125 Breast Cancer Essay Topic Ideas & Examples
🏆 best breast cancer topic ideas & essay examples, 💡 most interesting breast cancer topics to write about, 📌 simple & easy breast cancer essay titles, 👍 good essay topics on breast cancer.
- Breast Cancer: Concept Map and Case Study Each member of the interdisciplinary team involved in treating patients with cancer and heart disease should focus on educational priorities such as:
- Breast Cancer and Its Population Burden The other objectives that are central to this paper are highlighted below: To determine which group is at a high risk of breast cancer To elucidate the impact of breast cancer on elderly women and […] We will write a custom essay specifically for you by our professional experts 808 writers online Learn More
- Mindfulness Practice During Adjuvant Chemotherapy for Breast Cancer She discusses the significance of the study to the nursing field and how nurses can use the findings to help their patients cope with stress.
- Breast Cancer: The Effective Care Domain Information about how the patient is seen, how often the patient is seen, and whether she will return for mammograms can be collected and analyzed to verify the successful intervention to extend consistency with mammograms.
- Garden Pesticide and Breast Cancer Therefore, taking into account the basic formula, the 1000 person-years case, the number of culture-positive cases of 500, and culture-negative of 10000, the incidence rate will be 20 new cases.
- Breast Cancer as a Genetic Red Flag It is important to note that the genetic red flags in Figure 1 depicted above include heart disease, hypertension, and breast cancer.
- Breast Cancer Surveillance Consortium Analysis Simultaneously, the resource is beneficial because it aims to “improve the delivery and quality of breast cancer screening and related outcomes in the United States”.
- Drinking Green Tea: Breast Cancer Patients Therefore, drinking green tea regularly is just a necessity- it will contribute to good health and physical vigor throughout the day and prevent severe diseases.
- Breast Cancer Prevention: Ethical and Scientific Issues Such information can potentially impact the patient and decide in favor of sharing the information about the current condition and risks correlating with the family history.
- Breast Cancer: Epidemiology, Risks, and Prevention In that way, the authors discuss the topics of breast cancer and obesity and the existing methods of prevention while addressing the ethnic disparities persistent in the issue.
- Breast Cancer Development in Black Women With consideration of the mentioned variables and target population, the research question can be formulated: what is the effect of nutrition and lifestyle maintained on breast cancer development in black women?
- Breast Cancer in Miami Florida The situation with the diagnosis of breast cancer is directly related to the availability of medicine in the state and the general awareness of the non-population.
- Breast Cancer: Genetics and Malignancy In the presence of such conditions, the formation of atypical cells is possible in the mammary gland. In the described case, this aspect is the most significant since it includes various details of the patient’s […]
- Genes Cause Breast Cancer Evidence suggests the role of BRCA1 in DNA repair is more expansive than that of BRCA2 and involves many pathways. Therefore, it is suggested that BRCT ambit containing proteins are involved in DNA repair and […]
- Breast Cancer. Service Management The trial specifically looks at the effect on breast-cancer mortality of inviting women to screening from age 40 years compared with invitation from age 50 years as in the current NHS breast-screening programme.
- Fibrocystic Breast Condition or Breast Cancer? The presence of the fibrocystic breast condition means that the tissue of the breast is fibrous, and cysts are filled with the liquid or fluid. The main characteristic feature of this cancer is that it […]
- Coping With Stress in Breast Cancer Patients Therefore, it is important for research experts to ensure and guarantee adherence to methodologies and guidelines that define scientific inquiry. However, various discrepancies manifest with regard to the initiation and propagation of research studies.
- Breast Self-Examination and Breast Cancer Mortality Though it is harsh to dismiss self-exams entirely due to studies that indicate little in deaths of women who performed self-exams and those who did not, the self-exams should not be relied on exclusively as […]
- Breast Self-Exams Curbing Breast Cancer Mortality The results of the study were consistent with the findings of other studies of the same nature on the effectiveness of breast self-examination in detecting and curbing breast cancer.
- Taxol Effectiveness in Inhibiting Breast Cancer Cells The following were the objectives of this experiment: To determine the effectiveness of Taxol in inhibiting breast cancer cells and ovarian cancer cells using culture method.
- Control Breast Cancer: Nursing Phenomenon, Ontology and Epistemology of Health Management Then, the evidence received is presented in an expert way leading to implementation of the decision on the management of the disease.
- Breast Cancer: Effects of Breast Health Education The design of the research focused on research variables like skills, performance, self-efficacy, and knowledge as the researchers aimed at examining the effectiveness of these variables among young women who underwent training in breast cancer […]
- Community Nursing Role in Breast Cancer Prevention However, early detection still remains important in the prevention and treatment of breast cancer. The community has thus undertaken activities aimed at funding the awareness, treatment and research in order to reduce the number of […]
- Self-Examination and Knowledge of Breast Cancer Among Female Students Shin, Park & Mijung found that a quarter of the participants practiced breast self-examination and a half had knowledge regarding breast cancer.
- “Tracking Breast Cancer Cells on the Move” by Gomis The article serves the purpose of examining the role of NOG, a gene that is essential in bone development and its role in breast cancer.
- Breast Cancer Survivorship: Are African American Women Considered? The finding of the analysis is that the issue of cancer survivorship is exclusive, developing, and at the same time it depends on what individuals perceive to be cancer diagnosis as well as personal experiences […]
- Gaining Ground on Breast Cancer: Advances in Treatment The article by Esteva and Hortobagyi discusses breast cancer from the aspect of increased survival rates, the novel treatments that have necessitated this and the promise in even more enhanced management of breast cancer.
- Effects of Hypoxia, Surrounding Fibroblasts, and p16 Expression on Breast Cancer The study was conducted to determine whether migration and invasion of breast cancer cells were stimulated by hypoxia, as well as determining whether the expression of p16 ectopically had the potential to modulate the cell […]
- Breast Cancer: Preventing, Diagnosing, Addressing the Issue In contrast to the MRI, which presupposes that the image of the tissue should be retrieved with the help of magnetic fields, the mammography tool involves the use of x-rays.
- Dietary Fat Intake and Development of Breast Cancer This study aimed to determine the relationship between dietary fat intake and the development of breast cancer in women. The outcome of the study strongly suggests that there is a close relationship between a high […]
- The Detection and Diagnosis of Breast Cancer The severity of cancer depends on the movement of the cancerous cells in the body and the division and growth or cancerous cells.
- Breast Cancer: WMI Research and the Current Approaches Although the conclusions provided by the WHI in the study conducted to research the effects of estrogen and progesterone cessation on the chance of developing a breast cancer do not comply with the results of […]
- Breast Cancer Susceptibility Gene (BRCA2) The mechanisms underlying the genetic predisposition to a particular disease are manifold and this concept is the challenging one to the investigators since the advent of Molecular Biology and database resources.
- Prediction of Breast Cancer Prognosis It has been proposed that the fundamental pathways are alike and that the expression of gene sets, instead of that of individual genes, may give more information in predicting and understanding the basic biological processes.
- Breast Cancer Survivors: Effects of a Psychoeducational Intervention While the conceptual framework is justified in analysis of the quality of life, there is the likelihood of influence of the context with quality of life adopting different meanings to patients in different areas and […]
- Providers’ Role in Quality Assurance in Breast Cancer Screening In order to ensure the quality assurance of mammography, the providers involved in the procedure need to be aware of the roles they ought to play.
- Clinical Laboratory Science of Breast Cancer The word cancer is itself so much dreaded by people that the very occurrence of the disease takes half of the life away from the patient and the relatives.
- Induced and Spontaneous Abortion and Breast Cancer Incidence Among Young Women There is also no question as to whether those who had breast cancer was only as a result of abortion the cohort study does not define the total number of women in population.
- New Screening Guidelines for Breast Cancer On the whole, the Task Force reports that a 15% reduction in breast cancer mortality that can be ascribed to the use of mammograms seems decidedly low compared to the risks and harm which tend […]
- Breast Cancer in Afro- and Euro-Americans It is seen that in the age group of more than 50 years, EA was more at risk of contracting cancer, as compared to AA.
- Breast Cancer Assessment in London In light of these developments, it is therefore important that an evaluation of breast cancer amongst women in London be carried out, in order to explore strategies and policy formulations that could be implemented, with […]
- Breast Cancer: Crucial Issues The textbook also notes the significant racial differences in survival rates, mainly attributed to socioeconomic and cultural factors, including lack of available specialized care. Medical professionals and local communities highly appreciate the value of early […]
- Breast Cancer: At-Risk Population, Barriers, and Improvement Thus, the principal purpose of Part Two is to explain why older women face a higher risk of getting breast cancer, what barriers lead to this adverse state of affairs, and how to improve the […]
- Breast Cancer: Moral and Medical Aspects In addition to the question of the surgery, there is an ethical problem associated with the genetic characteristics of the disease.
- Breast Cancer and AIDS: Significant Issues in the United States in the Late 20th Century Thus, the given paper is going to explain why these activists challenged regulatory and scientific authorities and what they demanded. That is why the enthusiasts challenged their practices and made specific demands to improve the […]
- Breast Cancer Risk Factors: Genetic and Nutritional Influences However, the problems of genetics contribute to the identification of this disease, since the essence of the problem requires constant monitoring of the state of the mammary glands to detect cancer at an early stage.
- Breast Cancer Genetics & Chromosomal Analysis In this paper, the chromosomal analysis of breast cancer will be assessed, and the causes of the disorder will be detailed.
- Breast Cancer: The Case of Anne H. For this reason, even females with a high level of health literacy and awareness of breast cancer, such as Anne H, might still belong to the group risk and discover the issue at its late […]
- Breast Cancer Diagnosis Procedure in Saudi Arabia The fact is that, the health care program in this geographic area is associated with the encouragement of all the women in the area to be subjected to the examination for the breast cancer, as […]
- Breast Cancer and the Effects of Diet The information in noted clause is only a part of results of the researches spent in the field of the analysis of influence of a diet on a risk level of disease in cancer.
- Genetic Predisposition to Breast Cancer: Genetic Testing Their choice to have their first baby later in life and hormonal treatment for symptoms of menopause further increase the risk of breast cancer in women.
- Health Psychology: Going Through a Breast Cancer Diagnosis He is unaware that she has been diagnosed with depression and that she is going for breast screening Stress from work is also a contributing factor to her condition.
- Breast Cancer: Causes and Treatment According to Iversen et al this situation is comparable to the finding of abnormal cells on the surface of the cervix, curable by excision or vaporization of the tissue.
- Monoclonal Antibodies in Treating Breast Cancer The most important function of the lymph glands is that their tissue fluid carries the cancer cells that have been detached from the tumour to the closely located lymph gland.
- Breast Cancer: Women’s Health Initiative & Practices The new standard of care shows evidence that a low-fat diet, deemed insignificant by the WHI study, is beneficial to women for preventing or improving their risks of breast cancer.
- Hormone Receptor-Positive Breast Cancer Pathophysiology The contemporary understanding of the etiopathogenesis of breast cancer addresses the origin of invasive cancer through a substantive number of molecular alterations at the cellular level.
- Complex Fibroadenoma and Breast Cancer Risk Furthermore, KB decided that she did not need to remove the lump surgically she was advised to document changes after regular breast exams and return to the clinic in case of new concerns.
- Breast Cancer: Health Psychology Plan The goal of the plan is to identify the psychological issues and health priorities of the subject and propose a strategy for addressing them.
- Best Practices in Breast Cancer Care Based on this, the final stage of therapy should include comprehensive support for patients with breast cancer as one of the main health care practices within the framework of current treatment guidelines.
- Complementary and Alternative Medicine for Women With Breast Cancer The treatment of breast CA has developed over the past 20 years, and many treatment centers offer a variety of modalities and holistic treatment options in addition to medical management.
- Breast Cancer Screening in Young American Women It is proud to be at the forefront of widespread public health initiatives to improve the education and lives of young women.
- Screening for Breast Cancer The main goal of this paper is to describe the specific set of clinical circumstances under which the application of screening is the most beneficial for women aged 40 to 74 years.
- Annual Breast Cancer Awareness Campaign It may also need more time to be implemented as the development of the advertisement, and all visuals will take time.
- Breast Cancer Patients’ Life Quality and Wellbeing The article “Complementary Exercise and Quality of Life in Patients with Breast Cancer” examines the role of complementary exercises towards improving the lives of women with breast cancer.
- Breast Cancer Patients’ Functions and Suitable Jobs The key symptom of breast cancer is the occurrence of a protuberance in the breast. A screening mammography, scrutiny of the patient’s family history and a breast examination help in the diagnosis of breast cancer.
- Jordanian Breast Cancer Survival Rates in 1997-2002 This objective came from the realization that the best way to test the efficacy of breast cancer treatment and to uncover intervening factors influencing the efficacy of these treatments was to investigate the rates of […]
- Breast Cancer Awareness Among African Americans There are reasons that motivate women to seek mammography for example the belief that early detection will enable them treat the cancer in early stages, and their trust for the safety of mammogram. Social marketing […]
- Breast Cancer Screening Among Non-Adherent Women This is one of the aspects that can be identified. This is one of the short-comings that can be singled out, and this particular model may not be fully appropriate in this context.
- Breast Cancer: Treatment and Rehabilitation Options Depending on the site of occurrence, breast cancer can form ductal carcinomas and lobular carcinomas if they occur in the ducts and lobules of the breast, respectively. Breast cancer and treatment methods have significant effects […]
- Women Healthcare: Breast Cancer Reducing the levels of myoferlin alters the breast cancer cells’ mechanical properties, as it is evident from the fact that the shape and ability of breast cancer cells to spread is low with reduced production […]
- Breast Cancer Public Relations Campaign Audiences It is clear that the breast cancer campaign will target at women in their 30-40s as this is one of the most vulnerable categories of women as they often pay little attention to the […]
- Health Information Seeking and Breast Cancer Diagnosis Emotional support is also concerned with the kind of information given to patients and how the information is conveyed. It is equally significant to underscore the role of information in handling breast cancer patients immediately […]
- Current Standing of Breast Cancer and Its Effects on the Society It then places particular focus on the testing and treatment of breast cancer, the effects and conditions associated with it, from a financial point of view, and the possible improvements worth making in service or […]
- Breast Cancer: Disease Prevention The first indicator of breast cancer is the presence of a lump that feels like a swollen matter that is not tender like the rest of the breast tissues.
- Breast Cancer Definition and Treatment In the case where “the cells which appear like breast cancer are still confined to the ducts or lobules of the breast, it is called pre-invasive breast cancer”.”The most widespread pre-invasive type of breast cancer […]
- Breast Cancer Symptoms and Causes The mammogram is the first indication of breast cancer, even though other indications such as the presence of the lymph nodes in the armpits are also the early indications of breast cancer.
- Breast Cancer Incidence and Ethnicity This paper explores the different rates of breast cancer incidence as far as the different ethnic groups in the US are concerned as well as the most probable way of reducing the rates of incidence […]
- Treatment Options for Breast Cancer This type of breast cancer manifests itself in the tubes/ducts which form the channel for transporting milk from the breast to the nipple.”Lobular carcinoma: this type of cancer usually begins in the milk producing regions […]
- Risk Factors, Staging, and Treatment of Breast Cancer This is so because huge amounts of resources have been used in the research and the development of the breast cancer drugs that in effect help the body to combat the cancer by providing additional […]
- Case Management for Breast Cancer Patients In this respect, preventive measures should be taken in order to decrease the mortality rates all over the world in terms of cancer illness and breast cancer in particular.
- The Second Leading Cause of Death is the Breast Cancer
- The Benefits and Effects of Exercise on Post-Treatment Breast Cancer Patients
- Women’s Experiences Undergoing Reconstructive Surgery After Mastectomy Due To Breast Cancer
- Advanced Technology Of The Treatment Of Breast Cancer
- Using Genetic Testing For Breast Cancer
- The role of Perivascular Macrophages in Breast Cancer Metastasis
- The Psychological Aspect Of Coping With Breast Cancer
- An Analysis of an Alternative Prevention in Breast Cancer for Young Women in America
- The Complicated Biology of Breast Cancer
- The Impact Of Tamoxifen Adjuvant Therapy On Breast Cancer
- The Prevalence Of Breast Cancer Among Black Women
- The Embodiment Theory, Holistic Approach And Breast Cancer In The South African Context
- The Long-Term Evolution of Quality of Life for Breast Cancer Treated Patients
- The Signs and Early Prevention of Breast Cancer
- The Effect of Fast Food In Developing Breast Cancer among Saudi Populations
- The Effect Of Breastfeeding On Ovarian And Breast Cancer
- The Best Method Of Medicine For The Treatment Of Breast Cancer: Cam Or Drugs
- The Causes of Breast Cancer – Genetically or Environmentally Influenced
- The Symptoms, Causes and Treatment of Breast Cancer, a Malignant Disease
- The Risks, Characteristics and Symptoms of Breast Cancer, a Malignant Disease
- The Most Common Cancer In The UK: Breast Cancer
- Types Of Preventive Services For A Higher Risk Of Breast Cancer
- The Effect of Raloxifene on Risk of Breast Cancer in Postmenopausal Women
- The Impact of Culture and Location on Breast Cancer Around the World
- Understanding Breast Cancer, Its Triggers and Treatment Options
- The Risk, Development, Diagnosis, and Treatment of Breast Cancer in Women
- The Pathophysiology of Breast Cancer
- The Effects Of DNA Methylation On Breast Cancer
- The Treatment and Management Options for Breast Cancer Patients
- Alternative Forms Of Medicine For Breast Cancer Rates
- The Impact of Nutrition on Breast Cancer and Cervical Cancer
- The Economic Evaluation of Screening for Breast Cancer: A Tentative Methodology
- The Etymology of Breast Cancer, Types, Risk Factors, Early Detection Methods, and Demographics
- What Are The Symptoms And Treatments For Breast Cancer
- Treatments And Treatment Of Breast Cancer Therapy
- The Various Views and Approaches in the Treatment and Management of Breast Cancer
- The Growing Health Problem of Breast Cancer in the United States
- The Importance of Considering Breast Cancer Prevention Aside from Treatment
- The Different Ways That Can Reduce the Risk of Having Breast Cancer
- The Use of Radiation for Detection and Treatment of Breast Cancer
- The Condition Of Breast Cancer And Its Relevant Treatment
- The Relationship between a High-Dairy Diet and Breast Cancer in Women
- Treatment of Solid Tumors including Metastatic Breast Cancer
- Which Is More Effective In Reducing Arm Lymphoedema For Breast Cancer Patients
- The Use Of Telomerase In Diagnosis, Prognosis, And Treatment Of Cancer: With A Special Look At Breast Cancer
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 2). 125 Breast Cancer Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/breast-cancer-essay-topics/
"125 Breast Cancer Essay Topic Ideas & Examples." IvyPanda , 2 Mar. 2024, ivypanda.com/essays/topic/breast-cancer-essay-topics/.
IvyPanda . (2024) '125 Breast Cancer Essay Topic Ideas & Examples'. 2 March.
IvyPanda . 2024. "125 Breast Cancer Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/breast-cancer-essay-topics/.
1. IvyPanda . "125 Breast Cancer Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/breast-cancer-essay-topics/.
Bibliography
IvyPanda . "125 Breast Cancer Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/breast-cancer-essay-topics/.
- Cancer Essay Ideas
- Skin Cancer Questions
- Leukemia Topics
- Palliative Care Research Topics
- Pathogenesis Research Ideas
- Tuberculosis Questions
- DNA Essay Ideas
- Biochemistry Research Topics
- Gene Titles
- Human Papillomavirus Paper Topics
- Nursing Care Plan Paper Topics
- Hypertension Topics
- Stem Cell Essay Titles
- Osteoarthritis Ideas
- Diabetes Questions
- About Breast Cancer
- Find Support
- Get Involved
- Free Resources
- Mammogram Pledge
- Wall of Support
- In The News
- Recursos en Espa ñ ol
About Breast Cancer > Diagnosis > Breast Cancer Screening
- What Is Cancer?
- Causes of Breast Cancer
- Breast Cancer Facts & Stats
- Breast Tumors
- Breast Anatomy
- Male Breast Cancer
- Growth of Cancer
- Risk Factors
- Genetic Testing for Breast Cancer
- Other Breast Cancer Genes
- BRCA: The Breast Cancer Gene
- What To Do If You Tested Positive
- Breast Cancer Signs and Symptoms
- Breast Lump
- Breast Pain
- Breast Cyst

Breast Self-Exam
Clinical breast exam.
- How to Schedule a Mammogram
- Healthy Habits
Breast Cancer Screening
- Diagnostic Mammogram
- Breast Biopsy
- Waiting For Results
- Breast Cancer Stages
- Stage 2 (II) And Stage 2A (IIA)
- Stage 3 (III) A, B, And C
- Stage 4 (IV) Breast Cancer
- Ductal Carcinoma In Situ (DCIS)
- Invasive Ductal Carcinoma (IDC)
- Lobular Carcinoma In Situ (LCIS)
- Invasive Lobular Cancer (ILC)
- Triple Negative Breast Cancer (TNBC)
- Inflammatory Breast Cancer (IBC)
- Metastatic Breast Cancer (MBC)
- Breast Cancer During Pregnancy
- Other Types
- Choosing Your Doctor
- Lymph Node Removal & Lymphedema
- Breast Reconstruction
- Chemotherapy
- Radiation Therapy
- Hormone Therapy
- Targeted Therapy
- Side Effects of Breast Cancer Treatment and How to Manage Them
- Metastatic Breast Cancer Trial Search
- Standard Treatment vs. Clinical Trials
- Physical Activity, Wellness & Nutrition
- Bone Health Guide for Breast Cancer Survivors
- Follow-Up Care
- Myth: Finding a lump in your breast means you have breast cancer
- Myth: Men do not get breast cancer; it affects women only
- Myth: A mammogram can cause breast cancer or spread it
- Myth: If you have a family history of breast cancer, you are likely to develop breast cancer, too
- Myth: Breast cancer is contagious
- Myth: If the gene mutation BRCA1 or BRCA2 is detected in your DNA, you will definitely develop breast cancer
- Myth: Antiperspirants and deodorants cause breast cancer
- Myth: A breast injury can cause breast cancer
- Myth: Breast cancer is more common in women with bigger breasts
- Myth: Breast cancer only affects middle-aged or older women
- Myth: Breast pain is a definite sign of breast cancer
- Myth: Consuming sugar causes breast cancer
- Myth: Carrying a phone in your bra can cause breast cancer
- Myth: All breast cancers are the same
- Myth: Bras with underwire can cause breast cancer
- Can physical activity reduce the risk of breast cancer?
- Can a healthy diet help to prevent breast cancer?
- Does smoking cause breast cancer?
- Can drinking alcohol increase the risk of breast cancer?
- Is there a link between oral contraceptives and breast cancer?
- Is there a link between hormone replacement therapy (HRT) and breast cancer?
- How often should I do a breast self exam (BSE)?
- Does a family history of breast cancer put someone at a higher risk?
- Are mammograms painful?
- How does menstrual and reproductive history affect breast cancer risks?
- How often should I go to my doctor for a check-up?
- What kind of impact does stress have on breast cancer?
- What celebrities have or have had breast cancer?
- Where can I find a breast cancer support group?
- Can breastfeeding reduce the risk of breast cancer?
- Is dairy (milk) linked to a higher risk of breast cancer?
- Is hair dye linked to a higher risk of breast cancer?
- NEW! Smart Bites Cookbook: 7 Wholesome Recipes in 35 Minutes (or Less!)
- Weekly Healthy Living Tips: Volume 2
- Most Asked Questions: Breast Cancer Signs & Symptoms
- Cancer Caregiver Guide
- Breast Cancer Surgery eBook
- 10 Prompts to Mindfulness
- How to Talk About Breast Health
- Family Medical History Checklist
- Healthy Recipes for Cancer Patients eBook
- Chemo Messages
- Most Asked Questions About Breast Cancer Recurrence
- Breast Problems That Arent Breast Cancer eBook
- Nutrition Care for Breast Cancer Patients eBook
- Finding Hope that Heals eBook
- Dense Breasts Q&A Guide
- Breast Cancer Recurrence eBook
- What to Say to a Cancer Patient eBook
- Weekly Healthy Living Tips
- Bra Fit Guide
- Know the Symptoms Guide
- Breast Health Guide
- Mammogram 101 eBook
- 3 Steps to Early Detection Guide
- Abnormal Mammogram eBook
- Healthy Living & Personal Risk Guide
- What Every Woman Needs to Know eBook
- Breast Cancer Resources

Last updated on Jan 17, 2024
Breast cancer screening can detect cancer before signs or symptoms develop. While breast cancer screening cannot prevent breast cancer, it can help find breast cancer in its earliest and most treatable stage. When detected in the localized (early) stage, breast cancer has a 5-year relative survival rate of 99%, according to the American Cancer Society.
Regardless of your risk of breast cancer, it is important to talk with your healthcare provider about the best screening tests, recommendations, and timelines for screening.
Table of Contents
Use these links to jump to the breast cancer screening information you need:
What is Breast Cancer Screening? Breast Cancer Screening Recommendations Breast Cancer Screening Tests Breast Cancer Diagnostic Tests Benefits and Risks of Breast Cancer Screening Breast Cancer Screening for Men Breast Cancer Screening Facts Breast Cancer Screening FAQs
What is Breast Cancer Screening?
Breast cancer screening can detect breast cancer before it has spread and before there are symptoms to help reduce the number of people who die from cancer. Screening can also identify those who may need more frequent or additional tests to check for breast cancer.
There are different types of breast cancer screening tests, as well as different age recommendations to begin screenings. The different tests and recommendations are listed below, and you can also check with your doctor to determine which screenings are right for you and at what ages.
The more you know about breast cancer screening, the more you can take charge of your breast health.
Breast Cancer Screening Recommendations
The U.S. Preventative Services Task Force states that women should start receiving mammograms at the age of 40. However, women at higher risk of developing breast cancer may benefit from beginning regular mammography earlier than the age of 40. Family health history can inform the decision to undergo earlier breast cancer screening.
Below are general breast health screening recommendations for women at average risk of breast cancer. Please consult with your healthcare provider on when is the best time for you to begin breast health screenings based on your specific situation and any risk factors that may be present.
High Risk Breast Cancer Screening
Women at higher risk for breast cancer can benefit from screening at an earlier age, as well as from annual breast MRIs in addition to mammography. The American Cancer Society recommends most women at high risk begin screening at age 30, or upon your doctor’s recommendation.
Your doctor can help you assess if you are at higher risk of developing breast cancer. Risk factors include a personal or family history of breast cancer, a BRCA1 or BRCA2 inherited gene mutation , previous radiation to the chest area, and other gene mutations or health conditions.
In addition, breast cancer screening for dense breasts can be more challenging. The Food and Drug Administration (FDA) now requires mammogram providers to notify women if they have dense breast tissue and recommend consultation with a healthcare provider on potential additional screening, since dense breast tissue can make it more difficult to spot breast cancer.
Breast cancer screening after mastectomy is not needed on the side of the body where breast tissue was removed; breast cancer screening after double mastectomy should no longer be required since there likely won’t be enough breast tissue remaining for a mammogram.
Talk with your doctor or healthcare provider to assess breast cancer risk and determine the best age for you to begin breast cancer screening.
Breast Cancer Screening Tests
Although there are several types of breast cancer screening tests available, mammography is the most common and most accurate form of screening.
A breast self-exam involves looking at and feeling your breasts for potential lumps or swelling. If you are familiar with how your breasts typically look and feel, you will be more likely to notice any changes.
A breast self-exam should be performed once a month by all women. Premenopausal women should perform their self-exam the week after their cycle. Postmenopausal women should choose a consistent time each month to perform their self-exam.
While the majority of breast lumps are not breast cancer , all breast lumps should be investigated by a healthcare professional. If you’re not sure how to perform a breast self-exam, download the Know the Symptoms Guide for instructions.
During a clinical breast examination , a healthcare professional carefully looks and feels for any differences in breast shape and size, as well as lumps, dimpling, rashes, or anything else unusual. Clinical breast exams are often performed during your annual medical check-up or well-woman exam, beginning around the age of 20.
A low-dose x-ray of the breasts, mammograms are the best way to find breast cancer in its early stages. Mammograms can often find breast cancer or breast changes long before symptoms develop. If something is detected on an annual mammogram, typically known as a screening mammogram, additional tests, such as a diagnostic mammogram , will likely be ordered.
Mammograms are performed with a machine that has two plates that compress the breast and spread the tissue apart, providing a clearer picture of the breast.
2D screening mammography, which typically takes one picture of the breast from the side and one from above, was the standard for many years.
Today, 3D mammograms, also known as digital breast tomosynthesis, are more common and more accurate at detecting breast cancer. They also work well for women with dense breast tissue and reduce the need for follow-up screening. A more advanced type of imaging, a 3D mammogram takes multiple images of the breast from different angles. Not every insurance plan covers 3D mammography, although more are now doing so.
NBCF offers a free Mammogram 101 resource that helps you prepare for your mammogram.
Breast Cancer Diagnostic Tests
A breast MRI uses radio waves and magnets to take pictures of the breast and may be used in conjunction with mammograms for women at higher risk of breast cancer or those who have dense breast tissue . Likewise, if your initial breast screening exam is not conclusive, your doctor may order an MRI to take a closer look.
Breast MRI imaging creates detailed pictures of specific areas within the breast that can help your medical team distinguish between normal and potentially cancerous tissue.
Sometimes used in conjunction with other breast cancer screening tests, a breast ultrasound uses sound waves to view the inside of the breasts. The ultrasound generates a picture called a sonogram, which can help measure the size and location of a lump and determine if it is a cyst , which is not typically cancerous, or a cancerous tumor.
Genetic Screening
Genetic screening for breast cancer scans for mutations in the BRCA1 and BRCA2 genes . Some people inherit mutations in these genes, which can increase their risk of breast cancer as well as ovarian and pancreatic cancer.
Women with a family history of breast cancer are also at higher risk of getting breast cancer; however, most women with a family history of breast cancer do not have an inherited gene that increases their risk. It is important to weigh the pros and cons of genetic testing and screening with your family and doctor. To keep track of your family medical history to share with family members and your healthcare team, use NBCF’s free Family Medical History Checklist .
Benefits and Risks of Breast Cancer Screening
As with many medical tests, there are both benefits and risks. However, the benefits of breast cancer screening far outweigh the risks.
Benefits of Screening
The most significant benefit of breast cancer screening is reduced mortality. Women who receive annual mammograms from the ages of 40 to 84 experience a 40% lower breast cancer mortality rate than women with no screenings, according to research . Mammograms also decrease the number of women diagnosed with cancer in a later stage, when it is more difficult to treat and more likely to have spread.
Regular breast cancer screening also decreases healthcare costs, since cancer diagnosed at an earlier stage is usually less expensive to treat. Finally, breast cancer screening can provide peace of mind and a reminder of the importance of focusing on overall health and wellness.
Risks of Screening
The chief risk of screening is a false positive result, and the anxiety that may cause. A false positive is when something may initially look like cancer, but turns out not to be cancer upon further examination. Initial false-positive results may lead to additional testing, such as a biopsy, and can create unwarranted anxiety.
However, with recent advancements in mammogram technology, radiologists consider the risk of a false positive to be relatively small. The general consensus is that most women and doctors are willing to risk the small chance of a false positive over missing something suspicious found on a routine mammogram.
Radiation can be risky for women who are pregnant. Pregnant women should always let their doctor or x-ray technician know that they are expecting since pregnant women should limit or forgo any screenings or treatments involving radiation.
While no screening test is 100% accurate, regular mammograms have been repeatedly shown to significantly reduce the risk of dying from breast cancer.
Breast Cancer Screening for Men
Currently, there are no guidelines on screening men for breast cancer, and male breast cancer remains extremely rare, representing less than 1% of all breast cancer cases.
It is generally easier for men and their healthcare providers to feel a breast tumor since men have little breast tissue, yet men with breast cancer have a higher mortality rate than women due to lower awareness and likelihood of seeking treatment. Breast exams and occasionally mammograms and ultrasound may be appropriate for men who have a strong family history of male or female breast cancer or who have BRCA gene mutations .
Breast Cancer Screening Facts
In the United States, 1 in 8 women will develop breast cancer in her lifetime. It is the second most common type of cancer for women, following skin cancer.
About 65% of breast cancer cases are diagnosed in the localized stage, before the cancer has spread outside of the breast. The 5-year relative survival rate for breast cancer detected at this stage is 99%, which is why awareness and regular screenings are so critically important.
Unfortunately, there are notable disparities in breast cancer screening. Nearly half of uninsured women delay or go without care due to costs. In addition, the death rate for breast cancer among Black women is 40% higher than it is for white women, and it is the leading cause of cancer death for Hispanic women in the United States.
National Breast Cancer Foundation shares the latest statistics on breast cancer and breast cancer disparities. In addition, NBCF’s National Mammography Program provides resources on free mammograms and diagnostic services.
Breast Cancer Screening FAQs
When should you start screening for breast cancer .
Well-woman exams, which can include clinical breast exams, and Pap tests are recommended starting at age 20.
Mammograms are recommended starting at age 40 for women of average breast cancer risk. However, if you have a significant family history of breast cancer, such as one or more first-degree relatives diagnosed with breast cancer, or a first-degree relative diagnosed under the age of 50, then you may need to begin screening earlier. For example, if a mother was diagnosed with breast cancer at age 42, her biological daughter would likely benefit from breast cancer screening beginning at age 32. Talk with your healthcare provider about the best schedule for mammograms.
What are the screening tests for breast cancer?
In addition to mammograms, which are the best screening tests for finding breast cancer in its early stages , other screening tests for breast cancer include breast self-exams and clinical exams. Other forms of imaging studies for screening include ultrasounds and breast MRIs.
Can men get breast cancer?
While it is rare, men do get breast cancer. In 2023, an estimated 2,800 men will be diagnosed with breast cancer, according to the American Cancer Society. Men diagnosed with breast cancer may be encouraged to undergo genetic counseling and genetic testing to see if they carry a BRCA1 or BRCA2 gene mutation . The most common gene mutation for men is BRCA2.
What is the risk of radiation from mammograms?
Mammograms require very small doses of radiation, lower than that of a typical x-ray. The total radiation for a typical mammogram is about 0.4 millisieverts—the same amount women are exposed to in their natural environment in about seven weeks. Studies consistently show that the benefits of receiving mammograms outweigh the risks of radiation exposure for most women. However, always let your healthcare provider know if you are pregnant or could be pregnant as radiation exposure risk for pregnant women is higher.
American Cancer Society Centers for Disease Control and Prevention National Cancer Institute U.S. Preventative Services Task Force
Related reading:
We use cookies on our website to personalize your experience and improve our efforts. By continuing, you agree to the terms of our Privacy & Cookies Policies.

MUNEEZA KHAN, MD, AND ANNA CHOLLET, MD, MPH
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2021;103(1):33-41
Patient information: See related handout on mammogram screening for breast cancer , written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Breast cancer is the most common nonskin cancer in women and accounts for 30% of all new cancers in the United States. The highest incidence of breast cancer is in women 70 to 74 years of age. Numerous risk factors are associated with the development of breast cancer. A risk assessment tool can be used to determine individual risk and help guide screening decisions. The U.S. Preventive Services Task Force (USPSTF) and American Academy of Family Physicians (AAFP) recommend against teaching average-risk women to perform breast self-examinations. The USPSTF and AAFP recommend biennial screening mammography for average-risk women 50 to 74 years of age. However, there is no strong evidence supporting a net benefit of mammography screening in average-risk women 40 to 49 years of age; therefore, the USPSTF and AAFP recommend individualized decision-making in these women. For average-risk women 75 years and older, the USPSTF and AAFP conclude that there is insufficient evidence to recommend screening, but the American College of Obstetricians and Gynecologists and the American Cancer Society state that screening may continue depending on the woman's health status and life expectancy. Women at high risk of breast cancer may benefit from mammography starting at 30 years of age or earlier, with supplemental screening such as magnetic resonance imaging. Supplemental ultrasonography in women with dense breasts increases cancer detection but also false-positive results.
Breast cancer is the most common nonskin cancer in women and accounts for 30% of all new cancers in the United States. 1 From 2001 to 2016, more than 2.3 million women in the United States were diagnosed with breast cancer. 2 The incidence of breast cancer increases after 25 years of age, peaking between 70 and 74 years. 2 Approximately one in eight women will develop invasive breast cancer (12.8% lifetime risk). 1
WHAT'S NEW ON THIS TOPIC
Breast Cancer Screening
A 2016 meta-analysis calculated that per 10,000 women screened with mammography, three breast cancer deaths are avoided over 10 years in women 40 to 49 years of age, eight deaths are avoided in women 50 to 59 years, 21 deaths are avoided in women 60 to 69 years, and 13 deaths are avoided in women 70 to 74 years. [ corrected ]
One out of every eight women 40 to 49 years of age who has a screening mammogram will subsequently undergo additional imaging, and for every case of invasive breast cancer detected by screening mammography in this age group, 10 women will have had a biopsy.
In a large, multicenter trial, women with dense breasts and a negative standard mammogram result had two-year screening with MRI or standard mammography. The interval cancer rate was lower in the MRI group than in the mammography group; however, MRI had a high false-positive rate with hundreds of negative breast biopsy results among the 4,738 women who underwent MRI screening.
MRI = magnetic resonance imaging.
The overall mortality rate in U.S. women with breast cancer is about 20 per 100,000. Mortality rates are highest in women 85 years and older (170 per 100,000). 2 White women have the highest rate of breast cancer diagnosis, whereas Black women have the highest rate of breast cancer–related death. 2 Breast cancer is also the most common cause of cancer-related death in Hispanic women and the second leading cause of cancer-related death behind lung cancer among all women. 2
Cancer screening recommendations are determined by the patient's current anatomy. Transgender females with breast tissue and transgender males who have not undergone complete mastectomy should receive screening mammography based on guidelines for cisgender persons (see https://www.aafp.org/afp/2018/1201/p645.html#sec-4 ).
What Are the Risk Factors for Breast Cancer?
The strongest risk factors are a history of childhood chest radiation, older age, increased breast density, family history of breast cancer, and certain genetic mutations ( Table 1 ). 3 – 16 However, most women who develop invasive breast cancer do not have any of these risk factors . 3
EVIDENCE SUMMARY
A retrospective cohort study demonstrated a standardized incidence ratio (i.e., the ratio of observed to expected number of cases) of 21.9 for breast cancer in women who received chest radiation during childhood. 4 Higher doses of radiation were associated with higher risk, and the highest risk was in those who received whole lung radiation (standardized incidence ratio = 43.6). The overall cumulative risk of developing breast cancer by 50 years of age was 30%. 4
Increasing age is another strong risk factor. Invasive breast cancer will be diagnosed in one out of 42 women 50 to 59 years of age, and this rate increases to one out of 14 in women 70 years and older. 5
Breast density is the amount of glandular and stromal tissue compared with adipose tissue shown on a mammogram. A systematic review and meta-analysis found that compared with women who do not have dense breasts, the relative risk of developing breast cancer is 1.79 for women with breast density between 5% and 24% and 4.64 for those with breast density of 75% or higher. 6
Data from the Breast Cancer Surveillance Consortium and the Collaborative Breast Cancer Study showed that having a first-degree relative with breast cancer increases a woman's personal risk by a hazard ratio of 1.61 and odds ratio of 1.64. 7 For patients with BRCA mutations, the risk of developing breast cancer by 80 years of age is 60% to 63%, regardless of family history. 8
How Can Physicians Estimate the Risk of Developing Breast Cancer?
Several validated risk assessment tools are available to stratify breast cancer risk ( Table 2 ). 17 These tools can assist physicians and patients in developing individualized plans regarding screening, genetic testing, or chemoprevention .
A large retrospective cohort study compared the six-year accuracy of five validated risk assessment tools among 35,921 women 40 to 84 years of age who underwent screening mammography in the United States from 2007 to 2009. 17 The models were BRCAPRO ( https://projects.iq.harvard.edu/bayesmendel/bayesmendel-r-package ); Breast Cancer Risk Assessment Tool, or Gail model ( https://bcrisktool.cancer.gov , https://www.mdcalc.com/gail-model-breast-cancer-risk ); Tyrer-Cuzick model, or International Breast Cancer Intervention Study model ( http://www.ems-trials.org/riskevaluator ); Breast Cancer Surveillance Consortium model ( https://tools.bcsc-scc.org/BC5yearRisk/calculator.htm ); and Claus model (computer program).
Based on overall performance, the positive predictive values were 2.6% for BRCAPRO and the Tyrer-Cuzick model, 2.9% for the Breast Cancer Risk Assessment Tool and Breast Cancer Surveillance Consortium model, and 3.9% for the Claus model. The negative predictive values were high at 97% or more for all of the models. 17
Does Screening Mammography Reduce Breast Cancer–Related Mortality?
Screening mammography reduces breast cancer–related mortality, with larger reductions as women get older .
Modeling studies estimate that in women 40 to 49 years of age, the number needed to screen (NNS) with annual mammography to prevent one breast cancer death is 746. The NNS decreases to 351 in women 50 to 59 years and to 233 in women 60 to 69 years. The NNS is 377 in women 70 to 79 years of age. 18 However, randomized controlled trials have demonstrated a substantially higher NNS. A meta-analysis performed for the U.S. Preventive Services Task Force (USPSTF) calculated that per 10,000 women screened with mammography, only three breast cancer deaths are avoided over 10 years in women 40 to 49 years of age, eight deaths are avoided in women 50 to 59 years, 21 deaths are avoided in women 60 to 69 years, and 13 deaths are avoided in women 70 to 74 years. 19 [ corrected ]
Between 2008 and 2017, yearly rates of newly diagnosed breast cancer increased by 0.3%, and rates of breast cancer death fell by 1.5%. 20 This may be partly attributable to early detection of small, curable breast cancers that have a five-year relative survival rate of 98.8% posttreatment. 20 Studies have shown a reduction in the incidence of large tumors, which is also likely because of early detection of smaller tumors by mammography. 21
Lower death rates, however, may also reflect improved treatments. With older treatments, the reduction in mortality after screening mammography was approximately 12 deaths per 100,000 women. With improved treatments, the reduction in mortality after screening mammography is now about eight deaths per 100,000 women. 21
What Are the Potential Harms of Breast Cancer Screening?
False-positive results are common with screening mammography, especially in younger women, leading to further imaging and radiation exposure and subsequent breast biopsies that can be painful, can cause anxiety, and usually yield benign results. Furthermore, screening can lead to overdiagnosis and overtreatment of cancers that may never have become symptomatic or life-threatening .
According to the USPSTF, the false-positive rate of mammography is highest in women 40 to 49 years of age at 121 per 1,000 and decreases with age to 69.6 per 1,000 women 70 to 79 years of age. 22 About one of every eight women 40 to 49 years of age who has a screening mammogram will subsequently undergo additional imaging, and for every case of invasive breast cancer detected by screening mammography in this age group, 10 women will have had a biopsy, compared with only three women in their 70s. 22
False-positive results are associated with increased antidepressant and anxiolytic prescriptions, with a relative risk of 1.13 to 1.19. 23 Women at highest risk of needing antidepressant and anxiolytic therapy are those 40 to 49 years of age who underwent multiple tests, including a biopsy, and who had to wait more than one week to be told the results were false-positive. 23
Systematic reviews have found that screening mammography leads to an overdiagnosis rate of 10% to 30%. 24 , 26 [ corrected ] Overdiagnosis can lead to unnecessary treatments for screening-detected breast cancers. Sometimes this involves treating ductal carcinoma in situ that would have been inconsequential over a woman's lifetime. 3 A study based on a large U.S. cancer registry reported that out of 297,000 women 40 years and older who had a mastectomy in 2013, 18% may not have needed one. 25 Thus, the USPSTF concludes that there is no strong evidence supporting mammography screening of average-risk women in their 40s. 26
What Are the Screening Recommendations for Patients at Average Risk?
Recommendations for breast self-examinations, clinical breast examinations, and mammography vary among organizations . Table 3 summarizes recommendations from the USPSTF, the American Academy of Family Physicians (AAFP), the American College of Obstetricians and Gynecologists (ACOG), the American College of Radiology (ACR), the American Cancer Society (ACS), and the National Comprehensive Cancer Network (NCCN) . 3 , 26 – 33
Breast Self-Examination . The USPSTF and AAFP recommend against teaching patients to perform breast self-examinations because of a lack of supporting evidence. 26 , 27 ACOG, the NCCN, and the ACS encourage breast self-awareness (i.e., patient familiarity with how her breasts usually feel and look) and advise women to seek medical attention if they notice breast changes. 3 , 31 , 33 There may be some rationale for breast self-awareness based on the frequency of self-detection cited in some studies. For example, out of 361 breast cancer survivors who participated in the 2003 National Health Interview Survey, 43% reported detecting their own cancers. 34
Clinical Breast Examination . The USPSTF and AAFP state that there is insufficient evidence to assess the benefits and harms of clinical breast examinations. 26 , 28 The ACS recommends against these examinations because of insufficient evidence of benefit and a high rate of false-positive results (55 false-positives for every breast cancer detected). 31 , 35 For average-risk women 40 years and older, ACOG says that annual clinical breast examinations may be offered, and the NCCN recommends annual clinical breast examinations. 3 , 33
Mammography . Evidence of benefit varies with a woman's age. The USPSTF found lower mortality rates and a reduced risk of advanced breast cancer in women 50 years and older who had mammography screening (relative risk = 0.62; 95% CI, 0.46 to 0.83) but not in women 39 to 49 years of age (relative risk = 0.98; 95% CI, 0.74 to 1.37). 19 The number of breast cancer deaths prevented with screening over 10 years was 12.5 per 10,000 women 50 years and older but only 2.9 per 10,000 women in their 40s. 19 Overall, women 50 to 59 years of age have the best balance of risks and benefits from mammography. 3 , 19
ACS data, however, showed improved mortality benefit across all age groups, although the benefit was lower in younger women. The NNS to reduce mortality rates by 20% was 1,770 for women in their 40s, 1,087 for women in their 50s, and 835 for women in their 60s. 31
The USPSTF recommends biennial screening mammography for women 50 to 74 years of age. 26 This recommendation excludes women 40 to 49 years of age because the number needed to invite (NNI) of 1,904 and the NNS of 1,034 to detect one case of breast cancer with screening mammography were considered too high. The NNI of 1,339 and NNS of 455 in women 50 to 59 years of age and the NNI of 377 and NNS of 233 for women 60 to 69 years of age were considered acceptable. 18 The AAFP supports the USPSTF recommendation. 29
The ACS recommends annual screening mammography starting at 45 years of age and transitioning to biennial screening at 55 years of age. 31 This recommendation is based on multivariable analyses suggesting that women in the younger age group are more likely than older women to have advanced stage cancer when screened biennially rather than annually. 31
The NCCN recommends annual screening mammography. 33 , 36 ACOG recommends shared decision-making based on a discussion of benefits and harms when deciding between annual and biennial screening intervals. 3
At What Age Should Breast Cancer Screening Be Discontinued?
Women at average risk should continue screening mammography through 74 years of age . 3 , 26 , 29 – 31 , 33 Starting at 75 years of age, women should be involved in shared decision-making based on overall health status and life expectancy according to ACOG recommendations . 3 The ACS and NCCN recommend continued screening after 75 years of age if life expectancy is at least 10 years, and the ACR recommends continued screening if life expectancy is at least five to seven years . 30 , 31 , 33 The USPSTF states that there is insufficient evidence to assess the benefits and harms of screening past 74 years of age, and the AAFP supports this finding . 26 , 29
Randomized controlled trials have shown that when mammography screening prevents a death, the death would have occurred within five to seven years after screening; thus, screening women with limited life expectancy is not warranted. 36 In addition, the number of life-years gained from screening decreases from 7.8 to 11.4 per 1,000 mammograms at 74 years of age to 4.8 to 7.8 per 1,000 at 80 years and to 1.4 to 2.4 per 1,000 at 90 years. 37 When adjusted for quality of life, the number of life-years gained decreases even further, and by 90 to 92 years of age, all life-years gained are counter-balanced by a loss in quality of life, presumably because of treatment adverse effects. 37 Yet, despite these data and the corresponding recommendations, 62% of women 75 to 79 years of age and 50% of women 80 years or older get mammograms, and 70% to 86% of physicians recommend mammography for 80-year-old women. 38 , 39
What Are the Screening Recommendations for Patients at Increased Risk?
ACS recommends that women with a 20% or higher lifetime risk of breast cancer (assessed using a risk assessment tool [ Table 2 17 ] ) be offered annual mammography and magnetic resonance imaging (MRI), typically starting at 30 years of age . 32 For high-risk women 25 to 29 years of age, ACOG recommends a clinical breast examination every six to 12 months and annual breast MRI with contrast. For patients 30 years and older, ACOG recommends annual mammography and MRI with contrast . 40 The NCCN recommends that women with a lifetime risk of more than 20% have breast self-awareness and receive a clinical breast examination every six to 12 months starting at 21 years of age. Annual breast MRI is recommended starting at 25 years of age with annual screening mammography starting at 30 years . 33 Women younger than 25 years with a history of chest radiation should have breast self-awareness and receive a clinical breast examination every six to 12 months starting 10 years after radiation therapy. Once these women are 25 years old, annual breast MRI is recommended, then screening mammography starting at 30 years of age . 33 The USPSTF states that there is insufficient evidence to assess the benefits and harms of using MRI for breast cancer screening, and the AAFP supports this finding . 26 , 29
The evidence for adding annual MRI screening to mammography and clinical breast examinations in women with more than a 20% lifetime risk of breast cancer is based on nonrandomized screening trials and observational studies from the 1990s. 32 These studies showed that MRI has a sensitivity of 71% to 100% for detecting breast cancer in high-risk women vs. mammography's sensitivity of 16% to 40% in the same population. However, MRI is less specific (81% to 99%) compared with mammography (93% to more than 99%), resulting in higher rates of false-positives, subsequent medical appointments, and biopsies, with a positive predictive value of 20% to 40%. No data were collected on survival rates with MRI screening or on the optimal MRI screening interval. 32
Does Supplemental Imaging Have a Role in Evaluating Dense Breasts?
Almost 50% of women 40 to 74 years of age have dense breasts, which is a risk factor for breast cancer and for false-negative results on standard mammography . 41 Ultrasonography, MRI, and digital breast tomosynthesis (also known as 3D mammography) have been proposed as methods to detect breast cancers that might be missed on mammography in women with dense breasts .
The ACR recommends considering ultrasonography in addition to screening mammography based on a randomized multicenter trial showing improved cancer detection rates compared with mammography alone (1.9 vs. 4.2 per 1,000). 30 , 42 Ultrasonography may be particularly useful for women who have a 15% to 20% lifetime risk of breast cancer and dense breasts but no additional risk factors. 43
Data from the Connecticut Experiments showed an additional 2.3 cancers detected per 1,000 women with dense breasts who were screened with ultrasonography in addition to mammography. 43 By the fourth year of the study, the positive predictive value had increased from 7.3% to 20.1%, indicating an improved learning curve for the radiologists regarding which lesions to biopsy. Another study, involving 2,662 women with dense breasts plus one other risk factor for breast cancer, showed that adding ultrasonography to mammography increased the sensitivity of breast cancer detection compared with mammography alone (52% vs. 76%). 42
It is important to note, however, that the increased sensitivity comes at the cost of increasing false-positives. An observational cohort study of 6,081 women with varying risk of breast cancer showed that the false-positive rate was 22.2 per 1,000 screens for mammography alone vs. 52 per 1,000 screens for mammography plus ultrasonography (relative risk = 2.23). 44
MRI has also been studied as a screening option in women with dense breasts. A large multicenter trial randomized women with dense breasts and a negative result on standard mammography to two-year screening with either MRI or standard mammography. 45 The cancer detection rate during the two years was lower in the MRI group than in the mammography group (2.5 vs. 5 per 1,000 screens). More than 90% of MRI-detected cancers, however, were stage 0 or 1, and MRI screening resulted in a high false-positive rate (79.8 per 1,000 screens) with hundreds of negative breast biopsy results among the 4,738 women who underwent MRI screening.
MRI has also been compared with digital breast tomosynthesis. There were higher rates of cancer detection with MRI (11.8 per 1,000 screens) than with digital breast tomosynthesis (4.8 per 1,000 screens), but no data are available on long-term outcomes. 46 A study comparing standard mammography with digital breast tomosynthesis is underway. 47
The long-term survival of women whose breast cancers were detected with supplemental imaging modalities has not been studied.
This article updates previous articles on this topic by Tirona , 48 Knutson and Steiner , 49 and Apantaku . 50
Data Sources: A PubMed search was completed in Clinical Queries using the key terms breast cancer, breast cancer screening, risk factors for breast cancer, breast cancer risk assessment tools, breast cancer screening recommendations, breast density, mammography, supplemental screening. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Agency for Healthcare Research and Quality Effective Healthcare Reports, the Cochrane database, and Essential Evidence Plus. Search date: April 2020.
American Cancer Society. Cancer facts and figures 2020. Accessed April 4, 2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf
Centers for Disease Control and Prevention. United States cancer statistics: data visualizations. Accessed August 2, 2020. https://gis.cdc.gov/Cancer/USCS/DataViz.html
American College of Obstetricians and Gynecologists. Practice bulletin no. 179. Breast cancer risk assessment and screening in average-risk women. Obstet Gynecol. 2017;130(1):e1-e16.
Moskowitz CS, Chou JF, Wolden SL, et al. Breast cancer after chest radiation therapy for childhood cancer. J Clin Oncol. 2014;32(21):2217-2223.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30.
McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15(6):1159-1169.
Shiyanbola OO, Arao RF, Miglioretti DL, et al. Emerging trends in family history of breast cancer and associated risk. Cancer Epidemiol Biomarkers Prev. 2017;26(12):1753-1760.
Metcalfe KA, Lubinski J, Gronwald J, et al.; Hereditary Breast Cancer Clinical Study Group. The risk of breast cancer in BRCA1 and BRCA2 mutation carriers without a first-degree relative with breast cancer. Clin Genet. 2018;93(5):1063-1068.
Chen S, Iversen ES, Friebel T, et al. Characterization of BRCA1 and BRCA2 mutations in a large United States sample. J Clin Oncol. 2006;24(6):863-871.
American Cancer Society. Breast cancer facts and figures 2019–2020. Accessed August 2, 2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf
Schacht DV, Yamaguchi K, Lai J, et al. Importance of a personal history of breast cancer as a risk factor for the development of subsequent breast cancer. AJR Am J Roentgenol. 2014;202(2):289-292.
Dyrstad SW, Yan Y, Fowler AM, et al. Breast cancer risk associated with benign breast disease. Breast Cancer Res Treat. 2015;149(3):569-575.
Liu Y, Colditz GA, Rosner B, et al. Alcohol intake between menarche and first pregnancy. J Natl Cancer Inst. 2013;105(20):1571-1578.
Collaborative Group on Hormonal Factors in Breast Cancer. Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet. 2019;394(10204):1159-1168.
Collaborative Group on Hormonal Factors in Breast Cancer. Menarche, menopause, and breast cancer risk. Lancet Oncol. 2012;13(11):1141-1151.
Colditz GA, Rosner B. Cumulative risk of breast cancer to age 70 years according to risk factor status. Am J Epidemiol. 2000;152(10):950-964.
McCarthy AM, Guan Z, Welch M, et al. Performance of breast cancer risk-assessment models in a large mammography cohort. J Natl Cancer Inst. 2020;112(5):489-497.
Hendrick RE, Helvie MA. Mammography screening. AJR Am J Roentgenol. 2012;198(3):723-728.
Nelson HD, Fu R, Cantor A, et al. Effectiveness of breast cancer screening: systematic review and meta-analysis to update the 2009 U.S. Preventive Services Task Force recommendation. Ann Intern Med. 2016;164(4):244-255.
National Cancer Institute. Female breast cancer. Accessed August 2, 2020. https://seer.cancer.gov/statfacts/html/breast.html
Welch HG, Prorok PC, O'Malley AJ, et al. Breast-cancer tumor size, overdiagnosis, and mammography screening effectiveness. N Engl J Med. 2016;375(15):1438-1447.
Nelson HD, O'Meara ES, Kerlikowske K, et al. Factors associated with rates of false-positive and false-negative results from digital mammography screening. Ann Intern Med. 2016;164(4):226-235.
Segel JE, Balkrishnan R, Hirth RA. The effect of false-positive mammograms on antidepressant and anxiolytic initiation. Med Care. 2017;55(8):752-758.
Monticciolo DL, Helvie MA, Hendrick RE. Current issues in the overdiagnosis and overtreatment of breast cancer. AJR Am J Roentgenol. 2018;210(2):285-291.
Harding C, Pompei F, Burmistrov D, et al. Use of mastectomy for overdiagnosed breast cancer in the United States. J Cancer Epidemiol. ;2019:5072506.
U.S. Preventive Services Task Force. Breast cancer: screening. January 11, 2016. Accessed July 20, 2019. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/breast-cancer-screening
American Academy of Family Physicians. Breast cancer, breast self exam (BSE). Accessed July 20, 2019. https://www.aafp.org/patient-care/clinical-recommendations/all/breast-cancer-self-bse.html
American Academy of Family Physicians. Breast cancer, clinical breast examination (CBE). Accessed July 20, 2019. https://www.aafp.org/patient-care/clinical-recommendations/all/breast-cancer-cbe.html
American Academy of Family Physicians. Breast cancer. Accessed May 31, 2020. https://www.aafp.org/patient-care/clinical-recommendations/all/breast-cancer.html
Lee CH, Dershaw DD, Kopans D, et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol. 2010;7(1):18-27.
Oeffinger KC, Fontham ETH, Etzioni R, et al.; American Cancer Society. Breast cancer screening for women at average risk [published correction appears in JAMA . 2016;315(13):1406]. JAMA. 2015;314(15):1599-1614.
Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography [published correction appears in CA Cancer J Clin . 2007;57(3):185]. CA Cancer J Clin. 2007;57(2):75-89.
Bevers TB, Helvie M, Bonaccio E, et al. NCCN clinical practice guidelines in oncology. Breast cancer screening and diagnosis. Version 3.2019. May 17, 2019. Accessed May 31, 2019. https://www.nccn.org/professionals/physician_gls/pdf/breast-screening.pdf
Roth MY, Elmore JG, Yi-Frazier JP, et al. Self-detection remains a key method of breast cancer detection for U.S. women. J Womens Health (Larchmt). 2011;20(8):1135-1139.
Meyers ER, Moorman P, Gierisch JM, et al. Benefits and harms of breast cancer screening: a systematic review [published correction appears in JAMA . 2016;315(13):1406]. JAMA. 2015;314(15):1615-1634.
Helvie MA, Bevers TB. Screening mammography for average-risk women. J Natl Compr Canc Netw. 2018;16(11):1398-1404.
van Ravesteyn NT, Stout NK, Schechter CB, et al. Benefits and harms of mammography screening after age 74 years. J Natl Cancer Inst. 2015;107(7):djv103.
Bellizzi KM, Breslau ES, Burness A, et al. Prevalence of cancer screening in older, racially diverse adults. Arch Intern Med. 2011;171(22):2031-2037.
Leach CR, Klabunde CN, Alfano CM, et al. Physician over-recommendation of mammography for terminally ill women. Cancer. 2012;118(1):27-37.
American College of Obstetricians and Gynecologists. Hereditary breast and ovarian cancer syndrome. Practice bulletin no. 182. September 2017. Accessed August 2, 2020. https://bit.ly/37Kl2M4
Sprague BL, Gangnon RE, Burt V, et al. Prevalence of mammographically dense breasts in the United States. J Natl Cancer Inst. 2014;106(10):dju255.
Berg WA, Zhang Z, Lehrer D, et al.; ACRIN 6666 Investigators. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012;307(13):1394-1404.
Thigpen D, Kappler A, Brem R. The role of ultrasound in screening dense breasts. Diagnostics (Basel). 2018;8(1):20.
Lee JM, Arao RF, Sprague BL, et al. Performance of screening ultrasonography as an adjunct to screening mammography in women across the spectrum of breast cancer risk [published correction appears in JAMA Intern Med . 2019;179(5):733]. JAMA Intern Med. 2019;179(5):658-667.
Bakker MF, de Lange SV, Pijnappel RM, et al.; DENSE Trial Study Group. Supplemental MRI screening for women with extremely dense breast tissue. N Engl J Med. 2019;381(22):2091-2102.
Comstock CE, Gatsonis C, Newstead GM, et al. Comparison of abbreviated breast MRI vs digital breast tomosynthesis for breast cancer detection among women with dense breasts undergoing screening [published correction appears in JAMA . 2020;323(12):1194]. JAMA. 2020;323(8):746-756.
National Cancer Institute. TMIST (Tomosynthesis Mammographic Imaging Screening Trial). Accessed January 10, 2020. https://www.cancer.gov/about-cancer/treatment/clinical-trials/nci-supported/tmist
Tirona MT. Breast cancer screening update. Am Fam Physician. 2013;87(4):274-278. Accessed September 15, 2020. https://www.aafp.org/afp/2013/0215/p274.html
Knutson D, Steiner E. Screening for breast cancer. Am Fam Physician. 2007;75(11):1660-1666. Accessed September 15, 2020. https://www.aafp.org/afp/2007/0601/p1660.html
Apantaku LM. Breast cancer diagnosis and screening. Am Fam Physician. 2000;62(3):596-602. Accessed September 15, 2020. https://aafp.org/afp/2000/0801/p596.html
Continue Reading

More in AFP
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Bioethics in Medicine and Society
Ethical Concerns Regarding Breast Cancer Screening
Submitted: 04 June 2020 Reviewed: 23 September 2020 Published: 13 October 2020
DOI: 10.5772/intechopen.94159
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Bioethics in Medicine and Society
Edited by Thomas F. Heston and Sujoy Ray
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
749 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
The incidence and mortality of breast cancer are rising in the whole world in the past few decades, adding up to a total of around two million new cases and 620,000 deaths in 2018. Unlike what occurs in developed countries, most of the cases diagnosed in the developing world are already in advanced stages and also in women younger than 50 years old. As most screening programs suggest annual mammograms starting at the age of 50, we can infer that a considerable portion of the new breast cancer cases is missed with this strategy. Here, we will propose the adoption of an alternative hierarchical patient flow, with the creation of a diagnostic fast track with referral to timely treatment, promoting better resources reallocation favoring the least advantaged strata of the population, which is not only ethically acceptable but also a way of promoting social justice.
- breast cancer
- public health
Author Information
Rodrigo goncalves *.
- Breast Surgery Sector, Discipline of Gynecology, Department of Obstetrics and Gynecology, Hospital das Clinicas of the University of Sao Paulo Medical School, Brazil
Maria Carolina Formigoni
José maria soares.
- Discipline of Gynecology, Department of Obstetrics and Gynecology, Hospital das Clinicas of the University of Sao Paulo Medical School, Brazil
Edmund Chada Baracat
José roberto filassi.
*Address all correspondence to: [email protected]
1. Introduction
According to data from the World Health Organization (WHO), the number of deaths due to cancer will increase up to 45% between 2008 and 2030 and 70% of those deaths will occur in developing countries [ 1 ]. To try and change this scenario, the WHO recommends the implementation of cancer control programs that must include cost-effective measures on healthy life style, vaccination programs and screening programs [ 2 ]. A screening program consists in a set of coordinated actions with the objective of reducing cancer mortality through early stage diagnosis in an asymptomatic population, with adequate referral to diagnostic and treatment facilities. These programs have four main components: the definition and recruitment of the target population, adequate offer of diagnostic tests with quality assurance, guaranteed offer of follow up exams and biopsies to confirm findings from the initial diagnostic tests, and referral to treatment facilities and timely navigation through the health system [ 3 ]. Although screening programs present the potential benefit of reducing mortality, they are not risk-free. The main risks of such a program are the false-positive and false-negative results, and also the occurrence of over diagnosis. All these can lead to clinical and psychological repercussions and, also, to the increase in the health care system expenditure. To address this issue, the Public Health Agency of Canada performed a study to estimate the harms of the local breast cancer-screening program in 7 years, according to age, and the main results can be seen in Table 1 [ 4 ].
Benefits and harms of mammographic breast cancer screening [ 4 ].
In this text, we will use Brazil as a model to discuss screening programs in the developing countries. In the Brazilian setting, breast cancer is the most frequent type of cancer, responsible for 16,724 deaths in 2017 and with an estimate of 66,280 new cases in 2020 [ 5 ]. This scenario, however, has some peculiarities when compared to developed countries in the North America or Europe; 41.1% of all cases in Brazil happen in women younger than 50 years old and the majority of the operable cases is diagnosed in locally advanced stages, being 53.3% of the cases in stage II and 23.2% in stage III [ 6 ]. These characteristics are not typical of a country with a well-established breast cancer-screening program. The strategy adopted in Brazil states that women over 50 should get a mammogram every two years between 50 and 69 years old [ 7 ]. However, due to the early age of diagnosis that we observe in this developing country, we can argue that more than 40% of the diagnosed women are not eligible to the screening program in the first place. Moreover, the late presentation at diagnosis raises the hypothesis that the current screening program is not effective or that the patients do not have proper access to it. Added to that, the mortality due to breast cancer in Brazil has been increasing in the last decades [ 8 ]. All these issues taken together generate an ethical dilemma to be explored, once the investment of public resources in an ineffective program impacts negatively the whole society. This way, more effective resources reallocation strategies should be implemented to address this dilemma.
In this chapter we will discuss the breast cancer screening programs in developing countries and the main evidence regarding the barriers in the access to the healthcare system. Beyond that, we will address the main ethical questions related to breast cancer screening from the Rawls’s distributive justice [ 9 ] perspective, from the utilitarianism concepts [ 10 , 11 ] and from the principles of autonomy and non-maleficence. Lastly, we will propose the support to an alternative approach to breast cancer in developing countries, maximizing the cost–benefit ratio in the use of public resources.
2. Recommendations to breast cancer screening around the world
The U.S. Preventive Services Task Force (USPSTF) is an independent volunteer panel of American experts that develops recommendations regarding the efficacy of preventive services to asymptomatic patients. These recommendations are based on both benefits and harms that programs might cause, without consideration to the cost of the intervention. Current data about mammographic screening are solid regarding the benefits of this strategy when used in women over 50 years old and the USPSTF recommends a mammogram every two years, in women between 50 and 74; however, this same agency does not consider that there is enough evidence to support mammographic screening from 40 to 49 years old in asymptomatic patients without increased risk to breast cancer [ 12 ]. This recommendation is due to the fact that screening in this age range results in a smaller number of prevented deaths when compared to more advanced ages; also leads to a larger number of unnecessary biopsies; and to the possibility of psychological problems, like anxiety, because of the large number of false-positive results. While mammographic screening of 10,000 asymptomatic women between 50 and 59 years old can prevent 8 breast cancer deaths, the same strategy adopted in asymptomatic women between 40 and 49 years old would prevent only 3 breast cancer deaths [ 13 , 14 ]. Another harm associated with mammographic screening of an asymptomatic population considered by the USPSTF when issuing their recommendation is the occurrence of over diagnosis. Although it is extremely complex to calculate the proportion of diagnosed cases that would never evolve to cancer, the best estimates from randomized clinical trials suggest the occurrence of over diagnosis in 20% of the cases due to mammographic screening [ 15 ].
Another agency that carefully evaluated the cost–benefit ratio of mammographic screening in asymptomatic women between 40 and 49 years old was the Ontario Health Technology Advisory Committee through a systematic review of the literature [ 16 ]. This work included an evaluation of the USPSTF report [ 17 ], the Canadian Preventive Services Task Force (CPSTF) report [ 18 ], a Cochrane systematic review [ 19 ], five health technology assessments and eight randomized clinical trials [ 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 ] with the objective to assess the reduction of the breast cancer mortality in this age range attributable to mammographic screening. This agency reached a similar conclusion as the USPSTF that the mammographic screening in an asymptomatic population between 40 and 49 years old is not effective in reducing breast cancer mortality and that the harms associated with this intervention, like exposure to radiation, high rate of false-negatives leading to delays in diagnosis and high rate of false-positives with associated psychological harmful effects should not be overlooked.
The Brazilian College of Radiology (BCR) and Brazilian Society of Mastology (BSM) however issued a different recommendation, based on different published articles of international literature and methodologically inferior to the ones evaluated and with a clear selection bias [ 25 , 28 , 29 ]. In these studies, it was demonstrated a breast cancer mortality reduction between 18% and 38% in the studied populations. The main point to justify the recommendation of mammographic screening for asymptomatic women between 40 and 49 years old is to emphasize that in this developing country there is a higher proportion of breast cancer patients in this age range when compared to developed countries [ 30 ]. Despite the fact that it is a recommendation for Brazil, it did not include a single Brazilian study in the analysis. This scenario is repeated throughout Latin America as it has been shown in a report by The Economist Intelligence unit. Cancer care registries are lacking in Latin America due to insufficient coverage of the population and also due to low quality [ 31 ]. Without local high-quality data, it is impossible to perform local health technology assessments and the decision-making process is jeopardized.
3. Ethical implications of mammographic screening
Carefully considering the recommendations of these three different countries with very diverse populations, we can conclude that although mammographic screening in women between 40 and 49 provide a modest benefit in reducing breast cancer mortality, the occurrence of adverse effects is more pronounced.
We can also note that the BCR and BSM adopt a paternalistic approach, reflecting the principle of beneficence. In the meantime, the USPSTF and the CPSTF advocate that the screening decision should be shared with the patient. This way, patients that are more risk averse could opt out of the screening program and patients that value more the potential benefits could opt in, following the principles of non-maleficence and autonomy. However, what we must ask is whether it is possible to convey important information regarding the risks associated with a screening program in a clear and, more important, neutral manner. In this sense, it is of utmost importance that the autonomy principle is respected and that patients are not manipulated to undergo tests or treatments which they do not agree with, due to the use of biased information.
Addressing this issue, Biddle introduced the concept of epistemic risk, defined as the risk of error that comes up at any moment in the process of knowledge production [ 32 ]. These errors can happen because of biases during the data collection step and also because of decisions made in scenarios of uncertainty. These decisions reflect the set of values of the involved researchers and have consequences to human health and to the definition of public policies. Rudner agrees with this argument and suggests that it’s impossible to prove any hypothesis with full certainty, as there is always a possibility of error. This way, researchers must judge what is the necessary amount of data to accept or reject a hypothesis and this judgment depends on the set of values of the researcher and on the importance of the consequences an error can lead to [ 33 ]. Pramesh et al. discuss such a conflict in depth when they justify the necessity of a randomized clinical trial to prove a hypothesis raised by a cross-sectional study, as they believe the data gathered in the latter is not sufficient to support the decision-making process [ 34 ].
The reasoning to support a mammographic screening program for asymptomatic women below the age of 50 is not free of the risk of epistemic risks. One kind of epistemic risk associated with to mammographic screening is the inductive risk, defined as the risk of incorrectly accept or reject a hypothesis based on the available evidence [ 35 ]. Breast surgeons must accept or reject that a patient has a disease, frequently a ductal carcinoma in situ (DCIS), that will evolve causing symptoms and death based on evidence that does not guarantee the veracity of this hypothesis. That happens mostly because of the lack of evidence to predict which cases of DCIS will evolve to become invasive carcinomas. Another epistemic risk, the one in the gathering of data of breast biopsies, occurs in the evaluation of the differential diagnosis between atypical hyperplasia and DCIS. While the first ones are treated with a small surgical procedure, the latter requires surgical excision followed by radiation therapy and, in some cases, endocrine therapy for 5 years. This way, an error committed by the pathologist might lead to an enormous impact in the treatment of the patients. As pathologists have different formations and different experience backgrounds, and as the biopsy evaluation is a subjective process, this is an epistemic risk that is hard to be assessed. In order to try and decrease the odds of such an error is the development of image analyses software. Mercan et al. evaluated 240 breast biopsies comparing the performance of three experienced pathologists and an automated image analysis method. In this study, the automated method performed better than the pathologists in differentiating atypical hyperplasia and DCIS, becoming a promising alternative for the near future [ 36 ]. As we saw in these two examples, the information conveyed to the patients eligible to screening are not obtained in the absence of the researchers personal judgment and values. Thus, more than just respecting the autonomy principle in the shared decision-making process, healthcare workers must convey not only the necessary information but also their values and personal beliefs used by them to define their diagnostic and therapeutic decisions. As long as there is ambiguity in the results of mammographic screening studies in asymptomatic women below the age of 50, the priority should be debating the advantages and disadvantages of this strategy, instead of discrediting their opponents [ 37 ].
4. Current situation of mammographic screening
In Brazil, as in many developing countries, there is no public policy to the implementation of an organized mammographic screening program. As mentioned previously, there is a recommendation from the Brazilian National Cancer Institute (INCA) for mammogram every two years for women between 50 and 69 years old [ 7 ] and the main medical societies recommend an annual mammogram for women starting at 40 years of age [ 30 ].
This difference in recommendations happens due to complex interactions between the country’s decision makers’ interests, beliefs, perspectives and personal values. In the present scenario, with this disparity of recommendations, patients present late stage diagnosis, worse than the ones observed in Norway before the implementation of the local mammographic screening program ( Table 2 ) [ 38 ].
Prevalence of breast cancer according to stage in the state of São Paulo between 2000 and 2017, and in Norway before the implementation of mammographic screening.
Adapted from Tiezzi et al. [ 38 ].
To evaluate the necessity to expand the INCA’s recommendation to other age ranges, Brito et al. analyzed all breast cancer cases, all DCIS cases and all breast cancer related deaths in the city of Aracaju between 1998 and 2014, dividing pages according to age groups [ 39 ]. The breast cancer incidence trends remained stable over the studied period across all age groups. Both incidence and cancer-specific mortality in that municipality were similar to the ones observed in countries with the same human development index. The authors concluded that, as these rates remained stable in all age groups, including the ones in which screening is recommended, the investment of public resources to screen women below the age of 50 or over the age of 69 is not justifiable.
A broader study by Rodrigues et al. evaluated retrospective data regarding mammograms between 2008 and 2016 in the public health system [ 40 ]. Around nineteen million mammograms were performed in this period with an increase in coverage of 14.5% annually between 2008 and 2012 followed by a stable period between 2012 and 2017. The population coverage of mammogram varied in the period from 14.4% to 24.2% of the target population. This number is far from the 70% coverage recommended by the WHO, necessary to effectively reduce breast cancer-specific mortality [ 41 ]. Rodrigues et al. also evaluated the number of mammogram machines available in the country, their geographical distribution and the total number of exams performed in 2016 [ 42 ]. In this study, it was demonstrated that Brazil has 4628 machines with a capacity of 14,279,654 exams per year. In 2016, however, only 4,073,079 exams were performed, 29% of the total capacity, displaying a clear under-use of the available infrastructure. The low coverage of the target population with the stable trend in the past few years associated with the under-use of the available infrastructure raises the hypothesis of the existence of barriers to access to the healthcare system.
The Barretos Cancer Hospital adopted an alternative to improve the coverage of the screening program with the use of mobile mammogram machines in trucks reaching 108 municipalities in the northeastern region of São Paulo, targeting women between 40 and 69 years old. Greenwald et al. evaluated the efficacy of this initiative from 2010 to 2015 [ 43 ] and, in this period, 122,634 women were evaluated with a coverage of 54.8% of the target population, referral of 12.25% of these women were referred for additional exams with a cancer detection rate of 3,63/1000 women. 92.51% of the referrals to treatment centers were successfully accepted. The results obtained by this program are very promising, showing the potential to be expanded to other regions and other countries.
5. Barriers to access the healthcare system
Brazil is a developing country with a population of 209.3 million inhabitants with enormous social and economical disparities between its 5 regions [ 44 ]. Moreover, there are also inequalities in the distribution of human resources and health infrastructure with a significant variation in the number of hospital beds and physicians dedicated to oncological patients leading to significant differences in health outcomes [ 8 ]. Another source of outcome variability is the duality of access to the healthcare system. Every Brazilian citizen has unrestricted access to the public health system (PHS) and the richer portion of the population also has access to private healthcare providers through out-of-pocket direct expending or through healthcare insurance companies. This duality of the system is perverse in a way that it perpetuates the idea that a small portion of the population has access to state-of-the-art diagnostic and treatment facilities while the majority of the population, around 71%, depends exclusively on the PHS with all its limitations. When comparing this two scenarios, we observe a striking difference in the initial stage of the breast cancer patients; the majority of the patients seen in the private setting is diagnosed with early stage tumors, whereas the majority of patients that depend on the PHS is diagnosed with locally advanced tumors [ 45 ], a clear indication that difficulties to access the healthcare system are the main obstacles to early detection. 37% of the breast cancer cases diagnosed in the PHS are stage III or IV while in the private sector this number falls to 16.2% [ 46 ]. These data are corroborated by national studies that showed intervals of 75 to 185 days between initial symptom presentation and initial biopsy [ 45 ] and a median interval of 113.4 days between indication and initiation of radiation therapy [ 47 ]. For comparison purposes, patients seen in the private setting can have diagnostic tests and start treatment in less than 30 days.
To identify the main barriers to access to the PHS, Vieira et al. conducted a systematic review of the literature identifying 30 publications on this topic [ 48 ]. In a general analysis, it has been identified an underuse of mammogram machines on the north and northeast regions of the country and a mammogram coverage of only 35% of the Brazilian women, most of them in the private setting. The main issues related with not having a mammogram performed are non-white ethnicity, low educational level, low familiar income and not having health insurance. Another interesting finding of this study is that normally the treatment of breast cancer is performed in big cities and patients end up traveling more than 100 miles from their residences to the hospitals [ 49 ]. Even before the start of treatment, patients have to face delays of more than 60 days in 36.9% of the cases, because of inefficient referral and navigation. The main issues related with delays in the initiation of treatment were non-white ethnicity, not having a partner, low educational level, early stage breast cancer and dependence of the PHS [ 50 ]. Exclusive dependence on the PHS and non-white ethnicity were also associated with higher breast cancer-specific mortality [ 51 ].
6. Recommendation and discussion of the ethical dilemma
Considering the inefficacy of the screening programs in developing countries and the lack of solid evidence supporting screening of asymptomatic women below the age of 50 years old, we recommend resources reallocation to improve access to the healthcare system and the implementation of a fast track between diagnostic and treatment facilities to symptomatic patients, based on the hierarchical flow proposed by Migowski et al. ( Figure 1 ) [ 52 ]. This algorithm proposes three different actions: educational activities in primary care facilities to raise awareness regarding breast cancer and also the potential benefits and harms of mammographic screening; to offer the option of screening mammogram to asymptomatic women aged 50 to 69 during their visit to the primary healthcare provider; and to promote priority access to symptomatic patients, without the need of prior scheduling, in which the ones with suspicious lesions will be referred to diagnostic facilities. This recommendation is supported by Rawls’ two principles of justice [ 9 ]. The first principle governs that all persons have equal rights and freedoms. The second principle governs that the adoption of policies that generate social or economical inequalities is only acceptable if it favors the least advantaged portion of society. The promotion of educational activities proposed by Migowski et al. [ 52 ] is supported by Rawls’ first principle since it standardizes the access to a basic right, education. The second part of the recommendation is justified by Rawls’ second principle of justice. The adoption of a fast track to symptomatic patients, removing the need of a prior appointment or referral, promotes the reallocation of public resources to remove barriers in the access to care, reducing delays in diagnosis and treatment and, therefore, reducing inequalities in favor of the least advantaged part of the population that relies solely in the public health system. Although the recommendation favors a part of the population, it does not violate individual rights, as asymptomatic patients will still have access to screening mammogram in their routine visits to their primary healthcare providers. Moreover, the proposed recommendation promotes equal access to breast cancer diagnosis and treatment as it removes the age boundaries, starting to provide care to women below the age of 50 years old, an age range responsible for a large amount of new cases in developing countries and that were not previously included in the past recommendation [ 6 ].

Hierarchical flow to promote early diagnosis and treatment of breast cancer. Adapted from Migowski et al. [ 52 ].
Let us consider for a moment a hypothetical scenario in which the healthcare system works perfectly without any access barriers. Even in this setting, mammographic screening as it is currently suggested would not be ideal in developing countries. The current evidence that recommends mammographic screening is not unanimous and large randomized clinical trials did not show a robust mortality reduction attributable to it [ 13 , 53 ]. Moreover, even if these studies showed a significant mortality reduction attributable to screening mammogram, their results would hardly be applicable to the developing countries’ realities. Those studies were conducted in countries with high human development index (HDI) and in the context of organized screening. Brazil and most developing countries have lower HDIs and promote opportunistic screening due to the weak organizational structure of the healthcare system. This way, the international studies that assessed the effectiveness of mammographic screening lack the necessary external validity to be applied in developing countries. A recent article published by Vale et al. suggested, that the opportunistic screening program employed in the state of São Paulo, Brazil, promoted an increase in early stage diagnosis without, however, presenting data regarding mortality reduction [ 54 ]. Without data showing mortality reduction attributable to the screening program it is impossible to conclude whether this model is effective or not. Adding up to that data we have some concerning facts associated with screening women between the age of 40 and 49; we observe that less than one death from breast cancer is avoided for every one thousand screening mammograms performed; two hundred and ninety-four false-positive results ( Table 1 ) generate additional diagnostic procedures leading to economical impact to the health system and also physical and psychological impacts to the patients. Based on everything that was exposed in this paragraph, we can conclude is not adequate from Bentham’s and Mill’s utilitarianism perspective [ 10 , 11 ].
In this context, with the shortage of resources to invest in an organized mammographic screening program and without solid data to justify its implementation, can we accept a sub-optimal program? On the one hand, the inexistence of a screening program can lead to the increase in the number of cases diagnosed in late stages, for which the treatment options might be inaccessible and, sometimes, ineffective. On the other hand, developing countries, such as Brazil, sometimes lack the necessary infrastructure to perform timely screening mammograms to the whole eligible population and the consequent breast biopsies of lesions identified through screening [ 55 ]. In order to consider a screening program adequate, it must be acceptable, accessible, and sustainable, it must promote equity and it must be economically efficient to the target population [ 56 ]. As it has been demonstrated in this chapter, the Brazilian mammographic screening program is not accessible, since the coverage does not reach 30% of the target population [ 42 ]. This program is not sustainable either since there is a huge delay between the identification of an abnormal mammogram and the necessary biopsy to confirm the diagnostic. Due to the incapacity to adequately follow-up and refer patients with abnormal findings, the risk of a false-positive result must be considered clinically and ethically relevant. Finally, it’s been demonstrated that mammographic screening in developing countries is not cost-effective when compared to the alternative of treating patients with palpable initial lesions [ 57 , 58 ]. Contemplating all these issues, Sedhom et al. argued that clinical examination of the breast with fast referral to avoid delays in diagnosis and treatment, although not a screening program, must be considered a more pragmatic and adequate choice than screening mammogram in developing countries [ 59 ].
7. Conclusion
When weighing the benefits and harms of a mammographic screening program in a developing country, in a context where breast cancer-specific mortality has been increasing in the past few decades, it is extremely hard to justify increasing the age range to women aged 40 to 49 years old from an utilitarian perspective, since the amount of resources to establish and make the system work adequately is prohibitive. An alternative strategy that promotes easy access and fast referral of symptomatic patients, relegating a secondary role to mammographic screening, favors a larger and more vulnerable part of the population that depends solely on the PHS. This reallocation of resources to favor the least advantaged members of society is not only ethically justifiable but also a way of promoting social justice.
Conflict of interest
Rodrigo Goncalves has received consultation fees from EMS Pharmaceuticals in 2019 and 2020 and from Novartis in 2019, not related to the topics of this chapter.
The remaining authors do not have any conflicts of interest to disclose.
- 1. WHO. Key statistics on cancer. 29/02/2020]; Available from: https://www.who.int/cancer/resources/keyfacts/en/
- 2. WHO. National Cancer Control Programmes. Available from: https://www.who.int/cancer/nccp/en/
- 3. INCA, Rastreamento organizado do câncer de mama 2011
- 4. 1000 person tool. 2020 [cited 2020 09/11/2020]; Available from: https://canadiantaskforce.ca/tools-resources/breast-cancer-update/1000-person-tool/
- 5. INCA. Estatísticas de câncer. 2020 29/02/2020]; Available from: https://www.inca.gov.br/numeros-de-cancer
- 6. Simon, S.D., et al., Characteristics and prognosis of stage I-III breast cancer subtypes in Brazil: The AMAZONA retrospective cohort study. Breast, 2019. 44: p. 113-119
- 7. INCA, Diretrizes para a detecção precoce do câncer de mama no Brasil. 2015
- 8. da Mota Almeida Peroni, F., et al., Realizing the right to health in Brazil’s Unified Health System through the lens of breast and cervical cancer. Int J Equity Health, 2019. 18(1): p. 39
- 9. Rawls, J., A theory of justice. Rev. ed. 1999, Cambridge, Mass.: Belknap Press of Harvard University Press. xxii, 538 p
- 10. Bentham, J., An Introduction to the Principles of Morals and Legislation
- 11. Mill, J.S., Utilitarianism
- 12. Siu, A.L. and U.S.P.S.T. Force, Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med, 2016. 164(4): p. 279-96
- 13. Nelson, H.D., et al., Effectiveness of Breast Cancer Screening: Systematic Review and Meta-analysis to Update the 2009 U.S. Preventive Services Task Force Recommendation. Ann Intern Med, 2016. 164(4): p. 244-55
- 14. Nelson, H.D., et al., Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med, 2009. 151(10): p. 727-37, W237-42
- 15. Marmot, M.G., et al., The benefits and harms of breast cancer screening: an independent review. Br J Cancer, 2013. 108(11): p. 2205-40
- 16. Medical Advisory, S., Screening mammography for women aged 40 to 49 years at average risk for breast cancer: an evidence-based analysis. Ont Health Technol Assess Ser, 2007. 7(1): p. 1-32
- 17. Humphrey, L., et al., in Screening for Breast Cancer. 2002: Rockville (MD)
- 18. Ringash, J. and C. Canadian Task Force on Preventive Health, Preventive health care, 2001 update: screening mammography among women aged 40-49 years at average risk of breast cancer. CMAJ, 2001. 164(4): p. 469-76
- 19. Olsen, O. and P.C. Gotzsche, Screening for breast cancer with mammography. Cochrane Database Syst Rev, 2001(4): p. CD001877
- 20. Alexander, F.E., The Edinburgh Randomized Trial of Breast Cancer Screening. J Natl Cancer Inst Monogr, 1997(22): p. 31-5
- 21. Andersson, I. and L. Janzon, Reduced breast cancer mortality in women under age 50: updated results from the Malmo Mammographic Screening Program. J Natl Cancer Inst Monogr, 1997(22): p. 63-7
- 22. Bjurstam, N., et al., The Gothenburg breast screening trial: first results on mortality, incidence, and mode of detection for women ages 39-49 years at randomization. Cancer, 1997. 80(11): p. 2091-9
- 23. Frisell, J. and E. Lidbrink, The Stockholm Mammographic Screening Trial: Risks and benefits in age group 40-49 years. J Natl Cancer Inst Monogr, 1997(22): p. 49-51
- 24. Miller, A.B., et al., The Canadian National Breast Screening Study-1: breast cancer mortality after 11 to 16 years of follow-up. A randomized screening trial of mammography in women age 40 to 49 years. Ann Intern Med, 2002. 137(5 Part 1): p. 305-12
- 25. Moss, S.M., et al., Effect of mammographic screening from age 40 years on breast cancer mortality at 10 years’ follow-up: a randomised controlled trial. Lancet, 2006. 368(9552): p. 2053-60
- 26. Shapiro, S., Periodic screening for breast cancer: the HIP Randomized Controlled Trial. Health Insurance Plan. J Natl Cancer Inst Monogr, 1997(22):p. 27-30
- 27. Tabar, L., et al., The Swedish Two-County Trial twenty years later. Updated mortality results and new insights from long-term follow-up. Radiol Clin North Am, 2000. 38(4): p. 625-51
- 28. Hellquist, B.N., et al., Effectiveness of population-based service screening with mammography for women ages 40 to 49 years: evaluation of the Swedish Mammography Screening in Young Women (SCRY) cohort. Cancer, 2011. 117(4): p. 714-22
- 29. Jonsson, H., et al., Service screening with mammography in Northern Sweden: effects on breast cancer mortality - an update. J Med Screen, 2007. 14(2): p. 87-93
- 30. Urban, L., et al., Breast cancer screening: updated recommendations of the Brazilian College of Radiology and Diagnostic Imaging, Brazilian Breast Disease Society, and Brazilian Federation of Gynecological and Obstetrical Associations. Radiol Bras, 2017. 50(4): p. 244-249
- 31. Decision-making for cancer care: A review of current practice and opportunities for improvement in Latin America. 2019, The Economist Intelligence Unit
- 32. Biddle, J.B., Epistemic risks in cancer screening: Implications for ethics and policy. Stud Hist Philos Biol Biomed Sci, 2019: p. 101200
- 33. Rudner, R., The Scientist Qua Scientist Makes Value Judgments
- 34. Pramesh, C.S., et al., Ethics of “standard care” in randomised trials of screening for cervical cancer should not ignore scientific evidence and ground realities. Indian J Med Ethics, 2013. 10(4): p. 250-1
- 35. Douglas, H., Inductive risk and values in science
- 36. Mercan, E., et al., Assessment of Machine Learning of Breast Pathology Structures for Automated Differentiation of Breast Cancer and High-Risk Proliferative Lesions. JAMA Netw Open, 2019. 2(8): p. e198777
- 37. Ennis, R. and A. Jotkowitz, Good ethics begins with sound medicine: prostate cancer screening and chemoprevention. Am J Bioeth, 2011. 11(12): p. 26-7
- 38. Tiezzi, D.G., et al., Current Breast Cancer Screening Scenario in Brazil. Revista Brasileira de Ginecologia e Obstetrícia, 2019. 41: p. 633-635
- 39. Brito, E.A.C., et al., Assessing trends of breast cancer and carcinoma in situ to monitor screening policies in developing settings. Sci Rep, 2019. 9(1): p. 14144
- 40. Rodrigues, D.C.N., et al., Temporal changes in breast cancer screening coverage provided under the Brazilian National Health Service between 2008 and 2017. BMC Public Health, 2019. 19(1): p. 959
- 41. WHO, Cancer control: knowledge into action. WHO guide for effective programmes: prevention. 2007, Geneva: WHO
- 42. Rodrigues, D.C.N., et al., Difficult Access and Poor Productivity: Mammography Screening in Brazil. Asian Pac J Cancer Prev, 2019. 20(6): p. 1857-1864
- 43. Greenwald, Z.R., et al., The performance of mobile screening units in a breast cancer screening program in Brazil. Cancer Causes Control, 2018. 29(2): p. 233-241
- 44. Bank, W., Brazil - systematic country diagnostic. 2016
- 45. Werutsky, G., P. Nunes, and C. Barrios, Locally advanced breast cancer in Brazil: current status and future perspectives. Ecancermedicalscience, 2019. 13: p. 895
- 46. Lee, B.L., et al., Breast cancer in Brazil: present status and future goals. Lancet Oncol, 2012. 13(3): p. e95-e102
- 47. TCU, Relatório de Auditoria Operacional: Política Nacional de Atenção Oncológica. , S.d.F.e.A.d.P.d. Governo, Editor. 2011
- 48. Vieira, R., A. Formenton, and S.R. Bertolini, Breast cancer screening in Brazil. Barriers related to the health system. Rev Assoc Med Bras (1992), 2017. 63(5): p. 466-474
- 49. Oliveira, E.X., et al., [Access to cancer care: mapping hospital admissions and high-complexity outpatient care flows. The case of breast cancer]. Cad Saude Publica, 2011. 27(2): p. 317-26
- 50. Medeiros, G.C., et al., [Determinants of the time between breast cancer diagnosis and initiation of treatment in Brazilian women]. Cad Saude Publica, 2015. 31(6): p. 1269-82
- 51. Guerra, M.R., et al., Breast cancer survival and health iniquities. Cad Saude Publica, 2015. 31(8): p. 1673-84
- 52. Migowski, A., et al., Guidelines for early detection of breast cancer in Brazil. III - Challenges for implementation. Cad Saude Publica, 2018. 34(6): p. e00046317
- 53. Miller, A.B., et al., Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ, 2014. 348: p. g366
- 54. Vale, D.B., et al., Downstaging in opportunistic breast cancer screening in Brazil: a temporal trend analysis. BMC Cancer, 2019. 19(1): p. 432
- 55. Vizcaino, I., et al., Short-term follow-up results in 795 nonpalpable probably benign lesions detected at screening mammography. Radiology, 2001. 219(2): p. 475-83
- 56. Shah, S.C., et al., Cancer Control in Low- and Middle-Income Countries: Is It Time to Consider Screening? J Glob Oncol, 2019. 5: p. 1-8
- 57. Gelband, H., et al., Costs, affordability, and feasibility of an essential package of cancer control interventions in low-income and middle-income countries: key messages from Disease Control Priorities, 3rd edition. Lancet, 2016. 387(10033): p. 2133-2144
- 58. Groot, M.T., et al., Costs and health effects of breast cancer interventions in epidemiologically different regions of Africa, North America, and Asia. Breast J, 2006. 12 Suppl 1: p. S81-90
- 59. Sedhom, R. and B. Gyawali, When Is a Suboptimal Approach to Cancer Screening Better Than None? AMA J Ethics, 2020. 22(2): p. E93-101
© 2020 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Edited by Thomas F. Heston
Published: 19 May 2021
By Omur Sayligil
613 downloads
By Paulo Santos, Pedro Teixeira, Helena Beça and Albe...
823 downloads
By Neerja Aggarwal, Pawan Kumar Kare and Sudip Kumar ...
2142 downloads
What Is Breast Cancer Screening?
CDC’s Dr. Lisa Richardson talks about the best time for women to start getting mammograms in this video.
Breast cancer screening means checking a woman’s breasts for cancer before there are signs or symptoms of the disease. All women need to be informed by their health care provider about the best screening options for them. When you are told about the benefits and risks of screening and decide with your health care provider whether screening is right for you—and if so, when to have it—this is called informed and shared decision-making.
Although breast cancer screening cannot prevent breast cancer, it can help find breast cancer early, when it is easier to treat. Talk to your doctor about which breast cancer screening tests are right for you, and when you should have them.
Breast Cancer Screening Recommendations
The United States Preventive Services Task Force (USPSTF) is an organization made up of doctors and disease experts who look at research on the best way to prevent diseases and make recommendations on how doctors can help patients avoid diseases or find them early.
The USPSTF recommends that women who are 50 to 74 years old and are at average risk for breast cancer get a mammogram every two years. Women who are 40 to 49 years old should talk to their doctor or other health care provider about when to start and how often to get a mammogram. Women should weigh the benefits and risks of screening tests when deciding whether to begin getting mammograms before age 50.
Breast Cancer Screening Tests
Where can i go to get screened.
You can get screened for breast cancer at a clinic, hospital, or doctor’s office. If you want to be screened for breast cancer, call your doctor’s office. They can help you schedule an appointment.
Most health insurance plans are required to cover screening mammograms every one to two years for women beginning at age 40 with no out-of-pocket cost (like a co-pay, deductible, or co-insurance).
Find a mammography facility near you.
Are you worried about the cost? CDC offers free or low-cost mammograms. Find out if you qualify.
A mammogram is an X-ray of the breast. For many women, mammograms are the best way to find breast cancer early, when it is easier to treat and before it is big enough to feel or cause symptoms. Having regular mammograms can lower the risk of dying from breast cancer. At this time, a mammogram is the best way to find breast cancer for most women of screening age.
Breast Magnetic Resonance Imaging (MRI)
A breast MRI uses magnets and radio waves to take pictures of the breast. Breast MRI is used along with mammograms to screen women who are at high risk for getting breast cancer. Because breast MRIs may appear abnormal even when there is no cancer, they are not used for women at average risk.
Other Exams
Clinical breast exam.
A clinical breast exam is an examination by a doctor or nurse, who uses his or her hands to feel for lumps or other changes.
Breast Self-Awareness
Being familiar with how your breasts look and feel can help you notice symptoms such as lumps, pain, or changes in size that may be of concern. These could include changes found during a breast self-exam. You should report any changes that you notice to your doctor or health care provider.
Having a clinical breast exam or doing a breast self-exam has not been found to lower the risk of dying from breast cancer.
Benefits and Risks of Screening
Every screening test has benefits and risks, which is why it’s important to talk to your doctor before getting any screening test, like a mammogram.
Benefit of Screening
The benefit of screening is finding cancer early, when it’s easier to treat.
Risks of Screening
Harms can include false positive test results, when a doctor sees something that looks like cancer but is not. This can lead to more tests, which can be expensive, invasive, time-consuming, and may cause anxiety.
Tests also can lead to overdiagnosis, when doctors find a cancer that would not have gone on to cause symptoms or problems, or even may go away on its own. Treatment of these cancers is called overtreatment. Overtreatment can include treatments recommended for breast cancer, such as surgery or radiation therapy. These can cause unnecessary and unwanted side effects. Other potential harms from breast cancer screening include pain during procedures and radiation exposure from the mammogram test itself. While the amount of radiation in a mammogram is small, there may be risks with having repeated X-rays.
Mammograms may also miss some cancers, called false negative test results, which may delay finding a cancer and getting treatment.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Breast Cancer Prevention (PDQ®)–Patient Version
What is prevention.
Cancer prevention is action taken to lower the chance of getting cancer. By preventing cancer, the number of new cases of cancer in a group or population is lowered. Hopefully, this will reduce the burden of cancer and lower the number of deaths caused by cancer.
Cancer is not a single disease but a group of related diseases. Our genes , lifestyle, and the environment around us work together to increase or decrease our risk of getting cancer. Each person’s cancer risk is made up of a combination of these factors.
Anything that increases your chance of developing cancer is called a cancer risk factor ; anything that decreases your chance of developing cancer is called a cancer protective factor .
Some risk factors for cancer can be avoided, but many cannot. For example, both smoking and inheriting certain genes are risk factors for some types of cancer, but only smoking can be avoided. Regular exercise and a healthy diet may be protective factors for some types of cancer. Avoiding risk factors and increasing protective factors may lower your risk but it does not mean that you will not get cancer.
Different ways to prevent cancer are being studied, including:
- Changing lifestyle or eating habits.
- Avoiding things known to cause cancer.
- Taking medicine to treat a precancerous condition or to keep cancer from starting.
- Risk-reducing surgery .
General Information About Breast Cancer
Breast cancer is a disease in which malignant (cancer) cells form in the tissues of the breast., breast cancer is the second most common type of cancer in american women..
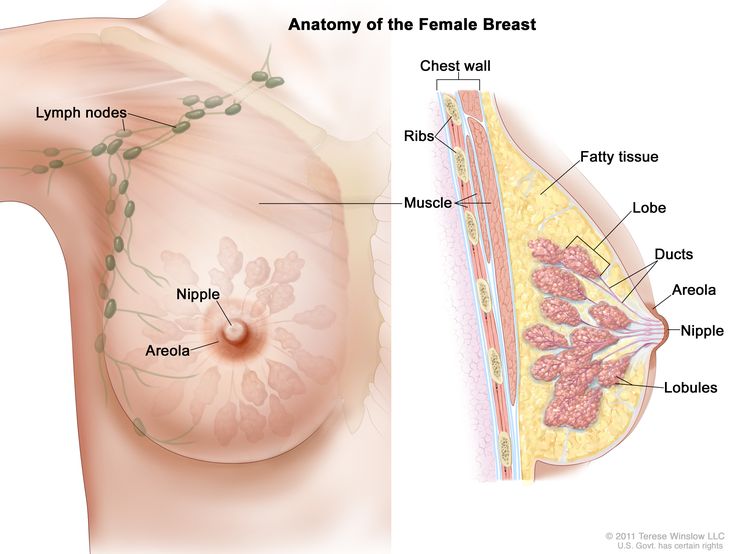
Each breast also has blood vessels and lymph vessels . The lymph vessels carry an almost colorless, watery fluid called lymph . Lymph vessels carry lymph between lymph nodes . Lymph nodes are small, bean-shaped structures that filter lymph and store white blood cells that help fight infection and disease. Groups of lymph nodes are found near the breast in the axilla (under the arm), above the collarbone , and in the chest.
See the following PDQ summaries for more information about breast cancer :
- Breast Cancer Screening
- Breast Cancer Treatment (Adult)
- Breast Cancer Treatment During Pregnancy
- Male Breast Cancer Treatment
- Genetics of Breast and Ovarian Cancer
Women in the United States get breast cancer more than any other type of cancer except skin cancer . Breast cancer is second to lung cancer as a cause of cancer death in American women. Breast cancer rates in women increased gradually for many years until the early 2000s and then decreased rapidly, coinciding with a drop in postmenopausal hormone therapy use. Deaths from breast cancer have declined by 42% as of 2019; however, breast cancer deaths in Black women remain 41% higher than in White women. Breast cancer also occurs in men, but the number of new cases is small.
Breast Cancer Prevention
Avoiding risk factors and increasing protective factors may help prevent cancer., a personal history of breast cancer or benign (noncancer) breast disease, inherited risk of breast cancer, dense breast tissue, reproductive history resulting in greater exposure to estrogen, taking hormone therapy for symptoms of menopause, radiation therapy to the breast or chest, drinking alcohol, reproductive history resulting in less exposure to estrogen, selective estrogen receptor modulators, aromatase inhibitors and inactivators, risk-reducing or prophylactic mastectomy, ovarian ablation, getting enough exercise, hormonal contraceptives, chemicals in the environment, studies have shown that some factors have little or no effect on the risk of breast cancer., cancer prevention clinical trials are used to study ways to prevent cancer., new ways to prevent breast cancer are being studied in clinical trials..
Avoiding cancer risk factors may help prevent certain cancers. Risk factors include smoking, having overweight , and not getting enough exercise. Increasing protective factors such as quitting smoking and exercising may also help prevent some cancers. Talk to your doctor or other health care professional about how you might lower your risk of cancer.
NCI's Breast Cancer Risk Assessment Tool uses a woman's risk factors to estimate her risk for breast cancer during the next five years and up to age 90. This online tool is meant to be used by a health care provider . For more information on breast cancer risk, call 1-800-4-CANCER.
The following are risk factors for breast cancer:
Besides being a woman, older age is the main risk factor for breast cancer. The chance of getting breast cancer increases as a woman gets older. A 30-year-old woman has about a 1 in 200 chance of being diagnosed with breast cancer in the next 10 years, while a 70-year-old woman has a 1 in 25 chance.
Women aged 50 to 69 years who have screening mammograms have a lower chance of dying from breast cancer than women who do not have screening mammograms. Screening by mammography decreases breast cancer mortality by identifying cases for treatment at an earlier stage.
Women with any of the following have an increased risk of breast cancer:
- A personal history of invasive breast cancer , ductal carcinoma in situ (DCIS), or lobular carcinoma in situ (LCIS).
- A personal history of benign (noncancer) breast disease.
Women with a family history of breast cancer in a first-degree relative (mother, sister, or daughter) have an increased risk of breast cancer.
Women who have inherited changes in the BRCA1 and BRCA2 genes or in certain other genes have a higher risk of breast cancer. The risk of breast cancer caused by inherited gene changes depends on the type of gene mutation , family history of cancer , and other factors.
Having breast tissue that is dense on a mammogram is a factor in breast cancer risk. The level of risk depends on how dense the breast tissue is. Women with very dense breasts have a higher risk of breast cancer than women with low breast density.
Increased breast density is often an inherited trait, but it may also occur in women who have not had children, have a first pregnancy late in life, take postmenopausal hormones , or drink alcohol . For more information, see Dense Breasts: Answers to Commonly Asked Questions .
Estrogen is a hormone made by the body. It helps the body develop and maintain female sex characteristics. Being exposed to estrogen over a long time may increase the risk of breast cancer. Estrogen levels are highest during the years a woman is menstruating .
The following factors in a woman's reproductive history increase the length of time her breast tissue is exposed to estrogen and may increase the risk of breast cancer:
- Early menstruation : Beginning to have menstrual periods before age 12 increases the number of years the breast tissue is exposed to estrogen.
- Starting menopause at a later age : The more years a woman menstruates, the longer her breast tissue is exposed to estrogen.
- Older age at birth of first child or never having given birth : Pregnancy lowers a woman’s lifetime number of menstrual cycles . Breast tissue is exposed to more estrogen for longer periods of time in women who become pregnant for the first time after age 35 or who never become pregnant.
Hormones, such as estrogen and progesterone , can be made into a pill form in a laboratory. Estrogen, progestin , or both may be given to replace the estrogen no longer made by the ovaries in postmenopausal women or women who have had their ovaries removed. This is called hormone replacement therapy (HRT) or hormone therapy (HT). Estrogen therapy that began close to the time of menopause is associated with an increased risk of developing breast cancer. Estrogen therapy that began at or after menopause is associated with an increased risk of developing endometrial cancer and total cardiovascular disease, especially stroke. The risk of breast cancer does not decrease after women stop taking estrogen. Combination HT is estrogen combined with progestin. This type of MHT increases the risk of breast cancer. Studies show that when women stop taking estrogen combined with progestin, the risk of breast cancer decreases.
Radiation therapy to the chest for the treatment of cancer increases the risk of breast cancer, starting 10 years after treatment. The risk of breast cancer depends on the dose of radiation and the age at which it is given. The risk is highest if radiation treatment was used during puberty , when breasts are forming.
Radiation therapy to treat cancer in one breast does not appear to increase the risk of cancer in the other breast.
For women who have inherited changes in the BRCA1 and BRCA2 genes, exposure to radiation, such as that from chest x-rays , may further increase the risk of breast cancer, especially in women who were x-rayed before 20 years of age.
Obesity increases the risk of breast cancer, especially in postmenopausal women who have not used hormone replacement therapy.
Drinking alcohol increases the risk of breast cancer. The level of risk rises as the amount of alcohol consumed rises.
The following are protective factors for breast cancer:
A woman’s reproductive history can affect the length of time her breast tissue is exposed to estrogen. Early onset of menstruation, late onset of menopause, later age at first pregnancy, and never having given birth have been linked to an increase in estrogen exposure and breast cancer risk. The following reproductive factors decrease the length of time a woman's breast tissue is exposed to estrogen and may help prevent breast cancer:
- Early pregnancy : Estrogen levels are lower during pregnancy. In one study, women who had a full-term pregnancy before age 20 had a lower risk of breast cancer than women who did not have children or who gave birth to their first child after age 35.
- Breast-feeding : Estrogen levels may remain lower while a woman is breast-feeding. Women who breastfed have a lower risk of breast cancer than women who have had children but did not breastfeed.

Taking selective estrogen receptor modulators or aromatase inhibitors and inactivators
Tamoxifen and raloxifene belong to the family of drugs called selective estrogen receptor modulators (SERMs). SERMs act like estrogen on some tissues in the body, but block the effect of estrogen on other tissues.
Treatment with tamoxifen lowers the risk of estrogen receptor-positive (ER-positive) breast cancer and ductal carcinoma in situ in premenopausal and postmenopausal women at high risk. Tamoxifen is also used to treat metastatic breast cancer and to prevent cancer from recurring after surgery to remove breast tumors . Treatment with raloxifene also lowers the risk of breast cancer in postmenopausal women. With either drug, the reduced risk lasts for several years or longer after treatment is stopped. Lower rates of broken bones have been noted in patients taking raloxifene.
Taking tamoxifen increases the risk of hot flashes , endometrial cancer , stroke, cataracts , and blood clots (especially in the lungs and legs). The risk of having these problems increases markedly in women older than 50 years compared with younger women. Women younger than 50 years who have a high risk of breast cancer may benefit the most from taking tamoxifen. The risk of endometrial cancer lasts for 5 years after tamoxifen is stopped, but the risk of cataracts or blood clots does not last long.. Talk with your doctor about the risks and benefits of taking this drug.
Taking raloxifene increases the risk of blood clots in the lungs and legs but does not appear to increase the risk of endometrial cancer. In postmenopausal women with osteoporosis (decreased bone density ), raloxifene lowers the risk of breast cancer for women who have a high or low risk of breast cancer. It is not known if raloxifene would have the same effect in women who do not have osteoporosis. Talk with your doctor about the risks and benefits of taking this drug.
Other SERMs are being studied in clinical trials.
Aromatase inhibitors ( anastrozole , letrozole ) and inactivators ( exemestane ) lower the risk of recurrence and of new breast cancers in women who have a history of breast cancer. Aromatase inhibitors also decrease the risk of breast cancer in women with the following conditions:
- Postmenopausal women with a personal history of breast cancer.
- Women with no personal history of breast cancer who are 60 years and older, have a history of ductal carcinoma in situ with mastectomy , or have a high risk of breast cancer based on the Gail model tool (a tool used to estimate the risk of breast cancer).
In women with an increased risk of breast cancer, taking aromatase inhibitors decreases the amount of estrogen made by the body. Before menopause, estrogen is made by the ovaries and other tissues in a woman's body, including the brain , fat tissue, and skin. After menopause, the ovaries stop making estrogen, but the other tissues do not. Aromatase inhibitors block the action of an enzyme called aromatase, which is used to make all of the body's estrogen. Aromatase inactivators stop the enzyme from working.
Possible harms from taking aromatase inhibitors include muscle and joint pain, osteoporosis, hot flashes, and feeling very tired.
Some women who have a high risk of breast cancer may choose to have a risk-reducing or prophylactic mastectomy (the removal of one or both breasts when there are no signs of cancer). After surgery, the risk of breast cancer becomes much lower in these women and most feel less anxious about their risk of breast cancer. Some women diagnosed with breast cancer may decide to have a healthy breast removed at the same time the breast with cancer is removed. This is called contralateral prophylactic mastectomy . However, it is very important to have a cancer risk assessment and counseling about the different ways to prevent breast cancer before making any decision about surgery.
The ovaries make most of the estrogen that is made by the body. Treatments that stop or lower the amount of estrogen made by the ovaries include surgery to remove the ovaries, radiation therapy, or taking certain drugs. This is called ovarian ablation .
Premenopausal women who have a high risk of breast cancer due to certain changes in the BRCA1 and BRCA2 genes may choose to have a risk-reducing oophorectomy (the removal of both ovaries when there are no signs of cancer). This decreases the amount of estrogen made by the body and lowers the risk of breast cancer. Risk-reducing oophorectomy also lowers the risk of breast cancer in average-risk premenopausal women and in women with an increased risk of breast cancer due to radiation to the chest. However, it is very important to have a cancer risk assessment and counseling before making this decision. The sudden drop in estrogen levels may cause the symptoms of menopause to begin. These include hot flashes, trouble sleeping, anxiety, and depression . Long-term effects include decreased sex drive , vaginal dryness, and decreased bone density.
Women who take part in physical exercise have a lower risk of breast cancer.
It is not clear whether the following affect the risk of breast cancer:
Hormonal contraceptives contain estrogen or estrogen and progestin. Some studies have shown that women who are current or recent users of hormonal contraceptives may have a slight increase in breast cancer risk. Other studies have not shown an increased risk of breast cancer in women using hormonal contraceptives.
In one study, the risk of breast cancer slightly increased the longer a woman used hormonal contraceptives. Another study showed that the slight increase in breast cancer risk decreased over time when women stopped using hormonal contraceptives.
More studies are needed to know whether hormonal contraceptives affect a woman's risk of breast cancer.
Scientists are studying whether exposure to chemicals in the environment may increase a woman's risk of breast cancer. Studies of this kind can be difficult to conduct and interpret for many reasons:
- It is hard to determine the specific chemicals people have been exposed to in the past. It can take decades after a potential exposure before cancer develops, and a person may not be aware of or remember the past exposure.
- Even if a chemical is shown in a laboratory test to cause cancer, this does not necessarily mean it will cause cancer in people exposed to that chemical in the environment. A chemical may cause cancer when tested at high levels in laboratory studies but not at the lower levels seen in the environment.
- Individual chemicals are likely to cause only a small increase in risk, and it can be difficult to detect that increase in the context of the other factors that may influence a woman's risk of breast cancer.
These reasons make it hard to know which chemicals, if any, may increase the risk of breast cancer. More studies are needed to know whether chemicals in the environment affect a woman's risk of breast cancer. For more information, see Environmental Carcinogens and Cancer Risk .
The following have little or no effect on the risk of breast cancer:
- Having an abortion.
- Making diet changes such as eating less fat or more fruits and vegetables.
- Taking vitamins , including fenretinide (a type of vitamin A ).
- Cigarette smoking, both active and passive ( inhaling secondhand smoke ).
- Using underarm deodorant or antiperspirant.
- Taking statins ( cholesterol -lowering drugs).
- Taking bisphosphonates (drugs used to treat osteoporosis and hypercalcemia ) by mouth or by intravenous infusion .
- Changes in your circadian rhythm (physical, mental, and behavioral changes that are mainly affected by darkness and light in 24 hour cycles), which may be affected by working night shifts or the amount of light in your bedroom at night.
Cancer prevention clinical trials are used to study ways to lower the risk of developing certain types of cancer. Some cancer prevention trials are conducted with healthy people who have not had cancer but who have an increased risk for cancer. Other prevention trials are conducted with people who have had cancer and are trying to prevent another cancer of the same type or to lower their chance of developing a new type of cancer. Other trials are done with healthy volunteers who are not known to have any risk factors for cancer.
The purpose of some cancer prevention clinical trials is to find out whether actions people take can prevent cancer. These may include exercising more or quitting smoking or taking certain medicines , supplements , vitamins, minerals , or food.
Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
About This PDQ Summary
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish .
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about breast cancer prevention. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board .
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website . For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Breast Cancer Prevention. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/breast/patient/breast-prevention-pdq . Accessed <MM/DD/YYYY>. [PMID: 26389410]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online . Visuals Online is a collection of more than 3,000 scientific images.
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us .
Home — Essay Samples — Nursing & Health — Oncology — Breast Cancer
Essays About Breast Cancer
Brief description of breast cancer.
Breast cancer is a type of cancer that forms in the cells of the breast. It is the second most common cancer in women and can also affect men. Breast cancer can be invasive or non-invasive and is often detected through screening and self-examination. Early detection and treatment are crucial for improving outcomes and survival rates.
Importance of Writing Essays on This Topic
Essays on breast cancer are significant for academic and personal exploration as they provide an opportunity to raise awareness about the disease, its risk factors, prevention, and treatment options. Writing about breast cancer also allows individuals to share personal experiences, advocate for research and support, and contribute to the ongoing dialogue surrounding this prevalent health issue.
Tips on Choosing a Good Topic
- Consider exploring the latest research and advancements in breast cancer treatment and prevention.
- Reflect on personal experiences or those of loved ones affected by breast cancer for a more personal and impactful essay.
- Investigate the societal and cultural impact of breast cancer, including awareness campaigns, advocacy, and support networks.
Essay Topics
- The Role of Genetic Testing in Breast Cancer Prevention
- The Impact of Lifestyle Choices on Breast Cancer Risk
- The Emotional and Psychological Effects of Breast Cancer Diagnosis and Treatment
- The Importance of Early Detection and Screening for Breast Cancer
- The Societal Stigma and Misconceptions Surrounding Breast Cancer
- Exploring Alternative and Complementary Therapies for Breast Cancer Patients
- The Influence of Support Networks and Advocacy Groups in Breast Cancer Awareness
- Analyzing the Economic and Social Burden of Breast Cancer on Patients and Families
- Debunking Common Myths and Misinformation about Breast Cancer
- The Role of Hormone Therapy in Breast Cancer Treatment
Concluding Thought
By writing essays on breast cancer, individuals can contribute to a better understanding of the disease, its impact, and the importance of ongoing research and support. Engaging with this topic through writing can help raise awareness, provide support, and inspire positive change within the community.
The Stages of Breast Cancer
Treatment and diagnosis of breast cancer, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Breast Cancer: The Physical and Mental Effects
The ways of raising awareness about breast cancer, breast cancer: an unending battle that brought us together, the treatment of breast cancer, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
The Benefits and Harmful Effects of Chemotherapy as a Treatment to Breast Cancer
Research on correlation of notch signaling pathway in the prognosis of breast cancer, hereditary breast and ovarian cancer, ultrasonography for the diagnosis of cancer, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
Mbmt Pilot Study: How This Affects The Breast Cancer Patient's Attention
Miracle in my life: my mother's battle with breast cancer, relevant topics.
- Mental Health
- Postpartum Depression
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Understanding...
Understanding inequalities in breast cancer screening uptake
Linked clinical review.
Advances in the care of breast cancer survivors
Linked research
Effect of invitation letter in language of origin on screening attendance
- Related content
- Peer review
- Elizabeth A Davies , clinical reader in cancer and public health ,
- Yueh-Hsin Wang , PhD student
- Cancer Epidemiology and Cancer Services Research, Centre for Cancer, Society and Public Health, Comprehensive Cancer Centre, King’s College London, UK
- Correspondence to: E A Davies Elizabeth.Davies{at}kcl.ac.uk
Language isn’t the only barrier for women from immigrant communities
Attendance for breast cancer screening tends to be considerably higher among women born in high income countries with established screening programmes than in women who migrate to and settle in these countries later in their lives. Norway’s breast screening programme began in 1996 and has one of the highest overall 10 year attendance rates in the world of 85%, yet the attendance rate for women who have migrated to Norway is only 67%. 1
Previous studies have suggested that language is a common barrier that women from culturally and linguistically diverse backgrounds face in accessing cancer screening. 2 So, in a linked paper (doi: 10.1136/bmj-2023-075465 ), Hofvind and colleagues report the first large scale, randomised controlled trial to investigate the effect of inviting women for breast screening by using letters translated into their language of origin and checked for sense by women from the same cultural group. 3 The authors invited for participation 11 347 women registered with the government as “immigrants” following migration from countries across North Africa and the Middle East, the Philippines, Poland, Somalia, and Pakistan, where official languages include Arabic, English, Polish, Somali, and Urdu. Women from each of these five groups were then randomised to receive either a postal invitation letter, leaflet, reminder, and screening result letter written in their language of origin as well as Norwegian (the intervention group) or letters and information written in Norwegian alone (the control group).
Somewhat surprisingly, the authors reported no difference in attendance for screening between women who received translated invitations and controls (46.5% (95% confidence interval 45.2% to 47.8%); 47.4% (46.0% to 48.7%)). The null result remained after stratification by country of birth, age at invitation, and years since migration. 3 This finding is critical because it overturns our understanding of language as one of the most important determining factors or barriers affecting decisions about screening made by women from a wide range of cultural backgrounds.
One way of making sense of this finding is to broaden our understanding of evidence on the mutifaceted nature of women’s experiences of migrating to and living in a different country and of negotiating new administrative, work, social, and health systems and cultures. Their experiences may include barriers to attending health appointments, differing perceptions of breast cancer risk, limited experience of the disease in family and friends owing to differing global incidence rates, and varying levels of understanding of or trust in the healthcare and other official systems.
Australia has one of the highest proportion of migrants among major high income countries and has sought to minimise health inequalities among migrant groups, particularly refugees and asylum seekers, who experience multiple social disadvantages, barriers to accessing healthcare, and difficulties in settling and gaining employment. 4 5 Against this backdrop, a woman’s struggle to achieve daily tasks may be more pressing than seeking early detection of a cancer she has little experience of or perceives as a low risk. 4
Research interviews suggest that the approach and sex of general practitioners or family doctors, women’s awareness and knowledge of cancer screening, financial problems, and language difficulties all contribute to low attendance for cancer screening. 6 Other qualitative work shows that previous healthcare experiences, personal or relatives’ cancer history, fatalistic beliefs about the inevitability of death, and media campaigns about screening can also be important. 7 Time lived in the country may be another factor.
In one study from the UK, women from white ethnic groups living in London were more likely to attend for breast screening than black Caribbean women, but these women attended more often than black African women and Bangladeshi women. 8 In another study, initiatives led by Bangladeshi general practitioners may have increased uptake among women in their communities. 9 Finally, the erroneous perception that breast cancer predominantly affects white women must be tackled worldwide. 10
The results of Hofvind and colleagues’ randomised trial are important as they remind us that simple interventions, such as translating letters to patients, do not always work as expected. Women face many challenges on multiple levels (individual, family, community, system, and policy) when they move to new countries. 11 In each country, local health services, screening services, and policy makers must actively engage with a wide range of communities in the long term to develop more nuanced, multifaceted, and targeted interventions collaboratively. One element of this may be for services to reconsider how long they label women as “immigrant” rather than viewing them as settled citizens from diverse cultural backgrounds.
Competing interests: The BMJ has judged that there are no disqualifying financial ties to commercial companies. The authors declare the following other interests: none.
Further details of The BMJ policy on financial interests is here: https://www.bmj.com/sites/default/files/attachments/resources/2016/03/16-current-bmj-education-coi-form.pdf .”
Provenance: Commissioned; not externally peer reviewed.
- Bhargava S ,
- Tsuruda K ,
- Bukholm I ,
- Scanlon B ,
- Hofvind S ,
- Chamberlain S
- Chandrakumar A ,
- MacMillan F ,
- Eilbert KW ,
- Carroll K ,
- Khatoon S ,
- Basnett I ,
- McCulloch N
- Jones CEL ,
- Davies EA ,
- Khatri RB ,
- Search Menu
- Advance Articles
- Editor's Choice
- CME Reviews
- Best of 2021 collection
- Abbreviated Breast MRI Virtual Collection
- Contrast-enhanced Mammography Collection
- Author Guidelines
- Submission Site
- Open Access
- Self-Archiving Policy
- Accepted Papers Resource Guide
- About Journal of Breast Imaging
- About the Society of Breast Imaging
- Guidelines for Reviewers
- Resources for Reviewers and Authors
- Editorial Board
- Advertising Disclaimer
- Advertising and Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Promoting and improving breast imaging patient care and outcomes.
- Article contents
- Figures & tables
- Supplementary Data
Wendy B DeMartini, Promoting and Improving Breast Imaging Patient Care and Outcomes, Journal of Breast Imaging , Volume 6, Issue 2, March-April 2024, Pages 113–115, https://doi.org/10.1093/jbi/wbae010
- Permissions Icon Permissions
Happy early spring, and welcome to volume 6, issue 2 of the Journal of Breast Imaging ( JBI ). I am extremely pleased to share that JBI has now received approval for inclusion in MEDLINE. With this important step, JBI article citations will now be indexed and searchable in PubMed. Thank you to our incredible editorial and publishing teams and our contributing authors, who have made this milestone possible through their many efforts in support of high-quality science. As always, please consider submitting your own work to JBI , now indexed and searchable in PubMed.
The spectrum articles in this issue highlight many ways we can continue to directly promote and improve breast imaging patient care and outcomes.
Please pay particular attention to our Science of Screening article by Hendrick and Monticciolo, an important review of the scientific concepts and evidence supporting screening mammography in women starting at age 40 years. Screening remains an essential component of our breast imaging care and value and has been well demonstrated to reduce breast cancer mortality and morbidity. In May 2023, the United States Preventive Services Task Force (USPSTF) updated its breast cancer screening recommendations and now recommends (in draft) initiation of screening mammography at age 40 years for all women at average risk of breast cancer ( 1). This update to initiation at age 40 years reflects USPSTF increased recognition by the USPSTF of the lifesaving screening benefits of mammography in younger women overall and in Black women because they are more likely to get aggressive breast cancer at younger ages. However, a subsequent New England Journal of Medicine Perspective article by Woloshin et al disagreed with this update ( 2). Of note, the questions and rationales in their Perspective dissent ignored important scientific concepts and data. Hendrick and Monticciolo directly refute the assumptions of Woloshin et al with a point-by-point review of the relevant data related to screening and breast cancer ( 3). This excellent article discusses key topics in support of screening starting at age 40, including breast cancer mortality trends, Cancer Intervention and Surveillance Modeling Network analyses, all-cause vs breast cancer mortality, overemphasis of the risks of screening, and the real risks of not screening.
Email alerts
Citing articles via.
- Recommend to your Librarian
- Journals Career Network
Affiliations
- Online ISSN 2631-6129
- Print ISSN 2631-6110
- Copyright © 2024 Society of Breast Imaging
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 31 March 2024
Association between sociodemographic factors and health beliefs related to breast cancer screening behavior among Northern Thai women: a hospital-based study
- Surin Jiraniramai 1 , 2 ,
- Kanokporn Pinyopornpanish 1 , 2 ,
- Nahathai Wongpakaran 3 ,
- Chaisiri Angkurawaranon 1 , 2 ,
- Victoria L. Champion 4 , 5 ,
- Imjai Chitapanarux 6 ,
- Wichuda Jiraporncharoen 1 , 2 &
- Tinakon Wongpakaran 3
Scientific Reports volume 14 , Article number: 7596 ( 2024 ) Cite this article
54 Accesses
1 Altmetric
Metrics details
- Health services
- Public health
Early diagnosis of breast cancer is crucial for reducing mortality rates. The purpose of this study is to determine the impact of demographics/social determinants of health on beliefs about the practice of self-breast examination, using mammogram and ultrasound in the context of breast cancer screening among Thai women in a hospital-based setting for implying program planning and future research. A cross-sectional study was conducted in two health centers in Chiang Mai Province from August 2021 to December 2021, involving 130 Thai women ages 40 to 70 years. Data were collected by a survey using a questionnaire to gather sociodemographic information, and health beliefs about breast cancer and screening behavior utilizing the modified Thai version of Champion's Health Belief Model Scale (MT-CHBMS). Descriptive statistics, t-tests, ANOVA, and linear regression models were employed for examining association between sociodemographic factors and health beliefs about the practice of self-breast examination (BSE), using mammogram (MG) and ultrasound (UTS). Health insurance schemes were associated with Benefit-MG, Barrier-BSE, Barrier-MG and Barrier-UTS subscales. Additionally, monthly income was associated with Barrier-MG and Barrier-UTS subscales. The most common barriers reported were “embarrassment”, “worry”, and “takes too much time”. To enhance breast cancer screening in Thailand, program planning and future research should focus on health insurance schemes, especially women with social security schemes, as they may be the most appropriate target group for intervention.
Similar content being viewed by others
Impact of a risk based breast screening decision aid on understanding, acceptance and decision making
Jocelyn Lippey, Louise Keogh, … Laura Elenor Forrest

Willingness to decrease mammogram frequency among women at low risk for hereditary breast cancer
Yue Guan, Eric Nehl, … Colleen M. McBride
Psychological impact of risk-stratified screening as part of the NHS Breast Screening Programme: multi-site non-randomised comparison of BC-Predict versus usual screening (NCT04359420)
David P. French, Lorna McWilliams, … D. Gareth Evans
Introduction
Female breast cancer is the most commonly diagnosed cancer, with approximately 2.3 million new cases and 685,000 deaths reported in 2020 1 . It is the leading or second leading cause of female cancer-related deaths in 95% of countries worldwide 2 . In 2022, breast cancer in Thailand accounted for 38,559 cases 3 , making it the most prevalent female cancer, and accounting for 32.64% of the top five cancers in the northern region of Thailand 4 . This region has been predicted to have the highest age-standardized incidence rate (ASR) and proportion of female cancer cases by 2025 5 . However, early diagnosis and treatment can significantly reduce breast cancer mortality rates and improve women's overall health 6 .
Globally, high-income countries have adopted mammography as the standard screening method for early diagnosis of breast cancer, which helps reduce rates of advanced and fatal breast cancer 7 . In contrast, low to moderate-income countries, including Thailand 8 , 9 , 10 , often rely on breast self-examination (BSE) due to its insufficient mammography resources, although it is considered less reliable 11 , 12 , 13 . Therefore, it is recommended that women regularly and accurately perform BSE and consult with their physicians, who might recommend mammography and/or ultrasound if a lump is found 9 . It's important to note that BSE alone is not an effective method for reducing breast cancer mortality 14 . However, a recent population-based study of 1,906,697 women participating in a breast cancer awareness program in Thailand reported that women who regularly practiced BSE had better survival rates compared to non-practicing women. Additionally, a significantly higher proportion of smaller tumor sizes and earlier stages of breast cancer were observed in the group that regularly performed BSE. This positive outcome was attributed to the strong collaboration between village health volunteers and the use of BSE record booklets. Village health volunteers played a vital role in reminding women to perform BSE consistently, while the BSE record booklets helped women accurately follow the instructions and document their BSE practices 15 . Many countries of low to moderate-income countries have BSE practice as the first line screening because it is easy, convenient, private safe and no specific equipment requirement. Its purpose is to make women familiar with both the appearance and feel of their breasts as early as possible, so that they will be able to easily detect changes in their breast 13 , 16 . The more practice of BSE, the more empower women health 8 , 13 , 17 Based on these evidence, initial BSE is deemed appropriate for Thailand as a low to moderate-income country. The practice of BSE among women is influenced by their knowledge and beliefs about breast cancer and screening methods 17 .
In Thailand, the current guidelines for breast cancer screening 18 include breast cancer screening according to age. For ages 20–39 years old, it is recommended that breast self-examination should be performed once a month. Women between 40 and 69 years should be examined by a doctor annually. If abnormalities are identified, a mammogram will be scheduled. For the age of 70 years old and over, mammography for breast cancer screening should be weighed in terms of benefits and risks based on individual’s life expectancy and preference. However, in the voluntary case of populations who wish to have breast cancer screening by mammogram in the first place, recommendations for screening have been added that are similar to those recommended by the American Cancer Society. This recommendation was caused by public health policy and public finance management in Thailand.
In some resource-limited areas, breast ultrasound has been proposed as a possible alternative for mammography in breast cancer screening because it is portable, less expensive than mammography, and versatile across a wider range of clinical applications. The use of ultrasound as an effective primary detection tool for breast cancer may be beneficial in low-resource settings where mammography is unavailable 19 . Furthermore, according to the findings of a multi-center randomized trial comparing ultrasound vs. mammography for screening breast cancer in high-risk Chinese women, ultrasound was superior to mammography for screening breast cancer in this group 19 . In Thailand, mammography is not available in most rural areas. Similarly, Thai women, like Chinese women, have smaller and denser breasts than Western women 20 . Additionally, ultrasound yields less pain or discomfort than a mammogram, which is one of the main problems preventing women from breast cancer screening. 21 .
In real-world practice, BSE is not widely adopted among most Thai women. From secondary data of the 2007 Health and Welfare Survey that comprised 18,474 women aged 20 years and older and the 2009 Reproductive Health Survey that comprised 26,951 women aged 30 to 59 years show that only 18.4% of women practice monthly BSE 21 , indicating a low level of knowledge and awareness about breast cancer and the importance of BSE, mammography, and ultrasound screening that are the steps for increasing diagnosis of breast cancer. Before planning effective interventions to motivate the use of these screening methods, it is important to understand Thai women's knowledge and beliefs about breast cancer screening. Previous studies have shown that the Health Belief Model is a reliable and valid tool for measuring individuals' knowledge and beliefs about breast cancer and screening methods 22 . This model predicts the behaviors of people who take action to prevent, screen for, or control illness conditions based on their personal beliefs or perceptions about a disease 23 . Champion's Health Belief Model Scale (CHBMS) is the first and most widely used tool in the literature across continents, countries, cultures, and ethnicities to measure women's beliefs about breast cancer screening 8 , 24 , 25 , 26 , 27 , 28 , 29 .
The CHBMS comprises six main constructs: susceptibility, seriousness, benefits, barriers, health motivation, and confidence (self-efficacy). This scale has also been developed to assess perceived benefits and barriers of BSE and mammogram screening 25 , 26 , 27 , 29 , 30 , 31 . Recently, a modified Thai version of Champion's Health Belief Model Scale (MT-CHBMS) 32 incorporated ultrasound items for breast cancer screening. The primary reason for this addition is that ultrasound can effectively detect small and dense tissue tumors, particularly in younger Asian women who tend to have denser breast tissue compared to Western women 19 . In terms of advanced technology, techniques such as artificial intelligence (e.g., deep-learning-enabled clinical decision support systems) and classification of ultrasound images have demonstrated superior accuracy in detecting breast cancers compared to various screening tools currently available 33 , 34 . The MT-CHBMS has been found to be valid and reliable among Thai women 32 . This scale can be comparing perceived benefits and barriers of BSE, mammogram and ultrasound screening from associate predictors of sociodemographic factors. These predictors could be implying the program design for increasing breast cancer screening.
Numerous studies have demonstrated the significant impact of sociodemographic factors on women's breast cancer screening behaviors, with results varying across cultures and values. For instance, research conducted in Middle Eastern countries revealed notable associations between age, title, giving birth, BC screening in the last 6 months, BSE training, chronic disease, mental illness, and BSE practice 35 . Conversely, a study in a similar cultural context showed that BSE and mammography practices among women were influenced by the only level of their knowledge about breast cancer 36 . In an African country, a study found significant associations between income status, marital status, age of first childbirth in the family, and perceived susceptibility, health motivation, convenience, perceived benefits, and self-efficacy for BSE 37 .
Despite these findings, there is currently a lack of information regarding the health perception of Thai women, the scope of their health beliefs, and how demographics/social determinants impact these beliefs. Additionally, these results have been integrated to plan for detecting and managing for breast cancer in primary care of hospital that is the one of strategic in Thailand’s sustainable development goals 38 , 39 . Therefore, the objective of this study is to determine the impact of demographics/social determinants of health on beliefs about the practice of self-breast examination, using mammogram and ultrasound in the context of breast cancer screening among Thai women in a hospital-based setting for implying program planning and future research.
Study design and participants
A cross-sectional study was conducted in Chiang Mai province, Kingdom of Thailand, from August 2021 to December 2021. One hundred and thirty participants recruited with convenience sampling method for the study, consisting of women from two health centers: Maharaj Nakorn Chiang Mai Hospital, located in an urban area, and San Pa Tong Hospital, situated in a rural area. A comprehensive description of the development of the MT-CHBMS has been previously published 32 .
Inclusion and exclusion criteria
The inclusion criteria for the study were as follows: individuals between the ages of 40 and 70 years (the recommended age for mammograms), no prior history of breast cancer or any other types of cancer, and not currently pregnant or breastfeeding. The exclusion criteria included individuals who were unable to communicate effectively due to language barriers and those who expressed unwillingness to complete the questionnaires.
Sample size
Sample size is calculated based on the following criteria.
Anticipated effect size ( f 2 ) was 0.15 (small). The desired statistical power level was 0.8
The number of predictors was 5. Therefore, the minimum required sample was 91. We recruited 130 participants for this study, indicating that it was sufficient.
The data collection tools
To collect data at the outpatient clinic, the researchers gathered socio-economic information by structured interviewing. The questions included items such as age, religion, marital status, education level, healthcare insurance schemes (including the three main public health insurance schemes: government or state enterprise officer, social security scheme, and universal coverage scheme), income, and residential area. Then paper questionnaires were provided to all participants. Prior to completing the questionnaires, all participants provided written informed consent.
The questionnaire addressing beliefs was the MT-CHBMS. The CHBMS was translated into Thai, validated by a panel of experts, back translated, modified by adding content about ultrasound for screening breast cancer, and pretested. Confirmatory factor analysis was used with a sample of 130 Thai women aged 40 to 70 years old. The scales were measured with an ordinal scale using a five-point Likert type 1: “Strongly disagree”, to 5: “Strongly agree”. Each subscale can be used independently. In the case of overall assessment of the awareness of breast cancer and screening methods, the total score can be adopted but the questions concerning barriers must be reversed before summing up.
The MT-CHBMS’s Cronbach’s alphas values were acceptable, ranging from 0.74 to 0.93 for the scales)and valid(Content validity using the CVI index from 3 experts showed that the average Item-CVI was 1.00, all factor loading coefficients in the confirmatory factor analysis were significant(p < 0.001) and ranged from 0.413 to 1.029) tool for measuring the Health Belief Model related to the practice of breast self-examination (BSE), as well as investigating attitudes towards mammograms and ultrasounds 32 . The confirmatory factor analysis results of the CHBMS and MT-CHBMS. Each item had sufficient factor loadings (estimated coefficients) on the designated factor. All factor loading coefficients were significant ( p < 0.001) and ranged from 0.413 to 1.029. The fit statistics were assessed to demonstrate how well the CFA model fitted the data. For the model MT-CHBM: chi-square = 2488.868, df = 1879, chi-square/df = 1.324, TLI = 0.961, CFI = 0.964, and RMSEA (90% CI) = 0.050(0.045–0.055). Except for the motivation subscale, 21 pairs of error terms in each subscale of T-CHBMS and 23 pairs of error terms of MT-CHBMS were correlated. All these error terms suggested a high correlation between items and became the potential sources of the model misfit.
The questionnaire consisted of 64 items distributed among 10 subscales: susceptibility (5 items), seriousness (7 items), benefits of BSE (6 items), barriers to BSE (6 items), benefits of mammogram (6 items), barriers to mammogram (5 items), benefits of ultrasound (6 items), barriers to ultrasound (5 items), confidence (11 items), and health motivation (7 items). All items were formatted using an ordinal scale with a 5-point Likert scale response: 1 = "Strongly disagree," 2 = "Disagree," 3 = "Neutral," 4 = "Agree," and 5 = "Strongly agree" for positive statements. Each subscale can be utilized independently. However, when conducting an overall assessment of awareness regarding breast cancer and screening methods, the total score may be used. It's important to note that questions pertaining to barriers must be reversed before summing up the scores.
Statistical analysis
The data were analysed using Stata version 15.0. Descriptive statistics, including mean, standard deviation (SD), frequency, and percentages, were used to describe the data. Internal consistency of the items within the health belief subscales was assessed using Cronbach's alpha. The association and comparison of items within the health belief subscales and across other variables were analysed using t-tests, analysis of variance (ANOVA), and linear regression models.
Ethical approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and under the review and approval of the Institutional Research Ethics Committee of the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand (No. FAM 2564-08138) and Sanpatong Hospital Ethics Committee (No. SPT/REC 012/2564). All procedures were conducted following the relevant institutional guidelines and regulations.
Distribution of sociodemographic factors of women (n = 130)
The sociodemographic characteristics of the 130 participants are presented in Table 1 . The average age of the participants was 52.33 years (SD = 7.28). The majority of participants were single (61.54%). About 37.69% of the participants had attained a college-level education, while 51.54% had a monthly income exceeding 10,000 Baht (270 US dollars). Additionally, 41.54% of the participants had health insurance schemes through government or state enterprise officers.
Distribution statistical data and Cronbach’s alphas for MT-CHBMS
Table 2 presents the mean ranged from 2.46 to 4.35 and SD ranged from 3.56 to 8.00. The overall Cronbach's alphas for the health belief model subscales were found to be within an acceptable range (0.70 or higher), indicating good internal consistency 40 .
Comparison of sociodemographic factors with MT-CHBMS
Table 3 presents the results of the statistical analyses conducted on various sociodemographic factors and their associations with the Health Belief Model subscales.
Participants with education less than secondary school exhibited higher scores in the Seriousness subscale compared to other education level groups ( F = 3.44, p = 0.035). Participants with a college educational level had higher scores in the Barrier-BSE subscale compared to other education level groups ( F = 5.32, p = 0.006).
In terms of monthly income, participants in the lower 10,000 Baht income group demonstrated higher scores in the Seriousness subscale compared to the more than 10,000 Baht income group ( t = 2.43, p = 0.017). Conversely, the more than 10,000 Baht income group had higher scores in the Barrier-BSE and Barrier-UTS subscales compared to the lower 10,000 Baht income group ( t = − 2.71, p = 0.008 and t = − 2.64, p = 0.009).
Participants with health insurance schemes through government or state enterprise officer schemes exhibited higher scores in the Barrier-BSE and Barrier-UTS subscales compared to other groups ( F = 8.50, p = 0.001 and F = 6.85, p = 0.002). Additionally, participants with health insurance schemes through government or state enterprise officer schemes and those covered under the universal coverage scheme had higher scores in the Barrier-MG subscale compared to the social security scheme group ( F = 5.94, p = 0.003).
Multiple linear regression model of MT-CHBMS
Table 4 presents the results of multiple linear regression analysis. None of the factors were found to be significant associated with of Seriousness subscale. However, health insurance schemes were found to be a significant associated with of the Benefit-MG and Barrier-BSE (β m = − 2.48, P = 0.023 and β m = − 3.38, P = 0.008, respectively). Both monthly income and health insurance schemes were significant associated with of the Barrier-MG and Barrier-UTS (β m = 2.65, P = 0.008, β h = − 3.11, P = 0.002 and β m = 2.49, P = 0.013, β h = − 3.40, P = 0.001, respectively).
BM= item from benefit to mammogram, BARB = item from barrier to breast self-examination, BARM = item from barrier to mammogram, BAU = item from barrier of ultrasound.
Comparison of monthly income and health insurance schemes with the significant subscales of MT-CHBMS
To delve deeper into the specifics, each subscale item, including those related to the benefits and barriers of mammograms, breast self-examination, and ultrasound, was compared among different monthly income groups and health insurance schemes using t-tests and ANOVA analyses (Table 5 ). For the Barrier-BSE subscale, the group with an income of 10,000 Baht or more demonstrated higher scores in Barrier-BSE compared to the less than 10,000 Baht income group across the BARB1 (funny), BARB3 (embarrassing), and BARB5 (unpleasant) items. Additionally, participants with health insurance schemes through government or state enterprise officer schemes exhibited higher scores in Barrier-BSE compared to other groups across all BARB (1–6) items.
Regarding the Barrier-MG subscale, participants with health insurance schemes through government or state enterprise officer schemes had higher scores in Barrier-MG compared to other groups across the BARM1 (worry), BARM2 (embarrassing), and BARM3 (take too much time) items.
In terms of the Barrier-UTS subscale, the group with an income of 10,000 Baht or more demonstrated higher scores in barrier-UTS compared to the less than 10,000 Baht income group across the BAU1 (worry), BAU2 (embarrassing), and BAU5 (cost too much money) items. Additionally, participants with health insurance schemes through government or state enterprise officer schemes had higher scores in Barrier-UTS compared to other groups across the BAU2 (embarrassing), BAU3 (take too much time), and BAU4 (painful) items.
The objective of the study was to investigate differences in beliefs related to breast examination among various sociodemographic variables in Thai women, and the results have confirmed their presence.
Using multiple linear regression analysis with the MT-CHBMS, the results indicated several findings. Health insurance schemes were associated with Benefit-MG, Barrier-BSE, Barrier-MG and Barrier-UTS subscales. Additionally, monthly income showed associations with the Barrier-MG and Barrier-UTS subscales. The most common barriers reported by participants were feeling “embarrassed”, “worry”, and feeling that it “takes too much time”.
Unlike population-based studies, the current study reveals a distinct finding: health beliefs were not associated with age, marital status, and education. This contrasts with findings from other related studies, such as those involving Turkish and Iranian women, where age, marital status, and education were significantly correlated with health beliefs scales. 41 , 42 .
Interestingly, our study observed that distinct income groups were associated with varying outcomes in the Barriers-MG and Barriers-UTS subscales. Notably, there is a dearth of similar literature available for direct comparison. However, Kirag and Kizilkaya et al. 35 reported correlations between income levels and Benefit-BSE, Barriers-BSE, Self-efficacy, and Benefit MG, while Altunkurek and Hassan Mohamed 37 also identified a relationship between income status and the Susceptibility and Health Motivation subscales. The connection between lower income and barriers to BSE is not easily explained. It is possible that there are intermediary variables requiring further investigation.
According to the Health Belief Model, perceived barriers have consistently been identified as the most influential predictor in various studies for practicing BSE and mammography 43 . Recent studies have also shown that perceiving more benefits, having higher confidence, and experiencing fewer barriers are positively associated with BSE practice 16 , 44 , 45 . Similarly, perceiving more benefits and fewer barriers is positively associated with mammography 44 . In this study, it was found that the social security scheme associated with Barrier-BSE, Barrier-MG and Barrier-UTS. In addition, the social security scheme had lower scores than the government or state enterprise officer and universal coverage scheme in the barrier to BSE, barrier to mammogram, and barrier to ultrasound subscales. It is to note that the government or state enterprise officer scheme beneficiaries benefit from a higher level of healthcare coverage compared to the other two schemes. It offers a high level of coverage and includes access to government hospitals and medical facilities. This scheme beneficiaries typically have access to a comprehensive range of medical services, often with little or no out-of-pocket expenses. The scheme provides coverage for both routine healthcare and specialized treatments, including access to government-run healthcare facilities. The social security scheme members often enjoy relatively comprehensive healthcare benefits, and the quality of care is generally good. However, it is limited to formal sector employees and their dependents, which means that informal sector workers and those not covered by formal employment arrangements are not eligible. The universal coverage scheme aims to provide equitable access to healthcare for all, emphasizing the principle of social justice. The scheme may have limitations on specialized or high-cost medical treatments, and there may be variations in the quality of care among different facilities.
The impact of the healthcare scheme type on barriers to BSE, MG, or UTS may be influenced by numerous factors. Nevertheless, the results suggests that women who have health coverage through the social security scheme may benefit from targeted interventions to improve detection. Evidence for program planning should be implement in health insurance schemes groups such as health education, skill training and confidence in performing for BSE, reminders to perform BSE, regular use of BSE record booklets 15 , 46 .
One of the general barriers observed in this study is the lack of knowledge and awareness of breast cancer among the participants, as evidenced by their low scores in the Susceptibility, Seriousness, and Confidence scales. Knowledge is identified as the most influential barrier affecting the engagement of participants in BSE, particularly in low to middle-income countries and rural areas where resources are limited 47 . Participants in this study perceived their ability to perform the BSE technique as low, indicating a lack of knowledge or a lack of regular practice. Susceptibility refers to participants' perception of their chances of being at risk for a disease. In this study, participants perceived their chances of having a risk or disease as low, indicating a potential lack of knowledge regarding the risk factors of breast cancer, such as young age, no family history of cancer, and the absence of breast lumps. Seriousness pertains to participants' perception of the severity of the consequences associated with the disease. In this study, participants may perceive breast cancer as not causing pain, exhibiting no symptoms or signs, and not posing a significant threat. This suggests a lack of knowledge or the use of defence mechanisms such as denial or rationalization, similar to behaviours observed in smokers and alcohol drinkers 48 , 49 . Consistent with many Thai studies, interventions focusing on health education and skill training for BSE are recommended to address these knowledge gaps 17 , 21 , 46 .
One of the most common barriers to early screening detection identified in this study is the feeling of “embarrassment” and “worry”. Similar to Amin MN et al. 50 , this study conducted a hospital survey. The feeling of embarrassment can be considered a cultural barrier, where women may feel too embarrassed to have their breasts examined by a male doctor. This cultural aspect can hinder their willingness to seek medical attention for abnormalities. Worry, on the other hand, is associated with feelings of anxiety. Women may experience worry related to breast lumps, the potential consequences of breast cancer, and concerns about health professionals and healthcare facilities. Additionally, the perception that screening “takes too much time” can be a deterrent. Women may feel that they are too busy, have limited time, or believe that they lack sufficient time to perform BSE and undergo screening procedures 47 . Interventions should focus on problem-solving approaches and aim to improve healthcare services in order to overcome barriers faced by the participants. By addressing these barriers and concerns, healthcare providers can create a more supportive and comfortable environment for women to engage in early screening and detection practices. Apart from the issue of “embarrassment”, “worry”, and “takes too much time”, which should be considered as one of the barriers to BSE, mammograms, and ultrasounds, there could be other contributing factors. Future research should incorporate qualitative studies to explore additional causal factors influencing the practice or non-practice of BSE, as well as the utilization or non-utilization of mammograms and ultrasounds. Additionally, it is recommended to compare interventions using a before-and-after study design involving the three main public health insurance schemes: government or state enterprise officer, social security scheme, and universal coverage scheme. This examination is necessary to identify effective interventions for women within each health insurance scheme who may face different barriers.
Participants in this study are to be more empowering their health. They have the highest score of Health Motivation and comparing Benefit-MG and Benefit-UTS more than Benefit-BSE. Conversely, Barrier-BSE when comparing Barrier-MG and Barrier-UTS is inverse. This is show that they would like to take investigate accuracy screening tools more than their manual. As health practitioners’ perspective of Thai study would like to drive a policy of national cancer act to enable women’s rights for accessing standardized screening tools 10 .
Evidence for planning and future research
There is associated between a monthly income and perceived Barriers-MG and Barriers-UTS. This predictor may be sensitive and difficult to approach regarding their monthly income when implementing intervention strategies targeting MG and UTS promotion. However, there is health insurance schemes which associated with Benefit-MG, Barrier-BSE, Barrier-MG and Barrier-UTS subscale. Also, health insurance schemes in the social security scheme is the predictor of perceived Barrier-BSE, Barrier-MG and Barrier-UTS. Specifically, the perceived barriers subscale can help identify the problems of implementation. Furthermore, attitudes toward BSE, mammograms, and ultrasounds can be compared in terms of their benefits and barriers. Such comparisons can yield valuable insights for the development of targeted interventions and approaches aimed at increasing breast cancer screening among Northern Thai women in a hospital-based setting. The design of programs and future research should take this evidence into account during implementation. Future research could employ a before-and-after study design, integrating health education and skill training for BSE, and incorporating qualitative studies to explore the additional causal factors influencing the practice or non-practice of BSE, using or non-using mammogram/ultrasound. Moreover, investigating how to improve healthcare services to ensure women's satisfaction would be beneficial.
Strength and limitations
This study is the first research project known to utilize the MT-CHBMS to study the association between sociodemographic factors and health beliefs of breast cancer and screening behaviors. Additionally, the inclusion of new items related to ultrasound in the MT-CHBMS holds promise for the assessment of breast cancer beliefs among Thai women with dense breast masses and the potential integration of advanced technologies such as artificial intelligence in the future.
However, it is important to acknowledge the limitations of this study. Firstly, the cross-sectional design employed cannot establish causal relationships between beliefs and screening practices. Secondly, the results may not be generalizable to the entire population due to the selection of participants from a single geographic area and hospital setting in Northern Thailand. Thirdly, convenience sampling may cause these study results to only generalize to this research's sampling group. Fourthly, small sample size may cause low statistical power, increased error rate, and less precise information. Fifthly, structured interviews may be subject to interviewer or social desirability bias. Sixthly, no external validation, e.g., concurrent validity, was conducted along with the construct validity. Test–retest reliability and predictive validity were not examined and should be included in future research. Lastly, certain factors such as family history of breast cancer and other breast masses were not specifically excluded from the study, which could potentially influence participants' beliefs regarding breast cancer and their practices related to screening methods.
This study marked the first use of the MT-CHBMS to investigate the association between sociodemographic factors and health beliefs related to breast cancer screening. The findings provide evidence for program design and future research aimed at increasing breast cancer screening among women in Northern Thailand in a hospital-based setting. By successfully implementing the interventions, the ssocial security scheme represents the most targeted interventions can serve as role models for other health insurance schemes and contribute to enhancing the effectiveness of screening among women.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71 (3), 209–249. https://doi.org/10.3322/caac.21660 (2021).
Article PubMed Google Scholar
Global breast cancer initiative implementation framework: assessing, strengthening and scaling up of serviecs for the early detection and management of breast cancer: executive summary eGeneva (World Health Organizaion) (2023).
Department of Health MoPH. The most Thai female cancer is breast cancer, suggested to breast self-examination every month. https://multimedia.anamai.moph.go.th/news/140366/ . Accessed 26 May 2023.
Department of Medical Service. Report of the Ministry of Public Health, Budget year 2023. Reducing illness, reducing death and health security, Cancer branch, Chiang Mai Province, Round 1/2023. http://www.chiangmaihealth.go.th/document/230305167799917158.pdf . Accessed 1 July 2023.
Virani, S. et al. National and subnational population-based incidence of cancer in Thailand: Assessing cancers with the highest burdens. Cancers (Basel) 9 (8), 108 (2017).
Duffy, S. et al. Annual mammographic screening to reduce breast cancer mortality in women from age 40 years: Long-term follow-up of the UK Age RCT. Health Technol. Assess. 24 (55), 1–24. https://doi.org/10.3310/hta24550 (2020).
Article PubMed PubMed Central Google Scholar
Tabár, L. & Dean, P. B. Recommendations for breast cancer screening. Lancet Oncol. 21 (11), e511. https://doi.org/10.1016/S1470-2045(20)30495-2 (2020).
Dewi, T. K. Validation of the Indonesian version of Champion’s Health Belief Model Scale for breast self-examination. Psychol. Res. Behav. Manag. 11 , 433–438. https://doi.org/10.2147/prbm.S177124 (2018).
Erbil, N. & Bölükbaş, N. Beliefs, attitudes, and behavior of Turkish women about breast cancer and breast self-examination according to a Turkish version of the Champion Health Belief Model Scale. Asian Pac. J. Cancer Prev. 13 (11), 5823–5828 (2012).
Pongthavornkamol, W. N. & Khuhaprema, T. Breast cancer prevention and screening system in Thailand in health practitioners’ perspectives. Thai Cancer J. 39 (3), 77–92 (2019).
Google Scholar
Birhane, N., Mamo, A., Girma, E. & Asfaw, S. Predictors of breast self - examination among female teachers in Ethiopia using health belief model. Arch. Public Health. 73 (1), 39. https://doi.org/10.1186/s13690-015-0087-7 (2015).
Nafissi, N., Saghafinia, M., Motamedi, M. H. & Akbari, M. E. A survey of breast cancer knowledge and attitude in Iranian women. J. Cancer Res. Ther. 8 (1), 46–49. https://doi.org/10.4103/0973-1482.95173 (2012).
Nde, F. P., Assob, J. C., Kwenti, T. E., Njunda, A. L. & Tainenbe, T. R. Knowledge, attitude and practice of breast self-examination among female undergraduate students in the University of Buea. BMC Res. Notes 8 , 43. https://doi.org/10.1186/s13104-015-1004-4 (2015).
Hackshaw, A. K. & Paul, E. A. Breast self-examination and death from breast cancer: A meta-analysis. Br. J. Cancer 88 (7), 1047–1053. https://doi.org/10.1038/sj.bjc.6600847 (2003).
Article CAS PubMed PubMed Central Google Scholar
Thaineua, V. et al. Impact of regular Breast Self-Examination on breast cancer size, stage, and mortality in Thailand. Breast J. 26 (4), 822–824. https://doi.org/10.1111/tbj.13611 (2020).
Dewi, T. K., Massar, K., Ruiter, R. A. C. & Leonardi, T. Determinants of breast self-examination practice among women in Surabaya, Indonesia: An application of the health belief model. BMC Public Health 19 (1), 1581. https://doi.org/10.1186/s12889-019-7951-2 (2019).
Pengpid, S. & Peltzer, K. Knowledge, attitude and practice of breast self-examination among female university students from 24 low, middle income and emerging economy countries. Asian Pac. J. Cancer Prev. 15 (20), 8637–8640. https://doi.org/10.7314/apjcp.2014.15.20.8637 (2014).
Thailand NCIo. Recommendations for Breast Cancer Screening in Thailand . National Cancer Institute; (2012).
Shen, S. et al. A multi-centre randomised trial comparing ultrasound vs mammography for screening breast cancer in high-risk Chinese women. Br. J. Cancer 112 (6), 998–1004. https://doi.org/10.1038/bjc.2015.33 (2015).
Office TNHS. Mammography and ultrasound breast cancer screening to be accessible for Thai women with high-risk. 2024. 07 Feb 2024. https://eng.nhso.go.th/view/1/DescriptionNews/Mammography-and-ultrasound-breast-cancer-screening-to-be-accessible-for-Thai-women-with-high-risk/592/EN-US . Accessed 04 March 2024.
Mukem, S., Sriplung, H., McNeil, E. & Tangcharoensathien, V. Breast cancer screening among women in Thailand: Analyses of population-based household surveys. J. Med. Assoc. Thai. 97 (11), 1106–1118 (2014).
PubMed Google Scholar
Liu, N., Wang, J., Chen, D. D., Sun, W. J. & Zhang, W. Tools for the assessment of breast cancer screening beliefs in women: A literature review. J. Comp. Eff. Res. 8 (9), 645–655. https://doi.org/10.2217/cer-2018-0142 (2019).
Rosenstock, I. M. Why people use health services. Milbank Mem. Fund Q. 44 (3), 94–127 (1966).
Article Google Scholar
Champion, V. L. Instrument development for health belief model constructs. ANS Adv. Nurs. Sci. 6 (3), 73–85. https://doi.org/10.1097/00012272-198404000-00011 (1984).
Article CAS PubMed Google Scholar
Lee, E. H., Kim, J. S. & Song, M. S. Translation and validation of champion’s health belief model scale with Korean women. Cancer Nurs. 25 (5), 391–395. https://doi.org/10.1097/00002820-200210000-00010 (2002).
Marmarà, D., Marmarà, V. & Hubbard, G. Maltese translation and adaptation of champion’s health belief model scale and the revised illness perception questionnaire for breast screening among Maltese women. J .Nurs. Meas. 25 (3), 486–503. https://doi.org/10.1891/1061-3749.25.3.486 (2017).
Medina-Shepherd, R. & Kleier, J. A. Spanish translation and adaptation of Victoria Champion’s Health Belief Model Scales for breast cancer screening–mammography. Cancer Nurs. 33 (2), 93–101. https://doi.org/10.1097/NCC.0b013e3181c75d7b (2010).
Noman, S. et al. Factor structure and internal reliability of breast cancer screening Champion’s Health Belief Model Scale in Yemeni women in Malaysia: A cross-sectional study. BMC Womens Health 21 (1), 437. https://doi.org/10.1186/s12905-021-01543-7 (2021).
Secginli, S. & Nahcivan, N. O. Reliability and validity of the breast cancer screening belief scale among Turkish women. Cancer Nurs. 27 (4), 287–294. https://doi.org/10.1097/00002820-200407000-00005 (2004).
Champion, V. L. Revised susceptibility, benefits, and barriers scale for mammography screening. Res. Nurs. Health 22 (4), 341–348. https://doi.org/10.1002/(sici)1098-240x(199908)22:4%3c341::aid-nur8%3e3.0.co;2-p (1999).
Parsa, P., Kandiah, M., Mohd Nasir, M. T., Hejar, A. R. & Nor Afiah, M. Z. Reliability and validity of Champion’s Health Belief Model Scale for breast cancer screening among Malaysian women. Singapore Med. J. 49 (11), 897–903 (2008).
CAS PubMed Google Scholar
Suriyong, P. et al. Translation, adaptation, and validation of the modified Thai version of champion’s health belief model scale (MT-CHBMS). Healthcare (Basel) 11 (1), 128. https://doi.org/10.3390/healthcare11010128 (2022).
Ragab, M., Albukhari, A., Alyami, J. & Mansour, R. F. Ensemble deep-learning-enabled clinical decision support system for breast cancer diagnosis and classification on ultrasound images. Biology (Basel) 11 (3), 439. https://doi.org/10.3390/biology11030439 (2022).
The, L. O. Can artificial intelligence improve cancer care?. Lancet Oncol. 24 (6), 577. https://doi.org/10.1016/s1470-2045(23)00240-1 (2023).
Kirag, N. & Kızılkaya, M. Application of the Champion Health Belief Model to determine beliefs and behaviors of Turkish women academicians regarding breast cancer screening: A cross sectional descriptive study. BMC Womens Health 19 (1), 132. https://doi.org/10.1186/s12905-019-0828-9 (2019).
Dundar, P. E. et al. The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer 6 , 43. https://doi.org/10.1186/1471-2407-6-43 (2006).
Altunkurek, ŞZ. & Hassan, M. S. Determine knowledge and belief of Somalian young women about breast cancer and breast self-examination with champion health belief model: A cross-sectional study. BMC Med. Inform. Decis. Mak. 22 (1), 326. https://doi.org/10.1186/s12911-022-02065-4 (2022).
Library UND. The future we want : outcome of the Conference on Sustainable Development, Rio de Janeiro, Brazil, 20–22 June 2012. https://digitallibrary.un.org/record/3826773?ln=en . Accessed 4 March 2024.
Organization WH. WHO package of essential noncommunicable (PEN) disease interventions for primary health care. https://www.who.int/publications/i/item/9789240009226 . Accessed 4 March 2024.
Danial, W. W. C. C. BIOSTATISTICS A Foundation for Analysis in the Health Sciences 10th edn. (Wiley, 2013).
Gumus, A. B., Cam, O. & Malak, A. T. Socio-demographic factors and the practice of breast self examination and mammography by Turkish women. Asian Pac. J. Cancer Prev. 11 (1), 57–60 (2010).
Esna-Ashari, F., Saffari, N., Parsapour, H. & Rezapur-Shahkolai, F. Factors associated with breast cancer mammographic screening behavior among Iranian Women. Asian Pac. J. Cancer Prev. 23 (12), 4073–4078. https://doi.org/10.31557/apjcp.2022.23.12.4073 (2022).
Champion, V. L. & Skinner, C. S. The health belief model. In Health Behavior and Health Education Theory, Research, and Practice 4th edn (eds Karen Glanz, B. K. R. & Viswanath, K.) (Jossey-Bass, 2008).
Darvishpour, A., Vajari, S. M. & Noroozi, S. Can health belief model predict breast cancer screening behaviors?. Open Access Maced. J. Med. Sci. 6 (5), 949–953. https://doi.org/10.3889/oamjms.2018.183 (2018).
Febriyanti, N. M. A., Lubis, D. S., Wirawan, D. N., Suariyani, N. L. P. & Karmaya, M. The Determinants of Early Breast Cancer Detection via Breast Self-Examination (BSE) in Denpasar (Public Health and Preventive Medicine Archive, 2018).
Satitvipawee, P. S. S., Pitiphat, W., Kalampakorn, S. & Parkin, D. M. Factors associated with breast self-examination among Thai women living in rural areas in Northeastern Thailand. J. Med. Assoc. Thai 92 , 29 (2009).
Francks, L., Murray, A. & Wilson, E. Barriers and facilitators to breast self-examination in women under 50 in an international context: A qualitative systematic review. Int. J. Health Promot. Educ. 03 (02), 1–18. https://doi.org/10.1080/14635240.2023.2185804 (2023).
Jiraniramai, S. et al. Functional beliefs and risk minimizing beliefs among Thai healthcare workers in Maharaj Nakorn Chiang Mai hospital: Its association with intention to quit tobacco and alcohol. Subst. Abuse Treat. Prev. Policy 12 (1), 34. https://doi.org/10.1186/s13011-017-0118-1 (2017).
Jiraniramai, S. et al. Risk-minimizing belief: Its association with smoking and risk of harm from smoking in Northern Thailand. J. Ethn. Subst. Abuse 14 (4), 364–378. https://doi.org/10.1080/15332640.2014.991468 (2015).
Amin, M. N. et al. A hospital based survey to evaluate knowledge, awareness and perceived barriers regarding breast cancer screening among females in Bangladesh. Heliyon 6 (4), e03753. https://doi.org/10.1016/j.heliyon.2020.e03753 (2020).
Download references
This research was self-funded.
Author information
Authors and affiliations.
Department of Family Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
Surin Jiraniramai, Kanokporn Pinyopornpanish, Chaisiri Angkurawaranon & Wichuda Jiraporncharoen
Global Health and Chronic Conditions Research Group, Chiang Mai University, Chiang Mai, 50200, Thailand
Department of Psychiatry, Faculty of Medicine, Chiang Mai University, 110 Inthawarorot Rd., Sriphum, Muang, Chiang Mai, 50200, Thailand
Nahathai Wongpakaran & Tinakon Wongpakaran
School of Nursing, Indiana University, Indianapolis, IN, 46202, USA
Victoria L. Champion
Melvin and Bren Simon Comprehensive Cancer Center, Indiana University, Indianapolis, IN, 46202, USA
Department of Radiology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
Imjai Chitapanarux
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to this study’s conceptualization and methodology. Validation, S.J., K.P.,V.L.C., N.W. and T.W.; Formal analysis,S.J.,K.P.,T.W.,N.W.and C.A.; investigation, all.; data curation, S.J., C.A.;The original draft was written by Surin Jiraniramai and reviewed and edited by all authors. Resources, S.J.,K.P.,C.A.,W.J.,and T.W.; supervision, T.W. and N.W.
Corresponding author
Correspondence to Tinakon Wongpakaran .
Ethics declarations
Competing interests.
Profs. Wongpakaran are the editorial board members of Scientific Reports, and all the rest of the authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Jiraniramai, S., Pinyopornpanish, K., Wongpakaran, N. et al. Association between sociodemographic factors and health beliefs related to breast cancer screening behavior among Northern Thai women: a hospital-based study. Sci Rep 14 , 7596 (2024). https://doi.org/10.1038/s41598-024-58155-y
Download citation
Received : 13 October 2023
Accepted : 26 March 2024
Published : 31 March 2024
DOI : https://doi.org/10.1038/s41598-024-58155-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
- Health beliefs
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Share full article
Advertisement
Supported by
Talking (or Not) About Your Cancer
More from our inbox:, ‘political anxieties’, a mystery from england’s bronze age.

To the Editor:
Re “ It’s Not Easy to Tell People You Have Cancer ,” by Daniela J. Lamas (Opinion guest essay, March 27):
As a cancer survivor myself, I understand the reluctance of Catherine, Princess of Wales, to speak out about her own diagnosis. However, she has the unique opportunity to alert and educate many people regarding symptoms and treatments. And by speaking calmly and frankly, she has the additional opportunity to help remove the fear and stigma of a cancer diagnosis.
Of course, she has no obligation to do this, but perhaps as time passes and she is no longer in the first stages of shock, she will be able to do a truly selfless thing and help educate people about cancer.
Barbara Mutterperl New York
My mother was diagnosed with breast cancer when I was 12 years old and she was 33. In the 1960s breast cancer was often fatal, and cancer was not discussed publicly. As the oldest child, I think I was told too much, not too little. Counseling would have been very helpful.
I am 75 and had early stage breast cancer four years ago. I was told my treatment would be over 90 percent successful; sharing that information normalized the situation and helped me get through the treatment. I am cancer free.
Some types of cancer have fairly good outcomes, while other types are almost always fatal. The more treatable a cancer is, the more comfortable a patient feels about telling friends about their diagnosis. And sharing information with children under 18 has to be done very carefully.
Catherine, Princess of Wales, has very young children. She and her husband will be careful about how much information to give them, hoping to be honest but not scare them unnecessarily. Expecting her to reveal her diagnosis in more detail would be inappropriate at this point.
Maureen Schild New York
The members of the royal family are funded by the people of Britain. If they do not abdicate their official roles, it is their duty to do good in this world for the people who afford them their sumptuous lifestyle (be it under press coverage under a microscope or not).
So if they are secretive about their cancer diagnosis, it sends a clear message — cancer is a secret, something to hide, to cover up, to be ashamed of — and that is simply awful for the millions of people who are diagnosed with cancer or who have some mysterious health condition that with proper attention is diagnosed, hopefully early, as cancer!
Catherine, Princess of Wales, is not an ordinary person. It is her duty in her role as a country’s figurehead to speak the truth and not cover up.
She and the crown mislead the public in calling her chemotherapy preventative. She is not taking chemo like a flu shot; you can’t go to your doctor and ask for some chemo to prevent you from getting cancer. Chemo kills cancer cells, plain and simple. It is a drug in the anticancer tool kit.
As a survivor of Stage 4 testicular cancer diagnosed 15 years ago, I know how such a diagnosis turns your world and that of those close to you upside down.
Catherine and the crown have the power, the responsibility and the duty to her employers — the people of Britain — and really to the world to speak the truth about her condition, to help them understand about cancer screening, about not shirking from the disease, about living with cancer and getting treatment for it, and about the many cases like mine that can be cured.
Roger S. Merians Simi Valley, Calif.
When I was growing up in the 1950s, people only whispered the letter C for cancer. And no one ever said out loud the possibility of someone being a homosexual. The word gay was never used.
Why do people keep secrets? Sometimes it’s shame; other times we don’t want to experience other people’s reaction to the news, or to worry our family or friends.
I have no trouble telling people about my 2019 cancer diagnosis. When I came out as a lesbian 46 years ago, I was thrilled to finally be out of the closet, but I told less than a handful of people. It took a while to be open about my sexuality.
Every person, famous or not, gets to decide what to reveal and when. But keeping a secret because of shame or embarrassment is very toxic.
Beth Rosen Bronx The writer is a psychotherapist.
Dr. Daniela J. Lamas’s article brought back memories from my diagnosis with spleen cancer in 2005.
I told adult family members and neighbors, but decided not to tell my daughters (then 14 and 9) any specifics, referring vaguely to an abdominal condition that required surgery.
I did not want to derail the ability of the 14-year-old to rebel and act like a normal teen, and I wanted to spare the 9-year-old, who was already a worrier who thought of me as vulnerable. I told myself that if I needed chemotherapy, I would tell my children at that point. Fortunately, I ended up not needing chemo.
What we did not count on was that the children of those adults we had told would see their parents’ emails or texts and inform our children that I had cancer.
It took years for me to regain my children’s trust that I would be truthful and not hide important information from them. So be mindful that your kids have a lot more access to information than we had at their age.
Barbara Quackenbos West Orange, N.J.
Re “ America’s Most Overlooked Political Divide ,” by David French (column, March 25):
I found Mr. French’s description of people on both sides of today’s political divide deciding to “unplug from the news” unsurprising.
Since 2016, patients in my practice, on both the left and the right of the political divide, have reported being distraught by a daily onslaught of political news. Consequently, I began including “political anxieties” as one problem distressing patients who could not tear themselves away from a favorite cable news network’s unending servings of doom and gloom punditry.
My response, and practical advice I follow myself, is suggesting to patients that rather than immersion in distressing cable news, just scan online headlines. Doing so provides a sense of what is going on in the world. However, I also advise not going into the weeds, as doing so only heightens political anxieties.
Some find this to be a reasonable balance between being an anxiously overstimulated citizen and a disengaged one.
Jack Drescher New York The writer, a psychiatrist and psychoanalyst, is past president of the Group for Advancement of Psychiatry.
Re “ Under Centuries of Silt, a Vivid View of Bronze Age Life ” (news article, March 21):
I have not been able to stop thinking about this extremely moving article about the surprisingly rich lives lived by the inhabitants of a Bronze Age village in England nearly 3,000 years ago. It makes one think that the high point of human existence may have actually occurred thousands of years ago.
These people were steeped in beauty, the bounties of nature, the satisfaction of craftsmanship and the joy of one another’s company. In stark contrast to humans today, they lived in quiet harmony with the earth.
The most fascinating mystery to me is why they never returned to salvage their things after, as you report, “a catastrophic fire tore through the compound.” Could it be that they felt no special attachment to their belongings?
As the article stated, these people had the skills to easily move and rebuild their compound. Perhaps they felt that their greatest possession was the earth itself.
Philip Dolin New York
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Breast cancer.
Fadi M. Alkabban ; Troy Ferguson .
Affiliations
Last Update: September 26, 2022 .
- Continuing Education Activity
Breast cancer is the most common cancer diagnosed in women, accounting for more than 1 in 10 new cancer diagnoses each year. It is the second most common cause of death from cancer among women in the world. Breast cancer evolves silently, and most disease is discovered on routine screening. This activity reviews the pathophysiology, presentation and diagnosis of breast cancer and highlights the role of the interprofessional team in its management.
- Review the risk factors for breast cancer.
- Describe the histopathology of the different types of breast cancer.
- Summarize the treatment options for breast cancer.
- Outline modalities for improving care coordination among interprofessional team members to optimize outcomes for patients affected by breast cancer.
- Introduction
Breast cancer is the most common cancer diagnosed in women, accounting for more than 1 in 10 new cancer diagnoses each year. It is the second most common cause of death from cancer among women in the world. Anatomically, the breast has milk-producing glands in front of the chest wall. They lie on the pectoralis major muscle, and there are ligaments support the breast and attach it to the chest wall. Fifteen to 20 lobes circularly arranged to form the breast. The fat that covers the lobes determines the breast size and shape. Each lobe is formed by lobules containing the glands responsible for milk production in response to hormone stimulation. Breast cancer always evolves silently. Most of the patients discover their disease during their routine screening. Others may present with an accidentally discovered breast lump, change of breast shape or size, or nipple discharge. However, mastalgia is not uncommon. Physical examination, imaging, especially mammography, and tissue biopsy must be done to diagnose breast cancer. The survival rate improves with early diagnosis. The tumor tends to spread lymphatically and hematologically, leading to distant metastasis and poor prognosis. This explains and emphasizes the importance of breast cancer screening programs. [1] [2] [3]
Identifying factors associated with an increased incidence of breast cancer development is important in general health screening for women. [4] [5] Risk factors for breast cancer can be divided into 7 broad categories:
- Age: The age-adjusted incidence of breast cancer continues to increase with the advancing age of the female population.
- Gender: Most breast cancers occur in women.
- Personal history of breast cancer: A history of cancer in one breast increases the likelihood of a second primary cancer in the contralateral breast.
- Histologic risk factors: Histologic abnormalities diagnosed by breast biopsy constitute an important category of breast cancer risk factors. These abnormalities include lobular carcinoma in situ (LCIS) and proliferative changes with atypia.
- The family history of breast cancer and genetic risk factors: First-degree relatives of patients with breast cancer have a 2-fold to 3-fold excess risk for developing the disease. Five percent to 10% of all breast cancer cases are due to genetic factors, but they may account for 25% of cases in women younger than 30 years. BRCA1 and BRCA2 are the 2 most important genes responsible for increased breast cancer susceptibility.
- Reproductive risk factors: Reproductive milestones that increase a woman’s lifetime estrogen exposure are thought to increase her breast cancer risk. These include the onset of menarche before 12 years of age, first live childbirth after age 30 years, nulliparity, and menopause after age 55 years.
- Exogenous hormone use: Therapeutic or supplemental estrogen and progesterone are taken for various conditions, with the two most common scenarios being contraception in premenopausal women and hormone replacement therapy in postmenopausal women.
- Epidemiology
Invasive breast cancer affects 1 in 8 women in the United States (12.4%) during their lifetime. [6] [7] [8] In the United States, about 266,120 women will have invasive breast carcinoma in 2018, and 63,960 will have in situ breast cancer. In 2018, approximately 2550 men will have invasive breast cancer. Approximately 1 in 1000 men will have breast cancer during their lifetime. In the year 2000, the incidence of breast cancer in the United States began decreasing. This decrease may be due to the reduced use of hormone replacement therapy (HRT) by women. A connection was suggested between HRT and increased breast cancer risk. About 40,920 US women may die in 2018 from breast cancer. Larger decreases occur in women younger than 50 years old. In 2008, there were an estimated 1.38 million new cases of invasive breast cancer worldwide. The 2008 incidence of female breast cancer ranged from 19.3 cases per 100,000 in Eastern Africa to 89.9 cases per 100,000 in Western Europe. With early detection and significant advances in treatment, death rates from breast cancer have been decreasing over the past 25 years in North America and parts of Europe. In many African and Asian countries (e.g., Uganda, South Korea, and India), however, breast cancer death rates are rising. The incidence rate of breast cancer increases with age, from 1.5 cases per 100,000 in women 20 to 24 years of age to a peak of 421.3 cases per 100,000 in women 75 to 79 years of age; 95% of new cases occur in women aged 40 years or older. The median age of women at the time of breast cancer diagnosis is 61 years. According to the American Cancer Society (ACS), breast cancer rates among women from various racial and ethnic groups are as follows:
- Non-Hispanic white: 128.1 in 100,000
- African American: 124.3 in 100,000
- Hispanic/Latina: 91.0 in 100,000
- American Indian/Alaska Native: 91.9 in 100,000
- Asian American/Pacific Islander: 88.3 in 100,000
- Pathophysiology
Breast cancer develops due to DNA damage and genetic mutations that can be influenced by exposure to estrogen. Sometimes there will be an inheritance of DNA defects or pro-cancerous genes like BRCA1 and BRCA2 . Thus the family history of ovarian or breast cancer increases the risk for breast cancer development. In a normal individual, the immune system attacks cells with abnormal DNA or abnormal growth. This fails in those with breast cancer disease leading to tumor growth and spread.
- Histopathology
Breast cancer can be invasive or non-invasive according to its relation to the basement membrane. Noninvasive neoplasms of the breast are broadly divided into two major types, lobular carcinoma in situ (LCIS) and ductal carcinoma in situ (DCIS).
LCIS is regarded as a risk factor for the development of breast cancer. LCIS is recognized by its conformity to the outline of the normal lobule, with expanded and filled acini. DCIS is more morphologically heterogeneous than LCIS, and pathologists recognize four broad types of DCIS: papillary, cribriform, solid, and comedo.
DCIS is recognized as discrete spaces filled with malignant cells, usually with a recognizable basal cell layer composed of presumably normal myoepithelial cells. The papillary and cribriform types of DCIS are generally lower grade lesions and may take longer to transform into invasive cancer.
The solid and comedo types of DCIS are generally higher-grade lesions. DCIS, if not treated, usually transforms into invasive cancer. Invasive breast cancers are recognized by their lack of overall architecture, infiltration of cells haphazardly into a variable amount of stroma, or formation of sheets of continuous and monotonous cells without respect for the form and function of a glandular organ. Pathologists broadly divide invasive breast cancer into ductal and lobular histologic types.
Invasive ductal cancer tends to grow as a cohesive mass; it appears as discrete abnormalities on mammograms and is often palpable as a discrete lump in the breast smaller than lobular cancers. Invasive lobular cancer tends to permeate the breast in a single-file nature, which explains why it remains clinically occult and often escapes detection on mammography or physical examination until the disease is extensive. Invasive ductal cancer, also known as infiltrating ductal carcinoma, is the most common form of breast cancer; it accounts for 50% to 70% of invasive breast cancers.
Invasive lobular carcinoma accounts for 10% of breast cancers, and mixed ductal and lobular cancers have been increasingly recognized and described in pathology reports. When invasive ductal carcinomas take on differentiated features, they are named according to the features that they display. If the infiltrating cells form small glands lined by a single row of the bland epithelium, they are called infiltrating tubular carcinoma. The infiltrating cells may secrete copious amounts of mucin and appear to float in this material. These lesions are called mucinous or colloid tumors.
Tubular and mucinous tumors are usually low-grade (grade I) lesions; these tumors account for approximately 2% to 3% of invasive breast carcinomas. Medullary cancer is characterized by bizarre invasive cells with high-grade nuclear features, many mitoses, and lack of an in situ component. The malignancy forms sheets of cells in an almost syncytial fashion, surrounded by an infiltrate of small mononuclear lymphocytes. The borders of the tumor push into the surrounding breast rather than infiltrate or permeate the stroma. In its pure form, medullary cancer accounts for only approximately 5% of breast cancers. [9] [10] [11]
- History and Physical
Most early breast cancer patients are asymptomatic and discovered during screening mammography. With increasing size, the patient may discover cancer as a lump that is felt accidentally, mostly during combing or showering. Breast pain is an unusual symptom that happens 5% of the time. The locally advanced disease may be presented with peau d'orange, frank ulceration, or fixation to the chest wall. Inflammatory breast cancer, an advanced form of breast cancer, frequently resembles breast abscess and presents with swelling, redness, and other local signs of inflammation. Paget disease of the nipple usually presents with nipple changes that must be differentiated from nipple eczema.
Evaluation of Patients with breast cancer needs a triple assessment using clinical evaluation, imaging, and tissue biopsy. Mammography is the most commonly used modality for the diagnosis of breast cancer. Most of the asymptomatic cases are diagnosed during screening mammography. Breast cancer always presents as calcifications, dense lump, with or without architecture distortion. However, mammography is not sensitive in young women for whom breast ultrasonography can be used. Ultrasonography is useful in assessing the consistency and size of breast lumps. It has a great role in guided needle biopsy. Magnetic resonance imaging has good sensitivity for describing abnormalities in soft tissues, including the breast. It is indicated if there are occult lesions, or suspicion of multifocal or bilateral malignancy, especially ILC, and in the assessment of response to neoadjuvant chemotherapy, or when planning for breast conservation surgery and screening in the high-risk patient. Tissue biopsy is an important step in the evaluation of a breast cancer patient. There are different ways to take a tissue specimen, and these include fine-needle aspiration cytology, core biopsy (Trucut), and incisional or excisional biopsy. [12] [13] [14]
- Treatment / Management
The 2 basic principles of treatment are to reduce the chance of local recurrence and the risk of metastatic spread. Surgery with or without radiotherapy achieves local control of cancer. When there is a risk for metastatic relapse, systemic therapy is indicated in the form of hormonal therapy, chemotherapy, targeted therapy, or any combination of these. In locally advanced disease, systemic therapy is used as a palliative therapy with a small or no role for surgery. [15] [16] [17]
- Differential Diagnosis
- Breast abscess
- Fat necrosis
- Fibroadenoma
- Surgical Oncology
Surgery has a major role in the treatment of breast cancer. It is the basic way to use for local control of the disease. Radical mastectomy of Halsted, which removed the breast with axillary lymph node dissection and excision of both pectoralis muscles, is no longer recommended due to the high rate of morbidity without a survival benefit. Now, the modified radical mastectomy of Patey is more famous. It entails removing the whole breast tissue with a large part of the skin and the axillary lymph nodes. The pectoralis major and minor muscles are preserved. Breast-only removal without axillary dissection is referred to as simple mastectomy. This procedure can be performed in small tumors with negative sentinel lymph nodes. Breast-conserving surgery (BCS) is aimed at removing the tumor plus a rim of at least 1 cm of normal breast tissue (wide local excision). A quadrantectomy involves removing the entire segment of the breast that contains the tumor. The last 2 procedures are usually combined with axillary clearance through a separate incision. Axillary procedures may include sentinel lymph node biopsy, sampling, partial (II), or complete (III) axillary lymph node dissection. Lumpectomy is the removal of a benign mass without excision of the normal breast tissue.
- Radiation Oncology
Radiation therapy has a significant role in local disease control. The risk of cancer recurrence decreases by about 50% at 10 years, and the risk of breast cancer death reduces by almost 20% at 15 years when radiation therapy follows BCS. However, radiation is not necessary for women 70 years of age and older with small, lymph node-negative, hormone receptor-positive (HR+) cancers because it has not been shown to improve survival in patients who take hormonal therapy for at least 5 years. Radiation therapy is beneficial in large tumors (greater to 5 cm) or if the tumor invades skin or chest wall and if there are positive lymph nodes. It can also be used as palliative therapy in advanced cases, such as a central nervous system (CNS) or bone metastasis. It can be delivered as external beam radiation, brachytherapy, or a combination of both. [18] [19]
- Medical Oncology
Chemotherapy, hormone therapy, and targeted therapy are the systemic therapies used in breast cancer management. A 25 percent reduction in the risk of relapse over a 10 to 15-year period using a first-generation chemotherapy regimen such as cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) in a 6-month cycle. Anthracyclines (doxorubicin or epirubicin) and the newer agents such as the taxanes are modern regimens used for breast cancer. Three to 6-month period is used for adjuvant and neoadjuvant chemotherapy. Adjuvant treatment of early-stage HR+ breast cancer with tamoxifen for at least 5 years has been shown to reduce the recurrence rate by about half throughout the first 10 years and reduces breast cancer mortality by about 30% throughout the first 15 years.
More recently, studies have shown that extended use of adjuvant tamoxifen (10 years versus 5 years) further reduces the risk of breast cancer recurrence and mortality, so clinical practice guidelines now recommend consideration of adjuvant tamoxifen therapy for 10 years. The mainstay of treatment for most premenopausal women with HR+ tumors is tamoxifen. Some women may also benefit from surgical removal (oophorectomy) or chemical suppression of the ovaries, which are the main source of estrogen before menopause. Treatment guidelines recommend aromatase inhibitors (AIs) such as anastrozole should usually be included in the treatment of postmenopausal women with HR+ breast cancer. Targeted therapy is usually indicated in about 17% of breast cancers that overproduce the growth-promoting protein HER2/neu. Trastuzumab, the first approved drug, is a monoclonal antibody that directly targets the HER2 protein. It reduces the risk of recurrence and death by 52% and 33%, respectively, if combined with chemotherapy in HER2+ early breast cancer if compared to chemotherapy alone. [20] [21]
Breast cancer staging is determined clinically by physical examination and imaging studies before treatment, and breast cancer stage is determined pathologically by pathologic examination of the primary tumor and regional lymph nodes after definitive surgical treatment. Staging is performed to group patients into risk categories that define prognosis and guide treatment recommendations for patients with a similar prognosis. Breast cancer is classified with the TNM classification system, which groups patients into 4 stage groupings based on the primary tumor size (T), the regional lymph nodes status (N), and if there is any distant metastasis (M). The most widely used system is that of the American Joint Committee on Cancer:
Primary Tumor (T)
Tis: Carcinoma in-situ, Paget‘s with no tumor
T1: Less than 2 cmT1a: 0.1 to 0.5 cmT1b: 0.5 to 1.0 cmT1c: 1.0 to 2.0 cm
T2: 2 to 5 cm
T3: Larger than 5 cm
T4 T4a: Chest wall involvementT4b: Skin involvementT4c: Both 4a and 4bT4d: Inflammatory ca
Regional Lymph Nodes (N)
N1: Mobile ipsilateral axillary nodes
N2: Fixed/matted ipsilateral axillary nodes
N3 N3a – Ipsilat infraclavicular nodesN3b – Ipsilat int mammary nodesN3c – Ipsilateral supraclavicular nodes
Distant Metastases (M)
M1: Distant metastases
Stage 0 Tis
Stage I T1N0
Stage II T2N0, T3N0 T0N1, T1N1, T2N1
Stage III
*skin, rib inv., matted LNs T3 N1 T0N2, T1N2, T2N2, T3N2 Any T, N3 T4, any N Locally advanced BC
The prognosis of early breast cancer is quietly good. Stage 0 and stage I both have a 100% 5-year survival rate. The 5-year survival rate of stage II and stage III breast cancer is about 93% and 72%, respectively. When the disease spreads systemically, its prognosis worsens dramatically. Only 22% of stage IV breast cancer patients will survive their next 5 years.
- Complications
Complications can arise from the treatment, whether chemotherapy, radiation, hormonal therapy, or surgery.
Surgical complications include:
- Cosmetic issues
- Permanent scarring
- Alteration or loss of sensation in the chest area and reconstructed breasts
Chemotherapy complications include:
- Nausea/vomiting and diarrhea
- Memory loss ("chemo brain")
- Vaginal dryness
- Menopausal symptoms/fertility issues
Complications accompanying hormonal therapy include:
- Hot flashes
- Vaginal discharge dryness
- Impotence in males with breast cancer
Radiation can result in the following complications:
- Pain and skin changes
- Heart and lung issues (long-term)
- Deterrence and Patient Education
Patients usually require counseling to deal with the condition and treatment. They should be put in touch with psychological counseling, and there are also support groups available.
- Pearls and Other Issues
Breast cancer patients are advised to be followed up for life to detect early recurrence and spread. Yearly or biannual follow-up mammography is recommended for the treated and the other breast. The patient must be informed that they must visit a breast clinic if they have any suspicious manifestations. Currently, there is no role for repeated measurements of tumor markers or doing follow-up imaging other than mammography.
- Enhancing Healthcare Team Outcomes
After the treatment of breast cancer, long-term follow-up is necessary. There is a risk of local and distant relapse, and hence an interprofessional team approach is necessary. The women need regular mammograms and a pelvic exam. Also, women with risk factors for osteoporosis need a bone density exam and monitoring for tumor markers for metastatic disease. For those who are about to undergo radiation therapy, a baseline echo and cardiac evaluation are necessary. Even though many types of integrative therapies have been developed to help women with breast cancer, evidence for the majority of these treatments is weak or lacking. [22]
Over the past four decades, the survival rates of most breast cancer patients have improved. Of note is that the presence of breast cancer has gradually slowed down over the past decade, which may be due to earlier detection and improved treatments. The prognosis for patients with breast cancer is highly dependent on the status of axillary lymph nodes. The higher the number of positive lymph nodes, the worse the outcome. In general, hormone-responsive tumors tend to have a better outcome. In breast cancer survivors, adverse cardiac events are common; this is partly due to the cardiotoxic drugs to treat cancer and the presence of traditional risk factors for heart disease. The onus is on the healthcare provider to reduce the modifiable risk factors and lower the risk of adverse cardiac events. [1] [23] [Level 5)
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Breast Cancer Metastasis Sites Medical Gallery of Mikael Häggström 2014, Public Domain, via Wikimedia Commons.
Breast Mammogram. A mammographic view of the left breast demonstrates skin thickening, diffusely increased breast density, and malignant type calcifications in this patient with biopsy-proven inflammatory breast cancer. Contributed by Hassana (more...)
Breast Cancer Risk Factors 5. Kerlikowske K, Gard CC, Tice JA, et al. for the Breast Cancer Surveillance Consortium. Risk factors that increase risk of estrogen receptor-positive and -negative breast cancer. J Natl Cancer Inst. 109(5): djw276, 2016.
Interprofessional care diagram Breast cancer patients Contributed by Kathryn Malherbe (PhD candidate)
Breast Estrogen Receptor Staining Contributed by Fabiola Farci, MD
Breast Cancer Axillary Lymphadenopathy Contributed by Sunil Munakomi, MD
Breast Cancer Fine Needle Aspiration Cytology Contributed by Sunil Munakomi, MD
Clinical Signs of Breast Carcinoma Contributed by Sunil Munakomi, MD
Disclosure: Fadi Alkabban declares no relevant financial relationships with ineligible companies.
Disclosure: Troy Ferguson declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Alkabban FM, Ferguson T. Breast Cancer. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Retrospective Analysis of Women with Only Mastalgia. [J Breast Health. 2016] Retrospective Analysis of Women with Only Mastalgia. Arslan M, Küçükerdem HS, Can H, Tarcan E. J Breast Health. 2016 Oct; 12(4):151-154. Epub 2016 Oct 1.
- Preventive health care, 1999 update: 3. Follow-up after breast cancer. Canadian Task Force on Preventive Health Care. [CMAJ. 1999] Preventive health care, 1999 update: 3. Follow-up after breast cancer. Canadian Task Force on Preventive Health Care. Temple LK, Wang EE, McLeod RS. CMAJ. 1999 Oct 19; 161(8):1001-8.
- Review Common Breast Problems. [Am Fam Physician. 2019] Review Common Breast Problems. Salzman B, Collins E, Hersh L. Am Fam Physician. 2019 Apr 15; 99(8):505-514.
- Responding to the challenges of breast cancer in egypt and other arab countries. [J Egypt Natl Canc Inst. 2008] Responding to the challenges of breast cancer in egypt and other arab countries. El Saghir NS. J Egypt Natl Canc Inst. 2008 Dec; 20(4):309-12.
- Review Overview of resistance to systemic therapy in patients with breast cancer. [Adv Exp Med Biol. 2007] Review Overview of resistance to systemic therapy in patients with breast cancer. Gonzalez-Angulo AM, Morales-Vasquez F, Hortobagyi GN. Adv Exp Med Biol. 2007; 608:1-22.
Recent Activity
- Breast Cancer - StatPearls Breast Cancer - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
COMMENTS
The article by Esteva and Hortobagyi discusses breast cancer from the aspect of increased survival rates, the novel treatments that have necessitated this and the promise in even more enhanced management of breast cancer. Effects of Hypoxia, Surrounding Fibroblasts, and p16 Expression on Breast Cancer.
ABSTRACT: Breast cancer is the most commonly diagnosed cancer in women in the United States and the second leading cause of cancer death in American women 1.Regular screening mammography starting at age 40 years reduces breast cancer mortality in average-risk women 2.Screening, however, also exposes women to harm through false-positive test results and overdiagnosis of biologically indolent ...
Breast cancer incidence and death rates have increased over the last three decades. Between 1990 and 2016 breast cancer incidence has more than doubled in 60/102 countries (e.g., Afghanistan, Philippines, Brazil, Argentina), whereas deaths have doubled in 43/102 countries (e.g., Yemen, Paraguay, Libya, Saudi Arabia) .
Screening is looking for signs of disease, such as breast cancer, before a person has symptoms.The goal of screening tests is to find cancer at an early stage when it can be treated and may be cured.Sometimes a screening test finds cancer that is very small or very slow growing. These cancers are unlikely to cause death or illness during the person's lifetime.
Breast Cancer Screening. Breast cancer screening can detect cancer before signs or symptoms develop. While breast cancer screening cannot prevent breast cancer, it can help find breast cancer in its earliest and most treatable stage. When detected in the localized (early) stage, breast cancer has a 5-year relative survival rate of 99% ...
Conclusion. The panel concludes that the current screening programmes in the United Kingdom, which invite women aged 50-70 every 3 years to undergo mammography, are likely to deliver about a 20% reduction in breast cancer mortality at ages 55-79 years. Clearly, there is uncertainty in this figure.
For women 40-74 years of age who actually participate in screening every 1-2 years, breast cancer mortality is reduced by 40%. With appropriate corrections, overdiagnosis accounts for 10% or fewer breast cancers. False positives occur in about 10% of screened women, 80% of which are resolved with additional imaging, and 10%, with breast biopsy.
The overall cumulative risk of developing breast cancer by 50 years of age was 30%. 4. Increasing age is another strong risk factor. Invasive breast cancer will be diagnosed in one out of 42 women ...
The American Cancer Society (ACS) breast cancer screening guidelines consider having had either a 2D or 3D mammogram as being in line with current screening recommendations. The ACS also believes that women should be able to choose between 2D and 3D mammography if they or their doctor believes one would be more appropriate, and that out-of ...
Breast Cancer Essay. Sort By: Page 1 of 50 - About 500 essays. Better Essays. Breast Cancer And Cancer Prevention. 2347 Words; 10 Pages ... 2017). In order to reach this goal, Komen has created many local outreach programs to educate the community about breast health and breast cancer screening (Susan G. Komen Greater Atlanta, 2017 ...
1514 Words. 7 Pages. Open Document. BREAST CANCER SCREENING DR. DANA MORTEZ ARLECIA PURVIS JULY 17, 2011. Current research shows mammograms are stronger than in the past. In a recent study it has confirmed that mammograms benefit for women in their forties and fifties. Women feel confident about the benefits that are associated with a regular ...
Breast cancer is a disease in which abnormal breast cells grow out of control and form tumours. If left unchecked, the tumours can spread throughout the body and become fatal. Breast cancer cells begin inside the milk ducts and/or the milk-producing lobules of the breast. The earliest form (in situ) is not life-threatening and can be detected ...
Mammograms are low-dose x-rays that can help detect breast cancer early. Explore in-depth information about mammograms. ... If you've been told you need a mammogram, or you're ready to start breast cancer screening, the topics below can help you know what to expect. Getting a mammogram. Find out what a mammogram is, why it's done, what doctors ...
The incidence and mortality of breast cancer are rising in the whole world in the past few decades, adding up to a total of around two million new cases and 620,000 deaths in 2018. Unlike what occurs in developed countries, most of the cases diagnosed in the developing world are already in advanced stages and also in women younger than 50 years old. As most screening programs suggest annual ...
Breast cancer screening means checking a woman's breasts for cancer before there are signs or symptoms of the disease. All women need to be informed by their health care provider about the best screening options for them. When you are told about the benefits and risks of screening and decide with your health care provider whether screening is ...
Breast cancer is the second most common type of cancer in American women. Women in the United States get breast cancer more than any other type of cancer except skin cancer.Breast cancer is second to lung cancer as a cause of cancer death in American women. Breast cancer rates in women increased gradually for many years until the early 2000s and then decreased rapidly, coinciding with a drop ...
Breast cancer screening guidelines could provide valuable tools for clinical decision making by reviewing the available evidence and providing recommendations. ... We included guidelines following inclusion criteria: (1) originally published guidelines, consensus, or position papers related to breast cancer screening; (2) the latest versions of ...
The Importance of Early Detection and Screening for Breast Cancer; ... By writing essays on breast cancer, individuals can contribute to a better understanding of the disease, its impact, and the importance of ongoing research and support. Engaging with this topic through writing can help raise awareness, provide support, and inspire positive ...
Mammography is a very common and widely accepted breast cancer-screening tool which was developed in the mid-1960s [3]. Several large clinical trials demonstrated that the detection of small tumors using mammography devices at an early stage reduces or delays mortality [4]. An X-ray image of the breast is called a mammogram.
Language isn't the only barrier for women from immigrant communities Attendance for breast cancer screening tends to be considerably higher among women born in high income countries with established screening programmes than in women who migrate to and settle in these countries later in their lives. Norway's breast screening programme began in 1996 and has one of the highest overall 10 ...
The Breast Screening Programme In The Uk Health Essay. Breast cancer is the most common cancer in women in the UK and is currently the second leading cause of cancer deaths after lung cancer1. In 1988, the National Health Service Breast Screening Programme (NHSBSP) was introduced in the UK with an aim to detect small invasive cancers as well as ...
Screening remains an essential component of our breast imaging care and value and has been well demonstrated to reduce breast cancer mortality and morbidity. In May 2023, the United States Preventive Services Task Force (USPSTF) updated its breast cancer screening recommendations and now recommends (in draft) initiation of screening mammography ...
Female breast cancer is the most commonly diagnosed cancer, with approximately 2.3 million new cases and 685,000 deaths reported in 2020 1.It is the leading or second leading cause of female ...
Breast cancer is the most common malignant tumor in women in the world. Breast cancer patients account for as much as 36% of oncological patients. An estimated 2.089 million women were diagnosed with breast cancer in 2018 [, ]. The incidence of this malignant tumor is increasing in all regions of the world, but the highest incidence occurs in ...
Conclusions: Beliefs about breast and colorectal cancers and screenings are influenced by family and social conversation and may respond to personalized contact from healthcare system representatives, including researchers. Screening campaigns to address both health beliefs as well as family and social discourse on these topics are needed.
Responses to an Opinion essay by Dr. Daniela J. Lamas. Also: "political anxieties"; a mystery from England's Bronze Age.
Background: To improve Shared decision-making (SDM) regarding personalized post-treatment surveillance, the Breast Cancer Surveillance Decision Aid (BCS-PtDA), integrating personalized risk information, was developed and implemented in eight hospitals. The aim of this mixed-methods study was to (1) assess the implementation and participation rates, (2) identify facilitators and barriers for ...
Breast cancer is the most common cancer diagnosed in women, accounting for more than 1 in 10 new cancer diagnoses each year. It is the second most common cause of death from cancer among women in the world. Anatomically, the breast has milk-producing glands in front of the chest wall. They lie on the pectoralis major muscle, and there are ligaments support the breast and attach it to the chest ...