An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Malays Fam Physician
- v.17(1); 2022 Mar 28

Case scenario: Management of major depressive disorder in primary care based on the updated Malaysian clinical practice guidelines
Uma visvalingam.
MBBS (MAHE), Master of Medicine (Psychiatry) (UKM), Department of Psychiatry and Mental Health, Hospital Putrajaya, Putrajaya, Malaysia
Umi Adzlin Silim
MD (UKM), M. Med (Psychiatry) (UKM), Department of Psychiatry and Mental Health, Hospital Serdang, Serdang, Selangor, Malaysia
Ahmad Zahari Muhammad Muhsin
MB., BCh., BAO (UCD, Ireland), M. Psych Med (Malaya), Department of Psychological Medicine, Faculty of Medicine Universiti Malaya, Kuala Lumpur, Malaysia
Firdaus Abdul Gani
MBBS (Malaya) M.Med (Psy) (USM) CMIA (NIOSH), Department of Psychiatry and Mental Health, Hospital Sultan Haji Ahmad Shah, Temerloh, Pahang, Malaysia
Noormazita Mislan
MB, BCh, BAO (Ireland), M Med. (Psychiatry) (UKM), Department of Psychiatry and Mental Health, Hospital Tuanku Ja'afar, Seremban, Negeri Sembilan, Malaysia
Noor Izuana Redzuan
MBBS (Malaya), Dr in Psychiatry (UKM), Department of Psychiatry and Mental Health, Hospital Raja Permaisuri Bainun, Ipoh, Perak, Malaysia
Peter Kuan Hoe Low
MB, BCh, BAO (Ireland), M.Psych Med (UM), Department of Psychiatry and Mental Health, Hospital Kuala Lumpur, Kuala Lumpur, Malaysia
Sing Yee Tan
MBBS (Malaya), M.Med (Family Med) (UM), Klinik Kesihatan Jenjarom, Jenjarom Selangor, Malaysia
Masseni Abd Aziz
MD (USM) M Med (Fammed) USM, Klinik Kesihatan Umbai, Merlimau, Melaka, Malaysia
Aida Syarinaz Ahmad Adlan
MBBS (Malaya), M. Psych Med (UM), PostGrad. Dip. (Dynamic Psychotherapy) (Mcgill University), Department of Psychological Medicine, Faculty of Medicine, Universiti Malaya Kuala, Lumpur, Malaysia
Suzaily Wahab
MD (UKM), MMed Psych (UKM), Hospital Canselor Tuanku Muhriz UKM, Kuala Lumpur, Malaysia
Aida Farhana Suhaimi
B. Psych (Adelaide), M. Psych (Clin. Psych) (Tasmania), PhD (Psychological Medicine) (UPM), Department of Psychiatry and Mental Health, Hospital Putrajaya, Putrajaya, Malaysia
Nurul Syakilah Embok Raub
BPharm (Hons) (CUCMS), MPH (Malaya), Pharmacy Enforcement Branch, Selangor Health State Department, Shah Alam, Selangor, Malaysia
Siti Mariam Mohtar
BPharm (UniSA), Malaysian Health Technology Assessment Section (MaHTAS), Ministry of Health Malaysia, Putrajaya, Malaysia
Mohd Aminuddin Mohd Yusof
MD (UKM), MPH (Epidemiology) (Malaya), Malaysian Health Technology Assessment Section (MaHTAS), Ministry of Health Malaysia, Putrajaya, Malaysia, Email: moc.oohay@rd2ma
Major depressive disorder (MDD) is a common but complex illness that is frequently presented in the primary care setting. Managing this disorder in primary care can be difficult, and many patients are underdiagnosed and/or undertreated. The Malaysian Clinical Practice Guidelines (CPG) on the Management of Major Depressive Disorder (MDD) (2nd ed.), published in 2019, covers screening, diagnosis, treatment and referral (which frequently pose a challenge in the primary care setting) while minimising variation in clinical practice.
Introduction
MDD is one of the most common mental illnesses encountered in primary care. It presents with a combination of symptoms that may complicate its management.
This mental disorder requires specific treatment approaches and is projected to be the leading cause of the disease burden in 2030. 1 Patients experiencing this ailment are at elevated risk for early mortality from physical disorders and suicide. 2 In Malaysia in particular, MDD contributes to 6.9% of total Years Living with Disability. 3
Ensuring full functional recovery and prevention of relapse makes remission the targeted outcome for treatment of MDD. In contrast, nonremission of depressive symptoms in MDD can impact functionality 4 and subsequently amplify the economic burden that the illness imposes.
About the new edition
The highlights of the updated CPG MDD (2nd ed.) are as follows:
- emphasis on psychosocial and psychological interventions, particularly for mild to moderate MDD
- inclusion of all second-generation antidepressants as the first-line pharmacotherapy
- introduction of new emerging treatments, ie. intravenous ketamine for acute phase and intranasal esketamine for next-step treatment/treatment-resistant MDD
- improvement in pre-treatment screening and monitoring of treatment
- integration of mental health into other health services with emphasis on collaborative care
- addition of 2 new chapters on special populations (pregnancy and postpartum, chronic medical illness) and table on safety profile of pharmacotherapy in pregnancy and breastfeeding
- comprehensive, holistic biopsychosocial-spiritual approaches addressing psychospirituality
Details of the evidence supporting the above statements can be found in Clinical Practice Guidelines on the Management of Major Depressive Disorder (2nd ed.) 2019, available on the following websites: http://www.moh.gov.my (Ministry of Health Malaysia) and http://www.acadmed.org.my (Academy of Medicine). Corresponding organisation: CPG Secretariat, Health Technology Assessment Section, Medical Development Division, Ministry of Health Malaysia; contactable at ym.vog.hom@aisyalamath .
Statement of intent
This is a support tool for implementation of CPG Management of Major Depressive Disorder (2nd ed.).
Healthcare providers are advised of their responsibility to implement this evidence-based CPG in their local context. Such implementation will lead to capacity building to ensure better accessibility of psychosocial and psychological services. More options in pharmacotherapy facilitate flexibility in prescribing antidepressants among clinicians. Further integration of mental health into other health services, upscaling of mental health service development in perinatal and medical services, and enhancement of collaborative care will incorporate holistic approaches into care.
Case Scenario
Tini is a female college student aged 24 years old. She comes to the health clinic accompanied by a friend and complains of several symptoms that she has experienced over the past 4 weeks. She reports:
- difficulty falling asleep, feeling tired after waking up in the morning and experiencing headaches
- difficulty staying focused during classes. These symptoms have led to deterioration in her study and prompted her to seek advice from the doctor.
Will you screen her for depression?
Yes, because the patient presents with multiple vague symptoms and sleep disturbance. 5 (Refer to Subchapter 2.1, page 3 in CPG.)
What tools are used to screen for depression?
Screening tools for depression are:
- Beck Depression Inventory (BDI)
- Depression Anxiety and Stress Scale (DASS)
- Patient Health Questionnaire-9 (PHQ-9)
- Hospital Anxiety and Depression Scale (HADS)
- Whooley Questions
Screening for depression using Whooley Questions in primary care may be considered in people at risk. 5
( Refer to Subchapter 2.1, pages 3 and 4 in CPG. )
- “During the past month, have you often been bothered by feeling down, depressed or hopeless?”
- “During the past month, have you often been bothered by having little interest or pleasure in doing things?
The doctor decides to use Whooley Questions, and Tini answers “yes” to both questions.
How would you proceed from here to further assess for depression?
Assessment of depression consists of:
- detailed history taking (Refer to Subchapter 2.2, page 4 in CPG.)
- mental state examination (MSE), including evaluation of symptom severity, presence of psychotic symptoms and risk of harm to self and others
- physical examination to rule out organic causes
- investigations where indicated — biological and psychosocial investigations
Upon further assessment, Tini reveals that she feels overwhelmingly sad. She is frequently tearful and reports feeling excessively guilty, blaming herself for not performing well enough in her studies. Her postings on social media have been revolving around themes of self-defeat. Despite feeling low, she still strives to attend classes and complete her assignments. However, her academic performance has exhibited a marked deterioration. There is no history to suggest hypomanic, manic or psychotic symptoms. She denies using any illicit substances or alcohol. Her menstrual cycle is normal and does not correspond to her mood changes.
MSE reveals a young lady who appears to be in distress. Rapport is easily established, but her eyes are downcast. Her speech is relevant, with low tone. She describes her mood as sad; she is tearful while talking about her poor results, with appropriate affect. She harbours multiple unhelpful thoughts, eg. “I’m a failure” and “I’m useless”. She exhibits no suicidal ideations, delusions or hallucinations. Her concentration is poor, and insight is partial.
Physical examination reveals no recent selfharm scars, and examination of other systems is unremarkable. Biological investigations such as full blood count and thyroid function test are within normal range. Corroborative history is taken from accompanying person to verify the symptoms.
How would you arrive at the diagnosis and severity?
Diagnosis of depression can be made using the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) or the 10th revision of the International Statistical Classification of Disease and Related Health Problems (ICD-10). 5 (Refer to Appendix 3 and 4, pages 73-76 in CPG.) 6 , 7
In the last 2 weeks, Tini has been experiencing:
- poor concentration
- excessive guilt
These symptoms have caused marked impairment in her academic functioning. Thus, she is diagnosed as having MDD with mild to moderate severity in acute phase and can be treated in primary care.
Severity according to DSM-5
- Five or more symptoms are present, which cause distress but are manageable
- Result in minor impairment in social or occupational functioning
- Symptom presentation and functional impairment between 2 severities
- Most of the symptoms are present with marked impairment in functioning
What can be offered to this patient?
Psychosocial interventions and psychotherapy with or without pharmacotherapy. 5 (Refer to Algorithm 1. Treatment of Major Depressive Disorder, page xii in CPG)
ALGORITHM 1. TREATMENT OF MAJOR DEPRESSIVE DISORDER

Psychosocial interventions include the following:
- symptoms and course of depression
- biopsychosocial model of aetiology
- pharmacotherapy for acute phase and maintenance
- drug side effects and complications
- importance of medication adherence
- early signs of recurrence
- management of relapse and recurrence
- counselling/non-directive supportive therapy - aims to guide the person in decision-making and allow to ventilate their emotions
- relaxation - a method to help a person attain a state of calmness, eg. breathing exercise, progressive muscle relaxation, relaxation imagery
- peer intervention - eg. peer support group
- exercise - activity of 45-60 minutes per session, up to 3 times per week, and prescribed for 10-12 weeks
(Refer to subchapter 4.1.1, pages 9-12 in CPG.)
However, the doctor may choose to start antidepressant medication as an initial measure in some situations, for example:
- past history of moderate to severe depression
- patient’s preference
- previous response to antidepressants
- lack of response to non-pharmacotherapy interventions
What are the types of psychotherapy that can be offered in mild to moderate MDD, and what factors should be considered before starting psychotherapy?
Psychotherapy for the treatment of MDD has been shown to reduce psychological distress and improve recovery through the therapeutic relationship between the therapist and the patient.
In mild to moderate MDD, psychosocial intervention and psychotherapy should be offered, based on resource availability, and may include but are not restricted to the following 5 :
- Cognitive behavioural therapy (CBT)
- Interpersonal therapy
- Problem-solving therapy
- Behavioural therapy
- Internet-based CBT
The type of psychotherapy offered to the patient will depend on various factors, including 5 :
- patient preference and attitude
- nature of depression
- availability of trained therapist
- therapeutic alliance
- availability of therapy
(Refer to Subchapter 4.1.1, page 17 in CPG.)
After shared-decision making, Tini receives psychosocial intervention, that includes:
- psychoeducation
- non-directive supportive therapy
- lifestyle modification, e.g. restoring healthy sleep hygiene and adopting healthy eating habits
- relaxation, e.g. progressive muscle relaxation, imagery and breathing technique
Tini will benefit from CBT due to her multiple unhelpful thoughts, for example, “I’m a failure” and “I’m useless”.
CBT helps improve understanding of the impact of a person’s unhelpful thoughts on current behaviour and functioning through cognitive restructuring and a behavioural approach. By learning to correctly identify these negative thinking patterns, Tini can then challenge such thoughts repeatedly to replace disordered thinking with more rational, balanced and healthy thinking. However, she is not able to commit to regular sessions of CBT due to a demanding academic schedule and upcoming final examination. After further discussion, Tini opts for pharmacotherapy.
What are the options for pharmacotherapy?
The choice of antidepressant medication will depend on various factors, including efficacy and tolerability, patient profile and comorbidities, concomitant medications and drug-drug interactions, cost and availability, as well as the patient’s preference. Taking into account efficacy and side effect profiles, most second-generation antidepressants, namely selective serotonin reuptake inhibitors (SSRIs), serotonin noradrenaline reuptake inhibitors (SNRIs), noradrenergic and specific serotonergic antidepressants (NaSSAs), melatonergic agonist and serotonergic antagonist, noradrenaline/dopamine-reuptake inhibitors (NDRIs) and a multimodal antidepressants may be considered as the initial treatment medication, while the older antidepressants such as tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) may be subsequently considered for a later choice. 5 (Refer to Subchapter 4.1.2, page 18 in CPG.)
Since Tini is being seen at a health clinic, the widely available SSRIs are sertraline and fluvoxamine. Sertraline has fewer gastrointestinal side effects and drug interactions compared with fluvoxamine. TCAs are not the treatment of choice due to prominent side effects. Tini is put on tablet sertraline 50 mg daily and educated on the anticipated onset of response and possible side effects. Short-term and low dose benzodiazepine, eg. alprazolam or lorazepam, may be offered as an adjunct to treat her insomnia. (Refer to Subchapter 4.1.2, page 24 in CPG.) Tini is given tablet lorazepam 0.5 mg at night for 2 weeks. She is asked to come in for a follow-up.
What is her follow-up and monitoring plan?
The following should be done:
(Refer to Appendix 8, page 81 in CPG.)
- Titrate up by 50 mg within 1-2 weeks (but may be done earlier based on clinical judgement)
- Monitor biological parameters if indicated (Refer to Table 5. Ongoing monitoring during treatment of MDD, page 57 in CPG.)
During follow-up at 2 weeks, she is noted to show partial response despite being compliant with good tolerability. She is not experienceing nausea, diarrhoea, headache, constipation, dry mouth or somnolence. She reports being less tearful. Her sleep and ability to focus have improved. Tini has started engaging in regular exercise and practises relaxation, especially before sleep. Tablet sertraline is optimised to 100 mg daily, while tablet lorazepam is reduced to 0.5 mg PRN.
Tini is reviewed again within 4 weeks; during this subsequent follow-up, she achieves full remission. Tablet lorazepam is stopped. She is then advised to continue tablet sertraline for at least 6-9 months in maintenance phase. The aim in this phase is to prevent relapse and recurrence of MDD. In view of her young age, no comorbidities and good tolerability, repeated electrolyte monitoring is not indicated.
(Refer to Algorithm 2. Pharmacotherapy for Major Depressive Disorder, page xiii in CPG.)
ALGORITHM 2. PHARMACOTHERAPY FOR MAJOR DEPRESSIVE DISORDER


Mental Health Case Study: Understanding Depression through a Real-life Example
Imagine feeling an unrelenting heaviness weighing down on your chest. Every breath becomes a struggle as a cloud of sadness engulfs your every thought. Your energy levels plummet, leaving you physically and emotionally drained. This is the reality for millions of people worldwide who suffer from depression, a complex and debilitating mental health condition.
Understanding depression is crucial in order to provide effective support and treatment for those affected. While textbooks and research papers provide valuable insights, sometimes the best way to truly comprehend the depths of this condition is through real-life case studies. These stories bring depression to life, shedding light on its impact on individuals and society as a whole.
In this article, we will delve into the world of mental health case studies, using a real-life example to explore the intricacies of depression. We will examine the symptoms, prevalence, and consequences of this all-encompassing condition. Furthermore, we will discuss the significance of case studies in mental health research, including their ability to provide detailed information about individual experiences and contribute to the development of treatment strategies.
Through an in-depth analysis of a selected case study, we will gain insight into the journey of an individual facing depression. We will explore their background, symptoms, and initial diagnosis. Additionally, we will examine the various treatment options available and assess the effectiveness of the chosen approach.
By delving into this real-life example, we will not only gain a better understanding of depression as a mental health condition, but we will also uncover valuable lessons that can aid in the treatment and support of those who are affected. So, let us embark on this enlightening journey, using the power of case studies to bring understanding and empathy to those who need it most.
Understanding Depression
Depression is a complex and multifaceted mental health condition that affects millions of people worldwide. To comprehend the impact of depression, it is essential to explore its defining characteristics, prevalence, and consequences on individuals and society as a whole.
Defining depression and its symptoms
Depression is more than just feeling sad or experiencing a low mood. It is a serious mental health disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities that were once enjoyable. Individuals with depression often experience a range of symptoms that can significantly impact their daily lives. These symptoms include:
1. Persistent feelings of sadness or emptiness. 2. Fatigue and decreased energy levels. 3. Significant changes in appetite and weight. 4. Difficulty concentrating or making decisions. 5. Insomnia or excessive sleep. 6. feelings of guilt, worthlessness, or hopelessness. 7. Loss of interest or pleasure in activities.
Exploring the prevalence of depression worldwide
Depression knows no boundaries and affects individuals from all walks of life. According to the World Health Organization (WHO), an estimated 264 million people globally suffer from depression. This makes depression one of the most common mental health conditions worldwide. Additionally, the WHO highlights that depression is more prevalent among females than males.
The impact of depression is not limited to individuals alone. It also has significant social and economic consequences. Depression can lead to impaired productivity, increased healthcare costs, and strain on relationships, contributing to a significant burden on families, communities, and society at large.
The impact of depression on individuals and society
Depression can have a profound and debilitating impact on individuals’ lives, affecting their physical, emotional, and social well-being. The persistent sadness and loss of interest can lead to difficulties in maintaining relationships, pursuing education or careers, and engaging in daily activities. Furthermore, depression increases the risk of developing other mental health conditions, such as anxiety disorders or substance abuse.
On a societal level, depression poses numerous challenges. The economic burden of depression is significant, with costs associated with treatment, reduced productivity, and premature death. Moreover, the social stigma surrounding mental health can impede individuals from seeking help and accessing appropriate support systems.
Understanding the prevalence and consequences of depression is crucial for policymakers, healthcare professionals, and individuals alike. By recognizing the significant impact depression has on individuals and society, appropriate resources and interventions can be developed to mitigate its effects and improve the overall well-being of those affected.
The Significance of Case Studies in Mental Health Research
Case studies play a vital role in mental health research, providing valuable insights into individual experiences and contributing to the development of effective treatment strategies. Let us explore why case studies are considered invaluable in understanding and addressing mental health conditions.
Why case studies are valuable in mental health research
Case studies offer a unique opportunity to examine mental health conditions within the real-life context of individuals. Unlike large-scale studies that focus on statistical data, case studies provide a detailed examination of specific cases, allowing researchers to delve into the complexities of a particular condition or treatment approach. This micro-level analysis helps researchers gain a deeper understanding of the nuances and intricacies involved.
The role of case studies in providing detailed information about individual experiences
Through case studies, researchers can capture rich narratives and delve into the lived experiences of individuals facing mental health challenges. These stories help to humanize the condition and provide valuable insights that go beyond a list of symptoms or diagnostic criteria. By understanding the unique experiences, thoughts, and emotions of individuals, researchers can develop a more comprehensive understanding of mental health conditions and tailor interventions accordingly.
How case studies contribute to the development of treatment strategies
Case studies form a vital foundation for the development of effective treatment strategies. By examining a specific case in detail, researchers can identify patterns, factors influencing treatment outcomes, and areas where intervention may be particularly effective. Moreover, case studies foster an iterative approach to treatment development—an ongoing cycle of using data and experience to refine and improve interventions.
By examining multiple case studies, researchers can identify common themes and trends, leading to the development of evidence-based guidelines and best practices. This allows healthcare professionals to provide more targeted and personalized support to individuals facing mental health conditions.
Furthermore, case studies can shed light on potential limitations or challenges in existing treatment approaches. By thoroughly analyzing different cases, researchers can identify gaps in current treatments and focus on areas that require further exploration and innovation.
In summary, case studies are a vital component of mental health research, offering detailed insights into the lived experiences of individuals with mental health conditions. They provide a rich understanding of the complexities of these conditions and contribute to the development of effective treatment strategies. By leveraging the power of case studies, researchers can move closer to improving the lives of individuals facing mental health challenges.
Examining a Real-life Case Study of Depression
In order to gain a deeper understanding of depression, let us now turn our attention to a real-life case study. By exploring the journey of an individual navigating through depression, we can gain valuable insights into the complexities and challenges associated with this mental health condition.
Introduction to the selected case study
In this case study, we will focus on Jane, a 32-year-old woman who has been struggling with depression for the past two years. Jane’s case offers a compelling narrative that highlights the various aspects of depression, including its onset, symptoms, and the treatment journey.
Background information on the individual facing depression
Before the onset of depression, Jane led a fulfilling and successful life. She had a promising career, a supportive network of friends and family, and engaged in hobbies that brought her joy. However, a series of life stressors, including a demanding job, a breakup, and the loss of a loved one, began to take a toll on her mental well-being.
Jane’s background highlights a common phenomenon – depression can affect individuals from all walks of life, irrespective of their socio-economic status, age, or external circumstances. It serves as a reminder that no one is immune to mental health challenges.
Presentation of symptoms and initial diagnosis
Jane began noticing a shift in her mood, characterized by persistent feelings of sadness and a lack of interest in activities she once enjoyed. She experienced disruptions in her sleep patterns, appetite changes, and a general sense of hopelessness. Recognizing the severity of her symptoms, Jane sought help from a mental health professional who diagnosed her with major depressive disorder.
Jane’s case exemplifies the varied and complex symptoms associated with depression. While individuals may exhibit overlapping symptoms, the intensity and manifestation of those symptoms can vary greatly, underscoring the importance of personalized and tailored treatment approaches.
By examining this real-life case study of depression, we can gain an empathetic understanding of the challenges faced by individuals experiencing this mental health condition. Through Jane’s journey, we will uncover the treatment options available for depression and analyze the effectiveness of the chosen approach. The case study will allow us to explore the nuances of depression and provide valuable insights into the treatment landscape for this prevalent mental health condition.
The Treatment Journey
When it comes to treating depression, there are various options available, ranging from therapy to medication. In this section, we will provide an overview of the treatment options for depression and analyze the treatment plan implemented in the real-life case study.
Overview of the treatment options available for depression
Treatment for depression typically involves a combination of approaches tailored to the individual’s needs. The two primary treatment modalities for depression are psychotherapy (talk therapy) and medication. Psychotherapy aims to help individuals explore their thoughts, emotions, and behaviors, while medication can help alleviate symptoms by restoring chemical imbalances in the brain.
Common forms of psychotherapy used in the treatment of depression include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and psychodynamic therapy. These therapeutic approaches focus on addressing negative thought patterns, improving relationship dynamics, and gaining insight into underlying psychological factors contributing to depression.
In cases where medication is utilized, selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed. These medications help rebalance serotonin levels in the brain, which are often disrupted in individuals with depression. Other classes of antidepressant medications, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) or tricyclic antidepressants (TCAs), may be considered in specific cases.
Exploring the treatment plan implemented in the case study
In Jane’s case, a comprehensive treatment plan was developed with the intention of addressing her specific needs and symptoms. Recognizing the severity of her depression, Jane’s healthcare team recommended a combination of talk therapy and medication.
Jane began attending weekly sessions of cognitive-behavioral therapy (CBT) with a licensed therapist. This form of therapy aimed to help Jane identify and challenge negative thought patterns, develop coping strategies, and cultivate more adaptive behaviors. The therapeutic relationship provided Jane with a safe space to explore and process her emotions, ultimately helping her regain a sense of control over her life.
In conjunction with therapy, Jane’s healthcare provider prescribed an SSRI medication to assist in managing her symptoms. The medication was carefully selected based on Jane’s specific symptoms and medical history, and regular follow-up appointments were scheduled to monitor her response to the medication and adjust the dosage if necessary.
Analyzing the effectiveness of the treatment approach
The effectiveness of treatment for depression varies from person to person, and it often requires a period of trial and adjustment to find the most suitable intervention. In Jane’s case, the combination of cognitive-behavioral therapy and medication proved to be beneficial. Over time, she reported a reduction in her depressive symptoms, an improvement in her overall mood, and increased ability to engage in activities she once enjoyed.
It is important to note that the treatment journey for depression is not always linear, and setbacks and challenges may occur along the way. Each individual responds differently to treatment, and adjustments might be necessary to optimize outcomes. Continuous communication between the individual and their healthcare team is crucial to addressing any concerns, monitoring progress, and adapting the treatment plan as needed.
By analyzing the treatment approach in the real-life case study, we gain insights into the various treatment options available for depression and how they can be tailored to meet individual needs. The combination of psychotherapy and medication offers a holistic approach, addressing both psychological and biological aspects of depression.
The Outcome and Lessons Learned
After undergoing treatment for depression, it is essential to assess the outcome and draw valuable lessons from the case study. In this section, we will discuss the progress made by the individual in the case study, examine the challenges faced during the treatment process, and identify key lessons learned.
Discussing the progress made by the individual in the case study
Throughout the treatment process, Jane experienced significant progress in managing her depression. She reported a reduction in depressive symptoms, improved mood, and a renewed sense of hope and purpose in her life. Jane’s active participation in therapy, combined with the appropriate use of medication, played a crucial role in her progress.
Furthermore, Jane’s support network of family and friends played a significant role in her recovery. Their understanding, empathy, and support provided a solid foundation for her journey towards improved mental well-being. This highlights the importance of social support in the treatment and management of depression.
Examining the challenges faced during the treatment process
Despite the progress made, Jane faced several challenges during her treatment journey. Adhering to the treatment plan consistently proved to be difficult at times, as she encountered setbacks and moments of self-doubt. Additionally, managing the side effects of the medication required careful monitoring and adjustments to find the right balance.
Moreover, the stigma associated with mental health continued to be a challenge for Jane. Overcoming societal misconceptions and seeking help required courage and resilience. The case study underscores the need for increased awareness, education, and advocacy to address the stigma surrounding mental health conditions.
Identifying the key lessons learned from the case study
The case study offers valuable lessons that can inform the treatment and support of individuals with depression:
1. Holistic Approach: The combination of psychotherapy and medication proved to be effective in addressing the psychological and biological aspects of depression. This highlights the need for a holistic and personalized treatment approach.
2. Importance of Support: Having a strong support system can significantly impact an individual’s ability to navigate through depression. Family, friends, and healthcare professionals play a vital role in providing empathy, understanding, and encouragement.
3. Individualized Treatment: Depression manifests differently in each individual, emphasizing the importance of tailoring treatment plans to meet individual needs. Personalized interventions are more likely to lead to positive outcomes.
4. Overcoming Stigma: Addressing the stigma associated with mental health conditions is crucial for individuals to seek timely help and access the support they need. Educating society about mental health is essential to create a more supportive and inclusive environment.
By drawing lessons from this real-life case study, we gain insights that can improve the understanding and treatment of depression. Recognizing the progress made, understanding the challenges faced, and implementing the lessons learned can contribute to more effective interventions and support systems for individuals facing depression.In conclusion, this article has explored the significance of mental health case studies in understanding and addressing depression, focusing on a real-life example. By delving into case studies, we gain a deeper appreciation for the complexities of depression and the profound impact it has on individuals and society.
Through our examination of the selected case study, we have learned valuable lessons about the nature of depression and its treatment. We have seen how the combination of psychotherapy and medication can provide a holistic approach, addressing both psychological and biological factors. Furthermore, the importance of social support and the role of a strong network in an individual’s recovery journey cannot be overstated.
Additionally, we have identified challenges faced during the treatment process, such as adherence to the treatment plan and managing medication side effects. These challenges highlight the need for ongoing monitoring, adjustments, and open communication between individuals and their healthcare providers.
The case study has also emphasized the impact of stigma on individuals seeking help for depression. Addressing societal misconceptions and promoting mental health awareness is essential to create a more supportive environment for those affected by depression and other mental health conditions.
Overall, this article reinforces the significance of case studies in advancing our understanding of mental health conditions and developing effective treatment strategies. Through real-life examples, we gain a more comprehensive and empathetic perspective on depression, enabling us to provide better support and care for individuals facing this mental health challenge.
As we conclude, it is crucial to emphasize the importance of continued research and exploration of mental health case studies. The more we learn from individual experiences, the better equipped we become to address the diverse needs of those affected by mental health conditions. By fostering a culture of understanding, support, and advocacy, we can strive towards a future where individuals with depression receive the care and compassion they deserve.
Similar Posts

Auvelity: Understanding the Link Between Auvelity and Depression
Auvelity: Understanding the Link Between Auvelity and Depression Imagine waking up every day with a heavy cloud weighing down on your mind, making it difficult to find joy, motivation, or even the will to get out…

Understanding Bipolar Seizure Symptoms: A Comprehensive Guide
Imagine living with two conditions that can cause extreme mood swings and unpredictable seizures. It may sound overwhelming, but for individuals with both bipolar disorder and epilepsy, it is a reality they face every day. Bipolar…

Understanding the Relationship Between PMDD and BPD: Common Misdiagnosis as Bipolar Disorder
Do you ever feel like your emotions are on a rollercoaster, leaving you unsure of what to expect from one day to the next? If so, you may be familiar with the challenges of dealing with…

Living with a Bipolar Husband: Finding Support and Understanding in Forums
Living with a Bipolar Husband: Finding Support and Understanding in Forums Navigating the challenges of bipolar disorder within a relationship can be an emotional rollercoaster, both for the individual living with the condition and their partner….

Can Low Testosterone Cause Anxiety? Exploring the Link and Related Effects
Imagine waking up every day with a sense of unease, your heart racing and your mind clouded with worry. This state of perpetual anxiety can be both mentally and physically exhausting, making even the simplest tasks…

How Much Money Do You Get for Bipolar Disability: A Guide to Understanding Bipolar Disability Benefits
Living with bipolar disorder can be a challenging journey. The highs and lows, the constant battle with your own mind, and the impact it has on your daily life can leave you feeling exhausted. But did…

- Fundamentals of Bipolar Disorder
Fundamentals of Major Depressive Disorder
- Fundamentals of Schizophrenia
- Fundamentals Certificate Program
- Clinical Article Summaries
- Events Calendar
- Interactive Case Study
- Psychopharmacology
- Test Your Knowledge
- Psychiatric Scale NPsychlopedia
- Psychotherapy NPsychlopedia
- Caregiver Resources
- Educate Your Patient
- Quick Guides
- Clinical Insights
- NP Spotlight
- Peer Exchanges
Top results
Patient case navigator: major depressive disorder.

Introduction
Learning Objectives
- How to perform a structured psychiatric interview
- Standardized psychiatric rating scales appropriate for patients with depressive symptoms
- Common barriers to adequate treatment response
- How to assess and monitor patients for treatment side effects and adequate treatment response
Watch the video:
History and Examination
Medical History
Examination
History of Present Illness
Eric is a 60-year-old man who presents to his primary care nurse practitioner, Tina, with irritability, excessive sleeping, and a lack of interest in his usual hobbies, such as attending baseball games and going to the movies with his wife. He also has been spending much time at home alone, watching television, rather than spending time with his friends or wife, as he usually does. Eric recently retired from his job as a general contractor remodeling people’s kitchens and bathrooms. He enjoyed his job very much and felt a sense of pride in helping people make their homes more functional and attractive. However, his job was very physical, and at times stressful, so Eric felt it was time to retire and find something new with which to occupy his time.
Eric was diagnosed with hypothyroidism 5 years ago and has been on medication ever since. Annual lab tests indicate his thyroid levels have remained within the normal range for the past few years. He also has mild hypertension, which is well-controlled at an adequate dose.
Psychosocial History
Eric reports that he has several close friends and that he got along well with people at work. He denies a history of substance misuse and reports that he occasionally drinks a glass of wine with dinner. He does not smoke. Eric describes his marriage as “very good.” He is also close with his adult daughter and enjoys spending time with his 2 grandchildren.
At age 33, Eric experienced a period of depressed mood after losing his job. During that time, he had problems getting out of bed in the morning because he felt hopeless and sad, stopped socializing with friends, and lost about 4 lbs of body weight in 4 weeks without intentionally dieting. He sought treatment from his primary care physician, who referred him to a psychiatrist for medication and a psychologist for outpatient cognitive-behavioral therapy (CBT). Eric worked with his psychiatrist and tried 4 different selective serotonin reuptake inhibitors (SSRIs) before he ultimately found one that seemed to work for him. He and his psychiatrist decided together that he could stop taking the medication after 1 year because his mood had improved and stabilized. He saw his therapist once weekly for approximately 2.5 years and reports that CBT also helped improve his mood and functioning.
Family History
Eric reports that, throughout his life, his mother had “very low periods” when she seemed extremely sad and had trouble functioning. However, she never sought treatment for these episodes.
Eric’s physical examination indicates he is generally healthy for his age. His vital signs are all within the normal range, and the mental status examination indicates he is fully oriented and alert. Eric’s appearance is that of an older man. His affect is flat, and he has trouble making eye contact, often staring at the floor instead.
Patient Interview
Quiz #1: initial presentation and diagnosis, dsm-5 diagnostic criteria for mdd.
MDE Diagnostic Criteria
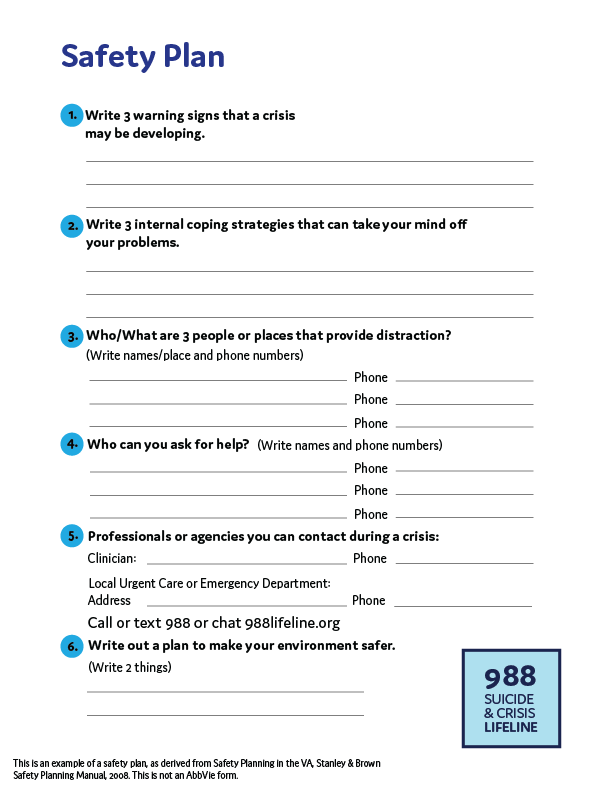
Safety Plan
Major Depressive Episode (MDE)
A. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous function; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure.
- Depressed mood most of the day, nearly every day, as indicated by either subjective report or observation made by others
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day
- Significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day
- Insomnia or hypersomnia nearly every day
- Psychomotor agitation or retardation nearly every day
- Fatigue or loss of energy nearly every day
- Feelings of worthlessness or excessive or inappropriate guilt nearly every day
- Diminished ability to think or concentrate, or indecisiveness, nearly every day
- Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide
B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of function
C. The episode is not attributable to the physiological effects of a substance or another medical condition
Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- It is important to thoroughly review each of these 9 symptoms with your patients when assessing them for MDD.
- Clinical rating scales can help identify which patients require more in-depth screening for depression.
Quiz #2: DSM-5 Diagnostic Criteria for MDD
Scales for mdd.
PHQ-9 Scale Scoring
QIDS Scale Scoring
Patient Health Questionnaire-9 (PHQ-9)
| Over the last 2 weeks, how often have you been bothered by any of the following problems? (Use "✓" to indicate your answer) | Not at all | Several days | More than half the days | Nearly every day |
|---|---|---|---|---|
| 1. Little interest or pleasure in doing things | 0 | 1 | 2 | 3 |
| 2. Feeling down, depressed, or hopeless | 0 | 1 | 2 | 3 |
| 3. Trouble falling or staying asleep, or sleeping too much | 0 | 1 | 2 | 3 |
| 4. Feeling tired or having little energy | 0 | 1 | 2 | 3 |
| 5. Poor appetite or overeating | 0 | 1 | 2 | 3 |
| 6. Feeling bad about yourself - or that you are a failure or have let yourself or your family down | 0 | 1 | 2 | 3 |
| 7. Trouble concentrating on things, such as reading the newspaper or watching television | 0 | 1 | 2 | 3 |
| 8. Moving or speaking slowly that other people could have noticed? Or the opposite - being so fidgety or restless that you have been moving around a lot more that usual | 0 | 1 | 2 | 3 |
| 9. Thoughts that you would be better off dead or of hurting yourself in some way | 0 | 1 | 2 | 3 |
| For Office Coding: | 0 | + | + | + |
| = | Total Score: | _____ |
| If you checked off any problems, how difficult have those problems made it for you to do your work, take care of things at home, or get along with other people? | |||
|---|---|---|---|
| Not difficult at all | Somewhat difficult | Very difficult | Extremely difficult |
This scale was developed by Drs Robert L. Spitzer, Janet B.W. Williams, Kurt Kroenke, and colleagues with an educational grant from Pfizer inc. No permission required.
Scoring Criteria
| 0-4 | No depression |
| 5-9 | Mild depression |
| 10-14 | Moderate depression |
| 15-19 | Moderately severe depression |
| 20-27 | Severe depression |
Kroenke K, Spitzer RL. Psychiatric Annals. 2002;32:509-521.
The Quick Inventory of Depressive Symptomatology (QIDS)
- The QIDS is a 16-item, multiple-choice questionnaire in which depressive symptoms are rated on a 0-3 scale according to severity
- Items are derived from the 9 diagnostic criteria for major depressive disorder used in the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV), including sadness, loss of interest or pleasure, poor concentration or decision-making, self-outlook, suicidal ideation, lack of energy, sleep disturbance, appetite change, and psychomotor agitation
- Although the QIDS was initially developed based on DSM-IV criteria, the scale is also compatible with the DSM-5. The core criteria for MDD are consistent across these editions
Rush AJ, et al. Biol Psychiatry. 2003;54(5):573-583.
| 0-5 | Normal |
| 6-10 | Mild |
| 11-15 | Moderate |
| 16-20 | Severe |
| ≥ 21 | Very Severe |
Bernstein IH, et al. Int J Methods Psychiatr Res. 2009;18(2):138-146.
Quiz #3: Scales for MDD
Treatment initiation and monitoring.
APA Guidelines
Eric's PHQ-9 Score
Treatment Options
American Psychiatric Association (APA) Guidelines for Treatment of MDD
1-2 weeks: Improvement from pharmacologic therapy can be seen as early as 1-2 weeks after starting treatment
2-4 weeks: Some patients may achieve improvement in 2-4 weeks
4-6 weeks: Short-term efficacy trials show antidepressant therapy appears to require 4-6 weeks to achieve maximum therapeutic effects
4-8 weeks: The APA recommends 4-8 weeks of adequate* treatment is needed before concluding that a patient is partially responsive or unresponsive to treatment *Adequate dose and duration Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
*Adequate dose and duration
Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
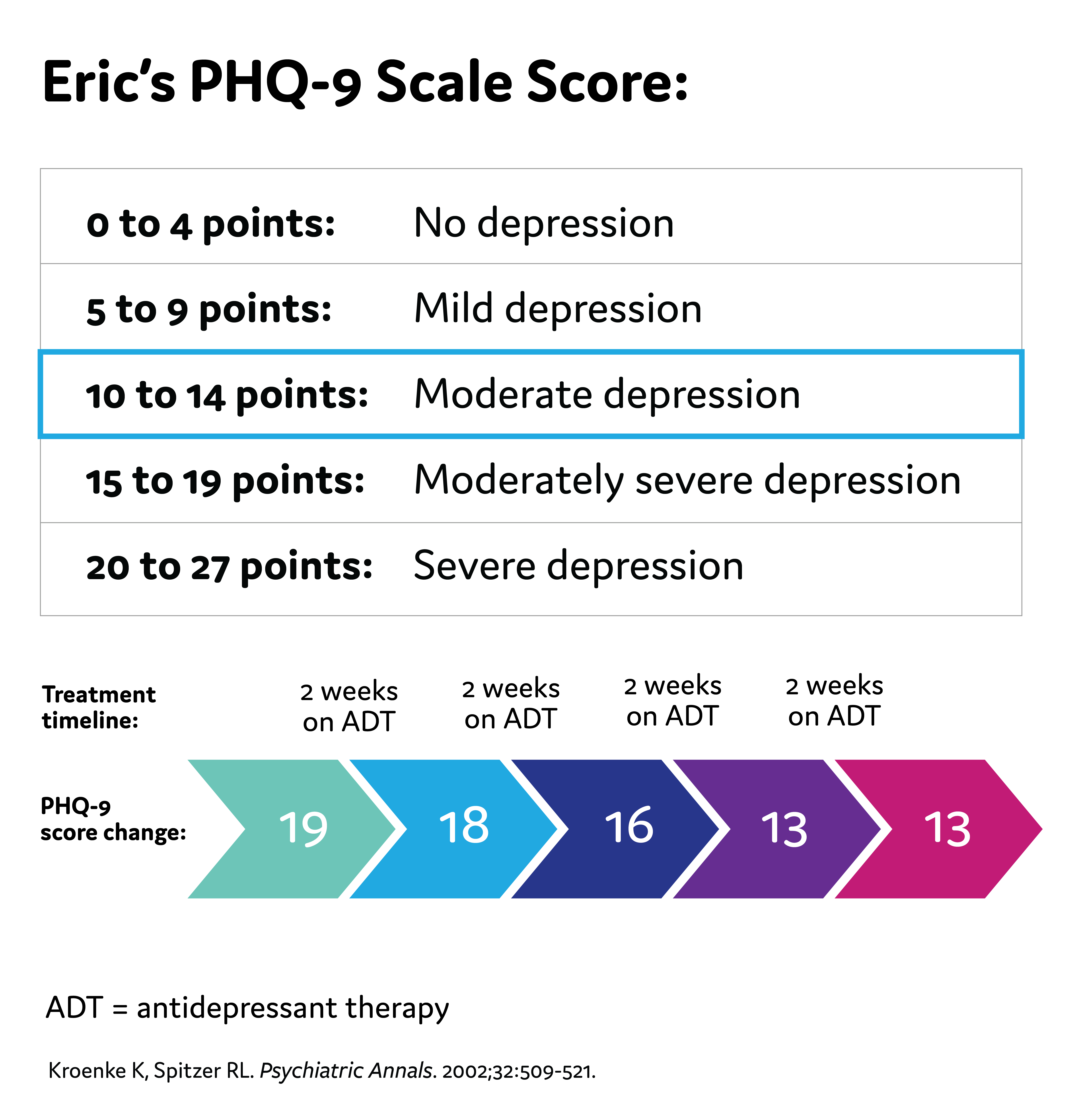
Quiz #4: Treatment Initiation and Monitoring
Assessing for treatment challenges.
Treatment Challenges
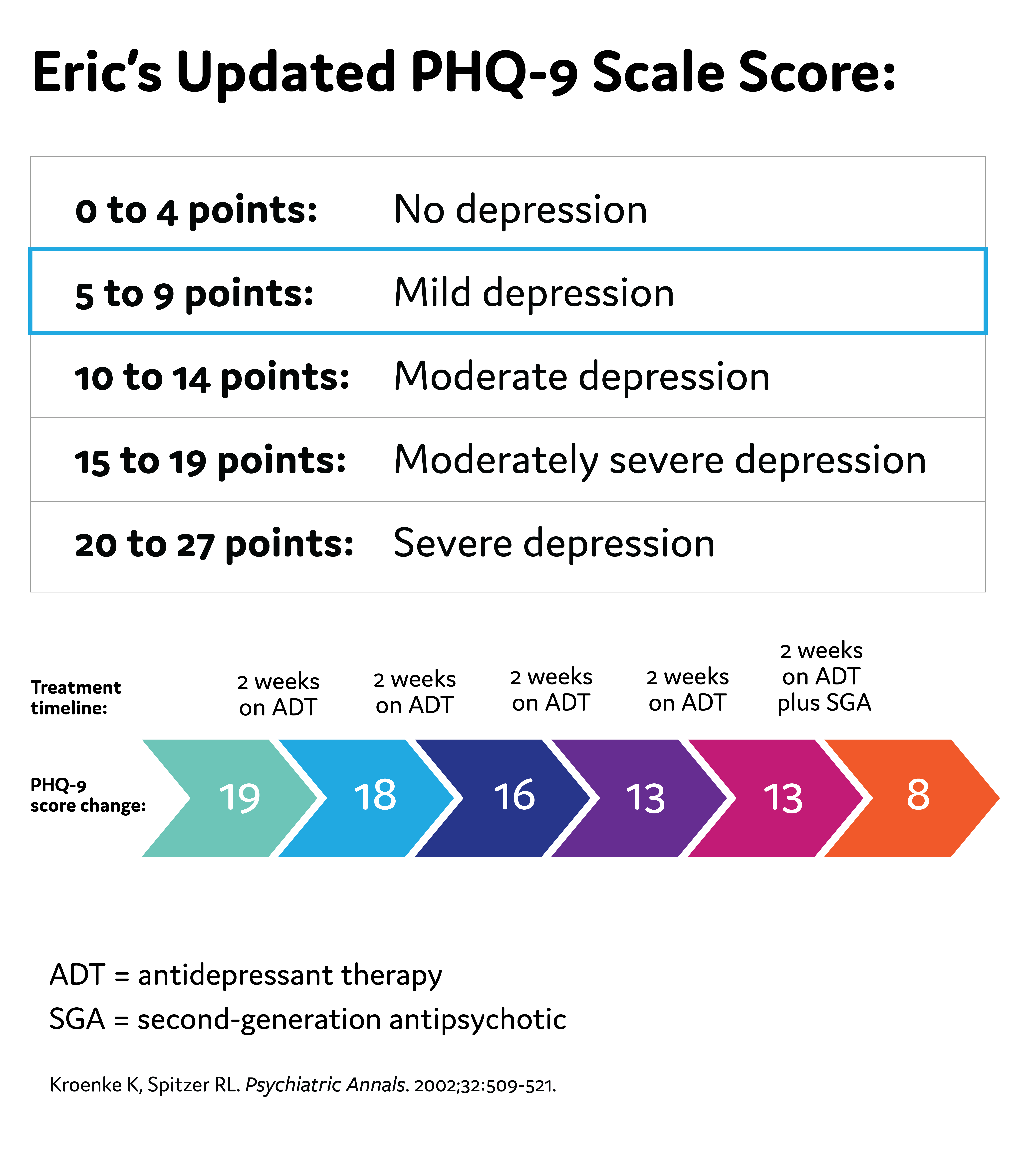
Eric's Updated PHQ-9 Score
Possible Challenges to Antidepressant Therapy
- Suboptimal efficacy due to the wrong dose, inadequate length of time on the medication, or the person's individual biology not being responsive to the medication
- Unpleasant side effects of antidepressants can occur, such as weight gain, insomnia, and sexual dysfunction
- Nonadherence to the antidepressant
- As a reminder, the American Psychiatric Association (APA) recommends 4-8 weeks of adequate* treatment is needed before concluding that a patient is partially responsive or unresponsive to treatment
Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
MDD Diagnosis
Clinical Probes
Treatment Assessment
Monitoring Considerations
Factors to Consider When Making a MDD Diagnosis
- Take a thorough patient history
- Previous or current depressive episodes
- Previous or current manic or hypomanic episodes
- Family history of MDD, bipolar disorder
- Medical comorbidities
- Consider a broad differential diagnosis
Clinical Queries That Aid in Diagnosing Major Depressive Episodes
| DSM-5 Criteria | Clinical Queries |
|---|---|
| 1. Depressed mood most of the day, nearly every day | 1. Have you been experiencing persistent feelings of low mood, sadness, or hopelessness? |
| 2. Markedly diminished interest or pleasure in activities most of the day, nearly every day | 2. Have you noticed a decrease in interest or pleasure in activities that you once enjoyed? |
| 3. Significant change in weight or appetite | 3. Have your eating habits changed, either with a decrease or increase in appetite? |
| 4. Insomnia or hypersomnia | 4. Have you noticed and changes in your sleep patterns? |
| 5. Psychomotor agitation or retardation | 5. Have you felt unusually restless or fidgety, or slower than usual in your movements or speech? |
| 6. Fatigue or loss of energy | 6. Have you been feeling more tired and consistently low on energy? |
| 7. Feelings of worthlessness or excessive or inappropriate guilt | 7. Have you been struggling with feelings of low self-worth? |
| 8. Diminished ability to think or concentrate, or indecisiveness | 8. Are you finding it difficult to concentrate or think clearly? |
| 9. Recurrent thoughts of death or suicidal ideation | 9. Have you been having thoughts about death or harming yourself? |
1. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. American Psychiatric Association; 2013. 2. Kroenke K, et al. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613.
APA Practice Guidelines on Treatment Assessment
- Wait 4 to 8 weeks to assess treatment response to antidepressants
- In patients without adequate response, clinicians can consider changing or augmenting with a second medication
- Changes to treatment plans, such as augmenting with a second-generation antipsychotic medication, are reasonable if a patient does not have adequate improvement in 6 weeks
- Consistently follow-up with patients to assess treatment effects, adverse medication effects, and risk of self-harm
APA Practice Guidelines note that the frequency of monitoring should be based on:
- Symptom severity (including suicidal ideation)
- Co-occurring disorders (including general medical conditions)
- Treatment adherence
- Availability of social supports
- Frequency and severity of side effects with medication

Tina Matthews-Hayes is a paid consultant for Abbvie Medical Affairs and was compensated for her time.
American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders . 5th ed. American Psychiatric Association; 2013.
- Kapfhammer HP. Somatic symptoms in depression. Dialogues Clin Neurosci . 2006;8(2):227-239.
- Bobo WV. The diagnosis and management of bipolar I and II disorders: clinical practice update. Mayo Clin Proc . 2017;92(10):1532-1551.
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med . 2001;16:606-613.
- Smarr KL, Keefer AL. Measures of depression and depressive symptoms. Arthritis Care Res . 2011;63(S11):S454-S466. doi:10.1002/acr.20556
- Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573-583.
- Brown ES, Murray M, Carmody TJ, et al. The Quick Inventory of Depressive Symptomatology–Self-report: a psychometric evaluation in patients with asthma and major depressive disorder. Ann Allergy Asthma Immunol. 2008;100(5):433-438. doi:10.1016/S1081-1206(10)60467-X
- Liu R, Wang F, Liu S, et al. Reliability and validity of the Quick Inventory of Depressive Symptomatology-Self-Report Scale in older adults with depressive symptoms. Front Psychiatry . 2021;12:686711. doi:10.3389/fpsyt.2021.686711
- Bernstein IH, Rush AJ, Suppes T, et al. A psychometric evaluation of the clinician-rated Quick Inventory of Depressive Symptomatology (QIDS-C16) in patients with bipolar disorder. Int J Methods Psychiatr Res . 2009;18(2):138-146. doi:10.1002/mpr.2855
- Bernstein IH, Rush AJ, Trivedi MH, et al. Psychometric properties of the Quick Inventory of Depressive Symptomatology in adolescents. Int J Methods Psychiatr Res. 2010;19(4):185-194. doi:10.1002/mpr.321
- Kroenke K. Enhancing the clinical utility of depression screening. CMAJ . 2012;184(3):281-282.doi:10.1503/cmaj.112004
- Levinstein MR, Samuels BA. Mechanisms underlying the antidepressant response and treatment resistance. Front Behav Neurosci . 2014;8:208. doi:10.3389/fnbeh.2014.00208
- Haddad PM, Talbot PS, Anderson IM, McAllister-Williams RH. Managing inadequate antidepressant response in depressive illness. Br Med Bull. 2015;115(1):183-201. doi:10.1093/bmb/ldv03
This resource is intended for educational purposes only and is intended for US healthcare professionals. Healthcare professionals should use independent medical judgment. All decisions regarding patient care must be handled by a healthcare professional and be made based on the unique needs of each patient.
This is not a diagnostic tool and is not intended to replace a clinical evaluation by a healthcare provider.
Reach out to your family or friends for help if you have thoughts of harming yourself or others, or call the National Suicide Prevention Helpline for information at 800-273-8255.
ABBV-US-00976-MC, V1.0 Approved 12/2023 AbbVie Medical Affairs
Recommended on NP Psych Navigator
Disease Primer
Major depressive disorder (MDD) is one of the most recognized mental disorders in the United States. Learn more about the prevalence, pathophysiology, diagnosis, and management of MDD here.
Clinical Article
State-Dependent Differences in Emotion Regulation Between Unmedicated Bipolar Disorder and Major Depressive Disorder
Rive et al use functional MRI to look at some of the differences between patients with bipolar depression and major depressive disorder.
Unrecognized Bipolar Disorder in Patients With Depression Managed in Primary Care: A Systematic Review and Meta-Analysis
Daveney et al explore the characteristics of patients with mixed symptoms, as compared to those without mixed symptoms, in both bipolar disorder and major depressive disorder.
Welcome To NP Psych Navigator
This website is intended for healthcare professionals inside the United States. Please confirm that you are a healthcare professional inside the US.
You are now leaving NP Psych Navigator
Links to sites outside of NP Psych Navigator are provided as a resource to the viewer. AbbVie Inc accepts no responsibility for the content of non-AbbVie linked sites.
Redirect to:

- myCME Login
- Monthly CME eNewsletter

Live Events
Text-based cme, journal cme, self-study cme, major depressive disorder, brian barnett, md jeremy weleff, do, case report.
A 24-year-old female presents to the outpatient clinic with abdominal pain. She describes vague symptoms of gastrointestinal distress. A physical examination reveals no emergent clinical signs.
In talking with her, the patient suddenly becomes tearful. She reports sadness for the last month, inability to experience pleasure, and trouble staying asleep at night. She is notably fatigued, lacks appetite, and skipped work multiple times in the last week, which is unusual for her. She ended a long-term romantic relationship during this period and notes that, “no one would want to be with me anyway.” She denies alcohol or drug use. She denies suicidal thoughts but notes that she is thinking more about death lately and increasingly feels that life may not be worth living.
Her only medication is an oral contraceptive pill. Past medical evaluations that included basic lab tests have shown no abnormalities.
What is the most likely clinical diagnosis?
- Hypothyroidism
- Alcohol use disorder
- Adjustment disorder with depressed mood
- Personality disorder
- Major depressive disorder
Correct! Answer:
Major depressive disorder (MDD) is one of the most common psychiatric illnesses and a common diagnosis in primary care clinics. Point prevalence of depression ranges around 5% (with considerable variation among countries), and it commonly ranks among the top conditions and causes considerable burden of disease. 1 Despite this, the rates of correct recognition of depression in primary care are only around 47%, with even fewer patients receiving adequate treatment or reaching remission. 2,3
The patient in this scenario meets at least six of the criteria for MDD — depressed mood, anhedonia, insomnia, fatigue, feelings of worthlessness, and recurrent thoughts of death. Importantly, during the past 2 weeks, she has at least one of the core diagnostic symptoms: depressed mood or loss of interest or pleasure (anhedonia). Symptoms should also cause clinically significant distress or impairment in social, occupational, or other important areas of functioning and not be caused by another psychiatric disorder. The full diagnostic criteria for MDD are listed on Table 1. 4
Another important diagnostic consideration is that the episode should not be attributable to the physiological effects of substance use or another medical condition. A complete medical workup for common mimics of depression and ruling out concurrent alcohol or drug use is key to diagnostic precision. Alcohol and drug use and withdrawal syndromes can mimic symptoms of depression, and treatment for these conditions requires much different steps than the treatment of MDD. The patient in this scenario didn’t present with any concerns for these diagnostic considerations. Because the patient meets criteria for a major depressive disorder, this cannot be classified as an adjustment disorder, which is milder.
| A. | Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning; at least 1 of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Which of the following best describes risk factor(s) for the development of MDD?
There are several risk factors for depression to consider when gathering clinical evidence to support (or suggest against) a diagnosis of MDD (Table 2). 4 A family history of depression in first-degree family members is thought to increase risk of MDD by 2- to 4-fold 5 and should always be obtained during the initial assessment of a patient with concerns of depression. Trauma and adverse childhood events are thought to be linked to increased incidence of many psychiatric illnesses, and they cause an earlier age of symptom onset, increased symptom severity, and worsened treatment responses in MDD. 6,7
What is another component of the patient’s history that should always be assessed during an initial clinical encounter for depression?
As always, diagnostic precision is a key to appropriate treatment and improved outcomes in depression care. Misdiagnosis of bipolar disorder I/II comes with considerable risk as rates of suicide with bipolar disorder are possibly 15 times greater than baseline, and suicide is one of the leading causes of death in this population. Clinical overlap between MDD and bipolar disorder is significant, as 90% of patients with a history of mania/bipolar I go on to have recurrent mood episodes. Approximately 60% of manic episodes occur before a major depressive episode, making questions about manic episodes a valuable tool for accurate diagnosis. In addition, the first-line treatments of bipolar depression are mood stabilizers and atypical antipsychotics rather than classic antidepressants. 4,8 A family history of bipolar disorder is thought to lead to an average 10-fold increased risk among adult relatives of individuals with bipolar disorders, making it one of the largest risk factors. Mania or hypomania that emerges during antidepressant treatment (eg, psychotropic medication, electroconvulsive therapy) should raise strong and immediate concern for a diagnosis of bipolar disorder rather than MDD. Traditionally, the introduction of antidepressants — first noticed with older tricyclic antidepressants and later with other classes such as selective serotonin reuptake inhibitors — in someone with bipolar disorder could precipitate mania. Although that remains an important treatment consideration, the incidence of this occurrence and the possible neurobiological causes is not clear. Mania is a psychiatric emergency that requires immediate psychiatric consultation and/or psychiatric admission. Patients who are manic often do not perceive that they are ill and will sometimes engage in uncharacteristically dangerous behaviors that can lead to interactions with police or other problems with serious potential for harm (eg, gambling, serious financial difficulties, physical assaults, suicide). Prominent delusions or psychotic symptoms can also put these patients at risk of harming themselves or others. The following define mania/hypomania:
An episode should not be attributable to the physiological effects of a substance (eg, drug of abuse, medication, other treatment) or another medical condition. By definition, during the period of mood disturbance and increased energy or activity, three (or more) of the following symptoms (four if the mood is only irritable) are present to a significant degree and represent a noticeable change from usual behavior:
For mania, the mood disturbance is sufficiently severe to cause marked impairment in social or occupational functioning, or to necessitate hospitalization to prevent harm to self or others, or if there are psychotic features. For hypomania, the episode is associated with an unequivocal change in functioning that is uncharacteristic of the individual when not symptomatic, but it does not cause marked impairment in functioning or lead to psychiatric admission. If the presence of psychotic features during hypomania emerges, then the diagnosis is then changed to mania (and subsequently bipolar I). Which of the following conditions should be on the differential diagnosis in a patient presenting with concerns about depression?
Many conditions can resemble MDD, so one should be attentive to its broad differential when considering MDD as a diagnosis. 4,9,10 Alcohol and many illicit substances can cause substance induced mood disorders, so screening patients for substance use is an important part of the workup. Additionally, some medications such as barbiturates, vigabatrin, topiramate, flunarizine, corticosteroids, mefloquine, efavirenz, and interferon-alpha can cause depression. Adjustment disorder with depressed mood is a condition that occurs in response to an identifiable stressor within 3 months of the stressor’s onset. Adjustment disorder is characterized by marked distress that is out of proportion to the severity or intensity of the stressor and causes significant impairment in social, occupational, or other important areas of functioning. Adjustment disorder does not persist for more than 6 months after a stressor or its consequences terminate. If a patient develops enough symptoms to meet the criteria for MDD, they cannot be diagnosed with an adjustment disorder because the MDD diagnosis takes precedence. Attention-deficit/hyperactivity disorder (ADHD) causes problems with concentration that can be similar to those produced by depression. ADHD is frequently misdiagnosed in people who have MDD. If a patient mentions attention problems, it is important to screen for ADHD as well as depression. Finally, the experience of sadness by itself does not constitute a psychiatric condition. It is only in the context of other symptoms recognized as part of MDD, along with impairment in function, that sadness becomes part of a psychiatric condition that should be treated. What is the first treatment step for mild MDD?
First-line treatments for individuals with mild depression include psychoeducation, self-management, and psychological treatments. Pharmacological treatments can be considered for mild depression in some situations, such as patient preference, previous improvement with antidepressants, or lack of response to other nonpharmacological interventions. 9,11 Assessment of severity and monitoring treatment response in depression care should incorporate the use of measurement-based outcomes (clinician-administered or patient-reported scales such as PHQ-9). The severity of MDD is determined by number of symptoms, symptom severity, depression scores on assessment tools, or by the practitioner’s clinical judgment of patient functioning. Of the following, which is the most appropriate first-line pharmacological treatment for moderate to severe MDD?
Table 3 shows the commonly used medications for first- and second-line treatment of moderate to severe MDD. The selective serotonin reuptake inhibitors are generally well-tolerated, which makes them the preferred first-line treatment for moderate to severe depression. 9,11 It should be noted that most patients will require an increase in dose or a change in medication. This is best exemplified by the remission rates found in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial, which were only 36.8% for the first treatment. 12 Thus, it is important for the practitioner to bring the patient to an adequate treatment dose before giving up on a medication. Common pitfalls in initiating treatment for MDD are inadequate dose adjustments, inadequate duration of medication trial (prescribe for at least 3 months at therapeutic dose), and diagnostic errors. There are a few additional considerations to make if there is suspicion for MDD with a specifier or other prominent clinical symptoms. These include the following:
Table 3: Commonly used first- and second-line pharmacological treatment of moderate and severe depression with treatment dose range.
NDRI = norepinephrine dopamine reuptake inhibitor; SNRIs = serotonin norepinephrine reuptake inhibitors; SSRIs = selective serotonin reuptake inhibitors A patient with MDD presents with positive suicidal ideation, what is the next step in care?
Patients with MDD are at increased risk of completing suicide or engaging in other suicidal behavior. Patients with depression, bipolar disorder, borderline personality disorder, and anorexia nervosa generally have the highest suicide risks. 13 There are many critical clinical steps to mitigate the risks for completing suicide and many standardized clinical assessment tools that can aid in determining risk and identifying modifiable risk factors. 14-17
While there is ongoing debate about how accurate these tools are in predicting suicide, clinically their importance remains paramount, and their use is recommended by the U.S. National Strategy for Suicide Prevention. 18 Using a standardized tool helps to identify important modifiable risk factors for suicide and to complete suicide risk documentation. Complete documentation of a risk assessment, as well as the steps that were taken to reduce risk, are key components of good clinical care and reducing liability risk. 19
Assessment of the nature of suicidal ideation — frequency, intensity, and characteristics of thoughts — as well as the presence of any planning or intent to suicide are the first steps. Suicide planning and intent generally require emergent psychiatric inpatient stabilization. Removing access to lethal means, treating underlying psychiatric disorders, and abstaining from alcohol and drug use are the three primary clinical targets in modifying suicide risk. In monitoring treatment response in depression, what is the definition of remission?
It is expected that symptom abatement should occur, generally, within the first 3 months of treatment with pharmacologic or psychological interventions. If the patient has an improvement in symptoms after 2 to 4 weeks, then treatment should continue for another 6 to 8 weeks. If the patient has remission of symptoms at that time, then the duration of antidepressant treatment is guided by the presence of risk factors for recurrence. If the patients has risk factors, then treatment should generally continue for 2 years or longer. Without risk factors, treatment should continue for approximately 6 to 9 months. Risk factors for recurrence that prompt longer antidepressant treatment include the following:
Other factors that contribute to lower rates of remission or recovery include multiple depressive episodes, younger age, episode severity, co-occurring personality disorders, presence of psychotic features, and prominent anxiety. The longer someone remains in remission, the lower the chances of recurrence. 9,11 Monitoring treatment response in depression should incorporate the use of clinician-administered or patient-reported scales. Assessment of symptom severity, severity scores, as well as functional improvement should be incorporated into routine clinical care. There are multiple well-validated scales to choose from and some examples are listed below. These scales provide quantification of symptoms and can be used to provide longitudinal comparison and evaluation of treatment. Many are quick to use in office and have become routine screening or severity tools in both clinical practice and research. Well-validated scales for monitoring treatment response in patients with depression include the following:
Which of the following is/are first- or second-line psychological treatment(s) for MDD?
All four of these psychological treatments are appropriate for managing a patient with MDD. 9,20 Table 4 shows their best use in clinical practice. Table 4. Common first and second line psychological treatments for MDD.
For a patient requesting the use of “alternative” or “complementary” treatment for their depression, which of the following treatments have sufficient evidence to be recommendation as first-line therapy for some forms of depression?
There are several alternative and complementary treatments that have evidence for use as monotherapy or as adjunctive therapy for the treatment of MDD (Table 5).21 Although there is evidence that some of these can be used as monotherapy for mild depression, for moderate or severe depression these should generally only be used an adjunctive treatment to other well-established treatments. Table 5. First-line and adjunctive alternative and complementary treatments for MDD.
It should be noted that unless there is a specific patient request for alternative or complementary treatment options, or other contraindications to well-established antidepressant treatment, these should not be used or offered as initial treatment for moderate to severe depression or where other clinically significant symptoms (eg, suicidal ideation, severe impairment) are present. Providers should be reminded that various forms of psychotherapy are available to those patients that may have contraindications to standard antidepressant therapy and that they should utilize consultation to psychiatry if treatment complications, nonresponse to medication trials, and other questions occur.
That answer is incorrect. Please try again. Rowan Digital Works
Home > ETD > 958 Theses and DissertationsCase study of a client diagnosed with major depressive disorder. Barbara Ann Marie Allison , Rowan University Date ApprovedEmbargo period, document type, degree name. M.A. in Applied Psychology College of Science & Mathematics Cahill, Janet Depressed persons--Case studies; Depression, Mental--Diagnosis
The purpose of this study was to determine the best practice for a client diagnosed with major depressive disorder who was referred for treatment at a community mental health facility. The client was assessed, diagnosed, and a treatment plan was developed. Implemented treatment consisted of combined cognitive behavioral oriented psychotherapy and psychotropic medication. The Beck Depression Inventory (BDI-II) was used to assess changes in depressive symptoms. Results indicated a significant decline in depressive symptoms over the course of treatment. At the onset of treatment, the client's BDI scores were in the clinically depressed range, while at the conclusion of treatment they had decreased to the borderline range. The client self-reported an improvement in mood. A comparison between the client's current treatment and what might be considered "best" treatment is presented. Suggestions for treatment improvements are made, with a particular emphasis on concerns regarding a potential relapse. Recommended CitationAllison, Barbara Ann Marie, "Case study of a client diagnosed with major depressive disorder" (2005). Theses and Dissertations . 958. https://rdw.rowan.edu/etd/958 Since April 10, 2016 Included inPsychology Commons  Advanced Search
Author Corner
ISSN 2689-0690 Home | About | FAQ | My Account | Accessibility Statement Privacy Copyright Ohio State nav barThe Ohio State University
PathophysiologyNormal Physiology Normal physiology of patient’s mood, perception, emotion and behavior focuses majorly on neurotransmitters in the brain. There are over 46 neurotransmitters in the brain and many have more than one function. Neurotransmitters are chemical messengers that are released and received by synapses of neurons to mediate intracellular communication in the nervous system. They use electrical signals to stimulate messages along the neurons where it affects ion channels and eventually performs a specific mechanism at a site of action (McCance & Huether, 2014). Serotonin is involved with mood, happiness, anxiety, and sleep induction. Raphe-Serotonin System normally modulates homeostasis, emotionality, and tolerance to aversive experiences. Norepinephrine in the brain helps regulate alertness, mood, functions in dream sleep, and maintains arousal. It also can help in the response to stressful situations. The locus ceruleus has a group of norepinephrine containing cells implicated in global psychologic processes including attention, vigilance and orientation to stimuli. Dopamine in the brain regulates reward and motivation which could explain the loss of interest in patients with depression. Dopamine motivates people to take action toward goals, desires, and needs, and issues a surge of reinforcing pleasure once they’ve been accomplished (Garcia-Arocena). Sufficient levels are needed for the brain to function properly and decreased levels have been found in patients with depression (McCance & Huether, 2014). 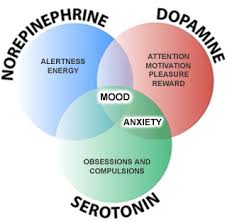 Major Depressive Disorder Major depression is classified as a unipolar mood disorder. Further, major depression can be classified as when an emotional state, such as sadness, becomes chronic and uncontrollable. It is the most common mood disorder (McCance & Huether, 2014). Mood disorders are still being studied due to the unclear nature of how they occur due to the difficult availability of human brain tissue for neurochemical measurement until patients are post-mortem. Each of the dysfunctions below focuses on what are thought to be the causes of major depressive disorder. Pathophysiology: Genetic Predisposition and Environmental Influences There is a genetic predisposition in major depression that runs in families. However, due to the large variance in symptoms, developmental and environmental factors also must be evaluated in the contributing factors to major depression. One view of mood disorders includes the connection between susceptible genes and environmental influence. The combination of life stressors and a potentially dysfunctional serotonin (5-HT) system. The serotonin transporter serves in the reuptake of serotonin at the synapse and may moderate the serotonergic response to stress. Individuals with 2 copies of the s allele were more likely to develop major depression and have suicidal thoughts in response to stressors than individuals homozygous for the l allele. As well as, individuals with 2 s alleles increased their risk for major depression episodes by twofold after experiencing 4 or more stressful events (McCance & Huether, 2014). Pathophysiology: Neurochemical dysregulation There are antidepressant drugs that can increase neurotransmitters in the body leading to another theory called the monoamine hypothesis of depression. In this hypothesis, there is a deficit in the concentration of the brain norepinephrine, dopamine, and/or serotonin resulting in depression. Antidepressant therapies focus on increasing the monoamine neurotransmitter levels within the synapses (McCance & Huether, 2014). 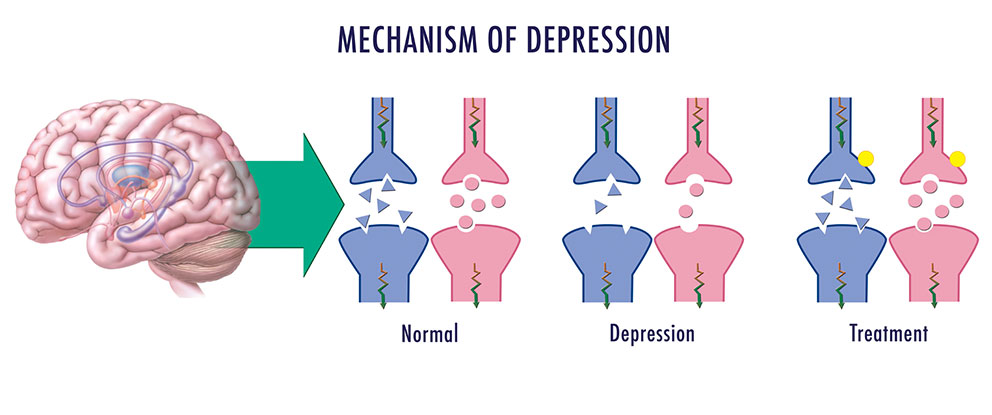 Pathophysiology: Neuroendocrine Dysregulation There are 2 theories in the pathophysiology of depression that involve dysregulation of the neuroendocrine system. The first one focuses on stress and the hypothalamic-Pituitary-Adrenal system. The hypothalamic-pituitary-adrenal system (HPA) plays an essential role in an individual’s ability to cope with stress. Chronic activation of the HPA system and chronic glucocorticoid secretion are found in 30-70% of individuals with major depression suggesting the correlation between the dysfunctional system and depression. Chronic cortisol release in the body results in secretion of pro-inflammatory cytokines which causes immunosuppression and inflammation. Also, there is a Neurotrophic Hypothesis of depression. It is thought to focus on neuronal atrophy of the hippocampus resulting in no cell growth consequently causing in a reduction of the hippocampal brain derived neurotrophic factor (BDNF) and has been proposed as an extension of the monoamine hypothesis of depression. The second neuroendocrine dysregulation is in the hypothalamic-pituitary-thyroid system. While this dysfunction is not completely understood, 20-30% cases of major depression have shown to have an altered hypothalamic-pituitary-thyroid (HPT) system. There is an increase in thyrotropin releasing hormone, blunted thyroid stimulating hormone in response to TRH challenge and decreased nocturnal rise in TSH level that normally occur. This all increases risk for relapse (McCance & Huether, 2014). Pathophysiology: Neuroanatomic and Function Abnormalities Depressed individuals post-mortem brains have shown widespread decrease in serotonin 5-HT1a receptor subtype binding in the frontal, temporal, and limbic cortex as well as serotonin transporter binding in the cerebral cortex and hippocampus, reflecting a dysfunction in the raphe-serotonin system. The activation of the locus ceruleus-norepinephrine system is capable of inhibiting the raphe-serotonin system. This suggests an indirect role in the modulation of serotonin function. Norepinephrine receptor alterations are found in the frontal cortex of some suicide victims with depression. Alterations in norepinephrine systems may be linked to attention or concentration difficulties as well as sleep and arousal disturbances in depression Alterations in frontal and limbic regions (such as the amygdala) have shown a decreased number of glial cells in people with unipolar disorders. As well as, a decreased prefrontal cortex functioning and decreased frontal lobe volume. Depressed individuals have also been found to have abnormalities in Cerebral blood flow and glucose metabolism. Dorsolateral prefrontal abnormalities in depression may be responsible for the retardation in cognitive processing and speech deficits similar to those found in schizophrenia. Dorsomedial frontal dysfunction may be associated with mnemonic and attentional impairments that accompany mood disorders. The frontal brain has increased blood flow and metabolism. It is positively related to negative affect in depressed individuals (McCance & Huether, 2014). Clinical Manifestations/Diagnostic Criteria To diagnosis depression, symptoms must be present for at least two weeks. There are unremitting feelings of sadness and despair. Depressive episodes may occur or recur suddenly, gradually or continue from a few weeks to months. Twenty percent of all people with depression exhibit chronic forms of depression. Symptoms vary widely depending on the individual. The timing and length of the depression also varies. To be diagnosed with Major Depressive Disorder, patients have to have several, usually five or more, symptoms including low mood that is present for at least two weeks (Depression, 2018). Other symptoms of major depressive disorder include:
Garcia-Arocena, D. (n.d.). Happy or SAD: The chemistry behind depression. Retrieved October 29, 2018, from https://www.jax.org/news-and-insights/jax-blog/2015/december/happy-or-sad-the-chemistry-behind-depression LA NEUROSCIENZA DEL CERVELLO CON ADHD. (2018, September 17). Retrieved from https://mondoadhd.blog/2018/09/17/la-neuroscienza-del-cervello-adhd/ (n.d.). Retrieved October 29, 2018, from https://www.nature.com/articles/nrdp201665/figures/3 What are neurotransmitters? (2017, November 09). Retrieved from https://qbi.uq.edu.au/brain/brain-physiology/what-are-neurotransmitters Major Depressive Disorder Case Queries: Where Do Rapid-Acting Therapies Fit Into Care?How soon is now? Identifying which patients with major depressive disorder (MDD) are candidates for treatment with a rapid-acting antidepressant . All Credits AvailableAMA PRA Category 1 Credit(s)™ ANCC Contact Hour(s) Target Audience and Goal StatementThis education is intended for psychiatrists, primary care physicians (PCPs), obstetricians and gynecologists (Ob/Gyns), nurse practitioners (NPs), nurses, and other clinicians who manage patients with MDD, as well as people living with depression and their care partners. The goal of this activity is for learners to be better able to navigate existing clinical evidence for novel, rapid-onset antidepressant therapy and incorporate novel agents into the treatment paradigm. Upon completion of this activity, participants will:
DisclosuresMedscape, LLC requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients. All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated. Others involved in the planning of this activity have no relevant financial relationships. Disclosures for additional planners can be found here .  Sagar V. Parikh, MD, FRCPCJohn F. Greden Professor of Depression and Clinical Neuroscience Professor of Psychiatry Michigan Medicine University of Michigan, Ann Arbor Ann Arbor, Michigan Clinton W. Wright, PharmD, BCPPMedical Education Director, Medscape, LLC Megan E. Breuer, PhDMedical Writer, WebMD Global, LLC Compliance Reviewer/Nurse PlannerLeigh schmidt, msn, rn, cne, chcp. Associate Director, Accreditation and Compliance, Medscape, LLC Peer ReviewerThis activity has been peer reviewed and the reviewer has no relevant financial relationships. Accreditation StatementsDeveloped through a strategic collaboration between Medscape and the Depression and Bipolar Support Alliance. In support of improving patient care, Medscape, LLC is jointly accredited with commendation by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team. For PhysiciansMedscape, LLC designates this enduring material for a maximum of 0.25 AMA PRA Category 1 Credit(s)™ . Physicians should claim only the credit commensurate with the extent of their participation in the activity. College of Family Physicians of Canada Mainpro+® participants may claim certified credits for any AMA PRA Category 1 credit(s) ™, up to a maximum of 50 credits per five-year cycle. Any additional credits are eligible as non-certified credits. College of Family Physicians of Canada (CFPC) members must log into Mainpro+ ® to claim this activity. Contact This Provider Awarded 0.25 contact hour(s) of nursing continuing professional development for RNs and APNs; 0.25 contact hours are in the area of pharmacology. Contact This Provider For questions regarding the content of this activity, contact the accredited provider for this CME/CE activity noted above. For technical assistance, contact [email protected] There are no fees for participating in or receiving credit for this online educational activity. For information on applicability and acceptance of continuing education credit for this activity, please consult your professional licensing board. This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity online during the valid credit period that is noted on the title page. To receive AMA PRA Category 1 Credit ™, you must receive a minimum score of 75% on the post-test. Follow these steps to earn CME/CE credit*:
You may now view or print the certificate from your CME/CE Tracker. You may print the certificate, but you cannot alter it. Credits will be tallied in your CME/CE Tracker and archived for 6 years; at any point within this time period, you can print out the tally as well as the certificates from the CME/CE Tracker. *The credit that you receive is based on your user profile. Supported by an educational grant from Axsome Therapeutics, Inc.  THIS ACTIVITY HAS EXPIRED FOR CREDITMedscape Education makes these downloadable slides available solely for non-commercial use by you as a reference tool. You may not use these slides for any commercial purpose or provide these slides to any third party for such party’s use for any commercial purpose. Please refer to the Medscape Terms of Use for additional details. Activity TranscriptAbbreviations.
The educational activity presented above may involve simulated, case-based scenarios. The patients depicted in these scenarios are fictitious and no association with any actual patient, whether living or deceased, is intended or should be inferred. The material presented here does not necessarily reflect the views of Medscape, LLC, or any individuals or commercial entities that support companies that support educational programming on medscape.org. These materials may include discussion of therapeutic products that have not been approved by the US Food and Drug Administration, off-label uses of approved products, or data that were presented in abstract form. These data should be considered preliminary until published in a peer-reviewed journal. Readers should verify all information and data before treating patients or employing any therapies described in this or any educational activity. A qualified healthcare professional should be consulted before using any therapeutic product discussed herein. Medscape Education © 2024 Medscape, LLC WebMD Network
Six distinct types of depression identified in Stanford Medicine-led studyBrain imaging, known as functional MRI, combined with machine learning can predict a treatment response based on one’s depression “biotype.” June 17, 2024 - By Rachel Tompa  Researchers have identified six subtypes of depression, paving the way toward personalized treatment. Damerfie - stock.adobe.com In the not-too-distant future, a screening assessment for depression could include a quick brain scan to identify the best treatment. Brain imaging combined with machine learning can reveal subtypes of depression and anxiety, according to a new study led by researchers at Stanford Medicine. The study , published June 17 in the journal Nature Medicine , sorts depression into six biological subtypes, or “biotypes,” and identifies treatments that are more likely or less likely to work for three of these subtypes. Better methods for matching patients with treatments are desperately needed, said the study’s senior author, Leanne Williams , PhD, the Vincent V.C. Woo Professor, a professor of psychiatry and behavioral sciences, and the director of Stanford Medicine’s Center for Precision Mental Health and Wellness . Williams, who lost her partner to depression in 2015, has focused her work on pioneering the field of precision psychiatry . Around 30% of people with depression have what’s known as treatment-resistant depression , meaning multiple kinds of medication or therapy have failed to improve their symptoms. And for up to two-thirds of people with depression, treatment fails to fully reverse their symptoms to healthy levels. That’s in part because there’s no good way to know which antidepressant or type of therapy could help a given patient. Medications are prescribed through a trial-and-error method, so it can take months or years to land on a drug that works — if it ever happens. And spending so long trying treatment after treatment, only to experience no relief, can worsen depression symptoms. “The goal of our work is figuring out how we can get it right the first time,” Williams said. “It’s very frustrating to be in the field of depression and not have a better alternative to this one-size-fits-all approach.” Biotypes predict treatment responseTo better understand the biology underlying depression and anxiety, Williams and her colleagues assessed 801 study participants who were previously diagnosed with depression or anxiety using the imaging technology known as functional MRI, or fMRI, to measure brain activity. They scanned the volunteers’ brains at rest and when they were engaged in different tasks designed to test their cognitive and emotional functioning. The scientists narrowed in on regions of the brain, and the connections between them, that were already known to play a role in depression. Using a machine learning approach known as cluster analysis to group the patients’ brain images, they identified six distinct patterns of activity in the brain regions they studied.  Leanne Williams The scientists also randomly assigned 250 of the study participants to receive one of three commonly used antidepressants or behavioral talk therapy. Patients with one subtype, which is characterized by overactivity in cognitive regions of the brain, experienced the best response to the antidepressant venlafaxine (commonly known as Effexor) compared with those who have other biotypes. Those with another subtype, whose brains at rest had higher levels of activity among three regions associated with depression and problem-solving, had better alleviation of symptoms with behavioral talk therapy. And those with a third subtype, who had lower levels of activity at rest in the brain circuit that controls attention, were less likely to see improvement of their symptoms with talk therapy than those with other biotypes. The biotypes and their response to behavioral therapy make sense based on what they know about these regions of the brain, said Jun Ma, MD, PhD, the Beth and George Vitoux Professor of Medicine at the University of Illinois Chicago and one of the authors of the study. The type of therapy used in their trial teaches patients skills to better address daily problems, so the high levels of activity in these brain regions may allow patients with that biotype to more readily adopt new skills. As for those with lower activity in the region associated with attention and engagement, Ma said it’s possible that pharmaceutical treatment to first address that lower activity could help those patients gain more from talk therapy. “To our knowledge, this is the first time we’ve been able to demonstrate that depression can be explained by different disruptions to the functioning of the brain,” Williams said. “In essence, it’s a demonstration of a personalized medicine approach for mental health based on objective measures of brain function.” In another recently published study , Williams and her team showed that using fMRI brain imaging improves their ability to identify individuals likely to respond to antidepressant treatment. In that study, the scientists focused on a subtype they call the cognitive biotype of depression, which affects more than a quarter of those with depression and is less likely to respond to standard antidepressants. By identifying those with the cognitive biotype using fMRI, the researchers accurately predicted the likelihood of remission in 63% of patients, compared with 36% accuracy without using brain imaging. That improved accuracy means that providers may be more likely to get the treatment right the first time. The scientists are now studying novel treatments for this biotype with the hope of finding more options for those who don’t respond to standard antidepressants. Further explorations of depressionThe different biotypes also correlate with differences in symptoms and task performance among the trial participants. Those with overactive cognitive regions of the brain, for example, had higher levels of anhedonia (inability to feel pleasure) than those with other biotypes; they also performed worse on executive function tasks. Those with the subtype that responded best to talk therapy also made errors on executive function tasks but performed well on cognitive tasks. One of the six biotypes uncovered in the study showed no noticeable brain activity differences in the imaged regions from the activity of people without depression. Williams believes they likely haven’t explored the full range of brain biology underlying this disorder — their study focused on regions known to be involved in depression and anxiety, but there could be other types of dysfunction in this biotype that their imaging didn’t capture. Williams and her team are expanding the imaging study to include more participants. She also wants to test more kinds of treatments in all six biotypes, including medicines that haven’t traditionally been used for depression. Her colleague Laura Hack , MD, PhD, an assistant professor of psychiatry and behavioral sciences, has begun using the imaging technique in her clinical practice at Stanford Medicine through an experimental protocol . The team also wants to establish easy-to-follow standards for the method so that other practicing psychiatrists can begin implementing it. “To really move the field toward precision psychiatry, we need to identify treatments most likely to be effective for patients and get them on that treatment as soon as possible,” Ma said. “Having information on their brain function, in particular the validated signatures we evaluated in this study, would help inform more precise treatment and prescriptions for individuals.” Researchers from Columbia University; Yale University School of Medicine; the University of California, Los Angeles; UC San Francisco; the University of Sydney; the University of Texas MD Anderson; and the University of Illinois Chicago also contributed to the study. Datasets in the study were funded by the National Institutes of Health (grant numbers R01MH101496, UH2HL132368, U01MH109985 and U01MH136062) and by Brain Resource Ltd.
About Stanford Medicine Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu . Hope amid crisisPsychiatry’s new frontiers 
Understanding Sleep, Activity, and Circadian Rhythms in Major Depressive DisorderA new study in JAMA Psychiatry aimed to understand how sleep, physical activity, and circadian rhythms relate to major depressive disorder (MDD). The study included adults with both current MDD and those with a history of MDD but who were symptom-free at the time of the study (remitted MDD). MDD is a serious mental health disorder with symptoms that include a lack of desire to enjoy life and difficulty doing simple things like eating and being socially engaged. The researchers found that the amount and quality of physical activity, and timing of both sleep and physical activity combined with the stability of their 24-hour circadian rhythm, was a better indicator of MDD than any of these factors individually. With this knowledge, doctors can provide potentially more efficient MDD interventions, jointly targeting these aspects of 24-hour behaviors. In a Q&A, lead author Vadim Zipunnikov, PhD, MS, MA , associate professor in the Department of Biostatistics, answers questions about the study, which shows the importance of looking at a person’s 24-hour behaviors comprehensively. Your study used a technology called accelerometry to measure sleep and activity. What exactly is it, and how did you use it? An accelerometer is a sensor that measures movement. It can be used to assess intensity and duration of physical activity, the amount of movement during sleep and for other things. Built-in accelerometers can be found in devices like Fitbits and smartphones. In the study, we used a research-grade device called GeneActiv to estimate both physical activity during the day and quality of sleep during the night. How are the research-grade devices you used similar to and different from common trackers such as Apple watches or Fitbits? Fitbit and similar devices have photoplethysmography (PPG) sensors that estimate heart rate and heart rate variability. Having a person’s heart rate, along with accelerometry information, makes the algorithms for estimating physical activity and sleep more accurate; this is a big advantage over research-grade devices that typically only record accelerometry data. A major advantage of research-grade accelerometer devices is that researchers have a lot more control over the algorithm processing pipeline. You found two key contributors that are both strongly associated with MDD: physical activity and the timing of sleep and physical activity. What does this mean in terms of the prevention and treatment of major depression? We found that the amount and quality of physical activity, and the timing of sleep and physical activity, were the two most important components of 24-hour behaviors, both for people with MDD and without it. People with MDD engaged in less physical activity and it was of poorer quality (more fragmented). They also had later timing of both sleep and physical activity. Thus, late timing of sleep and physical activity, or delayed circadian rhythm, is related to a higher chance of having current or remitted depression. We also found that people with current MDD tend to go to bed and be physically active even later than those with remitted MDD. Of course, later timing is relative to a person’s natural rhythm; for some people going to sleep at 11 p.m. naturally aligns with their internal clock, while for others it doesn’t. Our study adds to the existing literature that shows that not staying up too late and going to sleep at a regular time, based on your body’s natural clock, may be a healthy sleep routine. And the same may be equally applied to other daily routines including physical activity. How might these findings help clinicians treat people with MDD? Clinically, it means that intervention approaches jointly targeting these aspects of the 24-hour behaviors may potentially be more efficient in prevention/treatment of depression and beyond. It is important to understand what healthier behaviors are within the context of depression and how we could switch the person back if or when they fall out of them. What big questions was this study trying to answer? What is important to understand is that people working in the field of sleep are typically focused on sleep period, and physical activity experts primarily focus on daytime physical activity. In our work, we try to better understand the interplay between sleep and physical activity, looking at them as integral parts of the 24-hour daily cycle. In this study we focused on understanding the interdependencies between sleep, physical activity and circadian rhythms and seeing how these three domains related to current or remitted major depression. Interestingly, we learned that sleep timing, not duration, was related to MDD status, which indicates that circadian misalignment plays an important role in MDD. Were you surprised by any of the findings of the study? Some of the findings reconfirmed results that were previously published. That being said, our work used a novel methodological approach, which allowed us to jointly study the domains of sleep, physical activity, and circadian rhythmicity. Our approach allowed us to take a step forward, seeing which measures are closely related to each other and essentially allowing us to group these variables. What can the general public learn from this study? Understand your sleep, not just from a durational point of view but in terms of timing and how your sleep timing is related to the timing of other activities you do, such as physical activity. And there is no one right answer. Some people naturally stay up later or rise earlier. There is nothing wrong with either. But look at your history: Did you shift to this later timing? Additionally, any amount of physical activity takes you in the right direction, especially for those who are highly sedentary. How does this relate to other work you’ve done using accelerometry? Along with my colleagues at Johns Hopkins University and Motor Activity Research Consortium for Health (mMarch) at the National Institute of Mental Health (NIMH) I have been doing a lot of work to understand the role of sleep and physical activity across multiple diseases and disorders. Converging sleep and physical activity, and thinking about 24-hour behaviors jointly, is a very natural step both for me and these two fields. I think we will see more and more research approaching 24-hour behaviors in this comprehensive way of thinking. What’s next? This paper is based on our study in Switzerland with middle-aged to older people (the mean age was 61.79 years). Since then we have applied this approach across three continents (North America, Europe and Australia) and across the entire lifespan (from 5 to 85), and expanded to include people who experience ADHD, anxiety, and other mental health disorders. Our findings are very consistent across all three studies. Though these studies have not yet been published, we are in the process of doing so now and this will be our next step. We were really surprised in some sense to see such a consistency across continents and across lifespans. Related Content How to Offer Support and Find Strength on a Trauma Anniversary Mental Health in the Workplace: A Conversation Bridging Research and Practice Activity, Sleep & Dementia Rev. Pamula Yerby-Hammack Breaking the Stigma of Mental Health Inside the Movement to Transform Mental Health in Sierra LeoneThank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Gamma oscillations of visual cortex underlying emotion and cognition deficits associated with suicide attempt in major depressive disorder
Nature Mental Health ( 2024 ) Cite this article Metrics details
Altered neural oscillations in response to negative or positive emotional stimuli may be related to severe clinical symptoms in patients with major depressive disorder, particularly high suicidality. However, the underlying neurobiological mechanisms of this aberrant oscillatory activity and its potential emotional and cognitive functions remain unclear. Here we conducted a cross-sectional study of 107 participants, including 40 healthy controls and 67 patients with major depressive disorder (33 with suicide attempts and 34 without). All participants underwent an emotional expression recognition task during the magnetoencephalography scanning and completed neurocognitive assessments. Time–frequency characteristics and phase connections were analysed and compared between groups in sensor and source space using cluster-based permutation tests. The association between abnormal oscillatory features and neurocognitive performance was also evaluated. We found that increased gamma oscillations (50–70 Hz) of the visual cortices were considerably associated with suicide attempts in depression. Moreover, gamma-band source power in happy or sad conditions could predict individualized suicide risk. Gamma-band phase connections under the happy or sad condition were related to deficits in large-scale cognitive functions. Overall, gamma oscillations of the visual areas induced by the emotional stimuli were reliable biomarkers for identifying suicide attempts in depressive patients. Abnormal gamma-band connection involving visual cortex under both happy and sad expressions were significantly correlated with broad cognitive deficits. This is a preview of subscription content, access via your institution Access optionsSubscribe to this journal Receive 12 digital issues and online access to articles 55,14 € per year only 4,60 € per issue Buy this article
Prices may be subject to local taxes which are calculated during checkout 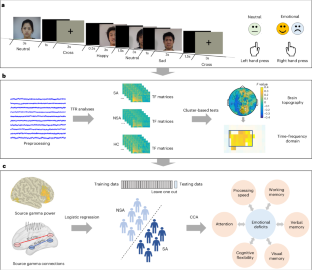 Data availabilityThe data that support the key findings are available from the Open Science Framework ( https://osf.io/q5zyg/ ). For any inquiries regarding the data, requests can be made to the corresponding authors. Code availabilityMEG data were preprocessed and analysed with the MATLAB r2016b based Fieldtrip (v.2017) toolbox ( https://github.com/fieldtrip/fieldtrip ) 55 . The sample size was estimated with G*Power_3.1.9.7 software ( https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower ) 47 . The statistical comparisons involving demographic variables, behavioral data were conducted with SPSS software (v.22) 59 . The data distribution plots were conducted with GraphPad Prism software (8.0.2) 60 . The brain maps were plotted with the BrainNet Viewer (v.2017) toolbox ( https://github.com/mingruixia/BrainNet-Viewer ) 32 . The custom codes are available from the Open Science Framework ( https://osf.io/q5zyg/ ). Millner, A. J., Robinaugh, D. J. & Nock, M. K. Advancing the understanding of suicide: the need for formal theory and rigorous descriptive research. Trends Cogn. Sci. 24 , 704–716 (2020). Article PubMed PubMed Central Google Scholar Séguin, M. Review of suicide risk management: a manual for health professionals. Can. Psychol. 53 , 255–257 (2012). Article Google Scholar Jung, J. et al. Alterations in functional brain networks in depressed patients with a suicide attempt history. Neuropsychopharmacology 45 , 964–974 (2020). Article PubMed Google Scholar Ruhe, H. G. et al. Emotional biases and recurrence in major depressive disorder. Results of 2.5 years follow-up of drug-free cohort vulnerable for recurrence. Front. Psychiatry 10 , 145 (2019). Stuhrmann, A., Suslow, T. & Dannlowski, U. Facial emotion processing in major depression: a systematic review of neuroimaging findings. Biol. Mood Anxiety Disord. 1 , 10 (2011). Dai, Z. et al. Attenuated alpha-gamma coupling in emotional dual pathways with right-amygdala predicting ineffective antidepressant response. CNS Neurosci. Ther. 28 , 401–410 (2022). Li, Y., Cao, D., Wei, L., Tang, Y. & Wang, J. Abnormal functional connectivity of EEG gamma band in patients with depression during emotional face processing. Clin. Neurophysiol. 126 , 2078–2089 (2015). Atallah, B. V. & Scanziani, M. Instantaneous modulation of gamma oscillation frequency by balancing excitation with inhibition. Neuron 62 , 566–577 (2009). Touboul, J. & Destexhe, A. Can power-law scaling and neuronal avalanches arise from stochastic dynamics? PLoS ONE 5 , e8982 (2010). Gladding, C. M., Fitzjohn, S. M. & Molnár, E. Metabotropic glutamate receptor-mediated long-term depression: molecular mechanisms. Pharmacol. Rev. 61 , 395–412 (2009). Uhlhaas, P. J. & Singer, W. Abnormal neural oscillations and synchrony in schizophrenia. Nat. Rev. Neurosci. 11 , 100–113 (2010). Arikan, M. K., Gunver, M. G., Tarhan, N. & Metin, B. High-gamma: a biological marker for suicide attempt in patients with depression. J. Affect. Disord. 254 , 1–6 (2019). Gilbert, J. R., Ballard, E. D., Galiano, C. S., Nugent, A. C. & Zarate, C. A. Jr Magnetoencephalographic correlates of suicidal ideation in major depression. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 5 , 354–363 (2020). PubMed Google Scholar Fitzgerald, P. J. & Watson, B. O. Gamma oscillations as a biomarker for major depression: an emerging topic. Transl. psychiatry 8 , 177 (2018). Dai, Z. et al. Disrupted fronto-parietal network and default-mode network gamma interactions distinguishing suicidal ideation and suicide attempt in depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 113 , 110475 (2022). Dai, Z. et al. Hampered gamma oscillations induced by sad emotion underlying suicide attempt in major depressive disorder. Psychiatry Clin. Neurosci. 77 , 20–29 (2023). Shestyuk, A. Y., Deldin, P. J., Brand, J. E. & Deveney, C. M. Reduced sustained brain activity during processing of positive emotional stimuli in major depression. Biol. Psychiatry 57 , 1089–1096 (2005). Silton, R. L. et al. Regulating positive emotions: implications for promoting well-being in individuals with depression. Emotion 20 , 93–97 (2020). Grent-‘t-Jong, T. et al. Association of magnetoencephalographically measured high-frequency oscillations in visual cortex with circuit dysfunctions in local and large-scale networks during emerging psychosis. JAMA Psychiatry 77 , 852–862 (2020). Liu, S. & Parvizi, J. Cognitive refractory state caused by spontaneous epileptic high-frequency oscillations in the human brain. Sci. Transl. Med. 11 , eaax7830 (2019). Lan, X. et al. Association between cognition and suicidal ideation in patients with major depressive disorder: a longitudinal study. J. Affect. Disord. 272 , 146–151 (2020). Fazakas-DeHoog, L. L., Rnic, K. & Dozois, D. J. A cognitive distortions and deficits model of suicide ideation. Eur. J. Psychol. 13 , 178–193 (2017). Westheide, J. et al. Executive performance of depressed suicide attempters: the role of suicidal ideation. Eur. Arch. Psychiatry Clin. Neurosci. 258 , 414–421 (2008). Gujral, S. et al. Impaired executive function in contemplated and attempted suicide in late life. Am. J. Geriatr. Psychiatry 22 , 811–819 (2014). Manor, I. et al. Possible association between attention deficit hyperactivity disorder and attempted suicide in adolescents—a pilot study. Eur. Psychiatry 25 , 146–150 (2010). Balazs, J. & Kereszteny, A. Attention-deficit/hyperactivity disorder and suicide: a systematic review. World J. Psychiatry 7 , 44–59 (2017). Ram, D., Chandran, S., Sadar, A. & Gowdappa, B. Correlation of cognitive resilience, cognitive flexibility and impulsivity in attempted suicide. Indian J. Psychol. Med. 41 , 362–367 (2019). Saffer, B. Y. & Klonsky, E. D. Do neurocognitive abilities distinguish suicide attempters from suicide ideators? A systematic review of an emerging research area. Clin. Psychol. 25 , e12227 (2018). Google Scholar Yin, Y. et al. Suicidal ideation, suicide attempts, and neurocognitive dysfunctions among patients with first‐episode schizophrenia. Suicide Life Threat. Behav. 50 , 1181–1188 (2020). Siems, M., Pape, A.-A., Hipp, J. F. & Siegel, M. Measuring the cortical correlation structure of spontaneous oscillatory activity with EEG and MEG. NeuroImage 129 , 345–355 (2016). Muthukumaraswamy, S. D. & Singh, K. D. Visual gamma oscillations: the effects of stimulus type, visual field coverage and stimulus motion on MEG and EEG recordings. Neuroimage 69 , 223–230 (2013). Xia, M., Wang, J. & He, Y. BrainNet Viewer: a network visualization tool for human brain connectomics. PLoS ONE 8 , e68910 (2013). Lewis, D. A., Curley, A. A., Glausier, J. R. & Volk, D. W. Cortical parvalbumin interneurons and cognitive dysfunction in schizophrenia. Trends Neurosci. 35 , 57–67 (2012). Murray, J. D. et al. Linking microcircuit dysfunction to cognitive impairment: effects of disinhibition associated with schizophrenia in a cortical working memory model. Cereb. Cortex 24 , 859–872 (2014). Schreiner, M. W., Klimes-Dougan, B. & Cullen, K. R. Neural correlates of suicidality in adolescents with major depression: resting-state functional connectivity of the precuneus and posterior cingulate cortex. Suicide Life Threat. Behav. 49 , 899–913 (2019). Vanderlind, W. M., Millgram, Y., Baskin-Sommers, A. R., Clark, M. S. & Joormann, J. Understanding positive emotion deficits in depression: from emotion preferences to emotion regulation. Clin. Psychol. Rev. 76 , 101826 (2020). Dai, Z. et al. Sub-second transient activated patterns to sad expressions in major depressive disorders discovered via hidden Markov model. J. Neurosci. Res. 99 , 3250–3260 (2021). Atlas, L. Y. How instructions shape aversive learning: higher order knowledge, reversal learning, and the role of the amygdala. Curr. Opin. Behav. Sci. 26 , 121–129 (2019). Farzan, F. et al. Evidence for gamma inhibition deficits in the dorsolateral prefrontal cortex of patients with schizophrenia. Brain 133 , 1505–1514 (2010). Yang, Y. et al. Atrophy of right inferior frontal orbital gyrus and frontoparietal functional connectivity abnormality in depressed suicide attempters. Brain Imag. Behav. 14 , 2542–2552 (2020). Zhu, R. et al. Discriminating suicide attempters and predicting suicide risk using altered frontolimbic resting-state functional connectivity in patients with bipolar II disorder. Front. Psychiatry 11 , 1352 (2020). Santamarina-Perez, P. et al. Visual memory improvement in adolescents at high risk for suicide who are receiving psychotherapy at a community clinic. Psychiatry Res. 298 , 113796 (2021). Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23 , 56–62 (1960). Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 32 , 50–55 (1959). Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR (American Psychiatric Association, 2003). Beck, A. T., Steer, R. A. & Ranieri, W. F. Scale for suicide ideation: psychometric properties of a self‐report version. J. Clin. Psychol. 44 , 499–505 (1988). Faul, F., Erdfelder, E., Buchner, A. & Lang, A.-G. Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods 41 , 1149–1160 (2009). Du, J., Yao, Z., XIE, S., Shi, J. & Teng, G. The primary development of Chinese facial expression video system. Chin. Ment. Health J. 21 , 333–337 (2007). Zhao, S. et al. Sex differences in the association between symptom profiles and cognitive functioning in patients with depressive disorder. J. Affect. Disord. 287 , 1–7 (2021). Reitan, R. M. Validity of the Trail Making Test as an indicator of organic brain damage. Percept. Mot. Skills 8 , 271–276 (1958). Wechsler, D. Wechsler Memory Scale-Revised (Psychological Corporation, 1987). Wechsler, D. Manual for the Wechsler Adult Intelligence Scale (Psychological Corporation, 1955). Wechsler, D. WMS-III: Wechsler Memory Scale Administration and Scoring Manual (Psychological Corporation, 1997). Liu, J. et al. Exploration of major cognitive deficits in medication-free patients with major depressive disorder. Front. Psychiatry 12 , 836 (2019). Oostenveld, R., Fries, P., Maris, E. & Schoffelen, J.-M. FieldTrip: open source software for advanced analysis of MEG, EEG, and invasive electrophysiological data. Comput. Intell. Neurosci. 2011 , 156869 (2011). Tallon-Baudry, C., Bertrand, O., Delpuech, C. & Pernier, J. Stimulus specificity of phase-locked and non-phase-locked 40 Hz visual responses in human. J. Neurosci. 16 , 4240–4249 (1996). Gross, J. et al. Dynamic imaging of coherent sources: studying neural interactions in the human brain. Proc. Natl Acad. Sci. USA 98 , 694–699 (2001). Vinck, M., Oostenveld, R., Van Wingerden, M., Battaglia, F. & Pennartz, C. M. An improved index of phase-synchronization for electrophysiological data in the presence of volume-conduction, noise and sample-size bias. Neuroimage 55 , 1548–1565 (2011). SPSS Statistics for Windows v.22.0 (IBM, 2013). GraphPad v.8.0.2. (GraphPad Software, 2019). Maris, E. & Oostenveld, R. Nonparametric statistical testing of EEG-and MEG-data. J. Neurosci. Methods 164 , 177–190 (2007). Download references AcknowledgementsThis research received support from the National Natural Science Foundation of China (grants 81871066, 81571639 and 81701784) awarded to Q.L.; the Fundamental Research Funds for the Central Universities (2242021k30014, 2242021k30059) awarded to Q.L.; the Jiangsu Provincial Medical Innovation Team of the Project of Invigorating Health Care through Science, Technology, and Education (grant CXTDC2016004) awarded to Z.Y.; and the Jiangsu Provincial key research and development program (grant BE2018609) awarded to Z.Y.; Z.D. was supported by the Chinese Scholarship Council. We are grateful to O. Jensen from the University of Birmingham and H. Jiang from Zhejiang University for their valuable comments on this work. We would also like to express our appreciation to Y. Pan and T. Ghafari from the University of Birmingham for their helpful suggestions. Additionally, we acknowledge the editing and proofreading services provided by American Journal Experts, which substantially contributed to improving the clarity and language of this paper. Author informationAuthors and affiliations. School of Biological Sciences and Medical Engineering, Child Development and Learning Science, Key Laboratory of Child Development and Learning Science, Ministry of Education, Research Center for Learning Science, Southeast University, Nanjing, China Zhongpeng Dai, Wei Zhang, Zhijian Yao & Qing Lu Centre for Human Brain Health, School of Psychology, University of Birmingham, Birmingham, UK Zhongpeng Dai Department of Psychiatry, Affiliated Brain Hospital of Nanjing Medical University, Nanjing, China Hongliang Zhou, Zhilu Chen & Zhijian Yao Institutes Sciences Cognitives Marc Jeannerod, CNRS UMR 5229, Lyon, France Nanjing Brain Hospital, Medical School of Nanjing University, Nanjing, China Zhijian Yao You can also search for this author in PubMed Google Scholar ContributionsQ.L. and Z.Y. were responsible for conceptualization. Z.D., W.Z. and S.Z. were responsible for methodology. Z.D., H.Z. and W.Z. were responsible for formal analysis. Z.D., H.Z., Z.C. and W.Z. were responsible for investigation. Z.D. wrote the orignal draft; Z.D., Q.L., H.Z. and S.Z. reviewed and edited the paper. Z.D. was responsible for visualization. Q.L. and Z.Y. supervised the project and acquired funding. Corresponding authorsCorrespondence to Zhijian Yao or Qing Lu . Ethics declarationsCompeting interests. The authors declare no competing interests. Peer reviewPeer review information. Nature Mental Health thanks the, anonymous, reviewer(s) for their contribution to the peer review of this work. Additional informationPublisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Supplementary informationSupplementary information. Supplementary Figs. 1–15 and Table 1. Reporting SummaryRights and permissions. Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law. Reprints and permissions About this articleCite this article. Dai, Z., Zhang, W., Zhou, H. et al. Gamma oscillations of visual cortex underlying emotion and cognition deficits associated with suicide attempt in major depressive disorder. Nat. Mental Health (2024). https://doi.org/10.1038/s44220-024-00269-3 Download citation Received : 26 January 2023 Accepted : 15 May 2024 Published : 21 June 2024 DOI : https://doi.org/10.1038/s44220-024-00269-3 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative Quick links
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Contributing studies for clinically elevated depression symptoms are presented in order of largest to smallest prevalence rate. Square data markers represent prevalence rates, with lines around the marker indicating 95% CIs. The diamond data marker represents the overall effect size based on included studies. Contributing studies for clinically elevated anxiety symptoms are presented in order of largest to smallest prevalence rate. Square data markers represent prevalence rates, with lines around the marker indicating 95% CIs. The diamond data marker represents the overall effect size based on included studies. eTable 1. Example Search Strategy from Medline eTable 2. Study Quality Evaluation Criteria eTable 3. Quality Assessment of Studies Included eTable 4. Sensitivity analysis excluding low quality studies (score=2) for moderators of the prevalence of clinically elevated depressive symptoms in children and adolescence during COVID-19 eTable 5. Sensitivity analysis excluding low quality studies (score=2) for moderators of the prevalence of clinically elevated anxiety symptoms in children and adolescence during COVID-19 eFigure 1. PRISMA diagram of review search strategy eFigure 2. Funnel plot for studies included in the clinically elevated depressive symptoms eFigure 3. Funnel plot for studies included in the clinically elevated anxiety symptoms
See More AboutSelect your interests. Customize your JAMA Network experience by selecting one or more topics from the list below.
Others Also Liked
Racine N , McArthur BA , Cooke JE , Eirich R , Zhu J , Madigan S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19 : A Meta-analysis . JAMA Pediatr. 2021;175(11):1142–1150. doi:10.1001/jamapediatrics.2021.2482 Manage citations:© 2024
Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19 : A Meta-analysis
Question What is the global prevalence of clinically elevated child and adolescent anxiety and depression symptoms during COVID-19? Findings In this meta-analysis of 29 studies including 80 879 youth globally, the pooled prevalence estimates of clinically elevated child and adolescent depression and anxiety were 25.2% and 20.5%, respectively. The prevalence of depression and anxiety symptoms during COVID-19 have doubled, compared with prepandemic estimates, and moderator analyses revealed that prevalence rates were higher when collected later in the pandemic, in older adolescents, and in girls. Meaning The global estimates of child and adolescent mental illness observed in the first year of the COVID-19 pandemic in this study indicate that the prevalence has significantly increased, remains high, and therefore warrants attention for mental health recovery planning. Importance Emerging research suggests that the global prevalence of child and adolescent mental illness has increased considerably during COVID-19. However, substantial variability in prevalence rates have been reported across the literature. Objective To ascertain more precise estimates of the global prevalence of child and adolescent clinically elevated depression and anxiety symptoms during COVID-19; to compare these rates with prepandemic estimates; and to examine whether demographic (eg, age, sex), geographical (ie, global region), or methodological (eg, pandemic data collection time point, informant of mental illness, study quality) factors explained variation in prevalence rates across studies. Data Sources Four databases were searched (PsycInfo, Embase, MEDLINE, and Cochrane Central Register of Controlled Trials) from January 1, 2020, to February 16, 2021, and unpublished studies were searched in PsycArXiv on March 8, 2021, for studies reporting on child/adolescent depression and anxiety symptoms. The search strategy combined search terms from 3 themes: (1) mental illness (including depression and anxiety), (2) COVID-19, and (3) children and adolescents (age ≤18 years). For PsycArXiv , the key terms COVID-19 , mental health , and child/adolescent were used. Study Selection Studies were included if they were published in English, had quantitative data, and reported prevalence of clinically elevated depression or anxiety in youth (age ≤18 years). Data Extraction and Synthesis A total of 3094 nonduplicate titles/abstracts were retrieved, and 136 full-text articles were reviewed. Data were analyzed from March 8 to 22, 2021. Main Outcomes and Measures Prevalence rates of clinically elevated depression and anxiety symptoms in youth. Results Random-effect meta-analyses were conducted. Twenty-nine studies including 80 879 participants met full inclusion criteria. Pooled prevalence estimates of clinically elevated depression and anxiety symptoms were 25.2% (95% CI, 21.2%-29.7%) and 20.5% (95% CI, 17.2%-24.4%), respectively. Moderator analyses revealed that the prevalence of clinically elevated depression and anxiety symptoms were higher in studies collected later in the pandemic and in girls. Depression symptoms were higher in older children. Conclusions and Relevance Pooled estimates obtained in the first year of the COVID-19 pandemic suggest that 1 in 4 youth globally are experiencing clinically elevated depression symptoms, while 1 in 5 youth are experiencing clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double of prepandemic estimates. An influx of mental health care utilization is expected, and allocation of resources to address child and adolescent mental health concerns are essential. Prior to the COVID-19 pandemic, rates of clinically significant generalized anxiety and depressive symptoms in large youth cohorts were approximately 11.6% 1 and 12.9%, 2 respectively. Since COVID-19 was declared an international public health emergency, youth around the world have experienced dramatic disruptions to their everyday lives. 3 Youth are enduring pervasive social isolation and missed milestones, along with school closures, quarantine orders, increased family stress, and decreased peer interactions, all potential precipitants of psychological distress and mental health difficulties in youth. 4 - 7 Indeed, in both cross-sectional 8 , 9 and longitudinal studies 10 , 11 amassed to date, the prevalence of youth mental illness appears to have increased during the COVID-19 pandemic. 3 However, data collected vary considerably. Specifically, ranges from 2.2% 12 to 63.8% 13 and 1.8% 12 to 49.5% 13 for clinically elevated depression and anxiety symptoms, respectively. As governments and policy makers deploy and implement recovery plans, ascertaining precise estimates of the burden of mental illness for youth are urgently needed to inform service deployment and resource allocation. Depression and generalized anxiety are 2 of the most common mental health concerns in youth. 14 Depressive symptoms, which include feelings of sadness, loss of interest and pleasure in activities, as well as disruption to regulatory functions such as sleep and appetite, 15 could be elevated during the pandemic as a result of social isolation due to school closures and physical distancing requirements. 6 Generalized anxiety symptoms in youth manifest as uncontrollable worry, fear, and hyperarousal. 15 Uncertainty, disruptions in daily routines, and concerns for the health and well-being of family and loved ones during the COVID-19 pandemic are likely associated with increases in generalized anxiety in youth. 16 When heterogeneity is observed across studies, as is the case with youth mental illness during COVID-19, it often points to the need to examine demographic, geographical, and methodological moderators. Moderator analyses can determine for whom and under what circumstances prevalence is higher vs lower. With regard to demographic factors, prevalence rates of mental illness both prior to and during the COVID-19 pandemic are differentially reported across child age and sex, with girls 17 , 18 and older children 17 , 19 being at greater risk for internalizing disorders. Studies have also shown that youth living in regions that experienced greater disease burden 2 and urban areas 20 had greater mental illness severity. Methodological characteristics of studies also have the potential to influence the estimated prevalence rates. For example, studies of poorer methodological quality may be more likely to overestimate prevalence rates. 21 The symptom reporter (ie, child vs parent) may also contribute to variability in the prevalence of mental illness across studies. Indeed, previous research prior to the pandemic has demonstrated that child and parent reports of internalizing symptoms vary, 22 with children/adolescents reporting more internalizing symptoms than parents. 23 Lastly, it is important to consider the role of data collection timing on potential prevalence rates. While feelings of stress and overwhelm may have been greater in the early months of the pandemic compared with later, 24 extended social isolation and school closures may have exerted mental health concerns. Although a narrative systematic review of 6 studies early in the pandemic was conducted, 8 to our knowledge, no meta-analysis of prevalence rates of child and adolescent mental illness during the pandemic has been undertaken. In the current study, we conducted a meta-analysis of the global prevalence of clinically elevated symptoms of depression and anxiety (ie, exceeding a clinical cutoff score on a validated measure or falling in the moderate to severe symptom range of anxiety and depression) in youth during the first year of the COVID-19 pandemic. While research has documented a worsening of symptoms for children and youth with a wide range of anxiety disorders, 25 including social anxiety, 26 clinically elevated symptoms of generalized anxiety are the focus of the current meta-analysis. In addition to deriving pooled prevalence estimates, we examined demographic, geographical, and methodological factors that may explain between-study differences. Given that there have been several precipitants of psychological distress for youth during COVID-19, we hypothesized that pooled prevalence rates would be higher compared with prepandemic estimates. We also hypothesized that child mental illness would be higher among studies with older children, a higher percentage of female individuals, studies conducted later in the pandemic, and that higher-quality studies would have lower prevalence rates. This systematic review was registered as a protocol with PROSPERO (CRD42020184903) and the Preferred Reporting Items for Systematic Reviews and Meta-analyses ( PRISMA ) reporting guideline was followed. 27 Ethics review was not required for the study. Electronic searches were conducted in collaboration with a health sciences librarian in PsycInfo, Cochrane Central Register of Controlled Trials (CENTRAL), Embase, and MEDLINE from inception to February 16, 2021. The search strategy (eTable 1 in the Supplement ) combined search terms from 3 themes: (1) mental illness (including depression and anxiety), (2) COVID-19, and (3) children and adolescents (age ≤18 years). Both database and subject headings were used to search keywords. As a result of the rapidly evolving nature of research during the COVID-19 pandemic, we also searched a repository of unpublished preprints, PsycArXiv . The key terms COVID-19 , mental health , and child/adolescent were used on March 8, 2021, and yielded 38 studies of which 1 met inclusion criteria. The following inclusion criteria were applied: (1) sample was drawn from a general population; (2) proportion of individuals meeting clinical cutoff scores or falling in the moderate to severe symptom range of anxiety or depression as predetermined by validated self-report measures were provided; (3) data were collected during COVID-19; (4) participants were 18 years or younger; (5) study was empirical; and (6) studies were written in English. Samples of participants who may be affected differently from a mental health perspective during COVID-19 were excluded (eg, children with preexisting psychiatric diagnoses, children with chronic illnesses, children diagnosed or suspected of having COVID-19). We also excluded case studies and qualitative analyses. Five (N.R., B.A.M., J.E.C., R.E. and J.Z.) authors used Covidence software (Covidence Inc) to review all abstracts and to determine if the study met criteria for inclusion. Twenty percent of abstracts reviewed for inclusion were double-coded, and the mean random agreement probability was 0.89; disagreements were resolved via consensus with the first author (N.R.). Two authors (N.R. and B.A.M.) reviewed full-text articles to determine if they met all inclusion criteria and the percent agreement was 0.80; discrepancies were resolved via consensus. When studies met inclusion criteria, prevalence rates for anxiety and depression were extracted, as well as potential moderators. When more than 1 wave of data was provided, the wave with the largest sample size was selected. For 1 study in which both parent and youth reports were provided, 26 the youth report was selected, given research that they are the reliable informants of their own behavior. 28 The following moderators were extracted: (1) study quality (see the next subsection); (2) participant age (continuously as a mean); (3) sex (% female in a sample); (4) geographical region (eg, East Asia, Europe, North America), (5) informant (child, parent), (6) month in 2020 when data were collected (range, 1-12). Data from all studies were extracted by 1 coder and the first author (N.R.). Discrepancies were resolved via consensus. Adapted from the National Institute of Health Quality Assessment Tool for Observation Cohort and Cross-Sectional Studies, a short 5-item questionnaire was used (eTable 2 in the Supplement ). 29 Studies were given a score of 0 (no) or 1 (yes) for each of the 5 criteria (validated measure; peer-reviewed, response rate ≥50%, objective assessment, sufficient exposure time) and summed to give a total score of 5. When information was unclear or not provided by the study authors, it was marked as 0 (no). All included studies are from independent samples. Comprehensive Meta-Analysis version 3.0 (Biostat) software was used for data analysis. Pooled prevalence estimates with associated 95% confidence intervals around the estimate were computed. We weighted pooled prevalence estimates by the weight of the inverse of their variance, which gives greater weight to large sample sizes. We used random-effects models to reflect the variations observed across studies and assessed between-study heterogeneity using the Q and I 2 statistics. Pooled prevalence is reported as an event rate (ie, 0.30) but interpreted as prevalence (ie, 30.0%). Significant Q statistics and I 2 values more than 75% suggest moderator analyses should be explored. 30 As recommended by Bornstein et al, 30 we examined categorical moderators when k of 10 or higher and a minimum cell size of k more than 3 were available. A P value of .05 was considered statistically significant. For continuous moderators, random-effect meta-regression analyses were conducted. Publication bias was examined using the Egger test 31 and by inspecting funnel plots for symmetry. Our electronic search yielded 3094 nonduplicate records (eFigure 1 in the Supplement ). Based on the abstract review, a total of 136 full-text articles were retrieved to examine against inclusion criteria, and 29 nonoverlapping studies 10 , 12 , 13 , 17 , 19 , 20 , 26 , 32 - 53 met full inclusion criteria. A total of 29 studies were included in the meta-analyses, of which 26 had youth symptom reports and 3 studies 39 , 42 , 48 had parent reports of child symptoms. As outlined in Table 1 , across all 29 studies, 80 879 participants were included, of which the mean (SD) perecentage of female individuals was 52.7% (12.3%), and the mean age was 13.0 years (range, 4.1-17.6 years). All studies provided binary reports of sex or gender. Sixteen studies (55.2%) were from East Asia, 4 were from Europe (13.8%), 6 were from North America (20.7%), 2 were from Central America and South America (6.9%), and 1 study was from the Middle East (3.4%). Eight studies (27.6%) reported having racial or ethnic minority participants with the mean across studies being 36.9%. Examining study quality, the mean score was 3.10 (range, 2-4; eTable 3 in the Supplement ). The pooled prevalence from a random-effects meta-analysis of 26 studies revealed a pooled prevalence rate of 0.25 (95% CI, 0.21-0.30; Figure 1 ) or 25.2%. The funnel plot was symmetrical (eFigure 2 in the Supplement ); however, the Egger test was statistically significant (intercept, −9.5; 95% CI, −18.4 to −0.48; P = .02). The between-study heterogeneity statistic was significant ( Q = 4675.91; P < .001; I 2 = 99.47). Significant moderators are reported below, and all moderator analyses are presented in Table 2 . As the number of months in the year increased, so too did the prevalence of depressive symptoms ( b = 0.26; 95% CI, 0.06-0.46). Prevalence rates were higher as child age increased ( b = 0.08; 95% CI, 0.01-0.15), and as the percentage of female individuals ( b = 0.03; 95% CI, 0.01-0.05) in samples increased. Sensitivity analyses removing low-quality studies were conducted (ie, scores of 2) 32 , 43 (eTable 4 in the Supplement ). Moderators remained significant, except for age, which became nonsignificant ( b = 0.06; 95% CI, −0.02 to 0.13; P = .14). The overall pooled prevalence rate across 25 studies for elevated anxiety was 0.21 (95% CI, 0.17-0.24; Figure 2 ) or 20.5%. The funnel plot was symmetrical (eFigure 3 in the Supplement ) and the Egger test was nonsignificant (intercept, −6.24; 95% CI, −14.10 to 1.62; P = .06). The heterogeneity statistic was significant ( Q = 3300.17; P < .001; I 2 = 99.27). Significant moderators are reported below, and all moderator analyses are presented in Table 3 . As the number of months in the year increased, so too did the prevalence of anxiety symptoms ( b = 0.27; 95% CI, 0.10-0.44). Prevalence rates of clinically elevated anxiety was higher as the percentage of female individuals in the sample increased ( b = 0.04; 95% CI, 0.01-0.07) and also higher in European countries ( k = 4; rate = 0.34; 95% CI, 0.23-0.46; P = .01) compared with East Asian countries ( k = 14; rate = 0.17; 95% CI, 0.13-0.21; P < .001). Lastly, the prevalence of clinically elevated anxiety was higher in studies deemed to have poorer quality ( k = 21; rate = 0.22; 95% CI, 0.18-0.27; P < .001) compared with studies with better study quality scores ( k = 4; rate = 0.12; 95% CI, 0.07-0.20; P < .001). Sensitivity analyses removing low quality studies (ie, scores of 2) 32 , 43 yielded the same pattern of results (eTable 5 in the Supplement ). The current meta-analysis provides a timely estimate of clinically elevated depression and generalized anxiety symptoms globally among youth during the COVID-19 pandemic. Across 29 samples and 80 879 youth, the pooled prevalence of clinically elevated depression and anxiety symptoms was 25.2% and 20.5%, respectively. Thus, 1 in 4 youth globally are experiencing clinically elevated depression symptoms, while 1 in 5 youth are experiencing clinically elevated anxiety symptoms. A comparison of these findings to prepandemic estimates (12.9% for depression 2 and 11.6% for anxiety 1 ) suggests that youth mental health difficulties during the COVID-19 pandemic has likely doubled. The COVID-19 pandemic, and its associated restrictions and consequences, appear to have taken a considerable toll on youth and their psychological well-being. Loss of peer interactions, social isolation, and reduced contact with buffering supports (eg, teachers, coaches) may have precipitated these increases. 3 In addition, schools are often a primary location for receiving psychological services, with 80% of children relying on school-based services to address their mental health needs. 54 For many children, these services were rendered unavailable owing to school closures. As the month of data collection increased, rates of depression and anxiety increased correspondingly. One possibility is that ongoing social isolation, 6 family financial difficulties, 55 missed milestones, and school disruptions 3 are compounding over time for youth and having a cumulative association. However, longitudinal research supporting this possibility is currently scarce and urgently needed. A second possibility is that studies conducted in the earlier months of the pandemic (February to March 2020) 12 , 51 were more likely to be conducted in East Asia where self-reported prevalence of mental health symptoms tends to be lower. 56 Longitudinal trajectory research on youth well-being as the pandemic progresses and in pandemic recovery phases will be needed to confirm the long-term mental health implications of the COVID-19 pandemic on youth mental illness. Prevalence rates for anxiety varied according to study quality, with lower-quality studies yielding higher prevalence rates. It is important to note that in sensitivity analyses removing lower-quality studies, other significant moderators (ie, child sex and data collection time point) remained significant. There has been a rapid proliferation of youth mental health research during the COVID-19 pandemic; however, the rapid execution of these studies has been criticized owing to the potential for some studies to sacrifice methodological quality for methodological rigor. 21 , 57 Additionally, several studies estimating prevalence rates of mental illness during the pandemic have used nonprobability or convenience samples, which increases the likelihood of bias in reporting. 21 Studies with representative samples and/or longitudinal follow-up studies that have the potential to demonstrate changes in mental health symptoms from before to after the pandemic should be prioritized in future research. In line with previous research on mental illness in childhood and adolescence, 58 female sex was associated with both increased depressive and anxiety symptoms. Biological susceptibility, lower baseline self-esteem, a higher likelihood of having experienced interpersonal violence, and exposure to stress associated with gender inequity may all be contributing factors. 59 Higher rates of depression in older children were observed and may be due to puberty and hormonal changes 60 in addition to the added effects of social isolation and physical distancing on older children who particularly rely on socialization with peers. 6 , 61 However, age was not a significant moderator for prevalence rates of anxiety. Although older children may be more acutely aware of the stress of their parents and the implications of the current global pandemic, younger children may be able to recognize changes to their routine, both of which may contribute to similar rates of anxiety with different underlying mechanisms. In terms of practice implications, a routine touch point for many youth is the family physician or pediatrician’s office. Within this context, it is critical to inquire about or screen for youth mental health difficulties. Emerging research 42 suggests that in families using more routines during COVID-19, lower child depression and conduct problems are observed. Thus, a tangible solution to help mitigate the adverse effects of COVID-19 on youth is working with children and families to implement consistent and predictable routines around schoolwork, sleep, screen use, and physical activity. Additional resources should be made available, and clinical referrals should be placed when children experience clinically elevated mental distress. At a policy level, research suggests that social isolation may contribute to and confer risk for mental health concerns. 4 , 5 As such, the closure of schools and recreational activities should be considered a last resort. 62 In addition, methods of delivering mental health resources widely to youth, such as group and individual telemental health services, need to be adapted to increase scalability, while also prioritizing equitable access across diverse populations. 63 There are some limitations to the current study. First, although the current meta-analysis includes global estimates of child and adolescent mental illness, it will be important to reexamine cross-regional differences once additional data from underrepresented countries are available. Second, most study designs were cross-sectional in nature, which precluded an examination of the long-term association of COVID-19 with child mental health over time. To determine whether clinically elevated symptoms are sustained, exacerbated, or mitigated, longitudinal studies with baseline estimates of anxiety and depression are needed. Third, few studies included racial or ethnic minority participants (27.6%), and no studies included gender-minority youth. Given that racial and ethnic minority 64 and gender-diverse youth 65 , 66 may be at increased risk for mental health difficulties during the pandemic, future work should include and focus on these groups. Finally, all studies used self- or parent-reported questionnaires to examine the prevalence of clinically elevated (ie, moderate to high) symptoms. Thus, studies using criterion standard assessments of child depression and anxiety disorders via diagnostic interviews or multimethod approaches may supplement current findings and provide further details on changes beyond generalized anxiety symptoms, such symptoms of social anxiety, separation anxiety, and panic. Overall, this meta-analysis shows increased rates of clinically elevated anxiety and depression symptoms for youth during the COVID-19 pandemic. While this meta-analysis supports an urgent need for intervention and recovery efforts aimed at improving child and adolescent well-being, it also highlights that individual differences need to be considered when determining targets for intervention (eg, age, sex, exposure to COVID-19 stressors). Research on the long-term effect of the COVID-19 pandemic on mental health, including studies with pre– to post–COVID-19 measurement, is needed to augment understanding of the implications of this crisis on the mental health trajectories of today’s children and youth. Corresponding Author: Sheri Madigan, PhD, RPsych, Department of Psychology University of Calgary, Calgary, AB T2N 1N4, Canada ( [email protected] ). Accepted for Publication: May 19, 2021. Published Online: August 9, 2021. doi:10.1001/jamapediatrics.2021.2482 Author Contributions: Drs Racine and Madigan had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Racine, Madigan. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Racine, McArthur, Eirich, Zhu, Madigan. Critical revision of the manuscript for important intellectual content: Racine, Cooke, Eirich, Madigan. Statistical analysis: Racine, McArthur. Administrative, technical, or material support: Madigan. Supervision: Racine, Madigan. Conflict of Interest Disclosures: Dr Racine reported fellowship support from Alberta Innovates. Dr McArthur reported a postdoctoral fellowship award from the Alberta Children’s Hospital Research Institute. Ms Cooke reported graduate scholarship support from Vanier Canada and Alberta Innovates Health Solutions outside the submitted work. Ms Eirich reported graduate scholarship support from the Social Science and Humanities Research Council. No other disclosures were reported. Additional Contributions: We acknowledge Nicole Dunnewold, MLIS (Research and Learning Librarian, Health Sciences Library, University of Calgary), for her assistance with the search strategy, for which they were not compensated outside of their salary. We also acknowledge the contribution of members of the Determinants of Child Development Laboratory at the University of Calgary, in particular, Julianna Watt, BA, and Katarina Padilla, BSc, for their contribution to data extraction, for which they were paid as research assistants.
An official website of the United States government The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Save citation to fileEmail citation, add to collections.
Add to My BibliographyYour saved search, create a file for external citation management software, your rss feed.
Evaluation of serum MIP-1β and MCP-2 levels in major depressive disorder: A case-control studyAffiliations.
Background: Major depressive disorder (MDD) is a common and debilitating mental illness characterized by persistent feelings of sadness, hopelessness, and a lack of interest in daily activities. The objective of this study was to investigate whether levels of macrophage inflammatory protein-1β (MIP-1β) and macrophage chemoattractant protein-2 (MCP-2) in the blood were associated with the pathophysiology and development of MDD compared to healthy controls (HCs). Methods: This case-control study was conducted involving 50 MDD patients and 38 HCs. We performed a comprehensive assessment to match age, sex, BMI, and socio-demographic profile between the groups. The study excluded participants with chronic infection, inflammatory diseases, coexisting psychiatric disorder, history of liver and kidney diseases, and individuals who are under antipsychotic medications. A professional psychiatrist diagnosed MDD patients and evaluated HCs based on the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) criteria. The severity of depression was assessed using the Hamilton Depression (Ham-D) rating scale. Commercially available enzyme-linked immunosorbent assay (ELISA) kits were used to quantify the serum MIP-1β and MCP-2 levels. Results: The results indicated elevated serum MIP-1β levels (207.73±24.24 pg/ml) in MDD patients compared to HCs (58.77±9.14 pg/ml). This difference in concentration is positively correlated with severity of disease symptoms (r = 0.451; p<0.001). Similarly, the levels of MCP-2 were found to be elevated in patients compared to controls (143.61±19.92 vs. 56.84±4.02 pg/ml; p = 0.003), with a positive correlation with the Ham-D scores (r = 0.373; p = 0.004). Conclusion: According to this study, elevated levels of MIP-1β and MCP-2 may be associated with the pathophysiology and development of MDD. These increased serum MIP-1β and MCP-2 levels could be used as risk assessment tools for MDD. The present findings urge further research and the development of therapeutic and diagnostic approaches for depression. Copyright: © 2024 Akter et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. PubMed Disclaimer Conflict of interest statementThe authors have declared that no competing interests exist. Fig 1. Comparison of serum MIP-1β and… Fig 1. Comparison of serum MIP-1β and MCP-2 levels between MDD patients and healthy controls. Receiver operating characteristic (ROC) curves… Receiver operating characteristic (ROC) curves of serum MIP-1β levels (a) and serum MCP-2…
Grants and fundingLinkout - more resources, full text sources.
Miscellaneous

NCBI Literature Resources MeSH PMC Bookshelf Disclaimer The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.  | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
IMAGES
VIDEO
COMMENTS
The adolescent was previously diagnosed with major depressive disorder and treated intermittently with supportive psychotherapy and antidepressants. ... Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response. Depression and Anxiety ...
In a study of 239 outpatients diagnosed with major depressive disorder in a NIMH. 16-week multi-center clinical trial, participants were assigned to interpersonal therapy, CBT, imipramine with clinical management, or placebo with clinical management. One. hundred sixty-two patients completed the trial.
Patient Case Presentation. Figure 1. Blue and silver stethoscope (Pixabay, N.D.) Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness.
Depression is a prevalent psychiatric disorder that often leads to poor quality of life and impaired functioning. Treatment during the acute phase of a major depressive episode aims to help the patient reach a remission state and eventually return to their baseline level of functioning. Pharmacotherapy, especially selective serotonin reuptake ...
With this case report, we underline the importance of diagnosing and treating OSA in patients with a depressive disorder, even when the depression is preceded by psychosocial stressors. As illustrated by our patient, proper diagnostics may improve quality of life and prevent misdiagnosing affective symptoms as a treatment-resistant depression.
Strengths and Assets: bright, attractive, personable, cooperative, collaborative, many good social skills Treatment Plan Goals (measures): Reduce symptoms of depression and anxiety (BDI, BAI). To feel more comfortable and less pressured in relationships, less guilty. To be less dependent in relationships.
The Malaysian Clinical Practice Guidelines (CPG) on the Management of Major Depressive Disorder (MDD) (2nd ed.), published in 2019, covers screening, diagnosis, treatment and referral (which frequently pose a challenge in the primary care setting) while minimising variation in clinical practice.
Introduction to the selected case study. In this case study, we will focus on Jane, a 32-year-old woman who has been struggling with depression for the past two years. Jane's case offers a compelling narrative that highlights the various aspects of depression, including its onset, symptoms, and the treatment journey.
A Comprehensive Overview of Major Depressive Disorder with Case Study. Depression affects 1 in 5 Americans. Home; Patient Case Presentation; Differential Diagnoses; Pathophysiology Description; Patient Education Video; Quiz (5 Q&A) References; Site contributors. October 21 2019 October 21, 2019. Alli Byers.
Items are derived from the 9 diagnostic criteria for major depressive disorder used in the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV), including sadness, loss of interest or pleasure, poor concentration or decision-making, self-outlook, suicidal ideation, lack of energy, sleep disturbance, appetite change, and psychomotor ...
Major depressive disorder (MDD) is one of the most common psychiatric illnesses and a common diagnosis in primary care clinics. Point prevalence of depression ranges around 5% (with considerable variation among countries), and it commonly ranks among the top conditions and causes considerable burden of disease. 1 Despite this, the rates of correct recognition of depression in primary care are ...
Disorders. Major depressive disorder is a situation that feeling low energy and high sadness in. everyday life that lasts at least two weeks (NIMH, 2016). 1.1 Criteria for Major Depressive ...
The purpose of this study was to determine the best practice for a client diagnosed with major depressive disorder who was referred for treatment at a community mental health facility. The client was assessed, diagnosed, and a treatment plan was developed. Implemented treatment consisted of combined cognitive behavioral oriented psychotherapy and psychotropic medication. The Beck Depression ...
Symptoms vary widely depending on the individual. The timing and length of the depression also varies. To be diagnosed with Major Depressive Disorder, patients have to have several, usually five or more, symptoms including low mood that is present for at least two weeks (Depression, 2018). Other symptoms of major depressive disorder include:
current issue. current issue; browse recently published; browse full issue index; learning/cme
Major Depressive Disorder Case Queries: Where Do Rapid-Acting Therapies Fit Into Care? How soon is now? Identifying which patients with major depressive disorder (MDD) are candidates for treatment with a rapid-acting antidepressant . ... Study the educational content online or print it out. Online, choose the best answer to each test question ...
Beyond Depression Case Studies 1 ase Studies from the "Other perinatal mental health concerns" module part A and part Case Study: Major Depressive Disorder Maria: I have a three month old baby and I have been waiting to feel like myself again, but I don't know whether I'll ever be me again. When I really look back on it, there were some
The patient's primary issue is major depression accompanied by severe suicidal thoughts. The underlying cause of this problem can be attributed to several challenging life events, including the loss of her daughter, her son's illness, and the absence of a healthy relationship with her husband.
Major Depressive Disorder Case Study. All the information given is important for me to evaluate because I am a Nurse. For me to understand the patient's depressive disorder, I need a broad perspective of her history. Especially considering she has been here for three weeks and most likely staying longer. However, the most important ...
Scientists may be a step closer to that reality, thanks to new research that has identified six subtypes — or "biotypes" — of major depression via brain imaging combined with machine learning.
In that study, the scientists focused on a subtype they call the cognitive biotype of depression, which affects more than a quarter of those with depression and is less likely to respond to standard antidepressants. By identifying those with the cognitive biotype using fMRI, the researchers accurately predicted the likelihood of remission in 63 ...
CASE STUDY Major Depressive Disorder Case Study 1. What information is pertinent to you as the nurse? As Mrs. Jones' health care nurse, I am interested in starting with the client's chief complaint where she says, "there is no point to my life, and I want to end it all." I would then like to set up trust to gain insight into whether Mrs ...
To the Editor: Manic symptoms are common in patients with major depressive disorder (MDD) with the prevalence of mixed depression approaching that observed for pure MDD in some studies. 1, 2 Compared with patients who have pure depression, those with mixed depression have higher rates of comorbid anxiety disorders, substance use disorders, and suicidal behavior. 3, 4 While there is increasing ...
A new study in JAMA Psychiatry aimed to understand how sleep, physical activity, and circadian rhythms relate to major depressive disorder (MDD). The study included adults with both current MDD and those with a history of MDD but who were symptom-free at the time of the study (remitted MDD). MDD is a serious mental health disorder with symptoms ...
Many of the studies cited likely did not evaluate lifetime depression history, this is often the case when diagnoses are obtained without using a diagnostic interview. Authors could enlighten current evidence by exploring effects based on depression history. ... including (1) presence of major depressive disorder indicated by self-report ...
Six subtypes of major depression have been identified in a new study. Here's what that could mean for the future of personalized mental health care.
Here we conducted a cross-sectional study of 107 participants, including 40 healthy controls and 67 patients with major depressive disorder (33 with suicide attempts and 34 without).
Study Selection Studies were included if they were published in English, had quantitative data, and reported prevalence of clinically elevated depression or anxiety in youth (age ≤18 years). Data Extraction and Synthesis A total of 3094 nonduplicate titles/abstracts were retrieved, and 136 full-text articles were reviewed. Data were analyzed ...
Background: Major depressive disorder (MDD) is a common and debilitating mental illness characterized by persistent feelings of sadness, hopelessness, and a lack of interest in daily activities. The objective of this study was to investigate whether levels of macrophage inflammatory protein-1β (MIP-1β) and macrophage chemoattractant protein-2 (MCP-2) in the blood were associated with the ...
Major Depressive Disorder Case Study. Charneise Nelson Arizona College of Nursing - Tempe NUR 356 Mental Health Theory & Application Professor Megan Graeff October 15, 2022 **Major Depressive Disorder Case Study. What information is pertinent to you as the nurse?** There are several pieces of information regarding Mrs. Jones that is ...