

Case Examples
Examples of recommended interventions in the treatment of depression across the lifespan.

Children/Adolescents
A 15-year-old Puerto Rican female
The adolescent was previously diagnosed with major depressive disorder and treated intermittently with supportive psychotherapy and antidepressants. Her more recent episodes related to her parents’ marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT).
Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response. Depression and Anxiety , 26, 98-103. https://doi.org/10.1002/da.20457
Sam, a 15-year-old adolescent
Sam was team captain of his soccer team, but an unexpected fight with another teammate prompted his parents to meet with a clinical psychologist. Sam was diagnosed with major depressive disorder after showing an increase in symptoms over the previous three months. Several recent challenges in his family and romantic life led the therapist to recommend interpersonal psychotherapy for adolescents (IPT-A).
Hall, E.B., & Mufson, L. (2009). Interpersonal Psychotherapy for Depressed Adolescents (IPT-A): A Case Illustration. Journal of Clinical Child & Adolescent Psychology, 38 (4), 582-593. https://doi.org/10.1080/15374410902976338
© Society of Clinical Child and Adolescent Psychology (Div. 53) APA, https://sccap53.org/, reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of the Society of Clinical Child and Adolescent Psychology (Div. 53) APA.
General Adults
Mark, a 43-year-old male
Mark had a history of depression and sought treatment after his second marriage ended. His depression was characterized as being “controlled by a pattern of interpersonal avoidance.” The behavior/activation therapist asked Mark to complete an activity record to help steer the treatment sessions.
Dimidjian, S., Martell, C.R., Addis, M.E., & Herman-Dunn, R. (2008). Chapter 8: Behavioral activation for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 343-362). New York: Guilford Press.
Reprinted with permission from Guilford Press.
Denise, a 59-year-old widow
Denise is described as having “nonchronic depression” which appeared most recently at the onset of her husband’s diagnosis with brain cancer. Her symptoms were loneliness, difficulty coping with daily life, and sadness. Treatment included filling out a weekly activity log and identifying/reconstructing automatic thoughts.
Young, J.E., Rygh, J.L., Weinberger, A.D., & Beck, A.T. (2008). Chapter 6: Cognitive therapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 278-287). New York, NY: Guilford Press.
Nancy, a 25-year-old single, white female
Nancy described herself as being “trapped by her relationships.” Her intake interview confirmed symptoms of major depressive disorder and the clinician recommended cognitive-behavioral therapy.
Persons, J.B., Davidson, J. & Tompkins, M.A. (2001). A Case Example: Nancy. In Essential Components of Cognitive-Behavior Therapy For Depression (pp. 205-242). Washington, D.C.: American Psychological Association. http://dx.doi.org/10.1037/10389-007
While APA owns the rights to this text, some exhibits are property of the San Francisco Bay Area Center for Cognitive Therapy, which has granted the APA permission for use.
Luke, a 34-year-old male graduate student
Luke is described as having treatment-resistant depression and while not suicidal, hoped that a fatal illness would take his life or that he would just disappear. His treatment involved mindfulness-based cognitive therapy, which helps participants become aware of and recharacterize their overwhelming negative thoughts. It involves regular practice of mindfulness techniques and exercises as one component of therapy.
Sipe, W.E.B., & Eisendrath, S.J. (2014). Chapter 3 — Mindfulness-Based Cognitive Therapy For Treatment-Resistant Depression. In R.A. Baer (Ed.), Mindfulness-Based Treatment Approaches (2nd ed., pp. 66-70). San Diego: Academic Press.
Reprinted with permission from Elsevier.
Sara, a 35-year-old married female
Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks.
Bleiberg, K.L., & Markowitz, J.C. (2008). Chapter 7: Interpersonal psychotherapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: a treatment manual (4th ed., pp. 315-323). New York, NY: Guilford Press.
Peggy, a 52-year-old white, Italian-American widow
Peggy had a history of chronic depression, which flared during her husband’s illness and ultimate death. Guilt was a driving factor of her depressive symptoms, which lasted six months after his death. The clinician treated Peggy with psychodynamic therapy over a period of two years.
Bishop, J., & Lane , R.C. (2003). Psychodynamic Treatment of a Case of Grief Superimposed On Melancholia. Clinical Case Studies , 2(1), 3-19. https://doi.org/10.1177/1534650102239085
Several case examples of supportive therapy
Winston, A., Rosenthal, R.N., & Pinsker, H. (2004). Introduction to Supportive Psychotherapy . Arlington, VA : American Psychiatric Publishing.
Older Adults
Several case examples of interpersonal psychotherapy & pharmacotherapy
Miller, M. D., Wolfson, L., Frank, E., Cornes, C., Silberman, R., Ehrenpreis, L.…Reynolds, C. F., III. (1998). Using Interpersonal Psychotherapy (IPT) in a Combined Psychotherapy/Medication Research Protocol with Depressed Elders: A Descriptive Report With Case Vignettes. Journal of Psychotherapy Practice and Research , 7(1), 47-55.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Healthcare (Basel)

Emotions, Feelings, and Experiences of Social Workers While Attending to Vulnerable Groups: A Qualitative Approach
María dolores ruiz-fernández.
1 Department of Nursing, Physiotherapy and Medicine, University of Almeria, 04120 Almeria, Spain; se.lau@757frm (M.D.R.-F.); moc.liamg@iicor92 (R.O.-A.); [email protected] (J.M.H.-P.); se.lau@nanrefc (C.F.-S.)
Rocío Ortiz-Amo
Elena andina-díaz.
2 Department of Nursing and Physiotherapy, University of León, 24071 León, Spain
3 SALBIS Research Group, University of León, 24071 León, Spain
4 EYCC Research Group, University of Alicante, 03690 Alicante, Spain
Isabel María Fernández-Medina
José manuel hernández-padilla.
5 Adult, Child and Midwifery Department, School of Health and Education, Middlesex University, London NW4 4BT, UK
Cayetano Fernández-Sola
6 Faculty of Health Sciences, University Autónoma of Chile, Temuco 3580000, Chile
Ángela María Ortega-Galán
7 Department of Nursing, University of Huelva, 21007 Huelva, Spain; moc.liamg@69agetroalegna
Associated Data
Not applicable.
Social workers in the community setting are in constant contact with the suffering experienced by the most vulnerable individual. Social interventions are complex and affect social workers’ emotional well-being. The aim of this study was to identify the emotions, feelings, and experiences social workers have while attending to individuals in situations of vulnerability and hardship. A qualitative methodology based on hermeneutic phenomenology was used. Six interviews and two focus group sessions were conducted with social workers from the community social services and health services of the Andalusian Public Health System in the province of Almería (Spain). Atlas.ti 8.0 software was used for discourse analysis. The professionals highlighted the vulnerability of certain groups, such as the elderly and minors, people with serious mental problems, and people with scarce or no economic resources. Daily contact with situations of suffering generates a variety of feelings and emotions (anger, sadness, fear, concern). Therefore, more attention should be paid to working with the emotions of social workers who are exposed to tense and threatening situations. Peer support, talking, and discussions of experiences are pointed out as relevant by all social workers. Receiving training and support (in formal settings) in order to learn how to deal with vulnerable groups could be positive for their work and their professional and personal quality of life.
1. Introduction
According to the World Health Organization (WHO), vulnerability is the degree to which a population, individual, or organization is unable to anticipate, cope with, resist, and recover from the impacts of disasters [ 1 ]. The concept of vulnerability refers to those sectors or groups of the population that, due to their age, sex, marital status, or ethnic origin, are in a risky condition that prevents them from accessing development and better welfare conditions [ 2 ]. These people are suffering or undergoing a painful experience [ 3 ] and turn to social services for a solution [ 4 , 5 ]. The care they receive may come from community social services [ 6 ] or, more specifically, from integrated social services in the health field [ 7 ].
Social workers are the frontline professionals of social services [ 8 ], that is, the first professionals in charge of meeting the demands of users upon arrival at care services [ 9 ]. They therefore play a fundamental role in the care trajectory of individuals in situations of need and social vulnerability [ 10 ].
The number of service users with very complex demands is quite high [ 11 ]. As a result, in daily practice, social work professionals find themselves in constant contact with individuals who are experiencing considerable social challenges [ 12 , 13 ]. Professionals are confronted with the task of promoting equality and well-being for individuals [ 14 ]. However, the interventions carried out with users are based on the traditional social intervention model of social services [ 15 ]. This strategy provides material and/or financial resources to users, which could help them to escape from that particular situation [ 16 ]. In this case, this means that the actual implementation of this model would be carried out to a greater or lesser extent, depending on the resources available to the state in question [ 17 ].
Professionals witness the suffering and despair of those most in need [ 18 , 19 ]. This situation triggers professionals’ emotions and feelings, the first being understood as the automatic and uncontrollable response to a stimulus and the feelings being the conscious evaluation of the emotion or experience suffered by the individual [ 20 ]. It is quite common that the demands made are greater than the resources available to manage them or that they need to be met faster than is possible due to the administrative procedures involved [ 21 ]. In addition, the vulnerability of some groups must be added to this context [ 22 ]. According to WHO, children, the elderly, and people who are ill are particularly vulnerable. Poverty is a major contributor to vulnerability [ 23 ]. In this sense, different studies establish that minors and the elderly are among the most vulnerable populations [ 24 ]. Thus, the occupational and professional commitment to these groups of individuals becomes even greater [ 25 ].
These repeated working conditions, alongside the contact with the person’s suffering, have repercussions on the professionals’ well-being [ 26 , 27 , 28 ], causing stress, emotional discomfort, and even vicarious trauma, defined as “those emotions and behaviours resulting from the interaction with traumatic events experienced by others” [ 29 , 30 ]. This is known as the cost of the emotional impact of caring [ 31 , 32 ], that is, the price professionals pay in the process of helping people in situations of intense suffering or trauma. According to the stress process models, some of the resources that potentially serve as a protective barrier include social support, the repertoire of confrontations, and some self-concepts such as self-esteem [ 33 , 34 , 35 ]. Other protective resources with the ability to significantly reduce the harmful consequences of existing stressors are the mastery and control of existing circumstances and mutual support among the professionals themselves [ 36 , 37 ].
According to the reviewed literature, research on social work has traditionally focused on professional performance and how this performance affects intervention subjects. However, there are fewer studies on the impact that the suffering of users has on social workers [ 38 , 39 , 40 , 41 ]. In recent years, there has been an increase in research, from a quantitative paradigm, in order to describe the working conditions of this group of professionals and their professional needs [ 42 , 43 , 44 ]. Despite this, research from a qualitative paradigm, from the perspective of social workers themselves, is still scarce. In particular, it reflects the emotional situation they experience in the development of their work, and seeks to delve into the experiences, the consequences, and what they would need, in order to continue helping in a sustainable way [ 45 , 46 , 47 ].
Bearing this in mind, the main objective of this research was to identify the social workers’ emotions, feelings, and experiences while attending to individuals in situations of vulnerability and hardship. Specifically, two secondary objectives were raised: to learn about the situations causing discomfort and suffering, as well as about the consequences of the same on the social workers themselves, and to inquire about the needs and resources of professionals so as to meet the demands of their work.
2. Materials and Methods
2.1. approach.
In the present study, a qualitative design based on a phenomenological–hermeneutic approach was used. According to Van Manen [ 48 ], this approach allows the study of non-conceptualized experiences lived by people, as well as the meaning of these experiences. Thus, it was possible to perform an in-depth analysis of the daily work experiences of social workers in community social services and health services. Their feelings and perceptions about the implementation of social interventions involving vulnerable groups of individuals were explored and interpreted.
2.2. Recruitment and Sampling
Participants in the study were the social workers at the community social services and health services of the Andalusian Public Health System in the province of Almería (Spain). Community social services in Andalusia are distributed as follows: In the capitals and cities of more than 20,000 inhabitants, the municipalities carry out the management of these services. In cities with less than 20,000 inhabitants, the provincial council carries out the management. Specifically, in Almeria city, there are 4 community social services centers managed by the city council. Regarding the Andalusian Health Service, in the capital city of Almería, there are 13 health centers (6 of these are centers with a full-time social worker). We selected social workers employed at three community social services centers in Almeria and social workers employed at the six health centers.
A total of 20 social workers participated. Of these, 11 worked in community social services centers and 9 worked in the Andalusian Health Service.
The inclusion criteria were the following: holding a stable position as a social work professional in community social services and/or the Andalusian Health Service, having a professional career or experience of no less than eight years, and regularly providing assistance to individuals in need of social services. The following professionals were excluded: professionals with temporary employment contracts or little work experience (less than eight years), professionals in managerial positions, professionals who had no contact with people in vulnerable situations, and professionals who had any psychological impairment that made it difficult for them to provide information.
Convenience sampling was the sampling method used. To recruit as many participants as possible, a snowball sampling procedure was used: a professional was contacted, who, in turn, would contact other professionals willing to participate [ 49 ]. First, the director of an urban community social services center was contacted by telephone. The study was explained to her, and a brief summary of the study, along with authorization from the Ethics and Research Commission, was sent to her via email. Subsequently, the director of the center informed her colleagues of the study and invited them to participate. Finally, the director contacted other directors of other centers, who then followed the same procedure.
The social workers at the health centers were contacted by a mental health social worker and a case manager nurse working at an urban health center. Both professionals were responsible for providing the health and social care workers with information about the study. Once they agreed to participate in the research, the participants were contacted to arrange a meeting.
When selecting participants, gender diversity was sought, although there were few male social workers among the centers’ staff. In Spain, the social work profession is predominantly female, so the sample (a larger number of women) could be considered representative. Equal representation of health and community social workers was also sought.
2.3. Data Collection
In-depth interviews and focus groups were the information-gathering techniques used. Two focus group sessions (with a total of seven people in each group) and six in-depth interviews were carried out. The two focus groups were conducted by a researcher and a collaborator, who had received specific training by specialists. The discourses were taped for transcription.
First, two focus group sessions were held in February 2019. One focus group session was held in the meeting room of an urban community social services center, and the other focus group was held in the multipurpose room of a social services center in the province of Almería (Spain). The groups comprised professionals working in both services (community and health services) to ensure that professionals from both sectors were included in each focus group. The researcher led the group, while the collaborator wrote down in a field notebook those observations that could be useful in subsequent analysis. The session began with an exercise that prompted discussion and dialogue among the members of the group: “Describe your day-to-day work experiences with individuals in vulnerable situations.” Finally, the conclusions were summarized, and the members were thanked for their participation. Each session lasted approximately 90 min.
Second, in-depth interviews were conducted by the researcher of this study in the professionals’ offices. Three interviews were undertaken with community services social workers and a further three with health and social care workers during the month of March 2019. None of them had participated before in the focus groups. In these interviews, those dimensions that had not been sufficiently explored in the focus groups were addressed. A list of interview questions was not used. Only an opening question was asked: “Tell me about your daily work. How does attending to individuals in situations of vulnerability on a daily basis affect you?” This question facilitated the participants’ discussion. The interviewer took all the necessary notes in a field notebook. The interviews lasted approximately one hour.
In the opinion of the researchers, the two focus groups and the six in-depth interviews were sufficient to achieve data saturation. The possibility of conducting one focus group session in the urban area and the other in a rural municipality was considered in order to identify the differences between community social services in the capital of the province and community social services in a rural setting. Furthermore, both focus groups included not only community social services professionals but also health services professionals in order to have discourses from both types of workers in the two settings studied. Once the focus group sessions were completed, in-depth interviews were conducted to investigate the emerging issues in the focus groups in order to obtain additional data.
2.4. Analysis
Giorgi’s method of analysis [ 50 ], which involves creating a series of categories and subcategories, was used to analyze the information from both the in-depth interviews and the focus groups. This procedure was carried out in several phases. The first one was an in-depth reading of all the discourses, which had already been transcribed verbatim. The second phase involved a second reading and the division of the data into parts. The basis of the division into parts is meaning discrimination, which presupposes the prior assumption of a disciplinary perspective (social work, in this case). These meaning discriminations constitute parts known as meaning units. The meaning units were examined, tested, and redefined so that the disciplinary value of each unit could be more explicit. These meaning units were then grouped into broader categories according to their shared characteristics and the disciplinary value. In the last phase, the contents of each of the categories were interpreted and analyzed based on the phenomenon or experience lived.
The theoretical–methodological approach was adequate to achieve the objectives of the study. The data obtained were relevant in the context and in other contexts, when compared to the literature.
As for the validity of the results of the analysis, contrast through triangulation was used to control for potential biases resulting from the heterogeneity of the data and the informants’ different points of view. To make a contrast between the differences and similarities conveyed in the discourses, the techniques of focus groups and in-depth interviews were used. In terms of triangulation between subjects, informants were selected from different settings and fields of work to diversify the information present in the discourses regarding the participants’ work experiences in these services. Two researchers began the analysis after the first interview in order to constantly verify that it was in line with the study’s objectives and in order to be prepared in case any change in the research design was needed (it was not). The main categories that researchers identified in the analysis were shared with the participants (by email) to confirm the discourses. In the participants’ discourses where contradictory information was detected, this moment was used to clarify it. The analysis was shared with the rest of the team to ratify the categories. At the same time, an external researcher (with expertise in the subject) validated the analysis.
Reflexivity and a self-critical attitude were maintained throughout the process by all the researchers. To avoid influencing data collection, sample recruitment, and location, the researchers only knew the topic in a superficial manner (as health professionals) and it was not their usual work/subject matter of research.
Atlas.ti 8.0 software (Scientific Software Development GmbH, Berlin, Germany) was used to analyze the discourses.
2.5. Ethical Aspects
This research obtained all the necessary authorization from the corresponding Research and Ethics Committee of the University of Almería, Spain (EFM-11/19). Previously, participants had been informed verbally and in writing of the purpose of the study, and their informed consent had been obtained in writing in a dedicated document. The confidentiality and anonymity of participants were preserved throughout this research, in compliance with the bioethical principles of the Declaration of Helsinki [ 51 ]. The data from the discourses were safeguarded and protected in accordance with the Spanish regulations in force regarding the official protection of personal data, i.e., the Spanish Organic Law 3/2018, of the 5th of December, on Personal Data Protection and Guarantee of Digital Rights [ 52 ].
The study population comprised 20 professionals: 11 professionals working in community social services and 9 professionals working in the Andalusian Health Service, with a mean age of 46.35 (SD = 7.36) years and with a mean work experience of 24.16 (SD = 7.87) years. Table 1 shows a summary of the sociodemographic characteristics of the sample of professionals who participated in this research.
Sociodemographic characteristics of participants.
| Variables | Focus Group ( = 14) | In-Depth Interviews ( = 6) |
|---|---|---|
| Gender | ||
| Female | 12 | 6 |
| Male | 2 | - |
| Marital status | ||
| Married | 10 | 5 |
| Single | 3 | 1 |
| Others | 1 | - |
| Work experience (years) | - | |
| 10–20 | 1 | 1 |
| 20–30 | 3 | 5 |
| 30–40 | 9 | 1 |
| >40 | 1 | |
| Area of work | ||
| Community Services | 8 | 3 |
| Health Services | 6 | 3 |
An analysis of the discourses was performed with the information gathered from the focus groups (FGs) and from the in-depth interviews (IDIs). Three categories with nine subcategories emerged from this analysis. All categories and subcategories were encompassed by a broader category relating to the social workers’ experience ( Table 2 ).
Categories and subcategories emerging from the study.
| Categories | Subcategories |
|---|---|
| Working with vulnerable groups | |
| Emotions emerging from working with vulnerable groups | |
| Need for spaces for self-care |
3.1. Working with Vulnerable Groups
In day-to-day practice, health and social care workers serve users with very different demands. The characteristics of the population visited by social services are highly varied. Certain settings and realities experienced by users are perceived by social workers as generators of further personal suffering or dismay. Moreover, the traditional social intervention model adopted by social services causes chronic frustration and professional burnout. The main element identified by the informants as a generator of further suffering in the person of the social worker was the intervention work carried out with vulnerable groups.
3.1.1. Minors and the Elderly
Two of the vulnerable groups that had an impact on participants were minors and the elderly, as they are fragile and innocent groups.
You can’t avoid being touched by the toughest situations, such as those involving minors or the elderly [who are] on their own… (IDIs, P3).
…then, well, that… what I always say when there are cases and cases, when you see the despair of a daughter because her mother is ill and the resources she needs do not arrive… There are cases that have an impact, and that no matter how professional you are, you can’t help it, of course not! Because I’m also a person… (FGs1, P11).
My weak point, so to speak, is the elderly, especially those who are alone… Many needs arise, and sometimes they cannot be met, and I cannot help but take work home with me… (FGs2, P17).
There are users who inevitably impact your situation, or groups such as minors who are still fragile and innocent… And, you find cases where these minors have a rather difficult context and that touches your heart… (IDIs, P5).
3.1.2. People with Serious Mental Problems
Another group mentioned by participants was people with serious mental problems. The fact of thinking that nobody understands them, that nobody believes them, that they are in danger, that they feel threatened, generates a lot of suffering.
…above all, patients with serious mental disorders, when they’re having delusions and hallucinations… and it’s so upsetting to think that nobody understands them, that nobody believes them, that they are in danger, that they feel threatened, and that causes me a lot of suffering, and to that, we must add the social aspect, when they see that the life project they had just like everybody else, their dreams… all is shattered… (IDIs, P5).
3.1.3. People with Scarce or a Lack of Economic Resources
There are also situations of poverty that become permanent for some people and that professionals attend to repeatedly. People with scarce or a lack of economic resources find themselves in very complex situations, and figuring out a way out of these situations has become almost impossible for them, so they visit social workers in a state of desperation, seeking help.
…these are people who come to my office in great distress because they don’t have the most basic things to eat. I mean, they can’t even pay for water [bills]; they can’t afford the most basic items. Besides, these are chronic situations; they no longer know how to get out of that labyrinth (IDIs, P3).
There are families with real hardships; they do not even have a snack for their children to eat at school, and they’ve had it for a long time, and that distresses them so much that they come looking for you again and again… (FGs1, P9).
We have many users who are poor, but really poor; they do not even have the most basic needs covered… (IDIs, P4).
The fight against poverty that leads to social exclusion must be prioritized. We have seen families with children, families who have suffered evictions, people who have reached a situation of poverty without the possibility of any intervention, and who are constantly visiting you out of desperation… (FGs2, P20).
3.2. Emotions Emerging from Working with Vulnerable Groups
Daily contact with situations of suffering can generate a variety of feelings and emotions among health and social care workers. The need arising in professionals to help users who find themselves in a complex situation is evident. However, sometimes social workers encounter a different reality, and aid does not arrive as expected, thus generating various emotions in them.
The most common emotions expressed by professionals, when facing users’ serious situations or when the outcome is not as expected, included anger, sadness, fear, and concern.
3.2.1. Anger
In relation to anger, participants commented on how seeing injustice, because things are not done as they should be, for example, made them feel helpless, and that helplessness generates anger.
…and many times, you feel angry and helpless; of course you feel that [way], and whoever says they don’t is lying, because we [usually] see very tough situations… (FGs2, P14).
…sometimes I get angry; other times I get sad… It’s a constant state of alertness. That’s my natural state, [and it has been] for some time now (FGs1, P12).
When you see injustice, I feel tremendous anger; it makes me very angry that things are not done as they should… or that the response to a user is not what he needs (IDIs, P6).
There are days when you get very angry or upset about certain situations that we have to deal with… (IDIs, P2).
3.2.2. Sadness
The fact of witnessing difficult times that other people go through, or the despair they experience, generates sadness in social workers.
…I feel like… how can I put it into words?… in a pyramid of dissatisfaction, in the sense that, you know, although you do everything you can, [you see] the outcome in the very long term, and then, in the meantime, you see those people here every day… (IDIs, P2).
…other times I have feelings of sadness… (FGs2, P19).
It is inevitable to feel sad on many occasions, when users are desperate and the answers do not come… (IDIs, P1).
Sometimes there are cases, people, who are in a difficult moment of their lives, and when they share their story with you, you feel a lot of sadness, although you cannot transmit it to them, but inside, you get sad… (FSs2, P18).
3.2.3. Fear
In some cases, some participants even mentioned the word “fear,” although they did not delve into that emotion.
…powerlessness, frustration, or even fear… (FGs2, P17).
…and so, it scares me… (FGs2, P15)
There are situations where you feel fear… (IDIs, P3)
3.2.4. Concern
Social workers disclosed that there are situations they cannot possibly stop thinking about, such as people who find themselves in very serious circumstances. These are extraordinary cases that social workers keep thinking about, even after their working hours, because, according to their accounts, some issues inevitably haunt them owing to their significance or complexity. The emotion that emerged related to this was concern about the problems of the users.
…but there are times and situations, quite exceptional ones, that I can’t help remembering; you definitely remember them… There are situations that I still do take home with me, although I’ve been [working this job] for many years, and you have to learn not to take [these situations] with you. Two, three…? or more [of these situations] a year, at least (FGs1, P13).
I guess situations stop shocking you with the passage of time, or you see it differently… But that does not mean that there are no cases that do not affect me, or that I [don’t] take them home, flitting around in my head… and you mull over them, or even after some time, you would remember that nothing could be done, you see that family member on the street and you remember. There are always situations that affect you…I don’t know… (IDIs, P1).
…I take problems home with me because [first] we’re people and then we’re professionals, and you’re there [trying to] figure out how to solve that situation… (FGs 1, P12).
Social workers identify the need and the urgency of some situations for some vulnerable groups. Not being able to respond adequately, because sometimes resolving a demand takes time, generates discomfort and concern among professionals.
…although you do everything you can, [you see] the outcome in the very long term… (IDIs, P2).
…when urgent cases arise and you can’t resolve them with the same urgency…you go home thinking “[hopefully] nothing [bad] happens by tomorrow,” and, well, you don’t even know if that’ll be resolved the next day (FGs2, P20).
…and when the user leaves, I think, what if by the time it’s resolved it’s too late…? And I know it’s not my fault, but I’m the one who’s facing the music… (FGs 2, P18).
…because I have cases [i.e., users] that you attend to and you tell them, “Come back tomorrow to finish this,” or that they have to wait for such-and-such… (FGs2, P18).
3.3. Need for Spaces for Self-Care
Health and social care workers recognized that working with vulnerable groups causes them many negative emotions, as we have previously described. They said that they feel the need to express and share those feelings.
3.3.1. Mutual Support
They end up developing more informal strategies, such as mutual support. Sharing complex cases and learning from the experience of other professionals and their way of dealing with different situations are two of the most valued strategies according to the discourses. Peer support, talking, and discussions of experiences are highlighted and widely accepted by all social workers. They agree that talking to peers and team support are essential to address certain cases or avoid being affected by them in one way or another. Sharing experiences with peers who have undergone similar situations is described as an informal therapy that social workers use to cope with daily work.
…we support each other here and help each other quite a lot; the director is always there… and that makes a big difference. Maybe peer support is a useful tool to deal with the most vulnerable situations, or so that the most complex cases don’t affect you that much (IDIs, P6).
…[having a] good relationship with my peers always helps; for me that’s my therapy (FGs2, P15).
Sharing experiences with colleagues is a mechanism that comes in handy so as to manage all these situations of frustration or in order to consider what [other] alternatives may exist, in addition to the ones you already know (IDIs, P4).
…we are like a kind of group therapy, and [I have] wonderful colleagues; we support each other, really, at least in my experience (FGs 2, P13).
If there is a case that worries me, she always asks me the first one, always, and I feel very supported. Also, in this office, [which] is shared with another colleague, if you arrive from a bad day, especially tired from so many kilometers, we can share how the day has gone and we can let off steam between us (IDIs, P4).
The truth is that relationships with colleagues are very good, and you find support, and of course that matters; just talking and venting our feelings already help (IDIs, P1).
…I have colleagues who may have [many] more years of experience or who have already undergone a similar case and similar experiences. It’s always good that they give you, like, their insight (FGs1, P12).
3.3.2. Formal Spaces to Work Emotions
Professionals talk about the benefits of peer support and report that it exists and is real. However, they also emphatically express the need for training and support in formal settings to learn how to deal with certain cases or not to bring those situations to their personal lives. They recognize the need to develop other types of skills to help them manage their own suffering and dissatisfaction in structured spaces dedicated to training, and emotional support. Receiving training and support in formal spaces can be positive. Working with emotions could favor their work and their professional and personal quality of life. Informants demand that social workers be cared for so that their work, which is in contact with suffering, is sustainable, without becoming exhausted or burned out.
…from the upper management, they have to think about the professionals; we lack the tools to face the current situations we are experiencing… (FGs2, P15).
Yeah, why not? Spaces to work on emotional education or other types of therapies and teachings so as to care for professionals, [and] formal spaces to talk to peers. These can be things that greatly facilitate and favor the work of social workers and their professional and personal quality of life. Psychologists and others to be within our reach… All professionals need their own space, and I think that in the long run it may prove useful, so why not? (IDIs, P1).
I believe that emotional education and self-care must be present… emotional education must always be present, on a professional and [a] personal level. Spaces where we can formally work with our colleagues… (FGs2, P12).
…maybe it would be good to have a structured space for the self-care of professionals (FGs1, P13).
A space to take care of oneself would be great, spending time with each other while learning to work with emotions (IDIs, P5).
4. Discussion
Social workers constantly provide care to people in vulnerable situations with complex demands. This scenario causes suffering in professionals.
In the literature consulted, social workers are portrayed as resource providers [ 17 ], that is, as mere intermediaries between the group of individuals with needs and the resources that the state decides to allocate. As a result, neither deadlines nor requirements depend on social workers themselves [ 53 ]. The professionals in our study and those in previous studies [ 54 ] agree that the bureaucratic processes faced by users represent obstacles for social workers as well, who have the feeling of not stepping in on time.
Social services users are very varied. The needs of each individual are different, and not all of these needs are equally demanding [ 9 ]. Among the plethora of cases, some groups are more vulnerable than others [ 38 ]. In concordance with our research, other studies have also shown that minors and the elderly are considered to be among the most vulnerable populations [ 24 ]. In addition, health and social care workers point out that individuals with mental illnesses [ 22 ] and individuals who are in a chronic situation from which they cannot get out are groups at greater risk [ 55 , 56 ].
As shown in this research, the emotions generated in professionals who are in constant contact with situations of suffering with a high emotional impact, such as the aforementioned, originate deep frustration, anger, and dissatisfaction, as well as sadness, fear, and concern. This is in consonance with the literature consulted, which also reports the great effect that working daily with the intense suffering of users has on social workers, along with a potentially poor response [ 26 , 27 , 57 , 58 ]. In fact, some studies conceptualize emotion as both a potential resource and a risk for social workers’ professional judgment and practice [ 59 ].
The social workers in our study considered that the most complex interventions with vulnerable people inevitably make it difficult for them to switch off from work. This aspect is consistent with other studies in which social workers had difficulties when switching off from work after attending to groups with complicated needs [ 55 , 60 ]. With regard to the reported resources for self-care, mutual support is virtually the only helping tool available to these professionals. In previous studies, professionals referred to social support as a key element [ 13 , 27 , 43 ] but did not specifically mention mutual peer support. Social workers ask for training and support in the face of complex social interventions, as proposed by different research studies that underline the importance of taking care, preparing, training, and supporting social workers in this regard [ 61 , 62 ]. Therefore, more attention should be paid to working with the emotions of social workers who are exposed to tense and threatening situations [ 63 , 64 ]. In this way, for instance, reflexivity strategies in order to build and rebuild emotions in social workers could be useful [ 65 ]. Receiving training and support in formal spaces, as social workers described in this study, could be positive for their work and their professional and personal quality of life.
As for the limitations of this study, we considered the possibility that the researchers’ personal positions on the matter may have introduced bias into the results. To control for bias, reflexivity and a self-critical attitude were maintained throughout the process by all the researchers. To avoid influencing data collection, sample recruitment, and location, the researchers only knew the topic in a superficial manner (as health professionals) and it was not their usual work/subject matter of research. We relied on the ultimate motivation for our work, which is to acquire knowledge to improve, rather than to demonstrate. Nevertheless, we have set out to conduct a release exercise to clarify our own assumptions and put them into perspective when designing our research.
Regarding future lines of research, a study with the methods combined regarding the quality of professional life of social workers should be conducted in order to identify related factors and to assess the levels of compassion fatigue. In addition, research should be undertaken on the concept of compassion among social workers and its relationship to suffering. Finally, interventions should be carried out with social work professionals to develop compassion as a protective element against compassion fatigue.
5. Conclusions
Social workers experience high levels of emotional discomfort when carrying out their work, which is exacerbated when the populations they attend to are particularly vulnerable groups, such as children, the elderly, individuals with mental health problems, or people with scarce or a lack of economic resources. The traditional hegemonic intervention model that lies within the structure of social services in this context results in all social work efforts revolving around the allocation of available resources, which are generally scarce. All aspects of the individual have been eliminated from the repertoire of interventions according to the comprehensive support approach. In this new model of care, based mainly on providing support to individuals, the professionals themselves are the main tools and resources. In the future, this will further enhance the role of social workers when supporting people experiencing social exclusion, poverty, and marginalization. More attention should be paid to working with the emotions of social workers who are exposed to tense and threatening situations. Peer support, talking, and discussions of experiences are highlighted as relevant to deal with their work. Receiving training and support (in formal spaces) in order to learn how to deal with vulnerable groups could be positive for their work and their professional and personal quality of life.
Acknowledgments
The authors thank the Health Sciences Research Group CTS-451 and the Health Research Center (CEINSA) of the University of Almería (Spain) for its support.
Author Contributions
Conceptualization, M.D.R.-F., E.A.-D., Á.M.O.-G. and R.O.-A.; methodology, R.O.-A. and E.A.-D.; validation, C.F.-S., I.M.F.-M. and J.M.H.-P.; formal analysis, Á.M.O.-G.; investigation, R.O.-A.; data curation, M.D.R.-F. and R.O.-A.; writing—original draft preparation, Á.M.O.-G. and R.O.-A.; writing—review and editing, M.D.R.-F. and E.A.-D.; visualization and supervision, C.F.-S., I.M.F.-M. and J.M.H.-P.; and funding acquisition, M.D.R.-F. All authors have read and agreed to the published version of the manuscript.
This research was funded by the University of Almería (project TRFE-SI-2019/010).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of University of Almería (protocol code EFM-11/19, 11/03/2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Social Work Practice with Carers

Case Study 2: Josef
Download the whole case study as a PDF file
Josef is 16 and lives with his mother, Dorota, who was diagnosed with Bipolar disorder seven years ago. Josef was born in England. His parents are Polish and his father sees him infrequently.
This case study looks at the impact of caring for someone with a mental health problem and of being a young carer , in particular the impact on education and future employment .
When you have looked at the materials for the case study and considered these topics, you can use the critical reflection tool and the action planning tool to consider your own practice.
- One-page profile
Support plan
Transcript (.pdf, 48KB)
Name : Josef Mazur
Gender : Male
Ethnicity : White European
Download resource as a PDF file
First language : English/ Polish
Religion : Roman Catholic
Josef lives in a small town with his mother Dorota who is 39. Dorota was diagnosed with Bi-polar disorder seven years ago after she was admitted to hospital. She is currently unable to work. Josef’s father, Stefan, lives in the same town and he sees him every few weeks. Josef was born in England. His parents are Polish and he speaks Polish at home.
Josef is doing a foundation art course at college. Dorota is quite isolated because she often finds it difficult to leave the house. Dorota takes medication and had regular visits from the Community Psychiatric Nurse when she was diagnosed and support from the Community Mental Health team to sort out her finances. Josef does the shopping and collects prescriptions. He also helps with letters and forms because Dorota doesn’t understand all the English. Dorota gets worried when Josef is out. When Dorota is feeling depressed, Josef stays at home with her. When Dorota is heading for a high, she tries to take Josef to do ‘exciting stuff’ as she calls it. She also spends a lot of money and is very restless.
Josef worries about his mother’s moods. He is worried about her not being happy and concerned at the money she spends when she is in a high mood state. Josef struggles to manage his day around his mother’s demands and to sleep when she is high. Josef has not told anyone about the support he gives to his mother. He is embarrassed by some of the things she does and is teased by his friends, and he does not think of himself as a carer. Josef has recently had trouble keeping up with course work and attendance. He has been invited to a meeting with his tutor to formally review attendance and is worried he will get kicked out. Josef has some friends but he doesn’t have anyone he can confide in. His father doesn’t speak to his mother.
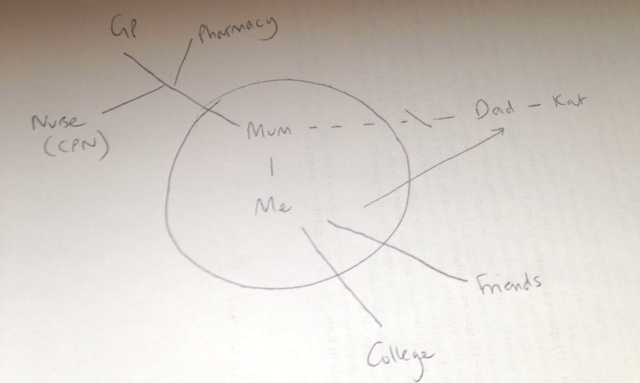
Josef sees some information on line about having a parent with a mental health problem. He sends a contact form to ask for information. Someone rings him and he agrees to come into the young carers’ team and talk to the social worker. You have completed the assessment form with Josef in his words and then done a support plan with him.
Back to Summary
Josef Mazur
What others like and admire about me
Good at football
Finished Arkham Asylum on expert level
What is important to me
Mum being well and happy
Seeing my dad
Being an artist
Seeing my friends
How best to support me
Tell me how to help mum better
Don’t talk down to me
Talk to me 1 to 1
Let me know who to contact if I am worried about something
Work out how I can have some time on my own so I can do my college work and see my friends
Don’t tell mum and my friends
Date chronology completed : 7 March 2016
Date chronology shared with person: 7 March 2016
| 1997 | Josef’s mother and father moved to England from Poznan. | Both worked at the warehouse – Father still works there. |
| 11.11.1999 | Josef born. | Mother worked for some of the time that Josef was young. |
| 2006 | Josef reports that his mother and father started arguing about this time because of money and Josef’s mother not looking after household tasks. | Josef started doing household tasks e.g. cleaning, washing and ironing. |
| 2008 | Josef reports that his mother didn’t get out of bed for a few months. | Josef managed the household during this period. |
| October 2008 | Josef reports that his mother spent lots of money in catalogues and didn’t sleep. She was admitted to hospital. | Mother was in hospital for 6 weeks and was diagnosed with bipolar disorder. Josef began looking after his mother’s medication and says that he started to ‘keep an eye on her.’ |
| May 2010 | Josef’s father moved out to live with his friend Kat. Josef stayed with his mother. | Josef reports that his mother was ‘really sad for a while and then she went round and shouted at them.’ Mother started on different medication and had regular visits from the Community Psychiatric Nurse. Josef said that the CPN told him about his mum’s illness and to let him know if he needed any help but he was managing ok. Josef saw his father every week for a few years and then it was more like every month. Father does not visit Josef or speak to his mother. |
| 2013/14 | Josef reports that his mother got into a lot of debt and they had eviction letters. | Josef’s father paid some of the bills and his mother was referred by the Community Mental Health Team for advice from CAB and started getting benefits. Josef started doing the correspondence. |
| 2015 | Josef left school and went to college. | Josef got an A (art), 4 Cs and 3 Ds GCSE. He says that he ‘would have done better but I didn’t do much work.’ |
| 26 Feb 2016 | Josef got a letter from his tutor at college saying he had to go to a formal review about attendance. | Josef saw information on-line about having a parent with a mental health problem and asked for some information. |
| 2 March 2016 | Phone call from young carer’s team to Josef. | Josef agreed to come in for an assessment. |
| 4 March 2016 | Social worker meets with Josef. | Carer’s assessment and support plan completed. |
| 7 March 2016 | Paperwork completed. | Sent to Josef. |
Young Carers Assessment
Do you look after or care for someone at home?
The questions in this paper are designed to help you think about your caring role and what support you might need to make your life a little easier or help you make time for more fun stuff.
Please feel free to make notes, draw pictures or use the form however is best for you.
What will happen to this booklet?
This is your booklet and it is your way to tell an adult who you trust about your caring at home. This will help you and the adult find ways to make your life and your caring role easier.
The adult who works with you on your booklet might be able to help you with everything you need. If they can’t, they might know other people who can.
Our Agreement
- I will share this booklet with people if I think they can help you or your family
- I will let you know who I share this with, unless I am worried about your safety, about crime or cannot contact you
- Only I or someone from my team will share this booklet
- I will make sure this booklet is stored securely
- Some details from this booklet might be used for monitoring purposes, which is how we check that we are working with everyone we should be
Signed: ___________________________________
Young person:
- I know that this booklet might get shared with other people who can help me and my family so that I don’t have to explain it all over again
- I understand what my worker will do with this booklet and the information in it (written above).
Signed: ____________________________________
Name : Josef Mazur Address : 1 Green Avenue, Churchville, ZZ1 Z11 Telephone: 012345 123456 Email: [email protected] Gender : Male Date of birth : 11.11.1999 Age: 16 School : Green College, Churchville Ethnicity : White European First language : English/ Polish Religion : Baptised Roman Catholic GP : Dr Amp, Hill Surgery
The best way to get in touch with me is:
Do you need any support with communication?
*Josef is bilingual – English and Polish. He speaks English at school and with his friends, and Polish at home. Josef was happy to have this assessment in English, however, another time he may want to have a Polish interpreter. It will be important to ensure that Josef is able to use the words he feels best express himself.
About the person/ people I care for
I look after my mum who has bipolar disorder. Mum doesn’t work and doesn’t really leave the house unless she is heading for a high. When Mum is sad she just stays at home. When she is getting hyper then she wants to do exciting stuff and she spends lots of money and she doesn’t sleep.
Do you wish you knew more about their illness?
Do you live with the person you care for?
What I do as a carer It depends on if my mum has a bad day or not. When she is depressed she likes me to stay home with her and when she is getting hyper then she wants me to go out with her. If she has new meds then I like to be around. Mum doesn’t understand English very well (she is from Poland) so I do all the letters. I help out at home and help her with getting her medication.
Tell us what an average week is like for you, what kind of things do you usually do?
Monday to Friday
Get up, get breakfast, make sure mum has her pills, tell her to get up and remind her if she’s got something to do.
If mum hasn’t been to bed then encourage her to sleep a bit and set an alarm
College – keep phone on in case mum needs to call – she usually does to ask me to get something or check when I’m coming home
Go home – go to shops on the way
Remind mum about tablets, make tea and pudding for both of us as well as cleaning the house and fitting tea in-between, ironing, hoovering, hanging out and bringing in washing
Do college work when mum goes to bed if not too tired
More chores
Do proper shop
Get prescription
See my friends, do college work
Sunday – do paper round
Physical things I do….
(for example cooking, cleaning, medication, shopping, dressing, lifting, carrying, caring in the night, making doctors appointments, bathing, paying bills, caring for brothers & sisters)
I do all the housework and shopping and cooking and get medication
Things I find difficult
Emotional support I provide…. (please tell us about the things you do to support the person you care for with their feelings; this might include, reassuring them, stopping them from getting angry, looking after them if they have been drinking alcohol or taking drugs, keeping an eye on them, helping them to relax)
If mum is stressed I stay with her
If mum is depressed I have to keep things calm and try to lighten the mood
She likes me to be around
When mum is heading for a high wants to go to theme parks or book holidays and we can’t afford it
I worry that mum might end up in hospital again
Mum gets cross if I go out
Other support
Please tell us about any other support the person you care for already has in place like a doctor or nurse, or other family or friends.
The GP sees mum sometimes. She has a nurse who she can call if things get bad.
Mum’s medication comes from Morrison’s pharmacy.
Dad lives nearby but he doesn’t talk to mum.
Mum doesn’t really have any friends.
Do you ever have to stop the person you care for from trying to harm themselves or others?
Some things I need help with
Sorting out bills and having more time for myself
I would like mum to have more support and to have some friends and things to do
On a normal week, what are the best bits? What do you enjoy the most? (eg, seeing friends, playing sports, your favourite lessons at school)
Seeing friends
When mum is up and smiling
Playing football
On a normal week, what are the worst bits? What do you enjoy the least? (eg cleaning up, particular lessons at school, things you find boring or upsetting)
Nagging mum to get up
Reading letters
Missing class
Mum shouting
Friends laugh because I have to go home but they don’t have to do anything
What things do you like to do in your spare time?
Do you feel you have enough time to spend with your friends or family doing things you enjoy, most weeks?
Do you have enough time for yourself to do the things you enjoy, most weeks? (for example, spending time with friends, hobbies, sports)
Are there things that you would like to do, but can’t because of your role as a carer?
Can you say what some of these things are?
See friends after college
Go out at the weekend
Time to myself at home
It can feel a bit lonely
I’d like my mum to be like a normal mum
School/ College Do you think being your caring role makes school/college more difficult for you in any way?
If you ticked YES, please tell us what things are made difficult and what things might help you.
Things I find difficult at school/ college
Sometimes I get stressed about college and end up doing college work really late at night – I get a bit angry when I’m stressed
I don’t get all my college work done and I miss days
I am tired a lot of the time
Things I need help with…
I am really worried they will kick me out because I am behind and I miss class. I have to meet my tutor about it.
Do your teachers know about your caring role?
Are you happy for your teachers and other staff at school/college to know about your caring role?
Do you think that being a carer will make it more difficult for you to find or keep a job?
Why do you think being a carer is/ will make finding a job more difficult?
I haven’t thought about it. I don’t know if I’ll be able to finish my course and do art and then I won’t be able to be an artist.
Who will look after mum?
What would make it easier for you to find a job after school/college?
Finishing my course
Mum being ok
How I feel about life…
Do you feel confident both in school and outside of school?
Somewhere in the middle
In your life in general, how happy do you feel?
Quite unhappy
In your life in general, how safe do you feel?
How healthy do you feel at the moment?
Quite healthy
Being heard
Do you think people listen to what you are saying and how you are feeling?
If you said no, can you tell us who you feel isn’t listening or understanding you sometimes (eg, you parents, your teachers, your friends, professionals)
I haven’t told anyone
I can’t talk to mum
My friends laugh at me because I don’t go out
Do you think you are included in important decisions about you and your life? (eg, where you live, where you go to school etc)
Do you think that you’re free to make your own choices about what you do and who you spend your time with?
Not often enough
Is there anybody who knows about the caring you’re doing at the moment?
If so, who?
I told dad but he can’t do anything
Would you like someone to talk to?
Supporting me Some things that would make my life easier, help me with my caring or make me feel better
I don’t know
Fix mum’s brain
People to help me if I’m worried and they can do something about it
Not getting kicked out of college
Free time – time on my own to calm down and do work or have time to myself
Time to go out with my friends
Get some friends for mum
I don’t want my mum to get into trouble
Who can I turn to for advice or support?
I would like to be able to talk to someone without mum or friends knowing
Would you like a break from your caring role?
How easy is it to see a Doctor if you need to?
To be used by social care assessors to consider and record measures which can be taken to assist the carer with their caring role to reduce the significant impact of any needs. This should include networks of support, community services and the persons own strengths. To be eligible the carer must have significant difficulty achieving 1 or more outcomes without support; it is the assessors’ professional judgement that unless this need is met there will be a significant impact on the carer’s wellbeing. Social care funding will only be made available to meet eligible outcomes that cannot be met in any other way, i.e. social care funding is only available to meet unmet eligible needs.
Date assessment completed : 7 March 2016
Social care assessor conclusion
Josef provides daily support to his mum, Dorota, who was diagnosed with bipolar disorder seven years ago. Josef helps Dorota with managing correspondence, medication and all household tasks including shopping. When Dorota has a low mood, Josef provides support and encouragement to get up. When Dorota has a high mood, Josef helps to calm her and prevent her spending lots of money. Josef reports that Dorota has some input from community health services but there is no other support. Josef’s dad is not involved though Josef sees him sometimes, and there are no friends who can support Dorota.
Josef is a great support to his mum and is a loving son. He wants to make sure his mum is ok. However, caring for his mum is impacting: on Josef’s health because he is tired and stressed; on his emotional wellbeing as he can get angry and anxious; on his relationship with his mother and his friends; and on his education. Josef is at risk of leaving college. Josef wants to be able to support his mum better. He also needs time for himself, to develop and to relax, and to plan his future.
Eligibility decision : Eligible for support
What’s happening next : Create support plan
Completed by Name : Role : Organisation :
Name: Josef Mazur
Address 1 Green Avenue, Churchville, ZZ1 Z11
Telephone 012345 123456
Email [email protected]
Gender: Male
Date of birth: 11.11.1999 Age: 16
School Green College, Churchville
Ethnicity White European
First language English/ Polish
Religion Baptised Roman Catholic
GP Dr Amp, Hill Surgery
My relationship to this person son
Name Dorota Mazur
Gender Female
Date of birth 12.6.79 Age 36
First language Polish
Religion Roman Catholic
Support plan completed by
Organisation
|
|
| |
|
|
| |
|
| ||
|
| ||
Date of support plan: 7 March 2016
This plan will be reviewed on: 7 September 2016
Signing this form
Please ensure you read the statement below in bold, then sign and date the form.
I understand that completing this form will lead to a computer record being made which will be treated confidentially. The council will hold this information for the purpose of providing information, advice and support to meet my needs. To be able to do this the information may be shared with relevant NHS Agencies and providers of carers’ services. This will also help reduce the number of times I am asked for the same information.
If I have given details about someone else, I will make sure that they know about this.
I understand that the information I provide on this form will only be shared as allowed by the Data Protection Act.
Josef has given consent to share this support plan with the CPN but does not want it to be shared with his mum.
Mental health
The social work role with carers in adult mental health services has been described as: intervening and showing professional leadership and skill in situations characterised by high levels of social, family and interpersonal complexity, risk and ambiguity (Allen 2014). Social work with carers of people with mental health needs, is dependent on good practice with the Mental Capacity Act where practitioner knowledge and understanding has been found to be variable (Iliffe et al 2015).
- Carers Trust (2015) Mental Health Act 1983 – Revised Code of Practice Briefing
- Carers Trust (2013) The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England
- Mind, Talking about mental health
- Tool 1: Triangle of care: self-assessment for mental health professionals – Carers Trust (2013) The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England Second Edition (page 23 Self-assessment tool for organisations)
Mental capacity, confidentiality and consent
Social work with carers of people with mental health needs, is dependent on good practice with the Mental Capacity Act where practitioner knowledge and understanding has been found to be variable (Iliffe et al 2015). Research highlights important issues about involvement, consent and confidentiality in working with carers (RiPfA 2016, SCIE 2015, Mental Welfare Commission for Scotland 2013).
- Beddow, A., Cooper, M., Morriss, L., (2015) A CPD curriculum guide for social workers on the application of the Mental Capacity Act 2005 . Department of Health
- Bogg, D. and Chamberlain, S. (2015) Mental Capacity Act 2005 in Practice Learning Materials for Adult Social Workers . Department of Health
- Department of Health (2015) Best Interest Assessor Capabilities , The College of Social Work
- RiPfA Good Decision Making Practitioner Handbook
- SCIE Mental Capacity Act resource
- Tool 2: Making good decisions, capacity tool (page 70-71 in good decision making handbook)
Young carers
A young carer is defined as a person under 18 who provides or intends to provide care for another person. The concept of care includes practical or emotional support. It is the case that this definition excludes children providing care as part of contracted work or as voluntary work. However, the local authority can ignore this and carry out a young carer’s need assessment if they think it would be appropriate. Young carers, young adult carers and their families now have stronger rights to be identified, offered information, receive an assessment and be supported using a whole-family approach (Carers Trust 2015).
- SCIE (2015) Young carer transition in practice under the Care Act 2014
- SCIE (2015) Care Act: Transition from children’s to adult services – early and comprehensive identification
- Carers Trust (2015) Rights for young carers and young adult carers in the Children and Families Act
- Carers Trust (2015) Know your Rights: Support for Young Carers and Young Adult Carers in England
- The Children’s Society (2015) Hidden from view: The experiences of young carers in England
- DfE (2011) Improving support for young carers – family focused approaches
- ADASS and ADCS (2015) No wrong doors: working together to support young carers and their families
- Carers Trust, Supporting Young Carers and their Families: Examples of Practice
- Refugee toolkit webpage: Children and informal interpreting
- SCIE (2010) Supporting carers: the cared for person
- SCIE (2015) Care Act Transition from children’s to adults’ services – Video diaries
- Tool 3: Young carers’ rights – The Children’s Society (2014) The Know Your Rights pack for young carers in England!
- Tool 4: Vision and principles for adults’ and children’s services to work together
Young carers of parents with mental health problems
The Care Act places a duty on local authorities to assess young carers before they turn 18, so that they have the information they need to plan for their future. This is referred to as a transition assessment. Guidance, advocating a whole family approach, is available to social workers (LGA 2015, SCIE 2015, ADASS/ADCS 2011).
- SCIE (2012) At a glance 55: Think child, think parent, think family: Putting it into practice
- SCIE (2008) Research briefing 24: Experiences of children and young people caring for a parent with a mental health problem
- SCIE (2008) SCIE Research briefing 29: Black and minority ethnic parents with mental health problems and their children
- Carers Trust (2015) The Triangle of Care for Young Carers and Young Adult Carers: A Guide for Mental Health Professionals
- ADASS and ADCS (2011) Working together to improve outcomes for young carers in families affected by enduring parental mental illness or substance misuse
- Ofsted (2013) What about the children? Joint working between adult and children’s services when parents or carers have mental ill health and/or drug and alcohol problems
- Mental health foundation (2010) MyCare The challenges facing young carers of parents with a severe mental illness
- Children’s Commissioner (2012) Silent voices: supporting children and young people affected by parental alcohol misuse
- SCIE, Parental mental health and child welfare – a young person’s story
Tool 5: Family model for assessment
- Tool 6: Engaging young carers of parents with mental health problems or substance misuse
Young carers and education/ employment
Transition moments are highlighted in the research across the life course (Blythe 2010, Grant et al 2010). Complex transitions required smooth transfers, adequate support and dedicated professionals (Petch 2010). Understanding transition theory remains essential in social work practice (Crawford and Walker 2010). Partnership building expertise used by practitioners was seen as particular pertinent to transition for a young carer (Heyman 2013).
- TLAP (2013) Making it real for young carers
- Learning and Work Institute (2018) Barriers to employment for young adult carers
- Carers Trust (2014) Young Adult Carers at College and University
- Carers Trust (2013) Young Adult Carers at School: Experiences and Perceptions of Caring and Education
- Carers Trust (2014) Young Adult Carers and Employment
- Family Action (2012) BE BOTHERED! Making Education Count for Young Carers

Download The Triangle of Care as a PDF file
The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England
The Triangle of Care is a therapeutic alliance between service user, staff member and carer that promotes safety, supports recovery and sustains wellbeing…

Download the Capacity Tool as a PDF file
Capacity Tool Good decision-making Practitioners’ Handbook
The Capacity tool on page 71 has been developed to take into account the lessons from research and the case CC v KK. In particular:
- that capacity assessors often do not clearly present the available options (especially those they find undesirable) to the person being assessed
- that capacity assessors often do not explore and enable a person’s own understanding and perception of the risks and advantages of different options
- that capacity assessors often do not reflect upon the extent to which their ‘protection imperative’ has influenced an assessment, which may lead them to conclude that a person’s tolerance of risks is evidence of incapacity.
The tool allows you to follow steps to ensure you support people as far as possible to make their own decisions and that you record what you have done.

Download Know your rights as a PDF file
Tool 3: Know Your Rights Young Carers in Focus
This pack aims to make you aware of your rights – your human rights, your legal rights, and your rights to access things like benefits, support and advice.
Need to know where to find things out in a hurry? Our pack has lots of links to useful and interesting resources that can help you – and help raise awareness about young carers’ issues!
Know Your Rights has been produced by Young Carers in Focus (YCiF), and funded by the Big Lottery Fund.
Tool 4: Vision and principles for adults’ and children’s services to work together to support young carers
Download the tool as a PDF file
You can use this tool to consider how well adults’ and children’s services work together, and how to improve this.
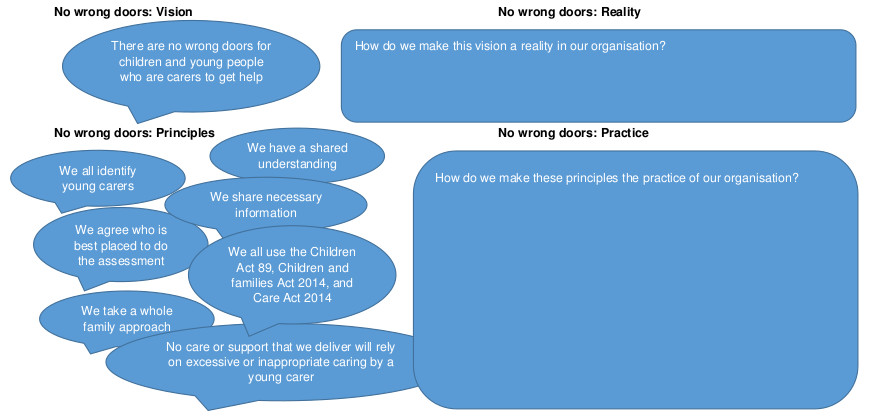
Click on the diagram to open full size in a new window
This is based on ADASS and ADCS (2015) No wrong doors : working together to support young carers and their families
Download the tool as a PDF file
You can use this tool to help you consider the whole family in an assessment or review.
What are the risk, stressors and vulnerability factors?
How is the child/ young person’s wellbeing affected?
How is the adult’s wellbeing affected?

What are the protective factors and available resources?
This tool is based on SCIE (2009) Think child, think parent, think family: a guide to parental mental health and child welfare
Tool 6: Engaging young carers
Young carers have told us these ten things are important. So we will do them.
- Introduce yourself. Tell us who you are and what your job is.
- Give us as much information as you can.
- Tell us what is wrong with our parents.
- Tell us what is going to happen next.
- Talk to us and listen to us. Remember it is not hard to speak to us we are not aliens.
- Ask us what we know and what we think. We live with our parents; we know how they have been behaving.
- Tell us it is not our fault. We can feel guilty if our mum or dad is ill. We need to know we are not to blame.
- Please don’t ignore us. Remember we are part of the family and we live there too.
- Keep on talking to us and keeping us informed. We need to know what is happening.
- Tell us if there is anyone we can talk to. Maybe it could be you.

- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility

A sample case study: Mrs Brown
On this page, social work report, social work report: background, social work report: social history, social work report: current function, social work report: the current risks, social work report: attempts to trial least restrictive options, social work report: recommendation, medical report, medical report: background information, medical report: financial and legal affairs, medical report: general living circumstances.
This is a fictitious case that has been designed for educative purposes.
Mrs Beryl Brown URN102030 20 Hume Road, Melbourne, 3000 DOB: 01/11/33
Date of application: 20 August 2019
Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke, which has left her with moderate weakness in her left arm and leg. A diagnosis of vascular dementia was also made, which is overlaid on a pre-existing diagnosis of Alzheimer’s disease (2016). Please refer to the attached medical report for further details.
I understand that Mrs Brown has been residing in her own home, a two-story terrace house in Melbourne, for almost 60 years. She has lived alone since her husband died two years ago following a cardiac arrest. She has two daughters. The youngest daughter Jean has lived with her for the past year, after she lost her job. The eldest daughter Catherine lives on the Gold Coast with her family. Mrs Brown is a retired school teacher and she and both daughters describe her as a very private woman who has never enjoyed having visitors in her home. Mrs Brown took much encouragement to accept cleaning and shopping assistance once a week after her most recent admission; however, she does not agree to increase service provision. Jean has Enduring Power of Attorney (EPOA) paperwork that indicates that Mrs Brown appointed her under an EPOA two years ago. She does not appear to have appointed a medical treatment decision maker or any other decision-supporter.
I also understand from conversations with her daughters that Jean and Mrs Brown have always been very close and that there is a history of long-standing conflict between Catherine and Jean. This was exacerbated by the death of their father. Both daughters state they understand the impact of the stroke on their mother’s physical and cognitive functioning, but they do not agree on a discharge destination. Mrs Brown lacks insight into her care needs and says she will be fine once she gets back into her own home. Repeated attempts to discuss options with all parties in the same room have not resulted in a decision that is agreeable to all parties.
Mrs Brown has a history of Alzheimer’s disease; type II diabetes – insulin dependent; hypertension; high cholesterol and osteoarthritis. She has had two recent admissions to hospital for a urinary tract infection and a fall in the context of low blood sugars. She is currently requiring one to two people to assist her into and out of bed and one person with managing tasks associated with post-toilet hygiene. She can walk slowly for short distances with a four-wheel frame with one person to supervise. She benefits from prompting to use her frame; she needs someone to cut her food and to set her up to eat and drink regularly and to manage her medication routine. She requires one person to assist her to manage her insulin twice daily.
The team believe that Mrs Brown’s capacity for functional improvement has plateaued in the last ten days. They recommend that it is in her best interests to be discharged to a residential care setting due to her need for one to two people to provide assistance with the core tasks associated with daily living. Mrs Brown is adamant that she wants to return home to live with Jean who she states can look after her. Jean, who has a history of chronic back pain, has required several admissions to hospital over the past five years, and states she wants to be able to care for her mother at home. Jean states she is reluctant to agree to extra services as her mother would not want this. Her sister Catherine is concerned that Jean has not been coping and states that given this is the third admission to hospital in a period of few months, believes it is now time for her mother to enter residential care. Catherine states that she is very opposed to her mother being discharged home.
Mrs Brown is at high risk of experiencing falls. She has reduced awareness of the left side of her body and her ability to plan and process information has been affected by her stroke. She is now requiring one to two people to assist with all her tasks of daily living and she lacks insight into these deficits. Mrs Brown is also at risk of further significant functional decline which may exacerbate Jean’s back pain. Jean has stated she is very worried about where she will live if her mother is to enter residential care.
We have convened two family meetings with Mrs Brown, both her daughters and several members of the multi-disciplinary team. The outcome of the first meeting saw all parties agree for the ward to provide personalised carer training to Jean with the aim of trialling a discharge home. During this training Jean reported significant pain when transferring her mother from the bed and stated she would prefer to leave her mother in bed until she was well enough to get out with less support.
The team provided education to both Jean and Catherine about the progressive impact of their mother’s multiple conditions on her functioning. The occupational therapist completed a home visit and recommended that the downstairs shower be modified so that a commode can be placed in it safely and the existing dining room be converted into a bedroom for Mrs Brown. Mrs Brown stated she would not pay for these modifications and Jean stated she did not wish to go against her mother’s wishes. The team encouraged Mrs Brown to consider developing a back-up plan and explore residential care options close to her home so that Jean could visit often if the discharge home failed. Mrs Brown and Jean refused to consent to proceed with an Aged Care Assessment that would enable Catherine to waitlist her mother’s name at suitable aged care facilities. We proceeded with organising a trial overnight visit. Unfortunately, this visit was not successful as Jean and Catherine, who remained in Melbourne to provide assistance, found it very difficult to provide care without the use of an accessible bathroom. Mrs Brown remains adamant that she will remain at home. The team is continuing to work with the family to maximise Mrs Brown’s independence, but they believe that it is unlikely this will improve. I have spent time with Jean to explore her adjustment to the situation, and provided her with information on community support services and residential care services. I have provided her with information on the Transition Care Program which can assist families to work through all the logistics. I have provided her with more information on where she could access further counselling to explore her concerns. I have sought advice on the process and legislative requirements from the Office of the Public Advocate’s Advice Service. I discussed this process with the treating team and we decided that it was time to lodge an application for guardianship to VCAT.
The treating team believe they have exhausted all least restrictive alternatives and that a guardianship order is required to make a decision on Mrs Brown’s discharge destination and access to services. The team recommend that the Public Advocate be appointed as Mrs Brown’s guardian of last resort. We believe that this is the most suitable arrangement as her daughters are not in agreement about what is in their mother’s best interests. We also believe that there is a potential conflict of interest as Jean has expressed significant concern that her mother’s relocation to residential care will have an impact on her own living arrangements.
Mrs Brown’s medical history includes Alzheimer’s disease; type II diabetes; hypertension; high cholesterol and osteoarthritis. She was admitted to Hume Hospital on 3 March 2019 following a stroke that resulted in moderate left arm and leg weakness. This admission was the third hospital admission in the past year. Other admissions have been for a urinary tract infection, and a fall in the context hypoglycaemia (low blood sugars), both of which were complicated by episodes of delirium.
She was transferred to the subacute site under my care, a week post her admission, for slow-stream rehabilitation, cognitive assessment and discharge planning.
Mrs Brown was diagnosed with Alzheimer’s disease by Dr Joanne Winters, Geriatrician, in April 2016. At that time, Mrs Brown scored 21/30 on the Standardised Mini-Mental State Examination (SMMSE). During this admission, Mrs Brown scored 15/30. I have undertaken cognitive assessment and agree with the diagnosis; further cognitive decline has occurred in the context of the recent stroke. There are global cognitive deficits, but primarily affecting memory, attention and executive function (planning, problem solving, mental flexibility and abstract reasoning). The most recent CT-Brain scan shows generalised atrophy along with evidence of the new stroke affecting the right frontal lobe. My assessments suggest moderate to severe mixed Alzheimer’s and vascular dementia.
While able to recall some key aspects of her financial affairs, including the general monetary value of her pension and regular expenses, Mrs Brown was unable to account for recent expenditure (for repairs to her home) or provide an estimate of its value, and had difficulty describing her investments. In addition, I consider that she would be unable to make complex financial decisions due to her level of cognitive impairment. Accordingly, I am of the view that Mrs Brown now lacks capacity to make financial decisions.
Mrs Brown states that she previously made an Enduring Power of Attorney (EPOA) but could no longer recall aspects of the EPOA, such as when it would commence and the nature of the attorney’s powers. Moreover, she confused the EPOA with her will. Her understanding of these matters did not improve with education, and therefore I consider that she no longer has capacity to execute or revoke an EPOA.
Mrs Brown acknowledges that she needs some assistance but lacks insight into the type of assistance that she requires, apart from home help for cleaning and shopping. She does not appreciate her risk of falling. She is unable to get in and out of bed without at least one person assisting her. She frequently forgets to use her gait aid when mobilising and is not able to describe how she would seek help in the event of falling. She is not able to identify or describe how she would manage her blood sugar levels, and this has not improved with education. Accordingly, I consider that she lacks capacity to make decisions about accommodation arrangements and services.
Mrs Brown does not agree with the treating team’s recommendation to move into residential care and maintains her preference to return home. This is in spite of a failed overnight trial at home with both her daughters assisting her. Unfortunately, she was unable to get out of bed to get to the toilet and required two people to assist her to do so in the morning. In light of these matters, and in the context of family disagreement regarding the matter, the team recommends that the Office of the Public Advocate be appointed as a guardian of last resort.
Reviewed 22 July 2022
- Hospitals & health services
- Public hospitals in Victoria
- Patient care
- Ambulance and patient transport
- Non-emergency patient transport
- Non-emergency patient transport review
- NEPT legislation and clinical practice protocols
- Non-emergency patient transport licensing
- NEPT licensing fees
- NEPT services information and guidance
- First Aid Services
- First aid licences
- First aid services information and guidance
- First aid service fees
- Victorian State Trauma System
- Acute medicine
- Emergency care
- Surgical services
- Better at Home
- Critical care
- Hospital in the Home
- Virtual care (Telehealth)
- Perinatal and reproductive services
- Rehabilitation and complex care
- Renal health
- Renal services in Victoria
- Funding for renal services
- Different approaches to haemodialysis
- Specialist clinics
- Access to non-admitted services
- Minimum referral information
- Communication toolkit
- Integrated care
- HealthLinks: Chronic Care
- Community Health Integrated Program (CHIP) guidelines
- Service coordination in Victoria
- Victorian integrated care online resources
- Specialist clinics programs
- Specialist clinics reform
- Specialty diagnostics, therapeutics and programs
- Older people in hospital
- End of life and palliative care in Victoria
- Voluntary assisted dying
- Quality, safety and service improvement
- Planned surgery recovery and reform program
- Digital Health
- Roadmap and Maturity Model
- Standards and guidelines
- Policies and frameworks
- Health Information Sharing Legislation Reform
- My Health Record
- Public hospital accreditation in Victoria
- Credentialing for senior medical staff in Victoria
- Clinical risk management
- Preventing infections in health services
- Healthy choices
- Victorian Perinatal Data Collection
- Rural health
- Improving Access to Primary Care in Rural and Remote Areas Initiative
- Rural x-ray services
- Rural health regions and locations
- Rural and regional medical director role
- Victorian Patient Transport Assistance Scheme
- Rural and isolated practice registered nurses
- Urgent care in regional and rural Victoria
- Private health service establishments
- Private hospitals
- Day procedure centres
- Mobile health services
- Fees for private health service establishments in Victoria
- Design resources for private health service establishments
- Professional standards in private health service establishments
- Legislation updates for private health service establishments
- Complaints about private health service establishments
- Cosmetic procedures
- Guideline for providers of liposuction
- Private hospital funding agreement
- Boards and governance
- About health service boards in Victoria
- Information and education
- Education resources for boards
- Sector leadership
- Data, reporting and analytics
- Health data standards and systems
- Funding, performance and accountability
- Statements of Priorities
- Performance monitoring framework
- Integrity governance framework and assessment tool
- Pricing and funding framework
- Patient fees and charges
- Fees and charges for admitted patients
- Non-admitted patients - fees and charges
- Other services
- Planning and infrastructure
- Sustainability in Healthcare
- Medical equipment asset management framework
- Health system design, service and infrastructure planning
- Complementary service and locality planning
- Primary & community health
- Primary care
- Community pharmacist pilot
- EOI - Victorian Community Pharmacist Statewide Pilot
- Victorian Community Pharmacist Statewide Pilot – Resources for pharmacists
- Emergency Response Planning Tool
- Working with general practice
- Victorian Supercare Pharmacies
- NURSE-ON-CALL
- Priority Primary Care Centres
- Local Public Health Units
- Community health
- Community health services
- Community health pride
- Registration and governance of community health centres
- Community Health Directory
- Community Health Program in Victoria
- Community health population groups
- Dental health
- Access to public dental care services
- Victoria's public dental care fees
- Victoria's public dental care waiting list
- Dental health for SRS residents
- Dental health program reporting
- Smile Squad school dental program
- Maternal and Child Health Service
- Nursery Equipment Program
- Maternal and Child Health Service Framework
- Maternal and Child Health Service resources
- Child Development Information System
- Early parenting centres
- Maternal Child and Health Reporting, Funding and Data
- Baby bundle
- Sleep and settling
- Maternal and Child Health Workforce professional development
- Aboriginal Maternal and Child Health
- Public Dental and Community Health Program funding model review
- Public health
- Women's Health and Wellbeing Program
- Inquiry into Women's Pain
- Inquiry into Women's Pain submissions
- Support groups and programs
- About the program
- Victorian Women's Health Advisory Council
- Cemeteries and crematoria
- Medicines and Poisons Regulation
- Patient Schedule 8 treatment permits
- Schedule 8 MDMA and Schedule 8 psilocybine
- Schedule 9 permits for clinical trials
- Documents and forms to print or download
- Legislation and Approvals
- Frequently Asked Questions - Medicines and Poisons Regulation
- Health practitioners
- Licences and permits to possess (& possibly supply) scheduled substances
- Medicinal cannabis
- Pharmacotherapy (opioid replacement therapy)
- Recent updates
- Environmental health
- Improving childhood asthma management in Melbourne's inner west
- Climate and weather, and public health
- Environmental health in the community
- Environmental health in the home
- Environmental health professionals
- Face masks for environmental hazards
- Human health risk assessments
- Lead and human health
- Per- and poly-fluoroalkyl substances (PFAS)
- Pesticide use and pest control
- Food safety
- Information for community groups selling food to raise funds
- Food businesses
- Food safety information for consumers
- Food regulation in Victoria
- Food safety library
- Food allergens
- Introducing Standard 3.2.2A: Food safety management tools
- Immunisation
- Respiratory syncytial virus (RSV) immunisation
- Seasonal influenza vaccine
- Immunisation schedule and vaccine eligibility criteria
- Ordering vaccine
- Immunisers in Victoria
- Immunisation provider information
- Cold chain management
- Adverse events following immunisation reporting
- Vaccine error management
- Vaccination for infants and children
- Vaccination for adolescents
- Vaccination program for adults
- Vaccination for special-risk groups
- Immunisation resources order form
- Victorian coverage rates for Victoria
- Infectious diseases guidelines & advice
- Infection control guidelines
- Disease information and advice
- Advice to the cruise industry: reporting infections
- Notifiable infectious diseases, conditions and micro-organisms
- Notification procedures for infectious diseases
- Infectious diseases surveillance in Victoria
- Germicidal ultraviolet light
- Protecting patient privacy in Victoria
- Population health systems
- Evidence and evaluation
- Health promotion
- Health status of Victorians
- Municipal public health and wellbeing planning
- Population screening
- Cancer screening
- Conditions not screened
- Improving outcomes in under-screened groups
- Infant hearing screening
- Newborn bloodspot screening
- Prenatal screening
- Screening registers
- Preventive health
- Type 2 diabetes and cardiovascular disease prevention
- Eye health promotion
- Injury prevention
- Healthy eating
- Oral health promotion
- Physical activity
- Sexual health
- Sex worker health
- Decriminalisation of sex work
- Automatic mutual recognition
- Domestic smoke detectors
- Lasers, IPL and LED devices for cosmetic treatments and beauty therapy
- Victoria's regulatory framework for radiation
- Radiation newsletter
- Tobacco reforms
- Tobacco reform legislation and regulations
- E-cigarettes and vaping
- Quitting smoking and vaping
- Smoke-free and vape-free areas
- Building entrances
- Children's indoor play centres
- Public hospitals and health centres
- Children's recreational areas
- Playground equipment
- Skate parks
- Swimming pools
- Under-age sporting events
- Enclosed workplaces
- Government buildings
- Learning environments
- Outdoor dining
- Outdoor drinking areas
- Patrolled beaches
- Train platforms and bus and tram shelters
- Under-age music or dance events
- Tobacco and e-cigarette retailers
- Making a report or complaint
- Resources and factsheets
- Alternative water supplies
- Aquatic facilities
- Blue-green algae (cyanobacteria)
- Drinking water in Victoria
- Legionella risk management
- Private drinking water
- Recreational water use and possible health risks
- Water fluoridation
- Chief Health Officer
- About the Chief Health Officer
- Chief Health Officer publications
- Health alerts and advisories
- Mental health
- Mental Health and Wellbeing Act 2022
- Mental Health and Wellbeing Act 2022 Handbook
- Community information
- Mental Health and Wellbeing Act 2022 in your language
- About Victoria's mental health services
- Area-based services
- Statewide and specialist mental health services
- Mental Health Community Support Services
- Support and intervention services
- Language services - when to use them
- Access to mental health services across areas
- Transport for people in mental health services
- Practice and service quality
- Medical Treatment Planning and Decisions Act
- Service quality
- Specialist responses
- Mental health and wellbeing reform
- Reform activity updates
- Priority areas
- Latest news
- Working with consumers and carers
- Consumer and carer engagement
- Consumer and Carer Experience Surveys
- Family support and crisis plans
- Consumer and carer financial support
- Supporting children whose parents have a mental illness
- Supporting parents with a mental illness
- Prevention and promotion
- Early intervention in mental illness
- Mental health promotion in Victoria
- Suicide prevention in Victoria
- Priorities and transformation
- Supporting the social and emotional wellbeing of Aboriginal and Torres Strait Islander Victorians
- National mental health strategy
- Rights and advocacy
- Making a complaint about a mental health service
- Chief Psychiatrist
- About the Chief Psychiatrist
- Principles in the Mental Health and Wellbeing Act and the Chief Psychiatrist's guidelines
- Obligations under the Mental Health and Wellbeing Act 2022
- Reporting a failure to comply with the Mental Health and Wellbeing Act 2022
- Governance and committees
- Reporting obligations for clinical mental health and wellbeing services
- Mental health and wellbeing support
- Making a complaint and seeking advocacy
- Second psychiatric opinion and process of review by Chief Psychiatrist
- Office of the Chief Psychiatrist's reform activities and news
- Oversight of forensic mental health and wellbeing services
- Resources and reports
- Chief psychiatrist guidelines
- Chief Mental Health Nurse
- About Victoria's Chief Mental Health Nurse
- Best practice
- Reducing restrictive interventions
- Research and reporting
- Mental health performance reports
- Reporting requirements and business rules for clinical mental health services
- Alcohol & drugs
- Alcohol and other drug treatment services
- Overview of Victoria's alcohol and drug treatment system
- Pathways into alcohol and other drugs treatment
- Prevention and harm reduction
- Medically supervised injecting room
- Victoria's Take-Home Naloxone Program
- Community-based AOD treatment services in Victoria
- Residential treatment services
- Mildura statewide alcohol and drug residential treatment service
- Drug rehabilitation plan
- Hospital-based services
- Forensic services
- Pharmacotherapy treatment
- Services for Aboriginal people
- Services for young people
- Statewide and specialist services
- Compulsory treatment
- Family and peer support
- Public intoxication reform
- New public intoxication response services
- Policy, research and legislation
- Alcohol and drug research and data
- Legislation governing alcohol and other drug treatment
- Alcohol and other drug service standards and guidelines
- Alcohol and other drug client charter and resources
- Alcohol and other drug treatment principles
- Service quality and accreditation
- Alcohol and other drug program guidelines
- Maintenance pharmacotherapy
- Specialist Family Violence Advisor capacity building program in mental health and alcohol and other drug services - Victoria
- Alcohol and other drug workforce
- Learning and development
- Alcohol and other drug workforce Minimum Qualification Strategy
- Workforce data and planning
- Funding and reporting for alcohol and other drug services
- Funding of alcohol and other drugs services in Victoria
- Reporting requirements and business rules for alcohol and other drug services
- Drug alerts
- 25C-NBOMe and 4-FA sold as '2C-B'
- Novel stimulants sold as MDMA, cocaine or speed
- Protonitazene sold as ketamine
- High potency benzodiazepine tablets
- MDMA adulterated with PMMA
- 25B-NBOH sold as powdered 'LSD'
- Green 'UPS' pills containing N-ethylpentylone (no MDMA)
- N-ethylpentylone in cocaine
- Ageing & aged care
- Supporting independent living
- Low cost accommodation support programs
- Personal Alert Victoria
- Dementia services
- Victorian Aids and Equipment Program
- Residential aged care services
- Public sector residential aged care services
- Safety and quality in public sector residential aged care
- Physical and social environments
- Emergency preparedness in residential aged care services
- My Aged Care assessment services
- Home and Community Care Program for Younger People
- HACC data reporting
- HACC PYP fees policy and schedule of fees
- Wellbeing and participation
- Age-friendly Victoria
- Healthy ageing
- Seniors participation
- Dementia-friendly environments
- Designing for people with dementia
- Maintaining personal identity
- Personal enjoyment
- Interior design
- Dining areas, kitchens and eating
- Bedrooms and privacy
- Gardens and outdoor spaces
- Assistive technology
- Staff education and support
- Strategies, checklists and tools
- Our Strategic Plan 2023-27
- Our organisation
- Our secretary
- Leadership charter
- Our services
- Our vision and values
- Specialist offices
- Senior officers in health
- Human Research Ethics Committee (HREC)
- Gifts, benefits and hospitality policy
- Information Asset Register
- Health legislation
- Health legislation overview
- Health Complaints legislation
- Health Records Act
- Human Tissue Act 1982
- Public Health and Wellbeing Act 2008
- Voluntary Assisted Dying Act
- Victoria's pandemic management framework
- Independent Pandemic Management Advisory Committee
- Pandemic Order Register
- Our ministers
- Our role in emergencies
- State Health Emergency Response Arrangements
- Emergency type
- Department's responsibilities in emergencies
- Health services’ responsibilities in emergencies
- Aboriginal employment
- Current vacancies
- Employment programs for students and graduates
- Rise program
- Inclusion and diversity at the Department of Health
- Health workforce
- Working in health
- Information sharing and MARAM
- Child Safe Standards
- Regulatory functions
- Reviews of decisions
- Victorian Public Healthcare Awards
- Aboriginal healthcare workers
- Mental health workforce
- Lived and living experience workforces
- Engaging with lived and living experience workforces
- Our workforce, our future
- Nursing and midwifery
- Free nursing and midwifery study
- Additional funding for nursing and midwifery positions
- Becoming a nurse or midwife
- Undergraduate nursing and midwifery scholarships
- Undergraduate student employment programs
- Nursing and midwifery graduates
- Nursing and midwifery graduate sign-on bonus
- Working as a nurse or midwife
- Enrolled nurse to registered nurse transition scholarships
- Support for new nurse practitioners
- Postgraduate scholarships for nurses and midwives
- Nurse practitioners
- Returning to nursing or midwifery
- Refresher pathway for nurses and midwives
- Re-entry pathway scholarships for nurses and midwives
- Nursing and midwifery - legislation and regulation
- Nursing and midwifery program - health sector
- Allied health workforce
- Education and training
- Enterprise agreements
- Worker health and wellbeing
- Working with us
- Grants and programs
- Freedom of Information
- Part II - Information Statements
- Procurement policies
- Protective markings
- Health and medical research
- Sponsorship application information
- Publications
- Annual reports
- Fact sheets
- Strategies, plans and charters
- Policies, standards and guidelines
- Research and reports
- Forms and templates
- Communities
- Designing for Diversity
- Vulnerable children
- Vulnerable children - responsibilities of health professionals
- Identifying and responding to children at risk
- Pathway to good health for children in care
- Older people
- Aboriginal health
- Improving health for Victorians from culturally and linguistically diverse backgrounds
- Asylum seeker and refugee health in Victoria
- News and media hub
- Media releases
- Health alerts
- Feedback and complaints
- Make a payment
- Fees, charges and penalties subject to automatic indexation
- Our campaigns
Share this page
- Facebook , opens a new window
- X (formerly Twitter) , opens a new window
- LinkedIn , opens a new window
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is a Case Study?
Weighing the pros and cons of this method of research
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
Verywell / Colleen Tighe
- Pros and Cons
What Types of Case Studies Are Out There?
Where do you find data for a case study, how do i write a psychology case study.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
The point of a case study is to learn as much as possible about an individual or group so that the information can be generalized to many others. Unfortunately, case studies tend to be highly subjective, and it is sometimes difficult to generalize results to a larger population.
While case studies focus on a single individual or group, they follow a format similar to other types of psychology writing. If you are writing a case study, we got you—here are some rules of APA format to reference.
At a Glance
A case study, or an in-depth study of a person, group, or event, can be a useful research tool when used wisely. In many cases, case studies are best used in situations where it would be difficult or impossible for you to conduct an experiment. They are helpful for looking at unique situations and allow researchers to gather a lot of˜ information about a specific individual or group of people. However, it's important to be cautious of any bias we draw from them as they are highly subjective.
What Are the Benefits and Limitations of Case Studies?
A case study can have its strengths and weaknesses. Researchers must consider these pros and cons before deciding if this type of study is appropriate for their needs.
One of the greatest advantages of a case study is that it allows researchers to investigate things that are often difficult or impossible to replicate in a lab. Some other benefits of a case study:
- Allows researchers to capture information on the 'how,' 'what,' and 'why,' of something that's implemented
- Gives researchers the chance to collect information on why one strategy might be chosen over another
- Permits researchers to develop hypotheses that can be explored in experimental research
On the other hand, a case study can have some drawbacks:
- It cannot necessarily be generalized to the larger population
- Cannot demonstrate cause and effect
- It may not be scientifically rigorous
- It can lead to bias
Researchers may choose to perform a case study if they want to explore a unique or recently discovered phenomenon. Through their insights, researchers develop additional ideas and study questions that might be explored in future studies.
It's important to remember that the insights from case studies cannot be used to determine cause-and-effect relationships between variables. However, case studies may be used to develop hypotheses that can then be addressed in experimental research.
Case Study Examples
There have been a number of notable case studies in the history of psychology. Much of Freud's work and theories were developed through individual case studies. Some great examples of case studies in psychology include:
- Anna O : Anna O. was a pseudonym of a woman named Bertha Pappenheim, a patient of a physician named Josef Breuer. While she was never a patient of Freud's, Freud and Breuer discussed her case extensively. The woman was experiencing symptoms of a condition that was then known as hysteria and found that talking about her problems helped relieve her symptoms. Her case played an important part in the development of talk therapy as an approach to mental health treatment.
- Phineas Gage : Phineas Gage was a railroad employee who experienced a terrible accident in which an explosion sent a metal rod through his skull, damaging important portions of his brain. Gage recovered from his accident but was left with serious changes in both personality and behavior.
- Genie : Genie was a young girl subjected to horrific abuse and isolation. The case study of Genie allowed researchers to study whether language learning was possible, even after missing critical periods for language development. Her case also served as an example of how scientific research may interfere with treatment and lead to further abuse of vulnerable individuals.
Such cases demonstrate how case research can be used to study things that researchers could not replicate in experimental settings. In Genie's case, her horrific abuse denied her the opportunity to learn a language at critical points in her development.
This is clearly not something researchers could ethically replicate, but conducting a case study on Genie allowed researchers to study phenomena that are otherwise impossible to reproduce.
There are a few different types of case studies that psychologists and other researchers might use:
- Collective case studies : These involve studying a group of individuals. Researchers might study a group of people in a certain setting or look at an entire community. For example, psychologists might explore how access to resources in a community has affected the collective mental well-being of those who live there.
- Descriptive case studies : These involve starting with a descriptive theory. The subjects are then observed, and the information gathered is compared to the pre-existing theory.
- Explanatory case studies : These are often used to do causal investigations. In other words, researchers are interested in looking at factors that may have caused certain things to occur.
- Exploratory case studies : These are sometimes used as a prelude to further, more in-depth research. This allows researchers to gather more information before developing their research questions and hypotheses .
- Instrumental case studies : These occur when the individual or group allows researchers to understand more than what is initially obvious to observers.
- Intrinsic case studies : This type of case study is when the researcher has a personal interest in the case. Jean Piaget's observations of his own children are good examples of how an intrinsic case study can contribute to the development of a psychological theory.
The three main case study types often used are intrinsic, instrumental, and collective. Intrinsic case studies are useful for learning about unique cases. Instrumental case studies help look at an individual to learn more about a broader issue. A collective case study can be useful for looking at several cases simultaneously.
The type of case study that psychology researchers use depends on the unique characteristics of the situation and the case itself.
There are a number of different sources and methods that researchers can use to gather information about an individual or group. Six major sources that have been identified by researchers are:
- Archival records : Census records, survey records, and name lists are examples of archival records.
- Direct observation : This strategy involves observing the subject, often in a natural setting . While an individual observer is sometimes used, it is more common to utilize a group of observers.
- Documents : Letters, newspaper articles, administrative records, etc., are the types of documents often used as sources.
- Interviews : Interviews are one of the most important methods for gathering information in case studies. An interview can involve structured survey questions or more open-ended questions.
- Participant observation : When the researcher serves as a participant in events and observes the actions and outcomes, it is called participant observation.
- Physical artifacts : Tools, objects, instruments, and other artifacts are often observed during a direct observation of the subject.
If you have been directed to write a case study for a psychology course, be sure to check with your instructor for any specific guidelines you need to follow. If you are writing your case study for a professional publication, check with the publisher for their specific guidelines for submitting a case study.
Here is a general outline of what should be included in a case study.
Section 1: A Case History
This section will have the following structure and content:
Background information : The first section of your paper will present your client's background. Include factors such as age, gender, work, health status, family mental health history, family and social relationships, drug and alcohol history, life difficulties, goals, and coping skills and weaknesses.
Description of the presenting problem : In the next section of your case study, you will describe the problem or symptoms that the client presented with.
Describe any physical, emotional, or sensory symptoms reported by the client. Thoughts, feelings, and perceptions related to the symptoms should also be noted. Any screening or diagnostic assessments that are used should also be described in detail and all scores reported.
Your diagnosis : Provide your diagnosis and give the appropriate Diagnostic and Statistical Manual code. Explain how you reached your diagnosis, how the client's symptoms fit the diagnostic criteria for the disorder(s), or any possible difficulties in reaching a diagnosis.
Section 2: Treatment Plan
This portion of the paper will address the chosen treatment for the condition. This might also include the theoretical basis for the chosen treatment or any other evidence that might exist to support why this approach was chosen.
- Cognitive behavioral approach : Explain how a cognitive behavioral therapist would approach treatment. Offer background information on cognitive behavioral therapy and describe the treatment sessions, client response, and outcome of this type of treatment. Make note of any difficulties or successes encountered by your client during treatment.
- Humanistic approach : Describe a humanistic approach that could be used to treat your client, such as client-centered therapy . Provide information on the type of treatment you chose, the client's reaction to the treatment, and the end result of this approach. Explain why the treatment was successful or unsuccessful.
- Psychoanalytic approach : Describe how a psychoanalytic therapist would view the client's problem. Provide some background on the psychoanalytic approach and cite relevant references. Explain how psychoanalytic therapy would be used to treat the client, how the client would respond to therapy, and the effectiveness of this treatment approach.
- Pharmacological approach : If treatment primarily involves the use of medications, explain which medications were used and why. Provide background on the effectiveness of these medications and how monotherapy may compare with an approach that combines medications with therapy or other treatments.
This section of a case study should also include information about the treatment goals, process, and outcomes.
When you are writing a case study, you should also include a section where you discuss the case study itself, including the strengths and limitiations of the study. You should note how the findings of your case study might support previous research.
In your discussion section, you should also describe some of the implications of your case study. What ideas or findings might require further exploration? How might researchers go about exploring some of these questions in additional studies?
Need More Tips?
Here are a few additional pointers to keep in mind when formatting your case study:
- Never refer to the subject of your case study as "the client." Instead, use their name or a pseudonym.
- Read examples of case studies to gain an idea about the style and format.
- Remember to use APA format when citing references .
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011;11:100.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011 Jun 27;11:100. doi:10.1186/1471-2288-11-100
Gagnon, Yves-Chantal. The Case Study as Research Method: A Practical Handbook . Canada, Chicago Review Press Incorporated DBA Independent Pub Group, 2010.
Yin, Robert K. Case Study Research and Applications: Design and Methods . United States, SAGE Publications, 2017.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
156 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health
At Tracking Happiness, we’re dedicated to helping others around the world overcome struggles of mental health.
In 2022, we published a survey of 5,521 respondents and found:
- 88% of our respondents experienced mental health issues in the past year.
- 25% of people don’t feel comfortable sharing their struggles with anyone, not even their closest friends.
In order to break the stigma that surrounds mental health struggles, we’re looking to share your stories.
Overcoming struggles
They say that everyone you meet is engaged in a great struggle. No matter how well someone manages to hide it, there’s always something to overcome, a struggle to deal with, an obstacle to climb.
And when someone is engaged in a struggle, that person is looking for others to join him. Because we, as human beings, don’t thrive when we feel alone in facing a struggle.
Let’s throw rocks together
Overcoming your struggles is like defeating an angry giant. You try to throw rocks at it, but how much damage is one little rock gonna do?
Tracking Happiness can become your partner in facing this giant. We are on a mission to share all your stories of overcoming mental health struggles. By doing so, we want to help inspire you to overcome the things that you’re struggling with, while also breaking the stigma of mental health.
Which explains the phrase: “Let’s throw rocks together”.
Let’s throw rocks together, and become better at overcoming our struggles collectively. If you’re interested in becoming a part of this and sharing your story, click this link!
Case studies
June 19, 2024
How Therapy, Self-Help and Medication Help Me Live With Depression and Anxiety
“When the next depressive episode hit in 2018, I was devastated. How could this happen again when I thought I had it all figured out? I experienced some of the darkest moments of my life and a nearly complete loss of hope.”
Struggled with: Anxiety Bipolar Disorder Depression Suicidal
Helped by: Medication Therapy
June 11, 2024
Sharing My Journey From Alcohol and Substance Abuse to Sobriety and Happiness
“I felt prettier, smarter, funnier when alcohol entered my body so I simply continued numbing through the years. The progression of this disease of alcoholism turned into a nasty drug habit and those feelings of insecurity turned into deep darkness when I was “off my meds”. Or in other words, without alcohol or drugs.”
Struggled with: Addiction Depression Suicidal
Helped by: Rehab Therapy
June 4, 2024
Finding Happiness and Self-Love After Escaping Death From Burning 90% Of My Body
“It was like starting life over again, except you know how to do things you physically can’t do, which emotionally drains you. There was definitely a sense of resentment and feeling sorry for myself, I think that is natural. You wonder what you did to deserve that, you wonder if things are ever going to get better, you wonder how people will treat you. When you are confined to a bed for weeks on end, really all you can do is wonder.”
Struggled with: Physical trauma
Helped by: Self-improvement Social support
May 28, 2024
Cognitive Reframing and Mindfulness Helped Me Overcome Depression and Suicidal Ideation
“After exploring ways to end my life, I resolved to slash my wrist. I retrieved a steak knife from the kitchen and pressed it against my skin. Yet, an unexpected sensation washed over me—a profound sense of peace, love, and joy.”
Struggled with: Depression Suicidal
Helped by: Meditation Mindfulness Self-improvement
May 21, 2024
Learning To Live With Postpartum Depression (PPD) Through Self-Acceptance and Coaching
“I absolutely did not want to talk to anyone about this. I found it easier to tell a stranger about my struggles because I knew I would not see them again. I felt that telling family or friends made my struggle real. I felt that they would now be able to hold me accountable.”
Struggled with: Postpartum depression
Helped by: Self-acceptance Social support
May 14, 2024
I’m Finding Luck After Trauma and Abuse Through Mindfulness
“I never mentioned the accident to anyone until I met my future husband at 22. He was sympathetic and supportive, and helped me understand the enormity of what I had been through.I still have not talked to my siblings about it.”
Struggled with: Abuse Depression Eating disorder Suicidal
Helped by: Meditation Mindfulness Reinventing yourself
May 7, 2024
My Journey From Hitting Rock Bottom to Overcoming Abuse, Addiction, and Eating Disorder
“Then something happened. On about day 3 or 4, the group spoke and I realized that their way of thinking around food, their rituals, and their tendencies, were all the same as the things I would do. It was wild because I thought I had made these things up myself and here I was with a room full of people who did the same things.”
Struggled with: Abuse Bullying Depression Divorce Eating disorder PTSD
Helped by: Self-Care Social support Therapy Treatment
May 2, 2024
How Yoga Became My Lifeline in Navigating Depression and Building Self-Love
“My relationship with myself was pretty broken and I had no self-belief, I had low self-esteem and I resented my family. It was through yoga that I found the truest feeling of comfort, self-compassion, and courage to move forward, grow as a person, and fall back in love with myself and life again.”
Struggled with: Depression Insomnia Stress Suicidal
Helped by: Exercise Meditation Mindfulness Self-Care
April 30, 2024
Finding Clarity After an ADHD Diagnosis and Bettering Myself With CBT and Medication
“Now as I was getting older, I felt I couldn’t trust my own thoughts in the same way as before, and self-doubt would creep in. I would constantly ask myself whether my emotions and thoughts were accurate or not when reacting to social situations. As you can imagine this was a huge challenge and draining emotionally.”
Struggled with: ADHD Autism
Helped by: Medication Social support Therapy
April 25, 2024
How I’m Seeking Moments of Happiness Despite Struggling With Depression
“The diagnosis I longed for finally arrived, but it didn’t bring the expected empowerment. While it sheds light on my struggles, it also serves as a reminder that this is a part of me that won’t simply vanish. Though mental health can be managed, I know it will always leave its mark. The most challenging part is not always pinpointing why I feel the way I do.”
Struggled with: Depression Negative body image
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
It’s a New Era for Mental Health at Work
- Kelly Greenwood

Research on how the past 18 months have affected U.S. employees — and how companies should respond.
In 2019, employers were just starting to grasp the prevalence of mental health challenges at work, the need to address stigma, and the emerging link to diversity, equity, and inclusion (DEI). One silver lining amid all the disruption and trauma over the last two years is the normalization of these challenges. In a follow-up study of their 2019 Mental Health at Work Report, Mind Share Partners’ 2021 Mental Health at Work Report, the authors offer a rare comparison of the state of mental health, stigma, and work culture in U.S. workplaces before and during the pandemic. They also present a summary of what they learned and their recommendations for what employers need to do to support their employees’ mental health.
When we published our research on workplace mental health in October 2019, we never could have predicted how much our lives would soon be upended by the Covid-19 pandemic. Then the murders of George Floyd and other Black Americans by the police; the rise in violence against Asian Americans and Pacific Islanders (AAPIs); wildfires; political unrest; and other major stressors unfolded in quick succession, compounding the damage to our collective mental health.
- Kelly Greenwood is the Founder and CEO of Mind Share Partners , a national nonprofit changing the culture of workplace mental health so both employees and organizations can thrive. Through movement building , custom training, and strategic advising, it normalizes mental health challenges and promotes sustainable ways of working to create a mentally healthy workforce. Follow her on LinkedIn and subscribe to her monthly newsletter.
- Julia Anas is the chief people officer at Qualtrics, the world’s #1 Experience Management (XM) provider and creator of the XM category. At Qualtrics, she is responsible for building a talented and diverse organization and driving employee development as well as organizational design, talent, and succession planning.
Partner Center

|
She has been treated for years with various antidepressants and mood stabilizers but has had only two short inpatient admissions. She has seen numerous therapists since childhood and, for the past five years, has been treated by a respected psychiatrist with a specialty in serious mental illness and psychopharmacology. Symptoms are similar to most major depressions: hopelessness, helplessness, self-directed angry outbursts, worthlessness, poor self-esteem, feelings of guilt, lack of motivation, excessive sleeping, poor hygiene, and tearfulness. She describes herself as a “terrible housekeeper.” She says she never cleans, never opens mail, and rarely eats at home. She once reported with sadness and disdain, “Sometimes, I make a bowl of cold cereal and milk, and I stand in the middle of the dining room and eat it. That’s so pitiful!” Because she is an exceptionally intelligent and articulate person, these negative characterizations are painful to hear—for her therapist, her doctor, and for Taylor.
Taylor’s descriptions of her father have always been more detailed and scathing. She describes her father as harsh and hypercritical with a history of severe teasing. “He never had to raise a hand against me. He is an expert at punishing with words,” Taylor explains. She has reported being called derogatory names critical of her mental health problems and physical appearance. Taylor does understand the connection between these experiences and her problems with depression, self-image, and self-esteem, but this insight does not seem to produce improvement. Unfortunately, due to the repeated episodes of depression, Taylor has had to depend on her father in the past eight years for financial assistance, which she bitterly resents. Periodically, Taylor had problems in school, especially high school. Eventually, her parents enrolled her in a private school that she loved and where she excelled. She was accepted into an Ivy League university but had difficulties due to a combination of social issues, an inability to organize her work, and a serious medical illness that led to a two-month hospitalization. Although she did not finish college, she transferred to a university in France where she stayed for several years, happily studying and traveling to many different countries. One of her major pastimes was mountain climbing, and she has climbed mountains all over Europe, Africa, and the United States. She sometimes talks about living in Europe permanently but has not pursued this beyond the most preliminary steps. Beginning in her mid-40s, Taylor began to suffer multiple health problems, some of which continue but are not life threatening. She has become more hopeless over her impending 50th birthday. The life review that this often engenders in people has become a major crisis for her as she reviews a life she believes to be worthless.
She had an unexpected monetary windfall and decided to reward herself with a three-week trip to Europe. She felt exceptionally energetic and returned to an old love of mountain climbing. On her return to the United States, she resumed treatment. She was full of stories about her trip, quickly found a new job, and felt reasonably content even though she had taken a pay cut. She resumed seeing her friends and talked about returning abroad to live permanently. This improvement was short lived. Over the next year and a half, the depression and its familiar distressing symptoms returned with increasing intensity. Taylor’s doctor actively managed her medications, but she continued to decline. During a session in my office one evening, she was so depressed that she sat practically mute with tears running down her face. She was still able to work but reported that her job was in jeopardy. After much consideration, she decided to try ECT again. However, this trial was unsuccessful, and Taylor had an unfortunate reaction and needed to be hospitalized for a few days. Since her discharge, sessions are dominated by Taylor’s depressive symptoms, self-hatred, and anger. She is frustrated with her inability to manage her home and is increasingly gloomy about her future. During our most recent session, she reported that she had lost her job. Taylor initially presented with a strong desire to get her life together, and she had two specific goals: to feel better about herself and to organize her home. “My doctor recommended you because he said you are a no-nonsense kind of person,” she told me. Taylor comes to therapy regularly, and she has been able to successfully discuss sensitive issues in her past such as a date rape in her late teens. Although she does not have an intimate relationship now and is not dating, she has several close friends with whom she sometimes goes out to dinner or to a movie when she agrees to call them. She often assumes it is their responsibility to call her. She has developed a trusting relationship with me as her therapist and is able to follow some basic cognitive therapy techniques to examine her thinking and structure her day. However, all attempts at permanent change have been met with only temporary success. Homework assignments are done only for a few days, and physical activity has the same duration. Suggestions such as focusing on her beloved Siamese cats, connecting with friends, revisiting former interests, and learning to manage anger and the relationship with her father have all worked for a while but are never entirely successful. There are times when she is able to draw on past accomplishments and see that she has some strengths and has done some positive things. Her life has been adventuresome and somewhat eccentric, but she resists seeing this as a genuine way to live and believes that she is a flawed person without a husband, children, a fine home, and living what she perceives to be a “normal” life. Despite her severe bouts of depression, she does not want to die and firmly states that she would never harm herself. Taylor is wedded to the idea that psychopharmacology or some other yet undiscovered miracle medical procedure will be the answer to her difficulties. She reports that she is more willing to try any medication or procedure (after careful assessment) rather than having to go through the harder, slower process of therapy. Her mantra about any new therapeutic process is “What good will this do?”
Taylor seems to be a study in contradictions. She wants a quick fix for her problems but has stayed in this therapy for at least a year and a half. She shifts from positive to negative feelings about her intelligence, and she sees herself as flawed for not having a “normal” life, though she is quite disparaging of her normal parents. One explanation for these contradictions could be her attachment to her negative feelings about herself, which seem quite profound. Her ability to tolerate positive feelings appears limited, perhaps because it could endanger her negative, but reliable, identity. Despite Taylor’s attachment to her negative persona, she has pursued this therapy, which suggests that there is a role for a therapist to play in helping her find a more self-accepting, positive identity. The key to working with Taylor could be helping her realize that someone understands how much she has suffered but is not empathically overwhelmed and/or emotionally harmed by the suffering she demonstrates in her sessions (i.e., mute despair with weeping and self-punitive comments). Taylor seems to be unaware that the way she treats herself is similar to the way she describes her father treating her, but in an internalized, self-imposed manner. The therapist’s role at this point in the treatment seems to be witnessing Taylor’s intense suffering. The description Taylor was given of her current therapist as “no-nonsense” could be a clue to what she thinks she needs (i.e., a therapist who doesn’t get lost in Taylor’s misery). This could also mean a therapist who sees that the suffering is a crucial part of Taylor’s identity and acknowledges the importance it has to her without seeing it as the only identity she could have. The therapist says, “Something very strong keeps her [Taylor] going in this world, helps her to survive.” I see this comment as encouraging Taylor to see herself as emotionally stronger than she feels, which could be overlooking how psychologically destroyed Taylor can feel at times during what sound like psychotic episodes. The desire to avoid these extremely painful episodes could be what leads Taylor to cling to her very difficult but reliable, negative self-images and to be financially dependent on her demeaning but reliable father. Over time, the therapeutic process could offer Taylor a different experience and new ways to avoid the experience of losing her identity in overwhelming depression. Taylor seems to be nonverbally asking the therapist to take responsibility for her awful feelings, just as she wants her friends to be the ones to reach out to her. Seeing the therapeutic process as a way to begin to own and contain her painful feelings would be a necessary precursor to helping Taylor look at the identity she has constructed and maintains. It would be a good idea for the therapist to explore Taylor’s question, “What good will this do?” and be clear that any change that comes from therapy will likely be a long process, as Taylor and the therapist build new ways for Taylor to own and contain her feelings. Empathizing with the frustration this is likely to cause Taylor would be an important part of building a therapeutic alliance. But simply tolerating the pain Taylor experiences and encouraging her to put it in words when she can, as the therapist seems to be doing, is also a crucial part of helping Taylor. Taylor appears to have built her identity on primarily negative images of herself, her mother, and her father, with little capacity to question the way she now projects these images onto herself and others. Despite her conscious wish to be different from her parents, who she felt were cruel and/or neglectful, Taylor nonetheless continues to expect to be treated in these hurtful ways. In the absence of others doing so, she treats herself cruelly. Her ability to form a connection to the therapist is a good sign, but the miserable internal world she has lived in needs to be identified and discussed, particularly the way it is expressed in the therapy. Managing the feelings Taylor stirs up in the therapist would be a major part of the therapist’s work. My primary goals for working with a patient like Taylor would be to look at her self-punitive comments as a way of avoiding critical comments about the therapist, helping her put her nonverbal anguish into words, and letting her know that this is a difficult process for both Taylor and the therapist but one that can be successful if Taylor is willing to work toward changing her self-punitive identity with the therapist’s help.
I utilize a biopsychosocial/spiritual perspective with most clients. As I explore developmental history, I focus on temperament and particularly on early personality development. Personality begins to show itself around the age of 3 and is thought to be malleable until somewhere in the third decade of life. I am most interested in attachment and bonding dynamics. From my vantage point, Taylor has introjected a “sterile” mother and a “dysfunctional” father in response to the early psychosocial climate and environment during her youth. So her “self” and “other” split object relations are negatively distorted. Through the lens of Erik Erikson, I look at the stages of psychosocial development: trust/mistrust, autonomy/shame or doubt, initiative/guilt, industry/inferiority, and identity and role integration/confusion or what I refer to as diffusion. Taylor has not mastered these opportunities. Drawing from John Bowlby, I look at the common reactions to as serious disruptions or fractures of significant relationships: shock, protest, despair, reattachment, or detachment. I see plenty of evidence of these dynamics, which Taylor projects onto current and future relationships. Taylor shows an insecure attachment with both aggressive/ambivalent and avoidant features. Globally, I consider her to show an “asocial” personality orientation. She likely feels vulnerable and fragile in close, intimate relationships. In my clinical experience, an early childhood onset of depression has been rare. We know that in adolescence and adulthood, women are at great risk of major depression. I am struck by Taylor’s suicide attempt during the latency period. I wonder if the presentation of puberty was a potential trigger. In terms of suicide, women are more likely the attempters and men the completers. What method did she use? I always explore the meaning of these incidents, questioning the client’s reaction to them then and now. I find it remarkable, considering her overall suffering, that she has not attempted again. I am very concerned about her degree of hopelessness. Aaron T. Beck and Judith S. Beck indicate this to be a high risk factor for suicide. I would also examine the degree of helplessness and worthlessness, as I have found this “suicidal triad” to be more predictive of risk. Taylor displays what the Becks refer to as the cognitive triad: negative view of past, self, and future. In addition, she clearly displays an external locus of control that leaves her vulnerable in facing psychosocial stressors. I would like to know more about her sibling position and her current and former connections to her sisters. I am curious about any dynamics related to having a father with no sons. I suspect that her siblings also feel vulnerable about intimacy. With all clients, I conduct a protection/risk inventory. Here is my assessment of Taylor’s: Her intellect and articulate qualities are assets. She has some friends. She used to really enjoy mountain climbing. Her therapy attendance is consistent. She showed a very positive response to her first series of ECT. Her risk factors include the degree of hopelessness she feels, her detachment from others, her persistent dysthymia, her marginal or poor response to appropriate psychotropic medication, and her long-standing negatively distorted self-concept. I am curious about her experiences with previous therapists, and I am especially interested in her transference to her present one. I would like to know more about the clinician’s countertransference to this client. My diagnosis is recurrent major depression with persisting dysthymia. When they occur together, some refer to this as double depression. In fact, some evidence shows that nine of 10 persons with dysthymia experience a major depressive episode. I also see Taylor as evidencing a mixed personality disorder in the “wary cluster (Cluster C), with avoidant and dependent features.” In my experience, persons with disordered personality respond marginally to the use of psychotropics. A course of cognitive behavioral therapy is appropriate for her. I also would consider a course of interpersonal therapy. Both approaches are known to be effective in treating major depression. More importantly for Taylor, I recommend a movement away from individual to group psychotherapy. In group therapy, clinicians have access to various therapeutic factors unique to group, which give them additional leverage to be useful to our clients. I think that it will be important to see her through menopause and beyond. Finally, I inquire about each person’s spiritual beliefs in terms of the meaning it gives to their life in times of suffering and in times of relative well-being. In summary, I see Taylor’s prognosis as guarded with continuing treatment and poor without it.
|
Social Work Today magazine

- Sign up and Get Listed
Be found at the exact moment they are searching. Sign up and Get Listed
- For Professionals
- Worksheets/Resources
Find a Therapist
- Find a Treatment Center
- Find a Marriage Counselor
- Find a Child Counselor
- Find a Support Group
- Find a Psychologist
- If You Are in Crisis
- Self-Esteem
- Sex Addiction
- Relationships
- Child and Adolescent Issues
- Eating Disorders
- How to Find the Right Therapist
- Explore Therapy
- Issues Treated
- Modes of Therapy
- Types of Therapy
- Famous Psychologists
- Psychotropic Medication
- What Is Therapy?
- How to Help a Loved One
- How Much Does Therapy Cost?
- How to Become a Therapist
- Signs of Healthy Therapy
- Warning Signs in Therapy
- The GoodTherapy Blog
- PsychPedia A-Z
- Dear GoodTherapy
- Share Your Story
- Therapy News
- Marketing Your Therapy Website
- Private Practice Checklist
- Private Practice Business Plan
- Practice Management Software for Therapists
- Rules and Ethics of Online Therapy for Therapists
- CE Courses for Therapists
- HIPAA Basics for Therapists
- How to Send Appointment Reminders that Work
- More Professional Resources
- List Your Practice
- List a Treatment Center
- Earn CE Credit Hours
- Student Membership
- Online Continuing Education
- Marketing Webinars
- GoodTherapy’s Vision
- Partner or Advertise
- GoodTherapy Blog >
The Important Role Social Workers Play in Mental Health

Who Are Social Workers?
Social workers are highly trained professionals working to improve the quality of life and well-being of others through direct practice, crisis intervention, research, community organizing, policy change, advocacy, and educational programs. Social workers are dedicated to the pursuit of social justice and strive to help those affected by poverty, disabilities, illnesses , divorce , unemployment, and other personal problems and social disadvantages.
Being a social worker requires extensive knowledge of human behavior and development, as well as social, cultural, and economic institutions and the ways in which they interact. Most social workers will hold at least a bachelor’s degree in social work or related field, though many (especially clinicians) will hold a master’s degree and valid license to practice.
A good social worker will often possess a high degree of compassion and empathy , a passion for helping others, strong interpersonal and problem-solving skills, and good listening and organizational skills.
What Do Social Workers Do?
Social workers fight for social justice, equality , and the overall well-being of people in need. Social workers are responsible for many of the liberties we have today. These include:
- Civil rights for all citizens regardless of race, sexual orientation , gender , faith, etc.
- Medicaid and Medicare programs that provide disadvantaged groups access to health care
- Child abuse and neglect prevention programs
- Unemployment insurance, disability pay, worker’s compensation, and social security
- Humane treatment for those with mental health conditions and developmental issues
Clinical social workers diagnose and treat mental health conditions as well. They provide individual, family, and couples therapy, and they assist with depression , anxiety , family problems , and other mental health or behavioral issues. They may work in private practice or at a mental health or therapeutic facility. Social workers host support groups, create treatment plans, and facilitate interventions when necessary.
Some common duties of a social worker include:
- Identifying and reaching out to those in need.
- Assessing people’s needs and implementing a plan of action.
- Helping people adjust to major life changes .
- Responding to crisis situations.
- Connecting people with important resources and support.
- Evaluating social services and support programs.
- Providing advocacy for people when needed.
- Following up with people to ensure circumstances are improving.
Where Do Social Workers Work?
There are several common areas of focus in the social work industry:
- Administration/supervision
- Alcohol, tobacco, and other drugs
- Children, adolescents , and young adults
- Child welfare
- Physical health
- Mental health
- Private practice
- School social work
- Social and economic justice and peace
- Social work and the courts
A good social worker will often possess a high degree of compassion and empathy, a passion for helping others, strong interpersonal and problem-solving skills, as well as good listening and organizational skills. Social work is unique in the way it can be found in most aspects of community life. Social workers are employed in schools, hospitals, rehabilitation facilities, hospices and nursing homes, private practices , government institutions, correctional facilities, law offices, military organizations, public welfare agencies, nonprofit organizations, and some private businesses and corporations.
Even when social workers are employed in office, they may spend time traveling to visit with people in need. School social workers may also travel from school to school or hospital social workers from hospital to hospital.
Why Social Work Is in Demand
According to the United States Bureau of Labor and Statistics, overall employment of social workers is expected to grow at a rate of 19% between 2012 and 2022. The demand for health care social workers is expected to grow by as much as 27% during this same time period—a rate much higher than the average growth rate for all occupations. One reason for the increase in demand is due to the aging of the baby boomers, who will soon need long-term care and assistance.
Social workers in the mental health and substance abuse fields will also be in high demand, with a 23% increase in employment expected by 2022. More people are expected to seek mental health treatment, and people who have a substance addiction are increasingly sent to treatment programs rather than jails or prisons.
How to Become a Social Worker
Those interested in entering the social work profession should first prepare for admission to the program of their choice by gaining valuable volunteer experience and obtaining professional references in the field.
A bachelor’s degree is the minimum requirement for an entry-level social work position, but most employers prefer a graduate degree. A master’s level education in social work is a requirement for clinical licensure in most states.
An undergraduate degree in social work is not necessary to gain admittance to a master’s program; virtually any bachelor’s degrees will suffice. Upon graduation, a few years of supervised work is necessary to gain licensure.
When to Reach Out to a Social Worker
- You’re seeking therapy or treatment for depression, anxiety, or another mental health condition.
- You’ve recently undergone a major life change (divorce, death of a loved one , etc.) and need support.
- You have witnessed child abuse or neglect.
- You need geriatric assistance for an elderly family member.
- You are coping with a drug or alcohol addiction .
- You are finding it difficult to cover the costs of basic needs (food, shelter, water, or others).
- You or a loved one is battling a major illness.
- You have recently become unemployed or disabled.
- Your child is experiencing behavior problems at school.
References:
- Bureau of Labor Statistics, U.S. Department of Labor, Occupational Outlook Handbook, 2014-15 Edition , Social Workers. Retrieved from http://www.bls.gov/ooh/community-and-social-service/social-workers.htm
- National Association of Social Workers. (NASW). Social Work Profession. Retrieved from https://www.socialworkers.org/pressroom/features/general/profession.asp
- National Association of Social Workers (NASW). Social Work History. Retrieved from http://socialworkers.org/pressroom/features/general/history.asp
- National Association of Social Workers (NASW). Who are Social Workers? We Help. Retrieved from http://www.naswdc.org/pressroom/2011/HSH-FactSheet2011.pdf

© Copyright 2015 GoodTherapy.org. All rights reserved.
The preceding article was solely written by the author named above. Any views and opinions expressed are not necessarily shared by GoodTherapy.org. Questions or concerns about the preceding article can be directed to the author or posted as a comment below.

Please fill out all required fields to submit your message.
Invalid Email Address.
Please confirm that you are human.
- 13 comments
Leave a Comment
These are the people who would be the most responsible with getting people with the resources that they need at any given point in time. They are literally a lifeline for a whole lot of people and yet they get very little praise and recognition overall.
They sure do have a lot of job responsibility without nearly enough in compensation
We do have a lot on our plate. Thanks for posting.
These are the people who advocate for those who tend to not have a voice of their own. I don’t think that we give enough credit to this group of professionals who typically go above and beyond the call of duty if they know that what they are doing is helping and serving another individual.
thanks for your recognition… It means a lot. I’ve been practicing social worker for over 30 years and were recently become an RM.
Think about all of the agencies and resources that they have to keep up with. They have to know where to refer which clients and who could benefit from what service but maybe not that one. I mean, that is a lot!
I do wish that there was a little more understanding about the work that most social workers find themselves engaged in. This is more than just about being a case manager. In many cases you are their link to normalcy, a counselor, and a friend. I think that in many instances families just need someone to talk to who really hears and understands their concerns and they do not get a lot of that. Social workers do a huge amount of work in filling that void for many families.
Good article but you need to be aware that licensure requirements vary from state to state. Some of what you describe here is very specific to “clinical licensure.” But there are other levels of licensure in most states, and those requirements are different from what you describe.
Most of the mass shootings have involved youth or adults with a history of mental illness. Too often families and individuals have fallen between the cracks because of the lack of services available or because there was no one to help them navigate the systems for help. In my former profession I often came in contact with numerous individuals and families who needed help accessing mental services. It was the mental health social workers who I contacted or referred them to. Because of the immense size of our state geographically, the weather barriers in many areas of the state, and number of very rural (Alaskan Bush) communities, it is often impossible for help to be available without a plane or boat ride to a larger community. We have to rely on the social workers in our schools or the village clinics to provide help 24/7. They have a tough job to do but they do it well.
It wasn’t until I looked over this list that I fully realized what kind of role social workers play in the lives of numerous amounts of people. There are those who rely on them for practically every service that they receive, there are those who receive a little help, and then pretty much anything in between. The spectrum that it appears that they deal with is massive and they should be commended much more often for the varying and taxing jobs that they must do.
Social workers are very essential to the growth of a Nation but most leaders fail to recognise that. They are are like a bedrock that should not be under-emphasized especially in Developing countries that’s always faced with series of social problems like poverty,juvenile delinquencydomestic violence to mention but a few. I look uptown that generation when Social work would be accorded the necessary recognition but I pray It comes early. I’m proud to be a social work student.
Hi, Thanks for the article and trying to contribute to the discourse. However, please clarify how could a Clinical/Psychiatric Social Worker diagnose and prescribe treatment? They can support with therapeutic and counselling interventions, yes, but how can they diagnose/treat? Social Worker are para-Health professionals working alongwith other professionals like Psychiatrist, Occupational Therapist, Therapist and so on. Yes, there could be some role overlaps, but certainly not when it comes to diagnosing/prescribing treatment. Social Workers can support the process. I work as a Psychiatric/Mental Health Social Worker in Mumbai, India. Please let me know if you beg to differ or if I have missed out something. Would be glad to recieve and listen:)
Stay safe and take care.
Clinical Social Workers are professionals that can diagnose and treat any mental illnesses. They do have a Master’s Degree in Clinical Social Work Practice and some of them are specialized in Mental Health and Addictions.
By commenting you acknowledge acceptance of GoodTherapy.org's Terms and Conditions of Use .
* Indicates required field.

Search Our Blog
Browse by category.
- Uncategorized
- GoodTherapy.org Announcements
- For Therapists by Therapist
- Find Therapist
- FAQ/What to Expect in Therapy
- Personal Growth
- Self-Concept
- Myths in Therapy
- Topic Expert Roundup
- Women's Issues
- Sex/Sexual Concerns
- Grief and Loss
- Separation and Divorce
- social media
Notice to users

- Children's mental health case studies
- Food, health and nutrition
- Mental wellbeing
- Mental health
Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and feedback for the user. Use these cases on your own or in classes and training events
Each case study:
- Explores the experiences of a child and family over time.
- Introduces theories, research and practice ideas about children's mental health.
- Shows the needs of a child at specific stages of development.
- Invites users to “try on the hat” of different specific professionals.
By completing a case study participants will:
- Examine the needs of children from an interdisciplinary perspective.
- Recognize the importance of prevention/early intervention in children’s mental health.
- Apply ecological and developmental perspectives to children’s mental health.
- Predict probable outcomes for children based on services they receive.
Case studies prompt users to practice making decisions that are:
- Research-based.
- Practice-based.
- Best to meet a child and family's needs in that moment.
Children’s mental health service delivery systems often face significant challenges.
- Services can be disconnected and hard to access.
- Stigma can prevent people from seeking help.
- Parents, teachers and other direct providers can become overwhelmed with piecing together a system of care that meets the needs of an individual child.
- Professionals can be unaware of the theories and perspectives under which others serving the same family work
- Professionals may face challenges doing interdisciplinary work.
- Limited funding promotes competition between organizations trying to serve families.
These case studies help explore life-like mental health situations and decision-making. Case studies introduce characters with history, relationships and real-life problems. They offer users the opportunity to:
- Examine all these details, as well as pertinent research.
- Make informed decisions about intervention based on the available information.
The case study also allows users to see how preventive decisions can change outcomes later on. At every step, the case content and learning format encourages users to review the research to inform their decisions.
Each case study emphasizes the need to consider a growing child within ecological, developmental, and interdisciplinary frameworks.
- Ecological approaches consider all the levels of influence on a child.
- Developmental approaches recognize that children are constantly growing and developing. They may learn some things before other things.
- Interdisciplinary perspectives recognize that the needs of children will not be met within the perspectives and theories of a single discipline.
There are currently two different case students available. Each case study reflects a set of themes that the child and family experience.
The About Steven case study addresses:
- Adolescent depression.
- School mental health.
- Rural mental health services.
- Social/emotional development.
The Brianna and Tanya case study reflects themes of:
- Infant and early childhood mental health.
- Educational disparities.
- Trauma and toxic stress.
- Financial insecurity.
- Intergenerational issues.
The case studies are designed with many audiences in mind:
Practitioners from a variety of fields. This includes social work, education, nursing, public health, mental health, and others.
Professionals in training, including those attending graduate or undergraduate classes.
The broader community.
Each case is based on the research, theories, practices and perspectives of people in all these areas. The case studies emphasize the importance of considering an interdisciplinary framework. Children’s needs cannot be met within the perspective of a single discipline.
The complex problems children face need solutions that integrate many and diverse ways of knowing. The case studies also help everyone better understand the mental health needs of children. We all have a role to play.
These case has been piloted within:
Graduate and undergraduate courses.
Discipline-specific and interdisciplinary settings.
Professional organizations.
Currently, the case studies are being offered to instructors and their staff and students in graduate and undergraduate level courses. They are designed to supplement existing course curricula.
Instructors have used the case study effectively by:
- Assigning the entire case at one time as homework. This is followed by in-class discussion or a reflective writing assignment relevant to a course.
- Assigning sections of the case throughout the course. Instructors then require students to prepare for in-class discussion pertinent to that section.
- Creating writing, research or presentation assignments based on specific sections of course content.
- Focusing on a specific theme present in the case that is pertinent to the course. Instructors use this as a launching point for deeper study.
- Constructing other in-class creative experiences with the case.
- Collaborating with other instructors to hold interdisciplinary discussions about the case.
To get started with a particular case, visit the related web page and follow the instructions to register. Once you register as an instructor, you will receive information for your co-instructors, teaching assistants and students. Get more information on the following web pages.
- Brianna and Tanya: A case study about infant and early childhood mental health
- About Steven: A children’s mental health case study about depression
Cari Michaels, Extension educator
Reviewed in 2023
© 2024 Regents of the University of Minnesota. All rights reserved. The University of Minnesota is an equal opportunity educator and employer.
- Report Web Disability-Related Issue |
- Privacy Statement |
- Staff intranet
- Find a Social Worker
About social work
Where social workers work
What social workers do
How social workers work
How to Find a Social Worker
Seeing a social worker
- Constitution & bylaws
Board of directors
AASW elections
Annual general meetings
Annual Reports
AASW structure
Strategic plan 22-23
Reconciliation action plan
Our history
- Practice & networking groups
Opportunities with AASW
Work with us
Volunteer with us
Employment partnerships
Sponsorships
Advertising
- Awards & grants
- Life Member
- AASW Fellow
Social Policy & Advocacy
Policy positions
Advocacy for the Profession
Registration of social work in Australia
Ethics and Standards
Code of ethics
Practice standards
Ethics consultation service
Making a complaint
Constitution & bylaws
Practice & networking groups
Awards & grants
Life member
AASW fellow
Become a member
- Membership FAQs
Credential Program
Renewal FAQs
Continuing professional development (CPD)
CPD overview
- Specialist learning programs & workshops
On Demand Learning
Live-online Webinars and Workshops
- Branch CPD & events
CPD Newsletter Subscription
Employer partnership program
Become an employer partner
Benefits to employers
Benefits to employees

Practice and careers
- Support & resources
Social work community
Mentoring program
AASW community hub
Credentials Program
- AASW credentials
Find CPD & Events
Specialist learning programs & workshops
Branch CPD & events
Support & resources
AASW Credentials
Higher education providers
Accredited Programs
Accreditation Process
Accreditation Roles
Additional Information
Migration & eligibility assessment (MEA)
Working Overseas
- Migration & eligibility assessment
International qualification recognition
New Zealand Mutual Recognition
International students studying an AASW accredited social work course in Australia
Temporary Graduate Visa Subclass 485
Renewals and reissue of Assessments
Optional migration assessments
Reassessment, internal review and external appeal
Horizon Career Centre
Mea online applications.
Migration & eligibility assessment
News and Media Releases
- News & media releases
- Information for the media
AASW in the media
Newsletters
Publications
Social Work Focus
Australian Social Work
News & media releases
Information for the Media
- Find a social worker
- AASW Accredited Mental Health Social Worker Application Criteria
- Credentials
- Mental Health
- Family Violence
- Child Protection
- Older Persons
In 2004, the Australian Government implemented the Enhanced Primary Care Program under which General Practitioners were able to refer patients with complex care requirements to a range of allied health services. Under this initiative social workers were recognised as one of the group of eligible mental health providers. In 2006, the Government introduced the ‘Better Access to Mental Health Care’ initiative, under which General Practitioners, Paediatricians and Private Psychiatrists could refer to suitably qualified and experienced allied health professionals namely: social workers; psychologists and occupational therapists for the provision of ‘Focussed Psychological Strategies’. This document explains the process which a social worker must undergo, should they wish to be considered by Medicare Australia as ‘suitably qualified and experienced allied health professional’.
Please refer to information below as to the 6 AMHSW criteria that must ALL be met to gain a successful outcome:
- Hold current eligible AASW membership
- Have at least 2 years’ full-time equivalent (FTE) post-qualifying social work experience* in a mental health setting within the last 5 years , totalling a minimum of 3,360 hours. The AASW recognises that full-time employment equates to 35 hours per week, for 48 weeks per year.
- Must be able to articulate your understanding and provide a case example on how your experience meets the AASW Practice Standards for Mental Health Social Workers 2014 . Where applicable, you must demonstrate the use of Focused Psychological Strategies (FPS), within your case example from your mental health practice position/s.
- Demonstrate at least 2 years’ full-time equivalent (FTE) post-qualifying supervision in a mental health setting/field within the last 5 years. You should be able to show that they have been formally supervised, in line with the AASW Supervision Standards . Generally, supervisors should have a higher level of practice experience than their supervisees and should have some training in supervision. For the purposes of this assessment, the supervisor does not necessarily need to have a social work background but should have provided the applicant/supervisee with appraisal and assessment in relation to practice in a mental health field (e.g. psychologist, medical practitioner or a mental health nurse).
- Have met the Continuing Professional Development requirements
- Demonstrate ability and knowledge of clinical Mental Health social work practice through Case study activities. Further information on the case study activity can be found on Case Study Activity
- Curriculum vitae: the CV or resume allows our assessor to get an overall picture of your social work experience. Please ensure the dates align with all the evidence you provide.
- Referee statement: You must provide the official AASW referee statement form completed, signed and dated by an employer or supervisor that validates your work and performance in a mental health setting/field using FPS. For the purposes of this credential, the referee must have appropriate qualifications and experience in mental health in order to provide appropriate assessment and appraisal of an applicants mental health practice and particularly your use of and competence in FPS. The form must also confirm the exact dates and hours per week of employment.
- Position description: an official agency position description on organisation letter head to confirm the key duties and responsibilities of the role.
Note for applicants who are self-employed in private practice
In addition to submitting a referee statement, you will need to provide a signed and declared statutory declaration outlining details of your roles and responsibilities in lieu of a position description. You will need to include the dates and approximate hours per week that you have worked in your private practice role, in particular, your clinical work with mental health clients, utilising FPS, and the percentage of time which is spent in this clinical mental health work.
Why be a member?
When you join the AASW you’ll become part of an active and vibrant community of more than 17,000 social work professionals. As the profession’s peak body, the AASW is committed to maintaining high standards, ethical practice and ongoing professional development.
Access on-demand content, live workshops and events at up to 50% discount as a member
National office
Level 7, 14-20 Blackwood St NORTH MELBOURNE 3051
PO Box 2008 Royal Melbourne Hospital VIC 3050
P: 03 9320 1000
Quick Links
Site information, get the latest cpd news & events, connect with us.
The AASW respectfully acknowledges Aboriginal and/or Torres Strait Islander peoples as the First Australians, and pay our respects to Elders past and present.
© 2023 - AASW Copyright
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Quality assurance in mental health-care: a case study from social work
Affiliation.
- 1 Calderdale and Huddersfield NHS Trust, Royal Infirmary, Lindley, Huddersfield HD3 3EA, UK. [email protected]
- PMID: 11846817
- DOI: 10.1046/j.0966-0410.2001.00324.x
The quality of health and social care is now a high priority for government, professionals, and the public. This is particularly true of mental health, where explicit standards lie at the centre of current policy, demanding the development of reliable means for quality assurance. These need to allow for the multiplicity of stakeholders in mental health-care, and their different constructions of "quality". The challenges presented are illustrated by this account of an action research programme, which was developed to improve social work practice in a multidisciplinary mental health service, and evaluated using a case study design. An action research approach was chosen in preference to an "off-the-shelf" quality assurance system, because it possessed features that appeared to match the context of the work. It involved feeding back the findings of a baseline assessment of service quality to four teams of social workers, who used the information to select priority areas for improvement. An action plan was developed with them, and its implementation and impact were examined. Substantial improvements were observed in only one of the chosen target areas--the quality of case recording. For the other--securing the clients' full involvement in their care plan--very limited improvements occurred. Interview data suggested that this was due to the presence of extensive organisational support for the first objective, but not the second. These findings suggest that while some features of action research can contribute to quality improvement, these must be incorporated into a more comprehensive programme of change, which commands the support of all the stakeholders involved.
PubMed Disclaimer
Similar articles
- Training to enhance user and carer involvement in mental health-care planning: the EQUIP research programme including a cluster RCT. Lovell K, Bee P, Bower P, Brooks H, Cahoon P, Callaghan P, Carter LA, Cree L, Davies L, Drake R, Fraser C, Gibbons C, Grundy A, Hinsliff-Smith K, Meade O, Roberts C, Rogers A, Rushton K, Sanders C, Shields G, Walker L. Lovell K, et al. Southampton (UK): NIHR Journals Library; 2019 Oct. Southampton (UK): NIHR Journals Library; 2019 Oct. PMID: 31647625 Free Books & Documents. Review.
- Information for mental health systems: an instrument for policy-making and system service quality. Lora A, Lesage A, Pathare S, Levav I. Lora A, et al. Epidemiol Psychiatr Sci. 2017 Aug;26(4):383-394. doi: 10.1017/S2045796016000743. Epub 2016 Oct 26. Epidemiol Psychiatr Sci. 2017. PMID: 27780495 Free PMC article. Review.
- Implementation of the care programme approach across health and social services for dual diagnosis clients. Kelly M, Humphrey C. Kelly M, et al. J Intellect Disabil. 2013 Dec;17(4):314-28. doi: 10.1177/1744629513508383. Epub 2013 Oct 16. J Intellect Disabil. 2013. PMID: 24132192
- The bigger picture. 'Outcome-focused provision' has become the latest buzzword, but what does it mean? Bogg D. Bogg D. Ment Health Today. 2008 Nov:24. Ment Health Today. 2008. PMID: 19058375 No abstract available.
- What is necessary to transform the quality of mental health care. Patel KK, Butler B, Wells KB. Patel KK, et al. Health Aff (Millwood). 2006 May-Jun;25(3):681-93. doi: 10.1377/hlthaff.25.3.681. Health Aff (Millwood). 2006. PMID: 16684732
- What Is Best for Esther? Building Improvement Coaching Capacity With and for Users in Health and Social Care--A Case Study. Vackerberg N, Levander MS, Thor J. Vackerberg N, et al. Qual Manag Health Care. 2016 Jan-Mar;25(1):53-60. doi: 10.1097/QMH.0000000000000084. Qual Manag Health Care. 2016. PMID: 26783868 Free PMC article.
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Recommended pages
- Undergraduate open days
- Postgraduate open days
- Accommodation
- Information for teachers
- Maps and directions
- Sport and fitness
Mental health practice case studies
Each of these short films presents a case study of a potentially difficult mental health situation that practitioners may need to deal with as part of their practice. Topics covered include appropriate listening skills, confidentiality, drug use, professional conduct, anger, social isolation, sexual advances and stereotyping. The aim of these films is to stimulate discussion and reflection about these particular situations and the issues that arise from them.
The following group of case studies form part of the Online Assessment Workbook.
See also Mental health case studies which were filmed as part of the SELF Project.
Return to film Index
The independent source for health policy research, polling, and news.
Key Data on Health and Health Care by Race and Ethnicity
Nambi Ndugga , Latoya Hill , and Samantha Artiga Published: June 11, 2024
Executive Summary
Introduction.
Racial and ethnic disparities in health and health care remain a persistent challenge in the United States. The COVID-19 pandemic’s uneven impact on people of color drew increased attention to inequities in health and health care, which have been documented for decades and reflect longstanding structural and systemic inequities rooted in historical and ongoing racism and discrimination. KFF’s 2023 Survey on Racism, Discrimination, and Health documents ongoing experiences with racism and discrimination, including in health care settings. While inequities in access to and use of health care contribute to disparities in health, inequities across broader social and economic factors that drive health, often referred to as social determinants of health , also play a major role. Using data to identify disparities and the factors that drive them is important for developing interventions and directing resources to address them, as well as for assessing progress toward achieving greater equity over time.
This analysis examines how people of color fare compared to White people across 64 measures of health, health care, and social determinants of health using the most recent data available from federal surveys and administrative sets as well as the 2023 KFF Survey on Racism, Discrimination, and Health , which provides unique nationally-representative measures of adults’ experiences with racism and discrimination, including in health care (see About the Data). Where possible, we present data for six groups: White, Asian, Hispanic, Black, American Indian or Alaska Native (AIAN), and Native Hawaiian or Pacific Islander (NHPI). People of Hispanic origin may be of any race, but we classify them as Hispanic for this analysis. We limit other groups to people who identify as non-Hispanic. When the same or similar measures are available in multiple datasets, we use the data that allow us to disaggregate for the largest number of racial and ethnic groups. Future analyses will reflect new federal standards that will utilize a combined race and ethnicity approach for collecting information and include a new category for people who identify as Middle Eastern or North African. Unless otherwise noted, differences described in the text are statistically significant at the p<0.05 level.
We include data for smaller population groups wherever available. Instances in which the unweighted sample size for a subgroup is less than 50 or the relative standard error is greater than 30% — which are outside of what we would typically include in analysis like this — are noted in the figures, and confidence intervals for those measures are included in the figure. Although these small sample sizes may impact the reliability, validity, and reproducibility of data, they are important to include because they point to potential underlying disparities that are hidden without disaggregated data. For some data measures throughout this brief we refer to “women” but recognize that other individuals also give birth, including some transgender men, nonbinary, and gender-nonconforming persons.
Key Takeaways
Black, Hispanic, and AIAN people fare worse than White people across the majority of examined measures of health and health care and social determinants of health (Figure 1). Black people fare better than White people for some cancer screening and incidence measures, although they have higher rates of cancer mortality. Despite worse measures of health coverage and access and social determinants of health, Hispanic people fare better than White people for some health measures, including life expectancy, some chronic diseases, and most measures of cancer incidence and mortality. These findings may, in part, reflect variation in outcomes among subgroups of Hispanic people , with better outcomes for some groups, particularly recent immigrants to the U.S. Examples of some key findings include:
- Nonelderly AIAN (19%) and Hispanic (18%) people were more than twice as likely as their White counterparts (7%) to be uninsured as of 2022.
- Among adults with any mental illness, Hispanic (40%), Black (38%), and Asian (36%) adults were less likely than White adults (56%) to receive mental health services as of 2022.
- Roughly, six in ten Hispanic (63%), AIAN (63%), and Black (58%) adults went without a flu vaccine in the 2022-2023 season, compared to less than half of White adults (49%).
- AIAN (67.9 years) and Black (72.8 years) people had a shorter life expectancy compared to White people (77.5 years) as of 2022, and AIAN, Hispanic, and Black people experienced larger declines in life expectancy than White people between 2019 and 2022; however, all racial and ethnic groups experienced a small increase in life expectancy between 2021 and 2022.
- Black (10.9 per 1,000) and AIAN (9.1 per 1,000) infants were at least two times as likely to die as White infants (4.5 per 1,000) as of 2022. Black and AIAN women also had the highest rates of pregnancy-related mortality.
- AIAN (24%) and Black (21%) children were more than three times as likely to have food insecurity as White children (6%), and Hispanic children (15%) were over twice as likely to have food insecurity than White children (6%) as of 2022.
Asian people in the aggregate fare the same or better compared to White people for most examined measures. However, they fare worse for some measures, including receipt of some routine care and screening services, and some social determinants of health, including home ownership, crowded housing, and experiences with racism. They also have higher shares of people who are noncitizens or who have limited English proficiency (LEP), which could contribute to barriers to accessing health coverage and care. Moreover, the aggregate data may mask underlying disparities among subgroups of the Asian population. Asian people also report experiences with discrimination in daily life, which is associated with adverse effects on mental health and well-being.
Data gaps largely prevent the ability to identify and understand health disparities for NHPI people. Data are insufficient or not disaggregated for NHPI people for a number of the examined measures. Among available data, NHPI people fare worse than White people for the majority of measures. There are no significant differences for some measures, but this largely reflects the smaller sample size for NHPI people in many datasets, which limits the power to detect statistically significant differences.
These data highlight the importance of continued efforts to address disparities in health and health care and show that it will be key for efforts to address factors both within and beyond the health care system. While these data provide insight into the status of disparities, ongoing data gaps and limitations hamper the ability to get a complete picture, particularly for smaller population groups and among subgroups of the broader racial and ethnic categories. As the share of people who identify as multiracial grows, it will be important to develop improved methods for understanding their experiences. How data are collected and reported by race and ethnicity is important for understanding disparities and efforts to address them. Recent changes to federal standards for collecting and reporting racial and ethnic data are intended to better represent the diversity of the population and will likely support greater disaggregation of data to identify and address disparities.
Racial Diversity Within the U.S. Today
Total population by race and ethnicity.
About four in ten people (42%) in the United States identify as people of color (Figure 2). This group includes 19% who are Hispanic, 12% who are Black, 6% who are Asian, 1% who are AIAN, less than 1% who are NHPI, and 5% who identify as another racial category, including individuals who identify as more than one race. The remaining 58% of the population are White. The share of the population who identify as people of color has been growing over time, with the largest growth occurring among those who identify as Hispanic or Asian. The racial diversity of the population is expected to continue to increase, with people of color projected to account for over half of the population by 2050. Recent changes to how data on race and ethnicity are collected and reported may also influence measures of the diversity of the population.
RACIAL DIVERSITY BY STATE
Certain areas of the country—particularly in the South, Southwest, and parts of the West—are more racially diverse than others (Figure 3). Overall, the share of the population who are people of color ranges from 10% or fewer in Maine, Vermont, and West Virginia to 50% or more of the population in California, District of Columbia, Georgia, Hawaii, Maryland, Nevada, New Mexico, and Texas. Most people of color live in the South and West. More than half (59%) of the Black population resides in the South, and nearly eight in ten Hispanic people live in the West (38%) or South (39%). About three quarters of the NHPI population (75%), almost half (49%) of the AIAN population, and 43% of the Asian population live in the Western region of the country.
TOTAL POPULATION BY AGE, RACE, AND ETHNICITY
People of color are younger compared to White people. Hispanic people are the youngest racial and ethnic group, with 31% ages 18 or younger and 56% below age 35 (Figure 4). Roughly half of Black (48%), AIAN (50%), and NHPI (51%) people are below age 35, compared to 42% of Asian people and 38% of White people.
Health Coverage, Access to and Use of Care
Racial disparities in health coverage, access, and use.
Overall, Hispanic and AIAN people fare worse compared to White people across most examined measures of health coverage, and access to and use of care (Figure 5). Black people fare worse than White people across half of these measures, and experiences for Asian people are mostly similar to or better than White people across these examined measures. NHPI people fare worse than White people across some measures, but several measures lacked sufficient data for a reliable estimate for NHPI people.
HEALTH COVERAGE
Despite gains in health coverage across racial and ethnic groups over time, nonelderly AIAN, Hispanic, NHPI, and Black people remain more likely to be uninsured compared to their White counterparts. After the Affordable Care Act (ACA), Medicaid, and Marketplace coverage expansions took effect in 2014, all racial and ethnic groups experienced large increases in coverage . Beginning in 2017, coverage gains began reversing and the number of uninsured people increased for three consecutive years. However, between 2019 and 2022, there were small gains in coverage across most racial and ethnic groups, with pandemic enrollment protections in Medicaid and enhanced ACA premium subsidies. Despite these gains over time, disparities in health coverage persist as of 2022. Nonelderly AIAN (19%) and Hispanic (18%) people have the highest uninsured rates (Figure 6). Uninsured rates for nonelderly NHPI (13%) and Black (10%) people are also higher than the rate for their White counterparts (7%). Nonelderly White (7%) and Asian (6%) people have the lowest uninsured rates.
ACCESS TO AND USE OF CARE
Most groups of nonelderly adults of color are more likely than nonelderly White adults to report not having a usual doctor or provider and going without care. Roughly one third (36%) of Hispanic adults, one quarter of AIAN (25%) and NHPI (24%) adults, and about one in five (21%) Asian adults report not having a personal health care provider compared to 17% of White adults (Figure 7). The share of Black adults who report not having a personal health care provider is the same as their White counterparts (17% for both). In addition, Hispanic (21%), NHPI (18%), AIAN (16%), and Black (14%) adults are more likely than White adults (11%) to report not seeing a doctor in the past 12 months because of cost, while Asian adults (8%) are less likely than White adults to say they went without a doctor visit due to cost. Hispanic (32%) and AIAN (31%) adults are more likely than White adults (28%) to say they went without a routine checkup in the past year, while Asian (26%), NHPI (24%), and Black (20%) adults are less likely to report going without a checkup. Hispanic and AIAN (both 45%) and Black (40%) adults are more likely than White adults (34%) to report going without a visit to a dentist or dental clinic in the past year.
In contrast to the patterns among adults, racial and ethnic differences in access to and use of care are more mixed for children. Nearly one in ten (9%) Hispanic children lack a usual source of care when sick compared to 5% of White children, but there are no significant differences for other groups for which data are available (Figure 8). Similar shares of Hispanic (7%), Asian (7%), and Black (4%) children went without a health care visit in the past year as White children (6%). However, higher shares of Asian (23%) and Black (21%) children went without a dental visit in the past year compared to White children (17%). Data are not available for NHPI children for these measures, and data for AIAN children should be interpreted with caution due to small sample sizes and large standard errors.
Among adults with any mental illness, Black, Hispanic, and Asian adults are less likely than White adults to report receiving mental health services. Roughly half (56%) of White adults with any mental illness report receiving mental health services in the past year. (Figure 9). In contrast, about four in ten (40%) Hispanic adults and just over a third of Black (38%) and Asian (36%) adults with any mental illness report receiving mental health care in the past year. Data are not available for AIAN and NHPI adults.
Experiences across racial and ethnic groups are mixed regarding receipt of recommended cancer screenings (Figure 10). Among women ages 50-74 (the age group recommended for screening prior to updates in 2024, which lowered the starting age to 40), Black people (24%) are less likely than White people (29%) to go without a recent mammogram. In contrast, AIAN (41%) and Hispanic (35%) people are more likely than White people (29%) to go without a mammogram. Among those recommended for colorectal cancer screening, Hispanic, Asian, AIAN, NHPI, and Black people are more likely than White people to not be up to date on their screening. Increases in cancer screenings, particularly for breast, colorectal, and prostate cancers, have been identified as one of the drivers of the decline in cancer mortality over the past few decades.
Racial and ethnic differences persist in flu and childhood vaccinations (Figure 11). Roughly six in ten Hispanic (63%), AIAN (63%), and Black (58%) adults went without a flu vaccine in the 2022-2023 season compared to about half (49%) of White adults. However, among children, White children (44%) are more likely than Asian (28%) and Hispanic (39%) children to go without the flu vaccine; data are not available to assess flu vaccinations among NHPI adults and children. In 2019-2020, AIAN (42%), Black (37%), and Hispanic (33%) children were more likely than White children (28%) to have not received all recommended childhood immunizations.
Health Status and Outcomes
Racial disparities in health status and outcomes.
Black and AIAN people fare worse than White people across the majority of examined measures of health status and outcomes (Figure 12). In contrast, Asian and Hispanic people fare better than White people for a majority of examined health measures. Nearly half of the examined measures did not have data available for NHPI people, limiting the ability to understand their experiences. Among available data, NHPI people fare worse than White people for more than half of the examined measures.
LIFE EXPECTANCY
AIAN and Black people have a shorter life expectancy at birth compared to White people, and AIAN, Hispanic, and Black people experienced larger declines in life expectancy than White people between 2019 and 2021. Life expectancy at birth represents the average number of years a group of infants would live if they were to experience the age-specific death rates prevailing during a specified period. Life expectancy declined by 2.7 years between 2019 and 2021, largely reflecting an increase in excess deaths due to COVID-19, which disproportionately impacted Black, Hispanic, and AIAN people. AIAN people experienced the largest life expectancy decline of 6.6 years, followed by Hispanic (4.2 years) and Black people (4.0 years), and a smaller decline of 2.4 years for White people. Asian people had the smallest decline in life expectancy of 2.1 years between 2019 and 2021. Provisional data from 2022 show that overall life expectancy increased across all racial and ethnic groups between 2021 and 2022, but racial disparities persist (Figure 13). Life expectancy is lowest for AIAN people at 67.9 years, followed by Black people at 72.8 years, while White and Hispanic people have higher life expectancies of 77.5 and 80 years, respectively, and Asian people have the highest life expectancy at 84.5 years. Life expectancies are even lower for AIAN and Black males, at 64.6 and 69.1 years, respectively. Data are not available for NHPI people.
SELF-REPORTED HEALTH STATUS
Black, Hispanic, and AIAN adults are more likely to report fair or poor health status than their White counterparts, while Asian adults are less likely to indicate fair or poor health. Nearly three in ten (29%) AIAN adults and roughly two in ten Hispanic (23%) and Black (21%) adults report fair or poor health status compared to 16% of White adults (Figure 14). One in ten Asian adults report fair or poor health status.
BIRTH RISKS AND OUTCOMES
NHPI (62.8 per 100,000), Black (39.9 per 100,000), and AIAN (32 per 100,000) women have the highest rates of pregnancy-related mortality (deaths within one year of pregnancy) between 2017-2019, while Hispanic women (11.6 per 100,000) have the lowest rate (Figure 15). More recent data for maternal mortality, which measures deaths that occur during pregnancy or within 42 days of pregnancy, shows that Black women (49.5 per 100,000) have the highest maternal mortality rate across racial and ethnic groups in 2022 (Figure 16). However, maternal mortality rates decreased significantly across most racial and ethnic groups between 2021 and 2022. Experts suggest the decline may reflect a return to pre-pandemic levels following the large increase in maternal death rates due to COVID-19 related deaths. The Dobbs decision eliminating the constitutional right to abortion could widen the already large disparities in maternal health as people of color may face disproportionate challenges accessing abortions due to state restrictions.
Black, AIAN, and NHPI women have higher shares of preterm births, low birthweight births, or births for which they received late or no prenatal care compared to White women (Figure 17). Additionally, Asian women are more likely to have low birthweight births than White women. Notably, NHPI women (22%) are four times more likely than White women (5%) to begin receiving prenatal care in the third trimester or to receive no prenatal care at all.
Teen birth rates have declined over time, but the birth rates among Black, Hispanic, AIAN, and NHPI teens are over two times higher than the rate among White teens (Figure 18). In contrast, the birth rate for Asian teens is more than four times lower than the rate for White teens.
Infants born to women of color are at higher risk for mortality compared to those born to White women. Infant mortality rates have declined over time although provisional 2022 data suggest a slight increase relative to 2021. As of 2022, Black (10.9 per 1,000) and AIAN (9.1 per 1,000) infants are at least two times as likely to die as White infants (4.5 per 1,000) (Figure 19). NHPI infants (8.5 per 1,000) are nearly twice as likely to die as White infants (4.5 per 1,000). Asian infants have the lowest mortality rate at 3.5 per 1,000 live births.
HIV AND AIDS DIAGNOSIS INDICATORS
Black, Hispanic, NHPI, and AIAN people are more likely than White people to be diagnosed with HIV or AIDS, the most advanced stage of HIV infection. In 2021, the HIV diagnosis rate for Black people is roughly eight times higher than the rate for White people, and the rate for Hispanic people is about four times higher than the rate for White people (Figure 20). AIAN and NHPI people also have higher HIV diagnosis rates compared to White people. Similar patterns are present in AIDS diagnosis rates, the most advanced stage of HIV, reflecting barriers to treatment. Black people have a roughly nine times higher rate of AIDS diagnosis compared to White people, and Hispanic, AIAN, and NHPI people also have higher rates of AIDS diagnoses. Most groups have seen decreases in HIV and AIDS diagnosis rates since 2013, although the HIV diagnosis rate has remained stable for Hispanic people and increased for AIAN and NHPI people.
Among people ages 13 and older living with diagnosed HIV infection, viral suppression rates are lower among AIAN (64%), Hispanic (64%), NHPI (63%), and Black (62%) people compared with White (72%) and Asian (70%) people (Figure 21) . Viral suppression refers to having less than 200 copies of HIV per milliliter of blood. Increasing the viral suppression rate among people with HIV is one of the key strategies of the Ending the HIV Epidemic in the U.S. initiative. Viral suppression promotes optimal health outcomes for people with HIV and also offers a preventive benefit as when someone is virally suppressed, they cannot sexually transmit HIV.
CHRONIC DISEASE AND CANCER
The prevalence of chronic disease varies across racial and ethnic groups and by type of disease. Diabetes rates for AIAN (18%), Black (16%), and Hispanic (13%) adults are all higher than the rate for White adults (11%). AIAN people (11%) are more likely to have had a heart attack or heart disease than White people (8%), while rates for Black (6%), NHPI (6%), Hispanic (4%) and Asian (3%) people are lower than White people. Black (12%) and AIAN (13%) adults have higher rates of asthma compared to their White counterparts (10%), while rates for Hispanic (8%) and Asian (5%) adults are lower, and the rate for NHPI is the same (10%). Among children, Black children (16%) are nearly twice as likely to have asthma compared to White children (9%), while Asian children (6%) have a lower asthma rate (Figure 22). Differences are not significant for other racial and ethnic groups, and data are not available for NHPI children.
AIAN, NHPI, and Black people are roughly twice as likely as White people to die from diabetes, and Black people are more likely than White people to die from heart disease (Figure 23). Hispanic people (28.3 per 100,000) also have a higher diabetes death rate compared to White people (21.3 per 100,000). In contrast, Asian people (17.2 per 100,000) are less likely than White people (21.3 per 100,000) to die from diabetes, and AIAN, Hispanic, and Asian people have lower heart disease death rates than their White counterparts.
People of color generally have lower rates of new cancer cases compared to White people, but Black people have higher incidence rates for some cancer types (Figure 24). Black people have lower rates of cancer incidence compared to White people for cancer overall, and most of the leading types of cancer examined. However, they have higher rates of new colon, and rectum, and prostate cancer. AIAN people have a higher rate of colon and rectum cancer than White people. Other groups have lower cancer incidence rates than White people across all examined cancer types.
Although Black people do not have higher cancer incidence rates than White people overall and across most types of cancer, they are more likely to die from cancer. Black people have a higher cancer death rate than White people for cancer overall and for most of the leading cancer types (Figure 25). In contrast, Hispanic, Asian and Pacific Islander, and AIAN people have lower cancer mortality rates across most cancer types compared to White people. The higher mortality rate among Black people despite similar or lower rates of incidence compared to White people could reflect a combination of factors , including more limited access to care, later stage of diagnosis, more comorbidities, and lower receipt of guideline-concordant care, which are driven by broader social and economic inequities.
COVID-19 DEATHS
AIAN, Hispanic, NHPI, and Black people have higher rates of COVID-19 deaths compared to White people. As of March 2024, provisional age-adjusted data from the Centers for Disease Control and Prevention (CDC) show that between 2020 and 2023, AIAN people are roughly two times as likely as White people to die from COVID-19, and Hispanic, NHPI and Black people are about 1.5 times as likely to die from COVID-19 (Figure 26). Asian people have lower COVID-19 death rates during this period compared to all other race and ethnicity groups.
Obesity rates vary across race and ethnicity groups. As of 2022, Black (43%), AIAN (39%), and Hispanic (37%) adults all have higher obesity rates than White adults (32%), while Asian adults (13%) have a lower obesity rate (Figure 27).
Mental Health and Drug Overdose Deaths
Overall rates of mental illness are lower for people of color compared to White people but could be underdiagnosed among people of color. About one in five Hispanic and Black (21% and 20%, respectively) adults and 17% of Asian adults report having a mental illness compared to 25% of White adults (Figure 28). Among adolescents , the share with symptoms of a past year major depressive episode were not significantly different across racial and ethnic groups, with roughly one in five White (21%) and Hispanic (20%) adolescents, 17% of Black, and about one in seven Asian (15%), and AIAN (14%) adolescents reporting symptoms. Data are not available for NHPI people. Research suggests that a lack of culturally sensitive screening tools that detect mental illness, coupled with structural barriers could contribute to underdiagnosis of mental illness among people of color.
AIAN and White people have the highest rates of deaths by suicide as of 2022. People of color have been disproportionately affected by recent increases in deaths by suicide compared with their White counterparts. As of 2022, AIAN (27.1 per 100,000) and White (17.6 per 100,000) people have the highest rates of deaths by suicide compared to all other racial and ethnic groups (Figure 29). Rates of deaths by suicide are also over three times higher among AIAN adolescents (32.9 per 100,000) than White adolescents (10.6 per 100,000). In contrast, Black, Hispanic, and Asian adolescents have lower rates of suicide deaths compared to their White peers.
Drug overdose death rates increased among AIAN, Black, Hispanic, and Asian people between 2021 and 2022. As of 2022, AIAN people continue to have the highest rates of drug overdose deaths (65.2 per 100,000 in 2022) compared with all other racial and ethnic groups. Drug overdose death rates among Black people (47.5 per 100,000) exceed rates for White people (35.6 per 100,000), reflecting larger increases among Black people in recent years (Figure 30). Hispanic (22.7 per 100,000), NHPI (18.8 per 100,000), and Asian (5.3 per 100,000) people have lower rates of drug overdose deaths than White people (35.6 per 100,000). Data on drug overdose deaths among adolescents show that while White adolescents account for the largest share of drug overdose deaths, Black and Hispanic adolescents have experienced the fastest increase in these deaths in recent years.
Social Determinants of Health
Racial disparities in social and economic factors.
Social determinants of health are the conditions in which people are born, grow, live, work, and age. They include factors like socioeconomic status, education, immigration status, language, neighborhood and physical environment, employment, and social support networks, as well as access to health care. There has been extensive research and recognition that addressing social, economic, and environmental factors that influence health is important for advancing health equity. Research also shows how racism and discrimination drive inequities across these factors and impact health and well-being.
Black, Hispanic, AIAN, and NHPI people fare worse compared to White people across most examined measures of social determinants of health (Figure 31). Experiences for Asian people are more mixed relative to White people across these examined measures. Reliable or disaggregated data for NHPI people are missing for a number of measures.
WORK STATUS, FAMILY INCOME, AND EDUCATION
Across racial and ethnic groups, most nonelderly people live in a family with a full-time worker, but Black, Hispanic, AIAN, and NHPI nonelderly people are more likely than White people to be in a family with income below poverty (Figure 32). While most people across racial and ethnic groups live in a family with a full-time worker, disparities persist. AIAN (68%), Black (73%), NHPI (77%), and Hispanic (81%) people are less likely than White people (83%) to have a full-time worker in the family. In contrast, Asian people (86%) are more likely than their White counterparts (83%) to have a full-time worker in the family. Despite the majority of people living in a family with a full-time worker, over one in five AIAN (25%) and Black (22%) people have family incomes below the federal poverty level, over twice the share as White people (10%), and rates of poverty were also higher among Hispanic (17%) and NHPI (16%) people.
Black, Hispanic, AIAN, and NHPI people have lower levels of educational attainment compared to their White counterparts. Among people ages 25 and older, over two thirds (69%) of White people have completed some post-secondary education, compared to less than half (45%) of Hispanic people, just over half of AIAN and NHPI people (both at 52%), and about six in ten Black people (58%) (Figure 33). Asian people are more likely than White people to have completed at least some post-secondary education, with 74% completing at least some college.
NET WORTH AND HOME OWNERSHIP
Black and Hispanic families have less wealth than White families. Wealth can be defined using net worth, a measure of the difference between a family’s assets and liabilities. The median net worth for White households is $285,000 compared to $44,900 for Black households and $61,600 for Hispanic households (Figure 34). Asian households have the highest median net worth of $536,000. Data are not available for AIAN and NHPI people.
People of color are less likely to own a home than White people (Figure 35). Nearly eight in ten (77%) White people own a home compared to 70% of Asian people, 62% of AIAN people, 55% of Hispanic people, and about half of Black (49%) and NHPI (48%) people.
FOOD SECURITY, HOUSING QUALITY, AND INTERNET ACCESS
Black and Hispanic adults and children are more likely to experience food insecurity compared to their White counterparts. Among adults, AIAN (18%), Black (14%), and Hispanic (12%) adults report low or very low food security compared to White adults (6%) (Figure 36). Among children, AIAN (24%), Black (21%) and Hispanic (15%) children are over twice as likely to be food insecure than White children (6%). Data are not available for NHPI adults and children.
People of color are more likely to live in crowded housing than their White counterparts (Figure 37). Among White people, 3% report living in a crowded housing arrangement, that is having more than one person per room, as defined by the American Community Survey. In contrast, almost three in ten (28%) NHPI people, roughly one in five (18%) Hispanic people, 16% AIAN people, and about one in ten Asian (12%) and Black (8%) people report living in crowded housing.
AIAN, NHPI, and Black people are less likely to have internet access than White people (Figure 38). Higher shares of AIAN (12%), and Black and NHPI people (both at 6%) say they have no internet access compared to their White counterparts (4%). In contrast, Asian people (2%) are less likely to report no internet access than White people (4%).
TRANSPORTATION
People of color are more likely to live in a household without access to a vehicle than White people (Figure 39) . About one in eight Black people (12%) and about one in ten AIAN (9%) and Asian (8%) people live in a household without a vehicle available followed by 7% of Hispanic and NHPI people. White people are the least likely to report not having access to a vehicle in the household (4%).
CITIZENSHIP AND ENGLISH PROFICIENCY
Asian, Hispanic, NHPI, and Black people include higher shares of noncitizen immigrants compared to White people. Asian and Hispanic people have the highest shares of noncitizen immigrants at 25% and 19%, respectively (Figure 40). Asian people are projected to become the largest immigrant group in the United States by 2055. Immigrants are more likely to be uninsured than citizens and face increased barriers to accessing health care.
Hispanic and Asian people are more likely to have LEP compared to White people. Almost one in three Asian (31%) and Hispanic (28%) people report speaking English less than very well compared to White people (1%)(Figure 41). Adults with LEP are more likely to report worse health status and increased barriers in accessing health care compared to English proficient adults.
EXPERIENCES WITH RACISM, DISCRIMINATION, AND UNFAIR TREATMENT
Racism is an underlying driver of health disparities, and repeated and ongoing exposure to perceived experiences of racism and discrimination can increase risks for poor health outcomes. Research has shown that exposure to racism and discrimination can lead to negative mental health outcomes and certain negative impacts on physical health, including depression, anxiety, and hypertension.
Black, AIAN, Hispanic, and Asian adults are more likely to report certain experiences with discrimination in daily life compared with their White counterparts, with the greatest frequency reported among Black and AIAN adults. A 2023 KFF survey shows that at least half of AIAN (58%), Black (54%), and Hispanic (50%) adults and about four in ten (42%) Asian adults say they experienced at least one type of discrimination in daily life in the past year (Figure 42). These experiences include receiving poorer service than others at restaurants or stores; people acting as if they are afraid of them or as if they aren’t smart; being threatened or harassed; or being criticized for speaking a language other than English. Data are not available for NHPI adults.
About one in five (18%) Black adults and roughly one in eight AIAN (12%) adults, followed by roughly one in ten Hispanic (11%), and Asian (10%) adults who received health care in the past three years report being treated unfairly or with disrespect by a health care provider because of their racial or ethnic background. These shares are higher than the 3% of White adults who report this (Figure 43). Overall, roughly three in ten (29%) AIAN adults and one in four (24%) Black adults say they were treated unfairly or with disrespect by a health care provider in the past three years for any reason compared with 14% of White adults.
About the Data
Data sources.
This chart pack is based on the KFF Survey on Racism, Discrimination, and Health and KFF analysis of a wide range of health datasets, including the 2022 American Community Survey, the 2022 Behavioral Risk Factor Surveillance System, the 2022 National Health Interview Survey, the 2022 National Survey on Drug Use and Health, and the 2022 Survey of Consumer Finances as well as from several online reports and databases including the Centers for Disease Control and Prevention (CDC) Morbidity and Mortality Weekly Report (MMWR) on vaccination coverage, the National Center for Health Statistics (NCHS) National Vital Statistics Reports, the CDC Influenza Vaccination Dashboard Flu Vaccination Coverage Webpage Report, the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP) Atlas, the United States Cancer Statistics Incidence and Mortality Web-based Report, the 2022 CDC Natality Public Use File, CDC Web-based Injury Statistics Query and Reporting System (WISQARS) database, and the CDC WONDER online database.
Methodology
Unless otherwise noted, race/ethnicity was categorized by non-Hispanic White (White), non-Hispanic Black (Black), Hispanic, non-Hispanic American Indian and Alaska Native (AIAN), non-Hispanic Asian (Asian), and non-Hispanic Native Hawaiian or Pacific Islander (NHPI). Some datasets combine Asian and NHPI race categories limiting the ability to disaggregate data for these groups. Non-Hispanic White persons were the reference group for all significance testing. All noted differences were statistically significant differences at the p<0.05. We include data for smaller population groups wherever available. Instances in which the unweighted sample size for a subgroup is less than 50 or the relative standard error is greater than 30% are noted in the figures, and confidence intervals for those measures are included in the figure.
This paper is in the following e-collection/theme issue:
Published on 25.6.2024 in Vol 8 (2024)
Leveraging Social Media to Predict COVID-19–Induced Disruptions to Mental Well-Being Among University Students: Modeling Study
Authors of this article:

Original Paper
- Vedant Das Swain 1 , BTECH, MS, PhD ;
- Jingjing Ye 2 , BS, MS ;
- Siva Karthik Ramesh 2 , BEng, MS ;
- Abhirup Mondal 2 , BTECH, MS ;
- Gregory D Abowd 3 , BS, MSc, DPhil ;
- Munmun De Choudhury 1 , BTECH, PhD
1 Khoury College of Computer Sciences, Northeastern University, Boston, MA, United States
2 College of Computing, Georgia Institute of Technology, Atlanta, GA, United States
3 College of Engineering, Northeastern University, Boston, MA, United States
Corresponding Author:
Vedant Das Swain, BTECH, MS, PhD
Khoury College of Computer Sciences
Northeastern University
#202, West Village Residence Complex H
440 Huntington Ave
Boston, MA, 02115
United States
Phone: 1 (404) 894 2000
Email: [email protected]
Background: Large-scale crisis events such as COVID-19 often have secondary impacts on individuals’ mental well-being. University students are particularly vulnerable to such impacts. Traditional survey-based methods to identify those in need of support do not scale over large populations and they do not provide timely insights. We pursue an alternative approach through social media data and machine learning. Our models aim to complement surveys and provide early, precise, and objective predictions of students disrupted by COVID-19.
Objective: This study aims to demonstrate the feasibility of language on private social media as an indicator of crisis-induced disruption to mental well-being.
Methods: We modeled 4124 Facebook posts provided by 43 undergraduate students, spanning over 2 years. We extracted temporal trends in the psycholinguistic attributes of their posts and comments. These trends were used as features to predict how COVID-19 disrupted their mental well-being.
Results: The social media–enabled model had an F1-score of 0.79, which was a 39% improvement over a model trained on the self-reported mental state of the participant. The features we used showed promise in predicting other mental states such as anxiety, depression, social, isolation, and suicidal behavior (F1-scores varied between 0.85 and 0.93). We also found that selecting the windows of time 7 months after the COVID-19–induced lockdown presented better results, therefore, paving the way for data minimization.
Conclusions: We predicted COVID-19–induced disruptions to mental well-being by developing a machine learning model that leveraged language on private social media. The language in these posts described psycholinguistic trends in students’ online behavior. These longitudinal trends helped predict mental well-being disruption better than models trained on correlated mental health questionnaires. Our work inspires further research into the potential applications of early, precise, and automatic warnings for individuals concerned about their mental health in times of crisis.
Introduction
The effects of global-scale crises on individual well-being often reach far beyond the actual incident. The onset of the COVID-19 pandemic highlighted this phenomenon. Within the first 7 months of COVID-19, we witnessed increased stress, anxiety, and depression across the world [ 1 ]. These outcomes can be explained by direct effects of the infection, for example, hospitalization [ 2 ], and indirect effects, for example, loss of family [ 3 ], anticipation of infection [ 4 ], or job loss [ 5 ]. Even the response to crises can exacerbate risks to well-being. One of the key interventions against the spread of COVID-19 was social isolation, but this recommendation also led to worsening mental health by increasing loneliness [ 6 ]. In addition, these disturbances can deteriorate an individual’s physical health by hindering his or her activity [ 7 ]. Not only do such disruptions worsen a person’s well-being but they may also discourage him or her to comply with crisis management guidelines, thereby worsening the crisis itself. During the severe acute respiratory syndrome epidemic, the anticipated distress of quarantining led to individuals deviating from recommended public health behaviors [ 8 ]. Infectious diseases are not the only kind of disasters that trigger depleted mental well-being. This phenomenon has been documented in other kinds of natural and man-made disasters [ 9 - 11 ]. Therefore, to preserve public well-being holistically, we need to enable ways to extend support and coping mechanisms to affected individuals during crises.
To prepare support for disaster well-being, it is important to identify the people whose lives were impacted as a consequence. Typically, this has been done through national-level reviews and surveys. However, meta-analyses have several inferential limitations [ 12 ], while surveys tend to have limited or biased coverage [ 13 ]. In commentary on mental health consequences after COVID-19 by Tušl et al [ 14 ], they posited that social media provides a unique opportunity to “identify and mitigate the immediate and long-term adverse psychological consequences associated with global crises.” People provide self-initiated perspectives on social media that can deepen our understanding of mental well-being states longitudinally [ 15 ]. Our paper demonstrates the efficacy of modeling individually contributed social media data to predict COVID-19–induced mental well-being disruptions.
The COVID-19 pandemic occurred at a time when activities on social media were already mainstream and so were the analyses of these activities. It represents an exemplary crisis scenario where we can leverage big data to gain a better understanding of the health impacts. Since the pandemic, we have already seen the use of social media analyses to explain population-level effects on mental well-being. Research on public social media, such as Twitter, has found an increase in psycholinguistic expressions of depression, anxiety, and stress pre- and post onset of COVID-19 [ 16 , 17 ]. Although public social media gives a strong signal of population-level sentiment, it is marred by self-presentation biases of the users posting the content, which can in turn misrepresent actual mental states [ 18 , 19 ]. Our research explores an alternative and complementary approach to provide individualized care by modeling longitudinal linguistic trends on users’ private social media contributed voluntarily. Private web-based personas (eg, on Facebook) have been noted to be less influenced by people’s impression management goals, and thus are likely to represent their actual selves, as opposed to idealized versions [ 20 - 22 ]. We specifically scoped our study to undergraduate students in the United States because these people have disproportionately suffered from worsening mental well-being challenges [ 23 ] and were more vulnerable to distress during COVID-19 [ 24 , 25 ]. We developed our machine learning model based on 4124 Facebook posts provided by 43 undergraduate students, spanning August 2019 through November 2021. We modeled and validated these data on an extensive ground truth battery that captured a variety of mental health states. We predicted self-reported mental well-being disruption with an F 1 -score of 0.79, which was a 34% improvement over predictions using correlated mental health questionnaires. In addition, to minimize data usage, we also discuss the varying data lengths required to make acceptable predictions. Through this study, we motivate future paradigms where concerned individuals can contribute private social media data to gain early insight into their risk of crisis-induced disruptions to mental health.
Recruitment
Historically, university students have been vulnerable to different mental health concerns such as anxiety, depression, and suicidality [ 23 ]. Crises such as COVID-19 have been shown to exacerbate mental health challenges among this group [ 25 ]. We recruited undergraduate students from a large urban university in the United States. All participants enrolled as students before the COVID-19–induced campus closure (March 15, 2020) and were students up until the time of recruitment. The recruitment was conducted between September and October of 2021. On joining, the participants were directed to our study portal hosted on the campus network. Participants signed in securely through their student credentials and were provided with a unique study identifier (eg, P112). The portal guided participants to complete an onboarding questionnaire and follow instructions to share their data. We provided participants with different mental health resources to access in case they were in need. Initially, we found that 87 students were interested to participate in the study. To minimize the sparsity of social media data, we retained only those students who had on average at least 1 post per month or 1 active event (such as reacting to someone else’s post). Finally, 43 students participated in the study.
Ethical Considerations
The study was approved by the Georgia Institute of Technology institutional review board (Protocol #H21051). The consent form was distributed online and potential participants were informed about the nature of data we required for the analysis and the type of analysis we would conduct. The participants were also informed of their ability to delete, or withhold, any part of their data they felt uncomfortable sharing, such as specific periods or types of data (eg, comments). All the data were deidentified using a unique study identifier and mapping to these IDs was kept on a separate server from the one that stored the data. We remunerated students with US $35 for participating in our study and providing their data.
Next, we describe the various types of data collected through the above recruitment and how they were processed for the ensuing machine learning modeling.
As a part of the data collection effort, the participants completed an extensive battery of survey questionnaires related to COVID-19 and general mental health. We used the Coronavirus Health and Impact Survey (CRISIS) [ 26 ] questionnaire to ask the participants how their health was before and after the COVID-19 pandemic. This instrument included 2 separate items to inquire about the participants’ mental health before and after COVID-19. The first item asked participants to rate their “overall Mental/Emotional health before the COVID-19 pandemic,” and the second item asked for them to rate the same but in a more recent frame, “overall Mental/Emotional health lately.” For our study, if the change in mental health scores reduced since their pre–COVID-19 ratings, they were assigned the disrupted label. Our machine learning (ML) model was designed to predict whether a user is in the disrupted class using his or her social media data. To validate our model, we used other instruments to measure participants’ psychosocial characteristics. Particularly, we used Patient Health Questionnaire-9 to measure depression [ 27 ], Suicidal Behaviors Questionnaire—Revised to measure suicidal behavior [ 2 ], Brief Resilience Scale to measure resilience [ 28 ] , and Patient-Reported Outcomes Measurement Information System to measure anxiety and social isolation [ 29 ]. Table 1 summarizes the different mental health constructs measured as a part of our data collection.
| Survey instrument | Class split | |
| Concerned | Unconcerned | |
| CRISIS —COVID Disruption | Stable: 23 | Disrupted: 20 |
| PROMIS —Anxiety | Low risk: 23 | Medium-high: 20 |
| PROMIS—Social Isolation | Low risk: 22 | Medium-high: 21 |
| PHQ-9 —Depression | No risk: 14 | Mild-severe: 29 |
| SBQ-R —Suicidal Behavior | Negative screen: 30 | Positive screen: 13 |
| BRS —Resilience | — | — |
a CRISIS: Coronavirus Health and Impact Survey.
b Target label for machine learning.
c PROMIS: Patient-Reported Outcomes Measurement Information System.
d Comparison: score used to model target as a baseline. Validation: class label used to benchmark features for machine learning.
e PHQ-9: Patient Health Questionnaire-9.
f SBQ-R: Suicidal Behaviors Questionnaire—Revised.
g BRS: Brief Resilience Scale.
h Comparison.
i Not applicable.
Social Media
After completing the survey, the participants were asked to visit their Facebook profile and download a subset of their information—posts, comments, and reactions. We neither requested nor stored any instant messages or media data (eg, images and videos). Then they submitted these data on our study portal. They were instructed to provide data only since August of 2019—1 semester before the events of COVID-19. The portal deidentified the participants’ name with their participant identifier. In addition, any other labeled name entities (such as the receiver of the comment) were also deidentified. The portal showed participants a sample of the information we stored for further analysis. These data were stored in a secure server hosted at the lead authors’ institute and for accessing these sensitive data, we followed the Principle of Least Privilege. We observed some gradual decline in posts and comments over the period, but we did not see any aberration due to the crisis itself ( Figure 1 ). On the other hand, engagement on Facebook remained relatively stable before and after the school closure. In totality, our data set included 4124 text-based posts (including status updates and comments).

Machine Learning
Feature engineering.
We built a primary feature set with the linguistic inquiry and word count (LIWC) lexicon, a validated dictionary of word categories that has been used extensively in prior research on social media [ 30 ]. This approach is inspired by other studies that have used both public and private social media data to predict mental states [ 17 , 31 ]. We referred to the selection of 50 LIWC categories by De Choudhury et al [ 32 ] to describe each post in our data set in terms of the occurrence of these 50 psycholinguistic attributes. To extract longitudinal trends in people’s behaviors and attitudes, we sought to assign psycholinguistic attributes temporally. College students use social media quite often, but not all usage involves posting content. Even though our data spanned over 2 years, a large number of days did not have any posts. Alternatively, on some days, users might even have multiple posts. About 51 days had the same user posting multiple times. On these days, we averaged the score for each feature. To account for days without posts, we used a 4-week rolling window that averaged feature values within that window. The window rolled by 1 day. The application of this rolling window technique assumes that people’s mental states gradually peak and trough and social media posts represent only an instance but not the people’s feelings across periods [ 31 ]. In this way, we obtained a time series for every user for each LIWC feature. Then, we extracted time series features such as absolute energy , kurtosis, longest strike above mean, number peaks, last location of maximum, and autocorrelation . We computed these features using the TSFRESH package for Python [ 33 ]. These time series–based features were our final set.
Model Parameters and Evaluation
Since we had more than 2 years of social media data, we decided to identify the optimal window of the above time series data to maximize the performance of our classifier. For this, we considered 2 parameters, the latest month (posts after this period were ignored) and number of months available (posts before this period were ignored). We built various models to predict mental health disruption by varying these parameters. We effectively performed a grid search varying these 2 parameters to find the best-performing combination. This document reports the best-performing models. All social media models used gradient boost [ 34 ] classifiers with 100 estimators, maximum depth of 10, and learning rate of 0.1. To evaluate these models, we used leave-one-participant-out validation—a decision stemming from the relatively smaller number of participants in our data set. As a result, our evaluation considered each participant as a test case while the classifier was trained on data from all other participants.
Baseline Model
A reasonable approach to anticipate mental health disruptions would be through survey to identify an individual’s mental state. People with anxiety and depression could find it difficult to cope with the external distress caused by a crisis event [ 25 , 35 ]. A community may consider using validated surveys to screen for these mental states [ 2 , 18 , 27 ]. However, it can be challenging to scale these surveys over large populations, such as an undergraduate campus. It can also be challenging to receive frequent responses to such surveys. Therefore, we compared the efficacy of our social media–enabled model against the self-reported baseline model. Our participants completed these surveys on recruitment. We used participant mental health scores for resilience, depression, anxiety, social isolation, and suicidal behavior to develop a baseline prediction model. We used gradient boost [ 35 ] along with a leave-one-participant-out validation method to test this model.
Validation Model
To provide external validity for our choice of features (derived from social media), we first tested the explanatory power of these features by building models to classify depression, anxiety, social isolation, and suicidal behavior. Prior research provides sufficient evidence of acceptable ML performance for similar constructs [ 36 , 37 ]. In our results, we report the performance of these models to validate that our features are meaningful to train ML models for predicting the mental well-being status of university students.
The key results from our study are summarized in Table 2 .
| Features and target | Precision | Recall | -score | |||||
| MH disruption | 0.60 | 0.59 | 0.59 | |||||
| MH disruption | 0.76 | 0.76 | 0.76 | |||||
| Anxiety | 0.92 | 0.92 | 0.92 | |||||
| Depression | 0.84 | 0.85 | 0.85 | |||||
| Social isolation | 0.88 | 0.88 | 0.89 | |||||
| Suicidal behavior | 0.92 | 0.92 | 0.93 | |||||
a Predictions with social media data performed better than the baseline to predict disruption to mental health, and we found it highly effective in predicting other psychosocial constructs.
b MH: mental health.
Social Media–Enabled ML Model
We first built baseline models using scores in self-reported survey instruments (anxiety, depression, social isolation, suicidal behavior, and resilience) to predict mental health disruptions. To compute the performance, we pooled all the predictions (1 per person) and compared it against the ground truth. We found that these predictions performed slightly better than chance ( F 1 -score=0.59). In comparison, features extracted from social media were much better at predicting disruptions ( F 1 -score=0.76). As described in Table 2 , we found that social media had a high positive predictive value (recall=0.76) and high true-positive rate (recall=0.76). Our results show that archival social media data can be provided by students to monitor their mental health during crises in a dynamic and scalable way. The 5 most important psycholinguistic trends were past tense ( Benford correlation ), certainty ( continuous strike below mean ), cognitive mechanism ( Benford correlation ), money ( Benford correlation ), and work ( Benford correlation ). Note that the prominent temporal trend in these models was the Benford correlation , which is known to identify anomalies in real data [ 38 ]. Among important linguistic attributes, past tense can indicate ruminating [ 18 ]; certainty, money, and work can all indicate changes in anxiety [ 39 ]. Figure 2 shows the top 10 features along with their contribution to the model.

Validity of Temporal Trends in Psycholinguistic Aspects of Speech
To ensure that our features are meaningful representations of users’ mental health, we developed additional models that predicted different mental health states.
Overall, we found commendable results in predicting students at risk of concerning mental health: anxiety ( F 1 -score=0.92), depression ( F 1 -score=0.98), social isolation ( F 1 -score=0.89), and suicidal behavior ( F 1 -score=0.93). Refer to Table 2 to see the performance of our validation models across other metrics. These results are comparable with results from other studies predicting mental health status with similar data sources. Saha et al [ 37 ] predicted mood instability of 23 college students with a maximum F 1 -score of 0.83. Islam et al [ 36 ] predicted depression markers in Facebook posts with a maximum F 1 -score of 0.73. Thus, extracting temporal psycholinguistic trends from personal social media can be a versatile source to approximate mental health states of individuals.
Post Hoc: Grid Search Analysis
In total, we had approximately 19 months of social media data since the campus went on lockdown because of the COVID-19 crisis. Participants reported their changes in well-being by reflecting over this entire period. As described in the Methods section, we searched through the entire time series and used variable lengths of data to understand when the signals for disruption emerge. Specifically, we were varying 2 parameters, latest month (April 2020 to October 2021) and number of months available (1-18 months). Figure 3 shows the F 1 -score for every combination of these 2 parameters. We ignored periods where we did not have sufficient data—particularly, when latest month was closer to October 2021 and number of months available were fewer. The sparsity of posts in this period could be due to the natural decline in Facebook posts over time ( Figure 1 ). Collectively, we trained 128 different versions of the ML model. We analyzed the findings from this grid search using an ordinary least squares regression to inspect whether the 2 parameters had any association with the F 1 -score. We found that neither latest month ( P =.31) nor number of months ( P =.62) had any relationship with the F 1 -score. Visually analyzing Figure 3 confirms this as increasing values on the x-axis do not indicate more accuracy. At the same time, the peak accuracy during earlier months is relatively lower. We observed this through the lack of bright spots in between April 2020 and October 2020. In comparison, after these 7 months, the data appear to have enough diversity for our ML model to identify the most predictive trends in the data.

Principal Findings
Large-scale crises can immediately lead to devastating consequences. In addition to the physical risk posed by a crisis event, individuals are likely to experience disruptions to their mental health as they try to cope with the disaster [ 1 , 6 - 11 ]. A key step in preparing for disaster well-being is to identify people whose mental well-being may have been impacted. Modeling activity on public social media already presents promise for building automatic models to infer trends in population well-being during times of crisis such as COVID-19 [ 16 , 17 ]. However, these applications are likely to ignore individual needs. Our research extends this body of work by demonstrating the feasibility of private social media, such as Facebook, as a potential indicator of disrupted well-being during crisis. We have shown that the psycholinguistic markers of the language used in personal social media can present temporal trends, which in turn help predict disruptions to mental well-being.
Through our study, we highlight the potential of personal social media to support disaster well-being. Additional training of ML models can help design applications where individuals can voluntarily choose to have their status dynamically monitored by providing a period of their social media data. As a result, health care providers can have precise information to help early and precise approximation of mental health disruptions, especially during crisis events. Nonetheless, these algorithmic applications need to be complemented with human follow-up to glean a holistic understanding of the individual’s needs. The automation provided by the ML models can help prioritize cases.
Our study also has implications for the use of private social media data in health research. Private social media could express the mental state of an individual more intimately; however, it is also likely to be more sensitive. Therefore, it is imperative to responsibly design data-sharing paradigms, especially since these data can be used to estimate an individual’s health. One possibility is to follow the paradigm in our study. First, the participants downloaded a full copy of their data. Then they submitted the data to us and our portal showed them a sample of tables we stored with deidentified information. They were able to download a full copy of the data we kept on the server as well. Through this approach, the participants were more mindful of the data provision process, and they had full transparency on what data are outside the social media platform itself. First responders and other clinical support can consider establishing similar mechanisms that ensure that enrollment is not only voluntary but also respects agency.
Limitations
Our study was aimed at demonstrating feasibility and our data included a long span of data, albeit for a small number of participants. The small number could lead to overfitting of our ML models. Given this concern, we took rigorous steps to reduce problems of overfitting, such as the use of leave-one-participant-out cross-validation, and presented pooled accuracy results (as opposed to mean accuracy). Having said that, our data set has too few participants to confidently claim that our models would work well off-the-shelf with new individuals. Instead, this paper provides evidence for larger recruitments to build more stable and generalizable models for prediction of crisis-induced mental health disruptions.
In addition, this study was conducted retrospectively in reference to the actual crisis. Social media is only one source of archival data. Future studies may consider leveraging other sources of data and, thus, provide a more holistic perspective on well-being in times of crisis. For instance, on-campus routers have been retroactively repurposed to understand student behaviors related to performance and health [ 23 , 40 , 41 ]. Combining multiple archival sources of data from the university infrastructure can help with situational preparedness.
Finally, the disruption to mental well-being was self-reported, but future studies may be able to complement these labels with complementary signals (eg, absenteeism or routine disruptions). Through these methods, researchers can mitigate the recall bias associated with self-reported labels. In fact, future studies can extend our temporal approach to identify anomalies in trends to not only identify whether an individual is vulnerable to health disruption but also pinpoint exactly when the disruptions are likely to take place.
Conclusions
The purpose of this research was to establish the feasibility of social media as a way to understand disruptions induced by a global crisis—COVID-19, among a particularly vulnerable population—college students. Our results indicate promise for larger and longer studies to understand the crisis-induced mental health disruptions. Given the retroactive nature of our approach, we stand to study a variety of crisis scenarios that may affect student populations.
Acknowledgments
We appreciate the assistance of Anjali Devakumar and Jay Modh for assisting in the development of the original institutional review board protocol. We also would like to thank Ursula Kelly and Dorian Lamis for their identifying the appropriate survey instruments for our study. This study was funded by Injury Prevention Research Center at Emory.
Data Availability
The de-identified data used in our analyses will be made available by the authors on reasonable request. The data are not publicly available because of the sensitive nature of mental health and private aspects of the social media data.
Authors' Contributions
VDS, GDA, and MDC conceived the study. VDS and AM conducted the recruitment and the data collection. VDS and SKR developed the feature engineering pipeline. VDS and JY trained all the machine learning models and analysis of findings.
Conflicts of Interest
None declared.
- Lakhan R, Agrawal A, Sharma M. Prevalence of depression, anxiety, and stress during COVID-19 pandemic. J Neurosci Rural Pract. Oct 2020;11(4):519-525. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. Dec 2001;8(4):443-454. [ CrossRef ] [ Medline ]
- Şimşir Z, Koç H, Seki T, Griffiths MD. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. Death Stud. 2022;46(3):515-523. [ CrossRef ] [ Medline ]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-920. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lin W, Shao Y, Li G, Guo Y, Zhan X. The psychological implications of COVID-19 on employee job insecurity and its consequences: the mitigating role of organization adaptive practices. J Appl Psychol. 2021;106(3):317-329. [ CrossRef ] [ Medline ]
- Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-1239. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hailey V, Fisher A, Hamer M, Fancourt D. Perceived social support and sustained physical activity during the COVID-19 pandemic. Int J Behav Med. 2023;30(5):651-662. [ FREE Full text ] [ CrossRef ] [ Medline ]
- DiGiovanni C, Conley J, Chiu D, Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur Bioterror. 2004;2(4):265-272. [ CrossRef ] [ Medline ]
- Gruebner O, Lowe SR, Sykora M, Shankardass K, Subramanian SV, Galea S. A novel surveillance approach for disaster mental health. PLoS One. 2017;12(7):e0181233. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Makwana N. Disaster and its impact on mental health: a narrative review. J Family Med Prim Care. 2019;8(10):3090-3095. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Miller K. The concept of crisis: current status and mental health implications. Hum Organ. 1963;22(3):195-201. [ CrossRef ]
- Metelli S, Chaimani A. Challenges in meta-analyses with observational studies. Evid Based Ment Health. 2020;23(2):83-87. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Laganà F, Elcheroth G, Penic S, Kleiner B, Fasel N. National minorities and their representation in social surveys: which practices make a difference? Qual Quant. 2011;47(3):1287-1314. [ CrossRef ]
- Tušl M, Thelen A, Marcus K, Peters A, Shalaeva E, Scheckel B, et al. Opportunities and challenges of using social media big data to assess mental health consequences of the COVID-19 crisis and future major events. Discov Ment Health. 2022;2(1):14. [ CrossRef ] [ Medline ]
- Gruebner O, Sykora M, Lowe SR, Shankardass K, Galea S, Subramanian SV. Big data opportunities for social behavioral and mental health research. Soc Sci Med. 2017;189:167-169. [ CrossRef ] [ Medline ]
- Guntuku SC, Sherman G, Stokes DC, Agarwal AK, Seltzer E, Merchant RM, et al. Tracking mental health and symptom mentions on Twitter during COVID-19. J Gen Intern Med. 2020;35(9):2798-2800. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Saha K, Torous J, Caine ED, De Choudhury M. Psychosocial effects of the COVID-19 pandemic: large-scale quasi-experimental study on social media. J Med Internet Res. 2020;22(11):e22600. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arntz A, Hawke LD, Bamelis L, Spinhoven P, Molendijk ML. Changes in natural language use as an indicator of psychotherapeutic change in personality disorders. Behav Res Ther. Mar 2012;50(3):191-202. [ CrossRef ] [ Medline ]
- Kivran-Swaine F, Naaman M. Network properties and social sharing of emotions in social awareness streams. 2011. Presented at: ACM 2011 Conference on Computer Supported Cooperative Work; March 19, 2011:379-382; Hangzhou, China. URL: https://dl.acm.org/doi/abs/10.1145/1958824.1958882 [ CrossRef ]
- Back MD, Stopfer JM, Vazire S, Gaddis S, Schmukle SC, Egloff B, et al. Facebook profiles reflect actual personality, not self-idealization. Psychol Sci. 2010;21(3):372-374. [ CrossRef ] [ Medline ]
- Bazarova NN, Taft JG, Choi YH, Cosley D. Managing impressions and relationships on Facebook. J Language Soc Psychol. 2012;32(2):121-141. [ CrossRef ]
- Waterloo SF, Baumgartner SE, Peter J, Valkenburg PM. Norms of online expressions of emotion: comparing Facebook, Twitter, Instagram, and WhatsApp. New Media Soc. 2018;20(5):1813-1831. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hall K, Yoo DW, Zhang W, Bin Morshed M, Das Swain V, Abowd G, et al. Supporting the contact tracing process with WiFi location data: opportunities and challenges. 2022. Presented at: Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems; Apr 27, 2022:1-14; New Orleans, LA. URL: https://dl.acm.org/doi/10.1145/3491102.3517703 [ CrossRef ]
- Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. 2010;46(1):3-10. [ CrossRef ] [ Medline ]
- Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110236. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nikolaidis A, Paksarian D, Alexander L, Derosa J, Dunn J, Nielson DM, et al. The Coronavirus Health and Impact Survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Sci Rep. 2021;11(1):8139. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194-200. [ CrossRef ] [ Medline ]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. PROMIS Cooperative Group. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63(11):1179-1194. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tausczik YR, Pennebaker JW. The psychological meaning of words: LIWC and computerized text analysis methods. J Lang Soc Psychol. 2009;29(1):24-54. [ CrossRef ]
- Das Swain V, Chen V, Mishra S, Mattingly S, Abowd G, De Choudhury M. Semantic gap in predicting mental wellbeing through passive sensing. 2022. Presented at: Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems; Apr 29 2022:1-16; New Orleans, LA. URL: https://dl.acm.org/doi/10.1145/3491102.3502037 [ CrossRef ]
- De Choudhury M, Gamon M, Counts S, Horvitz E. Predicting Depression via Social Media. In: ICWSM. 2021. Presented at: Proceedings of the international AAAI conference on web and social media (Vol. 7, No. 1); 2013:128-137; Washington, DC. URL: https://ojs.aaai.org/index.php/ICWSM/article/view/14432 [ CrossRef ]
- Christ M, Braun N, Neuffer J, Kempa-Liehr AW. Time Series FeatuRe Extraction on basis of Scalable Hypothesis tests (TSFRESH–a Python package). Neurocomputing. 2018;307:72-77. [ CrossRef ]
- Elith J, Leathwick JR, Hastie T. A working guide to boosted regression trees. J Anim Ecol. 2008;77(4):802-813. [ CrossRef ] [ Medline ]
- Sikaras C, Tsironi M, Zyga S, Panagiotou A. Anxiety, insomnia and family support in nurses, two years after the onset of the pandemic crisis. AIMS Public Health. 2023;10(2):252-267. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Islam MR, Kabir MA, Ahmed A, Kamal ARM, Wang H, Ulhaq A. Depression detection from social network data using machine learning techniques. Health Inf Sci Syst. 2018;6(1):8. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Saha K, Chan L, De Barbaro K, Abowd GD, De Choudhury M. Inferring mood instability on social media by leveraging ecological momentary assessments. 2017. Presented at: ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies; September 11, 2017:1-27; New York, NY. URL: https://dl.acm.org/doi/abs/10.1145/3130960 [ CrossRef ]
- Benford F. The law of anomalous numbers. 1938. Presented at: Proceedings of the American Philosophical Society; 1938 Mar 31:551-572; Philadelphia, PA. URL: https://www.jstor.org/stable/984802
- Low DM, Rumker L, Talkar T, Torous J, Cecchi G, Ghosh SS. Natural language processing reveals vulnerable mental health support groups and heightened health anxiety on Reddit during COVID-19: observational study. J Med Internet Res. 2020;22(10):e22635. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Das Swain V, Kwon H, Sargolzaei S, Saket B, Bin Morshed M, Tran K, et al. Leveraging WiFi network logs to infer student collocation and its relationship with academic performance. EPJ Data Sci. 2023;12(1):22. [ CrossRef ]
- Das Swain V, Xie J, Madan M, Sargolzaei S, Cai J, De Choudhury M, et al. Empirical networks for localized COVID-19 interventions using WiFi infrastructure at university campuses. Front Digit Health. 2023;5:1060828. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
| Coronavirus Health and Impact Survey |
| linguistic inquiry and word count |
| machine learning |
Edited by A Mavragani; submitted 30.08.23; peer-reviewed by V Girishan Prabhu, B Montezano, E Kawamoto; comments to author 02.12.23; revised version received 29.02.24; accepted 11.04.24; published 25.06.24.
©Vedant Das Swain, Jingjing Ye, Siva Karthik Ramesh, Abhirup Mondal, Gregory D Abowd, Munmun De Choudhury. Originally published in JMIR Formative Research (https://formative.jmir.org), 25.06.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Formative Research, is properly cited. The complete bibliographic information, a link to the original publication on https://formative.jmir.org, as well as this copyright and license information must be included.
- Share full article
Advertisement
Supported by
Guest Essay
Surgeon General: Why I’m Calling for a Warning Label on Social Media Platforms

By Vivek H. Murthy
Dr. Murthy is the surgeon general.
One of the most important lessons I learned in medical school was that in an emergency, you don’t have the luxury to wait for perfect information. You assess the available facts, you use your best judgment, and you act quickly.
The mental health crisis among young people is an emergency — and social media has emerged as an important contributor. Adolescents who spend more than three hours a day on social media face double the risk of anxiety and depression symptoms, and the average daily use in this age group, as of the summer of 2023, was 4.8 hours . Additionally, nearly half of adolescents say social media makes them feel worse about their bodies.
It is time to require a surgeon general’s warning label on social media platforms, stating that social media is associated with significant mental health harms for adolescents. A surgeon general’s warning label, which requires congressional action, would regularly remind parents and adolescents that social media has not been proved safe. Evidence from tobacco studies show that warning labels can increase awareness and change behavior. When asked if a warning from the surgeon general would prompt them to limit or monitor their children’s social media use, 76 percent of people in one recent survey of Latino parents said yes.
To be clear, a warning label would not, on its own, make social media safe for young people. The advisory I issued a year ago about social media and young people’s mental health included specific recommendations for policymakers, platforms and the public to make social media safer for kids. Such measures, which already have strong bipartisan support, remain the priority.
Legislation from Congress should shield young people from online harassment, abuse and exploitation and from exposure to extreme violence and sexual content that too often appears in algorithm-driven feeds. The measures should prevent platforms from collecting sensitive data from children and should restrict the use of features like push notifications, autoplay and infinite scroll, which prey on developing brains and contribute to excessive use.
Additionally, companies must be required to share all of their data on health effects with independent scientists and the public — currently they do not — and allow independent safety audits. While the platforms claim they are making their products safer, Americans need more than words. We need proof.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
- Skip to main content
- Keyboard shortcuts for audio player
Weekend Edition Sunday
- Latest Show
Sunday Puzzle
- Corrections
Listen to the lead story from this episode.
Politics chat: Trump and Biden's policy agendas will take center stage at the debate
by Ayesha Rascoe , Mara Liasson
Russia is finding new supporters after being isolated by the West
by Charles Maynes
State laws complicate the federal ban on gun possession for domestic abusers
by Paige Pfleger , Ayesha Rascoe
Middle East
Lebanon is home to the most refugees per capita. now it wants to send some of them back.
by Jane Arraf
Lebanon is home to the most number of refugees. Now it wants to send some of them back
Jonathan merritt's book reminds kids what makes them different makes them special.
by Jason DeRose
Republican lawmakers in Connecticut fight against a future ban on gas-powered vehicles
by Molly Ingram

Sunday Puzzle NPR hide caption
Sunday Puzzle: Summer movie blockbusters
by Will Shortz
Years before intimacy coordinators on Hollywood sets, there was the 1996 film Bound
by Isabella Gomez Sarmiento
Music Interviews
Agalisiga mackey reflects on writing songs in his native cherokee language.
by Ryan Benk , Ayesha Rascoe
Tsitsutsa Tsigesv reflects on writing songs in his native Cherokee language
How biden is getting ready for his high-stakes debate with former president trump.
by Asma Khalid
Young Black voters are feeling increasingly ambivalent about the Democratic Party
by Ayesha Rascoe
Hungary's far-right leader is set to take over rotating presidency of the EU
If ai provides false information, who takes the blame, the hottest new concert venue could be your local cemetery.
by Alison Cuddy
Health Care
'medicaid unwinding' can be dangerous for those who need opioid addiction medications.
by Stephanie Colombini
'Return to Rickwood' traces the history of the Major League's newest field
Author interviews, an incident at a grocery store set sadie dingfelder down the path of writing her book.
Searching for a song you heard between stories? We've retired music buttons on these pages. Learn more here.
- All health topics
Popular topics
- Communicable Diseases Department
- Vaccine preventable disease
- Department of Healthier Populations and Noncommunicable Diseases (HPN)
- Universal health coverage
- Research and Innovation
- Planning, Monitoring and Evaluation
- Publications
- News releases
- Media Statements
- Feature stories
- Opinion Editorials
- World Health Day 2024
- Emergency Operations
- Country Health Emergency Preparedness & IHR
- Infectious Hazard Management
- Health Emergency Information & Risk Assessment
- Public health Laboratory services
- Regional Strategic Roadmap for Health Security (2023-2027) endorsed by the Regional Committee
- Nepal Earthquake
- Thailand becomes first in SEAR with WHO classified emergency medical team
- Where we work
- Country Strategy and Support
- Regional Director
- Regional Committee
- Seventy-sixth Session of the Regional Committee
- Collaborating Centers
Regional Director’s Keynote Address at the Global Health Security 2024 (GHS2024) Conference, International Convention Centre (ICC), Sydney, Australia
- Lady Roslyn Morauta, Chair, Board of the Global Fund,
- Dr Magda Robalo, Co-Chair of the UHC2030 Steering Committee,
- Mr Joseph Simmonds-Issler, Chief of Staff and Executive Lead of Governance, Strategy and Portfolio Division, CEPI
- Dr Mika Salminen, Director General, Institute of Health and Welfare, Finland
Dignitaries, Partners, Colleagues and Friends
A very good morning to you all.
Thank you for inviting me to address you here today at this Global Health Security Conference.
Before I speak to you today about Leadership on Mental Health in Emergencies, I’d like to tell you a bit about myself.
I am from Bangladesh, a country which - as you may know - is very prone to extreme weather and climate events.
Over the past 22 years, I have worked on issues of mental health, neurodevelopmental disorders, and disability.
My career started as a licensed School Psychologist, when I worked in underprivileged communities in the USA. From there, I moved into public policy and worked as an advocate and a technical expert for public policy.
We all know that mental health issues are stigmatized in many societies. As an advocate, I worked to mainstream these matters - to break down taboos, and to start the necessary journey towards normalization. As a technical expert, I formulated public policy and advised national governments on developing legislative & technical frameworks. In my current role as WHO’s Regional Director for South-East Asia, I work on the public health policy for 11 countries and 2 billion people.
Therefore, I speak here today from a convergence of three distinct perspectives. First, as someone whose country knows all too well climate and weather emergencies. Second, as a mental health practitioner, and finally as a public policy specialist.
Emergencies create a wide range of problems experienced at the individual, family, community, and societal levels. They erode normally protective support, increase the risks of diverse problems, and tend to amplify pre-existing problems of social injustice and inequality. For example, natural disasters typically have a disproportionate impact on the poor, who may be living in relatively dangerous places.
Emergencies cause significant psychological and social suffering to the affected populations. These impacts may be acute in the short term, but they can also undermine long-term mental health and psychosocial well-being of the affected. This carries implications for peace, human rights and development.
After emergencies, people are more likely to suffer from a range of mental health problems. A minority may develop new and debilitating mental disorders, while many others may be in psychological distress. And those with pre-existing mental disorders often need even more help than before.
In the aftermath of the tragedy of an emergency situation, when we intervene to alleviate the human suffering created, we also have an opportunity to build better mental health care. The surge of aid, combined with sudden, focused attention on the mental health of the population, creates unparalleled opportunities to transform mental health care for the long term.
Our WHO South-East Asia Region represents some important case studies on this “Building Back Better” approach. It goes without saying that this approach requires leadership and guidance, to coordinate mental health and psychosocial support.
In Indonesia , in the Aceh province, there used to be a solitary mental health hospital. Yet, following the tsunami of 2004, the mental health services in were transformed in a matter of years. Aceh ‘built back better,’ and implemented a basic system of mental health care, grounded by primary health services, and supported by secondary care through district general hospitals.
In the aftermath of the very same 2004 tsunami, Sri Lanka made rapid progress in the development of basic mental health services. They extended these services beyond tsunami-affected zones, to most parts of the country. A national mental health policy has been guiding the development of decentralized and community-based care.
Building from a complete absence of mental health services in 1999, Timor-Leste now has a comprehensive community-based mental health system. They developed a National Mental Health Strategy and trained general nurses on mental health in approximately one quarter of the country’s community health centers.
As you may know, in Cox’s Bazaar, Bangladesh , there is an ongoing protracted emergency situation. A lot of special efforts and measures are being taken by the government and non-government entities to provide mental health and psychosocial support to the affected Rohingya populations in the camps.
In times of crisis, it is easy to overlook mental health concerns in favor of immediate physical needs. However, true leadership in mental health recognizes the interconnectedness of mental and physical well-being. By addressing mental health needs proactively, leaders can build stronger, more resilient communities that can withstand and recover from emergencies.
When emergencies do occur, strong and compassionate leadership is essential to guide individuals and communities towards recovery. This leadership requires empathy, understanding, and action. It involves fostering a culture of support, inclusivity, and empowerment. These leaders must communicate effectively, provide accurate information, and offer support to those in need. They should lead by example, showing vulnerability, openness, and a willingness to prioritize mental health as a priority.
The path is clear. We need to lead with compassion and empathy, and to create a culture of support and understanding. We need to prioritize mental health in emergencies. It is up to us to turn crises and emergencies, into a path for a better tomorrow.
I ask you all to join me in making that a reality. Thank you.

IMAGES
VIDEO
COMMENTS
Her more recent episodes related to her parents' marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT). Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response.
2. Significant impairment in social, occupational, or other important areas of functioning. C. The stress-related disturbance does not meet the criteria for another mental disorder and is not merely an exacerbation of a preexisting mental disorder. D. The symptoms do not represent normal bereavement.
The social workers at the health centers were contacted by a mental health social worker and a case manager nurse working at an urban health center. Both professionals were responsible for providing the health and social care workers with information about the study. ... The social workers in our study considered that the most complex ...
Grand Challenges Faculty Development Institute: Eradicate Social Isolation CSWE, Dallas, TX, Oct. 19, 2017 1 Case Studies The following case studies were included to highlight different ways that social workers can assess and intervene with issues of social isolation. These cases are free to you to use, modify, and incorporate into your teaching.
Case Study 2: Josef. Josef is 16 and lives with his mother, Dorota, who was diagnosed with Bipolar disorder seven years ago. Josef was born in England. His parents are Polish and his father sees him infrequently. This case study looks at the impact of caring for someone with a mental health problem and of being a young carer, in particular the ...
NCMHCE Sample Case Study. You are a licensed mental health counselor working in a community agency. Your client self-referred for services because "my mother won't stop bugging me for staying in bed all day. I can't help it. I am in a rut and cannot find a way out.".
Accessibility. Mental Health in Social Work: A Casebook on Diagnosis and Strengths-Based Assessment emphasizes gaining competency in the DSM-5 diagnoses of mental disorders that are commonly seen in clinical and social service settings. Using a case-based approach, the text helps you learn to understand clients holistically as you proceed with ...
Social work report: Background. Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke ...
Since 2005 the California Social Work Education Center (CalSWEC) Mental Health Program (MHP) has coor- dinated a stipend program through 17 schools of social work for almost 200 full-time 2nd-year MSW students. In return for their $18,500 stipend, students work for 1 year postgraduation in a county mental health agency or contract community ...
This case study portrays issues raised by social work students following a workshop with MHWLE as part of their graduate-level training. A workshop with MHWLE was designed for 24 social work graduate students during a mental health seminar. Following the workshop, a focus group was held.
A case study is an in-depth analysis of one individual or group. Learn more about how to write a case study, including tips and examples, and its importance in psychology. ... work, health status, family mental health history, family and social relationships, drug and alcohol history, life difficulties, goals, and coping skills and weaknesses ...
At Tracking Happiness, we're dedicated to helping others around the world overcome struggles of mental health. In 2022, we published a survey of 5,521 respondents and found: 88% of our respondents experienced mental health issues in the past year. 25% of people don't feel comfortable sharing their struggles with anyone, not even their ...
In a follow-up study of their 2019 Mental Health at Work Report, Mind Share Partners' 2021 Mental Health at Work Report, the authors offer a rare comparison of the state of mental health, stigma ...
3: 978--13-517190-5PrefaceMental Health in Social Work: A Casebook on Diagnosis and Strengths-Based Assessment is a graduate level textbook that will help students and professionals learn to understand clients holistically as they proceed with the assessm. nt and intervention process. A major purpose of Mental Health in Social Work is to ...
Mental health social workers remain a minority within a medically dominated workforce (Evans et al., 2012) meaning that when teams and services are faced with managing crises in an increasingly austere environment it might become more difficult for social workers to 'argue the importance of … a person's right to accommodation, building ...
July/August 2008 Issue. Therapist's Notebook: Case of Taylor Social Work Today Vol. 8 No. 4 P. 24. Social Work Today presents a case vignette with input from three social workers—a case presenter and two discussants who offer their insights on the presenting problem, background and family history, and the initial phase of treatment.. Case of Taylor
Social workers in the mental health and substance abuse fields will also be in high demand, with a 23% increase in employment expected by 2022. ... This is more than just about being a case ...
The LKSD school social work program is a long-standing mental health program. Staffed by itinerants and funded by the school district's general funds, the social work team provides each of LKSD's remote school communities with access to in-person supports and services at each tier of the MTSS framework. Community-based partnerships provide ...
The case studies are designed with many audiences in mind: Practitioners from a variety of fields. This includes social work, education, nursing, public health, mental health, and others. Professionals in training, including those attending graduate or undergraduate classes. The broader community.
Have at least 2 years' full-time equivalent (FTE) post-qualifying social work experience* in a mental health setting within the last 5 years, totalling a minimum of 3,360 hours. The AASW recognises that full-time employment equates to 35 hours per week, for 48 weeks per year. Must be able to articulate your understanding and provide a case ...
Will and Nikki have lived experience of mental health problems. In this video, they talk about when the influence and participation process wasn't too successful. Overcoming challenges 2. In this film, Sarah-Jane and Charlotte from Mind discuss some of the problems and challenges of lived experience work.
The quality of health and social care is now a high priority for government, professionals, and the public. This is particularly true of mental health, where explicit standards lie at the centre of current policy, demanding the development of reliable means for quality assurance. These need to allow for the multiplicity of stakeholders in ...
Lyndsey case study: Self-harm; sexual assault. Nicki and Gina case study: Poor interview / listening skills. Mr Singh case study: Poor listening skills. Ronnie case study: Social isolation, psychosis, suicide risk. Steve case study: Psychosis, drug and alcohol use. Sue case study: Confidentiality. Holly and Chris case study: Confidentiality and ...
The study of social media and mental health is complex and constantly evolving. In 2021, over 4.26 billion people worldwide classified themselves as active social media users (Social Media Fact Sheet, 2021).
This analysis examines how people of color fare compared to White people across 64 measures of health, health care, and social determinants of health using the most recent data available from ...
Warning: This episode contains mentions of bullying and suicide. A rising tide of mental health problems among teenagers has sent parents, teachers and doctors searching for answers.
Background: Large-scale crisis events such as COVID-19 often have secondary impacts on individuals' mental well-being. University students are particularly vulnerable to such impacts. Traditional survey-based methods to identify those in need of support do not scale over large populations and they do not provide timely insights. We pursue an alternative approach through social media data and ...
The advisory I issued a year ago about social media and young people's mental health included specific recommendations for policymakers, platforms and the public to make social media safer for ...
Hear the Weekend Edition Sunday program for Jun 23, 2024
- Lady Roslyn Morauta, Chair, Board of the Global Fund, - Dr Magda Robalo, Co-Chair of the UHC2030 Steering Committee, - Mr Joseph Simmonds-Issler, Chief of Staff and Executive Lead of Governance, Strategy and Portfolio Division, CEPI - Dr Mika Salminen, Director General, Institute of Health and Welfare, Finland Dignitaries, Partners, Colleagues and Friends A very good morning to you all.