
Related Expertise: Culture and Change Management , Business Strategy , Corporate Strategy

Five Case Studies of Transformation Excellence
November 03, 2014 By Lars Fæste , Jim Hemerling , Perry Keenan , and Martin Reeves
In a business environment characterized by greater volatility and more frequent disruptions, companies face a clear imperative: they must transform or fall behind. Yet most transformation efforts are highly complex initiatives that take years to implement. As a result, most fall short of their intended targets—in value, timing, or both. Based on client experience, The Boston Consulting Group has developed an approach to transformation that flips the odds in a company’s favor. What does that look like in the real world? Here are five company examples that show successful transformations, across a range of industries and locations.
VF’s Growth Transformation Creates Strong Value for Investors
Value creation is a powerful lens for identifying the initiatives that will have the greatest impact on a company’s transformation agenda and for understanding the potential value of the overall program for shareholders.
VF offers a compelling example of a company using a sharp focus on value creation to chart its transformation course. In the early 2000s, VF was a good company with strong management but limited organic growth. Its “jeanswear” and intimate-apparel businesses, although responsible for 80 percent of the company’s revenues, were mature, low-gross-margin segments. And the company’s cost-cutting initiatives were delivering diminishing returns. VF’s top line was essentially flat, at about $5 billion in annual revenues, with an unclear path to future growth. VF’s value creation had been driven by cost discipline and manufacturing efficiency, yet, to the frustration of management, VF had a lower valuation multiple than most of its peers.
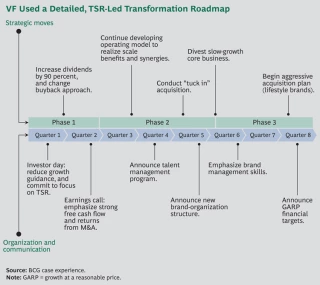
With BCG’s help, VF assessed its options and identified key levers to drive stronger and more-sustainable value creation. The result was a multiyear transformation comprising four components:
- A Strong Commitment to Value Creation as the Company’s Focus. Initially, VF cut back its growth guidance to signal to investors that it would not pursue growth opportunities at the expense of profitability. And as a sign of management’s commitment to balanced value creation, the company increased its dividend by 90 percent.
- Relentless Cost Management. VF built on its long-known operational excellence to develop an operating model focused on leveraging scale and synergies across its businesses through initiatives in sourcing, supply chain processes, and offshoring.
- A Major Transformation of the Portfolio. To help fund its journey, VF divested product lines worth about $1 billion in revenues, including its namesake intimate-apparel business. It used those resources to acquire nearly $2 billion worth of higher-growth, higher-margin brands, such as Vans, Nautica, and Reef. Overall, this shifted the balance of its portfolio from 70 percent low-growth heritage brands to 65 percent higher-growth lifestyle brands.
- The Creation of a High-Performance Culture. VF has created an ownership mind-set in its management ranks. More than 200 managers across all key businesses and regions received training in the underlying principles of value creation, and the performance of every brand and business is assessed in terms of its value contribution. In addition, VF strengthened its management bench through a dedicated talent-management program and selective high-profile hires. (For an illustration of VF’s transformation roadmap, see the exhibit.)
The results of VF’s TSR-led transformation are apparent. 1 1 For a detailed description of the VF journey, see the 2013 Value Creators Report, Unlocking New Sources of Value Creation , BCG report, September 2013. Notes: 1 For a detailed description of the VF journey, see the 2013 Value Creators Report, Unlocking New Sources of Value Creation , BCG report, September 2013. The company’s revenues have grown from $7 billion in 2008 to more than $11 billion in 2013 (and revenues are projected to top $17 billion by 2017). At the same time, profitability has improved substantially, highlighted by a gross margin of 48 percent as of mid-2014. The company’s stock price quadrupled from $15 per share in 2005 to more than $65 per share in September 2014, while paying about 2 percent a year in dividends. As a result, the company has ranked in the top quintile of the S&P 500 in terms of TSR over the past ten years.
A Consumer-Packaged-Goods Company Uses Several Levers to Fund Its Transformation Journey
A leading consumer-packaged-goods (CPG) player was struggling to respond to challenging market dynamics, particularly in the value-based segments and at the price points where it was strongest. The near- and medium-term forecasts looked even worse, with likely contractions in sales volume and potentially even in revenues. A comprehensive transformation effort was needed.
To fund the journey, the company looked at several cost-reduction initiatives, including logistics. Previously, the company had worked with a large number of logistics providers, causing it to miss out on scale efficiencies.
To improve, it bundled all transportation spending, across the entire network (both inbound to production facilities and out-bound to its various distribution channels), and opened it to bidding through a request-for-proposal process. As a result, the company was able to save 10 percent on logistics in the first 12 months—a very fast gain for what is essentially a commodity service.
Similarly, the company addressed its marketing-agency spending. A benchmark analysis revealed that the company had been paying rates well above the market average and getting fewer hours per full-time equivalent each year than the market standard. By getting both rates and hours in line, the company managed to save more than 10 percent on its agency spending—and those savings were immediately reinvested to enable the launch of what became a highly successful brand.
Next, the company pivoted to growth mode in order to win in the medium term. The measure with the biggest impact was pricing. The company operates in a category that is highly segmented across product lines and highly localized. Products that sell well in one region often do poorly in a neighboring state. Accordingly, it sought to de-average its pricing approach across locations, brands, and pack sizes, driving a 2 percent increase in EBIT.
Similarly, it analyzed trade promotion effectiveness by gathering and compiling data on the roughly 150,000 promotions that the company had run across channels, locations, brands, and pack sizes. The result was a 2 terabyte database tracking the historical performance of all promotions.
Using that information, the company could make smarter decisions about which promotions should be scrapped, which should be tweaked, and which should merit a greater push. The result was another 2 percent increase in EBIT. Critically, this was a clear capability that the company built up internally, with the objective of continually strengthening its trade-promotion performance over time, and that has continued to pay annual dividends.
Finally, the company launched a significant initiative in targeted distribution. Before the transformation, the company’s distributors made decisions regarding product stocking in independent retail locations that were largely intuitive. To improve its distribution, the company leveraged big data to analyze historical sales performance for segments, brands, and individual SKUs within a roughly ten-mile radius of that retail location. On the basis of that analysis, the company was able to identify the five SKUs likely to sell best that were currently not in a particular store. The company put this tool on a mobile platform and is in the process of rolling it out to the distributor base. (Currently, approximately 60 percent of distributors, representing about 80 percent of sales volume, are rolling it out.) Without any changes to the product lineup, that measure has driven a 4 percent jump in gross sales.
Throughout the process, management had a strong change-management effort in place. For example, senior leaders communicated the goals of the transformation to employees through town hall meetings. Cognizant of how stressful transformations can be for employees—particularly during the early efforts to fund the journey, which often emphasize cost reductions—the company aggressively talked about how those savings were being reinvested into the business to drive growth (for example, investments into the most effective trade promotions and the brands that showed the greatest sales-growth potential).
In the aggregate, the transformation led to a much stronger EBIT performance, with increases of nearly $100 million in fiscal 2013 and far more anticipated in 2014 and 2015. The company’s premium products now make up a much bigger part of the portfolio. And the company is better positioned to compete in its market.
A Leading Bank Uses a Lean Approach to Transform Its Target Operating Model
A leading bank in Europe is in the process of a multiyear transformation of its operating model. Prior to this effort, a benchmarking analysis found that the bank was lagging behind its peers in several aspects. Branch employees handled fewer customers and sold fewer new products, and back-office processing times for new products were slow. Customer feedback was poor, and rework rates were high, especially at the interface between the front and back offices. Activities that could have been managed centrally were handled at local levels, increasing complexity and cost. Harmonization across borders—albeit a challenge given that the bank operates in many countries—was limited. However, the benchmark also highlighted many strengths that provided a basis for further improvement, such as common platforms and efficient product-administration processes.
To address the gaps, the company set the design principles for a target operating model for its operations and launched a lean program to get there. Using an end-to-end process approach, all the bank’s activities were broken down into roughly 250 processes, covering everything that a customer could potentially experience. Each process was then optimized from end to end using lean tools. This approach breaks down silos and increases collaboration and transparency across both functions and organization layers.
Employees from different functions took an active role in the process improvements, participating in employee workshops in which they analyzed processes from the perspective of the customer. For a mortgage, the process was broken down into discrete steps, from the moment the customer walks into a branch or goes to the company website, until the house has changed owners. In the front office, the system was improved to strengthen management, including clear performance targets, preparation of branch managers for coaching roles, and training in root-cause problem solving. This new way of working and approaching problems has directly boosted both productivity and morale.
The bank is making sizable gains in performance as the program rolls through the organization. For example, front-office processing time for a mortgage has decreased by 33 percent and the bank can get a final answer to customers 36 percent faster. The call centers had a significant increase in first-call resolution. Even more important, customer satisfaction scores are increasing, and rework rates have been halved. For each process the bank revamps, it achieves a consistent 15 to 25 percent increase in productivity.
And the bank isn’t done yet. It is focusing on permanently embedding a change mind-set into the organization so that continuous improvement becomes the norm. This change capability will be essential as the bank continues on its transformation journey.
A German Health Insurer Transforms Itself to Better Serve Customers
Barmer GEK, Germany’s largest public health insurer, has a successful history spanning 130 years and has been named one of the top 100 brands in Germany. When its new CEO, Dr. Christoph Straub, took office in 2011, he quickly realized the need for action despite the company’s relatively good financial health. The company was still dealing with the postmerger integration of Barmer and GEK in 2010 and needed to adapt to a fast-changing and increasingly competitive market. It was losing ground to competitors in both market share and key financial benchmarks. Barmer GEK was suffering from overhead structures that kept it from delivering market-leading customer service and being cost efficient, even as competitors were improving their service offerings in a market where prices are fixed. Facing this fundamental challenge, Barmer GEK decided to launch a major transformation effort.
The goal of the transformation was to fundamentally improve the customer experience, with customer satisfaction as a benchmark of success. At the same time, Barmer GEK needed to improve its cost position and make tough choices to align its operations to better meet customer needs. As part of the first step in the transformation, the company launched a delayering program that streamlined management layers, leading to significant savings and notable side benefits including enhanced accountability, better decision making, and an increased customer focus. Delayering laid the path to win in the medium term through fundamental changes to the company’s business and operating model in order to set up the company for long-term success.
The company launched ambitious efforts to change the way things were traditionally done:
- A Better Client-Service Model. Barmer GEK is reducing the number of its branches by 50 percent, while transitioning to larger and more attractive service centers throughout Germany. More than 90 percent of customers will still be able to reach a service center within 20 minutes. To reach rural areas, mobile branches that can visit homes were created.
- Improved Customer Access. Because Barmer GEK wanted to make it easier for customers to access the company, it invested significantly in online services and full-service call centers. This led to a direct reduction in the number of customers who need to visit branches while maintaining high levels of customer satisfaction.
- Organization Simplification. A pillar of Barmer GEK’s transformation is the centralization and specialization of claim processing. By moving from 80 regional hubs to 40 specialized processing centers, the company is now using specialized administrators—who are more effective and efficient than under the old staffing model—and increased sharing of best practices.
Although Barmer GEK has strategically reduced its workforce in some areas—through proven concepts such as specialization and centralization of core processes—it has invested heavily in areas that are aligned with delivering value to the customer, increasing the number of customer-facing employees across the board. These changes have made Barmer GEK competitive on cost, with expected annual savings exceeding €300 million, as the company continues on its journey to deliver exceptional value to customers. Beyond being described in the German press as a “bold move,” the transformation has laid the groundwork for the successful future of the company.
Nokia’s Leader-Driven Transformation Reinvents the Company (Again)
We all remember Nokia as the company that once dominated the mobile-phone industry but subsequently had to exit that business. What is easily forgotten is that Nokia has radically and successfully reinvented itself several times in its 150-year history. This makes Nokia a prime example of a “serial transformer.”
In 2014, Nokia embarked on perhaps the most radical transformation in its history. During that year, Nokia had to make a radical choice: continue massively investing in its mobile-device business (its largest) or reinvent itself. The device business had been moving toward a difficult stalemate, generating dissatisfactory results and requiring increasing amounts of capital, which Nokia no longer had. At the same time, the company was in a 50-50 joint venture with Siemens—called Nokia Siemens Networks (NSN)—that sold networking equipment. NSN had been undergoing a massive turnaround and cost-reduction program, steadily improving its results.
When Microsoft expressed interest in taking over Nokia’s device business, Nokia chairman Risto Siilasmaa took the initiative. Over the course of six months, he and the executive team evaluated several alternatives and shaped a deal that would radically change Nokia’s trajectory: selling the mobile business to Microsoft. In parallel, Nokia CFO Timo Ihamuotila orchestrated another deal to buy out Siemens from the NSN joint venture, giving Nokia 100 percent control over the unit and forming the cash-generating core of the new Nokia. These deals have proved essential for Nokia to fund the journey. They were well-timed, well-executed moves at the right terms.
Right after these radical announcements, Nokia embarked on a strategy-led design period to win in the medium term with new people and a new organization, with Risto Siilasmaa as chairman and interim CEO. Nokia set up a new portfolio strategy, corporate structure, capital structure, robust business plans, and management team with president and CEO Rajeev Suri in charge. Nokia focused on delivering excellent operational results across its portfolio of three businesses while planning its next move: a leading position in technologies for a world in which everyone and everything will be connected.
Nokia’s share price has steadily climbed. Its enterprise value has grown 12-fold since bottoming out in July 2012. The company has returned billions of dollars of cash to its shareholders and is once again the most valuable company in Finland. The next few years will demonstrate how this chapter in Nokia’s 150-year history of serial transformation will again reinvent the company.

Managing Director & Senior Partner
San Francisco - Bay Area

Managing Director & Senior Partner, Chairman of the BCG Henderson Institute
ABOUT BOSTON CONSULTING GROUP
Boston Consulting Group partners with leaders in business and society to tackle their most important challenges and capture their greatest opportunities. BCG was the pioneer in business strategy when it was founded in 1963. Today, we work closely with clients to embrace a transformational approach aimed at benefiting all stakeholders—empowering organizations to grow, build sustainable competitive advantage, and drive positive societal impact.
Our diverse, global teams bring deep industry and functional expertise and a range of perspectives that question the status quo and spark change. BCG delivers solutions through leading-edge management consulting, technology and design, and corporate and digital ventures. We work in a uniquely collaborative model across the firm and throughout all levels of the client organization, fueled by the goal of helping our clients thrive and enabling them to make the world a better place.
© Boston Consulting Group 2024. All rights reserved.
For information or permission to reprint, please contact BCG at [email protected] . To find the latest BCG content and register to receive e-alerts on this topic or others, please visit bcg.com . Follow Boston Consulting Group on Facebook and X (formerly Twitter) .
Subscribe to our Business Transformation E-Alert.
JavaScript seems to be disabled in your browser. For the best experience on our site, be sure to turn on Javascript in your browser.
Hello! You are viewing this site in ${language} language. Is this correct?
Explore the Levels of Change Management
9 Successful Change Management Examples For Inspiration

Updated: February 9, 2024
Published: January 3, 2024
Welcome to our guide on change management examples, pivotal for steering through today's dynamic business terrain. Immerse yourself in the transformative power of change management, a tool for resilience, growth, innovation, and employee morale enhancement.
This guide equips you with strategies to promote an innovative, adaptable work environment and boost employee morale for lasting organizational success.
Uncover diverse types of change management with Prosci's established methodology and explore real-world examples that illustrate these principles in action.
What is Change Management?
Change management is a strategy for guiding an organization and its people through change. It goes beyond top-down orders, involving employees at all levels. This people-focused approach encourages everyone to participate actively, helping them adapt and use changes in their everyday work.
Effective change management aligns closely with a company's culture, values, and beliefs.
When change fits well with these cultural aspects, it feels more natural and is easier for employees to adopt. This contributes to smoother transitions and leads to more successful and lasting organizational changes.
Why is Change Management Important?
Change management is pivotal in guiding organizations through transitions, ensuring impactful and long-lasting results.
For example, a $28B electronic components and services company with 18,000 employees realized the importance of enhancing its processes. They knew to adopt more streamlined, efficient approaches, known as Lean initiatives .
However, they encountered challenges because they needed a more structured method for effectively managing the human aspects of these changes.
The company formed a specialized group focused on change to address their challenges and initiate key projects. These projects aligned with their culture of innovation and precision, which helped ensure that the changes were well-received and effectively implemented within the organization.
Matching change management to an organization's unique style and structure contributes to more effective transformations and strengthens the business for future challenges.
What Are the Main Types of Change Management?
Discover Prosci's change management models: from individual application and organizational strategies to enterprise-wide integration and effective portfolio management, all are vital for transformative success.
Individual change management
At Prosci, we understand that change begins with the individual.
The Prosci ADKAR ® Model ( Awareness, Desire, Knowledge, Ability and Reinforcement ) is expertly designed to equip change leaders with tools and strategies to engage your team.
This model is a framework that will guide and support you in confidently navigating and adapting to new changes.
Organizational change management
In organizational change management , we focus on the core elements of your company to fully understand and address each aspect of the change.
Our approach involves creating tailored strategies and detailed plans that benefit you and manage you to manage challenges effectively, which include:
- Clear communication
- Strong leadership support
- Personalized coaching
- Practical training
Our strategies are specifically aimed at meeting the diverse needs within your organization, ensuring a smooth and well-supported transition for everyone involved.
Enterprise change management capability
At the enterprise level, change management becomes an embedded practice, a core competency woven throughout the organization.
When you implement change capabilities:
- Employees know what to ask during change to reach success
- Leaders and managers have the training and skills to guide their teams during change
- Organizations consistently apply change management to initiatives
- Organizations embed change management in roles, structures, processes, projects and leadership competencies
It's a tactical effort to integrate change management into the very DNA of an organization—nurturing a culture that's ready and able to adapt to any change.
Change portfolio management
While distinct from project-level change management, managing a change portfolio is vital for an organization to stay flexible and responsive.

9 Dynamic Change Management Success Stories to Revolutionize Your Business
Prosci case studies reveal how diverse organizations spanning different sectors address and manage change. These cases illustrate how change management can provide transformative solutions from healthcare to finance:
1. Hospital system
A major healthcare organization implemented an extensive enterprise resource planning (ERP) system and adapted to healthcare reform. This case study highlights overcoming significant challenges through strategic change management:
Industry: Healthcare Revenue: $3.7 billion Employees: 24,000 Facilities: 11 hospitals
Major changes:
- Implemented a new ERP system across all hospitals
- Prepared for healthcare reform
Challenges:
- Managing significant, disruptive changes
- Difficulty in gaining buy-in for change management
- Align with culture: Strategically implemented change management to support staff, reflecting the hospital's core value of caring for people
- Focus on a key initiative: Applied change management in the electronic health record system implementation
- Integrate with existing competencies: Recognized change leadership as crucial at various leadership levels
This example shows that when change management matches a healthcare organization's values, it can lead to successful and smooth transitions.
2. Transportation department
A state government transportation department leveraged change management to effectively manage business process improvements amid funding and population challenges. This highlights the value of comprehensive change management in a public sector setting:
Industry: State Government Transportation Revenue: $1.3 billion Employees: 3,000 Challenges:
- Reduced funding
- Growing population
- Increasing transportation needs
Initiative:
- Major business process improvement
Hurdles encountered:
- Change fatigue
- Need for widespread employee adoption
- Focus on internal growth
- Implemented change management in process improvement
This department's experience teaches us the vital role of change management in successfully navigating government projects with multiple challenges.
3. Pharmaceuticals
A global pharmaceutical company navigated post-merger integration challenges. Using a proactive change management approach, they addressed resistance and streamlined operations in a competitive industry:
Industry: Pharma (Global Biopharmaceutical Company) Revenue: $6 billion Number of employees: 5,000
Recent activities: Experienced significant merger and acquisition activity
- Encountered resistance post-implementation of SAP (Systems, Applications and Products in Data Processing)
- They found themselves operating in a purely reactive mode
- Align with your culture: In this Lean Six Sigma-focused environment, where measurement is paramount, the ADKAR Model's metrics were utilized as the foundational entry point for initiating change management processes.
This company's journey highlights the need for flexible and responsive change management.
4. Home fixtures
A home fixtures manufacturing company’s response to the recession offers valuable insights on effectively managing change. They focused on aligning change management with their disciplined culture, emphasizing operational efficiency:
Industry: Home Fixtures Manufacturing Revenue: $600 million Number of employees: 3,000
Context: Facing the lingering effects of the recession
Necessity: Need to introduce substantial changes for more efficient operations
Challenge: Change management was considered a low priority within the company
- Align with your culture: The company's culture, characterized by discipline in projects and processes, ensured that change management was implemented systematically and disciplined.
This company’s experience during the recession proves that aligning change with company culture is key to overcoming tough times.

5. Web services
A web services software company transformed its culture and workspace. They integrated change management into their IT strategy to overcome resistance and foster innovation:
Industry : Web Services Software Revenue : $3.3 billion Number of employees : 10,000
Initiatives : Cultural transformation; applying an unassigned seating model
Challenges : Resistance in IT project management
- Focus on a key initiative: Applied change management in workspace transformation
- Go where the energy is: Establishing a change management practice within its IT department, developing self-service change management tools, and forming thoughtful partnerships
- I ntegrate with existing competencies: "Leading change" was essential to the organization's newly developed leadership competency model.
This case demonstrates the importance of weaving change management into the fabric of tech companies, especially for cultural shifts.
6. Security systems
A high-tech security company effectively managed a major restructuring. They created a change network that shifted change management from HR to business processes:
Industry : High-Tech (Security Systems) Revenue : $10 billion Number of employees: 57,000
Major changes : Company separation; division into three segments
Challenge : No unified change management approach
- Formed a network of leaders from transformation projects
- Go where the energy is: Shifted change management from HR to business processes
- Integrate with existing competencies: Included principles of change management in the training curriculum for the project management boot camp.
- Treat growing your capability like a change: Executive roadshow launch to gain support for enterprise-wide change management
This company’s innovative approach to restructuring shows h ow reimagining change management can lead to successful outcomes.
7. Clothing store
A major clothing retailer’s journey to unify its brand model. They overcame siloed change management through collaborative efforts and a community-driven approach:
Industry : Retail (Clothing Store) Revenue : $16 billion Number of employees : 141,000
Major change initiative : Strategic unification of the brand operating model
Historical challenge : Traditional management of change in siloes
- Build a change network : This retailer established a community of practice for change management, involving representatives from autonomous units to foster consensus on change initiatives.
The story of this retailer illustrates how collaborative efforts in change management can unify and strengthen a brand in the retail world.
A major Canadian bank initiative to standardize change management across its organization. They established a Center of Excellence and tailored communities of practice for effective change:
Industry : Financial Services (Canadian Bank) Revenue : $38 billion Number of employees : 78,000
Current state : Absence of enterprise-wide change management standards
Challenge :
- Employees, contractors, and consultants using individual methods for change management
- Reliance on personal knowledge and experience to deploy change management strategies
- Build a change network: The bank established a Center of Excellence and created federated communities of practice within each business unit, aiming to localize and tailor change management efforts.
This bank’s journey in standardizing change management offers valuable insights for large organizations looking to streamline their processes.
9. Municipality
You can learn from a Canadian municipality’s significant shift to enhance client satisfaction. They integrated change management across all levels to achieve profound organizational change and improved public service:
Industry : Municipal Government (Canadian Municipality) Revenue : $1.9 billion Number of employees : 3,000
New mandate:
- Implementing a new deliberate vision focusing on each individual’s role in driving client satisfaction
Nature of shift :
- A fundamental change within the public institution
Scope of impact :
- It affected all levels, from leadership to front-line staff
Solution :
- Treat growing your capability like a change: Change leaders promoted awareness and cultivated a desire to adopt change management as a standard enterprise-wide practice.
The municipality's strategy shows us how effective change management can significantly improve public services and organizational efficiency.
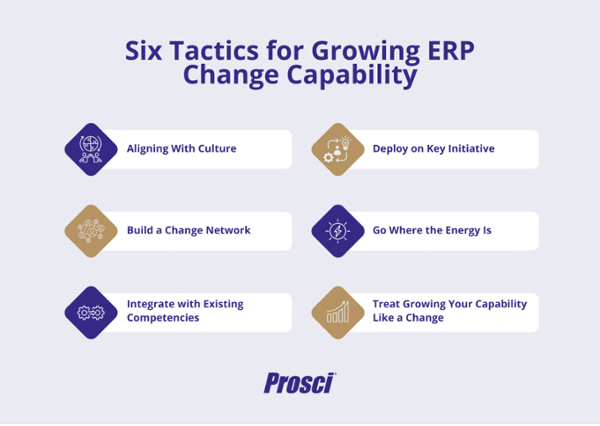
6 Tactics for Growing Enterprise Change Management Capability
Prosci's exploration with 10 industry leaders uncovered six primary tactics for enterprise change growth , demonstrating a "universal theme, unique application" approach.
This framework goes beyond standard procedures, focusing on developing a deep understanding and skill in managing change. It offers transformative tactics, guiding organizations towards excelling in adapting to change. Here, we uncover these transformative tactics, guiding organizations toward mastery of change.
1. Align with Your culture
Organizational culture profoundly influences how change management should be deployed.
Recognizing whether your organization leans towards traditional practices or innovative approaches is vital. This understanding isn't just about alignment; it's an opportunity to enhance and sometimes shift your cultural environment.
When effectively combined with an organization's unique culture, change management can greatly enhance key initiatives. This leads to widespread benefits beyond individual projects and promotes overall growth and development within the organization.
Embrace this as a fundamental tool to strengthen and transform your company's cultural fabric.
2. Focus on key initiatives
In the early phase of developing change management capabilities, selecting noticeable projects with executive backing is important.
This helps demonstrate the real-world impact of change management, making it easier for employees and leadership to understand its benefits. This strategy helps build support and maintain the momentum of change management initiatives within your organization.
Focus on capturing and sharing these successes to encourage buy-in further and underscore the importance of change management in achieving organizational goals.
3. Build a change network
Building change capability isn't just about a few advocates but creating a network of change champions across your organization.
This network, essential in spreading the message and benefits of change management, varies in composition but is universally crucial. It could include departmental practitioners, business unit leaders, or a mix of roles working together to enhance awareness, credibility, and a shared purpose.
Our Best Practices in Change Management study shows that 45% of organizations leverage such networks. These groups boost the effectiveness of change management and keep it moving forward.
4. Go where the energy is
To build change capabilities throughout an organization effectively, the focus should be on matching the organization's current readiness rather than just pushing new methods.
Identify and focus on parts of your organization that are ready for change. Align your change initiatives with these sectors. Involve senior leaders and those enthusiastic about change to naturally generate demand for these transformations.
Showcasing successful initiatives encourages a collaborative culture of change, making it an organic part of your organization's growth.
5. Integrate with existing competencies
Change management is a vital skill across various organizational roles.
Integrating it into competency models and job profiles is increasingly common, yet often lacks the necessary training and tools.
When change management skills expand beyond the experts, they become an integral part of the organization's culture—nurturing a solid foundation of effective change leadership.
This approach embeds change management deeper within the company and cultivates leaders who can support and sustain this essential practice.
6. Treat growing your capability like a change
Growing change capability is a transformative journey for your business and your employees. It demands a structured, strategic approach beyond telling your network that change is coming.
Applying the ADKAR Model universally and focusing on your organization's unique needs is pivotal. It's about building awareness, sparking a desire for change across the enterprise, and equipping employees with the knowledge and skills for effective, lasting change.
Treating capability-building like a change ensures that change management becomes a core part of your organization's fabric, benefitting every team member.
These six tactics are powerful tools for enhancing your organization's ability to adapt and remain resilient in a rapidly changing business environment.
Comprehensive Insights From Change Management Examples
These diverse change management examples provide field-tested savvy and offer a window into how varied organizations successfully manage change.
Case studies , from healthcare reform to innovative corporate restructuring, exemplify how aligning with organizational culture, building strong change networks, and focusing on tactical initiatives can significantly impact change management outcomes.
This guide, enriched with real-world applications, enhances understanding and execution of effective change management, setting a benchmark for future transformations.
To learn more about partnering with Prosci for your next change initiative, discover Prosci's Advisory services and enterprise training options and consider practitioner certification .
Founded in 1994, Prosci is a global leader in change management. We enable organizations around the world to achieve change outcomes and grow change capability through change management solutions based on holistic, research-based, easy-to-use tools, methodologies and services.
See all posts from Prosci
You Might Also Like
Enterprise - 8 MINS

What Is Change Management in Healthcare?

20 Change Management Questions Employees Ask and How To Answer Them
Subscribe here.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
What Really Makes Toyota’s Production System Resilient
- Willy C. Shih

“Just-in-time” only works as part of a comprehensive suite of strategies.
Toyota has fared better than many of its competitors in riding out the supply chain disruptions of recent years. But focusing on how Toyota had stockpiled semiconductors and the problems of other manufacturers, some observers jumped to the conclusion that the era of the vaunted Toyota Production System was over. Not the case, say Toyota executives. TPS is alive and well and is a key reason Toyota has outperformed rivals.
The supply chain disruptions triggered by the Covid-19 pandemic caused major headaches for manufacturers around the world. Nowhere was this felt more acutely than in the auto industry, which faced severe shortages of semiconductor chips and other components. This led many people to argue that just-in-time and lean production methods were dead and being superseded by “just-in-case” stocking of more inventory.
- Willy C. Shih is a Baker Foundation Professor of Management Practice at Harvard Business School.
Partner Center
Do people fear change?
Do people resist change?
If we do resist change, why and when do we resist change? How do we as leaders, change agents, project managers, coaches or scrum masters respond when we find resistance?
Change resistance is a positive for me!
It gives me a number of insights - maybe the change isn’t the correct one or perhaps the timing of bringing the change isn’t right or so many other reasons!
Pushing the change at people impacted by the change is not going to give me any additional benefit (unless I want to just put a check in the box - which I would not ofcourse!).
So, what do I do? What approaches could I take, given my unique context? What's your perspective?
Bringing you a real-life case study from my experience, along with a meaningful dialogue with you, around responding to change.
Join me Wednesday 15 June 1230 - 1330 CEST
A Lean Approach for Reducing Downtimes in Healthcare: A Case Study
- Conference paper
- First Online: 12 February 2023
- Cite this conference paper

- Stefano Frecassetti ORCID: orcid.org/0000-0002-9649-314X 19 ,
- Matteo Ferrazzi ORCID: orcid.org/0000-0001-9035-0773 19 &
- Alberto Portioli-Staudacher ORCID: orcid.org/0000-0002-9807-1215 19
Part of the book series: IFIP Advances in Information and Communication Technology ((IFIPAICT,volume 668))
Included in the following conference series:
- European Lean Educator Conference
447 Accesses
Lean Management is considered one of the most successful management paradigms for enhancing operational performance in the manufacturing environment. However, it has been applied throughout the years to several sectors and organisational areas, such as service, healthcare, and office departments. After the Covid-19 outbreak, increasing attention has been given to potential performance improvements in healthcare organisations by leveraging Lean. This paper intends to add further knowledge to this field by presenting a case study in a hospital. In this paper, a pilot project is presented carried out in a healthcare organisation. Lean methods were used to improve the operating room performance, particularly by reducing the operating room changeover time. The A3 template was used to drive the project and implement a new procedure using the Single Minute Exchange of Die (SMED) method. With the implementation of the new procedure, the changeover time between two different surgeries in the operating room was significantly reduced, together with a more stable and reliable process.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Lean Healthcare
Lean Healthcare: How to Start the Lean Journey

Lean Transformation in Healthcare: A French Case Study
Amati, M., et al.: Reducing changeover time between surgeries through lean thinking: an action research project. Front. Med. 9 (2022). https://doi.org/10.3389/fmed.2022.822964
Bharsakade, R.S., Acharya, P., Ganapathy, L., Tiwari, M.K.: A lean approach to healthcare management using multi criteria decision making. Opsearch 58 (3), 610–635 (2021). https://doi.org/10.1007/s12597-020-00490-5
Article Google Scholar
Costa, F., Kassem, B., Staudacher, A.P.: Lean office in a manufacturing company. In: Powell, D.J., Alfnes, E., Holmemo, M.D.Q., Reke, E. (eds.) Learning in the Digital Era. IFIP Advances in Information and Communication Technology, pp. 351–356. Springer, Cham (2021). https://doi.org/10.1007/978-3-030-92934-3_36
Chapter Google Scholar
Costa, F., Kassem, B., Portioli-Staudacher, A.: Lean thinking application in the healthcare sector. In: Powell, D.J., Alfnes, E., Holmemo, M.D.Q., Reke, E. (eds.) Learning in the Digital Era. IFIP Advances in Information and Communication Technology, pp. 357–364. Springer, Cham (2021). https://doi.org/10.1007/978-3-030-92934-3_37
Curatolo, N., Lamouri, S., Huet, J.C., Rieutord, A.: A critical analysis of Lean approach structuring in hospitals. Bus. Process Manag. J. 20 (3), 433–454 (2014)
D’Andreamatteo, A., Iannia, L., Lega, F., Sargiacomo, M.: Lean in healthcare: a comprehensive review. Health Policy 119 (9), 1197–1209 (2015)
Guercini, J., et al.: Application of SMED methodology for the improvement of operations in operating theatres. The case of the Azienda Ospedaliera Universitaria Senese. Mecosan 24 (98), 83–203 (2016). https://doi.org/10.3280/mesa2016-098005
Henrique, D.B., Godinho Filho, M.: A systematic literature review of empirical research in Lean and Six Sigma in healthcare. Total Qual. Manag. Bus. Excell. 31 (3–4), 429–449 (2020)
Henrique, D.B., Filho, M.G., Marodin, G., Jabbour, A.B.L.D.S., Chiappetta Jabbour, C.J.: A framework to assess sustaining continuous improvement in lean healthcare. Int. J. Prod. Res. 59 (10), 2885–2904 (2020)
Holweg, M.: The genealogy of lean production. J. Oper. Manag. 25 (2), 420–437 (2007). https://doi.org/10.1016/j.jom.2006.04.001
Sales-Coll, M., de Castro, R., Hueto-Madrid, J.A.: Improving operating room efficiency using lean management tools. Prod. Plan. Control 1–14 (2021). https://doi.org/10.1080/09537287.2021.1998932
Matos, I.A., Alves, A.C., Tereso, A.P.: Lean principles in an operating room environment: an action research study. J. Health Manag. 18 (2), 239–2577 (2016)
Portioli-Staudacher, A.: Lean healthcare. An experience in Italy. In: Koch, T. (ed.) APMS 2006. ITIFIP, vol. 257, pp. 485–492. Springer, Boston, MA (2008). https://doi.org/10.1007/978-0-387-77249-3_50
Rosa, A., Marolla, G., Lega, F., et al.: Lean adoption in hospitals: the role of contextual factors and introduction strategy. BMC Health Serv. Res. 21 , 889 (2021). https://doi.org/10.1186/s12913-021-06885-4
Rosa, C., Silva, F.J.G., Ferreira, L.P., Campilho, R.D.S.G.: SMED methodology: the reduction of setup times for Steel Wire-Rope assembly lines in the automotive industry. Procedia Manuf. 13 , 1034–1042 (2017)
Shah, R., Ward, P.T.: Lean manufacturing: context, practice bundles, and performance. J. Oper. Manag. 21 (2), 129–149 (2003)
Sunder, M.V., Mahalingam, S., Krishna, M.S.N.: Improving patients’ satisfaction in a mobile hospital using Lean Six Sigma – a design-thinking intervention. Prod. Plan. Control 31 (6), 512–526 (2020)
Torri, M., Kundu, K., Frecassetti, S., Rossini, M.: Implementation of Lean in IT SME company: an Italian case. Int. J. Lean Six Sigma (2021)
Google Scholar
Welsh, I., Lyons, C.M.: Evidence-based care and the case for intuition and tacit knowledge in clinical assessment and decision making in mental health nursing practice: an empirical contribution to the debate. J. Psychiatr. Ment. Health Nurs. 8 (4), 299–305 (2001)
Yin, R.K.: Case Study Research and Applications: Design and Methods, 6th edn. Sage, Los Angeles (2018)
Download references
Author information
Authors and affiliations.
Politecnico di Milano, Department of Management, Economics and Industrial Engineering, Milano, Italy
Stefano Frecassetti, Matteo Ferrazzi & Alberto Portioli-Staudacher
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Stefano Frecassetti .
Editor information
Editors and affiliations.
University of Galway, Galway, Ireland
Olivia McDermott
LUM University "Giuseppe Degennaro", Casamassima, Italy
Angelo Rosa
Instituto Superior de Engenharia do Porto, Porto, Portugal
José Carlos Sá
Aidan Toner
Rights and permissions
Reprints and permissions

Copyright information
© 2023 IFIP International Federation for Information Processing
About this paper
Cite this paper.
Frecassetti, S., Ferrazzi, M., Portioli-Staudacher, A. (2023). A Lean Approach for Reducing Downtimes in Healthcare: A Case Study. In: McDermott, O., Rosa, A., Sá, J.C., Toner, A. (eds) Lean, Green and Sustainability. ELEC 2022. IFIP Advances in Information and Communication Technology, vol 668. Springer, Cham. https://doi.org/10.1007/978-3-031-25741-4_8
Download citation
DOI : https://doi.org/10.1007/978-3-031-25741-4_8
Published : 12 February 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-25740-7
Online ISBN : 978-3-031-25741-4
eBook Packages : Computer Science Computer Science (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
Societies and partnerships

- Find a journal
- Track your research
Change Management Case Study- Toyota
Change management is a critical aspect of any organization’s success, especially in today’s fast-paced and constantly evolving business environment.
One company that has been widely recognized for its innovative and successful approach to change management is Toyota.
Over the years, Toyota has implemented a range of initiatives aimed at improving its operations, products, and services, from introducing the world’s first mass-produced hybrid car to adopting robots in its production lines.
In this blog post, we will explore Toyota’s approach to change management, looking at how the company’s philosophy and practices have enabled it to continuously innovate and improve.
Overview of Toyota and its history of innovation and improvement
Toyota is a Japanese multinational automotive manufacturer that was founded in 1937. The company is widely recognized for its innovative and efficient production system, known as the Toyota Production System (TPS), which has become a model for manufacturing excellence.
Toyota’s commitment to continuous improvement and innovation has resulted in many breakthroughs in the automotive industry, including the introduction of the first mass-produced hybrid car, the Toyota Prius, in 1997. The company has also been a pioneer in the use of robotics in production and has continuously worked to improve the safety and efficiency of its vehicles. Today, Toyota is one of the largest automakers in the world, with a reputation for quality, reliability, and innovation.
Toyota Production System
The Toyota Production System (TPS) is a lean manufacturing system developed by Toyota that focuses on reducing waste and maximizing efficiency in production. At the heart of TPS are two key principles: the first is to identify and eliminate all forms of waste in the production process, and the second is to continuously improve the production process.
TPS involves several key concepts and tools, including just-in-time (JIT) production, kanban (visual signals used to control the flow of materials), and andon (alerts used to signal production problems).
JIT involves producing only what is needed, when it is needed, and in the exact amount required. Kanban is a scheduling system that uses visual signals to control the flow of materials, while andon allows workers to stop production when a problem arises and signal for help.
TPS is not just a set of tools and concepts, but also a philosophy and way of working that involves change management at every level of the organization. All employees are encouraged to identify and suggest improvements to the production process, which are then tested and implemented on a small scale before being rolled out across the organization. This approach to continuous improvement is known as kaizen, and it has become a central part of Toyota’s culture and way of working.
Change Management at Toyota
Change management is also built into TPS through a system called Hoshin Kanri, which involves a top-down approach to strategic planning and goal setting. In this system, senior leaders set the direction for the organization, and then work with middle managers and front-line workers to implement changes and improvements that align with the overall strategy. This ensures that change is managed in a structured and coordinated way across the organization, with everyone working towards the same goals.
Examples of change management at Toyota
Toyota’s approach to change management is grounded in its core values of respect for people and continuous improvement. The company has a long history of successful change initiatives that have allowed it to stay at the forefront of the automotive industry. Here are two examples of successful change initiatives at Toyota:
- The Prius Hybrid: In 1997, Toyota introduced the world’s first mass-produced hybrid car, the Toyota Prius. The Prius was a radical departure from conventional gasoline-powered vehicles and represented a significant technological breakthrough. Toyota invested heavily in the development of the Prius, taking a long-term view of the potential for hybrid technology. The company faced numerous challenges in bringing the Prius to market, including concerns about the high cost of the hybrid system and doubts about consumer demand. However, Toyota remained committed to its vision of a more sustainable future and persisted in its efforts to improve and refine the Prius. Today, the Prius is a popular and widely recognized brand, with more than 10 million units sold worldwide.
- Introduction of Robots in Production: Toyota has been a pioneer in the use of robotics in production, starting with the introduction of the first industrial robot in 1967. Over the years, the company has continued to invest in robotics and automation, using these technologies to improve safety, quality, and efficiency in its production process. One example of a successful change initiative in this area was the introduction of collaborative robots, or “cobots,” in the assembly line. These robots work alongside human workers to perform repetitive or physically demanding tasks, freeing up workers to focus on more complex tasks that require human skills and judgment. This change has not only improved efficiency and safety but has also created a more engaging and satisfying work environment for employees.
These examples illustrate how Toyota’s commitment to continuous improvement and innovation has allowed it to successfully manage change and stay ahead of the curve in a rapidly evolving industry. By investing in new technologies and working collaboratively across the organization, Toyota has been able to achieve significant breakthroughs and maintain its position as a leader in the automotive industry.
Challenges faced by Toyota and how did it respond
Despite its many successes, Toyota has also faced several significant challenges in implementing change over the years. One of the most notable challenges was the series of recalls that the company experienced in the late 2000s and early 2010s.
These recalls were related to safety issues and quality problems with several models of Toyota vehicles, including issues with unintended acceleration and faulty brakes. These recalls had a significant impact on Toyota’s reputation and credibility, and the company faced intense scrutiny from regulators, consumers, and the media.
Toyota successfully implemented crisis management strategy in response to these challenges, Toyota implemented a number of changes to its production and quality control processes. The company established a new position of Chief Quality Officer and created a new division dedicated to product quality and safety.
Toyota also implemented new measures to improve communication and collaboration across the organization, including the creation of a global quality task force and the establishment of a new system for reporting and addressing quality issues.
Despite these challenges, Toyota has continued to innovate and improve, staying true to its commitment to continuous improvement and kaizen. The company has continued to invest in new technologies and has introduced several new models of hybrid and electric vehicles in recent years, including the Toyota Mirai hydrogen fuel cell vehicle.
Toyota has also continued to refine its production processes, implementing new systems and tools to improve efficiency and quality.
One notable example of Toyota’s continued innovation is the development of the Toyota New Global Architecture (TNGA) platform. This platform is designed to be more flexible and adaptable than previous platforms, allowing Toyota to build a wider range of vehicles with greater efficiency and quality.
The TNGA platform has already been used in several models, including the Toyota Camry and the Toyota Prius, and has received widespread praise for its performance and capabilities.
Results and Impact of successful implementation of change by Toyota
The successful implementation of change by Toyota has had a significant impact on the company, its employees, and the automotive industry as a whole. Here are some of the key results and impacts of Toyota’s successful change initiatives:
- Improved Efficiency and Quality : Toyota’s focus on continuous improvement and innovation has led to significant gains in efficiency and quality. The company’s production processes are now more streamlined and standardized, and its vehicles are known for their reliability and durability. This has helped Toyota to maintain its reputation as a leader in the automotive industry and has helped the company to remain competitive in a rapidly changing market.
- Increased Innovation: Toyota’s commitment to innovation has resulted in the development of several groundbreaking technologies, including the Prius hybrid, the Mirai fuel cell vehicle, and the TNGA platform. These innovations have not only helped to improve the performance and sustainability of Toyota’s vehicles but have also helped to push the entire industry forward, setting new standards and raising the bar for other automakers.
- Enhanced Employee Engagement and Satisfaction: Toyota’s focus on respect for people and employee engagement has created a culture of collaboration and teamwork within the organization. Employees are encouraged to contribute ideas and participate in continuous improvement initiatives, which has helped to create a more engaging and fulfilling work environment. This has contributed to high levels of employee satisfaction and retention at Toyota.
- Improved Safety and Sustainability: Toyota’s commitment to safety and sustainability has led to the development of several technologies and processes aimed at reducing the environmental impact of its vehicles and improving the safety of its customers. These efforts have helped to reduce carbon emissions and improve safety on the road, making Toyota a leader in corporate social responsibility and sustainability.
Final Words
The experience of Toyota demonstrates the critical importance of effective change management in driving success and growth in any organization. By committing to a culture of continuous improvement, Toyota has been able to maintain its position as a leader in the automotive industry and set new standards for efficiency, quality, and innovation.
Effective change management is essential to driving success and growth in any organization. By learning from Toyota’s experience and embracing the lessons outlined above, organizations can create a culture of continuous improvement and innovation that drives long-term success and sustainability.
About The Author
Tahir Abbas
Related posts.

Tesla Change Management Case Study

08 Ways Change Managers Benefit from Resistance to Change

Too Much Change in an Organization – Consequences and How to Avoid it?
- Research article
- Open access
- Published: 28 August 2021
Lean adoption in hospitals: the role of contextual factors and introduction strategy
- Angelo Rosa 1 ,
- Giuliano Marolla ORCID: orcid.org/0000-0002-2095-8641 1 ,
- Federico Lega 2 &
- Francesco Manfredi 1
BMC Health Services Research volume 21 , Article number: 889 ( 2021 ) Cite this article
4792 Accesses
14 Citations
2 Altmetric
Metrics details
In the scientific literature, many studies describe the application of lean methodology in the hospital setting. Most of the articles focus on the results rather than on the approach adopted to introduce the lean methodology. In the absence of a clear view of the context and the introduction strategy, the first steps of the implementation process can take on an empirical, trial and error profile. Such implementation is time-consuming and resource-intensive and affects the adoption of the model at the organizational level. This research aims to outline the role contextual factors and introduction strategy play in supporting the operators introducing lean methodology in a hospital setting.
Methodology
The methodology is revealed in a case study of an important hospital in Southern Italy, where lean has been successfully introduced through a pilot project in the pathway of cancer patients. The originality of the research is seen in the detailed description of the contextual elements and the introduction strategy.
The results show significant process improvements and highlight the spontaneous dissemination of the culture of change in the organization and the streamlined adoption at the micro level.
The case study shows the importance of the lean introduction strategy and contextual factors for successful lean implementation. Furthermore, it shows how both factors influence each other, underlining the dynamism of the organizational system.
Peer Review reports
Over the last decade, healthcare has been called upon to respond to the increasing pressures arising from changes in demand – due to epidemiological changes and the demand for quality and safety – and increased costs due to the introduction of new technologies [ 1 , 2 ]. These major challenges are exacerbated by the shrinking resources available in health systems and, for most countries, by the principle of universal access to patient care. In order to meet the patients’ needs, a hospital must utilize a number of scarce resources at the right time: beds, technological equipment, staff with appropriate clinical skills, medical devices, diagnostic reports, etc. [ 1 , 2 ].
One of the most relevant issues for the management of a healthcare provider is the management of patient flows in order to purchase, make available, and use these scarce resources at the right time and in the right way, and to ensure the best possible care [ 3 , 4 , 5 ]. In this scenario, hospitals need to focus on the patient pathways in order to ensure fast, safe, and high-quality service [ 3 , 6 , 7 , 8 ]. The search for solutions to these challenges has extended beyond the boundaries of healthcare practices to study organizational methods and paradigms that have been successfully implemented in other sectors [ 3 , 5 ]. Among these, lean thinking has proven to be one of the most effective solutions for improving operational performance and process efficiency and for reducing waste [ 5 , 9 ]. Lean is a process-based methodology focused on improving processes to achieve a customer ideal state and the elimination of waste [ 10 ]. Waste is defined as the results of unnecessary or wrong tasks, actions or process steps that do not directly benefit the patient. The taxonomy of waste is: overproduction, defects, waiting, transportation, inventory, motion, extra-processing and unused talent [ 3 , 4 , 5 ]. In addition, lean addresses other key service issues such as continuous improvement and employee empowerment, whether healthcare professionals or managers [ 1 , 11 , 12 ]. Lean healthcare is defined as a strategic approach to increasing the reliability and stability of healthcare processes [ 7 , 13 , 14 ].
The first documented cases of lean applications in a hospital setting (HS) date back to the late 1990s. These aimed at improving patient care processes, interdepartmental interaction, and employee satisfaction [ 1 , 2 ]. The Virginia Mason Medical Center is one of the first and most emblematic examples of a successful migration of lean methodology from the manufacturing sector to healthcare. The hospital, based on the principles of the Toyota Production System, created the Virginia Mason Production System, a holistic management model in continuous evolution that not only had a strong impact on the quality of the services provided and on the reduction of lead time, but it also led to a decrease in operating costs [ 14 , 15 ]. Over time, many hospitals have followed in the footsteps of the Virginia Mason Medical Center [ 8 , 16 , 17 ]. The lean paradigm crossed the US border and spread to other countries such as Canada and England [ 5 , 12 ]. It was not until the early 2000 that the model was introduced in European hospitals [ 12 , 16 ].
The implementation of the lean paradigm in HS environments has increasingly attracted the attention of researchers and professionals. The interest in lean in HSs was fostered by the idea that the paradigm was particularly suitable for hospitals because its concepts are intuitive, compelling, and, therefore, easy for medical staff to use [ 18 , 19 ]. However, over time, alongside the evidence of successful implementation of lean in HSs, much of the research has shown failures in adopting the paradigm [ 5 , 20 , 21 ]. Moreover, a literature review showed that most of the cases were characterized by a partial implementation of lean methodologies and concerned single processes in the value chain or restricted technical applications [ 20 , 22 ]. Even today, few hospitals apply lean principles at a systemic level [ 23 , 24 ].
The failure of lean implementation is a hot topic. Many authors who have focused their studies on social and managerial issues have highlighted the existence of factors that either enable or hinder the implementation of lean. These factors are mostly related to the context and the implementation strategies [ 5 , 16 , 25 , 26 , 27 ]. Lean implementation is not self-evident, and the process of transforming an organization into a lean organization requires a long-term strategic vision, a commitment by management, and a culture of change in the entire organization [ 5 , 16 , 26 ]. Contextual factors influence successful implementation and introduction strategy; lean adoption, in turn, changes contextual factors. A lean transformation must be planned and managed; it is not a quick solution, but a strategic plan in constant evolution [ 5 , 28 , 29 ]. From this point of view, the introduction phase plays a fundamental role in implementation because it facilitates the dissemination of the lean principle in hospitals and enables the contextual elements that support change. Although most researchers have recognized the role of the introduction step, the impact of this phase on contextual factors has been poorly reported on in the literature [ 5 , 12 , 20 ]. Most of the articles have focused more on the benefits of this phase than on how to manage it.
In light of this, it is necessary to examine how hospitals introduce lean into their clinical pathways in order to explain the success of the lean implementation. Starting with an in-depth analysis of the contextual factors discussed in the literature, the document helps to clarify what drives success in lean implementation within the hospital. The research has therefore undertaken a critical study of the introduction of lean in the case study of the haematology ward at a university hospital in the south of Italy. The objective is to highlight: (a) the role of contextual factors for successful lean introduction and implementation in a hospital ward; (b) how the pilot project has improved the pathway of a cancer patient undergoing chemotherapy infusion; and, (c) how the success of the pilot project modified the contextual factors, facilitating the spread of lean within the organization.
The study has the merit of detailing all the lean introduction phases. The analysis period is about 2 years. The lean introduction started in May 2018 and lasted 7 months. The pilot project results refer to the follow-up period of December 2018 to May 2020, while the dissemination results refer to the period from December 2019 to May 2020.
The paper is structured as follows: In the following section, the theoretical background is provided. Section 3 describes the research methods, while Section 4 presents the results of the pilot project. Finally, Section 5 presents the conclusion, highlights some limitations of this study, and proposes some directions for further research.
Theoretical background
Most authors point out that the introduction phase is a crucial moment in lean implementation [ 10 , 12 , 16 ]. This phase reduces distrust of the method and organizational resistance to change. It shows the benefits of lean and assesses the organization’s ability to undertake continuous improvement. Many case studies report the success of lean in HSs by describing the use of lean instruments [ 8 , 30 , 31 ]. They offer the practitioners some methodological support, but not in a structured way since they do not provide a clear implementation roadmap [ 5 , 32 , 33 ]. Some authors have tried to fill this gap in the literature by offering guidelines for implementation. Augusto and Tortorella [ 33 ] suggests carrying out a feasibility study focused on the desired performance before implementing continuous improvement activities. The author suggests defining the techniques, roles, and results related to the improvement path. Curatolo et al. [ 5 ] argue that the improvement procedure has to take into account six core operational activities of business process improvement and five support activities. The six core operational activities are: selecting projects, understanding process flows, measuring process performance, process analysis, process improvement, and implementing of lean solutions. The five support activities are: monitoring, managing change, organizing a project team, establishing top management support, and understanding the environment. These studies, while offering further guidance on the process of introducing lean into a hospital, do not describe either the organizational context in which the method is being implemented or the strategies for its implementation [ 5 , 12 , 25 ]. The introduction of lean into a HS is not an easy task; there are many organizational issues to be addressed. Among these, the analysis of the context and the definition of the implementation strategy are the ones with the greatest impact on the success of the introduction [ 16 , 26 , 34 ].
The contextual elements are the special organizational characteristics that must be considered to understand how a set of interventions may play out [ 35 , 36 ]. They interact and influence the intervention and its effectiveness [ 34 , 36 ]. Two of the most cited contextual element are the drive to improve processes and the level of maturity [ 5 , 10 ]. The drive for improvement is represented by the exogenous and endogenous needs that act as triggers for the introduction of improvement methodologies [ 25 , 26 , 35 , 37 ]. The level of maturity refers to knowledge and experience in process improvement initiatives. It includes knowledge of methodologies and tools, experience gained, confidence, trust, and dissemination within the organization. Where the maturity is low, there is a risk of lean introduction failure in both the processes and the organization as a whole [ 5 , 16 , 38 ]. As long as the organization does not reach a fair level of maturity, the rate of change tends to be slow and sometimes frustrating. However, as the degree of maturity increases, lean implementation becomes a “day-to-day job” rather than a series of projects that take place at discreet moments [ 10 , 21 , 39 ]. Hasle et al. [ 39 ] highlighted that a high level of maturity allows for the implementation of principle-driven lean. Contextual elements include organizational and technological barriers such as resistance to change, lack of motivation, skepticism, and a lack of time and resources that inhibits the introduction and the implementation process [ 4 , 8 , 21 , 40 ]. The lean introduction process in HS is also complicated by the organizational context and the double line of clinical and management authority in hospitals [ 41 , 42 ].
With regard to internal contextual factors, many authors explored the readiness and sustainability factors influencing the adoption of lean. Readiness factors are those elements that improve the chances of lean implementation success; they provide the necessary skills and knowledge to enable organizational change [ 23 , 43 , 44 , 45 ]. The readiness and sustainability factors include any practices or characteristics that allow organizational transformation by reducing or nullifying potential inhibitors of success. High commitment and strong leadership of managers and physicians, continuous training, value flow orientation, and the hospital’s involvement in continuous improvement are just some of the most discussed topics [ 5 , 10 , 16 , 43 ]. Other examples include understanding employees needs, identifying the organization’s strategic objectives, project management, and teamwork [ 5 , 12 , 16 , 46 ].
From the study of the contextual elements described so far, some authors have developed models to assess the impact of context on the implementation of organizational improvement activities. Kaplan et al. [ 36 ] put forth the Model for Understanding Success in Quality (MUSIQ). The authors identified 25 key contextual factors at different organizational levels that influence the success of quality improvement efforts. They defined five domains: the microsystem, the quality improvement team, quality improvement support and capacity, organization, and the external environment. Kaplan et al. [ 36 ] suggest that an organization that disregards contextual factors is doomed to fail in implementing an improvement program; an organization that adopts a context-appropriate implementation strategy can change the outcome by triggering implementation enablers. Previous studies of lean adoption in HSs suggest that the fit between the approach taken and the circumstances will influence the chances of success [ 3 , 12 , 34 ].
There are two strategies for introducing lean in a HS, and they are characterized by the implementation level. The level of implementation refers to either micro or meso implementation. Brandao de Souza [ 16 ] defined meso-level implementation as the condition under which lean is spread throughout the organization and is implemented at the strategic level, while micro-level implementation is where lean is implemented at a single process level in discrete moments. Meso-level implementation is crucial for long-term success because a lack of integration in a lean system can lead to the achievement of local rather than global objectives and can also affect the sustainability of the paradigm [ 23 , 26 , 47 ]. However, organizations that want to implement lean at the strategic level often do not recognize the need for a long-term implementation program and introduce lean as a “big-bang initiative”. This leads in many cases to a failure to introduce the method [ 16 , 47 ]. Many researchers suggest introducing the lean approach through a pilot project run by a specially formed lean team [ 12 , 16 , 48 , 49 ]. The pilot project should be challenging, involve a process relevant to the organization, and require the use of a systemic approach. In particular, it should not be limited to the application of “pockets of good practice” or lean tools, but should include the systemic adoption of improvement programs such as the Plan-Do-Check-Act (PDCA) cycle [ 21 , 48 ]. Brandao de Souza [ 16 ] asserts that the first initiative should be tested on a relevant patient pathway. The lean team should be composed of clinical and non-clinical staff actively involved in the patient pathway. A pilot project that meets these conditions is a useful tool for increasing the maturity of the method within the organization [ 21 , 39 ]. It can increase the confidence of the team and staff in the lean approach and can promote the learning of lean methodologies and techniques [ 21 , 39 ]. Moreover, the pilot project activates the contextual elements, enabling the introduction of the model [ 10 , 12 ]. The successes of the pilot initiative must be celebrated and communicated within the organization [ 10 ]. When the first initiative leads to visible and easily quantifiable results, the method has a greater chance of spreading throughout the organization [ 10 , 12 , 16 ]. In light of these considerations, the lean implementation requires that the contextual elements and the introduction strategy be assessed at the same time. In addition, it would seem fair to assume that as contextual factors influence the introduction strategy, the results of the implementation strategy will influence the contextual factors.
In Fig. 1 , we propose an adaptation of the MUSIQ model [ 36 ] that shows the impact that the lean implementation strategy has on the contextual elements.
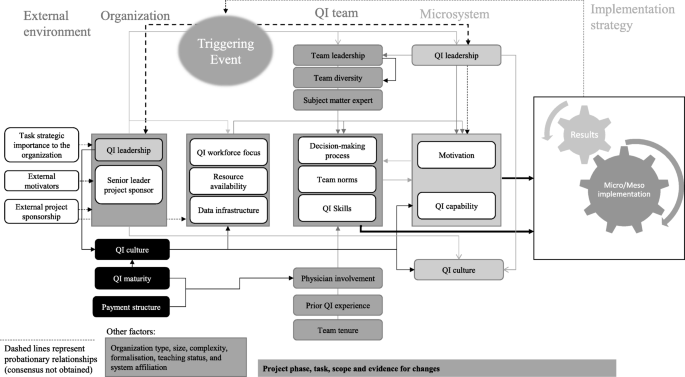
Our adaptation of the MUSIQ model
Study setting and design
This is an explanatory single-case study of the introduction of lean at a university hospital in Southern Italy. In particular, the introduction of lean in the pathway of a cancer patient undergoing infusion chemotherapy in a haematology ward will be discussed. This study was designed to evaluate how the contextual elements discussed so far have influenced the introduction of the method and how the successful pilot project has enhanced the internal context. We used the adaptation of the MUSIQ model [ 36 ] proposed in Fig. 1 to systematically trace the antecedents of the lean introduction and to explain how the success of the implementation strategy changes the contextual elements.
The work covers four periods over 2 years (Fig. 2 ). The first period concerns lean introduction and implementation strategy. The second is related to the pilot project implementation in the haematology ward. The third shows the pilot project results. The last assesses the impact of the pilot project on the dissemination of lean within the organization.
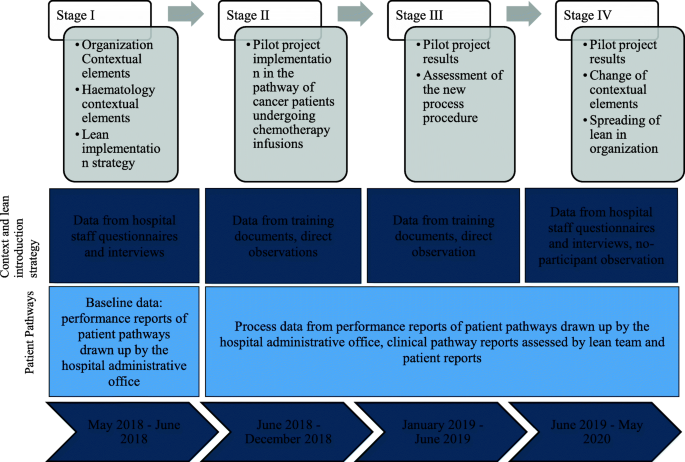
Stages of data analysis
Data collection
Different data sources and data collection methods are used with the aim of improving data validity through triangulation. The data sources are lean training documents, direct observations and nonparticipant observations, process performance reports, process data recorded by patients, and two questionnaires submitted to the hospital staff (the questionnaires assess the “pre” and “post” lean dissemination phases and the difference regards three open questions) (Fig. 2 ). The second author is the consultant who trained the lean team and coordinated the pilot project, and the first author conducted approximately 50 h of nonparticipant observations. The questionnaire was delivered to 25 medical department staff members in September 2018 and in May 2020. The first questionnaire focused on contextual factors that existed before the introduction of lean, and the second investigated changes in the contextual elements - in particular trust, maturity and lean dissemination. The semi-annual performance reports from 2017 to 2020 for the clinical pathway under examination include daily averages of the number of chemotherapies per chemo chair (MT), the patients’ length of stay (LOS), and the daily average of the percentage of patients undergoing chemotherapeutic infusion within 3 hours of hospital admission (P3). Each day, from September 2018, a document containing all the steps of the clinical pathway was given to each patient. For each activity, the patient recorded the start and end time, and a signature of the doctor or nurse was required. In the period of September 2018 – May 2020, the medical staff collected more than 1.250 reports from patients. The study also draws on 10 semi-structured interviews. The hospital CEO, the chief of the medical department, the nurse supervisor, the chief of the antiblastic chemotherapy handling units, and the chief of the clinical laboratory were interviewed in September 2018 and May 2020. The interviews focused on the contextual elements either enabling or inhibiting lean introduction or its dissemination, and ranged from 30 min to 1 hour in duration.
Data analysis
The factors described in Fig. 1 were used to systematically analyse the antecedents of the results and to understand their causal influence on the lean introduction. This data collection allows for the description of the case study. In addition, it simplifies the interpretation of the evidence that emerged through the study of the factors listed. The authors carried out a content analysis to classify the data by theme. The content analysis followed an inductive approach based on the identification of meaning units at the semantic level and the encoding of results [ 49 , 50 ]. Whenever researchers did not agree on semantic meaning, a new unit of analysis was proposed. The principle of consensus among all panel members was used to determine the interpretation, addition or deletion of elements of analysis. The discussion of the case study focuses on four themes: (a) contextual elements enabling or hindering lean introduction, (b) implementation strategy, (c) pilot project results, and (d) lean dissemination and adoption in hospital. These themes were submitted for review by the interviewees; their feedback was used to improve the accuracy of the case study description.
Case study presentation
The university hospital is a model of excellence in Italy for pre-clinical, translational, and clinical research and care activities. It is equipped with 110 beds to treat all types of oncological pathologies in adults. There are 115 researchers working there. The hospital is structured into six departments, of which three are clinical (Medical Area, Diagnosis and Imaging Therapy, Surgical Area), two are services, and one is an administrative/management department. The medical area includes four wards: medical oncology for thoracic pathology, medical oncology, haematology, medical oncology for oncology patient care. In 2015, the institute was accredited as a clinical cancer centre according to the Organization of European Cancer Institutes (OECI). Since 2015, evidence-based medicine and patient-centred care methodologies have been successfully implemented in the hospital, but no process improvement methodology has been used. In 2017, the hospital became a hub for oncological diseases, which led to an increased demand for care and services. The hospital has received national funds dedicated to hubs and has made investments in infrastructure improvements and the purchase of new innovative medical equipment.
Contextual factors enabling or hindering lean introduction
The description of the external and internal contextual factors, as revealed in the first questionnaire and the interviews, is given in Table 1 . Below is a brief description of each item.
External context and organizational elements driving lean introduction in the haematology ward
The analysis of the context revealed external and internal elements influencing the introduction of lean. Starting with the external elements, the most frequently discussed motivators that led to the search for methodologies for process improvement include the continuous increase in patient volume and the benchmark of process performance with other providers. Although the clinical results were above the national average, the increase in demand - especially in the medical area - highlighted the inability to manage the increasing flow of patients. The inability to manage the increasing number of patients also affected the performance of the process in the diagnostic area.
Internal elements driving the lean introduction were related to dissatisfaction with inefficient work practices within the medical area and the dissatisfaction of many patients who complained about long wait times and lengths of stay.
The choice of lean methodology derives from the desire to follow the example of certain Tuscan hospitals that have been using lean at a strategic level since 2015. These hospitals are considered the benchmark for continuous process improvement. One of these hospitals was already included in the 2013 OASI Report, edited by CERGAS - Bocconi, among the six Italian companies that were the first and best to successfully implement Lean Thinking in healthcare. In addition, the methodology was strongly sponsored by the clinical director and the general director of the hospital. They had participated in a 60-h regional training course on lean healthcare in the second half of 2017. During the training course, they studied case studies of excellence in lean implementation.
When, in May 2018, the hospital directorate proposed the introduction of lean methodology in the medical area, the head physicians showed strong resistance because of the resources that would need to be allocated to the implementation process. In addition, some doctors did not trust the method. This brought up some conflicts with the medical area managers. The haematology staff, represented by their head physician, were the only ones who explicitly agreed to implement the lean introduction. The department, as in most Italian hospitals, is structured as a clinical area where the physicians - in contrast to other professionals - were members of the ward organizationally. Haematology staff were strongly motivated to do research and achieve excellent process performance. They were interested in taking the opportunity to define excellent clinical pathways, as the ward was undergoing managerial and layout restructuring. In addition, the haematology staff believed that lean could further improve clinical performance and improve the patient-centred and evidence-based approach. Until mid-2017 the ward was part of oncology; afterward, it was made independent and new areas of the hospital were assigned to it. Since the ward became independent, one head physician, three doctors and four nurses have been hired. The department is equipped with the most modern medical equipment. The layout of the ward was not yet fully defined, and some rooms that could have potentially been assigned to medical, diagnostic and therapeutic activities had not been assigned to process activities. The ward shares the Antiblastic Chemotherapy Handling Unit (UMACA) and the analysis laboratory with the other four medical department wards in the hospital, so the staff needed to coordinate clinical processes so as not to create bottlenecks.
Since haematology is a strategic ward for the hospital, and in the last 2 years the demand for treatment has increased more than in other wards, the managers of the medical area have deemed it appropriate to introduce lean there. Haematology ward is considered strategic due to its high attractiveness and high immigration rates of patients from outside the region. These phenomena derive from the excellent reputation of the department in relation to the quality of care. Although the clinical pathways were characterized by excellent clinical outcomes, qualitative benchmarking activities (based on testimonials from physicians and patients) showed that the organization of the haematology patient pathway was very different compared to the benchmark (a Tuscan hospital) and that the patients’ perception of non-clinical service quality was lower. Although no investigation was carried out with respect to the ratio of equipment and personnel available per number of patients and amount of activities regarding the hospitals taken as benchmarks, the testimonials prompted management to come up with new specific, measurable, attainable, relevant and time - bound (SMART) goals (Table 2 ). The goals will be described in the next section.
Internal contextual elements enabling and hindering lean introduction in the haematology ward
At the organizational level, hospital management has strongly supported the introduction of the method. Since the haematology staff had no experience in process improvement activities, management provided the budget for an external consultant. In addition, three non-clinical personnel were allocated part-time to support the implementation of visual management systems and communication. The organizational structure of the ward has been modified to a matrix form. A team of three haematology ward physicians and two nurses was established and the ward’s head physician was elected project manager. The project manager had formal authority over the team and the personnel employed in the process to be improved; this reduced conflicts due to the double line of hierarchical authority. In this phase, the top-down decision-making approach was crucial to the successful restructuring of the organizational structure and the definition of the new organizational roles. The lean advisor supported the group for 8 months through training and project supervision. He coordinated two meetings per week and carried out Kata coaching activities. The theoretical training activity, lasting 5 week ends (in June 2018), was differentiated to accommodate technical and managerial competency needs. The team project manager and the medical area manager were trained on topics such as project management, team management, leadership, and the dissemination of lean. The members of the lean group were trained in lean techniques and tools. The key principles of lean thinking, the PDCA cycle methodology and lean assessment were taught to all participants. The most difficult barrier to overcome was the time available. The team agreed to spend 8 hours per week on training and pilot project implementation. The management of the team was facilitated by the experience gained with the implementation of the patient-centred care and evidence-based medicine. The motivation of the medical staff–microsystem element–and the focus on team management were key success factors for the involvement of team members. The culture of change introduced by patient-centred and evidence-based medicine was another enabling factor.
Implementation strategies
Pilot project definition.
Hospital managers and lean team members, who had experience in implementing patient-centred care methodologies, suggested starting a pilot project for the lean introduction. The consultant agreed. The team, with the support of the expert, analysed the clinical pathways in haematology. Six pathways emerged: a) diagnostic visits, b) biopsies, c) check-up visits, d) transfusions, e) infusion chemotherapies, and f) oral chemotherapies. Hospital managers argued that the pathway of the patient undergoing infusion chemotherapy was the most critical for patient and organization value. This process is the only one that involves several departments and requires a large amount of materials and time-consuming resources. In the first and second half of 2017 and 2018, there was a significant increase in the number of chemotherapeutic preparations. LOS, P3, and MT performance decreased during the same periods (Table 2 ). In addition, outpatient visits and the number of biopsies also increased. The medical staff stated that the increase in demand in the medical area had particularly affected the infusion therapy activities because they involved technical and instrumental resources that are shared with other departments (Table 2 ). The length of stay was analysed for patients undergoing short (LOS s ) and long-term infusion (LOS l ) chemotherapy. The first has a minimum duration of 90 min and a maximum of 180 min, and the second has a minimum duration of 181 min and a maximum of 360 min. Each patient was assigned to one of the infusion treatment classes. Process data were collected and analysed by the Department Management Control Office. The process performance data collection and reports were established in 2015 for the implementation of evidence-based medicine.
Pilot project implementation
The pilot project started in June 2018. The first month was dedicated to Gemba Walk, Methods-Time Measurement (MTM) and implementation of the 5S. In addition, the consultant trained the project manager, department managers and lean team members. There were many difficulties during the training period, especially with regard to process mapping and the concept of value, the latter being interpreted by doctors as clinical output. The non-medical staff dedicated to the project assisted the team in the drawing of the visual management material. A room in the medical department was dedicated for team meetings, and some notice boards were installed to post the materials developed during the project. The project activities were organized according to the Report A3 scheme. It followed the phases of the consolidated Deming cycle: Plan-Do-Check-Act (PDCA). Implementing the approach proposed by Deming allowed for the trial-and-error empirical method to be abandoned in favour of the “scientific” one. The PDCA allowed accurate planning of objectives and activities and their monitoring. The departmental managers and the consultant through the study of the national publications and explicit requests to colleagues in other hospitals - considered virtuous - identified the benchmark (Table 2 ). They took into account the hospital’s specific characteristics, such as the policy of not accepting haematochemical reports from outside for fragile patients. This choice is dictated by the risk management plan and affects P3 and MT performance. Time for blood sampling and haematochemical analysis is added to the cycle time; however, it eliminates many risks associated with clinical treatment.
The existing care process was mapped through Value Stream Mapping (VSM) based on the patient reports, Gemba walks, interviews, and direct observation. For instance, Fig. 3 shows the pathway of a patient undergoing short-term infusion chemotherapy. The cycle time in Fig. 3 was calculated over an observation period of 1 week and included 51 patients. In addition, the application of the Demand Map and the Spaghetti Chart were used to evaluate the ward nodes activated by the patients and the ward’s layout. These tools were useful in defining the possible sources of waste in the process. The application of these tools lasted more than 2 months and required several revisions. Once completed, the results were posted in the meeting room and were used for discussions with colleagues in the medical department. The lean team requested support from the consultant for the drafting of the VSM and for the layout analysis. In addition, the consultant was asked to simplify negotiations with staff from other departments who were reluctant to be subjected to time and method measurements. The negotiation activity required a degree of organizational effort. The facilitating elements were manifold: they enabled the involvement of staff opposed to the introduction of measuring instruments. In particular, the most effective were: the intervention of the directorate general, the delegation of hierarchical authority to the project manager and finally the endorsement of trade union committees. Moreover, during the planning phase, many difficulties emerged, including the selection of a unique and standardised measurement system, the coordination of work and meeting schedules, and the deadlines set by the project Gantt. Although the project manager was able to manage the team, he did not have enough experience in lean tools. The external consultant played a key role in managing these activities.
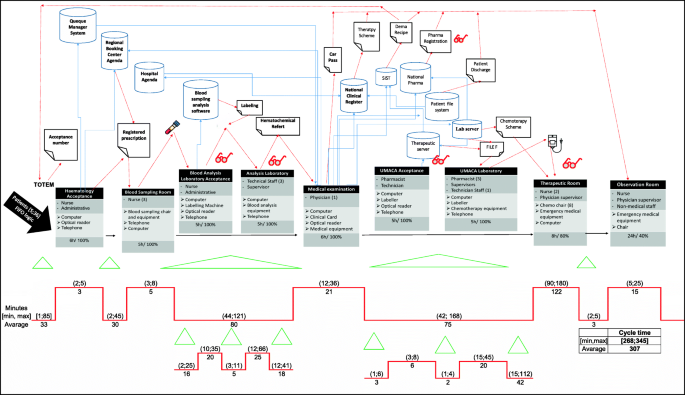
As-is process represented by VSM
At the end of the as-is analysis process, an Ishikawa diagram was used for the definition of root causes. Four root causes emerged from the meetings and interviews. They were patient flow management, coordination activities with other departments, layout, and Information Technology equipment (IT).
Patient flow management concerned the absence of priority in the management of patients based on the clinical path and the arrival of patients in the early hours of the morning. The lack of coordination with other departments led to delays in the preparation of infusion chemotherapy and blood test reports. The layout was such that the flow of doctors and nurses crossed the flow of patients, and this caused great inconvenience to the doctors and nurses. Also, the computer software was not compatible, which meant that the same data had to be recorded several times.
After some meetings and rigorous brainstorming, the lean team suggested changes to be made in the existing pathway. This was done by considering how patients could be divided into clusters so that the infusion activity could start as soon as possible without affecting other occurrences. Moreover, it is made possible to simplify the coordination between diagnostic units. The patient flow has been managed in such a way that long-term patients are given priority (first to be accepted and blood sampled), followed by patients needing biopsies, first visit, follow-up visit. Finally, short-term patients are treated in a way that limits waiting time and does not affect the activities of other departments. Theories of queues and operational research methodologies were implemented to address chemo chair saturation. A chemo chair activities plan was implemented through pull logic. In addition, the hospital engineer was involved in making sure the information systems were compatible. Whenever integrating the software was not possible, a data entry person was assigned to prevent medical staff from wasting their time on low-value activities. The ward layout has been modified to prevent patient flows from intersecting with the flows of doctors and nurses. In addition, the use of one room has been changed from a small warehouse to a blood collection room to increase the value of the activities carried out within it. The waiting rooms were moved outside the ward and, during the first 2 hours of the working day, the biopsy room was reassigned to blood collection activities to speed up the requests for therapies in UMACA. Patient intake, blood collection, and tube labelling activities have been paralleled to be performed simultaneously in the same room. The routes and modalities for the delivery of blood samples to the laboratories were revised in order to reduce the time and distance travelled by non-clinical staff. Tablet reporting systems were installed. Finally, a patient chemo chair allocation system was developed.
The resources needed for these changes were determined. The team tested and modified the changes during December 2018 and January 2019. The tests were evaluated based on the performance data, patient reports and the team’s expertise.
Pilot project results
In January 2019, it was decided to implement the new standard procedures that were tested in order to improve performance. The team met once a week for 6 months. On a monthly basis, performance was reviewed and new changes were tested. Clinical and nonclinical personnel from other wards and departments were invited to each weekly meeting to share with them the results of the pilot project, and to involve them in the lean methodology.
Every morning, the team leader investigated the impact of organizational changes in order to avoid conflicts. Organizational problems that emerged were discussed and resolved by consensus. In the follow-up phase, the consultant performed supervisory activities. Each week, the team leader performed the Kata coaching. During the first 6 months, the monitoring of activity was very frequent to prevent a return to old operating modes. Subsequently, when the staff had learned the new procedures, monitoring was reduced to once a month.
Table 2 and Fig. 4 shows the results achieved through the implementation of the pilot project. The objectives were not reached for all indicators; however, the results improved over time.
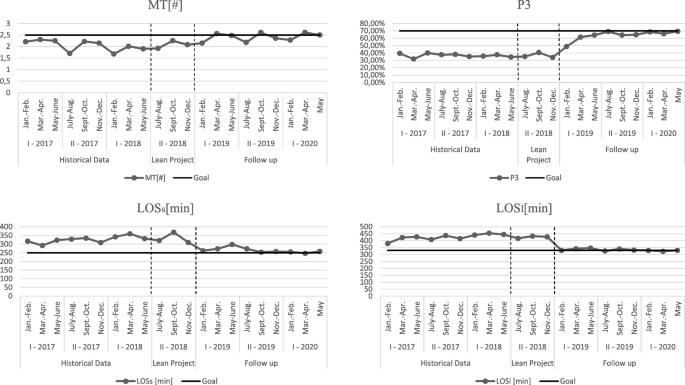
Figure 5 shows the to-be state of the same process analysed in Fig. 3 . From the cycle time analysis of each process step, the areas of waste eliminated are clear.
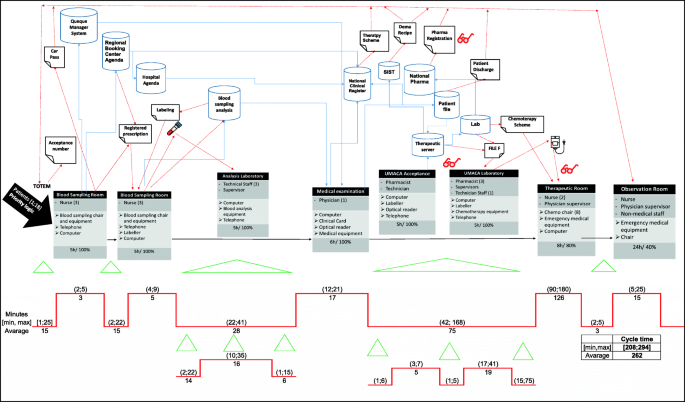
To-be process represented by VSM
The incremental improvements in process performance over time are explained by the need for staff to learn new procedures in the early period. In addition, the patients’ resistance to changing their habits also slowed down the improvement in performance. Patients have been educated over time, through an intense communication activity based on visual management systems and telephone reminders.
In addition to the results showed in Table 2 , the pilot project had a positive impact on the performance of other patient pathways in the medical department. The cycle time variability reduction and the levelling of the service demand allowed the UMACA and the analysis laboratory to better plan their activities. The new layout reduced waste due to unnecessary movement. Nurses walk 2 km less per day and doctors 1.5 km less per day. Software integration has reduced data logging time by 35 min per day for each doctor. Patients have evaluated the change positively. In particular, they have experienced a drastic reduction in wait times, and greater attention from the medical staff. Increased privacy and a precise time of service are other improvements reported by patients.
Finally, the clinical staff was satisfied with the new procedures because they reduce overloads and allowed for better planning of activities. They say that dividing patients into time slots based on clinical priority reduces stress and simplifies the coordination of activities with other departments. The success of the project was communicated internally and externally to the organization. In June 2019 the results were celebrated with a formal team award ceremony. The resulting Report A3 was posted on the bulletin boards in the hospital wards and in the reception area. By means of an internal circular sent to all medical directors, the directorate officially thanked the members of the lean team and highlighted the excellent results achieved in terms of waiting lists and process time reduction. In addition, the directorate funded the lean team’s participation to national conferences in order for the team to discuss the project. The improvement activities and results were described and summarized in an official report sent to the regional health authority and cancer patient associations (the latter were also given an evaluation form and an invitation to observe the optimised process in the field). Reporting was carried out by the hospital directorate and the project manager.
Lean dissemination and adoption in the hospital
Following several meetings between the directors and the primary doctors of the medical area, it became clear that there was a willingness to implement further improvement projects in other medical wards. The feedback from the pilot project team was a strong convincing factor. Moreover, the results of the external communication of the pilot project played a critical role in increasing the desire for emulation. The regional authorities requested for the project team to co-design the diagnostic and therapeutic care pathways (PDTA) of the haematology patient pathway inside the regional network. The patient association lobbied for similar projects to be implemented in other clinical oncology pathways. The change of internal context and enabling factors were of great importance at this stage. The drive to disseminate lean was characterized by both the need to improve process performance and to the desire to emulate the success of the project pilot. In addition, increased trust in the lean method has prompted the directors to provide a peer internal training program in the medical area. In June 2019, members of the pilot project lean team were promoted to the position of lean champions. Their role was to disseminate the lean methodology in the medical area and to train colleagues. The hospital directorate set up the Lean Support Office and assigned to it the three non-clinical resources that had already supported the pilot project. The first methodology to spread throughout the medical department was 5S. According to the lean sponsors, this methodology was a prerequisite for implementing lean methodologies in all wards and for facilitating inter-process lean implementation. Visual management systems have been implemented to facilitate changes and standardization of activities and to guide the patient through the hospital. The 5S methodology and visual management, which was initially underestimated by the medical staff, has solved many problems in the working environment. Increasing the availability of tools, simplifying the transmission of documentation, reducing errors in medical records and nursing diaries, reducing the duplication of requests and medical documentation, creating flexible workplaces, less movement and transportation in the hospital, and increasing patient autonomy are just some of the improvements achieved. However, the most important result to be achieved was an improvement in workplace wellbeing. Among the most used tools for 5S implementation and visual management are: checklists, one point lessons, kaizen forms, horizontal and vertical marking, red tags, Kanban, spaghetti charts. Finally, the demand map was implemented to trace the patient flow across the departments of the medical area and the vertical swim lanes and the resources/process matrix were utilized to identify staff involved in several processes and the potential bottlenecks (in addition to the UMACA and the blood chemistry laboratory). As of August 2019 many other lean projects have launched sometimes spontaneously and sometimes at the demand of department heads or project managers (Fig. 6 ). In August 2019, three projects were undertaken in the medical oncology for thoracic pathology and the medical oncology wards. Two of them concerned the same clinical pathway addressed in the pilot project, and the last one was the harmonization of protocols for caring for an oncological patient between departments. Each project has been implemented following the PDCA cycle (using the A3 report framework) with the support of one of the lean champions, who was assigned the role of project manager. Teams of three doctors and one nurse were dedicated to each project. In the planning phase, the tools adopted in each project were: spaghetti charts, VSM, Gemba Walk, standardized data collection sheets (both for patients and physicians), control charts, 5 Why or alternatively the Fishbone Diagram, definition of SMART objectives. In the “Do” phase, the solutions adopted for the resolution of problems are derived from Just in Time and agile approaches (especially for software’s’ integrations management). The pilot project A3 report was used as a knowledge management tool and resulted to be of great value to guide the implementation of the three projects. The members of the pilot project team supported their colleagues during the implementation of the three projects. This resulted in a positive impact on the quality and timing of the data collection activities, the drafting of the VSM, the definition of the KPIs and especially the root cause analysis. Even though the negotiation was simplified by peer training, support from more experienced colleagues and project management by a doctor, organizational and structural barriers emerged. The difficulty in getting the new procedures accepted, the impossibility of optimizing the layouts and the “not always respecting” the authority of the project manager limited the performance improvement. Although not all potential solutions have been implemented, the results obtained are evidence of the success of the projects.
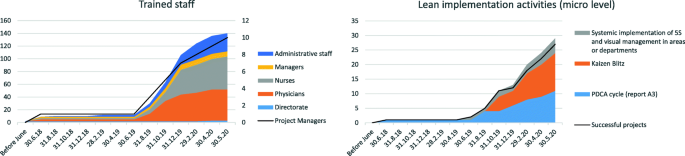
Lean projects and dissemination activities
In September 2019 the diagnostic department started 5S and visual management implementation initiatives. In October 2019 the same initiatives were undertaken in the surgical department. These initiatives were spontaneously implemented. The managers of these departments have asked the hospital director to introduce lean in their departments. Given the maturity of the method and the number of doctors trained, hospital managers did not consider it possible to undertake systemic improvement pathways in all departments. However, they have changed the organizational structures of the departments into matrix structures. Two doctors with lean experience, per department, have been assigned the role of project manager. The project managers have sponsored peer training and Kaizen blitz activities throughout the hospital departments. In the period October to December 2019 more than 60 doctors and nurses were trained in 40-h courses by their colleagues (Fig. 6 ). Three Kaizen blitz projects in the diagnostic department and two Kaizen blitz projects in the surgical area were carried out (Fig. 6 ). In addition, a PDCA cycle project was implemented in the medical area for the stocking and tracking of drugs and instruments. Moreover, the two bin Kanban systems, drug tracking tools, optimisation of the position in the storage layout and systems for the analysis of consumption time series were implemented.
In December 2019, in all the departments discussed so far, doctors were involved in continuous improvement activities, with projects structured through the use of both PDCA cycle and Kaizen blitz. The activities were undertaken spontaneously without the supervision of a manager and without any impact on daily clinical activity. The maturity of the methodology, the support of colleagues, and trust were enabling elements. However, some barriers such as infrastructural constraints and coordination of doctors and nurses and information systems have frequently affected the implementation of the method and two projects failed.
Due to the success of implementations at the micro level, managers have attempted to implement the lean methodology at the meso level. Hospital managers discussed, formalized and communicate in organization the Lean Strategic Plan. In January 2020, the Lean Support Office was transformed into a lean projects control room and renamed as the Operations Management Office. The role of this office is to define lean development policies and to supervise continuous improvement activities. The office has been placed in line with the strategic direction. Two lean project managers, two hospital managers, and three administrative officers have been assigned to it. Lean assessment, to evaluate the degree of lean maturity in organization, and Honshi Kanri, to strategically govern change activities, were implemented to the organizational level. While the lean assessment revealed an increase in both advance in the use of lean tools and the principles behind them, the governance of strategic implementation through Honshi Kanri did not seem to provide the foreseen results. Operations management office project managers did not always agree with hospital directorate on project prioritization. In addition, there often were disagreements between the Operations Management Office staff and departmental project managers about when to launch a project and how to manage it and communicate project results. Although there were many process improvement projects underway, these have not always been decided harmoniously between the Operation Management Office and the hospital departments. Moreover, many projects undertaken spontaneously by lean teams were not communicated to the Operations Management Office, which was therefore unable to govern the dissemination of the method. Medical leadership in departments seemed to dominate over managerial leadership; thus, there is great difficulty in strategically governing continuous improvement.
The marked differences in the responses to the closed questions of the questionnaires submitted provide significant evidence of how lean has spread throughout the organization (Fig. 7 ).
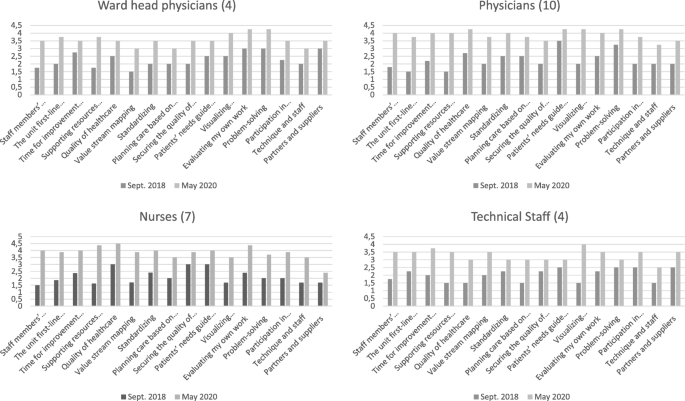
Responses to the closed questions of the questionnaire
The marked differences in the responses to the closed questions of the questionnaires presented provide significant evidence of how lean has spread throughout the organization. In particular, the results show how standardisation, self-assessment, time for improvement and peer-to-peer training have become part of everyday working practice. Furthermore, problem solving and collaborative decision-making show significant improvements. These improvements were witnessed not only by management but also by doctors, nurses and technical staff in the medical area.
After the pilot project and the initial push for implementation by management, internal contextual factors changed radically within the organization. While initially sponsorship and management involvement were necessary for lean implementation, today the methodology is independently disseminated. In particular, small improvement groups have emerged that are able to address various challenges. Process vision and patient focus have become part of the hospital culture. Doctors claim that continuous improvements simplify daily work, save time, and increase the level of service and the number of services provided. However, although these changes occurred at the micro level, the organization failed to direct change at the strategic level. Thus, harmonization of lean projects according to the strategic direction of the facility has yet to be achieved.
In accordance with the findings of many researchers [ 10 , 16 ], this case study showed how a careful, context-driven lean introduction strategy facilitated the dissemination of lean - at micro level - within the hospital. The decision to implement lean was precipitated by external factors, including the need to improve the performance of processes in the medical area and to follow the example of other successful hospitals. The in-depth training by an external specialist and the pilot project, characterized by interdepartmental activities, the need for a systemic approach based on the Deming Cycle and the constant support of the external consultant, allowed the participants to acquire the necessary skills to support - sufficiently - the lean implementation in the clinical pathways of the medical department and to train their colleagues. The results of this project have been manifold. At the process level, there was a significant reduction in the patients’ length of stay, the wait times for haematological patients, the process time variability, and an increase in the number of daily chemotherapy therapies performed. At the medical area level, a spontaneous spread of the culture of improvement has emerged. Directorate commitment, motivation of the medical department staff and management, and the presence of a consultant were the main enabling factors for the success of the pilot project. In turn, the results of the pilot project were the trigger for the spread of lean in the hospital. The pilot project itself, and the changes made to standard procedures that were inspired by the intervention, altered the contextual elements, mirroring the MUSIQ model [ 18 , 26 , 36 ]. Moreover, as trust and maturity raised, the speed of lean dissemination increased. This confirms that knowledge of the lean method tends to reduce organizational barriers and resistance [ 5 , 21 , 51 , 52 ]. Kata training and coaching were other key elements for the dissemination of the methodology. Initially, the consultant carried out the training activity, and after the pilot project, the team members became trainers and project managers; in this way, lean spread in the organization spontaneously. Moreover, as stated by many researchers [ 12 , 21 , 46 ], the matrix structure and project managers helped the staff to support and better coordinate process improvement. The many projects activated in the period July 2019–March 2020 are the measure of the diffusion itself.
However, some issues have arisen. For the new working procedures, the willingness of and the acceptance by the staff is crucial to achieving and sustaining the results of lean initiatives; where this did not occur, conflicts arose and the speed of change slowed. In addition, although in the early stages of implementation the bottom-up approach must prevail over a top-down approach to facilitate consensus and trust among physicians, nurses, and all workers, during the dissemination phase a greater equilibrium between the two decision-making approaches must be achieved. In accordance with [ 2 , 5 , 10 ], this case study demonstrates the importance of the right balance between bottom-up and top-down approaches. Medical leadership tends to dominate managerial leadership such that continuous improvement, even though it takes place in clinical processes, does not follow the strategic organizational guidelines. This leads to conflicts between managers and medical staff. Organizational, technical and infrastructural obstacles have hindered the adoption of the methodology. It is clear from what has been found that the introduction strategy was correct, but that the implementation at the strategic level has not yet taken place. The context has changed considerably from an organizational point of view, but some barriers have not been overcome. The management, which strongly sponsored and supported the introduction and implementation of lean, was subsequently unable to guide the implementation at the strategic level.
Our adaptation to the MUSIQ model is useful for interpreting the relationship between lean introduction strategies and changing contextual elements. Looking backward through this model allows us to understand the links between contextual elements, lean implementation and outcomes.
Conclusions
This study revealed that the strategy of introducing lean has improved readiness, sustainability and confidence in the method within the organization. The growing maturity of the organization has encouraged lean dissemination. However, the choice of strategy depends heavily on contextual factors. The two factors, therefore, influence each other. Although the introduction strategy may facilitate the introduction of lean, it may be less important when certain organizational, technical and infrastructural barriers remain. This is particularly relevant for systemic implementation. Contextual elements, which changed over time, influenced the success of the implementation at micro-level. At the meso-level, however, the organization has not reached the maturity for a systemic implementation of the method.
As has already been shown in the literature, the determining factors for introducing the methodology refer to external and internal pressures. The level of commitment of both the leadership and management are decisive for the success of the implementation only if the staff is motivated. Furthermore, the analysis shows that managing lean implementation at the micro and meso-levels requires different types of efforts. While the level of maturity speeds up the adoption of lean at the clinical level, it is not true that the dissemination of lean at the operational level inevitably translates into its application at the strategic level. Medical leadership, reinforced by the success of lean project implementations, could instead undermine proper implementation at the meso-level. This experience strengthens the MUSIQ model and complements it by showing the importance of the lean introduction strategy and its impact on contextual factors.
Limitations and future research
The main limitations concern the complexity of detecting and analysing all the relevant social and organizational aspects that have characterized the introduction and dissemination phases and the observation period of the dissemination phase. Moreover, the expert content analysis could introduce opportunities for misinterpretation of the data. The relationship between the contextual elements and the pilot project results were mainly assessed through participant and patient reports, document studies, and observations. The authors used data triangulation and a review of hospital staff to overcome the limits of the content analysis. Given the specificity of the hospital’s contextual factors and strategic choices, it is also clear that the case study cannot be generalized.
The sustainability aspect of lean was not considered because the observational study was conducted over a period of only 2 years. To understand this issue, the authors will investigate the socio-technical aspects of lean and how the context supports continuous improvement over time.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
Hospital Setting
Information Technology
Length of stay
Number of chemotherapies per chemo chair
Methods-Time Measurement
Model for Understanding Success in Quality
Organization of European Cancer Institutes
Patients undergoing chemotherapeutic infusion within three hours of hospital admission
Plan-Do-Check-Act
Antiblastic Chemotherapy Handling Unit
Value Stream Mapping
Godman B, Novakovic T, Tesic D, Oortwijn W, Martin AP, Parker M, et al. Addressing challenges for sustainable healthcare in central and Eastern Europe. Exp Rev Pharmacoecon Outcomes Res. 2016;16(6):685–7. https://doi.org/10.1586/14737167.2016.1165610 Epub 2016 Mar 30. PMID: 26966924 .
Article Google Scholar
Teisberg E, Wallace S, O’Hara S. Defining and implementing value-based health care: A strategic framework. Acad Med. 2020;95(5):682–5. https://doi.org/10.1097/ACM.0000000000003122 PMID: 31833857; PMCID: PMC7185050.
Article PubMed Google Scholar
Lum B, Png HM, Yap HL, Tan C, Sun B, Law YH. Streamlining workflows and redesigning job roles in the theatre sterile surgical unit. MJ Open Qual. 2019;8(3):e000583. https://doi.org/10.1136/bmjoq-2018-000583 .
Radnor Z, Holweg M, Waring J. Lean in healthcare: the unfilled promise? Soc Sci Med. 2012;74(3):364–71. https://doi.org/10.1016/j.socscimed.2011.02.011 .
Curatolo N, Lamouri S, Huet J, Rieutord A. A critical analysis of lean approach structuring in hospitals. Bus Process Manag J. 2014;20(3):433–54. https://doi.org/10.1108/BPMJ-04-2013-0051 .
Roemeling O, Land M, Ahaus K. Does lean cure variability in health care? Int J Oper Prod. 2017;37(9):1229–45. https://doi.org/10.1108/IJOPM-07-2015-0452 .
Chiarini A, Bracci E. Implementing lean six sigma in healthcare: issues from Italy. Public Money Manag. 2013;33(5):361–8. https://doi.org/10.1080/09540962.2013.817126 .
Parkhi SS. Lean management practices in healthcare sector: a literature review. Benchmarking. 2019;26(4):1275–89. https://doi.org/10.1108/BIJ-06-2018-0166 .
Joosten T, Bongers I, Janssen R. Application of lean thinking to health care: issues and observations. Int J Qual Health Care. 2009;21(5):341–7. https://doi.org/10.1093/intqhc/mzp036 .
Article PubMed PubMed Central Google Scholar
Womack JP, Jones DT. Lean consumption. Harv Bus Rev. 2005;83(3):58–68 148. PMID: 15768676 .
PubMed Google Scholar
Spear SJ. Fixing health care from the inside, today. Harv Bus Rev. 2005;83(9):78–91 158. PMID: 16171213 .
D’Andreamatteo A, Iannia L, Lega F, Sargiacomo M. Lean in healthcare: a comprehensive review. Health Policy. 2015;119(9):1197–209. https://doi.org/10.1016/j.healthpol.2015.02.002 .
Mazzocato P, Holden RJ, Brommels M, Aronsson H, Bäckman U, Elg M, et al. How does lean work in emergency care? A case study of a lean-inspired intervention at the Astrid Lindgren children’s hospital, Stockholm, Sweden. BMC Health Serv Res. 2012;12(28). https://doi.org/10.1186/1472-6963-12-28 .
Andersen H, Røvik KA. Lost in translation: a case-study of the travel of lean thinking in a hospital. BMC Health Serv Res. 2015;15(401). https://doi.org/10.1186/s12913-015-1081-z .
Goodridge D, Westhorp G, Rotter T, Dobson R, Bath B. Lean and leadership practices: development of an initial realist program theory. BMC Health Serv Res. 2015;15(1):362. https://doi.org/10.1186/s12913-015-1030-x .
Brandao de Souza L. Trends and approaches in lean healthcare. Leadersh Health Serv. 2009;22(2):121–39. https://doi.org/10.1108/17511870910953788 .
Ulhassan W, von Thiele SU, Thor J, Westerlund H. Interactions between lean management and the psychosocial work environment in a hospital setting - a multi-method study. BMC Health Serv Res. 2014;14(1):480. https://doi.org/10.1186/1472-6963-14-480 .
Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88(4):500–59. https://doi.org/10.1111/j.1468-0009.2010.00611.x .
Nelson-Peterson DL, Leppa CJ. Creating an environment for caring using lean principles of the Virginia Mason production system. J Nurs Adm. 2007;37(6):287–94. https://doi.org/10.1097/01.NNA.0000277717.34134.a9 .
Mazzocato P, Savage C, Brommels M, Aronsson H, Thor J. Lean thinking in healthcare: a realist review of the literature. Qual Saf Health Care. 2010;19(5):376–82. https://doi.org/10.1136/qshc.2009.037986 Epub 2010 Aug 19. PMID: 20724397 .
Brandao De Souza L, Pidd M. Exploring the barriers to lean health care implementation. Public Money Manag. 2011;31(1):59–66. https://doi.org/10.1080/09540962.2011.545548 .
Kaplan GS, Patterson SH, Ching JM, Blackmore CC. Why lean doesn’t work for everyone. BMJ Qual Saf. 2014;23(12):970–3. https://doi.org/10.1136/bmjqs-2014-003248 Epub 2014 Jul 23.
Al-Balushi S, Sohal AS, Singh PJ, Al Hajri A, Al Farsi YM, Al AR. Readiness factors for lean implementation in healthcare settings--a literature review. J Health Organ Manag. 2014;28(2):135–53. https://doi.org/10.1108/JHOM-04-2013-0083 .
Article CAS PubMed Google Scholar
Henrique DB, Filho MG. A systematic literature review of empirical research in lean and six sigma in healthcare. Total Qual Manag Bus Excell. 2020;31(3–4):429–49. https://doi.org/10.1080/14783363.2018.1429259 .
Coles E, Wells M, Maxwell M, Harris FM, Anderson J, Gray NM, et al. The influence of contextual factors on healthcare quality improvement initiatives: what works, for whom and in what setting? Syst Rev. 2017;6(1):168. https://doi.org/10.1186/s13643-017-0566-8 .
Kaplan HC, Froehle CM, Cassedy A, Provost LP, Margolis PA. An exploratory analysis of the model for understanding success in quality. Health Care Manag Rev. 2013;38(4):325–38. https://doi.org/10.1097/HMR.0b013e3182689772 .
Tay HL, Singh PJ, Bhakoo V, Al-Balushi S. Contextual factors: assessing their influence on flow or resource efficiency orientations in healthcare lean projects. Oper Manag Res. 2017;10(3–4):118–36. https://doi.org/10.1007/s12063-017-0126-3 .
Hussain M, Malik M. Prioritizing lean management practices in public and private hospitals. J Health Organ Manag. 2016;30(3):457–74. https://doi.org/10.1108/JHOM-08-2014-0135 PMID: 27119397 .
Fournier PL, Jobin MH. Understanding before implementing: the context of lean in public healthcare organizations. Public Money Manag. 2017;38(1):37–44. https://doi.org/10.1080/09540962.2018.1389505 .
Chiarini A. Risk management and cost reduction of cancer drugs using lean six sigma tools. Leadersh Health Serv. 2012;25(4):318–30. https://doi.org/10.1108/17511871211268982 .
Gonzalez ME. Improving customer satisfaction of a healthcare facility: reading the customers’ needs. Benchmarking. 2019;26(3):854–70. https://doi.org/10.1108/BIJ-01-2017-0007 .
Terra JDR, Berssaneti FT. Application of lean healthcare in hospital services: a review of the literature (2007 to 2017). Prod. 2018;28(0):e20180009. https://doi.org/10.1590/0103-6513.20180009 .
Augusto BP, Tortorella GL. Literature review on lean healthcare implementation: assessment methods and practices. Int J Serv Oper Manag. 2019;32(3):285–306. https://doi.org/10.1504/IJSOM.2019.10019746 .
Fournier PL, Jobin MH. Medical commitment to lean: an inductive model development. Leadersh Health Serv. 2018;31(3):326–42. https://doi.org/10.1108/LHS-02-2018-0015 Epub 2018 Jul 3. PMID: 30016920 .
Improta G, Romano M, Di Cicco MV, Ferrero A, Borrelli A, Verdolina C, et al. Lean thinking to improve emergency department throughput at AORN Cardarelli hospital. BMC Health Serv Res. 2018;18(1):265–78. https://doi.org/10.1186/s12913-018-3654-0 .
Kaplan HC, Provost LP, Froehle CM, Margolis PA. The model for understanding success in quality (MUSIQ): building a theory of context in healthcare quality improvement. BMJ Qual Saf. 2012;21(1):13–20. https://doi.org/10.1136/bmjqs-2011-000010 .
Kringos DS, Sunol R, Wagner C, Mannion R, Michel P, Klazinga NS, et al. The influence of context on the effectiveness of hospital quality improvement strategies: a review of systematic reviews. BMC Health Serv Res. 2015;15:277. https://doi.org/10.1186/s12913-015-0906-0 PMID: 26199147; PMCID: PMC4508989.
Hasle P, Bojesen A, Jensen PL, Bramming P. Lean and the working environment: a review of the literature. Int J Oper Prod. 2012;32(7):829–49. https://doi.org/10.1108/01443571211250103 .
Hasle P, Nielsen PA, Edwards K. Application of lean manufacturing in hospitals- the need to consider maturity, complexity, and the value concept. Hum Factors Ergon Manuf. 2016;26(4):430–42. https://doi.org/10.1002/hfm.20668 .
Narayanamurthy G, Gurumurthy A, Subramanian N, Moser R. Assessing the readiness to implement lean in healthcare institutions – a case study. Int J Prod Econ. 2018;197:123–42. https://doi.org/10.1016/j.ijpe.2017.12.028 .
Bijl A, Ahaus K, Ruël G, Gemmel P, Meijboom B. Role of lean leadership in the lean maturity - second-order problem-solving relationship: a mixed methods study. BMJ Open. 2019;9(6):e026737. https://doi.org/10.1136/bmjopen-2018-026737 .
Waring JJ, Bishop S. Lean healthcare: rhetoric, ritual and resistance. Soc Sci Med. 2010;71(7):1332–40. https://doi.org/10.1016/j.socscimed.2010.06.028 .
Arumugam V, Antony J, Kumar M. Linking learning and knowledge creation to project success in six sigma projects: an empirical investigation. Int J Prod Econ. 2013;141(1):388–402. https://doi.org/10.1016/j.ijpe.2012.09.003 .
Wilson WJ, Jayamaha N, Frater G. The effect of contextual factors on quality improvement success in a lean-driven New Zealand healthcare environment. Int J Lean Six Sigma. 2018;9(2):199–220. https://doi.org/10.1108/IJLSS-03-2017-0022 .
Gonzalez-Aleu F, Van Aken EM, Cross J, Glover WJ. Continuous improvement project within kaizen: critical success factors in hospitals. TQM J. 2018;30(8):335–55. https://doi.org/10.1108/TQM-12-2017-0175 .
Stanton P, Gough R, Ballardie R, Bertram T, Bamber GJ, Sohal A. Implementing lean management/six sigma in hospitals: beyond empowerment or work intensification? Int J Hum Res Manag. 2014;25(21):2926–40. https://doi.org/10.1080/09585192.2014.963138 .
McIntosh B, Sheppy B, Cohen I. Illusion or delusion--lean management in the health sector. Int J Health Care Qual Assur. 2014;27(6):482–92. https://doi.org/10.1108/IJHCQA-03-2013-0028 .
Jimmerson C, Weber D, Sobek DK 2nd. Reducing waste and errors: piloting lean principles at Intermountain Healthcare. Jt Comm J Qual Patient Saf. 2005;31(5):249–57. https://doi.org/10.1016/s1553-7250(05)31032-4 .
Drotz E, Poksinska B. Lean in healthcare from employees' perspectives. J Health Organ Manag. 2014;28(2):177–95. https://doi.org/10.1108/JHOM-03-2013-0066 .
Morgan SJ, Pullon SRH, Macdonald LM, McKinlay EM, Gray BV. Case study observational research: a framework for conducting case study research where observation data are the focus. Qual Health Res. 2017;27(7):1060–8. https://doi.org/10.1177/1049732316649160 Epub 2016 May 22. PMID: 27217290 .
van Rossum L, Aij KH, Simons FE, van der Eng N, Ten Have WD. Lean healthcare from a change management perspective. J Health Organ Manag. 2016;30(3):475–93. https://doi.org/10.1108/JHOM-06-2014-0090 .
Savage C, Parke L, von Knorring M, Mazzocato P. Does lean muddy the quality improvement waters? A qualitative study of how a hospital management team understands lean in the context of quality improvement. BMC Health Serv Res. 2016;16(588). https://doi.org/10.1186/s12913-016-1838-z .
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Management Studies, LUM University, S.S. 100 Km, 70010, Casamassima, Italy
Angelo Rosa, Giuliano Marolla & Francesco Manfredi
Center in Health Administration, and Center for Applied Health Economics and Management of IRCCS Galeazzi, University of Milan, Via Giacomo Venezian, 1, 20133, Milan, Italy
Federico Lega
You can also search for this author in PubMed Google Scholar
Contributions
All authors discussed the results and contributed to the final manuscript. GM conceived and designed the analysis, AR contributed data and analysis tools, FL and FM suggested the background reference model. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Giuliano Marolla .
Ethics declarations
Ethics approval and consent to participate.
Research project sheet describing the study purpose and procedures was provided and approved by Hospital Directorate. Hospital management informed potential participants and hospital staff about the study at its launch and before the interviews and questionnaires administration. It was disclosed that participation was voluntary and that voluntary participation in the study involved consent for publication. Fully informed verbal consent to participate was obtained from all participants prior to inclusion in the study. Anonymity was guaranteed as requested by the participants. The study was submitted to and approved by the LUM University Ethics Committee.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Rosa, A., Marolla, G., Lega, F. et al. Lean adoption in hospitals: the role of contextual factors and introduction strategy. BMC Health Serv Res 21 , 889 (2021). https://doi.org/10.1186/s12913-021-06885-4
Download citation
Received : 30 October 2020
Accepted : 09 August 2021
Published : 28 August 2021
DOI : https://doi.org/10.1186/s12913-021-06885-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lean implementation
- Contextual factors
- Introduction strategy
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
The Lean Post / Articles / Lean management case study series: Pediatric Hospital in Tough Market Pegs Growth to Lean Process Improvement
Lean management case study series: Pediatric Hospital in Tough Market Pegs Growth to Lean Process Improvement
June 2, 2011
Lean improvement projects at Akron Children’s Hospital have saved millions of dollars, increased utilization of expensive assets, and reduced wait times for patients and their families. While these gains are important, the learning and commitment that each project builds internally are crucial elements of the hospital’s drive to make continuous improvement not just a program but the overarching strategic imperative for the entire organization.Read an interview with hospital board member Bill Hopkins from LEI's lean leadership series.See all the executive interviews in the series.
Click to view/download file
Lean management case study series
Akron Children’s Hospital (ACH), a regional pediatric care system headquartered in Northeast Ohio, could be compared with David, the young lad who courageously brings down a giant in a classic Old Testament tale.
In this story, though, David battles two giants.
Akron is about 35 miles south of Cleveland, where two nationally ranked pediatric hospitals draw families from around the world who need specialized care for their children’s complex medical problems. Parents are attracted to the hospitals’ international reputations for being among the best: The Cleveland Clinic’s Children’s Hospital and University Hospital’s Rainbow Babies and Children’s Hospital are known for breakthrough research, life-saving surgeries and treatments, and other medical innovations. They also aggressively recruit gifted doctors, leading scientists, and other medical experts at the top of their professions.
But ACH, which certainly has a stellar regional reputation, is taking a unique weapon into the field as it battles for a bigger slice of the state’s pediatric care market. While the two Cleveland hospitals have continuous-improvement programs, neither has made continuous improvement a strategic imperative across its entire enterprise as ACH has.
The hospital’s Center for Operations Excellence (COE) is the engine that propels all employees and functions toward the growth goals set by executives and board members in hoshin kanri ( strategy deployment ) planning. Leaders are confident that the COE and its lean six sigma -focused training and project leadership give ACH enough competitive advantage to succeed, even in the same geographic market as two healthcare giants.
ACH’s expansion plan includes increasing the number of patients served both geographically and within certain sub-specialties; becoming the No. 1 choice for parents and referring physicians through quality achievements and availability of services; improving on infrastructure, quality, and clinical programs; and becoming the primary site for pediatric medical research in Northeast Ohio.
Already, the three-year-old COE has been widely embraced and highly effective. Projects have saved ACH millions of dollars, increased utilization of expensive assets, and reduced wait times and processing for patients and their families. The short-term gains are important, said Doug Dulin, the COE’s senior director, but the learning and commitment that each project builds internally are more crucial.
“What it comes down to is that we have to create a competitive advantage,” said Dulin, who learned the Toyota Production System at Aoyama Seisakusho, a Tier One supplier to Toyota Motor Manufacturing. “So how can we transfer what we’ve already done into every segment of the hospital? That’s how the Center for Operations Excellence fits in. This is a long-term journey.”
Akron Children’s Hospital at a Glance
- Largest pediatric healthcare system in northeast Ohio.
- Operating two freestanding pediatric hospitals and offering services at nearly 80 locations.
- Pediatric specialties draw half a million patients annually, including children, teens, and adults from all 50 states and around the world.
Level-Loading Schedule Improves Quality, Access, and Revenues
In addition to the challenge of having two highly regarded competitors in the market, ACH must do much more with much less. It doesn’t receive the numerous large grants and donations that the others do; and since all of the hospital’s patients are children, it can’t rely on Medicare reimbursements. Also, both the Clinic and UH are closely aligned with Case Western University Medical School in Cleveland, and so have access to more intellectual property, research programs, emerging technologies, and other assets than ACH has.
The hospital system’s smaller and less complex operation , however, seems to have been an advantage for quickly absorbing the lean culture. Evidence of how open all levels of the organization have been to lean is the speed with which a large number of employees — including doctors — have come together to identify problems, find the root causes, and then agree on countermeasures.
“There’s something about the culture at Children’s that allowed this to be very effective, very quickly,” said Board Member Bill Hopkins. “They were just primed for this. It speaks volumes about the commitment from everybody — the leadership, staff doctors, nurses.”
For example, MRI scheduling was one of the first areas the COE addressed because it had potential for significant and fast improvement, and because the hospital had not been able to effectively utilize a second MRI machine it had purchased. The most apparent barrier was a bottleneck in scheduling.
A kaizen event revealed that variability was the root cause : Children are more prone to move during exams when they need to be still, a reality that extends their appointment times because readings frequently need to be delayed or redone. On any given day, more than half of the hospital’s patients are five-years-old or younger, and so are particularly prone to moving during exams. Some children need to be sedated to keep them still. This causes more variability because a doctor needs to administer the sedation, and doctors’ schedules routinely change without notice because of emergencies and other unexpected events. The result was a backlog of patients with appointments, and long wait times for those needing new appointments.
The two-day kaizen — which included radiologists, radiology technologists, schedulers, nurses, and the employees who handle insurance authorization and registration — produced multiple solutions:
- Modifying the master schedule.
- Streamlining the insurance authorization process .
- Implementing standardized work instructions.
As is often the case with a level-loading solution, modifying the master schedule seemed counterintuitive, but it worked. More time was scheduled for each exam, a change that made it easier for the end-to-end process to absorb variability and remain level (on schedule). This eliminated the bottlenecks that were causing the long wait times for exams and results. In cycle-time terms, the “appointment-to-results” cycle shrunk drastically as the department got its scheduling process under control. As a result, more capacity opened, and this allowed an increase in throughput (appointments) without adding resources.
“Before the kaizen, the hospital was doing about 86 MRIs per week. Now, on average, we are doing 112,” Dulin said. “That is good news for our patients and the physicians who are waiting on the results of those tests. Instead of waiting 25 days for an uncomplicated exam, families can now schedule same-day appointments.” (See chart: Outpatient MRI Appointment Wait Times.)
The project significantly improved the hospital’s bottom line, with $1.2 million in additional revenue attributed to the better MRI scheduling.
It also earned ACH an honorary mention award at the International Quality and Productivity Center’s Lean Six Sigma & Process Improvement Summit in January, 2011. The award was in the category of “Best Process Improvement Project Under 90 Days,” with Akron Children’s competing against five other international companies and organizations that were selected as finalists.
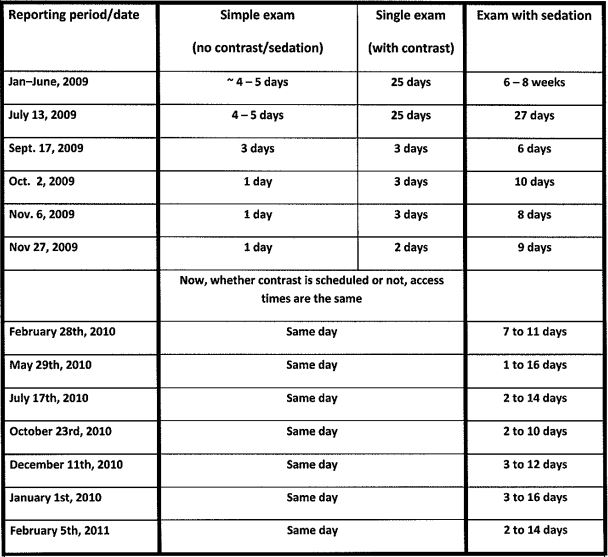
Surgery: Greater Capacity, Higher Quality without $3.5 Million Expansion
Perhaps the most striking example of how lean processes will feed ACH’s efficient growth is the avoidance of spending $3.5 million to enlarge the sterile processing area within the surgery department. According to Mark Watson, president of the ACH Regional Network, surgeons were performing 12,000 operations a year, and the number of cases was increasing. (They performed 14,000 in 2010.) Sterilization technicians had a hard time keeping up, but expanding space and staff would have been a problem.
“Our surgery area is landlocked,” explained Watson, who first introduced the idea of lean process improvement to the hospital. “In order to give sterile processing more, I would have to take away from someone else. So we started really looking at what was going on in the operating room, and we started with our flash-sterilization rate.”
The team decided this was the most urgent need — a flash sterilization rate of 10 percent was not acceptable, Watson said. (Flash sterilization is the immediate and unscheduled sterilization of instruments that have been dropped or otherwise contaminated during the surgery processes. It is a quality problem that creates variability and waste .) They scheduled a kaizen focused on reducing flash sterilization. The resulting improvements not only reduced flash sterilization to 2 percent, but also opened all the capacity needed to add an additional 4,000 surgeries a year.
“It was amazing what happened in the week-long program,” Watson said. “We fixed flash sterilization, and increased the capacity of the operating room to 16,000 cases. We invested in one flat-screen TV, and we took down one wall. We have a sterile processing department that could handle all the work that was there and more without expanding one square foot.
“And now, we’ve done two capacity studies on surgery, and we are running at 64 percent. It will take 2.5 years, but we want to get to 85 percent efficiency , which would mean around $15 million in additional revenue in the same operating room with essentially the same people.”
Low-Tech Solutions Increase Customer Value
In addition to increasing the number of procedures, the hospital is focusing on patient value in the form of decreasing wait times and increasing accessibility to doctors and services. This supports the goal of being the No. 1 choice for Northeast Ohio parents.
Outpatient doctor visits was an obvious place to start. If there is any customer who is most deserving of getting more from service providers, it’s a parent with a sick child. Emotionally drained and frequently exhausted, such parents value predictability and kept promises. Less time spent at the doctor’s office means more time to take care of themselves and their families.
The doctors, nurses, and other employees at ACH’s Locust Pediatric Care Group know this. When deciding on a process improvement goal, their focus was reducing the amount of time that established sick patients spend in the clinic. By its nature, the clinic is an unpredictable place as patients stream in from the city of Akron and surrounding urban and rural communities. Many of the children are poor, recent immigrants, or in foster care. All of them have potentially complex social and medical needs, and all of them receive care regardless of ability to pay.
Through a series of kaizens and A3 -based project planning and implementation, the Locust team identified and implemented a number of improvements that reduced patient in-clinic time from 70 minutes (2009) to 43 minutes (2011). Significant improvements included:
- Converting paper charts to electronic medical records, which helped to streamline the information flow .
- Implementing visual whiteboards that track patient flow during the appointment.
- Adding a team-wide “huddle” at the start of the day to prevent problems, such as scheduling issues.
- Eliminating triage rooms — where patients would be evaluated for priority of care — instead using mobile triage carts in the exam room.
The team is working on more definitive documentation, but early feedback is that customer value has increased.
“Office flow and access are the two biggest areas at Locust Peds where we can meet and exceed expectations from our patient families,” said Cindy Dormo, vice president for Pediatrics. “Now we’re measuring patient throughput and reviewing feedback from patients, which in the past has included complaints about long wait times, but is now turning favorable.”
Blue Belt Training Brings More People In
Dormo and other top-level executives said a key to the COE’s success is a focus on engaging all levels of the organization. Most recently, the COE team created a Blue Belt training program to focus on department and functional leaders, positions that would be considered “middle management” in a corporate setting. According to Dulin, the Blue Belt program is another example of how the COE program is directly supporting strategic growth goals.
“Our goal is to have this touch everyone. We then have everyone supporting the hospital’s goals, which then improves all of our major systems,” Dulin said.
Taking advantage of interest and enthusiasm generated by the MRI project’s success, the COE team chose the radiology department for the first Blue Belt training program. Every lead technologist, supervisor, manager, director, radiologist, the department chair and vice president participated.
Blue Belt participants learn how best to use the talents of their staff to streamline operations, improve the quality of care provided, and reduce variability and waste. Lessons focus on daily communication among staff members and leadership, learning how to track and improve daily metrics, and creation of standardized processes that stabilize patient flow.
The Blue Belt program is spreading to other departments. The plan is to begin with Dept. of Pediatrics employees, and then expand to surgical subspecialties, the Akron Children’s Heart Center, and Neurodevelopmental Sciences Center. In all at least 300 employees will have completed or been affected by Blue Belt training by the end of 2011.
Lessons Learned and a New Opportunity
Watson, the hospital executive who introduced continuous-improvement at ACH, identified these key factors as contributing to the COE’s early success:
Founding COE leaders: “After the decision was made to go with lean, I spent almost three months selecting people from our organization to help us on our lean journey,” he said.
Watson purposefully chose individuals who were successful, respected by their peers, and brought diverse backgrounds to the effort. These included a doctor with lean six sigma knowledge, a pharmacist who had just completed her Pharm.D., a medical technologist, a nurse, an M.B.A., and an administrator.

Watson also stressed the importance of having a practicing physician on the team. When Dr. David Chand joined ACH after working as a consultant, he dedicated 20% of his time to the COE and the rest to seeing patients. His role in the CEO has since expanded to about 90% of his time, but he will always see patients.
“When you are dealing with physicians, in order to be considered part of the club, you really need to have a stethoscope and see patients,” Watson said. “They like to interact with other physicians who are seeing patients. That’s just the way it is.”
Chand has been invited to work on improvement projects in many areas of the hospital and has become the go-to man for other doctors interested in learning more about the COE, some of whom are in the process of green-belt certification. His personal A3 projects have included removing non-value-add time from the residents’ patient-rounding process (daily in-person visits to patients).
Investing in education and training: Watson said an additional attribute that he looked for in team members was a quest for life-long learning.
After he assembled the team, Watson immediately sent them to a lean six sigma program at Johns Hopkins University, which included six weeks of learning over a four-month period of time (with project work done at ACH). The team then spent a week at Seattle Children’s Hospital to observe and learn from that CI program. In 2010, two team members received master’s degrees in operational efficiency and black belts from Ohio State University. Three others are now going through the course and will graduate in 2011.
Additionally, several department VPs have attended classes at Johns Hopkins and programs at Seattle Children’s Hospital.
“But we made a mistake,” Watson said. “When we started, we started with our front-line people working on projects with the A3 process. And we had very good engagement from the executive level, vice president and above. But what we left out was that middle manager level.
“Now the middle managers are really enjoying and learning with the Blue Belt program. The A3 process works much better now that we’ve covered the entire organization in terms of learning what we are doing. Our tagline is process improvement through people development. ”
Accepting failures/celebrating success: Not every project will be successful, Watson said, “and if they are all successful, you are not taking enough risks.”
ACH’s ambition is being noticed and rewarded outside of its own facilities. This year, it was awarded a contract by a third Cleveland hospital, MetroHealth Systems, to provide pediatric care in cardiology, gastroenterology, cancer and blood disorders, and critical care.
“We are impressed by how fully Akron Children’s is integrated into the region, how well it has partnered with other hospitals, and its growth, having added 77 individuals to its medical staff in 2009,” said Margaret Stager, chair of the Dept. of Pediatrics at MetroHealth. Previously, UH pediatric specialists were contracted to provide the services.
Akron Children’s Hospital Center for Operations Excellence
- Started in January of 2009
- Eight-week Lean Six Sigma Training designed for the people who do the work on a daily basis
- Projects are done on A3 paper using the DMAIC (Define, Measure, Analyze, Improve, Control) methodology
- Meet weekly for two hours of class time and one hour of coaching
Green Belt Program
- 10 Green Belts certified through Johns Hopkins Center for Innovation in Quality Patient Care
- Candidates and projects selected by hospital leadership
- Ten days of training and project work spread out over five months using DMAIC methodology
- Tollgate session at the end of each DMAIC step
Kaizen Program
- Two-to-five-day rapid process improvement events
- Strategically driven by hospital leadership
- Multi-disciplined teams that cross over value streams
- Key stakeholders from the value streams work together to solve problems and implement solutions
Blue Belt Program
- Manager/Leader Lean Six Sigma training for departmental certification
- Basic understanding of Lean Six Sigma principles and tools: gemba walks, daily huddles , value stream maps
Related Information
Akron Children’s Hospital: As the largest pediatric healthcare provider in northeast Ohio with hospital campuses in Akron and the Mahoning Valley, the dedicated team at Akron Children’s Hospital promotes the well-being of children now and in the future. We perform more than 600,000 patient visits each year at more than 85 locations. Our specialists care for infants, children, teens, and adults treating a wide range of conditions from routine primary care to the most complicated injuries and illnesses.
Akron Children’s earned the Gold Seal of Approval from the Joint Commission, as well as Magnet Recognition Status for nursing excellence from the American Nursing Credentialing Center. We are a major teaching affiliate of Northeastern Ohio Universities Colleges of Medicine and Pharmacy, and offer a number of pediatric subspecialty fellowship training programs. Our Rebecca D. Considine Research Institute is committed to advancing the prevention and treatment of pediatric illnesses and supporting the education and training of research staff. For more information, visit www.akronchildrens.org.
- Read an interview with Bill Hopkins, Akron Children’s Hospital Board member, as part of the Lean Enterprise Institute’s executive series on lean leadership.
- Akron Children’s Hospital is a member of the Healthcare Value Network, a network healthcare organizations share their lean methods and experiences to accelerating each organization’s “lean journey. The Healthcare Value Network was created as a partnership between the ThedaCare Center for Healthcare Value and the Lean Enterprise Institute.
- The Lean Enterprise Institute (LEI) teaches many of the lean management and lean healthcare concepts described above through workshops, Lean Summits, books and workbooks, and on its web site.
- Join LEI’s Lean Community for lean management case studies, webinars, newsletters, thought-leading columns, and e-letters, and many other resources for starting and sustaining a lean transformation.
Lean Enterprise Institute, Inc. was founded in 1997 by management expert James P. Womack, Ph.D., as a nonprofit research, education, publishing, and conference company with a mission to advance lean thinking around the world. We teach courses, hold management seminars, write and publish books and workbooks, and organize public and private conferences. We use the surplus revenues from these activities to conduct research projects and support other lean initiatives such as the Lean Education Academic Network, the Lean Global Network and the Healthcare Value Leaders Network. Visit LEI at www.lean.org for more information.
Leave a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

A New Era of Jidoka: How ChatGPT Could Alter the Relationship between Machines, Humans, and their Minds
Article by Matthew Savas
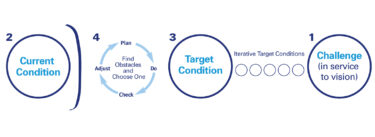
The Fundamentals of Improvement and Coaching Kata
Article by Lean Leaper

Ask Art: Why is a Lean Sensei Necessary?
Article by Art Byrne
Related books

The Power of Process – A Story of Innovative Lean Process Development
by Eric Ethington and Matt Zayko
The Gold Mine (Audio CD)
by Freddy Ballé and Michael Ballé
Related events
June 12, 2024 | Morgantown, PA
Building a Lean Operating and Management System
September 11, 2024 | Plant City, Florida and Gainesville, Florida
Lean Warehousing and Distribution Operations
Explore topics.
Subscribe to get the very best of lean thinking delivered right to your inbox
Privacy overview.

IMAGES
VIDEO
COMMENTS
The following case studies of lean management principles in action show you how a variety of real businesses solved real business problems under diverse conditions. ... After talking a lean tools approach to change, management re-organized the transformation around problem solving and process improvement to create a culture that engaged people ...
Historical context of Lean Change Management Model . ... Read more about: Change Management Case Study - Toyota. 2. Emergence of Lean Manufacturing (1980s): Lean principles gained global recognition after researchers at MIT studied Toyota's approach in the 1980s, coining the term 'Lean Manufacturing'. This methodology emphasized ...
Understand how to apply Agile and Lean techniques to Change Management. How to reframe resistance to change to response to change. Combine ideas from Lean Startup, Agile, OD and CM to develop your own contextual change framework. How to use light-weight planning and measurement tools such as Change Canvases, OKRs, Perspective Mapping and more.
Read more about: Change Management Case Study - Toyota. 3. Late 20th Century: Widespread Adoption and Evolution ... The Future Trends in Lean Change Management. The future of Lean Change Management is shaped by various evolving factors, especially technological advancements, changing business landscapes, and the evolving nature of work. ...
An Agile Approach to Change Management. Summary. In the wake of Covid-19, organizations are fundamentally rethinking their product and service portfolios, reinventing their supply chains, pursuing ...
Instead, you can rethink what it means to be in the retail-banking business, or the industrial-distribution business, or the office-cleaning business. Yet little did I know that some of the most ...
Five Case Studies of Transformation Excellence. November 03, 2014 By Lars Fæste , Jim Hemerling , Perry Keenan, and Martin Reeves. In a business environment characterized by greater volatility and more frequent disruptions, companies face a clear imperative: they must transform or fall behind. Yet most transformation efforts are highly complex ...
All files relevant for the case study
In theoretical terms, this study contributes by providing, from the lens of process effectiveness, the "seed" to facilitate the change to "become lean" in the public management area, as demonstrated by Radnor and Walley (2008). The findings of this study reveal a relevant relation between the two forms of management, and that Lean ...
Overview of the Case Study for the last session
Starbucks Change Management Case Study. Tahir Abbas March 4, 2023. Change is a constant in any business, and successful organizations must adapt to changes in the industry, market, and consumer preferences to remain competitive. The ability to manage change is crucial to the survival of businesses in today's dynamic market environment.
Change management is pivotal in guiding organizations through transitions, ensuring impactful and long-lasting results. For example, a $28B electronic components and services company with 18,000 employees realized the importance of enhancing its processes. They knew to adopt more streamlined, efficient approaches, known as Lean initiatives.
Save. Summary. Toyota has fared better than many of its competitors in riding out the supply chain disruptions of recent years. But focusing on how Toyota had stockpiled semiconductors and the ...
This section provides a brief overview of Lewin's Three-Step Model for Change and the Lean System Approach to change. Lewin's Three-Step Model for Change Healthcare organizations are complex adaptive systems where change is a complex process with varying degrees of complexity and agreement among disciplines. The Change Model.
To provide Perspectives and Points of View on how Lean can be Designed, Developed and Deployed in Large as well as Smaller and Medium sized organizations. 11:00 Kick-off the Webinar Debbie and Scott: Contextual Framework for thinking about Lean Transformations Gabe Case Sharing from Apache Helicopter Plant Jon Case Sharing from Sutphen
The researcher was not naive about lean, hence this was a case-study approach as opposed to a grounded theory approach. ... The second case (B) was a lean change management role for a business providing moderately customised products for the construction industry lasting 11 months with follow up 13 months after the embedment. These cases ...
In the case study, a Lean Management approach was pursued through the re-engineering of the production flow and the implementation of a pull-based system. Results from the case study show that it was a successful choice: efficiency KPIs, Works in Process, Cycle Time, etc. were dramatically improved.
Conversely, for lean construction, the lack of a clear vision, lack of leadership skills, low engagement of stakeholders, and poor communication are the main causes of change management failure. In the case study, the factors were scored differently by the interviewees, which explains why some factors may be more critical while others are less ...
Lean Change is revolutionizing the world of change management with lean, agile, and design thinking. We are leading the charge in AI change management solutions. ... Bringing you a real-life case study from my experience, along with a meaningful dialogue with you, around responding to change. Join me Wednesday 15 June 1230 - 1330 CEST.
Coherently with the aim of the research is to demonstrate a successful implementation of Lean tools in the healthcare sector for improving operational performance, a case study will be presented. The methodology used here is the single case study [ 20 ], considered the most appropriate one to address the starting research objective.
Change Management Case Study- Toyota. Tahir Abbas March 5, 2023. Change management is a critical aspect of any organization's success, especially in today's fast-paced and constantly evolving business environment. One company that has been widely recognized for its innovative and successful approach to change management is Toyota.
The case study shows the importance of the lean introduction strategy and contextual factors for successful lean implementation. Furthermore, it shows how both factors influence each other, underlining the dynamism of the organizational system. ... a commitment by management, and a culture of change in the entire organization [5, 16, 26 ...
The Lean Enterprise Institute (LEI) teaches many of the lean management and lean healthcare concepts described above through workshops, Lean Summits, books and workbooks, and on its web site. Join LEI's Lean Community for lean management case studies, webinars, newsletters, thought-leading columns, and e-letters, and many other resources for ...