
What is the Nursing Process?
Characteristics of the nursing process, history of the nursing process.

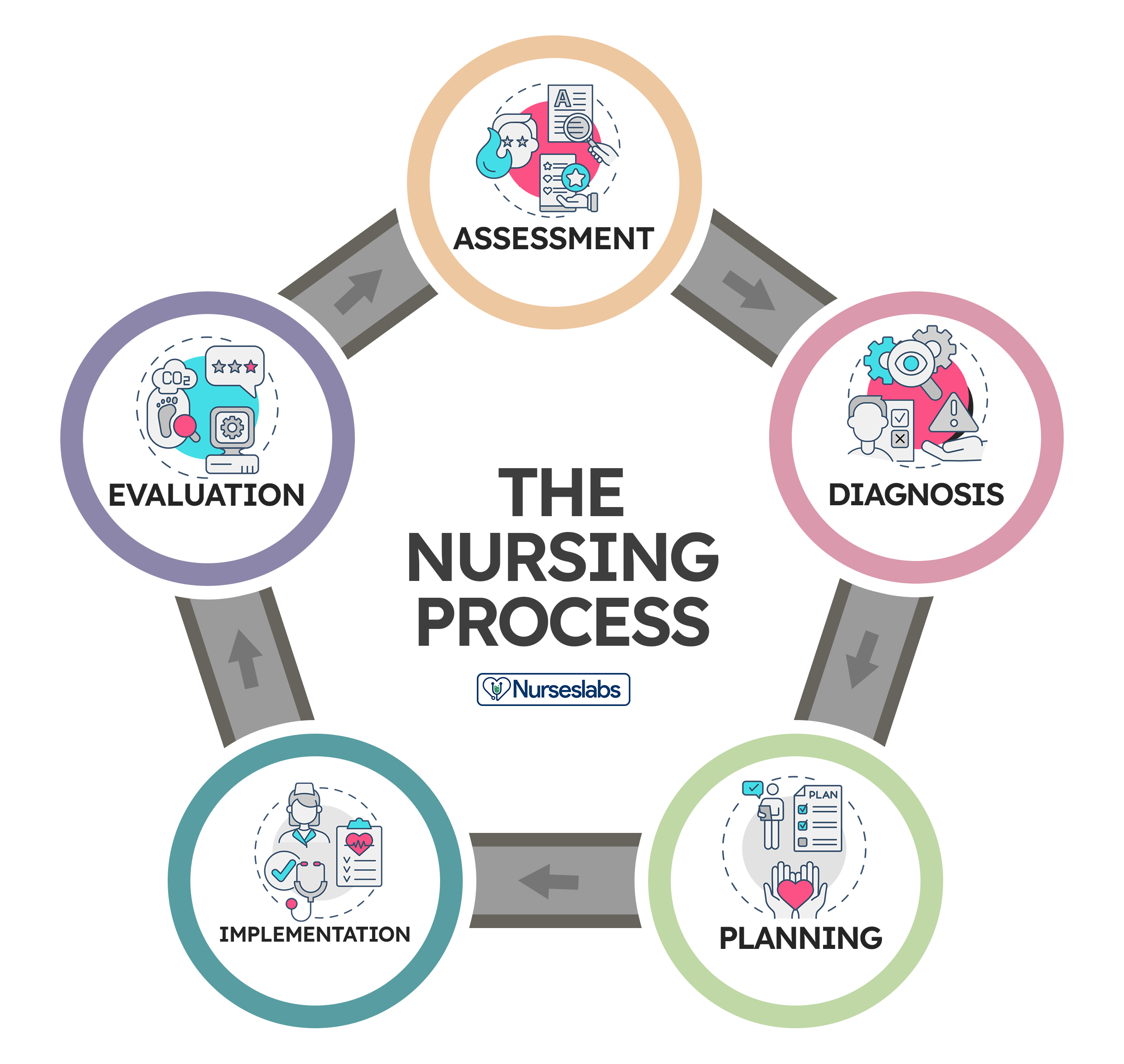
Understanding the nursing process is key to providing quality care to your patients. The nursing process is a cyclical process used to assess, diagnose, and care for patients as a nurse. It includes 5 progressive steps often referred to with the acronym:
- Planning/outcomes
- Implementation
In this article, we’ll discuss each step of the nursing process in detail and include some examples of how this process might look in your practice.
Find Nursing Programs
The nursing process is a patient-centered, systematic, evidence-based approach to delivering high-quality nursing care. It consists of five steps: assessment , diagnosis , outcomes/planning, implementation, and evaluation.
The Nursing Process (ADPIE)
1. Assessment
To begin the nursing process, assessment involves collecting information about the patient and their health. This information is used to identify any problems, or potential problems, that may need to be addressed while you’re caring for a patient.
Example: If you’re admitting an older patient who is falling and getting injured at home, you’ll want to do a thorough physical and mental health assessment, including a medical history to try and determine why this is happening.
Some important things you’ll want to find out are:
- What medications and over-the-counter products is the patient taking
- History of alcohol and recreational drug use
- Where the person lives and the layout of their home, including scatter rugs they may be tripping over: clutter, pets, stairs, slippery tubs they’re climbing into or out of, fluid or food spills on floors, lighting, mobility aids they use, etc.
2. Diagnosis
The Nursing Diagnosis is the second step in the nursing process and involves identifying real or potential health problems for a patient based on the information you gathered during the assessment.
Example: Using the falls patient example above, you may identify from your assessment that the patient is falling because they’re tripping on things in their environment that they don’t see, like their pet cat lying on the floor and loose scatter rugs.
Based on this, you might form a diagnosis such as “Falls related to poor vision, cluttered environment, unsteady gait, Lt. hip pain due to previous fall.”
3. Outcomes/Planning
Planning or Outcomes is the third step in the nursing process. This step involves developing a nursing care plan that includes goals and strategies to address the problems identified during the assessment and diagnosis steps.
Example: Continuing with the example above, you will likely recommend that the patient keep their environment,
- Free of scatter rugs
- Check to ensure the cat is not underfoot before they mobilize
- Suggest the patient use a walker for support when mobilizing
- Recommending that the patient schedule an eye exam to get their vision checked if they have not had one in the last year or two would also be a good idea or if they’ve noticed any changes in their vision lately.
4. Implementation
As the fourth step of the nursing process, implementation involves putting the plan of care into action.
Example In the above example, this would include:
- Making sure the patient’s environment is free of clutter and tripping hazards while in the hospital or a skilled nursing facility.
- Teaching the patient to wear proper footwear before mobilizing.
- Assisting the patient with mobility as needed, including putting proper footwear on the patient if needed.
- Speaking to the patient and family about removing scatter rugs from the patient’s home, scheduling an eye exam, and ensuring proper footwear is worn for mobilizing at home.
- Discussing with the patient and family about getting the patient a walker to assist with mobility on discharge and providing one while the patient is admitted.
5. Evaluation
The last step of the nursing process is evaluation , which involves determining whether or not the goals of care have been met.
Example Here you would look back at the patient’s medical record to see if the patient has had any further falls since implementing the preventative actions above.
If so, you would repeat the nursing process over and reassess why this is still happening and plan new actions to prevent future falls.
>> Show Me Online MSN Programs
The nursing process is also characterized by the following elements.
1. Dynamic and Cyclic
The nursing process is an evolving process that continues throughout a patient’s admission or illness and ends when the problems identified by the nurse are no longer an issue.
2. Patient-Centered and Goal-Directed
The entire nursing process is sensitive to and responsive to the patient's needs, preferences, and values. As nurses, we need to act as patient advocates and protect the patient’s right to make informed decisions while involving the patient in goal setting and attainment.
3. Collaborative and Interpersonal
This describes the level of interaction that may be required between nurses, patients, families and supports, and the interprofessional healthcare team. These aspects of the nursing process require mutual respect, cooperation, clear communication, and decision-making that is shared between all parties involved.
4. Universally Applicable
As a widely and globally accepted standard in nursing practice, the nursing process follows the same steps, regardless of where a nurse works.
5. Systematic and Scientific
The nursing process is also an objective and predictable process for planning, conducting, and evaluating patient care that is based on a large body of scientific evidence found in peer-reviewed nursing research.
6. Requires Critical Thinking
Most importantly, it’s essential that nurses use critical thinking when planning patient care using the nursing process. This means as nurses, we must use a combination of our knowledge and past experiences with the information we have about a current patient to make the best decisions we can about nursing care.
The nursing process was introduced in 1958 by Ida Jean Orlando. Today, it continues to be the most widely-accepted method of prioritizing, organizing, and providing patient care in the nursing profession.
It’s characterized by the key elements of:
- Critical thinking
- Client-centered methods for treatment
- Goal-oriented activities
- Evidence-based nursing research and findings
- The nursing process helps nurses to provide quality patient care by taking a holistic view of each patient they plan care for.
- The nursing process is an evidence-based approach to caring for patients that helps nurses provide quality care and improve patient outcomes.
- Ida Jean Orlando introduced the nursing process in 1958.
- The primary focus of the nursing process is the patient or client. The process is designed to meet the real and potential healthcare needs of the patient/client and to prevent possible illness or injury.

Leona Werezak BSN, MN, RN is the Director of Business Development at NCLEX Education. She began her nursing career in a small rural hospital in northern Canada where she worked as a new staff nurse doing everything from helping deliver babies to medevacing critically ill patients. Learning much from her patients and colleagues at the bedside for 15 years, she also taught in baccalaureate nursing programs for almost 20 years as a nursing adjunct faculty member (yes! Some of those years she did both!). As a freelance writer online, she writes content for nursing schools and colleges, healthcare and medical businesses, as well as various nursing sites.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
The Nursing Process: A Comprehensive Guide

In 1958, Ida Jean Orlando began developing the nursing process still evident in nursing care today. According to Orlando’s theory, the patient’s behavior sets the nursing process in motion. Through the nurse’s knowledge to analyze and diagnose the behavior to determine the patient’s needs.
Application of the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EBP) recommendations, and nursing intuition, the nursing process functions as a systematic guide to client-centered care with five subsequent steps. These are assessment , diagnosis, planning, implementation, and evaluation ( ADPIE ).
Table of Contents
What is the nursing process.
- What is the purpose of the nursing process?
Characteristics of the nursing process
Nursing process steps, collecting data, objective data or signs, subjective data or symptoms, verbal data, nonverbal data, primary source, secondary source, tertiary source, health interview, physical examination, observation, validating data, documenting data, 2. diagnosis: “what is the problem” , initial planning, ongoing planning, discharge planning, developing a nursing care plan, behavioral nursing interventions, community nursing interventions, family nursing interventions, health system nursing interventions, physiological nursing interventions, safety nursing interventions, skills used in implementing nursing care, 1. reassessing the client, 2. determining the nurse’s need for assistance, nursing intervention categories, independent nursing interventions, dependent nursing interventions, interdependent nursing interventions, 4. supervising the delegated care, 5. documenting nursing activities, 1. collecting data, 2. comparing data with desired outcomes, 3. analyzing client’s response relating to nursing activities, 4. identifying factors contributing to success or failure, 5. continuing, modifying, or terminating the nursing care plan, 6. discharge planning.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse’s critical thinking to provide the best care possible to the client.
What is the purpose of the nursing process?
The following are the purposes of the nursing process:
- To identify the client’s health status and actual or potential health care problems or needs (through assessment).
- To establish plans to meet the identified needs.
- To deliver specific nursing interventions to meet those needs.
- To apply the best available caregiving evidence and promote human functions and responses to health and illness (ANA, 2010).
- To protect nurses against legal problems related to nursing care when the standards of the nursing process are followed correctly.
- To help the nurse perform in a systematically organized way their practice.
- To establish a database about the client’s health status, health concerns, response to illness, and the ability to manage health care needs.
The following are the unique characteristics of the nursing process:
- Patient-centered . The unique approach of the nursing process requires care respectful of and responsive to the individual patient’s needs, preferences, and values. The nurse functions as a patient advocate by keeping the patient’s right to practice informed decision-making and maintaining patient-centered engagement in the health care setting.
- Interpersonal . The nursing process provides the basis for the therapeutic process in which the nurse and patient respect each other as individuals, both of them learning and growing due to the interaction. It involves the interaction between the nurse and the patient with a common goal.
- Collaborative . The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care.
- Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
- Requires critical thinking . The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation. The acronym ADPIE is an easy way to remember the components of the nursing process. Nurses need to learn how to apply the process step-by-step. However, as critical thinking develops through experience, they learn how to move back and forth among the steps of the nursing process.
The steps of the nursing process are not separate entities but overlapping, continuing subprocesses. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps of the nursing process are detailed below:
1. Assessment: “What data is collected?”
The first phase of the nursing process is assessment . It involves collecting, organizing, validating, and documenting the clients’ health status. This data can be obtained in a variety of ways. Usually, when the nurse first encounters a patient, the nurse is expected to assess to identify the patient’s health problems as well as the physiological, psychological, and emotional state and to establish a database about the client’s response to health concerns or illness and the ability to manage health care needs. Critical thinking skills are essential to the assessment, thus requiring concept-based curriculum changes.
Data collection is the process of gathering information regarding a client’s health status. The process must be systematic and continuous in collecting data to prevent the omission of important information concerning the client.
The best way to collect data is through head-to-toe assessment. Learn more about it at our guide: Head to Toe Assessment: Complete Physical Assessment Guide
Types of Data
Data collected about a client generally falls into objective or subjective categories, but data can also be verbal and nonverbal.
Objective data are overt, measurable, tangible data collected via the senses, such as sight, touch, smell, or hearing, and compared to an accepted standard, such as vital signs, intake and output , height and weight, body temperature, pulse, and respiratory rates, blood pressure, vomiting , distended abdomen, presence of edema , lung sounds, crying, skin color, and presence of diaphoresis.
Subjective data involve covert information, such as feelings, perceptions, thoughts, sensations, or concerns that are shared by the patient and can be verified only by the patient, such as nausea , pain , numbness, pruritus, attitudes, beliefs, values, and perceptions of the health concern and life events.
Verbal data are spoken or written data such as statements made by the client or by a secondary source. Verbal data requires the listening skills of the nurse to assess difficulties such as slurring, tone of voice, assertiveness, anxiety , difficulty in finding the desired word, and flight of ideas.
Nonverbal data are observable behavior transmitting a message without words, such as the patient’s body language, general appearance, facial expressions, gestures, eye contact, proxemics (distance), body language, touch, posture, clothing. Nonverbal data obtained can sometimes be more powerful than verbal data, as the client’s body language may not be congruent with what they really think or feel. Obtaining and analyzing nonverbal data can help reinforce other forms of data and understand what the patient really feels.
Sources of Data
Sources of data can be primary, secondary, and tertiary . The client is the primary source of data, while family members, support persons, records and reports, other health professionals, laboratory and diagnostics fall under secondary sources.
The client is the only primary source of data and the only one who can provide subjective data. Anything the client says or reports to the members of the healthcare team is considered primary.
A source is considered secondary data if it is provided from someone else other than the client but within the client’s frame of reference. Information provided by the client’s family or significant others are considered secondary sources of data if the client cannot speak for themselves, is lacking facts and understanding, or is a child. Additionally, the client’s records and assessment data from other nurses or other members of the healthcare team are considered secondary sources of data.
Sources from outside the client’s frame of reference are considered tertiary sources of data . Examples of tertiary data include information from textbooks, medical and nursing journals, drug handbooks, surveys, and policy and procedural manuals.
Methods of Data Collection
The main methods used to collect data are health interviews, physical examination, and observation.
The most common approach to gathering important information is through an interview. An interview is an intended communication or a conversation with a purpose, for example, to obtain or provide information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. One example of the interview is the nursing health history, which is a part of the nursing admission assessment. Patient interaction is generally the heaviest during the assessment phase of the nursing process so rapport must be established during this step.
Aside from conducting interviews, nurses will perform physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Establishing a good physical assessment would, later on, provide a more accurate diagnosis, planning, and better interventions and evaluation.
Observation is an assessment tool that depends on the use of the five senses (sight, touch, hearing, smell, and taste) to learn information about the client. This information relates to characteristics of the client’s appearance, functioning, primary relationships, and environment. Although nurses observe mainly through sight, most of the senses are engaged during careful observations such as smelling foul odors, hearing or auscultating lung and heart sounds and feeling the pulse rate and other palpable skin deformations.
Validation is the process of verifying the data to ensure that it is accurate and factual. One way to validate observations is through “double-checking,” and it allows the nurse to complete the following tasks:
- Ensures that assessment information is double-checked, verified, and complete. For example, during routine assessment, the nurse obtains a reading of 210/96 mm Hg of a client with no history of hypertension . To validate the data, the nurse should retake the blood pressure and if necessary, use another equipment to confirm the measurement or ask someone else to perform the assessment.
- Ensure that objective and related subjective data are valid and accurate. For example, the client’s perceptions of “feeling hot” need to be compared with the measurement of the body temperature.
- Ensure that the nurse does not come to a conclusion without adequate data to support the conclusion. A nurse assumes tiny purple or bluish-black swollen areas under the tongue of an older adult client to be abnormal until reading about physical changes of aging.
- Ensure that any ambiguous or vague statements are clarified. For example, a 86-year-old female client who is not a native English speaker says that “I am in pain on and off for 4 weeks,” would require verification for clarity from the nurse by asking “Can you describe what your pain is like? What do you mean by on and off?”
- Acquire additional details that may have been overlooked. For example, the nurse is asking a 32-year-old client if he is allergic to any prescription or non-prescription medications. And what would happen if he takes these medications.
- Distinguish between cues and inferences. Cues are subjective or objective data that can be directly observed by the nurse; that is, what the client says or what the nurse can see, hear, feel, smell, or measure. On the other hand, inferences are the nurse’s interpretation or conclusions made based on the cues. For example, the nurse observes the cues that the incision is red, hot, and swollen and makes an inference that the incision is infected.
Once all the information has been collected, data can be recorded and sorted. Excellent record-keeping is fundamental so that all the data gathered is documented and explained in a way that is accessible to the whole health care team and can be referenced during evaluation.
The second step of the nursing process is the nursing diagnosis . The nurse will analyze all the gathered information and diagnose the client’s condition and needs. Diagnosing involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements about a patient’s potential or actual health problem. More than one diagnosis is sometimes made for a single patient. Formulating a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care.
The types, components, processes, examples, and writing nursing diagnosis are discussed more in detail here “ Nursing Diagnosis Guide: All You Need To Know To Master Diagnosing ”
3. Planning: “How to manage the problem?”
Planning is the third step of the nursing process. It provides direction for nursing interventions. When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome.
The planning phase is where goals and outcomes are formulated that directly impact patient care based on evidence-based practice (EBP) guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual’s unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement, and continuity of care across the healthcare continuum.
Types of Planning
Planning starts with the first client contact and resumes until the nurse-client relationship ends, preferably when the client is discharged from the health care facility.
Initial planning is done by the nurse who conducts the admission assessment. Usually, the same nurse would be the one to create the initial comprehensive plan of care.
Ongoing planning is done by all the nurses who work with the client. As a nurse obtain new information and evaluate the client’s responses to care, they can individualize the initial care plan further. An ongoing care plan also occurs at the beginning of a shift. Ongoing planning allows the nurse to:
- determine if the client’s health status has changed
- set priorities for the client during the shift
- decide which problem to focus on during the shift
- coordinate with nurses to ensure that more than one problem can be addressed at each client contact
Discharge planning is the process of anticipating and planning for needs after discharge. To provide continuity of care, nurses need to accomplish the following:
- Start discharge planning for all clients when they are admitted to any health care setting.
- Involve the client and the client’s family or support persons in the planning process.
- Collaborate with other health care professionals as needed to ensure that biopsychosocial, cultural, and spiritual needs are met.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database .
4. Implementation: “Putting the plan into action!”
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect. It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This typically begins with the medical staff conducting any needed medical interventions.
Interventions should be specific to each patient and focus on achievable outcomes. Actions associated with a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks such as medication administration , educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
A taxonomy of nursing interventions referred to as the Nursing Interventions Classification (NIC) taxonomy, was developed by the Iowa Intervention Project. The nurse can look up a client’s nursing diagnosis to see which nursing interventions are recommended.
Nursing Interventions Classification (NIC) System
There are more than 550 nursing intervention labels that nurses can use to provide the proper care to their patients. These interventions are categorized into seven fields or classes of interventions according to the Nursing Interventions Classification system.
These are interventions designed to help a patient change their behavior. With behavioral interventions, in contrast, patient behavior is the key and the goal is to modify it. The following measures are examples of behavioral nursing interventions:
- Encouraging stress and relaxation techniques
- Providing support to quit smoking
- Engaging the patient in some form of physical activity , like walking, to reduce the patient’s anxiety, anger, and hostility
These are interventions that refer to the community-wide approach to health behavior change. Instead of focusing mainly on the individual as a change agent, community interventionists recognize a host of other factors that contribute to an individual’s capacity to achieve optimal health, such as:
- Implementing an education program for first-time mothers
- Promoting diet and physical activities
- Initiating HIV awareness and violence-prevention programs
- Organizing a fun run to raise money for breast cancer research
These are interventions that influence a patient’s entire family.
- Implementing a family-centered approach in reducing the threat of illness spreading when one family member is diagnosed with a communicable disease
- Providing a nursing woman support in breastfeeding her new baby
- Educating family members about caring for the patient
These are interventions that designed to maintain a safe medical facility for all patients and staff, such as:
- Following procedures to reduce the risk of infection for patients during hospital stays.
- Ensuring that the patient’s environment is safe and comfortable, such as repositioning them to avoid pressure ulcers in bed
These are interventions related to a patient’s physical health to make sure that any physical needs are being met and that the patient is in a healthy condition. These nursing interventions are classified into two types: basic and complex.
- Basic. Basic interventions regarding the patient’s physical health include hands-on procedures ranging from feeding to hygiene assistance.
- Complex. Some physiological nursing interventions are more complex, such as the insertion of an IV line to administer fluids to a dehydrated patient.
These are interventions that maintain a patient’s safety and prevent injuries, such as:
- Educating a patient about how to call for assistance if they are not able to safely move around on their own
- Providing instructions for using assistive devices such as walkers or canes, or how to take a shower safely.
When implementing care, nurses need cognitive, interpersonal, and technical skills to perform the care plan successfully.
- Cognitive Skills are also known as Intellectual Skills are skills involve learning and understanding fundamental knowledge including basic sciences, nursing procedures, and their underlying rationale before caring for clients. Cognitive skills also include problem-solving, decision-making, critical thinking, clinical reasoning, and creativity.
- Interpersonal Skills are skills that involve believing, behaving, and relating to others. The effectiveness of a nursing action usually leans mainly on the nurse’s ability to communicate with the patient and the members of the health care team.
- Technical Skills are purposeful “hands-on” skills such as changing a sterile dressing, administering an injection, manipulating equipment, bandaging, moving, lifting, and repositioning clients. All of these activities require safe and competent performance.
Process of Implementing
The process of implementing typically includes the following:
Prior to implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even if an order is written on the care plan, the client’s condition may have changed.
Other nursing tasks or activities may also be performed by non-RN members of the healthcare team. Members of this team may include unlicensed assistive personnel (UAP) and caregivers , as well as other licensed healthcare workers, such as licensed practical nurses/licensed vocational nurses (LPNs/LVNs). The nurse may need assistance when implementing some nursing intervention, such as ambulating an unsteady obese client, repositioning a client, or when a nurse is not familiar with a particular model of traction equipment needs assistance the first time it is applied.

3. Implementing the nursing interventions
Nurses must not only have a substantial knowledge base of the sciences, nursing theory , nursing practice, and legal parameters of nursing interventions but also must have the psychomotor skills to implement procedures safely. It is necessary for nurses to describe, explain, and clarify to the client what interventions will be done, what sensations to anticipate, what the client is expected to do, and what the expected outcome is. When implementing care, nurses perform activities that may be independent, dependent, or interdependent.
Nursing interventions are grouped into three categories according to the role of the healthcare professional involved in the patient’s care:
A registered nurse can perform independent interventions on their own without the help or assistance from other medical personnel, such as:
- routine nursing tasks such as checking vital signs
- educating a patient on the importance of their medication so they can administer it as prescribed
A nurse cannot initiate dependent interventions alone. Some actions require guidance or supervision from a physician or other medical professional, such as:
- prescribing new medication
- inserting and removing a urinary catheter
- providing diet
- Implementing wound or bladder irrigations
A nurse performs as part of collaborative or interdependent interventions that involve team members across disciplines.
- In some cases, such as post- surgery , the patient’s recovery plan may require prescription medication from a physician, feeding assistance from a nurse, and treatment by a physical therapist or occupational therapist.
- The physician may prescribe a specific diet to a patient. The nurse includes diet counseling in the patient care plan. To aid the patient, even more, the nurse enlists the help of the dietician that is available in the facility.
Delegate specific nursing interventions to other members of the nursing team as appropriate. Consider the capabilities and limitations of the members of the nursing team and supervise the performance of the nursing interventions. Deciding whether delegation is indicated is another activity that arises during the nursing process.
The American Nurses Association and the National Council of State Boards of Nursing (2006) define delegation as “the process for a nurse to direct another person to perform nursing tasks and activities.” It generally concerns the appointment of the performance of activities or tasks associated with patient care to unlicensed assistive personnel while retaining accountability for the outcome.
Nevertheless, registered nurses cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to unlicensed assistive personnel include assessment and evaluation of the impact of interventions on care provided to the patient.
Record what has been done as well as the patient’s responses to nursing interventions precisely and concisely.
5. Evaluation: “Did the plan work?”
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened.
Steps in Evaluation
Nursing evaluation includes (1) collecting data, (2) comparing collected data with desired outcomes, (3) analyzing client’s response relating to nursing activities, (4) identifying factors that contributed to the success or failure of the care plan, (5) continuing, modifying, or terminating the nursing care plan, and (6) planning for future nursing care.
The nurse recollects data so that conclusions can be drawn about whether goals have been fulfilled. It is usually vital to collect both objective and subjective data. Data must be documented concisely and accurately to facilitate the next part of the evaluating process.
The documented goals and objectives of the nursing care plan become the standards or criteria by which to measure the client’s progress whether the desired outcome has been met, partially met, or not met.
- The goal was met , when the client response is the same as the desired outcome.
- The goal was partially met , when either a short-term outcome was achieved but the long-term goal was not, or the desired goal was incompletely attained.
- The goal was not met.
It is also very important to determine whether the nursing activities had any relation to the outcomes whether it was successfully accomplished or not.
It is required to collect more data to confirm if the plan was successful or a failure. Different factors may contribute to the achievement of goals. For example, the client’s family may or may not be supportive, or the client may be uncooperative to perform such activities.
The nursing process is dynamic and cyclical. If goals were not sufficed, the nursing process begins again from the first step. Reassessment and modification may continually be needed to keep them current and relevant depending upon general patient condition. The plan of care may be adjusted based on new assessment data. Problems may arise or change accordingly. As clients complete their goals, new goals are set. If goals remain unmet, nurses must evaluate the reasons these goals are not being achieved and recommend revisions to the nursing care plan.
Discharge planning is the process of transitioning a patient from one level of care to the next. Discharge plans are individualized instructions provided as the client is prepared for continued care outside the healthcare facility or for independent living at home. The main purpose of a discharge plan is to improve the client’s quality of life by ensuring continuity of care together with the client’s family or other healthcare workers providing continuing care.
The following are the key elements of IDEAL discharge planning according to the Agency for Healthcare Research and Quality:
- I nclude the patient and family as full partners in the discharge planning process.
- Describe what life at home will be like
- Review medications
- Highlight warning signs and problems
- Explain test results
- Schedule follow-up appointments
- E ducate the patient and family in plain language about the patient’s condition, the discharge process, and next steps throughout the hospital stay.
- A ssess how well doctors and nurses explain the diagnosis, condition, and next steps in the patient’s care to the patient and family and use teach back.
- L isten to and honor the patient’s and family’s goals, preferences, observations, and concerns.
A discharge plan includes specific components of client teaching with documentation such as:
- Equipment needed at home. Coordinate home-based care and special equipment needed.
- Dietary needs or special diet . Discuss what the patient can or cannot eat at home.
- Medications to be taken at home. List the patient’s medications and discuss the purpose of each medicine, how much to take, how to take it, and potential side effects.
- Resources such as contact numbers and addresses of important people. Write down the name and contact information of someone to call if there is a problem.
- Emergency response: Danger signs. Identify and educate patients and families about warning signs or potential problems.
- Home care activities. Educate patient on what activities to do or avoid at home.
- Summary. Discuss with the patient and family about the patient’s condition, the discharge process, and follow-up checkups.
39 thoughts on “The Nursing Process: A Comprehensive Guide”
This article is helpful
So helpful And easy to understand A very good guide for nurses
I’m a clinical instructor teaching Fundamentals this semester. The article will be very helpful to give an in-depth explanation of “The Nursing Process” to students. Thank you.
Very detailed and easy to understand. Thx
Am a student I find it very educative
This is so helpful
Excellent information that is clearly outlined and user friendly.
This is so wonderful thank you
So helpful thank you
this is very helpful thank you
Helpful. So grateful
Is the nursing process the same as “critical thinking”?
Great information! Thanks!
This is very helpful. Thank you
Great explanation, in the understanding of Nursing process
Very Helpful to students, thank you for sharing
Excellent job. A great help to all nursing students. Thank you for sharing. God bless you.
Hi Joycelyn, Thank you so much for your kind words! It’s really rewarding to hear that it’s helping nursing students out there. We’re all about sharing knowledge and making things a bit easier. 😊 If there’s anything else you’d like to see or know, just let me know. And blessings right back at you!
Thank you so much…It’s a very comprehensive reference.
You’re very welcome, A.C! I’m glad you found the nursing process reference comprehensive and useful. Just out of curiosity, is there a particular step in the nursing process you’d like to explore more deeply, or do you have any specific areas where you’d like more detailed information?
I am a nursing student and I see this as a helpful tool, very detailed and easy to understand thanks for sharing
Hi Mawuli, I’m delighted to know that you’re finding our resources helpful! If you have any specific questions or if there’s a particular topic you’d like more information on, please feel free to ask. I’m here to assist you with any nursing-related inquiries you may have. Keep up the great work in your studies! 🩺📚🌟
Keep updating me about Nursing pdfs. You guys are really good at your work!!
Hey Mokete, Thank you so much for the kind words! We’re thrilled to hear that you’re finding our nursing resources helpful. We’ll do our best to keep you updated with more valuable nursing PDFs and information. If there’s anything specific you’d like to see or if you have any questions, feel free to let us know. Keep up the great work in your nursing journey! 👩⚕️📚🌟
Thanks it really helps alot
Glad to be of help! Thank you!
This guideline very useful for Nurses building their competency and practice quality of care of Nursing to use as reference please allow to download free especially to Nurses who live in developing countries since it is not affordable to buy it
You can download the articles by printing them as PDF :) You can use a service called printfriendly (google it) to make PDFs of our webpages.
Excellent work done I’m very happy to see this stuffs
Thank you so much…It’s a very comprehensive reference. God bless you
Hello Theophilus, You’re very welcome, and thank you for the blessings! 😊 I’m glad you found the reference on the nursing process comprehensive. Just out of curiosity, is there a particular part of the nursing process you’re most interested in, or any aspect you’d like to explore more deeply?
God bless you too, and if you have any more questions, feel free to ask!
Very helpful information. Thank you.
Thank you so much, Alisa. If you need more information or help regarding this, let us know.
You’re doing a great job here. Please can you do it in such a way for us to download it as a pdf?
Hi Millicent, Thank you so much for the kind words! 😊 I’m really glad you’re finding the site useful.
Regarding your request to download content as a PDF, a neat trick you can use is the “print” function in your web browser. Here’s how you can do it:
Open the page you want to save as a PDF. -Go to the “File” menu in your browser and select “Print,” or simply press Ctrl+P (Cmd+P on Mac). -In the print window, look for a destination option and select “Save as PDF” or something similar. -Adjust any settings as needed, then click “Save” or “Print,” and choose where you want to save the file on your computer.
This way, you can turn any page into a PDF for your personal use. If you have any more questions or need further assistance, feel free to ask. Always here to help!
Very helpful Thank you
Leave a Comment Cancel reply
The 5 Nursing Process Steps – (Learn Each Step in Detail)

One of the most important tools a nurse can use in practice is the nursing process. Although nursing schools teach first-year students about the nursing process, some nurses fail to grasp the impact its proper use can have on patient care. In this article, I will share information about the nursing process, its history, its purpose, its main characteristics, and the 5 steps involved in carrying out the nursing process. After reading this article, you will be able to answer the question, “what is the nursing process” and understand what is involved in each of the 5 steps of the nursing process. Additionally, throughout this article, after discussing a step of the nursing process, I will share an example of how the nurse would proceed with that step. For this article’s purposes, we will use information about the following patient: Mr. Collie, a fifty-four-year-old white male being admitted to the Medical-Surgical floor for acute congestive heart failure.
What Is The Nursing Process In Simple Words?
When was the nursing process developed, who developed the nursing process, what is the purpose of the nursing process, what are the 7 main characteristics of the nursing process, 1. within the legal scope of practice, 2. based on sound knowledge, 4. client-centered, 5. goal-directed, 6. prioritized, 7. dynamic and cyclical, how many steps are there in the nursing process, what are the 5 steps of the nursing process, step #1: assessment phase, step #2: diagnosis phase, step #3: planning phase, step #4: implementation phase, step #5: evaluation phase, useful resources to gain more information about the nursing process, blogs/websites, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. how is nursing process different from the scientific method, 2. do all nurses use the nursing process, 3. do doctors also use the nursing process, 4. what does adpie stand for, 5. is it always necessary for a nurse to follow all steps of the nursing process, 6. how does critical thinking impact the nursing process, 7. how does a health information system affect the nursing process, 8. how to use maslow hierarchy in the nursing process, 9. which nursing process step includes tasks that can be delegated, 10. which nursing process step includes tasks that cannot be delegated, 11. how does the nursing process apply to pharmacology.

Application deadline for pre-licensure programs: June 30th, 2024.

The Nursing Process: A Complete Guide to Using This Indispensable Nursing Tool
Posted on: Feb 27, 2022;

Nurses are guided by the nursing process through nursing school and their first clinicals, from their first nursing position to every other day of their nursing career. Such a ubiquitous and vital notion, it is essential for any aspiring nurse to master the nursing process.
That’s where we come in. In this article, we will walk you through everything you need to know about the nursing process: what it is, its five stages, and its clinical relevance . As a nurse, your main aim is to ensure that your patients receive the best possible care. Read on to find out how exactly the nursing process helps you achieve this goal.
What Is The Nursing Process?
The nursing process has been at the heart of nursing practice for more than six decades, from 1958, when Ida Orlando first introduced it. The American Nurses Association (ANA) defines the nursing process as “the essential core of practice for the registered nurse to deliver holistic, patient-focused care.” The principles that characterize it are critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice, and nursing intuition.
This valuable practice unites all different types of nurses working in various areas. Whether they work in the Emergency Room, NICU, Intensive Care Unit, or the Oncology Ward, all nurses use the nursing process daily. It helps them make clinical judgments, elaborate, and follow plans of care to ensure good patient outcomes.
At its core, the nursing process is an assertive, problem-solving approach that aids nurses in identifying and treating patient problems by providing them with a structured and easy-to-follow framework based on their practice, knowledge, judgments, and actions.

How Is a Nursing Plan Structured?
A nursing plan has five stages: assessment, diagnosis, planning, implementing, and evaluation. Taken together, they allow the nurse to think holistically and act accordingly. In this section, we’ll break down each of these steps individually.
Assessment Stage
Assessment is the first phase of the nursing process. It refers to the systematic collection of data about the patient’s condition , which nurses will further use in the care process. Nurses collect both subjective and objective data. Subjective data would be information learned directly from the patient or their caregiver. Objective data are the measurable, tangible information collected by the nurse firsthand. This can include taking vital signs, measuring input and output of oxygen, fluids, height, weight, and more.
As a nurse, you should pay close attention to more than just physiological factors in the assessment phase. Psychological data, sociocultural factors, spiritual, economic, and lifestyle components can be just as relevant to a patient’s wellbeing, thus, worthy of being accounted for.
For example, if a patient refuses to eat, the causes may run deeper than difficulty swallowing. They may be battling an eating disorder, or perhaps their reduced appetite is a sign of stress or depression. The nurse can only move to formulate a diagnosis and, later, a care plan after they have gathered a comprehensive enough set of information about the patient in the assessment stage.
In order to determine what details are essential to include in the assessment, the nurse needs to display excellent critical thinking skills.

Diagnosis Stage
After the nurse has assessed the patient and has enough information to work with, they can move on to the next step, diagnosis.
A nursing diagnosis consists of the nurse’s clinical judgment about the patient’s response to present or potential health conditions or needs. An RN diagnosis is different from a medical diagnosis. It is focused on the exact problems a patient faces (or my face) while they are in your care, like ineffective airway clearance or risk for adult falls. Formulating a nursing diagnosis based on assessments made in the first phase serves as a guide to patient care for the nurse, helping prioritize their needs and care options.
Prioritizing is an important skill in the diagnosis stage. That’s why an efficient nursing diagnosis will consider Maslow’s hierarchy of needs. According to the pyramid, basic physiological needs need to be fulfilled before moving to higher needs, like self-actualization or self-esteem. Thus, if a patient is experiencing severe trouble breathing, the nurse should deem this concern more urgent than their desire to meet their friends or go for a walk.
The nursing diagnosis will prove an invaluable tool to keep track of patients during your shift, anticipate their health needs and challenges, and provide optimal care.
For a complete guide on nursing diagnoses, check out our article .

Planning Stage
Once a nursing diagnosis has been formulated, the Registered Nurse can move to the next stage in the nursing process, planning. This is when the nurse formulates specific goals and desired outcomes that will directly impact patient care .
It is essential that the goal the nurse sets are:
- Measurable/ meaningful
- Achievable/ action-oriented
- Realistic/ Results-oriented
- Timely/ time-oriented
For example, some potential nursing goals can be: taking three short walks with the patient per day; helping the patient resolve conflict by setting a counseling meeting; ensuring patients get their necessary nutritional intake.
The care plan – the actual byproduct of the goal-setting phase – is unique to each patient, considering their individual needs and health challenges. Also, care plans enhance communication between different members of the healthcare team as well as nurse-patient relationships. They’re used for documentation or reimbursement purposes and allow for continuous care across the healthcare continuum.
Implementation Stage
The fourth step in the nursing process is implementation. In this stage, the nurse focuses on doing the actual interventions, activities, or actions indicated in the care plan. It’s an ongoing course of action that spreads to the entire duration of a patient’s hospitalization. Administering medication, offering feeding assistance, providing bedside care or postpartum support, monitoring vitals, and recovery practice – these are a few examples of possible interventions a nurse may do in the implementation stage.
Importantly, nursing interventions and care actions need to be listed in the patient’s record.

Evaluation Stage
The fifth and final step of the nursing process is the evaluation. The RN provides care throughout the nursing process with specific goals in mind (mentioned above). It’s essential to take a step back, reassess the patient’s situation and evaluate or observe if the initial goals have been fulfilled and if the desired outcomes have been achieved.
The evaluation stage doesn’t only happen once prior to discharging a patient. More evaluations may be needed to determine how the patient responds to specific interventions or actions. Thus, the plan of care can change based on new data.
Why Is The Nursing Plan Important?
In the intricate and dynamic world of nursing, the nursing process is an excellent tool for helping nurses navigate the intricacies of the healthcare system and offer optimal patient care.
The nursing process implies that patient-centered care is provided based on a plan. It’s an effective way for nurses to use their time more efficiently . It also promotes better communication practices between members of the healthcare team . The written resources generated from the nursing process increase the quality of care and provide evidence for nursing education and research.
Moreover, using the nursing process encourages nurses to practice critical thinking, creativity, and problem-solving and sharpens their decision-making abilities in clinical practice. As a result, the quality of nursing care increases, and so does the level of patient satisfaction .

Are You Ready to Utilize the Nursing Process in Practice?
A guide to systematic, compassionate, and qualitative care, the nursing process is one of the most critical instruments nurses have at their disposal. It is an efficient way to put nursing knowledge into practice and provide high-quality personalized care to patients. That’s why all nurses ought to utilize the nursing process in their day-to-day practice.
Your nursing education should give you the knowledge and skills to confidently apply the nursing process and all its steps in your future career. The nursing programs designed by Nightingale College will do just that: ensure that you step into nursing practice prepared to offer the best patient care via the nursing process.
Enroll today in our BSN program or advance your nursing degree with our RN-to-BSN program .
The nursing process
Cite this chapter.

- Peggy Martin
80 Accesses
The nursing process provides a problem-solving approach to nursing care based on the needs and problems of the individual patient. Whenever possible, the patient and his relatives are encouraged to participate in decisions relating to his care.
‘ Hopefully nurses will soon learn that nursing is a special case of loving. ’ (Jourard, 1971).
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Unable to display preview. Download preview PDF.
References and Further Reading
De La Cuesta, C. (1983), The nursing process: from development to implementation, Journal of Advanced Nursing , 8 , 365–371.
Article Google Scholar
Henderson, V. (1982), The nursing process—is the title right?, Journal of Advanced Nursing , 7 , 103–109.
Jourard, S. M. (1971), The Transparent Self , Van Nostrand Reinhold, New York.
Google Scholar
McGilloway, F. A. (1980), The nursing process: a problem solving approach to patient care, International Journal of Nursing Studies , 17 , 79–90.
Peplau, H. (1952), Interpersonal Relations in Nursing , G. P. Putnam, New York.
Smitherson, C. (1981), Nursing Actions for Health Promotion , F. A. Davis, Philadelphia, Pennsylvania.
Stanton, M., Paul, C., and Reeves, J. S. (1980), An overview of the nursing process. In: The Nursing Theories Conference Group. Nursing Theories: The Base for Professional Nursing Practice , Prentice-Hall, Englewood Cliffs, New Jersey.
Tierney, A. (1983), cited by Ross, T. (1983), Activities of living, Nursing Mirror , 156 , No. 6, 28–29.
Wainwright, P. (1984), Not the nursing process, Nursing Mirror , 158 , No. 21, 22–24.
Further reading
Aggleton, P., and Chalmers, H. (1986), Nursing research, nursing theory and the nursing process, Journal of Advanced Nursing , 11 , 197–202.
Glass, H. (1983), Interventions in nursing: goals or task orientated, International Nursing Review , 30 , No. 2, 52–56.
Johnson, J. (1984), The nursing process and psychiatry, Nursing Mirror, Mental Health Forum , 158 , No. 4, i–ii.
Keane, P. (1981), The nursing process in action 4. The nursing process in a psychiatric context, Nursing Times , 77 , No. 28, 1223–1224.
Martin, L., and Glasper, A. (1986), Core plans: nursing models and the nursing process in action, Nursing Practice , 1 , 268–273.
Miller, A. (1985), Are you using the nursing process?, Nursing Times , 81 , No. 50, 36–39.
Mitchell, J. R. A. (1984), Is nursing any business of doctors? A simple guide to the ‘nursing process’, British Medical Journal , 288 , 21 January, 216–219.
Roe, S., and Farrel, P. (1986), Shaping nursing process, Nursing Practice , 1 , 274–278.
Rowden, R. (1984), Doctors can work with the nursing process: a reply to Professor Mitchell, British Medical Journal , 288 , 21 January, 219–220.
Stockwell, F. (1985), The Nursing Process in Psychiatric Nursing , Croom Helm, London.
Syson Nibbs, L. (1980), Progress through a planned approach, Nursing Mirror , 150 , No. 7, 42–44.
Waters, K. (1985), The nursing process—methodology versus mythology, Nursing Practice , 1 , 92–97.
Further Reading
Bradley, J. C., and Edinberg, M. A. (1982), Communication in the Nursing Context , Appleton Century Crofts, Norwalk, Connecticut.
Collins, M. (1983), Communication in Health Care , C. V. Mosby, St Louis, Missouri.
Spradley, B. W. (1981), Community Health Nursing Concepts and Practice , Little, Brown, Boston, Massachusetts.
Altschul, A. T. (1977), Use of the nursing process in psychiatric care, Nursing Times , 73 , 1412–1413.
Banchik, D. (1983), Psychiatric assessment and case formulation. In: Handbook of Psychiatric Mental Health Nursing (eds Adams, C. G., and Macione, A.), John Wiley, Chichester, West Sussex.
Bermosk, L. S. (1966), Interviewing: a key to therapeutic communication in nursing practice, Nursing Clinics of North America , 1 , No. 2, 205–214.
Bootay, L. S. (1978), Interviewing your patient. In: Nursing Skillbook. Documenting Patient Care Responsibility , Nursing 78 Books, Horsham, Pennsylvania.
Burr, J., and Andrews, J. (1981), Nursing the Psychiatric Patient , 4th edn, Baillière Tindall, London.
Calnan, J. (1983), Talking with Patients , Heinemann Medical, London.
Cooper, J. (1979), Actions really do speak louder than words, American Journal of Nursing , 79 , No. 4, 29–32.
Crow, J. (1979), Assessment. In: The Nursing Process (ed. Kratz, C.), Baillière Tindall, London.
Duberley, J. (1979), Giving nursing care. In: The Nursing Process (ed. Kratz, C.), Bailltère Tindall, London.
Edwards, B. J., and Brilhart, J. K. (1981), Communication in Nursing Practice , C. V. Mosby, St Louis, Missouri.
Eisenman, E. J. P., and Dubbert, P. M. (1977), The mental health assessment interview. In: Psychiatric Mental Health Nursing Contemporary Readings (eds Backer, B. A., Dubbert, P. M., and Eisenman, E. J. P.), Van Nostrand Reinhold, New York.
French, P. (1983), Social Skills for Nursing Practice , Croom Helm, London.
Gillis, L. (1980), Human Behaviour in Illness , 3rd edn, Faber and Faber, London.
Haggerty, V. C. (1971), Listening, Nursing Forum , 10 , No. 4, 382–387.
Hayter, J. (1981), Territoriality as a universal need, Journal of Advanced Nursing , 6 , 79–85.
Hein, E. C. (1980), Communication in Nursing Practice , 2nd edn, Little, Brown, Boston, Massachusetts.
Kron, T. (1981), The Management of Patient Care , W. B. Saunders, Philadelphia, Pennsylvania.
Metz, E. L. (1978), Assessing the older psychiatric patient. In: Mental Health Concepts Applied to Nursing (ed. Dunlap, L. C.), John Wiley, Chichester, West Sussex.
Peplau, H. E. (1952), Interpersonal Relations in Nursing , G. P. Putnam, New York.
Price, B. (1983), Just a few forms to fill in, Nursing Times , 79 , No. 44, 26–29.
Rines, A. R., and Montag, M. L. (1976), Nursing Concepts and Nursing Care , John Wiley, New York.
Snyder, J. C., and Wilson, M. F. (1977), Elements of a psychological assessment, American Journal of Nursing , 77 , No. 2, 235–239.
Ujhely, G. B. (1966), Basic considerations for nurse-patient interaction in the prevention and treatment of emotional disorders, Nursing Clinics of North America , 1 , No. 2, 179–186.
Campbell, C. (1978), Nursing Diagnosis and Intervention in Nursing Practice , John Wiley, New York.
Frijda, N. H. (1982), The meanings of emotional expression. In: Non-verbal Communication Today (ed. Key, M. R.), Mouton, Berlin.
Hill, L. (1981), Don’t stereotype your patient, Journal of Practical Nursing , 31 , No. 8, 34–35.
Joel, L., and Davis, S. (1973), A proposal for baseline data collection for psychiatric care, Perspectives in Psychiatric Care , 11 , No. 2, 48–58.
Maguire, P. (1985), Deficiencies in key interpersonal skills. In: Interpersonal Skills in Nursing Research and Applications (ed. Kagan, C. M.), Croom Helm, London.
O’Brien, M. (1978), Communications and Relationships on Nursing , C. V. Mosby, St Louis, Missouri.
Prange, A. J., and Martin, H. W. (1962), Aids to understanding patients, American Journal of Nursing , 62 , 98–100.
Smitherman, C. (1981), Nursing Actions for Health Promotion , F. A. Davis, Philadelphia, Pennsylvania.
Tissier, J. (1986), The development of a psychiatric nursing assessment form. In: Psychiatric Nursing Research (ed. Brooking, J.), John Wiley, Chichester, West Sussex.
Tremlett, R. (1977), A dangerous practice, Nursing Mirror , 144 , No. 24, 33.
Whyte, L., and Youhill, G. (1984), The nursing process in the care of the mentally ill, Nursing Times , 80 , No. 5, 49–51.
Wilkinson, S. (1981), Factors influencing the relationship between the nurse and the client/patient. In: Process in Clinical Nursing (eds Leonard, B. J., and Redland, A. R.), Prentice-Hall, Englewood Cliffs, New Jersey.
Wilkinson, T. (1979), The problems and the values of objective nursing observations in psychiatric nursing care, Journal of Advanced Nursing , 4 , 151–159.
Bower, F. L. (1982), The Process of Planning Nursing Care , 3rd edn, C. V. Mosby, St Louis, Missouri.
Barnett, D. (1985), Making your plans work, Nursing Times , 81 , No. 2, 24–27.
Castledine, G. (1982), A poor record in writing, Nursing Mirror , 154 , No. 22, 31.
Duberley, J. (1979), Giving nursing care. In: The Nursing Process (ed. Kratz, C.), Baillifere Tindall, London.
Hampshire, G. (1984), Defining goals, Nursing Times , 80 , No. 11, 45–46.
Hunt, J. M., and Marks-Maran, D. J. (1980), Nursing Care Plans. The Nursing Process at Work , H. M. and M. Publishers, Aylesbury, Buckinghamshire.
Matthews, A. (1986), Patient-centred handovers, Nursing Times , 82 , No. 24, 47–48.
Schrock, R. A. (1980), Planning nursing care for the mentally ill, Nursing Times , 76 , No. 16, 704–707.
Vitale, B. A., and Schultz, N. V. (1974), A Problem Solving Approach to Nursing Care Plans: A Program , C. V. Mosby, St Louis, Missouri.
Wright, S. (1985), Real plans for real patients, Nursing Times , 81 , No. 34, 36–38.
Adams, D. M. (1980), Establishing therapeutic relationships. In: Psychiatric Nursing, A Basic Text (ed. Pothier, P. C.), Little, Brown, Boston, Massachusetts.
Anderson, M. L. (1983), Nursing interventions. What did you do that helped? Perspectives in Psychiatric Care , 21 , No. 1, 4–8.
Blondis, M. N., and Jackson, B. E. (1982), Non-verbal Communication with Patients , John Wiley, Chichester, West Sussex.
Brown, M. M., and Fowler, G. R. (1966), Psychodynamic Nursing , W. B. Saunders, Philadelphia, Pennsylvania.
Burgess, A. W., and Lazare, A. (1976), Psychiatric Nursing in the Hospital and the Community , Prentice-Hall, Englewood Cliffs, New Jersey.
Burton, G. (1977), Interpersonal Relations , 4th edn, Tavistock, London.
Butler, R. J., and Rosenthal, G. (1978), Behaviour and Rehabilitation , John Wright, Bristol.
Ellis, J. R., and Nowliss, E. A. (1981), Nursing, A Human Needs Approach , Houghton Mifflin, Boston, Massachusetts.
Grace, H. K., and Camelleri, D. (1981), Mental Health Nursing, A Socio-Psychological Approach , Wm. C. Brown, Dubuque, Iowa.
Marriner, A. (1983), The Nursing Process , C. V. Mosby, St Louis, Missouri.
Murray, R. (1975), Nursing Concepts for Health Promotion , Prentice-Hall, Englewood Cliffs, New Jersey.
Murray, R. B., and Huelskoetter, M. M. W. (1983), Psychiatric Mental Health Nursing: Giving Emotional Care , Prentice-Hall, Englewood Cliffs, New Jersey.
Paterson, J. G., and Zderad, L. T. (1976), Humanistic Nursing , John Wiley, Chichester, West Sussex.
Peplau, H. E. (1986), A celebration of skills, Paper presented at the Third International Congress of Psychiatric Nursing, Imperial College, London.
Robinson, L. (1983), Psychiatric Nursing as a Human Experience , W. B. Saunders, Philadelphia, Pennsylvania.
Travelbee, J. (1971), Interpersonal Aspects of Nursing , 2nd edn, F. A. Davis, Philadelphia, Pennsylvania.
Cooper, S. (1981), What is nursing?, Nursing Times, Occasional Papers , 77 , No. 34, 136.
Dirterle, J. A. (1983), Clinical validation of psychiatric nursing skills, Journal of Nursing Education , 22 , No. 9, 392–394.
Glass, H. (1983), Intervention in nursing: goals or task orientated, International Nursing Review , 30 , No. 2, 52–56.
Henderson, V. (1978), The concept of nursing, Journal of Advanced Nursing , 3 , 75–84.
McMahon, R. A. (1986), Nursing as a therapy, Professional Nurse , 1 , No. 10, 270–272.
Perry, J. (1985), Has the discipline of nursing developed to the stage where nurses do ‘think nursing’?, Journal of Advanced Nursing , 10 , 31–37.
Schoenhofer, S. O. (1984), Support as legitimate nursing action, Nursing Outlook , 32 , No. 4, 218–219.
Bergman, R. (1982), Evaluation of nursing care—could it make a difference?, International Journal of Nursing Studies , 19 , No. 2, 53–60.
Dye, M. C. (1963), Clarifying patient’s communication, American Journal of Nursing , 63 , 56–59.
Lowe, K. (1984), The fourth step of the nursing process evaluation. In: A Systematic Approach to Nursing Care , Open University, Milton Keynes, Buckinghamshire.
Ceccio, J. F., and Ceccio, C. M. (1982), Effective Communication in Nursing: Theory and Practice , John Wiley, New York.
Hargreaves, I. (1975), The nursing process. The key to individualised care, Nursing Times, Occasional Papers , 71 , No. 35, 89–92.
Kron, T. (1981), The Management of Patient Care , W. B. Standard.
Luker, K. (1979), Evaluating nursing care. In: The Nursing Process (ed. Kratz, C.), Bailliere Tindall, London.
Open University (1984), A Systematic Approach to Nursing Care , Open University, Milton Keynes, Buckinghamshire.
Waters, K. (1986), Cause and effect, Nursing Times , 82 , No. 5, 28–30.
Download references
You can also search for this author in PubMed Google Scholar
Editor information
Copyright information.
© 1987 Peggy Martin and the Individual Contributors
About this chapter
Martin, P. (1987). The nursing process. In: Martin, P. (eds) Psychiatric Nursing. Palgrave, London. https://doi.org/10.1007/978-1-349-09408-0_8
Download citation
DOI : https://doi.org/10.1007/978-1-349-09408-0_8
Publisher Name : Palgrave, London
Print ISBN : 978-0-333-43842-8
Online ISBN : 978-1-349-09408-0
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
The nursing process: a problem-solving approach to patient care
- PMID: 6902705
- DOI: 10.1016/0020-7489(80)90012-7
- Nursing Care / organization & administration
- Nursing Process*
- Problem Solving*

IMAGES
VIDEO
COMMENTS
The nursing process is a patient-centered, systematic, evidence-based approach to delivering high-quality nursing care. It consists of five steps: assessment, diagnosis, outcomes/planning, implementation, and evaluation. The Nursing Process (ADPIE) Assessment. Identify patients' health needs and collect subjective and objective nursing data ...
The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes. Nursing Process Steps. The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation.
The nursing process as we know it today is based upon the ... Critical thinking, problem-solving, and communication skills are necessary to work in this phase. Nurses must also demonstrate the ability to prioritize patient needs. ... Every step of the nursing process builds upon the previous step. Nurses must perform a thorough assessment and ...
The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). ... Depending on the severity of a problem, the steps of the nursing process may be performed in a matter of seconds for life-threatening concerns. ... A lifelong problem-solving approach that integrates the best ...
Nurses can implement the original nursing process to guide patient care for problem solving in nursing. These steps include: Assessment. Use critical thinking skills to brainstorm and gather information. Diagnosis. Identify the problem and any triggers or obstacles. Planning. Collaborate to formulate the desired outcome based on proven methods ...
In 1958, Ida Jean Orlando started the nursing process that still guides nursing care today. Defined as a systematic approach to care using the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EDP) recommendations, and nursing intuition. Holistic and scientific postulates are integrated to provide the basis for ...
Care is documented in the patient's record. Evaluation. Both the patient's status and the effectiveness of the nursing care must be continuously evaluated, and the care plan modified as needed. Learn more about the nursing process, including its five core areas (assessment, diagnosis, outcomes/planning, implementation, and evaluation).
The American Nurses Association (ANA) defines the nursing process as "the essential core of practice for the registered nurse to deliver holistic, patient-focused care.". The principles that characterize it are critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice, and nursing intuition.
The nursing process is a problem-solving activity. Problem-solving approaches to decision-making are not unique to nursing. The medical profession uses a specific format based upon an assessment of the body's systems. A number of questions are asked in a systematic manner to enable the doctor to make a diag nosis based upon the information ...
The nursing process provides a problem-solving approach to nursing care based on the needs and problems of the individual patient. Whenever possible, the patient and his relatives are encouraged to participate in decisions relating to his care.
Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues.
This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in nurse education curricula Further, it has attracted limited ...
To perform a clinical decision‐making process, it is necessary to examine and identify the problem, evaluate the existing solutions, and ultimately select the best option; this process is carried out at the clinic through the nursing process, and in fact, a nursing process is a tool for helping the nurse to make appropriate clinical decision ...
Memorization Reflection Assessment Evaluation, The nursing process is based upon the process of problem solving. The nurse attempts to obtain a blood pressure on the client's right arm, then on the left arm, then on the left leg, and finally on the right leg, where the blood pressure is obtained. What type of problem solving did the nurse use?
The purpose of the review is to heighten awareness amongst nurses in general, and nurse academics in particular about the theories developed, approaches taken and conclusions reached on how clinicians problem-solve. The nursing process, which is heavily used and frequently described as a problem-solving approach to nursing care, requires a ...
Prep U CH. 13 NRS 201. Get a hint. The nursing process is based upon the process of problem solving. The nurse attempts to obtain a blood pressure on the client's right arm, then on the left arm, then on the left leg, and finally on the right leg, where the blood pressure is obtained.
Study with Quizlet and memorize flashcards containing terms like The nursing process is based upon the process of problem solving. The nurse attempts to obtain a blood pressure on the client's right arm, then on the left arm, then on the left leg, and finally on the right leg, where the blood pressure is obtained. What type of problem solving did the nurse use? Intuitive thinking Trial-and ...
The nursing process is a systematic problem-solving approach used to identify, prevent and treat actual or potential health problems and promote wellness. ... The nursing process was initially an adapted form of problem-solving technique based on theory used by nurses every day to help patients improve their health and assist doctors in ...
Nursing Process (PrepU) The nursing process is based upon the process of problem solving. The nurse attempts to obtain a blood pressure on the client's right arm, then on the left arm, then on the left arm, then on the left leg, and finally on the right leg, where the blood pressure iis obtained. What type of problem solving did the nurse use?
The nursing process: a problem-solving approach to patient care. The nursing process: a problem-solving approach to patient care. The nursing process: a problem-solving approach to patient care Int J Nurs Stud. 1980;17(2):79-90. doi: 10.1016/0020-7489(80)90012-7. Author F A McGilloway ...
a) assessing b) implementing c) evaluating d) diagnosing, The nursing process is based upon the process of problem solving. What type of problem solving is the nurse using if she attempts to obtain a blood pressure on the patient's right arm, the left arm, the left leg, and then finally the right leg where a blood pressure is finally obtained ...
Study with Quizlet and memorize flashcards containing terms like The nursing process is based upon the process of problem solving. The nurse attempts to obtain a blood pressure on the client's right arm, then on the left arm, then on the left leg, and finally on the right leg, where the blood pressure is obtained. What type of problem solving did the nurse use? 1. Scientific problem solving 2 ...
Chapter 14. The nursing process is based upon the process of problem solving. The nurse attempts to obtain a blood pressure on the client's right arm, then on the left arm, then on the left leg, and finally on the right leg, where the blood pressure is obtained. What type of problem solving did the nurse use?