ 15 ].
Recent studies reported that depressed patients have a lower level of the pro-domain of BDNF (BDNF pro-peptide) than controls. This is located presynaptically and promotes long-term depression in the hippocampus, suggesting that it is a promising synaptic regulator [ 53 ].
Neuroinflammation
The immune-inflammation hypothesis has attracted much attention, suggesting that the interactions between inflammatory pathways and neural circuits and neurotransmitters are involved in the pathogenesis and pathophysiological processes of depression. Early evidence found that patients with autoimmune or infectious diseases are more likely to develop depression than the general population [ 54 ]. In addition, individuals without depression may display depressive symptoms after treatment with cytokines or cytokine inducers, while antidepressants relieve these symptoms [ 55 , 56 ]. There is a complex interaction between the peripheral and central immune systems. Previous evidence suggested that peripheral inflammation/infection may spread to the central nervous system in some way and cause a neuroimmune response [ 55 , 57 ]: (1) Some cytokines produced in the peripheral immune response, such as IL-6 and IL-1 β, can leak into the brain through the blood-brain barrier (BBB). (2) Cytokines entering the central nervous system act directly on astrocytes, small stromal cells, and neurons. (3) Some peripheral immune cells can cross the BBB through specific transporters, such as monocytes. (4) Cytokines and chemokines in the circulation activate the central nervous system by regulating the surface receptors of astrocytes and endothelial cells at the BBB. (5) As an intermediary pathway, the immune inflammatory response transmits peripheral danger signals to the center, amplifies the signals, and shows the external phenotype of depressive behavior associated with stress/trauma/infection. (6) Cytokines and chemokines may act directly on neurons, change their plasticity and promote depression-like behavior.
Patients with depression show the core feature of the immune-inflammatory response, that is, increased concentrations of pro-inflammatory cytokines and their receptors, chemokines, and soluble adhesion molecules in peripheral blood and cerebrospinal fluid [ 58 , 59 , 60 ]. Peripheral immune-inflammatory response markers not only change the immune activation state in the brain that affects explicit behavior, but also can be used as an evaluation index or biological index of antidepressant therapy [ 61 , 62 ]. Li et al . showed that the level of TNF-α in patients with depression prior to treatment was higher than that in healthy controls. After treatment with venlafaxine, the level of TNF-α in patients with depression decreased significantly, and the level of TNF-α in the effective group decreased more [ 63 ]. A recent meta-analysis of 1,517 patients found that antidepressants significantly reduced peripheral IL-6, TNF-α, IL-10, and CCL-2, suggesting that antidepressants reduce markers of peripheral inflammatory factors [ 64 ]. Recently, Syed et al . also confirmed that untreated patients with depression had higher levels of inflammatory markers and increased levels of anti-inflammatory cytokines after antidepressant treatment, while increased levels of pro-inflammatory cytokines were found in non-responders [ 62 ]. Clinical studies have also found that anti-inflammatory cytokines, such as monoclonal antibodies and other cytokine inhibitors, may play an antidepressant role by blocking cytokines. The imbalance of pro-inflammatory and anti-inflammatory cytokines may be involved in the pathophysiological process of depression.
In addition, a recent study showed that microglia contribute to neuronal plasticity and neuroimmune interaction that are involved in the pathophysiology of depression [ 65 ]. When activated microglia promote inflammation, especially the excessive production of pro-inflammatory factors and cytotoxins in the central nervous system, depression-like behavior can gradually develop [ 65 , 66 ]. However, microglia change polarization as two types under different inflammatory states, regulating the balance of pro- and anti-inflammatory factors. These two types are M1 and M2 microglia; the former produces large number of pro-inflammatory cytokines after activation, and the latter produces anti-inflammatory cytokines. An imbalance of M1/M2 polarization of microglia may contribute to the pathophysiology of depression [ 67 ].
Microbiome-Gut-Brain Axis
The microbiota-gut-brain axis has recently gained more attention because of its ability to regulate brain activity. Many studies have shown that the microbiota-gut-brain axis plays an important role in regulating mood, behavior, and neuronal transmission in the brain [ 68 , 69 ]. It is well established that comorbidity of depression and gastrointestinal diseases is common [ 70 , 71 ]. Some antidepressants can attenuate the symptoms of patients with irritable bowel syndrome and eating disorders [ 72 ]. It has been reported that gut microbiome alterations are associated with depressive-like behaviors [ 73 , 74 ], and brain function [ 75 ]. Early animal studies have shown that stress can lead to long-term changes in the diversity and composition of intestinal microflora, and is accompanied by depressive behavior [ 76 , 77 ]. Interestingly, some evidence indicates that rodents exhibit depressive behavior after fecal transplants from patients with depression [ 74 ]. On the other hand, some probiotics attenuated depressive-like behavior in animal studies, [ 78 ] and had antidepressant effects on patients with depression in several double-blind, placebo-controlled clinical trials [ 79 , 80 ].
The potential mechanism may be that gut microbiota can interact with the brain through a variety of pathways or systems, including the HPA axis, and the neuroendocrine, autonomic, and neuroimmune systems [ 81 ]. For example, recent evidence demonstrated that gut microbiota can affect the levels of neurotransmitters in the gut and brain, including serotonin, dopamine, noradrenalin, glutamate, and GABA [ 82 ]. In addition, recent studies showed that changes in gut microbiota can also impair the gut barrier and promote higher levels of peripheral inflammatory cytokines [ 83 , 84 ]. Although recent research in this area has made significant progress, more clinical trials are needed to determine whether probiotics have any effect on the treatment of depression and what the potential underlying mechanisms are.
Other Systems and Pathways
There is no doubt that several other systems or pathways are also involved in the pathophysiology of depression, such as oxidant-antioxidant imbalance [ 85 ], mitochondrial dysfunction [ 86 , 87 ], and circadian rhythm-related genes [ 88 ], especially their critical interactions ( e.g. interaction between the HPA and mitochondrial metabolism [ 89 , 90 ], and the reciprocal interaction between oxidative stress and inflammation [ 2 , 85 ]). The pathogenesis of depression is complex and all the hypotheses should be integrated to consider the many interactions between various systems and pathways.
Advances in Various Kinds of Research on Depressive Disorder
Genetic, molecular, and neuroimaging studies continue to increase our understanding of the neurobiological basis of depression. However, it is still not clear to what extent the results of neurobiological studies can help improve the clinical and functional prognosis of patients. Therefore, over the past 10 years, the neurobiological study of depression has become an important measure to understand the pathophysiological mechanism and guide the treatment of depression.
Genetic Studies
Previous twin and adoption studies have indicated that depression has relatively low rate of heritability at 37% [ 91 ]. In addition, environmental factors such as stressful events are also involved in the pathogenesis of depression. Furthermore, complex psychiatric disorders, especially depression, are considered to be polygenic effects that interact with environmental factors [ 13 ]. Therefore, reliable identification of single causative genes for depression has proved to be challenging. The first genome-wide association studies (GWAS) for depression was published in 2009, and included 1,738 patients and 1,802 controls [ 92 , 93 ]. Although many subsequent GWASs have determined susceptible genes in the past decade, the impact of individual genes is so small that few results can be replicated [ 94 , 95 ]. So far, it is widely accepted that specific single genetic mutations may play minor and marginal roles in complex polygenic depression. Another major recognition in GWASs over the past decade is that prevalent candidate genes are usually not associated with depression. Further, the inconsistent results may also be due to the heterogeneity and polygenic nature of genetic and non-genetic risk factors for depression as well as the heterogeneity of depression subtypes [ 95 , 96 ]. Therefore, to date, the quality of research has been improved in two aspects: (1) the sample size has been maximized by combining the data of different evaluation models; and (2) more homogenous subtypes of depression have been selected to reduce phenotypic heterogeneity [ 97 ]. Levinson et al . pointed out that more than 75,000 to 100,000 cases should be considered to detect multiple depression associations [ 95 ]. Subsequently, several recent GWASs with larger sample sizes have been conducted. For example, Okbay et al . identified two loci associated with depression and replicated them in separate depression samples [ 98 ]. Wray et al . also found 44 risk loci associated with depression based on 135,458 cases and 344,901 controls [ 99 ]. A recent GWAS of 807,553 individuals with depression reported that 102 independent variants were associated with depression; these were involved in synaptic structure and neural transmission, and were verified in a further 1,507,153 individuals [ 100 ]. However, even with enough samples, GWASs still face severe challenges. A GWAS only marks the region of the genome and is not directly related to the potential biological function. In addition, a genetic association with the indicative phenotype of depression may only be part of many pathogenic pathways, or due to the indirect influence of intermediate traits in the causal pathway on the final result [ 101 ].
Given the diversity of findings, epigenetic factors are now being investigated. Recent studies indicated that epigenetic mechanisms may be the potential causes of "loss of heritability" in GWASs of depression. Over the past decade, a promising discovery has been that the effects of genetic information can be directly influenced by environment factors, and several specific genes are activated by environmental aspects. This process is described as interactions between genes and the environment, which is identified by the epigenetic mechanism. Environmental stressors cause alterations in gene expression in the brain, which may cause abnormal neuronal plasticity in areas related to the pathogenesis of the disease. Epigenetic events alter the structure of chromatin, thereby regulating gene expression involved in neuronal plasticity, stress behavior, depressive behavior, and antidepressant responses, including DNA methylation, histone acetylation, and the role of non-coding RNA. These new mechanisms of trans-generational transmission of epigenetic markers are considered a supplement to orthodox genetic heredity, providing the possibility for the discovery of new treatments for depression [ 102 , 103 ]. Recent studies imply that life experiences, including stress and enrichment, may affect cellular and molecular signaling pathways in sperm and influence the behavioral and physiological phenotypes of offspring in gender-specific patterns, which may also play an important role in the development of depression [ 103 ].
Brain Imaging and Neuroimaging Studies
Neuroimaging, including magnetic resonance imaging (MRI) and molecular imaging, provides a non-invasive technique for determining the underlying etiology and individualized treatment for depression. MRI can provide important data on brain structure, function, networks, and metabolism in patients with depression; it includes structural MRI (sMRI), functional MRI (fMRI), diffusion tensor imaging, and magnetic resonance spectroscopy.
Previous sMRI studies have found damaged gray matter in depression-associated brain areas, including the frontal lobe, anterior cingulate gyrus, hippocampus, putamen, thalamus, and amygdala. sMRI focuses on the thickness of gray matter and brain morphology [ 104 , 105 ]. A recent meta-analysis of 2,702 elderly patients with depression and 11,165 controls demonstrated that the volumes of the whole brain and hippocampus of patients with depression were lower than those of the control group [ 106 ]. Some evidence also showed that the hippocampal volume in depressive patients was lower than that of controls, and increased after treatment with antidepressants [ 107 ] and electroconvulsive therapy (ECT) [ 108 ], suggesting that the hippocampal volume plays a critical role in the development, treatment response, and clinical prognosis of depression. A recent study also reported that ECT increased the volume of the right hippocampus, amygdala, and putamen in patients with treatment-resistant depression [ 109 ]. In addition, postmortem research supported the MRI study showing that dentate gyrus volume was decreased in drug-naive patients with depression compared to healthy controls, and was potentially reversed by treatment with antidepressants [ 110 ].
Diffusion tensor imaging detects the microstructure of the white matter, which has been reported impaired in patients with depression [ 111 ]. A recent meta-analysis that included first-episode and drug-naïve depressive patients showed that the decrease in fractional anisotropy was negatively associated with illness duration and clinical severity [ 112 ].
fMRI, including resting-state and task-based fMRI, can divide the brain into self-related regions, such as the anterior cingulate cortex, posterior cingulate cortex, medial prefrontal cortex, precuneus, and dorsomedial thalamus. Many previous studies have shown the disturbance of several brain areas and intrinsic neural networks in patients with depression which could be rescued by antidepressants [ 113 , 114 , 115 , 116 ]. Further, some evidence also showed an association between brain network dysfunction and the clinical correlates of patients with depression, including clinical symptoms [ 117 ] and the response to antidepressants [ 118 , 119 ], ECT [ 120 , 121 ], and repetitive transcranial magnetic stimulation [ 122 ].
It is worth noting that brain imaging provides new insights into the large-scale brain circuits that underlie the pathophysiology of depressive disorder. In such studies, large-scale circuits are often referred to as “networks”. There is evidence that a variety of circuits are involved in the mechanisms of depressive disorder, including disruption of the default mode, salience, affective, reward, attention, and cognitive control circuits [ 123 ]. Over the past decade, the study of intra-circuit and inter-circuit connectivity dysfunctions in depression has escalated, in part due to advances in precision imaging and analysis techniques [ 124 ]. Circuit dysfunction is a potential biomarker to guide psychopharmacological treatment. For example, Williams et al . found that hyper-activation of the amygdala is associated with a negative phenotype that can predict the response to antidepressants [ 125 ]. Hou et al . showed that the baseline characteristics of the reward circuit predict early antidepressant responses [ 126 ].
Molecular imaging studies, including single photon emission computed tomography and positron emission tomography, focus on metabolic aspects such as amino-acids, neurotransmitters, glucose, and lipids at the cellular level in patients with depression. A recent meta-analysis examined glucose metabolism and found that glucose uptake dysfunction in different brain regions predicts the treatment response [ 127 ].
The most important and promising studies were conducted by the ENIGMA (Enhancing NeuroImaging Genetics through Meta Analysis) Consortium, which investigated the human brain across 43 countries. The ENIGMA-MDD Working Group was launched in 2012 to detect the structural and functional changes associated with MDD reliably and replicate them in various samples around the world [ 128 ]. So far, the ENIGMA-MDD Working Group has collected data from 4,372 MDD patients and 9,788 healthy controls across 14 countries, including 45 cohorts [ 128 ]. Their findings to date are shown in Table 1 [ 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 ].
Objective Index for Diagnosis of MDD
To date, the clinical diagnosis of depression is subjectively based on interviews according to diagnostic criteria ( e.g. International Classification of Diseases and Diagnostic and Statistical Manual diagnostic systems) and the severity of clinical symptoms are assessed by questionnaires, although patients may experience considerable differences in symptoms and subtypes [ 138 ]. Meanwhile, biomarkers including genetics, epigenetics, peripheral gene and protein expression, and neuroimaging markers may provide a promising supplement for the development of the objective diagnosis of MDD, [ 139 , 140 , 141 ]. However, the development of reliable diagnosis for MDD using biomarkers is still difficult and elusive, and all methods based on a single marker are insufficiently specific and sensitive for clinical use [ 142 ]. Papakostas et al . showed that a multi-assay, serum-based test including nine peripheral biomarkers (soluble tumor necrosis factor alpha receptor type II, resistin, prolactin, myeloperoxidase, epidermal growth factor, BDNF, alpha1 antitrypsin, apolipoprotein CIII, brain-derived neurotrophic factor, and cortisol) yielded a specificity of 81.3% and a sensitivity of 91.7% [ 142 ]. However, the sample size was relatively small and no other studies have yet validated their results. Therefore, further studies are needed to identify biomarker models that integrate all biological variables and clinical features to improve the specificity and sensitivity of diagnosis for MDD.
Management of Depression
The treatment strategies for depression consist of pharmacological treatment and non-pharmacological treatments including psychotherapy, ECT [ 98 ], and transcranial magnetic stimulation. As psychotherapy has been shown to have effects on depression including attenuating depressive symptoms and improving the quality of life [ 143 , 144 ]; several practice guidelines are increasingly recommending psychotherapy as a monotherapy or in combination with antidepressants [ 145 , 146 ].
Current Antidepressant Treatment
Antidepressants approved by the US Food and Drug Administration (FDA) are shown in Table 2 . Due to the relatively limited understanding of the etiology and pathophysiology of depression, almost all the previous antidepressants were discovered by accident a few decades ago. Although most antidepressants are usually safe and effective, there are still some limitations, including delayed efficacy (usually 2 weeks) and side-effects that affect the treatment compliance [ 147 ]. In addition, <50% of all patients with depression show complete remission through optimized treatment, including trials of multiple drugs with and without simultaneous psychotherapy. In the past few decades, most antidepressant discoveries focused on finding faster, safer, and more selective serotonin or norepinephrine receptor targets. In addition, there is an urgent need to develop new approaches to obtain more effective, safer, and faster antidepressants. In 2019, the FDA approved two new antidepressants: Esketamine for refractory depression and Bresanolone for postpartum depression. Esmolamine, a derivative of the anesthetic drug ketamine, was approved by the FDA for the treatment of refractory depression, based on a large number of preliminary clinical studies [ 148 ]. For example, several randomized controlled trials and meta-analysis studies showed the efficacy and safety of Esketamine in depression or treatment-resistant depression [ 26 , 149 , 150 ]. Although both are groundbreaking new interventions for these debilitating diseases and both are approved for use only under medical supervision, there are still concerns about potential misuse and problems in the evaluation of mental disorders [ 151 ].
To date, although several potential drugs have not yet been approved by the FDA, they are key milestones in the development of antidepressants that may be modified and used clinically in the future, such as compounds containing dextromethorphan (a non-selective NMDAR antago–nist), sarcosine (N-methylglycine, a glycine reuptake inhibitor), AMPAR modulators, and mGluR modulators [ 152 ].
Neuromodulation Therapy
Neuromodulation therapy acts through magnetic pulse, micro-current, or neural feedback technology within the treatment dose, acting on the central or peripheral nervous system to regulate the excitatory/inhibitory activity to reduce or attenuate the symptoms of the disease.
ECT is one of most effective treatments for depression, with the implementation of safer equipment and advancement of techniques such as modified ECT [ 153 ]. Mounting evidence from randomized controlled trial (RCT) and meta-analysis studies has shown that rTMS can treat depressive patients with safety [ 154 ]. Other promising treatments for depression have emerged, such as transcranial direct current stimulation (tDCS) [ 155 ], transcranial alternating current stimulation (tACS)[ 156 ], vagal nerve stimulation [ 157 ], deep brain stimulation [ 158 ] , and light therapy [ 159 ], but some of them are still experimental to some extent and have not been widely used. For example, compared to tDCS, tACS displays less sensory experience and adverse reactions with weak electrical current in a sine-wave pattern, but the evidence for the efficacy of tACS in the treatment of depression is still limited [ 160 ]. Alexander et al . recently demonstrated that there was no difference in efficacy among different treatments (sham, 10-Hz and 40-Hz tACS). However, only the 10-Hz tACS group had more responders than the sham and 40-Hz tACS groups at week 2 [ 156 ]. Further RCT studies are needed to verify the efficacy of tACS. In addition, the mechanism of the effect of neuromodulation therapy on depression needs to be further investigated.
Precision Medicine for Depression
Optimizing the treatment strategy is an effective way to improve the therapeutic effect on depression. However, each individual with depression may react very differently to different treatments. Therefore, this raises the question of personalized treatment, that is, which patients are suitable for which treatment. Over the past decade, psychiatrists and psychologists have focused on individual biomarkers and clinical characteristics to predict the efficiency of antidepressants and psychotherapies, including genetics, peripheral protein expression, electrophysiology, neuroimaging, neurocognitive performance, developmental trauma, and personality [ 161 ]. For example, Bradley et al . recently conducted a 12-week RCT, which demonstrated that the response rate and remission rates of the pharmacogenetic guidance group were significantly higher than those of the non-pharmacogenetic guidance group [ 162 ].
Subsequently, Greden et al . conducted an 8-week RCT of Genomics Used to Improve Depression Decisions (GUIDED) on 1,167 MDD patients and demonstrated that although there was no difference in symptom improvement between the pharmacogenomics-guided and non- pharmacogenomics-guided groups, the response rate and remission rate of the pharmacogenomics-guided group increased significantly [ 163 ].
A recent meta-analysis has shown that the baseline default mode network connectivity in patients with depression can predict the clinical responses to treatments including cognitive behavioral therapy, pharmacotherapy, ECT, rTMS, and transcutaneous vagus nerve stimulation [ 164 ]. However, so far, the biomarkers that predict treatment response at the individual level have not been well applied in the clinic, and there is still a lot of work to be conducted in the future.
Future Perspectives
Although considerable progress has been made in the study of depression during a past decade, the heterogeneity of the disease, the effectiveness of treatment, and the gap in translational medicine are critical challenges. The main dilemma is that our understanding of the etiology and pathophysiology of depression is inadequate, so our understanding of depression is not deep enough to develop more effective treatment. Animal models still cannot fully simulate this heterogeneous and complex mental disorder. Therefore, how to effectively match the indicators measured in animals with those measured in genetic research or the development of new antidepressants is another important challenge.
Change history
17 may 2021.
A Correction to this paper has been published: https://doi.org/10.1007/s12264-021-00694-9
Dadi AF, Miller ER, Bisetegn TA, Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health 2020, 20: 173
Article PubMed PubMed Central Google Scholar
Zhu S, Zhao L, Fan Y, Lv Q, Wu K, Lang X. Interaction between TNF-alpha and oxidative stress status in first-episode drug-naive schizophrenia. Psychoneuroendocrinology 2020, 114: 104595
Article CAS PubMed Google Scholar
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390: 1211–1259
Article Google Scholar
Andrade L, Caraveo-Anduaga JJ, Berglund P, Bijl RV, De Graaf R, Vollebergh W, et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res 2003, 12: 3–21
Article PubMed Google Scholar
Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health 2013, 34: 119–138
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep 2018, 8: 2861
Liu J, Yan F, Ma X, Guo HL, Tang YL, Rakofsky JJ, et al. Prevalence of major depressive disorder and socio-demographic correlates: Results of a representative household epidemiological survey in Beijing, China. J Affect Disord 2015, 179: 74–81
Zhang YS, Rao WW, Cui LJ, Li JF, Li L, Ng CH, et al. Prevalence of major depressive disorder and its socio-demographic correlates in the general adult population in Hebei province, China. J Affect Disord 2019, 252: 92–98
Ma X, Xiang YT, Cai ZJ, Li SR, Xiang YQ, Guo HL, et al. Prevalence and socio-demographic correlates of major depressive episode in rural and urban areas of Beijing, China. J Affect Disord 2009, 115: 323–330
Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 2019, 6: 211–224
Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 2015, 54(37–44): e32
Google Scholar
Wang F, Zhang QE, Zhang L, Ng CH, Ungvari GS, Yuan Z, et al. Prevalence of major depressive disorder in older adults in China: A systematic review and meta-analysis. J Affect Disord 2018, 241: 297–304
Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature 2008, 455: 894–902
Article CAS PubMed PubMed Central Google Scholar
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry 2006, 163: 1905–1917
Li Z, Zhang Y, Wang Z, Chen J, Fan J, Guan Y, et al. The role of BDNF, NTRK2 gene and their interaction in development of treatment-resistant depression: data from multicenter, prospective, longitudinal clinic practice. J Psychiatr Res 2013, 47: 8–14
Murphy BE. Steroids and depression. J Steroid Biochem Mol Biol 1991, 38: 537–559
Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci 2008, 31: 464–468
Keller J, Gomez R, Williams G, Lembke A, Lazzeroni L, Murphy GM Jr, et al. HPA axis in major depression: cortisol, clinical symptomatology and genetic variation predict cognition. Mol Psychiatry 2017, 22: 527–536
Gomez RG, Fleming SH, Keller J, Flores B, Kenna H, DeBattista C, et al. The neuropsychological profile of psychotic major depression and its relation to cortisol. Biol Psychiatry 2006, 60: 472–478
Lamers F, Vogelzangs N, Merikangas KR, de Jonge P, Beekman AT, Penninx BW. Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression. Mol Psychiatry 2013, 18: 692–699
Nandam LS, Brazel M, Zhou M, Jhaveri DJ. Cortisol and major depressive disorder-translating findings from humans to animal models and back. Front Psychiatry 2019, 10: 974
Owashi T, Otsubo T, Oshima A, Nakagome K, Higuchi T, Kamijima K. Longitudinal neuroendocrine changes assessed by dexamethasone/CRH and growth hormone releasing hormone tests in psychotic depression. Psychoneuroendocrinology 2008, 33: 152–161
Mickey BJ, Ginsburg Y, Sitzmann AF, Grayhack C, Sen S, Kirschbaum C, et al. Cortisol trajectory, melancholia, and response to electroconvulsive therapy. J Psychiatr Res 2018, 103: 46–53
Stetler C, Miller GE. Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom Med 2011, 73: 114–126
Aubry JM. CRF system and mood disorders. J Chem Neuroanat 2013, 54: 20–24
Correia-Melo FS, Leal GC, Vieira F, Jesus-Nunes AP, Mello RP, Magnavita G, et al. Efficacy and safety of adjunctive therapy using esketamine or racemic ketamine for adult treatment-resistant depression: A randomized, double-blind, non-inferiority study. J Affect Disord 2020, 264: 527–534
Duman RS, Voleti B. Signaling pathways underlying the pathophysiology and treatment of depression: novel mechanisms for rapid-acting agents. Trends Neurosci 2012, 35: 47–56
Sanacora G, Zarate CA, Krystal JH, Manji HK. Targeting the glutamatergic system to develop novel, improved therapeutics for mood disorders. Nat Rev Drug Discov 2008, 7: 426–437
Hashimoto K. The role of glutamate on the action of antidepressants. Prog Neuropsychopharmacol Biol Psychiatry 2011, 35: 1558–1568
Gray AL, Hyde TM, Deep-Soboslay A, Kleinman JE, Sodhi MS. Sex differences in glutamate receptor gene expression in major depression and suicide. Mol Psychiatry 2015, 20: 1057–1068
Chandley MJ, Szebeni A, Szebeni K, Crawford JD, Stockmeier CA, Turecki G, et al. Elevated gene expression of glutamate receptors in noradrenergic neurons from the locus coeruleus in major depression. Int J Neuropsychopharmacol 2014, 17: 1569–1578
Musazzi L, Treccani G, Mallei A, Popoli M. The action of antidepressants on the glutamate system: regulation of glutamate release and glutamate receptors. Biol Psychiatry 2013, 73: 1180–1188
Kadriu B, Musazzi L, Henter ID, Graves M, Popoli M, Zarate CA Jr. Glutamatergic Neurotransmission: Pathway to Developing Novel Rapid-Acting Antidepressant Treatments. Int J Neuropsychopharmacol 2019, 22: 119–135
Beurel E, Grieco SF, Amadei C, Downey K, Jope RS. Ketamine-induced inhibition of glycogen synthase kinase-3 contributes to the augmentation of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA) receptor signaling. Bipolar Disord 2016, 18: 473–480
Gould TD, O’Donnell KC, Dow ER, Du J, Chen G, Manji HK. Involvement of AMPA receptors in the antidepressant-like effects of lithium in the mouse tail suspension test and forced swim test. Neuropharmacology 2008, 54: 577–587
Duman RS, Sanacora G, Krystal JH. Altered Connectivity in Depression: GABA and Glutamate Neurotransmitter Deficits and Reversal by Novel Treatments. Neuron 2019, 102: 75–90
Ghosal S, Hare B, Duman RS. Prefrontal Cortex GABAergic Deficits and Circuit Dysfunction in the Pathophysiology and Treatment of Chronic Stress and Depression. Curr Opin Behav Sci 2017, 14: 1–8
Fee C, Banasr M, Sibille E. Somatostatin-positive gamma-aminobutyric acid interneuron deficits in depression: Cortical microcircuit and therapeutic perspectives. Biol Psychiatry 2017, 82: 549–559
Schur RR, Draisma LW, Wijnen JP, Boks MP, Koevoets MG, Joels M, et al. Brain GABA levels across psychiatric disorders: A systematic literature review and meta-analysis of (1) H-MRS studies. Hum Brain Mapp 2016, 37: 3337–3352
Guilloux JP, Douillard-Guilloux G, Kota R, Wang X, Gardier AM, Martinowich K, et al. Molecular evidence for BDNF- and GABA-related dysfunctions in the amygdala of female subjects with major depression. Mol Psychiatry 2012, 17: 1130–1142
Karolewicz B, Maciag D, O’Dwyer G, Stockmeier CA, Feyissa AM, Rajkowska G. Reduced level of glutamic acid decarboxylase-67 kDa in the prefrontal cortex in major depression. Int J Neuropsychopharmacol 2010, 13: 411–420
Lener MS, Niciu MJ, Ballard ED, Park M, Park LT, Nugent AC, et al. Glutamate and gamma-aminobutyric acid systems in the pathophysiology of major depression and antidepressant response to ketamine. Biol Psychiatry 2017, 81: 886–897
Chen X, van Gerven J, Cohen A, Jacobs G. Human pharmacology of positive GABA-A subtype-selective receptor modulators for the treatment of anxiety. Acta Pharmacol Sin 2019, 40: 571–582
Ren Z, Pribiag H, Jefferson SJ, Shorey M, Fuchs T, Stellwagen D, et al. Bidirectional homeostatic regulation of a depression-related brain state by gamma-aminobutyric acidergic deficits and ketamine treatment. Biol Psychiatry 2016, 80: 457–468
Kolata SM, Nakao K, Jeevakumar V, Farmer-Alroth EL, Fujita Y, Bartley AF, et al. Neuropsychiatric phenotypes produced by GABA reduction in mouse cortex and hippocampus. Neuropsychopharmacology 2018, 43: 1445–1456
Duman RS, Li N. A neurotrophic hypothesis of depression: role of synaptogenesis in the actions of NMDA receptor antagonists. Philos Trans R Soc Lond B Biol Sci 2012, 367: 2475–2484
Albert PR, Benkelfat C, Descarries L. The neurobiology of depression—revisiting the serotonin hypothesis. I. Cellular and molecular mechanisms. Philos Trans R Soc Lond B Biol Sci 2012, 367: 2378–2381
Li K, Shen S, Ji YT, Li XY, Zhang LS, Wang XD. Melatonin augments the effects of fluoxetine on depression-like behavior and hippocampal BDNF-TrkB signaling. Neurosci Bull 2018, 34: 303–311
Zhang JJ, Gao TT, Wang Y, Wang JL, Guan W, Wang YJ, et al. Andrographolide exerts significant antidepressant-like effects involving the hippocampal BDNF system in mice. Int J Neuropsychopharmacol 2019, 22: 585–600
Wang JQ, Mao L. The ERK pathway: Molecular mechanisms and treatment of depression. Mol Neurobiol 2019, 56: 6197–6205
Chiou YJ, Huang TL. Serum brain-derived neurotrophic factors in taiwanese patients with drug-naive first-episode major depressive disorder: Effects of antidepressants. Int J Neuropsychopharmacol 2017, 20: 213–218
CAS PubMed Google Scholar
Youssef MM, Underwood MD, Huang YY, Hsiung SC, Liu Y, Simpson NR, et al. Association of BDNF Val66Met polymorphism and brain BDNF levels with major depression and suicide. Int J Neuropsychopharmacol 2018, 21: 528–538
Kojima M, Matsui K, Mizui T. BDNF pro-peptide: physiological mechanisms and implications for depression. Cell Tissue Res 2019, 377: 73–79
Jeon SW, Kim YK. Inflammation-induced depression: Its pathophysiology and therapeutic implications. J Neuroimmunol 2017, 313: 92–98
Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol 2016, 16: 22–34
Zhao G, Liu X. Neuroimmune advance in depressive disorder. Adv Exp Med Biol 2019, 1180: 85–98
Li Z, Wang Z, Zhang C, Chen J, Su Y, Huang J, et al. Reduced ENA78 levels as novel biomarker for major depressive disorder and venlafaxine efficiency: Result from a prospective longitudinal study. Psychoneuroendocrinology 2017, 81: 113–121
Ambrosio G, Kaufmann FN, Manosso L, Platt N, Ghisleni G, Rodrigues ALS, et al. Depression and peripheral inflammatory profile of patients with obesity. Psychoneuroendocrinology 2018, 91: 132–141
Mao R, Zhang C, Chen J, Zhao G, Zhou R, Wang F, et al. Different levels of pro- and anti-inflammatory cytokines in patients with unipolar and bipolar depression. J Affect Disord 2018, 237: 65–72
Enache D, Pariante CM, Mondelli V. Markers of central inflammation in major depressive disorder: A systematic review and meta-analysis of studies examining cerebrospinal fluid, positron emission tomography and post-mortem brain tissue. Brain Behav Immun 2019, 81: 24–40
Haroon E, Daguanno AW, Woolwine BJ, Goldsmith DR, Baer WM, Wommack EC, et al. Antidepressant treatment resistance is associated with increased inflammatory markers in patients with major depressive disorder. Psychoneuroendocrinology 2018, 95: 43–49
Syed SA, Beurel E, Loewenstein DA, Lowell JA, Craighead WE, Dunlop BW, et al. Defective inflammatory pathways in never-treated depressed patients are associated with poor treatment response. Neuron 2018, 99(914–924): e913
Li Z, Qi D, Chen J, Zhang C, Yi Z, Yuan C, et al. Venlafaxine inhibits the upregulation of plasma tumor necrosis factor-alpha (TNF-alpha) in the Chinese patients with major depressive disorder: a prospective longitudinal study. Psychoneuroendocrinology 2013, 38: 107–114
Kohler CA, Freitas TH, Stubbs B, Maes M, Solmi M, Veronese N, et al. Peripheral alterations in cytokine and chemokine levels after antidepressant drug treatment for major depressive disorder: systematic review and meta-analysis. Mol Neurobiol 2018, 55: 4195–4206
Innes S, Pariante CM, Borsini A. Microglial-driven changes in synaptic plasticity: A possible role in major depressive disorder. Psychoneuroendocrinology 2019, 102: 236–247
Sochocka M, Diniz BS, Leszek J. Inflammatory response in the CNS: Friend or foe? Mol Neurobiol 2017, 54: 8071–8089
Zhang L, Zhang J, You Z. Switching of the microglial activation phenotype is a possible treatment for depression disorder. Front Cell Neurosci 2018, 12: 306
Sandhu KV, Sherwin E, Schellekens H, Stanton C, Dinan TG, Cryan JF. Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry. Transl Res 2017, 179: 223–244
Gonzalez-Arancibia C, Urrutia-Pinones J, Illanes-Gonzalez J, Martinez-Pinto J, Sotomayor-Zarate R, Julio-Pieper M, et al. Do your gut microbes affect your brain dopamine? Psychopharmacology (Berl) 2019, 236: 1611–1622
Article CAS Google Scholar
Kennedy PJ, Cryan JF, Dinan TG, Clarke G. Irritable bowel syndrome: a microbiome-gut-brain axis disorder? World J Gastroenterol 2014, 20: 14105–14125
Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology 2002, 122: 1140–1156
Ruepert L, Quartero AO, de Wit NJ, van der Heijden GJ, Rubin G, Muris JW. Bulking agents, antispasmodics and antidepressants for the treatment of irritable bowel syndrome. Cochrane Database Syst Rev 2011: CD003460.
Marin IA, Goertz JE, Ren T, Rich SS, Onengut-Gumuscu S, Farber E, et al. Microbiota alteration is associated with the development of stress-induced despair behavior. Sci Rep 2017, 7: 43859
Zheng P, Zeng B, Zhou C, Liu M, Fang Z, Xu X, et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol Psychiatry 2016, 21: 786–796
Curtis K, Stewart CJ, Robinson M, Molfese DL, Gosnell SN, Kosten TR, et al. Insular resting state functional connectivity is associated with gut microbiota diversity. Eur J Neurosci 2019, 50: 2446–2452
O’Mahony SM, Marchesi JR, Scully P, Codling C, Ceolho AM, Quigley EM, et al. Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses. Biol Psychiatry 2009, 65: 263–267
Garcia-Rodenas CL, Bergonzelli GE, Nutten S, Schumann A, Cherbut C, Turini M, et al. Nutritional approach to restore impaired intestinal barrier function and growth after neonatal stress in rats. J Pediatr Gastroenterol Nutr 2006, 43: 16–24
Hao Z, Wang W, Guo R, Liu H. Faecalibacterium prausnitzii (ATCC 27766) has preventive and therapeutic effects on chronic unpredictable mild stress-induced depression-like and anxiety-like behavior in rats. Psychoneuroendocrinology 2019, 104: 132–142
Messaoudi M, Violle N, Bisson JF, Desor D, Javelot H, Rougeot C. Beneficial psychological effects of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in healthy human volunteers. Gut Microbes 2011, 2: 256–261
Rudzki L, Ostrowska L, Pawlak D, Malus A, Pawlak K, Waszkiewicz N, et al. Probiotic Lactobacillus Plantarum 299v decreases kynurenine concentration and improves cognitive functions in patients with major depression: A double-blind, randomized, placebo controlled study. Psychoneuroendocrinology 2019, 100: 213–222
Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci 2013, 36: 305–312
Mittal R, Debs LH, Patel AP, Nguyen D, Patel K, O’Connor G, et al. Neurotransmitters: The critical modulators regulating gut-brain axis. J Cell Physiol 2017, 232: 2359–2372
Diviccaro S, Giatti S, Borgo F, Barcella M, Borghi E, Trejo JL, et al. Treatment of male rats with finasteride, an inhibitor of 5alpha-reductase enzyme, induces long-lasting effects on depressive-like behavior, hippocampal neurogenesis, neuroinflammation and gut microbiota composition. Psychoneuroendocrinology 2019, 99: 206–215
Kiecolt-Glaser JK, Wilson SJ, Bailey ML, Andridge R, Peng J, Jaremka LM, et al. Marital distress, depression, and a leaky gut: Translocation of bacterial endotoxin as a pathway to inflammation. Psychoneuroendocrinology 2018, 98: 52–60
Lindqvist D, Dhabhar FS, James SJ, Hough CM, Jain FA, Bersani FS, et al. Oxidative stress, inflammation and treatment response in major depression. Psychoneuroendocrinology 2017, 76: 197–205
Czarny P, Wigner P, Galecki P, Sliwinski T. The interplay between inflammation, oxidative stress, DNA damage, DNA repair and mitochondrial dysfunction in depression. Prog Neuropsychopharmacol Biol Psychiatry 2018, 80: 309–321
Xie X, Yu C, Zhou J, Xiao Q, Shen Q, Xiong Z, et al. Nicotinamide mononucleotide ameliorates the depression-like behaviors and is associated with attenuating the disruption of mitochondrial bioenergetics in depressed mice. J Affect Disord 2020, 263: 166–174
Wang XL, Yuan K, Zhang W, Li SX, Gao GF, Lu L. Regulation of circadian genes by the MAPK pathway: Implications for rapid antidepressant action. Neurosci Bull 2020, 36: 66–76
Xie X, Shen Q, Yu C, Xiao Q, Zhou J, Xiong Z, et al. Depression-like behaviors are accompanied by disrupted mitochondrial energy metabolism in chronic corticosterone-induced mice. J Steroid Biochem Mol Biol 2020, 200: 105607
Zhang LF, Shi L, Liu H, Meng FT, Liu YJ, Wu HM, et al. Increased hippocampal tau phosphorylation and axonal mitochondrial transport in a mouse model of chronic stress. Int J Neuropsychopharmacol 2012, 15: 337–348
Flint J, Kendler KS. The genetics of major depression. Neuron 2014, 81: 1214
Sullivan PF, de Geus EJ, Willemsen G, James MR, Smit JH, Zandbelt T, et al. Genome-wide association for major depressive disorder: a possible role for the presynaptic protein piccolo. Mol Psychiatry 2009, 14: 359–375
Dunn EC, Brown RC, Dai Y, Rosand J, Nugent NR, Amstadter AB, et al. Genetic determinants of depression: recent findings and future directions. Harv Rev Psychiatry 2015, 23: 1–18
Major Depressive Disorder Working Group of the Psychiatric GC, Ripke S, Wray NR, Lewis CM, Hamilton SP, Weissman MM, et al. A mega-analysis of genome-wide association studies for major depressive disorder. Mol Psychiatry 2013, 18: 497–511.
Levinson DF, Mostafavi S, Milaneschi Y, Rivera M, Ripke S, Wray NR, et al. Genetic studies of major depressive disorder: why are there no genome-wide association study findings and what can we do about it? Biol Psychiatry 2014, 76: 510–512
Sullivan PF, Agrawal A, Bulik CM, Andreassen OA, Borglum AD, Breen G, et al. Psychiatric genomics: An update and an agenda. Am J Psychiatry 2018, 175: 15–27
Schwabe I, Milaneschi Y, Gerring Z, Sullivan PF, Schulte E, Suppli NP, et al. Unraveling the genetic architecture of major depressive disorder: merits and pitfalls of the approaches used in genome-wide association studies. Psychol Med 2019, 49: 2646–2656
Okbay A, Baselmans BM, De Neve JE, Turley P, Nivard MG, Fontana MA, et al. Genetic variants associated with subjective well-being, depressive symptoms, and neuroticism identified through genome-wide analyses. Nat Genet 2016, 48: 624–633
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet 2018, 50: 668–681
Howard DM, Adams MJ, Clarke TK, Hafferty JD, Gibson J, Shirali M, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci 2019, 22: 343–352
Ormel J, Hartman CA, Snieder H. The genetics of depression: successful genome-wide association studies introduce new challenges. Transl Psychiatry 2019, 9: 114
Uchida S, Yamagata H, Seki T, Watanabe Y. Epigenetic mechanisms of major depression: Targeting neuronal plasticity. Psychiatry Clin Neurosci 2018, 72: 212–227
Yeshurun S, Hannan AJ. Transgenerational epigenetic influences of paternal environmental exposures on brain function and predisposition to psychiatric disorders. Mol Psychiatry 2019, 24: 536–548
van Eijndhoven P, van Wingen G, Katzenbauer M, Groen W, Tepest R, Fernandez G, et al. Paralimbic cortical thickness in first-episode depression: evidence for trait-related differences in mood regulation. Am J Psychiatry 2013, 170: 1477–1486
Peng W, Chen Z, Yin L, Jia Z, Gong Q. Essential brain structural alterations in major depressive disorder: A voxel-wise meta-analysis on first episode, medication-naive patients. J Affect Disord 2016, 199: 114–123
Geerlings MI, Gerritsen L. Late-life depression, hippocampal volumes, and hypothalamic-pituitary-adrenal axis regulation: A systematic review and meta-analysis. Biol Psychiatry 2017, 82: 339–350
Maller JJ, Broadhouse K, Rush AJ, Gordon E, Koslow S, Grieve SM. Increased hippocampal tail volume predicts depression status and remission to anti-depressant medications in major depression. Mol Psychiatry 2018, 23: 1737–1744
Joshi SH, Espinoza RT, Pirnia T, Shi J, Wang Y, Ayers B, et al. Structural plasticity of the hippocampus and amygdala induced by electroconvulsive therapy in major depression. Biol Psychiatry 2016, 79: 282–292
Gryglewski G, Baldinger-Melich P, Seiger R, Godbersen GM, Michenthaler P, Klobl M, et al. Structural changes in amygdala nuclei, hippocampal subfields and cortical thickness following electroconvulsive therapy in treatment-resistant depression: longitudinal analysis. Br J Psychiatry 2019, 214: 159–167
Boldrini M, Santiago AN, Hen R, Dwork AJ, Rosoklija GB, Tamir H, et al. Hippocampal granule neuron number and dentate gyrus volume in antidepressant-treated and untreated major depression. Neuropsychopharmacology 2013, 38: 1068–1077
Liang S, Wang Q, Kong X, Deng W, Yang X, Li X, et al. White matter abnormalities in major depression biotypes identified by diffusion tensor imaging. Neurosci Bull 2019, 35: 867–876
Chen G, Guo Y, Zhu H, Kuang W, Bi F, Ai H, et al. Intrinsic disruption of white matter microarchitecture in first-episode, drug-naive major depressive disorder: A voxel-based meta-analysis of diffusion tensor imaging. Prog Neuropsychopharmacol Biol Psychiatry 2017, 76: 179–187
Brakowski J, Spinelli S, Dorig N, Bosch OG, Manoliu A, Holtforth MG, et al. Resting state brain network function in major depression - Depression symptomatology, antidepressant treatment effects, future research. J Psychiatr Res 2017, 92: 147–159
Dutta A, McKie S, Downey D, Thomas E, Juhasz G, Arnone D, et al. Regional default mode network connectivity in major depressive disorder: modulation by acute intravenous citalopram. Transl Psychiatry 2019, 9: 116
Meyer BM, Rabl U, Huemer J, Bartova L, Kalcher K, Provenzano J, et al. Prefrontal networks dynamically related to recovery from major depressive disorder: a longitudinal pharmacological fMRI study. Transl Psychiatry 2019, 9: 64
Muller VI, Cieslik EC, Serbanescu I, Laird AR, Fox PT, Eickhoff SB. Altered brain activity in unipolar depression revisited: Meta-analyses of neuroimaging studies. JAMA Psychiatry 2017, 74: 47–55
Connolly CG, Ho TC, Blom EH, LeWinn KZ, Sacchet MD, Tymofiyeva O, et al. Resting-state functional connectivity of the amygdala and longitudinal changes in depression severity in adolescent depression. J Affect Disord 2017, 207: 86–94
Godlewska BR, Browning M, Norbury R, Igoumenou A, Cowen PJ, Harmer CJ. Predicting treatment response in depression: The role of anterior cingulate cortex. Int J Neuropsychopharmacol 2018, 21: 988–996
Goldstein-Piekarski AN, Staveland BR, Ball TM, Yesavage J, Korgaonkar MS, Williams LM. Intrinsic functional connectivity predicts remission on antidepressants: a randomized controlled trial to identify clinically applicable imaging biomarkers. Transl Psychiatry 2018, 8: 57
Leaver AM, Vasavada M, Joshi SH, Wade B, Woods RP, Espinoza R, et al. Mechanisms of antidepressant response to electroconvulsive therapy studied with perfusion magnetic resonance imaging. Biol Psychiatry 2019, 85: 466–476
Miskowiak KW, Macoveanu J, Jorgensen MB, Stottrup MM, Ott CV, Jensen HM, et al. Neural response after a single ECT session during retrieval of emotional self-referent words in depression: A randomized, sham-controlled fMRI study. Int J Neuropsychopharmacol 2018, 21: 226–235
Du L, Liu H, Du W, Chao F, Zhang L, Wang K, et al. Stimulated left DLPFC-nucleus accumbens functional connectivity predicts the anti-depression and anti-anxiety effects of rTMS for depression. Transl Psychiatry 2018, 7: 3
Williams LM. Defining biotypes for depression and anxiety based on large-scale circuit dysfunction: a theoretical review of the evidence and future directions for clinical translation. Depress Anxiety 2017, 34: 9–24
Williams LM. Precision psychiatry: a neural circuit taxonomy for depression and anxiety. Lancet Psychiatry 2016, 3: 472–480
Williams LM, Korgaonkar MS, Song YC, Paton R, Eagles S, Goldstein-Piekarski A, et al. Amygdala reactivity to emotional faces in the prediction of general and medication-specific responses to antidepressant treatment in the randomized iSPOT-D trial. Neuropsychopharmacology 2015, 40: 2398–2408
Hou Z, Gong L, Zhi M, Yin Y, Zhang Y, Xie C, et al. Distinctive pretreatment features of bilateral nucleus accumbens networks predict early response to antidepressants in major depressive disorder. Brain Imaging Behav 2018, 12: 1042–1052
De Crescenzo F, Ciliberto M, Menghini D, Treglia G, Ebmeier KP, Janiri L. Is (18)F-FDG-PET suitable to predict clinical response to the treatment of geriatric depression? A systematic review of PET studies. Aging Ment Health 2017, 21: 889–894
Schmaal L, Pozzi E, T CH, van Velzen LS, Veer IM, Opel N, et al. ENIGMA MDD: seven years of global neuroimaging studies of major depression through worldwide data sharing. Transl Psychiatry 2020, 10: 172.
Schmaal L, Veltman DJ, van Erp TG, Samann PG, Frodl T, Jahanshad N, et al. Subcortical brain alterations in major depressive disorder: findings from the ENIGMA Major Depressive Disorder working group. Mol Psychiatry 2016, 21: 806–812
Schmaal L, Hibar DP, Samann PG, Hall GB, Baune BT, Jahanshad N, et al. Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA Major Depressive Disorder Working Group. Mol Psychiatry 2017, 22: 900–909
Frodl T, Janowitz D, Schmaal L, Tozzi L, Dobrowolny H, Stein DJ, et al. Childhood adversity impacts on brain subcortical structures relevant to depression. J Psychiatr Res 2017, 86: 58–65
Renteria ME, Schmaal L, Hibar DP, Couvy-Duchesne B, Strike LT, Mills NT, et al. Subcortical brain structure and suicidal behaviour in major depressive disorder: a meta-analysis from the ENIGMA-MDD working group. Transl Psychiatry 2017, 7: e1116
Tozzi L, Garczarek L, Janowitz D, Stein DJ, Wittfeld K, Dobrowolny H, et al. Interactive impact of childhood maltreatment, depression, and age on cortical brain structure: mega-analytic findings from a large multi-site cohort. Psychol Med 2020, 50: 1020–1031
de Kovel CGF, Aftanas L, Aleman A, Alexander-Bloch AF, Baune BT, Brack I, et al. No alterations of brain structural asymmetry in major depressive disorder: An ENIGMA consortium analysis. Am J Psychiatry 2019, 176: 1039–1049
Ho TC, Gutman B, Pozzi E, Grabe HJ, Hosten N, Wittfeld K, et al. Subcortical shape alterations in major depressive disorder: Findings from the ENIGMA major depressive disorder working group. Hum Brain Mapp 2020.
Han LKM, Dinga R, Hahn T, Ching CRK, Eyler LT, Aftanas L, et al. Brain aging in major depressive disorder: results from the ENIGMA major depressive disorder working group. Mol Psychiatry 2020.
van Velzen LS, Kelly S, Isaev D, Aleman A, Aftanas LI, Bauer J, et al. White matter disturbances in major depressive disorder: a coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. Mol Psychiatry 2020, 25: 1511–1525
Lv X, Si T, Wang G, Wang H, Liu Q, Hu C, et al. The establishment of the objective diagnostic markers and personalized medical intervention in patients with major depressive disorder: rationale and protocol. BMC Psychiatry 2016, 16: 240
Fabbri C, Hosak L, Mossner R, Giegling I, Mandelli L, Bellivier F, et al. Consensus paper of the WFSBP Task Force on Genetics: Genetics, epigenetics and gene expression markers of major depressive disorder and antidepressant response. World J Biol Psychiatry 2017, 18: 5–28
Li Z, Zhang C, Fan J, Yuan C, Huang J, Chen J, et al. Brain-derived neurotrophic factor levels and bipolar disorder in patients in their first depressive episode: 3-year prospective longitudinal study. Br J Psychiatry 2014, 205: 29–35
Gong Q, He Y. Depression, neuroimaging and connectomics: a selective overview. Biol Psychiatry 2015, 77: 223–235
Papakostas GI, Shelton RC, Kinrys G, Henry ME, Bakow BR, Lipkin SH, et al. Assessment of a multi-assay, serum-based biological diagnostic test for major depressive disorder: a pilot and replication study. Mol Psychiatry 2013, 18: 332–339
Kolovos S, Kleiboer A, Cuijpers P. Effect of psychotherapy for depression on quality of life: meta-analysis. Br J Psychiatry 2016, 209: 460–468
Park LT, Zarate CA Jr. Depression in the primary care setting. N Engl J Med 2019, 380: 559–568
Health N C C F M . Depression: The treatment and management of depression in adults (updated edition) 2010.
Qaseem A, Barry MJ, Kansagara D. Clinical Guidelines Committee of the American College of P. Nonpharmacologic versus pharmacologic treatment of adult patients with major depressive disorder: A clinical practice guideline from the american college of physicians. Ann Intern Med 2016, 164: 350–359
Dodd S, Mitchell PB, Bauer M, Yatham L, Young AH, Kennedy SH, et al. Monitoring for antidepressant-associated adverse events in the treatment of patients with major depressive disorder: An international consensus statement. World J Biol Psychiatry 2018, 19: 330–348
Cristea IA, Naudet F. US Food and Drug Administration approval of esketamine and brexanolone. Lancet Psychiatry 2019, 6: 975–977
Zheng W, Cai DB, Xiang YQ, Zheng W, Jiang WL, Sim K, et al. Adjunctive intranasal esketamine for major depressive disorder: A systematic review of randomized double-blind controlled-placebo studies. J Affect Disord 2020, 265: 63–70
Popova V, Daly EJ, Trivedi M, Cooper K, Lane R, Lim P, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: A Randomized Double-Blind Active-Controlled Study. Am J Psychiatry 2019, 176: 428–438
Turner EH. Esketamine for treatment-resistant depression: seven concerns about efficacy and FDA approval. Lancet Psychiatry 2019, 6: 977–979
Murrough JW, Abdallah CG, Mathew SJ. Targeting glutamate signalling in depression: progress and prospects. Nat Rev Drug Discov 2017, 16: 472–486
Gill SP, Kellner CH. Clinical practice recommendations for continuation and maintenance electroconvulsive therapy for depression: Outcomes from a review of the evidence and a consensus workshop held in Australia in May 2017. J ECT 2019, 35: 14–20
McClintock SM, Reti IM, Carpenter LL, McDonald WM, Dubin M, Taylor SF, et al. Consensus recommendations for the clinical application of repetitive transcranial magnetic stimulation (rTMS) in the treatment of depression. J Clin Psychiatry 2018, 79.
Chase HW, Boudewyn MA, Carter CS, Phillips ML. Transcranial direct current stimulation: a roadmap for research, from mechanism of action to clinical implementation. Mol Psychiatry 2020, 25: 397–407
Alexander ML, Alagapan S, Lugo CE, Mellin JM, Lustenberger C, Rubinow DR, et al. Double-blind, randomized pilot clinical trial targeting alpha oscillations with transcranial alternating current stimulation (tACS) for the treatment of major depressive disorder (MDD). Transl Psychiatry 2019, 9: 106
Akhtar H, Bukhari F, Nazir M, Anwar MN, Shahzad A. Therapeutic efficacy of neurostimulation for depression: Techniques, current modalities, and future challenges. Neurosci Bull 2016, 32: 115–126
Zhou C, Zhang H, Qin Y, Tian T, Xu B, Chen J, et al. A systematic review and meta-analysis of deep brain stimulation in treatment-resistant depression. Prog Neuropsychopharmacol Biol Psychiatry 2018, 82: 224–232
Li X, Li X. The antidepressant effect of light therapy from retinal projections. Neurosci Bull 2018, 34: 359–368
Shekelle PG, Cook IA, Miake-Lye IM, Booth MS, Beroes JM, Mak S. Benefits and harms of cranial electrical stimulation for chronic painful conditions, depression, anxiety, and insomnia: A systematic review. Ann Intern Med 2018, 168: 414–421
Kessler RC. The potential of predictive analytics to provide clinical decision support in depression treatment planning. Curr Opin Psychiatry 2018, 31: 32–39
Bradley P, Shiekh M, Mehra V, Vrbicky K, Layle S, Olson MC, et al. Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: A randomized clinical trial demonstrating clinical utility. J Psychiatr Res 2018, 96: 100–107
Greden JF, Parikh SV, Rothschild AJ, Thase ME, Dunlop BW, DeBattista C, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: A large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res 2019, 111: 59–67
Long Z, Du L, Zhao J, Wu S, Zheng Q, Lei X. Prediction on treatment improvement in depression with resting state connectivity: A coordinate-based meta-analysis. J Affect Disord 2020, 276: 62–68
Download references
Acknowledgments
This review was supported by the National Basic Research Development Program of China (2016YFC1307100), the National Natural Science Foundation of China (81930033 and 81771465; 81401127), Shanghai Key Project of Science & Technology (2018SHZDZX05), Shanghai Jiao Tong University Medical Engineering Foundation (YG2016MS48), Shanghai Jiao Tong University School of Medicine (19XJ11006), the Sanming Project of Medicine in Shenzhen Municipality (SZSM201612006), the National Key Technologies R&D Program of China (2012BAI01B04), and the Innovative Research Team of High-level Local Universities in Shanghai.
Author information
Authors and affiliations.
Clinical Research Center and Division of Mood Disorders of Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, 200030, China
Zezhi Li, Jun Chen & Yiru Fang
Department of Neurology, Ren Ji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, 200127, China
Shanghai Institute of Nutrition and Health, Shanghai Information Center for Life Sciences, Chinese Academy of Science, Shanghai, 200031, China
Meihua Ruan
Center for Excellence in Brain Science and Intelligence Technology, Chinese Academy of Science, Shanghai, 200031, China
Shanghai Key Laboratory of Psychotic Disorders, Shanghai, 201108, China
Jun Chen & Yiru Fang
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Yiru Fang .
Ethics declarations
Conflicts of interest.
The authors declare no conflicts of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Li, Z., Ruan, M., Chen, J. et al. Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications. Neurosci. Bull. 37 , 863–880 (2021). https://doi.org/10.1007/s12264-021-00638-3
Download citation
Received : 30 May 2020
Accepted : 30 September 2020
Published : 13 February 2021
Issue Date : June 2021
DOI : https://doi.org/10.1007/s12264-021-00638-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Major depressive disorder
- Pathogenesis
- Find a journal
- Publish with us
- Track your research
Incidence of depression among community-dwelling older adults: A systematic review
Affiliations.
- 1 Postgraduate Program in Collective Health, Federal University of Rio Grande do Norte (UFRN), Natal, Brazil.
- 2 Multicampi School of Medical Sciences, Federal University of Rio Grande do Norte (UFRN), Caicó, Brazil.
- 3 Department of Collective Health, Graduate Program in Collective Health, Federal University of Rio Grande do Norte, Natal, Brazil.
- 4 Graduate Program in Health Sciences, Federal University of Rio Grande do Norte, Natal, Brazil.
- 5 Research group on Methodology, Methods, Models and Outcomes of Health and Social Sciences (M3O), Faculty of Health Sciences and Welfare, Center for Health, and Social Care Research (CESS), University of Vic-Central University of Catalonia (UVic-UCC), Vic, Spain.
- 6 Institute for Research and Innovation in Life and Health Sciences in Central Catalonia (IRIS-CC), Vic, Spain.
- PMID: 38263357
- DOI: 10.1111/psyg.13081
We aimed to synthesise information related to the incidence of depression and depressive symptoms (DDS) in a community-dwelling older adult population at a global level. In this systematic review, we included articles with a cohort study design that evaluated the incidence of depression or depressive symptoms in older adults aged 60 years or more in a community-dwelling environment. Six databases were used: Web of Science, PubMed, Scopus, LILACS, SciELO, and Cochrane, and the entire selection process was independently performed by peers. We divided the included articles into subgroups according to the DDS assessment instrument: (i) Geriatric Depression Scale; (ii) Center for Epidemiologic Studies Depression Scale; (iii) miscellaneous scales; and (iv) diagnostic interviews. Each cumulative incidence value obtained per item was adjusted for a 1-year follow-up period, which generated an annual cumulative incidence (AcI). From 46 articles, 42 used scales to evaluate the depressive variable, with an AcI estimate of around 4.5%. The articles that assessed depression categorically observed a variation in AcI between 0.2% and 7.0%. Among all the materials included, the group that used the Geriatric Depression Scale observed the lowest and the highest AcI, 1.3% and 26.6% respectively. Most of the productions were from countries in the Asian continent (52.2%), followed by Europe (30.4%), the Americas (13%), and Oceania (4.4%). Despite the variation of AcI, we found a frequent occurrence of DDS in older adults in the community-dwelling environment, which highlights the need for preventive actions and better-targeted early care, especially in terms of primary health care.
Keywords: aged; cohort studies; depression; depressive disorder; incidence; systematic review.
© 2024 The Authors. Psychogeriatrics published by John Wiley & Sons Australia, Ltd on behalf of Japanese Psychogeriatric Society.
Publication types
- Systematic Review
- Depression* / diagnosis
- Depression* / epidemiology
- Independent Living*
- Social Environment
Grants and funding
- "Coordenação de Aperfeiçoamento de Pessoal de Nível Superior" - Brasil (CAPES)
- 308168/2020-8/CNPq (Brazilian National Council for Scientific and Technological Development)
Change Password
Your password must have 8 characters or more and contain 3 of the following:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
- Sign in / Register
Request Username
Can't sign in? Forgot your username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
An Exploratory Study of Students with Depression in Undergraduate Research Experiences
- Katelyn M. Cooper
- Logan E. Gin
- M. Elizabeth Barnes
- Sara E. Brownell
*Address correspondence to: Katelyn M. Cooper ( E-mail Address: [email protected] ).
Department of Biology, University of Central Florida, Orlando, FL, 32816
Search for more papers by this author
Biology Education Research Lab, Research for Inclusive STEM Education Center, School of Life Sciences, Arizona State University, Tempe, AZ 85281
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect graduate student depression, we know of no studies that have explored the relationship between depression and undergraduate research. In this study, we sought to understand how undergraduates’ symptoms of depression affect their research experiences and how research affects undergraduates’ feelings of depression. We interviewed 35 undergraduate researchers majoring in the life sciences from 12 research-intensive public universities across the United States who identify with having depression. Using inductive and deductive coding, we identified that students’ depression affected their motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing in undergraduate research experiences. We found that students’ social connections, experiencing failure in research, getting help, receiving feedback, and the demands of research affected students’ depression. Based on this work, we articulate an initial set of evidence-based recommendations for research mentors to consider in promoting an inclusive research experience for students with depression.
INTRODUCTION
Depression is described as a common and serious mood disorder that results in persistent feelings of sadness and hopelessness, as well as a loss of interest in activities that one once enjoyed ( American Psychiatric Association [APA], 2013 ). Additional symptoms of depression include weight changes, difficulty sleeping, loss of energy, difficulty thinking or concentrating, feelings of worthlessness or excessive guilt, and suicidality ( APA, 2013 ). While depression results from a complex interaction of psychological, social, and biological factors ( World Health Organization, 2018 ), studies have shown that increased stress caused by college can be a significant contributor to student depression ( Dyson and Renk, 2006 ).
Depression is one of the top undergraduate mental health concerns, and the rate of depression among undergraduates continues to rise ( Center for Collegiate Mental Health, 2017 ). While we cannot discern whether these increasing rates of depression are due to increased awareness or increased incidence, it is clear that is a serious problem on college campuses. The percent of U.S. college students who self-reported a diagnosis with depression was recently estimated to be about 25% ( American College Health Association, 2019 ). However, higher rates have been reported, with one study estimating that up to 84% of undergraduates experience some level of depression ( Garlow et al. , 2008 ). Depression rates are typically higher among university students compared with the general population, despite being a more socially privileged group ( Ibrahim et al. , 2013 ). Prior studies have found that depression is negatively correlated with overall undergraduate academic performance ( Hysenbegasi et al. , 2005 ; Deroma et al. , 2009 ; American College Health Association, 2019 ). Specifically, diagnosed depression is associated with half a letter grade decrease in students’ grade point average ( Hysenbegasi et al. , 2005 ), and 21.6% of undergraduates reported that depression negatively affected their academic performance within the last year ( American College Health Association, 2019 ). Provided with a list of academic factors that may be affected by depression, students reported that depression contributed to lower exam grades, lower course grades, and not completing or dropping a course.
Students in the natural sciences may be particularly at risk for depression, given that such majors are noted to be particularly stressful due to their competitive nature and course work that is often perceived to “weed students out”( Everson et al. , 1993 ; Strenta et al. , 1994 ; American College Health Association, 2019 ; Seymour and Hunter, 2019 ). Science course instruction has also been described to be boring, repetitive, difficult, and math-intensive; these factors can create an environment that can trigger depression ( Seymour and Hewitt, 1997 ; Osborne and Collins, 2001 ; Armbruster et al ., 2009 ; Ceci and Williams, 2010 ). What also distinguishes science degree programs from other degree programs is that, increasingly, undergraduate research experiences are being proposed as an essential element of a science degree ( American Association for the Advancement of Science, 2011 ; President’s Council of Advisors on Science and Technology, 2012 ; National Academies of Sciences, Engineering, and Medicine [NASEM], 2017 ). However, there is some evidence that undergraduate research experiences can add to the stress of college for some students ( Cooper et al. , 2019c ). Students can garner multiple benefits from undergraduate research, including enhanced abilities to think critically ( Ishiyama, 2002 ; Bauer and Bennett, 2003 ; Brownell et al. , 2015 ), improved student learning ( Rauckhorst et al. , 2001 ; Brownell et al. , 2015 ), and increased student persistence in undergraduate science degree programs ( Jones et al. , 2010 ; Hernandez et al. , 2018 ). Notably, undergraduate research experiences are increasingly becoming a prerequisite for entry into medical and graduate programs in science, particularly elite programs ( Cooper et al. , 2019d ). Although some research experiences are embedded into formal lab courses as course-based undergraduate research experiences (CUREs; Auchincloss et al. , 2014 ; Brownell and Kloser, 2015 ), the majority likely entail working with faculty in their research labs. These undergraduate research experiences in faculty labs are often added on top of a student’s normal course work, so they essentially become an extracurricular activity that they have to juggle with course work, working, and/or personal obligations ( Cooper et al. , 2019c ). While the majority of the literature surrounding undergraduate research highlights undergraduate research as a positive experience ( NASEM, 2017 ), studies have demonstrated that undergraduate research experiences can be academically and emotionally challenging for students ( Mabrouk and Peters, 2000 ; Seymour et al. , 2004 ; Cooper et al. , 2019c ; Limeri et al. , 2019 ). In fact, 50% of students sampled nationally from public R1 institutions consider leaving their undergraduate research experience prematurely, and about half of those students, or 25% of all students, ultimately leave their undergraduate research experience ( Cooper et al. , 2019c ). Notably, 33.8% of these individuals cited a negative lab environment and 33.3% cited negative relationships with their mentors as factors that influenced their decision about whether to leave ( Cooper et al. , 2019c ). Therefore, students’ depression may be exacerbated in challenging undergraduate research experiences, because studies have shown that depression is positively correlated with student stress ( Hish et al. , 2019 ).
While depression has not been explored in the context of undergraduate research experiences, depression has become a prominent concern surrounding graduate students conducting scientific research. A recent study that examined the “graduate student mental health crisis” ( Flaherty, 2018 ) found that work–life balance and graduate students’ relationships with their research advisors may be contributing to their depression ( Evans et al. , 2018 ). Specifically, this survey of 2279 PhD and master’s students from diverse fields of study, including the biological/physical sciences, showed that 39% of graduate students have experienced moderate to severe depression. Fifty-five percent of the graduate students with depression who were surveyed disagreed with the statement “I have good work life balance,” compared to only 21% of students with depression who agreed. Additionally, the study highlighted that more students with depression disagreed than agreed with the following statements: their advisors provided “real” mentorship, their advisors provided ample support, their advisors positively impacted their emotional or mental well-being, their advisors were assets to their careers, and they felt valued by their mentors. Another recent study identified that depression severity in biomedical doctoral students was significantly associated with graduate program climate, a perceived lack of employment opportunities, and the quality of students’ research training environment ( Nagy et al. , 2019 ). Environmental stress, academic stress, and family and monetary stress have also been shown to be predictive of depression severity in biomedical doctoral students ( Hish et al. , 2019 ). Further, one study found that self-esteem is negatively correlated and stress is positively correlated with graduate student depression; presumably research environments that challenge students’ self-esteem and induce stress are likely contributing to depressive symptoms among graduate students ( Kreger, 1995 ). While these studies have focused on graduate students, and there are certainly notable distinctions between graduate and undergraduate research, the research-related factors that affect graduate student depression, including work–life balance, relationships with mentors, research environment, stress, and self-esteem, may also be relevant to depression among undergraduates conducting research. Importantly, undergraduates in the United States have reported identical levels of depression as graduate students but are often less likely to seek mental health care services ( Wyatt and Oswalt, 2013 ), which is concerning if undergraduate research experiences exacerbate depression.
Based on the literature on the stressors of undergraduate research experiences and the literature identifying some potential causes of graduate student depression, we identified three aspects of undergraduate research that may exacerbate undergraduates’ depression. Mentoring: Mentors can be an integral part of a students’ research experience, bolstering their connections with others in the science community, scholarly productivity, and science identity, as well as providing many other benefits ( Thiry and Laursen, 2011 ; Prunuske et al. , 2013 ; Byars-Winston et al. , 2015 ; Aikens et al. , 2016 , 2017 ; Thompson et al. , 2016 ; Estrada et al. , 2018 ). However, recent literature has highlighted that poor mentoring can negatively affect undergraduate researchers ( Cooper et al. , 2019c ; Limeri et al. , 2019 ). Specifically, one study of 33 undergraduate researchers who had conducted research at 10 institutions identified seven major ways that they experienced negative mentoring, which included absenteeism, abuse of power, interpersonal mismatch, lack of career support, lack of psychosocial support, misaligned expectations, and unequal treatment ( Limeri et al. , 2019 ). We hypothesize negative mentoring experiences may be particularly harmful for students with depression, because support, particularly social support, has been shown to be important for helping individuals with depression cope with difficult circumstances ( Aneshensel and Stone, 1982 ; Grav et al. , 2012 ). Failure: Experiencing failure has been hypothesized to be an important aspect of undergraduate research experiences that may help students develop some the most distinguishing abilities of outstanding scientists, such as coping with failure, navigating challenges, and persevering ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, experiencing failure and the stress and fatigue that often accompany it may be particularly tough for students with depression ( Aldwin and Greenberger, 1987 ; Mongrain and Blackburn, 2005 ). Lab environment: Fairness, inclusion/exclusion, and social support within one’s organizational environment have been shown to be key factors that cause people to either want to remain in the work place and be productive or to want to leave ( Barak et al. , 2006 ; Cooper et al. , 2019c ). We hypothesize that dealing with exclusion or a lack of social support may exacerbate depression for some students; patients with clinical depression react to social exclusion with more pronounced negative emotions than do individuals without clinical depression ( Jobst et al. , 2015 ). While there are likely other aspects of undergraduate research that affect student depression, we hypothesize that these factors have the potential to exacerbate negative research experiences for students with depression.
Depression has been shown to disproportionately affect many populations that are underrepresented or underserved within the scientific community, including females ( American College Health Association, 2018 ; Evans et al. , 2018 ), first-generation college students ( Jenkins et al. , 2013 ), individuals from low socioeconomic backgrounds ( Eisenberg et al. , 2007 ), members of the LGBTQ+ community ( Eisenberg et al. , 2007 ; Evans et al. , 2018 ), and people with disabilities ( Turner and Noh, 1988 ). Therefore, as the science community strives to be more diverse and inclusive ( Intemann, 2009 ), it is important that we understand more about the relationship between depression and scientific research, because negative experiences with depression in scientific research may be contributing to the underrepresentation of these groups. Specifically, more information is needed about how the research process and environment of research experiences may affect depression.
Given the high rate of depression among undergraduates, the links between depression and graduate research, the potentially challenging environment of undergraduate research, and how depression could disproportionately impact students from underserved communities, it is imperative to begin to explore the relationship between scientific research and depression among undergraduates to create research experiences that could maximize student success. In this exploratory interview study, we aimed to 1) describe how undergraduates’ symptoms of depression affect their research experiences, 2) understand how undergraduate research affects students’ feelings of depression, and 3) identify recommendations based on the literature and undergraduates’ reported experiences to promote a positive research experience for students with depression.
This study was done with an approved Arizona State University Institutional Review Board protocol #7247.
In Fall 2018, we surveyed undergraduate researchers majoring in the life sciences across 25 research-intensive (R1) public institutions across the United States (specific details about the recruitment of the students who completed the survey can be found in Cooper et al. (2019c) ). The survey asked students for their opinions about their undergraduate research experiences and their demographic information and whether they would be interested in participating in a follow-up interview related to their research experiences. For the purpose of this study, we exclusively interviewed students about their undergraduate research experiences in faculty member labs; we did not consider students’ experiences in CUREs. Of the 768 undergraduate researchers who completed the survey, 65% ( n = 496) indicated that they would be interested in participating in a follow-up interview. In Spring 2019, we emailed the 496 students, explaining that we were interested in interviewing students with depression about their experiences in undergraduate research. Our specific prompt was: “If you identify as having depression, we would be interested in hearing about your experience in undergraduate research in a 30–60 minute online interview.” We did not define depression in our email recruitment because we conducted think-aloud interviews with four undergraduates who all correctly interpreted what we meant by depression ( APA, 2013 ). We had 35 students agree to participate in the interview study. The interview participants represented 12 of the 25 R1 public institutions that were represented in the initial survey.
Student Interviews
We developed an interview script to explore our research questions. Specifically, we were interested in how students’ symptoms of depression affect their research experiences, how undergraduate research negatively affects student depression, and how undergraduate research positively affects student depression.
We recognized that mental health, and specifically depression, can be a sensitive topic to discuss with undergraduates, and therefore we tried to minimize any discomfort that the interviewees might experience during the interview. Specifically, we conducted think-aloud interviews with three graduate students who self-identified with having depression at the time of the interview. We asked them to note whether any interview questions made them uncomfortable. We also sought their feedback on questions given their experiences as persons with depression who had once engaged in undergraduate research. We revised the interview protocol after each think-aloud interview. Next, we conducted four additional think-aloud interviews with undergraduates conducting basic science or biology education research who identified with having depression to establish cognitive validity of the questions and to elicit additional feedback about any questions that might make someone uncomfortable. The questions were revised after each think-aloud interview until no question was unclear or misinterpreted by the students and we were confident that the questions minimized students’ potential discomfort ( Trenor et al. , 2011 ). A copy of the final interview script can be found in the Supplemental Material.
All interviews were individually conducted by one of two researchers (K.M.C. and L.E.G.) who conducted the think-aloud interviews together to ensure that their interviewing practices were as similar as possible. The interviews were approximately an hour long, and students received a $15 gift card for their participation.
Personal, Research, and Depression Demographics
All student demographics and information about students’ research experiences were collected using the survey distributed to students in Fall 2018. We collected personal demographics, including the participants’ gender, race/ethnicity, college generation status, transfer status, financial stability, year in college, major, and age. We also collected information about the students’ research experiences, including the length of their first research experiences, the average number of hours they spend in research per week, how they were compensated for research, who their primary mentors were, and the focus areas of their research.
In the United States, mental healthcare is disproportionately unavailable to Black and Latinx individuals, as well as those who come from low socioeconomic backgrounds ( Kataoka et al. , 2002 ; Howell and McFeeters, 2008 ; Santiago et al. , 2013 ). Therefore, to minimize a biased sample, we invited anyone who identified with having depression to participate in our study; we did not require students to be diagnosed with depression or to be treated for depression in order to participate. However, we did collect information about whether students had been formally diagnosed with depression and whether they had been treated for depression. After the interview, all participants were sent a link to a short survey that asked them if they had ever been diagnosed with depression and how, if at all, they had ever been treated for depression. A copy of these survey questions can be found in the Supplemental Material. The combined demographic information of the participants is in Table 1 . The demographics for each individual student can be found in the Supplemental Material.
a Students reported the time they had spent in research 6 months before being interviewed and only reported on the length of time of their first research experiences.
b Students were invited to report multiple ways in which they were treated for their depression; other treatments included lifestyle changes and meditation.
c Students were invited to report multiple means of compensation for their research if they had been compensated for their time in different ways.
d Students were asked whether they felt financially stable, particularly during the undergraduate research experience.
e Students reported who they work/worked with most closely during their research experiences.
f Staff members included lab coordinators or lab managers.
g Other focus areas of research included sociology, linguistics, psychology, and public health.
Interview Analysis
The initial interview analysis aimed to explore each idea that a participant expressed ( Charmaz, 2006 ) and to identify reoccurring ideas throughout the interviews. First, three authors (K.M.C., L.E.G., and S.E.B.) individually reviewed a different set of 10 interviews and took detailed analytic notes ( Birks and Mills, 2015 ). Afterward, the authors compared their notes and identified reoccurring themes throughout the interviews using open coding methods ( Saldaña, 2015 ).
Once an initial set of themes was established, two researchers (K.M.C. and L.E.G.) individually reviewed the same set of 15 randomly selected interviews to validate the themes identified in the initial analysis and to screen for any additional themes that the initial analysis may have missed. Each researcher took detailed analytic notes throughout the review of an interview, which they discussed after reviewing each interview. The researchers compared what quotes from each interview they categorized into each theme. Using constant comparison methods, they assigned quotes to each theme and constantly compared the quotes to ensure that each quote fit within the description of the theme ( Glesne and Peshkin, 1992 ). In cases in which quotes were too different from other quotes, a new theme was created. This approach allowed for multiple revisions of the themes and allowed the authors to define a final set of codes; the researchers created a final codebook with refined definitions of emergent themes (the final coding rubric can be found in the Supplemental Material). Once the final codebook was established, the researchers (K.M.C. and L.E.G.) individually coded seven additional interviews (20% of all interviews) using the coding rubric. The researchers compared their codes, and their Cohen’s κ interrater score for these seven interviews was at an acceptable level (κ = 0.88; Landis and Koch, 1977 ). One researcher (L.E.G.) coded the remaining 28 out of 35 interviews. The researchers determined that data saturation had been reached with the current sample and no further recruitment was needed ( Guest et al. , 2006 ). We report on themes that were mentioned by at least 20% of students in the interview study. In the Supplemental Material, we provide the final coding rubric with the number of participants whose interview reflected each theme ( Hannah and Lautsch, 2011 ). Reporting the number of individuals who reported themes within qualitative data can lead to inaccurate conclusions about the generalizability of the results to a broader population. These qualitative data are meant to characterize a landscape of experiences that students with depression have in undergraduate research rather than to make claims about the prevalence of these experiences ( Glesne and Peshkin, 1992 ). Because inferences about the importance of these themes cannot be drawn from these counts, they are not included in the results of the paper ( Maxwell, 2010 ). Further, the limited number of interviewees made it not possible to examine whether there were trends based on students’ demographics or characteristics of their research experiences (e.g., their specific area of study). Quotes were lightly edited for clarity by inserting clarification brackets and using ellipses to indicate excluded text. Pseudonyms were given to all students to protect their privacy.
The Effect of Depressive Symptoms on Undergraduate Research
We asked students to describe the symptoms associated with their depression. Students described experiencing anxiety that is associated with their depression; this could be anxiety that precedes their depression or anxiety that results from a depressive episode or a period of time when an individual has depression symptoms. Further, students described difficulty getting out of bed or leaving the house, feeling tired, a lack of motivation, being overly self-critical, feeling apathetic, and having difficulty concentrating. We were particularly interested in how students’ symptoms of depression affected their experiences in undergraduate research. During the think-aloud interviews that were conducted before the interview study, graduate and undergraduate students consistently described that their depression affected their motivation in research, their creativity in research, and their productivity in research. Therefore, we explicitly asked undergraduate researchers how, if at all, their depression affected these three factors. We also asked students to describe any additional ways in which their depression affected their research experiences. Undergraduate researchers commonly described five additional ways in which their depression affected their research; for a detailed description of each way students’ research was affected and for example quotes, see Table 2 . Students described that their depression negatively affected their productivity in the lab. Commonly, students described that their productivity was directly affected by a lack of motivation or because they felt less creative, which hindered the research process. Additionally, students highlighted that they were sometimes less productive because their depression sometimes caused them to struggle to engage intellectually with their research or caused them to have difficulty remembering or concentrating; students described that they could do mundane or routine tasks when they felt depressed, but that they had difficulty with more complex and intellectually demanding tasks. However, students sometimes described that even mundane tasks could be difficult when they were required to remember specific steps; for example, some students struggled recalling a protocol from memory when their depression was particularly severe. Additionally, students noted that their depression made them more self-conscious, which sometimes held them back from sharing research ideas with their mentors or from taking risks such as applying to competitive programs. In addition to being self-conscious, students highlighted that their depression caused them to be overly self-critical, and some described experiencing imposter phenomenon ( Clance and Imes, 1978 ) or feeling like they were not talented enough to be in research and were accepted into a lab by a fluke or through luck. Finally, students described that depression often made them feel less social, and they struggled to socially engage with other members of the lab when they were feeling down.
The Effect of Undergraduate Research Experiences on Student Depression
We also wanted to explore how research impacted students’ feelings of depression. Undergraduates described how research both positively and negatively affected their depression. In the following sections, we present aspects of undergraduate research and examine how each positively and/or negatively affected students’ depression using embedded student quotes to highlight the relationships between related ideas.
Lab Environment: Relationships with Others in the Lab.
Some aspects of the lab environment, which we define as students’ physical, social, or psychological research space, could be particularly beneficial for students with depression.
Specifically, undergraduate researchers perceived that comfortable and positive social interactions with others in the lab helped their depression. Students acknowledged how beneficial their relationships with graduate students and postdocs could be.
Marta: “I think always checking in on undergrads is important. It’s really easy [for us] to go a whole day without talking to anybody in the lab. But our grad students are like ‘Hey, what’s up? How’s school? What’s going on?’ (…) What helps me the most is having that strong support system. Sometimes just talking makes you feel better, but also having people that believe in you can really help you get out of that negative spiral. I think that can really help with depression.”
Kelley: “I know that anytime I need to talk to [my postdoc mentors] about something they’re always there for me. Over time we’ve developed a relationship where I know that outside of work and outside of the lab if I did want to talk to them about something I could talk to them. Even just talking to someone about hobbies and having that relationship alone is really helpful [for depression].”
In addition to highlighting the importance of developing relationships with graduate students or postdocs in the lab, students described that forming relationships with other undergraduates in the lab also helped their depression. Particularly, students described that other undergraduate researchers often validated their feelings about research, which in turn helped them realize that what they are thinking or feeling is normal, which tended to alleviate their negative thoughts. Interestingly, other undergraduates experiencing the same issues could sometimes help buffer them from perceiving that a mentor did not like them or that they were uniquely bad at research. In this article, we use the term “mentor” to refer to anyone who students referred to in the interviews as being their mentors or managing their research experiences; this includes graduate students, postdoctoral scholars, lab managers, and primary investigators (PIs).
Abby: “One of my best friends is in the lab with me. A lot of that friendship just comes from complaining about our stress with the lab and our annoyance with people in the lab. Like when we both agree like, ‘Yeah, the grad students were really off today, it wasn’t us,’ that helps. ‘It wasn’t me, it wasn’t my fault that we were having a rough day in lab; it was the grad students.’ Just being able to realize, ‘Hey, this isn’t all caused by us,’ you know? (…) We understand the stresses in the lab. We understand the details of what each other are doing in the lab, so when something doesn’t work out, we understand that it took them like eight hours to do that and it didn’t work. We provide empathy on a different level.”
Meleana: “It’s great to have solidarity in being confused about something, and it’s just that is a form of validation for me too. When we leave a lab meeting and I look at [another undergrad] I’m like, ‘Did you understand anything that they were just saying?’ And they’re like, ‘Oh, no.’ (…) It’s just really validating to hear from the other undergrads that we all seem to be struggling with the same things.”
Developing positive relationships with faculty mentors or PIs also helped alleviate some students’ depressive feelings, particularly when PIs shared their own struggles with students. This also seemed to normalize students’ concerns about their own experiences.
Alexandra: “[Talking with my PI] is helpful because he would talk about his struggles, and what he faced. A lot of it was very similar to my struggles. For example, he would say, ‘Oh, yeah, I failed this exam that I studied so hard for. I failed the GRE and I paid so much money to prepare for it.’ It just makes [my depression] better, like okay, this is normal for students to go through this. It’s not an out of this world thing where if you fail, you’re a failure and you can’t move on from it.”
Students’ relationships with others in the lab did not always positively impact their depression. Students described instances when the negative moods of the graduate students and PIs would often set the tone of the lab, which in turn worsened the mood of the undergraduate researchers.
Abby: “Sometimes [the grad students] are not in a good mood. The entire vibe of the lab is just off, and if you make a joke and it hits somebody wrong, they get all mad. It really depends on the grad students and the leadership and the mood that they’re in.”
Interviewer: “How does it affect your depression when the grad students are in a bad mood?”
Abby: “It definitely makes me feel worse. It feels like, again, that I really shouldn’t go ask them for help because they’re just not in the mood to help out. It makes me have more pressure on myself, and I have deadlines I need to meet, but I have a question for them, but they’re in a bad mood so I can’t ask. That’s another day wasted for me and it just puts more stress, which just adds to the depression.”
Additionally, some students described even more concerning behavior from research mentors, which negatively affected their depression.
Julie: “I had a primary investigator who is notorious in the department for screaming at people, being emotionally abusive, unreasonable, et cetera. (…) [He was] kind of harassing people, demeaning them, lying to them, et cetera, et cetera. (…) Being yelled at and constantly demeaned and harassed at all hours of the day and night, that was probably pretty bad for me.”
While the relationships between undergraduates and graduate, postdoc, and faculty mentors seemed to either alleviate or worsen students’ depressive symptoms, depending on the quality of the relationship, students in this study exclusively described their relationships with other undergraduates as positive for their depression. However, students did note that undergraduate research puts some of the best and brightest undergraduates in the same environment, which can result in students comparing themselves with their peers. Students described that this comparison would often lead them to feel badly about themselves, even though they would describe their personal relationship with a person to be good.
Meleana: “In just the research field in general, just feeling like I don’t really measure up to the people around me [can affect my depression]. A lot of the times it’s the beginning of a little spiral, mental spiral. There are some past undergrads that are talked about as they’re on this pedestal of being the ideal undergrads and that they were just so smart and contributed so much to the lab. I can never stop myself from wondering like, ‘Oh, I wonder if I’m having a contribution to the lab that’s similar or if I’m just another one of the undergrads that does the bare minimum and passes through and is just there.’”
Natasha: “But, on the other hand, [having another undergrad in the lab] also reminded me constantly that some people are invested in this and meant to do this and it’s not me. And that some people know a lot more than I do and will go further in this than I will.”
While students primarily expressed that their relationships with others in the lab affected their depression, some students explained that they struggled most with depression when the lab was empty; they described that they did not like being alone in the lab, because a lack of stimulation allowed their minds to be filled with negative thoughts.
Mia: “Those late nights definitely didn’t help [my depression]. I am alone, in the entire building. I’m left alone to think about my thoughts more, so not distracted by talking to people or interacting with people. I think more about how I’m feeling and the lack of progress I’m making, and the hopelessness I’m feeling. That kind of dragged things on, and I guess deepened my depression.”
Freddy: “Often times when I go to my office in the evening, that is when I would [ sic ] be prone to be more depressed. It’s being alone. I think about myself or mistakes or trying to correct mistakes or whatever’s going on in my life at the time. I become very introspective. I think I’m way too self-evaluating, way too self-deprecating and it’s when I’m alone when those things are really, really triggered. When I’m talking with somebody else, I forget about those things.”
In sum, students with depression highlighted that a lab environment full of positive and encouraging individuals was helpful for their depression, whereas isolating or competitive environments and negative interactions with others often resulted in more depressive feelings.
Doing Science: Experiencing Failure in Research, Getting Help, Receiving Feedback, Time Demands, and Important Contributions.
In addition to the lab environment, students also described that the process of doing science could affect their depression. Specifically, students explained that a large contributor to their depression was experiencing failure in research.
Interviewer: “Considering your experience in undergraduate research, what tends to trigger your feelings of depression?”
Heather: “Probably just not getting things right. Having to do an experiment over and over again. You don’t get the results you want. (…) The work is pretty meticulous and it’s frustrating when I do all this work, I do a whole experiment, and then I don’t get any results that I can use. That can be really frustrating. It adds to the stress. (…) It’s hard because you did all this other stuff before so you can plan for the research, and then something happens and all the stuff you did was worthless basically.”
Julie: “I felt very negatively about myself [when a project failed] and pretty panicked whenever something didn’t work because I felt like it was a direct reflection on my effort and/or intelligence, and then it was a big glaring personal failure.”
Students explained that their depression related to failing in research was exacerbated if they felt as though they could not seek help from their research mentors. Perceived insufficient mentor guidance has been shown to be a factor influencing student intention to leave undergraduate research ( Cooper et al. , 2019c ). Sometimes students talked about their research mentors being unavailable or unapproachable.
Michelle: “It just feels like [the graduate students] are not approachable. I feel like I can’t approach them to ask for their understanding in a certain situation. It makes [my depression] worse because I feel like I’m stuck, and that I’m being limited, and like there’s nothing I can do. So then I kind of feel like it’s my fault that I can’t do anything.”
Other times, students described that they did not seek help in fear that they would be negatively evaluated in research, which is a fear of being judged by others ( Watson and Friend, 1969 ; Weeks et al. , 2005 ; Cooper et al. , 2018 ). That is, students fear that their mentor would think negatively about them or judge them if they were to ask questions that their mentor thought they should know the answer to.
Meleana: “I would say [my depression] tends to come out more in being more reserved in asking questions because I think that comes more like a fear-based thing where I’m like, ‘Oh, I don’t feel like I’m good enough and so I don’t want to ask these questions because then my mentors will, I don’t know, think that I’m dumb or something.’”
Conversely, students described that mentors who were willing to help them alleviated their depressive feelings.
Crystal: “Yeah [my grad student] is always like, ‘Hey, I can check in on things in the lab because you’re allowed to ask me for that, you’re not totally alone in this,’ because he knows that I tend to take on all this responsibility and I don’t always know how to ask for help. He’s like, ‘You know, this is my lab too and I am here to help you as well,’ and just reminds me that I’m not shouldering this burden by myself.”
Ashlyn: “The graduate student who I work with is very kind and has a lot of patience and he really understands a lot of things and provides simple explanations. He does remind me about things and he will keep on me about certain tasks that I need to do in an understanding way, and it’s just because he’s patient and he listens.”
In addition to experiencing failure in science, students described that making mistakes when doing science also negatively affected their depression.
Abby: “I guess not making mistakes on experiments [is important in avoiding my depression]. Not necessarily that your experiment didn’t turn out to produce the data that you wanted, but just adding the wrong enzyme or messing something up like that. It’s like, ‘Oh, man,’ you know? You can get really down on yourself about that because it can be embarrassing.”
Commonly, students described that the potential for making mistakes increased their stress and anxiety regarding research; however, they explained that how other people responded to a potential mistake was what ultimately affected their depression.
Briana: “Sometimes if I made a mistake in correctly identifying an eye color [of a fly], [my PI] would just ridicule me in front of the other students. He corrected me but his method of correcting was very discouraging because it was a ridicule. It made the others laugh and I didn’t like that.”
Julie: “[My PI] explicitly [asked] if I had the dedication for science. A lot of times he said I had terrible judgment. A lot of times he said I couldn’t be trusted. Once I went to a conference with him, and, unfortunately, in front of another professor, he called me a klutz several times and there was another comment about how I never learn from my mistakes.”
When students did do things correctly, they described how important it could be for them to receive praise from their mentors. They explained that hearing praise and validation can be particularly helpful for students with depression, because their thoughts are often very negative and/or because they have low self-esteem.
Crystal: “[Something that helps my depression is] I have text messages from [my graduate student mentor] thanking me [and another undergraduate researcher] for all of the work that we’ve put in, that he would not be able to be as on track to finish as he is if he didn’t have our help.”
Interviewer: “Why is hearing praise from your mentor helpful?”
Crystal: “Because a lot of my depression focuses on everybody secretly hates you, nobody likes you, you’re going to die alone. So having that validation [from my graduate mentor] is important, because it flies in the face of what my depression tells me.”
Brian: “It reminds you that you exist outside of this negative world that you’ve created for yourself, and people don’t see you how you see yourself sometimes.”
Students also highlighted how research could be overwhelming, which negatively affected their depression. Particularly, students described that research demanded a lot of their time and that their mentors did not always seem to be aware that they were juggling school and other commitments in addition to their research. This stress exacerbated their depression.
Rose: “I feel like sometimes [my grad mentors] are not very understanding because grad students don’t take as many classes as [undergrads] do. I think sometimes they don’t understand when I say I can’t come in at all this week because I have finals and they’re like, ‘Why though?’”
Abby: “I just think being more understanding of student life would be great. We have classes as well as the lab, and classes are the priority. They forget what it’s like to be a student. You feel like they don’t understand and they could never understand when you say like, ‘I have three exams this week,’ and they’re like, ‘I don’t care. You need to finish this.’”
Conversely, some students reported that their research labs were very understanding of students’ schedules. Interestingly, these students talked most about how helpful it was to be able to take a mental health day and not do research on days when they felt down or depressed.
Marta: “My lab tech is very open, so she’ll tell us, ‘I can’t come in today. I have to take a mental health day.’ So she’s a really big advocate for that. And I think I won’t personally tell her that I’m taking a mental health day, but I’ll say, ‘I can’t come in today, but I’ll come in Friday and do those extra hours.’ And she’s like, ‘OK great, I’ll see you then.’ And it makes me feel good, because it helps me take care of myself first and then I can take care of everything else I need to do, which is amazing.”
Meleana: “Knowing that [my mentors] would be flexible if I told them that I’m crazy busy and can’t come into work nearly as much this week [helps my depression]. There is flexibility in allowing me to then care for myself.”
Interviewer: “Why is the flexibility helpful given the depression?”
Meleana: “Because sometimes for me things just take a little bit longer when I’m feeling down. I’m just less efficient to be honest, and so it’s helpful if I feel like I can only go into work for 10 hours in a week. It declutters my brain a little bit to not have to worry about all the things I have to do in work in addition the things that I need to do for school or clubs, or family or whatever.”
Despite the demanding nature of research, a subset of students highlighted that their research and research lab provided a sense of stability or familiarity that distracted them from their depression.
Freddy: “I’ll [do research] to run away from those [depressive] feelings or whatever. (…) I find sadly, I hate to admit it, but I do kind of run to [my lab]. I throw myself into work to distract myself from the feelings of depression and sadness.”
Rose: “When you’re sad or when you’re stressed you want to go to things you’re familiar with. So because lab has always been in my life, it’s this thing where it’s going to be there for me I guess. It’s like a good book that you always go back to and it’s familiar and it makes you feel good. So that’s how lab is. It’s not like the greatest thing in the world but it’s something that I’m used to, which is what I feel like a lot of people need when they’re sad and life is not going well.”
Many students also explained that research positively affects their depression because they perceive their research contribution to be important.
Ashlyn: “I feel like I’m dedicating myself to something that’s worthy and something that I believe in. It’s really important because it contextualizes those times when I am feeling depressed. It’s like, no, I do have these better things that I’m working on. Even when I don’t like myself and I don’t like who I am, which is again, depression brain, I can at least say, ‘Well, I have all these other people relying on me in research and in this area and that’s super important.’”
Jessica: “I mean, it just felt like the work that I was doing had meaning and when I feel like what I’m doing is actually going to contribute to the world, that usually really helps with [depression] because it’s like not every day you can feel like you’re doing something impactful.”
In sum, students highlighted that experiencing failure in research and making mistakes negatively contributed to depression, especially when help was unavailable or research mentors had a negative reaction. Additionally, students acknowledged that the research could be time-consuming, but that research mentors who were flexible helped assuage depressive feelings that were associated with feeling overwhelmed. Finally, research helped some students’ depression, because it felt familiar, provided a distraction from depression, and reminded students that they were contributing to a greater cause.
We believe that creating more inclusive research environments for students with depression is an important step toward broadening participation in science, not only to ensure that we are not discouraging students with depression from persisting in science, but also because depression has been shown to disproportionately affect underserved and underrepresented groups in science ( Turner and Noh, 1988 ; Eisenberg et al. , 2007 ; Jenkins et al. , 2013 ; American College Health Association, 2018 ). We initially hypothesized that three features of undergraduate research—research mentors, the lab environment, and failure—may have the potential to exacerbate student depression. We found this to be true; students highlighted that their relationships with their mentors as well as the overall lab environment could negatively affect their depression, but could also positively affect their research experiences. Students also noted that they struggled with failure, which is likely true of most students, but is known to be particularly difficult for students with depression ( Elliott et al. , 1997 ). We expand upon our findings by integrating literature on depression with the information that students provided in the interviews about how research mentors can best support students. We provide a set of evidence-based recommendations focused on mentoring, the lab environment, and failure for research mentors wanting to create more inclusive research environments for students with depression. Notably, only the first recommendation is specific to students with depression; the others reflect recommendations that have previously been described as “best practices” for research mentors ( NASEM, 2017 , 2019 ; Sorkness et al. , 2017 ) and likely would benefit most students. However, we examine how these recommendations may be particularly important for students with depression. As we hypothesized, these recommendations directly address three aspects of research: mentors, lab environment, and failure. A caveat of these recommendations is that more research needs to be done to explore the experiences of students with depression and how these practices actually impact students with depression, but our national sample of undergraduate researchers with depression can provide an initial starting point for a discussion about how to improve research experiences for these students.
Recommendations to Make Undergraduate Research Experiences More Inclusive for Students with Depression
Recognize student depression as a valid illness..
Allow students with depression to take time off of research by simply saying that they are sick and provide appropriate time for students to recover from depressive episodes. Also, make an effort to destigmatize mental health issues.
Undergraduate researchers described both psychological and physical symptoms that manifested as a result of their depression and highlighted how such symptoms prevented them from performing to their full potential in undergraduate research. For example, students described how their depression would cause them to feel unmotivated, which would often negatively affect their research productivity. In cases in which students were motivated enough to come in and do their research, they described having difficulty concentrating or engaging in the work. Further, when doing research, students felt less creative and less willing to take risks, which may alter the quality of their work. Students also sometimes struggled to socialize in the lab. They described feeling less social and feeling overly self-critical. In sum, students described that, when they experienced a depressive episode, they were not able to perform to the best of their ability, and it sometimes took a toll on them to try to act like nothing was wrong, when they were internally struggling with depression. We recommend that research mentors treat depression like any other physical illness; allowing students the chance to recover when they are experiencing a depressive episode can be extremely important to students and can allow them to maximize their productivity upon returning to research ( Judd et al. , 2000 ). Students explained that if they are not able to take the time to focus on recovering during a depressive episode, then they typically continue to struggle with depression, which negatively affects their research. This sentiment is echoed by researchers in psychiatry who have found that patients who do not fully recover from a depressive episode are more likely to relapse and to experience chronic depression ( Judd et al. , 2000 ). Students described not doing tasks or not showing up to research because of their depression but struggling with how to share that information with their research mentors. Often, students would not say anything, which caused them anxiety because they were worried about what others in the lab would say to them when they returned. Admittedly, many students understood why this behavior would cause their research mentors to be angry or frustrated, but they weighed the consequences of their research mentors’ displeasure against the consequences of revealing their depression and decided it was not worth admitting to being depressed. This aligns with literature that suggests that when individuals have concealable stigmatized identities, or identities that can be hidden and that carry negative stereotypes, such as depression, they will often keep them concealed to avoid negative judgment or criticism ( Link and Phelan, 2001 ; Quinn and Earnshaw, 2011 ; Jones and King, 2014 ; Cooper and Brownell, 2016 ; Cooper et al. , 2019b ; Cooper et al ., unpublished data ). Therefore, it is important for research mentors to be explicit with students that 1) they recognize mental illness as a valid sickness and 2) that students with mental illness can simply explain that they are sick if they need to take time off. This may be useful to overtly state on a research website or in a research syllabus, contract, or agreement if mentors use such documents when mentoring undergraduates in their lab. Further, research mentors can purposefully work to destigmatize mental health issues by explicitly stating that struggling with mental health issues, such as depression and anxiety, is common. While we do not recommend that mentors ask students directly about depression, because this can force students to share when they are not comfortable sharing, we do recommend providing opportunities for students to reveal their depression ( Chaudoir and Fisher, 2010 ). Mentors can regularly check in with students about how they’re doing, and talk openly about the importance of mental health, which may increase the chance that students may feel comfortable revealing their depression ( Chaudoir and Quinn, 2010 ; Cooper et al ., unpublished data ).
Foster a Positive Lab Environment.
Encourage positivity in the research lab, promote working in shared spaces to enhance social support among lab members, and alleviate competition among undergraduates.
Students in this study highlighted that the “leadership” of the lab, meaning graduate students, postdocs, lab managers, and PIs, were often responsible for establishing the tone of the lab; that is, if they were in a bad mood it would trickle down and negatively affect the moods of the undergraduates. Explicitly reminding lab leadership that their moods can both positively and negatively affect undergraduates may be important in establishing a positive lab environment. Further, students highlighted how they were most likely to experience negative thoughts when they were alone in the lab. Therefore, it may be helpful to encourage all lab members to work in a shared space to enhance social interactions among students and to maximize the likelihood that undergraduates have access to help when needed. A review of 51 studies in psychiatry supported our undergraduate researchers’ perceptions that social relationships positively impacted their depression; the study found that perceived emotional support (e.g., someone available to listen or give advice), perceived instrumental support (e.g., someone available to help with tasks), and large diverse social networks (e.g., being socially connected to a large number of people) were significantly protective against depression ( Santini et al. , 2015 ). Additionally, despite forming positive relationships with other undergraduates in the lab, many undergraduate researchers admitted to constantly comparing themselves with other undergraduates, which led them to feel inferior, negatively affecting their depression. Some students talked about mentors favoring current undergraduates or talking positively about past undergraduates, which further exacerbated their feelings of inferiority. A recent study of students in undergraduate research experiences highlighted that inequitable distribution of praise to undergraduates can create negative perceptions of lab environments for students (Cooper et al. , 2019). Further, the psychology literature has demonstrated that when people feel insecure in their social environments, it can cause them to focus on a hierarchical view of themselves and others, which can foster feelings of inferiority and increase their vulnerability to depression ( Gilbert et al. , 2009 ). Thus, we recommend that mentors be conscious of their behaviors so that they do not unintentionally promote competition among undergraduates or express favoritism toward current or past undergraduates. Praise is likely best used without comparison with others and not done in a public way, although more research on the impact of praise on undergraduate researchers needs to be done. While significant research has been done on mentoring and mentoring relationships in the context of undergraduate research ( Byars-Winston et al. , 2015 ; Aikens et al. , 2017 ; Estrada et al. , 2018 ; Limeri et al. , 2019 ; NASEM, 2019 ), much less has been done on the influence of the lab environment broadly and how people in nonmentoring roles can influence one another. Yet, this study indicates the potential influence of many different members of the lab, not only their mentors, on students with depression.
Develop More Personal Relationships with Undergraduate Researchers and Provide Sufficient Guidance.
Make an effort to establish more personal relationships with undergraduates and ensure that they perceive that they have access to sufficient help and guidance with regard to their research.
When we asked students explicitly how research mentors could help create more inclusive environments for undergraduate researchers with depression, students overwhelmingly said that building mentor–student relationships would be extremely helpful. Students suggested that mentors could get to know students on a more personal level by asking about their career interests or interests outside of academia. Students also remarked that establishing a more personal relationship could help build the trust needed in order for undergraduates to confide in their research mentors about their depression, which they perceived would strengthen their relationships further because they could be honest about when they were not feeling well or their mentors might even “check in” with them in times where they were acting differently than normal. This aligns with studies showing that undergraduates are most likely to reveal a stigmatized identity, such as depression, when they form a close relationship with someone ( Chaudoir and Quinn, 2010 ). Many were intimidated to ask for research-related help from their mentors and expressed that they wished they had established a better relationship so that they would feel more comfortable. Therefore, we recommend that research mentors try to establish relationships with their undergraduates and explicitly invite them to ask questions or seek help when needed. These recommendations are supported by national recommendations for mentoring ( NASEM, 2019 ) and by literature that demonstrates that both social support (listening and talking with students) and instrumental support (providing students with help) have been shown to be protective against depression ( Santini et al. , 2015 ).
Treat Undergraduates with Respect and Remember to Praise Them.
Avoid providing harsh criticism and remember to praise undergraduates. Students with depression often have low self-esteem and are especially self-critical. Therefore, praise can help calibrate their overly negative self-perceptions.
Students in this study described that receiving criticism from others, especially harsh criticism, was particularly difficult for them given their depression. Multiple studies have demonstrated that people with depression can have an abnormal or maladaptive response to negative feedback; scientists hypothesize that perceived failure on a particular task can trigger failure-related thoughts that interfere with subsequent performance ( Eshel and Roiser, 2010 ). Thus, it is important for research mentors to remember to make sure to avoid unnecessarily harsh criticisms that make students feel like they have failed (more about failure is described in the next recommendation). Further, students with depression often have low self-esteem or low “personal judgment of the worthiness that is expressed in the attitudes the individual holds towards oneself” ( Heatherton et al. , 2003 , p. 220; Sowislo and Orth, 2013 ). Specifically, a meta-analysis of longitudinal studies found that low self-esteem is predictive of depression ( Sowislo and Orth, 2013 ), and depression has also been shown to be highly related to self-criticism ( Luyten et al. , 2007 ). Indeed, nearly all of the students in our study described thinking that they are “not good enough,” “worthless,” or “inadequate,” which is consistent with literature showing that people with depression are self-critical ( Blatt et al. , 1982 ; Gilbert et al. , 2006 ) and can be less optimistic of their performance on future tasks and rate their overall performance on tasks less favorably than their peers without depression ( Cane and Gotlib, 1985 ). When we asked students what aspects of undergraduate research helped their depression, students described that praise from their mentors was especially impactful, because they thought so poorly of themselves and they needed to hear something positive from someone else in order to believe it could be true. Praise has been highlighted as an important aspect of mentoring in research for many years ( Ashford, 1996 ; Gelso and Lent, 2000 ; Brown et al. , 2009 ) and may be particularly important for students with depression. In fact, praise has been shown to enhance individuals’ motivation and subsequent productivity ( Hancock, 2002 ; Henderlong and Lepper, 2002 ), factors highlighted by students as negatively affecting their depression. However, something to keep in mind is that a student with depression and a student without depression may process praise differently. For a student with depression, a small comment that praises the student’s work may not be sufficient for the student to process that comment as praise. People with depression are hyposensitive to reward or have reward-processing deficits ( Eshel and Roiser, 2010 ); therefore, praise may affect students without depression more positively than it would affect students with depression. Research mentors should be mindful that students with depression often have a negative view of themselves, and while students report that praise is extremely important, they may have trouble processing such positive feedback.
Normalize Failure and Be Explicit about the Importance of Research Contributions.
Explicitly remind students that experiencing failure is expected in research. Also explain to students how their individual work relates to the overall project so that they can understand how their contributions are important. It can also be helpful to explain to students why the research project as a whole is important in the context of the greater scientific community.
Experiencing failure has been thought to be a potentially important aspect of undergraduate research, because it may provide students with the potential to develop integral scientific skills such as the ability to navigate challenges and persevere ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, in the interviews, students described that when their science experiments failed, it was particularly tough for their depression. Students’ negative reaction to experiencing failure in research is unsurprising, given recent literature that has predicted that students may be inadequately prepared to approach failure in science ( Henry et al. , 2019 ). However, the literature suggests that students with depression may find experiencing failure in research to be especially difficult ( Elliott et al. , 1997 ; Mongrain and Blackburn, 2005 ; Jones et al. , 2009 ). One potential hypothesis is that students with depression may be more likely to have fixed mindsets or more likely to believe that their intelligence and capacity for specific abilities are unchangeable traits ( Schleider and Weisz, 2018 ); students with a fixed mindset have been hypothesized to have particularly negative responses to experiencing failure in research, because they are prone to quitting easily in the face of challenges and becoming defensive when criticized ( Forsythe and Johnson, 2017 ; Dweck, 2008 ). A study of life sciences undergraduates enrolled in CUREs identified three strategies of students who adopted adaptive coping mechanisms, or mechanisms that help an individual maintain well-being and/or move beyond the stressor when faced with failure in undergraduate research: 1) problem solving or engaging in strategic planning and decision making, 2) support seeking or finding comfort and help with research, and 3) cognitive restructuring or reframing a problem from negative to positive and engaging in self encouragement ( Gin et al. , 2018 ). We recommend that, when undergraduates experience failure in science, their mentors be proactive in helping them problem solve, providing help and support, and encouraging them. Students also explained that mentors sharing their own struggles as undergraduate and graduate students was helpful, because it normalized failure. Sharing personal failures in research has been recommended as an important way to provide students with psychosocial support during research ( NASEM, 2019 ). We also suggest that research mentors take time to explain to students why their tasks in the lab, no matter how small, contribute to the greater research project ( Cooper et al. , 2019a ). Additionally, it is important to make sure that students can explain how the research project as a whole is contributing to the scientific community ( Gin et al. , 2018 ). Students highlighted that contributing to something important was really helpful for their depression, which is unsurprising, given that studies have shown that meaning in life or people’s comprehension of their life experiences along with a sense of overarching purpose one is working toward has been shown to be inversely related to depression ( Steger, 2013 ).
Limitations and Future Directions
This work was a qualitative interview study intended to document a previously unstudied phenomenon: depression in the context of undergraduate research experiences. We chose to conduct semistructured interviews rather than a survey because of the need for initial exploration of this area, given the paucity of prior research. A strength of this study is the sampling approach. We recruited a national sample of 35 undergraduates engaged in undergraduate research at 12 different public R1 institutions. Despite our representative sample from R1 institutions, these findings may not be generalizable to students at other types of institutions; lab environments, mentoring structures, and interactions between faculty and undergraduate researchers may be different at other institution types (e.g., private R1 institutions, R2 institutions, master’s-granting institutions, primarily undergraduate institutions, and community colleges), so we caution against making generalizations about this work to all undergraduate research experiences. Future work could assess whether students with depression at other types of institutions have similar experiences to students at research-intensive institutions. Additionally, we intentionally did not explore the experiences of students with specific identities owing to our sample size and the small number of students in any particular group (e.g., students of a particular race, students with a graduate mentor as the primary mentor). We intend to conduct future quantitative studies to further explore how students’ identities and aspects of their research affect their experiences with depression in undergraduate research.
The students who participated in the study volunteered to be interviewed about their depression; therefore, it is possible that depression is a more salient part of these students’ identities and/or that they are more comfortable talking about their depression than the average population of students with depression. It is also important to acknowledge the personal nature of the topic and that some students may not have fully shared their experiences ( Krumpal, 2013 ), particularly those experiences that may be emotional or traumatizing ( Kahn and Garrison, 2009 ). Additionally, our sample was skewed toward females (77%). While females do make up approximately 60% of students in biology programs on average ( Eddy et al. , 2014 ), they are also more likely to report experiencing depression ( American College Health Association, 2018 ; Evans et al. , 2018 ). However, this could be because women have higher rates of depression or because males are less likely to report having depression; clinical bias, or practitioners’ subconscious tendencies to overlook male distress, may underestimate depression rates in men ( Smith et al. , 2018 ). Further, females are also more likely to volunteer to participate in studies ( Porter and Whitcomb, 2005 ); therefore, many interview studies have disproportionately more females in the data set (e.g., Cooper et al. , 2017 ). If we had been able to interview more male students, we might have identified different findings. Additionally, we limited our sample to life sciences students engaged in undergraduate research at public R1 institutions. It is possible that students in other majors may have different challenges and opportunities for students with depression, as well as different disciplinary stigmas associated with mental health.
In this exploratory interview study, we identified a variety of ways in which depression in undergraduates negatively affected their undergraduate research experiences. Specifically, we found that depression interfered with students’ motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing. We also identified that research can negatively affect depression in undergraduates. Experiencing failure in research can exacerbate student depression, especially when students do not have access to adequate guidance. Additionally, being alone or having negative interactions with others in the lab worsened students’ depression. However, we also found that undergraduate research can positively affect students’ depression. Research can provide a familiar space where students can feel as though they are contributing to something meaningful. Additionally, students reported that having access to adequate guidance and a social support network within the research lab also positively affected their depression. We hope that this work can spark conversations about how to make undergraduate research experiences more inclusive of students with depression and that it can stimulate additional research that more broadly explores the experiences of undergraduate researchers with depression.
Important note
If you or a student experience symptoms of depression and want help, there are resources available to you. Many campuses provide counseling centers equipped to provide students, staff, and faculty with treatment for depression, as well as university-dedicated crisis hotlines. Additionally, there are free 24/7 services such as Crisis Text Line, which allows you to text a trained live crisis counselor (Text “CONNECT” to 741741; Text Depression Hotline , 2019 ), and phone hotlines such as the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK). You can also learn more about depression and where to find help near you through the Anxiety and Depression Association of American website: https://adaa.org ( Anxiety and Depression Association of America, 2019 ) and the Depression and Biopolar Support Alliance: http://dbsalliance.org ( Depression and Biopolar Support Alliance, 2019 ).
ACKNOWLEDGMENTS
We are extremely grateful to the undergraduate researchers who shared their thoughts and experiences about depression with us. We acknowledge the ASU LEAP Scholars for helping us create the original survey and Rachel Scott for her helpful feedback on earlier drafts of this article. L.E.G. was supported by a National Science Foundation (NSF) Graduate Fellowship (DGE-1311230) and K.M.C. was partially supported by a Howard Hughes Medical Institute (HHMI) Inclusive Excellence grant (no. 11046) and an NSF grant (no. 1644236). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF or HHMI.
- Aikens, M. L., Robertson, M. M., Sadselia, S., Watkins, K., Evans, M., Runyon, C. R. , … & Dolan, E. L. ( 2017 ). Race and gender differences in undergraduate research mentoring structures and research outcomes . CBE—Life Sciences Education , 16 (2), ar34. Link , Google Scholar
- Aikens, M. L., Sadselia, S., Watkins, K., Evans, M., Eby, L. T., & Dolan, E. L. ( 2016 ). A social capital perspective on the mentoring of undergraduate life science researchers: An empirical study of undergraduate–postgraduate–faculty triads . CBE—Life Sciences Education , 15 (2), ar16. Link , Google Scholar
- Aldwin, C., & Greenberger, E. ( 1987 ). Cultural differences in the predictors of depression . American Journal of Community Psychology , 15 (6), 789–813. Medline , Google Scholar
- American Association for the Advancement of Science . ( 2011 ). Vision and change in undergraduate biology education: A call to action . Retrieved November 29, 2019, from http://visionandchange.org/files/2013/11/aaas-VISchange-web1113.pdf Google Scholar
- American College Health Association . ( 2018 ). Undergraduate reference group executive summary, Fall 2018 . Retrieved November 29, 2019, from www.acha.org/documents/ncha/NCHA-II_Fall_2018_Reference_Group_Executive_Summary.pdf Google Scholar
- American College Health Association . ( 2019 ). Retrieved November 29, 2019, from NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf www.acha.org/documents/ncha/NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf Google Scholar
- American Psychiatric Association . ( 2013 ). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. Google Scholar
- Aneshensel, C. S., & Stone, J. D. ( 1982 ). Stress and depression: A test of the buffering model of social support . Archives of General Psychiatry , 39 (12), 1392–1396. Medline , Google Scholar
- Anxiety and Depression Association of America . ( 2019 ). Home page . Retrieved November 29, 2019, from https://adaa.org Google Scholar
- Armbruster, P., Patel, M., Johnson, E., & Weiss, M. ( 2009 ). Active learning and student-centered pedagogy improve student attitudes and performance in introductory biology . CBE—Life Sciences Education , 8 (3), 203–213. Link , Google Scholar
- Ashford, S. J. ( 1996 ). Working with doctoral students: Rhythms of Academic Life: Personal Accounts of Careers in Academia . In Front, P. J.Taylor, M. S. (Eds.), Rhythms of Academic Life: Personal Accounts of Careers in Academia (pp. 153–158). Thousand Oaks, CA: Sage. Google Scholar
- Auchincloss, L. C., Laursen, S. L., Branchaw, J. L., Eagan, K., Graham, M., Hanauer, D. I. , … & Rowland, S. ( 2014 ). Assessment of course-based undergraduate research experiences: A meeting report . CBE—Life Sciences Education , 13 (1), 29–40. Link , Google Scholar
- Barak, M. E. M., Levin, A., Nissly, J. A., & Lane, C. J. ( 2006 ). Why do they leave? Modeling child welfare workers’ turnover intentions . Children and Youth Services Review , 28 (5), 548–577. Google Scholar
- Bauer, K. W., & Bennett, J. S. ( 2003 ). Alumni perceptions used to assess undergraduate research experience . Journal of Higher Education , 74 (2), 210–230. Google Scholar
- Birks, M., & Mills, J. ( 2015 ). Grounded theory: A practical guide . Thousand Oaks, CA: Sage. Google Scholar
- Blatt, S. J., Quinlan, D. M., Chevron, E. S., McDonald, C., & Zuroff, D. ( 1982 ). Dependency and self-criticism: Psychological dimensions of depression . Journal of Consulting and Clinical Psychology , 50 (1), 113. Medline , Google Scholar
- Brown, R. T., Daly, B. P., & Leong, F. T. ( 2009 ). Mentoring in research: A developmental approach . Professional Psychology: Research and Practice , 40 (3), 306. Google Scholar
- Brownell, S. E., Hekmat-Scafe, D. S., Singla, V., Seawell, P. C., Imam, J. F. C., Eddy, S. L. , … & Cyert, M. S. ( 2015 ). A high-enrollment course-based undergraduate research experience improves student conceptions of scientific thinking and ability to interpret data . CBE—Life Sciences Education , 14 (2), ar21. Link , Google Scholar
- Brownell, S. E., & Kloser, M. J. ( 2015 ). Toward a conceptual framework for measuring the effectiveness of course-based undergraduate research experiences in undergraduate biology . Studies in Higher Education , 40 (3), 525–544. Google Scholar
- Byars-Winston, A. M., Branchaw, J., Pfund, C., Leverett, P., & Newton, J. ( 2015 ). Culturally diverse undergraduate researchers’ academic outcomes and perceptions of their research mentoring relationships . International Journal of Science Education , 37 (15), 2533–2554. Medline , Google Scholar
- Cane, D. B., & Gotlib, I. H. ( 1985 ). Depression and the effects of positive and negative feedback on expectations, evaluations, and performance . Cognitive Therapy and Research , 9 (2), 145–160. Google Scholar
- Ceci, S. J., & Williams, W. M. ( 2010 ). Sex differences in math-intensive fields . Current Directions in Psychological Science , 19 (5), 275–279. Medline , Google Scholar
- Center for Collegiate Mental Health . ( 2017 ). Center for Collegiate Mental Health 2017 Annual Report . State College, PA: Penn State Universit. Google Scholar
- Charmaz, K. ( 2006 ). Constructing grounded theory: A practical guide through qualitative research . Thousand Oaks, CA: Sage. Google Scholar
- Chaudoir, S. R., & Fisher, J. D. ( 2010 ). The disclosure processes model: Understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity . Psychological Bulletin , 136 (2), 236. Medline , Google Scholar
- Chaudoir, S. R., & Quinn, D. M. ( 2010 ). Revealing concealable stigmatized identities: The impact of disclosure motivations and positive first-disclosure experiences on fear of disclosure and well-being . Journal of Social Issues , 66 (3), 570–584. Medline , Google Scholar
- Clance, P. R., & Imes, S. A. ( 1978 ). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention . Psychotherapy: Theory, Research & Practice , 15 (3), 241. Google Scholar
- Cooper, K. M., Ashley, M., & Brownell, S. E. ( 2017 ). A bridge to active learning: A summer bridge program helps students maximize their active-learning experiences and the active-learning experiences of others . CBE—Life Sciences Education , 16 (1), ar17. Link , Google Scholar
- Cooper, K. M., Blattman, J. N., Hendrix, T., & Brownell, S. E. ( 2019a ). The impact of broadly relevant novel discoveries on student project ownership in a traditional lab course turned CURE . CBE—Life Sciences Education , 18 (4), ar57. Link , Google Scholar
- Cooper, K. M., & Brownell, S. E. ( 2016 ). Coming out in class: Challenges and benefits of active learning in a biology classroom for LGBTQIA students . CBE—Life Sciences Education , 15 (3), ar37. https://doi.org/10.1187/cbe.16-01-0074 Link , Google Scholar
- Cooper, K. M., Brownell, S. E., & Gormally, C. C. ( 2019b ). Coming out to the class: Identifying factors that influence college biology instructor decisions about whether to reveal their LGBQ identity in class . Journal of Women and Minorities in Science and Engineering , 25 (3). Google Scholar
- Cooper, K. M., Downing, V. R., & Brownell, S. E. ( 2018 ). The influence of active learning practices on student anxiety in large-enrollment college science classrooms . International Journal of STEM Education , 5 (1), 23. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., Akeeh, B., Clark, C. E., Hunter, J. S., Roderick, T. B. , … & Brownell, S. E. ( 2019c ). Factors that predict life sciences student persistence in undergraduate research experiences . PLoS ONE , 14 (8). https://doi.org/10.1371/journal.pone.0220186 Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( 2019d ). Diagnosing differences in what introductory biology students in a fully online and an in-person biology degree program know and do regarding medical school admission . Advances in Physiology Education , 43 (2), 221–232. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( In press ). Depression as a concealable stigmatized identity: What influences whether students conceal or reveal their depression in undergraduate research experiences? International Journal of STEM Education , ( in press ). Google Scholar
- Depression and Biopolar Support Alliance . ( 2019 ). Home page . Retrieved November 28, 2019, from www.dbsalliance.org Google Scholar
- Deroma, V. M., Leach, J. B., & Leverett, J. P. ( 2009 ). The relationship between depression and college academic performance . College Student Journal , 43 (2), 325–335. Google Scholar
- Dweck, C. S. ( 2008 ). Mindset: The new psychology of success . New York, NY: Random House Digital. Google Scholar
- Dyson, R., & Renk, K. ( 2006 ). Freshmen adaptation to university life: Depressive symptoms, stress, and coping . Journal of Clinical Psychology , 62 (10), 1231–1244. Medline , Google Scholar
- Eddy, S. L., Brownell, S. E., & Wenderoth, M. P. ( 2014 ). Gender gaps in achievement and participation in multiple introductory biology classrooms . CBE—Life Sciences Education , 13 (3), 478–492. https://doi.org/10.1187/cbe.13-10-0204 Link , Google Scholar
- Eisenberg, D., Gollust, S. E., Golberstein, E., & Hefner, J. L. ( 2007 ). Prevalence and correlates of depression, anxiety, and suicidality among university students . American Journal of Orthopsychiatry , 77 (4), 534–542. Medline , Google Scholar
- Elliott, R., Sahakian, B. J., Herrod, J. J., Robbins, T. W., & Paykel, E. S. ( 1997 ). Abnormal response to negative feedback in unipolar depression: Evidence for a diagnosis specific impairment . Journal of Neurology, Neurosurgery & Psychiatry , 63 (1), 74–82. Medline , Google Scholar
- Eshel, N., & Roiser, J. P. ( 2010 ). Reward and punishment processing in depression . Biological Psychiatry , 68 (2), 118–124. Medline , Google Scholar
- Estrada, M., Hernandez, P. R., & Schultz, P. W. ( 2018 ). A longitudinal study of how quality mentorship and research experience integrate underrepresented minorities into STEM careers . CBE—Life Sciences Education , 17 (1), ar9. Link , Google Scholar
- Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., & Vanderford, N. L. ( 2018 ). Evidence for a mental health crisis in graduate education . Nature Biotechnology , 36 (3), 282. Medline , Google Scholar
- Everson, H. T., Tobias, S., Hartman, H., & Gourgey, A. ( 1993 ). Test anxiety and the curriculum: The subject matters . Anxiety, Stress, and Coping , 6 (1), 1–8. Google Scholar
- Flaherty, C. ( 2018 ). New study says graduate students’ mental health is a “crisis.” Retrieved November 29, 2019, from www.insidehighered.com/news/2018/03/06/new-study-says-graduate-students-mental-health-crisis Google Scholar
- Forsythe, A., & Johnson, S. ( 2017 ). Thanks, but no-thanks for the feedback . Assessment & Evaluation in Higher Education , 42 (6), 850–859. Google Scholar
- Garlow, S. J., Rosenberg, J., Moore, J. D., Haas, A. P., Koestner, B., Hendin, H., & Nemeroff, C. B. ( 2008 ). Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University . Depression and Anxiety , 25 (6), 482–488. Medline , Google Scholar
- Gelso, C. J., & Lent, R. W. ( 2000 ). Scientific training and scholarly productivity: The person, the training environment, and their interaction . In Brown, S. D.Lent, R. W. (Eds.), Handbook of counseling psychology (pp. 109–139). Hoboken, NJ: John Wiley & Sons Inc. Google Scholar
- Gilbert, P., Baldwin, M. W., Irons, C., Baccus, J. R., & Palmer, M. ( 2006 ). Self-criticism and self-warmth: An imagery study exploring their relation to depression . Journal of Cognitive Psychotherapy , 20 (2), 183. Google Scholar
- Gilbert, P., McEwan, K., Bellew, R., Mills, A., & Gale, C. ( 2009 ). The dark side of competition: How competitive behaviour and striving to avoid inferiority are linked to depression, anxiety, stress and self-harm . Psychology and Psychotherapy: Theory, Research and Practice , 82 (2), 123–136. Medline , Google Scholar
- Gin, L. E., Rowland, A. A., Steinwand, B., Bruno, J., & Corwin, L. A. ( 2018 ). Students who fail to achieve predefined research goals may still experience many positive outcomes as a result of CURE participation . CBE—Life Sciences Education , 17 (4), ar57. Link , Google Scholar
- Glesne, C., & Peshkin, A. ( 1992 ). Becoming qualitative researchers: An introduction . London, England, UK: Longman. Google Scholar
- Grav, S., Hellzèn, O., Romild, U., & Stordal, E. ( 2012 ). Association between social support and depression in the general population: The HUNT study, a cross-sectional survey . Journal of Clinical Nursing , 21 (1–2), 111–120. Medline , Google Scholar
- Guest, G., Bunce, A., & Johnson, L. ( 2006 ). How many interviews are enough? An experiment with data saturation and variability . Field Methods , 18 (1), 59–82. Google Scholar
- Hancock, D. R. ( 2002 ). Influencing graduate students’ classroom achievement, homework habits and motivation to learn with verbal praise . Educational Research , 44 (1), 83–95. Google Scholar
- Hannah, D. R., & Lautsch, B. A. ( 2011 ). Counting in qualitative research: Why to conduct it, when to avoid it, and when to closet it . Journal of Management Inquiry , 20 (1), 14–22. Google Scholar
- Heatherton, T. F., & Wyland, C. L. ( 2003 ). Assessing self-esteem . In Lopez, S. J.Snyder, C. R. (Eds.), Positive psychological assessment: A handbook of models and measures (pp. 219–233). Washington, DC: American Psychological Association. https://doi.org/10.1037/10612-014 . Google Scholar
- Henderlong, J., & Lepper, M. R. ( 2002 ). The effects of praise on children’s intrinsic motivation: A review and synthesis . Psychological Bulletin , 128 (5), 774. Medline , Google Scholar
- Henry, M. A., Shorter, S., Charkoudian, L., Heemstra, J. M., & Corwin, L. A. ( 2019 ). FAIL is not a four-letter word: A theoretical framework for exploring undergraduate students’ approaches to academic challenge and responses to failure in STEM learning environments . CBE—Life Sciences Education , 18 (1), ar11. Link , Google Scholar
- Hernandez, P. R., Woodcock, A., Estrada, M., & Schultz, P. W. ( 2018 ). Undergraduate research experiences broaden diversity in the scientific workforce . BioScience , 68 (3), 204–211. Google Scholar
- Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Applying the stress process model to stress–burnout and stress–depression relationships in biomedical doctoral students: A cross-sectional pilot study . CBE—Life Sciences Education , 18 (4), ar51. Link , Google Scholar
- Howell, E., & McFeeters, J. ( 2008 ). Children’s mental health care: Differences by race/ethnicity in urban/rural areas . Journal of Health Care for the Poor and Underserved , 19 (1), 237–247. Medline , Google Scholar
- Hysenbegasi, A., Hass, S. L., & Rowland, C. R. ( 2005 ). The impact of depression on the academic productivity of university students . Journal of Mental Health Policy and Economics , 8 (3), 145. Medline , Google Scholar
- Ibrahim, A. K., Kelly, S. J., Adams, C. E., & Glazebrook, C. ( 2013 ). A systematic review of studies of depression prevalence in university students . Journal of Psychiatric Research , 47 (3), 391–400. Medline , Google Scholar
- Intemann, K. ( 2009 ). Why diversity matters: Understanding and applying the diversity component of the National Science Foundation’s broader impacts criterion . Social Epistemology , 23 (3–4), 249–266. Google Scholar
- Ishiyama, J. ( 2002 ). Does early participation in undergraduate research benefit social science and humanities students? College Student Journal , 36 (3), 381–387. Google Scholar
- Jenkins, S. R., Belanger, A., Connally, M. L., Boals, A., & Durón, K. M. ( 2013 ). First-generation undergraduate students’ social support, depression, and life satisfaction . Journal of College Counseling , 16 (2), 129–142. Google Scholar
- Jobst, A., Sabass, L., Palagyi, A., Bauriedl-Schmidt, C., Mauer, M. C., Sarubin, N. , … & Zill, P. ( 2015 ). Effects of social exclusion on emotions and oxytocin and cortisol levels in patients with chronic depression . Journal of Psychiatric Research , 60 , 170–177. Medline , Google Scholar
- Jones, K. P., & King, E. B. ( 2014 ). Managing concealable stigmas at work: A review and multilevel model . Journal of Management , 40 (5), 1466–1494. Google Scholar
- Jones, M. T., Barlow, A. E., & Villarejo, M. ( 2010 ). Importance of undergraduate research for minority persistence and achievement in biology . Journal of Higher Education , 81 (1), 82–115. Google Scholar
- Jones, N. P., Papadakis, A. A., Hogan, C. M., & Strauman, T. J. ( 2009 ). Over and over again: Rumination, reflection, and promotion goal failure and their interactive effects on depressive symptoms . Behaviour Research and Therapy , 47 (3), 254–259. Medline , Google Scholar
- Judd, L. L., Paulus, M. J., Schettler, P. J., Akiskal, H. S., Endicott, J., Leon, A. C. , … & Keller, M. B. ( 2000 ). Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? American Journal of Psychiatry , 157 (9), 1501–1504. Medline , Google Scholar
- Kahn, J. H., & Garrison, A. M. ( 2009 ). Emotional self-disclosure and emotional avoidance: Relations with symptoms of depression and anxiety . Journal of Counseling Psychology , 56 (4), 573. Google Scholar
- Kataoka, S. H., Zhang, L., & Wells, K. B. ( 2002 ). Unmet need for mental health care among US children: Variation by ethnicity and insurance status . American Journal of Psychiatry , 159 (9), 1548–1555. Medline , Google Scholar
- Kreger, D. W. ( 1995 ). Self-esteem, stress, and depression among graduate students . Psychological Reports , 76 (1), 345–346. Medline , Google Scholar
- Krumpal, I. ( 2013 ). Determinants of social desirability bias in sensitive surveys: A literature review . Quality & Quantity , 47 (4), 2025–2047. Google Scholar
- Landis, J. R., & Koch, G. G. ( 1977 ). An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers . Biometrics , 33 (2), 363–374. Medline , Google Scholar
- Laursen, S., Hunter, A.-B., Seymour, E., Thiry, H., & Melton, G. ( 2010 ). Undergraduate research in the sciences: Engaging students in real science . Hoboken, NJ: Wiley. Google Scholar
- Limeri, L. B., Asif, M. Z., Bridges, B. H., Esparza, D., Tuma, T. T., Sanders, D. , … & Maltese, A. V. ( 2019 ). “Where’s my mentor?” Characterizing negative mentoring experiences in undergraduate life science research . CBE—Life Sciences Education , 18 (4), ar61. Link , Google Scholar
- Link, B. G., & Phelan, J. C. ( 2001 ). Conceptualizing stigma . Annual Review of Sociology , 27 (1), 363–385. Google Scholar
- Luyten, P., Sabbe, B., Blatt, S. J., Meganck, S., Jansen, B., De Grave, C. , … & Corveleyn, J. ( 2007 ). Dependency and self-criticism: Relationship with major depressive disorder, severity of depression, and clinical presentation . Depression and Anxiety , 24 (8), 586–596. Medline , Google Scholar
- Mabrouk, P. A., & Peters, K. ( 2000 ). Student perspectives on undergraduate research (UR) experiences in chemistry and biology . CUR Quarterly , 21 (1), 25–33. Google Scholar
- Maxwell, J. A. ( 2010 ). Using numbers in qualitative research . Qualitative Inquiry , 16 (6), 475–482. Google Scholar
- Mongrain, M., & Blackburn, S. ( 2005 ). Cognitive vulnerability, lifetime risk, and the recurrence of major depression in graduate students . Cognitive Therapy and Research , 29 (6), 747–768. Google Scholar
- Nagy, G. A., Fang, C. M., Hish, A. J., Kelly, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Burnout and mental health problems in biomedical doctoral students . CBE—Life Sciences Education , 18 (2), ar27. Link , Google Scholar
- National Academies of Sciences, Engineering, and Medicine (NASEM) . ( 2017 ). Undergraduate research experiences for STEM students: Successes, challenges, and opportunities . Washington, DC: National Academies Press. https://doi.org/10.17226/24622 Google Scholar
- NASEM . ( 2019 ). The science of effective mentorship in STEMM . Washington, DC: National Academies Press. Retrieved November 29, 2019, from www.nap.edu/download/25568 Google Scholar
- Osborne, J., & Collins, S. ( 2001 ). Pupils’ views of the role and value of the science curriculum: A focus-group study . International Journal of Science Education , 23 (5), 441–467. https://doi.org/10.1080/09500690010006518 Google Scholar
- Porter, S. R., & Whitcomb, M. E. ( 2005 ). Non-response in student surveys: The role of demographics, engagement and personality . Research in Higher Education , 46 (2), 127–152. Google Scholar
- President’s Council of Advisors on Science and Technology . ( 2012 ). Engage to excel: Producing one million additional college graduates with degrees in science, Technology, Engineering, and mathematics . Washington, DC: U.S. Government Office of Science and Technology. Google Scholar
- Prunuske, A. J., Wilson, J., Walls, M., & Clarke, B. ( 2013 ). Experiences of mentors training underrepresented undergraduates in the research laboratory . CBE—Life Sciences Education , 12 (3), 403–409. Link , Google Scholar
- Quinn, D. M., & Earnshaw, V. A. ( 2011 ). Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes . Social Issues and Policy Review , 5 (1), 160–190. Google Scholar
- Rauckhorst, W. H., Czaja, J. A., & Baxter Magolda, M. ( 2001 ). Measuring the impact of the undergraduate research experience on student intellectual development . Snowbird, UT: Project Kaleidoscope Summer Institute. Google Scholar
- Saldaña, J. ( 2015 ). The coding manual for qualitative researchers . Thousand Oaks, CA: Sage. Google Scholar
- Santiago, C. D., Kaltman, S., & Miranda, J. ( 2013 ). Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of Clinical Psychology , 69 (2), 115–126. Medline , Google Scholar
- Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., & Haro, J. M. ( 2015 ). The association between social relationships and depression: A systematic review . Journal of Affective Disorders , 175 , 53–65. Medline , Google Scholar
- Schleider, J., & Weisz, J. ( 2018 ). A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial . Journal of Child Psychology and Psychiatry , 59 (2), 160–170. Medline , Google Scholar
- Seymour, E., & Hewitt, N. M. ( 1997 ). Talking about leaving: Why undergraduates leave the sciences . Westview Press. Google Scholar
- Seymour, E., & Hunter, A.-B. ( 2019 ). Talking about leaving revisited . New York, NY: Springer. Google Scholar
- Seymour, E., Hunter, A.-B., Laursen, S. L., & DeAntoni, T. ( 2004 ). Establishing the benefits of research experiences for undergraduates in the sciences: First findings from a three-year study . Science Education , 88 (4), 493–534. Google Scholar
- Smith, D. T., Mouzon, D. M., & Elliott, M. ( 2018 ). Reviewing the assumptions about men’s mental health: An exploration of the gender binary . American Journal of Men’s Health , 12 (1), 78–89. Medline , Google Scholar
- Sorkness, C. A., Pfund, C., Ofili, E. O., Okuyemi, K. S., Vishwanatha, J. K., Zavala, M. E. , … & Deveci, A. ( 2017 ). A new approach to mentoring for research careers: The National Research Mentoring Network . BMC Proceedings , 11 , 22. Medline , Google Scholar
- Sowislo, J. F., & Orth, U. ( 2013 ). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies . Psychological Bulletin , 139 (1), 213. Medline , Google Scholar
- Steger, M. F. ( 2013 ). Experiencing meaning in life: Optimal functioning at the nexus of well-being, psychopathology, and spirituality . In Wong, P. T. P. (Ed.), The human quest for meaning (pp. 211–230). England, UK: Routledge. Google Scholar
- Strenta, A. C., Elliott, R., Adair, R., Matier, M., & Scott, J. ( 1994 ). Choosing and leaving science in highly selective institutions . Research in Higher Education , 35 (5), 513–547. Google Scholar
- Text Depression Hotline . ( 2019 ). Crisis text line . Retrieved November 29, 2019, from www.crisistextline.org/depression Google Scholar
- Thiry, H., & Laursen, S. L. ( 2011 ). The role of student–advisor interactions in apprenticing undergraduate researchers into a scientific community of practice . Journal of Science Education and Technology , 20 (6), 771–784. Google Scholar
- Thompson, J. J., Conaway, E., & Dolan, E. L. ( 2016 ). Undergraduate students’ development of social, cultural, and human capital in a networked research experience . Cultural Studies of Science Education , 11 (4), 959–990. Google Scholar
- Trenor, J. M., Miller, M. K., & Gipson, K. G. ( 2011 ). Utilization of a think-aloud protocol to cognitively validate a survey instrument identifying social capital resources of engineering undergraduates . 118th American Society for Engineering Education Annual Conference and Exposition, Vancouver, BC, Canada . Google Scholar
- Turner, R. J., & Noh, S. ( 1988 ). Physical disability and depression: A longitudinal analysis . Journal of Health and Social Behavior , 29 (1), 23–37. Medline , Google Scholar
- Watson, D., & Friend, R. ( 1969 ). Measurement of social-evaluative anxiety . Journal of Consulting and Clinical Psychology , 33 (4), 448. Medline , Google Scholar
- Weeks, J. W., Heimberg, R. G., Fresco, D. M., Hart, T. A., Turk, C. L., Schneier, F. R., & Liebowitz, M. R. ( 2005 ). Empirical validation and psychometric evaluation of the Brief Fear of Negative Evaluation Scale in patients with social anxiety disorder . Psychological Assessment , 17 (2), 179. Medline , Google Scholar
- World Health Organization . ( 2018 ). Depression . Retrieved November 29, 2019, from www.who.int/news-room/fact-sheets/detail/depression Google Scholar
- Wyatt, T., & Oswalt, S. B. ( 2013 ). Comparing mental health issues among undergraduate and graduate students . American Journal of Health Education , 44 (2), 96–107. Google Scholar
- Carly A. Busch ,
- Tala Araghi ,
- Jingyi He ,
- Katelyn M. Cooper , and
- Colin Harrison, Monitoring Editor
- Emma C. Goodwin ,
- Danielle Pais ,
- Logan E. Gin , and
- Derek Braun, Monitoring Editor
- Baylee A. Edwards ,
- Chloe Bowen ,
- M. Elizabeth Barnes , and
- Tati Russo-Tait, Monitoring Editor
- Sara E. Grineski ,
- Danielle X. Morales , and
- Timothy W. Collins
- Carly A. Busch , and
- Tasneem F. Mohammed ,
- Erika M. Nadile ,
- Madison L. Witt ,
- Cindy Vargas ,
- Missy Tran ,
- Joseph Gazing Wolf ,
- Danielle Brister , and
- Sehoya Cotner, Monitoring Editor
- Katelyn M. Cooper ,
- Sarah L. Eddy , and
- Coping behavior versus coping style: characterizing a measure of coping in undergraduate STEM contexts 14 February 2022 | International Journal of STEM Education, Vol. 9, No. 1
- Lisa A. Corwin ,
- Michael E. Ramsey ,
- Eric A. Vance ,
- Elizabeth Woolner ,
- Stevie Maiden ,
- Nina Gustafson and
- Joseph A. Harsh
- Erin Shortlidge, Monitoring Editor
- K. Supriya ,
- Brian Sato, Monitoring Editor
- Logan E. Gin ,
- Clark Coffman, Monitoring Editor
- Nicholas J. Wiesenthal , and
- Maryrose Weatherton and
- Elisabeth E. Schussler
- Erika Offerdahl, Monitoring Editor
- Eight Recommendations to Promote Effective Study Habits for Biology Students Enrolled in Online Courses Journal of Microbiology & Biology Education, Vol. 23, No. 1
- Fostering professional development through undergraduate research: supporting faculty mentors and student researchers 30 March 2022 | Mentoring & Tutoring: Partnership in Learning, Vol. 30, No. 2
- Jeffrey Maloy ,
- Monika B. Kwapisz , and
- Bryce E. Hughes
- Terrell Morton, Monitoring Editor
- Anxiety and depression among US college students engaging in undergraduate research during the COVID-19 pandemic 14 December 2021 | Journal of American College Health, Vol. 9
- Danielle Brister ,
- Sara E. Brownell ,
- Chade T. Claiborne ,
- Curtis Lunt ,
- Kobe M. Walker ,
- Tamiru D. Warkina ,
- Yi Zheng , and
- Rebecca Price, Monitoring Editor
- Dominant Learning Styles of Interior Design Students in Generation Z 26 July 2021 | Journal of Interior Design, Vol. 46, No. 4
- Linking Emotional Intelligence, Physical Activity and Aggression among Undergraduates 26 November 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 23
- Advancing undergraduate synthetic biology education: insights from a Canadian iGEM student perspective Canadian Journal of Microbiology, Vol. 67, No. 10
- Frank A. Guerrero ,
- Sara E. Brownell , and
- Jennifer Momsen, Monitoring Editor
- Nicholas J. Wiesenthal ,
- Isabella Ferreira , and
- Grant Ean Gardner, Monitoring Editor
- Carolyn E. Clark ,
- Deanna B. Elliott ,
- Travis B. Roderick ,
- Rachel A. Scott ,
- Denisse Arellano ,
- Diana Ramirez ,
- Kimberly Velarde ,
- Allyson Aeschliman ,
- Sarah T. Avalle ,
- Jessica Berkheimer ,
- Rachel Campos ,
- Michael Gerbasi ,
- Sophia Hughes ,
- Julie A. Roberts ,
- Quinn M. White ,
- Ehren Wittekind ,
- Rachelle Spell, Monitoring Editor
- Christine Pfund ,
- Janet L. Branchaw ,
- Melissa McDaniels ,
- Angela Byars-Winston ,
- Steven P. Lee ,, and
- Bruce Birren
- Vladimir Anokhin ,
- MacKenzie J. Gray ,
- Daniel E. Zajic ,
- Jason E. Podrabsky , and
- Erin E. Shortlidge
- Depression as a concealable stigmatized identity: what influences whether students conceal or reveal their depression in undergraduate research experiences? 4 June 2020 | International Journal of STEM Education, Vol. 7, No. 1
Submitted: 4 November 2019 Revised: 24 February 2020 Accepted: 6 March 2020
© 2020 K. M. Cooper, L. E. Gin, et al. CBE—Life Sciences Education © 2020 The American Society for Cell Biology. This article is distributed by The American Society for Cell Biology under license from the author(s). It is available to the public under an Attribution–Noncommercial–Share Alike 3.0 Unported Creative Commons License (http://creativecommons.org/licenses/by-nc-sa/3.0).
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Effect of exercise for...
Effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials
Linked editorial.
Exercise for the treatment of depression
- Related content
- Peer review
- Michael Noetel , senior lecturer 1 ,
- Taren Sanders , senior research fellow 2 ,
- Daniel Gallardo-Gómez , doctoral student 3 ,
- Paul Taylor , deputy head of school 4 ,
- Borja del Pozo Cruz , associate professor 5 6 ,
- Daniel van den Hoek , senior lecturer 7 ,
- Jordan J Smith , senior lecturer 8 ,
- John Mahoney , senior lecturer 9 ,
- Jemima Spathis , senior lecturer 9 ,
- Mark Moresi , lecturer 4 ,
- Rebecca Pagano , senior lecturer 10 ,
- Lisa Pagano , postdoctoral fellow 11 ,
- Roberta Vasconcellos , doctoral student 2 ,
- Hugh Arnott , masters student 2 ,
- Benjamin Varley , doctoral student 12 ,
- Philip Parker , pro vice chancellor research 13 ,
- Stuart Biddle , professor 14 15 ,
- Chris Lonsdale , deputy provost 13
- 1 School of Psychology, University of Queensland, St Lucia, QLD 4072, Australia
- 2 Institute for Positive Psychology and Education, Australian Catholic University, North Sydney, NSW, Australia
- 3 Department of Physical Education and Sport, University of Seville, Seville, Spain
- 4 School of Health and Behavioural Sciences, Australian Catholic University, Strathfield, NSW, Australia
- 5 Department of Clinical Biomechanics and Sports Science, University of Southern Denmark, Odense, Denmark
- 6 Biomedical Research and Innovation Institute of Cádiz (INiBICA) Research Unit, University of Cádiz, Spain
- 7 School of Health and Behavioural Sciences, University of the Sunshine Coast, Petrie, QLD, Australia
- 8 School of Education, University of Newcastle, Callaghan, NSW, Australia
- 9 School of Health and Behavioural Sciences, Australian Catholic University, Banyo, QLD, Australia
- 10 School of Education, Australian Catholic University, Strathfield, NSW, Australia
- 11 Australian Institute of Health Innovation, Macquarie University, Macquarie Park, NSW, Australia
- 12 Children’s Hospital Westmead Clinical School, University of Sydney, Westmead, NSW, Australia
- 13 Australian Catholic University, North Sydney, NSW, Australia
- 14 Centre for Health Research, University of Southern Queensland, Springfield, QLD, Australia
- 15 Faculty of Sport and Health Science, University of Jyvaskyla, Jyvaskyla, Finland
- Correspondence to: M Noetel m.noetel{at}uq.edu.au (or @mnoetel on Twitter)
- Accepted 15 January 2024
Objective To identify the optimal dose and modality of exercise for treating major depressive disorder, compared with psychotherapy, antidepressants, and control conditions.
Design Systematic review and network meta-analysis.
Methods Screening, data extraction, coding, and risk of bias assessment were performed independently and in duplicate. Bayesian arm based, multilevel network meta-analyses were performed for the primary analyses. Quality of the evidence for each arm was graded using the confidence in network meta-analysis (CINeMA) online tool.
Data sources Cochrane Library, Medline, Embase, SPORTDiscus, and PsycINFO databases.
Eligibility criteria for selecting studies Any randomised trial with exercise arms for participants meeting clinical cut-offs for major depression.
Results 218 unique studies with a total of 495 arms and 14 170 participants were included. Compared with active controls (eg, usual care, placebo tablet), moderate reductions in depression were found for walking or jogging (n=1210, κ=51, Hedges’ g −0.62, 95% credible interval −0.80 to −0.45), yoga (n=1047, κ=33, g −0.55, −0.73 to −0.36), strength training (n=643, κ=22, g −0.49, −0.69 to −0.29), mixed aerobic exercises (n=1286, κ=51, g −0.43, −0.61 to −0.24), and tai chi or qigong (n=343, κ=12, g −0.42, −0.65 to −0.21). The effects of exercise were proportional to the intensity prescribed. Strength training and yoga appeared to be the most acceptable modalities. Results appeared robust to publication bias, but only one study met the Cochrane criteria for low risk of bias. As a result, confidence in accordance with CINeMA was low for walking or jogging and very low for other treatments.
Conclusions Exercise is an effective treatment for depression, with walking or jogging, yoga, and strength training more effective than other exercises, particularly when intense. Yoga and strength training were well tolerated compared with other treatments. Exercise appeared equally effective for people with and without comorbidities and with different baseline levels of depression. To mitigate expectancy effects, future studies could aim to blind participants and staff. These forms of exercise could be considered alongside psychotherapy and antidepressants as core treatments for depression.
Systematic review registration PROSPERO CRD42018118040.

- Download figure
- Open in new tab
- Download powerpoint
Introduction
Major depressive disorder is a leading cause of disability worldwide 1 and has been found to lower life satisfaction more than debt, divorce, and diabetes 2 and to exacerbate comorbidities, including heart disease, 3 anxiety, 4 and cancer. 5 Although people with major depressive disorder often respond well to drug treatments and psychotherapy, 6 7 many are resistant to treatment. 8 In addition, access to treatment for many people with depression is limited, with only 51% treatment coverage for high income countries and 20% for low and lower-middle income countries. 9 More evidence based treatments are therefore needed.
Exercise may be an effective complement or alternative to drugs and psychotherapy. 10 11 12 13 14 In addition to mental health benefits, exercise also improves a range of physical and cognitive outcomes. 15 16 17 Clinical practice guidelines in the US, UK, and Australia recommend physical activity as part of treatment for depression. 18 19 20 21 But these guidelines do not provide clear, consistent recommendations about dose or exercise modality. British guidelines recommend group exercise programmes 20 21 and offer general recommendations to increase any form of physical activity, 21 the American Psychiatric Association recommends any dose of aerobic exercise or resistance training, 20 and Australian and New Zealand guidelines suggest a combination of strength and vigorous aerobic exercises, with at least two or three bouts weekly. 19
Authors of guidelines may find it hard to provide consistent recommendations on the basis of existing mainly pairwise meta-analyses—that is, assessing a specific modality versus a specific comparator in a distinct group of participants. 12 13 22 These meta-analyses have come under scrutiny for pooling heterogeneous treatments and heterogenous comparisons leading to ambiguous effect estimates. 23 Reviews also face the opposite problem, excluding exercise treatments such as yoga, tai chi, and qigong because grouping them with strength training might be inappropriate. 23 Overviews of reviews have tried to deal with this problem by combining pairwise meta-analyses on individual treatments. A recent such overview found no differences between exercise modalities. 13 Comparing effect sizes between different pairwise meta-analyses can also lead to confusion because of differences in analytical methods used between meta-analysis, such as choice of a control to use as the referent. Network meta-analyses are a better way to precisely quantify differences between interventions as they simultaneously model the direct and indirect comparisons between interventions. 24
Network meta-analyses have been used to compare different types of psychotherapy and pharmacotherapy for depression. 6 25 26 For exercise, they have shown that dose and modality influence outcomes for cognition, 16 back pain, 15 and blood pressure. 17 Two network meta-analyses explored the effects of exercise on depression: one among older adults 27 and the other for mental health conditions. 28 Because of the inclusion criteria and search strategies used, these reviews might have been under-powered to explore moderators such as dose and modality (κ=15 and κ=71, respectively). To resolve conflicting findings in existing reviews, we comprehensively searched randomised trials on exercise for depression to ensure our review was adequately powered to identify the optimal dose and modality of exercise. For example, a large overview of reviews found effects on depression to be proportional to intensity, with vigorous exercise appearing to be better, 13 but a later meta-analysis found no such effects. 22 We explored whether recommendations differ based on participants’ sex, age, and baseline level of depression.
Given the challenges presented by behaviour change in people with depression, 29 we also identified autonomy support or behaviour change techniques that might improve the effects of intervention. 30 Behaviour change techniques such as self-monitoring and action planning have been shown to influence the effects of physical activity interventions in adults (>18 years) 31 and older adults (>60 years) 32 with differing effectiveness of techniques in different populations. We therefore tested whether any intervention components from the behaviour change technique taxonomy were associated with higher or lower intervention effects. 30 Other meta-analyses found that physical activity interventions work better when they provide people with autonomy (eg, choices, invitational language). 33 Autonomy is not well captured in the taxonomy for behaviour change technique. We therefore tested whether effects were stronger in studies that provided more autonomy support to patients. Finally, to understand the mechanism of intervention effects, such as self-confidence, affect, and physical fitness, we collated all studies that conducted formal mediation analyses.
Our findings are presented according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses-Network Meta-analyses (PRISMA-NMA) guidelines (see supplementary file, section S0; all supplementary files, data, and code are also available at https://osf.io/nzw6u/ ). 34 We amended our analysis strategy after registering our review; these changes were to better align with new norms established by the Cochrane Comparing Multiple Interventions Methods Group. 35 These norms were introduced between the publication of our protocol and the preparation of this manuscript. The largest change was using the confidence in network meta-analysis (CINeMA) 35 online tool instead of the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) guidelines and adopting methods to facilitate assessments—for example, instead of using an omnibus test for all treatments, we assessed publication bias for each treatment compared with active controls. We also modelled acceptability (through dropout rate), which was not predefined but was adopted in response to a reviewer’s comment.
Eligibility criteria
To be eligible for inclusion, studies had to be randomised controlled trials that included exercise as a treatment for depression and included participants who met the criteria for major depressive disorder, either clinician diagnosed or identified through participant self-report as exceeding established clinical thresholds (eg, scored >13 on the Beck depression inventory-II). 36 Studies could meet these criteria when all the participants had depression or when the study reported depression outcomes for a subgroup of participants with depression at the start of the study.
We defined exercise as “planned, structured and repetitive bodily movement done to improve or maintain one or more components of physical fitness.” 37 Unlike recent reviews, 12 22 we included studies with more than one exercise arm and multifaceted interventions (eg, health and exercise counselling) as long as they contained a substantial exercise component. These trials could be included because network meta-analysis methods allows for the grouping of those interventions into homogenous nodes. Unlike the most recent Cochrane review, 12 we also included participants with physical comorbidities such as arthritis and participants with postpartum depression because the Diagnostic Statistical Manual of Mental Health Disorders , fifth edition, removed the postpartum onset specifier after that analysis was completed. 23 Studies were excluded if interventions were shorter than one week, depression was not reported as an outcome, and data were insufficient to calculate an effect size for each arm. Any comparison condition was included, allowing us to quantify the effects against established treatments (eg, selective serotonin reuptake inhibitors (SSRIs), cognitive behavioural therapy), active control conditions (usual care, placebo tablet, stretching, educational control, and social support), or waitlist control conditions. Published and unpublished studies were included, with no restrictions on language applied.
Information sources
We adapted the search strategy from the most recent Cochrane review, 12 adding keywords for yoga, tai chi, and qigong, as they met our definition for exercise. We conducted database searches, without filters or date limits, in The Cochrane Library via CENTRAL, SPORTDiscus via Embase, and Medline, Embase, and PsycINFO via Ovid. Searches of the databases were conducted on 17 December 2018 and 7 August 2020 and last updated on 3 June 2023 (see supplementary file section S1 for full search strategies). We assessed full texts of all included studies from two systematic reviews of exercise for depression. 12 22
Study selection and data collection
To select studies, we removed duplicate records in Covidence 38 and then screened each title and abstract independently and in duplicate. Conflicts were resolved through discussion or consultation with a third reviewer. The same methods were used for full text screening.
We used the Extraction 1.0 randomised controlled trial data extraction forms in Covidence. 38 Data were extracted independently and in duplicate, with conflicts resolved through discussion with a third reviewer.
For each study, we extracted a description of the interventions, including frequency, intensity, and type and time of each exercise intervention. Using the Compendium of Physical Activities, 39 we calculated the energy expenditure dose of exercise for each arm as metabolic equivalents of task (METs) min/week. Two authors evaluated each exercise intervention using the Behaviour Change Taxonomy version 1 30 for behaviour change techniques explicitly described in each exercise arm. They also rated the level of autonomy offered to participants, on a scale from 1 (no choice) to 10 (full autonomy). We also extracted descriptions of the other arms within the randomised trials, including other treatment or control conditions; participants’ age, sex, comorbidities, and baseline severity of depressive symptoms; and each trial’s location and whether or not the trial was funded.
Risk of bias in individual studies
We used Cochrane’s risk of bias tool for randomised controlled trials. 40 Risk of bias was rated independently and in duplicate, with conflicts resolved through discussion with a third reviewer.
Summary measures and synthesis
For main and moderation analyses, we used bayesian arm based multilevel network meta-analysis models. 41 All network meta-analytical approaches allow users to assess the effects of treatments against a range of comparisons. The bayesian arm based models allowed us to also assess the influence of hypothesised moderators, such as intensity, dose, age, and sex. Many network meta-analyses use contrast based methods, comparing post-test scores between study arms. 41 Arm based meta-analyses instead describe the population-averaged absolute effect size for each treatment arm (ie, each arm’s change score). 41 As a result, the summary measure we used was the standardised mean change from baseline, calculated as standardised mean differences with correction for small studies (Hedges’ g). In keeping with the norms from the included studies, effect sizes describe treatment effects on depression, such that larger negative numbers represent stronger effects on symptoms. Using National Institute for Health and Care Excellence guidelines, 42 we standardised change scores for different depression scales (eg, Beck depression inventory, Hamilton depression rating scale) using an internal reference standard for each scale (for each scale, the average of pooled standard deviations at baseline) reported in our meta-analysis. Because depression scores generally show regression to the mean, even in control conditions, we present effect sizes as improvements beyond active control conditions. This convention makes our results comparable to existing, contrast based meta-analyses.
Active control conditions (usual care, placebo tablet, stretching, educational control, and social support) were grouped to increase power for moderation analyses, for parsimony in the network graph, and because they all showed similar arm based pooled effect sizes (Hedges’ g between −0.93 and −1.00 for all, with no statistically significant differences). We separated waitlist control from these active control conditions because it typically shows poorer effects in treatment for depression. 43
Bayesian meta-analyses were conducted in R 44 using the brms package. 45 We preregistered informative priors based on the distributional parameters of our meta-analytical model. 46 We nested effects within arms to manage dependency between multiple effect sizes from the same participants. 46 For example, if one study reported two self-reported measures of depression, or reported both self-report and clinician rated depression, we nested these effect sizes within the arm to account for both pieces of information while controlling for dependency between effects. 46 Finally, we compared absolute effect sizes against a standardised minimum clinically important difference, 0.5 standard deviations of the change score. 47 From our data, this corresponded to a large change in before and after scores (Hedges’ g −1.16), a moderate change compared with waitlist control (g −0.55), or a small benefit when compared with active controls (g −0.20). For credibility assessments comparing exercise modalities, we used the netmeta package 48 and CINeMA. 49 We also used netmeta to model acceptability, comparing the odds ratio for drop-out rate in each arm.
Additional analyses
All prespecified moderation and sensitivity analyses were performed. We moderated for participant characteristics, including participants’ sex, age, baseline symptom severity, and presence or absence of comorbidities; duration of the intervention (weeks); weekly dose of the intervention; duration between completion of treatment and measurement, to test robustness to remission (in response to a reviewer’s suggestion); amount of autonomy provided in the exercise prescription; and presence of each behaviour change technique. As preregistered, we moderated for behaviour change techniques in three ways: through meta-regression, including all behaviour change techniques simultaneously for primary analysis; including one behaviour change technique at a time (using 99% credible intervals to somewhat control for multiple comparisons) in exploratory analyses; and through meta-analytical classification and regression trees (metaCART), which allowed for interactions between moderating variables (eg, if goal setting combined with feedback had synergistic effects). 50 We conducted sensitivity analyses for risk of bias, assessing whether studies with low versus unclear or high risk of bias on each domain showed statistically significant differences in effect sizes.
Credibility assessment
To assess the credibility of each comparison against active control, we used CINeMA. 35 49 This online tool was designed by the Cochrane Comparing Multiple Interventions Methods Group as an adaptation of GRADE for network meta-analyses. 35 In line with recommended guidelines, for each comparison we made judgements for within study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence. Similar to GRADE, we considered the evidence for comparisons to show high confidence then downgraded on the basis of concerns in each domain, as follows:
Within study bias —Comparisons were downgraded when most of the studies providing direct evidence for comparisons were unclear or high risk.
Reporting bias —Publication bias was assessed in three ways. For each comparison with at least 10 studies 51 we created funnel plots, including estimates of effect sizes after removing studies with statistically significant findings (ie, worst case estimates) 52 ; calculated an s value, representing how strong publication bias would need to be to nullify meta-analytical effects 52 ; and conducted a multilevel Egger’s regression test, indicative of small study bias. Given these tests are not recommended for comparisons with fewer than 10 studies, 51 those comparisons were considered to show “some concerns.”
Indirectness — Our primary population of interest was adults with major depression. Studies were considered to be indirect if they focused on one sex only (>90% male or female), participants with comorbidities (eg, heart disease), adolescents and young adults (14-20 years), or older adults (>60 years). We flagged these studies as showing some concerns if one of these factors was present, and as “major concerns” if two of these factors were present. Evidence from comparisons was classified as some concerns or major concerns using majority rating for studies directly informing the comparison.
Imprecision — As per CINeMA, we used the clinically important difference of Hedges’ g=0.2 to ascribe a zone of equivalence, where differences were not considered clinically significant (−0.2<g<0.2). Studies were flagged as some concerns for imprecision if the bounds of the 95% credible interval extended across that zone, and they were flagged as major concerns if the bounds extended to the other side of the zone of equivalence (such that effects could be harmful).
Heterogeneity — Prediction intervals account for heterogeneity differently from credible intervals. 35 As a result, CINeMA accounts for heterogeneity by assessing whether the prediction intervals and the credible intervals lead to different conclusions about clinical significance (using the same zone of equivalence from imprecision). Comparisons are flagged as some concerns if the prediction interval crosses into, or out of, the zone of equivalence once (eg, from helpful to no meaningful effect), and as major concerns if the prediction interval crosses the zone twice (eg, from helpful and harmful).
Incoherence — Incoherence assesses whether the network meta-analysis provides similar estimates when using direct evidence (eg, randomised controlled trials on strength training versus SSRI) compared with indirect evidence (eg, randomised controlled trials where either strength training or SSRI uses waitlist control). Incoherence provides some evidence the network may violate the assumption of transitivity: that the only systematic difference between arms is the treatment, not other confounders. We assessed incoherence using two methods: Firstly, a global design-by-treatment interaction to assess for incoherence across the whole network, 35 49 and, secondly, separating indirect and direct evidence (SIDE method) for each comparison through netsplitting to see whether differences between those effect estimates were statistically significant. We flagged comparisons as some concerns if either no direct comparisons were available or direct and indirect evidence gave different conclusions about clinical significance (eg, from helpful to no meaningful effect, as per imprecision and heterogeneity). Again, we classified comparisons as major concerns if the direct and indirect evidence changed the sign of the effect or changed both limits of the credible interval. 35 49
Patient and public involvement
We discussed the aims and design of this study with members of the public, including those who had experienced depression. Several of our authors have experienced major depressive episodes, but beyond that we did not include patients in the conduct of this review.
Study selection
The PRISMA flow diagram outlines the study selection process ( fig 1 ). We used two previous reviews to identify potentially eligible studies for inclusion. 12 22 Database searches identified 18 658 possible studies. After 5505 duplicates had been removed, two reviewers independently screened 13 115 titles and abstracts. After screening, two reviewers independently reviewed 1738 full text articles. Supplementary file section S2 shows the consensus reasons for exclusion. A total of 218 unique studies described in 246 reports were included, totalling 495 arms and 14 170 participants. Supplementary file section S3 lists the references and characteristics of the included studies.

Flow of studies through review
Network geometry
As preregistered, we removed nodes with fewer than 100 participants. Using this filter, most interventions contained comparisons with at least four other nodes in the network geometry ( fig 2 ). The results of the global test design-by-treatment interaction model were not statistically significant, supporting the assumption of transitivity (χ 2 =94.92, df=75, P=0.06). When net-splitting was used on all possible combinations in the network, for two out of the 120 comparisons we found statistically significant incoherence between direct and indirect evidence (SSRI v waitlist control; cognitive behavioural therapy v tai chi or qigong). Overall, we found little statistical evidence that the model violated the assumption of transitivity. Qualitative differences were, however, found for participant characteristics between different arms (see supplementary file, section S4). For example, some interventions appeared to be prescribed more frequently among people with severe depression (eg, 7/16 studies using SSRIs) compared with other interventions (eg, 1/15 studies using aerobic exercise combined with therapy). Similarly, some interventions appeared more likely to be prescribed for older adults (eg, mean age, tai chi=59 v dance=31) or women (eg, per cent female: dance=88% v cycling=53%). Given that plausible mechanisms exist for these systematic differences (eg, the popularity of tai chi among older adults), 53 there are reasons to believe that allocation to treatment arms would be less than perfectly random. We have factored these biases in our certainty estimates through indirectness ratings.

Network geometry indicating number of participants in each arm (size of points) and number of comparisons between arms (thickness of lines). SSRI=selective serotonin reuptake inhibitor
Risk of bias within studies
Supplementary file section S5 provides the risk of bias ratings for each study. Few studies explicitly blinded participants and staff ( fig 3 ). As a result, overall risk of bias for most studies was unclear or high, and effect sizes could include expectancy effects, among other biases. However, sensitivity analyses suggested that effect sizes were not influenced by any risk of bias criteria owing to wide credible intervals (see supplementary file, section S6). Nevertheless, certainty ratings for all treatments arms were downgraded owing to high risk of bias in the studies informing the comparison.

Risk of bias summary plot showing percentage of included studies judged to be low, unclear, or high risk across Cochrane criteria for randomised trials
Synthesis of results
Supplementary file section S7 presents a forest plot of Hedges’ g values for each study. Figure 4 shows the predicted effects of each treatment compared with active controls. Compared with active controls, large reductions in depression were found for dance (n=107, κ=5, Hedges’ g −0.96, 95% credible interval −1.36 to −0.56) and moderate reductions for walking or jogging (n=1210, κ=51, g −0.63, −0.80 to −0.46), yoga (n=1047, κ=33, g=−0.55, −0.73 to −0.36), strength training (n=643, κ=22, g=−0.49, −0.69 to −0.29), mixed aerobic exercises (n=1286, κ=51, g=−0.43, −0.61 to −0.25), and tai chi or qigong (n=343, κ=12, g=−0.42, −0.65 to −0.21). Moderate, clinically meaningful effects were also present when exercise was combined with SSRIs (n=268, κ=11, g=−0.55, −0.86 to −0.23) or aerobic exercise was combined with psychotherapy (n=404, κ=15, g=−0.54, −0.76 to −0.32). All these treatments were significantly stronger than the standardised minimum clinically important difference compared with active control (g=−0.20), equating to an absolute g value of −1.16. Dance, exercise combined with SSRIs, and walking or jogging were the treatments most likely to perform best when modelling the surface under the cumulative ranking curve ( fig 4 ). For acceptability, the odds of participants dropping out of the study were lower for strength training (n=247, direct evidence κ=6, odds ratio 0.55, 95% credible interval 0.31 to 0.99) and yoga (n=264, κ=5, 0.57, 0.35 to 0.94) than for active control. The rate of dropouts was not significantly different from active control in any other arms (see supplementary file, section S8).

Predicted effects of different exercise modalities on major depression compared with active controls (eg, usual care), with 95% credible intervals. The estimate of effects for the active control condition was a before and after change of Hedges’ g of −0.95 (95% credible interval −1.10 to −0.79), n=3554, κ =113. Colour represents SUCRA from most likely to be helpful (dark purple) to least likely to be helpful (light purple). SSRI=selective serotonin reuptake inhibitor; SUCRA=surface under the cumulative ranking curve
Consistent with other meta-analyses, effects were moderate for cognitive behaviour therapy alone (n=712, κ=20, g=−0.55, −0.75 to −0.37) and small for SSRIs (n=432, κ=16, g=−0.26, −0.50 to −0.01) compared with active controls ( fig 4 ). These estimates are comparable to those of reviews that focused directly on psychotherapy (g=−0.67, −0.79 to −0.56) 7 or pharmacotherapy (g=−0.30, –0.34 to −0.26). 25 However, our review was not designed to find all studies of these treatments, so these estimates should not usurp these directly focused systematic reviews.
Despite the large number of studies in the network, confidence in the effects were low ( fig 5 ). This was largely due to the high within study bias described in the risk of bias summary plot. Reporting bias was also difficult to robustly assess because direct comparison with active control was often only provided in fewer than 10 studies. Many studies focused on one sex only, older adults, or those with comorbidities, so most arms had some concerns about indirect comparisons. Credible intervals were seldom wide enough to change decision making, so concerns about imprecision were few. Heterogeneity did plausibly change some conclusions around clinical significance. Few studies showed problematic incoherence, meaning direct and indirect evidence usually agreed. Overall, walking or jogging had low confidence, with other modalities being very low.

Summary table for credibility assessment using confidence in network meta-analysis (CINeMA). SSRI=selective serotonin reuptake inhibitor
Moderation by participant characteristics
The optimal modality appeared to be moderated by age and sex. Compared with models that only included exercise modality (R 2 =0.65), R 2 was higher for models that included interactions with sex (R 2 =0.71) and age (R 2 =0.69). R 2 showed no substantial increase for models including baseline depression (R 2 =0.67) or comorbidities (R 2 =0.66; see supplementary file, section S9).
Effects appeared larger for women than men for strength training and cycling ( fig 6 ). Effects appeared to be larger for men than women when prescribing yoga, tai chi, and aerobic exercise alongside psychotherapy. Yoga and aerobic exercise alongside psychotherapy appeared more effective for older participants than younger people ( fig 7 ). Strength training appeared more effective when prescribed to younger participants than older participants. Some estimates were associated with substantial uncertainty because some modalities were not well studied in some groups (eg, tai chi for younger adults), and mean age of the sample was only available for 71% of the studies.

Effects of interventions versus active control on depression (lower is better) by sex. Shading represents 95% credible intervals

Effects of interventions versus active control on depression (lower is better) by age. Shading represents 95% credible intervals
Moderation by intervention and design characteristics
Across modalities, a clear dose-response curve was observed for intensity of exercise prescribed ( fig 8 ). Although light physical activity (eg, walking, hatha yoga) still provided clinically meaningful effects (g=−0.58, −0.82 to −0.33), expected effects were stronger for vigorous exercise (eg, running, interval training; g=−0.74, −1.10 to −0.38). This finding did not appear to be due to increased weekly energy expenditure: credible intervals were wide, which meant that the dose-response curve for METs/min prescribed per week was unclear (see supplementary file, section S10). Weak evidence suggested that shorter interventions (eg, 10 weeks: g=−0.53, −0.71 to −0.35) worked somewhat better than longer ones (eg, 30 weeks: g=−0.37, −0.79 to 0.03), with wide credible intervals again indicating high uncertainty (see supplementary file, section S11). We also moderated for the lag between the end of treatment and the measurement of the outcome. We found no indication that participants were likely to relapse within the measurement period (see supplementary file, section S12); effects remained steady when measured either directly after the intervention (g=−0.59, −0.80 to −0.39) or up to six months later (g=−0.63, −0.87 to −0.40).

Dose-response curve for intensity (METs) across exercise modalities compared with active control. METs=metabolic equivalents of task
Supplementary file section S13 provides coding for the behaviour change techniques and autonomy for each exercise arm. None of the behaviour change techniques significantly moderated overall effects. Contrary to expectations, studies describing a level of participant autonomy (ie, choice over frequency, intensity, type, or time) tended to show weaker effects (g=−0.28, −0.78 to 0.23) than those that did not (g=−0.75, −1.17 to −0.33; see supplementary file, section S14). This effect was consistent whether or not we included studies that used physical activity counselling (usually high autonomy).
Use of group exercise appeared to moderate the effects: although the overall effects were similar for individual (g=−1.10, −1.57 to −0.64) and group exercise (g=−1.16, −1.61 to −0.73), some interventions were better delivered in groups (yoga) and some were better delivered individually (strength training, mixed aerobic exercise; see supplementary file, section S15).
As preregistered, we tested whether study funding moderated effects. Models that included whether a study was funded did explain more variance (R 2 =0.70) compared with models that included treatment alone (R 2 =0.65). Funded studies showed stronger effects (g=−1.01, −1.19 to −0.82) than unfunded studies (g=−0.77, −1.09 to −0.46). We also moderated for the type of measure (self-report v clinician report). This did not explain a substantial amount of variance in the outcome (R 2 =0.66).
Sensitivity analyses
Evidence of publication bias was found for overall estimates of exercise on depression compared with active controls, although not enough to nullify effects. The multilevel Egger’s test showed significance (F 1,98 =23.93, P<0.001). Funnel plots showed asymmetry, but the result of pooled effects remained statistically significant when only including non-significant studies (see supplementary file, section S16). No amount of publication bias would be sufficient to shrink effects to zero (s value=not possible). To reduce effects below clinical significance thresholds, studies with statistically significant results would need to be reported 58 times more frequently than studies with non-significant results.
Qualitative synthesis of mediation effects
Only a few of the studies used explicit mediation analyses to test hypothesised mechanisms of action. 54 55 56 57 58 59 One study found that both aerobic exercise and yoga led to decreased depression because participants ruminated less. 54 The study found that the effects of aerobic exercise (but not yoga) were mediated by increased acceptance. 54 “Perceived hassles” and awareness were not statistically significant mediators. 54 Another study found that the effects of yoga were mediated by increased self-compassion, but not rumination, self-criticism, tolerance of uncertainty, body awareness, body trust, mindfulness, and attentional biases. 55 One study found that the effects from an aerobic exercise intervention were not mediated by long term physical activity, but instead were mediated by exercise specific affect regulation (eg, self-control for exercise). 57 Another study found that neither exercise self-efficacy nor depression coping self-efficacy mediated effects of aerobic exercise. 56 Effects of aerobic exercise were not mediated by the N2 amplitude from electroencephalography, hypothesised as a neuro-correlate of cognitive control deficits. 58 Increased physical activity did not appear to mediate the effects of physical activity counselling on depression. 59 It is difficult to infer strong conclusions about mechanisms on the basis of this small number of studies with low power.
Summary of evidence
In this systematic review and meta-analysis of randomised controlled trials, exercise showed moderate effects on depression compared with active controls, either alone or in combination with other established treatments such as cognitive behaviour therapy. In isolation, the most effective exercise modalities were walking or jogging, yoga, strength training, and dancing. Although walking or jogging were effective for both men and women, strength training was more effective for women, and yoga or qigong was more effective for men. Yoga was somewhat more effective among older adults, and strength training was more effective among younger people. The benefits from exercise tended to be proportional to the intensity prescribed, with vigorous activity being better. Benefits were equally effective for different weekly doses, for people with different comorbidities, or for different baseline levels of depression. Although confidence in many of the results was low, treatment guidelines may be overly conservative by conditionally recommending exercise as complementary or alternative treatment for patients in whom psychotherapy or pharmacotherapy is either ineffective or unacceptable. 60 Instead, guidelines for depression ought to include prescriptions for exercise and consider adapting the modality to participants’ characteristics and recommending more vigorous intensity exercises.
Our review did not uncover clear causal mechanisms, but the trends in the data are useful for generating hypotheses. It is unlikely that any single causal mechanism explains all the findings in the review. Instead, we hypothesise that a combination of social interaction, 61 mindfulness or experiential acceptance, 62 increased self-efficacy, 33 immersion in green spaces, 63 neurobiological mechanisms, 64 and acute positive affect 65 combine to generate outcomes. Meta-analyses have found each of these factors to be associated with decreases in depressive symptoms, but no single treatment covers all mechanisms. Some may more directly promote mindfulness (eg, yoga), be more social (eg, group exercise), be conducted in green spaces (eg, walking), provide a more positive affect (eg, “runner’s high”’), or be more conducive to acute adaptations that may increase self-efficacy (eg, strength). 66 Exercise modalities such as running may satisfy many of the mechanisms, but they are unlikely to directly promote the mindful self-awareness provided by yoga and qigong. Both these forms of exercise are often practised in groups with explicit mindfulness but seldom have fast and objective feedback loops that improve self-efficacy. Adequately powered studies testing multiple mediators may help to focus more on understanding why exercise helps depression and less on whether exercise helps. We argue that understanding these mechanisms of action is important for personalising prescriptions and better understanding effective treatments.
Our review included more studies than many existing reviews on exercise for depression. 13 22 27 28 As a result, we were able to combine the strengths of various approaches to exercise and to make more nuanced and precise conclusions. For example, even taking conservative estimates (ie, the least favourable end of the credible interval), practitioners can expect patients to experience clinically significant effects from walking, running, yoga, qigong, strength training, and mixed aerobic exercise. Because we simultaneously assessed more than 200 studies, credible intervals were narrower than those in most existing meta-analyses. 13 We were also able to explore non-linear relationships between outcomes and moderators, such as frequency, intensity, and time. These analyses supported some existing findings—for example, our study and the study by Heissel et al 22 found that shorter interventions had stronger effects, at least for six months; our study and the study by Singh et al 13 both found that effects were stronger with vigorous intensity exercise compared with light and moderate exercise. However, most existing reviews found various treatment modalities to be equally effective. 13 27 In our review, some types of exercise had stronger effect sizes than others. We attribute this to the study level data available in a network meta-analysis compared with an overview of reviews 24 and higher power compared with meta-analyses with smaller numbers of included studies. 22 28 Overviews of reviews have the ability to more easily cover a wider range of participants, interventions, and outcomes, but also risk double counting randomised trials that are included in separate meta-analyses. They often include heterogeneous studies without having as much control over moderation analyses (eg, Singh et al included studies covering both prevention and treatment 13 ). Some of those reviews grouped interventions such as yoga with heterogeneous interventions such as stretching and qigong. 13 This practise of combining different interventions makes it harder to interpret meta-analytical estimates. We used methods that enabled us to separately analyse the effects of these treatment modalities. In so doing, we found that these interventions do have different effects, with yoga being an intervention with strong effects and stretching being better described as an active control condition. Network meta-analyses revealed the same phenomenon with psychotherapy: researchers once concluded there was a dodo bird verdict, whereby “everybody has won, and all must have prizes,” 67 until network meta-analyses showed some interventions were robustly more effective than others. 6 26
Predictors of acceptability and outcomes
We found evidence to suggest good acceptability of yoga and strength training; although the measurement of study drop-out is an imperfect proxy of adherence. Participants may complete the study without doing any exercise or may continue exercising and drop out of the study for other reasons. Nevertheless, these are useful data when considering adherence.
Behaviour change techniques, which are designed to increase adherence, did not meaningfully moderate the effect sizes from exercise. This may be due to several factors. It may be that the modality explains most of the variance between effects, such that behaviour change techniques (eg, presence or absence of feedback) did not provide a meaningful contribution. Many forms of exercise potentially contain therapeutic benefits beyond just energy expenditure. These characteristics of a modality may be more influential than coexisting behaviour change techniques. Alternatively, researchers may have used behaviour change techniques such as feedback or goal setting without explicitly reporting them in the study methods. Given the inherent challenges of behaviour change among people with depression, 29 and the difficulty in forecasting which strategies are likely to be effective, 68 we see the identification of effective techniques as important.
We did find that autonomy, as provided in the methods of included studies, predicted effects, but in the opposite direction to our hypotheses: more autonomy was associated with weaker effects. Physical activity counselling, which usually provides a great deal of patient autonomy, was among the lowest effect sizes in our meta-analysis. Higher autonomy judgements were associated with weaker outcomes regardless of whether physical activity counselling was included in the model. One explanation for these data is that people with depression benefit from the clear direction and accountability of a standardised prescription. When provided with more freedom, the low self-efficacy that is symptomatic of depression may stop patients from setting an appropriate level of challenge (eg, they may be less likely to choose vigorous exercise). Alternatively, participants were likely autonomous when self-selecting into trials with exercise modalities they enjoyed, or those that fit their social circumstances. After choosing something value aligned, autonomy within the trial may not have helpful. Either way, data should be interpreted with caution. Our judgement of the autonomy provided in the methods may not reflect how much autonomy support patients actually felt. The patient’s perceived autonomy is likely determined by a range of factors not described in the methods (eg, the social environment created by those delivering the programme, or their social identity), so other studies that rely on patient reports of the motivational climate are likely to be more reliable. 33 Our findings reiterate the importance of considering these patient reports in future research of exercise for depression.
Our findings suggest that practitioners could advocate for most patients to engage in exercise. Those patients may benefit from guidance on intensity (ie, vigorous) and types of exercise that appear to work well (eg, walking, running, mixed aerobic exercise, strength training, yoga, tai chi, qigong) and be well tolerated (eg, strength training and yoga). If social determinants permit, 66 engaging in group exercise or structured programmes could provide support and guidance to achieve better outcomes. Health services may consider offering these programmes as an alternative or adjuvant treatment for major depression. Specifically, although the confidence in the evidence for exercise is less strong than for cognitive behavioural therapy, the effect sizes seem comparable, so it may be an alternative for patients who prefer not to engage in psychotherapy. Previous reviews on those with mild-moderate depression have found similar effects for exercise or SSRIs, or the two combined. 13 14 In contrast, we found some forms of exercise to have stronger effects than SSRIs alone. Our findings are likely related to the larger power in our review (n=14 170) compared with previous reviews (eg, n=2551), 14 and our ability to better account for heterogeneity in exercise prescriptions. Exercise may therefore be considered a viable alternative to drug treatment. We also found evidence that exercise increases the effects of SSRIs, so offering exercise may act as an adjuvant for those already taking drugs. We agree with consensus statements that professionals should still account for patients’ values, preferences, and constraints, ensuring there is shared decision making around what best suits the patient. 66 Our review provides data to help inform that decision.
Strengths, limitations, and future directions
Based on our findings, dance appears to be a promising treatment for depression, with large effects found compared with other interventions in our review. But the small number of studies, low number of participants, and biases in the study designs prohibits us from recommending dance more strongly. Given most research for the intervention has been in young women (88% female participants, mean age 31 years), it is also important for future research to assess the generalisability of the effects to different populations, using robust experimental designs.
The studies we found may be subject to a range of experimental biases. In particular, researchers seldom blinded participants or staff delivering the intervention to the study’s hypotheses. Blinding for exercise interventions may be harder than for drugs 23 ; however, future studies could attempt to blind participants and staff to the study’s hypotheses to avoid expectancy effects. 69 Some of our ratings are for studies published before the proliferation of reporting checklists, so the ratings might be too critical. 23 For example, before CONSORT, few authors explicitly described how they generated a random sequence. 23 Therefore, our risk of bias judgements may be too conservative. Similarly, we planned to use the Cochrane risk of bias (RoB) 1 tool 40 so we could use the most recent Cochrane review of exercise and depression 12 to calibrate our raters, and because RoB 2 had not yet been published. 70 Although assessments of bias between the two tools are generally comparable, 71 the RoB 1 tool can be more conservative when assessing open label studies with subjective assessments (eg, unblinded studies with self-reported measures for depression). 71 As a result, future reviews should consider using the latest risk of bias tool, which may lead to different assessments of bias in included studies.
Most of the main findings in this review appear robust to risks from publication bias. Specifically, pooled effect sizes decreased when accounting for risk of publication bias, but no degree of publication bias could nullify effects. We did not exclude grey literature, but our search strategy was not designed to systematically search grey literature or trial registries. Doing so can detect additional eligible studies 72 and reveal the numbers of completed studies that remain unpublished. 73 Future reviews should consider more systematic searches for this kind of literature to better quantify and mitigate risk of publication bias.
Similarly, our review was able to integrate evidence that directly compared exercise with other treatment modalities such as SSRIs or psychotherapy, while also informing estimates using indirect evidence (eg, comparing the relative effects of strength training and SSRIs when tested against a waitlist control). Our review did not, however, include all possible sources of indirect evidence. Network meta-analyses exist that directly focus on psychotherapy 7 and pharmacotherapy, 25 and these combined for treating depression. 6 Those reviews include more than 500 studies comparing psychological or drug interventions with controls. Harmonising the findings of those reviews with ours would provide stronger data on indirect effects.
Our review found some interesting moderators by age and sex, but these were at the study level rather than individual level—that is, rather than being able to determine whether women engaging in a strength intervention benefit more than men, we could only conclude that studies with more women showed larger effects than studies with fewer women. These studies may have been tailored towards women, so effects may be subject to confounding, as both sex and intervention may have changed. The same finding applied to age, where studies on older adults were likely adapted specifically to this age group. These between study differences may explain the heterogeneity in the effects of interventions, and confounding means our moderators for age and sex should be interpreted cautiously. Future reviews should consider individual patient meta-analyses to allow for more detailed assessments of participant level moderators.
Finally, for many modalities, the evidence is derived from small trials (eg, the median number of walking or jogging arms was 17). In addition to reducing risks from bias, primary research may benefit from deconstruction designs or from larger, head-to-head analyses of exercise modalities to better identify what works best for each candidate.
Clinical and policy implications
Our findings support the inclusion of exercise as part of clinical practice guidelines for depression, particularly vigorous intensity exercise. Doing so may help bridge the gap in treatment coverage by increasing the range of first line options for patients and health systems. 9 Globally there has been an attempt to reduce stigma associated with seeking treatment for depression. 74 Exercise may support this effort by providing patients with treatment options that carry less stigma. In low resource or funding constrained settings, group exercise interventions may provide relatively low cost alternatives for patients with depression and for health systems. When possible, ideal treatment may involve individualised care with a multidisciplinary team, where exercise professionals could take responsibility for ensuring the prescription is safe, personalised, challenging, and supported. In addition, those delivering psychotherapy may want to direct some time towards tackling cognitive and behavioural barriers to exercise. Exercise professionals might need to be trained in the management of depression (eg, managing risk) and to be mindful of the scope of their practice while providing support to deal with this major cause of disability.
Conclusions
Depression imposes a considerable global burden. Many exercise modalities appear to be effective treatments, particularly walking or jogging, strength training, and yoga, but confidence in many of the findings was low. We found preliminary data that may help practitioners tailor interventions to individuals (eg, yoga for older men, strength training for younger women). The World Health Organization recommends physical activity for everyone, including those with chronic conditions and disabilities, 75 but not everyone can access treatment easily. Many patients may have physical, psychological, or social barriers to participation. Still, some interventions with few costs, side effects, or pragmatic barriers, such as walking and jogging, are effective across people with different personal characteristics, severity of depression, and comorbidities. Those who are able may want to choose more intense exercise in a structured environment to further decrease depression symptoms. Health systems may want to provide these treatments as alternatives or adjuvants to other established interventions (cognitive behaviour therapy, SSRIs), while also attenuating risks to physical health associated with depression. 3 Therefore, effective exercise modalities could be considered alongside those intervention as core treatments for depression.
What is already known on this topic
Depression is a leading cause of disability, and exercise is often recommended alongside first line treatments such as pharmacotherapy and psychotherapy
Treatment guidelines and previous reviews disagree on how to prescribe exercise to best treat depression
What this study adds
Various exercise modalities are effective (walking, jogging, mixed aerobic exercise, strength training, yoga, tai chi, qigong) and well tolerated (especially strength training and yoga)
Effects appeared proportional to the intensity of exercise prescribed and were stronger for group exercise and interventions with clear prescriptions
Preliminary evidence suggests interactions between types of exercise and patients’ personal characteristics
Ethics statements
Ethical approval.
Not required.
Acknowledgments
We thank Lachlan McKee for his assistance with data extraction. We also thank Juliette Grosvenor and another librarian (anonymous) for their review of our search strategy.
Contributors: MN led the project, drafted the manuscript, and is the guarantor. MN, TS, PT, MM, BdPC, PP, SB, and CL drafted the initial study protocol. MN, TS, PT, BdPC, DvdH, JS, MM, RP, LP, RV, HA, and BV conducted screening, extraction, and risk of bias assessment. MN, JS, and JM coded methods for behaviour change techniques. MN and DGG conducted statistical analyses. PP, SB, and CL provided supervision and mentorship. All authors reviewed and approved the final manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: None received.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Data sharing Data and code for reproducing analyses are available on the Open Science Framework ( https://osf.io/nzw6u/ ).
The lead author (MN) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: We plan to disseminate the findings of this study to lay audiences through mainstream and social media.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- ↵ World Health Organization. Depression. 2020 [cited 2020 Mar 12]. https://www.who.int/news-room/fact-sheets/detail/depression
- ↵ Birkjær M, Kaats M, Rubio A. Wellbeing adjusted life years: A universal metric to quantify the happiness return on investment. Happiness Research Institute; 2020. https://www.happinessresearchinstitute.com/waly-report
- Jacobson NC ,
- Pinquart M ,
- Duberstein PR
- Cuijpers P ,
- Karyotaki E ,
- Vinkers CH ,
- Cipriani A ,
- Furukawa TA
- Strawbridge R ,
- Marwood L ,
- Santomauro D ,
- Collins PY ,
- Generaal E ,
- Lawlor DA ,
- Cooney GM ,
- Recchia F ,
- Miller CT ,
- Mundell NL ,
- Gallardo-Gómez D ,
- Del Pozo-Cruz J ,
- Álvarez-Barbosa F ,
- Alfonso-Rosa RM ,
- Del Pozo Cruz B
- Salcher-Konrad M ,
- ↵ National Collaborating Centre for Mental Health (UK). Depression: The Treatment and Management of Depression in Adults (Updated Edition). Leicester (UK): British Psychological Society; https://www.ncbi.nlm.nih.gov/pubmed/22132433
- Bassett D ,
- ↵ American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. Third Edition. Washington, DC: American Psychiatric Association; 2010. 87 p. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd-1410197717630.pdf
- ↵ NICE. Depression in adults: treatment and management. [cited 2023 Mar 13]. National Institute for Health and Care Excellence; 2022 https://www.nice.org.uk/guidance/ng222/resources
- Heissel A ,
- Brokmeier LL ,
- Ekkekakis P
- ↵ Chaimani A, Caldwell DM, Li T, Higgins JPT, Salanti G. Undertaking network meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane; 2022. www.training.cochrane.org/handbook
- Furukawa TA ,
- Salanti G ,
- Miller KJ ,
- Gonçalves-Bradley DC ,
- Areerob P ,
- Hennessy D ,
- Mesagno C ,
- Glowacki K ,
- Duncan MJ ,
- Gainforth H ,
- Richardson M ,
- Johnston M ,
- Abraham C ,
- Whittington C ,
- McAteer J ,
- French DP ,
- Olander EK ,
- Chisholm A ,
- Mc Sharry J
- Ntoumanis N ,
- Prestwich A ,
- Caldwell DM ,
- Nikolakopoulou A ,
- Higgins JPT ,
- Papakonstantinou T ,
- Caspersen CJ ,
- Powell KE ,
- Christenson GM
- ↵ Veritas Health Innovation. Covidence systematic review software. Melbourne, Australia; 2023. www.covidence.org
- Ainsworth BE ,
- Haskell WL ,
- Herrmann SD ,
- Altman DG ,
- Gøtzsche PC ,
- Cochrane Bias Methods Group ,
- Cochrane Statistical Methods Group
- Hodges JS ,
- ↵ Dias S, Welton NJ, Sutton AJ, Ades AE. NICE DSU technical support document 2: a generalised linear modelling framework for pairwise and network meta-analysis of randomised controlled trials. In: National Institute for Health and Care Excellence (NICE), editor. NICE Decision Support Unit Technical Support Documents. London: Citeseer; 2011. https://www.ncbi.nlm.nih.gov/books/NBK310366/
- Faltinsen E ,
- Todorovac A ,
- Staxen Bruun L ,
- ↵ R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2022. https://www.R-project.org/
- Hengartner MP ,
- Balduzzi S ,
- Dusseldorp E ,
- Sterne JAC ,
- Sutton AJ ,
- Ioannidis JPA ,
- Mathur MB ,
- VanderWeele TJ
- Leung LYL ,
- La Rocque CL ,
- Mazurka R ,
- Stuckless TJR ,
- Harkness KL
- Vollbehr NK ,
- Hoenders HJR ,
- Bartels-Velthuis AA ,
- Zeibig JM ,
- Seiffer B ,
- Ehmann PJ ,
- Alderman BL
- Bombardier CH ,
- Gibbons LE ,
- ↵ American Psychological Association. Clinical practice guideline for the treatment of depression across three age cohorts. American Psychological Association; 2019. https://www.apa.org/depression-guideline/
- van Straten A ,
- Reynolds CF 3rd .
- Johannsen M ,
- Nissen ER ,
- Lundorff M ,
- Coventry PA ,
- Schuch FB ,
- Deslandes AC ,
- Gosmann NP ,
- Fleck MP de A
- Saunders DH ,
- Phillips SM
- Teychenne M ,
- Hunsley J ,
- Di Giulio G
- Milkman KL ,
- Hecksteden A ,
- Savović J ,
- ↵ Richter B, Hemmingsen B. Comparison of the Cochrane risk of bias tool 1 (RoB 1) with the updated Cochrane risk of bias tool 2 (RoB 2). Cochrane; 2021. Report No.: 1. https://community.cochrane.org/sites/default/files/uploads/inline-files/RoB1_2_project_220529_BR%20KK%20formatted.pdf
- Chandler J ,
- Lefebvre C ,
- Glanville J ,
- Briscoe S ,
- Coronado-Montoya S ,
- Kwakkenbos L ,
- Steele RJ ,
- Turner EH ,
- Angermeyer MC ,
- van der Auwera S ,
- Schomerus G
- Al-Ansari SS ,
- Open access
- Published: 16 May 2024
Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress
- Anna Jochmann 1 ,
- Burkhard Gusy 1 ,
- Tino Lesener 1 &
- Christine Wolter 1
BMC Psychology volume 12 , Article number: 276 ( 2024 ) Cite this article
503 Accesses
Metrics details
It is generally assumed that procrastination leads to negative consequences. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. Therefore, the aim of our study was to examine the harmful consequences of procrastination on students’ stress and mental health. We selected the procrastination-health model as our theoretical foundation and tried to evaluate the model’s assumption that trait procrastination leads to (chronic) disease via (chronic) stress in a temporal perspective. We chose depression and anxiety symptoms as indicators for (chronic) disease and hypothesized that procrastination leads to perceived stress over time, that perceived stress leads to depression and anxiety symptoms over time, and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
To examine these relationships properly, we collected longitudinal data from 392 university students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models.
Procrastination did lead to depression and anxiety symptoms over time. However, perceived stress was not a mediator of this effect. Procrastination did not lead to perceived stress over time, nor did perceived stress lead to depression and anxiety symptoms over time.

Conclusions
We could not confirm that trait procrastination leads to (chronic) disease via (chronic) stress, as assumed in the procrastination-health model. Nonetheless, our study demonstrated that procrastination can have a detrimental effect on mental health. Further health outcomes and possible mediators should be explored in future studies.
Peer Review reports
Introduction
“Due tomorrow? Do tomorrow.”, might be said by someone who has a tendency to postpone tasks until the last minute. But can we enjoy today knowing about the unfinished task and tomorrow’s deadline? Or do we feel guilty for postponing a task yet again? Do we get stressed out because we have little time left to complete it? Almost everyone has procrastinated at some point when it came to completing unpleasant tasks, such as mowing the lawn, doing the taxes, or preparing for exams. Some tend to procrastinate more frequently and in all areas of life, while others are less inclined to do so. Procrastination is common across a wide range of nationalities, as well as socioeconomic and educational backgrounds [ 1 ]. Over the last fifteen years, there has been a massive increase in research on procrastination [ 2 ]. Oftentimes, research focuses on better understanding the phenomenon of procrastination and finding out why someone procrastinates in order to be able to intervene. Similarly, the internet is filled with self-help guides that promise a way to overcome procrastination. But why do people seek help for their procrastination? Until now, not much research has been conducted on the negative consequences procrastination could have on health and well-being. Therefore, in the following article we examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship on the basis of the procrastination-health model by Sirois et al. [ 3 ].
Procrastination and its negative consequences
Procrastination can be defined as the tendency to voluntarily and irrationally delay intended activities despite expecting negative consequences as a result of the delay [ 4 , 5 ]. It has been observed in a variety of groups across the lifespan, such as students, teachers, and workers [ 1 ]. For example, some students tend to regularly delay preparing for exams and writing essays until the last minute, even if this results in time pressure or lower grades. Procrastination must be distinguished from strategic delay [ 4 , 6 ]. Delaying a task is considered strategic when other tasks are more important or when more resources are needed before the task can be completed. While strategic delay is viewed as functional and adaptive, procrastination is classified as dysfunctional. Procrastination is predominantly viewed as the result of a self-regulatory failure [ 7 ]. It can be understood as a trait, that is, as a cross-situational and time-stable behavioral disposition [ 8 ]. Thus, it is assumed that procrastinators chronically delay tasks that they experience as unpleasant or difficult [ 9 ]. Approximately 20 to 30% of adults have been found to procrastinate chronically [ 10 , 11 , 12 ]. Prevalence estimates for students are similar [ 13 ]. It is believed that students do not procrastinate more often than other groups. However, it is easy to examine procrastination in students because working on study tasks requires a high degree of self-organization and time management [ 14 ].
It is generally assumed that procrastination leads to negative consequences [ 4 ]. Negative consequences are even part of the definition of procrastination. Research indicates that procrastination is linked to lower academic performance [ 15 ], health impairment (e.g., stress [ 16 ], physical symptoms [ 17 ], depression and anxiety symptoms [ 18 ]), and poor health-related behavior (e.g., heavier alcohol consumption [ 19 ]). However, most studies targeting consequences of procrastination are cross-sectional [ 4 ]. For that reason, it often remains unclear whether an examined outcome is a consequence or an antecedent of procrastination, or whether a reciprocal relationship between procrastination and the examined outcome can be assumed. Additionally, regarding negative consequences of procrastination on health, it is still largely unknown by which mechanisms they are mediated. Uncovering such mediators would be helpful in developing interventions that can prevent negative health consequences of procrastination.
The procrastination-health model
The first and only model that exclusively focuses on the effect of procrastination on health and the mediators of this effect is the procrastination-health model [ 3 , 9 , 17 ]. Sirois [ 9 ] postulates three pathways: An immediate effect of trait procrastination on (chronic) disease and two mediated pathways (see Fig. 1 ).
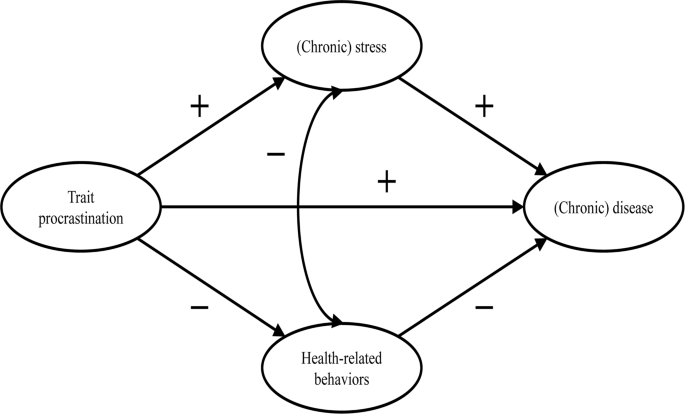
Adopted from the procrastination-health model by Sirois [ 9 ]
The immediate effect is not further explained. Research suggests that procrastination creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 ]. The described feelings could have a detrimental effect on mental health [ 23 , 24 , 25 ].
The first mediated pathway leads from trait procrastination to (chronic) disease via (chronic) stress. Sirois [ 9 ] assumes that procrastination creates stress because procrastinators are constantly aware of the fact that they still have many tasks to complete. Stress activates the hypothalamic-pituitary-adrenocortical (HPA) system, increases autonomic nervous system arousal, and weakens the immune system, which in turn contributes to the development of diseases. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress. She believes that, in the short term, single incidents of procrastination cause acute stress, which leads to acute health problems, such as infections or headaches. In the long term, chronic procrastination, as you would expect with trait procrastination, causes chronic stress, which leads to chronic diseases over time. There is some evidence in support of the stress-related pathway, particularly regarding short-term effects [ 3 , 17 , 26 , 27 , 28 ]. However, as we mentioned above, most of these studies are cross-sectional. Therefore, the causal direction of these effects remains unclear. To our knowledge, long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress have not yet been investigated.
The second mediated pathway leads from trait procrastination to (chronic) disease via poor health-related behavior. According to Sirois [ 9 ], procrastinators form lower intentions to carry out health-promoting behavior or to refrain from health-damaging behavior because they have a low self-efficacy of being able to care for their own health. In addition, they lack the far-sighted view that the effects of health-related behavior only become apparent in the long term. For the same reason, Sirois [ 9 ] believes that there are no short-term, but only long-term effects of procrastination on health mediated by poor health-related behavior. For example, an unhealthy diet leads to diabetes over time. The findings of studies examining the behavioral pathway are inconclusive [ 3 , 17 , 26 , 28 ]. Furthermore, since most of these studies are cross-sectional, they are not suitable for uncovering long-term effects of trait procrastination on (chronic) disease mediated by poor health-related behavior.
In summary, previous research on the two mediated pathways of the procrastination-health model mainly found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. However, only short-term effects have been investigated so far. Moreover, longitudinal studies are needed to be able to assess the causal direction of the relationship between trait procrastination, (chronic) stress, and (chronic) disease. Consequently, our study is the first to examine long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, using a longitudinal design. (Chronic) disease could be measured by a variety of different indicators (e.g., physical symptoms, diabetes, or coronary heart disease). We choose depression and anxiety symptoms as indicators for (chronic) disease because they signal mental health complaints before they manifest as (chronic) diseases. Additionally, depression and anxiety symptoms are two of the most common mental health complaints among students [ 29 , 30 ] and procrastination has been shown to be a significant predictor of depression and anxiety symptoms [ 18 , 31 , 32 , 33 , 34 ]. Until now, the stress-related pathway of the procrastination-health model with depression and anxiety symptoms as the health outcome has only been analyzed in one cross-sectional study that confirmed the predictions of the model [ 35 ].
The aim of our study is to evaluate some of the key assumptions of the procrastination-health model, particularly the relationships between trait procrastination, (chronic) stress, and (chronic) disease over time, surveyed in the following analysis using depression and anxiety symptoms.
In line with the key assumptions of the procrastination-health model, we postulate (see Fig. 2 ):
Procrastination leads to perceived stress over time.
Perceived stress leads to depression and anxiety symptoms over time.
Procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
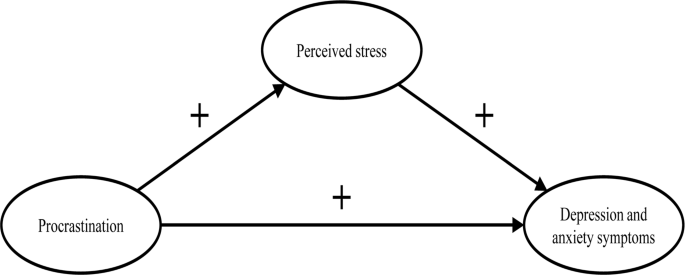
The section of the procrastination-health model we examined
Materials and methods
Our study was part of a health monitoring at a large German university Footnote 1 . Ethical approval for our study was granted by the Ethics Committee of the university’s Department of Education and Psychology. We collected the initial data in 2019. Two occasions followed, each at an interval of six months. In January 2019, we sent out 33,267 invitations to student e-mail addresses. Before beginning the survey, students provided their written informed consent to participate in our study. 3,420 students took part at the first occasion (T1; 10% response rate). Of these, 862 participated at the second (T2) and 392 at the third occasion (T3). In order to test whether dropout was selective, we compared sociodemographic and study specific characteristics (age, gender, academic semester, number of assessments/exams) as well as behavior and health-related variables (procrastination, perceived stress, depression and anxiety symptoms) between the participants of the first wave ( n = 3,420) and those who participated three times ( n = 392). Results from independent-samples t-tests and chi-square analysis showed no significant differences regarding sociodemographic and study specific characteristics (see Additional file 1: Table S1 and S2 ). Regarding behavior and health-related variables, independent-samples t-tests revealed a significant difference in procrastination between the two groups ( t (3,409) = 2.08, p < .05). The mean score of procrastination was lower in the group that participated in all three waves.
The mean age of the longitudinal respondents was 24.1 years ( SD = 5.5 years), the youngest participants were 17 years old, the oldest one was 59 years old. The majority of participants was female (74.0%), 7 participants identified neither as male nor as female (1.8%). The respondents were on average enrolled in the third year of studying ( M = 3.9; SD = 2.3). On average, the students worked about 31.2 h ( SD = 14.1) per week for their studies, and an additional 8.5 h ( SD = 8.5) for their (part-time) jobs. The average income was €851 ( SD = 406), and 4.9% of the students had at least one child. The students were mostly enrolled in philosophy and humanities (16.5%), education and psychology (15.8%), biology, chemistry, and pharmacy (12.5%), political and social sciences (10.6%), veterinary medicine (8.9%), and mathematics and computer science (7.7%).
We only used established and well evaluated instruments for our analyses.
- Procrastination
We adopted the short form of the Procrastination Questionnaire for Students (PFS-4) [ 36 ] to measure procrastination. The PFS-4 assesses procrastination at university as a largely stable behavioral disposition across situations, that is, as a trait. The questionnaire consists of four items (e.g., I put off starting tasks until the last moment.). Each item was rated on a 5-point scale ((almost) never = 1 to (almost) always = 5) for the last two weeks. All items were averaged, with higher scores indicating a greater tendency to procrastinate. The PFS-4 has been proven to be reliable and valid, showing very high correlations with other established trait procrastination scales, for example, with the German short form of the General Procrastination Scale [ 37 , 38 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.90.
Perceived stress
The Heidelberger Stress Index (HEI-STRESS) [ 39 ] is a three-item measure of current perceived stress due to studying as well as in life in general. For the first item, respondents enter a number between 0 (not stressed at all) and 100 (completely stressed) to indicate how stressed their studies have made them feel over the last four weeks. For the second and third item, respondents rate on a 5-point scale how often they feel “stressed and tense” and as how stressful they would describe their life at the moment. We transformed the second and third item to match the range of the first item before we averaged all items into a single score with higher values indicating greater perceived stress. We proved the scale to be one-dimensional and Cronbach’s alpha for our study was 0.86.
Depression and anxiety symptoms
We used the Patient Health Questionnaire-4 (PHQ-4) [ 40 ], a short form of the Patient Health Questionnaire [ 41 ] with four items, to measure depression and anxiety symptoms. The PHQ-4 contains two items from the Patient Health Questionnaire-2 (PHQ-2) [ 42 ] and the Generalized Anxiety Disorder Scale-2 (GAD-2) [ 43 ], respectively. It is a well-established screening scale designed to assess the core criteria of major depressive disorder (PHQ-2) and generalized anxiety disorder (GAD-2) according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). However, it was shown that the GAD-2 is also appropriate for screening other anxiety disorders. According to Kroenke et al. [ 40 ], the PHQ-4 can be used to assess a person’s symptom burden and impairment. We asked the participants to rate how often they have been bothered over the last two weeks by problems, such as “Little interest or pleasure in doing things”. Response options were 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day. Calculated as the sum of the four items, the total scores range from 0 to 12 with higher scores indicating more frequent depression and anxiety symptoms. The total scores can be categorized as none-to-minimal (0–2), mild (3–5), moderate (6–8), and severe (9–12) depression and anxiety symptoms. The PHQ-4 was shown to be reliable and valid [ 40 , 44 , 45 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.86.
Data analysis
To test our hypotheses, we performed structural equation modelling (SEM) using R (Version 4.1.1) with the package lavaan. All items were standardized ( M = 0, SD = 1). Due to the non-normality of some study variables and a sufficiently large sample size of N near to 400 [ 46 ], we used robust maximum likelihood estimation (MLR) for all model estimations. As recommended by Hu and Bentler [ 47 ], we assessed the models’ goodness of fit by chi-square test statistic, root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), Tucker-Lewis index (TLI), and comparative fit index (CFI). A non-significant chi-square indicates good model fit. Since chi-square is sensitive to sample size, we also evaluated fit indices less sensitive to the number of observations. RMSEA and SRMR values of 0.05 or lower as well as TLI and CFI values of 0.97 or higher indicate good model fit. RMSEA values of 0.08 or lower, SRMR values of 0.10 or lower, as well as TLI and CFI values of 0.95 or higher indicate acceptable model fit [ 48 , 49 ]. First, we conducted confirmatory factor analysis for the first occasion, defining three factors that correspond to the measures of procrastination, perceived stress, and depression and anxiety symptoms. Next, we tested for measurements invariance over time and specified the measurement model, before testing our hypotheses.
Measurement invariance over time
To test for measurement invariance over time, we defined one latent variable for each of the three occasions, corresponding to the measures of procrastination, perceived stress, and depression and anxiety symptoms, respectively. As recommended by Geiser and colleagues [ 50 ], the links between indicators and factors (i.e., factor loadings and intercepts) should be equal over measurement occasions; therefore, we added indicator specific factors. A first and least stringent step of testing measurement invariance is configural invariance (M CI ). It was examined whether the included constructs (procrastination, perceived stress, depression and anxiety symptoms) have the same pattern of free and fixed loadings over time. This means that the assignment of the indicators to the three latent factors over time is supported by the underlying data. If configural invariance was supported, restrictions for the next step of testing measurement invariance (metric or weak invariance; M MI ) were added. This means that each item contributes to the latent construct to a similar degree over time. Metric invariance was tested by constraining the factor loadings of the constructs over time. The next step of testing measurement invariance (scalar or strong invariance; M SI ) consisted of checking whether mean differences in the latent construct capture all mean differences in the shared variance of the items. Scalar invariance was tested by constraining the item intercepts over time. The constraints applied in the metric invariance model were retained [ 51 ]. For the last step of testing measurement invariance (residual or strict invariance; M RI ), the residual variables were also set equal over time. If residual invariance is supported, differences in the observed variables can exclusively be attributed to differences in the variances of the latent variables.
We used the Satorra-Bentler chi-square difference test to evaluate the superiority of a more stringent model [ 52 ]. We assumed the model with the largest number of invariance restrictions – which still has an acceptable fit and no substantial deterioration of the chi-square value – to be the final model [ 53 ]. Following previous recommendations, we considered a decrease in CFI of 0.01 and an increase in RMSEA of 0.015 as unacceptable to establish measurement invariance [ 54 ]. If a more stringent model had a significant worse chi-square value, but the model fit was still acceptable and the deterioration in model fit fell within the change criteria recommended for CFI and RMSEA values, we still considered the more stringent model to be superior.
Hypotheses testing
As recommended by Dormann et al. [ 55 ], we applied autoregressive time-lagged panel models to test our hypotheses. In the first step, we specified a model (M 0 ) that only included the stabilities of the three variables (procrastination, perceived stress, depression and anxiety symptoms) over time. In the next step (M 1 ), we added the time-lagged effects from procrastination (T1) to perceived stress (T2) and from procrastination (T2) to perceived stress (T3) as well as from perceived stress (T1) to depression and anxiety symptoms (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3). Additionally, we included a direct path from procrastination (T1) to depression and anxiety symptoms (T3). If this path becomes significant, we can assume a partial mediation [ 55 ]. Otherwise, we can assume a full mediation. We compared these nested models using the Satorra-Bentler chi-square difference test and the Akaike information criterion (AIC). The chi-square difference value should either be non-significant, indicating that the proposed model including our hypotheses (M 1 ) does not have a significant worse model fit than the model including only stabilities (M 0 ), or, if significant, it should be in the direction that M 1 fits the data better than M 0 . Regarding the AIC, M 1 should have a lower value than M 0 .
Table 1 displays the means, standard deviations, internal consistencies (Cronbach’s alpha), and stabilities (correlations) of all study variables. The alpha values of procrastination, perceived stress, and depression and anxiety symptoms are classified as good (> 0.80) [ 56 ]. The correlation matrix of the manifest variables used for the analyses can be found in the Additional file 1: Table S3 .
We observed the highest test-retest reliabilities for procrastination ( r ≥ .74). The test-retest reliabilities for depression and anxiety symptoms ( r ≥ .64) and for perceived stress ( r ≥ .54) were a bit lower (see Table 1 ). The pattern of correlations shows a medium to large but positive relationship between procrastination and depression and anxiety symptoms [ 57 , 58 ]. The association between procrastination and perceived stress was small, the one between perceived stress and depression and anxiety symptoms very large (see Table 1 ).
Confirmatory factor analysis showed an acceptable to good fit (x 2 (41) = 118.618, p < .001; SRMR = 0.042; RMSEA = 0.071; TLI = 0.95; CFI = 0.97). When testing for measurement invariance over time for each construct, the residual invariance models with indicator specific factors provided good fit to the data (M RI ; see Table 2 ), suggesting that differences in the observed variables can exclusively be attributed to differences of the latent variables. We then specified and tested the measurement model of the latent constructs prior to model testing based on the items of procrastination, perceived stress, and depression and anxiety symptoms. The measurement model fitted the data well (M M ; see Table 3 ). All items loaded solidly on their respective factors (0.791 ≤ β ≤ 0.987; p < .001).
To test our hypotheses, we analyzed the two models described in the methods section.
The fit of the stability model (M 0 ) was acceptable (see Table 3 ). Procrastination was stable over time, with stabilities above 0.82. The stabilities of perceived stress as well as depression and anxiety symptoms were somewhat lower, ranging from 0.559 (T1 -> T2) to 0.696 (T2 -> T3) for perceived stress and from 0.713 (T2 -> T3) to 0.770 (T1 -> T2) for depression and anxiety symptoms, respectively.
The autoregressive mediation model (M 1 ) fitted the data significantly better than M 0 . The direct path from procrastination (T1) to depression and anxiety symptoms (T3) was significant (β = 0.16; p < .001), however, none of the mediated paths (from procrastination (T1) to perceived stress (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3)) proved to be substantial. Also, the time-lagged paths from perceived stress (T1) to depression and anxiety symptoms (T2) and from procrastination (T2) to perceived stress (T3) were not substantial either (see Fig. 3 ).
To examine whether the hypothesized effects would occur over a one-year period rather than a six-months period, we specified an additional model with paths from procrastination (T1) to perceived stress (T3) and from perceived stress (T1) to depression and anxiety symptoms (T3), also including the stabilities of the three constructs as in the stability model M 0 . The model showed an acceptable fit (χ 2 (486) = 831.281, p < .001; RMSEA = 0.048; SRMR = 0.091; TLI = 0.95; CFI = 0.95), but neither of the two paths were significant.
Therefore, our hypotheses, that procrastination leads to perceived stress over time (H1) and that perceived stress leads to depression and anxiety symptoms over time (H2) must be rejected. We could only partially confirm our third hypothesis, that procrastination leads to depression and anxiety over time, mediated by perceived stress (H3), since procrastination did lead to depression and anxiety symptoms over time. However, this effect was not mediated by perceived stress.
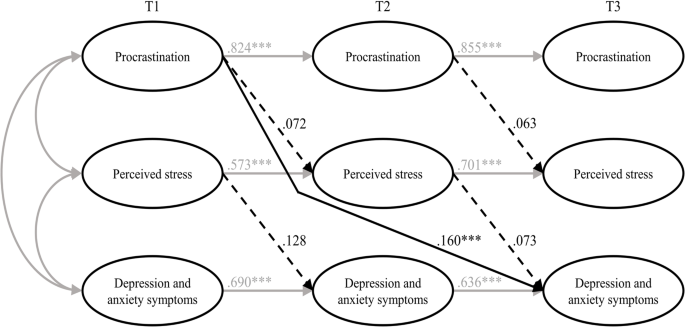
Results of the estimated model including all hypotheses (M 1 ). Note Non-significant paths are dotted. T1 = time 1; T2 = time 2; T3 = time 3. *** p < .001
To sum up, we tried to examine the harmful consequences of procrastination on students’ stress and mental health. Hence, we selected the procrastination-health model by Sirois [ 9 ] as a theoretical foundation and tried to evaluate some of its key assumptions in a temporal perspective. The author assumes that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and postulated, in line with the key assumptions of the procrastination-health model, that procrastination leads to perceived stress over time (H1), that perceived stress leads to depression and anxiety symptoms over time (H2), and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress (H3). To examine these relationships properly, we collected longitudinal data from students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models. Our first and second hypotheses had to be rejected: Procrastination did not lead to perceived stress over time, and perceived stress did not lead to depression and anxiety symptoms over time. However, procrastination did lead to depression and anxiety symptoms over time – which is in line with our third hypothesis – but perceived stress was not a mediator of this effect. Therefore, we could only partially confirm our third hypothesis.
Our results contradict previous studies on the stress-related pathway of the procrastination-health model, which consistently found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. Since most of these studies were cross-sectional, though, the causal direction of these effects remained uncertain. There are two longitudinal studies that confirm the stress-related pathway of the procrastination-health model [ 27 , 28 ], but both studies examined short-term effects (≤ 3 months), whereas we focused on more long-term effects. Therefore, the divergent findings may indicate that there are short-term, but no long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress.
Our results especially raise the question whether trait procrastination leads to (chronic) stress in the long term. Looking at previous longitudinal studies on the effect of procrastination on stress, the following stands out: At shorter study periods of two weeks [ 27 ] and four weeks [ 28 ], the effect of procrastination on stress appears to be present. At longer study periods of seven weeks [ 59 ], three months [ 28 ], six months, and twelve months, as in our study, the effect of procrastination on stress does not appear to be present. There is one longitudinal study in which procrastination was a significant predictor of stress symptoms nine months later [ 34 ]. The results of this study should be interpreted with caution, though, because the outbreak of the COVID-19 pandemic fell within the study period, which could have contributed to increased stress symptoms [ 60 ]. Unfortunately, Johansson et al. [ 34 ] did not report whether average stress symptoms increased during their study. In one of the two studies conducted by Fincham and May [ 59 ], the COVID-19 pandemic outbreak also fell within their seven-week study period. However, they reported that in their study, average stress symptoms did not increase from baseline to follow-up. Taken together, the findings suggest that procrastination can cause acute stress in the short term, for example during times when many tasks need to be completed, such as at the end of a semester, but that procrastination does not lead to chronic stress over time. It seems possible that students are able to recover during the semester from the stress their procrastination caused at the end of the previous semester. Because of their procrastination, they may also have more time to engage in relaxing activities, which could further mitigate the effect of procrastination on stress. Our conclusions are supported by an early and well-known longitudinal study by Tice and Baumeister [ 61 ], which compared procrastinating and non-procrastinating students with regard to their health. They found that procrastinators experienced less stress than their non-procrastinating peers at the beginning of the semester, but more at the end of the semester. Additionally, our conclusions are in line with an interview study in which university students were asked about the consequences of their procrastination [ 62 ]. The students reported that, due to their procrastination, they experience high levels of stress during periods with heavy workloads (e.g., before deadlines or exams). However, the stress does not last, instead, it is relieved immediately after these periods.
Even though research indicates, in line with the assumptions of the procrastination-health model, that stress is a risk factor for physical and mental disorders [ 63 , 64 , 65 , 66 ], perceived stress did not have a significant effect on depression and anxiety symptoms in our study. The relationship between stress and mental health is complex, as people respond to stress in many different ways. While some develop stress-related mental disorders, others experience mild psychological symptoms or no symptoms at all [ 67 ]. This can be explained with the help of vulnerability-stress models. According to vulnerability-stress models, mental illnesses emerge from an interaction of vulnerabilities (e.g., genetic factors, difficult family backgrounds, or weak coping abilities) and stress (e.g., minor or major life events or daily hassles) [ 68 , 69 ]. The stress perceived by the students in our sample may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. However, since we did not assess individual vulnerability and stress factors in our study, these considerations are mere speculation.
In our study, procrastination led to depression and anxiety symptoms over time, which is consistent with the procrastination-health model as well as previous cross-sectional and longitudinal evidence [ 18 , 21 , 31 , 32 , 33 , 34 ]. However, it is still unclear by which mechanisms this effect is mediated, as perceived stress did not prove to be a substantial mediator in our study. One possible mechanism would be that procrastination impairs affective well-being [ 70 ] and creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 , 62 , 71 ], which in turn could lead to depression and anxiety symptoms [ 23 , 24 , 25 ]. Other potential mediators of the relationship between procrastination and depression and anxiety symptoms emerge from the behavioral pathway of the procrastination-health model, suggesting that poor health-related behaviors mediate the effect of trait procrastination on (chronic) disease. Although evidence for this is still scarce, the results of one cross-sectional study, for example, indicate that poor sleep quality might mediate the effect of procrastination on depression and anxiety symptoms [ 35 ].
In summary, we found that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. For the most part, the relationships between procrastination, perceived stress, and depression and anxiety symptoms did not match the relationships between trait procrastination, (chronic) stress, and (chronic) disease as assumed in the procrastination-health model. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. In conclusion, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model.
Limitations and suggestions for future research
In our study, we tried to draw causal conclusions about the harmful consequences of procrastination on students’ stress and mental health. However, since procrastination is a trait that cannot be manipulated experimentally, we have conducted an observational rather than an experimental study, which makes causal inferences more difficult. Nonetheless, a major strength of our study is that we used a longitudinal design with three waves. This made it possible to draw conclusions about the causal direction of the effects, as in hardly any other study targeting consequences of procrastination on health before [ 4 , 28 , 55 ]. Therefore, we strongly recommend using a similar longitudinal design in future studies on the procrastination-health model or on consequences of procrastination on health in general.
We chose a time lag of six months between each of the three measurement occasions to examine long-term effects of procrastination on depression and anxiety symptoms mediated by perceived stress. However, more than six months may be necessary for the hypothesized effects to occur [ 72 ]. The fact that the temporal stabilities of the examined constructs were moderate or high (0.559 ≤ β ≤ 0.854) [ 73 , 74 ] also suggests that the time lags may have been too short. The larger the time lag, the lower the temporal stabilities, as shown for depression and anxiety symptoms, for example [ 75 ]. High temporal stabilities make it more difficult to detect an effect that actually exists [ 76 ]. Nonetheless, Dormann and Griffin [ 77 ] recommend using shorter time lags of less than one year, even with high stabilities, because of other influential factors, such as unmeasured third variables. Therefore, our time lags of six months seem appropriate.
It should be discussed, though, whether it is possible to detect long-term effects of the stress-related pathway of the procrastination-health model within a total study period of one year. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress, but does not address how long it might take for long-term effects to occur or when effects can be considered long-term instead of short-term. The fact that an effect of procrastination on stress is evident at shorter study periods of four weeks or less but in most cases not at longer study periods of seven weeks or more, as we mentioned earlier, could indicate that short-term effects occur within the time frame of one to three months, considering the entire stress-related pathway. Hence, it seems appropriate to assume that we have examined rather long-term effects, given our study period of six and twelve months. Nevertheless, it would be beneficial to use varying study periods in future studies, in order to be able to determine when effects can be considered long-term.
Concerning long-term effects of the stress-related pathway, Sirois [ 9 ] assumes that chronic procrastination causes chronic stress, which leads to chronic diseases over time. The term “chronic stress” refers to prolonged stress episodes associated with permanent tension. The instrument we used captures perceived stress over the last four weeks. Even though the perceived stress of the students in our sample was relatively stable (0.559 ≤ β ≤ 0.696), we do not know how much fluctuation occurred between each of the three occasions. However, there is some evidence suggesting that perceived stress is strongly associated with chronic stress [ 78 ]. Thus, it seems acceptable that we used perceived stress as an indicator for chronic stress in our study. For future studies, we still suggest the use of an instrument that can more accurately reflect chronic stress, for example, the Trier Inventory for Chronic Stress (TICS) [ 79 ].
It is also possible that the occasions were inconveniently chosen, as they all took place in a critical academic period near the end of the semester, just before the examination period began. We chose a similar period in the semester for each occasion for the sake of comparability. However, it is possible that, during this preparation periods, stress levels peaked and procrastinators procrastinated less because they had to catch up after delaying their work. This could have introduced bias to the data. Therefore, in future studies, investigation periods should be chosen that are closer to the beginning or in the middle of a semester.
Furthermore, Sirois [ 9 ] did not really explain her understanding of “chronic disease”. However, it seems clear that physical illnesses, such as diabetes or cardiovascular diseases, are meant. Depression and anxiety symptoms, which we chose as indicators for chronic disease, represent mental health complaints that do not have to be at the level of a major depressive disorder or an anxiety disorder, in terms of their quantity, intensity, or duration [ 40 ]. But they can be viewed as precursors to a major depressive disorder or an anxiety disorder. Therefore, given our study period of one year, it seems appropriate to use depression and anxiety symptoms as indicators for chronic disease. At longer study periods, we would expect these mental health complaints to manifest as mental disorders. Moreover, the procrastination-health model was originally designed to be applied to physical diseases [ 3 ]. Perhaps, the model assumptions are more applicable to physical diseases than to mental disorders. By applying parts of the model to mental health complaints, we have taken an important step towards finding out whether the model is applicable to mental disorders as well. Future studies should examine additional long-term health outcomes, both physical and psychological. This would help to determine whether trait procrastination has varying effects on different diseases over time. Furthermore, we suggest including individual vulnerability and stress factors in future studies in order to be able to analyze the effect of (chronic) stress on (chronic) diseases in a more differentiated way.
Regarding our sample, 3,420 students took part at the first occasion, but only 392 participated three times, which results in a dropout rate of 88.5%. At the second and third occasion, invitation e-mails were only sent to participants who had indicated at the previous occasion that they would be willing to participate in a repeat survey and provided their e-mail address. This is probably one of the main reasons for our high dropout rate. Other reasons could be that the students did not receive any incentives for participating in our study and that some may have graduated between the occasions. Selective dropout analysis revealed that the mean score of procrastination was lower in the group that participated in all three waves ( n = 392) compared to the group that participated in the first wave ( n = 3,420). One reason for this could be that those who have a higher tendency to procrastinate were more likely to procrastinate on filling out our survey at the second and third occasion. The findings of our dropout analysis should be kept in mind when interpreting our results, as lower levels of procrastination may have eliminated an effect on perceived stress or on depression and anxiety symptoms. Additionally, across all age groups in population-representative samples, the student age group reports having the best subjective health [ 80 ]. Therefore, it is possible that they are more resilient to stress and experience less impairment of well-being than other age groups. Hence, we recommend that future studies focus on other age groups as well.
It is generally assumed that procrastination leads to lower academic performance, health impairment, and poor health-related behavior. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. In consequence, the aim of our study was to examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship. We selected the procrastination-health model as a theoretical foundation and used the stress-related pathway of the model, assuming that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and collected longitudinal data from students at three occasions over a one-year period. This allowed us to draw conclusions about the causal direction of the effects, as in hardly any other study examining consequences of procrastination on (mental) health before. Our results indicate that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient on its own, that is, without the presence of other risk factors, to cause depression and anxiety symptoms. Overall, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model. Our study emphasizes the importance of identifying the consequences procrastination can have on health and well-being and determining by which mechanisms they are mediated. Only then will it be possible to develop interventions that can prevent negative health consequences of procrastination. Further health outcomes and possible mediators should be explored in future studies, using a similar longitudinal design.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
University Health Report at Freie Universität Berlin.
Abbreviations
Comparative fit index
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Generalized Anxiety Disorder Scale-2
Heidelberger Stress Index
Hypothalamic-pituitary-adrenocortical
Robust maximum likelihood estimation
Short form of the Procrastination Questionnaire for Students
Patient Health Questionnaire-2
Patient Health Questionnaire-4
Root mean square error of approximation
Structural equation modeling
Standardized root mean square residual
Tucker-Lewis index
Lu D, He Y, Tan Y, Gender S, Status. Cultural differences, Education, family size and procrastination: a sociodemographic Meta-analysis. Front Psychol. 2021. https://doi.org/10.3389/fpsyg.2021.719425 .
Article PubMed PubMed Central Google Scholar
Yan B, Zhang X. What research has been conducted on Procrastination? Evidence from a systematical bibliometric analysis. Front Psychol. 2022. https://doi.org/10.3389/fpsyg.2022.809044 .
Sirois FM, Melia-Gordon ML, Pychyl TA. I’ll look after my health, later: an investigation of procrastination and health. Pers Individ Dif. 2003;35:1167–84. https://doi.org/10.1016/S0191-8869(02)00326-4 .
Article Google Scholar
Grunschel C. Akademische Prokrastination: Eine qualitative und quantitative Untersuchung von Gründen und Konsequenzen [Unpublished doctoral dissertation]: Universität Bielefeld; 2013.
Steel P. The Nature of Procrastination: a Meta-Analytic and Theoretical Review of Quintessential Self-Regulatory failure. Psychol Bull. 2007;133:65–94. https://doi.org/10.1037/0033-2909.133.1.65 .
Article PubMed Google Scholar
Corkin DM, Yu SL, Lindt SF. Comparing active delay and procrastination from a self-regulated learning perspective. Learn Individ Differ. 2011;21:602–6. https://doi.org/10.1016/j.lindif.2011.07.005 .
Balkis M, Duru E. Procrastination, self-regulation failure, academic life satisfaction, and affective well-being: underregulation or misregulation form. Eur J Psychol Educ. 2016;31:439–59. https://doi.org/10.1007/s10212-015-0266-5 .
Schulz N. Procrastination und Planung – Eine Untersuchung zum Einfluss von Aufschiebeverhalten und Depressivität auf unterschiedliche Planungskompetenzen [Doctoral dissertation]: Westfälische Wilhelms-Universität Münster; 2007.
Sirois FM. Procrastination, stress, and Chronic Health conditions: a temporal perspective. In: Sirois FM, Pychyl TA, editors. Procrastination, Health, and well-being. London: Academic; 2016. pp. 67–92. https://doi.org/10.1016/B978-0-12-802862-9.00004-9 .
Harriott J, Ferrari JR. Prevalence of procrastination among samples of adults. Psychol Rep. 1996;78:611–6. https://doi.org/10.2466/pr0.1996.78.2.611 .
Ferrari JR, O’Callaghan J, Newbegin I. Prevalence of Procrastination in the United States, United Kingdom, and Australia: Arousal and Avoidance delays among adults. N Am J Psychol. 2005;7:1–6.
Google Scholar
Ferrari JR, Díaz-Morales JF, O’Callaghan J, Díaz K, Argumedo D. Frequent behavioral Delay tendencies by adults. J Cross Cult Psychol. 2007;38:458–64. https://doi.org/10.1177/0022022107302314 .
Day V, Mensink D, O’Sullivan M. Patterns of academic procrastination. JCRL. 2000;30:120–34. https://doi.org/10.1080/10790195.2000.10850090 .
Höcker A, Engberding M, Rist F, Prokrastination. Ein Manual Zur Behandlung Des Pathologischen Aufschiebens. 2nd ed. Göttingen: Hogrefe; 2017.
Kim KR, Seo EH. The relationship between procrastination and academic performance: a meta-analysis. Pers Individ Dif. 2015;82:26–33. https://doi.org/10.1016/j.paid.2015.02.038 .
Khalid A, Zhang Q, Wang W, Ghaffari AS, Pan F. The relationship between procrastination, perceived stress, saliva alpha-amylase level and parenting styles in Chinese first year medical students. Psychol Res Behav Manag. 2019;12:489–98. https://doi.org/10.2147/PRBM.S207430 .
Sirois FM. I’ll look after my health, later: a replication and extension of the procrastination–health model with community-dwelling adults. Pers Individ Dif. 2007;43:15–26. https://doi.org/10.1016/j.paid.2006.11.003 .
Reinecke L, Meier A, Aufenanger S, Beutel ME, Dreier M, Quiring O, et al. Permanently online and permanently procrastinating? The mediating role of internet use for the effects of trait procrastination on psychological health and well-being. New Media Soc. 2018;20:862–80. https://doi.org/10.1177/1461444816675437 .
Westgate EC, Wormington SV, Oleson KC, Lindgren KP. Productive procrastination: academic procrastination style predicts academic and alcohol outcomes. J Appl Soc Psychol. 2017;47:124–35. https://doi.org/10.1111/jasp.12417 .
Feyzi Behnagh R, Ferrari JR. Exploring 40 years on affective correlates to procrastination: a literature review of situational and dispositional types. Curr Psychol. 2022;41:1097–111. https://doi.org/10.1007/s12144-021-02653-z .
Rahimi S, Hall NC, Sticca F. Understanding academic procrastination: a longitudinal analysis of procrastination and emotions in undergraduate and graduate students. Motiv Emot. 2023. https://doi.org/10.1007/s11031-023-10010-9 .
Patrzek J, Grunschel C, Fries S. Academic procrastination: the perspective of University counsellors. Int J Adv Counselling. 2012;34:185–201. https://doi.org/10.1007/s10447-012-9150-z .
Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J Abnorm Psychol. 1988;97:346–53. https://doi.org/10.1037//0021-843x.97.3.346 .
Cândea D-M, Szentagotai-Tătar A. Shame-proneness, guilt-proneness and anxiety symptoms: a meta-analysis. J Anxiety Disord. 2018;58:78–106. https://doi.org/10.1016/j.janxdis.2018.07.005 .
Young CM, Neighbors C, DiBello AM, Traylor ZK, Tomkins M. Shame and guilt-proneness as mediators of associations between General Causality orientations and depressive symptoms. J Soc Clin Psychol. 2016;35:357–70. https://doi.org/10.1521/jscp.2016.35.5.357 .
Stead R, Shanahan MJ, Neufeld RW. I’ll go to therapy, eventually: Procrastination, stress and mental health. Pers Individ Dif. 2010;49:175–80. https://doi.org/10.1016/j.paid.2010.03.028 .
Dow NM. Procrastination, stress, and sleep in tertiary students [Master’s thesis]: University of Canterbury; 2018.
Sirois FM, Stride CB, Pychyl TA. Procrastination and health: a longitudinal test of the roles of stress and health behaviours. Br J Health Psychol. 2023. https://doi.org/10.1111/bjhp.12658 .
Hofmann F-H, Sperth M, Holm-Hadulla RM. Psychische Belastungen Und Probleme Studierender. Psychotherapeut. 2017;62:395–402. https://doi.org/10.1007/s00278-017-0224-6 .
Liu CH, Stevens C, Wong SHM, Yasui M, Chen JA. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: implications for addressing disparities in service use. Depress Anxiety. 2019;36:8–17. https://doi.org/10.1002/da.22830 .
Aftab S, Klibert J, Holtzman N, Qadeer K, Aftab S. Schemas mediate the Link between Procrastination and Depression: results from the United States and Pakistan. J Rat-Emo Cognitive-Behav Ther. 2017;35:329–45. https://doi.org/10.1007/s10942-017-0263-5 .
Flett AL, Haghbin M, Pychyl TA. Procrastination and depression from a cognitive perspective: an exploration of the associations among Procrastinatory Automatic thoughts, rumination, and Mindfulness. J Rat-Emo Cognitive-Behav Ther. 2016;34:169–86. https://doi.org/10.1007/s10942-016-0235-1 .
Saddler CD, Sacks LA. Multidimensional perfectionism and academic procrastination: relationships with Depression in University students. Psychol Rep. 1993;73:863–71. https://doi.org/10.1177/00332941930733pt123 .
Johansson F, Rozental A, Edlund K, Côté P, Sundberg T, Onell C, et al. Associations between procrastination and subsequent Health outcomes among University students in Sweden. JAMA Netw Open. 2023. https://doi.org/10.1001/jamanetworkopen.2022.49346 .
Gusy B, Jochmann A, Lesener T, Wolter C, Blaszcyk W. „Get it done – schadet Aufschieben Der Gesundheit? Präv Gesundheitsf. 2023;18:228–33. https://doi.org/10.1007/s11553-022-00950-4 .
Glöckner-Rist A, Engberding M, Höcker A, Rist F. Prokrastinationsfragebogen für Studierende (PFS): Zusammenstellung sozialwissenschaftlicher items und Skalen. ZIS - GESIS Leibniz Institute for the Social Sciences; 2014.
Klingsieck KB, Fries S. Allgemeine Prokrastination: Entwicklung Und Validierung Einer Deutschsprachigen Kurzskala Der General Procrastination Scale (Lay, 1986). Diagnostica. 2012;58:182–93. https://doi.org/10.1026/0012-1924/a000060 .
Lay CH. At last, my research article on procrastination. J Res Pers. 1986;20:474–95. https://doi.org/10.1016/0092-6566(86)90127-3 .
Schmidt LI, Obergfell J. Zwangsjacke Bachelor?! Stressempfinden Und Gesundheit Studierender: Der Einfluss Von Anforderungen Und Entscheidungsfreiräumen Bei Bachelor- Und Diplomstudierenden Nach Karaseks Demand-Control-Modell. Saarbrücken: VDM Verlag Dr. Müller; 2011.
Kroenke K, Spitzer RL, Williams JB, Löwe B. An Ultra-brief Screening Scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–21. https://doi.org/10.1016/S0033-3182(09)70864-3 .
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA. 1999;282:1737–44. https://doi.org/10.1001/jama.282.18.1737 .
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item Depression Screener. Med Care. 2003;41:1284–92.
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in Primary Care: prevalence, impairment, Comorbidity, and detection. Ann Intern Med. 2007;146:317–25. https://doi.org/10.7326/0003-4819-146-5-200703060-00004 .
Khubchandani J, Brey R, Kotecki J, Kleinfelder J, Anderson J. The Psychometric properties of PHQ-4 depression and anxiety screening scale among College Students. Arch Psychiatr Nurs. 2016;30:457–62. https://doi.org/10.1016/j.apnu.2016.01.014 .
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disorders. 2010;122:86–95. https://doi.org/10.1016/j.jad.2009.06.019 .
Boomsma A, Hoogland JJ. The robustness of LISREL modeling revisited. In: Cudeck R, Du Toit S, Sörbom D, editors. Structural equation modeling: Present and Future: a festschrift in honor of Karl Jöreskog. Lincolnwood: Scientific Software International; 2001. pp. 139–68.
Hu L, Bentler PM. Fit indices in Covariance structure modeling: sensitivity to Underparameterized Model Misspecification. Psychol Methods. 1998;3:424–53. https://doi.org/10.1037/1082-989X.3.4.424 .
Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: test of significance and descriptive goodness-of-fit measures. MPR. 2003;8:23–74.
Hu L, Bentler PM. Cutoff criteria for fit indexes in Covariance structure analysis: conventional criteria Versus New Alternatives. Struct Equ Model. 1999;6:1–55. https://doi.org/10.1080/10705519909540118 .
Geiser C, Eid M, Nussbeck FW, Courvoisier DS, Cole DA. Analyzing true change in Longitudinal Multitrait-Multimethod studies: application of a Multimethod Change Model to Depression and anxiety in children. Dev Psychol. 2010;46:29–45. https://doi.org/10.1037/a0017888 .
Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90. https://doi.org/10.1016/j.dr.2016.06.004 .
Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–14. https://doi.org/10.1007/BF02296192 .
Geiser C. Datenanalyse Mit Mplus: Eine Anwendungsorientierte Einführung. Wiesbaden: VS Verlag für Sozialwissenschaften; 2010.
Book Google Scholar
Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An empirical evaluation of the use of fixed cutoff points in RMSEA Test Statistic in Structural equation models. Sociol Methods Res. 2008;36:462–94. https://doi.org/10.1177/0049124108314720 .
Dormann C, Zapf D, Perels F. Quer- und Längsschnittstudien in der Arbeitspsychologie [Cross-sectional and longitudinal studies in occupational psychology.]. In: Kleinbeck U, Schmidt K-H,Enzyklopädie der Psychologie [Encyclopedia of psychology]:, Themenbereich D, Serie III, Band 1, Arbeitspsychologie [Subject Area, Series D. III, Volume 1, Industrial Psychology]. Göttingen: Hogrefe Verlag; 2010. pp. 923–1001.
Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994.
Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Pers Indiv Differ. 2016;102:74–8. https://doi.org/10.1016/j.paid.2016.06.069 .
Funder DC, Ozer DJ. Evaluating effect size in Psychological Research: sense and nonsense. Adv Methods Practices Psychol Sci. 2019;2:156–68. https://doi.org/10.1177/2515245919847202 .
Fincham FD, May RW. My stress led me to procrastinate: temporal relations between perceived stress and academic procrastination. Coll Stud J. 2021;55:413–21.
Daniali H, Martinussen M, Flaten MA. A Global Meta-Analysis of Depression, anxiety, and stress before and during COVID-19. Health Psychol. 2023;42:124–38. https://doi.org/10.1037/hea0001259 .
Tice DM, Baumeister RF. Longitudinal study of procrastination, performance, stress, and Health: the costs and benefits of Dawdling. Psychol Sci. 1997;8:454–8. https://doi.org/10.1111/j.1467-9280.1997.tb00460.x .
Schraw G, Wadkins T, Olafson L. Doing the things we do: a grounded theory of academic procrastination. J Educ Psychol. 2007;99:12–25. https://doi.org/10.1037/0022-0663.99.1.12 .
Slavich GM. Life Stress and Health: a review of conceptual issues and recent findings. Teach Psychol. 2016;43:346–55. https://doi.org/10.1177/0098628316662768 .
Phillips AC, Carroll D, Der G. Negative life events and symptoms of depression and anxiety: stress causation and/or stress generation. Anxiety Stress Coping. 2015;28:357–71. https://doi.org/10.1080/10615806.2015.1005078 .
Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. https://doi.org/10.1146/annurev.clinpsy.1.102803.143938 .
Blazer D, Hughes D, George LK. Stressful life events and the onset of a generalized anxiety syndrome. Am J Psychiatry. 1987;144:1178–83. https://doi.org/10.1176/ajp.144.9.1178 .
Southwick SM, Charney DS. The Science of Resilience: implications for the Prevention and Treatment of Depression. Science. 2012;338:79–82. https://doi.org/10.1126/science.1222942 .
Ingram RE, Luxton DD. Vulnerability-stress models. In: Hankin BL, Abela JR, editors. Development of psychopathology: a vulnerability-stress perspective. Thousand Oaks: Sage; 2005. pp. 32–46.
Chapter Google Scholar
Maercker A. Modelle Der Klinischen Psychologie. In: Petermann F, Maercker A, Lutz W, Stangier U, editors. Klinische psychologie – Grundlagen. Göttingen: Hogrefe; 2018. pp. 13–31.
Krause K, Freund AM. Delay or procrastination – a comparison of self-report and behavioral measures of procrastination and their impact on affective well-being. Pers Individ Dif. 2014;63:75–80. https://doi.org/10.1016/j.paid.2014.01.050 .
Grunschel C, Patrzek J, Fries S. Exploring reasons and consequences of academic procrastination: an interview study. Eur J Psychol Educ. 2013;28:841–61. https://doi.org/10.1007/s10212-012-0143-4 .
Dwyer JH. Statistical models for the social and behavioral sciences. New York: Oxford University Press; 1983.
Cohen JA, Power Primer. Psychol Bull. 1992;112:155–9. https://doi.org/10.1037//0033-2909.112.1.155 .
Ferguson CJ. An effect size primer: a Guide for clinicians and Researchers. Prof Psychol Res Pr. 2009;40:532–8. https://doi.org/10.1037/a0015808 .
Hinz A, Berth H, Kittel J, Singer S. Die zeitliche Stabilität (Test-Retest-Reliabilität) Von Angst Und Depressivität Bei Patienten Und in Der Allgemeinbevölkerung. Z Med Psychol. 2011;20:24–31. https://doi.org/10.3233/ZMP-2010-2012 .
Adachi P, Willoughby T. Interpreting effect sizes when controlling for stability effects in longitudinal autoregressive models: implications for psychological science. Eur J Dev Psychol. 2015;12:116–28. https://doi.org/10.1080/17405629.2014.963549 .
Dormann C, Griffin M. Optimal time lags in Panel studies. Psychol Methods. 2015;20:489–505. https://doi.org/10.1037/met0000041 .
Weckesser LJ, Dietz F, Schmidt K, Grass J, Kirschbaum C, Miller R. The psychometric properties and temporal dynamics of subjective stress, retrospectively assessed by different informants and questionnaires, and hair cortisol concentrations. Sci Rep. 2019. https://doi.org/10.1038/s41598-018-37526-2 .
Schulz P, Schlotz W, Becker P. TICS: Trierer Inventar Zum chronischen stress. Göttingen: Hogrefe; 2004.
Heidemann C, Scheidt-Nave C, Beyer A-K, Baumert J, Thamm R, Maier B, et al. Health situation of adults in Germany - results for selected indicators from GEDA 2019/2020-EHIS. J Health Monit. 2021;6:3–25. https://doi.org/10.25646/8459 .
Download references
Acknowledgements
Not applicable.
Open Access Funding provided by Freie Universität Berlin.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Division of Prevention and Psychosocial Health Research, Department of Education and Psychology, Freie Universität Berlin, Habelschwerdter Allee 45, 14195, Berlin, Germany
Anna Jochmann, Burkhard Gusy, Tino Lesener & Christine Wolter
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: A.J., B.G., T.L.; methodology: B.G., A.J.; validation: B.G.; formal analysis: A.J., B.G.; investigation: C.W., T.L., B.G.; data curation: C.W., T.L., B.G.; writing–original draft preparation: A.J., B.G.; writing–review and editing: A.J., T.L., B.G., C.W.; visualization: A.J., B.G.; supervision: B.G., T.L.; project administration: C.W., T.L., B.G.; All authors contributed to the article and approved the submitted version.
Corresponding authors
Correspondence to Anna Jochmann or Burkhard Gusy .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in line with the principles of the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Department of Education and Psychology, Freie Universität Berlin. All methods were carried out in accordance with relevant guidelines and regulations. The participants provided their written informed consent to participate in this study.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Selective dropout analysis and correlation matrix of the manifest variables
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jochmann, A., Gusy, B., Lesener, T. et al. Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress. BMC Psychol 12 , 276 (2024). https://doi.org/10.1186/s40359-024-01761-2
Download citation
Received : 25 May 2023
Accepted : 02 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s40359-024-01761-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Student health
- Longitudinal study
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Open access
- Published: 16 May 2024
Predictors for interest to participate in digital mental health therapy: a cross-sectional survey of individuals with anxiety and depression
- Tharidu Gunawardena 1 ,
- Marilyn M. Bartholmae 1 , 2 ,
- Matvey V. Karpov 1 ,
- Rohan Dod 1 ,
- Kripa Ahuja 1 ,
- Aishwarya Rajendran 1 ,
- Mayuri Kathrotia 1 &
- Sunita Dodani 1 , 3
BMC Digital Health volume 2 , Article number: 21 ( 2024 ) Cite this article
113 Accesses
Metrics details
Due to a multitude of factors, the onset of the COVID-19 pandemic resulted in a significant increase in mental health issues within society, including depression and anxiety. Due to the increased trend of mental health disorders in society, digital mental health therapies are more useful than ever. With the emergence of programs utilizing Internet Cognitive Behavioral Therapy (iCBT), mental health resources are easily accessible and can be widely implemented to those in need.
The aim of this study was to identify predictors for interest to participate in SilverCloud digital mental health therapy among individuals with mild to severe anxiety and/or depression based on preliminary findings from the COVIDsmart study.
COVIDSmart participants who had moderate to severe anxiety and/or depression based on the PHQ-9 and GAD-7 scores, and who consented to be contacted for future studies, were invited to complete a needs assessment survey via Research Electronic Data Capture (REDCap). This assessment used self-reported measures including medical diagnoses, mental health services received, reasons for anxiety and/or depression, the use of coping strategies, suicidal ideology using the Ask Suicide Questions tool, and whether they would be interested in receiving free digital mental therapy. Descriptive statistics were used to report participants’ demographics and a logistic regression was used to find predictors for interest in participation in SilverCloud. SAS 9.4 was used and p values < 0.05 were considered significant.
Out of the original 782 COVIDsmart participants, 634 consented to be contacted for future studies, 280 were subsequently invited to complete the SilverCloud needs assessment, and 120 individuals completed it. The largest demographic among these participants were females (70.83%) who identified as White (80.83%). The mean age was 48.74 years ( SD = 14.66). Results revealed that having a mental health comorbidity significantly predicted the likelihood of interest in participating in the SilverCloud digital mental health program ( p = 0.027).
Conclusions
In this study, mental illness comorbidities predicted the interest to participate in digital mental therapy. Fragmented healthcare and perceptions of unmet care needs are likely contributor factors. Further research with a diverse sample of participants is necessary for generalizability. Findings may have important implications for healthcare best practices.
Peer Review reports
Introduction
Repeatedly, it has been evident that periods of widespread human catastrophe or disaster often result in large-scale detrimental impacts on mental health. During the COVID-19 pandemic, there were not only new cases of mental health disorders but also an exacerbation of existing mental health conditions [ 1 ]. According to a briefing released by the World Health Organization in March 2022, during the first year of the COVID-19 pandemic, the prevalence of major depressive disorders and anxiety disorders had increased significantly [ 2 ]. There were multiple factors leading to a significant spike in mental health disorders. Common stressors were social isolationism, perpetual fear of COVID-19 infection, loss of employment, death of a loved one or friend and uncertainty about the future [ 3 ]. Despite many of the COVID-19 restrictions and lockdowns being relaxed since March of 2020, the damaging adverse mental health effects of the pandemic seem to have persisted throughout the United States (U.S). According to a CDC report, the prevalence of anxiety and depressive disorders has been three and four times higher, respectively, compared to pre-pandemic levels within the U.S.[ 4 ]. In 2021, mental health screenings were taken by over 5.4 million people, indicating a near 500% increase since 2019 and a 103% increase since 2020 [ 5 ].
In the state of Virginia, the COVIDsmart study was initiated to assess the effects of COVID-19 on health, behavioral and economic status of individuals in Virginia. The study gathered data from March 2021 to November 2021 through longitudinal surveys. The surveys comprised the Patient Health Questionnaire-9 (PHQ-9), Generalized Anxiety Disorder-7 (GAD-7), a condensed version of the UCLA Loneliness Scale, and a condensed version of the Social Network Index [ 6 ]. 782 Virginia residents, spanning from 18 to 87 years, registered in the COVIDsmart study. The COVIDsmart sample consisted of mostly White (81.5%), middle aged (mean age 51), middle income (51% with income of $100,000 or higher), college educated (62.6%) females (78.6%) [ 6 , 7 ]. The COVIDsmart preliminary results revealed that 21% of participants had moderate to severe anxiety and 25% had moderate to severe depression [ 7 ]. It was evident that there was a significant presence of mental disorders among Virginia residents after the COVID-19 pandemic. This prompted us to believe that there was a considerable number of individuals that required mental health services, but simply did not receive adequate counseling or therapy, leading to unmet health needs.
Based on these preliminary findings, a significant percentage of the participants of the COVIDsmart study had experienced some level of depression or anxiety, therefore the SilverCloud study was conceived and was funded by Eastern Virginia Medical School (EVMS) to alleviate the high rates of anxiety and depression among Virginians. Designed to alleviate depression and anxiety, SilverCloud is a digital mental health program that uses Internet Cognitive Behavioral Therapy (iCBT). CBT has been a highly effective form of psychological therapy for over 50 years. As patient requirements have increased, mental healthcare delivery has evolved significantly in the past decade with the introduction of new tools. Psychological interventions, specifically CBT, have become easier to implement in the form of iCBT [ 8 ]. The benefits of iCBT include cost effectiveness and global use [ 9 ]. Additionally, patients can utilize iCBT programs from the comfort of their homes, without the need for any in-person interaction. This can be particularly useful for those who have busy schedules or reside in more remote locations.
Although the mental health digital landscape is full of CBT-based apps and other digital interventions, meta-analyses and systematic reviews suggest that iCBT targeting anxiety and depression is not always effective. For example, a 2020 study by Etzelmueller et al., provided evidence for efficacy of iCBT interventions via randomized clinical trials [ 10 ] while Liu et al., 2022, suggested some iCBT-based modules are effective in treating anxiety and depression but other modules are not. Implementation science highlighting specialized needs, resources, and training to operate digital services is necessary for the success of digital therapeutics in healthcare [ 11 ]. SilverCloud Health has achieved global reach by using implementation science strategies and is the global leader in developing and delivering evidence-based mental health interventions across healthcare systems, payors such as insurance companies and government plans, providers, employer organizations, and charity/advocacy agencies [ 12 ]. SilverCloud delivers a vast array of personalized interventions to meet the specific mental health needs of individuals. Compared to other traditional digital platforms, SilverCloud offers self-guided programs, digital coaching, progress tracking tools and mobile accessibility in a secure environment. SilverCloud programs for anxiety and depression are recommended based on PHQ-9 and GAD-7 scores. These programs encourage the development of awareness and understanding of emotions, while increasing daily enjoyable activities and motivation. CBT is used to teach healthy thinking, feelings, behaviors, and to make positive changes to overcome anxiety and/or depression. SilverCloud programs include 10 modules: Getting Started, Understanding Depression and Anxiety, Noticing Feelings, Boosting Behavior, Spotting Thoughts, Challenging Thoughts, Managing Worry, Core Beliefs (unlockable by Coach), Facing Your Fears (unlockable by coach), and Bringing It All Together. SilverCloud coaches are licensed mental health professionals who provide weekly support to motivate users to engage in the SilverCloud programs, provide daily and weekly goals, and help users apply their learnings into everyday life [ 13 ]. The preliminary randomized controlled trials, which utilized SilverCloud, indicate that this therapy is effective as a stand-alone treatment for mild to moderate anxiety and depression [ 14 ].
The objective of this study was to determine the factors that can predict interest in participating in the SilverCloud program by COVIDsmart participants. Additionally, a secondary objective was to recognize the particular traits that enhance the probability of people seeking digital mental health care. This data could have significant clinical implications as it would enable healthcare professionals to gain better insights into the mental health needs of Virginians. With a greater understanding of the characteristics of these individuals in local communities, clinicians can customize digital interventions that cater to specific groups. This approach could enhance the rates of mental health screening and treatment accessibility among vulnerable populations, leading to better patient outcomes. Additionally, utilizing this information may enable digital mental health professionals to provide tailored and suitable treatment to their patients in the future. The implementation of these strategies could potentially have a notable effect in alleviating the continuous mental health emergency at a local, national, and conceivably worldwide scale.
Study design and recruitment
In order to conduct the SilverCloud study, the participants were recruited from the original COVIDSmart study. There were several recruitment strategies implemented in the COVIDSmart study, particularly to increase the likelihood of including ethnic minorities, individuals from rural areas, and individuals from lower socioeconomic backgrounds. The strategies implemented included online articles, employer e-newsletters, purchased email lists, social media posts, television, radio, paper flyers, and digital flyers. As an incentive, electronic gift cards were used to garner participation in the study. The data collection was conducted via an online HIPAA compliant platform designed by Vibrent Health Inc. The study was a joint effort with EVMS-Sentara Healthcare Analytics and Delivery Science Institute (HADSI), George Mason University, and Vibrent Health. 782 residents of Virginia enrolled in the COVIDSmart registry from March to May 2021.
The SilverCloud study was created to address the COVIDSmart study’s preliminary results showing 21% of participants had moderate to severe anxiety and 25% had moderate to severe depression [ 15 ]. Figure 1 shows the demographics for COVIDSmart participants.
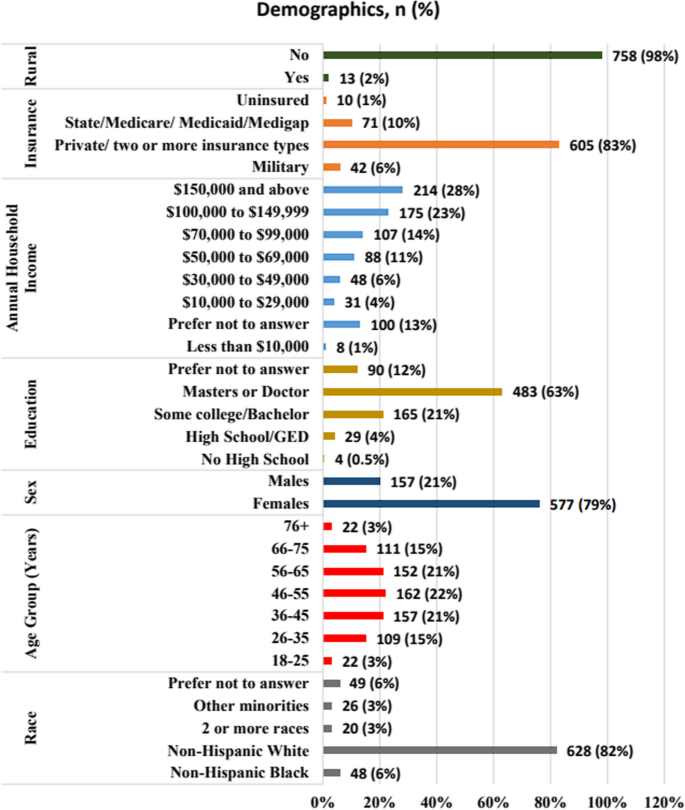
Demographics of COVIDsmart participants, N =771
Out of the 782 original COVIDsmart participants, 634 of them consented to be contacted for future studies. 280 of the COVIDSmart participants who had moderate to severe anxiety and/or depression based on the PHQ-9 and GAD-7 scores, and who consented to be contacted for future studies, were invited to complete a needs assessment questionnaire to further determine eligibility to the SilverCloud study. 120 individuals completed the SilverCloud needs assessment. The needs assessment (Appendix 1 ) evaluated self-reported measures such as medical diagnoses, mental health services received, reasons for anxiety and/or depression, the use of coping strategies, suicidal ideology (using the Ask Suicide Questions (ASQ) survey), and whether they would be interested in receiving free digital mental therapy.
Thus, the purpose of this survey was twofold: to determine their eligibility for the 8-week SilverCloud study and to assess the factors contributing to their elevated levels of anxiety and/or depression during the COVID-19 pandemic (Fig. 2 ).
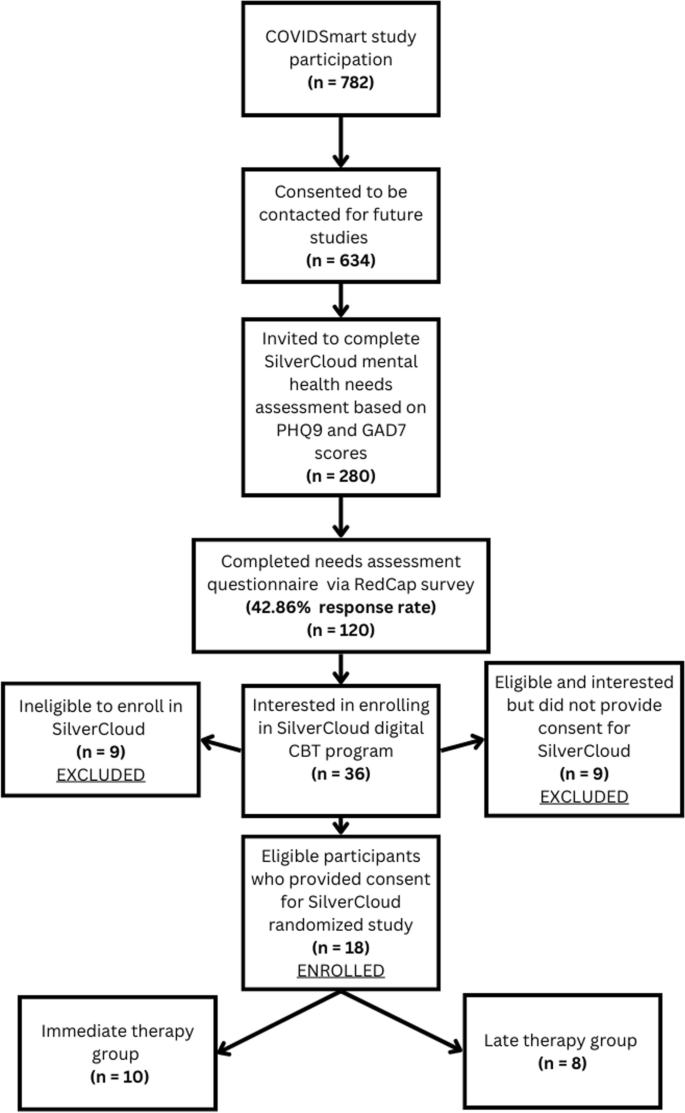
Procedure for participant recruitment and enrollment
COVIDsmart participants who had an acute suicide screening based on the ASQ survey or self-reported substance abuse and dependence were not eligible to participate in SilverCloud. However, they were provided with a list of resources they could reach for immediate assistance (Appendix 2 ). This study was approved by the Eastern Virginia Medical School Institutional Review Board (IRB# 21–07-FB-0185).
Data collection
The SilverCloud needs assessment survey was created using Research Electronic Data Capture (REDCap). REDCap is a secure web-based application used to create forms and manage databases in order to support data capture and surveys for research. REDCap data is stored securely at EVMS on private, protected servers, and meets requirements for the Health Insurance Portability and Accountability Act for collection of personal health information. The needs assessment was sent via REDcap to identified potential participants.
Statistical analysis
Descriptive statistics were used to analyze the demographics of participants. To find predictors for interest to participate in SilverCloud, we used a logistic regression including the independent variables: receiving mental health care (yes or no), having coping strategies (yes or no), severity categories for GAD-7 and PHQ-9 (moderate to severe), mental illness comorbidity (yes or no), current medications for anxiety and/or depression (yes or no), race, sex, and age. The dependent variable was interest to enroll in SilverCloud (yes or no). We conducted the analysis using SAS 9.4, and p values < 0.05 were considered significant.
A total of 120 participants who were part of the COVIDsmart program completed a needs assessment for SilverCloud. Table 1 shows that the majority of SilverCloud participants were female (70.83%) and White (80.83%). The mean age of participants was 48.74 years ( SD = 14.66, Table 2 ).
The study found that having a co-existing mental health condition was a significant predictor of the likelihood of showing interest in participating in the digital mental health SilverCloud program (p = 0.027). Among participants with moderate to severe anxiety and/or depression who were enrolled in COVIDsmart, those with a comorbidity of mental illness were 378% more inclined to be interested in SilverCloud as compared to those without a mental illness comorbidity. The mental health comorbidities reported by SilverCloud participants had a wide range, but the most common comorbidity was Posttraumatic Stress Disorder (PTSD) (28.6%), followed by eating disorder (21.4%) and Attention Deficit Hyperactivity Disorder (ADHD) (14.3%), as presented in Table 3 . These reported comorbidities were based off of self-reported survey data, and were not verified diagnoses.
However, factors such as race, gender, age, taking medication for anxiety or depression, anxiety severity, depression severity, use of coping strategies, and receiving mental health services did not have any predictive value in terms of interest in participating in SilverCloud ( p ≥ 0.05), as shown in Table 4 .
Principle results
This study showed that the only significant factor that led COVIDsmart participants to be interested in participating in SilverCloud for depression and anxiety treatment was a mental illness comorbidity. The most common comorbidities reported included PTSD, eating disorders, and ADHD. Individuals with comorbid mental illnesses experience a cumulative medical burden, often requiring multiple physical and mental health services [ 15 , 16 ]. These individuals are more likely to experience unintegrated and uncoordinated healthcare delivery [ 17 , 18 ]. Furthermore, individuals with multiple mental health comorbidities are more likely to have perceived unmet needs for care [ 19 , 20 ]. Thus, we hypothesize that individuals who experience fragmented healthcare and perceived unmet care needs may be more willing to accept mental health treatment for new conditions.
In addition, participants who had high levels of anxiety and/or depression, but no prior experience with mental health counseling, may be more apprehensive to receive treatment due to societal stigma about treatment for mental disorders. Participants with mental disorders with high levels of experienced stigma have lower rates of recovery since they are less likely to receive mental health services for their condition [ 21 ]. In this study, it seemed as if participants with multiple mental conditions were more likely to accept digital mental health treatment. The digital therapeutic setting may remove the stigma barrier for individuals with comorbid mental illnesses.
The PHQ-9 and GAD-7 scores did not have a significant predictive value for participating in mental health therapy. Unfortunately, it is unclear as to why this is. We hypothesize that since PHQ-9 and GAD-7 scores are only indicators for depression and anxiety alone, respectively, it is possible that despite a high level of depression and/or anxiety, the mental burden on these participants may not be as taxing as it is for participants with multiple mental health comorbidities, therefore, these participants were less likely to enroll in digital mental health therapy compared to participants with multiple comorbid mental illness. The individuals who chose to enroll in digital mental therapy may require integrated healthcare approaches to address their physical/mental multi-comorbidity healthcare needs. Additionally, participants who were already receiving mental health care services as well as those who were using coping strategies such as exercising and drinking less alcohol, were not likely to be interested in digital mental therapy.
The majority of participants in the COVIDsmart study were Non-Hispanic Whites and females, which explains why a similar demographic makeup was observed in the SilverCloud study. However, the SilverCloud study had a slightly higher percentage of female and Non-Hispanic White participants compared to the COVIDsmart study. Additionally, the greatest percentage of COVIDsmart participants fell into the 46–55 age range (Fig. 1 ). This corresponds accordingly with the mean age of SilverCloud participants being 48.74 years old (Table 2 ). Despite this, neither race nor gender nor age were significant predictors of participation in digital mental health therapy. It is not clear why these particular demographics were more likely to participate in both studies. Non-Hispanic Whites are known to have higher rates of mental disorders compared to people of color, although this may be due to various factors such as discriminatory medical practices, negative cultural attitudes towards mental illness, lack of insurance, and language barriers that minorities face [ 22 , 23 ].
Future directions
Our findings suggest healthcare workers should especially turn their attention towards individuals who are already suffering from coexisting mental conditions. It is very possible that the introduction of future large-scale stressors can result in new cases or the exacerbation of milder forms of depression and anxiety in these patients. Mental health counselors, psychiatrists, and therapists should regularly screen patients with existing mental health conditions with the PHQ-9 and GAD-7 for any new developments regarding depression and anxiety. Moreover, future research is needed to further evaluate the role of healthcare fragmentation and perceptions of unmet medical care needs in the enrollment of digital mental therapies. Findings could have important implications for healthcare best practices.
Future research should expand the scope and demographics of this study. While the cause of the increase in the percentage of highly-educated female and Non-Hispanic White participants in the SilverCloud study remains unknown, it is important to consider this metric on a global scale. Large nationally representative US surveys have found that mental health of Black, Hispanic, and Asian respondents worsened relative to White respondents during the pandemic, including significant increases in depression and anxiety among racialized minorities compared to White people [ 24 ]. These surveys also showed that White respondents were the most likely to receive professional mental health care before and during the pandemic, while minority respondents demonstrated higher levels of unmet mental health care needs during the pandemic than White respondents [ 24 ]. The findings of our study showed a similar trend, wherein there was an increase in the number of White participants seeking mental health care. Although our study was limited in size compared to a nationwide study, the outcomes are comparable. Securing a diverse socio-economic and racial participation is important for generalizability of future studies.
Limitations
The study has several limitations. Firstly, it only included participants from the COVIDsmart study, which means that the sample was restricted to residents of Virginia. Secondly, research fatigue from the six-month longitudinal COVIDsmart study could have deterred some participants from taking part in the SilverCloud study, thus resulting in a smaller sample size. Thirdly, the socioeconomic and racial diversity of the SilverCloud study participants did not accurately reflect the Virginia population, as there was an overrepresentation of highly educated White females and an underrepresentation of minority groups, including those living in rural areas. The lack of participant diversity and limited scope of this study may significantly hamper its generalizability to broader populations.
Fourthly, because the SilverCloud program was only accessible online, participants without internet access in Virginia may have been less likely to participate. In the future, alternative treatment options such as traditional in-person face-to-face therapy could be considered, although this would require additional resources and higher costs. Fifth, the mental illness comorbidity was self-reported. We included the variable comorbidity (yes or no) in the logistic regression model to determine whether having a mental illness comorbidity would influence the outcome: interest to participate in SilverCloud. Sixth, high risk respondents to the needs assessment could only be provided with available resources to receive help, rather than being provided with an on demand consultation with an available clinician.
Individuals with mental illness comorbidities may have a higher tendency to seek and participate in digital mental health programs amid the COVID-19 pandemic. Digital CBT-based programs can potentially improve the accessibility of care for this group. However, programs should prepare to address the needs of patients with mental illness comorbidities as they may require multidisciplinary healthcare services. Mental health professionals and researchers need to gain a deeper understanding of the unique needs of this population.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
Attention Deficit Hyperactive Disorder
Eastern Virginia Medical School
Internet cognitive behavioral therapy
Posttraumatic Stress Disorder
Research Electronic Data Capture
Jones EAK, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health. 2021;18(5):2470. https://doi.org/10.3390/ijerph18052470 . PMID: 33802278; PMCID: PMC7967607.
Article CAS PubMed PubMed Central Google Scholar
World Health Organization. Covid-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. World Health Organization. 2022. Retrieved February 1, 2023, from https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide
Panchal N, Kamal R, Cox C, & Garfield R. The implications of COVID-19 for mental health and substance use. KFF. 2021. Retrieved February 3, 2023, from https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/
Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049–57. https://doi.org/10.15585/mmwr.mm6932a1 .
Mental health and covid-19: Two years after the pandemic, mental health concerns continue to increase. Mental Health America. (n.d.). Retrieved February 3, 2023, from https://mhanational.org/mental-health-and-covid-19-two-years-after-pandemic
Bartholmae MM, Roess AA, Renshaw KD, Levy BL, Karpov MV, Sill JM, Dodani S. Evaluation of recruitment strategies on inclusiveness of populations at risk for health disparities in the statewide remote online COVID smart registry. Virginia J Publ Health. 2022;7(1):11–45 ( https://commons.lib.jmu.edu/vjph/vol7/iss1/5/ ).
Google Scholar
Schilling J, Klein D, Bartholmae MM, et al. COVID smart: A digital health initiative for remote data collection and study of COVID’s impact on the state of Virginia. J Med Internet Res. 2023. https://doi.org/10.2196/37550 .
Article PubMed PubMed Central Google Scholar
Karyotaki E, et al. Internet-based cognitive behavioral therapy for depression: a systematic review and individual patient data network meta-analysis. JAMA Psychiat. 2021;78(4):361–71. https://doi.org/10.1001/jamapsychiatry.2020.4364 . PMID: 33471111; PMCID: PMC8027916.
Article Google Scholar
Kumar V, Sattar Y, Bseiso A, Khan S, Rutkofsky IH. The effectiveness of internet-based cognitive behavioral therapy in treatment of psychiatric disorders. Cureus. 2017;9(8):e1626. https://doi.org/10.7759/cureus.1626 . PMID: 29098136; PMCID: PMC5659300.
Etzelmueller A, Vis C, Karyotaki E, Baumeister H, Titov N, Berking M, Cuijpers P, Riper H, & Ebert DD. Effects of internet-based cognitive behavioral therapy in routine care for adults in treatment for depression and anxiety: Systematic review and meta-analysis. Med Inter Res 2020;22(8). https://doi.org/10.2196/18100
Liu T, Xu J, Cheng H, Zhang Y, Wang S, Lin L, Tian L. Effects of internet-based cognitive behavioral therapy on anxiety and depression symptoms in cancer patients: a meta-analysis. Gen Hosp Psychiatry. 2022;79:135–45. https://doi.org/10.1016/j.genhosppsych.2022.09.003 .
Article PubMed Google Scholar
Richards D, Enrique A, Palacios J, et al. SilverCloud health: online mental health and wellbeing platform. In: Sverdlov O, van Dam J, eds. Digital Therapeutics Strategic, Scientific, Developmental, and Regulatory Aspects . 1st ed. CRS Press. 2022; 307–329. https://doi.org/10.1201/9781003017288-15
SilverCloud Program Guide. Anxiety depression, and co-morbid anxiety & depression. (n. d.). Retrieved June 22, 2023, from https://www.silvercloudhealth.com/programs/mental-health-wellbeing
Richards D, Enrique A, Eilert N, Franklin M, Palacios J, Duffy D, Earley C, Chapman J, Jell G, Sollesse S, Timulak L. Author correction: A pragmatic randomized waitlist-controlled effectiveness and cost-effectiveness trial of digital interventions for depression and anxiety. Npj Digit Med 2020;3(1). https://doi.org/10.1038/s41746-020-0298-3
Bartholmae MM, Karpov Sill JM, Karpov MV, Sunita D. The association between depression, anxiety, and COVID-19 symptoms. J Mental Health Clin Psychol. 2023;7(2):1–8. https://doi.org/10.29245/2578-2959/2023/2.1277 .
Doherty AM, Gaughran F. The interface of physical and mental health. Soc Psychiatry Psychiatr Epidemiol. 2014;49(5):673–82. https://doi.org/10.1007/s00127-014-0847-7 .
Pizzol D, Trott M, Butler L, et al. Relationship between severe mental illness and physical multimorbidity: a meta-analysis and call for action. BMJ Ment Health. 2023;26:e300870. Retrieved from: https://mentalhealth.bmj.com/content/26/1/e300870 .
Walker ER, Druss BG. Cumulative burden of comorbid mental disorders, substance use disorders, chronic medical conditions, and poverty on health among adults in the USA. Psychol Health Med. 2017;22(6):727–35. https://doi.org/10.1080/13548506.2016.1227855 Epub 2016 Sep 3. PMID: 27593083; PMCID: PMC5564203. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5564203/ .
Forman-Hoffman VL, Batts KR, Hedden SL, Spagnola K, Bose J. Comorbid mental disorders among adults in the mental health surveillance survey. Ann Epidemiol. 2018;28(7):468–74. Retrieved from: https://www.sciencedirect.com/science/article/pii/S104727971730889X .
Chen L-Y, Crum RM, Martins SS, Kaufmann CN, Strain EC, Mojtabai R. Service use and barriers to mental health care among adults with major depression and comorbid substance dependence. Psychiatric Services. 2013;64(9):863–70. Retrieved from https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201200289 .
Oexle N, Müller M, Kawohl W, Xu Z, Viering S, Wyss C, Vetter S, Rüsch N. Self-stigma as a barrier to recovery: A longitudinal study. Eur Arch Psychiatry Clin Neurosci. 2017;268(2):209–12. https://doi.org/10.1007/s00406-017-0773-2 .
Panchal N, Saunders H, & Ndugga N. Five key findings on Mental Health and Substance Use Disorders by race/ethnicity. KFF. 2022. Retrieved March 5, 2023, from https://www.kff.org/racial-equity-and-health-policy/issue-brief/five-key-findings-on-mental-health-and-substance-use-disorders-by-race-ethnicity/#:~:text=Overall%20rates%20of%20mental%20illness,to%20accessing%20mental%20health%20care .
Racial disparities in mental health treatment. SC-UMT. 2021. Retrieved March 5, 2023, from https://online.simmons.edu/blog/racial-disparities-in-mental-health-treatment/
Thomeer MB, Moody MD, Yahirun J. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J Racial Ethn Health Disparities. 2022:1–16. https://doi.org/10.1007/s40615-022-01284-9 . Epub ahead of print. PMID: 35318615; PMCID: PMC8939391.
Download references
Acknowledgements
We thank all of the participants who took part in the SilverCloud study. A preprint version of this manuscript has been published in JMIR Publications and is provided as #15 in the list of references.
SilverCloud did not provide any funding for this project. All funding was provided internally by Eastern Virginia Medical School.
Author information
Authors and affiliations.
EVMS-Sentara Healthcare Analytics and Delivery Science Institute, Norfolk, VA, USA
Tharidu Gunawardena, Marilyn M. Bartholmae, Matvey V. Karpov, Rohan Dod, Kripa Ahuja, Aishwarya Rajendran, Mayuri Kathrotia & Sunita Dodani
Department of Psychiatry and Behavioral Sciences, Eastern Virginia Medical School, Norfolk, VA, USA
Marilyn M. Bartholmae
Center 4 Health Research, University of Illinois College of Medicine Peoria, Peoria, IL, USA
Sunita Dodani
You can also search for this author in PubMed Google Scholar
Contributions
MB, MK, and SD contributed to the study design, data collection, and data analysis. TG, RD, KA, AR, MK, MB, MK, and SD wrote and revised the main manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Correspondence to Tharidu Gunawardena .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted in accordance with the ethical principles laid out in the Declaration of Helsinki. The participants gave informed consent to participate in the study. The study protocol was approved by the Eastern Virginia Medical School institutional review board (IRB# 21–07-FB-0185) and was conducted in compliance with all applicable laws and regulations.
Consent for publication
Not applicable.
Competing interests
None declared.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Gunawardena, T., Bartholmae, M.M., Karpov, M.V. et al. Predictors for interest to participate in digital mental health therapy: a cross-sectional survey of individuals with anxiety and depression. BMC Digit Health 2 , 21 (2024). https://doi.org/10.1186/s44247-024-00080-1
Download citation
Received : 24 September 2023
Accepted : 28 February 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s44247-024-00080-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- SilverCloud
- Digital mental health therapy
BMC Digital Health
ISSN: 2731-684X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Promot Chronic Dis Prev Can
- v.41(11); 2021 Nov
Original quantitative research - Symptoms of major depressive disorder during the COVID-19 pandemic: results from a representative sample of the Canadian population
Margot shields.
1 Public Health Agency of Canada, Ottawa, Ontario, Canada
Andrea Gonzalez
2 Department of Psychiatry and Behavioural Neurosciences, McMaster University, Hamilton, Ontario, Canada
Murray Weeks
Su-bin park, anne-marie robert, dawn-li blair, harriet l. macmillan, introduction:.
Since the outbreak of COVID-19, numerous studies from around the world have reported declines in mental health. However, most of these studies were of low-to-moderate quality and many were based on convenience samples or used mental health measures with low validity, or both. Consequently, it has been difficult to draw conclusions.
Both the 2020 Survey on COVID-19 and Mental Health (SCMH) and the Canadian Community Health Survey (CCHS) (2015–2019) used the Patient Health Questionnaire-9 to screen for major depressive disorder (MDD) in adults aged 18 or older. The prevalence of MDD was compared between the SCMH and the CCHS. Risk and protective factors for MDD in the SCMH were examined using bivariate and logistic regression analyses.
Based on SCMH data, 15.2% (95% CI: 14.2–16.2) of Canadians screened positive for MDD. The prevalence of MDD was more than two times higher in the SCMH (during COVID-19) than in the CCHS (predating COVID-19). In bivariate analysis, Canadians reporting five or more COVID-19-related risk factors were close to 30 times more likely to have MDD than those reporting no risk factors. Mastery and a sense of community belonging were protective factors for MDD.
Conclusion:
After remaining stable for two decades, the prevalence of depression among Canadians increased substantially with the onset of COVID-19. Ongoing monitoring of this common condition associated with major morbidity is vital to determine if elevated levels of MDD persist as we progress through and beyond future waves of COVID-19.
- During the second wave of COVID- 19 in the fall of 2020, the prevalence of major depressive disorder (MDD) among Canadians aged 18 or older (defined as the proportion screening positive for MDD using the Patient Health Questionnaire-9) was 15% (13% for males and 18% for females).
- Based on data from eight Canadian provinces, the prevalence of MDD during the fall of 2020 was more than double what it had been in pre-COVID times (16% vs. 7%).
- A dose-response relationship was observed between MDD and COVID- 19-related risk factors for poor mental health. Each increase in the number of COVID-19-related risk factors was associated with an increase in the prevalence of MDD, ranging from 2% among those reporting no risk factors to 62% among those reporting five or more risk factors.
- Mastery, the extent to which individuals perceive they have control over their life circumstances, was strongly associated with MDD. Those with low levels of mastery were 17 times more likely to screen positive for MDD than those with high mastery.
- Individuals reporting a very weak sense of community belonging were 10 times more likely to screen positive for MDD than those with a very strong sense of belonging.
Introduction
On March 11, 2020, the World Health Organization officially declared the COVID-19 outbreak to be a pandemic. 1 Since then, unprecedented public health measures have been implemented to contain the virus. In Canada, these have included closures of schools and childcare centres, physical distancing requirements, curfews, travel bans and the closure of many businesses. 2
COVID-19 and the measures imposed to reduce its spread have resulted in stressors and other negative effects for Canadians, including worries about personal health and the health of loved ones, job loss, income insecurity, family tension stemming from confinement and feelings of fear, loneliness and isolation. 3 , 4 As well, unhealthy lifestyle behaviour changes have been reported, such as greater consumption of alcohol and cannabis, 4 and some reports have suggested an increase in family violence. 4 , 5 These negative changes are concerning since research has found that experiencing stressful life events is the most important risk factor for depression. 6 - 13 Furthermore, problematic use of alcohol 14 and cannabis 15 has been shown to be related to depression.
Canadian data collected starting in the mid-1990s indicate that the prevalence of depression had been stable for two decades. 16 However, since the outbreak of the pandemic, studies from Canada and other countries reveal increases in negative psychological outcomes, including depression. 17 - 24 However, based on assessment of the target populations, sample sizes, methods of sample selection and instruments used for measuring mental health, most of these studies were of low-to-moderate quality—many were based on convenience samples or used mental health measures of low validity, or both, which makes it difficult to draw conclusions. 17 , 19 - 22 , 24
Psychosocial factors and resources such as mastery (the extent to which people perceive that they have control over their life circumstances), 25 coping mechanisms and a sense of community belonging have been shown to reduce the likelihood of depressive symptoms. 8 , 26 - 30 However, studies examining protective factors for depression during the pandemic are lacking. Identifying protective factors is essential for the development of intervention programs aimed at reducing depressive symptoms as Canadians live through multiple waves of COVID-19.
In this study, we examined depression in relation to COVID-19 using data from the nationally representative Canadian Survey on COVID-19 and Mental Health (SCMH) conducted during the second wave of the COVID-19 pandemic in the fall of 2020, and the Canadian Community Health Survey (CCHS)—Annual Component from 2015 to 2019 (conducted before the onset of COVID-19). In both surveys, symptoms of depression during the previous two weeks were measured using the Patient Health Questionnaire- 9 (PHQ-9), a nine-item instrument used as a screening tool for identifying probable cases of major depressive disorder, henceforth referred to as MDD for convenience. 31 - 33
The research questions addressed were:
- 1. Did the prevalence of MDD change between the pre-COVID period and the administration of the SCMH (during the second wave)? Did changes differ by sociodemographic characteristics?
- 2. What was the prevalence of COVID-19-related risk and protective factors during the second wave of COVID-19? The COVID-19-related risk factors include changes related to COVID-19 that have the potential to negatively impact mental health.
- 3. During the second wave of COVID-19, what were the risk factors (COVID-19-related and sociodemographic) and protective factors associated with MDD?
The unparalleled nature of the COVID-19 pandemic offers a unique opportunity to examine the mental health of Canadians during a public health emergency to understand the health consequences.
Data sources
Data are from the SCMH-2020 34 and the 2015 to 2019 CCHS—Annual Component. 35
The SCMH collected cross-sectional data from 11 September 2020 to 4 December 2020. The target population was individuals aged 18 years or older living in the 10 provinces or in the three territorial capital cities. Individuals living on reserves, in institutions and outside capital cities in the territories were excluded. These exclusions represented less than 2% of the Canadian population. In each province and in each territorial capital, a simple random sample of dwellings was selected from the Dwelling Universe File (a list of dwelling addresses based on various administrative data files created by Statistics Canada). One person aged 18 or older was randomly chosen from each occupied sampled dwelling to participate in the SCMH. Respondents completed the survey online or by telephone. The response rate was 53.3%—14689 respondents in total. SCMH respondents were asked for permission to share the information they provided with the Public Health Agency of Canada (PHAC); 12344 agreed to share. This study was based on records from the share file.
The target population of the CCHS was individuals aged 12 years or older living in the 10 provinces or three territories.35 Residents of reserves and other Indigenous settlements in the provinces, full-time members of the Canadian Forces, the institutionalized population and individuals living in some remote regions were excluded. These exclusions represented less than 3% of the Canadian population. In the CCHS, the Labour Force Survey area frame was used for the sampling of the adult population. The CCHS was completed by telephone or in person using a computer-assisted questionnaire.
In the annual CCHS, the PHQ-9 module is optional content; each year, the province or territory decides if this module will be administered. The years in which the CCHS depression module was most recently administered were: 2019 in Ontario and Manitoba; 2018 in Prince Edward Island; 2016 in Newfoundland and Labrador, Nova Scotia, New Brunswick and Saskatchewan; and 2015 in British Columbia. The PHQ-9 module has not been administered in Quebec and Alberta. The territories are excluded from the CCHS annual files because territorial data become representative of the population only after two years of data have been collected.
From 2015 to 2019, response rates to the CCHS ranged from a low of 54.4% in 2019 to a high of 62.8% in 2017. Similar to the SCMH, the CCHS asked respondents for permission to share their information with PHAC; each year, more than 90% agreed to share. For the eight provinces for which comparisons with the SCMH were made, the combined CCHS sample size of those aged 18 years or older on the share files was 31920.
Both surveys measured symptoms of MDD using the PHQ-9. 31 - 33 The PHQ-9 is not a diagnostic instrument, but a PHQ-9 score of 10 or higher suggests depressive symptoms of sufficient severity and persistence that additional assessment or treatment is required clinically. 31 - 33 Table 1 provides details on the items and scoring.
MDD was examined in relation to sociodemographic variables, COVID-19-related risk factors and protective factors.
The sociodemographic variables included were gender (female, male); age group (18–24, 25–34, 35–49, 50–64 and 65 years or older); racialized group member (non-White, White); immigrant status (yes, no [“non-immigrants” include those born in Canada and those who are Canadian citizens by birth]); place of residence (urban centre, rural); educational attainment (less than high school, high school, postsecondary certificate/degree/diploma, and university certificate, diploma or degree above the bachelor’s level); household income (divided into quintiles); and frontline worker (yes, no). In the SCMH questionnaire, a frontline worker was defined as “an individual who has the potential to come in direct contact with COVID-19 by assisting those who have been diagnosed with the virus.” Examples provided were “police officers, firefighters, paramedics, nurses or doctors.”
Nine COVID-19-related risk factors were examined: six COVID-19-related events or concerns, increases in the consumption of alcohol and cannabis since the onset of COVID-19, and concerns about family violence ( Table 1 ). An overall risk factor score (from 0–9) was created by summing the number of risk factors for each respondent.
The protective factors examined were sense of community belonging, mastery and coping mechanisms ( Table 1 ).
All analyses were run for the total sample and stratified by gender; separate analyses were not possible for gender-diverse individuals due to insufficient sample sizes, but gender-diverse individuals (n=20) are included in the total estimates.
Frequency estimates were produced to show the prevalence of MDD in the SCMH and the CCHS. Comparison of estimates between the two surveys was based on the eight provinces for which CCHS depression data were available. Overall comparisons (absolute and relative) were made, as well as comparisons by sociodemographic factors. The comparison by household income quintiles was based on three provinces because total household income was unavailable on the CCHS files for certain years. MDD prevalence estimates, and 95% confidence intervals (CIs), were produced for the SCMH and the CCHS, as well as absolute and relative differences in prevalence between the two surveys and the 95% CIs of the differences.
When making comparisons between the SCMH and the CCHS, we used CCHS data from the years 2015 to 2019 and implicitly assumed that the prevalence of MDD was stable across these years. Although Canadian data collected starting in the mid-1990s indicate that the prevalence of depression was stable for two decades,16 the final year in this time trend was prior to 2015. A sensitivity analysis was conducted to see if there is validity to the conjecture that the prevalence of MDD was stable over the years 2015 to 2019. For Ontario and Manitoba, three data points were available for these years, and we compared the prevalence estimates of MDD to see if they were stable.
All other analyses were based solely on SCMH data. Bivariate analysis was used to compare risk and protective factors for males and females.
Associations between COVID-19-related risk factors, protective factors and sociodemographic factors in relation to MDD were examined using cross-tabulations and logistic regression models while simultaneously controlling for the three groups of factors.
All analyses were based on weighted data. Weights created by Statistics Canada ensured that the data on the share files were representative of the population. Among other factors, the weights incorporate an adjustment for nonresponse. To account for the survey design effects of the SCMH and CCHS, standard errors, coefficients of variation and 95% CIs were estimated using the bootstrap technique.36 Differences between estimates were tested for statistical significance ( p <0.05) using chi-square tests. A Bonferroni adjustment for multiple comparisons was made when examining provincial/territorial differences. Analyses were conducted in SAS Enterprise Guide version 7.1 (SAS Institute Inc., Cary, NC, USA).
Changes in prevalence over time (research question 1)
Table 2 shows the prevalence of a positive screen for MDD for all Canadians based on data from the SCMH and compares estimates between the SCMH and the CCHS using data from eight provinces. In the fall of 2020, based on data from the SCMH, 15.2% of Canadians screened positive for MDD ( Table 2 ). The prevalence was higher among females than males (17.5% vs. 12.6%).
Based on data from the eight provinces where comparable data are available from the CCHS (2015 through 2019), the prevalence of MDD in the SCMH was 9.6 percentage points higher than it was in the CCHS (16.3% vs. 6.7%). A significant increase in the prevalence of MDD between CCHS and SCMH was observed for all sociodemographic variables except for males aged 65 years or older and males with less than high school education, among whom changes were not statistically significant.
Increases in the prevalence of MDD were similar among sociodemographic subgroups, with the following exceptions. Changes in the prevalence of MDD differed by age group: the largest increase was among young adults aged 18 to 24, for whom a 17.4 percentage point increase in MDD was observed (from 11.2% to 28.5%), and the smallest was among seniors aged 65 or older, for whom the increase was 4.1 percentage points (from 3.2% to 7.3%). A larger increase was observed among females in urban centres than among females living in rural areas. A smaller increase was observed among residents of Newfoundland and Labrador.
We also examined relative changes in the prevalence of MDD between the SCMH and the CCHS. Overall, the prevalence of MDD was 2.4 times higher in the SCMH compared with the CCHS. Although absolute changes differed among young adults aged 18 to 24 and seniors, the relative increases in the prevalence of MDD were similar (2.6 times higher vs. 2.3 times higher). The relative increase was larger for immigrants (3.3 times higher) than non-immigrants (2.2 times higher).
In our sensitivity analysis of the CCHS to assess the conjecture that the prevalence of MDD was stable from 2015 to 2019, we found that in the provinces of Ontario and Manitoba, the prevalence was 6.2% in 2015, 7.2% in 2016, and 6.8% in 2019, indicating stable rates over these years. This was followed by an increase to 16.5% in the 2020 SCMH.
Prevalence of COVID-19-related risk factors and protective factors (research question 2)
Based on SCMH data, among the nine COVID-19-related risk factors considered in the analysis ( Table 3 ), four factors were more prevalent among females than males: death of a family member, friend, or colleague (7.7% vs. 5.0%); feelings of loneliness or isolation (44.4% vs. 33.2%); physical concerns (28.7% vs. 19.8%); and challenges in personal relationships with household members (20.0% vs. 16.1%). Males were more likely to report loss of job or income due to COVID-19 (26.6% vs. 24.0%). Among people who increased their alcohol consumption, on the days they consumed alcohol, males reported an average of six drinks per day, and females, an average of four drinks per day. Among people who increased their cannabis use, 43% of males and 44% of females reported using it five or more days per week.
Females were more likely than males to report the use of several coping mechanisms. The average mastery score was higher for males than females (18.5 vs. 17.8). Estimates for a sense of community belonging were similar for males and females.
Associations between risk and protective factors and MDD (research question 3)
All nine COVID-19-related risk factors were individually associated with MDD among both males and females in the SCMH ( Table 4 ). A dose-response relationship was evident; each increase in the number of risk factors was associated with a significant increase in the prevalence of MDD. The prevalence of MDD was more than 60% among those reporting five or more risk factors, compared with 2.2% among those with no risk factors.
Individuals who reported using exercise and hobbies to promote health were less likely to have MDD. Meditating, changing food choices and changing sleep patterns to cope were associated with an increased risk of MDD. Mastery and a sense of community belonging were robust protective factors. People in the lowest mastery quartile were 17 times more likely to have MDD than were those in the highest quartile. Those with a very weak sense of community belonging were 10 times more likely to have MDD than were those with a very strong sense of belonging.
The prevalence of MDD was inversely associated with age, ranging from a high of 27.8% among those aged 18 to 24 to a low of 6.8% among seniors aged 65 or older. Non-immigrant females were at higher risk for MDD than were female immigrants (18.6% vs. 14.2%), as were females living in urban centres compared with those in rural areas (18.7% vs. 12.2%). For males, having less than high school education was associated with a lower risk of MDD. The same was true for having a university certificate, diploma or degree above bachelor’s level for both genders. Females with high school but no postsecondary education were at increased risk. MDD was inversely associated with household income quintile—the highest prevalence was for the bottom quintile (17.6%), and the lowest, for the top quintile (12.4%). Among females who had worked during the week before the survey, frontline workers were more likely than other workers to have MDD (24.0% vs. 17.3%). MDD was less common among residents of Quebec (10.5%) than other provinces/territories.
Table 5 presents the adjusted odds ratios for MDD, controlling for all factors simultaneously. Unadjusted odds are also included for ease of comparison between the bivariate and multivariate analyses.
Since a dose-response relationship was observed between COVID-19-related risk factors and MDD, in the logistic regression models, the number of COVID-19 risk factors was entered as a continuous variable. Based on the unadjusted odds, on average, each incremental increase in the number of risk factors was associated with a 2.1-fold increase in the odds of MDD. In the multivariate analysis, this finding persisted but was slightly attenuated to 1.7.
The regression models were rerun to examine effects of the nine risk factors individually. As expected, based on the unadjusted odds, all nine risk factors increased the odds of MDD. However, when we simultaneously controlled for all nine risk factors, there was some attenuation in odds, and the association with MDD for two risk factors no longer attained statistical significance: loss of job or income due to COVID-19 was no longer significant, and death of family member, friend or colleague due to COVID-19 only approached statistical significance (p=0.08). In the multivariate model for males, although the odds ratios remained elevated, the only risk factors that attained statistical significance were feelings of loneliness or isolation due to COVID-19 and physical health problems due to COVID-19.
For the protective factors, the associations observed in the bivariate analyses persisted in the multivariate analyses with two exceptions. The association with meditation was no longer statistically significant nor was changes in sleep patterns for females.
It was more common for associations between sociodemographic factors and MDD observed in the bivariate analysis to lose statistical significance in the multivariate analysis. For example, for the total population, the associations with education, income, living in an urban centre and living in Quebec did not persist in the multivariate analyses. For age group, in the gender stratified analysis, all associations failed to attain statistical significance in the multivariate analysis.
Based on SCMH data collected during the second wave of the COVID-19 pandemic, 15.2% of Canadians screened positive for MDD. Comparable estimates of the prevalence of MDD in various pre-COVID years (2015 through 2019) are available for eight Canadian provinces. SCMH results showed that in the fall of 2020, the prevalence of MDD in these eight provinces had more than doubled from what it had been in pre-COVID times.
For the most part, relative changes in the prevalence of MDD were similar among all sociodemographic subgroups. However, absolute changes in prevalence differed by age group; the largest increases in the prevalence of MDD were observed among young adults aged 18 to 24, and the smallest among seniors aged 65 or older. The 17.4 percentage point increase in the prevalence of MDD observed for young adults is concerning, and specific targeting of public health interventions may be warranted to deal with the excess burden of MDD for this age group.
All nine COVID-19-related risk factors examined in this study were individually associated with MDD, although in the multivariate analysis, loss of job or income due to COVID-19 and death of family member, friend or colleague due to COVID-19 did not attain statistical significance. Furthermore, a dose-response relationship was observed: each increase in the number of risk factors was associated with a significant increase in the prevalence of MDD. Research has found that stressful life events are the most important causal factor for first-time episodes of depression. 7 Although perception of what constitutes a stressful life event for an individual is subjective, many of the COVID-19-related risk factors considered in this analysis may be regarded as stressful life events. Indeed, the COVID-19 pandemic itself may be perceived as a stressful life event.
Although we observed that those who increased their use of cannabis and alcohol were more likely to screen positive for MDD, it is possible that they increased use to alleviate their depressive symptoms. However, longitudinal studies have shown that both alcohol use disorders and cannabis use (particularly heavy use) are associated with increased risk of subsequent depressive disorders. 14 , 15 Among those who increased their consumption of alcohol, on the days they consumed alcohol, males reported an average of six drinks per day, and females an average of four drinks per day. These consumption levels considerably surpass what is recommended in Canada’s low-risk drinking guidelines, which state that females should have no more than two drinks most days, and males no more than three drinks. 37 Among those who increased their cannabis use, 43% of males and 44% of females reported using it five or more days per week. According to Canada’s low-risk cannabis guidelines, frequent users (daily or near-daily) are more likely to develop health problems. 38 It will be important to continue to monitor consumption levels, given that increased use of these substances to deal with stress is a predictor of problem usage and dependence. 39 , 40
We observed that concern for family violence was associated with a higher risk of MDD. Longitudinal studies provide evidence of a bidirectional relationship between experiencing family violence and depressive symptoms. 41 Family violence has been shown to be associated with subsequent depression, but at the same time, depressive symptoms predict subsequent family violence.
As found in previous research, mastery 26 , 29 and a sense of community belonging 27 , 28 were protective factors for MDD. In our study, mastery was a potent protective factor; those in the lowest mastery quartile were 17 times more likely to have MDD than were those in the highest quartile. Those reporting a very weak sense of community belonging were 10 times more likely to have MDD than were those with a very strong sense of belonging. It is hypothesized that feeling “connected” to one’s community enhances social engagement. Having social ties can improve self-esteem, thereby enriching positive mental health. 27
Consistent with other studies, 30 , 42 we found some evidence that coping strategies aimed at promoting health were protective factors for MDD. Exercising and participating in hobbies were associated with a decreased risk of MDD. However, changes in food choices and sleep patterns to promote health did not emerge as protective factors and were unexpectedly associated with an increased risk of MDD. The higher prevalence of MDD among those who changed their food choices and sleep patterns to promote health may reflect the use of these strategies by those who have MDD and are using these strategies to combat their depressive symptoms. It is still plausible that these strategies may be useful in preventing MDD and reducing symptoms among those with MDD.
The increased risk of MDD among females and the negative association with age have been found in most community epidemiological studies. 43 - 45 The decreased risk for immigrants is consistent with the “healthy immigrant” effect. 46 However, while recent immigrants are healthier on their arrival, over time, the initial health advantage diminishes. 46 The comparison of estimates between the CCHS and the SCMH suggests that the gap between immigrants and non-immigrants has narrowed since the onset of COVID-19. Consistent with our findings, a rapid review of the psychological impact of COVID-19 on frontline health care workers identified many studies that reported increased levels of depression, with female nurses having higher risk than other frontline workers. 47
After more than two decades of stability,16 the prevalence of MDD among Canadians has increased substantially. It is estimated that a third to half of those with first-time depression will have a recurrence. 44 Since SCMH respondents were not asked about lifetime symptoms of depression, it is not possible to quantify the extent of first-time episodes, but likely a sizable proportion of Canadians have experienced MDD for the first time during COVD-19. Research suggests that the etiology of subsequent episodes of depression is highly variable. 6 , 7 , 9 , 11 - 13 While the first occurrence of a depressive episode is more commonly associated with a severe stressful life event, subsequent episodes often arise in the absence of severe stressful life events. 6 , 7 , 9 , 11 - 13 The stress sensitization model postulates that after an initial episode of depression, individuals are more sensitized to stress, and over time, less severe and even minor events such as daily hassles can trigger an episode. 12 , 13 Regardless of the cause of subsequent episodes, a larger percentage of Canadians may be more susceptible to episodes of depression in the near future.
Strengths and limitations
A major strength of this study is that it is based on a large representative sample from the 10 Canadian provinces as well as data from the capitals of the three territories. The scale used to measure MDD has good psychometric properties, and the cut-point used to define MDD has high sensitivity and specificity. 31 - 33 As well, we were able to examine how social and financial upheavals related to COVID-19, changes in behaviour since the onset of COVID-19 and protective factors (mastery, sense of community belonging) are related to MDD.
Nonetheless, some limitations should be considered when interpreting the results of this analysis:
- Changes in estimates of the prevalence of MDD over time were based only on certain provinces, and the baseline years for comparisons differ, ranging from 2015 to 2019. We implicitly assumed stable estimates of MDD across these years. Sensitivity analyses based on the provinces of Ontario and Manitoba supported the conjecture of stable estimates followed by an increase in the SCMH in the fall of 2020. These results suggest that the increases in MDD occurred after the onset of COVID-19.
- Methodological differences between the SCMH and the CCHS may influence comparisons. Data collection modes differed.
- CCHS data were collected throughout the year. SCMH data were collected during the fall months, and are, therefore, potentially subject to seasonality bias. 48
- For the comparison by household income, it should be noted that the SCMH is based on self-reported data, whereas the CCHS uses a combination of tax records, respondent-provided data and imputed data. It is unknown how this may have impacted the comparison of MDD estimates between the two surveys.
- The degree to which the response rates to the SCMH and the CCHS affect the prevalence of MDD in our study and the comparison of estimates between the two surveys is unknown.
- Marital status and social support were not collected in the SCMH. Being married and having social support have consistently been found to be protective factors for depression. 43 , 49
- The SCMH and CCHS excluded subpopulations among whom the prevalence of depression is likely higher, such as individuals experiencing homelessness, residents of reserves and other Indigenous settlements and residents of institutions. Depression is more common among seniors living in long-term care facilities. 50 Our study did not address the impact of COVID-19 on the mental health of seniors in long-term care.
- Although the PHQ-9 has been found to be a reliable and valid measure of MDD, 31 these are unprecedented times. New validity studies may be needed to assess whether the pandemic has increased the relative number of positive screens that are false positives based on a clinical diagnosis. Furthermore, trends based on the clinical diagnosis of MDD may differ.
- The cross-sectional nature of the SCMH data precludes establishing the temporal order of events and conclusions regarding the causal nature of associations.
Depression is a highly recurrent chronic condition that causes substantial suffering and results in increased mortality risk. 44 , 51 The World Health Organization has identified depression as a leading cause of disability worldwide and a major contributor to the overall burden of disease. 52 The SCMH was administered from September to December 2020, a period during which COVID-19 cases, hospitalizations and deaths were rising. The psychological impact of and economic fallout from lockdowns have yet to be fully understood. Given the recurrent nature of MDD and the likelihood that less severe events may result in subsequent episodes, 12 , 13 , 44 the recent increase, particularly among young adults, is cause for concern. Our findings highlight the need to identify evidence-based approaches for assessment and treatment of depressive disorders that can be delivered through public health programing to meet the increased numbers of those experiencing symptoms indicative of MDD during the pandemic, rather than relying solely on existing clinical services.
While delivery of mental health services is the responsibility of provinces and territories, planning should be based on up-to-date national estimates about the prevalence and associated risk factors of conditions such as MDD. This planning could include determining ways to make evidence-based treatments for depressive disorders, such as cognitive behavioural therapy, more broadly available, including remotely. Intervention strategies that enhance protective factors, such as identifying ways to promote community belonging, are important to consider. Ongoing monitoring is vital to determine if currently elevated levels of MDD persist.
Acknowledgements
The editorial assistance provided by Mary Sue Devereaux and Dawn Slawecki and the comments and support provided by the survey team at Statistics Canada (David Laferriere, Leslie Poon, Ayan Haji Egeh and Melanie Hoover) and Wendy Thompson (Acting Director at the Public Health Agency of Canada) are gratefully acknowledged. The excellent comments provided by Dr. Kathy Georgiades, the guest editor, and the anonymous peer reviewers considerably strengthened the paper.
Conflicts of interest
The authors have no conflicts of interest.
Authors’ contributions and statement
MS and LT conceived the project. MS and LT decided on the analytic approach. MS conducted the statistical analyses. MS, LT, AG, MW, SP, AMR, DLB and HM interpreted the results. MS drafted and revised the manuscript in response to feedback provided from LT, AG, MW, SP, AMR, DLB and HM.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
- World Health Organization (WHO) Geneva(CH): Rolling updates on coronavirus disease (COVID-19) [Internet] Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen . [ Google Scholar ]
- Canadian Institute for Health Information. Ottawa(ON): COVID-19 intervention timeline in Canada [Internet] Available from: https://www.cihi.ca/en/covid-19-intervention-timeline-in-canada . [ Google Scholar ]
- Galea S, Merchant RM, Lurie N, et al. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020:817–8. [ PubMed ] [ Google Scholar ]
- Government of Canada. Ottawa(ON): COVID-19 in Canada: a six-month update on social and economic impacts. Available from: https://www150.statcan.gc.ca/n1/en/pub/11-631-x/11-631-x2020003-eng.pdf?st=bxRrAnwr . [ Google Scholar ]
- Gunn H, McCormack S, et al. CADTH. Ottawa(ON): COVID-19 impact on intimate partner violence and child maltreatment: a summary of evidence. Available from: https://covid.cadth.ca/quickstarts/covid-19-impact-on-intimate-partner-violence-and-child-maltreatment . [ Google Scholar ]
- Brown GW, Harris TO, et al. Social origins of depression: a study of psychiatric disorder in women. Free Press. 1978 [ Google Scholar ]
- Kendler KS, Karkowski LM, Prescott CA, et al. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry. 1999:837–41. [ PubMed ] [ Google Scholar ]
- Kessler RC, et al. The effects of stressful life events on depression. Annu Rev Psychol. 1997:191–214. [ PubMed ] [ Google Scholar ]
- Monroe SM, Harkness KL, et al. Life stress, the “kindling” hypothesis, and the recurrence of depression: considerations from a life stress perspective. Psychol Rev. 2005; 112 ((2)):417–45. [ PubMed ] [ Google Scholar ]
- Monroe SM, Slavich GM, Torres LD, Gotlib IH, et al. Major life events and major chronic difficulties are differentially associated with history of major depressive episodes. J Abnorm Psychol. 2007; 116 ((1)):116–24. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Post RM, et al. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry. 1992; 149 ((8)):999–1010. [ PubMed ] [ Google Scholar ]
- Stroud CB, Davila J, Moyer A, et al. The relationship between stress and depression in first onsets versus recurrences: a meta-analytic review. J Abnorm Psychol. 2008; 117 ((1)):206–13. [ PubMed ] [ Google Scholar ]
- Stroud CB, Davila J, Hammen C, Vrshek-Schallhorn S, et al. Severe and nonsevere events in first onsets versus recurrences of depression: evidence for stress sensitization. J Abnorm Psychol. 2011; 120 ((1)):142–54. [ PubMed ] [ Google Scholar ]
- Li J, Wang H, Li M, et al, et al. Effect of alcohol use disorders and alcohol intake on the risk of subsequent depressive symptoms: a systematic review and meta-analysis of cohort studies. Addiction. 2020; 115 ((7)):1224–43. [ PubMed ] [ Google Scholar ]
- Lev-Ran S, Roerecke M, Foll B, George TP, McKenzie K, Rehm J, et al. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med. 2014; 44 ((4)):797–810. [ PubMed ] [ Google Scholar ]
- Patten SB, Williams JV, Lavorato DH, Fiest KM, Bulloch AG, Wang J, et al. The prevalence of major depression is not changing. Can J Psychiatry. 2015:31–4. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brooks SK, Webster RK, Smith LE, et al, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020; 395 ((10227)):912–20. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Capaldi CA, Liu L, Dopko RL, et al. Positive mental health and perceived change in mental health among adults in Canada during the second wave of the COVID-19 pandemic. Health Promot Chronic Dis Prev Can. 2021; 41 ((11)):359–77. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- nat JM, Blais-Rochette C, Kpolou CK, et al, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021:113599–77. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Flynn R, Riches E, Reid G, Rosenberg A, Niedzwiedz C, et al. Rapid review of the impact of COVID-19 on mental health. Rapid review of the impact of COVID-19 on mental health. Edinburgh: Public Health Scotland; 2020. 2020 Available from: http://www.healthscotland.scot/publications/rapid-review-of-the-impact-of-covid-19-on-mental-health . [ Google Scholar ]
- What is known about the impact of the COVID-19 pandemic on families with children. NCCMT. 2020 Available from: https://www.nccmt.ca/covid-19/covid-19-rapid-evidence-service/15 . [ Google Scholar ]
- Salari N, Hosseinian-Far A, Jalali R, et al, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020:57–77. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schmitz N, Holley P, Meng X, Fish L, Jedwab J, et al. COVID-19 and depressive symptoms: a community-based study in Quebec, Canada. Can J Psychiatry. 2020; 65 ((10)):733–5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Xiong J, Lipsitz O, Nasri F, et al, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020:55–64. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pearlin LI, Schooler C, et al. The structure of coping. J Health Soc Behav. 1978:2–21. [ PubMed ] [ Google Scholar ]
- Gadalla TM, et al. Determinants, correlates and mediators of psychological distress: a longitudinal study. Soc Sci Med. 2009; 68 ((12)):2199–205. [ PubMed ] [ Google Scholar ]
- Kitchen P, Williams A, Chowhan J, et al. Sense of community belonging and health in Canada: a regional analysis. Soc Indic Res. 2012:103–26. [ Google Scholar ]
- Michalski CA, Diemert LM, Helliwell JF, Goel V, Rosella LC, et al. Relationship between sense of community belonging and self-rated health across life stages. SSM Popul Health. 2020:100676–26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nicolaisen M, Moum T, Thorsen K, et al. Mastery and depressive symptoms: how does mastery influence the impact of stressors from midlife to old age. J Aging Health. 2018; 30 ((7)):1084–107. [ PubMed ] [ Google Scholar ]
- Wang J, Patten SB, et al. The moderating effects of coping strategies on major depression in the general population. Can J Psychiatry. 2002; 47 ((2)):167–73. [ PubMed ] [ Google Scholar ]
- Kroenke K, Spitzer RL, Williams JB, et al. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16 ((9)):606–13. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kroenke K, Spitzer RL, et al. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr Ann. 2002:509–15. [ Google Scholar ]
- Spitzer RL, Kroenke K, Williams JB, et al. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999; 282 ((18)):1737–44. [ PubMed ] [ Google Scholar ]
- Statistics Canada. Ottawa(ON): Survey on COVID- 19 and Mental Health (SCMH) [Internet] Available from: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5330 . [ Google Scholar ]
- Statistics Canada. Ottawa(ON): Canadian Community Health Survey (CCHS) - 2019 [Internet] Available from: https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=getInstrumentList&Item_Id=1207185&UL=1V . [ Google Scholar ]
- Rust KF, et al. Variance estimation for complex surveys using replication techniques. Stat Methods Med Res. 1996; 5 ((3)):283–310. [ PubMed ] [ Google Scholar ]
- Canadian Centre on Substance Use and Addiction (CCSA) Ottawa(ON): Canada’s low-risk alcohol drinking guidelines [Internet] Available from: https://www.ccsa.ca/canadas-low-risk-alcohol-drinking-guidelines-brochure . [ Google Scholar ]
- Fischer B, Russell C, Sabioni P, et al, et al. Lower-risk cannabis use guidelines: a comprehensive update of evidence and recommendations. Am J Public Health. 2017; 107 ((8)):e1–e12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Courtney KE, Mejia MH, Jacobus J, et al. Longitudinal studies on the etiology of cannabis use disorder: a review. Curr Addict Rep. 2017; 4 ((2)):43–52. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wu P, Liu X, Fang Y, et al, et al. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol Alcohol. 2008; 43 ((6)):706–12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bacchus LJ, Ranganathan M, Watts C, Devries K, et al. Recent intimate partner violence against women and health: a systematic review and meta-analysis of cohort studies. BMJ Open. 2018:e019995–12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Warheit GJ, et al. Life events, coping, stress, and depressive symptomatology. Am J Psychiatry. 1979; 136 ((4B)) [ PubMed ] [ Google Scholar ]
- rrez-Rojas L, Porras-Segovia A, Dunne H, Andrade-Gonzalez N, Cervilla JA, et al. Prevalence and correlates of major depressive disorder: a systematic review. Braz J Psychiatry. 2020:657–72. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kessler RC, Bromet EJ, et al. The epidemiology of depression across cultures. Annu Rev Public Health. 2013:119–38. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Patten SB, Wang JL, Williams JV, et al, et al. Descriptive epidemiology of major depression in Canada. Can J Psychiatry. 2006; 51 ((2)):84–90. [ PubMed ] [ Google Scholar ]
- Ng E, Zhang H, et al. The mental health of immigrants and refugees: Canadian evidence from a nationally linked database. Health Rep. 2020; 31 ((8)):3–12. [ PubMed ] [ Google Scholar ]
- Cabarkapa S, Nadjidai SE, Murgier J, Ng CH, et al. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: a rapid systematic review. Brain Behav Immun Health. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lukmanji A, Bhattarai A, Patten SB, et al. Seasonal variation in symptoms of depression: a Canadian population based study. J Affect Disord. 2019:142–9. [ PubMed ] [ Google Scholar ]
- Paykel ES, et al. Life events, social support and depression. Acta Psychiatr Scand Suppl. 1994:50–8. [ PubMed ] [ Google Scholar ]
- CIHI. Ottawa(ON): 2020. Depression among seniors in residential care. Available from: https://secure.cihi.ca/free_products/ccrs_depression_among_seniors_e.pdf . [ Google Scholar ]
- pine JP, Briley M, et al. The increasing burden of depression. Neuropsychiatr Dis Treat. 2011; 7 ((Suppl 1)):3–7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- World Health Organization (WHO) Geneva(CH): Depression [Internet] Available from: https://www.who.int/news-room/fact-sheets/detail/depression . [ Google Scholar ]
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Burden of Mental Disorders and Suicide Attributable to Childhood Maltreatment
- 1 The Matilda Centre for Research in Mental Health and Substance Use, The University of Sydney, Sydney, New South Wales, Australia
- 2 Department of Clinical, Educational, and Health Psychology, Division of Psychology and Language Sciences, University College London, London, United Kingdom
- 3 Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York
Question What proportion of mental health conditions and burden in Australia is attributable to childhood maltreatment?
Findings This meta-analysis found, after controlling for genetic and environmental confounding, that childhood maltreatment accounts for 21% to 41% of common mental health conditions in Australia, with the highest attributable proportion for suicide attempts and self-harm. More than 1.8 million cases of depressive, anxiety, and substance use disorders, 66 143 years of life lost, and 184 636 disability-adjusted life-years could be prevented if childhood maltreatment was eradicated in Australia.
Meaning Efforts to prevent child maltreatment exposure have the potential to improve mental health at a population level in Australia.
Importance The proportion of mental disorders and burden causally attributable to childhood maltreatment is unknown.
Objective To determine the contribution of child maltreatment to mental health conditions in Australia, accounting for genetic and environmental confounding.
Design, Setting, and Participants This meta-analysis involved an epidemiological assessment accounting for genetic and environmental confounding between maltreatment and mental health and 3 cross-sectional national surveys: the Australian Child Maltreatment Study (ACMS) 2023, National Study of Mental Health and Well-being 2020-2022, and Australian Burden of Disease Study 2023. Causal estimates were derived on the association between childhood maltreatment and mental health conditions from a meta-analysis of quasi-experimental studies. This was combined with the prevalence of maltreatment from the ACMS to calculate the population attributable fraction (PAF). The PAF was applied to the number and burden of mental health conditions in Australia, sourced from 2 population-based, nationally representative surveys of Australians aged 16 to 85 years, to generate the number and associated burden of mental disorders attributable to child maltreatment.
Exposure Physical abuse, sexual abuse, emotional abuse, or neglect prior to age 18 years.
Main Outcomes and Measures Proportion and number of cases, years of life lost, years lived with disability, and disability-adjusted life-years of mental health conditions (anxiety, depression, harmful alcohol and drug use, self-harm, and suicide attempt) attributable to childhood maltreatment.
Results Meta-analytic estimates were generated from 34 studies and 54 646 participants and applied to prevalence estimates of childhood maltreatment generated from 8503 Australians. Childhood maltreatment accounted for a substantial proportion of mental health conditions, ranging from 21% (95% CI, 13%-28%) for depression to 41% (95% CI, 27%-54%) of suicide attempts. More than 1.8 million cases of depressive, anxiety, and substance use disorders could be prevented if childhood maltreatment was eradicated. Maltreatment accounted for 66 143 years of life lost (95% CI, 43 313-87 314), primarily through suicide, and 184 636 disability-adjusted life-years (95% CI, 109 321-252 887).
Conclusions and Relevance This study provides the first estimates of the causal contribution of child maltreatment to mental health in Australia. Results highlight the urgency of preventing child maltreatment to reduce the population prevalence and burden of mental disorders.
Read More About
Grummitt L , Baldwin JR , Lafoa’i J , Keyes KM , Barrett EL. Burden of Mental Disorders and Suicide Attributable to Childhood Maltreatment. JAMA Psychiatry. Published online May 08, 2024. doi:10.1001/jamapsychiatry.2024.0804
Manage citations:
© 2024
Artificial Intelligence Resource Center
Psychiatry in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Depression articles from across Nature Portfolio
Depression refers to a state of low mood that can be accompanied with loss of interest in activities that the individual normally perceived as pleasurable, altered appetite and sleep/wake balance. Its severe form, major depression is classified as a mood disorder.
Latest Research and Reviews

Astrocytic ALKBH5 in stress response contributes to depressive-like behaviors in mice
The regulatory mechanism and function of astrocytic epigenetic effects on depression remain to be explored. Here, the authors show astrocytic ALKBH5 contributes to depressive-like behaviors via the m6A RNA methylation of GLT-1.
Severe mental illness and mortality in sepsis and septic shock: a systematic review and meta-analysis
- Ines Lakbar
- Eloise Maakaron
- Guillaume Fond
Improved implicit self-esteem is associated with extended antidepressant effects following a novel synergistic intervention
- H. Nur Eken
- Crystal Spotts
- Rebecca B. Price
Multiple paths to rumination within a network analytical framework
- Ernst H. W. Koster
- Kristof Hoorelbeke

Elevated SCN11A concentrations associated with lower serum lipid levels in patients with major depressive disorder
- Shuang Zhao
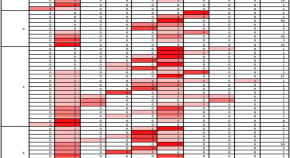
Occurrence and characteristics of suicidal ideation in psychiatrically healthy individuals based on ecological momentary assessment
- Maria A. Oquendo
- Hanga C. Galfalvy
- Barbara H. Stanley
News and Comment
Internet use and teen mental health: it’s about more than just screen time.
- Linxiao Zhang
Social-media influence on teen mental health goes beyond just cause and effect
- Michael A. Spikes
The personal brain
- Giovanni Stanghellini
- Luciano Mecacci
Interpersonal therapy can be an effective tool against the devastating effects of loneliness
- Myrna M. Weissman
- Jennifer J. Mootz
On assumptions and key issues in electric field modeling for ECT
- Zhi-De Deng
- Miklos Argyelan
- Christopher C. Abbott
Use fines from EU social-media act to fund research on adolescent mental health
- Christian Montag
- Benjamin Becker
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Depression rates among US adults reach new high: Gallup
Nearly 30% of adults say they've been diagnosed with depression at some point.
Depression rates in the United States are skyrocketing, particularly among young adults and women, a new poll shows.
The survey , published by Gallup on Wednesday, found 29% of U.S. adults report being diagnosed with depression at some point during their lifetimes, an increase from 19.6% in 2015.
Meanwhile, 17.8% of those aged 18 and older either currently have or are currently being treated for depression, up from 10.5% in 2015.
According to Gallup, both rates are the highest ever recorded by the analytics company since it began tracking depression rates.
MORE: Teen girls are experiencing record-high levels of sadness and violence: CDC
"I think the results are startling," Dan Witters, research director of the Gallup National Health and Well-Being, told ABC News. "The disproportionate manner in which some groups have been affected by this makes sense to me based upon what we know about other research and those sharp increases in those depression rates among those adults under 30, women too, Blacks and Hispanics, they are really eye-popping."
Although the COVID-19 pandemic can't be blamed completely for the increasing rates, it definitely was a major factor, Witters said.
"Both of these rates had kind of been coming up over the years pre-pandemic," he said. "And you don't want to get too far out in front of your skis as far as putting all the blame on the pandemic."
He went on, "There's plenty of other big factors out there that could be relevant to these increasing rates that we've been measuring but the pandemic's a big one and indeed the rates have really come up significantly in the years since COVID hit."

More than 5,100 adults were surveyed in all 50 states and the District of Columbia during the last week of February 2023. The results are part of the larger ongoing Gallup National Health and Well-Being Index, which seeks to track and understand factors that drive well-being.
Results showed rates are rising fastest among certain groups, particularly young adults and women.
Women's rates of depression during their lifetimes climbed from 26.2% in 2017 to 36.7% in 2023. Rates of those with current depression increased from 17.6% to 23.8% over the same period.
By comparison, men with depression during their lifetimes saw a smaller increase from 17.7% in 2017 to 20.4% in 2023. Current rates for depression rose from 9.3% to 11.3%.
Witters said women have historically had higher rates of depression than men. COVID, however, may have led to a jump in these rates due to women being disproportionately forced to leave the workforce to take care of children at home and that fact that they make up a higher percentage of frontline health care workers.
MORE: Suicides rose in 2021 after 2 years of declines, CDC report finds
Breakdowns by age showed one-third of younger adults between ages 18 to 29 reported being diagnosed with depression at some point in their lives, up from 20.4% in 2017. Additionally, 24.6% said they currently have depression, an increase from 13% in 2017.
Popular Reads

Smith suspected added obstruction effort by Trump
- May 21, 4:50 PM

Trump deletes clip mentioning 'Unified Reich'
- May 21, 9:27 AM

Johnson disappointed with chaotic House meeting
- May 17, 3:34 PM
Witters pointed to other research showing a growing mental health crisis among young people in the U.S.
"Obviously social media predates 2017, but social media had the effect on a lot of kids where they feel left out, they feel compelled to look at social media, and they see people out having fun, and they're not a part of it," he said. "They can get ostracized through social media."
Adults aged 65 and older had the smallest increase for depression and were the only group that saw a decrease in rates of current depression from 2021.
When it came to breakdowns by race/ethnicity, results showed rates for Black and Hispanic adults are rising at about twice the rate of white adults.
The percentage of Black adults diagnosed with depression at some point in their lifetime rose from 20.1% to 34.4% between 2017 and 2023. For Hispanic adults, the percentage jumped from 18.4% to 31.3% over the same period.

Comparatively, white adults saw their rates increase from 22.3% in 2017 to 29% in 2023.
"For a long time, white America and white adults were reporting a clinical diagnosis of depression at rates that exceed Black and Hispanic adults," Witters said. "These big increases ... really show the strain that Black and Hispanic Americans have been under since 2017."
Black and Hispanic Americans were more likely to lose their jobs in the early days of the pandemic, he said, and events such as the death of George Floyd in May 2020 may have also contributed to depression.
"When the pandemic first hit, across all adults, negative emotional experiences [tracked by Gallup] such as sadness and anger went up a little but didn't really change that much," Witters said. "You fast forward a couple of months and you get to kind of the latter part of May and into June, anger and sadness were up over 10 percentage points."
ABC News' Dr. Amanda Kravitz contributed to this report.
Related Topics
- Mental Health

10-year-old boy swept into storm drain
- May 20, 1:52 PM

Climber falls from highest peak in North America
- May 21, 3:29 AM
ABC News Live
24/7 coverage of breaking news and live events

IMAGES
VIDEO
COMMENTS
a. A data charting form was created to capture the data elements of interest, including the authors, titles, determinants (biological, psychological, social), and the type of depression assessed by the research (e.g., major depression, depressive symptoms, depressive behaviour). b.
Abstract. Depression is a prevalent psychiatric disorder that often leads to poor quality of life and impaired functioning. Treatment during the acute phase of a major depressive episode aims to help the patient reach a remission state and eventually return to their baseline level of functioning. ... and somatic approaches. Research on ...
Abstract. Major depressive disorder (MDD), also referred to as depression, is one of the most common psychiatric disorders with a high economic burden. The etiology of depression is still not clear, but it is generally believed that MDD is a multifactorial disease caused by the interaction of social, psychological, and biological aspects.
For the treatment of depression, targeting signaling transduction by BDNF and its receptor, tropomycin receptor kinase B (TrkB), is essential. 143,144 Recent research has shown a link between ...
Abstract. Background. Over the past 16 years, we have developed a 'Meta-analytic Research Domain' (MARD) of all randomized trials of psychological treatments of depression. ... Depression in most studies was moderate to severe. Response (50 % improvement between baseline and endpoint) was the main outcome. It was found that combined ...
Our lack of knowledge cannot be put down to a scarcity of research in existing treatments. In the past decades, more than 500 randomised trials have examined the effects of antidepressant medications, and more than 600 trials have examined the effects of psychotherapies for depression (although comparatively few are conducted for early-onset depression).
The idea that depression is the result of abnormalities in brain chemicals, particularly serotonin (5-hydroxytryptamine or 5-HT), has been influential for decades, and provides an important ...
Aim: This review explores current research on the effectiveness of IBIs for depression and anxiety. Results: For depression, therapist-guided cognitive behavioral therapy (CBT) had larger effect sizes consistently across studies, ranging from 0.6 to 1.9; while stand-alone CBT (without therapist guidance) had a more modest effect size of 0.3-0 ...
Abstract. Major depression is a mood disorder characterized by a sense of inadequacy, despondency, decreased activity, pessimism, anhedonia and sadness where these symptoms severely disrupt and ...
Depression is a common psychiatric disorder and a leading cause of disability worldwide. Here we conducted a genome-wide association study meta-analysis of six datasets, including >1.3 million ...
To improve our understanding, some research has been undertaken in which YP themselves are asked about their experience of depression. In a questionnaire study involving adolescents with depression in New Zealand, the researchers identified the aforementioned irritability as the most common characteristic alongside interpersonal problems and ...
In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety and depression can be traced back even earlier in life. For example, childhood behavioral inhibition in response to novelty or strangers, or an extreme anxious temperament ...
Abstract. Major depressive disorder (MDD), also referred to as depression, is one of the most common psychiatric disorders with a high economic burden. ... As shown in Fig. 1E, the hot research topics in depression are as follows: depression management in primary care, interventions to prevent depression, the pathogenesis of depression, ...
Abstract. We aimed to synthesise information related to the incidence of depression and depressive symptoms (DDS) in a community-dwelling older adult population at a global level. In this systematic review, we included articles with a cohort study design that evaluated the incidence of depression or depressive symptoms in older adults aged 60 ...
Abstract. Depression has become a major threat to human health, and researchers around the world are actively engaged in research on depression. ... A relationship network of depression research was established, highlighting the highly influential countries, journals, categories, authors, institutions, cited articles, and keywords in this ...
Abstract Objective—This report presents national estimates of self-reported feelings of depression among adults by whether they lived alone or with others. Methods—Data from the 2021 National Health Interview Survey were used to describe differences in self-reported feelings of depression and living arrangement by
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect ...
Following a title/abstract review and subsequent full-text review, 520 additional articles were excluded. ... The CES-D Scale: A self-report depression scale for research in the general population ...
Objective To identify the optimal dose and modality of exercise for treating major depressive disorder, compared with psychotherapy, antidepressants, and control conditions. Design Systematic review and network meta-analysis. Methods Screening, data extraction, coding, and risk of bias assessment were performed independently and in duplicate. Bayesian arm based, multilevel network meta ...
Background It is generally assumed that procrastination leads to negative consequences. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. Therefore, the aim of our study was to examine the harmful consequences of procrastination on students' stress and mental health. We selected the procrastination ...
Methods. PSY-CARE was a pragmatic single-center two arm randomized controlled trial (RCT) investigating the feasibility and effectiveness of providing outpatient cognitive-behavioral psychotherapy tailored for home-living vulnerable older adults with depression (Gellert et al., Citation 2020).This intervention was implemented in an urban environment (Berlin) under real-life conditions of the ...
After title/abstract screening, 215 studies were included for full-text screening. Finally, 47 publications were included in the final synthesis. ... Pouwer F. Depression and quality of life in patients with diabetes: A systematic review from the European depression in diabetes (EDID) research consortium. Curr. Diabetes Rev. 2009; 5:112-119 ...
Conclusion. The prevalence of depression among the older population in China is high. Those female, of older age, with a lower level of education, without a spouse, living in rural areas, with chronic diseases and comorbidities, self-rated poor health, suffering from insomnia, living alone, lack of physical exercise, and requiring full or partial assistance for daily living, are more likely to ...
Abstract Background: Numerous investigations indicate the presence of a reciprocal association between type 2 diabetes (T2D) and a range of mental health conditions. ... a systematic review from the European depression in diabetes (EDID) research consortium. Curr Diabetes Rev 2009; 5(2): 112-119. DOI: 10.2174/157339909788166828. Crossref. PubMed.
Depression is a disorder that increasingly affects different populations, with an estimated prevalence rate of 4.4% worldwide 1.This condition is defined as a mental disorder characterized by a ...
Due to a multitude of factors, the onset of the COVID-19 pandemic resulted in a significant increase in mental health issues within society, including depression and anxiety. Due to the increased trend of mental health disorders in society, digital mental health therapies are more useful than ever. With the emergence of programs utilizing Internet Cognitive Behavioral Therapy (iCBT), mental ...
Research suggests that the etiology of subsequent episodes of depression is highly variable. 6, 7, 9, 11-13 While the first occurrence of a depressive episode is more commonly associated with a severe stressful life event, subsequent episodes often arise in the absence of severe stressful life events. 6, 7, 9, 11-13 The stress sensitization ...
1 The Matilda Centre for Research in Mental Health and Substance Use, The University of Sydney ... years lived with disability, and disability-adjusted life-years of mental health conditions (anxiety, depression, harmful alcohol and drug use, self-harm, ... Research Ethics Topics and Collections Visual Abstracts War and Health Women's Health ...
Its severe form, major depression is classified as a mood disorder. Latest Research and Reviews Improved implicit self-esteem is associated with extended antidepressant effects following a novel ...
The survey, published by Gallup on Wednesday, found 29% of U.S. adults report being diagnosed with depression at some point during their lifetimes, an increase from 19.6% in 2015. Meanwhile, 17.8% ...