An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- AAS Open Res

- PMC7117957.1 ; 2018 Apr 18
- ➤ PMC7117957.2; 2019 Jan 24

Microbiological assessment of sachet water “pure water” from five regions in Ghana
1 West African Centre for Cell Biology of Infectious Pathogens, Department of Biochemistry, Cell and Molecular Biology, College of Basic and Applied Sciences, University of Ghana, Accra, P.O. Box LG 54, Ghana
Samuel Mawuli Adadey
Sandra akoley sowah.
2 Australian Institute for Bioengineering and Nanotechnology , University of Queensland, Brisbane , QLD, Australia
Charles Yeboah
3 Safe Water Network, Accra, Ghana
Associated Data
Underlying data for this study is available from Open Science Framework: Dataset 1. Microbiological assessment of sachet water “pure water” from five regions in Ghana. http://doi.org/10.17605/OSF.IO/J968K 16 under a CC0 1.0 Universal license
Version Changes
Revised. amendments from version 1.
The current manuscript is a revised version of the previous one based on the review comments. The ranking of samples based on their most probable number (MPN) was added to the abstract. The sampling period was added to the methods. The references of Table 1 and Figure 1 were corrected in the manuscript. There was an added text stating that the map was generated based on the field data. The contribution of the level of urbanization to microbial sachet water contamination was discussed in the new version of the manuscript. The aseptic techniques applied during the sample processing was updated in this new version. The title of figure 3 was changed. A conclusion session was added to the latest version as suggested by the reviewer. Aside from the above-mentioned updates, there were minor typographical errors that were corrected in the new version.
Peer Review Summary
| Review date | Reviewer name(s) | Version reviewed | Review status |
|---|---|---|---|
| Jonas A. Kengne-Ouafo and Bertrand Tatsinkou | Approved | ||
| Olusegun A. Olaoye | Approved | ||
| Jonas A. Kengne-Ouafo and Bertrand Tatsinkou | Approved with Reservations | ||
| Olusegun A. Olaoye | Approved with Reservations |
Background: Sachet water, popularly known as “pure water” has become an invaluable entity in most Ghanaian households. Despite its importance, there is no extensive nationwide investigations on its wholesomeness for consumption. The aim of this study was to determine the microbiological quality of 41 brands of sachet water sampled in 16 districts across 5 regions in Ghana.
Methods: The samples were analyzed for the presence of total and fecal coliform ( Escherichia coli ) using the Colilert*- 18 Test Kit.
Results: Majority of the samples (56.09%) were excellent, 4.87% satisfactory and 14.63% suspicious. Ten samples (24.4%) were unsatisfactory. For the degree of fecal contamination, (85.56%) were satisfactory, four (9.76%) were suspicious, and two others (4.88%) were unsatisfactory. The contaminations observed could be attributed to poor sanitary conditions (during and/or after production) and failure of some production facilities to adhere to standard manufacturing practices.
Conclusion: Our data suggest that microbiological quality sachet water from some sources have not yet attained levels that make it absolutely pure and wholesome for consumption in many areas.
Abbreviations
Ghana Water Company Limited (GWCL)
Most Probable Number (MPN)
Hazard Analysis Critical Control Point (HACCP)
Introduction
The occurrence of packaging water into sachets popularly referred to as “pure water” is one of the most lucrative business ventures in some West African countries including Ghana 1 . This business has gained much popularity and acceptance among the Ghanaian populace particularly because in the past, drinking water was sold in cups and plastic bags hand-tied at one end; a practice which was faced with a lot of sanitary issues 2 . Currently, the exact numbers of sachet water companies is unknown, as new ones spring up almost daily. There are more unregistered producers than registered ones, with the current estimate of registered producers reaching 3,000 2 .
“Pure water” contains 500ml of water in a clear plastic bag that is electrically heated and sealed at opposite ends. Water used for “pure water” is mostly obtained from ground water, springs and potable pipe-borne water. Prior to packaging, the water goes through a number of treatment processes, mainly filtration, in an attempt to make it cleaner and safer for consumption 3 . Most households and families depended greatly on tap water from the Ghana Water Company Limited (GWCL) for drinking and household activities including cooking 1 . However, with the frequent shortages associated with the supply of potable water across the country, and the questionable quality of the water supplied, many households and families in Ghana have resorted to using “pure water” mostly for drinking and cooking purposes 4 .
According to WHO guidelines, water for drinking must not present any significant risk to the health of the consumer over a lifetime of consumption 5 . Neither should the consumption of such water present different sensitivities that may arise between life stages. Invariably, safe drinking water should be colorless and tasteless, free from harmful chemicals as well as other suspended materials and most importantly should be devoid of disease-causing organisms 6 . Among many other concerns, the possibility of drinking water being the source of disease-causing organisms and related illnesses has been a huge hurdle to overcome, especially in parts of developing countries where availability, accessibility and affordability of potable and safe drinking water continues to be a challenge 2 , 5 .
Although the introduction of sachet water was intended to provide affordable and readily available safe drinking water for Ghanaians, investigations on its quality and wholesomeness for consumption have revealed considerable gaps especially with regards to microbial quality. Ngmekpele and Hawkins in 2015 analyzed the microbial and physicochemical properties of sachet water sold in Obuasi in the Ashanti region and found total coliform levels exceeding the WHO and the Ghana Standards Authority’s accepted levels for drinking water. In addition, fecal coliform was also detected in one of the samples.
In a study to investigate the bacteriological quality of sachet water produced and sold in Teshie-Nungua, a suburb known for perennial water shortages, Addo et al. (2009) reported sachet water sampled with suspicious microbial contaminations based on the most probable number (MPN) values. Fecal coliforms were detected in several samples while some of the samples were also contaminated with Escherichia coli . Given the vast number of people that rely on sachet water for their drinking needs, it is imperative that its quality is of the highest standard to avert any future waterborne outbreaks related to its consumption.
The quality of packaged water assessed in Nigeria showed some levels of microbial contamination 6 . The results of the study indicated that bottled water has lower microbial load than sachet water. E. coli, Clostridium perfringens spore and fecal Streptococcus were the most common isolated microbe from the packaged water. A similar study on the quality of potable water in Benin showed that some of the drinking water tested had microbiological pollution exceeding the approved levels, hence making the drinking water not wholesome for consumption 7 . Although packaged water is an improved source of drinking water, it is not totally free from microbial contaminations; hence the need for enhanced monitoring strategies to ensure that packaged water is always safe for human consumption 8 .
In this study we sought to examine the microbiological quality of sachet water sampled across Ghana, with primary focus on fecal contaminations. Although there have been several similar studies in the country 3 , 4 , 9 – 11 , our study has a wider geographic coverage (with samples from five regions out of the ten regions in Ghana) including mostly peri-urban and rural settings compared to previous studies where mostly urban settings were considered.
Study sites and design
Sachet water samples were collected from 41 selected communities within 16 districts in 5 out of the 10 regions in Ghana. The selection of the sample collection sites was based on a careful consideration of the sampling site of previous studies 1 , 3 which were all based in the Greater Accra Region. The water samples were collected between May to June 2015. The communities were selected from the southern/coastal belt (comprising communities in Central and Volta Regions), the middle belt (comprising communities in the Ashanti and Eastern Regions) and the northern belt (comprising communities in the Northern Region) of Ghana. These communities gave a fair representation of rural, urban as well as peri-urban communities in Ghana thus giving the study a wider geographic coverage ( Figure 1 ). The selected communities comprised towns and villages where sachet water is sold by retail shops and hawkers 12 . The study was designed to evaluate the microbial quality at the point of consumption of the most commonly sold sachet water.

The dots represents the sample collection sites and illustrate the wide geographical coverage of the study.
Sample collection
A total of 41 branded sachet water samples; one from each community (from different sachet water manufacturing companies), were randomly purchased from vendors on the streets. For each brand of sachet water, we tested 3 independent samples to correct for bias in sampling. The choice of purchase was based on the most commonly patronized sachet water by the inhabitants of a given community. The most commonly patronized sachet water was determined after interviewing a number of people in the community. The samples were stored on ice and transported (as described by Johnson et al. , 7 ) to central point laboratories within each region where the sample analyses were carried out.
Sample inoculation and incubation
We analyzed samples for the presence of total as well as fecal coliform ( E. coli ) using the Colilert*-18 Test Kit (with catalog number WP2001-8 from IDEXX Laboratories, Inc., Westbrook, Maine, USA) following the manufacturer’s protocol. A set of quality controls were run for the lot of sachet water sampled within each region ( Figure 2 ). Briefly, ATCC strains of Escherichia coli (ATCC 25922), Klebsiella pneumonia (ATCC 31488) and Pseudomonas aeriginosa (ATCC 10145) were each transferred with sterile loops into three sterile containers coated with sodium thiosulfate and each filled with 100 ml of sterile water. A similar set up with deionized water and Colilert*-18 substrate only served as negative control. After 18 hours of incubation at 35°C, each Quanti-Tray was compared with a Quanti-Tray comparator for the presence or absence of total coliform. E. coli enumeration was performed by observing wells under a 6-watt, 365-nm UV light in the dark. The results were read following the interpretations in Table 1 . Aseptic techniques were strictly followed to prevent laboratory based contaminations and this was confirmed by the negative controls.

Total coliform and Escherichia coli enumeration: Quality control test for ( A ) Pseudomonas aeriginosa (ATCC 10145), ( B ) Klebsiella pneumonia (ATCC 31488) and ( C ) Escherichia coli (ATCC 25922) to confirm negative result for both total coliform and fecal E. coli, positive results for total coliforms and positive results for fecal E. coli respectively. The positive wells for E. coli were observed under a 6-watt, 365-nm UV light in the dark.
| Appearance | Result |
|---|---|
| Yellow less than comparator | Negative for total coliform and |
| Yellow equal to or greater than comparator | Positive for total coliform |
| Yellow and fluorescence equal to or greater than | Positive for |
The number of positive wells in each Quanti-Tray was counted and the corresponding Most Probable Number (MPN) was obtained from the MPN table ( https://www.idexx.com/pdf/en_us/water/qt97mpntable.pdf ) provided by the manufacturer. With reference to the work done by Addo et al . in 2009, the WHO [4] and U.S. FDA 13 standards, the MPN values were used to categorize the samples.
Statistical analysis
Proportions of sachet water samples that were positive for E. coli and total coliform were compared across the five regions using Chi-square test with Yates correction for continuity using Microsoft excel (Microsoft Office 2013). The Marascuilo’s test of equality of several proportions was then used to compare pairs of proportions where the Chi-square test rejected the null hypothesis.
Sachet water microbiological quality
One branded sachet water with the most patronage was collected in triplicate from each of the 41 communities. Twenty-four (58.5%) samples tested positive for the presence of total coliforms with 7 (17.1%) of the positive samples positive for fecal E. coli. No E. coli was detected in the Central Region samples. The highest MPN for total coliform and fecal E. coli was estimated at 1299.7 and 27.5 respectively with samples from the Volta region having more positive total coliforms and E. coli compared to other regions ( Table 2 ). However, results from Chi-square and Marascuilo tests showed that, the proportion of sampled sachet water that was positive for E. coli was significantly different across the five regions while the proportion that were positive for total coliform did not differ significantly across the five regions ( Figure 3 and Supplementary File 1 ; Supplementary Table 1 and Supplementary Table 2 ).
| Region | District | Community | Fecal | |
|---|---|---|---|---|
| MPN/100mL | MPN/100mL | |||
| Ashanti | SEKYERE WEST | WORASO | 325.5 | 1 |
| Ashanti | SEKYERE WEST | APAAH | 2 | <1 |
| Ashanti | SEKYERE WEST | ADIDWAN | 1 | <1 |
| Ashanti | SEKYERE WEST | BUNUSU | <1 | <1 |
| Ashanti | SEKYERE WEST | NINTING | 2 | <1 |
| Ashanti | SEKYERE WEST | MPRIM | 24.3 | <1 |
| Ashanti | SEKYERE EAST | NAAMA | <1 | <1 |
| Ashanti | EJURA SEKYEDUMASE | KOBRITI | <1 | <1 |
| Ashanti | EJURA SEKYEDUMASE | AFRAMSO | <1 | <1 |
| Ashanti | EJURA SEKYEDUMASE | BABASO | 325.5 | 27.5 |
| Ashanti | EJURA SEKYEDUMASE | MBANAA | <1 | <1 |
| Ashanti | SEKYERE EAST | OGUAA | 1299.7 | <1 |
| Ashanti | EJURA SEKYEDUMASE | KASEI | <1 | <1 |
| Ashanti | EJURA SEKYEDUMASE | HIAWOANWU | <1 | <1 |
| Ashanti | SEKYERE EAST | ABOTANSO | 155.3 | <1 |
| Central | AWUTU-EFFUTU-SENYA | OSIMPO 1 | 1.5 | <1 |
| Central | GOMOA | GOMOA LOME | <1 | <1 |
| Eastern | AKWAPIM SOUTH | FOTOBI | 3.1 | <1 |
| Eastern | AKWAPIM SOUTH | OTU KWADJO | <1 | <1 |
| Eastern | YILO KROBO | TROM | <1 | <1 |
| Eastern | MANYA KROBO | AKOKOMA SISI | <1 | <1 |
| Eastern | MANYA KROBO | OBORPAH EAST | 1 | <1 |
| Eastern | KWAHU SOUTH | NTESO | 50.4 | <1 |
| Eastern | FANTEAKWA | ASIREBUSO | 3.1 | <1 |
| Eastern | FANTEAKWA | ODUMASI | <1 | <1 |
| Eastern | FANTEAKWA | MPAEM | <1 | <1 |
| Eastern | KWAHU SOUTH | SUMINAKESE | 6.3 | <1 |
| Eastern | KWAHU NORTH | KWAME DWAMENA | <1 | <1 |
| Eastern | KWAHU NORTH | FOSO (KWAWU FOSO) | 920.8 | <1 |
| Eastern | KWAHU NORTH | KOKROBUTA/ ADAMUKOPE | <1 | <1 |
| Northern | SAVELUGU-NANTON | SAVELUGU TOWNSHIP | 5.2 | <1 |
| Northern | WEST MAMPRUSI | LOAGRI NO.2 | <1 | <1 |
| Northern | WEST MAMPRUSI | ARIGU | 64 | 1 |
| Northern | KARAGA | TONG | 5.2 | <1 |
| Northern | KARAGA | KPATARIBORGU | <1 | <1 |
| Northern | KARAGA | TAMALEGU | 4.1 | <1 |
| Volta | KETU | TADZEWU | 5.2 | <1 |
| Volta | AKATSI | WUTE | 14.5 | <1 |
| Volta | KETU | HEDZRANAWO | 721.5 | 4.1 |
| Volta | SOUTH TONGU | AGBAKOPE | 9.7 | 3 |
| Volta | SOUTH TONGU | AGBOGBLA | 2 | 1 |

Of the 41 sachet water sampled, 58.5% tested positive for the presence of total coliforms while 17.1% of the total coliform- positive samples also tested positive for fecal Escherichia coli .
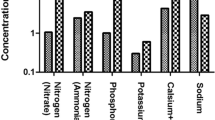
The results indicated that 11 out of the 41 (26.83%) sachet water brands sampled had coliforms exceeding the World Health Organization (WHO) and U.S. Food and Drugs Administration (U.S. FDA) approved limits of 9.2 MPN. The coliform MPN of the samples was used to grade the samples as Excellent (<2MPN/100), Satisfactory (2--3 MPN/100ml), Suspicious (4--10 MPN/100ml) and Unsatisfactory (>10MPN/100ml) ( Figure 4 ) 3 , 5 . The majority of the samples (56.09%) were excellent, with 4.87% and 14.63% as satisfactory and suspicious respectively. 10 samples (24.4%) however, were unsatisfactory ( Figure 4 ).
To determine the degree of fecal contamination, WHO and U.S. FDA standards were used to sort the samples based on the total fecal E. coli. The samples were graded Excellent (0 MPN/100ml), Suspicious (1--2 MPN/100ml) and Unsatisfactory (>2 MPN/100ml). The majority of the samples (85.56%) were satisfactory, however, 4 samples (9.76%) were suspicious and 2 others (4.88%) were unsatisfactory ( Figure 5 ).

Classification of sampled water for total coliform contamination was based on the total coliform MPN according to Addo et al . (2009), WHO (2011) and U.S. FDA standard for water purity. Approximately fifty six percent (56.09%) were excellent, 4.87% and 14.63% were satisfactory and suspicious respectively. The remaining samples (24.41%) were unsatisfactory.

Classification of sampled water for Escherichia coli contamination was based on the fecal E. coli MPN according to Addo et al . (2009), WHO (2011) and U.S. FDA standard for water purity. Majority of the samples (85.56%) were satisfactory, 9.76% were suspicious and 4.88% were unsatisfactory.
The study of the microbiological quality of sachet water has been a topic of interest to researchers since mid-1990s 14 . Nonetheless, publications on the microbial content of sachet water are still scarce, with only a few studies having a large sample size and are not representative of a nationwide study. Our study collected branded sachet water samples from 41 communities within 5 regions in Ghana to provide a better representation of the microbial water quality across the nation.
Based on the WHO 5 and U.S. FDA 13 standards, analytical samples should not have total coliform more than 9.2 MPN/100ml of water and must be free from fecal E. coli (thus 0 MPN/100ml). Our study revealed that 26.83% of our samples tested did not meet the above requirement as far as total coliform is concerned while 14.63% of the samples tested positive for fecal E. coli . Majority of the samples that had microbial contaminants were from the rural and peri-urban communities. These communities are often associated with poor sanitary conditions which could be a probable contributor to the above observations as well as failure of some production facilities to adhere to good sanitation practices. However, it is very important to further investigate the source of these contaminations.
Ideally, treated water should not have any coliform 10 , however, several studies have indicated the presence of microbial contamination in sachet water from different parts of the country 10 , 11 , 14 , 15 . Although the sachet water samples collected for this study were presumptively treated by the manufacturer, 58.5% of the samples tested positive for total coliforms which is indicative of the risk associated with their consumption. The presence of fecal E. coli in these samples point to fecal contamination. The trend observed in the contamination across the regions suggests more of a generalized rather than a centralized contamination. These microbial contaminants could have been either introduced during the manufacturing or post-manufacturing processes. Should these contaminants be as a result of gaps in the manufacturing processes, then it raises a lot of concern about the efficiency of the treatment processes involved in making the water wholesome for consumption.
We recommend that further studies be carried to investigate the efficiency of the treatment processes. Ngmekpele & Hawkins (2015) attributed the failure of most sachet water companies to adhere to the Hazard Analysis Critical Control Point (HACCP) system as another cause of contamination. The HACCP seeks to help check and eliminate the various levels of contamination that may occur in the sachet water production processes. Therefore, it is very essential that the manufacturing of sachet water be closely monitored by the regulatory bodies in charge to ensure strict adherence to the standard manufacturing procedures. Addo et al. (2009) randomly collected 30 sachets of 10 different brands of “pure water” from Teshie and Nungua, in the Greater Accra Region of Ghana. From their analysis none of the brands sampled met the WHO standards for drinking water based on their microbial contamination. Also, other related studies 10 implicated both vendors and poor production practices as the source of the microbial contamination. To effectively identify the sources of contamination of sachet water, a progressive study should be done with different brands of sachet water following them from production to consumers.
The strengths of this study include (1) obtaining random samples from each of the five regions, (2) accounting for overestimation of statistical significance for small samples using Yates correction for continuity in the Chi-squared test, and (3) the use of fisher’s exact test where cell counts are less than five.
The study identified microbial contamination; most alarming being contamination with E. coli in sachet water sampled in five regions across Ghana. As far as microbiological quality is concerned, sachet water has not yet attained levels that make it absolutely pure and wholesome for consumption.
Regulatory bodies in Ghana
There are two main regulatory bodies in Ghana that are responsible for the regulation of companies that produce drinking water. Ghana Food and Drugs Authority ( https://fdaghana.gov.gh ) which provides operational guidelines including codes of practice and good manufacturing practices for food, drug and other related manufacturing companies. The second regulatory body is Ghana Standards Authority ( https://www.gsa.gov.gh/ ) which has the vision of contributing towards growth of industry, protect consumers and facilitate trade through standardization, metrology and conformity assessment. These two regulatory ensure that drinking water producers meet all requirements for production before a permit is given. The regulatory bodies also have Quality Assessment departments that are responsible for quality check of licensed products including water. All the above efforts are towards the production of safe products for customer consumption.
Data availability
[version 2; peer review: 2 approved]
Funding Statement
This work was supported by the African Academy of Science (AAS) through a DELTAS African grant to GA [DEL-15-007] and by the BCAN Consult. The DELTAS Africa Initiative is an independent funding scheme of the AAS’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency), with funding from the Wellcome Trust to GA [107755/Z/15/Z]. Additional support was obtained from The South Africa Medical Research Council; self-initiated research to A.W.; and a National Institute of Health Grant to A.W. [U01 HG009716-01]. S.M.A. is supported by WACCBIP DELTAS PhD fellowship.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Supplementary material
Supplementary File 1 – file containing the following Supplementary Tables:
Supplementary Table 1: Chi-Square Test
Supplementary Table 2: Marascuilo test for Escherichia coli positive proportions
Reviewer response for version 2
Jonas a. kengne-ouafo.
1 Department of Microbiology and Parasitology, University of Buea, Buea, Cameroon
Bertrand Tatsinkou
2 Department of Microbiology and Parasitology, University of Buea, Buea, Cameroon
The authors have addressed the questions and comments raised. I, therefore, recommend the manuscript for indexing.
We confirm that we have read this submission and believe that we have an appropriate level of expertise to confirm that it is of an acceptable scientific standard.
Olusegun A. Olaoye
1 Department of Food Science and Technology, Michael Okpara University of Agriculture, Umudike, Nigeria
Authors have made significant improvement in the revised version of the manuscript based on reviewer's comments. I recommend acceptance of the manuscript for indexing.
I confirm that I have read this submission and believe that I have an appropriate level of expertise to confirm that it is of an acceptable scientific standard.
Reviewer response for version 1
Findings presented in this paper are of great public health importance. Mosi et al assessed the microbial content of different brands of sachet water produced, sold and consumed by the majority of the populations in different regions of Ghana with emphasis laid on coliforms and fecal E. coli. They showed that some sachet water brands in Ghana as a whole (since they sampled from 5 geographical distinct regions) are still contaminated by coliforms and fecal E. coli despite awareness-raising from previous reports. However, it would be good to specify the date of water sample collection in the study design to attest that what are referred to as previous reports are really previous reports in term of sample collection period. I will recommend this paper for indexing provided the authors address the comments raised below.
The authors present sachet water production and consumption at the beginning of the introduction as something specific to Ghana whereas it is common practice in many countries in Africa (West Africa mainly) (Nigeria, Cameroon). It would be good to move from general to specific.
Figure 1 and Table 1 are used in the method section to back up the wider geographic coverage of this study. But there is no link between what is found in table 1 and geographical coverage. The authors should clarify that. Was the map drawn by the authors or it is just an adaptation from another map? If that is the case, then the authors should specify that.
Study site and design
Sachet water samples were collected from 41 selected communities. How many samples were collected per community? The reader may have the impression that only one sample was collected per community. If that is the case, why? If many samples were collected then, your sample size should be 41 times the number of sample per brand. The authors should have collected more samples per community and even evaluate the storage conditions in each store, which information would have helped them discuss better their results. Did the authors collect each sachet water brands from the source (packaging company) to rule out the fact that water leaves the company already contaminated? If not, they should put that as a point in the discussion.
Giving the brand’s names as Obiri‐Danso et al (2003) 1 did in their paper “The microbiological quality of drinking water sold on the streets in Kumasi, Ghana” could be of great importance to the consumers in making the choice of which brands to take. Maybe ethically this is not correct but the authors should think about it.
“These communities gave a fair representation of rural, urban as well as peri-urban communities in Ghana thus giving the study a wider geographic coverage “ the authors mentioned this in their study design, the reader would expect them to present the results and discuss them with respect to level of urbanisation which is not the case in the current version of the paper.
-There is a word missing in the following sentence “The most commonly patronized sachet
water was determined after interviewing a number of people the community [...] to central point laboratories within each region where analysis were carried out." There seems to be a grammatical error in this sentence “where analysis was carried out or where analyses were”…
Again, in the methods, the authors did not describe clearly the measures taken to avoid contamination during sample transport and manipulation in the lab which could have contributed to the number of micro-organisms found.
……E. coli was estimated at 1299.7 and 27.5 respectively with samples from the Volta region having more positive total coliforms and E. coli compared to other regions (Table 1)
There is no link between the sentence and table1. The authors should make sure tables and figures are properly reference in the text.
The title of figure 3 :”Regional analysis of the samples” does not really describe the figure. The reader may think from the title that the figure summarizes the methods used to analyse the sample in different regions and not the analysis outcomes which the authors are referring to.
The authors could consider adding a small paragraph on the impact of used sachets on the environment, e.g. they constitute breeding sites for mosquitoes such as anopheles which transmit other diseases.
We confirm that we have read this submission and believe that we have an appropriate level of expertise to confirm that it is of an acceptable scientific standard, however we have significant reservations, as outlined above.
University of Ghana, Ghana
Comments addressed in manuscript
The study was designed to examine the wholesomeness of sachet water in Ghana. Therefore, the target was focused on microbial contaminants at the time it gets to the end user. It would have been interesting to sample water at the source (manufacturing treatment plant), and at the market but it was difficult to incorporate it in the study due to some technical challenges.
As rightly said, we considered the ethics of publishing the brand names and decided to leave them out.
Comments addressed in manuscript. In addition, transportation, as described by Johnson et al., was stated in the manuscript which gives reference to the aseptic measures used during the sample collection.
Since the publication was focused on the microbial contaminants and there was no result or evidence from our study on the environmental impact of sachet water, it would be difficult to discuss the effect of sachet water on the environment and it serving as breeding grounds for mosquitoes. This is however well noted for future studies.
The study presents microbiological analysis of sachet water samples across Ghana, with a view to ascertain their fitness for consumption. The research is an interesting one and of public health significance to the people that consume sachet water in Ghana.
The study reported occurrence of coliforms and useful microbial indicator of water quality, Escherichia coli in some of the water samples analyzed, signaling public health alarm to consumers.
Authors need to be consistent in their citations/references:, with the use of numbers ( 1,2 etc) or Surname with years, eg Ngmekpele and Hawkins (2015). Authors should choose a particular style of citation and use such throughout the manuscript.
Why did authors only take samples for analysis from 5 out of 10 regions? Why were the other regions not considered? Authors should be able to justify this.
Authors need to discuss briefly the efforts of the water regulatory body in Ghana in ensuring good quality drinking water, especially the regulations to companies involved. Are there laid down regulations by required body, are companies not adhering to such regulations? What possible sanctions can the regulatory body take on erring companies to serve as deterrent to others?
I suggest that the authors include a Conclusion section.
I recommend acceptance of the manuscript after the authors address the above points raised and other areas as highlighted in the reviewed PDF article, which can be downloaded here .
I confirm that I have read this submission and believe that I have an appropriate level of expertise to confirm that it is of an acceptable scientific standard, however I have significant reservations, as outlined above.
- Corpus ID: 67925695
Contamination of Sachet Water in Nigeria: Assessment and Health Impact
- Omalu Icj , GC Eze , +5 authors 1. Chukwuemeka
- Published 20 January 2011
- Environmental Science
Figures and Tables from this paper

49 Citations
Microbiological analysis of packaged drinking water sold in chennai, contamination of commercially packaged sachet water and the public health implications: an overview, assessment of bacteriological quality of vended water in jerry cans for domestic use in zaria, kaduna state, nigeria, microbiological quality of sachet packaged water vended in three local governments of oyo state, nigeria, parasitological evaluation of sachet drinking water in areas of lagos state , nigeria, overview of major bacterial contaminants of drinking water in nigeria: a review, detection and antibiogram of bacteriological contaminants in commonly consumed sachet water in dutse, jigawa state, nigeria, bacteriological assessment of bottled drinking water available at major transit places in mangalore city of south india, high fecal contamination and high levels of antibiotic-resistant enterobacteriaceae in water consumed in the city of maputo, mozambique, microbiological quality and contamination level of water sources in isiolo county in kenya, 15 references, pure water syndrome: bacteriological quality of sachet- packed drinking water sold in nigeria, bacteriology of sachet water sold in lagos, nigeria., quality of packaged waters sold in ibadan, nigeria, heavy metal hazards of sachet water in nigeria, the prevalence of bacteria in packaged sachets water sold in nnewi, south east, nigeria., waterborne disease: epidemiology and ecology, planning, anti-planning and the infrastructure crisis facing metropolitan lagos, related papers.
Showing 1 through 3 of 0 Related Papers
Advertisement
Contamination issues in sachet and bottled water in Nigeria: a mini-review
- Original Article
- Published: 05 November 2020
- Volume 6 , article number 112 , ( 2020 )
Cite this article

- Oluwaseun J. Ajala ORCID: orcid.org/0000-0002-0885-0910 1 , 3 ,
- Joshua O. Ighalo ORCID: orcid.org/0000-0002-8709-100X 2 , 4 ,
- Adewale George Adeniyi ORCID: orcid.org/0000-0001-6615-5361 2 ,
- Samuel Ogunniyi ORCID: orcid.org/0000-0003-3824-4273 2 &
- Comfort Abidemi Adeyanju ORCID: orcid.org/0000-0003-2968-8534 2
514 Accesses
20 Citations
4 Altmetric
Explore all metrics
Due to the unavailability of pipe-borne water in Nigeria, the idea of packaged drinking water in plastic bottles and sachets is now a common phenomenon in the country by private sector participation. The review aimed to evaluate and discuss the contamination issues on commercially available water in Nigeria. The review was conducted to synthesise the current body of knowledge in the research area to help present a proper perspective of the status quo. The result has shown that in most locations in the country, heavy metal pollution was still observable especially in sachet and bottled water. The result has shown that contamination by microbes, such as Escherichia coli , Enterococcus faecalis and Pseudomonas aeruginosa , was rampant. Furthermore, the microbial contamination issues were more widespread than for heavy metals. This was an indictment of the regulatory bodies that have not fully enforced stricter measures to ensure good quality of water is available to the Nigerian populace. It is recommended that integrated water management systems be set up in most urban and suburban locations to ensure the availability of pipe-borne water. Considering the significance of the current issue to the achievement of the sustainable development goals, efforts must be made to implement technological strategies for the separation and/or degradation of pollutants from commercial water during production.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
Wastewater Treatment and Reuse: a Review of its Applications and Health Implications
Drinking water contamination and treatment techniques.

Advantages and disadvantages of techniques used for wastewater treatment
Abdel-Satar AM, Ali MH, Goher ME (2017) Indices of water quality and metal pollution of Nile River Egypt. Egypt J Aquatic Res 43:21–29
Article Google Scholar
Abdullahi AA, Ighalo JO, Ajala OJ, Ayika S (2020) Physicochemical analysis and heavy metals remediation of pharmaceutical industry effluent using bentonite clay modified by H2SO4 and HCl. J Turkish Chem Soc Section A 7:727–744. https://doi.org/10.18596/jotcsa.703913
Adekunle L, Sridhar M, Ajayi A, Oluwade P, Olawuyi J (2004) An assessment of the health and social economc implications of satchet water in Ibadan, Nigeria: a public health challenge African. J Biomed Res 7:143–154
Google Scholar
Adelodun B, Ajibade FO, Ighalo JO, Odey G, Ibrahim RG, Kareem YF, Bakare HO, Tiamiyu AO, Ajibade TF, Abdulkadir TS, Adeniran KA, Choi KS (2020) Assessment of socioeconomic inequality based on virus-contaminated water usage in developing countries: a review. Environ Res. https://doi.org/10.1016/j.envres.2020.110309
Ajayi A, Sridhar M, Adekunle L, Oluwande P (2008) Quality of packaged waters sold in Ibadan, Nigeria African. J Biomed Res 11:7–13
Ajayi O, Adesida G (2009) Radioactivity in some sachet drinking water samples produced in Nigeria Iran. J Radiat Res 7:151–158
Akinbile C (2006) Hawked water quality and its health implications in Akure Nigeria Botswana. J Technol 15:70–75
Akinde SB, Nwachukwu MI, Ogamba AS (2011) Storage effects on the quality of sachet water produced within Port Harcourt Metropolis Nigeria Jordan. J Biol Sci 147:1–8
Akoteyon I, Omotayo A, Soladoye O, Olaoye H (2011) Determination of water quality index and suitability of urban river for municipal water supply in Lagos-Nigeria. Eur J Scient Res 54:263–271
Anake WU, Benson NU, Akinsiku AA, Ehi-Eromosele CO, Adeniyi IO (2014) Assessment of trace metals in drinking water and groundwater sources in Ota Nigeria. Internat J Scient Res Pub 4:1–4
Ariff S, Khan U, Turab A, Hussain I, Habib A, Mansoor T, Mallick D, Suhag Z, Bhatti Z, Ahmed I (2016) Evaluation of Solar Disinfection of water intervention delivered through Lady Health Workers in reduction of diarrheal episodes in under five children. Internat J Pediat Child Care 1:1
Bailey DM, Rasmussen P, Overgaard M, Evans KA, Bohm AM, Seifert T, Brassard P, Zaar M, Nielsen HB, Raven PB (2017) Nitrite and S-nitrosohemoglobin exchange across the human cerebral and femoral circulation: relationship to basal and exercise blood flow responses to hypoxia. Circulation 135:166–176
Chinedu SN, Nwinyi O, Oluwadamisi AY, Eze VN (2011) Assessment of water quality in Canaanland, Ota, Southwest Nigeria. Agri Biol J North Am 2:577–583
Chowdhury K, Khan S, Karim R, Obaid M, Hasan G (2011) Effect of moisture, water activity and packaging materials on quality and shelf life of some locally packed Chanachur Bangladesh. J Sci Ind Res 46:33–40
Dada AC (2009) Sachet water phenomenon in Nigeria: assessment of the potential health impacts. African J Microbiol Res 3:15–21
Daud M, Nafees M, Ali S, Rizwan M, Bajwa RA, Shakoor MB, Arshad MU, Chatha SAS, Deeba F, Murad W (2017) Drinking water quality status and contamination in Pakistan. BioMed Res Internat 1:6
Dunmade I (2017) Socioeconomic impacts of bottled water production and consumption system in a developing economy: a lifecycle approach. Internat J Business Manage Studies 6:471–484
Dunmade I, Onawumi S, Loto C, Oyawale F (2016) Social lifecycle assessment of sachet water: a case study on a Nigerian facility’s impacts on workers and the local community European international. J Sci Technol 5:31–45
Edema M, Atayese A, Bankole M (2011) Pure water syndrome: bacteriological quality of sachet-packed drinking water sold in Nigeria African. J Food Agri Nutr Dev 11:120–134
Edokpayi JN, Rogawski ET, Kahler DM, Hill CL, Reynolds C, Nyathi E, Smith JA, Odiyo JO, Samie A, Bessong P (2018) Challenges to sustainable safe drinking water: a case study of water quality and use across seasons in rural communities in Limpopo province. South Africa Water 10:159
Ekong PS, Ducheyne E, Carpenter TE, Owolodun OA, Oladokun AT, Lombin LH, Berkvens D (2012) Spatio-temporal epidemiology of highly pathogenic avian influenza (H5N1) outbreaks in Nigeria, 2006–2008. Prevent Vet Med 103:170–177
Ezeugwunne I, Agbakoba N, Nnamah N, Anahalu I (2009) The prevalence of bacteria in packaged sachets water sold in Nnewi South East, Nigeria. World J Dairy Food Sci 4:19–21
Igbeneghu OA, Lamikanra A (2014) The bacteriological quality of different brands of bottled water available to consumers in Ile-Ife, south-western Nigeria. BMC Res Notes 7:859
Ighalo JO, Adeniyi AG (2020) A comprehensive review of water quality monitoring and assessment in Nigeria. Chemosphere 260:127569. https://doi.org/10.1016/j.chemosphere.2020.127569
Ighalo JO, Adeniyi AG, Adeniran JA, Ogunniyi S (2020) A systematic literature analysis of the nature and regional distribution of water pollution sources in Nigeria. J Clean Prod. https://doi.org/10.1016/j.jclepro.2020.124566
Isikwue MO, Chikezie A (2014) Quality assessment of various sachet water brands marketed in Bauchi metropolis of Nigeria. Internat J Adv Eng Technol 6:2489–2495
Krishna RS, Mishra J, Ighalo JO (2020) Rising demand for rain water harvesting system in the world: a case study of Joda Town. India World Scient News 146:47–59
Kumar MD, Tortajada C (2020) Health Impacts of Water Pollution and ContaminationAssessing Wastewater Management in Indian. Springer, London
Kumpel E, Cock-Esteb A, Duret M, de Waal D, Khush R (2017) Seasonal variation in drinking and domestic water sources and quality in Port Harcourt Nigeria. Am J Trop Med Hyg 96:437–445
Muhamad SG, Esmail LS, Hasan SH (2011) Effect of storage temperature and sunlight exposure on the physicochemical properties of bottled water in Kurdistan region-Iraq. J Appl Sci Environ Manage 15:13–67
Musa D, Garba Y, Yusuf M, Ishaq A (2018) Assessment of water quality for selected boreholes and sachets water in Maigatari Town Jigawa State, Nigeria Bayero. J Pure Appl Sci 11:122–127
Olaoye O, Onilude A (2009) Assessment of microbiological quality of sachet-packaged drinking water in Western Nigeria and its public health significance. Public health 123:729–734
Omole DO, Ndambuki JM, Balogun K (2015) Consumption of sachet water in Nigeria: quality, public health and economic perspectives African. J Sci Technol Innov Dev 7:45–51
Onifade A, Ilori R (2008) Microbiological analysis of sachet water vended in Ondo State Nigeria. Environ Res J 2:107–110
Oparaocha E, Iroegbu O, Obi R (2010) Assessment of quality of drinking water sources in the federal university of technology Owerri, Imo state, Nigeria. J Appl Biosci 32:1964–1976
Orisakwe OE, Igwilo IO, Afonne OJ (2006) Heavy metal hazards of sachet water in Nigeria. Arch Environ Occup Health 61:209–213
Osikanmi BO, Mustapha M, Sridhar MKC, Coker AO (2020) Hazard identification and risk assessment-based water safety plan for packaged water production companies in Abeokuta South West Nigeria. J Environ Prot 11:48–63
Oyedeji O, Olutiola P, Moninuola M (2010) Microbiological quality of packaged drinking water brands marketed in Ibadan metropolis and Ile-Ife city in South Western Nigeria. African J Microbiol Res 4:096–102
Rendón-von Osten J, Dzul-Caamal R (2017) Glyphosate residues in groundwater, drinking water and urine of subsistence farmers from intensive agriculture localities: a survey in Hopelchén Campeche, Mexico. Internat J Environ Res Pub Health 14:595
Vunain E, Masoamphambe EF, Mpeketula PMG, Monjerezi M, Etale A (2019) Evaluation of coagulating efficiency and water borne pathogens reduction capacity of Moringa oleifera seed powder for treatment of domestic wastewater from Zomba Malawi. J Environ Chem Eng 7:103118
Yusuf KA, Majolagbe A, Sowemimo M (2018) Drinking water quality: physical and chemical evaluation of tap and packaged waters from eight local government areas in Lagos Nigeria. J Res Rev Sci 4:245–260
Download references
Author information
Authors and affiliations.
Department of Industrial Chemistry, University of Ilorin, P.M. B. 1515, Ilorin, Nigeria
Oluwaseun J. Ajala
Department of Chemical Engineering, University of Ilorin, P. M. B. 1515, Ilorin, Nigeria
Joshua O. Ighalo, Adewale George Adeniyi, Samuel Ogunniyi & Comfort Abidemi Adeyanju
Department of Pure and Applied Chemistry, Ladoke Akintola University of Technology, P. M. B. 4000, Ogbomoso, Nigeria
Department of Chemical Engineering, Nnamdi Azikiwe University, P. M. B. 5025, Awka, Nigeria
Joshua O. Ighalo
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Oluwaseun J. Ajala or Joshua O. Ighalo .
Ethics declarations
Conflict of interest.
The authors declare that there are no conflicts of interest.
Human or animal rights
This article does not contain any studies involving human or animal subjects.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Ajala, O.J., Ighalo, J.O., Adeniyi, A.G. et al. Contamination issues in sachet and bottled water in Nigeria: a mini-review. Sustain. Water Resour. Manag. 6 , 112 (2020). https://doi.org/10.1007/s40899-020-00478-5
Download citation
Received : 13 July 2020
Accepted : 27 October 2020
Published : 05 November 2020
DOI : https://doi.org/10.1007/s40899-020-00478-5

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bottled water
- Organic contaminants
- Inorganic contaminants
- Sachet water
- Find a journal
- Publish with us
- Track your research
Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Pathogenic Bacteria
Bacteriological Quality of Borehole and Sachet Water from a Community in Southeastern Nigeria
Submitted: 04 June 2019 Reviewed: 18 February 2020 Published: 20 August 2020
DOI: 10.5772/intechopen.91812
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Pathogenic Bacteria
Edited by Sahra Kırmusaoğlu and Sonia Bhonchal Bhardwaj
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
1,122 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Water from boreholes and packaged commercial sachet water from different areas in a community in southern Nigeria was analyzed with membrane filtration for a snapshot of heterotrophic count and coliforms. Two boreholes out of the 20 analyzed had counts of over 500 Cfu/mL and 7 boreholes indicated the presence of coliforms. Sixteen samples out of 20 sachet water brands analyzed showed a regulatory product registration code, whereas 4 samples had no number or code indicating that they were not registered. The heterotrophic count of all sachet water was well within the limit for all samples analyzed, and coliform was detected in only two samples. The overall quality of borehole water in the community studied was rated D (65%), whereas the sachet water was rated C (90%) according to the World Health Organization (WHO) surveillance guidelines. Improvements in water quality structure in the community studied are required to help achieve WHO sustainable development goals on water sanitation. The etiology, virulence properties, epidemiology, and pathogenicity of bacteria associated with borehole and sachet water are also discussed.
- sachet water
- heterotrophic count
Author Information
Ogueri nwaiwu *.
- School of Biosciences, University of Nottingham, Sutton Bonington Campus, United Kingdom
Chiugo Claret Aduba
- Department of Science Laboratory Technology, University of Nigeria, Nigeria
Oluyemisi Eniola Oni
- Department of Microbiology, Federal University of Agriculture, Nigeria
*Address all correspondence to: [email protected]
1. Introduction
Up to 2.1 billion people worldwide lack access to safe, readily available water at home according to a WHO/UNICEF report [ 1 ]. The report emphasized that majority of the people without good quality water are from developing countries and the lives of millions of children are at risk every day, with many dying from preventable diseases caused by poor water supply. The importance of good quality water is the reason why clean water and sanitation have been included as goal number 6 out of the 17 proposed sustainable development goals (SDGs) of the United Nations [ 2 ]. The proposal is that the SDGs will be the blueprint to achieving a better and more sustainable future for humanity by 2030.
In Nigeria, the public water supply is in a state of comatose in most towns and villages and dry taps without any hope of water running through the taps soon affect millions of homes. This has forced individuals and institutions to resort to self-help by using water from boreholes as the only source of water supply for drinking and general use. Use of borehole is a simple way of obtaining potable water from the aquifer below the ground, after which the water can be pumped into storage tanks before distribution.
Many people that went into borehole drilling business, which reduced the price of new boreholes, aided the proliferation of boreholes in Nigeria, and many citizens were ready to pay more money in rent for houses, which had boreholes. Furthermore, the dependence on groundwater, which is believed to be purified, is on the increase due to the increasing contamination of the surface water [ 3 ]. It is known that properly designed and constructed borehole both ensures the success of the borehole as an adequate supply of water and minimizes the risk of local pollution affecting the source [ 4 ]. If a borehole facility is not properly managed, contamination may occur in the process through the accumulation of physical, chemical, and biological agents in the pipelines and storage tanks of a distribution system or water packaging company. One direct use of boreholes is in the production and packaging of drinking water in sachets made from low-density polyethylene sheets. These products are popularly known as “pure water” in Nigeria. From the early 1990s, the production of sachet water increased exponentially and provided jobs for producers and sellers of the product. There is hardly any community in Nigeria without a sachet water facility. It is possibly the most widely consumed commercial liquid in Nigeria, and no sophistication is required for production. The quest for a cheap, readily available, and inexpensive source of potable water contributed to the emergence of sachet water [ 5 ], and it is far better and safer than the hand-filled, hand-tied packaged water in polyethylene bag [ 6 ] sold in Nigeria in the past. In developing countries, production and consumption of sachet water are rapidly on the rise [ 7 ], and many unregulated producers exist.
Packaged drinking water like the sachet water could be water from any potable source such as tap, well, and rain, which may be subjected to further treatments like decantation, filtration, demineralization, remineralization, and other methods to meet established drinking standards [ 8 , 9 ]. Packaged water is susceptible to microbial and chemical contamination regardless of their source [ 10 ]. Researchers have previously performed microbial analysis of sachet water in Nigeria using different laboratory techniques and found different bacteria and fungi. Occurrence of bacteria could lead to different disease conditions such as gastroenteritis, typhoid fever, cholera, bacillary dysentery, and hepatitis [ 11 ]. It has been reported [ 12 ] that waterborne diseases account for 80% of illnesses and diseases in developing countries, which leads to the death of several children every 8 seconds. In Nigeria, like most developing countries, various factors predispose packaged sachet water to contamination, and these include poor sanitation and source of raw material for food or water production [ 13 ]. Long storage of sachet under unfavorable environmental conditions and lack of good manufacturing practices (GMP) in general also contribute to contamination.
It has been found that the microbiome dynamically changes during different stages of water treatment distribution and the main important group in the past and present are fecal-associated bacterial pathogens like Escherichia coli [ 14 ]. However, opportunistic bacteria like Legionella and process-related bacteria, which form biofilms, are also a cause for concern [ 15 , 16 ]. A review [ 17 ] elucidated that drinking water comprises a complex microbiota that is influenced by disinfection and that members of the phylum Proteobacteria represent the most frequent bacteria in drinking water. It was also pointed out that their ubiquity has serious implications for human health and that the first step to address the persistent nature of bacteria in water would be to identify and characterize ubiquitous bacteria. The manifestation of bacterial contamination in drinking water can become known when outbreaks occur, and surveillance data provides insights on the microbial etiology of diseases and process failures that facilitated the outbreak [ 18 ]. Sometimes it can also be detected from laboratory results especially when water treatment facility is contaminated by bacterial biofilms [ 19 , 20 ].
In Nigeria, regulatory oversight is inadequate due to limited resources. Surveillance of bacteria in drinking water from boreholes and sachet water is necessary for the benefit of public health; hence, periodic surveys can help establish trends and identify where water quality of boreholes and sachet water is deficient. This chapter reports a survey, explores reports of bacteria associated with water from borehole and sachet water in Nigeria, and compares data found with WHO water standards. The organisms associated with boreholes and sachet water are discussed.
Water samples from boreholes were collected on different days using Whirl-Pak sampling bags (Nasco, Wisconsin, USA) and analyzed within 2 hours after collection. Twenty private boreholes and 20 different brands of commercial sachet water sold in four areas of a community were analyzed on different days. Sachet water was purchased (five each) from the different areas and were inspected for the inscription of an approved product registration code from the National Agency for Food and Drug Administration and Control (NAFDAC), the Nigerian national regulatory body. It was ensured that the same brand was not purchased twice from one area. The human population of the community (all 4 areas) was estimated to be over 5000 but less than 100,000.
Heterotrophic plate and total coliform count of bacteria were carried out using standard membrane filtration performed previously [ 21 ]. A slight modification of the method was introduced. Instead of using factory-made ready to use nutrient media sets, plate count agar (Oxoid, United Kingdom, CM0325) and violet red bile lactose agar (Oxoid, CM0107) for coliforms were prepared and used according to manufacturer’s instructions. Briefly, the filtration process involved placing of 100 ml of water sample in a sterile multibranched stainless steel manifold and filter holder system. A 0.45 μm membrane filter was fitted into the filter system after which water was drawn through to retain bacteria on the membrane. The membrane filter was placed on the media prepared and then incubated at 32°C over 48 h for membrane filters placed on plate count agar, whereas incubation at 30°C for 48 h was used for filters grown on violet red bile lactose agar. The heterotrophic count was noted, and estimated coliform results obtained for boreholes and sachet water were compared to WHO quality guidelines for drinking water [ 22 ].
3.1 Heterotrophic and total coliform count of borehole samples
This survey was carried out to have an overview of the bacterial load in water quality of some boreholes in the community surveyed. The borehole owners were apprehensive and thought they were being investigated for possible closure. To allow sample collection, it was agreed that the name of borehole owners and their location should remain anonymous when the findings were published. Results showed that borehole samples from area “C2” had the highest heterotrophic aerobic count. Two boreholes had counts of over 500 Cfu/mL, which is above the recommended heterotrophic limit [ 21 ]. All the other samples were below 500 Cfu/mL. Seven boreholes indicated the presence of coliforms because purple-pink colonies, which were 1–2 mm in diameter surrounded by a purple zone, were formed on the plates after incubation. Samples C2a, C2b, C2c, C2d, and C2e had coliform count of 17, 15, 9, 6, and 5 Cfu/mL, respectively, whereas samples C3b and C4b had coliform count of 4 and 2 Cfu/mL. The rest of the samples had no coliform on the plate used after incubation. A definitive trend was that samples with the highest heterotrophic count had the most coliform count ( Figure 1 ).

Heterotrophic plate count of borehole water sourced from different areas of the community studied (C1–C4). The letters a to e represent different samples.
3.2 Heterotrophic and total coliform count of sachet water samples
Periodic analysis of sachet water is important to public health because millions of people in Nigeria consume it. An ideal situation would be to analyze every borehole water from which sachet water is produced to establish water treatment effectiveness. Enquiries made to sachet water producers for access to their source of water for production were not successful. To refuse access some companies gave information and advice that they do not have a borehole and their water for production is sourced from the supply by water tankers. Hence, commercial samples of sachet water were purchased from different locations with unknown source of initial water for production of sachet water on sale. Sixteen samples out of the 20 analyzed showed a NAFDAC product registration code, whereas 4 samples had no number or code indicating that they were not registered. The heterotrophic count was well within the limit for all samples analyzed, and coliform was detected in only two samples. Sample SC1c and SC3c had a coliform count of 2 Cfu/mL each ( Figure 2 ).

Heterotrophic plate count of sachet water (S) sourced from different areas of the community studied (C1–C4). Letters a to e represent different samples.
3.3 Comparisons with WHO guidelines
The WHO standards and guidelines are usually used to monitor water quality. The WHO categorizes drinking water systems based on population size and quality rating to prioritize actions. A quality score from A to D is awarded (quality decreases A to D) based on the proportion (%) of samples negative for E. coli . However, the samples under study were assessed for total coliforms and not E.coli ; the scoring was carried out with the presumption that samples with high coliform count may contain E. coli . Total coliforms serve as a parameter to provide basic information on water quality [ 23 ]. On this basis, the overall quality of borehole water in the community studied (all areas combined) was rated D (proportion of samples negative for coliform =13; 65%), whereas the sachet water was rated C (18 = 90%).
4. Discussion
4.1 bacteria associated with boreholes in nigeria.
Pathogenic bacteria often occur in borehole water systems especially in developing nations [ 24 , 25 , 26 ]. Coliforms found in this study and other Gram-negative bacteria have been isolated from boreholes in different parts of Nigeria by many investigators [ 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 ]. The organisms mentioned in these studies include Enterobacter aerogenes , Escherichia coli , Klebsiella aerogenes , Klebsiella sp., Klebsiella pneumoniae , Klebsiella variicola , Proteus sp., and Proteus vulgaris . Other bacteria isolated are Providencia sneebia , Pseudomonas aeruginosa , Salmonella paratyphi , Salmonella sp., Salmonella typhi , Staphylococcus aureus , and Vibrio cholera .
The prevalence of the aforementioned species and genera may be due to the classical microbiological methods used for isolation. In most cases, MacConkey media was used for E.coli and coliform identification with no molecular studies that included 16S or whole-genome sequencing essential for establishing the actual prevalent bacteria species and strains in boreholes. An opportunity exists for regular molecular characterization of bacteria found in boreholes to help differentiate between harmless coliforms, fecal coliforms, and the deadly E. coli strain O157: H7. Borehole operators are required to deliver safe and reliable drinking water to their customers. If a community consistently consumes contaminated water, they may become unwell. Hence, regular monitoring and assessment of borehole water sources help maintain quality and provide data on groundwater management [ 35 , 36 , 37 , 38 ].
4.1.1 Bacteria contamination of groundwater
In Africa, many people rely on water from a borehole, but the purity of the drinking water from this source remains questionable [ 39 , 40 ]. The high heterotrophic count found in Area “2” of the community studied suggests that the groundwater of that area may be contaminated. The corresponding increased coliform count observed is consistent with the findings of Amanidaz et al. [ 41 ], which showed that when the concentration of coliforms and fecal Streptococci bacteria increased in a water network system, there was also an increased concentration of heterotrophic bacteria. These contrasts with the work of others [ 42 ] where it was shown that high heterotrophic count inhibits coliform proliferation. Despite increased heterotrophic count and coliforms in the study of Amanidaz et al. [ 41 ], it was concluded that no correlation exists, and increased numbers could be due to variability in nutrient composition [ 43 ]. Another factor could be biofilm formation because it has been shown that attached bacteria in biofilms of a water system are more metabolically active than the ones that are free-living [ 44 ]. Groundwater is susceptible to contamination by both organic and inorganic contaminants [ 45 , 46 , 47 , 48 ]. Contamination could happen through natural processes, such as geological weathering and dissolution of numerous minerals beneath the earth’s surface, which results in low natural concentrations of contaminants in groundwater [ 49 ]. Anthropogenic sources, such as seepages from agricultural wastewaters, domestic sewages, mining activities, and industrial effluents, can also affect the quality of groundwater in many parts of the world [ 50 , 51 , 52 ]. Other reports showed that borehole contamination may occur through domestic wastewater and livestock manure [ 53 ] industrialization and urbanization [ 54 ] and leakages from septic tanks [ 55 ] or pit latrines [ 56 ]. Seasonal environmental conditions may also contribute to increased bacteria count from borehole water because other investigators [ 57 , 58 ] have demonstrated that higher bacterial count in borehole water occurs during the rainy season. This has been attributed to flooding which may allow floodwater to get into borehole systems that are not properly constructed.
4.2 Cases of sachet water contamination in Nigeria
Postproduction improper handling [ 59 ] and compromising safety and quality for profit during production [ 60 ] are factors that can affect sachet water contamination in Nigeria. Sachet water producers are expected to be food safety conscious in order not to jeopardize the health of the public. A large number of sachet water-producing companies in Nigeria are not registered and do not practice good manufacturing practices or follow international quality standards of water treatment [ 61 ] despite the efforts of NAFDAC to improve standards. Up to 25% of samples analyzed in this study had no regulation or expiration date code as recommended previously [ 62 ]. However, the fact that 75% of sachet water analyzed had date codes is a remarkable improvement from what was the norm (0%) when sachet water production started in the country. Unlike a previous study with larger sample size [ 11 ], which reported isolation of bacterial species in 54 out of 720 (7.5%) from 6 different brands of sachet water in northern Nigeria, all the samples in this study (100%) showed heterotrophic growth that were within permissible limits (<500 Cfu/mL).
Sachet water analysis from other parts of Nigeria has shown different levels of contamination. In this study, 10% (2 out of 20) of samples contained coliforms. In other studies carried out on samples sourced from Aba in the southeast, an analysis of 20 sachet water samples showed that 32% of the samples reportedly tested positive for Staphylococcus spp., 23% for Pseudomonas , 20% for Klebsiella spp., 15% for Proteus , and 10% for Enterobacter [ 59 ]. Another study in the same region reported a contamination in 8 out of the 10 sachet water samples analyzed, isolated microorganisms included E. coli , Klebsiella spp., Pseudomonas spp., Bacillus spp., Proteus spp., and Staphylococcus spp. [ 5 ]. Also 66% and 73% prevalence of pathogens have been reported [ 63 ] in this region after two batches of 30 sachet water samples were analyzed. In Oyo, which is situated in the southwest of Nigeria, E. coli (13.3%), Pseudomonas aeruginosa (39.9%), and Enterobacter aerogenes (53.3%) were isolated from commercially sold sachet water [ 64 ]. Another report in this region [ 26 ] highlighted that all brands of sachet water (100%) analyzed had the presence of coliforms.
4.3 Compliance with world standards
A recent SDGs progress report [ 3 ] shows that between 2000 and 2017, the proportion of the global population using safely managed drinking water increased from 61 to 71%. The report highlighted that despite the increase, water stress affects people on every continent, requiring immediate and accelerated collective action to provide billions of people with safely managed drinking water. The quality score for the boreholes and sachet water from the community studied showed that the water needs improvement to achieve the desired “A” rating. In this study, the borehole water quality in Area “2” is a source of concern, and the owners in that area were advised to boil and filter the water before drinking. It is common knowledge in Nigeria that some boreholes are not deep enough to produce clean water from the aquifer; hence, such boreholes are used for other domestic purposes but not for cooking food or drinking. Owners of such boreholes normally boil and filter the water for drinking.
Water quality specifications may depend on the particular use, but the presence of coliforms in drinking water indicates that disease-causing organisms could be in the water system and may pose an immediate health risk to the water consumers. When coliforms and other bacteria are found, it is always recommended [ 65 ] that an investigation should be carried out to establish the sources of contamination. This confirmation will enable risk assessment and identification of solutions that will eliminate or reduce the risk of waterborne disease within a large population [ 66 ].
4.4 Etiology, virulence, epidemiology, and pathogenicity of bacteria associated with borehole and sachet water
From the studies reviewed, the organisms found in borehole water are well-known food- and waterborne bacteria that are constantly monitored by regulatory authorities in many parts of the world. Outbreaks can occur in a community and cause fatalities and economic losses. Hence, a constant review of the growth conditions that enable the bacteria to proliferate, the features that enable survival in different environments, infection mode, and prevalence pattern of these bacteria is important to reduce outbreaks.
4.4.1 Staphylococcus
The bacterium Staphylococcus aureus from the genus Staphylococcus is known for methicillin resistance of some strains. The bacterium is a major environmental contaminant of food and water, and the human skin and nose are known to be major sources of the organism. Nasal colonization [ 67 , 68 ] and atopic dermatitis of the skin [ 69 , 70 ] are considered risk factors. Environmental contamination may be the source of contamination in borehole water analyzed in this study, whereas humans or personnel involved in sachet water production are likely to be contributors to contamination. In Nigeria, sachet water producers are known to lack resources; hence, it is possible that respiratory protective equipment like nose masks are not worn during production in some facilities. Since it is possible to distinguish community-associated MRSA from healthcare-associated MRSA based on genetic, epidemiologic, or microbiological profiles [ 71 ], it would be beneficial to screen the strains found in this study to determine if they are methicillin resistant and community-related.
The pathogenicity, epidemiology, and virulence factors of Staphylococcus have been comprehensively reviewed [ 72 ]. It was highlighted that colonization is aided by biofilm formation that is housed in extracellular polymeric substance (EPS) found in many bacteria and that virulence factors are expressed with accessory gene regulator (agr) system in response to cell density [ 73 ]. To avoid formation of biofilms and EPS in the sachet water-producing environment, adequate personnel hygiene and good manufacturing practices that meet food safety standards must be implemented.
4.4.2 Pseudomonas
The genus Pseudomonas especially P. aeruginosa is known globally as endemic [ 74 ] and an opportunistic pathogen that causes several infections [ 75 ]. They are often isolated in clinics [ 76 ], and other sources may include residential, recreational, or surface water [ 77 ]. The colonies are usually heavily mucoid on solid media. It has been reported that mechanisms of antimicrobial resistance in Pseudomonas strains and most bacteria include multidrug efflux pumps and downregulation of outer membrane porins, whereas virulence may include secretion of toxins and the ability to form biofilms [ 78 , 79 ]. A natural property of Pseudomonas is the possession of multiple mechanisms for different forms of antibiotic resistance [ 80 ], and this may have facilitated its occurrence in boreholes and sachet water.
4.4.3 Klebsiella
Klebsiella causes many infections, which includes urinary tract infections, pneumonia, bacteremia, and liver abscesses [ 81 ]. The genus is associated with water, and this may be why it has been isolated in both borehole and sachet water. The organism is found in drinking water [ 82 ], rivers [ 83 ], and sewage water [ 84 ], which may encourage environmental spread. It has been reported that the organism has a variety of virulence and immune evasive factors, which contribute to uptake of genes associated with antimicrobial resistance and pathogenicity [ 85 ]. A report [ 86 ] suggested that the species K. pneumoniae acquired antimicrobial resistance genes independently and their population is highly diverse. An analysis of strains from human and animal isolates spanning four continents has shown convergence of virulence and resistance genes, which may lead to untreatable invasive K. pneumoniae infections [ 87 ].
4.4.4 Escherichia
The most studied species of the Escherichia genus is E. coli , a coliform bacteria used to verify hygiene status in food and water. Usually, the presence of various strains of pathogenic or nonpathogenic E. coli in food or water samples indicates fecal contamination [ 88 ]. It has been reported that [ 89 ] a comparative analysis show that avian and human E. coli isolates contain similar sets of genes encoding virulence factors and that they belong to the same phylogenetic groups, which may indicate the zoonotic origin of extraintestinal pathogenic E. coli .
A study of the prevalence of E. coli strain O157:H7 in England and Scotland showed that it has a seasonal dependency, with greater fecal shedding of the organism in the warmer months together with increased reporting of E. coli O157:H7 infection among hospitalized patients [ 90 ]. This finding is very worrying because it suggests that there could be high prevalence when applied to Nigeria because the country has a warm climate all year round. However, good manufacturing practices irrespective of the climate appear to be the key factor in producing packaged water free of coliforms. It has been shown that levels of coliform bacteria and E. coli detected in sachet water samples in Ghana, a country with similar climate to Nigeria, were statistically and significantly lower than levels detected from several water sources including public taps [ 91 ].
4.4.5 Enterobacter
The genus Enterobacter consists of coliforms that are known to be of non-fecal origin. It is believed [ 92 ] that many Enterobacter species, which could act as pathogens, are widely encountered in nature but are most frequently isolated in human clinical specimens possibly because phenotypic identification of all species belonging to this taxon is usually difficult and not always reliable. Therefore, the identification of this genus in borehole and sachet water may need a revisit since molecular methods were not used. The organism is known as a ubiquitous and persistent Gram-negative bacterium in drinking water [ 17 ], but there are few studies of its occurrence or prevalence in borehole and sachet water or other water sources in Nigeria.
To understand the carbapenemase-producing Enterobacter spp. and the development of molecular diagnostics, Chavda et al. [ 93 ] used genomic analysis of 447 sequenced strains to establish diverse mechanisms underlying the molecular evolutionary trajectory of drug-resistant Enterobacter spp. Their findings showed the acquisition of an antibiotic resistance plasmid, followed by clonal spread and horizontal transfer of blaKPC -harboring plasmids between different phylogenomic groups. The report also showed repeated transposition of the blaKPC gene among different plasmid backbones.
4.4.6 Proteus
Proteus species are Gram-negative opportunistic rod-shaped bacteria known for its swarming motility and contamination of agar plates. Furthermore, on agar plates, the bacteria undergoes a morphological conversion to a filamentous swarmer cell expressing hundreds of flagella, and during infection, histological damage is caused by cytotoxins including hemolysin and a variety of proteases [ 94 ]. The organism is reported to have negative and positive advantages. According to Drzewiecka [ 95 ], Proteus species may be indicators of fecal pollution, which may cause food poisoning when the contaminated water or seafood is consumed, and it could be used for bioremediation activity due to its tolerance and ability to utilize polluting compounds as sources of energy.
Virulence factors may include fimbriae, flagella, outer membrane proteins, lipopolysaccharide, capsule antigen, urease, immunoglobulin A, proteases, hemolysins, and amino acid deaminases [ 96 ]. The ability to swarm and survive is facilitated by the upregulation of FlhD(2)C(2) transcription activator, which activates the flagellar regulon [ 97 ]. The prevalence of Proteus spp. in borehole or sachet water may be aided by its ability to swarm and colonize the production environment.
4.4.7 Vibrio
In Nigeria, the most reported species among the Vibrio species that cause water-related infection is Vibrio cholerae . The organism causes cholera, which is an infection that is characterized by watery stooling. The disease has killed hundreds of people in Nigeria in the last decade. According to Faruque et al. [ 98 ], a lysogenic bacteriophage designated CTXΦ encodes the Cholera toxin (CT), which is strongly influenced by environmental conditions [ 99 ]. The organism is responsible for the profuse diarrhea, and molecular epidemiological surveillance has revealed clonal diversity among toxigenic V. cholerae strains with continuous emergence of new epidemic clones. It has not been established if the strains found in boreholes and sachet water are the V. cholerae O1 or O139 strains that cause cholera [ 100 ]. There is a possibility that they could be non-O1 or non-O139 strains that are common in the environment.
In 2017, the WHO launched a global strategy on cholera control with a target to reduce cholera deaths worldwide by 90% [ 101 ]. The strategy is to use safe oral cholera vaccines in conjunction with improvements in water and sanitation to control cholera outbreaks and for prevention in areas known to be high risk for cholera. Nigeria can be classified as a high-risk area, and the occurrence of Vibrio species in borehole or sachet water suggests that they could transmit cholera. Outbreaks occur regularly in Nigeria, and it is always difficult to bring it under control. An outbreak in 2018 was characterized by four epidemiological waves and led to 836 deaths out of 43,996 cases [ 102 ], whereas that of 2010 killed a total of 1716 out of 41, 787 cases [ 103 ]. In both cases, the case fatality rate was over 1% recommended by WHO.
4.4.8 Bacillus
Bacillus cereus is a food safety concern among several species of Bacillus . It is naturally widely distributed in nature, and it is known as a Gram-positive rod bacterium that is responsible for food poisoning [ 104 ]. It can proliferate because of unhygienic practices [ 105 ] and can attach to drinking water infrastructure [ 106 ]. This suggests that the ubiquity of the organism, poor hygiene, and attachment to equipment may be why Bacillus has been repeatedly isolated from boreholes and sachet water by previous investigators.
Bacillus growth is sometimes considered an insignificant contaminant. Some strains like B. subtilis is used for probiotics [ 107 ], whereas a strain like B. cereus which secrets toxins like hemolysins, phospholipases, an emesis-inducing toxin, and proteases [ 108 ] is not used due to obvious reasons. Toxin production in B. cereus requires the transcription factor PlcR , which controls expression of virulence factors [ 109 ]. Virulence-associated gene profiles have been used to evaluate the genetic backgrounds and relationships of food poisoning cases among other isolates from the environment, and it was concluded that both molecular and epidemiological surveillance studies could be used effectively to estimate virulence [ 110 ].
4.4.9 Salmonella
The species Salmonella typhi and Salmonella paratyphi cause typhoid fever and remain a major public health concern in Asia and Africa [ 111 ] due to antimicrobial resistance. For developed countries, it is believed that some non-typhoidal strains are zoonotic in origin and acquire their resistance in the food animal host before onward transmission to humans through the food chain [ 112 ]. It has been reported that the overall global burden of Salmonella infections is high and this may be the reason why in 2017, the WHO listed fluoroquinolone-resistant Salmonella spp. as priority pathogens for which new antibiotics were urgently needed [ 113 ].
The bacterium can survive in aquatic environments by a number of mechanisms, including entry into the viable but non-culturable state or residence within free-living protozoa [ 114 ]. Survival in water may have contributed to the isolation from borehole and sachet water in studies by others. It is not certain if the isolates encountered in this study cause typhoid fever or are the non-typhoid causing strains. Hence, additional studies are required to establish the prevalent type of Salmonella in water-producing facilities in Nigeria. A recent report found that typhoid fever still poses a serious health challenge in Nigeria and is a major health security issue [ 115 ]. It was recommended that a combined approach that includes the use of typhoid vaccines, improvements in sanitation, and safe water supply is essential.
5. Conclusions
The overall bacteria quality of the borehole and sachet water in the community studied needs improvement. An improvement can be achieved by focusing on areas with coliform contamination. Boreholes should be sited where pollutants will not easily contaminate them. Regular water testing should be carried out to ensure the attainment of WHO guidelines always. Where deviations are found, corrective actions should be undertaken. The literature on bacteria from boreholes and sachet water in Nigeria shows that not much molecular characterization has been carried out; hence an opportunity exists for more investigations. Regulatory oversight for sachet water production and the use of boreholes by large community populations requires improvement. It is recommended that universities should carry out periodic surveillance of boreholes and sachet water sold near them to support the SDG targets of the WHO.
Conflict of interest
The authors declare no conflict of interest.
- 1. United Nations International Children’s Emergency Fund (UNICEF). Water, sanitation and hygiene [Internet]. Available from: https://www.unicef.org/wash/ [Accessed: 03 November 2019]
- 2. United Nations. About the sustainable development goals [Internet]. Available from: https://www.un.org/sustainabledevelopment/sustainable-development-goals/ [Accessed: 03 November 2019]
- 3. Agwu A, Avoaja AG, Kalu AU. The assessment of drinking water sources in aba metropolis, Abia state, Nigeria. Resources and Environment. 2013; 3 (4):72-76
- 4. Ensure availability and sustainable management of water and sanitation for all [Internet]. Available from: https://unstats.un.org/sdgs/report/2019/goal-06/ [Accessed: 02 November 2019]
- 5. Anyamene NC, Ojiagu DK. Bacteriological analysis of sachet water sold in Awka Metropolis, Nigeria. International Journal of Agriculture and Biosciences. 2014; 3 (3):120-122
- 6. Manjaya D, Tilley E, Marks SJ. Informally vended sachet water: Handling practices and microbial water quality. Water. 2019; 11 (4):800. DOI: 10.3390/w11040800
- 7. Gangil R, Tripachi R, Patyal A, Dutta P, Mathur KN. Bacteriological evaluation of packaged bottled water sold at Jaipur city and its public health significance. Veterinary World. 2013; 6 :27-30
- 8. Aroh KN, Eze EM, Ukaji D, Wachuku CK, Gobo AE, Abbe SD, et al. Health and environmental components of sachet water consumption and trade in Aba and Port Harcourt, Nigeria. Journal of Chemical Engineering and Material Science. 2013; 4 :13-22
- 9. Isikwue MO, Chikezie A. Quality assessment of various sachet water brands marketed in Bauchi metropolis of Nigeria. International Journal of Advances in Engineering and Technology. 2014; 6 (6):2489-2495
- 10. Sudhakar MR, Mnatha P. Water quality in sustainable water management. Current Science. 2004; 87 :942-947
- 11. Thliza LA, Khan AU, Dangora DB, Yahaya A. Study of some bacterial load of some brands of sachet water sold in Ahmadu Bello University (Main campus), Zaria, Nigeria. International Journal of Current Science. 2015; 14 :91-97
- 12. Hughes JM, Koplan JP. Saving lives through global safe water. Journal of Infectious Diseases. 2011; 10 :1636-1637
- 13. Ashbolt NJ. Microbial contamination of drinking water and disease outcomes in developing regions. Toxicology. 2004; 198 :229-238
- 14. Proctor CR, Hammes F. Drinking water microbiology--from measurement to management. Current Opinion in Biotechnology. 2015; 33 :87-94. DOI: 10.1016/j.copbio.2014.12.014
- 15. Berry D, Xi C, Raskin L. Microbial ecology of drinking water distribution systems. Current Opinion in Biotechnology. 2006; 17 :297-302
- 16. Benner J, Helbling DE, Kohler HP, Wittebol J, Kaiser E, Prasse C, et al. Is biological treatment a viable alternative for micropollutant removal in drinking water treatment processes? Water Research. 2013; 47 (16):5955-5976
- 17. Vaz-Moreira I, Nunes OC, Manaia CM. Ubiquitous and persistent proteobacteria and other gram-negative bacteria in drinking water. Science of the Total Environment. 2017; 586 :1141-1149. DOI: 10.1016/j.scitotenv.2017.02.104
- 18. Hunter PR, Anderson Y, Von Bonsdorff CH, Chalmers RM, Cifuentes E, Deere D, et al. Surveillance and investigation of contamination incidents and water borne outbreaks. In: Dufour A, Snozzi M, Koster W, Bartram J, Ronchi E, Fewtrell L, editors. Microbial Safety of Drinking Water: Improving Approaches and Methods. Cornwall: IWA; 2003. pp. 205-236
- 19. Nwaiwu O, Nwachukwu MI. Detection and molecular identification of persistent water vessel colonizing bacteria in a table water factory in Nigeria. British Microbiology Research Journal. 2016; 13 (5):1-12
- 20. Nwaiwu O. Data on evolutionary relationships of Aeromonas hydrophila and Serratia proteamaculans that attach to water tanks. Data in Brief. 2018; 16 :10-14. DOI: 10.1016/j.dib.2017.10.073
- 21. Nwaiwu O, Ibekwe VI. Prevalence and risk of heterotrophic bacteria in a carbonated soft drink factory. African Journal of Microbiology Research. 2017; 11 (6):245-253
- 22. Guidelines for drinking-water quality: Fourth edition incorporating the first Addendum, Surveillance [Internet]. 2017. World Health Organization, pp. 89-91. Available from: https://www.who.int/water_sanitation_health/publications/drinking-water-quality-guidelines-4-including-1st-addendum/en/ [Accessed: 01 October 2019]
- 23. Shibata T, Solo-Gabriele HM, Fleming LE, Elmir S. Monitoring marine recreational water quality using multiple microbial indicators in an urban tropical environment. Water Research. 2004; 38 (13):3119-3131. DOI: 10.1016/j.watres.2004.04.004
- 24. Oludairo O, Aiyedun J. Contamination of commercially packaged sachet water and the public health implications: An overview. Bangladesh Journal of Veterinary Medicine. 2016; 13 (2):73-81
- 25. Aroh KN, Eze EM, Ukaji D, Wachukwu CK, Gobo AE, Abbe SD, et al. Health and environmental components of sachet water consumption and trade in aba and Port Harcourt, Nigeria. Journal of Chemical Engineering and Materials Science. 2013; 4 (2):13-22
- 26. Oyedeji O, Olutiola PO, Moninuola MA. Microbiological quality of packaged drinking water brands marketed in Ibadan metropolis and Ile-Ife city in South Western Nigeria. African Journal of Microbiology Research. 2010; 4 (1):096-102
- 27. Onuorah S, Nwoke J, Odibo F. Bacteriological assessment of the public hand-pump borehole water in Onueke, Ezza south local government area, Ebonyi state, Nigeria. International Journal of Photochemistry and Photobiology. 2018; 2 (2):39-48
- 28. Abdullahi M, Saidu BT, Salihu BA, Mohammed SA. Bacteriological and physicochemical properties of borehole water in Niger state polytechnic, Zungeru Campus. Indian Journal of Science Research. 2013; 4 (1):1-6
- 29. Akinola OT, Ogunbode TO, Akintunde EO. Borehole water quality characteristics and its potability in Iwo, Osun state Nigeria. Journal of Scientific Research and Reports. 2018; 18 (1):1-8
- 30. Ngele SO, Itumoh EJ, Onwa NC, Alobu F. Quality assessment of selected ground water samples in Amike-Aba, Abakaliki, Ebonyi State, Nigeria. Canadian Journal of Pure & Applied Science. 2014; 8 (1):2801-2805
- 31. Josiah JS, Nwangwu CO, Omage K, Akpanyung OE, Amaka DD. Physicochemical and microbiological properties of water samples used for domestic purposes in Okada Town, Edo State, Nigeria. International Journal of Current Microbiology and Applied Sciences. 2014; 3 (6):886-894
- 32. Ibe SN, Okpalenye JI. Bacteriological analysis of borehole water in Uli, Nigeria. African Journal of Applied Zoology and Environmental Biology. 2005; 7 :116-119
- 33. Uhuo CA, Uneke BI, Okereke CN, Nwele DE, Ogbanshi ME. The bacteriological survey of borehole waters in Peri-Urban areas of Abakaliki, Ebonyi State, Nigeria. International Journal of Bacteriology Research. 2014; 2 (2):28-31
- 34. Ukpong EC, Okon BB. Comparative analysis of public and private borehole water supply sources in Uruan local government area of AkwaIbom state, Nigeria. International Journal of Applied Science and Technology. 2013; 3 (1):76-88
- 35. Howard G, Bartram J, Pedley S, Schmoll O, Choros I, Berger P. Groundwater and public health. In: Schmoll O, Howard G, Chilton J, Chorus I, editors. Protecting Groundwater for Health: Managing the Quality of Drinking Water Sources. London: IWA Publishing; 2006. p. 17
- 36. Mogheir Y, Singh VP. Application of information theory to groundwater quality monitoring networks. Water Resources Management. 2002; 16 (1):37-49
- 37. Sundaram B, Feitz A, Caritat PD, Plazinska A, Brodie R, Coram J, et al. Groundwater sampling and analysis- A field guide, Geoscience Australia. Record: 2009/27. p. 95. Canberra [Internet]. Available from: http://www.cffet.net/env/uploads/gsa/BOOK-Groundwater-sampling-%26-analysis-A-field-guide.pdf [Accessed: 04 November 2019]
- 38. Suthar S, Chhimpa V, Singh S. Bacterial contamination in drinking water: A case study in rural areas of northern Rajasthan, India. Environmental Monitoring and Assessment. 2009; 159 :43 [Internet]. Available from: http://doi.org10.1007/s10661-008-0611-0 [Accessed: 05 November 2019]
- 39. Olalekan A, Abubakar B, Abdul-Mumini K. Physico-chemical characteristics of borehole water quality in Gassol, Taraba, State, Nigeria. African Journal of Environmental Science and Technology. 2015; 9 (2):143-154
- 40. Ncube EJ, Schutte CF. The occurrence of fluoride in south African groundwater: A water quality and health problem. Water SA. 2005; 31 (1):35-40
- 41. Amanidaz N, Zafarzadeh A, Mahvi AH. The interaction between heterotrophic bacteria and coliform, fecal coliform, Fecal streptococci bacteria in the water supply networks. Iranian Journal of Public Health. 2015; 44 (12):1685-1692
- 42. Clark JA. The influence of increasing numbers of nonindicator organisms upon the detection of indicator organisms by the membrane filter and presence-absence tests. Canadian Journal of Microbiology. 1980; 26 :827-832
- 43. LeChevallier MW, Schulz W, Lee RG. Bacterial nutrients in drinking water. Applied and Environmental Microbiology. 1991; 57 :857-862
- 44. Møller S, Kristensen CS, Poulsen L, Carstensen JM, Molin S. Bacterial growth on surfaces: Automated image analysis for quantification of growth rate-related parameters. Applied and Environmental Microbiology. 1995; 61 :741-748
- 45. Sun L, Peng W. Heavy metals in shallow groundwater of the urban area in Suzhou, northern Anhui Province, China. Water Practice and Technology. 2014; 9 (2):197-205
- 46. Abduljameel A, Sirajudeen J, Abdulvahith R. Studies on heavy metal pollution of groundwater sources between Tamilnadu and Pondicherry, India. Advances in Applied Science Research. 2012; 3 (1):424-429
- 47. Leung CM, Jiao JJ. Heavy metal and trace element distributions in groundwater in natural slopes and highly urbanized spaces in mid-levels areas, Hong Kong. Water Research. 2006; 40 (4):753-767
- 48. Nouri J, Mahvi AH, Babaei AA, Jahed GR, Ahmadpour E. Investigation of heavy metals in groundwater. Pakistan Journal of Biological Sciences. 2006; 9 (3):377-384
- 49. Rivett M, Drewes J, Barett M, Chilton J, Appleyard S, Dieter HH, et al. Chemicals: Health relevance, transport and attenuation. In: Schmoll O, Howard G, Chilton J, Chorus I, editors. Protecting Groundwater for Health: Managing the Quality of Drinking Water Sources. London: IWA Publishing; 2006. p. 123
- 50. Stamatis G, Voudouris K, Karefilakis F. Groundwater pollution by heavy metals in historical mining area of Kavrio, Attical, Greece. Water, Air, and Soil Pollution. 2001; 128 (2):61-83
- 51. Mahiknecht J, Steinich B, Navarro de Leon I. Groundwater chemistry and mass transfers in the independent aquifer, Central Mexico by using multivariate statistics and mass-balance models. Environmental Geology. 2004; 48 (6):781-795
- 52. Rajasekaran R, Abinaya M. Heavy metal pollution in groundwater: A review. International Journal of ChemTech Research. 2014; 6 (14):5661-5664
- 53. Obi CN, Okocha CO. Microbiological and physico-chemical of selected bore-hole waters in world bank housing estate, Umuahia, Abia state, Nigeria. Journal of Engineering and Applied Sciences. 2007; 2 (5):920-929
- 54. Longe EO, Balogun MR. Groundwater quality assessment near a municipal landfill, Lagos, Nigeria. Research Journal of Applied Sciences, Engineering and Technology. 2010; 2 (1):39-44
- 55. Fubara-Manuel I, Jumbo RB. The effects of septic tank locations on borehole water quality in Port Harcourt, Nigeria. International Journal of Engineering and Technology. 2014; 4 (5):236-264
- 56. Al-Sabahi E, Abdul RS, Wan Z, Al-Nozaily WY, Alshaebi F. The characteristics of leachate and ground water pollution at municipal solid waste landfill of Ibb city, Yemen. American Journal of Environmental Sciences. 2009; 5 (3):256-266
- 57. Onuorah S, Igwemadu N, Odibo F. Bacteriological quality assessment of borehole water in Ogbaru communities, Anambra state, Nigeria. Universal Journal of Clinical Medicine. 2019; 7 (1):1-10. DOI: 10.13189/ujcm.2019.070101
- 58. Adeyemi O, Oloyede OB, Olajidi AT. Physiochemical and microbial characteristics of leachate-contaminated groundwater. Asian Journal of Biochemistry. 2007; 2 (5):343-348
- 59. Adegoke OO, Bamigbowu EO, Oni ES, Ugbaja KN. Microbiological examination of sachet water sold in Aba, Abia State, Nigeria. Global Research Journal of Microbiology. 2012; 2 :62-66
- 60. Ackah-Arthur M, Amin AK, Gyamfi ET, Acquah J, Nyarko ES, Kpattah SE, et al. Assessment of the quality of sachet water consumed in urban townships of Ghana using physico-chemical indicators: A preliminary study. Advances in Applied Science Research. 2012; 3 :2120-2127
- 61. Falegan CR, Odeyemi AT, Ogunjobi LP. Bacteriological and Physico-chemicals studies of sachet water in locations at Ado- Ekiti, Ekiti State. Aquatic Biology. 2014; 2 :55-61
- 62. Adewoye AO, Adewoye SO, Opasola OA. Microbiological examination of sachet water experimentally exposed to sunlight. International Journal of Pure and Applied Sciences and Technology. 2013; 18 :36-42
- 63. Mgbakor C, Ojiegbe GC, Okonko IO, Odu NN, Alli JA, Nwaze JC, et al. Bacteriological evaluation of some sachet water on sales in Owerri metropolis, Imo State, Nigeria. Malaysian Journal of Microbiology. 2011; 7 :217-225
- 64. Onilude AA, Adesina FC, Oluboyede OA, Adeyemi BI. Micro-biological quality of sachet packaged water vended in three local government of Oyo State, Nigeria. African Journal of Food Science and Technology. 2013; 4 :195-200
- 65. Washington State Department of Health: Coliform bacteria in drinking water. 2019. Available from: https://www.doh.wa.gov/CommunityandEnvironment/DrinkingWater/Contaminants/Coliform [Accessed: 01 November 2019]
- 66. Edema MO, Omemu AM. Microbiology and physiochemical analysis of different water sources. International Journal of Microbiology. 2001; 15 (1):57-61
- 67. Botelho-Nevers E, Gagnaire J, Verhoeven PO, Cazorla C, Grattard F, Pozzetto B, et al. Decolonization of Staphylococcus aureus carriage. Médecine et Maladies Infectieuses. 2017; 47 (5):305-310
- 68. Verhoeven PO, Gagnaire J, Botelho-Nevers E, Grattard F, Carricajo A, Lucht F, et al. Detection and clinical relevance of Staphylococcus aureus nasal carriage: An update. Expert Review of Anti-Infective Therapy. 2014; 12 (1):75-89
- 69. Williams MR, Gallo RL. The role of the skin microbiome in atopic dermatitis. Current Allergy and Asthma Reports. 2015; 15 (11):65. DOI: 10.1007/s11882-015-0567-4
- 70. Alexander H, Paller AS, Traidl-Hoffmann C, Beck LA, De Benedetto A, Dhar S, et al. The role of bacterial skin infections in atopic dermatitis: Expert statement and review from the International Eczema Council Skin Infection Group. Brazilian Journal of Dermatology. 2019; 2019 :1-12. DOI: 10.1111/bjd.18643
- 71. Loewen K, Schreiber Y, Kirlew M, Bocking N, Kelly L. Community-associated methicillin-resistant Staphylococcus aureus infection: Literature review and clinical update. Canadian Family Physician. 2017; 63 (7):512-520
- 72. Kırmusaoğlu S. Staphylococcal biofilms: Pathogenicity, mechanism and regulation of biofilm formation by quorum-sensing system and antibiotic resistance mechanisms of biofilm-embedded microorganisms. In: Dhanasekaran D, Thajuddin N, editors. Microbial Biofilms - Importance and Applications. Rijeka: IntechOpen;
- 73. Arciola CR, Campoccia D, Ravaioli S, Montanaro L. Polysaccharide intercellular adhesin in biofilm: Structural and regulatory aspects. Frontiers in Cellular and Infection Microbiology. 2015; 5 :1-10
- 74. Karampatakis T, Antachopoulos C, Tsakris A, Roilides E. Molecular epidemiology of carbapenem-resistant Pseudomonas aeruginosa in an endemic area: Comparison with global data. European Journal of Clinical Microbiology and Infectious Diseases. 2018; 37 (7):1211-1220
- 75. Rehman A, Patrick WM, Lamont IL. Mechanisms of ciprofloxacin resistance in Pseudomonas aeruginosa : New approaches to an old problem. Journal of Medical Microbiology. 2019; 68 (1):1-10
- 76. Feng W, Sun F, Wang Q , Xiong W, Qiu X, Dai X, et al. Epidemiology and resistance characteristics of Pseudomonas aeruginosa isolates from the respiratory department of a hospital in China. Journal of Global Antimicrobial Resistance. 2017; 8 :142-147
- 77. English EL, Schutz KC, Willsey GG, Wargo MJ. Transcriptional responses of Pseudomonas aeruginosa to potable water and freshwater. Applied and Environmental Microbiology. 2018; 84 (6):1-12. DOI: 10.1128/AEM.02350-17
- 78. Driscoll JA, Brody SL, Kollef MH. The epidemiology, pathogenesis and treatment of Pseudomonas aeruginosa infections. Drugs. 2007; 67 (3):351-368
- 79. Kamali E, Jamali A, Ardebili A, Ezadi F, Mohebbi A. Evaluation of antimicrobial resistance, biofilm forming potential, and the presence of biofilm-related genes among clinical isolates of Pseudomonas aeruginosa . BMC Research Notes. 2020; 13 (1):27. DOI: 10.1186/s13104-020-4890-z
- 80. Moradali MF, Ghods S, Rehm BH. Pseudomonas aeruginosa lifestyle: A paradigm for adaptation, survival, and persistence. Frontiers in Cellular and Infection Microbiology. 2017; 7 :39. DOI: 10.3389/fcimb.2017.00039
- 81. Hennequin C, Robin F. Correlation between antimicrobial resistance and virulence in Klebsiella pneumoniae . European Journal of Clinical Microbiology and Infectious Diseases. 2016; 35 (3):333-341
- 82. Hamza E, Dorgham SM, Hamza DA. Carbapenemase-producing Klebsiella pneumoniae in broiler poultry farming in Egypt. Journal of Global Antimicrobial Resistance. 2016; 7 :8-10
- 83. Jelić M, Hrenović J, Dekić S, Goić-Barišić I, Tambić AA. First evidence of KPC-producing ST258 Klebsiella pneumoniae in river water. Journal of Hospital Infection. 2019; 103 (2):147-150
- 84. Ovejero CM, Delgado-Blas JF, Calero-Caceres W, Muniesa M, Gonzalez-Zorn B. Spread of mcr-1-carrying Enterobacteriaceae in sewage water from Spain. Journal of Antimicrobial Chemotherapy. 2017; 72 (4):1050-1053
- 85. Gomez-Simmonds A, Uhlemann AC. Clinical implications of genomic adaptation and evolution of carbapenem-resistant Klebsiella pneumoniae . Journal of Infectious Diseases. 2017; 215 (Suppl 1):S18-S27
- 86. Moradigaravand D, Martin V, Peacock SJ, Parkhill J. Evolution and epidemiology of multidrug-resistant Klebsiella pneumoniae in the United Kingdom and Ireland. MBio. 2017; 8 (1). pii: e01976-16. DOI: 10.1128/mBio.01976-16
- 87. Holt KE, Wertheim H, Zadoks RN, Baker S, Whitehouse CA, Dance D, et al. Genomic analysis of diversity, population structure, virulence, and antimicrobial resistance in Klebsiella pneumoniae , an urgent threat to public health. Proceedings of the National Academy of Sciences USA; 112 (27):E3574-E3581. DOI: 10.1073/pnas.1501049112
- 88. Carvalho F, George J, Sheikh HMA, Selvin R. Advances in screening, detection and enumeration of Escherichia coli using nanotechnology-based methods: A review. Journal of Biomedical Nanotechnology. 2018; 14 (5):829-846. DOI: 10.1166/jbn.2018.2549
- 89. Sarowska J, Futoma-Koloch B, Jama-Kmiecik A, Frej-Madrzak M, Ksiazczyk M, Bugla-Ploskonska G, et al. Virulence factors, prevalence and potential transmission of extraintestinal pathogenic Escherichia coli isolated from different sources: Recent reports. Gut Pathogenes. 2019; 11 :10. DOI: 10.1186/s13099-019-0290-0
- 90. Money P, Kelly AF, Gould SW, Denholm-Price J, Threlfall EJ, Fielder MD. Cattle, weather and water: Mapping Escherichia coli O157:H7 infections in humans in England and Scotland. Environmental Microbiology. 2010; 12 (10):2633-2644
- 91. Guzmán D, Stoler J. An evolving choice in a diverse water market: A quality comparison of sachet water with community and household water sources in Ghana. American Journal of Tropical Medicine and Hygiene. 2018; 99 (2):526-533
- 92. Mezzatesta ML, Gona F, Stefani S. Enterobacter cloacae complex: Clinical impact and emerging antibiotic resistance. Future Microbiology. 2012; 7 (7):887-902
- 93. Chavda KD, Chen L, Fouts DE, Sutton G, Brinkac L, Jenkins SG, et al. Comprehensive genome analysis of carbapenemase-producing Enterobacter spp.: New insights into phylogeny, population structure, and resistance mechanisms. mBio; 7 (6): e02093-16. DOI: 10.1128/mBio.02093-16
- 94. Armbruster CE, Mobley HLT, Pearson MM. Pathogenesis of Proteus mirabilis infection. EcoSal Plus. 2018; 8 (1). DOI: 10.1128/ecosalplus.ESP-0009-2017
- 95. Drzewiecka D. Significance and roles of Proteus spp. bacteria in natural environments. Microbial Ecology. 2016; 72 (4):741-758
- 96. Rózalski A, Sidorczyk Z, Kotełko K. Potential virulence factors of Proteus bacilli . Microbiology and Molecular Biology Reviews. 1997; 61 (1):65-89
- 97. Morgenstein RM, Szostek B, Rather PN. Regulation of gene expression during swarmer cell differentiation in Proteus mirabilis . FEMS Microbiology Reviews. 2010; 34 (5):753-763
- 98. Faruque SM, Albert MJ, Mekalanos JJ. Epidemiology, genetics, and ecology of toxigenic Vibrio cholerae . Microbiology and Molecular Biology Reviews. 1998; 62 :1301-1314
- 99. Zhu J, Miller MB, Vance RE, Dziejman M, Bassler BL, Mekalanos JJ. Quorum-sensing regulators control virulence gene expression in Vibrio cholerae . Proceedings of the National Academy of Sciences USA. 2002; 99 (5):3129-3134
- 100. Cabral JP. Water microbiology. Bacterial pathogens and water. International Journal of Environmental Research and Public Health. 2010; 7 (10):3657-3703
- 101. WHO cholera key facts 2019 [Internet]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/cholera [Accessed: 02 January 2020]
- 102. Elimian KO, Musah A, Mezue S, Oyebanji O, Yennan S, Jinadu A, et al. Descriptive epidemiology of cholera outbreak in Nigeria, January–November, 2018: Implications for the global roadmap strategy. BMC Public Health. 2019; 19 :1264. DOI: 10.1186/s12889-019-7559-6
- 103. Dalhat MM, Isa AN, Nguku P, Nasir S-G, Urban K, Abdulaziz M, et al. Descriptive characterization of the 2010 cholera outbreak in Nigeria. BMC Public Health. 2014; 14 :1167. DOI: 10.1186/1471-2458-14-1167
- 104. Ishida R, Ueda K, Kitano T, Yamamoto T, Mizutani Y, Tsutsumi Y, et al. Fatal community-acquired Bacillus cereus pneumonia in an immunocompetent adult man: A case report. BMC Infectious Diseases. 2019; 19 (1):197. DOI: 10.1186/s12879-019-3836-3
- 105. Chen D, Li Y, Lv J, Liu X, Gao P, Zhen G, et al. A foodborne outbreak of gastroenteritis caused by Norovirus and Bacillus cereus at a university in the Shunyi District of Beijing, China 2018: A retrospective cohort study. BMC Infectious Diseases. 2019; 19 (1):910. DOI: 10.1186/s12879-019-4570-6
- 106. Szabo JG, Meiners G, Heckman L, Rice EW, Hall J. Decontamination of bacillus spores adhered to iron and cement-mortar drinking water infrastructure in a model system using disinfectants. Journal of Environmental Management. 2017; 187 :1-7
- 107. Jeżewska-Frąckowiak J, Seroczyńska K, Banaszczyk J, Jedrzejczak G, Żylicz-Stachula A, Skowron PM. The promises and risks of probiotic bacillus species. Acta Biochimica Polonica. 2018; 65 (4):509-519
- 108. Bottone EJ. Bacillus cereus, a volatile human pathogen. Clinical Microbiology Reviews. 2010; 23 (2):382-398
- 109. Slamti L, Lereclus D. A cell–cell signaling peptide activates the PlcR virulence regulon in bacteria of the Bacillus cereus group. The EMBO Journal. 2002; 21 :4550-4559
- 110. Okutani A, Inoue S, Noguchi A, Kaku Y, Morikawa S. Whole-genome sequence-based comparison and profiling of virulence-associated genes of Bacillus cereus group isolates from diverse sources in Japan. BMC Microbiology. 2019; 19 (1):296. DOI: 10.1186/s12866-019-1678-1
- 111. Kariuki S, Gordon MA, Feasey N, Parry CM. Antimicrobial resistance and management of invasive salmonella disease. Vaccine. 2015; 33 (Suppl 3):C21-C29. DOI: 10.1016/j.vaccine.2015.03.102
- 112. Threlfall EJ. Antimicrobial drug resistance in Salmonella: Problems and perspectives in food- and water-borne infections. FEMS Microbiological Reviews. 2002; 26 (2):141-148
- 113. Cuypers WL, Jacobs J, Wong V, Klemm EJ, Deborggraeve S, Van Puyvelde S. Fluoroquinolone resistance in Salmonella: Insights by whole-genome sequencing. Microbial Genomics. 2018: 4 (7). DOI: 10.1099/mgen.0.000195
- 114. Liu H, Whitehouse CA, Li B. Presence and persistence of Salmonella in water: The impact on microbial quality of water and food safety. Frontiers in Public Health. 30 May 2018; 6 :159. DOI: 10.3389/fpubh.2018.00159
- 115. Akinyemi KO, Oyefolu AOB, Mutiu WB, Iwalokun BA, Ayeni ES, Ajose SO, et al. Typhoid fever: Tracking the trend in Nigeria. The American Journal of Tropical Medicine and Hygiene. 2018; 99 (Suppl 3):41-47
© 2020 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Edited by Sahra Kırmusaoğlu
Published: 09 December 2020
By Asma Bashir, Neha Farid, Kashif Ali and Kiran Fati...
767 downloads
By Nazish Mazhar Ali, Safia Rehman, Syed Abdullah Maz...
687 downloads
By Colleen M. Pike, Rebecca R. Noll and M. Ramona Neu...
782 downloads
A Comprehensive Review of Water Quality Monitoring and Assessment in Nigeria
- Chemosphere 260:127569

- Nnamdi Azikiwe University, Awka

- University of Ilorin
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
No full-text available
To read the full-text of this research, you can request a copy directly from the authors.

- O.T. Olurin
- Kazeem Agboola

- O O Fadairo
- Titus Olaniyi
- Nkechi Nwankwo
- U. E. U. E. Idahose

- Ibukun R Ogunbode

- Sergios Gerakidis

- Chinwe Nneamaka Atedhor

- Moshood Tijani

- Blessing Nkechi Emmanuel
- Abubakar Nuhu Ishaq

- Umar Faruk Saidu

- Adel Almaprok
- Jeetendra Kumar
- Rashmi Gupta
- Suvarna Sharma

- J CHEM TECHNOL BIOT

- CLEAN TECHNOL ENVIR

- Meghan Bygate

- Lingling Zhang
- Mya Myint Mo

- Segun A Adebisi

- J CHEM NEUROANAT
- Usende Ifukibot Levi

- Osinachi Chinonyerem Daniella
- Connor James
- Kwasi Gyau Baffour Awuah

- Godspower Imiete
- Hope Chizia Ebenezer
- Meelubari Barinua Tsaro Kpang

- Terna Austin

- Environ Dev Sustain

- Tolulope Adewunmi

- Oyindamola Olanrewaju
- Samson A. Oyetunji

- Uzairu Aminu

- Samuel Dzidefo Sagoe
- Water Pract Tech
- Ubechu Bridget

- Ajaegbu Ebuka Emmanuel

- Adolar Noernberg Júnior
- Bruna de Fátima Pereira Schmite
- Karine Andréa da Costa

- Elkin Dario Rojas-Marin
- Gustavo Andrés Angarita-Izaquita

- Esmaiel Rezazadeh
- Nedal Sawafta

- ENVIRON SCI POLLUT R

- Mohd Ghazali Mohd Nawawi
- Zaidi Jafaar Mohd
- Bayero Salih Farah
- M.Venkateswarlu, E.Ramachandra, A.Archana, V. Jaishnavi, Y. Malleswari
- Ojo Oluwole

- Mohamed Gamal EI-Din

- Yassine El-Ghoul

- L Huo Chong
- MV Prassana
- M A * Idris

- M N Almustapha

- emagbetere johnbull

- Abdurafiu Majolagbe

- Adedayo Badejo

- Temilola Oluseyi

- Emmanuel Amadi

- Fisayo Oyepeju Ayandele

- ENVIRON MONIT ASSESS

- O. Osarenotor

- EmmanuelA Ameh

- Adaeze Joseph

- F. A. Lawani

- Boluwatife Olusegun Osikanmi

- Mynepalli K. C. Sridhar

- Aondo Titus
- Tuma Joseph

- Adedokun T.

- Phani Brahma Somayajulu Rallapalli

- O.A. Oyetunde

- Emmanuel U Mboho

- Faith Ayakpo Miri

- Ebenezer IDOWU Oluwasola

- CHEMOSPHERE

- A O I Selemo

- E. E. Ikpeama

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Food and drinking water as sources of pathogenic protozoans: an update.

1. Introduction
3. waterborne and foodborne protozoan infections, 3.1. parasitic protozoans in the general population in different world regions, 3.2. parasitic protozoans in immunocompromised patients, 3.3. parasitic protozoans in food handlers, 3.4. pathogenic protozoans in drinking water, 3.5. pathogenic protozoans in raw vegetables, 4. cryptosporidium spp., 4.1. diseases caused by cryptosporidium spp ., 4.2. epidemiology of cryptosporidiosis, 4.3. cryptosporidium spp . in drinking water, 4.4. cryptosporidium spp . in food, 5. giardia intestinalis, 5.1. diseases caused by g. intestinalis, 5.2. epidemiology of giardiasis, 5.3. g. intestinalis infections from food and drinking water, 6. toxoplasma gondii, 6.1. diseases caused by t. gondii, 6.2. involvement of food and drinking water in t. gondii infections, 6.3. distribution of t. gondii in food producing animals and derived products, 7. entamoeba spp., 7.1. diseases caused by entamoeba spp ., 7.2. epidemiology of entamoeba spp ., 8. blastocystis hominis, 9. cyclospora cayetanensis, 9.1. diseases caused by c. cayetanensis, 9.2. epidemiology of c. cayetanensis, 9.3. dietary sources of c. cayetanensis, 10. trypanosoma cruzi, epidemiology and symptoms of t. cruzi infection, 11. sarcocystis, 11.1. diseases caused by sarcocystis spp ., 11.2. epidemiology of sarcocystis spp ., 11.3. prevalence of sarcocystis spp . in food-producing animals, 12. cystoisospora belli, 12.1. diseases caused by c. belli, 12.2. epidemiology of c. belli, 13. balantioides coli, 14. dientamoeba fragilis, 15. endolimax nana, 16. pentatrichomonas hominis, 17. methods for the detection/identification of protozoans in food and drinking water, 18. discussion, 19. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Yaeger, R.G. Chapter 77: Protozoa: Structure, Classification, Growth, and of the Development. In Medical Microbiology , 4th ed.; Baron, S., Ed.; University of Texas Medical Branch at Galveston: Galveston, TX, USA, 1996. Available online: https://www.ncbi.nlm.nih.gov/books/NBK7627/ (accessed on 1 December 2023).
- National Center for Biotechnology Information. Taxonomy Browser. Available online: https://www.ncbi.nlm.nih.gov/Taxonomy/Browser/wwwtax.cgi?mode=Info&id=2698737&lvl=3&lin=f&keep=1&srchmode=1&unlock (accessed on 1 December 2023).
- Baig, A.M.; Suo, X.; Liu, D. Chapter 148—Pathogenesis of protozoan infections. In Molecular Medical Microbiology , 3rd ed.; Tang, Y.-W., Hindiyeh, M.Y., Liu, D., Sails, A., Spearman, P., Zhang, J.-R., Eds.; Academic Press: Cambridge, MA, USA, 2024; pp. 2921–2940. [ Google Scholar ]
- Pignata, C.; Bonetta, S.; Bonetta, S.; Cacciò, S.M.; Sannella, A.R.; Gilli, G.; Carraro, E. Cryptosporidium Oocyst Contamination in Drinking Water: A Case Study in Italy. Int. J. Environ. Res. Public Health 2019 , 16 , 2055. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chique, C.; Hynds, P.D.; Andrade, L.; Burke, L.; Morris, D.; Ryan, M.P.; O’Dwyer, J. Cryptosporidium spp. in Groundwater Supplies Intended for Human Consumption—A Descriptive Review of Global Prevalence, Risk Factors and Knowledge Gaps. Water Res. 2020 , 176 , 115726. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hadjilouka, A.; Tsaltas, D. Cyclospora Cayetanensis -Major Outbreaks from Ready to Eat Fresh Fruits and Vegetables. Foods 2020 , 9 , 1703. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tharmaratnam, T.; Kumanan, T.; Iskandar, M.A.; D’Urzo, K.; Gopee-Ramanan, P.; Loganathan, M.; Tabobondung, T.; Tabobondung, T.A.; Sivagurunathan, S.; Patel, M.; et al. Entamoeba Histolytica and Amoebic Liver Abscess in Northern Sri Lanka: A Public Health Problem. Trop. Med. Health 2020 , 48 , 2. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rosenthal, B.M. Zoonotic Sarcocystis . Res. Vet. Sci. 2021 , 136 , 151–157. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Costa, D.; Razakandrainibe, R.; Basmaciyan, L.; Raibaut, J.; Delaunay, P.; Morio, F.; Gargala, G.; Villier, V.; Mouhajir, A.; Levy, B.; et al. A Summary of Cryptosporidiosis Outbreaks Reported in France and Overseas Departments, 2017–2020. Food Waterborne Parasitol. 2022 , 27 , e00160. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Helmy, Y.A.; Hafez, H.M. Cryptosporidiosis: From Prevention to Treatment, a Narrative review. Microorganisms 2022 , 10 , 2456. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- López Ureña, N.M.; Chaudhry, U.; Calero Bernal, R.; Cano Alsua, S.; Messina, D.; Evangelista, F.; Betson, M.; Lalle, M.; Jokelainen, P.; Ortega Mora, L.M.; et al. Contamination of Soil, Water, Fresh Produce, and Bivalve Mollusks with Toxoplasma Gondii Oocysts: A Systematic Review. Microorganisms 2022 , 10 , 517. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- López-García, A.; Gilabert, J.A. Oral Transmission of Chagas Disease from a One Health Approach: A Systematic Review. Trop. Med. Int. Health 2023 , 28 , 689–698. [ Google Scholar ] [ CrossRef ]
- Martín-Escolano, R.; Ng, G.C.; Tan, K.S.W.; Stensvold, C.R.; Gentekaki, E.; Tsaousis, A.D. Resistance of Blastocystis to Chlorine and Hydrogen Peroxide. Parasitol. Res. 2023 , 122 , 167–176. [ Google Scholar ] [ CrossRef ]
- Siwila, J.; Mwaba, F.; Chidumayo, N.; Mubanga, C. Food and Waterborne Protozoan Parasites: The African Perspective. Food Waterborne Parasitol. 2020 , 20 , e00088. [ Google Scholar ] [ CrossRef ]
- Brožová, K.; Jirků, M.; Lhotská, Z.; Květoňová, D.; Kadlecová, O.; Stensvold, C.R.; Samaš, P.; Petrželková, K.J.; Jirků, K. The Opportunistic Protist, Giardia Intestinalis , Occurs in Gut-Healthy Humans in a High-Income Country. Emerg. Microbes Infect. 2023 , 12 , 2270077. [ Google Scholar ] [ CrossRef ]
- World Health Organization Team Control of Neglected Tropical Diseases. Prevention and Control of Intestinal Parasitic Infections: WHO Technical Report Series N°749. Guideline. Available online: https://www.who.int/publications/i/item/WHO-TRS-749 (accessed on 16 November 2023).
- Das, R.; Palit, P.; Haque, M.A.; Levine, M.M.; Kotloff, K.L.; Nasrin, D.; Hossain, M.J.; Sur, D.; Ahmed, T.; Breiman, R.F.; et al. Symptomatic and Asymptomatic Enteric Protozoan Parasitic Infection and Their Association with Subsequent Growth Parameters in under Five Children in South Asia and Sub-Saharan Africa. PLoS Negl. Trop. Dis. 2023 , 17 , e0011687. [ Google Scholar ] [ CrossRef ]
- FAO/WHO. Multicriteria-Based Ranking for Risk Management of Food-Borne Parasites. Rome. Available online: http://www.who.int/iris/handle/10665/112672 (accessed on 16 February 2024).
- Iordanov, R.B.; Leining, L.M.; Wu, M.; Chan, G.; DiNardo, A.R.; Mejia, R. Case Report: Molecular Diagnosis of Cystoisospora Belli in a Severely Immunocompromised Patient with HIV and Kaposi Sarcoma. Am. J. Trop. Med. Hyg. 2021 , 106 , 678–680. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Noor, M.; Katzman, P.J.; Huber, A.R.; Findeis-Hosey, J.J.; Whitney-Miller, C.; Gonzalez, R.S.; Zhou, Z.; N’kodia, H.D.; Skonick, K.; Abell, R.L.; et al. Unexpectedly High Prevalence of Cystoisospora Belli Infection in Acalculous Gallbladders of Immunocompetent Patients. Am. J. Clin. Pathol. 2019 , 151 , 100–107. [ Google Scholar ] [ CrossRef ]
- Pietilä, J.-P.; Meri, T.; Siikamäki, H.; Tyyni, E.; Kerttula, A.-M.; Pakarinen, L.; Jokiranta, T.S.; Kantele, A. Dientamoeba Fragilis —The Most Common Intestinal Protozoan in the Helsinki Metropolitan Area, Finland, 2007 to 2017. Euro Surveill. 2019 , 24 , 1800546. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Popruk, S.; Adao, D.E.V.; Rivera, W.L. Epidemiology and Subtype Distribution of Blastocystis in Humans: A Review. Infect. Genet. Evol. 2021 , 95 , 105085. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Matovelle, C.; Tejedor, M.T.; Monteagudo, L.V.; Beltrán, A.; Quílez, J. Prevalence and Associated Factors of Blastocystis sp. Infection in Patients with Gastrointestinal Symptoms in Spain: A Case-Control Study. Trop. Med. Infect. Dis. 2022 , 7 , 226. [ Google Scholar ] [ CrossRef ]
- Cobuccio, L.G.; Laurent, M.; Gardiol, C.; Wampfler, R.; Poppert, S.; Senn, N.; Eperon, G.; Genton, B.; Locatelli, I.; de Vallière, S. Should We Treat Blastocystis sp.? A Double-Blind Placebo-Controlled Randomized Pilot Trial. J. Travel Med. 2023 , 30 , taac143. [ Google Scholar ] [ CrossRef ]
- Hooshyar, H.; Arbabi, M.; Rostamkhani, P. Checklist of Endolimax Species Recognized in Human and Animals, a Review on a Neglected Intestinal Parasitic Amoeba. Iraq Med. J. 2023 , 7 , 28–31. [ Google Scholar ] [ CrossRef ]
- Ryan, U.; Hijjawi, N.; Feng, Y.; Xiao, L. Giardia : An under-Reported Foodborne Parasite. Int. J. Parasitol. 2019 , 49 , 1–11. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bahrami, F.; Babaei, E.; Badirzadeh, A.; Riabi, T.R.; Abdoli, A. Blastocystis, Urticaria, and Skin Disorders: Review of the Current Evidences. Eur. J. Clin. Microbiol. Infect. Dis. 2020 , 39 , 1027–1042. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Carter, B.L.; Chalmers, R.M.; Davies, A.P. Health Sequelae of Human Cryptosporidiosis in Industrialised Countries: A Systematic Review. Parasit. Vectors 2020 , 13 , 443. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Thébault, A.; Favennec, L.; Kooh, P.; Cadavez, V.; Gonzales-Barron, U.; Villena, I. Risk Factors for Sporadic Giardiasis: A Systematic Review and Meta-Analysis. Microb. Risk Anal. 2021 , 17 , 100158. [ Google Scholar ] [ CrossRef ]
- Wadi, W.F.; Rathi, M.H.; Molan, A.-L. The Possible Link between Intestinal Parasites and Irritable Bowel Syndrome (IBS) in Diyala Province, Iraq. Ann. Parasitol. 2021 , 67 , 505–513. [ Google Scholar ] [ PubMed ]
- Abedi, S.H.; Fazlzadeh, A.; Mollalo, A.; Sartip, B.; Mahjour, S.; Bahadory, S.; Taghipour, A.; Rostami, A. The Neglected Role of Blastocystis sp. and Giardia Lamblia in Development of Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis. Microb. Pathog. 2022 , 162 , 105215. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ali, S.H.; Ismail, M.A.M.; El-Badry, A.A.; Abu-Sarea, E.Y.; Dewidar, A.M.; Hamdy, D.A. An Association between Blastocystis Subtypes and Colorectal Cancer Patients: A Significant Different Profile from Non-Cancer Individuals. Acta Parasitol. 2022 , 67 , 752–763. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mahmoud, A.M.; Ismail, K.A.; Khalifa, O.M.; Abdel-wahab, M.M.; Hagag, H.M.; Mahmoud, M.K. Molecular Identification of Blastocystis hominis Isolates in Patients with Autoimmune Diseases. Appl. Microbiol. 2023 , 3 , 417–428. [ Google Scholar ] [ CrossRef ]
- Issa, Y.A.; Ooda, S.A.; Salem, A.I.; Idris, S.N.; Elderbawy, M.M.; Tolba, M.M. Molecular Diagnosis and Subtyping of Blastocystis sp.: Association with Clinical, Colonoscopic, and Histopathological Findings. Trop. Parasitol. 2023 , 13 , 46–53. [ Google Scholar ] [ PubMed ]
- Zhang, N.; Yu, X.; Zhang, H.; Cui, L.; Li, X.; Zhang, X.; Gong, P.; Li, J.; Li, Z.; Wang, X.; et al. Prevalence and Genotyping of Cryptosporidium Parvum in Gastrointestinal Cancer Patients. J. Cancer 2020 , 11 , 3334–3339. [ Google Scholar ] [ CrossRef ]
- Certad, G. Is Cryptosporidium a Hijacker Able to Drive Cancer Cell Proliferation? Food Waterborne Parasitol. 2022 , 27 , e00153. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Berrouch, S.; Escotte-Binet, S.; Harrak, R.; Huguenin, A.; Flori, P.; Favennec, L.; Villena, I.; Hafid, J. Detection Methods and Prevalence of Transmission Stages of Toxoplasma Gondii , Giardia Duodenalis and Cryptosporidium spp. in Fresh Vegetables: A Review. Parasitology 2020 , 147 , 516–532. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Barlaam, A.; Temesgen, T.T.; Tysnes, K.R.; Rinaldi, L.; Ferrari, N.; Sannella, A.R.; Normanno, G.; Cacciò, S.M.; Robertson, L.J.; Giangaspero, A. Contamination of Fresh Produce Sold on the Italian Market with Cyclospora Cayetanensis and Echinococcus Multilocularis . Food Microbiol. 2021 , 98 , 103792. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sarzhanov, F.; Dogruman-Al, F.; Santin, M.; Maloney, J.G.; Gureser, A.S.; Karasartova, D.; Taylan-Ozkan, A. Investigation of Neglected Protists Blastocystis sp. and Dientamoeba fragilis in Immunocompetent and Immunodeficient Diarrheal Patients Using Both Conventional and Molecular Methods. PLoS Negl. Trop. Dis. 2021 , 15 , e0009779. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Barlaam, A.; Sannella, A.R.; Ferrari, N.; Temesgen, T.T.; Rinaldi, L.; Normanno, G.; Cacciò, S.M.; Robertson, L.J.; Giangaspero, A. Ready-to-Eat Salads and Berry Fruits Purchased in Italy Contaminated by Cryptosporidium spp., Giardia Duodenalis , and Entamoeba Histolytica . Int. J. Food Microbiol. 2022 , 370 , 109634. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- ISO 15553:2006 ; Water Quality. Isolation and Identification of Cryptosporidium Oocysts and Giardia Cysts from Water. International Organization for Standardization: Geneva, Switzerland, 2006. Available online: https://www.iso.org/standard/39804.html (accessed on 2 April 2024).
- Association Française de Normalisation, AFNOR. NF T90-455 Qualité de L’eau—Echantillonage et/ou Dénombrement des Oocystes de Cryptosporidium et des Kystes de Giardia—Méthode de Concentration et de Dénombrement. Available online: https://www.boutique.afnor.org/fr-fr/norme/nf-t90455/qualite-de-leau-echantillonage-et-ou-denombrement-des-oocystes-de-cryptospo/fa060794/46387#AreasStoreProductsSummaryView (accessed on 9 April 2024).
- El Bakri, A.; Hussein, N.M.; Ibrahim, Z.A.; Hasan, H.; AbuOdeh, R. Intestinal Parasite Detection in Assorted Vegetables in the United Arab Emirates. Oman Med. J. 2020 , 35 , e128. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dos Santos, T.L.; Medeiros de Carvalho Neto, A.; Da Silva Ferreira, J.R.; Azevedo, P.V.M.; Wallas Lins Da Silva, K.; Alencar dos Nascimento, C.M.; Calheiros, C.M.L.; Wanderley, F.S.G.; Dos Santos Cavalcanti, M.; Alencar Do Nascimento Rocha, M.; et al. Frequency of Intestinal Protozoan Infections Diagnosed in Patients from a Clinical Analysis Laboratory. Biosci. J. 2022 , 38 , e38001. [ Google Scholar ]
- Fortes, B.H.; Dilmaghani, S.; Ryan, S.M. 34-Year-Old Woman with Human Immunodeficiency Virus and Chronic Diarrhea. Mayo Clin. Proc. 2021 , 96 , 2474–2479. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Reh, L.; Muadica, A.S.; Köster, P.C.; Balasegaram, S.; Verlander, N.Q.; Chércoles, E.R.; Carmena, D. Substantial Prevalence of Enteroparasites Cryptosporidium spp., Giardia Duodenalis and Blastocystis sp. in Asymptomatic Schoolchildren in Madrid, Spain, November 2017 to June 2018. Euro Surveill. 2019 , 24 , 190024. [ Google Scholar ] [ CrossRef ]
- Trelis, M.; Sáez-Durán, S.; Puchades, P.; Castro, N.; Miquel, A.; Gozalbo, M.; Fuentes, M.V. Survey of the Occurrence of Giardia Duodenalis Cysts and Cryptosporidium spp. Oocysts in Green Leafy Vegetables Marketed in the City of Valencia (Spain). Int. J. Food Microbiol. 2022 , 379 , 109847. [ Google Scholar ] [ CrossRef ]
- Moreno-Mesonero, L.; Soler, L.; Amorós, I.; Moreno, Y.; Ferrús, M.A.; Alonso, J.L. Protozoan Parasites and Free-Living Amoebae Contamination in Organic Leafy Green Vegetables and Strawberries from Spain. Food Waterborne Parasitol. 2023 , 32 , e00200. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brown, A.B.; Miller, C.; Hamer, D.H.; Kozarsky, P.; Libman, M.; Huits, R.; Rizwan, A.; Emetulu, H.; Waggoner, J.; Chen, L.H.; et al. Travel-Related Diagnoses among U.s. Nonmigrant Travelers or Migrants Presenting to U.s. Geosentinel Sites—GeoSentinel Network, 2012–2021. MMWR Surveill. Summ. 2023 , 72 , 1–22. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Weitzel, T.; Brown, A.; Libman, M.; Perret, C.; Huits, R.; Chen, L.; Leung, D.; Leder, K.; Connor, B.A.; Menéndez, M.D.; et al. GeoSentinel Network. Intestinal protozoa in returning travellers: A GeoSentinel analysis from 2007 to 2019. J. Travel Med. 2024 , 31 , taae010. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kantzanou, M.; Karalexi, M.A.; Vrioni, G.; Tsakris, A. Prevalence of Intestinal Parasitic Infections among Children in Europe over the Last Five Years. Trop. Med. Infect. Dis. 2021 , 6 , 160. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Berhe, B.; Mardu, F.; Tesfay, K.; Legese, H.; Adhanom, G.; Haileslasie, H.; Gebremichail, G.; Tesfanchal, B.; Shishay, N.; Negash, H. More than Half Prevalence of Protozoan Parasitic Infections among Diarrheic Outpatients in Eastern Tigrai, Ethiopia, 2019; A Cross-Sectional Study. Infect. Drug Resist. 2020 , 13 , 27–34. [ Google Scholar ] [ CrossRef ]
- Tegen, D.; Damtie, D.; Hailegebriel, T. Prevalence and Associated Risk Factors of Human Intestinal Protozoan Parasitic Infections in Ethiopia: A Systematic Review and Meta-Analysis. J. Parasitol. Res. 2020 , 2020 , 8884064. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hijjawi, N.; Zahedi, A.; Ryan, U. Molecular Characterization of Entamoeba , Blastocystis and Cryptosporidium Species in Stool Samples Collected from Jordanian Patients Suffering from Gastroenteritis. Trop. Parasitol. 2021 , 11 , 122–125. [ Google Scholar ] [ PubMed ]
- Al-Sultany, A.K.; Al-Morshidy, K.A.H. An Epidemiological Study of Intestinal Parasites in Children Attending the Pediatric Teaching Hospital in the Holy City of Karbala, Iraq. Med. J. Babylon 2023 , 20 , 95–100. [ Google Scholar ] [ CrossRef ]
- Karim, A.; Zartashia, B.; Khwaja, S.; Akhter, A.; Raza, A.A.; Parveen, S. Prevalence and Risk Factors Associated with Human Intestinal Parasitic Infections (IPIs) in Rural and Urban Areas of Quetta, Pakistan. Braz. J. Biol. 2023 , 84 , e266898. [ Google Scholar ] [ CrossRef ]
- Tilahun, Y.; Gebreananiya, T.A. Prevalence of human intestinal parasitic infections and associated risk factors at Lay Armachiho District Tikildingay town health center, Northwest Ethiopia. Res. Sq. 2023 . [ Google Scholar ] [ CrossRef ]
- Candela, E.; Goizueta, C.; Periago, M.V.; Muñoz-Antoli, C. Prevalence of Intestinal Parasites and Molecular Characterization of Giardia Intestinalis , Blastocystis spp. and Entamoeba Histolytica in the Village of Fortín Mbororé (Puerto Iguazú, Misiones, Argentina). Parasit. Vectors 2021 , 14 , 510. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Deksne, G.; Krūmiņš, A.; Mateusa, M.; Morozovs, V.; Šveisberga, D.P.; Korotinska, R.; Bormane, A.; Vīksna, L.; Krūmiņa, A. Occurrence of Cryptosporidium spp. and Giardia spp. Infection in Humans in Latvia: Evidence of Underdiagnosed and Underreported Cases. Medicina 2022 , 58 , 471. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Laksemi, D.A.; Suwanti, L.T.; Mufasirin, M.; Suastika, K.; Sudarmaja, M. Opportunistic Parasitic Infections in Patients with Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome: A Review. Vet. World 2019 , 13 , 716–725. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chatterjee, R.; Mondal, T.; Barik, G.; Ghosh, S.; Pramanik, N.; Maji, A.; Ghosh, T. Multiple Protozoal Infections in a Single Immunocompromised Patient: A Case Report. Trop. Parasitol. 2023 , 13 , 121–125. [ Google Scholar ] [ PubMed ]
- Symmers, W.S.C. Opportunistic Infections: The Concept of ‘Opportunistic Infections’. Proc. R. Soc. Med. 1965 , 58 , 341–346. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Johnstone, S.L.; Erasmus, L.; Thomas, J.; Groome, M.J.; du Plessis, N.M.; Avenant, T.; de Villiers, M.; Page, N.A. Epidemiology and Aetiology of Moderate to Severe Diarrhoea in Hospitalised Patients ≥5 Years Old Living with HIV in South Africa, 2018–2021: A Case-Control Analysis. PLoS Glob. Public Health 2023 , 3 , e0001718. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mesfun, M.G.; Fuchs, A.; Holtfreter, M.C.; Tufa, T.B.; Orth, H.M.; Luedde, T.; Feldt, T. The Implementation of the Kinyoun Staining Technique in a Resource-Limited Setting Is Feasible and Reveals a High Prevalence of Intestinal Cryptosporidiosis in Patients with HIV. Int. J. Infect. Dis. 2022 , 122 , 130–135. [ Google Scholar ] [ CrossRef ]
- Younis, E.Z.; Elamami, A.H.; El-Salem, R.M. Intestinal Parasitic Infections among Patients with Type 2 Diabetes Mellitus in Benghazi, Libya. JCDO 2021 , 1 , 1–4. [ Google Scholar ] [ CrossRef ]
- Konadu, E.; Essuman, M.A.; Amponsah, A.; Agroh, W.X.K.; Badu-Boateng, E.; Gbedema, S.Y.; Boakye, Y.D. Enteric Protozoan Parasitosis and Associated Factors among Patients with and without Diabetes Mellitus in a Teaching Hospital in Ghana. Int. J. Microbiol. 2023 , 2023 , 5569262. [ Google Scholar ] [ CrossRef ]
- Taghipour, A.; Javanmard, E.; Rahimi, H.M.; Abdoli, A.; Matin, S.; Haghbin, M.; Olfatifar, M.; Mirjalali, H.; Zali, M.R. Prevalence of Intestinal Parasitic Infections in Patients with Diabetes: A Systematic Review and Meta-Analysis. Int. Health 2023 , 16 , 23–34. [ Google Scholar ] [ CrossRef ]
- Sror, S.M.; Galal, S.M.; Mohamed, Y.M.; Dyab, A.K. Prevalence of Intestinal Parasitic Infection among Children with Chronic Liver Diseases, Assiut Governorate, Egypt. Aljouf Univ. Med. J. 2019 , 6 , 1–8. [ Google Scholar ] [ CrossRef ]
- Łanocha, A.; Łanocha-Arendarczyk, N.; Wilczyńska, D.; Zdziarska, B.; Kosik-Bogacka, D. Protozoan Intestinal Parasitic Infection in Patients with Hematological Malignancies. J. Clin. Med. 2022 , 11 , 2847. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Patil, A.D.; Saxena, N.G.; Thakare, S.B.; Pajai, A.E.; Bajpai, D.; Jamale, T.E. Diarrhea after Kidney Transplantation: A Study of Risk Factors and Outcomes. J. Postgrad. Med. 2023 , 69 , 205–214. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Eslahi, A.V.; Olfatifar, M.; Zaki, L.; Karimipour Saryazdi, A.; Barikbin, F.; Maleki, A.; Abdoli, A.; Badri, M.; Karanis, P. Global Prevalence of Intestinal Protozoan Parasites among Food Handlers: A Systematic Review and Meta-Analysis. Food Control 2023 , 145 , 109466. [ Google Scholar ] [ CrossRef ]
- Yimam, Y.; Woreta, A.; Mohebali, M. Intestinal Parasites among Food Handlers of Food Service Establishments in Ethiopia: A Systematic Review and Meta-Analysis. BMC Public Health 2020 , 20 , 73. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hajare, S.T.; Gobena, R.K.; Chauhan, N.M.; Erniso, F. Prevalence of Intestinal Parasite Infections and Their Associated Factors among Food Handlers Working in Selected Catering Establishments from Bule Hora, Ethiopia. Biomed Res. Int. 2021 , 2021 , 6669742. [ Google Scholar ] [ CrossRef ]
- Lette, A.; Negash, G.; Kumbi, M.; Hussen, A.; Kassim, J.; Zenbaba, D.; Gezahgn, H.; Bonsa, M.; Aman, R.; Abdulkadir, A. Predictors of Intestinal Parasites among Food Handlers in, Southeast Ethiopia, 2020. J. Parasitol. Res. 2022 , 2022 , 3329237. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wondimu, H.; Mihret, M. Prevalence and Associated Factors of Intestinal Parasites among Food Handlers Working in Food Service Establishments in Northwest Ethiopia, 2022. J. Parasitol. Res. 2023 , 2023 , 3230139. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Muhammad Bunza, N.; Sale Kumurya, A.; Muhammad, A. Prevalence and Associated Risk Factors of Intestinal Parasitic Infections among Food Handlers in Kano Metropolis, Kano State, Nigeria. Microbes Infect. Dis. 2021 , 2 , 590–596. [ Google Scholar ] [ CrossRef ]
- Al-Daoody, A.A.K.A.; Ali, F.; Sadiq, L.B.; Samer Mamand, A.; Salah Ismail, R.; Fatah Muhammed, H. Investigation of Intestinal Protozoan Infections among Food-Handlers in Erbil City, Iraq. Plant Arch. 2021 , 21 (Suppl. S1), 1367–1372. [ Google Scholar ] [ CrossRef ]
- Alqarni, A.S.; Wakid, M.H.; Gattan, H.S. Prevalence, Type of Infections and Comparative Analysis of Detection Techniques of Intestinal Parasites in the Province of Belgarn, Saudi Arabia. PeerJ 2022 , 10 , e13889. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Şahin, M.; Ödemiş, N.; Yılmaz, H.; Beyhan, Y.E. Investigation of Parasites in Food Handlers in Turkey. Foodborne Pathog. Dis. 2023 , 20 , 381–387. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ma, J.-Y.; Li, M.-Y.; Qi, Z.-Z.; Fu, M.; Sun, T.-F.; Elsheikha, H.M.; Cong, W. Waterborne Protozoan Outbreaks: An Update on the Global, Regional, and National Prevalence from 2017 to 2020 and Sources of Contamination. Sci. Total Environ. 2022 , 806 Pt 2 , 150562. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bourli, P.; Eslahi, A.V.; Tzoraki, O.; Karanis, P. Waterborne Transmission of Protozoan Parasites: A Review of Worldwide Outbreaks—An Update 2017–2022. J. Water Health 2023 , 21 , 1421–1447. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Badri, M.; Olfatifar, M.; Karim, M.R.; Modirian, E.; Houshmand, E.; Abdoli, A.; Nikoonejad, A.; Sotoodeh, S.; Zargar, A.; Samimi, R.; et al. Global Prevalence of Intestinal Protozoan Contamination in Vegetables and Fruits: A Systematic Review and Meta-Analysis. Food Control 2022 , 133 , 108656. [ Google Scholar ] [ CrossRef ]
- Kifleyohannes, T.; Debenham, J.J.; Robertson, L.J. Is Fresh Produce in Tigray, Ethiopia a Potential Transmission Vehicle for Cryptosporidium and Giardia ? Foods 2021 , 10 , 1979. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Salamandane, C.; Lobo, M.L.; Afonso, S.; Miambo, R.; Matos, O. Occurrence of Intestinal Parasites of Public Health Significance in Fresh Horticultural Products Sold in Maputo Markets and Supermarkets, Mozambique. Microorganisms 2021 , 9 , 38. [ Google Scholar ] [ CrossRef ]
- El Safadi, D.; Osman, M.; Hanna, A.; Hajar, I.; Kassem, I.I.; Khalife, S.; Dabboussi, F.; Hamze, M. Parasitic Contamination of Fresh Leafy Green Vegetables Sold in Northern Lebanon. Pathogens 2023 , 12 , 1014. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chaudhary, A.; Rana, S.; Singh, R.; Gurian, P.L.; Betancourt, W.; Kumar, A.; Kumar, A. Non-Potable Water Reuse and the Public Health Risks from Protozoa and Helminths: A Case Study from a City with a Semi-Arid Climate. J. Water Health 2023 , 21 , 981–994. [ Google Scholar ] [ CrossRef ]
- Ryan, U.M.; Feng, Y.; Fayer, R.; Xiao, L. Taxonomy and Molecular Epidemiology of Cryptosporidium and Giardia —A 50 Year Perspective (1971–2021). Int. J. Parasitol. 2021 , 51 , 1099–1119. [ Google Scholar ] [ CrossRef ]
- Ryan, U.; Zahedi, A.; Feng, Y.; Xiao, L. An Update on Zoonotic Cryptosporidium Species and Genotypes in Humans. Animals 2021 , 11 , 3307. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ayres Hutter, J.; Dion, R.; Irace-Cima, A.; Fiset, M.; Guy, R.; Dixon, B.; Aguilar, J.L.; Trépanier, J.; Thivierge, K. Cryptosporidium spp.: Human Incidence, Molecular Characterization and Associated Exposures in Québec, Canada (2016–2017). PLoS ONE 2020 , 15 , e0228986. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Costa, D.; Razakandrainibe, R.; Valot, S.; Vannier, M.; Sautour, M.; Basmaciyan, L.; Gargala, G.; Viller, V.; Lemeteil, D.; Ballet, J.-J.; et al. Epidemiology of Cryptosporidiosis in France from 2017 to 2019. Microorganisms 2020 , 8 , 1358. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Garcia-R, J.C.; Pita, A.B.; Velathanthiri, N.; French, N.P.; Hayman, D.T.S. Species and Genotypes Causing Human Cryptosporidiosis in New Zealand. Parasitol. Res. 2020 , 119 , 2317–2326. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Omolabi, K.F.; Odeniran, P.O.; Soliman, M.E. A Meta-Analysis of Cryptosporidium Species in Humans from Southern Africa (2000–2020). J. Parasit. Dis. 2022 , 46 , 304–316. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Guy, R.A.; Yanta, C.A.; Muchaal, P.K.; Rankin, M.A.; Thivierge, K.; Lau, R.; Boggild, A.K. Molecular Characterization of Cryptosporidium Isolates from Humans in Ontario, Canada. Parasit. Vectors 2021 , 14 , 69. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Guo, Y.; Ryan, U.; Feng, Y.; Xiao, L. Emergence of Zoonotic Cryptosporidium Parvum in China. Trends Parasitol. 2022 , 38 , 335–343. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hijjawi, N.; Zahedi, A.; Al-Falah, M.; Ryan, U. A Review of the Molecular Epidemiology of Cryptosporidium spp. and Giardia Duodenalis in the Middle East and North Africa (MENA) Region. Infect. Genet. Evol. 2022 , 98 , 105212. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chen, Y.; Wu, Y.; Qin, H.; Xu, H.; Zhang, L. Prevalence of Cryptosporidium Infection in Children from China: A Systematic Review and Meta-Analysis. Acta Trop. 2023 , 244 , 106958. [ Google Scholar ] [ CrossRef ]
- Boughattas, S.; Behnke, J.M.; Al-Sadeq, D.; Ismail, A.; Abu-Madi, M. Cryptosporidium spp., Prevalence, Molecular Characterisation and Socio-Demographic Risk Factors among Immigrants in Qatar. PLoS Negl. Trop. Dis. 2019 , 13 , e0007750. [ Google Scholar ] [ CrossRef ]
- Lebbad, M.; Winiecka-Krusnell, J.; Stensvold, C.R.; Beser, J. High Diversity of Cryptosporidium Species and Subtypes Identified in Cryptosporidiosis Acquired in Sweden and Abroad. Pathogens 2021 , 10 , 523. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bujila, I.; Troell, K.; Fischerström, K.; Nordahl, M.; Killander, G.; Hansen, A.; Söderlund, R.; Lebbad, M.; Beser, J. Cryptosporidium Chipmunk Genotype I—An Emerging Cause of Human Cryptosporidiosis in Sweden. Infect. Genet. Evol. 2021 , 92 , 104895. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bujila, I.; Troell, K.; Ögren, J.; Hansen, A.; Killander, G.; Agudelo, L.; Lebbad, M.; Beser, J. Cryptosporidium species and subtypes identified in human domestic cases through the national microbiological surveillance programme in Sweden from 2018 to 2022. BMC Infect. Dis. 2024 , 24 , 146. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yang, X.; Guo, Y.; Xiao, L.; Feng, Y. Molecular Epidemiology of Human Cryptosporidiosis in Low- and Middle-Income Countries. Clin. Microbiol. Rev. 2021 , 34 , e00087-19. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lefebvre, M.; Razakandrainibe, R.; Villena, I.; Favennec, L.; Costa, D. Cryptosporidium -Biofilm Interactions: A Review. Appl. Environ. Microbiol. 2021 , 87 , e02483-20. [ Google Scholar ] [ CrossRef ]
- Huang, W.; Guo, Y.; Lysen, C.; Wang, Y.; Tang, K.; Seabolt, M.H.; Yang, F.; Cebelinski, E.; Gonzalez-Moreno, O.; Hou, T.; et al. Multiple Introductions and Recombination Events Underlie the Emergence of a Hyper-Transmissible Cryptosporidium Hominis Subtype in the USA. Cell Host Microbe 2023 , 31 , 112–123.e4. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jann, H.W.; Cabral-Castro, M.J.; Costa, J.V.B.; Alencar, A.C.M.d.B.; Peralta, J.M.; Peralta, R.H.S. Prevalence of Human Cryptosporidiosis in the Americas: Systematic Review and Meta-Analysis. Rev. Inst. Med. Trop. Sao Paulo 2022 , 64 , e70. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ahmadpour, E.; Safarpour, H.; Xiao, L.; Zarean, M.; Hatam-Nahavandi, K.; Barac, A.; Picot, S.; Rahimi, M.T.; Rubino, S.; Mahami-Oskouei, M.; et al. Cryptosporidiosis in HIV-Positive Patients and Related Risk Factors: A Systematic Review and Meta-Analysis. Parasite 2020 , 27 , 27. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cohn, I.S.; Henrickson, S.E.; Striepen, B.; Hunter, C.A. Immunity to Cryptosporidium : Lessons from Acquired and Primary Immunodeficiencies. J. Immunol. 2022 , 209 , 2261–2268. [ Google Scholar ] [ CrossRef ]
- Abdullah, R.; Azam, M.; Clement, D.; Al-Katib, S. Magnetic Resonance Cholangiopancreatography (MRCP) Findings in a Patient with AIDS Cholangiopathy and Cryptosporidiosis. Cureus 2023 , 15 , e45869. [ Google Scholar ] [ CrossRef ]
- Tie, X.; Zhang, Z.; Zhou, R.; Li, Y.; Xu, J.; Yin, W. A Case of Septic Shock Due to Delayed Diagnosis of Cryptosporidium Infection after Liver Transplantation. BMC Infect. Dis. 2023 , 23 , 260. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Khan, S.M.; Witola, W.H. Past, Current, and Potential Treatments for Cryptosporidiosis in Humans and Farm Animals: A Comprehensive Review. Front. Cell. Infect. Microbiol. 2023 , 13 , 1115522. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Korpe, P.; Ni, Z.; Kabir, M.; Alam, M.; Ferdous, T.; Ara, R.; Munday, R.M.; Haque, R.; Duggal, P. Prospective Cohort Study of Cryptosporidium Infection and Shedding in Infants and Their Households. Clin. Infect. Dis. 2023 , 76 , 2178–2186. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ghanadi, K.; Khalaf, A.K.; Jafrasteh, A.; Anbari, K.; Mahmoudvand, H. High Prevalence of Cryptosporidium Infection in Iranian Patients Suffering from Colorectal Cancer. Parasite Epidemiol. Control 2022 , 19 , e00271. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pielok, Ł.; Nowak, S.; Kłudkowska, M.; Frąckowiak, K.; Kuszel, Ł.; Zmora, P.; Stefaniak, J. Massive Cryptosporidium Infections and Chronic Diarrhea in HIV-Negative Patients. Parasitol. Res. 2019 , 118 , 1937–1942. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zahedi, A.; Ryan, U. Cryptosporidium —An Update with an Emphasis on Foodborne and Waterborne Transmission. Res. Vet. Sci. 2020 , 132 , 500–512. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hossain, M.J.; Saha, D.; Antonio, M.; Nasrin, D.; Blackwelder, W.C.; Ikumapayi, U.N.; Mackenzie, G.A.; Adeyemi, M.; Jasseh, M.; Adegbola, R.A.; et al. Cryptosporidium Infection in Rural Gambian Children: Epidemiology and Risk Factors. PLoS Negl. Trop. Dis. 2019 , 13 , e0007607. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Azami, M.; Amini Rarani, S.; Kiani, F. Treatment of Urticaria Caused by Severe Cryptosporidiosis in a 17-Month-Old Child—A Case Report. BMC Infect. Dis. 2023 , 23 , 461. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ahmed, S.A.; Karanis, P. Cryptosporidium and Cryptosporidiosis: The Perspective from the Gulf Countries. Int. J. Environ. Res. Public Health 2020 , 17 , 6824. [ Google Scholar ] [ CrossRef ]
- Levine, M.M.; Nasrin, D.; Acácio, S.; Bassat, Q.; Powell, H.; Tennant, S.M.; Sow, S.O.; Sur, D.; Zaidi, A.K.M.; Faruque, A.S.G.; et al. Diarrhoeal Disease and Subsequent Risk of Death in Infants and Children Residing in Low-Income and Middle-Income Countries: Analysis of the GEMS Case-Control Study and 12-Month GEMS-1A Follow-on Study. Lancet Glob. Health 2020 , 8 , e204–e214. [ Google Scholar ] [ CrossRef ]
- Johansen, Ø.H.; Abdissa, A.; Zangenberg, M.; Mekonnen, Z.; Eshetu, B.; Sharew, B.; Moyo, S.; Sommerfelt, H.; Langeland, N.; Robertson, L.J.; et al. A Comparison of Risk Factors for Cryptosporidiosis and Non-Cryptosporidiosis Diarrhoea: A Case-Case-Control Study in Ethiopian Children. PLoS Negl. Trop. Dis. 2022 , 16 , e0010508. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Alali, F.; Abbas, I.; Jawad, M.; Hijjawi, N. Cryptosporidium Infection in Humans and Animals from Iraq: A Review. Acta Trop. 2021 , 220 , 105946. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bouwknegt, M.; Devleesschauwer, B.; Graham, H.; Robertson, L.J.; van der Giessen, J.W.; Euro-FBP workshop participants. Prioritisation of Food-Borne Parasites in Europe, 2016. Euro Surveill. 2018 , 23 , 17-00161. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nic Lochlainn, L.M.; Sane, J.; Schimmer, B.; Mooij, S.; Roelfsema, J.; van Pelt, W.; Kortbeek, T. Risk Factors for Sporadic Cryptosporidiosis in the Netherlands: Analysis of a 3-Year Population Based Case-Control Study Coupled with Genotyping, 2013–2016. J. Infect. Dis. 2019 , 219 , 1121–1129. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Franceschelli, A.; Bonadonna, L.; Cacciò, S.M.; Sannella, A.R.; Cintori, C.; Gargiulo, R.; Coccia, A.M.; Paradiso, R.; Iaconelli, M.; Briancesco, R.; et al. An Outbreak of Cryptosporidiosis Associated with Drinking Water in North-Eastern Italy, August 2019: Microbiological and Environmental Investigations. Euro Surveill. 2022 , 27 , 2200038. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Watier-Grillot, S.; Costa, D.; Petit, C.; Razakandrainibe, R.; Larréché, S.; Tong, C.; Demont, G.; Billetorte, D.; Mouly, D.; Fontan, D.; et al. Cryptosporidiosis Outbreaks Linked to the Public Water Supply in a Military Camp, France. PLoS Negl. Trop. Dis. 2022 , 16 , e0010776. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Liu, A.; Gong, B.; Liu, X.; Shen, Y.; Wu, Y.; Zhang, W.; Cao, J. A Retrospective Epidemiological Analysis of Human Cryptosporidium Infection in China during the Past Three Decades (1987–2018). PLoS Negl. Trop. Dis. 2020 , 14 , e0008146. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Daraei, H.; Oliveri Conti, G.; Sahlabadi, F.; Thai, V.N.; Gholipour, S.; Turki, H.; Fakhri, Y.; Ferrante, M.; Moradi, A.; Mousavi Khaneghah, A. Prevalence of Cryptosporidium spp. in Water: A Global Systematic Review and Meta-Analysis. Environ. Sci. Pollut. Res. Int. 2021 , 28 , 9498–9507. [ Google Scholar ]
- Stokdyk, J.P.; Spencer, S.K.; Walsh, J.F.; de Lamber, J.R.; Firnstahl, A.D.; Anderson, A.C.; Rezania, L.I.W.; Borchardt, M.A. Cryptosporidium incidence and surface water influence of groundwater supplying public water systems in Minnesota, USA. Environ. Sci. Technol. 2019 , 53 , 3391–3398. [ Google Scholar ] [ CrossRef ]
- Nasser, A.M. Transmission of Cryptosporidium by Fresh Vegetables. J. Food Prot. 2022 , 85 , 1737–1744. [ Google Scholar ] [ CrossRef ]
- Kooh, P.; Thébault, A.; Cadavez, V.; Gonzales-Barron, U.; Villena, I. Risk Factors for Sporadic Cryptosporidiosis: A Systematic Review and Meta-Analysis. Microb. Risk Anal. 2021 , 17 , 100116. [ Google Scholar ] [ CrossRef ]
- Ursini, T.; Moro, L.; Requena-Méndez, A.; Bertoli, G.; Buonfrate, D. A Review of Outbreaks of Cryptosporidiosis Due to Unpasteurized Milk. Infection 2020 , 48 , 659–663. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- European Food Safety Authority. Scientific Opinion. The efficacy and safety of high-pressure processing of food. EFSA J. 2022 , 20 , e07128. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gopfert, A.; Chalmers, R.M.; Whittingham, S.; Wilson, L.; van Hove, M.; Ferraro, C.F.; Robinson, G.; Young, N.; Nozad, B. An Outbreak of Cryptosporidium Parvum Linked to Pasteurised Milk from a Vending Machine in England: A Descriptive Study, March 2021. Epidemiol. Infect. 2022 , 150 , e185. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Robertson, L.J.; Temesgen, T.T.; Tysnes, K.R.; Eikås, J.E. An Apple a Day: An Outbreak of Cryptosporidiosis in Norway Associated with Self-Pressed Apple Juice. Epidemiol. Infect. 2019 , 147 , e139. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ahlinder, J.; Svedberg, A.-L.; Nystedt, A.; Dryselius, R.; Jacobsson, K.; Hägglund, M.; Brindefalk, B.; Forsman, M.; Ottoson, J.; Troell, K. Use of Metagenomic Microbial Source Tracking to Investigate the Source of a Foodborne Outbreak of Cryptosporidiosis. Food Waterborne Parasitol. 2022 , 26 , e00142. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dankwa, K.; Nuvor, S.V.; Obiri-Yeboah, D.; Feglo, P.K.; Mutocheluh, M. Occurrence of Cryptosporidium Infection and Associated Risk Factors among HIV-Infected Patients Attending ART Clinics in the Central Region of Ghana. Trop. Med. Infect. Dis. 2021 , 6 , 210. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Certad, G.; Follet, J.; Gantois, N.; Hammouma-Ghelboun, O.; Guyot, K.; Benamrouz-Vanneste, S.; Fréalle, E.; Seesao, Y.; Delaire, B.; Creusy, C.; et al. Prevalence, Molecular Identification, and Risk Factors for Cryptosporidium Infection in Edible Marine Fish: A Survey across Sea Areas Surrounding France. Front. Microbiol. 2019 , 10 , 1037. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moratal, S.; Dea-Ayuela, M.A.; Martí-Marco, A.; Puigcercós, S.; Marco-Hirs, N.M.; Doménech, C.; Corcuera, E.; Cardells, J.; Lizana, V.; López-Ramon, J. Molecular Characterization of Cryptosporidium spp. In Cultivated and Wild Marine Fishes from Western Mediterranean with the First Detection of Zoonotic Cryptosporidium Ubiquitum . Animals 2022 , 12 , 1052. [ Google Scholar ] [ CrossRef ]
- Srisuphanunt, M.; Wilairatana, P.; Kooltheat, N.; Damrongwatanapokin, T.; Karanis, P. Occurrence of Cryptosporidium Oocysts in Commercial Oysters in Southern Thailand. Food Waterborne Parasitol. 2023 , 32 , e00205. [ Google Scholar ] [ CrossRef ]
- Ogbuigwe, P.; Biggs, P.J.; Garcia-Ramirez, J.C.; Knox, M.A.; Pita, A.; Velathanthiri, N.; French, N.P.; Hayman, D.T.S. Uncovering the Genetic Diversity of Giardia Intestinalis in Isolates from Outbreaks in New Zealand. Infect. Dis. Poverty 2022 , 11 , 49. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zajaczkowski, P.; Lee, R.; Fletcher-Lartey, S.M.; Alexander, K.; Mahimbo, A.; Stark, D.; Ellis, J.T. The Controversies Surrounding Giardia Intestinalis Assemblages A and B. Curr. Res. Parasitol. Vector Borne Dis. 2021 , 1 , 100055. [ Google Scholar ] [ CrossRef ]
- Fakhri, Y.; Daraei, H.; Ghaffari, H.R.; Rezapour-Nasrabad, R.; Soleimani-Ahmadi, M.; Khedher, K.M.; Rostami, A.; Thai, V.N. The Risk Factors for Intestinal Giardia spp. Infection: Global Systematic Review and Meta-Analysis and Meta-Regression. Acta Trop. 2021 , 220 , 105968. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shaima, S.N.; Das, S.K.; Ahmed, S.; Jahan, Y.; Khan, S.H.; Mamun, G.M.S.; Shahid, A.S.M.S.B.; Parvin, I.; Ahmed, T.; Faruque, A.S.G.; et al. Anthropometric Indices of Giardia -Infected under-Five Children Presenting with Moderate-to-Severe Diarrhea and Their Healthy Community Controls: Data from the Global Enteric Multicenter Study. Children 2021 , 8 , 1186. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Groudan, K.; Gupta, K.; Chalhoub, J.; Singhania, R. Giardia Lamblia Diagnosed Incidentally by Duodenal Biopsy. J. Investig. Med. High Impact Case Rep. 2021 , 9 , 23247096211001649. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hurník, P.; Žiak, D.; Dluhošová, J.; Židlík, V.; Šustíková, J.; Uvírová, M.; Urban, O.; Dvořáčková, J.; Nohýnková, E. Another Case of Coincidental Giardia Infection and Pancreatic Cancer. Parasitol. Int. 2019 , 71 , 160–162. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Loderstädt, U.; Frickmann, H. Antimicrobial Resistance of the Enteric Protozoon Giardia Duodenalis —A Narrative Review. Eur. J. Microbiol. Immunol. 2021 , 11 , 29–43. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- European Centre for Disease Prevention and Control (ECDC) Giardiasis (Lambliasis)—Annual Epidemiological Report for 2019. 2022. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/giardiasis-%20annual-epidemiological-report-2019_0.pdf (accessed on 22 February 2024).
- European Commission. Commission Implementing Decision (EU) 2018/945 of 22 June 2018 on the Communicable Diseases and Related Special Health Issues to be Covered by Epidemiological Surveillance as well as Relevant Case Definitions (Text with EEA Relevance.). Off. J. Eur. Union 2018 , 170 , 1–74. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=uriserv%3AOJ.L_.2018.170.01.0001.01.ENG (accessed on 16 January 2024).
- Dixon, B.R. Giardia Duodenalis in Humans and Animals—Transmission and Disease. Res. Vet. Sci. 2021 , 135 , 283–289. [ Google Scholar ] [ CrossRef ]
- Tembo, S.J.; Mutengo, M.M.; Sitali, L.; Changula, K.; Takada, A.; Mweene, A.S.; Simulundu, E.; Chitanga, S. Prevalence and Genotypic Characterization of Giardia Duodenalis Isolates from Asymptomatic School-Going Children in Lusaka, Zambia. Food Waterborne Parasitol. 2020 , 19 , e00072. [ Google Scholar ] [ CrossRef ]
- Muadica, A.S.; Balasegaram, S.; Beebeejaun, K.; Köster, P.C.; Bailo, B.; Hernández-de-Mingo, M.; Dashti, A.; Dacal, E.; Saugar, J.M.; Fuentes, I.; et al. Risk Associations for Intestinal Parasites in Symptomatic and Asymptomatic Schoolchildren in Central Mozambique. Clin. Microbiol. Infect. 2021 , 27 , 624–629. [ Google Scholar ] [ CrossRef ]
- Al-Jawabreh, A.; Ereqat, S.; Dumaidi, K.; Al-Jawabreh, H.; Abdeen, Z.; Nasereddin, A. Prevalence of Selected Intestinal Protozoan Infections in Marginalized Rural Communities in Palestine. BMC Public Health 2019 , 19 , 1667. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fusaro, C.; Chávez-Romero, Y.A.; Prada, S.L.G.; Serrano-Silva, N.; Bernal, J.E.; González-Jiménez, F.E.; Sarria-Guzmán, Y. Burden and Epidemiology of Human Intestinal Giardia Duodenalis Infection in Colombia: A Systematic Review. Trop. Med. Infect. Dis. 2022 , 7 , 325. [ Google Scholar ] [ CrossRef ]
- Bekele, D.; Reta, T. Prevalence and distribution of Giardia lamblia infection among patients of children aged 5–11years treated in Sheno town health centers, North Shoa Oromia region, Ethiopia. ClinicSearch 2023 . [ Google Scholar ] [ CrossRef ]
- Al-Yousofi, A.; Yan, Y.; Al Mekhlafi, A.M.; Hezam, K.; Abouelnazar, F.A.; Al-Rateb, B.; Almamary, H.; Abdulwase, R. Prevalence of Intestinal Parasites among Immunocompromised Patients, Children, and Adults in Sana’a, Yemen. J. Trop. Med. 2022 , 2022 , 5976640. [ Google Scholar ] [ CrossRef ]
- Resi, D.; Varani, S.; Sannella, A.R.; De Pascali, A.M.; Ortalli, M.; Liguori, G.; Benvenuti, M.; Re, M.C.; Pirani, R.; Prete, L.; et al. A Large Outbreak of Giardiasis in a Municipality of the Bologna Province, North-Eastern Italy, November 2018 to April 2019. Euro Surveill. 2021 , 26 , 2001331. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tawana, M.; Onyiche, T.E.; Ramatla, T.; Thekisoe, O. A “One Health” Perspective of Africa-Wide Distribution and Prevalence of Giardia Species in Humans, Animals and Waterbodies: A Systematic Review and Meta-Analysis. Parasitology 2023 , 150 , 769–780. [ Google Scholar ] [ CrossRef ]
- Gisbert Algaba, I.; Verhaegen, B.; Murat, J.B.; Coucke, W.; Mercier, A.; Cox, E.; Dorny, P.; Dierick, K.; De Craeye, S. Molecular Study of Toxoplasma Gondii Isolates Originating from Humans and Organic Pigs in Belgium. Foodborne Pathog. Dis. 2020 , 17 , 316–321. [ Google Scholar ] [ CrossRef ]
- Lobo, Y.; Holland, T.; Spelman, L. Toxoplasmosis in a Patient Receiving Ixekizumab for Psoriasis. JAAD Case Rep. 2020 , 6 , 204–206. [ Google Scholar ] [ CrossRef ]
- Papatsiros, V.G.; Athanasiou, L.V.; Kostoulas, P.; Giannakopoulos, A.; Tzika, E.; Billinis, C. Toxoplasma Gondii Infection in Swine: Implications for Public Health. Foodborne Pathog. Dis. 2021 , 18 , 823–840. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Friesema, I.H.M.; Hofhuis, A.; Hoek-van Deursen, D.; Jansz, A.R.; Ott, A.; van Hellemond, J.J.; van der Giessen, J.; Kortbeek, L.M.; Opsteegh, M. Risk Factors for Acute Toxoplasmosis in the Netherlands. Epidemiol. Infect. 2023 , 151 , e95. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cerutti, A.; Blanchard, N.; Besteiro, S. The Bradyzoite: A Key Developmental Stage for the Persistence and Pathogenesis of Toxoplasmosis. Pathogens 2020 , 9 , 234. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ducrocq, J.; Simon, A.; Lemire, M.; De Serres, G.; Lévesque, B. Exposure to Toxoplasma Gondii through Consumption of Raw or Undercooked Meat: A Systematic Review and Meta-Analysis. Vector Borne Zoonotic Dis. 2021 , 21 , 40–49. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dakroub, H.; Sgroi, G.; D’Alessio, N.; Russo, D.; Serra, F.; Veneziano, V.; Rea, S.; Pucciarelli, A.; Lucibelli, M.G.; De Carlo, E.; et al. Molecular Survey of Toxoplasma Gondii in Wild Mammals of Southern Italy. Pathogens 2023 , 12 , 471. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tawfik, O.; Hassan, A.; Mohamed, W.; Essmyer, C.; Ewing, E.; Lem, V.; Grobelny, B.; Breshears, J.; Akhtar, N. Disseminated Opportunistic Infections Masquerading as Central Nervous System Malignancies. Human Pathology Reports 2022 , 28 , 300629. [ Google Scholar ] [ CrossRef ]
- Rabaan, A.A.; Uzairue, L.I.; Alfaraj, A.H.; Halwani, M.A.; Muzaheed; Alawfi, A.; Alshengeti, A.; Al Kaabi, N.A.; Alawad, E.; Alhajri, M.; et al. Seroprevalence, Risk Factors and Maternal-Fetal Outcomes of Toxoplasma Gondii in Pregnant Women from WHO Eastern Mediterranean Region: Systematic Review and Meta-Analysis. Pathogens 2023 , 12 , 1157. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dini, F.M.; Morselli, S.; Marangoni, A.; Taddei, R.; Maioli, G.; Roncarati, G.; Balboni, A.; Dondi, F.; Lunetta, F.; Galuppi, R. Spread of Toxoplasma Gondii among Animals and Humans in Northern Italy: A Retrospective Analysis in a One-Health Framework. Food Waterborne Parasitol. 2023 , 32 , e00197. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hoshina, T.; Horino, T.; Saiki, E.; Aonuma, H.; Sawaki, K.; Miyajima, M.; Lee, K.; Nakaharai, K.; Shimizu, A.; Hosaka, Y.; et al. Seroprevalence and Associated Factors of Toxoplasma Gondii among HIV-Infected Patients in Tokyo: A Cross Sectional Study. J. Infect. Chemother. 2020 , 26 , 33–37. [ Google Scholar ] [ CrossRef ]
- Dong, W.; Zhong, Q.; Gu, Y.-L.; Liang, N.; Zhou, Y.-H.; Cong, X.-M.; Liang, J.-Y.; Wang, X.-M. Is Toxoplasma Gondii Infection a Concern in Individuals with Rheumatic Diseases? Evidence from a Case-Control Study Based on Serological Diagnosis. Microb. Pathog. 2023 , 182 , 106257. [ Google Scholar ] [ CrossRef ]
- Minuzzi, C.E.; Fernandes, F.D.; Portella, L.P.; Bräunig, P.; Sturza, D.A.F.; Giacomini, L.; Salvagni, E.; Ribeiro, J.D.S.; Silva, C.R.; Difante, C.M.; et al. Contaminated Water Confirmed as Source of Infection by Bioassay in an Outbreak of Toxoplasmosis in South Brazil. Transbound. Emerg. Dis. 2021 , 68 , 767–772. [ Google Scholar ] [ CrossRef ]
- Cabral Monica, T.; Pinto-Ferreira, F.; Martins, F.D.C.; de Matos, R.L.N.; de Matos, A.M.R.N.; Santos, A.C.; Nino, B.d.S.L.; Pereira, L.; Narciso, S.G.; Garcia, J.L.; et al. Epidemiology of a Toxoplasmosis Outbreak in a Research Institution in Northern Paraná, Brazil. Zoonoses Public Health 2020 , 67 , 760–764. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Da Costa, M.A.; Pinto-Ferreira, F.; de Almeida, R.P.A.; Martins, F.D.C.; Pires, A.L.; Mareze, M.; Mitsuka-Breganó, R.; Freire, R.L.; da Rocha Moreira, R.V.; Borges, J.M.; et al. Artisan Fresh Cheese from Raw Cow’s Milk as a Possible Route of Transmission in a Toxoplasmosis Outbreak, in Brazil. Zoonoses Public Health 2020 , 67 , 122–129. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rehman, F.; Shah, M.; Ali, A.; Ahmad, I.; Sarwar, M.T.; Rapisarda, A.M.C.; Cianci, A. Unpasteurised Milk Consumption as a Potential Risk Factor for Toxoplasmosis in Females with Recurrent Pregnancy Loss. J. Obstet. Gynaecol. 2020 , 40 , 1106–1110. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Schumacher, A.C.; Elbadawi, L.I.; DeSalvo, T.; Straily, A.; Ajzenberg, D.; Letzer, D.; Moldenhauer, E.; Handly, T.L.; Hill, D.; Dardé, M.-L.; et al. Toxoplasmosis Outbreak Associated with Toxoplasma Gondii -Contaminated Venison-High Attack Rate, Unusual Clinical Presentation, and Atypical Genotype. Clin. Infect. Dis. 2021 , 72 , 1557–1565. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Murata, R.; Kodo, Y.; Maeno, A.; Suzuki, J.; Mori, K.; Sadamasu, K.; Kawahara, F.; Nagamune, K. Detection of Toxoplasma Gondii and Sarcocystis sp. in the Meat of Common Minke Whale ( Balaenoptera Acutorostrata ): A Case of Suspected Food Poisoning in Japan. Parasitol. Int. 2023 , 99 , 102832. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Al-Adhroey, A.H.; Mehrass, A.A.-K.O.; Al-Shammakh, A.A.; Ali, A.D.; Akabat, M.Y.M.; Al-Mekhlafi, H.M. Prevalence and Predictors of Toxoplasma Gondii Infection in Pregnant Women from Dhamar, Yemen. BMC Infect. Dis. 2019 , 19 , 1089. [ Google Scholar ] [ CrossRef ]
- Sini, M.F.; Manconi, M.; Varcasia, A.; Massei, G.; Sandu, R.; Mehmood, N.; Ahmed, F.; Carta, C.; Cantacessi, C.; Scarano, C.; et al. Seroepidemiological and biomolecular survey on Toxoplasma gondii in Sardinian wild boar ( Sus scrofa ). Food Waterborne Parasitol. 2024 , 34 , e00222. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Marangi, M.; Lago, N.; Mancinelli, G.; Antonio, O.L.; Scirocco, T.; Sinigaglia, M.; Specchiulli, A.; Cilenti, L. Occurrence of the protozoan parasites Toxoplasma gondii and Cyclospora cayetanensis in the invasive Atlantic blue crab Callinectes sapidus from the Lesina Lagoon (SE Italy). Mar. Pollut. Bull. 2022 , 176 , 113428. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Çulbasan, V.; Gungor, C.; Gundog, D.A.; Koskeroglu, K.; Onmaz, N.E. Molecular surveillance of Toxoplasma gondii in raw milk and Artisan cheese of sheep, goat, cow and water buffalo origin. Int. J. Dairy Technol. 2023 , 76 , 948–954. [ Google Scholar ] [ CrossRef ]
- Maani, S.; Solhjoo, K.; Bagherzadeh, M.A.; Bazmjoo, A.; Barnaaji, H.G.; Mir, H.; Bahrami, F.; Khademi, S.Z.; Shams, M.; Abdoli, A.; et al. Prevalence of Toxoplasma Gondii and Neospora Caninum Contaminations in Poultry Eggs: Molecular Surveillance in Three Different Geographical Regions of Iran. Food Saf. Risk 2023 , 10 , 3. [ Google Scholar ] [ CrossRef ]
- Servián, A.; Lorena Zonta, M.; Navone, G.T. Differential Diagnosis of Human Entamoeba Infections: Morphological and Molecular Characterization of New Isolates in Argentina. Rev. Argent. Microbiol. 2023 , 56 , 16–24. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bao, X.; Wiehe, R.; Dommisch, H.; Schaefer, A.S. Entamoeba Gingivalis Causes Oral Inflammation and Tissue Destruction. J. Dent. Res. 2020 , 99 , 561–567. [ Google Scholar ] [ CrossRef ]
- Balarabe-Musa, B.; Onyeagba, K.D. Prevalence of Entamoeba Histolytica amongst Infants with Diarrhoea Visiting the University of Abuja Teaching Hospital. J. Vet. Biomed. Sci. 2020 , 2 , 128–134. [ Google Scholar ] [ CrossRef ]
- Leon-Coria, A.; Kumar, M.; Chadee, K. The Delicate Balance between Entamoeba Histolytica , Mucus and Microbiota. Gut Microbes 2020 , 11 , 118–125. [ Google Scholar ] [ CrossRef ]
- Singh, A.; Banerjee, T. Host-Parasite Interactions in Infections Due to Entamoeba Histolytica : A Tale of Known and Unknown. Trop. Parasitol. 2022 , 12 , 69–77. [ Google Scholar ]
- Das, K.; Sardar, S.K.; Ghosal, A.; Saito-Nakano, Y.; Dutta, S.; Nozaki, T.; Ganguly, S. Multilocus Sequence Typing (MLST) of Entamoeba Histolytica Identifies Kerp2 as a Genetic Marker Associated with Disease Outcomes. Parasitol. Int. 2021 , 83 , 102370. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Upadhyay, S.; Das, K.; Ghosal, A.; Manna, S.; Saito-Nakano, Y.; Dutta, S.; Nozaki, T.; Ganguly, S. Multi-Locus Sequence Analysis Reveals Phylogenetically Segregated Entamoeba Histolytica Population. Parasitol. Int. 2024 , 100 , 102861. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sardar, S.K.; Ghosal, A.; Haldar, T.; Prasad, A.; Mal, S.; Saito-Nakano, Y.; Kobayashi, S.; Dutta, S.; Nozaki, T.; Ganguly, S. Genetic Characterization of the Entamoeba Moshkovskii Population Based on Different Potential Genetic Markers. Parasitology 2024 , 151 , 429–439. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lin, F.-H.; Chen, B.-C.; Chou, Y.-C.; Chien, W.-C.; Chung, C.-H.; Hsieh, C.-J.; Yu, C.-P. The Epidemiology of Entamoeba histolytica Infection and Its Associated Risk Factors among Domestic and Imported Patients in Taiwan during the 2011–2020 Period. Medicina 2022 , 58 , 820. [ Google Scholar ] [ CrossRef ]
- Morán, P.; Serrano-Vázquez, A.; Rojas-Velázquez, L.; González, E.; Pérez-Juárez, H.; Hernández, E.G.; Padilla, M.d.L.A.; Zaragoza, M.E.; Portillo-Bobadilla, T.; Ramiro, M.; et al. Amoebiasis: Advances in Diagnosis, Treatment, Immunology Features and the Interaction with the Intestinal Ecosystem. Int. J. Mol. Sci. 2023 , 24 , 11755. [ Google Scholar ] [ CrossRef ]
- Tahir, M.; Sendzischew Shane, M.; Deshpande Amar, R.; Milikowski, C. An Unusual Case of Entamoeba Histolytica Infection in Miami Fl: Case Report and Review of the Literature. Res. Rev. Infect. Dis. 2020 , 3 , 40–43. [ Google Scholar ] [ CrossRef ]
- Samie, A.; Mahlaule, L.; Mbati, P.; Nozaki, T.; ElBakri, A. Prevalence and Distribution of Entamoeba Species in a Rural Community in Northern South Africa. Food Waterborne Parasitol. 2020 , 18 , e00076. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rahadiani, N.; Habiburrahman, M.; Putranto, A.S.; Handjari, D.R.; Stephanie, M.; Krisnuhoni, E. Fulminant Necrotizing Amoebic Colitis Presenting as Acute Appendicitis: A Case Report and Comprehensive Literature Review. J. Infect. Dev. Ctries. 2022 , 16 , 717–725. [ Google Scholar ] [ CrossRef ]
- Kumar, R.; Patel, R.; Priyadarshi, R.N.; Narayan, R.; Maji, T.; Anand, U.; Soni, J.R. Amebic liver abscess: An update. World J Hepatol. 2024 , 16 , 316–330. [ Google Scholar ] [ CrossRef ]
- Wang, H.; Kanthan, R. Multiple Colonic and Ileal Perforations Due to Unsuspected Intestinal Amoebiasis-Case Report and Review. Pathol. Res. Pract. 2020 , 216 , 152608. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- World Health Organization. Guidelines for Drinking-Water Quality. Fourth Edition Incorporating the First and Second Addenda ; WHO: Geneva, Switzerland, 2022; ISBN 978-92-4-004506-4. Available online: https://iris.who.int/bitstream/handle/10665/352532/9789240045064-eng.pdf?sequence=1&isAllowed=y#page=153 (accessed on 15 February 2024).
- Fichardt, H.J.; Rocha, J. S2741 Entamoeba Histolytica Dysentery Complicated by Amebic Liver Abscess and Type a Right Heart Thrombus: A Case Report. Am. J. Gastroenterol. 2020 , 115 , S1432. [ Google Scholar ] [ CrossRef ]
- Kaiser, R.W.J.; Allgeier, J.; Philipp, A.B.; Mayerle, J.; Rothe, C.; Wallrauch, C.; Op den Winkel, M. Development of Amoebic Liver Abscess in Early Pregnancy Years after Initial Amoebic Exposure: A Case Report. BMC Gastroenterol. 2020 , 20 , 424. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Usuda, D.; Tsuge, S.; Sakurai, R.; Kawai, K.; Matsubara, S.; Tanaka, R.; Suzuki, M.; Takano, H.; Shimozawa, S.; Hotchi, Y.; et al. Amebic Liver Abscess by Entamoeba Histolytica . World J. Clin. Cases 2022 , 10 , 13157–13166. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Herrera, G.C.; Herrera, A.C.; Pontón, P.; Molina, G.A.; Constante, J.E.; Delgado, J.A. Amebiasis, a Rare Cause of Acute Appendicitis. J. Surg. Case Rep. 2019 , 2019 , rjz076. [ Google Scholar ] [ CrossRef ]
- Patel, S.J.; Pathak, P.; Thejeswi, P.; Bandari, M. Acute Appendicitis Secondary to Entamoeba Histolytica Infestation. Trop. Parasitol. 2023 , 13 , 114–116. [ Google Scholar ]
- Dominic, C.; Kelly, S.; Melzer, M. Refractory Inflammatory Bowel Disease— Entamoeba Histolytica , the Forgotten Suspect. Clin. Infect. Pract. 2023 , 20 , 100245. [ Google Scholar ] [ CrossRef ]
- Müller, A.; Frickmann, H.; Tannich, E.; Poppert, S.; Hagen, R.M. Colitis Caused by Entamoeba Histolytica Identified by Real-Time-PCR and Fluorescence in Situ Hybridization from Formalin-Fixed, Paraffin-Embedded Tissue. Eur. J. Microbiol. Immunol. 2022 , 12 , 84–91. [ Google Scholar ] [ CrossRef ]
- Carrero, J.C.; Reyes-López, M.; Serrano-Luna, J.; Shibayama, M.; Unzueta, J.; León-Sicairos, N.; de la Garza, M. Intestinal Amoebiasis: 160 Years of Its First Detection and Still Remains as a Health Problem in Developing Countries. Int. J. Med. Microbiol. 2020 , 310 , 151358. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sardar, S.K.; Ghosal, A.; Haldar, T.; Maruf, M.; Das, K.; Saito-Nakano, Y.; Kobayashi, S.; Dutta, S.; Nozaki, T.; Ganguly, S. Prevalence and Molecular Characterization of Entamoeba Moshkovskii in Diarrheal Patients from Eastern India. PLoS Negl. Trop. Dis. 2023 , 17 , e0011287. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Flaih, M.H.; Khazaal, R.M.; Kadhim, M.K.; Hussein, K.R.; Alhamadani, F.A.B. The Epidemiology of Amoebiasis in Thi-Qar Province, Iraq (2015–2020): Differentiation of Entamoeba Histolytica and Entamoeba Dispar Using Nested and Real-Time Polymerase Chain Reaction. Epidemiol. Health 2021 , 43 , e2021034. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Aziz, K.T.; Rostam, R.A.; Nasir, K.; Qasem, A.O.; Azize, P.M. Epidemiological Study for Entamoeba Histolytica Infection and Their Risk Factors among Children in Pediatric Hospital in, Sulaimani Province-Iraq. Kufa J. Nurs. Sci. 2022 , 12 , 199–204. [ Google Scholar ]
- Roro, G.B.; Eriso, F.; Al-Hazimi, A.M.; Kuddus, M.; Singh, S.C.; Upadhye, V.; Hajare, S.T. Prevalence and Associated Risk Factors of Entamoeba Histolytica Infection among School Children from Three Primary Schools in Arsi Town, West Zone, Ethiopia. J. Parasit. Dis. 2022 , 46 , 776–784. [ Google Scholar ] [ CrossRef ]
- Tokijoh, N.I.; Bakar, A.A.; Othman, N.; Noordin, R.; Saidin, S. Assessing the Prevalence and Risk Factors Associated with Entamoeba Complex Infection among the Orang Asli School Children in Perak, Malaysia through Molecular Approach. Parasitol. Int. 2022 , 91 , 102638. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Atabati, H.; Kassiri, H.; Shamloo, E.; Akbari, M.; Atamaleki, A.; Sahlabadi, F.; Linh, N.T.T.; Rostami, A.; Fakhri, Y.; Khaneghah, A.M. The Association between the Lack of Safe Drinking Water and Sanitation Facilities with Intestinal Entamoeba spp. Infection Risk: A Systematic Review and Meta-Analysis. PLoS ONE 2020 , 15 , e0237102. [ Google Scholar ] [ CrossRef ]
- Azizi, H.; Davtalab-Esmaeili, E.; Mirzapour, M.; Karimi, G.; Rostampour, M.; Mirzaei, Y. A Case-Control Study of Timely Control and Investigation of an Entamoeba Histolytica Outbreak by Primary Health Care in Idahluy-e Bozorg Village, Iran. Int. J. Epidemiol. Res. 2019 , 6 , 120–127. [ Google Scholar ] [ CrossRef ]
- Chowdhury, R.; Esiobu, N.; Meeroff, D.; Bloetscher, F. Different Detection and Treatment Methods for Entamoeba histolytica and Entamoeba dispar in Water/Wastewater: A Review. J. Environ. Prot. 2022 , 13 , 126–149. [ Google Scholar ] [ CrossRef ]
- Khorshidvand, Z.; Khazaei, S.; Amiri, M.; Taherkhani, H.; Mirzaei, A. Worldwide Prevalence of Emerging Parasite Blastocystis in Immunocompromised Patients: A Systematic Review and Meta-Analysis. Microb. Pathog. 2021 , 152 , 104615. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wakid, M.H.; Aldahhasi, W.T.; Alsulami, M.N.; El-Kady, A.M.; Elshabrawy, H.A. Identification and Genetic Characterization of Blastocystis Species in Patients from Makkah, Saudi Arabia. Infect. Drug Resist. 2022 , 15 , 491–501. [ Google Scholar ] [ CrossRef ]
- Clark, C.G.; Diamond, L.S. Methods for Cultivation of Luminal Parasitic Protists of Clinical Importance. Clin. Microbiol. Rev. 2002 , 15 , 329–341. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Elsayad, M.H.; Tolba, M.M.; Argiah, H.A.; Gaballah, A.; Osman, M.M.; Lewis Mikhael, I. Electron microscopy of Blastocystis hominis and other diagnostic approaches. J. Egypt. Soc. Parasitol. 2019 , 49 , 373–380. [ Google Scholar ] [ CrossRef ]
- Maloney, J.G.; Molokin, A.; Seguí, R.; Maravilla, P.; Martínez-Hernández, F.; Villalobos, G.; Tsaousis, A.D.; Gentekaki, E.; Muñoz-Antolí, C.; Klisiowicz, D.R.; et al. Identification and Molecular Characterization of Four New Blastocystis Subtypes Designated ST35-ST38. Microorganisms 2023 , 11 , 46. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nguyen, L.D.N.; Gantois, N.; Hoang, T.T.; Do, B.T.; Desramaut, J.; Naguib, D.; Tran, T.N.; Truong, A.D.; Even, G.; Certad, G.; et al. First Epidemiological Survey on the Prevalence and Subtypes Distribution of the Enteric Parasite Blastocystis sp. in Vietnam. Microorganisms 2023 , 11 , 731. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Piubelli, C.; Soleymanpoor, H.; Giorli, G.; Formenti, F.; Buonfrate, D.; Bisoffi, Z.; Perandin, F. Blastocystis Prevalence and Subtypes in Autochthonous and Immigrant Patients in a Referral Centre for Parasitic Infections in Italy. PLoS ONE 2019 , 14 , e0210171. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cinek, O.; Polackova, K.; Odeh, R.; Alassaf, A.; Kramná, L.; Ibekwe, M.U.; Majaliwa, E.S.; Ahmadov, G.; Elmahi, B.M.E.; Mekki, H.; et al. Blastocystis in the Faeces of Children from Six Distant Countries: Prevalence, Quantity, Subtypes and the Relation to the Gut Bacteriome. Parasit. Vectors 2021 , 14 , 399. [ Google Scholar ] [ CrossRef ]
- Rauff-Adedotun, A.A.; Meor Termizi, F.H.; Shaari, N.; Lee, I.L. The Coexistence of Blastocystis spp. In Humans, Animals and Environmental Sources from 2010–2021 in Asia. Biology 2021 , 10 , 990. [ Google Scholar ] [ CrossRef ]
- Gureser, A.S.; Karasartova, D.; Sarzhanov, F.; Kosar, N.; Taylan-Ozkan, A.; Dogruman-Al, F. Prevalence of Blastocystis and Dientamoeba Fragilis in Diarrheal Patients in Corum, Türkiye. Parasitol. Res. 2023 , 122 , 2977–2987. [ Google Scholar ] [ CrossRef ]
- Marangi, M.; Boughattas, S.; De Nittis, R.; Pisanelli, D.; Delli Carri, V.; Lipsi, M.R.; La Bella, G.; Serviddio, G.; Niglio, M.; Lo Caputo, S.; et al. Prevalence and Genetic Diversity of Blastocystis sp. among Autochthonous and Immigrant Patients in Italy. Microb. Pathog. 2023 , 185 , 106377. [ Google Scholar ] [ CrossRef ]
- Rojas-Velázquez, L.; Maloney, J.G.; Molokin, A.; Morán, P.; Serrano-Vázquez, A.; González, E.; Pérez-Juárez, H.; Ximénez, C.; Santin, M. Use of Next-Generation Amplicon Sequencing to Study Blastocystis Genetic Diversity in a Rural Human Population from Mexico. Parasit. Vectors 2019 , 12 , 566. [ Google Scholar ] [ CrossRef ]
- Boutahar, M.; Belaouni, M.; Ibrahimi, A.; Eljaoudi, R.; Aanniz, T.; Er-Rami, M. Prevalence of Blastocystis sp. in Morocco: Comparative Assessment of Three Diagnostic Methods and Characterization of Parasite Forms in Jones’ Culture Medium. Parasite 2023 , 30 , 64. [ Google Scholar ] [ CrossRef ]
- Garcia-Montoya, G.M.; Galvan-Diaz, A.L.; Alzate, J.F. Metataxomics Reveals Blastocystis Subtypes Mixed Infections in Colombian Children. Infect. Genet. Evol. 2023 , 113 , 105478. [ Google Scholar ] [ CrossRef ]
- Rudzińska, M.; Sikorska, K. Epidemiology of Blastocystis Infection: A Review of Data from Poland in Relation to Other Reports. Pathogens 2023 , 12 , 1050. [ Google Scholar ] [ CrossRef ]
- Alamlih, L.; Abufaied, M.; Al-Allaf, A.-W. An Unusual Cause of Reactive Arthritis with Urticarial: A Case Report. Qatar Med. J. 2020 , 2020 , 25. [ Google Scholar ] [ CrossRef ]
- Ascuña-Durand, K.; Salazar-Sánchez, R.S.; Cartillo-Neyra, R.; Ballón-Echegaray, J. Molecular Epidemiology of Blastocystis in Urban and Periurban Human Populations in Arequipa, Peru. bioRxiv 2020 . [ Google Scholar ] [ CrossRef ]
- El-Zawawy, H.T.; Farag, H.F.; Tolba, M.M.; Abdalsamea, H.A. Improving Hashimoto’s Thyroiditis by Eradicating Blastocystis Hominis : Relation to IL-17. Ther. Adv. Endocrinol. Metab. 2020 , 11 , 2042018820907013. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rajamanikam, A.; Isa, M.N.M.; Samudi, C.; Devaraj, S.; Govind, S.K. Gut Bacteria Influence Blastocystis sp. Phenotypes and May Trigger Pathogenicity. PLoS Negl. Trop. Dis. 2023 , 17 , e0011170. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mayneris-Perxachs, J.; Arnoriaga-Rodríguez, M.; Garre-Olmo, J.; Puig, J.; Ramos, R.; Trelis, M.; Burokas, A.; Coll, C.; Zapata-Tona, C.; Pedraza, S.; et al. Presence of Blastocystis in Gut Microbiota Is Associated with Cognitive Traits and Decreased Executive Function. ISME J. 2022 , 16 , 2181–2197. [ Google Scholar ] [ CrossRef ]
- Sayed Ahmed Nasr, M.; Mohammed Abdellatif, M.; Belal, U.; Abdel-Hafeez, E.; Abdalgelil, N. Detection of Blastocystis Species in the Stool of Immuno-Compromised Patients by Using Two Different Diagnostic Techniques. Minia J. Med. Res. 2023 , 34 , 103–110. [ Google Scholar ] [ CrossRef ]
- Bhat Yellanthoor, R. Acute Gastroenteritis Due to Blastocystis Hominis in an Adolescent Boy. BMJ Case Rep. 2020 , 13 , e237810. [ Google Scholar ] [ CrossRef ]
- Permasutha, M.B.; Pranata, I.W.A.; Diptyanusa, A.; Murhandarwati, E.E.H. Blastocystis Hominis Infection in HIV/AIDS Children with Extraintestinal Symptom: A Case Report. Bali Med. J. 2022 , 11 , 498–500. [ Google Scholar ] [ CrossRef ]
- Hidalgo-Gonzalez, L.A.; Salgado-Lopez, J.; Pineda-Rodriguez, S.A.; Martinez, A.; Romero-Valdovinos, M.; Martinez-Hernandez, F.; Rendon-Franco, E.; Olivo-Diaz, A.; Maravilla, P.; Rodriguez-Bataz, E. Identification of Blastocystis sp. in School Children from a Rural Mexican Village: Subtypes and Risk Factors Analysis. Parasitol. Res. 2023 , 122 , 1701–1707. [ Google Scholar ] [ CrossRef ]
- Mathison, B.A.; Pritt, B.S. Cyclosporiasis-Updates on Clinical Presentation, Pathology, Clinical Diagnosis, and Treatment. Microorganisms 2021 , 9 , 1863. [ Google Scholar ] [ CrossRef ]
- Barratt, J.L.N.; Shen, J.; Houghton, K.; Richins, T.; Sapp, S.G.H.; Cama, V.; Arrowood, M.J.; Straily, A.; Qvarnstrom, Y. Cyclospora Cayetanensis Comprises at Least 3 Species That Cause Human Cyclosporiasis. Parasitology 2023 , 150 , 269–285. [ Google Scholar ] [ CrossRef ]
- Almeria, S.; Chacin-Bonilla, L.; Maloney, J.G.; Santin, M. Cyclospora Cayetanensis : A Perspective (2020–2023) with Emphasis on Epidemiology and Detection Methods. Microorganisms 2023 , 11 , 2171. [ Google Scholar ] [ CrossRef ]
- Durigan, M.; Ewing-Peeples, L.; Almeria, S.; Balan, K.V.; Grocholl, J.; Irizawa, S.; Mammel, M. Detection of Cyclospora cayetanensis in Food and Water Samples: Optimized Protocols for Specific and Sensitive Molecular Methods from a Regulatory Agency Perspective. J Food Prot. 2024 , 1 , 100291. [ Google Scholar ] [ CrossRef ]
- Sardar, S.K.; Goel, G.; Ghosal, A.; Deshmukh, R.; Bhattacharya, S.; Haldar, T.; Maruf, M.M.; Mahto, R.; Kumar, J.; Bhave, S.J.; et al. First Case Report of Cyclosporiasis from Eastern India: Incidence of Cyclospora Cayetanensis in a Patient with Unusual Diarrheal Symptoms. J. Infect. Dev. Ctries. 2023 , 17 , 1037–1040. [ Google Scholar ] [ CrossRef ]
- Lugo, R.; Angulo-Várguez, F.; Ávila-Nava, A.; Gutiérrez-Solis, A.L.; Reyes-Sosa, M.; Medina-Escobedo, M. Acute Kidney Injury Associated with Intestinal Infection by Cyclospora Cayetanensis in a Kidney Transplant Patient. A Case Report. Parasitol. Int. 2021 , 80 , 102212. [ Google Scholar ] [ CrossRef ]
- Alkorta, M.; Manzanal, A.; Zeberio, I. A Case of Severe Diarrhoea Caused by Cyclospora Cayetanensis in an Immunocompromised Patient in Northern Spain. Access Microbiol. 2022 , 4 , 000313. [ Google Scholar ] [ CrossRef ]
- Ahart, L.; Jacobson, D.; Rice, M.; Richins, T.; Peterson, A.; Zheng, Y.; Barratt, J.; Cama, V.; Qvarnstrom, Y.; Montgomery, S.; et al. Retrospective Evaluation of an Integrated Molecular-Epidemiological Approach to Cyclosporiasis Outbreak Investigations—United States, 2021. Epidemiol. Infect. 2023 , 151 , e131. [ Google Scholar ] [ CrossRef ]
- Chacin-Bonilla, L.; Santin, M. Cyclospora Cayetanensis Infection in Developed Countries: Potential Endemic Foci? Microorganisms 2023 , 11 , 540. [ Google Scholar ] [ CrossRef ]
- Ramezanzadeh, S.; Barzegar, G.; Osquee, H.O.; Pirestani, M.; Mahami-Oskouei, M.; Hajizadeh, M.; Hosseini, S.A.; Rodrigues Oliveira, S.M.; Agholi, M.; de Lourdes Pereira, M.; et al. Microscopic and Molecular Identification of Cyclospora Cayetanensis and Cystoisospora Belli in HIV-Infected People in Tabriz, Northwest of Iran. Trop. Med. Infect. Dis. 2023 , 8 , 368. [ Google Scholar ] [ CrossRef ]
- Ögren, J.; Dienus, O.; Beser, J.; Henningsson, A.J.; Matussek, A. Protozoan Infections Are Under-Recognized in Swedish Patients with Gastrointestinal Symptoms. Eur. J. Clin. Microbiol. Infect. Dis. 2020 , 39 , 2153–2160. [ Google Scholar ] [ CrossRef ]
- Berrouch, S.; Escotte-Binet, S.; Amraouza, Y.; Flori, P.; Aubert, D.; Villena, I.; Hafid, J. Cryptosporidium spp., Giardia Duodenalis and Toxoplasma Gondii Detection in Fresh Vegetables Consumed in Marrakech, Morocco. Afr. Health Sci. 2020 , 20 , 1669–1678. [ Google Scholar ] [ CrossRef ]
- Chacin-Bonilla, L.; Sanchez, Y.; Cardenas, R. Factors Associated with Cyclospora Infection in a Venezuelan Community: Extreme Poverty and Soil Transmission Relate to Cyclosporiasis. Trans. R. Soc. Trop. Med. Hyg. 2023 , 117 , 83–90. [ Google Scholar ] [ CrossRef ]
- Temesgen, T.T.; Stigum, V.M.; Robertson, L.J. Surveillance of berries sold on the Norwegian market for parasite contamination using molecular methods. Food Microbiol. 2022 , 104 , 103980. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lalonde, L.; Oakley, J.; Fries, P. Verification and Use of the US-FDA BAM 19b Method for Detection of Cyclospora cayetanensis in a Survey of Fresh Produce by CFIA Laboratory. Microorganisms 2022 , 10 , 559. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Almeria, S.; Shipley, A. Detection of Cyclospora cayetanensis on bagged pre-cut salad mixes within their shelf-life and after sell by date by the U.S. food and drug administration validated method. Food Microbiol. 2021 , 98 , 103802. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bruneto, E.G.; Fernandes-Silva, M.M.; Toledo-Cornell, C.; Martins, S.; Ferreira, J.M.B.; Corrêa, V.R.; da Costa, J.M.; Pinto, A.Y.d.N.; de Souza, D.d.S.M.; Pinto, M.C.G.; et al. Case-Fatality from Orally-Transmitted Acute Chagas Disease: A Systematic Review and Meta-Analysis. Clin. Infect. Dis. 2021 , 72 , 1084–1092. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Franco-Paredes, C.; Villamil-Gómez, W.E.; Schultz, J.; Henao-Martínez, A.F.; Parra-Henao, G.; Rassi, A., Jr.; Rodríguez-Morales, A.J.; Suarez, J.A. A Deadly Feast: Elucidating the Burden of Orally Acquired Acute Chagas Disease in Latin America—Public Health and Travel Medicine Importance. Travel Med. Infect. Dis. 2020 , 36 , 101565. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Velásquez-Ortiz, N.; Ramírez, J.D. Understanding the Oral Transmission of Trypanosoma Cruzi as a Veterinary and Medical Foodborne Zoonosis. Res. Vet. Sci. 2020 , 132 , 448–461. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Velásquez-Ortiz, N.; Herrera, G.; Hernández, C.; Muñoz, M.; Ramírez, J.D. Discrete Typing Units of Trypanosoma Cruzi : Geographical and Biological Distribution in the Americas. Sci. Data 2022 , 9 , 360. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brito, A.K.S.B.d.; Sousa, D.R.T.d.; Silva Junior, E.F.d.; Ruiz, H.J.d.S.; Arcanjo, A.R.L.; Ortiz, J.V.; Brito, S.S.d.; Jesus, D.V.; Lima, J.R.C.d.; Couceiro, K.d.N.; et al. Acute Micro-Outbreak of Chagas Disease in the Southeastern Amazon: A Report of Five Cases. Rev. Soc. Bras. Med. Trop. 2022 , 55 , e0687. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Esper, H.R.; Freitas, V.L.T.d.; Assy, J.G.P.L.; Shimoda, E.Y.; Berreta, O.C.P.; Lopes, M.H.; França, F.O.S. Fatal Evolution of Acute Chagas Disease in a Child from Northern Brazil: Factors That Determine Poor Prognosis. Rev. Inst. Med. Trop. Sao Paulo 2019 , 61 , e27. [ Google Scholar ] [ CrossRef ]
- De Oliveira, A.C.; Soccol, V.T.; Rogez, H. Prevention Methods of Foodborne Chagas Disease: Disinfection, Heat Treatment and Quality Control by RT-PCR. Int. J. Food Microbiol. 2019 , 301 , 34–40. [ Google Scholar ] [ CrossRef ]
- Zeng, H.; Van Damme, I.; Kabi, T.W.; Šoba, B.; Gabriël, S. Sarcocystis Species in Bovine Carcasses from a Belgian Abattoir: A Cross-Sectional Study. Parasit. Vectors 2021 , 14 , 271. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ota, T.; Nakano, Y.; Mizuno, T.; Shiozaki, A.; Hori, Y.; Yamanishi, K.; Hayakawa, K.; Hayakawa, T.; Fujimoto, T.; Nakamoto, C.; et al. First Case Report of Possible Sarcocystis Truncata -Induced Food Poisoning in Venison. Intern. Med. 2019 , 58 , 2727–2730. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rubiola, S.; Moré, G.; Civera, T.; Hemphill, A.; Frey, C.F.; Basso, W.; Colasanto, I.; Vercellino, D.; Fidelio, M.; Lovisone, M.; et al. Detection of Sarcocystis Hominis , Sarcocystis Bovifelis , Sarcocystis Cruzi , Sarcocystis Hirsuta and Sarcocystis Sigmoideus sp. Nov. in Carcasses Affected by Bovine Eosinophilic Myositis. Food Waterborne Parasitol. 2024 , 34 , e00220. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shams, M.; Shamsi, L.; Asghari, A.; Motazedian, M.H.; Mohammadi-Ghalehbin, B.; Omidian, M.; Nazari, N.; Sadrebazzaz, A. Molecular Epidemiology, Species Distribution, and Zoonotic Importance of the Neglected Meat-Borne Pathogen Sarcocystis spp. in Cattle ( Bos Taurus ): A Global Systematic Review and Meta-Analysis. Acta Parasitol. 2022 , 67 , 1055–1072. [ Google Scholar ] [ CrossRef ]
- Zhu, Z.; Ying, Z.; Feng, Z.; Liu, Q.; Liu, J. The Occurrence and Meta-Analysis of Investigations on Sarcocystis Infection among Ruminants (Ruminantia) in Mainland China. Animals 2022 , 13 , 149. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gazzonis, A.L.; Gjerde, B.; Villa, L.; Minazzi, S.; Zanzani, S.A.; Riccaboni, P.; Sironi, G.; Manfredi, M.T. Prevalence and Molecular Characterisation of Sarcocystis Miescheriana and Sarcocystis in Wild Boars ( Sus Scrofa ) in Italy. Parasitol. Res. 2019 , 118 , 1271–1287. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Prakas, P.; Kirillova, V.; Dzerkale, A.; Kirjušina, M.; Butkauskas, D.; Gavarāne, I.; Rudaitytė-Lukošienė, E.; Šulinskas, G. First Molecular Characterization of Sarcocystis Miescheriana in Wild Boars ( Sus Scrofa ) from Latvia. Parasitol. Res. 2020 , 119 , 3777–3783. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Helman, E.; Dellarupe, A.; Cifuentes, S.; Chang Reissig, E.; Moré, G. Identification of Sarcocystis spp. in Wild Boars ( Sus Scrofa ) from Argentina. Parasitol. Res. 2023 , 122 , 471–478. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Metwally, D.M.; Al-Damigh, M.A.; Al-Turaiki, I.M.; El-Khadragy, M.F. Molecular Characterization of Sarcocystis Species Isolated from Sheep and Goats in Riyadh, Saudi Arabia. Animals 2019 , 9 , 256. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Salehi, M.; Spotin, A.; Rostamian, M.; Adami, M. Prevalence and Molecular Assessment of Sarcocystis Infection in Livestock in Northeast Iran. Comp. Immunol. Microbiol. Infect. Dis. 2022 , 80 , 101738. [ Google Scholar ] [ CrossRef ]
- Feng, Y.; Guo, R.; Sang, X.; Zhang, X.; Li, M.; Li, X.; Yang, N.; Jiang, T. A Systematic Meta-Analysis of Global Sarcocystis Infection in Sheep and Goats. Pathogens 2023 , 12 , 902. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Galván-Díaz, A.L.; Alzate, J.C.; Villegas, E.; Giraldo, S.; Botero, J.; García-Montoya, G. Chronic Cystoisospora Belli Infection in a Colombian Patient Living with HIV and Poor Adherence to Highly Active Antiretroviral Therapy. Biomedica 2021 , 41 (Suppl. S1), 17–22. [ Google Scholar ]
- Özmen-Çapın, B.B.; Gürsoy, G.; Tortop, S.; Jabrayilov, J.; İnkaya, A.Ç.; Ergüven, S. Cystoisospora Belli Infection in a Renal Transplant Recipient: A Case Report and Review of Literature. J. Infect. Dev. Ctries. 2021 , 15 , 599–602. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tiryaki, T.O.; Anıl, K.U.; Büyük, M.; Yıldırım, A.Y.; Atasoy, A.; Çiftçibaşı Örmeci, A.; Kalayoğlu Beşışık, S. Prolonged Severe Watery Diarrhea in a Long-Term Myeloma Survivor: An Unforeseen Infection with Cystoisospora Belli . Turk. J. Hematol. 2021 , 38 , 171–173. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kanaujia, R.; Mewara, A. Cystoisospora Belli : A Cause of Chronic Diarrhea in Immunocompromised Patients. Am. J. Trop. Med. Hyg. 2023 , 108 , 1084–1085. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yi, F.; Li, F.; Chen, D.; Ma, Y. Cystoisospora Belli Infection in an AIDS Patient in China: Need for Cautious Interpretation of mNGS. Indian J. Med. Microbiol. 2022 , 40 , 163–165. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rial-Crestelo, D.; Otero, B.; Pérez-Ayala, A.; Pinto, A.; Pulido, F. Severe Diarrhea by Cystoisospora Belli in a Well Controlled HIV-Infected Patient. AIDS 2022 , 36 , 485–486. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rose, G.S.; Arnold, C.A.; Badizadegan, K.; Carter, C.M.; Conces, M.R.; Kahwash, S.B.; Nicol, K.K.; Arnold, M.A. Cytoplasmic Fibrillar Aggregates in Gallbladder Epithelium Are a Frequent Mimic of Cystoisospora in Pediatric Cholecystectomy Specimens. Arch. Pathol. Lab. Med. 2019 , 143 , 1259–1264. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gopinath, A.; Alkhasawneh, A.; Mubeen, A.; Makary, R.; Mohammed, I.; Baskovich, B. Pitfalls in Morphologic Diagnosis of Pathogens: Lessons Learned from the Pseudo- Cystoisospora Epidemic. Int. J. Surg. Pathol. 2021 , 29 , 169–173. [ Google Scholar ] [ CrossRef ]
- Ali, F.M. Detection of Cystoisospora belli among Children in Sulaimaniyah, Iraq. Res. Sq. 2014 . [ Google Scholar ] [ CrossRef ]
- Vizon, K.C.C.; Battad, Z.G., 2nd; Castillo, D.S.C. Contamination of Food-Borne Parasites from Green-Leafy Vegetables Sold in Public Markets of San Jose City, Nueva Ecija, Philippines. J. Parasit. Dis. 2019 , 43 , 651–657. [ Google Scholar ] [ CrossRef ]
- Barua, P.; Banik, K.S.; Saha, S.; Musa, S. Parasitic contamination of street food samples from schoolbased food vendors of Dhaka city, Bangladesh. Bangladesh J. Zool. 2023 , 51 , 217–229. [ Google Scholar ] [ CrossRef ]
- Almaw, A.; Berhan, A.; Solomon, Y.; Malkamu, B.; Eyayu, T.; Workineh, L.; Mekete, G.; Yayehrad, A.T. Balantidium coli ; Rare and Accidental Finding in the Urine of Pregnant Woman: Case Report. Int. Med. Case Rep. J. 2022 , 15 , 105–109. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Giarratana, F.; Nalbone, L.; Napoli, E.; Lanzo, V.; Panebianco, A. Prevalence of Balantidium coli (Malmsten, 1857) Infection in Swine Reared in South Italy: A Widespread Neglected Zoonosis. Vet. World 2021 , 14 , 1044–1049. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Martviset, P.; Sirisabhabhorn, K.; Pumpa, S.; Rhongbutsri, P.; Taylor, A.; Taylor, W.R.J. Urinary Balantidiasis in a Patient with Systemic Lupus Erythematosus and Lupus Nephritis: A Case Report. J. Med. Case Rep. 2020 , 14 , 63. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kennedy Souza Araújo, R.; Rios da Silva, A.; Souza, N.R.; Santos de Melo, K. Parasitological Analysis of Vegetables Sold in Supermarkets and Free Markets in the City of Taguatinga, Federal District, Brazil. Rev. Patol. Trop. 2022 , 51 , 225–234. [ Google Scholar ] [ CrossRef ]
- Calderaro, A.; Buttrini, M.; Montecchini, S.; Rossi, S.; Farina, B.; Arcangeletti, M.C.; De Conto, F.; Chezzi, C. Prevalence of Intestinal Parasitoses in a Non-Endemic Setting during a 10-Year Period (2011–2020): A Focus on Dientamoeba fragilis . Microorganisms 2022 , 10 , 426. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hall, L.M.; Munasinghe, V.S.; Vella, N.G.F.; Ellis, J.T.; Stark, D. Observations on the Transmission of Dientamoeba Fragilis and the Cyst Life Cycle Stage. Parasitology 2024 , 151 , 337–345. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Veraldi, S.; Angileri, L.; Rossi, L.C.; Nazzaro, G. Endolimax Nana and Urticaria. J. Infect. Dev. Ctries. 2020 , 14 , 321–322. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mahittikorn, A.; Udonsom, R.; Koompapong, K.; Chiabchalard, R.; Sutthikornchai, C.; Sreepian, P.M.; Mori, H.; Popruk, S. Molecular Identification of Pentatrichomonas Hominis in Animals in Central and Western Thailand. BMC Vet. Res. 2021 , 17 , 203. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Al-Hasnawy, M.H.; Rabee, A.H. A Review on Trichomonas Species Infection in Humans and Animals in Iraq. Iraqi J. Vet. Sci. 2023 , 37 , 305–313. [ Google Scholar ] [ CrossRef ]
- Abdo, S.M.; Ghallab, M.M.I.; Elhawary, N.M.; Elhadad, H. Pentatrichomonas hominis and other intestinal parasites in school-aged children: Coproscopic survey. J. Parasit. Dis. 2022 , 46 , 896–900. [ Google Scholar ] [ CrossRef ]
- Zhang, H.; Yu, Y.; Li, J.; Gong, P.; Wang, X.; Li, X.; Cheng, Y.; Yu, X.; Zhang, N.; Zhang, X. Changes of Gut Microbiota in Colorectal Cancer Patients with Pentatrichomonas Hominis Infection. Front. Cell. Infect. Microbiol. 2022 , 12 , 961974. [ Google Scholar ] [ CrossRef ]
- Murphy, H.R.; Almeria, S.; da Silva, A.J. BAM Chapter 19b: Molecular Detection of Cyclospora cayetanensis in Fresh Produce Using Real-Time PCR. Bacteriological Analytical Manual (BAM) Main Page. 2016, updated April 2022. Available online: https://www.fda.gov/food/laboratory-methods-food/bam-chapter-19b-molecular-detection-cyclospora-cayetanensis-fresh-produce-using-real-time-pcr (accessed on 2 April 2024).
- Balan, K.V.; Mammel, M.; Lipman, D.; Babu, U.; Harrison, L.M.; Almeria, S.; Durigan, M.; Leonard, S.R.; Jang, H.; Gebru, S.; et al. Development and Single Laboratory Evaluation of a Refined and Specific Real-Time PCR Detection Method, Using Mitochondrial Primers (Mit1C), for the Detection of Cyclospora Cayetanensis in Produce. J. Food Prot. 2023 , 86 , 100037. [ Google Scholar ] [ CrossRef ]
- ISO 18744:2016 ; Microbiology of the Food Chain. Detection and Enumeration of Cryptosporidium and Giardia in Fresh Leafy Green. International Organization for Standardization: Geneva, Switzerland, 2016. Available online: https://www.iso.org/standard/63252.html (accessed on 28 February 2024).
- Dashti, A.; Alonso, H.; Escolar-Miñana, C.; Köster, P.C.; Bailo, B.; Carmena, D.; González-Barrio, D. Evaluation of a Novel Commercial Real-Time PCR Assay for the Simultaneous Detection of Cryptosporidium spp., Giardia Duodenalis , and Entamoeba Histolytica . Microbiol. Spectr. 2022 , 10 , e0053122. [ Google Scholar ] [ CrossRef ]
- Mancusi, A.; Proroga, Y.T.R.; Giordano, A.; Girardi, S.; D’Orilia, F.; Pinto, R.; Sarnelli, P.; Rinaldi, L.; Capuano, F.; Maurelli, M.P. First Application of a Droplet Digital PCR to Detect Toxoplasma Gondii in Mussels. Front. Microbiol. 2023 , 14 , 1238689. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ligda, P.; Claerebout, E.; Robertson, L.J.; Sotiraki, S. Protocol Standardization for the Detection of Giardia Cysts and Cryptosporidium Oocysts in Mediterranean Mussels ( Mytilus Galloprovincialis ). Int. J. Food Microbiol. 2019 , 298 , 31–38. [ Google Scholar ] [ CrossRef ]
- Januskevicius, V.; Januskeviciene, G.; Prakas, P.; Butkauskas, D.; Petkevicius, S. Prevalence and Intensity of Sarcocystis spp. Infection in Animals Slaughtered for Food in Lithuania. Vet. Med. 2019 , 64 , 149–157. [ Google Scholar ] [ CrossRef ]
- Almeria, S.; Assurian, A.; Shipley, A. Modifications of the U.S. Food and Drug Administration Validated Method for Detection of Cyclospora Cayetanensis Oocysts in Prepared Dishes: Mexican-Style Salsas and Guacamole. Food Microbiol. 2021 , 96 , 103719. [ Google Scholar ] [ CrossRef ]
- Luka, G.; Samiei, E.; Tasnim, N.; Dalili, A.; Najjaran, H.; Hoorfar, M. Comprehensive Review of Conventional and State-of-the-Art Detection Methods of Cryptosporidium . J. Hazard. Mater. 2022 , 421 , 126714. [ Google Scholar ] [ CrossRef ]
- World Health Organization. Ending the Neglect to Attain the Sustainable Development Goals: A Global Strategy on Water, Sanitation and Hygiene to Combat Neglected Tropical Diseases, 2021–2030. World Health Organization. 2021. Available online: https://iris.who.int/handle/10665/340240 (accessed on 28 February 2024).
Click here to enlarge figure
| Infectious Agent | Dietary Infection Sources in Cases and Outbreaks * |
|---|---|
| Cryptosporidium spp. | Drinking water, unpasteurized or re-contaminated pasteurized milk, meat, dairy foods, dishes prepared outdoors, barbecued foods, raw foods, raw vegetables, raw fruits, unpasteurized drinks, apple juice, raw shellfish [ , , , , , , , , , , , , , , , ] |
| Entamoeba spp. | Drinking water, alcoholic fermented sap of the Palmyra toddy [ , ] |
| Toxoplasma gondii | Raw vegetables, fruits, raw or undercooked meats, unpasteurized milk, raw cow’s milk cheese, raw or undercooked crustaceans or shellfish, whale meat, drinking water [ , , , , , , , , , , , ] |
| Giardia intestinalis | Drinking water, fresh produce, composite ready-to-eat food, canned salmon, raw oysters, ice cream, noodle salad, chicken salad, dairy products, sandwiches, tripe soup, unpasteurized milk, shellfish, unidentified foods [ , , , , , ] |
| Trypanosoma cruzi | Açaí juice, sugar cane juice, palm, guanabana, guava, milpesillo, majo, mango, mandarin, orange juices, raw meat [ , ] |
| Balantioides coli | None reported |
| Cyclospora cayetanensis | Berries, cilantro, basil, lettuce, ready-to-eat bagged salads, sugar snap peas [ , , , ] |
| Cystoisospora belli | None reported |
| Sarcocystis spp. | Beef, pork, venison, whale meat [ , , ] |
| Blastocystis hominis | None reported |
| Endolimax nana | None reported |
| Dientamoeba fragilis | None reported |
| Pentatrichomonas hominis | None reported |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Rossi, F.; Santonicola, S.; Amadoro, C.; Marino, L.; Colavita, G. Food and Drinking Water as Sources of Pathogenic Protozoans: An Update. Appl. Sci. 2024 , 14 , 5339. https://doi.org/10.3390/app14125339
Rossi F, Santonicola S, Amadoro C, Marino L, Colavita G. Food and Drinking Water as Sources of Pathogenic Protozoans: An Update. Applied Sciences . 2024; 14(12):5339. https://doi.org/10.3390/app14125339
Rossi, Franca, Serena Santonicola, Carmela Amadoro, Lucio Marino, and Giampaolo Colavita. 2024. "Food and Drinking Water as Sources of Pathogenic Protozoans: An Update" Applied Sciences 14, no. 12: 5339. https://doi.org/10.3390/app14125339
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

IMAGES
VIDEO
COMMENTS
5.1 CONCLUSION. The brands of sachet water generally met the physical and chemical quality standards of the Ghana. Standards Board (1998) and World Health Organisation (2007), even though 90% ...
Bottled water quality is higher than for sachet water and the latter largely influenced by microbe contamination. Future perspectives in water quality monitoring and assessment are suggested in the evaluation of emerging contaminants and micro-pollutants and the utilisation of internet-enabled technologies.
This study assessed the physicochemical and microbiological quality of sachet drinking water samples in Kumasi, a major city in Ghana. Samples were collected from various sources within the city. Physicochemical properties, including pH, total dissolved solids, and concentrations of calcium, sodium, potassium, and magnesium ions, were analyzed following established protocols. Additionally ...
The study assessed the physicochemical quality of sachet water produced and/ or sold in some Local Government Areas of Kano State, Nigeria. Twenty-one (21) sachet water samples from seven (7 ...
Sachet water is now an important component of regional water security, although with attendant issues related to governance, quality control, environmental pollution, and social justice. This paper reviews the seminal literature on sachet water in West Africa, with particular emphasis on Ghana and Nigeria, where most studies have focused.
Background: Sachet water, popularly known as "pure water" has become an invaluable entity in most Ghanaian households.Despite its importance, there is no extensive nationwide investigations on its wholesomeness for consumption. The aim of this study was to determine the microbiological quality of 41 brands of sachet water sampled in 16 districts across 5 regions in Ghana.
As a form of packaged water, sachet water availability has helped bridge the gap in population access to drinking water [3, 6, 7]. However, concerns about the safety, microbial quality and public health implication of these products have been reported in the literature [8-11].
In general, sachet waters were within standards for all parameters except lead in batch A & B, iron in batch E, and E. coli in all water brands. Human health risk showed the order of THI as NO 3- > Pb > F - > Fe for batch A & B samples and NO 3- > F - > Pb > Fe for batch C, D & E. This showed nitrate constituting over 50% of the THI while batch ...
of packaged sachet water, previous work showed that there is a challenge associated with its quality as a result of isolation of some microbes and non-compliance with expected parameters.
Sachet water (SW) is a major source of drinking in most Nigerian homes, thus making it a possible conveyance medium for health risks due to contamination if persist rather than for replenishment of the body. This study collected SW from three busy neighborhoods in South-West Nigeria and investigated for the presence of indicator bacteria (Escherichia coli (E. coli), Total Coliform (TC), Total ...
Contamination of Sachet Water in Nigeria: Assessment and Health Impact. 1. Chukwuemeka. The quality of these 'pure water' is reviewed; its physical examination, microbial assessments, its impacts on health, and the various strategies adopted by the concerned authorities to regulate this thriving industry are reviewed.
The use of water is restrained by its quality which makes it unhealthy for a particular use. Water quality assessment is therefore an important aspect of water resource evaluation; as physical, biological and anthropogenic factors are important in water quality assessment (Eze and Abua, 2003). Hence, water quality depends on the physical ...
Sachet water is a fast growing source of drinking water and is widely accepted by the public due mainly to the low price, convenience, ubiquity, and perception of higher quality than tap water. Unfortunately, this often is not always the case, as about 50% of sachet water sold in the streets of Lagos Nigeria were reported not be potable ...
Sachet water. The flowchart in Fig. 2 illustrates the life cycle of production and consumption process of sachet water. There are various sources of water, such as well, borehole, river among others, and are used for production based on their availability (Dunmade et al. 2016).The water will be first pumped either from any of the listed sources of water into storage tanks for biological and ...
In this review study, over 50 articles were carefully analyzed. Collected data unveiled regional variations in the quality of sachet water across Nigeria. Noteworthy concerns revolve around levels of pH, total hardness, magnesium, calcium, nickel, iron, lead, mercury, arsenic, and cadmium.
Water from boreholes and packaged commercial sachet water from different areas in a community in southern Nigeria was analyzed with membrane filtration for a snapshot of heterotrophic count and coliforms. Two boreholes out of the 20 analyzed had counts of over 500 Cfu/mL and 7 boreholes indicated the presence of coliforms. Sixteen samples out of 20 sachet water brands analyzed showed a ...
6. Sabuz Sachet water C1-9053L Plot No.4 westerm bypass opposite Bafarawa flour mill Sokoto, Sokoto state - - 7. GB Nur Sachet water E1-5139L No.24 Behind GwiwaEka, water Board Sokoto - - 8. Deral Sachet water E1-0833L Opposite NBC Academy secondary school Sokoto + + 9. Aqua Solar Sachet water A1-4048L Gidansalanke area, behind
Abstract: This study presents the result obtained from the quality assessment of some sachet water produced in Irele, Ondo State, Nigeria. Eight different brands of sachet water certified by the National ... Reports from the literature have shown that eliminating or reducing water-borne diseases such as diarrhea, sleeping sickness, and guinea ...
The aim of this research is to investigate the effect of long-term storage conditions on the physicochemical and microbial quality of selected sachet water brands sold within the Samaru community and its health implication for consumers. Three brands of sachet water were subjected to different storage conditions and were analyzed for microbial and physicochemical parameters at intervals of 3 ...
The inadequacy of pipe borne water-supply in Nigeria is a growing problem; as a result people resort to buying water from vendors, and sachet or bottled water became a major source of drinking water.
Sachet water microbiological quality. One branded sachet water with the most patronage was collected in triplicate from each of the 41 communities. Twenty-four (58.5%) samples tested positive for the presence of total coliforms with 7 (17.1%) of the positive samples positive for fecal E. coli.
the Review. possibility provide information of testing a chemical on the fate tracers over time and in routinely understand as part waters if chemical or tracers program, identification of human sewage tracers is complicated by a number of variables a variety of environmental conditions. investigate monitoring.
Abstract. Nigeria is the most populated black nation in the world with about 199 million people. About 66.3 million Nigerians do not have access to safe drinking water. In this study, research ...
This narrative review was aimed at collecting updated knowledge on the risk factors, illnesses caused, and measures for the prevention of protozoan infections transmitted by food and drinking water. Reports screened dated from 2019 to the present and regarded global prevalence in food handlers, occurrence in food and drinking water, impact on human health, and recently reported outbreaks and ...