Medical Student Guide For Critical Thinking

Critical thinking is an essential cognitive skill for every individual but is a crucial component for healthcare professionals such as doctors, nurses and dentists. It is a skill that should be developed and trained, not just during your career as a doctor, but before that when you are still a medical student.
To be more effective in their studies, students must think their way through abstract problems, work in teams and separate high quality from low quality information. These are the same qualities that today's medical students are supposed to possess regardless of whether they graduate in the UK or study medicine in Europe .
In both well-defined and ill-defined medical emergencies, doctors are expected to make competent decisions. Critical thinking can help medical students and doctors achieve improved productivity, better clinical decision making, higher grades and much more.
This article will explain why critical thinking is a must for people in the medical field.

Definition of Critical Thinking
You can find a variety of definitions of Critical Thinking (CT). It is a term that goes back to the Ancient Greek philosopher Socrates and his teaching practice and vision. Critical thinking and its meaning have changed over the years, but at its core always will be the pursuit of proper judgment.
We can agree on one thing. Critical thinkers question every idea, assumption, and possibility rather than accepting them at once.
The most basic definition of CT is provided by Beyer (1995):
"Critical thinking means making reasoned judgements."
In other words, it is the ability to think logically about what to do and/or believe. It also includes the ability to think critically and independently. CT is the process of identifying, analysing, and then making decisions about a particular topic, advice, opinion or challenge that we are facing.
Steps to critical thinking
There is no universal standard for becoming a critical thinker. It is more like a unique journey for each individual. But as a medical student, you have already so much going on in your academic and personal life. This is why we created a list with 6 steps that will help you develop the necessary skills for critical thinking.
1. Determine the issue or question
The first step is to answer the following questions:
- What is the problem?
- Why is it important?
- Why do we need to find a solution?
- Who is involved?
By answering them, you will define the situation and acquire a deeper understanding of the problem and of any factors that may impact it.
Only after you have a clear picture of the issue and people involved can you start to dive deeper into the problem and search for a solution.
2. Research
Nowadays, we are flooded with information. We have an unlimited source of knowledge – the Internet.
Before choosing which medical schools to apply to, most applicants researched their desired schools online. Some of the areas you might have researched include:
- If the degree is recognised worldwide
- Tuition fees
- Living costs
- Entry requirements
- Competition for entry
- Number of exams
- Programme style
Having done the research, you were able to make an informed decision about your medical future based on the gathered information. Our list may be a little different to yours but that's okay. You know what factors are most important and relevant to you as a person.
The process you followed when choosing which medical school to apply to also applies to step 2 of critical thinking. As a medical student and doctor, you will face situations when you have to compare different arguments and opinions about an issue. Independent research is the key to the right clinical decisions. Medical and dentistry students have to be especially careful when learning from online sources. You shouldn't believe everything you read and take it as the absolute truth. So, here is what you need to do when facing a medical/study argument:
- Gather relevant information from all available reputable sources
- Pay attention to the salient points
- Evaluate the quality of the information and the level of evidence (is it just an opinion, or is it based upon a clinical trial?)
Once you have all the information needed, you can start the process of analysing it. It’s helpful to write down the strong and weak points of the various recommendations and identify the most evidence-based approach.
Here is an example of a comparison between two online course platforms , which shows their respective strengths and weaknesses.
When recommendations or conclusions are contradictory, you will need to make a judgement call on which point of view has the strongest level of evidence to back it up. You should leave aside your feelings and analyse the problem from every angle possible. In the end, you should aim to make your decision based on the available evidence, not assumptions or bias.
4. Be careful about confirmation bias
It is in our nature to want to confirm our existing ideas rather than challenge them. You should try your best to strive for objectivity while evaluating information.
Often, you may find yourself reading articles that support your ideas, but why not broaden your horizons by learning about the other viewpoint?
By doing so, you will have the opportunity to get closer to the truth and may even find unexpected support and evidence for your conclusion.
Curiosity will keep you on the right path. However, if you find yourself searching for information or confirmation that aligns only with your opinion, then it’s important to take a step back. Take a short break, acknowledge your bias, clear your mind and start researching all over.
5. Synthesis
As we have already mentioned a couple of times, medical students are preoccupied with their studies. Therefore, you have to learn how to synthesise information. This is where you take information from multiple sources and bring the information together. Learning how to do this effectively will save you time and help you make better decisions faster.
You will have already located and evaluated your sources in the previous steps. You now have to organise the data into a logical argument that backs up your position on the problem under consideration.
6. Make a decision
Once you have gathered and evaluated all the available evidence, your last step is to make a logical and well-reasoned conclusion.
By following this process you will ensure that whatever decision you make can be backed up if challenged
Why is critical thinking so important for medical students?
The first and most important reason for mastering critical thinking is that it will help you to avoid medical and clinical errors during your studies and future medical career.
Another good reason is that you will be able to identify better alternative options for diagnoses and treatments. You will be able to find the best solution for the patient as a whole which may be different to generic advice specific to the disease.
Furthermore, thinking critically as a medical student will boost your confidence and improve your knowledge and understanding of subjects.
In conclusion, critical thinking is a skill that can be learned and improved. It will encourage you to be the best version of yourself and teach you to take responsibility for your actions.
Critical thinking has become an essential for future health care professionals and you will find it an invaluable skill throughout your career.
We’ll keep you updated
Critical thinking in clinical medicine: what is it?
Affiliation.
- 1 Department of Psychiatry, University of Montreal, Montreal, PQ, Canada. [email protected]
- PMID: 22994988
- DOI: 10.1111/j.1365-2753.2012.01897.x
In this paper, we explore the recent emphasis, in various medical contexts, of the term 'critical' or the notion of 'being critical'. We identify various definitions of being critical and note that they differ strikingly. What are these different uses of the term trying to capture that is important in clinical medicine and medical education? We have analysed these qualities as responsibilist, epistemic virtues. We believe that a virtues approach is best able to make sense of the non-cognitive elements of 'being critical', such as the honesty and courage to question claims in the face of persuasion, authority or social pressure. Medical educators and professional bodies seem to agree that being critical is important and desirable. Yet, it is unclear how this quality can be optimally fostered and balanced with the constraints that act upon individual practitioners in the context of institutional medicine including professional standards and the demands of the doctor-patient relationship. Other constraints such as authoritarianism, intimidation and financial pressures may act against the expression of being critical or even the cultivation of critical thinking. The issue of the constraints on critical thinking and the potential hazards it entails will require further consideration by those who encourage being critical in medicine.
© 2012 Blackwell Publishing Ltd.
- Antidepressive Agents / adverse effects
- Clinical Medicine*
- Evidence-Based Medicine
- Physician-Patient Relations
- Antidepressive Agents
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Critical Thinking in medical education: When and How?
Rapid response to:
Critical thinking in healthcare and education
- Related content
- Article metrics
- Rapid responses
Rapid Response:
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from that of general cognitive abilities [1].
People cannot think critically about topics for which they have little knowledge. Critical thinking should be viewed as a domain-specific construct that evolves as an individual acquires domain-specific knowledge [1]. For instance, most common people have no basis for prioritizing patients in the emergency department to be shifted to the only bed available in the intensive care unit. Medical professionals who could thinking critically in their own discipline would have difficulty thinking critically about problems in other fields. Therefore, ‘domain-general’ critical thinking training and evaluation could be non-specific and might not benefit the targeted domain i.e. medical profession.
Moreover, the literature does not demonstrate that it is possible to train universally effective critical thinking skills [1]. As medical teachers, we can start building up student’s critical thinking skill by contingent teaching-learning environment wherein one should encourage reasoning and analytics, problem solving abilities and welcome new ideas and opinions [2]. But at the same time, one should continue rather tapering the critical skills as one ascends towards a specialty, thereby targeting ‘domain-specific’ critical thinking.
For the benefit of healthcare, tools for training and evaluating ‘domain-specific’ critical thinking should be developed for each of the professional knowledge domains such as doctors, nurses, lab technicians and so on. As the Authors rightly pointed out, this humongous task can be accomplished only with cross border collaboration among cognitive neuroscientists, psychologists, medical education experts and medical professionals.
References 1. National Research Council. (2011). Assessing 21st Century Skills: Summary of a Workshop. J.A. Koenig, Rapporteur. Committee on the Assessment of 21st Century Skills. Board on Testing and Assessment, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press. 2. Mafakheri Laleh M, Mohammadimehr M, Zargar Balaye Jame S. Designing a model for critical thinking development in AJA University of Medical Sciences. J Adv Med Educ Prof. 2016 Oct;4(4):179–87.
Competing interests: No competing interests
Critical Thinking in Medicine and Health
- First Online: 01 March 2020
Cite this chapter
- Louise Cummings 2
734 Accesses
1 Citations
This chapter addresses why there is a need for experts and lay people to think critically about medicine and health. It will be argued that illogical, misleading, and contradictory information in medicine and health can have pernicious consequences, including patient harm and poor compliance with health recommendations. Our cognitive resources are our only bulwark to the misinformation and faulty logic that exists in medicine and health. One resource in particular—reasoning—can counter the flawed thinking that pervades many medical and health issues. This chapter examines how concepts such as reasoning, logic and argument must be conceptualised somewhat differently (namely, in non-deductive terms) to accommodate the rationality of the informal fallacies. It also addresses the relevance of the informal fallacies to medicine and health and considers how these apparently defective arguments are a source of new analytical possibilities in both domains.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Albano, J. D., Ward, E., Jemal, A., Anderson, R., Cokkinides, V. E., Murray, T., et al. (2007). Cancer mortality in the United States by education level and race. Journal of the National Cancer Institute, 99 (18), 1384–1394.
Article Google Scholar
Coxon, J., & Rees, J. (2015). Avoiding medical errors in general practice. Trends in Urology & Men’s Health, 6 (4), 13–17.
Google Scholar
Croskerry, P. (2003). The importance of cognitive errors in diagnosis and strategies to minimize them. Academic Medicine, 78 (8), 775–780.
Cummings, L. (2002). Reasoning under uncertainty: The role of two informal fallacies in an emerging scientific inquiry. Informal Logic, 22 (2), 113–136.
Cummings, L. (2004). Analogical reasoning as a tool of epidemiological investigation. Argumentation, 18 (4), 427–444.
Cummings, L. (2009). Emerging infectious diseases: Coping with uncertainty. Argumentation, 23 (2), 171–188.
Cummings, L. (2010). Rethinking the BSE crisis: A study of scientific reasoning under uncertainty . Dordrecht: Springer.
Book Google Scholar
Cummings, L. (2011). Considering risk assessment up close: The case of bovine spongiform encephalopathy. Health, Risk & Society, 13 (3), 255–275.
Cummings, L. (2012a). Scaring the public: Fear appeal arguments in public health reasoning. Informal Logic, 32 (1), 25–50.
Cummings, L. (2012b). The public health scientist as informal logician. International Journal of Public Health, 57 (3), 649–650.
Cummings, L. (2013a). Public health reasoning: Much more than deduction. Archives of Public Health, 71 (1), 25.
Cummings, L. (2013b). Circular reasoning in public health. Cogency, 5 (2), 35–76.
Cummings, L. (2014a). Informal fallacies as cognitive heuristics in public health reasoning. Informal Logic, 34 (1), 1–37.
Cummings, L. (2014b). The ‘trust’ heuristic: Arguments from authority in public health. Health Communication, 29 (10), 1043–1056.
Cummings, L. (2014c). Coping with uncertainty in public health: The use of heuristics. Public Health, 128 (4), 391–394.
Cummings, L. (2014d). Circles and analogies in public health reasoning. Inquiry, 29 (2), 35–59.
Cummings, L. (2014e). Analogical reasoning in public health. Journal of Argumentation in Context, 3 (2), 169–197.
Cummings, L. (2015). Reasoning and public health: New ways of coping with uncertainty . Cham, Switzerland: Springer.
Fowler, F. J., Jr., Levin, C. A., & Sepucha, K. R. (2011). Informing and involving patients to improve the quality of medical decisions. Health Affairs, 30 (4), 699–706.
Graber, M. L., Franklin, N., & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165 (13), 1493–1499.
Hamblin, C. L. (1970). Fallacies . London: Methuen.
Johnson, R. H. (2011). Informal logic and deductivism. Studies in Logic, 4 (1), 17–37.
Kahane, H. (1971). Logic and contemporary rhetoric: The use of reason in everyday life . Belmont, CA: Wadsworth Publishing Company.
Loucks, E. B., Buka, S. L., Rogers, M. L., Liu, T., Kawachi, I., Kubzansky, L. D., et al. (2012). Education and coronary heart disease risk associations may be affected by early life common prior causes: A propensity matching analysis. Annals of Epidemiology, 22 (4), 221–232.
Saposnik, G., Redelmeier, D., Ruff, C. C., & Tobler, P. N. (2016). Cognitive biases associated with medical decisions: A systematic review. BMC Medical Informatics and Decision Making, 16, 138. https://doi.org/10.1186/s12911-016-0377-1 .
Trowbridge, R. L. (2008). Twelve tips for teaching avoidance of diagnostic errors. Medical Teacher, 30, 496–500.
Walton, D. N. (1985a). Are circular arguments necessarily vicious? American Philosophical Quarterly, 22 (4), 263–274.
Walton, D. N. (1985b). Arguer’s Position . Westport, CT: Greenwood Press.
Walton, D. N. (1987). The ad hominem argument as an informal fallacy. Argumentation, 1 (3), 317–331.
Walton, D. N. (1991). Begging the question: Circular reasoning as a tactic of argumentation . New York: Greenwood Press.
Walton, D. N. (1992). Plausible argument in everyday conversation . Albany: SUNY Press.
Walton, D. N. (1996). Argumentation schemes for presumptive reasoning . Mahwah, NJ: Erlbaum.
Walton, D. N. (2010). Why fallacies appear to be better arguments than they are. Informal Logic, 30 (2), 159–184.
Weingart, S. N., Wilson, R. M., Gibberd, R. W., & Harrison, B. (2000). Epidemiology of medical error. Western Journal of Medicine, 172 (6), 390–393.
Woods, J. (1995). Appeal to force. In H. V. Hansen & R. C. Pinto (Eds.), Fallacies: Classical and contemporary readings (pp. 240–250). University Park: The Pennsylvania State University Press.
Woods, J. (2004). The death of argument: Fallacies in agent-based reasoning . Dordrecht: Kluwer Academic.
Woods, J. (2007). Lightening up on the ad hominem. Informal Logic, 27 (1), 109–134.
Woods, J. (2008). Begging the question is not a fallacy. In C. Dégremont, L. Keiff, & H. Rükert (Eds.), Dialogues, logics and other strange things: Essays in honour of Shahid Rahman (pp. 523–544). London: College Publications.
Download references
Author information
Authors and affiliations.
Department of English, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong
Louise Cummings
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Louise Cummings .
Chapter Summary
Medicine and health have tended to be overlooked in the critical thinking literature . And yet robust critical thinking skills are needed to evaluate the large number and range of health messages that we are exposed to on a daily basis.
An ability to think critically helps us to make better personal health choices and to uncover biases and errors in health messages and other information. An ability to think critically allows us to make informed decisions about medical treatments and is vital to efforts to reduce medical diagnostic errors.
A key element in critical thinking is the ability to distinguish strong or valid reasoning from weak or invalid reasoning. When an argument is weak or invalid, it is called a ‘fallacy’ or a ‘fallacious argument’.
The informal fallacies are so-called on account of the presence of epistemic and dialectical flaws that cannot be captured by formal logic . They have been discussed by many generations of philosophers and logicians , beginning with Aristotle .
Historically, philosophers and logicians have taken a pejorative view of the informal fallacies. Much of the criticism of these arguments is related to a latent deductivism in logic , the notion that arguments should be evaluated according to deductive standards of validity and soundness . Against deductive standards and norms, many reasonable arguments are judged to be fallacies.
Developments in logic , particularly the teaching of logic, forced a reconsideration of the prominence afforded to deductive logic in the evaluation of arguments. New criteria based on presumptive reasoning and plausible argument started to emerge. Against this backdrop, non-fallacious variants of most of the informal fallacies began to be described for the first time.
Today, some argument analysts characterize non-fallacious variants of the informal fallacies in terms of cognitive heuristics . During reasoning , these heuristics function as mental shortcuts, allowing us to bypass knowledge and come to judgement about complex health problems.
Suggestions for Further Reading
Sharples, J. M., Oxman, A. D., Mahtani, K. R., Chalmers, I., Oliver, S., Collins, K., Austvoll-Dahlgren, A., & Hoffmann, T. (2017). Critical thinking in healthcare and education. British Medical Journal, 357 : j2234. https://doi.org/10.1136/bmj.j2234 .
The authors examine the role of critical thinking in medicine and healthcare, arguing that critical thinking skills are essential for doctors and patients. They describe an international project that involves collaboration between education and health. Its aim is to develop a curriculum and learning resources for critical thinking about any action that is claimed to improve health.
Hitchcock, D. (2017). On reasoning and argument: Essays in informal logic and on critical thinking . Cham: Switzerland: Springer.
This collection of essays provides more advanced reading on several of the topics addressed in this chapter, including the fallacies, informal logic , and the teaching of critical thinking . Chapter 25 considers if fallacies have a place in the teaching of critical thinking and reasoning skills.
Hansen, H. V., & Pinto, R. C. (Eds.). (1995). Fallacies: Classical and contemporary readings . University Park: The Pennsylvania State University Press.
This edited collection of 24 chapters contains historical selections on the fallacies, contemporary theory and criticism, and analyses of specific fallacies. It also examines fallacies and teaching. There are chapters on four of the fallacies that will be examined in this book: appeal to force; appeal to ignorance ; appeal to authority; and post hoc ergo propter hoc .
Diagnostic errors are a significant cause of death and serious injury in patients. Many of these errors are related to cognitive factors. Trowbridge ( 2008 ) has devised twelve tips to familiarize medical students and physician trainees with the cognitive underpinnings of diagnostic errors. One of these tips is to explicitly describe heuristics and how they affect clinical reasoning . These heuristics include the following:
Representativeness —a patient’s presentation is compared to a ‘typical’ case of specific diagnoses.
Availability —physicians arrive at a diagnosis based on what is easily accessible in their minds, rather than what is actually most probable.
Anchoring —physicians may settle on a diagnosis early in the diagnostic process and subsequently become ‘anchored’ in that diagnosis.
Confirmation bias —as a result of anchoring, physicians may discount information discordant with the original diagnosis and accept only that which supports the diagnosis.
Using the above information, identify any heuristics and biases that occur in the following scenarios:
Scenario 1: A 60-year-old man has epigastric pain and nausea. He is sitting forward clutching his abdomen. He has a history of several bouts of alcoholic pancreatitis. He states that he felt similar during these bouts to what he is currently feeling. The patient states that he has had no alcohol in many years. He has normal blood levels of pancreatic enzymes. He is given a diagnosis of acute pancreatitis. It is eventually discovered that he has had acute myocardial infarction.
Scenario 2: A 20-year-old, healthy man presents with sudden onset of severe, sharp chest pain and back pain. Based on these symptoms, he is suspected of having a dissecting thoracic aortic aneurysm. (In an aortic dissection, there is a separation of the layers within the wall of the aorta, the large blood vessel branching off the heart.) He is eventually diagnosed with pleuritis (inflammation of the pleura, the thin, transparent, two-layered membrane that covers the lungs).
Many of the logical terms that were introduced in this chapter also have non-logical uses in everyday language. Below are several examples of the use of these terms. For each example, indicate if the word in italics has a logical or a non - logical meaning or use:
University ‘safe spaces’ are a dangerous fallacy —they do not exist in the real world ( The Telegraph , 13 February 2017).
The MRI findings beg the question as to whether a careful ultrasound examination might have yielded some of the same information on haemorrhages ( British Medical Journal: Fetal & Neonatal , 2011).
The youth justice system is a slippery slope of failure ( The Sydney Morning Herald , 26 July 2016).
The EU countered with its own gastronomic analogy , saying that “cherry picking” the best bits of the EU would not be tolerated ( BBC News , 28 July 2017).
As Ebola spreads, so have several fallacies ( The New York Times , 23 October 2014).
Removing the statue of Confederacy Army General Robert E. Lee no more puts us on a slippery slope towards ousting far more nuanced figures from the public square than building the statue in the first place put us on a slippery slope toward, say, putting up statues of Hitler outside of Holocaust museums or of Ho Chi Minh at Vietnam War memorials ( Chicago Tribune , 16 August 2017).
We can expand the analogy a bit and think of a culture as something akin to a society’s immune system—it works best when it is exposed to as many foreign bodies as possible ( New Zealand Herald , 4 May 2010).
The Josh Norman Bowl begs the question : What’s an elite cornerback worth? ( The Washington Post , 17 December 2016).
The intuition behind these analogies is simple: As a homeowner, I generally have the right to exclude whoever I want from my property. I don’t even have to have a good justification for the exclusion. I can choose to bar you from my home for virtually any reason I want, or even just no reason at all. Similarly, a nation has the right to bar foreigners from its land for almost any reason it wants, or perhaps even no reason at all ( The Washington Post , 6 August 2017).
Legalising assisted suicide is a slippery slope toward widespread killing of the sick, Members of Parliament and peers were told yesterday ( Mail Online , 9 July 2014).
In the Special Topic ‘What’s in a name?’, an example of a question-begging argument from the author’s recent personal experience was used. How would you reconstruct the argument in this case to illustrate the presence of a fallacy?
On 9 July 2017, the effect of coconut oil on health was also discussed in an article in The Guardian entitled ‘Coconut oil: Are the health benefits a big fat lie?’ The following extract is taken from that article. (a) What type of reasoning is the author using in this extract? In your response, you should reconstruct the argument by presenting its premises and conclusion . Also, is this argument valid or fallacious in this particular context?
When it comes to superfoods, coconut oil presses all the buttons: it’s natural, it’s enticingly exotic, it’s surrounded by health claims and at up to £8 for a 500 ml pot at Tesco, it’s suitably pricey. But where this latest superfood differs from benign rivals such as blueberries, goji berries, kale and avocado is that a diet rich in coconut oil may actually be bad for us.
The article in The Guardian also makes extensive use of expert opinion. Two such opinions are shown below. (b) What three linguistic devices does the author use to confer expertise or authority on the individuals who advance these opinions?
Christine Williams, professor of human nutrition at the University of Reading, states: “There is very limited evidence of beneficial health effects of this oil”.
Tom Sanders, emeritus professor of nutrition and dietetics at King’s College London, says: “It is a poor source of vitamin E compared with other vegetable oils”.
The author of the article in The Guardian went on to summarize the findings of a study by two researchers that was published in the British Nutrition Foundation’s Nutrition Bulletin. The author’s summary included the following statement: There is no good evidence that coconut oil helps boost mental performance or prevent Alzheimer’s disease . (c) In what type of informal fallacy might this statement be a premise ?
Scenario 1: An anchoring error has occurred in which the patient is given a diagnosis of acute pancreatitis early in the diagnostic process. The clinician becomes anchored in this diagnosis, with the result that he overlooks two pieces of information that would have allowed this diagnosis to be disconfirmed—the fact that the patient has reported no alcohol use in many years and the presence of normal blood levels of pancreatic enzymes. By dismissing this information, the clinician is also showing a confirmation bias —he attends only to information that confirms his original diagnosis.
Scenario 2: A representativeness error has occurred. The patient’s presentation is typical of aortic dissection. However, this condition can be dismissed in favour of conditions like pleuritis or pneumothorax on account of the fact that aortic dissection is exceptionally rare in 20-year-olds.
(2) (a) non-logical; (b) non-logical; (c) non-logical; (d) non-logical; (e) non-logical; (f) logical; (g) logical; (h) non-logical; (i) logical; (j) logical
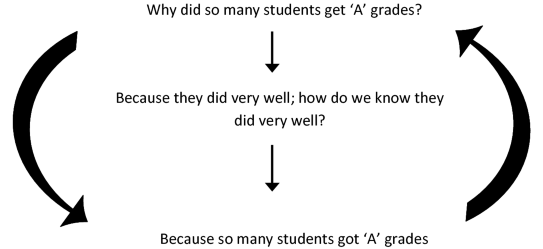
(3) The fallacy can be illustrated as follows. The head of department asks the question ‘Why did so many of these students get ‘A’ grades’? He receives the reply ‘Because they did very well’. But someone might reasonably ask ‘How do we know that they did very well?’ To which the reply is ‘Because so many students got ‘A’ grades’. The reasoning can be reconstructed in diagram form as follows:
The author is using an analogical argument , which has the following form:
P1: Blueberries, goji berries, kale, avocado and coconut oil are natural, exotic, pricey and surrounded by health claims.
P2: Blueberries, goji berries, kale and avocado have health benefits.
C: Coconut oil has health benefits.
This is a false analogy , or a fallacious analogical argument , because coconut oil does not share with these other superfoods the property or attribute < has health benefits >.
The author uses academic rank, field of specialization, and university affiliation to confer authority or expertise on individuals who advance expert opinions.
This statement could be a premise in an argument from ignorance .
Rights and permissions
Reprints and permissions
Copyright information
© 2020 The Author(s)
About this chapter
Cummings, L. (2020). Critical Thinking in Medicine and Health. In: Fallacies in Medicine and Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-28513-5_1
Download citation
DOI : https://doi.org/10.1007/978-3-030-28513-5_1
Published : 01 March 2020
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-28512-8
Online ISBN : 978-3-030-28513-5
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
Translate this page from English...
*Machine translated pages not guaranteed for accuracy. Click Here for our professional translations.

Our Concept and Definition of Critical Thinking
Critical Thinking Definition, Skills, and Examples
- Homework Help
- Private School
- College Admissions
- College Life
- Graduate School
- Business School
- Distance Learning
:max_bytes(150000):strip_icc():format(webp)/ADHeadshot-Cropped-b80e40469d5b4852a68f94ad69d6e8bd.jpg)
- Indiana University, Bloomington
- State University of New York at Oneonta
Critical thinking refers to the ability to analyze information objectively and make a reasoned judgment. It involves the evaluation of sources, such as data, facts, observable phenomena, and research findings.
Good critical thinkers can draw reasonable conclusions from a set of information, and discriminate between useful and less useful details to solve problems or make decisions. Employers prioritize the ability to think critically—find out why, plus see how you can demonstrate that you have this ability throughout the job application process.
Why Do Employers Value Critical Thinking Skills?
Employers want job candidates who can evaluate a situation using logical thought and offer the best solution.
Someone with critical thinking skills can be trusted to make decisions independently, and will not need constant handholding.
Hiring a critical thinker means that micromanaging won't be required. Critical thinking abilities are among the most sought-after skills in almost every industry and workplace. You can demonstrate critical thinking by using related keywords in your resume and cover letter, and during your interview.
Examples of Critical Thinking
The circumstances that demand critical thinking vary from industry to industry. Some examples include:
- A triage nurse analyzes the cases at hand and decides the order by which the patients should be treated.
- A plumber evaluates the materials that would best suit a particular job.
- An attorney reviews evidence and devises a strategy to win a case or to decide whether to settle out of court.
- A manager analyzes customer feedback forms and uses this information to develop a customer service training session for employees.
Promote Your Skills in Your Job Search
If critical thinking is a key phrase in the job listings you are applying for, be sure to emphasize your critical thinking skills throughout your job search.
Add Keywords to Your Resume
You can use critical thinking keywords (analytical, problem solving, creativity, etc.) in your resume. When describing your work history , include top critical thinking skills that accurately describe you. You can also include them in your resume summary , if you have one.
For example, your summary might read, “Marketing Associate with five years of experience in project management. Skilled in conducting thorough market research and competitor analysis to assess market trends and client needs, and to develop appropriate acquisition tactics.”
Mention Skills in Your Cover Letter
Include these critical thinking skills in your cover letter. In the body of your letter, mention one or two of these skills, and give specific examples of times when you have demonstrated them at work. Think about times when you had to analyze or evaluate materials to solve a problem.
Show the Interviewer Your Skills
You can use these skill words in an interview. Discuss a time when you were faced with a particular problem or challenge at work and explain how you applied critical thinking to solve it.
Some interviewers will give you a hypothetical scenario or problem, and ask you to use critical thinking skills to solve it. In this case, explain your thought process thoroughly to the interviewer. He or she is typically more focused on how you arrive at your solution rather than the solution itself. The interviewer wants to see you analyze and evaluate (key parts of critical thinking) the given scenario or problem.
Of course, each job will require different skills and experiences, so make sure you read the job description carefully and focus on the skills listed by the employer.
Top Critical Thinking Skills
Keep these in-demand critical thinking skills in mind as you update your resume and write your cover letter. As you've seen, you can also emphasize them at other points throughout the application process, such as your interview.
Part of critical thinking is the ability to carefully examine something, whether it is a problem, a set of data, or a text. People with analytical skills can examine information, understand what it means, and properly explain to others the implications of that information.
- Asking Thoughtful Questions
- Data Analysis
- Interpretation
- Questioning Evidence
- Recognizing Patterns
Communication
Often, you will need to share your conclusions with your employers or with a group of colleagues. You need to be able to communicate with others to share your ideas effectively. You might also need to engage in critical thinking in a group. In this case, you will need to work with others and communicate effectively to figure out solutions to complex problems.
- Active Listening
- Collaboration
- Explanation
- Interpersonal
- Presentation
- Verbal Communication
- Written Communication
Critical thinking often involves creativity and innovation. You might need to spot patterns in the information you are looking at or come up with a solution that no one else has thought of before. All of this involves a creative eye that can take a different approach from all other approaches.
- Flexibility
- Conceptualization
- Imagination
- Drawing Connections
- Synthesizing
Open-Mindedness
To think critically, you need to be able to put aside any assumptions or judgments and merely analyze the information you receive. You need to be objective, evaluating ideas without bias.
- Objectivity
- Observation
Problem Solving
Problem-solving is another critical thinking skill that involves analyzing a problem, generating and implementing a solution, and assessing the success of the plan. Employers don’t simply want employees who can think about information critically. They also need to be able to come up with practical solutions.
- Attention to Detail
- Clarification
- Decision Making
- Groundedness
- Identifying Patterns
More Critical Thinking Skills
- Inductive Reasoning
- Deductive Reasoning
- Noticing Outliers
- Adaptability
- Emotional Intelligence
- Brainstorming
- Optimization
- Restructuring
- Integration
- Strategic Planning
- Project Management
- Ongoing Improvement
- Causal Relationships
- Case Analysis
- Diagnostics
- SWOT Analysis
- Business Intelligence
- Quantitative Data Management
- Qualitative Data Management
- Risk Management
- Scientific Method
- Consumer Behavior
Key Takeaways
- Demonstrate that you have critical thinking skills by adding relevant keywords to your resume.
- Mention pertinent critical thinking skills in your cover letter, too, and include an example of a time when you demonstrated them at work.
- Finally, highlight critical thinking skills during your interview. For instance, you might discuss a time when you were faced with a challenge at work and explain how you applied critical thinking skills to solve it.
University of Louisville. " What is Critical Thinking ."
American Management Association. " AMA Critical Skills Survey: Workers Need Higher Level Skills to Succeed in the 21st Century ."
- Questions for Each Level of Bloom's Taxonomy
- Critical Thinking in Reading and Composition
- Bloom's Taxonomy in the Classroom
- Introduction to Critical Thinking
- How To Become an Effective Problem Solver
- Creativity & Creative Thinking
- Higher-Order Thinking Skills (HOTS) in Education
- 2020-21 Common Application Essay Option 4—Solving a Problem
- 6 Skills Students Need to Succeed in Social Studies Classes
- College Interview Tips: "Tell Me About a Challenge You Overcame"
- Types of Medical School Interviews and What to Expect
- The Horse Problem: A Math Challenge
- What to Do When the Technology Fails in Class
- What Are Your Strengths and Weaknesses? Interview Tips for Teachers
- A Guide to Business Letters Types
- How to Practice Critical Thinking in 4 Steps
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Greek and Roman Papyrology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Agriculture
- History of Education
- History of Emotions
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Variation
- Language Families
- Language Evolution
- Language Reference
- Lexicography
- Linguistic Theories
- Linguistic Typology
- Linguistic Anthropology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Culture
- Music and Media
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Oncology
- Medical Toxicology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Neuroscience
- Cognitive Psychology
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business History
- Business Ethics
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic Methodology
- Economic History
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Political Behaviour
- Political Economy
- Political Institutions
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
37 Medical Reasoning and Thinking
Vimla L. Patel, Center for Cognitive Studies in Medicine and Public Health, The New York Academy of Medicine, USA
Jose F. Arocha, Department of Health Studies and Gerontology, University of Waterloo, Waterloo, Ontario, Canada
Jiajie Zhang, Center for Cognitive Informatics and Decision Making, School of Biomedical Informatics, University of Texas at Houston, Houston, TX
- Published: 21 November 2012
- Cite Icon Cite
- Permissions Icon Permissions
The practice of medicine requires art as well as science. The latter argues for a deeper understanding of the mechanisms underlying disease processes and use of scientific evidence in making patient care decisions. The study of medical reasoning and thinking underlies much of medical cognition and has been the focus of research in cognitive science and artificial intelligence in medicine. Expertise and medical knowledge organization, the directionality of reasoning, and the nature of medical errors are intricately tied to thinking and decision-making processes in medicine. With the recent advancement of technology in medicine, technology-mediated reasoning and reasoning support systems will be a focus for future research. This chapter discusses these issues within historical and current research perspectives.
What Is Medical Reasoning?
Medical cognition refers to the study of cognitive structure and processes, such as perception and action, comprehension, problem solving, decision making, memory, and knowledge representation in medical practice or in tasks representative of medical practice. Medical reasoning research describes a form of qualitative and quantitative inquiry that examines the cognitive processes underlying medical decisions. Researchers study individuals at various levels of experience and in different roles in medical settings, including medical students, physicians, nurses, and biomedical scientists.
Medical problem solving, diagnostic reasoning, and decision making are all terms used in a growing body of literature that examines how clinicians understand biomedical information, solve clinical problems, and make clinical decisions. The study of medical reasoning underlies much of medical cognition, and it has been the focus of considerable research in cognitive science and artificial intelligence as applied to medicine.
Medical reasoning involves an inferential process for making diagnostic or therapeutic decisions or understanding the pathology of a disease process. On the one hand, medical reasoning is basic to all higher level cognitive processes in medicine, such as problem solving and medical text comprehension. On the other hand, the structure of medical reasoning is itself the subject of considerable scrutiny. For example, the directionality of reasoning in medicine has been an issue of considerable controversy in medical cognition, medical education, and artificial intelligence in medicine. It is typical to partition medical reasoning into clinical and biomedical or basic science reasoning. These are some of the central themes in this chapter.
Early Research on Medical Problem Solving and Reasoning
Understanding the thought processes involved in clinical reasoning to promote more effective practices has been the subject of inquiry for more than a century (Osler, 1906 ). However, it was not until the development of medical cognition, a subfield of cognitive science devoted to the study of cognitive processes in medical tasks, that major scientifically based advances were made. Studies of medical cognition include analyses of performance in “real-world” clinical environments as well as in experimental settings.
There have been two primary approaches to medical reasoning: the decision-analytic approach and the information-processing approach. Decision analysis uses formal models of decision making as the standard of comparison (Dowie & Elstein, 1988 ; see Chater & Oaksford, Chapter 2 ; LeBoeuf & Shafir, Chapter 16 ). Decision analysis research aims to compare the performance of a physician with a mathematical model that represents the ideal of rationality and focuses on the reasoning “fallacies” and biases inherent in human clinical decision making (Leaper, Horrocks, Staniland, & De Dombal, 1972 ). In contrast, the information-processing approach focuses on the description of cognitive processes in reasoning tasks and the development of information-processing models of performance, typically relying on protocol analysis (Ericsson & Simon, 1993 ) and other techniques, such as naturalistic observation. Human information-processing research has typically focused on the individual. A dual focus on in-depth task analysis and on the study of human performance is a central feature of the information-processing approach to medical cognition, which is the focus of this section.
The information-processing view of cognitive processes came into prominence in the early 1970s, spearheaded by the immensely influential work of Newell and Simon ( 1972 ) on problem solving (see Bassok & Novick, Chapter 21 ). Problem solving was conceived of as search in a problem space in which a problem solver was viewed as selecting an option (e.g., a hypothesis or an inference) or performing an operation (from a set of possible operations) in moving toward a problem solution or a goal state (e.g., diagnosis or treatment plan). This conceptualization had an enormous impact in both cognitive psychology and artificial intelligence (AI). It also led to rapid advances in medical reasoning and problem-solving research, as exemplified by the seminal work of Elstein, Shulman, and Sprafka ( 1978 ). These investigators studied the problem-solving processes of physicians, drawing on then contemporary methods and theories of cognition. Their view of problem solving had a substantial influence on both studies of medical reasoning and medical education. They were the first to use experimental methods and theories of cognitive science to investigate clinical competency. Their extensive empirical research led to the development of a model of hypothetico-deductive reasoning, which proposed that physicians reasoned by first generating and then testing a set of hypotheses to account for clinical data (i.e., reasoning from hypothesis to data). This model of problem solving had a substantial influence on studies of both medical cognition and medical education (Elstein, 2009 ; Elstein, Shulman, & Sprafka, 1978 ).
At the same time when empirical research in medical cognition was beginning, medical AI (particularly, expert systems technology) began development of methods and implementations of expert systems that mimic the way medical experts reasoned. AI in medicine and medical cognition mutually influenced each other in a number of ways, including (1) providing a basis for developing formal models of competence in problem-solving tasks; (2) elucidating the structure of medical knowledge and providing important epistemological distinctions, and (3) characterizing productive and less-productive lines of reasoning in diagnostic and therapeutic tasks. Gorry ( 1973 ) conducted a series of studies comparing a computational model of medical problem solving with the actual problem-solving behavior of physicians. This analysis provided a basis for characterizing a sequential process of medical decision making, one that differs in important respects from early diagnostic computational systems based on Bayes' theorem (Ledley & Lusted, 1959 ; see Chater & Oaksford, Chapter 2 ; Griffiths, Tenenbaum, & Kemp, Chapter 3 ), which describes the relations between conditional probabilities and provides a normative rule for updating belief in light of evidence. Pauker, Gorry, Kassirer, and Schwartz ( 1976 ) capitalized on some of the insights of Gorry's earlier work to develop the Present Illness Program (PIP), a program designed to take the history of a patient with edema. Several of the questions guiding this research, including the nature and organization of expert knowledge, were of central concern to both developers of medical expert systems and researchers in medical cognition. The development and refinement of the program was partially based on studies of clinical problem solving. Medical expert consultation systems, such as Internist (Miller, Pople, & Myers, 1984 ) and MYCIN (Shortliffe, 1976 ), introduced ideas about knowledge-based reasoning strategies across a range of cognitive tasks. MYCIN, in particular, had a substantial influence on cognitive science. It contributed several advances (e.g., representing reasoning under uncertainty) in the use of production systems as a representation scheme in a complex, knowledge-based domain. MYCIN also highlighted the difference between medical problem solving and the cognitive dimensions of medical explanation. Clancey's work (Clancey & Letsinger, 1984 ; Clancey 1985 ) in GUIDON and NEOMYCIN was particularly influential in the evolution of models of medical cognition. Clancey endeavored to reconfigure MYCIN in order to employ the system to teach medical students about meningitis and related disorders. NEOMYCIN was based on a more psychologically plausible model of medical diagnosis. This model differentiated data-directed and hypothesis-directed reasoning and separated control knowledge (rules) from the facts upon which it operated.
Feltovich Johnson, Moller, and Swanson ( 1984 ), drawing on models of knowledge representation from medical AI, characterized fine-grained differences in knowledge organization between subjects with different levels of expertise in the domain of pediatric cardiology. These differences accounted for subjects' inferences about diagnostic cues and their evaluation of competing hypotheses. Patel and Groen ( 1986 ), incorporating distinctions introduced by Clancey, studied the knowledge-based solution strategies of expert cardiologists as evidenced by their pathophysiological explanations of a complex clinical problem. The results indicated that subjects, who accurately diagnosed the problem, employed a forward-driven reasoning strategy—using patient data to lead toward a complete diagnosis (i.e., reasoning from data to hypothesis). In contrast, subjects who misdiagnosed or partially diagnosed the patient problem used a backward-driven reasoning strategy. These research findings presented a challenge to the hypothetico-deductive model of reasoning espoused by Elstein, Shulman, and Sprafka ( 1978 ), which did not differentiate expert from nonexpert reasoning strategies.
Much of the early research in the study of reasoning in domains such as medicine was carried out in laboratory or experimental settings. More recently, there has been a shift toward examining cognitive issues in naturalistic settings, such as medical teams in intensive care units (Patel, Kaufman, & Magder, 1996 ), anesthesiologists working in surgery (Gaba, 1992 ), nurses providing emergency telephone triage (Leprohon & Patel, 1995 ), and patients reasoning with the aid of technology in the health care system (Patel, Arocha, & Kushniruk, 2002 ). This research was been informed by work in the area of dynamic decision making (Salas & Klein, 2001 ), complex problem solving (Frensch & Funke, 1995 ), human factors (Hoffman & Deffenbacher, 1992 ; Vicente & Rasmussen, 1990 ), and cognitive engineering (Rasmussen, Pejtersen, & Goodstein, 1994 ).
Models of Medical Reasoning
The traditional view of medical reasoning has been to treat diagnosis as similar to the classical view of scientist's task of making a discovery or engaging in scientific experimentation. This classical view of scientific reasoning makes the same assumption that diagnostic inference follows a hypothetico-deductive process of reaching conclusions by testing hypotheses based on clinical evidence. Within a cognitive perspective, as we saw previously, this view of the diagnostic process in medicine was first proposed in the influential work of Elstein, Shulman, and Sprafka ( 1978 ). However, the view of medical reasoning as hypothetico-deductive has been challenged, as we will see in this section. Similarly, the classical view of scientific reasoning has been expanded to cover multiple types of reasoning strategies.
Toward a Model of Reasoning in Medicine: Induction, Deduction, and Abduction
It is generally agreed upon that there are two basic forms of reasoning. One is deductive reasoning (see Evans, Chapter 8 ), which in the context of medicine consists of deriving a particular conclusion (such as a diagnosis) from a hypothesis (such as a diagnostic category or a pathophysiological process). The other form is inductive reasoning, which consists of generating a likely general conclusion (such as a diagnosis) from patient data (see Rips et al., Chapter 11 ). However, reasoning in the “real world” does not appear to fit neatly into any of these basic types. For this reason, a third form of reasoning has been recognized as best capturing the generation of clinical hypotheses, where deduction and induction are intermixed. This corresponds to what Peirce ( 1955 ; see Lombrozo, Chapter 14 ) termed “abductive reasoning,” which in the medical context is illustrated by the clinician generating a plausible explanatory hypothesis through a process of heuristic rule utilization (Magnani, 1992 , 2001 ).
There are different uses of the term “abductive reasoning.” In our chapter, we use it to refer to a cyclical process of generating possible explanations (i.e., identification of a set of hypotheses that are able to account for the clinical case on the basis of the available data) from a set of data and testing those explanations (i.e., evaluation of each generated hypothesis on the basis of its expected consequences) for the abnormal state of the patient at hand (Elstein, Shulman, & Sprafka, 1978 ; Joseph & Patel, 1990 ; Kassirer 1989 ; Ramoni, Stefanelli, Magnani, & Barosi, 1992 ). Abductive reasoning is a data-driven process and also dependent on domain knowledge. 1 Within this generic framework, various models of diagnostic reasoning may be constructed. Following Patel and Ramoni ( 1997 ), we can distinguish between two major models of diagnostic reasoning: heuristic classification (Clancey, 1985 ) and cover and differentiate (Eshelman, 1988 ). However, these models can be seen as special cases of a more general model: the select and test model (Ramoni et al., 1992 ), where the processes of hypothesis generation and testing can be characterized in terms of four types of processes: abstraction, abduction, deduction, and induction. During abstraction , pieces of data in the data set are selected according to their relevance for the problem solution and chunked in schemas representing an abstract description of the problem at hand (e.g., abstracting that an adult male with hemoglobin concentration less than 14 g/dL is an anemic patient). Following this, hypotheses that could account for the current situation are related through a process of abduction , characterized by a “backward flow” of inferences across a chain of directed relations that identify those initial conditions from which the current abstract representation of the problem originates. This process provides tentative solutions to the problem at hand by way of hypotheses. For example, knowing that disease A will causes symptom b , by abduction one will try to identify the explanation for b , while through deduction one will forecast that a patient affected by disease A will manifest symptom b ; both inferences use the same relation along two different directions. These two types of clinical reasoning in medicine are described by Patel and Ramoni ( 1997 ).
In the testing phase, hypotheses are incrementally tested according to their ability to account for the whole problem, where deduction serves to build up the possible world described by the consequences of each hypothesis. This kind of reasoning is customarily regarded as a common way of evaluating diagnostic hypotheses (Joseph & Patel, 1990 ; Kassirer 1989 ; Patel, Arocha, & Kaufman, 1994 ; Patel, Evans, & Kaufman, 1989 ). As predictions are derived from hypotheses, they are matched to the case through a process of induction , where a prediction generated from a hypothesis can be matched with one specific aspect of the patient problem. The major feature of induction is, therefore, the ability to rule out those hypotheses whose expected consequences turn out to be not in agreement with the patient problem. This is because there is no way to logically confirm a hypothesis. We can only disconfirm or refute it in the presence of contrary evidence. This evaluation process closes the testing phase of the diagnostic cycle. Moreover, it determines which information is needed in order to discriminate among hypotheses and hence which information has to be collected.
Hypothesis Testing and Clinical Reasoning: A View From the Empirical Literature
A model such as one presented earlier can be used to explain the medical diagnostic process, while the empirical literature highlights aspects of medical reasoning that led support to the model. First, seasoned clinicians are selective in the data they collect ( abstraction ), focusing only on the data that are relevant to the generated hypotheses, while ignoring other less relevant data, as was found in the work of Patel and Groen ( 1986 ) and later supported in other studies. Successful clinicians focus on the fewest pieces of data and are better able to integrate these pieces of data into a coherent explanation for the problems (see Groves, O'Rourke, & Alexander 2003 , for an example). Second, typically physicians generate a small set of hypotheses very early in the case ( abduction ), as soon as the first pieces of data become available, as was first shown by Elstein, Shulman, and Sprafka ( 1978 ) and later corroborated by Feltovich et al.'s ( 1984 ) logical competitor set. Third, as also originally shown by Elstein, Shulman, and Sprafka ( 1978 ), physicians sometimes make use of the hypothetico-deductive process ( deduction ), which involved four stages: cue acquisition, hypothesis generation, cue interpretation, and hypothesis evaluation. Cues in the clinical case lead to the generation of a few selected hypotheses, and then each hypothesis is evaluated for consistency with the cues ( induction ).
The empirical research has also highlighted other aspects of medical reasoning that are independent of the general model. These include the directionality of diagnostic reasoning, the role of causal and analogical reasoning in clinical problem solving, and the development of medical expertise. A series of articles (Patel, Arocha, & Kaufman, 1994 , 2001 ; Patel, Kaufman, & Arocha, 2002 ) and other papers in edited volumes (Clancey & Shortliffe, 1984 ; Szolovits 1982 ) provide summaries of the different aspects of medical cognition. To some of these issues, we turn next.
Problem-Solving Strategies: Forward-Driven and Backward-Driven Reasoning
As indicated above, the study that Patel and Groen ( 1986 ) conducted on the knowledge-based solution strategies used by expert cardiologists showing that those physicians who accurately diagnosed the problem employed a forward-driven (also called data-driven) reasoning strategy. That is, they used patient data to generate a fully correct diagnosis; whereas those who did not diagnosed the problem accurately or failed to provide a correct solution to the patient problem used a backward or hypothesis-driven reasoning strategy. Such results challenged the hypothetico-deductive strategy proposed by Elstein, Shulman, and Sprafka ( 1978 ). Given the contrasting results of Patel and Groen with those of Elstein et al, it was necessary to search for an explanation that reconciled such empirical findings.
A hypothesis for reconciling these seemingly contradictory results is that forward-driven reasoning is used in clinical problems in which the physician has ample experience. In contrast, when reasoning through unfamiliar or difficult cases, physicians resort to backward-driven reasoning because their knowledge base does not support a pattern-matching process. To support this explanation, Patel, Groen, and Arocha ( 1990 ) looked for the conditions under which forward-driven reasoning breaks down. Cardiologists and endocrinologists were asked to solve diagnostic problems both in cardiology and in endocrinology. They showed that under conditions of case complexity and uncertainty, the pattern of forward-driven reasoning was disrupted. More specifically, the breakdown occurred when nonsalient cues in the case were tested for consistency against the main hypothesis, even by subjects who had generated the correct diagnosis. The results supported previous studies in that subjects with accurate diagnoses used pure forward-driven reasoning.
If forward-driven reasoning breaks down when case complexity is introduced, then experts and novices should reason differently because what are routine cases for experts would not be so for less-than-expert subjects. Investigating clinical reasoning in a range of contexts of varying complexity (Patel, Arocha, & Kaufman, 1994 ; Patel & Groen, 1991 a), the researchers found that novices and experts have different patterns of data-driven and hypothesis-driven reasoning. The use that experts make of data-driven reasoning, which depends on the physician possessing a highly organized knowledge base about the patient's disease (including sets of signs and symptoms). Furthermore, due to their extensive knowledge base and the high-level inferences they make, experts typically skip steps in their reasoning. In contrast, because of their lack of substantive knowledge or their inability to distinguish relevant from irrelevant knowledge, less-than-expert subjects (novices and intermediates) used more hypothesis-driven reasoning, resulting often in very complex reasoning patterns. Similar patterns of reasoning have been found in other domains (Larkin et al., 1980 ).
The fact that experts and novices reason differently suggests that they might reach different conclusions (e.g., decisions or understandings) when solving medical problems. Although data-driven reasoning is highly efficient, it is often error prone in the absence of adequate domain knowledge, since there are no built-in checks on the legitimacy of the inferences that a person makes. Pure data-driven reasoning is only successful in constrained situations, where one's knowledge of a problem can result in a complete chain of inferences from the initial problem statement to the problem solution. In contrast, hypothesis-driven reasoning is slower and requires high memory load, because one has to keep track of goals and hypotheses. It is therefore most likely to be used when domain knowledge is inadequate or the problem is complex. Hypothesis-driven reasoning is an example of a weak method of problem solving in the sense that it is used in the absence of relevant prior knowledge and when there is uncertainty about problem solutions (see Bassok & Novick, Chapter 21 ). In problem-solving terms, strong methods engage knowledge, whereas weak methods refer to general, knowledge-independent strategies. “Weak” does not necessarily imply ineffectual in this context.
Studies also showed that data-driven reasoning could break down due to uncertainty (Patel, Groen, & Arocha, 1990 ). These conditions include the presence of “loose ends” in explanations, where some particular piece of information remains unaccounted for and isolated from the overall explanation. Loose ends trigger explanatory processes that work by hypothesizing a disease, for instance, and trying to fit the loose ends within it, in a hypothesis-driven reasoning fashion. The presence of loose ends may foster learning, as the “reasoner” searches for an explanation for them. For example, a medical student or a physician may encounter a sign or a symptom in a patient problem and look for information that may account for the finding, by searching for similar cases seen in the past, reading a specialized medical book, or consulting a domain expert.
However, in some circumstances, the use of data-driven reasoning may lead to a heavy cognitive load (see van Merriënboer & Sweller, 2005 , for a recent review). For instance, when students are given problems to solve while they are being trained in the use of problem-solving strategies, the situation produces a heavy load on cognitive resources, which may diminish students' ability to focus on the task. The reason is that students have to share cognitive resources (e.g., attention, memory) between learning the problem-solving method and learning the content of the material. Research by Sweller ( 1988 ) suggested that when subjects use a strategy based on data-driven reasoning, they are more able to acquire a schema for the problem. In addition, other characteristics associated with expert performance were observed, such as a reduced number of moves to the solution. However, when subjects used a hypothesis-driven reasoning strategy, their problem-solving performance suffered.
The Role of Similarity of Cases in Diagnostic Reasoning
The fact that physicians make use of forward-driven reasoning in routine cases suggests a type of processing that is fast enough to be able to lead to the recognition of a set of signs and symptoms in a patient and generate a diagnosis based on such recognition. Most often this has been interpreted as a type of specific-to-general reasoning (e.g., reasoning from an individual case to a clinical schema or prototype). However, consistent with the model of abductive reasoning, some philosophers (Schaffner, 1986 ) and empirical researchers (Norman & Brooks, 1997 ) have supported an alternative hypothesis, which postulates specific-to-specific reasoning. That is, experts may use knowledge of specific instances (e.g., particular patients with specific disease presentations) to interpret particular cases, rather than relying only on general clinical knowledge (Kassirer & Kopelman, 1990 ). Similarity-based clinical reasoning has been informed by models of categorization, where the process of interpreting information, such as a clinical case, can be made by matching the case to a general, abstract category (e.g., a schema). However, in similarity-based reasoning a diagnosis may be reached through a process of matching the current case to similar cases seen in the past (Norman, Young, & Brooks, 2007 ).
Brooks and colleagues (Brooks, Norman, & Allen, 1991 ; Norman & Brooks, 1997 ) investigated clinicians' use of specific instances in order to compare and interpret a current clinical case. In these studies, mostly involving visual diagnosis based on X-rays, dermatological slides, and electrocardiograms, they showed that specific similarity to previous cases accounts for about 30% of diagnoses made. Furthermore, errors made by experts in identifying abnormalities in images were affected by the prior history of the patient. That is, if the prior history of the patient contained a possible abnormality, expert physicians more often identified those abnormalities in the images even when none were there, which was interpreted as the effect of specific past cases on the interpretation of the current case.
Norman and colleagues (Norman & Brooks, 1997 ; Norman, Young, & Brooks, 2007 ) have argued against the hypothesis that expert physicians always diagnose clinical cases by “analyzing” signs and symptoms and developing correspondences between those signs, symptoms, and diagnoses, in the manner that traditional cognitive research in medical reasoning suggests. They propose instead that medical diagnosis is often “nonanalytic.” By this, they mean that diagnostic reasoning is driven by the overall similarity between a previous case and the current case: A case previously seen in medical practice is retrieved unanalyzed from memory and compared to the current case (a kind of exemplar-based or case-based reasoning).
This discussion has its counterpart in the psychology of categorization, where two accounts have been proposed: Either categorization works by relying on prototypes or on exemplars (se Rips et al., Chapter 11 ). Exemplar-based thinking is certainly an important process in human cognition. There is ample evidence of conditions where reasoning by analogy to previous cases is used (Gentner & Holyoak, 1997 ; Holyoak & Thagard, 1997 ; see Holyoak, Chapter 13 ). Furthermore, given the complexity of natural reasoning in a highly dense knowledge domain such as medicine, it is very likely that more than one type of reasoning is actually employed. Seen in this light, the search for a single manner in which clinicians diagnose clinical problems may not be a reasonable goal. The inherent adaptability of humans to different kinds of knowledge domains, situations, problems, and cases may call for the use of a variety of reasoning modes, which is what, after all, the notion of abductive medical reasoning has tried to describe (Patel & Ramoni, 1997 ; see Lombrozo, Chapter 14 ). Similar conclusions appear to have been developed in the dual-process theory of reasoning (Evans, 2008 ; see Evans, Chapter 8 ). Thus, it seems that alongside a rule-based, more effortful prototype reasoning, clinical reasoning also allows for exemplar-based reasoning. However, it should be noted that not all reasoning from instances/analogs is nonanalytic. For example, analogical inferences may involve causal analysis of source analog in which similarity between particulars may be the main cognitive mechanism.
Reasoning and the Nature of Medical Knowledge
A reason for the variety of modes of reasoning used in actual diagnostic problems may be found in the inherent organization of medical knowledge. The prevalent view in the philosophy of medicine (Blois, 1988 ) has been that medical knowledge has an extremely complex organization, requiring the use of different reasoning strategies than those used in other formal scientific disciplines, such as physics. According to Blois, disciplines such as physics, chemistry, and some subfields of biology, are horizontally organized, where these domains are characterized by the construction of causal relations among concepts and by the application of general principles to specific instances (Blois, 1988 ). Furthermore, Blois asserts that such scientific fields are organized in a hypothetico-deductive manner such that particular cases are explained from first principles, where understanding the causal mechanisms plays a major role. In contrast, in medicine, reasoning from first principles does not play such an important role. He argued that reasoning in medicine instead requires vertical thinking. In this view, in the medical disciplines, notably clinical medicine, reasoning by analogy from case to case plays a more important role than reasoning causally from an understanding of the mechanism of disease. Based on this distinction, Blois argued that reasoning in the physical sciences and reasoning in the biomedical sciences are of different kinds.
Schaffner ( 1986 ) has argued that theories in the physical sciences can be conceptualized as a “deductive systematization of a broad class of generalizations under a small number of axioms” (Schaffner, 1986 , p. 69), but that such characterization cannot be applied to the biomedical sciences. The latter are characterized by what Schaffner ( 1986 , p. 68) calls “a series of overlapping interlevel temporal models.” Different level of aggregation (e.g., biochemical, cellular, organ), each with its own temporal development (e.g., some deterministic, others probabilistic, others still random) makes it difficult to develop deductive structures to explain biomedical reality. Rather, theories are based on the familiarization with shared exemplars to a much greater degree than is the case in the physical sciences. In biomedical research, an organism such as a Drosophila , for instance, is used as an exemplar embodying a given disease mechanism, which by analogy applies to other organisms, including humans. In the clinical sciences, the patient is seen as an exemplar to which generalizations based on multiple overlapping models are applied from disease mechanisms (e.g., physiological, biochemical, pathological) and from the population of similar patients (e.g., typical diagnostic categories described in clinical medicine).
A reason for the peculiar nature of biomedical knowledge may be that the field consists of two very different categories of knowledge: clinical knowledge, including knowledge of disease processes and associated findings; and basic science knowledge, incorporating subject matters such as biochemistry, anatomy, and physiology. Basic science or biomedical knowledge is supposed to provide a scientific foundation for clinical reasoning. The conventional view is that basic science knowledge can be seamlessly integrated into clinical knowledge, analogously to the way that learning the rules of the road can contribute to one's mastery of driving a car. A particular piece of biomedical knowledge could be automatically elicited in a range of clinical contexts and tasks in more or less the same fashion. However, the integration of these two types of knowledge has been difficult to demonstrate in empirical research.
Knowledge Organization and Changes in Directionality
Following Blois ( 1988 ) and Schaffner ( 1986 ), it can be argued that the way medical knowledge is organized can be a determinant factor explaining why experts do not use the hypothetico-deductive method of reasoning. Maybe the medical domain is too messy to allow neat partitioning and deductive use of reasoning strategies. Although the theory of reasoning in medicine is basically a theory of expert knowledge, reaching the level of efficient reasoning of the expert clinician reflects the extended continuum of training and levels of reasoning performance (Chi, Bassok, Lewis, Reiman, & Glaser, 1989 ; Dufresne, Gerace, Hardiman, & Mestre, 1992 ). This continuum is related to the nature of medical knowledge and its acquisition. Changes have been described in this process that serve to characterize the various phases medical trainees go through to become expert clinicians.
An important characteristic of this process is the intermediate effect . Although it generally seems reasonable to assume that performance will improve with training or time on task, there appear to be particular transitions in which subjects exhibit a certain drop in performance. This is an example of what is referred to in the developmental literature as nonmonotonicity (Strauss & Stavy, 1982 ), and it has also been observed in skill acquisition (Robertson & Glines, 1985 ). The result is a learning curve or developmental pattern that is shaped like either a U or an inverted U, as illustrated in Figure 37.1 . In the development of medical expertise, the performance of intermediates reflects the degradation in reasoning that results from the acquisition of knowledge during a period when such knowledge is not well organized and irrelevant associations abound in the learner's knowledge base. In contrast, the novice's knowledge base is sparse, containing very few associations, whereas the expert's knowledge base has been pruned of the irrelevancies that characterize intermediates.
It should be noted that not all intermediate performance is nonmonotonic; for example, on some global criteria such as diagnostic accuracy there appears to be a steady improvement (Patel & Groen, 1991 b). However, this increase in accuracy seems to be linked to a change in diagnostic strategy from hypothesis-driven reasoning to data-driven reasoning (Coderre, Mandin, Harasym, & Fick, 2003 ), and better organized knowledge in memory. Thus, knowledge acquisition results in changes in knowledge organization, which result in changes in the strategies used to solve clinical problems, which in turn lead to greater diagnostic accuracy. What the intermediate effect tells us is that the progression from a novice to an expert does not necessarily follow a linear improvement in performance, but a U-shaped pattern, where performance drops before it gets better. This is illustrated in Figure 37.1 , where medical students' recall of a clinical problem (after reading it once) showed an inverted U-shaped pattern with the third-year students recalling case information the most (Patel & Groen, 1991 b). Their inability to separate relevant from irrelevant information was consistently validated under various task conditions. This inability reflects in a decrease in diagnostic accuracy. Novices do not know enough, while experts know enough and have a well-developed schema for the problem to make accurate diagnoses. Intermediate-level subjects remember the most, but their knowledge is not organized in such a fashion that allows them to generate accurate diagnoses.
The “intermediate effect.” Recall of total and relevant information as a function of expertise, showing inverted U-shaped pattern, with intermediates recalling more relevant and irrelevant information. The performance level as a function of diagnostic accuracy and expertise shows a U-shaped phenomenon, where performance drops at the intermediate level (third year) before it gets better with training.
Now let us look at some details of the intermediate effect. The intermediate effect occurs with many tasks and at various levels of expertise. The tasks vary from recall of clinical cases (Claessen & Boshuizen, 1985 ), explanation of clinical problems (Arocha & Patel, 1995 ), to generating laboratory data (Patel, Groen, & Patel, 1997 ). For instance, when asked to recall clinical data from case descriptions, intermediates tend to recall more irrelevant information (Schmidt & Boshuizen, 1993 ) or generate more irrelevant hypotheses to account for a clinical case than novices or experts (Arocha & Patel, 1995 ). The phenomenon may be due to the fact that intermediates have acquired an extensive body of knowledge but have not yet reorganized this knowledge in a functional manner. Thus, intermediate knowledge has a sort of network structure that results in considerable search, which makes it more difficult for intermediates to set up structures for rapid encoding and selective retrieval of information (Patel & Groen, 1991 a). In contrast, expert knowledge is finely tuned to perform various tasks and experts can readily filter out irrelevant information using their hierarchically organized schemata. The difference is reflected both in the structural organization of knowledge and the extent to which it is proceduralized to perform different tasks.
Schmidt and Boshuizen ( 1993 ) reported that intermediate nonmonotonicity recall effects disappear by using short exposure times (about 30 seconds), which suggests that under time-restricted conditions, intermediates cannot engage in extraneous search. While a novice's knowledge base is likely to be sparse and an expert's knowledge base is intricately interconnected, the knowledge base of an intermediate possesses many of the pieces of knowledge in place but lacks the extensive connectedness of an expert. Until this knowledge becomes further consolidated, the intermediate is more likely to engage in unnecessary search. Whether this knowledge, painfully acquired during medical training, is really necessary for clinical reasoning has been a focus of intensive research and great debate. If expert clinicians do not explicitly use underlying biomedical knowledge, does that mean that it is not necessary? Or could it be simply the case that this knowledge remains “dormant” until it is really needed? This raises an important question of whether expert medical knowledge when applied to solving clinical problems is “deep” (e.g., making use of causal pathophysiological or basic science knowledge in clinical problem solving) or “shallow” (e.g., relying on the use of associations between disease categories and clinical manifestations of those categories, without considering the mechanism of the disease).
Causal Reasoning in Medicine
The differential role of basic science knowledge (e.g., physiology and biochemistry) in solving problems of varying complexity and the differences between subjects at different levels of expertise (Patel, Arocha, & Kaufman, 1994 ) have been a source of controversy in the study of medical cognition (Patel & Kaufman, 1994 ), as well as in medical education and artificial intelligence. As expertise develops, the disease knowledge of a clinician becomes more dependent on clinical experience, and clinical problem solving is increasingly guided by the use of exemplars and analogy and becomes less dependent on a functional understanding of the system in question. However, an in-depth conceptual understanding of basic science plays a central role in reasoning about complex problems and is also important in generating explanations and justifications for decisions.
Researchers in artificial intelligence were confronted with similar problems in extending the utility of systems beyond their immediate knowledge base. Biomedical knowledge can serve different functional roles depending on the goals of the system. Most models of diagnostic reasoning in medicine can be characterized as being “shallow.” For instance, a “shallow” medical expert system (e.g., MYCIN and INTERNIST) reasons by relating observations to intermediate hypotheses that partition the problem space, and further associating intermediate hypotheses with diagnostic hypotheses. This is consistent with the way physicians appear to reason. There are, however, other medical reasoning system models that propose a “deep” mode of reasoning as a main mechanism. Chandrasekeran, Smith, and Sticklen ( 1989 ) characterize a deep system as one that embodies a causal mental model of bodily function and malfunction, similar to the models used in qualitative physics (Bobrow, 1985 ). Systems such as MDX-2 (Chandrasakeran et al., 1989 ) or QSIM (Kuipers, 1987 ) have explicit representations of structural components and their relations, the functions of these components (in essence their purpose), and their relationship to behavioral states.
To become licensed physicians, medical trainees undergo a lengthy training process that includes learning of biomedical sciences, including biochemistry, physiology, and anatomy. There is an apparent contradiction between this type of training and the seeming absence of “deep” biomedical knowledge being used during expert medical reasoning. To account for such apparent inconsistency, Boshuizen and Schmidt ( 1992 ) proposed a learning mechanism, knowledge encapsulation . Knowledge encapsulation is a learning process that involves the organization of biomedical propositions and their interrelations in associative clusters, under a small number of higher level clinical propositions with the same explanatory power. Through exposure to clinical training, biomedical knowledge presumably becomes integrated with clinical knowledge. Biomedical knowledge can be “unpacked” when needed, but it is not used as a first line of explanation.
Boshuizen and Schmidt ( 1992 ) cite a wide range of clinical reasoning and recall studies that support this kind of learning process. Of particular importance is the well-documented finding that with increasing levels of expertise, physicians produce explanations at higher levels of generality, using fewer and fewer biomedical concepts while producing consistently accurate responses. The intermediate effect can also be accounted for as a stage in the encapsulation process in which a trainee's network of knowledge has not yet become sufficiently differentiated, thus resulting in more extensive processing of information.
Knowledge encapsulation provides an appealing account of a range of developmental phenomena in the course of acquiring medical expertise. However, the integration of basic science in clinical knowledge is a rather complex process, and encapsulation is likely to be only part of the knowledge development process. Basic science knowledge is likely to play a different role in different clinical domains. For example, clinical expertise in perceptual domains, such as dermatology and radiology, necessitates a relatively robust model of anatomical structures that is the primary source of knowledge for diagnostic classification. In other domains, such as cardiology and endocrinology, basic science knowledge has a more distant relationship with clinical knowledge. The misconceptions evident in physicians' biomedical explanations would argue against their having well-developed encapsulated knowledge structures in which basic science knowledge could easily be retrieved and applied when necessary.
The results of research into medical problem solving are consistent with the idea that clinical medicine and biomedical sciences constitute two distinct and not completely compatible “worlds,” with distinct modes of reasoning and quite different ways of structuring knowledge (see Patel et al., 1994 ). Clinical knowledge is based on a complex taxonomy that relates disease symptoms to underlying pathology. In contrast, biomedical sciences are based on general principles defining chains of causal mechanisms. Thus, learning to explain how a set of symptoms is consistent with a diagnosis may be very different from learning how to explain what causes a disease. Although basic science knowledge and clinical knowledge can be seen as worlds apart, this does not mean that basic biomedical knowledge is completely erased from an expert's disease schemata; rather, as suggested by the hypothesis of encapsulated knowledge, the two types of knowledge are not integrated into a whole (Rikers, Schmidt, & Moulaert, 2005 ). Thus, when physicians are trying to solve clinical cases at the limits of their expertise, they may resort to using biomedical knowledge to make sense of the clinical information and tie different concepts together, but in normal practice they seem to primarily use either schemata or exemplars that map directly onto clinical cases.
This “two worlds” position, although not incompatible with the notion of encapsulation, is supported in the study of conceptual understanding in biomedicine. The progression of mental models (White & Frederiksen, 1990 ) has been used as an alternative framework for characterizing the development of conceptual understanding in biomedical contexts. Mental models are dynamic knowledge structures that are composed to make sense of experience and to reason across spatial and/or temporal dimensions. An individual's mental models provide predictive and explanatory capabilities of the function of a given system. White and Frederiksen employed the progression of mental models to explain the process of understanding increasingly sophisticated electrical circuits. This notion can be used to account for differences between novices and experts in understanding circulatory physiology, describing misconceptions, and explaining the generation of spontaneous analogies in causal reasoning (Kaufman, Patel, & Magder, 1996 ).
Running a mental model is a potentially powerful form of reasoning, but it is also cognitively demanding. It may require an extended chain of reasoning and the use of complex representations. It is apparent that skilled individuals learn to circumvent long chains of reasoning and chunk or compile knowledge across intermediate states of inference (Chandrasekaran, 1994 ; Newell 1990 ). This results in shorter, more direct, inferences that are stored in long-term memory and are directly available to be retrieved in the appropriate contexts. Chandrasekaran ( 1994 ) refers to this sort of knowledge as compiled causal knowledge . This term refers to knowledge of causal expectations that people compile directly from experience and partly by chunking results from previous problem-solving endeavors. The goals of the individual and the demands of recurring situations largely determine which pieces of knowledge get stored and used. When a physician is confronted with a similar situation, she can employ this compiled knowledge in an efficient and effective manner. The development of compiled knowledge is an integral part of the acquisition of expertise.
The idea of compiling declarative knowledge bears a certain resemblance to the idea of knowledge encapsulation. However, the claim differs in two important senses. First, the process of compiling knowledge is not one of subsumption or abstraction, and the original knowledge (uncompiled mental model) may no longer be available in a similar form (Kuipers & Kassirer, 1984 ). Second, rather than being prestored unitary structures, mental models are composed dynamically out of constituent pieces of knowledge. The use of mental models is somewhat opportunistic and the learning process is less predictable. The compilation process can work in reverse as well. That is to say, discrete cause-and-effect relationships can be integrated into a mental model as a student reasons about complex physiological processes.
Errors in Medical Reasoning and Decision Making
One critical step toward understanding the cognitive mechanisms of performance problems in medical reasoning is to categorize medical errors along cognitively meaningful dimensions. Reason ( 1990 ) defines human error as a failure of achieving the intended outcome in a planned sequence of mental or physical activities. He divides human errors into two major categories: (1) slips that result from the incorrect execution of a correct action sequence, and (2) mistakes that result from the correct execution of an incorrect action sequence. Norman's theory of action (Norman, 1986 ) decomposes a human activity into seven stages. Based on Reason's definition of human error and Norman's action theory, Zhang, Patel, Johnson, and Shortliffe ( 2004 ) developed a cognitive taxonomy. In this cognitive taxonomy, goal and intention mistakes are mistakes about declarative knowledge (knowledge about factual statements and propositions), such as “Motrin is a pain reliever and fever reducer.” Action specification mistakes and action execution mistakes are mistakes about procedural knowledge (knowledge about procedures and rules), such as “give 1 tsp Motrin to a child per dosage up to 4 times a day if the child has fever or toothache and the weight of the child is 24–35 lb.”
Goal mistakes and intention mistakes are caused by many complex factors such as incorrect knowledge, incomplete knowledge, misuse of knowledge, biases, faulty heuristics, and information overload. For example, neglect of base rate information could result in incorrect diagnosis of a disease. This is a well-documented finding in human decision making (Tversky & Kahneman, 1974 ). As another example, the goal of “treating the disease as pneumonia” could be a mistake if it is a misdiagnosis based on incomplete knowledge (e.g., without X-ray images). Intention mistakes can be caused by similar factors. For example, a physician treating a patient with oxygen set the flow control knob between 1 and 2 liters per minute, not realizing that the scale numbers represented discrete rather than continuous settings. As a result, the patient did not receive any oxygen. This is a mistake due to incomplete knowledge.
The use of heuristics is another common source of goal and intention mistakes. A heuristic that is often used is the reliance on disease schemata during clinical diagnosis. Disease schemata are knowledge structures that have been formed from previous experience with diagnosing diseases and contain information about relevant and irrelevant signs and symptoms. When physicians and medical students diagnose patients, they tend to rely on their schemata and base their reasoning on the apparent similarity of patient information with these schemata, instead of a more objective analysis of patient data. The schemata that are used in diagnosis often guide future reasoning about the patient, affecting what tests are run and how data are interpreted. Arocha and Patel ( 1995 ) found that medical students and trainees maintained their initial hypotheses, even if subsequent data were contradictory. Therefore, if the initial hypothesis is wrong, errors in diagnosis and treatment are likely to occur. Preliminary presentation of the patient (e.g., signs and symptoms), then, becomes very important, because it can strongly suggest hypotheses that will be strongly held (i.e., lead to the use of schemata).
Medical Reasoning and Decision Research
Decision making is central to medical activity. Although health care professionals are generally highly proficient decision makers, their erroneous decisions have become the source of considerable public scrutiny, as described in three National Academy Press reports (Institute of Medicine, 1999 , 2001 , 2004 ).
Decisions involve the application of reasoning to select some course of action that achieves the desired goal. Hastie ( 2001 ) has identified three components of decision making: (a) choice options and courses of actions; (b) beliefs about objective states, processes, and events in the world, including outcomes states and means to achieve them; and (c) desires, values, or utilities that describe the consequences associated with the outcomes of each action-event combination. In this process, reasoning plays a major role. Research on hypothesis testing in the medical domain has shown the pervasiveness of confirmation bias (Patel, Groen, & Norman, 1993 ), which is evidenced by the generation of a hypothesis and the subsequent search for evidence consistent with the hypothesis, often leading to the failure to adequately consider alternative diagnostic possibilities. This bias may result in a less-than-thorough investigation with possible adverse consequences for the patient. A desire to confirm one's preferred hypothesis may moreover contribute to increased inefficiency and costs by leading to orders for additional laboratory tests that will do little to revise one's opinion, providing largely redundant data (Chapman & Elstein, 2000 ).
In natural setting of medicine, team decision making is the rule rather than the exception. Naturalistic decision making (NDM) is concerned with the study of cognition in “real-world” work environments that are often dynamic (e.g., rapidly changing; see Klein, Orasanu, Calderwood, & Zsambok, 1993 ). The majority of this research combines conventional protocol analytic methods with innovative methods designed to investigate reasoning and behavior in realistic settings (Rasmussen, Pejtersen, & Goodstein, 1994 ; Woods 1993 ). The study of decision making in the work context necessitates an extended cognitive science framework beyond typical characterizations of knowledge structures, processes, and skills, including modulating variables such as stress, time pressure, and fatigue as well as communication patterns that affect team performance.
Among the issues investigated in NDM are understanding how decisions are jointly negotiated and updated by participants differing substantially in their areas of expertise (e.g., pharmacology, respiratory medicine); how the complex communication process in these settings occurs; what role technology plays in mediating decisions and how it affects reasoning; and what the sources of error are in the decision-making process.
Research by Patel, Kaufman, and Magder ( 1996 ) studied decision making in a medical intensive care unit (ICU) with the objective of describing jointly negotiated decisions, communication processes, and the development of expertise. Intensive care decision making is characterized by a rapid, serial evaluation of options leading to immediate action, where reasoning is schema driven in a forward direction toward action with minimal inference or justification. However, when patients do not respond in a manner consistent with the original hypothesis, then the original decision comes under scrutiny. This strategy can result in a brainstorming session in which the team retrospectively evaluates and reconsiders the decision and considers possible alternatives. Various patterns of reasoning are used to evaluate alternatives in these brainstorming sessions, including probabilistic reasoning, diagnostic reasoning, and biomedical causal reasoning. Supporting decision making in clinical settings necessitates an understanding of communication patterns.
Another type of decision making that has attracted attention recently in medical cognition research is opportunistic decision making during task transitions. In medical settings (critical care in particular), the environment is stressful, time sensitive, interruption laden, and information rich. Franklin and colleagues (Franklin et al., 2011 studied how decisions are made when clinicians finished one task and transitioned to another task. The authors showed that the clinicians made two kinds of decisions: planned , in which they actively selected their next activity, and opportunistic , in which their next action in a series of behaviors was not determined by protocol but rather arose through unanticipated conditions (i.e., time, proximity or resources).
In summary, although traditional approaches to decision making have viewed decisions as choosing among known alternatives, real-world decision making involves reasoning that is constrained by dynamic factors, such as stress, time pressure, risk, and team interactions. Examining medical reasoning in social and collaborative settings is even more important when information technologies are part of the ebb and flow of clinical work.
Reasoning and Medical Education
The failures and successes of reasoning strategies and skills can be traced back to their sources: education. There is evidence suggesting that the way physicians reason results from the way they have been educated. Medical education in North America as well as in the rest of the world has followed a similar path: from practice-based training to an increasingly scientific training.
Motivated by the increasing importance of basic scientific knowledge in the context of clinical practice, problem-based learning (PBL) was developed on the premise that not only should physicians possess the ordered and systematic knowledge of science, but they should also think like scientists during their practices. Consistent with this idea, an attempt was made to teach hypothetico-deductive reasoning to medical students, as a way to provide an adequate structure to medical problem solving . After all, this was the way scientists were supposed to make discoveries.
However, based on cognitive research in other knowledge domains, some researchers argued that the hypothetico-deductive method might not be the most efficient way of solving clinical problems. To investigate how the kind of training medical students receive affected their reasoning patterns, Patel, Groen, and Norman ( 1993 ) looked at the problem-solving processes of students in two medical schools with different modes of instruction: classical and problem-based curricula. They found that students in the problem-based curriculum reasoned in a way that was consistent with their training methods, showing a preponderance of hypothetico-deductive reasoning and extensive elaborations of biomedical information. The PBL students used hypothesis-driven reasoning—from the hypothesis to explain the patient data—while non-PBL students used mainly data-driven reasoning—from data toward the hypothesis. In explaining clinical cases, PBL students produced extensive elaborations using detailed biomedical information, which was relatively absent from non-PBL students' explanations. It appears that PBL promotes the activation and elaboration of prior knowledge. However, these elaborations resulted in the generation of errors.
Patel, Arocha, and Lecissi ( 2001 ) also investigated the effects of non-PBL curricula on the use and integration of basic science and clinical knowledge and its impact on diagnostic explanation. The results showed that biomedical and clinical knowledge are not integrated and that very little biomedical information is used in routine problem-solving situations. There is significant use of expert-like data-driven strategies, however, in non-PBL students' explanations. The use of biomedical information increases when the clinical problems are complex; at the same time, hypothesis-driven strategies replace the data-driven strategies. Similar results were found in other professional domains such as law (Krieger, 2004 ).
Students from a PBL school integrated the two types of knowledge (biomedical sciences and clinical), and in contrast to the non-PBL students they spontaneously used biomedical information in solving even routine problems. It appeared that for students in the non-PBL curriculum, the clinical components of the problems are treated separately from the biomedical science components. The two components of the problem analysis seem to be viewed as serving different functions. However, when needed, the biomedical knowledge is utilized and seems to act as “glue” that ties the two kinds of information together.
In the PBL curriculum, the integration of basic science and clinical knowledge is so tight that students appear unable to separate the two types of knowledge. As a result, PBL students generate unnecessarily elaborate explanations, leading to errors of reasoning. PBL seems to promote a type of learning in which basic biomedical knowledge becomes so tightly tied to specific clinical problem types that it becomes difficult to decouple this knowledge in context in order to transfer to a new situation (Anderson, Reder, & Simon, 1996 ; Holyoak 1985 ).
This outcome is consistent with how biomedical information is taught in the classroom in PBL schools, namely, by encouraging use of the hypothetico-deductive method, resulting in a predominantly backward-directed mode of reasoning. Elaborations are accompanied by a tendency to generate errors of scientific fact and flawed patterns of explanation, such as circular reasoning. Even though a student's explanation may be riddled with bugs and misconceptions, their harmful effects may be dependent on the direction of reasoning. If they reason forward, then they are likely to view their existing knowledge as adequate. In this case, misconceptions may be long-lasting and difficult to eradicate. If they reason backward, misconceptions might best be viewed as transient hypotheses which, in the light of experience, are either refuted or else modified to form the kernel of a more adequate explanation. Interestingly, differences in the patterns of reasoning acquired in both PBL and non-PBL medical curricula are found to be quite stable, even after the students have completed medical school and are in residency training programs (Patel, Arocha, & Lecissi, 2001 ; Patel & Kaufman, 2001 ).
Instruction that emphasizes decontextualized abstracted models of phenomena has not yielded much success in medicine or in other spheres of science education. It is widely believed that the amount of transfer will be a function of the overlap between the original domain of learning and the target domain (Holyoak, 1985 ). The PBL's emphasis on real-world problems represents a very good source of transfer to clinical situations. However, it is very challenging to create a problem set that most effectively embodies certain biomedical concepts while maximizing transfer. Knowledge that is overly contextualized can actually reduce transfer.
Technology-Mediated Reasoning and Thinking in Medicine
All technologies mediate human performance. Technologies, whether they be computer-based or in some other form, transform the ways individuals and groups behave. They do not merely augment, enhance, or expedite performance, although a given technology may do all of these things. The difference is not one of quantitative change, but one that is qualitative in nature. Technology, tools, and artifacts not only enhance people's ability to perform tasks but also change the way they perform tasks. In cognitive science, this ubiquitous phenomenon is called the representational effect, which refers to the phenomenon that different representations of a common abstract structure can generate dramatically different representational efficiencies, task complexities, and behavioral outcomes (Zhang & Norman, 1994 ; see Markman, Chapter 4 ).
One approach to the study of how technology mediates thinking and reasoning is to consider technology as external representations (Zhang, 1997 ; Zhang & Norman, 1994 ). External representations are the knowledge and structure in the environment, as physical symbols, objects, or dimensions (e.g., written symbols, beads of abacuses, dimensions of a graph), and as external rules, constraints, or relations embedded in physical configurations (e.g., spatial relations of written digits, visual and spatial layouts of diagrams, physical constraints in abacuses). The information in external representations can be picked up, analyzed, and processed by perceptual systems alone, although the top-down participation of conceptual knowledge from internal representations can sometimes facilitate or inhibit the perceptual processes.
The mediating role of technology can be evaluated at several levels of analysis. For example, electronic medical records alter the practice of individual clinicians in significant ways, as discussed later. Changes to an information system substantially impacts organizational and institutional practices from research to billing to quality assurance. Even the introduction of patient-centered medical records early in the 20th century necessitated changes in hospital architecture and considerably effected work practices in clinical settings. Salomon, Perkins, and Globerson ( 1991 ) introduced a useful distinction in considering the mediating role of technology on individual performance, the effects with technology and the effects of technology. The former is concerned with the changes in performance displayed by users while equipped with the technology. For example, when using an effective medical information system, physicians should be able to gather information more systematically and efficiently. In this capacity, medical information technologies may alleviate some of the cognitive load associated with a given task and permit them to focus on higher order thinking skills, such as hypothesis generation and evaluation. The effects of technology refer to enduring changes in general cognitive capacities (knowledge and skills) as a consequence of interaction with a technology. For example, frequent use of information technologies may result in lasting changes in medical decision-making practices even in the absence of the system.
In several studies involving the mediating role of technology in clinical practice, Patel and her colleagues (Patel et al., 2000) observed the change of thinking and reasoning patterns caused by a change in methods of writing patient records from paper records to electronic medical records (EMRs). They found that before using EMRs, physicians focused on exploration and discovery, used complex propositions, and tended to use data-driven reasoning. After using EMRs, which have structured data, physicians focused on problem solving, used simple propositions, and tended to use problem-directed and hypothesis-driven reasoning. The change of behavior caused by the use of EMRs remained when the physicians went back to paper records, showing the enduring effects of technology on human reasoning in medicine.
As the basis for many medical decisions, diagnostic reasoning requires the collection, understanding, and use of many types of patient information, such as history, lab results, symptoms, prescriptions, images, and so on. It is affected by not just the expertise of the clinicians but also by the way the information is acquired, stored, processed, and presented. If we consider clinicians as rational decision makers, the format of a display, as long as it contains the same information, should not affect the outcome of the reasoning and decision-making process. But the formats of displays do affect many aspects of clinicians' task performance. Recently there have been several studies of how different displays of information in EMRs affect clinicians' behavior. Three major types of displays have been studied: source based, time based, and concept based. Source-based displays organize medical data by the sources of the data, such as encounter notes, lab reports, medications, lab results, radiology imaging and report, and physical exams. Time-based displays organize medical data as a temporal history of patient data. Concept-based displays organize medical data by clinically meaningful concepts or problems. In this case all data related to a specific problem are displayed together. For example, if a patient has symptoms such as coughing, chest pain, and fever, the lab results, imaging reports, prescriptions, assessments, and plans are displayed together. Zeng et al. ( 2002 ) found that different displays were useful for different tasks. For example, source-based displays aid clinicians in retrieving information for a specific test or procedure from a specific department, whereas concept-based displays aid the search of information related to a specific disease.
Medication management is always a challenging task for patients. How drug information is displayed can affect patients' understanding of the drug information, the way they manage their medication, and ultimately their health outcomes. For example, Day ( 1988 ) demonstrated how alternative representations should be used for different purposes for improving medication scheduling. With the rapid growth of computer-based information systems, people are interacting more and more with computer-generated health information displays. These displays need to be designed to effectively and accurately generate the information that people need for informed reasoning.
Conclusions and Future Directions
Advances in cognitive science have made significant contributions to investigations into the process of medical reasoning. However, there are a number of issues that could benefit from research, especially involving multidisciplinary approaches. At the theoretical level, an important issue for future theoretical and empirical development involves the integration of the diverse modes of medical reasoning. This includes the integration of the expertise and the decision-making approaches to expert cognition (see Kahneman & Klein, 2009 ), which has direct implications for establishing in more detail the role that intuitive and conscious reasoning play in the different medical tasks and in the commission of errors. Some attempts have been recently made (Croskerry, 2009 ; Norman 2009 ; Norman & Eva, 2010 ) to clarify their role, particularly through application of the dual-process view of thinking and reasoning (Evans, 2008 ) to clinical problem solving. As some have pointed out (GlÖckner & Witteman, 2010 ), both types of processes may involve different mechanisms, which remain to be empirically and theoretically established. In this regard, the medical environment may be used as a test bed for investigating these fundamental problems in an applied real-world arena.
As such an applied area, reasoning in a medical context involves complex compositions of various populations, settings, and a high degree of uncertainty (as in critical care environments). Compounded with constraints imposed by resource availability, these factors lead to increased use of heuristic strategies. The utility of heuristics lies in limiting the extent of purposeful search through data sets. By reducing redundancy, such heuristics have substantial practical value, as a significant part of a physician's cognitive effort is based on heuristic thinking. However, the use of heuristics introduces considerable bias in medical reasoning, often resulting in a number of conceptual and procedural errors. These include misconceptions about laws governing probability, instantiation of general rules to a specific patient at the point of care, incorrect use of prior probabilities and actions, as well as false confirmation of hypotheses.
With the increasing move of cognitive studies toward investigations in real-world settings, complex phenomena can be better studied. The constraints of laboratory-based work make it impossible to fully capture the dynamics of real-world problems. This issue is particularly salient in rapidly changing critical care environments. Studies of thinking and reasoning in medicine, which focus on medical errors and technology-mediated cognition, are increasingly paying attention to dimensions of medical work in clinical settings. The recent concern with understanding and reducing medical errors provides an opportunity for cognitive scientists to use cognitive theories and methodologies to address the pressing, practical problem of managing these errors under conditions of urgency and multitasking. A trend in health care, spurred partly by the advent of information technologies that foster communication, is the development of health care systems that are increasingly multidisciplinary and collaborative, often spanning geographic regions. Increasing costs of health care and rapid knowledge growth have accelerated the trend towards collaboration of health care professionals to share knowledge and skills. Comprehensive patient care necessitates the communication of health care providers in different medical domains, thereby optimizing the use of their expertise. Research on reasoning will need to continue to move toward a distributed model of cognition. This model will include a focus on both socially shared and technology-mediated reasoning. Finally, today medical applications from the domain of artificial intelligence span from molecular medicine to organizational aspects of work domain, the role of modeling human reasoning and cognitive science will need to be reevaluated. Modeling and reasoning will play a significant role as we strive to build successful systems to support reasoning processes (Patel, Shortliffe, Stefanelli, et al., 2009 ).
Acknowledgment
This chapter is dedicated to the memory of a close friend and a colleague, late Marco F. Ramoni, who was passionate about understanding the nature of reasoning in biomedicine, as he was passionate about life in general.
In contrast, early, precognitive, accounts of medical diagnosis (Rimoldi, 1961 ) described it in a way that was independent of the underlying structure of the domain knowledge, through the application of general reasoning strategies. These accounts simply made the assumption that some domain of knowledge existed and that all the hypotheses needed to explain a problem were available when the diagnostic process starts. For instance, skill in diagnosing patients was assumed to be the result of the application of knowledge-independent strategies to clinical problems (e.g., by following the scientific method).
Anderson, J. R., Reder, L. M., & Simon, H. A. ( 1996 ). Situated learning and education. Educational Researcher , 25 (4), 5–11.
Arocha, J. F., & Patel, V. L. ( 1995 b). Novice diagnostic reasoning in medicine: Accounting for evidence. Journal of the Learning Sciences , 4 (4), 355–384.
Blois, M. S. ( 1988 ). Medicine and the nature of vertical reasoning. New England Journal of Medicine , 318 , 847–851.
Bobrow, D. G. (Ed.). ( 1985 ). Qualitative reasoning about physical systems . Cambridge, MA: MIT Press.
Google Scholar
Google Preview
Boshuizen, H. P. A., & Schmidt, H. G. ( 1992 ). On the role of biomedical knowledge in clinical reasoning by experts, intermediates, and novices. Cognitive Science , 16 (2), 153–184.
Brooks, L. R., Norman, G. R., & Allen, S. W. ( 1991 ). Role of specific similarity in a medical diagnostic task. Journal of Experimental psychology: General , 120 (3), 278–287.
Chandrasekaran, B. ( 1994 ). The functional representation and causal process. In M. Yovitz (Ed.), Advances in computing (pp. 73–143). New York: Academic Press.
Chandrasekeran, B., Smith, J. W., & Sticklen, J. ( 1989 ). Deep models and their relation to diagnosis. Artificial Intelligence in Medicine , 1 , 29–40.
Chapman, G. B., & Elstein, A. S. ( 2000 ). Cognitive processes and biases in medical decision making. In G. B. Chapman & F.A. Sonnenberg (Eds.), Decision making in health care: Theory, psychology, and applications (pp. 183–210). New York: Cambridge University Press.
Chi, M. T. H., Bassok, M., Lewis, M. W., Reiman, P., & Glaser, R. ( 1989 ). Self explanations: How students study and use examples in learning to solve problems. Cognitive Science , 13 , 145–182.
Claessen, H. F. A., & Boshuizen, H. P. A. ( 1985 ). Recall of medical information by students and doctors. Medical Education , 19 , 61–67.
Clancey, W. J. ( 1985 ). Heuristic classification. Artificial Intelligence , 27 , 289–350.
Clancey, W. J., & Letsinger, R. ( 1984 ). NEOMYCIN: Reconfiguring a rule-based expert system for application to teaching. In W. J. Clancey & E. H. Shortliffe (Eds.), Readings in medical artificial intelligence: The first decade (pp. 361–381). Reading, MA: Addison-Wesley.
Clancey, W. J., & Shortliffe, E. H. ( 1984 ) (Eds.). Readings in medical artificial intelligence: The first decade . Reading, MA: Addison-Wesley.
Coderre, S., Mandin, H., Harasym, P. H., & Fick, G. H. ( 2003 ). Diagnostic reasoning strategies and diagnostic success. Medical Education , 37 (8), 695–703.
Croskerry, P. ( 2009 ). Clinical cognition and diagnostic error: Applications of a dual process model of reasoning. Advances in Health Sciences Education , 14 , 27–35.
Day, R. S. ( 1988 ) Alternative representations. The Psychology of Learning and Motivation , 22 , 261–305.
Dowie, J., & Elstein, A. S. (Eds.). ( 1988 ). Professional judgment: A reader in clinical decision making . Cambridge, England: Cambridge University Press.
Dufresne, R. J., Gerace, W. J., Hardiman, P. T., & Mestre, J. P. T. ( 1992 ). Constraining novices to perform expertlike problem analyses: Effects on schema acquisition. The Journal of the Learning Sciences , 2 (3), 307–331.
Elstein, A. S. ( 2009 ). Thinking about diagnostic thinking: A 30-year perspective. Advances in Health Science Education, Theory and Practice , 14 (Suppl. 1), 7–18.
Elstein, A. S., Shulman, L. S., & Sprafka, S. A. ( 1978 ). Medical problem solving: An analysis of clinical reasoning . Cambridge, MA: Harvard University Press.
Ericsson, K. A., & Simon, H. A. ( 1993 ). Protocol analysis: Verbal reports as data (Rev. ed.). Cambridge, MA: MIT Press.
Eshelman, L. ( 1988 ). MOLE: A knowledge acquisition tool for Cover-and-Differentiatiate systems. In S. C. Marcus (Ed.), Automating knowledge acquistion for expert systems (pp. 37–80). Boston, MA: Kluwer.
Evans, J. St. B. T ( 2008 ). Dual-processing accounts of reasoning, judgement, and social cognition. Annual Review of Psychology , 59 , 255–278.
Feltovich, P. J., Johnson, P. E., Moller, J. H., & Swanson, D. B. ( 1984 ). LCS: The role and development of medical knowledge in diagnostic expertise. In W. J. Clancey & E. H. Shortliffe (Eds.), Readings in medical artificial intelligence: The first decade (pp. 275–319). Reading, MA: Addison-Wesley.
Frensch, P. A., & Funke, J. ( 1995 ). Complex problem solving: The European perspective . Hillsdale, NJ: Erlbaum.
Franklin, A., Liua, Y., Li, Z., Nguyen, V., Johnson, R.R., Robinson, D., Okafor, N., King, B., Patel, V.L., Zhang, J. ( 2011 ). Opportunistic decision making and complexity in emergency care. Journal of Biomedical Informatics. 44 (3), 469–476.
Gaba, D. M. ( 1992 ). Dynamic decision-making in anesthesiology: Cognitive models and training approaches. In D. A. Evans & V. L. Patel (Eds.), Advanced models of cognition for medical training and practice (pp. 123–147). New York: Springer-Verlag.
Gentner, D., & Holyoak, K. J. ( 1997 ). Reasoning and learning by analogy: Introduction. American Psychologist , 52 (1), 32–34.
Glöckner, A., & Witteman, C. ( 2010 ). Beyond dual-process models: A categorisation of processes underlying intuitive judgement and decision making. Thinking and Reasoning , 16 , 1–25.
Gorry, G. A. ( 1973 ). Computer-assisted clinical decision-making. Methods of Information in Medicine , 12 (1), 45–51.
Groves, M., O'Rourke, P., & Alexander, H. ( 2003 ). The clinical reasoning characteristics of diagnostic experts. Medical Teacher , 25 (3), 308–313.
Hastie, R. ( 2001 ). Problems for judgment and decision making. Annual Review of Psychology , 52 , 653–683.
Hoffman, R., & Deffenbacher, K. ( 1992 ). A brief history of applied cognitive psychology. Applied Cognitive Psychology , 6 (1), 1–48.
Holyoak, K. J. ( 1985 ). The pragmatics of analogical transfer. The Psychology of Learning and Motivation , 19 , 59–87.
Holyoak, K. J., & Thagard, P. ( 1997 ). The analogical mind. American Psychologist , 52 (1), 35–44.
Institute of Medicine. ( 1999 ). To err is human: Building a safer health system . Washington, DC: National Academy Press.
Institute of Medicine. ( 2001 ). Crossing the quality chasm: A new health system for the 21st century . Washington, DC: National Academy Press.
Institute of Medicine. ( 2004 ). Patient safety . Washington, DC: National Academy Press.
Joseph, G. M., & Patel, V. L. ( 1990 ). Domain knowledge and hypothesis generation in diagnostic reasoning. Medical Decision Making , 10 (1), 31–46.
Kahneman, D., & Klein, G. ( 2009 ). Conditions for intuitive expertise: A failure to disagree. American Psychologist , 64 , 515–526.
Kassirer, J. P. ( 1989 ). Diagnostic reasoning. Annals of Internal Medicine , 110 (11), 893–900.
Kassirer, J. P., & Kopelman, R. I. ( 1990 ). Diagnosis and the structure of memory. 2. Exemplars, scripts, and simulation. Hospital Practice (Office Edition) , 25 (11), 29–33, 36.
Kaufman, D. R., Patel, V. L., & Magder, S. ( 1996 ). The explanatory role of spontaneously generated analogies in reasoning about physiological concepts. International Journal of Science Education , 18 , 369–386.
Klein, G. A. Orasanu, J., Calderwood, R., & Zsambok, C. E. (Eds.). ( 1993 ). Decision making in action: Models and methods . Norwood, NJ: Ablex.
Krieger, S. H. ( 2004 ). Domain knowledge and the teaching of creative legal problem solving, Clinical Law Review , 11, 149–207.
Kuipers, B. ( 1987 ). Qualitative simulation as causal explanation. IEEE Transactions on Systems, Man, and Cybernetics , 17 , 432–444.
Kuipers, B., & Kassirer, J. P. ( 1984 ). Causal reasoning in medicine: Analysis of a protocol. Cognitive Science , 8 (4), 363–385.
Larkin, J. H., McDermott, J., Simon, H. A., & Simon, D. P. ( 1980 ). Expert and novice performance in solving physics problems. Science , 208 , 1335–1342.
Leaper, D. J., Horrocks, J. C., Staniland, J. R., & De Dombal, F. T. ( 1972 ). Computer-assisted diagnosis of abdominal pain using “estimates” provided by clinicians. British Medical Journal , 4 (836), 350–354.
Ledley, R. S., & Lusted, L. B. ( 1959 ). Reasoning foundations of medical diagnosis. Science , 130 , 9–21.
Leprohon, J., & Patel, V. L. ( 1995 ). Decision-making strategies for telephone triage in emergency medical services. Medical Decision Making , 15 (3), 240–253.
Magnani, L. ( 1992 ). Abductive reasoning: Philosophical and educational perspectives in medicine. In D. A. Evans & V. L. Patel (Eds.), Advanced models of cognition for medical training and practice (pp. 21–41). Berlin, Germany: Springer-Verlag.
Magnani, L. ( 2001 ). Abduction, reason, and science: Processes of discovery and explanation . London: Kluwer Academic-Plenum.
Miller, R. A., Pople, H. E., & Myers, J. D. ( 1984 ). Internist-I, an experimental computer-based diagnostic for general internal medicine. In W. J. Clancey & E. H. Shortliffe (Eds.), Readings in medical artificial intelligence: The first decade (pp. xvi, p. 512). Reading, MA: Addison-Wesley.
Newell, A. ( 1990 ). Unified theories of cognition . Cambridge, MA: Harvard University Press.
Newell, A., & Simon, H. A. ( 1972 ). Human problem solving . Englewood Cliffs, NJ: Prentice-Hall.
Norman, D. A. ( 1986 ). Cognitive engineering. In D. A. Norman & S. W. Draper (Eds.), User centered system design: New perspectives on human-computer interaction (pp. 31–61). Hillsdale, NJ: Erlbaum.
Norman, G. R. ( 2009 ). Dual processing and diagnostic errors. Advances in Health Sciences Education , 14 , 37–49.
Norman, G. R., & Brooks, L. R. ( 1997 ). The non-analytical basis of clinical reasoning. Advances in Health Sciences Education , 2 (2), 173–184.
Norman, G. R., & Eva, K. W. ( 2010 ). Diagnostic error and clinical reasoning. Medical Education , 44 , 94–100.
Norman, G. R., Brooks, L. R., & Allen, S. W. ( 1989 ). Recall by expert medical practitioners and novices as a record of processing attention. Journal of Experimental Psychology: Learning, Memory, and Cognition , 15 (6), 1166–1174.
Norman, G., Young, M., & Brooks, L. ( 2007 ). Non-analytical models of clinical reasoning: The role of experience. Medical Education , 41 (12), 1140–1145.
Osler, W. ( 1906 ). Aequanimitas. With other addresses to medical students, nurses and practitioners of medicine . Philadelphia, PA: Blakiston's.
Patel, V. L., Arocha, J. F., & Kaufman, D. R. ( 1994 ). Diagnostic reasoning and expertise. Psychology of Learning and Motivation , 31 , 137–252.
Patel, V. L., Arocha, J. F., & Kaufman, D. R. ( 2001 ). A primer on aspects of cognition for medical informatics. Journal of the American Medical Informatics Association , 8 (4), 324–343.
Patel, V. L., Arocha, J. F., & Kushniruk, A. W. ( 2002 ). Patients’ and physicians’ understanding of health and biomedical concepts: relationship to the design of EMR systems. Journal of Biomedical Informatics , 35 (1), 8–16.
Patel, V. L., Arocha, J., & Lecissi, M. ( 2001 ). Impact of undergraduate medical training on housestaff problem solving performance: Implications for health education in problem-based curricula. Journal of Dental Education , 65 (11), 1199–1218.
Patel, V. L., Evans, D. A., & Kaufman, D. R. ( 1989 ). Cognitive framework for doctor-patient communication. In D. A. Evans & V. L. Patel (Eds.), Cognitive science in medicine: Biomedical modeling (pp. 257–312). Cambridge, MA: MIT Press.
Patel, V. L., & Groen, G. J. ( 1986 ). Knowledge-based solution strategies in medical reasoning. Cognitive Science , 10 , 91–116.
Patel, V. L., & Groen, G. J. ( 1991 a). The general and specific nature of medical expertise: A critical look. In K. A. Ericsson & J. Smith (Eds.), Toward a general theory of expertise: Prospects and limits (pp. 93–125). New York: Cambridge University Press.
Patel, V. L., & Groen, G. J. ( 1991 b). Developmental accounts of the transition from medical student to doctor: Some problems and suggestions. Medical Education , 25 (6), 527–535.
Patel, V. L., Groen, G. J., & Arocha, J. F. ( 1990 ). Medical expertise as a function of task difficulty. Memory and Cognition , 18 (4), 394–406.
Patel, V. L., Groen, G. J., & Norman, G. R. ( 1993 ). Reasoning and instruction in medical curricula. Cognition and Instruction , 10 (4), 335–378.
Patel, V. L., Groen, C., & Patel, Y. ( 1997 ). Cognitive aspects of clinical performance during patient workup: The role of medical expertise. Advances in Health Sciences Education , 2 (2), 95–114.
Patel, V. L., & Kaufman, D. R. ( 1994 ). On poultry expertise, precocious kids, and diagnostic reasoning. Academic Medicine , 69 (12), 971–972.
Patel, V. L., & Kaufman, D. R. (2001, Feb 02). Medical education isn't just about solving problems. The Chronicle of Higher Education , p. B12.
Patel, V. L., Kaufman, D. R., & Arocha, J. F. ( 2002 ). Emerging paradigms of cognition in medical decision-making. Journal of Biomedical Informatics , 35 , 52–75.
Patel, V. L., Kaufman, D. R., & Magder, S. ( 1996 ). The acquisition of medical expertise in complex dynamic decision-making environments. In K. A. Ericsson (Ed.), The road to excellence: The acquisition of expert performance in the arts and sciences, sports and games (pp. 127–165). Hillsdale, NJ: Elrbaum.
Patel, V. L., & Ramoni, M. F. ( 1997 ). Cognitive models of directional inference in expert medical reasoning. In P. J. Feltovich & K. M. Ford (Eds.), Expertise in context: Human and machine (pp. 67–99). Cambridge, MA: MIT Press.
Patel, V. L., Shortliffe, E. H., Stefanelli, M., Szolovits, P., Berthold, M. R., Bellazzi, R., & Abu-Hanna, A. ( 2009 ), The coming of age of artificial intelligence in medicine. Artificial Intelligence in Medicine , 46 , 5–17.
Pauker, S. G., Gorry, G. A., Kassirer, J. P., & Schwartz, W. B. ( 1976 ). Towards the simulation of clinical cognition. American Journal of Medicine , 60 , 981–996.
Peirce, C. S. ( 1955 ). Abduction and induction. In C. S. Peirce & J. Buchler (Eds.), Philosophical writings of Peirce (pp. 150–156). New York: Dover.
Ramoni, M. F., Stefanelli, M., Magnani, L., & Barosi, G. ( 1992 ). An epistemological framework for medical knowledge based system. IEEE Transactions on Systems, Man, and Cybernetics , 22 , 1361–1375.
Rasmussen, J., Pejtersen, A. M., & Goodstein, L. P. ( 1994 ). Cognitive systems engineering . New York: Wiley.
Reason, J. T. ( 1990 ). Human error . Cambridge, England: Cambridge University Press.
Rikers, R. M. J. P., Schmidt, H. G., & Moulaert, V. ( 2005 ). Biomedical knowledge: Encapsulated or two worlds apart? Applied Cognitive Psychology , 19 (2), 223–231.
Rimoldi, H. J. A. ( 1961 ). The test of diagnostic skills. Journal of Medical Education , 36 , 73–79.
Robertson, R. J. & Glines, L. A. ( 1985 ). The phantom plateau returns. Perceptual and Motor Skills , 61 , 55–64.
Salas, E., & Klein, G. A. ( 2001 ). Linking expertise and naturalistic decision making . Mahwah, NJ: Erlbaum.
Salomon, G., Perkins, D., & Globerson, T. ( 1991 ). Partners in cognition: Extending human intelligence with intelligent technologies. Educational Researcher , 20 (4), 2–9.
Schaffner, K. F. ( 1986 ). Exemplar reasoning about biological models and diseases: A relation between the philosophy of medicine and philosophy of science. Journal of Medicine and Philosophy , 11 , 63–80.
Schmidt, H. G., & Boshuizen, H. P. A. ( 1993 ). On the origin of intermediate effects in clinical case recall. Memory and Cognition , 21 , 338–351.
Shortliffe, E. H. ( 1976 ). Computer-based medical consultations, MYCIN . New York: Elsevier.
Strauss, S., & Stavy, R. ( 1982 ). U-shaped behavioral growth . New York: Academic Press.
Sweller, J. ( 1988 ). Cognitive load during problem solving: Effects on learning. Cognitive Science , 12 , 257–285.
Szolovits, P. (Ed.). ( 1982 ). Artificial intelligence in medicine (Vol. 51). Boulder, CO: Westview Press.
Tversky, A., & Kahneman, D. ( 1974 ). Judgment under uncertainty: Heuristics and biases. Science , 185 (4157), 1124–1131.
van Merriënboer, J. J. G., & Sweller, J. ( 2005 ). Cognitive load theory and complex learning: Recent developments and future directions. Educational Psychology Review , 17 (2), 147–176.
Vicente, K. J., & Rasmussen, J. ( 1990 ). The ecology of human-machine systems. II: Mediating “direct perception” in complex work domains. Ecological Psychology , 2 , 207–250.
White, B. Y., & Frederiksen, J. R. ( 1990 ). Causal model progressions as a foundation for intelligent learning environments. In W. J. Clancey & E. Soloway (Eds.), Artificial Intelligence : Artificial intelligence and learning environments [Special issue]. 42(1) , 99–157.
Woods, D. D. ( 1993 ). Process-tracing methods for the study of cognition outside of the experimental psychology laboratory. In G. A. Klein, J. Orasanu R. Calderwood, & C. E. Zsambok (Eds.), Decision making in action: Models and methods (pp. 228–251). Norwood, NJ: Ablex.
Zeng, Q., Cimino, J. J., & Zou, K. H. ( 2002 ). Providing concept-oriented views for clinical data using a knowledge-based system: an evaluation. Journal of the American Medical Informatics Association , 9 (3), 294–305.
Zhang, J. ( 1996 ). A representational analysis of relational information displays. International Journal of Human-Computer Studies , 45 (1), 59–74.
Zhang, J. ( 1997 ). The nature of external representations in problem solving. Cognitive Science , 21 (2), 179–217.
Zhang, J., & Norman, D. A. ( 1994 ). Representations in distributed cognitive tasks. Cognitive Science , 18 , 87–122.
Zhang, J., Patel, V. L, Johnson, T. R., & Shortliffe, E. H. ( 2004 ). A cognitive taxonomy of medical errors, Journal of Biomedical Informatics , 37 , 193–204.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- To save this word, you'll need to log in. Log In
critical thinking
Definition of critical thinking
Examples of critical thinking in a sentence.
These examples are programmatically compiled from various online sources to illustrate current usage of the word 'critical thinking.' Any opinions expressed in the examples do not represent those of Merriam-Webster or its editors. Send us feedback about these examples.
Word History
1815, in the meaning defined at sense 1
Dictionary Entries Near critical thinking
critical temperature
critical value
Cite this Entry
“Critical thinking.” Merriam-Webster.com Dictionary , Merriam-Webster, https://www.merriam-webster.com/dictionary/critical%20thinking. Accessed 2 May. 2024.
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!

Can you solve 4 words at once?
Word of the day.
See Definitions and Examples »
Get Word of the Day daily email!
Popular in Grammar & Usage
What’s the difference between ‘hillbilly’ and ‘redneck’, more commonly misspelled words, commonly misspelled words, how to use em dashes (—), en dashes (–) , and hyphens (-), absent letters that are heard anyway, popular in wordplay, the words of the week - apr. 26, 9 superb owl words, 'gaslighting,' 'woke,' 'democracy,' and other top lookups, 10 words for lesser-known games and sports, your favorite band is in the dictionary, games & quizzes.

- Dictionaries home
- American English
- Collocations
- German-English
- Grammar home
- Practical English Usage
- Learn & Practise Grammar (Beta)
- Word Lists home
- My Word Lists
- Recent additions
- Resources home
- Text Checker
Definition of critical thinking noun from the Oxford Advanced Learner's Dictionary
critical thinking
- The school encourages critical thinking and problem-solving.
- Students are encouraged to develop critical thinking instead of accepting opinions without questioning them.
- The book shows you how to apply critical thinking to your studies.
- Critical thinking skills enable students to evaluate information.
Take your English to the next level
The Oxford Learner’s Thesaurus explains the difference between groups of similar words. Try it for free as part of the Oxford Advanced Learner’s Dictionary app

By Daniela J. Lamas
Dr. Lamas, a contributing Opinion writer, is a pulmonary and critical-care physician at Brigham and Women’s Hospital in Boston.
I arrived at the hospital one recent morning to find a team of doctors gathered just outside a patient room. The patient was struggling — his breaths too fast and too shallow. For days we had been trying to walk the line between treating the pain caused by his rapidly growing cancer and prolonging his life.
Overnight he had worsened. His family, wrestling with the inevitability of his death, had come to a tentative plan, and I needed to make sure that his wife understood what was ahead. I explained that if we inserted a breathing tube, as she had decided overnight, her husband would be sedated. When the rest of their family arrived in Boston, we would take out the tube and he would die. We would not be able to wake him up — to do so would only cause him to suffer.
At this, his wife stiffened. Why wouldn’t he be able to wake up? I explained that his cancer was so advanced that to wake him would be to give him the conscious awareness of drowning. I watched as she took me in, this doctor she had never met before, telling her something she did not want to hear. Her expression shifted. “Why should I believe you?” she asked me. And then, her voice toughening: “I don’t think that I do.”
The room was silent. My patient’s wife looked into her bag, rooting around for a tissue. I glanced down at my feet. Why should she believe me? I was wearing sneakers with my scrub pants, and I found myself wondering whether she would have trusted me without question if I appeared more professional, or if I were older or male. Perhaps, but there was so much more at play in that moment. This was not just about one doctor and one family member, but instead, about a public for whom the medical system is no longer an institution to be trusted.
We are at a crossroads in medicine when it comes to public trust. After a pandemic that twisted science for political gain, it is not surprising that confidence in medicine is eroding. In fact, trust in medical scientists has fallen to its lowest levels since January 2019. As a result, more people are seeking out less conventional voices of “authority” that hew closer to their beliefs. Robert F. Kennedy Jr., a longtime vaccine skeptic campaigning for the presidency, is finding double-digit support in some polls and has made medical freedom a recurring theme of his candidacy.
But our medical system relies on trust — in face-to-face meetings as well as public health bulletins. Distrust can lead doctors to burnout and can encourage avoidable negative outcomes for our patients. This is partly what is driving increasing rates of measles among unvaccinated children , failure to follow recommended cancer screening and refusal to take lifesaving preventive medications . There are no easy solutions here. But if we do not find ways to restore and strengthen trust with our patients, more lives will be lost.
This is relatively new terrain for American physicians. When I was in medical training, we did not talk much about trust. During my early years as a doctor, I barely trusted myself and in fact felt uncomfortable with the responsibility I had to keep my patients alive. Only recently have I found myself thinking about what happens when this ephemeral ingredient in the doctor-patient relationship is lost.
Medical skepticism is not the same as medical nihilism. The data behind the drugs doctors prescribe and the decisions we make need not be the purview of us alone; the public has the right to review the numbers and to make their own decisions about risk and benefit. But when that skepticism shifts into abject and irreparable disbelief, we see some patients make dangerous decisions. And when doctors respond with frustration, that only further separates us from those patients.
Trust can sometimes be repaired by clearly presenting facts and figures, but it is about more than explaining numbers. We tell patients things about the body that are unseen. We recommend lifestyle changes and medication to treat or to prevent problems that may not be felt. Surgeons refer to a profound version of trust called the surgical contract: the idea that when people go under the knife, they are allowing their surgeon to make them sicker — to cut them open — in order to make them better. That trust must be earned.
In emergencies, patients don’t have the luxury to choose whom to trust, and medical decisions must happen hastily, in minutes even. So part of our job is to build rapport quickly. That becomes harder, impossible even, when we enter into the climax of a medical crisis to find that whatever trust our patient may have once had long ago has been eroded. Many of our patients started their medical journeys wanting to believe in their doctors. But then the medical system that they wanted to trust failed them, in small ways and large, from haphazardly rescheduled appointments to real medical error. How do we begin the process of repair, both as a profession and as individuals, when time is short?
In medicine, we talk about the idea of shared decision-making, in which medical decisions are arrived at jointly by doctor and patient, in contrast to the paternalistic tone of years gone by. As doctors, we do not tell our patients what to do — instead we offer them the information necessary for them to choose the path that is right for them.
For all our training, our medical knowledge is useless if our patients are unwilling or unable to believe what we have to offer. And that isn’t a fault of our patients, no matter how bothered we might become. This is a fault of a system that does not deserve our patients’ blind faith, of a surrounding political milieu that has turned scientific fact into fiction in many people’s minds.
That is how I found myself in that room, early that one morning, with my patient’s wife, her disbelief and the weight of the decision hanging between us. I knew so little about her. I did not know her history or her interactions with the medical system. I did not know the story of her husband’s diagnosis and treatment, or whether he had struggled to find care for his cancer. In our fractured system, I was just meeting her that day. I had no way to make her trust me, except to sit with her, to give her what little time with her husband we could. And to hope that regardless of what came before, she would choose to believe what I was telling her.
I am not certain what she believed, but she chose against intubation. Her husband lived until the rest of his family came anyway. And when he died, they left without a word, carrying with them his bags of belongings and — I can only hope — faith that we had done the best we could.
Daniela Lamas is a contributing Opinion writer and a pulmonary and critical-care physician at Brigham and Women’s Hospital in Boston.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Critical thinking definition

Critical thinking, as described by Oxford Languages, is the objective analysis and evaluation of an issue in order to form a judgement.
Active and skillful approach, evaluation, assessment, synthesis, and/or evaluation of information obtained from, or made by, observation, knowledge, reflection, acumen or conversation, as a guide to belief and action, requires the critical thinking process, which is why it's often used in education and academics.
Some even may view it as a backbone of modern thought.
However, it's a skill, and skills must be trained and encouraged to be used at its full potential.
People turn up to various approaches in improving their critical thinking, like:
- Developing technical and problem-solving skills
- Engaging in more active listening
- Actively questioning their assumptions and beliefs
- Seeking out more diversity of thought
- Opening up their curiosity in an intellectual way etc.
Is critical thinking useful in writing?
Critical thinking can help in planning your paper and making it more concise, but it's not obvious at first. We carefully pinpointed some the questions you should ask yourself when boosting critical thinking in writing:
- What information should be included?
- Which information resources should the author look to?
- What degree of technical knowledge should the report assume its audience has?
- What is the most effective way to show information?
- How should the report be organized?
- How should it be designed?
- What tone and level of language difficulty should the document have?
Usage of critical thinking comes down not only to the outline of your paper, it also begs the question: How can we use critical thinking solving problems in our writing's topic?
Let's say, you have a Powerpoint on how critical thinking can reduce poverty in the United States. You'll primarily have to define critical thinking for the viewers, as well as use a lot of critical thinking questions and synonyms to get them to be familiar with your methods and start the thinking process behind it.
Are there any services that can help me use more critical thinking?
We understand that it's difficult to learn how to use critical thinking more effectively in just one article, but our service is here to help.
We are a team specializing in writing essays and other assignments for college students and all other types of customers who need a helping hand in its making. We cover a great range of topics, offer perfect quality work, always deliver on time and aim to leave our customers completely satisfied with what they ordered.
The ordering process is fully online, and it goes as follows:
- Select the topic and the deadline of your essay.
- Provide us with any details, requirements, statements that should be emphasized or particular parts of the essay writing process you struggle with.
- Leave the email address, where your completed order will be sent to.
- Select your prefered payment type, sit back and relax!
With lots of experience on the market, professionally degreed essay writers , online 24/7 customer support and incredibly low prices, you won't find a service offering a better deal than ours.

IMAGES
VIDEO
COMMENTS
Here are five ways to nurture your critical-thinking skills: Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice. That knowledge helps you make informed decisions in stressful moments. Practice reflection.
Critical thinking can help medical students and doctors achieve improved productivity, better clinical decision making, higher grades and much more. This article will explain why critical thinking is a must for people in the medical field. Definition of Critical Thinking. You can find a variety of definitions of Critical Thinking (CT).
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses' continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
We believe that a virtues approach is best able to make sense of the non-cognitive elements of 'being critical', such as the honesty and courage to question claims in the face of persuasion, authority or social pressure. Medical educators and professional bodies seem to agree that being critical is important and desirable.
Key words: Critical thinking, medical education, quality patient care, fostering critical thinking. Introduction ... The simplest definition is offered by Beyer (1995): "Critical thinking means making reasoned judgments". In other words, critical thinking is a disciplined manner
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient's sex and age, and you begin to think about what ...
Critical thinking is the ability to effectively analyze information and form a judgment. To think critically, you must be aware of your own biases and assumptions when encountering information, and apply consistent standards when evaluating sources. Critical thinking skills help you to: Identify credible sources. Evaluate and respond to arguments.
After completing this chapter, you should be able to: 1. Describe critical thinking (CT), clinical reasoning, and clinical judgment in your own words, based on the descriptions in this chapter. 2. Give at least three reasons why CT skills are essential for stu- dents and nurses. 3.
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from ...
Abstract. This chapter addresses why there is a need for experts and lay people to think critically about medicine and health. It will be argued that illogical, misleading, and contradictory information in medicine and health can have pernicious consequences, including patient harm and poor compliance with health recommendations.
Introduction. Even though the term critical thinking is ubiquitous in educational settings, there is significant disagreement about what it means to 'think critically' [].Predominantly, authors have attempted to develop consensus definitions of critical thinking that would finally put these disagreements to rest (e. g. [2-5]).They define critical thinking variously, but tend to focus on ...
For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
thinking [thingk´ing] ideational mental activity (in contrast to emotional activity); the flow of ideas, symbols, and associations that brings forth concepts and reasons. autistic thinking self-absorption; preoccupation with inner thoughts, daydreams, fantasies, delusions, drives, and personal logic. It is egocentric, subjective thinking lacking ...
The term "critical thinking" has its roots in the mid-late 20th century. Below, we offer overlapping definitions which together form a substantive and trans-disciplinary conception of critical thinking. ... A Definition Critical thinking is that mode of thinking - about any subject, content, or problem - in which the thinker improves the ...
A Definition. Critical thinking is that mode of thinking — about any subject, content, or problem — in which the thinker improves the quality of his or her thinking by skillfully analyzing, assessing, and reconstructing it. Critical thinking is self-directed, self-disciplined, self-monitored, and self-corrective thinking.
The visual image is then altered "illogically" to link the word part to its meaning. Medical Terminology 350 postulates that the "crazier" or "more illogical" an association, the better it is to help recall, retain, and remember over a long period of time and in essence "learn" the meanings of word parts comprising medical terms.
Critical thinking refers to the ability to analyze information objectively and make a reasoned judgment. It involves the evaluation of sources, such as data, facts, observable phenomena, and research findings. Good critical thinkers can draw reasonable conclusions from a set of information, and discriminate between useful and less useful ...
According to the University of the People in California, having critical thinking skills is important because they are [ 1 ]: Universal. Crucial for the economy. Essential for improving language and presentation skills. Very helpful in promoting creativity. Important for self-reflection.
Abstract. The practice of medicine requires art as well as science. The latter argues for a deeper understanding of the mechanisms underlying disease processes and use of scientific evidence in making patient care decisions. The study of medical reasoning and thinking underlies much of medical cognition and has been the focus of research in ...
The meaning of CRITICAL THINKING is the act or practice of thinking critically (as by applying reason and questioning assumptions) in order to solve problems, evaluate information, discern biases, etc.. How to use critical thinking in a sentence.
Critical thinking is the analysis of available facts, evidence, observations, and arguments in order to form a judgement by the application of rational, skeptical, and unbiased analyses and evaluation. The application of critical thinking includes self-directed, self-disciplined, self-monitored, and self-corrective habits of the mind, thus a critical thinker is a person who practices the ...
The school encourages critical thinking and problem-solving. Students are encouraged to develop critical thinking instead of accepting opinions without questioning them. The book shows you how to apply critical thinking to your studies. Critical thinking skills enable students to evaluate information.
Dr. Lamas, a contributing Opinion writer, is a pulmonary and critical-care physician at Brigham and Women's Hospital in Boston. I arrived at the hospital one recent morning to find a team of ...
Critical thinking, as described by Oxford Languages, is the objective analysis and evaluation of an issue in order to form a judgement. Active and skillful approach, evaluation, assessment, synthesis, and/or evaluation of information obtained from, or made by, observation, knowledge, reflection, acumen or conversation, as a guide to belief and ...