Case Studies on Maternal Death Surveillance and Response

Para ver esta página en español y descargar los estudios de caso, hacer clic aquí .
Of the almost 5 million women that experienced complications during pregnancy and childbirth around the world, 303,000 died in 2017. This represents an estimated global maternal mortality ratio (MMR) of 216 maternal deaths per 100,000 live births, a reduction of 44% from 1990 (385 per 100,000 live births) (WHO, 2015).
In Latin America and the Caribbean (LAC), the estimated maternal mortality ratio in 2015 was 59 deaths per 100,000 live births (PAHO/WHO). Thirteen countries in LAC have MMRs above the regional average: Bahamas, Brazil, Colombia, Guatemala, Haiti, Jamaica, Paraguay, Dominican Republic, Saint Kitts and Nevis, Saint Martin, Suriname and Venezuela. However, the actual number of deaths is most likely significantly higher due to under-registration and given that several countries with high mortality ratios, have not presented data over the last 5 years. Overall, the LAC region has seen a reduction of its MMR by 39% between 1990 and 2015 (WHO, 2015).
Efforts to strengthen data and accountability, especially in recent years, have helped fuel this improvement. Developing evidence-based care which responds to factual, timely and disaggregated information on how many women die, where, why and when in the reproductive process are essential steps in an effective epidemiological surveillance cycle that helps to prevent future deaths. However, much more is needed, particularly in terms of implementing comprehensive maternal death audits, understanding the cause of death and making structural health systems changes to avoid similar deaths in the future.
In 2015, the Regional Task Force for Maternal Mortality Reduction (GTR) released an updated version of the Guidelines for Maternal Death Surveillance and Response in the Americas to assist national efforts to identify and timely notify all maternal deaths, followed by review of their causes (maternal death reviews) and the implementation of actions to prevent future deaths. To complement these guidelines, case studies were conducted in five countries in the region which have made the greatest strides in improving their maternal mortality surveillance and response systems: Brazil, Colombia, El Salvador, Jamaica and Mexico.
The case studies presented are meant to accompany the guidelines. They present the maternal morbidity and mortality landscape in each of the five countries, along with describing the surveillance system structure and the system’s strengths and challenges. The case studies are targeted to maternal mortality surveillance systems managers, and are meant to foster greater national proficiency in maternal morbidity and mortality monitoring and response.

Related Content
Estudios de Caso de la Vigilancia de la Mortalidad Materna
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
News Release
Thursday, August 12, 2021
NIH-funded study highlights stark racial disparities in maternal deaths
Racial and ethnic disparities in maternal mortality — deaths related to pregnancy or childbirth — in the United States may be larger than previously reported, suggests a study funded by the National Institutes of Health. By re-examining information on death certificates from 2016 and 2017, researchers found that the maternal mortality rate among non-Hispanic Black women was 3.5 times higher than among non-Hispanic white women. Previously, standard analyses had indicated a 2.5-times-higher death rate for Black women.
The new analysis also revealed that these disparities were concentrated among a few causes of death. Postpartum cardiomyopathy (disease of the heart muscle) and the blood pressure disorders preeclampsia and eclampsia were leading causes of maternal death for Black women, with mortality rates five times higher than those for white women. Pregnant and postpartum Black women were two to three times more likely than white women to die of hemorrhage (severe bleeding) or embolisms (blood vessel blockages).
The study was funded by NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and led by Marian MacDorman, Ph.D., of the Maryland Population Research Center at the University of Maryland. It appears in the American Journal of Public Health .
“These sobering findings highlight the urgent need to address racial and ethnic disparities in maternal deaths,” said NICHD Director Diana W. Bianchi, M.D. “Accurate data are essential to guide efforts to reduce maternal deaths, many of which are preventable, and to improve the equity of healthcare for women during and after pregnancy.”
U.S. maternal mortality statistics are determined from death certificates completed by a physician, coroner or medical examiner and reported to state vital records offices. Information about the cause of death is translated into medical codes, which the Centers for Disease Control and Prevention compile into national datasets. In 2003, states began adding a checkbox to the certificates to indicate whether a woman was pregnant or postpartum at the time of death. However, validation studies revealed frequent checkbox errors and found that maternal deaths often are coded to poorly defined causes.
In the current study, researchers re-examined death certificates from 2016 and 2017, carefully evaluating the text on the death certificates that describes in detail the factors that led to death. This allowed the researchers to identify deaths that could be clearly confirmed as maternal ones. In most cases, they also were able to determine the primary cause of death, reducing the percentage of deaths attributed to poorly defined causes from 43% in standard datasets to 2.5% among their set of confirmed maternal deaths.
In their analysis, embolisms and preeclampsia/eclampsia tied for the leading overall cause of maternal death across all racial and ethnic groups during pregnancy or within six weeks after pregnancy. These were followed by postpartum cardiomyopathy, hemorrhage and complications from obstetric surgeries such as cesarean sections . Rankings were similar among white and Hispanic women. For Black women, preeclampsia/eclampsia was the leading cause of maternal death, followed by postpartum cardiomyopathy, embolism and hemorrhage. Ectopic pregnancy was the fifth leading cause of maternal death for Black women but was not a leading cause for white or Hispanic women.
Late maternal deaths — those occurring between six weeks and one year postpartum — were 3.5 times more likely among Black women than white women. Postpartum cardiomyopathy was the leading overall cause of late maternal deaths, with Black women having a six-times-higher risk than white women.
“We conclude that the prominence of cardiovascular conditions among the leading causes of maternal deaths, particularly for Black women, highlights the importance of increased vigilance to improve early diagnosis and treatment of these complications,” said Dr. MacDorman.
The study was funded by NICHD under award number R21HD095236. A summary of the findings was presented at the Population Association of America Annual Meeting in May 2021.
About the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD): NICHD leads research and training to understand human development, improve reproductive health, enhance the lives of children and adolescents, and optimize abilities for all. For more information, visit https://www.nichd.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
MacDorman MF, Thoma M, Declercq E, and Howell EA. Racial and ethnic disparities in maternal mortality in the United States using enhanced vital records, 2016-2017. American Journal of Public Health DOI: 10.2105/AJPH.2021.306375 (2021).
Connect with Us
- More Social Media from NIH
- Introduction
- Conclusions
- Article Information
Q indicates quarter.
The 2021 US maternal mortality rate is more than 10 times the rate of other high-income countries, according to a March 2023 CDC report. In this Q&A, JAMA Editor in Chief Kirsten Bibbins-Domingo, PhD, MD, MAS, is joined by Monica McLemore, PhD, MPH, RN, University of Washington, Audra Meadows, MD, MPH, UC San Diego, and Joia Crear-Perry, MD, founder and president of the National Birth...
eTable 1. ICD-9-CM and ICD-10-CM Diagnosis and Procedure Codes Used for Patient Inclusion and Exclusion
eTable 2. ICD-9-CM and ICD-10-CM Diagnosis and Procedure Codes Used to Identify Severe Maternal Morbidities
eTable 3. ICD-9-CM and ICD-10-CM Diagnosis Codes Used to Identify Maternal Comorbidities
eTable 4. Rates of Adjusted Mortality for American Indian Patients with 95% Poisson CIs
Data Sharing Statement
- US Maternal Mortality Is Unacceptably High, Unequal, and Getting Worse—What Can Be Done About It? JAMA Medical News & Perspectives July 25, 2023 This Medical News article is an interview by JAMA Editor in Chief Kirsten Bibbins-Domingo, PhD, MD, MAS, about maternal deaths and disparities in the US. Jennifer Abbasi
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Fink DA , Kilday D , Cao Z, et al. Trends in Maternal Mortality and Severe Maternal Morbidity During Delivery-Related Hospitalizations in the United States, 2008 to 2021. JAMA Netw Open. 2023;6(6):e2317641. doi:10.1001/jamanetworkopen.2023.17641
Manage citations:
© 2024
- Permissions
Trends in Maternal Mortality and Severe Maternal Morbidity During Delivery-Related Hospitalizations in the United States, 2008 to 2021
- 1 Office on Women’s Health, US Department of Health & Human Services, Washington, DC
- 2 Premier Inc, Charlotte, North Carolina
- 3 Now with Office on Women’s Health, US Department of Health & Human Services, Washington, DC
- 4 Now with Attentive Mobile, New York, New York
- Medical News & Perspectives US Maternal Mortality Is Unacceptably High, Unequal, and Getting Worse—What Can Be Done About It? Jennifer Abbasi JAMA
Question What were trends of and risk factors associated with maternal mortality and severe maternal morbidity (SMM) among women giving birth in US hospitals during 2008 to 2021?
Findings In this cross-sectional study of more than 11.6 million delivery-related hospitalizations, regression-adjusted in-hospital maternal delivery-related mortality per 100 000 discharges declined from 10.6 to 4.6, while the prevalence of SMM per 10 000 discharges increased from 146.8 to 179.8 during 2008 to 2021. Differences were found across racial and ethnic groups, age, mode of delivery, and comorbidities for mortality and SMM.
Meaning In this study, in-hospital maternal mortality improved between 2008 and 2021 despite increases in SMM prevalence and presence of comorbidities for the overall population.
Importance Maternal mortality and severe maternal morbidity (SMM) are important focus areas in public health. Further understanding trends, health disparities, and risk factors for these adverse outcomes is vital to public health decision-making.
Objective To describe trends and risk factors for delivery-related maternal deaths and SMM in the United States.
Design, Setting, and Participants This is a retrospective cross-sectional study using data from a large, geographically diverse, all-payer hospital administrative database. Hospital discharges from January 2008 to December 2021 with any Medicare Severity Diagnosis Related Group, International Classification of Diseases, Ninth Revision, Clinical Modification , or International Classification of Diseases, Tenth Revision, Clinical Modification delivery diagnosis or procedure code were included. Data analysis took place from February 2021 to March 2023.
Exposures Year, quarter (Q), age, race and ethnicity, delivery method.
Main Outcomes and Measures Maternal mortality, SMM during delivery-related hospitalization.
Results Overall, 11 628 438 unique hospital discharges were analyzed, with a mean (SD) age of 28 (6) years. There were 437 579 (3.8%) Asian, 92 547 (0.8%) American Indian, 1 640 355 (14.1%) Black, 1 762 392 (15.2%) Hispanic, 83 189 (0.7%) Pacific Islander, and 6 194 139 (53.3%) White patients. Regression-adjusted maternal mortality per 100 000 discharges declined from 10.6 deaths in Q1 2008 to 4.6 deaths in Q4 2021. Mortality was significantly higher among patients with advanced maternal age (eg, age 35-44 years vs 25-34 years: adjusted odds ratio [aOR], 1.49; 95% CI, 1.22-1.84). Other significant risk factors for mortality included cesarean delivery, comorbid conditions, complications, and COVID-19 diagnosis (eg, cesarean delivery: aOR, 2.28; 95% CI, 1.87-2.79). The prevalence of any SMM increased from 146.8 per 10 000 discharges in Q1 of 2008 to 179.8 per 10 000 discharges in Q4 of 2021. SMM risk factors included age 24 years or younger or age 35 years or older, belonging to a racial or ethnic minority group, cesarean delivery, Medicaid insurance, and having 1 or more comorbidities (eg, age 10-19 years: aOR, 1.39; 95% CI, 1.36-1.42).
Conclusions and Relevance This cross-sectional study found that delivery-related mortality in US hospitals decreased for all racial and ethnic groups, age groups, and modes of delivery during 2008 to 2021, likely demonstrating the impact of national strategies focused on improving maternal quality of care provided during delivery-related hospitalizations. SMM prevalence increased for all patients, with higher rates for racial and ethnic minority patients of any age. Advanced maternal age, racial or ethnic minority group status, cesarean delivery, and comorbidities were associated with higher odds of mortality and SMM.
Complications from pregnancy and childbirth are leading contributors to mortality and severe morbidities, resulting in significant burden on pregnant patients and their babies. Among developed countries, the United States has the highest maternal mortality ratio. 1 In 2019, there were 3 747 540 births in the United States, with an estimated birth rate of 11.4 per 1000 population. 2 According to US Pregnancy Mortality Surveillance System (PMSS) data, the pregnancy-related mortality ratio in the United States had increased since 1987 from 7.2 deaths per 100 000 live births to 17.3 deaths per 100 000 live births in 2017, although the trend slowed substantially after 2008. 3
Maternal mortality has been described as the “tip of the iceberg” and maternal morbidity as a larger problem, “the base.” 4 For every individual who dies as a result of their pregnancy, it is estimated that 20 or 30 more experience significant lifelong complications that affect their health and well-being. 5 , 6 Severe maternal morbidity (SMM), which the US Centers for Disease Control and Prevention (CDC) defines as “unexpected outcomes of labor and delivery that result in significant short- or long-term consequences to a woman’s health,” 1 has steadily increased in the United States in recent years and is estimated to affect more than 50 000 patients annually.
Causes of maternal deaths and SMM at the time of delivery are multifactorial and are not well documented. 7 Measuring specific outcomes occurring during delivery and hospitalization could improve understanding of how to predict, manage, and mitigate maternal outcomes. In addition, enhanced understanding of the causes of delivery-related death and SMM can inform potential strategies to improve overall maternal health outcomes in the United States. This study aimed to provide evidence to enhance understanding of patterns, trends, and risk factors associated with delivery-related deaths and SMM in US hospitals using a large maternal sample in the hospital setting.
This retrospective cross-sectional study was conducted to examine trends associated with delivery-related maternal in-hospital mortality and SMM between January 2008 and December 2021, using data from the Premier PINC AI Healthcare Database (PHD). All data were statistically deidentified and adherent to the Health Insurance Portability and Accountability Act. Based on US Title 45 Code of Federal Regulations, Part 46, this study was exempted from institutional review board approval and informed consent. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
The PHD is a large, all-payer (including Medicaid), geographically diverse administrative database comprising more than 1200 US hospitals and health systems. 8 This database represents approximately 25% of all US inpatient admissions. All data were validated at both facility and patient levels. The CDC, the National Institute of Health, and academic and industry researchers have used PHD data for studies in a variety of disease areas. 9 - 15
This study reviewed inpatient hospitalizations between January 1, 2008, and December 31, 2021, with any Medicare Severity Diagnosis Related Group (MS-DRG) or International Classification of Diseases, Ninth Revision, Clinical Modification ( ICD-9-CM ) diagnosis or procedure codes (on or before September 30, 2015) or International Classification of Diseases and Related Health Problems, Tenth Revision, Clinical Modification ( ICD-10-CM ) codes (on or after October 1, 2015) indicating delivery (eTable 1 in Supplement 1 ). Hospitalizations for patients younger than 10 years at time of admission and those with evidence of abortive outcomes were excluded from the study. The index date was defined as the discharge date for the qualifying hospitalization. Missing data for categorical variables were included in the other or unknown group. Only a small percentage of patients had missing data, which should not have affected the trend analysis.
Complications or procedures indicative of SMMs were examined during the delivery-related hospitalization; these included acute myocardial infarction, acute kidney failure, amniotic fluid embolism, aneurysm, cardiac arrest or ventricular fibrillation, cardioversion, disseminated intravascular coagulation, eclampsia, heart failure or arrest during procedure, puerperal cerebrovascular disorders, acute heart failure or pulmonary edema, severe anesthesia complications, sepsis, shock, sickle cell anemia with crisis, air and thrombotic embolism, blood transfusion, hysterectomy, temporary tracheostomy, and ventilation. The diagnosis and procedure codes to identify the complications are listed in eTable 2 in Supplement 1 . The presence of any SMM was used as a measure for the adverse event occurring during delivery. Morbidities were reported as number of patients with each SMM or any SMM of interest per 10 000 eligible discharges.
Death was defined as having delivery-related hospitalization discharge status as deceased. In-hospital mortality was reported as the number of patients who died during index hospitalization per 100 000 eligible discharges.
Patient characteristics included age (10-19, 20-24, 25-34, 35-44, ≥45 years), race and ethnicity (categorized as American Indian, Asian, Black, Hispanic, Pacific Islander, White, and other or unknown), and primary insurance payer. The other or unknown category captures all patients who selected other category for race, had missing data for race or ethnicity, or had a hospital-reported race that could not be matched to the standard race categories used in this article. Race and ethnicity were reported by the hospital. For the purposes of this study, we defined racial or ethnic minority patients as those with race or ethnicity classifications other than White. Hospital characteristics included population served (urban, rural), teaching status, US census divisions (ie, Middle Atlantic, Mountain, East North Central, East South Central, New England, Pacific, South Atlantic, West North Central, and West South Central), and hospital size (1-299, 300-499, and ≥500 beds). Visit information, such as index year, quarter (Q), admission type (elective, emergency, urgent, or trauma center), and an indicator for pre– ICD-10-CM or post– ICD-10-CM coding system change on October 1, 2015, were also examined.
The individual conditions in the Maternal Comorbidity Index (MCI) 16 were assessed as potential risk factors of maternal mortality or morbidity, including pulmonary hypertension, placenta previa, sickle cell disease, gestational hypertension, mild or unspecified preeclampsia, severe preeclampsia, chronic kidney disease, preexisting hypertension, chronic ischemic heart disease, congenital heart disease, systemic lupus erythematosus, HIV, multiple gestation, substance use disorder, alcohol abuse, tobacco use, cardiac valvular disease, chronic congestive heart failure, asthma, preexisting diabetes, gestational diabetes, obesity, cystic fibrosis, and previous cesarean delivery (eTable 3 in Supplement 1 ). The type of delivery (vaginal, cesarean) and COVID-19 status were also examined.
All SMMs were included as covariates for the mortality analysis. Because of overlap across comorbid conditions, certain SMMs were grouped together. Per CDC recommendations, cardiac conditions (including acute myocardial infarction, cardiac arrest or ventricular fibrillation, conversion of cardiac rhythm, heart failure or arrest during surgery or procedure, and pulmonary edema or acute heart failure) were grouped into 1 binary variable called cardiovascular complications for multivariable modeling. Acute respiratory conditions (including acute respiratory distress syndrome, temporary tracheostomy, and ventilation) were grouped into a binary variable called respiratory complications. 17 Hemorrhage and blood transfusion were combined into bleeding complications with 3 categories: no bleeding, hemorrhage with no blood transfusion, and blood transfusion. Eclampsia, severe preeclampsia without eclampsia, mild or unspecified preeclampsia without eclampsia, or severe preeclampsia, and no preeclampsia or eclampsia were grouped into one 4-level covariate.
Descriptive analysis was performed to assess the distribution of demographics and hospital and clinical characteristics for each year. Categorical variables were expressed as counts and percentages. Owing to space limitations, we only included specific descriptive results for 2008, 2014 (ie, the year before the ICD-9-CM to ICD-10-CM coding change), 2016 (ie, the year after the ICD-9-CM to ICD-10-CM coding change), 2019 (ie, the year before the COVID-19 pandemic), 2020, and 2021 (ie, years during the COVID-19 pandemic), rather than for all years in this study.
Two separate multivariable logistic regression models were created to assess the independent associations of potential risk factors with delivery-related maternal mortality and SMM, adjusting for confounders. For both models, patient demographics, hospital and visit characteristics, and MCI conditions were included as covariates. In the mortality regression, the SMM complications were added to the model to account for disease conditions that happened during the delivery-related hospitalization before the occurrence of mortality. In addition, a logistic regression of mortality without SMMs as covariates was performed as a sensitivity analysis. Backward selection with P < .05 was used to select final models, with the exception that patient age, race and ethnicity, delivery type, and study year and Q were kept in the model regardless of P values. For the mortality model, SMM conditions that were closely related to each other were combined. Combined variables included bleeding complications, cardiovascular complications, respiratory complications, and an eclampsia or preeclampsia category. In the regression of SMM, eclampsia was 1 component of the SMM outcome, while the preeclampsia conditions were used as separate covariates in the model.
Adjusted mortality and SMM rates for the overall study population were calculated using recycled prediction methods 16 , 18 based on estimates from the regressions. Adjusted mortality and SMM rates were also reported by age group, race and ethnicity, and type of delivery, based on additional regression models that included interaction terms between year and the variable of interest.
All analyses were conducted using Python Scikit-Learn package version 0.22.1 (Python Software Foundation). Analysis of the data took place from February 2021 through March 2023. P values were 2-sided, and statistical significance was set at P < .05.
Among the 11 628 438 eligible discharges related to delivery, more than half (6 498 217 [55.9%]) were among patients aged 25 to 34 years, 1 885 571 (16.2%) were among patients aged 35 years or older, and 759 301 (6.5%) were among patients aged 10 to 19 years. There were 437 579 (3.8%) Asian patients, 92 547 (0.8%) American Indian patients, 1 640 355 (14.1%) Black patients, 1 762 392 (15.2%) Hispanic patients, 83 189 (0.7%) Pacific Islander patients, and 6 194 139 (53.3%) White patients. Medicaid was identified as the primary payer for 4 958 174 discharges (42.6%). The census region distribution reflected the geographic distribution of the PHD patient population. Approximately one-third of the sample underwent cesarean delivery. The proportion of discharges in younger age groups decreased while the proportion in older age groups increased over the study period. The distribution of race and ethnicity, primary payer type, census region, and delivery type did not differ significantly across years ( Table 1 ).
As shown in Table 1 , obesity (91.0 per 1000 discharges), gestational diabetes (74.3 per 1000 discharges), and tobacco use (58.2 per 1000 discharges) were the most common comorbidities, followed by gestational hypertension, asthma, preeclampsia, preexisting hypertension, and substance use disorder. Compared with the prevalence in 2008, higher prevalence of sickle cell disease, gestational hypertension, severe preeclampsia, preexisting hypertension, substance use disorder, asthma, gestational diabetes, obesity, and hemorrhage were observed in 2021 ( Table 1 ).
The unadjusted prevalence of any SMM was estimated to be 163.3 per 10 000 discharges for the overall sample from 2008 to 2021, with higher prevalence observed in 2021 (206.1 per 10 000 discharges) compared with 2008 (135.2 per 10 000 discharges). Blood transfusion was the most common SMM observed, with a prevalence of 108.4 per 10 000 discharges. Other relatively common SMMs included disseminated intravascular coagulation (24.7 per 10 000 discharges), hysterectomy (11.0 per 10 000 discharges), acute respiratory distress syndrome (9.8 per 10 000 discharges), acute kidney failure (9.7 per 10 000 discharges), sepsis (7.4 per 10 000 discharges), eclampsia (7.2 per 10 000 discharges), shock (6.1 per 10 000 discharges), and acute heart failure or pulmonary edema (5.6 per 10 000 discharges). Prevalence of acute kidney failure, acute respiratory distress syndrome, sepsis, shock, mechanical ventilation, blood transfusion, and hysterectomy were higher in 2021 than in 2008 ( Table 1 ).
As seen in Figure 1 A, the adjusted prevalence of any SMM increased from Q1 2008 (146.8 per 10 000 discharges) to Q4 2021 (179.8 per 10 000 discharges). The increasing trend was observed in all age groups with the greatest change observed in patients aged 45 years or older and those aged 10 to 19 years ( Figure 1 B). Consistent increasing trend was also observed in all racial and ethnic groups, with the biggest increase observed among Pacific Islander patients (from 132.0 per 10 000 discharges in Q1 2008 to 298.8 per 10 000 discharges in Q4 2021), American Indian patients (from 156.5 per 10 000 discharges in Q1 2008 to 245.0 per 10 000 discharges in Q4 2021), and Asian patients (from 133.4 per 10 000 discharges in Q1 2008 to 238.2 per 10 000 discharges in Q4 2021) ( Figure 1 C). A significant increase in adjusted SMM prevalence was observed in patients undergoing cesarean delivery (from 252.4 per 10 000 discharges in Q1 of 2008 to 312.1 per 10 000 discharges in Q4 of 2021), and a similarly increasing trend was seen in patients with vaginal delivery (from 84.4 per 10 000 discharges in Q1 of 2008 to 108.4 per 10 000 discharges in Q4 of 2021) ( Figure 1 D).
As shown in Figure 2 A, a downward trend was observed for in-hospital mortality among deliveries after adjusting for changes in patient demographic, visit, hospital, and clinical characteristics. From Q1 of 2008 to Q4 of 2021, the adjusted in-hospital mortality decreased from 10.6 per 100 000 discharges to 4.6 per 100 000 discharges. Each subsequent year after 2008 had an 11% decrease in odds of death compared with the previous year (adjusted odds ratio [aOR], 0.89; 95% CI, 0.87-0.92) ( Table 2 ). There was an increase in mortality from Q2 of 2020 through Q4 of 2021 that may be associated with the COVID-19 pandemic. However, after controlling for COVID-19 diagnosis, the adjusted trend decreased consistently across the full study period. The downward trend for in-hospital mortality was observed in all age groups, with the biggest decrease occurring in patients aged 45 years or older ( Figure 2 B). A decreasing trend for in-hospital mortality was observed in all racial and ethnic groups. In particular, the greatest decrease in adjusted mortality was observed for American Indian patients: from 34.8 per 100 000 discharges in Q1 of 2008 to 2.7 per 100 000 discharges in Q4 of 2021 ( Figure 2 C; the 95% CI for mortality among American Indian patients is provided in eTable 4 in Supplement 1 ). In-hospital mortality consistently decreased during the study period for patients with cesarean delivery (from 12.6 per 100 000 discharges in Q1 of 2008 to 5.2 per 100 000 discharges in Q4 of 2021) and also for patients with vaginal delivery (from 6.6 per 100 000 discharges in Q1 of 2008 to 3.0 per 100 000 discharges in Q4 of 2021) ( Figure 2 D).
Compared with patients aged 25 to 34 years, those between 35 and 44 years had higher odds of dying during the index hospitalization (aOR, 1.49; 95% CI, 1.22-1.84). Although the association between race and mortality was not statistically significant in the regression in which SMMs were included as covariates, a sensitivity analysis showed that American Indian (aOR, 1.93, 95% CI, 1.10-3.39), Black (aOR, 1.78; 95% CI, 1.47-2.15), and Asian patients (aOR, 1.61, 95% CI, 1.11-2.34) had increased risk of death compared with White patients, suggesting that the racial disparity was partly attributable to the difference in the SMM rates across racial and ethnic groups. The mortality of Pacific Islander patients and Hispanic patients was not statistically significantly different from White patients in the sensitivity analysis. Patients with cesarean delivery had 2-fold higher odds of death than those with vaginal delivery (aOR, 2.28; 95% CI, 1.87-2.79). Patients with a COVID-19 diagnosis had a 13-fold increased odds of mortality compared with those without COVID-19 (aOR, 13.31; 95% CI, 8.95-19.79). Among comorbidity and acute complications assessed, cardiac complications, cystic fibrosis, aneurysm, trauma, and puerperal cerebrovascular disorder were among the risk factors associated with death during delivery-related hospitalization ( Table 2 ).
As seen in Table 2 , after adjusting for other risk factors and compared with patients aged 25 to 34 years, both patients younger than 24 years (eg, age 10-19 years: aOR, 1.39; 95% CI, 1.36-1.42) and older than 35 years (eg, age ≥45 years: aOR, 1.76; 95% CI, 1.65-1.88) had increased odds of SMM. All minority racial and ethnic groups were associated with increased odds of experiencing any SMM (Pacific Islander: aOR, 1.53; 95% CI, 1.45-1.61; American Indian: aOR, 1.41; 95% CI, 1.35-1.48; Black: aOR, 1.39; 95% CI, 1.38-1.41; Asian: aOR, 1.33; 95% CI, 1.30-1.36; Hispanic: aOR, 1.22; 95% CI, 1.20-1.24). Cesarean delivery (aOR, 3.00; 95% CI, 2.97- 3.03) and COVID-19 diagnosis (aOR, 4.44; 95% CI, 4.23-4.66) were also associated with substantially higher adjusted odds of SMM. Among all the chronic comorbidities assessed, placenta previa (aOR, 6.32; 95% CI, 6.17-6.47), chronic kidney disease (aOR, 5.21; 95% CI, 4.99-5.44), severe preeclampsia (aOR, 4.55; 95% CI, 4.48-4.62), cardiac valvular disease (aOR, 3.50; 95% CI, 3.32-3.69), chronic ischemic heart disease (aOR, 3.92; 95% CI, 3.50-4.39), and sickle cell disease (aOR, 2.93; 95% CI, 2.82-3.05) were associated with the highest odds of experiencing SMM ( Table 2 ).
This cross-sectional study examined rates of delivery-related in-hospital maternal mortality and SMM in a large national inpatient database. In this sample encompassing more than 11 million inpatient discharges, delivery-related in-hospital mortality was found to decrease significantly over a period of 14 years. The adjusted mortality per 100 000 discharges decreased by more than 50% from Q1 of 2008 to Q4 of 2021, likely demonstrating the impact of national strategies focused on improving the maternal quality of care provided by the hospitals during delivery-related hospitalizations. In contrast, the rates of overall SMM increased over time for the overall population, which may be attributable to preexisting conditions and the increasing trend in the age of delivering patients in the past decade. The increasing trend of adjusted SMM rates was seen in all racial and ethnic minority groups and was most prominent in Asian, American Indian, and Pacific Islander patients. The fact that many of the comorbid conditions are risk factors for mortality and SMM indicates that it is essential to consider comorbid conditions when assessing SMM and mortality and that better management of patients’ comorbid conditions during pregnancy may help reduce SMM occurrence and ultimately decrease mortality risk. Further improvement in patient outcomes could be achieved if patients with known risk factors could access improved care during pregnancy and during hospital delivery.
Delivery-related in-hospital maternal mortality in this study was lower than that reported in PMSS data, which defined pregnancy-related death as death during pregnancy or within 1 year of the end of pregnancy, from a cause related to pregnancy or its management. 3 PMSS data showed an increasing trend in pregnancy-related mortality during 1987 to 2017, which differs from our findings. A plausible explanation for these differences is that the timeframe for assessing mortality was substantially different between our study and the PMSS. Our study focused on mortality during delivery-related hospitalizations, which was associated with the change in quality of care for all patients in a hospital setting. In contrast, the PMSS estimates cover the entire pregnancy and postpartum period, which are associated with the overall burden of deaths among pregnant patients. Because a proportion of pregnancy-related deaths occur during delivery hospitalization, the differences between our findings and the PMSS estimates reinforced the importance of examining mortality separately for different stages of pregnancy and postpartum.
The study found that mortality risk was associated with several factors, including advanced maternal age, Medicaid as primary insurance, cesarean delivery, comorbid conditions, and severe complications during delivery. Similarly, a maternal age younger than 19 years or older than 35 years; being Asian, American Indian, Black, Hispanic, Pacific Islander; cesarean delivery; Medicaid enrollment; and maternal comorbid conditions were associated with higher risk of developing SMM during delivery. The racial and ethnic differences observed in delivery-related maternal mortality seem to be at least partly attributable to the racial and ethnic variation observed in SMM based on the main and sensitivity analyses of this study. Therefore, further research and understanding on the causes of both mortality and SMM, including the impact of comorbidities on maternal outcomes, is needed. Additionally, developing a national hospital measure to more clearly identify and reduce SMMs will likely have a beneficial impact on improving national quality strategies aimed at improving maternal health outcomes in the United States.
The study has limitations. The PHD is a hospital administrative database and does not include as much clinical details as electronic health records. Identifying clinical conditions and procedures relied on the accuracy of hospital-reported diagnosis and procedure codes. Coding errors may lead to misclassification of variables. The definition of mortality was based on in-hospital death during the visit for delivery, without accounting for death before delivery admission or after discharge.
Maternal comorbid conditions were defined based on diagnosis during the visit for delivery. Conditions occurring before admission may not have been captured. Since the study spanned 14 years, there were changes in how hospitals collected and reported race and ethnicity. Hispanic was reported as a race category before 2011, while ethnicity was listed as a separate field in the patient admission form in later years. Hispanic race or ethnicity as defined in this study included patients who reported Hispanic as their race before 2011 and those who reported Hispanic as their ethnicity in 2012 and later, regardless of their reported race.
This large national study found a decreasing trend of in-hospital delivery-related maternal mortality during 2008 to 2021, regardless of racial or ethnic group, age, or mode of delivery, likely demonstrating the impact of national and local strategies focused on improving the maternal quality of care provided by hospitals during delivery-related hospitalizations. Risk factors for in-hospital delivery-related mortality included cesarean delivery, COVID-19 diagnosis, and comorbidities and acute complications. Analysis indicated that American Indian, Black, and Asian patients had a statistically significant increased risk of death compared with White patients only when not controlling for SMMs, suggesting that the racial difference in mortality could be at least partly attributable to the differences in SMM rates across racial groups (analysis of Pacific Islander and Hispanic patients were not statistically significant).
From 2008 to 2021, there was an increasing trend of SMM rates, and chronic comorbid conditions were associated with higher rates. SMMs are known risk factors of maternal deaths and impose substantial social and economic burdens. Notably, disparities in both mortality and SMM remained across age, delivery mode, and racial and ethnic groups. These characteristics should be considered when designing maternal care quality improvement programs. As current national strategies increasingly focus on improving delivery-related maternal outcomes among high-risk groups, including racial and ethnic minority groups, it will become important to evaluate the effectiveness of these strategies in reducing occurrences of maternal mortality and SMM.
Accepted for Publication: April 12, 2023.
Published: June 22, 2023. doi:10.1001/jamanetworkopen.2023.17641
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Fink DA et al. JAMA Network Open .
Corresponding Authors: Dorothy A. Fink, MD ( [email protected] ), and Deborah Kilday ( [email protected] ), US Department of Health & Human Services, 1101 Wootton Pkwy, Rockville, MD 20852.
Author Contributions: Messers Lipkin and Perigard had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Fink, Kilday, Cao, Larson, Smith, Perigard, Marshall, Deirmenjian, Rosenthal.
Acquisition, analysis, or interpretation of data: Fink, Kilday, Cao, Larson, Smith, Lipkin, Perigard, Finke, Tatum, Deirmenjian, Rosenthal.
Drafting of the manuscript: Fink, Kilday, Cao, Smith, Perigard, Tatum, Deirmenjian, Rosenthal.
Critical revision of the manuscript for important intellectual content: Fink, Kilday, Cao, Larson, Smith, Lipkin, Perigard, Marshall, Finke, Deirmenjian, Rosenthal.
Statistical analysis: Kilday, Cao, Lipkin, Tatum, Deirmenjian, Rosenthal.
Obtained funding: Kilday, Marshall.
Administrative, technical, or material support: Kilday, Larson, Smith, Marshall, Finke, Deirmenjian, Rosenthal.
Supervision: Kilday, Smith, Marshall, Deirmenjian, Rosenthal.
Conflict of Interest Disclosures: Ms Kilday, Dr Cao, Ms Larson, Mr Lipkin, Mr Perigard, Ms Finke, Mr Tatum, Ms Deirmenjian, and Dr Rosenthal reported having a contract with the Department of Health and Human Services Maternal Morbidity and Mortality Data and Analysis Project during the conduct of the study and outside the submitted work. No other disclosures were reported.
Funding/Support: This project was supported by the US Department of Health & Human Services Office on Women’s Health (contract No. 75P00120C00066).
Role of the Funder/Sponsor: Under the leadership of the HHS Office on Women’s Health team, this study was designed and conducted; data were collected, managed, analyzed, and interpreted; the manuscript was prepared, reviewed, and approved; and decision to submit the manuscript for publication was made.
Disclaimer: The opinions expressed in this article are the authors’ own and do not reflect the view of the Department of Health and Human Services.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: Margaret Snyder, MALD, and Alain Moluh, MSc (Department of Health and Human Services); and Amy Karon, DVM, MPH, MA, and Cate Polacek, MLIS (Premier, Inc), assisted with manuscript editing. Alex Kartashov, PhD, MS, Ben Davis, MS, Antony Vibin, BS, Himanshu Jayswal, MS (Premier, Inc), assisted with conducting statistical analyses and generating descriptive tables. Ashley Wilkes, BS (Premier Inc), assisted with project management, manuscript revision, and analysis and technology support.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Maternal Mortality Rates in the United States, 2021
Data source and methods, suggested citation.
by Donna L. Hoyert, Ph.D., Division of Vital Statistics
PDF Version [PDF – 462 KB]
This report presents maternal mortality rates for 2021 based on data from the National Vital Statistics System. A maternal death is defined by the World Health Organization as “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes” ( 1 ). Maternal mortality rates, which are the number of maternal deaths per 100,000 live births, are shown in this report by age group and race and Hispanic origin.
This report updates a previous one that showed maternal mortality rates for 2018–2020 ( 2 ). In 2021, 1,205 women died of maternal causes in the United States compared with 861 in 2020 and 754 in 2019 ( 2 ). The maternal mortality rate for 2021 was 32.9 deaths per 100,000 live births, compared with a rate of 23.8 in 2020 and 20.1 in 2019 ( Table ).
In 2021, the maternal mortality rate for non-Hispanic Black (subsequently, Black) women was 69.9 deaths per 100,000 live births, 2.6 times the rate for non-Hispanic White (subsequently, White) women (26.6) ( Figure 1 and Table ). Rates for Black women were significantly higher than rates for White and Hispanic women. The increases from 2020 to 2021 for all race and Hispanic-origin groups were significant.
Rates increased with maternal age. Rates in 2021 were 20.4 deaths per 100,000 live births for women under age 25, 31.3 for those aged 25–39, and 138.5 for those aged 40 and over ( Figure 2 and Table ). The rate for women aged 40 and over was 6.8 times higher than the rate for women under age 25. Differences in the rates between age groups were statistically significant. The increases in the rates between 2020 and 2021 for each of these age groups were statistically significant.
Data are from the National Vital Statistics System mortality file ( 3 ). Consistent with previous reports, the number of maternal deaths does not include all deaths occurring to pregnant or recently pregnant women, but only deaths with the underlying cause of death assigned to International Statistical Classification of Diseases, 10th Revision code numbers A34, O00–O95, and O98–O99. Maternal mortality rates are per 100,000 live births, based on data from the National Vital Statistics System natality file. Maternal mortality rates fluctuate from year to year because of the relatively small number of these events and possibly due to issues with the reporting of maternal deaths on death certificates ( 4 ) . Efforts to improve data quality are ongoing, and these data will continue to be evaluated for possible errors. Data are shown for only the three largest race and Hispanic-origin groups for which statistically reliable rates can be calculated.
- World Health Organization. International statistical classification of diseases and related health problems, 10th revision (ICD–10). 2008 ed. Geneva, Switzerland. 2009.
- Hoyert DL. Maternal mortality rates in the United States, 2020. NCHS Health E-Stats. 2022. DOI: https://doi.org/10.15620/cdc:113967 .
- Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2021. NCHS Data Brief, no 456. Hyattsville, MD: National Center for Health Statistics. 2022. DOI: https://dx.doi.org/10.15620/cdc:122516 .
- Hoyert DL, Miniño AM. Maternal mortality in the United States: Changes in coding, publication, and data release, 2018. National Vital Statistics Reports; vol 69 no 2. Hyattsville, MD: National Center for Health Statistics. 2020.
Hoyert DL. Maternal mortality rates in the United States, 2021. NCHS Health E-Stats. 2023. DOI: https://dx.doi.org/10.15620/cdc:124678 .
Table. Number of live births, maternal deaths, and maternal mortality rates, by race and Hispanic origin and age: United States, 2018–2021
* Rate does not meet National Center for Health Statistics standards of reliability. 1 Maternal mortality rates are deaths per 100,000 live births. 2 Includes deaths for race and Hispanic-origin groups not shown separately, including women of multiple races and origin not stated. 3 Race groups are single race.
NOTES: Maternal causes are those assigned to code numbers A34, O00–O95, and O98–O99 of the International Classification of Diseases, 10th Revision . Maternal deaths occur while pregnant or within 42 days of being pregnant.
SOURCE: National Center for Health Statistics, National Vital Statistics System, Natality and Mortality.
Figure 1. Maternal mortality rates, by race and Hispanic origin: United States, 2018–2021
Figure 2. Maternal mortality rates, by age group: United States, 2018–2021
- Data Visualization Gallery
- MMWR QuickStats
- Printed Publications
- Birth, Death, Marriage and Divorce Certificates
- Government Printing Office Bookstore
- How to Order from the National Technical Information Service
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
Public Health
How bad is maternal mortality in the u.s. a new study says it's been overestimated.

Selena Simmons-Duffin

The new analysis of death certificates says the U.S. maternal mortality rate is in line with other wealthy countries, contradicting an earlier report from the CDC. muratkoc/Getty Images hide caption
The new analysis of death certificates says the U.S. maternal mortality rate is in line with other wealthy countries, contradicting an earlier report from the CDC.
This story has been updated to include additional comment from the Centers for Disease Control and Prevention.
The CDC's National Center for Health Statistics' most recent report put the U.S. maternal mortality rate at a whopping 32.9 deaths per 100,000 births. That number garnered a great deal of attention, including being covered by NPR and other news outlets.
A new study suggests the national U.S. maternal mortality rate is actually much lower than that: 10.4 deaths per 100,000 births.
The widely reported issue of racial disparities in U.S. maternal mortality persists, even with the lower overall rate. Black pregnant patients are still three times more likely to die than white patients, according to data in the study published in the American Journal of Obstetrics and Gynecology on Wednesday.
"We have to prevent these deaths," says K.S. Joseph , a physician and epidemiologist in the OB-GYN department of the University of British Columbia. Joseph is the lead author of the peer-reviewed paper. "Even if we say that the rate is 10 per 100,000 and not 30 per 100,000, it does not mean that we have to stop trying."
The fact that the rate of maternal mortality in the U.S. seems to have been significantly inflated may be disconcerting. Experts NPR spoke with about the data explain that measuring maternal deaths is complex, and that CDC was not intentionally misleading the public. They also emphasize that most maternal deaths are preventable .

Shots - Health News
Health department medical detectives find 84% of u.s. maternal deaths are preventable.
The trouble with the data started about 20 years ago, when the national death certificate was updated to include a pregnancy checkbox that the person certifying someone's death could tick. This checkbox created problems, which CDC analysts have acknowledged in their own papers , and changes were made in 2018 to CDC's methods for calculating maternal deaths. But Joseph and other researchers suspected the data was still not reliable.
"We felt that the pregnancy checkbox was misclassifying a lot of such deaths and adding them to maternal deaths," he explains.
In the new paper, Joseph and colleagues redid the CDC's National Center for Health Statistics analysis of data from 1999-2002 and 2018-2021, skipping over years when the data was in flux. Then they disregarded the deaths with only the pregnancy checkbox ticked. "We would only consider deaths to be a maternal death if there was a pregnancy-related cause mentioned by the physician who was certifying the death," he explains. "There are several lines in the certificate where a pregnancy-related cause can be mentioned, and if any of those lines mentioned a pregnancy-related cause, we would call it that."
That approach yielded a rate of 10.4 per 100,000. It also showed that the rate did not change much between 1999 and 2021. That rate is much closer to those reported in other wealthy countries , although Joseph warns that every country uses a different process and so international comparisons are unreliable.
"I think it's a very important study – I was happy to see it," says Steven L. Clark , an OB-GYN at Baylor College of Medicine who was not involved in the research. "It confirms statistically what most of us who actually deal with critically ill pregnant women on a regular basis thought for years. We are bombarded with these statistics saying how horrible maternal care is in the United States, and yet we just don't see it."
Clark does not blame the CDC for putting the maternal mortality rate so high. "They can only analyze the data that they're provided with, and that data starts at the individual hospitals and individual places in the United States," Clark says. "CDC gets these numbers, and I think they probably do a great job – I don't think there's any conspiracy here to hide anything from the public."
Joseph agrees. "The point I would like to make is that, yes, the [National Vital Statistics System] is overestimating rates and that's because of the pregnancy checkbox," Joseph says. "But this issue of assessing the actual maternal mortality rate is not a simple issue."
Deciding what time frame to consider, which conditions to include, and more, makes the task challenging. Joseph's study does not count suicides in the post-partum period, for instance.
The CDC's National Center for Health Statistics declined NPR's initial request for comment on the study. After publication, a spokesperson for the agency emailed a written statement. "CDC disagrees with the findings," the statement reads, and goes on to assert that the methods used by the researchers "are known to produce a substantial undercount of maternal mortality." The CDC declined to provide anyone for an interview.
Dr. Veronica Gillispie-Bell is an OB-GYN and the medical director of Louisiana's maternal mortality review committee. She also was not involved in the study. She says the findings do not surprise her – her committee finds checkbox errors all the time. "When we're validating the cases, it's very common that a 70 year old man – somebody checked the pregnancy checkbox and it will appear that that was a pregnancy-associated death when it was more of a clerical error."
She says in committees like hers in states all over the country – supported and funded by CDC – experts are looking closely at each of these maternal deaths and validating them. "We don't just look at the numbers," she says. "We review cases to determine, first of all, was this death pregnancy-related or not? Was this death preventable? And if so, what could we have done to prevent the death?"
She worries this new study will encourage some to dismiss the issue. "Anybody that was doubting is going to be like, 'I knew it wasn't that bad of a problem.'" She thinks the study should instead be a "call to action" to support state review committees like hers that validate the data and investigate each death.
Dr. Louise King , an OB-GYN and bioethicist at Harvard Medical School, agrees. "It's really important to dig down into this," she says. "Maternal deaths may be related to poor health coming into pregnancy, but that's still on us."
King notes that maternal mortality rates are still too high in the U.S., and the disproportionate effect on Black patients "is just plain scary," she says.
Joseph agrees that the racial disparities in the data make clear that there's a long way to go before the problem of maternal mortality is addressed. He adds, "this study does not mean that you can take your eye off the ball."
- maternal mortality
- death certificates

Maternal Deaths Rose Dramatically During Pandemic, CDC Study Shows
The maternal death rate rose 89% from 2018 to 2021, and racial disparities continued to widen, according to a new CDC study.
Maternal Deaths Rose During Pandemic

Getty Stock Images
The maternal mortality rate among non-Hispanic Black women rose by 26% from 2020 to 2021, from 55.3 deaths per 100,000 live births to 69.9 deaths per 100,000.
New figures offer a grim picture of the state of maternal health in the U.S. during the COVID-19 pandemic, with the maternal mortality rate increasing by 38% from 2020 to 2021 as racial disparities in outcomes continued to widen.
The latest figures on maternal mortality released Thursday by the Centers for Disease Control and Prevention show the overall maternal death rate increased from 23.8 deaths per 100,000 live births in 2020 to 32.9 deaths per 100,000 in 2021, marking a 89% increase since 2018.
A total of 1,205 women in 2021 reportedly died either during or within 42 days of the end of their pregnancy, according to the analysis, compared with 861 women in 2020 and 754 in 2019. Before COVID-19, the average number of women who died each year from complications related to pregnancy or delivery had remained around 700.
Findings of the report are based on data collected from the CDC’s National Vital Statistics System, which includes only maternal deaths linked to a pregnancy or its management and not deaths from accidental or incidental causes.
The rate of maternal deaths increased across all racial and ethnic groups in 2021, but has disproportionately affected women of color, particularly Black women, who had the highest mortality rate compared to Hispanic and non-Hispanic white women.
The maternal mortality rate among non-Hispanic Black women rose by 26% from 2020 to 2021, from 55.3 deaths per 100,000 live births to 69.9 deaths per 100,000. Among non-Hispanic white women, rates increased by 39% from 2020 to 2021, from 19.1 deaths per 100,000 to 26.6 deaths per 100,000.
Andria Cornell, associate director for Women’s and Infant Health at the Association of Maternal and Child Programs, says such racial disparities are rooted in a system based in structural racism that stakeholders have only just begun to acknowledge and address.
“There is an environment now where public health professionals, knowledgeable about this influence, can’t confront antiquated or harmful institutional practices and policies and propose changes they know will help because they are being hamstrung by the politicization of terms and different interpretations of events in history,” Cornell says. “We are overdue in confronting hard truths, and until we do, we as a nation will continue to nibble at the edges of this crisis.”
For the second straight year, Hispanic women had the largest increase in maternal mortality rates, rising 54%, from 18.2 deaths per 100,000 in 2020 to 28 deaths per 100,000 in 2021, according to the study.
The study found maternal mortality increased by age, with the rate among women 40 and older increasing by 28% in 2021 to 138.5 deaths per 100,000 live births. The rate among women ages 25 to 39 increased by 37% to 31.1 deaths per 100,000 in 2021, while the rate among women under age 25 had the largest increase of any age group studied in 2021, rising 48% to 20.4 deaths per 100,000 compared to 13.8 deaths per 100,000 in 2020.
Study researchers say COVID-19 likely accelerated the rise in maternal mortality in 2021. “Both the number and percentage of maternal death records mentioning COVID-19 among the causes of death were greater in 2021 than in 2020,” a CDC spokesperson said in an email response to questions.
A 2022 report by the U.S. Government Accountability Office found COVID-19 contributed to a quarter of all maternal deaths in 2020 and 2021.
Highest Fetal Mortality Rates by State

Experts say the pandemic had an indirect role in disrupting health care services as hospitals and clinics temporarily canceled many routine services like prenatal and perinatal care visits , which likely put vulnerable women at a greater health risk.
“Prior to the pandemic there was a growing consensus in health care and public health that accountability for health needed to be in the hands of birthing people – driving respect and holistic care and support,” Cornell says. “Many of the gains that were being made were upended by the pandemic and hospital and health care institution policies that prioritized protection from COVID-19. We’re likely seeing these impacts, especially for birthing persons with chronic or more complex health conditions.”
Preliminary signs do, however, seem to indicate maternal mortality has fallen as the severity of the pandemic has eased. A provisional count of maternal mortality deaths for a 12-month period ending October 2022 shows there were 830 maternal deaths, according to CDC data. While slightly higher, that figure is still closer to the annual number of maternal deaths that occurred in the years leading up to the pandemic.
However, as the Biden administration prepares to end the public health emergency related to the pandemic on May 11, some of the coverage protections and flexibilities provided during the emergency for Medicaid beneficiaries could make it more difficult for women to access maternal health care services. After the declaration expires, states will go back to pre-pandemic Medicaid eligibility requirements, which could remove pregnant women from coverage. Medicaid is the single largest payer of pregnancy-related care services in the U.S., covering the cost of nearly half of all births .
“We need to think about who is not going to have access to insurance coverage, who is not going to have access to key supports that have been critical to helping people live their lives,” says Dr. Laurie Zephyrin, senior vice president for advancing health equity for the Commonwealth Fund, a private foundation that promotes high-performing health care in the U.S.
Efforts to reduce maternal mortality could be further complicated by the U.S. Supreme Court’s decision in June 2022 to overturn Roe v. Wade , the landmark case that established a right to abortion. A Commonwealth Fund report from last December found fewer maternity care providers and resources and higher rates of maternal and infant mortality in states that have imposed or planned to impose restrictions on abortion compared to states where there were fewer restrictions.
“Given where we are today in terms of deaths, looking at just the different outcomes currently, people are at risk and it’s pretty scary,” Zephyrin says.
Previous evidence has ranked the U.S. near the bottom compared to other wealthy countries in terms of maternal health outcomes. A 2022 Commonwealth Fund report found women of reproductive age in the U.S. were more likely to delay or cancel medical visits due to cost and to spend more out of pocket for their health care. They were also less likely to have regular doctor visits or a place of care than women in most other countries.
Join the Conversation
Tags: CDC , pregnancy , birth , women's health , death , public health , Coronavirus , pandemic , race
Recommended Articles
Healthiest communities.

Healthiest Communities Health News

Best States

America 2024

- # 1 Los Alamos County, NM
- # 2 Falls Church city, VA
- # 3 Douglas County, CO
- # 4 Morgan County, UT
- # 5 Carver County, MN
Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

Inflation a Stubborn Foe for the Fed
Tim Smart April 26, 2024

The Curse of the Modern Vice President
Cecelia Smith-Schoenwalder April 26, 2024

‘A Rule for the Ages’
Lauren Camera April 25, 2024

Sale? Ban? What’s Next for TikTok?
Laura Mannweiler April 25, 2024

The Status of the Cases Against Trump
Lauren Camera and Kaia Hubbard April 25, 2024

Economy Slows in First Quarter
Tim Smart April 25, 2024

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 22 October 2020
Epidemiology and Population Health
Understanding maternal mortality in women with obesity and the role of care they receive: a national case-control study
- Monica Saucedo ORCID: orcid.org/0000-0003-1213-5693 1 ,
- Ana Paula Esteves-Pereira ORCID: orcid.org/0000-0002-0236-2043 1 , 2 ,
- Lucile Pencolé 3 ,
- Agnès Rigouzzo 4 ,
- Alain Proust 5 ,
- Marie-Hélène Bouvier-Colle 1 ,
- CNEMM study group &
- Catherine Deneux-Tharaux 1
International Journal of Obesity volume 45 , pages 258–265 ( 2021 ) Cite this article
11k Accesses
21 Citations
102 Altmetric
Metrics details
- Epidemiology
- Risk factors
Obesity has significant implications for the health of pregnant women. However, few studies have quantified its association with maternal mortality or examined the relevant underlying causes and the role of care, although this remains the most severe maternal outcome. Our objectives were to quantify the risk of maternal death by prepregnancy body mass index and to determine whether obesity affected the quality of care of the women who died.
This is a national population-based case–control study in France. Cases were 364 maternal deaths from the 2007–2012 National Confidential Enquiry. Controls were 14,681 parturients from the nationally representative 2010 perinatal survey. We studied the association between categories of prepregnancy BMI and maternal death by multivariable logistic regression, estimating adjusted odds ratios and 95% confidence intervals, overall and by specific causes of death. Individual case reviews assessed the quality of care provided to the women who died, by obesity status.
Compared with women with normal BMI, underweight women (<18.5 kg/m 2 ) had an adjusted OR of death of 0.75 (95% CI, 0.42–1.33), overweight women (25–29.9 kg/m 2 ) 1.65 (95% CI, 1.24–2.19), women with class 1 obesity (30–34.9 kg/m 2 ) 2.22 (95% CI, 1.55–3.19) and those with class 2–3 obesity (≥35 kg/m 2 ) 3.40 (95% CI, 2.17–5.33). Analysis by cause showed significant excess risk of maternal death due to cardiovascular diseases, venous thromboembolism, hypertensive complications and stroke in women with obesity. Suboptimal care was as frequent among women with (35/62, 57%) as without obesity (136/244, 56%), but this inadequate management was directly related to obesity among 14/35 (40%) obese women with suboptimal care. Several opportunities for improvement were identified.
Conclusions
The risk of maternal death increases with BMI; it multiplied by 1.6 in overweight women and more than tripled in pregnant women with severe obesity. Training clinicians in the specificities of care for pregnant women with obesity could improve their outcomes.
Similar content being viewed by others

Obstetric outcomes during delivery hospitalizations among obese pregnant women in the United States

Adverse perinatal outcomes for obese women are influenced by the presence of comorbid diabetes and hypertensive disorders
Maternal infection and antibiotic use in pregnancy and the risk of childhood obesity in offspring: a birth cohort study, introduction.
As obesity (body mass index, that is, BMI, ≥30 kg/m 2 ) increases in both low- and high-income countries [ 1 ], so does its prevalence in pregnant women. It affects about 20% of those in England [ 2 ] and 25% in the United States [ 3 , 4 ]. In France, the proportion of parturient women with prepregnancy obesity grew from 7.5% in 2003 to 11.8% in 2016 [ 5 ]. These trends have aggravated concerns about its associated adverse maternal and neonatal outcomes.
Maternal obesity is a risk factor for pregnancy-related disorders, including gestational hypertension, preeclampsia, and gestational diabetes [ 6 , 7 , 8 ]. The risk of maternal complications is also increased during the postpartum period, including postpartum haemorrhage [ 8 , 9 ], postpartum infection, and longer post-delivery hospital stays [ 10 ]. Recent studies show that obesity is associated with severe maternal morbidity [ 8 , 11 , 12 ], but fewer investigations have explored or quantified its association with maternal mortality or examined the relevant underlying causes of death, although this remains the most severe maternal outcome [ 13 , 14 , 15 ]. Documentation of the role in this association of these women’s other characteristics and of the quality of care they receive remains sparse. To prevent these severe outcomes, we must examine, beyond mortality, whether obesity results in gaps of treatment of pregnancy complications and if specific aspects of medical care for these women require improvement.
Our first aim was to quantify the risk of maternal death independently associated with prepregnancy obesity, overall and by underlying cause of death, after controlling for individual confounders. Second, and the novelty of our study, we sought to determine whether their obesity affected the quality of care of the women who died and identify opportunities to improve care.
Materials and methods
This population-based case–control study used cases and controls from nationwide surveys in France.
Cases came from the French National Confidential Enquiry into Maternal Deaths (ENCMM, Enquête Confidentielle sur les Morts Maternelles ) [ 16 , 17 ]. This permanent survey has studied all deaths since 1996 of women during pregnancy or within 1 year of its end. The sources used to identify these deaths and the procedures for investigating and assessing them have been described in detail [ 16 , 18 ]. In brief, besides spontaneous notifications by clinicians, deaths are identified from three sources: (1) death certificates of women of reproductive age; (2) computer-based national linkage of the death register with the birth register, from death and birth certificates; and (3) hospital discharge databases. Two assessors (an obstetrician or midwife and an anaesthetist) conduct a confidential enquiry of each pregnancy-associated death identified, collecting relevant clinical information about the woman and her death through interviews and review of the medical records and autopsy reports. The ENCMM national expert committee analyses the anonymised deaths and consensually determines for each: (1) its underlying cause, i.e., the illness or complication triggering the chain of events until death; (2) whether it was a maternal death, defined as a woman’s death during pregnancy or within 1 year of its end, regardless of its duration and site, from any cause related to or aggravated by the pregnancy or its management (but not accidental or incidental); and (3) the quality of care provided (optimal or non-optimal) and the preventability of maternal deaths. This study includes maternal deaths identified by the ENCMM for 2007–2012 (the six most recent years available) in mainland France ( n = 441). After the exclusion of 77 maternal deaths before 22 weeks’ gestation (during pregnancy or post-abortion), for consistency with the definition of controls below, this analysis included 364 maternal deaths.
Controls came from a representative sample of births in France, the 2010 French National Perinatal Survey (NPS), a repeated cross-sectional study conducted periodically since 1995 to produce statistics about perinatal indicators [ 19 ]. These surveys cover all live- and stillbirths at or after 22 weeks of gestation or with a birth weight of at least 500 g in every maternity unit in France for a complete 1-week period (1/52nd of births in France). Midwives interview mothers before discharge to obtain data on maternal social and demographic characteristics and prenatal care. Data about the pregnancy, delivery and newborns are collected from medical records. The 2010 version of the NPS, in the middle of the 2007–2012 case inclusion period, served as the source population for the control women in this analysis ( n = 14 681). Its methods have been detailed elsewhere [ 19 ]. By definition, the control group should not include women who died in the postpartum period. Although it is possible that some died after discharge, the reported maternal mortality ratio in France is low enough (10.3/100,000 live births 2007–2012) to consider the number of such cases, about one or two expected maternal deaths after discharge among the 14,681 women, negligible [ 17 ].
Ethical approval for both the ENCMM and NPS surveys was granted by the French Commission on Information Technology and Liberties.
The primary predictor variable was categorical prepregnancy body mass index (BMI; kg/m2) as underweight: BMI < 18.5; normal weight: BMI 18.5–24.9; overweight: BMI 25–29.9; class 1 obesity: BMI 30–34.9; class 2–3 obesity: BMI ≥ 35. BMI was calculated from self-reported prepregnancy weight and height in the medical records of cases and controls. BMI categories for class 2 and class 3 obesity were combined because of the small number of cases in these groups. The precise BMI for some women was not available because either weight or height or both were missing, but the prepregnancy obesity status (yes/no) was reported from another questionnaire item. The following covariates were examined: mother’s country of birth (France or other European country, North Africa, sub-Saharan Africa, other), mother’s age (≤24, 25–29, 30–34, 35–39, ≥40 years), educational level of zip-code of residence (proportion of adults 20–45 years who did not complete high school, grouped into quintiles based on data available from the French census) as a proxy for socioeconomic status, severe pre-existing chronic conditions (a composite binary variable including hypertension, diabetes, cardiac diseases, and other notable chronic conditions), previous deliveries (nulliparous, only vaginal deliveries, one or more caesarean deliveries), multiple pregnancy and median gestational age (weeks).
Statistical analysis
The characteristics of cases and controls were compared by chi-square or Wilcoxon tests. The association between prepregnancy BMI and maternal mortality was assessed by univariate and multivariable logistic regression models. We selected potential confounders from the literature and the univariate analysis and adjusted for them. Pre-existing chronic conditions were not included in the main adjusted models because they were considered potential mediators rather than confounders of the link between obesity and maternal death [ 20 ]. The analysis by causal condition used the main cause of death, exclusive categorization, determined by the ENCMM expert committee. To assess the cause-specific risk of maternal mortality associated with maternal body mass, we used a binary obesity (yes/no) exposure variable, because of the limited numbers of maternal deaths by cause. Crude and adjusted odds ratios were calculated with 95% confidence intervals. Interactions between obesity and covariables were systematically tested.
The proportion of women with missing information was 15.9% for obesity status and 33.0% for BMI among maternal deaths, and 7.0 and 7.5% respectively among controls. We handled missing values by multiple imputation with chained equations (10 datasets) on the missing-at-random hypothesis [ 21 ]. The multiple imputation prediction model was composed of the outcome variable, prepregnancy BMI, maternal age, country of birth, quintile of zip-code education level, pre-existing chronic conditions, previous deliveries, multiple pregnancy and duration of pregnancy. Results are presented with imputed data.
Post-hoc calculations showed that with a significance level of 5% and obesity prevalence of 10% among controls, this sample would have >90% power to detect a doubled risk of death in obese versus non-obese women (OR ≥ 2.0).
We performed several sensitivity analyses. The first tested the impact of adjusting for severe chronic conditions before pregnancy together with confounders in the multivariate logistic regression model; although we primarily considered this variable an intermediate factor (see above), it might also affect maternal risk directly, regardless of obesity status. Second, we assessed the relevance of the multiple imputation for missing data and performed an analysis of the association between BMI and maternal mortality with non-imputed data.
The second part of the analysis was restricted to women who died. Here we compared the proportion of suboptimal care, assessed by the ENCMM expert committee, by obesity status. To isolate the components of suboptimal care directly related to obesity, we reviewed each death of an obese woman with suboptimal care, relying on the ENCMM committee determinations given the absence of specific clinical guidelines in France for managing pregnancy in women with obesity.
Analyses used STATA 14.0 (StataCorp LP, College Station, TX, USA).
Compared with controls, cases were more often born outside France (or Europe), older, and more likely to have severe chronic conditions before pregnancy, at least one previous caesarean delivery and a multiple pregnancy (Table 1 ). The distribution of BMI differed significantly between cases and controls. The proportion of overweight and obesity was significantly higher among women who died than among controls (Table 2 ).
After adjustment for confounders, the risk of maternal death increased with categories of BMI, with an adjusted OR of 1.65 for overweight women and of 3.40 for women with class 2–3 obesity, compared with women with a normal BMI. The risk in underweight women did not significantly differ from that of normal-weight women. The analysis with non-imputed data provided similar results (Table S1 ). The addition of pre-existing medical conditions as covariates in the multivariable model provided similar results although the associations were attenuated (Table S2 ).
We further analysed the risk of cause-specific maternal mortality associated with prepregnancy obesity. Women with obesity had a statistically significantly higher risk of maternal death from cardiovascular disease (CVD), thromboembolism, hypertensive complications and stroke, after adjustment for confounders, compared with non-obese women (Table 3 ).
The ENCMM expert committee considered it had sufficient information to judge the quality of care for 306 of the 364 maternal deaths. The proportion of suboptimal care did not differ between the obese and non-obese women who died (35/62, 57%, vs 136/244, 56%, P = 0.9). Among the 35 women with obesity who died after receiving suboptimal care, this care involved factors related to obesity for 14/35 (40%), 8 with class 1 obesity and 6 with class 2–3. Thes causes of these 14 deaths were 4 pulmonary embolisms 2 uterine ruptures, 2 amniotic fluid embolisms, 2 cardiomyopathies, 2 brain anoxia secondary to complicated endotracheal intubation, 1 sepsis and 1 HELLP syndrome. Specifically, there were technical difficulties with clinical examinations or procedures for diagnosis or treatment (abdominal ultrasound, venous access, intubation, tracheotomy, extracorporeal membrane oxygenation) and treatment underdosing (antibiotics, anticoagulants). Table 4 reports these factors. The two vignettes in supplementary material briefly illustrate some of these factors
Principal findings of the study
This national study shows that after adjustment for confounders the risk of maternal death increases as BMI rises, multiplying by 1.6 in women with overweight and more than tripling in women with severe obesity, compared with normal weight women. This excess risk is mainly explained by increased maternal mortality due to CVDs, hypertensive complications, thromboembolism and stroke. Suboptimal care among the women with obesity who died often involved inadequate management directly related to obesity; opportunities for improvement therefore exist.
Interpretation
Although several studies have addressed the association between obesity and diverse adverse pregnancy outcomes, evidence for the link with maternal mortality has been sparse and inconsistent. A California study found prepregnancy obesity more frequent among women who died than among a reference parturient population (30 vs 16%); [ 14 ] in Florida, relative ratios of maternal death showed a rising trend with severity of obesity (from a 2.8-fold increase for class 1 to sevenfold for class 3, compared with women with normal weight) [ 22 ]. Confounders may, however, have biased these crude associations because neither study considered any of the women’s other individual characteristics. In contrast, a UK national case–control study assessing risk factors for maternal mortality found that it was not significantly associated with obesity after controlling for other individual characteristics, including pre-existing chronic conditions [ 23 ]. Because some comorbidities are likely consequences of obesity and thus intermediate rather than confounding factors in this association, their analysis strategy might have masked obesity’s actual role. Our analysis treated pre-existing chronic conditions as an intermediate factor instead of a confounder, and our sensitivity analysis, which included severe chronic conditions before pregnancy in the multivariable model, showed an attenuated but still significant association between BMI and maternal mortality.
The risk of maternal mortality from CVD was four times higher in women with than without obesity. Although the link between obesity and CVD in the general adult population is well known [ 24 , 25 , 26 ], an associated increase in mortality risk is less clear [ 27 , 28 ]. This issue has been studied still less among pregnant women. A population-based study in the state of Washington found a risk of severe cardiac morbidity three times higher among women with class 3 obesity than among those without obesity during hospitalisation for delivery [ 11 ]. While this association might indirectly reflect the higher prevalence of chronic conditions in women with obesity, the excess risk for cardiovascular mortality remained significant in our sensitivity analysis after controlling for severe chronic conditions before pregnancy. This adverse outcome may reflect a reduced capacity to respond to pregnancy-induced cardiovascular changes, including cardiovascular compliance and maximum heart rate, among other biological effects, induced by obesity [ 29 , 30 ]. In our study, one-third of the women with obesity who died of CVD had been diagnosed with it before pregnancy. Risk stratification is needed for these women before or early in pregnancy, together with joint management by a cardiologist and an obstetrician. Inversely, CVD developed or was revealed during pregnancy or the postpartum for the remaining two-thirds. This suggests that clinicians involved in antenatal care of women with obesity must pay particular attention to screening for cardiovascular clinical signs during pregnancy and after delivery.
Women with obesity also had a risk almost three times higher than those without it of maternal death from thromboembolism, hypertensive complications and stroke. The incidence of these conditions is known to be increased in women with obesity [ 6 , 31 , 32 , 33 ]. Our analysis shows that this susceptibility persists along the continuum of morbidity and translates into increased mortality. In addition, factors related to the quality of care provided to women with obesity might aggravate this disparity; these include the adequacy of blood pressure monitoring among women with obesity or the failure to take body mass into account when adjusting the dose of thromboprophylaxis.
One original aspect of our study is the case review conducted to assess care received by women with obesity and identify opportunities for improvement. This approach can and should be developed beyond assessing these women’s risk of severe maternal complications. This detailed case review suggests that some of these outcomes might have been prevented by improvement of some aspects of the care they received during pregnancy and delivery. Our results, by showing that improvement opportunities in obese women who died often involve aspects of care directly related to obesity, highlight the need to customise their care before and during pregnancy and in the peripartum period. This has several implications for care improvement: first, screening for clinical signs suggestive of cardiac conditions such as dyspnoea should be part of routine prenatal care in pregnant women with obesity; second, initial and continuing training of professionals involved in prenatal care should ensure that they know the specificities of clinical management of pregnant women with obesity and help them to anticipate challenging medical procedures (diagnostic, anaesthesiological, or surgical) and dosing strategies for specific treatments, such as anticoagulants or antibiotics. Those results provide scientific support to some of the recommendations for care of women with obesity (such as the recent “Care of Women with Obesity in Pregnancy” NICE guideline), and also highlight some aspects not mentioned in those recommendations and that may usefully be added, in particular the need for careful screening for cardiac clinical signs during pregnancy and after delivery [ 34 ].
Several strengths characterised our study. We assessed the risk of maternal mortality according to BMI class with cases and controls from nationwide population-based sources providing comprehensive individual data for pregnant women. The availability of detailed data on maternal deaths enabled further analysis of the care these women received so that we could isolate the aspects of inadequate management directly related to obesity and propose areas for improvement.
Limitations
This study has some limitations. First, some maternal BMI data were missing. Nonetheless, we were able to include all women in the analysis by using multiple imputation for missing data, and the results of the sensitivity analysis with non-imputed data were similar to those with imputed data. Another limitation, due to case number constraints, was the need to study obesity with a binary variable, rather than classes of BMI, in the risk assessment by specific causes of maternal mortality. Because this binary obesity variable combines women with underweight, normal weight, and overweight women in the same reference class, it may result in underestimating the association studied, but does not challenge our main conclusions. Additionally, prepregnancy BMI may be inaccurate because height and weight were self-reported. Nevertheless, a recent meta-analysis showed that self-reported weight of women of reproductive age differs only slightly from direct measures [ 35 ]. Finally, beyond BMI, gestational weight gain, a recently highlighted risk factor for adverse pregnancy outcomes [ 36 ], was not taken into account in our analysis, because related data were not available. Nonetheless, a noteworthy study from the state of Washington did not show any substantial modification in the associations between BMI and maternal outcomes after controlling for gestational weight gain [ 11 ].
The risk of maternal death increases with BMI. Public health interventions promoting lifestyle changes for obesity management remain a major challenge. Identifying modifiable factors related to the health care provide to women with obesity might produce a more positive effect. The opportunities for improvement identified in this study in a substantial proportion of women emphasise the need for optimal screening and management of CVD in women with obesity before and during pregnancy and for training clinicians in the specificities of their care.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Article Google Scholar
Heslehurst N, Rankin J, Wilkinson JR, Summerbell CD. A nationally representative study of maternal obesity in England, UK: trends in incidence and demographic inequalities in 619 323 births, 1989–2007. Int J Obesity. 2010;34:420–8.
Article CAS Google Scholar
Branum AM, Kirmeyer SE, Gregory EC. Prepregnancy body mass index by maternal characteristics and state: data from the birth certificate, 2014. Natl Vital Stat. 2016;65:1–11.
Google Scholar
Deputy NP, Dub B, Sharma AJ. Prevalence and trends in prepregnancy normal weight - 48 States, New York City, and District of Columbia, 2011–2015. MMWR Morbidity and Mortality Weekly Report. 2018;66:1402–7.
Blondel B, Coulm B, Bonnet C, Goffinet F, Le Ray C. National Coordination Group of the National Perinatal STrends in perinatal health in metropolitan France from 1995 to 2016: results from the French National Perinatal Surveys. J Gynecol Obstet Human Reproduct. 2017;46:701–13.
O’Brien TE, Ray JG, Chan WS. Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology. 2003;14:368–74.
Guelinckx I, Devlieger R, Beckers K, Vansant G. Maternal obesity: pregnancy complications, gestational weight gain and nutrition. Obes Rev. 2008;9:140–50.
Schummers L, Hutcheon JA, Bodnar LM, Lieberman E, Himes KP. Risk of adverse pregnancy outcomes by prepregnancy body mass index: a population-based study to inform prepregnancy weight loss counseling. Obstet Gynecol. 2015;125:133–43.
Knight M, Kurinczuk JJ, Spark P, Brocklehurst P. Extreme obesity in pregnancy in the United Kingdom. Obstet Gynecol. 2010;115:989–97.
Heslehurst N, Simpson H, Ells LJ, Rankin J, Wilkinson J, Lang R, et al. The impact of maternal BMI status on pregnancy outcomes with immediate short-term obstetric resource implications: a meta-analysis. Obesity Rev. 2008;9:635–83.
Lisonkova S, Muraca GM, Potts J, Liauw J, Chan WS, Skoll A, et al. Association between prepregnancy body mass index and severe maternal morbidity. JAMA. 2017;318:1777–86.
Siddiqui A, Azria E, Howell EA, Deneux-Tharaux C, Group ES. Associations between maternal obesity and severe maternal morbidity: findings from the French EPIMOMS population-based study. Paediatr Perinat Epidemiol. 2019;33:7–16.
Campbell KH, Savitz D, Werner EF, Pettker CM, Goffman D, Chazotte C, et al. Maternal morbidity and risk of death at delivery hospitalization. Obstet Gynecol. 2013;122:627–33.
Main EK, McCain CL, Morton CH, Holtby S, Lawton ES. Pregnancy-related mortality in California: causes, characteristics, and improvement opportunities. Obstet Gynecol. 2015;125:938–47.
Heyl PS, Sappenfield WM, Burch D, Hernandez LE, Kavanaugh VM, Hill WC. Pregnancy-related deaths due to pulmonary embolism: findings from two state-based mortality reviews. Matern Child Health J. 2013;17:1230–5.
Saucedo M, Deneux-Tharaux C, Bouvier-Colle MH. Ten years of confidential inquiries into maternal deaths in France, 1998–2007. Obstet Gynecol. 2013;122:752–60.
Deneux-Tharaux C, Saucedo M. Epidemiology of maternal mortality in France, 2010–2012. Gynecol Obstet Fert Senol. 2017;45:S8–21.
CAS Google Scholar
Deneux-Tharaux C, Saucedo M. Enhanced system for maternal mortality surveillance in France, context and methods. Gynecol Obstet Fert Senol. 2017;45:S3–7.
Blondel B, Lelong N, Kermarrec M, Goffinet F. Trends in perinatal health in France from 1995 to 2010. Results from the French National Perinatal Surveys. J Gynecol Obstet Biol Reprod. 2012;41:e1–15.
Ananth CV, Schisterman EF. Confounding, causality, and confusion: the role of intermediate variables in interpreting observational studies in obstetrics. Am J Obstet Gynecol. 2017;217:167–75.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30:377–99.
Hernandez LE, Sappenfield WM, Harris K, Burch D, Hill WC, Clark CL, et al. Pregnancy-related deaths, Florida, 1999–2012: opportunities to improve maternal outcomes. Matern Child Health J. 2018;22:204–15.
Nair M, Knight M, Kurinczuk JJ. Risk factors and newborn outcomes associated with maternal deaths in the UK from 2009 to 2013: a national case-control study. BJOG. 2016;123:1654–62.
Dowd JB, Zajacova A. Long-term obesity and cardiovascular, inflammatory, and metabolic risk in U.S. adults. Am J Prevent Med. 2014;46:578–84.
Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–74.
Ortega FB, Lavie CJ. Introduction and update on obesity and cardiovascular diseases 2018. Progr Cardiovasc Dis. 2018;61:87–8.
Shah R, Gayat E, Januzzi JL Jr., Sato N, Cohen-Solal A, diSomma S, et al. Body mass index and mortality in acutely decompensated heart failure across the world: a global obesity paradox. J Am College Cardiol. 2014;63:778–85.
Lavie CJ, McAuley PA, Church TS, Milani RV, Blair SN. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox. J Am College Cardiol. 2014;63:1345–54.
Hall ME, George EM, Granger JP. The heart during pregnancy. Revista espanola de cardiologia. 2011;64:1045–50.
Alpert MA, Omran J, Bostick BP. Effects of obesity on cardiovascular hemodynamics, cardiac morphology, and ventricular function. Curr Obesity Reports. 2016;5:424–34.
Larsen TB, Sorensen HT, Gislum M, Johnsen SP. Maternal smoking, obesity, and risk of venous thromboembolism during pregnancy and the puerperium: a population-based nested case-control study. Thrombosis Res. 2007;120:505–9.
Abdul Sultan A, West J, Tata LJ, Fleming KM, Nelson-Piercy C, Grainge MJ. Risk of first venous thromboembolism in pregnant women in hospital: population based cohort study from England. BMJ. 2013;347:f6099.
Poorolajal J, Jenabi E. The association between body mass index and preeclampsia: a meta-analysis. J Maternal fetal Neonatal Med. 2016;29:3670–6.
Denison FC, Aedla NR, Keag O, Hor K, Reynolds RM, Milne A, et al. Care of women with obesity in pregnancy: green-top guideline No. 72. BJOG: Int J Obstet Gynaecol. 2019;126:e62–106.
Seijo M, Minckas N, Cormick G, Comande D, Ciapponi A, BelizAn JM. Comparison of self-reported and directly measured weight and height among women of reproductive age: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2018;97:429–39.
Platner MH, Ackerman C, Howland RE, Xu X, Pettker CM, Illuzzi JL, et al. Gestational weight gain and severe maternal morbidity at delivery hospitalization. Obstet Gynecol. 2019;133:515–24.
Download references
Acknowledgements
We thank the obstetricians, midwives, and anaesthetists of the French Confidential Enquiry into Maternal Deaths who collected information for the case reviews and the national centre for cause-of-death statistics and epidemiology (CépiDc) for assistance in case identification. We also acknowledge the team and all the participants of the French National Perinatal Survey. We also thank Jo Ann Cahn for editorial assistance.
CNEMM study group
Dominique Chassard 6 , Henri Cohen 7 , Michel Dreyfus 8 , Jean-Claude Ducloy 9 , Irina Guseva-Canu 10 , Jean-Pierre Laplace 11 , Véronique Le Guern 12 , Sylvie Leroux 13 , Estelle Morau 14 , Claire Rondet 15 , Mathias Rossignol 16 , Véronique Tessier 17 , Éric Verspyck 18 , Philippe Weber 19 , Laurent Zieleskiewicz 20
The French Confidential Enquiry into Maternal Deaths was funded by the French National Public Health agency (Santé Publique France) and the French National Institute of Health and Medical Research (Inserm). The French National Perinatal Survey was funded by the Ministry of Health
Author information
Authors and affiliations.
Université de Paris, CRESS, Obstetrical, Perinatal and Pediatric Epidemiology Research Team, EPOPé, INSERM, INRA, DHU Risks in pregnancy, Paris, France
Monica Saucedo, Ana Paula Esteves-Pereira, Marie-Hélène Bouvier-Colle & Catherine Deneux-Tharaux
Department of Epidemiology and Quantitative Methods in Health, Sérgio Arouca National School of Public Health, Oswaldo Cruz Foundation, Rio de Janeiro, Brazil
Ana Paula Esteves-Pereira
Department of Obstetrics and Gynecology, Armand Trousseau Hospital, Assistance publique des hôpitaux de Paris, Paris, France
Lucile Pencolé
Department of Anesthesiology, Armand Trousseau University Hospital, Assistance publique des hôpitaux de Paris, Paris, France
Agnès Rigouzzo
Department of Obstetrics and Gynecology, Hôpital Privé d’Antony, Antony, France
Alain Proust
Department of Anesthesia and Intensive Care, Femme Mère Enfant Hospital, Hospices Civiles de Lyon, Lyon, France
- Dominique Chassard
Department of Obstetrics and Gynecology, Institut Mutuliste Montsouris, Paris, France
Henri Cohen
Department of Obstetrics and Gynecology, CHU de Caen, Caen, France
Michel Dreyfus
Department of Anesthesia, Hôpital privé Villeneuve d’Ascq, Villeneuve d’Ascq, France
Jean-Claude Ducloy
Non-communicable diseases and trauma division, Santé publique France, Saint-Maurice, France
Irina Guseva-Canu
Department of Obstetrics and Gynecology, Polyclinique Bordeaux Nord Aquitaine, Bordeaux, France
Jean-Pierre Laplace
Centre de Référence Maladies Auto-Immunes et Systémiques Rares, Service de Médecine Interne Pôle Médecine, Hôpital Cochin, AP-HP, Paris, France
Véronique Le Guern
Department of Obstetrics and Gynecology, Centre Hospitalier Annecy-Genevois, Annecy, France
Sylvie Leroux
Department of Anaesthesia, CHU de Nimes, Nimes, France
Estelle Morau
Centre for Epidemiology on Medical Causes of Death (CépiDc-Inserm), Le Kremlin-Bicêtre, France
Claire Rondet
Department of Intensive Care, Hôpital Lariboisière, Assistance Publique Hôpitaux de Paris, University of Paris, Paris, France
Mathias Rossignol
DHU Risques et Grossesse, Maternité Port Royal, Hôpitaux Universitaires Paris Centre, Hôpital Cochin, AP-HP, Paris, France
Véronique Tessier
Department of Obstetrics and Gynecology, CHU de Rouen, Rouen, France
Éric Verspyck
Department of Obstetrics and Gynecology, Centre Hospitalier de Mulhouse, Mulhouse, France
Philippe Weber
Département Anesthésie-Réanimation, Assistance publique-Hôpitaux de Marseille, Hôpital Nord, Marseille, France
Laurent Zieleskiewicz
You can also search for this author in PubMed Google Scholar
- , Henri Cohen
- , Catherine Deneux-Tharaux
- , Michel Dreyfus
- , Jean-Claude Ducloy
- , Irina Guseva-Canu
- , Jean-Pierre Laplace
- , Véronique Le Guern
- , Sylvie Leroux
- , Estelle Morau
- , Alain Proust
- , Claire Rondet
- , Agnès Rigouzzo
- , Mathias Rossignol
- , Véronique Tessier
- , Éric Verspyck
- , Philippe Weber
- & Laurent Zieleskiewicz
Corresponding author
Correspondence to Monica Saucedo .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the CNEMM study group are listed below Acknowledgements
Supplementary information
Suplementary tables and vignettes, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Saucedo, M., Esteves-Pereira, A.P., Pencolé, L. et al. Understanding maternal mortality in women with obesity and the role of care they receive: a national case-control study. Int J Obes 45 , 258–265 (2021). https://doi.org/10.1038/s41366-020-00691-4
Download citation
Received : 25 February 2020
Revised : 11 September 2020
Accepted : 25 September 2020
Published : 22 October 2020
Issue Date : January 2021
DOI : https://doi.org/10.1038/s41366-020-00691-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The 90% effective dose of intrathecal hyperbaric bupivacaine for cesarean delivery under combined spinal–epidural anesthesia in parturients with super obesity: an up-down sequential allocation study.
- Hon Sen Tan
- Matthew E. Fuller
- Ashraf S. Habib
Canadian Journal of Anesthesia/Journal canadien d'anesthésie (2024)
Maternal Morbidity Predicted by an Intersectional Social Determinants of Health Phenotype: A Secondary Analysis of the NuMoM2b Dataset
- Elise N Erickson
- Nicole S Carlson
Reproductive Sciences (2022)
Cardio-Obstetrics: the Next Frontier in Cardiovascular Disease Prevention
- Aarti Thakkar
- Tigist Hailu
- Garima Sharma
Current Atherosclerosis Reports (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Loading metrics
Open Access
Peer-reviewed
Research Article
Infection-related severe maternal outcomes and case fatality rates in 43 low and middle-income countries across the WHO regions: Results from the Global Maternal Sepsis Study (GLOSS)
Roles Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft
* E-mail: [email protected]
Affiliations Biomedical and Public Health Department, Institut de Recherche en Sciences de la Santé (IRSS), Ouagadougou, Burkina Faso, Doctoral School, Saint Thomas d’Aquin University, Ouagadougou, Burkina Faso
Roles Conceptualization, Methodology, Writing – review & editing
Affiliation Department of Reproductive Health and Research, UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), World Health Organization, Geneva, Switzerland
Roles Methodology, Writing – review & editing
Roles Writing – review & editing
Affiliation Faculty of Economics and Statistics, National University of Rosario, Rosario, Argentina
Affiliation Nuffield Department of Population Health, National Perinatal Epidemiology Unit, University of Oxford, Oxford, United Kingdom
Affiliation Faculty of Medicine, Department of Obstetrics and Gynaecology, Khon Kaen University, Khon Kaen, Thailand
Affiliation Centro Rosarino de Estudios Perinatales (CREP), Rosario, Argentina
¶ Membership of WHO Global Maternal Sepsis Study Research Group is provided in S1 Acknowledgments
- Adama Baguiya,
- Mercedes Bonet,
- Vanessa Brizuela,
- Cristina Cuesta,
- Marian Knight,
- Pisake Lumbiganon,
- Edgardo Abalos,
- Séni Kouanda,
- WHO Global Maternal Sepsis Study Research Group

- Published: April 25, 2024
- https://doi.org/10.1371/journal.pgph.0003109
- Peer Review
- Reader Comments
The highest toll of maternal mortality due to infections is reported in low and middle-income countries (LMICs). However, more evidence is needed to understand the differences in infection-related severe maternal outcomes (SMO) and fatality rates across the WHO regions. This study aimed to compare the burden of infection-related SMO and case fatality rates across the WHO regions using the Global Maternal Sepsis Study (GLOSS) data. GLOSS was a hospital-based one-week inception prospective cohort study of pregnant or recently pregnant women admitted with suspected or confirmed infection in 2017. Four hundred and eight (408) hospitals from 43 LMICs in the six WHO regions were considered in this analysis. We used a logistic regression model to compare the odds of infection-related SMOs by region. We then calculated the fatality rate as the proportion of deaths over the total number of SMOs, defined as maternal deaths and near-misses. The proportion of SMO was 19.6% (n = 141) in Africa, compared to 18%(n = 22), 15.9%(n = 50), 14.7%(n = 48), 12.1%(n = 95), and 10.8%(n = 21) in the Western Pacific, European, Eastern Meditteranean, Americas, and South-Eastern Asian regions, respectively. Women in Africa were more likely to experience SMO than those in the Americas (aOR = 2.41, 95%CI: [1.78 to 2.83]), in South-East Asia (aOR = 2.60, 95%CI: [1.57 to 4.32]), and the Eastern Mediterranean region (aOR = 1.58, 95%CI: [1.08 to 2.32]). The case fatality rate was 14.3%[3.05% to 36.34%] (n/N = 3/21) and 11.4%[6.63% to 17.77%] (n/N = 16/141) in the South-East Asia and Africa, respectively. Infection-related SMOs and case fatality rates were highest in Africa and Southeast Asia. Specific attention and actions are needed to prevent infection-related maternal deaths and severe morbidity in these two regions.
Citation: Baguiya A, Bonet M, Brizuela V, Cuesta C, Knight M, Lumbiganon P, et al. (2024) Infection-related severe maternal outcomes and case fatality rates in 43 low and middle-income countries across the WHO regions: Results from the Global Maternal Sepsis Study (GLOSS). PLOS Glob Public Health 4(4): e0003109. https://doi.org/10.1371/journal.pgph.0003109
Editor: Hannah Tappis, Jhpiego, UNITED STATES
Received: December 5, 2023; Accepted: March 29, 2024; Published: April 25, 2024
Copyright: © 2024 Baguiya et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data used for this analysis can be made available upon request. Contact of the GLOSS coordinator [email protected] .
Funding: AB received funding from the HRP Alliance, part of the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development, and Training in Human Reproduction (HRP), a cosponsored program executed by the World Health Organization (WHO), to complete his studies. The main study was financially supported by the UNDP–UNFPA–UNICEF–WHO–World Bank Special Programme of Research, Development and Research Training in Human Reproduction, Department of Sexual and Reproductive Health and Research, WHO, Geneva, Switzerland (project A65787), Merck Sharp & Dohme, a wholly owned subsidiary of Merck (Kenilworth, NJ, USA), through its Merck for Mothers programme, and the United States Agency for International Development (grant GHA-G-00-09-00003). The funders had no role in study design, data collection and analysis, decision to publish, or manuscript preparation. The named authors alone are responsible for the views expressed in this publication and do not necessarily represent the decisions or the policies of the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP) or the World Health Organization (WHO) or the other affiliated institutions.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Maternal sepsis is defined as “ a life-threatening condition defined as organ dysfunction resulting from infection during pregnancy , childbirth , post-abortion , or post-partum period” [ 1 ]. It can complicate all types of infection, including pregnancy-related ones, and lead to severe maternal outcomes. The incidence of direct obstetric infections in late pregnancy and the postpartum period in sub-Saharan Africa is 3.5% and 2.4%, respectively. In South Asia and sub-Saharan Africa, women with infection in the postpartum period are 1.8 times more likely to die compared to those without infection [ 2 ]. Globally, direct obstetric infections represent the third cause of maternal mortality. They are responsible for almost 11% of all maternal deaths worldwide; specific to sub-Saharan Africa and South Asia, these numbers rise to 12% and 14%, respectively [ 3 , 4 ].
Previous publications from the Global Maternal Sepsis Study (GLOSS) indicated that for every 1000 live births to women with suspected or confirmed infection, 11 women experience infection-related severe maternal outcomes (SMO), which include maternal near-misses and deaths. Out of those SMOs, the global case fatality rate is 6.8%. The highest rates and proportions are observed in low-income countries, with SMO in 15 women per 1000 live births and a 15% fatality rate among infection-related SMOs [ 5 ].
There is a growing literature on maternal infection and sepsis, particularly with country-specific data in high- [ 6 – 8 ], low, and middle-income countries [ 9 – 12 ]. Previous comparisons across regions or income levels used mathematical models such as the Global Burden of Diseases [ 13 – 15 ] or systematic reviews [ 16 ]. However, they were often limited by insufficient data in resource-constrained settings. Nevertheless, these studies highlighted inequalities related to the burden of maternal infections and hospital readiness for their identification and treatment between low- and high-income countries and across levels of sociodemographic indexes [ 5 , 14 , 16 , 17 ]. Based on the high burden of all-cause maternal mortality in sub-Saharan Africa (70% of the global burden) [ 18 ], we hypothesized that there could be disparities across the WHO regions, and women could be more likely to experience severe morbidity or die from maternal infections in Africa than in the other regions.
The maternal mortality ratio is an indicator of poor quality of care provided to women during and after pregnancy [ 19 ]; hence, the provision of optimal care for maternal and neonatal infection is part of the priorities in maternal and child health service delivery [ 20 ]. When systems fail to prevent maternal infections, the capacity of facilities to respond becomes crucial for women’s survival. Country and region-level data on SMO could be helpful for policymakers and health systems managers to understand and assess hospitals’ performance in caring for women with infection during pregnancy or in the postpartum period [ 21 ]. Therefore, GLOSS data give a unique opportunity to explore the regional disparities in hospitals’ capacity to identify and manage maternal infections and assess the burden of infection-related SMOs among LMICs in each region. In this study, we aimed to describe the hospitals’ capacity for identifying and managing maternal infections and to compare the proportion of infection-related SMOs and their associated case fatality rate in the African region versus the other regions based on the WHO classification of the countries, using GLOSS data.
Materials and methods
Study design and setting.
The GLOSS was a hospital-based one-week inception prospective cohort study. Forty-three (43) LMICs (out of 52 countries involved in the entire GLOSS) were included in this analysis.
There were 13 countries in the African Region (AFR) and five in Europe. The other four regions were the Americas (AMR: 10 countries), South-East Asia (SEAR: 5 countries), Eastern Mediterranean (EMR: 6 countries), and the Western Pacific (WPR: 4 countries) [ 12 ]. Nine (09) high-income countries of the GLOSS, including eight (08) in Europe [ 22 ] and one (01) in the Americas, were excluded from this analysis.
The GLOSS identified and included all women with confirmed or suspected infection during any stage of pregnancy and up to the 42 nd day after the end of the pregnancy who were admitted or already hospitalized for at least 12 hours in participating health facilities.
Women were enrolled between November 28 and December 4, 2017, in geographical areas within 52 purposively selected countries in all six WHO regions. The study procedures are described elsewhere [ 12 ].
Data sources
Briefly, data were collected on the characteristics of the study’s geographical areas, hospitals, and individual participants. Information on the geographical area’s characteristics, including its population, was captured at the area level. At the hospital level, data were collected on the hospital size, level of care, type (public or private), the number of deliveries in the year before the study, and staff availability by category. It also included a set of equipment and services, among others. Individual-level data were extracted from patients’ records by health workers in the participating hospitals. Individual information included women’s sociodemographics, obstetric background, clinical profile, pregnancy outcomes, and clinical management data. All procedures and diagnoses were based on the staff’s routine clinical activities. Data collectors did not have to interact with the patients except when seeking consent. No additional resources, guidelines, or interventions were provided for the study, except that GLOSS was accompanied by an awareness campaign fully described elsewhere [ 23 ].
Variables and measurement
The primary outcome variable in this analysis is an infection-related SMO, including infection-related maternal death and near-miss. Maternal deaths were either directly linked to the infection or had an infection as a contributing cause. For maternal near-miss, we applied the WHO definition: a woman who nearly died but survived a life-threatening condition during pregnancy, childbirth, or postpartum or post-abortion period [ 24 ]. Participants were classified as near-miss cases if they had at least one of the WHO near-miss criteria [ 25 ]. The independent variable was the region. Participants were classified according to the region to which their country belonged. Six categories represented the WHO regions: AFR, AMR, EMR, EUR, SEAR, and WPR [ 26 ].
Data on the hospital capacity were collected using a dedicated form, which gathered information on the availability of medical and laboratory equipment, drugs, staff, and infection prevention and control procedures and protocols in the facility. We used the variables related to the country’s level of income (upper middle, lower middle, and low income), hospitals’ location (urban or rural/peri-urban), level of care (primary, secondary, or tertiary), type of facility (public or private/non-governmental organization/faith-based), capacity to provide Emergency Obstetric and Newborn Care (basic -BEmONC-, comprehensive -CEmONC-, or neither), affiliation to a university or not, facility size (number of births the previous, year with, 2016, with four categories: <1000 livebirths, 1000–2499 livebirths, 2500–4499 livebirths, and ≥4500 livebirths), staff availability 24/7 (either physically or on call), availability of infection prevention and control (IPC) committee (yes or no), of a surveillance system for antibiotics and antimicrobials (yes or no), and a training or continuing education system on IPC and hospital hygiene (yes or no). In addition, we computed three composite variables related to i) availability of services and equipment, ii) identification capacity, and iii) management capacity. For each of these variables, we used a set of dummy variables presented in S1 Table to create an index (score) for each hospital using a Principal Component Analysis (PCA). Hospitals were then ranged and divided into three groups of equal size (each group contains one-third of the hospitals), namely the lowest (coded 1), medium (coded 2), and highest (coded 3) level of hospital service availability, capacity, or management index [ 27 ].
Data analysis
We used descriptive statistics to present data on the facility’s general characteristics, including the availability of services and equipment, identification, and management capacity.
We then calculated the proportion of women who had SMO among all women with infection and the rate of infection-related SMO per 1000 live births with their 95% confidence intervals (95%CI), stratified by region. Cases Fatality Rates by region were computed as the proportion of deaths due to infections over the total number of women with SMO.
Finally, we fitted a logistic regression model to assess the association between the WHO region and the occurrence of SMO. We computed crude and adjusted odds ratios (aOR) with their 95%CI using a backward stepwise approach with facility-level characteristics. The final model was adjusted based on facility size, location, capacity to manage maternal infections, and the availability of a routine training program on infection management. We used the Akaike Information Criteria (AIC) and the “ linktest ” command to compare the models and assess the goodness of fit. All analyses were performed using Stata 18.
Ethical considerations
During the GLOSS, written informed consent or waiver of consent was obtained to extract data from the patient’s records (based on the requirements of each local institutional or national ethics committee). We also explained to participants that they could opt out of the study at any time and request the withdrawal of their data. All study records, forms, logs, and data were kept confidential. Data were entered with hospitals and participants’ sequential numbers. No identifiable information was entered into the system. Data were anonymized for all the analysis. The study protocol was submitted to and approved by the WHO Ethics Review Committee (protocol ID A65787) and the ethics committees of the respective countries and facilities according to national regulations.
This analysis included 2466 women from 408 facilities in 43 LMICs. Most women were from the Americas (31.2%, n = 788) and Africa (30.2%, n = 718). Overall, 577 women had infections with complications, and 377 had severe maternal outcomes ( Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0003109.t001
Services availability and hospital capacity
Table 2 presents the general characteristics of the facilities, staff, services, and equipment availability and their capacity to identify and manage maternal infections. Most of the facilities were located in urban areas (77.9%, n = 317 in total) and were comprehensive EmONC facilities (80.4%, n = 328), except in the Western Pacific (48.2%, n = 27). One out of four facilities (27.4%, n = 111) had more than 4500 births annually. Regarding staff availability, midwives were available in at least 80% of the facilities (85.6%, n = 107, in Africa), except in the Americas (40.9%, n = 36). But, the availability of internal medicine and infectious disease specialists was lower in Africa (26.6%, n = 33) and higher in the Americas (72.4%, n = 63). In Africa, the antibiotic/antimicrobial use surveillance system was available only in 43.6% (n = 55) of the facilities. In all the other regions, more than 60% of the facilities had a surveillance system. The highest percentage was in the Western Pacific, with 80.4% (n = 45). Regarding the availability of an IPC Committee and a training/continuing education system on IPC/hospital hygiene, the highest percentages were reported in Europe (93.0%, n = 53 and 90.9%, n = 50, respectively) and the lowest in Africa (73%, n = 92 and 76%, n = 95, respectively). In addition, Africa (43.7%, n = 55) and the Western Pacific (55.4%, n = 31) were the two regions where most facilities fell in the group of the lowest level of services and equipment availability, compared to the Americas (8%, n = 7) and South-East Asia (17.1%, n = 6).
https://doi.org/10.1371/journal.pgph.0003109.t002
The distribution of the individual items related to service availability is presented in S2 Table . More than half of the facilities in the Western Pacific (51.8%, n = 29) and over one-third in Africa (36.5%; n = 46) fell in the category of the lowest level of identification capacity, whereas two-thirds in the Americas (65.9%, n = 58) were in the category of the highest level. The lowest management capacity level was represented by 38.1% (n = 48) in Africa and 10.2% (n = 9) in the Americas. The percentages of the individual items of the capacity of identification and management are presented in S3 and S4 Tables .
Severe maternal outcome and associated fatality rate
In total, infection-related severe maternal outcomes were experienced by 15.3% (n = 377, 95%CI:13.9% to 16.8%) of the women. Fig 1 shows that Africa had the highest percentage of SMO (19.6%, 95%CI:16.8% to 22.7%), followed by the Western Pacific (18%, 95%CI:11.7% to 26%). The confidence intervals presented in S1 Fig indicate that the percentage in Africa was statistically higher than the ones in the Americas (12.1%, 95%CI: 9.9 to 14.5) and South-East Asia (10.7%, 95%CI: 6.8 to 16.0), where the lowest percentages were reported.
https://doi.org/10.1371/journal.pgph.0003109.g001
Fig 2 shows that the rates of SMO per 1000 live births were also higher in Africa (16.58; 95%CI:10.38 to 22.78), the Americas (16.26; 95%CI:10.47 to 22.05), and Europe (16.19; 95%CI:8.34 to 24.04).
https://doi.org/10.1371/journal.pgph.0003109.g002
The forest plot in Fig 3 shows the overall and regional SMO fatality rate in percentage. In total, 26 women died, and the global case fatality rate was 6.9% (n/N = 26/377). In Africa and South-East Asia, it was 11.4% (n/N = 16/141) and 14.3% (n/N = 3/21) respectively.
https://doi.org/10.1371/journal.pgph.0003109.g003
Association between the region and the occurrence of severe maternal outcome
We fitted a logistic regression model with women as units of analysis to explore the difference in the likelihood of experiencing a severe maternal outcome in Africa compared to the other five WHO regions. The results are presented in Table 3 .
https://doi.org/10.1371/journal.pgph.0003109.t003
The unadjusted model showed that women in Africa were more likely to experience severe maternal outcomes than those living in the Americas (OR = 1.78, 95%CI: [1.34 to 2.36]) and in Southeast Asia (OR = 2.02, 95%CI: [1.24, 3.30]). After adjustment, women in Africa were more likely to experience SMO than those in the Americas (aOR = 2.41, 95%CI: [1.78 to 2.83]), the Eastern Mediterranean (aOR = 1.58, 95%CI: [1.08 to 2.32]), and South-East Asia (aOR = 2.60, 95%CI: [1.57 to 4.32]).
This analysis highlights differences in infection-related SMOs and case fatality rates across the WHO regions, using data from 43 LMICs of the GLOSS. One-fifth of women hospitalized with a suspected or confirmed infection in Africa experienced an SMO, the highest proportion among all the regions. Case fatality rates were also higher in South-East Asia and Africa. In addition, hospitals’ readiness to identify and manage maternal infections was relatively lower in Africa than in the other regions.
This is the first analysis with global primary data that used standardized definitions related to maternal infectious complications across such a large number of hospitals. It adds to the previous analysis of the GLOSS [ 5 , 17 ] and the AMANHI study [ 2 , 4 ].
The low level of equipment, availability, and capacity for identification and the management of maternal infection in Africa is somehow related to the high incidence of SMO. Previous authors warned that some sepsis-related guidelines could not be implemented in sub-Saharan Africa due to the low availability of required facilities, equipment, and drugs [ 28 ]. Previous GLOSS analysis on the availability of resources and services by Brizuela et al. found differences in the availability of certain practices and resources across the country’s income level. The lowest level of availability was reported in the group of low-income countries to which most African countries belonged [ 17 ]. Hospital management and women’s clinical profile at admission are determinants of the burden of SMO in the regions. The differences in the proportion of SMOs across the regions could reflect low quality of care and weaknesses in health systems management [ 20 , 29 ].
All the global estimates indicate that sub-Saharan Africa and Asia (Central and South) have the highest maternal mortality ratios. But sub-Africa alone bears 70% of the global number of maternal deaths. With 545 deaths per 100,000 live births, the region has the highest maternal mortality ratio compared to any other region of the world, including South-East Asia [ 18 ]. Although the difference was not statistically significant, in our findings, the infection-related fatality rate was higher in South-East Asia than in Africa, which is quite surprising. There were contradictory findings in the literature in this regard. Some studies have shown that the proportion of maternal deaths attributable to maternal infections is higher in South Asia than in sub-Saharan Africa [ 2 , 4 ]. However, Chen et al. reported in their global estimates of the burden and trends of maternal sepsis and other maternal infections, that maternal mortality ratio in sub-Saharan Africa ranged from 19.40 (Western sub-Saharan Africa) to 71.54 (Central sub-Saharan Africa) deaths per 100 000 live births, and in Asia from 0.38 (East Asia) to 8.37 (South Asia) deaths per 100 000 live births [ 14 ]. There are differences in the definition and the measurements of these estimates. Still, the findings in our study could imply that the distribution of cause-specific (infection in particular) maternal mortality across the regions may differ from the overall mortality figure [ 30 ]. Therefore, assigning a death to a single cause can be problematic when weighing the importance of other concurrent causes [ 31 ]. Future studies on causes of maternal deaths, especially for maternal sepsis across the regions, could consider a more robust sample to explore differences in infection-related fatality rates across the regions because our study was somehow limited by the number of deaths identified during the follow-up.
Nonetheless, across all regions, preventing maternal infection-related morbidity and mortality will require further and specific actions. A critical aspect of prevention and management will be to improve hospitals’ capacity to identify and manage infections, quality of care, and health system governance. The global community can assist countries in reviewing and improving their identification and treatment capacity [ 32 ], improving maternal infection surveillance, and investing in skilled health workers’ availability, equipment, and supply [ 10 , 33 , 34 ].
This study has some limitations. First, the included facilities may not be fully representative of the regions. Second, the generalisability of the GLOSS findings is limited to intra-hospital outcomes and geographical areas similar to those included in the study. Third, our sample size was not powered to compare death rates; therefore, we could not accurately explore the association between the region and death rates. In addition, the availability of the services and equipment and the hospital’s capacity to identify and manage maternal infections were based on the hospital’s managers’ self-reports. Therefore, these measures may be overestimated to show better performance. However, this cohort study included participants prospectively. They were evaluated by the hospital’s medical staff. In addition, the study was supported by an awareness campaign that helped improve the identification of the case and reduce the measurement and selection biases.
This study showed disparities between Africa and the other regions regarding maternal infection-related SMO to the disadvantage of Africa. The hospitals in this region are relatively less equipped compared to others. The increased utilization of health services in recent years continually promoted through Universal Health Coverage, is an opportunity to treat complications and avert preventable maternal deaths, such as deaths due to infections. Therefore, the quality of in-hospital care is the main driver of women’s and newborns’ survival. Hospitals should, thus, be prepared for the prevention, early identification, and treatment of maternal infections with any severity level to significantly reduce the burden of severe maternal outcomes and intra-hospital fatality rate, particularly in the most disadvantaged regions.
Supporting information
S1 fig. percentage (%) of women with infection-related severe maternal outcome by region..
https://doi.org/10.1371/journal.pgph.0003109.s001
S1 Table. List of binary variables used to compute the composite variables.
https://doi.org/10.1371/journal.pgph.0003109.s002
S2 Table. Services and equipment available in the facility.
https://doi.org/10.1371/journal.pgph.0003109.s003
S3 Table. Identification and diagnostic capacity.
https://doi.org/10.1371/journal.pgph.0003109.s004
S4 Table. Infection management-related characteristics of the facilities by region.
https://doi.org/10.1371/journal.pgph.0003109.s005
S1 Acknowledgments.
https://doi.org/10.1371/journal.pgph.0003109.s006
Acknowledgments
We sincerely thank the women who participated in this study. WHO is grateful to the extensive network of institutions and individuals who contributed to the project design and implementation, including researchers, study coordinators, data collectors, data clerks, and other partners, including the staff from the Ministries of Health and WHO offices. We would like to acknowledge the contribution and lifelong achievements of our late colleague Bukola Fawole, who passed away before the publication of this Article.
- View Article
- PubMed/NCBI
- Google Scholar
- 18. WHO, UNICEF, UNFPA, World Bank Group, UNDESA/PopulationDivision. Trends in maternal mortality 2000 to 2020. Geneva: World Health Organization; 2023.
- 21. World Health Organization. Global report on the epidemiology and burden of sepsis: current evidence, identifying gaps and future directions. Geneva: WHO; 2020 p. 56. Available: https://apps.who.int/iris/bitstream/handle/10665/334216/9789240010789-eng.pdf .
- 34. World Health Organization. Maternal death surveillance and response: technical guidance information for action to prevent maternal death. Geneva: WHO; 2013 p. 128.

Who are dying and why? A case series study of maternal deaths in Nepal
Affiliations.
- 1 School of Public Health and Community Medicine, BP Koirala Institute of Health Sciences, Dharan, Sunsari, Nepal [email protected].
- 2 Mother and Infant Research Activities, Kathmandu, Nepal.
- PMID: 33986042
- PMCID: PMC8126278
- DOI: 10.1136/bmjopen-2020-042840
Objectives: To identify delays and associated factors for maternal deaths in Nepal.
Design: A cross-sectional case series study of maternal deaths. An integrated verbal and social autopsy tool was used to collect quantitative and qualitative information regarding three delays. We recorded death accounts and conducted social autopsy by means of community Focus Group Discussions for each maternal death; and analysed data by framework analysis.
Setting: Sixty-two maternal deaths in six districts in three provinces of Nepal.
Results: Nearly half of the deceased women (45.2%) were primiparous and one-third had no formal education. About 40% were from Terai/Madhesi and 30.6% from lower caste. The most common place of death was private hospitals (41.9%), followed by public hospitals (29.1%). Nearly three-fourth cases were referred to higher health facilities and median time (IQR) of stay at the lower health facility was 120 (60-180) hours. Nearly half of deaths (43.5%) were attributable to more than one delay while first and third delay each contributed equally (25.8%). Lack of perceived need; perceived cost and low status; traditional beliefs and practices; physically inaccessible facilities and lack of service readiness and quality care were important factors in maternal deaths.
Conclusions: The first and third delays were the equal contributors of maternal deaths. Interventions related to birth preparedness, economic support and family planning need to be focused on poor and marginalised communities. Community management of quick transportation, early diagnosis of pregnancy risks, accommodation facilities near the referral hospitals and dedicated skilled manpower with adequate medicines, equipment and blood supplies in referral hospitals are needed for further reduction of maternal deaths in Nepal.
Keywords: health policy; international health services; social medicine.
© Author(s) (or their employer(s)) 2021. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
Publication types
- Research Support, Non-U.S. Gov't
- Cross-Sectional Studies
- Health Services Accessibility
- Maternal Death*
- Maternal Health Services*
- Maternal Mortality
Connection denied by Geolocation Setting.
Reason: Blocked country: Russia
The connection was denied because this country is blocked in the Geolocation settings.
Please contact your administrator for assistance.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Acad Forensic Pathol
- v.8(4); 2018 Dec
Maternal Death and Its Investigation
Maternal deaths are a leading cause of death in young females worldwide, particularly in developing countries. Maternal mortality ratio, the number of maternal deaths per 100 000 live births, averages 240 in developing regions, but only 16 in developed regions.
Causes of maternal and pregnancy-related deaths can be subdivided into three broad categories. Direct maternal deaths result from obstetric complications of the pregnant state (i.e., pregnancy, labor, and puerperium) from interventions, omissions, incorrect treatment, or from a chain of events resulting from any of the above. Indirect maternal deaths result from previously existing diseases or diseases that developed during pregnancy, and which are not due to a direct obstetric cause, but are aggravated by the physiologic effects of pregnancy. Incidental maternal deaths are those from causes unrelated to pregnancy or the puerperium, including accidental deaths and homicide.
Maternal deaths carry significant short- and long-term impacts for family members and the role of the pathologist is an important part of the wider knowledge-gathering process that can contribute to changes in maternal mortality rates. This paper reviews the clinical and pathological features of common pregnancy-related disorders and gives guidelines for performing an autopsy related to maternal death.
Introduction
The World Health Organization (WHO) defines maternal death as:
…the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes ( 1 ).
Pregnancy-related death is similarly defined by the WHO as “ the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the cause of death ” ( 1 ). Given their closely-related definitions, many papers and investigative bodies use the term maternal death when referring to the WHO definition of pregnancy-related deaths.
Worldwide, maternal mortality is unevenly distributed with the vast majority of maternal deaths taking place in developing countries, particularly across Southern Asia and Sub-Saharan Africa where 30% and 57% of global maternal deaths in 2008 occurred, respectively ( 2 – 4 ). Maternal deaths are a leading cause of death in young females (10-24 years of age) worldwide at 15%, with most of these deaths occurring in developing countries ( 5 ). A common international measure of maternal mortality rates is via maternal mortality ratio (MMR), which is defined as the number of maternal deaths per 100 000 live births ( 2 , 6 ). Due to issues such as local registration of death reporting quality, chosen datasets, and differences in statistical analysis, MMRs are at risk of underestimation and can vary between studies ( 2 , 7 ). In a 2012 joint review involving the WHO and the United Nations International Children’s Emergency Fund (UNICEF), 40 countries had a high MMR (≥300 maternal deaths per 100 000 live births), the highest of which were Chad and Somalia, with respective MMRs at 1100 and 1000 ( 3 ). Contrasting with developing regions where the average MMR was 240, the average MMR in developed regions was 16, although a range of MMRs was noted between developed countries, such as Italy (n = 4), Australia (n = 7), the United Kingdom (n = 12), and the United States of America (n = 21) ( 3 ).
The Millennium Development Goals established by the United Nations in 2000 aimed to reduce maternal mortality by 75% between 1990 and 2015 as part of a general global trend of reduction in maternal mortality ( 8 ). Contrary to the global overall reduction in maternal mortality of 44% over this time period ( 8 ), maternal mortality in the United States of America (USA) is amongst the highest in the developed world and has actually increased over this same period ( 2 , 3 , 9 ). Whilst MMRs in most other developed countries have decreased or remained stable over this period ( 2 , 3 ), the Centers for Disease Control and Prevention (CDC) estimate an increase in USA MMR between 1987 and 2014 from 7.2 to 18.0 ( 9 ). A systematic analysis for the Global Burden of Disease Study had higher estimates of an increase in USA MMR from 16.9 to 26.4 from 1990 to 2015 ( 2 ).
The precise causes for the apparent increase in USA maternal mortality over this period are not clear, although increased identification through computerized data gathering and reporting are thought to have contributed to these figures ( 9 , 10 ). Increases in comorbidities that affect the risk of pregnancy complications such as hypertension, diabetes, and heart disease are also suspected to have contributed to an increase in USA MMR, whilst a 15-month spike in MMR between 2009 and 2010 was attributed to the H1N1 influenza A pandemic at that time ( 9 ). Maternal deaths in the USA are also not evenly distributed, with black women having a MMR that is approximately four times greater than that of white women ( 9 – 12 ). Over the period of 2011 to 2013, the MMR of non-Hispanic black women was estimated as 43.5 compared to 12.7 for non-Hispanic white women ( 10 ). Socioeconomic factors such as education and access to healthcare in addition to medical comorbidities are considered to contribute to much of this difference ( 12 ).
Causes of maternal and pregnancy-related deaths can be subdivided into three broad categories: direct maternal deaths, indirect maternal deaths, and incidental maternal deaths ( 1 , 6 , 13 ) ( Table 1 ).
Causes of Maternal Death.
Worldwide, direct causes account for 86% of maternal deaths, with the most common causes being hemorrhage and hypertensive disorders, whilst death from maternal hemorrhage is overwhelmingly more common in developing compared to developed countries ( 2 ). Factors such as access to safe health care, antibiotics, and maternal monitoring, where available, contribute to lower rates of maternal complications leading to death ( 6 , 8 ). In the USA, the most common causes of maternal death are indirect, with the most frequent being cardiovascular diseases (15.2%), noncardiovascular medical diseases (14.7%), infection (12.8%), hemorrhage (11.5%), cardiomyopathy (10.3%), pulmonary embolism (9.1%), cerebrovascular accident (7.4%), hypertensive disorders of pregnancy (6.8%), and amniotic fluid embolism (5.5%) ( 9 ). The most common causes of maternal death in the USA differ depending on pregnancy outcome, where in cases of stillbirth or ectopic pregnancy, hemorrhage is the most common cause of death and makes up 21.4% and 94.4% of maternal deaths respectively ( 7 ).
Race and sociodemographic factors also influence the common causes of maternal death, with hemorrhage being the most common cause of death in the USA for foreign-born white, black, and Hispanic women and USA-born Hispanic women compared to the higher rates of cardiovascular death amongst white and black USA-born women ( 12 ). Despite increasing rates of USA maternal mortality and the influence of sociodemographic factors on maternal death, the low percentage of maternal deaths compared to mortality in the wider population means that maternal autopsies are a rare encounter for any individual pathologist.
Maternal deaths carry particularly significant shortand long-term impacts for family members and the role of the pathologist is an important part of the wider knowledge-gathering process that can contribute to changes in maternal mortality rates. The purpose of this paper is to review the clinical and pathological features of common pregnancy-related disorders and to give guidelines for performing an autopsy related to maternal death.
Direct Maternal Deaths
Pregnancy-induced hypertensive disease (preeclampsia, eclampsia, and hellp syndrome).
The diagnostic criteria for preeclampsia were changed in 2014 by the International Society for the Study of Hypertension in Pregnancy (ISSHP) to:
…de novo hypertension developing after 20 weeks of gestation combined with proteinuria (>300 mg per day), other maternal organ dysfunction, such as renal insufficiency, liver involvement, neurological or hematological complications, uteroplacental dysfunction or fetal growth restriction ( 14 , 15 ).
Eclampsia is progression of the disorder with development of cerebral symptoms such as visual disturbance, headache, dizziness, seizure, decreased level of consciousness, or coma. It occurs in approximately 0.5% of pregnancies ( 16 ). Intracerebral hemorrhage is the most common cause of death, particularly in older women, accounting for approximately 60% of fatalities ( 17 ).
Preeclampsia occurs in approximately 3-8% of pregnancies globally ( 18 – 20 ). There is a higher rate in developing countries ( 15 ) where it is responsible for up to 20% of maternal fatalities ( 21 ). In the USA in 2010, 3.8% pregnancies were affected by preeclampsia ( 18 ) and the rate is not deceasing with time ( 14 , 16 ). Risk factors for preeclampsia include primiparity, age greater than 40 years, obesity, diabetes mellitus, multi-fetal pregnancy, and positive family history ( 14 , 19 ).
The pathophysiology of preeclampsia is not completely understood. However, it is thought that abnormal placental vascular remodelling may result in placental ischemia with release of inflammatory factors to the maternal blood, causing vascular endothelial dysfunction with generalized vasoconstriction and subsequent multiorgan dysfunction ( 15 , 18 ). There are no reliable clinical screening tests to predict risk of preeclampsia ( 14 ).
Pathology of Preeclampsia
Histology of the uterus in preeclampsia shows fibrinoid necrosis in the vessel walls with numerous lipophages cuffed by mononuclear inflammatory cells ( Image 1 ). This change is seen especially in the spiral arteries of the decidua parietalis, the basal arteries of the decidua basalis and myometrium, and in the myometrial segments of the spiral arteries in the placental bed ( 22 ). In addition, there is failure of the normal physiological adaptive changes in the spiral arteries of the placental bed to extend beyond the deciduo-myometrial junction ( 22 ). In contrast, in uncomplicated essential hypertension, although there is hyperplastic arteriosclerosis especially in the myometrial segments of the spiral arteries, vascular changes are otherwise normal, including the depth of endovascular trophoblastic invasion.

Fibrinoid necrosis with lipophage cuffing in placental bed vessel walls in a case of preeclampsia (H&E, x100). Image courtesy of Dr. TY Khong, Adelaide, Australia.
Other pathological changes which may be seen include glomerular capillary endotheliosis (swelling of endothelial cells with occlusion of capillary lumens) in the kidneys, “flame” hemorrhages in the left ventricular outflow tract of the heart, and adrenal hemorrhage and necrosis ( 20 ).
HELLP Syndrome
HELLP stands for hemolysis, elevated liver enzymes, low platelets, which is descriptive of the features of this disorder, first described in 1982. Two-thirds of cases occur in the third trimester and one third are postpartum ( 23 ).
HELLP occurs in approximately 5-12% of patients with severe preeclampsia ( 17 , 21 ). At risk groups are very old or young maternal age, multi-fetus gestation, multiparity, and a past history of preeclampsia or HELLP. The pathogenesis is thought to be damage to vascular endothelial cells by activated platelets and inflammatory factors which activate the coagulation cascade with development of thrombotic microangiopathy ( 23 , 24 ).
One percent of patients develop severe disease with complications including disseminated intravascular coagulation (21%), placental abruption (16%), acute kidney disease (8%), and spontaneous rupture of the liver. It is thought that spontaneous rupture of the liver may be a result of inflammation with blood flow obstruction which causes liver swelling and hepatocellular necrosis (particularly peri-portal) with intrahepatic hemorrhage and development of a subcapsular hematoma that may rupture spontaneously to cause hemoperitoneum ( 17 , 21 , 23 ).
In preeclampsia, eclampsia, and HELLP syndrome, particular efforts must be made to obtain relevant clinical history, examination notes, and antemortem investigation results, due to the high importance of clinical information in assisting the diagnosis of these conditions.
Peripartum Hemorrhage
Peripartum hemorrhage is commonly due to placental abnormalities, but may also be caused by genital tract tears, either spontaneously-occurring during parturition or iatrogenic. Placental abnormalities include placenta previa, abnormally adherent placenta (e.g., accreta, increta, percreta), placental abruption, and retained placenta. These may be related to a previous cesarean section scar.
Placenta previa is the implantation of the placenta in the uterine lining near or over the cervical opening and is usually diagnosed clinically. Its demonstration at autopsy in the undelivered patient requires removal of the uterus en bloc with the cervix and upper vagina to show the placenta covering the lower segment of the uterus and/or across the internal os. Abnormally adherent placenta ( Image 2 ) occurs in one in 540 to one in 93 000 pregnancies ( 22 ). It is often associated with placenta previa and/or previous uterine surgery. Examination shows direct apposition between villous and trophoblastic elements and the myometrium without an intervening layer of decidua. Placenta percreta is the most severe form and villi can penetrate through the uterine or cervical wall to adjacent structures, such as the bladder.

Placenta accreta – the placenta is firmly attached to the uterine wall. Courtesy of Dr T. Y. Khong, Adelaide, Australia.
Placental abruption is the early detachment of the placenta from the uterus wall prior to delivery. This may be traumatic or nontraumatic in etiology. In traumatic placental abruption, for example caused by blunt force trauma to the abdomen secondary to a fall, motor vehicle collision, or homicide, there may be little or no external evidence of injury despite the internal trauma. It is important to look for patterned imprint injuries to the abdomen in these cases. Nontraumatic placental abruption may be associated with maternal hypertension, cigarette smoking, or use of stimulant drugs (such as cocaine and amphetamines). In the latter case, the placenta may appear normal on microscopy.
Pulmonary Embolism and Venous Thrombosis
Venous thrombosis has a five times increased risk in pregnancy due to the hypercoagulable state in pregnancy, vascular trauma (during normal vaginal birth and/or with medical intervention procedures), and venous stasis (particularly if there is immobility due to bed rest). Hypercoagulability persists until about two months postpartum. It is a normal pregnancy change that protects against excessive hemorrhage during delivery. There is an increase in clotting factors and fibrinogen along with decrease in components of the fibrinolytic system ( 17 , 20 ). The risks are increased if there is an underlying mutation in prothrombin or Factor V Leiden and in cesarean section compared to vaginal birth. There is also an increased risk of cerebral venous sinus thrombosis, particularly of the superior sagittal sinus.
Amniotic Fluid Embolism
Amniotic fluid embolism (AFE) presents as sudden onset shortness of breath and circulatory collapse in a previously asymptomatic woman during or shortly after delivery. Amniotic fluid embolism occurs in approximately one in 25 000 deliveries ( 22 ). The death rate is 60-85% and accounts for approximately 5-10% of all maternal deaths ( 20 , 25 ).
Amniotic fluid embolism is caused by a tear in the placental membranes and uterine body, cervix, or vagina which allows amniotic fluid to enter the maternal venous system. The tear may be difficult to demonstrate at autopsy. The amniotic fluid can cause physical obstruction of the pulmonary microvasculature and vasospasm with resultant right heart failure and hypoxia ( 17 , 22 , 25 ). There may also be activation of complement system and/or anaphylactoid reaction to the amniotic fluid ( 25 , 26 ). If there is a period of survival, there is development of dissemination intravascular coagulation (DIC) and acute renal failure develops.
Risk factors include uterine hypercontractility, instrumental procedures (e.g., cesarean section, use of forceps, vacuum extraction), high maternal age, placental abruption, uterine rupture, maternal diabetes mellitus, and fetal macrosmia. Amniotic fluid embolism requires a pathological diagnosis. There are no clinical diagnostic tests for the condition. Amniotic fluid emboli are rarely seen macroscopically and may include lanugo hairs, vernix caseosa, and/or meconium.
The maternal lung should be examined histologically for components of amniotic fluid in the pulmonary arterial system such as epithelial squames from fetal skin (which must be differentiated from sloughed maternal endothelial cells, the latter having nuclei, unlike the squames), lanugo hairs (which may be seen under polarised light [20]), vernix caseosa (fatty), mucin from the fetal intestine and bile from meconium ( Image 3 ). Sections should be taken from all lobes of both lungs. Stains have been developed to show all of these amniotic fluid components, such as the modified Attwood stain (alcian green/blue-phloxine-tartrazine). Immunohistochemical stains on may also be performed on the maternal lung looking for components of amniotic fluid. These include cytokeratin to show epithelial squames ( 17 ) and zinc coproporphyrin 1 (ZnCP-1) for meconium ( 25 ). Zinc coproporphyrin 1 and sialyl-Tn, components of meconium, may also be assayed in the maternal blood ( 25 ).

Maternal lung arteriole in amniotic fluid embolism showing epithelial squames in the lumen (H&E, x400). Courtesy of Dr T. Y. Khong, Adelaide, Australia.
Peripartum Cardiomyopathy
Peripartum cardiomyopathy is defined as:
…the development of cardiac failure between the last month of pregnancy and five months postpartum, the absence of an identifiable cause, the absence of recognisable heart disease prior to the last month of pregnancy, and left ventricular systolic dysfunction demonstrated by echocardiographic criteria ( 27 ).
Peripartum cardiomyopathy occurs in one in 2289-4000 live births in the USA ( 27 – 29 ) and it carries high mortality and morbidity rates (up to 50% mortality) ( 17 ).
The cause of peripartum cardiomyopathy is unknown, but is probably multifactorial, including myocarditis, micro-chimerism, increased apoptosis with inflammation, and maladaptive response to pregnancy-induced hemodynamic changes. There may be a genetic basis, but no specific genetic defects have been yet identified ( 27 – 29 ).
The risk of peripartum cardiomyopathy is increased in multiparity, high maternal age, multi-fetal pregnancy, preeclampsia, black women, and women with high prolactin levels ( 27 – 29 ).
Peripartum cardiomyopathy is a type of dilated cardiomyopathy, and this reflected in the morphology of the condition. Pulmonary congestion and edema may be present, and cardiomegaly with left ventricular hypertrophy in particular may also be demonstrated ( 29 ). Pathological examination of the heart shows four chamber dilatation with myocyte hypertrophy, interstitial fibrosis, and scattered inflammatory cells on microscopy ( 17 , 27 ).
Complications of Early Pregnancy
Complications of early pregnancy include ruptured ectopic pregnancy ( Image 4 ) and problems related to termination of pregnancy.

Ectopic pregnancy (H&E, x50). Image courtesy of Dr. C Milroy, Ottawa, Canada.
Approximately 2% of pregnancies occur in an ectopic site – other than in the normal intrauterine location ( 30 ). The most common site (90%) ( 30 ) is the fallopian tube, but ectopic pregnancies can also occur in the ovary and peritoneal cavity. Autopsy requires careful examination of the uterus, adnexa, and peritoneal cavity in women of childbearing age in order to identify ectopic pregnancies.
Macroscopically, the fallopian tube is enlarged and filled with blood. If rupture has occurred, there may be massive hemorrhage into the peritoneal cavity.
Microscopy shows an embryonal sac and chorionic villi with invasion of the wall of the fallopian tube by trophoblast. Collection of DNA specimens from the gestational material, or, at minimum, preservation of the ectopic tissue in a block, should be performed should potential paternity questions arise.
Deaths related to termination of pregnancy are more common in countries with restrictive policies regarding legal termination of pregnancy where infection and/or hemorrhage are the most common causes of death. Risk factors include younger women and gestation over 14 weeks ( 3 ).
In the USA, for therapeutic terminations of pregnancy the death rate is approximately 0.7/100 000 procedures. The risk increases with increasing gestational age and is three times greater for black women ( 30 ). Most deaths over 13 weeks gestation are associated with complications of anesthesia ( 17 ) or infection. Deaths under 13 weeks gestation are associated with infection and/or hemorrhage ( 31 ).
Puerperal Sepsis
Puerperal sepsis occurs in 2.7-5.2% of pregnancies, depending on the region in the world ( 19 ). It is frequently Gram-negative bacterial sepsis caused by extension of local infections into the systemic circulation (for example from endometritis, intramyometrial abscess, uterine gas gangrene, or pyomyoma) that causes shock and DIC ( 20 ). Sepsis may be difficult to diagnose early on routine blood tests as neutrophilia is a normal pregnancy change.
Venous Air Embolism
Venous air embolism may occur in normal labor, during operative procedures such as termination of pregnancy or cesarean section, secondary to douching, or due to sexual activity.
Venous air embolism requires introduction of a large volume of air into the systemic venous system (at least 150 mL) via distended uterine or cervical veins. This leads to frothing of the blood in right side of the heart which then blocks the pulmonary arteries ( 17 ).
Diagnosis of air embolism at autopsy is enhanced by radiological imaging to detect the presence of air in the vasculature and heart and to exclude pneumothorax. Diagnostic changes may be evident on chest radiograph, but can be more readily seen with computed tomography (CT). Imaging needs to be performed as soon as possible after death to avoid decomposition gas artifact, such as gas seen in liver.
At autopsy, the body is opened without incising the neck blood vessels. The inferior vena cava is checked for froth or bubbles. The pericardium is opened and filled with water before opening the right atrium underwater to check for escaping bubbles which indicate the presence of air in the heart ( 17 , 22 ).
Acute Fatty Liver of Pregnancy
Acute fatty liver of pregnancy (AFLP) occurs in approximately one in 7-15 000 pregnancies ( 17 , 21 , 23 , 32 , 33 ). It has a 10-20% fatality rate, the higher rates being seen in developing countries ( 20 , 21 , 23 , 32 ).
The clinical presentation is frequently of abdominal pain, vomiting, and jaundice. There may be associated renal failure. Diagnosis is complicated by a significant overlap in clinical and biochemical features with the HELLP syndrome ( 33 ). Acute fatty liver of pregnancy typically occurs in the third trimester of pregnancy ( 17 , 23 , 32 ), but may develop postpartum ( 33 ). Risk factors include primparity, multi-fetus gestation, and male fetus ( 23 , 33 ).
The cause of AFLP is unknown but is thought to be due to mitochondrial fatty acid beta-oxidation dysfunction in the fetus – particularly deficiency of the enzyme long-chain 3-hydroxyacyl-CoA dehydrogenase (LCHAD) ( 17 , 21 , 23 , 32 – 34 ). A fetus that is homozygous for this autosomal recessive disorder causes placental production of fatty acids and their metabolites, which then accumulate in the liver of the heterozygous mother, having a toxic effect on her liver function ( 33 ).
Complications include hepatic failure, severe coagulopathy, coma, and death. At autopsy, the liver is macroscopically soft and yellow. Histology of the liver shows severe centrilobular microvesicular steatosis with inflammation and hepatocyte necrosis. In more severe cases, the whole hepatic lobule may be affected ( 17 ). Special stains for lipid, such as oil-red-O, may confirm the presence of fat.
Acute Myocardial Infarction
Acute myocardial infarction occurs in approximately one in 10 000 pregnancies. The main risk factor is high maternal age (over 33 years).
Pathological examination of the heart shows 43% with coronary atherosclerosis with or without thrombosis, 21% with coronary thrombosis alone, 16% with coronary artery dissection, and 29% of cases with apparently normal coronary arteries ( 25 ).
Pregnancy-Associated Spontaneous Coronary Artery Dissection
Pregnancy-associated spontaneous coronary artery dissection usually occurs in the third trimester or postpartum in a previously healthy woman ( Image 5 ) ( 35 ). It is an important cause of acute coronary syndrome that predominantly affects young patients with no atherosclerotic coronary artery disease ( 36 ).

Coronary artery dissection (H&E, x25).
It carries a higher-risk presentation than non-pregnancy-associated spontaneous coronary artery dissection, with patients being more likely to present with ST segment elevation and left main or multi-vessel coronary artery dissection ( 36 ). The overall incidence of the disease is likely to be underestimated, as most diagnoses are made at autopsy ( 35 ).
Although the pathophysiology of pregnancy-associated spontaneous coronary artery dissection is poorly understood, there are some typical postmortem findings in addition to coronary artery dissection in the absence of atherosclerotic disease ( 35 , 37 ). Periadventitial eosinophilic infiltrate is present in many cases, although it is unclear whether this may be reactive or causative of medial wall weakness ( 37 ). Antemortem blood tests may also demonstrate an elevated eosinophil to lymphocyte ratio ( 37 ).
Pituitary Gland Infarction
Pituitary gland infarction in the postpartum patient, can be due to Sheehan syndrome, whereby the pituitary undergoes ischemic necrosis as a result of hypoperfusion from hypotension and blood loss during or after childbirth. Signs of acute necrosis may be noted macroscopically with a grey-red appearance to the cut surface and it may be soft to the touch. Later, microscopic evaluation can demonstrate extensive necrosis with ghost cells, necrotic debris, and inflammatory infiltrate ( 38 ).
Anesthetic Complications
Anesthetic complications in the pregnant patient encompass those which may occur as a result of any anesthesia, such as anaphylaxis, aspiration of gastric contents, or intubation complications, including malplacement of the endotracheal tube and damage to the trachea or larynx.
Additionally, there are conditions that are more specific to the pregnant patient, for example iatrogenic pulmonary edema from drugs used to suppress premature labor (especially ritodrine plus betamethasone) ( 39 ), bronchospasm in an asthmatic woman secondary to administration of ergometrine ( 40 ), and water intoxication following infusion of electrolyte-free, glucose only solutions plus syntocinon ( 41 ). The latter is particularly a problem if there is preexisting cardiac disease.
Multifactorial Conditions and Generalized Complications of Direct Maternal Deaths
Hemoperitoneum.
Causes of hemoperitoneum include uterine rupture, ruptured subcapsular hematoma of liver (in HELLP syndrome), and ruptured aneurysms, particularly of the splenic artery.
Uterine rupture accounts for approximately 5% of maternal deaths per annum in the USA and has a death rate of about 15% ( 17 ). Uterine rupture may be due to trauma, for example during obstetric interventional procedures or secondary to an assault, motor vehicle collision, or fall. In these cases, the site of rupture is often at the fundus of the uterus.
In nontrauma-associated uterine rupture, the rupture is frequently at a site of scarring, for example the lower segment of the uterus through a previous cesarean section scar. The risk of nontrauma-associated uterine rupture is increased in multiparity, with increased maternal age, and following the use of uterotonic drugs such as oxytocin. A study by Miller et al. showed that 142 of 153 cases of nontrauma-associated uterine rupture were related to previous cesarean section ( 42 ).
Disseminated Intravascular Coagulation
Disseminated intravascular coagulation occurs most often in the following complications of obstetrics: placental abruption, saline-induced therapeutic abortion, retained dead fetus or products of conception, amniotic fluid embolism, Gram-negative sepsis, and preeclampsia. Placental tissue with tissue factor activity enters or is exposed to the maternal circulation. Clinically, the subsequent rapidly evolving DIC results in severe thrombocytopenia, prolonged prothrombin time and partial thromboplastin time, rapidly declining plasma fibrinogen concentration, and high plasma d-dimer concentration. Disseminated intravascular coagulation causes hemorrhage and shock and can result in death.
Macroscopically at autopsy, purpura are seen and there is evidence of generalized bleeding ( 43 , 44 ).
Microscopy shows the presence of microthrombi in organs, but particularly in the lungs and kidneys ( 45 , 46 ). The microthrombi may be confirmed by a fibrin stain, such as Martius scarlet blue.
Thrombotic Microangiopathy of Pregnancy
Thrombotic microangiopathy is the primary or secondary development of microthrombi in blood vessels.
Included under the direct causes of thrombotic microangiopathy of pregnancy are thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS) ( 47 ).
Secondary causes include preeclampsia/eclampsia/ HELLP syndrome, acute fatty liver of pregnancy, systemic lupus erythematosus, and antiphospholipid antibody syndromes.
For definite diagnosis of the etiology, a detailed clinical history is required with antemortem laboratory testing ( 17 , 47 ).
In the case of TTP, the most common clinical symptoms are neurological, with headache, paresis, speech abnormalities and confusion. Antemortem laboratory testing reveals thrombocytopenia, anemia, and raised lactate dehydrogenase, and creatinine, whilst antemortem urine analysis demonstrates proteinuria and hematuria ( 47 ). On postmortem evaluation, TTP microthrombi are widespread and typically affect multiple organs such as the heart, kidneys, skin, and adrenal glands. ( 47 ).
In HUS, the classical clinical presentation and laboratory findings involve the triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure, with initial symptoms of vomiting and diarrhea and rapidly progressing oliguric renal failure ( 47 ). The kidney is the primary affected organ, although thrombosis of small vessels is also commonly found in the colon.
Diffuse Alveolar Damage
Diffuse alveolar damage may occur secondary to a number of conditions complicating pregnancy, such as prolonged artificial ventilation, DIC, sepsis, and amniotic fluid embolism.
Indirect Maternal Deaths
Preexisting maternal diseases that may be aggravated by the pregnant state are listed in Table 2 .
Maternal Diseases Associated with Indirect Maternal Death.
Cardiovascular Disease and Pregnancy
Pregnancy may cause aggravation of preexisting cardiac or vascular disease, particularly congenital heart disease, inherited cardiomyopathy, ischemic heart disease, valvular heart disease, channelopathies (such as Long QT syndrome), hypertension, and connective tissue diseases with risk of aortic dissection ( 17 ).
Aortic dissection typically occurs in the third trimester of pregnancy or postpartum in a woman with an underlying genetic predisposition or known connective tissue disorder such as Ehlers-Danlos syndrome or Marfan syndrome. It is thought that aortic dissection is triggered by a combination of pregnancy-induced hormonally-mediated biochemical changes and the effects of pregnancy-induced hemodynamic stresses on an at risk aortic wall ( 17 ).
Incidental Maternal Deaths
Incidental maternal deaths are those which occur from unrelated causes that happen to occur during pregnancy or in the puerperium.
These may be due to accidental causes (frequently as a result of a traffic collision, fall, or drug overdose) ( Image 6 ), preexisting advanced neoplastic disorder, or homicide. In the latter case, it should be noted that in some jurisdictions it is a criminal act to injure a fetus by injuring the mother and can result in more serious charges.

Uterine rupture after motor vehicle collision with expulsion of fetus into the maternal abdominal cavity. Courtesy of Dr. K Collins, South Carolina, USA.
The Maternal Autopsy
The maternal autopsy should be a full three cavity autopsy with appropriate ancillary testing including full histopathology and toxicological analysis and other ancillary tests appropriate to the pathological abnormalities found.
The autopsy should be performed as per usual practice for an adult autopsy with special consideration of specific potential lethal complications associated with pregnancy.
As pregnancy may not be suspected prior to autopsy, especially if the woman is in the early stages of pregnancy, the uterus, adnexa, and peritoneal cavity should be examined carefully in all autopsies on women of child-bearing age. For example, this may reveal an ectopic pregnancy which has caused death.
If there has been medical intervention, it is important to look for general complications of any anesthetic or surgical procedure, including esophageal intubation, trauma to the upper airways and/or esophagus, evidence of anaphylaxis to drugs administered, wound dehiscence and/or infection, and trauma to adjacent organs or tissues.
A full clinical history is needed before the autopsy begins. This includes a full obstetric history and antenatal records of the current pregnancy. Cardiotocographic and obstetric ultrasound data should be obtained for expert review if subsequently required. All records relating to any anesthetic or surgical procedures performed should also be obtained, including the drugs given and the dosage.
Prior to autopsy, consideration should be given to radiological examination (plain radiograph or CT) to look for evidence of air embolism.
External Examination
A routine adult external examination should be performed, including evidence of trauma and medical procedures.
Evidence of jaundice (skin and scleral icterus) and hemorrhagic diatheses should be specifically sought, since they may be present in pregnancy-related deaths.
Typical pregnancy skin changes which may be seen include striae gravidarum on the abdomen, thighs, and breasts; hyperpigmentation of the nipples; and linea nigra on the abdomen.
Internal Examination
Routine adult internal examination should be performed, including evidence of trauma and medical procedures.
The fetus and placenta should be examined if they are still in utero .
If delivery has already occurred, the placenta should be obtained and examined. Specialist gynecological pathology referral may be requested.
If there is a suspected or possible diagnosis of air embolism the body should be opened without incising the neck blood vessels. The inferior vena cava should be checked for froth or bubbles in the blood. The pericardium is opened and filled with water. The right atrium is then incised under water and checked for escaping bubbles ( 17 , 22 ).
Specific abnormalities which should be sought to exclude pregnancy-related complications are listed in Table 3 .
Pathological Conditions Which Should be Specifically Investigated on Internal Examination in a Maternal Autopsy.
Histopathology
If amniotic fluid embolism is suspected or a possibility, sections should be taken from all lobes of both lungs with special stains performed to detect the components of amniotic fluid (such as a modified Attwood stain and/or immunohistochemistry for cytokeratin and zinc coproporphyrin 1).
The placental bed vasculature of the uterus should always be examined histologically. Normal physiological changes to the spiral arteries in the placental bed of uterus seen on microscopy include replacement of the endothelium by endovascular trophoblast (which spreads to the myometrial segments during the second trimester), fibrinoid change in the arterial walls, and hypertrophy of the radial and arcuate vessels. The basal arteries, however, remain normal.
Examination of the placenta should include sections from the central and marginal areas of the placenta, any macroscopically abnormal areas, the umbilical cord, and the membranes. Chorioamnionitis and funisitis should be specifically excluded.
If there has been development of DIC, microthrombi may be seen in the tissues. These may be highlighted by special stains such as Martius scarlet blue.
Ancillary Tests
If puerperal sepsis is suspected, aerobic and anaerobic blood cultures and swabs should be taken.
DNA specimens may be taken from the fetus and mother (e.g., a blood spot card), particularly in homicides, cases where there may be issues regarding paternity, and for investigation of potentially inherited disorders (such as connective tissue disorders in aortic dissection or coagulation disorders in pulmonary thromboembolism).
Maternal deaths can pose a particular challenge to the forensic pathologist and carry significant short- and long-term implications for family members and wider medical and legal practice. The role of the forensic pathologist has an important contribution to wider surveillance and research processes that can contribute to changes in clinical practice, policy, and subsequent changes in maternal mortality rates.
In the USA in particular, recent trends in maternal mortality have demonstrated increases in maternal mortality, which contrast with the overall decrease in maternal mortality in the developed world. With the USA carrying one of the highest maternal mortality ratios in the developed world, the role of the forensic pathologist in maternal deaths is important, despite the overall rarity of such cases.
The purpose of this paper has been to review the clinical and pathological features of common pregnancy-related disorders and to give guidelines for performing an autopsy related to maternal death. Whilst there are extensive documented causes of maternal mortality, the pathophysiology of many maternal conditions remains poorly understood or under-researched and careful postmortem evaluation is necessary.
Jack Garland BMed, Hornsby and Ku-ring-gai Hospital
Roles : Project conception and/or design, manuscript creation and/or revision, approved final version for publication, accountable for all aspects of the work, writing assistance and/or technical editing.
Dianne Little MBBS FRCPA, Department of Forensic Medicine, Sydney
Ethical Approval: As per Journal Policies, ethical approval was not required for this manuscript
Statement of Human and Animal Rights: This article does not contain any studies conducted with animals or on living human subjects
Statement of Informed Consent: No identifiable personal data were presented in this manuscript
Disclosures & Declaration of Conflicts of Interest: The authors, reviewers, editors, and publication staff do not report any relevant conflicts of interest
Financial Disclosure: The authors have indicated that they do not have financial relationships to disclose that are relevant to this manuscript
- women's health
Women are more likely to survive health issues with female doctors, new study finds

CHICAGO -- A new study suggests women are more likely to survive health issues when their doctors are also women.
The study, which was published in Annals of Internal Medicine , looked at Medicare patients over three years, and noted findings may be different for younger populations. The patients in the study had been hospitalized with medical conditions between 2016 and 2019 and were treated in the hospital.
Researchers also found that women are less likely to be re-admitted to the hospital under a female doctor's care.
The difference is just a quarter percent, but researchers said that even such a small difference is statistically significant and noteworthy.
Related Topics
- HEALTH & FITNESS
- WOMEN'S HEALTH
Women's Health

3 GOP House members join Dems in vote to repeal 1864 abortion ban

What are Texas-sized implications following the Idaho abortion case?

AZ GOP block another Democratic effort to repeal 1864 abortion ban

Join hundreds of walkers at UH to support Black breast cancer patients
Top stories.

Man accused in road rage shooting says he didn't intend to kill anyone

Woman steals ambulance after asking paramedics for a ride, police say
- 42 minutes ago

Woman ran red light before major rollover crash in Midtown, police say
- 3 hours ago

13 Investigates: Is mail being stolen inside a Houston USPS facility?

River Oaks street sees back-to-back SWAT scenes in 2 weeks
Small rain chance Friday, higher storm chances Sunday
- 2 hours ago
Woman surrenders to police after 2 hour standoff in west Houston
Houston police officer subject of 4th deadly investigation since 2022
- Open access
- Published: 22 April 2024
The influence of maternal prepregnancy weight and gestational weight gain on the umbilical cord blood metabolome: a case–control study
- Xianxian Yuan ORCID: orcid.org/0000-0001-8762-8471 1 ,
- Yuru Ma 1 ,
- Jia Wang 2 ,
- Yan Zhao 1 ,
- Wei Zheng 1 ,
- Ruihua Yang 1 ,
- Lirui Zhang 1 ,
- Xin Yan 1 &
- Guanghui Li ORCID: orcid.org/0000-0003-2290-1515 1
BMC Pregnancy and Childbirth volume 24 , Article number: 297 ( 2024 ) Cite this article
63 Accesses
Metrics details
Maternal overweight/obesity and excessive gestational weight gain (GWG) are frequently reported to be risk factors for obesity and other metabolic disorders in offspring. Cord blood metabolites provide information on fetal nutritional and metabolic health and could provide an early window of detection of potential health issues among newborns. The aim of the study was to explore the impact of maternal prepregnancy overweight/obesity and excessive GWG on cord blood metabolic profiles.
A case control study including 33 pairs of mothers with prepregnancy overweight/obesity and their neonates, 30 pairs of mothers with excessive GWG and their neonates, and 32 control mother-neonate pairs. Untargeted metabolomic profiling of umbilical cord blood samples were performed using UHPLC‒MS/MS.
Forty-six metabolites exhibited a significant increase and 60 metabolites exhibited a significant reduction in umbilical cord blood from overweight and obese mothers compared with mothers with normal body weight. Steroid hormone biosynthesis and neuroactive ligand‒receptor interactions were the two top-ranking pathways enriched with these metabolites ( P = 0.01 and 0.03, respectively). Compared with mothers with normal GWG, in mothers with excessive GWG, the levels of 63 metabolites were increased and those of 46 metabolites were decreased in umbilical cord blood. Biosynthesis of unsaturated fatty acids was the most altered pathway enriched with these metabolites ( P < 0.01).
Conclusions
Prepregnancy overweight and obesity affected the fetal steroid hormone biosynthesis pathway, while excessive GWG affected fetal fatty acid metabolism. This emphasizes the importance of preconception weight loss and maintaining an appropriate GWG, which are beneficial for the long-term metabolic health of offspring.
Peer Review reports
The obesity epidemic is an important public health problem in developed and developing countries [ 1 ] and is associated with the emergence of chronic noncommunicable diseases, including type 2 diabetes mellitus (T2DM), hypertension, cardiovascular disease, nonalcoholic fatty liver disease (NAFLD), and cancer [ 2 , 3 , 4 ]. Maternal obesity is the most common metabolic disturbance in pregnancy, and the prevalence of obesity among women of childbearing age is 7.1% ~ 31.9% in some countries [ 5 ]. In China, the prevalence of overweight and obesity has also increased rapidly in the past four decades. Based on Chinese criteria, the latest national prevalence estimates for 2015–2019 were 34.3% for overweight and 16.4% for obesity in adults (≥ 18 years of age) [ 6 ].
Increasing evidence implicates overnutrition in utero as a major determinant of the health of offspring during childhood and adulthood, which is compatible with the developmental origins of health and disease (DOHaD) framework [ 7 ]. Maternal obesity and excessive gestational weight gain (GWG) are important risk factors for several adverse maternal outcomes, including gestational diabetes and hypertensive disorders, fetal death, and preterm birth [ 8 , 9 , 10 ]. More importantly, they have negative implications for offspring, both perinatally and later in life. Evidence from cohort studies focusing on offspring development confirms the relationship between maternal obesity/excessive GWG and offspring obesity programming [ 11 , 12 , 13 ]. Currently, there is no unified mechanism to explain the adverse outcomes associated with maternal obesity and excessive GWG, which may be the independent and interactive effects of the obese maternal phenotype itself and the diet associated with this phenotype. In addition to genetic and environmental factors, metabolic programming may also lead to the intergenerational transmission of obesity through epigenetic mechanisms.
Metabolomics, which reflects the metabolic phenotype of human subjects and animals, is the profiling of metabolites in biofluids, cells and tissues using high-throughput platforms, such as mass spectrometry. It has unique potential in identifying biomarkers for predicting occurrence, severity, and progression of diseases, as well as exploring underlying mechanistic abnormalities [ 14 , 15 ]. Umbilical cord metabolites can provide information about fetal nutritional and metabolic health, and may provide an early window for detection of potential health issues in newborns [ 16 ]. Previous studies have reported differences in umbilical cord metabolite profiles associated with maternal obesity [ 17 , 18 ]. However, the results were inconsistent due to differences in sample sizes, ethnicity and region, and mass spectrometry. In addition, most studies have not considered the difference in the effects of prepregnancy body mass index (BMI) and GWG on cord blood metabolites.
To investigate the relationship between early metabolic programming and the increased incidence of metabolic diseases in offspring, we studied the associations between elevated prepregnancy BMI/excessive GWG and umbilical cord metabolic profiles. Another purpose of this study was to explore whether there were differences in the effects of prepregnancy overweight/obesity and excessive GWG on cord blood metabolites.
Study population
This was a hospital-based, case control study that included singleton pregnant women who received prenatal care and delivered vaginally at Beijing Obstetrics and Gynecology Hospital, Capital Medical University, from January 2022 to March 2022. We selected 33 pregnant women with a prepregnancy BMI ≥ 24.0 kg/m 2 regardless of their gestational weight gain as the overweight/obese group, 30 pregnant women with a prepregnancy BMI of 18.5–23.9 kg/m 2 and a GWG > 14.0 kg as the excessive GWG group, and 32 pregnant women with a BMI of 18.5–23.9 kg/m 2 and a GWG of 8.0–14.0 kg as the control group. The ages of the three groups were matched (± 1.0 years), and the prepregnancy BMIs of the excessive GWG and control groups were matched (± 1.0 kg/m 2 ).
The inclusion criteria were women with singleton pregnancies, those aged between 20 and 45 years, those with full-term delivery (gestational age ≥ 37 weeks), those with a prepregnancy BMI ≥ 18.5 kg/m 2 , those without prepregnancy diabetes mellitus (DM) or hypertension, and those without gestational diabetes mellitus (GDM). The exclusion criteria were women with multiple pregnancies, those less than 20 years or more than 45 years old, those with a prepregnancy BMI < 18.5 kg/m 2 , those with prepregnancy DM, hypertension or GDM, and those without cord blood samples.
We classified pregnant women into BMI categories based on Chinese guidelines [ 19 ]: normal weight (prepregnancy BMI 18.5–23.9 kg/m 2 ), overweight (prepregnancy BMI 24.0–27.9 kg/m 2 ), and obese (prepregnancy BMI ≥ 28.0 kg/m 2 ). GWG guideline concordance was defined by the 2021 Chinese Nutrition Society recommendations according to prepregnancy BMI. The upper limits of GWG for normal weight, overweight, and obesity were 14.0 kg, 11.0 kg, and 9.0 kg, respectively.
Ethical approval and written informed consent were obtained from all participants. The study has been performed according to the Declaration of Helsinki, and the procedures have been approved by the ethics committees of Beijing Obstetrics and Gynecology Hospital, Capital Medical University (2021-KY-037).
Sample and data collection
Maternal and neonatal clinical data were collected from the electronic medical records system of Beijing Obstetrics and Gynecology Hospital. Maternal clinical characteristics included age, height, prepregnancy and predelivery weight, education level, smoking and drinking status during pregnancy, parity, conception method, comorbidities and complications of pregnancy, family history of DM and hypertension, gestational age, mode of delivery, and biochemical results during pregnancy. Prepregnancy BMI was calculated as prepregnancy weight in kilograms divided by the square of height in meters. GWG was determined by subtracting the prepregnancy weight in kilograms from the predelivery weight in kilograms. GDM was defined using the IAPDSG’s diagnostic criteria at 24 to 28 +6 weeks gestation and the fasting glucose and 1- and 2-h glucose concentrations at the time of the oral glucose tolerance test (OGTT). Neonatal clinical characteristics included sex, birth weight and length. Macrosomia was defined as a birth weight of 4,000 g or more [ 20 ]. Low birth weight (LBW) was defined as a birth weight less than 2,500 g [ 21 ].
Umbilical cord blood samples were obtained by trained midwives after clamping the cord at delivery. Whole blood samples were collected in EDTA tubes, refrigerated for < 24 h, and centrifuged at 2,000 r.p.m. at 4 ℃ for 10 min. Plasma aliquots were stored at -80 ℃ until shipment on dry ice to Novogene, Inc. (Beijing, China) for untargeted metabolomic analysis.
Untargeted metabolomic analyses
Ultrahigh-performance liquid chromatography tandem mass spectrometry (UHPLC‒MS/MS) analyses were performed using a Vanquish UHPLC system (Thermo Fisher, Germany) coupled with an Orbitrap Q Exactive™ HF mass spectrometer (Thermo Fisher, Germany) at Novogene Co., Ltd. (Beijing, China). Detailed descriptions of the sample preparation, mass spectrometry and automated metabolite identification procedures are described in the Supplementary materials .
Statistical analysis
Clinical data statistical analysis.
Quantitative data are shown as the mean ± standard deviation (SD) or median (interquartile range), and categorical data are presented as percentages. The Mann‒Whitney U test, chi-square test, and general linear repeated-measures model were used to assess the differences between the control and study groups when appropriate. A P value < 0.05 was considered statistically significant. All analyses were performed using Statistical Package of Social Sciences version 25.0 (SPSS 25.0) for Windows (SPSS Inc).
Umbilical cord metabolome statistical analysis
These metabolites were annotated using the Human Metabolome Database (HMDB) ( https://hmdb.ca/metabolites ), LIPIDMaps database ( http://www.lipidmaps.org/ ), and Kyoto Encylopaedia of Genes and Genomes (KEGG) database ( https://www.genome.jp/kegg/pathway.html ). Principal component analysis (PCA) and partial least-squares discriminant analysis (PLS-DA) were performed at metaX. We applied univariate analysis ( T test) to calculate the statistical significance ( P value). Metabolites with a variable importance for the projection (VIP) > 1, a P value < 0.05 and a fold change (FC) ≥ 2 or FC ≤ 0.5 were considered to be differential metabolites. A false discovery rate (FDR) control was implemented to correct for multiple comparisons. The q -value in the FDR control was defined as the FDR analog of the P -value. In this study, the q -value was set at 0.2. For clustering heatmaps, the data were normalized using z scores of the intensity areas of differential metabolites and were plotted by the Pheatmap package in R language.
The correlations among differential metabolites were analyzed by cor () in R language (method = Pearson). Statistically significant correlations among differential metabolites were calculated by cor.mtest () in R language. A P value < 0.05 was considered statistically significant, and correlation plots were plotted by the corrplot package in R language. The functions of these metabolites and metabolic pathways were studied using the KEGG database. The metabolic pathway enrichment analysis of differential metabolites was performed when the ratio was satisfied by x/n > y/N, and the metabolic pathway was considered significantly enriched when P < 0.05.
Demographic characteristics of study participants
The demographic and clinical characteristics of the three population groups enrolled in the study are summarized in Table 1 . Mothers had no significant difference regarding their ages or gestational ages. Compared to the mothers in the excessive GWG and control groups, those in the prepregnancy overweight/obesity group had a significantly higher prepregnancy BMI (25.6 (24.5, 27.2) kg/m 2 ). However, there was no significant difference in prepregnancy BMI between mothers in the excessive GWG group (20.3 ± 1.2 kg/m 2 ) and mothers in the control group (20.6 ± 1.5 kg/m 2 ). Mothers in the excessive GWG group had the highest GWG (17.0 (15.5, 19.1) kg) among the three groups. The mean GWG of the mothers in the prepregnancy overweight/obesity group was 12.9 ± 3.8 kg, which was similar to that of the control group (11.8 ± 1.5 kg). It was noteworthy that among the 33 prepregnancy overweight/obese pregnant women, 20 of them had appropriate GWG, 1 had insufficient GWG, and 12 had excessive GWG. The proportion of mothers who underwent invitro fertilization and embryo transfer (IVF-ET) in the prepregnancy overweight/obesity group (15.2%) was significantly higher than that in the excessive GWG and control groups. There were no statistically significant differences in the proportions of pregnancy outcomes among the three groups, including preeclampsia, premature rupture of membranes, postpartum hemorrhage, macrosomia, and LBW. The babies in the three groups showed no significant difference regarding their birth weights or lengths.
The biochemical parameters of the mothers during pregnancy are shown in Table 2 . The levels of triglyceride (TG) and uric acid (UA) of mothers in the prepregnancy overweight/obesity group were significantly higher than those of the mothers in the excessive GWG and control groups in the first trimester. However, there was no significant difference in the blood glucose and lipid levels in the second and third trimesters of pregnancy among the three groups.
PCA and PLS-DA analysis of cord blood metabolites
Functional and taxonomic annotations of the identified metabolites included the HMDB classification annotations, LIPID MAPS classification annotations, and KEGG pathway annotations. Those cord blood metabolites included lipids and lipid-like molecules, organic acids and their derivatives, and organoheterocyclic compounds, which were mainly involved in metabolism. To better understand the structure of the cord blood metabolome in cases versus controls, we used unsupervised PCA to identify metabolites contributing the most to observed differences in the dataset. PCA did not clearly separate the three groups. We next used PLS-DA to identify metabolites that were predictive of case versus control status. PLS-DA clearly distinguished the cases from the controls (Fig. 1 ), the prepregnancy overweight/obesity group vs. the control group (R2Y = 0.82, Q2Y = 0.37; R2Y = 0.77, Q2Y = 0.13, respectively) (Fig. 1 A), and the excessive GWG group vs. the control group (R2Y = 0.76, Q2Y = 0.16; R2Y = 0.81, Q2Y = 0.41) (Fig. 1 B).
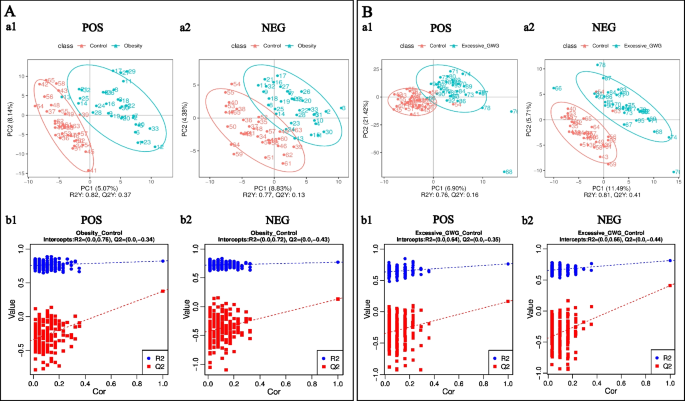
PLS-DA of identified cord blood metabolites. A the prepregnancy overweight/obesity group vs. the control group; B the excessive GWG group vs. the control group. (a) PLS-DA score. The horizontal coordinates are the score of the sample on the first principal component; the longitudinal coordinates are the score of the sample on the second principal component; R2Y represents the interpretation rate of the model, and Q2Y is used to evaluate the predictive ability of the PLS-DA model, and when R2Y is greater than Q2Y, it means that the model is well established. (b) PLS-DA valid. Horizontal coordinates represent the correlation between randomly grouped Y and the original group Y, and vertical coordinates represent the scores of R2 and Q2. (1) POS, positive metabolites; (2) NEG, negative metabolites
Maternal prepregnancy overweight/obesity
Screening differential metabolites according to a PLS-DA VIP > 1.0, a FC > 1.2 or < 0.833 and a P value < 0.05, a total of 106 cord blood metabolites (77 positive metabolites and 29 negative metabolites) differed between the prepregnancy overweight/obesity group and the control group. Compared with those in the control group, the levels of 46 metabolites (19 positive metabolites and 27 negative metabolites) were increased in the prepregnancy overweight/obesity group, among which octopamine was the metabolite with the largest increase, followed by (2S)-4-Oxo-2-phenyl-3,4-dihydro-2H-chromen-7-yl beta-D-glucopyranoside, N-tetradecanamide, stearamide, and methanandamide (Fig. 2 A). Compared with the control group, in the prepregnancy overweight/obesity group, there were 60 metabolites (58 positive metabolites and 2 negative metabolites) with reduced concentrations, among which senecionine was the metabolite with the largest decrease, followed by 3-(methylsulfonyl)-2H-chromen-2-one, methyl EudesMate, cuminaldehyde, and 2-(tert-butyl)-1,3-thiazolane-4-carboxylic acid (Fig. 2 A).
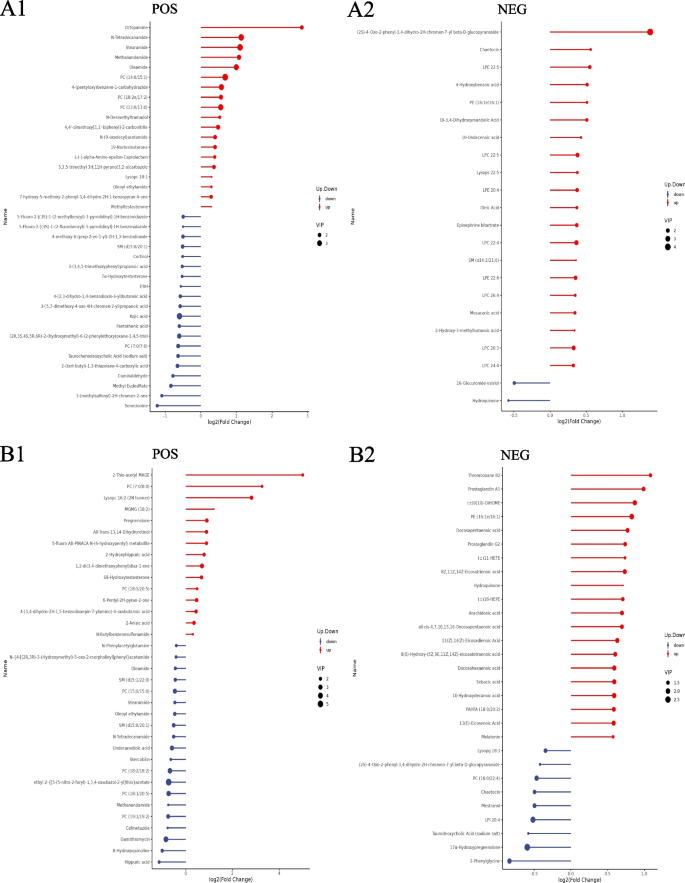
Stem plots of differential cord blood metabolites. A the prepregnancy overweight/obesity group vs. the control group; B the excessive GWG group vs. the control group. (1) positive metabolites; (2) negative metabolites. Notes: The color of the dot in the stem plots represents the upward and lower adjustment, the blue represents downward, and the red represents upward. The length of the rod represents the size of log2 (FC), and the size of the dot represents the size of the VIP value
A hierarchical analysis of the two groups of differential metabolites obtained was carried out, and the difference in metabolic expression patterns between the two groups and within the same comparison was obtained, which is shown in Fig. 3 . KEGG pathway analysis of differential cord blood metabolites associated with the prepregnancy overweight/obesity group versus the control group is shown in Table 3 and Fig. 4 A. The metabolite enrichment analysis revealed that steroid hormone biosynthesis ( P value = 0.01) and neuroactive ligand‒receptor interactions ( P value = 0.03) were the two pathways that were most altered between the prepregnancy overweight/obesity group and the control group. 19 metabolites were distributed in the pathway of steroid hormone biosynthesis, and 4 metabolites were distributed in the pathway of neuroactive ligand‒receptor interactions. In the steroid hormone biosynthesis pathway, the levels of corticosterone, 11-deoxycortisol, cortisol, testosterone, and 7α-hydroxytestosterone were decreased in the prepregnancy overweight/obesity group relative to those in the control group. In the neuroactive ligand‒receptor interaction pathway, the level of cortisol was decreased and the levels of trace amines were increased in the prepregnancy overweight/obesity group relative to the control group.
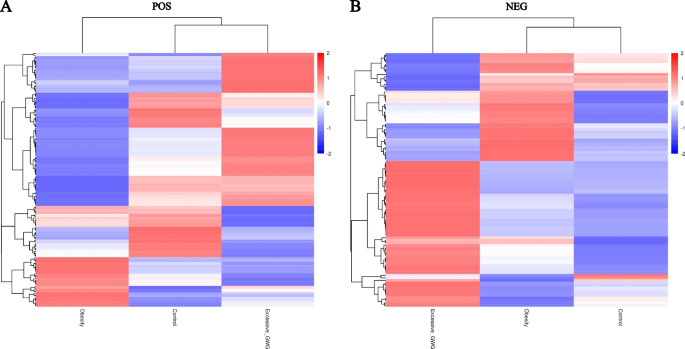
Clustering heat maps of differential cord blood metabolites of the three groups. A positive metabolites; B negative metabolites. Notes: Longitudinal clustering of samples and trans-verse clustering of metabolites. The shorter the clustering branches, the higher the similarity. Through horizontal comparison, we can see the relationship between groups of metabolite content clustering
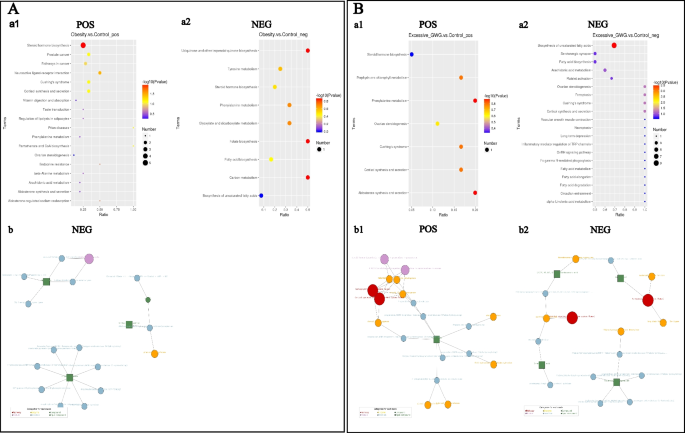
KEGG enrichment scatterplots (a) and net (b) of differential cord blood metabolites. A the prepregnancy overweight/obesity group vs. the control group; B the excessive GWG group vs. the control group. (1) positive metabolites; (2) negative metabolites. Notes: (a) The horizontal co-ordinates in the figure are x/y (the number of differential metabolites in the corresponding metabolic pathway/the total number of total metabolites identified in this pathway). The value represents the enrichment degree of differential metabolites in the pathway. The color of the point rep-resents the P -value of the hypergeometric test, and the size of the point represents the number of differential metabolites in the corresponding pathway. (b) The red dot represents a metabolic pathway, the yellow dot represents a substance-related regulatory enzyme information, the green dot represents the background substance of a metabolic pathway, the purple dot represents the molecular module information of a class of substances, the blue dot represents a substance chemical reaction, and the green square represents the differential substance obtained by this comparison
Maternal excessive GWG
A total of 109 cord blood metabolites (52 positive metabolites and 57 negative metabolites) differed between the excessive GWG group and the control group. Compared with the control group, in the excessive GWG group, there were 63 metabolites (15 positive metabolites and 48 negative metabolites) with increased concentrations, among which 2-thio-acetyl MAGE was the metabolite with the largest increase, followed by PC (7:0/8:0), lysopc 16:2 (2 N isomer), MGMG (18:2), and thromboxane B2 (Fig. 2 B). Compared with the levels in the control group, the levels of 46 metabolites (37 positive metabolites and 9 negative metabolites) in the excessive GWG group were reduced, among which hippuric acid had the largest decrease, followed by 8-hydroxyquinoline, gamithromycin, 2-phenylglycine, and cefmetazole (Fig. 2 B).
A hierarchical analysis of differential metabolites obtained in the two groups was carried out, and the difference in metabolic expression patterns between the two groups and within the same comparison was obtained, which is shown in Fig. 3 . KEGG pathway analysis of the cord blood metabolites associated with the excessive GWG group versus the control group is shown in Table 4 and Fig. 4 B. The metabolite enrichment analysis revealed that biosynthesis of unsaturated fatty acids was the most altered pathway between the excessive GWG and control groups ( P value < 0.01). There were 13 metabolites distributed in the enriched pathway. The levels of docosapentaenoic acid (DPA), docosahexaenoic acid (DHA), arachidonic acid, adrenic acid, palmitic acid, stearic acid, behenic acid, lignoceric acid, and erucic acid were increased in the excessive GWG group relative to those in the control group.
Our present study found that both maternal prepregnancy overweight/obesity and excessive GWG could affect umbilical cord blood metabolites, and they had different effects on these metabolites. Regardless of their gestational weight gain, the umbilical cord blood of prepregnancy overweight and obese mothers had 46 metabolites increased and 60 metabolites decreased compared with the umbilical cord blood of mothers with normal body weight and appropriate GWG. Steroid hormone biosynthesis and neuroactive ligand‒receptor interactions were the two top-ranking pathways enriched with these metabolites. Compared with mothers with normal prepregnancy BMI and appropriate GWG, in mothers with normal prepregnancy BMI but excessive GWG, the levels of 63 metabolites were increased and those of 46 metabolites were decreased in umbilical cord blood. Biosynthesis of unsaturated fatty acids was the most altered pathway enriched with these metabolites.
There were many differential metabolites in the cord blood between the prepregnancy overweight/obesity group and the control group and between the excessive GWG group and the control group. However, the roles of most of these differential metabolites are unknown. The levels of stearamide and methanandamide were increased in the prepregnancy overweight/obesity group. Stearamide, also known as octadecanamide or kemamide S, belongs to the class of organic compounds known as carboximidic acids. Stearamide, which is increased in the serum of patients with hepatic cirrhosis and sepsis, may be associated with the systemic inflammatory state [ 22 , 23 ]. Methanandamide is a stable analog of anandamide that participates in energy balance mainly by activating cannabinoid receptors. Methanandamide dose-dependently inhibits and excites tension-sensitive gastric vagal afferents (GVAs), which play a role in appetite regulation [ 24 ]. In mice fed a high-fat diet, only an inhibitory effect of methanandamide was observed, and GVA responses to tension were dampened [ 24 , 25 ]. These changes may contribute to the development and/or maintenance of obesity. Moreover, methanandamide can produce dose-related hypothermia and attenuate cocaine-induced hyperthermia by a cannabinoid 1-dopamine D2 receptor mechanism [ 26 ].
Metabolomic pathway analysis of the cord blood metabolite features in the prepregnancy overweight and obesity group identified two filtered significant pathways: steroid hormone biosynthesis and neuroactive ligand‒receptor interaction pathways. In the steroid hormone biosynthesis pathway, the levels of several glucocorticoids (including corticosterone, 11-deoxycortisol, cortisol, testosterone, and 7α-hydroxytestosterone) were decreased in the prepregnancy overweight/obesity group. In addition to the physiological role of glucocorticoids in the healthy neuroendocrine development and maturation of fetuses and babies, glucocorticoids are essential to human health by regulating different physiological events in mature organs and tissues, such as glucose metabolism, lipid biosynthesis and distribution, food intake, thermogenesis, and mood and learning patterns [ 27 ]. Glucocorticoids have been considered as a link between adverse early-life conditions and the development of metabolic disorders in later life [ 28 , 29 , 30 ]. However, there is still much controversy regarding the role of maternal obesity in the fetal–steroid hormone biosynthesis pathway. Studies of maternal obesity animal models showed that corticosterone and cortisol levels were increased in the offspring of obese mothers [ 31 , 32 ]. A study reported by Satu M Kumpulainen et al. showed that young adults born to mothers with higher early pregnancy BMIs show lower average levels of diurnal cortisol, especially in the morning [ 33 ]. Laura I. Stirrat et al. found that increased maternal BMI was associated with lower maternal cortisol, corticosterone, and 11-dehydrocorticosterone levels. However, there were no associations between maternal BMI and glucocorticoid levels in the cord blood [ 34 ]. The differences in the study protocols of these previous studies may explain the mixed findings, such as cortisol measured from peripheral blood, cord blood or saliva; variation in measurement time points; the number of samples. Although the effect of maternal obesity on fetal steroid hormone levels is controversial, dysregulation of glucocorticoids may be a plausible mechanism by which maternal obesity can increase the risk of metabolic disorders and mental health disorders in offspring.
The effect of excessive GWG on umbilical cord blood metabolites is different from that of maternal overweight and obesity. Compared with the control group, in the excessive GWG group, the level of thromboxane B2 was increased and the level of hippuric acid was decreased. Thromboxane B2, which is important in the platelet release reaction, is a stable, physiologically active compound formed in vivo from prostaglandin endoperoxides. Hippuric acid is an acyl glycine formed from the conjugation of benzoic acid with glycine. Several studies have confirmed that both thromboxane B2 and hippuric acid levels are associated with diet. Dietary fatty acids affect platelet thromboxane production [ 35 , 36 , 37 ]. In our study, several fatty acids (e.g., palmitic acid, stearic acid, behenic acid, and lignoceric acid) in the excessive GWG group were also increased, which may have led to the increase in thromboxane B2 levels. Hippuric acid can be detected after the consumption of whole grains and anthocyanin-rich bilberries [ 38 , 39 ]. A healthy diet intervention increased the signals for hippuric acid to incorporate polyunsaturated fatty acids [ 38 ], and the low level of hippuric acid was associated with lower fruit-vegetable intakes [ 39 ]. Maternal overnutrition and unhealthy dietary patterns are the main reasons for excessive GWG [ 40 , 41 ]. Therefore, we speculated that the differences in thromboxane B2 and hippuric acid between the excessive GWG and control groups were associated with maternal diet during pregnancy. The effect of these differential metabolites on the long-term metabolic health of offspring after birth needs further study.
Metabolomic pathway analysis of the cord blood metabolite features in the excessive GWG group identified that biosynthesis of unsaturated fatty acids was the filtered significant pathway. The levels of several fatty acids in this pathway were increased in the excessive GWG group, including long-chain saturated fatty acids (e.g., palmitic acid (C 16:0), stearic acid (C 18:0), behenic acid (C 22:0), and lignoceric acid (C 23:0)), monounsaturated fatty acids (erucic acid), and polyunsaturated fatty acids (e.g., DPA, DHA, arachidonic acid, and adrenic acid). Because perinatal fatty acid status can be influenced by maternal dietary modifications or supplementation [ 42 ], we speculated that maternal diet during pregnancy caused the difference in umbilical cord blood fatty acids between the excessive GWG and control groups. A large body of evidence from mechanistic studies supports the potential of fatty acids to influence later obesity. However, the possible mechanisms and observed relationships are complex and related to the types and patterns of fatty acids [ 43 , 44 ]. Maternal dietary fatty acids have been found to induce hypothalamic inflammation, cause epigenetic changes, and alter the mechanisms of energy control in offspring [ 43 ]. Evidence from cell culture and rodent studies showed that polyunsaturated fatty acids might serve several complex roles in fetuses, including the stimulation and/or inhibition regulation of adipocyte differentiation [ 44 ]. The questions of whether lower n-6 long-chain polyunsaturated fatty acid levels or higher n-3 long-chain polyunsaturated fatty acid levels are of more relevance and whether the long-term effects differ with different offspring ages remain [ 44 ]. Although there is a biologically plausible case for the relevance of perinatal fatty acid status in later obesity risk, available data in humans suggest that the influence of achievable modification of perinatal n-3/n-6 status is not sufficient to influence offspring obesity risk in the general population [ 45 ]. Further studies seem justified to clarify the reasons.
The advantage of our present study is that we simultaneously analyzed the effects of prepregnancy overweight/obesity and excessive GWG on cord blood metabolites and explored their differences. In addition, to exclude the effect of hyperglycemia on cord blood metabolites, both women with prepregnancy diabetes mellitus and gestational diabetes mellitus were excluded from our study. The limitation of our study is that it was a single-center study with a small sample, especially in the prepregnancy overweight/obesity group. In the future, we can expand the sample size and conduct a subgroup analysis of the prepregnancy overweight/obesity group and analyze the differences in the effects of different degrees of obesity on cord blood metabolites. The prepregnancy overweight/obesity group can be further divided into an appropriate GWG group and an excessive GWG group, and the differences in the effects of these two groups on umbilical cord blood metabolites can be analyzed. Moreover, the dietary pattern of the pregnant woman could affect the production of cord blood metabolites. We did not investigate the dietary patterns of the mothers in this study, which is another limitation of this study. In future studies, we should investigate maternal dietary patterns as a very important confounding variable.
In conclusion, our present study confirmed that both prepregnancy overweight/obesity and excessive GWG could affect umbilical cord blood metabolites, and they had different effects on these metabolites. Prepregnancy overweight and obesity affected the fetal steroid hormone biosynthesis pathway, while normal prepregnancy body weight but excessive GWG affected fetal fatty acid metabolism. This emphasizes the importance of preconception weight loss and maintaining an appropriate GWG, which are beneficial for the long-term metabolic health of offspring.
Availability of data and materials
Data sets generated during the current study are not publicly available but will be available from the corresponding author at a reasonable request. Responses to the request for the raw data will be judged by a committee including XXY and GHL.
Abbreviations
Excessive gestational weight gain
Ultrahigh-performance liquid chromatography tandem mass spectrometry
Type 2 diabetes mellitus
Nonalcoholic fatty liver disease
The developmental origins of health and disease
Body mass index
Diabetes mellitus
Gestational diabetes mellitus
Oral glucose tolerance test
Low birth weight
Standard deviation
The Human Metabolome Database
Kyoto Encylopaedia of Genes and Genomes
Principal component analysis
Partial least-squares discriminant analysis
Importance for the projection
Fold change
Invitro fertilization and embryo transfer
Triglyceride
Docosapentaenoic acid
Docosahexaenoic acid
Gastric vagal afferents
Collaborators GBDO, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Article Google Scholar
Bjerregaard LG, Jensen BW, Angquist L, Osler M, Sorensen TIA, Baker JL. Change in overweight from childhood to early adulthood and risk of type 2 diabetes. N Engl J Med. 2018;378(14):1302–12.
Article PubMed Google Scholar
Sharma V, Coleman S, Nixon J, Sharples L, Hamilton-Shield J, Rutter H, Bryant M. A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes Rev. 2019;20(10):1341–9.
Article PubMed PubMed Central Google Scholar
Llewellyn A, Simmonds M, Owen CG, Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev. 2016;17(1):56–67.
Article CAS PubMed Google Scholar
Poston L, Caleyachetty R, Cnattingius S, Corvalan C, Uauy R, Herring S, Gillman MW. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016;4(12):1025–36.
Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9(6):373–92.
Barker DJ. The developmental origins of adult disease. J Am Coll Nutr. 2004;23(6 Suppl):588S-595S.
LifeCycle Project-Maternal O, Childhood Outcomes Study G, Voerman E, Santos S, Inskip H, Amiano P, Barros H, Charles MA, Chatzi L, Chrousos GP, et al. Association of gestational weight gain with adverse maternal and infant outcomes. JAMA. 2019;321(17):1702–15.
Aune D, Saugstad OD, Henriksen T, Tonstad S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. JAMA. 2014;311(15):1536–46.
Ukah UV, Bayrampour H, Sabr Y, Razaz N, Chan WS, Lim KI, Lisonkova S. Association between gestational weight gain and severe adverse birth outcomes in Washington State, US: a population-based retrospective cohort study, 2004–2013. PLoS Med. 2019;16(12):e1003009.
Starling AP, Brinton JT, Glueck DH, Shapiro AL, Harrod CS, Lynch AM, Siega-Riz AM, Dabelea D. Associations of maternal BMI and gestational weight gain with neonatal adiposity in the Healthy Start study. Am J Clin Nutr. 2015;101(2):302–9.
Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H, Bergstrom A, Charles MA, Chatzi L, Chevrier C, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. 2019;16(2):e1002744.
Heslehurst N, Vieira R, Akhter Z, Bailey H, Slack E, Ngongalah L, Pemu A, Rankin J. The association between maternal body mass index and child obesity: a systematic review and meta-analysis. PLoS Med. 2019;16(6):e1002817.
Newgard CB. Metabolomics and metabolic diseases: where do we stand? Cell Metab. 2017;25(1):43–56.
Johnson CH, Ivanisevic J, Siuzdak G. Metabolomics: beyond biomarkers and towards mechanisms. Nat Rev Mol Cell Biol. 2016;17(7):451–9.
Article CAS PubMed PubMed Central Google Scholar
Hivert MF, Perng W, Watkins SM, Newgard CS, Kenny LC, Kristal BS, Patti ME, Isganaitis E, DeMeo DL, Oken E, et al. Metabolomics in the developmental origins of obesity and its cardiometabolic consequences. J Dev Orig Health Dis. 2015;6(2):65–78.
Schlueter RJ, Al-Akwaa FM, Benny PA, Gurary A, Xie G, Jia W, Chun SJ, Chern I, Garmire LX. Prepregnant obesity of mothers in a multiethnic cohort is associated with cord blood metabolomic changes in offspring. J Proteome Res. 2020;19(4):1361–74.
Shokry E, Marchioro L, Uhl O, Bermudez MG, Garcia-Santos JA, Segura MT, Campoy C, Koletzko B. Impact of maternal BMI and gestational diabetes mellitus on maternal and cord blood metabolome: results from the PREOBE cohort study. Acta Diabetol. 2019;56(4):421–30.
Chen C, Lu FC, Department of Disease Control Ministry of Health PRC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17(Suppl):1–36.
PubMed Google Scholar
The American College of Obstetricians and Gynecologists. Macrosomia: ACOG practice bulletin, number 216. Obstet Gynecol. 2020;135(1):e18–e35.
Goldenberg RL, Culhane JF. Low birth weight in the United States. Am J Clin Nutr. 2007;85(2):584S-590S.
Lian JS, Liu W, Hao SR, Guo YZ, Huang HJ, Chen DY, Xie Q, Pan XP, Xu W, Yuan WX, et al. A serum metabonomic study on the difference between alcohol- and HBV-induced liver cirrhosis by ultraperformance liquid chromatography coupled to mass spectrometry plus quadrupole time-of-flight mass spectrometry. Chin Med J (Engl). 2011;124(9):1367–73.
CAS PubMed Google Scholar
Ding W, Xu S, Zhou B, Zhou R, Liu P, Hui X, Long Y, Su L. Dynamic plasma lipidomic analysis revealed cholesterol ester and amides associated with sepsis development in critically Ill patients after cardiovascular surgery with cardiopulmonary bypass. J Pers Med. 2022;12(11):1838.
Christie S, O’Rielly R, Li H, Nunez-Salces M, Wittert GA, Page AJ. Modulatory effect of methanandamide on gastric vagal afferent satiety signals depends on nutritional status. J Physiol. 2020;598(11):2169–82.
Christie S, O’Rielly R, Li H, Wittert GA, Page AJ. High fat diet induced obesity alters endocannabinoid and ghrelin mediated regulation of components of the endocannabinoid system in nodose ganglia. Peptides. 2020;131:170371.
Rasmussen BA, Kim E, Unterwald EM, Rawls SM. Methanandamide attenuates cocaine-induced hyperthermia in rats by a cannabinoid CB1-dopamine D2 receptor mechanism. Brain Res. 2009;1260:7–14.
Facchi JC, Lima TAL, Oliveira LR, Costermani HO, Miranda GDS, de Oliveira JC. Perinatal programming of metabolic diseases: the role of glucocorticoids. Metabolism. 2020;104:154047.
Reynolds RM, Walker BR, Syddall HE, Andrew R, Wood PJ, Whorwood CB, Phillips DI. Altered control of cortisol secretion in adult men with low birth weight and cardiovascular risk factors. J Clin Endocrinol Metab. 2001;86(1):245–50.
Valtat B, Dupuis C, Zenaty D, Singh-Estivalet A, Tronche F, Breant B, Blondeau B. Genetic evidence of the programming of beta cell mass and function by glucocorticoids in mice. Diabetologia. 2011;54(2):350–9.
Jia Y, Li R, Cong R, Yang X, Sun Q, Parvizi N, Zhao R. Maternal low-protein diet affects epigenetic regulation of hepatic mitochondrial DNA transcription in a sex-specific manner in newborn piglets associated with GR binding to its promoter. PLoS ONE. 2013;8(5):e63855.
Rodriguez JS, Rodriguez-Gonzalez GL, Reyes-Castro LA, Ibanez C, Ramirez A, Chavira R, Larrea F, Nathanielsz PW, Zambrano E. Maternal obesity in the rat programs male offspring exploratory, learning and motivation behavior: prevention by dietary intervention pre-gestation or in gestation. Int J Dev Neurosci. 2012;30(2):75–81.
Tuersunjiang N, Odhiambo JF, Long NM, Shasa DR, Nathanielsz PW, Ford SP. Diet reduction to requirements in obese/overfed ewes from early gestation prevents glucose/insulin dysregulation and returns fetal adiposity and organ development to control levels. Am J Physiol Endocrinol Metab. 2013;305(7):E868-878.
Kumpulainen SM, Heinonen K, Kaseva N, Andersson S, Lano A, Reynolds RM, Wolke D, Kajantie E, Eriksson JG, Raikkonen K. Maternal early pregnancy body mass index and diurnal salivary cortisol in young adult offspring. Psychoneuroendocrinology. 2019;104:89–99.
Stirrat LI, Just G, Homer NZM, Andrew R, Norman JE, Reynolds RM. Glucocorticoids are lower at delivery in maternal, but not cord blood of obese pregnancies. Sci Rep. 2017;7(1):10263.
Prisco D, Filippini M, Francalanci I, Paniccia R, Gensini GF, Serneri GG. Effect of n-3 fatty acid ethyl ester supplementation on fatty acid composition of the single platelet phospholipids and on platelet functions. Metabolism. 1995;44(5):562–9.
Kaapa P, Uhari M, Nikkari T, Viinikka L, Ylikorkala O. Dietary fatty acids and platelet thromboxane production in puerperal women and their offspring. Am J Obstet Gynecol. 1986;155(1):146–9.
Teng KT, Chang CY, Kanthimathi MS, Tan AT, Nesaretnam K. Effects of amount and type of dietary fats on postprandial lipemia and thrombogenic markers in individuals with metabolic syndrome. Atherosclerosis. 2015;242(1):281–7.
Hanhineva K, Lankinen MA, Pedret A, Schwab U, Kolehmainen M, Paananen J, de Mello V, Sola R, Lehtonen M, Poutanen K, et al. Nontargeted metabolite profiling discriminates diet-specific biomarkers for consumption of whole grains, fatty fish, and bilberries in a randomized controlled trial. J Nutr. 2015;145(1):7–17.
Brunelli L, Davin A, Sestito G, Mimmi MC, De Simone G, Balducci C, Pansarasa O, Forloni G, Cereda C, Pastorelli R, et al. Plasmatic hippuric acid as a hallmark of frailty in an Italian cohort: the mediation effect of fruit-vegetable intake. J Gerontol A Biol Sci Med Sci. 2021;76(12):2081–9.
Ferreira LB, Lobo CV, Miranda A, Carvalho BDC, Santos LCD. Dietary patterns during pregnancy and gestational weight gain: a systematic review. Rev Bras Ginecol Obstet. 2022;44(5):540–7.
Tielemans MJ, Garcia AH, Peralta Santos A, Bramer WM, Luksa N, Luvizotto MJ, Moreira E, Topi G, de Jonge EA, Visser TL, et al. Macronutrient composition and gestational weight gain: a systematic review. Am J Clin Nutr. 2016;103(1):83–99.
Lewis RM, Wadsack C, Desoye G. Placental fatty acid transfer. Curr Opin Clin Nutr Metab Care. 2018;21(2):78–82.
Cesar HC, Pisani LP. Fatty-acid-mediated hypothalamic inflammation and epigenetic programming. J Nutr Biochem. 2017;42:1–6.
Demmelmair H, Koletzko B. Perinatal polyunsaturated fatty acid status and obesity risk. Nutrients. 2021;13(11):3882.
Hauner H, Brunner S. Early fatty acid exposure and later obesity risk. Curr Opin Clin Nutr Metab Care. 2015;18(2):113–7.
Download references
Acknowledgements
The authors thank the study participants for their involvement and research assistants for their help conducting the study.
This research was funded by the Beijing Natural Science Foundation, grant number 7214231.
Author information
Authors and affiliations.
Division of Endocrinology and Metabolism, Department of Obstetrics, Beijing Obstetrics and Gynecology Hospital, Capital Medical University, Beijing Maternal and Child Health Care Hospital, No. 251, Yaojiayuan Road, Chaoyang District, Beijing, 100026, China
Xianxian Yuan, Yuru Ma, Yan Zhao, Wei Zheng, Ruihua Yang, Lirui Zhang, Xin Yan & Guanghui Li
Department of Obstetrics and Gynecology, The Second Hospital of Jilin University, Changchun, 130041, Jilin, China
You can also search for this author in PubMed Google Scholar
Contributions
XXY designed the study. XXY, WZ, LRZ and XY analyzed the data. YRM, JW, YZ and RHY took part in data collection and management. XXY wrote the manuscript. XXY and GHL reviewed the manuscript and contributed to manuscript revision. All authors contributed to the article and approved the submitted version. All authors reviewed the manuscript.
Corresponding author
Correspondence to Guanghui Li .
Ethics declarations
Ethics approval and consent to participate.
This study has been performed in accordance with the Declaration of Helsinki and has been approved by the ethics committee of Beijing Obstetrics and Gynecology Hospital, Capital Medical University (2021-KY-037). Informed consent was obtained from all subjects involved in the study to publish this paper. All methods were carried out in accordance with relevant guidelines and regulations in the declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yuan, X., Ma, Y., Wang, J. et al. The influence of maternal prepregnancy weight and gestational weight gain on the umbilical cord blood metabolome: a case–control study. BMC Pregnancy Childbirth 24 , 297 (2024). https://doi.org/10.1186/s12884-024-06507-x
Download citation
Received : 30 September 2023
Accepted : 11 April 2024
Published : 22 April 2024
DOI : https://doi.org/10.1186/s12884-024-06507-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Maternal obesity
- Gestational weight gain
- Offspring health
- Metabolites
- Umbilical cord blood
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
COMMENTS
From the 1999-2002 to the 2018-2021 period, case fatality rates increased by 130% (95% confidence interval [CI], 47-260) ... A study of maternal deaths from 2016 to 2017, which required mention of pregnancy among the multiple causes of death on the death certificate, yielded a maternal mortality rate of 7.88, as opposed to the NCHS ...
Although women of all backgrounds may be at risk, poverty is linked to the higher rates of maternal deaths.4 Most heartbreaking is the CDC's conclusion that six of every 10 maternal deaths that occur can be prevented. Bluntly stated, with better and more accessible health care for all, many would be alive today.
Introduction. Maternal mortality is defined as deaths occurring in women, while pregnant or within 42 days of termination of pregnancy irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes ().Maternal mortality continues to be a great concern with almost (99%) all maternal ...
Maternal Mortality Review Committees (MMRCs) are multidisciplinary committees that convene at the state or local level to comprehensively review deaths during or within a year of pregnancy (pregnancy-associated deaths). ... MMRIA supports standardized record abstraction, case summary development, documentation of committee decisions, and ...
Multiple studies have concluded that improvements in reporting and case ascertainment explain some of the recent increase in maternal mortality in the United States. ( 7 )( 11 )( 12 )( 13 ) One study estimated that about 80% of the reported increase in maternal mortality between 2000 and 2014 could be attributed to improvements in data linkages ...
Data from the CDC shows that for each year from 2018 to 2021, Black women have maternal mortality rates double that of women overall and 2.5 to 3 times higher than white women. The new study ...
Of the almost 5 million women that experienced complications during pregnancy and childbirth around the world, 303,000 died in 2017. This represents an estimated global maternal mortality ratio (MMR) of 216 maternal deaths per 100,000 live births, a reduction of 44% from 1990 (385 per 100,000 live births) (WHO, 2015).
The National Center for Health Statistics reported 658 maternal deaths, 277 late maternal deaths, and 3,791,712 live births in 2018, yielding an maternal mortality rate of 17.4 per 100,000 live births and a late maternal mortality rate of 7.2 per 100,000 live births. 8 There was a strong age-mortality gradient between age 20 and 44 years but no ...
A maternal death is defined as a death due to complications related to pregnancy or childbirth, occurring when a woman is pregnant, or within six weeks of the end of the pregnancy. Every two minutes, a woman dies during pregnancy or childbirth, according to the latest estimates released in a report by United Nations agencies today.
Maternal mortality is unacceptably high. About 287 000 women died during and following pregnancy and childbirth in 2020. Almost 95% of all maternal deaths occurred in low and lower middle-income countries in 2020, and most could have been prevented. Sustainable Development Goal (SDG) regions and sub-regions are used here.
Racial and ethnic disparities in maternal mortality — deaths related to pregnancy or childbirth — in the United States may be larger than previously reported, suggests a study funded by the National Institutes of Health. By re-examining information on death certificates from 2016 and 2017, researchers found that the maternal mortality rate ...
Delivery-related in-hospital maternal mortality in this study was lower than that reported in PMSS data, which defined pregnancy-related death as death during pregnancy or within 1 year of the end of pregnancy, from a cause related to pregnancy or its management. 3 PMSS data showed an increasing trend in pregnancy-related mortality during 1987 ...
The maternal mortality rate for 2021 was 32.9 deaths per 100,000 live births, compared with a rate of 23.8 in 2020 and 20.1 in 2019 ( Table ). In 2021, the maternal mortality rate for non-Hispanic Black (subsequently, Black) women was 69.9 deaths per 100,000 live births, 2.6 times the rate for non-Hispanic White (subsequently, White) women (26. ...
The estimates represent the most up to date, internationally-comparable MMEIG estimates of maternal mortality, using refined input data and methods from previous rounds. The report presents internationally comparable global, regional and country-level estimates and trends for maternal mortality between 2000 and 2020.
The causes of maternal death vary considerably and depend on when mothers die. These data are based on a report from maternal mortality review committees. During pregnancy, hemorrhage and cardiovascular conditions are the leading causes of death. At birth and shortly after, infection is the leading cause.
The peer-reviewed study in the American Journal of Obstetrics and Gynecology says a pregnancy checkbox on national death certificates inflates the death rate. The CDC "disagrees with the findings."
The study found maternal mortality increased by age, with the rate among women 40 and older increasing by 28% in 2021 to 138.5 deaths per 100,000 live births. ... Roe v. Wade, the landmark case ...
Another limitation, due to case number constraints, was the need to study obesity with a binary variable, rather than classes of BMI, in the risk assessment by specific causes of maternal mortality.
The highest toll of maternal mortality due to infections is reported in low and middle-income countries (LMICs). However, more evidence is needed to understand the differences in infection-related severe maternal outcomes (SMO) and fatality rates across the WHO regions. This study aimed to compare the burden of infection-related SMO and case fatality rates across the WHO regions using the ...
Like the new study suggests, Texas has seen general stability in maternal mortality rates in recent years. "From 2013 to 2019, we're looking at fluctuation between 17 deaths per 100,000 live ...
Design: A cross-sectional case series study of maternal deaths. An integrated verbal and social autopsy tool was used to collect quantitative and qualitative information regarding three delays. We recorded death accounts and conducted social autopsy by means of community Focus Group Discussions for each maternal death; and analysed data by ...
The state's maternal mortality review committee reported that there were 35.6 pregnancy-related deaths per 100,000 live births in the state between 2019 and 2021. Idaho became the only state without a maternal mortality review committee after the previous ended due to legislation it was tied to expiring last year. House Majority Leader Megan ...
This paper will explore the complexities preventing an understanding of and expedient solution to maternal mortality in the United States. Although maternal mortality rates vary by state and region, the nation's capital city, Washington, D.C., is an excellent case study. One thing implied by this case study is that lack of funding for or ...
Maternal deaths are a leading cause of death in young females worldwide, particularly in developing countries. Maternal mortality ratio, the number of maternal deaths per 100 000 live births, averages 240 in developing regions, but only 16 in developed regions. Causes of maternal and pregnancy-related deaths can be subdivided into three broad ...
stand the factors associated with maternal mortality, this is a cross-sectional case series study of maternal deaths (cases). We aimed to identify maternal deaths that would occur for the period of 6 months and that had occurred in previous 9 months from the start of field work in May, 2019. Maternal deaths that occurred in the last year in the
Pregnancy and delivery deaths represent a risk to women, particularly those living in low- and middle-income countries (LMICs). This population-based survey was conducted to provide estimates of the maternal mortality ratio (MMR) in Lagos Nigeria. A community-based, cross-sectional study was conducted in mapped Wards and Enumeration Areas (EA) of all Local Government Areas (LGAs) in Lagos ...
Studies show multiple factors contribute to preventable maternal deaths. For example, the amount of blood a woman loses during delivery is routinely underestimated, research shows. That can lead to delays in diagnosis and effective treatment, which may contribute to nearly a third of all hemorrhage-related pregnancy deaths, according to a 2018 ...
The patients in the study had been hospitalized with medical conditions between 2016 and 2019 and were treated in the hospital. Researchers also found that women are less likely to be re-admitted ...
The aim of the study was to explore the impact of maternal prepregnancy overweight/obesity and excessive GWG on cord blood metabolic profiles. A case control study including 33 pairs of mothers with prepregnancy overweight/obesity and their neonates, 30 pairs of mothers with excessive GWG and their neonates, and 32 control mother-neonate pairs.
Without timely and appropriate intervention, malaria in pregnancy can have devastating consequences, including severe anaemia, maternal death, stillbirth, premature delivery, and low-birth-weight babies.Refugees, migrants, internally displaced people, and indigenous people are also at heightened risk of malaria, often excluded from disease ...