- Utility Menu
- Get Involved
- News & Events

qualtrics survey
New research finds that pandemic learning loss impacted whole communities, regardless of student race or income.
Analysis of prior decade shows that learning loss will become permanent if schools and parents do not expand learning time this summer and next year
(May 11, 2023) – Today, The Education Recovery Scorecard , a collaboration with researchers at the Center for Education Policy Research at Harvard University (CEPR) and Stanford University’s Educational Opportunity Project, released 12 new state reports and a research brief to provide the most comprehensive picture yet of how the pandemic affected student learning. Building on their previous work, their findings reveal how school closures and local conditions exacerbated inequality between communities — and how little time school leaders have to help students catch up.
The research team reviewed data from 8,000 communities in 40 states and Washington, D.C., including 2022 NAEP scores and Spring 2022 assessments, COVID death rates, voting rates and trust in government, patterns of social activity and survey data from Facebook/Meta on family activities and mental health during the pandemic.
They found that where children lived during the pandemic mattered more to their academic progress than their family background, income, or internet speed. Moreover, after studying instances where test scores rose or fell in the decade before the pandemic, the researchers found that the impacts lingered for years.
“Children have resumed learning, but largely at the same pace as before the pandemic. There’s no hurrying up teaching fractions or the Pythagorean theorem,” said CEPR faculty director Thomas Kane. “The hardest hit communities—like Richmond, VA, St. Louis, MO, and New Haven, CT, where students fell behind by more than 1.5 years in math—would have to teach 150 percent of a typical year’s worth of material for three years in a row—just to catch up. That is simply not going to happen without a major increase in instructional time. Any district that lost more than a year of learning should be required to revisit their recovery plans and add instructional time—summer school, extended school year, tutoring, etc.—so that students are made whole. ”
“It’s not readily visible to parents when their children have fallen behind earlier cohorts, but the data from 7,800 school districts show clearly that this is the case,” said Sean Reardon, Professor of Poverty and Inequality, Stanford Graduate School of Education. “The educational impacts of the pandemic were not only historically large, but were disproportionately visited on communities with many low-income and minority students. Our research shows that schools were far from the only cause of decreased learning—the pandemic affected children through many ways – but they are the institution best suited to remedy the unequal impacts of the pandemic.”
The new research includes:
- A research brief that offers insights into why students in some communities fared worse than others.
- An update to the Education Recovery Scorecard, including data from 12 additional states whose 2022 scores were not available in October. The project now includes a district-level view of the pandemic’s effects in 40 states (plus DC).
- A new interactive map that highlights examples of inequity between neighboring school districts.
Among the key findings:
- Within the typical school district, the declines in test scores were similar for all groups of students, rich and poor, white, Black, Hispanic. And the extent to which schools were closed appears to have had the same effect on all students in a community, regardless of income or race.
- Test scores declined more in places where the COVID death rate was higher, in communities where adults reported feeling more depression and anxiety during the pandemic, and where daily routines of families were most significantly restricted. This is true even in places where schools closed only very briefly at the start of the pandemic.
- Test score declines were smaller in communities with high voting rates and high Census response rates—indicators of what sociologists call “institutional trust.” Moreover, remote learning was less harmful in such places. Living in a community where more people trusted the government appears to have been an asset to children during the pandemic.
- The average U.S. public school student in grades 3-8 lost the equivalent of a half year of learning in math and a quarter of a year in reading.
The researchers also looked at data from the decade prior to the pandemic to see how students bounced back after significant learning loss due to disruption in their schooling. The evidence shows that schools do not naturally bounce back: Affected students recovered 20-30% of the lost ground in the first year, but then made no further recovery in the subsequent 3-4 years.
“Schools were not the sole cause of achievement losses,” Kane said. “Nor will they be the sole solution. As enticing as it might be to get back to normal, doing so will just leave the devastating increase in inequality caused by the pandemic in place. We must create learning opportunities for students outside of the normal school calendar, by adding academic content to summer camps and after-school programs and adding an optional 13th year of schooling.”
The Education Recovery Scorecard is supported by funds from Citadel founder and CEO Kenneth C. Griffin , Carnegie Corporation of New York, and the Walton Family Foundation.
About the Center for Education Policy Research at Harvard University The Center for Education Policy Research at Harvard University, based at the Harvard Graduate School of Education, seeks to transform education through quality research and evidence. CEPR and its partners believe all students will learn and thrive when education leaders make decisions using facts and findings, rather than untested assumptions. Learn more at cepr.harvard.edu.
Contact: Jeff Frantz, [email protected] , 614-204-7438 (mobile)
News by Focus Area
- COVID-19 Impact (69)
- Postsecondary Access & Success (27)
- School Improvement & Redesign (64)
- Teacher Effectiveness (57)
News by Type
- Press Releases (40)
- Newsletters (5)
- Insights (5)
- Announcements (6)
- In the News (225)
News by Project
News by year.
Public school educators are calling for a post-pandemic reset. Can it be done?
Four years after COVID-19 forced schools to close, educators want an overhaul.
Four years after the coronavirus pandemic closed much of the nation's education system, thousands of the more than 50 million U.S. public school students and teachers are returning to school this month.
In interviews with ABC News, education experts suggest the impact school closures had on the public education model could leave students with long-term developmental issues from lost learning time.
It has already exacerbated issues such as chronic absenteeism and teacher burnout, and now the persistent problems public educators face are causing leaders, experts and caregivers to sound the alarm.
MORE: Where COVID cases are increasing in the US amid summer 'bump'
One prominent educator told ABC that "public education is on life support." Another said the greatest current education challenge is the need for it to "reset," which the educator projected could take five to 10 years to achieve. And, polling suggests the American public also believes there could be grave consequences if nothing is done to fix public education.
Pew Research Center found about half of Americans think the public education system is going in the wrong direction. Eighty-two percent of people surveyed by Pew said it has been trending that way over the past five years -- even before the pandemic hit.
"It's needed restructuring for a while," STEM Equity Alliance Executive Director Arthur Mitchell told ABC News. "Education as it exists is unsustainable."
MORE: Teachers want the public to know their job is difficult, new survey finds
Mitchell shares the viewpoint of many educators ABC News spoke with -- that the issues facing school districts predate COVID-19. However, the pandemic exposed the need for an education reboot.
"The message that the pandemic sent was that you're not going to be successful teaching math and reading and science and social studies if kids haven't eaten, they haven't slept, they're worried about their dad's job or their grandmother's recent death," FutureEd Director Thomas Toch said.
'These kids aren't going to learn'
During his first year as Education Secretary in 2021, Miguel Cardona said the system is "missing the point" if school districts fail to restructure schools with better social and emotional support such as mental health resources.

Emphasizing the need for Social Emotional Learning (SEL) curriculums could serve as a start, according to Katie Kirby, a principal and experienced educator in Union City, New Jersey.
"These kids aren't going to learn," Kirby told ABC News, adding "All they're thinking about [is] the trauma that happened in their house. Or, even during COVID, just being isolated is a trauma."
"I feel like more could be done to address the mental health issues and social emotional things around, you know, not just the students but the teachers also," Kirby said about post-COVID schooling.
The New Jersey elementary school principal said more mental health practitioners and teachers will energize school communities.
Experts told ABC that innovative models, such as communities in schools, have worked with local agencies to provide positive SEL results over the years.
Toch said these communities in schools structure is a solution to the typical public education framework because it is a "difficult" time to grow up in America.
"We need to recognize that students need a range of supports in order to be successful academically," he said.
Due to the complexity of American children, Toch said the community is responsible for helping raise students.
"These models, at best, they are partnerships where other agencies are contributing resources to the partnership so that schools don't have to shoulder the entire burden, financial burden, of a more comprehensive model on behalf of the whole child."
Jonte Lee, a science teacher in the nation's capital, also said a reboot is enhanced by community partnerships.
MORE: Despite opposition, Arkansas Gov. Sarah Sanders the latest Republican to push 'school choice'
"We need parental support as well and we need other entities in the community to support [teachers]," he said. "It's like we support you, you support us -- we need to come together as a community and a culture."
Lee said a public education overhaul isn't necessary though. The system only needs minor "tweaks" such as hiring and paying more teachers, according to Lee.
"Hasn't the model been recreated multiple times?" Lee told ABC News, adding "When we say recreate the public school education model, it has already been recreated multiple times, which is why I believe in school choice, because 'this model may not work for me.'"

Injecting "choice" into education refers to a largely conservative movement that supports charter schools. Public charter schools are taxpayer funded and state-run, but the schools have the ability to turn students away, according to the National Center for Education Statistics. Their curriculums are agreed upon or chartered by local or state government, which gives the school more freedom than a traditional public school.
In contrast, tuition-free public education is schooling provided under the public's supervision or direction, according to the Cornell Law School.
'Education is always about the economy'
With several school districts back in full swing this summer, experts told ABC News that challenges stretch beyond academic and social emotional learning.
"Education is always about the economy," Mitchell said. "We just don't discuss those two things together."
In the wake of an educator shortage, Mitchell described school vacancies as an economic issue since workforce trends have outpaced the public education sector. Therefore, leaders such as Cardona and Harvard Center for Education Policy Research Executive Director Dr. Christina Grant stress the need to make public high school a pathway to careers for students. Research supports these proposals. After graduation, adults are a "direct reflection" of the preparation given to them by the school system, according to Mitchell.
For the most part, experts said they believe some reconfiguring of the education system should occur. Christina Grant, who was Washington, D.C.'s state superintendent during the pandemic, said she fully supports large-scale adjustments such as adding high-impact tutoring for all, utilizing federal investments and resources, and rethinking the high school structure.

Meanwhile, many conservative policymakers are pushing to defund the U.S. Department of Education as a whole. They argue that the word "education" doesn't appear in the Constitution, so the individual states have to work through issues on a case-by-case basis.
At CEPR, Grant is researching evidence-based solutions for students across the country. She said intentional revisions are required for improving public education.
"The data is telling us that we have work to do," she told ABC News. "Do I think that that means we need a whole system overhaul? I don't think that you can eat a whole elephant at one time. I think you have to be laser-like focused on which chunks you would attack in which ways."
Toch warns changes, whether sweeping or incremental, could take up to a decade on a widespread scale.
He and Grant agree the roughly $190 billion in elementary and secondary school emergency relief from the federal government during COVID has been helpful in tackling these concerns -- particularly student recovery -- over the last three years. But the Biden administration's American Rescue Plan (ARP) money expires on Sept. 30.
With that deadline looming, Grant hopes more investments will move the needle.
"I do think that the federal government still has to make seismic commitments in public education because we are far from out of this," she said.
Related Topics
Trending reader picks.

Today's Amazon Deals: 14 picks starting at 40% off
- Aug 9, 1:47 PM

What to know about the Olympics closing ceremony
- Aug 7, 1:10 PM

3rd arrest over plot targeting Taylor Swift shows
- Aug 9, 4:55 AM

Chemical substances at home of Austrian suspect
- Aug 8, 4:03 PM

Skinner asks Biles to 'put a stop' to bullying
- Aug 6, 4:43 PM
ABC News Live
24/7 coverage of breaking news and live events
How is COVID-19 affecting student learning?
Subscribe to the brown center on education policy newsletter, initial findings from fall 2020, megan kuhfeld , megan kuhfeld senior research scientist - nwea jim soland , jim soland assistant professor, school of education and human development - university of virginia, affiliated research fellow - nwea beth tarasawa , bt beth tarasawa executive vice president of research - nwea angela johnson , aj angela johnson research scientist - nwea erik ruzek , and er erik ruzek research assistant professor, curry school of education - university of virginia karyn lewis karyn lewis director, center for school and student progress - nwea.
December 3, 2020
The COVID-19 pandemic has introduced uncertainty into major aspects of national and global society, including for schools. For example, there is uncertainty about how school closures last spring impacted student achievement, as well as how the rapid conversion of most instruction to an online platform this academic year will continue to affect achievement. Without data on how the virus impacts student learning, making informed decisions about whether and when to return to in-person instruction remains difficult. Even now, education leaders must grapple with seemingly impossible choices that balance health risks associated with in-person learning against the educational needs of children, which may be better served when kids are in their physical schools.
Amidst all this uncertainty, there is growing consensus that school closures in spring 2020 likely had negative effects on student learning. For example, in an earlier post for this blog , we presented our research forecasting the possible impact of school closures on achievement. Based on historical learning trends and prior research on how out-of-school-time affects learning, we estimated that students would potentially begin fall 2020 with roughly 70% of the learning gains in reading relative to a typical school year. In mathematics, students were predicted to show even smaller learning gains from the previous year, returning with less than 50% of typical gains. While these and other similar forecasts presented a grim portrait of the challenges facing students and educators this fall, they were nonetheless projections. The question remained: What would learning trends in actual data from the 2020-21 school year really look like?
With fall 2020 data now in hand , we can move beyond forecasting and begin to describe what did happen. While the closures last spring left most schools without assessment data from that time, thousands of schools began testing this fall, making it possible to compare learning gains in a typical, pre-COVID-19 year to those same gains during the COVID-19 pandemic. Using data from nearly 4.4 million students in grades 3-8 who took MAP ® Growth™ reading and math assessments in fall 2020, we examined two primary research questions:
- How did students perform in fall 2020 relative to a typical school year (specifically, fall 2019)?
- Have students made learning gains since schools physically closed in March 2020?
To answer these questions, we compared students’ academic achievement and growth during the COVID-19 pandemic to the achievement and growth patterns observed in 2019. We report student achievement as a percentile rank, which is a normative measure of a student’s achievement in a given grade/subject relative to the MAP Growth national norms (reflecting pre-COVID-19 achievement levels).
To make sure the students who took the tests before and after COVID-19 school closures were demographically similar, all analyses were limited to a sample of 8,000 schools that tested students in both fall 2019 and fall 2020. Compared to all public schools in the nation, schools in the sample had slightly larger total enrollment, a lower percentage of low-income students, and a higher percentage of white students. Since our sample includes both in-person and remote testers in fall 2020, we conducted an initial comparability study of remote and in-person testing in fall 2020. We found consistent psychometric characteristics and trends in test scores for remote and in-person tests for students in grades 3-8, but caution that remote testing conditions may be qualitatively different for K-2 students. For more details on the sample and methodology, please see the technical report accompanying this study.
In some cases, our results tell a more optimistic story than what we feared. In others, the results are as deeply concerning as we expected based on our projections.
Question 1: How did students perform in fall 2020 relative to a typical school year?
When comparing students’ median percentile rank for fall 2020 to those for fall 2019, there is good news to share: Students in grades 3-8 performed similarly in reading to same-grade students in fall 2019. While the reason for the stability of these achievement results cannot be easily pinned down, possible explanations are that students read more on their own, and parents are better equipped to support learning in reading compared to other subjects that require more formal instruction.
The news in math, however, is more worrying. The figure below shows the median percentile rank in math by grade level in fall 2019 and fall 2020. As the figure indicates, the math achievement of students in 2020 was about 5 to 10 percentile points lower compared to same-grade students the prior year.
Figure 1: MAP Growth Percentiles in Math by Grade Level in Fall 2019 and Fall 2020
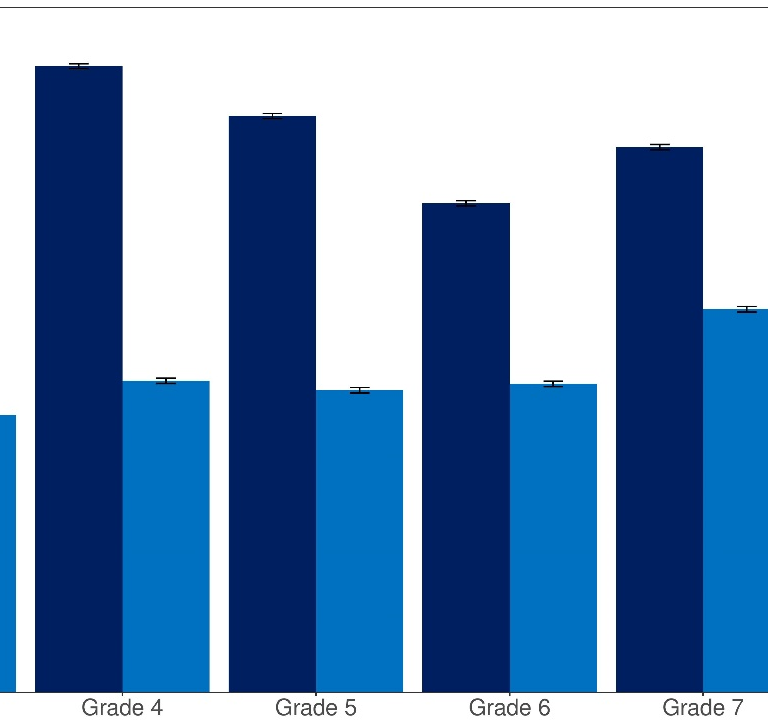
Source: Author calculations with MAP Growth data. Notes: Each bar represents the median percentile rank in a given grade/term.
Question 2: Have students made learning gains since schools physically closed, and how do these gains compare to gains in a more typical year?
To answer this question, we examined learning gains/losses between winter 2020 (January through early March) and fall 2020 relative to those same gains in a pre-COVID-19 period (between winter 2019 and fall 2019). We did not examine spring-to-fall changes because so few students tested in spring 2020 (after the pandemic began). In almost all grades, the majority of students made some learning gains in both reading and math since the COVID-19 pandemic started, though gains were smaller in math in 2020 relative to the gains students in the same grades made in the winter 2019-fall 2019 period.
Figure 2 shows the distribution of change in reading scores by grade for the winter 2020 to fall 2020 period (light blue) as compared to same-grade students in the pre-pandemic span of winter 2019 to fall 2019 (dark blue). The 2019 and 2020 distributions largely overlapped, suggesting similar amounts of within-student change from one grade to the next.
Figure 2: Distribution of Within-student Change from Winter 2019-Fall 2019 vs Winter 2020-Fall 2020 in Reading

Source: Author calculations with MAP Growth data. Notes: The dashed line represents zero growth (e.g., winter and fall test scores were equivalent). A positive value indicates that a student scored higher in the fall than their prior winter score; a negative value indicates a student scored lower in the fall than their prior winter score.
Meanwhile, Figure 3 shows the distribution of change for students in different grade levels for the winter 2020 to fall 2020 period in math. In contrast to reading, these results show a downward shift: A smaller proportion of students demonstrated positive math growth in the 2020 period than in the 2019 period for all grades. For example, 79% of students switching from 3 rd to 4 th grade made academic gains between winter 2019 and fall 2019, relative to 57% of students in the same grade range in 2020.
Figure 3: Distribution of Within-student Change from Winter 2019-Fall 2019 vs. Winter 2020-Fall 2020 in Math

It was widely speculated that the COVID-19 pandemic would lead to very unequal opportunities for learning depending on whether students had access to technology and parental support during the school closures, which would result in greater heterogeneity in terms of learning gains/losses in 2020. Notably, however, we do not see evidence that within-student change is more spread out this year relative to the pre-pandemic 2019 distribution.
The long-term effects of COVID-19 are still unknown
In some ways, our findings show an optimistic picture: In reading, on average, the achievement percentiles of students in fall 2020 were similar to those of same-grade students in fall 2019, and in almost all grades, most students made some learning gains since the COVID-19 pandemic started. In math, however, the results tell a less rosy story: Student achievement was lower than the pre-COVID-19 performance by same-grade students in fall 2019, and students showed lower growth in math across grades 3 to 8 relative to peers in the previous, more typical year. Schools will need clear local data to understand if these national trends are reflective of their students. Additional resources and supports should be deployed in math specifically to get students back on track.
In this study, we limited our analyses to a consistent set of schools between fall 2019 and fall 2020. However, approximately one in four students who tested within these schools in fall 2019 are no longer in our sample in fall 2020. This is a sizeable increase from the 15% attrition from fall 2018 to fall 2019. One possible explanation is that some students lacked reliable technology. A second is that they disengaged from school due to economic, health, or other factors. More coordinated efforts are required to establish communication with students who are not attending school or disengaging from instruction to get them back on track, especially our most vulnerable students.
Finally, we are only scratching the surface in quantifying the short-term and long-term academic and non-academic impacts of COVID-19. While more students are back in schools now and educators have more experience with remote instruction than when the pandemic forced schools to close in spring 2020, the collective shock we are experiencing is ongoing. We will continue to examine students’ academic progress throughout the 2020-21 school year to understand how recovery and growth unfold amid an ongoing pandemic.
Thankfully, we know much more about the impact the pandemic has had on student learning than we did even a few months ago. However, that knowledge makes clear that there is work to be done to help many students get back on track in math, and that the long-term ramifications of COVID-19 for student learning—especially among underserved communities—remain unknown.
Related Content
Jim Soland, Megan Kuhfeld, Beth Tarasawa, Angela Johnson, Erik Ruzek, Jing Liu
May 27, 2020
Amie Rapaport, Anna Saavedra, Dan Silver, Morgan Polikoff
November 18, 2020
Education Access & Equity K-12 Education
Governance Studies
Brown Center on Education Policy
Kelly Rosinger, Robert Kelchen, Justin Ortagus, Dominique J. Baker, Mitchell Lingo
August 9, 2024
Carolyn Esswein, Justin Hegarty
August 8, 2024
Nicol Turner Lee

The World Bank Group is the largest financier of education in the developing world, working in 94 countries and committed to helping them reach SDG4: access to inclusive and equitable quality education and lifelong learning opportunities for all by 2030.
World Bank Education and COVID-19 (coronavirus) Response

The State of Global Learning Poverty: 2022 Update
Report: The RAPID Framework and a Guide for Learning Recovery and Acceleration

Education Finance Watch 2022

Western and Central Africa Education Strategy 2022-2025
The State of the Global Education Crisis: A Path to Recovery
Report: The Most Effective Ways to Keep Children Learning During and Post-Pandemic
Remote Learning During COVID-19: Lessons from Today, Principles for Tomorrow
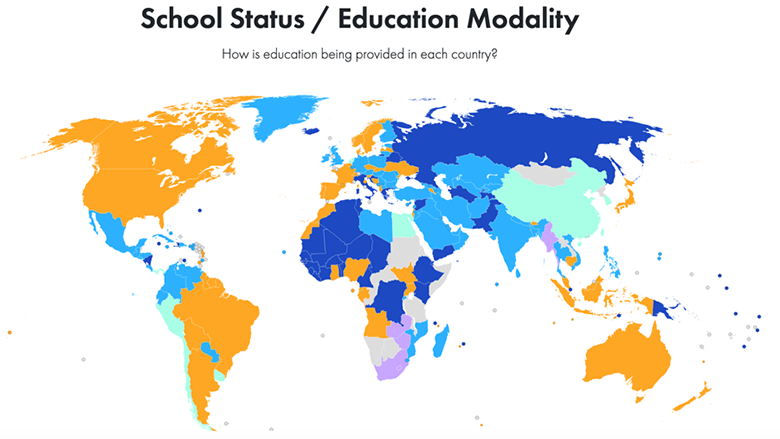
COVID-19 Global Education Recovery Tracker
The World Bank’s education team worked to support countries as they managed the changing education landscape during the pandemic. They advised on remote learning at scale and supported operations to facilitate post-pandemic learning recovery . The World Bank provides support to systemic education reform to ensure that schools can provide the necessary environments to ensure children learn effectively. Estimates indicate that the impacts of the pandemic on the human capital of young children, school-age children, and youth require urgent action to reverse the damage.
COVID-RELATED EDUCATION BLOGS
| | | | | | |
Education Systems' Response to COVID-19 (coronavirus)
: The world was living a learning crisis, even before the pandemic, but now the crisis is even deeper.
| The World Bank releases global simulations of the impact of the crisis on education outcomes. The debate on reopening schools safely continues. World Bank and UNICEF join debate on high stakes exams with a webinar. |
: The sourced by teams across the World Bank, Johns Hopkins, and UNICEF, monitors recovery planning efforts in more than 200 countries and territories. | : Impact of school closures on education attainment and the economy are becoming more evident. Brief summarizing latest studies from around the world. |
: As schools begin reopening, some students have been out of learning nearly 300 days, learning losses have only increased. | : 1.19 billion students (68% of the world’s learners) are in countries that are still with full school lockdowns. COVID19 is impacting education financing. The World Bank offers resources on the topic. |
: Latest data from the shows that most countries have already opened schools partially (rural areas or parts of the country) and mostly with hybrid (combining remote and in-person) or mixed approaches. | : Nearly 20 countries including China have moved to gradually reopen schools while others announce cancellation of school year. Still 1.2 billion students are in countries with full school lockdowns- 70% of world learners. |
New year, new school closures as COVID-19 surges in many countries. Distance Learning 2.0 with lessons from Spring 2020. | : World Bank introduces a country tool or estimating COVID-19 impacts on learning and student outcomes. Schools are still closed or partly closed in 178 countries, with about 73% of students out of school. |
: A summary of the growing evidence suggesting learning losses are climbing. The World Bank sounds the alarm on the looming long term crisis of a generation to be lost. | The COVID-19 Global Education Tracker is now live. It monitors recovery planning efforts in more than 200 countries and territories. |
: Annex – Latest on countries reopening schools. | : Schools are closed in 185 countries, with 85% of the world’s learners still shut out. Those reopening are doing so for select classes and with significant safety measures. |
More than 40% of the world’s learners are in countries with school closures still. The World Bank, UNESCO, UNICEF release the second-round results from the global survey on education responses-all aspects of the education systems are impacted. | : 175 or just about every system that was not on extended holiday shutters its schools. The debate emerges on school closures as University College releases a report indicating that keeping kids at home has little impact. Decisions on delay or examination cancellation also begin to emerge. |
: All school systems in Europe and Central Asia (ECA) have reopened and returned to mostly traditional schooling with safety measures. The World Bank introduced a supplement to the WB, UNESCO, UNICEF Framework on reopening schools. A summary of studies on affects of COVID-19 on children’s mental health. | | : Schools are now closed in 168 countries. World Bank produces a guidance note synthesizing developments around the globe, a dashboard to track closures, and summaries of education technology solutions repository. |
: Countries move to reopen schools under a new normal, many with delays as a new wave of the virus is likely looming. A summary of the latest evidence and debates on school reopening. | : 161 countries (out of 181 reporting cases) declare national school closures, leaving 1.1 students without schools globally; UK, which originally said they would schools open, reverses policy. |
| : About 2/3 of the world’s learners are still impacted by closures. While some countries have reopened, others announce a remote-only start to the new school year. | : 172 countries announce closures or extension of existing closures while China begins to reopen some schools. Number of Students out of school is 1.5 billion. Remote learning is now heavily introduced, with varying success across systems. |
: 1.13 billion students remain out of school. The first round of World Bank, UNESCO, UNICEF Survey of governments on the education response is released. |
PAPERS AND GUIDANCE NOTES
| | | l |
| l |
| l |
| : | | |
| : | |

Collapse & Recovery: How COVID-19 Eroded Human Capital and What to Do About It
Education and COVID-19 Blogs
News Releases
70% of 10-Year-Olds now in Learning Poverty, Unable to Read and Understand a Simple Text, June 23, 2022
Financing for Education Stagnant or Declining Despite Chronic Learning Needs Post-COVID-19 , June 28, 2022
Learning Losses from COVID-19 Could Cost this Generation of Students Close to $17 Trillion in Lifetime Earnings , Dec 6, 2021
Pandemic Threatens to Push 72 Million More Children into Learning Poverty—World Bank outlines a New Vision to ensure that every child learns, everywhere , Dec 2, 2021
Two-Thirds of Poorer Countries Are Cutting Education Budgets Due to COVID-19 , Feb 22, 2021
Pandemic Threatens to Push 72 Million More Children into Learning Poverty—World Bank outlines a New Vision to ensure that every child learns, everywhere , Dec 2, 2020
More press releases
Blog Collections:
COVID-19 (Coronavirus) & Education: A World Bank Group Perspective
Supporting teachers during the COVID-19 (Coronavirus) pandemic and beyond
COVID-19 (Coronavirus) & Education: A World Bank Group Perspective, part 2
COVID-19 (Coronavirus) Impact on Tertiary Education
2022: AFR | EAP | ECA | LAC | MENA | SAR
2021 : AFR | EAP | ECA | LAC | MENA | SAR
2020 : AFR | EAP | ECA | ECA long | LAC | MENA | SAR
COUNTRY BRIEFS
China ECE | Colombia (ES) | Turkey | Brazil l China | South Korea
REGIONAL RESPONSE
Learning Recovery after COVID-19 in Europe and Central Asia : Policy and Practice | RUSSIAN
Response Note to COVID-19 (Coronavirus) in Europe and Central Asia l RUSSIAN
Video: The COVID-19 pandemic threatens education systems worldwide – but also offers a chance to build back better
Video: COVID-19 has brought the Future of Learning to Now
Video: Accelerating Progress to Reducing Learning Poverty During COVID-19
Infographic: Simulating COVID-19 impacts on learning and schooling outcomes: A set of global estimates
Infographic: Realizing the Future of Learning
Brief: Mission: Recovering Education in 2021
Policy Actions for School Reopening and Learning Recovery
Around the bank group.
Resilient Recovery Series: Re-Imagining Post-Pandemic Education
Realizing the Future of Learning Today
Global Education Evidence Advisory Panel’s “Smart Buys” to Improve Global Learning Levels
Joint UNESCO-UNICEF-World Bank webinar series on the reopening of schools, June 8-30
Watch : Education Global Director interview
The impact of COVID-19 on education in Brazil
STAY CONNECTED

Global Education Newsletter - June 2024
What's happening in the World Bank Education Global Practice? Read to learn more.

Learning Can't Wait: A commitment to education in Latin America and the ...
A new IDB-World Bank report describes challenges and priorities to address the educational crisis.
Human Capital Project
The Human Capital Project is a global effort to accelerate more and better investments in people for greater equity and economic growth.

Impact Evaluations
Research that measures the impact of education policies to improve education in low and middle income countries.

Education Videos
Watch our latest videos featuring our projects across the world
Additional Resources
Media inquiries.
This site uses cookies to optimize functionality and give you the best possible experience. If you continue to navigate this website beyond this page, cookies will be placed on your browser. To learn more about cookies, click here .
- Election 2024
- Entertainment
- Newsletters
- Photography
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Delegate Tracker
- AP & Elections
- 2024 Paris Olympic Games
- Auto Racing
- Movie reviews
- Book reviews
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Texas schools got billions in federal pandemic relief, but it is coming to an end as classes begin
- Copy Link copied
The $43 million infusion the Port Arthur Independent School District received in federal COVID-19 pandemic relief funds accomplished more than Phyllis Geans could have ever imagined.
The money allowed the district to upgrade antiquated heating, ventilation and air conditioning systems. Teachers earned retention stipends at a time when many were leaving the profession. Students received new band instruments. An ambitious summer program taught them about photography, robots and skydiving.
“We were excited, really excited, because we started thinking about things that we knew were almost impossible,” said Geans, Port Arthur ISD’s assistant superintendent of operations. “It was unreal.”
Districts like Port Arthur ISD , where roughly 85% of students are economically disadvantaged, received a level of financial support they likely wouldn’t have received otherwise — and they took advantage of it by investing in community health, learning, infrastructure and safety.
But the more than $19 billion Texas schools received in Elementary and Secondary School Emergency Relief funds over the last four years will expire on Sept. 30, with a few exceptions .
The money will go away at a time when Texas schools are already struggling to keep the lights on. A number of districts are planning to enter the next school year with multimillion-dollar holes in their budgets as inflation has sent costs soaring. The Texas Legislature failed last year to approve a significant boost to the base amount of money every school receives per student — an amount that hasn’t changed since 2019 — as lawmakers fought over whether to fund private education with taxpayer dollars.
School administrators say losing the pandemic relief funds not only threatens the programs they paid for but also highlights how precarious their districts’ situation has become after years of clamoring for more state funding.
“It’s not about making up ESSER, because we all knew that was one-time funding,” said La Joya ISD Superintendent Marcey Sorensen. “I just would ask, without getting political whatsoever, that everybody just look in the mirror and say, OK, if we really haven’t provided additional funding since 2019, maybe it’s time that we just give school districts a little bit more of what they need, knowing that kids have different needs now.”
Congress established the ESSER program in 2020 to help schools address the devastating impacts of the COVID-19 pandemic. In Texas, districts experienced significant enrollment declines and the number of burnt-out teachers exiting the profession skyrocketed. Years of educational gains unraveled as kids, parents and teachers struggled with school closures and the hurried transition to online learning.
District leaders say the federal pandemic relief funds helped them address learning disruptions and provide additional academic support for students.
“They helped us ride out the five years of no new funding from the state,” said Ronald Wilson, Hearne ISD’s chief financial officer.
Recent studies show the relief funds helped schools across the country improve test scores . For districts where most students come from low-income households, the funds were particularly meaningful, and not just for academics.
In Port Arthur ISD, where most students are Black and Hispanic and the four-year graduation rate is well below the state average, the Brilliance Academy summer program took students on an indoor skydiving trip , where they learned about wind resistance, speed and velocity. The district created a program that paid high school seniors to provide supplemental classroom instruction to elementary kids. Geans said some of the students who participated in the program later expressed interest in pursuing a career in teaching.
Meanwhile, Paris ISD established income incentives for teachers to mentor students. Hearne ISD hired behavioral specialists and social workers to assist students and their families during the pandemic. San Elizario ISD built spaces for recreational activities like playing the piano and hosted family fitness, literacy and math events.
“I think we were more successful in growing the whole child, on the part where we’re growing young ladies and young men,” said Jerrica Liggins, Paris ISD’s secondary education director and college transition coordinator. “We gave them things that they need to be successful in the next grade level or whether they were graduating and going out into the workforce. We gave them things that helped make them a better person.”
Schools across the country have faced questions about how they’ve spent federal relief funds. District officials who used them for things like hiring more staff for their central offices, purchasing pool passes or renovating sports stadiums have received the harshest criticism .
Texas schools will likely face similar spending questions next year. Lt. Gov. Dan Patrick , who presides over the Texas Senate, recently directed that chamber’s education committee to review how public schools spent the massive influx of federal COVID-19 relief money. The review will likely focus on how districts used the funds to improve student outcomes.
Standardized test scores are one of the main ways in which student achievement and growth are measured in the state, and the same is true for how the use of pandemic relief funds has been evaluated in national studies .
In Texas, the pandemic caused a dramatic decline in learning, with reading and math scores hit particularly hard. The effects were even more profound for students who participated in online classes. Math scores have yet to rebound to pre-pandemic levels.
How to hold schools accountable for Texas students’ academic performance has also been a contentious issue in recent years. School districts have fought with the Texas Education Agency over its letter grade accountability system, claiming recent changes would hurt their ratings. School officials have argued that testing scores alone are not enough to measure school systems’ effectiveness.
What ESSER spending evaluations sometimes miss is the extent to which the relief funds helped school districts stay alive, said Amanda Brownson, deputy executive director of the Texas Association of School Business Officials.
The funds “helped them keep the doors open, helped them make sure staff were in classrooms ready to greet kids when they came back; it helped them not … collapse,” Brownson said. “What we don’t have is the counterfactual: What shape would school districts be in right now if they had to manage the pandemic and had not had ESSER funding available?”
Maintaining the programs Texas schools created with federal relief funds will likely be difficult without them.
A recent survey conducted by the TASBO found that out of 313 school districts across the state, nearly 80% reported deficit budgets or a lack of resources as one of their top challenges. Ninety percent of respondents said they have less than a quarter of pandemic relief funds remaining.
Gov. Greg Abbott has faced sharp criticism from public school advocates for his unwillingness to support standalone legislation to significantly boost school funding.
Since last year, Abbott has pushed for education savings accounts, which would allow families to use tax dollars to pay for their children’s private education and other school-related expenses. Opponents in the Texas House, citing worries that such a program would siphon funds away from public schools, successfully blocked the measure. But it meant public schools wouldn’t get the funding boost they wanted: Abbott had said he would veto any school funding proposal that did not include an education savings accounts program.
The governor has vowed to make a similar push when the Legislature reconvenes next year.
The uncertainty around state funding for public schools has created a situation where school districts are spending more time worrying about their financial sustainability and less about what’s best for students, said Monty Exter, governmental relations director of the Association of Texas Professional Educators.
But for low-income districts, money difficulties are not unfamiliar. And they plan to do what they’ve always done: find ways to provide for students and families with their limited resources.
Some school districts are encouraging their staff to be on the lookout for local grant opportunities. Others are thinking of asking voters to increase the tax revenue going to schools or support school bonds. Few say they are looking to the Legislature for solutions.
”We’re taking as much of the funding issues on ourselves and moving forward,” said Hearne ISD Superintendent Adrian Johnson, adding that he is still hopeful that legislators will do more to fund public schools.
“But we’re not waiting on that to happen,” he said.
This story was originally published by The Texas Tribune and distributed through a partnership with The Associated Press.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Medical Student Education in the Time of COVID-19
- 1 Perelman School of Medicine, University of Pennsylvania, Philadelphia
- Editorial Medical Students and Public Health Service for the COVID-19 Pandemic Howard Bauchner, MD; Joshua Sharfstein, MD JAMA
- Viewpoint How Academic Health Systems Can Move Forward Once COVID-19 Wanes Steven D. Shapiro, MD; Paul B. Rothman, MD JAMA
- Viewpoint Potential Implications of COVID-19 for the 2020-2021 Residency Application Cycle Maya M. Hammoud, MD, MBA; Taylor Standiford, BS; J. Bryan Carmody, MD, MPH JAMA
These are unprecedented times. Although the necessary focus has been to care for patients and communities, the emergence of severe acute respiratory syndrome coronavirus 2 has disrupted medical education and requires intense and prompt attention from medical educators. The need to prepare future physicians has never been as focused as it is now in the setting of a global emergency. The profound effects of coronavirus disease 2019 (COVID-19) may forever change how future physicians are educated.
This pandemic presents practical and logistical challenges and concerns for patient safety, recognizing that students may potentially spread the virus when asymptomatic and may acquire the virus in the course of training. This Viewpoint discusses the current status of medical education, describes how COVID-19 may affect preclerkship and clerkship learning environments, and explores potential implications of COVID-19 for the future of medical education.
Medical Student Education in 2020
For more than a decade, medical schools have been working to transform pedagogy by eliminating/reducing lectures; using technology to replace/enhance anatomy and laboratories; implementing team-facilitated, active, and self-directed learning; and promoting individualized and interprofessional education. 1 , 2 The development of entrustable professional activities and competency-based learning with identified milestones for achievement have transformed assessment. Many schools have decreased the basic science curriculum to 12 or 18 months while integrating clinical medicine within this timeframe and revisiting the basic sciences later in medical school. 3
Today, in most medical schools, students convene in physical settings during the first 12 to 18 months for interactive problem-solving or discussions in small groups; their physical presence in both inpatient and outpatient settings has been an unquestioned tenet of early clinical immersion experiences and the clerkship curriculum. The last 18 months of medical school may be individualized, with students participating in advanced clinical rotations, subinternships prior to residency, or scholarly projects. COVID-19 has the potential to affect students throughout the educational process.
How COVID-19 Affects the Preclerkship Learning Environment
Social distancing is the most effective preventative strategy since the emergence of COVID-19 pending development of a vaccine, treatment, or both. 4 By definition, this precludes students from gathering in learning studios, lecture halls, or small-group rooms. Within the past few years, many faculty were already “flipping” the classroom to provide individualized instruction for asynchronous learning “anytime/anywhere.” However, students still convened for small-group interactions, laboratory sessions, simulations, and technology sessions (eg, learning bedside ultrasonography), as well as for clinical instruction with standardized patients and in authentic patient care environments.
In response to COVID-19, medical education faculty have quickly transitioned the entire preclerkship curriculum to online formats that include content in the basic sciences, health systems sciences, and even in behavioral sciences. Small-group formats convene online in virtual team settings, and clinical skills sessions may occur online or, in some cases, may be deferred. Examinations have also transitioned to online settings. Updating content material may be a benefit of the online format and virtual activities seem functional, but outcomes of these changes will require subsequent evaluation. The transition from the workplace or medical school setting to home results in isolation, an increased use of email, and struggles with establishing boundaries between work and home, which could affect faculty, students, and support staff.
How COVID-19 Affects the Clerkship Learning Environment
What exactly is the role of the medical student in the clinical environment? Ideally, the student is part of the team as a learner who requires supervision. Formation of students’ professional identity relies on teaching and role modeling in these settings as students learn to prioritize patients and aspire to altruism. The next question then is what level of student involvement during a crisis best represents this prioritization? In other disaster circumstances, including natural disasters, blackouts, fires, and the September 11 attacks, students were able to continue their education and help in the effort. However, with the emergence of a highly contagious pandemic, students may transmit the virus unknowingly or contract the disease. Other contributing factors that limit the role of students in this clinical environment include lack of COVID-19 testing; diminished value of education, with cancelation of surgical procedures and routine appointments and the transition to telehealth formats; and lack of adequate personal protective equipment (PPE).
With the initial emergence of COVID-19, students were not involved in the care of patients with suspected or confirmed COVID-19, especially with the shortage of PPE. As infection rates increased, schools began to remove students from the clerkship environment and on March 17, 2020, the Association of American Medical Colleges provided guidelines suggesting that medical schools support pausing clinical rotations for medical students. 5 However, specific geographic differences may lead schools to make individualized decisions based on unique circumstances.
What then could educators do to create experiences for students who are usually assigned to inpatient or outpatient rotations? The options are continually evolving but may include consolidating and moving clinical didactic sessions online earlier to allow for later entry into the clinical environment; creating and using available virtual cases; modifying the academic calendar to exchange later experiences (eg, scholarly work) and defer clinical rotations; and involving students in the telehealth environment, including electives based on experiences students are pursuing to enable them to assist and learn in this critical situation.
There is uncertainty regarding how long this situation will persist and increasing recognition that there may be periods in the future after reengagement in a “new normal” environment, in which quarantines and social distancing may again be required. The challenge is in providing authentic patient experiences for medical students as a key component of medical education under these circumstances. If schools defer clinical immersion experiences, there could be 2 full cohort classes of students in the clinical environment simultaneously and education could be adversely affected by the density of learners (which is already a problem in many geographic locations). Regarding accreditation, the Liaison Committee on Medical Education has provided resources to help medical schools. 6
What Does the Future Hold?
The medical education environment is cross-generational. The former mindset that physicians would work when they were ill was considered to be altruistic and professional, with prioritization of the patient above the physician. However, the situation that COVID-19 represents is different. Clinicians who come to work while they are ill, as well as those who may be asymptomatic and silently incubating the virus, might facilitate transmitting the virus to others. Therefore, the culture of professionalism and altruism must be redefined and take into consideration the effects of potential actions, even with good intentions. This is all the more difficult because of the lack of COVID-19 testing and limited availability of PPE.
Additional unknown academic issues will require attention, including standardized examinations when testing centers are closed, the timeline for residency applications for current third-year students, and the ability to meet requirements for certain subspecialties prior to applying to residency (eg, away rotations).
However, learners across the continuum of education have participated in many ways to care for patients and communities in this crisis. In medical schools across the country, students are volunteering in call centers, creating patient education materials, and helping with grocery shopping, among other activities, while adhering to physical separation, safe travel (walking, biking, or personal car), and supervision.
Recognizing the possibility that the COVID-19 pandemic could result in a health care worker shortage, students may need to be engaged as part of the workforce and embedded in the clinical environment. This situation could change rapidly, and medical schools will need to be nimble and flexible in their response. Some schools are considering early graduation with preparation of fourth-year students to engage as either volunteers or as residents earlier in the clinical environment. The latter may require university flexibility with regard to the conferring of degrees as well as revised processes for licensure.
Conclusions
While in the midst of this COVID-19 crisis, it is crucial that the academic educational community learns from the experience and prioritizes a forward-thinking and scholarly approach as practical solutions are implemented. Reflection and evaluation must follow. For educators, the expression “make your work count twice” (the first time for the job you are doing and the second to get the work published and disseminated [eg, creating a curriculum that you plan to use for scholarship by publishing it]) and the plan for educational scholarship has never been more imperative. One area in which students can serve and have a positive effect is as educators to their peers, patients, and communities, using the tools available through social media and other modalities to help influence behaviors in a positive way.
The COVID-19 epidemic may represent an enduring transformation in medicine with the advancement of telehealth, adaptive research protocols, and clinical trials with flexible approaches to achieve solutions. There are many examples whereby learning from difficult experiences (eg, emergence of HIV, response to disasters) changed discovery, science, and patient care. Students and educators can help document and analyze the effects of current changes to learn and apply new principles and practices to the future. This is not only a time to contribute to the advancement of medical education in the setting of active curricular innovation and transformation, but it may be a seminal moment for many disciplines in medicine.
Corresponding Author: Suzanne Rose, MD, MSEd, Perelman School of Medicine, University of Pennsylvania, 3400 Civic Center Blvd, Philadelphia, PA 19104 ( [email protected] ).
Published Online: March 31, 2020. doi:10.1001/jama.2020.5227
Conflict of Interest Disclosures: Dr Rose reported receiving honoraria for educational consulting from another medical school and from organizations for speaking on mentoring and leadership and leading a course; receiving royalties for 2 books on topics unrelated to the content of this article; and leading the team at her prior institution to receive an American Medical Association Accelerating Change in Medical Education grant in the second call for proposals for a project related to electronic health record training.
See More About
Rose S. Medical Student Education in the Time of COVID-19. JAMA. 2020;323(21):2131–2132. doi:10.1001/jama.2020.5227
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

Infectious diseases spike when kids return to school − here’s what you can do about it
Professor of Nursing, Purdue University
Disclosure statement
Libby Richards receives funding from the American Nurses Foundation, National Institutes of Health, and Indiana Clinical and Translational Sciences Institute.
Purdue University provides funding as a member of The Conversation US.
View all partners
Ready or not, back-to-school season is here, and kids will be bringing home more than homework. They’ll be carrying germs, too.
These viruses and bacteria will be agents that cause the common cold, influenza, norovirus, COVID-19, strep throat and more. There’s a reason why boxes of tissues and sanitizing wipes show up on most school supply lists.
As a nursing professor with experience in public health promotion , I have spent the past several years helping the public understand how to prevent the spread of infectious diseases, especially the flu and COVID-19 .
Here are some ways to minimize illness transmission from school to home.
COVID-19 cases likely to rise
In what health care providers call the summer wave , COVID-19 infections have been increasing throughout the summer of 2024. As of July 30, 2024, the number of COVID-19 infections has grown or is likely to grow in 35 states and territories .
Summer heat waves force people inside and into close proximity . And as record-setting temperatures continue driving this trend, the number of COVID-19 cases is expected to increase. This increase is expected to extend into the 2024–25 school year.
Currently, COVID-19 variants KP.3 and KP.3.1.1 are the dominant circulating virus strains . These variants are among the FLiRT variants , nicknamed after the locations of their spike protein mutations . These variants spread more easily from person to person and are able to evade vaccine-induced immunity better than previous strains .
These highly contagious COVID-19 strains, combined with the relaxed isolation guidelines that the Centers for Disease Control and Prevention released in March 2024, are likely to increase classroom disease transmission this coming school year. These updated CDC guidelines apply to all respiratory viruses, not just COVID-19.
The new guidelines recommend that everyone stay home when they are sick but also suggest that a person can return to normal activities once symptoms are improving and the person is fever-free for at least 24 hours without the use of fever-reducing medication. While it is too early to know the transmission impact of these guidelines, they may lead to more people coming out of isolation while still infectious.
Children play a large role in transmitting the COVID-19 virus. Children often do not have overt symptoms when they are infected with COVID-19, leading to increased contact and spread.
A two-year study following over 160,000 households composed of both adults and children found that just over 70% of viral transmissions , including COVID-19, in these households were pediatric index cases, meaning they started with a child. Further, these pediatric index cases were reduced by 60% to 80% during school breaks. This data suggests that COVID-19 infections will continue to increase once the school year starts.
Good hygiene habits reduce the spread
In May 2024, the CDC also released guidance for preventing classroom spread of infectious disease , including COVID-19 and other common infectious diseases such as the flu, norovirus and strep throat. This guidance places emphasis on proper respiratory etiquette, hand-washing and vaccination.

Proper cough and sneeze hygiene is especially important to reduce transmission of diseases such as COVID-19 and the flu, which are commonly transmitted through respiratory droplets . Coughs and sneezes create respiratory droplets that can be full of viruses or bacteria. Because these droplets are forcefully expelled, they can be spread around the environment and inhaled by another person.
That’s why it is important to turn your face away from others and cover up coughing or sneezing with a tissue and then quickly dispose of the tissue. If a tissue is not available, your sleeve is the next best option. Whichever method you use, it is important to wash your hands afterward. In addition to encouraging proper respiratory etiquette, classrooms should also have appropriate ventilation .
The CDC’s classroom guidance also focuses on proper hand-washing . Up to 80% of infectious diseases are spread through touch. Classrooms have countless high-touch surfaces , including light switches, tabletops, shared supplies, doorknobs, sports equipment and toys.
Proper hand-washing can prevent about 30% of diarrhea-related illness and about 20% of respiratory infections, such as colds and flu. The CDC also reports that proper hand-washing reduces absenteeism due to gastrointestinal illness by up to 57%.
Health care providers recommend COVID-19 and flu vaccines
Another important part of reducing classroom spread of infectious disease is keeping children up to date on vaccinations . Proper vaccination can reduce disease transmission rates 40% to 50% for flu and COVID-19 , 80% for child pneumococcal cases , upward of 90% for chickenpox and 100% for diseases such as polio and smallpox .

For the past several years, the CDC has recommended receiving the flu and COVID-19 vaccine at the same time when possible . Despite this recommendation, there has been some hesitancy in the uptake of both vaccines at the same time.
A 2024 Canadian study found that 20% of respondents did not see the benefit in co-administration, and another 17% were concerned about adverse reactions of receiving both vaccines together. However, several years of CDC data demonstrates the safety of receiving the flu and COVID-19 vaccines together .
Moderna recently released Phase 3 clinical trial data on a new combination vaccine against both the flu and COVID-19. This combination vaccine, currently called mRNA-1083, has demonstrated higher effectiveness when compared with individual vaccines for the flu or COVID-19. Moderna is expected to seek FDA approval soon. This combination vaccine may increase vaccine uptake because only one shot will be required instead of two.
Sick kids should stay home
The most important way to reduce the spread of germs in school is to follow the principle of keeping kids home when they’re sick . When sick kids go to school, they infect not only other students but teachers and staff too. When teachers get sick, it affects student learning and costs the U.S. billions of dollars each year.
Most schools and day care centers have guidelines on when to keep a child at home . As a general rule, a child should stay home from school or day care if they have a fever, vomiting, diarrhea or if they are generally unwell and unable to fully participate in school.
Without the presence of a fever, it is OK to go to school with a cough or runny nose, as long as the child feels well enough to participate in class. To return to school or day care , the child should be fever-free for at least 24 hours without the use of fever-reducing medications. When a student is returning to school with respiratory symptoms, consider having them take extra precautions, such as using a mask to protect others for the next five days.
If you have concerns about whether to send your child to school, it’s always a good idea to seek advice from your health care provider.
Healthy habits boost the immune system
Last but not least, focusing on healthy habits such as getting enough sleep and exercise , as well as eating nutritious meals , helps boost the immune system .
These actions should be practiced by family members of all ages.
- Infectious diseases
- Back to school
- Centers for Disease Control and Prevention (CDC)
- COVID-19 variants
- CDC guidelines
- Virus variants
- COVID isolation requirements
- Subvariants
- FLiRT variants


Service Delivery Consultant

Newsletter and Deputy Social Media Producer

College Director and Principal | Curtin College

Head of School: Engineering, Computer and Mathematical Sciences

Educational Designer
- Voter Guide
- Crime & Courts
- Special Reports
- Faith & Values
- National Politics
- The American South
- Women of the Century
- Coronavirus
WHO raises concerns for COVID-19 surge as school heads back into session
As the new school year starts in Tennessee, the World Health Organization warns that COVID-19 cases could soon become an issue once school is back in session and flu season is upon us.
The latest COVID-19 variant has infections surging worldwide, including at the Olympics where 40 athletes from various countries have tested positive. And they are unlikely to decline anytime soon, WHO warned during a United Nations press conference on Tuesday.
“In recent months, regardless of the season, many countries have experienced surges of COVID-19, including at the Olympics where at least 40 athletes have tested positive,” said Dr. Maria Van Kerkhove, director of epidemic and pandemic preparedness and prevention at the World Health Organization, on Tuesday.
Globally, the test positivity rate is about 10%, but it's 20% in Europe, Van Kerkhove said. In the United States, there was a dip in reported positive COVID-19 tests, but that has changed in the last several months. The Centers for Disease Control reported around a 2% increase in positive tests as of the week of July 27 with a 16.3% positive test rate.
Here's everything to know about the latest variant and how Tennessee is being affected.
What is the dominant COVID-19 variant?
The latest dominant COVID-19 variant is KP.3.1.1, according to the latest projections from the Centers for Disease Control and Prevention (CDC) .
"The KP.3.1.1 variant is very similar to other circulating variants in the United States. All current lineages are descendants of JN.1, which emerged in late 2023," Rosa Norman, a spokesperson at the CDC, previously told USA TODAY.
CDC's Nowcast data tracker , which displays COVID-19 estimates and projections for two-week periods, projects the KP.3.1.1 variant accounting for 27.8% of positive infections, followed by KP.3 at 20.1% in the two-week stretch starting July 21 and ending Aug. 3.
COVID-19 in Tennessee
As of July 30, COVID-19 infections were growing in 35 states or territories , including Tennessee and much of the South, according to the CDC.
Tennessee's latest COVID-19 statistics from the last 180 days finishing on Aug. 3, has seen more than 63,000 positive COVID-19 cases reported, of that 602 people have been hospitalized and 399 deaths related to COVID-19 have been reported to the state .
Since July 1, the number of daily cases reported has nearly doubled from 341 cases on July 1 to 747 cases on July 29.
Should I get a COVID-19 vaccine booster shot?
It may be time to get an updated COVID-19 vaccine for 2023-2024. Here's what the CDC recommends if you are wondering if you need to get an updated vaccine:
- Everyone aged 5 years and older should get one dose of an updated COVID-19 vaccine to protect against serious illness from COVID-19.
- Children aged 6 months to 4 years may need multiple doses of COVID-19 vaccines to be current, including at least 1 dose of updated COVID-19 vaccine.
- People who are moderately or severely immunocompromised may get additional doses of the updated COVID-19 vaccine.
- People aged 65 years and older who received one dose of any updated 2023-2024 COVID-19 vaccine (Pfizer-BioNTech, Moderna or Novavax) should receive an additional dose of an updated COVID-19 vaccine at least four months after the previous updated dose.
USA TODAY contributed to this report.
New UNESCO global survey reveals impact of COVID-19 on higher education

In the wake of the unprecedented COVID-19 education disruptions which affected more than 220 million tertiary-level students around the world, UNESCO conducted a global survey aimed at providing an evidence-based overview of the current situation of the higher education system at national and global levels.
The results provide insights on how some countries were able to transform challenges, brought by the rapid digitalization of education, into opportunities through strong government support and international cooperation.
The survey attempts to assess the varying impact the pandemic had on higher education systems in terms of access, equity and quality of teaching and learning, university operation, national challenges, emerging issues, and strategic responses.
The key findings for the various assessment dimensions are:
Mode of teaching and learning: The major impact of COVID-19 on teaching and learning is the increase in online education. The hybrid mode of teaching has become the most popular form.
- Access : The impact of COVID-19 on enrollment varies by regional and income levels. High income and Europe and North American countries are better able to cope with the disruption due to government funding support and increase in domestic enrollment.
- International mobility : Mobility took a major hit, affecting international students significantly, but virtual mobility could compensate or even replace physical mobility.
- University staff : Despite the closure of many universities, the impact of COVID-19 on university staff compared to the previous academic year is limited.
- Disruption of research and extension activities : COVID-19 caused suspension and cancellation of teaching and research activities globally.
- Widening inequality : The mixed impact of the pandemic on university finance shed a light on the exacerbation of inequality in higher education. Financial support from the government and external sources are crucial to the survival of HEIs.
- University operations : The strong impact of the pandemic on HEIs operations caused reduced maintenance and services on campus and campuses closures worldwide.
- National challenges : Health and adaptation to new modes and models of teaching are the top concerns for students and institutions.
- Transition from higher education to work : The significant reduction of job opportunities makes the transition from higher education to the labor market more difficult. Employers are also seeking applicants with higher technology skills.
- National priority : Strategic options for country-specific response are to improve infrastructure and availability of digital devices for online or distance learning as well as support for teachers and more international collaboration in research and policy dialogues.
The global survey was addressed to the 193 UNESCO Member States and 11 Associate Members. Sixty-five countries submitted responses, fifty-seven of which were used for the analysis that informed the report.
- Access the full report
- More on UNESCO’s work in higher education
Related items
- Higher education

Other recent news

Color Scheme
- Use system setting
- Light theme
Montana State University doesn’t owe students tuition from COVID-19 closures

Montana State University doesn’t owe a student any refunds from tuition or fees when it shut down in-person education in response to the COVID-19 pandemic, the Montana Supreme Court said in an order this week.
MSU did have an “express contract,” one stated in words, with Anthony Cordero, who had sued the Bozeman university alleging it should have paid him back when it transitioned to distance learning.
But the institution never promised a complete in-person education, and it didn’t promise to never shut down the campus if it had a good reason to do so, the justices said.
Cordero had, “at most, a presumption” of in-person education, but MSU retained its right to respond to emergencies, the Supreme Court said.
Additionally, MSU is governed by the Board of Regents, which has full authority in the Montana Constitution to supervise all campuses.
“We cannot fathom upholding a prorated refund of tuition and fees for MSU being forced to close due to inclement weather that prohibits classes, which frequently occurs due to Montana winters,” the order said. “Here, Cordero was never deprived of classes, which were still conducted, albeit online.”
The District Court had found there was no express contract between Cordero and MSU – contrary to the findings of the Supreme Court – and also no “implied contract.”
However, in a unanimous decision by a five-judge panel, the Supreme Court said the overall conclusion the lower court reached in favor of MSU was still correct because MSU didn’t breach “contractual duties with respect to tuition.”
Adrian Miller, a lawyer at Sullivan Miller who represents Cordero, said MSU should have done better for students.
“It is disappointing that the Supreme Court does not believe MSU had an obligation to provide even a prorated refund for services and facilities that were unavailable during its COVID campus closure,” Miller said in an email. “We respect the Supreme Court’s decision, but students deserve better from the university.”
MSU spokesperson Tracy Ellig, however, said the order affirms the university’s actions during the emergency.
“The court’s ruling speaks clearly,” Ellig said in an email. “This ruling vindicates the university against these unfounded claims and reinforces that the university did everything in its power to provide education to students fairly and effectively during the pandemic.”
After COVID-19 hit the country in 2020 and many campuses closed, lawsuits popped up from students alleging various campuses owed them refunds. But courts came to different conclusions.
“Because this is a matter of first impression in Montana, we note other jurisdictions have considered nearly identical agreements between students and universities,” the Montana justices said. “Across the country, the precedent varies with some jurisdictions finding there to be enough evidence to maintain a claim for a contract, and others finding insufficient evidence to maintain a claim for a contract between student and university.”
Cordero never disputed MSU had the right to halt in-person instruction. However, he alleged he shouldn’t have had to pay MSU the same amount, some $19,901 that semester, according to the order, including many fees, for online classes.
As part of his argument, Cordero pointed to numerous marketing materials from MSU that show students making friends in residence halls, working together in labs and the library, and engaging in other community activities.
He alleged those materials reflected a commitment from MSU that included in-person education, but the Supreme Court disagreed.
The materials he provided don’t create a contract, the justices said. Rather, the language “informs students they have access to opportunities on campus,” which aren’t a promise in a contract, the order said.
“Although he did not get the experience he expected to get during the final half of the Spring 2020 semester, Cordero still progressed in his academic program and was able to graduate,” the order said.
The Supreme Court said Cordero doesn’t get any of his fees back either. It said even though the fitness center was temporarily closed, it was maintained, and even though the library was closed, its online services were available, for example.
“Mandatory fees are charged to everybody as a condition of enrollment, and they do not promise anything in return, according to MSU,” the order said.
It said MSU may have encouraged students to go home, but it also made accommodations for students who decided to stay on campus, “including keeping its campus operational so that students could progress and complete their academic programs.”
In its order, the Supreme Court also disagreed that MSU was “unjustly enriched” by keeping tuition and fees from students without giving them their expected benefit. It said Montana law doesn’t allow recovery under “unjust enrichment” if the parties have a written contract.
Daily Montanan is part of States Newsroom, a nonprofit news network supported by grants and a coalition of donors as a 501c(3) public charity. Daily Montanan maintains editorial independence.
Hydropower remains essential to affordable, reliable electricity in Idaho
We all love Idaho for its natural beauty, homegrown agriculture and great outdoor recreation.
- Skip to Main Content
- Skip to audio player to listen live
Enter the username on file and we'll send you a code to reset your password.
A verification code has been emailed to
6 facts about Walz’s education track record in Minnesota

Create an account or log in to save stories.
Thanks for liking this story! We have added it to a list of your favorite stories.
Minnesota Gov. Tim Walz loves talking about the more than two decades he spent as a classroom teacher. Much of that time was in Mankato in southern Minnesota where he taught social studies and coached football.
He’s made public education a key part of his political identity, holding news conferences at schools and talking frequently about making Minnesota the kid-friendliest state in the country.
Here are six facts to know about his work as a self-styled education governor.
1) Walz signed into law a universal school meals bill
In 2023 the Minnesota Legislature passed a universal school meals bill, which meant that, for about a year now, all students attending Minnesota public and charter schools are required to provide breakfast and lunch free of charge to all their students, regardless of income.
Support the News you Need
Gifts from individuals keep MPR News accessible to all - free of paywalls and barriers.
The program has been incredibly popular in Minnesota. The number of students eating cafeteria lunches and breakfasts has gone up anywhere from 10 to 50 percent. As a result, the program is costing more than expected. Authorities, though, say it’s also significantly reduced the stigma for students around accessing food when they need it.
In a recent interview with a New York Times columnist, Walz said after the free meal policy went into effect, “attendance went up, we saw huge usage of this and we saw classroom behaviors go down.”
Walz’s communications team says that the feedback he’s hearing anecdotally from teachers backs up his statement.
While research generally shows behavior and achievement improve when kids have access to free meals, the research isn’t there yet to back up Walz’s statements specifically in Minnesota.
“I would love to get to a point where we can validate some of the things that he’s saying directly to this program,” said Leah Gardner, policy director for Hunger Solutions, a nonprofit focused on fighting hunger in Minnesota that’s in the middle of a two-year evaluation of the new program.
2) Walz has poured big money into K-12 schools
Last year, Walz and the DFL-controlled Legislature backed historic spending on K-12 and early education . At the end of the 2023 legislative session, he signed into law a bill that put $2.2 billion in new funding toward K-12 education. This was a significant hike in education spending for the state — about $400 per student per year more than previous spending.
That bill also tied state education funding to inflation, something school administrators had been asking for for decades.
School leaders have expressed excitement and appreciation over that, but they also say the hike wasn’t enough to cover some of the requirements from the federal government on spending for special education services as well as newly passed requirements from the state government on new initiatives related to reading instruction, discipline and other issues, as well as the loss of federal pandemic money.
3) Walz’s COVID-19 policies made it difficult for many schools to operate in-person during the pandemic
Like many other governors, Walz closed in-person education across the state in March 2020 as the pandemic took hold. Over the next year he backed a policy created by his education commissioner that saw schools open fully in-person, fully-remote or a hybrid combination of those two options, depending on what COVID case counts looked like in various regions of the state.
Closing schools was especially difficult for administrators living in rural communities where a majority of parents wanted schools open, said Deb Henton, executive director of the Minnesota Association of School Administrators.
“Our knowledge of what to do in a pandemic was extremely limited at the time, so I believe he (Walz) acted on the best information possible,” she said. “It was difficult for our school districts that at first were not experiencing any COVID cases in their districts and yet they needed to close schools and they had a community that maybe was not supportive.”
Like other parts of the country, Minnesota saw student mental health and test scores fall during the pandemic. Four years later, Minnesota’s most recent graduation numbers appear to be on the rise again . New K-12 test score data comes out this month.
Critics, though, believe Walz’s decision-making around schools and the pandemic was too restrictive and that more schools should have been encouraged to remain open and offer in-person learning sooner.
4) Walz has spent record amounts on early childhood
Walz and the DFL Legislature last year passed record spending in early child care and learning. As part of a $1.3 billion package of child care spending for families and providers, Walz used $316 million to boost wages for child care providers through the Great Start Compensation Support Program.
“He [Walz] didn’t just sit back and sign bills into law, but he actually was out there working to get these bills taken care of,” said Burnsville child care director Amanda Schillinger. “It made huge changes for our ability to pay living wages to our staff, increasing the early learning scholarship, increasing funding for child care assistance. Those things have been just, they’ve made such huge changes in our industry.”
In addition to raising wages for child care providers, Walz passed a major paid family and medical leave bill. He also supported the creation of a brand new state agency, the Department of Children, Youth and Families, which combines state agency programs for young children under one jurisdiction, a change Schillinger and other child care advocates had been seeking.
“He sat at the table with us. He sat at the table and heard what we had to say, he actually listened to us and then worked to make those things come true,” Schillinger said.
Most recently, Walz named the commissioner for this new department and launched a new initiative for military families to receive child care funding vouchers in Minnesota. But Monique Stumon, a child care director in north Minneapolis, said his work started before the most recent child care legislative wins.
“The support that he gave day care providers during the pandemic of COVID, I mean he made sure that we were recognized, he made sure that we received different types of compensation,” Stumon said.
“We still have things that we want to get accomplished, but the first steps have been enormous for us, and they have impacted so many lives, particularly little Black and brown children that so many times get left behind,” Stumon added. “And so I think he’s going to be a good leader in making sure that we have a more even playing ground.”
5) The Feeding Our Future scandal brought scrutiny of Walz’s Education Department
Critics have attacked Walz and his Education Department for not doing enough to uncover a massive $250 million child nutrition fraud in Minnesota.
The agency distributed that federal money largely through the local nonprofit Feeding Our Future. But prosecutors later alleged Feeding Our Future was a conduit for illegal payments sent to people who used the money to buy cars, luxury goods and property instead of feeding children.
The Education Department is not accused of wrongdoing, but a recent report from the Office of the Legislative Auditor found “actions and inactions” by the department created opportunities for this fraud.
6) Minnesota public colleges have seen an increase in enrollment under Walz
As part of the One Minnesota budget plan, Walz and lawmakers approved an additional $650 million for higher education in 2023 for the implementation of new programs for financial aid and workforce initiatives in the 2024-25 school year. He also passed the North Star Promise program which covers tuition and fees for Minnesota familiars earning less than $80,000 a year.
Since the funding passed, Minnesota public colleges and universities have seen a slight increase in enrollment for the first time in a decade.
- Special education support staff can get fully licensed teaching degrees through new apprenticeship program
- State Appeals Court rules Indus School closure legal
- What children learn when they play
Supporting the campus community
Our goal is to ensure that you have the right to an education and to work and advance in employment on the basis of merit, ability, and potential without fear of discrimination.

NSHE and its member institutions do not discriminate on the basis of sex in their education programs and activities. Title IX of the Education Amendments Act of 1972, 20 U.S.C. § 1861(a), provides: “No person in the United States shall, on the basis of sex, be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any education program or activity receiving Federal financial assistance.”
Explore Title IX
View more information about Title IX
More in Title IX
Related links for Title IX resources
- Title IX complaint process
- Title IX Staff
- Title IX reporting statistics
- Filing a Concern

Unlawful discrimination and harassment
The University of Nevada, Reno, does not discriminate on the basis of protected classes in any education program or activity that it operates. Non-discrimination on the basis of protected classes is mandated by Federal law. The University’s commitment to nondiscrimination in its education programs and activities extends to applicants for admission and employment.
Investigations
EO/TIX does not advocate on behalf of any party. When we receive a complaint of sexual harassment, sexual violence, or of unlawful discrimination or retaliation, we act as an independent fact-finder.
Prevention & compliance
Provides training and various workshops for students, employees, and campus organizations related to the prevention of sexual misconduct, discrimination, and harassment.
Serves as a resource and leader in furthering the University’s commitment to equity and diversity working to promote equal opportunity for all members of the Wolf Pack Community. Through educational programming, policy review, and collaborative campus initiatives.
NSHE is committed to providing a place of work and learning free of discrimination on the basis of a person’s age (40 or older), disability, whether actual or perceived by others (including service-connected disabilities), gender (including pregnancy-related conditions), military status or military obligations, sexual orientation, gender identity or expression, genetic information, national origin, race (including hair texture and protected hairstyles such as natural hairstyles, afros, bantu knots, curls, braids, locks and twists), color, or religion (protected classes).
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

COVID-19 and excess mortality in Russia: Regional estimates of life expectancy losses in 2020 and excess deaths in 2021
Sergei scherbov.
1 Population and Just Societies Program, International Institute of Applied Systems and Analysis, Laxenburg, Austria
Stuart Gietel-Basten
2 Division of Social Science, The Hong Kong University of Science and Technology, Kowloon, Hong Kong SAR, China
3 Department of Humanities and Social Science, Khalifa University of Science and Technology, Abu Dhabi, United Arab Emirates
Dalkhat Ediev
4 North-Caucasian State Academy, Institute for Applied Mathematics and Information Technologies, Cherkessk, Russia
Sergey Shulgin
5 International Laboratory of Demography and Human Capital, Russian Presidential Academy of National Economy and Public Administration, Moscow, Russia
Warren Sanderson
6 Department of Economics, Stony Brook University, Stony Brook, NY, United States of America
Associated Data
All data used in this paper are publicly accessible, and are listed in the Materials and Methods section with links to the datasets to be found in the bibliography. The full datasets generated and behind the summary tables in this article have been uploaded as part of the Supplementary Material. For clarity, the dataset links are reproduced here: ROSSTAT. 2021 INFORMATION ON THE NUMBER OF REGISTERED BIRTHS, DEADS, MARRIAGES AND DIVORCE for January - December 2021. See https://rosstat.gov.ru/storage/mediabank/2021_edn12_t1_2.xlsx . ROSSTAT. 2021 Natural movement of the population of the Russian Federation in 2020. See https://rosstat.gov.ru/compendium/document/13269 . ROSSTAT. 2021 Estimate Of Life Expectancy At Birth By Regions Of the Russian Federation for 2020. See https://rosstat.gov.ru/folder/12781 . ROSSTAT. 2022 Operational information about the natural movement of the population. See https://rosstat.gov.ru/storage/mediabank/2021_edn12.htm . Center for Demographic Research. 2017 Russian Fertility and Mortality Database. See http://demogr.nes.ru/index.php/ru/demogr_indicat/data .
Accurately counting the human cost of the COVID-19 at both the national and regional level is a policy priority. The Russian Federation currently reports one of the higher COVID-19 mortality rates in the world; but estimates of mortality differ significantly. Using a statistical method accounting for changes in the population age structure, we present the first national and regional estimates of excess mortality for 2021; calculations of excess mortality by age, gender, and urban/rural status for 2020; and mean remaining years of life expectancy lost at the regional level. We estimate that there were 351,158 excess deaths in 2020 and 678,022 in 2021 in the Russian Federation; and, in 2020, around 2.0 years of life expectancy lost. While the Russian Federation exhibits very high levels of excess mortality compared to other countries, there is a wide degree of regional variation: in 2021, excess deaths expressed as a percentage of expected deaths at the regional level range from 27% to 52%. Life expectancy loss is generally greater for males; while excess mortality is greater in urban areas. For Russia as whole, an average person who died due to the pandemic in 2020 would have otherwise lived for a further 14 more years (and as high as 18 years in some regions), disproving the widely held view that excess mortality during the pandemic period was concentrated among those with few years of life remaining–especially for females. At a regional level, less densely populated, more remote regions, rural regions appear to have fared better regarding excess mortality and life expectancy loss–however, a part of this differential could be owing to measurement issues. The calculations demonstrate more clearly the true degree of the human cost of the pandemic in the Russian Federation.
Introduction
Counting the human cost of the COVID-19 pandemic is clearly a demographic, policy and epidemiological priority. The particular circumstances in the Russian Federation have come to international attention because of the especially high levels of mortality compared to other parts of the world [ 1 ]. There are, however, many challenges to producing what appear to be a simple estimate of mortality derived from COVID-19. For example, differences in the adequacy and completeness of registration data around the world, as well as the definition and specification of causes of death represent a key challenge. According to the recommendations of the World Health Organization (WHO), death from COVID-19 is defined ‘for surveillance purposes as a death resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID disease (e.g. trauma)… There should be no period of complete recovery from COVID-19 between illness and death’ [ 2 ]. This definition, however, is not universally applied across all WHO member states, not least because of the challenges associated with determining a primary cause of death. The situation is even more complicated in the current pandemic, where a relatively mild infection can trigger a series of events resulting in death from an underlying condition. Such problems with defining cause of death result in wide variations in estimates of ‘deaths due to COVID-19’ at the global and national level [ 3 ].
In the Russian Federation (hereafter Russia), there appears to be an especially high degree of uncertainty concerning mortality due to COVID-19 [ 4 ]. The number of deaths due to COVID-19 reported by the Russian Federal State Statistical Service for 2020 (163,325) was three times that produced by the Russian Virus Response Center [ 5 ]. In other parts of the world, there have been marked differences between regions in terms of their mortality experience of COVID-19 [ 6 , 7 ]. Such uncertainty is expected to be amplified when considering the regional heterogeneity and different experiences of COVID-19 across the country [ 8 ].
Against this backdrop, the concept of ‘excess mortality’ has been set out as a possible ‘gold standard’ of measuring the human cost of the COVID-19 pandemic [ 9 ]. Excess mortality is estimated as the difference between the number of deaths that occurred during the COVID-19 pandemic in a particular period and the number of deaths that estimated to have occurred in the same period if there were no pandemic. The latter number is often referred to as the ‘baseline death count’. A major benefit of the excess mortality approach is that it is not sensitive to variations in cause of death reporting, and encompasses deaths relating directly to COVID-19 as well as those due to related causes and issues which may have stemmed from lockdowns, restriction on movement, postponed operations and so on [ 5 ]. This approach to measurement has been adopted in various datasets [ 10 , 11 ], by various international organizations (such as WHO [ 12 ], OECD [ 13 ], and by national statistical agencies (e.g. [ 14 ]).
Despite this consensus on the benefits of the excess mortality approach, there are still variations in the final calculated numbers of such deaths at the global and national level [ 3 ]. A recent paper by Kobak [ 8 ] produces various estimates for excess mortality stemming from COVID-19 in Russia, with one as high as 380,000 deaths (as of 1 January 2021), corresponding to 0.26% of the population. For the period April to November 2021, Kobak [ 8 ] estimates a total of 264,100 excess deaths (95% interval: [232,000, 296,200]), which is higher than the total number of COVID-19 related deaths reported to WHO for the entire period from January 2020 to December 2021 [ 15 ]. Kobak’s figures show Russia to have the second highest absolute number of estimated excess deaths in the world after the United States (over 400,000), and one of the highest numbers per capita. More recently, Aburto et al. [ 16 ] found that that life expectancy losses among females were the largest in Russia, and losses among males stand only behind the USA (2.2 years) and Lithuania (1.7 years), although Islam et al [ 20 ] estimate that Russian losses in life expectancy are highest for both men and women. Kobak [ 8 ] also produced estimates of excess mortality by Federal Region, and finds 23,500 cases of excess mortality in Moscow alone, with the highest excess mortality rate found in Samara Oblast: a 22% yearly mortality increase.
Part of the reason for the discrepancy in figures of excess mortality presented for Russia above stems from alternative methods of calculating this projected death count. As the recent study by Nepomuceno et al. [ 17 ] describes, there can be differences in measured outcomes based on a variety of factors such as the mortality index; the method used to estimate the baseline; the number of years included in the reference period; and the time unit of the death data (weekly and monthly). In addition, the jump-off effect of the previous year’s data for trend models must also be considered. Turning back to studies of excess mortality in Russia, in the first approach an average count of deaths for a particular time interval is calculated (e.g. five years before the pandemic began) and these numbers are compared to the number of deaths that occur during the pandemic [ 18 ]. In the second approach, used in Kobak [ 8 ], deaths are extrapolated. In this method, the average monthly number of deaths for each year are computed for 2006–19; then a linear trend is fitted to the 2015–2019 values which is then extrapolated to provide the predicted baseline value for 2020.
Neither approach accounts for changes in mortality and population age structure over time and can lead to a biased estimation of excess mortality from the COVID-19 pandemic. This can be especially true for an aging population with an irregular age structure–such as Russia. In each case, the dynamics of mortality and waves in the demographic structure will affect the assessment of deaths in the absence of a pandemic and, accordingly, affect the assessment of demographic losses due to the coronavirus pandemic.
For a more accurate assessment of the number of deaths in the absence of a pandemic, it is possible to use predicted values of the number of deaths that consider the peculiarities of the age structure of the population. To estimate the number of deaths in 2020–21 in the absence of a pandemic—and therefore to calculate excess mortality in comparison—it is necessary to make a population forecast for one year from the beginning of 2020 to 2021 or for two years from the beginning of 2020 to 2022. The population forecast can be made either with the mortality rate of 2019 or considering the dynamics of mortality in previous years to predict the expected mortality for 2020/2021. Both versions of the forecast allow us to estimate the number of deaths that would have occurred in 2020/2021 in the absence of the COVID-19 pandemic. Excess mortality, in this vein, is defined as the difference between the recorded number of deaths in 2020/2021 and the projected estimate of the number of deaths in the absence of the COVID-19. In this paper we followed the second approach. Projecting the number of deaths in the absence of the pandemic, we assumed that life expectancy would have increased at the same pace as it has been increasing recently. Such an approach was also performed in Islam et al. [ 19 , 20 ]. Timonin et al. calculated excess mortality for Russia and its regions for 2020 [ 5 ]. They found that Russia had one of the highest levels of excess mortality in the world and matched most closely those found in other central and eastern European countries. At the regional level, they found that excess mortality began to increase in Moscow and St. Petersburg in the Spring of 2020, and then spread to all regions of Russia by the end of 2020. They concluded by arguing that the observed negative association between excess mortality and reported cases was explained by under-recording of the latter.
In this paper, using the latest data released from ROSSTAT [ 19 – 22 ], we are able to calculate excess mortality for Russia and its regions for 2020 by age, sex, and rural-urban residence. For 2021, we produce estimates for regions only (because more granular data have not yet been released). In doing so, we build on the extant literature in the following ways: firstly, we are able to go beyond the estimates produced for 2020 in Kobak [ 8 ] by deploying this alternative methodology which takes into account projected changes in the age structure. Secondly, we produce the first estimates for 2021 using a variation of the enhanced method deployed by Timonin et al. [ 5 ] (building on Islam et al. [ 23 ]). Finally, we are able to go beyond the analysis performed in Timonin et al. [ 5 ] by producing estimates for rural and urban excess mortality for 2020.
Islam et al. [ 24 ] further applied an important measure of losses due to the pandemic, namely, the Years of Life Lost ( YLL ). Following WHO methodology [ 25 ], they calculated YLL based on expected remaining years of life from a standard life table for all countries. Such an approach, as useful as it may be for international comparisons, does not adequately express losses of expected years of life in countries like Russia where actual remaining life expectancies deviate substantially from those of the standard life table used in Islam et al. [ 23 ]. As such, we calculate a related indicator using life tables based on actual mortality data and extrapolations for Russia and its regions, relating the life years lost to those very people who perished due to the pandemic. To avoid confusion with YLL , we term our indicator Mean Remaining Life Expectancy of the Deceased ( RLED ).
Materials and methods
The primary sources of data are derived from official ROSSTAT publications for the 2021 [ 19 – 22 ]; the Russian Economic School database [ 26 ] for the 2020; and calculations and population projections which were used in the Russian Demographic Data Sheet 2019 [ 27 ]. The database of the Russian Economic School provides death rates for 2020 by gender, region, urban and rural residence and single years of age as well as population exposures. The time series of observed life expectancies for the regions of Russia were obtained from Federal State Statistics Service [ 28 ].
Our approach builds on that of Islam et al. [ 20 ] who used the Lee-Carter model [ 29 ] to extrapolate age-specific mortality rates based on trends over the period 2005–2019. We do not, however, use that extrapolation method, because it relies on the existence of extended log-linear temporal trends of age-specific mortality rates, an assumption that may not be applied to the volatile and complex dynamics of mortality in Russia and its regions. Instead, we extrapolate the life expectancies at birth and then adjust the baseline 2019 death rates so as to fit to the extrapolated life expectancies (graduation and adjustment procedures come from an earlier projection for Russia [ 27 ]). Our method is somewhat similar to the one employed by UN [ 30 , 31 ] who also extrapolate life expectancy first and then disaggregate it into age-specific rates. There are important differences, though. In predicting the counterfactual life expectancy in the absence of the pandemic, given the short projection horizon and linear trends in the life expectancy since 2010, we use linear trend model fit to data for the years 2010 to 2019. To check relevance of the linear trend to our data, we calculated determination coefficients (R2). Among the regions included in our tabulations, the average determination coefficient was 94.1%, and only in one region (Arkhangelsk Region less autonomous area) was it below 70% (67%). When disaggregating the life expectancy into age-specific death rates, we use Ediev’s [ 32 , 33 ] approach to preserve consistent age-sex patterns of the projected mortality. To this end, we fit log-linear trends to age-sex-specific death rates in the period 2010–2019 (controlling for regional effects and interaction of age-sex with rurality)
where M x , t i – are the age-specific death rates in year t in population i (rates are calculated separately by region, rurality, and sex), a x , s R E G – age-sex- federal district (REG)-specific effects, b i −population-specific effects, b x −age-specific rates of mortality improvement over time. From the modelling outcomes, we obtained age-specific rates of mortality improvement similar to the b x of the Lee-Carter model [ 25 ]. The age-specific rates of mortality improvement are then adjusted to form an age-monotone (increasing with age) profile b x * that, being used in the projection, assures consistency of age profiles of the mortality rates. In the projection, the baseline death rates of 2019 are updated by applying the age-specific improvement rates b x * :
where M x , t 0 i are the age-specific death rates in the base year; and k t i are scaling factors that are matched to the projected life expectancy for a given population. The described procedure is technically similar to what has been recently introduced as the ‘rotation’ technique used, for example, in the UN’s World Population Prospects [ 34 ].
A standard cohort-component method-based system for producing multiregional population projections was used. To estimate excess mortality, we needed to project the deaths only for two years: 2020 and 2021. In this short time interval, the influence of migration and fertility on the total number of deaths would likely be insignificant (see below). Although we used a multiregional package to produce the number of deaths, similar results would have been obtained had we applied a cohort-component projection model to each region and urban settlement independently.
The population projection approach has several advantages over approaches that average the number of deaths over the previous five years or extrapolate the annual number of deaths from the years preceding pandemics. First, the change in the age structure of the population and its impact on the number of deaths is considered. Second, it is possible to reduce random fluctuations in the expected number of deaths, since the population forecasts produce graduated structures of mortality. In fact, the primary reason why the traditional method uses a five-year interval to average the number of deaths is the need to reduce the random component in estimating the number of deaths. Finally, because of the need to obtain time-series data on which to draw the projections—we used data from 2010- we excluded regions with short series of data available, and with small death count as described below (see Appendix for full list).
In this paper, to estimate excess mortality, we use a population forecast for all regions of Russia, that assumes the observed recent trend in life expectancy would have continued in the absence of the COVID-19 pandemic. The base population estimate is taken as of January 1, 2020. To estimate the number of excess deaths in 2020 and 2021, the population forecast is made for two years. As the impact of fertility and migration on the number of deaths in 2020–21 is extremely small, so the baseline scenario of fertility and migration, similar to the level of fertility and migration in 2019, was considered. Finally, to mitigate against high levels of fluctuations resulting from small numbers, we only consider populations where our calculated number of expected deaths is greater than 3,000 per year. Although this particular threshold was chosen rather arbitrarily, our decision was based on earlier experience with sampling errors of life expectancy estimates [ 34 ]. Given a Russian Crude Death Rate of roughly 12.8, 3,000 deaths correspond to around 235,000 people which, at life expectancy around 73 years, yields a sampling standard error of about 0.27 years (see Appendix 1 of [ 34 ]). This approximately corresponds to 95% CI (±0.5 years). Because the COVID-19 related losses to life expectancy are measured in years, we considered such a threshold to be reasonable for the current study.
To produce estimates of RLED in Russia and its regions in 2020 we use the following procedure. For each age group with non-negative excess mortality, we multiply the excess deaths by the corresponding remaining life expectancy in the absence of the COVID-19, sum up those products and divide by the total excess deaths in those age groups:
where D x o b s is the number of deaths that was observed in the age group x in 2020, D x e x p is the number of deaths that would be expected in the absence of COVID-19 in age group x in 2020, e x is life expectancy at age x from the baseline life table in 2020 which would hold in the absence of pandemic. RLED is calculated for each region, urbanization status, and gender. We do not estimate RLED for 2021 because the required data have not been published yet.
Calculations were produced using packages written by authors in FORTRAN and R.
Excess deaths at the regional level for 2020 and 2021
Based on our population projections, we estimate that there were 351,158 excess deaths in 2020 and 678,022 in 2021 in the Russian Federation (see Tables Tables1 1 and S1 )—a total of 1,029,181 excess deaths over the period 2020–2021. This figure represents an excess of 19.65% and 38.36% over the expected number of deaths for 2020 and 2021 respectively. Our results are not much different from those that might have been obtained for Russia as a whole based on the official population projection by ROSSTAT that was conducted in 2019 [ 35 ]. Comparing deaths projected by ROSSTAT for 2020 and 2021 to actual figures, yield estimates of excess mortality 350,600 for 2020 and 657,800 for 2021 (1,007,400 in total over two years). ROSSTAT’s projection, however, do not provide the regional details that are studied here.
| Region | Expected deaths in thousands | Observed deaths | Excess deaths | Excess deaths as % of expected deaths |
|---|---|---|---|---|
| | ||||
| Chechen Republic | 6.4 | 9.4 | 2.9 | 45.97 |
| Republic of Dagestan | 15.2 | 19.8 | 4.6 | 30.21 |
| Republic of Tatarstan | 42.3 | 54.3 | 12.0 | 28.41 |
| Lipetzk oblast | 15.8 | 20.2 | 4.4 | 27.92 |
| Republic of Mordovia | 10.3 | 13.1 | 2.8 | 26.95 |
| , . | , . | . | . | |
| Sakhalin oblast | 5.9 | 6.7 | 0.8 | 13.07 |
| Arkhangelsk Region (less NAA) | 14.5 | 16.2 | 1.7 | 11.82 |
| Zabaikalsk kray | 12.9 | 14.4 | 1.5 | 11.58 |
| Republic of Buryatia | 10.6 | 11.8 | 1.2 | 11.26 |
| Republic of Adygeya | 5.6 | 6.2 | 0.6 | 10.37 |
| | ||||
| Lipetzk oblast | 15.5 | 23.6 | 8.1 | 52.14 |
| Saratov oblast | 32.4 | 49.1 | 16.6 | 51.25 |
| Ryazan oblast | 16.0 | 24.0 | 8.0 | 50.00 |
| Orenburg oblast | 24.7 | 36.6 | 11.9 | 48.00 |
| Volgograd oblast | 31.6 | 46.6 | 15.0 | 47.35 |
| , . | , . | . | . | |
| Moscow | 132.5 | 172.8 | 40.3 | 30.39 |
| Sakhalin oblast | 5.8 | 7.6 | 1.8 | 30.29 |
| Zabaikalsk kray | 12.7 | 16.5 | 3.8 | 30.04 |
| Kemerovo oblast | 36.9 | 47.6 | 10.7 | 29.04 |
| Primorsky kray | 25.1 | 31.9 | 6.8 | 27.25 |
S1 Table shows the numbers of excess deaths per region for all regions with greater than 3,000 predicted deaths per year. Table 1 gives a snapshot of this regional data showing the five regions with the highest and lowest percentage of excess deaths. While the figures show a wide variation between provinces, no specific regional patterns (e.g. an east-west gradient) could be observed. In 2021, the highest percentages of excess mortality can be found in Lipetzk oblast (52.14%) in the Central Federal District, while the lowest can be found in Primorsky kray (27.25%) in the Far East of the country. In terms of the regional distribution, the patterns are far from clear cut. In 2020, for example, the range was from an 10.37% excess in the Republic of Adygeya in the Northern Caucasus up to a 45.97% excess in the Chechen Republic. In other words, some of the highest and lowest percentages of excess mortality can be found in the Caucasus–a feature which warrants further investigation. Similarly, while four of the six regions with the lowest excess mortality (Republic of Buryatia, Sakhalin oblast, Zabaikalsk kray and Promorsky oblast) can be found in the Far Eastern Federal District, so too can the 9 th highest ranking region (Republic of Sakha). Indeed, the regions with the highest excess mortality in 2021 are to be found around the country: four in the Central Federal District (Lipetzk oblast, Ryazan oblast, Voronezh oblast and Kursk oblast); three in the Volga Federal District (Saratov oblast, Orenburg oblast and Republic of Mordovia) and one each in the Southern Federal District (Volgorad oblast), Northwestern Federal District (Republic of Karelia) and Far Eastern Federal District (Republic of Sakha). Among the regions with the lowest excess mortality, the majority are to be found in the sparsely populated regions of the Far Eastern Federal District and Siberia. Moscow City, however, is also in this low ranked groups.
Finally, there is a high degree of change both between the two years and across the regions of Russia. In the Republic of Karelia, for example, excess mortality rose from 17.11% in 2020 to 46.3%, propelling it from a middle-ranking position to one of the highest in the country. A further five regions saw increases in excess mortality of greater than 25% (Kursk oblast, Kostroma oblast, Novgorod oblast, Voronezh oblast and Saratov oblast). Other states, meanwhile, saw much less dramatic changes. Eleven regions saw increases of 10–15% (Khabarovsk kray, Kabardian-Balkar Republic, Primorsky kray, Novosibirsk oblast, Chelyabinsk oblast, Chuvash Republic, Samara oblast, Udmurt Republic, Perm kray, Republic of Bashkortostan, and Kemerovo oblast). Excess mortality in the Republic of Dagestan, meanwhile, stayed almost constant between 2020 and 2021. Because of the sharp increases across the country, this meant the region dropped in the national rankings from second top to eighth last. Mortality in the Chechen Republic appears to have fallen between 2020 and 2021.
Excess deaths and life expectancy loss at the regional level for 2020 by urban-rural residence, gender and age
S2 Table shows excess mortality in urban and rural areas. As expected, the percentage of excess deaths is higher in urban areas due to the much higher population density. A summary of this table is presented in Table 2 . In 2020, there were 274,520 excess deaths in urban areas compared to 76,640 in rural areas. Our results for Russia are consistent with other studies [ 16 , 20 ]. The Republic of Dagestan has the highest excess mortality of either rural or urban areas (34.8%), and the highest number of years in terms of life expectancy lost (3.5). Despite this, it is apparent that the highest levels of excess mortality were, indeed, higher in the urban areas than in rural areas. The top five urban areas (Lipetzk oblast, Republic of Mordovia, Churvash Republic, Republic of Tatartstan and Orenburg oblast) all reported excess mortality greater than 30% than expected mortality. In rural areas, meanwhile, only the Republic of Dagestan reported excess mortality of greater than 30%; the remaining four areas in the top five (Samara Oblast, Kabardian-Blakar Republic, Astrakhan oblast and Leningrad oblast) all reported excess mortality between 23.7 and 24.7. The lowest excess mortality in urban areas was found in Vologda oblast, Republic of Buryatia, Sakhalin oblast, Moscow city and Kaliningrad oblast. In these areas, excess mortality was between 13.6% and 15.3%. In the ‘best performing’ rural areas, however (Irkutsk oblast, Kemerovo oblast, Zabaikalsk oblast, Arkhangelsk Region less autonomous area and the Chechen Republic), excess mortality was comparatively much lower (below 6%). Rural areas within the Chechen Republic, in fact, reported negative excess mortality. However, these data bring out one of the main caveats relating to measurements of excess mortality in rural areas–namely that deaths may have been registered in urban areas. This, then, will lead to an inflation of urban excess mortality, and an undercount of rural mortality. As such, extreme caution should be exercised in the interpretation of these results.
| Region | Excess deaths in thousands | Excess deaths as a percent of expected | Life expectancy loss |
|---|---|---|---|
| | |||
| Lipetzk oblast | 3.04 | 32.6 | 2.9 |
| Republic of Mordovia | 1.73 | 31.1 | 2.4 |
| Chuvash Republic | 2.35 | 31.0 | 2.3 |
| Republic of Tatarstan | 9.06 | 30.8 | 2.5 |
| Orenburg oblast | 4.30 | 29.5 | 2.4 |
| . | . | . | |
| Vologda oblast | 1.60 | 15.3 | 1.0 |
| Republic of Buryatia | 0.86 | 15.2 | 1.0 |
| Sakhalin oblast | 0.67 | 14.5 | 1.0 |
| Moscow city | 17.72 | 13.7 | 0.9 |
| Kaliningrad oblast | 1.27 | 13.6 | 0.6 |
| | |||
| Republic of Dagestan | 3.19 | 34.8 | 3.5 |
| Samara oblast | 2.15 | 24.7 | 2.9 |
| Kabardian-Balkar Republic | 0.81 | 24.5 | 2.6 |
| Astrakhan oblast | 0.84 | 23.8 | 2.4 |
| Leningrad oblast | 1.51 | 23.7 | 3.6 |
| . | . | . | |
| Irkutsk oblast | 0.39 | 5.6 | 1.3 |
| Kemerovo oblast | 0.29 | 5.3 | 1.4 |
| Zabaikalsk kray | 0.19 | 4.0 | 1.1 |
| Arkhangelsk Region less autonomous area | 0.02 | 0.4 | 0.6 |
| Chechen Republic* | -0.01 | -0.4 | -0.1 |
* Note: For the case of the Chechen Republic (as also in some other areas), it is likely that COVID-19 deaths were registered in urban areas, hence leading to very low levels of excess mortality. However, the urban data is not described here as the expected number of deaths in urban area was less then 3000.
S3 Table show the excess deaths and life expectancy lost by gender for the regions of Russia. This is summarized in Table 3 , which again gives a snapshot of variation showing the regions with the highest and lowest mortality by gender. Nationally in 2020, there were 171,600 excess deaths for males compared to 179,560 for females. For both males and females, the Chechen Republic returns the highest percentage of excess mortality (48.2% for males, 43.5% for females). For males, the next highest percentages of excess mortality can be found in Republic of Dagestan (33.1%), Lipetzk oblast (28.0%), Republic of Tatarstan (27.7%), and Moscow oblast (25.7%); while the lowest can be found in Kaliningrad oblast (12.3%), Sakhalin oblast (12.1%), Moscow city (10.1%), Republic of Buryatia (10.1%) and Zabaikalsk kray (9.9%). For females, the highest excess mortality (after Chechen Republic) can be found in Khanty-Mansi Autonomous Area–Yugra (32.9%), Orenburg oblast (30.2%), Republic of Tatarstan (29.1%), and Samara oblast (28.4%). The lowest, meanwhile, can be found in Republic of Komi (13.1%), Ivanovo oblast (12.8%), Republic of Buryatia (12.6%), Novgorod oblast (11.5%), and Arkhangelsk Region less autonomous area (10.8%). The data show that while the differences by gender at the national level were modest (comparing 20.1% with 19.2% excess mortality for males and females respectively), this masks important regional differences. For example, in Moscow City, the percentage of excess deaths for males is one of the very lowest in the country at 10.1%. For females, however, it is closer to the national average at 17.7%. In the Khanty-Mansi Autonomous Area, meanwhile, the gap is even greater, 21.6%, for females and 32.9% for males.
| Region | Excess deaths in thousands | Excess deaths as a percent of expected | Life expectancy loss |
|---|---|---|---|
| Chechen Republic | 1.63 | 48.2 | 4.7 |
| Republic of Dagestan | 2.63 | 33.1 | 3.9 |
| Lipetzk oblast | 2.17 | 28.0 | 3.3 |
| Republic of Tatarstan | 5.93 | 27.7 | 3.0 |
| Moscow oblast | 11.07 | 25.7 | 2.9 |
| . | . | . | |
| Kaliningrad oblast | 0.70 | 12.3 | 0.9 |
| Sakhalin oblast | 0.39 | 12.1 | 1.0 |
| Moscow city | 6.53 | 10.1 | 0.7 |
| Republic of Buryatia | 0.58 | 10.1 | 0.7 |
| Zabaikalsk kray | 0.71 | 9.9 | 0.9 |
| | |||
| Chechen Republic | 1.32 | 43.5 | 3.8 |
| Khanty-Mansi Autonomous Area–Yugra | 1.36 | 32.9 | 2.7 |
| Orenburg oblast | 3.69 | 30.2 | 2.9 |
| Republic of Tatarstan | 6.08 | 29.1 | 2.5 |
| Samara oblast | 5.96 | 28.4 | 2.7 |
| . | . | . | |
| Republic of Komi | 0.60 | 13.1 | 1.0 |
| Ivanovo oblast | 1.06 | 12.8 | 1.1 |
| Republic of Buryatia | 0.62 | 12.6 | 1.4 |
| Novgorod oblast | 0.57 | 11.5 | 1.2 |
| Arkhangelsk Region less autonomous area | 0.76 | 10.8 | 0.7 |
Next, we turn to the distribution of excess mortality by age. This is represented in Fig 1 –a box plot of excess deaths as a percentage of the expected number of deaths, with the unit of measurement distribution being the regional territories of Russia. Fig 1 shows a number of distinct patterns. Firstly, we see a different relationship between age and excess mortality for males and females. For males, the relationship is generally linear. For females, however, there is an increase from age group 40–50 to 60–70, but then a dropping away towards the highest ages. Turning to the distribution, we can see there is a high degree of variation between regions for both males and females. However, it is clear that the range of the distribution is higher for females than for males. S4 Table shows excess mortality for those aged above and below 65. The details for other age groups are available on request from the authors.

Mean Remaining Life Expectancy of Deceased (RLED)
Finally, we present the results for the Mean Remaining Life Expectancy of the Deceased (RLED) for all regions in S5 Table . Table 4 shows the top and bottom five regions by RLED for 2020. For males in two regions (Khanty-Mansi Autonomous Area–Yugra and Kabardian-Balkar Republic), this RLED was greater than 17 years, and in the Republic of Sakha in the Far East it was 18.4. For females, meanwhile, three regions (Republic of Buryatia and Khanty-Mansi Autonomous Area–Yugra) saw RLED greater than 16 years while, again, the Republic of Sakha had the highest RLED at 17.9 years. Other regions, meanwhile, saw lower levels of RLED . Amongst males, Khabarovsk kray reported a RLED of 12.4 years, while Omsk oblast, Chelyabinsk oblast, Republic of Buryatia and Altai kray all reported RLED s between 10.9 and 11.8 years. For females, the lower RLED in Omsk oblast, Republic of Tatarstan, Udmurt Republic, Chelyabinsk oblast and Kirov oblast were all rather narrowly distributed between 11.9 and 12.2 years.
| Region | Excess deaths as a percent of expected | |
|---|---|---|
| | ||
| Republic of Sakha (Yakutia) | 22.5 | 18.4 |
| Khanty-Mansi Autonomous Area–Yugra | 22.6 | 17.2 |
| Kabardian-Balkar Republic | 25.8 | 17.1 |
| Republic of Dagestan | 34.4 | 16.8 |
| Leningrad oblast | 20.9 | 16.5 |
| . | . | |
| Khabarovsk kray | 19.2 | 12.4 |
| Omsk oblast | 24.1 | 11.8 |
| Chelyabinsk oblast | 22.5 | 11.8 |
| Republic of Buryatia | 10.7 | 11.7 |
| Altai kray | 18.0 | 10.9 |
| | ||
| Republic of Sakha (Yakutia) | 21.8 | 17.9 |
| Republic of Buryatia | 12.7 | 16.3 |
| Khanty-Mansi Autonomous Area–Yugra | 33.9 | 16.3 |
| Republic of Dagestan | 28.2 | 16.0 |
| Kabardian-Balkar Republic | 20.1 | 15.3 |
| . | . | |
| Omsk oblast | 25.7 | 12.2 |
| Republic of Tatarstan | 29.6 | 12.1 |
| Udmurt Republic | 21.4 | 12.1 |
| Chelyabinsk oblast | 23.8 | 12.0 |
| Kirov oblast | 20.8 | 11.9 |
Table 4 shows clearly how the data dramatically diverge from the widespread notion that the pandemic might have had a limited effect on people’s lifespans, because it primarily kills those who would anyway die in a near future. For Russia as whole, an average person who died due to the pandemic in 2020, would have otherwise lived for almost a further 14 more years. Our RLED estimates are relatively similar to estimates for other countries. Based on evidence from the Human Mortality Database [ 36 ], we estimate RLED for Sweden as 8.1 years in 2020 and 16.2 years in 2021.
Our calculations found significant degrees of regional divergence in terms of the experience of COVID-19 related excess mortality. This is important for two reasons. Firstly, this reveals the very unequal experience of COVID-19 across the country and may reflect the heterogeneity of the degree to which medical and public health systems at the regional level may have been affected by the pandemic and other local factors which shaped the regional pandemic experience [ 37 , 38 ]. Secondly, this regional divergence further justifies our methodological approach. Given the fact that the regions of Russia differ substantially in age structure and the dynamics and level of life expectancy, the use of the average number of deaths, as an estimate of the number of deaths in the absence of a pandemic, can lead to a distortion in the estimation of excess mortality. Naïve linear extrapolations of deaths, similarly, may be biased in regions, like Moscow, where the combination of population aging and mortality decline results in complex non-monotonic changes in the number of deaths. Indeed, due to the age structure shifts of the population of Russia, it is expected that the number of deaths will start rising soon, also making linear trend assumptions questionable. While historic trends were demonstrating a close to linear decline in the number of deaths on the national level, there is no evidence that this is happening on the regional level. Furthermore, the estimates of expected deaths using linear regression (and any other type of regression as well) depend on the length of historical time series used in the regression and is affected by outliers in the observations where, in the case of Russia, years like 2010 and 2017 returned relatively low numbers of deaths).
Our results point to considerable regional variation in excess mortality that deserves further analysis. Tentatively, one may note several factors that might have played their role in forming the regional differences in losses to the pandemics. First, we find that there is substantial positive correlation between the regional demographic losses and the life expectancy projected in the absence of the pandemic. Both life expectancy loss and excess mortality show correlation with the projected life expectancy of around 0.45 for males and 0.57 for females ( Table 5 ). On this basis, one may speculate that regions leading in life expectancy improvements before the pandemic may have suffered more because of accumulation of population with poorer health status who were hit harder during the pandemic. The pandemic appears to have played a levelling role by cutting down the advantages in life expectancy of regions leading in mortality reduction.
| Indicator | Female | Male |
|---|---|---|
| Excess deaths as a percent of expected | 0.44 (1.2e-4) | 0.58 (7.6e-8) |
| Loss in life expectancy | 0.46 (4.4e-5) | 0.57 (1.5e-7) |
Note: Numbers in the parentheses indicate p-values.
Secondly, in addition to purely demographic factors, one may also expect socio-cultural, economic and, perhaps, geographic differentials also to contribute to differences in the impact of the pandemics. Regions of the Northern Caucasus, for example, are known for their tradition of elderly living in larger households of extended families together with their children and descendants. While this is generally considered a health-protective behavior, such a tradition might have contributed to higher social exposure and, hence, higher losses in the Northern Caucasus.
A preliminary analysis of association between average regional income in 2019 was performed, and number of beds per capita in regional hospitals in 2019 as independent variables and regional excess deaths as a percent of expected as dependent. We run a multiple regression for 2020, 2021 and a combination of 2020–21 data. In all cases the influence of regional income was statistically insignificant, while number of hospital beds per capita was significant at 0.001 level in 2020 while nonsignificant in 2021. An explanation could be that in 2021, the number of hospital beds drastically increased in the regions due to temporarily organized treatment facilities and thus linking excess death in 2021 with the number of hospital beds per capita loses its meaning. Correlation between the number of hospital beds per capita and excess mortality in 2020 was -0.37 and significant at p-value = 0.001 level. We also found a negative correlation between female education and excess mortality in 2020, but no such correlation with the male education, although these results are preliminary and need further investigation. We intend a thorough study of factors of regional variation in excess mortality in the future.
Of course, infrastructure of the region—especially in terms of health facilities—would also contribute to the differences in excess mortality. There is, for instance, a huge disparity in excess mortality between Moscow city and the surrounding Moscow oblast. Life expectancy in Moscow oblast is considerably lower than in Moscow (expected life expectancy for males 67.7 versus 73.1). Moscow city, following the arguments introduced above, should have higher excess mortality. On the contrary, excess deaths measured as a percent of expected for men in 2020 was more than two-time higher in Moscow oblast compared to Moscow (25.7% versus 10.1%). Residents of these two places are not especially different in terms of culture, although that does not mean that there are not large behavioral differences. Health care in Moscow city is more advanced than in Moscow oblast, but under normal circumstances for advanced medical treatments people in Moscow oblast would not need to travel far to get treatment in Moscow city. However, in the case of a pandemic, when most health facilities in Moscow were running at (or near) full capacity, there were fewer opportunities for patients from Moscow oblast to be treated in Moscow city.
Policies to prevent the spread of COVID-19 and the implementation of measures also played a role in the number of infections. The central government delegated much of the responsibilities in this field to regional administrations and those policies were diverse in the regions of Russia. At the initial stage of the COVID-19 pandemic, there was a high degree of misinformation related to the spread and severity of COVID-19 in Russian media. Sometimes public figures and even medical doctors on TV programs downplayed the danger of COVID-19 [ 39 ]. That influenced the efficiency of vaccination policies which, in turn, contributed to the number of COVID-19 cases and the excess number of deaths. A recent study by Roschina et al. has highlighted a high degree of ‘vaccine hesitancy’ in Russia, with only 45% of those surveyed in 2021 demonstrating positive attitudes towards the vaccination program [ 40 ]. As of March 2022, the total vaccination rate remains relatively low in Russia (around 55%, with around 20% in some regions) [ 41 ]. This compares unfavourably to even the global figure of around 60%, and is lower than in Pakistan and The Philippines. Maleva et al. [ 42 ] found that Russian young people and people with low levels of education are the least likely to be vaccinated.
So, in general there are many social, political, cultural and epidemiological factors and their interactions contributed to the diversity of patterns of excess mortality. In each region, the combination of those factors must be studied. In the Chechen Republic, for example, we observed a sharp drop in excess mortality between 2020 and 2021. This may be related to the hardline rhetoric and measures put in place in 2021 by the Chechen leader Ramzan Kadyrov. In May 2021, for example, it is reported that Kadyrov warned citizens that those who refused to be vaccinated would be treated last and will ‘feel how terrible the lack of oxygen feels’ [ 43 ]. Meanwhile in July 2021, it was decreed that unvaccinated residents in the Chechen Republic were banned from attending mosques. Citizens also stated that it was impossible to buy bread without a vaccine certificate [ 44 ].
Stepping back, our data presents clear evidence of the very high levels of excess mortality seen in Russia over the past two years; and that this level has significantly accelerated between 2020 and 2021. In a comparative sense, this overall finding accords with previous analyses of Russia which suggest it may come out of the COVID-19 experience with one of the very highest levels of excess mortality in the world. Using our RLED measure, however, we clearly disprove the widely held concept that such deaths were ‘going to happen anyway’ because of the relatively large number of remaining years of life expectancy of a deceased. Together, it appears that COVID-19 has further added to traumatic recent history of mortality–especially among males–in Russia [ 45 , 46 ].
Our study does, however, have several limitations. Firstly, the restricted data we have for 2021 means we cannot provide an analysis on the level of granularity which we would wish for this year. Secondly, as with all studies of mortality in Russia, there will inevitably be challenges concerning both completeness of registration as well as discrepancies in the place of registration of a death because of migration and different living/working patterns [ 47 ]. This is especially likely to be the case of the Republics in the Caucasus, and perhaps also the areas surrounding major cities such as Moscow and St. Petersburg. Such issues relating to death registration also impact upon the potential validity of comparisons between urban and rural excess mortality (as discussed above).
The human cost of the COVID-19 pandemic is well known. Quantifying this carefully, however, is a high priority to not only measure this impact, but to ensure adequate policy responses. In this paper, we have identified the high levels of excess mortality in the regions of Russia during the COVID-19 pandemic. To do so, we have deployed a rigorous method which accounts more accurately for underlying demographic change. We estimate that more than a million lives were lost to the pandemic. Contrary to the popular belief that such deaths were ‘likely to occur anyway’, our analysis shows that COVID-19 in Russia has had a significant impact upon remaining life expectancy. We have also, for the first, time, been able to present regional figures of excess mortality for 2021, as well as an analysis by age, gender and urban and rural status. These figures showed a higher impact on life expectancy for males who also had rising excess mortality (as a percent of expected) with age, unlike females where there was a non-linear relationship, and in general higher level of excess mortality in urban areas compared to rural areas and little difference is observed in male versus female excess mortality. Higher urban excess mortality could be driven by a higher density of population in urban areas, and thus higher infection transmission rate. As mentioned earlier, another source of bias towards higher urban excess mortality may be caused by registration of deaths of rural residents transferred to urban hospitals. While there is a wide variation in mortality rates between regions, there is no clear regional distribution (e.g. an east-west gradient).
While national figures show that excess mortality in Russia is perhaps amongst the highest in the world, there is a wide degree of regional variation. Such variation–and its interaction with age, gender, and rural/urban status–is key to better consideration and formulation of public health strategies to mitigate both the ongoing impact of COVID-19, and to rebuild and reshape health systems after the pandemic is over. As such, the determinants of mortality and the experience of (and response) to the pandemic at the regional level is a critical future avenue of research. This would enable more precise policy recommendations to be generated from our research. At this stage, however, some outcomes are clear. The regional disparities in infrastructure–especially in health–appear to be a key factor in determining levels of excess mortality. These disparities become amplified when the circumstances of the pandemic disrupted access. Higher levels of excess mortality in urban areas may have resulted from greater levels of infection in spaces of higher population density. This may mean that alternative strategies for infection control and management need to be in pace for urban and rural areas. Finally, we must look at the broader picture of how such mortality is so high in the first place. In this, the role of (mis)information and communication concerning both the severity of the public health emergency appears to have played a critical role. Ensuring the public have access to objective, honest, impartial, and accurate information about their circumstances is of the highest priority. For their part, scientists should be providing clear transparent assessments of mortality to inform government, media and other stakeholders.
Supporting information
Funding statement.
This work was supported by a joint the International Institute for Applied Systems Analysis (IIASA) and the Russian Foundation for Basic Research (RFBR) project, "Demographic consequences of COVID-19 for short and long term population dynamics in Russia and its regions” [20-510-82002].
Data Availability
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
COVID-19 and excess mortality in Russia: Regional estimates of life expectancy losses in 2020 and excess deaths in 2021
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Population and Just Societies Program, International Institute of Applied Systems and Analysis, Laxenburg, Austria
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Division of Social Science, The Hong Kong University of Science and Technology, Kowloon, Hong Kong SAR, China, Department of Humanities and Social Science, Khalifa University of Science and Technology, Abu Dhabi, United Arab Emirates
Roles Conceptualization, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing
Affiliations Population and Just Societies Program, International Institute of Applied Systems and Analysis, Laxenburg, Austria, North-Caucasian State Academy, Institute for Applied Mathematics and Information Technologies, Cherkessk, Russia
Roles Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Validation, Writing – original draft, Writing – review & editing
Affiliation International Laboratory of Demography and Human Capital, Russian Presidential Academy of National Economy and Public Administration, Moscow, Russia
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing
Affiliations Population and Just Societies Program, International Institute of Applied Systems and Analysis, Laxenburg, Austria, Department of Economics, Stony Brook University, Stony Brook, NY, United States of America
- Sergei Scherbov,
- Stuart Gietel-Basten,
- Dalkhat Ediev,
- Sergey Shulgin,
- Warren Sanderson

- Published: November 2, 2022
- https://doi.org/10.1371/journal.pone.0275967
- Reader Comments
Accurately counting the human cost of the COVID-19 at both the national and regional level is a policy priority. The Russian Federation currently reports one of the higher COVID-19 mortality rates in the world; but estimates of mortality differ significantly. Using a statistical method accounting for changes in the population age structure, we present the first national and regional estimates of excess mortality for 2021; calculations of excess mortality by age, gender, and urban/rural status for 2020; and mean remaining years of life expectancy lost at the regional level. We estimate that there were 351,158 excess deaths in 2020 and 678,022 in 2021 in the Russian Federation; and, in 2020, around 2.0 years of life expectancy lost. While the Russian Federation exhibits very high levels of excess mortality compared to other countries, there is a wide degree of regional variation: in 2021, excess deaths expressed as a percentage of expected deaths at the regional level range from 27% to 52%. Life expectancy loss is generally greater for males; while excess mortality is greater in urban areas. For Russia as whole, an average person who died due to the pandemic in 2020 would have otherwise lived for a further 14 more years (and as high as 18 years in some regions), disproving the widely held view that excess mortality during the pandemic period was concentrated among those with few years of life remaining–especially for females. At a regional level, less densely populated, more remote regions, rural regions appear to have fared better regarding excess mortality and life expectancy loss–however, a part of this differential could be owing to measurement issues. The calculations demonstrate more clearly the true degree of the human cost of the pandemic in the Russian Federation.
Citation: Scherbov S, Gietel-Basten S, Ediev D, Shulgin S, Sanderson W (2022) COVID-19 and excess mortality in Russia: Regional estimates of life expectancy losses in 2020 and excess deaths in 2021. PLoS ONE 17(11): e0275967. https://doi.org/10.1371/journal.pone.0275967
Editor: Zhuo Chen, University of Georgia, UNITED STATES
Received: April 19, 2022; Accepted: September 27, 2022; Published: November 2, 2022
Copyright: © 2022 Scherbov et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All data used in this paper are publicly accessible, and are listed in the Materials and Methods section with links to the datasets to be found in the bibliography. The full datasets generated and behind the summary tables in this article have been uploaded as part of the Supplementary Material. For clarity, the dataset links are reproduced here: ROSSTAT. 2021 INFORMATION ON THE NUMBER OF REGISTERED BIRTHS, DEADS, MARRIAGES AND DIVORCE for January - December 2021. See https://rosstat.gov.ru/storage/mediabank/2021_edn12_t1_2.xlsx . ROSSTAT. 2021 Natural movement of the population of the Russian Federation in 2020. See https://rosstat.gov.ru/compendium/document/13269 . ROSSTAT. 2021 Estimate Of Life Expectancy At Birth By Regions Of the Russian Federation for 2020. See https://rosstat.gov.ru/folder/12781 . ROSSTAT. 2022 Operational information about the natural movement of the population. See https://rosstat.gov.ru/storage/mediabank/2021_edn12.htm . Center for Demographic Research. 2017 Russian Fertility and Mortality Database. See http://demogr.nes.ru/index.php/ru/demogr_indicat/data .
Funding: This work was supported by a joint the International Institute for Applied Systems Analysis (IIASA) and the Russian Foundation for Basic Research (RFBR) project, "Demographic consequences of COVID-19 for short and long term population dynamics in Russia and its regions” [20-510-82002].
Competing interests: The authors have declared that no competing interests exist.
Introduction
Counting the human cost of the COVID-19 pandemic is clearly a demographic, policy and epidemiological priority. The particular circumstances in the Russian Federation have come to international attention because of the especially high levels of mortality compared to other parts of the world [ 1 ]. There are, however, many challenges to producing what appear to be a simple estimate of mortality derived from COVID-19. For example, differences in the adequacy and completeness of registration data around the world, as well as the definition and specification of causes of death represent a key challenge. According to the recommendations of the World Health Organization (WHO), death from COVID-19 is defined ‘for surveillance purposes as a death resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID disease (e.g. trauma)… There should be no period of complete recovery from COVID-19 between illness and death’ [ 2 ]. This definition, however, is not universally applied across all WHO member states, not least because of the challenges associated with determining a primary cause of death. The situation is even more complicated in the current pandemic, where a relatively mild infection can trigger a series of events resulting in death from an underlying condition. Such problems with defining cause of death result in wide variations in estimates of ‘deaths due to COVID-19’ at the global and national level [ 3 ].
In the Russian Federation (hereafter Russia), there appears to be an especially high degree of uncertainty concerning mortality due to COVID-19 [ 4 ]. The number of deaths due to COVID-19 reported by the Russian Federal State Statistical Service for 2020 (163,325) was three times that produced by the Russian Virus Response Center [ 5 ]. In other parts of the world, there have been marked differences between regions in terms of their mortality experience of COVID-19 [ 6 , 7 ]. Such uncertainty is expected to be amplified when considering the regional heterogeneity and different experiences of COVID-19 across the country [ 8 ].
Against this backdrop, the concept of ‘excess mortality’ has been set out as a possible ‘gold standard’ of measuring the human cost of the COVID-19 pandemic [ 9 ]. Excess mortality is estimated as the difference between the number of deaths that occurred during the COVID-19 pandemic in a particular period and the number of deaths that estimated to have occurred in the same period if there were no pandemic. The latter number is often referred to as the ‘baseline death count’. A major benefit of the excess mortality approach is that it is not sensitive to variations in cause of death reporting, and encompasses deaths relating directly to COVID-19 as well as those due to related causes and issues which may have stemmed from lockdowns, restriction on movement, postponed operations and so on [ 5 ]. This approach to measurement has been adopted in various datasets [ 10 , 11 ], by various international organizations (such as WHO [ 12 ], OECD [ 13 ], and by national statistical agencies (e.g. [ 14 ]).
Despite this consensus on the benefits of the excess mortality approach, there are still variations in the final calculated numbers of such deaths at the global and national level [ 3 ]. A recent paper by Kobak [ 8 ] produces various estimates for excess mortality stemming from COVID-19 in Russia, with one as high as 380,000 deaths (as of 1 January 2021), corresponding to 0.26% of the population. For the period April to November 2021, Kobak [ 8 ] estimates a total of 264,100 excess deaths (95% interval: [232,000, 296,200]), which is higher than the total number of COVID-19 related deaths reported to WHO for the entire period from January 2020 to December 2021 [ 15 ]. Kobak’s figures show Russia to have the second highest absolute number of estimated excess deaths in the world after the United States (over 400,000), and one of the highest numbers per capita. More recently, Aburto et al. [ 16 ] found that that life expectancy losses among females were the largest in Russia, and losses among males stand only behind the USA (2.2 years) and Lithuania (1.7 years), although Islam et al [ 20 ] estimate that Russian losses in life expectancy are highest for both men and women. Kobak [ 8 ] also produced estimates of excess mortality by Federal Region, and finds 23,500 cases of excess mortality in Moscow alone, with the highest excess mortality rate found in Samara Oblast: a 22% yearly mortality increase.
Part of the reason for the discrepancy in figures of excess mortality presented for Russia above stems from alternative methods of calculating this projected death count. As the recent study by Nepomuceno et al. [ 17 ] describes, there can be differences in measured outcomes based on a variety of factors such as the mortality index; the method used to estimate the baseline; the number of years included in the reference period; and the time unit of the death data (weekly and monthly). In addition, the jump-off effect of the previous year’s data for trend models must also be considered. Turning back to studies of excess mortality in Russia, in the first approach an average count of deaths for a particular time interval is calculated (e.g. five years before the pandemic began) and these numbers are compared to the number of deaths that occur during the pandemic [ 18 ]. In the second approach, used in Kobak [ 8 ], deaths are extrapolated. In this method, the average monthly number of deaths for each year are computed for 2006–19; then a linear trend is fitted to the 2015–2019 values which is then extrapolated to provide the predicted baseline value for 2020.
Neither approach accounts for changes in mortality and population age structure over time and can lead to a biased estimation of excess mortality from the COVID-19 pandemic. This can be especially true for an aging population with an irregular age structure–such as Russia. In each case, the dynamics of mortality and waves in the demographic structure will affect the assessment of deaths in the absence of a pandemic and, accordingly, affect the assessment of demographic losses due to the coronavirus pandemic.
For a more accurate assessment of the number of deaths in the absence of a pandemic, it is possible to use predicted values of the number of deaths that consider the peculiarities of the age structure of the population. To estimate the number of deaths in 2020–21 in the absence of a pandemic—and therefore to calculate excess mortality in comparison—it is necessary to make a population forecast for one year from the beginning of 2020 to 2021 or for two years from the beginning of 2020 to 2022. The population forecast can be made either with the mortality rate of 2019 or considering the dynamics of mortality in previous years to predict the expected mortality for 2020/2021. Both versions of the forecast allow us to estimate the number of deaths that would have occurred in 2020/2021 in the absence of the COVID-19 pandemic. Excess mortality, in this vein, is defined as the difference between the recorded number of deaths in 2020/2021 and the projected estimate of the number of deaths in the absence of the COVID-19. In this paper we followed the second approach. Projecting the number of deaths in the absence of the pandemic, we assumed that life expectancy would have increased at the same pace as it has been increasing recently. Such an approach was also performed in Islam et al. [ 19 , 20 ]. Timonin et al. calculated excess mortality for Russia and its regions for 2020 [ 5 ]. They found that Russia had one of the highest levels of excess mortality in the world and matched most closely those found in other central and eastern European countries. At the regional level, they found that excess mortality began to increase in Moscow and St. Petersburg in the Spring of 2020, and then spread to all regions of Russia by the end of 2020. They concluded by arguing that the observed negative association between excess mortality and reported cases was explained by under-recording of the latter.
In this paper, using the latest data released from ROSSTAT [ 19 – 22 ], we are able to calculate excess mortality for Russia and its regions for 2020 by age, sex, and rural-urban residence. For 2021, we produce estimates for regions only (because more granular data have not yet been released). In doing so, we build on the extant literature in the following ways: firstly, we are able to go beyond the estimates produced for 2020 in Kobak [ 8 ] by deploying this alternative methodology which takes into account projected changes in the age structure. Secondly, we produce the first estimates for 2021 using a variation of the enhanced method deployed by Timonin et al. [ 5 ] (building on Islam et al. [ 23 ]). Finally, we are able to go beyond the analysis performed in Timonin et al. [ 5 ] by producing estimates for rural and urban excess mortality for 2020.
Islam et al. [ 24 ] further applied an important measure of losses due to the pandemic, namely, the Years of Life Lost ( YLL ). Following WHO methodology [ 25 ], they calculated YLL based on expected remaining years of life from a standard life table for all countries. Such an approach, as useful as it may be for international comparisons, does not adequately express losses of expected years of life in countries like Russia where actual remaining life expectancies deviate substantially from those of the standard life table used in Islam et al. [ 23 ]. As such, we calculate a related indicator using life tables based on actual mortality data and extrapolations for Russia and its regions, relating the life years lost to those very people who perished due to the pandemic. To avoid confusion with YLL , we term our indicator Mean Remaining Life Expectancy of the Deceased ( RLED ).
Materials and methods
The primary sources of data are derived from official ROSSTAT publications for the 2021 [ 19 – 22 ]; the Russian Economic School database [ 26 ] for the 2020; and calculations and population projections which were used in the Russian Demographic Data Sheet 2019 [ 27 ]. The database of the Russian Economic School provides death rates for 2020 by gender, region, urban and rural residence and single years of age as well as population exposures. The time series of observed life expectancies for the regions of Russia were obtained from Federal State Statistics Service [ 28 ].
A standard cohort-component method-based system for producing multiregional population projections was used. To estimate excess mortality, we needed to project the deaths only for two years: 2020 and 2021. In this short time interval, the influence of migration and fertility on the total number of deaths would likely be insignificant (see below). Although we used a multiregional package to produce the number of deaths, similar results would have been obtained had we applied a cohort-component projection model to each region and urban settlement independently.
The population projection approach has several advantages over approaches that average the number of deaths over the previous five years or extrapolate the annual number of deaths from the years preceding pandemics. First, the change in the age structure of the population and its impact on the number of deaths is considered. Second, it is possible to reduce random fluctuations in the expected number of deaths, since the population forecasts produce graduated structures of mortality. In fact, the primary reason why the traditional method uses a five-year interval to average the number of deaths is the need to reduce the random component in estimating the number of deaths. Finally, because of the need to obtain time-series data on which to draw the projections—we used data from 2010- we excluded regions with short series of data available, and with small death count as described below (see Appendix for full list).
In this paper, to estimate excess mortality, we use a population forecast for all regions of Russia, that assumes the observed recent trend in life expectancy would have continued in the absence of the COVID-19 pandemic. The base population estimate is taken as of January 1, 2020. To estimate the number of excess deaths in 2020 and 2021, the population forecast is made for two years. As the impact of fertility and migration on the number of deaths in 2020–21 is extremely small, so the baseline scenario of fertility and migration, similar to the level of fertility and migration in 2019, was considered. Finally, to mitigate against high levels of fluctuations resulting from small numbers, we only consider populations where our calculated number of expected deaths is greater than 3,000 per year. Although this particular threshold was chosen rather arbitrarily, our decision was based on earlier experience with sampling errors of life expectancy estimates [ 34 ]. Given a Russian Crude Death Rate of roughly 12.8, 3,000 deaths correspond to around 235,000 people which, at life expectancy around 73 years, yields a sampling standard error of about 0.27 years (see Appendix 1 of [ 34 ]). This approximately corresponds to 95% CI (±0.5 years). Because the COVID-19 related losses to life expectancy are measured in years, we considered such a threshold to be reasonable for the current study.
Calculations were produced using packages written by authors in FORTRAN and R.
Excess deaths at the regional level for 2020 and 2021
Based on our population projections, we estimate that there were 351,158 excess deaths in 2020 and 678,022 in 2021 in the Russian Federation (see Tables 1 and S1 )—a total of 1,029,181 excess deaths over the period 2020–2021. This figure represents an excess of 19.65% and 38.36% over the expected number of deaths for 2020 and 2021 respectively. Our results are not much different from those that might have been obtained for Russia as a whole based on the official population projection by ROSSTAT that was conducted in 2019 [ 35 ]. Comparing deaths projected by ROSSTAT for 2020 and 2021 to actual figures, yield estimates of excess mortality 350,600 for 2020 and 657,800 for 2021 (1,007,400 in total over two years). ROSSTAT’s projection, however, do not provide the regional details that are studied here.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0275967.t001
S1 Table shows the numbers of excess deaths per region for all regions with greater than 3,000 predicted deaths per year. Table 1 gives a snapshot of this regional data showing the five regions with the highest and lowest percentage of excess deaths. While the figures show a wide variation between provinces, no specific regional patterns (e.g. an east-west gradient) could be observed. In 2021, the highest percentages of excess mortality can be found in Lipetzk oblast (52.14%) in the Central Federal District, while the lowest can be found in Primorsky kray (27.25%) in the Far East of the country. In terms of the regional distribution, the patterns are far from clear cut. In 2020, for example, the range was from an 10.37% excess in the Republic of Adygeya in the Northern Caucasus up to a 45.97% excess in the Chechen Republic. In other words, some of the highest and lowest percentages of excess mortality can be found in the Caucasus–a feature which warrants further investigation. Similarly, while four of the six regions with the lowest excess mortality (Republic of Buryatia, Sakhalin oblast, Zabaikalsk kray and Promorsky oblast) can be found in the Far Eastern Federal District, so too can the 9 th highest ranking region (Republic of Sakha). Indeed, the regions with the highest excess mortality in 2021 are to be found around the country: four in the Central Federal District (Lipetzk oblast, Ryazan oblast, Voronezh oblast and Kursk oblast); three in the Volga Federal District (Saratov oblast, Orenburg oblast and Republic of Mordovia) and one each in the Southern Federal District (Volgorad oblast), Northwestern Federal District (Republic of Karelia) and Far Eastern Federal District (Republic of Sakha). Among the regions with the lowest excess mortality, the majority are to be found in the sparsely populated regions of the Far Eastern Federal District and Siberia. Moscow City, however, is also in this low ranked groups.
Finally, there is a high degree of change both between the two years and across the regions of Russia. In the Republic of Karelia, for example, excess mortality rose from 17.11% in 2020 to 46.3%, propelling it from a middle-ranking position to one of the highest in the country. A further five regions saw increases in excess mortality of greater than 25% (Kursk oblast, Kostroma oblast, Novgorod oblast, Voronezh oblast and Saratov oblast). Other states, meanwhile, saw much less dramatic changes. Eleven regions saw increases of 10–15% (Khabarovsk kray, Kabardian-Balkar Republic, Primorsky kray, Novosibirsk oblast, Chelyabinsk oblast, Chuvash Republic, Samara oblast, Udmurt Republic, Perm kray, Republic of Bashkortostan, and Kemerovo oblast). Excess mortality in the Republic of Dagestan, meanwhile, stayed almost constant between 2020 and 2021. Because of the sharp increases across the country, this meant the region dropped in the national rankings from second top to eighth last. Mortality in the Chechen Republic appears to have fallen between 2020 and 2021.
Excess deaths and life expectancy loss at the regional level for 2020 by urban-rural residence, gender and age
S2 Table shows excess mortality in urban and rural areas. As expected, the percentage of excess deaths is higher in urban areas due to the much higher population density. A summary of this table is presented in Table 2 . In 2020, there were 274,520 excess deaths in urban areas compared to 76,640 in rural areas. Our results for Russia are consistent with other studies [ 16 , 20 ]. The Republic of Dagestan has the highest excess mortality of either rural or urban areas (34.8%), and the highest number of years in terms of life expectancy lost (3.5). Despite this, it is apparent that the highest levels of excess mortality were, indeed, higher in the urban areas than in rural areas. The top five urban areas (Lipetzk oblast, Republic of Mordovia, Churvash Republic, Republic of Tatartstan and Orenburg oblast) all reported excess mortality greater than 30% than expected mortality. In rural areas, meanwhile, only the Republic of Dagestan reported excess mortality of greater than 30%; the remaining four areas in the top five (Samara Oblast, Kabardian-Blakar Republic, Astrakhan oblast and Leningrad oblast) all reported excess mortality between 23.7 and 24.7. The lowest excess mortality in urban areas was found in Vologda oblast, Republic of Buryatia, Sakhalin oblast, Moscow city and Kaliningrad oblast. In these areas, excess mortality was between 13.6% and 15.3%. In the ‘best performing’ rural areas, however (Irkutsk oblast, Kemerovo oblast, Zabaikalsk oblast, Arkhangelsk Region less autonomous area and the Chechen Republic), excess mortality was comparatively much lower (below 6%). Rural areas within the Chechen Republic, in fact, reported negative excess mortality. However, these data bring out one of the main caveats relating to measurements of excess mortality in rural areas–namely that deaths may have been registered in urban areas. This, then, will lead to an inflation of urban excess mortality, and an undercount of rural mortality. As such, extreme caution should be exercised in the interpretation of these results.
https://doi.org/10.1371/journal.pone.0275967.t002
S3 Table show the excess deaths and life expectancy lost by gender for the regions of Russia. This is summarized in Table 3 , which again gives a snapshot of variation showing the regions with the highest and lowest mortality by gender. Nationally in 2020, there were 171,600 excess deaths for males compared to 179,560 for females. For both males and females, the Chechen Republic returns the highest percentage of excess mortality (48.2% for males, 43.5% for females). For males, the next highest percentages of excess mortality can be found in Republic of Dagestan (33.1%), Lipetzk oblast (28.0%), Republic of Tatarstan (27.7%), and Moscow oblast (25.7%); while the lowest can be found in Kaliningrad oblast (12.3%), Sakhalin oblast (12.1%), Moscow city (10.1%), Republic of Buryatia (10.1%) and Zabaikalsk kray (9.9%). For females, the highest excess mortality (after Chechen Republic) can be found in Khanty-Mansi Autonomous Area–Yugra (32.9%), Orenburg oblast (30.2%), Republic of Tatarstan (29.1%), and Samara oblast (28.4%). The lowest, meanwhile, can be found in Republic of Komi (13.1%), Ivanovo oblast (12.8%), Republic of Buryatia (12.6%), Novgorod oblast (11.5%), and Arkhangelsk Region less autonomous area (10.8%). The data show that while the differences by gender at the national level were modest (comparing 20.1% with 19.2% excess mortality for males and females respectively), this masks important regional differences. For example, in Moscow City, the percentage of excess deaths for males is one of the very lowest in the country at 10.1%. For females, however, it is closer to the national average at 17.7%. In the Khanty-Mansi Autonomous Area, meanwhile, the gap is even greater, 21.6%, for females and 32.9% for males.
https://doi.org/10.1371/journal.pone.0275967.t003
Next, we turn to the distribution of excess mortality by age. This is represented in Fig 1 –a box plot of excess deaths as a percentage of the expected number of deaths, with the unit of measurement distribution being the regional territories of Russia. Fig 1 shows a number of distinct patterns. Firstly, we see a different relationship between age and excess mortality for males and females. For males, the relationship is generally linear. For females, however, there is an increase from age group 40–50 to 60–70, but then a dropping away towards the highest ages. Turning to the distribution, we can see there is a high degree of variation between regions for both males and females. However, it is clear that the range of the distribution is higher for females than for males. S4 Table shows excess mortality for those aged above and below 65. The details for other age groups are available on request from the authors.
https://doi.org/10.1371/journal.pone.0275967.g001
Mean Remaining Life Expectancy of Deceased (RLED)
Finally, we present the results for the Mean Remaining Life Expectancy of the Deceased (RLED) for all regions in S5 Table . Table 4 shows the top and bottom five regions by RLED for 2020. For males in two regions (Khanty-Mansi Autonomous Area–Yugra and Kabardian-Balkar Republic), this RLED was greater than 17 years, and in the Republic of Sakha in the Far East it was 18.4. For females, meanwhile, three regions (Republic of Buryatia and Khanty-Mansi Autonomous Area–Yugra) saw RLED greater than 16 years while, again, the Republic of Sakha had the highest RLED at 17.9 years. Other regions, meanwhile, saw lower levels of RLED . Amongst males, Khabarovsk kray reported a RLED of 12.4 years, while Omsk oblast, Chelyabinsk oblast, Republic of Buryatia and Altai kray all reported RLED s between 10.9 and 11.8 years. For females, the lower RLED in Omsk oblast, Republic of Tatarstan, Udmurt Republic, Chelyabinsk oblast and Kirov oblast were all rather narrowly distributed between 11.9 and 12.2 years.
https://doi.org/10.1371/journal.pone.0275967.t004
Table 4 shows clearly how the data dramatically diverge from the widespread notion that the pandemic might have had a limited effect on people’s lifespans, because it primarily kills those who would anyway die in a near future. For Russia as whole, an average person who died due to the pandemic in 2020, would have otherwise lived for almost a further 14 more years. Our RLED estimates are relatively similar to estimates for other countries. Based on evidence from the Human Mortality Database [ 36 ], we estimate RLED for Sweden as 8.1 years in 2020 and 16.2 years in 2021.
Our calculations found significant degrees of regional divergence in terms of the experience of COVID-19 related excess mortality. This is important for two reasons. Firstly, this reveals the very unequal experience of COVID-19 across the country and may reflect the heterogeneity of the degree to which medical and public health systems at the regional level may have been affected by the pandemic and other local factors which shaped the regional pandemic experience [ 37 , 38 ]. Secondly, this regional divergence further justifies our methodological approach. Given the fact that the regions of Russia differ substantially in age structure and the dynamics and level of life expectancy, the use of the average number of deaths, as an estimate of the number of deaths in the absence of a pandemic, can lead to a distortion in the estimation of excess mortality. Naïve linear extrapolations of deaths, similarly, may be biased in regions, like Moscow, where the combination of population aging and mortality decline results in complex non-monotonic changes in the number of deaths. Indeed, due to the age structure shifts of the population of Russia, it is expected that the number of deaths will start rising soon, also making linear trend assumptions questionable. While historic trends were demonstrating a close to linear decline in the number of deaths on the national level, there is no evidence that this is happening on the regional level. Furthermore, the estimates of expected deaths using linear regression (and any other type of regression as well) depend on the length of historical time series used in the regression and is affected by outliers in the observations where, in the case of Russia, years like 2010 and 2017 returned relatively low numbers of deaths).
Our results point to considerable regional variation in excess mortality that deserves further analysis. Tentatively, one may note several factors that might have played their role in forming the regional differences in losses to the pandemics. First, we find that there is substantial positive correlation between the regional demographic losses and the life expectancy projected in the absence of the pandemic. Both life expectancy loss and excess mortality show correlation with the projected life expectancy of around 0.45 for males and 0.57 for females ( Table 5 ). On this basis, one may speculate that regions leading in life expectancy improvements before the pandemic may have suffered more because of accumulation of population with poorer health status who were hit harder during the pandemic. The pandemic appears to have played a levelling role by cutting down the advantages in life expectancy of regions leading in mortality reduction.
https://doi.org/10.1371/journal.pone.0275967.t005
Secondly, in addition to purely demographic factors, one may also expect socio-cultural, economic and, perhaps, geographic differentials also to contribute to differences in the impact of the pandemics. Regions of the Northern Caucasus, for example, are known for their tradition of elderly living in larger households of extended families together with their children and descendants. While this is generally considered a health-protective behavior, such a tradition might have contributed to higher social exposure and, hence, higher losses in the Northern Caucasus.
A preliminary analysis of association between average regional income in 2019 was performed, and number of beds per capita in regional hospitals in 2019 as independent variables and regional excess deaths as a percent of expected as dependent. We run a multiple regression for 2020, 2021 and a combination of 2020–21 data. In all cases the influence of regional income was statistically insignificant, while number of hospital beds per capita was significant at 0.001 level in 2020 while nonsignificant in 2021. An explanation could be that in 2021, the number of hospital beds drastically increased in the regions due to temporarily organized treatment facilities and thus linking excess death in 2021 with the number of hospital beds per capita loses its meaning. Correlation between the number of hospital beds per capita and excess mortality in 2020 was -0.37 and significant at p-value = 0.001 level. We also found a negative correlation between female education and excess mortality in 2020, but no such correlation with the male education, although these results are preliminary and need further investigation. We intend a thorough study of factors of regional variation in excess mortality in the future.
Of course, infrastructure of the region—especially in terms of health facilities—would also contribute to the differences in excess mortality. There is, for instance, a huge disparity in excess mortality between Moscow city and the surrounding Moscow oblast. Life expectancy in Moscow oblast is considerably lower than in Moscow (expected life expectancy for males 67.7 versus 73.1). Moscow city, following the arguments introduced above, should have higher excess mortality. On the contrary, excess deaths measured as a percent of expected for men in 2020 was more than two-time higher in Moscow oblast compared to Moscow (25.7% versus 10.1%). Residents of these two places are not especially different in terms of culture, although that does not mean that there are not large behavioral differences. Health care in Moscow city is more advanced than in Moscow oblast, but under normal circumstances for advanced medical treatments people in Moscow oblast would not need to travel far to get treatment in Moscow city. However, in the case of a pandemic, when most health facilities in Moscow were running at (or near) full capacity, there were fewer opportunities for patients from Moscow oblast to be treated in Moscow city.
Policies to prevent the spread of COVID-19 and the implementation of measures also played a role in the number of infections. The central government delegated much of the responsibilities in this field to regional administrations and those policies were diverse in the regions of Russia. At the initial stage of the COVID-19 pandemic, there was a high degree of misinformation related to the spread and severity of COVID-19 in Russian media. Sometimes public figures and even medical doctors on TV programs downplayed the danger of COVID-19 [ 39 ]. That influenced the efficiency of vaccination policies which, in turn, contributed to the number of COVID-19 cases and the excess number of deaths. A recent study by Roschina et al. has highlighted a high degree of ‘vaccine hesitancy’ in Russia, with only 45% of those surveyed in 2021 demonstrating positive attitudes towards the vaccination program [ 40 ]. As of March 2022, the total vaccination rate remains relatively low in Russia (around 55%, with around 20% in some regions) [ 41 ]. This compares unfavourably to even the global figure of around 60%, and is lower than in Pakistan and The Philippines. Maleva et al. [ 42 ] found that Russian young people and people with low levels of education are the least likely to be vaccinated.
So, in general there are many social, political, cultural and epidemiological factors and their interactions contributed to the diversity of patterns of excess mortality. In each region, the combination of those factors must be studied. In the Chechen Republic, for example, we observed a sharp drop in excess mortality between 2020 and 2021. This may be related to the hardline rhetoric and measures put in place in 2021 by the Chechen leader Ramzan Kadyrov. In May 2021, for example, it is reported that Kadyrov warned citizens that those who refused to be vaccinated would be treated last and will ‘feel how terrible the lack of oxygen feels’ [ 43 ]. Meanwhile in July 2021, it was decreed that unvaccinated residents in the Chechen Republic were banned from attending mosques. Citizens also stated that it was impossible to buy bread without a vaccine certificate [ 44 ].
Stepping back, our data presents clear evidence of the very high levels of excess mortality seen in Russia over the past two years; and that this level has significantly accelerated between 2020 and 2021. In a comparative sense, this overall finding accords with previous analyses of Russia which suggest it may come out of the COVID-19 experience with one of the very highest levels of excess mortality in the world. Using our RLED measure, however, we clearly disprove the widely held concept that such deaths were ‘going to happen anyway’ because of the relatively large number of remaining years of life expectancy of a deceased. Together, it appears that COVID-19 has further added to traumatic recent history of mortality–especially among males–in Russia [ 45 , 46 ].
Our study does, however, have several limitations. Firstly, the restricted data we have for 2021 means we cannot provide an analysis on the level of granularity which we would wish for this year. Secondly, as with all studies of mortality in Russia, there will inevitably be challenges concerning both completeness of registration as well as discrepancies in the place of registration of a death because of migration and different living/working patterns [ 47 ]. This is especially likely to be the case of the Republics in the Caucasus, and perhaps also the areas surrounding major cities such as Moscow and St. Petersburg. Such issues relating to death registration also impact upon the potential validity of comparisons between urban and rural excess mortality (as discussed above).
The human cost of the COVID-19 pandemic is well known. Quantifying this carefully, however, is a high priority to not only measure this impact, but to ensure adequate policy responses. In this paper, we have identified the high levels of excess mortality in the regions of Russia during the COVID-19 pandemic. To do so, we have deployed a rigorous method which accounts more accurately for underlying demographic change. We estimate that more than a million lives were lost to the pandemic. Contrary to the popular belief that such deaths were ‘likely to occur anyway’, our analysis shows that COVID-19 in Russia has had a significant impact upon remaining life expectancy. We have also, for the first, time, been able to present regional figures of excess mortality for 2021, as well as an analysis by age, gender and urban and rural status. These figures showed a higher impact on life expectancy for males who also had rising excess mortality (as a percent of expected) with age, unlike females where there was a non-linear relationship, and in general higher level of excess mortality in urban areas compared to rural areas and little difference is observed in male versus female excess mortality. Higher urban excess mortality could be driven by a higher density of population in urban areas, and thus higher infection transmission rate. As mentioned earlier, another source of bias towards higher urban excess mortality may be caused by registration of deaths of rural residents transferred to urban hospitals. While there is a wide variation in mortality rates between regions, there is no clear regional distribution (e.g. an east-west gradient).
While national figures show that excess mortality in Russia is perhaps amongst the highest in the world, there is a wide degree of regional variation. Such variation–and its interaction with age, gender, and rural/urban status–is key to better consideration and formulation of public health strategies to mitigate both the ongoing impact of COVID-19, and to rebuild and reshape health systems after the pandemic is over. As such, the determinants of mortality and the experience of (and response) to the pandemic at the regional level is a critical future avenue of research. This would enable more precise policy recommendations to be generated from our research. At this stage, however, some outcomes are clear. The regional disparities in infrastructure–especially in health–appear to be a key factor in determining levels of excess mortality. These disparities become amplified when the circumstances of the pandemic disrupted access. Higher levels of excess mortality in urban areas may have resulted from greater levels of infection in spaces of higher population density. This may mean that alternative strategies for infection control and management need to be in pace for urban and rural areas. Finally, we must look at the broader picture of how such mortality is so high in the first place. In this, the role of (mis)information and communication concerning both the severity of the public health emergency appears to have played a critical role. Ensuring the public have access to objective, honest, impartial, and accurate information about their circumstances is of the highest priority. For their part, scientists should be providing clear transparent assessments of mortality to inform government, media and other stakeholders.
Supporting information
S1 table. expected, observed and excess deaths (expressed in absolute and percentage terms), highest and lowest five regions of the russian federation with greater than 3,000 predicted deaths per year, 2021 and 2020..
https://doi.org/10.1371/journal.pone.0275967.s001
S2 Table. Expected, observed and excess deaths (expressed in absolute and percentage terms) and life expectancy lost, regions of the Russian Federation with greater than 3,000 predicted deaths per year, 2020, urban and rural areas.
https://doi.org/10.1371/journal.pone.0275967.s002
S3 Table. Expected, observed and excess deaths (expressed in absolute and percentage terms), regions of the Russian Federation with greater than 3,000 predicted deaths per year, 2020, males and females.
https://doi.org/10.1371/journal.pone.0275967.s003
S4 Table. Expected, observed and excess deaths (expressed in absolute and percentage terms), regions of the Russian Federation with greater than 3,000 predicted deaths per year, 2020, aged below and above 65.
https://doi.org/10.1371/journal.pone.0275967.s004
S5 Table. Remaining life expectancy in regions of the Russian Federation with greater than 3,000 predicted deaths per year, 2020, males and females.
https://doi.org/10.1371/journal.pone.0275967.s005
- View Article
- Google Scholar
- 2. WHO. International Guidelines for Certification and Classification (Coding) of COVID-19 as Cause of Death: Based on ICD International Statistical Classification of Diseases. WHO; 2020. Report No.: WHO/HQ/DDI/DNA/CAT. Available: https://www.who.int/classifications/icd/Guidelines_Cause_of_Death_COVID-19.pdf .
- PubMed/NCBI
- 12. World Health Organization. The true death toll of COVID-19: estimating global excess mortality. In: WHO [Internet]. 2021 [cited 17 Feb 2022]. Available: https://www.who.int/data/stories/the-true-death-toll-of-covid-19-estimating-global-excess-mortality .
- 13. OECD. Excess mortality. OECD; 2020 Oct. https://doi.org/10.1787/c5dc0c50-en
- 15. WHO. WHO Coronavirus (COVID-19) Dashboard. In: WHO [Internet]. 2022 [cited 18 Feb 2022]. Available: https://covid19.who.int/ .
- 20. ROSSTAT. Natural movement of the population of the Russian Federation in 2020. In: ROSSTAT [Internet]. 2021 [cited 1 Feb 2022]. Available: https://rosstat.gov.ru/compendium/document/13269 .
- 21. ROSSTAT. Estimate Of Life Expectancy At Birth By Regions Of the Russian Federation for 2020. In: ROSSTAT [Internet]. 2021 [cited 1 Feb 2022]. Available: https://rosstat.gov.ru/folder/12781 .
- 22. ROSSTAT. Operational information about the natural movement of the population. In: ROSSTAT [Internet]. 2022 [cited 1 Feb 2022]. Available: https://rosstat.gov.ru/storage/mediabank/2021_edn12.htm .
- 25. WHO. Years of life lost from mortality (YLL). In: WHO [Internet]. 2022 [cited 12 Sep 2022]. Available: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/159 .
- 27. Scherbov S, Shulgin S, Andruchowitz S, Arkhangelsky V, Ediev D, Efremov I, et al. Russian Demographic Data Sheet 2019. Moscow: RANEPA, Rosstat and IIASA; 2019. Available: http://pure.iiasa.ac.at/id/eprint/15652/ .
- 31. Ševčíková H, Li N, Kantorová V, Gerland P, Raftery AE. Age-specific mortality and fertility rates for probabilistic population projections. Dynamic Demographic Analysis. Cham: Springer International Publishing; 2016. pp. 285–310. https://doi.org/10.1007/978-3-319-26603-9_15
- 35. ROSSTAT. Demography. In: ROSSTAT [Internet]. 2021 [cited 1 Feb 2022]. Available: https://rosstat.gov.ru/folder/12781 .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
ABO blood type analysis of the donors of convalescent plasma after COVID-19 infection in Chelyabinsk region, Russia
Affiliations.
- 1 Blood Transfusion Station, Chief Physician, Chelyabinsk Oblast Ministry of Health, Chelyabinsk, Russia.
- 2 Department of Microbiology, Immunology and General Biology, Faculty of Biology, Chelyabinsk State University, Chelyabinsk, Russia.
- 3 Neonatology Division, Department of Pediatrics, Columbia University, New York, New York, USA.
- PMID: 34268789
- PMCID: PMC8447374
- DOI: 10.1111/vox.13178
PubMed Disclaimer
Conflict of interest statement
The authors declare no conflicts of interest.
Similar articles
- Correlation between ABO blood group and neutralizing anti-SARS-CoV-2 antibody titers in convalescent plasma donations. Franchini M, Mengoli C, Ballotari A, Glingani C. Franchini M, et al. Transfus Clin Biol. 2022 May;29(2):186-187. doi: 10.1016/j.tracli.2021.10.002. Epub 2021 Oct 12. Transfus Clin Biol. 2022. PMID: 34690072 Free PMC article. No abstract available.
- COVID-19 convalescent plasma from Norwegian blood donors. Nissen-Meyer LSH, Hervig T, Fevang B, Norheim G, Kran AB, Vaage JT, Flesland Ø. Nissen-Meyer LSH, et al. Tidsskr Nor Laegeforen. 2022 Jun 13;142(9). doi: 10.4045/tidsskr.22.0057. Print 2022 Jun 14. Tidsskr Nor Laegeforen. 2022. PMID: 35699539 English, Norwegian.
- Absence of correlation between ABO Rh(D) blood group and neutralizing antibody titers in SARS-CoV-2 convalescent plasma donors. Hirani R, Hoad V, Gosbell IB, Irving DO. Hirani R, et al. Transfusion. 2022 Feb;62(2):292-297. doi: 10.1111/trf.16781. Epub 2021 Dec 22. Transfusion. 2022. PMID: 34936102
- Regulatory challenges of convalescent plasma collection during the evolving stages of COVID-19 pandemic in the United States. Hassan S, West KA, Conry-Cantilena K, De Giorgi V. Hassan S, et al. Transfusion. 2022 Feb;62(2):483-492. doi: 10.1111/trf.16751. Epub 2021 Dec 3. Transfusion. 2022. PMID: 34778974 Free PMC article. Review. No abstract available.
- Potential mechanisms of action of convalescent plasma in COVID-19. Franchini M, Glingani C, Liumbruno GM. Franchini M, et al. Diagnosis (Berl). 2021 Mar 1;8(4):413-420. doi: 10.1515/dx-2020-0161. Print 2021 Nov 25. Diagnosis (Berl). 2021. PMID: 33652503 Review.
- Goel R, Bloch EM, Pirenne F, Al‐Riyami AZ, Crowe E, Dau L, et al. ABO blood group and COVID‐19: a review on behalf of the ISBT COVID‐19 working group. Vox Sang. 2021; 10.1111/vox.13076 - DOI - PMC - PubMed
- Levi JE, Telles PR, Scrivani H, Campana G. Lack of association between ABO blood groups and susceptibility to SARS‐CoV‐2 infection. Vox Sang. 2021;116:251–2. - PubMed
- Padhi S, Suvankar S, Dash D, Panda VK, Pati A, Panigrahi J, et al. ABO blood group system is associated with COVID‐19 mortality: an epidemiological investigation in the Indian population. Transfus Clin Biol. 2020;27:253–8. - PMC - PubMed
- Abdollahi A, Mahmoudi‐Aliabadi M, Mehrtash V, Jafarzadeh B, Salehi M. The novel coronavirus SARS‐CoV‐2 vulnerability association with ABO/Rh blood types. Iran J Pathol. 2020;15:156–60. - PMC - PubMed
- Khalil A, Feghali R, Hassoun M. The Lebanese COVID‐19 cohort; a challenge for the ABO blood group system. Front Med. 2020;7:1–7. - PMC - PubMed
Publication types
- Search in MeSH
Grants and funding
- R01 NS112381/NS/NINDS NIH HHS/United States
- RO1 NS112381/GF/NIH HHS/United States
- 20-44-740004/Chelyabinsk Region
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- Ovid Technologies, Inc.
- PubMed Central
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
COMMENTS
When the World Health Organization declared COVID-19 to be a pandemic on 11 March 2020, few could have foreseen the catastrophic effects the virus would have on the education of the world's children. During the first 12 months of the pandemic, lockdowns led to 1.5 billion students in 188 countries being unable to attend school in person ...
The transition to an online education during the coronavirus disease 2019 (COVID-19) pandemic may bring about adverse educational changes and adverse health consequences for children and young adult learners in grade school, middle school, high school, college, and professional schools. The effects may differ by age, maturity, and socioeconomic ...
Education: From COVID-19 school closures to recovery. After the historic disruption of the COVID-19 pandemic, most schools are back open worldwide but education is still in recovery assessing the damage done and lessons learned. Education: The pandemic affected more than 1.6 billion students and youth globally, with the most vulnerable learners ...
Today, The Education Recovery Scorecard, a collaboration with researchers at the Center for Education Policy Research at Harvard University (CEPR) and Stanford University's Educational Opportunity Project, released 12 new state reports and a research brief to provide the most comprehensive picture yet of how the pandemic affected student learning. Building on their previous work, their ...
U.S. Education in the Time of COVID. Beginning in March 2020, the American education system was confronted with unprecedented challenges as the COVID-19 pandemic caused the closures of many U.S. schools to in-person learning. Schools quickly transitioned to remote learning models, and the most lingering question—for parents, students, and ...
UNESCO's education response to COVID-19. After the historic disruption of the COVID-19 pandemic, most schools are back open worldwide but education is still in recovery assessing the damage done and lessons learned. The pandemic affected more than 1.5 billion students and youth with the most vulnerable learners were hit hardest.
(May 11, 2023) - Today, The Education Recovery Scorecard, a collaboration with researchers at the Center for Education Policy Research at Harvard University (CEPR) and Stanford University's Educational Opportunity Project, released 12 new state reports and a research brief to provide the most comprehensive picture yet of how the pandemic affected student learning. Building on their ...
The COVID-19 pandemic has caused abrupt and profound changes around the world. This is the worst shock to education systems in decades, with the longest school closures combined with looming recession. It will set back progress made on global development goals, particularly those focused on education. The economic crises within countries and ...
The rapid and unexpected onset of the COVID-19 global pandemic has generated a great degree of uncertainty about the future of education and has required teachers and students alike to adapt to a new normal to survive in the new educational ecology. Through ...
The COVID-19 pandemic has had a considerable impact on female education. Female education relates to the unequal social norms and the specific forms of discrimination that girls face. In 2018, 130 million girls worldwide were out of school, and only two out of three girls were enrolled in secondary education.
Four years after COVID-19 forced schools to close, educators want an overhaul. Four years after the coronavirus pandemic closed much of the nation's education system, thousands of the more than 50 ...
The COVID-19 pandemic has introduced uncertainty into major aspects of national and global society, including for schools. For example, there is uncertainty about how school closures last spring ...
COVID-19 has devastated the education sector. School closures have disrupted learning for more than 1.6 billion students around the world. As of January 2021, UNESCO estimates that more than 234 million children and youth remain affected by school closures in 33 countries, equaling more than 13 percent of enrolled learners worldwide.An estimated 11 million girls may never return to schooling ...
COVID-19 Global Education Recovery Tracker The World Bank's education team worked to support countries as they managed the changing education landscape during the pandemic. They advised on remote learning at scale and supported operations to facilitate post-pandemic learning recovery.
COVID-19 stands for "coronavirus disease 2019." It is caused by a virus called SARS-CoV-2. The virus first appeared in late 2019 and quickly spread around the world. There are different "variants," or strains, of the virus that causes COVID-19. Some variants seem to spread more easily than the original virus.
COVID Data The U.S. Department of Education worked across the federal government to track the pandemic and ensure schools, families and communities had the most relevant and current data to keep everyone safe. The Centers for Disease Control and Prevention (CDC) in partnership with the U.S. Department of Health and Human Services (HHS) provided real-time data tracking of the COVID-19 pandemic ...
The $43 million infusion the Port Arthur Independent School District received in federal COVID-19 pandemic relief funds accomplished more than Phyllis Geans could have ever imagined.
This Viewpoint discusses ways the coronavirus pandemic is forcing change onto graduate medical education, including online implementation of preclerkship curricula and alternatives to in-person patient experiences in clinical clerkship rotations.
These highly contagious COVID-19 strains, combined with the relaxed isolation guidelines that the Centers for Disease Control and Prevention released in March 2024, are likely to increase ...
The World Health Organization raises concerns for COVID-19 spike as schools go back in session and flu season nears.
In the wake of the unprecedented COVID-19 education disruptions which affected more than 220 million tertiary-level students around the world, UNESCO conducted a global survey aimed at providing an evidence-based overview of the current situation of the higher education system at national and global levels.
Montana State University doesn't owe a student any refunds from tuition or fees when it shut down in-person education in response to the COVID-19 pandemic, the Montana Supreme Court said in an ...
Health and education services have been critical challenges during the COVID-19 pandemic for children with invisible disabilities in Thailand due to their disab...
Minnesota Gov. Tim Walz often touts his experience teaching high school and his focus on education as governor. Here's a look at what he's done in the five-plus years he's led the state.
Learn more about the work done by the Equal Opportunity and Title IX office at the University of Nevada, Reno and find out where to go if you need resources or support.
The meteor that exploded over Chelyabinsk, Russia in February 2013 was "a wake-up call," according to a UC Davis scientist who participated in analyzing the event.
Accurately counting the human cost of the COVID-19 at both the national and regional level is a policy priority. The Russian Federation currently reports one of the higher COVID-19 mortality rates in the world; but estimates of mortality differ significantly. ...
Accurately counting the human cost of the COVID-19 at both the national and regional level is a policy priority. The Russian Federation currently reports one of the higher COVID-19 mortality rates in the world; but estimates of mortality differ significantly. Using a statistical method accounting for changes in the population age structure, we present the first national and regional estimates ...
ABO blood type analysis of the donors of convalescent plasma after COVID-19 infection in Chelyabinsk region, Russia