
- Register-org
- Subscriptions

Recent Posts
- How an Artificial Intelligence Model Simulates Randomized Clinical Trials to Determine the Optimal Treatment for Stroke Prevention
- The Pros and Cons of Dental Veneers: Is It the Right Choice for You?
- Comparing Dental Veneers and Teeth Whitening: Which Option is Right for You?
- Exploring 8 Prominent Careers with an Associate’s Degree in Medicine
- How To Overcome Addiction and Make a Fresh Start in Life
- Entries feed
- Comments feed
- WordPress.org
- Allergy and Immunology
- Anesthesiology
- Basic Science
- Cardiothoracic Surgery
- Cardiovascular
- Complementary Medicine
- Critical Care Medicine
- Dermatology
- Emergency Medicine
- Endocrinology, Diabetes and Metabolism
- Gastroenterology and Hepatology
- Hematology, Oncology and Palliative Medicine
- Internal Medicine
- Medical Education
- Neonatal – Perinatal Medicine
- Neurosurgery
- Nursing & Midwifery & Medical Assistant
- Obstetrics & Gynecology
- Opthalmology
- Orthopaedics
- Otolaryngology
- Physical Medicine and Rehabilitation
- Plastic Reconstructive Surgery
- Pulmolory and Respiratory
- Rheumatology
Search Engine
Upper respiratory tract infections (case 48).
Published on 24/06/2015 by admin
Filed under Internal Medicine
Last modified 24/06/2015
This article have been viewed 4600 times
Chapter 56 Upper Respiratory Tract Infections (Case 48)
Patricia D. Brown MD
Case: A previously healthy 33-year-old woman presents with a 4-day history of sneezing and runny nose accompanied by nasal congestion, sore throat, and a feeling of fullness in the ears. For the past 2 days she has had a cough, which was initially dry but is now productive of yellowish sputum. She denies fever, chills, or dyspnea. She does complain of generalized myalgias and malaise. Her toddler is currently recovering from a “cold.” She states that she feels she has a cold as well and would normally not seek medical attention, but she is leaving on a business trip in the morning and would like to begin antibiotic therapy “just in case” she has a bacterial infection that could worsen while she is on her trip. Her physical exam reveals normal vital signs; she has erythema of the posterior pharynx with tonsillar enlargement but no exudates. The tympanic membranes are mildly erythematous bilaterally, with no evidence of fluid or retraction. There is no palpable lymphadenopathy in the neck, and the lung examination reveals only a few scattered expiratory wheezes bilaterally.
Differential Diagnosis
Speaking Intelligently
Infections of the respiratory tract are extremely common in both children and adults and are a leading cause of acute-care visits to the physician. Most of these are infections of the upper respiratory tract (URIs), but the possibility of community-acquired pneumonia must also be considered in patients with an illness characterized by acute cough. URIs are more common in the fall to early spring, and the vast majority are due to viruses. Adults can be expected to have two to four colds per year; parents of preschool and young school-aged children experience the highest incidence of URI.
PATIENT CARE
Clinical thinking.
• My first task is to try to differentiate URIs such as the common cold, sinusitis, acute bronchitis, pharyngitis, and OM from lower respiratory tract infections (pneumonia).
• Once I have determined that my patient has an infection confined to the upper respiratory tract (URI), the next challenge is to differentiate viral infection from bacterial infection. This differentiation is important, as viral infections will not require antibiotic therapy, although many patients—such as the woman in the case presented here—will present to the physician with an expectation for an antibiotic prescription.
• The single exception is influenza, which may be treated with antiviral therapy, although the benefits in otherwise healthy adults are very modest.
• Acute respiratory tract infections account for the majority of antibiotic prescriptions given to adults in ambulatory practices in the United States, and many of these prescriptions are given for infections that are viral in etiology.
• In addition to increasing costs and exposing patients to unnecessary risk of untoward medication effects, inappropriate antibiotic use is believed to be an important factor in increasing the prevalence of antimicrobial resistance among bacteria that cause both upper and lower respiratory tract infections, especially Streptococcus pneumoniae .
• Focus on careful elucidation of the constellation of symptoms and the temporal course of the illness.
• The constellation of symptoms is important in pharyngitis, for example, where the presence of cough makes the likelihood of viral infection much greater.
• The temporal course of illness is of critical importance in trying to differentiate VRS from ACABS. Patients with purulent nasal discharge and facial pain or tenderness (especially if unilateral), who are not improving or are worsening after 7 days of illness, are more likely to have a bacterial sinusitis.
• History of sick contacts is also important; sick contacts with URI symptoms support a diagnosis of viral infection, while an adult patient with pharyngitis who has been exposed to a person with documented streptococcal pharyngitis is at higher risk for having this pathogen as the etiology of his or her infection.
• Emphasize that the presence of purulent respiratory secretions simply reflects inflammation (the presence of polymorphonuclear neutrophils [PMNs]), which may be elicited by either viral or bacterial infection.
• In patients with acute coughing illness, the presence of pleuritic chest pain should prompt further investigation to exclude pneumonia.
• Influenza virus can cause VRS and acute pharyngitis.
Physical Examination
• Evaluate the temperature, respiratory rate, and pulse.
• Examine the upper respiratory tract, including palpation over the maxillary and frontal sinuses, and carefully examine the posterior pharynx for the presence of tonsillar enlargement, erythema, and exudates.
• Note conjunctival injection.
• Examine the tympanic membranes in adults whose complaints include ear pain or fullness, and palpate the neck for the presence of adenopathy.
• Perform careful auscultation and percussion of the lungs to exclude the presence of focal findings that would suggest pneumonia.
• In patients with severe symptoms suggestive of sinusitis, the presence of periorbital swelling, conjunctival injection, proptosis, or deficits of the extraocular movements suggests extension of infection beyond the sinuses and requires emergent evaluation.
• In a patient with severe symptoms of pharyngitis, diffuse swelling on one side of the neck or asymmetric tonsillar enlargement with medial displacement suggests a suppurative complication such as a peritonsillar abscess.
Tests for Consideration
Share this:.
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
Medicine A Competency-Based Companion With STUDENT CONSULT Onlin


KATHARINE C. DEGEORGE, MD, MS, DANIEL J. RING, MD, AND SARAH N. DALRYMPLE, MD
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2019;100(5):281-289
Patient information: See related handouts on treating common colds in adults and treating common colds in children , written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Acute upper respiratory tract infections are extremely common in adults and children, but only a few safe and effective treatments are available. Patients typically present with nasal congestion, rhinorrhea, sore throat, cough, general malaise, and/or low-grade fever. Informing patients about the self-limited nature of the common cold can help manage expectations, limit antibiotic use, and avoid over-the-counter purchases that may not help. Treatments with proven effectiveness for cold symptoms in adults include over-the-counter analgesics, zinc, nasal decongestants with or without antihistamines, and ipratropium for cough. Lower-quality evidence suggests that Lactobacillus casei may be beneficial in older adults. The only established safe and effective treatments for children are acetylcysteine, honey (for children one year and older), nasal saline irrigation, inhaled ipratropium, and topical application of ointment containing camphor, menthol, and eucalyptus oils. Over-the-counter cold medications should not be used in children younger than four years. Counseling patients about the importance of good hand hygiene is the best way to prevent transmission of cold viruses.
Acute upper respiratory tract infection (URI), also called the common cold, is the most common acute illness in the United States and the industrialized world. 1 Patients typically present with nasal congestion, rhinorrhea, sore throat, cough, general malaise, and/or low-grade fever. Symptoms are self-limited, often lasting up to 10 days. In children, the median duration is eight days in those who receive medical care, and 90% of cases resolve within 23 days. 2 Viruses such as rhinovirus are the predominant cause of acute URI; transmission occurs through contact with the nasal secretions and saliva of infected people. 3 The common cold should be distinguished from allergic rhinitis, isolated pharyngitis, acute bronchitis (which generally has a longer duration, with a mean of 18 days in adults and 12 days in children 2 , 4 ), influenza, bacterial sinusitis, and pertussis ( Table 1 ) . The primary goals of treatment are reduction of symptom duration and severity. Over-the-counter cold medications should not be used to treat children younger than four years because of lack of benefit and low but significant mortality rates associated with their use in this population. 5 , 6 Informing patients about the natural course of the common cold can help manage expectations, limit antibiotic use, 7 and avoid unnecessary over-the-counter purchases ( Table 2 ) .
Good hand hygiene is the most effective and practical way to prevent URIs in children and adults. 8 The use of hand sanitizer is more protective than hand washing and is associated with shorter duration of symptoms and fewer school absences. 9 , 10 Washing hands several times per day for at least 15 to 30 seconds can help prevent illness. 8 , 11 , 12 Regular soap is as effective as antibacterial soap. 13
Interventions with limited or no effectiveness for the prevention of the common cold include ginseng and echinacea, 14 adenovirus vaccination, 15 vitamin C or D, 16 – 19 probiotics, 20 and water gargles. 21
Treatment for Adults
Effective symptomatic treatments.
Effective treatments for symptoms of the common cold in adults are limited to inhaled ipratropium (Atrovent), over-the-counter analgesics, decongestants with or without antihistamines, and zinc ( Table 3 ) . 22 – 30 [corrected]
Analgesics . Nonsteroidal anti-inflammatory drugs—mainly ibuprofen—have been shown to reduce headache, ear pain, muscle pain, joint pain, and sneezing but do not improve cough, cold duration, or total symptom score. 27 Ibuprofen is more effective than acetaminophen for reducing fever-related discomfort. 31 Acetaminophen may provide short-term relief of rhinorrhea and nasal obstruction but has no effect on sore throat, malaise, sneezing, or cough. 22
Decongestants . Nasal decongestants (oral and intranasal) may relieve nasal congestion , 25 but there is no evidence that they reduce cough. Topical oxymetazoline, which is included in many over-the-counter intranasal decongestants, reduces the duration and severity of nasal congestion after multiple doses. 32 Patients should be warned about the risk of rhinitis when intranasal oxymetazoline is used for more than three days. 33
Antihistamines in Combination Medications . Antihistamines combined with oral decongestants and/or analgesics may provide some relief of cold symptoms, although the effect on cough is limited. 6 , 23 This benefit is most pronounced in the first two days of treatment. 34 When started on the first day of symptoms, medications containing ibuprofen and pseudoephedrine may reduce the severity of cold symptoms. 35 Antihistamine monotherapy is not effective for relieving cough. 6 , 23
Ipratropium . Inhaled ipratropium is the only medication that improves persistent cough related to URI in adults. 24 , 36 Inhaled ipratropium in combination with albuterol improves cough during the first 10 days of treatment, but there is no benefit at 20 days compared with placebo. 37
Complementary and Alternative Treatments . Several meta-analyses and a randomized controlled trial suggest that taking at least 75 mg of zinc acetate or gluconate lozenges per day relieves cough and nasal discharge more quickly when treatment is started within 24 hours of symptom onset. 28 – 30 , 38 Probiotics may have a role in the treatment of URIs. A randomized controlled trial showed that three months of daily use of a fermented dairy product containing Lactobacillus casei reduced the duration of URI symptoms by 1.5 days in older adults. 26
TREATMENTS WITH UNCERTAIN BENEFIT
Although nasal saline irrigation is effective for the treatment of chronic rhinosinusitis, only low-quality evidence supports its benefit in URIs. 39 Increased fluid intake is commonly recommended, but low-quality data suggest that it may not provide benefit and in rare cases can cause hyponatremia. 40 Good evidence is similarly lacking for acetylcysteine, 41 garlic, 42 , 43 and Chinese medicinal herbs. 44 , 45
INEFFECTIVE TREATMENTS
There are more ineffective treatments for the common cold than effective treatments, and some may even be harmful ( Table 4 ) . 6 , 16 , 19 , 34 , 46 – 54 Treatments that are not recommended include antibiotics, antivirals, most cough medications, antihistamine monotherapy, intranasal corticosteroids, steam, vitamins D and E, echinacea, and Pelargonium sidoides (African geranium).
Antibiotics . Antibiotics have no role in the treatment of the common cold. They do not reduce the severity or duration of symptoms, even when purulent rhinitis is present. 46 , 47 Antibiotic prescriptions for patients with URI are a major source of inappropriate prescribing in the outpatient setting. 55 Informing patients about the natural course of URIs and recommending appropriate treatments will improve antibiotic stewardship in the United States. 7
Antihistamine Monotherapy . When used alone, antihistamines are no more effective than placebo for the treatment of cold symptoms. 6 , 34
Antitussives and Expectorants . Antitussives and expectorants have little benefit in the treatment of cough due to the common cold. 6 , 54 Codeine and other opioid antitussives have not been studied extensively for the treatment of acute cough in adults. 6 One trial of 82 adults found that codeine was no more effective than placebo for cough; however, both groups had significant reductions in cough frequency and severity during the first two days of treatment. 48
Antivirals . Antivirals are not indicated or effective for the treatment of URIs, and they have been associated with clinical syndromes similar to the common cold. Because of their effectiveness in preventing other conditions, several antivirals (e.g., interferons, dipyridamole [Persantine], palmitate) have been studied for the treatment of URIs. However, no benefit was found, and none are licensed for this use.
Intranasal Corticosteroids . Three small trials found no evidence that intranasal corticosteroids relieve symptoms of the common cold. 50
Complementary and Alternative Treatments . Neither steam 31 , 56 nor vitamin D supplementation 19 improves symptoms of the common cold. Once symptoms have developed, vitamin C has no effect on symptom duration or severity. 16 Vitamin E can actually make symptoms worse in older adults. 53 Although echinacea was previously thought to provide benefit, high-quality studies have not shown that it reduces the duration or severity of cold symptoms. 49 , 52 , 57 , 58 Based on low-quality evidence, P. sidoides does not shorten time to resolution of cold symptoms in adults. 51
Safe and effective treatment options for symptoms of the common cold in children vary somewhat from those for adults. Nasal saline irrigation, analgesics, and time are the mainstays of treatment for URIs in children. Other effective treatments are summarized in Table 5 . 6 , 16 , 41 , 59 – 64
Analgesics . Although ibuprofen and acetaminophen reduce fever-related discomfort, ibuprofen may be more effective. 59 Alternating these medications may reduce daycare absences in children with fever.
Acetylcysteine . The mucolytic acetylcysteine may safely decrease cough after six to seven days in children two years and older. 41
Ipratropium . Intranasal ipratropium may decrease rhinorrhea but not congestion related to URIs in children five years and older. It should not be used in children younger than five years. The main adverse effects are nosebleeds, nasal dryness, and headache, although these are self-limited. 62
Nasal Saline Irrigation . One large trial found that children who use saline nasal washes six times per day have faster resolution of nasal secretions and nasal obstruction and reduced use of antipyretics, decongestants, and antibiotics. 63 This regimen also reduces school absences.
Complementary and Alternative Treatments . Application of ointment containing camphor, menthol, and eucalyptus oils on the chest and neck of children at bedtime can relieve nasal congestion and reduce nighttime cough frequency and severity, improving sleep for both the child and parents. 64 The use of menthol alone may also improve perceived nasal patency but may not help with cough. 65 Menthol is safe for use in children two years and older. The use of honey before bedtime may also reduce the frequency and severity of cough. 60 , 61 Honey should not be given to children younger than 12 months because of the risk of exposure to botulinum spores.
The use of antihistamines, either alone or in combination with a decongestant, is no more effective than placebo, and the risk of harm is significant. 6 There is insufficient evidence on the use of oral or intranasal decongestants as monotherapy for symptoms of the common cold in children. 25 Guaifenesin and other expectorants have not been studied in this population. P. sidoides may help with symptoms of acute bronchitis in children, but it has not been studied in children with the common cold. 51 Two small trials demonstrated little or no clinically significant benefit of zinc in children, even with frequent doses that were started within 24 hours of symptom onset. 66 , 67 A Cochrane review that previously reported benefit of zinc in children has been withdrawn. 68
Table 6 summarizes the evidence of ineffective treatments for children with the common cold. 6 , 18 , 31 , 46 , 47 , 49 , 69
Antibiotics . Antibiotics provide no benefit for URI symptoms in terms of severity or duration. 46 , 47 There is no role for antibiotics in the treatment of URIs in children.
Antitussives . Neither dextromethorphan nor codeine relieves cough in children with URIs. 70 , 71
Bronchodilators . In a randomized controlled trial of 59 children without asthma, oral albuterol did not improve acute cough at seven days compared with placebo, but it was associated with increased adverse effects. 72 Beta agonists have no benefit for cough in children without airflow restriction. 72 , 73
Increased Fluid Intake . Low-quality studies suggest that increasing fluid intake in children with URIs actually causes harm. 40
Intranasal and Oral Corticosteroids . Intranasal corticosteroids do not reduce symptom duration or severity in children with the common cold; oral corticosteroids have not been studied for the treatment of URIs in children. 50 , 69
Complementary and Alternative Treatments . Steam does not improve cold symptoms in children, and caution must be used to prevent burns. 31 Data do not support the use of vitamin D 18 or echinacea 49 , 74 in children with the common cold.
This article updates previous articles on this topic by Fashner, et al. , 75 and by Simasek and Blandino . 76
Data Sources: A primary search of PubMed, the Cochrane database, the TRIP database, clinical guidelines from the American College of Chest Physicians, the National Institute for Health and Clinical Excellence, DynaMed Plus, and Essential Evidence Plus was completed using the key words cold, cough, respiratory tract infection, upper respiratory infection, nasal congestion, and rhinorrhea. We also searched the U.S. Food and Drug Administration website for specific information regarding changes in recommendations for the use of cough and cold medications in children. Search dates: September 5 to November 28, 2018, and February 18 to July 17, 2019.
Centers for Disease Control and Prevention. National Center for Health Statistics. Current estimates from the National Health Interview Survey, 1996. Accessed July 17, 2019. https://www.cdc.gov/nchs/data/series/sr_10/sr10_200.pdf
Hay AD, Anderson E, Ingle S, et al. Respiratory tract infections in children in the community: prospective online inception cohort study. Ann Fam Med. 2019;17(1):14-22.
Kirkpatrick GL. The common cold. Prim Care. 1996;23(4):657-675.
Ebell MH, Lundgren J, Youngpairoj S. How long does a cough last? Comparing patients' expectations with data from a systematic review of the literature. Ann Fam Med. 2013;11(1):5-13.
U.S. Food Drug Administration. Use caution when giving cough and cold products to kids. Accessed November 21, 2018. https://www.fda.gov/Drugs/ResourcesForYou/SpecialFeatures/ucm263948.htm
Smith SM, Schroeder K, Fahey T. Over-the-counter (OTC) medications for acute cough in children and adults in community settings. Cochrane Database Syst Rev. 2014(11):CD001831.
Centers for Disease Control and Prevention. Antibiotic use in the United States, 2017: progress and opportunities. Accessed June 19, 2019. https://www.cdc.gov/antibiotic-use/stewardship-report/pdf/stewardship-report.pdf
Jefferson T, Del Mar CB, Dooley L, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev. 2011(7):CD006207.
Hübner NO, Hübner C, Wodny M, et al. Effectiveness of alcohol-based hand disinfectants in a public administration: impact on health and work performance related to acute respiratory symptoms and diarrhoea. BMC Infect Dis. 2010;10:250.
Dyer DL, Shinder A, Shinder F. Alcohol-free instant hand sanitizer reduces elementary school illness absenteeism. Fam Med. 2000;32(9):633-638.
Chamberlain AN, Halablab MA, Gould DJ, et al. Distribution of bacteria on hands and the effectiveness of brief and thorough decontamination procedures using non-medicated soap. Zentralbl Bakteriol. 1997;285(4):565-575.
Todd EC, Michaels BS, Smith D, et al. Outbreaks where food workers have been implicated in the spread of foodborne disease. Part 9. Washing and drying of hands to reduce microbial contamination. J Food Prot. 2010;73(10):1937-1955.
Aiello AE, Coulborn RM, Perez V, et al. Effect of hand hygiene on infectious disease risk in the community setting: a meta-analysis. Am J Public Health. 2008;98(8):1372-1381.
Seida JK, Durec T, Kuhle S. North American ( Panax quinquefolius ) and Asian ginseng ( Panax ginseng ) preparations for prevention of the common cold in healthy adults: a systematic review. Evid Based Complement Alternat Med. 2011;2011:282151.
Simancas-Racines D, Franco JV, Guerra CV, et al. Vaccines for the common cold. Cochrane Database Syst Rev. 2017(5):CD002190.
Hemilä H, Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev. 2013(1):CD000980.
Martineau AR, Jolliffe DA, Hooper RL, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583.
Aglipay M, Birken CS, Parkin PC, et al.; TARGet Kids! Collaboration. Effect of high-dose vs standard-dose wintertime vitamin D supplementation on viral upper respiratory tract infections in young healthy children. JAMA. 2017;318(3):245-254.
Murdoch DR, Slow S, Chambers ST, et al. Effect of vitamin D3 supplementation on upper respiratory tract infections in healthy adults: the VIDARIS randomized controlled trial. JAMA. 2012;308(13):1333-1339.
Hao Q, Dong BR, Wu T. Probiotics for preventing acute upper respiratory tract infections. Cochrane Database Syst Rev. 2015(2):CD006895.
Satomura K, Kitamura T, Kawamura T, et al.; Great Cold Investigators-I. Prevention of upper respiratory tract infections by gargling: a randomized trial. Am J Prev Med. 2005;29(4):302-307.
Li S, Yue J, Dong BR, et al. Acetaminophen (paracetamol) for the common cold in adults. Cochrane Database Syst Rev. 2013(7):CD008800.
De Sutter AI, van Driel ML, Kumar AA, et al. Oral antihistamine-decongestant-analgesic combinations for the common cold. Cochrane Database Syst Rev. 2012(2):CD004976.
Holmes PW, Barter CE, Pierce RJ. Chronic persistent cough: use of ipratropium bromide in undiagnosed cases following upper respiratory tract infection. Respir Med. 1992;86(5):425-429.
Deckx L, De Sutter AI, Guo L, et al. Nasal decongestants in monotherapy for the common cold. Cochrane Database Syst Rev. 2016(10):CD009612.
Guillemard E, Tondu F, Lacoin F, et al. Consumption of a fermented dairy product containing the probiotic Lactobacillus casei DN-114001 reduces the duration of respiratory infections in the elderly in a randomised controlled trial. Br J Nutr. 2010;103(1):58-68.
Kim SY, Chang YJ, Cho HM, et al. Non-steroidal anti-inflammatory drugs for the common cold. Cochrane Database Syst Rev. 2015(9):CD006362.
Hemilä H, Chalker E. The effectiveness of high dose zinc acetate lozenges on various common cold symptoms: a meta-analysis. BMC Fam Pract. 2015;16:24.
Hemilä H. Zinc lozenges and the common cold: a meta-analysis comparing zinc acetate and zinc gluconate, and the role of zinc dosage. JRSM Open. 2017;8(5):2054270417694291.
Science M, Johnstone J, Roth DE, et al. Zinc for the treatment of the common cold: a systematic review and meta-analysis of randomized controlled trials. CMAJ. 2012;184(10):E551-E561.
Little P, Moore M, Kelly J, et al.; PIPS Investigators. Ibuprofen, paracetamol, and steam for patients with respiratory tract infections in primary care: pragmatic randomised factorial trial. BMJ. 2013;347:f6041.
Reinecke S, Tschaikin M. Investigation of the effect of oxymetazoline on the duration of rhinitis. results of a placebo-controlled double-blind study in patients with acute rhinitis [in German]. MMW Fortschr Med. 2005;147(suppl 3):113-118.
Dykewicz MS, Fineman S, Skoner DP, et al.; American Academy of Allergy, Asthma, and Immunology. Diagnosis and management of rhinitis: complete guidelines of the Joint Task Force on Practice Parameters in Allergy, Asthma and Immunology. Ann Allergy Asthma Immunol. 1998;81(5 pt 2):478-518.
DeSutter AI, Saraswat A, van Driel ML. Antihistamines for the common cold. Cochrane Database Syst Rev. 2015(11):CD009345.
Klimek L, Schumacher H, Schütt T, et al. Factors associated with efficacy of an ibuprofen/pseudoephedrine combination drug in pharmacy customers with common cold symptoms. Int J Clin Pract. 2017;71(2):e12907.
Bolser DC. Cough suppressant and pharmacologic protussive therapy: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 suppl):238S-249S.
Zanasi A, Lecchi M, Del Forno M, et al. A randomized, placebo-controlled, double-blind trial on the management of post-infective cough by inhaled ipratropium and salbutamol administered in combination. Pulm Pharmacol Ther. 2014;29(2):224-232.
Prasad AS, Fitzgerald JT, Bao B, et al. Duration of symptoms and plasma cytokine levels in patients with the common cold treated with zinc acetate. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2000;133(4):245-252.
King D, Mitchell B, Williams CP, et al. Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database Syst Rev. 2015(4):CD006821.
Guppy MP, Mickan SM, Del Mar CB, et al. Advising patients to increase fluid intake for treating acute respiratory infections. Cochrane Database Syst Rev. 2011(2):CD004419.
Chalumeau M, Duijvestijn YC. Acetylcysteine and carbocysteine for acute upper and lower respiratory tract infections in paediatric patients without chronic broncho-pulmonary disease. Cochrane Database Syst Rev. 2013(5):CD003124.
Josling P. Preventing the common cold with a garlic supplement: a double-blind, placebo-controlled survey. Adv Ther. 2001;18(4):189-193.
Lissiman E, Bhasale AL, Cohen M. Garlic for the common cold. Cochrane Database Syst Rev. 2014(11):CD006206.
Li G, Cai L, Jiang H, et al. Compound formulas of traditional Chinese medicine for the common cold: systematic review of randomized, placebo-controlled trials. Altern Ther Health Med. 2015;21(6):48-57.
Zhang X, Wu T, Zhang J, et al. Chinese medicinal herbs for the common cold. Cochrane Database Syst Rev. 2007(1):CD004782.
Spurling GK, Del Mar CB, Dooley L, et al. Delayed antibiotic prescriptions for respiratory infections. Cochrane Database Syst Rev. 2017(9):CD004417.
Kenealy T, Arroll B. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database Syst Rev. 2013(6):CD000247.
Freestone C, Eccles R. Assessment of the antitussive efficacy of codeine in cough associated with common cold. J Pharm Pharmacol. 1997;49(10):1045-1049.
Karsch-Völk M, Barrett B, Kiefer D, et al. Echinacea for preventing and treating the common cold. Cochrane Database Syst Rev. 2014(2):CD000530.
Hayward G, Thompson MJ, Perera R, et al. Corticosteroids for the common cold. Cochrane Database Syst Rev. 2015(10):CD008116.
Timmer A, Günther J, Motschall E, et al. Pelargonium sidoides extract for treating acute respiratory tract infections. Cochrane Database Syst Rev. 2013(10):CD006323.
Barrett BP, Brown RL, Locken K, et al. Treatment of the common cold with unrefined echinacea. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2002;137(12):939-946.
Graat JM, Schouten EG, Kok FJ. Effect of daily vitamin E and multivitamin-mineral supplementation on acute respiratory tract infections in elderly persons: a randomized controlled trial. JAMA. 2002;288(6):715-721.
Malesker MA, Callahan-Lyon P, Ireland B, et al.; CHEST Expert Cough Panel. Pharmacologic and nonpharmacologic treatment for acute cough associated with the common cold. Chest. 2017;152(5):1021-1037.
Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA. 2016;315(17):1864-1873.
Singh M, Singh M, Jaiswal N, et al. Heated, humidified air for the common cold. Cochrane Database Syst Rev. 2017(8):CD001728.
Woelkart K, Linde K, Bauer R. Echinacea for preventing and treating the common cold. Planta Med. 2008;74(6):633-637.
Yale SH, Liu K. Echinacea purpurea therapy for the treatment of the common cold: a randomized, double-blind, placebo-controlled clinical trial. Arch Intern Med. 2004;164(11):1237-1241.
Wong T, Stang AS, Ganshorn H, et al. Combined and alternating paracetamol and ibuprofen therapy for febrile children. Cochrane Database Syst Rev. 2013(10):CD009572.
Paul IM, Beiler J, McMonagle A, et al. Effect of honey, dextromethorphan, and no treatment on nocturnal cough and sleep quality for coughing children and their parents. Arch Pediatr Adolesc Med. 2007;161(12):1140-1146.
Oduwole O, Udoh EE, Oyo-Ita A, et al. Honey for acute cough in children. Cochrane Database Syst Rev. 2018(4):CD007094.
AlBalawi ZH, Othman SS, Alfaleh K. Intranasal ipratropium bromide for the common cold. Cochrane Database Syst Rev. 2013(6):CD008231.
Slapak I, Skoupá J, Strnad P, et al. Efficacy of isotonic nasal wash (sea-water) in the treatment and prevention of rhinitis in children. Arch Otolaryngol Head Neck Surg. 2008;134(1):67-74.
Paul IM, Beiler JS, King TS, et al. Vapor rub, petrolatum, and no treatment for children with nocturnal cough and cold symptoms. Pediatrics. 2010;126(6):1092-1099.
Kenia P, Houghton T, Beardsmore C. Does inhaling menthol affect nasal patency or cough?. Pediatr Pulmonol. 2008;43(6):532-537.
Eby GA, Davis DR, Halcomb WW. Reduction in duration of common colds by zinc gluconate lozenges in a double-blind study. Antimicrob Agents Chemother. 1984;25(1):20-24.
Macknin ML, Piedmonte M, Calendine C, et al. Zinc gluconate lozenges for treating the common cold in children: a randomized controlled trial. JAMA. 1998;279(24):1962-1967.
Singh M, Das RR. Withdrawn: zinc for the common cold. Cochrane Database Syst Rev. 2015(4):CD001364.
McKean M, Ducharme F. Inhaled steroids for episodic viral wheeze of childhood. Cochrane Database Syst Rev. 2000(2):CD001107.
Taylor JA, Novack AH, Almquist JR, et al. Efficacy of cough suppressants in children. J Pediatr. 1993;122(5 pt 1):799-802.
Paul IM, Yoder KE, Crowell KR, et al. Effect of dextromethorphan, diphenhydramine, and placebo on nocturnal cough and sleep quality for coughing children and their parents. Pediatrics. 2004;114(1):e85-e90.
Bernard DW, Goepp JG, Duggan AK, et al. Is oral albuterol effective for acute cough in non-asthmatic children?. Acta Paediatr. 1999;88(4):465-467.
Becker LA, Hom J, Villasis-Keever M, et al. Beta2-agonists for acute cough or a clinical diagnosis of acute bronchitis. Cochrane Database Syst Rev. 2015(9):CD001726.
Taylor JA, Weber W, Standish L, et al. Efficacy and safety of echinacea in treating upper respiratory tract infections in children: a randomized controlled trial. JAMA. 2003;290(21):2824-2830.
Fashner J, Ericson K, Werner S. Treatment of the common cold in children and adults. Am Fam Physician. 2012;86(2):153-159. Accessed June 19, 2019. https://www.aafp.org/afp/2012/0715/p153.html
Simasek M, Blandino DA. Treatment of the common cold. Am Fam Physician. 2007;75(4):515-520. Accessed June 19, 2019. https://www.aafp.org/afp/2007/0215/p515.html
Continue Reading
More in AFP
More in pubmed.
Copyright © 2019 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 79, Issue 3
- Systematic review of the treatment of upper respiratory tract infection
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Tom Fahey a ,
- Nigel Stocks a ,
- Toby Thomas b
- a Division of Primary Care, University of Bristol, Canynge Hall, Whiteladies Road, Bristol BS8 2PR, UK, b United Medical and Dental Schools, London SE11 6SP, UK
- Dr Fahey. email: tom.fahey{at}bris.ac.uk
OBJECTIVES To assess the risks and benefits of antibiotic treatment in children with symptoms of upper respiratory tract infection (URTI).
DESIGN Quantitative systematic review of randomised trials that compare antibiotic treatment with placebo.
DATA SOURCES Twelve trials retrieved from a systematic search (electronic databases, contact with authors, contact with drug manufacturers, reference lists); no restriction on language.
MAIN OUTCOME MEASURES The proportion of children in whom the clinical outcome was worse or unchanged; the proportion of children who suffered complications or progression of illness; the proportion of children who had side effects.
RESULTS 1699 children were randomised in six trials that contributed to the meta-analysis. Six trials were not used in the meta-analysis because of different outcomes or incomplete data. Clinical outcome was not improved by antibiotic treatment (relative risk 1.01, 95% confidence interval (CI) 0.90 to 1.13), neither was the proportion of children suffering from complications or progression of illness (relative risk 0.71, 95% CI 0.45 to 1.12). Complications from URTI in the five trials that reported this outcome was low (range 2–15%). Antibiotic treatment was not associated with an increase in side effects compared with placebo (relative risk 0.8, 95% CI 0.54 to 1.21).
CONCLUSIONS In view of the lack of efficacy and low complication rates, antibiotic treatment of children with URTI is not supported by current evidence from randomised trials.
Antibiotic treatment did not alter clinical outcome or reduce complication rates in children with upper respiratory tract infections
Side effects were similar in antibiotic treatment and placebo groups
Complications from upper respiratory tract infections are low (2–15%)
Larger trials are needed to establish whether antibiotic treatment reduces complications in children with upper respiratory tract infections
- respiratory tract infections
- systematic review
- meta-analysis
- antibiotics
https://doi.org/10.1136/adc.79.3.225
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Upper respiratory tract infection (URTI) in children is a common illness and accounts for a substantial proportion of consultations to family doctors in the UK. The fourth National Morbidity Survey reports consultation rates of 3103 and 1002 per 10 000 years at risk in children aged 0–4 and 5–15 years, respectively. 1 The clinical syndrome of URTI comprises a variety of symptoms—most frequently cough and coryza associated with fever. The cause is usually viral, with fewer than 10% of cases caused by bacteria. 2 URTI forms a continuum with lower respiratory tract infection, which is more often associated with bacterial infection. Haemophilus influenzae and Streptococcus pneumoniae are cultured in approximately 20% of children with lower respiratory tract infection in the community. 3
Despite the predominantly viral cause, antibiotics are frequently prescribed to children with symptoms of URTI. 4 On average, 40% of children with URTI are prescribed an antibiotic, but this varies substantially between doctors, with some general practitioners prescribing to as many as 60% of children who present with URTI. 4 Such prescribing is initiated by general practitioners in the belief that antibiotics may either ameliorate symptoms, shorten the illness, or prevent further complications, such as pneumonia or acute otitis media. This belief is not based on any firm evidence from clinical trials. In fact, previous narrative reviews have suggested that for most children URTI is a self limiting condition that requires symptomatic treatment alone, and that antibiotic treatment is more likely to cause harm than benefit. 5 6
In view of the persistence of antibiotic prescribing for this condition and the uncertainty concerning the risks and benefits from treatment, we performed a quantitative systematic review of randomised controlled trials (RCTs) that compared antibiotic treatment with placebo in children with URTI managed in community settings.
INCLUSION AND EXCLUSION CRITERIA
We included studies of infants and children aged 0–12 years who were attending a family practice clinic, hospital based outpatient department, or community based health clinic, with onset of acute upper respiratory illness in the previous two weeks. The definition of URTI was a pragmatic one. We included studies of children with non-specific symptoms referable to the respiratory tract, which had not been treated in the preceding week with antibiotics. Therefore, we accorded with the definition of the International Classification of Health Problems in Primary Care (ICHPPC-2), which defines URTI as the acute inflammation of nasal or pharyngeal mucosa in the absence of other specifically defined respiratory infection. 7 The studies included were prospective RCTs where antibiotic was allocated by formal randomisation or by quasi-randomisation such as alternation, to treatment and placebo groups. Only placebo controlled trials were included, comparative studies between different classes of antibiotics were excluded. The outcomes in this review were: the proportion of children in whom clinical outcome was worse or unchanged at day 5–7; the proportion of children who suffered complications or progression of illness (defined in individual trials as either otitis media or progression of respiratory symptoms including pharyngitis, bronchitis or pneumonia); and the proportion of children who had side effects (including diarrhoea and vomiting, rashes, hyperactivity, and stomatitis).
SYSTEMATIC SEARCH
We searched medline and embase databases from 1966 and 1982, respectively, using the recommended Cochrane Collaboration search strategy, 8 using the following Medical Subject Headings ( mesh ) terms: cough, bronchitis, sputum, respiratory tract infection. The search was not restricted to the English language. We also searched for references from published research by using Science Citation Index and searching references in published studies and abstracts, particularly for those published before 1966. We conducted a search on the controlled trials register from the Cochrane Library, 9 using the search terms bronchitis, chest infection or common cold. We contacted authors of published RCTs requesting knowledge of any unpublished studies. We also wrote to all UK drug companies who manufacture antibiotics according to the British National Formulary requesting unpublished RCTs.
QUALITY ASSESSMENT AND EXTRACTION OF DATA
Each trial was read independently by two authors who then assessed the quality of each study according to the four criteria outlined in the Cochrane collaboration handbook . 10 Each criterion—selection bias, performance bias, attrition bias, and detection bias—was scored from 1 to 3, so the highest score for an individual trial was 12. Measurement of agreement between reviewers was calculated by means of the κ statistic and disagreement resolved by consensus. Data were extracted independently and where data were missing or incomplete the authors of the trial were contacted and clarification was sought.
Statistical and clinical significance was evaluated by means of estimating relative risk. 11 The magnitude of baseline risk and heterogeneity between studies was explored by means of a L’Abbe graph. 12 Pooled relative risks were estimated with 95% confidence intervals (CI) by means of a fixed effects model. 13 Relative risks and pooling of data were calculated with REVMAN 3.0 (Update Software 1996, Oxford, UK).
TRIALS FOUND AND QUALITY RATING
We found 12 randomised trials that matched the inclusion criteria of the study (tables 1 and 2 ). A further unpublished RCT from the 1950s was mentioned in a report from a conference proceeding, 14 but we were unable to secure any data from this study (unable to contact authors). Of the 12 studies, two were concerned with management of URTI in children with persistent cough (> 10 days), 15 16 and in view of the different characteristics of the children at the time of recruitment these were not included in the principal results of the meta-analysis. Both of these trials reported that antibiotic treatment has a beneficial effect on clinical outcome (table 2 ).
- View inline
Characteristics of population, diagnostic labels, and clinical features
Interventions, outcomes, and quality of trials
Of the 10 remaining RCTs, six contributed data to the meta-analysis. 17-22 The other four RCTs did not contribute data because the outcome was reported as a rate, with no actual data on the number of children assessed at the end of the trial. 23-26 Three of these four trials reported that antibiotic treatment had no effect on either relief of symptoms or subsequent complications in children (table 2 ). 23 24 26
The quality of RCTs was variable, with a range of 4 to 10 in terms of overall quality score. The κ score for the between-investigator assessment of RCT quality was 0.79 indicating a substantial agreement in quality rating of the separate RCTs.
BASELINE RISK AND DIAGNOSIS
There was a substantial difference between individual RCTs in the proportion of children in whom the clinical outcome was worse or unchanged (range in placebo arms of individual trials 5–69%) (fig 1 ). This finding highlights the heterogeneous nature of the participants in each of the studies in terms of the natural resolution from URTI. In contrast, the baseline risk for progression of illness or further complications was less variable (range 2–15%) (fig 1 ).
- Download figure
- Open in new tab
- Download powerpoint
L’Abbe plots of the proportion of children in whom (A) the clinical outcome was worse or unchanged and (B) who suffered complications or progression of illness.
EFFICACY AND SIDE EFFECTS OF ANTIBIOTIC
Clinical condition worse or unchanged at follow up (relative risk 1.01, 95% CI 0.90 to 1.13) and complications or progression of illness (relative risk 0.71, 95% CI 0.45 to 1.12) were different for antibiotic treatment and placebo groups (figs 2 and 3 ). The complications from illness were not reported at a uniform time interval in all studies, the maximum time of reporting after initial treatment was two weeks. 17 Side effects from treatment were not significantly associated with antibiotic use (relative risk 0.8, 95% CI 0.54 to 1.21) (fig 4 ).
Clinical outcome worse or unchanged in children with upper respiratory tract infection treated with antibiotic v placebo.
Subsequent complications or progression of illness in children with upper respiratory tract infection treated with antibiotic v placebo.
Side effects of treatment in children with upper respiratory tract infection treated with antibiotic v placebo.
This review demonstrates that antibiotic treatment of children with URTI does not alter the clinical outcome of the illness or prevent further complications (figs 2 and 3 ). Furthermore, the reported complication rate in the placebo arms of the RCTs included confirms that most cases of URTI resolve without further problems, with complications ranging from 2% to 15% in the four trials that examined this outcome (fig 1 ). Antibiotic treatment was not associated with a significant risk of side effects but the range of reported side effects in the antibiotic arms of included RCTs was wide (1% to 28%).
These results are consistent with previous reviews of URTI in children that questioned the role of antibiotic treatment. 5 6 Observational research in a cohort of 965 children in UK general practice 4 reported no correlation between antibiotic treatment and subsequent complication rate. The complication rate of 6% in observational research is consistent with the range of complications reported in the individual RCTs in this systematic review (fig 1 ).
There are shortcomings to this systematic review that need to be addressed. First, with the exception of Sutrisna et al , 22 all trials that contributed to the meta-analysis were small with inadequate power to detect clinically important differences between antibiotic treatment and placebo. Pooling a small number of trials each of which has not recruited many subjects makes a systematic review of such trials prone to error and potential bias. 27 This systematic review cannot rule out a small but possibly clinically important treatment effect with antibiotics. A larger fully powered study is required to determine the size and precision of any effects of antibiotics on complications of URTI or progression of disease. Of the complications that occurred, 30% were diagnosed as otitis media, 17% as pneumonia, and the rest classified as a variety of upper respiratory complications. The efficacy of antibiotic treatment may indeed be greater in a subgroup of children who have a higher baseline risk of developing complications. Further study is needed to test the hypothesis that children at higher risk of complications benefit from antibiotic treatment. Second, the range of clinical outcome at follow up in the individual RCTs (fig 1 ) shows that the clinical diagnosis of URTI is imprecise in terms of the likely resolution of illness. Further studies are needed to delineate the symptoms and signs of URTI and their prognostic significance. Third, four of 10 trials did not provide any data, principally because authors could not be contacted as the trial had been published some years ago and the published report did not contain usable data. 23-26 Only one of these trials reported a positive effect of antibiotic treatment. 25 Lastly, two trials reported a beneficial effect of antibiotic treatment but were not included in the pooled analysis in this review. 15 16 In view of the small number of patients recruited to these two RCTs and the fact that one trial was an unblinded study, assessment of efficacy in children with persistent cough requires further evaluation before antibiotic treatment can be recommended for these children.
Why do general practitioners continue to prescribe antibiotics for URTI? First, they may be too cautious when managing URTI, overestimating the likely complications, with a lowered threshold for antibiotic prescribing. Second, general practitioners may feel that parents of children with URTI expect a prescription for an antibiotic. Evidence from adults presenting with URTI refutes this assumption. 28 Patients with URTI are more satisfied when doctors explain the nature of likely course of their illness. 28 Qualitative work has demonstrated that parents of young children with acute illness were more dissatisfied when doctors provided inadequate information about the likely course of the illness. 29 Thus, like the management of acute otitis media, the management of URTI should be reassessed in terms of the natural course of the illness and the low rate of complications. 30
There are other serious consequences that need to be considered in the context of a policy of prescribing antibiotics for URTI. Observational research has shown that 24% of children are re-evaluated by a general practitioner during the same episode of URTI. 4 Antibiotic use in adults with sore throat “medicalises” a self limiting condition and increases patient expectation for reattendance and antibiotic treatment when a recurrent episode of illness occurs. 31 It seems likely that continuing to prescribe antibiotics for URTI is likely to increase parental expectations, influencing both prescribing and reattendance rates. Lastly, antibiotic use in the UK is increasing and is associated with the emergence of resistant organisms. 32 33 These considerations emphasise that antibiotic treatment is not a risk free policy 34 ; careful measurement of the likely benefit and harm of treatment is required for all cases of URTI. 35
In conclusion, URTI in children is usually a self limiting condition with complications occurring in approximately 10% of cases. Antibiotic treatment does not influence either the course of illness or the likelihood of suffering complications. In view of the adverse effects on reattendance, “medicalisation” of a self limiting condition, costs of treatment, and impact on antibiotic resistant organisms, the management of URTI should be based on a full explanation of the likely course of the illness to the child’s parents, and symptomatic treatment in the first instance.
Acknowledgments
We thank Matthias Egger, David Jewell, and Debbie Sharp for helpful comments on this paper, and Johan Darelid for clarification concerning data from his study. This study was funded by The Royal College of General Practitioners Scientific Foundation Board.
- Royal College of General Practitioners OPCS and Department of Health
- Mandell GL ,
- Bennet JE ,
- Gwaltney JM
- Turner RB ,
- Wedgwood RJ
- Robinson DS ,
- Lachant N ,
- World Organisation of National Colleges and Academies of General Practice
- Chalmers I ,
- Dickerson K ,
- Scherer R ,
- Cochrane Collaboration
- The Cochrane Collaboration
- Mulrow CD ,
- Hennekens C ,
- L’Abbe KA ,
- Detsky AS ,
- Eichenwald HF ,
- Darelid J ,
- Lofgren S ,
- Gottfarb P ,
- Traisman HS
- Lexomboon U ,
- Duangmani C ,
- Kusalasai V ,
- Sunakorn P ,
- Abbott GD ,
- Kerr MMcK ,
- Fergusson DM
- Sutrisna B ,
- Frerichs RR ,
- Reingold AL
- Townsend EH ,
- Radebaugh JF
- Townsend EH
- Wynn-Williams N
- Davey Smith G ,
- Schneider M ,
- Culpepper L ,
- Williamson I ,
- Gantley M ,
- Kinmonth AL
- Arason VA ,
- Kristinsson KG ,
- Sigurdsson JA ,
- Stefánsdóttir G ,
- Mölstad S ,
- Gudmundsson S
- Gilbert R ,
Toby Thomas died in a road traffic accident on 26 November 1996.
Read the full text or download the PDF:
Explore NYSORA knowledge base for free:

Upper respiratory tract infection
Learning objectives.
- Recognize the signs and symptoms of an upper respiratory tract infection
- Decide whether or not surgery should be postponed in children with an acute upper respiratory tract infection
- Anesthetic management of pediatric patients with upper respiratory tract infections
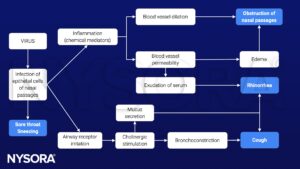
Definition and mechanisms
- An upper respiratory tract infection (URTI) is an illness caused by an acute infection, which involves the upper respiratory tract, including the nose, sinuses, pharynx, larynx, or trachea
- URTIs are characterized by cough, nasal congestion and discharge, sore throat, and sneezing
- URTIs include the common cold, epiglottitis, tonsillitis, rhinitis, pharyngitis, laryngitis, sinusitis, and otitis media
- Children experience 6 to 8 URTIs per year
- Risk of perioperative adverse respiratory complications (i.e., coughing, breath holding, laryngospasm , bronchospasm , airway obstruction, oxygen desaturation <90%, atelectasis, post-extubation stridor, pneumonia, and unanticipated tracheal intubation or reintubation) is greatest during acute infection but remains increased for 2-6 weeks after URTI
- Independent risk factors for adverse respiratory events in children with active URTI include intubation, prematurity (<37 weeks), child <1 year, history of asthma or atopy, passive smoking , airway surgery, presence of copious secretions, nasal congestion, parental confirmation “my child has a cold”, snoring, and use of an endotracheal tube (ETT)
- Airway hyperreactivity is present for up to 6-8 weeks following a URTI
Signs and symptoms
- Nasal congestion
- Sore throat
- Low-grade fever
- Facial pressure
- Hoarse voice
- Fatigue and lack of energy
- Swollen lymph nodes
- 95% of URTIs are secondary to viral causes, with rhinoviruses accounting for 30-40% of infections
Pathophysiology
- Fluids to stay hydrated
- Over-the-counter pain medications
- Antibiotics in case of bacterial origin (i.e., penicillin or amoxicillin)

Preoperative assessment
- Parents statement
- Check for the presence of respiratory and cardiovascular comorbidities
- Monitor vital signs and baseline saturation
- Anticipate perioperative adverse respiratory events
- Chest X-ray if physical examination suggests signs of lower respiratory tract involvement
- Mild URTIs: Clear runny nose, dry cough, appear healthy otherwise, clear lungs to auscultation, no fever
- Moderate URTIs: Green runny nose, mild moist cough, no wheezing or involvement of lower respiratory tract, no fever or irritability for 1-2 days
- Severe URTIs: Green runny nose, productive cough, mucopurulent secretion, nasal congestion, fever >38°C, severe sore or scratchy throat, pulmonary involvement (lower respiratory tract), wheezing, and lethargy
Anesthetic management
- Goal: Minimize secretions and avoid or limit stimulation of a potentially irritable airway
- Experienced pediatric anesthesia team
- Preoperative bronchodilators 10-30 min before surgery to reduce bronchoconstriction and perioperative respiratory events
- Humidifiers may help to clear secretions and prevent bronchial mucus plugging
- Combining β2-agonist (e.g., salbutamol) with inhaled corticosteroids is more effective in minimizing bronchoconstriction due to intubation compared to inhaled β2-agonist alone
- Avoid tracheal intubation, particularly in children <5 years
- A laryngeal mask airway or facemask is preferred
- IV lidocaine may be helpful in reducing the laryngospasm reflex
- Less adverse respiratory events with propofol than sevoflurane as induction agent
- Maintenance of anesthesia: Intravenous or inhalation techniques, anesthesia should be deep enough
- Suction airway only under deep anesthesia
Keep in mind
- Children with active and recent URTI are at increased risk of perioperative respiratory complications
- Assessment of suitability of any child with URTI symptoms for surgery includes the child’s age and presenting symptoms, frequency of URTIs, urgency and type of procedure, and presence of comorbidities
- The decision to postpone or proceed with surgery for children with URTI should be made on an individual basis by considering the presence of identified risk factors and the anesthesiologist’s experience
Suggested reading
- Lema GF, Berhe YW, Gebrezgi AH, Getu AA. Evidence-based perioperative management of a child with upper respiratory tract infections (URTIs) undergoing elective surgery; A systematic review. International Journal of Surgery Open. 2018;12:17-24.
- Regli A, Becke K, von Ungern-Sternberg BS. An update on the perioperative management of children with upper respiratory tract infections. Curr Opin Anaesthesiol. 2017;30(3):362-367.
- Tait AR, Malviya S. Anesthesia for the child with an upper respiratory tract infection: still a dilemma?. Anesth Analg. 2005;100(1):59-65.
We would love to hear from you. If you should detect any errors, email us [email protected]

- Case report
- Open access
- Published: 12 September 2018
A 2-year-old girl with chronic crackles after respiratory syncytial virus infection: a case report
- Katarzyna Woicka-Kolejwa 1 ,
- Henryk Mazurek 2 &
- Iwona Stelmach 1 , 3
Journal of Medical Case Reports volume 12 , Article number: 258 ( 2018 ) Cite this article
5328 Accesses
Metrics details
Respiratory syncytial virus is the most common cause of lower respiratory tract infections in infants and young children. While the majority of infants display only mild upper respiratory tract infection or occasionally otitis media, around one-third will develop an infection of the lower respiratory tract, usually bronchiolitis. There is now convincing evidence from a number of cohorts that respiratory syncytial virus is a significant, independent risk factor for later wheezing, at least within the first decade of life. The wide variation in response to respiratory syncytial virus infection suggests that susceptibility and disease are influenced by multiple host-intrinsic factors.
Case presentation
A 2-year-old white girl presented to our Pediatric Allergy Clinic with recurrent crackles in addition to cough, fevers, and labored breathing since her first respiratory syncytial virus infection at the age of 7 months. She had been under the care of pulmonologists, who suspected childhood interstitial lung disease. She was hospitalized eight times due to exacerbation of symptoms and prescribed systemic and inhaled steroids, short-acting β2-mimetics, and antileukotriene. There was no short-term clinical improvement at that time between hospitalizations.
During her hospital stay at the Pneumonology and Cystic Fibrosis Department in Rabka a bronchoscopy with bronchoalveolar lavage was performed. Laboratory bacteriological tests found high colony count of Moraxella catarrhalis (β-lactamase positive), sensitive to amoxicillin-clavulanate, in bronchial secretions and swabs from her nose. After this, infections were treated with antibiotics; she remained in good condition without symptoms. Crackles and wheezing recurred only during symptoms of infections. Therefore, we hypothesize that respiratory syncytial virus infection at an early age might cause severe damage of the lung epithelium and prolonged clinical symptoms, mainly crackles and wheezing, each time the child has a respiratory infection.
Conclusions
This case illustrates the importance of respiratory syncytial virus infection in an immunocompetent child. Pediatricians need to have a high index of suspicion and knowledge of recurrent symptoms associated with severe damage of the lung epithelium to establish the correct diagnosis.
Peer Review reports
Respiratory syncytial virus (RSV) is the most common cause of lower respiratory tract infections (LRTIs) in infants and young children [ 1 ]. By the age of 2 years, over 80% of children have experienced at least one RSV infection, two-thirds of these occurring in the first year of life. Strong epidemiologic evidence suggests that early-life infections with this virus predispose to chronic respiratory dysfunction and even asthma, possibly related to persistence of the virus itself or to its effects on lung development [ 2 ]. While the majority of infants display only mild upper respiratory tract infection (URTI) or occasionally otitis media, around one-third will develop an LRTI, usually bronchiolitis. This is caused by an infiltration of inflammatory cells into the air spaces, mucus hyper-production, shedding of necrotic airway epithelial cells, and edema of the airway wall. These processes lead to a narrowing of the airway lumen, airflow obstruction, overinflation, and impaired gas exchange. In more severe RSV disease, crackles and wheeze occur with labored breathing, tachypnea, and hypoxia; a small percentage of cases require intensive care and may result in death [ 3 ]. There is now convincing evidence from a number of cohorts that RSV is a significant, independent risk factor for later wheezing, at least within the first decade of life. The wide variation in response to RSV infection suggests that susceptibility and disease are influenced by multiple host-intrinsic factors.
We present a case of 2-year-old white girl with chronic crackles admitted to our Pediatric and Allergy Clinic. The pregnancy was unremarkable and after birth the child was healthy until the seventh month of life, when she developed RSV infection. From then on she had a LRTI every month treated with antibiotics, mainly macrolides for presumed bacterial pneumonia; symptoms persisted daily. She had been under the care of pulmonologists from a different department, who suspected childhood interstitial lung disease (chILD) and prescribed systemic and inhaled steroids, short-acting β2-mimetics, and antileukotriene. This treatment, however, did not lead to any clinical improvement; symptoms of crackles were present at all times. She was hospitalized eight times due to exacerbation of symptoms such as dyspnea, cough, and persistent crackles during physical examination. At the age of 11 months she had high resolution computed tomography (HRCT) which revealed lung areas of uneven aeration in the middle lobe of her right lung and small areas of densities which indicated postinflammatory changes. Due to suspected Pneumocystis jirovecii ( carinii ) infection, she was unsuccessfully treated with sulfamethoxazole and trimethoprim.
She was admitted to our clinic at 23 months of age with intense cough, dyspnea, and chronic crackles. A chest X-ray showed areas of density due to parenchymal and interstitial inflammatory changes. Autoimmune disease and atypical inflammatory infections ( Mycoplasma pneumoniae, Chlamydia pneumoniae, and Bordetella pertussis ) were excluded by use of a multiplex assay; immunodeficiency was also excluded. An echocardiogram revealed no abnormalities. Next, she was referred to the Pneumonology and Cystic Fibrosis Department in Rabka for bronchoscopy with bronchoalveolar lavage (BAL). The result showed: copious purulent secretions in her lower throat; mucosal edema of the larynx (Fig. 1a ), trachea, and bronchial tree; and retention of the purulent mucus in bronchi (Fig. 1b ) with normal movement of bronchial cilia (high frequency video microscopy). Microbiological testing with growth on blood/chocolate agar isolated high colony count of Moraxella catarrhalis in the BAL fluid. It was beta-lactamase producer sensitive to amoxicillin-clavulanate. The BAL also showed epithelial cells, macrophages, and neutrophils under high power field. She was administered amoxicillin-clavulanate for 14 days with good clinical improvement in respiratory rate, labored breathing, and cough and she was discharged. She was observed for 2 months after discharge from the hospital and showed no signs of recurrence. Then, she had a few more respiratory tract infections (usually every other month) treated with antibiotics (crackles were present at each time during infection); between infections she remained healthy, without any crackles or wheezing.
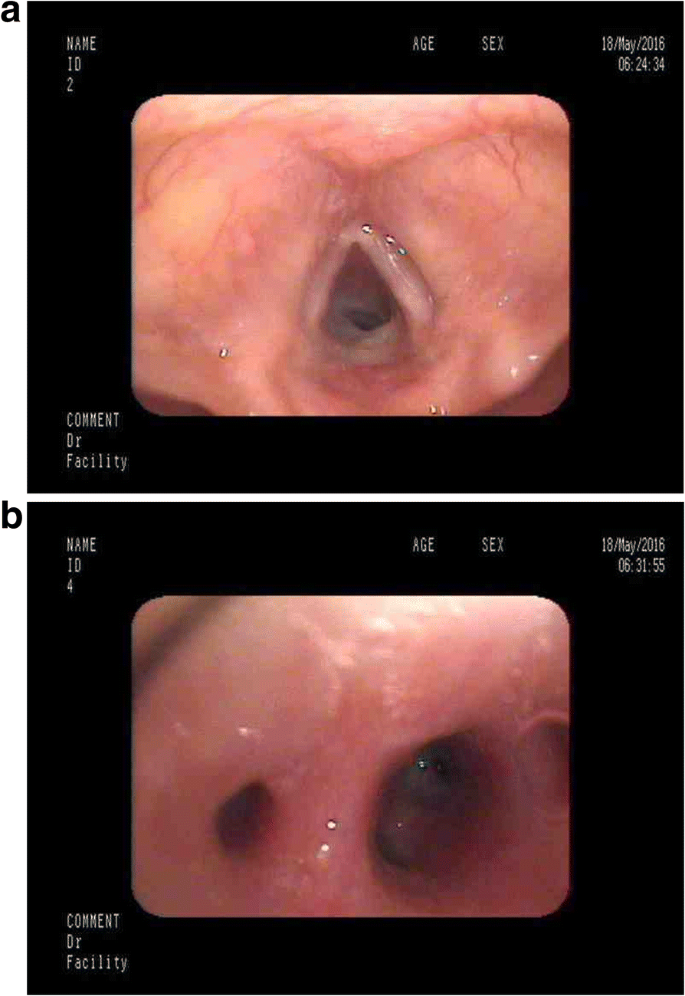
a Bronchoscopy image – mucosal edema of the larynx. b Bronchoscopy image – purulent mucus in bronchi
This case illustrates RSV pneumonia in an immunocompetent child. The chronic character of symptoms, persistent crackles, and the lack of improvement after treatment with systemic and inhaled steroids, short-acting β2-mimetics, and antileukotriene at first suggested interstitial lung disease. Interstitial lung disease is a rare condition in childhood, with an estimated prevalence of 0.36/100,000; therefore, pediatricians may be less familiar with interstitial lung disease [ 4 ]. To diagnose chILD at least three of four criteria should be fulfilled [ 5 , 6 ]. Our patient does not meet the criteria for chILD as the symptoms were not present since birth and there was no hypoxia. In addition, computed tomography (CT) findings did not show signs such as septal thickening, ground glass opacification, geographic hyperlucency or mosaic attenuation, lung cysts or nodules, and consolidation suggestive of chILD. What is more, CT scans did not suggest bronchiolitis obliterans, neuroendocrine cell hyperplasia of infancy, or other airway pathology. Later, a bronchoscopy with BAL revealed M. catarrhalis infection. M. catarrhalis is a common commensal as well as a pathogen of the human respiratory tract. In our patient, after this infection was treated with an antibiotic, she remained in good condition without symptoms; crackles and wheezing recurred only during infection. Pulmonary function testing was not done due to her young age. We hypothesize that RSV infection at an early age might cause severe damage of the lung epithelium and prolonged clinical symptoms, mainly crackles and wheezing, each time the child has respiratory infection. In this case, the main prophylactic of recurrent clinical symptoms is to avoid exogenous infections by additional prophylactic vaccination. Symptoms resolution after treatment with antibiotics of this and later infections suggest that initial RSV infection in early childhood has a role.
This case illustrates the importance of RSV infection in an immunocompetent child. Pediatricians need to have a high index of suspicion and knowledge of symptoms associated with severe damage of the lung epithelium to establish the correct diagnosis.
Abbreviations
Bronchoalveolar lavage
Childhood interstitial lung disease
Computed tomography
High resolution computed tomography
Lower respiratory tract infection
Respiratory syncytial virus
Upper respiratory tract infection
Piedimonte G, Walton C, Samsell L. Vertical Transmission of Respiratory Syncytial Virus Modulates Pre- and Postnatal Innervation and Reactivity of Rat Airways. PLoS One. 2013;8(4):e61309. Published online 2013 Apr 18
Article PubMed PubMed Central CAS Google Scholar
High M, Cho HY, Marzec J. Determinants of host susceptibility to murine respiratory syncytial virus (RSV) disease identify a role for the innate immunity scavenger receptor MARCO gene in human infants. EBioMedicine. 2016;11:73–84. Published online 2016 Aug 6
Article PubMed PubMed Central Google Scholar
Lambert L, Sagfors A, Openshaw P, Culley F. Immunity to RSV in Early-Life. Front Immunol. 2014;5:466. Published online 2014 Sep 29
Hines EJ, Walsh M, Armes JE, Douglas T, Chawla J. Interstitial lung disease in infancy: a general approach. J Paediatr Child Health. 2016;52(4):370–6.
Article PubMed Google Scholar
Spagnolo P, Bush A. Interstitial Lung Disease in Children Younger Than 2 Years. Pediatrics. 2016;137(6) https://doi.org/10.1542/peds.2015-2725 .
Fuger M, Clair MP, Ibrahim NE, L'Excellent S, Nizery L, O'Neill C, Tabone L, Truffinet O, Yakovleff C, de Blic J. Chronic interstitial lung disease in children: diagnostic approach and management. Archives De Pediatrie. 2016;23(5):525–53.
Article PubMed CAS Google Scholar
Download references
Self-funded.
Availability of data and materials
Please contact author for data requests. The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Department of Pediatrics and Allergy, Medical University of Lodz, Lodz, Poland
Katarzyna Woicka-Kolejwa & Iwona Stelmach
Department of Pneumonology and Cystic Fibrosis, Institute of Tuberculosis and Lung Disorders, Rabka–Zdrój, Poland
Henryk Mazurek
Copernicus Memorial Hospital, Korczak Paediatric Center, Piłsudskiego 71 Str, 90-329, Lodz, Poland
Iwona Stelmach
You can also search for this author in PubMed Google Scholar
Contributions
IS concept of the study; KW-K manuscript writing, completing data; HM critical review and final accept. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Iwona Stelmach .
Ethics declarations
Ethics approval and consent to participate.
The consent from the caregivers was obtained.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian(s) for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Woicka-Kolejwa, K., Mazurek, H. & Stelmach, I. A 2-year-old girl with chronic crackles after respiratory syncytial virus infection: a case report. J Med Case Reports 12 , 258 (2018). https://doi.org/10.1186/s13256-018-1797-6
Download citation
Received : 09 September 2017
Accepted : 09 August 2018
Published : 12 September 2018
DOI : https://doi.org/10.1186/s13256-018-1797-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Interstitial lung disease (ILD)
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 126: Upper Respiratory Tract Infections
Christopher R. Frei; Bradi L. Frei
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Chapter summary from the pharmacotherapy handbook, key concepts, preclass activity, introduction, acute otitis media.
- PATIENT CARE PROCESS
- ACUTE BACTERIAL RHINOSINUSITIS
- ACUTE PHARYNGITIS
- POSTCLASS ACTIVITY
- ABBREVIATIONS
- LEARNING OBJECTIVES
- SELF-ASSESSMENT QUESTIONS
- Full Chapter
- Supplementary Content
For the Chapter in the Schwinghammer, Handbook (not Wells Handbook anymore) please go to Chapter 45, Respiratory Tract Infections, Upper .
Create a summary table of first-line drug treatment options, including recommended treatment if the patient has a penicillin allergy, for the upper respiratory tract infections discussed in this chapter: acute otitis media, rhinosinusitis, and pharyngitis. The table should include columns for type of upper respiratory tract infection, first-line treatment, dose, route, and duration of treatment. The table should also include important counseling points and adverse effects.
More patients present to physicians’ offices and emergency departments for upper respiratory tract infections than any other infectious disease. There are over 25 million office visits per year for acute upper respiratory tract infections. 1 Otitis media, rhinosinusitis, and pharyngitis are the three most common upper respiratory tract infections. Because they are so common, community and emergency healthcare workers must be familiar with the diagnosis, assessment, and management of patients with these infections. Furthermore, antibiotics used for the treatment of upper respiratory tract infections serve as catalysts for the emergence and spread of antibiotic resistance, thereby making prudent antibiotic use critically important.
The term otitis media comes from the Latin oto - for “ear,” itis for “inflammation,” and medi - for “middle”; otitis media, then, is an inflammation of the middle ear. There are three subtypes of otitis media: acute otitis media, otitis media with effusion, and chronic otitis media. Acute otitis media is the subtype with the greatest role for antibiotics and will be discussed in detail.
Epidemiology
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Bird flu: US confirms...
Bird flu: US confirms first case with respiratory symptoms
- Related content
- Peer review
- Mun-Keat Looi
The US has recorded the first person with H5N1 flu to have respiratory symptoms, in what is thought to be the third human case in an ongoing outbreak among dairy farms. All previous confirmed cases of the infection in people had symptoms of conjunctivitis but no respiratory problems.
“The patient reported upper respiratory tract symptoms, including cough without fever, and eye discomfort with watery discharge,” said the US Centers for Disease Control and Prevention (CDC). 1 “The patient was given antiviral treatment with oseltamivir, is isolating at home, and their symptoms are resolving.”
The CDC added that household contacts of the patient have not developed symptoms but are being monitored for illness and have also been offered oseltamivir. “No other workers at the same farm have reported symptoms, and all staff are being monitored. There is no indication of person-to-person spread of A(H5N1) viruses at this time.”
The new case, confirmed by Michigan state officials on Thursday 30 May, 2 came after another human infection from cows on a different Michigan farm last week. 3
Natasha Bagdasarian, chief medical executive at the Michigan Department of Health and Human Services, said in a statement, “With the first case in Michigan, eye symptoms occurred after a direct splash of infected milk to the eye. With this case, respiratory symptoms occurred after direct exposure to an infected cow.” She added that “neither individual was wearing full personal protective equipment (PPE).”
Bagdasarian continued: “This tells us that direct exposure to infected livestock poses a risk to humans and that PPE is an important tool in preventing spread among individuals who work on dairy and poultry farms. We have not seen signs of sustained human-to-human transmission, and the current health risk to the general public remains low.”
Nevertheless, the development has worried experts, given that influenza virus spreads through the airways, raising the risk of the virus mutating to achieve person-to-person transmission.
“Simply put, someone who’s coughing may be more likely to transmit the virus than someone who has an eye infection like conjunctivitis,” said CDC deputy director Nirav Shah at a press conference on 30 May. “The presence of respiratory symptoms tells us that the exposure risk is higher.”
Shah told the news website STAT that at least 40 people have been tested for the virus, and roughly 350 workers are being monitored, many of them in Michigan. Bagdasarian added that several people in Michigan had refused to be tested and several had refused the offer of antiviral drugs. 4
On 30 May the US Department of Agriculture announced a further $824m for more testing and surveillance for bird flu on dairy farms. 5
In a separate outbreak Australia recorded its first ever human case of H5N1 bird flu, although this was from chickens and not cows. 6
“A child acquired the infection while overseas and became unwell on returning to Australia earlier this year,” said the Victoria Department of Health on 18 May. “The child has now made a full recovery, and no family members in Australia or overseas have reported symptoms.”
The department emphasised that the case in Victoria was not the same strain as those recently been found in dairy cattle in the US and was a different strain from one previously detected at a poultry farm in Victoria.
- ↵ CDC. CDC confirms second human H5 bird flu case in Michigan; third case tied to dairy outbreak. 30 May 2024. https://www.cdc.gov/media/releases/2024/p0530-h5-human-case-michigan.html
- ↵ Department of Health and Human Services. Additional influenza A (H5) case detected in Michigan. 30 May 2024. https://www.michigan.gov/mdhhs/inside-mdhhs/newsroom/2024/05/30/h5n1-updates
- ↵ Branswell H. Stat. 30 May 2024. A third US farmworker infected with bird flu is the first to experience respiratory symptoms. https://www.statnews.com/2024/05/30/bird-flu-third-case-human-infection-caused-respiratory-symptoms
- ↵ US Department of Agriculture. USDA announces $824 million in new funding to protect livestock health; launches voluntary H5N1 dairy herd status pilot program. 30 May 2024. https://www.usda.gov/media/press-releases/2024/05/30/usda-announces-824-million-new-funding-protect-livestock-health
- ↵ Australian Centre for Disease Control. Human case of bird flu in Victoria. 23 May 2024. https://www.cdc.gov.au/newsroom/news-and-articles/media-release-human-case-bird-flu-victoria
Individualized Supplementation of Immunoactive Micronutrients and Severity of Upper Respiratory Infection Symptoms-A Randomized Intervention Study
Affiliations.
- 1 ZIEL-Institute for Food and Health, Core Facility Human Studies, Technical University Munich, Gregor-Mendel-Straße 2, 85354 Freising, Germany.
- 2 School of Medicine and Health, Technical University of Munich, Ismaninger Straße 22, 81675 Munich, Germany.
- PMID: 38794638
- PMCID: PMC11123851
- DOI: 10.3390/nu16101400
Certain micronutrients exhibit immunomodulatory effects. However, no intervention has yet investigated the effect of individualized supplementation on the severity of upper respiratory tract infections (URIs). Therefore, we investigated whether a personalized supplementation moderates the incidence and severity of URI. Selenium, zinc, and vitamin D were measured in dried blood spots from 59 healthy participants. Accordingly, a personalized supplement was provided with or without the respective micronutrients. We used WURSS-21 questionnaires to assess the disease status. The blood values converged during the intervention and micronutrients no longer differed between treated and untreated volunteers at the end of the intervention period. The incidence and severity of the illness did not significantly differ between the groups. However, when analyzing the WURSS-21 scores by the intention to treat, the initially randomized treatment arm revealed a significantly higher score than the placebo arm. Upon acute administration, individualized combinations of selenium, zinc and vitamin D do not reduce the number, or contribute to a milder course of URIs. Therefore, supplementation in acute infectious situations seems questionable. Further studies must address the habitual diet in more detail, to better understand the impact of individual micronutrient status on the prevention of URI.
Keywords: WURSS-21; dried blood spots; personalized nutrition; selenium; upper respiratory tract infections; vitamin D; zinc.
Publication types
- Randomized Controlled Trial
- Dietary Supplements*
- Micronutrients* / administration & dosage
- Middle Aged
- Respiratory Tract Infections* / prevention & control
- Selenium* / administration & dosage
- Selenium* / blood
- Severity of Illness Index
- Vitamin D* / administration & dosage
- Vitamin D* / blood
- Young Adult
- Zinc* / administration & dosage
- Zinc* / blood
- Micronutrients

Grants and funding
- Covid-19 Rapid Response Call - Innovation ID20398/European Institute of Innovation and Technology

- Free Case Studies
- Business Essays
Write My Case Study
Buy Case Study
Case Study Help
- Case Study For Sale
- Case Study Service
- Hire Writer
Case Study on Upper Respiratory Tract Infection
Upper respiratory tract infection case study:.
Upper respiratory tract infections are the groups of inflammation processes in the respiratory tract, which cause harm to the organism and are caused by viruses. URTI are the most widespread groups of diseases in the world, because nearly everyone suffers from it at least once every year, especially in cold periods. URTI includes such diseases as influenza, parainfluenza, respiratory syncytial virus, rhinovirus and adenovirus infections and other infections of the upper respiratory tract. When the disease is progressing, the condition of the patient may be damaged even more because of the activity of various bacteria. URTI are considered to be the most widespread infections in the world, that is why it is impossible to predict epidemics in the definite parts of the world. Speaking about babies, they do not fall ill with URTI due to the isolated way of life and strong immune system, but when they get older and go to kindergarten or school, they will fall ill very often, sometimes more than ten times per year.
Grownups fall ill with URTI more seldom, because they have developed a specific immunity and resistance from these infections. The possibility of URTI depends on the age of a person, the epidemic situation and her lifestyle. If a person spends much time in crowded places, the risk to fall ill is higher, because the infections are transmitted through coughing, sneezing, kissing, direct contact with the infected object, etc. Sometimes it is possible to catch the infection just having a contact with an animal, a dog, cat and a bird. The most effective ways to prevent URTI are to avoid crowded placed during epidemics, consume much vitamin C and wash hands often etc.
We Will Write a Custom Case Study Specifically For You For Only $13.90/page!
The topic on URTI is very important and interesting for everyone, because one falls ill with the diseases of this group several times a year. It is important to know how to prevent and cure the disease effectively and understand its nature. In order to solve the puzzle of a case study one will need to research the case site and interview the patient to collect information about the cause of the URTI for the profound analysis. When the data is collected it is possible to value the effect of the disease and define the most appropriate ways of the solution of the problem.The process of case study writing requires time and efforts; moreover, one should know everything about writing to complete a highquality paper. It is easy to find in the web a free sample case study on upper respiratory tract infection and understand how to compose a good paper well.
On the basis of a free example case study on acute upper respiratory tract infection it is possible to learn about the process of analysis, formatting and composition of the correct structure.
Related posts:
- Pneumonia is an acute respiratory infection
- Pneumonia is a serious infection
- Abdominal Infection Case Study
- Case Study on Respiratory System
- Respiratory System Case Study
- Title of Paper Uses Upper and Lower Case
- Respiratory System Study Guide
Quick Links
Privacy Policy
Terms and Conditions
Testimonials
Our Services
Case Study Writing Service
Case Studies For Sale
Our Company
Welcome to the world of case studies that can bring you high grades! Here, at ACaseStudy.com, we deliver professionally written papers, and the best grades for you from your professors are guaranteed!
[email protected] 804-506-0782 350 5th Ave, New York, NY 10118, USA
Acasestudy.com © 2007-2019 All rights reserved.

Hi! I'm Anna
Would you like to get a custom case study? How about receiving a customized one?
Haven't Found The Case Study You Want?
For Only $13.90/page
Phone Numbers
Routine and emergency care.
Companion Animal Hospital in Ithaca, NY for cats, dogs, exotics, and wildlife
Equine and Nemo Farm Animal Hospitals in Ithaca, NY for horses and farm animals
Cornell Ruffian Equine Specialists, on Long Island for every horse
Ambulatory and Production Medicine for service on farms within 30 miles of Ithaca, NY
Animal Health Diagnostic Center New York State Veterinary Diagnostic Laboratory
General Information
Cornell University College of Veterinary Medicine Ithaca, New York 14853-6401

Baker Institute for Animal Health
Dedicated to the study of veterinary infectious diseases, immunology, cancer, reproduction, genomics and epigenomics, feline calicivirus.
Feline calicivirus is a highly contagious virus that causes a mild to severe respiratory infection and oral disease in cats. It is especially common in shelters and breeding colonies, and often infects young cats. Most cats recover completely after a calicivirus infection, but rare strains can be especially deadly. The virus poses no threat to humans.
Cause Symptoms and complications Tests and diagnosis Treatment Prevention Additional resources Baker Institute and calicivirus
What causes calicivirus infection?
Feline calicivirus (FCV) belongs to a large family of viruses named Caliciviridae, whose members infect a wide range of vertebrate animals, including rabbits, livestock, reptiles, birds and amphibians. The human virus norovirus, which causes a brief but unpleasant gastrointestinal disease, is also a member of the Caliciviridae family.
Several strains of FCV circulate in domestic and wild cats. The virus mutates readily, leading to new strains that may not be fully covered by existing vaccines. Strains vary in the severity of the disease that they cause, with the majority causing only mild disease. The ability of the virus to mutate likely explains why after 40 years of vaccinating against FCV, outbreaks still frequently occur.
Rarely, a mutant strain of FCV will spontaneously arise that causes very serious disease with multiple organ damage or even death, called FCV-associated virulent systemic disease or FCV-VSD. The first known outbreak of FCV-VSD occurred in Northern California in 1998. Outbreaks of FCV-VSD are unusual and unrelated to each other.
Why and how might my cat become infected?
FCV occurs most commonly in multi-cat environments. A cat’s risk of exposure is higher in shelters, pet stores, and catteries, where 25 to 40 percent of cats may be carriers.
The virus spreads through direct contact with the saliva, nasal mucus and eye discharge of infected cats and through aerosol droplets that spread when cats sneeze. Lab tests have also detected the virus in urine, feces and blood. Cats typically shed the virus for about two or three weeks after infection, but some cats become long-term carriers, and continue to shed the virus on and off for months.
FCV is a hardy virus that survives on surfaces for up to a month in certain environments. Humans that handle infected cats can inadvertently transfer the virus to new animals. Objects that come in contact with a cat’s bodily fluids, such as food bowls, litter boxes or bedding, can also be a source of infection.
What happens during infection?
After being exposed to FCV, the incubation period is two to 14 days before symptoms appear. The virus likely initially infects the lining of the back of the mouth. After the virus replicates there, it likely spreads through the bloodstream to other organs. However, FCV preferentially infects the lining of the mouth and the tissues within the lungs. Most cats develop an upper respiratory tract infection and in more severe cases, the virus travels into the lungs where it causes pneumonia.
Symptoms and complications
A cat’s symptoms will depend on the strain of FCV it contracts. At first the cat will have symptoms that look like a cold, with sneezing, nasal congestion, fever and sometimes drooling. Large amounts of discharge can come from the eyes and nose. In more severe cases, cats can also develop inflammation and ulcers on the tongue, and the lining of the mouth. Lethargy, mild lameness and lack of appetite may also occur.
These symptoms can persist from five to 10 days in mild cases and up to six weeks in more severe ones. During the course of the illness, opportunistic bacterial infections can also occur. Cats may lose weight, and the infection can also cause abortions in pregnant cats. Most cats recover completely, but some will go on to develop a chronic form of gingivitis that causes thick and inflamed gums, which makes eating painful. Elderly cats and young kittens are more likely to suffer more severe symptoms. Fortunately, it is quite rare for cats to succumb to FCV infection.
Cats that develop FCV-VSD will have much more severe symptoms, including a high fever, swelling of the head and legs, as well as crusting sores and hair loss on the nose, eyes, ears and footpads. The mouth and ears may turn yellowish from liver damage, and there may be bleeding under the skin and in the gastrointestinal tract. FCV-VSD is fatal in up to 60 percent of cats that develop the disease.
Tests and diagnosis
How will my vet diagnose calicivirus.
Pet owners should always bring their cat to see the veterinarian if it shows signs of respiratory disease. FCV causes about half of the respiratory infections that occur in cats, but feline alphaherpesvirus1 (sometimes called feline rhinotracheitis virus) is another common cause and sometimes dual infections occur. The bacterial species Chlamydia felis and Mycoplasma felis also cause respiratory disease, and may complicate FCV infections.
A veterinarian will examine the cat for symptoms. In most cases, there is no need to make a definite diagnosis, as these infections are common and will resolve with supportive treatment. However, if multiple cats are infected or the cats are housed with others, the veterinarian may take swabs from the eyes, nose or mouth. These swabs will be sent to the lab to test for the presence of the virus. Labs can also test tissue or serum samples.
Commercial labs detect the presence of FCV in two ways: by growing the virus in cells in a petri dish, or through reverse transcriptase PCR (RT-PCR), a procedure that detects a segment of genetic material that is specific to calicivirus. Both tests are equally effective, though the RT-PCR test may be more common in some areas, as part of a panel that tests for several organisms that cause respiratory disease.
Test results should be interpreted carefully. Many cats that appear healthy, especially ones recently adopted from a shelter, pet store or breeder, will test positive for the virus due to previous exposure, so a positive result does not necessarily indicate that FCV is the cause of the problem. Recent vaccination with a modified live strain of the virus can also cause a false positive result. Incorrect negative results are more likely if the cat is swabbed more than a week after the start of the infection.
Commercial testing cannot distinguish between mild strains of FCV and the more virulent strains that cause FCV-VSD.
What are the treatment options for cats with calicivirus?
Currently there is no treatment to stop the virus, but pet owners can offer supportive care for their cat while its immune system fights the infection. Most cats can recover at home, but severely affected cats may need intensive nursing care.
Keep the nose and eyes of the cat clean and use vaporizers and saline nose drops to help clear the nasal passages. A drug that breaks down mucus, like bromhexine, also can help reduce congestion. Non-steroidal anti-inflammatory drugs can lower the fever and reduce mouth pain, and broad-spectrum antibiotics can be used to treat opportunistic bacterial infections, when necessary.
Cats often lose their appetite and stop eating due to congestion and the sores in their mouths. Owners should provide strong-smelling, soft foods, which can be pureed to make them easier to swallow and heated slightly to increase their odor. If cats have not eaten for more than three days, they may need hospitalization to receive fluids and IV nutrition.
If a cat develops FCV-VSD, it should receive intensive care, which could include IV fluids, antibiotics and other treatments as needed.
How do I vaccinate my pet against calicivirus?
Vaccines do not protect against FCV entirely, but they can greatly reduce the severity of the infection if your cat is exposed. Several combination vaccines against FCV, feline herpesvirus type 1 and feline panleukopenia virus (the cause of feline distemper) are available, which can be given nasally or as an injection. The vaccines given nasally contain a modified live form of the virus, while injected vaccines can be modified live viruses or inactivated ones. Cats that receive the nasal vaccine may sneeze for four to seven days after vaccination.
Once kittens reach six to eight weeks of age, they should receive a vaccine every three to four weeks, with the final booster being given after 16 weeks of age. If the cat is already older than 16 weeks, give two doses of the vaccine, three to four weeks apart. Cats should receive boosters every three years, unless they are in a high-risk, multi-cat environment, in which case they should be revaccinated annually. Even cats that have recovered from a calicivirus infection should receive boosters, because they may not be protected against other strains of the virus.
Studies suggest that the nasal form of the vaccine leads to more rapid protection against the virus, which may be helpful in containing outbreaks in shelters.
A vaccine called Calicivax™ is available that includes modified forms of a strain of FCV that causes FCV-VSD, and a typical strain of FCV. This vaccine may offer some protection against outbreaks of FCV-VSD, but since the virulent strains that cause these outbreaks arise from different mutations in less aggressive strains, it is unknown how effective Calicivax™ will be against future outbreaks. Calicivax™ is not part of the set of core vaccines recommended for all cats.
How else can I help prevent the disease?
If you have multiple cats and one or more are being treated for FCV, then you should quarantine the infected animals and clean food and water bowls, the litter box and other items that may be contaminated with the virus. A dilute bleach solution made up of one half cup of bleach per gallon of water is effective at killing the virus. Cleaning solutions that contain phenol, like Lysol, also are effective, but should not be used around cats because they cause irritation and are toxic. Owners may wish to remove other cats from the home during this period to prevent exposure. The virus will die off naturally after one month.
Cats that become carriers will continue to shed the virus in the home, even after they recover from the infection. Owners may need to re-home carrier cats before disinfecting the home to protect the remaining animals from exposure.
Whenever you bring a new cat into the home, it is wise to isolate the animal from other cats in the household for one to two weeks while you watch for signs of disease.
Additional resources
For veterinarians, the Merck Veterinary Manual provides information on calicivirus and other feline respiratory infections. The American Association of Feline Practitioners publishes a detailed fact sheet from their advisory panel.
Baker Institute and calicivirus
Dr. John S.L. Parker , associate professor of virology at the Baker Institute for Animal Health has worked with calicivirus for 15 years. He wants to know why some cats experience a short flu-like illness, while others develop a chronic gingivitis or the more severe life-threatening form of the disease.
Parker’s research group has investigated different strains of the virus that cause outbreaks of FCV-VSD. Studies in his lab have shown that these viruses can’t be identified based on their genetics, but there are detectable differences among the strains when they grow in cells in the lab.
Parker is also looking into the finer details of how FCV gets inside feline cells, where it copies itself using the cell’s machinery. The virus must shape-shift to attach to a receptor molecule on the surface of cells, which allows it to gain entry. By understanding this interaction, Parker hopes to identify an “Achilles heel” that will lead to the development of more effective vaccines.
These investigations into FCV not only give us a better understanding of this common feline infection, but can also help advance the study of similar caliciviruses, such as human norovirus.
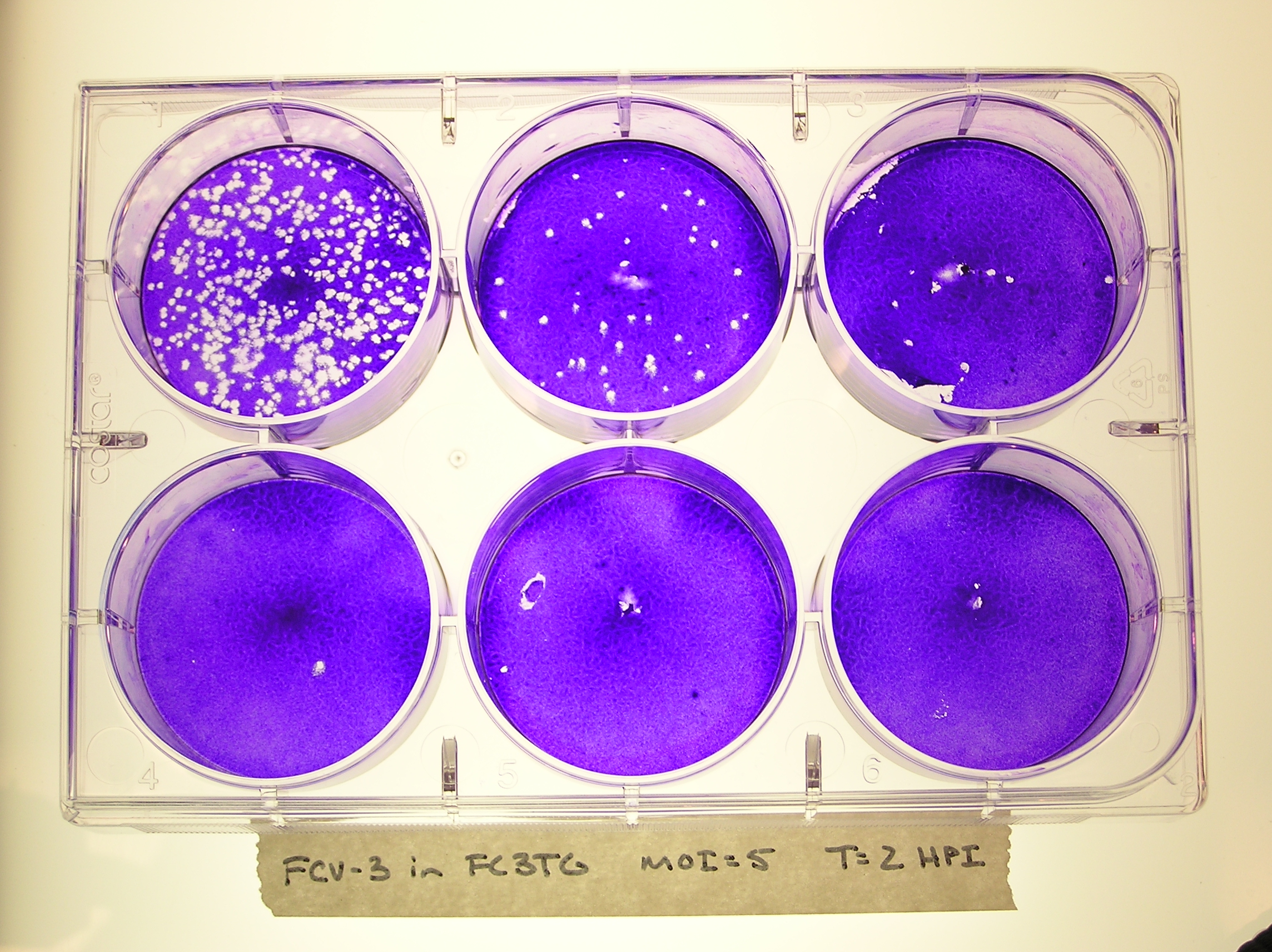
Connect with the Baker Institute on Twitter and Facebook:
- Correspondence
- Open access
- Published: 20 May 2024
PD-1 blockade immunotherapy as a successful rescue treatment for disseminated adenovirus infection after allogeneic hematopoietic stem cell transplantation
- Fei Zhou 1 ,
- Feng Du 2 ,
- Ziyan Wang 2 ,
- Mengxing Xue 1 ,
- Depei Wu 1 ,
- Suning Chen 1 &
- Xuefeng He 1
Journal of Hematology & Oncology volume 17 , Article number: 34 ( 2024 ) Cite this article
433 Accesses
1 Altmetric
Metrics details
Disseminated adenovirus infection is a complication with a relatively high mortality rate among patients undergoing hematopoietic stem cell transplantation. The low efficacy and poor availability of current treatment options are of major concern. Programmed cell death 1 (PD-1) blockade has been used to treat several chronic viral infections. Herein, we report a case of disseminated adenovirus infection in the early posttransplant period. The patient was diagnosed with diffuse large B-cell lymphoma at first and underwent 8 cycles of chemotherapy, including rituximab. She was subsequently diagnosed with acute myeloid leukemia and received haploidentical transplantation. She was diagnosed with Epstein‒Barr virus (EBV)-positive posttransplant lymphoproliferative disorder (PTLD) 2 months after the transplant, and 3 doses of rituximab were administered. The patient was diagnosed with disseminated adenovirus infection with upper respiratory tract, gastrointestinal tract and blood involved at 3 months after transplantation. She was first treated with a reduction in immunosuppression, cidofovir and ribavirin. Then, the patient received salvage treatment with the PD-1 inhibitor sintilimab (200 mg) after achieving no response to conventional therapy. The adenovirus was cleared 3 weeks later, and concomitant EBV was also cleared. Although the patient developed graft-versus-host disease of the liver after the administration of the PD-1 inhibitor, she was cured with steroid-free therapy. Therefore, PD-1 blockade immunotherapy can be considered a promising treatment option for patients with disseminated adenovirus infection after transplantation, with fully weighing the hazards of infection and the side effects of this therapy.
To the Editor,
The reported prevalence rate of Human adenovirus (HAdV) infection after hematopoietic stem cell transplantation (HSCT) ranges from 5–21% [ 1 ]. Approximately 10–20% of patients with HAdV infection may develop disseminated adenovirus disease (dAdV), with mortality rates ranging from 20 to 80% [ 2 ]. DAdV infection is characterized by systemic symptoms with adenoviruses detected in two or more organs, or adenoviruses detected in one organ accompanied by high viral copy numbers in blood (> 10E4 per milliliter) [ 3 ]. Reducing immunosuppression and using antiviral drugs, including cidofovir, are still the main treatment methods. The prognosis of patients with dAdV remains poor even if they are treated with combined therapy [ 3 , 4 , 5 ]. Herein, we report a patient with dAdV who was successfully treated with a PD-1 inhibitor rapidly and effectively. This is the first report of PD-1 inhibitors being applied to treat dAdV patients after transplantation.
Case presentation
The patient was a 54-year-old female who was diagnosed with diffuse large B-cell lymphoma in March 2020. She underwent 8 cycles of chemotherapy, including rituximab, and reached complete remission. The patient was subsequently diagnosed with MLL-ELL-positive acute myeloid leukemia, presumed to be treatment-related, in October 2022 and underwent 3 cycles of chemotherapy. She reached morphological remission and received haploidentical transplantation from her son on June 14, 2023. Unfortunately, she was diagnosed with EBV-positive PTLD at 2 months posttransplant. Immunosuppressive agents were rapidly tapered, and 3 doses of rituximab (375 mg/m 2 ) were administered. The number of EBV copies in the blood decreased from 4.1*10E5 to 4.5*10E3 per milliliter after treatment. Moreover, the patient got intermittent fever, nausea, vomiting, diarrhea, and cough, and HAdV was detected positive in blood, throat swabs and stool specimens, at 3.7*10E4 copies/ml (cp/ml) in blood and 4.0*10E8 cp/ml in stool at 3 months posttransplant. She was diagnosed with dAdV disease, with upper respiratory tract, gastrointestinal tract and peripheral blood involved. After administration of 2 doses of cidofovir (5 mg/kg per week), the patient’s clinical symptoms and inflammatory indicators worsened, and her HAdV copy number continued to increase to 1.7*10E6 cp/ml in blood. Since PD-1 inhibitors have been successfully used to treat several chronic viral infections [ 6 , 7 , 8 ], it is speculated that PD-1 inhibitors might be effective for HAdV clearance. Therefore, 200 mg of sintilimab (a recombinant human IgG4 monoclonal antibody against PD-1) was administered as a salvage treatment with the prior informed consent of the patient. The viral copy numbers in blood and stool both decreased gradually and finally became negative 3 weeks later (Fig. 1 ). The patient developed acute graft-versus-host disease (GVHD) grade III in the liver. She was treated with cyclosporine and 3 doses of basiliximab (20 mg, twice a week) and showed a complete response. Surprisingly, the patient also became negative for peripheral EBV soon after receiving sintilimab. Routine bone marrow exams at 4 months posttransplant showed molecular relapse of leukemia, with MLL-ELL being positive, so the patient was treated with 100 mg of sintilimab again. MLL-ELL turned negative 1 month later and no recurrence of GHVD occurred. At 9 months posttransplant, the patient was in good condition with no recurrence of leukemia, HAdV infection or GVHD.

Treatment process and development trends of viral copy numbers in the patient
Discussion and conclusions
We treated the dAdV patient with sintilimab as a salvage therapy successfully and rapidly, though the additional efficacy of cidofovir cannot be completely ruled out. Concomitant EBV infection also seemed to respond to PD-1 blockade. Chen et al. reported that inhibitors targeting the PD-1 pathway could rescue T cells from an exhausted state and revive the immune response against EBV [ 9 ]. You et al. reported a successful case of sintilimab in the treatment of chronic active EBV infection after allogeneic HSCT [ 10 ], which, together with our case, suggests that PD-1 blockade has a curative effect on viral infections in HSCT setting.
The administration of PD-1 inhibitors in patients posttransplant has the risk of inducing GVHD, with one study showing that the incidence of GVHD can reach 55% [ 11 ]; hence the use of PD-1 inhibitors in the treatment of transplant recipients needs to be carefully managed. However, considering the relatively high mortality rate of dAdV infection, treatment with PD-1 inhibitors is still worth trying in patients with dAdV infection after HSCT.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Programmed cell death 1
Epstein-Barr virus
Posttransplant lymphoproliferative disorders
Human adenovirus
- Hematopoietic stem cell transplantation
- Disseminated adenovirus disease
Copies per milliliter
Graft-versus-host disease
Chakrabarti S, Mautner V, Osman H, et al. Adenovirus infections following allogeneic stem cell transplantation: incidence and outcome in relation to graft manipulation, immunosuppression, and immune recovery. Blood. 2002;100(5):1619–27.
Article CAS PubMed Google Scholar
Robin M, Marque-Juillet S, Scieux C, et al. Disseminated adenovirus infections after allogeneic hematopoietic stem cell transplantation: incidence, risk factors and outcome. Haematologica. 2007;92(9):1254–7.
Article PubMed Google Scholar
Inamoto Y, Takeda W, Hirakawa T, et al. Adenovirus disease after hematopoietic cell transplantation: a Japanese transplant registry analysis. Am J Hematol. 2022;97(12):1568–79.
Hiwarkar P, Kosulin K, Cesaro S, et al. Management of adenovirus infection in patients after haematopoietic stem cell transplantation: state-of-the-art and real-life current approach: a position statement on behalf of the Infectious Diseases Working Party of the European Society of Blood and marrow transplantation. Rev Med Virol. 2018;28(3):e1980.
Cesaro S, Berger M, Tridello G, et al. A survey on incidence and management of adenovirus infection after allogeneic HSCT. Bone Marrow Transpl. 2019;54(8):1275–80.
Article Google Scholar
Li B, Yan C, Zhu J, et al. Anti-PD-1/PD-L1 blockade immunotherapy employed in treating Hepatitis B Virus infection-related Advanced Hepatocellular Carcinoma: A literature review. Front Immunol. 2020;11:1037.
Article CAS PubMed PubMed Central Google Scholar
Liu P, Pan X, Chen C, et al. Nivolumab treatment of relapsed/refractory Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis in adults. Blood. 2020;135(11):826–33.
Chen R, Lin Q, Zhu Y, et al. Sintilimab treatment for chronic active Epstein-Barr virus infection and Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis in children. Orphanet J Rare Dis. 2023;18(1):297.
Article PubMed PubMed Central Google Scholar
Chen RY, Zhu Y, Shen YY, et al. The role of PD-1 signaling in health and immune-related diseases. Front Immunol. 2023;14:1163633.
You Y, Wang J, Wang Z. Programmed death 1 monoclonal antibody helped to treat mixed chimeric and reactivation of Epstein–Barr virus in a patient with adult-onset chronic active Epstein–Barr virus infection after allogeneic hematopoietic stem cell transplantation: a case report. Med (Baltim). 2022;101:e28542.
Haverkos BM, Abbott D, Hamadani M, et al. PD-1 blockade for relapsed lymphoma post-allogeneic hematopoietic cell transplant: high response rate but frequent GVHD. Blood. 2017;130(2):221–8.
Download references
Acknowledgements
We thank the patient, and her relatives, for their participation in this study, and the staff at The First Affiliated Hospital of Soochow University and Soochow Hopes Hematonosis Hospital who offered help to finish this report.
Not applicable.
Author information
Authors and affiliations.
The First Affiliated Hospital of Soochow University, National clinical research center for hematologic diseases, Jiangsu Institute of Hematology, 188 Shizi Street, Suzhou, 215006, China
Fei Zhou, Mengxing Xue, Depei Wu, Suning Chen & Xuefeng He
Soochow Hopes Hematonosis Hospital, Suzhou, 215006, China
Feng Du & Ziyan Wang
You can also search for this author in PubMed Google Scholar
Contributions
In the author list, FZ, XH, SC wrote the main text, FD, ZW, and MX provide clinical materials of the patients, DW gave suggestions for polish and revise, XH and SC were responsible for staff management and workflow for the project. XH and SC initiated and was responsible for the whole work. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Suning Chen or Xuefeng He .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Consents from the patient has been obtained.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhou, F., Du, F., Wang, Z. et al. PD-1 blockade immunotherapy as a successful rescue treatment for disseminated adenovirus infection after allogeneic hematopoietic stem cell transplantation. J Hematol Oncol 17 , 34 (2024). https://doi.org/10.1186/s13045-024-01557-2
Download citation
Received : 16 April 2024
Accepted : 09 May 2024
Published : 20 May 2024
DOI : https://doi.org/10.1186/s13045-024-01557-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Programmed cell death 1 inhibitor
Journal of Hematology & Oncology
ISSN: 1756-8722
- General enquiries: [email protected]
- My View My View
- Following Following
- Saved Saved
Bird flu infects third US dairy worker; Michigan set to expand testing
- Medium Text

'A MILD CASE'
Sign up here.
Reporting by Leah Douglas in Washington and Julie Steenhuysen and Tom Polansek in Chicago; Editing by Bill Berkrot
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

Thomson Reuters
Washington-based award-winning journalist covering agriculture and energy including competition, regulation, federal agencies, corporate consolidation, environment and climate, racial discrimination and labour, previously at the Food and Environment Reporting Network.

Tom has been a journalist for Reuters in Chicago since 2011. He writes primarily about food and agriculture, and has reported on disruptions to global fertilizer and grain supplies from Russia's invasion of Ukraine. He also covers U.S. livestock production and meatpacking companies including Tyson Foods, Smithfield Foods and JBS. Tom was part of a team of reporters that Reuters named as Journalists of the Year in 2016 for coverage of Monsanto. He also won awards from the North American Agricultural Journalists.

Business Chevron

Boeing executives unlikely to be charged over 737 MAX crashes, source says
The statute of limitations has likely passed, Justice Department officials told victims' families.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Management of upper respiratory tract infections in children
Upper respiratory tract infection (URTI) occurs commonly in both children and adults and is a major cause of mild morbidity. It has a high cost to society, being responsible for absenteeism from school and work and unnecessary medical care, and is occasionally associated with serious sequelae. URTIs are usually caused by several families of virus; these are the rhinovirus, coronavirus, parainfluenza, respiratory syncytial virus (RSV), adenovirus, human metapneumovirus, influenza, enterovirus and the recently discovered bocavirus. This review will mainly focus on the rhinovirus, where significant advances have been made in understanding the epidemiology, natural history and relationship with other pathogens.
Introduction
Upper respiratory tract infection (URTI) or “the common cold” is a symptom complex usually caused by several families of virus; these are the rhinovirus, coronavirus, parainfluenza, respiratory syncytial virus (RSV), adenovirus, human metapneumovirus and influenza. Occasionally the enterovirus is implicated in summer. Recently, the newly discovered bocavirus (related to the parvovirus) has also been linked to URTI. 1 The term “URTI” is probably a misnomer as it incorrectly implies an absence of lower respiratory tract symptoms. URTI occurs commonly in both children and adults and is a major cause of mild morbidity. URTIs have a high cost to society, being responsible for missed work and unnecessary medical care. Occasionally they have serious sequelae. Often regarded as trivial, URTIs do not receive serious attention in medical school curricula.
Bacterial complications such as otitis media and acute sinusitis and inflammatory sequelae such as asthma, however, are well described. Readers are referred to a recent review of symptomatic management of URTI in children in this journal. 2 This review will mainly focus on the rhinovirus, where significant advances have been made in understanding the epidemiology, natural history and relationship with other pathogens. Where relevant, features specific to other causes of URTI will be mentioned. By understanding the natural history, spectrum of complications and awareness of “warning signs”, the family practitioner may be better equipped to manage the most common human viral infection. Management issues include the correct use of antibiotics, new information warning against over the counter medication for URTI in children under two years of age, emerging data on complementary and alternate medications (CAM) and other low-cost evidence-based interventions.
Epidemiology of URTI
In industrial United States of America (USA), adults have two to four, and children have between six and eight URTIs a year. 3 , 4 There is little data from developing countries. In a cross-sectional study from rural Uganda where data was collected from 300 women with children under two years of age, 37% of children had a current URTI. 5
Recent studies from Kenya in the rural Kilifi district on RSV epidemiology in a birth cohort demonstrated that almost 70% of RSV infections were of the upper respiratory tract only with no seasonality. 6
The majority of infections are spread through contact with infected secretions and can be interrupted through hand hygiene. Rhinoviral infections occur throughout the year, most commonly in spring and autumn. Influenza peaks in winter have been noted universally. 7 – 9
The rhinovirus, a single-stranded RNA virus, has more than 100 antigenic types and is the most common cause of URTIs in adults and children. As the rhinovirus grows best in tissue culture at 33 °C, it was believed earlier that it would not infect the lower airways. However, it was recently found to replicate in the lower respiratory tract. 10
Symptoms and signs
The symptoms and signs of the common cold have been well delineated in adult natural history studies since the 1960s. 11 Onset is heralded by nasal stuffiness and throat irritation, usually accompanied by low-grade fever, anorexia and myalgia. Sneezing is accompanied by a watery nasal discharge, which after one to three days becomes mucopurulent and can persist for up to ten days in over a third of patients. Coughing occurs commonly probably due to inflammation of the lower respiratory tract ( Figure 1 ). Rhinovirus infection causes concomitant inflammation of the paranasal sinuses. 12

Natural history and symptoms of rhinovirus infection
The natural history of URTI in children has been less well defined because of reliance on parent recall or physician referral. As the rhinovirus is difficult to culture, only with the advent of sensitive and specific reverse transcriptase polymerase chain reaction techniques has the natural history been better documented. The first major community-based natural history study in children was published in 2008. Pappas and colleagues conducted a survey in Virginia, USA. 13 Children between five and ten years of age were enrolled and data was collected on 81 cases from the onset of symptoms through day ten. Rhinoviruses were responsible for 37 (almost 50%) of cases.
The most common signs were coughing and sneezing and the most common symptoms were congestion and a runny nose. These signs and symptoms persisted for the first week. Coughing was present in 46% at onset, peaking at 69% on day one and still present in ≥ 50% at day seven. Rhinorrhoea occurred in 71% on day one and was still present in ≥ 50% by day five. Sneezing occurred in 36% at onset, peaking at 55% on day one and still noted in 35% by day five. Fever was uncommon, reported in only 15% on day one and declining even further. Headache was reported in 15% on day one and declined thereafter. Vomiting and diarrhoea were extremely uncommon. None of the children received antibiotics. A comparison between the course of URTI in children and adults is shown in Table I . 11 , 13
Comparison of signs and symptoms in adults and children 11 , 13
Important management points from natural history data are that coughing is extremely common in children and adults and can persist with high frequency until day nine. In contrast, fever is uncommon especially after the first day, and its presence suggests either another cause such as influenza and/or a bacterial complication such as otitis media or sinusitis.
Lower respiratory disease associated with the rhinovirus
Two studies of hospitalised children have recently documented considerable lower respiratory disease caused by the rhinovirus. In the USA, the rhinovirus was implicated in 26% of children younger than five years of age hospitalised for acute respiratory disease. 14 The rhinovirus was detected more frequently than RSV, the virus traditionally linked to most lower airway morbidity and was highly associated with a history of asthma. In infants under six months of age, apnoea was common (7 out of 62). In a similar study from Spain in children under two years of age, the rhinovirus was associated with 25% of admissions for respiratory disease. 15 Diagnoses included recurrent wheezing, bronchiolitis and pneumonia. Sixty per cent of children were febrile. Multiple viruses were isolated in almost 40% of children, suggesting a role for co-infection in the pathogenesis of respiratory disease.
Treatment of URTIs
Symptomatic treatment.
The main emphasis of management is symptom relief of fever, nasal congestion and coughing. A variety of adrenergic agonist, anticholinergic, antihistamine preparations, antitussives and expectorants are marketed for these purposes. Common constituents of such medication include first generation antihistamines, antipyretics (paracetamol) or anti-inflammatory agents (ibuprofen), cough suppressants such as dextromethorphan, expectorants (guaifenesin) and decongestants such as pseudoephedrine and phenylpropanolamine. 16
Although they provide symptom relief, there is no conclusive evidence that they shorten the duration of symptoms. 17 , 18 Recently, the Food and Drug Administration issued an advisory statement warning against using over the counter medications for URTIs in children under two years of age. 19 This arose from a report of three infants under six months of age who died after receiving these medications, possibly linked to the pseudoephedrine component. Since there is no proven benefit over placebo of these medications in children of any age, and the risks of side effects in children are great, practitioners should be cautious in recommending or prescribing such therapies.
Antibiotics
Antibiotic use in childhood URTIs remains contentious since more than 90% of the infections are of viral aetiology. The reasons cited for prescribing antibiotics include diagnostic uncertainty, socio-cultural and economic pressures, concern over malpractice litigation and parental expectations of an antibiotic. 20 Antibiotics are overprescribed for URTIs and promote antibiotic resistance. 21 However, there is a role for defined indications, such as severe acute rhinosinusitis lasting more than ten days and severe acute otitis media. 22
Fahey et al’s quantitative systematic review of randomised controlled trials comparing antibiotics to placebo for paediatric URTIs concluded that antibiotic treatment did not alter clinical outcome or reduce complication rates. 23 The authors do, however, make the point that the efficacy of antibiotic treatment may be greater in a subgroup with a higher baseline risk of developing complications.
Complementary and alternative medicine (CAM) for URTI
There is growing interest in the use of complementary and alternative medicines for URTIs. Herbal remedies have been studied and conflicting results found. Two of the most commonly used and studied herbs are Echinacea and Andrographis paniculata , both of which are believed to be immunostimulants. Propolis (bee resin) has also been studied and stimulates antibody production. 24 A major problem with the investigation and use of herbal products is the lack of standardisation. 25
A recent meta-analysis by Shah et al found that Echinacea decreased the odds of developing the common cold by 58% and the duration of a cold by 1.4 days. 26 At least two of the fourteen studies reviewed included children. The authors call for large randomised trials using standardised preparations and measuring well-defined endpoints. There is still insufficient data on safety, especially with prolonged use. The effects on blood pressure and rate-corrected QT interval are not known. As Echinacea inhibits cytochrome P450 3A4 enzymes, there is considerable potential for drug interaction. Rash, including anaphylaxis, has also been reported. 27 , 28
A review of safety and efficacy of six CAM studies for prevention and treatment of URTIs in children found that Echinacea did not reduce the duration and severity of URTIs, but that both Echinacea and Andrographis paniculata decreased nasal secretions. Echinacea was associated with a higher frequency of rash compared with placebo (p = 0.008). This review also found that a combination of these herbs with propolis and ascorbic acid reduced the number of URTI episodes, duration of symptoms and the number of days of illness. The review concludes, however, that data are inadequate to support CAM use for the prevention or treatment of URTIs in children. 29 The impact of herbal immunostimulants on the immature immune system is unknown.
Other practical interventions
Saline nasal spray may be beneficial. For example, in a study of Swedish military recruits, daily spraying with physiological saline significantly reduced the incidence of the common cold and nasal symptoms. 30 In a recent study of children with URTIs, daily nasal wash with a sea water-based preparation significantly reduced symptoms in comparison to standard medications. 31 Regrettably, the study agent was not compared to physiological saline.
Although zinc supplementation is ineffective for treatment of URTIs, 32 iron supplementation is remarkably effective in areas where iron deficiency is endemic and easy to implement. 33
Honey is superior to both dextromethorphan and no treatment for night-time coughing associated with URTIs. 34 Although the authors hypothesise that the effect could be due to its anti-oxidant or antimicrobial effects, another hypothesis is that a sweet taste might induce endogenous opioids. 35 Honey should not be given to infants under 12 months of age, however, because of a real danger of infant botulism. 36
The promotion of hand washing in households significantly reduces the incidence of both respiratory and gastrointestinal infections in children from both impoverished and well-resourced communities. 8 , 37
Parental smoking exacerbates respiratory infections in children and predisposes to asthma. 38 Tobacco is a highly addictive substance and is a major health problem requiring concerted efforts to assist addicts to wean themselves. 39
Influenza virus 40
The influenza A, B and C are double-stranded RNA orthomyxoviruses; A and B are usually responsible for influenza outbreaks in humans. The influenza viruses are classified according to haemagglutinin (HA) protein and neuraminidase (NA) proteins.
Fever is the most common sign and is higher and of longer duration than in rhinovirus infection. 41 Rhinorrhoea occurs commonly. The classic symptoms are sudden onset of fever, with or without chills, headache, malaise, and cough. Older children may complain of myalgia. The upper respiratory symptoms usually have a later onset and include conjunctivitis, otitis media, and gastrointestinal symptoms. Influenza can lead to serious sequelae such as pneumonia, encephalopathy or encephalitis, myocarditis, and secondary bacterial infections.
Epidemiology
Patients are infectious for 24 hours prior to symptoms, and continue to be for about one week, or longer in young children or immunocompromised hosts. Children under four years of age and those older with bronchopulmonary dysplasia, asthma, cardiac abnormalities, cystic fibrosis, malignancy, diabetes, chronic renal failure and HIV are at risk for complications.
Both influenza A and B viruses cause epidemics almost annually in many parts of the world. Community outbreaks usually affect school children first. These epidemics are due to antigenic drift.
Rapid diagnostic tests are becoming more available and can be very useful in determining whether influenza is circulating in the community and also in individual patients. 42 Rapid tests are helpful in decision making with regard to antibiotics. 43 , 44
Treatment and prevention
The adamantanes (amantadine and rimantadine) M2 ion channel blockers are only effective against influenza A, and therefore of no use unless influenza A has been identified. Two neuraminidase inhibitors (oseltamivir [oral] and zanamivir [inhaled]) are active against influenza A and B. 45 If taken within 48 hours of onset, the duration of the disease and complications are reduced. They are also useful for post-exposure prophylaxis during outbreaks. Both drugs are licensed in South Africa for children older than one year of age. A presumptive diagnosis can be made in adults during epidemics or after close contact with a known case. Adults with an influenza-like illness with cough and fever in the first 48 hours are likely to have influenza. 46 Children at risk for serious disease exposed to adults with the typical symptom complex may benefit from prophylaxis during winter outbreaks.
As bacterial infections can complicate influenza, practitioners should have a low threshold for use of antibiotics if complications are suspected.
Influenza is vaccine-preventable. Licensed vaccines include the live, attenuated influenza vaccine (LAIV), and the trivalent inactivated vaccine (TIV). Only the TIV is available in South Africa. Both are adapted every year for the recommended strains. The vaccines contain one influenza A (H3N2) and one (H1N1) virus, and also one influenza B virus.
Individuals at high risk for influenza complications should be vaccinated. 40 Additionally, people of any age with chronic underlying medical conditions, including HIV, should be immunised. The Centers for Disease Control and Prevention recommends that all children six months to eight years of age receive two doses of TIV separated by ≥ 4 weeks if they have not been vaccinated previously. Children who receive two doses in their first vaccination year can get a single annual dose in subsequent years. If they only received one dose in their first year of vaccination, they need two doses the following year, with single annual doses in subsequent years. Vaccination should be encouraged, particularly if there are high-risk people in the home.
Management of pharyngitis – syndromic or targeted
The two most important causes of pharyngitis requiring antibiotics are diphtheria and Streptococcus pyogenes . Fortunately diphtheria is extremely rare but can occur where public immunisation programmes have waned.
Pharyngitis due to S pyogenes may be easy to recognise, as it manifests as a febrile, purulent pharyngitis without rhinitis or cough. However, milder cases can be confused with viral URTI. The most important consequence of not treating pharyngitis is rheumatic fever, which can occur in all settings, but is far more common in resource-poor communities. 47 – 49
There are two approaches to managing pharyngitis. In the USA the emphasis is on limiting antibiotics to those with bacteriological confirmation. A streptococcal antigen test, which gives a rapid answer and is highly specific, is followed by a culture, in the event of a negative antigen test. 50
In the resource-limited primary healthcare settings where both laboratory tests and follow-up are unreliable, it is more appropriate to use a syndromic approach. In Costa Rica a single-dose of intramuscular benzathine penicillin for all infants and children with pharyngitis has been used very effectively since the 1970s to reduce the incidence of acute rheumatic fever from 90 to 1 per 100 000. 51 Any patient presenting with fever or a sore throat who had halitosis, red throat, and tonsillar hypertrophy with a white exudate was treated. Over a 20-year period, Streptococcus pneumoniae remained fully susceptible to penicillin. This represents a major success in reducing the lifetime disease burden of rheumatic heart disease.
In infants and young children, the catarrhal stage of pertussis typically presents as a “common cold”. Complications are most severe in infants under six months of age, especially if preterm or unimmunised. Therefore, a “common cold” presenting in this age group should raise suspicion of pertussis. Infants are especially at risk until all three primary doses of vaccine have been given at 6, 10 and 14 weeks. Adolescents and adults are susceptible to pertussis due to waning immunity. A useful clinical case definition for adults is an acute cough illness lasting at least seven days, especially if associated with posttussive vomiting or gagging beyond two weeks. 52 Any infant with URTI symptoms and in contact with an adult or adolescent fulfilling the case definition of pertussis should receive a macrolide antibiotic. As pertussis remains a formidable disease with high morbidity and significant mortality in young infants, current recommendations still urge practitioners to consider pertussis in young infants and to give antibiotic prophylaxis to household contacts. 53
Azithromycin is now recommended for infants below a month of age at a dosage of 10 mg/kg/day for five days because of the risk of hypertrophic pyloric stenosis with erythromycin in neonates. However, erythromycin at a dosage of 50 mg/kg/day for 14 days can still be used. For older infants and adults, clarithromycin can also be used. 54
Conclusions
Knowledge of the natural history of rhinovirus infection and awareness of influenza, pertussis and S. pyogenes will help the clinician to make clinically relevant decisions. There is already a large body of evidence-based practical information that can easily be applied to diagnosis, management and prevention.

IMAGES
VIDEO
COMMENTS
On examination, the temperature was 37.9°C, the blood pressure 157/95 mm Hg, the pulse 112 beats per minute, the respiratory rate 30 breaths per minute, and the oxygen saturation 91% while the ...
There has been extensive research showing that upper respiratory tract infections (URTIs), such as the common cold and influenza, can impair mental performance. ... The present paper reports a case study of a primary school student who normally had very high academic grades and did very badly on the 11+ examination, which is used to determine ...
A variety of viruses and bacteria can cause upper respiratory tract infections. These cause a variety of patient diseases including acute bronchitis, the common cold, influenza, and respiratory distress syndromes. Defining most of these patient diseases is difficult because the presentations connected with upper respiratory tract infections (URIs) commonly overlap and their causes are similar.
Chapter 56. Upper Respiratory Tract Infections (Case 48) Patricia D. Brown MD. Case: A previously healthy 33-year-old woman presents with a 4-day history of sneezing and runny nose accompanied by nasal congestion, sore throat, and a feeling of fullness in the ears. For the past 2 days she has had a cough, which was initially dry but is now ...
Acute respiratory infections (ARIs) are classified as upper respiratory tract infections (URIs) or lower respiratory tract infections (LRIs). The upper respiratory tract consists of the airways from the nostrils to the vocal cords in the larynx, including the paranasal sinuses and the middle ear. The lower respiratory tract covers the continuation of the airways from the trachea and bronchi to ...
Acute upper respiratory tract infections are extremely common in adults and children, but only a few safe and effective treatments are available. Patients typically present with nasal congestion ...
Background: There has been extensive research showing that upper respiratory tract infections (URTIs), such as the common cold and influenza, can impair mental performance. Much of this research has involved studies of experimentally induced URTIs or laboratory studies of naturally occurring illnesses. ... This case study shows that information ...
Practice Essentials. Upper respiratory tract infection (URI) represents the most common acute illness evaluated in the outpatient setting. URIs range from the common cold—typically a mild, self-limited, catarrhal syndrome of the nasopharynx—to life-threatening illnesses such as epiglottitis (see the image below).
Acute viral (upper) respiratory tract infections (ARTIs) are among the most common reasons for a healthcare encounter in the United States, with over 43 million ambulatory visits yearly for cough or sore throat. ... Encyclopedia of Case Study Research. 2010. SAGE Knowledge. Entry . Disease Management. Show details Hide details. Sarah E ...
Over 2.8 million people are infected with, and 35,000 people die from antibiotic-resistant bacteria annually in the United States.1 Injudicious outpatient use of antibiotics contributes to the growth of antibiotic-resistant bacteria and reduced efficacy of antibiotics. Approximately 30% of all antibiotic prescriptions and 50% of prescriptions for upper respiratory tract infections (URTIs) in ...
Investigator-reported respiratory infection events occurred at a significantly lower incidence in patients treated with dupilumab versus placebo, in both asthma (22% lower; P < .0001; 95% CI 0.71-0.85) and CRSwNP (38% lower; P <.0001; 95% CI 0.51-0.75). Reported upper and lower respiratory tract infection events were numerically or significantly lower in dupilumab-treated patients in both ...
OBJECTIVES To assess the risks and benefits of antibiotic treatment in children with symptoms of upper respiratory tract infection (URTI). DESIGN Quantitative systematic review of randomised trials that compare antibiotic treatment with placebo. DATA SOURCES Twelve trials retrieved from a systematic search (electronic databases, contact with authors, contact with drug manufacturers, reference ...
Box 1. Choosing Wisely is a clinician-led campaign, present in more than 20 countries, which encourages conversations between clinicians and patients about overuse of antibiotic medication. Below is a sample of statements from different countries' Choosing Wisely campaigns pertaining to avoiding antibiotics for viral respiratory tract infection.
Upper respiratory tract infection (URTI) is the commonest reason for consulting. Inappropriate antibiotics promote resistant bacteria. Nurse management of URTI is an ideal opportunity to promote self-care and nonantibiotic management. Aims: To describe the effects of a specially trained practice nurse managing URTI in a general practice in ...
An upper respiratory tract infection (URTI) is an illness caused by an acute infection, which involves the upper respiratory tract, including the nose, sinuses, pharynx, larynx, or trachea. URTIs are characterized by cough, nasal congestion and discharge, sore throat, and sneezing. URTIs include the common cold, epiglottitis, tonsillitis ...
January 3, 2018. A 44-year-old man with no significant medical history presents to his local urgent care center after 3 days of fevers, sore throat, rhinitis, coughing, and myalgia. He reports that his girlfriend who works at a daycare center has had similar flu-like symptoms for the past week and that she has noted something has been going ...
A. paniculata may be a safe and efficacious treatment for the relief of symptoms of uncomplicated upper respiratory tract infection; ... a slight increase in the incidence of skin rash among patients randomized to echinacea. 169 While there is a modest case control study finding no adverse effects in pregnancy, 170 I caution against its use as ...
Respiratory syncytial virus is the most common cause of lower respiratory tract infections in infants and young children. While the majority of infants display only mild upper respiratory tract infection or occasionally otitis media, around one-third will develop an infection of the lower respiratory tract, usually bronchiolitis. There is now convincing evidence from a number of cohorts that ...
Provides rich case studies of historical ... SARS-CoV-2 is shed mainly from deep in the lungs, not the upper respiratory tract, ... Laboratory-confirmed viral respiratory infections and clinical respiratory infections. Study tents were visited twice daily. Nasal swabs were obtained from those who had flu-like symptoms.
KEY CONCEPTS. Many upper respiratory tract infections will resolve spontaneously without pharmacologic therapy. The most common bacterial causes are Streptococcus pneumoniae (acute otitis media and acute rhinosinusitis) and group A β-hemolytic Streptococcus (acute pharyngitis).. Vaccination against influenza and pneumococcus may decrease the risk of acute otitis media.
URI Case Study. Directions: This is an "unfolding" case study. Answer all of the questions in order and submit your answers to D2L. Scenario: Mom calls the pediatrician's office stating that her 2-year-old son woke up screaming in the middle of the night with a fever. You are the telephone triage nurse today.
The US has recorded the first person with H5N1 flu to have respiratory symptoms, in what is thought to be the third human case in an ongoing outbreak among dairy farms. All previous confirmed cases of the infection in people had symptoms of conjunctivitis but no respiratory problems. "The patient reported upper respiratory tract symptoms, including cough without fever, and eye discomfort ...
Certain micronutrients exhibit immunomodulatory effects. However, no intervention has yet investigated the effect of individualized supplementation on the severity of upper respiratory tract infections (URIs). Therefore, we investigated whether a personalized supplementation moderates the incidence …
Upper Respiratory Tract Infection Case Study: Upper respiratory tract infections are the groups of inflammation processes in the respiratory tract, which cause harm to the organism and are caused by viruses. URTI are the most widespread groups of diseases in the world, because nearly everyone suffers from it at least once every year, especially in cold periods.
In this light, an oral spray based on propolis, traditionally used to maintain oral cavity and upper respiratory tract health due to its antimicrobial and anti-inflammatory properties, was tested in a randomized, double-blind, placebo-controlled clinical study in adults with MURTIs ( n =122).
After the virus replicates there, it likely spreads through the bloodstream to other organs. However, FCV preferentially infects the lining of the mouth and the tissues within the lungs. Most cats develop an upper respiratory tract infection and in more severe cases, the virus travels into the lungs where it causes pneumonia.
Disseminated adenovirus infection is a complication with a relatively high mortality rate among patients undergoing hematopoietic stem cell transplantation. The low efficacy and poor availability of current treatment options are of major concern. Programmed cell death 1 (PD-1) blockade has been used to treat several chronic viral infections. Herein, we report a case of disseminated adenovirus ...
A third U.S. dairy worker tested positive for bird flu after exposure to infected cows, and was the first to suffer respiratory problems, U.S. officials said on Thursday.
Upper respiratory tract infection (URTI) occurs commonly in both children and adults and is a major cause of mild morbidity. It has a high cost to society, being responsible for absenteeism from school and work and unnecessary medical care, and is occasionally associated with serious sequelae. URTIs are usually caused by several families of ...
But unlike the earlier two cases, the case reported on May 30 had "more typical symptoms of acute respiratory illness associated with influenza virus infection, including A(H5N1) viruses".