- Advisory Board
- Publications
- Data & Tools
- News & Analysis
- Stepping Up
- Justice Reinvestment
- Reentry 2030
- Justice & Mental Health Collaboration Program (JMHCP)
- More Projects
- Career Opportunities
- Partner With Us
- Stay Connected


Addressing Misconceptions about Mental Health and Violence
Despite public perception that there is a direct connection between mental health and violence, research shows that this relationship is complex and that the presence of a mental illness doesn’t automatically predispose a person to violent behavior. As criminal justice professionals work to protect public safety, it’s important that their policies and practices reflect accurate information, not common misperceptions. This brief addresses these misconceptions, presents important information about risk factors for violence, and offers ways that criminal justice professionals can help mitigate such risks.
Project Credits
About the author.
When incidents of violence occur, the public is sometimes quick to assume that the person (or people) involved has a mental illness. This can be for numerous reasons, but largely, it is that misconceptions about mental health and violence are often perpetuated in media and public discourse. In fact, despite prevailing beliefs about a direct connection between the two, research shows that the relationship between violence and mental illness is complex, and the presence of a mental illness does not automatically predispose a person to violent behavior. 1
As criminal justice professionals work to protect public safety, it is important that their policies and practices reflect accurate information, not common misperceptions. Additionally, they need to understand the real risk factors and warning signs of violence to minimize the risk of violence among the people they supervise or encounter. This brief addresses common misconceptions about the relationship between mental illness and violence, presents important information about risk factors for violence, and offers ways that criminal justice professionals can help mitigate these risks.
Dispelling Misconceptions
Many people are not familiar with the signs, symptoms, and effects of various mental illnesses, and therefore sometimes use mental illness as an explanation when seeking reasons for seemingly senseless acts of violence. The public also often does not understand the complex nature of the relationship between mental illness and violence. Below are three important facts people should know.
1. People with mental illnesses are not more likely to be violent than the general public.
The perception that people with mental illnesses are more prone to violence is based on the stigma surrounding mental illnesses and the ways in which researchers study this relationship. For example, most research on mental illness is conducted in inpatient treatment settings, but evidence indicates that people receiving inpatient treatment have a higher risk of violence than people in outpatient settings. 2
The National Council for Mental Wellbeing says that having a diagnosed mental illness is not, in the absence of other factors, a sufficient risk to warrant fear of mass violence. 3
2. People with mental illnesses are more likely to cause self-harm or be victims of violence than to inflict harm on others. 4
Serious mental illnesses (SMI) such as depression, bipolar disorder, and borderline personality disorder may at times increase the risk of danger to oneself. 5
This can include suicidal ideation, parasuicidal behaviors, 6 and self-harm. However, there are no accurate data to support the belief that people with mental illnesses are more likely to be violent toward others. Indeed, research shows the opposite—people with mental illnesses account for only about 4 percent of violent crime in the United States. 7 When there is a direct relationship between people with SMI and violence, factors such as substance use 8 and environmental stressors, such as poverty and housing instability are associated with the connection. 9
3. Clinical assessments are not the most effective way to determine a person’s risk of violence.
Although clinical behavioral health practitioners have often been asked to determine the risk of violence a person with mental illness poses, research shows that clinicians’ judgment regarding risk is no better than chance. 10 Instead, the use of actuarial violence risk assessment tools are more accurate, and tools have been developed to determine risk for specific types of violence including sexual violence 11 and workplace violence. 12 It is also important to keep in mind that clinicians and violence risk assessment tools , like most people and tools used in the criminal justice system, have inherent biases, even when there are good intentions. Criminal justice professionals should receive implicit bias training even when using violence risk assessment tools to mitigate some of these concerns.
Risk factors for violence
While people with mental illnesses are not predisposed to violent behavior, criminal justice professionals should still understand key risk factors for violence. These factors include:
Prior history of violent behavior
Previous acts of violence can be a risk factor for future violence, especially if other risk factors were and are present.13
Times of crisis
During times of crisis, anyone can be at an increased risk for acting out violently because they may have a lower tolerance for frustrations when stressed. For some people, this tolerance can drop so low that they are less able to control their behaviors. It is important to distinguish between a diagnosable mental illness and someone with mental health needs, however.14 For example, if someone is experiencing a time of stress, trauma, or crisis, such as being fired from a job, the breakdown of a relationship, or the loss of a loved one, it can be a risk factor for violence regardless of whether they have been diagnosed with a mental illness.15
Command auditory hallucinations
When someone is experiencing auditory hallucinations telling them to act in violence, this is considered a risk because they may follow the command.16 This may be especially true if the person has a history of acting on these types of commands. Increased stress may make this risk even more acute.
Substance use
Substance use can be a stand-alone risk factor or increase other risk factors for violence, especially co-occurring substance use and mental illness.17 Intoxication by some substances can increase the risk for violence, especially stimulants.18 Agitation, due to withdrawal or intoxication, is a sign someone should be assessed for risk of violence.
Mitigating Risks of Violence: Practical Steps
1. understand the research. .
Becoming familiar with the research and data on the relationship between mental illness and violence—as well as the general causes and risk factors for violent behavior—can help criminal justice professionals recognize warning signs and avoid misconceptions and biases. Understanding the research can also help agencies choose the most appropriate actuarial violence risk assessment tool, as well as help focus resources on people at highest risk for becoming violent based on the chosen assessment instrument.
2. Provide ongoing training.
Staff who may encounter people at risk of committing violence should be trained on recognizing risk factors and intervention methods, like de-escalation techniques. They should also receive implicit bias training and education on stereotypes so that they do not assume a person is dangerous simply because of a mental illness. This is especially important for Black, Indigenous, and People of Color (BIPOC) with mental illnesses, who can be seen as intimidating to some staff due to premature judgments, limited personal experiences, or prejudices.
3. Leverage community resources and their clinical expertise.
Criminal justice professionals should partner with local behavioral health treatment providers and access resources that can help them recognize people who are at risk to act violently. This can also help facilitate referrals when people are experiencing a mental health crisis. As partners, clinicians may be able to provide trainings to criminal justice staff on ways to identify signs and symptoms of risk. This partnership can also help make criminal justice staff aware of all the mental health resources that exist in their community, such as diversion programs, Assertive Community Treatment (ACT) Teams, or as a last resort, civil commitment .
The Council of State Governments Justice Center offers free in-depth subject matter expertise and can connect you to jurisdictions that are supporting people with serious mental illness to help them avoid violent behavior. Visit the Center for Justice and Mental Health Partnerships to learn more.
Additional Resources
Mass Violence in America: Causes, Impacts, and Solutions by National Council for Mental Wellbeing
Understanding and Managing Risks for People with Behavioral Health Needs by The Council of State Governments Justice Center
1 Seena Fazel et al., “Schizophrenia and Violence: Systematic Review and Meta-Analysis,” PLOS Medicine 6, no. 8 (2009).
2 Solveig Osborg Ose et al., “Risk of Violence Among Patients in Psychiatric Treatment: Results from a National Census,” Nordic Journal of Psychiatry 71, no. 8 (2017): 551.
3 Note that the National Council for Mental Wellbeing defines an act of mass violence as an event in which four or more people are killed. See National Council for Mental Wellbeing, Mass Violence in America Executive Summary (Washington, DC: National Council for Mental Wellbeing, 2019), v.
4 Jeanne Y Choe et al., “Perpetration of Violence, Violent Victimization, and Severe Mental Illness: Balancing Public Health Concerns,” Psychiatric Services 59, no. 2 (2008): 153–64; Kimberlie Dean et al., “Risk of Being Subjected to Crime, Including Violent Crime, After Onset of Mental Illness: A Danish National Registry Study Using Police Data,” JAMA Psychiatry 75, no. 7 (2018): 689–696.
5 “Mental Illness and Suicide,” Suicide Awareness Voices of Education, accessed August 18, 2021 .
6 Virpi Leppanen et al., “Association of Parasuicidal Behavior to Early Maladaptive Schemas and Schema Modes in Patients with BPD: The Oulu BPD Study,” Personality and Mental Health 10 (2016): 61.
7 “This means that even if all of the association between mental illness and violence could somehow be eliminated, we would still have to confront 96 percent of the violence in the United States.” See John S. Rozel and Edward P. Mulvey, “The Link Between Mental Illness and Firearm Violence: Implications for Social Policy and Clinical Practice,” Annual Review of Clinical Psychology 13, (2017): 445–69.
8 Seena Fazel et al., “Schizophrenia and Violence: Systematic Review and Meta-Analysis,” PLOS Medicine 6, no. 8 (2009); Because substance use disorder is a criminogenic risk factor, which increases the likelihood someone will commit another crime, a high criminogenic risk level may increase the risk of violent crime. See also Fred Osher et al., Adults with Behavioral Health Needs Under Correctional Supervision: A Shared Framework for Reducing Recidivism and Promoting Recovery (New York: The Council of State Governments Justice Center, 2012) .
9 Eric B. Elbogen and Sally C. Johnson, “The Intricate Link Between Violence and Mental Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions,” Arch Gen Psychiatry 66, no. 2 (2009): 152–161.
10 Claudia C. Hurducas et al., “Violence Risk Assessment Tools: A Systematic Review of Surveys,” International Journal of Forensic Mental Health 13, no. 3 (2014): 182 ; J. Monahan, The Clinical Prediction of Violent Behavior: An Assessment of Clinical Techniques (Lanham, MD: Jason Aronson, 1981).
12 Dr. J. Reid Meloy, Dr. Stephen G. White, and Dr. Stephen Hart, “Workplace Assessment of Targeted Violence Risk: The Development and Reliability of the WAVR-21,” Journal of Forensic Sciences 58, no. 5 (2013): 1353.
13 Mairead Dolan and Regine Blattner, “The Utility of the Historical Clinical Risk-20 Scale as a Predictor of Outcomes in Decisions to Transfer Patients from High to Lower Levels of Security –A UK Perspective,” BMC Psychiatry 10, no. 76 .
14 In times of transition or stress, many people may experience some mental health needs that don’t rise to the level of a diagnosable mental illness. They may benefit from behavioral health supports like talk therapy or skill-building exercises to strengthen coping skills. See American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (Arlington, VA: American Psychiatric Association, 2013).
15 In one study of 28 acts of violence, every person who committed the act had recent stressors reported. See National Council for Mental Wellbeing, Mass Violence in America Executive Summary (Washington, DC: National Council for Mental Wellbeing, 2019), 11.
16 R. Upthegrove et al., “Understanding Auditory Verbal Hallucinations: A Systematic Review of Current Evidence,” Acta Pschiatrica Scandanavica 188 (2016): 355.
17 Elbogen and Johnson, “The Intricate Link Between Violence and Mental Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions.”
18 Rebecca McKetin et al., “Does Methamphetamine Use Increase Violent Behavior? Evidence From a Prospective Longitudinal Study,” Addiction 109 (2014): 901.7. “This means that even if all of the association between mental illness and violence could somehow be eliminated, we would still have to confront 96 percent of the violence in the United States.” See John S. Rozel and Edward P. Mulvey, “The Link Between Mental Illness and Firearm Violence: Implications for Social Policy and Clinical Practice,” Annual Review of Clinical Psychology 13, (2017): 445–69.
Writing: Deirdra Assey, CSG Justice Center
Research : Deirdra Assey, CSG Justice Center
Advising: Julia Kessler and Demetrius Thomas, CSG Justice Center
Editing: Darby Baham and Emily Morgan, CSG Justice Center
Design: Michael Bierman
Public Affairs: Ruvi Lopez, CSG Justice Center
Web Development : Andrew Currier
This project was supported by Grant No. 2019-MO-BX-K001 awarded by the Bureau of Justice Assistance. The Bureau of Justice Assistance is a component of the Department of Justice’s Office of Justice Programs, which also includes the Bureau of Justice Statistics, the National Institute of Justice, the Office of Juvenile Justice and Delinquency Prevention, the Office for Victims of Crime, and the SMART Office. Points of view or opinions in this document are those of the author and do not necessarily represent the official position or policies of the U.S. Department of Justice.

With support from the U.S. Department of Justice’s Office of Justice Programs’ Bureau of Justice Assistance, The Council…

Unlike drug courts, which have been informed by national standards for 10 years, mental health courts (MHCs)…

With support from the U.S. Department of Justice’s Office of Justice Programs’…
On March 9, 2024, President Joe Biden signed a $460 billion spending…
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- Winter 2024 | VOL. 36, NO. 1 CURRENT ISSUE pp.A5-81
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Neurobiology of Violence
- Jan Volavka , M.D., Ph.D.
Search for more papers by this author
Clinical correlates of violent behavior are known, but the underlying mechanisms are not well understood. This article reviews recent progress in the understanding of such mechanisms involving complex interactions between genes, prenatal and perinatal environmental factors, and rearing conditions. Violent behavior is heterogeneous; that is, impulsive and premeditated violent acts differ in their origins, mechanisms, and management. Recent molecular genetic studies of neurotransmitter regulation are providing new insights into pathophysiology of violent behavior. Functional anatomy of neurotransmitters involved in the regulation of violent behavior is being studied with recently developed brain imaging methods. Increasing evidence indicates commonalities between the neurobiology of violent and suicidal behavior. Progress in the prevention and management of violent behavior depends on studies that address biological factors in their social context. This article updates a previous review.
In the United States, homicide accounts for approximately 20,000 deaths annually. 1 A victimization survey estimated that approximately 4.2 violent crimes (assaults, robberies, and rapes) occur annually for each 100 persons older than 12 years. 1 Another survey of the general adult population found a 3.7% annual rate of self-reported violent behavior against other persons. 2 Thus, violent crime and violent behavior in general cause a major public health problem.
Societal and cultural factors play an important role in the development of violent behavior. However, these environmental factors and their fluctuations elicit different responses in different people. Violent behavior develops as a result of complex interactions between neurobiological and environmental factors. This review will focus primarily on neurobiology. Some of the neurobiological mechanisms of violent behavior are similar or identical to those that operate in suicidal behavior. 3
Substance use, personality disorders, major mental disorders, head injuries, and other diagnosable disorders contribute to the level of community violence. However, recent evidence points to neurobiological mechanisms that affect the development and the control of violent behavior but that are not clearly linked to the existing diagnostic categories. These mechanisms involve neurotransmitters that are in part under genetic control; the details are emerging in current research efforts. The main purpose of this article is to update a previous review, 4 stressing the neurobiological commonalities between aggressive and suicidal behavior.
DEFINITION AND SUBTYPES OF VIOLENT BEHAVIOR
For the purpose of this review, violent behavior is defined as overt and intentional physically aggressive behavior against another person. Examples include beating, kicking, choking, pushing, grabbing, throwing objects, using a weapon, threatening to use a weapon, and forcing sex. The definition does not include aggression against self. Violent crimes include murder, robbery, assault, and rape. In this review, I will not deal with organized state violence or ethnic warfare.
Violent behavior is heterogeneous in its origins and manifestations. Nevertheless, most violent acts can be classified as impulsive or premeditated, and many perpetrators can be classified as committing predominantly impulsive or predominantly premeditated violent acts. There is increasing evidence for the validity of this distinction. Phenytoin reduced impulsive, but not premeditated, violent acts among prisoners. 5 Impulsive violent offenders had lower verbal skills than those committing premeditated violent acts. 6 Persons who committed impulsive murders differed from those who committed premeditated ones in their pattern of brain glucose utilization. 7 Premeditated violent acts may be either predatory (committed for one's own gain; for example, a robbery) or pathological (committed, for example, by mentally ill people acting on their delusions or hallucinations). The mentally ill, however, may also commit predatory or impulsive violent acts.
CLINICAL CORRELATES OF VIOLENT BEHAVIOR
Substance use disorders (alcohol and drugs) play a major role in violent and suicidal behavior. In the United States, 34% of the risk of violence self-reported by community residents is attributable to substance abuse. 2 Urine tests were positive for illicit drugs in 37% to 59% of males arrested for violent crimes in U.S.cities. 8 Among Finnish males, 40% of the risk for homicide is attributable to alcoholism. 9 There are two types of alcoholism. 10 Type 2 accounts for most of the violence associated with alcohol abuse. This type, transmitted from fathers to sons, develops early in life. Type 2 abusers frequently fight under the influence of alcohol and show features of antisocial personality disorder. Personality disorders, particularly the antisocial personality and the borderline personality disorders, are frequently manifested by violent behavior.
A proportion of violent acts occurring in the community are committed by persons diagnosed with major mental disorders such as schizophrenia or mood disorders. Although these disorders carry an elevated risk for violent crime, 9 , 11 only about 4% of the risk for violence self-reported by community residents in the United States is attributable to such disorders. 2 However, major mental disorders are frequently comorbid with substance abuse, 12 and this comorbidity further elevates the risk for violent behavior. 2 , 13 Patients with major mental disorders who stop taking their medication are at a higher risk for developing violent behavior than those who adhere to the treatment. 14 The combination of substance abuse and nonadherence to treatment places patients at a particularly high risk for violence. 15 Brain injuries, particularly those affecting the frontal ventromedial areas 16 or the temporal lobes, are frequently associated with violent behavior. Dementia, mental retardation, and essentially any other disease or disorder affecting the brain may elicit impulsive violent behavior through cognitive impairment and a failure of inhibitory control.
Rearing environment has a powerful effect on behavior, including violence ( Figure 1 ). At least one-third of victims of child abuse grow up to continue the pattern of inept, neglectful, or abusive rearing as parents. 17 Many aspects of the rearing environment are determined by the parents' behavior; that behavior is of course not independent of the parents' genes (a factor not shown in Figure 1). Furthermore, the rearing environment is partly shaped by the child's behavior. Thus, genetic and environmental factors continuously interact in child development.
It is clear that maladaptive behaviors can be learned, but this is not the only mechanism of the intergenerational transfer of violence. Well before any teaching or role modeling takes place, the development of the brain may be affected by various factors in the prenatal and perinatal environment. Fetal exposure to alcohol may contribute to the development of violent behavior. 18 , 19 Early maternal rejection of the child interacts with obstetrical complications to predispose the individual to later (adult) violence. 20 Aggressive behavior is heritable, 21 , 22 and these pre- and perinatal events interact with genetic factors. Some of these complex relationships are depicted in Figure 1 .
The clinical correlates of suicidal and violent behavior overlap: alcohol and drug abuse, personality disorders, schizophrenia, early life experiences, and various brain disorders predispose to both types of behavior. 3
NEUROTRANSMITTERS, THEIR GENETIC CONTROL, AND VIOLENCE
Many neurotransmitters and hormones, including vasopressin, 23 steroids, opioids, and other substances, are involved in the modulation of aggressive behavior. Most of the current evidence strongly supports the roles of serotonin and catecholamines.
Serotonin (5-hydroxytryptamine; 5-HT) exerts inhibitory control over impulsive aggression. It is formed in the body by hydroxylation and decarboxylation of the essential amino acid tryptophan. The hydroxylation is the rate-limiting step in 5-HT synthesis; it is catalyzed by tryptophan hydroxylase (TPH). The gene for TPH has been cloned and mapped to the short arm of chromosome 11; two polymorphisms have been identified. The levels of a serotonin metabolite, 5-hydroxyindoleacetic acid (5-HIAA) in the cerebrospinal fluid (CSF) of impulsive offenders were associated with TPH genotype. 24 In general, these levels are believed to reflect presynaptic serotonergic activity in the brain. Reduced CSF 5-HIAA levels thus indicate a reduction in central serotonergic activity. At the synaptic level, reuptake is a mechanism for the termination of the action of serotonin. This reuptake is accomplished by a plasma membrane carrier called serotonin transporter (5HTT). The gene for 5HTT has been mapped to chromosome 17; a polymorphism has been described. 25 Thus, in summary, serotonin synthesis and activity regulation are under genetic control.
These indices of serotonergic transmission were examined in relation to violent and suicidal behavior. TPH genotype was associated with impulsive-aggressive behavior in male (but not female) patients who had personality disorders 26 as well as with suicide attempts in impulsive offenders 24 and in nonoffenders. 27 Low levels of CSF 5-HIAA have been reported in persons who attempted suicide (particularly by violent means) 28 and in persons with personality disorders who showed high levels of lifetime aggressiveness. 29 In these subjects, there was an association between aggressiveness and suicidal behavior. 29 This trivariate relationship between low levels of CSF 5-HIAA, impulsive aggression, and suicide has been replicated in various other populations. 3 , 4 As mentioned above, type 2 alcoholics frequently exhibit violent behavior; there is a common predisposition underlying the transmission of both alcoholism and violent behavior in families. Type 2 alcoholism is associated with a serotonergic deficit. 30 – 32 An association between low-activity 5HTT promoter genotype and early-onset alcoholism with habitual impulsive violent behavior has been observed. 33 Furthermore, a polymorphism of the 5-HT 1B receptor gene was linked to alcoholism with aggressive and impulsive behavior. 34 A nonhuman primate model confirmed that the serotonergic deficit, assessed by CSF 5-HIAA concentrations, is an antecedent (not a consequence) of alcohol consumption. 35
Neuroendocrine challenges offer another method of indirectly studying central serotonergic activity. A single dose of fenfluramine elevates the plasma levels of prolactin. This response is mediated by serotonergic action, and the prolactin elevation thus measures central serotonin activity. Prolactin response is reduced in aggressive subjects; this measure may be more sensitive than the CSF 5-HIAA. 36
These measures demonstrated a central serotonergic deficit associated with violence, but they could not locate the deficit to any area within the brain. Such localization has now become possible. Localized reductions of the 5HTT-specific binding were visualized in the living human brain. 37 I will return to these results in the section on brain imaging.
Thus, in summary, the association between impulsive violent behavior and central serotonin deficit has been demonstrated by using varied measures of serotonin function. The subjects in these studies were largely diagnosed with personality disorders and alcoholism. The role of serotonergic mechanisms in violent behavior accompanying other disorders is not clear; a small study has failed to detect low levels of CSF 5-HIAA in violent schizophrenic patients. 38
Norepinephrine systems also play a role in aggression. Similar to suicidal behavior, aggression is associated with increased noradrenergic activity. Stress-elicited noradrenergic activity is linked to irritable aggression in animals. The evidence for noradrenergic involvement in human aggression is indirect. Plasma levels of epinephrine and norepinephrine were related to experimentally induced hostile behavior in normal subjects. 39 Growth hormone response to clonidine, an alpha-2-adrenergic receptor agonist, was related to irritability (but not to assaultiveness) in normal subjects and in patients with personality disorders. 40 Furthermore, beta-adrenergic blocking agents have been used clinically to suppress violent behavior in patients with a variety of neuropsychiatric disorders. 41
Two enzymes are important in the catabolism of catecholamines, including norepinephrine: monoamine oxidase (MAO) and catechol- O -methyltransferase (COMT). MAO exists in two forms, A and B. Both types are present in the brain; type B is also in the platelets where it can be assayed. Genes for both types are located at the X chromosome. Several lines of evidence link MAO to aggressive behavior. Low MAO activity was found in the platelets of violent offenders. 42 In a large kindred, several males showed consistent impulsive violent behavior and mental retardation; each of these males had a point mutation in the MAO-A structural gene that resulted in a complete and selective deficiency of the activity of this enzyme. 43 Male “knockout” (genetically altered) mice lacking the MAO-A gene showed aggressive behavior. 44 Thus, low levels of MAO activity were associated with impulsive aggression.
COMT activity is governed by a common polymorphism that results in 3- to 4-fold variations in enzymatic activity. Two studies have demonstrated an association between the allele coding for the less active form of the enzyme and violent behavior in schizophrenic and schizoaffective patients. 45 , 46 This association seemed more expressed in males. These small association studies need to be replicated in larger samples of schizophrenic patients and extended to nonschizophrenic subjects. Male (but not female) knockout mice deficient in the COMT gene exhibited aggressive behavior. 47 Thus, in summary, high noradrenergic activity and low activity of the enzymes that catabolize catecholamines are associated with aggressive behavior. The roles of dopaminergic mechanisms in relation to alcoholism and personality traits are being studied; the results have not yet provided a generally accepted pattern of association with violence.
In the preceding paragraphs, I discussed various polymorphisms that contribute to the control of neurotransmission. These polymorphisms are genetically transmitted; this is the template function of the gene. This function is not amenable to any changes due to environmental effects except for mutations. However, the transcriptional function that determines the gene expression (i.e., the manufacture of specific proteins) does depend on environmental and social factors. 48 Gene expression can be modified, for example, by the rearing environment: CSF 5-HIAA in monkeys varies depending on whether they were reared by their mothers or by peers 49 (see Figure 1 ).
GENDER AND VIOLENCE
Gender is a very robust predictor of violent behavior 4 and of suicide. 3 In the United States, male suspects account for 85% of arrests for violent crimes. 1 Victimization surveys as well as self-reports by adults living in the community 2 have generally supported the predominance of males among perpetrators of violence. However, this gender difference is reduced among community residents with major mental disorders and those with substance use disorders, 2 and it disappears among hospitalized psychiatric patients. 4
The gender difference in aggressiveness develops in preschool years, and it is fully expressed by puberty. The difference is partly due to societal causes, including child-rearing practices. Numerous lines of evidence suggest biological origins of the gender difference. As noted above, the TPH, MAO-A, and COMT genotypes show associations with violent behavior that are largely limited to males. Males are more likely than females to develop alcoholism, particularly type 2 alcoholism that is associated with aggression. Elevated circulating testosterone level may be associated with aggression in young males, 50 and perhaps even in young females, 51 but these findings have not been consistently replicated; furthermore, it is not clear whether the hormonal level is an antecedent or a consequence of violent behavior. 52
BRAIN STRUCTURE AND FUNCTION
The orbitomedial prefrontal cortex is involved in controlling and inhibiting impulsive actions, and lesions to this area may result in disinhibited aggressive 4 , 16 or suicidal behaviors. 3 Furthermore, literature on aggression points to a dysfunction of parts of the limbic system, particularly the amygdala and the hippocampus, the two limbic structures within the temporal lobe. 53 There is some evidence that the frontal and temporal abnormalities associated with violence may be more expressed in the dominant hemisphere. Until recently, electroencephalography was the main method of studying the function of these systems in humans; this approach was useful in confirming frontotemporal abnormalities in violent individuals (particularly in impulsive violence), but the information was relatively nonspecific in terms of the nature of the dysfunction and its subcortical localization. 54 , 55 More recent imaging methods such as positron emission tomography (PET) and single-photon emission computed tomography (SPECT) are providing more specific information. Glucose utilization and blood flow measurements using PET showed abnormality in the left temporal lobe and in the frontal lobes of violent psychiatric patients. 56 Mentally ill murderers showed selective reductions in prefrontal glucose utilization during a continuous performance task. 57 A reanalysis of the data obtained in this study showed that the murderers who had no history of early psychosocial deprivation (e.g., no childhood abuse or family neglect) had lower prefrontal glucose metabolism than murderers with early psychosocial deprivation and a group of normal controls. 58 Thus, these results suggest the existence of two paths toward the development of violent behavior: abnormal neurobiology (prefrontal cortical dysfunction), or abnormal rearing environment. Another reanalysis of these data 57 determined that the impulsive (but not the predatory) offenders had lower prefrontal glucose metabolism in comparison with the control subjects. 7 Thus, prefrontal cortical functioning that controls aggressive behavior was impaired specifically in persons who exhibit impulsive (but not premeditated) violence.
The PET results discussed have revealed brain dysfunctions that were localized, but not specifically linked to any neurotransmitter system. A recent SPECT study reported such specific findings. The 5HTT binding in the midbrain and in the occipital and the frontal mesial cortex of alcoholic impulsive violent offenders was lower than that in healthy control subjects or in nonviolent alcoholics. 37 Interestingly, autoradiographic studies of suicide victims' postmortem brain tissue have also revealed serotonin receptor abnormalities in the ventral prefrontal cortex. 3 The recent PET and SPECT results discussed above will have to be replicated.
If these studies are correct, what are the origins of the brain dysfunctions they reveal? They may be genetic, or due to noxious environmental influences disturbing prenatal neurodevelopment, or related to perinatal complications, or an interaction among these factors. Some structural changes, such as a reduction of the temporal lobe volume, may be caused by child abuse; this effect could be mediated by chronic elevations of glucocorticoids and catecholamines associated with the stress of being maltreated. 59 Similarly, a quantitative EEG study provided preliminary evidence for aberrant cortical development in abused children. 60
PREVENTION AND TREATMENT OF VIOLENCE
Improvements in prenatal and perinatal care and prevention of head injuries may reduce the level of violence in the community. Since substance use disorders play such an important role in violence, it seems that recidivistic violent crime could be substantially reduced if the treatment of substance use disorders were routinely available to prisoners. In the United States, the availability is inadequate. Facilities that care for schizophrenic and manic patients need to focus on the diagnosis and treatment of the frequently comorbid substance use disorders. Adherence to treatment must be strongly encouraged and monitored in patients with major mental disorders who have a history of recidivistic violence after they discontinue their medication.
Pharmacological treatment of violent behavior in patients with mental disorders is somewhat similar to the treatment of patients with suicidal ideation. Selective serotonin reuptake inhibitors (SSRIs) that are routinely used to treat depression were also effective against impulsive aggression in patients with personality disorders who were not suffering from major depression. 61 Clozapine, an atypical antipsychotic medication, is more effective than other antipsychotics in reducing both aggressive 41 and suicidal 3 behaviors in schizophrenia. Pharmacological reduction of violent behavior in persons without mental disorders might be possible, but it could raise ethical issues that have not been addressed. Lithium, a medication that appears to reduce suicide risk for bipolar patients, 3 also reduced impulsive aggressive behavior in prisoners who were not psychotic; 62 both effects could be mediated by an enhancement of serotonergic activity. The administration of an SSRI for 4 weeks to persons without mental disorders has reduced their feelings of hostility. 63 Pharmacological treatments of aggression have been recently reviewed in detail elsewhere. 41 , 64 , 65
FUTURE DIRECTIONS
Phenotypic heterogeneity of violent behaviors is a principal problem of this research area. Efforts at subtyping of violence (e.g., impulsive versus premeditated violence) are in progress, but much remains to be done. Most of the neurobiological tools I discussed have separated, one tool at a time, a group of violent subjects from a group of control subjects. Very rarely has a single tool been used to define subgroups of violent patients; using more than one tool for such grouping is even rarer. But even violent behaviors that are phenotypically identical may be heterogeneous from the standpoint of underlying neurobiology.
A fundamental challenge is to translate the recognition of this heterogeneity into research, prevention, and treatment. This requires using the available tools of molecular genetics, neuropharmacology, brain imaging, and psychopharmacology in the same subjects. In this way, it may, for example, become possible to identify patients with specific serotonergic or noradrenergic deficits that could be corrected pharmacologically, or, in the future, perhaps using gene therapy. Furthermore, such a multidisciplinary approach would enable a search for protective factors that might explain, for example, why some patients with very low CSF 5-HIAA do not become violent. Knowledge of such protective factors would be useful in developing strategies for prevention and treatment.
Testing the efficacy of antiaggressive treatments will require substantial modifications of the classic trial designs that have been used in psychopharmacology for the past three decades. The problems to be addressed include the need for precise definition of violent behavior, the difficulty of measuring outcome because of the relative rarity of violent incidents, bias in the selection of patients for study, inadequate and inappropriate control groups, and inattention to comorbidities and concomitant medications in analyzing results. 66
Neurobiological and environmental (e.g., social) factors continuously interact and influence each other. For example, obstetrical complications and maternal rejection interact to raise the propensity for violence, and they may influence each other (e.g., a child with brain dysfunction resulting from obstetrical complications may behave in a way that provokes maternal rejection). To understand the neurobiology of violence, we need to study it in the context of such biosocial interactions.
CONCLUSIONS
The past five years have brought significant progress in our understanding of the neurobiology of violence. The field has been enriched by numerous contributions in the areas of molecular genetics and brain imaging. With deeper understanding of the underlying neurobiology, commonalities between violent and suicidal behaviors can be seen more clearly now.
Up until recently, the assessment of biosocial interactions that result in violent behavior was largely limited to acknowledgments of their existence; we have now progressed to formal statistical demonstrations of these interactions. The “nature or nurture” controversy inherited from Francis Galton has been an underlying philosophical basis of numerous political problems that have plagued the field of violence research during the past decade. 67 The recent studies of biosocial interactions have rendered the controversy of nature and nurture moot; nature is nurture.
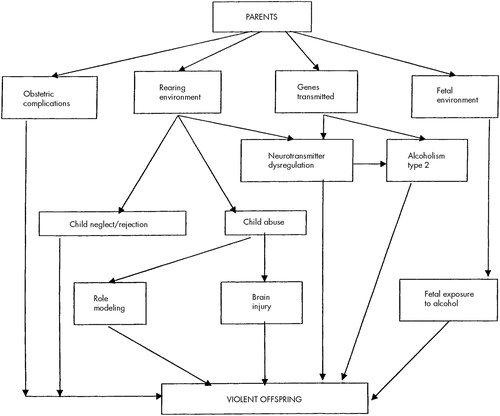
FIGURE 1. Mechanisms for the intergenerational transmission of propensity for violence
1 Sourcebook of Criminal Justice Statistics Online. Washington, DC, U.S. Department of Justice, Bureau of Justice Statistics, 1997 Google Scholar
2 Swanson JW: Mental disorder, substance abuse, and community violence: an epidemiological approach, in Violence and Mental Disorder: Developments in Risk Assessment, edited by Monahan J, Steadman HJ. Chicago, University of Chicago Press, 1994, pp 101–136 Google Scholar
3 Mann JJ: The neurobiology of suicide. Nat Med 1998 ; 4:25–30 Crossref , Medline , Google Scholar
4 Volavka J: Neurobiology of Violence. Washington, DC, American Psychiatric Press, 1995 Google Scholar
5 Barratt ES, Stanford MS, Felthous AR, et al: The effects of phenytoin on impulsive and premeditated aggression: a controlled study. J Clin Psychopharmacol 1997 ; 17:341–349 Crossref , Medline , Google Scholar
6 Barratt ES, Stanford MS, Kent TA, et al: Neuropsychological and cognitive psychophysiological substrates of impulsive aggression. Biol Psychiatry 1997; 41:1045– 1061 Google Scholar
7 Raine A, Meloy JR, Bihrle S, et al: Reduced prefrontal and increased subcortical brain functioning assessed using positron emission tomography in predatory and affective murderers. Behavioral Sciences and the Law 1998 ; 16:319–332 Crossref , Medline , Google Scholar
8 Maguire K, Pastore AL, Flanagan TJ (eds): Sourcebook of Criminal Justice Statistics 1992. Washington, DC, U.S. Department of Justice, Bureau of Justice Statistics, 1993 Google Scholar
9 Eronen M, Hakola P, Tiihonen J: Mental disorders and homicidal behavior in Finland. Arch Gen Psychiatry 1996 ; 53:497–501 Crossref , Medline , Google Scholar
10 Cloninger CR, Bohman M, Sigvardsson S: Inheritance of alcohol abuse: cross-fostering analysis of adopted men. Arch Gen Psychiatry 1981 ; 38:861–868 Crossref , Medline , Google Scholar
11 Hodgins S, Mednick SA, Brennan PA, et al: Mental disorder and crime: evidence from a Danish birth cohort. Arch Gen Psychiatry 1996 ; 53:489–496 Crossref , Medline , Google Scholar
12 Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) Study. JAMA 1990; 264:2511– 2518 Google Scholar
13 Steadman HJ, Mulvey EP, Monahan J, et al: Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry 1998 ; 55:393–401 Crossref , Medline , Google Scholar
14 Torrey EF: Violent behavior by individuals with serious mental illness. Hospital and Community Psychiatry 1994 ; 45:653–662 Medline , Google Scholar
15 Swartz MS, Swanson JW, Hiday VA, et al: Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry 1998 ; 155:226–231 Medline , Google Scholar
16 Grafman J, Schwab K, Warden D, et al: Frontal lobe injuries, violence, and aggression: a report of the Vietnam head injury study. Neurology 1996; 46:1231– 1238 Google Scholar
17 Oliver JE: Intergenerational transmission of child abuse: rates, research, and clinical implications. Am J Psychiatry 1993; 150:1315– 1324 Google Scholar
18 Brown RT, Coles CD, Smith IE, et al: Effects of prenatal alcohol exposure at school age, II: attention and behavior. Neurotoxicology and Teratology 1991 ; 13:369–376 Crossref , Medline , Google Scholar
19 Streissguth AP, Randels SP, Smith DF: A test-retest study of intelligence in patients with fetal alcohol syndrome: implications for care. J Am Acad Child Adolesc Psychiatry 1991 ; 30:584–587 Crossref , Medline , Google Scholar
20 Raine A, Brennan P, Mednick SA: Interaction between birth complications and early maternal rejection in predisposing individuals to adult violence: specificity to serious, early-onset violence. Am J Psychiatry 1997; 154:1265– 1271 Google Scholar
21 Coccaro EF, Bergeman CS, Kavoussi RJ, et al: Heritability of aggression and irritability: a twin study of the Buss-Durkee aggression scales in adult male subjects. Biol Psychiatry 1997 ; 41:273–284 Crossref , Medline , Google Scholar
22 Bergeman CS, Seroczynski AD: Genetic and environmental influences on aggression and impulsivity, in Neurobiology and Clinical Views on Aggression and Impulsivity, edited by Maes M, Coccaro EF. Chichester, UK, Wiley, 1998, pp 63–80 Google Scholar
23 Coccaro EF, Kavoussi RJ, Hauger RL, et al: Cerebrospinal fluid vasopressin levels: correlates with aggression and serotonin function in personality-disordered subjects. Arch Gen Psychiatry 1998 ; 55:708–714 Crossref , Medline , Google Scholar
24 Nielsen DA, Goldman D, Virkkunen M, et al: Suicidality and 5-hydroxyindoleacetic acid concentration associated with a tryptophan hydroxylase polymorphism. Arch Gen Psychiatry 1994 ; 51:34–38 Crossref , Medline , Google Scholar
25 Collier DA, Stober G, Li T, et al: A novel functional polymorphism within the promoter of the serotonin transporter gene: possible role in susceptibility to affective disorders. Molecular Psychiatry 1996 ; 1:453–460 Medline , Google Scholar
26 New AS, Gelernter J, Yovell Y, et al: Tryptophan hydroxylase genotype is associated with impulsive-aggression measures: a preliminary study. American Journal of Medical Genetics 1998 ; 81:13–17 Crossref , Medline , Google Scholar
27 Courtet P, Buresi C, Abbar M, et al: Association between the tryptophan hydroxylase gene and suicidal behavior (abstract 146). Presented at the American Psychiatric Association 151st annual meeting, Toronto, Ontario, Canada, May 30–June 4, 1998 Google Scholar
28 Åsberg M, Traskman L, Thoren P: 5-HIAA in the cerebrospinal fluid: a biochemical suicide predictor? Arch Gen Psychiatry 1976; 33:1193– 1197 Google Scholar
29 Brown GL, Goodwin FK, Ballenger JC, et al: Aggression in humans correlates with cerebrospinal fluid amine metabolites. Psychiatry Res 1979 ; 1:131–139 Crossref , Medline , Google Scholar
30 Virkkunen M, Linnoila M: Serotonin in early-onset, male alcoholics with violent behaviour. Ann Med 1990 ; 22:327–331 Crossref , Medline , Google Scholar
31 LeMarquand D, Pihl RO, Benkelfat C: Serotonin and alcohol intake, abuse, and dependence: clinical evidence. Biol Psychiatry 1994 ; 36:326–337 Crossref , Medline , Google Scholar
32 Cloninger CR: The psychobiological regulation of social cooperation. Nat Med 1995 ; 1:623–625 Crossref , Medline , Google Scholar
33 Hallikainen T, Saito T, Lachman HM, et al: Association between low activity serotonin transporter promoter genotype with habitual impulsive behavior among antisocial early onset alcoholics. Molecular Psychiatry 1999 (in press) Google Scholar
34 Lappalainen J, Long JC, Eggert M, et al: Linkage of antisocial alcoholism to the serotonin 5-HT 1B receptor gene in 2 populations. Arch Gen Psychiatry 1998 ; 55:989–994 Crossref , Medline , Google Scholar
35 Higley JD, Suomi SJ, Linnoila M: A nonhuman primate model of type II excessive alcohol consumption? Part I: low cerebrospinal fluid 5-hydroxyindoleacetic acid concentrations and diminished social competence correlate with excessive alcohol consumption. Alcohol Clin Exp Res 1996 ; 20:629–642 Crossref , Medline , Google Scholar
36 Coccaro EF, Kavoussi RJ, Cooper TB, et al: Central serotonin activity and aggression: inverse relationship with prolactin response to d -fenfluramine, but not CSF 5-HIAA concentration, in human subjects. Am J Psychiatry 1997; 154:1430– 1435 Google Scholar
37 Tiihonen J, Kuikka JT, Bergstrom KA, et al: Single-photon emission tomography imaging of monoamine transporters in impulsive violent behaviour. European Journal of Nuclear Medicine 1997; 24:1253– 1260 Google Scholar
38 Kunz M, Sikora J, Krakowski M, et al: Serotonin in violent patients with schizophrenia. Psychiatry Res 1995 ; 59:161–163 Crossref , Medline , Google Scholar
39 Gerra G, Zaimovic A, Avanzini P, et al: Neurotransmitter-neuroendocrine responses to experimentally induced aggression in humans: influence of personality variable. Psychiatry Res 1997 ; 66:33–43 Crossref , Medline , Google Scholar
40 Coccaro EF, Lawrence T, Trestman R, et al: Growth hormone responses to intravenous clonidine challenge correlate with behavioral irritability in psychiatric patients and healthy volunteers. Psychiatry Res 1991 ; 39:129–139 Crossref , Medline , Google Scholar
41 Citrome L, Volavka J: Psychopharmacology of violence, II: beyond the acute episode. Psychiatric Annals 1997 ; 27:696–703 Crossref , Google Scholar
42 Belfrage H, Lidberg L, Oreland L: Platelet monoamine oxidase activity in mentally disordered violent offenders. Acta Psychiatr Scand 1992 ; 85:218–221 Crossref , Medline , Google Scholar
43 Brunner HG, Nelen M, Breakefield XO, et al: Abnormal behavior associated with a point mutation in the structural gene for monoamine oxidase A. Science 1993 ; 262:578–580 Crossref , Medline , Google Scholar
44 Cases O, Seif I, Grimsby J, et al: Aggressive behavior and altered amounts of brain serotonin and norepinephrine in mice lacking MAOA. Science 1995; 268:1763– 1766 Google Scholar
45 Strous RD, Bark N, Parsia SS, et al: Analysis of a functional catechol O -methyltransferase gene polymorphism in schizophrenia: evidence for association with aggressive and antisocial behavior. Psychiatry Res 1997 ; 69:71–77 Crossref , Medline , Google Scholar
46 Lachman HM, Nolan KA, Mohr P, et al: Association between catechol O -methyltransferase genotype and violence in schizophrenia and schizoaffective disorder. Am J Psychiatry 1998 ; 155:835–837 Medline , Google Scholar
47 Gogos JA, Morgan M, Luine V, et al: Catechol- O -methyltransferase-deficient mice exhibit sexually dimorphic changes in catecholamine levels and behavior. Proc Natl Acad Sci USA 1998; 95:9991– 9996 Google Scholar
48 Kandel ER: A new intellectual framework for psychiatry. Am J Psychiatry 1998 ; 155:457–469 Crossref , Medline , Google Scholar
49 Higley JD, Suomi SJ, Linnoila M: A longitudinal assessment of CSF monoamine metabolite and plasma cortisol concentrations in young rhesus monkeys. Biol Psychiatry 1992 ; 32:127–145 Crossref , Medline , Google Scholar
50 Dabbs JM Jr, Carr TS, Frady RL, et al: Testosterone, crime, and misbehavior among 692 male prison inmates. Personality and Individual Differences 1995 ; 18:627–633 Crossref , Google Scholar
51 Dabbs JM Jr, Hargrove MF: Age, testosterone, and behavior among female prison inmates. Psychosom Med 1997 ; 59:477–480 Crossref , Medline , Google Scholar
52 Susman EJ, Worrall BK, Murowchick E, et al: Experience and neuroendocrine parameters of development: aggressive behavior and competencies, in Aggression and Violence: Genetic, Neurobiological, and Biosocial Perspectives, edited by Stoff DM, Cairns RB. Mahwah, NJ, Lawrence Erlbaum, 1996, pp 267–289 Google Scholar
53 Bear D: Neurological perspectives on aggressive behavior. J Neuropsychiatry Clin Neurosci 1991; 3:S3–S8 Google Scholar
54 Volavka J: Aggression, electroencephalography, and evoked potentials: a critical review. Neuropsychiatry Neuropsychol Behav Neurol 1990 ; 3:249–259 Google Scholar
55 Convit A, Douyon R, Yates K, et al: Frontotemporal abnormalities and violent behavior, in Aggression and Violence: Genetic, Neurobiological, and Biosocial Perspectives, edited by Stoff DM, Cairns RB. Mahwah, NJ, Lawrence Erlbaum, 1996, pp 169–194 Google Scholar
56 Volkow ND, Tancredi L: Neural substrates of violent behaviour: a preliminary study with positron emission tomography. Br J Psychiatry 1987 ; 151:668–673 Crossref , Medline , Google Scholar
57 Raine A, Buchsbaum M, LaCasse L: Brain abnormalities in murderers indicated by positron emission tomography. Biol Psychiatry 1997 ; 42:495–508 Crossref , Medline , Google Scholar
58 Raine A, Phil D, Stoddard J, et al: Prefrontal glucose deficits in murderers lacking psychosocial deprivation. Neuropsychiatry Neuropsychol Behav Neurol 1998 ; 11:1–7 Medline , Google Scholar
59 DeBellis MD, Casey BJ, Clark DB, et al: Anatomical MRI in maltreated children with PTSD (abstract). Biol Psychiatry 1998 ; 43:16S Crossref , Google Scholar
60 Ito Y, Teicher MH, Glod CA: Preliminary evidence for aberrant cortical development in abused children: a quantitative EEG study. J Neuropsychiatry Clin Neurosci 1998 ; 10:298–307 Link , Google Scholar
61 Coccaro EF, Kavoussi RJ: Fluoxetine and impulsive aggressive behavior in personality-disordered subjects. Arch Gen Psychiatry 1997; 54:1081– 1088 Google Scholar
62 Sheard MH, Marini JL, Bridges CI, et al: The effect of lithium on impulsive aggressive behavior in man. Am J Psychiatry 1976; 133:1409– 1413 Google Scholar
63 Knutson B, Wolkowitz OM, Cole SW, et al: Selective alteration of personality and social behavior by serotonergic intervention. Am J Psychiatry 1998 ; 155:373–379 Crossref , Medline , Google Scholar
64 Citrome L, Volavka J: Psychopharmacology of violence, I: assessment and acute treatment. Psychiatric Annals 1997 ; 27:691–695 Crossref , Google Scholar
65 Citrome L, Volavka J: The efficacy of pharmacological treatments in preventing crime and violence among persons with psychotic disorders, in Violence, Crime, and Mentally Disordered Offenders: Concepts and Methods for Effective Treatment and Prevention, edited by Hodgins S, Muller-Isberner R. New York, Wiley (in press) Google Scholar
66 Volavka J, Citrome L: Atypical antipsychotics in the treatment of the persistently aggressive psychotic patient: methodological concerns. Schizophr Res 1999 (in press) Google Scholar
67 Touchette N: Genetics and crime: It's not over. Till it's over. Journal of NIH Research 1993 ; 5:32–34 Google Scholar
- Examining the cognitive contributors to violence risk in forensic samples: A systematic review and meta-analysis Aggression and Violent Behavior, Vol. 74
- Assessing attentional bias to emotions in adolescent offenders and nonoffenders 24 November 2023 | Frontiers in Psychology, Vol. 14
- Prediction of violence: Part contagious disease, part unpredictable individual: Is a public health assessment approach an additional option and at what cost? 3 March 2023 | Behavioral Sciences & the Law, Vol. 41, No. 5
- Low oxytocin levels in schizophrenia patients involved in crime and the relationship of these levels to aggression, empathy and forgiveness 15 December 2022 | The Journal of Forensic Psychiatry & Psychology, Vol. 34, No. 1
- Effects of Psychiatric Disease Severity and Clinical Characteristics on Duration of High Violence Risk: A Perspective on Violence Prevention in the Psychiatric Ward 1 March 2023 | Neuropsychiatric Disease and Treatment, Vol. Volume 19
- Assessment and Management of Violent Behavior 1 July 2023
- A Machine Learning Approach to the Analytics of Representations of Violence in Khaled Hosseini's Novels
- Violent crimes and homicide in New York City: The role of weather and pollution Journal of Forensic and Legal Medicine, Vol. 91
- Personality Factors Predicting Cyberbullying and Online Harassment
- Biochemical Factors in Aggression and Violence
- Anger Experience and Anger Expression Through Drawing in Schizophrenia: An fNIRS Study 1 September 2021 | Frontiers in Psychology, Vol. 12
- Reprint of "Executive dysfunction, violence and aggression" Aggression and Violent Behavior, Vol. 54
- Sex Differences in QEEG in Psychopath Offenders 6 September 2019 | Clinical EEG and Neuroscience, Vol. 51, No. 3
- Executive dysfunction, violence and aggression Aggression and Violent Behavior, Vol. 51
- Psychometric properties of the Impulsive/Premeditated Aggression Scale in Portuguese community and forensic samples 1 June 2019 | Trends in Psychiatry and Psychotherapy, Vol. 41, No. 2
- Aggression and Violent Behavior, Vol. 47
- Workplace violence perpetrated by clients of health care: A need for safety and trauma‐informed care 30 October 2018 | Journal of Clinical Nursing, Vol. 28, No. 1-2
- Neurobiology of Brain Injury and its Link with Violence and Extreme Single and Multiple Homicides 16 February 2018
- Applied Nursing Research, Vol. 43
- Revue Neurologique, Vol. 174, No. 4
- Criminal Justice and Behavior, Vol. 45, No. 4
- Preventing aggressive/violent behavior: a role for biomarkers? Biomarkers in Medicine, Vol. 11, No. 9
- Psychological Medicine, Vol. 47, No. 7
- Prevalence and Correlates of Aggression and Hostility in Hospitalized Schizophrenic Patients 11 July 2016 | Journal of Interpersonal Violence, Vol. 32, No. 2
- Doriana Chialant , Ph.D. ,
- Judith Edersheim , M.D., J.D. ,
- Bruce H. Price , M.D.
- Journal of Veterinary Behavior, Vol. 16
- Psychology of Sport and Exercise, Vol. 22
- Serotonin and Dopamine Candidate Gene Variants and Alcohol- and Non-Alcohol-Related Aggression 3 June 2015 | Alcohol and Alcoholism, Vol. 50, No. 6
- Treatment of Aggressive and Violent Behavior 20 February 2015
- Cognitive Systems Research, Vol. 34-35
- L'Encéphale, Vol. 41, No. 5
- Safety Science, Vol. 78
- Val158Met COMT polymorphism and risk of aggression in alcohol dependence 3 October 2013 | Addiction Biology, Vol. 20, No. 1
- Impulsivity and Physical Aggression: Examining the Moderating Role of Anxiety The American Journal of Psychology, Vol. 127, No. 2
- Rousseau, Happiness and Human Nature 13 November 2012 | Political Studies, Vol. 62, No. 1
- Neurology and Neurochemistry of Crime 27 November 2018
- Aggression and Violent Behavior, Vol. 19, No. 1
- Aggression and Violent Behavior, Vol. 19, No. 3
- Journal of Psychiatric Research, Vol. 58
- The COMT Met158 allele and violence in schizophrenia: A meta-analysis Schizophrenia Research, Vol. 140, No. 1-3
- Journal of Family Violence, Vol. 27, No. 1
- International Review of Economics, Vol. 59, No. 4
- Persönlichkeitsstörungen
- Schizophrenia Bulletin, Vol. 38, No. 1
- Foreign Policy Analysis, Vol. 8, No. 2
- Genomic architecture of aggression: Rare copy number variants in intermittent explosive disorder 2 August 2011 | American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, Vol. 156, No. 7
- Manganese Exposure from Drinking Water and Children’s Classroom Behavior in Bangladesh Environmental Health Perspectives, Vol. 119, No. 10
- Current Psychology, Vol. 30, No. 4
- Aggression and Violent Behavior, Vol. 16, No. 6
- Journal of Criminal Justice, Vol. 39, No. 1
- Research in Veterinary Science, Vol. 91, No. 3
- An Exploratory Analysis of Factors Associated With Repeat Homicide in Canada 22 March 2010 | Homicide Studies, Vol. 14, No. 2
- Journal of Neural Transmission, Vol. 117, No. 3
- Neuroethics, Vol. 3, No. 1
- The Combative Patient
- États dangereux et troubles mentaux
- Accident Analysis & Prevention, Vol. 42, No. 6
- Medical Hypotheses, Vol. 74, No. 3
- Brain, Vol. 133, No. 12
- Low Resting Heart Rate and Antisocial Behavior 10 August 2009 | Criminal Justice and Behavior, Vol. 36, No. 11
- Evil: Illusion of 15 September 2009
- Influence of Functional Variant of Neuronal Nitric Oxide Synthase on Impulsive Behaviors in Humans Archives of General Psychiatry, Vol. 66, No. 1
- Psychiatry Research: Neuroimaging, Vol. 171, No. 3
- Polypharmacy With Second-Generation Antipsychotics: A Review of Evidence Journal of Psychiatric Practice, Vol. 14, No. 6
- The Neural Basis of Moral Cognition 3 April 2008 | Annals of the New York Academy of Sciences, Vol. 1124, No. 1
- Psychiatrie und Psychotherapie, Vol. 4, No. 2
- Aggression and Violent Behavior, Vol. 13, No. 5
- Physiology & Behavior, Vol. 94, No. 4
- Seyed Mohammad Assadi, M.D.
- Maryam Noroozian, M.D.
- Seyed Vahid Shariat, M.D.
- Omid Yahyazadeh, M.D.
- Mahdi Pakravannejad, M.D.
- Shahrokh Aghayan, M.D.
- Contrary to popular belief, a lack of behavioural inhibitory control may not be associated with aggression 27 June 2007 | Criminal Behaviour and Mental Health, Vol. 17, No. 3
- Aggression and Violent Behavior, Vol. 12, No. 1
- Schizophrenia Research, Vol. 97, No. 1-3
- Neuropsychopharmacology, Vol. 32, No. 11
- Steven G. Sugden, M.D.
- Shawn J. Kile, M.D.
- Robert L. Hendren, D.O.
- Journal of Family Violence, Vol. 21, No. 7
- Child and Adolescent Psychiatric Clinics of North America, Vol. 15, No. 2
- Psychiatry Research: Neuroimaging, Vol. 147, No. 2-3
- International Journal of Nursing Studies, Vol. 42, No. 2
- Journal of Abnormal Psychology, Vol. 114, No. 3
- Serial murder by children and adolescents 16 June 2004 | Behavioral Sciences & the Law, Vol. 22, No. 3
- Association of serotonin transporter promoter gene polymorphism with violence: relation with personality disorders, impulsivity, and childhood ADHD psychopathology 16 June 2004 | Behavioral Sciences & the Law, Vol. 22, No. 3
- Role of experience in processing bias for aggressive words in forensic and non-forensic populations 1 January 2004 | Aggressive Behavior, Vol. 30, No. 2
- Australian Emergency Nursing Journal, Vol. 7, No. 2
- Biological Psychiatry, Vol. 55, No. 5
- Aggression, psychopathology, and delinquency: influences of gender and maturation – where did all the good girls go?
- Antiaggressive Action of Combined Risperidone and Quetiapine in a Patient with Schizophrenia 1 July 2003 | The Canadian Journal of Psychiatry, Vol. 48, No. 6
- Expanding Evolutionary Psychology: toward a Better Understanding of Violence and Aggression 29 June 2016 | Social Science Information, Vol. 42, No. 1
- Journal of Psychiatric Research, Vol. 37, No. 6
- Experimental and Clinical Psychopharmacology, Vol. 11, No. 2
- International Journal of Men's Health, Vol. 2, No. 1
- Annotation: The role of prefrontal deficits, low autonomic arousal, and early health factors in the development of antisocial and aggressive behavior in children 21 April 2002 | Journal of Child Psychology and Psychiatry, Vol. 43, No. 4
- Biological Psychiatry, Vol. 52, No. 1
- VIOLENCE against Psychiatric Nurses: An Untreated Epidemic? Journal of Psychosocial Nursing and Mental Health Services, Vol. 40, No. 1
- Orbitofrontal and anterior cingulate cortex neurofibrillary tangle burden is associated with agitation in Alzheimer disease 1 March 2001 | Annals of Neurology, Vol. 49, No. 3
- Epilepsy & Behavior, Vol. 1, No. 3
- Child and Adolescent Psychiatric Clinics of North America, Vol. 9, No. 4
- Research article
- Open access
- Published: 23 January 2017
Mental illness and violent behavior: the role of dissociation
- Aliya R. Webermann 1 &
- Bethany L. Brand 2
Borderline Personality Disorder and Emotion Dysregulation volume 4 , Article number: 2 ( 2017 ) Cite this article
43k Accesses
12 Citations
67 Altmetric
Metrics details
The role of mental illness in violent crime is elusive, and there are harmful stereotypes that mentally ill people are frequently violent criminals. Studies find greater psychopathology among violent offenders, especially convicted homicide offenders, and higher rates of violence perpetration and victimization among those with mental illness. Emotion dysregulation may be one way in which mental illness contributes to violent and/or criminal behavior. Although there are many stereotyped portrayals of individuals with dissociative disorders (DDs) being violent, the link between DDs and crime is rarely researched.
We reviewed the extant literature on DDs and violence and found it is limited to case study reviews. The present study addresses this gap through assessing 6-month criminal justice involvement among 173 individuals with DDs currently in treatment. We investigated whether their criminal behavior is predicted by patient self-reported dissociative, posttraumatic stress disorder and emotion dysregulation symptoms, as well as clinician-reprted depressive disorders and substance use disorder.
Past 6 month criminal justice involvement was notably low: 13% of the patients reported general police contact and 5% reported involvement in a court case, although either of these could have involved the DD individual as a witness, victim or criminal. Only 3.6% were recent criminal witnesses, 3% reported having been charged with an offense, 1.8% were fined, and 0.6% were incarcerated in the past 6 months. No convictions or probations in the prior 6 months were reported. None of the symptoms reliably predicted recent criminal behavior.
Conclusions
In a representative sample of individuals with DDs, recent criminal justice involvement was low, and symptomatology did not predict criminality. We discuss the implications of these findings and future directions for research.
Stereotypes abound in the media regarding violent behavior and crimes among those with mental illness. One need not look further than popular crime television shows, the latest blockbuster film or news stories on perpetrators of atrocities such as school shootings or terrorist attacks. Researchers have worked to unpack the complex question of what role mental illness plays in violence, if any, especially in light of mass shootings in the United States at Sandy Hook Elementary, Virginia Tech University and Pulse Nightclub, among others. Researchers generally agree that there is some relationship between mental illness and the risk for violence, such that mental illness increases the risk for violence perpetration as well as victimization, but there is less consensus on the specific psychopathology and symptoms that contribute to violence.
A brief literature review on mental illness and violent behavior
Stereotypes about mental illness and violence are common among the general public. Link, Phelan, Bresnahan, Stueve and Pescosolido [ 1 ] presented a large sample ( N = 1444) with vignettes of people with mental illness, in which no violent behavior or thoughts were described, and inquired how likely it was that the “patient” would be violent. Many participants believed it likely that the hypothetical mentally ill individual would perpetrate violence: 17% of respondents endorsed violence as likely among those with minor interpersonal problems, and 33% and 61% thought violence was likely among people with major depression or schizophrenia, respectively. Individuals with mental illness are frequently aware of others’ negative perceptions of them, which can worsen isolation, negative affect and treatment adherence [ 2 , 3 ].
Individuals with psychological disorders that are highly stigmatized and misunderstood, such as schizophrenia, borderline personality disorder (BPD) and dissociative identity disorder (DID), often face harmful and inaccurate stereotypes which portray them as dangerous and untreatable menaces who require psychiatric or forensic institutionalization. However, as we will review in this study, it is a myth that individuals with DID are the most likely patients in the mental health system to be violent. Various methodologies have been used to study the link between mental illness and violence including: reporting on the prevalence of mental illness among convicted violent offenders, typically homicide defendants; examining violent behavior and crime among clinical populations; and assessing prevalence of violent behavior and crime among those with mental illness in the general population (see Tables 1 , 2 , 3 , 4 and 5 below for the results of studies utilizing each of these methodologies). Many studies examine only violence perpetration, but some examine victimization as well [ 4 – 6 ] (Table 1 ).
In research on the prevalence of mental illness among violent offenders, multiple studies have found the highest rates of violence among individuals with substance use disorders, rather than schizophrenia, BPD and other psychotic disorders [ 7 – 11 ] (Tables 2 and 3 ). Rates of substance use disorders (including alcohol use disorders and illicit substance use disorders) among self-reported violent offenders range from 20 to 42% [ 7 , 11 , 12 ] (Table 2 ). Rates of substance use disorders among convicted homicide offenders are lower but still noteworthy, ranging from 1 to 20% [ 8 , 9 , 13 , 14 ] (Table 3 ).
Other studies have approached the question of how mental illness intersects with violence through examining rates of violent behavior among clinical populations. These studies tend to focus on severe/serious mental illness (SMI), that is, disorders which cause or are associated with serious functional impairment or limitations on major life activities [ 15 ]. The majority of studies on violent behavior among SMI patients focus on schizophrenia, although some also include other SMIs such as bipolar disorder and antisocial personality disorder (Table 4 ). Studies on violent behavior and homicide among individuals with schizophrenia indicate these individuals are at increased risk for both violence perpetration and victimization, but that violence is often predicted by comorbid substance use, medication noncompliance and a recent history of being assaulted [ 16 – 18 ]. Studies on violent behavior among individuals with BPD indicate that emotion dysregulation is a longitudinal mediator of violent behavior and may be a primary mechanism that increases risk for violence in this population [ 19 , 20 ]. The complex DDs, including DID, have been conceptualized as disorders of emotional dysregulation and are often highly comorbid with BPD [ 21 ]. The association of emotion dysregulation with violence in DDs should be further examined.
Dissociative disorders and violent behavior
Notably missing from almost all studies on the intersection of mental illness and violent crime are individuals with dissociative disorders (DDs), including DID and DD not otherwise specified (DDNOS in DSM-IV)/other specified DD (OSDD in DSM-5). This is true of mixed clinical population studies [ 22 – 25 ], studies on violence and mental illness in the general population [ 7 , 11 , 12 , 26 ], as well as forensic studies of convicted violent offenders [ 8 , 9 , 13 , 14 , 27 ]. Although DID is missing from almost all the research on mental illness and violence, it gets an inordinate amount of focus in films about mental illness, particularly those in the horror and thriller genres such as Split , Psycho, Fight Club or Secret Window which portray people with dissociative self-states as prone to violence including homicide, or within comedies that poke fun at the “outlandishness” of dissociative self-states, such as Me, Myself and Irene. Given the paucity of research on violent behavior among individuals with DDs, coupled with the saturation of stereotypic portrayals of DDs in the media, misunderstanding abounds regarding what role dissociation plays in violent behavior, if any.
A few studies have examined dissociative symptoms, rather than DDs, as a predictor of violent interpersonal behavior within mixed clinical populations (Table 4 ). They typically focus on trait dissociation, that is, chronic and enduring dissociative experiences across multiple contexts [ 28 ], compared to state dissociation, e.g., transient, not enduring and time-limited dissociative experiences [ 29 ], the latter of which are often anecdotally reported by violent offenders, such as amnesia for a violent episode and violence-related dissociative episodes [ 30 ]. Quimby and Putnam [ 31 ] found that among adult psychiatric inpatients, trait dissociation was positively correlated with patient sexual aggression via staff reports. Kaplan and colleagues [ 32 ] found a positive correlation between trait dissociation and patient-reported general aggression among psychiatric outpatients. Dissociation has also been posited to play a role in the intergenerational transmission of domestic violence: grouping young mothers who were survivors of childhood maltreatment based on whether or not they abused their own children, Egeland and Susman-Stillman [ 33 ] found significantly greater trait dissociation among mothers who were abusive as compared to those who were not.
A number of case study reviews, conducted nearly three decades ago, reported high rates of violent behavior among patients with DID, according to reports by their treating clinicians [ 34 – 38 ] (Table 5 ). These studies were typically conducted with small samples derived from the authoring clinician’s case load, relied on clinician reports rather than patient self-report, utilized adult lifetime reporting timeframes rather than specified time frames (the latter is more typical of current studies on violence and mental illness), and did not attempt to objectively verify violent behavior through criminal records or other official documentation. Many studies inquired about DID patients’ violent and/or homicidal dissociative self-states. Footnote 1 Therapists reported that between 33 and 70% of DID patients had violent self-states [ 34 – 37 ]. At times, aggressive self-states within individuals with DID threaten other self-states, which some patients perceive to be internalized homicidal ideation and/or threats, but if carried out, would result in suicide and not homicide. Some of the studies reviewed above did not distinguish violent self-states who were violent towards the individual themselves versus those who were externally violent toward others [ 34 – 36 ]. Putnam and colleagues [ 37 ] make the distinction that while 70% of those with DID had violent or homicidal self-states, 53% of the aggressive self-states were “internally homicidal,” that is, with homicidal ideation toward another self-state. Some DID patients may misperceive these internally aggressive self-states as external violent people, rather than the patient being self-destructive or suicidal [ 39 ]. Putnam and colleagues [ 37 ] describe internalized homicidal behavior as occurring among 53% of their 100 DID patient sample. Some DID patients may also experience flashbacks of past violence perpetrated by another person against them and mistakenly believe they are perpetrating violence against someone else when in fact they are experiencing an intrusive recollection of the past [ 39 ].
Within these aforementioned case studies, clinicians reported that 38–55% of their DID patients had a history of any violent behavior [ 34 , 36 – 38 ]. Ross and Norton [ 38 ] reported that of 236 DID patients, 29% of the males and 10% of females reported being convicted of a crime, and the same percentage reported a history of incarceration. While the type of conviction and reason for incarceration were not specified, Ross and Norton [ 38 ] describe more antisocial behavior among men than women. Loewenstein and Putnam [ 36 ] and Putnam and colleagues [ 37 ] report high rates of sexual assault perpetration among their DID patient samples. Among an all-male sample, Loewenstein and Putnam [ 36 ] reported 13% of patients reported having perpetrated a sexual assault, while in a predominately female sample, Putnam and colleagues [ 37 ] reported 20% of patients reported having perpetrated sexual assault. Lewis, Yeager, Swica, Pincus and Lewis [ 40 ] reported severe childhood maltreatment and adult psychopathology among 12 DID inmates who were incarcerated for homicide. Two studies found 19% of DID patients had completed homicide [ 36 , 37 ]. Loewenstein and Putnam [ 36 ] attribute this extremely high rate of violent behavior to the childhood maltreatment these patients experienced which increases their risk for aggression and violence, as well as their reliance on an all-male sample, who have higher rates of violence. Alternatively, Putnam and colleagues [ 37 ] describe confusion about “personified intraphysic conflicts” among the patients leading to misperceptions about the degree of actual violence among DID patients, as described above.
These numbers are concerning, but they are not consistent with more recent studies of DD patients and clinicians that utilize different sampling techniques and designs. Within the international prospective Treatment of Patients with DD (TOP DD) Network Study, only 2% of clinicians and 4–7% of patients report that DD (including both DID and DDNOS/OSDD) patients perpetrated sexual coercion or sexual assault toward a partner in their adult lifetime [ 41 ]. Additionally, rates of perpetration of intimate partner violence were low among DD patients, according to therapists: only 3.5% of DD patients were reported by their TOP DD therapists as having perpetrated physical or sexual abuse toward a partner in their adult lifetime [ 6 ].
To date, no studies have examined the variables that might contribute to violence and/or criminal behavior among individuals with DDs. Given the important role that emotion dysregulation has had in predicting violence among individuals with BPD, emotion dysregulation should be examined as a possible contributing factor among individuals with DDs. Dissociative and PTSD symptoms may also be associated with violence or criminal behavior due to the possibility that when highly symptomatic, individuals with DDs may be overwhelmed and unable to manage their symptoms such that they become vulnerable to dyscontrol. Lastly, potential psychological comordities to DDs related to violent behavior within the literature, such as mood and substance use disorders, should be examined as potential explanatorty variables for recent criminal justice involvement.
The present study
Many questions remain regarding what role mental illness plays in violence. Are mentally ill individuals more likely to perpetrate violence compared to people who do not have mental illness? What psychiatric diagnoses are most highly associated with violent behavior and crime? Are individuals with DDs particularly likely to engage in violent and/or criminal behavior? The present study attempts to provide evidence on violent behavior and crime among individuals with DDs engaged in outpatient treatment.
The purpose of our study was threefold; first, to provide a review of the extant literature on DDs and violent behavior; second, to describe the prevalence of recent criminal justice involvement among a sample of treatment-engaged individuals with DDs; and third, to assess symptomatic predictors of violent behavior and crime among individuals with DDs, including dissociative, emotion dysregulation, posttraumatic stress disorder (PTSD) and depressive symptoms, as well as problematic substance use. We hypothesized that crime rates would be low in our sample of individuals with DDs, with the majority of patients reporting no recent criminal history or involvement with the criminal justice system, unless their involvement was as victims of crime. Additionally, we hypothesized that the aforementioned symptoms (dissociation, emotion dysregulation, PTSD, depression and substance use) would not be significantly associated with recent criminal behavior and justice system involvement.
Overview and recruitment
Clinician and patient participants were recruited through the Treatment of Patients with Dissociative Disorders (TOP DD) Network study. The TOP DD Network study is a longitudinal educational intervention study of patients with DDs who are diagnosed with either DID or DDNOS/OSDD. Over the course of 1 year, patients and clinicians watched weekly 7–15 min psychoeducational and skills training videos and completed written reflection and behavioral exercises. Additionally, therapist and patient participants completed surveys every 6 months (at baseline, 6, 12, 18 and 24 months) that provided additional clinical and behavioral data.
Clinicians were recruited through listservs for mental health professionals, professional trauma conferences and emails to participated in the first TOP DD study [ 42 , 43 ]. Clinicians were asked to enroll as a dyad with one DD patient from their caseload. All clinician and patient participants completed a voluntary consent process, and the study was approved by the Towson University Institutional Review Board. Eligibility requirements for patients in the TOP DD Network study included a DD diagnosis (DID, DDNOS or OSDD); being in treatment with their current clinician for at least 3 months prior to starting the study; reading English at an 8 th grade level; being willing to continue in individual therapy and complete approximately 2 ½ hours weekly of study activities; and being able to tolerate references to trauma, dissociation and safety struggles.
Participants
The total TOP DD Network study included 242 patients who completed baseline measures, presented after the screening measures which verified study eligibility. TOP DD Network study patient participants were majority female (88.6%), Caucasian (82.1%), middle-aged ( Median = 41), highly-educated (50.9% had at least a college diploma), and primarily resided in the United States (42.3%), although the study recruited internationally with a sizeable portion derived from Norway (27.5%) as well as other countries (30.2%). About half of participants (55.2%) were either in a dating or married relationship. Patients were primarily diagnosed by their therapists as having DID (63.4%). Clinician participants were primarily female (80%) and Caucasian (91.3%). Most reported years of experience as therapists ( Median = 15), as well as in treating trauma ( Median = 13), and dissociation ( Median = 8). Clinicians primarily worked in private practice (81.1%) or in an outpatient clinic or hospital (41.6%).
Patient measures
Criminal justice involvement.
DD patients were asked about involvement with the criminal justice system in the last 6 months including contact with the police, charges, convictions, court cases, fines, incarceration, probation, referral to mental health through the criminal justice system, and serving as a criminal witness. Participants could respond yes or no to these questions. Clinicians were not asked about their patients’ recent criminal justice involvement.
Trait dissociation
Trait dissociation was measured at baseline by the Dissociative Experiences Scale-II (DES) [ 28 ]. DES is a 28-item, 10-point scale (ranging from 0 to 100% of the time) where the participant indicates what percentage of the time a particular dissociative experience occurred within the past month. A meta-analysis by van Ijzendoorn and Schuengel [ 44 ] demonstrated test-retest reliability of .78–.93, α = .93, and convergent validity of r = .67. The measure was scored by adding the item frequency values and dividing by the total number of items, yielding an average summary score for each participant.
- Emotion dysregulation
Emotional dysregulation was measured at baseline by the Difficulties with Emotion Regulation Scale (DERS) [ 45 ]. DERS is a 36-item, 5-point scale (ranging from almost never [0–10% of the time] to almost always [91–100% of the time]) where the participant indicates what percentage of the time a particular difficulty with emotion regulation applies to them. The DERS has six subscales encompassing difficulties with accepting emotions, goal-directed behavior, impulse control, as well as lack of emotional awareness, emotional clarity and emotion regulation strategies. Gratz and Roemer [ 45 ] reported α > .80 for the six DERS subscales, while Mitsopoulou, Kafetsios, Karademas, Papastefanakis & Simos [ 46 ] demonstrated a test-retest reliability ranging from .63 to 81 for the six DERS subscales. The measure was scored by summing the item frequency values.
Posttraumatic stress disorder
PTSD symptomatology and severity was measured with PTSD Checklist-Civilian (PCL-C) [ 47 ]. The PCL-C is a 17-item, 5-point scale (ranging from not at all to extremely) where a participant indicates how often they have experienced a particular PTSD symptom within the past month. A total score of 50 points is the typical cutoff indicating a possible PTSD diagnosis [ 48 ]. Weathers and colleagues [ 47 ] reported a test–retest reliability of .96 with a retest interval of 2 to 3 days [ 47 ]. The measure was scored by summing all items together.
Depressive disorders were assessed by having clinicians report whether their patient currently had a diagnosis of either dysthymia or major depression (yielding answers of yes or no). Major depressive disorder and persistent depressive disorder (e.g., dysthymia) were assessed as potential predictors of criminal behavior.
Substance use
Substance use disorders were assessed by having clinicians report whether their patient currently had a diagnosis of a substance use disorder (differentiated from a substance/medication-induced mental disorder; answers were yes or no.)
Binary logistic regression was utilized to assess symptomatic predictors of recent criminal justice involvement in individuals with DDs. Logistic regression was chosen because it predicts membership for a dichotomous dependent variable (i.e., criminal justice involvement) from multiple independent variables, and is appropriate in cases of unequal group sample sizes. We ran eight separate logistic regressions to assess symptomatic predictors of each of the eight criminal justice involvement variables. We report Nagelkerke R squared effect sizes on the significant omnibus models. We adjusted alpha levels to account for multiple hypothesis testing, and the critical p -value = 0.0062. The sample size for the logistic regression models was N = 125, as variables were used from both clinician and patient surveys, and both pre-baseline screening and baseline surveys, which each contained slightly different sample sizes.
Prevalence of recent criminal justice involvement
Among 173 DD patients, 12.7% reported contact with the police within the last 6 months; the reasons for this contact were not queried. The patients reported low rates of recent criminal behavior in the last 6 months (Table 6 ): 4.8% reported involvement in a court case, although it is unknown what role the patient played in the court proceedings (e.g., witness, victim, alleged criminal); 3.6% were witnesses in a criminal case; 3% reported a legal charge; 1.8% reported a fine (s); 1.2% reported a criminal justice mental health referral; and 0.6% reported having been incarcerated. None of the 173 DD patients reported convictions or probation during the most recent 6 months.
Regarding the nature of criminal justice involvement, patients had the option of explaining criminal justice involvement they labeled as “other.” Eight individuals elected to complete the “other” open text box, indicating the following: calling the non-emergency police due to loud neighbors; reporting a substance abusing child to the police; reporting criminal offenses; participating in divorce court and domestic violence orders; receiving a traffic ticket; “[meeting] with secret service;” reporting a suspicious vehicle; and being admitted to the hospital with police involvement.
Symptomatic predictors of criminal justice involvement
Within binary logistic regressions assessing symptomatic predictors of eight types of recent criminal justice involvement, symptomatology significantly predicted recent contact with police, χ 2 (6) = 13.28, p < .05, Nagelkerke R 2 = 0.17. Post-hoc tests indicated that only PTSD symptoms (via the PCL-C) significantly predicted recent contact with police, p < .01. However, after applying the critical p -value = 0.0062, neither the omnibus model nor the post-hoc tests remained significant.
Symptomatology also significantly predicted recent contact with the court system, χ 2 (6) = 26.18, p < .001, Nagelkerke R 2 = 0.59. Post-hoc tests indicated that PTSD symptoms (via the PCL-C) significantly predicted recent contact with the court system, p < 01, as well as a substance use disorder diagnosis (via clinician report), p < .01. However, after applying the critical p -value = 0.0062, the post-hoc tests did not remain significant.
The present study had three aims: first, to provide a review of the extant literature on DDs and violent behavior; second, to describe the prevalence of recent criminal justice involvement among a sample of treatment-engaged individuals with DDs; and third, to assess symptomatic predictors of recent criminal justice involvement within the DD sample.
As we hypothesized, criminal justice involvement among individuals with DDs within the prior 6 months was low, according to patient self-reports. Specifically, patients reported the following in the prior 6 months: 4.8% were involved in a court proceeding, 3.6% were witnesses in a criminal case, 3% had a legal charge, 1.8% received a fine (s), 1.2% received a criminal justice mental health referral, and only 0.6% had been incarcerated. None of the DD patients reported convictions or probation during the past 6 months. This contrasts with prior case study reviews of DID patients in which clinicians reported a history of violent behavior among 29–55% of DID patients, and severely violent crime (e.g., homicide and sexual assault) among upwards of 20% of patients [ 34 , 36 – 38 ]. While the prior studies assess lifetime rates, as compared to the present study’s 6-month time frame, and relied on clinician reports rather than patient self-reports, the inconsistencies are instructive. The contrasting results may mean that as sampling and assessment techniques develop, research on individuals with DDs will increasingly suggest they are not as prone to violence or crime as initially thought, as violence towards self may have been conflated with violence towards others. Individuals with DD seem to pose a greater threat to themselves then to anyone else, as reflected in their very high rates of self-injurious behavior and frequent suicide attempts [ 42 , 43 , 49 ].
Additionally, our hypothesis that symptoms of emotion dysregulation, dissociation, PTSD, depression (major depressive disorder and persistent depressive disorder), and substance use disorder were not associated with criminal justice involvement in our sample was supported. Out of eight different types of recent criminal justice involvement, symptoms were able to significantly predict only DD patients’ recent contact with police, as well as recent court involvement, but the former omnibus model did not remain significant after applying the critical alpha which adjusted for Type I error due to multiple hypothesis testing. Regarding recent court involvement, PTSD symptoms and substsance use disorder symptoms significantly predicted recent court involvement, but again, these post-hoc tests did not remain significant after applying the critical alpha. Thus, no symptoms reliably predicted criminal behavior among those with DDs. More importantly, dissociative symptoms did not significantly predict any type of criminal justice involvement among our sample of DD patients. This counters the notion that dissociative symptoms increase risk for criminal and violent behavior. It is also possible that given the high level of dissociation and PTSD among our sample, the strength of the relationships could have been attenuated due to a ceiling effect.
Our study’s major limitations concern selection bias and the nature of data available on patients’ criminal justice involvement. First, our participants are in psychotherapeutic treatment and thus may not be representative of those with DDs who do not present to treatment, nor of those in the criminal justice system who have DDs and dissociation. Additionally, by definition, our sample experience severe and chronic trait dissociation, but some criminal behavior may be more related to state dissociation [ 29 , 30 ]. Second, our data on patients’ criminal justice system involvement was limited: we did not collect clinician reports of patients’ recent criminal justice involvement, details regarding the nature of patients’ recent criminal justice involvement (i.e., our data on police contact and court cases are ambiguous as to whether they indicate possible criminal behavior or being involved as a witness or victim), nor data on lifetime criminal justice involvement. Many studies on mental illness and violent behavior use lifetime rates, and thus this would facilitate comparisons across studies.
Using patient self-reports of criminal justice involvement in the present study may have provided more accurate responses than only using clinician reports, as it is possible that patients would not report criminal behavior to their clinicians due to social desirability concerns and taboos around criminality, although clinician reports would have been a useful adjunct to patient self-reports. Future studies should review criminal justice records for this population because lifetime memories can be difficult to accurately solicit due to amnesia, and due to the confusion some patients may experience between past and present as well as internal versus external events [ 39 ]. Future studies should assess both lifetime and recent criminal justice involvement, utilizing clinician reports and criminal justice records in addition to patient self-reports.
Studies on psychopathology and violent behavior should include DD individuals in their samples. Small forensic studies have assessed DDs in violent offenders [ 40 ] but larger epidemiological studies of violent offenders have not included DDs, despite assessing a range of psychopathology among offenders [ 7 – 9 , 11 – 14 , 26 , 27 ].
In summary, recent criminal justice involvement among our DD clinical sample is low, according to patient self-reports and is not predicted by dissociative, PTSD or emotion dysregulation symptoms, nor by clinician reported substance abuse disorders or mood disorders. This provides compelling evidence contradicting public and media misconceptions and stereotypes of those with DDs as highly prone to criminality and violence. Public awareness about DDs needs to improve through thoughtful and accurate portrayals of DD, as well as all mental illnesses, in media and literature so that stereotypes and stigma are replaced with understanding and scientifically based knowledge. Enduring stigmas portraying those with mental illness as violent may have considerable negative impacts on their treatment engagement, ability to seek out social support, and overall quality of life [ 2 , 3 ]. Reductions in stereotypes and stigma will allow those with mental illness to live more comfortably and safely and allow the general public to also be less fearful and more compassionate towards those with DDs and all forms of mental illness.
Sometimes referred to as personalities, identities or parts.
Abbreviations
Borderline personality disorder
- Dissociative disorders
Dissociative disorder not otherwise specified
Difficulties with Emotion Regulation Scale
Dissociative Experiences Scale
Dissociative identity disorder
Diagnostic and Statistical Manual of Mental Disorders
Other specified dissociative disorder
PTSD Checklist-Civilian
Severe mental illness
Treatment of Patients with Dissociative Disorders Network Study
Link BG, Phelan JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: Labels, causes, dangerousness, and social distance. Am J Public Health. 1999;89(9):1328–33.
Article CAS PubMed PubMed Central Google Scholar
Gonzales L, Davidoff KC, Nadal KL, Yanos PT. Microaggressions experienced by persons with mental illnesses: An exploratory study. Psychiatr Rehabil J. 2015;38(3):234–41.
Article PubMed Google Scholar
Stuart H. Media portrayal of mental illness and its treatments: What effect does it have on people with mental illness? CNS Drugs. 2006;20(2):99–106.
Crisanti AS, Frueh BC, Archambeau O, Steffen JJ, Wolff N. Prevalence and correlates of criminal victimization among new admissions to outpatient mental health services in Hawaii. Community Ment Health J. 2014;50(3):296–304.
Teplin LA, McClelland GM, Abram KM, Weiner DA. Crime victimization in adults with severe mental Illness: Comparison with the National Crime Victimization Survey. Arch Gen Psychiatry. 2005;62(8):911–21.
Article PubMed PubMed Central Google Scholar
Webermann AR, Brand BL, Chasson GS. Childhood maltreatment and intimate partner violence in dissociative disorder patients. Eur J Psychotraumatol. 2014;5:1–8.
Article Google Scholar
Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2009;66(2):152–61.
Fazel S, Grann M. Psychiatric morbidity among homicide offenders: A Swedish population study. Am J Psychiatry. 2004;161(11):2129–31.
Flynn S, Abel KM, While D, Mehta H, Shaw J. Mental illness, gender and homicide: A population-based descriptive study. Psychiatry Res. 2011;185(3):368–75.
González RA, Igoumenou A, Kallis C, Coid JW. Borderline personality disorder and violence in the UK population: Categorical and dimensional trait assessment. BMC Psychiatry. 2016;16:1–10.
Swanson JW, Holzer CE, Ganju VK, Jono RT. Violence and psychiatric disorder in the community: Evidence from the Epidemiologic Catchment Area surveys. Hosp Community Psychiatry. 1990;41(7):761–70.
CAS PubMed Google Scholar
Coker KL, Smith PH, Westphal A, Zonana HV, McKee SA. Crime and psychiatric disorders among youth in the US population: An analysis of the national comorbidity survey–adolescent supplement. J Am Acad Child Adolesc Psychiatry. 2014;53(8):888–98.
Rodway C, Flynn S, While D, Rahman MS, Kapur N, Appleby L, Shaw J. Patients with mental illness as victims of homicide: A national consecutive case series. Lancet Psychiatry. 2014;1(2):129–34.
Simpson AF, McKenna B, Moskowitz A, Skipworth J, Barry-Walsh J. Homicide and mental illness in New Zealand, 1970–2000. British J Psychiatry. 2004;185(5):394–8.
Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15–4927, NSDUH Series H-50). Center for Behavioral Health Statistics and Quality. 2015. https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf . Retrieved 3 Aug 2016.
Gourion D. Schizophrenia and violence: A common developmental pathway? In: Verrity PM, editor. Violence and aggression around the globe. Hauppauge: Nova; 2007. p. 29–44.
Google Scholar
Swanson JW, Borum R, Swartz MS, Monahan J. Psychotic symptoms and disorders and the risk of violent behaviour in the community. Crim Behav Ment Health. 1996;6(4):309–29.
Walsh E, Gilvarry C, Samele C, Harvey K, Manley C, Tattan T, Tyrer P, Creed F, Murray R, Fahy T. Predicting violence in schizophrenia: A prospective study. Schizophr Res. 2004;67(2–3):247–52.
Newhill CE, Eack S, Mulvey EP. A growth curve analysis of emotion dysregulation as a mediator for violence in individuals with and without borderline personality disorder. J Pers Disord. 2012;26(3):452–67.
Scott LN, Stepp SD, Pilkonis PA. Prospective associations between features of borderline personality disorder, emotion dysregulation, and aggression. Pers Disord. 2014;5(3):278–88.
Brand BL, Lanius RA. Chronic complex dissociative disorders and borderline personality disorder: Disorders of emotion dysregulation? Borderline Personal Disord Emot Dysregul. 2014;1:13.
Bruce M, Cobb D, Clisby H, Ndegwa D, Hodgins S. Violence and crime among male inpatients with severe mental illness: Attempting to explain ethnic differences. Soc Psychiatry Psychiatr Epidemiol. 2014;49(4):549–58.
Hodgins S, Alderton J, Cree A, Aboud A, Mak T. Aggressive behaviour, victimisation and crime among severely mentally ill patients requiring hospitalisation. British J Psychiatry. 2007;191(4):343–50.
Matejkowski JC, Cullen SW, Solomon PL. Characteristics of persons with severe mental illness who have been incarcerated for murder. J Am Acad Psychiatry Law. 2008;36(1):74–86.
PubMed Google Scholar
Jordan B, Schlenger WE, Fairbank JA, Caddell JM. Prevalence of psychiatric disorders among incarcerated women: Convicted felons entering prison. Arch Gen Psychiatry. 1996;53(6):513–9.
Article CAS PubMed Google Scholar
Crime in the United States, 2014. United States Department of Justice, Federal Bureau of Investigation.2015. https://ucr.fbi.gov/crime-in-the-u.s/2014/crime-in-the-u.s.-2014/cius-home . Retrieved 3 Aug 2016.
Wilcox DE. The relationship of mental illness to homicide. Am J Forensic Psychiatry. 1985;6(1):3–15.
Carlson EB, Putnam FW. An update on the Dissociative Experiences Scale. Dissociation. 1993;6(1):16–27.
Kruger C, Mace CJ. Psychometric validation of the State Scale of Dissociation (SSD). Psychol Psychother Theory Res Pract. 2002;75:33–51.
Moskowitz A. Dissociation and violence: A review of the literature. Trauma Violence Abuse. 2004;5(1):21–46.
Quimby LG, Putnam FW. Dissociative symptoms and aggression in a state mental hospital. Diss. 1991;4(1):21–4.
Kaplan ML, Erensaft M, Sanderson WC, Wetzler S, Foote B, Asnis GM. Dissociative symptomatology and aggressive behavior. Compr Psychiatry. 1998;39(5):271–6.
Egeland B, Susman-Stillman A. Dissociation as a mediator of child abuse across generations. Child Abuse Negl. 1996;20(11):1123–32.
Dell PF, Eisenhower JW. Adolescent multiple personality disorder: A preliminary study of eleven cases. J Am Acad Child Adolesc Psychiatry. 1990;29(3):359–66.
Kluft RP. The parental fitness of mothers with multiple personality disorder: A preliminary study. Child Abuse Negl. 1987;11(2):273–80.
Loewenstein RJ, Putnam FW. The clinical phenomenology of males with MPD: A report of 21 cases. Dissociation. 1990;3(3):135–43.
Putnam FW, Guroff JJ, Silberman EK, Barban L, Post RM. Clinical phenomenology of multiple personality disorder: review of 100 recent cases. J Clin Psychiatry. 1986;47(6):285–93.
Ross CA, Norton GR. Differences between men and women with multiple personality disorder. Hosp Community Psychiatry. 1989;40(2):186–8.
International Society for the Study of Trauma and Dissociation. Guidelines for treating dissociative identity disorder in adults, third revision. J Trauma Dissociation. 2011;12(2):115–87.
Lewis D, Yeager CA, Swica Y, Pincus JH, Lewis M. Objective documentation of child abuse and dissociation in 12 murderers with dissociative identity disorder. Am J Psychiatry. 1997;154(12):1703–10.
Webermann AR, Brand BL. The sitting duck syndrome: What contributes to dissociative patients’ being victims and perpetrators of violence? Symposium to be presented to the 33rd Annual International Society for the Study of Trauma and Dissociation (ISSTD) Conference. 2016.
Brand BL, Classen C, Lanius R, Loewenstein R, McNary S, Pain C, Putnam FW. A naturalistic study of dissociative identity disorder and dissociative disorder not otherwise specified patients treated by community clinicians. Psychol Trauma. 2009;1(2):153–71.
Brand BL, McNary SW, Myrick AC, Classen CC, Lanius R, Loewenstein RJ, Pain C, Putnam FW. A longitudinal naturalistic study of patients with dissociative disorders treated by community clinicians. Psychol Trauma. 2013;5(4):301–8.
van Ijzendoorn MH, Schuengel C. The measurement of dissociation in normal and clinical populations: Meta-analytic validation of the Dissociative Experiences Scale (DES). Clin Psychol Rev. 1996;16(5):365–82.
Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26(1):41–54.
Mitsopoulou E, Kafetsios K, Karademas E, Papastefanakis E, Simos PG. The Greek version of the Difficulties in Emotion Regulation Scale: Testing the factor structure, reliability and validity in an adult community sample. J Psychopathol Behav Assess. 2013;35(1):123–31.
Weathers FW, Litz BT, Huska JA, Keane TM. The PTSD Checklist—Civilian Version (PCL-C). Boston: National Center for PTSD; 1994.
Weathers FW, Ford J. Psychometric review of PTSD Checklist. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville: Sidran Press; 1996. p. 250–1.
Webermann AR, Myrick AC, Taylor CL, Chasson GS, Brand BL. Dissociative, depressive, and PTSD severity as correlates of non-suicidal self-injury and suicidality in dissociative disorder patients. J Trauma Dissociation. 2016;17(1):67–80.
Download references
Acknowledgements
The authors warmly thank the patients and therapists who generously donated their time to participate in the TOP DD Network study.
The authors declare that this research was funded by foundations (i.e., ANS Research, Constantinidas Family Foundation), private donations (including from Anne Bartello and family, Brad Foote, M.D. and gifts made to Sheppard Pratt Health System’s Trauma Disorders Research Program and Towson University’s Foundation), and grants from Towson University.
Availability of data and materials
Please contact corresponding author for data requests.
Authors’ contributions
ARW conducted the literature review, analyzed the data and drafted the manuscript. BLB is the Principal Investigator for the study from which the data is derived (the TOP DD Network Study), developed the methods and assisted in manuscript writing. Both authors read and approved the final manuscript.
Authors’ information
Aliya R. Webermann, M.A., is a clinical/community doctoral student at University of Maryland, Baltimore County (UMBC), USA and a graduate of the clinical psychology master’s program at Towson University. Ms. Webermann’s research primarily concerns the links between intimate partner violence, complex trauma and trauma and dissociative disorders. Bethany L. Brand, Ph.D., is the Martha A. Mitten Professor of Psychology at Towson University and maintains an independent practice in clinical psychology on Towson, Maryland, USA. She serves as an expert witness in criminal, civil, disability and employment matters. Dr. Brand conducts research on the assessment and treatment of trauma disorders, including the assessment of feigned dissociative disorders.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The TOP DD Network Study received approval from the Towson University Institutional Review Board in 2014, IRB number IRB00002844. All particpants completed an informed consent process before participating in the study.
Author information
Authors and affiliations.
University of Maryland Baltimore County, 1000 Hilltop Circle, Math/Psychology Building Rm. 312, Baltimore County, Baltimore, MD, 21250, USA
Aliya R. Webermann
Department of Psychology, Towson University, Towson, 21252, MD, USA
Bethany L. Brand
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Aliya R. Webermann .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Webermann, A.R., Brand, B.L. Mental illness and violent behavior: the role of dissociation. bord personal disord emot dysregul 4 , 2 (2017). https://doi.org/10.1186/s40479-017-0053-9
Download citation
Received : 30 October 2016
Accepted : 13 January 2017
Published : 23 January 2017
DOI : https://doi.org/10.1186/s40479-017-0053-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Criminal behavior
- Dissociation
- Violent crime
Borderline Personality Disorder and Emotion Dysregulation
ISSN: 2051-6673
- General enquiries: [email protected]
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Mental Illness Too Often Wrongly Associated With Gun Violence
- Katie O'Connor
Search for more papers by this author
People with mental illness are more likely to be the victims of violence than perpetrators, but mass shootings are often incorrectly associated with psychiatric illnesses. Psychiatrists can help educate the public about evidence-based strategies that reduce gun violence.

Only 4% of the violence that occurs in the United States can be attributed to people with mental illness, yet when incidents of gun violence occur, they are almost immediately associated with psychiatric illnesses.
Words such as “psycho,” “crazy,” and “insane” are often used in media coverage of events such as mass shootings, explained Dhruv Gupta, M.D., a PGY-3 psychiatry resident at the Icahn School of Medicine at Mount Sinai Hospital. That media coverage perpetuates a stigma that people with mental illness are inherently dangerous was addressed by Gupta and his colleagues during the session “Why Blaming Violence on Mental Illness Is Misleading: A Call for Multifaceted and Evidence-Based Strategies to Reduce Gun Violence” at APA’s online 2021 Annual Meeting in May.

Psychiatrists are often asked to predict who may become perpetrators of violence, but often family members are in a better position to report when an individual may do something violent, says Alisa Gutman, M.D.
The presenters pointed out that people with mental illness are far more likely to be the victims of violence than the perpetrators. Research shows that of all the violence that occurs in the United States, 96% is due to risk factors other than mental illness, said Alisa Gutman, M.D., Ph.D., the founder and medical director of the Philadelphia Human Rights Clinic. Referring to mental illness during every conversation about violence “further stigmatizes what is already a marginalized group of individuals who are suffering with severe symptoms,” Gutman said. “That’s unacceptable, and as psychiatrists, we need to take a public stand.”
In some circumstances, psychiatric patients may have a high risk of violence perpetration compared with the general population, including when in emergency departments or involuntarily committed. First-episode psychosis patients also have a higher risk of violence. Yet the risk of violence may be correlated with other systemic concerns, such as poverty, crime victimization, involvement with illegal drugs, and early life trauma, which people with serious mental illness also commonly experience, Gutman explained.
“We must ask ourselves: When we’re looking at the perpetration of violence in individuals with serious mental illness, what’s the actual factor here that’s resulting in violent actions?” Gutman said. In most cases, the data support that, outside of high-risk periods, the violence perpetration risk is not higher than that of individuals in the general population, she said.

“While restricting firearm access on the basis of certain dangerous behaviors is supported by evidence, restricting access on the basis of a mental illness diagnosis is not,” says Jessica Bayner, M.D.
There are a number of risk factors for gun violence, including being young, male, and disadvantaged and misusing drugs or alcohol, explained Jessica Bayner, M.D., a recent graduate of the child and adolescent psychiatry track of the Forensic Psychiatry Fellowship at the University of Pennsylvania. She is a consultant and forensic psychiatrist in Auckland, New Zealand. “Evidence points to the fact that violence risk is better characterized by behaviors than diagnoses,” Bayner said.
She pointed to examples of this theory being used effectively to reduce gun violence. A California law passed in 1991 that prohibits firearm ownership among people charged with a violent misdemeanor resulted in a 29% reduction in arrests for new crimes involving guns and other violence. Similarly, cities and states with laws prohibiting people who are subject to domestic violence restraining orders from having guns had 25% fewer intimate-partner homicides.
The most prevalent question that audience members asked after the presentation was “Can psychiatrists effectively predict who may commit acts of violence?” “It’s not for us to predict all the violence that will occur,” Gutman said. “Ultimately, the people who spend time with an individual every day, such as family members, are in a better position to notice high-risk times when an individual may become violent.”
Yet, Bayner pointed out, as of April 2020, only 19 states and Washington, D.C., had some type of red-flag law, which allows family members to petition a court to temporarily remove firearms from people deemed a danger to themselves or others.
Gun violence is a hugely complex issue and requires a variety of stakeholders to address, said Ahmar Mannan Butt, M.D., an adult and child psychiatrist at Broadlawns Medical Center in Des Moines, Iowa. “One discipline cannot address this multifaceted issue,” Butt said. “We need help from all disciplines, and education is the first step.” ■


Is Mental Illness the Cause or the Result of Violence?
Research calls for us to know the difference..
Posted August 25, 2022 | Reviewed by Lybi Ma
By David Spiegel, M.D., with Sarah Sherwood, M.A.
The recent horrific shootings in Philadelphia, Buffalo, and at Robb Elementary School in Uvalde, Texas, perfectly illustrate some of the reasons that many children and their parents are experiencing troubling mental health issues. They're living in a very frightening world that feels out of control. We watch as Russia invades its neighbor Ukraine. Sars-Co-V-2 infects, kills, and mutates around the world. Wildfires spread as the globe heats. And for parents, who want to model the right response for their kids, the levels of fear and anxiety are also higher than ever recorded.
Earlier this Spring, the U.S. Department of Health and Human Services (HHS) published a study in the American Medical Association’s journal JAMA Pediatrics that reports significant increases in the number of children diagnosed with mental health conditions. The study, conducted by the Health Resources and Services Administration (HRSA), finds that between 2016 and 2020, the number of children ages 3-17 years diagnosed with anxiety grew by 29 percent and those with depression by 27 percent. According to the American Psychological Association (APA), adults and parents are experiencing anxiety as well. 1 In a mental health study we conducted early in the pandemic, we found that young people and women were the most profoundly affected. 1
Mental Illness Vs. Just Plain Violent
Our country pays a high price for each act of mass violence. Not only the immediate victims, survivors, their families and friends, but our communities, children, and families suffer. How do we explain the violence that the perpetrator inflicted? It has become popular to assert that mental illness is the cause. But is it?
The APA asserts that diagnosis alone cannot determine who may commit violence. 2 In fact, the vast majority of violent offenders are not mentally ill, as years of research have proven. According to research published by the APA, of all crimes committed by people with serious mental disorders, only 7.5 percent were directly related to symptoms of mental illness. 3 Furthermore, in the study, there was no relationship between mental illness symptoms and the crime . Yet, we continue to associate mental illness and criminality, often with intense debate. 4
In fact, more often than not, we are blaming the victims. We know that people with mental illness are actually more likely to be a victim of violent crime than a perpetrator of a crime. 5 Many of the symptoms of psychiatric conditions are behaviors considered antisocial or criminal. 6 As a result, we have the false perception of a causal relationship between psychiatric illness and criminality.
People naturally want to feel safer, and they have turned to owning guns themselves as a solution, attempting to calm their stress and anxiety over the increase in violence in the country. In a Stanford study of 26.3 million California residents published in the New England Journal of Medicine (NEJM), among those who had acquired handguns, the risk of suicide by firearm was 7.8 times higher for men and 35 times higher for women compared with non-handgun owners. 2 Suicide rates by other means were not any higher among handgun owners. This study confirmed a previous case-control study also published in the New England Journal of Medicine , that showed that in homes containing firearms, the odds of dying by suicide are three to five times greater than among non-gun owners. 7
In a more recent study, the Stanford team addressed the question of whether possession of firearms at home provides protection against homicide. 3 In this study of 17.6 million California residents, the researchers found that the rates of death by homicide were more than twice as high among those who lived in homes with guns, and the risk of being killed by a spouse or intimate partner was seven-fold higher; 84 percent of these victims were women. Thus, the presence of a firearm in the home provided risk, not protection.
This is especially important because one in three homes in the U.S. contain at least one firearm, and the evidence from ecological and case-controlled research suggests that gun access has the opposite effect. It is clear that gun violence is a cause of mental illness, not the product of it. Easy access to guns increases the risk of suicide, homicide, and serious injury. The threat of such tragedies and their occurrence causes substantial mental stress, and prevention is always preferable. Direct and indirect exposure to such dangers has deleterious effects on our mental health.
How We Can Respond to the Stress of Violence in Our Society
Still, those who witness violence can be greatly affected by what they see, even on the evening news. All of us need, at the very least, remedies for our fear and anxiety, ones that really work. These solutions should involve a plan of daily mental health maintenance. Having a daily practice of de-compressing after watching the news or whenever one is stressed by societal troubles is paramount. It is wise to limit the daily amount of traumatic input from social and other media. Verbal and physical conflict is now a constant reality in our culture, with cult-like characters who shock us, almost daily. We must make sure we take good care of ourselves.

As a researcher and psychiatrist, I have spent my career talking about stress and the benefits of hypnosis and self-hypnosis to relieve stress. Because of years of close examination and study, we know that hypnosis, the oldest known therapy , helps with the stress and anxiety we’ve been experiencing. Think of hypnosis as a natural anesthesia for stress. Proven by years of science, it provides deep relaxation and the state of flow we need to reset our busy, worried brains. Like meditation practice, many people are capable of doing hypnosis on their own.
Other therapeutic tools that may help, when used regularly, are:
- Self-hypnosis via technology can be more convenient and private than a hypnosis session
- Calming music can create a hypnotic state as well
- Cognitive therapy or talking through what you feel
- Talking with a close friend you feel you can confide in
- Meaningful volunteer work
We need this reset because stress and anxiety have become all too common. You can set up a healthy, daily practice of reversing stress that is proven by science. Better yet, you want to have a household that is more stress and anxiety resistant for years to come.
Co-author Sarah Sherwood is a science writer and social scientist based in San Mateo, California.
1.Adamson MM, Phillips A, Seenivasan S, Martinez J, Grewal H, Kang X, Coetzee J, Luttenbacher I, Jester A, Harris OA, Spiegel D. International Prevalence and Correlates of Psychological Stress during the Global COVID-19 Pandemic. International journal of environmental research and public health. 2020;17(24). Epub 2020/12/17. PubMed PMID: 33321950; PMCID: PMC7763004.
2.Studdert DM, Zhang Y, Swanson SA, Prince L, Rodden JA, Holsinger EE, Spittal MJ, Wintemute GJ, Miller M. Handgun Ownership and Suicide in California . N Engl J Med. 2020;382(23):2220-9. PubMed PMID: 32492303.
3.Studdert DM, Zhang Y, Holsinger EE, Prince L, Holsinger AF, Rodden JA, Wintemute GJ, Miller M. Homicide Deaths Among Adult Cohabitants of Handgun Owners in California , 2004 to 2016: A Cohort Study. Annals of internal medicine. 2022;175(6):804-11. Epub 20220405. PubMed PMID: 35377715.

David Spiegel, M.D. , is Willson Professor and Associate Chair of Psychiatry and Behavioral Sciences at Stanford University School of Medicine, and a co-founder of stress reduction app, Reveri.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Opportunities & Announcements
- Funding Strategy for Grants
- Grant Writing & Approval Process
- Managing Grants
- Clinical Research
- Small Business Research
Research on the Mental Health Consequences of Violence and Trauma
Program Announcement
The National Institute of Mental Health (NIMH) encourages investigator-initiated research to enhance scientific understanding about the etiology of psychopathology related to violence and trauma, as well as studies to develop and test effective treatments, services, and prevention strategies in this area. The NIMH mission encompasses the conduct and support of biomedical and behavioral research, and the translation of scientifically generated information into clinical applications and interventions implemented in the community.
The populations and phenomenon of concern include children, youth, adults, and the elderly, males and females, and all racial and ethnic groups. Studies of interest can focus on victims/survivors of interpersonal violence and crime, such as child abuse and neglect, rape, sexual assault, family violence, community violence and victims/survivors of major traumatic events, such as combat and war, mass shootings, terrorism, natural and technological disaster, refugee trauma and relocation, and torture.
Because the consequences of violence and traumatic stress typically involve several factors, the portfolio of NIMH research is multidisciplinary in nature. For example, the portfolio encompasses animal studies of the biological and behavioral effects of unpredictable and uncontrollable stress, mechanistic and descriptive studies of behavioral and biological dysregulation in humans, and clinical studies examining how the severity of post traumatic symptoms is linked to neural functioning, processing of memories, and interpretations of trauma. It also encompasses research to develop, test, and disseminate effective interventions addressing the sequelae of violence and trauma. NIMH encourages research that incorporates genetic, environmental, and neurobiological parameters as they relate to adjustment and psychopathology throughout life, as well as studies of implementation of proven treatments at the individual, clinic, organizational, and systems levels.
Areas of interest include:
- Studies of interactions among psychosocial and biological risk factors that increase or decrease risk for and course (escalation, persistence, and cessation) of psychopathology.
- Studies of the type and incidence of mental disorders resulting from exposure to violence and traumatic events, including studies of psychological or biological changes; also studies of the diagnosis, assessment, and course of PTSD and other trauma-related disorders and the appropriate threshold for clinical significance.
- Studies of psychosocial and psychobiological risk factors associated with differential risk of negative effects in different victim subgroups, as well as studies of psychosocial and psychobiological mechanisms by which interventions work and for whom.
- Research on the contributions of sleep patterns and pathophysiological indicators of stress and anxiety, including the failure to extinguish negative imagery, on risk and resilience.
- Development of assessment and screening instruments to guide treatment planning and management plans for victims of violence and traumatic events.
- Intervention studies testing the efficacy and refinement of individual, family, and/or community-level models and methods of prevention, treatment and services.
- Studies of system level effects of post-disaster service delivery.
- Studies of the effectiveness of interventions for victimization in various social and community settings, and the influence of social, institution, and community settings on the availability of interventions, program participation, and outcomes; use of different conceptual and intervention models with various social and cultural groups.
- Development of innovative, effective, and ethical methods of obtaining and maintaining the participation in research of victims of violence and traumatic events.
Potential applicants are encouraged to consult with program contacts regarding relevant research announcements and grant types.
Farris Tuma, Sc.D. Division of Adult Translational Research and Treatment Development National Institute of Mental Health 6001 Executive Boulevard, Room 5197, MSC 9589 Bethesda, MD 20892-9589 Telephone: 301-443-5944 Fax: 301-480-4415 Email: [email protected]
Steven J. Zalcman, M.D. Division of Adult Translational Research and Treatment Development National Institute of Mental Health 6001 Executive Boulevard, Room 7177 MSC 9639 Bethesda, MD 20892-9639 301-443-1692 Fax: 301-402-4740 Email: [email protected]
Denise Juliano-Bult, MSW Division of Services and Intervention Research National Institute of Mental Health 6001 Executive Boulevard, Room 7146 MSC 963 Bethesda, MD 20892-9639 Phone: 301-443-1638 Fax: 301-443-4045 Email: [email protected]
Criminal Psychology and the Criminal Justice System in India and Beyond pp 69–92 Cite as
Mental Disorders, Violence, and Crime
- Sanjeev P. Sahni 3 &
- Karishma 3
- First Online: 02 October 2021
542 Accesses
Mental disorders are identified by a set of signs and symptoms causing significant clinical distress or impairment in an individual’s functioning. The relationship between mental disorders and crime has been a topic of research and heated controversy since many decades. There is a consensus advocating a link between the two. However, the exact nature of the relationship is quite complex. Though individuals with mental disorders are frequently perceived as the perpetrators of crime, emerging research shows that they are more likely to be victimized than committing a crime. Moreover, mental disorders cannot be perceived as a singular variable and need to be understood as distinct categories with different levels of sense of judgement, touch with reality, decision-making, and so forth. To understand the culpability of such individuals, these aspects need to be established clearly. This chapter elaborates upon the categories of mental disorders that are frequently associated with crime namely psychotic spectrum disorders, addiction disorders, personality disorders, dissociative disorders, and sexual disorders, and their respective association with criminal offending.
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Ahlers, C. J., Schaefer, G. A., Mundt, I. A., Roll, S., Englert, H., Willich, S. N., & Beier, K. M. (2011). How unusual are the contents of paraphilias? Paraphilia-associated sexual arousal patterns in a community-based sample of men. The Journal of Sexual Medicine, 8 (5), 1362–1370.
Article Google Scholar
Alavi, S. S., Ferdosi, M., Jannatifard, F., Eslami, M., Alaghemandan, H., & Setare, M. (2012). Behavioral addiction versus substance addiction: Correspondence of psychiatric and psychological views. International Journal of Preventive Medicine, 3 (4), 290.
Google Scholar
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. BMC Medicine, 17 , 133–137.
Andreasen, N. C. (1986). Scale for the assessment of thought, language, and communication (TLC). Schizophrenia Bulletin, 12 (3), 473.
Angermeyer, M. C., Dietrich, S., Pott, D., & Matschinger, H. (2005). Media consumption and desire for social distance towards people with schizophrenia. European Psychiatry, 20 (3), 246–250.
Arasi, N. K. (2016). Internet addiction and cyber crime engagement () f undergraduate students. Journal of Gducational Research S 6xtension , 55 (5).
Bo, S., Abu-, A., Kongerslev, M., Haahr, U. H., & Simonsen, E. (2011). Risk factors for violence among patients with schizophrenia. Clinical Psychology Review, 31 (5), 711–726.
Bourget, D., Gagne, P., & Wood, S. F. (2007). Dissociation: Defining the concept in criminal forensic psychiatry. Journal of the American Academy of Psychiatry and the Law, 45 (2), 147–160.
Brand, B. L., Sar, V., Stavropoulos, P., Krüger, C., Korzekwa, M., Martínez-Taboas, A., & Middleton, W. (2016). Separating fact from fiction: An empirical examination of six myths about dissociative identity disorder. Harvard review of psychiatry .
Brand, M., Young, K. S., & Laier, C. (2014). Prefrontal control and Internet addiction: A theoretical model and review of neuropsychological and neuroimaging findings. Frontiers in Human Neuroscience, 8 , 375.
Coid, J., Yang, M., Roberts, A., Ullrich, S., Moran, P., Bebbington, P., … & Singleton, N. (2006). Violence and psychiatric morbidity in a national household population—a report from the British Household Survey. American Journal of Epidemiology , 164 (12), 1199-1208.
Copes, H., Hochstetler, A., & Sandberg, S. (2015). Using a narrative framework to understand the drugs and violence nexus. Criminal Justice Review, 40 (1), 32–46.
Darke, S., Torok, M., Kaye, S., Ross, J., & McKetin, R. (2010). Comparative rates of violent crime among regular methamphetamine and opioid users: Offending and victimization. Addiction, 105 (5), 916–919.
De la Rosa, M., Lambert, E., & Cropper, B. (1990). Drugs and Violence: Causes, Correlates, and Consequences, National Institute of Drug Abuse Research Monograph 103. Rockville, Maryland: National Institute on Drug Abuse .
Degenhardt, L., Charlson, F., Ferrari, A., Santomauro, D., Erskine, H., Mantilla-Herrara, A., ... & Rehm, J. (2018). The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet Psychiatry , 5 (12), 987–1012.
Dennis, M. L., Chan, Y. F., & Funk, R. R. (2006). Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. American Journal on Addictions, 15 (sup1), 80–91.
Dobbert, D. L. (2007). Understanding Personality Disorders: An Introduction: An Introduction . ABC-CLIO.
Dorahy, M. J., Brand, B. L., Şar, V., Krüger, C., Stavropoulos, P., Martínez-Taboas, A., ... & Middleton, W. (2014). Dissociative identity disorder: An empirical overview. Australian & New Zealand Journal of Psychiatry , 48 (5), 402–417.
Dreger, A. (2010). Of kinks, crimes, and kinds: The paraphilias proposal for the DSM-5. Science and Society
Dressing, H., Sartorius, A., & Meyer-, A. (2008). Implications of fMRI and genetics for the law and the routine practice of forensic psychiatry. Neurocase, 14 (1), 7–14.
Eher, R., Rettenberger, M., & Schilling, F. (2010). Psychiatric diagnoses of sexual offenders: An empirical investigation of 807 delinquents imprisoned for child abuse and rape. Z Sexualforsch, 23 , 23–35.
Farrell, H. M. (2011). Dissociative identity disorder: Medicolegal challenges. Journal of the American Academy of Psychiatry and the Law Online, 39 (3), 402–406.
Fazel, S., Gulati, G., Linsell, L., Geddes, J. R., & Grann, M. (2009). Schizophrenia and violence: systematic review and meta-analysis. PLoS medicine , 6 (8), e1000120.
Fish, F. J., Casey, P. R., & Kelly, B. (2007). Fish's clinical psychopathology: signs and symptoms in psychiatry . RCPsych Publications.
Fitzgerald, P. B., De Castella, A. R., Filia, K. M., Filia, S. L., Benitez, J., & Kulkarni, J. (2005). Victimization of patients with schizophrenia and related disorders. Australian and New Zealand Journal of Psychiatry, 39 (3), 169–174.
Galbicsek, C. (2019, July). Alcohol Related Crimes . Retrieved from https://www.alcoholrehabguide.org/alcohol/crimes/
Gask, L., Evans, M., & Kessler, D. (2013). Personality disorder. Bmj , 347 , f5276.
Gentile, J. P., Snyder, M., & Gillig, P. M. (2014). Stress and trauma: Psychotherapy and pharmacotherapy for depersonalization/derealization disorder. Innovations in Clinical Neuroscience, 11 (7–8), 37.
Ghiasi, N., & Singh, J. (2019). Psychiatric illness and criminality. In StatPearls [Internet] . StatPearls Publishing.
Goldstein, P. J. (1985). The drugs/violence nexus: A tripartite conceptual framework. Journal of Drug Issues, 15 (4), 493–506.
Goodman, A. (1990). Addiction: Definition and implications. British Journal of Addiction, 85 (11), 1403–1408.
Graff-Radford, J., Whitwell, J. L., Geda, Y. E., & Josephs, K. A. (2012). Clinical and imaging features of Othello’s syndrome. European Journal of Neurology, 19 (1), 38–46.
Grant, J. E., Potenza, M. N., Weinstein, A., & Gorelick, D. A. (2010). Introduction to behavioral addictions. The American Journal of Drug and Alcohol Abuse, 36 (5), 233–241.
Hammersley, R., Forsyth, A., Morrison, V., & Davies, J. B. (1989). The relationship between crime and opioid use⋆. British Journal of Addiction, 84 (9), 1029–1043.
Hartman, R. L., & Huestis, M. A. (2013). Cannabis effects on driving skills. Clinical Chemistry, 59 (3), 478–492.
Harvard health Publishing (2019, March). Schizotypal Personality Disorder . Retrieved from https://www.health.harvard.edu/a_to_z/schizotypal-personality-disorder-a-to-z
Havnes, I. A., Clausen, T., Brux, C., & Middelthon, A. L. (2014). The role of substance use and morality in violent crime-a qualitative study among imprisoned individuals in opioid maintenance treatment. Harm Reduction Journal, 11 (1), 24.
Hodgins, S. (1998). Epidemiological investigations of the associations between major mental disorders and crime: Methodological limitations and validity of the conclusions. Social Psychiatry and Psychiatric Epidemiology, 33 (1), S29–S37.
Holden, C. (2001). ‘Behavioral'addictions: do they exist?.
India Today. (2018, October). Delhi teen who stabbed parents 26 times was addicted to online game: Police. Retrieved from https://www.indiatoday.in/india/story/delhi-teen-who-stabbed-parents-26-times-was-addicted-to-online-game-police-1366758-2018-10-12
Janofsky, J. S., Hanson, A., Candilis, P. J., Myers, W. C., Zonana, H., Irving, B., ... & Merideth, P. (2014). AAPL practice guideline for forensic psychiatric evaluation of defendants raising the insanity defense. Journal of the American Academy of Psychiatry and the Law , 42 , S3–S76.
Johnson, S. C., & Elbogen, E. B. (2013). Personality disorders at the interface of psychiatry and the law: Legal use and clinical classification. Dialogues in Clinical Neuroscience, 15 (2), 203.
Joyal, C. C., & Carpentier, J. (2017). The prevalence of paraphilic interests and behaviors in the general population: A provincial survey. The Journal of Sex Research, 54 (2), 161–171.
Kandel, E. R., & Kandel, D. B. (2014). A molecular basis for nicotine as a gateway drug. New England Journal of Medicine, 371 (10), 932–943.
Karishma, P. N. & Kumar, K. (2017). Is it Personality or the Alcohol that makes one an addict? In Chikkara, B.S. & Shanwal, V.K. (Eds), Alcoholism: Causes, symptoms effects and treatment . Manakin Press.
Kay, S. R., Fiszbein, A., & Opler, L. A. (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin, 13 (2), 261–276.
Kendell, R. E. (2002). The distinction between personality disorder and mental illness. The British Journal of Psychiatry, 180 (2), 110–115.
King, D. L., & Delfabbro, P. H. (2014). Internet gaming disorder treatment: A review of definitions of diagnosis and treatment outcome. Journal of Clinical Psychology, 70 (10), 942–955.
Kiran, & & Chaudhary. (2009). Understanding delusions. Indian Journal of Psychiatry., 18 (1), 3–18.
Kircher, T., Bröhl, H., Meier, F., & Engelen, J. (2018). Formal thought disorders: From phenomenology to neurobiology. The Lancet Psychiatry, 5 (6), 515–526.
Kirkpatrick, B., Fenton, W. S., Carpenter, W. T., & Marder, S. R. (2006). The NIMH-MATRICS consensus statement on negative symptoms. Schizophrenia Bulletin, 32 (2), 214–219.
Kumar, A. (2017, December). Experts examine if internet addiction led to Noida Teenage boy killing family members . Retrieved from https://www.news18.com/news/india/experts-examine-if-internet-addiction-led-to-noida-teenage-boy-killing-family-members-1602619.html
Kuss, J. D., Griffiths, D. M., Karila, L., & Billieux, J. (2014). Internet addiction: A systematic review of epidemiological research for the last decade. Current Pharmaceutical Design, 20 (25), 4026–4052.
Lawyer Monthly. (2019, October). 10 countries where gambling is completely illegal . Retrieved from https://www.lawyer-monthly.com/2018/02/10-countries-where-gambling-is-completely-illegal/
Lowenstein, J., Purvis, C., & Rose, K. (2016). A systematic review on the relationship between antisocial, borderline and narcissistic personality disorder diagnostic traits and risk of violence to others in a clinical and forensic sample. Borderline Personality Disorder and Emotion Dysregulation, 3 (1), 14.
Lincoln, T. M., & Hodgins, S. (2008). Is lack of insight associated with physically aggressive behavior among people with schizophrenia living in the community? The Journal of Nervous and Mental Disease, 196 (1), 62–66.
M. H. S. A. U., & Office of the Surgeon General (US. (2016). Facing addiction in America: The Surgeon General's report on alcohol, drugs, and health .
Marzuk, P. M. (1996). Violence, crime, and mental illness: How strong a link? .
Mayo Clinic. (n.d). Personality Disorders . Retrived from https://www.mayoclinic.org/diseases-conditions/personality-disorders/symptoms-causes/syc-20354463
McManus, M. A., Hargreaves, P., & Lee Rainbow, L. J. A. (2013). Paraphilias: Definition, diagnosis and treatment. F1000prime reports , 5 .
Medrano, K. (2019). 30 places where weed is legal . Retrieved from https://www.thrillist.com/vice/30-places-where-weed-is-legal-cities-and-countries-with-decriminalized-marijuana
Meier, M. H., Caspi, A., Ambler, A., Harrington, H., Houts, R., Keefe, R. S., … & Moffitt, T. E. (2012). Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of the National Academy of Sciences , 109 (40), E2657–E2664.
Mental Health Daily. (2015). Delusions of Persecution: Causes, Symptoms, Treatment. Retrieved from https://mentalhealthdaily.com/2015/05/13/delusions-of-persecution-causes-symptoms-treatment/
Mitra, S., Mahintamani, T., Kavoor, A. R., & Nizamie, S. H. (2016). Negative symptoms in schizophrenia. Industrial Psychiatry Journal, 25 (2), 135.
Morgan, V. A., Morgan, F., Valuri, G., Ferrante, A., Castle, D., & Jablensky, A. (2013). A whole-of-population study of the prevalence and patterns of criminal offending in people with schizophrenia and other mental illness. Psychological Medicine, 43 (9), 1869–1880.
National Collaborating Centre for Mental Health (UK). (2010). Antisocial Personality Disorder: Treatment, Management and Prevention. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK55350/
National Institute of Health. (2011, November). Why Nicotine is a Gateway Drug. Retrieved from https://www.nih.gov/news-events/nih-research-matters/why-nicotine-gateway-drug
National Institute of Mental Health. (n.d). Schizophrenia. Retrieved from https://www.nimh.nih.gov/health/statistics/schizophrenia.shtml
National Mental Health Survey of India, 2015–2016. (2016). Prevalence, Patterns and Outcomes, Supported by Ministry of Health and Family Welfare, Government of India, and Implemented by National institute of Mental Health and Neurosciences (NIMHANS) Bengaluru: In Collaboration with Partner Institutions. Retrieved from http://indianmhs.nimhans.ac.in/Docs/Report2.pdf
Noll, R. (2009). The encyclopedia of schizophrenia and other psychotic disorders . Infobase Publishing.
Nykodym, N., Ariss, S., & Kurtz, K. (2008). Computer addiction and cyber crime. Journal of Leadership, Accountability and Ethics , 78.
Oser, C. B., Mooney, J. L., Staton-Tindall, M., & Leukefeld, C. G. (2009). The drugs—violence nexus among rural felony probationers. Journal of Interpersonal Violence, 24 (8), 1285–1303.
Owen, P. R. (2012). Portrayals of schizophrenia by entertainment media: A content analysis of contemporary movies. Psychiatric Services, 63 (7), 655–659.
Paris, J. (2019). Dissociative identity disorder: Validity and use in the criminal justice system. Bjpsych Advances, 25 (5), 287–293.
Pastwa-Wojciechowska, B. (2011). The relationship of pathological gambling to criminality behavior in a sample of Polish male offenders. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research , 17 (11), CR669.
Patel, J., & Marwaha, R. (2019). Cannabis Use Disorder. In StatPearls [Internet] . StatPearls Publishing.
Pedersen, W., & Skardhamar, T. (2010). Cannabis and crime: Findings from a longitudinal study. Addiction, 105 (1), 109–118.
Peele, S., & Brodsky, A. (1975). Love and addiction.
Pickard, H. (2015). Choice, deliberation, violence: Mental capacity and criminal responsibility in personality disorder. International Journal of Law and Psychiatry, 40 , 15–24.
Porter, S., Birt, A. R., Yuille, J. C., & Hervé, H. F. (2001). Memory for murder: A psychological perspective on dissociative amnesia in legal contexts. International Journal of Law and Psychiatry, 24 (1), 23–42.
Rasmussen, S. A., Mazurek, M. F., & Rosebush, P. I. (2016). Catatonia: Our current understanding of its diagnosis, treatment and pathophysiology. World Journal of Psychiatry, 6 (4), 391.
Rohde, D. (October, 1999). Witness Tearfully Describe Fatal Subway shoving, The New York Times . Retrieved from https://www.nytimes.com/1999/10/09/nyregion/witness-tearfully-describes-fatal-subway-shoving.html
Rose, S. (January, 2017). From Split to Psycho: why cinema fails dissociative identity disorder . The Guardian . Retrieved from https://www.theguardian.com/film/2017/jan/12/cinema-dissociative-personality-disorder-split-james-mcavoy
Rosenthal, R. J., & Lorenz, V. C. (1992). The pathological gambler as criminal offender: Comments on evaluation and treatment. Psychiatric Clinics, 15 (3), 647–660.
Sadock, B. J., Sadock, V. A., & Ruiz, P. (2017). Comprehensive textbook of psychiatry (10th ed.).
Sar, V. (2011). Epidemiology of dissociative disorders: An overview. Epidemiology Research International , 2011 .
Şar, V. (2014). The many faces of dissociation: Opportunities for innovative research in psychiatry. Clinical Psychopharmacology and Neuroscience, 12 (3), 171.
Sestoft, D. (2006). Crime and mental illness: It is time to take action. World Psychiatry, 5 (2), 95.
Sheil, W. (2018). Medical definition of psychotropic drug . Retrived from https://www.medicinenet.com/script/main/art.asp?articlekey=30807
Sitarz, R., Rogers, M., Bentley, L., & Jackson, E. (2014). Internet addiction to child pornography .
Soyka, M. (2000). Substance misuse, psychiatric disorder and violent and disturbed behaviour. The British Journal of Psychiatry, 176 (4), 345–350.
Sperry, L. (2016). Handbook of diagnosis and treatment of DSM-5 personality disorders: Assessment, case conceptualization, and treatment . Routledge.
Book Google Scholar
Spiegel, D., Lewis-, R., Lanius, R., Vermetten, E., Simeon, D., & Friedman, M. (2013). Dissociative disorders in DSM-5. Annual Review of Clinical Psychology, 9 , 299–326.
Stone, M. H. (2007). Violent crimes and their relationship to personality disorders. Personality and Mental Health, 1 (2), 138–153.
Taborda, J. G., & Michalski-Jaeger, C. A. (2012). Sexual disorders and crime. Current Opinion in Psychiatry, 25 (5), 370–374.
Tappan, P. W. (1960). Crime, justice, and correction . McGraw-Hill Companies.
The Economic Times. (2018, Septempber). Section 377: Here is everything you need to know. Retrieved from https://economictimes.indiatimes.com/news/politics-and-nation/sc-delivers-historic-verdict-heres-everything-you-need-to-know-about-section-377/articleshow/65698429.cms?from=mdr
TNM Staff. (2019, September). Karnataka Shocker: 21-year-old allegedly beheads father for not letting play him PUBG. Retrieved from https://www.thenewsminute.com/article/karnataka-shocker-21-yr-old-allegedly-beheads-father-not-letting-him-play-pubg-108613
Tyrer, P., & Simonsen, E. (2003). Personality disorder in psychiatric practice. World Psychiatry, 2 (1), 41.
Varshney, M., Mahapatra, A., Krishnan, V., Gupta, R., & Deb, K. S. (2016). Violence and mental illness: What is the true story? Journal of Epidemiology and Community Health, 70 (3), 223–225.
Wehring, H. J., & Carpenter, W. T. (2011). Violence and schizophrenia .
World Health Organization. (1992). The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines . World Health Organization.
World Health Organization. (2017). Alcohol and drug disorders: Global Health Estimates. Retrieved from https://www.who.int/substance_abuse/activities/fadab/msb_adab_2017_GHE_23June2017.pdf
Young, K. S. (1998). Internet addiction: The emergence of a new clinical disorder. Cyberpsychology & Behavior, 1 (3), 237–244.
Download references
Author information
Authors and affiliations.
Jindal Institute of Behavioural Sciences, O.P. Jindal Global University, Sonipat, Haryana, India
Sanjeev P. Sahni & Karishma
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sanjeev P. Sahni .
Editor information
Editors and affiliations.
Sanjeev P. Sahni
Poulomi Bhadra
Rights and permissions
Reprints and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter.
Sahni, S.P., Karishma (2021). Mental Disorders, Violence, and Crime. In: Sahni, S.P., Bhadra, P. (eds) Criminal Psychology and the Criminal Justice System in India and Beyond. Springer, Singapore. https://doi.org/10.1007/978-981-16-4570-9_5
Download citation
DOI : https://doi.org/10.1007/978-981-16-4570-9_5
Published : 02 October 2021
Publisher Name : Springer, Singapore
Print ISBN : 978-981-16-4569-3
Online ISBN : 978-981-16-4570-9
eBook Packages : Law and Criminology Law and Criminology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Science Reveals a Silver Lining to Dark Behaviors
For psychological scientists, exploring the less pleasant aspects of individual and social nature is an occasional necessity.

Research Topic: Aggression and Violence
In the first webinar of APS’s Science for Society series on September 20, 2023, scientists and advocates shared their expertise and perspectives on the relationship between gun violence and anxiety.

How Owning a Gun Raises Anxiety
In the first webinar of APS's Science for Society series on September 20, 2023, scientists and advocates shared their expertise and perspectives on the relationship between gun-violence and anxiety.

Science for Society: Insights from Psychological Science on Gun Violence and Anxiety
Podcast: Dr. Amanda Nickerson joins Under the Cortex to explore the developmental pathways and risk factors for being exposed to gun-related violence.

Do Lockdown Drills Create Anxiety? New Research Says No
A group activity can help students reflect on different kinds of dehumanization and brainstorm a more prosocial path forward.


Teaching: Understanding Our Inner Darkness May Shed Light into Humanity’s Common Good
“The one gene, one disease idea is a thing of the past.” Scientists aren’t simply trying to identify people who are innately predisposed to incivility, immorality, or lawlessness. They’re examining how parenting, education, and other life experiences trigger those biological leanings.

The Bad-Behavior Blend
Research on war, conflict, and authoritarianism published in various APS journals between 2008 and 2020.

Collected Research on War, Conflict, and Authoritarianism
As of December 2021, a record 82.4 million people have been forced to flee their homes to escape war, violence, or persecution. Here’s a look at some recent research (2017–2021) on refugee integration and well-being.

New Research on Refugee Integration and Well-Being
Addressing a crisis like this means looking directly at the problem-solving needs that arise in times of war, danger, or difficulty and empowering ourselves to meet these needs.

Trauma and Ukraine: The World Health Organization Leveraged Psychological Science to Help Prepare Us for This Moment
Arielle Baskin-Sommers explores the cognitive-affective processes associated with disinhibition and community violence.

Back Page: Environment and Disinhibition
We’ve all been on the receiving end of an angry glare, whether from a teacher, parent, boss, or significant other. These angry expressions seem to boost the effectiveness of threats without actual aggression, according to

Angry Faces Back Up Verbal Threats, Making Them Seem More Credible
Most research on negotiations has shown that showing anger can win you larger concessions, but a psychological study shows it can hurt your cause when used in certain cultural environments.

Cultural Reactions to Anger Expression can Affect Negotiation Outcomes
Research reveals unequivocal evidence that exposure to media violence increases the likelihood of aggressive and violent behavior in both immediate and long-term contexts.
Does Onscreen Violence Beget Real-World Violence?
Long thought to result from fragile self-esteem, bullying may instead stem from grandiose, inflated, and narcissistic self-assessment, some psychological scientists argue.

Back-to-school dilemma: Why do bullies bully?
Using eye-tracking technology, researchers have found that women with a history of depression tend to spend more time looking at the angry faces compared to women with no history of depression.

Attention to Angry Faces May Predict Future Depression
Violent individuals are often assumed to suffer from a long history of mental illness that compels them to act destructively, but the link between psychosis and aggressive acts may be weak.

Psychosis and Violence Aren’t Strongly Linked
A large data analysis shows only minimal impact of violent video games on aggressive behavior, but scientists say they need better measures to confirm those findings.

Researchers Delve Into Data on Video Games and Aggression in Kids
A mix of behavioral research, economic studies, and time-series data portend some unsettling effects of climate change on human social interactions.
Global Warming and Violent Behavior
Findings from a longitudinal study suggest that childhood bullying may lead to long-lasting health consequences, impacting psychosocial risk factors for cardiovascular health well into adulthood.

Childhood Bullying Linked to Health Risks in Adulthood
The latest issue of Perspectives on Psychological Science is dedicated to the singular topic of microaggressions: statements, policies, and environmental cues that carry racial and prejudicial overtones.

Current Understandings of Microaggressions: Impacts on Individuals and Society
Angry negotiators can make irrational decisions that lead to lower offers, but researchers from Saarland University demonstrate that a simple self-regulation plan can help cooler heads prevail.

Anger Derails Negotiations, Unless You Have a Plan
If you are worried about violent video games triggering aggressive behavior in children, new research may help to alleviate your concerns.

Violent Video Games and Aggression: The Connection is Dubious, at Best
Hot weather seems to amplify people’s responses to provocation, ultimately increasing rates of aggressive behavior and violence.

Does Hot Weather Fuel Road Rage?
A meta-analysis finds no clear link between video game violence and aggression in children.
Violent Video Games and Aggression: The Connection Is Dubious, at Best
People tend to view a social media comment that calls out offensive behavior positively, but not when it's echoed by several other commenters.

When Moral Outrage Goes Viral, It Can Come Across as Bullying
Instructors should be prepared to listen for —and challenge — belief perseverance, and can use this myth to highlight how automatic and difficult belief perseverance can be to overcome.

Myth: People With Mental Illness Are More Prone to Violence
A study involving Dutch Police Academy recruits suggests that aggressive individuals may be more sensitive to the effects of testosterone when faced with emotionally charged situations.

Testosterone May Dampen Police Recruits’ Emotional Control
Aggression appears to relate to superior anger-identification abilities.

Physically Aggressive People Spot Anger in Ambiguity
New findings raise the possibility that men with a specific mix of biology and personality traits may be prone to aggressive driving as well as other fiery behavior.
How DNA and Testosterone May Affect Men’s Driving
Spanking at age 5 is associated with increased behavior problems 1 and 3 years later -- an increase that cannot be attributed to characteristics of the child or the family environment

Spanking Linked to Increase in Children’s Behavior Problems
Narrative interventions using storytelling may provide impactful solutions for shifting behavioral intentions, beliefs, and attitudes around extremist violence.

Extremism Threatened. Radio “Narratives” Intervened.
Civil unrest and political violence may be related to the psychological burden of the COVID-19 pandemic.

The Burden of the COVID-19 Pandemic May Motivate Outbreaks of Violent Protest and Antigovernment Sentiment
The National Institutes of Health (NIH) has issued an invitation to researchers who currently hold an R01 or R21 grant to expand the focus of their research to include firearms research.

NIH Grant Funding for Firearms Injury and Mortality Prevention Research
The very same technologies that make social distancing bearable in the age of COVID-19 have also been cited among leading causes of social isolation and mental health issues. Psychological research suggests a more nuanced reality.
Technology in Context: The Surprising Social Upsides of Constant Connectivity
Repeated incidences of racial discrimination and violence have far reaching consequences for mental health.

Student Notebook: Police Brutality and Mental Health in the African-American Community
With the passage of the 2020 US funding bill in December, US federal funding dollars will finally be allocated for research on gun violence and ways to prevent it.

Funding for Gun-Violence Research Ends 20-Year Drought
NIH has issued a new funding opportunity to support research on injuries and death resulting from firearms. This cross-NIH opportunity is another in a line of new grants that support research on this topic.
New NIH Grant Opportunity to Study Firearms Injury and Mortality Prevention
A study shows the role that “plausible deniability" may in discriminatory behavior against marginalized groups.

“But I Didn’t Know!” People Show Prejudice-Based Aggression When It’s Easily Deniable
A longitudinal twin study suggests that victimization makes general and far-reaching contributions to mental disorders.

Unpacking the Link Between Teen Victimization and Mental Illness
Learn what researchers have discovered about the factors that lead to bullying and the long-term consequences it can have.
A new study links workplace bullying to negative health outcomes for employees, including increases in long-term sick leave and prescriptions for antidepressants.

Workplace Bullying May Be Linked to Long-Term Health Issues
Leaders who view themselves as less competent are much more likely to act out aggressively towards their subordinates.

What To Do When the Boss is a Bully?
Research exploring factors that contribute to wrongful convictions reveals a path for addressing the serious consequences of wrongful incarceration.

Convicted by Memory, Exonerated by Science
Research in psychological science reveals the causes and consequences of bullying behavior in the office.
Workplace Bullying
New research associates early life adversity with the presentation of social anxiety disorder later in life.

The Emerging Self: Social Anxiety Disorder and Emotional Maltreatment in Childhood
Kitty Genovese's murder caught the attention of the public and psychological scientists alike, but new research indicates we’ve had the story all wrong for the last 50 years.

A New Look at the Killing of Kitty Genovese: The Science of False Confessions
Psychological science on the effects of prejudice, and how to counter these beliefs.

Bias and Stigma
People who score high on a measure of sadism seem to derive pleasure from behaviors that hurt others, and are even willing to expend extra effort to make someone else suffer, a study shows.

Everyday Sadists Take Pleasure In Others’ Pain
Why are we scared of some things and not others? Psychological scientists are exploring the many facets of fear and the mechanisms that drive it.

Victims of workplace bullying often become stressed and anxious, making them easy targets for additional abuse.

The Vicious Cycle of Workplace Bullying
The intense exhaustion of parental burnout can lead parents to feel detached from their children and unsure of their parenting abilities.

Parental Burnout Can Lead to Harmful Outcomes for Parent and Child
Research aimed at understanding men who sexually harass subordinates in the workplace suggest these individuals are able to convince themselves they're not to blame for their behavior.

Harassers Tend to Deflect Blame for Their Behavior, Study Suggests
A look at several researchers who have studied racism in recent years. Collectively, they address the nature of racism and the social processes that maintain it; examine the issues of structural and institutional racism; explore the consequences of various forms of racism; and suggest possible paths of action to combat racism.

Racism: Further Considerations from Psychological Science
Privacy overview.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- BOOK REVIEW
- 29 March 2024
The great rewiring: is social media really behind an epidemic of teenage mental illness?
- Candice L. Odgers 0
Candice L. Odgers is the associate dean for research and a professor of psychological science and informatics at the University of California, Irvine. She also co-leads international networks on child development for both the Canadian Institute for Advanced Research in Toronto and the Jacobs Foundation based in Zurich, Switzerland.
You can also search for this author in PubMed Google Scholar
You have full access to this article via your institution.

Social-media platforms aren’t always social. Credit: Getty
The Anxious Generation: How the Great Rewiring of Childhood is Causing an Epidemic of Mental Illness Jonathan Haidt Allen Lane (2024)
Two things need to be said after reading The Anxious Generation . First, this book is going to sell a lot of copies, because Jonathan Haidt is telling a scary story about children’s development that many parents are primed to believe. Second, the book’s repeated suggestion that digital technologies are rewiring our children’s brains and causing an epidemic of mental illness is not supported by science. Worse, the bold proposal that social media is to blame might distract us from effectively responding to the real causes of the current mental-health crisis in young people.
Haidt asserts that the great rewiring of children’s brains has taken place by “designing a firehose of addictive content that entered through kids’ eyes and ears”. And that “by displacing physical play and in-person socializing, these companies have rewired childhood and changed human development on an almost unimaginable scale”. Such serious claims require serious evidence.

Collection: Promoting youth mental health
Haidt supplies graphs throughout the book showing that digital-technology use and adolescent mental-health problems are rising together. On the first day of the graduate statistics class I teach, I draw similar lines on a board that seem to connect two disparate phenomena, and ask the students what they think is happening. Within minutes, the students usually begin telling elaborate stories about how the two phenomena are related, even describing how one could cause the other. The plots presented throughout this book will be useful in teaching my students the fundamentals of causal inference, and how to avoid making up stories by simply looking at trend lines.
Hundreds of researchers, myself included, have searched for the kind of large effects suggested by Haidt. Our efforts have produced a mix of no, small and mixed associations. Most data are correlative. When associations over time are found, they suggest not that social-media use predicts or causes depression, but that young people who already have mental-health problems use such platforms more often or in different ways from their healthy peers 1 .
These are not just our data or my opinion. Several meta-analyses and systematic reviews converge on the same message 2 – 5 . An analysis done in 72 countries shows no consistent or measurable associations between well-being and the roll-out of social media globally 6 . Moreover, findings from the Adolescent Brain Cognitive Development study, the largest long-term study of adolescent brain development in the United States, has found no evidence of drastic changes associated with digital-technology use 7 . Haidt, a social psychologist at New York University, is a gifted storyteller, but his tale is currently one searching for evidence.
Of course, our current understanding is incomplete, and more research is always needed. As a psychologist who has studied children’s and adolescents’ mental health for the past 20 years and tracked their well-being and digital-technology use, I appreciate the frustration and desire for simple answers. As a parent of adolescents, I would also like to identify a simple source for the sadness and pain that this generation is reporting.
A complex problem
There are, unfortunately, no simple answers. The onset and development of mental disorders, such as anxiety and depression, are driven by a complex set of genetic and environmental factors. Suicide rates among people in most age groups have been increasing steadily for the past 20 years in the United States. Researchers cite access to guns, exposure to violence, structural discrimination and racism, sexism and sexual abuse, the opioid epidemic, economic hardship and social isolation as leading contributors 8 .

How social media affects teen mental health: a missing link
The current generation of adolescents was raised in the aftermath of the great recession of 2008. Haidt suggests that the resulting deprivation cannot be a factor, because unemployment has gone down. But analyses of the differential impacts of economic shocks have shown that families in the bottom 20% of the income distribution continue to experience harm 9 . In the United States, close to one in six children live below the poverty line while also growing up at the time of an opioid crisis, school shootings and increasing unrest because of racial and sexual discrimination and violence.
The good news is that more young people are talking openly about their symptoms and mental-health struggles than ever before. The bad news is that insufficient services are available to address their needs. In the United States, there is, on average, one school psychologist for every 1,119 students 10 .
Haidt’s work on emotion, culture and morality has been influential; and, in fairness, he admits that he is no specialist in clinical psychology, child development or media studies. In previous books, he has used the analogy of an elephant and its rider to argue how our gut reactions (the elephant) can drag along our rational minds (the rider). Subsequent research has shown how easy it is to pick out evidence to support our initial gut reactions to an issue. That we should question assumptions that we think are true carefully is a lesson from Haidt’s own work. Everyone used to ‘know’ that the world was flat. The falsification of previous assumptions by testing them against data can prevent us from being the rider dragged along by the elephant.
A generation in crisis
Two things can be independently true about social media. First, that there is no evidence that using these platforms is rewiring children’s brains or driving an epidemic of mental illness. Second, that considerable reforms to these platforms are required, given how much time young people spend on them. Many of Haidt’s solutions for parents, adolescents, educators and big technology firms are reasonable, including stricter content-moderation policies and requiring companies to take user age into account when designing platforms and algorithms. Others, such as age-based restrictions and bans on mobile devices, are unlikely to be effective in practice — or worse, could backfire given what we know about adolescent behaviour.
A third truth is that we have a generation in crisis and in desperate need of the best of what science and evidence-based solutions can offer. Unfortunately, our time is being spent telling stories that are unsupported by research and that do little to support young people who need, and deserve, more.
Nature 628 , 29-30 (2024)
doi: https://doi.org/10.1038/d41586-024-00902-2
Heffer, T., Good, M., Daly, O., MacDonell, E. & Willoughby, T. Clin. Psychol. Sci. 7 , 462–470 (2019).
Article Google Scholar
Hancock, J., Liu, S. X., Luo, M. & Mieczkowski, H. Preprint at SSRN https://doi.org/10.2139/ssrn.4053961 (2022).
Odgers, C. L. & Jensen, M. R. J. Child Psychol. Psychiatry 61 , 336–348 (2020).
Article PubMed Google Scholar
Orben, A. Soc . Psychiatry Psychiatr. Epidemiol. 55 , 407–414 (2020).
Valkenburg, P. M., Meier, A. & Beyens, I. Curr. Opin. Psychol. 44 , 58–68 (2022).
Vuorre, M. & Przybylski, A. K. R. Sci. Open Sci. 10 , 221451 (2023).
Miller, J., Mills, K. L., Vuorre, M., Orben, A. & Przybylski, A. K. Cortex 169 , 290–308 (2023).
Martínez-Alés, G., Jiang, T., Keyes, K. M. & Gradus, J. L. Annu. Rev. Publ. Health 43 , 99–116 (2022).
Danziger, S. Ann. Am. Acad. Pol. Soc. Sci. 650 , 6–24 (2013).
US Department of Education. State Nonfiscal Public Elementary/Secondary Education Survey 2022–2023 (National Center for Education Statistics, 2024).
Google Scholar
Download references
Competing Interests
The author declares no competing interests.
Related Articles

- Public health
Use fines from EU social-media act to fund research on adolescent mental health
Correspondence 09 APR 24

AI-fuelled election campaigns are here — where are the rules?
World View 09 APR 24

Why loneliness is bad for your health
News Feature 03 APR 24

Circulating myeloid-derived MMP8 in stress susceptibility and depression
Article 07 FEB 24

Only 0.5% of neuroscience studies look at women’s health. Here’s how to change that
World View 21 NOV 23

Bird flu outbreak in US cows: why scientists are concerned
News Explainer 08 APR 24
Adopt universal standards for study adaptation to boost health, education and social-science research
Correspondence 02 APR 24

Abortion-pill challenge provokes doubt from US Supreme Court
News 26 MAR 24
Junior Group Leader Position at IMBA - Institute of Molecular Biotechnology
The Institute of Molecular Biotechnology (IMBA) is one of Europe’s leading institutes for basic research in the life sciences. IMBA is located on t...
Austria (AT)
IMBA - Institute of Molecular Biotechnology
Open Rank Faculty, Center for Public Health Genomics
Center for Public Health Genomics & UVA Comprehensive Cancer Center seek 2 tenure-track faculty members in Cancer Precision Medicine/Precision Health.
Charlottesville, Virginia
Center for Public Health Genomics at the University of Virginia
Husbandry Technician I
Memphis, Tennessee
St. Jude Children's Research Hospital (St. Jude)
Lead Researcher – Department of Bone Marrow Transplantation & Cellular Therapy
Researcher in the center for in vivo imaging and therapy.
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Epidemiol Rev

Drug Use Disorders and Violence: Associations With Individual Drug Categories
We conducted a systematic review that examined the link between individual drug categories and violent outcomes. We searched for primary case-control and cohort investigations that reported risk of violence against others among individuals diagnosed with drug use disorders using validated clinical criteria, following Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. We identified 18 studies published during 1990–2019, reporting data from 591,411 individuals with drug use disorders. We reported odds ratios of the violence risk in different categories of drug use disorders compared with those without. We found odds ratios ranging from 0.8 to 25.0 for most individual drug categories, with generally higher odds ratios among individuals with polydrug use disorders. In addition, we explored sources of between-study heterogeneity by subgroup and meta-regression analyses. Cohort investigations reported a lower risk of violence than case-control reports (odds ratio = 2.7 (95% confidence interval (CI): 2.1, 3.5) vs. 6.6 (95% CI: 5.1, 8.6)), and associations were stronger when the outcome was any violence rather than intimate partner violence (odds ratio = 5.7 (95% CI: 3.8, 8.6) vs. 1.7 (95% CI: 1.4, 2.1)), which was consistent with results from the meta-regression. Overall, these findings highlight the potential impact of preventing and treating drug use disorders on reducing violence risk and associated morbidities.
Abbreviations
Introduction.
Drug misuse is a global public health concern ( 1 , 2 ). Worldwide, around 70 million individuals were diagnosed with a drug use disorder ( 1 ). Drug use disorders have been associated with a wide range of adverse outcomes, including suicide, comorbid mental illness, and premature mortality ( 3–5 ). In addition, drug use disorders increase risk of violence against others ( 3 , 6–9 ). Further, the prevalence of drug use disorder in prison ranges from 10% to 61% in men and 30% to 69% in women ( 10 ), which is substantially elevated compared with the prevalence, ranging from 0.6% to 4.0% in men and 0.3% to 2.9% in women, in the general population ( 11 ).
The prevalence differs between individual categories of drug use disorders. Globally, the prevalence rate per 100,000 people is 65 for stimulants such as amphetamines, 78 for cocaine, 290 for cannabis, 353 for opioids, and less than 52 for other drugs including hallucinogens and sedatives ( 12 ). Although research has consistently found increased violence risk in drug use disorders, individual studies have shown that the magnitude of this increased risk varies depending on the drug category. For example, when compared with the general population, odds ratios of violence in cannabis use disorder have ranged from 1 to 7 ( 13–17 ), and in cocaine, they have varied from 2 to 11 ( 18–21 ). This might be due to different methodologies adopted and specific outcomes used in different studies. Furthermore, it has been suggested that certain type of stimulants, such as crack cocaine, that are associated with irritability and aggressiveness ( 7 , 22 ), might have a higher risk of criminal behavior than others, including less-strong forms of cannabis that might reduce risks due to sedative and calming effects ( 23 , 24 ). This is important to clarify further in that more precise estimates would allow for risk stratification, better treatment allocation (especially if liaison with criminal justice agencies is required), and more evidence-based estimates of the population impact of certain drug policies.
Previous reviews have explored associations between general drug misuse and violence against others but have mostly investigated selected samples, such as prisoners ( 25 ) or psychiatric patients ( 26–29 ). In addition, most existing reviews have not used standardized clinical criteria to identify drug use disorders ( 22 , 30 ). This could introduce bias given that self-report of the extent of drug use is often unreliable ( 31 ). Validated diagnostic tools based on validated criteria (such as the Diagnostic and Statistical Manual of Mental Disorders or International Classification of Diseases ) can identify individuals with a severe form of drug misuse, who might present to clinical and addiction services, and for whom there is evidence-based treatment available. In addition, diagnostic categories enable consistent communication between clinicians and researchers because the criteria are widely known and validated cross-culturally with decent reliability measures ( 32 , 33 ). Furthermore, the most recent review that examined the link between general drug use disorders and violence was conducted more than 2 decades ago ( 34 ) and did not explore potential source of between-study heterogeneity or differences between individual categories of druguse.
The link between drug use and violent outcomes is complex; a wide range of factors—such as experiences of violence including both as victim and perpetrator, the comorbidity of other mental disorders, and social determinants such as sex, ethnicity, and poverty—might moderate and mediate this link. For instance, previous violence victimization might trigger development of drug use disorders, which might in turn lead to later perpetration of violence ( 35–39 ). Moreover, structural causes of drug use problems are relevant, given that they have been linked to criminalization ( 23 ), as well as factors such as poverty ( 40 ), poor mental health ( 4 , 41 ), treatment availability ( 42 ), and homelessness ( 43 ). In addition, physical and psychological effects of drugs can lead to agitation, aggression, and cognitive impairment that might in turn heighten risk of violence. Individuals with drug use disorders might also turn to violence to finance their drug use, and disputes within illegal drug markets might be associated with violence ( 44 ). To address these gaps in the evidence, in this review, we aimed to synthesize the odds of violence in individual drug use disorders and explore sources of heterogeneity between studies.
We conducted this review following the Meta-analyses of Observational Studies in Epidemiology (MOOSE) ( 45 ) and Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines ( 46 ). The study was registered with an international prospective register of systematic reviews (PROSPERO CRD42019119533).
Search strategy
We conducted searches in the following digital databases from the inception of the databases (dated from January 1, 1927) to February 18, 2019: PubMed, Web of Science, Embase, Ovid MEDLINE, PsycINFO, Global Health, and US National Criminal Justice Reference Service Abstract Database. We used a combination of search terms related to drug misuse (i.e., illegal drug OR illegal substance OR marijuana OR cocaine OR cannabis OR opioid OR heroin OR methamphetamine OR stimulant*) AND violence (i.e., violen* OR crim* OR homicide OR aggress* OR offen*) AND study design (i.e., cohort OR longitudinal OR follow-up OR prospective OR case-control). We included studies of both illegally and legally obtained drugs. There were no language restrictions, and non-English-language articles were translated. We also scanned reference lists in an attempt to identify additional articles. We searched for unpublished literature including conference proceedings, theses, and dissertations. The first author (S.Z.) conducted the initial screening of the titles and abstracts for inclusion and exclusion. S.Z. and R.Y. screened full-text publications for eligibility. Any uncertainties were discussed with S.F.
Study selection
Inclusion criteria were: 1) cohort and case-control studies that examined link between individual categories of drug use disorders and violent outcomes and provided data for calculation of odds ratio between individuals with and without the drug use disorder being studied, and eligible case-control studies were those that reported prevalence of drug use disorders in cases with and without violence perpetration; 2) investigations that reported drug use disorders (or, in older studies, equivalent diagnostic categories of drug abuse or dependence) meeting diagnostic criteria for Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases ; and 3) studies that reported violent outcomes, including any violence and not being limited to context (e.g., community, domestic, intimate partner), type of crime (e.g., homicide, assault, threat or intimidation, and all sexual offenses), and measures (self-report, family report, or official/criminal records).
We excluded: 1) animal investigations; 2) experimental, cross-sectional, qualitative studies, or randomized controlled trials; 3) investigations with within-individual designs; 4) studies that used self-report ( 47 ) (e.g., Addiction Severity Index) or urine tests to identify drug use or that did not separate drug misuse from alcohol and nicotine misuse; 5) reports with recidivism or reoffending as outcomes ( 48 ); 6) studies in selected samples (e.g., offenders, cohorts with mental disorders) so we could increase the generalizability of risk estimates to the general population; 7) investigations that used the nonspecific outcome of all criminal behavior, antisocial behavior, or delinquency, which was not broken down for violence specifically; 8) studies that reported selected participants under medication (e.g., antidepressant, antipsychotic drugs, or other prescription drugs) or individuals undergoing other interventions for drug use disorders; or 9) case-series studies or reviews.
In case of duplicate samples, we included the study that was most recent, used the most common outcome, or had the largest sample. If a study reported outcomes at multiple time points, outcomes with the longest follow-up period were included.
Data extraction
We used a standardized form to extract data. The following information was recorded: study design, country, sample characteristics, diagnostic criteria, category of drug use disorders, type of drugs, comparison group, sex, age, years of follow-up, and study period. S.Z. conducted the initial data extraction. In case of uncertainties, R.Y. and S.F. were consulted.
Statistical analysis
Quality of the individual study was assessed using the Newcastle-Ottawa Quality Assessment Scale ( 49 ). Heterogeneity was estimated using I 2 . I 2 is reported as a percentage out of 100%, where 0%–40% represents low heterogeneity, 30%–60% might indicate moderate heterogeneity, 50%–90% might denote substantial heterogeneity, and 75%–100% might indicate considerable heterogeneity ( 50 , 51 ). All effect sizes were converted into odds ratios and converted from Pearson’s r and Cohen’s d using standard approaches ( 52 ). Sources of heterogeneity were explored using subgroup analyses and meta-regression analyses. Meta-regression was conducted to estimate the extent to which one or more measured covariates (the same variables as used in the subgroup analysis) explained the observed heterogeneity in risk estimates between primary studies ( 50 ). The same variables were used in the subgroup and meta-regression analyses, and only nonoverlapping samples were included in the analyses. When testing the effect of sample size, we excluded 2 studies that were disproportionately large ( 53 , 54 ). We set the years of follow-up as a continuous variable and also a dichotomous variable using the median period as the cut-off. Other analyses included estimating associations between drug use disorders and violence while excluding studies published before 2000 and subgroup analyses by different comparison groups. We tested publication bias using Egger’s test ( 55 ), with P < 0.05 indicating publication bias. Analyses were performed using STATA, version 13 (StataCorp LP, College Station, Texas).
We identified 18 eligible studies (for details, see Figure 1 and Table 1 ) that included 591,411 individuals with drug use disorders. Studies were from 5 countries: 14 from the United States ( n = 542,393, 91.7%) ( 53 , 54 , 56–67 ) and 1 each from New Zealand ( n = 182, 0.03%) ( 68 ), Denmark ( n = 43,403, 7.3%) ( 69 ), the Netherlands ( n = 5,303, 0.9%) ( 70 ), and Turkey ( n = 130, 0.02%) ( 71 ). Eight studies used case–control designs ( 53 , 54 , 56 , 58 , 63 , 66 , 67 , 71 ); the remaining 10 studies were longitudinal cohorts with a median follow-up of 9.5 years.

Flowchart of systematic search strategy of primary studies on drug use disorders and violence in multiple countries, 1990–2019.
Summary of Included Studies on Risk of Violence in Drug Use Disorders
Abbreviations: DSM, Diagnostic and Statistical Manual of Mental Disorders ; ICD, International Classification of Diseases ; N/A, not available; WHO-CIDI; World Health Organization’s Composite International Diagnostic Interview.
a Non–drug, non–drug use disorder, and non–drug addicts served as a control group and they refer to people who might have used drugs before but did not meet diagnostic criteria for any drug use disorders. “Healthy volunteers without substance use disorders” refers to healthy volunteers without drug or alcohol use disorders.
In 16 investigations, diagnosis was made using the Diagnostic and Statistical Manual of Mental Disorders (version 3 onward). One study adopted the International Classification of Diseases , Eighth Revision ( 69 ), and 1 provided both International Classification of Diseases , Tenth Revision , and Diagnostic and Statistical Manual of Mental Disorders–IV diagnoses ( 63 ).
For outcome measurement, 2 studies used violent conviction from official records ( 65 , 69 ) and 1 reported intimate partner violence from the partner’s report ( 62 ). Most used self-report items in the Diagnostic Interview Schedule ( 56 ), PPC Delinquency and Criminal Behavior inventory ( 57 ), Aggression Questionnaire ( 58 ), Conflict Tactics Scale ( 63 ), physical aggression subscale in Buss-Perry Scale ( 71 ), and specially developed questionnaires ( 53 , 54 , 60 , 61 , 66 , 67 , 70 ). A combination of several measures (e.g., official records and self-report) was applied in 3 studies ( 59 , 64 , 68 ).
Any drug or polydrug use disorder
We identified 6 cohort investigations ( 57 , 60 , 64 , 65 , 69 , 70 ) and 6 case-control reports ( 53 , 54 , 56 , 63 , 66 , 67 ) that examined the risk of violence in any or polydrug use disorder. The odds ratios ranged from 1.3 (95% confidence interval (CI): 0.1, 13.0) to 25.0 (95% CI: 16.1–39.0) ( Figure 2 ). When excluding the 2 studies that were published prior to 2000, the odds ratio was 4.1 (95% CI: 3.0, 5.7).

Odds ratios (ORs) and confidence interval (CIs) for the association between drug use disorders and violent outcome. Weights are from random effects analysis.
Cannabis/marijuana use disorder
Six cohort studies ( 57 , 59 , 61 , 62 , 64 , 68 ) and 5 case-control investigations ( 53 , 54 , 56 , 67 , 71 ) examined the link between cannabis/marijuana use disorder and violence. The odds ratios ranged from 1.3 (95% CI: 1.1, 1.7) to 11.5 (95% CI: 7.8, 17.2). When excluding studies prior to 2000, the odds ratios ranged from 1.3 (95% CI: 1.1, 1.7) to 9.1 (95% CI: 8.5, 9.7). (See Figure 2 ).
Hallucinogen use disorder
Two cohort investigations ( 59 , 62 ) and 1 case-control report ( 54 ) tested the association between hallucinogen use disorder and violence. The odds ratios varied from 1.4 (95% CI: 1.3, 1.4) to 18.3 (95% CI: 14.9, 22.5). (See Figure 2 ).
Stimulant use disorder
We identified 5 studies that reported risk estimates for violence in stimulant use disorder, with 3 studies ( 59 , 61 , 62 ) using a cohort study design and 2 ( 54 , 58 ) using a case-control study design. All of these studies were conducted in the United States. The odds ratios ranged from 1.9 (95% CI: 1.4, 2.6) to 10.8 (95% CI: 9.3, 12.5). (See Figure 2 ).
Opioid use disorder
Three cohort investigations ( 59 , 61 , 62 ) and 2 case-control studies ( 54 , 67 ) reported the risk of violence in opioid use disorder, all of which were conducted in the United States. The risk estimates ranged from an odds ratio of 0.8 (95% CI: 0.5, 1.1) to 9.5 (95% CI: 8.7, 10.4). (See Figure 2 ).
Sedative use disorder
Two cohort investigations ( 59 , 62 ) and 1 case-control study ( 54 ) examined the association between sedative use disorder and violence. Odds ratios varied from 1.1 (95% CI: 1.1, 1.2) to 10.5 (95% CI: 9.1, 12.2). (See Figure 2 ).
Heterogeneity
No significant differences were found in risk estimates by sex, country, outcome measures, years of follow-up, and sample size in subgroup analyses ( Table 2 ). The risk estimates in cohort investigations (odds ratio (OR) = 2.7, 95% CI: 2.1, 3.5) were lower than in the case-control reports (OR = 6.6, 95% CI: 5.1, 8.6). No differences were found among violence by self-report (OR = 4.6, 95% CI: 3.0, 7.2), informant report/official records (OR = 3.2, 95% CI: 1.3, 7.8), and combined measures (OR = 4.4, 95% CI: 1.3, 14.5).
Risk Estimates for Violence in Drug Use Disorders According to Sample or Study Characteristics, Multiple Countries, 1990–2019
Abbreviations: CI, confidence interval; DSM, Diagnostic and Statistical Manual of Mental Disorders ; OR, odds ratio.
Main findings
This systematic review examined the association between drug use disorders and violence. We identified 18 eligible studies from 5 countries, with 591,411 individuals meeting diagnostic criteria for drug use disorders. There were 2 main findings. First, we found that individuals with a diagnosed drug use disorder have a 4- to 10-fold higher risk of perpetrating violence compared with general population or individuals without the drug use disorder being studied. All of the examined categories of drug use disorders—including cannabis, hallucinogens, stimulants, opioids, and sedatives—were associated with elevated violence risks. Of the total of 37 included studies, we found increased risk of violence in 34 studies with confidence intervals that did not cross 1. To examine the population impact, the odds of violence perpetration need to be seen in the context of general population prevalence of these disorders—which varies from 52 cases (per 100,000) of hallucinogen use disorders to 353 cases (per 100,000) of opioid use disorders ( 12 ). Second, there was substantial heterogeneity between studies, which was partially explained by study design and the type of outcome. Violence risk in drug use disorders was lower in cohort than in case-control studies, and when intimate partner violence was the outcome rather than general violence.
Implications
Although the odds of increased risk of violence in drug use disorders are not dissimilar to those in other neuropsychiatric conditions ( 72 ), their importance is greater from a public health perspective as drug use disorders are more prevalent than severe mental illnesses, such as schizophrenia or bipolar disorder. In addition, although drug use disorders are not more prevalent than disorders such as depression and anxiety, their risk of violence is usually higher ( 67 , 73 ). Therefore, drug use disorders have greater population impact when taking into account both prevalence and relative risk. This underscores the importance of treating drug use disorders as part of any public health approach to violence prevention. Notably, long-term methadone maintenance programs and behavioral treatments can reduce crime ( 74 ). In addition, there are studies that demonstrate reduced crime after drug treatment (e.g., opioid maintenance treatment, methadone, buprenorphine, and naltrexone) and nonmedical treatment (e.g., therapeutic communities, drug courts), among individuals using cocaine (75) and opioids ( 76–79 ), as well as with general drug use disorders ( 80–83 ). Moreover, prison-based interventions—such as therapeutic communities, opiate maintenance treatment, and pharmacotherapies for drug use disorders—are effective in reducing recidivism in prisoners ( 84–86 ). Despite this, most individuals with drug use disorders do not receive treatment. In the United States, among individuals with 12-month and lifetime drug use disorders, only 14% and 25% received treatment, respectively ( 87 ). Thus, more efforts should be made to improve accessibility of treatment for individuals with drug use disorders. Together, the treatability of drug use disorders, unmet needs, and risk of adverse outcomes present an opportunity to improve public health and safety.
A second implication, regarding study design, is that 2 aspects of design explained some of the between-study heterogeneity. Cohort studies had lower risk estimates than case-control investigations. This difference is likely because cohort studies are more likely to take into account the temporal sequence between drug use disorders and violent outcome. This allowed for a more accurate estimation of the associations than case-control studies. Future observational research should prioritize cohort designs to longitudinally follow individuals with drug use disorders and examine their violent outcomes. We also found that the association with intimate partner violence was less strong than with general violence. This might be because individuals with drug use disorders are less likely to have partners ( 87 , 88 ) and those who have partners might present with less severe symptoms of drug use disorders ( 89 ).
Strengths, limitations, and future directions
This review has several strengths. First, we included only studies that used validated diagnostic criteria to identify drug use disorders and excluded studies using self-report or other measures that might reflect short-term or recreational use. Second, we carefully explored heterogeneity using 2 methods (subgroup analyses and meta-regression). Third, we excluded studies examining drug use disorders and violent outcomes in selected samples such as offenders, cohorts with mental disorders, and individuals under treatment for drug use disorders, because not all individuals with drug use disorders are offenders or have other mental disorders, and the majority will not be subject to treatment. This likely increases the generalizability of our findings.
However, a number of limitations should be noted. First, all but one of the studies we included were conducted in high-income countries. We found an investigation from a middle-income country—Turkey—but no others, and none in Central Latin America, Tropical Latin America, and Southern sub-Saharan Africa, where violence is among the top 10 leading causes of disability-adjusted life-years ( 90 ). Many countries in these regions account for the majority of global drug manufacture, trafficking, and consumption ( 91 , 92 ). Therefore, more research on the link in these settings is needed. A second limitation was that the amount of information on individual categories was not sufficient to draw definite conclusions about differences by drug class. We identified 3 studies ( 54 , 59 , 62 ) of sedative use disorder and 5 each for stimulant use disorder ( 54 , 58 , 59 , 61 , 62 ) and opioid use disorder ( 54 , 59 , 61 , 62 , 67 ). Furthermore, we found a limited literature on polydrug use, although it is common and linked to poorer treatment outcomes, social maladjustment, and overdose lethality ( 93–95 ). Future studies should investigate more carefully the different categories of drug use disorders, polydrug use, and links with novel psychoactive substances. Third, it is not possible to meta-analyze studies of selected populations because the effects of mediators cannot be modeled. Therefore, our findings are not necessarily risk estimates in specific subpopulations, such as prisoners or individuals who are participating in treatment programs. For example, our estimates might be overestimates given that we excluded studies of individuals under drug treatment, which could decrease risk of violence ( 96 , 97 ). Fourth, we found links between hallucinogen use and violence in the general population, but there appears to be heterogeneity in their associations by population. For example, in criminal justice populations, recent work has found decreased associations between hallucinogen use and repeated offending in substance-involved offenders under community corrections supervision ( 48 ), which is also reported among intimate partner violence perpetrators ( 47 , 98 ). Among individuals with schizophrenia, there is an increased risk ( 99 ). Finally, due to lack of data, we identified only a few factors that might explain heterogeneity between studies. For example, we were not able to examine whether some factors moderate the link between drug use disorders and violence, such as being subjected to violence, comorbidity of other substance use disorders (including alcohol) and mental health conditions, time between onset of drug use and violent outcome, and other social determinants (including poverty and access to services). In addition, the heterogeneity analyses were based on different drug categories and limited by variations in primary study settings. The results should therefore be interpreted with caution and read in the context of implications for future research rather than clinical practice.
Moreover, some factors could be associated with, could mediate, or could modify links between drug misuse and violence. For instance, an umbrella review of 22 meta-analyses based on over 120,000 individuals has shown that a range of neuropsychiatric disorders—including schizophrenia, personality disorders, and bipolar disorders—and perpetration, being a witness, or being a victim of violence during childhood are linked to increased risk of violence ( 72 ), suggesting that all of these comorbidities can be confounders. In addition, individuals who are victims of violence might use drugs as a coping mechanism, and victimization itself might in turn lead to later violence ( 35–39 ). Therefore, more research accounting for these factors is necessary.
Conclusions
This systematic review has synthesized evidence on associations between individual categories of drug use disorder and violent outcomes. The findings suggest that all categories of drug use disorder have an elevated risk of violence, and that study design and type of violent outcome partly explain variation in risk estimates between studies.
ACKNOWLEDGMENTS
Author affiliations: Department of Psychiatry, National Clinical Research Center for Mental Disorders, Second Xiangya Hospital of Central South University, Changsha, China (Shaoling Zhong); and Department of Psychiatry, University of Oxford, Oxford, United Kingdom (Rongqin Yu, Seena Fazel).
This work was funded by the China Scholarship Council (grant 201806370093 to S.Z) and the Wellcome Trust Senior Research Fellowship (grant 202836/Z/16/Z to S.F.).
Conflict of interest: none declared.

IMAGES
VIDEO
COMMENTS
A growing body of research is helping to tease apart why some people with serious mental illness are prone to violence while others are not, and how clinicians and others can help through improved treatment and informed myth-busting. DeAngelis, T. (2022, July 11). Mental illness and violence: Debunking myths, addressing realities.
In this Review, we summarise evidence on the association between different mental disorders and violence, with emphasis on high quality designs and replicated findings. Relative risks are typically increased for all violent outcomes in most diagnosed psychiatric disorders compared with people without psychiatric disorders, with increased odds in the range of 2-4 after adjustment for familial ...
Abstract. The debate about addressing mental illness and violence often ignores key facts. Many people experience mental illnesses, so having had a diagnosed illness is not a very specific predictor of violent behavior. This means that many proposed policy approaches, from expanded screening to more institutionalization, are unlikely to be ...
Mentally ill population. Most patients with stable mental illness do not present an increased risk of violence. Asnis, et al., 8 found that 21 of 517 outpatients (4%) in an urban setting reported a history of homicide attempts. Steadman and colleagues 9 followed several cohorts of recently discharged American psychiatric patients for one year and compared rates of violence with violence rates ...
The relationship between mental health and violence is complex and often misunderstood, with a number of misperceptions around risk of violence and victimization. Speakers discussed the stigma and discrimination that people with mental illness experience, particularly in the media. They also discussed the need for additional research on the intersection of mental health and violence, noting ...
Mitigating Risks of Violence: Practical Steps. 1. Understand the research. Becoming familiar with the research and data on the relationship between mental illness and violence—as well as the general causes and risk factors for violent behavior—can help criminal justice professionals recognize warning signs and avoid misconceptions and biases.
People with mental illness are generally considered to be more likely to perpetrate violence than the general population; 2 however, evidence of significant levels of physical victimization is increasingly recognized. 3 Although violence towards people diagnosed with mental illness is common, there is little evidence that it is decreasing: A ...
This paper offers a criminologically informed framework to guide research on the relationship between mental disorder and violence. Criminological theories examined include social learning, social stress, social control, rational choice, and social disorganization. In addition, the "criminal careers" and "local life circumstance" methodologies are reviewed. It is argued that adopting a ...
Some of the neurobiological mechanisms of violent behavior are similar or identical to those that operate in suicidal behavior. 3. Substance use, personality disorders, major mental disorders, head injuries, and other diagnosable disorders contribute to the level of community violence. However, recent evidence points to neurobiological ...
In research on the prevalence of mental illness among violent offenders, multiple studies have found the highest rates of violence among individuals with substance use disorders, rather than schizophrenia, BPD and other psychotic disorders [7-11] (Tables 2 and 3).Rates of substance use disorders (including alcohol use disorders and illicit substance use disorders) among self-reported violent ...
The presenters pointed out that people with mental illness are far more likely to be the victims of violence than the perpetrators. Research shows that of all the violence that occurs in the United States, 96% is due to risk factors other than mental illness, said Alisa Gutman, M.D., Ph.D., the founder and medical director of the Philadelphia Human Rights Clinic.
Purpose A general consensus exists that severe mental illness (SMI) increases violence risk. However, a recent report claimed that SMI "alone was not statistically related to future violence in bivariate or multivariate analyses." We reanalyze the data used to make this claim with a focus on causal relationships between SMI and violence, rather than the statistical prediction of violence ...
Donald Trump, US President, Feb. 22, 2018 3. Are people with psychiatric disorders violent? The relevant data are influenced by reporting biases (e.g., changing willingness to report assaults) and the varying likelihood of being caught, convicted, and diagnosed, but there is compelling evidence that those with mental health problems are more ...
According to research published by the APA, of all crimes committed by people with serious mental disorders, only 7.5 percent were directly related to symptoms of mental illness. 3 Furthermore, in ...
Throughout history and in all known societies, people have believed that mental disorder and violence were somehow related. The consensus of modern scholarly opinion, however, has been that no such relationship exists. Recent epidemiological studies cast doubt on this no-relationship position. Evidence now indicates that mental disorder may be a consistent, albeit modest, risk factor for the ...
The National Institute of Mental Health (NIMH) encourages investigator-initiated research to enhance scientific understanding about the etiology of psychopathology related to violence and trauma, as well as studies to develop and test effective treatments, services, and prevention strategies in this area.
Abstract. Mental disorders are identified by a set of signs and symptoms causing significant clinical distress or impairment in an individual's functioning. The relationship between mental disorders and crime has been a topic of research and heated controversy since many decades. There is a consensus advocating a link between the two.
Science for Society: Insights from Psychological Science on Gun Violence and Anxiety. In the first webinar of APS's Science for Society series on September 20, 2023, scientists and advocates shared their expertise and perspectives on the relationship between gun-violence and anxiety. Podcast: Dr. Amanda Nickerson joins Under the Cortex to ...
Our results indicate that people with alcohol dependence, depressive disorder, panic disorder, social phobia or GAD are at risk of psychological victimisation after adjustment for childhood trauma. ... Elbogen EB and Johnson SC (2009) The intricate link between violence and mental disorder: results from the national epidemiologic survey on ...
b. Those with psychological disorders are much more prone to random violent crime than others. c. Studies have found that those with psychological disorders are more likely than those without a psychological disorder to be a victim of crime. d. Focusing gun restrictions only on mentally ill people will likely reduce gun violence.
The Anxious Generation: How the Great Rewiring of Childhood is Causing an Epidemic of Mental Illness Jonathan Haidt Allen Lane (2024) Two things need to be said after reading The Anxious Generation .
BACKGROUND. Interpersonal violence is one of the major causes of death and disability worldwide. [] For every death, many more people are exposed to nonfatal violence: for example, in national, population-based surveys, estimates of violence exposure before age 18 range from 14.0% for family violence, [2,3] 49.6-53.1% for physical assault, 6.7-8% for sexual victimization, and 24.8-29.7% ...
Psychology questions and answers. Research on psychological disorders and violence indicates that Select one: a. the majority of violent crimes are committed by those with a psychological disorder. b. having a diagnosed psychological disorder is a better predictor of violence than the use of alcohol or drugs. c.
INTRODUCTION. Drug misuse is a global public health concern (1, 2).Worldwide, around 70 million individuals were diagnosed with a drug use disorder ().Drug use disorders have been associated with a wide range of adverse outcomes, including suicide, comorbid mental illness, and premature mortality ().In addition, drug use disorders increase risk of violence against others (3, 6-9).