- Login | Register
- Repository Home
- Electronic Theses and Dissertations
- Doctoral Papers

Distributive Justice and Social Policy: A Case Study
View file(s).

- Swider, Susan
- Susan Swider, PhD, PHNA-BC
- Sigma Affiliation
- Alpha Lambda
Visitor Statistics
Visits vs downloads, visitors - world map, top visiting countries, top visiting cities, visits (last 6 months), downloads (last 6 months), popular works for swider, susan by view, popular works for swider, susan by download, view citations.
All rights reserved by the author(s) and/or publisher(s) listed in this item record unless relinquished in whole or part by a rights notation or a Creative Commons License present in this item record.
All permission requests should be directed accordingly and not to the Sigma Repository.
All submitting authors or publishers have affirmed that when using material in their work where they do not own copyright, they have obtained permission of the copyright holder prior to submission and the rights holder has been acknowledged as necessary.
Related items
Showing items related by title, author, creator and subjects.

Moral development and public health nursing

Determining the impact of using a social determinants of health screening tool in identifying unmet needs, barriers to care, and basic awareness of social resources

A policy pathway: Nursing’s role in advancing diversity and health equity

Fostering a supportive moral climate for health care providers: Toward cultural safety and equity

Political astuteness and beliefs among senior-level baccalaureate nursing students: A mixed-methods approach
New questions start here.
- Research article
- Open access
- Published: 18 July 2018
Supporting shared decision making for older people with multiple health and social care needs: a realist synthesis
- Frances Bunn ORCID: orcid.org/0000-0002-5885-918X 1 ,
- Claire Goodman 1 ,
- Bridget Russell 1 ,
- Patricia Wilson 2 ,
- Jill Manthorpe 3 ,
- Greta Rait 4 ,
- Isabel Hodkinson 5 &
- Marie-Anne Durand 6
BMC Geriatrics volume 18 , Article number: 165 ( 2018 ) Cite this article
19k Accesses
89 Citations
66 Altmetric
Metrics details
Health care systems are increasingly moving towards more integrated approaches. Shared decision making (SDM) is central to these models but may be complicated by the need to negotiate and communicate decisions between multiple providers, as well as patients and their family carers; particularly for older people with complex needs. The aim of this review was to provide a context relevant understanding of how interventions to facilitate SDM might work for older people with multiple health and care needs, and how they might be applied in integrated care models.
Iterative, stakeholder driven, realist synthesis following RAMESES publication standards. It involved: 1) scoping literature and stakeholder interviews (n = 13) to develop initial programme theory/ies, 2) systematic searches for evidence to test and develop the theories, and 3) validation of programme theory/ies with stakeholders ( n = 11). We searched PubMed, The Cochrane Library, Scopus, Google, Google Scholar, and undertook lateral searches. All types of evidence were included.
We included 88 papers; 29 focused on older people or people with complex needs. We identified four context-mechanism-outcome configurations that together provide an account of what needs to be in place for SDM to work for older people with complex needs. This includes: understanding and assessing patient and carer values and capacity to access and use care, organising systems to support and prioritise SDM, supporting and preparing patients and family carers to engage in SDM and a person-centred culture of which SDM is a part. Programmes likely to be successful in promoting SDM are those that allow older people to feel that they are respected and understood, and that engender confidence to engage in SDM.
Conclusions
To embed SDM in practice requires a radical shift from a biomedical focus to a more person-centred ethos. Service providers will need support to change their professional behaviour and to better organise and deliver services. Face to face interactions, permission and space to discuss options, and continuity of patient-professional relationships are key in supporting older people with complex needs to engage in SDM. Future research needs to focus on inter-professional approaches to SDM and how families and carers are involved.
Peer Review reports
Shared decision making (SDM) involves patients and health and social care practitioners (HSCPs) jointly offering treatment, care and support packages to reflect, respect and accommodate the patient’s preferences, priorities and goals [ 1 , 2 ]. Although the original underlying ethos for sharing decisions between patients and HSCPs is based on values, i.e. people have the right to self-determination and autonomy, there is evidence that SDM can lead to better outcomes and care for people [ 3 ]. For example, patients who feel involved in the decision and in accord with the HSCP are less likely to need other services such as extra tests or referrals to other HSCPs [ 4 ]. More recently SDM has been envisaged as part of person and family centred care and integrated care [ 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 ].
Decision making becomes more complex for older people with multiple health and care needs as the capacity to self-manage is affected by the cumulative effects of long-term conditions. The nature of decisions is complicated by resource availability, polypharmacy, decline in decision making abilities and concordance, availability of support networks, suitability of treatment, safeguarding and the increased likelihood of depression [ 17 , 18 , 19 , 20 ]. Moreover, decision making may need to be negotiated between, and communicated to, multiple health and social care practitioners, as well as patients and their families. Whilst there is evidence that many older people and their family carers would like to be involved in decision making [ 21 , 22 ], there is little evidence relating specifically to SDM with older people with complex health needs.
The skills for sharing and discussing personal information with vulnerable patients, and their families, can be hard to embed in services. There is a need to establish the mechanisms that preserve and foster shared decision making (SDM) between professionals, patients and carers and how they achieve improvements in patient outcomes [ 23 , 24 ]. Approaches are needed that aim to address the complexity of life when living with, and managing, multiple long-term conditions [ 25 , 26 ] or recognise the need to consider the abilities of patients and their families to attend to the demands of each condition [ 19 , 27 , 28 ]. Such approaches require the building of relationships, meaningful discussion and SDM between a range of different providers, patients and carers [ 29 ].
To develop an understanding of the realities of working in and across complex, overlapping systems of care, it is necessary to synthesise evidence from diverse strands of research [ 30 , 31 ]. Realist methodology allows the deconstruction of component theories underpinning different interventions and enables us to consider relevant contextual data to test our understanding of the applicability of different approaches for older people with multi-morbidity and how SDM might achieve desired outcomes such as improvements in; patient safety, clinical effectiveness, quality of life and patient experience [ 23 ] within the context of integration. The aim of this review was to develop an explanatory account of how interventions to facilitate SDM might work for older people with multiple health and care needs, and how they might be applied to integrated care models.
Realist synthesis is a systematic, iterative, theory-driven approach designed to make sense of diverse evidence about complex interventions applied in different settings [ 32 , 33 , 34 ]. The rationale for using a realist synthesis approach for this review is that interventions to promote shared decision making (SDM) in older people with complex health and care needs are likely to be multi-component and are contingent on the behaviours and choices of those delivering or receiving the care.
A realist synthesis assumes a ‘generative’ approach to causation, that is, “to infer a causal outcome (O) between two events (X and Y), one needs to understand the underlying mechanism (M) that connects them and the context (C) in which the relationship occurs. It is typically used to understand complex interventions that ‘often have multiple components (which interact in non-linear ways) and outcomes (some intended and some not) and long pathways to the desired outcome(s)” [ 32 , 35 ]. Central to the realist review process is the development of programme theory, i.e. what a programme or intervention comprises and how it is expected to work. The review followed the Realist and Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) publication standards for realist syntheses [ 36 ]. A fuller version of the methods is published elsewhere [ 37 ].
The synthesis focuses on community dwelling older people with complex health and care needs, for example, people with frailty, multi-morbidity and long-term conditions. The rationale for focusing on this group is that they often use several health and social care services, their needs change over time and/or suddenly, sometimes with progressive loss of cognitive and/or physical function, a family carer is frequently involved in their care, and they are often at risk of exacerbation of their illness and death [ 17 ]. In addition, many find it difficult to navigate complicated and under-resourced services and are particularly vulnerable to fragmented care [ 38 ]. The focus was generally on those aged 65 years or over, although for certain groups (e.g. people from black and minority ethnic groups (BME), those with mental health problems) we included some younger participants (≥55 years) if the issues were similar. We used an iterative, stakeholder driven approach with three phases.
Phase 1: Development of initial programme theory/ies
In Phase 1 we sought to develop candidate theories about why programmes that seek to promote SDM do, or do not, work. The starting point was systematic reviews of SDM and related topics (such as person-centred care). To identify reviews we searched PubMed and the Cochrane library using the following MESH terms: shared decision making, patient participation, patient decision making, decision support, decision aid, expert patient, proxy decision making, collaborative care, co-construction, coproduction and minimally disruptive medicine. These terms were combined with methodological search terms for systematic reviews. In addition, we undertook key word searches on Google Scholar for both reviews and primary studies and looked for relevant papers published by key authors in the area. We identified 39 systematic reviews and 35 primary studies. In addition, we undertook face to face or telephone interviews with stakeholders in England including user/patient representatives, health care professionals and commissioners/funders, and service providers in integrated care sites. We recruited 13 stakeholders rather than the 20 specified in the protocol. Interviews were conducted using realist principles [ 39 ] and participants were a convenience sample recruited for their known expertise in SDM and care of older people. The purpose of the stakeholder consultation was to explore key assumptions about what needs to be in place for effective SDM and identify relevant outcomes. Ethical approval was obtained from the University of Hertfordshire Health and Human Sciences Ethics Committee with delegated authority (ECDA), reference number HSK/SF/UH/02387.
The literature and stakeholder interviews were used to develop preliminary hypotheses in the form of five ‘If-Then’ statements (Table 1 ). These if-then statements, which helped to specify context and mechanism, were illustrated with supporting evidence from the interviews and literature. ‘If-Then’ statements are the identification of an intervention/activity linked to outcome(s), and contain references to contexts and mechanisms (though these may not be very explicit at this stage), and/or barriers and enablers (which can be both mechanism and context) [ 40 ]. The ‘If-Then’ statements helped to focus the process of taking ideas and assumptions about how interventions work and testing them against the evidence we found.
The ‘If-Then’ statements were further developed through discussions at a workshop attended by eight members of the research team and consultation with the Project Advisory Group. The Advisory Group included experts in the field of older people’s health, primary care, patient involvement and realist methods, and experts by experience (Public Involvement representatives).
Phase 2: Retrieval, review and synthesis
In Phase 2 we undertook systematic searches of the evidence to test and develop the theories identified in Phase 1. The focus of the review was on community dwelling older people with complex health and care needs, such as those with frailty, multi-morbidity, dementia. However, we also included other populations where the study was considered to offer opportunities for transferrable learning. Other inclusion criteria were as follows:
Older people with complex health needs living in their own homes, in sheltered housing or extra care housing.
Any intervention or strategy designed to promote the ongoing engagement of older people with complex health needs, and/or their family carers, in decision making relating to their health or social care needs (e.g. decision aids, physician or patient coaching, education or training, personalised care planning, joint goal setting). The focus was on complex decision making and personal goals rather than single issues (such as whether to have a hip replacement). This included:
○ Interprofessional SDM where at least two health care professionals collaborate to achieve SDM with the patient and/or family carer either concurrently or sequentially [ 41 ]
○ Studies that provide evidence relating to the implementation and uptake of interventions designed to promote SDM for older people with complex health needs.
Published and unpublished studies of any design.
Data sources included: Medline (PubMed), SCOPUS, The Cochrane Database of Systematic Reviews, DARE (Database of Abstracts of Reviews of Effects), the HTA Database, NHS EED (NHS Economic Evaluation Database), Google and Google Scholar. The searches were designed to reflect the five ‘If-Then’ statements identified in Phase 1. Date limits and search terms used in PubMed can be seen in Table 2 . In addition, we undertook lateral searching such as forward and backward citation tracking. The purpose of the searches was not to identify an exhaustive set of studies but rather to identify sufficient sources for building and testing our programme theory [ 42 ]. As is usual with a realist review, the process of identifying relevant information and deciding what to include was iterative involving tracking backwards and forwards between the literature and our review questions [ 43 ].
Selection and appraisal of documents
Search results were downloaded into bibliographic software. Two reviewers independently screened titles and abstracts identified by electronic search and applied the selection criteria to potentially relevant full-text papers. Decisions on inclusion were recorded in an excel spreadsheet. Consistent with a realist review approach, items were assessed for inclusion on the basis of whether they were considered ‘good enough and relevant enough’ [ 44 , 45 ]. This was an iterative process that involved discussion between team members. Good enough was based on the reviewers’ own assessment of the quality of evidence, for example was it considered to be of a sufficient standard for the type of research, and whether the claims made were considered trustworthy. Relevance related to whether the authors provided sufficient descriptive detail and/or theoretical discussion to contribute to the theories generated in Phase 1. Studies considered by the team to be poorly executed could still be included if the study was considered to contribute to understanding about how a programme was thought to work.
Data extraction and synthesis
A data extraction form was developed, piloted on five records and further refined as necessary. Once the final fields for data extraction were agreed, an electronic version was created in MS Access. The data extraction form included fields relating to study aims, design and methods; the types of participants (e.g. older people, people with long-term health conditions, HSCPs); outcomes; information relevant to the theory areas; and emerging CMOs. Data were extracted by one reviewer with 20% checked by a second reviewer. PDFs in Mendeley were also annotated and relevant sections highlighted. Data in a realist sense are not just restricted to the study results or outcomes measured but also include author explanations and discussions, which can provide a rich source of ‘data’ that makes explicit how an intervention was thought to work or not. The query feature in the ACCESS database was used to create tables to facilitate the identification of prominent recurrent patterns of contexts and outcomes (demi-regularities) in the data and the possible means (mechanisms) by which they occurred [ 46 ]. This deliberative and iterative process enabled iteration from plausible explanations to the uncovering of potential context-mechanism-outcome (CMO) configurations.
Phase 3: Testing and refining of programme theory
In Phase 3, we tested the programme theory via interviews with 11 stakeholders and through discussions with the research team and Project Advisory Group. An interview schedule, based on the four CMOs, was used to elicit stakeholders’ views on their meaningfulness, both from practice and service user/carer perspectives. The interview data were used to test the CMOs.
We included 88 items that included 26 evidence reviews, [ 3 , 30 , 31 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 ] 46 primary research studies, [ 41 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 ] seven guidelines, cases studies or reports, [ 8 , 14 , 117 , 118 , 119 , 120 , 121 ] and nine discussion/opinion papers [ 79 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 ]. Of the 46 primary research papers, 25 were qualitative studies, five were RCTs and the rest included a variety of study designs. Of the evidence reviews, 20 were systematic reviews, [ 3 , 30 , 31 , 47 , 48 , 49 , 50 , 52 , 53 , 54 , 55 , 56 , 58 , 60 , 62 , 63 , 64 , 65 , 66 , 69 ] five were literature reviews, [ 51 , 57 , 61 , 67 , 68 ] and one was a realist synthesis [ 59 ]. The study selection process can be seen in Fig. 1 . Thirty-three papers from Phase 1 were excluded at Phase 2 because they were not considered to be of high enough rigour or relevance.
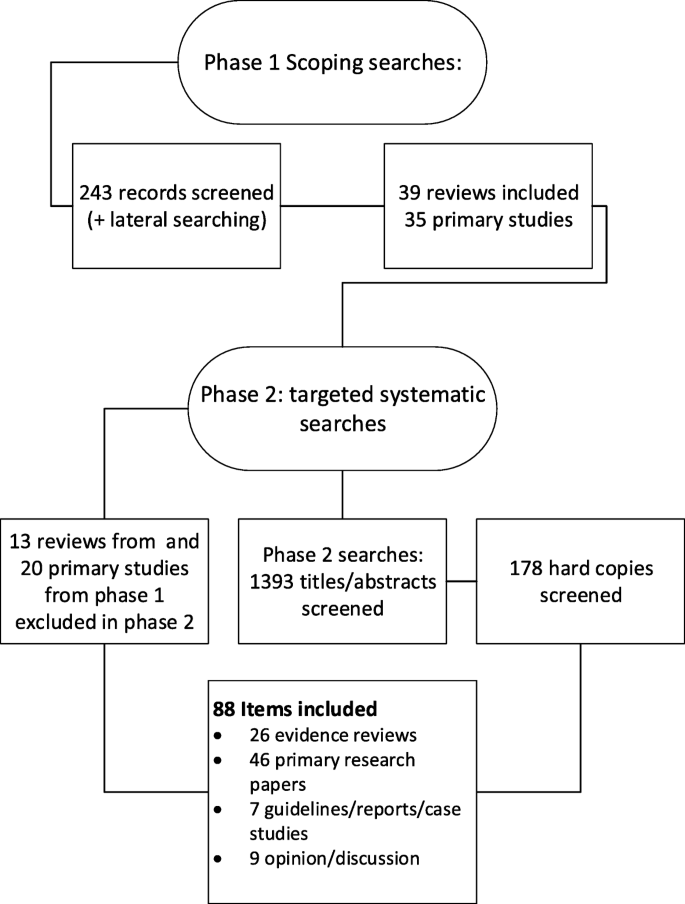
Flow chart summarising study identification
The included literature either focused specifically on SDM or on aspects of care, such as person-centred care or personalised care planning, in which SDM plays an essential if not specified part with the patient or their proxy. We categorised the included reviews and other items according to the focus of the paper. The numbers in each category can be seen in Table 3 . Twenty-five primary studies and four systematic reviews focused on older people or those with complex health and care needs. Of those 19 focused on older people or had a population with a mean or median age over 65, nine specified that people had multi-morbidities and 11 that they had long-term conditions.
Sixteen reviews were evaluating an intervention, such as decision aids or tools, coaching, and interventions to increase or promote the adoption of SDM amongst health care professionals. Nineteen of the other papers described or evaluated an intervention. Interventions included care planning, training and education for professionals, the use of decision aids or integrated/collaborative care practices that involved SDM. More details of the reviews can be seen in Additional file 1 and of other items (e.g. primary studies) in Additional file 2 .
The theory development, refinement and testing process led to the development of four context-mechanism-outcome (CMO) configurations (see Table 4 ). Together, these explanations or hypotheses constitute a programme theory about ‘what works’ (or ‘what might work’) to facilitate shared decision-making (SDM) for older people with multiple health and care needs or conditions, and how they might be applied within models of integrated working. Supporting evidence from the stakeholder interviews can be seen in Table 5 .
CMO1: Reflecting patient and carer values
Understanding the needs and priorities of service users/patients/carers.
Considering patients’ and, where appropriate, family carers’ preferences and values is seen as key to the decision-making process [ 51 , 59 , 67 , 102 , 103 , 124 ]. Systematic review evidence suggests that interventions to promote a patient-centred approach in clinical consultations can have a positive effect on a range of measures although the impacts on satisfaction, behaviour and health status were mixed [ 56 ]. Despite this, individual needs and circumstances of patients and their family carers are frequently not taken into account [ 53 , 74 , 96 , 98 ]. Reasons for information sharing difficulties, and goal divergence include health care professionals having difficulty identifying patient preferences, [ 47 , 50 ] differences in the way patients and clinicians interpret and frame the patient’s health problems [ 94 , 110 ] and clinicians being reluctant to engage in SDM when the patient’s preferences are not in line with clinical guidelines [ 106 ] or when there are concerns about safety or cognitive function [ 98 ].
Developing relationships
Achieving collaborative approaches to care, such as SDM, depends on building a good relationship in the clinical encounter [ 59 , 74 , 83 , 90 , 97 , 101 , 103 , 104 , 109 , 115 , 128 ]. This impacts on patient and carer perceptions of the quality of care, [ 55 , 80 , 82 ] and may improve adherence to medical treatments [ 55 ]. Increased trust was associated with longer consultations, physician verbal behaviour (such as exploring the impact of the condition or illness on the patient) [ 130 ] and continuity of care. [ 47 , 59 , 93 ]. The importance of ongoing relationships and the ability to reassess changing priorities were highlighted in several studies [ 47 , 103 ]. This was particularly important for people with complex needs or dementia as ‘the dominant chronic illness shifts over time as conditions and treatments change, and re-prioritization occurs’ [ 51 ] and decision-making responsibility may shift over time, from the person with dementia to the family carer [ 91 ].
Interprofessional working
Partnership working between different health and care professionals was seen as key to decision making for older adults with complex needs [ 73 , 78 , 91 , 97 ]. Facilitators of interprofessional working include a history of working together, mutual knowledge and understanding of disciplinary roles, trust and respect, a shared understanding of SDM, and effective communication between individuals (including different health and social care practitioners and patients & carers) [ 41 , 64 , 80 , 100 , 120 ]. However, few studies addressed an interprofessional approach to SDM, with most studies targeting a single professional group [ 41 , 65 ].
Patient and carer outcomes
Systematic reviews suggest that interventions to promote SDM may lead to patients and carers feeling more involved in decision making [ 63 , 67 ]. There is also evidence of improved quality of life and reduced depression in carers, [ 67 ] and improved affective cognitive outcomes for patients, such as increased satisfaction and reduced decisional conflict [ 47 ]. These impacts (particularly on patient satisfaction) are echoed in many of the other studies we accessed. There is also some evidence that SDM leads to better treatment adherence [ 118 ]. There is little evidence, however, to suggest that there is an association between empirical measures of SDM and health outcomes [ 47 ].
CMO2: Systems to support SDM
Studies support a link between organisational ‘buy-in’ (e.g. identifying SDM as an organisational priority) and an increase in health and social care practitioner engagement with, and prioritisation of, SDM. However, whilst SDM is a core part of policy in many countries, including the UK, [ 131 ] at a service level, systems are not in place to incentivise or appropriately reward patient-centred practice and SDM [ 96 , 128 ]. Furthermore, for older people with complex conditions SDM is hindered by the risk and uncertainty associated with complex conditions and by systems and structures that block communication between patients and the different professional groups involved in their care [ 96 ]. The literature outlines several system based approaches to improve SDM. For example, preparatory work to support the patient’s involvement in decision making, e.g. an initial appointment with a nurse or health care assistant before a meeting with the GP [ 14 ], longer appointments, [ 85 , 86 ] and annual reviews which include monitoring for all chronic conditions [ 14 , 110 , 121 ]. However, little data on patient outcomes are available.
The need for enhanced communication skills among clinicians was a common theme across the papers [ 30 , 47 , 53 , 56 , 59 , 87 ]. This included the ability to address with patients the uncertainty involved in many medical and care decisions [ 103 , 122 ]. Several studies reported that training to promote person-centred approaches and SDM had positive impacts on SDM skills and engagement [ 56 , 65 , 85 , 86 ]; there was less evidence of changes in patient focused outcomes [ 85 , 86 , 96 ]. A UK based study reported that interactive skills training workshops based on a SDM model helped build coherence, improving skills, and promoting positive attitudes. It was also considered important that clinical teams were able to develop a shared understanding of how SDM might differ from their current practice [ 96 ].
CMO3: Preparing for the SDM encounter
Decision support.
Much of the literature on preparing patients and carers relates to the use of patient decision aids; tools designed to help people participate in decision making about health care options [ 132 ]. Systematic reviews provide good evidence that patient decision aids can have a positive impact on patient knowledge, decisional conflict, informed choice, participation in SDM and decision self-efficacy, [ 3 , 48 , 49 , 54 , 62 , 69 ] including for those who are socially disadvantaged [ 48 ]. Potential mechanisms relating to the likely benefits of decision aids include patients becoming more engaged, [ 48 ] developing greater decisional self-efficacy, [ 48 ] feeling more involved in decisions, [ 85 , 86 ] and increased mutuality [ 90 ]. However, the reviews provide little evidence that decision aids improve health outcomes or patient adherence.
Older age, depressive symptoms and difficulties with activities of daily living are associated with decreased patient activation [ 89 ]. There is some evidence that decision aids can enhance older adults’ participation in SDM [ 54 , 69 ]. However, most evidence relates to younger older people (70 years and under) rather than the oldest old (80+) and most tools are not tailored to the needs of people with multi-morbidity [ 69 ]. Moreover, there is unlikely to ever be a patient decision aid for every decision, not all patients will find them acceptable or helpful [ 96 ], and they may not address the entry level factors to SDM, such as subjective norms and patients’ roles [ 62 , 90 ]. There is some evidence that the use of coaching or guidance may support patients in the process of thinking about a decision and in communicating their values and preferences with others [ 68 , 70 , 92 ]. The mechanisms inferred from these papers are that improving patients’ deliberation and communication skills will lead to empowerment and thus patients will feel better supported. However, the impact on other outcomes, such as participation in decision making or satisfaction with option chosen, is mixed [ 68 ].
Permission/space to discuss option
Key to CMO 3 is that SDM is undertaken in a context where patients and their families can discuss the value and effectiveness of proposed treatments without feeling judged. Longer consultations are linked to greater patient satisfaction and improved SDM, [ 14 , 53 , 74 , 83 , 85 , 101 , 104 , 113 ] which is likely to be related to the opportunity for patients to ask questions, and feel listened to [ 83 , 101 ] and respected [ 97 , 109 ]. However, clinicians’ attitudes may act as a barrier to SDM with older people feeling unable to make their needs heard [ 76 ] or reluctant or unable to discuss relevant context or preferences during a consultation [ 75 , 76 ]. Moreover older people may not always be aware that there is a choice to be made [ 76 ]. Research has underscored the importance of family-centred approaches for older people with complex needs [ 18 , 133 ]. However, similar to a realist review on engaging older adults in healthcare decision making [ 59 ], we found few studies that considered the involvement of family members and friends in SDM.
CMO 4: SDM as part of a wider culture change
Time and resources.
The programme theory outlined in CMOs 1–3 outlines many barriers to SDM and it is clear that relying on individual clinicians or patients to implement SDM without system-based support is unlikely to be successful or sustainable [ 60 , 62 , 65 ]. Several included papers described system-based changes that involve person-centred, integrated approaches to people with long-term conditions, [ 8 , 14 , 82 , 121 ] of which SDM is an integral part. These initiatives reported increased staff and patient satisfaction [ 8 , 14 , 121 ] although the impact on clinical outcomes is not clear. One report suggested that changing patient and professional habits may need a number of care planning cycles [ 121 ]. This is reflected in our programme theory which argues that familiarity and a shared expectation of new ways of working (which include SDM) are likely to take time to develop.
Patient activation or engagement
The willingness or ability of patients to participate in SDM is a key contextual factor in our programme theory (see also CMO3). This was supported by the literature, [ 53 ] and underscored by our interviews with stakeholders. In general, the consensus from the literature is that although the majority of older people would wish to be involved in decision-making in practice they are often not encouraged, or enabled, to participate in SDM [ 50 , 62 , 96 ]. Reasons for this include limited time, poor continuity of care, environmental conditions, organisational inertia, a biomedical focus, concern about disruption to routines, clinicians’ belief that they are already practicing SDM, and power imbalances [ 60 , 62 , 87 , 122 , 134 ]. Whilst many SDM initiatives involve giving patients more information, this alone is not enough. Patients need knowledge and power to participate in SDM [ 62 , 135 ]. A systematic review of patient reported barriers and facilitators to SDM suggested that power may be linked to perceptions of permission to participate in decision making, perceived influence on decision making, confidence in own knowledge and self-efficacy in SDM [ 62 ].
Summary of the findings
We have developed an explanatory account of what SDM should look like for older people with complex health and care needs (see Fig. 2 ). Our theory suggests that programmes that are likely to be successful in fostering SDM between older people with complex needs, their family carers and service providers are those that create trust between those involved, that allow older people to feel that they are respected and understood, that are accessible to older people and that engender confidence to engage in SDM. Confidence is likely to take time to develop as, we suggest, it is related to the development of a shared understanding and expectation of SDM between patients and HSCPs. The cultural shift that is needed to embed SDM in practice may require new ways of working for professionals and a shift away from a biomedical focus to a more person-centred ethos that goes beyond the individual patient encounter. To achieve this, health care professionals are likely to need support, both in terms of the way services are organised and delivered and in terms of their own continuing professional development. Older people with complex needs and their family carers may also need support to engage in SDM, which includes interventions that are adapted to their needs (in terms of literacy, health literacy and computer literacy, among other things). How this support might best be provided needs to be further explored, although face to face interactions and ongoing patient-professional relationships are clearly key.
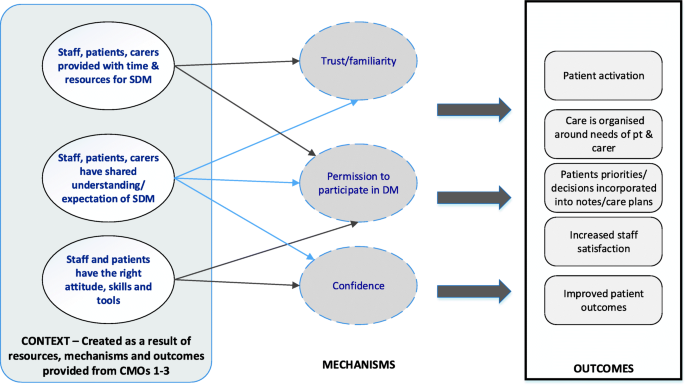
Summary of programme theory: the figure depicts how the context is created as result of the resources, mechanisms and outcomes provided by CMOs 1–3
Strengths and weaknesses of the study
One of the main limitations of this review is the lack of evidence around interventions to promote SDM in older people with complex health and care needs. The lack of evidence is compounded by little evidence around SDM in integrated care teams. However, in realist methodology, the unit of analysis is the programme theory, or underpinning mechanism of action, rather than the intervention [ 43 ]. This meant we were able to draw on a wider literature that provided opportunities for transferable learning, for example studies involving people with long-term conditions or mental health problems. This enabled us to develop a programme theory which can inform initiatives to promote SDM for older people with complex needs. Whilst our searches were systematic the broad nature of our inclusion criteria means that we may have missed potentially relevant literature. However, the nature of realist methodology means that there is not a finite set of relevant papers to be found. Instead the reviewer is able to take a more purposive approach to sampling that aims to identify sufficient sources for theory building and testing rather than identify an exhaustive set of documents [ 42 , 43 ].
Strengths and weaknesses in relation to other studies
Person-centred approaches to health and care and considering each patient’s preferences and values are central to the SDM process [ 12 ]. For older people with complex needs eliciting preferences is likely to involve regularly revisiting decisions because the dominant illness, and priorities, may shift over time [ 51 , 91 ]. However, the evidence suggests that doctors are better at recognising and discussing options than eliciting patient preferences (see CMO 1). This may reflect the fact that different health and social care practitioners conceptualise person-centred care in different ways [ 136 , 137 ]. A review of literature on person-centred care suggests that whilst the nursing literature tends to focus more on respecting patients’ values and beliefs in promoting person-centred care, the medical literature has devoted more attention to understanding the nature of the informed decision-making process between the doctor and the patient [ 136 ]. What is not explored in the literature is whether integrated care and interprofessional working might enable different members of the multi-disciplinary team to draw on the skills of others in order to promote effective person-centred approaches to SDM.
Meaning of the study
The quality of individual clinicians’ communication skills, and their ability to foster trusting relationships with older people and their families, is fundamental to SDM. SDM education and training should be focused on all members of the multidisciplinary team and not just doctors or lead clinicians. It should be part of undergraduate training programmes but also part of ongoing professional development and should include exploring what matters to patients and how to elicit their goals and priorities. In addition, there is also a need for systems that foster continuity of care. Continuity can be achieved through an ongoing relationship with one clinician (relationship continuity) or a system based approach that develops ways of working whereby the patient is linked to multiple professionals (management and informational continuity) [ 138 , 139 , 140 ]. The evidence would suggest that both need to be in place. Informational continuity is, however, often hindered by electronic systems not set up to record information relating to patient preferences and goals [ 110 ]. The evidence highlights key contextual factors to facilitate SDM for older people, including consultation length, clinicians’ communication skills, and whether it is possible to create a culture that allows people to ask questions without feeling judged. A culture that allows people time to ask questions and to discuss options, and staff with positive attitudes towards SDM are likely to be more important than decision support tools for older people with complex health and care needs. These resources are likely to lead to an increased ability and willingness to engage in SDM through mechanisms such as feeling respected and understood.
Unanswered questions and future research
Evidence from stakeholders and from the literature suggests that older people with complex and competing health and care demands (and where depression is a common comorbidity) may need considerable support to enable them to engage in SDM. This can be exacerbated by factors such as deprivation, low health literacy or cognitive impairment. There is a need for more work to specifically focus on older people with complex needs, for example, more research looking at what is happening in SDM conversations involving older people with complex needs, how patient decision aids are being used and to what effect? More research is needed on family-centred approaches to SDM. For example, what is the impact of making it the default option (with consent from the older person) to involve designated family members in consultations and discussions about treatment options? In addition, whilst models for health care delivery are moving towards a more interprofessional healthcare team-based approach, [ 24 ] most evidence concerns decision making involving a single doctor and a patient, and there is a lack of studies addressing interprofessional approaches to SDM [ 65 ]. For interprofessional SDM to work the development and involvement of all staff are important [ 8 , 100 ].
Models of SDM for older people with complex health and care needs should move away from thinking about SDM purely in terms of one doctor/patient encounter. Rather SDM should be conceptualised as a series of conversations that each patient, and their family carers, may have with a variety of different health and care professionals. Such an approach relies on continuity of care fostered through good relationships between practitioners and patients, and systems that facilitate the communication of information, including that about patient goals and preferences, between different health and care professionals. The literature on SDM involving older people or those with complex needs is largely qualitative or descriptive and there are very few evaluations of interventions specifically designed to promote SDM with this group, and with their family carers. This review suggests there is need for further work to establish how organisational structures can be better aligned to the needs of older people with complex needs. This includes a need to define and evaluate the contribution that different members of the health and care team can make to SDM for older people with complex health and care needs.
Abbreviations
Context-Mechanism-Outcome
Health and Social Care Practitioner
Patient Decision Aid
Shared Decision Making
Coulter A, Collins A. Making shared decision-making a reality no decision about me, without me. London: The King's Fund; 2011.
Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997/03/01. 1997;44(5):681–92.
Article PubMed CAS Google Scholar
Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017; Issue 4, Art No. CD001431.
Elwyn G, Edwards A, Kinnersley P. Shared decision-making in primary care: the neglected second half of the consultation. Br J Gen Pr. 1999;49:477–82.
CAS Google Scholar
Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision-making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pr. 2000;50:892–9.
Barry MJ, Edgman-Levitan S. Shared decision making — the pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–1.
National Diabetes Support Team. Getting to Grips with the Year of Care: A Practical Guide. 2008;(October):4–5.
Diabetes UK. Department of Health. The Health Foundation. NHS diabetes. Year of care report of findings from the pilot programme. 2011.
Taylor A, Neal D, Jones S, Oliver L, Tipper E, Collins A, et al. Building the House of Care. London; 2015.
Coulter A, Kramer G, Warren T, Salisbury C. Building the house of care for people with long-term conditions: the foundation of the house of care framework. Br J Gen Pract. 2016;66(645):e288–90.
Article PubMed PubMed Central Google Scholar
Mathers N, Paynton D. Rhetoric and reality in person-centred care: introducing the house of care framework. Br J Gen Pract. 2016;66(644):124–5.
Google Scholar
NHS Health Educ England, Skills for Care, Skills for Health. Person-Centred Approaches: Empowering people in their lives and communities to enable an upgrade in prevention, wellbeing, health, care and support. 2017.
RCGP. Collaborative Care and Support Planning: Ready to be a reality. 2014.
Glenpark Medical Practice. The Glenpark story implementing care and support planning for people with long term conditions. Gateshead: Year of Care Partnership; 2016.
Hannan R, Thompson R. The Triangle of Care Carers Included: A Guide to Best Practice for Dementia Care. London: Carer’s Trust; 2013.
Year of Care Partnerships. The Year of Care Partnership Programme: Working Together for Better Healthcare and Self Care. Tyneside; 2014.
Banerjee S. Multimorbidity - older adults need health care that can count past one. Lancet Elsevier. 2017;385(9968):587–9.
Article Google Scholar
Bunn F, Burn A-M, Goodman C, Robinson L, Rait G, Norton S, et al. Comorbidity and dementia: a mixed-method study on improving health care for people with dementia (CoDem). Health Serv Deliv Res. 2016;4(8).
Leppin AL, Montori VM, Gionfriddo MR. Minimally Disruptive Medicine: A Pragmatically Comprehensive Model for Delivering Care to Patients with Multiple Chronic Conditions. Healthcare. 2015/01/01. 2015;3(1):50–63.
Gagnon LM, Patten SB. Major depression and its association with long-term medical conditions. Can J Psychiatr. 2002;47(2):149–52.
Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G. Patient preferences for shared decisions: A systematic review. Patient Educ Couns. Elsevier Ireland Ltd; 2012;86(1):9–18. Available from: https://doi.org/10.1016/j.pec.2011.02.004
Wolff JL, Boyd CM. A Look at person-centered and family-centered care among older adults: results from a National Survey. J Gen Intern Med. 2015;30(10):1497–504.
Goodman C, Drennan V, Manthorpe J, Gage H, D. T, Shah D, et al. A study of the effectiveness of inter-professional working for community dwelling older people: Final Report – NIHR Service Delivery and Organisation Programme. 2011.HMSO; 2012.
NHS England. Five year forward view. 2014.
Sinclair AJ, Hillson R, Bayer AJ. National Expert Working G. Diabetes and dementia in older people: a best clinical practice statement by a multidisciplinary National Expert Working Group. Diabet Med. 2014;31(9):1024–31.
Sinclair A, Morley JE, Rodriguez-Manas L, Paolisso G, Bayer T, Zeyfang A, et al. Diabetes mellitus in older people: position statement on behalf of the International Association of Gerontology and Geriatrics (IAGG), the European diabetes working Party for Older People (EDWPOP), and the international task force of experts in diabetes. J Am Med Dir Assoc Elsevier. 2012;13(6):497–502.
Demain S, Goncalves AC, Areia C, Oliveira R, Marcos AJ, Marques A, et al. Living with, managing and minimising treatment burden in long term conditions: a systematic review of qualitative research. PLoS One. 2015;10(5):e0125457.
Article PubMed PubMed Central CAS Google Scholar
May C, Montori VM, Mair FS. We need minimally disruptive medicine. BMJ. 2009;339
Ridgeway JL, Egginton JS, Tiedje K, Linzer M, Boehm D, Poplau S, et al. Factors that lessen the burden of treatment in complex patients with chronic conditions: a qualitative study. Patient prefer adherence. Dove Press. 2014;8:339–51.
Coulter A, Entwistle VA, Eccles A, Ryan S, Shepperd S, Perera R. Personalised care planning for adults with chronic or long-term health conditions. Cochrane Database Syst Rev. 2015;3:CD010523.
Sinnott C, Mc Hugh S, Browne J, Bradley CGP. Perspectives on the management of patients with multimorbidity: systematic review and synthesis of qualitative research. BMJ Open. 2013;3(9):e003610.
Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med. 2013;11(1):21.
Pawson R. Evidence-based policy: a realist perspective. London: Sage publicaitons; 2006.
Book Google Scholar
Pawson R, Walshe K, Greenhalgh T. Realist synthesis: an introduction. 2004.
Kastner M, Estey E, Perrier L, Graham ID, Grimshaw J, Straus SE, et al. Understanding the relationship between the perceived characteristics of clinical practice guidelines and their uptake: protocol for a realist review. Implement Sci. 2011;6(1):1–9.
Wong G, Westhorp G, Pawson R, Greenhalgh T. Realist synthesis. RAMESES training materials. RAMESES Proj. 2013:55.
Bunn F, Goodman C, Manthorpe J, Durand M-A, Hodkinson I, Rait G, et al. Supporting shared decision-making for older people with multiple health and social care needs: a protocol for a realist synthesis to inform integrated care models. BMJ Open. 2017;7(2):e014026.
Wong G, Westhorp G, Pawson R, Greenhalgh T. Realist Synthesis. RAMESES Training Materials. NIHR HSDR. 2013:55.
Manzano A. The craft of interviewing in realist evaluation. Evaluation. 2016;22(3):342–60.
Pearson M, Brand SL, Quinn C, Shaw J, Maguire M, Michie S, et al. Using realist review to inform intervention development: methodological illustration and conceptual platform for collaborative care in offender mental health. Implement Sci Implementation Science. 2015;10(1):134.
Legare F, Stacey D, Pouliot S, Gauvin FP, Desroches S, Kryworuchko J, et al. Interprofessionalism and shared decision-making in primary care: a stepwise approach towards a new model. J Interprof Care. 2011;25(1):18–25.
Article PubMed Google Scholar
Ford JA, Wong G, Jones AP, Steel N. Access to primary care for socioeconomically disadvantaged older people in rural areas: a realist review. BMJ Open. 2016:1–14.
Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review--a new method of systematic review designed for complex policy interventions. J Heal Serv Res Policy. 2005;10(Suppl 1):21–34. Available from: https://doi.org/10.1258/1355819054308530%0A
Rycroft-Malone J, Burton C, Hall B, McCormack B, Nutley S, Seddon D, et al. Improving skills and care standards in the support workforce for older people: a realist review. BMJ Open. 2014;4(5):e005356.
Pawson R. Evidence-based policy: the promise of ‘realist synthesis’. Evaluation. 2002;8(3):340–58.
Wong G, Pawson R, Owen L. Policy guidance on threats to legislative interventions in public health: a realist synthesis. BMC Public Health. 2011;11:222.
Shay AL, Lafata JE. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med Decis Mak. 2015;35(1):114–31.
Durand M-A, Carpenter L, Dolan H, Bravo P, Mann M, Bunn F, et al. Do interventions designed to support shared decision- making reduce health inequalities? A systematic review and meta-analysis. PLoS One. 2014;9(4):1–13.
Austin CA, Mohottige D, Sudore RL, Smith AK, Hanson LC. Tools to promote shared decision making in serious illness. JAMA Intern Med. 2015;175(7):1213.
Belanger E, Rodriguez C, Groleau D. Shared decision-making in palliative care: a systematic mixed studies review using narrative synthesis. Palliat Med. 2011;25(3):242–61.
Bratzke LC, Muehrer RJ, Kehl KA, Lee KS, Ward EC, Kwekkeboom KL. Self-management priority setting and decision-making in adults with multimorbidity: a narrative review of literature. Int J Nurs Stud Elsevier Ltd. 2015;52(3):744–55.
Clayman ML, Bylund CL, Chewning B, Makoul G. The impact of patient participation in health decisions within medical encounters: a systematic review. Med Decis Mak. 2016;36:427–52.
Couët N, Desroches S, Robitaille H, Vaillancourt H, Leblanc A, Turcotte S, et al. Assessments of the extent to which health-care providers involve patients in decision making: a systematic review of studies using the OPTION instrument. Health Expect. 2015;18(4):542–61.
Coylewright M, Branda M, Inselman JW, Shah N, Hess E, LeBlanc A, et al. Impact of sociodemographic patient characteristics on the efficacy of decision aids a patient-level meta-analysis of 7 randomized trials. Circ Cardiovasc Qual Outcomes. 2014;7(3):360–7.
Doyle C, Lennox L. Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):1–18.
Dwamena F, Holmes-Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012/12/14. 2012;12:Cd003267.
PubMed Google Scholar
Dy SM, Purnell TS. Key concepts relevant to quality of complex and shared decision-making in health care: a literature review. Soc Sci Med Elsevier Ltd. 2012;74(4):582–7.
Edwards M, Davies M, Edwards A. What are the external influences on information exchange and shared decision-making in healthcare consultations: a meta-synthesis of the literature. Patient Educ Couns Ireland. 2009;75(1):37–52.
Elliott J, McNeil H, Ashbourne J, Huson K, Boscart V, Stolee P. Engaging Older Adults in Health Care Decision-Making: A Realist Synthesis. Patient. 2016;9:383–93.
Elwyn G, Scholl I, Tietbohl C, Mann M, Edwards AG, Clay C, et al. “Many miles to go ...”: a systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med Inf Decis Mak. 2013;13(Suppl 2):S14.
Fagerlin A, Pignone M, Abhyankar P, Col N, Feldman-Stewart D, Gavaruzzi T, et al. Clarifying values: an updated review. BMC Med Inform Decis Mak. 2013;13(Suppl 2):S8.
Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94(3):291–309.
Land V, Parry R, Seymour J. Communication practices that encourage and constrain shared decision making in health-care encounters: Systematic review of conversation analytic research. Health Expect. 2017;20:1228–47. https://doi.org/10.1111/hex.12557 .
Legare F, Ratte S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73(3):526–35.
Légaré F, Stacey D, Turcotte S, Cossi MJ, Kryworuchko J, Graham ID, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2014;9:CD006732.
Légaré F, Turcotte S, Stacey D, Ratté S, Kryworuchko J, Graham ID. Patients’ perceptions of sharing in decisions. Patient - Patient-Centered Outcomes Res. 2012;5(1):1–19.
Miller LM, Whitlatch CJ, Lyons KS. Shared decision-making in dementia: a review of patient and family carer involvement. Dementia. 2014;15(5):1141–57.
Stacey D, Kryworuchko J, Belkora J, Davison BJ, Durand MA, Eden KB, et al. Coaching and guidance with patient decision aids: a review of theoretical and empirical evidence. BMC Med Inform Decis Mak. 2013;13(Suppl 2):S11.
van Weert JC, van Munster BC, Sanders R, Spijker R, Hooft L, Jansen J. Decision aids to help older people make health decisions: a systematic review and meta-analysis. BMC Med Inform Decis Mak. 2016;16:45.
Belkora JK, Loth MK, Chen DF, Chen JY, Volz S, Esserman LJ. Monitoring the implementation of consultation planning, recording, and summarizing in a breast care center. Patient Educ Couns. 2008;73(3):536–43.
Berntsen GKR, Gammon D, Steinsbekk A, Salamonsen A, Foss N, Ruland C, et al. How do we deal with multiple goals for care within an individual patient trajectory? A document content analysis of health service research papers on goals for care. BMJ Open. 2015;5(12):e009403.
Blom J, den Elzen W, van Houwelingen AH, Heijmans M, Stijnen T, Van den Hout W, et al. Effectiveness and cost-effectiveness of a proactive, goal-oriented, integrated care model in general practice for older people. A cluster randomised controlled trial: integrated systematic care for older people--the ISCOPE study. Age ageing. England. 2016;45(1):30–41.
Bookey-Bassett S, Markle-Reid M, Mckey CA, Akhtar-Danesh N. Understanding interprofessional collaboration in the context of chronic disease management for older adults living in communities: a concept analysis. J Adv Nurs England. 2017;73(1):71–84.
Bridges J, Hughes J, Farrington N, Richardson A. Cancer treatment decision-making processes for older patients with complex needs: a qualitative study. BMJ Open England. 2015;5(12):e009674.
Bugge C, Entwistle VA, Watt IS. The significance for decision-making of information that is not exchanged by patients and health professionals during consultations. Soc Sci Med. 2006;63(8):2065–78.
Bynum J, Barre L, Reed Catherine PH. Participation of very old adults in healthcare decisions. Med Decis Mak. 2014;34(2):216–30.
Chong WW, Aslani P, Chen TF. Shared decision-making and interprofessional collaboration in mental healthcare: a qualitative study exploring perceptions of barriers and facilitators. J Interprof Care. 2013;27(5):373–9.
Chong WW, Aslani P, Chen TF. Multiple perspectives on shared decision-making and interprofessional collaboration in mental healthcare. J Interprof Care. 2013;27(3):223–30.
Col N, Bozzuto L, Kirkegaard P, Koelewijnvan Loon M, Majeed H, Jen Ng C, et al. Interprofessional education about shared decision making for patients in primary care settings. J Interprof Care. 2011;25(6):409–15.
Cramm JM, Nieboer AP. The changing nature of chronic care and coproduction of care between primary care professionals and patients with COPD and their informal caregivers. Int J COPD. 2016;11:175–82.
Article CAS Google Scholar
Cramm JM, Nieboer AP. In the Netherlands, rich interaction among professionals conducting disease management led to better chronic care. Health Aff (Millwood). United States. 2012;31(11):2493–500.
Cramm JM, Nieboer AP. A longitudinal study to identify the influence of quality of chronic care delivery on productive interactions between patients and (teams of) healthcare professionals within disease management programmes. BMJ Open. England. 2014;4(9):e005914.
Dardas AZ, Stockburger C, Boone S, An T, Calfee RP. Preferences for shared decision making in older adult patients with orthopedic hand conditions. J Hand Surg Am United States. 2016;41(10):978–87.
Durand M-A, Barr PJ, Walsh T, Elwyn G. Incentivizing shared decision making in the USA – where are we now? Healthc (Amsterdam, Netherlands). Netherlands. 2015;3(2):97–101.
Edwards A, Elwyn G, Hood K, Atwell C, Robling M, Houston H, et al. Patient-based outcome results from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Fam Pract. 2004;21(4):347–54.
Elwyn G, Edwards A, Hood K, Robling M, Atwell C, Russell I, et al. Achieving involvement: process outcomes from a cluster randomized trial of shared decision-making skill development and use of risk communication aids in general practice. Fam Pr. 2004;21:337–46.
Farrelly S, Lester H, Rose D, Birchwood M, Marshall M, Waheed W, et al. Barriers to shared decision making in mental health care: qualitative study of the joint crisis plan for psychosis. Health Expect. 2016;19(2):448–58.
Fried TR, O’Leary J, Van Ness P, Fraenkel L. Inconsistency over time in the preferences of older persons with advanced illness for life-sustaining treatment. J Am Geriatr Soc. 2007;55(7):1007–14.
Gleason KT, Tanner EK, Boyd CM, Saczynski JS, Szanton SL. Factors associated with patient activation in an older adult population with functional difficulties. Patient Educ Couns Elsevier Ireland Ltd. 2016;99(8):1421–6.
Grim K, Rosenberg D, Svedberg P, Schön UK. Shared decision-making in mental health care – A user perspective on decisional needs in community-based services. Int J Qual Stud Health Well-being. 2016;11:30563.
Groen-van de Ven L, Smits C, Span M, Jukema J, Coppoolse K, de Lange J, et al. The challenges of shared decision making in dementia care networks [published online ahead of print 9 September 2016]. Int Psychogeriatr; 2016.
Hacking B, Wallace L, Scott S, Kosmala-Anderson J, Belkora J, McNeill A. Testing the feasibility, acceptability and effectiveness of a “decision navigation” intervention for early stage prostate cancer patients in Scotland - a randomised controlled trial. Psychooncology. 2013;22(5):1017–24.
Hart JL, Pflug E, Madden V, Halpern SD. Thinking forward: future-oriented thinking among patients with tobacco-associated thoracic diseases and their surrogates. Am J Respir Crit Care Med. 2016;193(3):321–9.
Herlitz A, Munthe C, Törner M, Forsander G. The counseling, self-care, adherence approach to person-centered care and shared decision making: moral psychology, executive autonomy, and ethics in multi-dimensional care decisions. Health Commun. 2016;31(8):964–73.
Jones JB, Bruce CA, Shah NR, Taylor WF, Stewart WF. Shared decision making: using health information technology to integrate patient choice into primary care. Transl Behav Med United States. 2011;1(1):123–33.
Joseph-Williams N, Lloyd A, Edwards A, Stobbart L, Tomson D, Macphail S, et al. Implementing shared decision making in the NHS: lessons from the MAGIC programme. BMJ. 2017;1744:j1744.
Körner M, Ehrhardt H, Steger A-K. Designing an interprofessional training program for shared decision making. J Interprof Care. 2013;27(2):146–54.
Kuluski K, Gill A, Naganathan G, Upshur R, Jaakkimainen RL, Wodchis WP. A qualitative descriptive study on the alignment of care goals between older persons with multi-morbidities, their family physicians and informal caregivers. BMCFamPract. 2013;14:133.
Ladin K, Lin N, Hahn E, Zhang G, Koch-Weser S, Weiner DE. Engagement in decision-making and patient satisfaction: a qualitative study of older patients’ perceptions of dialysis initiation and modality decisions. Nephrol Dial Transplant England. 2016;32(8):1–8.
Légaré F, Stacey D, Gagnon S, Dunn S, Pluye P, Frosch D, et al. Validating a conceptual model for an inter-professional approach to shared decision making: a mixed methods study. J Eval Clin Pract. 2011;17(4):554–64.
Mercer SW, O’Brien R, Fitzpatrick B, Higgins M, Guthrie B, Watt G, et al. The development and optimisation of a primary CARE-based whole system complex intervention (CARE plus) for patients with multimorbidity living in areas of high socioeconomic deprivation. Chronic Illn. 2016;12(3):165–81.
Naik AD, Martin LA, Moye J, Health Values KMJ. Treatment goals of older, multimorbid adults facing life-threatening illness. J Am Geriatr Soc. 2016;64(3):625–31.
Politi MC, Street RL. The importance of communication in collaborative decision making: facilitating shared mind and the management of uncertainty. J Eval Clin Pract. 2011;17(4):579–84.
Robben S, van Kempen J, Heinen M, Zuidema S, Olde Rikkert M, Schers H, et al. Preferences for receiving information among frail older adults and their informal caregivers: a qualitative study. Fam Pr. 2012/04/26. 2012;29(6):742–7.
Ruggiano N, Whiteman K, Shtompel N. “If I Don’t like the way I feel with a certain drug, I’ll tell them.”: older adults’ experiences with self-determination and health self-advocacy. J Appl Gerontol 2014/04/23. 2016;35(4):401–20.
Sanders ARJ, Bensing JM, Essed MALU, Magnée T, de Wit NJ, Verhaak PF. Does training general practitioners result in more shared decision making during consultations? Patient Educ Couns. Elsevier Ireland Ltd; 2016;100(3):563–574.
Schaller S, Marinova-Schmidt V, Setzer M, Kondylakis H, Griebel L, Sedlmayr M, et al. Usefulness of a tailored eHealth Service for Informal Caregivers and Professionals in the dementia treatment and care setting: the eHealthMonitor dementia portal. JMIR Res Protoc. 2016;5(2):e47.
Schaller S, Marinova-Schmidt V, Gobin J, Criegee-Rieck M, Griebel L, Engel S, et al. Tailored e-health services for the dementia care setting: a pilot study of “eHealthMonitor”. BMC med inform Decis Mak. England. 2015;15:58.
Shay LA, Lafata JE. Understanding patient perceptions of shared decision making. Patient Educ Couns. 2014;96(3):295–301.
Sheaff R, Halliday J, Byng R, Øvretveit J, Exworthy M, Peckham S, et al. Bridging the discursive gap between lay and medical discourse in care coordination. Sociol Health Illn. 2017;39:1019–34.
Schuling J, Gebben H, Veehof LJG, Haaijer-Ruskamp FM. Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Fam Pract England. 2012;13:56.
Baqir W, Hughes J, Jones T, Barrett S, Desai N, Copeland R, et al. Impact of medication review, within a shared decision-making framework, on deprescribing in people living in care homes. Eur J Hosp Pharm. 2016;24(1):30. LP-33
van JJGT S, Haaijer-Ruskamp FM, Schuling J. Eliciting preferences of multimorbid elderly adults in family practice using an outcome prioritization tool. J Am Geriatr Soc Netherlands. 2016;64(11):e143–8.
Wrede-Sach J, Voigt I, Diederichs-Egidi H, Hummers-Pradier E, Dierks M-L, Junius-Walker U. Decision-making of older patients in context of the doctor-patient relationship: a typology ranging from “self-determined” to “doctor-trusting” patients. Int J Family Med. 2013;2013:478498.
Tietbohl CK, Rendle KAS, Halley MC, May SG, Lin GA, Frosch DL. Implementation of patient decision support interventions in primary care: the role of relational coordination. Med Decis Making United States. 2015;35(8):987–98.
Zoffmann V, Harder I. Kirkevold M. A person-centered communication and reflection model: sharing decision-making in chronic care. Qual Health Res. 2008;18(5):670–85.
Foot C, Gilburt H, Dunn P, Jabbal J, Seale B, Goodrich J, Buck D TJ. People in control of their own health and care: the state of involvement. London; 2014.
Nunes V, Neilson J, O’Flynn N, Calvert N, Kuntze S, Smithson H, et al. Medicines Adherence: involving patients in decisions about prescribed medicines and supporting adherence full guideline January 2009 National Collaborating Centre for primary. London; 2009.
Health Foundation. The Power of People. [cited 14 Jul 2017]. Available from: http://www.health.org.uk/node/10181
Lown BA, Kryworuchko J, Bieber C, Lillie DM, Kelly C, Berger B, et al. Continuing professional development for interprofessional teams supporting patients in healthcare decision making. J Interprof Care. 2011;25(6):401–8.
Holmside Medical Group. The Holmside story person centred primary care: care and support planning. Newcastle-upon-Tyne: Quality Care Commission; 2014.
Berger Z. Navigating the unknown: shared decision-making in the face of uncertainty. J Gen Intern Med. 2015;30(5):675–8.
Agoritsas T, Heen AF, Brandt L, Alonso-Coello P, Kristiansen A, Akl EA, et al. Decision aids that really promote shared decision making: the pace quickens. BMJ. 2015;350:g7624.
Barrett B, Ricco J, Wallace M, Kiefer D, Rakel D. Communicating statin evidence to support shared decision-making. BMC fam Pract. England. 2016;17:41.
Eaton S, Roberts S, Turner B. Delivering person centred care in long term conditions. BMJ. 2015;350(h181):4.
Clayman ML, Gulbrandsen P, Morris MA. A patient in the clinic; a person in the world. Why shared decision making needs to center on the person rather than the medical encounter. Patient Educ Couns. Elsevier Ireland Ltd. 2017;100(3):600–4.
Cooper Z, Koritsanszky LA, Cauley CE, Frydman JL, Bernacki RE, Mosenthal AC, et al. Recommendations for best communication practices to facilitate goal-concordant Care for Seriously ill Older Patients with Emergency Surgical Conditions. Ann Surg. 2016;263(1):1–6.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med 2012/05/24. 2012;27(10):1361–7.
Gorin M, Joffe S, Dickert N, Halpern S. Justifying clinical nudges. Hast Cent Rep. 2017;47(2):32–8.
Fiscella K, Meldrum S, Franks P, Shields CG, Duberstein P, McDaniel SH, et al. Patient trust: is it related to patient-centered behavior of primary care physicians? Med Care. 2004;42(11):1049–55.
Depatment of Health. The NHS constitution. Dh; 2015.
IPDAS. International Patient Decision Aid Standards (IPDAS) Collaboration: What are patient decision aids. [cited 8 Jul 2017]. Available from: http://ipdas.ohri.ca/what.html
Bunn F, Burn A, Robinson L, Poole M, Rait G, Brayne C, et al. Healthcare organisation and delivery for people with dementia and comorbidity: a qualitative study exploring the views of patients, carers and professionals. BMJ Open. 2017;7(1):e013067.
Joseph-Williams N, Edwards A, Elwyn G. Power imbalance prevents shared decision making. BMJ. 2014;348(3):g3178.
Mavis B, Holmes Rovner M, Jorgenson S, Coffey J, Anand N, Bulica E, et al. Patient participation in clinical encounters: a systematic review to identify self-report measures. Health Expect. 2015;18(6):1827–43.
Kitson A, Marshall A, Bassett K, Zeitz K. What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J Adv Nurs. 2013;69(1):4–15.
Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–110.
Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–21. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=274066&tool=pmcentrez&rendertype=abstract
Freeman GK, Woloshynowych M, Baker R, Boulton M, Guthrie B, Car J, et al. Continuity of care 2006: what have we learned since 2000 and what are policy imperatives now?. National Co-ordinating Centre for NHS Service Delivery and Organisation (NCCSDO). London; 2007 [cited 20 Nov 2017]. Available from: http://www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1609-138_V01.pdf
Parker G, Corden A, Heaton J. Experiences of and influences on continuity of care for service users and carers: synthesis of evidence from a research programme. Health Soc Care Community. Blackwell Publishing Ltd. 19(6):576–601. Available from: https://doi.org/10.1111/j.1365-2524.2011.01001.x
Download references
Acknowledgments
We would like to acknowledge the contribution of Ms. Sue Davies who worked as a researcher on the project. We thank our Project Advisory Group, Dr. Geoff Wong (Chair), Ms. Jane Hopkins, Mrs. Jeanne Carlin, Ms. Natalie Koussa and patient and public involvement members, Dr. Paul Millac and Ms. Marion Cowe, for their support and guidance.
Study registration: This study is registered as PROSPERO CRD42016039013.
This work is supported by the National Institute for Health Research (NIHR) HS&DR project reference: 15/77/25.
This report presents independent research commissioned by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Frances Bunn is the guarantor for the manuscript
She affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Author information
Authors and affiliations.
Centre for Research in Public Health and Community Care, University of Hertfordshire, College Lane, Hatfield, Hertfordshire, AL10 9AB, UK
Frances Bunn, Claire Goodman & Bridget Russell
Centre for Health Service Studies, University of Kent, George Allen Wing, Canterbury, Kent, CT2 7NF, UK
Patricia Wilson
Social Care Workforce Research Unit, King’s College London, Strand, London, WC2B 4LL, UK
Jill Manthorpe
Research Department of Primary Care and Population Health, UCL Medical School (Royal Free Campus), Rowland Hill Street, London, NW3 2PF, UK
Tower Hamlets Clinical Commissioning Group, The Tredegar Practice, London, E3 5JD, UK
Isabel Hodkinson
The Preference Laboratory, The Dartmouth Institute for Health Policy & Clinical Practice, Level 5, Williamson Translational Research Building, Lebanon, New Hampshire, USA
Marie-Anne Durand
You can also search for this author in PubMed Google Scholar
Contributions
FB was the principal investigator, led the study, was involved in all aspects of the review process and wrote the manuscript, CG was a coapplicant on the grant, was involved in study design, was involved in research team meetings and workshops, gave feedback between meetings and participated in the synthesis process and preparation of the manuscript, BR was involved in all aspects of the review process and participated in the preparation of the final report, PW was a coapplicant on the grant, was involved in review processes, attended research team meetings and workshops and participated in the preparation of the manuscript, GM was a coapplicant on the grant, was involved in review processes, attended research team meetings and workshops and participated in the preparation of the manuscript, GR was a coapplicant on the grant, was involved in study design, attended workshops and meetings and participated in the preparation of the manuscript, IH was a coapplicant on the grant, was involved in study design, attended workshops and meetings and commented on the final manuscript, MAD was a coapplicant on the grant, was involved in review processes and participated in the preparation of the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Frances Bunn .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the University of Hertfordshire Health and Human Sciences Ethics Committee with delegated authority (ECDA), reference number HSK/SF/UH/02387. Written informed consent was obtained from all participants.
Consent for publication
Competing interests.
All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/conflicts-of-interest/ and declare: all authors had financial support from National Institute for Health Research (NIHR) HS&DR for the submitted work, Rait is a member of the HTA Commissioning Board, HTA Methods Group and Panel, Goodman is an NIHR Senior Investigator. Goodman and Manthorpe are Trustees of the Order of St John Care Trust, Manthorpe is Chair of the NIHR Policy Research Programme Board, and Durand reports personal fees from EBSCO Health and ACCESS Community Health Network outside the submitted work. There are no other financial relationships with any organisations that might have an interest in the submitted work in the previous three years.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
Table summarising details of included systematic reviews. (DOCX 21 kb)
Additional file 2:
Table summarising details of included primary studies. (DOCX 79 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Bunn, F., Goodman, C., Russell, B. et al. Supporting shared decision making for older people with multiple health and social care needs: a realist synthesis. BMC Geriatr 18 , 165 (2018). https://doi.org/10.1186/s12877-018-0853-9
Download citation
Received : 20 March 2018
Accepted : 28 June 2018
Published : 18 July 2018
DOI : https://doi.org/10.1186/s12877-018-0853-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Shared decision making
- Person-centred care
- Realist synthesis
- Multimorbidity
- Older people
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Understanding the dynamics of sustainable change: A 20-year case study of integrated health and social care
Affiliations.
- 1 Department of Learning, Informatics, Management and Ethics (LIME), Medical Management Centre (MMC) | Karolinska Institutet, 171 77, Stockholm, Sweden. [email protected].
- 2 Department of Learning, Informatics, Management and Ethics (LIME), Medical Management Centre (MMC) | Karolinska Institutet, 171 77, Stockholm, Sweden.
- PMID: 29866114
- PMCID: PMC5987399
- DOI: 10.1186/s12913-018-3061-6
Background: Change initiatives face many challenges, and only a few lead to long-term sustainability. One area in which the challenge of achieving long-term sustainability is particularly noticeable is integrated health and social care. Service integration is crucial for a wide range of patients including people with complex mental health and social care needs. However, previous research has focused on the initiation, resistance and implementation of change, while longitudinal studies remain sparse. The objective of this study was therefore to gain insight into the dynamics of sustainable changes in integrated health and social care through an analysis of local actions that were triggered by a national policy.
Methods: A retrospective and qualitative case-study research design was used, and data from the model organisation's steering-committee minutes covering 1995-2015 were gathered and analysed. The analysis generated a narrative case description, which was mirrored to the key elements of the Dynamic Sustainability Framework (DSF).
Results: The development of inter-sectoral cooperation was characterized by a participatory approach in which a shared structure was created to support cooperation and on-going quality improvement and learning based on the needs of the service user. A key management principle was cooperation, not only on all organisational levels, but also with service users, stakeholder associations and other partner organisations. It was shown that all these parts were interrelated and collectively contributed to the creation of a structure and a culture which supported the development of a dynamic sustainable health and social care.
Conclusion: This study provides valuable insights into the dynamics of organizational sustainability and understanding of key managerial actions taken to establish, develop and support integration of health and social care for people with complex mental health needs. The service user involvement and regular reviews of service users' needs were essential in order to tailor services to the needs. Another major finding was the importance of continuously adapting the content of the change to suit its context. Hence, continuous refinement of the change content was found to be more important than designing the change at the pre-implementation stage.
Keywords: Change management; Implementation; Integrated care; Mental health; Organisational sustainability.
Publication types
- Research Support, Non-U.S. Gov't
- Delivery of Health Care, Integrated* / organization & administration
- Health Services Research
- Mental Health Services / organization & administration*
- Mental Health Services / standards
- Middle Aged
- Organizational Culture
- Organizational Innovation
- Qualitative Research
- Quality Improvement / organization & administration*
- Quality Improvement / standards
- Retrospective Studies
- Social Work / organization & administration*
- Social Work / standards
Grants and funding
- 2014-0303/FORTE/International
- 521-2014-2710/The Swedish Research Council/International
- Research article
- Open access
- Published: 04 June 2018
Understanding the dynamics of sustainable change: A 20-year case study of integrated health and social care
- Charlotte Klinga ORCID: orcid.org/0000-0003-0512-8719 1 ,
- Henna Hasson 1 ,
- Magna Andreen Sachs 1 &
- Johan Hansson 1
BMC Health Services Research volume 18 , Article number: 400 ( 2018 ) Cite this article
4107 Accesses
21 Citations
3 Altmetric
Metrics details
Change initiatives face many challenges, and only a few lead to long-term sustainability. One area in which the challenge of achieving long-term sustainability is particularly noticeable is integrated health and social care. Service integration is crucial for a wide range of patients including people with complex mental health and social care needs. However, previous research has focused on the initiation, resistance and implementation of change, while longitudinal studies remain sparse. The objective of this study was therefore to gain insight into the dynamics of sustainable changes in integrated health and social care through an analysis of local actions that were triggered by a national policy.
A retrospective and qualitative case-study research design was used, and data from the model organisation’s steering-committee minutes covering 1995-2015 were gathered and analysed. The analysis generated a narrative case description, which was mirrored to the key elements of the Dynamic Sustainability Framework (DSF).
The development of inter-sectoral cooperation was characterized by a participatory approach in which a shared structure was created to support cooperation and on-going quality improvement and learning based on the needs of the service user. A key management principle was cooperation, not only on all organisational levels, but also with service users, stakeholder associations and other partner organisations. It was shown that all these parts were interrelated and collectively contributed to the creation of a structure and a culture which supported the development of a dynamic sustainable health and social care.
This study provides valuable insights into the dynamics of organizational sustainability and understanding of key managerial actions taken to establish, develop and support integration of health and social care for people with complex mental health needs. The service user involvement and regular reviews of service users’ needs were essential in order to tailor services to the needs. Another major finding was the importance of continuously adapting the content of the change to suit its context. Hence, continuous refinement of the change content was found to be more important than designing the change at the pre-implementation stage.
Peer Review reports
Because organisational change requires investments of time, money and human resources, the lasting impact of this type of change is generally of great interest to care providers, funders and other stakeholders. Change initiatives, however, face many challenges, and only a few of them lead to long-term sustainability [ 1 ]. Knowledge of whether program outcomes are beneficial and sustainable is also valuable when spreading and supporting such programs across several settings [ 2 ]. In the health sector, the prior research has mainly been focused on the early stages of the change process – initiation, resistance and implementation [ 3 , 4 , 5 ] – and longitudinal studies are sparse [ 1 , 5 , 6 ] . The research on strategies for achieving sustainability in change initiatives is rather scant [ 7 ], and studies that explicitly address sustainability are almost absent [ 8 ]. Therefore, knowledge on how to achieve long-term maintenance of organisational changes is needed [ 2 , 9 ].
The recent research highlights several factors’ influences on sustainability, including the content of the change and its contextual, political, organisational, processual and temporal factors [ 5 , 10 ]. Certain enabling factors have been highlighted, including a supportive context, capacity building, effective relationships among the actors, and rigorous planning and decision making [ 11 ]. However, few investigations of these factors or of the possible interrelationships between them have been conducted [ 12 ]. Thus, the ways in which these factors interact and impact sustainable change remain unclear.
A conventional way to study sustainability is to describe the extent to which the change content is maintained over a period of time – for instance, after initial or external support is removed [ 2 , 13 ]. This approach assumes that the change content is constant over time. However, adaptations to changes in local conditions are common and sometimes necessary. Thus, interventions are rarely implemented as they were originally intended, and their content often varies over time [ 14 ]. This makes the concepts of fidelity and adaptation to intervention important in sustainability studies [ 13 ]. These two concepts are inherently linked [ 15 ] ways of overcoming organisational inertia while adapting to contemporary environmental changes [ 16 ].
Chambers [ 13 ] recently proposed a more dynamic view on sustainability called the Dynamic Sustainability Framework (DSF); in this view, change is an ongoing adaptation process in which the intervention is continuously refined and improved in relation to its context. The context comprises the practice setting, its surroundings and the ecological system [ 13 ]. Thus, the DSF addresses the paradox of sustainability amid ongoing change. The fit between the intervention and the local context can be optimized by continuously matching the characteristics of the intervention to the practice setting and the ecological system through appropriate improvements [ 13 ]. This is an iterative, dynamic process in which continued learning and development are central. Thus, ongoing quality improvement is the ultimate goal of such interventions.
One area in which the challenge of achieving long-term sustainability is particularly noticeable is integrated health and social care. In the contemporary system, which was constructed to provide diverse, unconnected health and social care services, those who protect these systems’ separate regulations and policies may constantly challenge the idea that the systems should be integrated [ 17 ]. Additional challenges include organisations’ conflicting objectives and values as well as professionals’ distinct cultures [ 18 ]. Hence, there is neither a universal definition of integrated care nor a one-size-fits-all model [ 19 , 20 ]. However, evidence has demonstrated that integrated health and social care leads to care that is more people-centric and holistic; this can be achieved by developing cross-sectoral and inter-professional collaboration [ 21 ]. Such services is of great value for people who have complex health and social care needs, such as those who are suffering from mental illness. One major objective that the World Health Organisation (WHO) set forth in its Mental Health Action Plan 2013-2020 [ 22 ] was to provide comprehensive, integrated mental health and social care services in community-based settings . Hence, innovative approaches are needed in both technical and relational aspects [ 23 ]. To facilitate long-term organisational sustainability, policies must address the entire health system, including incentive structures and performance measures [ 17 ]. A 2016 review concluded that no complete, peer-evaluated longitudinal studies have been conducted on integrated health and social care [ 24 ], so the uncertainty regarding long-term effects remains.
In Sweden, the responsibility for the provision of health and social care services is managed on three levels: the government (national level), the 21 county councils (regional level) and the 290 municipalities (local level). The county councils have the responsibility for provision of health care and the municipalities for the provision of care for elderly and disabled people, as well people in need of long-term mental health care. Municipalities and county councils have a substantial freedom to organise health and social care services [ 25 ]. Since the 1990s several structural changes have aimed to move from inpatient care towards outpatient care [ 26 ]. That was also the case in 1995 when Sweden launched a national policy which was manifested in the Health and Medical Care Act, Social Services Act and The Swedish Act concerning Support and Service for Persons with Certain Functional Impairments to create more integrated services for people with mental illnesses. The policy’s goals were to improve the coordination and individualisation of care and by service user involvement integrate them into society. The policy clarified the municipality’s responsibility for planning and coordinating interventions and for developing housing and employment for those who suffer from mental disorders. As before, the county council’s responsibilities were the prevention, investigation and treatment of psychiatric conditions [ 27 ]. The continued sectoral division of care and support meant that the county and municipal social care organisations have to develop cooperation to meet the service users’ complex needs. However, the authorities in Sweden interpreted the policy differently.
More than 20 years have passed since the policy was introduced. In that time, much has changed, but the division of responsibilities between the municipality and the county remains a key challenge in providing cohesive health and social care [ 28 ]. A recent study found that, at a policy level, establishing an overall perspective on healthcare and social support for people with mental illness has been difficult. The reasons for this include shortcomings in cooperation between the levels of care and inadequate coordination between social services, primary care, employment services and the nation’s social insurance agency. The focus remains split among various components rather than on the whole picture [ 29 ].
Nevertheless, examples of sector-related barriers being overcome exist. For instance, one geographical area has sustained its extensive integration of mental health and social care services since the policy was implemented [ 30 ]. For the purpose of this paper we use the definition from WHO for integrated health services [ 18 ].
“Integrated health services are health services that are managed and delivered in a way that ensures people receive a continuum of health promotion, disease prevention, diagnosis, treatment, disease management, rehabilitation and palliative care services, at the different levels and sites of care within the health system, and according to their needs throughout their life course ”.
The abbreviation IC will be used, referring to integrated mental health and social care services. Based on our previous research [ 30 , 31 , 32 ], we anticipated that this case would be particularly interesting to study from a sustainability perspective. By viewing sustainability as a process in a constantly changing context, the DSF is a relevant means through which to explore the mechanisms of sustainability in this integrated mental health and social care organisation.
The specific objective of this study is to gain insight into the dynamics of sustainable changes in integrated health and social care through an analysis of local actions that were trigged by a national policy.
To study inter-sectoral cooperation, a retrospective and qualitative case-study research design was applied based on data from the model organisation’s steering-committee minutes from 1995 through 2015.
Study setting
The area of Sweden in which the inter-sectoral cooperation took place has a long record of providing integrated health and social care, with the county council providing psychiatric care and the municipality providing social services. The population in this urban area is just over 96,000; the proportion of the population with a foreign background is 51%; the average age is 39 years; the employment rate of 20-64 years is 72% [ 33 ]. This case was chosen because it represented a unique example of long-lasting, inter-sectoral cooperation. Since the introduction of the national psychiatric policy, the cooperating agencies have striven to overcome fragmented health and social care. Through the policy, the obligation of people for those with long-term psychiatric disorders upon their discharge from closed-environment mental health institutions was transferred from the county council to the municipality. During the policy’s establishment period (1996-1998), funding was available for both the county council and the municipality, provided that they presented a shared plan for how the money would be used to facilitate organisational and operational changes.
The original idea behind this integration was to create a single point at which all service users could receive help and support, regardless of which authority had the competence or means to address the problem. Initially, this plan was to offer services to those over 18 years old who had chronic, severe mental illnesses that caused permanent disabilities, as well as to those who were in need of both psychiatric treatment and social services. Today, the integration has evolved to also include people with neuropsychiatric diagnoses, people with addiction problems and other target groups. Since 1995, a steering committee has governed the integrated organisation, with representatives from the county council’s psychiatric care and the municipality’s social services. The committee’s mission is to develop cooperation between the municipality’s social care and the county council’ psychiatric care . The services consist of geographically dispersed co-located centres and mobile units for specific target groups. Although separate legislation regulates the services, they are all organised based on inter-professional teams and are managed, at all levels, through co-leadership of two leaders, one from each organisation. Access to services is mainly via primary care but also from emergency care. Inpatient care is provided by the regional hospital.
Data collection and data characteristics
Data were collected from the minutes of all steering-committee meetings held from 1995 through 2015. The minutes were available in digital form ( n = 98; approximately 3-5 meetings per semester, fewer in recent years) and followed the same basic structure. However, some variation regarding the content occurred due to the relevance of certain topics and questions at certain times. This variation in content determined the committee’s composition; in addition to the permanent members – representatives from the county, the municipality and the stakeholder associations (e.g. patients’ and relatives’ associations) – other relevant stakeholders were invited. The same person wrote all the minutes, which were primarily for the internal use of the organisation’s managers and professionals. However, the minutes were also available to cooperating partners outside the organisation and to other interested stakeholders.
Data analysis
Thematic analysis, as Braun and Clarke [ 34 ] described, is used to handle extensive data sets. This study’s data included a large amount of information generated over twenty years, which required condensation; a semantic approach was used to handle this rich data set. Based on the study’s objective, an initial orientation was developed, and a search for codes and meaningful groups was performed. Based on the predetermined area of interest, actions not directly linked to integration were excluded. This first stage of the analysis was explorative and inductive [ 35 ]; data were used to map the steering committee’s actions. The resulting analysis was intended to illustrate the trend in integration over time and to serve as a basis for the subsequent analysis in stage 2, which was intended to mirror the findings regarding the key elements of the DSF. This procedure resulted in a detailed data analysis that would aid in identifying the empirical themes from the narrative description. The thematic analysis-process is illustrated in Table 1 .
The results are presented in two parts. The first, Case findings , provides a chronological case narrative of the key events related to the integration. The second, Empirical themes , is based on identified chains of actions that are reflected in DSF.
Case findings
The individual organisations had a history of collaboration prior to the launch of the psychiatric policy. That policy, however, triggered the development of an integrated health and social care organisation, with project funding provided for both the county council and the municipality. In 1995, both the inter-sectoral steering committee and the two project managers (one from each organisation) were put in place. One guiding principle was that all service users should be at the centre of – and participate in – the planning of care and support. The integrated organisation started by inventorying the need for staff training and for a cooperative model to apply with each service user. Stakeholder associations were involved, and the central role of the service users (i.e. the patients and clients), their families and the stakeholder associations was emphasised. A co-leadership model was created in which the leaders from each sector jointly managed all services. Joint trainings, information sessions, outdoor excursions and conferences were arranged. The continuous exchange of competencies and experiences was given high priority, and co-run projects targeted to specific groups, such as people with substance abuse, were initiated.
In 1996 and 1997, several changes were introduced to integrate the services. For instance, three co-located and jointly managed centres were opened, mainly for persons with psychosis and complex needs. Furthermore, each service user received coordinators from each organisation; these coordinators shared the responsibility for all of the user’s health and social care planning. Data on the service users’ needs (the Camberwell Assessment of Needs [CAN] scale) were used for these purposes. Individualised care and rehabilitation plans were introduced to personalise care and to support service users. In addition, shared clinical guidelines and agreements concerning financial issues were established. The overarching vision, in which service users would be active co-producers, triggered the development of a consistent terminology; the term ‘customer’, instead of ‘patient’ or ‘client’, was suggested. Nevertheless, the term ‘customer’ was incompatible with then-current national regulations, and the terms ‘patient’ (for psychiatric care) and ‘client’ (for social care) were kept. The importance of a shared IT system was recognised, and much effort was spent in trying to achieve this. However, the Swedish Data Protection Authority did not permit the use of such a shared register for service-users assessment data (using the CAN scale) because of questions regarding data ownership. Thereafter, the possibility of digitally sharing care and rehabilitation plans was examined.
In 1998, challenges related to financing surfaced, partly because the initial funding had ended. In addition, difficulties concerning the management of the integrated services were noted, as differences in managers’ decision-making mandates varied between the organisations. To meet these challenges, additional training in integration was offered; for instance, the two project managers received support in how to manage integrated projects, and the coordinators were trained in case management. The expansion of integration to include new groups of service users (e.g. those with severe mental disabilities) was considered. In addition, a new organisation was proposed that would be aimed at outsourcing cooperative units to the municipal districts, but the steering committee rejected this proposal due to the risk of losing coordination and the knowledge required for rehabilitation in the event of a disruption in the organisation’s integration.
In 1999, the steering committee reviewed the integrated organisation’s costs. Savings from the previous year enabled the financing of additional training to facilitate the handover of service users from external locations to the local municipality’s care. Actions were planned to simplify the practical work and to increase collaboration. For instance, the plan was for decisions about housing support to be transferred to the unit level (i.e. as close to the service users as possible) with the goal of improving collaboration among social workers, assistance officers and occupational therapists. The integrated organisation continued to grow; it initiated a mobile team and developed the coordinator role to enhance focus on the entire rehabilitation process. The shared use of the CAN data was further developed to tailor both health and social care to meet the service users’ individual needs.
In 2000 and 2001, efforts were made to make the two organisations’ economic steering mechanisms equivalent. The steering committee also expanded to include members who represented areas that had recently been integrated, such as elder care. It was agreed that all new projects within the integrated organisation would be managed in close collaboration and based on formal agreements – in contrast to earlier, verbal agreements. An example of concrete integration was the announcement of a vacant manager position on a psychiatric addiction team. The organisational affiliation for that position was decided based on the selected candidate’s profession (nurse or social worker) rather than in advance, when announcing the position. The integrated services were expanded with the opening of a day centre for people with borderline personality disorder.
During 2002 and 2003, the integrated services were further expanded by developing services for elderly people and for some new target groups (e.g. those with long-lasting depression and those who were unemployed or on sick leave due to mental health problems). Furthermore, a joint home-support group with staff from both organisations was proposed. In addition, several structural changes were made in the integrated organisation. For instance, social workers and assistance officers were decentralised and sent to the individual units, and co-location was planned for some administrators. The steering committee proposed further expansion to include a representative for service users who were covered by the law that regulated support and service for people with certain functional impairments.
During 2004 and 2005, actions were taken to further develop the practical work such as by opening a new coach position. The coach would support the managers in designing processes for shared service planning. New groups in need of integrated services were identified: people with Asperger’s disease or ADHD, those at risk of criminality or with addiction problems, asylum seekers with mental health problems, and individuals facing deportation. In addition, the organisation expanded by establishing a neuropsychiatric team and new accommodations for people with double diagnoses. The question was raised over whether to institute a common title – coordinator – for all employees, regardless of profession. This was considered to have a symbolic importance, as it would indicate that cooperation was central and that responsibilities could not be transferred across organisations. The steering committee continued to expand, this time with representatives from child and adolescent psychiatry.
In 2006, efforts were made to overcome evolving macro-level challenges. The integration agreement was revised to further clarify the organisations’ equal status and responsibilities concerning costs. Participation in further education became compulsory for all inter-professional team members, and opportunities for shared research and improvement activities were investigated. The senior county council managers decided to close one of the units. However, to avoid the closure, the municipality took over responsibility for the unit. Another example of integration development was the evolution of the coordinator role into the case manager role, as advocated in the national clinical guidelines on psychosis.
In 2007, a statement was made regarding the importance of giving equal value to the service users’ existential, medical, psychological and social well-being rather than emphasising only some of these depending on the organisation. The steering committee and the stakeholder associations presented a revised vision that highlighted how service users and the two organisations would cooperate to provide flexible and need-based support. This vision also specified the planning, development and evaluation of the units and the teams, emphasising that the professionals’ roles needed to be streamlined so that they would become experts. All service users’ needs were analysed to inform the organisation about whether its services should be revised. Some changes in the needs were noticed; consequently, the units revised their services to better suit people who lacked long histories of inpatient care. The organisation continued to expand by including services for young, self-harming people; the focus was on improving cooperation regarding young people and those with bipolar disorder or complex needs.
In 2008, the integration agreement was once again revised, and the shared routines for risk assessments were included. The steering committee actively requested the stakeholders’ views on the integrated services. They invited partners, stakeholder associations and service-user representatives to discuss these issues. In addition, services continued to be developed for people with neuropsychiatric diagnoses and elderly people with mental illnesses or health problems related to drug abuse and addiction. For the latter, local guidelines clarifying the shared responsibility were developed. The neuropsychiatric staff members were trained accordingly.
In 2009, the stakeholder associations’ roles were strengthened by increasing their participation in the meetings and by gathering their views on the new integration agreement. Substantial work was done to develop integrated services for new user groups. For instance, an initiative was launched to develop collective, overall support for users of the care and habilitation service for people with disabilities. In addition, this service expanded to handle the increasing number of service users with neuropsychiatric disorders. A growing group in need of health and social care comprised traumatised refugees, who required new and well-adjusted integrated services. To treat this group, the organisations co-applied for project funding to develop a care program.
In 2010, continual efforts were made towards the improvement of stakeholder associations. This action was consistent with the search for shared and streamlined service activities focusing on cost reduction. The efforts to increase the service users’ involvement in care and support were also on the agenda. The overall integration agreement was again revised, this time to clarify the steering committee’s responsibilities. In addition, attention was drawn to subgroups that were not yet included in the target population of the integrated organisation. Planning for the housing of people with long-term substance abuse and extensive care needs started with a guiding principle that these individuals would be able to maintain the accommodation regardless of which organisation had the formal responsibility for the individual. Further contacts were made with the primary health care to develop care for elderly people with mental illness, substance abuse and drug addiction. Another central group was people with ADHD, for whom integrated health and social care were considered to be essential. Cooperation was under development with the municipal unit around disabled people and a correctional care unit.
In 2011, the ability to cooperate with primary care was hampered as the number of private care providers increased. Nonetheless, new forms of cooperation within subgroups, such as people with substance abuse and within the neuropsychiatry, were successfully established. In this development work, a mobile team was launched for supporting young people with neuropsychiatric diagnoses, and the care centre for addicts was advanced. The steering committee continued to find solutions to the funding of the integrated services. An example was a new, integrated type of employment form where a manager was formally employed by the municipality, but the costs were shared through the county council purchasing the manager’s services.
In 2012, a regional agreement on how to support people with a mental illness and disability was reached, which strengthened the integration of focusing on the needs and shared responsibilities of service users. The integrated organisation was reviewed in two evaluations. An external evaluation concluded that cost-effective and high quality care was provided and that the steering committee served an important role in overviewing the integration. The internal evaluation underlined that the resources of the relatives and the families could be more optimally used. Consequently, stakeholder associations were invited to take part in discussions of their role and the revision of the services. A new function, a multi-case manager, was also established to handle service users with highly complex needs. Furthermore, clarification of the shared responsibility for service users with psychiatric diagnoses and substance abuse was made, and a newly diagnosed psychiatric patients’ team was initiated to provide integrated services at a care centre for addicts. Further, an operational management group of representatives from the units for adults and elderly people was created and supplemented with a representative from the psychiatry centre.
In 2013, attention was drawn to savings opportunities by further developing the integration. For instance, integration of services with the neighbouring municipalities was discussed. The cooperation agreements were revised regarding elderly users, children and adolescents, and efforts were made to improve cooperation between the psychiatry centre for adults and a centre for children and adolescents to better meet the needs of children, young people and their families. Other areas of improvement included clarifying the primary care and psychiatry responsibilities and reorganising neuropsychiatric care in order to make it more cost-effective. An inter-sectoral co-located neuropsychiatric outpatient clinic was proposed. Despite the economic challenges, the willingness to further integrate health and social care for people with mental illness continued. For example, a “house of health” with all services co-located at one place was planned together with web-based network-gathering activities.
In 2014, the steering committee decided to only meet once per semester. The role of the committee had become more “consultative” and less of a working group due to an increased number of members, which in turn was an effect of the increased number of services included in the organisation. Meanwhile, the steering committee function changed, however, the practical integrated work at the unit levels continued intensively. For instance, procedures for coordinated individual rehabilitation plans were developed, and various improvement projects were launched.
In 2015, attention was again drawn to the needs of elderly service users and to unaccompanied refugee children. Integration with geriatric psychiatry care, primary care and elder care continued to be of high priority but challenging. The economy was strained for both organisations. A new review of the services and the service users’ needs was made. The number of service users in need of health and social care had decreased, while some changes in their needs were also noticed. As a consequence, efforts were made to reduce costs by streamlining the integrated processes. At the end of the year, the steering committee decided to schedule two meetings per semester since the time between the meetings was concluded to be too long.
Empirical themes
Shared structure and ongoing refinement.
The services of the municipality and county were interlinked at both structural and functional levels, and the foundation was built on shared mission and agreements, co-leadership and by creating inter-professional teams in co-located services. The question of how the integration would take place was not predetermined; rather, by involving stakeholder associations and other key actors, the organisational development was co-created in a dynamic process through the years. The integration work was characterised by continuous adaptations of interventions on multiple levels. Adjustments were made in order to continuously adapt the organisation and the services to changes in context. For instance, new services were started based on the change in service users’ needs. When financial savings were required, the two organisations streamlined the processes together. All internal improvement work was also made with participation in various improvement projects and with external partners. The thorough work carried out aimed at bringing the municipality and county closer in the pursuit of a shared IT system, aligned steering mechanisms (score cards), service outcome measures, shared routines, common referral forms and shared clinical guidelines. External influences recognised to cause fragmentation were handled by strengthening cooperation, for example, by underlining the equal state of the organisations in the cooperation agreement and by emphasising the equal value to the service users’ existential issues of medical, psychological and social well-being. The following excerpt from the steering committee minutes exemplifies this:
The county council and the municipality are two organizations that complement each other. […] The things we do, we do together. […] The reform requires functioning forms of cooperation and creation of shared goals along with a union of our cultures and decision-making systems. But still, the two cooperating organisations need to continuously develop their own working methods.
Continuous learning
The integration of health and social care emerged as a fusion of norms, values, assumptions and behaviours from two different sectors, which had certain challenges to overcome. A mutual understanding of the differences, including the mission of each sector, was recognised and respected. Formal structures for learning were created by allowing employees, managers and service users to exchange experiences and knowledge. The financial support of learning activities was strategically used over the years to promote and develop integration. The development of new ways of working such as teamwork and case management was given financial support. Managers’ need for development was also recognised, and their professional development was among other things supported through the coaches who provided support in managing shared service planning. The managers were also innovative in implementing new working methods and functions before these methods and functions were decreed by the national government. Data from all levels of the organisation were continuously collected to assess progress. These measurements enabled immediate reactions, which in turn contributed to continuous optimisation of the conditions for sustainability of the inter-sectoral cooperation. The following excerpt from the steering committee minutes exemplifies this:
The psychiatric reform requires mutual respect and trust for the cooperating health and social care professionals’ different conditions, tasks and methods. Only thus, it is possible to achieve a common set of values upon which the concrete work should rest. In order for this respect and understanding to be maintained, ongoing, mutual knowledge development is required.
Cooperation as a guiding principle for management
The composition of the steering committee could be described as dynamic since it constantly adapted to match the service users. Permanent members were representatives from the mental health services at the municipality and the county, along with the stakeholder associations. The continuity among the core members was high, and other temporary members were determined by the content of each meeting. The two project managers had a central role for the creation of the integration. They, representing both municipality and county council, made key contributions in the creation of a culture and shared values. Also, the line managers (i.e., co-leaders) functioned as opinion leaders and cultural carriers and therefore had a strong symbolic value. In addition, they worked closely together in applying co-leadership, as all leaders on all levels, and thereby served as role models. The decision-making process was based on dialogue and negotiation, and all solutions were consensus-based. The following excerpt from the steering committee minutes exemplifies this:
Cooperation is necessary to realize the reform. It applies to several levels, county, municipality, team and at the individual level. [...] In our services, service users, municipality and county council cooperate for flexible and needs-based support for the different target groups. The cooperation includes planning, development and evaluation of operations.
Service user centeredness
Over the years, the steering committee recognised the interdependence of physical, psychological and social factors in health and illness, which was manifested in the committee early on and set the goal to collaborate around each service user. The formal agreements stated that service users should be at the centre. The services were therefore organised around each service users’ personal needs, rather than from the perspective of the organisations. For instance, this was achieved by having ongoing stakeholder involvement through representatives from the stakeholder associations in the steering committee and local service user groups at the service centres. Thus, the service users took part in co-creating the services. On an individual level, coordinators were introduced early on in the process, and a multi-case manager was appointed for service users with complex needs. The content of the care and support was also co-produced according to individual rehabilitation plans, and health and social care interventions were continuously followed up by the use of CAN data. As new service user groups were added over time, new inter-professional teams were arranged to meet the specific needs of the new groups. The following excerpt from the steering committee minutes exemplifies this:
The services should be formed and developed based on the service users’ needs. [...] The organisational and economical conditions should therefore be arranged to enable long-term care and support, based on the service users´ need of continuity.
The study aimed to gain insights into the dynamics of the sustainable change of integrated health and social care. Five main factors were found to be essential for the achievement of the 20 years of inter-sectoral cooperation.
First, the integration was characterised by ongoing adaptations. The services provided and the work of the steering committee was constantly improved based on changes in the surrounding context. The needs of the service users were frequently reviewed in order to create new services or to adapt the existing ones. Service users and stakeholder associations were considered important partners in this. This also applied to the view of other collaborators (e.g., Primary Care, Social Insurance Agency, Public Employment Service etc.) who came to change over time depending on the service users’ needs. The importance of using bottom-up strategies for implementation of new intervention has been emphasised by others [ 36 ]. In this case, the steering committee worked actively to align the organisational characteristics with actual needs, meaning that inappropriate structures were removed. This is in line with the DSF, which also recommends contextualising or removing non-outcome-focused intervention components [ 13 ].
Secondly, the ambition for ongoing learning among all stakeholders was highly present. Continuous feedback on performance was provided with the measures on the organisational, professional and service user level, which was one step in the creation of a culture for learning. Previous studies on collaboration have shown that arenas for dialogues and exchange of relevant knowledge is important [ 35 ], and we found that the decision to co-locate all health and social services in co-run centres required interdisciplinary teamwork on a very practical level, which also surfaced as an important step in the continuous learning and integration of the services. The issue of culture is highly relevant for multi-sectoral collaboration (e.g., between health and social care), since the organisations often have different cultural lenses. In a similar manner, each professional group tends to have its own professional culture, which makes this type of organisation even more multicultural [ 37 ]. Protectionism and scepticism towards other professional groups are common in integrated services [ 38 ]. The current organisation was no exception to this, but it had a clear ambition on tackling these challenges together through collaboration, education and experience exchange, which has been shown to contribute to successful multidisciplinary integration [ 39 ].
Thus, the third issue characterising this sustained integration of services was the emphasis on collaboration. This was one of the most essential guiding principles in the steering group’s work over time. This manifested in considering the dissimilarities, conditions and needs of each organisation in decision making. Thereby, the steering committee was long-term-oriented with collaboration in mind, while also continuously solving the problems at hand to enable collaboration on a practical level. The many actions that the steering committee took initially and the persistent work for the continuation of cooperation reflect a firm belief in inter-sectoral cooperation. These findings relate to prior research showing a relation between committed leaders across the organisation and successful long-term change [ 40 ]. The role of managers and leadership, together with the leadership system, is repeatedly highlighted as crucial for change, especially for sustainable change [ 41 ]. The leadership system in this case was based on co-leadership and cooperation. The work tasks were regarded as a joint responsibility, which is consistent with previous research on shared leadership showing that a close leadership created space for forward thinking and a long-term approach to work [ 42 ].
Fourthly, the service users, their families and the stakeholder associations were key partners in the collaboration and in forming the services. Their engagement in the development of processes was a core strategy used by the steering committee to align interventions to the service users’ needs and to create empowerment. Furthermore, equal importance was given to all of the service users’ needs (medical, psychological, social etc.) rather than prioritising one of these based on sectorial priorities. The shared holistic view on service users and, consequently, an identified need to organise health and social care in a cohesive manner enabled the creation of a shared vision and strategy formulation, which in turn set the direction for the organisation and its priorities. It also seemed that the two organisations could always make up for the needs by putting the service users’ needs first, which helped them to solve potentially sensitive issues in funding and managing the integrated services. This may have caused them to become more solution focused and less protective, enabling the establishment of a shared organisational culture that includes roles, norms and values, which is also underlined by Schein as important [ 43 ]. In the research examples of service users being active, the contributors of skills and knowledge in the development of healthcare services can be found [ 44 , 45 ]. The interaction between service users and health and social care providers forming a partnership is referred to as co-production [ 46 ], co-creation [ 47 ], experienced based co-design [ 48 ] and patient and public involvement [ 49 ], to mention a few. Hence, research has shown that the consultative approaches are more common than partnership [ 50 ]. However, it seems that this integrated health and social care organisation was an early adopter of this involvement approach enabling service user participation.
Lastly, the steering committee’s work was dynamic, and new members were invited to participate depending on what services were included in the integrated organisation. At the same time, their work was characterised by a low turnover since the core individuals in the steering group were the same during the entire 20-year period. For instance, the minutes were written by the same person in all cases. The stable step of individuals with a shared vision certainly had a great impact on the sustained integration. Furthermore, the two project managers, holding key functions in the process of integration, were the same individuals throughout the years. These functions, called opinion leaders or program leaders in other studies [ 51 ], have had a great impact on integration. Previous research has also highlighted the importance of stability on a strategic and operational level to overcome sector-related challenges in integrated health and social care [ 52 ]. However, the current study does not reveal whether the impact of the stakeholders derives from what they did, the fact that they were the same people over the years or a combination of these factors.
Methodological considerations
The main strength of the study was the long time period in which we were able to complete a thorough document analysis. This provided valuable insight into the steering committees’ work over time. A potential limitation with the minutes afforded for study in each meeting was that we were restricted to the information provided in the documents. It’s possible that other data sources such as interviews could have provided a broader picture of the actions taken by the steering committee. Nevertheless, the minutes were rich and provided insights into how the committee members perceived their context, the organisation and their actions rather than only consisting of decisions and actions. As these minutes were not designed with research in mind, the bias from leaving out certain information such as disagreements and conflicts must be considered. Furthermore, the same person wrote out the minutes of the meeting throughout the study period. This can be considered a strength since the minutes followed the same structure and had an equal amount of information throughout the years. At the same time, it can limit the type and information provided since one person made decisions on what to note, although the minutes were always reviewed by the other committee members. Generally, the overall framework helped to identify several factors related to the dynamics of sustainable change. More precisely, the framework was found useful as a tool to limit the scope of relevant data and in interpreting our findings. While the framework focused our attention to some specific components we still strived to remain open for unexpected findings and alternative explanations. One example was the identification of service user centeredness as an enabling factor for the achievement of long-lasting cooperation. By this the services were organised around each service users’ personal needs, rather than from the perspective of the organisations. A limitation to generalisability of the findings can be that the study was conducted in one specific geographical area, which was characterised by long-term integrated health and social care services.
Suggestions for future research and implications for practice
As this study primarily addresses the steering committee decisions and actions, future research could build on our findings by including perspectives on organisational champions and the meaning of organising networks for achieving sustainability. As the knowledge on champions and networks increases, we stress that organisations and services adjust accordingly. We suggest three main areas of future research: 1) studies on the sustainability of change; 2) studies on the interrelatedness of factors impacting sustainable change; and 3) longitudinal studies on the impact of different factors on sustainability (e.g., to explore the importance of leadership during different stages of change). In regard to practical implications, the findings suggest that service user involvement and the critical review of service users’ needs on a regular basis are essential in order to tailor to the current needs and services. Furthermore the importance of continuously adapting the content of the change to suit its context, was clear, and it’s suggested that continuous refinement of the change content was found to be more important than designing the change at the pre-implementation stage.
This study provides some valuable insight into the dynamics of sustainable change and the understanding of key managerial actions in order to establish, develop and support the integration of health and social care for people with complex mental health needs. The development of inter-sectoral cooperation was characterised by a participatory approach in which a shared structure was created to support cooperation and ongoing quality improvement and learning focused on the service user’s needs. The key management principle included cooperation on all organisational levels as well as with service users, stakeholder associations and other partner organisations. This study shows that all these parts were interrelated and collectively contributed to the creation of a structure and a culture that supported the development of dynamic and sustainable health and social care.
Abbreviations
the Camberwell Assessment of Needs scale
Dynamic Sustainability Framework
Wiltsey Stirman S, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci. 2012;7:17. https://doi.org/10.1186/1748-5908-7-17 .
Article PubMed PubMed Central Google Scholar
Scheirer MA, Dearing JW. An Agenda for Research on the Sustainability of Public Health Programs. Am J Public Health. 2011;101:2059–67. https://doi.org/10.2105/AJPH.2011.300193 .
Martin GP, Currie G, Finn R, McDonald R. The medium-term sustainability of organisational innovations in the national health service. Implement Sci. 2011;6:19. https://doi.org/10.1186/1748-5908-6-19 .
Arends I, Baer N, Miranda V, Prinz C, Singh S. Mental Health and Work: Achieving Well-integrated Policies and Service Delivery. OECD Soc Employ Migr Work Pap. 2014;161:1–39. https://doi.org/10.1787/1815199X .
Article Google Scholar
Buchanan DA, Fitzgerald L, Ketley D, editors. The sustainability and spread of organizational change: Modernizing healthcare. London: Routledge; 2006.
Google Scholar
May CR, Johnson M, Finch T. Implementation, context and complexity. Implement Sci. 2016;11:141. https://doi.org/10.1186/s13012-016-0506-3 .
Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: translating science to practice. Oxford: Oxford University Press; 2012. https://doi.org/10.1093/acprof:oso/9780199751877.001.0001 .
Greenhalgh T, Robert G, Bate P, Kyriakidou O, Macfarlane F, Peacock R. How to spread good ideas - A systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organisation. 2004. http://www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1201-038_V01.pdf .
Proctor E, Luke D, Calhoun A, McMillen C, Brownson R, McCrary S, et al. Sustainability of evidence-based healthcare: research agenda, methodological advances, and infrastructure support. Implement Sci. 2015;10:88. https://doi.org/10.1186/s13012-015-0274-5 .
Buchanan D, Fitzgerald L, Ketley D, Gollop R, Jones JL, Saint LS, et al. No going back: A review of the literature on sustaining organizational change. Int J Manag Rev. 2005;7:189–205. https://doi.org/10.1111/j.1468-2370.2005.00111.x .
Whelan J, Love P, Pettman T, Doyle J, Booth S, Smith E, et al. Cochrane update: Predicting sustainability of intervention effects in public health evidence: identifying key elements to provide guidance. J Public Health (Oxf). 2014;36:347–51. https://doi.org/10.1093/pubmed/fdu027 .
Campbell M. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–6. https://doi.org/10.1136/bmj.321.7262.694 .
Article PubMed PubMed Central CAS Google Scholar
Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117. https://doi.org/10.1186/1748-5908-8-117 .
Dusenbury L. A review of research on fidelity of implementation: implications for drug abuse prevention in school settings. Health Educ Res. 2003;18:237–56. https://doi.org/10.1093/her/18.2.237 .
Article PubMed Google Scholar
Pérez D, Van der Stuyft P, Zabala M del C, Castro M, Lefèvre P, Sorensen G, et al. A modified theoretical framework to assess implementation fidelity of adaptive public health interventions. Implement Sci. 2015;11:91. https://doi.org/10.1186/s13012-016-0457-8 .
Sisaye S. Ecological systems approaches to sustainability and organizational development. Leadersh Organ Dev J. 2011;32:379–98. https://doi.org/10.1108/01437731111134652 .
Plochg T, Delnoij DMJ, Hoogedoorn NPC, Klazinga NS. Collaborating while competing? The sustainability of community-based integrated care initiatives through a health partnership. BMC Health Serv Res. 2006;6:37. https://doi.org/10.1186/1472-6963-6-37 .
World Health Organization. WHO Global Strategy on People-centred and Integrated Health Services. Interim Report. Switzerland: Geneva; 2015. http://apps.who.int/iris/bitstream/handle/10665/155002/WHO_HIS_SDS_2015.6_eng.pdf;jsessionid=3BBDDBC72FF786E5623D3540E9F06326?sequence=1
Sun X, Tang W, Ye T, Zhang Y, Wen B, Zhang L. Integrated care: a comprehensive bibliometric analysis and literature review. Int J Integr Care. 2014;14:1–12. https://doi.org/10.5334/ijic.1437 .
Ouwens M. Integrated care programmes for chronically ill patients: a review of systematic reviews. Int J Qual Heal Care. 2005;17:141–6. https://doi.org/10.1093/intqhc/mzi016 .
Stein V, Barbazza ES, Tello J, Kluge H. Towards people-centred health services delivery: a Framework for Action for the World Health Organisation (WHO) European Region. Int J Integr Care. 2013;13 https://doi.org/10.5334/ijic.1514 .
World Health Organization. Mental Health Action Plan 2013-2020. Geneva, Switzerland; 2013. http://apps.who.int/iris/bitstream/handle/10665/89966/9789241506021_eng.pdf?sequence=1
Goodwin N. Understanding and Evaluating the Implementation of Integrated Care: A “Three Pipe” Problem. Int J Integr Care. 2016;16:1–2. https://doi.org/10.5334/ijic.2609 .
Mackie S, Darvill A. Factors enabling implementation of integrated health and social care: a systematic review. Br J Community Nurs. 2016;21:82–7. https://doi.org/10.12968/bjcn.2016.21.2.82 .
Anell A. Swedish healthcare under pressure. Health Econ. 2005;14:S237–54. https://doi.org/10.1002/hec.1039 .
Anell A, Glenngård AH, Merkur S. Sweden health system review. Health Syst Transit. 2012;14:1–159. http://www.euro.who.int/__data/assets/pdf_file/0008/164096/e96455.pdf
PubMed Google Scholar
Patana P. Mental Health Analysis Profiles (MhAPs): Sweden. OECD Health Working Papers, No. 82, OECD Publishing, Paris; 2015. doi: https://doi.org/10.1787/5jrxr7qx6ctb-en .
Silfverhielm H, Kamis-Gould E. The Swedish Mental Health System. Past, Present, and Future Int J Law Psychiatry. 2000;23:293–307. https://doi.org/10.1016/S0160-2527(00)00039-X .
Article PubMed CAS Google Scholar
Lindqvist R, Rosenberg D, Fredén L. [Den svenska psykiatrireformen i nordisk belysning] (Swedish). Soc Tidskr. 2011;88:524–33.
Hansson J, Øvretveit J, Brommels M. Case study of how successful coordination was achieved between a mental health and social care service in Sweden. Int J Health Plann Manag. 2012;27:e132–45. https://doi.org/10.1002/hpm.1099 .
Hansson J, Ovretveit J, Askerstam M, Gustafsson C, Brommels M. Coordination in networks for improved mental health service. Int J Integr Care. 2010;10 August:1–9. doi: https://doi.org/10.5334/ijic.511 .
Klinga C, Hansson J, Hasson H, Sachs MA. Co-Leadership – A Management Solution for Integrated Health and Social Care. Int J Integr Care. 2016;16:1–9. https://doi.org/10.5334/ijic.2236 .
Statistics Sweden, Statistical Database. 2017. http://www.statistikdatabasen.scb.se/pxweb/en/ssd/?rxid=86abd797-7854-4564-9150-c9b06ae3ab07 . Accessed 27 Feb 2018.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. https://doi.org/10.1191/1478088706qp063oa .
Widmark C, Sandahl C, Piuva K, Bergman D. What do we think about them and what do they think about us? Social representations of interprofessional and interorganizational collaboration in the welfare sector. J Interprof Care. 2016;30:50–5. https://doi.org/10.3109/13561820.2015.1055716 .
Carlfjord S, Festin K. Primary health care staff’s opinions about changing routines in practice: a cross-sectional study. BMC Fam Pract. 2014;15:2. https://doi.org/10.1186/1471-2296-15-2 .
Ferlie EB, Shortell SM. Improving the Quality of Health Care in the United Kingdom and the United States: A Framework for Change. Milbank Q. 2001;79:281–315. https://doi.org/10.1111/1468-0009.00206 .
Cameron A, Bostock L, Lart R. Service user and carers perspectives of joint and integrated working between health and social care. J Integr Care. 2014;22:62–70. https://doi.org/10.1108/JICA-10-2013-0042 .
Robertson H. Integration of health and social care A review of literature and models Implications for Scotland. Scotland: Royal College of Nursing; 2011. https://my.rcn.org.uk/__data/assets/pdf_file/0008/455633/Hilarys_Paper.pdf . Accessed 27 Feb 2017.
Fleiszer AR, Semenic SE, Ritchie JA, Richer M-C, Denis J-L. The sustainability of healthcare innovations: a concept analysis. J Adv Nurs. 2015;71(7) https://doi.org/10.1111/jan.12633 .
Metcalf L, Benn S. Leadership for Sustainability: An Evolution of Leadership Ability. J Bus Ethics. 2013;112:369–84. https://doi.org/10.1007/s10551-012-1278-6 .
Döös M. Together as One: Shared Leadership Between Managers. Int J Bus Manag. 2015;10:46–59. https://doi.org/10.5539/ijbm.v10n8p46 .
Schein EH. Organizational culture and leadership. Vol. 2. New Jersey: Wiley; 2010.
Elg M, Engström J, Witell L, Poksinska B. Co-creation and learning in health-care service development. J Serv Manag. 2012;23:328–43. https://doi.org/10.1108/09564231211248435 .
Boyd H, McKernon S, Mullin B, Old A. Improving healthcare through the use of co-design. N Z Med J. 2012;125:76–87. https://scholar.google.se/scholar?hl=sv&as_sdt=0%2C5&q=Improving+healthcare+through+the+use+of+co-design&btnG= . Accessed 14 Sept 2017.
Realpe A, Wallace LM. What is co-production? London: The Health Foundation; 2010. http://personcentredcare.health.org.uk/sites/default/files/resources/what_is_co-production.pdf . Accessed 27 Feb 2017.
Sanders EB-N, Stappers PJ. Co-creation and the new landscapes of design. CoDesign. 2008;4:5–18. https://doi.org/10.1080/15710880701875068 .
Donetto S, Pierri P, Tsianakas V, Robert G. Experience-based Co-design and Healthcare Improvement: Realizing Participatory Design in the Public Sector. Des J. 2015;18:227–48. https://doi.org/10.2752/175630615X14212498964312 .
Renedo A, Marston CA, Spyridonidis D, Barlow J. Patient and Public Involvement in Healthcare Quality Improvement: How organizations can help patients and professionals to collaborate. Public Manag Rev. 2015;17:17–34. https://doi.org/10.1080/14719037.2014.881535 .
Rutter D, Manleya C, Weaver T, Crawford MJ, Fulop N. Patients or partners? Case studies of user involvement in the planning and delivery of adult mental health services in London. Soc Sci Med. 2004;58:1973–84. https://doi.org/10.1016/S0277-9536(03)00401-5 .
Vermeer AJM, Van Assema P, Hesdahl B, Harting J, De Vries NK. Factors influencing perceived sustainability of Dutch community health programs. Health Promot Int. 2015;30:473–83. https://doi.org/10.1093/heapro/dat059 .
Cameron A. What have we learnt about joint working between health and social care? Public Money Manag. 2016;36:7–14. https://doi.org/10.1080/09540962.2016.1103411 .
Download references
Acknowledgements
We would like to thank the municipality for providing us with all the Steering Committee minutes. In addition we would like to thank Karin Solberg Carlsson for helping with the initial assortment of the collected data.
This research was funded by a grant from The Swedish Research Council (521-2014-2710), the involvement of the second author was funded by a research grant from FORTE (2014-0303).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Department of Learning, Informatics, Management and Ethics (LIME), Medical Management Centre (MMC) | Karolinska Institutet, 171 77, Stockholm, Sweden
Charlotte Klinga, Henna Hasson, Magna Andreen Sachs & Johan Hansson
You can also search for this author in PubMed Google Scholar
Contributions
CK, MAS, HH, JH: conception and design of the study; CK: data collection; CK, MAS, HH, JH: data analysis; CK, MAS, HH, JH: drafting the article. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Charlotte Klinga .
Ethics declarations
Ethics approval and consent to participate.
This study has been reviewed and approved by The Regional Ethics Committee in Stockholm (Dnr 2014/612-31/5). The data in the study consists of public documents, no files containing personal data were compiled and the results are presented at aggregated level.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Klinga, C., Hasson, H., Andreen Sachs, M. et al. Understanding the dynamics of sustainable change: A 20-year case study of integrated health and social care. BMC Health Serv Res 18 , 400 (2018). https://doi.org/10.1186/s12913-018-3061-6
Download citation
Received : 29 September 2017
Accepted : 26 March 2018
Published : 04 June 2018
DOI : https://doi.org/10.1186/s12913-018-3061-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Implementation
- Organisational sustainability
- Change management
- Integrated care
- Mental health
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

Children and Families Policy Research Unit
NIHR Children and Families Policy Research Unit

Case Study: Sociology of health and illness
Pathways for young people leaving care: what helps.

What are the experiences of young people leaving residential or foster care?
For looked-after children, the transition from care can be a daunting time, as they navigate the complexities of adult life. Government guidance is designed to ensure smooth transitions, but there can be a gap between national and local aspirations, and young peoples' own hopes and priorities.
Exploring transitions from care was a recent focus of the sociology of health and illness cross-cutting theme of the CPRU. As Professor Helen Roberts, medical sociology lead explained, this theme "undertakes research into social aspects of children and young people's health to inform policy."
Key Points:
- This qualitative research explored the priorities for young people leaving foster or residential care seekers and those with disabilities
- Collaborative work with and between young people and professionals is important for understanding the experiences of care leavers
- Two groups of care leavers were identified as having a particularly hard time: asylum
This case study is from Sociology of health and illness Cross-cutting themes.
- Download pdf
- Download plain text version pdf
- Helping young people say no
- Cutting the risk
- Mental health in children
- Type 2 diabetes in children
- Family finances and disability
- Stories from data and young people
- Growing up happy in England
Integrated care in practice: a case study of health and social care for adults considered to be at high risk of hospital admission
Integrated care is pursued globally as a strategy to manage health and social care resources more effectively. It offers the promise of meeting increasingly complex needs, particularly those of aging populations, in a person-centred, co-ordinated way that addresses fragmentation and improves quality.
However, policy to integrate health and social care in England has led to programmes which have had disappointing effects on reducing hospital admissions and costs. My concern with the...
Email this record
Please enter the email address that the record information will be sent to.
Please add any additional information to be included within the email.
Cite this record
Chicago style, access document.
- HUGHES 2018 thesis.pdf (pdf, 3.1MB)
Why is the content I wish to access not available via ORA?
Content may be unavailable for the following four reasons.
- Version unsuitable We have not obtained a suitable full-text for a given research output. See the versions advice for more information.
- Recently completed Sometimes content is held in ORA but is unavailable for a fixed period of time to comply with the policies and wishes of rights holders.
- Permissions All content made available in ORA should comply with relevant rights, such as copyright. See the copyright guide for more information.
- Clearance Some thesis volumes scanned as part of the digitisation scheme funded by Dr Leonard Polonsky are currently unavailable due to sensitive material or uncleared third-party copyright content. We are attempting to contact authors whose theses are affected.
Alternative access to the full-text
Request a copy.
We require your email address in order to let you know the outcome of your request.
Provide a statement outlining the basis of your request for the information of the author.
Please note any files released to you as part of your request are subject to the terms and conditions of use for the Oxford University Research Archive unless explicitly stated otherwise by the author.
Contributors
Bibliographic details, item description, terms of use, views and downloads.
If you are the owner of this record, you can report an update to it here: Report update to this record
Report an update
We require your email address in order to let you know the outcome of your enquiry.
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Architecture
- Theory of Architecture
- Browse content in History
- History of Education
- Regional and National History
- Browse content in Philosophy
- Feminist Philosophy
- Philosophy of Language
- Browse content in Religion
- Religious Studies
- Browse content in Society and Culture
- Cultural Studies
- Ethical Issues and Debates
- Technology and Society
- Browse content in Law
- Comparative Law
- Criminal Law
- Environment and Energy Law
- Human Rights and Immigration
- Browse content in International Law
- Public International Law
- Legal System and Practice
- Medical and Healthcare Law
- Browse content in Medicine and Health
- Browse content in Public Health and Epidemiology
- Public Health
- Browse content in Science and Mathematics
- Browse content in Earth Sciences and Geography
- Environmental Geography
- Urban Geography
- Environmental Science
- Browse content in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Browse content in Business and Management
- Business Ethics
- Business History
- Corporate Social Responsibility
- Human Resource Management
- Industry Studies
- Information and Communication Technologies
- Knowledge Management
- Criminology and Criminal Justice
- Browse content in Economics
- Behavioural Economics and Neuroeconomics
- Economic History
- Economic Systems
- Economic Development and Growth
- Financial Markets
- History of Economic Thought
- Public Economics
- Browse content in Education
- Educational Strategies and Policy
- Higher and Further Education
- Philosophy and Theory of Education
- Browse content in Human Geography
- Political Geography
- Browse content in Politics
- Asian Politics
- Comparative Politics
- Conflict Politics
- Environmental Politics
- European Union
- Indian Politics
- International Relations
- Middle Eastern Politics
- Political Economy
- Political Sociology
- Political Theory
- Public Policy
- Russian Politics
- Security Studies
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- Asian Studies
- Browse content in Social Work
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Urban and Rural Studies
- Reviews and Awards
- Journals on Oxford Academic
- Books on Oxford Academic

Social Determinantsof Health: An Interdisciplinary Approach to Social Inequality and Wellbeing

- Cite Icon Cite
This book examines the social determinants of health from an interdisciplinary perspective, focusing on social inequalities and well-being. It analyses the key factors which can lead to poor quality of life, homelessness and reduced mortality. The book begins by looking at early life experiences, which in combination with social networks, exert a strong influence on health and well-being in later life, which in turn are mediated by the development of prosocial behaviour, coping skills, resilience, and optimal cognitive functioning. This requires a healthy mind and body and the motivation to benefit and learn from a supportive environment. The book provides an overview of neuropsychological development and the role of affection, fear and anxiety in early development before discussing social anxiety, communication and socialisation, and the well-being of children. It considers the interrelationships between poverty, child abuse and neglect, with an assessment of social inclusion strategies, troubled families, deviant and anti-social behaviour, and the link between mental health and human distress. Ultimately, the book shows that relative poverty and social capital will provide the resilience for an individual to experience a sense of well-being and lead to successful ageing, while lifestyle choices and the support of a healthy community will reduce vulnerability to negative health behaviours. It explains how personal well-being is related to the availability of personal, family and community resources. The book will enable researchers, front-line workers, managers, service commissioners and politicians to identify and employ the most appropriate health care, social and economic interventions to support those at the edge of the community.
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Coronavirus (COVID-19) Updates For the latest information and advice see: Coronavirus (COVID-19) frequently asked questions

Scottish Graduate School of Social Science
Improving person-centred care communication in health and social care settings.

PHD STUDENT: Natalia Rodriguez UNIVERSITY: Heriot-Watt COMPANY: Healthcare Improvement Scotland
In January 2019 Healthcare Improvement Scotland welcomed Natalia Rodriguez to undertake a 3 month internship. Natalia is studying for a PhD with a focus on interpreting in mental healthcare settings at Heriot Watt University. During her time at Healthcare Improvement Scotland she worked within the Evidence and Evaluation for Improvement Team (EEvIT), supporting them to evaluate the ‘What Matters to You? Day’ (WMTY) initiative that is facilitated by the Person Centred Care Team. Natalia was happy to share information about her experience below.
"It has been an absolute joy working with Natalia. She has been a breath of fresh air. She picked it up quickly and I didn't feel that I had to direct her too much. I think we really lucked out on Natalia's skill set." Colleague from HIS
What attracted you to this internship?
When I first saw the advertisement for an internship position for PhD candidates with Healthcare Improvement Scotland (HIS) I was both thrilled and hesitant about applying. On paper, I was a good candidate, but I wondered if my academic background would be the right fit for the organisation. On the other hand, I was sure that it would be a great opportunity for me and that I definitely wanted to put my research skills to use in public healthcare.
My PhD had already given me the chance to witness the work of the NHS first-hand. For data collection purposes, I observed consultations conducted through spoken-language interpreters in two psychiatric wards within NHS Lothian for over a year. During this time, I not only collected data but also learnt lessons about human resilience that I will always carry with me. Having finished the data-collection work in December, I have now a year of funding left to convert my data into a thesis. So, the chance to work with HIS in this transition stage could not have come at a better time!
What did you do?
During my time at HIS, I supported the Evidence and Evaluation for Improvement Team (EEvIT). Specifically, I supported EEvIT to evaluate the ‘What matters to you? day’ initiative that is facilitated by the Person-Centred Care Team within HIS. For this purpose, I conducted primary and secondary research to produce an evidence report called: “‘What matters to you?’ Embedding the question in everyday practice: a multiple case-study”.
Did the internship meet your expectations?
It definitely exceeded my expectations. When I applied for the post, I was expecting that I would be doing some kind of work for a public health organisation, which in itself was to enough to make me feel excited. What I did not know then was that I would be applying my whole range of research skills to explore a topic fully in line with my PhD aims. I really was not expecting that before I started.

How did you utilise your research skills and knowledge during the internship?
There was clear common ground between my PhD topic and the aims of my internship project, which made it possible for me to use my knowledge and apply the research skills required to fulfil my internship aims. My PhD is about how linguistically and culturally diverse patients access healthcare services when they do not share a language with the service provider. During my internship, I evaluated the impact of a campaign that aims to promote a communication model in which patients and practitioners are encouraged to interact as equal partners in the planning of care. Methodologically speaking, for my PhD I have adopted a single case-study research design and for my internship, I adopted a multiple-case study design. In summary, my knowledge on the topic and the methodology required to explore was useful as a starting point, but the internship aims required me to take my expertise a step further.
How has it impacted your professional and personal development?
I am not sure about what type of work I will conduct after my PhD but public health and social care provision is definitely a research and personal interest that I am going to carry with me for life after my internship.
I do believe that my internship will help open up a new range of future possibilities that I would have never even thought about until now. The National Health Service is such a complex organisation that encompasses so many different departments, teams and staff with different backgrounds. Particularly, Healthcare Improvement Scotland contains different portfolios that have different objectives but pursue the common aim of driving improvement in the provision of health and social care services. This is an excellent area of work and definitely worth considering in the future.
Are there any outputs from the internship that you would like to share?
It was key for me to meet other people in the organisation outside from the team that I was allocated to work with as that provided me with unintended benefits. E.g. I was able to meet the Equality and Diversity advisor from HIS whose work is closely connected with my research interests and PhD aims. Because of his support, I was able to provide some feedback on a policy document draft around my area of expertise (healthcare interpreting) that will soon be published. That was not part of my internship aims but I definitely count that as one my main internship accomplishments.
What transferable skills did you learn?
Communicate clearly with a wide audience. During my internship I worked with a multidisciplinary team made up of health service researchers, a health economist and an information scientist. During data-collection, I interviewed people with a wide range of backgrounds including consultant, nurses, health service managers, etc. Developing appropriate timescales and sticking to them which was key to success as I was fully responsible for the development of the project. Being flexible: we had to consider different study designs as we depended on data availability.
How did you find coming back to your research after the internship?
I feel more confident now when approaching my PhD dataset. I did my internship during a transition time, right in between finishing data collection and starting data analysis and subsequent reporting. During my internship, I had to analyse and report data and that gave me a small-scale taster of what would come after. A team of health service researchers supported my work and provided guidance at all times so that I could fulfil my internship study aims. I am going to keep using that guidance to safeguard rigour in my own research work. I feel that I have more research tools and resources now.
What advice would you give other PhD students thinking about an internship?
1- Be more confident in their own potential contribution to the hosting organisation. I think that they might find it refreshing to work with someone new who brings a unique set of research skills to their organisation. 2- Remember that you do not need to know everything from the beginning as people want you to do well and will train you and you learn on the job 3- Your co-workers are engaged in their own routine so speak up if you need anything from them as they may not be used to having an intern. It is important to be self-directed (within limits and guidance)
Subscribe to our Newsletter

Privacy Policy
© 2023 All rights reserved
Scottish Graduate School of Social Science, proudly funded by

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Integr Care
- v.21(4); Oct-Dec 2021

Integrated Health and Social Care in the United States: A Decade of Policy Progress
Sahil sandhu.
1 Duke-Margolis Center for Health Policy, Duke University, NC, US
2 Population Health Sciences Institute, Newcastle University, UK
Rushina Cholera
3 National Clinicians Scholars Program, Department of Pediatrics, School of Medicine, Duke University, NC, US
Janet Prvu Bettger
4 Department of Orthopaedic Surgery, School of Medicine, Duke University, NC, US
5 Duke Global Health Institute, Duke University, NC, US
Introduction:
Over the last decade in the United States (US), the burden of chronic disease, health care costs, and fragmented care delivery have increased at alarming rates. To address these challenges, policymakers have prioritized new payment and delivery models to incentivize better integrated health and social services.
Policy practice:
This paper outlines three major national and state policy initiatives to improve integrated health and social care over the last ten years in the US, with a focus on the Medicaid public insurance program for Americans with low incomes. Activities supported by these initiatives include screening patients for social risks in primary care clinics; building new cross-sector collaborations; financing social care with healthcare dollars; and sharing data across health, social and community services. Stakeholders from the private sector, including health systems and insurers, have partnered to advance and scale these initiatives. This paper describes the implementation and effectiveness of such efforts, and lessons learned from translating policy to practice.
Discussion and Conclusion:
National policies have catalyzed initiatives to test new integrated health and social care models, with the ultimate goal of improving population health and decreasing costs. Preliminary findings demonstrated the need for validated measures of social risk, engagement across levels of organizational leadership and frontline staff, and greater flexibility from national policymakers in order to align incentives across sectors.
Introduction
Health in the United States (US) is remarkably poor given the personal and societal costs for healthcare. Despite spending nearly double of its gross domestic product on health care compared to the average Organization for Economic Co-operation and Development (OECD) country, the US has the highest chronic disease burden, highest rate of avoidable deaths, and lowest life expectancy among high-income countries [ 1 ]. This misalignment has sparked a range of policy reforms over the last ten years, including innovative efforts to reduce fragmentation, improve coordination across systems and sectors, and address the social determinants of health (SDOH).
The purpose of this paper is to describe national and state policy initiatives over the last ten years in the US aimed to integrate health and social care for Americans with health insurance provided by the public Medicaid insurance program. We also contextualize the US experience in the broader international landscape using an integrated care framework. Policy reform in the US can inform and be informed by other countries in an effort to globally advance integrated health and social care.
Healthcare System Context
The US is a country of fifty states, a federal district, five major territories, multiple minor islands, and nearly 330 million people. The healthcare system is a mixture of public and private providers and healthcare insurers. In 2019, about 56% of Americans were covered through private insurance (mostly employer-sponsored); 35% were covered through public insurance (e.g., “Medicare” predominantly for older adults; “Medicaid” for Americans with low incomes; and other public programs for active military, veterans, American Indians, and Alaskan Natives), and 9% were uninsured [ 2 ].
Traditionally, health services in the US have been paid in a fee-for-service model. In this model, providers, office visits, tests, procedures, and treatments are each paid for separately. This structure incentivizes quantity of services rather than quality of care. In 2010, President Obama signed into law the Affordable Care Act, one of the most comprehensive healthcare reform policies in American history. The law aimed to achieve universal health care coverage, while controlling costs and improving quality of care through new payment structures [ 3 ]. The Affordable Care Act supported new value-based payment models in which payment for health care services is tied to quality and cost rather than volume [ 4 ]. Examples of value-based payment models include giving health systems global budgets to care for patient populations rather than linking payments to individual services for each patient, and making payments conditional on meeting specific quality measures [ 5 ]. Providers and insurers have financial flexibility in value-based payment models to develop creative solutions for improving access, coordination, and integration across settings and sectors.
Innovative approaches to integrate health and social services expanded rapidly with the shift towards value-based payment models and the growing evidence that adverse social determinants of health (SDOH) are major drivers of poor health. Research showing that health care alone only shapes 10–20% of an individual’s health status led to greater attention on upstream SDOH including economic stability, housing stability, neighborhood environment, educational attainment, and food security [ 6 , 7 , 8 ]. A meta-analysis concluded that the number of deaths in 2000 in the US attributable to low education, racial segregation, and low social support, were comparable to those attributed to myocardial infarctions, cerebrovascular disease, and lung cancer respectively [ 9 ]. In addition to impacts on mortality, research has demonstrated clear links between adverse SDOH and a multitude of outcomes, including health expenditures, healthcare utilization, physical health, mental health, chronic disease management, and health-related behaviors (e.g., exercise, diet, sleep, smoking, drug use) [ 7 , 10 ].
In response, the health sector expanded implementation and evaluation of a variety of integration efforts to identify and address individuals’ social risks and unmet social needs. Social risks refer to the adverse social conditions associated with an individual’s poor health, such as food insecurity and housing instability [ 10 , 11 ]. Social needs refer to the specific social risks that a patient perceives as most pressing to them. Both these terms are more precise than the broader term of social determinants of health which refer to a community’s underlying social and economic conditions that affect everyone and can both be positive or negative. Health system approaches to address social risks and needs have spanned from individual-level activities, such as screening patients for social risks and referring them to external social services, to community-level approaches, such as cross-sector technology referral platforms and health clinic-food bank partnerships [ 12 ]. In 2019, the National Academies of Sciences, Engineering, and Medicine released a consensus report proposing a framework for activities to integrate social care into healthcare delivery and outlining recommendations to guide future practice and policy efforts [ 13 , 14 ].
US government agencies, and the Medicaid program as part of the Centers for Medicare and Medicaid Services (CMS) in particular, have played a critical role in advancing integrated health and social care through policy and payment reform. The Medicaid insurance program is a public insurance program for people with low incomes, covering about 20% of Americans (70+ million) [ 15 ]. Specifically, Medicaid covers 49% of births, 38% of all children, 45% of non-elderly adults with disabilities, and 62% of nursing home residents [ 15 ]. Created in 1965, Medicaid is a jointly financed federal and state partnership, in which the federal government sets core requirements for eligibility and benefits, and individual states administer the program. The Affordable Care Act further expanded the Medicaid program to cover over 12 million additional Americans [ 16 ]. Given Americans covered by Medicaid face greater socioeconomic challenges compared to Americans with private insurance, and are traditionally at highest risk for unmet social needs and societal inequities, the Medicaid program has been uniquely poised and motivated to integrate social care into health care delivery.
Recent Integrated Care Reforms in the United States Medicaid Program
Three major policy initiatives in the last decade aimed to advance integrated care and improve health for populations with Medicaid health insurance coverage. First, we describe the Accountable Health Communities demonstration program to integrate health, social and community-based organizations funded by the federal government for Medicaid recipients in selected regions. Then, we describe two policy tools leveraged by state Medicaid agencies to integrate health and social care: 1115 waivers, which give state Medicaid agencies flexibility to test novel approaches to service delivery and payment and managed care contracts, under which state Medicaid services are delivered by risk-based private insurance companies. Table 1 provides an overview of each of the three integrated care reforms. Figure 1 shows the geographic distribution of these integrated care programs and efforts.

Map of Integrated Care Reforms in the US Medicaid Program.
Overview of Integrated Health and Social Care Reforms in the US Medicaid Program.
Accountable Health Communities
Description.
The Affordable Care Act funded the new Center for Medicare and Medicaid Innovation (CMMI) to design and test innovations in payment and care delivery. In 2016, CMMI announced a five year, $157 million program to scale and evaluate the “Accountable Health Communities” model, which aims to address health-related social needs through improved coordinated efforts between health care organizations and community services [ 17 ]. CMMI funded 29 organizations in 21 states across the country to implement this model and bring together diverse stakeholders ( Figure 1 ). Funded organizations varied in type, including county governments, hospitals, universities, and public health departments. CMMI provides organizations with funding and technical assistance, in addition to outlining program requirements.
The foundation of the model for all sites rested on universal and standardized screening of all Medicare and Medicaid beneficiaries for five social needs domains: housing, food insecurity, utility, interpersonal violence, and transportation. CMMI convened a Technical Expert Panel to create a standardized 10-question social needs screening tool to be used in the model [ 18 ].
Individual sites applied to participate in one of three tracks: “awareness,” “assistance” or “alignment.” Each track had distinct program requirements and funding amounts. Healthcare organizations in the awareness track were required to screen patients for social needs and refer patients to community services. Those in the assistance track provided intensive community navigation (e.g., follow-up support) to help high-risk patients connect to referrals. Organizations in the alignment track focused on aligning with community partners at the community level to build capacity for integrated health social care. Each track was linked to payment methods including start-up funds and additional funds for ongoing services (e.g., $2 per person per year for the awareness track, $86 dollars per person per year for the assistance track, and annual lump-sum payments of $350,000 per year for the alignment track).
CMMI will complete a federal evaluation of the Accountable Health Communities program by 2022 across the 29 funded sites. To facilitate evaluation activities, sites are required to follow rigorous research designs and standardized metrics. Sites in assistance tracks must randomize participants into an intervention group that receives both a list of community resources and intensive community service navigation or a control group that only receives a list of community resources. Sites in the alignment track must use a matched controlled design [ 19 ]. CMMI also set evaluation metrics, including total cost of care and health care utilization, including emergency department visits, inpatient admissions, readmissions, and utilization of outpatient services.
Early experiences have revealed a number of important insights related to process measures, infrastructure and implementation. In the first 750,000 completed screenings across programs across the country, 33% of patients reported at least one social need, with food being the most common need identified [ 20 ]. Eighteen percent of patients were eligible for navigation services, and 76% of eligible patients accepted navigation services. From the patient perspective, quantitative and qualitative studies have shown that patients find screening for social needs using the Accountable Health Communities tool appropriate and acceptable [ 21 , 22 ]. Case studies of providers identified that some perceive risks of collaboration between health and social services, including power dynamics between sector stakeholders, financial sustainability, and competition for employees [ 23 ].
Medicaid 1115 Waivers Program
While the federal government sets the core requirements and benefits covered by Medicaid, individual states can request the federal government waive specific Medicaid requirements and “approve experimental, pilot, or demonstration (state-level) projects…likely to assist in promoting the objectives of the Medicaid program” [ 24 ]. Since the 1960’s, these “Section 1115” waivers have been instrumental in giving state Medicaid agencies the flexibility to test innovative approaches aimed at improving care delivery and access to services to meet their beneficiaries’ unique needs.
Over the past decade, the Accountable Care Act and push towards value-based care models has catalyzed use of 1115 waivers for integrated care [ 25 ]. Sixteen states were granted 1115 waivers to pilot programs specifically focused on addressing social drivers of health ( Figure 1 ), [ 26 ]. For example, California’s Whole Person Care (WPC) program is a $3 billion effort aimed to integrate physical health, behavioral health, and social service delivery for Medicaid beneficiaries who utilize acute and high-cost services [ 27 ]. WPC was granted 1115 waiver authority in 2016 because it used Medicaid funding to address social needs, which is beyond the scope of what is typically covered by Medicaid. During this five-year program, 25 WPC pilots across the state of California were approved to leverage data sharing infrastructure and strengthen cross-sector coordination, many partnering with county housing agencies, to improve health outcomes for their target population. Similarly, in 2018, North Carolina received an 1115 waiver to launch its Health Opportunities Pilots, a program that will use $650 million Medicaid health dollars to pay for non-medical services to address food insecurity, housing instability, transportation issues, and interpersonal violence across four regions in North Carolina [ 28 ]. These pilots will have standardized screening for social needs and pay for social services through value-based arrangements. The Healthy Opportunities Pilot will be supported by North Carolina’s NCCARE360, a technology solution for health and social service providers to refer and initiate appropriate services for individuals with identified needs across the state, and monitor the outcomes of the referral in order to optimize health outcomes [ 29 ]. Medicaid 1115 waivers have been instrumental in supporting pilot demonstration programs like these focused on delivery system reform to address social drivers of health across different states. Table 2 lists other exemplar 1115 waiver demonstration programs that have included initiatives to address social determinants of health.
Examples of SDOH-Related Activities Implemented Via 1115 Waivers.
The demonstration projects supported by 1115 waivers are evaluated by states and independent evaluators [ 35 ]. However, several issues have impeded rigorous state-led evaluations including a limited budget for evaluation, methodological challenges such as identifying appropriate comparison groups and inconsistent reporting of outcomes [ 36 ]. This has made it difficult for states to learn from each other’s approaches in a timely manner and for the federal government to identify innovations that have the potential to improve quality and costs.
Due to these concerns, the Centers for Medicare and Medicaid Services (CMS) has begun to conduct more robust evaluations on the national level and institute more rigorous evaluation criteria for states in recent years. First, in 2014, CMS began conducting meta-analyses to track performance and evaluate the outcomes of 1115 waivers implemented in similar domains across states [ 37 ]. From an integrated care perspective, key findings from these federal reports indicated that 1115 waiver programs have led to increased provider collaboration to support physical and behavioral health integration [ 38 ]. Furthermore, in 2019, CMS began providing states with evaluation tools tailored to their interventions and requiring states to report on performance measures that are specific to the type of demonstration project being evaluated (e.g., reporting on mental health services utilization for pilot projects on Substance Use Disorders) [ 35 ]. Thus, while evaluation remains a challenge, recent trends seem to indicate an increased focus on rigorous, transparent, and timely processes at the federal level.
Medicaid Managed Care
In 40 US states, the Medicaid program is administered by risk-based managed care organizations (MCOs), or private insurance companies that receive per-member, per-month payments from state Medicaid agencies to provide comprehensive services to their enrollees [ 39 ]. If MCOs spend more on services than they are paid by the state, they are at financial “risk” and undergo financial losses. From 2003 to 2018, as states have increasingly transitioned their Medicaid programs to the managed care model, the number of Medicaid beneficiaries enrolled in these risk-based managed care organizations has increased from 16 million to nearly 60 million [ 40 ]. This rise coupled with the growing evidence base linking unmet social needs with health has led Medicaid agencies to push MCOs to identify and address beneficiaries’ social needs as part of broader prevention efforts around reducing costs and improving health outcomes [ 41 ].
Between 2010 and 2020, 35 state Medicaid agencies have included efforts to integrate health and social care into managed care through contract requirements or incentives with the MCOs [ 39 ]. Six state examples are highlighted in Table 3 . While there is tremendous variation in states’ approaches, there are common elements and patterns. In contract requirements, states often embed addressing social needs within broader care coordination and care management requirements. States may require MCOs to screen individuals for social risks and develop care plans to identify needs related to food, housing, or employment [ 42 ]. Similarly, some may require using SDOH data to inform risk stratification frameworks for targeting interventions and allocating resources [ 43 ]. Others may require MCOs to coordinate with community-based organizations or government social services [ 44 ]. This coordination may be through designated “community service coordinators” who can ensure linkage to social services, a community advisory committee to develop strategies for improved integrated care, or contracts between MCOs and social services [ 43 ]. States may also create new value-based payment models, in which MCOs are given incentive payments or bonuses for meeting SDOH-related target measures [ 45 ].
Examples of SDOH-Related Activities Supported Via Managed Care Contracts.
Formal process or outcome evaluations of Medicaid Managed Care contracts that attempt to integrate health and social care have not yet been conducted to our knowledge. Early survey and qualitative research has shown that state Medicaid agencies worry about including SDOH performance measures into contracts without well-validated measures or processes for assuring data quality. Similarly, Medicaid agencies have described how privacy and confidentiality policies limit sharing individual data across health and social service agencies (e.g., insurers, health systems, schools, justice system, non-profits, housing assistance, employment services), and thus limit cross-sector integration [ 49 ]. Medicaid managed care organizations reported that a lack of designated funding streams have made it difficult to adopt social interventions [ 41 , 50 ]. Researchers have an opportunity to partner with state Medicaid agencies and managed care organizations to co-develop studies to evaluate the implementation and effectiveness of efforts to address adverse SDOH within MCOs and identify best practices.
Policy reform and progress made over the last 10 years in the US have advanced the integration of health and social care. In this paper we focused on examples that target the 1 in 5 most socially vulnerable Americans insured through the Medicaid program, including one nationally funded demonstration and two state policy tools. These developments resulted from a policy opportunity that emerged from (1) new value-based payment models in healthcare that prioritize individual and population health outcomes over volume of services and (2) a growing evidence base linking social risk factors with health outcomes. Implementation of these new policy initiatives have required a complex web of actors including government health agencies, private payers, health care organizations, and community-based organizations. While research on integrating health and social care in the US has focused on small interventions implemented in individual clinics and hospitals and is limited by poor study quality and a focus on process measures [ 51 , 52 ], efforts from these broader policy initiatives have reached millions of Americans. Comprehensive evaluation, with a focus on implementation and effectiveness, is still needed.
Although the US has historically lagged in efforts to integrate health and social care compared to other high-income countries, the US is not alone in its recent commitment to this area. To identify cross-cutting learnings across various US initiatives and contextualize them globally, we applied an adapted SELFIE framework for integrated care for multi-morbidity [ 53 ]. Developed from the World Health Organization’s building blocks for health systems, this framework aims to aid the development, implementation, description, and evaluation of integrated care programs. We use the framework here to guide a more conceptual discussion of policy and program components for integrated health and social care. Specifically, we draw on international literature to discuss five main framework concepts: (1) governance and culture, (2) financing, (3) service delivery, (4) workforce, and (5) information & research.
Governance & Culture
Over the last decade, federal and state governments in the US have demonstrated a newfound and robust commitment to health and social care integration [ 54 ]. However, given that service delivery is largely driven by the private hospitals and clinics in the US, policy action from public actors has primarily focused on changes in financing and payment structures. In addition, given the Medicaid program is administered at the state level, the federal government has focused on giving states flexibility in the types of service delivery models each state employs and what benefits are afforded to beneficiaries. This has resulted in a “bottom up” or decentralized approach to health and social care integration, in which the government provides incentives and flexibility for care re-design, and private actors and community-based organizations implement changes in services, workforce, and health information technology [ 55 ].
This is in contrast to the United Kingdom (UK) and Germany, which have taken a more “top down” approach, led by the central government, by aligning goals and setting standards across medical and social service agencies [ 55 ]. For example, in 2013, the UK government partnered with health and social care organizations to create a national policy framework called “Integrated Care and Support: Our Shared Commitment” that outlined a shared vision for reform and available government resources [ 56 ]. While the US’s predominantly “bottom up” healthcare governance model allows for integrated care efforts to be better tailored to local needs, lack of alignment on overarching goals at a national level may hinder collective action on building the workforce or information technology to implement successful strategies more broadly.
Often a hybrid approach which combines the “top down” and “bottom up” governance structures is the most effective. This model ensures that there is national guidance to drive integrated care but it is not overly prescriptive as to preclude adapting models to local context [ 57 , 58 ]. Across approaches and countries, efforts to improve integrated care should actively engage patients, local communities, and the social care sector in the co-design of new care delivery models [ 59 ]. If the health sector alone leads integrated care reforms, it could unintentionally “medicalize” SDOH, in which social needs are viewed like a pathology to diagnose and treat at the point of care, with little acknowledgement of the root causes.
Policy efforts to finance integrated health and social care in the US have focused on providing flexibility to use healthcare dollars to address SDOH and social needs through capacity-building and direct service delivery. This approach resulted from the US’ lopsided health-to-social service spending ratio. That is, for every $1 spent on health care in the US, $0.90 is spent on social services [ 14 ]. In contrast, in OECD countries, for every $1 spend on healthcare, an average of $2 is spent on social services. As a result, federal healthcare dollars in the US are funding cross-sector partnerships between health and social services, as seen in the “Accountable Health Communities” model. At the state level, Medicaid agencies are using payment levers to incentivize or reward private healthcare payers to invest in social care interventions. The state of North Carolina is even using Medicaid healthcare dollars to directly pay social service providers (e.g., food banks, housing agencies, etc.) [ 28 ]. Some experts worry that health care-centered integration efforts may inadvertently medicalize social care [ 60 ] or overburden underfunded social services [ 10 ]. Additionally, financing interventions that target individual-level social needs fail to address the upstream, community-level or systemic root causes that lead to health-related inequities [ 61 ].
In contrast, other countries have experimented with more bi-directional financing mechanisms between health and social services. Models may include aligning budgets across sectors to meet agreed-upon objectives; pooling funds and management staff across sectors into common buckets; or even integrating health and social services under a single management body [ 62 ]. In Sweden, the Norrtalje model brought together the local health care governance structure (“Stockholm County Council”) and local social care governance structure (“Norrtalje Local Authority”) to form a new join Governing Committee that pooled funding from both original structures [ 63 ]. The US should consider this model and other international examples, as it moves to adopt more advanced budgeting tools for cross-sector integration [ 64 ].
Service Delivery
In the US, efforts to integrate health and social care have mainly focused on identifying and responding to individual patients’ social needs. All three Medicaid policy examples described in this paper include requirements or incentives for standardized screenings for social needs. Once patients are screened, health care organizations can help patients connect to social services [ 51 ]. These individual-level programs have been complemented by broader collaborations between healthcare organizations and social services, such as medical-legal partnerships and clinic-based food pantries [ 12 ].
Globally, this model of linking patients with non-medical services for social needs has been coined “social prescribing” and is often associated with primary care [ 65 ]. In March 2019, 11 countries celebrated the world’s first Social Prescribing Day, including Finland, UK, Brazil, and Canada [ 66 ]. There are important distinctions between American social prescribing schemes and those from other countries. The US has developed standardized screening questions that have been used across primary, secondary, and tertiary care settings [ 67 ]. Simple and standardized approaches allow for patient self-administered screening; scalable pathways for responding to reported needs; population-level tracking of social needs; and consistent measures for program evaluation and research. Common questions in the US include screening for transportation, food insecurity, housing instability, utilities, and interpersonal violence [ 68 ].
Other international models often implement broader individually-tailored approaches. Patients may be asked about overall social and mental well-being, and social prescribing staff may co-create strength-based care plans with patients [ 69 ]. Thus, while US social prescribing initiatives supported through Medicaid mostly target basic material needs (e.g., food and housing), international models more often include more holistic referrals (e.g., exercise, volunteering, parks, recreation centers, and art museums) [ 70 ]. Despite policy support globally, social prescribing initiatives within and outside individual countries greatly vary in intervention components, intensity, target populations, and settings. More international research is needed to study the effectiveness and value for money of social prescribing programs, particularly under different financing and governance structures.
The US policy efforts have not outlined a comprehensive workforce strategy for integrating health and social care, including for the Medicaid population. The workforce used for social prescribing activities in the US has been heterogenous and include both the traditional health care workforce (e.g., doctors and nurses) and the social care workforce (e.g., case managers, social workers, and volunteers) [ 71 ]. Although research of workforce models suggest interprofessional care teams in clinical settings and community health workers in community and home-based settings could be possible in the US [ 14 ], barriers to reimbursement remain a challenge.
In contrast, other countries have focused on policies to deploy a standardized workforce to integrate health and social care. For example, the UK National Health Service (NHS) aims to fund 1,000 social prescribing “link workers” to work in primary care practices by 2021 [ 72 ]. The NHS is working to ensure that link workers have clinical supervisors, access to peer support and regional learning coordinators, and online training packages [ 72 ]. Similarly, Germany has instituted a training program at the national level for nurses to gain the skills and expertise to serve as case managers and care coordinators to support integrated care [ 55 ]. In contrast, in the US such roles are hired and trained at the local level. Future efforts to develop a workforce to integrate health and social care in the US should look to such global examples to gain insight into recruitment, training, and team integration.
Information & Research
Emerging evidence in the US has focused on local health-system interventions to integrate health and social care rather than the policies that support them [ 73 ]. Studies in the US have demonstrated the feasibility and patient acceptability of screening for social needs [ 21 , 22 , 74 , 75 ], as well as the need for further studies on the psychometric and pragmatic properties of various screening tools [ 76 ]. More research in the US and internationally is needed to evaluate the effectiveness and cost-effectiveness of social prescribing programs that link patients with community resources, particularly under different financing and governance structures [ 52 , 68 ]. However, evaluating integrated care efforts like social prescribing presents many challenges. First, determining the impact of these programs can be difficult given lack of alignment on measures and measure specifications [ 77 , 78 , 79 ]. Historically, there has been little standardization of social needs screening questions or the measures for evaluating the “success” of interventions (e.g., process measures, social care impacts such as income or food insecurity, health and well-being impacts, healthcare costs and utilization impacts, provider outcomes related to burnout or efficiency). Certain initiatives in the US, such as the Gravity Project initiated by the University of California-San Francisco, are making headway in standardizing how social risk data is captured in electronic health records (EHR) [ 80 ]. Second, few studies have used rigorous study designs or evaluate impact beyond process measures or improvements in specific social needs or subpopulations (e.g., high healthcare utilizers). At the policy level, governments globally can support national evaluation frameworks and better fund research to fill evidence gaps.
Another necessary component of analyzing patient and population-level data is appropriate information technology. In 2009, the US passed a new law to increase the adoption of EHRs among healthcare providers and systems [ 81 ]. Widespread uptake of EHRs created an opportunity to routinely collect measures of patients’ social risks in the clinic setting. However, there has been little policy guidance on which SDOH screening tools to embed in the EHR or which codes to use to classify social risks [ 82 ]. Furthermore, while health systems can document and aggregate data related to social risk screening and referrals to community resources, social service providers often do not have access to patients’ EHRs due to privacy and confidentiality laws. These challenges fragment care, and prevent the ability to generate real world evidence or evaluate innovative models without external funds for research or additional investment on measurement.
To overcome the limitations in US informational continuity across settings, recent efforts have created new technology platforms that both health and social service partners can access to make bi-directional referrals and monitor care management [ 83 ]. Medicaid state agencies or Medicaid managed care organizations can license these software products from private companies or foundations. For example, as part of its Medicaid reform, North Carolina has launched NCCARE360, “a statewide coordinated care network” which contains a resource directory and referral system that is accessible to health and social service providers, and an ability to track outcomes [ 29 ]. Implementation research is in its earliest stage and state-level evaluation is likely to align with the previously mentioned Healthy Opportunities Pilots.
Similar pushes for digital platforms to facilitate cross-sector integration have emerged in the UK [ 84 ]. Private companies have started to contract with health care organizations and community-based organizations to implement their platforms across a range of providers [ 85 , 86 , 87 ]. Additionally, some health information technology efforts in the UK have focused on increasing interoperability between healthcare systems, enabling national audits and secondary analysis of public health systems. In 2017, the NHS chose eight regions across England to transition to accountable care systems (ACS) to better integrate and coordinate care at the community level [ 88 ]. As part of these efforts, each ACS has designed its own digital shared care record that is interoperable across different NHS entities and accessible to a patients primary, community, secondary and social care providers. While information technology efforts in the US mirror many of the efforts in the UK to integrate care, future efforts in the US should focus on increasing data interoperability across sectors and health systems.
The Decade Ahead
Table 4 summarizes the main lessons learned from the three integrated health and social care policy initiatives over the last decade and highlights priority areas for future work. The start of the 2020s, with the COVID-19 pandemic and a new presidential administration, has created a new opportunity to build upon and sustain recent progress towards integrated care [ 89 ]. The COVID-19 pandemic has further exposed the role that social inequalities play in shaping health inequalities [ 90 ]. Americans from low-income communities have been more likely to contract and become hospitalized from COVID-19, and suffer from the pandemic’s economic repercussions, such as unemployment and increased food insecurity [ 89 , 91 ]. As the country realizes the need for a coordinated response to intertwined social and health challenges, the new Democratic administration can prioritize integrated health and social care in their broader “Build Back Better” strategy, already demonstrated by their interest in adding 150,000 community health workers to underserved communities and creating a new Public Health Job Corps to address SDOH [ 92 ]. While previous policy efforts for integrated care have largely been state-driven, the new administration could provide leadership to create a bold national strategy around data infrastructure, workforce, financing, and service delivery [ 93 ].
Lessons Learned.
Over the last decade, new policies in the US have catalyzed initiatives to test innovative integrated health and social care models, with the ultimate goal of improving population health and decreasing costs. The examples from the US Medicaid insurance program highlighted in this paper describe the country’s progress in an international context. Continued investment is needed into each building block to ensure a sustainable approach to integrated care. Cross-nation collaboration is needed to globally advance policies and research that improve population health and address individuals’ needs.
Dr Julia Vera Pescheny, MPH., European Institute of Innovation and Technology (EIT) Health.
Two anonymous reviewers.
Competing Interests
The authors have no competing interests to declare.

Get inspired with empowering stories from across the health sector.
Speaking the same language
Seeing through wards, super-efficiency saves lives, case studies.
Read our healthcare case studies and discover powerful solutions.
Barking, Havering and Redbridge University NHS Trust
Cambridge university hospitals nhs foundation trust, guy’s and st thomas’ nhs foundation trust, leeds teaching hospitals nhs trust.
- Uncategorised
- Procurement
- Medical records
- Diagnostics
Recent Articles
- Harnessing GS1 standards to reduce unwarranted clinical variation View Case Study
- Harnessing the clinical benefits of point-of-care scanning View Case Study
- CareScan+: Enabling safer more efficient care View Case Study
- Terms and conditions
- Privacy Policy
- Cookie policy
- Competition policy
Department of Health and Social Care introduces Scan4Safety to revolutionise patient care
Key results, gs1 standards allow clinical staff to build a complete patient picture that is easily accessible, increased data visibility can aid efficiencies in catalogue management and staffing, the problem.
The Department of Health and Social Care (DHSC) needed to support the NHS in improving the delivery of patient care through process standardisation and efficiency.
The 2014 NHS eProcurement strategy highlighted that investment in digital platforms, staff organisation, and standardised purchasing could make a huge difference in the way the NHS operates. It calculated that these changes could contribute to cost savings of up to £5 billion per year.
But with varying degrees of readiness across NHS trusts, the challenge to roll out a completely new system across the service was huge.
The solution
With support from GS1 UK, the DHSC announced six NHS acute trusts in England that would act as Scan4Safety demonstrator sites.
£12 million of funding was made available to the six trusts, and teams were asked to focus on three core enablers: patient identification, catalogue management, and location numbering. In addition to this, three use cases were highlighted including purchase to pay, inventory management, and product recall.
GS1 UK also put together an advisory board of industry leaders, senior clinical staff and regulators from across the UK. This team would support all activities in order to ensure success.

"GS1 standards enable everything that happens to a patient to be recorded accurately and with minimal impact on patient or clinical staff. "
The results
The adoption of the Scan4Safety initiative clearly demonstrated that GS1 standards are key in building a more efficient, future-proofed NHS.
Through the use of barcodes and handheld scanners, clinicians are provided with an accurate and real-time record of exactly who did what to the patient, when it happened, and where it took place.
Hosting patient data electronically and accessing it via barcoded wristbands means that any potential problems can be flagged before they happen. For example, if a patient is mistakenly prescribed a treatment that does not tally with their record, the scanning device will flag it immediately.
Submit a case study
If you would like to submit a case study demonstrating how your trust has implemented GS1 standards, email us at [email protected]
- Download the PDF
- icon-share Contact us
- icon-share Submit a case study
Related case studies
Helping nhs organisations better manage non-pay spend, salisbury nhs foundation trust.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- NHS and the whole of...
NHS and the whole of society must act on social determinants of health for a healthier future
Read the full series: the bmj commission on the future of the nhs.
- Related content
- Peer review
- Lucinda Hiam , Clarendon scholar 1 ,
- Bob Klaber , director of strategy 2 3 ,
- Annabel Sowemimo , consultant in sexual and reproductive health 4 ,
- Michael Marmot , director 5
- 1 University of Oxford, Oxford, UK
- 2 Research, Innovation, Imperial College Healthcare NHS Trust, London, UK
- 3 School of Public Health, Imperial College London, London, UK
- 4 Lewisham and Greenwich NHS Trust, London, UK
- 5 UCL Institute of Health Equity, London, UK
- Correspondence to: L Hiam lucinda.hiam{at}kellogg.ox.ac.uk
Health is going in the wrong direction in the UK, and reversing the trend requires political and societal commitment to deal with the underlying causes
The UK is facing a prolonged and serious health crisis. At a time when the future of the NHS is in jeopardy after over a decade of austerity, and with public satisfaction at an all time low, 1 it must pick up the pieces of failures across government. Attaining good health requires more than healthcare, and improvements in the provision of healthcare by the NHS alone is inadequate to address the health crisis—action is needed on the social determinants of health 2 ( box 1 ).
Definition of social determinants of health 3
The social determinants of health are defined by the World Health Organization as: “the conditions in which people are born, grow, live, work, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, and political systems.”
In this paper, we propose evidence based solutions to the worsening health and widening inequalities in the UK through action on the social determinants of health. (A separate article within the commission is focused on health equity. 4 ) We first outline the problem of deteriorating health across the UK. We then provide an overview of the evidence, showing how action on the social determinants can improve health. We confront the challenging political nature of this area, including rebuttal of criticisms of interventions as actions of a “nanny state” and the neoliberal focus on individualism. Finally, we offer action focused solutions and recommendations on what NHS workers, leaders of NHS organisations and integrated care systems, and the government can do to urgently deal with the deteriorating health of the population.
Although much of the evidence we draw on is focused on England, or England and Wales, we suggest that the overall findings and recommendations are relevant to all of the UK nations, and we emphasise where these might differ. Furthermore, throughout we highlight that health is inherently political, but it is not party political. Politicians from any party can choose to act on the ample evidence available to them.
The problem: why is action needed?
Among European countries, the UK is a relatively poor, sick country with some rich, healthy people. 5 Summary measures of the health of the population are going in the wrong direction for all four nations of the UK. The UK consistently ranks poorly for infant mortality, 6 and its global ranking for life expectancy has fallen, with only the US faring worse of the G7 countries. 7 The public health system in the UK has been decimated over the past decade, 8 particularly in England and Northern Ireland, with the unexpected abolition of Public Health England in 2020, and a 27% real terms per person cut to the public health grant since 2015-16, 9 with greater cuts in poorer areas of England. In contrast, both Public Health Scotland, reformed in 2019, 10 and Public Health Wales and are making progress in improving the health of the populations they serve. 8 11
Shorter lives spent in poorer health
People in the UK are dying earlier. Life expectancy can be calculated at any age and provides an estimate of the average age a person would live if the current mortality rates were applied over their lifespan. Since 2010, the long history of improvements in life expectancy have plateaued and, for some groups, declined. 12 13 14 15 16 As of early 2024, the latest figures from the Office for National Statistics show that the combination of slow improvements for the past decade and the covid-19 pandemic have decreased overall life expectancy, returning to 2010-12 levels for women and below the 2010-12 level for men, and falling in all four nations for 2020-22 compared with 2017-19. 17 Furthermore, people are spending less of their lives in good health. Health Equity in England: The Marmot Review 10 Years On reported that healthy life expectancy has reduced for women since 2010, and the proportion of life spent in poor health has increased for both sexes. 14 A 2024 report found 9.6 million households are living on incomes below the minimum income standard and in some of the least well insulated, cold, damp homes in industrialised countries, 18 with negative consequences for the health of children and adults. 19
The decline in health shows marked inequalities across factors such as ethnic group, race, sex, and deprivation, many of which intersect with each other. Life expectancy and healthy life expectancy are closely linked to deprivation: the greater the deprivation, the shorter the life expectancy. Those living in deprived areas spend more of their shorter lives in poor health. 14 This relation represents a social gradient: each increase in socioeconomic level results in an increase in health and lower mortality rates. Health Inequalities: Lives Cut Short found that that one million lives were cut short between 2011 and the start of the pandemic in 90% of areas in England. 20 Figure 1 , from the Marmot Review 10 Years On, shows how deprivation and region overlap, with regional differences greater in the most deprived group (divided by deciles) than in the least deprived group. 14 In every region outside of London, life expectancy has fallen in the most deprived group. Acknowledging the overlap and intersections in the groups affected is important. Those living in the most deprived areas are often affected by multiple factors, such as structural racism and the consequences of the climate emergency, and are often more likely to lack the resources to mitigate the subsequent health consequences.

Life expectancy at birth by sex for the least and most deprived groups in each region, England, 2010-12 and 2016-18 14
- Download figure
- Open in new tab
- Download powerpoint
Health is deteriorating from the cradle to the grave
Older women were among the first groups to have an unprecedented fall in life expectancy. 15 21 Older people have been particularly affected because of a greater reliance on a functioning health and social care system. The golden generation, those born between 1925 and 1934, saw remarkable improvements in mortality throughout their lifetimes, 22 but the remainder of their lives were cut short since 2010. 23 Over time, in more and more groups, health has worsened and lives have been shortened, 12 13 including a rise in deaths of despair in middle age, reflecting the US experience, of deaths from suicide and from causes related to alcohol and drugs. 24 These findings are reflected across Scotland, 25 26 27 and in Northern Ireland, life expectancy in men has been declining since 2016-18, with increased mortality in those aged 30-39 years making the greatest contribution. 28
Of particular concern is the “appalling decline” in both physical and mental health of children aged <5 years, detailed in the 2024 report from the Academy of Medical Sciences. The report described children as being “betrayed” by a failure to be provided with a healthy start in life. 29 30 The accompanying statistics include that infant mortality increased between 2014 and 2017, with the UK ranking 30th out of 49 OECD (Organisation for Economic Cooperation and Development) countries; child vaccination levels are currently below WHO coverage targets; and a quarter of all children aged 5 years are affected by preventable tooth decay, the main reason for hospital admissions in children aged 6-10 years. These problems are entirely preventable and disproportionately affect the most deprived communities.
Figures 2 and 3 show that infant and child death rates increased between 2020 and 2023, with infant deaths almost three times as high for black/black British babies than white babies, and marked regional inequalities in child deaths. 31 Similar trends have been seen in the rates of stillbirths, with increasing rates linked to worsening areas of deprivation and ethnic groups. 32 Other inequalities in early child development exist: cognitive, linguistic, emotional, and behavioural. 14 These inequalities are important because they are correlated with behavioural problems in children and predict the subsequent development of health inequalities. Another marker of poor health in children in the UK is height. In 1985, the height of boys and girls aged 5 years in the UK was lower than in 68 other countries. Height in children aged 5 years increased more slowly in the UK than in many other countries. By 2019, in the UK, boys ranked 102 and girls ranked 96. The average height of children aged 5 years fell from 2015 onwards, suggesting that austerity, which began in 2010, might have had an effect. 33

Estimated infant death rate per 1000 live births by ethnic group 31

Estimated child death rate per 100 000 population, by region. Population is children aged 0-17 years 31
Rising poverty, worsening health
A wide body of evidence has indicated a link between deterioration in health in the UK and cuts in public spending through austerity policies introduced in 2010, policies that are continuing into 2024. 12 13 14 23 25 34 35 36 The effect of austerity on poverty in the UK has been so great that two successive United Nations special rapporteurs on extreme poverty have called on the government to take action on the problem. 37 The first, Philip Alston, visiting in 2018, called the policies of austerity “punitive, mean spirited, and callous” and the levels of child poverty both a disgrace and an economic disaster. 38 The second, Olivier de Schutter, visiting in 2023, commented that the warning signs his predecessor had given had not been acted upon, that universal credit was too low to protect people from poverty, and that “There’s a huge gap, which is increasingly troubling, between the kinds of indicators the government chooses to assess its progress on one hand, and the lived experience of people living in poverty.” 39 Currently, government policy does not provide enough money for people to live healthily. 40 41
Evidence to support action on social determinants of health
Without a change in policy, there is no reason to think that the worsening trajectory of health in the UK will improve. Here, we summarise the key evidence on how action on the social determinants of health can improve the health of the population.
How do social determinants of health cause ill health?
The WHO Commission on Social Determinants of Health synthesised the evidence on social determinants of health. 42 Building on this global body of work, in 2010, Fair Society Healthy Lives: the Marmot Review , re-examined the evidence as it applied to England. 43 The review categorised the determinants of health inequality into six domains: early childhood, education, employment and working conditions, having enough money for a healthy life, environmental and living conditions, including housing, and health behaviours. Health Equity in England: the Marmot Review 10 Years On , published in 2020, indicated the health picture summarised above and showed worsening in most of these six domains, the likely cause of which was austerity. 14 Relative child poverty, after housing costs, increased from 27% to 30%, and 1000 Sure Start Children’s Centres closed; spending on education per pupil was reduced by 8%; the gig economy increased; poverty increased, as summarised above; little was done to solve the housing crisis; and spending to improve the thermal property of housing was reduced. Looking at one key marker of future ill health, inequalities in childhood obesity increased.
Each of these domains was made worse by the pandemic and the cost-of-living crisis. For example, the Joseph Rowntree Foundation defined destitution as doing without two or more of six essential items: housing, heat, light, food, clothing, and toiletries. 44 In the UK in 2022, 3.8 million people, including one million children, were destitute. The figure for children increased by 2.9-fold since 2017. Food poverty and food insecurity rose, linked to austerity, 45 46 including for children, with the number of children in food poverty doubling between 2022 and 2023 to four million. 47 Between April 2022 and March 2023, the Trussell Trust’s network of food banks delivered almost three million emergency food parcels (a 37% rise compared with the same period the year before); one million food parcels went to children. 48 The lack of these essential items will damage health and increase health inequalities. Living in these conditions has a huge social, emotional, and psychological effect, which will in turn affect mental and physical health.
Much has been reported on the commercial determinants of health. 49 A review of how industry can affect health and health inequalities summarised the evidence into three areas: employment and working conditions, unhealthy goods and services, and the wider effect on society and communities, including procurement, employment, and the environmental and social impact. 50 The 2010 Marmot review developed the concept of proportionate universalism: universal policies with effort proportional to need. Spending by local government in the decade after 2010 was regressive, showing effort inversely proportionate to need. The greater the deprivation of the area, the greater was the reduction in spending per person. Spending was reduced by 17% in the least deprived 20% of areas (quintile) and by 32% in the most deprived areas (quintile). Spending on adult social care was also regressive, with a reduction of 3% in the least deprived areas and 16% in the most deprived areas. Evidence indicated that the greater the reduction in local authority spending, the worse the mortality trends after 2010. 12
Action on social determinants of health improves health
Recognising that the action needed to improve the health of the population is outside the provision of health services is not new, but some political factions reject such action, favouring an individualistic approach more consistent with a libertarian ideology. The great health gains made during the 19th and early 20th century were not because of the therapeutic revolutions of modern medicine but more a result of the sanitary and social reforms that provided people with better living conditions, such as uncontaminated food, clean water, waste disposal, improved housing, and education of children. The marked improvements in life expectancy in the 1940s and 1950s were thought to be a result of a combination of improved housing and nutrition after rationing during the second world war, which improved understanding of the importance of childhood nutrition, free secondary education for all (Butler Education Act of 1944), advancement of public health measures, including in sanitation and access to clean water, introduction of antibiotics and immunisations and, eventually, the introduction of the NHS in 1948. Although the NHS was established after the initial acceleration in improving life expectancy, substantial health gains have been made since, thanks to greater access to effective care that it enabled.
Politics of health
Given the repeated warnings and attention from international bodies, 37 39 why has the UK government failed to act on the social determinants of health? Here, we briefly outline what has been known for centuries: health is political.
Improving health is a political choice
Ten years ago, in 2014, experts wrote an open letter in the Lancet to the then prime minister, David Cameron, highlighting concerns about food poverty. 51 Since then (and before then), multiple reports, research papers, and editorials have called for government action on rising infant mortality rates, child poverty, and growing inequalities. 6 15 21 36 52 Many other reports on these problems exist, spanning over a decade, all indicating that the state of health in the UK in 2024 is not unexpected, has not happened without warning, and could feasibly have been prevented. More research is not needed; action is needed. Action to reduce poverty can be taken almost immediately. For example, the decision by the then chancellor, Rishi Sunak, to reverse the temporary increase of £20/week in universal credit during the covid-19 pandemic, which had helped 400 000 children out of poverty, returned the number of children living in poverty to levels before the pandemic of 4.2 million. 53 Notably, fewer children are living in poverty in Scotland than in England, 54 where child benefit payments for more than two children in a family have been maintained, and the Scottish child weekly payment was raised to £25 for any child aged <16 years in a household receiving benefits, a move the children’s commissioner in Wales is advocating to replicate. 55 56 Child poverty in the UK is a political choice.
The economic decline of the UK, exacerbated by Brexit, must be confronted. The Institute for Fiscal Studies has forecast that real household disposable income will not return to pre-pandemic levels before the next election in 2024, after “another terrible decade” of poor economic growth. 57 The number of people signed off sick from work has tripled in the past decade, because Britain is sicker than it was a decade ago. 58 Investing in the social determinants of health will improve health, productivity, and thus economic growth. The move from health in all policies to health for all policies acknowledges that progress and improvement in health and health outcomes has substantial benefits for other sectors. 59 We cannot afford inaction.
We know what to do
Focused, evidence based recommendations exist on how to improve health in the UK. The 2010 Marmot review called for action on six policy objectives (the first six in box 2 ), and publication of a framework of indicators and economic analysis followed one year later. 43 Inequalities in Health: the Black Report was commissioned by a Labour government and published under Margaret Thatcher’s Conservative government. The report detailed inequalities in poor health and mortality in Britain. 60 Similarly, the Marmot review was commissioned by a Labour government and published under the Conservative-Liberal Democrat coalition government. The coalition focused on implementing austerity, “doing more for less,” 61 and the recommendations were not acted upon.
The Marmot principles
Give every child the best start in life
Create fair employment and good work for all
Enable all children, young people, and adults to maximise their capabilities and have control over their lives
Ensure a healthy standard of living for all
Create and develop healthy and sustainable places and communities
Strengthen the role and impact of ill health prevention
Tackle discrimination, racism, and their outcomes
Pursue environmental sustainability and health equity together
From 2020 onwards, the covid-19 pandemic intensified and increased the existing inequalities. The UK fared comparatively badly, in part because of the condition of the country before the pandemic. 62 63 The Build Back Fairer: COVID-19 Marmot Review detailed short, medium, and long term actions needed on each of the six Marmot principles to reduce inequalities and improve health to build, or rebuild, a healthy society. 64 The profound effect of structural racism on the outcomes of covid-19 led to the addition of the seventh Marmot principle, and the eighth was added in consideration of the climate emergency ( box 2 ). 65 These additional principles are based on empirical observation, but regrettably are often politically partisan. Although central government has failed to act on the robust evidence available, some local governments have acted decisively 66 ; for example, Coventry and Manchester are Marmot cities, acting on the Marmot principles to improve health. 67 68
Challenging individualism and the nanny state
Two related areas of political ideology, individualism and accusations of the nanny state, act as powerful rhetoric against public health interventions intended to improve the health of the population. Every day, people make decisions that affect their health and wellbeing, but not under conditions of their own choosing. The individualistic approach to health assigns blame to those who show behaviours associated with ill health, and is a convenient mechanism for those in and with power, and wider society, to abrogate responsibility for creating the conditions for a healthy society. Instead, those with the worst health are blamed for their conditions. For example, during the peak of the covid-19 pandemic, people from lower income households, frequently with frontline roles, were unable to work from home and had greater loss of income during quarantine when infected with the virus. 62 69 People infected with the virus, including those who died, were frequently blamed for not taking adequate precautions or having weaker immune systems or pre-existing conditions (also linked to deprivation) rather than the wider social context being acknowledged. The pandemic is just one example.
Low income, racial, and sex discrimination, commercial exploitation, poor housing (or lack of housing), and lack of access to high quality education are some of the social conditions that diminish the ability of people to live healthy and fulfilling lives. Action to improve these social and economic conditions can and will improve health and reduce the burden on healthcare.
If public health is seen as simply instructing people on how to behave, then accusations of the nanny state are understandable. But what is necessary for public health is ensuring that people have a roof over their heads, have sufficient money to buy food to feed their families, can afford heating when the weather turns cold, and can face the weeks and months without fear of eviction, which is different from instructing people on how to behave. Disputes at the margin, however, are inevitable. Some will see Prime Minister Sunak’s ambition for a smoke-free generation as a bold step towards improving the public health (although a substantial health problem is looming from the growth in vaping, now shown to markedly increase risks of cardiovascular disease 70 ). Others will see it as a step too far. We should see the key social determinants of health as the responsibility of government and other social actors, not simply individual responsibility. Asking individuals to make choices that their circumstances do not allow almost guarantees persisting health inequalities.
Weakening of the public health system across UK
Because of the political climate, at least in part, the public health system across the UK is now arguably weaker than at any point in history, going back as far as the 1870s, with substantial reductions to public health budgets and staffing levels. Northern Ireland and England have seen significant changes, with the functions of public health severely weakened at local, regional, and national levels.
In England, the abolition of the regional tier of government has seen the end of regional development agencies, regional assemblies, strategic health authorities, and government offices for the regions, among other subnational infrastructure. The abolition of regional emergency planning and response functions, which had worked effectively during crises, such as foot and mouth disease and the fuel tanker drivers’ action, was a weakness in the poor response to covid-19 in the UK. The role of public health has been curtailed, with major reductions in resources and expertise, and changes in the role of directors of public health. The abolition of Public Health England and creation of the UK Health Security Agency as an executive component of the Westminster government’s Department of Health and Social Care not only saw the disappearance of the term public health but cast the new and undefined function of health security as part of the country’s security system. This change has been accompanied by attempts to replace the term health inequalities with the ill defined and obscure health disparities.
In Northern Ireland, local director of public health posts have disappeared entirely, and the public health function has been severely weakened. The absence of a functioning government for several years has created something that resembles a failed state. 71 The re-establishment of the Northern Ireland Executive offers a mechanism to begin to deal with these problems, and the current health minister is familiar with his brief. The legislative agenda is enormous, however, and health might not be a priority. Northern Ireland’s unique position with regard to the European single market is a further advantage as it limits the ability of the government at Westminster to enact health damaging policies, such as relaxation of restrictions on harmful chemicals. 72 The Good Friday Agreement also offers opportunities to learn from and expand joint programmes with Ireland, where in marked contrast with the UK, life expectancy is improving.
Recommendations
Just as the health of people served by the NHS is determined by their economic and societal conditions, the future of the NHS is inextricable from the future of society and policies that provide for good health. Our recommendations focus on what the NHS can do in each of the four nations of the UK and what the whole of society can do, to act on the social determinants of health.
Restore, revitalise, and prioritise the public health system in the UK
We recommend urgent restoration of the public health system across all four nations of the UK. The evidence base for what needs to be done to improve population health continues to strengthen, as we have highlighted, even while the capacity in the UK to carry out the necessary actions to improve health is depleted. The deterioration in health and the social determinants of health, such as housing, have been accompanied by the dismantling and the imposed disorganisation of the public health system, particularly in England and Northern Ireland. Thus, we recommend that the government should restore the public health grant to at least 2015-16 levels 73 and re-establish Public Health England.
Dealing with the population health crisis in the UK requires urgent, in-depth consideration and substantial commitment to creating a system that can deliver all WHO defined essential public health functions. One way to engage in this task would be the formation of a cross party task force accountable for public health, enabling non-partisan consideration of the necessary actions. The task force should cover the whole of the UK and seek to learn from the positive experiences of public health structures in Wales and Scotland. Because of the long term nature of public health change, there would also be value in creating this cross party task force as a standing body so that it could review the implementation of its recommendations and measure the results.
Role of the NHS
The NHS is predominantly focused on providing clinical care and support to those needing treatment for health conditions. It is because of its role in the delivery of care that the NHS can do much more as both a health service provider and the country’s largest employer 74 to ensure that fewer people are burdened with poor health and that many more enjoy healthy lives.
What individuals working in the NHS can do —Recognising that improving the social determinants of health will improve health, and thus reduce the burden on healthcare, those working in the NHS might consider the effect they can have as individuals. Box 3 shows some examples.
Examples of actions on social determinants of health by individuals working in the NHS
As an individual healthcare worker.
Focus on co-production for service design, development, and evaluation. 75
Use clinical encounters with patients and their families to ask about, and listen to, some of the wider problems that might be affecting the patient’s health.
Consider if adaptations to how care is delivered could be helpful (eg, adapting the follow-up conversation to a time and method that saves travel and thus has less impact on time, carbon, and money), and fit around the patient’s work (which might be paid by the hour or on a zero hours contract) and their children’s schooling (education being a critical social determinant)?
As a community member
Consider and mitigate for the effect of all activities on the environment, such as changing methods of travel, reducing waste, and switching off unused desktops/lights.
Support initiatives on anti-oppression and raise awareness on how intersecting factors can worsen health outcomes.
As an organisation member
Advocate for a more thoughtful, intentional, and effective organisation in its role as a partner in civil society (eg, explore the organisation’s role in working with multi-agency partners such as housing departments of the local council, voluntary sector, public health teams, schools, and police).
As a member of the electorate
Build knowledge on policies that can affect the social determinants of health, while supporting organisations and voting for policies that proactively deal with these concerns.
What the NHS can do as a health system —Leaders of NHS organisations and systems can act on the social determinants of health: firstly, as an employer, considering their staff as a key population; secondly, on staff recruitment, development, and training, working towards self-sufficiency in the workforce; thirdly, as important social partners within local communities; fourthly, as a procurer of goods in its supply chain; and finally, in reducing its environmental impact ( box 4 ). These actions are linked to recommendations to enhance the NHS’s role as an anchor institution (ie, an institution that can positively contribute to the wellbeing of the population it serves and the communities it is based in). 77 Healthcare leaders might draw inspiration from the East London NHS Foundation Trust, which is working with University College London Institute of Health Equity to become the first Marmot Trust, exploring how trusts can work upstream to tackle the drivers of poor health and implement the Marmot principles ( box 2 ). 78
What the NHS can do as a health system
As an organisation or system that employs staff.
Build and maintain a workforce environment that is conducive to improving the health of patients, and protecting and enhancing the health of staff
Ensure staff have the pay, conditions, and opportunities to learn and develop, and have inclusive working environments where they can thrive
Take a proactive approach to workplace health and wellbeing
Encourage an open and supportive culture for the early recognition and proactive management of mental health problems
Ensure a continued commitment to educational programmes that raise awareness on how factors such as race, sex, sexuality, and deprivation can affect health outcomes
As an NHS workforce
Work towards a model of workforce self-sufficiency for the UK
Ensure adequate support structures are in place for international staff, because marked inequalities also exist in access to healthcare for staff and their families 76
Support local communities to explore the roles available in the health service, and support apprenticeship schemes in the NHS
Increase training opportunities and skills development for all staff
As an organisational partner in civil society
Learn from others, share and adopt ideas that improve health and care, and model broader civic responsibility
Build relationships and partnerships with organisations (eg, local authorities, voluntary sector organisations, local businesses, sports club foundations, community groups, healthcare providers)
Harness these relationships to work in multi-agency partnerships within a defined place, forming a strong collective power to tackle barriers to good health
As a procurer of goods and services
Ensure contracted service providers have fair working conditions for their employees.
Where possible, procure goods and services locally that benefit the community and minimise harm to the environment
As a sustainable healthcare system
Continue to work to reduce the environmental impact, working in partnership with others on key concerns
Continue progress towards the NHS becoming the world’s first net zero health service
Role of policy makers
The health crisis cannot be solved by the NHS alone. Action on the social determinants of health requires changes in policies and political support from local and central governments. We know what to do. The political will to implement the recommended measures has, so far, been missing. The UK lost a decade between the government commissioned 2010 and 2020 Marmot reviews; the findings and recommendations were not acted upon by successive governments. 79 Since then, the covid-19 pandemic has worsened the crisis, 64 and life expectancy has regressed to 2010-12 levels. 17 Time is of the essence.
We are not recommending further reviews, research, or commissions; these processes would delay urgently needed action. Instead, from the Marmot reports, 14 19 43 64 we highlight three recommendations ( box 5 ): implement policies to tackle poverty so that individuals and families can lead healthy lives; invest in housing that is compatible with good health; and prioritise children and young people. These recommendations are, of course, related. Reducing child poverty and improving child health will, in turn, improve the physical and mental health of families, strengthening the workforce and productivity, as well as reducing costs to the NHS. Although managing poverty does not level the social gradient, proportional universalism does, and a focus on housing and childhood can help deal with the gradient, as will further action on the Marmot principles ( box 2 ). Similarly, by dealing with key policy areas, such as working and housing conditions, people experiencing intersecting factors are most likely to benefit, because the data consistently show that they are over-represented in these areas.
Recommendations for the government 19 64
Implement policies to tackle poverty so that individuals and families can lead healthy lives
Ensure the national minimum wage and national living wage are sufficient to lead a healthy life
Adopt more equitable redistribution of profits in companies to reduce in-work poverty
Support the Joseph Rowntree Foundation and Trussell Trust campaign (Essentials Guarantee) 40 to raise universal credit to ensure that essentials are covered, with at least an annual review
Invest in housing compatible with good health
Introduce schemes to increase the supply of affordable, good quality, sustainable housing (eg, by reform of the private housing market and by increased investment in building social housing)
Commit to a 10 year retro-fit programme targeted to people on low incomes in energy inefficient housing, tackling both the negative effects of poor housing on health and the effects on the climate
Prioritise children and young people, giving every child the best start in life
Reverse the deterioration in mental and physical health of children and young people, and improve levels of wellbeing from the current low rankings internationally, as a national aspiration
Reduce levels of child poverty to 10% (comparable with the lowest rates in Europe)
Prioritise reducing inequalities in early years development (eg, allocating additional spending to early years in more deprived areas)
Implement policies to tackle poverty so that individuals and families can lead healthy lives —Poverty causes poor health. 80 Treating people in a health service that returns them to conditions that are making them sick is futile. Policies to deal with poverty will, evidently, improve health.
Invest in sustainable housing compatible with good health —The standard of housing in the UK is poor, and homelessness is rising to record levels. Cold, energy inefficient homes cause poor health and cost billions a year, directly and indirectly, through costs to the NHS of associated health problems, energy bills, lost productivity from poor health, and carbon emissions. 19
Prioritise children and young people, giving every child the best start in life —The government must act immediately to reduce child poverty and improve child health, with proportionate universalism, ensuring that those doing worst receive appropriate support. This approach requires acknowledgment of racial, ethnic, and geographical inequalities, as well as their interaction. In addition to the recommendations in box 5 , the government should remove the two-child restriction on child benefit and benefit cap, increase child benefit for lower income families, and extend free school provision for all children in households that receive universal credit, as set out in the Build Back Fairer review . 64
For any recommendations to be meaningful, an acknowledgment that the UK has a problem is crucial. Thus we call on the leaders of all political parties to recognise the scale of the problem and the need for action, and to commit to acting on the available evidence ( box 6) . Support for this initiative must come from an informed, unified general voting population, who are also considering those who cannot vote (eg, those who are too young to vote).
Call for leaders of all political parties to acknowledge the problem and act on the evidence
Austerity has harmed health, including through worsening of many social determinants of health, including housing, income, and education
Action on the social determinants of health will improve health
Inequalities are rising in the UK, based on factors such as deprivation, race, ethnic group, and sex, which overlap and interact
Conclusions
Improving the health of the population and reducing avoidable health inequalities must be a national priority. So strong is the evidence on social determinants of health that the health of the population is a good measure of how well society is meeting the needs of its members. If health inequalities are increasing, inequalities in society are increasing, and dealing with these inequalities is urgently needed. Action will include an NHS, free at the point of use, that delivers high quality care proportionate to need.
But much more will be needed. A common response is that we cannot afford such action—we argue, we cannot afford inaction. We call on all political leaders to acknowledge the problem and the urgent need for action on the social determinants of health. This action can be a story of hope: we can change the direction of health in the UK if we use the robust, broad evidence on how to act.
Form a cross-party task force accountable for public health
Re-establish Public Health England and restore the public health grant to 2015-16 levels
Build and maintain a workforce environment in the NHS that supports action on the social determinants of health and that is conducive to protecting and enhancing the health of staff, as well as patients
Invest in sustainable housing compatible with good health
We thank Gabriel Scally for his significant contribution to the first iteration of the paper, including the section on the weakening of the public health system; Martin McKee for contributing on public health in Northern Ireland and providing further informal review and support in the final version of the paper; and Sophie Cook from The BMJ for her constant support throughout.
Contributors and sources: LH, BK, and MM are members of the BMJ commission. LH is a general practitioner and public health doctor. She is studying for a DPhil in geography and the environment focused on the change in health outcomes in the UK from 2010 onwards. BK is a consultant paediatrician who also leads his organisation’s work on its role as an anchor institution, as it tries to play a part in improving the social determinants of health. MM has had a longstanding research programme on health inequalities and led several commissions and reviews on social determinants of health. AS is studying part time for a PhD in the department of global health and social medicine at King’s College London. Her research and writing focus on health inequalities. All authors contributed to ideas, writing, and revision of this article. LM is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of The BMJ Commission on the Future of the NHS ( https://www.bmj.com/nhs-commission ). The purpose of the commission is to identify key areas for analysis, lay out a vision for a future NHS, and make recommendations as to how we get there. The BMJ convened this commission, which was chaired independently by Victor Adebowale, Parveen Kumar, and Liam Smeeth. The BMJ was responsible for the peer review, editing, and publication of the papers of the commission. The BMA, which owns The BMJ , grants editorial freedom to the editor in chief of The BMJ . The views expressed are those of the authors and may not necessarily comply with BMA policy.
- ↵ National Centre for Social Research. Public attitudes to the NHS and social care. 2023 . https://natcen.ac.uk/publications/public-attitudes-nhs-and-social-care
- ↵ Marmot M, Wilkinson R. Social determinants of health. Oxford University Press, 2006.
- ↵ World Health Organization. Social determinants of health. 2024. https://www.who.int/health-topics/social-determinants-of-health
- Wormersley K ,
- ↵ Mortimer J. ‘A poor country with a few rich people in it’: renowned inequalities expert speaks out as bereaved families give their accounts of ‘the unequal pandemic’. Byline Times 14 Sep 2023. https://bylinetimes.com/2023/09/14/a-poor-country-with-a-few-rich-people-in-it-renowned-inequalities-expert-speaks-out-as-bereaved-families-give-their-accounts-of-the-unequal-pandemic/
- ↵ Royal College of Paediatrics and Child Health. State of Child Health: Infant Mortality. https://stateofchildhealth.rcpch.ac.uk/evidence/mortality/infant-mortality/ (2021).
- Dorling D ,
- Hunter DJ ,
- Littlejohns P ,
- ↵ Finch D, Gazzillo A, Vriend M. Investing in the public health grant. Health Foundation , 2024. https://www.health.org.uk/news-and-comment/charts-and-infographics/public-health-grant-what-it-is-and-why-greater-investment-is-needed
- The Public Health Scotland Order
- Alexiou A ,
- Bennett JE ,
- Paciorek CJ ,
- ↵ Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J. Health equity in England: the Marmot review 10 years on . 2020. health.org.uk/publications/reports/the-marmot-review-10-years-on
- ↵ Public Health England. A review of recent trends in mortality in England . https://www.gov.uk/government/publications/recent-trends-in-mortality-in-england-review-and-data-packs . 2018.
- ↵ Office for National Statistics. National life tables–life expectancy in the UK. 2024. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/bulletins/nationallifetablesunitedkingdom/2020to2022
- ↵ Resolution Foundation. Britain’s housing stock offers worst value for money of any advanced economy. 2024. https://www.resolutionfoundation.org/press-releases/britains-housing-stock-offers-worst-value-for-money-of-any-advanced-economy/
- ↵ Donkin A, Marmot M. Left out in the cold: the hidden impact of cold homes . 2024. https://www.instituteofhealthequity.org/resources-reports/left-out-in-the-cold-the-hidden-impact-of-cold-homes
- ↵ Goldblatt P. Health inequalities, lives cut short . 2024. https://www.instituteofhealthequity.org/resources-reports/health-inequalities-lives-cut-short/read-the-report.pdf
- ↵ Dorling D. Why are old people in Britain dying before their time? New Statesman Feb 2014. https://www.newstatesman.com/politics/2014/02/why-are-old-people-britain-dying-their-time
- Goldring S ,
- Henretty N ,
- Johnson K ,
- Smallwood S
- McCartney G ,
- Parkinson J ,
- Shipton D ,
- ↵ McCartney G, Walsh D, Fenton L, Devine R. Resetting the course for population health: evidence and recommendations to address stalled mortality improvements in Scotland and the rest of the UK . 2022. https://www.gcph.co.uk/assets/0000/8723/Stalled_Mortality_report_FINAL_WEB.pdf .
- ↵ Department of Health. Life expectancy in Northern Ireland 2020-22. 2023. https://www.health-ni.gov.uk/news/life-expectancy-northern-ireland-2020-22 .
- Iacobucci G
- ↵ Academy of Medical Sciences. Prioritising Early Childhood to Promote the Nation’s Health, Wellbeing and Prosperity . 2024. https://acmedsci.ac.uk/file-download/16927511
- ↵ National Child Mortality Database. Child death data release 2023. 2023. https://www.ncmd.info/publications/child-death-data-2023/ .
- ↵ Sands and Tommy’s Policy Unit. Saving Babies’ Lives 2023: A report on progress. 2023. https://www.sands.org.uk/sites/default/files/JPU_Saving_Babies_Lives_Report_2023.pdf
- ↵ British children shorter than other five-year-olds in Europe. ITV News 21 Jun 2023. https://www.itv.com/news/2023-06-21/british-children-shorter-than-other-five-year-olds-in-europe
- McMaster R ,
- Darlington-Pollock F ,
- Taylor-Robinson D ,
- Wickham S ,
- ↵ Booth R, Butler P. UK austerity has inflicted ‘great misery’ on citizens, UN says. Guardian 16 Nov 2018. https://www.theguardian.com/society/2018/nov/16/uk-austerity-has-inflicted-great-misery-on-citizens-un-says
- ↵ Booth RUK. ‘in violation of international law’ over poverty levels, says UN envoy. Guardian 5 Nov 2023. https://www.theguardian.com/society/2023/nov/05/uk-poverty-levels-simply-not-acceptable-says-un-envoy-olivier-de-schutter
- ↵ Joseph Rowntree Foundation. Guarantee our essentials: reforming Universal Credit to ensure we can all afford the essentials in hard times. 2023. https://www.jrf.org.uk/report/guarantee-our-essentials
- ↵ Marmot M. [@MichaelMarmot]. Creating the conditions for ill health by denying minimum income for a healthy life. It is government policy that people who need benefits, Universal Credit, will have only 70% of the money they need to live healthily. Twitter, 27 Feb 2023. https://twitter.com/MichaelMarmot/status/1630177367137058817
- ↵ Commission on Social Determinants of Health. Closing the gap in a generation : health equity through action on the social determinants of health : final report of the Commission on Social Determinants of Health . (2008). https://iris.who.int/handle/10665/43943
- ↵ Marmot M, Goldblatt P, Allen J. Fair society healthy lives (The Marmot Review) . 2008. https://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review .
- ↵ Joseph Rowntree Foundation. Deep poverty and destitution. 2024. https://www.jrf.org.uk/deep-poverty-and-destitution
- ↵ Francis-Devine B, Danechi S, Malik X, Zayed Y. Food poverty: Households, food banks and free school meals. 2023. https://commonslibrary.parliament.uk/research-briefings/cbp-9209/
- Jenkins RH ,
- Aliabadi S ,
- ↵ Butler P. Number of UK children in food poverty nearly doubles in a year to 4m. Food poverty. Guardian 1 Mar 2023. https://www.theguardian.com/society/2023/mar/01/number-of-uk-children-in-food-poverty-nearly-doubles-in-a-year-to-4m
- ↵ Trussell Trust UK. End of year stats. 2023. https://www.trusselltrust.org/news-and-blog/latest-stats/end-year-stats/
- ↵ Lancet. Commercial determinants of health. 2023. https://www.thelancet.com/series/commercial-determinants-health
- ↵ Marmot M, Alexander M, Allen J, Munro A. The business of health equity: the Marmot review for industry . 2022. https://www.instituteofhealthequity.org/resources-reports/the-business-of-health-equity-the-marmot-review-for-industry
- Ashton JR ,
- Middleton J ,
- 170 signatories
- ↵ Action for Children. Where is child poverty increasing in the UK? 2023. https://www.actionforchildren.org.uk/blog/where-is-child-poverty-increasing-in-the-uk/
- ↵ End Child Poverty Coalition. Child poverty statistics. 2022. https://endchildpoverty.org.uk/child-poverty/
- ↵ Scottish Government. Scottish child payment. 2022. https://www.mygov.scot/scottish-child-payment
- ↵ Lewis R, Glyn Jones T. Child poverty: could Wales cut rates by copying Scotland? BBC News 29 Oct 2023. https://www.bbc.co.uk/news/uk-wales-67238317#
- ↵ Institute for Fiscal Studies. Spring Budget 2024: IFS analysis. 2024. https://ifs.org.uk/events/spring-budget-2024-ifs-analysis
- ↵ Hiam L, Marmot M. Is Britain sicker than a decade ago? 2024. https://www.prospectmagazine.co.uk/politics/policy/health/64510/is-britain-sicker-than-a-decade-ago
- Falkenbach M ,
- Siciliani L ,
- ↵ Black SD. Inequalities in health: the Black report. 1982. https://repository.library.georgetown.edu/handle/10822/792483
- ↵ Summers D. David Cameron warns of ‘new age of austerity’. Guardian 26 Apr 2009. https://www.theguardian.com/politics/2009/apr/26/david-cameron-conservative-economic-policy1
- ↵ Build back fairer: the covid-19 Marmot review. Health Foundation, 2020. https://www.health.org.uk/publications/build-back-fairer-the-covid-19-marmot-review .
- ↵ Marmot M. Build back fairer: social determinants, ethnicity and health. NHS Race and Health Observatory, 2022. https://www.nhsrho.org/news/build-back-fairer-social-determinants-ethnicity-and-health/
- ↵ Munro A. Coventry Marmot city evaluation 2020 . 2020. https://www.instituteofhealthequity.org/resources-reports/coventry-marmot-city-evaluation-2020
- ↵ Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J. Build Back Fairer in Greater Manchester: Health Equity and Dignified Lives . 2021. https://www.instituteofhealthequity.org/resources-reports/build-back-fairer-in-greater-manchester-health-equity-and-dignified-lives
- Glantz SA ,
- Oliveira da Silva AL
- ↵ McCullough F. Is Northern Ireland a failed state. The Fitzwilliam 11 Dec 2023. https://www.thefitzwilliam.com/p/is-northern-ireland-a-failed-state
- ↵ Monbiot G. Britain is becoming a toxic chemical dumping ground – yet another benefit of Brexit. Guardian 18 Mar 2024. https://www.theguardian.com/commentisfree/2024/mar/18/britain-toxic-chemical-dump-brexit-europe
- ↵ Health Foundation. Investing in public health grant. 2024. https://www.health.org.uk/news-and-comment/charts-and-infographics/public-health-grant-what-it-is-and-why-greater-investment-is-needed
- ↵ Rolewicz L, Palmer B, Lobont C. The NHS workforce in numbers. Nuffield Trust 2024. https://www.nuffieldtrust.org.uk/resource/the-nhs-workforce-in-numbers
- ↵ NHS England. Co-production. 2024. https://www.england.nhs.uk/always-events/co-production/
- ↵ The NHS as an anchor institution. https://www.health.org.uk/news-and-comment/charts-and-infographics/the-nhs-as-an-anchor-institution .
- ↵ East London NHS Foundation Trust. Being a Marmot Trust. 2023. https://www.elft.nhs.uk/information-about-elft/our-strategy-vision-and-values/population-health/being-marmot-trust
- ↵ King’s Fund. Poverty taking a heavy toll on NHS services. 2024. https://www.kingsfund.org.uk/insight-and-analysis/press-releases/poverty-health-nhs-services
This paper is in the following e-collection/theme issue:
Published on 11.4.2024 in Vol 26 (2024)
Evaluating the Digital Health Experience for Patients in Primary Care: Mixed Methods Study
Authors of this article:

Original Paper
- Melinda Ada Choy 1, 2 , BMed, MMed, DCH, MD ;
- Kathleen O'Brien 1 , BSc, GDipStats, MBBS, DCH ;
- Katelyn Barnes 1, 2 , BAPSC, MND, PhD ;
- Elizabeth Ann Sturgiss 3 , BMed, MPH, MForensMed, PhD ;
- Elizabeth Rieger 1 , BA, MClinPsych, PhD ;
- Kirsty Douglas 1, 2 , MBBS, DipRACOG, Grad Cert HE, MD
1 School of Medicine and Psychology, College of Health and Medicine, The Australian National University, Canberra, Australia
2 Academic Unit of General Practice, Office of Professional Leadership and Education, ACT Health Directorate, Canberra, Australia
3 School of Primary and Allied Health Care, Monash University, Melbourne, Australia
Corresponding Author:
Melinda Ada Choy, BMed, MMed, DCH, MD
School of Medicine and Psychology
College of Health and Medicine
The Australian National University
Phone: 61 51244947
Email: [email protected]
Background: The digital health divide for socioeconomic disadvantage describes a pattern in which patients considered socioeconomically disadvantaged, who are already marginalized through reduced access to face-to-face health care, are additionally hindered through less access to patient-initiated digital health. A comprehensive understanding of how patients with socioeconomic disadvantage access and experience digital health is essential for improving the digital health divide. Primary care patients, especially those with chronic disease, have experience of the stages of initial help seeking and self-management of their health, which renders them a key demographic for research on patient-initiated digital health access.
Objective: This study aims to provide comprehensive primary mixed methods data on the patient experience of barriers to digital health access, with a focus on the digital health divide.
Methods: We applied an exploratory mixed methods design to ensure that our survey was primarily shaped by the experiences of our interviewees. First, we qualitatively explored the experience of digital health for 19 patients with socioeconomic disadvantage and chronic disease and second, we quantitatively measured some of these findings by designing and administering a survey to 487 Australian general practice patients from 24 general practices.
Results: In our qualitative first phase, the key barriers found to accessing digital health included (1) strong patient preference for human-based health services; (2) low trust in digital health services; (3) high financial costs of necessary tools, maintenance, and repairs; (4) poor publicly available internet access options; (5) reduced capacity to engage due to increased life pressures; and (6) low self-efficacy and confidence in using digital health. In our quantitative second phase, 31% (151/487) of the survey participants were found to have never used a form of digital health, while 10.7% (52/487) were low- to medium-frequency users and 48.5% (236/487) were high-frequency users. High-frequency users were more likely to be interested in digital health and had higher self-efficacy. Low-frequency users were more likely to report difficulty affording the financial costs needed for digital access.
Conclusions: While general digital interest, financial cost, and digital health literacy and empowerment are clear factors in digital health access in a broad primary care population, the digital health divide is also facilitated in part by a stepped series of complex and cumulative barriers. Genuinely improving digital health access for 1 cohort or even 1 person requires a series of multiple different interventions tailored to specific sequential barriers. Within primary care, patient-centered care that continues to recognize the complex individual needs of, and barriers facing, each patient should be part of addressing the digital health divide.
Introduction
The promise of ehealth.
The rapid growth of digital health, sped up by the COVID-19 pandemic and associated lockdowns, brings the promise of improved health care efficiency, empowerment of consumers, and health care equity [ 1 ]. Digital health is the use of information and communication technology to improve health [ 2 ]. eHealth, which is a type of digital health, refers to the use of internet-based technology for health care and can be used by systems, providers, and patients [ 2 ]. At the time of this study (before COVID-19), examples of eHealth used by patients in Australia included searching for web-based health information, booking appointments on the web, participating in online peer-support health forums, using mobile phone health apps (mobile health), emailing health care providers, and patient portals for electronic health records.
Digital health is expected to improve chronic disease management and has already shown great potential in improving chronic disease health outcomes [ 3 , 4 ]. Just under half of the Australian population (47.3%) has at least 1 chronic disease [ 5 ]. Rates of chronic disease and complications from chronic disease are overrepresented among those with socioeconomic disadvantage [ 6 ]. Therefore, patients with chronic disease and socioeconomic disadvantage have a greater need for the potential benefits of digital health, such as an improvement in their health outcomes. However, there is a risk that those who could benefit most from digital health services are the least likely to receive them, exemplifying the inverse care law in the digital age by Hart [ 7 ].
Our Current Understanding of the Digital Health Divide
While the rapid growth of digital health brings the promise of health care equity, it may also intensify existing inequities [ 8 ]. The digital health divide for socioeconomic disadvantage describes a pattern in which patients considered socioeconomically disadvantaged who are already marginalized through poor access to traditional health care are additionally hindered through poor access to digital health [ 9 ]. In Australia, only 67.4% of households in the lowest household income quintile have home internet access, compared to 86% of the general population and 96.9% of households in the highest household income quintile [ 10 ]. Survey-based studies have also shown that even with internet access, effective eHealth use is lower in populations considered disadvantaged, which speaks to broader barriers to digital health access [ 11 ].
The ongoing COVID-19 global pandemic has sped up digital health transitions with the rapid uptake of telephone and video consultations, e-prescription, and the ongoing rollout of e-mental health in Australia. These have supported the continuation of health care delivery while limiting physical contact and the pandemic spread; however, the early evidence shows that the digital health divide remains problematic. A rapid review identified challenges with reduced digital access and digital literacy among the older adults and racial and ethnic minority groups, which are both groups at greater health risk from COVID-19 infections [ 12 ]. An Australian population study showed that the rapid uptake of telehealth during peak pandemic was not uniform, with the older adults, very young, and those with limited English language proficiency having a lower uptake of general practitioner (GP) telehealth services [ 13 ].
To ensure that digital health improves health care outcome gaps, it is essential to better understand the nature and nuance of the digital health divide for socioeconomic disadvantage. The nature of the digital health divide for socioeconomic disadvantage has been explored primarily through quantitative survey data, some qualitative papers, a few mixed methods papers, and systematic reviews [ 11 , 14 - 16 ]. Identified barriers include a lack of physical hardware and adequate internet bandwidth, a reduced inclination to seek out digital health, and a low ability and confidence to use digital health effectively [ 16 ]. The few mixed methods studies that exist on the digital health divide generally triangulate quantitative and qualitative data on a specific disease type or population subgroup to draw a combined conclusion [ 17 , 18 ]. These studies have found digital health access to be associated with education, ethnicity, and gender as well as trust, complementary face-to-face services, and the desire for alternative sources of information [ 17 , 19 ].
What This Work Adds
This project sought to extend previous research by using an exploratory mixed methods design to ensure that the first step and driver of our survey of a larger population was primarily shaped by the experiences of our interviewees within primary care. This differs from the triangulation method, which places the qualitative and quantitative data as equal first contributors to the findings and does not allow one type of data to determine the direction of the other [ 18 ]. We qualitatively explored the experience of digital health for patients with socioeconomic disadvantage and chronic disease and then quantitatively measured some of the qualitative findings via a survey of the Australian general practice patient population. Our key objective was to provide comprehensive primary mixed methods data, describing the experience and extent of barriers to accessing digital health and its benefits, with a focus on the digital health divide. We completed this research in a primary care context to investigate a diverse community-based population with conceivable reasons to seek digital help in managing their health. Findings from this mixed methods study were intended to provide health care providers and policy makers with a more detailed understanding of how specific barriers affect different aspects or steps of accessing digital health. Ultimately, understanding digital health access can influence the future design and implementation of digital health services by more effectively avoiding certain barriers or building in enablers to achieve improved digital health access not only for everyone but also especially for those in need.
Study Design
We conducted a sequential exploratory mixed methods study to explore a complex phenomenon in depth and then measure its prevalence. We qualitatively explored the experience of digital health for patients with chronic disease and socioeconomic disadvantage in the first phase. Data from the first phase informed a quantitative survey of the phenomenon across a wider population in the second phase [ 18 ]. Both stages of research were conducted before the COVID-19 pandemic in Australia.
Recruitment
Qualitative phase participants.
The eligibility criteria for the qualitative phase were as follows: English-speaking adults aged ≥18 years with at least 1 self-reported chronic disease and 1 marker of socioeconomic disadvantage (indicated by ownership of a Health Care Card or receiving a disability pension, unemployment, or a user of public housing). A chronic disease was defined to potential participants as a diagnosed long-term health condition that had lasted at least 6 months (or is expected to last for at least 6 months; examples are listed in Multimedia Appendix 1 ). The markers of socioeconomic disadvantage we used to identify potential participants were based on criteria typically used by local general practices to determine which patients can have lower or no out-of-pocket expenses. Apart from unemployment, the 3 other criteria to identify socioeconomic disadvantage are means-tested government-allocated public social services [ 20 ]. Qualitative phase participants were recruited from May to July 2019 through 3 general practices and 1 service organization that serve populations considered socioeconomically disadvantaged across urban, regional, and rural regions in the Australian Capital Territory and South Eastern New South Wales. A total of 2 recruitment methods were used in consultation with and as per the choice of the participating organizations. Potential participants were either provided with an opportunity to engage with researchers (KB and MAC) in the general practice waiting room or identified by the practice or organization as suitable for an interview. Interested participants were given a detailed verbal and written description of the project in a private space before providing written consent to be interviewed. All interview participants received an Aus $50 (US $32.68) grocery shopping voucher in acknowledgment of their time.
Quantitative Phase Participants
Eligibility for the quantitative phase was English-speaking adults aged ≥18 years. The eligibility criteria for the quantitative phase were deliberately broader than those for the qualitative phase to achieve a larger sample size within the limitations of recruitment and with the intention that the factors of socioeconomic disadvantage and having a chronic disease could be compared to the digital health access of a more general population. The quantitative phase participants were recruited from November 2019 to February 2020. Study information and paper-based surveys were distributed and collected through 24 general practices across the Australian Capital Territory and South Eastern New South Wales regions, with an option for web-based completion.
Ethical Considerations
Qualitative and quantitative phase research protocols, including the participant information sheet, were approved by the Australian Capital Territory Health Human Research Ethics Committee (2019/ETH/00013) and the Australian National University Human Research Ethics Committee (2019/ETH00003). Qualitative phase participants were given a verbal and written explanation of the study, including how and when they could opt out, before they provided written consent. All interview participants received an Aus $50 (US $32.68) grocery shopping voucher in acknowledgment of their time. Quantitative participants were given a written explanation and their informed consent was implied by return of a completed survey. Participants in both phases of the study were told that all their data was deidentified. Consent was implied through the return of a completed survey.
Qualitative Data Collection and Analysis
Participants were purposively sampled to represent a range in age, gender, degree of socioeconomic disadvantage, and experience of digital health. The sampling and sample size were reviewed regularly by the research team as the interviews were being completed to identify potential thematic saturation.
The interview guide was developed by the research team based on a review of the literature and the patient dimensions of the framework of access by Levesque et al [ 21 ]. The framework by Levesque et al [ 21 ] is a conceptualization of health care access comprising 5 service and patient dimensions of accessibility and ability. The patient dimensions are as follows: (1) ability to perceive, (2) ability to seek, (3) ability to reach, (4) ability to pay, and (5) ability to engage [ 21 ]. The key interview topics included (1) digital health use and access, including facilitators and barriers; (2) attitudes toward digital health; and (3) self-perception of digital health skills and potential training. The interview guide was reviewed for face and content validity by the whole research team, a patient advocate, a digital inclusion charity representative, and the general practices where recruitment occurred. The questions and guide were iteratively refined by the research team to ensure relevance and support reaching data saturation. The interview guide has been provided as Multimedia Appendix 1 . The interviews, which took 45 minutes on average, were taped and transcribed. An interview summary sheet and reflective journal were completed by the interviewer after each interview to also capture nonverbal cues and tone.
Interview transcriptions were coded and processed by inductive thematic analysis. Data collection and analysis were completed in parallel to support the identification of data saturation. Data saturation was defined as no significant new information arising from new interviews and was identified by discussion with the research team [ 22 ]. The 2 interviewers (MAC and KB) independently coded the first 5 transcripts and reflected on them with another researcher (EAS) to ensure intercoder validity and reliability. The rest of the interviews were coded independently by the 2 interviewers, who regularly met to reflect on emerging themes and thematic saturation. Data saturation was initially indicated after 15 interviews and subsequently confirmed with a total of 19 interviews. Coding disagreements and theme development were discussed with at least 1 other researcher (EAS, ER, and KD). Thematic saturation and the final themes were agreed upon by the entire research team.
Quantitative Survey Development
The final themes derived in the qualitative phase of the project guided the specific quantitative phase research questions. The final themes were a list of ordered cumulative barriers experienced by participants in accessing digital health and its benefits ( Figure 1 ). The quantitative survey was designed to test the association between barriers to access and the frequency of use of digital health as a proxy measure for digital health access.

In the survey, the participants were asked about their demographic details, health and chronic diseases, knowledge, use and experience of digital health tools, internet access, perception of digital resource affordability, trust in digital health and traditional health services, perceived capability, health care empowerment, eHealth literacy, and relationship with their GP.
Existing scales and questions from the literature and standardized Australian-based surveys were used whenever possible. We used selected questions and scales from the Australian Bureau of Statistics standards, the eHealth Literacy Scale (eHEALS), the eHealth Literacy Questionnaire, and the Southgate Institute for Health Society and Equity [ 17 , 23 - 26 ]. We adapted other scales from the ICEpop Capability Measure for Adults, the Health Care Empowerment Inventory (HCEI), the Patient-Doctor Relationship Questionnaire, and the Chao continuity questionnaire [ 23 , 27 - 29 ]. Where an existing scale to measure a barrier or theme did not exist, the research team designed the questions based on the literature. Our questions around the frequency of digital health use were informed by multiple existing Australian-based surveys on general technology use [ 30 , 31 ]. Most of the questions used a Likert scale. Every choice regarding the design, adaptation, or copy of questions for the survey was influenced by the qualitative findings and decided on by full agreement among the 2 researchers who completed and coded the interviews. A complete copy of the survey is provided in Multimedia Appendix 2 .
Pilot-testing of the survey was completed with 5 patients, 2 experts on digital inclusion, and 3 local GPs for both the paper surveys and web-based surveys via Qualtrics Core XM (Qualtrics LLC). The resulting feedback on face and content validity, functionality of the survey logic, and feasibility of questionnaire completion was incorporated into the final version of the survey.
The survey was offered on paper with a participant information sheet, which gave the patients the option to complete the web-based survey. The survey was handed out to every patient on paper to avoid sampling bias through the exclusion of participants who could not complete the web-based survey [ 32 ].
Quantitative Data Treatment and Analysis
Data were exported from Qualtrics Core XM to an SPSS (version 26; IBM Corp) data set. Data cleaning and screening were undertaken (KB and KO).
Descriptive statistics (number and percentage) were used to summarize participant characteristics, preference measures, and frequency of eHealth use. Significance testing was conducted using chi-square tests, with a threshold of P <.05; effect sizes were measured by the φ coefficient for 2×2 comparisons and Cramer V statistic for all others. Where the cells sizes were too small, the categories were collapsed for the purposes of significance testing. The interpretation of effect sizes was as per the study by Cohen [ 33 ]. The analysis was conducted in SPSS and SAS (version 9.4; SAS Institute).
Participant Characteristics
Participants’ self-reported characteristics included gender, indigenous status, income category, highest level of education, marital status, and language spoken at home.
Age was derived from participant-reported year of birth and year of survey completion as of 2019 and stratified into age groups. The state or territory of residence was derived from the participant-reported postcode. The remoteness area was derived using the postcode reported by the participants and mapped to a modified concordance from the Australian Bureau of Statistics. Occupation-free text responses were coded using the Australian Bureau of Statistics Census statistics level 1 and 2 descriptors. The country of birth was mapped to Australia, other Organisation for Economic Cooperation and Development countries, and non–Organisation for Economic Cooperation and Development countries.
Frequency of eHealth Use
A summary measure of the frequency of eHealth use was derived from the questions on the use of different types of eHealth.
Specifically, respondents were asked if they had ever used any form of web-based health (“eHealth“) and, if so, to rate how often (never, at least once, every now and then, and most days) against 6 types of “eHealth” (searching for health information online, booking appointments online, emailing health care providers, using health-related mobile phone apps, accessing My Health Record, and accessing online health forums). The frequency of eHealth use was then classified as follows:
- High user: answered “most days” to at least 1 question on eHealth use OR answered “every now and then” to at least 2 questions on eHealth use
- Never user: answered “no” to having ever used any form of eHealth OR “never” to all 6 questions on eHealth use
- Low or medium user: all other respondents.
The frequency of eHealth use was reported as unweighted descriptive statistics (counts and percentages) against demographic characteristics and for the elements of each of the themes identified in phase 1.
Overview of Key Themes
Data were reported against the 6 themes from the phase 1 results of preference, trust, cost, structural access, capacity to engage, and self-efficacy. Where the components of trust, cost, capacity to engage, and self-efficacy had missing data (for less than half of the components only), mean imputation was used to minimize data loss. For each theme, the analysis excluded those for whom the frequency of eHealth use was unknown.
Preference measures (survey section D1 parts 1 to 3) asked participants to report against measures with a 4-point Likert scale (strongly disagree, disagree, agree, and strongly agree). Chi-square tests were conducted after the categories were condensed into 2 by combining strongly disagree and as well as combining strongly agree and agree.
Summary measures for trust were created in 4 domains: trust from the eHealth Literacy Questionnaire (survey section D1 parts 4 to 8), trust from Southgate—GPs, specialists, or allied health (survey section D2 parts 1 to 5), trust from Southgate—digital health (survey section D2 parts 6, 7, 9, and 10), and trust from Southgate—books or pamphlets (survey section D2 part 8). The data were grouped as low, moderate, and high trust based on the assigned scores from the component data. Chi-square tests were conducted comparing low-to-moderate trust against high trust for GP, specialists, or allied health and comparing low trust against moderate-to-high trust for book or pamphlet.
Summary measures for cost were created from survey item C10. To measure cost, participants were asked about whether they considered certain items or services to be affordable. These included cost items mentioned in the qualitative phase interviews relating to mobile phones (1 that connects to the internet, 1 with enough memory space to download apps, downloads or apps requiring payment, repairs, and maintenance costs), having an iPad or tablet with internet connectivity, a home computer or laptop (owning, repairs, and maintenance), home fixed internet access, and an adequate monthly data allowance. These 9 items were scored as “yes definitely”=1 or 0 otherwise. Chi-square tests were conducted with never and low or medium eHealth users combined.
Structural Access
Structural access included asking where the internet is used by participants (survey section C8) and factors relating to internet access (survey section C8 parts 1-3) reporting against a 4-point Likert scale (strongly disagree, disagree, agree, and strongly agree). Chi-square tests were conducted with strongly disagree, disagree, agree, or strongly agree, and never, low, or medium eHealth use combined.
Capacity to Engage
Summary measures for capacity to engage were created from survey section E1. To measure the capacity to engage, participants were asked about feeling “settled and secure,” “being independent,” and “achievement and progress” as an adaptation of the ICEpop Capability Measure for Adults [ 27 ], reporting against a 4-point Likert-like scale. Responses were scored from 1 (“I am unable to feel settled and secure in any areas of my life”) to 4 (“I am able to feel settled and secure in all areas of my life”).
The summary capacity measure was derived by the summation of responses across the 3 questions, which were classified into 4 groups, A to D, based on these scores. Where fewer than half of the responses were missing, mean imputation was used; otherwise, the record was excluded. Groups A and B were combined for significance testing.
Self-Efficacy
Summary measures for self-efficacy were adapted from the eHEALS (E3) and the HCEI (E2) [ 23 , 24 ].
Survey section E3—eHEALS—comprised 8 questions, with participants reporting against a 5-point Likert scale for each (strongly disagree, disagree, neither, agree, and strongly agree). These responses were assigned 1 to 5 points, respectively. The summary eHEALS measure was derived by the summation of responses across the 8 questions, which were classified into 5 groups, A to E, based on these scores. Where fewer than half of the responses were missing, mean imputation was used; otherwise, the record was excluded. Groups A to C and D to E were combined for significance testing.
Survey section E2—HCEI—comprised 5 questions, with participants reporting against a 5-point Likert scale for each (strongly disagree, disagree, neither, agree, and strongly agree). Strongly disagree and disagree and neither were combined, and similarly agree and strongly agree were combined for significance testing.
Qualitative Results
The demographic characteristics of the patients that we interviewed are presented in Table 1 .
The key barriers found to accessing digital health included (1) strong patient preference for human-based health services; (2) low trust in digital health services; (3) high financial costs of necessary tools, maintenance, and repairs; (4) poor publicly available internet access options; (5) reduced capacity to engage due to increased life pressures; and (6) low self-efficacy and confidence in using digital health.
Rather than being an equal list of factors, our interviewees described these barriers as a stepped series of cumulative hurdles, which is illustrated in Figure 1 . Initial issues of preference and trust were foundational to a person even when considering the option of digital health, while digital health confidence and literacy were barriers to full engagement with and optimal use of digital health. Alternatively, interviewees who did use digital health had been enabled by the same factors that were barriers to others.
a GP: general practitioner.
b Multiple answers per respondent.
Strong Patient Preference for Human-Based Health Services
Some patients expressed a strong preference for human-based health services rather than digital health services. In answer to a question about how digital health services could be improved, a patient said the following:
Well, having an option where you can actually bypass actually having to go through the app and actually talk directly to someone. [Participant #10]
For some patients, this preference for human-based health services appeared to be related to a lack of exposure to eHealth. These patients were not at all interested in or had never thought about digital health options. A participant responded the following to the interviewer’s questions:
Interviewer: So when...something feels not right, how do you find out what’s going on?
Respondent: I talk to Doctor XX.
Interviewer: Do you ever Google your symptoms or look online for information?
Respondent: No, I have never even thought of doing that actually. [Participant #11]
For other patients, their preference for human-based health care stemmed from negative experiences with technology. These patients reported actively disliking computers and technology in general and were generally frustrated with what they saw as the pitfalls of technology. A patient stated the following:
If computers and internet weren’t so frigging slow because everything is on like the slowest speed network ever and there’s ads blocking everything. Ads, (expletive) ads. [Participant #9]
A patient felt that he was pushed out of the workforce due his inability to keep up with technology-based changes and thus made a decision to never own a computer:
But, you know, in those days when I was a lot younger those sorts of things weren’t about and they’re just going ahead in leaps and bounds and that’s one of the reasons why I retired early. I retired at 63 because it was just moving too fast and it’s all computers and all those sorts of things and I just couldn’t keep up. [Participant #17]
Low Trust in Digital Health Services
Several patients described low trust levels for digital and internet-based technology in general. Their low trust was generally based on stories they had heard of other people’s negative experiences. A patient said the following:
I don’t trust the internet to be quite honest. You hear all these stories about people getting ripped off and I’ve worked too hard to get what I’ve got rather than let some clown get it on the internet for me. [Participant #11]
Some of this distrust was specific to eHealth. For example, some patients were highly suspicious of the government’s motives with regard to digital health and were concerned about the privacy of their health information, which made them hesitant about the concept of a universal electronic health record. In response to the interviewer’s question, a participant said the following:
Interviewer: Are there any other ways you think that eHealth might help you?
Respondent: I’m sorry but it just keeps coming back to me, Big Brother. [Participant #7]
Another participant said the following:
I just would run a mile from it because I just wouldn’t trust it. It wouldn’t be used to, as I said, for insurance or job information. [Participant #16]
High Financial Costs of the Necessary Tools, Maintenance, and Repairs
A wide variety of patients described affordability issues across several different aspects of the costs involved in digital health. They expressed difficulty in paying for the following items: a mobile phone that could connect to the internet, a mobile phone with enough memory space to download apps, mobile phone apps requiring extra payment without advertisements, mobile phone repair costs such as a broken screen, a computer or laptop, home internet access, and adequate monthly data allowance and speeds to functionally use the internet. Current popular payment systems, such as plans, were not feasible for some patients. A participant stated the following:
I don’t have a computer...I’m not in the income bracket to own a computer really. Like I could, if I got one on a plan kind of thing or if I saved up for x-amount of time. But then like if I was going on the plan I’d be paying interest for having it on like lay-buy kind of thing, paying it off, and if it ever got lost or stolen I would still have to repay that off, which is always a hassle. And yeah. Yeah, I’m like financially not in the state where I’m able to...own a computer right now as I’m kind of paying off a number of debts. [Participant #9]
Poor Publicly Available Internet Access Options
Some patients described struggling without home internet access. While they noted some cost-free public internet access points, such as libraries, hotel bars, and restaurants, they often found these to be inconvenient, lacking in privacy, and constituting low-quality options for digital health. A patient stated the following:
...it’s incredibly slow at the library. And I know why...a friend I went to school with used to belong to the council and the way they set it up, they just got the raw end of the stick and it is really, really slow. It’s bizarre but you can go to the X Hotel and it’s heaps quicker. [Participant #15]
In response to the interviewer's question, a participant said the following:
Interviewer: And do you feel comfortable doing private stuff on computers at the library...?
Respondent: Not really, no, but I don’t have any other choice, so, yeah. [Participant #9]
Reduced Capacity to Engage Due to Increased Life Pressures
When discussing why they were not using digital health or why they had stopped using digital health, patients often described significant competing priorities and life pressures that affected their capacity to engage. An unemployed patient mentioned that his time and energy on the internet were focused primarily on finding work and that he barely had time to focus on his health in general, let alone engage in digital health.
Other patients reported that they often felt that their ability to learn about and spend time on digital health was taken up by caring for sick family members, paying basic bills, or learning English. Some patients said that the time they would have spent learning digital skills when they were growing up had been lost to adverse life circumstances such as being in jail:
So we didn’t have computers in the house when I was growing up. And I didn’t know I’ve never...I’ve been in and out of jail for 28 odd years so it sort of takes away from learning from this cause it’s a whole different… it’s a whole different way of using a telephone from a prison. [Participant #11]
Low Self-Efficacy and Confidence in Starting the Digital Health Process
Some patients had a pervasive self-perception of being slow learners and being unable to use technology. Their stories of being unconfident learners seemed to stem from the fact that they had been told throughout their lives that they were intellectually behind. A patient said the following:
The computer people...wouldn’t take my calls because I’ve always been dumb with that sort of stuff. Like I only found out this later on in life, but I’m actually severely numerically dyslexic. Like I have to triple-check everything with numbers. [Participant #7]
Another patient stated the following:
I like went to two English classes like a normal English class with all the kids and then another English class with about seven kids in there because I just couldn’t I don’t know maybe because I spoke another language at home and they sort of like know I was a bit backward. [Participant #6]
These patients and others had multiple missing pieces of information that they felt made it harder to engage in digital health compared to “easier” human-based services. A patient said the following:
Yeah I’ve heard of booking online but I just I don’t know I find it easier just to ring up. And I’ll answer an email from a health care provider but I wouldn’t know where to start to look for their email address. [Participant #11]
In contrast, the patients who did connect with digital health described themselves as independent question askers and proactive people. Even when they did not know how to use a specific digital health tool, they were confident in attempting to and asking for help when they needed it. A patient said the following:
I’m a “I will find my way through this, no matter how long it takes me” kind of person. So maybe it’s more my personality...If I have to ask for help from somewhere, wherever it is, I will definitely do that. [Participant #3]
Quantitative Results
A total of 487 valid survey responses were received from participants across 24 general practices. The participant characteristics are presented in detail in Table S1 in Multimedia Appendix 3 .
The mean age of the participants was approximately 50 years (females 48.9, SD 19.4 years; males 52.8, SD 20.0 years), and 68.2% (332/487) of the participants identified as female. Overall, 34.3% (151/439) of respondents reported never using eHealth, and 53.8% (236/439) reported high eHealth use.
There were statistically significant ( P <.05) differences in the frequency of eHealth use in terms of age group, gender, state, remoteness, highest level of education, employment status, occupation group, marital status, and language spoken at home, with effect sizes being small to medium. Specifically, high eHealth characteristics were associated with younger age, being female, living in an urban area, and being employed.
Table 2 presents the frequency of eHealth use against 3 internet preference questions.
Preference for using the internet and technology in general and for health needs in particular were significantly related to the frequency of eHealth use ( P <.05 for each), with the effect sizes being small to medium.
a Excludes those for whom frequency of eHealth use is unknown.
b Chi-square tests conducted with strongly disagree and disagree combined, and agree and strongly agree combined.
Table 3 presents the frequency of eHealth use against 4 measures of trust.
The degree of trust was not statistically significantly different for the frequency of eHealth use for any of the domains.
b eHLQ: eHealth Literacy Questionnaire.
c Derived from survey question D1, parts 4 to 8. Mean imputation used where ≤2 responses were missing. If >2 responses were missing, the records were excluded.
d Derived from survey question D2, parts 1 to 5. Mean imputation used where ≤2 responses were missing. If >2 responses were missing, the records were excluded.
e Chi-square test conducted comparing low-to-moderate trust against high trust.
f Derived from survey question D2, parts 6, 7, 9, and 10. Mean imputation used where ≤2 responses were missing. If >2 responses were missing, the records were excluded.
g Derived from survey question D2 part 8.
h Chi-square test conducted comparing low trust against moderate-to-high trust.
Affordability of items and services was reported as No cost difficulty or Cost difficulty. eHealth frequency of use responses were available for 273 participants; among those with no cost difficulty , 1% (2/204) were never users, 14.2% (29/204) were low or medium users, and 84.8% (173/204) were high users of eHealth; among those with cost difficulty , 1% (1/69) were never users, 26% (18/69) were low or medium users, and 73% (50/69) were high users. There was a statistically significant difference in the presence of cost as a barrier between never and low or medium eHealth users compared to high users ( χ 2 1 =5.25; P =.02), although the effect size was small.
Table 4 presents the frequency of eHealth use for elements of structural access.
Quality of internet access and feeling limited in access to the internet were significantly associated with frequency of eHealth use ( P <.05), although the effect sizes were small.
b N/A: not applicable (cell sizes insufficient for chi-square test).
c Chi-square tests conducted with strongly disagree and disagree combined, agree and strongly agree combined, and never and low or medium categories combined.
Table 5 presents the frequency of eHealth use against respondents’ capacity to engage.
Capacity to engage was not significantly different for the frequency of eHealth use ( P =.54).
b Derived from survey item E1. Where 1 response was missing, the mean imputation was used. If >1 response was missing, the record was excluded.
c Chi-square tests conducted with groups A and B combined.
Table 6 presents the frequency of eHealth use for elements of self-efficacy.
Statistically significant results were observed for the relationship between self-efficacy by eHEALS (moderate effect size) and frequency of eHealth use as well as for some of the questions from the HCEI (reliance on health professionals or others to access and explain information; small effect size; P <.05).
b eHEALS: eHealth Literacy Scale.
c eHEALS derived from item E3 (8 parts). Where ≤ 4 responses were missing, mean imputation was used. If >4 responses were missing, the records were excluded. Groups A to C as well as groups D to E were combined for the chi-square test.
d Strongly disagree, disagree, neither, and agree or strongly agree combined for significance testing.
Principal Findings
This paper reports on the findings of a sequential exploratory mixed methods study on the barriers to digital health access for a group of patients in Australian family medicine, with a particular focus on chronic disease and socioeconomic disadvantage.
In the qualitative first phase, the patients with socioeconomic disadvantage and chronic disease described 6 cumulative barriers, as demonstrated in Figure 1 . Many nonusers of digital health preferred human-based services and were not interested in technology, while others were highly suspicious of the technology in general. Some digitally interested patients could not afford quality hardware and internet connectivity, a barrier that was doubled by low quality and privacy when accessing publicly available internet connections. Furthermore, although some digitally interested patients had internet access, their urgent life circumstances left scarce opportunity to access digital health and develop digital health skills and confidence.
In our quantitative second phase, 31% (151/487) of the survey participants from Australian general practices were found to have never used a form of digital health. Survey participants were more likely to use digital health tools frequently when they also had a general digital interest and a digital health interest. Those who did not frequently access digital health were more likely to report difficulty affording the financial costs needed for digital access. The survey participants who frequently accessed digital health were more likely to have high eHealth literacy and high levels of patient empowerment.
Comparison With Prior Work
In terms of general digital health access, the finding that 31% (151/487) of the survey participants had never used one of the described forms of eHealth is in keeping with an Australian-based general digital participation study that found that approximately 9% of the participants were nonusers and 17% rarely engaged with the internet at all [ 34 ]. With regard to the digital health divide, another Australian-based digital health divide study found that increased age, living in a lower socioeconomic area, being Aboriginal or Torres Strait Islander, being male, and having no tertiary education were factors negatively associated with access to digital health services [ 17 ]. Their findings correspond to our findings that higher-frequency users of eHealth were associated with younger age, being female, living in an urban area, and being employed. Both studies reinforce the evidence of the digital health divide based on gender, age, and socioeconomic disadvantage in Australia.
With regard to digital health barriers, our findings provide expanded details on the range of digital health items and services that present a cost barrier to consumers. Affordability is a known factor in digital access and digital health access, and it is measured often by general self-report or relative expenditure on internet access to income [ 30 ]. Our study revealed the comprehensive list of relevant costs for patients. Our study also demonstrated factors of cost affordability beyond the dollar value of an item, as interviewees described the struggle of using slow public internet access without privacy features and the risks involved in buying a computer in installments. When we reflected on the complexity and detail of the cost barrier in our survey, participants demonstrated a clear association between cost and the frequency of digital health use. This suggests that a way to improve digital health access for some people is to improve the quality, security, and accessibility of public internet access options as well as to provide free or subsidized hardware, internet connection, and maintenance options for those in need, work that is being done by at least 1 digital inclusion charity in the United Kingdom [ 35 ].
Many studies recognize the factors of eHealth literacy and digital confidence for beneficial digital health access [ 36 ]. Our interviews demonstrated that some patients with socioeconomic disadvantage have low digital confidence, but that this is often underlined by a socially reinforced lifelong low self-confidence in their intellectual ability. In contrast, active users, regardless of other demographic factors, described themselves as innately proactive question askers. This was reinforced by our finding of a relationship between health care empowerment and the frequency of eHealth use. This suggests that while digital health education and eHealth literacy programs can improve access for some patients, broader and deeper long-term solutions addressing socioeconomic drivers of digital exclusion are needed to improve digital health access for some patients with socioeconomic disadvantage [ 8 ]. The deep permeation of socially enforced low self-confidence and lifelong poverty experienced by some interviewees demonstrate that the provision of free hardware and a class on digital health skills can be, for some, a superficial offering when the key underlying factor is persistent general socioeconomic inequality.
The digital health divide literature tends to identify the digital health divide, the factors and barriers that contribute to it, and the potential for it to widen if not specifically addressed [ 16 ]. Our findings have also identified the divide and the barriers, but what this study adds through our qualitative phase in particular is a description of the complex interaction of those barriers and the stepped nature of some of those barriers as part of the individual’s experience in trying to access digital health.
Strengths and Limitations
A key strength of this study is the use of a sequential exploratory mixed methods design. The initial qualitative phase guided a phenomenological exploration of digital health access experiences for patients with chronic disease and socioeconomic disadvantage. Our results in both study phases stem from the patients’ real-life experiences of digital health access. While some of our results echo the findings of other survey-based studies on general digital and digital health participation, our method revealed a greater depth and detail of some of these barriers, as demonstrated in how our findings compare to prior work.
As mentioned previously, the emphasis of this study on the qualitative first phase is a strength that helped describe the interactions between different barriers. The interviewees described their experiences as cumulative unequal stepped barriers rather than as producing a nonordered list of equal barriers. These findings expand on the known complexity of the issue of digital exclusion and add weight to the understanding that improving digital health access needs diverse, complex solutions [ 17 ]. There is no panacea for every individual’s digital health access, and thus, patient-centered digital health services, often guided by health professionals within the continuity of primary care, are also required to address the digital health divide [ 37 ].
While the sequential exploratory design is a strength of the study, it also created some limitations for the second quantitative phase. Our commitment to using the qualitative interview findings to inform the survey questions meant that we were unable to use previously validated scales for every question and that our results were less likely to lead to a normal distribution. This likely affected our ability to demonstrate significant associations for some barriers. We expect that further modeling is required to control for baseline characteristics and determine barrier patterns for different types of users.
One strength of this study is that the survey was administered to a broad population of Australian family medicine patients with diverse patterns of health via both paper-based and digital options. Many other digital health studies use solely digital surveys, which can affect the sample. However, we cannot draw conclusions from our survey about patients with chronic disease due to the limitations of the sample size for these subgroups.
Another sample-based limitation of this study was that our qualitative population did not include anyone aged from 18 to 24 years, despite multiple efforts to recruit. Future research will hopefully address this demographic more specifically.
While not strictly a limitation, we recognize that because this research was before COVID-19, it did not include questions about telehealth, which has become much more mainstream in recent years. The patients may also have changed their frequency of eHealth use because of COVID-19 and an increased reliance on digital services in general. Future work in this area or future versions of this survey should include telehealth and acknowledge the impact of COVID-19. However, the larger concept of the digital health divide exists before and after COVID-19, and in fact, our widespread increased reliance on digital services makes the digital divide an even more pressing issue [ 12 ].
Conclusions
The experience of digital health access across Australian primary care is highly variable and more difficult to access for those with socioeconomic disadvantage. While general digital interest, financial cost, and digital health literacy and empowerment are clear factors in digital health access in a broad primary care population, the digital health divide is also facilitated in part by a stepped series of complex and cumulative barriers.
Genuinely improving digital health access for 1 cohort or even 1 person requires a series of multiple different interventions tailored to specific sequential barriers. Given the rapid expansion of digital health during the global COVID-19 pandemic, attention to these issues is necessary if we are to avoid entrenching inequities in access to health care. Within primary care, patient-centered care that continues to recognize the complex individual needs of, and barriers facing, each patient should be a part of addressing the digital health divide.
Acknowledgments
The authors are thankful to the patients who shared their experiences with them via interview and survey completion. The authors are also very grateful to the general practices in the Australian Capital Territory and New South Wales who kindly gave their time and effort to help organize interviews, administer, and post surveys in the midst of the stress of day-to-day practice life and the bushfires of 2018-2019. The authors thank and acknowledge the creators of the eHealth Literacy Scale, the eHealth Literacy Questionnaire, the ICEpop Capability Measure for Adults, the Health Care Empowerment Inventory, the Patient-Doctor Relationship Questionnaire, the Chao continuity questionnaire, and the Southgate Institute for Health Society and Equity for their generosity in sharing their work with the authors [ 17 , 19 - 25 ]. This study would not have been possible without the support of the administrative team of the Academic Unit of General Practice. This project was funded by the Royal Australian College of General Practitioners (RACGP) through the RACGP Foundation IPN Medical Centres Grant, and the authors gratefully acknowledge their support.
Data Availability
The data sets generated during this study are not publicly available due to the nature of our original ethics approval but are available from the corresponding author on reasonable request.
Authors' Contributions
MAC acquired the funding, conceptualized the project, and organized interview recruitment. MAC and KB conducted interviews and analyzed the qualitative data. EAS, ER, and KD contributed to project planning, supervision and qualitative data analysis. MAC, KB and KO wrote the survey and planned quantitative data analysis. MAC and KB recruited practices for survey administration. KO and KB conducted the quantitative data analysis. MAC and KO, with KB drafted the paper. EAS, ER, and KD helped with reviewing and editing the paper.
Conflicts of Interest
None declared.
Phase 1 interview guide.
Phase 2 survey: eHealth and digital divide.
Phase 2 participant characteristics by frequency of eHealth use.
- Eysenbach G. What is e-health? J Med Internet Res. 2001;3(2):E20. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Iyawa GE, Herselman M, Botha A. Digital health innovation ecosystems: from systematic literature review to conceptual framework. Procedia Comput Sci. 2016;100:244-252. [ FREE Full text ] [ CrossRef ]
- Berrouiguet S, Baca-García E, Brandt S, Walter M, Courtet P. Fundamentals for future mobile-health (mHealth): a systematic review of mobile phone and web-based text messaging in mental health. J Med Internet Res. Jun 10, 2016;18(6):e135. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shen H, van der Kleij RM, van der Boog PJ, Chang X, Chavannes NH. Electronic health self-management interventions for patients with chronic kidney disease: systematic review of quantitative and qualitative evidence. J Med Internet Res. Nov 05, 2019;21(11):e12384. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Australia's health 2018. Australian Institute of Health and Welfare. 2018. URL: https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/table-of-contents [accessed 2024-04-04]
- Australian Institute of Health and Welfare. Chronic Diseases and Associated Risk Factors in Australia, 2006. Canberra, Australia. Australian Institute of Health and Welfare; 2006.
- Hart JT. The inverse care law. The Lancet. Feb 27, 1971;297(7696):405-412. [ CrossRef ]
- Davies AR, Honeyman M, Gann B. Addressing the digital inverse care law in the time of COVID-19: potential for digital technology to exacerbate or mitigate health inequalities. J Med Internet Res. Apr 07, 2021;23(4):e21726. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Choi NG, Dinitto DM. The digital divide among low-income homebound older adults: internet use patterns, eHealth literacy, and attitudes toward computer/internet use. J Med Internet Res. May 02, 2013;15(5):e93. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Household use of information technology. Australian Bureau of Statistics. 2018. URL: https://tinyurl.com/4efm6u92 [accessed 2024-03-24]
- Kontos E, Blake KD, Chou WY, Prestin A. Predictors of eHealth usage: insights on the digital divide from the health information national trends survey 2012. J Med Internet Res. Jul 16, 2014;16(7):e172. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Litchfield I, Shukla D, Greenfield S. Impact of COVID-19 on the digital divide: a rapid review. BMJ Open. Oct 12, 2021;11(10):e053440. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Butler DC, Joshy G, Douglas KA, Sayeed MS, Welsh J, Douglas A, et al. Changes in general practice use and costs with COVID-19 and telehealth initiatives: analysis of Australian whole-population linked data. Br J Gen Pract. Apr 27, 2023;73(730):e364-e373. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arsenijevic J, Tummers L, Bosma N. Adherence to electronic health tools among vulnerable groups: systematic literature review and meta-analysis. J Med Internet Res. Feb 06, 2020;22(2):e11613. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kontos EZ, Bennett GG, Viswanath K. Barriers and facilitators to home computer and internet use among urban novice computer users of low socioeconomic position. J Med Internet Res. Oct 22, 2007;9(4):e31. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Latulippe K, Hamel C, Giroux D. Social health inequalities and eHealth: a literature review with qualitative synthesis of theoretical and empirical studies. J Med Internet Res. Apr 27, 2017;19(4):e136. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Foley K, Freeman T, Ward P, Lawler A, Osborne R, Fisher M. Exploring access to, use of and benefits from population-oriented digital health services in Australia. Health Promot Int. Aug 30, 2021;36(4):1105-1115. [ CrossRef ] [ Medline ]
- Cresswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA. SAGE Publications; 2007.
- Tappen RM, Cooley ME, Luckmann R, Panday S. Digital health information disparities in older adults: a mixed methods study. J Racial Ethn Health Disparities. Feb 2022;9(1):82-92. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Who can get a card. Services Australia. URL: https://www.servicesaustralia.gov.au/who-can-get-health-care-card?context=21981 [accessed 2023-11-03]
- Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. Mar 11, 2013;12:18. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bryant A, Charmaz K. The SAGE Handbook of Grounded Theory, Paperback Edition. Thousand Oaks, CA. SAGE Publications; 2010.
- Johnson MO, Rose CD, Dilworth SE, Neilands TB. Advances in the conceptualization and measurement of health care empowerment: development and validation of the health care empowerment inventory. PLoS One. 2012;7(9):e45692. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res. Nov 14, 2006;8(4):e27. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kayser L, Karnoe A, Furstrand D, Batterham R, Christensen KB, Elsworth G, et al. A multidimensional tool based on the eHealth literacy framework: development and initial validity testing of the eHealth Literacy Questionnaire (eHLQ). J Med Internet Res. Feb 12, 2018;20(2):e36. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Standards. Australian Bureau of Statistics. URL: https://www.abs.gov.au/statistics/standards [accessed 2024-04-04]
- Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res. Feb 2012;21(1):167-176. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Van der Feltz-Cornelis CM, Van Oppen P, Van Marwijk HW, De Beurs E, Van Dyck R. A patient-doctor relationship questionnaire (PDRQ-9) in primary care: development and psychometric evaluation. Gen Hosp Psychiatry. 2004;26(2):115-120. [ CrossRef ] [ Medline ]
- Chao J. Continuity of care: incorporating patient perceptions. Fam Med. 1988;20(5):333-337. [ Medline ]
- Wilson CK, Thomas J, Barraket J. Measuring digital inequality in Australia: the Australian digital inclusion index. JTDE. Jun 30, 2019;7(2):102-120. [ CrossRef ]
- Digital participation: a view of Australia's online behaviours. Australia Post. Jul 2017. URL: https://auspost.com.au/content/dam/auspost_corp/media/documents/white-paper-digital-inclusion.pdf [accessed 2024-04-04]
- Poli A, Kelfve S, Motel-Klingebiel A. A research tool for measuring non-participation of older people in research on digital health. BMC Public Health. Nov 08, 2019;19(1):1487. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences Second Edition. London, UK. Routledge; 1988.
- Borg K, Smith L. Digital inclusion and online behaviour: five typologies of Australian internet users. Behav Inf Technol. Feb 15, 2018;37(4):367-380. [ CrossRef ]
- Mathers A, Richardson J, Vincent S, Joseph C, Stone E. Good Things Foundation COVID-19 response report. Good Things Foundation. 2020. URL: https://tinyurl.com/2peu3kak [accessed 2024-04-04]
- Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res. Jun 16, 2006;8(2):e9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Neves AL, Burgers J. Digital technologies in primary care: implications for patient care and future research. Eur J Gen Pract. Dec 11, 2022;28(1):203-208. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by T Leung; submitted 03.07.23; peer-reviewed by T Freeman, H Shen; comments to author 16.08.23; revised version received 30.11.23; accepted 31.01.24; published 11.04.24.
©Melinda Ada Choy, Kathleen O'Brien, Katelyn Barnes, Elizabeth Ann Sturgiss, Elizabeth Rieger, Kirsty Douglas. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 11.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

IMAGES
VIDEO
COMMENTS
In this booklet, you will find: • The marking criteria - so you know how you will get awarded Pass, Merit and Distinction • Scenario - sets the tone of your work • Task - looks at what you need to do in the assignment • Writing frame - to help you complete ALL of the assignment • Case studies to choose from Component 1 - Learning Aim B
Introduction. Many populations across the globe are ageing, with growing numbers of people living with multiple long-term conditions, leading to increased complexity of care provision and rising demand for services [].Integrated Health and Social Care (IHSC) services offer a potential solution to support individual citizens across these populations [].
Introduction: International policies and legislation set a precedence of person-centred sustainable integrated Health and Social Care (HSC) that meets the health and wellbeing needs of service users through improved experiences. However, current research focuses on service models, with fewer studies investigating experiences and needs. ...
Unit number and title 7: Principles of Safe Practice in Health and Social Care. ... Produce materials for an essay on a Duty of Care and Safe Practice, in a health or social care setting, based on case study of your choice. Please refer to the case studies attached to this assignment brief.
This research focused on explicating the conceptions of just distribution of resources underlying one example of health policy. The policy used as a case study was federal funding of home health care under Medicare, during the period 1965-1984. The data consisted of the public records of debate on federal policy for home health care during this ...
people using health and social care - can sometimes seem more complicated than it really is. As part of Scotland's National Action Plan for Human Rights (SNAP), the Scottish Human Rights Commission, the Health and Social Care Alliance and NHS Health Scotland have developed this guide to help organisations learn from others who have put human
Shared decision making (SDM) involves patients and health and social care practitioners (HSCPs) jointly offering treatment, care and support packages to reflect, respect and accommodate the patient's preferences, priorities and goals [1, 2].Although the original underlying ethos for sharing decisions between patients and HSCPs is based on values, i.e. people have the right to self ...
Conclusion: This study provides valuable insights into the dynamics of organizational sustainability and understanding of key managerial actions taken to establish, develop and support integration of health and social care for people with complex mental health needs. The service user involvement and regular reviews of service users' needs were ...
The abbreviation IC will be used, referring to integrated mental health and social care services. Based on our previous research [30,31,32], we anticipated that this case would be particularly interesting to study from a sustainability perspective.By viewing sustainability as a process in a constantly changing context, the DSF is a relevant means through which to explore the mechanisms of ...
1 INTRODUCTION. Over the past decade, an increased focus on the way that integrated health and social care (IHSC) services are delivered and a growing demand for improved service user experience have driven forward improvements in worldwide health and social care (HSC; World Health Organization, 2016a).Person-centred IHSC systems aim to follow principles of participatory care and governance ...
Exploring transitions from care was a recent focus of the sociology of health and illness cross-cutting theme of the CPRU. As Professor Helen Roberts, medical sociology lead explained, this theme "undertakes research into social aspects of children and young people's health to inform policy." Key Points:
Case Studies in Community Health presents 14 classroom-tested case study scenarios, including background information and discussion questions. Written for students in public health and community health courses, these cases help integrate the basic concepts of public health into an applied setting. The case studies provide an opportunity for students to apply those basic concepts to a "real ...
The Equality and Human Rights commission has launched a new website. Visit our new website. You can continue to use our archived website until Spring 2024. Please note, it will not be updated after 30 October 2023. Continue to our archived website. Public Sector Equality Duty case study - Increasing awareness of bowel cancer symptoms among the ...
Validation of the abbreviated Lubben Social Network Scale (LSNS-6) and its association with self-rated health amongst older adults in Puerto Rico. Thomas D. Buckley PhD, Todd D. Becker LMSW, Denise Burnette PhD. , Pages: e5527-e5538. First Published: 30 August 2022.
Integrated care is pursued globally as a strategy to manage health and social care resources more effectively. It offers the promise of meeting increasingly complex needs, particularly those of aging populations, in a person-centred, co-ordinated way that addresses fragmentation and improves quality.
It explains how personal well-being is related to the availability of personal, family and community resources. The book will enable researchers, front-line workers, managers, service commissioners and politicians to identify and employ the most appropriate health care, social and economic interventions to support those at the edge of the ...
Introduction. Efforts to address social determinants of health (SDOH), long a priority for public health professionals (), have been re-energized by recent attention and investment from the healthcare sector, spurred by a range of opportunities, initiatives and incentives, including the Affordable Care Act ().This paper reviews the rich and rapidly growing body of research driving the efforts ...
Methodologically speaking, for my PhD I have adopted a single case-study research design and for my internship, I adopted a multiple-case study design. In summary, my knowledge on the topic and the methodology required to explore was useful as a starting point, but the internship aims required me to take my expertise a step further.
In this special theme issue of NEJM Catalyst Innovations in Care Delivery on social determinants of health and health-related social needs, we highlight important ongoing work on both the barriers to addressing these challenging topics and overcoming them. This double issue results from a call for submissions that began in April 2022, followed by rigorous review of the many papers submitted by ...
Introduction. Health in the United States (US) is remarkably poor given the personal and societal costs for healthcare. Despite spending nearly double of its gross domestic product on health care compared to the average Organization for Economic Co-operation and Development (OECD) country, the US has the highest chronic disease burden, highest rate of avoidable deaths, and lowest life ...
Case Study. Department of Health and Social Care introduces Scan4Safety to revolutionise patient care. Scroll. Key Results. GS1 standards allow clinical staff to build a complete patient picture that is easily accessible. Increased data visibility can aid efficiencies in catalogue management and staffing. The problem.
University of Portsmouth case studies Case study 1 Mental health issues that are not to do with doctoral study but may have an impact on it. Clara is a first year PhD student who is experiencing symptoms of depression following several negative life events, and has just started seeing a University-based counsellor. As part of her
Health is going in the wrong direction in the UK, and reversing the trend requires political and societal commitment to deal with the underlying causes The UK is facing a prolonged and serious health crisis. At a time when the future of the NHS is in jeopardy after over a decade of austerity, and with public satisfaction at an all time low,1 it must pick up the pieces of failures across ...
Background: The digital health divide for socioeconomic disadvantage describes a pattern in which patients considered socioeconomically disadvantaged, who are already marginalized through reduced access to face-to-face health care, are additionally hindered through less access to patient-initiated digital health. A comprehensive understanding of how patients with socioeconomic disadvantage ...