Clinical Presentation: Case History # 1 Ms. C is a 35 year old white female. She came to Neurology Clinic for evaluation of her long-term neurologic complaints. The patient relates that for many years she had noticed some significant changes in neurologic functions, particularly heat intolerance precipitating a stumbling gait and a tendency to fall. Her visual acuity also seemed to change periodically during several years. Two months ago the patient was working very hard and was under a lot of stress. She got sick with a flu and her neurologic condition worsened. At that time, she could not hold objects in her hands, had significant tremors and severe exhaustion. She also had several bad falls. Since that time she had noticed arthralgia on the right and subsequently on the left side of her body. Then, the patient abruptly developed a right hemisensory deficit after several days of work. The MRI scan was performed at that time and revealed a multifocal white matter disease - areas of increased T2 signal in both cerebral hemispheres. Spinal tap was also done which revealed the presence of oligoclonal bands in CSF. Visual evoked response testing was abnormal with slowed conduction in optic nerves. (Q.1) (Q. 2) (Q.3) Today, the patient has multiple problems related to her disease: she remains weak and numb on the right side; she has impaired urinary bladder function which requires multiple voids in the mornings, and nocturia times 3. She became incontinent and now has to wear a pad during the day. (Q.4) She also has persistent balance problems with some sensation of spinning, and she is extremely fatigued. REVIEW OF SYSTEMS is also significant for a number of problems related to her suspected MS. The patient has a tendency to aspirate liquids and also solids. (Q.5) (Q.6) She complains of tinnitus which is continuous and associated with hearing loss, more prominent on the left. She has decreased finger dexterity and weakness of the hands bilaterally. She also complains of impaired short-term memory and irritability. FAMILY HISTORY is significant for high blood pressure, cancer and heart disease in the immediate family. PERSONAL HISTORY is significant for mumps and chicken pox as a child, and anemia and allergies with hives later in life. She also had a tubal ligation. NEUROLOGIC EXAMINATION: Cranial Nerve II - disks are sharp and of normal color. Funduscopic examination is normal. Cranial Nerves III, IV, VI - no extraocular motor palsy or difficulties with smooth pursuit or saccades are seen. Remainder of the cranial nerve exam is normal except for decreased hearing on the left, and numbness in the right face, which extends down into the entire right side. The Weber test reveals greater conductance to the right. Rinne's test reveals air greater than bone bilaterally. (Q.7) The palate elevates well. Swallow appears to be intact. Tongue movements are slowed, but tongue power appears to be intact. Motor examination reveals relatively normal strength in the upper extremities throughout. However, rapid alternating movements are decreased in both upper extremities and the patient has dysdiadochokinesia in the left hand. (Q.8) Mild paraparesis is noted in both legs without severe spasticity. Deep tendon reflexes are +2 and symmetrical in the arms, +3 at the ankles and at the knees. Bilateral extensor toe sign are present. Sensory exam reveals paresthesia on the right to touch and decreased pin sensation on the right diffusely. The patient has mild vibratory sense loss in the distal lower extremities. Romberg's is negative. (Q.9) Tandem gait is mildly unstable. Ambulation index is 7.0 seconds for 25 feet. (The patient takes 7.0 seconds to walk 25 feet.) Diagnosis: Multiple Sclerosis with laboratory support. © John W.Rose, M.D., Maria Houtchens, MSIII, Sharon G. Lynch, M.D.


Case Studies in Multiple Sclerosis
- © 2017
- Paul S. Giacomini 0
McGill University , MONTREAL, Canada
You can also search for this editor in PubMed Google Scholar
- A collection of case studies illustrating the complex, unpredictable nature of multiple sclerosis and its many presentations and disease courses
- Case studies submitted from clinicians from some of the world's leading neurology departments
- Edited by Dr Paul Giacomini of McGill University, a leading expert in the field of multiple sclerosis
- Includes supplementary material: sn.pub/extras
19k Accesses
2 Citations
1 Altmetric
This is a preview of subscription content, log in via an institution to check access.
Access this book
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Other ways to access
Licence this eBook for your library
Institutional subscriptions
Table of contents (19 chapters)
Front matter, clinically isolated syndrome, optic neuritis.
- Mahtab Ghadiri
Early Multiple Sclerosis
Disease-modifying therapies.
- Anne-Marie Trudelle
Management of relapses with corticosteroids
Established relapsing-remitting multiple sclerosis, breakthrough disease.
- Chris Eckstein
Progressive multifocal leukoencephalopathy
Induction therapy, primary progressive multiple sclerosis, diagnosing primary progressive multiple sclerosis.
- Scott D. Newsome
Symptomatic care in primary progressive multiple sclerosis
Secondary progressive multiple sclerosis, diagnosing secondary progressive multiple sclerosis.
- Sarah Morrow
Walking disability in multiple sclerosis
Cognitive impairment, pediatric multiple sclerosis and related disorders, acute disseminated encephalomyelitis.
- Sunita Venkateswaran
- Case studies
- Clinically isolated syndrome
- Multiple sclerosis
- Primary progressive multiple sclerosis
- Relapse remitting multiple sclerosis
About this book
Editors and affiliations.
Paul S. Giacomini
About the editor
Bibliographic information.
Book Title : Case Studies in Multiple Sclerosis
Editors : Paul S. Giacomini
DOI : https://doi.org/10.1007/978-3-319-31190-6
Publisher : Adis Cham
eBook Packages : Medicine , Medicine (R0)
Copyright Information : Springer International Publishing Switzerland 2017
Softcover ISBN : 978-3-319-31188-3 Published: 21 October 2016
eBook ISBN : 978-3-319-31190-6 Published: 06 October 2016
Edition Number : 1
Number of Pages : XVII, 149
Number of Illustrations : 14 b/w illustrations
Topics : Neurology , Neuroradiology , Primary Care Medicine
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Campus Directory
- Current Students
- Faculty & Staff

Multiple Sclerosis Case Study
Janet has experienced periodic episodes of tingling in her extremities, dizziness, and even episodes of blindness. After 12 years, doctors have finally given her a diagnosis. Follow Janet through her journey and find out why her disease is so difficult to diagnose.
Module 3: Multiple Sclerosis

Janet, age 22, was preparing for her 6-week postpartum checkup...
MS - Page 1
Three years later, at 34, Janet awoke to a prickly tingling feeling...
MS - Page 2
The neurologist made a diagnosis of multiple sclerosis based on the MRI...
MS - Page 3
Case Summary
Summary of the Case
MS - Summary

Answers to Case Questions
MS - Answers

Professionals
Health Professionals Introduced in Case
MS - Professionals
Additional Links
Optional Links to Explore Further
- Future Leaders in Neurology
- ACTRIMS 2024
- Treating NMOSD: What's Next?

- Conferences
- Publications
Patient Case #1: 37-Year-Old Female With RRMS
- Gabriel Pardo, MD, FAAN
Expert neurologists review treatment options for a young female with relapsing remitting multiple sclerosis (RRMS).

EP: 1 . Advances in the Management of Relapsing-Remitting Multiple Sclerosis (RRMS)

EP: 2 . Unmet Needs in the RRMS Treatment Landscape

EP: 3 . Generic Disease-Modifying Therapies (DMTs) in RRMS
Ep: 4 . fda approval process for rrms therapies, ep: 5 . treatment selection in rrms.

EP: 6 . Generic DMTs as First-Line Treatment in RRMS
Ep: 7 . patient case #1: 37-year-old female with rrms, ep: 8 . switching dmts in patients with rrms, ep: 9 . patient case #2: 36-year-old female with rrms with lesions in the spine and brain, ep: 10 . treatment options for a patient with rrms and psoriasis, ep: 11 . use of generic dmts in clinical practice in rrms, ep: 12 . challenges in use of generic dmts for treatment of ms, ep: 13 . the future of rrms treatment, ep: 14 . recommendations for rrms management.
Ahmed Zayed Obeidat MD, PhD: The first case we’re going to talk about is a 37-year-old female with 2 young children. We’re going to talk about some factors about what you would select as a treatment. The patient presented to the neurology clinic for first time with fatigue, weakness, tremors in the right hand, so that’s 1 side. And then medical history was significant for previous numbness and tingling in the lower extremity which was both and the result spontaneously about 2 years ago—not an uncommon scenario where people had maybe a pinched disc or something and they didn’t get medical attention because it went away on a physical exam. She had mild right upper extremity weakness and then increased tone in her right hand, already with increased tone, and some mild intention tremor. That’s important to keep in mind. And then gait was stable but had some hyperreflexia on examination. So those are some of the symptoms she presented with.
You did an MRI, and there were some lesions consistent with demyelination, and then spinal fluid showed unique oligoclonal bands. So, the diagnosis was consistent with what appears to be a relapsing remitting MS [multiple sclerosis].I’ll start with you, Dr Dukkipati. What’s your impression of this case and the initial treatment recommendation? How would you treat this patient?
Ravi Dukkipati, MD: Based on the vignette given, this is a relatively young woman, still of childbearing age with 2 young children, who I’m presuming is fairly active, and by all means has relapsing remitting multiple sclerosis based on the clinical presentation. And the brain MRI demonstrates multiple areas of demyelination, which is concerning, and I would characterize this woman as having a moderate disease burden both clinically and radiographically.
This is the type of patient whom I would not hesitate in terms of being aggressive from the beginning because the concern is that time is brain matter. And so, I generally don’t start new patients on platform therapies any longer, so the real decision-making in my mind would be between one of the oral therapies vs monoclonal antibodies with a patient like this or natalizumab.
Ahmed Zayed Obeidat MD, PhD: Dr Pardo?
Gabriel Pardo, MD, FAAN: Yes, I completely agree. I think there are some concerning signs already in this patient. I assume she’s right-hand dominant just by statistics and that’s where she has most of her symptoms. She already has dexterity problems spasticity problems weakness problems, and it’s not harboring good things for the future. The burden of disease seems to be high, and the diagnosis is straightforward. So, I am concerned about this patient. I think that there is no time to waste with platform therapies; there is no doubt about that.
Other elements we were discussing to individualize the decision-making along with the patient will be, as Dr Dukkipati mentioned, as she is still of childbearing age, is she planning on having more children? That will be a very important aspect in the counseling of this patient regarding the selection of the different agents that we have. And each one of them will have different characteristics in that regard. Some of them will allow her to be treated with 4 courses and then be free of treatment if she is able to delay pregnancy for 2 years, for example, maybe 2½ years 1½ years, or 18 months. Or she might imply the decision of having to stop treatment to pursue pregnancy with the risk of a potential rebound if she does not become pregnant promptly. So, a lot of elements again become important in individual patients, and for this patient, we’ll have to get that in the conversation to be able to counsel her in addition. But from the get-go, I am concerned about the patient, and she should definitely be on high-efficacy therapies. There’s no time to beat around the bush.
Ahmed Zayed Obeidat MD, PhD: Yes, and I agree because as you mentioned, there are already signs of incomplete recovery. There are signs of maybe brain stem involvement here, right? There’s a tremor, there is maybe cerebellar involvement. And that’s concerning when we think about her young age and that it was previously untreated for probably over 2 years because the first episode was over 2 years ago with what appears to be transgressed myelitis, which is again another spinal cord involvement which carries a poor prognosis sometimes. So I would do the same. I would start with a highly effective therapy for her. And then maybe, again, considering other factors; when she wants, if she wants more children, when the plan is. And we’ll work around many of these factors.
So I’m going to tell you a little bit of what happened. Maybe she was not started on highly effective therapy. So despite receiving disease-modifying therapy [DMT], she had 2 more relapses in the past year. She reported increased fatigue, difficulty with memory and concentration. And her exam showed right-sided weakness and wrist reflexes are still there, but more weakness. Another MRI of the brain shows multiple new and enhancing lesions while on a disease-modifying therapy, suggestive of ongoing disease activity. Her fatigue and memory issues are interfering with job performance. Now her symptoms are starting to affect her day-to-day and then maybe threatening her job or maybe could result in her losing her job. So this is now even more concerning. So now the patient comes back to you and asks, “How would you monitor? How would you treat me? What else can I do?" Dr Dukkipati, I’ll start with you for this one now, and then we’ll see what Dr Pardo has to say.
Ravi Dukkipati, MD: Well, this is clearly the worst-case scenario, what we had talked about earlier. This woman unfortunately is progressing. Clinically she’s had several relapses. She’s exhibiting signs of progression and her MRI studies clearly demonstrate a very active disease, involving both the brain and the spinal cord. Now, we don’t necessarily know what her initial disease-modifying therapy was, but clearly, she’s failing with that initial therapy. And this patient would need close monitoring both clinically and radiographically and imminent or immediate change or escalation of therapy to a different class.
Ahmed Zayed Obeidat MD, PhD: Dr Pardo, do you agree, and do you have any other additional thoughts?
Gabriel Pardo, MD, FAAN: Absolutely. I agree completely. And just this case highlights the fact that in addition to our selection of the disease-modifying therapy, we need to be always in tune with the patient’s needs and the fact that MS is multifaceted, it has a lot of manifestations, and that it does require comprehensive management of the disease. We need to go beyond the selection of the DMT. We need to explore all these other possibilities.
The threat of potentially losing her job has tremendous social, familial, and personal implications. And it brings then the conversation of the complementary things that we do to the DMTs, which are symptom management and trying to improve function, something that we also need to monitor closely. It is not just the markers that we use for failing a treatment as clearly evident in this case with relapses, and new MRI additions, but all these other ancillary ways of assessing how the patient is functioning and what else should we do, and can we do to improve that function, and to improve the ability of the patient to continue to live their life the best they can?
Ahmed Zayed Obeidat MD, PhD: Yes, and what strikes me in this case is also that she had 2 relapses in the past year, so she was left to relapse again after 1 relapse. So we didn’t have to even wait for that, right? You see 1 relapse, and for me, it’s sufficient to just switch to a different mechanism of action, and in this case, perhaps going higher; something with known higher efficacy.
Transcript edited for clarity

This Week on NeurologyLive® — May 6 2024
Episode 112: Exploring Dimethyl Fumarate to Treat Friedreich Ataxia

FDA Allows Additional Enrollment to Foralumab Expanded Access Program
Episode 111: Reviewing ACTRIMS 2024

Ocrelizumab Gains EU CHMP Positive Opinion for Subcutaneous Formulation to Treat MS
NeuroVoices: Eoin P. Flanagan, MB, BCh, on the Potential Significance of Spinal Fluid Testing for MOGAD Diagnosis
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Chief complaint: “When I woke up yesterday my legs felt so stiff, I could barely walk. My hands shake every time I try to paint. I feel uncoordinated, exhausted, and just not like myself lately.”
History of present illness: Ms. N.S. is a 29 yo white female, who was referred to the neurology clinic by her PCP after complaining of frequent episodes of weakness, fatigue, and a tingling sensation in different areas of her body. She states she first started noticing symptoms about 2 weeks ago and has been feeling progressively worse. Patient has also reported some urinary frequency, but she has been attributing it to her recent childbirth.

Past medical history
- Tonsillectomy, age 5 years
- Epstein-Barr virus, age 14 years
- Reports a “precancerous mole” that was removed at age 18 years with no complications
- Gave birth to first child 3 months ago with no complications
Pertinent family history:
- Mother alive and healthy at age 58 years
- Father alive, patient reports he takes medication for blood pressure but otherwise is healthy at age 59 years
- Patient has no siblings
- Maternal Aunt alive, living with multiple sclerosis, age 54 years
- Paternal grandfather died after suffering a stroke 2 years ago
Pertinent social history:
- Former smoker, patient quit at age 23
- Recently moved to Columbus, Ohio from Toronto, Canada
- Social drinker with approx. 1-2 alcoholic beverages per week
- Patient is an artist, enjoys going to the gym 2-3 times per week, and is currently working part time in an art gallery
- Patient likes being outdoors and states she recently returned from a several day hiking trip
- None known to patient
Medications:
- Pt states takes Tylenol “occasionally only for headaches”
Focused physical exam:
- Height 5′ 6″
- Weight 135 lb.
- Skin: clear with no lesions or rashes
- Heart Sounds: S1, S2 Regular
- Lungs: Clear in all fields, respirations regular and unlabored
- Abdomen: Soft, nontender, active bowel sounds. Pt reports last BM was this morning.
- Genitourinary: Patient reports urinary frequency, states urine is clear and yellow with no foul odor
- Patient is alert, oriented x 4 to person, place, time, situation
- Pupils are equal, round, and reactive
- Strength equal bilaterally in all extremities, patient has a slight intention tremor present in both hands
- Patient reports feeling “pins and needles” in her left and right lower legs
- Distal pulses are palpable in all extremities with no abnormalities
Vital Signs:
- Temperature: 37.0 degrees celsius
- Respiratory rate: 18
- Blood pressure: 108/76
- Oxygen saturation: 99% on room air
- Pain: 0/10 pt states: “No pain, I just feel tired and my legs are tingling”
Lab Values/Imaging:
- CBC: unremarkable
- Antinuclear antibodies (ANA) test: negative
- Enzyme-linked immunosorbent assay (ELISA) test: negative
- Urinary analysis: unremarkable
- Urine culture: pending
- CT Scan: unremarkable
- MRI with IV contrast: results are positive for inflammation in areas of the brain and spinal cord
Patient perspectives on patient-reported outcomes in multiple sclerosis treatment trajectories: A qualitative study of why, what, and how?
Affiliations.
- 1 The Danish Multiple Sclerosis Society, Valby, Denmark; The Danish Multiple Sclerosis Registry, Copenhagen University Hospital Rigshospitalet, Denmark. Electronic address: [email protected].
- 2 The Danish Multiple Sclerosis Society, Valby, Denmark.
- 3 Danish Multiple Sclerosis Center, Department of Neurology, Copenhagen University Hospital Rigshospitalet, Denmark; The Danish Multiple Sclerosis Registry, Copenhagen University Hospital Rigshospitalet, Denmark.
- 4 Department of Public Health & Center for Healthy Aging, University of Copenhagen, Copenhagen, Denmark.
- PMID: 34995975
- DOI: 10.1016/j.msard.2021.103475
Background: Interest in patient-reported outcomes has been growing in multiple sclerosis research and clinical care in recent years. This situation reflects the need for developing, testing, and integrating measures that adequately capture patients' perspectives on symptoms, functional capacity, health status, and health-related quality of life. However, the patient perspective on the relevance, content, and use of patient-reported outcomes is yet to be investigated. Hence, this study aims to investigate the perspectives of people with multiple sclerosis on the value of patient-reported outcomes in clinical encounters, the most important aspects of living with multiple sclerosis that should be reflected in these reports, and possible opportunities and barriers for integrating this data into clinical care.
Methods: A qualitative study was conducted to capture patient perspectives in a Danish population of people with multiple sclerosis. Initially, two focus group interviews were conducted with a total of 11 participants to explore their perspectives on patient-reported outcomes and related prospects and barriers. Subsequently, nine individual interviews were conducted to further investigate the identified aspects, opportunities, and barriers to use patient-reported outcomes in clinical care and treatment.
Results: In general, the informants were motivated to report patient-reported outcomes, and they believed these reports to be relevant in clinical encounters as well as to have potential to promote patient involvement by focusing on current challenges for others with this disease. However, differences in the perceived need for reporting patient-reported outcomes were detected regarding the stage in the multiple sclerosis care trajectory and in relation to the disease phenotypes. In terms of domains to be incorporated into patient-reported outcomes, a total of 28 were identified by the informants, including neurological symptoms, cognitive impairments, mental health and well-being, self-care activities, and social challenges. Several factors for integrating patient-reported outcomes into clinical care emerged as important, in particular related to timing and frequency of reporting patient reported outcomes, considerations of cognitive impairments, the need for individualized approaches to patient-reported outcomes, and the need for active use of these reports for adjustment of treatment approaches in clinical encounters.
Conclusion: From the perspective of people with multiple sclerosis, patient-reported outcomes hold important potential for enhanced patient involvement leading to a more multifaceted agenda in clinical consultations. However, patient-reported outcomes need to be comprehensive and encompass a broad range of measures regarding neurological symptoms, cognitive impairments, mental health and well-being, self-care activities, and social challenges to adequately capture and support the needs of people with multiple sclerosis in clinical encounters. It is important to address barriers for integration of patient-reported outcomes into clinical care, with the aim of preventing misuse. Future studies should focus on the synergy between perspectives from both patients and clinicians to understand how integration of patient-reported outcomes in clinical care can succeed.
Keywords: Clinician-patient relationship; Multiple sclerosis; Patient involvement; Patient perspective; Patient-reported outcomes.
Copyright © 2022 Elsevier B.V. All rights reserved.
- Mental Health
- Multiple Sclerosis* / therapy
- Patient Reported Outcome Measures
- Qualitative Research
- Quality of Life*

Case Study: Use of Disease-Modifying Therapy in Elderly Patients With Multiple Sclerosis
With the advent of disease-modifying therapies, the life span of patients with multiple sclerosis has increased dramatically.
CM is a 65-year-old female presenting to the neurology clinic with a past medical history of relapsing/remitting multiple sclerosis (MS). Her initial symptoms at diagnosis were sensory loss in her left leg and optic neuritis.
After diagnosis, it was decided to start disease-modifying therapy (DMT) on interferon beta-1a. CM remained on this therapy for 13 years. She suffered from multiple relapses, including a relapse that resulted in hospitalization and steroid treatments.
The MRI results showed multiple enhancing lesions. The provider switched therapy to fingolimod. After 7 years of fingolimod therapy, CM suffered another severe relapse, resulting in hospitalization requiring treatment with SoluMedrol.
After multiple severe relapses and complications surrounding a car accident, CM is no longer ambulatory. She is in an assisted living facility, has an indwelling catheter, and has multiple reoccurring infections. Her EDSS score is 8.
In 2021, the provider discontinued all DMTs due to the risk of infection outweighing the benefits of prevention of relapses and disease progression due to the high EDSS score.
Today, a year later, she is presenting to the neurology clinic with the question of whether to restart a DMT to prevent relapses.What is your recommendation to the provider?
Mental Status
- Oriented to person, place, and time.
- Follows 3 step commands.
- Attention: normal.
- Concentration: normal.
- Speech: normal
- Level of consciousness: alert
- Knowledge: good.
- Able to name object. Able to read. Normal comprehension.
- Nurse advocate: She has good cognitive function and can feed herself if her meal is set up for her, uses her arms for daily tasks that are important for her quality of life.
- Gait: wheelchair bound
Coordination
Finger to nose coordination: normal
- Left deltoid: 4/5
- Right wrist flexion: 4/5
- Right wrist extension: 4/5
- Right interossei: 4/5
- Right abdominals: 1/5
- Left abdominals: 0/5
- AST, ALT, WBC – Within normal limits
- CrCl – 94 mL/min
- JCVaB – Negative
Medications
- Baclofen 10 mg oral BID
- Bupropion XL 300 mg QD
- Eliquis 5 mg QD
- Sulfamethoxazole-trimethoprim 400/80 mg as needed
Immunizations
Up to date on all vaccines.
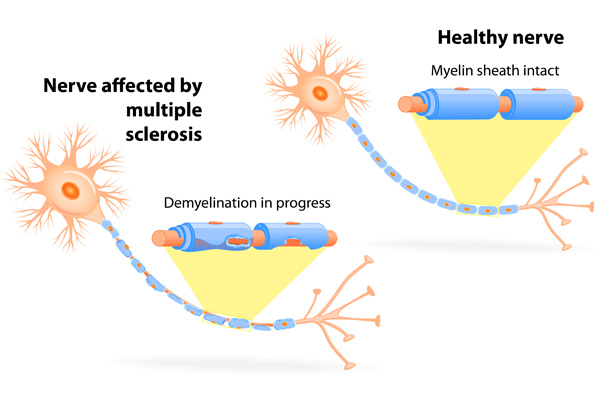
MS is an autoimmune disease characterized by inflammation, demyelination, and axonal degeneration. MS primarily affects women with a ratio of 3:1 compared to men with an initial diagnosis age ranging from 20 to 40 years. 1
According to the International Advisory Committee on Clinical Trials of MS, there are 4 main disease courses—clinically isolated syndrome (CIS), relapsing/remitting MS (RRMS), secondary progressive MS (SPMS), and primary progressive MS (PPMS). RRMS is the most common disease course, with approximately 85% of patients initially diagnosed in this stage. Patients with RRMS form cycles between relapses followed by periods of complete or partial recovery. 1
With the advent of DMTs, the life span of patients with MS has increased dramatically. Approximately 25% of patients with MS are adults over 65 years of age. 2
Health care providers face unique challenges in treating an elderly patient with MS. Elderly patients suffer from age-related and MS-related comorbidities with the disease course shifting from an inflammatory to a neurodegenerative phenotype. Among older adults, limited data exist for prescribing patterns of DMTs.
A retrospective longitudinal cohort study examined the prescribing patterns of DMTs in older adults with MS. 3 The study cohort consisted of 12,922 patients with MS aged 60 years and older, with 2455 patients receiving DMT therapy.
The most commonly prescribed DMTs were injectables (10.46%), orals (6.06%), and infusions (2.40%). The authors concluded nearly 1 in 5 older adults with MS were prescribed DMTs, with injectables being the most common form.
CMs condition has deteriorated over time and her EDSS score is currently 8. Clinical trials routinely exclude patients of CM’s age and with her degree of disability.
Hence, health care providers face a lack of knowledge of the safety and efficacy of DMTs in the elderly population. Often, providers will discontinue treatment because of increased risk and decreased benefit to the patient.
CM and her nurse advocate favor preserving and maintaining her quality of life. CM is still very functional cognitively and has fine upper extremity mobility.
Because future relapses could affect CM’s quality of life—after discussions with the patient, and the patient advocate—the provider decided to initiate CM on diroximel fumarate. Although the platform therapies of glatiramer acetate and interferon-beta1a are safest in the elderly population, CM was not interested in any injectable forms.
DMTs can cause varying degrees of lymphopenia, which is classified as grade 1 (mild lymphopenia) ALC < lower limit of normal to 800/mm 3 , grade 2 (moderate lymphopenia) ALC < 800–500/mm 3 , grade 3 (severe lymphopenia) ALC < 500–200/mm 3 and grade 4 < 200/mm 3 .
In the general population, lymphopenia is associated with increased risk of hospitalization and increased risk of infection-related death. 4 In patients with MS, this increased risk of infection is likely to be elevated due to comorbidities and the immunocompromised state.
Diroximel fumarate is used to treat both RRMS and active SPMS. 5 It has an unknown mechanism of action but does activate the nuclear factor (erythroid-derived 2)-like 2 (Nrf2) pathway reducing cellular oxidative stress.
CM is at a high risk of infection due to her baseline wheelchair status, prior infections, and indwelling catheter. In clinical trials with dimethyl fumarate (has the same active metabolite as diroximel fumarate), mean lymphocyte counts decreased by 30% during the first year of treatment, and then remained stable thereafter. 5
CM requires close monitoring—she will need CBC including lymphocyte count at baseline, and every 6 months thereafter, and MRI at baseline and then for routine monitoring. 5 If CM exhibits any disease activity (either clinical or on radiograph) after initiating diroximel fumarate, the provider should stop the medication due to the altered risk versus benefit scenario. Diroximel fumarate can cause liver toxicity—serum aminotransferase, alkaline phosphates, and total bilirubin levels must be checked before initiation and during treatment as clinically indicated.
The starting dose of diroximel fumarate is 231 mg twice a day orally. 5 The dose is increased to 462 mg twice a day after 7 days.
The pharmacist should counsel CM to take the medication with a meal or snack containing no more than 700 calories and 30 grams of fat to reduce flushing. Although diroximel fumarate causes less GI distress compared to dimethyl fumarate, CM should be counseled on abdominal pain, diarrhea, and nausea.5
PML is an opportunistic infection caused by the JC virus in immunocompromised patients. CM has tested negative for the JCV virus, but she should be counseled on the signs and symptoms of PML which include progressive weakness on one side of the body or clumsiness of limbs, visual changes, changes in memory, and orientation leading to confusion and personality changes. Patients may also develop herpes zoster or other opportunistic infections while on therapy.
The safety and efficacy of live or live-attenuated vaccines with diroximel fumarate has not been assessed. 5 According to the National MS Society guidelines, no adjustments are required with diroximel fumarate and COVID-19 vaccine administration. 6
About the Authors
Justin Bivona is a specialty clinical pharmacist working in multiple sclerosis and rare diseases at the Outpatient Pharmacy Services (OPS).
Bisni Narayanan, PharmD, MS is the supervisor for operations at OPS. OPS is a specialty pharmacy integrated within the Yale New Health System.
- What is MS? National Multiple Sclerosis Society 2022. Accessed on Nov 17, 2022. What is MS? | National Multiple Sclerosis Society (nationalmssociety.org)
- Vaughn CB, Jakimovski D, Kavak KS, et al. Epidemiology and treatment of multiple sclerosis in elderly populations. Nat Rev Neurol. 2019;15(6):329-342
- Talwar A, Earla JR, Hutton GJ, et al. Prescribing of disease modifying agents in older adults with multiple sclerosis. Mult Scler Relat Disord. 2022;57:103308
- Warny M, Helby J, Nordestgaard BG, et al. Lymphopenia and risk of infection and infection-related death in 98,344 individuals from a prospective Danish population-based study. PLoS Med. 2018;15(11):e1002685.
- Vumerity [package insert] Biogen; 2019
- COVID-19 VACCINE GUIDANCE FOR PEOPLE LIVING WITH MS. National Multiple Sclerosis Society. 2022. Accessed on Nov 17, 2022. COVID-19 Vaccine Guidance for People Living with MS | National MS Society | National Multiple Sclerosis Society .

Elevating Pharmacists, Empowering Pharmacy Technicians: A Symbiotic Journey in Health Care Excellence

Pharmacy Focus - Pharmacist-Led Initiatives on C diff Rates
FCRL5-Directed CAR T-Cell Therapy: A Novel Therapeutic Approach for Multiple Myeloma

Public Health Matters: Seacrest Studios’ Impact on Children’s Hospitals and Healing Through Broadcasting

The Biomedical Footprint of the Iraq War, Resulting Medical Innovation

Navigating the Long, Bumpy Road to Rare Disease Diagnosis and Treatment
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

- Open access
- Published: 02 May 2024
Risk factors and long-term outcomes of oropharyngeal dysphagia in persons with multiple sclerosis: a systematic review protocol
- Zahra Sadeghi 1 ,
- Mohamadreza Afshar 2 ,
- Asefeh Memarian 3 &
- Heather L. Flowers ORCID: orcid.org/0000-0001-6742-9459 3
Systematic Reviews volume 13 , Article number: 121 ( 2024 ) Cite this article
195 Accesses
Metrics details
Oropharyngeal dysphagia (OPD) can be functionally debilitating in persons with multiple sclerosis (pwMS). OPD induces alterations in safety and efficiency of food and/or liquid ingestion and may incur negative sequalae such as aspiration pneumonia or malnutrition/dehydration. Early detection and timely management of OPD in pwMS could prevent such complications and reduce mortality rates. Identifying risk factors of OPD relative to its onset or repeat manifestation will enable the development of care pathways that target early assessment and sustained management. The aims of this systematic review are to compile, evaluate, and summarize the existing literature reporting potential risk factors and associated long-term outcomes (e.g., aspiration pneumonia, malnutrition, dehydration, and/or death) of OPD in pwMS.
We will undertake a systematic review to identify studies that describe patterns and complications of OPD in pwMS. Variables of interest include predictors of OPD along with long-term outcomes. We will search MEDLINE, Embase, CINAHL, AMED, the Cochrane Library, Web of Science, and Scopus. We will consider studies for inclusion if they involve at least 30 adult participants with MS and report risk factors for OPD and/or its long-term outcomes. Studies will be excluded if they refer to esophageal or oropharyngeal dysphagia induced by causes other than multiple sclerosis. Study selection and data extraction will be performed by two independent assessors for abstract and full article review. We will present study characteristics in tables and document research findings for dysphagia-related risk factors or its complications via a narrative format or meta-analysis if warranted (e.g., mean difference and/or risk ratio measurements). All included studies will undergo risk-of-bias assessment conducted independently by two authors with consensus on quality ratings.
There is a lacune for systematic reviews involving risk factors and long-term outcomes of dysphagia in pwMS to date. Our systematic review will provide the means to develop accurate and efficient management protocols for careful monitoring and evaluation of dysphagia in pwMS. The results of this systematic review will be published in a peer-reviewed journal.
Systematic review registration
PROSPERO CRD42022340625.
Peer Review reports
Oropharyngeal dysphagia (OPD) is common in multiple sclerosis (MS) [ 1 ] due to injury to the corticobulbar tracts, potentially involving the brainstem, the cerebellum [ 2 , 3 ], and the cortex [ 4 ]. There may be a differing clinical course across types of MS, classified based on disease onset and progression over time [ 5 ]. The most frequent includes relapsing–remitting MS (RRMS), usually beginning with acute exacerbation and detrimental impacts that recover fully or partially over time. The other forms of MS are all defined as progressive, including secondary progressive MS (SPMS), primary progressive MS (PPMS), and progressive relapsing MS (PRMS). Patients with RRMS develop SPMS within 10 years of the onset of RRMS. PPMS is the least frequent type of MS and is characterized by deteriorating neurological function from disease onset coupled with a lack of remittance. Nevertheless, superimposed relapses are also evidenced in this type. Overall, the course of MS is unpredictable, and depending on the severity, the diversity of anatomic impacts, and the onset of associated lesions, its clinical manifestations are also heterogeneous.
Symptoms of OPD in MS may include coughing and/or choking on saliva or other liquid and food boluses, feelings of bolus sticking in the throat, the need to swallow multiple times per bolus, difficulty initiating a swallow (accompanied by drooling), and alterations to usual eating patterns (such as viscosity or texture changes) [ 3 , 4 , 6 ]. Oropharyngeal dysphagia may incur severe and multifaceted poor outcomes, such as aspiration pneumonia, malnutrition/dehydration [ 3 , 4 , 6 ], increased psychosocial comorbidities [ 7 , 8 ], and even death during periods of medical instability [ 9 ]. Identifying risk factors for OPD in pwMS will provide the means to develop accurate and efficient management protocols for careful monitoring and evaluation by dysphagia experts. By extension, sustained management will permit timely and comprehensive care to mitigate potential serious complications.
In two recent systematic reviews, the authors provided an estimate of the pooled frequency of dysphagia in pwMS based on a range of evaluation methods, whether screening, clinical, or instrumental examination [ 1 , 10 ]. Guan et al. [ 1 ] reported a pooled frequency estimate of 36% based on subjective screenings or cursory evaluations (such as the Dysphagia in Multiple Sclerosis Questionnaire, the water swallowing test, and various dysphagia checklists from individual clinical swallowing centers) and 81% based on objective measurements (such as videofluoroscopy or fiber-optic nasoendoscopy). More specifically, the frequency of dysphagia was 46% in pwMS when Expanded Disability Status Scale (EDSS) scores were stratified as 4.5 or higher and 40% for those below 3.0. Similarly, patients with longer disease duration (over 10 years) were more likely to have dysphagia symptoms compared with shorter disease duration.
Various individual studies have also shown a higher frequency of dysphagia with greater disability [ 11 , 12 , 13 , 14 , 15 ] and/or disease duration [ 15 , 16 ]. Nevertheless, a few studies have reported that pwMS with low EDSS scores still had dysphagia [ 15 , 17 , 18 ]. To illustrate, Abraham et al. [ 18 ] reported that 43% of pwMS in their sample had dysphagia including 17% with low levels of disability (EDSS score lower than 2.5). Aghaz et al. [ 10 ] estimated the pooled frequency of dysphagia as 37% based on subjective evaluations or cursory checklists versus 47% for objective instrumental evaluations respectively. In contrast to the findings of Abraham et al. [ 18 ], they failed to demonstrate associations for the presence of dysphagia according to EDSS-based disease severity, duration of disease, or MS stage.
Taken together, reported frequencies of dysphagia hover around one-third of pwMS at a given point in time [ 1 , 10 ], whereby varied frequencies relate primarily to evaluation methods, whether screening, clinical assessment, or instrumental evaluation. The most common patient-report tool used to identify dysphagia in pwMS is the Dysphagia in Multiple Sclerosis Questionnaire (DYMUS) [ 1 , 10 , 19 ], involving 10 items with very good reliability and internal consistency. However, frequencies of reported dysphagia based on questionnaires are lower than those based on standardized tools or instrumental evaluations [ 1 ]. In general, instrumental assessment remains the gold standard for dysphagia and aspiration detection, whether by videofluoroscopy or fiber-optic nasoendoscopy rather than various types of screening tools, bedside evaluations, or patient-reported questionnaires. Some pwMS may underestimate their dysphagia severity due to altered sensory appreciation of symptoms, despite instrumental evidence to the contrary.
In addition to our poor understanding of the frequency of dysphagia in pwMS, gaps exist regarding patterns of associations between disease severity, duration, or stage. Notwithstanding, certain predictive factors may well routinely accompany the expression of dysphagia in pwMS. Elucidating such information would require a comprehensive profile of patient groups with known disease severity, duration, and stage alongside MS type, neuroanatomical impacts, and concomitant deficits or disorders. For example, dysphagia may be precipitated by coexisting psychological or cognitive impairments [ 11 , 18 , 20 ]. Therefore, continual monitoring for risk of dysphagia in pwMS who also experience negative mental health symptoms or cognitive disorders [ 4 , 20 ] is warranted. Furthermore, speech impairments (e.g., dysarthria) may provide good and readily identifiable clinical indicators for the presence of dysphagia in persons with neuromuscular diseases [ 21 ]. A systematic appraisal of the literature is required to identify the best available evidence for risk factors of dysphagia along with ensuing long-term sequelae in pwMS.
A systematic review constitutes the highest level of research evidence, especially if there is a quality evaluation and meta-analysis. Therefore, a comprehensive systematic review, aimed at establishing the predictors of dysphagia in pwMS, ideally identified with gold standard evaluation methods (such as instrumental assessment), could facilitate the development of new tools for screening or assessing dysphagia and inform practice guidelines. In addition, a close consideration of associated outcomes over the long term (e.g., pneumonia, poor social participation, death) could contribute to our understanding of prognostic indicators for particular patient groups. Consequently, our purpose is to search the existing literature to systematically identify the risk factors and associated outcomes of oropharyngeal dysphagia over the long term in persons with pwMS.
The protocol of this systematic review has been registered in PROSPERO (registration number: CRD42022340625). We have applied PRISMA-P guidelines to develop this review protocol further. It served to direct our search strategy of databases and the gray literature as well as our data extraction and compilation methods. We will document our article selection results using the PRISMA flow diagram to delineate reasons for abstract and article exclusion until the final set of articles is identified. Our investigation of risk factors is in keeping with recommendations from the Cochrane Prognostic Methods Group ( https://methods.cochrane.org/prognosis/ ) [ 22 ]. We are submitting the protocol prior to undertaking the full search or any subsequent processes such as abstract screening and full article evaluation.
Operational definitions
Oropharyngeal dysphagia is defined as body and structure impairment [ 23 ] in swallowing physiology evidenced by expert clinical or instrumental assessment of function from the anterior aspect of the lips to inferior aspect of the upper esophageal sphincter. Diagnosis of multiple sclerosis is based on accepted criteria for both definite and probable MS, according to a classification scheme that involves expert clinical and objective evaluations (such as neuroimaging) [ 24 ].
Data sources
We will conduct an electronic search in the following databases for abstracts in languages that the co-authors can read (English, French, German, Persian, Portuguese, Spanish, and Turkish). No publication date or study design restrictions will be imposed. Relevant databases will include MEDLINE, Embase, CINAHL, AMED, the Cochrane Library (CENTRAL), Web of Science, and Scopus. The MeSH and search terms used in the search strategy were developed a priori (Table 1 ). A research librarian will consult to enable valid adaptations of the MEDLINE terms into the other databases. Our MEDLNE search was conducted in OVID, revealing 189 citations (April 2023). We will also search international gray literature sources (e.g., OpenGrey and Dissertation Abstracts) and review the bibliographies and citations for all included articles in a reiterative manner until no further possible references are identified.
Eligibility criteria
Studies will be considered for inclusion if they have observational intent and involve retrospective or prospective consecutive or randomly selected sampling (either from a particular cohort or population). Study designs may include case series, cross-sectional, longitudinal, case–control, and/or other observational investigations as well as the control arm (i.e., participants who are not receiving trial-related interventions for MS or dysphagia) of randomized controlled trials. We will consider studies with at least 30 adults (18 years or older) with MS. Studies must include an aim to identify risk factors (e.g., MS subtype, disease duration, EDSS score, age, gender, smoking or alcohol use, psychological symptoms, cognitive impairments, and/or dysarthria) that may precipitate oropharyngeal dysphagia (OPD). We have chosen not to prespecify all possible risk factors as we seek to identify new potential risk factors. The body of evidence is small, and risk factors are likely underrepresented at present. Any potential new risk factors will provide a path for future researchers to investigate them in a comprehensive way and thus extend the literature and knowledge base in this respect.
Corresponding studies that include follow-up time points will contribute to our interest in long-term outcomes (e.g., detrimental medical, activity/participation, or quality-of-life outcomes). Ideally, such studies would have comparable follow-up periods (e.g., yearly) that span the course of the disease and document the outcomes relative to the absence/presence and/or severity classifications of OPD. However, we will not exclude any studies based on their follow-up points or overall time horizon.
During our review of abstracts and full articles, we will apply pre-defined exclusion criteria. That is, we will exclude studies involving convenience samples, those without extractable data (e.g., studies involving aggregate results for multiple etiologies rather than pwMS alone) for our outcomes of interest, and those reporting duplicate data. Any abstracts without corresponding full study publications will be excluded. We will also exclude articles without a clear sample of at least 30 pwMS and corresponding OPD (for at least a declared portion of the sample), identified by clinical or instrumental swallowing assessments. Finally, articles will be excluded if they do not conform to our operational definitions of OPD and MS or if they refer to oropharyngeal dysphagia induced by causes other than multiple sclerosis. We will contact authors when we cannot find full articles or when we wish to elucidate study characteristics such as method of dysphagia assessment. Our full systematic review reporting will conform to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist [ 27 ].
Data collection
Study selection from primary articles will be performed in two stages:
Initial screening and coding of titles and abstracts whereby relevant abstracts (stage 1) will undergo full article review (stage 2) (Table 2 )
Evaluation and coding of full articles for inclusion in the final sample (Table 2 )
The review process will be conducted by two independent reviewers (blind to each other’s coding) across the two stages. Any discrepancies will be resolved by consensus discussion between the two reviewers, and, when agreement is not possible, a third reviewer (also a member of the research team) will read the abstract or article independently and contribute to a decision. All references for the excluded articles will be retained for documentation purposes.
One data extractor will identify pertinent information from the final set of included articles and compile it into a table or spreadsheet. Extracted data will be verified by a second independent reviewer to ensure the accuracy of information from the following categories:
Study characteristics: First author’s name, year of publication, country in which the study was conducted, study design, and size of the sample
Study population and participant characteristics: Age, gender, MS type, disease duration, and EDSS score
Diagnostic assessments for MS and dysphagia
Risk factors for dysphagia whether related to MS (e.g., MS type, disease duration, and EDSS score), to patient characteristics (e.g., age, gender, and smoking or alcohol abuse), and/or to comorbidities (e.g., psychological symptoms, cognitive impairments, or dysarthria)
Follow-up assessments of dysphagia in terms of type and timing
Frequency and impact (e.g., severity) of detrimental medical (e.g., aspiration pneumonia, dehydration, malnutrition, institutionalization, and mortality), activity/participation (e.g., fewer social engagements around meals), or quality-of-life outcomes.
Risk of bias in individual studies
We will apply appropriate risk-of-bias evaluations [ 22 , 28 ] such as the Newcastle–Ottawa scale (NOS) [ 29 ] as a quality evaluation of included obserervational studies. To illustrate, the NOS contains grading for categories of selection (e.g., sample representativeness), comparability (e.g., evaluation of confounders), and outcome (adequacy of follow-up period). Further, if warranted, the Cochrane Collaboration’s risk-of-bias tool will be used for randomized controlled trials, based on the domains: sequence generation, blinding of participants, blinding of outcome measurement, allocation sequence concealment, missing data, selective outcome reporting, and other biases such as sources of funding and conflicts of interest [ 30 ]. Additionally, the Quality in Prognosis Studies (QUIPS) tool will facilitate assessment for the risk factor studies [ 22 ]. For any type of quality appraisal (observational study quality scale, Cochrane’s risk-of-bias tool, or QUIPS), two authors will independently review the included studies and resolve discrepancies by discussion and consensus agreement within the review team.
Data analysis
We will provide a descriptive synthesis of the findings from the included studies, structured around target population characteristics, type of assessments, and outcomes of interest. We will consider meta-analyses if there is an adequate number of studies and homogeneity of study populations and assessment methods. Otherwise, we will present a narrative synthesis of the results. We anticipate that there will be restricted scope for meta-analysis due to differing study populations and/or assessment methods along with a paucity of existing literature. Where studies have similar sample characteristics (including potential comparison groups), assessment methods, and corresponding outcomes, we will pool the results and apply various types of meta-analyses such as mean difference, standard mean difference, or Cox regression for continuous outcomes and risk ratio measurement or logistic regression for categorical outcomes depicted in forest plots along with their 95% confidence intervals (CIs). Finally, we will evaluate the overall strength of the evidence based on discussion among authors through application of a tool such as GRADE.
Assessment of heterogeneity
If there is reason to consider meta-analysis, analyses will be performed using Cochrane’s Review Manager tool (Review Manager: RevMan [computer program]. The Cochrane Collaboration, 2024). We plan to assess study features such as participant age and sex, MS subtype, time course for follow-up, and primary outcome measures as the basis for determining if data pooling for meta-analysis is warranted. Subsequently, if meta-analysis is undertaken, we will apply and interpret the I 2 statistic [ 30 ] as an indictor of heterogeneity relative to the number of studies and direction of effect using the following guide: mild (between 0 and < 25%), moderate (between 25 and < 50%), severe (between 50 and < 75%), and highly severe (between 75 and 100%). If there is moderate heterogeneity, we will present a supplementary qualitative synthesis of the findings.
Analysis of subgroups or subsets
If sufficient data are available, subgroup analyses may be conducted for different OPD assessment methods (e.g., clinical bedside evaluation, fiber-optic nasoendoscopic evaluation, and/or videofluoroscopic evaluation) relative to MS type and risk factors. Similarly, long-term outcomes based on dysphagia status or severity levels will be analyzed according to follow-up periods or comparable overall time horizon.
Assessment of publication bias
Publication bias will be evaluated using a funnel plot (i.e., plots of study results against precision) and Begg’s [ 31 ] and Egger’s [ 32 ] tests if an adequate number of studies (≥ 10) are identified. Additionally, we will incorporate Deek’s asymmetry test [ 33 ] to mitigate overestimation of effects when predictive modeling with odds ratios is applied for the determination of OPD across studies that involve low event proportions. However, if meta-analysis is not possible, publication bias will be assessed descriptively and involve documentation of direction of results across risk factors (whether significant or not) as well as potential follow-up time lags across studies.
Our search strategy is extensive compared to other recent systematic reviews in the field of multiple sclerosis [ 1 , 34 ] given the inclusion of numerous sources and comprehensive search terms. We believe that it will yield a broad capture of abstracts internationally, but that many articles will derive from western or developed countries. This may be an important limitation because many underrepresented countries, such as Iran, have a high and increasing prevalence of pwMS in certain regions [ 35 , 36 ].
Other systematic reviews have undertaken different lines of inquiry such as investigating the prevalence of dysphagia in pwMS without considering risk factors [ 1 ] or long-term outcomes [ 1 , 10 ]. Thus, we will extend the knowledge base in a new content area (involving predictors and long-term outcomes of dysphagia in pwMS). Our identification of literature in the field of MS will provide new insights into the repercussions of dysphagia and offer direction for the development of screening protocols, assessment methods, and improved therapeutic management in pwMS. In the event that our findings elucidate multiple predictors (e.g., related to MS, patient characteristics, and/or comorbidities) and varied outcomes (e.g., medical, activity/participation, or quality of life), they may warrant publication in multiple peer-reviewed papers.
We anticipate that various limitations will result during our search of the literature. First, studies may not report the timeframe between dysphagia onset, assessments, and associated outcomes. Second, dysphagia identification in specific studies might be based on cursory screenings, patient self-report (and potentially non-standardized) questionnaires, and/or subjective clinical assessments rather than on instrumental reference tests such as videofluoroscopy and fiber-optic nasoendoscopy. Finally, it may be difficult to pool results from the existing literature for some of the risk factors or outcomes if investigations restrict enrolment to particular types of pwMS, involving subsamples of larger studies, or if they fail to incorporate shared definitions and research methods in the field of multiple sclerosis [ 36 ].
Although the frequency of dysphagia in pwMS has been a topic of inquiry within the past two decades [ 1 , 10 ], a poor understanding of associations to disease-related risk factors and negative outcomes remains. Our proposed systematic review will address such a gap in the literature, as we will attempt to elucidate risk factors of dysphagia and long-term outcomes from observational studies reporting frequencies of dysphagia over the long term. Where relevant, we will pool results across studies or extract individual-level data that may permit us to model risk factors of dysphagia and/or its associated long-term outcomes in pwMS. Our inquiry will offer the means to inform best practices in the early detection of dysphagia and provide information that can be incorporated into guidelines and clinical practice initiatives for the management of dysphagia in pwMS.
Availability of data and materials
Not applicable.
Abbreviations
- Oropharyngeal dysphagia
Persons with multiple sclerosis
- Multiple sclerosis
Expanded Disability Status Scale
Dysphagia in Multiple Sclerosis Questionnaire
Strengthening the Reporting of Observational Studies in Epidemiology
Newcastle-Ottawa scale
Guan X-L, Wang H, Huang H-S, Meng L. Prevalence of dysphagia in multiple sclerosis: a systematic review and meta-analysis. Neurol Sci. 2015;36:671–81.
Article PubMed Google Scholar
Tassorelli C, Bergamaschi R, Buscone S, Bartolo M, Furnari A, Crivelli P, et al. Dysphagia in multiple sclerosis: from pathogenesis to diagnosis. Neurol Sci. 2008;29:360–3.
Article Google Scholar
Marchese-Ragona R, Restivo D, Marioni G, Ottaviano G, Masiero S, Staffieri A. Evaluation of swallowing disorders in multiple sclerosis. Neurol Sci. 2006;27:s335–7.
Calcagno P, Ruoppolo G, Grasso M, De Vincentiis M, Paolucci S. Dysphagia in multiple sclerosis–prevalence and prognostic factors. Acta Neurol Scand. 2002;105(1):40–3.
Article CAS PubMed Google Scholar
Katz Sand IB, Lublin FD. Diagnosis and differential diagnosis of multiple sclerosis. Continuum. 2013;19(4 Multiple Sclerosis):922-43. https://doi.org/10.1212/01.CON.0000433290.15468.21 .
Prosiegel M, Schelling A, Wagner-Sonntag E. Dysphagia and multiple sclerosis. Int MS J. 2004;11:22–31.
CAS PubMed Google Scholar
Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia. 2002;17:139–46.
Verdonschot RJ, Baijens LW, Vanbelle S, van de Kolk I, Kremer B, Leue C. Affective symptoms in patients with oropharyngeal dysphagia: a systematic review. J Psychosom Res. 2017;97:102–10.
Sadovnick A, Eisen K, Ebers GC, Paty DW. Cause of death in patients attending multiple sclerosis clinics. Neurology. 1991;41(8):1193.
Aghaz A, Alidad A, Hemmati E, Jadidi H, Ghelichi L. Prevalence of dysphagia in multiple sclerosis and its related factors: systematic review and meta-analysis. Iran J Neurol. 2018;17(4):180.
PubMed PubMed Central Google Scholar
Thomas FJ, Wiles C. Dysphagia and nutritional status in multiple sclerosis. J Neurol. 1999;246:677–82.
Hartelius L, Svensson P. Speech and swallowing symptoms associated with Parkinson’s disease and multiple sclerosis: a survey. Folia Phoniatr Logop. 1994;46(1):9–17.
De Pauw A, Dejaeger E, D’hooghe B, Carton H. Dysphagia in multiple sclerosis. Clin Neurol Neurosurg. 2002;104(4):345–51.
Herrera W, Zeligman BE, Gruber J, Jones MC, Pautler R, Wriston R, et al. Dysphagia in multiple sclerosis: clinical and videofluoroscopic correlations. J Neurol Rehabil. 1990;4(1):1–8.
Google Scholar
Sadeghi Z, Afshar M, Ebadi A, Baghban K, Qureshi ZS. Swallowing disorder in multiple sclerosis: modified version of the screening tool. Arch Rehabil. 2020;21(2):236–55.
Tarameshlu M, Azimi AR, Ghelichi L, Ansari NN. Prevalence and predictors of dysphagia in Iranian patients with multiple sclerosis. Med J Islam Repub Iran. 2017;31:133.
Article PubMed PubMed Central Google Scholar
Pajouh SD, Moradi N, Yazdi MJS, Latifi SM, Mehravar M, Majdinasab N, et al. Diagnostic evaluation of dysphagia in multiple sclerosis patients using a Persian version of DYMUS questionnaire. Mult Scler Relat Disord. 2017;17:240–3.
Abraham S, Scheinberg LC, Smith CR, LaRocca NG. Neurologic impairment and disability status in outpatients with multiple sclerosis reporting dysphagia symptomatology. J Neurol Rehabil. 1997;11(1):7–13.
Bergamaschi R, Crivelli P, Rezzani C, Patti F, Solaro C, Rossi P, et al. The DYMUS questionnaire for the assessment of dysphagia in multiple sclerosis. J Neurol Sci. 2008;269(1–2):49–53.
Sadeghi Z, Ghoreishi ZS, Flowers H. et al. Depression, anxiety, and stress relative to swallowing impairment in persons with multiple sclerosis. Dysphagia. 2021;36:902–9. https://doi.org/10.1007/s00455-020-10207-x .
Wang BJ, Carter FL, Altman KW. Relationship between dysarthria and oral-oropharyngeal dysphagia: the present evidence. Ear Nose Throat J. 2020:145561320951647. https://doi.org/10.1177/0145561320951647 .
Riley RD, Ridley G, Williams K, Altman DG, Hayden J, de Vet HC. Prognosis research: toward evidence-based results and a Cochrane methods group. J Clin Epidemiol. 2007;60(8):863-5.
World Health Organization. International classification of functioning, disability and health: ICF. World Health Organization; 2001. https://iris.who.int/handle/10665/42407.
Poser CM, Paty DW, Scheinberg L, McDonald WI, Davis FA, Ebers GC, et al. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol. 1983;13(3):227–31.
Flowers H, Bérubé D, Ebrahimipour M, Perrier M-F, Moloci S, Skoretz S. Swallowing behaviours and feeding environment in relation to communication development from early infancy to 6 years of age: a scoping review protocol. BMJ Open. 2019;9(8):e028850.
Farinotti M, Vacchi L, Simi S, Di Pietrantonj C, Brait L, Filippini G. Dietary interventions for multiple sclerosis. Cochrane Database Syst Rev. 2012;12:CD004192.
PubMed Google Scholar
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
Ma L-L, Wang Y-Y, Yang Z-H, Huang D, Weng H, Zeng X-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020;7:1–11.
Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2011. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101. https://doi.org/10.2307/2533446 .
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629 .
Article CAS PubMed PubMed Central Google Scholar
Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58(9):882–93. https://doi.org/10.1016/j.jclinepi.2005.01.016 . PMID: 16085191.
Mirmosayyeb O, Ebrahimi N, Shekarian A, Afshari-Safavi A, Shaygannejad V, Barzegar M, Bagherieh S. Prevalence of dysphagia in patients with multiple sclerosis: a systematic review and meta-analysis. J Clin Neurosci. 2023;108:84–94.
Bagherieh S, Mirmosayyeb O, Vaheb S, Afshari-Safavi A, Barzegar M, Ashtari F, Shaygannejad V. Prevalence and incidence of multiple sclerosis in Isfahan Province, Iran: a 25-year population-based study. Mult Scler Relat Disord. 2023;71:104310.
Cohen JA, Trojano M, Mowry EM, Uitdehaag BM, Reingold SC, Marrie RA. Leveraging real-world data to investigate multiple sclerosis disease behavior, prognosis, and treatment. Mult Scler J. 2020;26(1):23–37.
Download references
Acknowledgements
Author information, authors and affiliations.
Department of Speech Therapy, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Zahra Sadeghi
Department of Speech Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran
Mohamadreza Afshar
School of Rehabilitation Sciences, Faculty of Health Sciences, University of Ottawa, 200 Lees Avenue, Ottawa, ON, K1S 5S9, Canada
Asefeh Memarian & Heather L. Flowers
You can also search for this author in PubMed Google Scholar
Contributions
ZS conceptualized, designed, and wrote much manuscript. HF conceptualized, designed, wrote, and edited the manuscript. MA conceptualized, designed, and wrote parts of the manuscript. AM developed the search terms and wrote parts of the manuscript.
Corresponding author
Correspondence to Heather L. Flowers .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sadeghi, Z., Afshar, M., Memarian, A. et al. Risk factors and long-term outcomes of oropharyngeal dysphagia in persons with multiple sclerosis: a systematic review protocol. Syst Rev 13 , 121 (2024). https://doi.org/10.1186/s13643-024-02530-3
Download citation
Received : 13 September 2023
Accepted : 11 April 2024
Published : 02 May 2024
DOI : https://doi.org/10.1186/s13643-024-02530-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Online First
- Active and non-active progression independent of relapse activity within the first 20 years of relapsing multiple sclerosis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-6755-496X Adil Maarouf 1 , 2 ,
- Jan Patrick Stellmann 2 , 3 ,
- Audrey Rico 1 , 2 ,
- Clemence Boutiere 1 ,
- http://orcid.org/0000-0002-8513-5443 Sarah Demortiere 1 ,
- Pierre Durozard 4 ,
- Wafaa Zaaraoui 2 ,
- Jean-Philippe Ranjeva 2 ,
- Jean Pelletier 1 , 2 ,
- http://orcid.org/0000-0002-9860-7657 Bertrand Audoin 1 , 2
- 1 Pôle de Neurosciences Cliniques, Service de Neurologie , Assistance Publique Hopitaux de Marseille , Marseille , France
- 2 Aix-Marseille Univ, CRMBM, CNRS UMR 7339 , Marseille , France
- 3 Département de Neuroradiologie, Assistance Publique Hopitaux de Marseille , Marseille , France
- 4 Centre Hospitalier d'Ajaccio , Ajaccio , France
- Correspondence to Dr Bertrand Audoin, Assistance Publique Hopitaux de Marseille, Marseille, France; bertrand.audoin{at}ap-hm.fr
Background Progression independent of relapse activity (PIRA) has been described since the early stage of relapsing multiple sclerosis (RMS). However, little is known about the relation between PIRA and inflammatory activity that is particularly important at this stage of the disease.
Method We included 110 patients in a prospective study within 18 months of RMS onset. MRI examinations and clinical visits were scheduled on the same day for months 0, 6, 12, 24, 36, 60, 84, 120, 180 and 240.
Results The mean (SD) age of patients was 30 (6.7) years at inclusion and median (range) follow-up 15 (9–20) years. Analysis of 1118 between-visit intervals revealed 93 confirmed disability accumulation events in 68 (62%) patients: 50 (54%) events related to relapse activity worsening and 43 (46%) PIRA events, including 17 (18%) with MRI activity. The risk of PIRA between two visits (stable event as the reference category) was associated with Expanded Disability Status Scale (EDSS) score (HR: 1.41; 95% CI: 1.18 to 1.69; p<0.001), disease duration (HR: 0.75; 95% CI: 0.62 to 0.90; p<0.005) and new lesions between the visits (HR: 1.09 per lesion; 95% CI: 1.01 to 1.17; p<0.05). As compared with PIRA events with MRI activity, PIRA events without such activity occurred in patients with more disability (mean EDSS score 3, p<0.05), longer disease duration (mean 11 years, p<0.001) and greater number of T2-weighted lesions (p<0.05).
Conclusion This study evidenced that inflammatory activity increases the risk of PIRA in early RMS, arguing that a significant part of PIRA is accessible to treatment targeting inflammation in these patients.
- MULTIPLE SCLEROSIS
https://doi.org/10.1136/jnnp-2024-333597
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Disease progression independent of relapse activity (PIRA) was described in patients with relapsing multiple sclerosis (RMS) treated with high-efficacy therapy, which suggested that PIRA could occur independent of disease activity. 1 Hence, PIRA was interpreted as the clinical counterpart of the neurodegenerative component of MS. However, in patients without full control of disease activity, lesion accumulation could also contribute to PIRA. 2–5 In these patients, non-active PIRA (naPIRA), defining patients free of relapse but also free of MRI activity, could better reflect the neurodegenerative component of MS as compared with those with active PIRA (aPIRA). Nevertheless, to what extent aPIRA contributes to PIRA in early RMS remains largely unknown because, in previous studies, MRI explorations were missing or not performed at the same time as clinical visits. 2 3
In the present study, we analysed data from a prospective MRI study of 129 patients with RMS enrolled after their first clinical event and followed up to 20 years (median 15 years). Importantly, all clinical visits and MRI examinations (>1100) were scheduled on the same day, which allowed for qualifying each confirmed disability accumulation (CDA) event as aPIRA, naPIRA or relapse-associated worsening (RAW).
Participants
From 2001 to 2011, 129 patients were included in a prospective MRI study based on the following criteria: (1) age 18–45 years; (2) occurrence of a first inflammatory demyelinating event in the central nervous system in the last 18 months; (3) presence of oligoclonal bands in cerebral spinal fluid and (4) presence of at least two demyelinating lesions in the brain or spinal cord detected at the initial MRI performed before inclusion. All participants gave informed consent to participate in the study before taking part. 6 7
Study design
Brain MRI examinations and clinical visits were scheduled on the same day for months 0, 6, 12, 24, 36, 60, 84, 120, 180 and 240. Disability level was rated with the Expanded Disability Status Scale (EDSS). 8 All relapses since the last visit were recorded.
CDA was considered according to the used three strata definitions (increase in EDSS score by 1.5 points if the last EDSS score was 0, increase by 1 point if the EDSS score was 1–5.5 or increase by 0.5 points if the EDSS score was >5.5), confirmed after at least 6 months. The existence of a PIRA event was defined at each visit considering the presence of CDA during the interval and the absence of any relapse during the same interval. With new T2-weighted lesions and PIRA during the same interval, we retained an aPIRA event. If PIRA occurred in an interval without new lesions, we retained an naPIRA event. PIRA events had to be present in all longitudinal follow-up data. With the presence of CDA and relapse during the same interval, we retained a RAW event. If no CDA occurred in an interval, we retained a STABLE event.
We compared patient characteristics at the beginning of each intervisit interval associated with an episode of CDA (RAW, aPIRA and naPIRA), including age, disease duration, EDSS score and number of brain T2 lesions, by using linear mixed-effects models accounting for recurrent measurements in patients. To explore factors associated with PIRA between two consecutive visits (with STABLE events as the reference category), we computed Cox proportional-hazards regression models for recurrent events with patient ID used as a cluster variable and first clinical event or the next visit as the end time, estimating HRs and 95% CIs. The initial Cox proportional-hazards model included age, EDSS score, disease duration, total lesion number, type of treatment (no vs high/moderate/low efficacy therapy) at the beginning of the intervisit interval and number of new T2-weighted lesions in the intervisit interval and in the previous intervisit interval. The model was then reduced by backward selection of variables. We used the Akaike Information Criterion to select variables. All analyses were performed with Statistics in R V.4.2.1.
Data availability
All data will be shared anonymised by reasonable request of a qualified investigator to the corresponding author.
Characteristics of the cohort
At the time of the analysis, 110 of 129 (85%) patients were still being followed (88 women, mean (SD) age 30 (6.7) years at the first MRI/clinical visit); 14 patients dropped out after the first MRI and 5 before 5 years. At the first MRI/clinical visit, the mean (SD) time since the first MS symptoms was 0.48 (0.35) years. At the last MRI/clinical visit, the median (range) follow-up of patients was 15 (9–20) years, corresponding to 1569 patient-years. The number of combined MRI/clinical visits was 1120, corresponding to a median (range) of 10 (4–19) visits per patient.
During the same period of inclusion (2001–2011), 571 patients visited the MS centre of Marseille for a first demyelinating MS event. These patients represented 87% of the estimated number of patients with a first demyelinating MS event during this period (n=657) according to the incidence of MS in the Provence region. 9 The 110 patients followed and the 571 who visited the centre did not differ in demographic characteristics (sex ratio and age) (p=0.28 and p=0.11).
CDA during follow-up
Analysis of the 1118 between-visit intervals revealed 93 CDA events in 68 of 110 (62%) patients: 50 (54%) RAW and 43 PIRA (46%) ( table 1 and figure 1 ). PIRA events included 26 naPIRA (60%) and 17 aPIRA (40%) events. As compared with aPIRA events, naPIRA events occurred in patients with more disability (mean EDSS score 3, p<0.05), longer disease duration (mean 11 years, p<0.001) and greater number of T2-weighted lesions (mean 55, p<0.05) ( tables 1 and 2 ). The final model included only EDSS score (HR: 1.41; 95% CI: 1.18 to 1.69; p<0.005), disease duration (HR: 0.75; 95% CI: 0.62 to 0.90; p<0.005) and number of new T2-weighted lesions during the intervisit interval (HR: 1.09 per lesion; 95% CI: 1.01 to 1.17; p<0.05) ( table 3 ).
- View inline
Patient characteristics by type of event
- Download figure
- Open in new tab
- Download powerpoint
(A) Individual disease course for 110 patients ordered from bottom to top by their last documented Expanded Disability Status Scale (EDSS) score. The colour of the bar represents the EDSS at the beginning of each intervisit interval. Filled dots represent the timepoint of confirmed progression events classified as relapse-associated worsening (RAW), active progression independent of relapse activity (PIRA) or non-active PIRA. (B) Boxplots illustrating the difference in selected characteristics at the beginning of each intervisit interval with a confirmed progression event. Horizontal line is median, box edges are IQR and whiskers are range. DDS, Disease Durations.
Disease characteristics at the beginning of episodes with confirmed EDSS score progression labelled as RAW (the reference category), active PIRA or non-active PIRA
Predictors for a PIRA event
Events related to disease activity (RAW and aPIRA) contribute to almost 75% of all CDA events occurring within the first 20 years of RMS. naPIRA contributed to the remaining CDA events and occurred more frequently after several years of disease evolution (mean 11 years) in patients with significant disability (mean EDSS score 3) and a high number of lesions.
In the present study, we selected patients younger than 45 years at inclusion to limit the risk of including patients not at the real first stage of MS and patients with progressive MS erroneously classified as RMS. Therefore, the association found between lesion accumulation and risk of concomitant PIRA could not be generalised to late-onset RMS.
The present study indicates that PIRA events in early RMS could not be exclusively related to diffuse inflammation and/or secondary degeneration and that the accumulation of asymptomatic demyelinating lesions in the brain was observed in 40% of all PIRA events. Crucially, the association found between lesion accumulation during the intervisit interval and risk of PIRA at the end of the intervisit interval suggests that the accumulation of demyelinating lesions independent from relapse may be involved in the pathogenesis of PIRA. The risk of PIRA at each visit was increased to a mean of 9% for each new single brain T2 lesion that occurred since the last visit. This association between MRI activity and subsequent disability worsening can partly explain the elevation of neurofilament light chain observed more than one year before disability worsening independent of clinical relapses. 10 One may suppose that subclinical relapse activity could result in disability worsening as the central nervous system reserve is lost. 5 Moreover, the contribution of aPIRA events was probably under-estimated here because of lack of available spinal-cord MRI images. Indeed, previous studies found that lesion accumulation in the spinal cord contributed highly to disability. 11 12 Finally, we found that naPIRA events occurred generally after several years of disease in patients with a high number of lesions and more disability. All these findings suggest that many PIRA events occurring in RMS could be accessible to early treatment with high-efficacy therapy that fully controls disease activity and reduces early disability accumulation. 13 14 In the present study, we did not find an association between treatment and risk of PIRA. However, the interpretation of this result is difficult because the decision to treat and the choice of therapy were based on the physician’s preference and highly depended on the level of disease activity. Thus, the design of the present study allowed for depicting an association between disease activity and risk of PIRA but not the potential effect of therapy on risk of PIRA.
The strengths of the study are its prospective design, the long-term follow-up, the high number of standardised clinical and MRI examinations performed concomitantly, the inclusion of patients right after RMS onset and the low number of patients lost to follow-up. Limitations are lack of spinal-cord MRI images, the relatively small sample size and the monocentric design. Moreover, the effect of EDSS levels on the risk of progression needs to be interpreted with caution because the non-continuous character of the EDSS scale might bias our analyses, in which EDSS score was used as a continuous variable.
Conclusions
APIRA and naPIRA may have different pathophysiologies, and full control of disease activity from disease onset may significantly reduce the risk of PIRA in RMS.
Ethics statements
Patient consent for publication.
Consent obtained directly from patient(s).
Ethics approval
This study involves human participants and was approved. This study involves human participants and was approved by local ethics committee (Timone Hospital, Marseille and Comité de Protection des Personnes Sud-Méditerranée), number CCPPRB Marseille 2: 99-47 for patients explored with 1.5T MR system and CPP Sud Méditerranée 1: 08-45 for patients explored with 3T MR system. Participants gave informed consent to participate in the study before taking part.
- Wolinsky JS ,
- Giovannoni G , et al
- Carbonell-Mirabent P ,
- Cobo-Calvo Á , et al
- Portaccio E ,
- Bellinvia A ,
- Fonderico M , et al
- Lorscheider J , et al
- Zaaraoui W ,
- Reuter F , et al
- Wybrecht D ,
- Pariollaud F , et al
- Fromont A ,
- Binquet C ,
- Sauleau EA , et al
- Abdelhak A ,
- Benkert P ,
- Schaedelin S , et al
- Kerbrat A ,
- Badji A , et al
- Brownlee WJ ,
- Altmann DR ,
- Prados F , et al
- Harding K ,
- Williams O ,
- Willis M , et al
- Spelman T ,
- Magyari M ,
- Piehl F , et al
Contributors AM played a major role in the acquisition of the data and the gathering of data. JPS played a major role in the acquisition of the data and conducted statistical analysis. AR, CB, SD and WZ played a major role in the acquisition of the data. J-PR and JP planned the study and played a major role in the acquisition of the data. BA planned and conducted the study, conducted statistical analysis and wrote the manuscript.
Funding This study was supported by Fondation pour l’Aide à la Recherche sur la Sclérose En Plaques (ARSEP Fondation)
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Updated Terms of Use
- New Privacy Policy
- Your Privacy Choices
- Closed Caption Policy
- Accessibility Statement
This material may not be published, broadcast, rewritten, or redistributed. ©2024 FOX News Network, LLC. All rights reserved. Quotes displayed in real-time or delayed by at least 15 minutes. Market data provided by Factset . Powered and implemented by FactSet Digital Solutions . Legal Statement . Mutual Fund and ETF data provided by Refinitiv Lipper .
‘Liquid gold’ could bring new hope to multiple sclerosis patients, study suggests: ‘Profound benefit’
In phase 2 trials, drinkable medication with gold nanocrystals significantly reduced symptoms.

Fox News Flash top headlines for April 29
Fox News Flash top headlines are here. Check out what's clicking on Foxnews.com.
Researchers may have hit "gold" when it comes to the treatment of multiple sclerosis .
An experimental medication called CNM-Au8 — a drinkable liquid with gold nanocrystals — has shown promising results in clinical trials in terms of improvements in MS symptoms.
The "catalytically active" liquid, developed by Clene Nanomedicine in North East, Maryland, can cross the blood-brain barrier to help improve cellular energy and restore neurological function, according to researchers.
BREAKTHROUGH FOR MULTIPLE SCLEROSIS SUFFERERS MAY INVOLVE HELPFUL HORMONE: ‘PATIENTS SHOULD REMAIN OPTIMISTIC’
Doctors at the University of Sydney presented the Phase 2 clinical trial findings at the American Academy of Neurology’s annual meeting earlier in April 2024.
The clinical trials included 78 patients who had relapsing multiple sclerosis.

An experimental medication called CNM-Au8 — a drinkable liquid with gold nanocrystals — has shown promising results in clinical trials for improving MS symptoms. (Clene Nanomedicine)
The gold liquid suspension was found to have a "profound clinical benefit," with the patients experiencing physical improvements not achieved in prior trials.
A need for new MS drugs
Multiple sclerosis is an autoimmune disease of the central nervous system, brain, spinal cord and optic nerve.
In people with MS, white cells called lymphocytes infiltrate the central nervous system and trigger inflammation.
That often causes them to feel off balance or lose their vision , according to Dr. Robert C. Sergott, chief of the neuro-ophthalmology service at Wills Eye Hospital and professor of ophthalmology, neurology and neurosurgery at Sidney Kimmel Medical College in Philadelphia.
The MS medications that are currently available work by addressing inflammation — but there is a subset of patients that continue to experience symptoms even without inflammation, he said. This is a condition called progression independent of relapse activity (PIRA).
RESEARCHERS FIND SOURCES OF FOUR BRAIN DISORDERS, WHICH COULD LEAD TO NEW TREATMENTS
"This is a non-inflammatory component of the disease, where patients would worsen in vision and cognitive abilities," Sergott, who was involved in the clinical trial for CNM-Au8, told Fox News Digital.
Researchers suspected that something to do with mitochondria — parts of cells that are responsible for supplying those cells with energy — was causing these patients’ symptoms.
"The theory was that if we could give the mitochondria an extra boost, the neurons, axons and other cells in the central nervous system may work better," said Sergott.
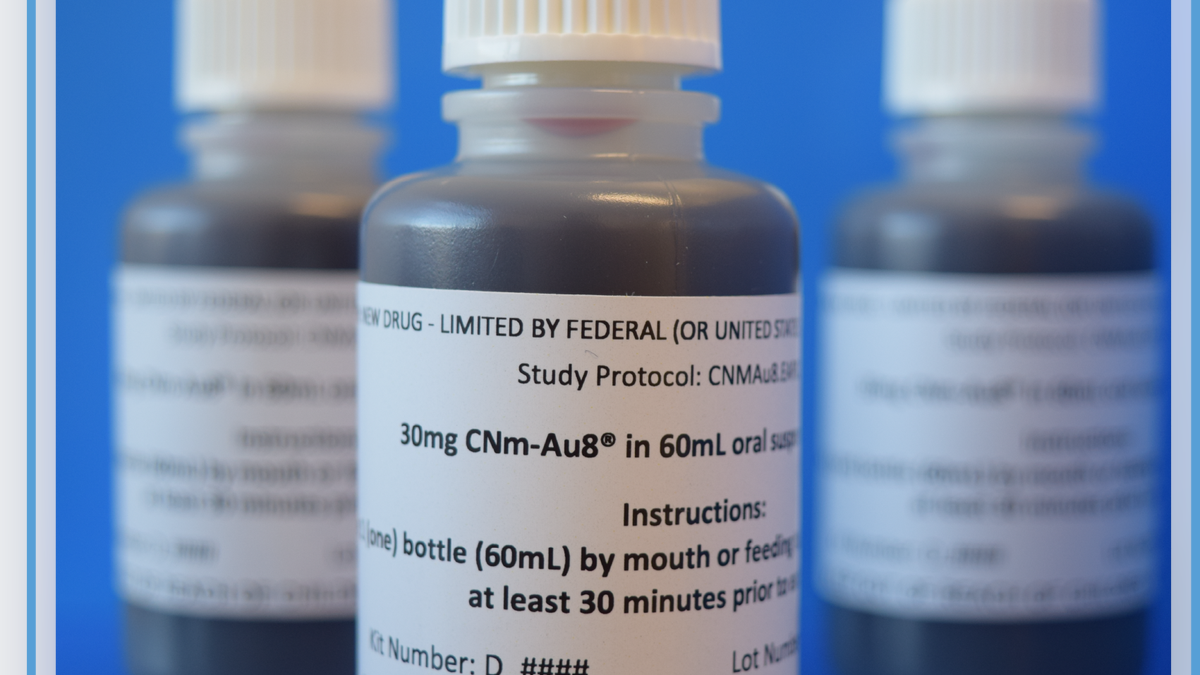
The "catalytically active" liquid can cross the blood-brain barrier to help improve cellular energy and restore neurological function, according to researchers. (Clene Nanomedicine)
"In other words, maybe these cells aren't dead, but they're hibernating."
Gold nanoparticles were originally used to treat rheumatoid arthritis many years ago, according to Sergott.
"Clene innovated a novel electrochemical method to make gold particles and [got] them to a very highly purified nanoparticle state — into very small particles, so they can get through the blood-brain barrier to the cells that need it to work better."
‘Significant result’
Among the 78 participants in the randomized clinical trial performed in Australia, two-thirds of them received the gold treatment and the other third received a placebo over a three-year period.
"We had hoped to enroll more patients, but COVID intervened ," Sergott said.
Neither the patients nor the neurologist overseeing the trial knew who was receiving the actual medicine.
"We're very encouraged and ready to take the next step. It's going to help a lot of people."
"Patients saw a clinical improvement in the function of their vision and their cognitive ability," Sergott reported.
Doctors also noted an improvement in the electrophysiology, he said — "the patients’ MRIs looked better, which is a special measure."

"The theory was that if we could give the mitochondria an extra boost, the neurons, axons and other cells in the central nervous system may work better," a doctor said. (iStock)
The patients who received the medicine had no decline in retinal thickness, but those on the placebo did see a decline, he said.
"This was a very significant result, and gives us a lot of hope that we may be able to help patients who have deficits from MS and have had progression independent of relapse activity — or maybe they had an attack and didn't get complete recovery from it," Sergott said.
TO LIVE LONGER, DO THESE 5 THINGS EVERY DAY, SAYS A BRAIN HEALTH EXPERT
None of the trial participants reported any adverse side effects, he said.
"The safety profile is excellent," Sergott told Fox News Digital. "I can't say this doesn't have any side effects — but no patients discontinued the trial because of a side effect that was significant."

None of the trial participants reported any adverse side effects from the gold treatment, the researchers said. (iStock)
With the successful Phase 2 trials complete, researchers are now looking ahead to Phase 3 trials.
"We're very encouraged and we're ready to take the next step," said Sergott. "It's really going to help a lot of people."
Patients taking CNM-Au8 would still need to continue with the standard regimen of anti-inflammatory medications, the doctor noted.
CAN WE REVERSE ALZHEIMER’S DISEASE? EXPERTS SUGGEST ‘NEW PARADIGM’ FOR COMBATING DEMENTIA
Looking ahead, there is the potential for the "liquid gold" medication to help treat symptoms of other neurological disorders, including amyotrophic lateral sclerosis (ALS), Alzheimer’s and Parkinson’s , according to Sergott — but the focus is on MS for now.
"We don't want to get too far ahead of ourselves, but there is plenty of information to support trying this in other diseases."
Patient shares his experience
Damian Kunko of Arlington, Virginia, was one of the MS patients who participated in the trial. He had previously taken disease-modifying therapies that included Zeposia and Tecfidera.
"These drugs reduced the risk of relapse, but had no effect on progressive symptom worsening," Kunko told Fox News Digital.

Damian Kunko of Arlington, Virginia, was one of the MS patients who participated in the trial. (Clene Nanomedicine)
Kunko’s primary symptoms included heat intolerance, foot drop/limping, numbness, balance issues, double vision and minor decline of cognitive function and energy.
After four months of taking CNM-Au8, Kunko found that his walking speed was 14% faster.
"I was also able to do short 5-10-yard jogs without falling, which was impossible prior to taking [the drug]," he said.
"The best ‘side effect’ was knowing that this drug will fix my MS issues."
"I also experienced improved visual acuity, less severe double vision, zero cognitive fog issues and increased energy levels."
Later in the trial, Kunko was able to withstand high heat and humidity for several hours and did not experience any double vision, foot drop, excessive numbness or fatigue issues .
"It was nice to be able to go up and down stairs without having to hold the railing," he said.

Clinical improvements were seen in both the visual system and on patients' MRI scans, according to doctors. (iStock)
The patient said he did not experience any negative side effects or adverse reactions.
"The best ‘side effect’ was knowing that this drug will fix my MS issues," Kunko said.
"I am very disappointed that this therapy is not yet commercially available for those who need to restore function and alleviate MS symptoms," he added.
Doctors weigh in
Dr. Marc Siegel, clinical professor of medicine at NYU Langone Medical Center and a Fox News medical contributor, was not involved in the drug’s development but commented on the potential of gold therapies.
"Gold-containing analogies have long been treatments for rheumatoid arthritis — what is known as disease-modifying anti-rheumatic drugs," he told Fox News Digital.
"And now gold-containing agents are being studied in MS and ALS."
While the latest study is small, Siegel said, it "looks promising in terms of modifying disease and improving thinking and vision, which can be affected in the early stages of MS."
He added, " More research with larger numbers needs to be done to be conclusive."

"Gold-containing analogies have long been treatments for rheumatoid arthritis — what is known as disease-modifying anti-rheumatic drugs," one doctor told Fox News Digital. (Clene Nanomedicine)
Dr. James Kuo, vice president of R&D at Silo Pharma in New Jersey, was also not involved in the drug’s development but said the trial results are "encouraging."
"These new long-term results from the Phase 2 clinical trial support the therapeutic hypothesis that CNM-Au8 is remyelinating nerve cells in MS patients," Kuo told Fox News Digital.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
"What is further encouraging is that both the primary and secondary endpoints showed continued improvement," he added. "There was physiological enhancement in the visual neural pathway, a biomarker of nerve health. Further MRI measurements support remyelination occurring."
"If further clinical data supports these initial findings, MS patients could well have a new, well-tolerated oral therapy that is not based upon immune system modulation."

Ensuring proper dosing, monitoring patients for potential side effects and following proper follow-up protocols are "essential aspects" of bringing this therapy into clinical practice, a doctor said. (iStock)
Dr. Sameea Husain Wilson, director of movement disorder neurology at Marcus Neuroscience Institute, at Boca Raton Regional Hospital in Florida, said that CNM-Au8 offers hope for patients and their families.
"It shows promise in the possibility of slowing disease progression, improving symptoms and enhancing quality of life," she told Fox News Digital in a statement.
Wilson noted, however, that it is important to "approach the drug development cautiously and be aware of potential risks."
"The complexity of neurodegenerative diseases necessitates a comprehensive understanding of individual patient profiles," she said.
CLICK HERE TO GET THE FOX NEWS APP
"It's essential to recognize that not all patients may respond uniformly to treatment, and factors such as disease stage, comorbidities and genetic predispositions may influence outcomes."
Ensuring proper dosing, monitoring patients for potential side effects and following proper follow-up protocols are "essential aspects" of bringing this therapy into clinical practice, Wilson added.
For more Health articles, visit www.foxnews.com/health .
Melissa Rudy is health editor and a member of the lifestyle team at Fox News Digital. Story tips can be sent to [email protected].

Stay up-to-date on the biggest health and wellness news with our weekly recap.
You've successfully subscribed to this newsletter!
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 8, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Study shows how sepsis can affect vascular smooth muscle cells on an acute and long-term basis
by Jonas Machner, Universitätsmedizin Halle
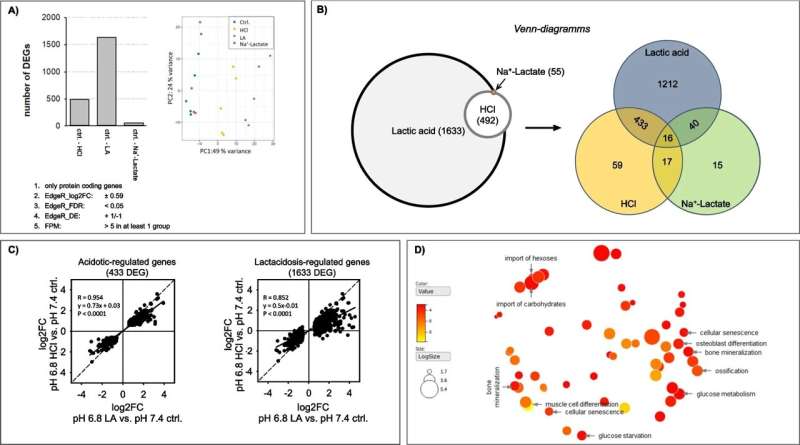
A recent study by University Medicine Halle shows how sepsis can lead to dysfunction of vascular smooth muscle cells. The researchers found that elevated lactate levels and acidosis, which can occur acutely during sepsis due to metabolic derailment, only have a disrupting effect in synergistic combination.
The study, published in the Journal of Biomedical Science , also provides a possible explanation for why some sepsis survivors experience long-lasting impairments.
Treating sepsis poses a major challenge worldwide. Early diagnosis is crucial, as advanced stages can only be treated to a limited degree and up to half of all cases are fatal.
"Sepsis is a serious complication that often leads to multiple organ failure. Circulatory disorders play a decisive role. However, the pathogenetic mechanisms are still poorly understood," explains Dr. Stefanie Ruhs, a biochemist at University Medicine Halle and one of the first authors of the study. Sepsis is known to lead to metabolic changes. Two thirds of affected individuals have extremely high lactate levels with concurrent metabolic acidosis—a low blood pH.
At University Medicine Halle, the University Clinic and Outpatient Clinic for Anesthesiology and Operative Intensive Care and the Julius Bernstein Institute of Physiology joined forces to better understand the pathogenesis of sepsis.
"In our study, we investigated the effects that lactate, acidosis on its own, and both in combination ( lactic acidosis ), have on the vascular smooth muscle cells in blood vessels. The latter, lactic acidosis, is clinically associated with low survival rates," explains Ruhs.
In their experiments, the researchers used isolated vascular smooth muscle cells from the aorta, which were propagated in the laboratory. These were treated for 48 hours either with lactate at a normal pH, with acid without lactate, and with both in combination (lactic acidosis).
Fatigue and stiffening of blood vessel cells caused by lactic acidosis
Lactate at a normal pH has shown to cause a few relevant changes in the vascular smooth muscle cells. Acidosis without lactate led to changes at the genetic level: under acidic conditions, nearly 500 genes were expressed differently. However, the cells investigated in this study were able to compensate to a large degree for any adverse effects on function.
"Only the combination of lactate and acidic conditions, i.e. lactic acidosis, led to extensive changes at the genetic level, in energy metabolism , and to the phenotype," says Philipp Terpe, Ph.D. student and first author.
"Around 1,500 genes exhibited an altered expression linked to metabolism and cell appearance. This can lead to the impairment of various processes related to energy balance that could no longer be compensated for. We were also able to demonstrate a restructuring of the vascular smooth muscle cells as a result of mineralization."
All in all, these effects indicate that, during sepsis, blood vessels partially lose their function and stiffen due to restructuring. This can restrict blood flow in both short and long term. According to the authors of the study, this lasting impairment could also explain why patients who survive sepsis continue to experience symptoms on a physical and cognitive level.
"In the future, we want to analyze further types of vascular cells and investigate whether cells undergo repeated stress once blood values normalize after sepsis. A better understanding of the underlying mechanisms might help to develop new bio markers that could help indicate the severity of sepsis at an early stage, thereby shortening clinical response times.
"After all, every minute counts during the intensive care treatment of sepsis and septic shock. And if we succeed in identifying the long-term effects at the molecular level, we may be able to use new approaches for treating survivors," says Terpe.
Sepsis can occur after a bacterial, viral or fungal infection. The cause of this life-threatening condition is a dysregulated immune reaction. This is characterized by vasodilation and decreased systemic vascular resistance, resulting in circulatory disorders. It often leads to the failure of one or more organs.
Even if the patient receives intensive care treatment, sepsis can be fatal in 30 to 50% of all cases. Some studies have also reported a mortality rate of more than 50% in the case of septic shock.
Explore further
Feedback to editors

Research team identifies four new genetic risk factors for multiple system atrophy
6 minutes ago

About 90% of US adults are on the way to heart disease, study suggests
7 minutes ago

Researchers identify what drives PARP inhibitor resistance in advanced breast cancer
53 minutes ago

How infections influence our social empathy

Health risks of using cannabis are higher in adolescents than in adults, study finds
2 hours ago

Study finds THC lingers in breastmilk with no clear peak point

New study offers insight into genesis of spina bifida

Serotonergic neuron findings suggest possible treatment for depression-related infertility

Strengthening CAR-T therapy to work against solid tumors
3 hours ago

Study reveals role of iron in allergic asthma and points to potential new therapies
Related stories.

Blood stem cells unlock clues for helping sepsis patients fight recurring infections
Apr 11, 2024

Sepsis signature shifts speed of diagnosis
Apr 10, 2024

New device can treat injury from sepsis
Apr 13, 2024

Consumer health: What do you know about sepsis?
Sep 14, 2022

Advances in pediatric sepsis biomarkers: A pediatric investigation review
Feb 6, 2024

What to know about treating sepsis
Sep 14, 2021
Recommended for you

Team develops computational approach to redesign antibodies for broader effectiveness against viral pandemics
4 hours ago

Researchers may have found an Achilles heel for Hepatitis B
5 hours ago

Researchers outline how cells activate to cause fibrosis and organ scarring
6 hours ago

Mouse study shows intermittent fasting protects against liver inflammation and liver cancer
May 7, 2024

New genetic mutation identified for congenital thyroid condition
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
Clinical Presentation: Case History # 1. Ms. C is a 35 year old white female. She came to Neurology Clinic for evaluation of her long-term neurologic complaints. The patient relates that for many years she had noticed some significant changes in neurologic functions, particularly heat intolerance precipitating a stumbling gait and a tendency to ...
The mean age of onset is from 28 to 31 years. The age of onset varies among the clinical subtypes (phenotypes). RRMS has an earlier onset, averaging between 25 and 29 years, with SPMS presenting at a mean age between 40 and 49 years of age. The estimated male to female ratio is 1.4-2.3 to 1.
Oct 2017. Case Studies in Multiple Sclerosis. pp.27-32. A 28-year-old woman with known relapsing-remitting multiple sclerosis (RRMS) for 2 years was seen in the emergency room for a subacute onset ...
This case report involved one patient; having more participants in this case study would have produced more information for analysis. Longer treatment durations are shown to be more effective in chronic conditions. ... Doig J, Premkumar K. The effects of massage therapy on multiple sclerosis patients' quality of life and leg function. Evid ...
The PROs, related to domains that most care to multiple sclerosis patients (case study) defined by the PROMOPROMS initiative (manual ability, bladder functions, motor, cognitive, psychosocial fatigue, anxiety, and depression, quality of life), are currently used to measure disease progression and the efficacy of treatments (drugs and/or ...
Multiple sclerosis (MS) is the most common disabling neurologic disease in people ages 18 to 60, second overall only to trauma. This prevalence is more than matched by the complexity of the disease, which is compounded by the dearth of definitive evidence to guide clinical decision making and leaves physicians to rely on their judgment and anecdotal experience.
A collection of case studies illustrating the complex, unpredictable nature of multiple sclerosis and its many presentations and disease courses. Case studies submitted from clinicians from some of the world's leading neurology departments. Edited by Dr Paul Giacomini of McGill University, a leading expert in the field of multiple sclerosis.
Patient 2drelapsing remitting multiple sclerosis on disease-modifying therapy with breakthrough relapses A 39-year-old woman suffers an episode of optic neuritis and is found to have multiple white matter lesions consistent with MS on MRI. A course of intravenous (IV) steroids is given with subsequent recovery of vision after 2 weeks.
Multiple Sclerosis (MS) is a chronic, inflammatory, demyelinating disease of CNS that afects cerebral cortex and grey matter including basal ganglia and Cerebellar cortex [1]. MS prevails in a total of 2.8 million people worldwide according to a study conducted in 2020 with an estimation of one person being diagnosed with MS every five minutes [2].
A CASE STUDY OF MULTIPLE SCLEROSIS (MS) YEAR/BLOCK . YEAR 1 BLOCK 3 2017/2018 . ... patients are more likely than controls to have EBV-specific cytotoxic T cells. MS patients are .
Multiple Sclerosis Case Study. Janet has experienced periodic episodes of tingling in her extremities, dizziness, and even episodes of blindness. After 12 years, doctors have finally given her a diagnosis. Follow Janet through her journey and find out why her disease is so difficult to diagnose.
Multiple sclerosis (MS) is an incurable, heterogeneous, chronic, degenerative, demyelinating, immune-mediated neurological disease of the central nervous system. 1,2 Indeed, the disease burden of MS affects the physical, mental, emotional, psychosocial, and spiritual dimensions of the patient and their family. A plethora of studies highlight the symptoms, stressors, financial demands, and ...
Hence, this study aims to investigate the perspectives of people with multiple sclerosis on the value of patient-reported outcomes in clinical encounters, the most important aspects of living with multiple sclerosis that should be reflected in these reports, and possible opportunities and barriers for integrating this data into clinical care ...
Ahmed Zayed Obeidat MD, PhD: The first case we're going to talk about is a 37-year-old female with 2 young children. We're going to talk about some factors about what you would select as a treatment. The patient presented to the neurology clinic for first time with fatigue, weakness, tremors in the right hand, so that's 1 side.
Pertinent family history: Mother alive and healthy at age 58 years. Father alive, patient reports he takes medication for blood pressure but otherwise is healthy at age 59 years. Patient has no siblings. Maternal Aunt alive, living with multiple sclerosis, age 54 years. Paternal grandfather died after suffering a stroke 2 years ago.
Bilateral internuclear ophthalmoplegia is pathognomonic of MS. The diagnosis of MS is based on the clinical features of the attacks including the history and examination findings. The guiding principle of the diagnosis is that of dissemination in time (DIT) and dissemination in space (DIS). There is no single diagnostic laboratory test for MS.
Background: Interest in patient-reported outcomes has been growing in multiple sclerosis research and clinical care in recent years. This situation reflects the need for developing, testing, and integrating measures that adequately capture patients' perspectives on symptoms, functional capacity, health status, and health-related quality of life.
Case Study: Adult with Multiple Sclerosis 1. CASE AUTHORS Name Department of Nursing - NP Programs Phone FAX Name Department of NP Phone FAX 2. TOPIC OF THE CASE: Adult with Multiple Sclerosis ... Advise Patient of Diagnosis 2 min. [X] Feedback from SP 5 min. Development of this content was partially supported by a grant from HRSA (D09HP18998 ...
What is MS? | National Multiple Sclerosis Society (nationalmssociety.org) Vaughn CB, Jakimovski D, Kavak KS, et al. Epidemiology and treatment of multiple sclerosis in elderly populations. Nat Rev Neurol. 2019;15(6):329-342; Talwar A, Earla JR, Hutton GJ, et al. Prescribing of disease modifying agents in older adults with multiple sclerosis.
Multiple sclerosis is an autoinflammatory condition that results in damage to myelinated neurons in affected patients. While disease-modifying treatments have been successful in slowing the progression of relapsing-remitting disease, most patients still progress to secondary progressive disease that is largely unresponsive to disease-modifying treatments. Similarly, there is currently no ...
Patients with Multiple Sclerosis (pwMS) treated with anti-CD20 (cluster of differentiation) monoclonal antibodies (mAbs) such as ocrelizumab (OCR) and ofatumumab (OFA) show a reduction mainly of B-lymphocytes, but also other lymphocyte subsets can be affected by these treatments. ... This study was approved by the responsible ethic committees ...
Finally, we enrolled 101 patients in our study as a case group. All patients have been visited by an expert neurologist and psychologist. For each patient, we considered two healthy individuals with age and sex matched as controls. ... Personality factors in recently diagnosed multiple sclerosis patients: a preliminary investigation with the ...
Oropharyngeal dysphagia (OPD) is common in multiple sclerosis (MS) [] due to injury to the corticobulbar tracts, potentially involving the brainstem, the cerebellum [2, 3], and the cortex [].There may be a differing clinical course across types of MS, classified based on disease onset and progression over time [].The most frequent includes relapsing-remitting MS (RRMS), usually beginning ...
Background Progression independent of relapse activity (PIRA) has been described since the early stage of relapsing multiple sclerosis (RMS). However, little is known about the relation between PIRA and inflammatory activity that is particularly important at this stage of the disease. Method We included 110 patients in a prospective study within 18 months of RMS onset. MRI examinations and ...
The clinical trials included 78 patients who had relapsing multiple sclerosis. ... While the latest study is small, Siegel said, it "looks promising in terms of modifying disease and improving ...
Multiple sclerosis (MS) is a chronic neurodegenerative condition characterised by a wide range of symptoms and a highly unpredictable prognosis, which can severely affect patient QoL. 6-8 Patients with MS tend to report lower QoL than the general population. 9-12 This diminished QoL may be due to their impaired functioning in daily living ...
This Multiple Sclerosis Discovery Could Be a Breakthrough A new blood test reveals signs of the disease years before symptoms occur. It could change how MS is diagnosed, treated and studied.
Even if the patient receives intensive care treatment, sepsis can be fatal in 30 to 50% of all cases. Some studies have also reported a mortality rate of more than 50% in the case of septic shock.