- Open access
- Published: 22 March 2021

Patient safety from the perspective of quality management frameworks: a review
- Amrita Shenoy ORCID: orcid.org/0000-0001-8355-7792 1
Patient Safety in Surgery volume 15 , Article number: 12 ( 2021 ) Cite this article
22k Accesses
3 Citations
1 Altmetric
Metrics details
Patient safety is one of the overarching goals of patient care and quality management. Of the many quality management frameworks, Beauchamp and Childress’s four principles of biomedical ethics presents aspects of patient centeredness in clinical care. The Institute of Medicine’s six aims for improvement encapsulates elements of high-quality patient care. The Institute of Healthcare Improvement’s Triple Aim focuses on three aspects of care, cost, and health. Given the above frameworks, the present review was designed to emphasize the initiatives the system has taken to address various efforts of improving quality and patient safety. We, hereby, present a contemplative review of the concepts of informed consent, informed refusal, healthcare laws, policy programs, and regulations. The present review, furthermore, outlines measures and policies that management and administration implement and enforce, respectively, to ensure patient centered care. We, conclusively, explore prototype policies such as the Delivery System Reform Incentive Payment Program that imbues the elements of quality management frameworks, Hospital-Acquired Conditions Reduction Program that supports patient safety, and Hospital Readmissions Reduction Program that focuses on curbing readmissions.
The logistics of patient care and healthcare management revolve around many aspects of optimized high-quality care. The Joint Commission (TJC), Malcolm Baldrige National Quality Award (MBNQA), and The Magnet Recognition Program signify healthcare accreditation, performance excellence, and nursing excellence, respectively [ 1 , 2 , 3 ]. TJC is the recognized global leader of healthcare accreditation [ 4 ]. It is an independent not-for-profit organization that offers an unbiased assessment of quality achievement in patient care and safety [ 4 ]. MBNQA is the nation’s highest presidential honor for performance excellence [ 5 ]. The Magnet Recognition Program designates organizations worldwide where nursing leaders successfully align their nursing strategic goals to improve the organization’s patient outcomes [ 6 ]. In addition to the above healthcare recognition, the Institute of Medicine (IOM) categorizes aspects of care delivery with its six aims for improvement [ 7 ]. The Institute of Healthcare Improvement’s (IHI's) Triple Aim comprises of three aspects: improving the experience of care, improving the health of populations, and reducing per capita costs of healthcare.
We, hereby, present a synthesis of how the perspectives of biomedical ethics, six aims for improvement, and the Triple Aim converge into a focal point of preserving patient safety and promoting improvement in care delivery. The present review elaborates and explains the clinical and managerial roles inherent in the logistics of patient safety in emergencies and non-emergencies. The impetus here is to exemplify existing policies supporting patient centeredness while preserving the parameters that improve patient care, preserve quality, and promote patient safety.
As one of the cornerstones of high-quality healthcare, patient safety is intrinsic to all healthcare professionals. Clinicians are involved in direct patient care. However, does that imply that policymakers, leadership, and managers are separate and distinct components not involved in patient safety? The answer to the above question is not likely because these entities devise and enforce policies to preserve and augment patient safety in communities, institutions, and departments. At the macro-level, policymakers devise and recommend healthcare policies that at the micro-level, leadership, management, and clinicians enforce, adopt, and practice, respectively, at the point of patient care.
Research questions and objectives
Past literature establishes quality management frameworks such as Beauchamp and Childress’s Principles of Biomedical Ethics, six aims for improvement and the Triple Aim. The above frameworks, broadly, capture the patient’s needs/preferences while aligning with improvement in care delivery. However, there are instances in which patients when presented in an unconscious or inebriated state cannot communicate their treatment preferences. Given the above case, the first research question is: what are some recourses that providers can choose to adopt as safe harbors while treating such patients? The second research question is: what are the practices that clinicians could potentially adhere when the patient consents or refuses to consent? As a close follow-up, the third research question is: what is the role of administration in implementing policies that fall outside the purview of already enforced laws? The objective of the present review is threefold. First, we aim to propose answers to the dos and don’ts that clinicians could potentially adopt in emergency and non-emergency cases, given the concepts of informed consent and informed refusal. Second, we attempt to explain how hospital leadership can best facilitate patient safety and manage risk while facilitating high-quality patient care. Finally, we explore prototype policies such as the Delivery System Reform Incentive Payment program, Quadruple Aim, Hospital-Acquired Conditions Reduction Program, and Hospital Readmissions Reduction Program which have been implemented more recently as systemic initiatives to preserve patient safety and promote measures in care delivery.
Literature review
Quality management frameworks preserving patient safety: an overview of three established frameworks, beauchamp and childress’s principles of biomedical ethics.
Faculty in medicine and surgery have a substantial role in ethically creating a culture of safety via medical and surgical treatments for patients. In this context, four principles of biomedical ethics come into the picture. Those principles are autonomy, non-maleficence, beneficence, and justice [ 9 ]. The above four principles are the four pillars of medical ethics and form the basis of ethical practice in medicine and surgery. Some more aspects of biomedical ethics stemming from the above four principles are considered in ethical medical and surgical decision making [ 10 ]. A list of those additional aspects are as follows: [ 10 ].
Truthfulness, Full Disclosure, and Confidentiality: On the one hand, truthfulness is not distorting facts while presenting information to the patient; full disclosure is accurately and completely informing the details of the patient’s medical condition. On the other hand, confidentiality is the principle of not revealing information about the patient’s medical condition to third parties [ 10 ].
Autonomy and Freedom: Autonomy is the principle of providing the patient discretion, freedom, and independence to choose treatment preferences. This concept particularly comes into the spotlight in end-of-life hospice treatments and medical terminations of pregnancies [ 10 ].
Beneficence is the principle of doing good and inflicting the least harm to the patient.
The Institute of medicine’s six aims for improvement model
The Agency for Healthcare Research and Quality (AHRQ) Patient Safety Network expands upon the definition of prevention of harm as, “freedom from accidental or preventable injuries produced by medical care” [ 11 ]. Furthermore, the IOM introduced six aims for improvement in healthcare to meet the patient’s healthcare needs and preserve patient safety. Those six aims are as follows: [ 7 ].
Safe: avoiding injuries to patients from the care that is intended to help them. Patient safety can be a system-wide approach when patients see measures adopted and practiced that create a safe environment [ 7 ].
Efficient: avoiding waste including waste from equipment, supplies, ideas, and energy. Healthcare wastes are also in the form of defensive medicine, malpractice litigation, systemic complexities, and administrative fraud and abuse. Cost-effective care potentially supports efficiency in healthcare [ 7 ].
Effective: providing services based on scientific knowledge to all those who could benefit. In this context, Evidence Based Medicine is incorporating scientific knowledge into treatment and procedure options [ 7 ].
Patient-centered: providing care that is respectful of and responsive to the patient’s needs, preferences, and values. Delivery of care is considered to be patient-centered when the patient can choose certain aspects of care. This approach towards patient care prospectively ingrains elements of cooperation and collaboration [ 7 ].
Timely: reducing waiting times and detrimental delays for both, recipients and providers of care. Waits and harmful delays potentially produce life threatening illnesses worsening quality outcomes throughout the continuum of a patient care [ 7 ].
Equitable: providing care that is consistent and does not vary in quality based on personal aspects such as gender, ethnicity, geographic location, and socioeconomic status, etc. [ 7 ].
As per the IOM’s six aims for improvement, first, healthcare processes need to be safe which implies the provider makes an active attempt to ensure patient safety. Second, patient care prospectively needs to be aligned with recent developments to be potentially effective. Third, patient-centered care takes into consideration the patient’s culture, dietary and personal preferences incorporated into care delivery methods. The above concept plays an important role in end-of-life or hospice care provided to the elderly. Fourth, timeliness is providing and receiving care in a manner that reduces waiting times and delays. On the one hand, unforeseen wait periods may delay care and result in serious unintended harm to patients. On the other hand, the provision of timely care is essential to patient safety. Fifth, focusing on eliminating wastes and redundant processes could potentially help conserving resources and making care more affordable. Finally, providing equitable care is that which does not vary in terms of race, ethnicity, socioeconomic status, and income [ 7 ].
The Institute of healthcare improvement’s triple aim model
The Institute of Healthcare Improvement’s (IHI’s) Triple Aim model synthesizes and incorporates aspects of care, cost, and health [ 8 ]. The IHI’s Triple Aim model involves the following three components: [ 8 ].
Improving the experience of care: Implementing Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) and Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys are few of the many ways of recording patient experience of care [ 12 , 13 ]. The National Practitioner Data Bank (NPDB), additionally, assists in promoting quality health care and deterring fraud and abuse within health care delivery systems [ 14 ].
Reducing per capita costs of care: Cost of care could be reduced with the help of using generic drugs instead of brand name drugs for prescriptions, as an example [ 8 ].
Improving the health of populations [ 8 ].
The IHI's Triple Aim is a framework that describes an approach with a threefold purpose. First, improving the experience of care regarding healthcare quality, second, decreasing per capita costs of care that aims at reducing wastes and variation in healthcare, and third, improving the health of populations. The IHI’s Triple Aim model has universal applications that cover medical treatment, surgical care, therefore, opening avenues to solve administrative complexities for preserving health and wellness in populations.
The first component of the Triple Aim, improving the experience of care applies to advances in medical technology making a positive impact in the patient experience of care [ 8 ]. The second component of the Triple Aim, reducing per capita costs of care, applies to implementing telemedicine and telehealth projects, as an example. Telemedicine brings to fruition, efficient and timely care when physicians may not be in the vicinity of the patient [ 8 ]. On the one hand, one of pros of telemedicine is the potential to enhance access to care. On the other hand, it introduces this concept to some practitioners and patients who have little to no experience with e-health. The third component of the Triple Aim, improving the overall health of the population applies to facilitating a combination of the above two aims. The IHI’s Triple Aim model, therefore, is a three-pointed framework in which the first two aims are intrinsic to the third aim, improving population health [ 8 ].
The roles of clinical faculty and administration in patient safety: adoption and implementation of best practices in emergency and non-emergency cases
Emergency Medical Treatment and Active Labor Act (EMTALA) is a federal law that requires anyone coming to an emergency department to be stabilized and treated, regardless of their insurance status or ability to pay [ 15 ]. As per EMTALA, the patient has a right to be treated and clinicians are bound to provide treatment [ 15 ]. In this context, let us consider an example of an unconscious patient in the emergency department that does not culturally prefer receiving blood transfusions. In the above case, hypothetically, if the treating provider is not knowledgeable of the cultural preference of the unconscious patient and proceeds to revive the patient via a blood transfusion, then, was patient centered care provided? The answer likely lies in the provider’s assessment in the context of EMTALA. The assessment, first and foremost, relates to the binding duty of the clinician to provide care to every patient, especially in times of emergencies.
The dynamics of the above hypothetical scenario entirely changes in non-emergency situations in which patients can choose a provider to treat them; and reciprocally, even providers can choose whom to treat. The rationale behind this is the physician-patient relationship that specifies the terms and conditions of a physician-patient contract [ 16 ]. This legal relationship is based on contract principles because the physician agrees to provide treatment in return for payment in the presence of the contract [ 16 ]. The law usually imposes no duty on the physician to treat the patient in the absence of a physician-patient contract [ 16 ].
In the process of providing treatment, obtaining informed consent is the concept in which the clinician explains the proposed line of treatment, duration, benefits, risks of opting in as well as opting out of the treatment, alternatives to the proposed treatment with an opportunity to answer patient questions [ 17 ]. In 1914, an American judge Benjamin Cardozo composed the foundational principle of informed consent as, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault for which he is liable in damages” [ 18 ]. An interesting aspect of treatment in non-emergency cases is when the patient does not agree to informed consent which brings forth the concept of “Informed Refusal” [ 19 , 20 ]. A living will is an example of an informed refusal document in which the patient states his or her end of life preferences [ 21 ]. In the above case, the provider honors the patient’s end of life preferences and/or withholds treatment for the patient as specified in the living will.
The role of leadership is to enforce EMTALA and help clinicians' awareness of informed consent and informed refusal processes in organizations. Moreover, they ensure that providers implement the above policies regarding patient preferences. In medical cases that fall outside the purview of the already enforced laws, leadership can prospectively make rules but with caution that those rules are not against public policy.
Macro-level healthcare programs focusing on patient safety: prototype policies
Delivery system reform incentive payment program: focusing on alignment with quality management frameworks.
The Delivery System Reform Incentive Payment (DSRIP) program is one prototype policy that incorporates six aims for improvement and the Triple Aim model. DSRIP has multiple healthcare projects that improve health statuses incorporating numerous metrics and milestones in primary care, specialty care, chronic care, navigation and case management, disease prevention and wellness, and general categories [ 23 , 24 ]. These projects are reimbursed by the State Department of Health in a systematic manner when adopted by healthcare institutions [ 22 , 23 , 24 , 25 , 26 ].
DSRIP’s framework involves four components: (1) Infrastructure Development, (2) Program Innovation and Redesign, (3) Quality Improvement, and (4) Improvement in Population Health in states where its projects are implemented [ 22 , 23 , 24 , 25 , 26 ]. In its third year of implementation, the Texas DSRIP program in the southeastern county region had about 172 projects in eight cohorts those being, primary care, emergency care, chronic care, navigation/case management, disease prevention and wellness, behavioral health/substance abuse prevention, and general.[ 22 , 23 , 25 ] Each cohort had a set number of projects that involve meeting patient care milestones and metrics, simultaneously incorporating IOM’s six patient care aims of medical care being safe, efficient, effective, patient centered, timely, and equitable [ 22 , 23 , 24 , 25 ].
DSRIP, with all its projects implemented in the adopted regions and counties has been measured to improve population health [ 25 ]. A metric of measuring improvement in population health within the DSRIP program was preventable hospitalization rate [ 24 ]. The decrease in preventable hospitalization rates may have been attributed to the inherent design and dynamics of the DSRIP policy [ 23 , 24 ]. Those dynamics comprised of factors such as physician-administrator collaboration, mechanisms of incentive payments, types of measures for reporting outcomes in quality, and interplaying healthcare externalities [ 24 ]. In the adopted regions and counties, a statistically significant decrease in preventable hospitalization rates was observed when tested with an interrupted time series method [ 25 ].
There were two phases of the Texas DSRIP program, DSRIP 1.0 and 2.0. It was in DSRIP 2.0 that comprehensive Diabetes Care: eye exam metric improved by 16 % while Influenza immunization improved by 12 % in the latter [ 27 ]. Researchers Revere et al. have identified that in DSRIP 2.0, the metrics for Central Line Associated Bloodstream Infection (CLABSI) rates, Catheter Associated Urinary Tract Infections (CAUTI), and Surgical Site Infection (SSI) rates improved by 26 %, 10 %, and 9 %, respectively [ 27 ].
Quadruple aim framework: focusing on the evolution of the triple aim
The Triple Aim, formulated in 2008, drew focus on three aims which were based on care, cost, and health. Sikka and colleagues, in 2015, constructed a fourth aim, improving the experience of providing care. This was made to acknowledge the importance of physicians, nurses, and all employees in “finding joy and meaning in their work and in doing so improving the experience of providing care” [ 28 ]. At the core of the fourth aim is the experience of joy and meaning in providing care making it synonymous with acquiring accomplishment and meaning in their contributions. The Quadruple Aim has broad implications in theory and practice factoring inclusiveness in terms of all members in the healthcare workforce [ 28 ].
Hospital-Acquired conditions reduction program: focusing on patient safety
The Hospital-Acquired Conditions Reduction Program (HACRP) is a Medicare pay-for-performance program that supports the CMS’ long-standing effort to link Medicare payments to healthcare quality in the inpatient hospital setting [ 29 ]. HACRP focuses on specific conditions that the Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) healthcare- associated infection (HAI) measures which are: [ 30 ] (1) Central Line Associated Blood Stream Infection (CLABSI), (2) Catheter Associated Urinary Tract Infection (CAUTI), (3) Surgical Site Infection (SSI) for colon and hysterectomy, (4) Methicillin-Resistant Staphylococcus Aureus (MRSA) bacteremia, (5) Clostridium Difficile Infection (CDI).
Additionally, eight Patient Safety Indicators (PSIs) included in the program comprise of: [ 31 ] (1) PSI 03 - Pressure Ulcer Rate, (2) PSI 06 - Iatrogenic Pneumothorax Rate (3) PSI 07 - Central Venous Catheter-Related Bloodstream Infection Rate, (4) PSI 08 - Postoperative Hip Fracture Rate, (5) PSI 12 - Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate, (6) PSI 13 - Postoperative Sepsis Rate, (7) PSI 14 - Postoperative Wound Dehiscence Rate, (8) PSI 15 - Accidental Puncture or Laceration Rate.
Hospital readmissions reduction program: focusing on patient safety
The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that reduces payments to hospitals with excess readmissions. The program supports the national goal of improving healthcare by linking payment to the quality of hospital care [ 32 ]. HRRP has a specific focus on the following conditions to reduce readmissions that in turn improve patient safety [ 32 ]. Those conditions are as follows: [ 32 ] (1) Acute Myocardial Infarction (AMI), (2) Chronic Obstructive Pulmonary Disease (COPD), (3) Heart Failure (HF), (4) Pneumonia (5) Coronary Artery Bypass Graft (CABG) surgery, and (6) Elective Primary Total Hip Arthroplasty and/or Total Knee Arthroplasty (THA/TKA) [ 32 ].
The purpose of the present review was to analyze patient safety through the lens of the above quality management frameworks. We, specifically, illuminated policies and laws such as EMTALA, informed consent, informed refusal, and living will as examples. In emergency cases, the rules of EMTALA apply whereas in non-emergency cases, the same applies to obtaining informed consent from the patient. In the event the patient refuses treatment, documenting the informed refusal would be ideal. We underscored selective new prototype policies percolating from national policymaking to institutional levels with a focus on the initiatives the system has actively taken to preserve patient safety and promote improvement in care delivery.
Facts about The Joint Commission. Retrieved from https://www.jointcommission.org/about_us/about_the_joint_commission_main.aspx . Accessed 16 Feb 2021
Malcolm Baldrige Award. Retrieved from https://baldrigefoundation.org/ . Accessed 16 Feb 2021
Magnet Recognition Criteria. Retrieved from https://www.mghpcs.org/PCS/Magnet/Documents/Education_Toolbox/01_Intro-Ovrvw/Magnet-Overview-2017.pdf . Accessed 16 Feb 2021.
The Joint Commission is the recognized global leader of healthcare accreditation and offers an unbiased assessment of quality achievement in patient care and safety Retrieved from: https://www.jointcommission.org/accreditation-and-certification/why-the-joint-commission/ . Accessed 16 Feb 2021
The Malcolm Baldrige National Quality Award being the nation's highest presidential honor for performance excellence. Retrieved from: https://asq.org/quality-resources/malcolm-baldrige-national-quality-award . Accessed 16 Feb 2021
The Magnet Recognition Program’s alignment of nursing strategic goals to improve the organization’s patient outcomes. Retrieved from: https://www.nursingworld.org/organizational-programs/magnet/ . Accessed 16 Feb 2021
The Institute of Medicine Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academies Press (US); 2001.
Google Scholar
Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff. 2008;27(3):759–69.
Article Google Scholar
Page K. The four principles: Can they be measured and do they predict ethical decision making? BMC Med Ethics. 2012;13(1):10.
Landau R, Osmo R. Professional and personal hierarchies of ethical principles. Int J Soc Welfare. 2003;12(1):42–9.
Mitchell PH. Defining patient safety and quality care. In: Hughes RG, editor Patient safety and quality: An evidence-based handbook for nurses. Rockville: Agency for Healthcare Research and Quality (US); 2008. Chapter 1. NBK2681.
Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Survey of Patient Perspectives. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS . Accessed 16 Feb 2021.
Consumer Assessment of Healthcare Providers and Systems (CAHPS) Survey assessing patient experience. Retrieved from https://www.ahrq.gov/cahps/about-cahps/cahps-program/index.html . Accessed 16 Feb 2021
National Practitioner Data Bank Web site. Retrieved from: https://www.npdb.hrsa.gov/topNavigation/aboutUs.jsp . Accessed 16 Feb 2021.
Emergency Medical Treatment and Labor Act (EMTALA). Retrieved from https://www.acep.org/life-as-a-physician/ethics--legal/emtala/emtala-fact-sheet/ . Accessed 16 Feb 2021.
Showalter JS. The Law of Healthcare Administration. Eighth Edition. Chicago, Washington, DC: Health Administration Press; 2017.
Boland GL. The doctrines of lack of consent and lack of informed consent in medical procedures in Louisiana. La L Rev. 1984;45:1.
Alexis O, Caldwell J. Administration of medicines–the nurse’s role in ensuring patient safety. Brit J Nurs. 2013;22(1):32–5.
Wagner RF Jr, Torres A, Proper S. Informed consent and informed refusal. Dermatol Surg. 1995;21(6):555–9.
Ridley DT. Informed consent, informed refusal, informed choice–what is it that makes a patient’s medical treatment decisions informed? Med Law. 2001;20(2):205–14.
CAS PubMed Google Scholar
Emanuel L. Living wills can help doctors and patients talk about dying. West J Med. 2000;173(6):368–9. https://doi.org/10.1136/ewjm.173.6.368 .
Article CAS PubMed PubMed Central Google Scholar
Shenoy A, Revere L, Begley C, Linder S, Daiger S. The Texas DSRIP program: An exploratory evaluation of its alignment with quality assessment models in healthcare. Int J Healthcare Manage. 2017;12(2):165–72. https://doi.org/10.1080/20479700.2017.1397339 .
Begley C, Hall J, Shenoy A, Hanke J, Wells R, Revere L, Lievsay N. Design and implementation of the Texas Medicaid DSRIP program. Popul Health Manag. 2017;20(2):139–45.
Shenoy A, Begley C, Revere L, Linder S, Daiger SP. Delivery system innovation and collaboration: A case study on influencers of preventable hospitalizations. Int J Healthcare Manage. 2017:1–8. DOI: https://doi.org/10.1080/20479700.2017.14057772017.1405777
Shenoy AG, Begley CE, Revere L, Linder SH, Daiger SP. Innovating patient care delivery: DSRIP’s interrupted time series analysis paradigm. Healthcare. 2019;7(1):44–50. https://doi.org/10.1016/j.hjdsi.2017.11.004 .
Article PubMed Google Scholar
Shenoy AG. DSRIP’s innovation and collaboration in population health management: A cross-sectional segmented time series model. Health Serv Manage Res. 2020;33(1):2–12. https://doi.org/10.1177/0951484819868679 .
Revere L, Kavarthapu N, Hall J, Begley C. Achieving triple aim outcomes: An evaluation of the Texas medicaid waiver. Inquiry. 2020;57:46958020923547. https://doi.org/10.1177/0046958020923547 .
Sikka R, Morath JM, Leape L. The Quadruple aim: care, health, cost and meaning in work. BMJ Qual Safety. 2015;24:608–10.
Hospital Acquired Conditions Reduction Program. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-ServicePayment/AcuteInpatientPPS/HAC-Reduction-Program . Accessed 16 Feb 2021.
HACRP List of Conditions. Retrieved from https://qualitynet.cms.gov/inpatient/hac Accessed 16 Feb 2021.
List of PSI 90. Retrieved from https://www.qualityindicators.ahrq.gov/Modules/PSI_TechSpec_ICD10_v2020.aspx . Accessed 16 Feb 2021
Hospital Readmissions Reduction Program. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program . Accessed 16 Feb 2021
Download references
Acknowledgements
Not applicable.
Conflict of interest and financial disclosure statement
The authors collectively declare that there is no conflict of interest and have no financial interests with any sponsoring organization, for-profit or not-for-profit.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
College of Public Affairs, School of Health and Human Services, Healthcare Administration Program, University of Baltimore, 1420 N. Charles Street, MD, 21201, Baltimore, USA
Amrita Shenoy
You can also search for this author in PubMed Google Scholar
Contributions
The author read and approved the final manuscript. AS conducted the literature search and review, drafted the manuscript and responded the reviewer's comments.
Authors' information
Dr. Amrita Shenoy is an Assistant Professor of Healthcare Admin-istration at the University of Baltimore and the Winner of the 2011 McGraw-Hill/Irwin Distinguished Paper Award. She leverageseconometrics to quantify policy impact and qualitatively exploreshealthcare laws and policies for a deeper comprehension of its ana-lytical spectra. Dr. Shenoy received her PhD from the University ofTexas Health Science Center at Houston School of Public Health,MHA/MBA from the University of Houston — Clear Lake and MScfrom Nottingham Trent University, United Kingdom. Her researchareas spotlight topics in healthcare law, policy, and quality with abroad emphasis on public health and healthcare management.
Corresponding author
Correspondence to Amrita Shenoy .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval and consent to participate on data involving the use of any animal/human tissue Not applicable
Consent for publication
Not applicable
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shenoy, A. Patient safety from the perspective of quality management frameworks: a review. Patient Saf Surg 15 , 12 (2021). https://doi.org/10.1186/s13037-021-00286-6
Download citation
Received : 04 January 2021
Accepted : 23 February 2021
Published : 22 March 2021
DOI : https://doi.org/10.1186/s13037-021-00286-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality management frameworks
- IOM’s six aims for improvement
- IHI’s Triple Aim
- Patient safety
- Patient centeredness
- High‐quality clinical care
Patient Safety in Surgery
ISSN: 1754-9493
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 05 December 2019
Networked information technologies and patient safety: a protocol for a realist synthesis
- Justin Keen 1 ,
- Joanne Greenhalgh 2 ,
- Rebecca Randell 3 ,
- Peter Gardner 4 ,
- Justin Waring 5 ,
- Roberta Longo 1 ,
- Jon Fistein 1 ,
- Maysam Abdulwahid 1 ,
- Natalie King 1 &
- Judy Wright 1
Systematic Reviews volume 8 , Article number: 307 ( 2019 ) Cite this article
1852 Accesses
3 Citations
1 Altmetric
Metrics details
There is a widespread belief that information technologies will improve diagnosis, treatment and care. Evidence about their effectiveness in health care is, however, mixed. It is not clear why this is the case, given the remarkable advances in hardware and software over the last 20 years. This review focuses on interoperable information technologies, which governments are currently advocating and funding. These link organisations across a health economy, with a view to enabling health and care professionals to coordinate their work with one another and to access patient data wherever it is stored. Given the mixed evidence about information technologies in general, and current policies and funding, there is a need to establish the value of investments in this class of system. The aim of this review is to establish how, why and in what circumstances interoperable systems affect patient safety.
A realist synthesis will be undertaken, to understand how and why inter-organisational systems reduce patients’ clinical risks, or fail to do so. The review will follow the steps in most published realist syntheses, including (1) clarifying the scope of the review and identifying candidate programme and mid-range theories to evaluate, (2) searching for evidence, (3) appraising primary studies in terms of their rigour and relevance and extracting evidence, (4) synthesising evidence, (5) identifying recommendations, based on assessment of the extent to which findings can be generalised to other settings.
The findings of this realist synthesis will shed light on how and why an important class of systems, that span organisations in a health economy, will contribute to changes in patients’ clinical risks. We anticipate that the findings will be generalizable, in two ways. First, a refined mid-range theory will contribute to our understanding of the underlying mechanisms that, for a range of information technologies, lead to changes in clinical practices and hence patients’ risks (or not). Second, many governments are funding and implementing cross-organisational IT networks. The findings can inform policies on their design and implementation.
Systematic review registration
PROSPERO CRD42017073004
Peer Review reports
There is a widespread belief, particularly among policy makers, that information technologies will improve diagnosis, treatment and care [ 1 ]. Evidence about the effectiveness of a range of IT applications is, however, mixed [ 2 , 3 , 4 , 5 ]. A comprehensive review by Brenner and colleagues covered a number of technologies and focused on safety-related end-points including mortality, infection rates and medication error rates [ 2 ]. Twenty-five out of 69 studies included in their review reported a statistically significant positive effect. The other 44 studies reported no or negative effects. More recent systematic reviews report broadly similar findings [ 6 , 7 ]. Authors stress that evidence is uneven in both coverage and quality, and care needs to be taken in interpreting the findings, but the general picture is clear.
There is, therefore, a need to understand why the evidence has, to date, fallen short of expectations. We seek to shed light on the question in this systematic review. It focuses on the effects of a particular class of IT systems, interoperable systems, on patient safety. The term ‘system’ here refers to the combination of technologies and the people who used them. In a well-designed system, technologies are seamlessly integrated into users’ working practices. In poorly designed systems, in contrast, the technologies do not fit easily into users’ working practices, and in the worst cases can make it more difficult to deliver safe treatment and care. The term ‘interoperable’ refers to the ability of any two or more IT systems to exchange data, and for the receiving system to make use of the data. The IT systems of interest in this protocol allow professionals to access patients’ records held in other organisations.
Policy makers’ assumptions
Many people who live in their own homes, and who are frail or have chronic health problems, need support from a range of professionals. These include general (or family) practitioners, community nurses, therapists, social workers, and planned and emergency hospital services. There is good evidence that treatment and care is often fragmented [ 8 , 9 , 10 ]. Linking IT systems across a health economy can, policy makers reason, help to improve the coordination of services. Professionals can, the thinking goes, use the IT networks to communicate with one another, and hence effectively coordinate a patient’s treatment and care. The value of this function might be particularly evident at transition points, for example in a health emergency or at the point of returning from hospital to home. The IT systems can also be designed to enable access to all parts of a patient’s record, so that professionals can search for and locate information wherever it is held. The Obama administration in the USA committed considerable sums to linking hospital, family physician, pharmacy and other IT systems. Similarly, and more recently, the National Health Service in England has emphasised the importance of linking hitherto fragmented IT systems across organisations in local health economies [ 11 , 12 ].
- Realist synthesis
This protocol describes a realist synthesis, which seeks to understand how and why inter-organisational IT systems reduce patients’ clinical risks, or fail to do so. The realist synthesis method involves opening up the ‘black box’ of events that lie between an intervention and its effects [ 13 , 14 ]. It does so by identifying programme theories: these are sequences of decisions and actions that capture the intended effects of an intervention, and the underlying logic that links them together. A number of initial theories are typically identified.
Literature searches are then designed. It is not usually feasible to identify evidence about all of the sequences in all of the theories. Searches therefore focus on two or three theories, or on key sequences within those theories. Empirical evidence is then identified, assessed and synthesised, in order to evaluate the actual steps in the sequences. The evidence can, in addition, lead teams to realise that a programme is effective, but not in the way originally envisaged. A programme theory therefore needs to be reformulated. More searches may then be needed, to evaluate elements of the revised theory. That is, the cycle of programme theory formulation and evaluation can be iterative and—resources permitting—pursued until a settled, evidence-based account has been identified [ 15 ].
There are literatures that will enable us to develop and evaluate programme theories [ 16 ]. For example, the computer-supported cooperative work literature sits at the intersection of computer science and psychology, and is a source of evidence about the inter-relationships of IT systems and peoples’ working practices. A comprehensive review suggests that we have a reasonable understanding of the design features and organisational settings that are associated with the effective integration of systems into clinical working practices [ 17 ]. Similarly, there are literatures on health professionals’ decisions and actions, and their consequences for patients’ clinical risks. In particular, there is a substantial literature based on retrospective analysis of adverse events, both in health care and other sectors [ 18 ].
This protocol has been written in accordance with PRISMA-P guidelines [ 19 ].
We will undertake a realist synthesis. The aim of the study is to establish how, why and in what circumstances networked, inter-organisational IT systems affect patient safety. The objectives of the study are to:
Identify initial programme theories and prioritise theories to review;
Search systematically for evidence to test and refine the theories;
Undertake quality appraisal and use included texts to support, refine or reject programme theories;
Synthesise the findings;
Disseminate the findings to a range of audiences.
The following sections focus on the first four objectives.
Stage 1: Identification of programme and mid-range theories
This stage is essentially developmental in nature. The first step in this review will be to construct one or more programme theories, concerning the use of networked IT systems and their effects on patient safety. Mid-range theories, which are usefully thought of as a broader class of theory than programme theories, and which will be used to generalise findings at the end of the review, will also be identified. We will supplement our existing knowledge of candidate theories with literature searches to define and develop them. The programme theories will determine the scope (inclusion and exclusion criteria) for the searches and synthesis in the following stages, which will be used to support, refine or reject each theory examined.
Search strategy and information resources
Theories can be explicitly mentioned in research articles and policy documents, or they can be implied in the introductory or discussion sections of documents. They can also be found in commentaries and opinion pieces. We will use conventional literature searching using free text words, synonyms and subject index terms, and some CLUSTER searching techniques (identifying a few key relevant studies and finding further relevant studies via forwards and backwards citation searches, author searches, searching for reports of a particular project) [ 20 ]. Using this combined approach, we aim to identify literature that leads us to theories or fragments of theories that can be used to construct programme and mid-range theories.
We anticipate that three searches will supplement the policy documents and academic literature already known to the project team. MEDLINE (1946–present) and EMBASE (1947–present) will be searched as a core set of databases for all of the theory generating searches.
Background search of systematic reviews . We will search for systematic reviews that link IT systems and patient safety. This will identify any reviews on this topic that have been published since our scoping review, undertaken before the start of the project. The reviews may describe programme theories or fragments in their introduction or discussion sections, providing insights into the sequences of events linking the intervention and outcomes. We will search the core databases plus the Cochrane Database of Systematic Reviews, the Epistemonikos database and Health Systems Evidence (McMaster University). An example MEDLINE search strategy containing a full set of search terms is available in the Additional file 1 (Search 1).
Policies, opinion pieces and research reports . We will search the core databases plus Health Management Information Consortium (1983–present) and Web of Science - Science Citation Index (1990–present) for policy documents, opinion pieces (e.g. editorials) and reports describing leading theories about the relationships between IT systems and patient safety (Additional file 1 Search 2). We will also undertake Google searches to locate reports on key policies, e.g. about the Health Information Technology for Economic and Clinical Health (HITECH) Act 2009, a major US initiative promoting the implementation of cross-organisational IT networks.
Author search and Citation search . We will search for reports and articles authored by influential commentators in the core databases plus Health Management Information Consortium (1983–present), Web of Science - Science Citation Index (1990–present), Google Scholar and Scopus (1823–present). Literature by David Bates, the most cited author in the health informatics literature, and Robert Wachter, the author of an influential report on IT in the NHS in England, will be searched (Additional file 1 Search 3). Citation searching may be required due to the iterative nature of developing searches for a realist synthesis.
Inclusion, analysis and synthesis
The records identified in the searches will be saved and managed in an EndNote library. Details of all search activities (databases, websites, date of search, number of records found, search strategies) will be recorded in a timeline spreadsheet. The inclusion criteria for the three searches will be:
IT networks that link two or more organisations outside (but possibly including) hospitals;
IT networks that support direct treatment and care;
Arguments that identify relationships between IT networks and patient safety;
Published in the English language between 2000 and 2018.
Non-English language articles will not be included. The project does not have sufficient resources to translate the full text of articles that may be relevant. In conventional systematic reviews, it is not necessary to translate whole papers, as it is only necessary to identify defined data. In this review, however, we will be looking for data that might occur anywhere in a paper, and a full translation would be needed.
The exclusion criteria will be for studies that:
Describe hospital-only IT systems;
Describe systems that do not link two or more distinct services;
Focus on IT systems that support secondary uses of data, e.g for service planning, research;
are published before 2000;
are published in languages other than English.
Two reviewers (MA and JK) will first independently screen the titles and abstracts of the records for relevance and then assess full-text reports. Any discrepancies will be solved by discussion, and if needed consultation with a third author (JG or RR). Data extraction forms will be developed to capture basic details of studies—authors, publication year, etc.—and passages on theories and theory fragments.
The selected studies will be used to develop visual representations of programme theories, with accompanying text that explains the reasoning that underpins those theories. Experience gained in earlier reviews suggests that there are likely to be several programme theories at this point, and that some of them will be partial, in the sense that the chains of reasoning are ‘high level’ and not fully articulated, or only cover some of the steps linking networked information technologies and patient safety. Where available, claims about the reasons why programmes succeed or fail in practice will be used to annotate the representations.
The programme theories will be used as the basis for consultation with three groups of stakeholders—policy makers, senior IT managers and frontline clinicians. We will use the nominal group technique, which has been used in a previous realist study [ 21 ]. At the nominal group meetings participants will be asked to comment critically on the programme theories, on the basis of their knowledge and experience. They will also be asked to develop and then prioritise theories, or particular chains of reasoning within theories, for further study. The prioritisation will take into account the potential to provide learning for the NHS, and the types of networked systems that NHS organisations are implementing. The groups will be re-convened for consultation by email at the end of stage 4 (see below).
The outputs of the three groups will be further reviewed by a patient and public involvement (PPI) group, and discussed with our project steering group. Following these meetings, we will decide on the programme theories, and key elements of those theories, that we will explore in depth in stages 2–4.
Stage 2: Systematic search for evidence
The next stage of the review is a search for empirical studies to test and refine the leading programme theories identified in stage 1. The initial searches will be designed to identify evidence about the steps in the chains of reasoning in each theory. Literatures often focus on one or other section in a chain of reasoning, and as a result, individual searches will often focus on sections rather than a whole programme theory [ 22 ]. We will undertake searches using resources which span health and computing literatures including—but not limited to—MEDLINE (1946–present), EMBASE (1947–present), Web of Science Core Collection (1900–present) and INSPEC (1896–present).
We anticipate hand searching papers from leading conferences which are not indexed, for example Software Engineering in Healthcare workshops papers, from the International Conference on Software Engineering. The search strategies for identifying empirical evidence for programme theories can only be fully developed once the programme theories are agreed. However, we anticipate they will contain search concepts for an aspect of patient safety such as medication reconciliation, inter-organisational IT networks and evaluative studies.
The search results will be reviewed in stage 3 (evidence review, see below) and further searches will develop iteratively to follow lines of enquiry. Initial searches may not identify empirical evidence that supports or rejects a programme theory. If that happens, the search will be re-designed to capture empirical evidence that may be found in a different discipline or information resource. For example, we could extend the scope of our searches to look for evidence about other IT applications, including hospital-based systems, and/or extend the scope of the populations of interest. As in stage 1, these searches may use CLUSTER search techniques as an efficient method for finding relevant papers [ 20 ].
The results of the electronic searches and all references that are retrieved for stage 2 will be kept in the same EndNote library as those found during stage 1. Details of all search activities during stage 2 will be recorded in the timeline spreadsheet.
Stage 3: Evidence review and quality appraisal
Titles and abstracts of records identified, and the full-text papers selected in stage 2, will be independently screened by two reviewers (MA and JK) to identify those which contain evidence that sheds light on one or more elements of the programme theories identified in stage 1. The RAMESES I guidance states that:
An appraisal of the contribution of any section of data (within a document) should be made on two criteria: • Relevance – whether it can contribute to theory building and/or testing; and • Rigour – whether the method used to generate that particular piece of data is credible and trustworthy [ 14 ].
We will follow Rycroft-Malone and colleagues in developing criteria for judging relevance [ 23 ]. We will, further, use the mid-range theory developed in stage 1 to refine the criteria. Rigour refers to the requirement for an investigation to be of sufficient standard within type , whether that is a process evaluation, an ethnography or other type of study [ 14 ].
The empirical data for supporting and/or refuting programme theories will be extracted from the included studies. It is anticipated that a significant proportion of the evidence will be in the form of narrative data and will accordingly be copied into Word files. To maximise accuracy and transparency, a proportion of data extraction will be performed independently by two members of the research team.
Stage 4: Synthesis
Synthesis involves two distinct, but linked, activities. In the first, the empirical evidence identified in stages 2 and 3 will be used to evaluate the programme theories developed in stage 1. In the most straightforward case, the evidence will support the chains of reasoning in one programme theory and serve to reject alternative or competing theories. Less straightforwardly, the evidence might provide support for one part of a programme theory and adverse evidence for another part of the same theory. Or, it might not ‘fit’ a programme theory, neither supporting nor undermining it. Both instances suggest that there may be a problem with the programme theory itself and will lead us to refine it, to achieve a better fit between evidence and theory. On the basis of experience of earlier realist syntheses, we expect that at least one of the selected theories—or theory fragments—will be reasonably well supported by empirical evidence, and at least one will not be not supported.
Second, when a settled programme theory or theories have been produced, they will be interpreted in the broader context of the mid-range theory. This involves abduction, where inferences that lead to the best available explanation are identified. The details of the abductive reasoning processes vary from review to review, but a key point is that it involves inter-play between situation-specific programme theories and broader mid-range theory [ 24 ]. In the simplest case, the (now evidence-based) programme theories will be consistent with the mid-range theory. If we find that a programme theory holds across a number of settings (e.g. different combinations of health services and/or different patient groups), this will increase our confidence in it. Alternatively, evidence or argument (or both) may point in different directions, and the wider project team will use the mid-range theory to ‘adjudicate’ between contending programme theories.
Nominal group email consultation
The nominal groups will be re-convened for email consultation. We will summarise our findings to this point, including our provisional syntheses, and present them to the groups. They will be asked to comment on the findings, including whether any of the theories can be rejected, and whether any further searches are merited. The PPI group will also meet at the end of this stage and review the findings and interpretations of the three nominal groups. We will refine our interpretations on the basis of the comments of all four groups.
Policy makers in many countries believe that IT systems can contribute to safer patient care. Interoperable systems are currently being promoted by governments, and funding made available for their development, in many countries. As noted above, though, the empirical evidence about this belief is mixed, and it is not clear why this is the case. We are using the realist synthesis method because we believe that it will shed light on how and why interoperable systems contribute to reductions in patients’ clinical risks, and hence help to explain why the evidence is so mixed.
As with any evidence synthesis, there are risks and limitations associated with the method. The most obvious risk, in common with other review methods that focus on effectiveness, is that we are not able to identify high-quality effectiveness evidence. This will necessarily limit the extent to which we are able to explain ‘what works’ when interoperable systems are deployed. Another significant risk is the flip side of a potential strength. The explicit inclusion of theory in the method means that the basis for interpreting the available evidence is clear. But, there must be a risk that—however much care is taken—a sub-optimal theoretical framework will be used, and valuable insights foregone. If we are able to mitigate these risks in the course of the review, though, it should produce two main outcomes. First, the refined mid-range theory will contribute to our understanding of the underlying mechanisms that lead to changes in clinical practices and hence patients’ risks (or not). Second, many governments are funding and implementing cross-organisational IT networks. The findings can be used to inform policies on their design and implementation.
Availability of data and materials
This is a protocol for a systematic review. We will make all searches, and the results of those searches, available publicly when the review is completed. This will, again, require clearance by NIHR—but we do not anticipate any problems, given the nature of the study.
Agboola SO, Bates DW, Kvedar JC. Digital health and patient safety. JAMA. 2016;315(16):1697–8.
Article CAS Google Scholar
Brenner SK, et al. Effects of health information technology on patient outcomes: a systematic review. J Am Med Inform Assoc. 2016;23(5):1016–36.
Article Google Scholar
Black AD, et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med. 2011;8(1):e1000387.
Kruse CS, Beane A. Health information technology continues to show positive effect on medical outcomes: systematic review. J Med Internet Res. 2018;20(2):e41.
Chaudhry B, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–52.
Feldman SS, Buchalter S, Hayes LW. Health information technology in healthcare quality and patient safety: literature review. JMIR Med Inform. 2018;6(2):e10264.
Garavand A, et al. Factors influencing the adoption of health information technologies: a systematic review. Electron Physician. 2016;8(8):2713–8.
O’Hara JK, Aase K, Waring J. Scaffolding our systems? Patients and families ‘reaching in’ as a source of healthcare resilience. BMJ Qual Saf. 2019;28(1):3–6.
Care Quality Commission, Building bridges, breaking barriers. Newcastle upon Tyne: CQC, 2017.
Leigh Johnston DR, Dorrans S, Dussin L. A.T. Barker, Integration 2020: Scoping research. p. 2017.
Jacob JA. On the road to interoperability, public and private organizations work to connect health care data. JAMA. 2015;314(12):1213–5.
Bates DW. Health information technology and care coordination: the next big opportunity for informatics? Yearb Med Inform. 2015;10(1):11–4.
Pawson R. Evidence Based Policy: A Realist Perspective. London: Sage; 2006.
Book Google Scholar
Wong G, et al. Development of methodological guidance, publication standards and training materials for realist and meta-narrative reviews: the RAMESES (Realist And Meta-narrative Evidence Syntheses – Evolving Standards) project. Health Serv Del Res. 2014;2:30.
Google Scholar
Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage; 2013.
Pollock N, Williams R. Software and organisations. The biography of the enterprise-wide system or how SAP conquered the world. London: Routledge; 2009.
Fitzpatrick G, Ellingsen G. A review of 25 years of CSCW research in healthcare: contributions, challenges and future agendas. Comput Supp Coop Work (CSCW). 2013;22(4-6):609–65.
Vincent, C. and R. Amalberti, Safety strategies in hospitals, in Safer Healthcare. SpringerOpen, 2016, p. 73-91.
Moher D, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Booth A, et al. Towards a methodology for cluster searching to provide conceptual and contextual “richness” for systematic reviews of complex interventions: case study (CLUSTER). BMC Med Res Methodol. 2013;13:118.
Tolson D, et al. Developing a managed clinical network in palliative care: a realistic evaluation. Int J Nurs Stud. 2007;44(2):183–95.
Ball SL, Greenhalgh J, Roland M. Referral management centres as a means of reducing outpatients attendances: how do they work and what influences successful implementation and perceived effectiveness? BMC Fam Pract. 2016;17:37.
Rycroft-Malone J, et al. Improving skills and care standards in the support workforce for older people: a realist review. BMJ Open. 2014;4(5):e005356.
Pawson R. Evidence and policy and naming and shaming. Policy Stud. 2002;23(3):211–30.
Download references
Acknowledgements
This project is funded by the NIHR Health Services and Delivery Research programme, project 16/53/03. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
National Institute for Health Research, Health Services and Delivery Research programme, project 16/53/03.
Author information
Authors and affiliations.
Leeds Institute of Health Sciences, University of Leeds, Worsley Building, Clarendon Way, Leeds, LS2 9NL, England
Justin Keen, Roberta Longo, Jon Fistein, Maysam Abdulwahid, Natalie King & Judy Wright
School of Sociology and Social Policy, University of Leeds, Leeds, England
Joanne Greenhalgh
School of Healthcare, University of Leeds, Leeds, England
Rebecca Randell
School of Psychology, University of Leeds, Leeds, England
Peter Gardner
Health Services Management Centre, University of Birmingham, Birmingham, England
Justin Waring
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to writing the paper. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Justin Keen .
Ethics declarations
Ethics approval and consent to participate.
Ethics letter provided.
Consent for publication
The National Institute for Health Research operates a ‘negative consent’ model, whereby papers are submitted and if—after 30 days—no objections are raised, consent is deemed to have been given. This draft paper has been submitted to NIHR.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Search strategies to identify reports for generating theory.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Keen, J., Greenhalgh, J., Randell, R. et al. Networked information technologies and patient safety: a protocol for a realist synthesis. Syst Rev 8 , 307 (2019). https://doi.org/10.1186/s13643-019-1223-1
Download citation
Received : 13 February 2019
Accepted : 06 November 2019
Published : 05 December 2019
DOI : https://doi.org/10.1186/s13643-019-1223-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient safety
- Information technology
- Systems integration
- Health information exchange
- Health services research
- Systematic review
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Help & FAQ
Patient safety risks associated with telecare: A systematic review and narrative synthesis of the literature
Research output : Contribution to journal › Article › Research › peer-review
Background: Patient safety risk in the homecare context and patient safety risk related to telecare are both emerging research areas. Patient safety issues associated with the use of telecare in homecare services are therefore not clearly understood. It is unclear what the patient safety risks are, how patient safety issues have been investigated, and what research is still needed to provide a comprehensive picture of risks, challenges and potential harm to patients due to the implementation and use of telecare services in the home. Furthermore, it is unclear how training for telecare users has addressed patient safety issues. A systematic review of the literature was conducted to identify patient safety risks associated with telecare use in homecare services and to investigate whether and how these patient safety risks have been addressed in telecare training. Methods: Six electronic databases were searched in addition to hand searches of key items, reference tracking and citation tracking. Strict inclusion and exclusion criteria were set. All included items were assessed according to set quality criteria and subjected to a narrative synthesis to organise and synthesize the findings. A human factors systems framework of patient safety was used to frame and analyse the results. Results: 22 items were included in the review. 11 types of patient safety risks associated with telecare use in homecare services emerged. These are in the main related to the nature of homecare tasks and practices, and person-centred characteristics and capabilities, and to a lesser extent, problems with the technology and devices, organisational issues, and environmental factors. Training initiatives related to safe telecare use are not described in the literature. Conclusions: There is a need to better identify and describe patient safety risks related to telecare services to improve understandings of how to avoid and minimize potential harm to patients. This process can be aided by reframing known telecare implementation challenges and user experiences of telecare with the help of a human factors systems approach to patient safety.
- Human factors
- Narrative synthesis
- Patient safety
- Systematic review
This output contributes to the following UN Sustainable Development Goals (SDGs)
Access to Document
- 10.1186/s12913-014-0588-z Licence: CC BY
Other files and links
- Link to publication in Scopus
T1 - Patient safety risks associated with telecare
T2 - A systematic review and narrative synthesis of the literature
AU - Guise, Veslemøy
AU - Anderson, Janet
AU - Wiig, Siri
N1 - Funding Information: We would like to thank Grete Mortensen, special librarian at the University of Stavanger, for valuable assistance during the literature search process. We would also like to acknowledge The Research Council of Norway for funding the Safer@Home research project of which this study is a part (grant number 210799) and thank our partners in the project. Publisher Copyright: © 2014 Guise et al.; licensee BioMed Central Ltd.
PY - 2014/11
Y1 - 2014/11
N2 - Background: Patient safety risk in the homecare context and patient safety risk related to telecare are both emerging research areas. Patient safety issues associated with the use of telecare in homecare services are therefore not clearly understood. It is unclear what the patient safety risks are, how patient safety issues have been investigated, and what research is still needed to provide a comprehensive picture of risks, challenges and potential harm to patients due to the implementation and use of telecare services in the home. Furthermore, it is unclear how training for telecare users has addressed patient safety issues. A systematic review of the literature was conducted to identify patient safety risks associated with telecare use in homecare services and to investigate whether and how these patient safety risks have been addressed in telecare training. Methods: Six electronic databases were searched in addition to hand searches of key items, reference tracking and citation tracking. Strict inclusion and exclusion criteria were set. All included items were assessed according to set quality criteria and subjected to a narrative synthesis to organise and synthesize the findings. A human factors systems framework of patient safety was used to frame and analyse the results. Results: 22 items were included in the review. 11 types of patient safety risks associated with telecare use in homecare services emerged. These are in the main related to the nature of homecare tasks and practices, and person-centred characteristics and capabilities, and to a lesser extent, problems with the technology and devices, organisational issues, and environmental factors. Training initiatives related to safe telecare use are not described in the literature. Conclusions: There is a need to better identify and describe patient safety risks related to telecare services to improve understandings of how to avoid and minimize potential harm to patients. This process can be aided by reframing known telecare implementation challenges and user experiences of telecare with the help of a human factors systems approach to patient safety.
AB - Background: Patient safety risk in the homecare context and patient safety risk related to telecare are both emerging research areas. Patient safety issues associated with the use of telecare in homecare services are therefore not clearly understood. It is unclear what the patient safety risks are, how patient safety issues have been investigated, and what research is still needed to provide a comprehensive picture of risks, challenges and potential harm to patients due to the implementation and use of telecare services in the home. Furthermore, it is unclear how training for telecare users has addressed patient safety issues. A systematic review of the literature was conducted to identify patient safety risks associated with telecare use in homecare services and to investigate whether and how these patient safety risks have been addressed in telecare training. Methods: Six electronic databases were searched in addition to hand searches of key items, reference tracking and citation tracking. Strict inclusion and exclusion criteria were set. All included items were assessed according to set quality criteria and subjected to a narrative synthesis to organise and synthesize the findings. A human factors systems framework of patient safety was used to frame and analyse the results. Results: 22 items were included in the review. 11 types of patient safety risks associated with telecare use in homecare services emerged. These are in the main related to the nature of homecare tasks and practices, and person-centred characteristics and capabilities, and to a lesser extent, problems with the technology and devices, organisational issues, and environmental factors. Training initiatives related to safe telecare use are not described in the literature. Conclusions: There is a need to better identify and describe patient safety risks related to telecare services to improve understandings of how to avoid and minimize potential harm to patients. This process can be aided by reframing known telecare implementation challenges and user experiences of telecare with the help of a human factors systems approach to patient safety.
KW - Homecare
KW - Human factors
KW - Narrative synthesis
KW - Patient safety
KW - Systematic review
KW - Telecare
UR - http://www.scopus.com/inward/record.url?scp=84988602909&partnerID=8YFLogxK
U2 - 10.1186/s12913-014-0588-z
DO - 10.1186/s12913-014-0588-z
M3 - Article
C2 - 25421823
AN - SCOPUS:84988602909
SN - 1472-6963
JO - BMC Health Services Research
JF - BMC Health Services Research
- Research article
- Open access
- Published: 12 March 2019
A systematic literature review and narrative synthesis on the risks of medical discharge letters for patients’ safety
- Christine Maria Schwarz 1 ,
- Magdalena Hoffmann ORCID: orcid.org/0000-0003-1668-4294 1 , 2 ,
- Petra Schwarz 3 ,
- Lars-Peter Kamolz 1 ,
- Gernot Brunner 1 &
- Gerald Sendlhofer 1 , 2
BMC Health Services Research volume 19 , Article number: 158 ( 2019 ) Cite this article
27k Accesses
45 Citations
5 Altmetric
Metrics details
The medical discharge letter is an important communication tool between hospitals and other healthcare providers. Despite its high status, it often does not meet the desired requirements in everyday clinical practice. Occurring risks create barriers for patients and doctors. This present review summarizes risks of the medical discharge letter.
The research question was answered with a systematic literature research and results were summarized narratively. A literature search in the databases PubMed and Cochrane Library for Studies between January 2008 and May 2018 was performed. Two authors reviewed the full texts of potentially relevant studies to determine eligibility for inclusion. Literature on possible risks associated with the medical discharge letter was discussed.
In total, 29 studies were included in this review. The major identified risk factors are the delayed sending of the discharge letter to doctors for further treatments, unintelligible (not patient-centered) medical discharge letters, low quality of the discharge letter, and lack of information as well as absence of training in writing medical discharge letters during medical education.
Conclusions
Multiple risks factors are associated with the medical discharge letter. There is a need for further research to improve the quality of the medical discharge letter to minimize risks and increase patients’ safety.
Peer Review reports
The medical discharge letter is an important communication medium between hospitals and general practitioners (GPs) and an important legal document for any queries from insurance carriers, health insurance companies, and lawyers [ 1 ]. Furthermore, the medical discharge letter is an important document for the patient itself.
A timely transmission of the letter, a clear documentation of findings, an adequate assessment of the disease as well as understandable recommendations for follow-up care are essential aspects of the medical discharge letter [ 2 ]. Despite this importance, medical discharge letters are often insufficient in content and form [ 3 ]. It is also remarkable that writing of medical discharge letters is often not a particular subject in the medical education [ 4 ]. Nevertheless, the medical discharge letter is an important medical document as it contains a summary of the patient’s hospital admission, diagnosis and therapy, information on the patient’s medical history, medication, as well as recommendations for continuity of treatment. A rapid transmission of essential findings and recommendations for further treatment is of great interest to the patient (as well as relatives and other persons that are involved in the patients’ caring) and their current and future physicians. In most acute care hospitals, patients receive a preliminary medical discharge letter (short discharge letter) with diagnoses and treatment recommendations on the day of discharge [ 5 ]. Unfortunately, though, the full hospital medical discharge letter, which is often received with great delay, is an area of constant conflict between GPs and hospital doctors [ 1 ]. Thus the medical discharge letter does not only represent a feature of process and outcome quality of a clinic, but also influences confidence building and binding of resident physicians to the hospital [ 6 ].
Beside the transmission of patients’ findings from physician to physician, the delivery of essential information to the patient is an underestimated purpose of the medical discharge letter [ 7 ]. The medical discharge letter is often characterized by a complex medical language that is often not understood by the patients. In recent years, patient-centered/patient-directed medical discharge letters are more in discussion [ 8 ]. Thus, the medical discharge letter points out risks for patients and physicians while simultaneously creating barriers between them.
A systematic review of the literature was undertaken to identify patient safety risks associated with the medical discharge letter.
Search strategy
A systematic literature search was conducted using the electronic databases PubMed and Cochrane Database. Additionally, we scanned the reference lists of selected articles (snowballing). The following search terms were used: “discharge summary AND risks”, “discharge summary AND risks AND patient safety” and “discharge letter AND risks” and “discharge letter AND risks AND patient safety”. We reviewed relevant titles and abstracts on English and German literature published between January 2008 and May 2018 and started the search at the beginning of February 2018 and finished it at the end of May 2018.
Eligibility criteria
In this systematic review, articles were included if the title and/or abstract indicated the report of results of original research studies using quantitative, qualitative, or mixed method approaches. Studies in paediatric settings or studies that do not handle possible risks of the medical discharge letter were excluded, as well as reports, commentaries and letters. Electronic citations, including available abstracts of all articles retrieved from the search, were screened by two authors to select reports for full-text review. Duplicates were removed from the initial search. Nevertheless, during the search of articles the selection, publication as well as language bias must be considered. Thereafter, full-texts of potentially relevant studies were reviewed to determine eligibility for inclusion. In the following Table 1 inclusion and exclusion criteria for the studies are listed. Afterwards, key outcomes and main results were summarized. Differences were resolved by consensus. Finally, a narrative synthesis of studies meeting the inclusion criteria was conducted. Reference management software MENDELEY (Version 1.19.3) was used to organise and store the literature.
Data extraction
The data extraction in form of a table was used to summarize study results. The two authors extracted the data relating to author, country, year, study design, and outcome measure as well as potential risk factors to patient safety directly into a pre-formatted data collection form. After data extraction, the literature was discussed and synthesized into themes. The evaluation of the single studies was done using checklists [STROBE (combined) and the Cochrane Data collection form for intervention reviews (RCTs and non-RCTs)]. Meta-analysis was not considered appropriate for this body of literature because of the wide variability of studies in relation to research design, study population, types of interventions and outcomes.
Then a narrative synthesis was performed to synthesize the findings of the different studies. Because of the range of very different studies that were included in this systematic review, we have decided that a narrative synthesis constitutes the best instrument to synthesise the findings of the studies. First, a preliminary synthesis was undertaken in form of a thematic analysis involving searching of studies, listing and presenting results in tabular form. Then the results were discussed again and structured into themes. Afterwards, summarizing of included studies in a narrative synthesis within a framework was performed by one author.
This framework consisted of the following factors: the individuals and the environment involved in the studies (doctors, hospitals), the tools and technology (such as discharge letter delivery systems), the content of the medical discharge letter (such as missing content, quality of content), the accuracy and timeliness of transfer. These themes were discussed in relation to potential risks for patient’s safety. All articles that were included in this review were published before. The framework of this study was chosen following a previously published systematic review dealing with patient risks associated with telecare [ 9 ].
The initial literature search in the two online databases identified 940 records. From these records, 65 full text articles were screened for eligibility. Then 36 full-text articles were excluded because they pertained to patient transfer within the hospital or to another hospital, or to patient hand-over situations. Finally, 29 studies were included in this review. Included studies are listed in Table 2 . All document types were searched with a focus on primary research studies. The results of the search strategy are shown in Fig. 1 .
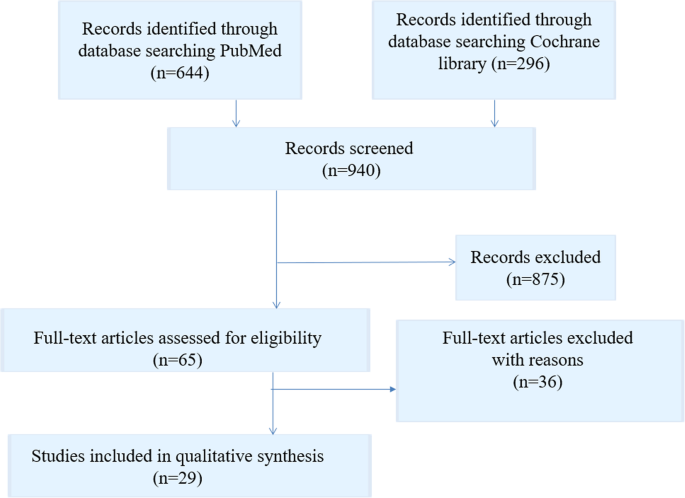
Flow chart literature search strategy
From these 29 studies, 13 studies dealt with the quality analysis of discharge letters, 12 studies with delayed transmission of medical discharge letters and just as many with the lack of information in medical discharge letters. Only few studies dealt with training on writing medical discharge letters and with understanding of patients of their medical discharge letters. The descriptive information of the included articles is presented in Table 2 . Overall quality of the articles was found to be acceptable, with clearly stated research questions and appropriate used methods.
Risk factors
In the following the identified major risk factors concerning the medical discharge letter are presented in a narrative summary.
Delayed delivery
The medical discharge letters should arrive at the GP soon after hospital discharge to ensure the quickest possible further treatment [ 4 ]. If letters are delivered weeks after the hospital stay, a continuous treatment of the patient cannot be ensured. Furthermore, the author of the medical discharge letter will no longer have current data after the discharge of the patient, which may result in a loss of important information [ 10 ]. Interfaces between different treatment areas and organizational units are known to cause a loss of information and a lack of quality in patient handling [ 11 ]. The improvement of information transfer between different healthcare providers during the transition of patients has been recommended to improve patient care [ 12 , 13 ]. Delayed communication of findings may lead to a lack of continuity of care and suboptimal outcomes, as well as decreased satisfaction levels for both patients and GPs [ 14 , 15 , 16 ]. In a review of Kripalani et al., it was shown that 25% of discharge summaries were never received by GPs [ 17 ]. This has several negative consequences for patients. Li et al. [ 18 ] found that a delayed transmission or absence of the medical discharge summary is related to patient readmission, and a study by Gilmore-Bykovskyi [ 19 ] found a strong relationship between patients whose discharge summaries omitted designation of a responsible clinician/clinic for follow-up care and re-hospitalisation and/or death. A Swedish study by Carlsson et al. [ 20 ] points out that a lack of accuracy and continuity in discharge information on eating difficulties may increase risk of undernutrition and related complications. A study of Were et al. [ 18 ] investigated pending lab results in medical discharge summaries and found that only 16% of tests with pending results were mentioned in the discharge summaries, and Walz et al. [ 21 ] found that approximately one third of the sub-acute care patients had pending lab results at discharge, but only 11% of these were documented in the medical discharge summaries.
Quality, lack of information
Medical discharge letters are a key communication tool for patient safety issues [ 17 ]. Incomplete and insufficient medical discharge letters increase the risks of readmission and myriad other complications [ 22 ]. Langelaan et al. (2017) evaluated more than 2000 medical discharge letters and found that in about 60% of the letters essential information was missing, such as a change of the existing medication, laboratory data, and even data on the patients themselves [ 23 ]. Accurate and complete medical discharge summaries are essential for patient safety [ 17 , 24 , 25 ]. Addresses; patient data, including duration of stay; diagnoses; procedures; operations; epicrisis and therapy recommendations; as well as findings in the appendix; are minimum requirements that are supposed to be included in the medical discharge letter [ 4 ]. However, it was found that key components are often lacking in medical discharge letters, including information about follow-up and management plans [ 23 , 26 ], test results [ 27 , 28 , 29 ], and medication adjustments [ 30 , 31 , 32 , 33 , 34 , 35 ]. In a review of Wimsett et al. [ 36 ] key components of a high-quality medical discharge summary were identified in 32 studies. These important components were discharge diagnosis, the received treatment, results of investigations as well as follow-up plans.
Accuracy of patients’ medication information is important to ensure patient safety. Hospital doctors expect GPs to continue with the prescribed (or modified) drug therapy. However, the selection of certain drugs is not always transparent for the GPs. A study by Grimes et al. [ 30 ] found that a discrepancy in medication documentation at discharge occurred in 10.8% of patients. From these patients nearly 65.5% were affected by discrepancies in medication documentation. The most prevalent inconsistency was drug omission (20.9%). Only 2% of patients were contacted, although general patient harm was assessed. A Swedish study of 2009 [ 37 ] investigated the quality improvement of medical discharge summaries. A higher quality of discharge letter led to an average of 45% fewer medication errors per patient.
A recent study by Tong et al. [ 38 ] revealed a reduced rate of medication errors in medical discharge summaries that were completed by a hospital pharmacist. Hospital pharmacists play a key role in preparing the discharge medication information transferred to GPs upon patient discharge and should work closely with hospital doctors to ensure accurate medication information that is quickly communicated to GPs at transitions of care [ 39 ]. Most hospitals have introduced electronic systems to improve the discharge communication, and many studies found a significant overall improvement in electronic transfer systems due to better documentation of information about follow-up care, pending test results, and information provided to patients and relatives [ 40 , 41 , 42 ]. Mehta et al. [ 43 ] found that the changeover to a new electronic system resulted in an increased completeness of discharge summaries from 60.7 to 75.0% and significant improvements in levels of completeness in certain categories.
Writing of medical discharge letter is missing in medical education
Both junior doctors as well as medical students reported that they received inadequate guidance and training on how to write medical discharge summaries [ 44 , 45 ] and recognized that higher priority is often given to pressing clinical tasks [ 46 ]. Research into the causes of prescribing errors by junior doctors at hospitals in the UK has revealed that latent conditions like organizational processes, busy environments, and medical care for complex patients can lead to medication errors in the medical discharge summary [ 47 ].
Fortunately, some study results demonstrate that information and education on writing medical discharge letters would enhance communication to the GPs and prevent errors during the patient discharge process [ 37 ]. Minimal formal teaching about writing medical discharge summaries is common in most medical schools [ 39 , 46 ]; however, a study by Shivji et al. has shown that simple, intensive educational sessions can lead to an improvement in the writing process of medical discharge summaries and communication with primary care [ 48 ].
Since the medical discharge letter should meet specific quality criteria, senior physicians and/or the head physician correct(s) and validate(s) the letter. The medical discharge letter therefore represents an essential learning target [ 8 ]. Training activities and workshops are necessary for junior doctors to improve writing medical discharge letters [ 44 , 49 ]. It might be also useful for young doctors to use checklists or other structured procedures to improve writing [ 4 ]. Maher et al. showed that the use of a checklist enhanced the quality (content, structure, and clarity) of medical discharge letters written by medical students [ 50 ].
In the following Table 3 main risk factors of the medical discharge letter are summarized.
The results of this systematic literature research indicate notable risk factors relating to the medical discharge letter. In a study by Sendlhofer et al., 360 risks were identified in hospital settings [ 51 ]. From these, 176 risks were scored as strategic and clustered into “top risks”. Top risks included medication errors, information errors, and lack of communication, among others. During this review, these potential risk factors were also identified in terms of the medical discharge letter.
Delayed sending and low quality of medical discharge letters to the referring physicians, may adversely affect the further course of treatment. However, a study of Spencer et al. has determined rates of failures in processing actions requested in hospital discharge summaries in general practice. It was found that requested medication changes were not made in 17% and patient harm occurred in 8% in relation to failures [ 52 ].
Despite the existence of reliable standards [ 53 ] many physicians are not adequately trained for writing medical discharge letters during their studies. Regular trainings and workshops and standardized checklists may optimize the quality of the medical discharge letter. Furthermore, electronic discharge letters have the potential to easily and quickly extract important information such as diagnoses, medication, and test results into a structured discharge document, and offer important advantages such as reliability, speed of information transfer, and standardization of content. Comprehensive discharge letters reduce the readmission rate and increase safety and quality by discharging of the patient. A missing structure, as well as a complex language, illegible handwriting, and unknown abbreviations, make reading medical discharge letters more complicated [ 4 ]. At least, poor patient understanding of their diagnosis and treatment plans and incomprehensible recommendations can adversely impact clinical outcome following hospital discharge. Many studies confirm that inadequate communication of findings [ 3 , 39 , 54 ] is an important risk factor in patients’ safety [ 51 ].
Most medical information in the discharge letter is not understood by patients (as well as relatives and other persons that are involved in the patients’ caring) and patients themselves do not receive a comprehensible medical discharge letter. The content of the medical discharge letter is often useless for the patient due to its medical terminology and content that is not matching with the patient’s level of knowledge or health literacy [ 55 , 56 , 57 ]. Poor understanding of diagnoses and related discharge plans are common among patients and family members and often accompanied by unplanned hospital readmissions [ 58 , 59 , 60 , 61 ]. In a study by Lin et al., it was shown that a patient-directed discharge letter enhanced understanding for hospitalization and for recommendations. Furthermore, verbal communication of the letter contents, explanation of every section of the medical discharge letter, and the opportunity for discussion and asking questions improved patient comprehension [ 7 ]. A study by O’Leary et al. showed that roughly 80–95% of patients with breast tumours want to be informed and educated about their illness, treatment, and prognosis [ 62 ].
High quality of care is characterized by a patient-centered communication, where the patient’s personal needs are also in focus [ 63 ]. Translation of medical terms in reports and letters leads to a better understanding of the disease and, interestingly, the avoidance of medical terms did not lead to deterioration in the transmission of information between the treating physicians. Moreover, it was found that the minimisation of medical terminology in medical discharge letters improved understanding and perception of patients’ ability to manage chronic health conditions [ 64 ]. In effect, it is clear that patient-centered communication improves outcome, mental health, patient satisfaction and reduces the use of health services [ 65 ].
Strengths and limitations
We have identified key problems with the medical discharge summaries that negatively impact patients’ safety and wellbeing. However, there is a heterogeneous nature of the included studies in terms of study design, sample size, outcomes, and language. Only two reviewers screened the studies for eligibility and only full-text articles were included in the literature review; furthermore, only the databases Pubmed and Cochrane library were screened for appropriate studies. Due to these constraints, there is a chance that other relevant studies may have been missed.
High-quality medical discharge letters are essential to ensure patient safety. To address this, the current review identified the major risk factors as delayed sending and low quality of medical discharge letters, lack of information and patient understanding, and inadequate training in writing medical discharge letters. In future, research studies should focus on improving the communication of pending test results and findings at discharge, and on evaluating the impact that this improved communication has on patient outcomes. Moreover, a simple patient-centered medical discharge letter may improve the patient’s (as well as family members’ and other caregivers’) understanding of disease, treatment and post-discharge recommendations.

Abbreviations
General practitioner
Randomized Controlled Trial
STrengthening the Reporting of OBservational studies in Epidemiology
United Kingdom
Kreße B, Dinser R. Anforderungen an Arztberichte- ein haftungsrechtlicher Ansatz. Medizinrecht. 2010;28(6):396–400.
Google Scholar
Möller K-H, Makoski K. Der Arztbrief - Rechtliche Rahmen- Bedingungen. 2015;5:186–94.
Van Walraven C, Weinberg AL. Quality assessment of a discharge summary system. CMAJ. 1995;152(9):1437–42.
PubMed Google Scholar
Unnewehr M, Schaaf B, Friederichs H. Die Kommunikation optimieren. Dtsch Arztebl Int. 2013;110(37):831–4.
Roth-Isigkeit A, Harder S. Die Entlassungsmedikation im Arztbrief. Eine explorative Befragung von Hausärzten/−innen. Vol. 100, Medizinische Klinik. 2005. p. 87–93.
Bohnenkamp B. Arbeitsorganisation: Der Arztbrief - Viel mehr als nur lästige Pflicht. Vol. 113, Deutsches Ärzteblatt International. 2016. p. 2–4.
Lin R, Tofler G, Spinaze M, Dennis C, Clifton-Bligh R, Nojoumian H, Gallagher R, et al. Patient-directed discharge letter (PADDLE)-a simple and brief intervention to improve patient knowledge and understanding at time of hospital discharge. Hear Lung Circ. 2012;21:S312.
Hammerer P. Patientenverständliche Arztbriefe und Befunde. Springer Medizin. 2018;33(2):119–23.
Guise V, Anderson J, Wiig S. Patient safety risks associated with telecare: a systematic review and narrative synthesis of the literature. BMC Health Serv Res. 2014;14(1):588.
Raab, A., & Drissner A. Einweiserbeziehungsmanagement: Wie Krankenhäuser erfolgreich Win-Win-Beziehungen zu niedergelassenen Ärzten aufbauen. Kohlhammer Verlag; 2011. 240 p.143.
Hart D. Vertrauen, Kooperation, Organisation. Berlin Heidelberg: Springer Verlag; 2006. p. 845–7.
Cook RI. Gaps in the continuity of care and progress on patient safety. BMJ. 2000;320(7237):791–4.
CAS PubMed Google Scholar
Duggan C, Feldman R, Hough J, Bates I. Reducing adverse prescribing discrepancies following hospital discharge. Int J Pharm Pract. 1998;6(2):77–82.
Polyzotis PA, Suskin N, Unsworth K, Reid RD, Jamnik V, Parsons C, et al. Primary care provider receipt of cardiac rehabilitation discharge summaries are they getting what they want to promote long-term risk reduction. Circ Cardiovasc Qual Outcomes. 2013;6(1):83–9.
Poon EG, Gandhi TK, Sequist TD, Murff HJ, Karson AS, Bates DW. “I wish i had seen this test result earlier!”: Dissatisfaction with test result management systems in primary care. Vol. 164, Archives of Internal Medicine. 2004. p. 2223–8.
Coleman EA, Berenson RA. Lost in transition: Challenges and opportunities for improving the quality of transitional care. Vol. 141, Annals of Internal Medicine. 2004. p. 533–6.
Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–41.
Were MC, Li X, Kesterson J, Cadwallader J, Asirwa C, Khan B, et al. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow-up providers. J Gen Intern Med. 2009;24(9):1002–6.
Gilmore-Bykovskyi AL, Kennelty KA, Dugoff E, Kind AJH. Hospital discharge documentation of a designated clinician for follow-up care and 30-day outcomes in hip fracture and stroke patients discharged to sub-acute care. BMC Health Serv Res. 2018;18(1).
Carlsson E, Ehnfors M, Eldh AC, Ehrenberg A. Accuracy and continuity in discharge information for patients with eating difficulties after stroke. J Clin Nurs. 2012;21(1–2):21–31.
Walz SE, Smith M, Cox E, Sattin J, Kind AJH. Pending laboratory tests and the hospital discharge summary in patients discharged to sub-acute care. J Gen Intern Med. 2011;26(4):393–8.
Horwitz LI, Jenq GY, Brewster UC, Chen C, Kanade S, Van Ness PH, et al. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. 2013;8(8):436–43.
Alderton M, Callen JL. Are general practitioners satisfied with electronic discharge summaries? Vol. 36, Health Information Management Journal. 2007. p. 7–12.
Harel Z, Wald R, Perl J, Schwartz D, Bell CM. Evaluation of deficiencies in current discharge summaries for dialysis patients in Canada. J Multidiscip Healthc. 2012;5:77–84.
Philibert I, Barach P. The European HANDOVER Project: A multi-nation program to improve transitions at the primary care - Inpatient interface. BMJ Quality and Safety. 2012;21(SUPPL. 1).
Greer RC, Liu Y, Crews DC, Jaar BG, Rabb H, Boulware LE. Hospital discharge communications during care transitions for patients with acute kidney injury: a cross-sectional study. BMC Health Serv Res. 2016;16:449.
Belleli E, Naccarella L, Pirotta M. Communication at the interface between hospitals and primary care: a general practice audit of hospital discharge summaries. Aust Fam Physician. 2013;42(12):886–90.
Roy CL, Poon EC, Karson AS, Ladak-Merchant Z, Johnson RE, Maviglia SM, et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143(2):121–8.
Gandara E, Moniz T, Ungar J, Lee J, Chan-Macrae M, O’Malley T, et al. Communication and information deficits in patients discharged to rehabilitation facilities: an evaluation of five acute care hospitals. J Hosp Med. 2009;4(8):E28–33.
Grimes T, Delaney T, Duggan C, Kelly JG, Graham IM. Survey of medication documentation at hospital discharge: implications for patient safety and continuity of care. Ir J Med Sci. 2008;177(2):93–7.
Uitvlugt EB, Siegert CEH, Janssen MJA, Nijpels G, Karapinar-Çarkit F. Completeness of medication-related information in discharge letters and post-discharge general practitioner overviews. Int J Clin Pharm. 2015;37(6):1206–12.
Ooi CE, Rofe O, Vienet M, Elliott RA. Improving communication of medication changes using a pharmacist-prepared discharge medication management summary. Int J Clin Pharm. 2017;39(2):394–402.
Perren A, Previsdomini M, Cerutti B, Soldini D, Donghi D, Marone C. Omitted and unjustified medications in the discharge summary. Qual Saf Heal Care. 2009;18(3):205–8.
CAS Google Scholar
Garcia BH, Djønne BS, Skjold F, Mellingen EM, Aag TI. Quality of medication information in discharge summaries from hospitals: an audit of electronic patient records. Int J Clin Pharm. 2017;39(6):1331–7.
Monfort AS, Curatolo N, Begue T, Rieutord A, Roy S. Medication at discharge in an orthopaedic surgical ward: quality of information transmission and implementation of a medication reconciliation form. Int J Clin Pharm. 2016;38(4):838–47.
Wimsett J, Harper A, Jones P. Review article: Components of a good quality discharge summary: A systematic review. Vol. 26, EMA - Emergency Medicine Australasia. 2014. p. 430–8.
Bergkvist A, Midlöv P, Höglund P, Larsson L, Bondesson Å, Eriksson T. Improved quality in the hospital discharge summary reduces medication errors-LIMM: Landskrona integrated medicines management. Eur J Clin Pharmacol. 2009;65(10):1037–46.
Tong EY, Roman CP, Mitra B, Yip GS, Gibbs H, Newnham HH, et al. Reducing medication errors in hospital discharge summaries: a randomised controlled trial. Med J Aust. 2017;206(1):36–9.
Yemm R, Bhattacharya D, Wright D, Poland F. What constitutes a high quality discharge summary? A comparison between the views of secondary and primary care doctors. Int J Med Educ. 2014;5:125–31.
O’Leary KJ, Liebovitz DM, Feinglass J, Liss DT, Evans DB, Kulkarni N, et al. Creating a better discharge summary: improvement in quality and timeliness using an electronic discharge summary. J Hosp Med. 2009;4(4):219–25.
Chan S. P Maurice a, W pollard C, Ayre SJ, Walters DL, Ward HE. Improving the efficiency of discharge summary completion by linking to preexisiting patient information databases. BMJ Qual Improv Reports. 2014;3(1):1–5.
Lehnbom EC, Raban MZ, Walter SR, Richardson K, Westbrook JI. Do electronic discharge summaries contain more complete medication information? A retrospective analysis of paper versus electronic discharge summaries. Heal Inf Manag J. 2014;43(3):4–12.
Mehta RL, Baxendale B, Roth K, Caswell V, Le Jeune I, Hawkins J, et al. Assessing the impact of the introduction of an electronic hospital discharge system on the completeness and timeliness of discharge communication: A before and after study. BMC Health Serv Res. 2017;17(1).
Heaton A, Webb DJ, Maxwell SRJ. Undergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol. 2008;66(1):128–34.
Maxwell S, Walley T. Teaching safe and effective prescribing in UK medical schools: A core curriculum for tomorrow’s doctors. Vol. 55, British Journal of Clinical Pharmacology. 2003. p. 496–503.
Frain JP, Frain AE, Carr PH. Experience of medical senior house officers in preparing discharge summaries. Br Med J. 1996;312(7027):350.
Dornan T, Investigator P, Ashcroft D, Lewis P, Miles J, Taylor D, et al. An in depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education. EQUIP study. Vol. 44, Methods. 2010.
Shivji FS, Ramoutar DN, Bailey C, Hunter JB. Improving communication with primary care to ensure patient safety post-hospital discharge. Br J Hosp Med. 2015;76(1):46–9.
Cresswell A, Hart M, Suchanek O, Young T, Leaver L, Hibbs S. Mind the gap: Improving discharge communication between secondary and primary care. BMJ Qual Improv Reports. 2015;4(1):u207936.w3197.
Maher B, Drachsler H, Kalz M, Hoare C, Sorensen H, Lezcano L, et al. Use of Mobile applications for hospital discharge letters - improving handover at point of practice. Int J Mob Blended Learn. 2013;5(4):29.
Sendlhofer G, Brunner G, Tax C, Falzberger G, Smolle J, Leitgeb K, et al. Systematic implementation of clinical risk management in a large university hospital: the impact of risk managers. Wien Klin Wochenschr [Internet]. 2015; 127:1–11. Available from: https://doi.org/10.1007/s00508-014-0620-7
Spencer RA, Spencer SEF, Rodgers S, Campbell SM, Avery AJ. Processing of discharge summaries in general practice: a retrospective record review. Br J Gen Pract. 2018;68(673):e576–85.
Carpenter I. A Clinician’s guide to record standards - part 2: standards for the structure and content of medical records and communications when patients are admitted to hospital. Acad Med R Coll R Coll Physicians. 2008;10(5):24.
GMC. Good practice in prescribing and managing medicines and devices. Good Medical Practice. 2013. p. 1–11.
Jolly BT, Scott JL, Sanford SM. Simplification of emergency department discharge instructions improves patient comprehension. Ann Emerg Med. 1995;26(4):443–6.
Williams DM, Counselman FL, Caggiano CD. Emergency department discharge instructions and patient literacy: a problem of disparity. Am J Emerg Med. 1996;14(1):19–22.
Jolly BT, Scott JL, Feied CF, Sanford SM. Functional illiteracy among emergency department patients: a preliminary study. Ann Emerg Med. 1993;22(3):573–8.
Soler RS, Juvinyà Canal D, Noguer CB, Poch CG, Brugada Motge N, Garcia D m, Gil M. Continuity of care and monitoring pain after discharge: patient perspective. J Adv Nurs. 2010;66(1):40–8.
Grover G, Berkowitz CD, Lewis RJ. Parental recall after a visit to the emergency department. Clin Pediatr (Phila). 1994;33(4):194–201.
Witherington EMA, Pirzada OM, Avery AJ. Communication gaps and readmissions to hospital for patients aged 75 years and older: observational study. Qual Saf Heal Care. 2008;17(1):71–5.
Marcantonio ER, McKean S, Goldfinger M, Kleefield S, Yurkofsky M, Brennan T. a. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan. Am J Med. 1999;107(1):13–7.
O’Leary KA, Estabrooks CA, Olson K, Cumming C. Information acquisition for women facing surgical treatment for breast cancer: Influencing factors and selected outcomes. Vol. 69, Patient Education and Counseling. 2007. p. 5–19.
Vogel BA, Helmes AW, Bengel J. Arzt-Patienten-Kommunikation in der Tumorbehandlung: Erwartungen und Erfahrungen aus Patientensicht. Zeitschrift für Medizinische Psychol. 2006;15(4):149–61.
Wernick M, Hale P, Anticich N, Busch S, Merriman L, King B, et al. A randomised crossover trial of minimising medical terminology in secondary care correspondence in patients with chronic health conditions: impact on understanding and patient reported outcomes. Intern Med J. 2016;46(5):596–601.
Woods SS, Schwartz E, Tuepker A, Press NA, Nazi KM, Turvey CL, et al. Patient experiences with full electronic access to health records and clinical notes through the my healthevet personal health record pilot: Qualitative study. J Med Internet Res. 2013;(15, 3).
Weiskopf NG, Rusanov A, Weng C. Sick patients have more data: the non-random completeness of electronic health records. MIA Symp. 2013;2013:1472–7.
Choudhry AJ, Baghdadi YMK, Wagie AE, Habermann EB, Heller SF, Jenkins DH, et al. Readability of discharge summaries: with what level of information are we dismissing our patients? In: Am J Surg. 2016. p. 631–6.
Li JYZ, Yong TY, Hakendorf P, Ben-Tovim D, Thompson CH. Timeliness in discharge summary dissemination is associated with patients’ clinical outcomes. J Eval Clin Pract. 2013;19(1):76–9.
Download references
Acknowledgements
Not applicable.
This research project was part of a project funded by the Gesundheitsfonds Steiermark. The funders had no role in study design, data collection and analyses, decision to publish, or preparation of the manuscript.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Author information
Authors and affiliations.
Research Unit for Safety in Health, c/o Division of Plastic, Aesthetic and Reconstructive Surgery, Department of Surgery, Medical University of Graz, Graz, Austria
Christine Maria Schwarz, Magdalena Hoffmann, Lars-Peter Kamolz, Gernot Brunner & Gerald Sendlhofer
Executive Department for Quality and Risk Management, University Hospital Graz, Auenbruggerplatz 1/3, 8036, Graz, Austria
Magdalena Hoffmann & Gerald Sendlhofer
Carinthia University of Applied Science, Feldkirchen, Austria
Petra Schwarz
You can also search for this author in PubMed Google Scholar
Contributions
CS wrote the manuscript; CS, MH and PS performed the literature search; LK contributed to the conception of this work; GB contributed to the interpretation of data and GS supervised the project. All authors were critically revising the manuscript and all authors have read and approved the final manuscript.
Corresponding author
Correspondence to Magdalena Hoffmann .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Schwarz, C.M., Hoffmann, M., Schwarz, P. et al. A systematic literature review and narrative synthesis on the risks of medical discharge letters for patients’ safety. BMC Health Serv Res 19 , 158 (2019). https://doi.org/10.1186/s12913-019-3989-1
Download citation
Received : 09 August 2018
Accepted : 06 March 2019
Published : 12 March 2019
DOI : https://doi.org/10.1186/s12913-019-3989-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Discharge letter
- Discharge summary
- Patient safety
- Hospital discharge
- Systematic review
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
A systematic literature review and narrative synthesis on the risks of medical discharge letters for patients' safety
Affiliations.
- 1 Research Unit for Safety in Health, c/o Division of Plastic, Aesthetic and Reconstructive Surgery, Department of Surgery, Medical University of Graz, Graz, Austria.
- 2 Research Unit for Safety in Health, c/o Division of Plastic, Aesthetic and Reconstructive Surgery, Department of Surgery, Medical University of Graz, Graz, Austria. [email protected].
- 3 Executive Department for Quality and Risk Management, University Hospital Graz, Auenbruggerplatz 1/3, 8036, Graz, Austria. [email protected].
- 4 Carinthia University of Applied Science, Feldkirchen, Austria.
- 5 Executive Department for Quality and Risk Management, University Hospital Graz, Auenbruggerplatz 1/3, 8036, Graz, Austria.
- PMID: 30866908
- PMCID: PMC6417275
- DOI: 10.1186/s12913-019-3989-1
Background: The medical discharge letter is an important communication tool between hospitals and other healthcare providers. Despite its high status, it often does not meet the desired requirements in everyday clinical practice. Occurring risks create barriers for patients and doctors. This present review summarizes risks of the medical discharge letter.
Methods: The research question was answered with a systematic literature research and results were summarized narratively. A literature search in the databases PubMed and Cochrane Library for Studies between January 2008 and May 2018 was performed. Two authors reviewed the full texts of potentially relevant studies to determine eligibility for inclusion. Literature on possible risks associated with the medical discharge letter was discussed.
Results: In total, 29 studies were included in this review. The major identified risk factors are the delayed sending of the discharge letter to doctors for further treatments, unintelligible (not patient-centered) medical discharge letters, low quality of the discharge letter, and lack of information as well as absence of training in writing medical discharge letters during medical education.
Conclusions: Multiple risks factors are associated with the medical discharge letter. There is a need for further research to improve the quality of the medical discharge letter to minimize risks and increase patients' safety.
Keywords: Discharge letter; Discharge summary; Hospital discharge; Patient safety; Risk; Systematic review.
Publication types
- Systematic Review
- Communication
- Health Personnel
- Medical Records / standards*
- Patient Discharge / standards*
- Patient Safety / standards*
- Professional Practice / standards
Grants and funding
- -/Gesundheitsfonds Steiermark
Perceptions of Patient Safety Culture Dimensions among Hospital Nurses: A Systematic Review
- Review Article
- Open access
- Published: 04 July 2022
- Volume 4 , pages 103–125, ( 2022 )
Cite this article
You have full access to this open access article

- Sultan Almutairi 1 ,
- Abdulrahman Aljohani 2 ,
- Mansour Awad 3 ,
- Chandni Saha 4 ,
- Hamed Alhobaishi 3 ,
- Ahmad Almutairi 5 &
- Abbas Al Mutair ORCID: orcid.org/0000-0002-9471-2767 6 , 7 , 8 , 9 nAff4
3505 Accesses
2 Citations
Explore all metrics
Patient safety culture, an important aspect in the field of patient safety, plays an important role in the promotion of healthcare quality. Improved patient safety culture decreases patient readmission rates, lengths of hospital stay, and patient safety issues. Patient safety culture includes a set of dimensions. This review focuses on the differing perceptions of these dimensions among healthcare providers in hospitals.
This study aimed to identify studies examining healthcare providers’ perceptions of patient safety culture in hospitals and to summarize the data from these studies.
Electronic database searching was based on the research question. Two electronic databases were used: CINHAL and Scopus. The search was limited to the period 2005–2012, and studies examining healthcare providers’ perceptions of patient safety culture were identified. Key terms were used to search the articles that were selected on the basis of inclusion and exclusion criteria. Articles examining healthcare providers’ perceptions of patient safety culture in hospitals without comparison between nurses and other healthcare professionals were selected.
Eight articles were reviewed. Several questionnaires were used to assess healthcare providers’ perceptions of patient safety culture in these articles. Our review indicated differences in healthcare providers’ perceptions. In two articles, participants reported a high positive response to teamwork. In addition, participants in the other two articles reported a high positive response to job satisfaction.
The results of the current review reveal healthcare providers’ perceptions of patient safety culture. The results highlight that careful recognition and committed work on various scales/dimensions of patient safety culture can improve healthcare quality and consequently decrease patient safety issues associated with nursing care. Our findings also encourage hospital management and decision-makers to focus on and establish improvements in areas that will positively affect the quality of healthcare.
Similar content being viewed by others

Perceived patient safety culture and its associated factors among clinical managers of tertiary hospitals: a cross-sectional survey
Hospital survey on patient safety culture in ethiopian public hospitals: a cross-sectional study.

Predictors and outcomes of patient safety culture at King Abdulaziz Medical City, Jeddah, Saudi Arabia. A nursing perspective
Avoid common mistakes on your manuscript.
1 Introduction
Patient safety culture is an integral part of healthcare services. Healthcare has become complex, with the development of therapeutic interventions and new technologies. Such factors may negatively affect the level of healthcare provided and patient safety, according to the World Health Organization [ 1 ]. The Agency for healthcare Research and Quality (AHRQ) [ 2 ] has defined patient safety as “freedom from accidental or preventable injuries produced by medical care” and patient safety culture as “the extent to which an organization's culture supports and promotes patient safety” [ 3 ]. Patients are admitted to hospitals to be treated for health problems, but in some cases, patients are exposed to adverse events, such as medication errors, incorrect surgeries, nosocomial infections, falls in hospitals, and pressure ulcers. These events may injure patients and even lead to death, according to the World Health Organization [ 1 ]. Consequently, patient safety has become an important concern, owing to the prevalence of such adverse events, which have negatively affected patients and healthcare organizations.
The Harvard Medical Practice study has found that 4% of patients are exposed to adverse events. Of these adverse events, 70% of cause disability, and 14% lead to death, as reported by the World Health Organization [ 1 ]. The Department of Health and Children [ 4 ] of the Institute of Medicine has released a report called “To Err is Human: Building a Safer Health System,” which states that “there are between 44,000 and 98,000 preventable deaths annually due to medical error in hospitals.” Such adverse events not only affect patients (primary victims) but also have been reported to have psychological and psychosomatic effects, such as distress, anxiety, anger, and emotional stress, on healthcare providers as secondary victims [ 5 ]. Positive patient safety culture can reduce the occurrence of adverse effects [ 6 ].
Patient safety culture is one of several important aspects of patient safety. According to AHRQ, patient safety culture refers to the beliefs, values, and norms shared by healthcare and other staff in an organization that influence their conduct related to patient safety. Patient safety culture is measured by the values, beliefs, norms, and behaviors that are recognized, rewarded, expected, and accepted in an organization [ 3 ]. Additionally, AHRQ underscores the presence of patient safety culture at multiple levels, from the unit, department, and organization levels to the system level [ 3 ]. Hammer et al. [ 7 ] have stated that, because of the importance of patient safety culture, healthcare institutions perform improvement activities that create a positive culture. Patient safety culture assessment and interventions can improve the overall perceptions of patient safety [ 8 ]. Improvements in patient safety culture positively influence healthcare services. Positive patient safety culture decreases the readmission rate for patients and the length of hospital stay. Hospitals with a positive safety culture have reported low rates of adverse events [ 9 , 10 ]. Patient safety culture is measured by several tools. According to The Health Foundation [ 9 , 10 ], three main tools are used to assess patient safety culture. The first tool is the Hospital Surveys On Patient Safety Culture (HSOPSC), developed by the AHRQ in the United States. Its validity and reliability have been examined in several studies. The survey includes 12 dimensions for patient safety culture, measured by 42 items [ 11 ]. The dimensions are communication openness, feedback and communication about errors, handoffs and transitions, management support for patient safety, nonpunitive response to errors, organizational learning, overall perceptions of patient safety, staffing, supervisor/manager expectations, and actions promoting safety, teamwork across units, teamwork within units, and frequency of events reported [ 12 ]. The second tool is the Manchester patient safety culture assessment tool developed by the National Patient Safety Agency in the United Kingdom. It was developed to enable the National Health Service to assess patient safety culture improvement within healthcare organizations. The tool includes ten dimensions [ 13 ]: continual improvement, priority given to safety, system errors and individual responsibility, recording incidents, evaluating incidents, learning and effecting change, communication, personnel management, staff education, and teamwork [ 14 ]. The validity and reliability of this tool were tested in several studies on patient safety culture [ 9 , 10 ]. The third tool is the Safety Attitudes Questionnaire (SAQ), which originated from the Flight Management Attitude Questionnaire used to assess safety culture in cockpits in airplanes [ 15 ]. This tool includes six domains focusing on the safety climate: safety climate, teamwork climate, stress recognition, perceptions of management, working conditions, and job satisfaction [ 14 ]. This questionnaire is valid and reliable according to previous studies [ 9 , 10 ].
To gauge patient safety culture, it is crucial to consider nurses. Nurses make up the majority of healthcare professionals [ 16 ]. In addition, nurses play a pivotal role in healthcare settings, such as through ensuring steady bedside care and communicating with other healthcare providers, such as physicians and the pharmacists [ 17 ]. Nurse staffing and empowerment have been significantly associated with patient safety and patient safety culture, respectively [ 17 , 18 ]. Consequently, the issues affecting nursing care should be examined and addressed in the assessment of patient safety culture in healthcare organizations.
Interest in patient safety culture assessment among nurses has become important [ 19 ]. Amiri et al. [ 18 ] have described patient safety culture as a culture in which nurses are cognizant of errors and are supported to discuss them. Several articles have assessed nurses’ perceptions of dimensions of patient safety culture in hospitals [ 16 , 19 , 20 , 21 , 22 , 23 , 24 , 25 ]. However, no published reviews have systematically analyzed and summarized nurses’ perceptions of various patient safety culture dimensions and the differences in their perceptions across several descriptive socio-demographic variables. Such a comprehensive systematic review is essential to estimating and improving patient safety culture in healthcare settings. Therefore, in this study, articles associated with nurses’ perceptions of patient safety culture were systematically reviewed and summarized. This review also aims to present the differences in perceptions across various respondent characteristics, such as age, education, experience, hospital unit, and position at work.
2 Materials and Methods
2.1 formulation of the research question.
The research question was formulated on the basis of the following process. The area of interest was nurses’ perceptions of patient safety culture dimensions in hospitals. This area was selected because of its effects on healthcare services. The Patient/Population, Intervention, Comparison, and Outcomes (PICO) method was not appropriate for the formulation of the research question, because it is suitable for clinical research using interventions. Sample, Phenomenon of Interest, Design, Evaluation, Research type (SPIDER) is another method for research question formulation. The research question was formulated by using the items in the SPIDER framework, as shown in Table 1 .
The research question was formulated as follows: What are nurses’ perceptions of patient safety culture in hospitals, according to questionnaires?
2.2 Inclusion Criteria
The specific inclusion criteria were as follows:
Type of studies studies focusing on nurses’ perceptions of patient safety culture in hospitals, studies based on a descriptive design, studies using questionnaires to measure patient safety culture among nurses, regardless of questionnaire type.
Country of studies studies focusing on measuring healthcare nurses’ perceptions of patient safety culture in any country worldwide.
Place of studies studies measuring nurses’ perceptions of patient safety culture in one hospital, more than one hospital, all departments of a hospital, specific departments of a hospital, or one unit in a hospital, regardless of hospital type.
Type of participants studies whose participants are nurses occupying various positions throughout a hospital.
Qualification of participants studies in which participants are healthcare providers with qualifications such as a diploma, bachelor's degree, master’s degree or PhD.
Experience of participants in work studies in which participants have different experiences, included without limitation.
Nationality of participants studies on participants of all nationalities, included without limitation.
Gender studies focusing on one gender or men and women, included without limitation.
Age studies in all age groups, included without limitation.
Outcome studies examining some or all dimensions of patient safety culture, for example, manager expectations, frequency of event reporting, rating overall perceptions of safety, number of events reported, patient safety grade, organizational learning, communication openness, communication, nonpunitive response to error, teamwork, hospital handoffs, and transitions, and staffing and hospital management support for patient safety.
2.3 Search Strategies
The search in the electronic database was based on the research question. Two electronic databases were used: Cumulative Index of Nursing and Allied Health Literature (CINHAL) and Scopus. Key terms and synonyms in the questions were used in the electronic search. Searching by using statements (patient safety culture nurses) provided 106 results in the CINHAL database and 609 results in the Scopus database. Another statement was used in searching, “patient safety culture charge nurses,” which yielded 17 results in the CINHAL database and 234 results in the Scopus Database. The advanced search in CINHAL using the terms “perception AND patient safety culture AND nurses” yielded zero results, whereas searching “perception OR patient safety culture OR nurses” yielded 1817 results. Using “perception patient safety culture nurses” and “patient safety culture survey nurses” in the Scopus database provided 99 and 135 results, respectively. An advanced search in the CINHAL database with “evaluation AND patient safety culture AND nurses” yielded zero results, whereas “evaluation OR patient safety culture OR nurses” provided 3255 results. The combined words “evaluation patient safety culture healthcare providers” in the Scopus database yielded 74 results. An advanced search in the CINHAL database by using “patient safety culture AND survey AND healthcare providers” yielded zero results, whereas “patient safety culture OR survey OR healthcare providers” gave 2680 results. A search in the Scopus database by using the combined words “patient safety culture survey nurses” provided 135 results. Using “patient safety culture AND registered nurses” gave 1 result, and using “patient safety culture OR registered nurses” gave 14 results. Scopus database searching using the combined words “patient safety culture registered nurses” yielded zero results, whereas using “evaluation patient safety culture” gave 74 results. An advanced search in the CINHAL database for “patient safety culture AND assessment AND nurses” provided 1 result. Using “patient safety culture OR assessment OR nurses” gave 3077 results. In the Scopus database, using “patient safety culture assessment nurses” provided 139 results (see Figs. 1 and 2 ).
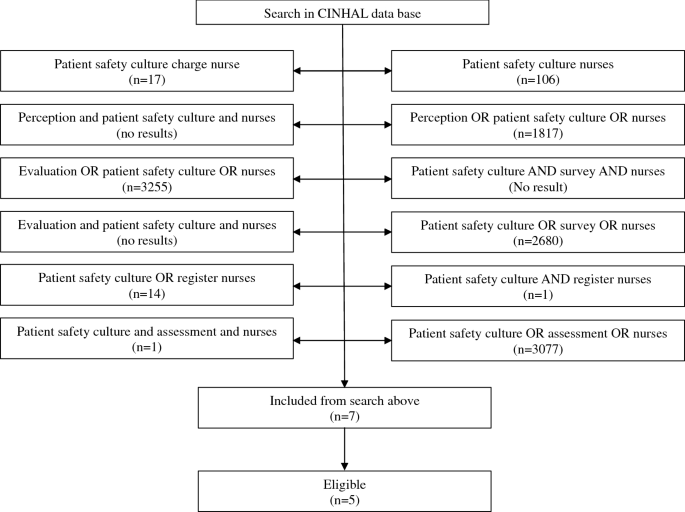
Search strategy in the CINHAL electronic database
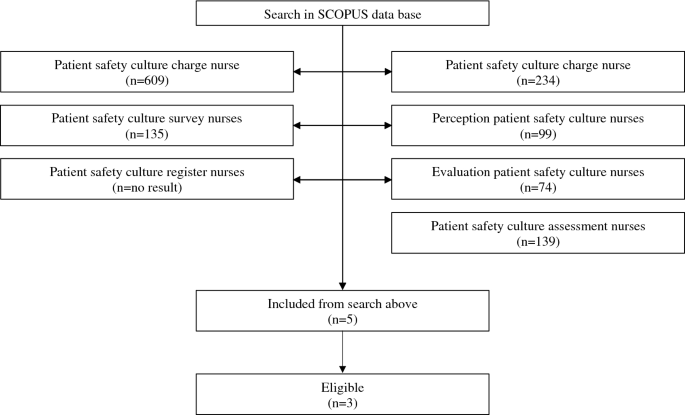
Search strategy in the Scopus electronic database
No restriction was applied to search for articles according to the country of study, whereas restrictions were applied to the language of articles and period of publication. The language of the articles was limited to English, and the period of publication was limited to 2005–2012. In addition, the search was limited to studies with full text and abstract availability.
2.4 Study Selection Procedures
Studies were selected according to the following procedures. The title and abstract in each article were scanned, and articles were assessed according to the inclusion criteria. Articles measuring nurses’ perceptions of patient safety culture in hospitals, in specific departments, or in one department in a hospital, were included. Articles not associated with the review topic, such as those examining the relationship between patient safety culture and the level of healthcare, articles measuring the effects of patient safety culture improvement programs, and articles in which the full text or abstract was not available were excluded from this systematic review.
2.5 Data Extraction and Synthesis
Data were extracted from each eligible article. The key aspects of each article were extracted, including the location of the study, sample size, response rate, healthcare providers' work experience, healthcare providers' age, nurses’ qualification, study design, type of questionnaire, method of data analysis, patient safety culture dimensions, and duration of data collection. In addition, data associated with the results were extracted, which included healthcare providers’ perceptions of patient safety culture. Because the articles included in this review presented the perceptions of nurses according to multiple questionnaires (Fig. 3 ), data comparability was important for identifying the direction and the gaps of the patient safety culture perception. On the basis of the commonalities among surveys, we grouped the results from these studies into seven patient safety culture dimensions, as shown in Fig. 4 [ 26 ].
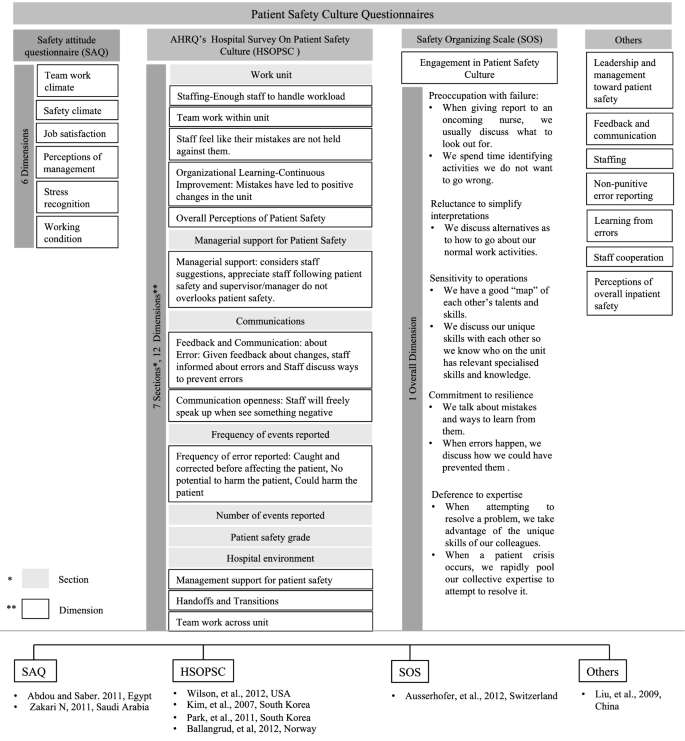
Various patient safety culture surveys. Commonly used patient safety culture surveys and dimensions covered in each survey. Articles using a specific survey are listed
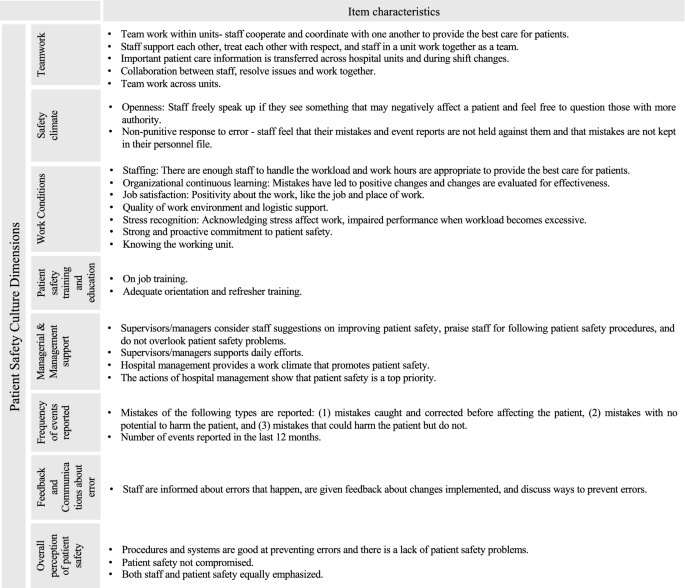
Patient safety culture dimensions. Some common dimensions and their item characteristics are summarized from various patient safety culture surveys, and grouped and described along with their specific item characteristics
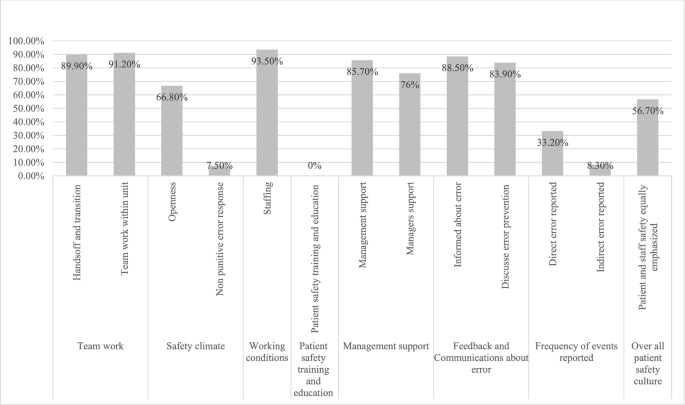
Nurses’ perceptions of patient safety culture by Liu et al. [ 16 ]: the percentage of nurses ( y -axis) agreeing to various items across each patient safety culture dimension ( x -axis)
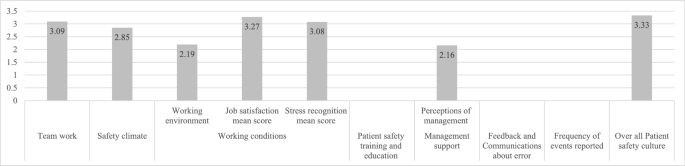
Nurses’ perceptions of patient safety culture by Abdou and Saber [ 19 ]: the mean scores ( y -axis) of the patient safety culture dimensions ( x -axis)
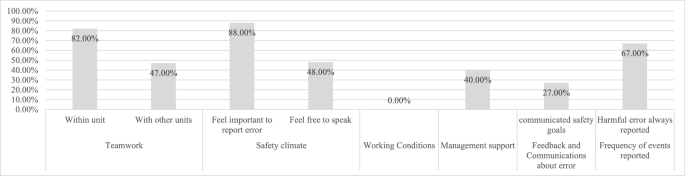
Nurses’ perceptions of patient safety culture by Kim et al. [ 21 ]: the percentage of nurses ( y -axis) strongly agreeing with various items across each patient safety culture dimension ( x -axis)
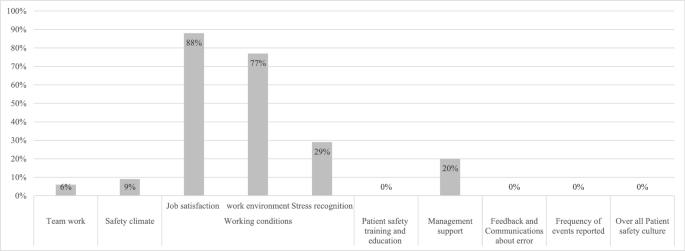
Nurses’ perceptions of patient safety culture by Zakari [ 22 ]: the percentage of nurses with a positive patient safety attitude ( y -axis) toward the various patient safety dimensions ( x -axis)
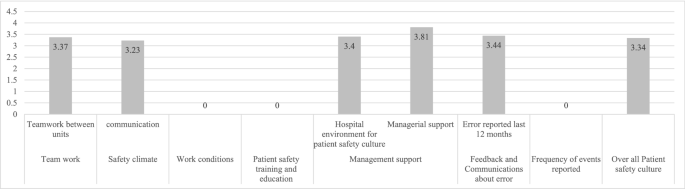
Nurses’ perceptions of patient safety culture by Park et al. [ 23 ]: the mean scores of some items ( y -axis) of the patient safety culture dimensions ( x -axis)
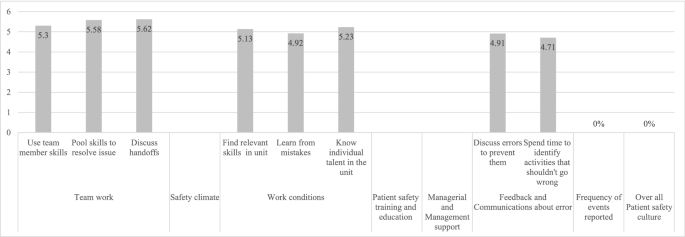
Nurses’ perceptions of patient safety culture by Ausserhofer et al. [ 12 ]: the mean scores of various items ( y -axis) of the patient safety culture dimensions ( x -axis)
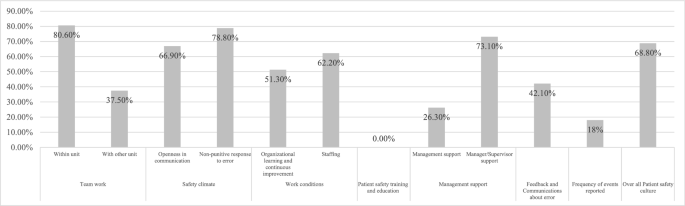
Nurses’ perceptions of patient safety culture by Ballangrud et al. [ 25 ]: the registered nurses' positive scores ( y -axis) for various items of the patient safety culture dimensions ( x -axis)
The extracted data were synthesized in a simple manner. Attitude was considered highly positive if the article reported the score as positive or having a scale score > 75; attitude was considered positive/desirable if an item had a mean score > 3 on a 5-point Likert scale or > 4 on a 7-point Likert scale, i.e., “strongly agree,” “agree,” or “somewhat agree” [ 22 , 26 ].
Quality assessment strategy The quality of selected articles was assessed on the basis of questions in the critical appraisal tool for cross-sectional designs (Joanna Briggs Institute’s critical appraisal tool available on the website of the University of Adelaide) [ 27 ]. This tool provides a checklist for assessing the quality, relevance, and reliability of analytical cross-sectional studies. Questions in the checklist focus on the inclusion relevance, appropriateness of study design, appropriateness of the population in the study, response rate, validity of questionnaires, and statistical methods used for analysis of results. The assessment of the quality of selected articles indicated that all eight articles [ 16 , 19 , 20 , 21 , 22 , 23 , 24 , 25 ] were relevant to this project. In the selected articles, researchers provided background and overviews of previous articles associated with the area of research. Moreover, the aim of the study was stated in each article; this aspect was important to ensure that the findings were relevant to the aim of this study and that no bias was present. No systematic bias was present in the selected articles, because of their appropriate study design. All eight articles used a cross-sectional design, which was suitable for the aim of each study. In addition, articles were assessed on the basis of other criteria. Samples in eight articles were considered representative, because the target population in each article was hospital nurses. Seven articles measured nurses’ perceptions of patient safety culture in a hospital [ 16 , 19 , 20 , 21 , 22 , 23 , 24 ]; one study targeted the population of nurses in an intensive care unit (ICU) in a hospital [ 25 ]. The participant selection procedure in each article was explained. In some articles, researchers randomly selected the place of the study and targeted the entire population. All healthcare providers in selected departments were included, thus ensuring no bias in the participant selection procedure [ 9 ]. Confounding factors were not identified during bias assessment, because the studies included measured behavioral and attitudinal factors [ 27 ]. The appraisal was scored as “yes,” “no,” “unclear,” and “not applicable,” and was later converted to a percentage. For measuring the risk of bias, a score above 70 indicated low bias, a score of 50–69 indicated moderate bias, and a score < 49 indicated high bias [ 6 ]. A summary is presented in Table 2 .
3.1 Characteristics of the Included Studies
The selected studies showed marked diversity with respect to study location, encompassing four continents: Asia [ 16 , 21 , 22 , 23 ], Europe [ 24 , 25 ], North America [ 20 ], and Africa [ 19 ]. These studies also varied in hospital number and size. The included studies presented the perceptions of respondents from a single hospital [ 19 , 20 , 22 , 23 ] to as many as 35 hospitals [ 24 ]. Respondent nurses with roles as diverse as clinical or ambulatory nurses, and nurse managers were included in these studies (Table 3 ). Differences in sample size, response rate, and participants’ characteristics were observed among the selected articles. Ausserhofer et al. [ 24 ] had the largest study sample size among the selected articles ( n = 1633), with a response rate of 72%. The second highest sample size was n = 886, with a response rate of 92.3%, in a study by Kim et al. [ 21 ]. The lowest sample size was n = 126, but the study had a response rate of 100% [ 23 ]. Data are provided in Table 2 .
Participants in these eight articles had different characteristics with respect to age, working experience, hospital unit, and qualifications. In some articles, the researchers did not report some of the participants’ characteristics, for example, the age of participants [ 20 ]. Data are shown in Table 3 .
3.2 Assessment of Patient Safety Culture
The studies included in this review assessed the nurses’ overall perceptions of patient safety culture through surveys. The most common survey questionnaire used was the HSOPSC [ 20 , 25 ]. The survey measured patient safety culture under 12 dimensions, as described above. Two studies used the Korean translated version of the same survey [ 21 , 23 ]. The SAQ, typically measuring six domains (as listed above) of patient safety culture, was also used by some included studies [ 19 , 22 ]. The Safety Organizing Scale (SOS) questionnaire, which assesses engagement in patient safety culture through nine items under the single domain of engagement in patient safety culture was also used in one of the studies [ 24 ]. Liu et al. [ 16 ] used a custom two-part survey constructed from existing surveys, which was tested before being administered to the respondents. That study assessed patient safety culture under the following domains: leadership and management regarding patient safety, feedback and communication about errors, staffing, nonpunitive error reporting, learning from errors, staff cooperation, and perceptions of overall inpatient safety. Although different questionnaires were used, and some were translated into the respondents’ language [ 19 , 21 , 23 , 24 , 25 ], all were verified for reliability/validity. Most of the studies scored the items of patient safety culture dimensions on a 5-point Likert scale [ 19 , 20 , 21 , 22 , 23 , 25 ], with reverse scoring for negative questions. One study used a 7-point Likert scale [ 24 ], and one study used a yes/no format [ 16 ]. Data are shown in Table 4 . The results of nurses’ perceptions of patient safety culture dimensions, as reported by the authors, are represented herein through bar graphs in Figs. 5 , 6 , 7 , 8 , 9 , 10 and 11 in which the x -axis represents assessed dimensions of patient safety culture and the y -axis represents the percentage of positive responses [ 16 , 21 , 22 , 25 ] or the mean score of a dimension [ 19 , 23 , 24 ].
Because different patient safety culture assessment questionnaires were used in the reviewed articles, for ease of understanding and discussion, the observations are discussed under the following dimensions: teamwork, safety climate, working conditions, management support, frequency of errors reported, feedback and communication, and overall patient safety culture [ 26 ]. The characteristic items of these dimensions that were considered in reviewing the articles are shown in Fig. 4 .
3.3 Teamwork
On the basis of the HSOPSC survey, between 80.6% [ 25 ] and 82.6% [ 21 ] of nurses strongly agreed that staff were supported within the working unit, and 30% of nurses strongly agreed that physicians and nurses worked well as a team, whereas only 39.3% strongly agreed about teamwork between units [ 21 ]. Additionally, the perceptions of handling handoff and transition during shift changes were considered positive by only 57.3% [ 25 ] of nurses, whereas approximately 56.8% considered the shift change problematic [ 21 ]. A total of 58% of nurses expressed that important patient care information is often lost during shift changes, and 56% found difficulty in approaching physicians [ 21 ]; 47.1% indicated that hospital units do not coordinate, and 49.5% indicated unpleasant feelings in working with other units [ 21 ]. In a study from South Korea, collaboration between units received a mean score of 3.37 ± 0.40 [ 23 ], thus suggesting fairly good and positive cooperation between units. Similarly, the teamwork perceptions inferred through the SAQ received a mean score of 3.09 ± 0.78 [ 19 ], whereas the perspective of ambulatory nurses’ regarding teamwork was lowest, with only 6% positive perception [ 22 ]. The SOS questionnaire revealed that discussion during handoffs received a mean score of 5.62 ± 1.074, with nurses agreeing to a good extent [ 24 ]. Considerable agreement, with mean scores of 5.34 ± 1.154 and 5.58 ± 1.060, was observed for using one another’s skills to resolve an issue and teams acting collectively during crises, respectively [ 24 ]. According to other questionnaires, teamwork within a unit was perceived to be positive by 91.2% of the nurses [ 16 ]. The shift change procedure was considered to promote patient safety by 89.9% [ 16 ].
3.4 Safety Climate
According to the HSOPSC survey, only 15% of nurses perceived feeling free to reporting an error [ 21 ]; 66.9% expressed a positive attitude to openness to communication [ 25 ], whereas communication among clinicians was fair, with a mean score of 3.23 ± 0.40 [ 23 ]. A total of 78.8% felt positive about the nonpunitive response to error reporting [ 25 ], 88% believed in the importance of reporting errors, and 77.3% felt that errors must be reported even if they cause no harm [ 21 ]. A total of 48% felt free to speak regarding errors, 27% felt free to question authority, and 38% felt free to voice opinions different from those in authority [ 21 ]. By contrast, with the SAQ, safety climate received a mean score of 2.85 ± 0.97 [ 19 ], which translated to a neutral positive attitude, and organizational commitment toward patient safety was expressed positively by only 9% [ 23 ]. Through the other questionnaire, 66.8% of staff reported feeling free to report errors [ 16 ], 92.2% believed that the person committing the error would be punished, and 90.3% believed that the person making the error was responsible for the consequences [ 16 ]. Here, making an error was also considered shameful by 69.11% [ 16 ]. The SOS questionnaire did not assess the safety climate dimension.
3.5 Working Conditions
Through the SAQ, perceptions of job satisfaction and stress recognition were reported positively by 88% and 29% of nurses, respectively [ 22 ]. In another study using the SAQ, job satisfaction received a mean score of 3.27 ± 0.61 [ 19 ], reflecting a neutral attitude among nurses. Similarly, stress recognition received a mean score of 3.08 ± 1.02 [ 19 ]. The working conditions were perceived positively by 77% of nurses [ 22 ] and received a mean score of 2.19 ± 0.79 in another study [ 19 ]. According to the HSOPSC questionnaire, organizational learning and continual improvement were positively perceived by 51.3% [ 25 ], whereas 62% considered that the working unit had sufficient staff for the given workload [ 25 ]. Through the other questionnaire, the number of staff present to handle the workload was considered sufficient by 93.5% of nurses [ 16 ]. Some characteristic perceptions emerged through the SOS questionnaire. A discussion to identify the suitable skills among the working unit staff was agreed upon to a considerable extent by responding nurses, with a mean score of 5.13 ± 1.237. Similarly, having a map of the abilities of the staff in the working unit received a mean score of 5.23 ± 1.073 [ 24 ], and learning from mistakes received a mean score of 4.92 ± 1.25.
3.6 Management Support
According to the HSOPSC questionnaire, six Norwegian hospitals reported a low rate of 26.3% positivity regarding management support [ 25 ], whereas 40% indicated that management cared more about cutting costs than patient safety culture [ 21 ]. The mean score for hospital work environment promoting patient safety was 3.4 ± 0.62, whereas that for managerial support was 3.81 ± 0.54, inclining toward “agree” [ 23 ]. Managerial support for patient safety was perceived positively by 73.1% [ 25 ]. The perception of management support for patient safety culture according to the SAQ questionnaire revealed that 9% of nurses had a positive attitude [ 22 ]; another article reported a mean of 2.16 ± 0.59 for perceptions regarding management [ 19 ], thus indicating agreement to a very limited extent. In the article using the other questionnaire, 85.7% considered hospital administrators to have patient safety as a priority, and 76% indicated managerial support for patient support [ 16 ]. The SOS questionnaire did not address the dimension of management support for establishing patient safety culture.
3.7 Frequency of Errors Reported
Results obtained with the HSOPSC questionnaire indicated that 18% of nurses had a positive attitude toward reporting an error [ 25 ]; 67% [ 21 ] of nurses considered reporting errors that harmed patients, whereas 66% [ 21 ] always reported mistakes that resulted in patient harm. For the number of errors reported in the previous 12 months, the mean was 3.44 for one or two events being reported [ 23 ]. However, 50% were unclear on what type of errors to report [ 21 ]. The other questionnaire highlighted direct and indirect patient safety error reporting systems [ 16 ], wherein 33.3% agreed that direct errors were always reported, and 8.3% agreed that indirect errors were always reported. With the SAQ and the SOS questionnaires, the perceptions of nurses regarding the frequency of error reporting were not documented.
3.8 Feedback and Communication
According to the HSOPSC questionnaire, 52% reported receiving feedback on errors committed, whereas 66% of respondents felt that their suggestions to improve patient safety were ignored [ 21 ]. A total of 42.1% indicated a positive attitude toward feedback and communication [ 25 ]. A total of 27% reported that hospital leaders successfully communicated patient safety goals [ 21 ]. Other questionnaires revealed that 88.5% of respondents agreed that they were informed when an error occurred in their unit [ 16 ]. The SOS and another questionnaire shed light on openness toward discussing error causes and prevention, which was affirmed by 70.1% [ 24 ] and 83.9% [ 16 ] of respondents, respectively, whereas 67.3% [ 24 ] affirmed discussions on identifying activities that should never occur through the SOS questionnaire. The SAQ questionnaire did not elaborate on the feedback and communication dimension of patient safety culture.
3.9 Overall Patient Safety Culture
According to the HSOPSC questionnaire, 68.8% [ 25 ] indicated that nurses showed a positive attitude toward overall patient safety culture. However, 83% strongly agreed or agreed that more serious errors did not occur only because of chance, expressed negative perceptions of overall patient safety [ 21 ], and had negative perceptions of overall patient safety culture. The SAQ questionnaire results indicated that the mean for overall perceptions of safety culture was 3.33 ± 0.58, indicating near neutral opinions toward patient safety culture [ 19 ]. The other questionnaire revealed that 56.7% agreed to equal emphasis on patient and staff safety [ 16 ] and 67% expressed that no safety committee (system) is present in the hospital [ 16 ].
3.10 Differences in Perceptions Across Descriptive Variables
Differences in respondents’ perceptions of patient safety culture dimensions were reported across descriptive variables, such as the hospital unit or hospital, position at work, age, experience, education level, marital status, working hours, and language region of the respondents. All the reported differences in perceptions are presented in Table 5 . The perceptions of overall patient safety culture dimensions among healthcare providers in the ICU were reported to be higher (3.38 ± 0.51) than those among coronary care unit (CCU) nurses (3.34 ± 0.46) followed by general unit nurses (3.32 ± 0.60) [ 19 ]. CCU unit nurses were more perceptive to stress recognition [ 19 ]. Technical healthcare providers showed higher positivity for overall patient safety culture dimensions (mean score of 3.41 ± 0.54) than professional nurses (3.23 ± 0.61) [ 19 ]. Similarly, regarding job satisfaction, the mean scores among technical nurses were higher (3.07 ± 0.0.91) than those among professional nurses (2.56 ± 0.98) [ 19 ]. Registered nurses had more positive attitudes toward stress recognition and acknowledgment of the effects of stress on patient safety than nurse managers [ 22 ]. In addition, perceptions of management were higher among nurse managers than registered nurses [ 22 ]. A significant difference ( P < 0.05) was found between work position and job satisfaction dimension. The nurse managers had greater positive attitudes than registered nurses [ 19 ]. In addition, significant differences ( P < 0.05) were observed among head nurses, staff nurses, and charge nurses. Head nurses reported higher positive perceptions of patient safety culture in their units [ 21 ]. They also reported more errors [ 21 ]. Respondent age significantly influenced perceptions [ 19 , 21 ]. Nurses above 40 years of age responded more positively toward patient safety culture dimensions than younger nurses [ 19 , 21 ]. Respondent experience also influenced overall patient safety culture perceptions [ 20 , 21 ], job satisfaction [ 19 ], communication [ 23 ], and the frequency of error reporting [ 21 ]. Education level and marital status have been reported to affect respondents’ job satisfaction [ 19 ]. Moreover, working hours influenced the perceptions of job satisfaction, teamwork, safety climate, and overall patient safety [ 19 ]. Notably, an influence of language region on the perceptions of the respondents was observed [ 24 ]. Data are shown in Table 5 .
4 Discussion
In this systematic review, eight articles were selected, on the basis of specific criteria of showing different healthcare providers’ perceptions of patient safety culture. The participants in the selected articles reported high perceptions regarding several characteristic items of patient safety culture dimensions, such as teamwork within a unit, discussing handoff during shift change, discussing and preventing errors, job satisfaction, and having sufficient staff for the workload in a unit and managerial support. Similarities were observed among several selected articles concerning several findings. The respondents’ perceptions of teamwork within the unit were reported to be highly positive across all studies except those using the SAQ [ 19 , 22 ]. Moreover, a positive attitude toward teamwork within the unit was reported to be highest in one study using the HSOPSC questionnaire [ 25 ]. However, teamwork across units was perceived comparatively less positively [ 21 , 25 ]. Ineffective teamwork in hospitals negatively affects healthcare, and this aspect was one cause of adverse events in the ICU, as reported by Ballangrud et al. [ 25 ]. Nurses reported the highest positive perceptions of effective teamwork at the unit level and not across units because they might experience feelings of being part of a team, which seldom occur with other teams, which are often viewed critically [ 24 ]. The finding was in agreement with those of a study reported by Georgiou et al. [ 28 ], wherein teamwork within a unit was perceived more positively than safety climate, because of the implementation of quality systems at the unit level. In a study involving multicultural nurses, negative perceptions of nurses toward teamwork have been reported to be due to language and cultural differences [ 22 ]. Job satisfaction, an item in the work condition dimension, has been perceived positively by nurses [ 19 ]. Glendon and Mckenna, in 1995, expressed that the characteristics of an organization with high patient safety culture are high positive job satisfaction and effective communication [ 19 ]. This aspect has also emerged in studies conducted through the SAQ questionnaire, wherein the perceptions of job satisfaction ranked first [ 22 ] and second [ 19 ] among other dimensions of patient safety culture. In the dimension of managerial and management support, the analyzed results indicated positive managerial perceptions but low perceptions of management regarding patient safety culture, according to the SAQ questionnaire [ 19 , 22 ], and of management support, according to the HSOPSC questionnaire [ 21 , 23 , 25 ]. The not very positive attitude toward management support for patient safety culture might be attributable to management decisions not to form patient safety committees [ 16 ]. Among these articles, a study conducted in Norway [ 25 ] has shown low positive attitudes toward management support, because the health personnel had undergone considerable reorganization and efficiency improvement in the past few years [ 29 ], and the management was more focused on production than communication [ 30 ]. By contrast, a study on Chinese hospitals has reported high positive perceptions among nurses regarding hospital management support [ 16 ]. Huang et al. [ 31 ] have also recognized the importance of management and organizational commitment in improving patient safety culture. The Department of Health and Children (Dublin, Ireland) [ 4 ] has noted a strong association between the management of healthcare institutions and positive patient safety culture. However, the SOS questionnaire does not cover the perceptions of management while assessing the dimensions of patient safety culture. In addition, it does not address several aspects of the safety climate dimension. Findings for other dimensions indicated the close link between the dimensions of safety climate and frequency of errors reported: the results showed low positive perceptions of the frequency of error reporting along with negative perceptions toward nonpunitive responses to errors (an item of the safety climate dimension). Although the importance of reporting errors was perceived positively by 88% of the respondents, as expressed through the HSOPSC questionnaire [ 21 ], the frequency of error reporting was low among the nurses [ 25 ], and negative perceptions of nonpunitive response to error were observed [ 16 ]. The reason for this behavior might be a fear of repercussions from colleagues and punishment from management [ 19 ]. Making errors was considered shameful by 69.11% of the respondents [ 16 ]. A closely related factor involves feedback and communication regarding errors. That dimension also received a low positive response [ 21 , 25 ], as expressed through the HSOPSC questionnaire. However, negligence in patient safety and risks to critically ill patients can be effectively diminished through fostering communication and the flow of information [ 32 ]. The low error reporting frequency was also associated with low feedback and communication about errors [ 25 ]. Discussing the possible causes of error and establishing an effective feedback system are essential for patient safety [ 16 ]. Positive attitudes toward feedback and communication, and reporting of errors can be increased if a working unit’s reporting system is blame-free and considers errors as system failures [ 30 ]. Finally, this review highlights variations in perceptions of patient safety culture dimensions across multiple descriptive variables, such as the hospital unit or hospital, position at work, experience, age, education, marital status, working hours, and language region. The differences in perceptions of patient safety across working units in a hospital are attributable to variations in culture across units [ 31 ]. The variations in perceptions due to differences in position may be explained by their direct effects on patients. Technical nurses did not directly affect patients, unlike professional nurses; thus, they felt more positive toward patient safety culture [ 19 ]. Nurses who had less experience and were young perceived patient safety culture negatively, because of high perceptions of stress and low job satisfaction [ 21 ]. Finally, the effects of the language region on positive perceptions were considered to be due to more patient safety programs being introduced in certain regions [ 25 ].
Interestingly, although prominent safety culture assessment questionnaires were used, some important patient safety culture dimensions were not measured. The SAQ [ 19 , 22 ] and SOS [ 24 ] questionnaires do not report the frequency of error reporting—an important dimension to assess overall patient safety. Moreover, the SOS questionnaire does not report management support and items of safety climate, and the SAQ does not cover feedback and communication aspects of patient safety culture. However, a customized questionnaire used by Liu et al . [ 16 ] has been used to investigate all dimensions of patient safety culture missed by the other questionnaires. In addition, the SOS survey includes questions not covered by other surveys. In the future, a notable practice to enhance patient safety culture will be encouraging and fostering on-job training and educational programs. The studies included in this review unexpectedly did not analyze the importance of on-job training and education while assessing various patient safety culture dimensions. The importance of on job training programs has effectively been documented by Ginsburg et al. [ 30 ], and an interventional training program has been found to enhance the perceptions of patient safety culture among nurse leaders [ 33 ]. Similarly, Al Mutair et al. have reported a decrease in hospital-acquired pressure ulcers through the implementation of an educational program. The educational program significantly decreased the number of hospital-acquired pressure ulcers, even though the number of inpatients tripled in 2018 [ 34 ]. Morello et al. [ 35 ] have stated that educational activities in hospitals positively affect patient safety culture. Involving staff in the implementation of updated policy and procedures and setting documentation requirements in addition to key performance indicator tracking will reinforce new behaviors in a strong care culture [ 36 ]. A lack of knowledge and information among healthcare workers can also weaken healthcare delivery [ 37 ]. Results from the reviewed studies by AlJohani et al. have shown that high-level knowledge of precautionary measures affects compliance with needle safety precautions. Thus, updating knowledge and information greatly affects patient safety in several ways. On-job training, appropriate programs, and an effective feedback system are critical to incident reporting and overall patient safety [ 38 ]. In addition, health organizations must use an effective reporting environment for the process of medication use to ensure sounder practice [ 39 ].
4.1 Limitations
This review has several limitations. One is the limited number of articles in the electronic database associated with nurses’ perceptions of patient safety culture in hospitals, given that the field of patient safety culture is considerably new, and researchers have only recently begun conducting studies in this area, in the past few years. Another limitation is the unavailability of published reviews on nurses’ perceptions of patient safety culture in hospitals. Therefore, we were unable to compare the results of this review. In addition, the association between descriptive variables and patient safety culture dimensions was not calculated in some selected articles. The included studies were also characterized by specific limitations, such as limited sample sizes and nurses belonging to a single hospital, thus making the overall results difficult to generalize [ 19 , 20 , 22 , 23 ]. Similarly, a limitation was also observed for a study based in a single city [ 16 ]. The self-reporting survey design is also considered a limitation, because of potential doubts regarding the trustworthiness of the respondents’ answers [ 22 ]. The risk of bias is also a limitation, owing to the lack of random sampling [ 24 ]. The SOS provides information on patient safety behavior but not other patient safety culture dimensions, such as a blame-free environment or management support for patient safety [ 24 ]. Despite these limitations, including the small sample sizes, the results provided information regarding the level of patient safety culture in hospitals. These findings may be considered by decision-makers in other small hospitals.
5 Conclusion
Patient safety culture is an important component of patient safety. Improvement in patient safety culture positively affects the quality of healthcare. The perceptions of patient safety culture dimensions among nurses are dissimilar; however, promoting patient safety culture can minimize issues that affect patient safety and consequently errors in patient safety. Through this systematic review, we presented substantial observations that may help foster patient safety culture in healthcare organizations. First, a comprehensive assessment of patient safety culture requires rigorous considerations while selecting an assessment tool that encompasses most, if not all, patient safety culture dimensions. In the future, although teamwork within a unit is generally perceived positively, improvement in teamwork across units in a healthcare organization can additionally contribute to the building of patient safety culture. Furthermore, management support is another key contributor to patient safety culture and must be improved. In addition, to ameliorate error reporting, a nonpunitive attitude toward error reporting must be fostered simultaneously with strengthened communication. Ultimately, substantial improvements in the availability and accessibility of on-job training and continuing education are necessary to achieve and sustain a robust patient safety culture. In conclusion, careful recognition and committed work on various scales/dimensions of patient safety culture can lead to improvements in the quality of healthcare and consequently decrease patient safety issues associated with nursing care. These results may provide direction and guidance for healthcare management and decision-makers in focusing and establishing improvement in areas that will positively affect the quality of healthcare.
Data availability
Data used and analyzed in this study are available on request.
Abbreviations
Cumulative Index of Nursing and Allied Health Literature
Safety Attitudes Questionnaire
Sample, Phenomenon of Interest, Design, Evaluation, Research type
Hospital Survey on Patient Safety Culture survey
Safety Organizing Scale
Intensive care unit
Coronary care unit
World Health Organization. World alliance for patient safety: WHO draft guidelines for adverse event reporting and learning systems: from information to action. 2005. https://apps.who.int/iris/handle/10665/69797 . Accessed 2 Mar 2022.
Zrelak PA, Utter GH, Sadeghi B, Cuny J, Baron R, Romano PS. Using the Agency for Healthcare Research and Quality patient safety indicators for targeting nursing quality improvement. J Nurs Care Qual. 2012;27(2):99–108.
Article Google Scholar
Agency for Healthcare Research and Quality. What Is Patient Safety Culture? [Internet]. [cited 2022 May 23]. https://www.ahrq.gov/sops/about/patient-safety-culture.html . Accessed 23 May 2022.
Building a Culture of Patient Safety: Report of the Commission on Patient Safety and Quality Assurance [Internet]. 2008 [cited 2022 Feb 22]. https://www.gov.ie/en/publication/5d9570-building-a-culture-of-patient-safety-report-of-the-commission-on-pat/ . Accessed 22 Feb 2022.
Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Psychological and psychosomatic symptoms of second victims of adverse events: a systematic review and meta-analysis. J Patient Saf [Internet]. 2020 Jun [cited 2022 Feb 22];16(2):61–74. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386870/ . Accessed 22 Feb 2022.
Alanazi FK, Sim J, Lapkin S. Systematic review: Nurses’ safety attitudes and their impact on patient outcomes in acute-care hospitals. Nurs Open. 2022;9(1):30–43.
Hammer A, Ernstmann N, Ommen O, Wirtz M, Manser T, Pfeiffer Y, et al. Psychometric properties of the Hospital Survey on Patient Safety Culture for hospital management (HSOPS_M). BMC Health Serv Res [Internet]. 2011;11(1):165. https://doi.org/10.1186/1472-6963-11-165 .
Adams-Pizarro I, Walker Z, Robinson J, Kelly S, Toth M. Using the AHRQ Hospital Survey on Patient Safety Culture as an Intervention Tool for Regional Clinical Improvement Collaboratives. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol 2: Culture and Redesign) [Internet]. 2008 [cited 2022 Feb 22]; http://www.ncbi.nlm.nih.gov/books/NBK43728/ . Accessed 22 Feb 2022.
Lachman P, Linkson L, Evans T, Clausen H, Hothi D. Developing person-centred analysis of harm in a paediatric hospital: a quality improvement report. BMJ Qual Saf. 2015;24(5):337–44.
Pittet D, Donaldson L. Challenging the world: patient safety and health care-associated infection. Int J Qual Health Care. 2006;18(1):4–8.
Sorra J, Gray L, Streagle S, Famolaro T, Yount N, Behm J. AHRQ Hospital Survey on Patient Safety Culture: User’s Guide [Internet]. AHRQ Publication; 2016 [cited 2022 Feb 22]. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/patientsafetyculture/hospital/userguide/hospcult.pdf . Accessed 22 Feb 2022.
Hao HS, Gao H, Li T, Zhang D. Assessment and Comparison of Patient Safety Culture Among Health-Care Providers in Shenzhen Hospitals. RMHP [Internet]. 2020 Sep 11 [cited 2022 May 23];13:1543–52. https://www.dovepress.com/assessment-and-comparison-of-patient-safety-culture-among-health-care--peer-reviewed-fulltext-article-RMHP . Accessed 23 May 2022.
NPSA: Manchester Patient Safety Framework (2006) [Internet]. Patient Safety Learning - the hub. [cited 2022 Mar 2]. https://www.pslhub.org/learn/culture/safety-culture-programmes/incentives-and-techniques/npsa-manchester-patient-safety-framework-2006-r753/ . Accessed 02 Mar 2022.
Measuring safety culture-The Health Foundation [Internet]. 2011 [cited 2022 May 23]. https://www.health.org.uk/publications/measuring-safety-culture . Accessed 23 May 2022.
Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res [Internet]. 2006;6(1):44. https://doi.org/10.1186/1472-6963-6-44 .
Article PubMed PubMed Central Google Scholar
Liu Y, Kalisch BJ, Zhang L, Xu J. Perception of safety culture by nurses in hospitals in china. J Nurs Care Qual. 2009;24(1):63–8.
Malliaris AP, Phillips J, Bakerjian D. Nursing and Patient Safety [Internet]. Patient Safety Network. 2021 [cited 2022 Feb 22]. https://psnet.ahrq.gov/primer/nursing-and-patient-safety . Accessed 22 Feb 2022.
Amiri M, Khademian Z, Nikandish R. The effect of nurse empowerment educational program on patient safety culture: a randomized controlled trial. BMC Medical Educ [Internet]. 2018. https://doi.org/10.1186/s12909-018-1255-6 .
Abdou H, Saber K. A baseline assessment of patient safety culture among nurses at Student University Hospital. World J Med Sci. 2011;1(6):17–26.
Google Scholar
Wilson D, Redman RW, Talsma A, Aebersold M. Differences in perceptions of patient safety culture between charge and noncharge nurses: implications for effectiveness outcomes research. Nurs Res Pract. 2012;2012:847626. https://doi.org/10.1155/2012/847626
Kim J, An K, Kim MK, Yoon SH. Nurses’ perception of error reporting and patient safety culture in Korea. West J Nurs Res. 2007;29(7):827–44.
Zakari N. Attitude of Academic Ambulatory Nurses toward Patient Safety Culture in Saudi Arabia. undefined [Internet]. 2011 [cited 2022 Feb 20]; https://www.semanticscholar.org/paper/Attitude-of-Academic-Ambulatory-Nurses-toward-in-Zakari/fd932a8b140f31f8742d99a4b9dc125fec837962 . Accessed 20 Feb 2022.
Park SA, Lee SJ, Choi GU. Survey of factors associated with nurses’ perception of patient safety. Asian Pac J Cancer Prev. 2011;12(8):2129–32.
PubMed Google Scholar
Ausserhofer D, Schubert M, Engberg S, Blegen M, De G, Schwendimann R. Nurse-reported patient safety climate in Swiss hospitals: a descriptive-explorative substudy of the Swiss RN4CAST study. Swiss Med Wkly. 2012;142: w13501.
CAS PubMed Google Scholar
Ballangrud R, Hedelin B, Hall-Lord ML. Nurses’ perceptions of patient safety climate in intensive care units: a cross-sectional study. Intensive Crit Care Nurs. 2012;28(6):344–54.
Tocco Tussardi I, Benoni R, Moretti F, Tardivo S, Poli A, Wu AW, et al. Patient safety in the eyes of aspiring healthcare professionals: a systematic review of their attitudes. Int J Environ Res Public Health. 2021;18(14):7524.
Joanna Briggs Institute. Critical Appraisal Tools [Internet]. [cited 2022 Mar 2]. https://jbi.global/critical-appraisal-tools . Accessed 02 Mar 2022.
Kyriacou Georgiou M, Merkouris A, Hadjibalassi M, Sarafis P, Kyprianou T. Correlation Between Teamwork and Patient Safety in a Tertiary Hospital in Cyprus. Cureus [Internet]. 2021 [cited 2022 Mar 1];13(11):e19244. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8642670/ . Accessed 01 Mar 2022.
Lægreid P, Opedal S, Stigen IM. The Norwegian Hospital reform: balancing political control and enterprise autonomy. J Health Polit Policy Law. 2005;30:1027–64.
McFadden KL, Stock GN, Gowen CR. Implementation of patient safety initiatives in US hospitals. Int J Oper Prod Manag [Internet]. 2006;26(3):326–47. https://doi.org/10.1108/01443570610651052 .
Huang DT, Clermont G, Sexton JB, Karlo CA, Miller RG, Weissfeld LA, et al. Perceptions of safety culture vary across the intensive care units of a single institution. Crit Care Med. 2007;35(1):165–76.
Valentin A, Capuzzo M, Guidet B, Moreno R, Metnitz B, Bauer P, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ [Internet]. 2009;338(mar12 1):b814–b814. https://doi.org/10.1136/bmj.b814 .
Ginsburg L, Norton PG, Casebeer A, Lewis S. An educational intervention to enhance nurse leaders’ perceptions of patient safety culture. Health Serv Res [Internet]. 2005 Aug [cited 2022 Mar 1];40(4):997–1020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1361187/ . Accessed 01 Mar 2022.
Al Mutairi A, Schwebius D, Al MA. Hospital-acquired pressure ulcer incident rates among hospitals that implement an education program for staff, patients, and family caregivers inclusive of an after discharge follow-up program in Saudi Arabia. Int Wound J [Internet]. 2020;17(5):1135–41. https://doi.org/10.1111/iwj.13459 .
Morello RT, Lowthian JA, Barker AL, McGinnes R, Dunt D, Brand C. Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf. 2013;22(1):11–8.
Al Mutair A, Al Mutairi A, Schwebius D. The retention effect of staff education program: sustaining a decrease in hospital-acquired pressure ulcers via culture of care integration. Int Wound J. 2021;18(6):843–9.
AlJohani A, Karuppiah K, Al Mutairi A, Al Mutair A. Narrative Review of Infection Control Knowledge and Attitude among Healthcare Workers. J Epidemiol Glob Health [Internet]. 2021 Mar [cited 2022 Feb 22];11(1):20–5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7958281/ . Accessed 22 Feb 2022.
Cullen DJ, Bates DW, Small SD, Cooper JB, Nemeskal AR, Leape LL. The incident reporting system does not detect adverse drug events: a problem for quality improvement. Jt Comm J Qual Improv. 1995;21(10):541–8.
Mutair AA, Alhumaid S, Shamsan A, Zaidi ARZ, Mohaini MA, Al Mutairi A, et al. The effective strategies to avoid medication errors and improving reporting systems. Medicines [Internet]. 2021 Sep [cited 2022 Feb 22];8(9):46. https://www.mdpi.com/2305-6320/8/9/46 . Accessed 22 Feb 2022.
Download references
Acknowledgements
The research team and the authors extend sincere thanks and appreciation to all respondents for their patience in cooperation.
Author information
Abbas Al Mutair
Present address: Research Center, Almoosa Specialist Hospital, Alahsa, Saudi Arabia
Authors and Affiliations
Quality and Patients Safety Department, King Fahd General Hospital, Ministry of Health, Jeddah, Saudi Arabia
Sultan Almutairi
Occupational Health & Safety Department, Faculty of Nursing, Taibah University, Medina, Saudi Arabia
Abdulrahman Aljohani
Commitment Administration, General Directorate of Health Affairs, Medina, Saudi Arabia
Mansour Awad & Hamed Alhobaishi
Research Center, Almoosa Specialist Hospital, Alahsa, Saudi Arabia
Chandni Saha
General Directorate of Commitment Administration, Ministry of Health, Riyadh, Saudi Arabia
Ahmad Almutairi
School of Nursing, University of Wollongong, Wollongong, NSW, 2522, Australia
Princess Nourah Bint Abdul Rahman University, Riyadh, Saudi Arabia
Almoosa College of Health Sciences, Al-ahsa, Saudi Arabia
Department of Nursing, Prince Sultan Military College of Health Sciences, Al Dhahran, Saudi Arabia
You can also search for this author in PubMed Google Scholar
Contributions
SA, MA, AA: methodology; CS; validation and formal analysis; SA, MA, AA, CS: data curation; SA, ABA, MA, CS, HA, AAL, AA: original draft preparation, writing, review and editing.
Corresponding author
Correspondence to Abbas Al Mutair .
Ethics declarations
Conflicts of interest.
The authors declare no conflicts of interest.
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the institutional review board.
Consent for publication
All authors have read and approved the manuscript for publication.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Almutairi, S., Aljohani, A., Awad, M. et al. Perceptions of Patient Safety Culture Dimensions among Hospital Nurses: A Systematic Review. Dr. Sulaiman Al Habib Med J 4 , 103–125 (2022). https://doi.org/10.1007/s44229-022-00012-z
Download citation
Received : 14 March 2022
Accepted : 25 May 2022
Published : 04 July 2022
Issue Date : September 2022
DOI : https://doi.org/10.1007/s44229-022-00012-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient safety culture
- Healthcare providers
- Healthcare services
- Healthcare quality
- Hospital management
- Find a journal
- Publish with us
- Track your research

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
A model framework for patient safety training in chiropractic: a literature synthesis.
Zaugg B, Wangler M. A model framework for patient safety training in chiropractic: a literature synthesis. J Manipulative Physiol Ther. 2009;32(6):493-499. doi:10.1016/j.jmpt.2009.06.004.
This systematic review synthesizes prior literature to develop a framework for learning from adverse events and building a safety culture in chiropractic care.
Effect of genetic diagnosis on patients with previously undiagnosed disease. November 7, 2018
Causes of use errors in ventilation devices--systematic review. November 10, 2021
Patient and caregiver factors in ambulatory incident reports: a mixed-methods analysis. November 24, 2021
Nurse staffing levels and patient-reported missed nursing care. October 14, 2015
Errors of omission: missed nursing care. May 28, 2014
The impact of teamwork on missed nursing care. October 27, 2010
Interruptions and multitasking in nursing care. March 3, 2010
Nurse and nurse assistant perceptions of missed nursing care: what does it tell us about teamwork? November 25, 2009
Health care serial murder: a patient safety orphan. March 31, 2010
Do staffing levels predict missed nursing care? June 29, 2011
Patient-reported missed nursing care correlated with adverse events. October 30, 2013
Near-miss events are really missed! Reflections on incident reporting in a department of pediatric surgery. May 9, 2012
Patient perceptions of missed nursing care. April 4, 2012
Missed nursing care: a concept analysis. July 8, 2009
Development and psychometric testing of a tool to measure missed nursing care. June 3, 2009
Patient safety implications of wearing a face mask for prevention in the era of COVID-19 pandemic: a systematic review and consensus recommendations. February 15, 2023
Experience of hospital-initiated medication changes in older people with multimorbidity: a multicentre mixed-methods study embedded in the OPtimising thERapy to prevent Avoidable hospital admissions in Multimorbid older people (OPERAM) trial. December 7, 2022
What does nursing teamwork look like? A qualitative study. May 6, 2009
Overcoming barriers to patient safety. July 5, 2006
An intervention to enhance nursing staff teamwork and engagement. February 21, 2007
Improving nursing unit teamwork. January 4, 2006
Assessing the impact of the anesthesia medication template on medication errors during anesthesia: a prospective study. April 26, 2017
Failure events in transition of care for surgical patients. March 5, 2014
A decade after Francis: is the NHS safer and more open? April 5, 2023
Healthcare-associated infections in Veterans Affairs acute-care and long-term healthcare facilities during the coronavirus disease 2019 (COVID-19) pandemic. April 5, 2023
Undertaking risk and relational work to manage vulnerability: acute medical patients' involvement in patient safety in the NHS. March 15, 2023
More than an apple a day: factors associated with avoidance of doctor visits among transgender, gender nonconforming, and nonbinary people in the USA. September 23, 2020
Seroprevalence of SARS-CoV-2 among frontline health care personnel in a multistate hospital network--13 academic medical centers, April-June 2020. September 23, 2020
Chronic hospital nurse understaffing meets COVID-19: an observational study. September 9, 2020
Why do hospital prescribers continue antibiotics when it is safe to stop? Results of a choice experiment survey. September 2, 2020
What has been the impact of Covid-19 on safety culture? A case study from a large metropolitan healthcare trust. September 2, 2020
Work-related factors, cognitive skills, unsafe behavior and safety incident involvement among emergency medical services crew members: relationships and indirect effects. May 5, 2021
Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: a multinational cross-sectional study. May 5, 2021
The randomized AMBORA trial: impact of pharmacological/pharmaceutical care on medication safety and patient-reported outcomes during treatment with new oral anticancer agents. April 21, 2021
Patients and relatives as auditors of safe practices in oncology and hematology day hospitals. March 31, 2021
Association of physician burnout with suicidal ideation and medical errors. January 27, 2021
Barriers to and facilitators of bedside nursing handover: a systematic review and meta-synthesis. July 7, 2021
The role of the informal and formal organisation in voice about concerns in healthcare: a qualitative interview study. June 16, 2021
Medication errors during treatment with new oral anticancer agents: consequences for clinical practice based on the AMBORA Study. November 3, 2021
Why do systems for responding to concerns and complaints so often fail patients, families and healthcare staff? September 29, 2021
A machine learning-based clinical decision support system to identify prescriptions with a high risk of medication error. October 21, 2020
Performance of a trigger tool for detecting drug-related hospital admissions in older people: analysis from the OPERAM trial. February 16, 2022
What counts as a voiceable concern in decisions about speaking out in hospitals: a qualitative study. January 19, 2022
Evaluation of clinical practice guidelines on fall prevention and management for older adults: a systematic review. January 12, 2022
Optimizing Therapy to Prevent Avoidable Hospital Admissions in Multimorbid Older Adults (OPERAM): cluster randomised controlled trial. August 18, 2021
A 6-year thematic review of reported incidents associated with cardiopulmonary resuscitation calls in a United Kingdom hospital. April 27, 2022
Investigating the impact of cognitive bias in nursing documentation on decision-making and judgement. April 20, 2022
Predictive power of the "trigger tool" for the detection of adverse events in general surgery: a multicenter observational validation study. March 9, 2022
A systematic review of methods for medical record analysis to detect adverse events in hospitalized patients. March 2, 2022
Adverse safety events in emergency medical services care of children with out-of-hospital cardiac arrest. January 31, 2024
E-prescribing and medication safety in community settings: a rapid scoping review. January 24, 2024
Sleep deprivation and medication administration errors in registered nurses- a scoping review. December 20, 2023
Quality and reporting of large-scale improvement programmes: a review of maternity initiatives in the English NHS, 2010–2023. December 13, 2023
Patients who die by suicide: a study of treatment patterns and patient safety incidents in Norway. November 9, 2022
Causes of adverse events in home mechanical ventilation: a nursing perspective. October 12, 2022
Misdiagnosis of thoracic aortic emergencies occurs frequently among transfers to aortic referral centers: an analysis of over 3700 patients. October 12, 2022
Understanding teamwork in rapidly deployed interprofessional teams in intensive and acute care: a systematic review of reviews. September 28, 2022
The impact of transition to a digital hospital on medication errors (TIME study). August 16, 2023
Associations between self-reported healthcare disruption due to COVID-19 and avoidable hospital admission: evidence from seven linked longitudinal studies for England. August 9, 2023
Student mistakes and teacher reactions in bedside teaching. July 19, 2023
Medication-related problems in critical care survivors: a systematic review. June 28, 2023
Moving beyond implicit bias in antiracist academic medicine initiatives. September 7, 2022
Strength of safety measures introduced by medical practices to prevent a recurrence of patient safety incidents: an observational study. September 7, 2022
Pediatric musculoskeletal radiographs: anatomy and fractures prone to diagnostic error among emergency physicians. August 3, 2022
Who killed patient safety? July 20, 2022
Adverse drug events caused by three high-risk drug-drug interactions in patients admitted to intensive care units: a multicentre retrospective observational study. October 18, 2023
What can safety cases offer for patient safety? A multisite case study. October 11, 2023
Towards diagnostic excellence on academic ward teams: building a conceptual model of team dynamics in the diagnostic process. September 20, 2023
Improving critical incident reporting in primary care through education and involvement. October 16, 2019
Diagnostic errors reported in primary healthcare and emergency departments: a retrospective and descriptive cohort study of 4830 reported cases of preventable harm in Sweden. October 9, 2019
Is disruptive behavior inherent to the surgeon or the environment? Analysis of 314 events at a single academic medical center. September 4, 2019
Eight years of decreased methicillin-resistant Staphylococcus aureus health care–associated infections associated with a Veterans Affairs prevention initiative. February 22, 2017
Incident and long-term opioid therapy among patients with psychiatric conditions and medications: a national study of commercial health care claims. January 25, 2017
Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006–2015. March 29, 2017
Evidence-based guidelines for fatigue risk management in EMS: formulating research questions and selecting outcomes. December 7, 2016
ASPEN Safe Practices for Enteral Nutrition Therapy. December 14, 2016
Imperfect practice makes perfect: error management training improves transfer of learning. April 26, 2017
Electronic patient identification for sample labeling reduces wrong blood in tube errors. March 20, 2019
Clinical decision support in the era of artificial intelligence. November 21, 2018
Effect of a pharmacist-led educational intervention on inappropriate medication prescriptions in older adults: the D-PRESCRIBE randomized clinical trial. November 21, 2018
Predictors of adverse events and medical errors among adult inpatients of psychiatric units of acute care general hospitals. January 30, 2019
Impact of interactions between drugs and laboratory test results on diagnostic test interpretation—a systematic review. November 21, 2018
Defining and classifying terminology for medication harm: a call for consensus. December 19, 2018
Association of cataract surgical outcomes with late surgeon career stages: a population-based cohort study. October 24, 2018
Ten principles for more conservative, care-full diagnosis. October 10, 2018
Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. November 28, 2018
Nurses' perspectives regarding the disclosure of errors to patients: a qualitative study. December 17, 2014
A prospective cohort study of medication reconciliation using pharmacy technicians in the emergency department to reduce medication errors among admitted patients. January 21, 2015
Identifying hospital-wide harm: a set of ICD-9–CM-coded conditions associated with increased cost, length of stay, and risk of mortality. December 17, 2014
Medical harm: patient perceptions and follow-up actions. December 10, 2014
Systematic review of patient safety interventions in dentistry. December 9, 2015
Sleep deprivation and starvation in hospitalised patients: how medical care can harm patients. October 21, 2015
Clinical communities at Johns Hopkins Medicine: an emerging approach to quality improvement. September 2, 2015
Reducing errors through discharge medication reconciliation by pharmacy services. August 26, 2015
What to expect when you're evaluating healthcare improvement: a concordat approach to managing collaboration and uncomfortable realities. April 29, 2015
'Sorry, I meant the patient's left side': impact of distraction on left-right discrimination. May 13, 2015
Reducing inappropriate polypharmacy: the process of deprescribing. April 1, 2015
The Safer Delivery of Surgical Services Program (S3): explaining its differential effectiveness and exploring implications for improving quality in complex systems. February 24, 2016
Best practices for chemotherapy administration in pediatric oncology: quality and safety process improvements (2015). January 20, 2016
Association of safety culture with surgical site infection outcomes. January 13, 2016
World Patient Safety Day. April 22, 2024
Annual Perspective
Defining the landscape of patient harm after osteopathic manipulative treatment: synthesis of an adverse event model. December 13, 2023
Assertive communication training for nurses to speak up in cases of medical errors: a systematic review and meta-analysis. June 14, 2023
"It's probably an STI because you're gay": a qualitative study of diagnostic error experiences in sexual and gender minority individuals. May 24, 2023
Cognitive bias and dissonance in surgical practice: a narrative review. April 26, 2023
Ten years of online incident reporting and learning using CPiRLS: implications for improved patient safety. March 15, 2023
Effect on diagnostic accuracy of cognitive reasoning tools for the workplace setting: systematic review and meta-analysis. September 14, 2022
Patterns of error in interpretive pathology. August 17, 2022
Stigma and healthcare access among transgender and gender-diverse people: a qualitative meta-synthesis. July 20, 2022
Simulation Articles of Influence. June 8, 2022
‘Almost like malpractice’: to shed bias, doctors get schooled to look beyond obesity. June 1, 2022
How Discrimination in Health Care Affects Older Americans, and What Health Systems and Providers Can Do. May 4, 2022
The Joint Commission's new and revised workplace violence prevention standards for hospitals: a major step forward toward improved quality and safety. May 4, 2022
Diagnostic reasoning in cardiovascular medicine. January 19, 2022
Prevalence, contributory factors and severity of medication errors associated with direct-acting oral anticoagulants in adult patients: a systematic review and meta-analysis. January 12, 2022
Misdiagnosis of acute myocardial infarction: a systematic review of the literature. October 6, 2021
New Horizons in Patient Safety. Safe Communication: Evidence-based Core Competencies with Case Studies from Nursing. August 17, 2021
Effectiveness of communication interventions in obstetrics--a systematic review. April 21, 2021
Implicit bias in healthcare: clinical practice, research and decision making. April 21, 2021
Education and training of nurses in the use of advanced medical technologies in home care related to patient safety: a cross-sectional survey. March 24, 2021
Patient safety. Factors for and perceived consequences of nursing errors by nursing staff in home care services. March 3, 2021
Misdiagnosis and failure to diagnose in emergency care: causes and empathy as a solution. November 11, 2020
Assessing adverse events after chiropractic care at a chiropractic teaching clinic: an active-surveillance pilot study. November 4, 2020
Understanding context specificity: the effect of contextual factors on clinical reasoning. September 2, 2020
Response of practicing chiropractors during the early phase of the COVID-19 pandemic: a descriptive report. July 8, 2020
'Whatever you cut, I can fix it': clinical supervisors' interview accounts of allowing trainee failure while guarding patient safety. November 20, 2019
What causes prescribing errors in children? Scoping review. August 28, 2019

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.

IMAGES
VIDEO
COMMENTS
Background: Quality-of-care improvement and prevention of practice errors is dependent on nurses' adherence to the principles of patient safety.Aims: This paper aims to provide a systematic review of the international literature, to synthesise knowledge and explore factors that influence nurses' adherence to patient-safety principles.Methods: Electronic databases in English, Norwegian, and ...
Improving communication with primary care to ensure patient safety post-hospital discharge. Interventional study, ... Guise V, Anderson J, Wiig S. Patient safety risks associated with telecare: a systematic review and narrative synthesis of the literature. BMC Health Serv Res. 2014; 14 (1):588.
Patient safety is one of the overarching goals of patient care and quality management. Of the many quality management frameworks, Beauchamp and Childress's four principles of biomedical ethics presents aspects of patient centeredness in clinical care. The Institute of Medicine's six aims for improvement encapsulates elements of high-quality patient care. The Institute of Healthcare ...
The patient safety culture is an accumulation of shared values and policies shared by all professionals in the professionals of organization's professionals [ 45 ]. Patient safety training is an ongoing process, not a one-time event. Healthcare worker and patient safety is a connected problem, especially in hospitals.
Abstract. This integrative literature review was conducted to examine the relationships between safety culture and patient safety and quality of care outcomes in hospital settings and to identify directions for future research. Using a search of six electronic databases, 17 studies that met the study criteria were selected for review.
Barriers and facilitators to patient engagement in patient safety from patients and healthcare professionals' perspectives: A systematic review and meta‐synthesis August 2021 Nursing Forum 56(4 ...
The aim of this review is to establish how, why and in what circumstances interoperable systems affect patient safety. A realist synthesis will be undertaken, to understand how and why inter-organisational systems reduce patients' clinical risks, or fail to do so. ... Literature searches are then designed. It is not usually feasible to ...
Design and methods: A comprehensive review of the culture of safety literature within the U.S. hospital setting. The review was a qualitative meta-analysis from which we generated a conceptual culture of safety framework and developed a typology of the safety culture literature. Findings: Seven subcultures of patient safety culture were ...
nising and reporting patient safety incidents in this popu-lation.13-15 Therefore, the need to bring together what is known about the safety of people with learning disabili-ties receiving healthcare, is clear. In this review, we aimed to produce a narrative synthesis of published academic and grey literature focusing on
A systematic literature review is undertaken to identify the main constructs of leading indicators (both passive leading indicators and active leading indicators). •. Interpretivism and critical realism philosophical stances are utilised together with inductive reasoning to generate new perspectives and insight in leading indicators. •.
Furthermore, it is unclear how training for telecare users has addressed patient safety issues. A systematic review of the literature was conducted to identify patient safety risks associated with telecare use in homecare services and to investigate whether and how these patient safety risks have been addressed in telecare training.
A literature search in the databases PubMed and Cochrane Library for Studies between January 2008 and May 2018 was performed. Two authors reviewed the full texts of potentially relevant studies to determine eligibility for inclusion. Literature on possible risks associated with the medical discharge letter was discussed.
Literature Synthesis: 2004‐2009: Acute care: RN hours of direct care per patient day. ... The Association Between Patient Safety Outcomes and Nurse/healthcare Assistant Skill Mix and Staffing Levels and Factors that may Influence Staffing Requirements. Southampton: University of Southampton Centre for Innovation and Leadership in Health ...
Due to the lack of updated synthesis and appraisal of these challenges, a synthesis of findings from the literature was deemed timely and significant. Hence, a literature review was carried out to comprehensively understand the challenges. ... What Do Nursing Students Learn About Patient Safety? An Integrative Literature Review.
This literature review found that the relationship between safety culture and patient safety outcomes is inconsistent across studies. Researchers recommend use of a theoretical framework and validated safety culture instruments to shed light on the correlation between safety culture and patient harm. PubMed citation. Available at.
A systematic literature review and narrative synthesis on the risks of medical discharge letters for patients' safety ... Literature on possible risks associated with the medical discharge letter was discussed. Results: In total, 29 studies were included in this review. The major identified risk factors are the delayed sending of the discharge ...
Results: Our review yielded 13 instruments, covering a total of 23 individual dimensions of patient safety grouped into the broad categories of management/supervision, risk, work pressure, competence, rules, and miscellaneous. The instruments varied substantially in content (number of dimensions addressed), emphasis, and length.
Background Patient safety culture, an important aspect in the field of patient safety, plays an important role in the promotion of healthcare quality. Improved patient safety culture decreases patient readmission rates, lengths of hospital stay, and patient safety issues. Patient safety culture includes a set of dimensions. This review focuses on the differing perceptions of these dimensions ...
This article summarizes a systematic review of bedside shift reports and relates the support for improving quality of care, patient safety, and patient-centered care. A computer-assisted search using MEDLINE, PubMed, and Ovid databases produced a total of 33 studies that met all inclusion criteria.
A patient safety learning system (also called a critical incident reporting system) refers to structured reporting, collation, and analysis of such incidents. 2 Potential benefits of using this system are as follows: learning from adverse events. monitoring of underlying trends and patterns to allow early detection of future adverse events.
Speaking up for patient safety by hospital-based health care professionals: a literature review. March 5, 2014 Responding to clinicians who fail to follow patient safety practices: perceptions of physicians, nurses, trainees, and patients.
Tipping the balance: a systematic review and meta-ethnography to unfold the complexity of surgical antimicrobial prescribing behavior in hospital settings. August 10, 2022. The relationship between patient safety culture and the intentions of the nursing staff to report a near-miss event during the COVID-19 crisis.
This systematic review synthesizes prior literature to develop a framework for learning from adverse events and building a safety culture in chiropractic care. A model framework for patient safety training in chiropractic: a literature synthesis. | PSNet