Our range of over 180 online courses are fully accredited, trusted by more than 3 million learners and ideal for training you and your team.
- Food Hygiene
- Health and Safety
- Safeguarding
- Asbestos Awareness
- Fire Safety
- Mental Health
- Health and Social Care
- Business Essentials
- Team training

Welcome to the Hub, the company blog from High Speed Training.
Select a topic to find the most up to date, practical information and resources produced by our experts to support you in your professional life.
- Health & Safety

Promoting Effective Communication in Health and Social Care
Communication plays an instrumental role in health and social care and is a core aspect of your working relationships. Being able to communicate effectively is a skill that has a range of benefits, perhaps most importantly that it helps you to deliver person-centred, high-quality care.
However, communication isn’t as straightforward as it might first appear. It’s not simply about what we say, but about relationships, understanding, and ensuring that our needs are met and our wishes are addressed. It is a two-way process involving one person expressing themselves and being understood by another.
This article outlines the role of communication in health and social care, examining its benefits and providing you with the knowledge you need to overcome any barriers and communicate effectively.
What is the Role of Communication in Health and Social Care?
The role of communication in health and social care is an incredibly important one. The nature of health and social care environments means that you will be interacting with multiple people on a daily basis, and it’s essential that you are able to communicate effectively with them.
It’s important to remember that communication looks different to everyone. There are many ways that people communicate, including verbal communication (speaking aloud), written communication, such as sending emails or keeping records, and non-verbal communication, such as hand gestures or facial expressions. However, there are also many additional ways that people communicate, depending on what works best for them and their needs. For example, individuals may communicate using sign language, Makaton or Braille. It’s important that all types of communication are supported.
Interested in Learning More?
If you’re looking for an in-depth and effective way to improve communication in a health care setting, our Communication Skills in Health & Social Care Course will provide you with the information and guidance you need to develop your existing skills and use a variety of communication methods.
Finally, developing good communication skills is essential if health and social care workers are to develop other skills. For example, you would be unable to offer person-centred care if you couldn’t communicate well with the individual in your care and understand their needs and preferences. Similarly, you need to be able to communicate well with individuals in order to uphold their privacy and dignity and promote their independence.

Why is It Important for Healthcare Professionals to Have Effective Communication?
Being able to communicate well helps to ensure that you can carry out your role effectively. It is central to finding out service users’ needs and wishes, delivering high-quality care, and building good relationships with service users, any visitors and your colleagues.
Service Users
Being able to communicate effectively is crucial for having good relationships with your service users. You will be able to find out their needs and wishes and avoid any potentially distressing misunderstandings and miscommunications. What’s more, if you communicate effectively with a service user, they are much more likely to have confidence in what you tell them and put their trust in you.
Communicating poorly with service users can have a range of consequences. For example, if you adopt closed body language such as crossing your arms, they may feel like you are unapproachable or unfriendly. Similarly, if you miscommunicate and share inaccurate information, a person’s care and support could be affected – for example, if they have an allergy and you miscommunicate this to kitchen staff.
Your Colleagues
Communication is also the foundation of your working relationships. Your job role will likely involve you sharing relevant information with colleagues about service users, making decisions, listening to the views of others and acting on them.
Communicating effectively with colleagues is key if you are to deliver your mutual goal of providing high-quality care to individuals. For example, if an individual wants to change something about how their care is delivered, then it is also important that you share this information effectively with colleagues who care for the individual so that they are aware and meet the individual’s needs. Additionally, it’s crucial that you communicate this change formally in the individual’s care plan so that it is documented and everyone who cares for them can see it.
Finally, being able to communicate effectively is central to the relationship you have with visitors, such as an individual’s family. A key part of communication is confidentiality – respecting all individuals’ personal data and protecting it by ensuring that it is only shared with others on a need-to-know basis and with consent.
If an individual gives you consent to share information with somebody, it’s crucial that you communicate this information in a professional manner. Speak to the person out of earshot of other people to avoid sharing information with those who don’t need to know.
It’s also important that your communication is empathetic and understanding. There may be times when you have to deliver bad news to a service user’s family and it’s crucial that you communicate sensitive topics in a suitable and professional manner.

What are the Barriers to Communication in Health and Social Care?
While it’s clear to see how important communication is, there are a number of barriers that may prevent you, and those who you care for and support, from communicating effectively. These can include:
- Emotions and attitudes – these can play a large role in communication. For example, if you rush a conversation with a service user because you are busy, or come across as abrupt, you may make them feel frustrated and unlikely to want to communicate. Similarly, if an individual feels upset or angry, they may not want to communicate with you or may struggle to communicate without letting their emotions take over.
- Language – if you and the service user speak different languages, this may make it difficult to communicate. Additionally, even having a strong accent or speaking in a dialect associated with where you live can make it difficult for others to understand you.
- Health conditions – some individuals in your care may have a health condition that makes it difficult for them to communicate. For example, if they have had a stroke, or if they have dementia, this may have affected their ability to think rationally and reason clearly. Additionally, if someone is experiencing a mental health condition such as depression, they may find it difficult to express how they are feeling.
- Physical barriers – someone may be physically unable to communicate, such as if they are breathless or in pain. Additionally, the use of PPE, such as face coverings, can make it especially difficult for some people to communicate -for example, if they are deaf and rely on lip reading, if they use facial expressions to help them understand, or if they have hearing difficulties and can’t hear people clearly through the face covering.
- Environment – certain environments can make it difficult to communicate in – for example, if the room is noisy and you struggle to hear others. Additionally, if the environment is uncomfortable for the service user, such as if it is too dark or too warm/cold, they may be less likely to want to communicate.

How to Promote Effective Communication in Health and Social Care
While there are many barriers to effective communication, you need to overcome them if you are to offer person-centred care. Recognising when someone is struggling to communicate and putting actions into place that will help them can vastly improve their quality of life.
Remember that communication is a two-way process: it involves both giving and receiving messages. Therefore, to be able to promote effective communication, you need to consider the way you give messages as well as receive them from others. If you are wanting to promote more effective communication, you should think about the following:
Consider the Environment and Distance
Think about the way that you position yourself in relation to a service user. For example, your chairs should be facing each other if you are sitting and having a conversation. Additionally, it’s important to think about how close you are to them in distance. If you are too close, they may feel uncomfortable and as though you are invading their personal space.
The nature of health and social care means that you may sometimes have to get closer to an individual, such as if you are taking a blood sample or providing personal care. Ensure you always inform the individual of what you are about to do before you move closer to them.
Listen Actively
When an individual communicates with you, it’s important that you employ active listening skills. This means listening closely to what they are saying and then employing certain techniques, such as nodding to encourage them to keep talking, changing your facial expression so that you are smiling or raising your eyebrows in response to what they have said, and adopting open body language such as open arms and uncrossed legs. This is important for making an individual feel valued and as though they are being listened to.

Give Them Time
Give people enough time to communicate and don’t rush them. For certain individuals, such as some who have learning disabilities, they may take longer to process information and gather their thoughts, so giving them plenty of time is crucial. Additionally, there may be some people who have reduced energy levels, such as if they are in hospital with illness, who may need a bit longer to think before they respond. Ensure that you are guided by the individual and communicate at a pace that is comfortable for them.
Ask Questions
Don’t be afraid to ask if you don’t quite understand what someone is saying, rather than guessing what you think they mean or making assumptions about what you think they’ve said. For example, concluding that someone has expressed they want their care to be delivered in a certain way based on assumptions can be damaging if they meant something completely different.
Similarly, if you haven’t heard someone, ask them to repeat themselves rather than pretending to hear or guessing what you think they said. Physical barriers to communication, such as the use of face masks, can make this especially difficult, so ensure that you ask questions to avoid any miscommunications or misunderstandings.
Listen to More Than Just Words
Communication is about so much more than simply what somebody says. It also includes:
- Tone of voice – this is about the way somebody speaks. Tone of voice is important for conveying meaning; if somebody is feeling low they may speak in a monotonous tone, or if somebody is excited their tone may be more varied and enthusiastic.
- Pace – this refers to the speed at which somebody speaks. For example, somebody may speak quickly if they are excited.
- Body language – this can be open or closed. Closed body language, such as fiddling or turning away, can indicate that someone is disinterested or nervous.
- Gestures – these can emphasise what is being said or act as an alternative to speech. For example, somebody may use hand movements to express or emphasise what they are feeling.
- Facial expressions – these can show emotions or reactions, such as smiling when you are happy or raising your eyebrows when you’re interested.
However, it’s important not to make assumptions about how somebody is feeling or what they’re trying to communicate. For example, we may think that if somebody is maintaining eye contact they are engaged, and if they are looking away they are disengaged. However, in some cultures eye contact is considered impolite. Avoid making assumptions and ensure you take the interaction as a whole, asking questions if you are unsure.
Communication is a central part of health and social care, and being able to communicate effectively with service users, colleagues and visitors is a crucial part of delivering high-quality and person-centred care. Avoid making assumptions about what you think people mean, address any barriers to communication, and remember that communication is a two-way process.
Further Resources:
- Person-Centred Care Training
- Compassion in Care: What are the Six Cs?
- What is Person-Centred Care and Why is it Important?
- How to Maintain Confidentiality in Health and Social Care
- Champions in Healthcare: Role and Responsibilities
- Using a Personal Development Plan in Health and Social Care
- Guidance on Complaints Procedures in Health and Social Care
- Defining the Different Types of Discrimination in Health and Social Care
- What are Difficult Conversations in Health and Social Care?
- Duty of Care in Health and Social Care: Responsibilities & Examples
- What are Inequalities in Health and Social Care?
- How to Promote Empowerment in Health and Social Care
- What is the Role of Active Participation in Health and Social Care?
- How to Support Professional Development in Health and Social Care

Post Author

Her favourite article is Promoting Effective Communication in Health and Social Care
The National Weather Service has issued an alert. Visit the KatSafe site for details.
COVID-19 Community Level: Low
- SHSU Online
- Academic Affairs
- Academic Calendar
- Academic Community Engagement (ACE)
- Academic Planning and Program Development
- Academic Success Center
- Accepted Students and Bearkat Orientation
- Admissions (Undergraduate)
- Admissions (Graduate)
- Admission Requirements
- Advising (SAM Center)
- Agricultural Sciences
- Alumni Association
- American Association of University Professors
- Analytical Laboratory
- Application for Admission
- Army ROTC - Military Science
- Arts & Media
- Auxiliary Services
- Bearkat Bundle
- Bearkat Camp
- Bearkat EduNav (BEN)
- Bearkat Express Payment
- Bearkat Kickoff
- Bearkat Marching Band
- Bearkat OneCard
- Bearkat Transfer Scholarship
- Blinn College Transfers
- Budget Office
- Business Administration
- Campus Activities & Traditions
- Campus Recreation
- Career Success Center
- Cashier's Office
- Charter School
- Class Schedule
- Computer Account Creation
- Computer Labs
- Continuing Education
- Controller's Office
- Counseling Center
- Criminal Justice
- Current Students
- Data Analytics and Decision Support
- Dean of Students' Office
- Departments
- Department of Dance
- Dining Services
- Disbursements Services
- Educator Preparation Services
- Emergency Management
- Employee Services Center
- Employment Opportunities
- Engineering Technology
- Enrollment Success
- Enrollment Marketing and Communication
- Enrollment Services - TWC
- Exchange Mail
- Facilities Management
- Faculty Senate
- Faculty/Staff Directory
- Final Exam Schedule
- Finance and Operations
- Financial Aid
- Food & Housing Access Network
- First-Generation Center
- First-Year Experience
- Free Speech & Expressive Activity
- General Information
- Garrett Center
- Global Engagement
- Golf Course
- Graduate Admissions
- The Graduate School
- Great Names
- Health Sciences
- Honors College
- Human Resources
- Humanities and Social Sciences
- IT@Sam Service Desk
- Institutional Animal Care & Use Committee (IACUC)
- Internal Grant Program
- Institutional Review Board (IRB)
- Integrated Marketing & Communications
- Internal Audit
- Joint Admission Students
- Jr. Bearkats
- Leadership Academy
- Leadership Initiatives
- LEAP Center
- Library (NGL)
- Lone Star College Transfers
- Lowman Student Center
- Mail Services
- Map - Campus
- Marketing & Communications
- McNair Program
- Military Science
- Music Choir
- MyGartner Portal
- National Student Exchange
- Office of the President
- Ombuds Office
- Online Information Request
- Organization Chart
- Orientation - New Student
- Osteopathic Medicine
- Parent & Family Relations
- Payroll Office
- PGA Golf Management
- Pre-Health Professional Student Services
- Procurement and Business Services
- Procurement Opportunities
- Program Analytics
- Prospective Students
- Quality Enhancement Plan
- Reading Center
- Registration
- Registrar's Office
- Research Administration (Post-Award)
- Research and Sponsored Programs
- Residence Life
- SACSCOC Reaffirmation
- Sam Houston Memorial Museum
- Services for Students with Disabilities
- Schedule of Classes
- Scholarships
- SHSU MarketPlace
- Spirit Programs
- Smith-Hutson Endowed Chair of Banking
- Smith-Hutson Scholarship Program
- Staff Senate
- Student Affairs
- Student Government Association
- Student Health Center
- Student Legal Services
- Student Money Management Center
- Student Success Technologies
- Study Abroad
- Summer Camps
- Supplemental Instruction
- Technology Tutorials
- Testing Center
- Theatre and Musical Theatre
- Title IX (Sexual Misconduct)
- Tour the University
- Transcripts
- Transfer Equivalency Guide
- Transfer Students (Articulation)
- Travel Services
- Undergraduate Research Symposium
- University Advancement
- University Hotel
- University Police Department
- Visitor Services
- The Woodlands Center
Communication for Health and Social Care Professionals , Undergraduate Certificate
Available: On Campus and Online
The Undergraduate Certificate in Communication for Health and Social Care Professionals helps students develop professional communication skills in the health and social care industries. The curriculum combines courses from the department’s existing curriculum to serve students interested in a health and social care career, such as nurses, health technicians, patient ambassadors, health care managers, human service specialists, counselors, therapists, and nutritionists.
The certificate is a freestanding credential that can be earned as a stand-alone certification or awarded on the way toward a bachelor's degree.
Gain In-Demand Skills
Students in the Undergraduate Certificate in Communication for Health and Social Care Professionals program develop and refine in-demand, marketable skills, including:
- Communication Skills. Students will be able to demonstrate effective verbal and nonverbal communication skills in health contexts.
- Leadership. Students will be able to demonstrate effective leadership of small groups in health contexts.
- Problem Solving. Students will synthesize information and present different viewpoints related to health communication.
- Planning. Students will gather and evaluate health information critically.
- Interpersonal Communication. Students will be able to demonstrate interpersonal competence in health contexts.
Program Breakdown
| Category | Summary |
|---|---|
| 18 Credit Hours | |
| Fall, Spring, Summer | |
Current SHSU Students
Current students have an opportunity to gain a valuable certificate upon completion of the courses.
To enroll, schedule an appointment or virtual drop-in with your advisor as soon as possible and let them know you would like to apply for this certificate program.
Go to the SAM Center

- Reading List
- Upload Document

6 – HSC CM4: Communication in Health and Social Care
1.1 explain the use of communication in health and social care settings..
Communication is the exchange of information or interaction between two or more people. It is also a way of sending and receiving information from one person to another. There are several ways for people to interact, such as verbal communication (speaking out), written communication (such as emails), and non-verbal communication (gestures, facial expressions).
Communication in health and social care entails passing on and understanding information between care workers and care receivers. It is a useful tool to inform care receivers on how to maintain their health conditions and what steps to take when having any health issues.
Communication is extremely important in the health/social care environment because it gives more space for openness and transparency. This means that it helps care receivers to open up more about their health to the health and social care workers and for care workers to talk more transparently to patients about how they are doing, whether they are getting better or offering them comfort and reassurance. For example, service users may feel like they are not in control when in a health and social care facility. But through good communication, transparency, and openness from care workers, they can understand that the service they are receiving is actually person-centred.
Communication is also effective in improving health care services as team members are able to pass information within the organization.
If team members are able to communicate effectively, it will lead to improved health care services. This is because team members will be able to share important information within the organization, which will help to improve the overall quality of care. Additionally, effective communication can help to reduce errors and improve patient safety.
Other answers in the full document:
- 1.2. Explain the impact of communication on service delivery outcomes.
- 2.1. Outline theories of communication.
- 2.2. Describe communication and language needs and preferences of individuals.
- 2.3. Explain factors that influence communication and interactions.
- 2.4. Explain how barriers to communication can be overcome.
- 2.5. Explain how to communicate to meet the needs of others.
- 2.6. Explain how to access additional support or services to enable individuals to communicate effectively.
- 3.1. Explain the meaning of the term confidentiality.
- 3.2. Summarise legislation, policies, procedures and codes of practice relating to the management of information
- 3.3. Explain the potential tension between maintaining confidentiality and the need to disclose information.
- 4.1. Describe how to ensure the security of data when accessing and storing records.
- 4.2. Describe how to ensure the security of data when sharing information.
- 4.3. Explain how to maintain records
Related Documents
3 – hsc cm3: safeguarding in health and social care, 9 – hsc cm1: equality, diversity and rights in health and social care, 1 – unit 18: cleaning, decontamination and waste management.
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Featured Campaigns
Take a look at what CDC programs are doing to reach their target audiences. Explore these links to current campaigns, health communication and social marketing materials, and interventions. Knowing what has worked may help you develop your health promotion materials and campaigns.

Getting older doesn’t have to mean giving up the activities you enjoy.

CDC’s Let’s Stop HIV Together (Together) campaign is the national campaign of the Ending the HIV Epidemic in the U.S. (EHE) initiative and the National HIV/AIDS Strategy . Together is an evidence-based campaign created in English and Spanish. It aims to empower communities, partners, and health care providers to reduce HIV stigma and promote HIV testing , prevention , and treatment .

Over 700 women die each year in this country from problems related to pregnancy or delivery complications. Every death is a tragedy, especially when we know that two thirds of pregnancy-related deaths could be prevented. As many as 50,000 women experience severe, unexpected health problems related to pregnancy that may have long-term health consequences.
The Centers for Disease Control and Prevention (CDC) launched the first-ever federally paid national tobacco education campaign— Tips From Former Smokers ® ( Tips ® ) – in March 2012. The Tips campaign profiles real people living with serious long-term health effects from smoking and secondhand smoke exposure. Tips also features compelling stories of the toll these smoking-related conditions have taken on family members .
The Tips campaign engages doctors, nurses, dentists, pharmacists, and many other healthcare providers so they can encourage their smoking patients to quit for good.
How Right Now: Getting Resources to Manage Stress, Stay Healthy in COVID-19 Pandemic
The Clean Hands Count campaign aims to:
- Improve healthcare provider adherence to CDC hand hygiene recommendations
- Address the myths and misperceptions about hand hygiene
- Empower patients to play a role in their care by asking or reminding healthcare providers to clean their hands
To help prevent chronic disease and promote healthy living, CDC works with communities, states, tribes, territories, and a variety of federal and nongovernmental partners. This website shares information and resources for communities to make healthy living easier where people live, learn, work, and play.
Medicines are used to treat diseases, manage conditions, and relieve symptoms. Medicines are generally safe when used as prescribed or as directed on the label, but there are risks in taking any medicine.
Our campaigns provide crucial information on prediabetes, type 2 diabetes prevention, and diabetes management to empower people to safeguard and improve their health. Campaign messaging reaches our key audiences through their preferred communication channels, including social media and other digital platforms, print, radio, and broadcast TV.
A health communications campaigns that promote physical activity as a method of arthritis self-management. These campaigns are for general use by state health departments, their partners, and other community organizations.
A broad awareness campaign to promote self-management education (SME) interventions as a chronic disease self-management strategy. SME refers to programs that help people who have ongoing health conditions learn how to live life to the fullest.
To receive email updates about this page, enter your email address:

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Big Data for Social Good
Big social problems require big data solutions.
Using real-world data and policy interventions as applications, this Harvard Online course will teach core concepts in data science, economics, and statistics and equip you to tackle some of the most pressing social challenges of our time.

What You'll Learn
The American Dream—the idea that through hard work any child can rise up and achieve a higher standard of living than their parents—is fading: only half of kids today will go on to earn more than their parents did. Why has this happened? And, how can we reverse the fading of the American Dream? “Big data” is often associated with corporations seeking to improve products by collecting data on customers. What if we could use big data for social good—to address problems such as the fading American Dream, growing income inequality, or persistent racial disparities? Big Data for Social Good will teach you how to use big data, coupled with the tools of data science and economics, to solve some of the most important social problems of our time. Big data can help us cut through politically charged debates and find out what policies actually work from a scientific perspective, making the often-discussed notion of “evidence-based policymaking” a reality. Using big data, we can see how the specific neighborhoods in which we grow up and the schools we attend shape our life outcomes—and how we can take these insights to create better opportunities for all.
The course will be delivered via HBS Online’s course platform and immerse learners in real-world examples from experts at industry-leading organizations. By the end of the course, participants will be able to:
- Examine historical income, education and family support, and geography to understand how these economic factors lead to upward mobility
- Understand how big data is used to identify the causes of socioeconomic disparities and how data can lead to evidence-based action and outcomes
- Explore economic methodologies, such as statistical models, regression analysis, and quasi-experiments in data set combinations
- Utilize economic frameworks and apply them to your work
- Use evidence to engage and gain support of communities and constituents to drive systemic policy developments and changes
Your Instructor
Raj Chetty, PhD, is the William A. Ackman Professor of Public Economics at Harvard University and Director of Opportunity Insights. His research uses “big data” to understand how we can give children from disadvantaged backgrounds better chances of succeeding. Chetty's research combines empirical evidence and economic theory to help design more effective government policies. His work on topics ranging from tax policy and unemployment insurance to education and affordable housing has been widely cited in academia, media outlets, and Congressional testimony. He has received numerous awards for his research, including a MacArthur "Genius" Fellowship and the John Bates Clark medal, given to the economist under 40 whose work is judged to have made the most significant contribution to the field.
Real World Case Studies
Affiliations are listed for identification purposes only.

Geoffrey Canada
Hear from Geoffrey Canada, an educator, social activist, and author, about his pioneering work in helping children and families in Harlem and about place-based innovations.

Sarah Oppenheimer
Learn how Sarah Oppenheimer’s work bridges research with applied policy and practice to address poverty and support families’ outcomes.

Nathaniel Hendren
Explore research based on the core question “Do markets provide opportunity?”
Available Discounts and Benefits for Groups and Individuals
Experience Harvard Online by utilizing our wide variety of discount programs for individuals and groups.
Past participant discounts.
Learners who have enrolled in at least one qualifying Harvard Online program hosted on the HBS Online platform are eligible to receive a 30% discount on this course, regardless of completion or certificate status in the first purchased program. Past Participant Discounts are automatically applied to the Program Fee upon time of payment. Learn more here .
Learners who have earned a verified certificate for a HarvardX course hosted on the edX platform are eligible to receive a 30% discount on this course using a discount code. Discounts are not available after you've submitted payment, so if you think you are eligible for a discount on a registration, please check your email for a code or contact us .
Nonprofit, Government, Military, and Education Discounts
For this course we offer a 30% discount for learners who work in the nonprofit, government, military, or education fields.
Eligibility is determined by a prospective learner’s email address, ending in .org, .gov, .mil, or .edu. Interested learners can apply below for the discount and, if eligible, will receive a promo code to enter when completing payment information to enroll in a Harvard Online program. Click here to apply for these discounts.
Gather your team to experience Data Privacy and Technology and other Harvard Online courses to enjoy the benefits of learning together:
- Single invoicing for groups of 10 or more
- Tiered discounts and pricing available with up to 50% off
- Growth reports on your team's progress
- Flexible course and partnership plans
Learn more and enroll your team !
Who Will Benefit
Community activists and nonprofits
Use big data and economic principles to gain support and advocate for change in underserved communities.
Policy advocates and public sector employees
Serve the needs and requests of your communities better through evidence-based research and defined policy outcomes.
Students and Recent Graduates
Learn how to combine disparate data sets that lead to key findings, insights, and solutions for addressing economic societal problems.
Course Syllabus
Learning requirements: In order to earn a Certificate of Completion from Harvard Online and Harvard Business School Online, participants must thoughtfully complete all 8 modules, including satisfactory completion of the associated assignments, by stated deadlines.
Download Full Syllabus
- Study The Opportunity Atlas and Brownsville, Brooklyn cases
- Recognize some of the statistical techniques used to measure and map opportunity
- Explore granular variation in levels of upward mobility
- Study the moving to opportunity experiment
- Consider the ethical and societal impacts of social experiments
- Explore two methods for causal inference
- Interpret methods for establishing statistical significance
- Study cases like Creating Moves to Opportunity and the Harlem Children's Zone
- Describe the factors that are correlated with differences in upward mobility across places
- Understand the relationship between supply and demand
- Explain the distinction between constraints and barriers
- Study the American Dream and social capital
- Understand the concept of social capital
- Understand how economic policies can "pay for themselves" in the long terms
- Identify different statistical approaches to measuring upward mobility
- Investigate both redistributive policies and policies that invest in human capital
- Study the effect of mentorship
- Explain the relationship between economic growth and equality of opportunity
- Identify data sources for studying innovation
- Explore innovation as a potential path for increasing both equality of opportunity and economic growth
- Understand how to use propensity score reweighting
- Study college mobility rates
- Explore the extent to which colleges and universities in the US either promote or hinder upward mobility
- Understand how to measure the causal effect of college on a student’s outcomes
- Recognize the importance of both access and outcomes in determining a college’s Mobility Rate
- Understand methods for standardizing data from across different sources
- Study the importance of class size and teacher quality in determining students’ outcomes
- Understand dynamic models and steady states
- Explore differences in upward mobility by race/ethnicity and gender
- Explain that differences in upward mobility lead to the persistence of mobility gaps in “steady state”
Earn Your Certificate
Enroll today in Harvard Online's Big Data for Social Good course.

Still Have Questions?
Are there discounts available for this course? What are the learning requirements? How do I list my certificate on my resume? Learn the answers to these and more in our FAQs.
Related Courses
Reducing racial disparities in health care.
In partnership with the Disparities Solutions Center at MGH, this course will help you deliver high-quality health care to all through organizational change.
Data Privacy and Technology
Explore legal and ethical implications of one’s personal data, the risks and rewards of data collection and surveillance, and the needs for policy, advocacy, and privacy monitoring.
Outsmarting Implicit Bias
Designed for individuals and teams, this Harvard Online course taught by preeminent Harvard Professor Mahzarin Banaji teaches the science of implicit bias and strategies to counter the impact of bias in the workplace.
The independent source for health policy research, polling, and news.
Disparities in Health and Health Care: 5 Key Questions and Answers
Nambi Ndugga and Samantha Artiga Published: Apr 21, 2023
Introduction
The COVID-19 pandemic and nationwide racial justice movement over the past several years have heightened the focus on health disparities and their underlying causes and contributed to the increased prioritization of health equity. These disparities are not new and reflect longstanding structural and systemic inequities rooted in racism and discrimination. Although growing efforts have focused recently on addressing disparities, the ending of some policies implemented during the COVID-19 pandemic, including continuous enrollment for Medicaid and the Children’s Health Insurance Program (CHIP), may reverse progress and widen disparities. Addressing health disparities is not only important from an equity standpoint, but also for improving the nation’s overall health and economic prosperity. This brief provides an introduction to what health and health care disparities are, why it is important to address disparities, what the status of disparities is today, recent federal actions to address disparities, and key issues related to addressing disparities looking ahead.
What are health and health care disparities?
Health and health care disparities refer to differences in health and health care between groups that stem from broader inequities . There are multiple definitions of health disparities. Healthy People 2030 defines a health disparity, as “a particular type of health difference that is linked with social, economic, and/or environmental disadvantage,” and that adversely affects groups of people who have systematically experienced greater obstacles to health. The Centers for Disease Control and Prevention (CDC) defines health disparities as, “preventable differences in the burden, disease, injury, violence, or in opportunities to achieve optimal health experienced by socially disadvantaged racial, ethnic, and other population groups and communities.” A health care disparity typically refers to differences between groups in health insurance coverage, affordability, access to and use of care, and quality of care. The terms “health inequality” and “inequity” are also sometimes used to describe unjust differences. Racism, which the CDC defines as the structures, policies, practices, and norms that assign value and determine opportunities based on the way people look or the color of their skin, results in conditions that unfairly advantage some and disadvantage others, placing people of color at greater risk for poor health outcomes.
Health equity generally refers to individuals achieving their highest level of health through the elimination of disparities in health and health care. Healthy People 2030 defines health equity as the attainment of the highest level of health for all people and notes that it requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and health and health care disparities. The CDC describes health equity as when everyone has the opportunity to be as healthy as possible.
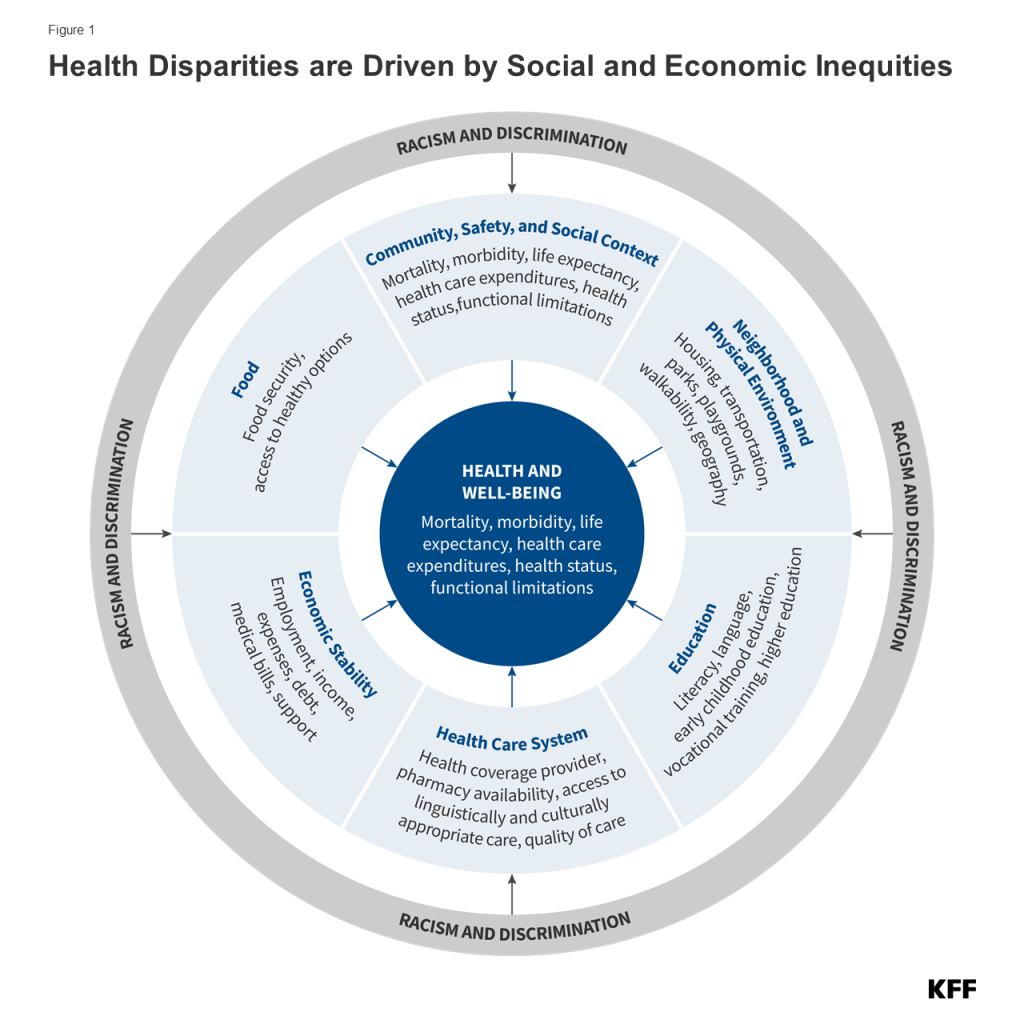
A broad array of factors within and beyond the health care system drive disparities in health and health care (Figure 1) . Though health care is essential to health, research shows that health outcomes are driven by multiple factors, including underlying genetics, health behaviors, social and environmental factors, and access to health care. While there is currently no consensus in the research on the magnitude of the relative contributions of each of these factors to health, studies suggest that health behaviors and social and economic factors, often referred to as social determinants of health , are the primary drivers of health outcomes and that social and economic factors shape individuals’ health behaviors. Moreover, racism negatively affects mental and physical health both directly and by creating inequities across the social determinants of health.
Health and health care disparities are often viewed through the lens of race and ethnicity, but they occur across a broad range of dimensions. For example, disparities occur across socioeconomic status, age, geography, language, gender, disability status, citizenship status, and sexual identity and orientation. Research also suggests that disparities occur across the life course, from birth, through mid-life, and among older adults. Federal efforts to reduce disparities focus on designated priority populations , including, “members of underserved communities: Black, Latino, and Indigenous and Native American persons, Asian Americans and Pacific Islanders and other persons of color; members of religious minorities; lesbian, gay, bisexual, transgender, and queer (LGBT+) persons; persons with disabilities; persons who live in rural areas; and persons otherwise adversely affected by persistent poverty or inequality.” These groups are not mutually exclusive and often intersect in meaningful ways. Disparities also occur within subgroups of populations. For example, there are differences among Hispanic people in health and health care based on length of time in the country, primary language, and immigration status . Data often also mask underlying disparities among subgroups within the Asian population.
Why is it important to address disparities?
Addressing disparities in health and health care is important not only from an equity standpoint but also for improving the nation’s overall health and economic prosperity . People of color and other underserved groups experience higher rates of illness and death across a wide range of health conditions, limiting the overall health of the nation. Research further finds that health disparities are costly, resulting in excess medical care costs and lost productivity as well as additional economic losses due to premature deaths each year.
What is the status of disparities today?
Disparities in health and health care are persistent and prevalent. Major recognition of health disparities began more than three decades ago with the Report of the Secretary’s Task Force on Black and Minority Health (Heckler Report) in 1985, which documented persistent health disparities that accounted for 60,000 excess deaths each year and synthesized ways to advance health equity. The Heckler Report led to the creation of the U.S. Department of Health and Human Services Office of Minority Health and influenced federal recognition of and investment in many aspects of health equity. In 2003, the Institute of Medicine’s Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care released the report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care , which identified systemic racism as a major cause of health disparities in the United States. Despite the recognition and documentation of disparities for decades and overall improvements in population health over time, many disparities have persisted, and, in some cases, widened over time.
Beyond coverage, people of color and other marginalized and underserved groups continue to experience many disparities in accessing and receiving care . For example, people in rural areas face barriers to accessing care due to low density of providers and longer travel times to care, as well as more limited access to health coverage. There also are inequities in experiences receiving health care across groups. For example, the KFF/The Undefeated 2020 Survey on Race and Health , found that one in five Black adults and one in five Hispanic adults report being treated unfairly treatment due to their race or ethnicity while getting health care for themselves or a family member in the past year. Nearly one-quarter (24%) of Hispanic adults and over one in three (34%) potentially undocumented Hispanic adults reported that it was very or somewhat difficult to find a doctor who explains this in a way that is easy to understand in a 2021 KFF survey. Other KFF survey data from 2022 found that nearly one in ten (9%) of nonelderly adult women who visited a health care provider in the past two years said they experienced discrimination because of their age, gender, race, sexual orientation, religion, or some other personal characteristic during a health care visit. KFF data also showed that LGBT+ people were more likely than their non-LGBT+ counterparts to report certain negative experiences while getting health care, including a doctor not believing they were telling the truth, suggesting they are personally to blame for a health problem, assuming something about them without asking, and/or dismissing their concerns. The 2023 KFF/The Washington Post Trans Survey found that trans adults were more likely to report having difficulty finding affordable health care or a provider who treated them with dignity and respect compared to cisgender adults.
The COVID-19 pandemic has taken a disproportionate toll on the health and well-being of people of color and other underserved groups. Cumulative age-adjusted data showed that AIAN and Hispanic people have had a higher risk for COVID-19 infection and AIAN, Hispanic, and Black people have had a higher risk for hospitalization and death due to COVID-19. Beyond these direct health impacts, the pandemic has negatively impacted the mental health, well-being, and social and economic factors that drive health for people of color and other underserved groups, including LGBT+ people . As such, the pandemic may contribute to worsening health disparities going forward.
Concerns about mental health and substance use have increased since the onset of the pandemic, particularly among some groups. According to a 2022 KFF/CNN survey , 90% of the public think there is a mental health crisis in the U.S. today. Over the course of the pandemic, many adults reported symptoms consistent with anxiety and depression. Additionally, drug overdose deaths have sharply increased – largely due to fentanyl – and after a brief period of decline, suicide deaths are once again on the rise. These negative mental health and substance use outcomes have disproportionately affected some populations, particularly communities of color and youth. Drug overdose death rates were highest among AIAN and Black people as of 2021. Alcohol-induced death rates increased substantially during the pandemic, with rates increasing the fastest among people of color and people living in rural areas. From 2019 to 2021, many people of color experienced a larger growth in suicide death rates compared to their White counterparts. Additionally, self-harm and suicidal ideation has increased faster among adolescent females compared to their male peers. Findings from a 2023 KFF/The Washington Post survey found that more trans adults reported struggling with serious mental health issues compared to cisgender adults and were six times as likely as cisgender adults to have engaged in self-harm in the previous year (17% vs. 3%). There are also substantial disparities in mental health, including suicidality, among LGBT+ youth compared to their non-LGBT+ peers.
What are recent federal actions to address disparities?
In the wake of the COVID-19 pandemic, there has been a heightened awareness of and focus on addressing health disparities. The disparate impacts of COVID-19 and coinciding racial reckoning following the police killing of George Floyd contributed to a growing awareness of racial disparities in health and their underlying causes, including racism. Early in his presidency, President Biden issued a series of executive orders focused on advancing health equity, including orders that outlined equity as a priority for the federal government broadly and as part of the pandemic response and recovery efforts . Federal agencies were directed with developing Equity Action Plans that outlined concrete strategies and commitments to addressing systemic barriers across the federal government. In its Health Equity Plan, the Department of Health and Human Services (HHS) outlined a series of new strategies, including addressing increased pregnancy and postpartum morbidity and mortality among Black and AIAN women; addressing barriers that individuals with limited English proficiency face in obtaining information, services, and benefits from HHS programs; leveraging grants to incorporate equity consideration into funding opportunities, implementing equity assessments across its major policies and programs; investing in resources to advance civil rights; and expanding contracting opportunities for small, disadvantaged businesses. The plan builds on earlier efforts that included increasing stakeholder engagement, establishing the Office of Climate Change and Health Equity , and establishing the National Institutes of Health UNITE Initiative to address structural racism and racial inequities in biomedical research. Since the release of its Equity Action Plan, HHS has taken actions to extend postpartum coverage through Medicaid and CHIP; issued rules to strengthen patient protections, including nondiscrimination protections; and issued nondiscrimination guidance to ensure that telehealth services are accessible to people with disabilities and those with limited English proficiency.
The Centers for Medicare and Medicaid Services (CMS) released an updated framework to advance health equity, expand health coverage, and improve health outcomes for people covered by Medicare, Medicaid, CHIP, and the Health Insurance Marketplaces. The framework outlined five priorities including expanding the collecting, reporting, and analysis of standardized data on demographics and social determinants of health; assessing the causes of disparities within CMS programs and addressing inequities in policies and operations; building capacity of health care organizations and the workforce to reduce disparities; advancing language access, health literacy, and the provision of culturally tailored services; and increasing all forms of accessibility to health services and coverage. The Administration has also identified advancing health equity and addressing social determinants of health as key priorities within Medicaid and has encouraged states to propose Section 1115 Medicaid waivers that expand coverage, reduce health disparities, and/or advance “whole-person care.” States have increasingly requested and/or received approval for waivers that aim to advance equity . Further, a growing number of states have approved or pending waivers with provisions related to addressing health-related social needs , such as food and housing, often focused on specific populations with high needs or risks.
The Administration and Congress have taken a range of actions to stabilize and increase access to health coverage amid the pandemic. Early in the pandemic, Congress passed the Families First Coronavirus Response Act (FFCRA), which included a temporary requirement that Medicaid programs keep people continuously enrolled during the COVID-19 Public Health Emergency in exchange for enhanced federal funds. Primarily due to the continuous enrollment provision, Medicaid enrollment has grown substantially compared to before the pandemic, and the uninsured rate has dropped with differences in uninsured rates between people of color and White people narrowing. Coverage gains also likely reflected enhanced ACA Marketplace subsidies made available by the American Rescue Plan Act (ARPA) of 2021 and renewed for another three years in the Inflation Reduction Act of 2022, boosted outreach and enrollment efforts, a Special Enrollment Period for the Marketplaces provided in response to the pandemic, and low Marketplace attrition . Additionally, in 2019, the Biden Administration reversed changes the Trump Administration had previously made to public charge immigration policies that increased reluctance among some immigrant families to enroll in public programs, including health coverage. Most recently, the Consolidated Appropriations Act of 2023 included a requirement for all states to implement 12 months of continuous coverage for children, supporting their coverage stability. However, it also set the end of the broader Medicaid continuous enrollment provision for March 31, 2023, which could lead to coverage losses for millions of people, reversing recent coverage gains.
There have been growing federal efforts to address disparities in maternal health. Over the past few years, the Administration launched several initiatives focused on addressing inequities in maternal health. In April 2021, President Biden issued a proclamation to recognize the importance of addressing the high rates of maternal mortality and morbidity among Black people. At the end of 2021, the White House hosted its inaugural White House Maternal Health Day of Action during which areas of concern in maternal health outcomes were identified and the Administration announced actions aimed at solving the maternal health crisis. In June 2022, the Biden Administration released the Blueprint for Addressing the Maternal Health Crisis . The Blueprint outlines priorities and actions across federal agencies to improve access to coverage and care, expand and enhance data collection and research, grow and diversify the perinatal workforce, strengthen social and economic support, and increase trainings and incentives to support women being active participants in their care before, during and after pregnancy. In July 2022, CMS announced a Maternity Care Action Plan to support the implementation of the Biden-Harris Administration’s Blueprint for Addressing the Maternal Health Crisis. The action plan takes a holistic and coordinated approach across CMS to improve health outcomes and reduce inequities for people during pregnancy, childbirth, and the postpartum period. ARPA included an option, made permanent in the Consolidated Appropriations Act , to allow states to extend Medicaid postpartum coverage from 60 days to 12 months. As of April 2023, the majority of states have taken steps to extend postpartum coverage. The Human Resources and Services Administration also announced $12 million in awards for the Rural Maternal and Obstetrics Management Strategies Program (RMOMS), which is designed to develop models and implement strategies to improve maternal health in rural communities.
The Administration has also taken steps to address health disparities and discrimination experienced among LGBT+ people. On his first day in office, President Biden signed an Executive Order on “Preventing and Combating Discrimination on the Basis of Gender Identity or Sexual Orientation.” Since then, the Administration has taken multiple actions to address discrimination within health care specifically. In May 2021, the Biden Administration announced that the HHS Office for Civil Rights (OCR) would include gender identity and sexual orientation as it interprets and enforces the ACA’s prohibition against sex discrimination (Section 1557), reversing the approach taken by the Trump Administration. Additionally, the Administration has spoken out against state actions aimed at curtailing access to gender affirming care for transgender and gender nonconforming people, particularly policies targeting youth. In January 2023, the Administration released its Federal Evidence Agenda on LGBTQI+ Equity , a “roadmap for federal agencies as they work to create their own data-driven and measurable SOGI Data,” which the Administration views as central to understanding disparities and discrimination facing this community.
What are key issues related to health disparities looking ahead?
The end of the Medicaid continuous enrollment provision may lead to coverage losses and widening disparities. Following the ending of the Medicaid continuous enrollment provision on March 31, 2023, states resumed Medicaid redeterminations. KFF estimates that between 5 and 14 million people could lose Medicaid coverage, including many who newly gained coverage during the pandemic. Other research shows that Hispanic and Black people are likely to be disproportionately impacted by the expiration of the continuous enrollment provision. Moreover, some groups, such as individuals with limited English proficiency and people with disabilities may face increased challenges in completing the Medicaid renewal process increasing their risk of coverage loss even if they remain eligible for coverage. OCR has reminded states of their obligations under federal civil rights laws to take reasonable steps to provide meaningful language access for individuals with limited English proficiency and ensure effective communication with individuals with disabilities to prevent lapses in coverage amid the unwinding of the continuous enrollment provision. CMS issued guidance that provides a roadmap for states to streamline processes and implement strategies to reduce the number of people who lose coverage even though they remain eligible. The extent to which states simplify processes to renew or transition to other coverage and provide outreach and assistance to individuals more likely to face challenges completing renewal processes will impact coverage losses and potential impacts on coverage disparities.
The end of the COVID-19 Public Health Emergency (PHE) and the potential depletion of the federally purchased supply of COVID-19 vaccines, treatments, and tests may curtail access to these supplies for some individuals, particularly those who are uninsured. In response to the COVID-19 pandemic, the federal government spent billions of dollars in emergency funds to purchase COVID-19 vaccines, including boosters, treatments, and tests to provide free of charge to the public. In addition, Congress enacted legislation that included special requirements for their coverage by both public and private insurers, and the Administration issued guidance and regulations to protect patient access and promote equitable distribution. The upcoming end to the PHE on May 11, 2023, as well as the potential depletion of federally purchased supplies in the absence of any additional funding, could result in new or higher cost-sharing and/or reduced access to these products although these impacts may vary by product and the type of health coverage an individual has. People who are uninsured or underinsured face the greatest risk of access challenges, including limited access to free vaccines and no coverage for treatment or tests. Since people of color and people with lower incomes are more likely to be uninsured, they may be at a disproportionate risk of facing barriers to accessing COVID-19 vaccines, tests, and treatments once the PHE ends and the federal supply is depleted.
The overturning of Roe v. Wade may exacerbate the already large racial disparities in maternal and infant health. The decision to overturn the longstanding Constitutional right to abortion and elimination of federal standards on abortion access has resulted in growing variation across states in laws protecting or restricting abortion. These changes may disproportionately impact women of color, as they are more likely to obtain abortions, have more limited access to health care, and face underlying inequities that would make it more difficult to travel out of state for an abortion compared to their White counterparts. Restricted access to abortions may widen the already stark racial disparities in maternal and infant health, as some groups of color are at higher risk of dying from pregnancy-related reasons and during infancy and are more likely to experience birth risks and adverse birth outcomes compared to White people. It may also have negative economic consequences associated with the direct costs of raising children and impacts on educational and employment opportunities. Further, women from underserved communities may be at increased risk for criminalization in a post-Roe environment, as prior to the ruling, there were already cases of women being criminalized for their miscarriages, stillbirths, or infant death, many of whom were low-income or women of color.
Many states have implemented policies banning or limiting access to gender affirming care, especially for youth, as well as other legal actions that threaten access to care for LGBT+ people . Policies aimed at limiting access to gender affirming care may have significant negative implications for the health of trans and nonconforming people, particularly young people, including negative mental health impacts, and an increased risk of suicidality . Additionally, the recent Braidwood case on preventive care access directly affects LGBT+ people in its treatment of Pre-Exposure Prophylaxis (PrEP). It relies, in part, on religious protections arguments to limit access to the drug based on the plaintiff’s claim that it “facilitate[s] and encourage[s] homosexual behavior, prostitution, sexual promiscuity, and intravenous drug use.” If PrEP use declines as a result of the Braidwood decision, HIV incidence could increase , likely disproportionally impacting people of color and LGBT+ people. Efforts to curtail access to gender affirming care and the Braidwood decision are at odds with the Administration’s stated approach to health equity for LGBT+ people. How such policies play out in the longer term will be determined largely by the courts.
Evolving immigration policies may impact the health and well-being of immigrant families. When the PHE ends on May 11, 2023, Title 42 restrictions that suspended the entry of individuals at the U.S. border to protect public health during the COVID-19 emergency are expected to terminate. It is anticipated that when the authority ends, there will be an increase in immigrant activity at the U.S. border. The Biden Administration has announced plans to increase security and enforcement at the border to reduce unlawful crossings, expand “legal pathways for orderly migration”, invest additional resources in the border region, and partner with Mexico to implement the aforementioned plans. However, it remains to be seen how shifting policies will impact trends at the border and health and health care in that region. The future of the Deferred Action for Childhood Arrivals (DACA) program remains uncertain, and its implementation is currently limited subject to court orders . If the DACA program is found to be unlawful in pending court rulings, individuals would lose their DACA status and subsequently their work authorizations. The loss of status and work authorization may result in loss of employer-based health coverage, leaving people uninsured and unable to qualify for Medicaid, CHIP, or to purchase coverage through the Marketplaces. Additionally, although the Biden Administration reversed public charge regulations implemented by the Trump Administration as part of an effort to address immigration-related fears that limited immigrant families’ participation in government assistance programs, including Medicaid and CHIP, many families continue to have fears and concerns about enrolling in these programs, contributing to ongoing gaps in coverage for immigrants and children of immigrants.
Growing mental health and substance use concerns and ongoing racism, discrimination, and violence may contribute to health disparities. As previously noted, mental health and substance use concerns have increased since the onset of the pandemic, with some groups particularly affected. These trends may lead to new and widening disparities. For example, people of color have experienced larger increases in drug overdose death rates than White people, resulting in the death rate for Black people newly surpassing that of White people by 2020. Further, Black and Asian people have reported negative mental health impacts due to heightened anti-Black and anti-Asian racism and violence in recent years. Research has documented the negative health impacts, including negative impacts on mental health and well-being, of exposure to violence, including police and violence. Research shows African American and AIAN men and women, and Latino men are at increased risk of being killed by police compared to their White peers. Black and Hispanic adults also are more likely than White adults to worry about gun violence according to 2023 KFF survey data . Other KFF analysis shows that firearm death rates increased sharply among Black and Hispanic youth during the pandemic driven primarily by gun assaults and suicide by firearm. Research further shows that repeated and chronic exposure to racism and discrimination is associated with negative physical and mental health outcomes , including premature aging and associated health risks, referred to as “ weathering ,” as well as higher mortality .
Despite growing mental health concerns, people of color continue to face disproportionate barriers to accessing mental health care. Research suggests that structural inequities may contribute to disparities in use of mental health care, including lack of health insurance coverage and financial and logistical barriers to accessing care, stemming from broader inequities in social and economic factors . Lack of a diverse mental health care workforce, the absence of culturally informed treatment options, and stereotypes and discrimination associated with poor mental health may also contribute to limited mental health treatment among people of color. Amid the pandemic, many states implemented telehealth behavioral health services to expand access to behavioral health care, and most states intend to keep these services. States are also adopting strategies to address workforce shortages in behavioral health. As states seek to expand access to behavioral health care, it will be important to ensure that services address the cultural and linguistic needs of diverse populations. Further, in 2022, the federal government mandated the suicide and crisis lifeline number that provides a single three-digit number (988) to access a network of over 200 local and state-funded crisis centers. The 988 number is expected to improve the delivery of mental health crisis care; however, it is unknown how well it will address the needs of people of color and other underserved populations.
In sum, disparities in health and health care for people of color and other underserved groups are longstanding challenges, many of which are driven by underlying structural and economic disparities rooted in racism. Addressing disparities is key not only from an equity standpoint but for improving the nation’s overall health and economic prosperity. Amid the COVID-19 pandemic, the federal government identified health equity as a priority and has since launched initiatives to address disparities wrought by the COVID-19 pandemic and more broadly. Alongside the federal government, states, local communities, private organizations, and providers have engaged in efforts to reduce health disparities. Moving forward, a broad range of efforts both within and beyond the health care system will be instrumental in reducing disparities and advancing equity.
- Racial Equity and Health Policy
- Coronavirus (COVID-19)
- Women's Health Policy
- Access to Care
- American Indian/Alaska Native
- Race/Ethnicity
Also of Interest
- How History Has Shaped Racial and Ethnic Health Disparities: A Timeline of Policies and Events
- Key Data on Health and Health Care by Race and Ethnicity
- Health Coverage by Race and Ethnicity, 2010-2022
We're sorry but you will need to enable Javascript to access all of the features of this site.
Stanford Online
Artificial intelligence in healthcare.
Stanford School of Medicine , Stanford Center for Health Education
Monthly subscription: $79
Get Started
Artificial intelligence (AI) has transformed industries around the world, and has the potential to radically alter the field of healthcare. Imagine being able to analyze data on patient visits to the clinic, medications prescribed, lab tests, and procedures performed, as well as data outside the health system -- such as social media, purchases made using credit cards, census records, Internet search activity logs that contain valuable health information, and you’ll get a sense of how AI could transform patient care and diagnoses. In this specialization, we'll discuss the current and future applications of AI in healthcare with the goal of learning to bring AI technologies into the clinic safely and ethically. This specialization is designed for both healthcare providers and computer science professionals, offering insights to facilitate collaboration between the disciplines.
- Identify problems healthcare providers face that machine learning can solve
- Analyze how AI affects patient care safety, quality, and research
- Relate AI to the science, practice, and business of medicine
- Apply the building blocks of AI to help you innovate and understand emerging technologies
- Preview Image
- Course/Course #
- Time Commitment
- Availability

Introduction to Healthcare

Introduction to Clinical Data

Fundamentals of Machine Learning for Healthcare

Evaluations of AI Applications in Healthcare

AI in Healthcare Capstone
Flexible enrollment options, monthly subscription: $79.
View and complete course materials, video lectures, assignments, and exams, at your own pace with a monthly subscription to the Artificial Intelligence in Healthcare Specialization.
What Our Learners Are Saying
AI in Healthcare is an incredible program offering content related to the Healthcare System, Clinical Data, Machine Learning, & Artificial Intelligence Applications in Healthcare. After completing this program, one choose more advanced study in the aforementioned topics and/or take a deeper dive in the numerous interrelated subjects such as computational math, stats, programming/coding and algorithms. Simply outstanding!!
John S., Clinical Specialist
Upcoming Events

Health & Medicine Programs Information Session
- Engineering
- Computer Science & Security
- Business & Management
- Energy & Sustainability
- Data Science
- Medicine & Health
- Explore All
- Technical Support
- Master’s Application FAQs
- Master’s Student FAQs
- Master's Tuition & Fees
- Grades & Policies
- Graduate Application FAQs
- Graduate Student FAQs
- Graduate Tuition & Fees
- Community Standards Review Process
- Academic Calendar
- Exams & Homework FAQs
- Enrollment FAQs
- Tuition, Fees, & Payments
- Custom & Executive Programs
- Free Online Courses
- Free Content Library
- School of Engineering
- Graduate School of Education
- Stanford Doerr School of Sustainability
- School of Humanities & Sciences
- Stanford Human Centered Artificial Intelligence (HAI)
- Graduate School of Business
- Stanford Law School
- School of Medicine
- Learning Collaborations
- Stanford Credentials
- What is a digital credential?
- Grades and Units Information
- Our Community
- Get Course Updates
- The Open University
- Study with The Open University
My OpenLearn Profile
Personalise your OpenLearn profile, save your favourite content and get recognition for your learning

See where curiosity takes you
Everything on the multi-award winning OpenLearn is free to everyone!
Get inspired and learn something new today
Crime fiction
Explore the world of crime fiction with The Open University, a world leader in distance learning. Discover free courses, articles, video and audio resources, and interactive activities, free to study and available to start right away.
Nature & Environment
Learning our way to a better environment
How can our capacity for learning help us understand more about managing our environment? This short video looks at developing a more sustainable relationship between humans and the environment.
Health, Sports & Psychology
The 2024 UEFA European Championships start on 14 June in Germany. Check out our expert insights and free resources in our Euro 2024 hub.

Getting started with German 1
Almost 100 million people speak German as their main language. Most of them live in Germany, Austria and Switzerland, making German one of the most widely-used languages in Europe. Although now associated with economic success and advances in science and technology, German has a long-standing reputation as the language of poets and thinkers, die...

Education & Development
What do you think about OpenLearn? Take the survey
Let us know what you think! We are running a survey to find out more about how you use OpenLearn, what’s great and what could be improved. The aim is to provide a better free learning experience for everyone.

Heroes and villains: the presentation of the outlaw in early twentieth-century American folk music
This article will consider how the figure of the outlaw is presented in early twentieth-century American folk music. What is constant, and what changes? What lies behind these strands of imitation and innovation?

Understanding ADHD
This free course, Understanding Attention Deficit Hyperactivity Disorder (ADHD), explores the experience of ADHD from the perspective of those who are diagnosed with the condition, and those who care for them. It covers the contribution of scientific research to understanding ADHD, with a focus on assessing the effectiveness and mechanism of ...

D-Day, the Battle of Normandy, and the British Military Nursing Services
Operation Overlord, the invasion of Europe known as D-Day, began on 6 June 1944. 12,000 British military nurses served during World War II, many of these during the aftermath of D-Day and the Battle of Normandy. In this article, explore what it was like to be a nurse at this time.
You can use OpenLearn to
Study free courses.
From 1 to 100 hours of learning - discover hundreds of free courses to inspire and inform everyone.
Earn while you learn
Earn a free digital badge or Statement of Participation as evidence of your learning to share with employers, friends and family.
Study skills
Improve your study skills and get acquainted with student life with our expertly created courses and resources.
Work skills
Boost your employability skills and find useful resources to help you with your life outside of work.
Pick a subject and start learning
Get the most out of openlearn.
Anyone can learn for free on OpenLearn but creating an account lets you set up a personal learning profile which tracks your course progress and gives you access to Statements of Participation and digital badges you earn along the way. Sign-up now!
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Economic strain, social relations, gender, and binge drinking in Moscow

2008, Social Science & Medicine
Related Papers
Lyudmila Saburova
To estimate the prevalence of hazardous drinking and its socio-economic distribution among Russian men. Participants were an age-stratified, population-based random sample of men aged 25-54 years living in Izhevsk, a city in the Urals, Russia. Interviewers administered questionnaires to cohabiting proxy respondents about behavioural indicators of hazardous drinking derived from frequency of hangover, frequency of drinking beverage spirits, episodes in the last year of extended periods of drunkenness during which the participant withdraws from normal life (zapoi), consumption of alcoholic substances not intended to be drunk (surrogates) and socio-economic position. Logistic regression was used to examine associations between socio-economic position and indicators of hazardous drinking in the past year. Of 1750 men, 79% drank spirits and 8% drank surrogates at least sometimes in the past year; 25% drank spirits and 4% drank surrogates at least weekly and 10% had had an episode of zapo...
Richard Rose
Alcohol and Alcoholism
S. Malyutina
The European Journal of Public Health
Andrey Korotayev
During the study period, Russia’s public health crisis, which was characterised in the 1990s and until 2005 by dramatic fluctuations of all-cause mortality and of mortality from alcohol-related causes, has continued. Research carried out during the past two decades suggested that this public health crisis was driven by excessive and hazardous alcohol consumption, by high rates of smoking, by deterioration of the health system and of other broader social-economic determinants in the country, with alcohol playing a substantial proximal role among them. However, after 2005 mortality trends began to decline, and this decline has continued up to 2013. The amendments to alcohol legislation introduced since 2001, and especially those in 2006 and later in 2011, have likely played a positive role in diminishing the production and consumption of illegal and unrecorded spirits, which has subsequently led to an improvement in alcohol-driven health indicators. However, life expectancy in Russia still remains 10–15 years lower than in Western countries and corresponds closely to the previous 1960-levels in the Soviet Union, suggesting that the quality and implementation of recent alcohol control measures has not led to significant improvements in the health status of Russian citizens, which would be expected to correspond to the level of other modern industrialised countries.
Katherine Keenan
Journal of epidemiology and community health
Hynek Pikhart
Health Education and Care
Sergei Jargin
The problem of excessive alcohol consumption in Russia is well known; however, there is a tendency to exaggerate it, which seems to be used to disguise shortages of the healthcare and the fact of legal trade with falsified beverages and surrogates. In this way, responsibility for the relatively low life expectancy is shifted upon patients, that is, supposedly self-inflicted diseases due to excessive alcohol consumption.
Hans van Oers , Inge Bongers , Henk Garretsen , Ien Am Goor
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
International Journal of High Risk Behaviors and Addiction
David H Leon
Journal of Economic and Business Studies
BMC Public …
Yury Razvodovsky
Arşiv Kaynak Tarama Dergisi
Population and Economics
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

IMAGES
VIDEO
COMMENTS
A piece of coursework that I passed alice lacy 661723 p4 demonstrate effective communication skills in interaction to build positive relationship in health,
A.1 Effective communication. Communication is a two-way process, and the key elements needed are as follows: sender - the person starting the communication. message - what the sender wishes to communicate. medium - the method of communication: verbal, written, signed, electronic, telephone, etc. receiver - the person who receives the ...
outline. Care workers require effective communication skills in order to work with the diverse range of people they meet in health and social care settings. This unit will introduce you to: different forms of communication factors that affect communication in care settings ways of overcoming barriers to effective communication.
interest to social workers, not least because the author is deeply involved in social work education, and has many years' experience in helping students develop their communication skills for this important work.
Understand the importance of communication in health and social care, including the principles of confidentiality. Know the different types of communication used within and between health and social care settings. Be able to adapt communication to meet individual needs, wishes and preferences using different methods.
The course "Communication for Health and Social Care" is essential for healthcare professionals and social care workers to improve patient outcomes and provide exceptional support. Effective communication skills, including active listening, empathy, and cultural sensitivity, are crucial in establishing trust and understanding with patients and ...
• Understand the importance of communication in health and social care, including the principles of confidentiality. • Know the different types of communication used within and between health and social care settings. • Be able to adapt communication to meet individual needs, wishes and preferences using different methods.
Effective communication plays an instrumental role in health and social care. Learn about its importance and how to overcome any barriers here.
Promoting communication in health and social care T he Social Care Institute for Excellence states that good communication skills are the starting point for all the other skills that health and social care workers need. The other skills that you will need in order to work in health and social care cannot be developed unless you have good
Enhance your skills in Communication for Health and Social Care with this comprehensive course. Learn effective communication techniques and strategies tailored for the healthcare and social care sectors.
Written communication Care report: ... Medical procedure: a medical procedure is a course of action intended to achieve a result in a care of persons with health problems for example when an elderly person goes for an operation and receives ... Year 10 health and social care controlled assessment
Writing coursework on health and social care communication and values can be challenging due to the complex subject matter. It requires extensive research, a thorough understanding of theoretical concepts, and applying them to real-world scenarios. Some difficulties include navigating diverse disciplines, addressing intricate topics in-depth, conducting intensive research, engaging in critical ...
Syllabus and Upcoming Calendars. Reducing Racial Disparities in Health Care is a health equity course introduces strategies that advance policy and practice to eliminate racial and ethnic disparities in health care. The course begins with understanding our history (Module 1), followed by learning about the foundations of this type of work ...
The Undergraduate Certificate in Communication for Health and Social Care Professionals helps students develop professional communication skills in the health and social care industries. The curriculum combines courses from the department's existing curriculum to serve students interested in a health and social care career, such as nurses ...
Good luck on your coursework journey. The document discusses the challenges of writing coursework, especially on complex topics like health and social care. It can involve extensive research, planning, and finding the right words.
1.1 Explain the use of communication in health and social care settings. Communication is the exchange of information or interaction between two or more people. It is also a way of sending and receiving information from one person to another. There are several ways for people to interact, such as verbal communication (speaking out), written ...
Introduction (Briefly explain the context/background and what you will discuss in assignment ) Task 1: Role of communication in effective health and social care practice AC 1.1 Describe the methods used to communicate in health and social care. AC 1.2 Discuss the strengths and weaknesses of both formal and informal communication methods.
Core Skills Communication (Level 3) Health and social care learning resources for adults, children, parents and teachers.
The document discusses some of the challenges of writing coursework, especially on complex topics like health and social care. It notes that such topics involve intricate concepts that require in-depth knowledge and research to understand and present coherently. Producing quality coursework also requires extensive research, proper formatting and structure, strong time management skills to ...
Our campaigns provide crucial information on prediabetes, type 2 diabetes prevention, and diabetes management to empower people to safeguard and improve their health. Campaign messaging reaches our key audiences through their preferred communication channels, including social media and other digital platforms, print, radio, and broadcast TV.
Harvard Online presents curated online courses that combine faculty and disciplines ... Deepen perspectives and advance insights into the strategic issues facing health care organizations today. ... this course will teach core concepts in economics and statistics and equip you to tackle some of the most pressing social challenges of our time. ...
Enrol to our free online medical courses with top universities to dive into the complex world of healthcare and get professional development training.
A three-day workshop, Introduction to Advocacy, Communication and Social Mobilization, was conducted in Moscow, Russian Federation, March 14-16, 2005. Participants represented national TB programs in Russia, Ukraine, Moldova, Georgia, Azerbaijan, Uzbekistan and Kazakhstan, as well as non-governmental organizations such as the Red Cross.
Using real-world data and policy interventions as applications, this Harvard Online course will teach core concepts in data science, economics, and statistics and equip you to tackle some of the most pressing social challenges of our time.
By Mark Warschauer, University of California, Irvine. Of Digital Divides and Social Multipliers: Combining Language and Technology for Human Development. The purpose of language teaching goes beyond memorization of grammar rules. and vocabulary, or even the development of individual communication skills. Rather, the.
Disparities in health and health care for people of color and underserved groups are longstanding challenges. This brief provides an introduction to what health and health care disparities are ...
on social networks affect not only those who are facing the problem, but also their friends and family. Previous studies of depression-related social networks can be divided into two groups. The first includes projects aimed at identifying the markers of depression by analyzing the users' behavior, the content on their pages, and communication
Artificial intelligence (AI) has transformed industries around the world, and has the potential to radically alter the field of healthcare. Imagine being able to analyze data on patient visits to the clinic, medications prescribed, lab tests, and procedures performed, as well as data outside the health system -- such as social media, purchases made using credit cards, census records, Internet ...
Explore a wide range of free courses on OpenLearn, from science and health to arts and humanities, and earn badges and certificates.
Economic strain, social relations, gender, and binge drinking in Moscow. Tanya Jukkala ...