Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 15 April 2021

A unified model of the pathophysiology of bipolar disorder
- Paola Magioncalda ORCID: orcid.org/0000-0003-4985-4819 1 , 2 , 3 na1 &
- Matteo Martino ORCID: orcid.org/0000-0002-3783-707X 1 , 2 na1
Molecular Psychiatry volume 27 , pages 202–211 ( 2022 ) Cite this article
5424 Accesses
27 Citations
3 Altmetric
Metrics details
- Bipolar disorder
- Neuroscience
This work provides an overview of the most consistent alterations in bipolar disorder (BD), attempting to unify them in an internally coherent working model of the pathophysiology of BD. Data on immune-inflammatory changes, structural brain abnormalities (in gray and white matter), and functional brain alterations (from neurotransmitter signaling to intrinsic brain activity) in BD were reviewed. Based on the reported data, (1) we hypothesized that the core pathological alteration in BD is a damage of the limbic network that results in alterations of neurotransmitter signaling. Although heterogeneous conditions can lead to such damage, we supposed that the main pathophysiological mechanism is traceable to an immune/inflammatory-mediated alteration of white matter involving the limbic network connections, which destabilizes the neurotransmitter signaling, such as dopamine and serotonin signaling. Then, (2) we suggested that changes in such neurotransmitter signaling (potentially triggered by heterogeneous stressors onto a structurally-damaged limbic network) lead to phasic (and often recurrent) reconfigurations of intrinsic brain activity, from abnormal subcortical–cortical coupling to changes in network activity. We suggested that the resulting dysbalance between networks, such as sensorimotor networks, salience network, and default-mode network, clinically manifest in combined alterations of psychomotricity, affectivity, and thought during the manic and depressive phases of BD. Finally, (3) we supposed that an additional contribution of gray matter alterations and related cognitive deterioration characterize a clinical–biological subgroup of BD. This model may provide a general framework for integrating the current data on BD and suggests novel specific hypotheses, prompting for a better understanding of the pathophysiology of BD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

The serotonin theory of depression: a systematic umbrella review of the evidence
Joanna Moncrieff, Ruth E. Cooper, … Mark A. Horowitz

Emotions and brain function are altered up to one month after a single high dose of psilocybin
Frederick S. Barrett, Manoj K. Doss, … Roland R. Griffiths

A systems identification approach using Bayes factors to deconstruct the brain bases of emotion regulation
Ke Bo, Thomas E. Kraynak, … Tor D. Wager
A.P.A. Diagnostic and statistical manual for mental disorders. 5th ed. (DSM-5). Washington: American Psychiatric Association; 2013.
Kraepelin E. Clinical psychiatry. London: Macmillan; 1902.
Savitz JB, Rauch SL, Drevets WC. Clinical application of brain imaging for the diagnosis of mood disorders: the current state of play. Mol Psychiatry. 2013;18:528–39.
Article CAS PubMed PubMed Central Google Scholar
Savitz J, Drevets WC. Bipolar and major depressive disorder: neuroimaging the developmental-degenerative divide. Neurosci Biobehav Rev. 2009;33:699–771.
Article PubMed PubMed Central Google Scholar
Mechawar N, Savitz J. Neuropathology of mood disorders: do we see the stigmata of inflammation? Transl Psychiatry. 2016;6:e946.
Nikolaus S, Antke C, Muller HW. In vivo imaging of synaptic function in the central nervous system: II. Mental and affective disorders. Behav Brain Res. 2009;204:32–66.
Article PubMed Google Scholar
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506.
Northoff G, Hirjak D, Wolf RC, Magioncalda P, Martino M. All roads lead to the motor cortex: psychomotor mechanisms and their biochemical modulation in psychiatric disorders. Mol Psychiatry. 2021;26:92–102.
Martino M, Magioncalda P. Tracing the psychopathology of bipolar disorder to the functional architecture of intrinsic brain activity and its neurotransmitter modulation: a three-dimensional model. Mol Psychiatry. 2021; [Online ahead of print].
Irwin M, Smith TL, Gillin JC. Low natural killer cytotoxicity in major depression. Life Sci. 1987;41:2127–33.
Article CAS PubMed Google Scholar
Maes M, Bosmans E, Suy E, Minner B, Raus J. Impaired lymphocyte stimulation by mitogens in severely depressed patients. A complex interface with HPA-axis hyperfunction, noradrenergic activity and the ageing process. Br J Psychiatry. 1989;155:793–8.
Anderson G, Maes M. Bipolar disorder: role of immune-inflammatory cytokines, oxidative and nitrosative stress and tryptophan catabolites. Curr Psychiatry Rep. 2015;17:8.
Reus GZ, Fries GR, Stertz L, Badawy M, Passos IC, Barichello T, et al. The role of inflammation and microglial activation in the pathophysiology of psychiatric disorders. Neuroscience. 2015;300:141–54.
Kupka RW, Hillegers MH, Nolen WA, Breunis N, Drexhage HA. Immunological aspects of bipolar disorder. Acta Neuropsychiatr. 2000;12:86–90.
Barbosa IG, Machado-Vieira R, Soares JC, Teixeira AL. The immunology of bipolar disorder. Neuroimmunomodulation. 2014;21:117–22.
Sayana P, Colpo GD, Simoes LR, Giridharan VV, Teixeira AL, Quevedo J, et al. A systematic review of evidence for the role of inflammatory biomarkers in bipolar patients. J Psychiatr Res. 2017;92:160–82.
Article Google Scholar
Fernandes BS, Steiner J, Molendijk ML, Dodd S, Nardin P, Goncalves CA, et al. C-reactive protein concentrations across the mood spectrum in bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3:1147–56.
Tsai SY, Chung KH, Chen PH. Levels of interleukin-6 and high-sensitivity C-reactive protein reflecting mania severity in bipolar disorder. Bipolar Disord. 2017;19:708–9.
Barbosa IG, Rocha NP, Assis F, Vieira EL, Soares JC, Bauer ME, et al. Monocyte and lymphocyte activation in bipolar disorder: a new piece in the puzzle of immune dysfunction in mood disorders. Int J Neuropsychopharmacol. 2015;18:pyu021.
Breunis MN, Kupka RW, Nolen WA, Suppes T, Denicoff KD, Leverich GS, et al. High numbers of circulating activated T cells and raised levels of serum IL-2 receptor in bipolar disorder. Biol Psychiatry. 2003;53:157–65.
Tsai SY, Chen KP, Yang YY, Chen CC, Lee JC, Singh VK, et al. Activation of indices of cell-mediated immunity in bipolar mania. Biol Psychiatry. 1999;45:989–94.
do Prado CH, Rizzo LB, Wieck A, Lopes RP, Teixeira AL, Grassi-Oliveira R, et al. Reduced regulatory T cells are associated with higher levels of Th1/TH17 cytokines and activated MAPK in type 1 bipolar disorder. Psychoneuroendocrinology. 2013;38:667–76.
Brambilla P, Bellani M, Isola M, Bergami A, Marinelli V, Dusi N, et al. Increased M1/decreased M2 signature and signs of Th1/Th2 shift in chronic patients with bipolar disorder, but not in those with schizophrenia. Transl Psychiatry. 2014;4:e406.
Kohler O, Sylvia LG, Bowden CL, Calabrese JR, Thase M, Shelton RC, et al. White blood cell count correlates with mood symptom severity and specific mood symptoms in bipolar disorder. Aust N Z J Psychiatry. 2017;51:355–65.
Wu W, Zheng YL, Tian LP, Lai JB, Hu CC, Zhang P, et al. Circulating T lymphocyte subsets, cytokines, and immune checkpoint inhibitors in patients with bipolar II or major depression: a preliminary study. Sci Rep. 2017;7:40530.
Magioncalda P, Martino M, Tardito S, Sterlini B, Conio B, Marozzi V, et al. White matter microstructure alterations correlate with terminally differentiated CD8+ effector T cell depletion in the peripheral blood in mania: Combined DTI and immunological investigation in the different phases of bipolar disorder. Brain Behav Immun. 2018;73:192–204.
Kempton MJ, Geddes JR, Ettinger U, Williams SC, Grasby PM. Meta-analysis, database, and meta-regression of 98 structural imaging studies in bipolar disorder. Arch Gen Psychiatry. 2008;65:1017–32.
Birur B, Kraguljac NV, Shelton RC, Lahti AC. Brain structure, function, and neurochemistry in schizophrenia and bipolar disorder-a systematic review of the magnetic resonance neuroimaging literature. NPJ Schizophr. 2017;3:15.
Vita A, De Peri L, Sacchetti E. Gray matter, white matter, brain, and intracranial volumes in first-episode bipolar disorder: a meta-analysis of magnetic resonance imaging studies. Bipolar Disord. 2009;11:807–14.
Bora E, Fornito A, Yucel M, Pantelis C. Voxelwise meta-analysis of gray matter abnormalities in bipolar disorder. Biol Psychiatry. 2010;67:1097–105.
Lim CS, Baldessarini RJ, Vieta E, Yucel M, Bora E, Sim K. Longitudinal neuroimaging and neuropsychological changes in bipolar disorder patients: review of the evidence. Neurosci Biobehav Rev. 2013;37:418–35.
Hibar DP, Westlye LT, Doan NT, Jahanshad N, Cheung JW, Ching CRK, et al. Cortical abnormalities in bipolar disorder: an MRI analysis of 6503 individuals from the ENIGMA Bipolar Disorder Working Group. Mol Psychiatry. 2018;23:932–42.
Mahon K, Burdick KE, Szeszko PR. A role for white matter abnormalities in the pathophysiology of bipolar disorder. Neurosci Biobehav Rev. 2010;34:533–54.
Sexton CE, Mackay CE, Ebmeier KP. A systematic review of diffusion tensor imaging studies in affective disorders. Biol Psychiatry. 2009;66:814–23.
Vederine FE, Wessa M, Leboyer M, Houenou J. A meta-analysis of whole-brain diffusion tensor imaging studies in bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1820–6.
Nortje G, Stein DJ, Radua J, Mataix-Cols D, Horn N. Systematic review and voxel-based meta-analysis of diffusion tensor imaging studies in bipolar disorder. J Affect Disord. 2013;150:192–200.
Wise T, Radua J, Nortje G, Cleare AJ, Young AH, Arnone D. Voxel-based meta-analytical evidence of structural disconnectivity in major depression and bipolar disorder. Biol Psychiatry. 2016;79:293–302.
Heng S, Song AW, Sim K. White matter abnormalities in bipolar disorder: insights from diffusion tensor imaging studies. J Neural Transm. 2010;117:639–54.
Favre P, Pauling M, Stout J, Hozer F, Sarrazin S, Abe C, et al. Widespread white matter microstructural abnormalities in bipolar disorder: evidence from mega- and meta-analyses across 3033 individuals. Neuropsychopharmacology. 2019;44:2285–93.
Magioncalda P, Martino M, Conio B, Piaggio N, Teodorescu R, Escelsior A, et al. Patterns of microstructural white matter abnormalities and their impact on cognitive dysfunction in the various phases of type I bipolar disorder. J Affect Disord. 2016;193:39–50.
Martino M, Magioncalda P, Saiote C, Conio B, Escelsior A, Rocchi G, et al. Abnormal functional-structural cingulum connectivity in mania: combined functional magnetic resonance imaging-diffusion tensor imaging investigation in different phases of bipolar disorder. Acta Psychiatr Scand. 2016;134:339–49.
Savitz JB, Price JL, Drevets WC. Neuropathological and neuromorphometric abnormalities in bipolar disorder: view from the medial prefrontal cortical network. Neurosci Biobehav Rev. 2014;42:132–47.
Bellani M, Boschello F, Delvecchio G, Dusi N, Altamura CA, Ruggeri M, et al. DTI and myelin plasticity in bipolar disorder: integrating neuroimaging and neuropathological findings. Front Psychiatry. 2016;7:21.
Benedetti F, Poletti S, Hoogenboezem TA, Mazza E, Ambree O, de Wit H, et al. Inflammatory cytokines influence measures of white matter integrity in bipolar disorder. J Affect Disord. 2016;202:1–9.
Savitz J. Musings on mania: A role for T-lymphocytes? Brain Behav Immun. 2018;73:151–2.
Pape K, Tamouza R, Leboyer M, Zipp F. Immunoneuropsychiatry—novel perspectives on brain disorders. Nat Rev Neurol. 2019;15:317–28.
Schiffer RB, Wineman NM, Weitkamp LR. Association between bipolar affective disorder and multiple sclerosis. Am J Psychiatry. 1986;143:94–5.
Perugi G, Quaranta G, Belletti S, Casalini F, Mosti N, Toni C, et al. General medical conditions in 347 bipolar disorder patients: clinical correlates of metabolic and autoimmune-allergic diseases. J Affect Disord. 2015;170:95–103.
Rosenblat JD, McIntyre RS. Bipolar disorder and immune dysfunction: epidemiological findings, proposed pathophysiology and clinical implications. Brain Sci. 2017;7:144.
Turner AP, Alschuler KN, Hughes AJ, Beier M, Haselkorn JK, Sloan AP, et al. Mental health comorbidity in MS: depression, anxiety, and bipolar disorder. Curr Neurol Neurosci Rep. 2016;16:106.
Marrie RA, Reingold S, Cohen J, Stuve O, Trojano M, Sorensen PS, et al. The incidence and prevalence of psychiatric disorders in multiple sclerosis: a systematic review. Mult Scler. 2015;21:305–17.
Pender MP. CD8+ T-cell deficiency, epstein-barr virus infection, vitamin d deficiency, and steps to autoimmunity: a unifying hypothesis. Autoimmune Dis. 2012;2012:189096.
PubMed PubMed Central Google Scholar
Melzer N, Meuth SG, Wiendl H. CD8+ T cells and neuronal damage: direct and collateral mechanisms of cytotoxicity and impaired electrical excitability. FASEB J. 2009;23:3659–73.
Baecher-Allan C, Kaskow BJ, Weiner HL. Multiple sclerosis: mechanisms and immunotherapy. Neuron. 2018;97:742–68.
Roosendaal SD, Geurts JJ, Vrenken H, Hulst HE, Cover KS, Castelijns JA, et al. Regional DTI differences in multiple sclerosis patients. Neuroimage. 2009;44:1397–403.
Willing A, Friese MA. CD8-mediated inflammatory central nervous system disorders. Curr Opin Neurol. 2012;25:316–21.
Piaggio N, Schiavi S, Martino M, Bommarito G, Inglese M, Magioncalda P. Exploring mania-associated white matter injury by comparison with multiple sclerosis: a diffusion tensor imaging study. Psychiatry Res Neuroimaging. 2018;281:78–84.
Martino M, Magioncalda P, El Mendili MM, Droby A, Paduri S, Schiavi S, et al. Depression is associated with disconnection of neurotransmitter-related nuclei in multiple sclerosis. Mult Scler. 2020; [Online ahead of print].
Purves D, Augustine GJ, Fitzpatrick D, Katz LC, LaMantia AS, McNamara JO. The limbic system, in Neuroscience, 2nd ed. Sunderland, MA: Sinauer Associates; 2001.
Yeo BT, Krienen FM, Sepulcre J, Sabuncu MR, Lashkari D, Hollinshead M, et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106:1125–65.
Drevets WC, Savitz J, Trimble M. The subgenual anterior cingulate cortex in mood disorders. CNS Spectr. 2008;13:663–81.
Ongur D, Ferry AT, Price JL. Architectonic subdivision of the human orbital and medial prefrontal cortex. J Comp Neurol. 2003;460:425–49.
Drevets WC, Ongur D, Price JL. Neuroimaging abnormalities in the subgenual prefrontal cortex: implications for the pathophysiology of familial mood disorders. Mol Psychiatry. 1998;3:220–6.
Mayberg HS. Limbic-cortical dysregulation: a proposed model of depression. J Neuropsychiatry Clin Neurosci. 1997;9:471–81.
Drevets WC, Price JL, Simpson JR Jr., Todd RD, Reich T, Vannier M, et al. Subgenual prefrontal cortex abnormalities in mood disorders. Nature. 1997;386:824–7.
Ongur D, Drevets WC, Price JL. Glial reduction in the subgenual prefrontal cortex in mood disorders. Proc Natl Acad Sci USA. 1998;95:13290–5.
Leow A, Ajilore O, Zhan L, Arienzo D, GadElkarim J, Zhang A, et al. Impaired inter-hemispheric integration in bipolar disorder revealed with brain network analyses. Biol Psychiatry. 2013;73:183–93.
O’Donoghue S, Holleran L, Cannon DM, McDonald C. Anatomical dysconnectivity in bipolar disorder compared with schizophrenia: a selective review of structural network analyses using diffusion MRI. J Affect Disord. 2017;209:217–28.
Belvederi Murri M, Prestia D, Mondelli V, Pariante C, Patti S, Olivieri B, et al. The HPA axis in bipolar disorder: Systematic review and meta-analysis. Psychoneuroendocrinology. 2016;63:327–42.
Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45:651–60.
Pani L, Porcella A, Gessa GL. The role of stress in the pathophysiology of the dopaminergic system. Mol Psychiatry. 2000;5:14–21.
Lanfumey L, Mongeau R, Cohen-Salmon C, Hamon M. Corticosteroid-serotonin interactions in the neurobiological mechanisms of stress-related disorders. Neurosci Biobehav Rev. 2008;32:1174–84.
Bali A, Randhawa PK, Jaggi AS. Stress and opioids: role of opioids in modulating stress-related behavior and effect of stress on morphine conditioned place preference. Neurosci Biobehav Rev. 2015;51:138–50.
Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5:243–51.
Elenkov IJ. Neurohormonal-cytokine interactions: implications for inflammation, common human diseases and well-being. Neurochem Int. 2008;52:40–51.
Zheng H, Ford BN, Bergamino M, Kuplicki R, Hunt PW, Bodurka J, et al. A hidden menace? Cytomegalovirus infection is associated with reduced cortical gray matter volume in major depressive disorder. Mol Psychiatry. 2020; [Online ahead of print].
Savitz J. The kynurenine pathway: a finger in every pie. Mol Psychiatry. 2020;25:131–47.
Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol. 2016;16:22–34.
Myint AM, Kim YK. Network beyond IDO in psychiatric disorders: revisiting neurodegeneration hypothesis. Prog Neuropsychopharmacol Biol Psychiatry. 2014;48:304–13.
Carlsson A, Waters N, Holm-Waters S, Tedroff J, Nilsson M, Carlsson ML. Interactions between monoamines, glutamate, and GABA in schizophrenia: new evidence. Annu Rev Pharmacol Toxicol. 2001;41:237–60.
Felger JC, Li Z, Haroon E, Woolwine BJ, Jung MY, Hu X, et al. Inflammation is associated with decreased functional connectivity within corticostriatal reward circuitry in depression. Mol Psychiatry. 2016;21:1358–65.
Salomon RM, Cowan RL. Oscillatory serotonin function in depression. Synapse. 2013;67:801–20.
Anand A, Li Y, Wang Y, Lowe MJ, Dzemidzic M. Resting state corticolimbic connectivity abnormalities in unmedicated bipolar disorder and unipolar depression. Psychiatry Res. 2009;171:189–98.
Anticevic A, Cole MW, Repovs G, Murray JD, Brumbaugh MS, Winkler AM, et al. Characterizing thalamo-cortical disturbances in schizophrenia and bipolar illness. Cereb Cortex. 2014;24:3116–30.
Skatun KC, Kaufmann T, Brandt CL, Doan NT, Alnaes D, Tonnesen S, et al. Thalamo-cortical functional connectivity in schizophrenia and bipolar disorder. Brain Imaging Behav. 2018;12:640–52.
Tu PC, Bai YM, Li CT, Chen MH, Lin WC, Chang WC, et al. Identification of common thalamocortical dysconnectivity in four major psychiatric disorders. Schizophr Bull. 2019;45:1143–51.
Martino M, Magioncalda P, Conio B, Capobianco L, Russo D, Adavastro G, et al. Abnormal functional relationship of sensorimotor network with neurotransmitter-related nuclei via subcortical-cortical loops in manic and depressive phases of bipolar disorder. Schizophr Bull. 2020;46:163–74.
Ongur D, Lundy M, Greenhouse I, Shinn AK, Menon V, Cohen BM, et al. Default mode network abnormalities in bipolar disorder and schizophrenia. Psychiatry Res. 2010;183:59–68.
Khadka S, Meda SA, Stevens MC, Glahn DC, Calhoun VD, Sweeney JA, et al. Is aberrant functional connectivity a psychosis endophenotype? A resting state functional magnetic resonance imaging study. Biol Psychiatry. 2013;74:458–66.
Magioncalda P, Martino M, Conio B, Escelsior A, Piaggio N, Presta A, et al. Functional connectivity and neuronal variability of resting state activity in bipolar disorder−reduction and decoupling in anterior cortical midline structures. Hum Brain Mapp. 2015;36:666–82.
Doucet GE, Bassett DS, Yao N, Glahn DC, Frangou S. The role of intrinsic brain functional connectivity in vulnerability and resilience to bipolar disorder. Am J Psychiatry. 2017;174:1214–22.
Baker JT, Dillon DG, Patrick LM, Roffman JL, Brady RO Jr., Pizzagalli DA, et al. Functional connectomics of affective and psychotic pathology. Proc Natl Acad Sci USA. 2019;116:9050–9.
Vargas C, Lopez-Jaramillo C, Vieta E. A systematic literature review of resting state network-functional MRI in bipolar disorder. J Affect Disord. 2013;150:727–35.
Shiah IS, Yatham LN. Serotonin in mania and in the mechanism of action of mood stabilizers: a review of clinical studies. Bipolar Disord. 2000;2:77–92.
Mosienko V, Beis D, Pasqualetti M, Waider J, Matthes S, Qadri F, et al. Life without brain serotonin: reevaluation of serotonin function with mice deficient in brain serotonin synthesis. Behav Brain Res. 2015;277:78–88.
Dalley JW, Roiser JP. Dopamine, serotonin and impulsivity. Neuroscience. 2012;215:42–58.
Winter C, von Rumohr A, Mundt A, Petrus D, Klein J, Lee T, et al. Lesions of dopaminergic neurons in the substantia nigra pars compacta and in the ventral tegmental area enhance depressive-like behavior in rats. Behav Brain Res. 2007;184:133–41.
van Enkhuizen J, Geyer MA, Minassian A, Perry W, Henry BL, Young JW. Investigating the underlying mechanisms of aberrant behaviors in bipolar disorder from patients to models: rodent and human studies. Neurosci Biobehav Rev. 2015;58:4–18.
Cosgrove VE, Kelsoe JR, Suppes T. Toward a valid animal model of bipolar disorder: how the research domain criteria help bridge the clinical-basic science divide. Biol Psychiatry. 2016;79:62–70.
Altinay MI, Hulvershorn LA, Karne H, Beall EB, Anand A. Differential resting-state functional connectivity of striatal subregions in bipolar depression and hypomania. Brain Connect. 2016;6:255–65.
Brady RO Jr., Masters GA, Mathew IT, Margolis A, Cohen BM, Ongur D, et al. State dependent cortico-amygdala circuit dysfunction in bipolar disorder. J Affect Disord. 2016;201:79–87.
Brady RO Jr., Margolis A, Masters GA, Keshavan M, Ongur D. Bipolar mood state reflected in cortico-amygdala resting state connectivity: A cohort and longitudinal study. J Affect Disord. 2017;217:205–9.
Martino M, Magioncalda P, Huang Z, Conio B, Piaggio N, Duncan NW, et al. Contrasting variability patterns in the default mode and sensorimotor networks balance in bipolar depression and mania. Proc Natl Acad Sci USA. 2016;113:4824–9.
Zuo XN, Di Martino A, Kelly C, Shehzad ZE, Gee DG, Klein DF, et al. The oscillating brain: complex and reliable. NeuroImage. 2010;49:1432–45.
Zhang J, Magioncalda P, Huang Z, Tan Z, Hu X, Hu Z, et al. Altered global signal topography and its different regional localization in motor cortex and hippocampus in mania and depression. Schizophr Bull. 2019;45:902–10.
Russo D, Martino M, Magioncalda P, Inglese M, Amore M, Northoff G. Opposing changes in the functional architecture of large-scale networks in bipolar mania and depression. Schizophr Bull. 2020;46:971–80.
Brady RO Jr., Tandon N, Masters GA, Margolis A, Cohen BM, Keshavan M, et al. Differential brain network activity across mood states in bipolar disorder. J Affect Disord. 2017;207:367–76.
Lee I, Nielsen K, Nawaz U, Hall MH, Ongur D, Keshavan M, et al. Diverse pathophysiological processes converge on network disruption in mania. J Affect Disord. 2019;244:115–23.
Spielberg JM, Beall EB, Hulvershorn LA, Altinay M, Karne H, Anand A. Resting state brain network disturbances related to hypomania and depression in medication-free bipolar disorder. Neuropsychopharmacology. 2016;41:3016–24.
Liu CH, Li F, Li SF, Wang YJ, Tie CL, Wu HY, et al. Abnormal baseline brain activity in bipolar depression: a resting state functional magnetic resonance imaging study. Psychiatry Res. 2012;203:175–9.
Liu CH, Ma X, Li F, Wang YJ, Tie CL, Li SF, et al. Regional homogeneity within the default mode network in bipolar depression: a resting-state functional magnetic resonance imaging study. PloS ONE. 2012;7:e48181.
Wang Y, Wang J, Jia Y, Zhong S, Zhong M, Sun Y, et al. Topologically convergent and divergent functional connectivity patterns in unmedicated unipolar depression and bipolar disorder. Transl Psychiatry. 2017;7:e1165.
Syan SK, Smith M, Frey BN, Remtulla R, Kapczinski F, Hall GBC, et al. Resting-state functional connectivity in individuals with bipolar disorder during clinical remission: a systematic review. J Psychiatry Neurosci. 2018;43:298–316.
Conio B, Martino M, Magioncalda P, Escelsior A, Inglese M, Amore M, et al. Opposite effects of dopamine and serotonin on resting-state networks: review and implications for psychiatric disorders. Mol Psychiatry. 2020;25:82–93.
Floreani A, Leung PS, Gershwin ME. Environmental basis of autoimmunity. Clin Rev Allergy Immunol. 2016;50:287–300.
Rocchi G, Sterlini B, Tardito S, Inglese M, Corradi A, Filaci G, et al. Opioidergic system and functional architecture of intrinsic brain activity: implications for psychiatric disorders. Neuroscientist. 2020;26:343–58.
Horrobin DF, Lieb J. A biochemical basis for the actions of lithium on behaviour and on immunity: relapsing and remitting disorders of inflammation and immunity such as multiple sclerosis or recurrent herpes as manic-depression of the immune system. Med Hypotheses. 1981;7:891–905.
Zuo XN, Xu T, Milham MP. Harnessing reliability for neuroscience research. Nat Hum Behav. 2019;3:768–71.
Gong ZQ, Gao P, Jiang C, Xing XX, Dong HM, White T, et al. DREAM: a toolbox to decode rhythms of the brain system. Neuroinformatics. 2021; [Online ahead of print].
Dong HM, Castellanos FX, Yang N, Zhang Z, Zhou Q, He Y, et al. Charting brain growth in tandem with brain templates at school age. Sci Bull. 2020;65:1924–34.
Download references
Author information
These authors contributed equally: Paola Magioncalda, Matteo Martino
Authors and Affiliations
Graduate Institute of Mind Brain and Consciousness, Taipei Medical University, Taipei, Taiwan
Paola Magioncalda & Matteo Martino
Brain and Consciousness Research Center, Taipei Medical University - Shuang Ho Hospital, New Taipei City, Taiwan
Department of Psychiatry, Taipei Medical University - Shuang Ho Hospital, New Taipei City, Taiwan
- Paola Magioncalda
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Paola Magioncalda or Matteo Martino .
Ethics declarations
Conflict of interest.
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary_material, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Magioncalda, P., Martino, M. A unified model of the pathophysiology of bipolar disorder. Mol Psychiatry 27 , 202–211 (2022). https://doi.org/10.1038/s41380-021-01091-4
Download citation
Received : 07 December 2020
Revised : 17 March 2021
Accepted : 29 March 2021
Published : 15 April 2021
Issue Date : January 2022
DOI : https://doi.org/10.1038/s41380-021-01091-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Motor performance and functional connectivity between the posterior cingulate cortex and supplementary motor cortex in bipolar and unipolar depression.
- Lara E. Marten
- Aditya Singh
- Roberto Goya-Maldonado
European Archives of Psychiatry and Clinical Neuroscience (2024)
Prefrontal, parietal, and limbic condition-dependent differences in bipolar disorder: a large-scale meta-analysis of functional neuroimaging studies
- Maya C. Schumer
- Henry W. Chase
- Mary L. Phillips
Molecular Psychiatry (2023)
Circulating cytotoxic immune cell composition, activation status and toxins expression associate with white matter microstructure in bipolar disorder
- Veronica Aggio
- Lorena Fabbella
- Francesco Benedetti
Scientific Reports (2023)
A three-dimensional model of neural activity and phenomenal-behavioral patterns
- Matteo Martino
Mania-related effects on structural brain changes in bipolar disorder – a narrative review of the evidence
- Christoph Abé
- Benny Liberg
- Mikael Landén
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- Spring 2024 | VOL. 22, NO. 2 Autism Across the Lifespan CURRENT ISSUE pp.147-262
- Winter 2024 | VOL. 22, NO. 1 Reproductive Psychiatry: Postpartum Depression is Only the Tip of the Iceberg pp.1-142
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Abstracts for B ipolar D isorder
Given space limitations and varying reprint permission policies, not all of the influential publications the editors considered reprinting in this issue could be included. This section contains abstracts from additional articles the editors deemed well worth reviewing.
Clinical Course of Children and Adolescents with Bipolar Spectrum Disorders
Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Ivengar S, Keller M
Archives of General Psychiatry February 2006 ; 63(2):175–183
Context: Despite the high morbidity associated with bipolar disorder (BP), few studies have prospectively studied the course of this illness in youth. Objective: To assess the longitudinal course of BP spectrum disorders (BP-I, BP-II, and not otherwise specified [BP-NOS]) in children and adolescents. Design: Subjects were interviewed, on average, every 9 months for an average of 2 years using the Longitudinal Interval Follow-up Evaluation. Setting: Outpatient and inpatient units at 3 university centers. Participants: Two hundred sixty-three children and adolescents (mean age, 13 years) with BP-I (n = 152), BP-II (n = 19), and BP-NOS (n = 92). Main Outcome Measures: Rates of recovery and recurrence, weeks with syndromal or subsyndromal mood symptoms, changes in symptoms and polarity, and predictors of outcome. Results: Approximately 70% of subjects with BP recovered from their index episode, and 50% had at least 1 syndromal recurrence, particularly depressive episodes. Analyses of weekly mood symptoms showed that 60% of the follow-up time, subjects had syndromal or subsyndromal symptoms with numerous changes in symptoms and shifts of polarity, and 3% of the time, psychosis. Twenty percent of BP-II subjects converted to BP-I, and 25% of BP-NOS subjects converted to BP-I or BP-II. Early-onset BP, BP-NOS, long duration of mood symptoms, low socioeconomic status, and psychosis were associated with poorer outcomes and rapid mood changes. Secondary analyses comparing BP-I youths with BP-I adults showed that youths significantly more time symptomatic and had more mixed/cycling episodes, mood symptom changes, and polarity switches. Conclusions: Youths with BP spectrum disorders showed a continuum of BP symptom severity from subsyndromal to full syndromal with frequent mood fluctuations. Results of this study provide preliminary validation for BP-NOS.
Genetic Variation of Brain-derived Neurotrophic Factor (BDNF) in Bipolar Disorder: Case-control Study of Over 3000 Individuals From the UK
Green EK, Raybould R, Macqregor S, Hyde S, Young AH, O’Donovan MC, Owen MJ, Kirov G, Jones L, Jones I, Craddock N
The British Journal of Psychiatry January 2006 ; 188:21–25
Background: Brain-derived neurotrophic factor (BDNF) influences neuronal survival, proliferation and plasticity. Three family-based studies have shown association of the common Valine (Val) allele of the Val66Met polymorphism of the BDNF gene with susceptibility to bipolar disorder. Aims: To replicate this finding. Method: We genotyped the Val66Met polymorphism in our UK White bipolar case-control sample (n = 3062). Results: We found no overall evidence of allele or genotype association. However, we found association with disease status in the subset of 131 individuals that had experienced rapid cycling at some time (P = 0.004). We found a similar association on re-analysis of our previously reported family-based association sample (P < 0.03, one-tailed test). Conclusions: Variation at the Val66Met polymorphism of BDNF does not play a major role in influencing susceptibility to bipolar disorder as a whole, but is associated with susceptibility to the rapid-cycling subset of the disorder.
Relationship of Mania Symptomatology to Maintenance Treatment Response with Divalproex, Lithium, or Placebo
Bowden CL, Collins MA, McElrov SL, Calabrese JR, Swann AC, Weisler RH, Wozniak PJ
Neuropsychopharmacology October 2005 ; 30(10):1932–1939
Euphoric and mixed (dysphoric) manic symptoms have different response patterns to divalproex and lithium in acute mania treatment, but have not been studied in relationship to maintenance treatment outcomes. We examined the impact of initial euphoric or dysphoric manic symptomatology on maintenance outcome. Randomized maintenance treatment with divalproex, lithium, or placebo was provided for 372 bipolar I patients, who met improvement criteria during open phase treatment for an index manic episode. The current analysis grouped patients according to the index manic episode subtype (euphoric or dysphoric), and evaluated the impact on maintenance treatment outcome. The rate of early discontinuation due to intolerance during maintenance treatment was higher for initially dysphoric patients (N = 249) than euphoric patients (N = 123; 15.7 vs 7.3%, respectively; p = 0.032). Both lithium (23.2%) and divalproex (17.1%) were associated with more premature discontinuations due to intolerance than placebo (4.8%; p = 0.003 and 0.02, respectively) in the initially dysphoric patients. Among initially euphoric patients, treatment with lithium was associated with significantly more premature discontinuations due to intolerance compared to placebo (18.2 vs 0%; p = 0.03), and divalproex was significantly (p = 0.05) more effective than lithium, but not placebo in delaying time to a depressive episode. Initial euphoric mania appeared to predispose to better outcomes on indices of depression and overall function with divalproex maintenance than with either placebo or lithium. Dysphoric mania appeared to predispose patients to more side effects when treated with either divalproex or lithium during maintenance therapy.
Dermatology Precautions and Slower Titration Yield Low Incidence of Lamotrigine Treatment-emergent Rash
Ketter TA, Wang PW, Chandler RA, Alarcon AM, Becker OV, Nowakowska C, O’Keeffe CM, Schumacher MR
The Journal of Clinical Psychiatry May 2005 ; 66(5):642–645
Objective: To assess treatment-emergent rash incidence when using dermatology precautions (limited antigen exposure) and slower titration during lamotrigine initiation. Method: We assessed rash incidence in 100 patients with DSM-IV bipolar disorder instructed, for their first 3 months taking lamotrigine, to avoid other new medicines and new foods, cosmetics, conditioners, deodorants, detergents, and fabric softeners, as well as sunburn and exposure to poison ivy/oak. Lamotrigine was not started within 2 weeks of a rash, viral syndrome, or vaccination. In addition, lamotrigine was titrated more slowly than in the prescribing information. Patients were monitored for rash and clinical phenomena using the Systematic Treatment Enhancement Program for Bipolar Disorder Clinical Monitoring Form. Descriptive statistics were compiled. Results: No patient had serious rash. Benign rash occurred in 5 patients (5%) and resolved uneventfully in 3 patients discontinuing and 2 patients continuing lamotrigine. Two patients with rash were found to be not adherent to dermatology precautions. Therefore, among the remaining patients, only 3/98 (3.1%) had benign rashes. Conclusion: The observed rate of benign rash was lower than the 10% incidence in other clinical studies. The design of this study confounds efforts to determine the relative contributions of slower titration versus dermatology precautions to the low rate of rash. Systematic studies are needed to confirm these preliminary findings, which suggest that adhering to dermatology precautions with slower titration may yield a low incidence of rash with lamotrigine.
Two-year Outcomes for Interpersonal and Social Rhythm Therapy in Individuals with Bipolar I Disorder
Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz HA, Fagiolini AM, Grochocinski V, Houck P, Scott J, Thompson W, Monk T
Archives of General Psychiatry September 2005 ; 62(9):996–1004
Context: Numerous studies have pointed to the failure of prophylaxis with pharmacotherapy alone in the treatment of bipolar I disorder. Recent investigations have demonstrated benefits from the addition of psychoeducation or psychotherapy to pharmacotherapy in this population. Objective: To compare 2 psychosocial interventions: interpersonal and social rhythm therapy (IPSRT) and an intensive clinical management (ICM) approach in the treatment of bipolar I disorder. Design: Randomized controlled trial involving 4 treatment strategies: acute and maintenance IPSRT (IPSRT/IPSRT), acute and maintenance ICM (ICM/ICM), acute IPSRT followed by maintenance ICM (IPSRT/ICM), or acute ICM followed by maintenance IPSRT (ICM/IPSRT). The preventive maintenance phase lasted 2 years. Setting: Research clinic in a university medical center. Participants: One hundred seventy-five acutely ill individuals with bipolar I disorder recruited from inpatient and outpatient settings, clinical referral, public presentations about bipolar disorder, and other public information activities. Interventions: Interpersonal and social rhythm therapy, an adaptation of Klerman and Weissman’s interpersonal psychotherapy to which a social rhythm regulation component has been added, and ICM. Main Outcome Measures: Time to stabilization in the acute phase and time to recurrence in the maintenance phase. Results: We observed no difference between the treatment strategies in time to stabilization. After controlling for covariates of survival time, we found that participants assigned to IPSRT in the acute treatment phase survived longer without a new affective episode (P = .01), irrespective of maintenance treatment assignment. Participants in the IPSRT group had higher regularity of social rhythms at the end of acute treatment (P<.001). Ability to increase regularity of social rhythms during acute treatment was associated with reduced likelihood of recurrence during the maintenance phase (P = .05). Conclusion: Interpersonal and social rhythm therapy appears to add to the clinical armamentarium for the management of bipolar I disorder, particularly with respect to prophylaxis of new episodes.
A Placebo-controlled 18-month Trial of Lamotrigine and Lithium Maintenance Treatment in Recently Manic or Hypomanic Patients with Bipolar I Disorder
Bowden CL, Calabrese JR, Sachs G, Yatham LN, Asghar SA, Hompland M, Montgomery P, Earl N, Smoot TM, DeVeaugh-Geiss J; Lamictal 606 Study Group
Archives of General Psychiatry April 2003 ; 60(4):392–400
Background: Lamotrigine has been shown to be an effective treatment for bipolar depression and rapid cycling in placebo-controlled clinical trials. This double-blind, placebo-controlled study was conducted to assess the efficacy and tolerability of lamotrigine and lithium compared with placebo for the prevention of relapse or recurrence of mood episodes in recently manic or hypomanic patients with bipolar I disorder. Methods: After an 8- to 16-week open-label phase during which treatment with lamotrigine was initiated and other psychotropic drug regimens were discontinued, patients were randomized to lamotrigine (100–400 mg daily), lithium (0.8–1.1 mEq/L), or placebo as double-blind maintenance treatment for as long as 18 months. Results: Of 349 patients who met screening criteria and entered the open-label phase, 175 met stabilization criteria and were randomized to double-blind maintenance treatment (lamotrigine, 59 patients; lithium, 46 patients; and placebo, 70 patients). Both lamotrigine and lithium were superior to placebo at prolonging the time to intervention for any mood episode (lamotrigine vs placebo, P = .02; lithium vs placebo, P = .006). Lamotrigine was superior to placebo at prolonging the time to a depressive episode (P = .02). Lithium was superior to placebo at prolonging the time to a manic, hypomanic, or mixed episode (P = .006). The most common adverse event reported for lamotrigine was headache. Conclusions: Both lamotrigine and lithium were superior to placebo for the prevention of relapse or recurrence of mood episodes in patients with bipolar I disorder who had recently experienced a manic or hypomanic episode. The results indicate that lamotrigine is an effective, well-tolerated maintenance treatment for bipolar disorder, particularly for prophylaxis of depression.
A Randomized Trial on the Efficacy of Group Psychoeducation in the Prophylaxis of Recurrences in Bipolar Patients whose Disease is in Remission
Colom F, Vieta E, Martinez-Aran A, Reinares M, Goikolea JM, Benabarre A, Torrent C, Comes M, Corbella B, Parramon G, Corominas J
Archives of General Psychiatry April 2003 ; 60(4):402–407
Background: Studies on individual psychotherapy indicate that some interventions may reduce the number of recurrences in bipolar patients. However, there has been a lack of structured, well-designed, blinded, controlled studies demonstrating the efficacy of group psychoeducation to prevent recurrences in patients with bipolar I and II disorder. Methods: One hundred twenty bipolar I and II outpatients in remission (Young Mania Rating Scale score <6, Hamilton Depression Rating Scale-17 score <8) for at least 6 months prior to inclusion in the study, who were receiving standard pharmacologic treatment, were included in a controlled trial. Subjects were matched for age and sex and randomized to receive, in addition to standard psychiatric care, 21 sessions of group psychoeducation or 21 sessions of nonstructured group meetings. Subjects were assessed monthly during the 21-week treatment period and throughout the 2-year follow-up. Results: Group psychoeducation significantly reduced the number of relapsed patients and the number of recurrences per patient, and increased the time to depressive, manic, hypomanic, and mixed recurrences. The number and length of hospitalizations per patient were also lower in patients who received psychoeducation. Conclusion: Group psychoeducation is an efficacious intervention to prevent recurrence in pharmacologically treated patients with bipolar I and II disorder.
A Randomized Controlled Study of Cognitive Therapy for Relapse Prevention for Bipolar Affective Disorder: Outcome of the First Year
Lam DH, Watkins ER, Hayward P, Bright J, Wright K, Kerr N, Parr-Davis G, Sham P
Archives of General Psychiatry February 2003 ; 60(2):145–152
Background: Despite the use of mood stabilizers, a significant proportion of patients with bipolar affective disorder experience frequent relapses. A pilot study of cognitive therapy (CT) specifically designed to prevent relapses for bipolar affective disorder showed encouraging results when used in conjunction with mood stabilizers. This article reports the outcome of a randomized controlled study of CT to help prevent relapses and promote social functioning. Methods: We randomized 103 patients with bipolar 1 disorder according to the DSM-IV, who experienced frequent relapses despite the prescription of commonly used mood stabilizers, into a CT group or control group. Both the control and CT groups received mood stabilizers and regular psychiatric follow-up. In addition, the CT group received an average of 14 sessions of CT during the first 6 months and 2 booster sessions in the second 6 months. Results: During the 12-month period, the CT group had significantly fewer bipolar episodes, days in a bipolar episode, and number of admissions for this type of episode. The CT group also had significantly higher social functioning. During these 12 months, the CT group showed less mood symptoms on the monthly mood questionnaires. Furthermore, there was significantly less fluctuation in manic symptoms in the CT group. The CT group also coped better with manic prodromes at 12 months. Conclusion: Our findings support the conclusion that CT specifically designed for relapse prevention in bipolar affective disorder is a useful tool in conjunction with mood stabilizers.
The Long-term Natural History of the Weekly Symptomatic Status of Bipolar I Disorder
Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, Leon AC, Rice JA, Keller MB
Archives of General Psychiatry June 2002 ; 59(6):530–537
Background: To our knowledge, this is the first prospective natural history study of weekly symptomatic status of patients with bipolar I disorder (BP-I) during long-term follow-up. Methods: Analyses are based on ongoing prospective follow-up of 146 patients with Research Diagnostic Criteria BP-I, who entered the National Institute of Mental Health (Bethesda, Md) Collaborative Depression Study from 1978 through 1981. Weekly affective symptom status ratings were analyzed by polarity and severity, ranging from asymptomatic, to subthreshold levels, to full-blown major depression and mania. Percentages of follow-up weeks at each level as well as number of shifts in symptom status and polarity during the entire follow-up period were examined. Finally, 2 new measures of chronicity were evaluated in relation to previously identified predictors of chronicity for BP-I. Results: Patients with BP-I were symptomatically ill 47.3% of weeks throughout a mean of 12.8 years of follow-up. Depressive symptoms (31.9% of total follow-up weeks) predominated over manic/hypomanic symptoms (8.9% of weeks) or cycling/mixed symptoms (5.9% of weeks). Subsyndromal, minor depressive, and hypomanic symptoms combined were nearly 3 times more frequent than syndromal-level major depressive and manic symptoms (29.9% vs 11.2% of weeks, respectively). Patients with BP-I changed symptom status an average of 6 times per year and polarity more than 3 times per year. Longer intake episodes and those with depression-only or cycling polarity predicted greater chronicity during long-term follow-up, as did comorbid drug-use disorder. Conclusions: The longitudinal weekly symptomatic course of BP-I is chronic. Overall, the symptomatic structure is primarily depressive rather than manic, and subsyndromal and minor affective symptoms predominate. Symptom severity levels fluctuate, often within the same patient over time. Bipolar I disorder is expressed as a dimensional illness featuring the full range (spectrum) of affective symptom severity and polarity.
- Cited by None

- Search by keyword
- Search by citation
Page 1 of 8
Longitudinal studies of bipolar patients and their families: translating findings to advance individualized risk prediction, treatment and research
Bipolar disorder is a broad diagnostic construct associated with significant phenotypic and genetic heterogeneity challenging progress in clinical practice and discovery research. Prospective studies of well-c...
- View Full Text
Sociodemographic, clinical and treatment characteristics of current rapid-cycling bipolar disorder: a multicenter Chinese study
Rapid cycling bipolar disorder (RCBD), characterized by four or more episodes per year, is a complex subtype of bipolar disorder (BD) with poorly understood characteristics.
Type of cycle, temperament and childhood trauma are associated with lithium response in patients with bipolar disorders
Lithium stands as the gold standard in treating bipolar disorders (BD). Despite numerous clinical factors being associated with a favorable response to lithium, comprehensive studies examining the collective i...
How effective are mood stabilizers in treating bipolar patients comorbid with cPTSD? Results from an observational study
Multiple traumatic experiences, particularly in childhood, may predict and be a risk factor for the development of complex post-traumatic stress disorder (cPTSD). Unfortunately, individuals with bipolar disord...
Perceived loneliness and social support in bipolar disorder: relation to suicidal ideation and attempts
The suicide rate in bipolar disorder (BD) is among the highest across all psychiatric disorders. Identifying modifiable variables that relate to suicidal thoughts and behaviors (STBs) in BD may inform preventi...
Effectiveness of ultra-long-term lithium treatment: relevant factors and case series
The phenomenon of preventing the recurrences of mood disorders by the long-term lithium administration was discovered sixty years ago. Such a property of lithium has been unequivocally confirmed in subsequent ...
Prevention of suicidal behavior with lithium treatment in patients with recurrent mood disorders
Suicidal behavior is more prevalent in bipolar disorders than in other psychiatric illnesses. In the last thirty years evidence has emerged to indicate that long-term treatment of bipolar disorder patients wit...
Correlations between multimodal neuroimaging and peripheral inflammation in different subtypes and mood states of bipolar disorder: a systematic review
Systemic inflammation-immune dysregulation and brain abnormalities are believed to contribute to the pathogenesis of bipolar disorder (BD). However, the connections between peripheral inflammation and the brai...
Lithium: how low can you go?
Why is lithium [not] the drug of choice for bipolar disorder a controversy between science and clinical practice.
During over half a century, science has shown that lithium is the most efficacious treatment for bipolar disorder but despite this, its prescription has consistently declined internationally during recent deca...
Biomarkers for neurodegeneration impact cognitive function: a longitudinal 1-year case–control study of patients with bipolar disorder and healthy control individuals
Abnormalities in cerebrospinal fluid (CSF)-amyloid-beta (Aβ)42, CSF-Aβ40, CSF-Aβ38, CSF-soluble amyloid precursor proteins α and β, CSF-total-tau, CSF-phosphorylated-tau, CSF-neurofilament light protein (NF-L)...
Cognitive behavioural therapy for social anxiety disorder in people with bipolar disorder: a case series
Social anxiety disorder increases the likelihood of unfavourable outcomes in people with bipolar disorder. Cognitive behavioural therapy (CBT) is the first-line treatment for social anxiety disorder. However, ...
Lithium prescription trends in psychiatric inpatient care 2014 to 2021: data from a Bavarian drug surveillance project
Lithium (Li) remains one of the most valuable treatment options for mood disorders. However, current knowledge about prescription practices in Germany is limited. The objective of this study is to estimate the...
Lifetime risk of severe kidney disease in lithium-treated patients: a retrospective study
Lithium is an essential psychopharmaceutical, yet side effects and concerns about severe renal function impairment limit its usage.
Factors associated with suicide attempts in the antecedent illness trajectory of bipolar disorder and schizophrenia
Factors associated with suicide attempts during the antecedent illness trajectory of bipolar disorder (BD) and schizophrenia (SZ) are poorly understood.
Behavioral lateralization in bipolar disorders: a systematic review
Bipolar disorder (BD) is often seen as a bridge between schizophrenia and depression in terms of symptomatology and etiology. Interestingly, hemispheric asymmetries as well as behavioral lateralization are shi...
High lithium concentration at delivery is a potential risk factor for adverse outcomes in breastfed infants: a retrospective cohort study
Neonatal effects of late intrauterine and early postpartum exposure to lithium through mother’s own milk are scarcely studied. It is unclear whether described symptoms in breastfed neonates are caused by place...
Key questions on the long term renal effects of lithium: a review of pertinent data
For over half a century, it has been widely known that lithium is the most efficacious maintenance treatment for bipolar disorder. Despite thorough research on the long-term effects of lithium on renal functio...
Controversies regarding lithium-associated weight gain: case–control study of real-world drug safety data
The impact of long-term lithium treatment on weight gain has been a controversial topic with conflicting evidence. We aim to assess reporting of weight gain associated with lithium and other mood stabilizers c...
Differential diagnosis of unipolar versus bipolar depression by GSK3 levels in peripheral blood: a pilot experimental study
The differential diagnosis of patients presenting for the first time with a depressive episode into unipolar disorder versus bipolar disorder is crucial to establish the correct pharmacological therapy (antide...
Supra-second interval timing in bipolar disorder: examining the role of disorder sub-type, mood, and medication status
Widely reported by bipolar disorder (BD) patients, cognitive symptoms, including deficits in executive function, memory, attention, and timing are under-studied. Work suggests that individuals with BD show imp...
Association between childhood trauma, cognition, and psychosocial function in a large sample of partially or fully remitted patients with bipolar disorder and healthy participants
Childhood trauma (CT) are frequently reported by patients with bipolar disorder (BD), but it is unclear whether and how CT contribute to patients’ cognitive and psychosocial impairments. We aimed to examine th...
Countering the declining use of lithium therapy: a call to arms
For over half a century, it has been widely known that lithium is the most efficacious treatment for bipolar disorder. Yet, despite this, its prescription has consistently declined over this same period of tim...
Paediatric bipolar disorder: an age-old problem
Nrx-101 (d-cycloserine plus lurasidone) vs. lurasidone for the maintenance of initial stabilization after ketamine in patients with severe bipolar depression with acute suicidal ideation and behavior: a randomized prospective phase 2 trial.
We tested the hypothesis that, after initial improvement with intravenous ketamine in patients with bipolar disorder (BD) with severe depression and acute suicidal thinking or behavior, a fixed-dose combinatio...
The IBER study: a feasibility randomised controlled trial of imagery based emotion regulation for the treatment of anxiety in bipolar disorder
Intrusive mental imagery is associated with anxiety and mood instability within bipolar disorder and therefore represents a novel treatment target. Imagery Based Emotion Regulation (IBER) is a brief structured...
Mitochondrial genetic variants associated with bipolar disorder and Schizophrenia in a Japanese population
Bipolar disorder (BD) and schizophrenia (SZ) are complex psychotic disorders (PSY), with both environmental and genetic factors including possible maternal inheritance playing a role. Some studies have investi...
Differential characteristics of bipolar I and II disorders: a retrospective, cross-sectional evaluation of clinical features, illness course, and response to treatment
The distinction between bipolar I and bipolar II disorder and its treatment implications have been a matter of ongoing debate. The aim of this study was to examine differences between patients with bipolar I a...
Neonatal admission after lithium use in pregnant women with bipolar disorders: a retrospective cohort study
Lithium is the preferred treatment for pregnant women with bipolar disorders (BD), as it is most effective in preventing postpartum relapse. Although it has been prescribed during pregnancy for decades, the sa...
Rates and associations of relapse over 5 years of 2649 people with bipolar disorder: a retrospective UK cohort study
Evidence regarding the rate of relapse in people with bipolar disorder (BD), particularly from the UK, is lacking. This study aimed to evaluate the rate and associations of clinician-defined relapse over 5 yea...
Exploratory study of ultraviolet B (UVB) radiation and age of onset of bipolar disorder
Sunlight contains ultraviolet B (UVB) radiation that triggers the production of vitamin D by skin. Vitamin D has widespread effects on brain function in both developing and adult brains. However, many people l...
Characteristics of rapid cycling in 1261 bipolar disorder patients
Rapid-cycling (RC; ≥ 4 episodes/year) in bipolar disorder (BD) has been recognized since the 1970s and associated with inferior treatment response. However, associations of single years of RC with overall cycl...
Clinicians’ preferences and attitudes towards the use of lithium in the maintenance treatment of bipolar disorders around the world: a survey from the ISBD Lithium task force
Lithium has long been considered the gold-standard pharmacological treatment for the maintenance treatment of bipolar disorders (BD) which is supported by a wide body of evidence. Prior research has shown a st...
Phenotype fingerprinting of bipolar disorder prodrome
Detecting prodromal symptoms of bipolar disorder (BD) has garnered significant attention in recent research, as early intervention could potentially improve therapeutic efficacy and improve patient outcomes. T...
Predictors of adherence to electronic self-monitoring in patients with bipolar disorder: a contactless study using Growth Mixture Models
Several studies have reported on the feasibility of electronic (e-)monitoring using computers or smartphones in patients with mental disorders, including bipolar disorder (BD). While studies on e-monitoring ha...
Racial differences in the major clinical symptom domains of bipolar disorder
Across clinical settings, black individuals are disproportionately less likely to be diagnosed with bipolar disorder compared to schizophrenia, a traditionally more severe and chronic disorder with lower expec...
Methylomic biomarkers of lithium response in bipolar disorder: a clinical utility study
Response to lithium (Li) is highly variable in bipolar disorders (BD). Despite decades of research, no clinical predictor(s) of response to Li prophylaxis have been consistently identified. Recently, we develo...
A compelling need to empirically validate bipolar depression
Structured physical exercise for bipolar depression: an open-label, proof-of concept study.
Physical exercise (PE) is a recommended lifestyle intervention for different mental disorders and has shown specific positive therapeutic effects in unipolar depressive disorder. Considering the similar sympto...
Experiences that matter in bipolar disorder: a qualitative study using the capability, comfort and calm framework
When assessing the value of an intervention in bipolar disorder, researchers and clinicians often focus on metrics that quantify improvements to core diagnostic symptoms (e.g., mania). Providers often overlook...
Emotion regulation in bipolar disorder type-I: multivariate analysis of fMRI data
Bipolar disorder type-I (BD-I) patients are known to show emotion regulation abnormalities. In a previous fMRI study using an explicit emotion regulation paradigm, we compared responses from 19 BD-I patients a...
Lithium levels and lifestyle in patients with bipolar disorder: a new tool for self-management
Patients should get actively involved in the management of their illness. The aim of this study was to assess the influence of lifestyle factors, including sleep, diet, and physical activity, on lithium levels...
Reduced parenting stress following a prevention program decreases internalizing and externalizing symptoms in the offspring of parents with bipolar disorder
Offspring of parents with bipolar disorder (OBD) are at risk for developing mental disorders, and the literature suggests that parenting stress may represent an important risk factor linking parental psychopat...
Stigma in people living with bipolar disorder and their families: a systematic review
Stigma affects different life aspects in people living with bipolar disorder and their families. This study aimed to examining the experience of stigma and evaluating predictors, consequences and strategies to...
Lithium use in childhood and adolescence, peripartum, and old age: an umbrella review
Lithium is one of the most consistently effective treatment for mood disorders. However, patients may show a high level of heterogeneity in treatment response across the lifespan. In particular, the benefits o...
Risk of childhood trauma exposure and severity of bipolar disorder in Colombia
Bipolar disorder (BD) is higher in developing countries. Childhood trauma exposure is a common environmental risk factor in Colombia and might be associated with a more severe course of bipolar disorder in Low...
A systematic review on the effectiveness of dialectical behavior therapy for improving mood symptoms in bipolar disorders
Evidence-based psychotherapies available to treat patients with bipolar disorders (BD) are limited. Dialectical behavior therapy (DBT) may target several common symptoms of BD. We conducted a systematic review...
Bipolar disorder and sexuality: a preliminary qualitative pilot study
Individuals with mental health disorders have a higher risk of sexual problems impacting intimate relations and quality of life. For individuals with bipolar disorder (BD) the mood shifts might to a particular...
Long-term lithium therapy and risk of chronic kidney disease, hyperparathyroidism and hypercalcemia: a cohort study
Lithium is well recognized as the first-line maintenance treatment for bipolar disorder (BD). However, besides therapeutic benefits attributed to lithium therapy, the associated side effects including endocrin...
The association of genetic variation in CACNA1C with resting-state functional connectivity in youth bipolar disorder
CACNA1C rs1006737 A allele, identified as a genetic risk variant for bipolar disorder (BD), is associated with anomalous functional connectivity in adults with and without BD. Studies have yet to investigate the ...
- Editorial Board
- Sign up for article alerts and news from this journal
- ISSN: 2194-7511 (electronic)
- Open access
- Published: 18 April 2024
A bibliometric and visual analysis of cognitive function in bipolar disorder from 2012 to 2022
- Xiaohong Cui 4 , 5 na1 ,
- Tailian Xue 1 na1 ,
- Zhiyong Zhang 1 ,
- Hong Yang 2 &
- Yan Ren 3
Annals of General Psychiatry volume 23 , Article number: 13 ( 2024 ) Cite this article
43 Accesses
Metrics details

Introduction
Bipolar disorder (BD) is a chronic psychiatric disorder that combines hypomania or mania and depression. The study aims to investigate the research areas associated with cognitive function in bipolar disorder and identify current research hotspots and frontier areas in this field.
Methodology
Publications related to cognitive function in BD from 2012 to 2022 were searched on the Web of Science Core Collection (WoSCC) database. VOSviewer, CiteSpace, and Scimago Graphica were used to conduct this bibliometric analysis.
A total of 989 articles on cognitive function in BD were included in this review. These articles were mainly from the United States, China, Canada, Spain and the United Kingdom. Our results showed that the journal “ Journal of Affective Disorders ” published the most articles. Apart from “Biploar disorder” and “cognitive function”, the terms “Schizophrenia”, “Meta analysis”, “Rating scale” were also the most frequently used keywords. The research on cognitive function in bipolar disorder primarily focused on the following aspects: subgroup, individual, validation and pathophysiology.
Conclusions
The current concerns and hotspots in the filed are: “neurocognitive impairment”, “subgroup”, “1st degree relative”, “mania”, “individual” and “validation”. Future research is likely to focus on the following four themes: “Studies of the bipolar disorder and cognitive subgroups”, “intra-individual variability”, “Validation of cognitive function tool” and “Combined with pathology or other fields”.
Bipolar disorder presents a complex clinical presentation. It is characterized by alternating episodes of mania and depression, and is a serious mental health problem with a high rate of disability and difficult to cure [ 1 ]. The phenotypic manifestations of BD include not only core abnormalities in mood regulation, but also cognitive impairments, sleep/wake disturbances, and a high prevalence of comorbidities in both internal medicine and psychiatry. Cognitive function, also known as neurocognitive function, refers to the ability of the human brain to process information, including memory, executive function, space, time, language comprehension and expression. The current cognitive dysfunction in patients with bipolar disorder primarily affects memory, attention, executive function and so on [ 2 ].
In recent years, there has been increasing attention on cognitive functioning in patients with bipolar disorder. For example, a study has shown that individuals with bipolar disorder experience cognitive impairments during periods of remission as well as during acute episodes of depression or mania. Cognitive impairment is associated with multiple factors, including age of onset, duration of remission, and cognitive impairment, which are also intrinsic phenotypes of the disease [ 3 ]. Different diseases cause varying degrees of cognitive impairment. Patients with schizophrenia exhibit comprehensive cognitive decline, while those with bipolar disorder primarily experience impairment in memory, attention, and executive function, especially during acute episodes. The classification of bipolar disorder also corresponds to different areas of cognitive impairment. The impact of medication treatment on the cognitive function of bipolar disorder patients is contradictory, requiring a combined approach with other therapeutic methods to improve patient cognition [ 4 ]. The assessment of cognitive function is also a research prominent topic in this field. The assessment of cognitive function in bipolar disorder includes both objective and subjective aspects. Various neuropsychological tests, such as the Rey Auditory Verbal Learning Test (RAVLT) and Rapid Visual Information Processing (RVP) test, are used to assess objective cognitive function in individuals with bipolar disorder. Subjective cognitive function assessment can be performed using the Cognitive and Physical Functioning Questionnaire (CPFQ) [ 5 ]. In addition to the above assessment tools, the results of another study showed: for patients with BD in partial or full remission, the Screen for Cognitive Impairment in Psychiatry (SCIP) and the Cognitive Complaints in Bipolar Disorder Rating Scale (COBRA) are effective tools for screening objective and subjective cognitive impairments, respectively [ 6 ]. These findings indicate that we need to assess different aspects of cognitive impairment in patients using various scales. This will help us better understand their cognitive performance and provide assistance for clinical treatment.
Bibliometrics is the analysis of published information (books, journal articles, datasets, blogs) and associated metadata (abstracts, keywords, citations). It describes or shows the relationship between published works by using statistical data [ 7 ]. The characteristics of publications and the relationships between publications can be described by qualitative and quantitative analysis. Cognitive function is currently a hot topic of research in bipolar disorder, but there are no bibliometric articles yet, although there are many articles on cognitive function in bipolar disorder.
In this article, we use CiteSpace and VOSviewer software to review the research of cognitive function in bipolar disorder in the past 12 years (from 2012 to 2022) to learn the status of international research, the shift in research hotspots and emerging trends in this field.
Research methodology
Data sources and search strategy.
This study searched the related literature of cognitive function in bipolar disorder from the Web of Science (core collection) database, The reason for choosing WoSCC is that it is a high-quality digital literature resources database, suitable for the quantitative analysis of literature. The retrieval formula is TS="bipolar disorder” OR “bipolar affective disorder” OR “bipolar depressive disorder” OR “bipolar spectrum disorder” OR “biphasic disorder” AND TS = cognition OR “cognitive impairment” OR “cognitive decline” OR “cognitive function” OR “cognitive dysfunction” OR cognitive, selected over a period of 2012–2022, analyzed the type of literature as articles and reviews, and included the studies without regard to language. Through the analysis of the titles, abstracts and keywords of the article, a total of 4939 articles were searched, 1005 articles were preliminarily screened out, 989 articles were obtained (865 articles, 124 reviews) (Fig. 1 ).
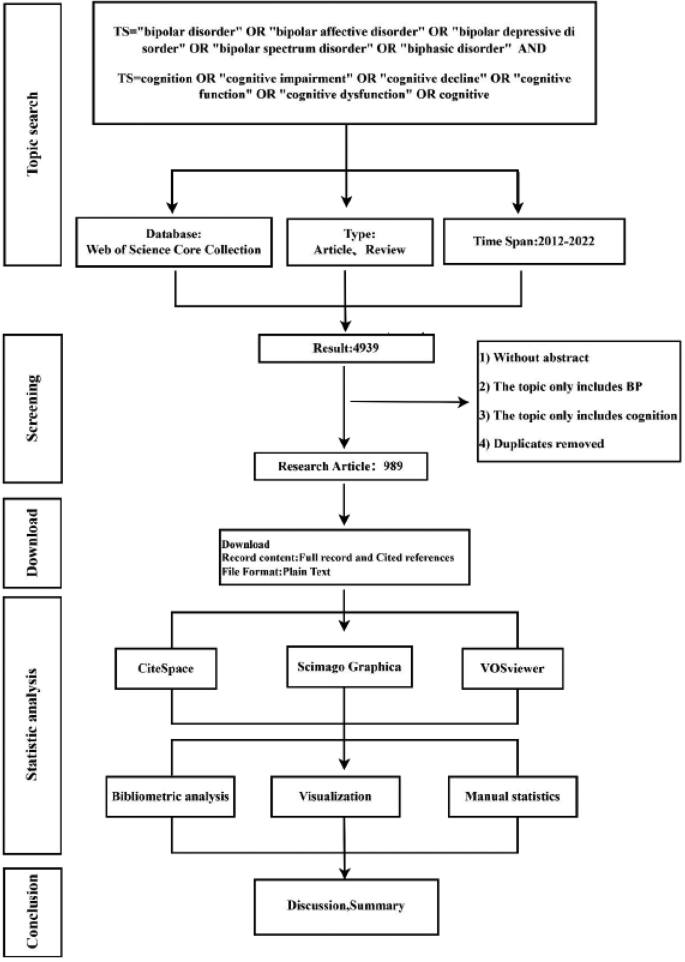
Flow chart of scientometric analysis
Research tools
In this study, VOSviewer software (version 1.6.18) on WoSCC database is applied to conduct co-occurrence analysis, combined with Scimago Graphica software to achieve a country map visualization analysis. Using CiteSpace (version of 6.1.R6) software for the database author co-operation analysis, keyword cluster analysis, literature co-citations and keyword mutation analysis. VOSviewer application developed by Nees Jan van Eck and Ludo Waltman (Leiden University) in 2010, can be used for a variety of network analysis, including collaborative analysis, keyword co-occurrence analysis, citation and co-citation analysis, and bibliographic coupling. It can be used to conduct co-authorship analysis, keyword co-occurrence analysis, citation and co-citation analysis, and bibliographic coupling [ 8 ]. Citespace is a software developed by Professor Chaomei Chen of Drexel University (Philadelphia, USA) for the visual analysis of scientific references. With the software, we can generate a series of visual knowledge atlases to understand the research hotspots in the field, delve into the forefront of its development, and ascertain emerging trends [ 9 ].
The parameters used for co-occurrence analysis using VOSviewer are the default parameters for the software, and the parameters used in CiteSpace are as follows: time slices (2012–2022), number of years per slice (1), node types (author collaborations, co-citations, and keywords), pruning (pathfinder, pruning sliced network, pruning the merged network), g-index (k = 25, literature co-citations are k = 15).
Analysis of publication years
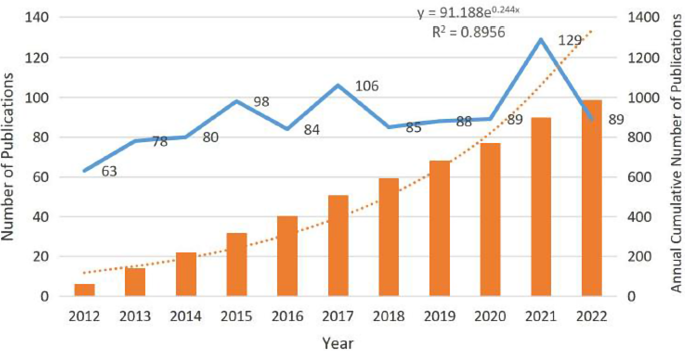
Distribution of publication from 2012 to 2022
There are a total of 989 articles were used in this study from 57 countries. Figure 2 shows the distribution of publication years for articles in the field of cognitive function in bipolar disorder. Overall, the volume of articles in this field is relatively balanced, with more than 60 articles published annually starting from 2012. The number of articles published in 2018–2020 remained relatively stable. The highest volume of articles was in 2021, with 129 articles published. The annual cumulative volume model aligns with the annual growth data y = 91.188e 0.244x (R 2 = 0.8956). This also shows that the field of cognitive function in bipolar disorder has garnered significant attention from scholars, with the development of society and technology, the study of cognition in the context of bipolar disorder has become an important and hot topic.
Analysis of author
By analyzing the authors of the literature cited in this paper, we aimed to gain insights into the prominent scholars and core strength within this research area. Famous scholar Price pointed out that, in the same subject, half of the papers are written by a group of high-productivity authors, and the number of authors in this group is approximately equal to the square root of the total number of authors [ 10 ].
According to the Price’s Law, the minimum number of core authors in the field is m = 4.79, so authors with 5 or more posts (including 5) are positioned as core authors in the field, where they are active professionals. Table 1 shows the top five productivity authors with contributions in this area. Top of the list was Vieta E, professor and chair of psychiatry at the University of Barcelona, with the highest number of published articles (41). He spearheads research focused on investigating cognitive function, cognitive impairment, and clinical manifestations associated with bipolar disorder, leading the Bipolar Disorder and Depression Project in Barcelona, Catalonia, Spain.
We then analyzed the author’s cooperation relationship. These studies published between 2012 and 2022, the year per slice for analysis is 1 year. The author cooperation network is shown in Fig. 3 (N = 419, E = 862). The circle size of the node represents the number of publications.
The centrality indicates that an author has a close cooperation relationship with other authors. According to Table 1 , the centrality of Vieta E is 0.14 (centrality > 0.1), indicating that the author has cooperation with multiple authors in the field, while the centrality of Vinberg M is 0.02. The author’s cooperation network graph also shows that Vinberg M is far away from other high-yielding authors, indicating that the author has less cooperation with other high-yielding authors in the research of cognitive function in bipolar disorder.
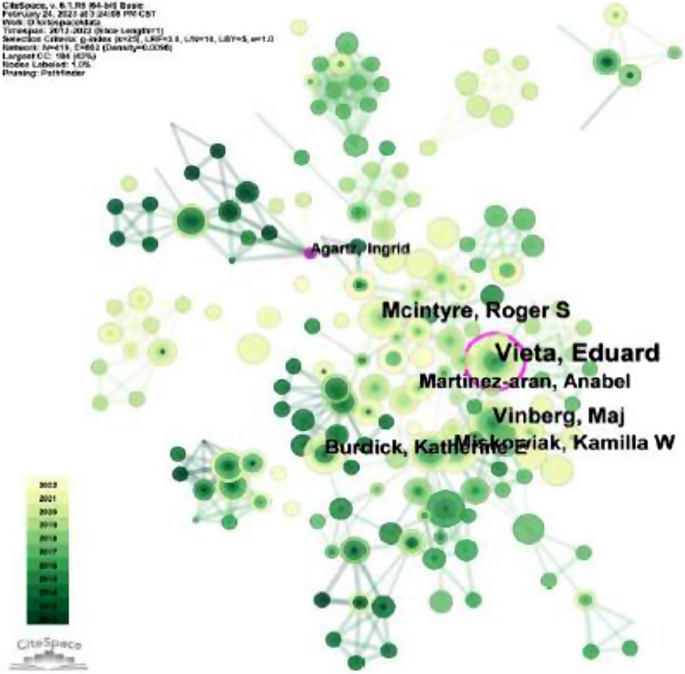
Author collaboration network analysis. The shorter the distance between two nodes the thicker the connection, indicating a higher level of collaboration between the two authors. Green nodes represent earlier published studies, while yellow nodes represent more recent studies
Analysis of the most productive journals
The analysis of the journals in literature shows that journals published in this field belong to the medical field except a few comprehensive journals in the past ten years. The top 10 most publication journals have shown in Table 2 . Journals with more than 60 published articles were Journal of Affective Disorders , Psychiatry Research and Bipolar Disorders , with 185, 72, and 66 articles, respectively. Among them, PLOS ONE is an open-source journal, with 20 citations, ranking 10th in the number of published journals.
Analyzing of journal citation founds that (Table 2 ) the most cited journals are the top medical journal “ Acta Psychiatrica Scandinavica ”, with a total of 27 articles cited up to 47 times. It indicates that the journal publishes high-quality articles and is of widespread interest in the field of cognitive function in bipolar disorder. The contents published in this journal include: empirical studies, factor studies, and the influence of variable indicators on cognitive function in patients with bipolar disorder.
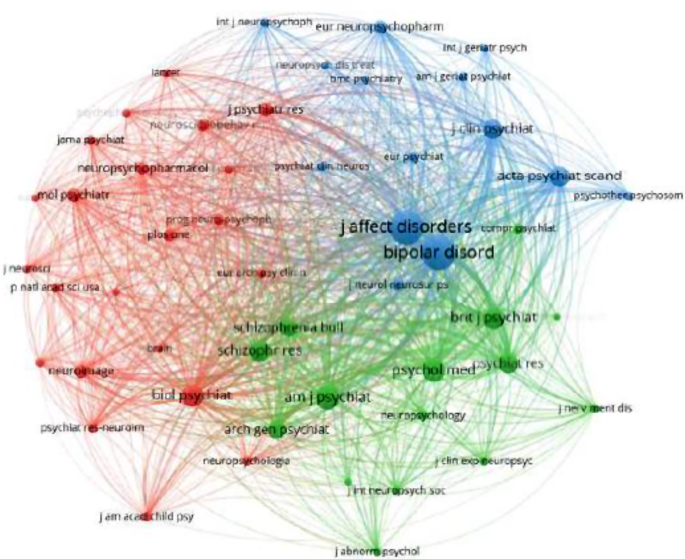
Furthermore, a visual analysis of the journal co-citation network reveals the presence of three clusters (Fig. 4 , in supplementary material). According to the subject of the co-citation literature clustering, it divided into three different themes. The top 3 most cited journals are Journal of Affective Disorders (3807 citations), Bipolar Disorders (2186 citations), and American Journal of Psychiatry (1284 citations). All three of these journals are in the JCR1. The most cited journal, Journal of Affective Disorders , which includes articles on affective disorder. It covers a wide range of subjects, including neuroimaging, cognitive neuroscience, genetics, molecular biology, etc. This is in line with the research focus on cognitive function in bipolar disorder.
Co-citation resource
Analysis of the most productive countries/regions
In 2012–2022, a total of 57 countries have published articles on cognitive function in bipolar disorder. To gain an understanding of the countries that have made significant contributions to this field, the study utilized VOSviewer to visualize the countries with 5 or more articles, a total of 33 countries met this criterion. The data was then exported in HTML format and imported into Scimago Graphica for visual analysis to generate map. The result is shown in the Fig. 5 .
As we can see, most of articles are written by scholars from a few countries. Other countries such as Chile, Ireland, Colombia, etc. They have published fewer articles related to cognitive function in bipolar disorder in 2012–2022.
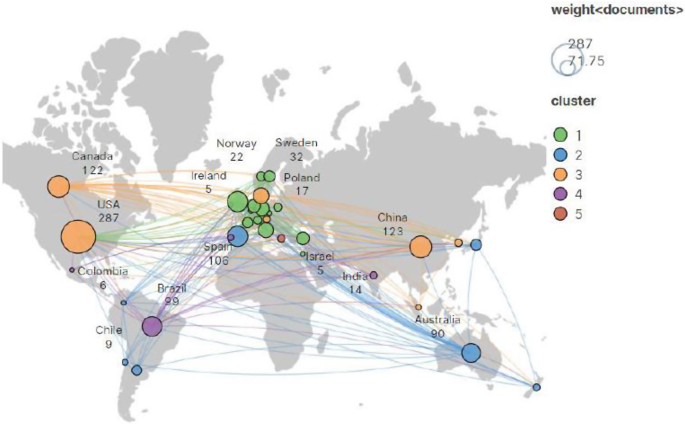
The visual map of countries. ( A ) The size of each node represents the number of publications from that country. ( B ) The number displayed below each country indicates the total number of publications
A further analysis of high-productivity countries in the field is presented in Table 3 , showing the Top 5 countries in the field. According to the data in Table 3 , American scholars have contributed the most research articles (287 articles published), accounting for 29% of the total number of articles published in this field. The second largest country is China, with 123 articles. The USA and the United Kingdom with a centrality value above 0.1, with centrality ratios of 0.25 and 0.36, respectively, indicating that these countries work closely with other countries in the study of cognitive function in bipolar disorder.
Analysis of keywords
We can classify keywords according to their frequency of occurrence and point out the links between high-frequency keywords. The analysis of keywords can help us understand the academic structure of a field and reveal the frontiers of research in the discipline. Figure 6 ( in supplementary material) presents the network and density of keywords that are referenced in the top 50. Keywords that are close to each other are classified into the same cluster, providing an overview of the main topics related to cognitive function in bipolar disorder.
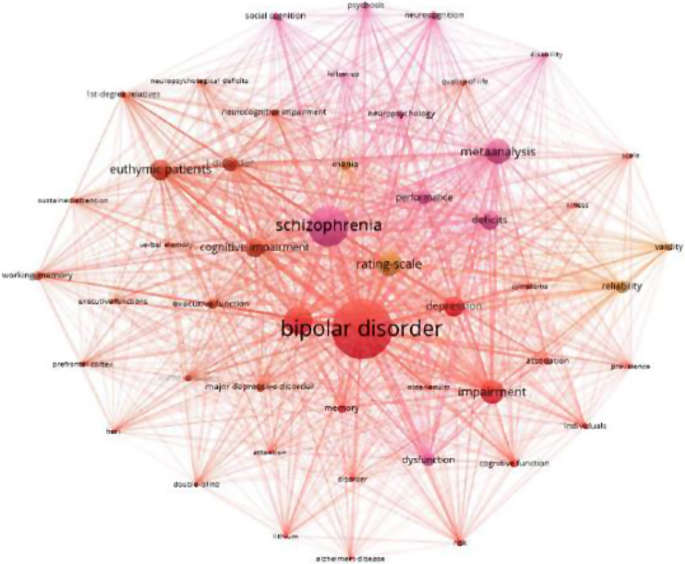
Co-occurrence analysis of keywords. ( A ) The size of the node represets the frequency of the keyword. ( B ) The distance between two node represets the strength of their association
In terms of co-occurrence frequency, the most frequent keyword was “Biploar disorder” with 712 citation times, followed by “Schizophrenia”, “Cognition”, “Meta analysis”, “Rating scale”, “Impairment”, “Euthymic patients”, “Deficits”, “Depression” and “Cognitive impairment” (Table 4 ). These high-frequency keywords reflect the hot spots of cognitive function in bipolar disorder.
In CiteSpace, the LLR method was used to cluster the keywords (N = 473, E = 947) (Fig. 7 , in supplementary material). All keywords were divided into 15 clusters with co-citation relationship, including the largest cluster “cognitive function” (#0), followed by “Alzheimer disease” (#1), “cognitive control” (#2) and “executive function” (#3). Clustering results point to clinical symptoms (including #0 cognitive function, #1 Alzheimer disease, #2 cognitive control, #3 executive function, #15 affective response inhibition) and diagnostic and intervention strategies (#5 psychological testing, #10 clinical staging model, #11 antipsychotic).
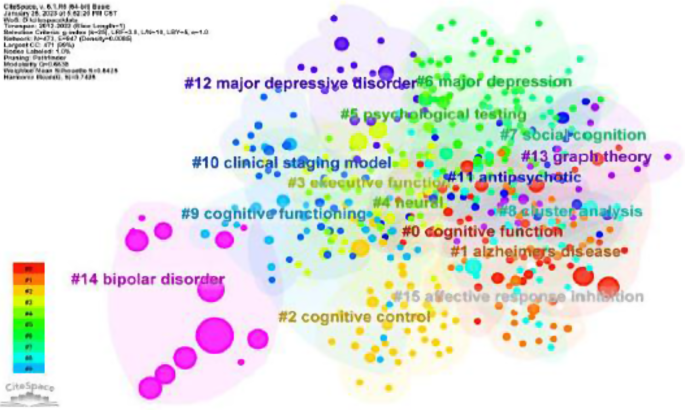
The cluster map of keywords
Generally, Q = 0.6638 (Q > 0.3) means that the clustering structure is significant. Silhouette: S value is the average contour value of clustering, it is generally believed that S > 0.5 clustering is reasonable, and S = 0.8425 (S > 0.7) means clustering is convincing (Fig. 7 ).
Analysis of reference co-citation
The CiteSpace software analysis was used to analyze studies published between 2012 and 2022, with 1-year time slice for analysis. The network diagram of the document is shown in Fig. 8 , which consists of 216 nodes and 235 connections. The more times a document is cited, the greater the circle of the node. A circle with a purple outer ring indicates the document of intermediary centrality, meaning it is cited by several documents simultaneously. The color of the circle corresponds directly to the time slice, with yellow representing the earlier year and green representing more recent years. For example, light yellow represents co-cited studies in 2012, while dark green represents more recent co-references.
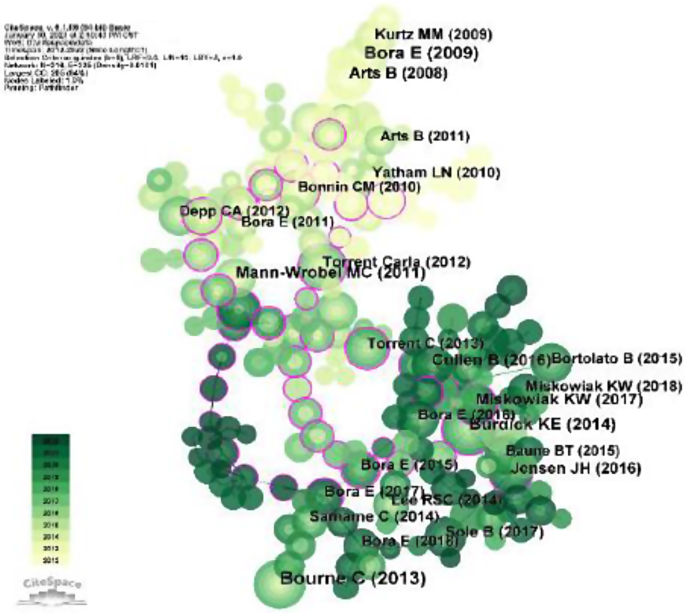
Co-occurrence analysis of references. ( A ) The nodes represent references. ( B ) The lines represent the relationships between the references and the common references of the collected studies
Table 5 shows the top 10 references, the most frequently cited is “Bourne C (2013)”, and the title of the article is “Neuropsychological testing of cognitive impairment in euthymic bipolar disorder: an individual patient data meta-analysis”, with 104 citations. This article is a meta-analysis describing reliable measures of cognitive impairment in bipolar patients: VLT, Digit Span, and TMT. Among the top ten cited articles, the highest centrality is “Bora E (2017)”, with the title “Meta-analysis of longitudinal studies of cognition in bipolar disorder: comparison with healthy controls and schizophrenia”, with a centrality of 0.22, which indicates that the article has important reference value in cognitive research of bipolar disorder.
Burst analysis of keywords
Burst words are the keywords that are frequently quoted and regarded as frontier topic indicators in a certain period. Figure 9 shows the top 25 keywords which are the most burst between 2012 and 2022. The most recent keywords are “pathophysiology”, “subgroup”, “individual”, “cognitive control” and “cluster analysis”. The keyword “neurocognitive impairment”, shows the reference burst to 5.55 began in 2012.
As can be seen from the figure, the research hotspots can be divided into the following three stages. The first stage was from 2012 to 2016. Focused on exploring cognitive impairment in patients with bipolar disorder, with keywords such as “neurocognitive impairment”, “cognitive impairment”, and“internal phenotype”,. The second stage was from 2016 to 2019, the keywords include “cognitive control”, “executive function”, “task”, and “risk factors”. This stage focused on investigating specific cognitive domains affected in bipolar disorder, utilizing cognitive task procedures and further integrating cognition with neurology. In the third stage, from 2019 to 2022, the keywords with bursts include “subgroup”、 “individual”、 “validation”、 “pathophysiology”. This stage emphasized the study of the neurocognitive subgroup within bipolar disorder, validating the scale for measuring cognitive function, and combining with pathophysiology. These studies provide practical evidence for the treatment of bipolar disorder.
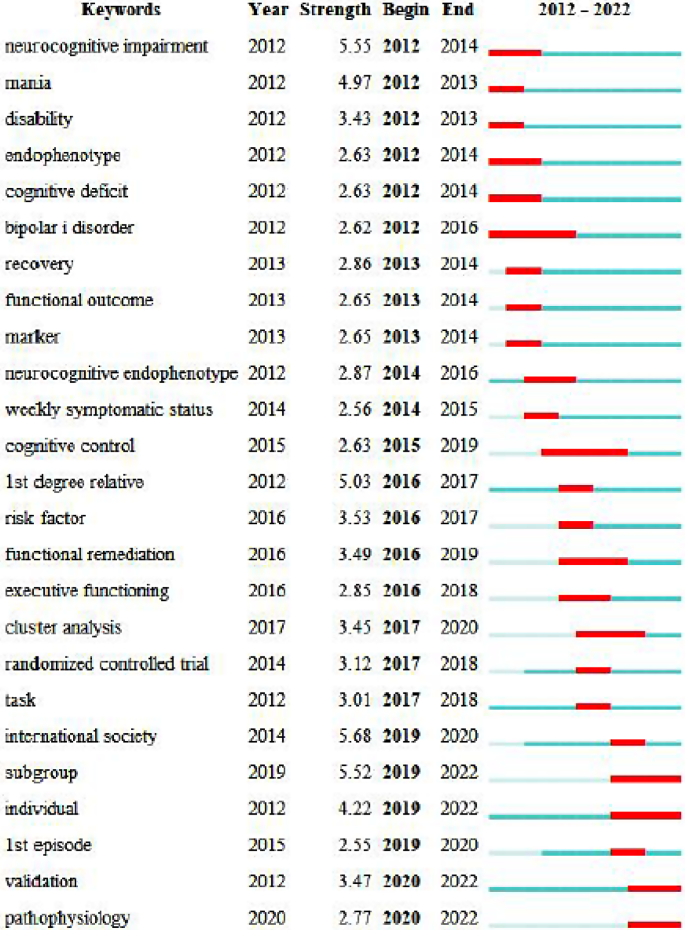
Top 25 Keyword with the strongest citation. The blue and white squares in each row on the right side of the figure correspond to the year of hotspot. Red squares represent the year of hotspot, and blue squares represent non-hotspot year. The recent successive red squares represent the research hotspots in recent wears
This is the first bibliometric analysis of cognitive function in bipolar disorder. Our investigation covered 989 publications from WoSCC, most of them are original articles, and a few are review articles. The results show that during 2012–2022, the number of related publications increased significantly.
From the perspective of the authors. Vieta E, McIntyre RS, Vinberg M, and Miskowiak KW have published 20 or more articles. The articles published by Professor Eduard focus on cognitive dysfunction of schizophrenia and bipolar disorder. One of these articles points out that there is a widespread cognitive impairment in the first episode of mania, and its severity is lower than that of individuals with schizophrenia in their first episode. BD patients performed better than schizophrenia patients in verbal working memory, mental speed, executive control, and immediate verbal memory [ 11 ]. Both diseases have cognitive impairments, albeit with varying degrees of severity. Exploring the comorbidities between the two can lead to the development of more treatment options. In McIntyre RS’s articles, two of them examined the impact of obesity on the cognitive function of BD patients. The result shows that overweight/obese BD patients have significant cognitive defects and experience more severe cognitive impairment than normal-weight BD patients [ 12 , 13 ]. Approved for obesity treatment, Liraglutide, a GLP-1R agonist, has shown promise in enhancing objective measures of cognitive function in adults diagnosed with mood disorders. This research suggests that Liraglutide could potentially serve as a therapeutic intervention to improve cognitive function in individuals with mood disorders [ 14 ]. This research finding highlights the possibility of investigating factors like obesity, which contribute to cognitive abnormalities in patients, as potential avenues for developing interventions to enhance cognitive function.
According to the analysis of centrality and author’s cooperative relationship, it can be known that Miskowiak KW cooperated with two productive authors, Vieta E and Vinberg M. The five articles, produced in collaboration with Vieta E, are systematic reviews or meta-analyses. Two of them focus on cognitive dysfunction in patients with bipolar disorder across different age groups. Euthymic youths with BD exhibit significant cognitive dysfunction in verbal learning and memory, working memory, visual learning, and memory domains. Further research has shown that euthymic adults with BD have more widespread cognitive impairment [ 15 ]. Euthymic older adults with BD have important deficits in almost all cognitive domains, particularly in the memory domain [ 16 ]. The impact of the disease varies among different age groups, with cognitive decline typically occurring as individuals grow older, resulting in irreversible damage. Treatment options can only enhance cognitive performance in patients to a certain extent. One article explores the effects of various medications on cognitive function of BD patients. The efficacy of N-acetyl cysteine, pregnenolone, ketamine, and pramipexole did not demonstrate any cognitive benefits, while mifepristone, galantamine, and insulin were shown to improve different areas of cognition [ 17 ]. In addition, they also conducted a functional magnetic resonance imaging study on individuals with BD, and the results showed that the neural basis of cognitive impairment in BD patients was a failure to recruit key regions in the CCN and to suppress task-irrelevant DMN activity during cognitive performance [ 18 ]. Miskowiak KW has published eight articles with Vinberg M, one of which is meta-analysis. From the perspective of the ‘cold’ and ‘hot’ cognition and neuroimaging, they found that the most promising specific endophenotypic marker for BD is the abnormalities within ‘hot’ cognition, which is represented by impairments in emotion processing and regulation and reward processing [ 19 ]. The remaining seven articles are experimental studies. There are four articles related to cognitive remediation. They first conducted erythropoietin (EPO) trials, which showed that EPO effectively promotes cognitive recovery in patients [ 20 ]. Then based on the above research, they conducted a study on Action-Based Cognitive Remediation (ABCR). The result showed that the ABCR can improve executive function and subjective cognitive functioning in BD patients [ 21 , 22 ]. In another study, cognitive remediation (CR) was shown to improve subjective sharpness/mental acuity, verbal fluency and psychological quality of life in BD patients [ 23 ].
Most of the research on cognitive functioning in bipolar disorder was published in Journal of Affective Disorders (IF = 6.533, Q1), indicating it is currently the most popular journal in this research field. Among these journals, the journal with the highest impact factor is Psychiatry Research (IF = 11.225, Q1), followed by Psychological Medicine (IF = 10.592, Q1). Besides, PLOS ONE , which ranks 10th in terms of the number of published articles, is an open-source journal. This indicates that the presence of open-source journals has also promoted the development of this field, and it can obtain full-text documents for free, which facilitates knowledge dissemination and allows researchers to stay updated with the latest findings in the field of cognitive function in bipolar disorder. Through the co-citation analysis of journals, it can be found that the top cited journals are Q1 journals, which provide support for the study of cognitive function in bipolar disorder. More importantly, the most of research on cognitive function in bipolar disorder is published in clinical journals, which indicates that current research is in the clinical research stage.
In this bibliometric analysis, the majority of the related articles were published by authors from the United States, China, Canada, Spain, and Britain. According to the centrality, the United States and Britain had more cooperation with other countries, indicating their higher level of international cooperation. Although the number of articles published by China ranks second, showed that it had made extensive development in this field. However, due to a lack of collaboration with other productive countries, its influence is relatively low. Therefore, more international cooperation is needed in China. Spain ranks third in the number of articles published and had a significant presence due to the most active scholar, “Vieta E”, from the University of Barcelona. Vieta E set up a group to study bipolar disorder and depression, through experimental design and clinical trials, research on medication treatments, psychological therapy, and biophysical therapy, investigate the clinical development and progression of these disorders.
Keywords can be regarded as the core content of a specific article. Thus, keyword frequencies provide important clues about major trends in a research area [ 24 ]. Through the co-occurrence analysis of keywords, it can be found that apart from bipolar disorder and cognition, schizophrenia is also a high-frequency cited keyword, which indicates that one direction of research in this field is a comparative study of schizophrenia and bipolar disorder. This study compares the evolution of cognitive functioning in the same intervention mode and explores the fields of cognitive impairment. The research has shown that people with schizophrenia also perform significantly worse than people with bipolar disorder on social cognitive tasks such as theory of mind (ToM) and emotion recognition [ 25 ]. The keyword “Rating Scale” is also frequently cited, reflecting that a research topic in this research field is the analysis and measurement of cognitive scale for bipolar disorder, such as evaluating the degree of cognitive impairment in patients with bipolar disorder using different scales. Through cluster analysis, it can be found that the research mainly focuses on the cognitive impairments, diagnosis, and treatment of bipolar affective disorder in clinical settings.
Highly co-cited references are those that are frequently cited together by other articles, and thus, can be regarded as knowledge bases in a particular field [ 26 ]. In this article, the top ten cited literature are listed. The total number of citations can be regarded as an important indicator of interest in a specific research field. Nine of the articles in the top 10 co-cited references are meta-analyses. The tenth article is an empirical study published by Torrent Carla in 2012. This study points out the changes in cognitive impairment in BD patients during a longitudinal study: except for a worsening of executive function and slight improvement of attention, other cognitive fields remained stable [ 27 ]. The most frequently cited documents have been mentioned before and will not be explained here. The second most cited article is a meta-analysis published by Bora E in 2009. The results of this analysis show that response inhibition, set- shifting, verbal memory, and target detection impairments are potential candidate endophenotypes for BD. Euthymic patients may be associated with the medication they are taking and can also be influenced by disease-related factors [ 28 ]. The top 10 co-cited references focus on the following topics: meta-analysis, cognitive impairment, endophenotype, memory, executive function, neuropsychological test, and neurocognition. These are the research bases of cognitive function in bipolar disorder.
The burst detection analysis can show the interests of the research field and the changes in research hotspots over time. If a keyword is a high-frequency cited burst word, it indicates that the keyword has been actively discussed or used in a certain period [ 29 ]. From the citation bursts, we can conclude that the research on cognitive function in bipolar disorder mainly focuses on the following aspects: subgroup, individual, validation, and pathophysiology.
“subgroup”. There are three neurocognitive subgroups of BD. The “cognitively intact group” does not differ from HCs. The “Selective cognitive impairment group” has a lower cognitive score compared to HCs and one or two cognitive fields are damaged. The “Global cognitive impairment group” shows overall cognitive impairment [ 30 , 31 , 32 ]. There are differences in cognitive performance between subgroups of BD. BD-I performs significantly worse than BD-II in some cognitive performance, such as verbal memory, and processing speed [ 33 ]. However, BD-II has larger impairments in inhibition [ 34 ]. The study of cognitive subgroups and the varying impairments of the cognitive function in different subtypes of bipolar disorder will emerge as a prominent research focus in this field.
“individual”. Bipolar patients demonstrate increased intra-individual variability in cognitive processing, which can be observed through dispersion across tests within a single testing session or relative variability compared to their average performance over time [ 35 , 36 ]. In the future, we can study the intra-individual variability of cognitive ability of BD patients and its clinical significance。.
“validation”. The related content is the validation of cognitive assessment for bipolar disorder. The effectiveness of a cognitive assessment tool may vary among different individuals or regions, so it is necessary to verify its validity when applied in new situations. ICAT, an internet-based cognitive assessment tool, has been found to be feasible for large-scale assessment and monitoring of cognition in the clinical management of bipolar disorder [ 37 ]. The reliability and validity of the new cognitive assessment tools may be verified in future research. By utilizing existing cognitive assessment tools, we can determine the extent of cognitive impairment in BD patients, which can help identify therapeutic targets. For instance, a study has shown that many patients with BD have sleep problems, which can impact the process of cognitive testing and the accuracy of test results. It indicates that sleep maybe a potential target for treating cognitive disturbances in BD [ 38 ].
“pathophysiology”, major depressive disorder (MDD) and BD exhibit similar microstructural abnormalities in anterior callosal fibers, which can be considered as a basis for the neuropathy physiology of these two disorder [ 39 ]. Additionally, some evidence indicates that there is a connection between the dysfunction of the the hypothalamic-pituitary-adrenal (HPA) axis and impairments in neurocognitive function in BD. Dopamine neurotransmission is also believed to play an important role in the pathophysiology of BD [ 40 ]. By incorporating these findings into a coherent pathophysiological model, future research can generate testable hypotheses.
Strengths and limitations
Firstly, this study analyzes the research on the cognitive function of bipolar disorder using a bibliometrics system for the first time, providing valuable guidance for scholars interested in related research. Secondly, this article uses two bibliometrics tools, VOSviewer and CiteSpace, which have been widely used in the field of bibliometrics, ensuring an objective data analysis process.
At the same time, there are certain limitations. The data of this study only comes from the WoSCC database, other databases are ignored, and language restriction to English may result in the omission of relevant studies. Additionally, the time span considered in this study is from 2012 to 2022, excluding the year 2023 due to insufficient data.
Cognitive function has important research value and promising prospects for application in bipolar disorder. In general, the number of research papers is increasing, and there is a need for stronger collaboration among countries. Each journal has its scope, and researchers can choose an appropriate journal based on their article. On the one hand, the study of the neurocognitive subgroup of bipolar disorder helps us determine cognitive domains that are impaired in individuals with the disorder. This knowledge is valuable for diagnosing the disease process of bipolar disorder. On the other hand, with the development of society, the cognitive function assessment tools of bipolar disorder are also constantly updated, and these tools can help us understand the general situation of the patient before formal treatment. Therefore, it is of great application value to continuously verify the reliability and validity of new cognitive assessment tools. In addition, more treatment options can be explored in combination with other areas.
Data availability
No datasets were generated or analysed during the current study.
Balanzá-Martínez V, Selva G, Martínez-Arán A, Prickaerts J, Salazar J, González-Pinto A, Vieta E, Tabarés-Seisdedos R. Neurocognition in bipolar disorders–a closer look at comorbidities and medications. Eur J Pharmacol. 2010;626(1):87–96. https://doi.org/10.1016/j.ejphar.2009.10.018 . Epub 2009 Oct 18. PMID: 19836378.
Article CAS PubMed Google Scholar
Solé B, Jiménez E, Torrent C, Reinares M, Bonnin CDM, Torres I, Varo C, Grande I, Valls E, Salagre E, Sanchez-Moreno J, Martinez-Aran A, Carvalho AF, Vieta E. Cognitive impairment in bipolar disorder: treatment and Prevention Strategies. Int J Neuropsychopharmacol. 2017;20(8):670–80. https://doi.org/10.1093/ijnp/pyx032 . PMID: 28498954; PMCID: PMC5570032.
Article CAS PubMed PubMed Central Google Scholar
Mann-Wrobel MC, Carreno JT, Dickinson D. Meta-analysis of neuropsychological functioning in euthymic bipolar disorder: an update and investigation of moderator variables. Bipolar Disord. 2011;13(4):334 – 42. https://doi.org/10.1111/j.1399-5618.2011.00935.x . PMID: 21843273.
Xu N, Huggon B, Saunders KEA. Cognitive Impairment in Patients with Bipolar Disorder: Impact of Pharmacological Treatment. CNS Drugs. 2020;34(1):29–46. https://doi.org/10.1007/s40263-019-00688-2 . PMID: 31808104.
Demant KM, Vinberg M, Kessing LV, Miskowiak KW. Assessment of subjective and objective cognitive function in bipolar disorder: Correlations, predictors and the relation to psychosocial function. Psychiatry Res. 2015;229(1–2):565 – 71. https://doi.org/10.1016/j.psychres.2015.05.022 . Epub 2015 Jun 3. PMID: 26073281.
Jensen JH, Støttrup MM, Nayberg E, Knorr U, Ullum H, Purdon SE, Kessing LV, Miskowiak KW. Optimising screening for cognitive dysfunction in bipolar disorder: validation and evaluation of objective and subjective tools. J Affect Disord. 2015;187:10–9. Epub 2015 Aug 1. PMID: 26301477.
Article PubMed Google Scholar
Ninkov A, Frank JR, Maggio LA, Bibliometrics. Methods for studying academic publishing. Perspect Med Educ. 2022;11(3):173–6. https://doi.org/10.1007/s40037-021-00695-4 . Epub 2021 Dec 16. PMID: 34914027; PMCID: PMC9240160.
Arruda H, Silva ER, Lessa M, Proença D Jr. VOSviewer and Bibliometrix. J Med Libr Assoc. 2022;110(3):392–5. https://doi.org/10.5195/jmla.2022.1434 . PMID: 36589296; PMCID: PMC9782747.
Article PubMed PubMed Central Google Scholar
Luo H, Cai Z, Huang Y, Song J, Ma Q, Yang X, Song Y. Study on Pain Catastrophizing from 2010 to 2020: a bibliometric analysis via CiteSpace. Front Psychol. 2021;12:759347. https://doi.org/10.3389/fpsyg.2021.759347 . PMID: 34975649; PMCID: PMC8718514.
Price DJ. Little science, big science. Columbia University; 1963.
Bortolato B, Miskowiak KW, Köhler CA, Vieta E, Carvalho AF. Cognitive dysfunction in bipolar disorder and schizophrenia: a systematic review of meta-analyses. Neuropsychiatr Dis Treat. 2015;11:3111–25. https://doi.org/10.2147/NDT.S76700 . PMID: 26719696; PMCID: PMC4689290.
McIntyre RS, Mansur RB, Lee Y, Japiassú L, Chen K, Lu R, Lu W, Chen X, Li T, Xu G, Lin K. Adverse effects of obesity on cognitive functions in individuals at ultra high risk for bipolar disorder: Results from the global mood and brain science initiative. Bipolar Disord. 2017;19(2):128–134. https://doi.org/10.1111/bdi.12491 . Epub 2017 May 11. PMID: 28493605.
Bora E, McIntyre RS, Ozerdem A. Neurococognitive and neuroimaging correlates of obesity and components of metabolic syndrome in bipolar disorder: a systematic review. Psychol Med. 2019;49(5):738–49. Epub 2018 Oct 17. PMID: 30326979.
Mansur RB, Lee Y, Subramaniapillai M, Brietzke E, McIntyre RS. Cognitive dysfunction and metabolic comorbidities in mood disorders: a repurposing opportunity for glucagon-like peptide 1 receptor agonists? Neuropharmacology. 2018;136(Pt B):335–42. https://doi.org/10.1016/j.neuropharm.2018.01.048 . Epub 2018 Feb 23. PMID: 29481915.
Elias LR, Miskowiak KW, Vale AM, Köhler CA, Kjærstad HL, Stubbs B, Kessing LV, Vieta E, Maes M, Goldstein BI, Carvalho AF. Cognitive impairment in Euthymic Pediatric Bipolar disorder: a systematic review and Meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(4):286–96. Epub 2017 Feb 2. PMID: 28335872.
Montejo L, Torrent C, Jiménez E, Martínez-Arán A, Blumberg HP, Burdick KE, Chen P, Dols A, Eyler LT, Forester BP, Gatchel JR, Gildengers A, Kessing LV, Miskowiak KW, Olagunju AT, Patrick RE, Schouws S, Radua J, Bonnín CDM, Vieta E. International Society for Bipolar Disorders (ISBD) older adults with bipolar disorder (OABD) Task Force. Cognition in older adults with bipolar disorder: an ISBD task force systematic review and meta-analysis based on a comprehensive neuropsychological assessment. Bipolar Disord. 2022;24(2):115–36. https://doi.org/10.1111/bdi.13175 . Epub 2022 Jan 7. PMID: 34978124.
Miskowiak KW, Carvalho AF, Vieta E, Kessing LV. Cognitive enhancement treatments for bipolar disorder: a systematic review and methodological recommendations. Eur Neuropsychopharmacol. 2016;26(10):1541–61. https://doi.org/10.1016/j.euroneuro.2016.08.011 . Epub 2016 Sep 1. PMID: 27593623.
Zarp Petersen J, Varo C, Skovsen CF, Ott CV, Kjaerstad HL, Vieta E, Harmer CJ, Knudsen GM, Kessing LV, Macoveanu J, Miskowiak KW. Neuronal underpinnings of cognitive impairment in bipolar disorder: a large data-driven functional magnetic resonance imaging study. Bipolar Disord. 2022;24(1):69–81. https://doi.org/10.1111/bdi.13100 . Epub 2021 Jun 18. PMID: 33955648.
Miskowiak KW, Kjærstad HL, Meluken I, Petersen JZ, Maciel BR, Köhler CA, Vinberg M, Kessing LV, Carvalho AF. The search for neuroimaging and cognitive endophenotypes: a critical systematic review of studies involving unaffected first-degree relatives of individuals with bipolar disorder. Neurosci Biobehav Rev. 2017;73:1–22. Epub 2016 Dec 12. PMID: 27979650.
Ott CV, Vinberg M, Kessing LV, Miskowiak KW. The effect of erythropoietin on cognition in affective disorders - associations with baseline deficits and change in subjective cognitive complaints. Eur Neuropsychopharmacol. 2016;26(8):1264–73. https://doi.org/10.1016/j.euroneuro.2016.05.009 . Epub 2016 Jun 24. PMID: 27349944.
Ott CV, Vinberg M, Kessing LV, Bowie CR, Forman JL, Miskowiak KW. Effect of action-based cognitive remediation on cognitive impairment in patients with remitted bipolar disorder: a randomized controlled trial. Bipolar Disord. 2021;23(5):487–99. https://doi.org/10.1111/bdi.13021 . Epub 2020 Oct 29. PMID: 33053258.
Ott CV, Vinberg M, Bowie CR, Christensen EM, Knudsen GM, Kessing LV, Miskowiak KW. Effect of action-based cognitive remediation on cognition and neural activity in bipolar disorder: study protocol for a randomized controlled trial. Trials. 2018;19(1):487. https://doi.org/10.1186/s13063-018-2860-8 . Erratum in: Trials. 2019;20(1):201. PMID: 30208971; PMCID: PMC6134776.
Demant KM, Vinberg M, Kessing LV, Miskowiak KW. Effects of short-term cognitive remediation on cognitive dysfunction in partially or fully remitted individuals with bipolar disorder: results of a Randomised Controlled Trial. PLoS ONE. 2015;10(6):e0127955. https://doi.org/10.1371/journal.pone.0127955 . PMID: 26070195; PMCID: PMC4467086.
Sun HL, Feng Y, Zhang Q, Li JX, Wang YY, Su Z, Cheung T, Jackson T, Sha S, Xiang YT. The Microbiome-Gut-Brain Axis and Dementia: a bibliometric analysis. Int J Environ Res Public Health. 2022;19(24):16549. https://doi.org/10.3390/ijerph192416549 . PMID: 36554429; PMCID: PMC9779855.
Bora E, Veznedaroğlu B, Vahip S. Theory of mind and executive functions in schizophrenia and bipolar disorder: a cross-diagnostic latent class analysis for identification of neuropsychological subtypes. Schizophr Res. 2016;176(2–3):500–5. https://doi.org/10.1016/j.schres.2016.06.007 . Epub 2016 Jun 14. PMID: 27317360.
Zhu X, Hu J, Deng S, Tan Y, Qiu C, Zhang M, Ni X, Lu H, Wang Z, Li L, Luo Y, Huang S, Xiao T, Liu S, Li X, Shang D, Wen Y. Comprehensive Bibliometric Analysis of the Kynurenine Pathway in Mood disorders: Focus on Gut Microbiota Research. Front Pharmacol. 2021;12:687757. https://doi.org/10.3389/fphar.2021.687757 . PMID: 34239441; PMCID: PMC8258344.
Torrent C, Martinez-Arán A, del Mar Bonnin C, Reinares M, Daban C, Solé B, Rosa AR, Tabarés-Seisdedos R, Popovic D, Salamero M, Vieta E. Long-term outcome of cognitive impairment in bipolar disorder. J Clin Psychiatry. 2012;73(7):e899-905. https://doi.org/10.4088/JCP.11m07471 . PMID: 22901360.
Bora E, Yucel M, Pantelis C. Cognitive endophenotypes of bipolar disorder: a meta-analysis of neuropsychological deficits in euthymic patients and their first-degree relatives. J Affect Disord. 2009;113(1–2):1–20. https://doi.org/10.1016/j.jad.2008.06.009 . Epub 2008 Aug 5. PMID: 18684514.
Sun HL, Bai W, Li XH, Huang H, Cui XL, Cheung T, Su ZH, Yuan Z, Ng CH, Xiang YT. Schizophrenia and Inflammation Research: a bibliometric analysis. Front Immunol. 2022;13:907851. https://doi.org/10.3389/fimmu.2022.907851 . PMID: 35757702; PMCID: PMC9219580.
Jensen JH, Knorr U, Vinberg M, Kessing LV, Miskowiak KW. Discrete neurocognitive subgroups in fully or partially remitted bipolar disorder: associations with functional abilities. J Affect Disord. 2016;205:378–86. https://doi.org/10.1016/j.jad.2016.08.018 . Epub 2016 Aug 22. PMID: 27573491.
Lima F, Rabelo-da-Ponte FD, Bücker J, Czepielewski L, Hasse-Sousa M, Telesca R, Solé B, Reinares M, Vieta E, Rosa AR. Identifying cognitive subgroups in bipolar disorder: A cluster analysis. J Affect Disord. 2019;246:252–261. https://doi.org/10.1016/j.jad.2018.12.044 . Epub 2018 Dec 18. Erratum in: J Affect Disord. 2019;: PMID: 30590288.
Karantonis JA, Rossell SL, Carruthers SP, Sumner P, Hughes M, Green MJ, Pantelis C, Burdick KE, Cropley V, Van Rheenen TE. Cognitive validation of cross-diagnostic cognitive subgroups on the schizophrenia-bipolar spectrum. J Affect Disord. 2020;266:710–21. Epub 2020 Jan 25. PMID: 32056949.
Bora E. Neurocognitive features in clinical subgroups of bipolar disorder: a meta-analysis. J Affect Disord. 2018;229:125–34. https://doi.org/10.1016/j.jad.2017.12.057 . Epub 2017 Dec 29. PMID: 29306692.
Cotrena C, Damiani Branco L, Ponsoni A, Samamé C, Milman Shansis F, Paz Fonseca R. Executive functions and memory in bipolar disorders I and II: new insights from meta-analytic results. Acta Psychiatr Scand. 2020;141(2):110–30. https://doi.org/10.1111/acps.13121 . Epub 2019 Nov 14. PMID: 31697843.
Krukow P, Szaniawska O, Harciarek M, Plechawska-Wójcik M, Jonak K. Cognitive inconsistency in bipolar patients is determined by increased intra-individual variability in initial phase of task performance. J Affect Disord. 2017;210:222–5. https://doi.org/10.1016/j.jad.2016.12.050 . Epub 2017 Jan 2. PMID: 28063384.
Depp CA, Savla GN, de Dios LA, Mausbach BT, Palmer BW. Affective symptoms and intra-individual variability in the short-term course of cognitive functioning in bipolar disorder. Psychol Med. 2012;42(7):1409–16. https://doi.org/10.1017/S0033291711002662 . Epub 2011 Dec 9. PMID: 22152983; PMCID: PMC3536028.
Miskowiak KW, Jespersen AE, Obenhausen K, Hafiz P, Hestbæk E, Gulyas L, Kessing LV, Bardram JE. Internet-based cognitive assessment tool: sensitivity and validity of a new online cognition screening tool for patients with bipolar disorder. J Affect Disord. 2021;289:125–34. Epub 2021 Apr 27. PMID: 33979722.
Bradley AJ, Anderson KN, Gallagher P, McAllister-Williams RH. The association between sleep and cognitive abnormalities in bipolar disorder. Psychol Med. 2020;50(1):125–32. Epub 2019 Jan 16. PMID: 30646966.
Yamada S, Takahashi S, Ukai S, Tsuji T, Iwatani J, Tsuda K, Kita A, Sakamoto Y, Yamamoto M, Terada M, Shinosaki K. Microstructural abnormalities in anterior callosal fibers and their relationship with cognitive function in major depressive disorder and bipolar disorder: a tract-specific analysis study. J Affect Disord. 2015;174:542–8. Epub 2014 Dec 16. PMID: 25556672.
Young AH. The effects of HPA axis function on cognition and its implications for the pathophysiology of bipolar disorder. Harv Rev Psychiatry. 2014 Nov-Dec;22(6):331-3. https://doi.org/10.1097/HRP.0000000000000020 . PMID: 25377604.
Download references
Acknowledgements
We thank all authors who participated in the study.
The study was supported by the Research Project Supported by Shanxi Scholarship Council of China (2021 − 167) and the Scientific Research Project of Health Commission of Shanxi Province (2019007).
Author information
Xiaohong Cui and Tailian Xue contributed equally to this work.
Authors and Affiliations
Department of Psychology, School of Humanities and Social Sciences, Shanxi Medical University, Taiyuan, Shanxi, China
Tailian Xue & Zhiyong Zhang
Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Taiyuan, 030032, China
Department of Psychiatry, Third Hospital of Shanxi Medical University, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences,Tongji Shanxi Hospital, Taiyuan, 030032, China
Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Third Hospital of Shanxi Medical University, Taiyuan, 030032, China
Xiaohong Cui
Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430030, China
You can also search for this author in PubMed Google Scholar
Contributions
Study design: YR, HY; data collection, analysis, and interpretation: TLX, XHC, YZZ; drafting of the manuscript: TLX; critical revision of the manuscript: XHC. All authors contributed to the article and approved the submitted version.
Corresponding authors
Correspondence to Zhiyong Zhang or Yan Ren .
Ethics declarations
Ethical approval.
Not applicable.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Cui, X., Xue, T., Zhang, Z. et al. A bibliometric and visual analysis of cognitive function in bipolar disorder from 2012 to 2022. Ann Gen Psychiatry 23 , 13 (2024). https://doi.org/10.1186/s12991-024-00498-x
Download citation
Received : 10 January 2024
Accepted : 25 March 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12991-024-00498-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bipolar disorder
- Cognitive function
- Bibliometric
Annals of General Psychiatry
ISSN: 1744-859X
- Submission enquiries: [email protected]
Bipolar disorders: An overview of current literature
Research output : Contribution to journal › Article › peer-review
- Bipolar disorders
- Epidemiology
- Pharmacology
- Psychosocial interventions
This output contributes to the following UN Sustainable Development Goals (SDGs)
Access to Document
- 10.1046/j.1365-2850.2001.00416.x
Fingerprint
- Bipolar Disorder Psychology 100%
- Groups Psychology 66%
- Client Group Nursing and Health Professions 66%
- Psychosocial Intervention Psychology 33%
- Reading Psychology 33%
- Coping Strategy Psychology 33%
- Research Psychology 33%
- Diseases Nursing and Health Professions 33%
T1 - Bipolar disorders: An overview of current literature
AU - Baker, John
AU - Baker, J. A.
N2 - This paper aims to review current literature around bipolar disorder from a multidisciplinary stance. As a result of a literature search, several key themes have been identified which will be discussed during this paper: first, the definition of bipolar disorders, their epidemiology and the effect of the illness on outcome, and secondly pharmacological interventions, psychosocial interventions and the use of coping strategy enhancement for this client group. The paper attempts to direct clinicians towards relevant further reading and research for the development of interventions when working with this client group.
AB - This paper aims to review current literature around bipolar disorder from a multidisciplinary stance. As a result of a literature search, several key themes have been identified which will be discussed during this paper: first, the definition of bipolar disorders, their epidemiology and the effect of the illness on outcome, and secondly pharmacological interventions, psychosocial interventions and the use of coping strategy enhancement for this client group. The paper attempts to direct clinicians towards relevant further reading and research for the development of interventions when working with this client group.
KW - Bipolar disorders
KW - Epidemiology
KW - Pharmacology
KW - Psychosocial interventions
U2 - 10.1046/j.1365-2850.2001.00416.x
DO - 10.1046/j.1365-2850.2001.00416.x
M3 - Article
SN - 1351-0126
JO - Journal of Psychiatric and Mental Health Nursing
JF - Journal of Psychiatric and Mental Health Nursing
Advances in functional MRI research in bipolar disorder: from the perspective of mood states
Affiliations.
- 1 Department of Clinical Psychopharmacology, Peking University Sixth Hospital, Peking University Institute of Mental Health, NHC Key Laboratory of Mental Health (Peking University), National Clinical Research Center for Mental Disorders (Peking University Sixth Hospital), Beijing, China.
- 2 Peking University Sixth Hospital, Peking University Institute of Mental Health, NHC Key Laboratory of Mental Health (Peking University), National Clinical Research Center for Mental Disorders (Peking University Sixth Hospital), Beijing, China.
- PMID: 38292862
- PMCID: PMC10826570
- DOI: 10.1136/gpsych-2023-101398
Bipolar disorder is characterised by recurrent and alternating episodes of mania/hypomania and depression. Current breakthroughs in functional MRI techniques have uncovered the functional neuroanatomy of bipolar disorder. However, the pathophysiology underlying mood instability, mood switching and the development of extreme mood states is less well understood. This review presents a comprehensive overview of current evidence from functional MRI studies from the perspective of mood states. We first summarise the disrupted brain activation patterns and functional connectivity that have been reported in bipolar disorder, irrespective of the mood state. We next focus on research that solely included patients in a single mood state for a better understanding of the pathophysiology of bipolar disorder and research comparing patients with different mood states to dissect mood state-related effects. Finally, we briefly summarise current theoretical models and conclude this review by proposing potential avenues for future research. A comprehensive understanding of the pathophysiology with consideration of mood states could not only deepen our understanding of how acute mood episodes develop at a neurophysiological level but could also facilitate the identification of biological targets for personalised treatment and the development of new interventions for bipolar disorder.
Keywords: Bipolar Disorder; Brain; Emotions.
© Author(s) (or their employer(s)) 2024. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
Publication types
- Search Menu
- Advance Articles
- Supplements
- Editor's Choice
- Virtual Issues
- Virtual Roundtables
- Abstract Supplements
- Basic Science
- Circadian Disorders
- Cognitive, Affective and Behavioral Neuroscience of Sleep
- Neurological Disorders
- Sleep Across the Lifespan
- Sleep and Metabolism
- Sleep Disordered Breathing
- Sleep Health and Safety
- Author Guidelines
- Instructions for Reviewers
- Submission Site
- Open Access Options
- Additional Resources
- Self-Archiving Policy
- About SLEEP
- Editorial Board
- Dispatch Dates
- Permissions
- Advertising & Corporate Services
- Journals Career Network
- Reprints and ePrints
- Sponsored Supplements
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- < Previous
0965 Investigating Cardiac Autonomic Activity During Sleep in Individuals with Major Depression and Bipolar Disorder
- Article contents
- Figures & tables
- Supplementary Data
Chloe Leveille, Mysa Saad, Daniel Brabant, David Birnie, Elliott Lee, Alan Douglass, Georg Northoff, Katerina Nikolitch, Julie Carrier, Stuart Fogel, Caitlin Higginson, Tetyana Kendzerska, Rebecca Robillard, 0965 Investigating Cardiac Autonomic Activity During Sleep in Individuals with Major Depression and Bipolar Disorder, Sleep , Volume 47, Issue Supplement_1, May 2024, Page A414, https://doi.org/10.1093/sleep/zsae067.0965
- Permissions Icon Permissions
Autonomic nervous system dysfunction and reduced heart rate variability (HRV) have been reported in individuals with mood disorders, a phenomenon likely to be influenced by sleep disturbances. Several studies have previously assessed HRV in individuals with major depression or bipolar disorder across the entire sleep period. This study investigated whether distinct heart rate (HR) and HRV profiles across wake, rapid eye movement (REM) sleep, and non-REM (NREM) sleep are linked to unipolar versus bipolar mood disorders in individuals with sleep complaints.
Polysomnographic data was retrospectively collated for 120 adult patients with sleep complaints and depressive symptoms referred to a specialized sleep clinic for sleep assessment [60 diagnosed with bipolar disorder (70% female, mean age= 43.4±11.6 years) and 60 age-matched cases diagnosed with a unipolar depressive disorder (68.3% female, mean age= 43.2±11.6 years)], and 60 age-matched healthy controls (68.3% female, mean age= 43.4±12.6 years). HR and time-based HRV parameters were computed on 30-second segments and averaged across the night for wake and sleep stages.
Significant group by sleep stage interactions showed that the unipolar and bipolar groups had lower standard deviation of normal-to-normal intervals (SDNN) and vagal tone root mean square of successive R-R interval differences (RMSSD) compared to controls during NREM sleep ( p≤.001) and REM sleep (p≤.003), but not during wake (p>.050). The unipolar group had significantly higher heart rate than controls regardless of sleep stages (all, p≤ .042), while the bipolar group had higher heart rate than controls only during NREM 2 (p=.012) and NREM 3 (p=.009) sleep. These interactions persisted after excluding individuals taking antipsychotic, lithium, anticonvulsant, and cardiovascular medications.
While additional research is required to account for manic and euthymic states, as well as the impact of psychotropic and cardiac medications, and potential confounders like variations in body mass index, the present findings suggest that the sleep-based autonomic signature of depressive states differs across different types of mood disorders and could potentially inform the development of biomarkers and therapeutic targets.
This project was supported by the Ottawa Region for Advanced Cardiovascular Research Excellence (ORACLE) funding program.
Email alerts
Citing articles via, looking for your next opportunity.
- Recommend to Your Librarian
- Advertising and Corporate Services
Affiliations
- Online ISSN 1550-9109
- Print ISSN 0161-8105
- Copyright © 2024 Sleep Research Society
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Diagnosis and...
Diagnosis and management of bipolar disorders
- Related content
- Peer review
- Fernando S Goes , associate professor of psychiatry and behavioral sciences 1 2
- 1 Precision Medicine Center of Excellence in Mood Disorders, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
- 2 Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA
- Correspondence to: F S Goes fgoes1{at}jhmi.edu
Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that affect around 2% of the world’s population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a leading cause of disability and premature mortality. The clinical manifestations of bipolar disorder can be markedly varied between and within individuals across their lifespan. Early diagnosis is challenging and misdiagnoses are frequent, potentially resulting in missed early intervention and increasing the risk of iatrogenic harm. Over 15 approved treatments exist for the various phases of bipolar disorder, but outcomes are often suboptimal owing to insufficient efficacy, side effects, or lack of availability. Lithium, the first approved treatment for bipolar disorder, continues to be the most effective drug overall, although full remission is only seen in a subset of patients. Newer atypical antipsychotics are increasingly being found to be effective in the treatment of bipolar depression; however, their long term tolerability and safety are uncertain. For many with bipolar disorder, combination therapy and adjunctive psychotherapy might be necessary to treat symptoms across different phases of illness. Several classes of medications exist for treating bipolar disorder but predicting which medication is likely to be most effective or tolerable is not yet possible. As pathophysiological insights into the causes of bipolar disorders are revealed, a new era of targeted treatments aimed at causal mechanisms, be they pharmacological or psychosocial, will hopefully be developed. For the time being, however, clinical judgment, shared decision making, and empirical follow-up remain essential elements of clinical care. This review provides an overview of the clinical features, diagnostic subtypes, and major treatment modalities available to treat people with bipolar disorder, highlighting recent advances and ongoing therapeutic challenges.
Introduction
Abnormal states of mood, ranging from excesses of despondency, psychic slowness, diminished motivation, and impaired cognitive functioning on the one hand, and exhilaration, heightened energy, and increased cognitive and motoric activity on the other, have been described since antiquity. 1 However, the syndrome in which both these pathological states occur in a single individual was first described in the medical literature in 1854, 2 although its fullest description was made by the German psychiatrist Emil Kraepelin at the turn of the 19th century. 3 Kraepelin emphasized the periodicity of the illness and proposed an underlying trivariate model of mood, thought (cognition), and volition (activity) to account for the classic forms of mania and depression and the various admixed presentations subsequently know as mixed states. 3 These initial descriptions of manic depressive illness encompassed most recurrent mood syndromes with relapsing remitting course, minimal interepisode morbidity, and a wide spectrum of “colorings of mood” that pass “without a sharp boundary” from the “rudiment of more severe disorders…into the domain of personal predisposition.” 3 Although Kraepelin’s clinical description of bipolar disorder (BD) remains the cornerstone of today’s clinical description, more modern conceptions of bipolar disorder have differentiated manic depressive illness from recurrent depression, 4 partly based on differences in family history and the relative specificity of lithium carbonate and mood stabilizing anticonvulsants as anti-manic and prophylactic agents in bipolar disorder. While the boundaries of bipolar disorder remain a matter of controversy, 5 this review will focus on modern clinical conceptions of bipolar disorder, highlighting what is known about its causes, prognosis, and treatments, while also exploring novel areas of inquiry.
Sources and selection criteria
PubMed and Embase were searched for articles published from January 2000 to February 2023 using the search terms “bipolar disorder”, “bipolar type I”, “bipolar type II”, and “bipolar spectrum”, each with an additional search term related to each major section of the review article (“definition”, “diagnosis”, “nosology”, “prevalence”, “epidemiology”, “comorbid”, “precursor”, “prodrome”, “treatment”, “screening”, “disparity/ies”, “outcome”, “course”, “genetics”, “imaging”, “treatment”, “pharmacotherapy”, “psychotherapy”, “neurostimulation”, “convulsive therapy”, “transmagnetic”, “direct current stimulation”, “suicide/suicidal”, and “precision”). Searches were prioritized for systematic reviews and meta-analyses, followed by randomized controlled trials. For topics where randomized trials were not relevant, searches also included narrative reviews and key observational studies. Case reports and small observations studies or randomized controlled trials of fewer than 50 patients were excluded.
Modern definitions of bipolar disorder
In the 1970s, the International Classification of Diseases and the Diagnostic and Statistical Manual of Mental Disorders reflected the prototypes of mania initially described by Kraepelin, following the “neo-Kraepelinian” model in psychiatric nosology. To meet the primary requirement for a manic episode, an individual must experience elevated or excessively irritable mood for at least a week, accompanied by at least three other typical syndromic features of mania, such as increased activity, increased speed of thoughts, rapid speech, changes in esteem, decreased need for sleep, or excessive engagement in impulsive or pleasurable activities. Psychotic symptoms and admission to hospital can be part of the diagnostic picture but are not essential to the diagnosis. In 1994, Diagnostic and Statistical Manual of Mental Disorders , fourth edition (DSM-IV) carved out bipolar disorder type II (BD-II) as a separate diagnosis comprising milder presentations of mania called hypomania. The diagnostic criteria for BD-II are similar to those for bipolar disorder type I (BD-I), except for a shorter minimal duration of symptoms (four days) and the lack of need for significant role impairment during hypomania, which might be associated with enhanced functioning in some individuals. While the duration criteria for hypomania remain controversial, BD-II has been widely accepted and shown to be as common as (if not more common than) BD-I. 6 The ICD-11 (international classification of diseases, 11th revision) included BD-II as a diagnostic category in 2019, allowing greater flexibility in its requirement of hypomania needing to last several days.
The other significant difference between the two major diagnostic systems has been their consideration of mixed symptoms. Mixed states, initially described by Kraepelin as many potential concurrent combinations of manic and depressive symptoms, were more strictly defined by DSM as a week or more with full syndromic criteria for both manic and depressive episodes. In DSM-5, this highly restrictive criterion was changed to encompass a broader conception of subsyndromal mixed symptoms (consisting of at least three contrapolar symptoms) in either manic, hypomanic, or depressive episodes. In ICD-11, mixed symptoms are still considered to be an episode, with the requirement of several prominent symptoms of the countervailing mood state, a less stringent requirement that more closely aligns with Kraepelin's broader conception of mixed states. 7
Epidemiology
Using DSM-IV criteria, the National Comorbidity Study replication 6 found similar lifetime prevalence rates for BD-I (1.0%) and BD-II (1.1%) among men and women. Subthreshold symptoms of hypomania (bipolar spectrum disorder) were more common, with prevalence rate estimates of 2.4%. 6 Incidence rates, which largely focus on BD-I, have been estimated at approximately 6.1 per 100 000 person years (95% confidence interval 4.7 to 8.1). 8 Estimates of the incidence and lifetime prevalence of bipolar disorder show moderate variations according to the method of diagnosis (performed by lay interviewers in a research context v clinically trained interviews) and the racial, ethnic, and demographic context. 9 Higher income, westernized countries have slightly higher rates of bipolar disorder, 10 which might reflect a combination of westernized centricity in the specific idioms used to understand and elicit symptoms, as well as a greater knowledge, acceptance, and conceptualization of emotional symptoms as psychiatric disorders.
Causes of bipolar disorder
Like other common psychiatric disorders, bipolar disorder is likely caused by a complex interplay of multiple factors, both at the population level and within individuals, 11 which can be best conceptualized at various levels of analysis, including genetics, brain networks, psychological functioning, social support, and other biological and environmental factors. Because knowledge about the causes of bipolar disorder remains in its infancy, for pragmatic purposes, most research has followed a reductionistic model that will ultimately need to be synthesized for a more coherent view of the pathophysiology that underlies the condition.
Insights from genetics
From its earliest descriptions, bipolar disorder has been observed to run in families. Indeed, family history is the strongest individual risk factor for developing the disorder, with first degree relatives having an approximately eightfold higher risk of developing bipolar disorder compared with the baseline population rates of ~1%. 12 While family studies cannot separate the effects of genetics from behavioral or cultural transmission, twin and adoption studies have been used to confirm that the majority of the familial risk is genetic in origin, with heritability estimates of approximately 60-80%. 13 14 There have been fewer studies of BD-II, but its heritability has been found to be smaller (~46%) 15 and closer to that of more common disorders such as major depressive disorder or generalized anxiety. 15 16 Nevertheless, significant heritability does not necessarily imply the presence of genes of large effect, since the genetic risk for bipolar disorder appears likely to be spread across many common variants of small effect sizes. 16 17 Ongoing studies of rare variations have found preliminary evidence for variants of slightly higher effect sizes, with initial evidence of convergence with common variations in genes associated with the synapse and the postsynaptic density. 18 19
While the likelihood that the testing of single variants or genes will be useful for diagnostic purposes is low, analyses known as polygenic risk studies can sum across all the risk loci and have some ability to discriminate cases from controls, albeit at the group level rather than the individual level. 20 These polygenic risk scores can also be used to identify shared genetic risk factors across other medical and psychiatric disorders. Bipolar disorder has strong evidence for common variant based coheritability with schizophrenia (genetic correlation (r g ) 0.69) and major depressive disorder (r g 0.48). BD-I has stronger coheritability with schizophrenia compared with BD-II, which is more strongly genetically correlated with major depressive disorder (r g 0.66). 16 Lower coheritability was observed with attention deficit hyperactivity disorder (r g 0.21), anorexia nervosa (0.20), and autism spectrum disorder (r g 0.21). 16 These correlations provide evidence for shared genetic risk factors between bipolar disorder and other major psychiatric syndromes, a pattern also corroborated by recent nationwide registry based family studies. 12 14 Nevertheless, despite their potential usefulness, polygenic risk scores must currently be interpreted with caution given their lack of populational representation and lingering concerns of residual confounds such as gene-environment correlations. 21
Insights from neuroimaging
Similarly to the early genetic studies, small initial studies had limited replication, leading to the formation of large worldwide consortiums such as ENIGMA (enhancing neuroimaging genetics through meta-analysis) which led to substantially larger sample sizes and improved reproducibility. In its volumetric analyses of subcortical structures from MRI (magnetic resonance imaging) of patients with bipolar disorder, the ENIGMA consortium found modest decreases in the volume of the thalamus (Cohen’s d −0.15), the hippocampus (−0.23), and the amygdala (−0.11), with an increased volume seen only in the lateral ventricles (+0.26). 22 Meta-analyses of cortical regions similarly found small reductions in cortical thickness broadly across the parietal, temporal, and frontal cortices (Cohen’s d −0.11 to −0.29) but no changes in cortical surface area. 23 In more recent meta-analyses of white matter tracts using diffuse tension imaging, widespread but modest decreases in white matter integrity were found throughout the brain in bipolar disorder, most notably in the corpus callosum and bilateral cinguli (Cohen’s d −0.39 to −0.46). 24 While these findings are likely to be highly replicable, they do not, as yet, have clinical application. This is because they reflect differences at a group level rather than an individual level, 25 and because many of these patterns are also seen across other psychiatric disorders 26 and could be either shared risk factors or the effects of confounding factors such as medical comorbidities, medications, co-occurring substance misuse, or the consequences (rather than causes) of living with mental illness. 27 Efforts to collate and meta-analyze large samples utilizing longitudinal designs 28 task based, resting state functional MRI measurents, 29 as well as other measures of molecular imaging (magnetic resonance spectroscopy and positron emission tomography) are ongoing but not as yet synthesized in large scale meta-analyses.
Environmental risk factors
Because of the difficulty in measuring and studying the relevant and often common environmental risk factors for a complex illness like bipolar disorder, there has been less research on how environmental risk factors could cause or modify bipolar disorder. Evidence for intrauterine risk factors is mixed and less compelling than such evidence in disorders like schizophrenia. 30 Preliminary evidence suggests that prominent seasonal changes in solar radiation, potentially through its effects on circadian rhythm, can be associated with an earlier onset of bipolar disorder 31 and a higher likelihood of experiencing a depressive episode at onset. 31 However, the major focus of environmental studies in bipolar disorder has been on traumatic and stressful life events in early childhood 32 and in adulthood. 33 The effects of such adverse events are complex, but on a broad level have been associated with earlier onset of bipolar disorder, a worse illness course, greater prevalence of psychotic symptoms, 34 substance misuse and psychiatric comorbidities, and a higher risk of suicide attempts. 32 35 Perhaps uniquely in bipolar disorder, evidence also indicates that positive life events associated with goal attainment can also increase the risk of developing elevated states. 36
Comorbidity
Bipolar disorder rarely manifests in isolation, with comorbidity rates indicating elevated lifetime risk of several co-occurring symptoms and comorbid disorders, particularly anxiety, attentional disorders, substance misuse disorders, and personality disorders. 37 38 The causes of such comorbidity can be varied and complex: they could reflect a mixed presentation artifactually separated by current diagnostic criteria; they might also reflect independent illnesses; or they might represent the downstream effects of one disorder increasing the risk of developing another disorder. 39 Anxiety disorders tend to occur before the frank onset of manic or hypomanic symptoms, suggesting that they could in part reflect prodromal symptoms that manifest early in the lifespan. 37 Similarly, subthreshold and syndromic symptoms of attention deficit/hyperactivity disorder are also observed across the lifespan of people with bipolar disorder, but particularly in early onset bipolar disorder. 40 On the other hand, alcohol and substance misuse disorders occur more evenly before and after the onset of bipolar disorder, consistent with a more bidirectional causal association. 41
The association between bipolar disorder and comorbid personality disorders is similarly complex. Milder manifestations of persistent mood instability (cyclothymia) or low mood (dysthymia) have previously been considered to be temperamental variants of bipolar disorder, 42 but are now classified as related but separate disorders. In people with persistent emotional dysregulation, making the diagnosis of bipolar disorder can be particularly challenging, 43 since the boundaries between longstanding mood instability and phasic changes in mood state can be difficult to distinguish. While symptom overlap can lead to artificially inflated prevalence rates of personality disorders in bipolar disorder, 44 the elevated rates of most personality disorders in bipolar disorder, particularly those related to emotional instability, are likely reflective of an important clinical phenomenon that is understudied, particularly with regard to treatment implications. 45 In general, people with comorbidities tend to have greater symptom burden and functional impairment and have lower response rates to treatment. 46 47 Data on approaches to treat specific comorbid disorders in bipolar disorder are limited, 48 49 and clinicians are often left to rely on their clinical judgment. The most parsimonious approach is to treat primary illness as fully as possible before considering additional treatment options for remaining comorbid symptoms. For certain comorbidities, such as anxiety symptoms and disorders of attention, first line pharmacological treatment—namely, antidepressants and stimulants, should be used with caution, since they might increase the long term risks of mood switching or overall mood instability. 50 51
Like other major mental illnesses, bipolar disorder is also associated with an increased prevalence of common medical disorders such as obesity, hyperlipidemia, coronary artery disease, chronic obstructive pulmonary disease, and thyroid dysfunction. 52 These have been attributed to increase risk factors such as physical inactivity, poor nutrition, smoking, and increased use of addictive substances, 53 but some could also be consequences of specific treatments, such as the atypical antipsychotics and mood stabilizers. 54 Along with poor access to care, this medical burden likely accounts for much of the increased standardized mortality (approximately 2.6 times higher) in people with bipolar disorder, 55 highlighting the need to utilize treatments with better long term side effect profiles, and the need for better integration with medical care.
Precursors and prodromes: who develops bipolar disorder?
While more widespread screening and better accessibility to mental health providers should in principle shorten the time to diagnosis and treatment, early manifestation of symptoms in those who ultimately go on to be diagnosed with bipolar disorder is generally non-specific. 56 In particular, high risk offspring studies of adolescents with a parent with bipolar disorder have found symptoms of anxiety and attentional/disruptive disorders to be frequent in early adolescence, followed by higher rates of depression and sleep disturbance in later teenage years. 56 57 Subthreshold symptoms of mania, such as prolonged increases in energy, elated mood, racing thoughts, and mood lability are also more commonly found in children with prodromal symptoms (meta-analytic prevalence estimates ranging from 30-50%). 58 59 Still, when considered individually, none of these symptoms or disorders are sensitive or specific enough to accurately identify individuals who will transition to bipolar disorder. Ongoing approaches to consider these clinical factors together to improve accuracy have a promising but modest ability to identify people who will develop bipolar disorder, 60 emphasizing the need for further studies before implementation.
Screening for bipolar disorder
Manic episodes can vary from easily identifiable prototypical presentations to milder or less typical symptoms that can be challenging to diagnose. Ideally, a full diagnostic evaluation with access to close informants is performed on patients presenting to clinical care; however, evaluations can be hurried in routine clinical care, and the ability to recall previous episodes might be limited. In this context, the use of screening scales can be a helpful addition to clinical care, although screening scales must be regarded as an impetus for a confirmatory clinical interview rather than a diagnostic instrument by themselves. The two most widely used and openly available screening scales are the mood disorders questionnaire (based on the DSM-IV criteria for hypomania) 61 and the hypomania check list (HCL-32), 62 that represent a broader overview of symptoms proposed to be part of a broader bipolar spectrum.
Racial/ethnic disparities
Although community surveys using structured or semi-structured diagnostic instruments, have provided little evidence for variation across ethnic groups, 63 64 observational studies based on clinical diagnoses in healthcare settings have found a disproportionately higher rate of diagnosis of schizophrenia relative to bipolar disorder in black people. 65 Consistent with similar disparities seen across medicine, these differences in clinical diagnoses are likely influenced by a complex mix of varying clinical presentations, differing rates of comorbid conditions, poorer access to care, greater social and economic burden, as well as the potential effect of subtle biases of healthcare professionals. 65 While further research is necessary to identify driving factors responsible for diagnostic disparities, clinicians should be wary of making a rudimentary diagnosis in patients from marginalized backgrounds, ensuring comprehensive data gathering and a careful diagnostic formulation that incorporates shared decision making between patient and provider.
Bipolar disorder is a recurrent illness, but its longitudinal course is heterogeneous and difficult to predict. 46 66 The few available long term studies of BD-I and BD-II have found a consistent average rate of recurrence of 0.40 mood episodes per year in historical studies 67 and 0.44 mood episodes per year in more recent studies. 68 The median time to relapse is estimated to be 1.44 years, with higher relapse rates seen in BD-I (0.81 years) than in BD-II (1.63 years) and no differences observed with respect to age or sex. 1 2 In addition to focusing on episodes, an important development in research and clinical care of bipolar disorder has been the recognition of the burden of subsyndromal symptoms. Although milder in severity, these symptoms can be long lasting, functionally impairing, and can themselves be a risk factor for episode relapse. 69 Recent cohort studies have also found that a substantial proportion of patients with bipolar disorder (20-30%) continue to have poor outcomes even after receiving guideline based care. 46 70 Risk factors that contribute to this poor outcome include transdiagnostic indicators of adversity such as substance misuse, low educational attainment, socioeconomic hardship, and comorbid disorders. As expected, those with more severe past illness activity, including those with rapid cycling, were also more likely to remain symptomatically and psychosocially impaired. 46 71 72
The primary focus of treating bipolar disorder has been to manage the manic, mixed, or depressive episodes that present to clinical care and to subsequently prevent recurrence of future episodes. Owing to the relapse remitting nature of the illness, randomized controlled trials are essential to determine treatment efficacy, as the observation of clinical improvement could just represent the ebbs and flows of the natural history of the illness. In the United States, the FDA (Food and Drug Administration) requires at least two large scale placebo controlled trials (phase 3) to show significant evidence of efficacy before approving a treatment. Phase 3 studies of bipolar disorder are generally separated into short term studies of mania (3-4 weeks), short term studies for bipolar depression (4-6 weeks), and longer term maintenance studies to evaluate prophylactic activity against future mood episodes (usually lasting one year). Although the most rigorous evaluation of phase 3 studies would be to require two broadly representative and independent randomized controlled trials, the FDA permits consideration of so called enriched design trials that follow participants after an initial response and tolerability has been shown to an investigational drug. Because of this initial selection, such trials can be biased against comparator agents, and could be less generalizable to patients seen in clinical practice.
A summary of the agents approved by the FDA for treatment of bipolar disorder is in table 1 , which references the key clinical trials demonstrating efficacy. Figure 1 and supplementary table 1 are a comparison of treatments for mania, depression, and maintenance. Effect sizes reflect the odds ratios or relative risks of obtaining response (defined as ≥50% improvement from baseline) in cases versus controls and were extracted from meta-analyses of randomized controlled trials for bipolar depression 86 and maintenance, 94 as well as a network meta-analysis of randomized controlled trials in bipolar mania. 73 Effect sizes are likely to be comparable for each phase of treatment, but not across the different phases, since methodological differences exist between the three meta-analytic studies.
FDA approved medications for bipolar disorder
- View inline

Summary of treatment response rates (defined as ≥50% improvement from baseline) of modern clinical trials for acute mania, acute bipolar depression, and long term recurrence. Meta-analytic estimates were extracted from recent meta-analyses or network meta-analyses of acute mania, 73 acute bipolar depression, 86 and bipolar maintenance studies 94
- Download figure
- Open in new tab
- Download powerpoint
Acute treatment of mania
As mania is characterized by impaired judgment, individuals can be at risk for engaging in high risk, potentially dangerous behaviors that can have substantial personal, occupational, and financial consequences. Therefore, treatment of mania is often considered a psychiatric emergency and is, when possible, best performed in the safety of an inpatient unit. While the primary treatment for mania is pharmacological, diminished insight can impede patients' willingness to accept treatment, emphasizing the significance of a balanced therapeutic approach that incorporates shared decision making frameworks as much as possible to promote treatment adherence.
The three main classes of anti-manic treatments are lithium, mood stabilizing anticonvulsants (divalproate and carbamazepine), and antipsychotic medications. Almost all antipsychotics are effective in treating mania, with the more potent dopamine D2 receptor antagonists such as risperidone and haloperidol demonstrating slightly higher efficacy ( fig 1 ). 73 In the United States, the FDA has approved the use of all second generation antipsychotics for treating mania except for lurasidone and brexpriprazole. Compared with mood stabilizing medications, second generation antipsychotics have a faster onset of action, making them a first line treatment for more severe manic symptoms that require rapid treatment. 99 The choice of which specific second generation antipsychotic to use depends on a balance of efficacy, tolerability concerns, and cost considerations (see table 1 ). Notably, the FDA has placed a black box warning on all antipsychotics for increasing the risk of cerebral vascular accidents in the elderly. 100 While this was primarily focused on the use of antipsychotics in dementia, this likely class effect should be taken into account when considering the use of antipsychotics in the elderly.
Traditional mood stabilizers, such as lithium, divalproate, and carbamazepine are also effective in the treatment of active mania ( fig 1 ). Since lithium also has a robust prophylactic effect (see section on prevention of mood episodes below) it is often recommended as first line treatment and can be considered as monotherapy when rapid symptom reduction is not clinically indicated. On the other hand, other anticonvulsants such as lamotrigine, gabapentin, topiramate, and oxcarbazepine have not been found to be effective for the treatment of mania or mixed episodes. 101 Although the empirical evidence for polypharmacy is limited, 102 combination treatment in acute mania, usually consisting of a mood stabilizer and a second generation antipsychotic, is commonly used in clinical practice despite the higher burden of side effects. Following resolution of an acute mania, consideration should be given to transitioning to monotherapy with an agent with proven prophylactic activity.
Pharmacological approaches to bipolar depression
Depressed episodes are usually more common than mania or hypomania, 103 104 and often represent the primary reason for individuals with bipolar disorder to seek treatment. Nevertheless, because early antidepressant randomized controlled trials did not distinguish between unipolar and bipolar depressive episodes, it has only been in the past two decades that large scale randomized controlled trials have been conducted specifically for bipolar depression. As such trials are almost exclusively funded by pharmaceutical companies, they have focused on the second generation antipsychotics and newer anticonvulsants still under patent. These trials have shown moderate but robust effects for most recent second generation antipsychotics, five of which have received FDA approval for treating bipolar depression ( table 1 ). No head-to-head trials have been conducted among these agents, so the choice of medication depends on expected side effects and cost considerations. For example, quetiapine has robust antidepressant efficacy data but is associated with sedation, weight gain, and adverse cardiovascular outcomes. 105 Other recently approved medications such as lurasidone, cariprazine, and lumateperone have better side effect profiles but show more modest antidepressant activity. 106
Among the mood stabilizing anticonvulsants, lamotrigine has limited evidence for acute antidepressant activity, 107 possibly owing to the need for an 8 week titration to reach the full dose of 200 mg. However, as discussed below, lamotrigine can still be considered for mild to moderate acute symptoms owing to its generally tolerable side effect profile and proven effectiveness in preventing the recurrence of depressive episodes. Divalproate and carbamazepine have some evidence of being effective antidepressants in small studies, but as there has been no large scale confirmatory study, they should be considered second or third line options. 86 Lithium has been studied for the treatment of bipolar depression as a comparator to quetiapine and was not found to have a significant acute antidepressant effect. 88
Antidepressants
Owing to the limited options of FDA approved medications for bipolar depression and concerns of metabolic side effects from long term second generation antipsychotic use, clinicians often resort to the use of traditional antidepressants for the treatment of bipolar depression 108 despite the lack of FDA approval for such agents. Indeed, recent randomized clinical trials of antidepressants in bipolar depression have not shown an effect for paroxetine, 89 109 bupropion, 109 or agomelatine. 110 Beyond the question of efficacy, another concern regarding antidepressants in bipolar disorder is their potential to worsen the course of illness by either promoting mixed or manic symptoms or inducing more subtle degrees of mood instability and cycle acceleration. 111 However, the risk of switching to full mania while being treated with mood stabilizers appears to be modest, with a meta-analysis of randomized clinical trials and clinical cohort studies showing the rates of mood switching over an average follow-up of five months to be approximately 15.3% in people with bipolar disorder treated on antidepressants compared with 13.8% in those without antidepressant treatment. 111 The risk of switching appears to be higher in the first 1-2 years of treatment in people with BD-I, and in those treated with a tricyclic antidepressant 112 or the dual reuptake inhibitor venlafaxine. 113 Overall, while the available data have methodological limitations, most guidelines do not recommend the use of antidepressants in bipolar disorder, or recommend them only after agents with more robust evidence have been tried. That they remain so widely used despite the equivocal evidence base reflects the unmet need for treatment of depression, concerns about the long term side effects of second generation antipsychotics, and the challenges of changing longstanding prescribing patterns.
Pharmacological approaches to prevention of recurrent episodes
Following treatment of the acute depressive or manic syndrome, the major focus of treatment is to prevent future episodes and minimize interepisodic subsyndromal symptoms. Most often, the medication that has been helpful in controlling the acute episode can be continued for prevention, particularly if clinical trial evidence exists for a maintenance effect. To show efficacy for prevention, studies must be sufficiently long to allow the accumulation of future episodes to occur and be potentially prevented by a therapeutic intervention. However, few long term treatment studies exist and most have utilized enriched designs that likely favor the drug seeking regulatory approval. As shown in figure 1 , meta-analyses 94 show prophylactic effect for most (olanzapine, risperidone, quetiapine, aripiprazole, asenapine) but not all (lurasidone, paliperidone) recently approved second generation antipsychotics. The effect sizes are generally comparable with monotherapy (odds ratio 0.42, 95% confidence interval 0.34 to 0.5) or as adjunctive therapy (odds ratio 0.37, 95% confidence interval 0.25 to 0.55). 94 Recent studies of lithium, which have generally used it as a (non-enriched) comparator drug, show a comparable protective effect (odds ratio 0.46, 95% confidence interval 0.28 to 0.75). 94 Among the mood stabilizing anticonvulsant drugs, a prophylactic effect has also been found for both divalproate and lamotrigine ( fig 1 and supplementary table 1), although only the latter has been granted regulatory approval for maintenance treatment. While there are subtle differences in effect sizes in drugs approved for maintenance ( fig 1 and table 1 ), the overlapping confidence intervals and methodological differences between studies prevent a strict comparison of the effect measures.
Guidelines often recommend lithium as a first line agent given its consistent evidence of prophylaxis, even when tested as the disadvantaged comparator drug in enriched drug designs. Like other medications, lithium has a unique set of side effects and ultimately the decision about which drug to use among those which are efficacious should be a decision carefully weighed and shared between patient and provider. The decision might be re-evaluated after substantial experience with the medication or at different stages in the long term treatment of bipolar disorder (see table 1 ).
Psychotherapeutic approaches
The frequent presence of residual symptoms, often associated with psychosocial and occupational dysfunction, has led to renewed interest in psychotherapeutic and psychosocial approaches to bipolar disorder. Given the impairment of judgment seen in mania, psychotherapy has more of a supportive and educational role in the treatment of mania, whereas it can be more of a primary focus in the treatment of depressive states. On a broad level, psychotherapeutic approaches effective for acute depression, such as cognitive behavioral therapy, interpersonal therapy, behavioral activation, and mindfulness based strategies, can also be recommended for acute depressive states in individuals with bipolar disorder. 114 Evidence for more targeted psychotherapy trials for bipolar disorder is more limited, but meta-analyses have found evidence for decreased recurrence (odds ratio 0.56; 95% confidence interval 0.43 to 0.74) 115 and improvement of subthreshold interepisodic depressive and manic symptoms with cognitive behavioral therapy, family based therapy, interpersonal and social rhythm therapy, and psychoeducation. 115 Recent investigations have also focused on targeted forms of psychotherapy to improve cognition 116 117 118 as well as psychosocial and occupational functioning. 119 120 Although these studies show evidence of a moderate effect, they remain preliminary, methodologically diverse, and require replication on a larger scale. 121
The implementation of evidence based psychotherapy as a treatment faces several challenges, including clinical training, fidelity monitoring, and adequate reimbursement. Novel approaches, leveraging the greater tractability of digital tools 122 and allied healthcare workers, 123 are promising means of lessening the implementation gap; however, these approaches require validation and evidence of clinical utility similar to traditional methods.
Neurostimulation approaches
For individuals with bipolar disorder who cannot tolerate or do not respond well to standard pharmacotherapy or psychotherapeutic approaches, neurostimulation techniques such as repetitive transcranial magnetic stimulation or electric convulsive therapy should be considered as second or third line treatments. Electric convulsive therapy has shown response rates of approximately 60-80% in severe acute depressions 124 125 and 50-60% in cases with treatment resistant depression. 126 These response rates compare favorably with those of pharmacological treatment, which are likely to be closer to ~50% and ~30% in subjects with moderate to severe depression and treatment resistant depression, respectively. 127 Although the safety of electric convulsive therapy is well established, relatively few medical centers have it available, and its acceptability is limited by cognitive side effects, which are usually short term, but which can be more significant with longer courses and with bilateral electrode placement. 128 While there have been fewer studies of electric convulsive therapy for bipolar depression compared with major depressive disorder, it appears to be similarly effective and might show earlier response. 129 Anecdotal evidence also suggests electric convulsive therapy that is useful in refractory mania. 130
Compared with electric convulsive therapy, repetitive transcranial magnetic stimulation has no cognitive side effects and is generally well tolerated. Repetitive transcranial magnetic stimulation acts by generating a magnetic field to depolarize local neural tissue and induce excitatory or inhibitory effects depending on the frequency of stimulation. The most studied FDA approved form of repetitive transcranial magnetic stimulation applies high frequency (10 Hz) excitatory pulses to the left prefrontal cortex for 30-40 minutes a day for six weeks. 131 Like electric convulsive therapy, repetitive transcranial magnetic stimulation has been primarily studied in treatment resistant depression and has been found to have moderate effect, with about one third of patients having a significant treatment response compared with those treated with pharmacotherapy. 131 Recent innovations in transcranial magnetic stimulation have included the use of a novel, larger coil to stimulate a larger degree of the prefrontal cortex (deep transcranial magnetic stimulation), 132 and a shortened (three minutes), higher frequency intermittent means of stimulation known as theta burst stimulation that appears to be comparable to conventional (10 Hz) repetitive transcranial magnetic stimulation. 133 A preliminary trial has recently assessed a new accelerated protocol of theta burst stimulation marked by 10 sessions a day for five days. It found that theta burst stimulation had a greater effect on people with treatment resistant depression compared with treatment as usual, although larger studies are needed to confirm these findings. 134
Conventional repetitive transcranial magnetic stimulation (10 Hz) studies in bipolar disorder have been limited by small sample sizes but have generally shown similar effects compared with major depressive disorder. 135 However, a proof of concept study of single session theta burst stimulation did not show efficacy in bipolar depression, 136 reiterating the need for specific trials for bipolar depression. Given the lack of such trials in bipolar disorder, repetitive transcranial magnetic stimulation should be considered a potentially promising but as yet unproven treatment for bipolar depression.
The other major form of neurostimulation studied in both unipolar and bipolar depression is transcranial direct current stimulation, an easily implemented method of delivering a low amplitude electrical current to the prefrontal area of the brain that could lead to local changes in neuronal excitability. 137 Like repetitive transcranial magnetic stimulation, transcranial direct current stimulation is well tolerated and has been mostly studied in unipolar depression, but has not yet generated sufficient evidence to be approved by a regulatory agency. 138 Small studies have been performed in bipolar depression, but the results have been mixed and require further research before use in clinical settings. 137 138 139 Finally, the evidence for more invasive neurostimulation studies such as vagal nerve stimulation and deep brain stimulation remains extremely limited and is currently insufficient for clinical use. 140 141
Treatment resistance in bipolar disorder
As in major depressive disorder, the use of term treatment resistance in bipolar disorder is controversial since differentiating whether persistent symptoms are caused by low treatment adherence, poor tolerability, the presence of comorbid disorders, or are the result of true treatment resistance, is an essential but often challenging clinical task. Treatment resistance should only be considered after two or three trials of evidence based monotherapy, adjunctive therapy, or both. 142 In difficult-to-treat mania, two or more medications from different mechanistic classes are typically used, with electric convulsive therapy 143 and clozapine 144 being considered if more conventional anti-manic treatments fail. In bipolar depression, it is common to combine antidepressants with anti-manic agents, despite limited evidence for efficacy. 145 Adjunctive therapies such as bright light therapy, 146 the dopamine D2/3 receptor agonist pramipexole, 147 and ketamine 148 149 have shown promising results in small open label trials that require further study.
Treatment considerations to reduce suicide in bipolar disorder
The risk of completed suicide is high across the subtypes of bipolar disorder, with estimated rates of 10-15% across the lifespan. 150 151 152 Lifetime rates of suicide attempts are much higher, with almost half of all individuals with bipolar disorder reporting at least one attempt. 153 Across a population and, often within individuals, the causes of suicide attempts and completed suicides are likely to be multifactorial, 154 affected by various risk factors, such as symptomatic illness, environmental stressors, comorbidities (particularly substance misuse), trait impulsivity, interpersonal conflict, loneliness, or socioeconomic distress. 155 156 Risk is highest in depressive and dysphoric/mixed episodes 157 158 and is particularly high in the transitional period following an acute admission to hospital. 159 Among the available treatments, lithium has potential antisuicidal properties. 160 However, since suicide is a rare event, with very few to zero suicides within a typical clinical trial, moderate evidence for this effect emerges only in the setting of meta-analyses of clinical trials. 160 Several observational studies have shown lower mortality in patients on lithium treatment, 161 but such associations might not be causal, since lithium is potentially fatal in overdose and is often avoided by clinicians in patients at high risk of suicide.
The challenge of studying scarce events has led most studies to focus on the reduction of the more common phenomena of suicidal ideation and behavior as a proxy for actual suicides. A recent such multisite study of the Veterans Affairs medical system included a mixture of unipolar and bipolar disorder and was stopped prematurely for futility, indicating no overall effect of moderate dose lithium. 162 Appropriate limitations of this study have been noted, 163 164 including difficulties in recruitment, few patients with bipolar disorder (rather than major depressive disorder), low levels of compliance with lithium therapy, high rates of comorbidity, and a follow-up of only one year. Nevertheless, while the body of evidence suggests that lithium has a modest antisuicidal effect, its degree of protection and utility in complex patients with comorbidities and multiple risk factors remain matters for further study. Treatment of specific suicidal risk in patients with bipolar disorder must therefore also incorporate broader interventions based on the individual’s specific risk factors. 165 Such an approach would include societal interventions like means restriction 166 and a number of empirically tested suicide focused psychotherapy treatments. 167 168 Unfortunately, the availability of appropriate training, expertise, and care models for such treatments remains limited, even in higher income countries. 169
More scalable solutions, such as the deployment of shortened interventions via digital means could help to overcome this implementation gap; however, the effectiveness of such approaches cannot be assumed and requires empirical testing. For example, a recent large scale randomized controlled trial of an abbreviated online dialectical behavioral therapy skills training program was paradoxically associated with slightly increased risk of self-harm. 170
Treatment consideration in BD-II and bipolar spectrum conditions
Because people with BD-II primarily experience depressive symptoms and appear less likely to switch mood states compared with individuals with BD-I, 50 171 there has been a greater acceptance of the use of antidepressants in BD-II depression, including as monotherapy. 172 However, caution should be exercised when considering the use of antidepressants without a mood stabilizer in patients with BD-II who might also experience high rates of mood instability and rapid cycling. Such individuals can instead respond better to newer second generation antipsychotic agents such as quetiapine 173 and lumateperone, 93 which are supported by post hoc analyses of these more recent clinical trials with more BD-II patients. In addition, despite the absence of randomized controlled trials, open label studies have suggested that lithium and other mood stabilizers can have similar efficacy in BD-II, especially in the case of lamotrigine. 174
Psychotherapeutic approaches such as psychoeducation, cognitive behavioral therapy, and interpersonal and social rhythm therapy have been found to be helpful 115 and can be considered as the primary form of treatment for BD-II in some patients, although in most clinical scenarios BD-II is likely to occur in conjunction with psychopharmacology. While it can be tempting to consider BD-II a milder variant of BD-I, high rates of comorbid disorders, rapid cycling, and adverse consequences such as suicide attempts 175 176 highlight the need for clinical caution and the provision of multimodal treatment, focusing on mood improvement, emotional regulation, and better psychosocial functioning.
Precision medicine: can it be applied to improve the care of bipolar disorder?
The recent focus on precision medicine approaches to psychiatric disorders seeks to identify clinically relevant heterogeneity and identify characteristics at the level of the individual or subgroup that can be leveraged to identify and target more efficacious treatments. 1 177 178
The utility of such an approach was originally shown in oncology, where a subset of tumors had gene expression or DNA mutation signatures that could predict response to treatments specifically designed to target the aberrant molecular pathway. 179 While much of the emphasis of precision medicine has been on the eventual identification of biomarkers utilizing high throughput approaches (genetics and other “omics” based measurements), the concept of precision medicine is arguably much broader, encompassing improvements in measurement, potentially through the deployment of digital tools, as well as better conceptualization of contextual, cultural, and socioeconomic mechanisms associated with psychopathology. 180 181 Ultimately, the goal of precision psychiatry is to identify and target driving mechanisms, be they molecular, physiological, or psychosocial in nature. As such, precision psychiatry seeks what researchers and clinicians have often sought: to identify clinically relevant heterogeneity to improve prediction of outcomes and increase the likelihood of therapeutic success. The novelty being not so much the goals of the overarching approach, but the increasing availability of large samples, novel digital tools, analytical advances, and an increasing armamentarium of biological measurements that can be deployed at scale. 177
Although not unique to bipolar disorder, several clinical decision points along the life course of bipolar disorder would benefit from a precision medicine approach. For example, making an early diagnosis is often not possible based on clinical symptoms alone, since such symptoms are usually non-specific. A precision medicine approach could also be particularly relevant in helping to identify subsets of patients for whom the use of antidepressants could be beneficial or harmful. Admittedly, precision medicine approaches to bipolar disorder are still in their infancy, and larger, clinically relevant, longitudinal, and reliable phenotypes are needed to provide the infrastructure for precision medicine approaches. Such data remain challenging to obtain at scale, leading to renewed efforts to utilize the extant clinical infrastructure and electronic medical records to help emulate traditional longitudinal analyses. Electronic medical records can help provide such data, but challenges such as missingness, limited quality control, and potential biases in care 182 need to be resolved with carefully considered analytical designs. 183
Emerging treatments
Two novel atypical antipsychotics, amilsupride and bifeprunox, are currently being tested in phase 3 trials ( NCT05169710 and NCT00134459 ) and could gain approval for bipolar depression in the near future if these pivotal trials show a significant antidepressant effect. These drugs could offer advantages such as greater antidepressant effects, fewer side effects, and better long term tolerability, but these assumptions must be tested empirically. Other near term possibilities include novel rapid antidepressant treatments, such as (es)ketamine that putatively targets the glutamatergic system, and has been recently approved for treatment resistant depression, but which have not yet been tested in phase 3 studies in bipolar depression. Small studies have shown comparable effects of intravenous ketamine, 149 184 in bipolar depression with no short term evidence of increased mood switching or mood instability. Larger phase 2 studies ( NCT05004896 ) are being conducted which will need to be followed by larger phase 3 studies. Other therapies targeting the glutamatergic system have generally failed phase 3 trials in treatment resistant depression, making them unlikely to be tested in bipolar depression. One exception could be the combination of dextromethorphan and its pharmacokinetic (CYP2D6) inhibitor bupropion, which was recently approved for treatment resistant depression but has yet to be tested in bipolar depression. Similarly, the novel GABAergic compound zuranolone is currently being evaluated by the FDA for the treatment of major depressive disorder and could also be subsequently studied in bipolar depression.
Unfortunately, given the general efficacy for most patients of available treatments, few scientific and financial incentives exist to perform large scale studies of novel treatment in mania. Encouraging results have been seen in small studies of mania with the selective estrogen receptor modulator 185 tamoxifen and its active metabolite endoxifen, both of which are hypothesized to inhibit protein kinase C, a potential mechanistic target of lithium treatment. These studies remain small, however, and anti-estrogenic side effects have potentially dulled interest in performing larger studies.
Finally, several compounds targeting alternative pathophysiological mechanisms implicated in bipolar disorder have been trialed in phase 2 academic studies. The most studied has been N -acetylcysteine, a putative mitochondrial modulator, which initially showed promising results only to be followed by null findings in larger more recent studies. 186 Similarly, although small initial studies of anti-inflammatory agents provided impetus for further study, subsequent phase 2 studies of the non-steroidal agent celecoxib, 187 the anti-inflammatory antibiotic minocycline, 187 and the antibody infliximab (a tumor necrosis factor antagonist) 188 have not shown efficacy for bipolar depression. Secondary analyses have suggested that specific anti-inflammatory agents might be effective only for a subset of patients, such as those with elevated markers of inflammation or a history of childhood adversity 189 ; however, such hypotheses must be confirmed in adequately powered independent studies.
Several international guidelines for the treatment of bipolar disorder have been published in the past decade, 102 190 191 192 providing a list of recommended treatments with efficacy in at least one large randomized controlled trial. Since effect sizes tend to be moderate and broadly comparable across classes, all guidelines allow for significant choice among first line agents, acknowledging that clinical characteristics, such as history of response or tolerability, severity of symptoms, presence of mixed features, or rapid cycling can sometimes over-ride guideline recommendations. For acute mania requiring rapid treatment, all guidelines prioritize the use of second generation antipsychotics such as aripiprazole, quetiapine, risperidone, asenapine, and cariprazine. 102 192 193 Combination treatment is considered based on symptom severity, tolerability, and patient choice, with most guidelines recommending lithium or divalproate along with a second generation antipsychotic for mania with psychosis, severe agitation, or prominent mixed symptoms. While effective, haloperidol is usually considered a second choice option owing to its propensity to cause extrapyramidal symptoms. 102 192 193 Uniformly, all guidelines agree on the need to taper antidepressants in manic or mixed episodes.
For maintenance treatment, guidelines are generally consistent in recommending lithium if tolerated and without relative contraindications, such as baseline renal disease. 194 The second most recommended maintenance treatment is quetiapine, followed by aripiprazole for patients with prominent manic episodes and lamotrigine for patients with predominant depressive episodes. 194 Most guidelines recommend considering prophylactic properties when initially choosing treatment for acute manic episodes, although others suggests that acute maintenance treatments can be cross tapered with maintenance medications after several months of full reponse. 193
For bipolar depression, recent guidelines recommend specific second generation antipsychotics such as quetiapine, lurasidone, and cariprazine 102 192 193 For more moderate symptoms, consideration is given to first using lamotrigine and lithium. Guidelines remain cautious about the use of antidepressants (selective serotonin reuptake inhibitors, venlafaxine, or bupropion) in patients with BP-I, restricting them to second or third line treatments and always in the context of an anti-manic agent. However, for patients with BP-II and no rapid cycling, several guidelines allow for the use of carefully monitored antidepressant monotherapy.
Bipolar disorder is a highly recognizable syndrome with many effective treatment options, including the longstanding gold standard therapy lithium. However, a significant proportion of patients do not respond well to current treatments, leading to negative consequences, poor quality of life, and potentially shortened lifespan. Several novel treatments are being developed but limited knowledge of the biology of bipolar disorder remains a major challenge for novel drug discovery. Hope remains that the insights of genetics, neuroimaging, and other investigative modalities could soon be able to inform the development of rational treatments aimed to mitigate the underlying pathophysiology associated with bipolar disorder. At the same time, however, efforts are needed to bridge the implementation gap and provide truly innovative and integrative care for patients with bipolar disorder. 195 Owing to the complexity of bipolar disorder, few patients can be said to be receiving optimized care across the various domains of mental health that are affected in those with bipolar disorder. Fortunately, the need for improvement is now well documented, 196 and concerted efforts at the scale necessary to be truly innovative and integrative are now on the horizon.
Questions for future research
Among adolescents and young adults who manifest common mental disorders such as anxiety or depressive or attentional disorders, who will be at high risk for developing bipolar disorder?
Can we predict the outcomes for patients following a first manic or hypomanic episode? This will help to inform who will require lifelong treatment and who can be tapered off medications after sustained recovery.
Are there reliable clinical features and biomarkers that can sufficiently predict response to specific medications or classes of medication?
What are the long term consequences of lifelong treatments with the major classes of medications used in bipolar disorder? Can we predict and prevent medical morbidity caused by medications?
Can we understand in a mechanistic manner the pathophysiological processes that lead to abnormal mood states in bipolar disorder?
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: FSG performed the planning, conduct, and reporting of the work described in the article. FSG accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Competing interests: I have read and understood the BMJ policy on declaration of interests and declare no conflicts of interest.
Patient involvement: FSG discussed of the manuscript, its main points, and potential missing points with three patients in his practice who have lived with longstanding bipolar disorder. These additional viewpoints were incorporated during the drafting of the manuscript.
Provenance and peer review: Commissioned; externally peer reviewed.
- ↵ . Falret’s discovery: the origin of the concept of bipolar affective illness. Translated by M. J. Sedler and Eric C. Dessain. Am J Psychiatry 1983;140:1127-33. doi: 10.1176/ajp.140.9.1127 OpenUrl CrossRef PubMed Web of Science
- ↵ Kraepelin E. Manic-depressive Insanity and Paranoia. Translated by R. Mary Barclay from the Eighth German. Edition of the ‘Textbook of Psychiatry.’ 1921.
- Merikangas KR ,
- Akiskal HS ,
- Koukopoulos A ,
- Jongsma HE ,
- Kirkbride JB ,
- Rowland TA ,
- Kessler RC ,
- Kazdin AE ,
- Aguilar-Gaxiola S ,
- WHO World Mental Health Survey collaborators
- Bergen SE ,
- Kuja-Halkola R ,
- Larsson H ,
- Lichtenstein P
- Smoller JW ,
- Lichtenstein P ,
- Sjölander A ,
- Mullins N ,
- Forstner AJ ,
- O’Connell KS ,
- Palmer DS ,
- Howrigan DP ,
- Chapman SB ,
- Pirooznia M ,
- Murray GK ,
- McGrath JJ ,
- Hickie IB ,
- ↵ Mostafavi H, Harpak A, Agarwal I, Conley D, Pritchard JK, Przeworski M. Variable prediction accuracy of polygenic scores within an ancestry group. Loos R, Eisen MB, O’Reilly P, eds. eLife 2020;9:e48376. doi: 10.7554/eLife.48376 OpenUrl CrossRef PubMed
- Westlye LT ,
- van Erp TGM ,
- Costa Rica/Colombia Consortium for Genetic Investigation of Bipolar Endophenotypes
- Pauling M ,
- ENIGMA Bipolar Disorder Working Group
- Schnack HG ,
- Ching CRK ,
- ENIGMA Bipolar Disorders Working Group
- Goltermann J ,
- Hermesdorf M ,
- Dannlowski U
- Gurholt TP ,
- Suckling J ,
- Lennox BR ,
- Bullmore ET
- Marangoni C ,
- Hernandez M ,
- Achtyes ED ,
- Agnew-Blais J ,
- Gilman SE ,
- Upthegrove R ,
- ↵ Etain B, Aas M. Childhood Maltreatment in Bipolar Disorders. In: Young AH, Juruena MF, eds. Bipolar Disorder: From Neuroscience to Treatment . Vol 48. Current Topics in Behavioral Neurosciences. Springer International Publishing; 2020:277-301. doi: 10.1007/7854_2020_149
- Johnson SL ,
- Weinberg BZS
- Stinson FS ,
- Costello CG
- Klein & Riso LP DN
- Sandstrom A ,
- Perroud N ,
- de Jonge P ,
- Bunting B ,
- Nierenberg AA
- Hantouche E ,
- Vannucchi G
- Zimmerman M ,
- Ruggero CJ ,
- Chelminski I ,
- Leverich GS ,
- McElroy S ,
- Mignogna KM ,
- Balling C ,
- Dalrymple K
- Kappelmann N ,
- Stokes PRA ,
- Jokinen T ,
- Baldessarini RJ ,
- Faedda GL ,
- Offidani E ,
- Viktorin A ,
- Launders N ,
- Osborn DPJ ,
- Roshanaei-Moghaddam B ,
- De Hert M ,
- Detraux J ,
- van Winkel R ,
- Lomholt LH ,
- Andersen DV ,
- Sejrsgaard-Jacobsen C ,
- Skjelstad DV ,
- Gregersen M ,
- Søndergaard A ,
- Brandt JM ,
- Van Meter AR ,
- Youngstrom EA ,
- Taylor RH ,
- Ulrichsen A ,
- Strawbridge R
- Hafeman DM ,
- Merranko J ,
- Hirschfeld RM ,
- Williams JB ,
- Spitzer RL ,
- Adolfsson R ,
- Benazzi F ,
- Regier DA ,
- Johnson KR ,
- Akinhanmi MO ,
- Biernacka JM ,
- Strakowski SM ,
- Goldberg JF ,
- Schettler PJ ,
- Coryell W ,
- Scheftner W ,
- Endicott J ,
- Zarate CA Jr . ,
- Matsuda Y ,
- Fountoulakis KN ,
- Zarate CA Jr .
- Bowden CL ,
- Brugger AM ,
- The Depakote Mania Study Group
- Calabrese JR ,
- Depakote ER Mania Study Group
- Weisler RH ,
- Kalali AH ,
- Ketter TA ,
- SPD417 Study Group
- Keck PE Jr . ,
- Cutler AJ ,
- Caffey EM Jr . ,
- Grossman F ,
- Eerdekens M ,
- Jacobs TG ,
- Grundy SL ,
- The Olanzipine HGGW Study Group
- Versiani M ,
- Ziprasidone in Mania Study Group
- Sanchez R ,
- Aripiprazole Study Group
- McIntyre RS ,
- Panagides J
- Calabrese J ,
- McElroy SL ,
- EMBOLDEN I (Trial 001) Investigators
- EMBOLDEN II (Trial D1447C00134) Investigators
- Lamictal 606 Study Group
- Lamictal 605 Study Group
- Keramatian K ,
- Chakrabarty T ,
- Nestsiarovich A ,
- Gaudiot CES ,
- Neijber A ,
- Hellqvist A ,
- Paulsson B ,
- Trial 144 Study Investigators
- Schwartz JH ,
- Szegedi A ,
- Cipriani A ,
- Salanti G ,
- Dorsey ER ,
- Rabbani A ,
- Gallagher SA ,
- Alexander GC
- Cerqueira RO ,
- Yatham LN ,
- Kennedy SH ,
- Parikh SV ,
- Højlund M ,
- Andersen K ,
- Correll CU ,
- Ostacher M ,
- Schlueter M ,
- Geddes JR ,
- Mojtabai R ,
- Nierenberg AA ,
- Goodwin GM ,
- Agomelatine Study Group
- Vázquez G ,
- Baldessarini RJ
- Altshuler LL ,
- Cuijpers P ,
- Miklowitz DJ ,
- Efthimiou O ,
- Furukawa TA ,
- Strawbridge R ,
- Tsapekos D ,
- Hodsoll J ,
- Vinberg M ,
- Kessing LV ,
- Forman JL ,
- Miskowiak KW
- Lewandowski KE ,
- Sperry SH ,
- Torrent C ,
- Bonnin C del M ,
- Martínez-Arán A ,
- Bonnín CM ,
- Tamura JK ,
- Carvalho IP ,
- Leanna LMW ,
- Karyotaki E ,
- Individual Patient Data Meta-Analyses for Depression (IPDMA-DE) Collaboration
- Vipulananthan V ,
- Hurlemann R ,
- UK ECT Review Group
- Haskett RF ,
- Mulsant B ,
- Trivedi MH ,
- Wisniewski SR ,
- Espinoza RT ,
- Vazquez GH ,
- McClintock SM ,
- Carpenter LL ,
- National Network of Depression Centers rTMS Task Group ,
- American Psychiatric Association Council on Research Task Force on Novel Biomarkers and Treatments
- Levkovitz Y ,
- Isserles M ,
- Padberg F ,
- Blumberger DM ,
- Vila-Rodriguez F ,
- Thorpe KE ,
- Williams NR ,
- Sudheimer KD ,
- Bentzley BS ,
- Konstantinou G ,
- Toscano E ,
- Husain MM ,
- McDonald WM ,
- International Consortium of Research in tDCS (ICRT)
- Sampaio-Junior B ,
- Tortella G ,
- Borrione L ,
- McAllister-Williams RH ,
- Gippert SM ,
- Switala C ,
- Bewernick BH ,
- Hidalgo-Mazzei D ,
- Mariani MG ,
- Fagiolini A ,
- Swartz HA ,
- Benedetti F ,
- Barbini B ,
- Fulgosi MC ,
- Burdick KE ,
- Diazgranados N ,
- Ibrahim L ,
- Brutsche NE ,
- Sinclair J ,
- Gerber-Werder R ,
- Miller JN ,
- Vázquez GH ,
- Franklin JC ,
- Ribeiro JD ,
- Turecki G ,
- Gunnell D ,
- Hansson C ,
- Pålsson E ,
- Runeson B ,
- Pallaskorpi S ,
- Suominen K ,
- Ketokivi M ,
- Hadzi-Pavlovic D ,
- Stanton C ,
- Lewitzka U ,
- Severus E ,
- Müller-Oerlinghausen B ,
- Rogers MP ,
- Li+ plus Investigators
- Manchia M ,
- Michel CA ,
- Auerbach RP
- Altavini CS ,
- Asciutti APR ,
- Solis ACO ,
- Casañas I Comabella C ,
- Riblet NBV ,
- Young-Xu Y ,
- Shortreed SM ,
- Rossom RC ,
- Amsterdam JD ,
- Brunswick DJ
- Gustafsson U ,
- Marangell LB ,
- Bernstein IH ,
- Karanti A ,
- Kardell M ,
- Collins FS ,
- Armstrong K ,
- Concato J ,
- Singer BH ,
- Ziegelstein RC
- ↵ Holmes JH, Beinlich J, Boland MR, et al. Why Is the Electronic Health Record So Challenging for Research and Clinical Care? Methods Inf Med 2021;60(1-02):32-48. doi: 10.1055/s-0041-1731784
- García Rodríguez LA ,
- Cantero OF ,
- Martinotti G ,
- Dell’Osso B ,
- Di Lorenzo G ,
- REAL-ESK Study Group
- Palacios J ,
- DelBello MP ,
- Husain MI ,
- Chaudhry IB ,
- Subramaniapillai M ,
- Jones BDM ,
- Daskalakis ZJ ,
- Carvalho AF ,
- ↵ Goodwin GM, Haddad PM, Ferrier IN, et al. Evidence-based guidelines for treating bipolar disorder: revised third edition Recommendations from the British Association for Psychopharmacology. J Psychopharmacol 2016;30:495-553. doi: 10.1177/0269881116636545 OpenUrl CrossRef PubMed
- Verdolini N ,
- Del Matto L ,
- Regeer EJ ,
- Hoogendoorn AW ,
- Harris MG ,
- WHO World Mental Health Survey Collaborators
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Focus (Am Psychiatr Publ)
- v.17(3); Summer 2019

Evidence-Based Psychotherapies for Bipolar Disorder
This literature review focuses on randomized controlled trials of psychotherapy for bipolar disorder. Evidence-based psychotherapies are shown to play an important role in the development of skills needed to manage the persistent and lifelong consequences of bipolar disorder.
Bipolar disorder is a recurrent psychiatric disorder marked by waxing and waning affective symptoms and impairment in functioning. Some of the morbidity and mortality associated with the illness may be reduced with evidence-based psychotherapies (EBPs) along with pharmacotherapy. To enhance clinicians’ understanding of which therapy modalities have evidence supporting their use, the authors conducted a systematic literature review to identify randomized controlled trials (RCTs) of psychotherapy for adults with bipolar disorder. A strong evidence base exists for psychoeducation, cognitive-behavioral therapy, family-focused therapy, interpersonal and social rhythm therapy, and peer-support programs. Promising modalities include functional remediation, mindfulness-based cognitive therapy, illness management and recovery, and technology-assisted strategies. RCTs demonstrate a consistent advantage of these psychotherapies plus pharmacotherapy, compared with the use of pharmacotherapy alone. Adjunctive EBPs hasten time to remission, delay time to recurrence, and improve functional outcomes. EBPs play an important role in helping individuals develop skills needed to manage the persistent and lifelong psychosocial, neurocognitive, vocational, and interpersonal consequences of bipolar disorder. Continued efforts to improve the effectiveness of EBPs for adults with bipolar disorder are warranted.
Clinical Context
Bipolar disorder is a recurrent psychiatric disorder that is marked by waxing and waning affective symptoms and impairment in functioning, even during well intervals ( 1 , 2 ). Approximately 2.4% of the world’s population is affected, resulting in a staggering disease burden and substantial years lost to disability ( 3 , 4 ).
Over the past few decades, there has been increasing attention to the development of bipolar disorder–specific psychotherapies ( 5 ). In part, this resurgence is related to disappointingly low remission and recovery rates, despite more pharmacotherapy options and growing efforts to personalize treatment ( 4 , 6 ). Pharmacological interventions are essential to the management of bipolar disorder, needed for all except a subset of individuals with bipolar disorder type II, for whom psychotherapy may be an adequate monotherapy ( 7 ). However, even when pharmacotherapy follows best-practice guidelines, it is effective in reducing only some symptoms, some relapses, and some suicides ( 8 – 10 ). A comprehensive treatment approach that includes pharmacotherapy and an evidence-based psychotherapy (EBP) may provide the strongest foundation for increasing self-efficacy, reducing symptoms and recurrences, and restoring functioning and quality of life.
In this clinical synthesis, we present the rationale for psychotherapy’s integration in the management of bipolar disorder. We then discuss the results of a systematic literature review focused on randomized controlled trials (RCTs) of psychotherapy for bipolar disorder. For modalities with the strongest level of evidence, as defined by the Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines ( 4 ), we review their core objectives and strategies and summarize the data supporting their efficacy. Next, we highlight promising psychotherapy modalities, including technology-assisted strategies. We conclude with a discussion of recommendations for clinical practice and future directions.
Rationale for Adjunctive Psychotherapy in Bipolar Disorder
In 1949, John Cade’s introduction of lithium carbonate for the management of bipolar disorder was revolutionary, and the field reconceptualized bipolar disorder as a medical illness amenable to biochemical intervention ( 11 ). Pharmacotherapy has fallen short of Cade’s promise of a cure for bipolar disorder, providing only partial relief from symptoms with the attendant risk of significant side-effect burden, such as sexual dysfunction and metabolic changes ( 7 , 10 , 12 ).
Recurrent episodes of mania, hypomania, and depression, coupled with pervasive interepisode subthreshold symptoms, lead to substantial mortality and morbidity of patients with bipolar disorder. Poorly managed symptoms may even result in death from suicide ( 13 ). Even when this endpoint is avoided, all-cause mortality is increased, with women and men with bipolar disorder dying 9.0 and 8.5 years earlier, on average, respectively, than the general population ( 3 ). Bipolar disorder is associated with a high likelihood of significant impairment across domains of living, and this is even more pronounced with early-onset bipolar disorder ( 14 , 15 ). Psychotherapies that help individuals develop skills needed to manage the persistent and lifelong psychosocial, neurocognitive, vocational, and interpersonal consequences of bipolar disorder may decrease illness burden and limit impairment in ways that pharmacotherapy cannot ( 16 ). EBPs should be considered for the management of bipolar disorder, even as early as the first episode ( 4 , 5 ).
Treatment Strategies and Evidence
To identify EBPs for adults with bipolar disorder, we conducted a systematic literature review of RCTs investigating the efficacy or effectiveness of individual and group interventions for bipolar disorder. We excluded RCTs targeting comorbid conditions or health behaviors, such as insomnia or smoking cessation, as well as RCTs developed primarily for caregivers and other supportive persons. Results were restricted to those focused on adulthood and published between January 2014 and March 2019, in a journal, and in English. We restricted the lower limit of the search parameters for publication date to January 2014, because we had conducted a similar review of psychotherapy for bipolar disorder through December 2013 ( 11 ), and we incorporated previous findings with the current search results. We conducted our searches by applying Boolean algorithms with PsycINFO databases. We searched for the following terms paired with the term bipolar: psychotherapy or psychosocial, psychoeducation, cognitive-behavior or cognitive-behavioral, dialectical, family, functional remediation, acceptance, integrated, unified or transdiagnostic, interpersonal, mobile, and internet or online.
We identified 273 reports for possible inclusion. We reviewed each abstract and, when unclear, the full article to determine whether the report should be included as evidence. Most often, the reason for excluding a report was that it was a secondary analysis of an RCT already identified or did not have a control group. The samples comprised individuals with bipolar disorder and other serious mental illnesses, type I only, type II only, or a combination. All interventions were manualized, and some manuals are available to clinicians.
A strong evidence base exists for psychoeducation (N=14 trials), cognitive-behavioral therapy (CBT; N=13 trials), family-focused therapy (FFT; N=4 trials), interpersonal and social rhythm therapy (IPSRT; N=5 trials), and peer-support (N=4 trials) programs. There is some promising evidence for other modalities, including functional remediation (N=2 trials), mindfulness-based cognitive therapy (MBCT; N=3 trials), illness management and recovery (N=4 trials), and technology-assisted strategies (N=12 trials).
Psychoeducation
The core objective of psychoeducation is to foster a clear rationale for individuals with bipolar disorder to seek, adhere to, and remain in treatment ( 17 – 19 ). Whereas early psychoeducation was narrowly oriented toward simply improving medication adherence, today’s psychoeducation is more comprehensive ( 20 ). It often includes structured sessions that focus on empowering an individual to better understand his or her illness, recognize and manage symptoms, resolve stressful situations, and adhere to pharmacotherapy. It can be administered individually or in a group format—or, more recently, remotely through a telephone, smartphone, or Web platform ( Table 1 ). Psychoeducation can be delivered by professionals of different backgrounds, including psychiatric nurse practitioners and trained peer supports ( 21 , 22 ). Psychoeducation can be administered as a stand-alone treatment or combined with strategies from other evidence-based interventions. In fact, all the evidence-based psychotherapies include at least a modest amount of psychoeducation, suggesting that it is a core, common therapeutic element across interventions for bipolar disorder.
Evidence-based psychotherapies for bipolar disorder
We identified 14 RCTs with in-person psychoeducation as the experimental condition. The number of psychoeducation sessions was as few as four and as many as 21. Here, we provide brief summaries of each report and describe particularly noteworthy findings.
Perry and colleagues conducted the first trial of individual psychoeducation ( 19 ). The goal of individual psychoeducation is to help patients identify prodromal symptoms and respond to prodromes with an “action plan.” The median number of one-hour sessions was nine. Compared with treatment as usual (i.e., pharmacotherapy alone), individual psychoeducation was associated with a significant extension of time to first manic relapse, reduction in the number of manic relapses, and improved social and occupational functioning over 18 months.
In another seminal trial, Colom and colleagues compared group psychoeducation to an unstructured support group ( 23 ). Group psychoeducation was a manualized, structured program of 21 sessions ( 18 ). The program targeted treatment compliance, illness awareness, early detection of prodromes, and lifestyle regularity. Compared with treatment as usual, group psychoeducation was associated with significantly longer time to recurrence, fewer relapses and hospitalizations, and shorter hospital stays at two- and five-year follow-ups ( 23 , 24 ). Zaretsky and colleagues compared seven sessions of individual psychoeducation with or without 13 sessions of CBT ( 25 ). Compared with psychoeducation alone, psychoeducation with the addition of CBT was associated with significantly fewer days of depressed mood and fewer increases in antidepressant dosage over one year.
D’Souza and colleagues evaluated 12 sessions of group psychoeducation for companion and patient dyads compared with treatment as usual ( 26 ). Group psychoeducation was based on the same principles of Colom and Vieta ( 18 ) and was modified to reflect the premise that companions might recognize and detect prodromes too. Group psychoeducation was associated with significantly decreased likelihood of relapse, longer time to relapse, decreased manic symptoms, and improved medication adherence over 60 weeks compared with treatment as usual.
Candini and colleagues demonstrated that Colom and Vieta’s ( 18 ) 21-session group psychoeducation program significantly reduced risk of, time to, and length of hospitalization compared with treatment as usual over one year ( 27 ).
Javadpour and colleagues found that, compared with treatment as usual, eight sessions of group psychoeducation were associated with significantly greater improvement in all areas of quality of life, fewer relapses and affective symptoms, and greater medication adherence over 18 months ( 28 ).
Kessing and colleagues demonstrated that, compared with treatment as usual, 12 sessions of group psychoeducation provided in a specialized outpatient mood disorder clinic significantly reduced the rehospitalization rate and increased satisfaction with care over two years ( 29 ).
Parikh and colleagues found no significant group difference between six weeks of group psychoeducation and 20 weeks of individual CBT as an adjunct to naturalistic pharmacotherapy ( 30 ). This suggests that a brief course of group psychoeducation may be as effective as a full course of individual CBT. The group psychoeducation program was a manualized, structured program of six sessions based on Bauer and McBride’s life goals program ( 17 ). It was designed to teach illness recognition and coping strategies and assist with the creation of an action plan for an individual to use when experiencing prodromes or illness triggers. Individual CBT included traditional CBT techniques in addition to an emphasis on understanding the diagnosis and course of bipolar disorder, personal warning signs, and a “relapse drill” of actions to take to reduce full-episode recurrence.
Morris and colleagues reported no significant differences between Colom and Vieta’s ( 18 ) 21-session group psychoeducation and unstructured peer-support groups ( 31 ), although attendance was higher for group psychoeducation and was associated with improved outcomes for individuals with fewer episodes. Group psychoeducation was more costly than peer support ( 32 ).
Kallestad and colleagues ( 33 ) compared three sessions of individual psychoeducation and 10 sessions of group psychoeducation, on the basis of Colom and Vieta’s ( 18 ) model. Although there were no significant group differences, there was a significant interaction between group and diagnosis. Compared with individuals with bipolar disorder type I, individuals with bipolar disorder type II benefited less from either intervention, and individuals with bipolar disorder type II receiving individual psychoeducation fared significantly worse than those receiving group psychoeducation.
Not all investigations have reported positive effects of psychoeducation. de Barros Pellegrini and colleagues ( 34 ), de Azevedo Cardoso and colleagues ( 35 ), and Gumus and colleagues ( 21 ) all compared group psychoeducation to treatment as usual and found no significant group differences. Of note, de Barros Pellegrinelli et al. reduced Colom and Vieta’s program from 21 weekly sessions to 16 sessions held twice weekly, resulting in a shorter intervention duration ( 34 ). They noted that, although the intervention did not result in a decreased risk of recurrence, the interventions were perceived as beneficial by both clinicians and patients. Gumus and colleagues decreased psychoeducation to only four sessions ( 21 ).
In aggregate, there is a strong level of evidence for psychoeducation as a maintenance treatment ( 4 ), and psychoeducation may be one of the most effective psychotherapies for bipolar disorder, especially type I ( 36 ). Psychoeducation appears to be most effective when administered in a group format ( 23 , 26 , 30 , 33 ), when delivered over several months ( 23 , 34 ), and when administered early in the course of illness ( 31 ). When resources are limited, psychoeducation may be a reasonable alternative to more costly individual modalities ( 30 ). Readers are referred to Colom and Vieta’s ( 18 ) and Bauer and McBride’s ( 17 ) manuals for full descriptions of psychoeducation.
The core objectives of CBT are to identify and change maladaptive thoughts, beliefs, and behaviors that contribute to and escalate symptoms ( 37 ). CBT for bipolar disorder rests on the premise that thoughts, feelings, and behaviors are interconnected and that shifts in mood and cognitive processes during affective episodes influence behavior, all of which can lead to a vicious cycle that contributes to illness burden. Modification of automatic thoughts and elimination of distorted thinking interrupt the problematic affective cycle. CBT includes psychoeducation, thought records, mood diaries, and activity schedules. In CBT, the clinician helps an individual link mood and thoughts, recognize and monitor symptoms and prodromes, develop behavioral strategies for symptoms, learn basic CBT techniques, improve sleep and activity routines, improve medication adherence, and resolve psychosocial problems ( 38 , 39 ) ( Table 1 ). CBT can be administered individually or in a group format (CBT-G) and has been adapted in many ways to include other strategies, such as MBCT, or to target comorbid conditions, such as integrated group therapy (IGT) for substance use in bipolar disorder.
We identified 13 RCTs with in-person CBT or cognitive therapy (CT) as the experimental condition. Two studies were described earlier in the section on psychoeducation and are not repeated here ( 25 , 30 ). For this review, we did not include variants of CBT, such as MBCT or IGT. Below, we provide brief summaries of each report and detail particularly noteworthy findings. We also discuss results of a recent meta-analysis, which included CBT and modifications.
In the earliest trial of CBT for bipolar disorder, Cochran and colleagues compared six sessions of CBT with treatment as usual ( 40 ). At six months, compared with treatment as usual, CBT was associated with significantly lower rates of discontinuing lithium against medical advice, fewer hospitalizations, and fewer episodes precipitated by lithium noncompliance.
Scott ( 41 ) investigated 25 sessions of individual CT versus a wait-list (WL) control group. At six months, CT was associated with significantly greater improvements in symptoms and functioning, compared with those of the WL group. In the WL group, relapse rates in the 18 months after commencing CT were 60% lower than those in the 18 months before commencing CT.
Lam and colleagues investigated 12–20 sessions of individual CT over six months versus treatment as usual ( 42 ). At 12 months, compared with treatment as usual, CT was associated with significantly fewer affective episodes, higher social functioning, fewer mood fluctuations, and better medication compliance. In a larger follow-up study, Lam and colleagues again compared individual CT with treatment as usual ( 38 , 43 ). CT was administered in 12 to 18 sessions over six months, followed by two booster sessions. At 12 and 30 months, the risk of relapse was significantly lower in the CT group compared with the treatment-as-usual group. At 30 months, CT was associated with a significantly longer time to depressive but not manic or hypomanic relapse.
Ball and colleagues found that, after six months of 20 sessions of CT or treatment as usual, individuals receiving CT had lower depression scores compared with individuals in treatment as usual, but the benefits of CT diminished somewhat over 12 months ( 44 ).
Miklowitz and colleagues conducted STEP-BD, a multisite project that compared the efficacy of three individual psychotherapies—CBT, IPSRT, and FFT—to a three-session psychoeducation control intervention as treatment for acute bipolar disorder depression ( 39 ). For the psychoeducation control condition, participants received an informational video and companion workbook, and sessions focused on a review of these materials. After controlling for site, family involvement, and bipolar disorder subtype, assignment to any one of the three intensive psychotherapies—compared with psychoeducation—was associated with significantly higher rates of recovery, shorter time to recovery, and greater improvement in functioning. CBT, IPSRT, and FFT were equally efficacious for both bipolar disorder types I and II.
Scott and colleagues compared 22 sessions of CBT to treatment as usual ( 45 ). They reported that, by 18 months, there were no group differences in recurrence, duration of illness episodes, or mean symptom severity. CBT was significantly more effective than treatment as usual in delaying recurrences for individuals with fewer than 12 previous episodes and significantly less effective for individuals with more than 12 episodes.
Gomes and colleagues investigated the effects of 18 sessions of CBT-G and treatment as usual over a period of 12–24 months ( 46 ). There were no group differences in time to recurrence or number of episodes, although median time to relapse was shorter in the treatment-as-usual group than in the CBT-G group.
Meyer and Hautzinger compared 20 sessions of CBT and supportive therapy ( 47 ). There were no significant group differences. Bipolar disorder subtype was a nonspecific predictor of outcomes. Those with bipolar disorder type II had a higher risk of recurrence and increased risk of depressive relapse. That is, CBT and supportive therapy were both less effective for the management of bipolar disorder type II compared with bipolar disorder type I.
Costa and colleagues found that, compared with treatment as usual, 14 sessions of CBT-G significantly reduced mood symptoms and number of episodes and improved quality of life ( 48 , 49 ).
Similarly, González Isasi and colleagues investigated the effects of group psychoeducation with CBT-G and treatment as usual over five years ( 50 ). Psychoeducation with CBT-G was associated with fewer hospitalizations at 12 months and lower rates of depression and anxiety at 12 months and five years. Over five years, 89% of the treatment-as-usual group had experienced persistent affective symptoms, compared with only 20% for group psychoeducation with CBT-G.
In sum, there is a strong level of support for CBT as an acute treatment for bipolar depression and as a maintenance treatment. Our findings are consistent with Chiang and colleagues’ meta-analysis, which concluded, with small to medium effect sizes, that CBT lowers relapse rates, improves depressive symptoms, reduces mania severity, and improves psychosocial functioning ( 51 ). They included 19 RCTs evaluating CBT-based treatments for bipolar disorder, including variants such as MBCT and IGT. They found that CBT was more effective in reducing relapse rates in bipolar disorder type I groups than in combined bipolar disorder type I and type II groups and when the session duration was 90 minutes or longer. Readers are referred to Basco and Rush ( 37 ) for a full description of CBT for bipolar disorder.
FFT is a manualized treatment developed by Miklowitz to decrease overall stress for individuals with bipolar disorder by improving family and primary relationship functioning ( 52 ) ( Table 1 ). FFT posits that unsupportive and negative interactions and high expressed emotion within the family or primary relationships increase an individual’s stress—which, in turn, increases vulnerability to developing affective symptoms and episodes. FFT involves three core phases: psychoeducation, communication enhancement training, and problem solving. First, the clinician promotes an understanding of the illness, the vulnerability-stress model, and the importance of medication adherence with the individual and his or her family member or other support. Next, the clinician helps them improve their communications through role plays and skill practice. Finally, the clinician strengthens the problem-solving abilities of both the individual and the family member or other support. FFT is typically delivered to a single individual and family (vs. multifamily).
We identified four RCTs evaluating in-person FFT as an acute treatment, a maintenance treatment, or both. One trial, which found similar benefit across active psychotherapies (IPSRT, CBT, and FFT), was discussed within the CBT results section and is not repeated here ( 39 ). In the following text, we provide brief summaries of each RCT and findings.
Miklowitz and colleagues conducted the first trial of FFT and compared 21 sessions of FFT to a comparison condition involving two psychoeducation sessions and crisis management delivered over nine months ( 53 , 54 ). At one and two years, compared with crisis management, FFT was associated with significantly fewer relapses, longer time before relapse, decreased depressive symptoms, and better medication adherence. Families with high expressed emotion benefited most.
In another study, Rea and colleagues compared nine months of FFT to individual treatment ( 55 ). At two years, compared with individual treatment, FFT was associated with significantly fewer hospitalizations and recurrences; both treatments had similar effects on time to first relapse.
Fiorillo and colleagues compared an adaptation of FFT for nontertiary settings in Italy to treatment as usual ( 56 ). FFT was associated with significantly greater improvement in social functioning and reduction of family burden, compared with treatment as usual.
There is a strong level of support for FFT as an acute treatment for depression and as a maintenance treatment ( 57 ). FFT is an efficacious and effective treatment that reduces illness burden for not only the individual but also the family. Readers are referred to Miklowitz’s ( 52 ) manual for a full description of FFT.
IPSRT is a manualized treatment developed by Frank to improve mood and stability by resolving interpersonal problems and regulating social rhythms ( 58 ). Social rhythms are those daily activities—such as time getting out of bed, first contact with another person, the start of daily activity, dinner, and time going to bed—that are thought to exert an effect on underlying biological rhythms and serve as anchors for dysregulated circadian rhythms. IPSRT is a hybrid treatment, combining the core elements of interpersonal psychotherapy for unipolar depression (IPT) ( 59 ) with a behavioral intervention, social rhythm therapy, targeting disrupted social rhythms. IPSRT includes psychoeducation and emphasizes mood and activity monitoring with the Social Rhythm Metric ( 60 ) (see Table 1 ). IPSRT rests on an “instability model” that defines three interconnected pathways to bipolar recurrences: stressful life events, medication nonadherence, and social rhythm disruption. Accordingly, life events contribute to unstable or disrupted daily routines, which lead to circadian rhythm instability and, in turn, the initiation, maintenance, or worsening of affective symptoms ( 61 , 62 ). In IPSRT, the clinician helps an individual link mood and life events, identify and manage symptoms, mourn the loss of the healthy self ( i.e., who the person would have been without bipolar disorder), resolve a primary problem area (e.g., role transitions, role disputes, interpersonal sensitivities, or grief), maintain regular daily rhythms, and predict and troubleshoot potential precipitants of rhythm dysregulation (e.g., interpersonal triggers). IPSRT typically is administered individually but can be provided in a group format ( 63 ), and the therapy has been modified for bipolar disorder type II ( 64 ). Changes include increased attention to the rationale for making changes to social rhythms; identification of mood states; regulation of levels of stimulation; and management of grandiosity, emotional dysregulation, and comorbid substance use.
We identified five RCTs evaluating in-person IPSRT as an acute treatment, a maintenance individual treatment, or both. One trial, which found similar benefit across active psychotherapies (IPSRT, CBT, and FFT), was discussed within the CBT results and is not repeated here ( 39 ). Here, we provide brief summaries of each RCT and findings.
Frank and colleagues randomly assigned acutely ill individuals to pharmacotherapy with IPSRT or intensive clinical monitoring (ICM) ( 65 ). Once stabilized, individuals were randomly reassigned to two years of monthly IPSRT or ICM maintenance treatment. Individuals assigned to IPSRT during the acute phase survived significantly longer without a new episode, regardless of maintenance treatment assignment.
Swartz and colleagues compared 12 sessions of IPSRT to flexibly dosed quetiapine for depression in an unmedicated bipolar disorder type II sample ( 66 ). Over 12 weeks, both groups experienced improvements in depressive and manic symptoms, and there were no significant differences between groups. In a follow-up study, Swartz and colleagues compared IPSRT plus placebo to IPSRT plus quetiapine for treatment of bipolar disorder type II depression ( 7 ). IPSRT plus quetiapine was associated with significantly faster improvements in depression and manic symptoms, albeit with more side effects than IPSRT alone.
Inder and colleagues compared IPSRT and specialist supportive care for a sample of young adults (ages 15 to 36 years) ( 67 , 68 ). Specialist supportive care was a manualized treatment of psychoeducation with supportive psychotherapy. After 78 weeks, there were no significant group differences. Both groups had improved depressive symptoms, social functioning, and manic symptoms.
There is a strong level of support for IPSRT as an acute treatment for depression and as a maintenance treatment. Evidence shows that IPSRT is an efficacious treatment that may be most potent during the acute phase of illness ( 39 , 65 ). When adapted for bipolar disorder type II, IPSRT may be an effective monotherapy for a subset of patients ( 7 , 66 ). Readers are referred to Frank’s manual ( 58 ) and www.ipsrt.org for more information about IPSRT.
Peer Support
Peer support includes group and one-on-one support and encompasses a variety of heterogeneous interventions. It is founded in the belief that a peer’s experiential knowledge and example of recovery is a valuable resource for an individual with a serious mental illness ( 69 , 70 ). Peer support follows a resource- versus deficit-oriented approach (see Table 1 ). Of late, the field has been moving peer support from a supportive, user-led program to a structured, supported, and trained intervention ( 71 ). Peer support may be administered as a stand-alone adjunctive treatment or combined with other strategies ( 72 ).
We identified four RCTs evaluating in-person or virtual peer support with an identified bipolar population. To clarify, there are reviews and meta-analyses of other RCTs of peer support ( 73 , 74 ), but these interventions are for severe mental illness in general and not necessarily bipolar specific. One peer-support trial was previously discussed in the context of psychoeducation trials (discussed earlier) and is not repeated here ( 31 ). In the following text, we provide brief summaries of the RCTs and findings.
Proudfoot and colleagues compared an attentional control condition and an eight-week online psychoeducation program completed alone or with the virtual support of a peer ( 72 ). Virtual support was provided entirely by e-mail and focused on self-management across three domains: medical, emotional, and role. E-mails from the peer were restricted to two 300-word communications each week. Outcomes did not differ across the three conditions. Adherence, however, was significantly higher for women, individuals over age 30, and those who had peer support.
Mahlke and colleagues compared one-on-one in-person peer support and treatment as usual over one year among individuals experiencing severe mental illness for the past two years ( 70 ). Individuals with peer support attended structured training totaling 192 hours. At one year, compared with treatment as usual, peer support was associated with greater improvements in self-efficacy. There were no group differences for quality of life, social functioning, or number of hospitalizations.
Salzer and colleagues evaluated the effectiveness of trained peer support in comparison with that of treatment as usual in a community living center for individuals with schizophrenia spectrum and affective disorders ( 75 ). Over 80% of individuals made at least one contact with peer support, but only about half had at least a second contact. Despite limited participation, engagement with peer support led to a new resource (e.g., employment, education, leisure information, referral, or support) for over half of the participants.
Overall, evidence supports the utility of peer support as a maintenance treatment; however, there are not enough data to evaluate its efficacy as an acute intervention ( 4 ). Peer support may be most helpful for improving self-efficacy and reducing isolation and stigma. When resources are limited, peer-support groups may be a reasonable alternative to more costly clinician-led group psychoeducation ( 31 ). Peer support may work best when peers receive ongoing training and support. Emerging models of peer support include online resources sponsored by peer advocacy groups such as the Depression and Bipolar Support Alliance ( www.dbsalliance.org ).
Questions and Controversy
Overall, even when clinical trials yield largely positive findings for any EBP, there are also negative results, and the benefits conferred may be limited to a few domains. In general, the extant literature suggests that adjunctive EBPs, especially psychoeducation, CBT, FFT, and IPSRT, hasten time to remission, delay time to recurrence, and improve functional outcomes. EBPs play their most important role in helping individuals develop the higher order skills needed to manage the persistent and lifelong psychosocial, neurocognitive, vocational, and interpersonal consequences of bipolar disorder.
In addition to psychoeducation, CBT, FFT, IPSRT, and peer support, several other psychotherapeutic modalities have been tested in a preliminary manner as interventions for bipolar disorder. Here, we describe additional psychosocial approaches to bipolar disorder, although each has been identified in the recent CANMAT and ISBD guidelines for bipolar disorder as interventions for which insufficient evidence exists to make treatment recommendations ( 4 ). Thus, these are approaches that do not yet have established efficacy and likely should be used after one of the interventions for which better evidence exists or in the absence of availability of one of the first-line psychotherapies.
One promising intervention is functional remediation. This is a neurocognitive intervention designed specifically to target attention, memory, and executive functioning deficits associated with bipolar disorder ( 76 ). Functional remediation includes 21 structured group sessions providing neurocognitive techniques, psychoeducation on cognition-related issues, and problem solving to enhance functioning. We found two trials of functional remediation demonstrating its positive effects on bipolar disorder outcomes ( 76 , 77 ).
Another potentially useful intervention is MBCT, a “third-wave” behavioral therapy centered on tenets of mindfulness and acceptance. In MBCT the emphasis is on noticing (versus changing) the thinking process and formal mindfulness practices, including meditations and yoga ( 78 , 79 ). MBCT varies in structure and content and may be delivered individually or in a group format. There are some bipolar-disorder-specific modifications within individual RCTs ( 78 ). We identified three trials with encouraging findings in support of MBCT for bipolar disorder ( 79 ).
Illness management and recovery has promise as a treatment for bipolar disorder. This is a structured program developed to help improve illness outcomes and recovery among individuals with serious mental illness, including bipolar disorder ( 80 ). The treatment includes skills training and components of psychoeducation, CBT, and peer support. We found four trials of illness management and recovery ( 81 – 84 ), three of which demonstrated the advantages of that treatment over treatment as usual.
Last, adjunctive psychotherapies that utilize modern technologies are promising and may help increase access to efficacious treatments. We identified 12 trials of technology-assisted interventions for bipolar disorder. Most of the interventions included both psychoeducation and mood monitoring, and some included elements of CBT ( 85 – 87 ). Additionally, some include personalized interactions with a health care provider in a clinical setting, either through a technology platform or in person ( 88 – 91 ). Results have been mixed and inconsistent, and one study found that a technology-assisted intervention worsened depression ( 89 ). Nonetheless, the proliferation of Internet and mobile phone use, coupled with the limited access to EBPs for bipolar disorder, underscores the importance of pursuing technology-assisted interventions ( 92 ).
Recommendations
Overall, our systematic review demonstrates that clinicians who treat individuals with bipolar disorder have more options at their disposal than just pharmacotherapy. The evidence base supporting the efficacy of bipolar disorder–specific psychotherapies is substantial ( 4 , 16 , 93 , 94 ). Although the utility of adding antidepressant medication to a mood stabilizer for the management of bipolar depression remains a controversial strategy ( 95 , 96 ), adding psychotherapy is clearly beneficial and well supported by the evidence. Clinicians should consider adjunctive psychoeducation, CBT, FFT, or IPSRT for acute depression and maintenance treatments, as well as peer support for maintenance treatment. Although insufficient, there is some preliminary but positive evidence for functional remediation, MBCT, illness management and recovery, and technology-assisted strategies. At a minimum, psychoeducation should be offered to all, especially for relapse prevention, and the addition of another EBP should be based on individual concerns, characteristics, or deficits ( 4 ). To date, the literature provides little information about which treatment works for whom, and choice of treatment most likely will be driven by availability and patient preference. Indeed, there is some evidence that individuals with bipolar disorder do better when they receive the treatment they prefer, inclusive of psychotherapy ( 7 ).
Previously, we have argued that several strategies are common to almost all of the EBPs for bipolar disorder ( 97 ). These include education about the illness, education about medications, a review of medication side effects, promotion of regular sleep-wake cycles, daily monitoring of mood, discussion of prodromes and related approaches to relapse prevention, and direct involvement of family members and significant others or, at a minimum, consideration of their role in the maintenance of wellness. Although these therapy elements have not been tested apart from their parent EBPs, it would be reasonable to conceptualize these strategies as core components of bipolar disorder illness management. They may, for instance, be incorporated into psychopharmacology visits when separate psychotherapy sessions are not available or not acceptable to the patient.
Unmet Needs and Future Directions
Although therapy clearly plays an important role in the management of bipolar disorder, there is more to be done. EBPs, though efficacious, remain difficult to access for many individuals with the disorder. Technology-enabled solutions offer the promise of extending the reach of these very helpful treatments, but remote access therapies remain in the early stages of testing. In addition, one size does not fit all. Despite the availability of several EBPs, more treatments are needed to address the complex needs of individuals with bipolar disorder. Specifically, treatments that are designed to target common psychiatric comorbidities (e.g., alcohol use disorders, personality disorders, and anxiety disorders), medical comorbidities (e.g., cardiovascular disease and cerebrovascular disease), treatment resistance, and bipolar disorder in an aging population are needed to round out the therapeutic armamentarium ( 5 , 16 ).
In summary, although pharmacotherapy remains the cornerstone of bipolar disorder treatment, medication alone rarely suffices to bring about a full and enduring recovery. Psychotherapy is increasingly recognized as a central component of care, providing patients with much needed skills to assist with illness management and social functioning. In the past decade, sufficient evidence has accumulated to allow recommendations for the use of therapy in the maintenance (e.g., psychoeducation, CBT, FFT, IPSRT, and peer support) and depressive (CBT, FFT, and IPSRT) phases of illness, according to international clinical treatment guidelines ( 4 ). When used in conjunction with medication, bipolar disorder–specific therapies hasten time to remission, delay time to recurrence, and improve functional outcomes. They should be considered a key strategy in evidence-based approaches to caring for individuals with bipolar disorder.
Dr. Novick reports no financial relationships with commercial interests. Dr. Swartz has received consulting fees from Otsuka and Myriad Genetics, grant support from Myriad Genetics, royalties from UpToDate, and an editorial stipend from American Psychiatric Association Publishing for her role as editor of the American Journal of Psychotherapy .

IMAGES
VIDEO
COMMENTS
Abstract. Bipolar disorder is a severe, complicated, and often misunderstood disorder that can have serious impacts on a person's quality of life, sense of self-worth, and overall health. This ...
Abstract. Objective: This article reviews the epidemiology, etiology, assessment, and management of bipolar disorder. Special attention is paid to factors that complicate treatment, including nonadherence, comorbid disorders, mixed mania, and depression. Methods: A Medline search was conducted from January of 1990 through December of 2005 using ...
Prevalence. Lifetime and 12 month prevalence for bipolar I disorder have been estimated at 2.1% and 1.5%, respectively, based on criteria from the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) Citation 4; rates for men and women are similar Citation 3.The prevalence of bipolar disorder decreases with increasing age and education level, while its prevalence ...
The Bipolar Illness Onset (BIO) study is the first study aiming to identify (1) a composite blood-based biomarker, (2) a composite electronic smartphone-based biomarker and (3) a neurocognitive signature for bipolar disorder. The same biomarkers will be measured longitudinally in newly diagnosed/first-episode patients with bipolar disorder and ...
Abstract. Bipolar disorders are a complex group of severe and chronic disorders that includes bipolar I disorder, defined by the presence of a syndromal, manic episode, and bipolar II disorder, defined by the presence of a syndromal, hypomanic episode and a major depressive episode. Bipolar disorders substantially reduce psychosocial ...
Bipolar I disorder is defined by the presence of a syndromal, manic episode, and has an estimated global lifetime prevalence of 0·6-1·0%. 1. Bipolar II disorder is defined by the presence of a syndromal, hypomanic episode and a major depressive episode, and has an estimated global lifetime prevalence of 0·4-1·1%. 1.
Introduction. Bipolar disorder (BD) is a chronic illness associated with severely debilitating symptoms that can have profound effects on both patients and their caregivers (Miller, 2006).BD typically begins in adolescence or early adulthood and can have life‐long adverse effects on the patient's mental and physical health, educational and occupational functioning, and interpersonal ...
Cosgrove VE, Kelsoe JR, Suppes T. Toward a valid animal model of bipolar disorder: how the research domain criteria help bridge the clinical-basic science divide. Biol Psychiatry. 2016;79:62-70.
Context: Despite the high morbidity associated with bipolar disorder (BP), few studies have prospectively studied the course of this illness in youth. Objective: To assess the longitudinal course of BP spectrum disorders (BP-I, BP-II, and not otherwise specified [BP-NOS]) in children and adolescents. Design: Subjects were interviewed, on ...
Abstract. Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that afect around 2% of the world's population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a ...
Bipolar disorder is a broad diagnostic construct associated with significant phenotypic and genetic heterogeneity challenging progress in clinical practice and discovery research. Prospective studies of well-c... Anne Duffy and Paul Grof. International Journal of Bipolar Disorders 2024 12 :12.
Bipolar disorder (BD) is a severe psychiatric illness with an increasing prevalence worldwide. Although the pathological mechanism of and pharmacological interventions for BD have been extensively investigated in preclinical and clinical studies, a scientometric analysis of the developmental trends, interdisciplinary frontiers, and research hotspots in this field has not yet been conducted.
Abstract. Bipolar disorder (BD) is a leading cause of global disability. Its biological basis is unknown, and its treatment unsatisfactory. Here, we review two recent areas of progress. First, the discovery of risk genes and their implications, with a focus on voltage-gated calcium channels as part of the disease process and as a drug target.
Abstract Objectives: Over the past two decades, there has been tremendous growth in research regarding bipolar disorder (BD) among children and adolescents (ie, pediatric BD [PBD]). The primary purpose of this article is to distill the extant literature, dispel myths or exaggerated assertions in the field, and disseminate clinically relevant ...
Bipolar disorder (BD) is a chronic psychiatric disorder that combines hypomania or mania and depression. The study aims to investigate the research areas associated with cognitive function in bipolar disorder and identify current research hotspots and frontier areas in this field. Publications related to cognitive function in BD from 2012 to 2022 were searched on the Web of Science Core ...
Abstract and Figures. Bipolar disorder is a mental illness that causes dramatic shifts in a person's mood, energy and ability to think clearly. People with bipolar experience high and low moods ...
abstract = "This paper aims to review current literature around bipolar disorder from a multidisciplinary stance. As a result of a literature search, several key themes have been identified which will be discussed during this paper: first, the definition of bipolar disorders, their epidemiology and the effect of the illness on outcome, and secondly pharmacological interventions, psychosocial ...
Abstract. Bipolar disorder is characterised by recurrent and alternating episodes of mania/hypomania and depression. Current breakthroughs in functional MRI techniques have uncovered the functional neuroanatomy of bipolar disorder. However, the pathophysiology underlying mood instability, mood switching and the development of extreme mood ...
Introduction. Bipolar affective disorder (bipolar) is a multicomponent illness involving episodes of severe mood disturbance, neuropsychological deficits, immunological and physiological changes, and disturbances in functioning. 1 It is one of the leading causes of disability worldwide 2 and is associated with high rates of premature mortality from both suicide and medical comorbidities. 3,4
Abstract. Bipolar disorder is a common psychiatric condition that is one of the leading causes of disability worldwide. As a dynamic, recurrent, and chronic illness, it can be complex to identify and manage. In this Primer on text, leading international authors explore aspects of clinical presentation epidemiology, etiology, neurobiology, and ...
Bipolar Disorders publishes research of relevance to the basic mechanisms, clinical aspects, or treatment of bipolar disorders and related illnesses. Abstract Introduction Alterations in motor activity are well-established symptoms of bipolar disorder, and time series of motor activity can be considered complex dynamical systems.
Polysomnographic data was retrospectively collated for 120 adult patients with sleep complaints and depressive symptoms referred to a specialized sleep clinic for sleep assessment [60 diagnosed with bipolar disorder (70% female, mean age= 43.4±11.6 years) and 60 age-matched cases diagnosed with a unipolar depressive disorder (68.3% female, mean age= 43.2±11.6 years)], and 60 age-matched ...
Current status of depression in bipolar disorder. Depression in bipolar disorder (BD) is the major residual psychiatric morbidity with available treatments, accounting for three-quarters of the 40-50% long-term time-ill. Unresolved morbidity, and especially depression, is associated with excess medical morbidity, including metabolic syndrome ...
Abstract Bipolar Disorder is a mental illness in which a person's mood alternates between extreme mania and depression. The present study reviewed recent research to determine the trends in bipolar disorder to promote a better understanding of and response to the problem. The main issues discussed in the study include the definition of bipolar disorder, causes, sign and symptoms of this mental ...
Abstract. Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that affect around 2% of the world's population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a ...
Abstract. Bipolar disorder is a recurrent psychiatric disorder marked by waxing and waning affective symptoms and impairment in functioning. Some of the morbidity and mortality associated with the illness may be reduced with evidence-based psychotherapies (EBPs) along with pharmacotherapy. To enhance clinicians' understanding of which therapy ...