

Handbook of Clinical Teaching
- © 2016
- Somnath Mookherjee 0 ,
- Ellen M. Cosgrove 1
Division of General Internal Medicine Department of Medicine, University of Washington School of Medicine, Seattle, USA
You can also search for this editor in PubMed Google Scholar
Department of Medicine, University of Nevada Las Vegas School of Medicine, Las Vegas, USA
Includes the most relevant topics for new clinical teachers in an easy-to-access format
Provides tips for using observations and feedback to improve teaching
Emphasizes key points with frequent use of tables and boxed practical content
Conducive to quick reference before meeting with learners or engaging in a specific teaching situation
Includes supplementary material: sn.pub/extras
55k Accesses
18 Citations
2 Altmetric
This is a preview of subscription content, log in via an institution to check access.
Access this book
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Other ways to access
Licence this eBook for your library
Institutional subscriptions
About this book
Targeting the practical needs of clinical teachers who do not have extensive time to undergo additional training, this book provides an accessible, on-the-spot resource to bolster teaching skills and optimize the education of trainees. A massive transformation takes place every summer in the United States: thousands of trainees in graduate medical education are appointed as attending physicians responsible for effectively teaching the next generation of medical students and residents. This handbook includes only the most relevant topics for new clinical teachers, and covers the basics of clinical teaching, teaching in specific situations, teaching different audiences, and best practices for handling challenging situations. The format is conducive to “just in time” learning, perfect for quick reference before meeting with learners or engaging in specific teaching situations, such as in an ambulatory clinic or at the bedside. Key points are emphasized with frequent use of tables and boxed practical content. Applicable to all teaching attendings regardless of specialty, the Handbook of Clinical Teaching is a valuable aid for individuals who wish to improve their teaching, and serves as a practical guide for faculty development in clinical teaching.
Similar content being viewed by others

Clinical Teaching: The Bedside and Beyond

How to Teach in Busy Clinical Settings

- bedside teaching
- clinical teaching
- medical education
- teaching end-of-life care
- teaching error disclosure
- teaching hospitals
Table of contents (27 chapters)
Front matter, introduction.
Somnath Mookherjee
How to Become a Learner-Centered Teacher
- Kristen N. Hayward
How to Optimize Teaching by Using Observation and Feedback
How to use learning preferences to optimize teaching effectiveness.
- Paul R. Sutton, Heather A. McPhillips
How to Effectively Teach Millennials: Understanding Intergenerational Factors
- Byron D. Joyner
How to Use Reflective and Deliberate Practice to Maximize Learning
- Thomas E. McNalley
How to Use Teaching Scripts to Make Teaching More Effective and Efficient
- Ellen M. Cosgrove, Somnath Mookherjee, Lynne Robins
How to Give a Great PowerPoint Presentation
- Tiffany M. Bridges, Andrew M. Luks
How to Give a Great “Chalk Talk”
- Gabrielle N. Berger, Patricia A. Kritek
How to Teach at the Bedside
- Paul B. Cornia
How to Teach Beginning Students in the Clinical Setting
- Molly Blackley Jackson
How to Teach Medical Students in an Ambulatory Clinic
- Jennifer J. Wright
How to Teach in Free Clinics: Brief Encounters with Learners and Patients in Vulnerable Communities
- L. Renata Thronson
How to Teach Students on an Inpatient Clerkship
- Tiffany Chen, Susan Merel
How to Use Entrustable Professional Activities to Evaluate and Teach Physician Trainees
- John H. Choe
How to Teach in the Emergency Department
- Joshua Jauregui, Anne K. Chipman
How to Teach in the Operating Room
- Morgan K. Richards, Erik G. Van Eaton
How to Teach Procedures
- Amy E. Morris, Kristen K. Patton
How to Teach Quality Improvement and Patient Safety
- Alvin S. Calderon
Editors and Affiliations
Ellen M. Cosgrove
About the editors
Somnath Mookherjee, MD
Assistant Professor of Medicine
University of Washington School of Medicine
Department of Medicine
Division of General Internal Medicine
Seattle, WA, USA
Ellen M. Cosgrove, MD, FACP
Vice Dean, Academic Affairs & Education
University of Nevada, Las Vegas, School of Medicine
Las Vegas, NV, USA
Bibliographic Information
Book Title : Handbook of Clinical Teaching
Editors : Somnath Mookherjee, Ellen M. Cosgrove
DOI : https://doi.org/10.1007/978-3-319-33193-5
Publisher : Springer Cham
eBook Packages : Medicine , Medicine (R0)
Copyright Information : Springer International Publishing Switzerland 2016
Softcover ISBN : 978-3-319-33191-1 Published: 10 October 2016
eBook ISBN : 978-3-319-33193-5 Published: 28 September 2016
Edition Number : 1
Number of Pages : XIV, 256
Number of Illustrations : 7 b/w illustrations, 33 illustrations in colour
Topics : Internal Medicine , Medical Education , Public Health
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Why are Case Studies Important for Developing Clinical Judgment?

Related Reading
- Defining Clinical Judgment and Why it’s So Important
Frameworks to Teach Clinical Judgment
- Faculty Guide to Develop Clinical Judgment
Keith Rischer – Ph.D., RN, CCRN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.
Sign up to receive a free KeithRN NextGen Case Study!
Develop clinical judgment skills with this innovative new case study on asthma to prepare your students for nextgen nclex and practice.
" * " indicates required fields
Keith Rischer
Recommended for you.
Case method teaching has been found to improve student learning, to increase students’ perception of learning gains, and to meet learning objectives 8 9 . Faculty have noted the instructional benefits of cases including greater student engagement in their learning 10 , deeper student understanding of concepts, stronger critical thinking skills, and an ability to make connections across content areas and view an issue from multiple perspectives 11 .
Through case-based learning, students are the ones asking questions about the case, doing the problem-solving, interacting with and learning from their peers, “unpacking” the case, analyzing the case, and summarizing the case. They learn how to work with limited information and ambiguity, think in professional or disciplinary ways, and ask themselves “what would I do if I were in this specific situation?”
The case method bridges theory to practice, and promotes the development of skills including: communication, active listening, critical thinking, decision-making, and metacognitive skills 12 , as students apply course content knowledge, reflect on what they know and their approach to analyzing, and make sense of a case.
Though the case method has historical roots as an instructor-centered approach that uses the Socratic dialogue and cold-calling, it is possible to take a more learner-centered approach in which students take on roles and tasks traditionally left to the instructor.
Cases are often used as “vehicles for classroom discussion” 13 . Students should be encouraged to take ownership of their learning from a case. Discussion-based approaches engage students in thinking and communicating about a case. Instructors can set up a case activity in which students are the ones doing the work of “asking questions, summarizing content, generating hypotheses, proposing theories, or offering critical analyses” 14 .
The role of the instructor is to share a case or ask students to share or create a case to use in class, set expectations, provide instructions, and assign students roles in the discussion. Student roles in a case discussion can include:
- discussion “starters” get the conversation started with a question or posing the questions that their peers came up with;
- facilitators listen actively, validate the contributions of peers, ask follow-up questions, draw connections, refocus the conversation as needed;
- recorders take-notes of the main points of the discussion, record on the board, upload to CourseWorks, or type and project on the screen; and
- discussion “wrappers” lead a summary of the main points of the discussion.
Prior to the case discussion, instructors can model case analysis and the types of questions students should ask, co-create discussion guidelines with students, and ask for students to submit discussion questions. During the discussion, the instructor can keep time, intervene as necessary (however the students should be doing the talking), and pause the discussion for a debrief and to ask students to reflect on what and how they learned from the case activity.
Note: case discussions can be enhanced using technology. Live discussions can occur via video-conferencing (e.g., using Zoom ) or asynchronous discussions can occur using the Discussions tool in CourseWorks (Canvas) .
Table 2 includes a few interactive case method approaches. Regardless of the approach selected, it is important to create a learning environment in which students feel comfortable participating in a case activity and learning from one another. See below for tips on supporting student in how to learn from a case in the “getting started” section and how to create a supportive learning environment in the Guide for Inclusive Teaching at Columbia .
Table 2. Strategies for Engaging Students in Case-Based Learning
Approaches to case teaching should be informed by course learning objectives, and can be adapted for small, large, hybrid, and online classes. Instructional technology can be used in various ways to deliver, facilitate, and assess the case method. For instance, an online module can be created in CourseWorks (Canvas) to structure the delivery of the case, allow students to work at their own pace, engage all learners, even those reluctant to speak up in class, and assess understanding of a case and student learning. Modules can include text, embedded media (e.g., using Panopto or Mediathread ) curated by the instructor, online discussion, and assessments. Students can be asked to read a case and/or watch a short video, respond to quiz questions and receive immediate feedback, post questions to a discussion, and share resources.
For more information about options for incorporating educational technology to your course, please contact your Learning Designer .
To ensure that students are learning from the case approach, ask them to pause and reflect on what and how they learned from the case. Time to reflect builds your students’ metacognition, and when these reflections are collected they provides you with insights about the effectiveness of your approach in promoting student learning.
Well designed case-based learning experiences: 1) motivate student involvement, 2) have students doing the work, 3) help students develop knowledge and skills, and 4) have students learning from each other.
Designing a case-based learning experience should center around the learning objectives for a course. The following points focus on intentional design.
Identify learning objectives, determine scope, and anticipate challenges.
- Why use the case method in your course? How will it promote student learning differently than other approaches?
- What are the learning objectives that need to be met by the case method? What knowledge should students apply and skills should they practice?
- What is the scope of the case? (a brief activity in a single class session to a semester-long case-based course; if new to case method, start small with a single case).
- What challenges do you anticipate (e.g., student preparation and prior experiences with case learning, discomfort with discussion, peer-to-peer learning, managing discussion) and how will you plan for these in your design?
- If you are asking students to use transferable skills for the case method (e.g., teamwork, digital literacy) make them explicit.
Determine how you will know if the learning objectives were met and develop a plan for evaluating the effectiveness of the case method to inform future case teaching.
- What assessments and criteria will you use to evaluate student work or participation in case discussion?
- How will you evaluate the effectiveness of the case method? What feedback will you collect from students?
- How might you leverage technology for assessment purposes? For example, could you quiz students about the case online before class, accept assignment submissions online, use audience response systems (e.g., PollEverywhere) for formative assessment during class?
Select an existing case, create your own, or encourage students to bring course-relevant cases, and prepare for its delivery
- Where will the case method fit into the course learning sequence?
- Is the case at the appropriate level of complexity? Is it inclusive, culturally relevant, and relatable to students?
- What materials and preparation will be needed to present the case to students? (e.g., readings, audiovisual materials, set up a module in CourseWorks).
Plan for the case discussion and an active role for students
- What will your role be in facilitating case-based learning? How will you model case analysis for your students? (e.g., present a short case and demo your approach and the process of case learning) (Davis, 2009).
- What discussion guidelines will you use that include your students’ input?
- How will you encourage students to ask and answer questions, summarize their work, take notes, and debrief the case?
- If students will be working in groups, how will groups form? What size will the groups be? What instructions will they be given? How will you ensure that everyone participates? What will they need to submit? Can technology be leveraged for any of these areas?
- Have you considered students of varied cognitive and physical abilities and how they might participate in the activities/discussions, including those that involve technology?
Student preparation and expectations
- How will you communicate about the case method approach to your students? When will you articulate the purpose of case-based learning and expectations of student engagement? What information about case-based learning and expectations will be included in the syllabus?
- What preparation and/or assignment(s) will students complete in order to learn from the case? (e.g., read the case prior to class, watch a case video prior to class, post to a CourseWorks discussion, submit a brief memo, complete a short writing assignment to check students’ understanding of a case, take on a specific role, prepare to present a critique during in-class discussion).
Andersen, E. and Schiano, B. (2014). Teaching with Cases: A Practical Guide . Harvard Business Press.
Bonney, K. M. (2015). Case Study Teaching Method Improves Student Performance and Perceptions of Learning Gains†. Journal of Microbiology & Biology Education , 16 (1), 21–28. https://doi.org/10.1128/jmbe.v16i1.846
Davis, B.G. (2009). Chapter 24: Case Studies. In Tools for Teaching. Second Edition. Jossey-Bass.
Garvin, D.A. (2003). Making the Case: Professional Education for the world of practice. Harvard Magazine. September-October 2003, Volume 106, Number 1, 56-107.
Golich, V.L. (2000). The ABCs of Case Teaching. International Studies Perspectives. 1, 11-29.
Golich, V.L.; Boyer, M; Franko, P.; and Lamy, S. (2000). The ABCs of Case Teaching. Pew Case Studies in International Affairs. Institute for the Study of Diplomacy.
Heath, J. (2015). Teaching & Writing Cases: A Practical Guide. The Case Center, UK.
Herreid, C.F. (2011). Case Study Teaching. New Directions for Teaching and Learning. No. 128, Winder 2011, 31 – 40.
Herreid, C.F. (2007). Start with a Story: The Case Study Method of Teaching College Science . National Science Teachers Association. Available as an ebook through Columbia Libraries.
Herreid, C.F. (2006). “Clicker” Cases: Introducing Case Study Teaching Into Large Classrooms. Journal of College Science Teaching. Oct 2006, 36(2). https://search.proquest.com/docview/200323718?pq-origsite=gscholar
Krain, M. (2016). Putting the Learning in Case Learning? The Effects of Case-Based Approaches on Student Knowledge, Attitudes, and Engagement. Journal on Excellence in College Teaching. 27(2), 131-153.
Lundberg, K.O. (Ed.). (2011). Our Digital Future: Boardrooms and Newsrooms. Knight Case Studies Initiative.
Popil, I. (2011). Promotion of critical thinking by using case studies as teaching method. Nurse Education Today, 31(2), 204–207. https://doi.org/10.1016/j.nedt.2010.06.002
Schiano, B. and Andersen, E. (2017). Teaching with Cases Online . Harvard Business Publishing.
Thistlethwaite, JE; Davies, D.; Ekeocha, S.; Kidd, J.M.; MacDougall, C.; Matthews, P.; Purkis, J.; Clay D. (2012). The effectiveness of case-based learning in health professional education: A BEME systematic review . Medical Teacher. 2012; 34(6): e421-44.
Yadav, A.; Lundeberg, M.; DeSchryver, M.; Dirkin, K.; Schiller, N.A.; Maier, K. and Herreid, C.F. (2007). Teaching Science with Case Studies: A National Survey of Faculty Perceptions of the Benefits and Challenges of Using Cases. Journal of College Science Teaching; Sept/Oct 2007; 37(1).
Weimer, M. (2013). Learner-Centered Teaching: Five Key Changes to Practice. Second Edition. Jossey-Bass.
Additional resources
Teaching with Cases , Harvard Kennedy School of Government.
Features “what is a teaching case?” video that defines a teaching case, and provides documents to help students prepare for case learning, Common case teaching challenges and solutions, tips for teaching with cases.
Promoting excellence and innovation in case method teaching: Teaching by the Case Method , Christensen Center for Teaching & Learning. Harvard Business School.
National Center for Case Study Teaching in Science . University of Buffalo.
A collection of peer-reviewed STEM cases to teach scientific concepts and content, promote process skills and critical thinking. The Center welcomes case submissions. Case classification scheme of case types and teaching methods:
- Different types of cases: analysis case, dilemma/decision case, directed case, interrupted case, clicker case, a flipped case, a laboratory case.
- Different types of teaching methods: problem-based learning, discussion, debate, intimate debate, public hearing, trial, jigsaw, role-play.
Columbia Resources
Resources available to support your use of case method: The University hosts a number of case collections including: the Case Consortium (a collection of free cases in the fields of journalism, public policy, public health, and other disciplines that include teaching and learning resources; SIPA’s Picker Case Collection (audiovisual case studies on public sector innovation, filmed around the world and involving SIPA student teams in producing the cases); and Columbia Business School CaseWorks , which develops teaching cases and materials for use in Columbia Business School classrooms.
Center for Teaching and Learning
The Center for Teaching and Learning (CTL) offers a variety of programs and services for instructors at Columbia. The CTL can provide customized support as you plan to use the case method approach through implementation. Schedule a one-on-one consultation.
Office of the Provost
The Hybrid Learning Course Redesign grant program from the Office of the Provost provides support for faculty who are developing innovative and technology-enhanced pedagogy and learning strategies in the classroom. In addition to funding, faculty awardees receive support from CTL staff as they redesign, deliver, and evaluate their hybrid courses.
The Start Small! Mini-Grant provides support to faculty who are interested in experimenting with one new pedagogical strategy or tool. Faculty awardees receive funds and CTL support for a one-semester period.
Explore our teaching resources.
- Blended Learning
- Contemplative Pedagogy
- Inclusive Teaching Guide
- FAQ for Teaching Assistants
- Metacognition
CTL resources and technology for you.
- Overview of all CTL Resources and Technology
- The origins of this method can be traced to Harvard University where in 1870 the Law School began using cases to teach students how to think like lawyers using real court decisions. This was followed by the Business School in 1920 (Garvin, 2003). These professional schools recognized that lecture mode of instruction was insufficient to teach critical professional skills, and that active learning would better prepare learners for their professional lives. ↩
- Golich, V.L. (2000). The ABCs of Case Teaching. International Studies Perspectives. 1, 11-29. ↩
- Herreid, C.F. (2007). Start with a Story: The Case Study Method of Teaching College Science . National Science Teachers Association. Available as an ebook through Columbia Libraries. ↩
- Davis, B.G. (2009). Chapter 24: Case Studies. In Tools for Teaching. Second Edition. Jossey-Bass. ↩
- Andersen, E. and Schiano, B. (2014). Teaching with Cases: A Practical Guide . Harvard Business Press. ↩
- Lundberg, K.O. (Ed.). (2011). Our Digital Future: Boardrooms and Newsrooms. Knight Case Studies Initiative. ↩
- Heath, J. (2015). Teaching & Writing Cases: A Practical Guide. The Case Center, UK. ↩
- Bonney, K. M. (2015). Case Study Teaching Method Improves Student Performance and Perceptions of Learning Gains†. Journal of Microbiology & Biology Education , 16 (1), 21–28. https://doi.org/10.1128/jmbe.v16i1.846 ↩
- Krain, M. (2016). Putting the Learning in Case Learning? The Effects of Case-Based Approaches on Student Knowledge, Attitudes, and Engagement. Journal on Excellence in College Teaching. 27(2), 131-153. ↩
- Thistlethwaite, JE; Davies, D.; Ekeocha, S.; Kidd, J.M.; MacDougall, C.; Matthews, P.; Purkis, J.; Clay D. (2012). The effectiveness of case-based learning in health professional education: A BEME systematic review . Medical Teacher. 2012; 34(6): e421-44. ↩
- Yadav, A.; Lundeberg, M.; DeSchryver, M.; Dirkin, K.; Schiller, N.A.; Maier, K. and Herreid, C.F. (2007). Teaching Science with Case Studies: A National Survey of Faculty Perceptions of the Benefits and Challenges of Using Cases. Journal of College Science Teaching; Sept/Oct 2007; 37(1). ↩
- Popil, I. (2011). Promotion of critical thinking by using case studies as teaching method. Nurse Education Today, 31(2), 204–207. https://doi.org/10.1016/j.nedt.2010.06.002 ↩
- Weimer, M. (2013). Learner-Centered Teaching: Five Key Changes to Practice. Second Edition. Jossey-Bass. ↩
- Herreid, C.F. (2006). “Clicker” Cases: Introducing Case Study Teaching Into Large Classrooms. Journal of College Science Teaching. Oct 2006, 36(2). https://search.proquest.com/docview/200323718?pq-origsite=gscholar ↩
This website uses cookies to identify users, improve the user experience and requires cookies to work. By continuing to use this website, you consent to Columbia University's use of cookies and similar technologies, in accordance with the Columbia University Website Cookie Notice .
- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Instructional Materials
- Free Resources
- American Rescue Plan
- For Preservice Teachers
NCCSTS Case Collection
- Science and STEM Education Jobs
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning
MyNSTA Community
- My Collections
Case Study Listserv
Permissions & Guidelines
Submit a Case Study
Resources & Publications
Enrich your students’ educational experience with case-based teaching
The NCCSTS Case Collection, created and curated by the National Center for Case Study Teaching in Science, on behalf of the University at Buffalo, contains over a thousand peer-reviewed case studies on a variety of topics in all areas of science.
Cases (only) are freely accessible; subscription is required for access to teaching notes and answer keys.
Subscribe Today
Browse Case Studies
Latest Case Studies

Development of the NCCSTS Case Collection was originally funded by major grants to the University at Buffalo from the National Science Foundation , The Pew Charitable Trusts , and the U.S. Department of Education .
- Open access
- Published: 15 May 2024
Learning together for better health using an evidence-based Learning Health System framework: a case study in stroke
- Helena Teede 1 , 2 na1 ,
- Dominique A. Cadilhac 3 , 4 na1 ,
- Tara Purvis 3 ,
- Monique F. Kilkenny 3 , 4 ,
- Bruce C.V. Campbell 4 , 5 , 6 ,
- Coralie English 7 ,
- Alison Johnson 2 ,
- Emily Callander 1 ,
- Rohan S. Grimley 8 , 9 ,
- Christopher Levi 10 ,
- Sandy Middleton 11 , 12 ,
- Kelvin Hill 13 &
- Joanne Enticott ORCID: orcid.org/0000-0002-4480-5690 1
BMC Medicine volume 22 , Article number: 198 ( 2024 ) Cite this article
498 Accesses
2 Altmetric
Metrics details
In the context of expanding digital health tools, the health system is ready for Learning Health System (LHS) models. These models, with proper governance and stakeholder engagement, enable the integration of digital infrastructure to provide feedback to all relevant parties including clinicians and consumers on performance against best practice standards, as well as fostering innovation and aligning healthcare with patient needs. The LHS literature primarily includes opinion or consensus-based frameworks and lacks validation or evidence of benefit. Our aim was to outline a rigorously codesigned, evidence-based LHS framework and present a national case study of an LHS-aligned national stroke program that has delivered clinical benefit.
Current core components of a LHS involve capturing evidence from communities and stakeholders (quadrant 1), integrating evidence from research findings (quadrant 2), leveraging evidence from data and practice (quadrant 3), and generating evidence from implementation (quadrant 4) for iterative system-level improvement. The Australian Stroke program was selected as the case study as it provides an exemplar of how an iterative LHS works in practice at a national level encompassing and integrating evidence from all four LHS quadrants. Using this case study, we demonstrate how to apply evidence-based processes to healthcare improvement and embed real-world research for optimising healthcare improvement. We emphasize the transition from research as an endpoint, to research as an enabler and a solution for impact in healthcare improvement.
Conclusions
The Australian Stroke program has nationally improved stroke care since 2007, showcasing the value of integrated LHS-aligned approaches for tangible impact on outcomes. This LHS case study is a practical example for other health conditions and settings to follow suit.
Peer Review reports
Internationally, health systems are facing a crisis, driven by an ageing population, increasing complexity, multi-morbidity, rapidly advancing health technology and rising costs that threaten sustainability and mandate transformation and improvement [ 1 , 2 ]. Although research has generated solutions to healthcare challenges, and the advent of big data and digital health holds great promise, entrenched siloes and poor integration of knowledge generation, knowledge implementation and healthcare delivery between stakeholders, curtails momentum towards, and consistent attainment of, evidence-and value-based care [ 3 ]. This is compounded by the short supply of research and innovation leadership within the healthcare sector, and poorly integrated and often inaccessible health data systems, which have crippled the potential to deliver on digital-driven innovation [ 4 ]. Current approaches to healthcare improvement are also often isolated with limited sustainability, scale-up and impact [ 5 ].
Evidence suggests that integration and partnership across academic and healthcare delivery stakeholders are key to progress, including those with lived experience and their families (referred to here as consumers and community), diverse disciplines (both research and clinical), policy makers and funders. Utilization of evidence from research and evidence from practice including data from routine care, supported by implementation research, are key to sustainably embedding improvement and optimising health care and outcomes. A strategy to achieve this integration is through the Learning Health System (LHS) (Fig. 1 ) [ 2 , 6 , 7 , 8 ]. Although there are numerous publications on LHS approaches [ 9 , 10 , 11 , 12 ], many focus on research perspectives and data, most do not demonstrate tangible healthcare improvement or better health outcomes. [ 6 ]
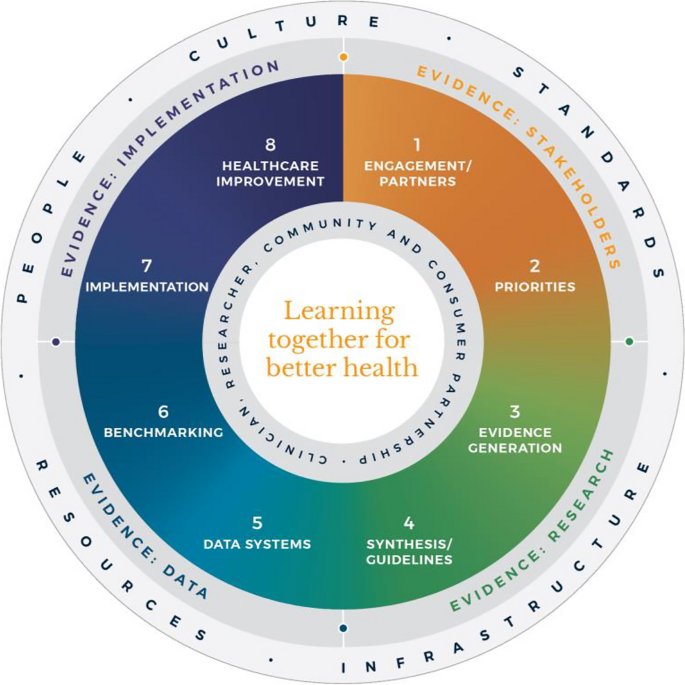
Monash Learning Health System: The Learn Together for Better Health Framework developed by Monash Partners and Monash University (from Enticott et al. 2021 [ 7 ]). Four evidence quadrants: Q1 (orange) is evidence from stakeholders; Q2 (green) is evidence from research; Q3 (light blue) is evidence from data; and, Q4 (dark blue) is evidence from implementation and healthcare improvement
In developed nations, it has been estimated that 60% of care provided aligns with the evidence base, 30% is low value and 10% is potentially harmful [ 13 ]. In some areas, clinical advances have been rapid and research and evidence have paved the way for dramatic improvement in outcomes, mandating rapid implementation of evidence into healthcare (e.g. polio and COVID-19 vaccines). However, healthcare improvement is challenging and slow [ 5 ]. Health systems are highly complex in their design, networks and interacting components, and change is difficult to enact, sustain and scale up. [ 3 ] New effective strategies are needed to meet community needs and deliver evidence-based and value-based care, which reorients care from serving the provider, services and system, towards serving community needs, based on evidence and quality. It goes beyond cost to encompass patient and provider experience, quality care and outcomes, efficiency and sustainability [ 2 , 6 ].
The costs of stroke care are expected to rise rapidly in the next decades, unless improvements in stroke care to reduce the disabling effects of strokes can be successfully developed and implemented [ 14 ]. Here, we briefly describe the Monash LHS framework (Fig. 1 ) [ 2 , 6 , 7 ] and outline an exemplar case in order to demonstrate how to apply evidence-based processes to healthcare improvement and embed real-world research for optimising healthcare. The Australian LHS exemplar in stroke care has driven nationwide improvement in stroke care since 2007.
An evidence-based Learning Health System framework
In Australia, members of this author group (HT, AJ, JE) have rigorously co-developed an evidence-based LHS framework, known simply as the Monash LHS [ 7 ]. The Monash LHS was designed to support sustainable, iterative and continuous robust benefit of improved clinical outcomes. It was created with national engagement in order to be applicable to Australian settings. Through this rigorous approach, core LHS principles and components have been established (Fig. 1 ). Evidence shows that people/workforce, culture, standards, governance and resources were all key to an effective LHS [ 2 , 6 ]. Culture is vital including trust, transparency, partnership and co-design. Key processes include legally compliant data sharing, linkage and governance, resources, and infrastructure [ 4 ]. The Monash LHS integrates disparate and often siloed stakeholders, infrastructure and expertise to ‘Learn Together for Better Health’ [ 7 ] (Fig. 1 ). This integrates (i) evidence from community and stakeholders including priority areas and outcomes; (ii) evidence from research and guidelines; (iii) evidence from practice (from data) with advanced analytics and benchmarking; and (iv) evidence from implementation science and health economics. Importantly, it starts with the problem and priorities of key stakeholders including the community, health professionals and services and creates an iterative learning system to address these. The following case study was chosen as it is an exemplar of how a Monash LHS-aligned national stroke program has delivered clinical benefit.
Australian Stroke Learning Health System
Internationally, the application of LHS approaches in stroke has resulted in improved stroke care and outcomes [ 12 ]. For example, in Canada a sustained decrease in 30-day in-hospital mortality has been found commensurate with an increase in resources to establish the multifactorial stroke system intervention for stroke treatment and prevention [ 15 ]. Arguably, with rapid advances in evidence and in the context of an ageing population with high cost and care burden and substantive impacts on quality of life, stroke is an area with a need for rapid research translation into evidence-based and value-based healthcare improvement. However, a recent systematic review found that the existing literature had few comprehensive examples of LHS adoption [ 12 ]. Although healthcare improvement systems and approaches were described, less is known about patient-clinician and stakeholder engagement, governance and culture, or embedding of data informatics into everyday practice to inform and drive improvement [ 12 ]. For example, in a recent review of quality improvement collaborations, it was found that although clinical processes in stroke care are improved, their short-term nature means there is uncertainty about sustainability and impacts on patient outcomes [ 16 ]. Table 1 provides the main features of the Australian Stroke LHS based on the four core domains and eight elements of the Learning Together for Better Health Framework described in Fig. 1 . The features are further expanded on in the following sections.
Evidence from stakeholders (LHS quadrant 1, Fig. 1 )
Engagement, partners and priorities.
Within the stroke field, there have been various support mechanisms to facilitate an LHS approach including partnership and broad stakeholder engagement that includes clinical networks and policy makers from different jurisdictions. Since 2008, the Australian Stroke Coalition has been co-led by the Stroke Foundation, a charitable consumer advocacy organisation, and Stroke Society of Australasia a professional society with membership covering academics and multidisciplinary clinician networks, that are collectively working to improve stroke care ( https://australianstrokecoalition.org.au/ ). Surveys, focus groups and workshops have been used for identifying priorities from stakeholders. Recent agreed priorities have been to improve stroke care and strengthen the voice for stroke care at a national ( https://strokefoundation.org.au/ ) and international level ( https://www.world-stroke.org/news-and-blog/news/world-stroke-organization-tackle-gaps-in-access-to-quality-stroke-care ), as well as reduce duplication amongst stakeholders. This activity is built on a foundation and culture of research and innovation embedded within the stroke ‘community of practice’. Consumers, as people with lived experience of stroke are important members of the Australian Stroke Coalition, as well as representatives from different clinical colleges. Consumers also provide critical input to a range of LHS activities via the Stroke Foundation Consumer Council, Stroke Living Guidelines committees, and the Australian Stroke Clinical Registry (AuSCR) Steering Committee (described below).
Evidence from research (LHS quadrant 2, Fig. 1 )
Advancement of the evidence for stroke interventions and synthesis into clinical guidelines.
To implement best practice, it is crucial to distil the large volume of scientific and trial literature into actionable recommendations for clinicians to use in practice [ 24 ]. The first Australian clinical guidelines for acute stroke were produced in 2003 following the increasing evidence emerging for prevention interventions (e.g. carotid endarterectomy, blood pressure lowering), acute medical treatments (intravenous thrombolysis, aspirin within 48 h of ischemic stroke), and optimised hospital management (care in dedicated stroke units by a specialised and coordinated multidisciplinary team) [ 25 ]. Importantly, a number of the innovations were developed, researched and proven effective by key opinion leaders embedded in the Australian stroke care community. In 2005, the clinical guidelines for Stroke Rehabilitation and Recovery [ 26 ] were produced, with subsequent merged guidelines periodically updated. However, the traditional process of periodic guideline updates is challenging for end users when new research can render recommendations redundant and this lack of currency erodes stakeholder trust [ 27 ]. In response to this challenge the Stroke Foundation and Cochrane Australia entered a pioneering project to produce the first electronic ‘living’ guidelines globally [ 20 ]. Major shifts in the evidence for reperfusion therapies (e.g. extended time-window intravenous thrombolysis and endovascular clot retrieval), among other advances, were able to be converted into new recommendations, approved by the Australian National Health and Medical Research Council within a few months of publication. Feedback on this process confirmed the increased use and trust in the guidelines by clinicians. The process informed other living guidelines programs, including the successful COVID-19 clinical guidelines [ 28 ].
However, best practice clinical guideline recommendations are necessary but insufficient for healthcare improvement and nesting these within an LHS with stakeholder partnership, enables implementation via a range of proven methods, including audit and feedback strategies [ 29 ].
Evidence from data and practice (LHS quadrant 3, Fig. 1 )
Data systems and benchmarking : revealing the disparities in care between health services. A national system for standardized stroke data collection was established as the National Stroke Audit program in 2007 by the Stroke Foundation [ 30 ] following various state-level programs (e.g. New South Wales Audit) [ 31 ] to identify evidence-practice gaps and prioritise improvement efforts to increase access to stroke units and other acute treatments [ 32 ]. The Audit program alternates each year between acute (commencing in 2007) and rehabilitation in-patient services (commencing in 2008). The Audit program provides a ‘deep dive’ on the majority of recommendations in the clinical guidelines whereby participating hospitals provide audits of up to 40 consecutive patient medical records and respond to a survey about organizational resources to manage stroke. In 2009, the AuSCR was established to provide information on patients managed in acute hospitals based on a small subset of quality processes of care linked to benchmarked reports of performance (Fig. 2 ) [ 33 ]. In this way, the continuous collection of high-priority processes of stroke care could be regularly collected and reviewed to guide improvement to care [ 34 ]. Plus clinical quality registry programs within Australia have shown a meaningful return on investment attributed to enhanced survival, improvements in quality of life and avoided costs of treatment or hospital stay [ 35 ].
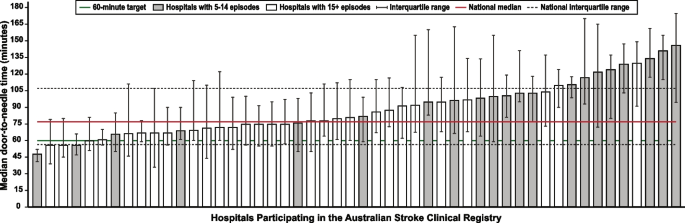
Example performance report from the Australian Stroke Clinical Registry: average door-to-needle time in providing intravenous thrombolysis by different hospitals in 2021 [ 36 ]. Each bar in the figure represents a single hospital
The Australian Stroke Coalition endorsed the creation of an integrated technological solution for collecting data through a single portal for multiple programs in 2013. In 2015, the Stroke Foundation, AuSCR consortium, and other relevant groups cooperated to design an integrated data management platform (the Australian Stroke Data Tool) to reduce duplication of effort for hospital staff in the collection of overlapping variables in the same patients [ 19 ]. Importantly, a national data dictionary then provided the common data definitions to facilitate standardized data capture. Another important feature of AuSCR is the collection of patient-reported outcome surveys between 90 and 180 days after stroke, and annual linkage with national death records to ascertain survival status [ 33 ]. To support a LHS approach, hospitals that participate in AuSCR have access to a range of real-time performance reports. In efforts to minimize the burden of data collection in the AuSCR, interoperability approaches to import data directly from hospital or state-level managed stroke databases have been established (Fig. 3 ); however, the application has been variable and 41% of hospitals still manually enter all their data.
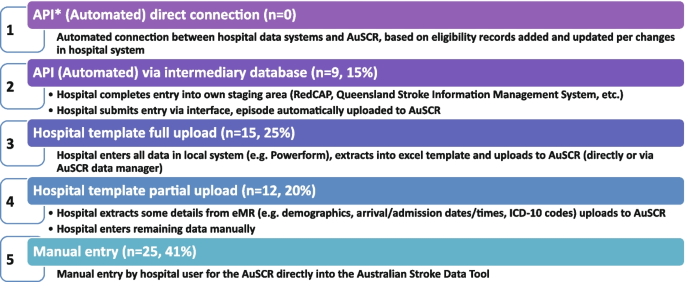
Current status of automated data importing solutions in the Australian Stroke Clinical Registry, 2022, with ‘ n ’ representing the number of hospitals. AuSCR, Australian Stroke Clinical Registry; AuSDaT, Australian Stroke Data Tool; API, Application Programming Interface; ICD, International Classification of Diseases; RedCAP, Research Electronic Data Capture; eMR, electronic medical records
For acute stroke care, the Australian Commission on Quality and Safety in Health Care facilitated the co-design (clinicians, academics, consumers) and publication of the national Acute Stroke Clinical Care Standard in 2015 [ 17 ], and subsequent review [ 18 ]. The indicator set for the Acute Stroke Standard then informed the expansion of the minimum dataset for AuSCR so that hospitals could routinely track their performance. The national Audit program enabled hospitals not involved in the AuSCR to assess their performance every two years against the Acute Stroke Standard. Complementing these efforts, the Stroke Foundation, working with the sector, developed the Acute and Rehabilitation Stroke Services Frameworks to outline the principles, essential elements, models of care and staffing recommendations for stroke services ( https://informme.org.au/guidelines/national-stroke-services-frameworks ). The Frameworks are intended to guide where stroke services should be developed, and monitor their uptake with the organizational survey component of the Audit program.
Evidence from implementation and healthcare improvement (LHS quadrant 4, Fig. 1 )
Research to better utilize and augment data from registries through linkage [ 37 , 38 , 39 , 40 ] and to ensure presentation of hospital or service level data are understood by clinicians has ensured advancement in the field for the Australian Stroke LHS [ 41 ]. Importantly, greater insights into whole patient journeys, before and after a stroke, can now enable exploration of value-based care. The LHS and stroke data platform have enabled focused and time-limited projects to create a better understanding of the quality of care in acute or rehabilitation settings [ 22 , 42 , 43 ]. Within stroke, all the elements of an LHS culminate into the ready availability of benchmarked performance data and support for implementation of strategies to address gaps in care.
Implementation research to grow the evidence base for effective improvement interventions has also been a key pillar in the Australian context. These include multi-component implementation interventions to achieve behaviour change for particular aspects of stroke care, [ 22 , 23 , 44 , 45 ] and real-world approaches to augmenting access to hyperacute interventions in stroke through the use of technology and telehealth [ 46 , 47 , 48 , 49 ]. The evidence from these studies feeds into the living guidelines program and the data collection systems, such as the Audit program or AuSCR, which are then amended to ensure data aligns to recommended care. For example, the use of ‘hyperacute aspirin within the first 48 h of ischemic stroke’ was modified to be ‘hyperacute antiplatelet…’ to incorporate new evidence that other medications or combinations are appropriate to use. Additionally, new datasets have been developed to align with evidence such as the Fever, Sugar, and Swallow variables [ 42 ]. Evidence on improvements in access to best practice care from the acute Audit program [ 50 ] and AuSCR is emerging [ 36 ]. For example, between 2007 and 2017, the odds of receiving intravenous thrombolysis after ischemic stroke increased by 16% 9OR 1.06 95% CI 1.13–1.18) and being managed in a stroke unit by 18% (OR 1.18 95% CI 1.17–1.20). Over this period, the median length of hospital stay for all patients decreased from 6.3 days in 2007 to 5.0 days in 2017 [ 51 ]. When considering the number of additional patients who would receive treatment in 2017 in comparison to 2007 it was estimated that without this additional treatment, over 17,000 healthy years of life would be lost in 2017 (17,786 disability-adjusted life years) [ 51 ]. There is evidence on the cost-effectiveness of different system-focussed strategies to augment treatment access for acute ischemic stroke (e.g. Victorian Stroke Telemedicine program [ 52 ] and Melbourne Mobile Stroke Unit ambulance [ 53 ]). Reciprocally, evidence from the national Rehabilitation Audit, where the LHS approach has been less complete or embedded, has shown fewer areas of healthcare improvement over time [ 51 , 54 ].
Within the field of stroke in Australia, there is indirect evidence that the collective efforts that align to establishing the components of a LHS have had an impact. Overall, the age-standardised rate of stroke events has reduced by 27% between 2001 and 2020, from 169 to 124 events per 100,000 population. Substantial declines in mortality rates have been reported since 1980. Commensurate with national clinical guidelines being updated in 2007 and the first National Stroke Audit being undertaken in 2007, the mortality rates for men (37.4 deaths per 100,000) and women (36.1 deaths per 100,0000 has declined to 23.8 and 23.9 per 100,000, respectively in 2021 [ 55 ].
Underpinning the LHS with the integration of the four quadrants of evidence from stakeholders, research and guidelines, practice and implementation, and core LHS principles have been addressed. Leadership and governance have been important, and programs have been established to augment workforce training and capacity building in best practice professional development. Medical practitioners are able to undertake courses and mentoring through the Australasian Stroke Academy ( http://www.strokeacademy.com.au/ ) while nurses (and other health professionals) can access teaching modules in stroke care from the Acute Stroke Nurses Education Network ( https://asnen.org/ ). The Association of Neurovascular Clinicians offers distance-accessible education and certification to develop stroke expertise for interdisciplinary professionals, including advanced stroke co-ordinator certification ( www.anvc.org ). Consumer initiative interventions are also used in the design of the AuSCR Public Summary Annual reports (available at https://auscr.com.au/about/annual-reports/ ) and consumer-related resources related to the Living Guidelines ( https://enableme.org.au/resources ).
The important success factors and lessons from stroke as a national exemplar LHS in Australia include leadership, culture, workforce and resources integrated with (1) established and broad partnerships across the academic-clinical sector divide and stakeholder engagement; (2) the living guidelines program; (3) national data infrastructure, including a national data dictionary that provides the common data framework to support standardized data capture; (4) various implementation strategies including benchmarking and feedback as well as engagement strategies targeting different levels of the health system; and (5) implementation and improvement research to advance stroke systems of care and reduce unwarranted variation in practice (Fig. 1 ). Priority opportunities now include the advancement of interoperability with electronic medical records as an area all clinical quality registry’s programs needs to be addressed, as well as providing more dynamic and interactive data dashboards tailored to the need of clinicians and health service executives.
There is a clear mandate to optimise healthcare improvement with big data offering major opportunities for change. However, we have lacked the approaches to capture evidence from the community and stakeholders, to integrate evidence from research, to capture and leverage data or evidence from practice and to generate and build on evidence from implementation using iterative system-level improvement. The LHS provides this opportunity and is shown to deliver impact. Here, we have outlined the process applied to generate an evidence-based LHS and provide a leading exemplar in stroke care. This highlights the value of moving from single-focus isolated approaches/initiatives to healthcare improvement and the benefit of integration to deliver demonstrable outcomes for our funders and key stakeholders — our community. This work provides insight into strategies that can both apply evidence-based processes to healthcare improvement as well as implementing evidence-based practices into care, moving beyond research as an endpoint, to research as an enabler, underpinning delivery of better healthcare.
Availability of data and materials
Not applicable
Abbreviations
Australian Stroke Clinical Registry
Confidence interval
- Learning Health System
World Health Organization. Delivering quality health services . OECD Publishing; 2018.
Enticott J, Braaf S, Johnson A, Jones A, Teede HJ. Leaders’ perspectives on learning health systems: A qualitative study. BMC Health Serv Res. 2020;20:1087.
Article PubMed PubMed Central Google Scholar
Melder A, Robinson T, McLoughlin I, Iedema R, Teede H. An overview of healthcare improvement: Unpacking the complexity for clinicians and managers in a learning health system. Intern Med J. 2020;50:1174–84.
Article PubMed Google Scholar
Alberto IRI, Alberto NRI, Ghosh AK, Jain B, Jayakumar S, Martinez-Martin N, et al. The impact of commercial health datasets on medical research and health-care algorithms. Lancet Digit Health. 2023;5:e288–94.
Article CAS PubMed PubMed Central Google Scholar
Dixon-Woods M. How to improve healthcare improvement—an essay by Mary Dixon-Woods. BMJ. 2019;367: l5514.
Enticott J, Johnson A, Teede H. Learning health systems using data to drive healthcare improvement and impact: A systematic review. BMC Health Serv Res. 2021;21:200.
Enticott JC, Melder A, Johnson A, Jones A, Shaw T, Keech W, et al. A learning health system framework to operationalize health data to improve quality care: An Australian perspective. Front Med (Lausanne). 2021;8:730021.
Dammery G, Ellis LA, Churruca K, Mahadeva J, Lopez F, Carrigan A, et al. The journey to a learning health system in primary care: A qualitative case study utilising an embedded research approach. BMC Prim Care. 2023;24:22.
Foley T, Horwitz L, Zahran R. The learning healthcare project: Realising the potential of learning health systems. 2021. Available from https://learninghealthcareproject.org/wp-content/uploads/2021/05/LHS2021report.pdf . Accessed Jan 2024.
Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Washington: The National Academies Press; 2013.
Google Scholar
Zurynski Y, Smith CL, Vedovi A, Ellis LA, Knaggs G, Meulenbroeks I, et al. Mapping the learning health system: A scoping review of current evidence - a white paper. 2020:63
Cadilhac DA, Bravata DM, Bettger J, Mikulik R, Norrving B, Uvere E, et al. Stroke learning health systems: A topical narrative review with case examples. Stroke. 2023;54:1148–59.
Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: The 60–30-10 challenge. BMC Med. 2020;18:1–8.
Article Google Scholar
King D, Wittenberg R, Patel A, Quayyum Z, Berdunov V, Knapp M. The future incidence, prevalence and costs of stroke in the UK. Age Ageing. 2020;49:277–82.
Ganesh A, Lindsay P, Fang J, Kapral MK, Cote R, Joiner I, et al. Integrated systems of stroke care and reduction in 30-day mortality: A retrospective analysis. Neurology. 2016;86:898–904.
Lowther HJ, Harrison J, Hill JE, Gaskins NJ, Lazo KC, Clegg AJ, et al. The effectiveness of quality improvement collaboratives in improving stroke care and the facilitators and barriers to their implementation: A systematic review. Implement Sci. 2021;16:16.
Australian Commission on Safety and Quality in Health Care. Acute stroke clinical care standard. 2015. Available from https://www.safetyandquality.gov.au/our-work/clinical-care-standards/acute-stroke-clinical-care-standard . Accessed Jan 2024.
Australian Commission on Safety and Quality in Health Care. Acute stroke clinical care standard. Sydney: ACSQHC; 2019. Available from https://www.safetyandquality.gov.au/publications-and-resources/resource-library/acute-stroke-clinical-care-standard-evidence-sources . Accessed Jan 2024.
Ryan O, Ghuliani J, Grabsch B, Hill K, G CC, Breen S, et al. Development, implementation, and evaluation of the Australian Stroke Data Tool (AuSDaT): Comprehensive data capturing for multiple uses. Health Inf Manag. 2022:18333583221117184.
English C, Bayley M, Hill K, Langhorne P, Molag M, Ranta A, et al. Bringing stroke clinical guidelines to life. Int J Stroke. 2019;14:337–9.
English C, Hill K, Cadilhac DA, Hackett ML, Lannin NA, Middleton S, et al. Living clinical guidelines for stroke: Updates, challenges and opportunities. Med J Aust. 2022;216:510–4.
Cadilhac DA, Grimley R, Kilkenny MF, Andrew NE, Lannin NA, Hill K, et al. Multicenter, prospective, controlled, before-and-after, quality improvement study (Stroke123) of acute stroke care. Stroke. 2019;50:1525–30.
Cadilhac DA, Marion V, Andrew NE, Breen SJ, Grabsch B, Purvis T, et al. A stepped-wedge cluster-randomized trial to improve adherence to evidence-based practices for acute stroke management. Jt Comm J Qual Patient Saf. 2022.
Elliott J, Lawrence R, Minx JC, Oladapo OT, Ravaud P, Jeppesen BT, et al. Decision makers need constantly updated evidence synthesis. Nature. 2021;600:383–5.
Article CAS PubMed Google Scholar
National Stroke Foundation. National guidelines for acute stroke management. Melbourne: National Stroke Foundation; 2003.
National Stroke Foundation. Clinical guidelines for stroke rehabilitation and recovery. Melbourne: National Stroke Foundation; 2005.
Phan TG, Thrift A, Cadilhac D, Srikanth V. A plea for the use of systematic review methodology when writing guidelines and timely publication of guidelines. Intern Med J . 2012;42:1369–1371; author reply 1371–1362
Tendal B, Vogel JP, McDonald S, Norris S, Cumpston M, White H, et al. Weekly updates of national living evidence-based guidelines: Methods for the Australian living guidelines for care of people with COVID-19. J Clin Epidemiol. 2021;131:11–21.
Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7:50.
Harris D, Cadilhac D, Hankey GJ, Hillier S, Kilkenny M, Lalor E. National stroke audit: The Australian experience. Clin Audit. 2010;2:25–31.
Cadilhac DA, Purvis T, Kilkenny MF, Longworth M, Mohr K, Pollack M, et al. Evaluation of rural stroke services: Does implementation of coordinators and pathways improve care in rural hospitals? Stroke. 2013;44:2848–53.
Cadilhac DA, Moss KM, Price CJ, Lannin NA, Lim JY, Anderson CS. Pathways to enhancing the quality of stroke care through national data monitoring systems for hospitals. Med J Aust. 2013;199:650–1.
Cadilhac DA, Lannin NA, Anderson CS, Levi CR, Faux S, Price C, et al. Protocol and pilot data for establishing the Australian Stroke Clinical Registry. Int J Stroke. 2010;5:217–26.
Ivers N, Jamtvedt G, Flottorp S, Young J, Odgaard-Jensen J, French S, et al. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev . 2012
Australian Commission on Safety and Quality in Health Care. Economic evaluation of clinical quality registries. Final report. . 2016:79
Cadilhac DA, Dalli LL, Morrison J, Lester M, Paice K, Moss K, et al. The Australian Stroke Clinical Registry annual report 2021. Melbourne; 2022. Available from https://auscr.com.au/about/annual-reports/ . Accessed 6 May 2024.
Kilkenny MF, Kim J, Andrew NE, Sundararajan V, Thrift AG, Katzenellenbogen JM, et al. Maximising data value and avoiding data waste: A validation study in stroke research. Med J Aust. 2019;210:27–31.
Eliakundu AL, Smith K, Kilkenny MF, Kim J, Bagot KL, Andrew E, et al. Linking data from the Australian Stroke Clinical Registry with ambulance and emergency administrative data in Victoria. Inquiry. 2022;59:469580221102200.
PubMed Google Scholar
Andrew NE, Kim J, Cadilhac DA, Sundararajan V, Thrift AG, Churilov L, et al. Protocol for evaluation of enhanced models of primary care in the management of stroke and other chronic disease (PRECISE): A data linkage healthcare evaluation study. Int J Popul Data Sci. 2019;4:1097.
CAS PubMed PubMed Central Google Scholar
Mosalski S, Shiner CT, Lannin NA, Cadilhac DA, Faux SG, Kim J, et al. Increased relative functional gain and improved stroke outcomes: A linked registry study of the impact of rehabilitation. J Stroke Cerebrovasc Dis. 2021;30: 106015.
Ryan OF, Hancock SL, Marion V, Kelly P, Kilkenny MF, Clissold B, et al. Feedback of aggregate patient-reported outcomes (PROs) data to clinicians and hospital end users: Findings from an Australian codesign workshop process. BMJ Open. 2022;12:e055999.
Grimley RS, Rosbergen IC, Gustafsson L, Horton E, Green T, Cadigan G, et al. Dose and setting of rehabilitation received after stroke in Queensland, Australia: A prospective cohort study. Clin Rehabil. 2020;34:812–23.
Purvis T, Middleton S, Craig LE, Kilkenny MF, Dale S, Hill K, et al. Inclusion of a care bundle for fever, hyperglycaemia and swallow management in a national audit for acute stroke: Evidence of upscale and spread. Implement Sci. 2019;14:87.
Middleton S, McElduff P, Ward J, Grimshaw JM, Dale S, D’Este C, et al. Implementation of evidence-based treatment protocols to manage fever, hyperglycaemia, and swallowing dysfunction in acute stroke (QASC): A cluster randomised controlled trial. Lancet. 2011;378:1699–706.
Middleton S, Dale S, Cheung NW, Cadilhac DA, Grimshaw JM, Levi C, et al. Nurse-initiated acute stroke care in emergency departments. Stroke. 2019:STROKEAHA118020701.
Hood RJ, Maltby S, Keynes A, Kluge MG, Nalivaiko E, Ryan A, et al. Development and pilot implementation of TACTICS VR: A virtual reality-based stroke management workflow training application and training framework. Front Neurol. 2021;12:665808.
Bladin CF, Kim J, Bagot KL, Vu M, Moloczij N, Denisenko S, et al. Improving acute stroke care in regional hospitals: Clinical evaluation of the Victorian Stroke Telemedicine program. Med J Aust. 2020;212:371–7.
Bladin CF, Bagot KL, Vu M, Kim J, Bernard S, Smith K, et al. Real-world, feasibility study to investigate the use of a multidisciplinary app (Pulsara) to improve prehospital communication and timelines for acute stroke/STEMI care. BMJ Open. 2022;12:e052332.
Zhao H, Coote S, Easton D, Langenberg F, Stephenson M, Smith K, et al. Melbourne mobile stroke unit and reperfusion therapy: Greater clinical impact of thrombectomy than thrombolysis. Stroke. 2020;51:922–30.
Purvis T, Cadilhac DA, Hill K, Reyneke M, Olaiya MT, Dalli LL, et al. Twenty years of monitoring acute stroke care in Australia from the national stroke audit program (1999–2019): Achievements and areas of future focus. J Health Serv Res Policy. 2023.
Cadilhac DA, Purvis T, Reyneke M, Dalli LL, Kim J, Kilkenny MF. Evaluation of the national stroke audit program: 20-year report. Melbourne; 2019.
Kim J, Tan E, Gao L, Moodie M, Dewey HM, Bagot KL, et al. Cost-effectiveness of the Victorian Stroke Telemedicine program. Aust Health Rev. 2022;46:294–301.
Kim J, Easton D, Zhao H, Coote S, Sookram G, Smith K, et al. Economic evaluation of the Melbourne mobile stroke unit. Int J Stroke. 2021;16:466–75.
Stroke Foundation. National stroke audit – rehabilitation services report 2020. Melbourne; 2020.
Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. 2023. Webpage https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts/contents/about (accessed Jan 2024).
Download references
Acknowledgements
The following authors hold National Health and Medical Research Council Research Fellowships: HT (#2009326), DAC (#1154273), SM (#1196352), MFK Future Leader Research Fellowship (National Heart Foundation #105737). The Funders of this work did not have any direct role in the design of the study, its execution, analyses, interpretation of the data, or decision to submit results for publication.
Author information
Helena Teede and Dominique A. Cadilhac contributed equally.
Authors and Affiliations
Monash Centre for Health Research and Implementation, 43-51 Kanooka Grove, Clayton, VIC, Australia
Helena Teede, Emily Callander & Joanne Enticott
Monash Partners Academic Health Science Centre, 43-51 Kanooka Grove, Clayton, VIC, Australia
Helena Teede & Alison Johnson
Stroke and Ageing Research, Department of Medicine, School of Clinical Sciences at Monash Health, Monash University, Level 2 Monash University Research, Victorian Heart Hospital, 631 Blackburn Rd, Clayton, VIC, Australia
Dominique A. Cadilhac, Tara Purvis & Monique F. Kilkenny
Stroke Theme, The Florey Institute of Neuroscience and Mental Health, University of Melbourne, Heidelberg, VIC, Australia
Dominique A. Cadilhac, Monique F. Kilkenny & Bruce C.V. Campbell
Department of Neurology, Melbourne Brain Centre, Royal Melbourne Hospital, Parkville, VIC, Australia
Bruce C.V. Campbell
Department of Medicine, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia
School of Health Sciences, Heart and Stroke Program, University of Newcastle, Hunter Medical Research Institute, University Drive, Callaghan, NSW, Australia
Coralie English
School of Medicine and Dentistry, Griffith University, Birtinya, QLD, Australia
Rohan S. Grimley
Clinical Excellence Division, Queensland Health, Brisbane, Australia
John Hunter Hospital, Hunter New England Local Health District and University of Newcastle, Sydney, NSW, Australia
Christopher Levi
School of Nursing, Midwifery and Paramedicine, Australian Catholic University, Sydney, NSW, Australia
Sandy Middleton
Nursing Research Institute, St Vincent’s Health Network Sydney and and Australian Catholic University, Sydney, NSW, Australia
Stroke Foundation, Level 7, 461 Bourke St, Melbourne, VIC, Australia
Kelvin Hill
You can also search for this author in PubMed Google Scholar
Contributions
HT: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. DAC: conception, design and initial draft, provided essential literature and case study examples, approved the submitted version. TP: revised the manuscript critically for important intellectual content, approved the submitted version. MFK: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. BC: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. CE: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. AJ: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. EC: revised the manuscript critically for important intellectual content, approved the submitted version. RSG: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. CL: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. SM: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. KH: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. JE: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. All authors read and approved the final manuscript.
Authors’ Twitter handles
@HelenaTeede
@DominiqueCad
@Coralie_English
@EmilyCallander
@EnticottJo
Corresponding authors
Correspondence to Helena Teede or Dominique A. Cadilhac .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Teede, H., Cadilhac, D.A., Purvis, T. et al. Learning together for better health using an evidence-based Learning Health System framework: a case study in stroke. BMC Med 22 , 198 (2024). https://doi.org/10.1186/s12916-024-03416-w
Download citation
Received : 23 July 2023
Accepted : 30 April 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12916-024-03416-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Evidence-based medicine
- Person-centred care
- Models of care
- Healthcare improvement
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Predictors of effective clinical teaching – nursing educators’ perspective
O. m. al-rawajfah.
1 College of Nursing, Sultan Qaboos University, P.O. Box 66, Al Khoud, Muscat, Oman
L. Al Hadid
2 Faculty of Nursing, Al Balqa Applied University, P.O. Box 206, Salt, 19117 Jordan
G. K. Madhavanprabhakaran
3 Faculty of Health Sciences, Kristianstad University, Elmetorpsvägen 15, SE-291 88 Kristianstad, Sweden
Associated Data
The datasets generated and/or analysed during the current study are not publicly available due [restrictions by the Research and Ethics Committee in the College of Nursing at Sultan Qaboos University to protect the participants’ privacy] but are available from the Principal Investigator (Omar Al-Rawajfah) on reasonable request.
The clinical teaching is the core component of the nursing curriculum, the alarming pandemic rates brought uncertainty to clinical teaching, weighing the safety of patients, students, and faculty, which demanded essential modification in clinical teaching and resulted in challenges in relation to effective response to clinical teaching requirements. This study aimed to assess the effective clinical teaching from the nurse educators’ perspective during the remote teaching that followed the COVID-19 pandemic.
This study is a national Web-based descriptive study. Participants were recruited from five major Nursing Colleges in Oman. Descriptive and inferential as well as multiple linear regression analyses were conducted.
A total of 127 nurse educators completed the survey with mean age of 43.9 (SD = 6.9) years. The overall effective clinical teaching score was 54.4 (SD = 10.9) which is considered acceptable, although the nurse educators in Oman reported the highest score on the safety dimension of the effective clinical teaching. Furthermore, females, doctoral prepared nurse educators, and those who acted as preceptors reported higher effective clinical teaching levels compared to their counterparts. The regression analysis showed that age, gender, and attending infection control training are significant predictors of effective clinical teaching.
The paradigm shift in clinical teaching requires adequate measures including identification and appropriate training of clinical instructors and preceptors to meet clinical teaching demands in remote teaching. It is also important to take actions that promote and maintain the safety prioritization in bedside clinical teaching. These measures might positively impact on the nursing education process.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12912-022-00836-y.
The outbreak of coronavirus disease 2019 (COVID-19) erupted in Wuhan, China in December 2019 and reached pandemic level in March 2020 [ 1 ]. According to the latest statistics published by the WHO on January 22, 2022, there were more than 323 million confirmed cases with more than 5.5 million deaths globally. In the Eastern Mediterranean region, the pandemic’s effects were also disastrous, with more than 17.5 million confirmed cases and 318,268 deaths [ 2 ]. Furthermore, the Sultanate of Oman has been greatly affected by the pandemic. With the total lockdown of societies including educational facilities, the extensive spread of the pandemic has resulted in drastic challenges and changes in nursing education including suspension of training of nursing students in clinical settings.
One of the most important challenges is the quick and effective response of nursing educators to modify the learning experience to be compatible with safety requirements for patients, students, and nursing educators [ 3 – 5 ]. The response to these challenges was managed at institutional and global levels. For example, in January 2020, the WHO published its first COVID-19 course through its OpenWHO platform. According to the weekly operational update on COVID-19 published by the WHO, more than 6 million people had enrolled on 39 courses, and more than 3.2 million certificates had been issued by the platform [ 6 ]. The purpose of these courses is to improve the response to health emergencies and obtain the latest scientific and operational know-how. Although many of these courses are directed to the public, some are directed to health-care educators and professionals [ 6 ].
Regulatory and nursing education accreditation bodies such as the Commission on Collegiate Nursing Education [ 7 ], the Accreditation Commission for Education in Nursing [ 8 ], and the Canadian Association of Schools of Nursing [ 9 ] have issued their statements concerning the required changes to nursing education programs to adapt to the pandemic situation. These changes have stressed the concept of flexibility along with maintaining program outcomes and safety for all educational process stakeholders. Effective clinical teaching (ECT) within the pandemic context became a core concept to maintaining nursing program outcomes and safety [ 3 – 5 ]. The preliminary research on COVID-19 has shown that health-care professionals, including nurses, are putting their efforts into fighting the pandemic with less consciousness of their personal safety [ 10 ]. Indeed, one initial report of 44,672 COVID-19 cases from China showed a prevalence rate of 3.8% among health-care professionals [ 10 ].
In clinical teaching, the development of professional identity and expansion of clinical skills is offered through appropriate clinical learning and conducive clinical environment where theoretical knowledge is applied into the practical aspects [ 11 ]. Wider exposures in the clinical units are key factors for developing the cognitive and affective activities including the psychomotor mastery of skills [ 12 ]. The emergence of the pandemic has put the clinical nursing practice at crossroads leaving behind the concern of how to teach the clinical courses in an environment of social distancing and quarantine measures [ 3 ]. Many factors contribute to shape an effective clinical instructor such as sound preparation, awareness of attributes needed for a clinical teacher, integrating evidence-based knowledge into teaching, enhancing good communication skills, and adapting to different environmental factors. These are major components required for an ECT [ 13 ]. COVID-19 pandemic has left behind a lesson about why it is important to future-proof the clinical learning for nursing students and has highlighted the need to recalibrate the organization and facilitation of clinical education and thus produce competent and confident nurses [ 14 ]. In addition to it, the pandemic has also shown how important it is to integrate technology for clinical training and develop a variety of teaching methods to continue the clinical education. The situation has demanded the clinical trainers to be committed and develop teaching practices that would allow application of critical thinking. Trainers are expected to leave their comfort zones and have readiness to face scenarios that constantly keep changing. Updating the teaching skills is a good practice to achieve positive clinical learning outcomes [ 15 ]. Perceived characteristics for clinical instructors that are considered best are possessing a thorough knowledge and refined skills, good communication styles, being compassionate and respectful. Competent and professional clinical teachers also exhibit humanistic behaviors [ 13 ]. Awareness of those characteristics creates a path for reinforcing, modifying, and developing teaching strategies and attitudes, which in turn promotes clinical learning making it a worthy enjoyable experience [ 16 ].
In Oman, there are four nursing programs that offer a bachelor’s degree of nursing and only one (College of Nursing at Sultan Qaboos University) that offers three masters of nursing programs, and one program that offers a one-year postgraduate nursing specialized diploma (the Higher Institute of Health Specialties). Nurse educators in these programs have been largely affected by the pandemic and have created their own innovative methods to maintain ECT for their nursing students. Assessing ECT within the remote teaching situation is critical to maintaining an optimal learning experience for students. No previous studies have been conducted to assess ECT in Oman. Hence, this study aimed to assess ECT and its associated factors from nurse educators’ perspectives during the remote teaching that followed the COVID-19 pandemic.
This study was a national web-based descriptive study. The study involved data collection using an online survey. For the purpose of this study, “nurse educator” was defined as a professional nurse engaged in teaching activities for nursing students at the time of the study or who has been engaged in teaching activities within the last 6 months.
Settings and sampling
The study participants were recruited from four major colleges in Oman that offer a bachelor’s degree in nursing. Two of the study settings were governmental colleges, whereas the other two were private colleges. The two governmental colleges are the largest in the country. All the colleges are offering the bachelor’s degree of nursing science. Only the college affiliated to the principal investigator is offering the master’s degree of nursing science. This study utilized the convenient sampling technique. Faculty members in the study settings were invited to participate in the study based on individual invitation through their official emails. The study hyperlink was initially sent to about 400 nurse educators. A reminder was sent after 1 week from the initial invitation. The electronic survey was designed to be completed only once to prevent possible duplication of responses. No specific exclusion criteria were applied in the study. Ethical approval was secured from an affiliated university of the principal investigator as well as from the Ministry of Health research ethics committee. The survey was anonymous and no participant’s identification data were collected. On the front page of the survey, participants were given a full explanation about the study and asked to voluntarily click on the “starting” icon to commence the survey.
The current study was conducted during the initial period of the pandemic, in which the bedside-clinical teaching was suspended and replaced by online clinical teaching sessions. Data collection started on August 2020 and was finalized in December 2020. In the current study setting, the online-clinical sessions included different approaches such as online-case study discussions, watching clinical-based videos followed by online discussion, and reviewing de-identified clinical cases as well as developing an appropriate care plan. For most of the above-mentioned teaching approaches, the clinical educators were interacting with the students using both synchronous and asynchronous online modes. In the current study setting, the clinical educators were responsible for supervising a number of students ranging from 2 to 10 students, where the number of the students is reduced in the introductory clinical courses. After resuming the face-to-face clinical teaching, students were given a refreshing period where the clinical components during the lockdown period were reviewed before introducing the new clinical components.
Sample size calculation
For the current study, a ratio of 1:10 and 1:15 subject for each predictor was used based on sample size recommendations by different researchers [ 17 – 19 ]. Accordingly, with a moderate effect size (R 2 = 0.13) and a power of 0.80 and α = 0.05, and 10 predictors, the required sample size was 119 subjects. Given the fact that 127 nurse educators have filled the survey, the sample size in the current study was considered adequate for performing multiple linear regression analysis.
Study instrument
The Effective Clinical Teaching Inventory (ECTI) was developed to meet the objective of the study. This newly developed tool was mainly based on the previous Effective Clinical Instructor Characteristics Inventory [ 20 ] and the Preceptor’s Clinical Teaching Learning Inventory [ 21 ]. Essential modifications were made based on current literature to be more relevant to major concepts of clinical teaching adhering to COVID-19 prevention and control protocols. The instrument items were stated to reflect the extent to which nurse educators were ready to conduct clinical teaching, taking into consideration the pandemic requirement. Content validity was established by obtaining expert opinion from six clinical educators (3 PhD and 3 MSN) currently in the field of clinical teaching. For the purpose of the current study, clinical educators are PhD or Master-prepared nurses who are engaged in teaching clinical courses at the time of conducting the study. In the current study setting, MSN-prepared nurse educators are primary responsible for direct supervising of students in the bedside clinical settings. Whereas PhD-prepared nurse educators are responsible for clinical course development and participating in students’ evaluation based on scheduled clinical site visits. The final version of the inventory was composed of 17 items scored on a four-point Likert scale that ranged from four (to a greater extent) to one (to a lesser extent). The items were categorized into four main dimensions including: support (5 items), professional qualities (5 items), safety (3 items), and feedback (4 items). The categorization of the tool was done based on the agreement and expertise of the research team. The tool was pilot tested among five clinical nurse educators who approved the final version for clarity and readability. All of the clinical nurse educators participated in the pilot testing were Master-prepared nurse. Along with the ECTI, biographical information of the participants was collected via a biographical information sheet. Based on the current study sample, the final modified version had a Cronbach’s alpha reliability coefficient of 0.95, which demonstrates an excellent level of internal consistency. The Cronbach’s alpha for the subscales were 0.86, 0.85, 0.82, and 0.89 for support, professional qualities, safety, and feedback subscales, respectively (see Supplement I for the complete list of the items).
The total score of the tool is ranging between 17 to 68. For the current study, the total score was categorized into 3 categories: (a) total scores less than the 50th percentile (range 17 to 43) were classified as “suboptimal effective”; (b) scores between the 50th and 75th percentiles (range 44 to 56) were classified as “satisfactory effective”; and (c) scores exceeding the 75th percentile (range 57 to 68) were classified as “highly effective”. The categorization was validated by 3 PhD-prepared nursing educators.
Data analysis
Data were analyzed using SPSS®-PC Version 23. Descriptive statistics, including frequencies, percentages, means, and standard deviations were used to describe the study sample. The mean score of ECT was compared across different variables using an independent t-test and one-way ANOVA (with post-hoc correction where applicable), as appropriate. The normality assumption was validated before running the analysis and no serious violation was found. In order to compare the scores at the subscale level, a mean score out of four was computed for each subscale. Finally, multiple linear regression analysis was used to test possible predictors of “ECT”. For the regression modeling, we have used the “enter” method for selecting the predictors in the final model. No missing data were found for any of the study variables.
Sample characteristics
A total of 127 nursing educators completed the electronic survey, with an overall response rate of 31.8%. The mean age of participants was 43.9 (SD = 6.9) years with a range of 30–60 years. The majority of participants (78%, n = 99) were female, had academic experience of more than 10 years (70.1%, n = 89), had a master’s degree (68.5%, n = 87), and a role in the training process in clinical settings (76.4%, n = 97). The majority of participants (78%, n = 99) had previous training related to infection control. However, 41.7% ( n = 53) reported that they did not receive any training concerning teaching methods during the COVID-19 pandemic. The WHO website was the most common first choice source of information for participants (39.4%, n = 50) (Table 1 ).
Sample characteristics of the nurse educators, n = 127
a Missing data for clinician = 5, Academician = 1
b Clinical instructor: A Master-prepared nurse educator who is responsible for direct supervision of the students in the clinical settings. Course coordinator: A PhD-prepared nurse educator who is responsible for clinical course development and participating in students’ evaluation based on scheduled clinical site visits. Preceptor: is a clinically active nurse who provides an in-depth clarification/education of specific procedures
Factors associated with effective clinical teaching
The mean scores for the subscale out of four were ( M = 3.31, SD = 0.67) for safety; ( M = 3.25, SD = 0.76) for feedback; ( M = 3.20, SD = 0.66) for professional qualities; and ( M = 3.21, SD = 0.71) for support. The overall ECT score was 54.4 ( SD = 10.9), which represented 80% of the highest possible score. According to the total score categories, the majority of the nurse educators (48.8%, n = 62) were classified as highly effective.
Female nurse educators reported a greater ECT level ( M = 58.0, SD = 9.5) than males ( M = 53.4, SD = 11.0, p = 0.046). The total ECT score was statistically significant across different academic levels ( F = 6.60, p = 0.002). The Tukey post hoc comparison showed that doctoral prepared nurse educators reported higher ECT ( M = 56.0, SD = 8.4) than masters prepared nurse educators ( M = 55.3, SD = 10.1, p = 0.002) and bachelor prepared nurse educators ( M = 44.1, SD = 15.6, p = 0.003). Further, masters prepared nurse educators reported a higher ECT score ( M = 55.3, SD = 10.1) than bachelor prepared nurse educators ( M = 44.1, SD = 15.6, p = 0.002).
The overall ECT score was statistically different across different teaching roles ( F = 3.40, p = 0.033). Post hoc analysis with unequal variance was assumed (Tamhane procedure) and revealed that preceptors reported higher ECT score ( M = 62.7, SD = 4.6), than clinical instructor ( M = 53.2, SD = 11.4, p = 0.005). No other significant differences were detected. Moreover, nurse educators who acted as preceptors, reported a higher ECT ( M = 62.7, SD = 4.6) than course coordinators ( M = 57.7, SD = 8.0) and clinical instructors ( M = 53.2, SD = 1.4, p = 0.033) (Table 2 ).
Effective Clinical Training, mean scores and the associated factors
# Tamhane post-hoc procedure (preceptors vs clinical instructors, p = 0.005)
*Tukey post hoc (doctoral vs masters prepared nurse educators, p = 0.002; doctoral vs bachelor prepared nurse educators, p = 0.003; masters vs bachelor prepared nurse educators, p = 0.002)
Predictors of effective clinical teaching
A linear regression analysis was conducted to identify possible predictors of ECT. Variables entered in the model were age, gender, teaching role, academic level, experience as an academic, experience as a clinician, attending infection control training, attending staff development related to teaching during the COVID-19 pandemic, and first sources of information. The results revealed that age, gender, and attending infection control training were significant predictors of ECT (Table 3 ). The overall model was statistically significant (F = 3.00, p = 0.004, with an overall R = 0.45, R 2 = 0.20, and adjusted R 2 = 0.14).
Linear Regression for Predictors of Effective Clinical Teaching
reference group for the Dummy variables were as the following: male (gender), clinical instructor (teaching role), BSN (academic level), No (attended infection control training), No (attended staff development), and other sources (first source of information)
This study aimed to assess the ECT from the nurse educators’ perspective. Gender and academic degree were identified as significantly important factors associated with different levels of ECT in that female and doctoral prepared educators were found to have higher levels of ECT. In addition, age, gender, and attending infection control training were identified as significant predictors of ECT. Clinical preceptors (bedside nurses), who acted as nurse educators reported higher ECT compared to full time faculty clinical instructors and nurse educators who acted as course coordinators. The most commonly reported source of information for participants was the formal WHO website. This finding suggests that academic staff are genuinely updated on infection control with ongoing WHO reports, guidelines, and recommendations related to the pandemic. However, we can hardly make conclusions as this could possibly be associated with the current situation of COVID-19, and not necessarily a common practice among nurse educators.
Although the current study revealed an acceptable level of ECT, about half of the participants (41.8%) reported that they did not receive any training concerning teaching methods adopted during the COVID-19 pandemic, including the use of electronic platforms and the range of options available within these platforms such as the use of shared material, the whiteboard, or the use of dynamic teaching material. In addition, knowledge about the COVID-19 pandemic and how to manage patients with this infection were not addressed nor had the educators received any training in relation to this. Although clinical teaching is the core component of the nursing curriculum, the alarming pandemic rates brought uncertainty to clinical teaching, weighing the safety of patients, students, and faculty, which demanded essential modification in clinical teaching to ensure safety of stakeholders involved in the clinical teaching process. Indeed, a substantial motion has emerged to redefine clinical teaching and how this core component of health-care education can be conducted and evaluated [ 3 – 5 ]. With the paradigm shift in clinical teaching during this pandemic, the role of restorative supervision and professional resilience enhancement programs became essential for ECT [ 22 ].
This study is probably one of the earliest studies focusing on the concept of ECT during the COVID-19 pandemic. The traditional view of ECT within nursing is mainly focused on nurse educators’ behaviors and their professional qualities that promote effective transfer of clinical knowledge to students [ 23 – 25 ]. During the current period of widespread COVID-19, this concept has become even more important for all stakeholders of the clinical teaching process [ 3 , 26 ]. In the current study, among different dimensions of ECT, nurse educators in Oman reported the highest score on the safety dimension of the ECT. This reflects that the nurse educators are valuing safety among the highest priorities during bedside clinical teaching. However, the data collected in this study are limited and we could not determine the level of knowledge about COVID-19 among the educators.
The pandemic has imposed many changes to healthcare and nursing curricula. Shifting to remote and online teaching has created a new dimension to the concept of ECT [ 27 ]. Before the pandemic, the nursing curricula were based on direct supervision of the students, especially for the clinical courses. Whereas, after the pandemic different new approaches became essential competent of the nursing curricula. For example, electronic platforms to explain theoretical material, the use of educational videos, virtual simulation, and other innovative methods were used as alternative methods over traditional clinical teaching [ 28 , 29 ]. Although these methods have been used in the past, the intensity of their use was much less than the current situation. This extensive use was not accompanied by appropriate assessment of the ability of health-care educators to deliver ECT. Therefore, future research should consider exploring the effects of these innovative approaches on the ECT. In addition, there were no reports on training of educators on the use of these methods to cover all clinical course objectives. Hence, future research may consider assessing the readiness of nurse educators to integrate the new innovative approaches in the clinical teaching modalities. Furthermore, reports showed that nursing students have become more independent self-leaners [ 30 ]. Students become less dependent on their nurse educators on finding the information and switch to unclassical sources of information even when it is less reliable sources [ 31 ]. Future research may consider exploring the role of nurse educators in supporting the self-learning in the ECT.
During the COVID-19 pandemic, many changes and challenges were introduced to academia and have surely influenced nursing students’ psychological status. Students have reported a high level of anxiety and stress related to the shift in their teaching methods as well as lockdown consequences [ 32 – 34 ]. With this stressful learning environment, students need educators who are available for support. In the current study, about 86% of nurse educators reported that they could provide the appropriate psychological support to students during their clinical teaching. However, no specific elements of this support were assessed during this study. Different reports have shown that psychological support from different parties, including educators, is a critical element to overcome students’ psychological distress associated with COVID-19 consequences, including stress associated with graduation and joining the workforce to care for patients with COVID-19 [ 34 – 36 ].
The unforeseen circumstances of COVID-19 has raised questions concerning the current practices of clinical training during clinical placement, whether students could go to the setting or be trained using electronic platforms [ 37 ]. In addition, other questions have been raised regarding whether clinical training would be the same after COVID-19 has been controlled or not. Therefore, it is important for nursing programs to gain insight into these perceived feelings within nurse educators and to assess areas that require optimizing, especially in clinical training strategies [ 3 ]. With this uncertainty, students need a role model to follow and guide them in this difficult leaning environment. Professional qualities of nurse educators are critical in creating a role model for students. In the current study, the majority of nurse educators (83%) reported that they can act as a role model for their students when providing direct patient care and demonstrating clinical skills while maintaining safety requirements. Different reports have stressed the importance of the role model during clinical education [ 38 – 40 ]. Students have always acknowledged the role model of the nurse educator as an effective method of transferring knowledge and clinical experience to them [ 38 , 41 ]. Furthermore, the current study showed that preceptor nurse educators reported a higher level of ECT than other nursing educators. This finding is consistent with previous studies [ 16 , 42 , 43 ]. Preceptors are usually practicing nurses. Therefore, they are more engaged in direct patient care and are more aware of patient and professional safety requirements during this pandemic. This makes them excellent role models for students, who can be an effective solution for staff shortages especially when regular academic educators are unable to be available with students at the bedside level.
Many published studies have addressed the impact of COVID-19 on students’ safety, preparedness, and clinical placements. However, this study examined nurse educators’ preparedness and how well they are expected to perform as the pandemic exists. Staff development and continuing education are essential factors for ECT [ 44 , 45 ]. The current study demonstrated that staff who have engaged in infection control educational programs reported a higher level of ECT. During this pandemic, the WHO have created different educational programs for health-care providers and educators [ 46 ]. These programs are aimed to enhance patient and professional safety. In the current study, more than half of the nurse educators reported that the WHO website is their first source of information. This reflects that the majority of nurse educators seek reliable sources of information in order to deliver ECT.
Methodological aspects
The current study’s response rate is about 32%, which is relatively low for an academic community. The low response rate is commonly reported in online survey methodologies [ 47 , 48 ]. Different reports have suggested that a response rate for online survey is normally ranged between 25 and 30% [ 49 , 50 ]. Nevertheless, one possible reason for the low response rate in the current study could be the timing of the data collection, which was at the peak of the pandemic when academic institutions, in the country and globally, had shifted to remote and online teaching. Faculty members were mostly busy in shifting a lot of the educational material into online format, which may have resulted in survey fatigue and reduced the interest in taking part of this survey.
The univariate analysis showed that four factors were significantly associated with the overall ECT score for the nursing educators. However, using the multiple regression modeling, three significant predictors for ECT were identified with an overall adjusted R2 = 0.14. This is relatively low explanatory power. As discussed early, this study was conducted at the early stage of the pandemic. It seems the survey has not captured many different aspects related to ECT during the pandemic. For example, previous reports have suggested that providing different types of support is an essential component of ECT [ 51 ]. The current study did not tap many aspects and types of support by the nurse educators. Further, as the available information about COVID-19 in terms of prognosis, treatment, vaccines, and other related issues were still evolving, nurse educators may lack sufficient knowledge about the disease. However, the current study did not assess the knowledge about COVID-19 and hence knowledge was not included in the regression model.
Limitations
As it was introduced earlier, the pandemic has forced nurse educators to utilize different teaching methods to supplement the clinical teaching. Although this study has explored the perspective of nurse educators about the ECT, it did not investigate the influence of these methods on the ECT because of the nature of the study design (cross-sectional). Hence, we recommend strongly that future studies investigate different teaching methods’ effect on the ECT to gain better insight into and understanding of the ECT.
This study focused on ECT from the nurse educator perspective. However, it is important to investigate students’ perspectives about ECT during the COVID-19 pandemic. Future research may consider comparing the perceptions of both parties (students and educators). Moreover, future research may consider conducting multi-country studies comparing and contrasting experiences in which global understanding of ECT during pandemic or disaster situations can be achieved. Furthermore, this study did not examine the psychological impact of this pandemic on nurse educators as they had to change many of their academic and clinical plans to accommodate the lockdowns associated with it. Many studies have investigated the impact of the pandemic on students; however, this study addressed nurse educators’ perspectives. Yet, the findings from the current study should be taken in the context of the convenient sampling and the relatively low response rate (32%) which may limit the generalizability of the findings. Finally, although the current study tool has achieved the initial psychometric properties (i.e. internal consistency and content validity), it requires further assessment by conducting an Exploratory Factor Analysis. Because of the relatively small sample size, assessing the dimensions of the tool using the factor analysis method was not feasible. Future research can consider a further assessment of the tool.
Nursing education in Middle Eastern countries during COVID-19 has taught important lessons. Pandemic preparedness and mitigation plans need to be in place not only to meet the health care demands but also the training of students on health-care professional courses, especially nursing. Adequate measures including identification and appropriate training of clinical instructors and preceptors to meet clinical teaching demands during the pandemic will bring a positive impact to the education process. Therefore, it is imperative to emphasize the need to ensure educators’ readiness to use electronic platforms and methods of education, to reflect both knowledge and experience to students during limited clinical training opportunities. Sound implementation of educational policies in developing countries will help in responding to, coping with, and quickly recovering from future occurrences like emergency disasters or pandemics.
Acknowledgements
Not applicable.
Abbreviations
Authors’ contributions.
OAR is the Principal Investigator and responsible for data collection, analysis, and drafting the manuscript. LAH contributed to tool development, discussion and reviewing of the manuscript. GKM contributed to tool development, data collection, and writing the manuscript. FF contributed to data collection and writing the manuscript. AK critically reviewed and revised the manuscript, including the results section, and is the corresponding author. All authors approved the final version of the manuscript.
Open access funding provided by Kristianstad University.
Availability of data and materials
Declarations.
Ethical approval was obtained from the affiliated university of the principal investigator as well as from the Ministry of Health research ethics committee. In addition, all methods were performed in accordance with the ethical guidelines and regulations for research among human subjects following the Helsinki Declaration [ 52 ]. The survey was anonymous and no participant’s identification data were collected. On the front page of the survey, participants were given a full explanation about the study and asked to voluntarily click on the “starting” icon to commence the survey. With other words, the participants actively gave informed consent once they chose to proceed to the survey.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
O. M. Al-Rawajfah, Email: mo.ude.uqs@hafjawar .
L. Al Hadid, Email: [email protected] .
G. K. Madhavanprabhakaran, Email: mo.ude.uqs@ajirig .
F. Francis, Email: [email protected] .
A. Khalaf, Email: [email protected] .

Quality and Safety Education for Nurses
Strategy submission, using unfolding case studies to develop clinical forethought in novice nursing students.
Brenda Moench
RN, MS, CNE
Nursing Instructor
Institution:
University of Wisconsin Milwaukee
Competency Categories:
Patient-Centered Care, Safety
Learner Level(s):
Pre-Licensure ADN/Diploma, Pre-Licensure BSN
Learner Setting(s):
Strategy Type:
Case Studies
Learning Objectives:
Strategy Overview:
Submitted Materials:
Teaching-Strategy-QSEN-TS-241-1.docx - https://drive.google.com/open?id=1AECA5dGZdE6YPXxF0DmMMC8M9maipFe5&usp=drive_copy
Additional Materials:
Benner, P., Hughes, R.G., & Sutphen, M., (2008). Patient safety and quality: An evidence-based handbook for nurses. Rockville, MD: Agency for Healthcare Research and Quality. Tanner, C.A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45, 204-211.
Evaluation Description:
- Open access
- Published: 22 May 2024
Preparedness for a first clinical placement in nursing: a descriptive qualitative study
- Philippa H. M. Marriott 1 ,
- Jennifer M. Weller-Newton 2 nAff3 &
- Katharine J. Reid 4
BMC Nursing volume 23 , Article number: 345 ( 2024 ) Cite this article
162 Accesses
2 Altmetric
Metrics details
A first clinical placement for nursing students is a challenging period involving translation of theoretical knowledge and development of an identity within the healthcare setting; it is often a time of emotional vulnerability. It can be a pivotal moment for ambivalent nursing students to decide whether to continue their professional training. To date, student expectations prior to their first clinical placement have been explored in advance of the experience or gathered following the placement experience. However, there is a significant gap in understanding how nursing students’ perspectives about their first clinical placement might change or remain consistent following their placement experiences. Thus, the study aimed to explore first-year nursing students’ emotional responses towards and perceptions of their preparedness for their first clinical placement and to examine whether initial perceptions remain consistent or change during the placement experience.
The research utilised a pre-post qualitative descriptive design. Six focus groups were undertaken before the first clinical placement (with up to four participants in each group) and follow-up individual interviews ( n = 10) were undertaken towards the end of the first clinical placement with first-year entry-to-practice postgraduate nursing students. Data were analysed thematically.
Three main themes emerged: (1) adjusting and managing a raft of feelings, encapsulating participants’ feelings about learning in a new environment and progressing from academia to clinical practice; (2) sinking or swimming, comprising students’ expectations before their first clinical placement and how these perceptions are altered through their clinical placement experience; and (3) navigating placement, describing relationships between healthcare staff, patients, and peers.
Conclusions
This unique study of first-year postgraduate entry-to-practice nursing students’ perspectives of their first clinical placement adds to the extant knowledge. By examining student experience prior to and during their first clinical placement experience, it is possible to explore the consistency and change in students’ narratives over the course of an impactful experience. Researching the narratives of nursing students embarking on their first clinical placement provides tertiary education institutions with insights into preparing students for this critical experience.
Peer Review reports
First clinical placements enable nursing students to develop their professional identity through initial socialisation, and where successful, first clinical placement experiences can motivate nursing students to persist with their studies [ 1 , 2 , 3 , 4 ]. Where the transition from the tertiary environment to learning in the healthcare workplace is turbulent, it may impact nursing students’ learning, their confidence and potentially increase attrition rates from educational programs [ 2 , 5 , 6 ]. Attrition from preregistration nursing courses is a global concern, with the COVID-19 pandemic further straining the nursing workforce; thus, the supply of nursing professionals is unlikely to meet demand [ 7 ]. The COVID-19 pandemic has also impacted nursing education, with student nurses augmenting the diminishing nursing workforce [ 7 , 8 ].
The first clinical placement often triggers immense anxiety and fear for nursing students [ 9 , 10 ]. Research suggests that among nursing students, anxiety arises from perceived knowledge deficiencies, role ambiguity, the working environment, caring for ‘real’ people, potentially causing harm, exposure to nudity and death, and ‘not fitting in’ [ 2 , 3 , 11 ]. These stressors are reported internationally and often relate to inadequate preparation for entering the clinical environment [ 2 , 10 , 12 ]. Previous research suggests that high anxiety before the first clinical placement can be related to factors likely to affect patient outcomes, such as self-confidence and efficacy [ 13 ]. High anxiety during clinical placement may impair students’ capacity to learn, thus compromising the value of the clinical environment for learning [ 10 ].
The first clinical placement often occurs soon after commencing nursing training and can challenge students’ beliefs, philosophies, and preconceived ideas about nursing. An experience of cultural or ‘reality’ shock often arises when entering the healthcare setting, creating dissonance between reality and expectations [ 6 , 14 ]. These experiences may be exacerbated by tertiary education providers teaching of ‘ideal’ clinical practice [ 2 , 6 ]. The perceived distance between theoretical knowledge and what is expected in a healthcare placement, as opposed to what occurs on clinical placement, has been well documented as the theory-practice gap or an experience of cognitive dissonance [ 2 , 3 ].
Given the pivotal role of the first clinical placement in nursing students’ trajectories to nursing practice, it is important to understand students’ experiences and to explore how the placement experience shapes initial perceptions. Existing research focusses almost entirely either on describing nursing students’ projected emotions and perceptions prior to undertaking a first clinical placement [ 3 ] or examines student perceptions of reflecting on a completed first placement [ 15 ]. We wished to examine consistency and change in student perception of their first clinical placement by tracking their experiences longitudinally. We focused on a first clinical placement undertaken in a Master of Nursing Science. This two-year postgraduate qualification provides entry-to-practice nursing training for students who have completed any undergraduate qualification. The first clinical placement component of the course aimed to orient students to the clinical environment, support students to acquire skills and develop their clinical reasoning through experiential learning with experienced nursing mentors.
This paper makes a significant contribution to understanding how nursing students’ perceptions might develop over time because of their clinical placement experiences. Our research addresses a further gap in the existing literature, by focusing on students completing an accelerated postgraduate two-year entry-to-practice degree open to students with any prior undergraduate degree. Thus, the current research aimed to understand nursing students’ emotional responses and expectations and their perceptions of preparedness before attending their first clinical placement and to contrast these initial perceptions with their end-of-placement perspectives.
Study design
A descriptive qualitative study was undertaken, utilising a pre- and post-design for data collection. Focus groups with first-year postgraduate entry-to-practice nursing students were conducted before the first clinical placement, with individual semi-structured interviews undertaken during the first clinical placement.
Setting and participants
All first-year students enrolled in the two-year Master of Nursing Science program ( n = 190) at a tertiary institution in Melbourne, Australia, were eligible to participate. There were no exclusion criteria. At the time of this study, students were enrolled in a semester-long subject focused on nursing assessment and care. They studied the theoretical underpinnings of nursing and science, theoretical and practical nursing clinical skills and Indigenous health over the first six weeks of the course. Students completed a preclinical assessment as a hurdle before commencing a three-week clinical placement in a hospital setting, a subacute or acute environment. Overall, the clinical placement aimed to provide opportunities for experiential learning, skill acquisition, development of clinical reasoning skills and professional socialisation [ 16 , 17 ].
In total, sixteen students participated voluntarily in a focus group of between 60 and 90 min duration; ten of these students also participated in individual interviews of between 30 and 60 min duration, a number sufficient to reach data saturation. Table 1 shows the questions used in the focus groups conducted before clinical placement commenced and the questions for the semi-structured interview questions conducted during clinical placement. Study participants’ undergraduate qualifications included bachelor’s degrees in science, arts and business. A small number of participants had previous healthcare experience (e.g. as healthcare assistants). The participants attended clinical placement in the Melbourne metropolitan, Victorian regional and rural hospital locations.
Data collection
The study comprised two phases. The first phase comprised six focus groups prior to the first clinical placement, and the second phase comprised ten individual semi-structured interviews towards the end of the first clinical placement. Focus groups (with a maximum of four participants) and individual interviews were conducted by the lead author online via Zoom and were audio-recorded. Capping group size to a relatively small number considered diversity of perceptions and opportunities for participants to share their insights and to confirm or contradict their peers, particularly in the online environment [ 18 , 19 ].
Focus groups and interview questions were developed with reference to relevant literature, piloted with volunteer final-year nursing students, and then verified with the coauthors. All focus groups and interviewees received the same structured questions (Table 1 ) to ensure consistency and to facilitate comparison across the placement experience in the development of themes. Selective probing of interviewees’ responses for clarification to gain in-depth responses was undertaken. Nonverbal cues, impressions, or observations were noted.
The lead author was a registered nurse who had a clinical teaching role within the nursing department and was responsible for coordinating clinical placement experiences. To ensure rigour during the data collection process, the lead author maintained a reflective account, exploring her experiences of the discussions, reflecting on her interactions with participants as a researcher and as a clinical educator, and identifying areas for improvement (for instance allowing participants to tell their stories with fewer prompts). These reflections in conjunction with regular discussion with the other authors throughout the data collection period, aided in identifying any researcher biases, feelings and thoughts that possibly influenced the research [ 20 ].
To maintain rigour during the data analysis phase, we adhered to a systematic process involving input from all authors to code the data and to identify, refine and describe the themes and subthemes reported in this work. This comprehensive analytic process, reported in detail in the following section, was designed to ensure that the findings arising from this research were derived from a rigorous approach to analysing the data.
Data analysis
Focus groups and interviews were transcribed using the online transcription service Otter ( https://otter.ai/ ) and then checked and anonymised by the first author. Preliminary data analysis was carried out simultaneously by the first author using thematic content analysis proposed by Braun and Clarke [ 21 ] using NVivo 12 software [ 22 ]. All three authors undertook a detailed reading of the first three transcripts from both the focus groups and interviews and independently identified major themes. This preliminary coding was used as the basis of a discussion session to identify common themes between authors, to clarify sources of disagreement and to establish guidelines for further coding. Subsequent coding of the complete data set by the lead author identified a total of 533 descriptive codes; no descriptive code was duplicated across the themes. Initially, the descriptive codes were grouped into major themes identified from the literature, but with further analysis, themes emerged that were unique to the current study.
The research team met frequently during data analysis to discuss the initial descriptive codes, to confirm the major themes and subthemes, to revise themes on which there was disagreement and to identify any additional themes. Samples of quotes were reviewed by the second and third authors to decide whether these quotes were representative of the identified themes. The process occurred iteratively to refine the thematic categories, to discuss the definitions of each theme and to identify exemplar quotes.
Ethical considerations
The lead author was a clinical teacher and the clinical placement coordinator in the nursing department at the time of the study. Potential risks of perceived coercion and power imbalances were identified because of the lead author’s dual roles as an academic and as a researcher. To manage these potential risks, an academic staff member who was not part of the research study informed students about the study during a face-to-face lecture and ensured that all participants received a plain language statement identifying the lead author’s role and how perceived conflicts of interest would be managed. These included the lead author not undertaking any teaching or assessment role for the duration of the study and ensuring that placement allocations were completed prior to undertaking recruitment for the study. All students who participated in the study provided informed written consent. No financial or other incentives were offered. Approval to conduct the study was granted by the University of Melbourne Human Research Ethics Committee (Ethics ID 1955997.1).
Three main themes emerged describing students’ feelings and perceptions of their first clinical placement. In presenting the findings, before or during has been assigned to participants’ quotes to clarify the timing of students’ perspectives related to the clinical placement.
Major theme 1: Adjusting and managing a raft of feelings
The first theme encompassed the many positive and negative feelings about work-integrated learning expressed by participants before and during their clinical placement. Positive feelings before clinical placement were expressed by participants who were comfortable with the unknown and cautiously optimistic.
I am ready to just go with the flow, roll with the punches (Participant [P]1 before).
Overwhelmingly, however, the majority of feelings and thoughts anticipating the first clinical placement were negatively oriented. Students who expressed feelings of fear, anxiety, lack of knowledge, lack of preparedness, uncertainty about nursing as a career, or strong concerns about being a burden were all classified as conveying negative feelings. These negative feelings were categorised into four subthemes.
Subtheme 1.1 I don’t have enough knowledge
All participants expressed some concerns and anxiety before their first clinical placement. These encompassed concerns about knowledge inadequacy and were linked to a perception of under preparedness. Participants’ fears related to harming patients, responsibility for managing ‘real’ people, medication administration, and incomplete understanding of the language and communication skills within a healthcare setting. Anxiety for many participants merged with the logistics and management of their life during the clinical placement.
I’m scared that they will assume that I have more knowledge than I do (P3 before). I feel quite similar with P10, especially when she said fear of unknown and fear that she might do something wrong (P9 before).
Subtheme 1.2 Worry about judgment, being seen through that lens
Participants voiced concerns that they would be judged negatively by patients or healthcare staff because they perceived that the student nurse belonged to specific social groups related to their cultural background, ethnicity or gender. Affiliation with these groups contributed to students’ sense of self or identity, with students often describing such groups as a community. Before the clinical placement, participants worried that such judgements would impact the support they received on placement and their ability to deliver patient care.
Some older patients might prefer to have nurses from their own background, their own ethnicity, how they would react to me, or if racism is involved (P10 before). I just don’t want to reinforce like, whatever negative perceptions people might have of that community (P16 before).
Participants’ concerns prior to the first clinical placement about judgement or poor treatment because of patients’ preconceived ideas about specific ethnic groups did not eventuate.
I mean, it didn’t really feel like very much of a thing once I was actually there. It is one of those things you stress about, and it does not really amount to anything (P16 during).
Some students’ placement experiences revealed the positive benefits of their cultural background to enhancing patient care. One student affirmed that the placement experience reinforced their commitment to nursing and that this was related to their ability to communicate with patients whose first language was not English.
Yeah, definitely. Like, I can speak a few dialects. You know, I can actually see a difference with a lot of the non-English speaking background people. As soon as you, as soon as they’re aware that you’re trying and you’re trying to speak your language, they, they just open up. Yeah, yes. And it improves the care (P10 during).
However, a perceived lack of judgement was sometimes attributed to wearing the full personal protective equipment required during the COVID-19 pandemic, which meant that their personal features were largely obscured. For this reason, it was more difficult for patients to make assumptions or attributions about students’ ethnic or gender identity based on their appearance.
People tend to assume and call us all girls, which was irritating. It was mostly just because all of us were so covered up, no one could see anyone’s faces (P16 during).
Subtheme 1.3 Is nursing really for me?
Prior to their first clinical placement experience, many participants expressed ambivalence about a nursing career and anticipated that undertaking clinical placement could determine their suitability for the profession. Once exposed to clinical placement, the majority of students were completely committed to their chosen profession, with a minority remaining ambivalent or, in rare cases, choosing to leave the course. Not yet achieving full commitment to a nursing career was related to not wishing to work in the ward they had for their clinical placement, while remaining open to trying different specialities.
I didn’t have an actual idea of what I wanted to do after arts, this wasn’t something that I was aiming towards specifically (P14 before). I think I’m still not 100%, but enough to go on, that I’m happy to continue the course as best as I can (P11 during).
Subtheme 1.4 Being a burden
Before clinical placement, participants had concerns about being burdensome and how this would affect their clinical placement experiences.
If we end up being a burden to them, an extra responsibility for them on top of their day, then we might not be treated as well (P10 before).
A sense of burden remained a theme during the clinical placement for participants for the first five to seven days, after which most participants acknowledged that their role became more active. As students contributed more productively to their placement, their feelings of being a burden reduced.
Major theme 2: Sinking or swimming
The second major theme, sinking or swimming, described participants’ expectations about a successful placement experience and identified themes related to students’ successes (‘swimming’) or difficulties (‘sinking’) during their placement experience. Prior to clinical placement, without a realistic preview of what the experience might entail, participants were uncertain of their role, hoped for ‘nice’ supervising nurses and anticipated an observational role that would keep them afloat.
I will focus on what I want to learn and see if that coincides with what is expected, I guess (P15 before).
During the clinical placement, the reality was very different, with a sense of sinking. Participants discovered, some with shock, that they were expected to participate actively in the healthcare team.
I got the sense that they were not going to muck around, and, you know, they’re ‘gonna’ use the free labour that came with me (P1 during).
Adding to the confusion about the expected placement experience, participants believed that healthcare staff were unclear about students’ scope of practice for a postgraduate entry-to-practice degree, creating misalignment between students’ and supervising nurses’ expectations.
It seems to me like the educators don’t really seem to have a clear picture of what the scope is, and what is actually required or expected of us (P10 during).
In exploring perceived expectations of the clinical placement and the modifying effect of placement on initial expectations, three subthemes were identified: translation to practice is overwhelming, trying to find the rhythm or jigsaw pieces, and individual agency.
Subtheme 2.1 Translation to practice is overwhelming
Before clinical placement, participants described concerns about insufficient knowledge to enable them to engage effectively with the placement experience.
If I am doing an assessment understanding what are those indications and why I would be doing it or not doing it at a certain time (P1 before).
Integrating and applying theoretical content while navigating an unfamiliar clinical environment created a significant gap between theory and practice during clinical placement. As the clinical placement experience proceeded and initial fears dissipated, students became more aware of applying their theoretical knowledge in the clinical context.
We’re learning all this theory and clinical stuff, but then we don’t really have a realistic idea of what it’s like until we’re kind of thrown into it for three weeks (P10 during).
Subtheme 2.2 Trying to find the rhythm or the jigsaw pieces
Before clinical placement, participants described learning theory and clinical skills with contextual unfamiliarity. They had the jigsaw pieces but did not know how to assemble it; they had the music but did not know the final song. When discussing their expectations about clinical placement, the small number of participants with a healthcare background (e.g. as healthcare assistants) proposed realistic answers, whereas others struggled to answer or cited stories from friends or television. With a lack of context, feelings of unpreparedness were exacerbated. Once in the clinical environment, participants further emphasised that they could not identify what they needed to know to successfully prepare for clinical placement.
It was never really pieced together. We’ve learned bits and pieces, and then we’re putting it together ourselves (P8 during). On this course I feel it was this is how you do it, but I did not know how it was supposed to be played, I did not know the rhythm (P4 during).
Subtheme 2.3 Individual agency
Participants’ individual agency, their attitude, self-efficacy, and self-motivation affected their clinical placement experiences. Participant perceptions in advance of the clinical placement experience remained consistent with their perspectives following clinical placement. Before clinical placement, participants who were highly motivated to learn exhibited a growth mindset [ 23 ] and planned to be proactive in delivering patient care. During their clinical placement, initially positive students remained positive and optimistic about their future. Participants who believed that their first clinical placement role would be largely observational and were less proactive about applying their knowledge and skills identified boredom and a lack of learning opportunities on clinical placement.
A shadowing position, we don’t have enough skills and authority to do any work, not do any worthwhile skills (P3 before). I thought it would be a lot busier, because we’re limited with our scope, so there’s not much we can do, it’s just a bit slower than I thought (P12 during).
Individual agency appears to influence a successful first clinical placement; other factors may also be implicated but were not the focus of this study. Further research exploring the relationships between students’ age, life experience, resilience, individual agency, and the use of coping strategies during a first clinical placement would be useful.
Major theme 3: The reality of navigating placement relationships
The third main theme emphasised the reality of navigating clinical placement relationships and explored students’ relationships with healthcare staff, patients, and peers. Before clinical placement, many participants, especially those with healthcare backgrounds, expressed fears about relationships with supervising nurses. They perceived that the dynamics of the team and the healthcare workplace might influence the support they received. Several participants were nervous about attending placement on their own without peers for support, especially if the experience was challenging. Participants identified expectations of being mistreated, believing that it was unavoidable, and prepared themselves to not take it personally.
For me it’s where we’re going to land, are we going to be in a supportive, kind of nurturing environment, or is it just kind of sink or swim? (P5 before). If you don’t really trust them, you’re nervous the entire time and you’ll be like what if I get it wrong (P16 before).
Despite these concerns, students strongly emphasised the value of relationships during their first clinical placement, with these perceptions unchanged by their clinical placement experience. Where relationships were positive, participants felt empowered to be autonomous, and their self-confidence increased.
You get that that instant reaction from the patients. And that makes you feel more confident. So that really got me through the first week (P14 during). I felt like I was intruding, then as I started to build a bit of rapport with the people, and they saw that I was around, I don’t feel that as much now (P1 during).
Such development hinged on the receptiveness and support of supervising nurses, the team on the ward, and patients and could be hindered by poor relationships.
He was the old-style buddy nurse in his fifties, every time I questioned him, he would go ssshh, just listen, no questions, it was very stressful (P10 during). It depends whether the buddy sees us as an extra pair of hands, or we’re learners (P11 during).
Where students experienced poor behaviour from supervising nurses, they described a range of emotional responses to these interactions and also coping strategies including avoiding unfriendly staff and actively seeking out those who were more inclusive.
If they weren’t very nice, it wouldn’t be very enjoyable and if they didn’t trust you, then it would be a bit frustrating, that like I can do this, but you won’t let me (P12 during). If another nurse was not nice to me, and I was their buddy, I would literally just not buddy with them and go and follow whoever was nice to me (P4 during).
Relationships with peers were equally important; students on clinical placement with peers valued the shared experience. In contrast, students who attended clinical placement alone at a regional or rural hospital felt disconnected from the opportunities that learning with peers afforded.
Our research explored the emotional responses and perceptions of preparedness of postgraduate entry-to-practice nursing students prior to and during their first clinical placement. In this study, we described how the perceptions of nursing students remained consistent or were modified by their clinical placement experiences. Our analysis of students’ experiences identified three major themes: adjusting and managing a raft of feelings; sinking or swimming; and the reality of navigating placement relationships. We captured similar themes identified in the literature; however, our study also identified novel aspects of nursing students’ experiences of their first clinical placement.
The key theme, adjusting and managing a raft of feelings, which encapsulates anxiety before clinical placement, is consistent with previous research. This theme included concerns in communicating with healthcare staff and managing registered nurses’ negative attitudes and expectations, in addition to an academic workload [ 11 , 24 ]. Concerns not previously identified in the literature included a fear of judgement or discrimination by healthcare staff or patients that might impact the reputation of marginalised communities. Fortunately, these initial fears largely dissipated during clinical placement. Some students discovered that a diverse cultural background was an asset during their clinical placement. Although these initial fears were ameliorated by clinical placement experiences, evidence of such fears before clinical placement is concerning. Further research to identify appropriate support for nursing students from culturally diverse or marginalised communities is warranted. For example, a Finnish study highlighted the importance of mentoring culturally diverse students, creating a pedagogical atmosphere during clinical placement and integrating cultural diversity into nursing education [ 25 ].
Preclinical expectations of being mistreated can be viewed as an unavoidable phenomenon for nursing students [ 26 ]. The existing literature highlights power imbalances and hierarchical differences within the healthcare system, where student nurses may be marginalised, disrespected, and ignored [ 9 , 27 , 28 ]. During their clinical placement, students in our study reported unintentional incivility by supervising nurses: feeling not wanted, ignored, or asked to remain quiet by supervising nurses who were unfriendly or highly critical. These findings were similar to those of Thomas et al.’s [ 29 ] UK study and were particularly heightened at the beginning of clinical placement. Several students acknowledged that nursing staff fatigue from a high turnover of students on their ward and the COVID-19 pandemic could be contributing factors. In response to such incivility, students reported decreased self-confidence and described becoming quiet and withdrawing from active participation with their patients. Students oriented their behaviour towards repetitive low-level tasks, aiming to please and help their supervising nurse, to the detriment of learning opportunities. Fortunately, these incidents did not appear to impact nursing students’ overall experience of clinical placement. Indeed, students found positive experiences with different supervising nurses and their own self-reflection assisted with coping. Other active strategies to combat incivility identified in the current study that were also identified by Thomas et al. [ 29 ] included avoiding nurses who were uncivil, asking to work with nurses who were ‘nice’ to them, and seeking out support from other staff as a coping strategy. The nursing students in our study were undertaking a postgraduate entry-to-practice qualification and already had an undergraduate degree. The likely greater levels of experience and maturity of this cohort may influence their resilience when working with unsupportive supervising nurses and identifying strategies to manage challenging situations.
The theory-practice gap emerged in the theme of sinking or swimming. A theory-practice gap describes the perceived dissonance between theoretical knowledge and expectations for the first clinical placement, as opposed to the reality of the experience, and has been reported in previous studies (see, for instance, 24 , 30 , 31 , 32 ). Existing research has shown that when the first clinical placement does not meet inexperienced student nurses’ expectations, a disconnect between theory and practice occurs, creating feelings of being lost and insecure within the new environment, potentially impacting students’ motivation and risk of attrition [ 19 , 33 ]. The current study identified further areas exacerbating the theory-practice gap. Before the clinical placement, students without a healthcare background lacked context for their learning. They lacked understanding of nurses’ shift work and were apprehensive about applying clinical skills learned in the classroom. Hence, some students were uncertain if they were prepared for their first clinical placement or even how to prepare, which increased their anxiety. Prior research has demonstrated that applying theoretical knowledge more seamlessly during clinical placement was supported when students knew what to expect [ 6 ]. For instance, a Canadian study exposed students as observers to the healthcare setting before starting clinical placement, enabling early theory to practice connections that minimised misconceptions and false assumptions during clinical placement [ 34 ].
In the current study, the theory-practice gap was further exacerbated during clinical placement, where healthcare staff were confused about students’ scope of practice and the course learning objectives and expectations in a postgraduate entry-to-practice nursing qualification. The central booking system for clinical placements classifies first-year nursing students who participated in this study as equivalent to second-year undergraduate nursing students. Such a classification could create a misalignment between clinical educators’ expectations and their delivery of education versus students’ actual learning needs and capacity [ 3 , 31 ]. Additional communication to healthcare partners is warranted to enhance understanding of the scope of practice and expectations of a first-year postgraduate entry-to-practice nursing student. Educating and empowering students to communicate their learning needs within their scope of practice is also required.
Our research identified a link between students’ personality traits or individual agency and their first clinical placement experience. The importance of a positive orientation towards learning and the nursing profession in preparedness for clinical placement has been highlighted in previous studies [ 31 ]. Students’ experience of their first clinical placement in our study appeared to be strongly influenced by their mindset [ 23 ]. Some students demonstrated motivation to learn, were happy to ‘roll with the punches’, yet remain active in their learning requirements, whereas others perceived their role as observational and expected supervising nurses to provide learning opportunities. Students who anticipated a passive learning approach prior to their first clinical placement reported boredom, limited activity, and lack of opportunities during their first clinical placement. These students could have a lowered sense of self-efficacy, which may lead to a greater risk of doubt, stress, and reduced commitment to the profession [ 35 ]. Self-efficacy theory explores self-perceived confidence and competence around people’s beliefs in their ability to influence events, which is associated with motivation and is key to nursing students progressing in their career path confidently [ 35 , 36 ]. In the current study, students who actively engaged in their learning process used strategies such as self-reflection and sought support from clinical educators, peers and family. Such active approaches to learning appeared to increase their resilience and motivation to learn as they progressed in their first clinical placement.
Important relationships with supervising nurses, peers, or patients were highlighted in the theme of the reality of navigating placement relationships. This theme links with previous research findings about belongingness. Belongingness is a fundamental human need and impacts students’ behaviour, emotions, cognitive processes, overall well-being, and socialisation into the profession [ 37 , 38 ]. Nursing students who experience belongingness feel part of a team and are more likely to report positive experiences. Several students in the current study described how feeling part of a team improved self-confidence and empowered work-integrated learning. Nonetheless, compared with previous literature (see for instance, 2), working as a team and belongingness were infrequent themes. Such infrequency could be related to the short duration of the clinical placement. In shorter clinical placements, nursing students learn a range of technical skills but have less time to develop teamwork skills and experience socialisation to the profession [ 29 , 39 ].
Positive relationships with supervising nurses appeared fundamental to students’ experiences. Previous research has shown that in wards with safe psycho-social climates, where the culture tolerates mistakes, regarding them as learning opportunities, a pedagogical atmosphere prevails [ 25 , 39 ]. Whereas, if nursing students experience insolent behaviours or incivility, this not only impacts learning it can also affect career progression [ 26 ]. Participants who felt safe asking questions were given responsibility, had autonomy to conduct skills within their scope of practice and thrived in their learning. This finding aligns with previous research affirming that a welcoming and supportive clinical placement environment, where staff are caring, approachable and helpful, enables student nurses to flourish [ 36 , 40 , 41 , 42 ]. Related research highlights that students’ perception of a good clinical placement is linked to participation within the community and instructor behaviour over the quality of the clinical environment and opportunities [ 27 , 28 ]. Over a decade ago, a large European study found that the single most important element for students’ clinical learning was the supervisory relationship [ 39 ]. In our study, students identified how supervising nurses impacted their emotions and this was critical to their experience of clinical placement, rather than how effective they were in their teaching, delivery of feedback, or their knowledge base.
Students’ relationships with patients were similarly important for a successful clinical placement. Before the clinical placement, students expressed anxiety and fears in communicating and interacting with patients, particularly if they were dying or acutely unwell, which is reflective of the literature [ 2 , 10 , 11 ]. However, during clinical placement, relationships with patients positively impacted nursing students’ experiences, especially at the beginning when they felt particularly vulnerable in a new environment. Towards the end of clinical placement, feelings of incompetence, nervousness and uncertainty had subsided. Students were more active in patient care, which increased self-confidence, empowerment, and independence, in turn further improving relationships with patients and creating a positive feedback loop [ 36 , 42 , 43 ].
Limitations
This study involved participants from one university and a single course, thus limiting the generalisability of the results. Thus, verification of the major themes identified in this research in future studies is needed. Nonetheless, the purpose of this study was to explore in detail the way in which the experiences of clinical placement for student nurses modified initial emotional responses towards undertaking placement and their perceptions of preparedness. Participants in this study undertook their clinical placement in a variety of different hospital wards in different specialties, which contributed to the rigour of the study in identifying similar themes in nursing students’ experiences across diverse placement contexts.
This study explored the narratives of first-year nursing students undertaking a postgraduate entry-to-practice qualification on their preparedness for clinical placement. Exploring students’ changing perspectives before and during the clinical placement adds to extant knowledge about nursing students’ emotional responses and perceptions of preparedness. Our research highlighted the role that preplacement emotions and expectations may have in shaping nursing students’ clinical placement experiences. Emerging themes from this study highlighted the importance students placed on relationships with peers, patients, and supervising nurses. Significant anxiety and other negative emotions experienced by nursing students prior to the first clinical placement suggests that further research is needed to explore the impact of contextual learning to scaffold students’ transition to the clinical environment. The findings of this research also have significant implications for educational practice. Additional educational support for nursing students prior to entering the clinical environment for the first time might include developing students’ understanding of the clinical environment, such as through increasing students’ understanding of the different roles of nurses in the clinical context through pre-recorded interviews with nurses. Modified approaches to simulated teaching prior to the first clinical placement would also be useful to increase the emphasis on students applying their learning in a team-based, student-led context, rather than emphasising discrete clinical skill competencies. Finally, increasing contact between students and university-based educators throughout the placement would provide further opportunities for students to debrief, to receive support and to manage some of the negative emotions identified in this study. Further supporting the transition to the first clinical placement could be fundamental to reducing the theory-practice gap and allaying anxiety. Such support is crucial during their first clinical placement to reduce attrition and boost the nursing workforce.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to the conditions of our ethics approval but may be available from the corresponding author on reasonable request and subject to permission from the Human Research Ethics Committee.
Alshahrani Y, Cusack L, Rasmussen P. Undergraduate nursing students’ strategies for coping with their first clinical placement: descriptive survey study. Nurse Educ Today. 2018;69:104–8.
Article PubMed Google Scholar
Brady M, Price J, Bolland R, Finnerty G. Needing to belong: first practice placement experiences of childrens’ nursing students. Compr Child Adolesc Nurs. 2019;421:24–39.
Article Google Scholar
Levett-Jones T, Pitt V, Courtney-Pratt H, Harbrow G, Rossiter R. What are the primary concerns of nursing students as they prepare for and contemplate their first clinical placement experience? Nurse Educ Pract. 2015;154:304–9.
McCloughen A, Levy D, Johnson A, Nguyen H, McKenzie H. Nursing students’ socialisation to emotion management during early clinical placement experiences: a qualitative study. J Clin Nurs. 2020;2913–14:2508–20.
Andrew N, McGuinness C, Reid G, Corcoran T. Greater than the sum of its parts: transition into the first year of undergraduate nursing. Nurse Educ Pract. 2009;91:13–21.
Leducq M, Walsh P, Hinsliff-Smith. K McGarry J. A key transition for student nurses: the first placement experience. Nurse Educ Today. 2012;327:779–81.
Spurlock D Jr. The nursing shortage and the future of nursing education is in our hands. J Nurs Educ. 2020;596:303–4.
Agu CF, Stewart J, McFarlane-Stewart N, Rae T. COVID‐19 pandemic effects on nursing education: looking through the lens of a developing country. Int Nurs Rev. 2021;682:153–8.
Nejad FM, Asadizaker M, Baraz S, Malehi AS. Investigation of nursing student satisfaction with the first clinical education experience in universities of medical sciences in Iran. J Med Life. 2019;121:75–82.
Sun FK, Long A, Tseng YS, Huang HM, You JH, Chiang CY. Undergraduate student nurses’ lived experiences of anxiety during their first clinical practicum: a phenomenological study. Nurse Educ Today. 2016;37:21–6.
Article CAS PubMed Google Scholar
Gurková E, Zeleníková R. Nursing students perceived stress coping strategies health and supervisory approaches in clinical practice: a Slovak and Czech perspective. Nurse Educ Today. 2018;65:4–10.
Hanson J, Walsh S, Mason M, Wadsworth D, Framp A, Watson K. Speaking up for safety: a graded assertiveness intervention for first year nursing students in preparation for clinical placement: thematic analysis. Nurse Educ Today. 2020;84:104252.
Khalaila R. Simulation in nursing education: an evaluation of students outcomes at their first clinical practice combined with simulations. Nurse Educ Today. 2014;342:252–8.
Cummins AM, Catling C, Hogan R, Homer CS. Addressing culture shock in first year midwifery students: maximising the initial clinical experience. Women Birth. 2014;274:271–5.
Chesser-Smyth PA. The lived experiences of general student nurses on their first clinical placement: a phenomenological study. Nurse Educ Pract. 2005;56:320–7.
Arkan B, Ordin Y, Yılmaz D. Undergraduate nursing students experience related to their clinical learning environment and factors affecting to their clinical learning process. Nurse Educ Pract. 2018;29:127–32.
Cowen KJ, Hubbard LJ, Hancock DC. Expectations and experiences of nursing students in clinical courses: a descriptive study. Nurse Educ Today. 2018;67:15–20.
Krueger RA, Casey MA. Focus groups: a practical guide for applied research. 5th ed. Thousand Oaks, California: Sage; 2014.
Jonsén E, Melender HL, Hilli Y. Finnish and Swedish nursing students experiences of their first clinical practice placement—A qualitative study. Nurse Educ Today. 2013;333:297–302.
Watt D. On becoming a qualitative researcher: the value of reflexivity. Qual Rep. 2007;121:82–101.
Google Scholar
Braun V, Clarke V. Thematic analysis. In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf DK, Sher J, editors. APA handbook of research methods in psychology Vol. 2. Research designs: quantitative qualitative neuropsychological and biological. Washington, DC: American Psychological Association; 2012. pp. 57–71.
Chapter Google Scholar
Lumivero. - Software Solutions for Data Analysis & Management [Internet]. Lumivero. http://www.lumivero.com .
Yeager DS, Dweck CS. Mindsets that promote resilience: when students believe that personal characteristics can be developed. Educ Psychol. 2012;47(4):302–14.
Kol E, İnce S. Determining the opinions of the first-year nursing students about clinical practice and clinical educators. Nurse Educ Pract. 2018;31:35–40.
Mikkonen K, Merilainen M, Tomietto M. Empirical model of clinical learning environment and mentoring of culturally and linguistically diverse nursing students. J Clin Nurs. 2020;29(3–4):653–61.
Ahn YH, Choi J. Incivility experiences in clinical practicum education among nursing students. Nurse Educ Today. 2019;73:48–53.
Molesworth M. Nursing students first placement: peripherality and marginality within the community of practice. J Nurs Educ. 2017;561:31–8.
Rafati F, Nouhi E, Sabzehvari S, Dehghan-Nayyeri N. Iranian nursing students’ experience of stressors in their first clinical experience. J Prof Nurs. 2017;333:250–7.
Thomas J, Jinks A, Jack B. Finessing incivility: the professional socialisation experiences of student nurses first clinical placement a grounded theory. Nurse Educ Today. 2015;3512:e4–9.
Astin F, McKenna L, Newton J, Moore-Coulson L. Registered nurses–expectations and experiences of first year students–clinical skills and knowledge. Contemp Nurse. 2005;183:279–91.
Kalyani MN, Jamshidi N, Molazem Z, Torabizadeh C, Sharif F. How do nursing students experience the clinical learning environment and respond to their experiences? A qualitative study. BMJ Open. 2019;97:e028052.
Maginnis C, Croxon L. Transfer of learning to the nursing clinical practice setting. Rural Remote Health. 2010;102:334–40.
Soler OM, Aguayo-González M, Gutiérrez SSR, Pera MJ, Leyva-Moral JM. Nursing students’ expectations of their first clinical placement: a qualitative study. Nurse Educ Today. 2021;98:104736.
Powell TL, Cooke J, Brakke A. Altered nursing student perspectives: impact of a pre-clinical observation experience at an outpatient oncology setting. Can Oncol Nurs J. 2019;291:34–9.
Bandura AJJW. Self-efficacy. In: Weiner IB, Craighead WE, editors. The Corsini encyclopedia of psychology. Hoboken, NJ: John Wiley & Sons Inc; 2010.
Porteous DJ, Machin A. The lived experience of first year undergraduate student nurses: a hermeneutic phenomenological study. Nurse Educ Today. 2018;60:56–61.
Cooper J, Courtney-Pratt H, Fitzgerald M. Key influences identified by first year undergraduate nursing students as impacting on the quality of clinical placement: a qualitative study. Nurse Educ Today. 2015;359:1004–8.
Levett-Jones T, Lathlean J. The ascent to competence conceptual framework: an outcome of a study of belongingness. J Clin Nurs. 2009;1820:2870–9.
Warne T, Johansson UB, Papastavrou E, Tichelaar E, Tomietto M, Van den Bossche K. Saarikoski M. An exploration of the clinical learning experience of nursing students in nine European countries. Nurse Educ Today. 2010;308:809–15.
Laugaland K, Kaldestad K, Espeland E, McCormack B, Akerjordet K, Aase I. Nursing students experience with clinical placement in nursing homes: a focus group study. BMC Nurs. 2021;201:1–13.
Manninen K, Henriksson EW, Scheja M, Silén C. Authenticity in learning–nursing students experiences at a clinical education ward. Health Educ. 2013;1132:132–43.
Teskereci G, Boz İ. I try to act like a nurse: a phenomenological qualitative study. Nurse Educ Pract. 2019;37:39–44.
Chesser-Smyth PA, Long T. Understanding the influences on self‐confidence among first‐year undergraduate nursing students in Ireland. J Adv Nurs. 2013;691:145–57.
Download references
Acknowledgements
The authors wish to thank the first-year nursing students who participated in this study and generously shared their experiences of undertaking their first clinical placement.
No funding was received for this study.
Author information
Jennifer M. Weller-Newton
Present address: School of Nursing and Midwifery, University of Canberra, Kirinari Drive, Bruce, Canberra, ACT, 2617, Australia
Authors and Affiliations
Department of Nursing, The University of Melbourne, Grattan St, Parkville, VIC, 3010, Australia
Philippa H. M. Marriott
Department of Rural Health, The University of Melbourne, Grattan St, Shepparton, VIC, 3630, Australia
Present address: Department of Medical Education, Melbourne Medical School, The University of Melbourne, Grattan St, Parkville, VIC, 3010, Australia
Katharine J. Reid
You can also search for this author in PubMed Google Scholar

Contributions
All authors made a substantial contribution to conducting the research and preparing the manuscript for publication. P.M., J.W-N. and K.R. conceptualised the research and designed the study. P.M. undertook the data collection, and all authors were involved in thematic analysis and interpretation. P.M. wrote the first draft of the manuscript, K.R. undertook a further revision and all authors contributed to subsequent versions. All authors approved the final version for submission. Each author is prepared to take public responsibility for the research.
Corresponding author
Correspondence to Katharine J. Reid .
Ethics declarations
Ethics approval and consent to participate.
The research was undertaken in accordance with the National Health and Medical Research Council of Australia’s National Statement on Ethical Conduct in Human Research and the Australian Code for the Responsible Conduct of Research. Ethical approval to conduct the study was obtained from the University of Melbourne Human Research Ethics Committee (Ethics ID 1955997.1). All participants received a plain language statement that described the requirements of the study. All participants provided informed written consent to participate, which was affirmed verbally at the beginning of focus groups and interviews.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Marriott, P.H.M., Weller-Newton, J.M. & Reid, K.J. Preparedness for a first clinical placement in nursing: a descriptive qualitative study. BMC Nurs 23 , 345 (2024). https://doi.org/10.1186/s12912-024-01916-x
Download citation
Received : 17 November 2023
Accepted : 04 April 2024
Published : 22 May 2024
DOI : https://doi.org/10.1186/s12912-024-01916-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Postgraduate nursing education
- Nursing students
- Nursing schools
- Clinical skills
- Qualitative research
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 14 May 2024
Protocol for a scoping review study on learning plan use in undergraduate medical education
- Anna Romanova ORCID: orcid.org/0000-0003-1118-1604 1 ,
- Claire Touchie 1 ,
- Sydney Ruller 2 ,
- Victoria Cole 3 &
- Susan Humphrey-Murto 4
Systematic Reviews volume 13 , Article number: 131 ( 2024 ) Cite this article
189 Accesses
Metrics details
The current paradigm of competency-based medical education and learner-centredness requires learners to take an active role in their training. However, deliberate and planned continual assessment and performance improvement is hindered by the fragmented nature of many medical training programs. Attempts to bridge this continuity gap between supervision and feedback through learner handover have been controversial. Learning plans are an alternate educational tool that helps trainees identify their learning needs and facilitate longitudinal assessment by providing supervisors with a roadmap of their goals. Informed by self-regulated learning theory, learning plans may be the answer to track trainees’ progress along their learning trajectory. The purpose of this study is to summarise the literature regarding learning plan use specifically in undergraduate medical education and explore the student’s role in all stages of learning plan development and implementation.
Following Arksey and O’Malley’s framework, a scoping review will be conducted to explore the use of learning plans in undergraduate medical education. Literature searches will be conducted using multiple databases by a librarian with expertise in scoping reviews. Through an iterative process, inclusion and exclusion criteria will be developed and a data extraction form refined. Data will be analysed using quantitative and qualitative content analyses.
By summarising the literature on learning plan use in undergraduate medical education, this study aims to better understand how to support self-regulated learning in undergraduate medical education. The results from this project will inform future scholarly work in competency-based medical education at the undergraduate level and have implications for improving feedback and supporting learners at all levels of competence.
Scoping review registration:
Open Science Framework osf.io/wvzbx.
Peer Review reports
Competency-based medical education (CBME) has transformed the approach to medical education to focus on demonstration of acquired competencies rather than time-based completion of rotations [ 1 ]. As a result, undergraduate and graduate medical training programs worldwide have adopted outcomes-based assessments in the form of entrustable professional activities (EPAs) comprised of competencies to be met [ 2 ]. These assessments are completed longitudinally by multiple different evaluators to generate an overall impression of a learner’s competency.
In CBME, trainees will progress along their learning trajectory at individual speeds and some may excel while others struggle to achieve the required knowledge, skills or attitudes. Therefore, deliberate and planned continual assessment and performance improvement is required. However, due to the fragmented nature of many medical training programs where learners rotate through different rotations and work with many supervisors, longitudinal observation is similarly fragmented. This makes it difficult to determine where trainees are on their learning trajectories and can affect the quality of feedback provided to them, which is a known major influencer of academic achievement [ 3 ]. As a result, struggling learners may not be identified until late in their training and the growth of high-performing learners may be stifled [ 4 , 5 , 6 ].
Bridging this continuity gap between supervision and feedback through some form of learner handover or forward feeding has been debated since the 1970s and continues to this day [ 5 , 7 , 8 , 9 , 10 , 11 ]. The goal of learner handover is to improve trainee assessment and feedback by sharing their performance and learning needs between supervisors or across rotations. However, several concerns have been raised about this approach including that it could inappropriately bias subsequent assessments of the learner’s abilities [ 9 , 11 , 12 ]. A different approach to keeping track of trainees’ learning goals and progress along their learning trajectories is required. Learning plans (LPs) informed by self-regulated learning (SRL) theory may be the answer.
SRL has been defined as a cyclical process where learners actively control their thoughts, actions and motivation to achieve their goals [ 13 ]. Several models of SRL exist but all entail that the trainee is responsible for setting, planning, executing, monitoring and reflecting on their learning goals [ 13 ]. According to Zimmerman’s SRL model, this process occurs in three stages: forethought phase before an activity, performance phase during an activity and self-reflection phase after an activity [ 13 ]. Since each trainee leads their own learning process and has an individual trajectory towards competence, this theory relates well to the CBME paradigm which is grounded in learner-centredness [ 1 ]. However, we know that medical students and residents have difficulty identifying their own learning goals and therefore need guidance to effectively partake in SRL [ 14 , 15 , 16 , 17 ]. Motivation has also emerged as a key component of SRL, and numerous studies have explored factors that influence student engagement in learning [ 18 , 19 ]. In addition to meeting their basic psychological needs of autonomy, relatedness and competence, perceived learning relevance through meaningful learning activities has been shown to increase trainee engagement in their learning [ 19 ].
LPs are a well-known tool across many educational fields including CBME that can provide trainees with meaningful learning activities since they help them direct their own learning goals in a guided fashion [ 20 ]. Also known as personal learning plans, learning contracts, personal action plans, personal development plans, and learning goals, LPs are documents that outline the learner’s roadmap to achieve their learning goals. They require the learner to self-identify what they need to learn and why, how they are going to do it, how they will know when they are finished, define the timeframe for goal achievement and assess the impact of their learning [ 20 ]. In so doing, LPs give more autonomy to the learner and facilitate objective and targeted feedback from supervisors. This approach has been described as “most congruent with the assumptions we make about adults as learners” [ 21 ].
LP use has been explored across various clinical settings and at all levels of medical education; however, most of the experience lies in postgraduate medical education [ 22 ]. Medical students are a unique learner population with learning needs that appear to be very well suited for using LPs for two main reasons. First, their education is often divided between classroom and clinical settings. During clinical training, students need to be more independent in setting learning goals to meet desired competencies as their education is no longer outlined for them in a detailed fashion by the medical school curriculum [ 23 ]. SRL in the workplace is also different than in the classroom due to additional complexities of clinical care that can impact students’ ability to self-regulate their learning [ 24 ]. Second, although most medical trainees have difficulty with goal setting, medical students in particular need more guidance compared to residents due to their relative lack of experience upon which they can build within the SRL framework [ 25 ]. LPs can therefore provide much-needed structure to their learning but should be guided by an experienced tutor to be effective [ 15 , 24 ].
LPs fit well within the learner-centred educational framework of CBME by helping trainees identify their learning needs and facilitating longitudinal assessment by providing supervisors with a roadmap of their goals. In so doing, they can address current issues with learner handover and identification as well as remediation of struggling learners. Moreover, they have the potential to help trainees develop lifelong skills with respect to continuing professional development after graduation which is required by many medical licensing bodies.
An initial search of the JBI Database, Cochrane Database, MEDLINE (PubMed) and Google Scholar conducted in July–August 2022 revealed a paucity of research on LP use in undergraduate medical education (UGME). A related systematic review by van Houten–Schat et al. [ 24 ] on SRL in the clinical setting identified three interventions used by medical students and residents in SRL—coaching, LPs and supportive tools. However, only a couple of the included studies looked specifically at medical students’ use of LPs, so this remains an area in need of more exploration. A scoping review would provide an excellent starting point to map the body of literature on this topic.
The objective of this scoping review will therefore be to explore LP use in UGME. In doing so, it will address a gap in knowledge and help determine additional areas for research.
This study will follow Arksey and O’Malley’s [ 26 ] five-step framework for scoping review methodology. It will not include the optional sixth step which entails stakeholder consultation as relevant stakeholders will be intentionally included in the research team (a member of UGME leadership, a medical student and a first-year resident).
Step 1—Identifying the research question
The overarching purpose of this study is to “explore the use of LPs in UGME”. More specifically we seek to achieve the following:
Summarise the literature regarding the use of LPs in UGME (including context, students targeted, frameworks used)
Explore the role of the student in all stages of the LP development and implementation
Determine existing research gaps
Step 2—Identifying relevant studies
An experienced health sciences librarian (VC) will conduct all searches and develop the initial search strategy. The preliminary search strategy is shown in Appendix A (see Additional file 2). Articles will be included if they meet the following criteria [ 27 ]:
Participants
Medical students enrolled at a medical school at the undergraduate level.
Any use of LPs by medical students. LPs are defined as a document, usually presented in a table format, that outlines the learner’s roadmap to achieve their learning goals [ 20 ].
Any stage of UGME in any geographic setting.
Types of evidence sources
We will search existing published and unpublished (grey) literature. This may include research studies, reviews, or expert opinion pieces.
Search strategy
With the assistance of an experienced librarian (VC), a pilot search will be conducted to inform the final search strategy. A search will be conducted in the following electronic databases: MEDLINE, Embase, Education Source, APA PsycInfo and Web of Science. The search terms will be developed in consultation with the research team and librarian. The search strategy will proceed according to the JBI Manual for Evidence Synthesis three-step search strategy for reviews [ 27 ]. First, we will conduct a limited search in two appropriate online databases and analyse text words from the title, abstracts and index terms of relevant papers. Next, we will conduct a second search using all identified key words in all databases. Third, we will review reference lists of all included studies to identify further relevant studies to include in the review. We will also contact the authors of relevant papers for further information if required. This will be an iterative process as the research team becomes more familiar with the literature and will be guided by the librarian. Any modifications to the search strategy as it evolves will be described in the scoping review report. As a measure of rigour, the search strategy will be peer-reviewed by another librarian using the PRESS checklist [ 28 ]. No language or date limits will be applied.
Step 3—Study selection
The screening process will consist of a two-step approach: screening titles/abstracts and, if they meet inclusion criteria, this will be followed by a full-text review. All screening will be done by two members of the research team and any disagreements will be resolved by an independent third member of the team. Based on preliminary inclusion criteria, the whole research team will first pilot the screening process by reviewing a random sample of 25 titles/abstracts. The search strategy, eligibility criteria and study objectives will be refined in an iterative process. We anticipate several meetings as the topic is not well described in the literature. A flowchart of the review process will be generated. Any modifications to the study selection process will be described in the scoping review report. The papers will be excluded if a full text is not available. The search results will be managed using Covidence software.
Step 4—Charting the data
A preliminary data extraction tool is shown in Appendix B (see Additional file 3 ). Data will be extracted into Excel and will include demographic information and specific details about the population, concept, context, study methods and outcomes as they relate to the scoping review objectives. The whole research team will pilot the data extraction tool on ten articles selected for full-text review. Through an iterative process, the final data extraction form will be refined. Subsequently, two members of the team will independently extract data from all articles included for full-text review using this tool. Charting disagreements will be resolved by the principal and senior investigators. Google Translate will be used for any included articles that are not in the English language.
Step 5—Collating, summarising and reporting the results
Quantitative and qualitative analyses will be used to summarise the results. Quantitative analysis will capture descriptive statistics with details about the population, concept, context, study methods and outcomes being examined in this scoping review. Qualitative content analysis will enable interpretation of text data through the systematic classification process of coding and identifying themes and patterns [ 29 ]. Several team meetings will be held to review potential themes to ensure an accurate representation of the data. The PRISMA Extension for Scoping Reviews (PRISMA-ScR) will be used to guide the reporting of review findings [ 30 ]. Data will be presented in tables and/or diagrams as applicable. A descriptive summary will explain the presented results and how they relate to the scoping review objectives.
By summarising the literature on LP use in UGME, this study will contribute to a better understanding of how to support SRL amongst medical students. The results from this project will also inform future scholarly work in CBME at the undergraduate level and have implications for improving feedback as well as supporting learners at all levels of competence. In doing so, this study may have practical applications by informing learning plan incorporation into CBME-based curricula.
We do not anticipate any practical or operational issues at this time. We assembled a team with the necessary expertise and tools to complete this project.
Availability of data and materials
All data generated or analysed during this study will be included in the published scoping review article.
Abbreviations
- Competency-based medical education
Entrustable professional activity
- Learning plan
- Self-regulated learning
- Undergraduate medical education
Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638–45.
Article PubMed Google Scholar
Shorey S, Lau TC, Lau ST, Ang E. Entrustable professional activities in health care education: a scoping review. Med Educ. 2019;53(8):766–77.
Hattie J, Timperley H. The power of feedback. Rev Educ Res. 2007;77(1):81–112.
Article Google Scholar
Dudek NL, Marks MB, Regehr G. Failure to fail: the perspectives of clinical supervisors. Acad Med. 2005;80(10 Suppl):S84–7.
Warm EJ, Englander R, Pereira A, Barach P. Improving learner handovers in medical education. Acad Med. 2017;92(7):927–31.
Spooner M, Duane C, Uygur J, et al. Self-regulatory learning theory as a lens on how undergraduate and postgraduate learners respond to feedback: a BEME scoping review : BEME Guide No. 66. Med Teach. 2022;44(1):3–18.
Frellsen SL, Baker EA, Papp KK, Durning SJ. Medical school policies regarding struggling medical students during the internal medicine clerkships: results of a National Survey. Acad Med. 2008;83(9):876–81.
Humphrey-Murto S, LeBlanc A, Touchie C, et al. The influence of prior performance information on ratings of current performance and implications for learner handover: a scoping review. Acad Med. 2019;94(7):1050–7.
Morgan HK, Mejicano GC, Skochelak S, et al. A responsible educational handover: improving communication to improve learning. Acad Med. 2020;95(2):194–9.
Dory V, Danoff D, Plotnick LH, et al. Does educational handover influence subsequent assessment? Acad Med. 2021;96(1):118–25.
Humphrey-Murto S, Lingard L, Varpio L, et al. Learner handover: who is it really for? Acad Med. 2021;96(4):592–8.
Shaw T, Wood TJ, Touchie T, Pugh D, Humphrey-Murto S. How biased are you? The effect of prior performance information on attending physician ratings and implications for learner handover. Adv Health Sci Educ Theory Pract. 2021;26(1):199–214.
Artino AR, Brydges R, Gruppen LD. Chapter 14: Self-regulated learning in health professional education: theoretical perspectives and research methods. In: Cleland J, Duning SJ, editors. Researching Medical Education. 1st ed. John Wiley & Sons; 2015. p. 155–66.
Chapter Google Scholar
Cleland J, Arnold R, Chesser A. Failing finals is often a surprise for the student but not the teacher: identifying difficulties and supporting students with academic difficulties. Med Teach. 2005;27(6):504–8.
Reed S, Lockspeiser TM, Burke A, et al. Practical suggestions for the creation and use of meaningful learning goals in graduate medical education. Acad Pediatr. 2016;16(1):20–4.
Wolff M, Stojan J, Cranford J, et al. The impact of informed self-assessment on the development of medical students’ learning goals. Med Teach. 2018;40(3):296–301.
Sawatsky AP, Halvorsen AJ, Daniels PR, et al. Characteristics and quality of rotation-specific resident learning goals: a prospective study. Med Educ Online. 2020;25(1):1714198.
Article PubMed PubMed Central Google Scholar
Pintrich PR. Chapter 14: The role of goal orientation in self-regulated learning. In: Boekaerts M, Pintrich PR, Zeidner M, editors. Handbook of self-regulation. 1st ed. Academic Press; 2000. p. 451–502.
Kassab SE, El-Sayed W, Hamdy H. Student engagement in undergraduate medical education: a scoping review. Med Educ. 2022;56(7):703–15.
Challis M. AMEE medical education guide No. 19: Personal learning plans. Med Teach. 2000;22(3):225–36.
Knowles MS. Using learning contracts. 1 st ed. San Francisco: Jossey Bass; 1986.
Parsell G, Bligh J. Contract learning, clinical learning and clinicians. Postgrad Med J. 1996;72(847):284–9.
Article CAS PubMed PubMed Central Google Scholar
Teunissen PW, Scheele F, Scherpbier AJJA, et al. How residents learn: qualitative evidence for the pivotal role of clinical activities. Med Educ. 2007;41(8):763–70.
Article CAS PubMed Google Scholar
van Houten-Schat MA, Berkhout JJ, van Dijk N, Endedijk MD, Jaarsma ADC, Diemers AD. Self-regulated learning in the clinical context: a systematic review. Med Educ. 2018;52(10):1008–15.
Taylor DCM, Hamdy H. Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach. 2013;35(11):e1561–72.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalol H. Chapter 11: Scoping reviews. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. JBI; 2020. https://synthesismanual.jbi.global. . Accessed 30 Aug 2022.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Venables M, Larocque A, Sikora L, Archibald D, Grudniewicz A. Understanding indigenous health education and exploring indigenous anti-racism approaches in undergraduate medical education: a scoping review protocol. OSF; 2022. https://osf.io/umwgr/ . Accessed 26 Oct 2022.
Download references
Acknowledgements
Not applicable.
This study will be supported through grants from the Department of Medicine at the Ottawa Hospital and the University of Ottawa. The funding bodies had no role in the study design and will not have any role in the collection, analysis and interpretation of data or writing of the manuscript.
Author information
Authors and affiliations.
The Ottawa Hospital – General Campus, 501 Smyth Rd, PO Box 209, Ottawa, ON, K1H 8L6, Canada
Anna Romanova & Claire Touchie
The Ottawa Hospital Research Institute, Ottawa, Canada
Sydney Ruller
The University of Ottawa, Ottawa, Canada
Victoria Cole
The Ottawa Hospital – Riverside Campus, Ottawa, Canada
Susan Humphrey-Murto
You can also search for this author in PubMed Google Scholar
Contributions
AR designed and drafted the protocol. CT and SH contributed to the refinement of the research question, study methods and editing of the manuscript. VC designed the initial search strategy. All authors reviewed the manuscript for final approval. The review guarantors are CT and SH. The corresponding author is AR.
Authors’ information
AR is a clinician teacher and Assistant Professor with the Division of General Internal Medicine at the University of Ottawa. She is also the Associate Director for the internal medicine clerkship rotation at the General campus of the Ottawa Hospital.
CT is a Professor of Medicine with the Divisions of General Internal Medicine and Infectious Diseases at the University of Ottawa. She is also a member of the UGME Competence Committee at the University of Ottawa and an advisor for the development of a new school of medicine at Toronto Metropolitan University.
SH is an Associate Professor with the Department of Medicine at the University of Ottawa and holds a Tier 2 Research Chair in Medical Education. She is also the Interim Director for the Research Support Unit within the Department of Innovation in Medical Education at the University of Ottawa.
CT and SH have extensive experience with medical education research and have numerous publications in this field.
SR is a Research Assistant with the Division of General Internal Medicine at the Ottawa Hospital Research Institute.
VC is a Health Sciences Research Librarian at the University of Ottawa.
SR and VC have extensive experience in systematic and scoping reviews.
Corresponding author
Correspondence to Anna Romanova .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. prisma-p 2015 checklist., 13643_2024_2553_moesm2_esm.docx.
Additional file 2: Appendix A. Preliminary search strategy [ 31 ].
Additional file 3: Appendix B. Preliminary data extraction tool.
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Romanova, A., Touchie, C., Ruller, S. et al. Protocol for a scoping review study on learning plan use in undergraduate medical education. Syst Rev 13 , 131 (2024). https://doi.org/10.1186/s13643-024-02553-w
Download citation
Received : 29 November 2022
Accepted : 03 May 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s13643-024-02553-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 21 May 2024
A modern way to teach and practice manual therapy
- Roger Kerry 1 ,
- Kenneth J. Young ORCID: orcid.org/0000-0001-8837-7977 2 ,
- David W. Evans 3 ,
- Edward Lee 1 , 4 ,
- Vasileios Georgopoulos 1 , 5 ,
- Adam Meakins 6 ,
- Chris McCarthy 7 ,
- Chad Cook 8 ,
- Colette Ridehalgh 9 , 10 ,
- Steven Vogel 11 ,
- Amanda Banton 11 ,
- Cecilia Bergström 12 ,
- Anna Maria Mazzieri 13 ,
- Firas Mourad 14 , 15 &
- Nathan Hutting 16
Chiropractic & Manual Therapies volume 32 , Article number: 17 ( 2024 ) Cite this article
113 Altmetric
Metrics details
Musculoskeletal conditions are the leading contributor to global disability and health burden. Manual therapy (MT) interventions are commonly recommended in clinical guidelines and used in the management of musculoskeletal conditions. Traditional systems of manual therapy (TMT), including physiotherapy, osteopathy, chiropractic, and soft tissue therapy have been built on principles such as clinician-centred assessment , patho-anatomical reasoning, and technique specificity. These historical principles are not supported by current evidence. However, data from clinical trials support the clinical and cost effectiveness of manual therapy as an intervention for musculoskeletal conditions, when used as part of a package of care.
The purpose of this paper is to propose a modern evidence-guided framework for the teaching and practice of MT which avoids reference to and reliance on the outdated principles of TMT. This framework is based on three fundamental humanistic dimensions common in all aspects of healthcare: safety , comfort , and efficiency . These practical elements are contextualised by positive communication , a collaborative context , and person-centred care . The framework facilitates best-practice, reasoning, and communication and is exemplified here with two case studies.
A literature review stimulated by a new method of teaching manual therapy, reflecting contemporary evidence, being trialled at a United Kingdom education institute. A group of experienced, internationally-based academics, clinicians, and researchers from across the spectrum of manual therapy was convened. Perspectives were elicited through reviews of contemporary literature and discussions in an iterative process. Public presentations were made to multidisciplinary groups and feedback was incorporated. Consensus was achieved through repeated discussion of relevant elements.
Conclusions
Manual therapy interventions should include both passive and active, person-empowering interventions such as exercise, education, and lifestyle adaptations. These should be delivered in a contextualised healing environment with a well-developed person-practitioner therapeutic alliance. Teaching manual therapy should follow this model.
Musculoskeletal (MSK) conditions are leading contributors to the burden of global disability and healthcare [ 1 ]. Amongst other interventions, manual therapy (MT) has been recommended for the management of people with MSK conditions in multiple clinical guidelines, for example [ 2 , 3 ].
MT has been described as the deliberate application of externally generated force upon body tissue, typically via the hands, with therapeutic intent [ 4 ]. It includes touch-based interventions such as thrust manipulation, joint mobilisation, soft-tissue mobilisation, and neurodynamic movements [ 5 ]. For people with MSK conditions, this therapeutic intent is usually to reduce pain and improve movement, thus facilitating a return to function and improved quality of life [ 6 ]. Patient perceptions of MT are, however, vague and sit among wider expectations of treatment including education, self-efficacy and the role of exercise, and prognosis [ 7 ].
Although the teaching and practice of MT has invariably changed over time, its foundations arguably remain unaltered and set in biomedical and outdated principles. This paper sets out to review contemporary literature and propose a revised model to inform the teaching and practice of MT.
The aim of this paper is to stimulate debate about the future teaching and practice of manual therapy through the proposal of an evidence-informed re-conceptualised model of manual therapy. The new model dismisses traditional elements of manual therapy which are not supported by research evidence. In place, the model offers a structure based on common humanistic principles of healthcare.
Consenus methodology
We present the literature synthesis and proposed framework as a consensus document to motivate further professional discussion developed through a simple three-stage iterative process over a 5-year period. The consensus methodology was classed as educational development which did not require ethical approval. Stage 1: a change of teaching practice was adopted by some co-authors (VG, RK, EL) on undergraduate and postgraduate Physiotherapy programmes at a UK University in 2018. This was a result of standard institutional teaching practice development which includes consideration of evidence-informed teaching. Stage 2: Input from a broader spectrum of stakeholders was sought, so a group of experienced, internationally-based educators, clinicians, and researchers from across the spectrum of manual therapy was convened. Perspectives were elicited through discussions in an iterative process. Stage 3: Presentations were made by some of the co-authors (VG, RK, SV, KY) to multidisciplinary groups (UK, Europe, North America) and feedback via questions and discussions was incorporated into further co-author discussions on the development of the framework. Consensus was achieved through repeated discussion of relevant elements. Figure 1 summarises the consensus methodology.
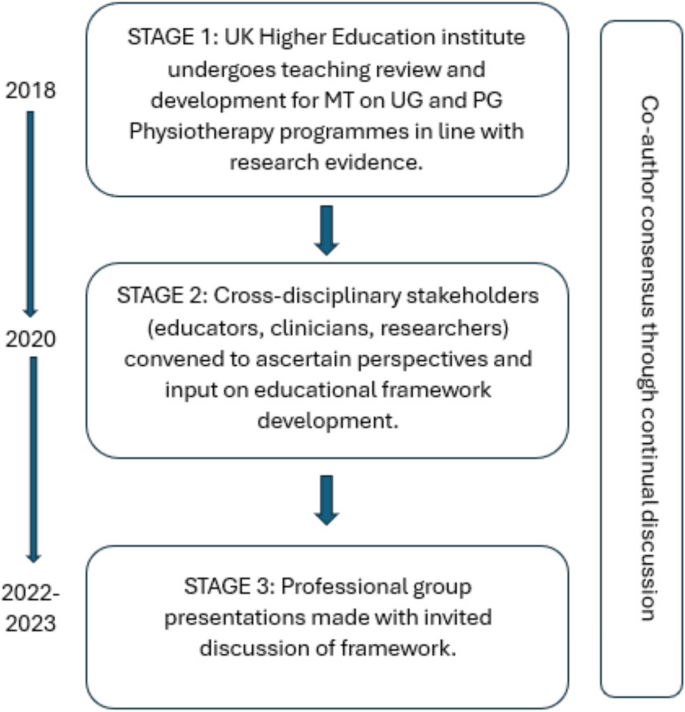
Summary and timeline of iterative consensus process for development of framework (MT: Manual Therapy; UG: Undergraduate; PG: Postgraduate)
Clinical & cost effectiveness of manual therapy
Manual therapy has been suggested to be a valuable part of a multimodal approach to managing MSK pain and disability, for example [ 8 ]. The majority of recent systematic reviews of clinical trials report a beneficial effect of MT for a range of MSK conditions, with at least similar effect sizes to other recommended approaches, for example [ 9 ]. Some systematic reviews report inconclusive findings, for example [ 10 ], and a minority report effects that were no better than comparison or sham treatments, for example [ 11 ].
Potential benefits must always be weighed against potential harms, of course. Mild to moderate adverse events from MT (e.g. mild muscle soreness) are common and generally considered acceptable [ 12 ], whilst serious adverse events are very rare and their risk may be mitigated by good practice [ 13 ]. MT has been reported by people with MSK disorders as a preferential and effective treatment with accepted levels of post-treatment soreness [ 14 ].
MT is considered cost-effective [ 15 ] and the addition of MT to exercise packages has been shown to increase clinical and cost-effectiveness compared to exercise alone in several MSK conditions [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 ]. Further, manual therapy has been shown to be less costly and more beneficial than evidence-based advice to stay active [ 24 ].
In summary, MT is considered a useful evidence-based addition to care packages for people experiencing pain and disability associated with MSK conditions. As such, MT continues to be included in national and international clinical guidelines for a range of MSK conditions as part of multimodal care.
Principles of traditional manual therapy (TMT)
Manual therapy has been used within healthcare for centuries [ 4 ] with many branches of MT having appeared (and disappeared) over time [ 25 ]. In developed nations today, MT is most commonly utilised by the formalised professional groups of physiotherapy, osteopathy, chiropractic, as well as groups such as soft tissue therapists. All of these groups have a history that borrows heavily from traditional healers and bone-setters [ 26 ].
Although there are many elements of MT, three principles appear to have become ubiquitous within what we shall now refer to as ‘traditional manual therapy’ (TMT): clinician-centred assessment , patho-anatomical reasoning , and technique specificity [ 27 , 28 , 29 , 30 ]. These principles continue to influence the teaching and practice of manual therapy over recent years, for example [ 31 ].
However, they have become increasingly difficult to defend given a growing volume of empirical evidence to the contrary.
Traditional manual therapy (TMT) principles: origins and problems
Clinician-centred assessment.
TMT has long had an emphasis on what we shall refer to as clinician-centred assessments . Within this, we claim, is an assumption that clinical information is both highly accurate and diagnostically important, for example [ 32 ]. Clinician-centred assessments include, for example, routine imaging, the search for patho-anatomical 'lesions’ and asymmetries, and specialised palpation. Although the focus of this paper is on the ‘hands-on’ examples of client-centred assessment, the notion of imaging is presented below to expose some of the flaws in the underlying belief system for TMT.
The emphasis on clinician-centred assessments has probably been driven, in part, by a desire for objective diagnostic tests which align well with gold-standard imaging. Indeed, since the discovery of x-rays, radiological imaging been used as an assessment for spinal pain – and a justification for using spinal manipulation – particularly in the chiropractic profession [ 33 ]. Contrary to many TMT claims, X-ray imaging is not without risk [ 34 ]. Additionally, until relatively recently (with the advent of magnetic resonance imaging) it was not widely appreciated that patho-anatomical ‘lesions’ believed to explain MSK pain conditions were nearly as common in pain-free individuals as those with pain [ 35 ]. Accordingly, the rates of unnecessary treatments, including surgery, are known to increase when imaging is used routinely [ 36 ]. For patients with non-specific low back pain, for example, imaging does not improve outcomes and risks overdiagnosis and overtreatment [ 37 ]. Hence, despite being objective in nature, the value of imaging for many MSK pain conditions (particularly spinal pain) has reduced drastically with clinical guidelines across the globe recommending against routine imaging for MSK pain of non-traumatic origin [ 38 ]. Even so, the practice of routine imaging continues [ 39 ].
Hands-on interventions are inextricably related to hands-on assessment [ 40 ], and often associated with claims of ‘specialisation’ [ 41 ]. By this we mean where a great level of training and precision are claimed to be necessary for influencing the interpretation of assessment findings, treatment decisions, and/or treatment outcomes. Implicit within this claim is that therapists who are unable to achieve such precision are not able to perform MT to an acceptable level (and thereby are not able to provide benefit to patients).
There are numerous studies that cast doubt over claims of highly specialised palpation skills. Palpation of anatomical landmarks does not reach a clinically acceptable level of validity [ 42 ]. Specialised motion palpation does not appear to be a good method for differentiating people with or without low back pain [ 43 ]. Poor content validity of specialised motion tests have been reported, in line with a lack of acceptable reference standards [ 44 ]. Palpable sensations reported by therapists are unlikely to be due to tissue deformation [ 45 ]. Furthermore, the delivery of interventions based on specialised palpatory findings is no better than non-specialised palpation [ 46 ]. Generally poor reliability of motion palpation skills has been reported, for example [ 47 ] and appear to be independent of clinician experience or training, for example [ 48 ]. Notably, person-centred palpation—for pain and tenderness for example—has slightly higher reliability, but is still fair at best [ 49 ].
This does not mean that palpation is of no use at all though; just that effective manual therapy does not depend upon it. For example, expert therapists can display high levels of interrater reliability during specialised motion palpation [ 50 ]. Focused training can improve the interrater reliability of specialised skills [ 51 ]. However, the validity of the phenomenon remains poor. Given the weight of the evidence and consistency of data over recent decades, we suggest that the role of clinician-centred hands-on assessment is no longer central to contemporary manual therapy.
Patho-anatomical reasoning
The justification for selecting particular MT interventions has historically been based upon the patho-anatomical status of local peripheral tissue [ 52 , 53 , 54 , 55 ]. Patho-anatomical reasoning, we propose, is the framework that links clinician-centred assessments to the desire for highly specific delivery of MT interventionsKey to this is the relationship between a patho-anatomic diagnosis and the assumed mechanisms of action of the intervention employed.
Theories for the mechanisms of action of MT interventions are many. Some of the most prominent include reductions of disc herniations [ 56 ], re-positioning of a bone or joint [ 32 ], removal of intra-articular adhesions [ 57 ], changes in the biomechanical properties of soft tissues [ 58 ], central pain modulation [ 59 ], and biochemical changes [ 60 ]. These theories have been used to justify the choice of certain interventions: a matching of diagnosis (i.e., existence of a lesion) to the effect of treatment takes place. However, most of these mechanistic theories either lack evidence or have been directly contested [ 61 ].
The causal relationship between proposed tissue-based factors such as posture, ergonomic settings, etc. and painful experience has also been disputed [ 62 ]. Although local tissue stiffness has been observed in people with pain, this is typically associated with neuromuscular responses, rather than patho-anatomical changes at local tissue level [ 63 , 64 , 65 , 66 ]. Overall, although some local tissue adaptions have been identified in people with recurrent MSK pain, this is inconsistent and the evidence is currently of low quality [ 67 ] are generally limited to short-term follow-up measures [ 68 ].
Technique specificity
TMT techniques have been taught with an emphasis that a particular direction, ‘grade’ of joint movement, or deformation of tissue at a very specific location in a certain way, is required to achieve a successful treatment outcome.
One problem with a demand for technique specificity in manual therapy is that an intervention does not always result in the intended effect. For example, posteroanterior forces applied during spinal mobilization consistently induce sagittal rotation, as opposed to the assumed posteroanterior translation, for example [ 69 ]. Furthermore, irrespective of the MT intervention chosen, restricting movements to a particular spinal segment is difficult and a regional, non-specific motion is typically induced, for example [ 70 ].
To support technique specificity, comparative data must repeatedly and reproducibly show superiority of outcome from specific MT interventions over non-specific MT, which is consistently not observed [ 71 , 72 , 73 ]. Some studies have demonstrated localised effects of targeted interventions [ 74 ] but there appears to be no difference in outcome related to: the way in which techniques are delivered [ 75 ]; whether technique selection is random or clinician-selected [ 41 ]; or variations in the direction of force or targeted spinal level [ 76 ]. Conversely, there is evidence that non-specific technique application may improve outcomes [ 77 , 78 , 79 ]. Further, sham techniques produce comparable results to specialised approaches [ 11 ].
Passive movement and localised touch have been associated with significant analgesic responses [ 80 ]. These data indicate the presence of an analgesic mechanism. Unfortunately, mechanistic explanation for the therapeutic effects of MT upon pain and disability still remain largely in a ‘black box’ state [ 81 ]. Nevertheless, there are several plausible mechanisms of action to explain the analgesic action of MT interventions, including the activation of modulatory spinal and supraspinal responses [ 82 , 83 , 84 , 85 ]. In support of this, MT interventions have been associated with a variety of neurophysiological responses [ 61 ]. However, it must be acknowledged that these studies provide mechanistic evidence based on association, which is insufficient to make causal claims [ 86 ]. Importantly, none of these neurophysiological responses have been directly related to either the analgesic mechanisms or clinical outcome and may therefore be incidental.
There is evidence that MT does not provide analgesia in injured tissues [ 87 , 88 ]. Conversely, MT has been shown to decrease inflammatory biomarkers [ 89 , 90 , 91 , 92 , 93 ], although these changes have not been evaluated in the longer-term, nor associated with clinical outcomes.
A modern framework for manual therapy
We propose a new direction for the future of MT in which the teaching and practice of this core dimension of MSK care are no longer based on the traditional principles of clinician-centred assessment , patho-anatomical reasoning , and technique specificity .
In doing so, this framework places MT more explicitly as part of person-centred care and appeals to common principles of healthcare, best available evidence, and contemporary theory which avoids unnecessary and over-complicated explanations of observed effects. The framework is simple in terms of implementation and delivery and contextualised by common elements of best practice for healthcare, in line with regulated standard of practice, e.g., [ 94 , 95 , 96 , 97 ]. Our proposal simply illustrates the operationalisation of these common elements through manual therapy.
Too much emphasis has been given to clinician-centred assessments and this should be rebalanced with an increased use of patient-centred assessments, such as a thorough case history, the use of validated patient-reported outcome measures (PROMS), and real-time patient feedback during assessments.
The new framework considers fundamental and humanistic dimensions of touch-based therapies, such as non-specific neuromodulation, communication and sense-making, physical education, and contextual clinical effectiveness. This aligns to contemporary ideas regarding therapeutic alliance and a move towards genuinely holistic healthcare [ 98 , 99 ]. The framework needs to be “open” in order to represent and allow expression of the complexity of the therapeutic encounter. However, to prevent the exploitation of this openness the framework is underpinned by evidence, and any manual therapy approaches without plausible and measurable mechanisms are not supported.
To provide the best care, common healthcare elements such as the safety and comfort of the person seeking help and therapist must be considered, and care should be provided as efficiently as possible. Our framework embraces these dimensions and employs an integration of current evidence. It is transdisciplinary in nature and may be adopted by all MT professions. Figure 1 provides a graphical representation of the framework. It is acknowledged that all components overlap, relate, and influence each. There are two main components: the practical elements on the inside, comprised of safety, comfort, and efficiency, and the conceptual themes on the outer regions, consisting of communication, context, and person-centred care Fig. 2 .
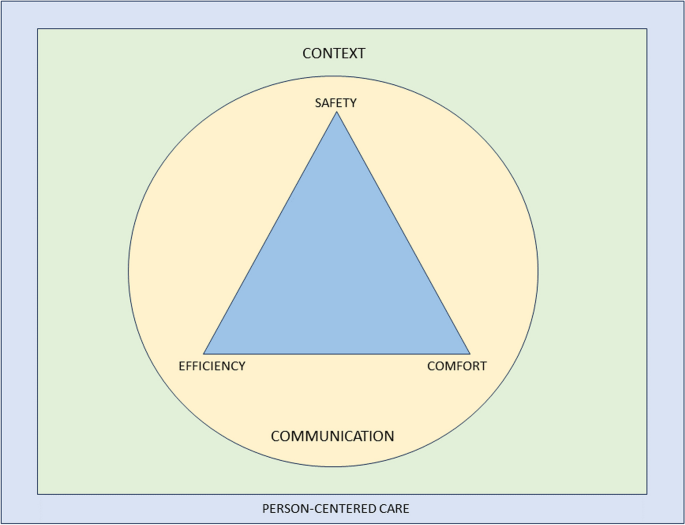
Representation of a modern teaching and practice framework for manual therapy. The image is purposefully designed to be simple, and has been developed primarily to be used as a teaching aid. When displayed in a learning environment, learners and clinicians can quickly refer to the image to check their practice against each element. To keep the image clear, each element of the image is described in detail in the text below”
Practical elements
Safety for people seeking help is a primary concern for all healthcare providers, with the aims to “ prevent and reduce risks, errors and harm that occur to patients [sic] during provision of health care… and to deliver quality essential health services ” [ 100 ]. This, and the notion of safety more generally (including that of the therapist), should be central to way MT is taught and practised.
A fundamentally safe context should be created where there is an absence of any obvious danger or risk of harm to physical or mental health. Consideration should be given to ensuring that communication and consent processes are orientated towards the safety of both the person seeking help and the therapist. The therapist should pay attention to any sense of threat that could be present in the physical, emotional, cognitive and environmental domains of the clinical encounter, and use skilful communication to mitigate anxiety about the assessment or therapeutic process.
Safety should also be considered in the clinical context of the assessment and treatment approach, ensuring that relevant and meaningful safety screenings have been undertaken [ 67 , 101 ]. There remains a need for good, skilful practice and development of manually applied techniques, but this can be achieved without reference to the principles of TMT and without the dogma of a proprietary therapeutic approach.
Comfort suggests that both the person seeking help and the therapist are physically and emotionally content during the assessment and therapeutic process. For example, the person seeking help is agreeable with any necessary state of dress (sociocultural difference should be considered); the person is relaxed and untroubled in whatever position they are in, and is adequately supported whether sitting, standing or recumbent during assessment and treatment; the therapist is comfortable with their positioning and posture; any discomfort produced by the therapeutic process is negotiated and agreed. Any physical mobilisation or touch should be applied with respect to the feedback from the person in relation to their comfort, rather than a pre-determined force based on the notion of resistance. This process requires clinical phronesis, sensitivity, responsivity, dexterity, and embodied communication [ 102 ].
The therapeutic process should be undertaken in a well-organised, competent manner aiming to achieve maximum therapeutic benefit with minimum waste of effort, time, or expense. To enhance the efficiency dimension, the assessment and therapeutic process should be an integral part of a holistic educational and/or activity-based approach to the management of the people which might also address psychological, nutritional, or ergonomic aspects of care, while being aware of social determinants to health. Recommendations exist which serve as a useful guide for enhancing care and promoting self-management in an efficient way [ 103 ].
A principle of this new model of MT is that therapists should not lose sight of the goals they develop with the people they help and ensure that there is coherence between their management aims and their techniques. Therapists should aim to support a person’s self-efficacy and use active approaches to empower them in their recovery. The overall number of therapeutic applications should be made in the context of fostering therapeutic alliance and supporting people to make sense of their situation and symptoms. This should be informed by contemporary views of the effects of manual therapy, emphasising a “physical education process” to promote sense-making and self-efficacy in alliance with the people they aim to help.
Clinical interactions need to be reproducible under a person’s own volition, serving to enhance self-empowerment. For example, someone could be taught how to “self-mobilise” if a positive effect is found with a particular therapeutic application. This should be appropriately scaffolded with behavioural change principles and functional contextualism that promote autonomy and self-management, rather than inappropriate reliance on the therapist [ 103 , 104 ].
An important and emergent notion from the proposed model is to question what constitutes indications for MT given that the model excludes traditional factors which would have informed whether manual therapy is indicated or not for a particular person. The response to this sits within the efficiency and safety dimensions: MT can be beneficial as part of a multi-dimensional approach to management across a broad population of people with musculoskeletal dysfunction, with no evidence to suggest any clinician-centered or patho-anatomical finding influences outcomes. The choice of whether or not to include MT as part of a management strategy should therefore be a product of a lack of contraindications and shared-decision making.
This framework aligns with evidence-based propositions that effectiveness and efficiency in assessment, diagnosis, and outcomes are not reliant on the therapist’s skill set of specialised elements of TMT, but rather other factors—for example variations in pain phenotypes [ 5 ].
Conceptual themes
Communication.
Communication is the overriding critical dimension to the whole therapeutic process and should be aimed at addressing peoples’ fundamental needs to make sense of their symptoms and path to recovery. The delivery and uptake of the therapy should therefore be operationalised in a communication process that meaningfully represents shared-decision making and the best possible attempt to contextualise the therapy in positive and evidence-informed explanations of the process and desired effects [ 105 ].
Within a therapeutic encounter, practitioners must give the time to listen to peoples’ accounts and explanations of their symptoms, including their ideas about their cause [ 106 ]. The assessment and diagnostic process should be a shared endeavour, for example, the negotiation of symptom reproduction. This should be done in a manner that facilitates sense-making, and which simultaneously encourages people to move on from unhelpful beliefs about their symptoms [ 107 , 108 ], encouraging understanding of the uncertain nature of pain and injury. Person-centered communication requires attention to what we communicate and how we communicate across the entire clinical interaction including interview, examination, and management planning [ 109 ]. Therapists need to be open, reflective, aware and responsive to verbal and non-verbal cues, and demonstrate a balance between engaging with people (e.g. eye-gaze) and writing/typing notes during the interview [ 110 , 111 , 112 ].
People should be given the opportunity to discuss their understanding of the diagnosis and options for treatment and rehabilitation. The decision-making process is dialogical, in which alternative options to the offered therapy should also be discussed with the comparative risks and benefits of all available management options, including doing nothing [ 113 , 114 ].
The therapist must fully appreciate the potential consequences of touch without consent. Continual dialogue should ensure that all parties are moving towards mutually agreed goals. The context of the therapy should be explicitly communicated to give appropriate context for any particular intervention as part of a holistic, evidence-based approach [ 115 , 116 , 117 ]. Therapists should be aware that their own beliefs can affect the way they communicate with their people; in the same way, a person’s context affects how they communicate what they expect from their treatment [ 107 , 118 , 119 , 120 ]. The construction of contextual healing scenarios which support positive outcomes, whilst minimising nocebic effects, is critical to effective healthcare [ 121 , 122 , 123 ].
There is a growing academic interest in the nature, role, and purpose of social and affective touch, and any re-framing of MT should consider touch as a means of communication to develop and enhance cooperative communications and strengthen the therapeutic relationship [ 124 , 125 , 126 , 127 , 128 , 129 ]. It can be soothing for a person in pain to experience the caring touch of a professional therapist [ 130 ]; on the other hand, probing, diagnostic, and touch can be experienced as alienating [ 131 , 132 , 133 ]. Touch can alter a person’s sense of body ownership and their ability to recognise and process their emotions by modulating interoceptive precision [ 129 , 134 , 135 ], and intentional touch may be perceived differently from casual, unfocussed touch [ 136 , 137 ]. There is also a thesis that touch generates shared understanding and meaning [ 138 , 139 , 140 ]. This wider appreciation of touch should be embedded in modern MT communication.
The contextual quality of a person’s experience of the therapeutic encounter can affect satisfaction and clinical outcomes [ 141 , 142 , 143 , 144 , 145 ]. The context in which therapeutic care takes place should therefore be developed to enhance this experience. There could be very local, practical aspects of the context, such as the type of passive information available in the clinical space, e.g. replacing biomedical and pathological imagery and objects with positive, active artefacts; judicious and thoughtful organisation and use of treatment tables to discourage a sense of passivity and disempowerment; allocating a comfortable space where communication can take place; colour schemes and light sources which facilitate positivity; ensuring consistency through all clinical and administrative staff promoting encouraging and non-nocebic messages. Importantly, the way the therapist dresses influences peoples’ perception of their healthcare experience [ 146 , 147 ], and that in turn should be contextually and culturally sensitive [ 148 , 149 , 150 ].
Beyond the local clinical space is the broader social environment. The undertaking of MT should serve a role in a person’s engagement with their social environment. For example, someone returning home after engaging with their therapist and disseminating positive health messages within their home and social networks; people acting as advocates for self-empowered healthcare. Furthermore, early data have demonstrated that aligning treatment with the beliefs and values of culturally and linguistically diverse communities enhances peoples’ engagement with their healthcare [ 151 ].
Person-centred care
Here we borrow directly from one of the most established and clinically useful definitions of Person-Centered Medicine [ 152 ]:
“(Person-Centered Medicine is) an affordable biomedical and technological advance to be delivered to patients [sic] within a humanistic framework of care that recognises the importance of applying science in a manner that respects the patients [sic] as a whole person and takes full account of [their] values, preferences, aspirations, stories, cultural context, fears, worries and hopes and thus that recognises and responds to [their] emotional, social and spiritual necessities in addition to [their] physical needs” [ 152 ] , p219.
Person-centred care incorporates a person’s perspective as part of the therapeutic process. In practice, therapists need to communicate in a manner that creates adequate conversational space to elicit a person’s agenda (i.e. understanding, impact of pain, concerns, needs, and goals), which guides clinical interactions. This approach encourages greater partnership in management [ 109 , 153 , 154 ].
A roadmap outlining key actions to implement person-centeredness in clinical practice has been outlined in detail elsewhere [ 155 ]. This includes screening for serious pathology, health co-morbidities and psychosocial factors; adopting effective communication; providing positive health education; coaching and supporting people towards active self-management; and facilitating and managing co-care (when needed) [ 154 ].
It is critical and necessary now to make these features explicit and central to the revised model of MT proposed in this paper. We wish to identify common ground across all MT professions in order to achieve a trans-disciplinary understanding of the evidence supporting the use of MT.
We acknowledge that our arguments here are rooted in empiricism and deliberately based on available research data from within the health science disciplines. We also acknowledge that there is a wider debate about future directions in person-centred care arising from the current evolution of the evidence-based health care movement, which has pointed to the need to learn more about peoples’ lived experiences, to redefine the model of the therapeutic relationship. Although beyond the scope of this paper, a full exploration of modern health care provision involves reconsideration of the ethics and legal requirements of communication and shared decision-making [ 156 , 157 , 158 , 159 ]. The authors envision this paper as a stimulus for self-reflection, stakeholder discussions, and ultimately change that can positively impact outcomes for people who seek manual therapy interventions.
Manual therapy has long been part of MSK healthcare and, given that is likely to continue. Current evidence suggests that effectiveness does not rely on the traditional principles historically developed in any of the major manual therapies. Therefore, the continued teaching and practice based on the principles of clinician-centred palpation , patho-anatomical reasoning , and technique specificity are no longer justified and may well even limit the value of MT.
A revised and reconceptualised framework of MT, based on the humanistic domains of safety, comfort and efficiency and underpinned by the dimensions of communication, context and person-centred care will ensure an empowering, biopsychosocial, evidence-informed approach to MSK care. We propose that the future teaching and practice of MT in physiotherapy, osteopathy, chiropractic, and all associated hands-on professions working within the healthcare field should be based on this new framework.
Availability of data and materials
Young C, Argáez C. CADTH Rapid Response Reports. Manual Therapy for Chronic Non-Cancer Back and Neck Pain: A Review of Clinical Effectiveness. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health. Copyright © 2020 Canadian Agency for Drugs and Technologies in Health.; 2020.
Blanpied PR, Gross AR, Elliott JM, Devaney LL, Clewley D, Walton DM, et al. Neck Pain: Revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1-a83.
Article PubMed Google Scholar
NICE. Low back pain and sciatica in over 16s: assessment and management. NICE guideline [NG59]. 2016.
Pettman E. A history of manipulative therapy. J Man Manip Ther. 2007;15(3):165–74.
Article PubMed PubMed Central Google Scholar
Damian K, Chad C, Kenneth L, David G. Time to evolve: the applicability of pain phenotyping in manual therapy. J Man Manip Ther. 2022;30(2):61–7.
McCarthy CJ. Combined Movement Theory: Rational Mobilization and Manipulation of the Vertebral Column. London, UK: Churchill Livingstone; 2010.
Google Scholar
Subialka JA, Smith K, Signorino JA, Young JL, Rhon DI, Rentmeester C. What do patients referred to physical therapy for a musculoskeletal condition expect? A qualitative assessment. Musculoskel Sci Pract. 2022;59:102543.
Article Google Scholar
Louw A, Nijs J, Puentedura EJ. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017;25(3):160–8.
Wilhelm M, Cleland J, Carroll A, Marinch M, Imhoff M, Severini N, et al. The combined effects of manual therapy and exercise on pain and related disability for individuals with nonspecific neck pain: A systematic review with meta-analysis. J Man Manip Ther. 2023;31(6):393–407.
Schenk R, Donaldson M, Parent-Nichols J, Wilhelm M, Wright A, Cleland JA. Effectiveness of cervicothoracic and thoracic manual physical therapy in managing upper quarter disorders - a systematic review. J Man Manipulative Therap. 2021:1–10.
Lavazza C, Galli M, Abenavoli A, Maggiani A. Sham treatment effects in manual therapy trials on back pain patients: a systematic review and pairwise meta-analysis. BMJ Open. 2021;11(5):e045106.
Funabashi M, Pohlman KA, Goldsworthy R, Lee A, Tibbles A, Mior S, et al. Beliefs, perceptions and practices of chiropractors and patients about mitigation strategies for benign adverse events after spinal manipulation therapy. Chiropr Man Therap. 2020;28(1):46.
Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for Examination of the Cervical Region for Potential of Vascular Pathologies of the Neck Prior to Musculoskeletal Intervention: International IFOMPT Cervical Framework. J Orthop Sports Phys Ther. 2022;53(1):7–22.
Thomas M, Thomson OP, Kolubinski DC, Stewart-Lord A. The attitudes and beliefs about manual therapy held by patients experiencing low back pain: a scoping review. Musculoskelet Sci Pract. 2023;65:102752.
Lilje S, van Tulder M, Wykman A, Aboagye E, Persson U. Cost-effectiveness of specialised manual therapy versus orthopaedic care for musculoskeletal disorders: long-term follow-up and health economic model. Ther Adv Musculoskelet Dis. 2023;15:1759720x221147751.
Article CAS PubMed PubMed Central Google Scholar
Abbott JH, Robertson MC, Chapple C, Pinto D, Wright AA, Leon de la Barra S, et al. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial. 1: clinical effectiveness. Osteoarthritis Cartilage. 2013;21(4):525–34.
Article CAS PubMed Google Scholar
Bove AM, Smith KJ, Bise CG, Fritz JM, Childs JD, Brennan GP, et al. Exercise, Manual Therapy, and Booster Sessions in Knee Osteoarthritis: Cost-Effectiveness Analysis From a Multicenter Randomized Controlled Trial. Phys Ther. 2018;98(1):16–27.
Leininger B, McDonough C, Evans R, Tosteson T, Tosteson AN, Bronfort G. Cost-effectiveness of spinal manipulative therapy, supervised exercise, and home exercise for older adults with chronic neck pain. Spine J. 2016;16(11):1292–304.
Tsertsvadze A, Clar C, Court R, Clarke A, Mistry H, Sutcliffe P. Cost-effectiveness of manual therapy for the management of musculoskeletal conditions: a systematic review and narrative synthesis of evidence from randomized controlled trials. J Manipulative Physiol Ther. 2014;37(6):343–62.
UK Beam Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ. 2004;329(7479):1377.
Article PubMed Central Google Scholar
UK Beam Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: cost effectiveness of physical treatments for back pain in primary care. BMJ (Clinical research ed). 2004;329(7479):1381.
van Dongen JM, Groeneweg R, Rubinstein SM, Bosmans JE, Oostendorp RA, Ostelo RW, et al. Cost-effectiveness of manual therapy versus physiotherapy in patients with sub-acute and chronic neck pain: a randomised controlled trial. Eur Spine J. 2016;25(7):2087–96.
Woods B, Manca A, Weatherly H, Saramago P, Sideris E, Giannopoulou C, et al. Cost-effectiveness of adjunct non-pharmacological interventions for osteoarthritis of the knee. PLoS ONE. 2017;12(3):e0172749.
Aboagye E, Lilje S, Bengtsson C, Peterson A, Persson U, Skillgate E. Manual therapy versus advice to stay active for nonspecific back and/or neck pain: a cost-effectiveness analysis. Chiropr Man Therap. 2022;30(1):27.
Paris SV. A History of Manipulative Therapy Through the Ages and Up to the Current Controversy in the United States. J Man Manipulative Ther. 2000;8(2):66–77.
MacDonald CW, Osmotherly PG, Parkes R, Rivett DA. The current manipulation debate: historical context to address a broken narrative. J Man Manipulative Therap. 2019;27(1):1–4.
Fryer G. Intervertebral dysfunction: a discussion of the manipulable spinal lesion. J Am Osteopath Assoc. 2003;6(2):64–73.
McCarthy CJ. Spinal manipulative thrust technique using combined movement theory. Man Ther. 2001;6(4):197–204.
Vickers A, Zollman C. ABC of complementary medicine Massage therapies. BMJ (Clinical research ed). 1999;319(7219):1254–7.
Evans DW. Osteopathic principles: More harm than good? Int J Osteopath Med. 2013;16(1):46–53.
Mourad F, Yousif MS, Maselli F, Pellicciari L, Meroni R, Dunning J, et al. Knowledge, beliefs, and attitudes of spinal manipulation: a cross-sectional survey of Italian physiotherapists. Chiropr Man Therap. 2022;30(1):38.
Cyriax JH, Cyriax PJ. Cyriax's Illustrated Manual of Orthopaedic Medicine. 3rd ed: Butterworth-Heinemann; 1996.
Young KJ. Words matter: the prevalence of chiropractic-specific terminology on Australian chiropractors’ websites. Chiropr Man Therap. 2020;28(1):18.
Jenkins HJ, Downie AS, Moore CS, French SD. Current evidence for spinal X-ray use in the chiropractic profession: a narrative review. Chiropr Man Therap. 2018;26:48.
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811–6.
Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573–81.
Hall AM, Aubrey-Bassler K, Thorne B, Maher CG. Do not routinely offer imaging for uncomplicated low back pain. BMJ (Clinical research ed). 2021;372:n291.
PubMed Google Scholar
Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79.
Hall AM, Scurrey SR, Pike AE, Albury C, Richmond HL, Matthews J, et al. Physician-reported barriers to using evidence-based recommendations for low back pain in clinical practice: a systematic review and synthesis of qualitative studies using the Theoretical Domains Framework. Implement Sci. 2019;14(1):49.
Eriksson L, Ekenberg L, Melander-Wikman A. The concept of palpation of the shoulder – A basic element of physiotherapy practice: A focus group study with physiotherapists. Adv Physiother. 2012;14(4):183–93.
Nim CG, Downie A, O’Neill S, Kawchuk GN, Perle SM, Leboeuf-Yde C. The importance of selecting the correct site to apply spinal manipulation when treating spinal pain: Myth or reality? A systematic review. Sci Rep. 2021;11(1):23415.
Alexander N, Rastelli A, Webb T, Rajendran D. The validity of lumbo-pelvic landmark palpation by manual practitioners: A systematic review. Int J Osteopath Med. 2021;39:10–20.
Leboeuf-Yde C, van Dijk J, Franz C, Hustad SA, Olsen D, Pihl T, et al. Motion palpation findings and self-reported low back pain in a population-based study sample. J Manipulative Physiol Ther. 2002;25(2):80–7.
Najm WI, Seffinger MA, Mishra SI, Dickerson VM, Adams A, Reinsch S, et al. Content validity of manual spinal palpatory exams - A systematic review. BMC Complement Altern Med. 2003;3:1.
Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, Findley T. Three-dimensional mathematical model for deformation of human fasciae in manual therapy. J Am Osteopath Assoc. 2008;108(8):379–90.
Gabriel A, Konrad A, Roidl A, Queisser J, Schleip R, Horstmann T, et al. Myofascial Treatment Techniques on the Plantar Surface Influence Functional Performance in the Dorsal Kinetic Chain. J Sports Sci Med. 2022;21(1):13–22.
PubMed PubMed Central Google Scholar
Nolet PS, Yu H, Côté P, Meyer A-L, Kristman VL, Sutton D, et al. Reliability and validity of manual palpation for the assessment of patients with low back pain: a systematic and critical review. Chiropr Man Therap. 2021;29(1):33.
Seffinger MA, Najm WI, Mishra SI, Adams A, Dickerson VM, Murphy LS, et al. Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature. Spine. 2004;29(19):E413–25.
Beynon AM, Hebert JJ, Walker BF. The interrater reliability of static palpation of the thoracic spine for eliciting tenderness and stiffness to test for a manipulable lesion. Chiropr Man Therap. 2018;26:49.
Petersen EJ, Thurmond SM, Shaw CA, Miller KN, Lee TW, Koborsi JA. Reliability and accuracy of an expert physical therapist as a reference standard for a manual therapy joint mobilization trial. J Man Manip Ther. 2021;29(3):189–95.
Petersen EJ, Thurmond SM, Buchanan SI, Chun DH, Richey AM, Nealon LP. The effect of real-time feedback on learning lumbar spine joint mobilization by entry-level doctor of physical therapy students: a randomized, controlled, crossover trial. J Man Manip Ther. 2020;28(4):201–11.
Abbott JH, Flynn TW, Fritz JM, Hing WA, Reid D, Whitman JM. Manual physical assessment of spinal segmental motion: intent and validity. Man Ther. 2009;14(1):36–44.
Bialosky JE, Simon CB, Bishop MD, George SZ. Basis for spinal manipulative therapy: a physical therapist perspective. J Electromyogr Kinesiol. 2012;22(5):643–7.
Henderson CN. The basis for spinal manipulation: chiropractic perspective of indications and theory. J Electromyogr Kinesiol. 2012;22(5):632–42.
Sizer PS Jr, Felstehausen V, Sawyer S, Dornier L, Matthews P, Cook C. Eight critical skill sets required for manual therapy competency: a Delphi study and factor analysis of physical therapy educators of manual therapy. J Allied Health. 2007;36(1):30–40.
Ombregt L. A System of Orthopaedic Medicine: Elsevier; 2013.
Cramer GD, Henderson CN, Little JW, Daley C, Grieve TJ. Zygapophyseal joint adhesions after induced hypomobility. J Manipulative Physiol Ther. 2010;33(7):508–18.
George JW, Tunstall AC, Tepe RE, Skaggs CD. The Effects of Active Release Technique on Hamstring Flexibility: A Pilot Study. J Manipulative Physiol Ther. 2006;29(3):224–7.
Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–8.
Plaza-Manzano G, Molina-Ortega F, Lomas-Vega R, Martínez-Amat A, Achalandabaso A, Hita-Contreras F. Changes in biochemical markers of pain perception and stress response after spinal manipulation. J Orthop Sports Phys Ther. 2014;44(4):231–9.
Zusman M. Mechanism of mobilization. Physical Therapy Reviews. 2011;16(4):233–6.
De Carvalho DE, de Luca K, Funabashi M, Breen A, Wong AYL, Johansson MS, et al. Association of Exposures to Seated Postures With Immediate Increases in Back Pain: A Systematic Review of Studies With Objectively Measured Sitting Time. J Manipulative Physiol Ther. 2020;43(1):1–12.
Colloca CJ, Keller TS. Stiffness and neuromuscular reflex response of the human spine to posteroanterior manipulative thrusts in patients with low back pain. J Manipulative Physiol Ther. 2001;24(8):489–500.
Colloca CJ, Keller TS, Gunzburg R. Biomechanical and neurophysiological responses to spinal manipulation in patients with lumbar radiculopathy. J Manipulative Physiol Ther. 2004;27(1):1–15.
Reed WR, Long CR, Kawchuk GN, Sozio RS, Pickar JG. Neural Responses to Physical Characteristics of a High-velocity, Low-amplitude Spinal Manipulation: Effect of Thrust Direction. Spine. 2018;43(1):1–9.
Reed WR, Pickar JG, Sozio RS, Liebschner MAK, Little JW, Gudavalli MR. Characteristics of Paraspinal Muscle Spindle Response to Mechanically Assisted Spinal Manipulation: A Preliminary Report. J Manipulative Physiol Ther. 2017;40(6):371–80.
Devecchi V, Rushton AB, Gallina A, Heneghan NR, Falla D. Are neuromuscular adaptations present in people with recurrent spinal pain during a period of remission? a systematic review. PLoS ONE. 2021;16(4):e0249220.
Pagé I, Nougarou F, Lardon A, Descarreaux M. Changes in spinal stiffness with chronic thoracic pain: Correlation with pain and muscle activity. PLoS ONE. 2018;13(12):e0208790.
Lee RY, McGregor AH, Bull AM, Wragg P. Dynamic response of the cervical spine to posteroanterior mobilisation. Clin Biomech (Bristol, Avon). 2005;20(2):228–31.
Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific? Spine. 2004;29(13):1452–7.
Donaldson M, Petersen S, Cook C, Learman K. A Prescriptively Selected Nonthrust Manipulation Versus a Therapist-Selected Nonthrust Manipulation for Treatment of Individuals With Low Back Pain: A Randomized Clinical Trial. J Orthop Sports Phys Ther. 2016;46(4):243–50.
McCarthy CJ, Potter L, Oldham JA. Comparing targeted thrust manipulation with general thrust manipulation in patients with low back pain. A general approach is as effective as a specific one. A randomised controlled trial. BMJ Open Sport Exerc Med. 2019;5(1):e000514.
Sutlive TG, Mabry LM, Easterling EJ, Durbin JD, Hanson SL, Wainner RS, et al. Comparison of short-term response to two spinal manipulation techniques for patients with low back pain in a military beneficiary population. Mil Med. 2009;174(7):750–6.
Tuttle N, Evans K, Sperotto dos Santos Rocha C. Localised manual therapy treatment has a preferential effect on the kinematics of the targeted motion segment. Musculoskelet Sci Pract. 2021;56:102457.
Ali MN, Sethi K, Noohu MM. Comparison of two mobilization techniques in management of chronic non-specific low back pain. J Bodyw Mov Ther. 2019;23(4):918–23.
de Oliveira RF, Costa LOP, Nascimento LP, Rissato LL. Directed vertebral manipulation is not better than generic vertebral manipulation in patients with chronic low back pain: a randomised trial. J Physiother. 2020;66(3):174–9.
Gevers-Montoro C, Provencher B, Northon S, Stedile-Lovatel JP, Ortega de Mues A, Piché M. Chiropractic Spinal Manipulation Prevents Secondary Hyperalgesia Induced by Topical Capsaicin in Healthy Individuals. Front Pain Res (Lausanne, Switzerland). 2021;2:702429.
Provencher B, Northon S, Piché M. Segmental Chiropractic Spinal Manipulation Does not Reduce Pain Amplification and the Associated Pain-Related Brain Activity in a Capsaicin-Heat Pain Model. Front Pain Res (Lausanne, Switzerland). 2021;2:733727.
Watanabe N, Piché M. Editorial: Mechanisms and Effectiveness of Complementary and Alternative Medicine for Pain Management. Front Pain Res (Lausanne, Switzerland). 2022;3:863751.
Muhsen A, Moss P, Gibson W, Walker B, Jacques A, Schug S, et al. The Association Between Conditioned Pain Modulation and Manipulation-induced Analgesia in People With Lateral Epicondylalgia. Clin J Pain. 2019;35(5):435–42.
Howick J, Glasziou P, Aronson JK. Evidence-based mechanistic reasoning. J Roy Soc Med. 2010;103(11):433–41.
Haavik Taylor H, Murphy B. The effects of spinal manipulation on central integration of dual somatosensory input observed after motor training: a crossover study. J Manipulative Physiol Ther. 2010;33(4):261–72.
Haavik-Taylor H, Murphy B. Cervical spine manipulation alters sensorimotor integration: a somatosensory evoked potential study. ClinNeurophysiol. 2007;118(2):391–402.
Ogura T, Tashiro M, Masud M, Watanuki S, Shibuya K, Yamaguchi K, et al. Cerebral metabolic changes in men after chiropractic spinal manipulation for neck pain. Altern Ther Health Med. 2011;17(6):12–7.
Sparks C, Cleland JA, Elliott JM, Zagardo M, Liu WC. Using functional magnetic resonance imaging to determine if cerebral hemodynamic responses to pain change following thoracic spine thrust manipulation in healthy individuals. J Orthop Sports Phys Ther. 2013;43(5):340–8.
Evans DW. How to gain evidence for causation in disease and therapeutic intervention: from Koch’s postulates to counter-counterfactuals. Med Health Care Philos. 2022;25(3):509–21.
Lascurain-Aguirrebeña I, Newham D, Critchley DJ. Mechanism of Action of Spinal Mobilizations: A Systematic Review. Spine. 2016;41(2):159–72.
Parravicini G, Bergna A. Biological effects of direct and indirect manipulation of the fascial system Narrative review. J Bodyw Mov Ther. 2017;21(2):435–45.
Crane JD, Ogborn DI, Cupido C, Melov S, Hubbard A, Bourgeois JM, et al. Massage therapy attenuates inflammatory signaling after exercise-induced muscle damage. Sci Transl Med. 2012;4(119):119ra13.
Degenhardt BF, Darmani NA, Johnson JC, Towns LC, Rhodes DC, Trinh C, et al. Role of osteopathic manipulative treatment in altering pain biomarkers: a pilot study. J Am Osteopath Assoc. 2007;107(9):387–400.
Kovanur-Sampath K, Mani R, Cotter J, Gisselman AS, Tumilty S. Changes in biochemical markers following spinal manipulation-a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;29:120–31.
Lohman EB, Pacheco GR, Gharibvand L, Daher N, Devore K, Bains G, et al. The immediate effects of cervical spine manipulation on pain and biochemical markers in females with acute non-specific mechanical neck pain: a randomized clinical trial. J Man Manip Ther. 2019;27(4):186–96.
Teodorczyk-Injeyan JA, McGregor M, Triano JJ, Injeyan SH. Elevated Production of Nociceptive CC Chemokines and sE-Selectin in Patients With Low Back Pain and the Effects of Spinal Manipulation: A Nonrandomized Clinical Trial. Clin J Pain. 2018;34(1):68–75.
Council GC. The Code: Standards of conduct, performance and ethics for chiropractors. GCC; 2019.
Council HaCP. Standards of Proficiency - Physiotherapists. HCPC; 2013.
Council GO. Osteopathic Practice Standards. GOC; 2023.
Therapies TCfST. GCMT Code of Practice, Ethics and Proficiency for Professional Associations. GCMT; 2023.
Daluiso-King G, Hebron C. Is the biopsychosocial model in musculoskeletal physiotherapy adequate? An evolutionary concept analysis. Physiotherapy theory and practice. 2020:1–17.
Søndenå P, Dalusio-King G, Hebron C. Conceptualisation of the therapeutic alliance in physiotherapy: is it adequate? Musculoskelet Sci Pract. 2020;46:102131.
World Health Organisation. Patient Safety 2019 [Available from: https://www.who.int/news-room/fact-sheets/detail/patient-safety#:~:text=Patient%20Safety%20is%20a%20health,during%20provision%20of%20health%20care .
Vogel S, Mars T, Keeping S, Barton T, Marlin N, Froud R, et al. Clinical Risk Osteopathy and Management Scientific Report. 2012.
Ekerholt K, Bergland A. Learning and knowing bodies: Norwegian psychomotor physiotherapists’ reflections on embodied knowledge. Physiother Theory Pract. 2019;35(1):57–69.
Hutting N, Johnston V, Staal JB, Heerkens YF. Promoting the Use of Self-management Strategies for People With Persistent Musculoskeletal Disorders: The Role of Physical Therapists. J Orthop Sports Phys Ther. 2019;49(4):212–5.
Kongsted A, Ris I, Kjaer P, Hartvigsen J. Self-management at the core of back pain care: 10 key points for clinicians. Braz J Phys Therap. 2021.
Elwyn G, Durand MA, Song J, Aarts J, Barr PJ, Berger Z, et al. A three-talk model for shared decision making: multistage consultation process. BMJ (Clinical research ed). 2017;359:j4891.
Broom B. The Practice of Whole Person-Centred Healthcare. In: Anjum RL, Copeland S, Rocca E, editors. Rethinking Causality, Complexity and Evidence for the Unique Patient: A CauseHealth Resource for Healthcare Professionals and the Clinical Encounter. Cham: Springer International Publishing; 2020. p. 215–26.
Chapter Google Scholar
Darlow B, Dowell A, Baxter GD, Mathieson F, Perry M, Dean S. The enduring impact of what clinicians say to people with low back pain. Ann Fam Med. 2013;11(6):527–34.
Stewart M, Loftus S. Sticks and Stones: The Impact of Language in Musculoskeletal Rehabilitation. J Orthop Sports Phys Ther. 2018;48(7):519–22.
Lin I, Wiles L, Waller R, Caneiro JP, Nagree Y, Straker L, et al. Patient-centred care: the cornerstone for high-value musculoskeletal pain management. Br J Sports Med. 2020;54(21):1240–2.
Cowell I, O’Sullivan P, O’Sullivan K, Poyton R, McGregor A, Murtagh G. Perceptions of physiotherapists towards the management of non-specific chronic low back pain from a biopsychosocial perspective: A qualitative study. Musculoskelet Sci Pract. 2018;38:113–9.
Edmond SN, Keefe FJ. Validating pain communication: current state of the science. Pain. 2015;156(2):215–9.
O’Keeffe M, Cullinane P, Hurley J, Leahy I, Bunzli S, O’Sullivan PB, et al. What Influences Patient-Therapist Interactions in Musculoskeletal Physical Therapy? Qualitative Systematic Review and Meta-Synthesis. Phys Ther. 2016;96(5):609–22.
Copnell G. Informed consent in physiotherapy practice: it is not what is said but how it is said. Physiotherapy. 2018;104(1):67–71.
Lee A. Bolam’ to “Montgomery” is result of evolutionary change of medical practice towards ’patient-centred care. Postgrad Med J. 2017;93(1095):46–50.
Lewis J, O’Sullivan P. Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br J Sports Med. 2018;52(24):1543–4.
Lewis J, Ridehalgh C, Moore A, Hall K. This is the day your life must surely change: Prioritising behavioural change in musculoskeletal practice. Physiotherapy. 2021.
Lewis JS, Stokes EK, Gojanovic B, Gellatly P, Mbada C, Sharma S, et al. Reframing how we care for people with persistent non-traumatic musculoskeletal pain. Suggestions for the rehabilitation community. Physiotherapy. 2021.
Bishop A, Foster NE, Thomas E, Hay EM. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health care practitioners? A survey of UK general practitioners and physiotherapists. Pain. 2008;135(1–2):187–95.
Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain (London, England). 2012;16(1):3–17.
Article CAS Google Scholar
Lakke SE, Soer R, Krijnen WP, van der Schans CP, Reneman MF, Geertzen JH. Influence of Physical Therapists’ Kinesiophobic Beliefs on Lifting Capacity in Healthy Adults. Phys Ther. 2015;95(9):1224–33.
Howe LC, Leibowitz KA, Crum AJ. When Your Doctor “Gets It” and “Gets You”: The Critical Role of Competence and Warmth in the Patient-Provider Interaction. Front Psych. 2019;10:475.
Newell D, Lothe LR, Raven TJL. Contextually Aided Recovery (CARe): a scientific theory for innate healing. Chiropr Man Therap. 2017;25:6.
Rossettini G, Camerone EM, Carlino E, Benedetti F, Testa M. Context matters: the psychoneurobiological determinants of placebo, nocebo and context-related effects in physiotherapy. Arch Physiother. 2020;10:11.
Gallace A. Social Touch. In: Olausson H, Wessberg J, Morrison I, McGlone F, editors. Affective Touch and the Neurophysiology of CT Afferents: Springer; 2016.
Gallace A, Spence C. The science of interpersonal touch: an overview. Neurosci Biobehav Rev. 2010;34(2):246–59.
Kelly MA, Nixon L, McClurg C, Scherpbier A, King N, Dornan T. Experience of Touch in Health Care: A Meta-Ethnography Across the Health Care Professions. Qual Health Res. 2018;28(2):200–12.
McGlone F, Cerritelli F, Walker S, Esteves J. The role of gentle touch in perinatal osteopathic manual therapy. Neurosci Biobehav Rev. 2017;72:1–9.
Olausson H, Wessberg J, Morrison I, McGlone F. Affective Touch and the Neurophysiology of CT Afferents: Springer; 2016.
McParlin Z, Cerritelli F, Rossettini G, Friston KJ, Esteves JE. Therapeutic Alliance as Active Inference: The Role of Therapeutic Touch and Biobehavioural Synchrony in Musculoskeletal Care. Front Behav Neurosci. 2022;16:897247.
Meijer LL, Ruis C, van der Smagt MJ, Scherder EJA, Dijkerman HC. Neural basis of affective touch and pain: A novel model suggests possible targets for pain amelioration. J Neuropsychol. 2021.
Allen-Collinson J, Pavey A. Touching moments: phenomenological sociology and the haptic dimension in the lived experience of motor neurone disease. Sociol Health Illn. 2014;36(6):793–806.
Bjorbækmo WS, Mengshoel AM. “A touch of physiotherapy” - the significance and meaning of touch in the practice of physiotherapy. Physiother Theory Pract. 2016;32(1):10–9.
Nummenmaa L, Tuominen L, Dunbar R, Hirvonen J, Manninen S, Arponen E, et al. Social touch modulates endogenous μ-opioid system activity in humans. Neuroimage. 2016;138:242–7.
Calsius J, De Bie J, Hertogen R, Meesen R. Touching the Lived Body in Patients with Medically Unexplained Symptoms. How an Integration of Hands-on Bodywork and Body Awareness in Psychotherapy may Help People with Alexithymia. Front Psychol. 2016;7:253.
Gentsch A, Crucianelli L, Jenkinson P, Fotopoulou A. The touched self: Affective touch and body awareness in health and disease. Affective touch and the neurophysiology of CT afferents Springer; 2016.
Cerritelli F, Chiacchiaretta P, Gambi F, Ferretti A. Effect of Continuous Touch on Brain Functional Connectivity Is Modified by the Operator’s Tactile Attention. Front Hum Neurosci. 2017;11:368.
Tramontano M, Cerritelli F, Piras F, Spanò B, Tamburella F, Piras F, et al. Brain Connectivity Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Brain Sci. 2020;10(12):969.
Øberg GK, Blanchard Y, Obstfelder A. Therapeutic encounters with preterm infants: interaction, posture and movement. Physiother Theory Pract. 2014;30(1):1–5.
Øberg GK, Normann B, Gallagher S. Embodied-enactive clinical reasoning in physical therapy. Physiother Theory Pract. 2015;31(4):244–52.
Consedine S, Standen C, Niven E. Knowing hands converse with an expressive body – An experience of osteopathic touch. Int J Osteopath Med. 2016;19:3–12.
Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39–48.
Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41–8.
Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201–3.
Sherriff B, Clark C, Killingback C, Newell D. Musculoskeletal practitioners’ perceptions of contextual factors that may influence chronic low back pain outcomes: a modified Delphi study. Chiropr Man Therap. 2023;31(1):12.
Sherriff B, Clark C, Killingback C, Newell D. Impact of contextual factors on patient outcomes following conservative low back pain treatment: systematic review. Chiropr Manual Therap. 2022;30(1):20.
Mercer E, Mackay-Lyons M, Conway N, Flynn J, Mercer C. Perceptions of outpatients regarding the attire of physiotherapists. Physiother Can. 2008;60(4):349–57.
Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature— targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578.
Beach MC, Fitzgerald A, Saha S. White Coat Hype: Branding Physicians With Professional Attire. JAMA Intern Med. 2013;173(6):467–8.
Bearman G, Bryant K, Leekha S, Mayer J, Munoz-Price LS, Murthy R, et al. Healthcare Personnel Attire in Non-Operating-Room Settings. Infect Control Hosp Epidemiol. 2014;35(2):107–21.
Rehman SU, Nietert PJ, Cope DW, Kilpatrick AO. What to wear today? Effect of doctor’s attire on the trust and confidence of patients. Am J Med. 2005;118(11):1279–86.
Brady B, Veljanova I, Schabrun S, Chipchase L. Integrating culturally informed approaches into physiotherapy assessment and treatment of chronic pain: a pilot randomised controlled trial. BMJ Open. 2018;8(7):e021999.
Miles A, Mezzich JE. The care of the patient and the soul of the clinic: person-centered medicine as an emergent model of clinical practice. Int J Person Centred Med. 2012;1(2):207–22.
Cowell I, McGregor A, O’Sullivan P, O’Sullivan K, Poyton R, Schoeb V, et al. How do physiotherapists solicit and explore patients’ concerns in back pain consultations: a conversation analytic approach. Physiother Theory Pract. 2021;37(6):693–709.
Hutting N, Caneiro JP, Ong'wen MO, Miciak M, Roberts LE. Patient-centered care in musculoskeletal practice: key elements to support clinicians to focus on the person. 2021.
Caneiro JP, Roos EM, Barton CJ, O’Sullivan K, Kent P, Lin I, et al. It is time to move beyond “body region silos” to manage musculoskeletal pain: five actions to change clinical practice. Br J Sports Med. 2020;54(8):438–9.
Greenhalgh T, Howick J, Maskrey N, EBM Renaissance Group. Evidence based medicine: a movement in crisis? Brit Med J. 2014;348:g3725.
Greenhalgh T, Snow R, Ryan S, Rees S, Salisbury H. Six ‘biases’ against patients and carers in evidence-based medicine. Bmc Med. 2015;13(1):200.
Loughlin M, Fuller J, Bluhm R, Buetow S, Borgerson K. Theory, experience and practice. J Eval Clin Pract. 2016;22(4):459–65.
Simpson JK, Innes S. Informed consent, duty of disclosure and chiropractic: where are we? Chiropr Man Therap. 2020;28(1):60.
Download references
Acknowledgements
Use of any animal or human data or tissue.
No funding was received for this paper.
Author information
Authors and affiliations.
School of Health Sciences, Queens Medical Centre, University of Nottingham, Nottingham, NG7 2HA, UK
Roger Kerry, Edward Lee & Vasileios Georgopoulos
Allied Health Research Unit, University of Central Lancashire, Preston, PR1 2HE, UK
Kenneth J. Young
Centre of Precision Rehabilitation for Spinal Pain, School of Sport, Exercise and Rehabilitation Sciences, University of Birmingham, Edgbaston, Birmingham, B15 2TT, UK
David W. Evans
Nottingham CityCare Partnership, Bennerley Rd, Nottingham, NG6 8WR, UK
School of Medicine, University of Nottingham, Queens Medical Centre, Nottingham, NG7 2HA, UK
Vasileios Georgopoulos
Department of Orthopaedics, West Herts Hospitals Trust, Watford, WD18 0HB, UK
Adam Meakins
School of Physiotherapy, Manchester Metropolitan University, Manchester, M15 6GX, UK
Chris McCarthy
Department of Orthopaedics, Duke University, 200 Morris Street, Durham, NC, 27701, USA
School of Sport and Health Sciences, University of Brighton, Darley Rd, Eastbourne, BN20 7UR, UK
Colette Ridehalgh
Clinical Neuroscience, Trafford Building, Brighton and Sussex Medical School, University of Sussex, Brighton, BN1 9PX, UK
University College of Osteopathy, 275 Borough High St, London, SE1 1JE, UK
Steven Vogel & Amanda Banton
Department of Clinical Sciences, Obstetrics and Gynecology, Umeå University, S-90187, Umeå, Sweden
Cecilia Bergström
The School of Soft Tissue Therapy, Exmouth, Devon, EX8 1DQ, UK
Anna Maria Mazzieri
Department of health, LUNEX, Differdange, 4671, Luxembourg
Firas Mourad
Luxembourg Health & Sport Sciences Research Institute A.s.b.l., 50, Avenue du Parc des Sports, Differdange, 4671, Luxembourg
Department of Occupation and Health, School of Organization and Development, HAN University of Applied Sciences, Nijmegen, the Netherlands
Nathan Hutting
You can also search for this author in PubMed Google Scholar
Contributions
Concept and research design: RK, KJY, DWE, EL, AM, VG. Data collection: All authors. Data analysis: All authors. Writing and editing of the manuscript: All authors.
Corresponding author
Correspondence to Kenneth J. Young .
Ethics declarations
Ethics approval and consent to participate.
All participants are co-authors. Ethical approval was not necessary.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kerry, R., Young, K.J., Evans, D.W. et al. A modern way to teach and practice manual therapy. Chiropr Man Therap 32 , 17 (2024). https://doi.org/10.1186/s12998-024-00537-0
Download citation
Received : 18 October 2023
Accepted : 17 April 2024
Published : 21 May 2024
DOI : https://doi.org/10.1186/s12998-024-00537-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Manual Therapy
- Evidence-based healthcare
- Person-centred healthcare
- Physiotherapy
- Chiropractic
- Soft-tissue therapy
Chiropractic & Manual Therapies
ISSN: 2045-709X
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Case Study Research Method in Psychology
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews).
The case study research method originated in clinical medicine (the case history, i.e., the patient’s personal history). In psychology, case studies are often confined to the study of a particular individual.
The information is mainly biographical and relates to events in the individual’s past (i.e., retrospective), as well as to significant events that are currently occurring in his or her everyday life.
The case study is not a research method, but researchers select methods of data collection and analysis that will generate material suitable for case studies.
Freud (1909a, 1909b) conducted very detailed investigations into the private lives of his patients in an attempt to both understand and help them overcome their illnesses.
This makes it clear that the case study is a method that should only be used by a psychologist, therapist, or psychiatrist, i.e., someone with a professional qualification.
There is an ethical issue of competence. Only someone qualified to diagnose and treat a person can conduct a formal case study relating to atypical (i.e., abnormal) behavior or atypical development.
Famous Case Studies
- Anna O – One of the most famous case studies, documenting psychoanalyst Josef Breuer’s treatment of “Anna O” (real name Bertha Pappenheim) for hysteria in the late 1800s using early psychoanalytic theory.
- Little Hans – A child psychoanalysis case study published by Sigmund Freud in 1909 analyzing his five-year-old patient Herbert Graf’s house phobia as related to the Oedipus complex.
- Bruce/Brenda – Gender identity case of the boy (Bruce) whose botched circumcision led psychologist John Money to advise gender reassignment and raise him as a girl (Brenda) in the 1960s.
- Genie Wiley – Linguistics/psychological development case of the victim of extreme isolation abuse who was studied in 1970s California for effects of early language deprivation on acquiring speech later in life.
- Phineas Gage – One of the most famous neuropsychology case studies analyzes personality changes in railroad worker Phineas Gage after an 1848 brain injury involving a tamping iron piercing his skull.
Clinical Case Studies
- Studying the effectiveness of psychotherapy approaches with an individual patient
- Assessing and treating mental illnesses like depression, anxiety disorders, PTSD
- Neuropsychological cases investigating brain injuries or disorders
Child Psychology Case Studies
- Studying psychological development from birth through adolescence
- Cases of learning disabilities, autism spectrum disorders, ADHD
- Effects of trauma, abuse, deprivation on development
Types of Case Studies
- Explanatory case studies : Used to explore causation in order to find underlying principles. Helpful for doing qualitative analysis to explain presumed causal links.
- Exploratory case studies : Used to explore situations where an intervention being evaluated has no clear set of outcomes. It helps define questions and hypotheses for future research.
- Descriptive case studies : Describe an intervention or phenomenon and the real-life context in which it occurred. It is helpful for illustrating certain topics within an evaluation.
- Multiple-case studies : Used to explore differences between cases and replicate findings across cases. Helpful for comparing and contrasting specific cases.
- Intrinsic : Used to gain a better understanding of a particular case. Helpful for capturing the complexity of a single case.
- Collective : Used to explore a general phenomenon using multiple case studies. Helpful for jointly studying a group of cases in order to inquire into the phenomenon.
Where Do You Find Data for a Case Study?
There are several places to find data for a case study. The key is to gather data from multiple sources to get a complete picture of the case and corroborate facts or findings through triangulation of evidence. Most of this information is likely qualitative (i.e., verbal description rather than measurement), but the psychologist might also collect numerical data.
1. Primary sources
- Interviews – Interviewing key people related to the case to get their perspectives and insights. The interview is an extremely effective procedure for obtaining information about an individual, and it may be used to collect comments from the person’s friends, parents, employer, workmates, and others who have a good knowledge of the person, as well as to obtain facts from the person him or herself.
- Observations – Observing behaviors, interactions, processes, etc., related to the case as they unfold in real-time.
- Documents & Records – Reviewing private documents, diaries, public records, correspondence, meeting minutes, etc., relevant to the case.
2. Secondary sources
- News/Media – News coverage of events related to the case study.
- Academic articles – Journal articles, dissertations etc. that discuss the case.
- Government reports – Official data and records related to the case context.
- Books/films – Books, documentaries or films discussing the case.
3. Archival records
Searching historical archives, museum collections and databases to find relevant documents, visual/audio records related to the case history and context.
Public archives like newspapers, organizational records, photographic collections could all include potentially relevant pieces of information to shed light on attitudes, cultural perspectives, common practices and historical contexts related to psychology.
4. Organizational records
Organizational records offer the advantage of often having large datasets collected over time that can reveal or confirm psychological insights.
Of course, privacy and ethical concerns regarding confidential data must be navigated carefully.
However, with proper protocols, organizational records can provide invaluable context and empirical depth to qualitative case studies exploring the intersection of psychology and organizations.
- Organizational/industrial psychology research : Organizational records like employee surveys, turnover/retention data, policies, incident reports etc. may provide insight into topics like job satisfaction, workplace culture and dynamics, leadership issues, employee behaviors etc.
- Clinical psychology : Therapists/hospitals may grant access to anonymized medical records to study aspects like assessments, diagnoses, treatment plans etc. This could shed light on clinical practices.
- School psychology : Studies could utilize anonymized student records like test scores, grades, disciplinary issues, and counseling referrals to study child development, learning barriers, effectiveness of support programs, and more.
How do I Write a Case Study in Psychology?
Follow specified case study guidelines provided by a journal or your psychology tutor. General components of clinical case studies include: background, symptoms, assessments, diagnosis, treatment, and outcomes. Interpreting the information means the researcher decides what to include or leave out. A good case study should always clarify which information is the factual description and which is an inference or the researcher’s opinion.
1. Introduction
- Provide background on the case context and why it is of interest, presenting background information like demographics, relevant history, and presenting problem.
- Compare briefly to similar published cases if applicable. Clearly state the focus/importance of the case.
2. Case Presentation
- Describe the presenting problem in detail, including symptoms, duration,and impact on daily life.
- Include client demographics like age and gender, information about social relationships, and mental health history.
- Describe all physical, emotional, and/or sensory symptoms reported by the client.
- Use patient quotes to describe the initial complaint verbatim. Follow with full-sentence summaries of relevant history details gathered, including key components that led to a working diagnosis.
- Summarize clinical exam results, namely orthopedic/neurological tests, imaging, lab tests, etc. Note actual results rather than subjective conclusions. Provide images if clearly reproducible/anonymized.
- Clearly state the working diagnosis or clinical impression before transitioning to management.
3. Management and Outcome
- Indicate the total duration of care and number of treatments given over what timeframe. Use specific names/descriptions for any therapies/interventions applied.
- Present the results of the intervention,including any quantitative or qualitative data collected.
- For outcomes, utilize visual analog scales for pain, medication usage logs, etc., if possible. Include patient self-reports of improvement/worsening of symptoms. Note the reason for discharge/end of care.
4. Discussion
- Analyze the case, exploring contributing factors, limitations of the study, and connections to existing research.
- Analyze the effectiveness of the intervention,considering factors like participant adherence, limitations of the study, and potential alternative explanations for the results.
- Identify any questions raised in the case analysis and relate insights to established theories and current research if applicable. Avoid definitive claims about physiological explanations.
- Offer clinical implications, and suggest future research directions.
5. Additional Items
- Thank specific assistants for writing support only. No patient acknowledgments.
- References should directly support any key claims or quotes included.
- Use tables/figures/images only if substantially informative. Include permissions and legends/explanatory notes.
- Provides detailed (rich qualitative) information.
- Provides insight for further research.
- Permitting investigation of otherwise impractical (or unethical) situations.
Case studies allow a researcher to investigate a topic in far more detail than might be possible if they were trying to deal with a large number of research participants (nomothetic approach) with the aim of ‘averaging’.
Because of their in-depth, multi-sided approach, case studies often shed light on aspects of human thinking and behavior that would be unethical or impractical to study in other ways.
Research that only looks into the measurable aspects of human behavior is not likely to give us insights into the subjective dimension of experience, which is important to psychoanalytic and humanistic psychologists.
Case studies are often used in exploratory research. They can help us generate new ideas (that might be tested by other methods). They are an important way of illustrating theories and can help show how different aspects of a person’s life are related to each other.
The method is, therefore, important for psychologists who adopt a holistic point of view (i.e., humanistic psychologists ).
Limitations
- Lacking scientific rigor and providing little basis for generalization of results to the wider population.
- Researchers’ own subjective feelings may influence the case study (researcher bias).
- Difficult to replicate.
- Time-consuming and expensive.
- The volume of data, together with the time restrictions in place, impacted the depth of analysis that was possible within the available resources.
Because a case study deals with only one person/event/group, we can never be sure if the case study investigated is representative of the wider body of “similar” instances. This means the conclusions drawn from a particular case may not be transferable to other settings.
Because case studies are based on the analysis of qualitative (i.e., descriptive) data , a lot depends on the psychologist’s interpretation of the information she has acquired.
This means that there is a lot of scope for Anna O , and it could be that the subjective opinions of the psychologist intrude in the assessment of what the data means.
For example, Freud has been criticized for producing case studies in which the information was sometimes distorted to fit particular behavioral theories (e.g., Little Hans ).
This is also true of Money’s interpretation of the Bruce/Brenda case study (Diamond, 1997) when he ignored evidence that went against his theory.
Breuer, J., & Freud, S. (1895). Studies on hysteria . Standard Edition 2: London.
Curtiss, S. (1981). Genie: The case of a modern wild child .
Diamond, M., & Sigmundson, K. (1997). Sex Reassignment at Birth: Long-term Review and Clinical Implications. Archives of Pediatrics & Adolescent Medicine , 151(3), 298-304
Freud, S. (1909a). Analysis of a phobia of a five year old boy. In The Pelican Freud Library (1977), Vol 8, Case Histories 1, pages 169-306
Freud, S. (1909b). Bemerkungen über einen Fall von Zwangsneurose (Der “Rattenmann”). Jb. psychoanal. psychopathol. Forsch ., I, p. 357-421; GW, VII, p. 379-463; Notes upon a case of obsessional neurosis, SE , 10: 151-318.
Harlow J. M. (1848). Passage of an iron rod through the head. Boston Medical and Surgical Journal, 39 , 389–393.
Harlow, J. M. (1868). Recovery from the Passage of an Iron Bar through the Head . Publications of the Massachusetts Medical Society. 2 (3), 327-347.
Money, J., & Ehrhardt, A. A. (1972). Man & Woman, Boy & Girl : The Differentiation and Dimorphism of Gender Identity from Conception to Maturity. Baltimore, Maryland: Johns Hopkins University Press.
Money, J., & Tucker, P. (1975). Sexual signatures: On being a man or a woman.
Further Information
- Case Study Approach
- Case Study Method
- Enhancing the Quality of Case Studies in Health Services Research
- “We do things together” A case study of “couplehood” in dementia
- Using mixed methods for evaluating an integrative approach to cancer care: a case study
Related Articles
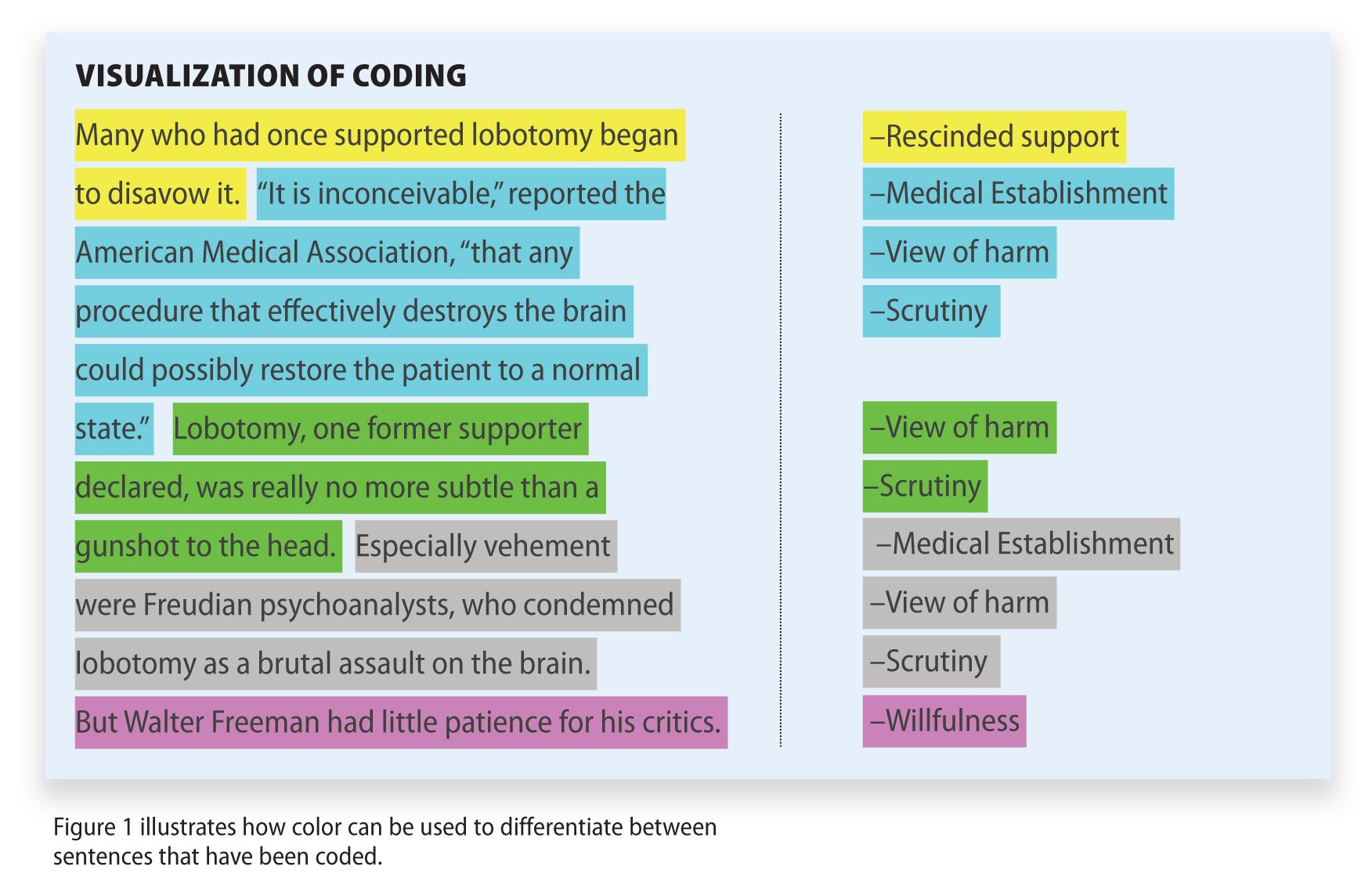
Research Methodology
Qualitative Data Coding

What Is a Focus Group?
Cross-Cultural Research Methodology In Psychology
What Is Internal Validity In Research?

Research Methodology , Statistics
What Is Face Validity In Research? Importance & How To Measure

Criterion Validity: Definition & Examples
- Open access
- Published: 22 May 2024
Enhancing clinical skills in pediatric trainees: a comparative study of ChatGPT-assisted and traditional teaching methods
- Hongjun Ba 1 , 2 ,
- Lili zhang 1 &
- Zizheng Yi 1
BMC Medical Education volume 24 , Article number: 558 ( 2024 ) Cite this article
201 Accesses
Metrics details
As artificial intelligence (AI) increasingly integrates into medical education, its specific impact on the development of clinical skills among pediatric trainees needs detailed investigation. Pediatric training presents unique challenges which AI tools like ChatGPT may be well-suited to address.
This study evaluates the effectiveness of ChatGPT-assisted instruction versus traditional teaching methods on pediatric trainees’ clinical skills performance.
A cohort of pediatric trainees ( n = 77) was randomly assigned to two groups; one underwent ChatGPT-assisted training, while the other received conventional instruction over a period of two weeks. Performance was assessed using theoretical knowledge exams and Mini-Clinical Evaluation Exercises (Mini-CEX), with particular attention to professional conduct, clinical judgment, patient communication, and overall clinical skills. Trainees’ acceptance and satisfaction with the AI-assisted method were evaluated through a structured survey.
Both groups performed similarly in theoretical exams, indicating no significant difference ( p > 0.05). However, the ChatGPT-assisted group showed a statistically significant improvement in Mini-CEX scores ( p < 0.05), particularly in patient communication and clinical judgment. The AI-teaching approach received positive feedback from the majority of trainees, highlighting the perceived benefits in interactive learning and skill acquisition.
ChatGPT-assisted instruction did not affect theoretical knowledge acquisition but did enhance practical clinical skills among pediatric trainees. The positive reception of the AI-based method suggests that it has the potential to complement and augment traditional training approaches in pediatric education. These promising results warrant further exploration into the broader applications of AI in medical education scenarios.
Peer Review reports
Introduction
The introduction of ChatGPT by OpenAI in November 2022 marked a watershed moment in educational technology, heralded as the third major innovation following Web 2.0’s emergence over a decade earlier [ 1 ] and the rapid expansion of e-learning driven by the COVID-19 pandemic [ 2 ]. In medical education, the integration of state-of-the-art Artificial Intelligence (AI) has been particularly transformative for pediatric clinical skills training—a field where AI is now at the forefront.
Pediatric training, with its intricate blend of extensive medical knowledge and soft skills like empathetic patient interaction, is pivotal for effective child healthcare. The need for swift decision-making, especially in emergency care settings, underscores the specialty’s complexity. Traditional teaching methods often fall short, hindered by logistical challenges and difficulties in providing a standardized training experience. AI tools such as ChatGPT offer a promising solution, with their ability to simulate complex patient interactions and thus improve pediatric trainees’ communication, clinical reasoning, and decision-making skills across diverse scenarios [ 3 , 4 ].
ChatGPT’s consistent, repeatable, and scalable learning experiences represent a significant advancement over traditional constraints, such as resource limitations and standardization challenges [ 5 ], offering a new paradigm for medical training. Its proficiency in providing immediate, personalized feedback could revolutionize the educational journey of pediatric interns. Our study seeks to investigate the full extent of this potential revolution, employing a mixed-methods approach to quantitatively and qualitatively measure the impact of ChatGPT on pediatric trainees’ clinical competencies.
Despite AI’s recognized potential within the academic community, empirical evidence detailing its influence on clinical skills development is limited [ 6 ]. Addressing this gap, our research aims to contribute substantive insights into the efficacy of ChatGPT in enhancing the clinical capabilities of pediatric trainees, establishing a new benchmark for the intersection of AI and medical education.
Participants and methods
Participants.
Our study evaluated the impact of ChatGPT-assisted instruction on the clinical skills of 77 medical interns enrolled in Sun Yat-sen University’s five-year program in 2023. The cohort, consisting of 42 males and 35 females, was randomly allocated into four groups based on practicum rotation, using a computer-generated randomization list. Each group, composed of 3–4 students, was assigned to either the ChatGPT-assisted or traditional teaching group for a two-week pediatric internship rotation. Randomization was stratified by baseline clinical examination scores to ensure group comparability.
Study design
A controlled experimental design was implemented with blind assessment. The interns were randomly assigned to the ChatGPT-assisted group (39 students) or the traditional group (38 students), with no significant differences in gender, age, or baseline clinical examination scores ( p > 0.05). The ChatGPT-assisted group received instruction supplemented with ChatGPT version 4.0, while the traditional group received standard bedside teaching (as depicted in Fig. 1 ). Both groups encountered identical clinical case scenarios involving common pediatric conditions: Kawasaki disease, gastroenteritis, congenital heart disease, nephrotic syndrome, bronchopneumonia, and febrile convulsion. All interns had equal access to the same teaching materials, instructors, and intensity of courses. The core textbook was the 9th edition of “Pediatrics” published by the People’s Medical Publishing House. Ethical approval was obtained from the institutional review board, and informed consent was secured, with special attention to privacy concerns due to the involvement of pediatric patient data.
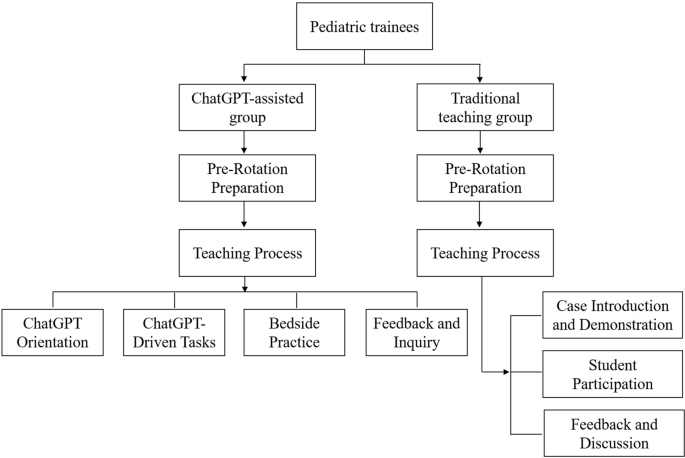
Study design and flow chart
Instructional implementation
Traditional teaching group, pre-rotation preparation.
Instructors designed typical cases representing common pediatric diseases and updated knowledge on the latest diagnostic and therapeutic advancements. They developed multimedia presentations detailing the presentation, diagnostic criteria, and treatment plans for each condition.
Teaching process
The teaching method during the rotation was divided into three stages:
Case introduction and demonstration
Instructors began with a detailed introduction of clinical cases, explaining diagnostic reasoning and emphasizing key aspects of medical history-taking and physical examination techniques.
Student participation
Students then conducted patient interviews and physical assessments independently, with the instructor observing. For pediatric patients, particularly infants, history was provided by the guardians.
Feedback and discussion
At the end of each session, instructors provided personalized feedback on student performance and answered questions, fostering an interactive learning environment.
ChatGPT-assisted teaching group
Educators prepared structured teaching plans focusing on common pediatric diseases and representative cases. The preparation phase involved configuring ChatGPT (version 4.0) settings to align with the educational objectives of the rotation.
The rotation was executed in four consecutive steps:
ChatGPT orientation
Students were familiarized with the functionalities and potential educational applications of ChatGPT version 4.0.
ChatGPT-driven tasks
In our study, ChatGPT version 4.0 was used as a supplementary educational tool within the curriculum. Students engaged with the AI to interactively explore dynamically generated clinical case vignettes based on pediatric medicine. These vignettes encompassed clinical presentations, history taking, physical examinations, diagnostic strategies, differential diagnoses, and treatment protocols, allowing students to query the AI to enhance their understanding of various clinical scenarios.
Students accessed clinical vignettes in both text and video formats, with video particularly effective in demonstrating physical examination techniques and communication strategies with guardians, thereby facilitating a more interactive learning experience.
ChatGPT initially guided students in forming assessments, while educators critically reviewed their work, providing immediate, personalized feedback to ensure proper development of clinical reasoning and decision-making skills. This blend of AI and direct educator involvement aimed to improve learning outcomes by leveraging AI’s scalability alongside expert educators’ insights.
Bedside clinical practice
Students practiced history-taking and physical examinations at the patient’s bedside, with information about infants provided by their guardians.
Feedback and inquiry
Instructors offered feedback on performance and addressed student queries to reinforce learning outcomes.
Assessment methods
The methods used to evaluate the interns’ post-rotation performance included three assessment tools:
Theoretical knowledge exam
Both groups completed the same closed-book exam to test their pediatric theoretical knowledge, ensuring consistency in cognitive understanding assessment.
Mini-CEX assessment
The Mini-CEX has been widely recognized as an effective and reliable method for assessing clinical skills [ 7 , 8 ]. Practical skills were evaluated using the Mini-CEX, which involved students taking histories from parents of pediatric patients and conducting physical examinations on infants, supervised by an instructor. Mini-CEX scoring utilized a nine-point scale with seven criteria, assessing history-taking, physical examination, professionalism, clinical judgment, doctor-patient communication, organizational skills, and overall competence.
History taking
This assessment measures students’ ability to accurately collect patient histories, utilize effective questioning techniques, respond to non-verbal cues, and exhibit respect, empathy, and trust, while addressing patient comfort, dignity, and confidentiality.
Physical examination
This evaluates students on informing patients about examination procedures, conducting examinations in an orderly sequence, adjusting examinations based on patient condition, attending to patient discomfort, and ensuring privacy.
Professionalism
This assesses students’ demonstration of respect, compassion, and empathy, establishment of trust, attention to patient comfort, maintenance of confidentiality, adherence to ethical standards, understanding of legal aspects, and recognition of their professional limits.
Clinical judgment
This includes evaluating students’ selection and execution of appropriate diagnostic tests and their consideration of the risks and benefits of various treatment options.
Doctor-patient communication
This involves explaining test and treatment rationales, obtaining patient consent, educating on disease management, and discussing issues effectively and timely based on disease severity.
Organizational efficiency
This measures how students prioritize based on urgency, handle patient issues efficiently, demonstrate integrative skills, understand the healthcare system, and effectively use resources for optimal service.
Overall competence
This assesses students on judgment, integration, and effectiveness in patient care, evaluating their overall capabilities in caring and efficiency.
The scale ranged from below expectations (1–3 points), meeting expectations (4–6 points), to exceeding expectations (7–9 points). To maintain assessment consistency, all Mini-CEX evaluations were conducted by a single assessor.
ChatGPT method feedback survey
Only for the ChatGPT-assisted group, the educational impact of the ChatGPT teaching method was evaluated post-rotation through a questionnaire. This survey used a self-assessment scale with a Cronbach’s Alpha coefficient of 0.812, confirming its internal consistency and reliability. Assessment items involved active learning engagement, communication skills, empathy, retention of clinical knowledge, and improvement in diagnostic reasoning. Participant satisfaction was categorized as (1) very satisfied, (2) satisfied, (3) neutral, or (4) dissatisfied.
Statistical analysis
Data were analyzed using R software (version 4.2.2) and SPSS (version 26.0). Descriptive statistics were presented as mean ± standard deviation (x ± s), and independent t-tests were performed to compare groups. Categorical data were presented as frequency and percentage (n[%]), with chi-square tests applied where appropriate. A P -value of < 0.05 was considered statistically significant. All assessors of the Mini-CEX were blinded to the group assignments to minimize bias.
Theoretical knowledge exam scores for both groups of trainees
The theoretical knowledge exam revealed comparable results between the two groups, with the ChatGPT-assisted group achieving a mean score of 92.21 ± 2.37, and the traditional teaching group scoring slightly higher at 92.38 ± 2.68. Statistical analysis using an independent t-test showed no significant difference in the exam scores (t = 0.295, p = 0.768), suggesting that both teaching methods similarly supported the trainees’ theoretical learning.
Mini-CEX evaluation results for both groups of trainees
All trainees completed the Mini-CEX evaluation in 38 ± 0.5 min on average, with immediate post-evaluation feedback averaging 5.8 ± 0.6 min per student. The ChatGPT group demonstrated statistically significant improvement in professional conduct, clinical judgment, patient communication, and overall clinical skills compared to the traditional group. A detailed comparison of the CEX scoring for both student groups is presented in Table 1 ; Fig. 2 .
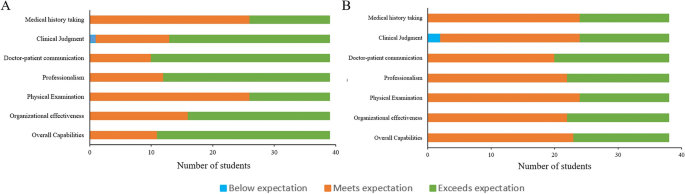
The scale scores of Mini-CEX assessment between the two groups. A : ChatGPT-assisted group; B : Traditional teaching group
Satisfaction survey results of trainees in the ChatGPT-assisted teaching
Feedback from the trainees regarding the ChatGPT-assisted teaching method was overwhelmingly positive. High levels of satisfaction and interest were reported, with no instances of dissatisfaction noted. The summary of these findings, including specific aspects of the teaching method that were rated highly by the students, is detailed in Table 2 .
The integration of ChatGPT into pediatric medical education represents a significant stride in leveraging artificial intelligence (AI) to enhance the learning process. Our findings suggest that while AI does not substantially alter outcomes in theoretical knowledge assessments, it plays a pivotal role in the advancement of clinical competencies.
The parity in theoretical examination scores between the ChatGPT-assisted and traditionally taught groups indicates that foundational medical knowledge can still be effectively acquired through existing educational frameworks. This underscores the potential of ChatGPT as a complementary, rather than a substitutive, educational instrument [ 9 , 10 ].
Mini-CEX evaluations paint a different picture, revealing the ChatGPT group’s superior performance in clinical realms. These competencies are crucial for the comprehensive development of a pediatrician and highlight the value of an interactive learning environment in bridging the gap between theory and practice [ 11 , 12 ].
The unanimous satisfaction with ChatGPT-assisted learning points to AI’s capacity to enhance student engagement. This positive response could be attributed to the personalized and interactive nature of the AI experience, catering to diverse learning styles [ 13 , 14 ]. However, it is critical to consider the potential for overreliance on technology and the need for maintaining an appropriate balance between AI and human interaction in medical training.
The ChatGPT group’s ascendency in clinical skillfulness could be a testament to the repetitive, adaptive learning scenarios proffered by AI technology. ChatGPT’s proficiency in tailoring educational content to individual performance metrics propels a more incisive and efficacious learning journey. Furthermore, the on-site, real-time feedback from evaluators is likely instrumental in consolidating clinical skillsets, echoing findings on the potency of immediate feedback in clinical education [ 15 , 16 ].
The study’s strength lies in its pioneering exploration of ChatGPT in pediatric education and the structured use of Mini-CEX for appraising clinical competencies, but it is not without limitations. The ceiling effect may have masked subtle differences in theoretical knowledge, and our small, single-center cohort limits the generalizability of our findings. The transitory nature of the study precludes assessment of long-term retention, a factor that future research should aim to elucidate [ 17 , 18 ].
Moreover, the ongoing evolution of AI and medical curricula necessitates continuous reevaluation of ChatGPT’s role in education. Future studies should explore multicenter trials, long-term outcomes, and integration strategies within existing curricula to provide deeper insights into AI’s role in medical education. Ethical and practical considerations, including data privacy, resource allocation, and cost, must also be carefully navigated to ensure that AI tools like ChatGPT are implemented responsibly and sustainably.
In conclusion, ChatGPT’s incorporation into pediatric training did not significantly affect the acquisition of theoretical knowledge but did enhance clinical skill development. The high levels of trainee satisfaction suggest that ChatGPT is a valuable adjunct to traditional educational methods, warranting further investigation and thoughtful integration into medical curricula.
Availability of data and materials
All data sets generated for this study were included in the manuscript.
Hollinderbäumer A, Hartz T, Uckert F. Education 2.0 — how has social media and web 2.0 been integrated into medical education? A systematical literature review. GMS Z Med Ausbild. 2013;30(1):Doc14. https://doi.org/10.3205/zma000857 .
Article Google Scholar
Turnbull D, Chugh R, Luck J. Transitioning to E-Learning during the COVID-19 pandemic: how have higher education institutions responded to the challenge? Educ Inf Technol (Dordr). 2021;26(5):6401–19. https://doi.org/10.1007/s10639-021-10633-w .
Bright TJ, Wong A, Dhurjati R, Bristow E, Bastian L, Coeytaux RR, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29–43. https://doi.org/10.7326/0003-4819-157-1-201207030-00450 .
Chan KS, Zary N. Applications and challenges of implementing artificial intelligence in medical education: integrative review. JMIR Med Educ. 2019;5(1):e13930. https://doi.org/10.2196/13930 .
Geoffrey Currie. A conversation with ChatGPT. J Nucl Med Technol. 2023;51(3):255–60. https://doi.org/10.2967/jnmt.123.265864 .
Hossain E, Rana R, Higgins N, Soar J, Barua PD, Pisani AR, et al. Natural language processing in electronic health records in relation to healthcare decision-making: a systematic review. Comput Biol Med. 2023;155:106649. https://doi.org/10.1016/j.compbiomed.2023.106649 .
Mortaz Hejri S, Jalili M, Masoomi R, Shirazi M, Nedjat S, Norcini J. The utility of mini-clinical evaluation Exercise in undergraduate and postgraduate medical education: a BEME review: BEME guide 59. Med Teach. 2020;42(2):125–42. https://doi.org/10.1080/0142159X.2019.1652732 .
Motefakker S, Shirinabadi Farahani A, Nourian M, Nasiri M, Heydari F. The impact of the evaluations made by Mini-CEX on the clinical competency of nursing students. BMC Med Educ. 2022;22(1):634. https://doi.org/10.1186/s12909-022-03667-2 .
Eysenbach G. The role of ChatGPT, generative language models, and artificial intelligence in medical education: a conversation with ChatGPT and a call for papers. JMIR Med Educ. 2023;9:e46885. https://doi.org/10.2196/46885 .
Guo J, Bai L, Yu Z, Zhao Z, Wan B. An AI-application-oriented In-Class teaching evaluation model by using statistical modeling and ensemble learning. Sens (Basel). 2021;21(1):241. https://doi.org/10.3390/s21010241 .
Vishwanathaiah S, Fageeh HN, Khanagar SB, Maganur PC. Artificial Intelligence its uses and application in pediatric dentistry: a review. Biomedicines. 2023;11(3):788. https://doi.org/10.3390/biomedicines11030788 .
Cooper A, Rodman A. AI and Medical Education - A 21st-Century Pandora’s Box. N Engl J Med. 2023;389(5):385–7. https://doi.org/10.1056/NEJMp2304993 .
Arif TB, Munaf U, Ul-Haque I. The future of medical education and research: is ChatGPT a blessing or blight in disguise? Med Educ Online. 2023;28(1):2181052. https://doi.org/10.1080/10872981.2023.2181052 .
Nagi F, Salih R, Alzubaidi M, Shah H, Alam T, Shah Z, et al. Applications of Artificial Intelligence (AI) in medical education: a scoping review. Stud Health Technol Inf. 2023;305:648–51. https://doi.org/10.3233/SHTI230581 .
van de Ridder JM, Stokking KM, McGaghie WC, ten Cate OT. What is feedback in clinical education? Med Educ. 2008;42(2):189–97. https://doi.org/10.1111/j.1365-2923.2007.02973.x .
Wilbur K, BenSmail N, Ahkter S. Student feedback experiences in a cross-border medical education curriculum. Int J Med Educ. 2019;10:98–105. https://doi.org/10.5116/ijme.5ce1.149f .
Morrow E, Zidaru T, Ross F, Mason C, Patel KD, Ream M, et al. Artificial intelligence technologies and compassion in healthcare: a systematic scoping review. Front Psychol. 2023;13:971044. https://doi.org/10.3389/fpsyg.2022.971044 .
Soong TK, Ho CM. Artificial intelligence in medical OSCEs: reflections and future developments. Adv Med Educ Pract. 2021;12:167–73. https://doi.org/10.2147/AMEP.S287926 .
Download references
Acknowledgements
Author information, authors and affiliations.
Department of Pediatric Cardiology, Heart Center, First Affiliated Hospital of Sun Yat-sen University, 58# Zhongshan Road 2, Guangzhou, 510080, China
Hongjun Ba, Lili zhang & Zizheng Yi
Key Laboratory on Assisted Circulation, Ministry of Health, 58# Zhongshan Road 2, Guangzhou, 510080, China
You can also search for this author in PubMed Google Scholar
Contributions
H-JB conceived and designed the ideas for the manuscript. H-JB, L-LZ, and Z-ZY participated in all data collection and processing. H-JB was the major contributors in organizing records and drafting the manuscript. All authors proofread and approved the manuscript.
Corresponding author
Correspondence to Hongjun Ba .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the the Ethics Committee of The First Affiliated Hospital, Sun Yat-sen University, and informed consent was secured, with special attention to privacy concerns due to the involvement of pediatric patient data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ba, H., zhang, L. & Yi, Z. Enhancing clinical skills in pediatric trainees: a comparative study of ChatGPT-assisted and traditional teaching methods. BMC Med Educ 24 , 558 (2024). https://doi.org/10.1186/s12909-024-05565-1
Download citation
Received : 01 March 2024
Accepted : 16 May 2024
Published : 22 May 2024
DOI : https://doi.org/10.1186/s12909-024-05565-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pediatric training
- Clinical skills
- Medical education
- AI in healthcare
- Mini-clinical evaluation exercise
- Interactive learning
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Using Trauma-Informed Teaching to Handle Sensitive Topics in Online Teaching: A Case Study from Divinity
How can Christian faith influence the practice of mental health care? How do we define mental health and mental illness — and what are the limitations of these concepts? How can Christian theology provide us with tools to ethically engage with challenges related to mental health care? When developing their new graduate-level course, Christian Approaches to Mental Health Care , Professors Warren Kinghorn and John Swinton created a course where students could explore these questions.
“Theology provides us with a language, a worldview and a set of practices that are vital for mental health care,” Swinton said. “The intention of this course is to help people to think theologically and provide people with other ideas and tools to help them care more fully and more faithfully.”
A hybrid, nine-week course, Christian Approaches to Mental Health Care is part of a new mental health track in the Divinity School’s Certificate in Theology and Health Care . Students attended an immersive week on Duke’s campus where they were introduced to key concepts; they attended course sessions the following eight weeks via Zoom.
“In the Theology, Medicine, and Culture Initiative, we invite students into deep engagement with the practices of health care in light of Christian theology and practice,” Kinghorn said. “This class is a natural extension of that aim, but now focused specifically on the practices of mental health care.”
This Divinity course was aimed at both professionals who work in any context related to mental health care (e.g., counselors, social workers) and those who may have a personal interest in the material. First taught in Spring 2024 to over 30 students, the course covered a wide-range of topics that needed to be handled with care, including trauma, anxiety, and dementia.
Challenges and Affordances of Teaching Online
How does one approach teaching sensitive topics online? Are there challenges unique to this environment?
Swinton noted that the structure of a course using a web conferencing software like Zoom can present challenges.
“When you are in a standard class situation and difficult issues come up, people have the opportunity to find immediate support either from us as tutors or from classmates,” he said. “When you are doing a course online, that support is often not available. You switch off the camera and you are on your own.”
That being said, knowing this can be an issue without the buffer space at the beginning or end of the class session, Swinton and Kinghorn have worked to ensure their online sessions do offer support. Kinghorn noted that during his first foray into online teaching during the onset of the COVID-19 pandemic, he was concerned about engaging with sensitive topics in a virtual class setting.
“But I learned that if the class is structured in a way that leaves time and space for self-care, Zoom-based instruction has advantages,” he said. “Students generally join class from a space where they feel safe. They can titrate their own exposure in class, shifting position or even briefly turning off camera or microphone if necessary. If done well and in a trauma-informed way, I think that even the hardest topics can be addressed well through online pedagogy.”
Strategies to Teach a Trauma-Informed Course
What does it mean to be a trauma-informed instructor? How can Kinghorn and Swinton’s course act as an example for other courses?
“Adopting a trauma-informed approach is not accomplished through any single particular technique or checklist,” the CDC’s 6 Guiding Principles To A Trauma-Informed Approach reminds us, “It requires constant attention, caring awareness, sensitivity, and possibly a cultural change at an organizational level.”
Kinghorn and Swinton, however, do have specific strategies that worked for the specific context of their course. Given that this course covered topics such as depression, suicide, substance use issues, and more during the online weeks, the instructors informed students about upcoming content and encouraged them to approach these topics with care for themselves and for others. While there are different approaches to creating a trauma-informed environment, Kinghorn and Swinton focused on harm reduction in suggesting how instructors can think about this during a live course.
“My belief (as others have argued in the trauma-informed teaching literature) is that it should be a last resort for professors to invite students to opt out of a class due to difficult past experiences, as this kind of approach (if made systematic) can compound educational differences and marginalization— effectively giving educational access to those fortunate not to have particular trauma histories and excluding (even if student-driven) those who do,” Kinghorn said. “I would much rather structure courses (as I think we did this semester) with the goal that every student, including those with recent loss or difficult trauma histories, feels a sense of welcome and belonging that enables them to participate in the good, hard work of the course.”
Swinton shared that choice is important to him in thinking about student participation.
“For example, if an online student has had someone close to them die by suicide either recently or historically and they feel that a class on this subject could be problematic for them, we would want to make sure that the person involved does not feel compelled to participate in the class if it is going to be harmful,” Swinton said of a hypothetical scenario. “It’s always going to be difficult with sensitive issues online, but we do the best we can to minimize the possibility of harm.”
Other strategies to help students feel like the course was a safe place for student learning included:
- Focusing on helping students create a connected community, which included putting them in consistent breakout room groups of 5-6 students for the semester
- Modelling honesty and humility as instructors when receiving difficult questions during the immersive week
- Starting each class session with grounding practices (e.g., reading a psalm and pausing in silent reflection)
- Staying after class in Zoom to be available to students and ensuring presence and privacy by turning off recording features
- Providing clear guidelines about evaluations and deadlines, as well as sharing how students should communicate with faculty and teaching assistants
- Granting structured flexibility (e.g., offering a no-questions-asked 72-hour extension for one assignment over the semester)
- Respecting students’ privacy (e.g., not asking students to disclose why they need to turn in late work)
Teaching with Care
How might you begin to integrate trauma-informed practices into your own teaching?
The first step, Swinton said, is to recognize that this is an issue instructors should take note of in all of their teaching.
Using Duke as an example, Kinghorn elaborated that while instructors should not be asking students to disclose their trauma, they can assume “that a majority or near-majority of every class of Duke students have survived trauma of some sort (recognizing the challenges of defining that term).”
“Assume that all students, including trauma survivors, are at Duke because they want to learn, want to engage difficult material well, and generally want to do good, hard work together,” he said. “Then ask: how specific to my subject matter can I invite students to do good, hard work in a way that respects their lived experience? That’s going to differ by class and by student but is the place to start.”
If you’d like to learn more about trauma-informed teaching, here are a few resources where you could start are:
- Trauma-Informed Teaching – University of Wisconsin, Lacrosse
- Trauma-Informed Pedagogy, Montclair State University
- Karen Costa’s Trauma Informed Pedagogy Course
- A feature of a recent Coursera course that integrated trauma-informed frameworks into its design
- SAMHSA, Trauma and Violence
- The Missouri Model: A Developmental Framework for Trauma-Informed Approaches
- CDC, 6 Guiding Principles to a Trauma-Informed Approach
- Potentially Perilous Pedagogies: Teaching Trauma Is Not the Same as Trauma-Informed Teaching
If you’d like to learn more about Warren Kinghorn and John Swinton’s work, here are a few places to start are:
- Finding Jesus in the Storm: The Spiritual Lives of Christians with Mental Health Challenges (2020)
- Wayfaring: A Christian Approach to Mental Health Care by Warren Kinghorn (July 2024)
- Developing Best Practices for Trauma-Informed Teaching and Learning

COMMENTS
These study findings add to the existing body of knowledge that places case study based teaching as a tested method that promotes perception learning where students' senses are engaged as a result of the real-life and authentic clinical scenarios (Malesela, 2009), resulting in deeper learning and achievement of long-lasting knowledge (Fiscus ...
Systematic review of homogenous case-control studies: 3b: Individual case-control study ** 4: Case series or low-quality cohort or case-control study *** 5: Expert opinion: Open in a separate window * <80% follow-up; ... Clinical teaching should never hinder or delay care for patients, ...
There are many teaching strategies that are effective in developing students' clinical judgment and other cognitive skills. These strategies include questions, simulation with debriefing, think-aloud activities, discussions, cases and unfolding cases, reflection, and clinical practice. For these strategies to be effective, students need to ...
Basic nursing course is the core course of nursing major, and it is one of the main courses to cultivate the core competence of nursing students. 1 Basic nursing course is a comprehensive subject in clinical nursing with coverage of a wide range of content. Previous studies 2,3 have reported that students in nursing colleges have poor cultural foundations, unclear learning motivation, weak ...
White Paper Using Case Studies to Develop Clinical Judgment and Ensure Next eneration NCLEX ® NGN) Success 2 Background In 2010, the results of a large study of nursing education in the United States were summarized in Educating Nurses: A Call for Radical Transformation (Benner, et al., 2010).One of the key findings was that nurses entering practice do not
All schools reported using at least one strategy to teach clinical judgment. The number of strategies used ranged from 1 to 9; the median number was 6 for ADN programs, 7 for BSN programs, and 99.6% of all programs reported using multiple strategies. Of all schools surveyed, 98% use case studies to teach clinical judgment, 97% use simulation ...
Other teaching strategies to develop clinical judgment included the use of a clinical preparation guide (Rusch, 2010), expert observation (Kim et al., 2022), clinical reasoning web worksheet (Bartlett et al., 2008), role playing (Kim et al., 2022), and case-study presentations (Hannah, 2006).
Clinical Teaching Somnath Mookherjee Ellen M. Cosgrove Editors 123. Handbook of Clinical Teaching . Somnath Mookherjee Ellen Cosgrove M. Editors Handbook of Clinical Teaching . ISBN 978-3-319-33191-1 ISBN 978-3-319-33193-5 (eBook) DOI 10.1007/978-3-319-33193-5 Library of Congress Control Number: 2016948572 ...
To bridge the gap, educators need to bring clinical practice realities into the classroom, with salient practice-based case studies to develop clinical judgment. This simple teaching strategy can empower educators to better prepare students for both practice and Next Gen licensure. We have emphasized CBC (Concept-Based Curriculum) in nursing ...
Clinical teaching practice of nurse educators is important in the development of clinical competence of undergraduate nursing students, but it is often not done according to best practice standards. ... Berragan, L., 2014, ' Learning nursing through simulation: A case study approach towards an expansive model of learning ', Nurse Education ...
Teaching with real patients in the clinical setting lies at the heart of health professional education, providing an essential component to clinical training. This is true of all the health disciplines - particularly medicine, nursing, dentistry, physiotherapy, and dietetics. Clinical tutorials orientate students to the culture and social aspects of the healthcare environment, and shape ...
Teaching with Case Studies to Develop Clinical Reasoning. By Ann Horigan. Owen, M.I. (2017). A case study scavenger hunt for senior nursing students. Journal of Nursing Education, 56 (3), 191. doi: 10.3928/01484834-20170222-13. Describes the use of a case study and simulation used with a group of senior nursing students in a synthesis seminar.
Case-based learning with situated cognition theory (CBL-SCT) combines knowledge and clinical skills through problem-solving cases to develop clinical judgment (Wang et al., 2023). Using case studies and other activities, such as active learning and flipped classrooms, moves the focus from the presentation of content by the instructor to student ...
This paper examines the use of case studies as teaching strategies to promote critical thinking. Critical thinking and case studies are defined as teaching method. ... Using case studies for clinical problem solving. The case study as a method in problem-based learning is defined by Rideout (2001): "Problem-based learning (PBL) ...
Depending on the subject area and the 'case' used, many methods can be used to describe case-based learning (CBL). The majority of health professional education is patient-centered. As a result, clinical presentations and diseases are combined with social and clinical sciences, and student learning is linked to real-world applications. The purpose of this study was to evaluate how medical ...
This study explores the integration of 3DP with CBL teaching for clinical medical undergraduates. Sixty senior clinical medical undergraduates were randomly assigned to the CBL group and the CBL-3DP group. Computed tomography imaging data from a typical TOF case were exported, processed, and utilized to create four TOF models with a color 3D ...
Clinical simulation: An evolving teaching pedagogy for the education of entry-level health care students. Melissa Brown, Corresponding Author ... The aim of this chapter is to provide the reader with a broad overview of clinical simulation using case examples to highlight the evolving multidomain teaching pedagogy in healthcare professional ...
The Value of Case Studies. Six Steps for Creating an Effective Case Study. Step 1. Identify the Learners and Write Educational Objectives. Step 2. Describe the Patient and Develop Sufficient Case Detail. Step 3. Focus the Learner on Discrete Clinical Decision Points. Step 4.
Case method 1 teaching is an active form of instruction that focuses on a case and involves students learning by doing 2 3. Cases are real or invented stories 4 that include "an educational message" or recount events, problems, dilemmas, theoretical or conceptual issue that requires analysis and/or decision-making.
The NCCSTS Case Collection, created and curated by the National Center for Case Study Teaching in Science, on behalf of the University at Buffalo, contains over a thousand peer-reviewed case studies on a variety of topics in all areas of science. Cases (only) are freely accessible; subscription is required for access to teaching notes and ...
In developed nations, it has been estimated that 60% of care provided aligns with the evidence base, 30% is low value and 10% is potentially harmful [].In some areas, clinical advances have been rapid and research and evidence have paved the way for dramatic improvement in outcomes, mandating rapid implementation of evidence into healthcare (e.g. polio and COVID-19 vaccines).
The Effective Clinical Teaching Inventory (ECTI) was developed to meet the objective of the study. This newly developed tool was mainly based on the previous Effective Clinical Instructor Characteristics Inventory and the Preceptor's Clinical Teaching Learning Inventory . Essential modifications were made based on current literature to be ...
Safety Unfolding Case Study Purpose: The purpose of this assignment is for students to describe patient-centered care, to identify safety interventions, to explain clinical forethought and to value seeing health care through the patient's eyes. Instructions: This strategy can be used with individual students or with groups of students.
First clinical placements enable nursing students to develop their professional identity through initial socialisation, and where successful, first clinical placement experiences can motivate nursing students to persist with their studies [1,2,3,4].Where the transition from the tertiary environment to learning in the healthcare workplace is turbulent, it may impact nursing students' learning ...
Background The current paradigm of competency-based medical education and learner-centredness requires learners to take an active role in their training. However, deliberate and planned continual assessment and performance improvement is hindered by the fragmented nature of many medical training programs. Attempts to bridge this continuity gap between supervision and feedback through learner ...
However, data from clinical trials support the clinical and cost effectiveness of manual therapy as an intervention for musculoskeletal conditions, when used as part of a package of care. The purpose of this paper is to propose a modern evidence-guided framework for the teaching and practice of MT which avoids reference to and reliance on the ...
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews). The case study research method originated in clinical medicine (the case history, i.e., the patient's personal history). In psychology, case studies are ...
Clinical teaching is the primary educational tool use to train learners from day one of medical school all the way to the completion of fellowship. However, concerns over time constraints and patient census ... 3b Individual case-control study** 4 Case series or low-quality cohort or case-control study*** 5 Expert opinion Table 1. Oxford Centre ...
As artificial intelligence (AI) increasingly integrates into medical education, its specific impact on the development of clinical skills among pediatric trainees needs detailed investigation. Pediatric training presents unique challenges which AI tools like ChatGPT may be well-suited to address. This study evaluates the effectiveness of ChatGPT-assisted instruction versus traditional teaching ...
"My belief (as others have argued in the trauma-informed teaching literature) is that it should be a last resort for professors to invite students to opt out of a class due to difficult past experiences, as this kind of approach (if made systematic) can compound educational differences and marginalization— effectively giving educational ...