Persuasive Essay Guide
Persuasive Essay About Covid19

How to Write a Persuasive Essay About Covid19 | Examples & Tips
11 min read

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Free Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Persuasive Essay About Smoking - Making a Powerful Argument with Examples
Are you looking to write a persuasive essay about the Covid-19 pandemic?
Writing a compelling and informative essay about this global crisis can be challenging. It requires researching the latest information, understanding the facts, and presenting your argument persuasively.
But don’t worry! with some guidance from experts, you’ll be able to write an effective and persuasive essay about Covid-19.
In this blog post, we’ll outline the basics of writing a persuasive essay . We’ll provide clear examples, helpful tips, and essential information for crafting your own persuasive piece on Covid-19.
Read on to get started on your essay.
- 1. Steps to Write a Persuasive Essay About Covid-19
- 2. Examples of Persuasive Essay About Covid19
- 3. Examples of Persuasive Essay About Covid-19 Vaccine
- 4. Examples of Persuasive Essay About Covid-19 Integration
- 5. Examples of Argumentative Essay About Covid 19
- 6. Examples of Persuasive Speeches About Covid-19
- 7. Tips to Write a Persuasive Essay About Covid-19
- 8. Common Topics for a Persuasive Essay on COVID-19
Steps to Write a Persuasive Essay About Covid-19
Here are the steps to help you write a persuasive essay on this topic, along with an example essay:
Step 1: Choose a Specific Thesis Statement
Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example:
Step 2: Research and Gather Information
Collect reliable and up-to-date information from reputable sources to support your thesis statement. This may include statistics, expert opinions, and scientific studies. For instance:
- COVID-19 vaccination effectiveness data
- Information on vaccine mandates in different countries
- Expert statements from health organizations like the WHO or CDC
Step 3: Outline Your Essay
Create a clear and organized outline to structure your essay. A persuasive essay typically follows this structure:
- Introduction
- Background Information
- Body Paragraphs (with supporting evidence)
- Counterarguments (addressing opposing views)
Step 4: Write the Introduction
In the introduction, grab your reader's attention and present your thesis statement. For example:
Step 5: Provide Background Information
Offer context and background information to help your readers understand the issue better. For instance:
Step 6: Develop Body Paragraphs
Each body paragraph should present a single point or piece of evidence that supports your thesis statement. Use clear topic sentences, evidence, and analysis. Here's an example:
Step 7: Address Counterarguments
Acknowledge opposing viewpoints and refute them with strong counterarguments. This demonstrates that you've considered different perspectives. For example:
Step 8: Write the Conclusion
Summarize your main points and restate your thesis statement in the conclusion. End with a strong call to action or thought-provoking statement. For instance:
Step 9: Revise and Proofread
Edit your essay for clarity, coherence, grammar, and spelling errors. Ensure that your argument flows logically.
Step 10: Cite Your Sources
Include proper citations and a bibliography page to give credit to your sources.
Remember to adjust your approach and arguments based on your target audience and the specific angle you want to take in your persuasive essay about COVID-19.
Paper Due? Why Suffer? That's our Job!
Examples of Persuasive Essay About Covid19
When writing a persuasive essay about the Covid-19 pandemic, it’s important to consider how you want to present your argument. To help you get started, here are some example essays for you to read:
Check out some more PDF examples below:
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
If you're in search of a compelling persuasive essay on business, don't miss out on our “ persuasive essay about business ” blog!
Examples of Persuasive Essay About Covid-19 Vaccine
Covid19 vaccines are one of the ways to prevent the spread of Covid-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others.
A persuasive essay about the Covid-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects.
Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Covid19 Vaccine Persuasive Essay
Persuasive Essay on Covid Vaccines
Interested in thought-provoking discussions on abortion? Read our persuasive essay about abortion blog to eplore arguments!
Examples of Persuasive Essay About Covid-19 Integration
Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. However, people have started to learn to live with Covid19.
Writing a persuasive essay about it shouldn't be stressful. Read the sample essay below to get idea for your own essay about Covid19 integration.
Persuasive Essay About Working From Home During Covid19
Searching for the topic of Online Education? Our persuasive essay about online education is a must-read.
Examples of Argumentative Essay About Covid 19
Covid-19 has been an ever-evolving issue, with new developments and discoveries being made on a daily basis.
Writing an argumentative essay about such an issue is both interesting and challenging. It allows you to evaluate different aspects of the pandemic, as well as consider potential solutions.
Here are some examples of argumentative essays on Covid19.
Argumentative Essay About Covid19 Sample
Argumentative Essay About Covid19 With Introduction Body and Conclusion
Looking for a persuasive take on the topic of smoking? You'll find it all related arguments in out Persuasive Essay About Smoking blog!
Examples of Persuasive Speeches About Covid-19
Do you need to prepare a speech about Covid19 and need examples? We have them for you!
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus.
Check out some examples of persuasive speeches on Covid-19:
Persuasive Speech About Covid-19 Example
Persuasive Speech About Vaccine For Covid-19
You can also read persuasive essay examples on other topics to master your persuasive techniques!
Tips to Write a Persuasive Essay About Covid-19
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively.
Here are some tips to help you craft a compelling persuasive essay on this topic:
Choose a Specific Angle
Start by narrowing down your focus. COVID-19 is a broad topic, so selecting a specific aspect or issue related to it will make your essay more persuasive and manageable. For example, you could focus on vaccination, public health measures, the economic impact, or misinformation.
Provide Credible Sources
Support your arguments with credible sources such as scientific studies, government reports, and reputable news outlets. Reliable sources enhance the credibility of your essay.
Use Persuasive Language
Employ persuasive techniques, such as ethos (establishing credibility), pathos (appealing to emotions), and logos (using logic and evidence). Use vivid examples and anecdotes to make your points relatable.
Organize Your Essay
Structure your essay involves creating a persuasive essay outline and establishing a logical flow from one point to the next. Each paragraph should focus on a single point, and transitions between paragraphs should be smooth and logical.
Emphasize Benefits
Highlight the benefits of your proposed actions or viewpoints. Explain how your suggestions can improve public health, safety, or well-being. Make it clear why your audience should support your position.
Use Visuals -H3
Incorporate graphs, charts, and statistics when applicable. Visual aids can reinforce your arguments and make complex data more accessible to your readers.
Call to Action
End your essay with a strong call to action. Encourage your readers to take a specific step or consider your viewpoint. Make it clear what you want them to do or think after reading your essay.
Revise and Edit
Proofread your essay for grammar, spelling, and clarity. Make sure your arguments are well-structured and that your writing flows smoothly.
Seek Feedback
Have someone else read your essay to get feedback. They may offer valuable insights and help you identify areas where your persuasive techniques can be improved.
Tough Essay Due? Hire Tough Writers!
Common Topics for a Persuasive Essay on COVID-19
Here are some persuasive essay topics on COVID-19:
- The Importance of Vaccination Mandates for COVID-19 Control
- Balancing Public Health and Personal Freedom During a Pandemic
- The Economic Impact of Lockdowns vs. Public Health Benefits
- The Role of Misinformation in Fueling Vaccine Hesitancy
- Remote Learning vs. In-Person Education: What's Best for Students?
- The Ethics of Vaccine Distribution: Prioritizing Vulnerable Populations
- The Mental Health Crisis Amidst the COVID-19 Pandemic
- The Long-Term Effects of COVID-19 on Healthcare Systems
- Global Cooperation vs. Vaccine Nationalism in Fighting the Pandemic
- The Future of Telemedicine: Expanding Healthcare Access Post-COVID-19
In search of more inspiring topics for your next persuasive essay? Our persuasive essay topics blog has plenty of ideas!
To sum it up,
You have read good sample essays and got some helpful tips. You now have the tools you needed to write a persuasive essay about Covid-19. So don't let the doubts stop you, start writing!
If you need professional writing help, don't worry! We've got that for you as well.
MyPerfectWords.com is a professional persuasive essay writing service that can help you craft an excellent persuasive essay on Covid-19. Our experienced essay writer will create a well-structured, insightful paper in no time!
So don't hesitate and place your ' write my essay online ' request today!
Frequently Asked Questions
Are there any ethical considerations when writing a persuasive essay about covid-19.
Yes, there are ethical considerations when writing a persuasive essay about COVID-19. It's essential to ensure the information is accurate, not contribute to misinformation, and be sensitive to the pandemic's impact on individuals and communities. Additionally, respecting diverse viewpoints and emphasizing public health benefits can promote ethical communication.
What impact does COVID-19 have on society?
The impact of COVID-19 on society is far-reaching. It has led to job and economic losses, an increase in stress and mental health disorders, and changes in education systems. It has also had a negative effect on social interactions, as people have been asked to limit their contact with others.
Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading
How to Write About Coronavirus in a College Essay
Students can share how they navigated life during the coronavirus pandemic in a full-length essay or an optional supplement.
Writing About COVID-19 in College Essays

Getty Images
Experts say students should be honest and not limit themselves to merely their experiences with the pandemic.
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many – a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.
Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them – and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic – and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
10 Ways to Discover College Essay Ideas

Tags: students , colleges , college admissions , college applications , college search , Coronavirus
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
College Admissions: Get a Step Ahead!
Sign up to receive the latest updates from U.S. News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
Ask an Alum: Making the Most Out of College
You May Also Like
Federal vs. private parent student loans.
Erika Giovanetti May 9, 2024

14 Colleges With Great Food Options
Sarah Wood May 8, 2024

Colleges With Religious Affiliations
Anayat Durrani May 8, 2024

Protests Threaten Campus Graduations
Aneeta Mathur-Ashton May 6, 2024

Protesting on Campus: What to Know
Sarah Wood May 6, 2024

Lawmakers Ramp Up Response to Unrest
Aneeta Mathur-Ashton May 3, 2024

University Commencements Must Go On
Eric J. Gertler May 3, 2024

Where Astronauts Went to College
Cole Claybourn May 3, 2024

College Admitted Student Days
Jarek Rutz May 3, 2024

Universities, the Police and Protests
John J. Sloan III May 2, 2024

I Thought We’d Learned Nothing From the Pandemic. I Wasn’t Seeing the Full Picture

M y first home had a back door that opened to a concrete patio with a giant crack down the middle. When my sister and I played, I made sure to stay on the same side of the divide as her, just in case. The 1988 film The Land Before Time was one of the first movies I ever saw, and the image of the earth splintering into pieces planted its roots in my brain. I believed that, even in my own backyard, I could easily become the tiny Triceratops separated from her family, on the other side of the chasm, as everything crumbled into chaos.
Some 30 years later, I marvel at the eerie, unexpected ways that cartoonish nightmare came to life – not just for me and my family, but for all of us. The landscape was already covered in fissures well before COVID-19 made its way across the planet, but the pandemic applied pressure, and the cracks broke wide open, separating us from each other physically and ideologically. Under the weight of the crisis, we scattered and landed on such different patches of earth we could barely see each other’s faces, even when we squinted. We disagreed viciously with each other, about how to respond, but also about what was true.
Recently, someone asked me if we’ve learned anything from the pandemic, and my first thought was a flat no. Nothing. There was a time when I thought it would be the very thing to draw us together and catapult us – as a capital “S” Society – into a kinder future. It’s surreal to remember those early days when people rallied together, sewing masks for health care workers during critical shortages and gathering on balconies in cities from Dallas to New York City to clap and sing songs like “Yellow Submarine.” It felt like a giant lightning bolt shot across the sky, and for one breath, we all saw something that had been hidden in the dark – the inherent vulnerability in being human or maybe our inescapable connectedness .
More from TIME
Read More: The Family Time the Pandemic Stole
But it turns out, it was just a flash. The goodwill vanished as quickly as it appeared. A couple of years later, people feel lied to, abandoned, and all on their own. I’ve felt my own curiosity shrinking, my willingness to reach out waning , my ability to keep my hands open dwindling. I look out across the landscape and see selfishness and rage, burnt earth and so many dead bodies. Game over. We lost. And if we’ve already lost, why try?
Still, the question kept nagging me. I wondered, am I seeing the full picture? What happens when we focus not on the collective society but at one face, one story at a time? I’m not asking for a bow to minimize the suffering – a pretty flourish to put on top and make the whole thing “worth it.” Yuck. That’s not what we need. But I wondered about deep, quiet growth. The kind we feel in our bodies, relationships, homes, places of work, neighborhoods.
Like a walkie-talkie message sent to my allies on the ground, I posted a call on my Instagram. What do you see? What do you hear? What feels possible? Is there life out here? Sprouting up among the rubble? I heard human voices calling back – reports of life, personal and specific. I heard one story at a time – stories of grief and distrust, fury and disappointment. Also gratitude. Discovery. Determination.
Among the most prevalent were the stories of self-revelation. Almost as if machines were given the chance to live as humans, people described blossoming into fuller selves. They listened to their bodies’ cues, recognized their desires and comforts, tuned into their gut instincts, and honored the intuition they hadn’t realized belonged to them. Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. “The way I dress, the way I love, and the way I carry myself have both shrunk and expanded,” she shared. “I don’t love myself very well with an audience.” Without the daily ritual of trying to pass as “normal” in public, Tamar, a queer mom in the Netherlands, realized she’s autistic. “I think the pandemic helped me to recognize the mask,” she wrote. “Not that unmasking is easy now. But at least I know it’s there.” In a time of widespread suffering that none of us could solve on our own, many tended to our internal wounds and misalignments, large and small, and found clarity.
Read More: A Tool for Staying Grounded in This Era of Constant Uncertainty
I wonder if this flourishing of self-awareness is at least partially responsible for the life alterations people pursued. The pandemic broke open our personal notions of work and pushed us to reevaluate things like time and money. Lucy, a disabled writer in the U.K., made the hard decision to leave her job as a journalist covering Westminster to write freelance about her beloved disability community. “This work feels important in a way nothing else has ever felt,” she wrote. “I don’t think I’d have realized this was what I should be doing without the pandemic.” And she wasn’t alone – many people changed jobs , moved, learned new skills and hobbies, became politically engaged.
Perhaps more than any other shifts, people described a significant reassessment of their relationships. They set boundaries, said no, had challenging conversations. They also reconnected, fell in love, and learned to trust. Jeanne, a quilter in Indiana, got to know relatives she wouldn’t have connected with if lockdowns hadn’t prompted weekly family Zooms. “We are all over the map as regards to our belief systems,” she emphasized, “but it is possible to love people you don’t see eye to eye with on every issue.” Anna, an anti-violence advocate in Maine, learned she could trust her new marriage: “Life was not a honeymoon. But we still chose to turn to each other with kindness and curiosity.” So many bonds forged and broken, strengthened and strained.
Instead of relying on default relationships or institutional structures, widespread recalibrations allowed for going off script and fortifying smaller communities. Mara from Idyllwild, Calif., described the tangible plan for care enacted in her town. “We started a mutual-aid group at the beginning of the pandemic,” she wrote, “and it grew so quickly before we knew it we were feeding 400 of the 4000 residents.” She didn’t pretend the conditions were ideal. In fact, she expressed immense frustration with our collective response to the pandemic. Even so, the local group rallied and continues to offer assistance to their community with help from donations and volunteers (many of whom were originally on the receiving end of support). “I’ve learned that people thrive when they feel their connection to others,” she wrote. Clare, a teacher from the U.K., voiced similar conviction as she described a giant scarf she’s woven out of ribbons, each representing a single person. The scarf is “a collection of stories, moments and wisdom we are sharing with each other,” she wrote. It now stretches well over 1,000 feet.
A few hours into reading the comments, I lay back on my bed, phone held against my chest. The room was quiet, but my internal world was lighting up with firefly flickers. What felt different? Surely part of it was receiving personal accounts of deep-rooted growth. And also, there was something to the mere act of asking and listening. Maybe it connected me to humans before battle cries. Maybe it was the chance to be in conversation with others who were also trying to understand – what is happening to us? Underneath it all, an undeniable thread remained; I saw people peering into the mess and narrating their findings onto the shared frequency. Every comment was like a flare into the sky. I’m here! And if the sky is full of flares, we aren’t alone.
I recognized my own pandemic discoveries – some minor, others massive. Like washing off thick eyeliner and mascara every night is more effort than it’s worth; I can transform the mundane into the magical with a bedsheet, a movie projector, and twinkle lights; my paralyzed body can mother an infant in ways I’d never seen modeled for me. I remembered disappointing, bewildering conversations within my own family of origin and our imperfect attempts to remain close while also seeing things so differently. I realized that every time I get the weekly invite to my virtual “Find the Mumsies” call, with a tiny group of moms living hundreds of miles apart, I’m being welcomed into a pocket of unexpected community. Even though we’ve never been in one room all together, I’ve felt an uncommon kind of solace in their now-familiar faces.
Hope is a slippery thing. I desperately want to hold onto it, but everywhere I look there are real, weighty reasons to despair. The pandemic marks a stretch on the timeline that tangles with a teetering democracy, a deteriorating planet , the loss of human rights that once felt unshakable . When the world is falling apart Land Before Time style, it can feel trite, sniffing out the beauty – useless, firing off flares to anyone looking for signs of life. But, while I’m under no delusions that if we just keep trudging forward we’ll find our own oasis of waterfalls and grassy meadows glistening in the sunshine beneath a heavenly chorus, I wonder if trivializing small acts of beauty, connection, and hope actually cuts us off from resources essential to our survival. The group of abandoned dinosaurs were keeping each other alive and making each other laugh well before they made it to their fantasy ending.
Read More: How Ice Cream Became My Own Personal Act of Resistance
After the monarch butterfly went on the endangered-species list, my friend and fellow writer Hannah Soyer sent me wildflower seeds to plant in my yard. A simple act of big hope – that I will actually plant them, that they will grow, that a monarch butterfly will receive nourishment from whatever blossoms are able to push their way through the dirt. There are so many ways that could fail. But maybe the outcome wasn’t exactly the point. Maybe hope is the dogged insistence – the stubborn defiance – to continue cultivating moments of beauty regardless. There is value in the planting apart from the harvest.
I can’t point out a single collective lesson from the pandemic. It’s hard to see any great “we.” Still, I see the faces in my moms’ group, making pancakes for their kids and popping on between strings of meetings while we try to figure out how to raise these small people in this chaotic world. I think of my friends on Instagram tending to the selves they discovered when no one was watching and the scarf of ribbons stretching the length of more than three football fields. I remember my family of three, holding hands on the way up the ramp to the library. These bits of growth and rings of support might not be loud or right on the surface, but that’s not the same thing as nothing. If we only cared about the bottom-line defeats or sweeping successes of the big picture, we’d never plant flowers at all.
More Must-Reads From TIME
- What Student Photojournalists Saw at the Campus Protests
- How Far Trump Would Go
- Why Maternity Care Is Underpaid
- Saving Seconds Is Better Than Hours
- Welcome to the Golden Age of Ryan Gosling
- Scientists Are Finding Out Just How Toxic Your Stuff Is
- The 100 Most Influential People of 2024
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
8 Lessons We Can Learn From the COVID-19 Pandemic
BY KATHY KATELLA May 14, 2021

Note: Information in this article was accurate at the time of original publication. Because information about COVID-19 changes rapidly, we encourage you to visit the websites of the Centers for Disease Control & Prevention (CDC), World Health Organization (WHO), and your state and local government for the latest information.
The COVID-19 pandemic changed life as we know it—and it may have changed us individually as well, from our morning routines to our life goals and priorities. Many say the world has changed forever. But this coming year, if the vaccines drive down infections and variants are kept at bay, life could return to some form of normal. At that point, what will we glean from the past year? Are there silver linings or lessons learned?
“Humanity's memory is short, and what is not ever-present fades quickly,” says Manisha Juthani, MD , a Yale Medicine infectious diseases specialist. The bubonic plague, for example, ravaged Europe in the Middle Ages—resurfacing again and again—but once it was under control, people started to forget about it, she says. “So, I would say one major lesson from a public health or infectious disease perspective is that it’s important to remember and recognize our history. This is a period we must remember.”
We asked our Yale Medicine experts to weigh in on what they think are lessons worth remembering, including those that might help us survive a future virus or nurture a resilience that could help with life in general.
Lesson 1: Masks are useful tools
What happened: The Centers for Disease Control and Prevention (CDC) relaxed its masking guidance for those who have been fully vaccinated. But when the pandemic began, it necessitated a global effort to ensure that everyone practiced behaviors to keep themselves healthy and safe—and keep others healthy as well. This included the widespread wearing of masks indoors and outside.
What we’ve learned: Not everyone practiced preventive measures such as mask wearing, maintaining a 6-foot distance, and washing hands frequently. But, Dr. Juthani says, “I do think many people have learned a whole lot about respiratory pathogens and viruses, and how they spread from one person to another, and that sort of old-school common sense—you know, if you don’t feel well—whether it’s COVID-19 or not—you don’t go to the party. You stay home.”
Masks are a case in point. They are a key COVID-19 prevention strategy because they provide a barrier that can keep respiratory droplets from spreading. Mask-wearing became more common across East Asia after the 2003 SARS outbreak in that part of the world. “There are many East Asian cultures where the practice is still that if you have a cold or a runny nose, you put on a mask,” Dr. Juthani says.
She hopes attitudes in the U.S. will shift in that direction after COVID-19. “I have heard from a number of people who are amazed that we've had no flu this year—and they know masks are one of the reasons,” she says. “They’ve told me, ‘When the winter comes around, if I'm going out to the grocery store, I may just put on a mask.’”
Lesson 2: Telehealth might become the new normal
What happened: Doctors and patients who have used telehealth (technology that allows them to conduct medical care remotely), found it can work well for certain appointments, ranging from cardiology check-ups to therapy for a mental health condition. Many patients who needed a medical test have also discovered it may be possible to substitute a home version.
What we’ve learned: While there are still problems for which you need to see a doctor in person, the pandemic introduced a new urgency to what had been a gradual switchover to platforms like Zoom for remote patient visits.
More doctors also encouraged patients to track their blood pressure at home , and to use at-home equipment for such purposes as diagnosing sleep apnea and even testing for colon cancer . Doctors also can fine-tune cochlear implants remotely .
“It happened very quickly,” says Sharon Stoll, DO, a neurologist. One group that has benefitted is patients who live far away, sometimes in other parts of the country—or even the world, she says. “I always like to see my patients at least twice a year. Now, we can see each other in person once a year, and if issues come up, we can schedule a telehealth visit in-between,” Dr. Stoll says. “This way I may hear about an issue before it becomes a problem, because my patients have easier access to me, and I have easier access to them.”
Meanwhile, insurers are becoming more likely to cover telehealth, Dr. Stoll adds. “That is a silver lining that will hopefully continue.”
Lesson 3: Vaccines are powerful tools
What happened: Given the recent positive results from vaccine trials, once again vaccines are proving to be powerful for preventing disease.
What we’ve learned: Vaccines really are worth getting, says Dr. Stoll, who had COVID-19 and experienced lingering symptoms, including chronic headaches . “I have lots of conversations—and sometimes arguments—with people about vaccines,” she says. Some don’t like the idea of side effects. “I had vaccine side effects and I’ve had COVID-19 side effects, and I say nothing compares to the actual illness. Unfortunately, I speak from experience.”
Dr. Juthani hopes the COVID-19 vaccine spotlight will motivate people to keep up with all of their vaccines, including childhood and adult vaccines for such diseases as measles , chicken pox, shingles , and other viruses. She says people have told her they got the flu vaccine this year after skipping it in previous years. (The CDC has reported distributing an exceptionally high number of doses this past season.)
But, she cautions that a vaccine is not a magic bullet—and points out that scientists can’t always produce one that works. “As advanced as science is, there have been multiple failed efforts to develop a vaccine against the HIV virus,” she says. “This time, we were lucky that we were able build on the strengths that we've learned from many other vaccine development strategies to develop multiple vaccines for COVID-19 .”
Lesson 4: Everyone is not treated equally, especially in a pandemic
What happened: COVID-19 magnified disparities that have long been an issue for a variety of people.
What we’ve learned: Racial and ethnic minority groups especially have had disproportionately higher rates of hospitalization for COVID-19 than non-Hispanic white people in every age group, and many other groups faced higher levels of risk or stress. These groups ranged from working mothers who also have primary responsibility for children, to people who have essential jobs, to those who live in rural areas where there is less access to health care.
“One thing that has been recognized is that when people were told to work from home, you needed to have a job that you could do in your house on a computer,” says Dr. Juthani. “Many people who were well off were able do that, but they still needed to have food, which requires grocery store workers and truck drivers. Nursing home residents still needed certified nursing assistants coming to work every day to care for them and to bathe them.”
As far as racial inequities, Dr. Juthani cites President Biden’s appointment of Yale Medicine’s Marcella Nunez-Smith, MD, MHS , as inaugural chair of a federal COVID-19 Health Equity Task Force. “Hopefully the new focus is a first step,” Dr. Juthani says.
Lesson 5: We need to take mental health seriously
What happened: There was a rise in reported mental health problems that have been described as “a second pandemic,” highlighting mental health as an issue that needs to be addressed.
What we’ve learned: Arman Fesharaki-Zadeh, MD, PhD , a behavioral neurologist and neuropsychiatrist, believes the number of mental health disorders that were on the rise before the pandemic is surging as people grapple with such matters as juggling work and childcare, job loss, isolation, and losing a loved one to COVID-19.
The CDC reports that the percentage of adults who reported symptoms of anxiety of depression in the past 7 days increased from 36.4 to 41.5 % from August 2020 to February 2021. Other reports show that having COVID-19 may contribute, too, with its lingering or long COVID symptoms, which can include “foggy mind,” anxiety , depression, and post-traumatic stress disorder .
“We’re seeing these problems in our clinical setting very, very often,” Dr. Fesharaki-Zadeh says. “By virtue of necessity, we can no longer ignore this. We're seeing these folks, and we have to take them seriously.”
Lesson 6: We have the capacity for resilience
What happened: While everyone’s situation is different (and some people have experienced tremendous difficulties), many have seen that it’s possible to be resilient in a crisis.
What we’ve learned: People have practiced self-care in a multitude of ways during the pandemic as they were forced to adjust to new work schedules, change their gym routines, and cut back on socializing. Many started seeking out new strategies to counter the stress.
“I absolutely believe in the concept of resilience, because we have this effective reservoir inherent in all of us—be it the product of evolution, or our ancestors going through catastrophes, including wars, famines, and plagues,” Dr. Fesharaki-Zadeh says. “I think inherently, we have the means to deal with crisis. The fact that you and I are speaking right now is the result of our ancestors surviving hardship. I think resilience is part of our psyche. It's part of our DNA, essentially.”
Dr. Fesharaki-Zadeh believes that even small changes are highly effective tools for creating resilience. The changes he suggests may sound like the same old advice: exercise more, eat healthy food, cut back on alcohol, start a meditation practice, keep up with friends and family. “But this is evidence-based advice—there has been research behind every one of these measures,” he says.
But we have to also be practical, he notes. “If you feel overwhelmed by doing too many things, you can set a modest goal with one new habit—it could be getting organized around your sleep. Once you’ve succeeded, move on to another one. Then you’re building momentum.”
Lesson 7: Community is essential—and technology is too
What happened: People who were part of a community during the pandemic realized the importance of human connection, and those who didn’t have that kind of support realized they need it.
What we’ve learned: Many of us have become aware of how much we need other people—many have managed to maintain their social connections, even if they had to use technology to keep in touch, Dr. Juthani says. “There's no doubt that it's not enough, but even that type of community has helped people.”
Even people who aren’t necessarily friends or family are important. Dr. Juthani recalled how she encouraged her mail carrier to sign up for the vaccine, soon learning that the woman’s mother and husband hadn’t gotten it either. “They are all vaccinated now,” Dr. Juthani says. “So, even by word of mouth, community is a way to make things happen.”
It’s important to note that some people are naturally introverted and may have enjoyed having more solitude when they were forced to stay at home—and they should feel comfortable with that, Dr. Fesharaki-Zadeh says. “I think one has to keep temperamental tendencies like this in mind.”
But loneliness has been found to suppress the immune system and be a precursor to some diseases, he adds. “Even for introverted folks, the smallest circle is preferable to no circle at all,” he says.
Lesson 8: Sometimes you need a dose of humility
What happened: Scientists and nonscientists alike learned that a virus can be more powerful than they are. This was evident in the way knowledge about the virus changed over time in the past year as scientific investigation of it evolved.
What we’ve learned: “As infectious disease doctors, we were resident experts at the beginning of the pandemic because we understand pathogens in general, and based on what we’ve seen in the past, we might say there are certain things that are likely to be true,” Dr. Juthani says. “But we’ve seen that we have to take these pathogens seriously. We know that COVID-19 is not the flu. All these strokes and clots, and the loss of smell and taste that have gone on for months are things that we could have never known or predicted. So, you have to have respect for the unknown and respect science, but also try to give scientists the benefit of the doubt,” she says.
“We have been doing the best we can with the knowledge we have, in the time that we have it,” Dr. Juthani says. “I think most of us have had to have the humility to sometimes say, ‘I don't know. We're learning as we go.’"
Information provided in Yale Medicine articles is for general informational purposes only. No content in the articles should ever be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider with any questions you have regarding a medical condition.
More news from Yale Medicine

The complexity of managing COVID-19: How important is good governance?
- Download the essay
Subscribe to Global Connection
Alaka m. basu , amb alaka m. basu professor, department of global development - cornell university, senior fellow - united nations foundation kaushik basu , and kaushik basu nonresident senior fellow - global economy and development @kaushikcbasu jose maria u. tapia jmut jose maria u. tapia student - cornell university.
November 17, 2020
- 13 min read
This essay is part of “ Reimagining the global economy: Building back better in a post-COVID-19 world ,” a collection of 12 essays presenting new ideas to guide policies and shape debates in a post-COVID-19 world.
The COVID-19 pandemic has exposed the inadequacy of public health systems worldwide, casting a shadow that we could not have imagined even a year ago. As the fog of confusion lifts and we begin to understand the rudiments of how the virus behaves, the end of the pandemic is nowhere in sight. The number of cases and the deaths continue to rise. The latter breached the 1 million mark a few weeks ago and it looks likely now that, in terms of severity, this pandemic will surpass the Asian Flu of 1957-58 and the Hong Kong Flu of 1968-69.
Moreover, a parallel problem may well exceed the direct death toll from the virus. We are referring to the growing economic crises globally, and the prospect that these may hit emerging economies especially hard.
The economic fall-out is not entirely the direct outcome of the COVID-19 pandemic but a result of how we have responded to it—what measures governments took and how ordinary people, workers, and firms reacted to the crisis. The government activism to contain the virus that we saw this time exceeds that in previous such crises, which may have dampened the spread of the COVID-19 but has extracted a toll from the economy.
This essay takes stock of the policies adopted by governments in emerging economies, and what effect these governance strategies may have had, and then speculates about what the future is likely to look like and what we may do here on.
Nations that build walls to keep out goods, people and talent will get out-competed by other nations in the product market.
It is becoming clear that the scramble among several emerging economies to imitate and outdo European and North American countries was a mistake. We get a glimpse of this by considering two nations continents apart, the economies of which have been among the hardest hit in the world, namely, Peru and India. During the second quarter of 2020, Peru saw an annual growth of -30.2 percent and India -23.9 percent. From the global Q2 data that have emerged thus far, Peru and India are among the four slowest growing economies in the world. Along with U.K and Tunisia these are the only nations that lost more than 20 percent of their GDP. 1
COVID-19-related mortality statistics, and, in particular, the Crude Mortality Rate (CMR), however imperfect, are the most telling indicator of the comparative scale of the pandemic in different countries. At first glance, from the end of October 2020, Peru, with 1039 COVID-19 deaths per million population looks bad by any standard and much worse than India with 88. Peru’s CMR is currently among the highest reported globally.
However, both Peru and India need to be placed in regional perspective. For reasons that are likely to do with the history of past diseases, there are striking regional differences in the lethality of the virus (Figure 11.1). South America is worse hit than any other world region, and Asia and Africa seem to have got it relatively lightly, in contrast to Europe and America. The stark regional difference cries out for more epidemiological analysis. But even as we await that, these are differences that cannot be ignored.
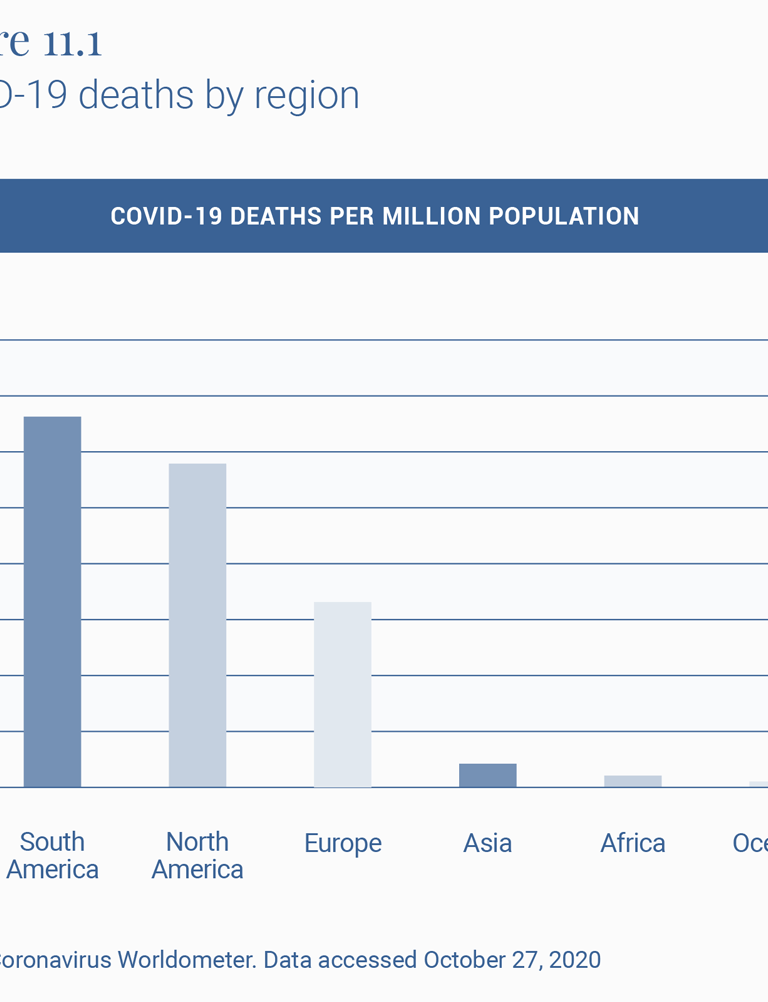
To understand the effect of policy interventions, it is therefore important to look at how these countries fare within their own regions, which have had similar histories of illnesses and viruses (Figure 11.2). Both Peru and India do much worse than the neighbors with whom they largely share their social, economic, ecological and demographic features. Peru’s COVID-19 mortality rate per million population, or CMR, of 1039 is ahead of the second highest, Brazil at 749, and almost twice that of Argentina at 679.
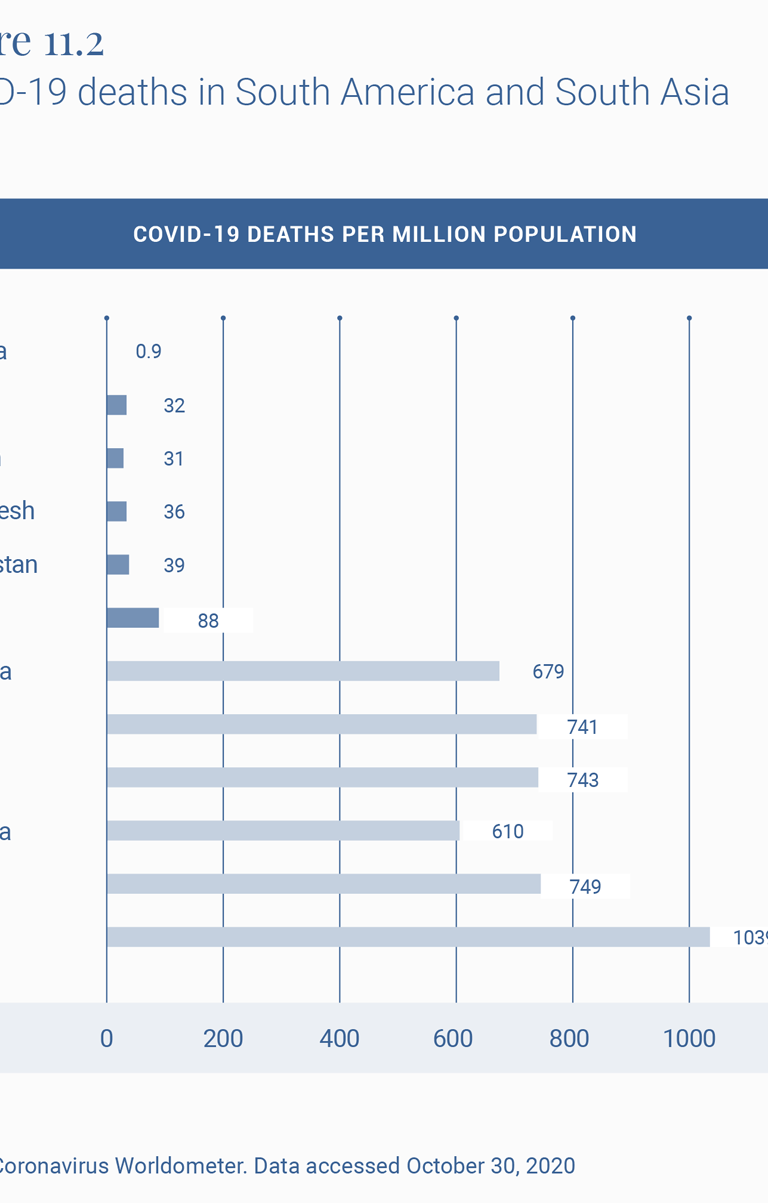
Similarly, India at 88 compares well with Europe and the U.S., as does virtually all of Asia and Africa, but is doing much worse than its neighbors, with the second worst country in the region, Afghanistan, experiencing less than half the death rate of India.
The official Indian statement that up to 78,000 deaths 2 were averted by the lockdown has been criticized 3 for its assumptions. A more reasonable exercise is to estimate the excess deaths experienced by a country that breaks away from the pattern of its regional neighbors. So, for example, if India had experienced Afghanistan’s COVID-19 mortality rate, it would by now have had 54,112 deaths. And if it had the rate reported by Bangladesh, it would have had 49,950 deaths from COVID-19 today. In other words, more than half its current toll of some 122,099 COVID-19 deaths would have been avoided if it had experienced the same virus hit as its neighbors.
What might explain this outlier experience of COVID-19 CMRs and economic downslide in India and Peru? If the regional background conditions are broadly similar, one is left to ask if it is in fact the policy response that differed markedly and might account for these relatively poor outcomes.
Peru and India have performed poorly in terms of GDP growth rate in Q2 2020 among the countries displayed in Table 2, and given that both these countries are often treated as case studies of strong governance, this draws attention to the fact that there may be a dissonance between strong governance and good governance.
The turnaround for India has been especially surprising, given that until a few years ago it was among the three fastest growing economies in the world. The slowdown began in 2016, though the sharp downturn, sharper than virtually all other countries, occurred after the lockdown.
On the COVID-19 policy front, both India and Peru have become known for what the Oxford University’s COVID Policy Tracker 4 calls the “stringency” of the government’s response to the epidemic. At 8 pm on March 24, 2020, the Indian government announced, with four hours’ notice, a complete nationwide shutdown. Virtually all movement outside the perimeter of one’s home was officially sought to be brought to a standstill. Naturally, as described in several papers, such as that of Ray and Subramanian, 5 this meant that most economic life also came to a sudden standstill, which in turn meant that hundreds of millions of workers in the informal, as well as more marginally formal sectors, lost their livelihoods.
In addition, tens of millions of these workers, being migrant workers in places far-flung from their original homes, also lost their temporary homes and their savings with these lost livelihoods, so that the only safe space that beckoned them was their place of origin in small towns and villages often hundreds of miles away from their places of work.
After a few weeks of precarious living in their migrant destinations, they set off, on foot since trains and buses had been stopped, for these towns and villages, creating a “lockdown and scatter” that spread the virus from the city to the town and the town to the village. Indeed, “lockdown” is a bit of a misnomer for what happened in India, since over 20 million people did exactly the opposite of what one does in a lockdown. Thus India had a strange combination of lockdown some and scatter the rest, like in no other country. They spilled out and scattered in ways they would otherwise not do. It is not surprising that the infection, which was marginally present in rural areas (23 percent in April), now makes up some 54 percent of all cases in India. 6
In Peru too, the lockdown was sudden, nationwide, long drawn out and stringent. 7 Jobs were lost, financial aid was difficult to disburse, migrant workers were forced to return home, and the virus has now spread to all parts of the country with death rates from it surpassing almost every other part of the world.
As an aside, to think about ways of implementing lockdowns that are less stringent and geographically as well as functionally less total, an example from yet another continent is instructive. Ethiopia, with a COVID-19 death rate of 13 per million population seems to have bettered the already relatively low African rate of 31 in Table 1. 8
We hope that human beings will emerge from this crisis more aware of the problems of sustainability.
The way forward
We next move from the immediate crisis to the medium term. Where is the world headed and how should we deal with the new world? Arguably, that two sectors that will emerge larger and stronger in the post-pandemic world are: digital technology and outsourcing, and healthcare and pharmaceuticals.
The last 9 months of the pandemic have been a huge training ground for people in the use of digital technology—Zoom, WebEx, digital finance, and many others. This learning-by-doing exercise is likely to give a big boost to outsourcing, which has the potential to help countries like India, the Philippines, and South Africa.
Globalization may see a short-run retreat but, we believe, it will come back with a vengeance. Nations that build walls to keep out goods, people and talent will get out-competed by other nations in the product market. This realization will make most countries reverse their knee-jerk anti-globalization; and the ones that do not will cease to be important global players. Either way, globalization will be back on track and with a much greater amount of outsourcing.
To return, more critically this time, to our earlier aside on Ethiopia, its historical and contemporary record on tampering with internet connectivity 9 in an attempt to muzzle inter-ethnic tensions and political dissent will not serve it well in such a post-pandemic scenario. This is a useful reminder for all emerging market economies.
We hope that human beings will emerge from this crisis more aware of the problems of sustainability. This could divert some demand from luxury goods to better health, and what is best described as “creative consumption”: art, music, and culture. 10 The former will mean much larger healthcare and pharmaceutical sectors.
But to take advantage of these new opportunities, nations will need to navigate the current predicament so that they have a viable economy once the pandemic passes. Thus it is important to be able to control the pandemic while keeping the economy open. There is some emerging literature 11 on this, but much more is needed. This is a governance challenge of a kind rarely faced, because the pandemic has disrupted normal markets and there is need, at least in the short run, for governments to step in to fill the caveat.
Emerging economies will have to devise novel governance strategies for doing this double duty of tamping down on new infections without strident controls on economic behavior and without blindly imitating Europe and America.
Here is an example. One interesting opportunity amidst this chaos is to tap into the “resource” of those who have already had COVID-19 and are immune, even if only in the short-term—we still have no definitive evidence on the length of acquired immunity. These people can be offered a high salary to work in sectors that require physical interaction with others. This will help keep supply chains unbroken. Normally, the market would have on its own caused such a salary increase but in this case, the main benefit of marshaling this labor force is on the aggregate economy and GDP and therefore is a classic case of positive externality, which the free market does not adequately reward. It is more a challenge of governance. As with most economic policy, this will need careful research and design before being implemented. We have to be aware that a policy like this will come with its risk of bribery and corruption. There is also the moral hazard challenge of poor people choosing to get COVID-19 in order to qualify for these special jobs. Safeguards will be needed against these risks. But we believe that any government that succeeds in implementing an intelligently-designed intervention to draw on this huge, under-utilized resource can have a big, positive impact on the economy 12 .
This is just one idea. We must innovate in different ways to survive the crisis and then have the ability to navigate the new world that will emerge, hopefully in the not too distant future.
Related Content
Emiliana Vegas, Rebecca Winthrop
Homi Kharas, John W. McArthur
Anthony F. Pipa, Max Bouchet
Note: We are grateful for financial support from Cornell University’s Hatfield Fund for the research associated with this paper. We also wish to express our gratitude to Homi Kharas for many suggestions and David Batcheck for generous editorial help.
- “GDP Annual Growth Rate – Forecast 2020-2022,” Trading Economics, https://tradingeconomics.com/forecast/gdp-annual-growth-rate.
- “Government Cites Various Statistical Models, Says Averted Between 1.4 Million-2.9 Million Cases Due To Lockdown,” Business World, May 23, 2020, www.businessworld.in/article/Government-Cites-Various-Statistical-Models-Says-Averted-Between-1-4-million-2-9-million-Cases-Due-To-Lockdown/23-05-2020-193002/.
- Suvrat Raju, “Did the Indian lockdown avert deaths?” medRxiv , July 5, 2020, https://europepmc.org/article/ppr/ppr183813#A1.
- “COVID Policy Tracker,” Oxford University, https://github.com/OxCGRT/covid-policy-tracker t.
- Debraj Ray and S. Subramanian, “India’s Lockdown: An Interim Report,” NBER Working Paper, May 2020, https://www.nber.org/papers/w27282.
- Gopika Gopakumar and Shayan Ghosh, “Rural recovery could slow down as cases rise, says Ghosh,” Mint, August 19, 2020, https://www.livemint.com/news/india/rural-recovery-could-slow-down-as-cases-rise-says-ghosh-11597801644015.html.
- Pierina Pighi Bel and Jake Horton, “Coronavirus: What’s happening in Peru?,” BBC, July 9, 2020, https://www.bbc.com/news/world-latin-america-53150808.
- “No lockdown, few ventilators, but Ethiopia is beating Covid-19,” Financial Times, May 27, 2020, https://www.ft.com/content/7c6327ca-a00b-11ea-b65d-489c67b0d85d.
- Cara Anna, “Ethiopia enters 3rd week of internet shutdown after unrest,” Washington Post, July 14, 2020, https://www.washingtonpost.com/world/africa/ethiopia-enters-3rd-week-of-internet-shutdown-after-unrest/2020/07/14/4699c400-c5d6-11ea-a825-8722004e4150_story.html.
- Patrick Kabanda, The Creative Wealth of Nations: Can the Arts Advance Development? (Cambridge: Cambridge University Press, 2018).
- Guanlin Li et al, “Disease-dependent interaction policies to support health and economic outcomes during the COVID-19 epidemic,” medRxiv, August 2020, https://www.medrxiv.org/content/10.1101/2020.08.24.20180752v3.
- For helpful discussion concerning this idea, we are grateful to Turab Hussain, Daksh Walia and Mehr-un-Nisa, during a seminar of South Asian Economics Students’ Meet (SAESM).
Global Economy and Development
Tedros Adhanom-Ghebreyesus
May 9, 2024
Robin Brooks
Emily Gustafsson-Wright, Elyse Painter
May 8, 2024
- Research article
- Open access
- Published: 04 June 2021
Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews
- Israel Júnior Borges do Nascimento 1 , 2 ,
- Dónal P. O’Mathúna 3 , 4 ,
- Thilo Caspar von Groote 5 ,
- Hebatullah Mohamed Abdulazeem 6 ,
- Ishanka Weerasekara 7 , 8 ,
- Ana Marusic 9 ,
- Livia Puljak ORCID: orcid.org/0000-0002-8467-6061 10 ,
- Vinicius Tassoni Civile 11 ,
- Irena Zakarija-Grkovic 9 ,
- Tina Poklepovic Pericic 9 ,
- Alvaro Nagib Atallah 11 ,
- Santino Filoso 12 ,
- Nicola Luigi Bragazzi 13 &
- Milena Soriano Marcolino 1
On behalf of the International Network of Coronavirus Disease 2019 (InterNetCOVID-19)
BMC Infectious Diseases volume 21 , Article number: 525 ( 2021 ) Cite this article
16k Accesses
29 Citations
13 Altmetric
Metrics details
Navigating the rapidly growing body of scientific literature on the SARS-CoV-2 pandemic is challenging, and ongoing critical appraisal of this output is essential. We aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Nine databases (Medline, EMBASE, Cochrane Library, CINAHL, Web of Sciences, PDQ-Evidence, WHO’s Global Research, LILACS, and Epistemonikos) were searched from December 1, 2019, to March 24, 2020. Systematic reviews analyzing primary studies of COVID-19 were included. Two authors independently undertook screening, selection, extraction (data on clinical symptoms, prevalence, pharmacological and non-pharmacological interventions, diagnostic test assessment, laboratory, and radiological findings), and quality assessment (AMSTAR 2). A meta-analysis was performed of the prevalence of clinical outcomes.
Eighteen systematic reviews were included; one was empty (did not identify any relevant study). Using AMSTAR 2, confidence in the results of all 18 reviews was rated as “critically low”. Identified symptoms of COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%) and gastrointestinal complaints (5–9%). Severe symptoms were more common in men. Elevated C-reactive protein and lactate dehydrogenase, and slightly elevated aspartate and alanine aminotransferase, were commonly described. Thrombocytopenia and elevated levels of procalcitonin and cardiac troponin I were associated with severe disease. A frequent finding on chest imaging was uni- or bilateral multilobar ground-glass opacity. A single review investigated the impact of medication (chloroquine) but found no verifiable clinical data. All-cause mortality ranged from 0.3 to 13.9%.
Conclusions
In this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic were of questionable usefulness. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards.
Peer Review reports
The spread of the “Severe Acute Respiratory Coronavirus 2” (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [ 1 ]. The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [ 2 ], causing massive economic strain, and escalating healthcare and public health expenses [ 3 , 4 ].
The research community has responded by publishing an impressive number of scientific reports related to COVID-19. The world was alerted to the new disease at the beginning of 2020 [ 1 ], and by mid-March 2020, more than 2000 articles had been published on COVID-19 in scholarly journals, with 25% of them containing original data [ 5 ]. The living map of COVID-19 evidence, curated by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), contained more than 40,000 records by February 2021 [ 6 ]. More than 100,000 records on PubMed were labeled as “SARS-CoV-2 literature, sequence, and clinical content” by February 2021 [ 7 ].
Due to publication speed, the research community has voiced concerns regarding the quality and reproducibility of evidence produced during the COVID-19 pandemic, warning of the potential damaging approach of “publish first, retract later” [ 8 ]. It appears that these concerns are not unfounded, as it has been reported that COVID-19 articles were overrepresented in the pool of retracted articles in 2020 [ 9 ]. These concerns about inadequate evidence are of major importance because they can lead to poor clinical practice and inappropriate policies [ 10 ].
Systematic reviews are a cornerstone of today’s evidence-informed decision-making. By synthesizing all relevant evidence regarding a particular topic, systematic reviews reflect the current scientific knowledge. Systematic reviews are considered to be at the highest level in the hierarchy of evidence and should be used to make informed decisions. However, with high numbers of systematic reviews of different scope and methodological quality being published, overviews of multiple systematic reviews that assess their methodological quality are essential [ 11 , 12 , 13 ]. An overview of systematic reviews helps identify and organize the literature and highlights areas of priority in decision-making.
In this overview of systematic reviews, we aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Methodology
Research question.
This overview’s primary objective was to summarize and critically appraise systematic reviews that assessed any type of primary clinical data from patients infected with SARS-CoV-2. Our research question was purposefully broad because we wanted to analyze as many systematic reviews as possible that were available early following the COVID-19 outbreak.
Study design
We conducted an overview of systematic reviews. The idea for this overview originated in a protocol for a systematic review submitted to PROSPERO (CRD42020170623), which indicated a plan to conduct an overview.
Overviews of systematic reviews use explicit and systematic methods for searching and identifying multiple systematic reviews addressing related research questions in the same field to extract and analyze evidence across important outcomes. Overviews of systematic reviews are in principle similar to systematic reviews of interventions, but the unit of analysis is a systematic review [ 14 , 15 , 16 ].
We used the overview methodology instead of other evidence synthesis methods to allow us to collate and appraise multiple systematic reviews on this topic, and to extract and analyze their results across relevant topics [ 17 ]. The overview and meta-analysis of systematic reviews allowed us to investigate the methodological quality of included studies, summarize results, and identify specific areas of available or limited evidence, thereby strengthening the current understanding of this novel disease and guiding future research [ 13 ].
A reporting guideline for overviews of reviews is currently under development, i.e., Preferred Reporting Items for Overviews of Reviews (PRIOR) [ 18 ]. As the PRIOR checklist is still not published, this study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 statement [ 19 ]. The methodology used in this review was adapted from the Cochrane Handbook for Systematic Reviews of Interventions and also followed established methodological considerations for analyzing existing systematic reviews [ 14 ].
Approval of a research ethics committee was not necessary as the study analyzed only publicly available articles.
Eligibility criteria
Systematic reviews were included if they analyzed primary data from patients infected with SARS-CoV-2 as confirmed by RT-PCR or another pre-specified diagnostic technique. Eligible reviews covered all topics related to COVID-19 including, but not limited to, those that reported clinical symptoms, diagnostic methods, therapeutic interventions, laboratory findings, or radiological results. Both full manuscripts and abbreviated versions, such as letters, were eligible.
No restrictions were imposed on the design of the primary studies included within the systematic reviews, the last search date, whether the review included meta-analyses or language. Reviews related to SARS-CoV-2 and other coronaviruses were eligible, but from those reviews, we analyzed only data related to SARS-CoV-2.
No consensus definition exists for a systematic review [ 20 ], and debates continue about the defining characteristics of a systematic review [ 21 ]. Cochrane’s guidance for overviews of reviews recommends setting pre-established criteria for making decisions around inclusion [ 14 ]. That is supported by a recent scoping review about guidance for overviews of systematic reviews [ 22 ].
Thus, for this study, we defined a systematic review as a research report which searched for primary research studies on a specific topic using an explicit search strategy, had a detailed description of the methods with explicit inclusion criteria provided, and provided a summary of the included studies either in narrative or quantitative format (such as a meta-analysis). Cochrane and non-Cochrane systematic reviews were considered eligible for inclusion, with or without meta-analysis, and regardless of the study design, language restriction and methodology of the included primary studies. To be eligible for inclusion, reviews had to be clearly analyzing data related to SARS-CoV-2 (associated or not with other viruses). We excluded narrative reviews without those characteristics as these are less likely to be replicable and are more prone to bias.
Scoping reviews and rapid reviews were eligible for inclusion in this overview if they met our pre-defined inclusion criteria noted above. We included reviews that addressed SARS-CoV-2 and other coronaviruses if they reported separate data regarding SARS-CoV-2.
Information sources
Nine databases were searched for eligible records published between December 1, 2019, and March 24, 2020: Cochrane Database of Systematic Reviews via Cochrane Library, PubMed, EMBASE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Web of Sciences, LILACS (Latin American and Caribbean Health Sciences Literature), PDQ-Evidence, WHO’s Global Research on Coronavirus Disease (COVID-19), and Epistemonikos.
The comprehensive search strategy for each database is provided in Additional file 1 and was designed and conducted in collaboration with an information specialist. All retrieved records were primarily processed in EndNote, where duplicates were removed, and records were then imported into the Covidence platform [ 23 ]. In addition to database searches, we screened reference lists of reviews included after screening records retrieved via databases.
Study selection
All searches, screening of titles and abstracts, and record selection, were performed independently by two investigators using the Covidence platform [ 23 ]. Articles deemed potentially eligible were retrieved for full-text screening carried out independently by two investigators. Discrepancies at all stages were resolved by consensus. During the screening, records published in languages other than English were translated by a native/fluent speaker.
Data collection process
We custom designed a data extraction table for this study, which was piloted by two authors independently. Data extraction was performed independently by two authors. Conflicts were resolved by consensus or by consulting a third researcher.
We extracted the following data: article identification data (authors’ name and journal of publication), search period, number of databases searched, population or settings considered, main results and outcomes observed, and number of participants. From Web of Science (Clarivate Analytics, Philadelphia, PA, USA), we extracted journal rank (quartile) and Journal Impact Factor (JIF).
We categorized the following as primary outcomes: all-cause mortality, need for and length of mechanical ventilation, length of hospitalization (in days), admission to intensive care unit (yes/no), and length of stay in the intensive care unit.
The following outcomes were categorized as exploratory: diagnostic methods used for detection of the virus, male to female ratio, clinical symptoms, pharmacological and non-pharmacological interventions, laboratory findings (full blood count, liver enzymes, C-reactive protein, d-dimer, albumin, lipid profile, serum electrolytes, blood vitamin levels, glucose levels, and any other important biomarkers), and radiological findings (using radiography, computed tomography, magnetic resonance imaging or ultrasound).
We also collected data on reporting guidelines and requirements for the publication of systematic reviews and meta-analyses from journal websites where included reviews were published.
Quality assessment in individual reviews
Two researchers independently assessed the reviews’ quality using the “A MeaSurement Tool to Assess Systematic Reviews 2 (AMSTAR 2)”. We acknowledge that the AMSTAR 2 was created as “a critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both” [ 24 ]. However, since AMSTAR 2 was designed for systematic reviews of intervention trials, and we included additional types of systematic reviews, we adjusted some AMSTAR 2 ratings and reported these in Additional file 2 .
Adherence to each item was rated as follows: yes, partial yes, no, or not applicable (such as when a meta-analysis was not conducted). The overall confidence in the results of the review is rated as “critically low”, “low”, “moderate” or “high”, according to the AMSTAR 2 guidance based on seven critical domains, which are items 2, 4, 7, 9, 11, 13, 15 as defined by AMSTAR 2 authors [ 24 ]. We reported our adherence ratings for transparency of our decision with accompanying explanations, for each item, in each included review.
One of the included systematic reviews was conducted by some members of this author team [ 25 ]. This review was initially assessed independently by two authors who were not co-authors of that review to prevent the risk of bias in assessing this study.
Synthesis of results
For data synthesis, we prepared a table summarizing each systematic review. Graphs illustrating the mortality rate and clinical symptoms were created. We then prepared a narrative summary of the methods, findings, study strengths, and limitations.
For analysis of the prevalence of clinical outcomes, we extracted data on the number of events and the total number of patients to perform proportional meta-analysis using RStudio© software, with the “meta” package (version 4.9–6), using the “metaprop” function for reviews that did not perform a meta-analysis, excluding case studies because of the absence of variance. For reviews that did not perform a meta-analysis, we presented pooled results of proportions with their respective confidence intervals (95%) by the inverse variance method with a random-effects model, using the DerSimonian-Laird estimator for τ 2 . We adjusted data using Freeman-Tukey double arcosen transformation. Confidence intervals were calculated using the Clopper-Pearson method for individual studies. We created forest plots using the RStudio© software, with the “metafor” package (version 2.1–0) and “forest” function.
Managing overlapping systematic reviews
Some of the included systematic reviews that address the same or similar research questions may include the same primary studies in overviews. Including such overlapping reviews may introduce bias when outcome data from the same primary study are included in the analyses of an overview multiple times. Thus, in summaries of evidence, multiple-counting of the same outcome data will give data from some primary studies too much influence [ 14 ]. In this overview, we did not exclude overlapping systematic reviews because, according to Cochrane’s guidance, it may be appropriate to include all relevant reviews’ results if the purpose of the overview is to present and describe the current body of evidence on a topic [ 14 ]. To avoid any bias in summary estimates associated with overlapping reviews, we generated forest plots showing data from individual systematic reviews, but the results were not pooled because some primary studies were included in multiple reviews.
Our search retrieved 1063 publications, of which 175 were duplicates. Most publications were excluded after the title and abstract analysis ( n = 860). Among the 28 studies selected for full-text screening, 10 were excluded for the reasons described in Additional file 3 , and 18 were included in the final analysis (Fig. 1 ) [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Reference list screening did not retrieve any additional systematic reviews.
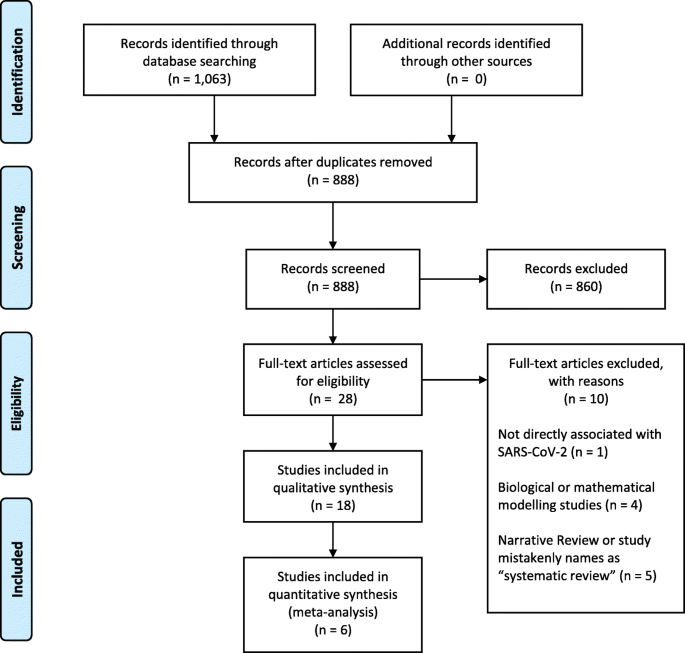
PRISMA flow diagram
Characteristics of included reviews
Summary features of 18 systematic reviews are presented in Table 1 . They were published in 14 different journals. Only four of these journals had specific requirements for systematic reviews (with or without meta-analysis): European Journal of Internal Medicine, Journal of Clinical Medicine, Ultrasound in Obstetrics and Gynecology, and Clinical Research in Cardiology . Two journals reported that they published only invited reviews ( Journal of Medical Virology and Clinica Chimica Acta ). Three systematic reviews in our study were published as letters; one was labeled as a scoping review and another as a rapid review (Table 2 ).
All reviews were published in English, in first quartile (Q1) journals, with JIF ranging from 1.692 to 6.062. One review was empty, meaning that its search did not identify any relevant studies; i.e., no primary studies were included [ 36 ]. The remaining 17 reviews included 269 unique studies; the majority ( N = 211; 78%) were included in only a single review included in our study (range: 1 to 12). Primary studies included in the reviews were published between December 2019 and March 18, 2020, and comprised case reports, case series, cohorts, and other observational studies. We found only one review that included randomized clinical trials [ 38 ]. In the included reviews, systematic literature searches were performed from 2019 (entire year) up to March 9, 2020. Ten systematic reviews included meta-analyses. The list of primary studies found in the included systematic reviews is shown in Additional file 4 , as well as the number of reviews in which each primary study was included.
Population and study designs
Most of the reviews analyzed data from patients with COVID-19 who developed pneumonia, acute respiratory distress syndrome (ARDS), or any other correlated complication. One review aimed to evaluate the effectiveness of using surgical masks on preventing transmission of the virus [ 36 ], one review was focused on pediatric patients [ 34 ], and one review investigated COVID-19 in pregnant women [ 37 ]. Most reviews assessed clinical symptoms, laboratory findings, or radiological results.
Systematic review findings
The summary of findings from individual reviews is shown in Table 2 . Overall, all-cause mortality ranged from 0.3 to 13.9% (Fig. 2 ).
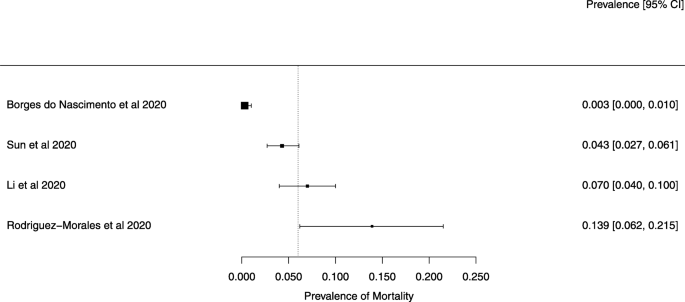
A meta-analysis of the prevalence of mortality
Clinical symptoms
Seven reviews described the main clinical manifestations of COVID-19 [ 26 , 28 , 29 , 34 , 35 , 39 , 41 ]. Three of them provided only a narrative discussion of symptoms [ 26 , 34 , 35 ]. In the reviews that performed a statistical analysis of the incidence of different clinical symptoms, symptoms in patients with COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%), gastrointestinal disorders, such as diarrhea, nausea or vomiting (5.0–9.0%), and others (including, in one study only: dizziness 12.1%) (Figs. 3 , 4 , 5 , 6 , 7 , 8 and 9 ). Three reviews assessed cough with and without sputum together; only one review assessed sputum production itself (28.5%).
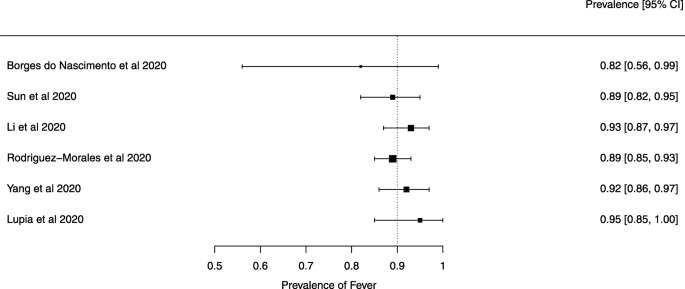
A meta-analysis of the prevalence of fever
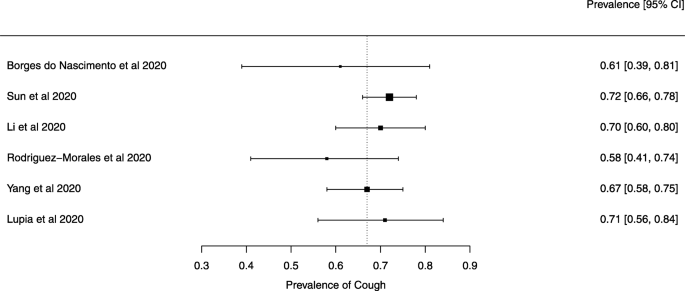
A meta-analysis of the prevalence of cough
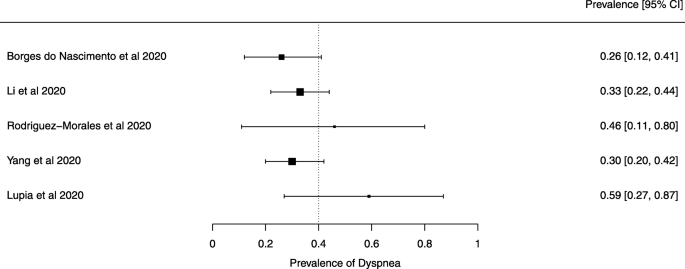
A meta-analysis of the prevalence of dyspnea
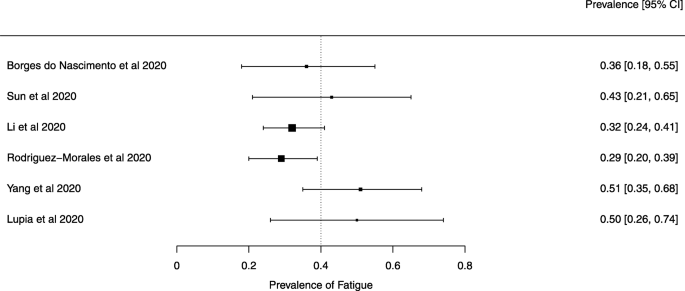
A meta-analysis of the prevalence of fatigue or myalgia
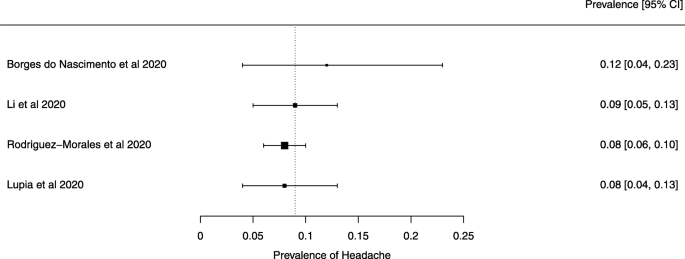
A meta-analysis of the prevalence of headache
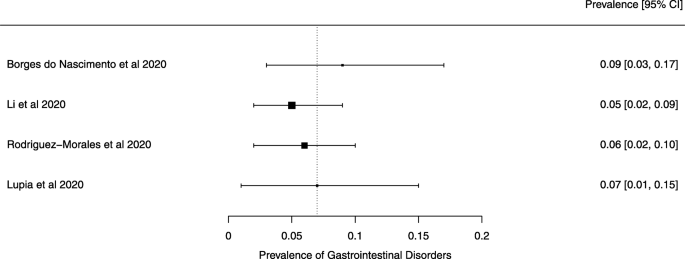
A meta-analysis of the prevalence of gastrointestinal disorders
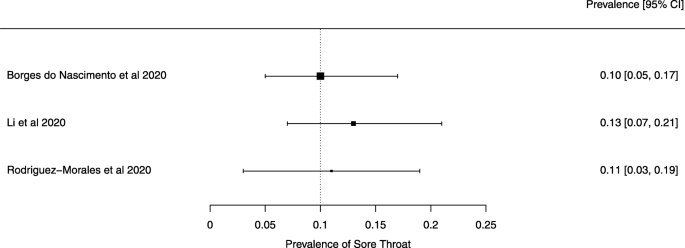
A meta-analysis of the prevalence of sore throat
Diagnostic aspects
Three reviews described methodologies, protocols, and tools used for establishing the diagnosis of COVID-19 [ 26 , 34 , 38 ]. The use of respiratory swabs (nasal or pharyngeal) or blood specimens to assess the presence of SARS-CoV-2 nucleic acid using RT-PCR assays was the most commonly used diagnostic method mentioned in the included studies. These diagnostic tests have been widely used, but their precise sensitivity and specificity remain unknown. One review included a Chinese study with clinical diagnosis with no confirmation of SARS-CoV-2 infection (patients were diagnosed with COVID-19 if they presented with at least two symptoms suggestive of COVID-19, together with laboratory and chest radiography abnormalities) [ 34 ].
Therapeutic possibilities
Pharmacological and non-pharmacological interventions (supportive therapies) used in treating patients with COVID-19 were reported in five reviews [ 25 , 27 , 34 , 35 , 38 ]. Antivirals used empirically for COVID-19 treatment were reported in seven reviews [ 25 , 27 , 34 , 35 , 37 , 38 , 41 ]; most commonly used were protease inhibitors (lopinavir, ritonavir, darunavir), nucleoside reverse transcriptase inhibitor (tenofovir), nucleotide analogs (remdesivir, galidesivir, ganciclovir), and neuraminidase inhibitors (oseltamivir). Umifenovir, a membrane fusion inhibitor, was investigated in two studies [ 25 , 35 ]. Possible supportive interventions analyzed were different types of oxygen supplementation and breathing support (invasive or non-invasive ventilation) [ 25 ]. The use of antibiotics, both empirically and to treat secondary pneumonia, was reported in six studies [ 25 , 26 , 27 , 34 , 35 , 38 ]. One review specifically assessed evidence on the efficacy and safety of the anti-malaria drug chloroquine [ 27 ]. It identified 23 ongoing trials investigating the potential of chloroquine as a therapeutic option for COVID-19, but no verifiable clinical outcomes data. The use of mesenchymal stem cells, antifungals, and glucocorticoids were described in four reviews [ 25 , 34 , 35 , 38 ].
Laboratory and radiological findings
Of the 18 reviews included in this overview, eight analyzed laboratory parameters in patients with COVID-19 [ 25 , 29 , 30 , 32 , 33 , 34 , 35 , 39 ]; elevated C-reactive protein levels, associated with lymphocytopenia, elevated lactate dehydrogenase, as well as slightly elevated aspartate and alanine aminotransferase (AST, ALT) were commonly described in those eight reviews. Lippi et al. assessed cardiac troponin I (cTnI) [ 25 ], procalcitonin [ 32 ], and platelet count [ 33 ] in COVID-19 patients. Elevated levels of procalcitonin [ 32 ] and cTnI [ 30 ] were more likely to be associated with a severe disease course (requiring intensive care unit admission and intubation). Furthermore, thrombocytopenia was frequently observed in patients with complicated COVID-19 infections [ 33 ].
Chest imaging (chest radiography and/or computed tomography) features were assessed in six reviews, all of which described a frequent pattern of local or bilateral multilobar ground-glass opacity [ 25 , 34 , 35 , 39 , 40 , 41 ]. Those six reviews showed that septal thickening, bronchiectasis, pleural and cardiac effusions, halo signs, and pneumothorax were observed in patients suffering from COVID-19.
Quality of evidence in individual systematic reviews
Table 3 shows the detailed results of the quality assessment of 18 systematic reviews, including the assessment of individual items and summary assessment. A detailed explanation for each decision in each review is available in Additional file 5 .
Using AMSTAR 2 criteria, confidence in the results of all 18 reviews was rated as “critically low” (Table 3 ). Common methodological drawbacks were: omission of prospective protocol submission or publication; use of inappropriate search strategy: lack of independent and dual literature screening and data-extraction (or methodology unclear); absence of an explanation for heterogeneity among the studies included; lack of reasons for study exclusion (or rationale unclear).
Risk of bias assessment, based on a reported methodological tool, and quality of evidence appraisal, in line with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method, were reported only in one review [ 25 ]. Five reviews presented a table summarizing bias, using various risk of bias tools [ 25 , 29 , 39 , 40 , 41 ]. One review analyzed “study quality” [ 37 ]. One review mentioned the risk of bias assessment in the methodology but did not provide any related analysis [ 28 ].
This overview of systematic reviews analyzed the first 18 systematic reviews published after the onset of the COVID-19 pandemic, up to March 24, 2020, with primary studies involving more than 60,000 patients. Using AMSTAR-2, we judged that our confidence in all those reviews was “critically low”. Ten reviews included meta-analyses. The reviews presented data on clinical manifestations, laboratory and radiological findings, and interventions. We found no systematic reviews on the utility of diagnostic tests.
Symptoms were reported in seven reviews; most of the patients had a fever, cough, dyspnea, myalgia or muscle fatigue, and gastrointestinal disorders such as diarrhea, nausea, or vomiting. Olfactory dysfunction (anosmia or dysosmia) has been described in patients infected with COVID-19 [ 43 ]; however, this was not reported in any of the reviews included in this overview. During the SARS outbreak in 2002, there were reports of impairment of the sense of smell associated with the disease [ 44 , 45 ].
The reported mortality rates ranged from 0.3 to 14% in the included reviews. Mortality estimates are influenced by the transmissibility rate (basic reproduction number), availability of diagnostic tools, notification policies, asymptomatic presentations of the disease, resources for disease prevention and control, and treatment facilities; variability in the mortality rate fits the pattern of emerging infectious diseases [ 46 ]. Furthermore, the reported cases did not consider asymptomatic cases, mild cases where individuals have not sought medical treatment, and the fact that many countries had limited access to diagnostic tests or have implemented testing policies later than the others. Considering the lack of reviews assessing diagnostic testing (sensitivity, specificity, and predictive values of RT-PCT or immunoglobulin tests), and the preponderance of studies that assessed only symptomatic individuals, considerable imprecision around the calculated mortality rates existed in the early stage of the COVID-19 pandemic.
Few reviews included treatment data. Those reviews described studies considered to be at a very low level of evidence: usually small, retrospective studies with very heterogeneous populations. Seven reviews analyzed laboratory parameters; those reviews could have been useful for clinicians who attend patients suspected of COVID-19 in emergency services worldwide, such as assessing which patients need to be reassessed more frequently.
All systematic reviews scored poorly on the AMSTAR 2 critical appraisal tool for systematic reviews. Most of the original studies included in the reviews were case series and case reports, impacting the quality of evidence. Such evidence has major implications for clinical practice and the use of these reviews in evidence-based practice and policy. Clinicians, patients, and policymakers can only have the highest confidence in systematic review findings if high-quality systematic review methodologies are employed. The urgent need for information during a pandemic does not justify poor quality reporting.
We acknowledge that there are numerous challenges associated with analyzing COVID-19 data during a pandemic [ 47 ]. High-quality evidence syntheses are needed for decision-making, but each type of evidence syntheses is associated with its inherent challenges.
The creation of classic systematic reviews requires considerable time and effort; with massive research output, they quickly become outdated, and preparing updated versions also requires considerable time. A recent study showed that updates of non-Cochrane systematic reviews are published a median of 5 years after the publication of the previous version [ 48 ].
Authors may register a review and then abandon it [ 49 ], but the existence of a public record that is not updated may lead other authors to believe that the review is still ongoing. A quarter of Cochrane review protocols remains unpublished as completed systematic reviews 8 years after protocol publication [ 50 ].
Rapid reviews can be used to summarize the evidence, but they involve methodological sacrifices and simplifications to produce information promptly, with inconsistent methodological approaches [ 51 ]. However, rapid reviews are justified in times of public health emergencies, and even Cochrane has resorted to publishing rapid reviews in response to the COVID-19 crisis [ 52 ]. Rapid reviews were eligible for inclusion in this overview, but only one of the 18 reviews included in this study was labeled as a rapid review.
Ideally, COVID-19 evidence would be continually summarized in a series of high-quality living systematic reviews, types of evidence synthesis defined as “ a systematic review which is continually updated, incorporating relevant new evidence as it becomes available ” [ 53 ]. However, conducting living systematic reviews requires considerable resources, calling into question the sustainability of such evidence synthesis over long periods [ 54 ].
Research reports about COVID-19 will contribute to research waste if they are poorly designed, poorly reported, or simply not necessary. In principle, systematic reviews should help reduce research waste as they usually provide recommendations for further research that is needed or may advise that sufficient evidence exists on a particular topic [ 55 ]. However, systematic reviews can also contribute to growing research waste when they are not needed, or poorly conducted and reported. Our present study clearly shows that most of the systematic reviews that were published early on in the COVID-19 pandemic could be categorized as research waste, as our confidence in their results is critically low.
Our study has some limitations. One is that for AMSTAR 2 assessment we relied on information available in publications; we did not attempt to contact study authors for clarifications or additional data. In three reviews, the methodological quality appraisal was challenging because they were published as letters, or labeled as rapid communications. As a result, various details about their review process were not included, leading to AMSTAR 2 questions being answered as “not reported”, resulting in low confidence scores. Full manuscripts might have provided additional information that could have led to higher confidence in the results. In other words, low scores could reflect incomplete reporting, not necessarily low-quality review methods. To make their review available more rapidly and more concisely, the authors may have omitted methodological details. A general issue during a crisis is that speed and completeness must be balanced. However, maintaining high standards requires proper resourcing and commitment to ensure that the users of systematic reviews can have high confidence in the results.
Furthermore, we used adjusted AMSTAR 2 scoring, as the tool was designed for critical appraisal of reviews of interventions. Some reviews may have received lower scores than actually warranted in spite of these adjustments.
Another limitation of our study may be the inclusion of multiple overlapping reviews, as some included reviews included the same primary studies. According to the Cochrane Handbook, including overlapping reviews may be appropriate when the review’s aim is “ to present and describe the current body of systematic review evidence on a topic ” [ 12 ], which was our aim. To avoid bias with summarizing evidence from overlapping reviews, we presented the forest plots without summary estimates. The forest plots serve to inform readers about the effect sizes for outcomes that were reported in each review.
Several authors from this study have contributed to one of the reviews identified [ 25 ]. To reduce the risk of any bias, two authors who did not co-author the review in question initially assessed its quality and limitations.
Finally, we note that the systematic reviews included in our overview may have had issues that our analysis did not identify because we did not analyze their primary studies to verify the accuracy of the data and information they presented. We give two examples to substantiate this possibility. Lovato et al. wrote a commentary on the review of Sun et al. [ 41 ], in which they criticized the authors’ conclusion that sore throat is rare in COVID-19 patients [ 56 ]. Lovato et al. highlighted that multiple studies included in Sun et al. did not accurately describe participants’ clinical presentations, warning that only three studies clearly reported data on sore throat [ 56 ].
In another example, Leung [ 57 ] warned about the review of Li, L.Q. et al. [ 29 ]: “ it is possible that this statistic was computed using overlapped samples, therefore some patients were double counted ”. Li et al. responded to Leung that it is uncertain whether the data overlapped, as they used data from published articles and did not have access to the original data; they also reported that they requested original data and that they plan to re-do their analyses once they receive them; they also urged readers to treat the data with caution [ 58 ]. This points to the evolving nature of evidence during a crisis.
Our study’s strength is that this overview adds to the current knowledge by providing a comprehensive summary of all the evidence synthesis about COVID-19 available early after the onset of the pandemic. This overview followed strict methodological criteria, including a comprehensive and sensitive search strategy and a standard tool for methodological appraisal of systematic reviews.
In conclusion, in this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all the reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic could be categorized as research waste. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards to provide patients, clinicians, and decision-makers trustworthy evidence.
Availability of data and materials
All data collected and analyzed within this study are available from the corresponding author on reasonable request.
World Health Organization. Timeline - COVID-19: Available at: https://www.who.int/news/item/29-06-2020-covidtimeline . Accessed 1 June 2021.
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available at: https://coronavirus.jhu.edu/map.html . Accessed 1 June 2021.
Anzai A, Kobayashi T, Linton NM, Kinoshita R, Hayashi K, Suzuki A, et al. Assessing the Impact of Reduced Travel on Exportation Dynamics of Novel Coronavirus Infection (COVID-19). J Clin Med. 2020;9(2):601.
Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. https://doi.org/10.1126/science.aba9757 .
Article CAS PubMed PubMed Central Google Scholar
Fidahic M, Nujic D, Runjic R, Civljak M, Markotic F, Lovric Makaric Z, et al. Research methodology and characteristics of journal articles with original data, preprint articles and registered clinical trial protocols about COVID-19. BMC Med Res Methodol. 2020;20(1):161. https://doi.org/10.1186/s12874-020-01047-2 .
EPPI Centre . COVID-19: a living systematic map of the evidence. Available at: http://eppi.ioe.ac.uk/cms/Projects/DepartmentofHealthandSocialCare/Publishedreviews/COVID-19Livingsystematicmapoftheevidence/tabid/3765/Default.aspx . Accessed 1 June 2021.
NCBI SARS-CoV-2 Resources. Available at: https://www.ncbi.nlm.nih.gov/sars-cov-2/ . Accessed 1 June 2021.
Gustot T. Quality and reproducibility during the COVID-19 pandemic. JHEP Rep. 2020;2(4):100141. https://doi.org/10.1016/j.jhepr.2020.100141 .
Article PubMed PubMed Central Google Scholar
Kodvanj, I., et al., Publishing of COVID-19 Preprints in Peer-reviewed Journals, Preprinting Trends, Public Discussion and Quality Issues. Preprint article. bioRxiv 2020.11.23.394577; doi: https://doi.org/10.1101/2020.11.23.394577 .
Dobler CC. Poor quality research and clinical practice during COVID-19. Breathe (Sheff). 2020;16(2):200112. https://doi.org/10.1183/20734735.0112-2020 .
Article Google Scholar
Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. 2010;7(9):e1000326. https://doi.org/10.1371/journal.pmed.1000326 .
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231. https://doi.org/10.1186/s13643-017-0617-1 .
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane. 2020. Available from www.training.cochrane.org/handbook .
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane. 2020; Available from www.training.cochrane.org/handbook .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18. https://doi.org/10.1186/s13643-018-0914-3 .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):29. https://doi.org/10.1186/s13643-018-0768-8 .
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39. https://doi.org/10.1186/s13643-018-0695-8 .
Pollock M, Fernandes RM, Pieper D, Tricco AC, Gates M, Gates A, et al. Preferred reporting items for overviews of reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):335. https://doi.org/10.1186/s13643-019-1252-9 .
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009;3(3):e123–30.
Krnic Martinic M, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol. 2019;19(1):203. https://doi.org/10.1186/s12874-019-0855-0 .
Puljak L. If there is only one author or only one database was searched, a study should not be called a systematic review. J Clin Epidemiol. 2017;91:4–5. https://doi.org/10.1016/j.jclinepi.2017.08.002 .
Article PubMed Google Scholar
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254. https://doi.org/10.1186/s13643-020-01509-0 .
Covidence - systematic review software. Available at: https://www.covidence.org/ . Accessed 1 June 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Borges do Nascimento IJ, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med. 2020;9(4):941.
Article PubMed Central Google Scholar
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. https://doi.org/10.1186/s40249-020-00646-x .
Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279–83. https://doi.org/10.1016/j.jcrc.2020.03.005 .
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–8. https://doi.org/10.1007/s00392-020-01626-9 .
Article CAS PubMed Google Scholar
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577–83. https://doi.org/10.1002/jmv.25757 .
Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63(3):390–1. https://doi.org/10.1016/j.pcad.2020.03.001 .
Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med. 2020;75:107–8. https://doi.org/10.1016/j.ejim.2020.03.014 .
Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020;505:190–1. https://doi.org/10.1016/j.cca.2020.03.004 .
Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–8. https://doi.org/10.1016/j.cca.2020.03.022 .
Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–95. https://doi.org/10.1111/apa.15270 .
Lupia T, Scabini S, Mornese Pinna S, di Perri G, de Rosa FG, Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J Glob Antimicrob Resist. 2020;21:22–7. https://doi.org/10.1016/j.jgar.2020.02.021 .
Marasinghe, K.M., A systematic review investigating the effectiveness of face mask use in limiting the spread of COVID-19 among medically not diagnosed individuals: shedding light on current recommendations provided to individuals not medically diagnosed with COVID-19. Research Square. Preprint article. doi : https://doi.org/10.21203/rs.3.rs-16701/v1 . 2020 .
Mullins E, Evans D, Viner RM, O’Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586–92. https://doi.org/10.1002/uog.22014 .
Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JIP, et al. Potential Rapid Diagnostics, Vaccine and Therapeutics for 2019 Novel coronavirus (2019-nCoV): a systematic review. J Clin Med. 2020;9(3):623.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. https://doi.org/10.1016/j.tmaid.2020.101623 .
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. https://doi.org/10.2214/AJR.20.23034 .
Sun P, Qie S, Liu Z, Ren J, Li K, Xi J. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis. J Med Virol. 2020;92(6):612–7. https://doi.org/10.1002/jmv.25735 .
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. https://doi.org/10.1016/j.ijid.2020.03.017 .
Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Investig. 2020;50(3):e13209. https://doi.org/10.1111/eci.13209 .
Article CAS Google Scholar
Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwanica. 2006;15(1):26–8.
Google Scholar
Suzuki M, Saito K, Min WP, Vladau C, Toida K, Itoh H, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope. 2007;117(2):272–7. https://doi.org/10.1097/01.mlg.0000249922.37381.1e .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7. https://doi.org/10.1016/S1473-3099(20)30244-9 .
Wolkewitz M, Puljak L. Methodological challenges of analysing COVID-19 data during the pandemic. BMC Med Res Methodol. 2020;20(1):81. https://doi.org/10.1186/s12874-020-00972-6 .
Rombey T, Lochner V, Puljak L, Könsgen N, Mathes T, Pieper D. Epidemiology and reporting characteristics of non-Cochrane updates of systematic reviews: a cross-sectional study. Res Synth Methods. 2020;11(3):471–83. https://doi.org/10.1002/jrsm.1409 .
Runjic E, Rombey T, Pieper D, Puljak L. Half of systematic reviews about pain registered in PROSPERO were not published and the majority had inaccurate status. J Clin Epidemiol. 2019;116:114–21. https://doi.org/10.1016/j.jclinepi.2019.08.010 .
Runjic E, Behmen D, Pieper D, Mathes T, Tricco AC, Moher D, et al. Following Cochrane review protocols to completion 10 years later: a retrospective cohort study and author survey. J Clin Epidemiol. 2019;111:41–8. https://doi.org/10.1016/j.jclinepi.2019.03.006 .
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. 2015;13(1):224. https://doi.org/10.1186/s12916-015-0465-6 .
COVID-19 Rapid Reviews: Cochrane’s response so far. Available at: https://training.cochrane.org/resource/covid-19-rapid-reviews-cochrane-response-so-far . Accessed 1 June 2021.
Cochrane. Living systematic reviews. Available at: https://community.cochrane.org/review-production/production-resources/living-systematic-reviews . Accessed 1 June 2021.
Millard T, Synnot A, Elliott J, Green S, McDonald S, Turner T. Feasibility and acceptability of living systematic reviews: results from a mixed-methods evaluation. Syst Rev. 2019;8(1):325. https://doi.org/10.1186/s13643-019-1248-5 .
Babic A, Poklepovic Pericic T, Pieper D, Puljak L. How to decide whether a systematic review is stable and not in need of updating: analysis of Cochrane reviews. Res Synth Methods. 2020;11(6):884–90. https://doi.org/10.1002/jrsm.1451 .
Lovato A, Rossettini G, de Filippis C. Sore throat in COVID-19: comment on “clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis”. J Med Virol. 2020;92(7):714–5. https://doi.org/10.1002/jmv.25815 .
Leung C. Comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1431–2. https://doi.org/10.1002/jmv.25912 .
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. Response to Char’s comment: comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1433. https://doi.org/10.1002/jmv.25924 .
Download references
Acknowledgments
We thank Catherine Henderson DPhil from Swanscoe Communications for pro bono medical writing and editing support. We acknowledge support from the Covidence Team, specifically Anneliese Arno. We thank the whole International Network of Coronavirus Disease 2019 (InterNetCOVID-19) for their commitment and involvement. Members of the InterNetCOVID-19 are listed in Additional file 6 . We thank Pavel Cerny and Roger Crosthwaite for guiding the team supervisor (IJBN) on human resources management.
This research received no external funding.
Author information
Authors and affiliations.
University Hospital and School of Medicine, Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
Israel Júnior Borges do Nascimento & Milena Soriano Marcolino
Medical College of Wisconsin, Milwaukee, WI, USA
Israel Júnior Borges do Nascimento
Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare, College of Nursing, The Ohio State University, Columbus, OH, USA
Dónal P. O’Mathúna
School of Nursing, Psychotherapy and Community Health, Dublin City University, Dublin, Ireland
Department of Anesthesiology, Intensive Care and Pain Medicine, University of Münster, Münster, Germany
Thilo Caspar von Groote
Department of Sport and Health Science, Technische Universität München, Munich, Germany
Hebatullah Mohamed Abdulazeem
School of Health Sciences, Faculty of Health and Medicine, The University of Newcastle, Callaghan, Australia
Ishanka Weerasekara
Department of Physiotherapy, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka
Cochrane Croatia, University of Split, School of Medicine, Split, Croatia
Ana Marusic, Irena Zakarija-Grkovic & Tina Poklepovic Pericic
Center for Evidence-Based Medicine and Health Care, Catholic University of Croatia, Ilica 242, 10000, Zagreb, Croatia
Livia Puljak
Cochrane Brazil, Evidence-Based Health Program, Universidade Federal de São Paulo, São Paulo, Brazil
Vinicius Tassoni Civile & Alvaro Nagib Atallah
Yorkville University, Fredericton, New Brunswick, Canada
Santino Filoso
Laboratory for Industrial and Applied Mathematics (LIAM), Department of Mathematics and Statistics, York University, Toronto, Ontario, Canada
Nicola Luigi Bragazzi
You can also search for this author in PubMed Google Scholar
Contributions
IJBN conceived the research idea and worked as a project coordinator. DPOM, TCVG, HMA, IW, AM, LP, VTC, IZG, TPP, ANA, SF, NLB and MSM were involved in data curation, formal analysis, investigation, methodology, and initial draft writing. All authors revised the manuscript critically for the content. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Livia Puljak .
Ethics declarations
Ethics approval and consent to participate.
Not required as data was based on published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Search strategies used in the study.
Additional file 2: Appendix 2.
Adjusted scoring of AMSTAR 2 used in this study for systematic reviews of studies that did not analyze interventions.
Additional file 3: Appendix 3.
List of excluded studies, with reasons.
Additional file 4: Appendix 4.
Table of overlapping studies, containing the list of primary studies included, their visual overlap in individual systematic reviews, and the number in how many reviews each primary study was included.
Additional file 5: Appendix 5.
A detailed explanation of AMSTAR scoring for each item in each review.
Additional file 6: Appendix 6.
List of members and affiliates of International Network of Coronavirus Disease 2019 (InterNetCOVID-19).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions

About this article
Cite this article.
Borges do Nascimento, I.J., O’Mathúna, D.P., von Groote, T.C. et al. Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect Dis 21 , 525 (2021). https://doi.org/10.1186/s12879-021-06214-4
Download citation
Received : 12 April 2020
Accepted : 19 May 2021
Published : 04 June 2021
DOI : https://doi.org/10.1186/s12879-021-06214-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Coronavirus
- Evidence-based medicine
- Infectious diseases
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]
/media/video/upload/Opener_rt.mp4)
How Science Beat the Virus
And what it lost in the process

Listen to this article
Listen to more stories on audm
This article was published online on December 14, 2020.
In fall of 2019, exactly zero scientists were studying COVID‑19, because no one knew the disease existed. The coronavirus that causes it, SARS‑CoV‑2, had only recently jumped into humans and had been neither identified nor named. But by the end of March 2020, it had spread to more than 170 countries, sickened more than 750,000 people, and triggered the biggest pivot in the history of modern science. Thousands of researchers dropped whatever intellectual puzzles had previously consumed their curiosity and began working on the pandemic instead. In mere months, science became thoroughly COVID-ized.
As of this writing, the biomedical library PubMed lists more than 74,000 COVID-related scientific papers—more than twice as many as there are about polio, measles, cholera, dengue, or other diseases that have plagued humanity for centuries. Only 9,700 Ebola-related papers have been published since its discovery in 1976; last year, at least one journal received more COVID‑19 papers than that for consideration. By September, the prestigious New England Journal of Medicine had received 30,000 submissions—16,000 more than in all of 2019. “All that difference is COVID‑19,” Eric Rubin, NEJM ’s editor in chief, says. Francis Collins, the director of the National Institutes of Health, told me, “The way this has resulted in a shift in scientific priorities has been unprecedented.”
Much like famous initiatives such as the Manhattan Project and the Apollo program, epidemics focus the energies of large groups of scientists. In the U.S., the influenza pandemic of 1918, the threat of malaria in the tropical battlegrounds of World War II, and the rise of polio in the postwar years all triggered large pivots. Recent epidemics of Ebola and Zika each prompted a temporary burst of funding and publications . But “nothing in history was even close to the level of pivoting that’s happening right now,” Madhukar Pai of McGill University told me.
That’s partly because there are just more scientists: From 1960 to 2010, the number of biological or medical researchers in the U.S. increased sevenfold , from just 30,000 to more than 220,000. But SARS-CoV-2 has also spread farther and faster than any new virus in a century. For Western scientists, it wasn’t a faraway threat like Ebola. It threatened to inflame their lungs. It shut down their labs. “It hit us at home,” Pai said.
In a survey of 2,500 researchers in the U.S., Canada, and Europe, Kyle Myers from Harvard and his team found that 32 percent had shifted their focus toward the pandemic. Neuroscientists who study the sense of smell started investigating why COVID‑19 patients tend to lose theirs. Physicists who had previously experienced infectious diseases only by contracting them found themselves creating models to inform policy makers. Michael D. L. Johnson at the University of Arizona normally studies copper’s toxic effects on bacteria. But when he learned that SARS‑CoV‑2 persists for less time on copper surfaces than on other materials, he partially pivoted to see how the virus might be vulnerable to the metal. No other disease has been scrutinized so intensely, by so much combined intellect, in so brief a time.
These efforts have already paid off. New diagnostic tests can detect the virus within minutes. Massive open data sets of viral genomes and COVID‑19 cases have produced the most detailed picture yet of a new disease’s evolution. Vaccines are being developed with record-breaking speed. SARS‑CoV‑2 will be one of the most thoroughly characterized of all pathogens, and the secrets it yields will deepen our understanding of other viruses, leaving the world better prepared to face the next pandemic.
But the COVID‑19 pivot has also revealed the all-too-human frailties of the scientific enterprise . Flawed research made the pandemic more confusing, influencing misguided policies. Clinicians wasted millions of dollars on trials that were so sloppy as to be pointless. Overconfident poseurs published misleading work on topics in which they had no expertise. Racial and gender inequalities in the scientific field widened.
Amid a long winter of sickness , it’s hard not to focus on the political failures that led us to a third surge. But when people look back on this period, decades from now, they will also tell stories, both good and bad, about this extraordinary moment for science. At its best, science is a self-correcting march toward greater knowledge for the betterment of humanity. At its worst, it is a self-interested pursuit of greater prestige at the cost of truth and rigor. The pandemic brought both aspects to the fore. Humanity will benefit from the products of the COVID‑19 pivot. Science itself will too, if it learns from the experience.
In February, Jennifer Doudna, one of America’s most prominent scientists, was still focused on CRISPR—the gene-editing tool that she’d co-discovered and that won her a Nobel Prize in October. But when her son’s high school shut down and UC Berkeley, her university, closed its campus, the severity of the impending pandemic became clear. “In three weeks, I went from thinking we’re still okay to thinking that my whole life is going to change,” she told me. On March 13, she and dozens of colleagues at the Innovative Genomics Institute, which she leads, agreed to pause most of their ongoing projects and redirect their skills to addressing COVID‑19. They worked on CRISPR-based diagnostic tests. Because existing tests were in short supply, they converted lab space into a pop-up testing facility to serve the local community. “We need to make our expertise relevant to whatever is happening right now,” she said.
Scientists who’d already been studying other emerging diseases were even quicker off the mark. Lauren Gardner, an engineering professor at Johns Hopkins University who has studied dengue and Zika, knew that new epidemics are accompanied by a dearth of real-time data. So she and one of her students created an online global dashboard to map and tally all publicly reported COVID‑19 cases and deaths. After one night of work, they released it, on January 22. The dashboard has since been accessed daily by governments, public-health agencies, news organizations, and anxious citizens.
Studying deadly viruses is challenging at the best of times, and was especially so this past year. To handle SARS‑CoV‑2, scientists must work in “biosafety level 3” labs, fitted with special airflow systems and other extreme measures; although the actual number is not known, an estimated 200 such facilities exist in the U.S. Researchers often test new drugs and vaccines on monkeys before proceeding to human trials, but the U.S. is facing a monkey shortage after China stopped exporting the animals, possibly because it needed them for research. And other biomedical research is now more difficult because of physical-distancing requirements. “Usually we had people packed in, but with COVID, we do shift work,” Akiko Iwasaki, a Yale immunologist, told me. “People are coming in at ridiculous hours” to protect themselves from the very virus they are trying to study.
Recommended Reading

What the Chaos in Hospitals Is Doing to Doctors

How the Pandemic Defeated America

Uber’s Self-Driving Car Didn’t Malfunction, It Was Just Bad
Experts on emerging diseases are scarce: These threats go neglected by the public in the lulls between epidemics. “Just a year ago I had to explain to people why I was studying coronaviruses,” says Lisa Gralinski of the University of North Carolina at Chapel Hill. “That’s never going to be a concern again.” Stressed and stretched, she and other emerging-disease researchers were also conscripted into unfamiliar roles. They’re acting as makeshift advisers to businesses, schools, and local governments. They’re barraged by interview requests from journalists. They’re explaining the nuances of the pandemic on Twitter, to huge new follower counts. “It’s often the same person who’s helping the Namibian government to manage malaria outbreaks and is now being pulled into helping Maryland manage COVID‑19,” Gardner told me.
But the newfound global interest in viruses also means “you have a lot more people you can talk through problems with,” Pardis Sabeti, a computational geneticist at the Broad Institute of MIT and Harvard, told me. Indeed, COVID‑19 papers are more likely than typical biomedical studies to have authors who had never published together before, according to a team led by Ying Ding, who works at the University of Texas at Austin.
Fast-forming alliances could work at breakneck speed because many researchers had spent the past few decades transforming science from a plodding, cloistered endeavor into something nimbler and more transparent. Traditionally, a scientist submits her paper to a journal, which sends it to a (surprisingly small) group of peers for (several rounds of usually anonymous) comments; if the paper passes this (typically months-long) peer-review gantlet, it is published (often behind an expensive paywall). Languid and opaque, this system is ill-suited to a fast-moving outbreak. But biomedical scientists can now upload preliminary versions of their papers, or “preprints,” to freely accessible websites, allowing others to immediately dissect and build upon their results. This practice had been slowly gaining popularity before 2020, but proved so vital for sharing information about COVID‑19 that it will likely become a mainstay of modern biomedical research. Preprints accelerate science, and the pandemic accelerated the use of preprints. At the start of the year, one repository, medRxiv (pronounced “med archive”), held about 1,000 preprints. By the end of October, it had more than 12,000.
Open data sets and sophisticated new tools to manipulate them have likewise made today’s researchers more flexible. SARS‑CoV‑2’s genome was decoded and shared by Chinese scientists just 10 days after the first cases were reported. By November, more than 197,000 SARS‑CoV‑2 genomes had been sequenced. About 90 years ago, no one had even seen an individual virus; today, scientists have reconstructed the shape of SARS‑CoV‑2 down to the position of individual atoms. Researchers have begun to uncover how SARS‑CoV‑2 compares with other coronaviruses in wild bats, the likely reservoir; how it infiltrates and co-opts our cells; how the immune system overreacts to it, creating the symptoms of COVID‑19. “We’re learning about this virus faster than we’ve ever learned about any virus in history,” Sabeti said.
By March, the odds of quickly eradicating the new coronavirus looked slim. A vaccine became the likeliest endgame, and the race to create one was a resounding success. The process normally takes years, but as I write this, 54 different vaccines are being tested for safety and efficacy, and 12 have entered Phase 3 clinical trials—the final checkpoint. As of this writing, Pfizer/BioNTech and Moderna have announced that, based on preliminary results from these trials, their respective vaccines are roughly 95 percent effective at preventing COVID‑19. * “We went from a virus whose sequence was only known in January, and now in the fall, we’re finishing— finishing —a Phase 3 trial,” Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases and a member of the White House’s coronavirus task force, told me. “Holy mackerel.”
Most vaccines comprise dead, weakened, or fragmented pathogens, and must be made from scratch whenever a new threat emerges. But over the past decade, the U.S. and other countries have moved away from this slow “one bug, one drug” approach. Instead, they’ve invested in so-called platform technologies, in which a standard chassis can be easily customized with different payloads that target new viruses. For example, the Pfizer/BioNTech and Moderna vaccines both consist of nanoparticles that contain pieces of SARS‑CoV‑2’s genetic material—its mRNA. When volunteers are injected with these particles, their cells use the mRNA to reconstruct a noninfectious fragment of the virus, allowing their immune system to prepare antibodies that neutralize it. No company has ever brought an mRNA vaccine to market before, but because the basic platform had already been refined, researchers could quickly repurpose it with SARS‑CoV‑2’s mRNA. Moderna got its vaccine into Phase 1 clinical trials on March 16, just 66 days after the new virus’s genome was first uploaded—far faster than any pre-COVID vaccine.
Meanwhile, companies compressed the process of vaccine development by running what would normally be sequential steps in parallel, while still checking for safety and efficacy. The federal government’s Operation Warp Speed, an effort to accelerate vaccine distribution, funded several companies at once—an unusual move. It preordered doses and invested in manufacturing facilities before trials were complete, reducing the risk for pharmaceutical companies looking to participate. Ironically, federal ineptitude at containing SARS‑CoV‑2 helped too. In the U.S., “the fact that the virus is everywhere makes it easier to gauge the performance of a vaccine,” says Natalie Dean of the University of Florida, who studies vaccine trials. “You can’t do a [Phase 3] vaccine trial in South Korea,” because the outbreak there is under control.
Read: How the pandemic will end
Vaccines will not immediately end the pandemic . Millions of doses will have to be manufactured, allocated, and distributed ; large numbers of Americans could refuse the vaccine ; and how long vaccine-induced immunity will last is still unclear. In the rosiest scenario, the Pfizer/BioNTech and Moderna vaccines are approved and smoothly rolled out over the next 12 months. By the end of the year, the U.S. achieves herd immunity, after which the virus struggles to find susceptible hosts. It still circulates, but outbreaks are sporadic and short-lived. Schools and businesses reopen. Families hug tightly and celebrate joyously over Thanksgiving and Christmas.
And the next time a mystery pathogen emerges, scientists hope to quickly slot its genetic material into proven platforms, and move the resulting vaccines through the same speedy pipelines that were developed during this pandemic. “I don’t think the world of vaccine development will ever be the same again,” says Nicole Lurie of the Coalition for Epidemic Preparedness Innovations.
As fast as the vaccine-development process was, it could have been faster. Despite the stakes, some pharmaceutical companies with relevant expertise chose not to enter the race, perhaps dissuaded by intense competition. Instead, from February to May, the sector roughly tripled its efforts to develop drugs to treat COVID‑19, according to Kevin Bryan, an economist at the University of Toronto. The decades-old steroid dexamethasone turned out to reduce death rates among severely ill patients on ventilators by more than 12 percent. Early hints suggest that newer treatments such as the monoclonal-antibody therapy bamlanivimab, which was just approved for emergency use by the FDA, could help newly infected patients who have not yet been hospitalized. But although these wins are significant, they are scarce. Most drugs haven’t been effective. Health-care workers became better at saving hospitalized patients more through improvements in basic medical care than through pharmaceutical panaceas—a predictable outcome, because antiviral drugs tend to offer only modest benefits.
The quest for COVID‑19 treatments was slowed by a torrent of shoddy studies whose results were meaningless at best and misleading at worst. Many of the thousands of clinical trials that were launched were too small to produce statistically solid results. Some lacked a control group—a set of comparable patients who received a placebo, and who provided a baseline against which the effects of a drug could be judged. Other trials needlessly overlapped. At least 227 involved hydroxychloroquine—the antimalarial drug that Donald Trump hyped for months. A few large trials eventually confirmed that hydroxychloroquine does nothing for COVID‑19 patients, but not before hundreds of thousands of people were recruited into pointlessly small studies . More than 100,000 Americans have also received convalescent plasma—another treatment that Trump touted. But because most were not enrolled in rigorous trials, “we still don’t know if it works—and it likely doesn’t,” says Luciana Borio, the former director for medical and biodefense preparedness at the National Security Council. “What a waste of time and resources.”
Read: How we survive the winter
In the heat of a disaster, when emergency rooms are filling and patients are dying, it is hard to set up one careful study, let alone coordinate several across a country. But coordination is not impossible. During World War II , federal agencies unified private companies, universities, the military, and other entities in a carefully orchestrated effort to speed pharmaceutical development from benchtop to battlefield. The results—revolutionary malaria treatments, new ways of mass-producing antibiotics, and at least 10 new or improved vaccines for influenza and other diseases—represented “not a triumph of scientific genius but rather of organizational purpose and efficiency,” Kendall Hoyt of Dartmouth College has written.
Similar triumphs occurred last year—in other countries. In March, taking advantage of the United Kingdom’s nationalized health system, British researchers launched a nationwide study called Recovery, which has since enrolled more than 17,600 COVID‑19 patients across 176 institutions. Recovery offered conclusive answers about dexamethasone and hydroxychloroquine and is set to weigh in on several other treatments. No other study has done more to shape the treatment of COVID‑19. The U.S. is now catching up. In April, the NIH launched a partnership called ACTIV , in which academic and industry scientists prioritized the most promising drugs and coordinated trial plans across the country. Since August, several such trials have started. This model was late, but is likely to outlast the pandemic itself, allowing future researchers to rapidly sort medical wheat from pharmaceutical chaff. “I can’t imagine we’ll go back to doing clinical research in the future the way we did in the past,” the NIH’s Francis Collins said.
Even after the COVID‑19 pandemic, the fruits of the pivot will leave us better equipped for our long and intensifying war against harmful viruses. The last time a virus caused this much devastation—the flu pandemic of 1918—scientists were only just learning about viruses, and spent time looking for a bacterial culprit. This one is different. With so many scientists observing intently as a virus wreaks its horrible work upon millions of bodies, the world is learning lessons that could change the way we think about these pathogens forevermore.
Consider the long-term consequences of viral infections. Years after the original SARS virus hit Hong Kong in 2003, about a quarter of survivors still had myalgic encephalomyelitis—a chronic illness whose symptoms, such as extreme fatigue and brain fogs, can worsen dramatically after mild exertion. ME cases are thought to be linked to viral infections, and clusters sometimes follow big outbreaks. So when SARS‑CoV‑2 started spreading, people with ME were unsurprised to hear that tens of thousands of COVID‑19 “long-haulers” were experiencing incapacitating symptoms that rolled on for months . “Everyone in my community has been thinking about this since the start of the pandemic,” says Jennifer Brea, the executive director of the advocacy group #MEAction.
ME and sister illnesses such as dysautonomia, fibromyalgia, and mast cell activation syndrome have long been neglected, their symptoms dismissed as imaginary or psychiatric. Research is poorly funded, so few scientists study them. Little is known about how to prevent and treat them. This negligence has left COVID‑19 long-haulers with few answers or options, and they initially endured the same dismissal as the larger ME community. But their sheer numbers have forced a degree of recognition. They started researching, cataloging their own symptoms. They gained audiences with the NIH and the World Health Organization. Patients who are themselves experts in infectious disease or public health published their stories in top journals. “Long COVID” is being taken seriously, and Brea hopes it might drag all post-infection illnesses into the spotlight. ME never experienced a pivot. COVID‑19 might inadvertently create one.
Anthony Fauci hopes so. His career was defined by HIV, and in 2019 he said in a paper he co-wrote that “the collateral advantages of” studying HIV “have been profound.” Research into HIV/AIDS revolutionized our understanding of the immune system and how diseases subvert it. It produced techniques for developing antiviral drugs that led to treatments for hepatitis C. Inactivated versions of HIV have been used to treat cancers and genetic disorders. From one disease came a cascade of benefits. COVID‑19 will be no different. Fauci had personally seen cases of prolonged symptoms after other viral infections, but “I didn’t really have a good scientific handle on it,” he told me. Such cases are hard to study, because it’s usually impossible to identify the instigating pathogen. But COVID‑19 has created “the most unusual situation imaginable,” Fauci said—a massive cohort of people with long-haul symptoms that are almost certainly caused by one known virus. “It’s an opportunity we cannot lose,” he said.
Read: The core lesson of the COVID-19 heart debate
COVID‑19 has developed a terrifying mystique because it seems to behave in unusual ways. It causes mild symptoms in some but critical illness in others. It is a respiratory virus and yet seems to attack the heart, brain, kidneys, and other organs. It has reinfected a small number of people who had recently recovered. But many other viruses share similar abilities; they just don’t infect millions of people in a matter of months or grab the attention of the entire scientific community. Thanks to COVID‑19, more researchers are looking for these rarer sides of viral infections, and spotting them.
At least 20 known viruses, including influenza and measles, can trigger myocarditis—inflammation of the heart. Some of these cases resolve on their own, but others cause persistent scarring, and still others rapidly progress into lethal problems. No one knows what proportion of people with viral myocarditis experience the most mild fate, because doctors typically notice only those who seek medical attention. But now researchers are also intently scrutinizing the hearts of people with mild or asymptomatic COVID‑19 infections, including college athletes, given concerns about sudden cardiac arrest during strenuous workouts. The lessons from these efforts could ultimately avert deaths from other infections.
Respiratory viruses, though extremely common, are often neglected. Respiratory syncytial virus, parainfluenza viruses, rhinoviruses, adenoviruses, bocaviruses, a quartet of other human coronaviruses—they mostly cause mild coldlike illnesses, but those can be severe. How often? Why? It’s hard to say, because, influenza aside, such viruses attract little funding or interest. “There’s a perception that they’re just colds and there’s nothing much to learn,” says Emily Martin of the University of Michigan, who has long struggled to get funding to study them. Such reasoning is shortsighted folly. Respiratory viruses are the pathogens most likely to cause pandemics, and those outbreaks could potentially be far worse than COVID‑19’s.
Read: We need to talk about ventilation
Their movements through the air have been poorly studied, too. “There’s this very entrenched idea,” says Linsey Marr at Virginia Tech, that viruses mostly spread through droplets (short-range globs of snot and spit) rather than aerosols (smaller, dustlike flecks that travel farther). That idea dates back to the 1930s, when scientists were upending outdated notions that disease was caused by “bad air,” or miasma. But the evidence that SARS‑CoV‑2 can spread through aerosols “is now overwhelming,” says Marr, one of the few scientists who, before the pandemic, studied how viruses spread through air. “I’ve seen more acceptance in the last six months than over the 12 years I’ve been working on this.”
Another pandemic is inevitable, but it will find a very different community of scientists than COVID‑19 did. They will immediately work to determine whether the pathogen—most likely another respiratory virus—moves through aerosols, and whether it spreads from infected people before causing symptoms. They might call for masks and better ventilation from the earliest moments, not after months of debate. They will anticipate the possibility of an imminent wave of long-haul symptoms, and hopefully discover ways of preventing them. They might set up research groups to prioritize the most promising drugs and coordinate large clinical trials. They might take vaccine platforms that worked best against COVID‑19, slot in the genetic material of the new pathogen, and have a vaccine ready within months.
For all its benefits, the single-minded focus on COVID‑19 will also leave a slew of negative legacies. Science is mostly a zero-sum game, and when one topic monopolizes attention and money, others lose out. Last year, between physical-distancing restrictions, redirected funds, and distracted scientists, many lines of research slowed to a crawl. Long-term studies that monitored bird migrations or the changing climate will forever have holes in their data because field research had to be canceled. Conservationists who worked to protect monkeys and apes kept their distance for fear of passing COVID‑19 to already endangered species. Roughly 80 percent of non-COVID‑19 clinical trials in the U.S.—likely worth billions of dollars—were interrupted or stopped because hospitals were overwhelmed and volunteers were stuck at home. Even research on other infectious diseases was back-burnered. “All the non-COVID work that I was working on before the pandemic started is now piling up and gathering dust,” says Angela Rasmussen of Georgetown University, who normally studies Ebola and MERS. “Those are still problems.”
The COVID‑19 pandemic is a singular disaster, and it is reasonable for society—and scientists—to prioritize it. But the pivot was driven by opportunism as much as altruism. Governments, philanthropies, and universities channeled huge sums toward COVID‑19 research. The NIH alone received nearly $3.6 billion from Congress. The Bill & Melinda Gates Foundation apportioned $350 million for COVID‑19 work. “Whenever there’s a big pot of money, there’s a feeding frenzy,” Madhukar Pai told me. He works on tuberculosis, which causes 1.5 million deaths a year—comparable to COVID‑19’s toll in 2020. Yet tuberculosis research has been mostly paused. None of Pai’s colleagues pivoted when Ebola or Zika struck, but “half of us have now swung to working on COVID‑19,” he said. “It’s a black hole, sucking us all in.”
While the most qualified experts became quickly immersed in the pandemic response, others were stuck at home looking for ways to contribute. Using the same systems that made science faster, they could download data from free databases, run quick analyses with intuitive tools, publish their work on preprint servers, and publicize it on Twitter. Often, they made things worse by swerving out of their scholarly lanes and plowing into unfamiliar territory. Nathan Ballantyne, a philosopher at Fordham University, calls this “ epistemic trespassing .” It can be a good thing: Continental drift was championed by Alfred Wegener, a meteorologist; microbes were first documented by Antonie van Leeuwenhoek, a draper. But more often than not, epistemic trespassing just creates a mess, especially when inexperience couples with overconfidence.
On March 28, a preprint noted that countries that universally use a tuberculosis vaccine called BCG had lower COVID‑19 mortality rates. But such cross-country comparisons are infamously treacherous. For example, countries with higher cigarette-usage rates have longer life expectancies, not because smoking prolongs life but because it is more popular in wealthier nations. This tendency to draw faulty conclusions about individual health using data about large geographical regions is called the ecological fallacy. Epidemiologists know to avoid it. The BCG-preprint authors, who were from an osteopathic college in New York, didn’t seem to . But their paper was covered by more than 70 news outlets, and dozens of inexperienced teams offered similarly specious analyses. “People who don’t know how to spell tuberculosis have told me they can solve the link between BCG and COVID‑19,” Pai said. “Someone told me they can do it in 48 hours with a hackathon.”

Other epistemic trespassers spent their time reinventing the wheel. One new study, published in NEJM , used lasers to show that when people speak, they release aerosols. But as the authors themselves note, the same result—sans lasers—was published in 1946, Marr says. I asked her whether any papers from the 2020 batch had taught her something new. After an uncomfortably long pause, she mentioned just one.
In some cases, bad papers helped shape the public narrative of the pandemic. On March 16, two biogeographers published a preprint arguing that COVID‑19 will “marginally affect the tropics” because it fares poorly in warm, humid conditions. Disease experts quickly noted that techniques like the ones the duo used are meant for modeling the geographic ranges of animal and plant species or vector-borne pathogens, and are ill-suited to simulating the spread of viruses like SARS-CoV-2. But their claim was picked up by more than 50 news outlets and echoed by the United Nations World Food Program. COVID‑19 has since run rampant in many tropical countries, including Brazil, Indonesia, and Colombia—and the preprint’s authors have qualified their conclusions in later versions of the paper. “It takes a certain type of person to think that weeks of reading papers gives them more perspective than someone with a Ph.D. on that subject, and that type of person has gotten a lot of airtime in this pandemic,” says Colin Carlson of Georgetown.
The incentives to trespass are substantial. Academia is a pyramid scheme: Each biomedical professor trains an average of six doctoral students across her career, but only 16 percent of the students get tenure-track positions . Competition is ferocious, and success hinges on getting published—a feat made easier by dramatic results. These factors pull researchers toward speed, short-termism, and hype at the expense of rigor—and the pandemic intensified that pull. With an anxious world crying out for information, any new paper could immediately draw international press coverage—and hundreds of citations.
The tsunami of rushed but dubious work made life harder for actual experts, who struggled to sift the signal from the noise. They also felt obliged to debunk spurious research in long Twitter threads and relentless media interviews—acts of public service that are rarely rewarded in academia. And they were overwhelmed by requests to peer-review new papers. Kristian Andersen, an infectious-disease researcher at Scripps Research, told me that journals used to send him two or three such requests a month. Now “I’m getting three or five a day,” he said in September.
The pandemic’s opportunities also fell inequitably upon the scientific community. In March, Congress awarded $75 million to the National Science Foundation to fast-track studies that could quickly contribute to the pandemic response. “That money just went ,” says Cassidy Sugimoto of Indiana University, who was on rotation at the agency at the time. “It was a first-come, first-served environment. It advantaged people who were aware of the system and could act upon it quickly.” But not all scientists could pivot to COVID‑19, or pivot with equal speed.
Among scientists, as in other fields, women do more child care, domestic work, and teaching than men, and are more often asked for emotional support by their students. These burdens increased as the pandemic took hold, leaving women scientists “less able to commit their time to learning about a new area of study, and less able to start a whole new research project,” says Molly M. King, a sociologist at Santa Clara University. Women’s research hours fell by nine percentage points more than did men’s because of the pressures of COVID‑19. And when COVID‑19 created new opportunities, men grabbed them more quickly. In the spring, the proportion of papers with women as first authors fell almost 44 percent in the preprint repository medRxiv, relative to 2019. And published COVID‑19 papers had 19 percent fewer women as first authors compared with papers from the same journals in the previous year. Men led more than 80 percent of national COVID‑19 task forces in 87 countries . Male scientists were quoted four times as frequently as female scientists in American news stories about the pandemic.
American scientists of color also found it harder to pivot than their white peers, because of unique challenges that sapped their time and energy. Black, Latino, and Indigenous scientists were most likely to have lost loved ones, adding mourning to their list of duties. Many grieved, too, after the killings of Breonna Taylor, George Floyd, Ahmaud Arbery, and others. They often faced questions from relatives who were mistrustful of the medical system, or were experiencing discriminatory care. They were suddenly tasked with helping their predominantly white institutions fight racism. Neil Lewis Jr. at Cornell, who studies racial health disparities, told me that many psychologists had long deemed his work irrelevant. “All of a sudden my inbox is drowning,” he said, while some of his own relatives have become ill and one has died.
Science suffers from the so-called Matthew effect, whereby small successes snowball into ever greater advantages, irrespective of merit. Similarly, early hindrances linger. Young researchers who could not pivot because they were too busy caring or grieving for others might suffer lasting consequences from an unproductive year. COVID‑19 “has really put the clock back in terms of closing the gap for women and underrepresented minorities,” Yale’s Akiko Iwasaki says. “Once we’re over the pandemic, we’ll need to fix it all again.”
COVID-19 has already changed science immensely, but if scientists are savvy, the most profound pivot is still to come—a grand reimagining of what medicine should be. In 1848, the Prussian government sent a young physician named Rudolf Virchow to investigate a typhus epidemic in Upper Silesia. Virchow didn’t know what caused the devastating disease, but he realized its spread was possible because of malnutrition, hazardous working conditions, crowded housing, poor sanitation, and the inattention of civil servants and aristocrats—problems that require social and political reforms. “Medicine is a social science,” Virchow said, “and politics is nothing but medicine in larger scale.”
This viewpoint fell by the wayside after germ theory became mainstream in the late 19th century. When scientists discovered the microbes responsible for tuberculosis, plague, cholera, dysentery, and syphilis, most fixated on these newly identified nemeses. Societal factors were seen as overly political distractions for researchers who sought to “be as ‘objective’ as possible,” says Elaine Hernandez, a medical sociologist at Indiana University. In the U.S., medicine fractured. New departments of sociology and cultural anthropology kept their eye on the societal side of health, while the nation’s first schools of public health focused instead on fights between germs and individuals. This rift widened as improvements in hygiene, living standards, nutrition, and sanitation lengthened life spans: The more social conditions improved, the more readily they could be ignored.
The ideological pivot away from social medicine began to reverse in the second half of the 20th century. The women’s-rights and civil-rights movements, the rise of environmentalism, and anti-war protests created a generation of scholars who questioned “the legitimacy, ideology, and practice of any science … that disregards social and economic inequality,” wrote Nancy Krieger of Harvard . Beginning in the 1980s, this new wave of social epidemiologists once again studied how poverty, privilege, and living conditions affect a person’s health—to a degree even Virchow hadn’t imagined. But as COVID‑19 has shown, the reintegration is not yet complete.
Politicians initially described COVID‑19 as a “great equalizer,” but when states began releasing demographic data, it was immediately clear that the disease was disproportionately infecting and killing people of color . These disparities aren’t biological. They stem from decades of discrimination and segregation that left minority communities in poorer neighborhoods with low-paying jobs, more health problems, and less access to health care—the same kind of problems that Virchow identified more than 170 years ago.
From the September 2020 issue: How the pandemic defeated America
Simple acts like wearing a mask and staying at home, which rely on people tolerating discomfort for the collective good, became society’s main defenses against the virus in the many months without effective drugs or vaccines. These are known as nonpharmaceutical interventions—a name that betrays medicine’s biological bias. For most of 2020, these were the only interventions on offer, but they were nonetheless defined in opposition to the more highly prized drugs and vaccines.
In March, when the U.S. started shutting down, one of the biggest questions on the mind of Whitney Robinson of UNC at Chapel Hill was: Are our kids going to be out of school for two years? While biomedical scientists tend to focus on sickness and recovery, social epidemiologists like her “think about critical periods that can affect the trajectory of your life,” she told me. Disrupting a child’s schooling at the wrong time can affect their entire career, so scientists should have prioritized research to figure out whether and how schools could reopen safely. But most studies on the spread of COVID‑19 in schools were neither large in scope nor well-designed enough to be conclusive. No federal agency funded a large, nationwide study, even though the federal government had months to do so. The NIH received billions for COVID‑19 research , but the National Institute of Child Health and Human Development—one of its 27 constituent institutes and centers—got nothing.
The horrors that Rudolf Virchow saw in Upper Silesia radicalized him, pushing the future “father of modern pathology” to advocate for social reforms. The current pandemic has affected scientists in the same way. Calm researchers became incensed as potentially game-changing innovations like cheap diagnostic tests were squandered by a negligent administration and a muzzled Centers for Disease Control and Prevention. Austere publications like NEJM and Nature published explicitly political editorials castigating the Trump administration for its failures and encouraging voters to hold the president accountable. COVID‑19 could be the catalyst that fully reunifies the social and biological sides of medicine, bridging disciplines that have been separated for too long.
“To study COVID‑19 is not only to study the disease itself as a biological entity,” says Alondra Nelson, the president of the Social Science Research Council. “What looks like a single problem is actually all things, all at once. So what we’re actually studying is literally everything in society, at every scale, from supply chains to individual relationships.”
The scientific community spent the pre-pandemic years designing faster ways of doing experiments, sharing data, and developing vaccines, allowing it to mobilize quickly when COVID‑19 emerged. Its goal now should be to address its many lingering weaknesses. Warped incentives, wasteful practices, overconfidence, inequality, a biomedical bias—COVID‑19 has exposed them all. And in doing so, it offers the world of science a chance to practice one of its most important qualities: self-correction.
* The print version of this article stated that the Moderna and Pfizer/BioNTech vaccines were reported to be 95 percent effective at preventing COVID-19 infections. In fact, the vaccines prevent disease, not infection.
This article appears in the January/February 2021 print edition with the headline “The COVID-19 Manhattan Project.”
- Share full article
Advertisement
Supported by
current events
12 Ideas for Writing Through the Pandemic With The New York Times
A dozen writing projects — including journals, poems, comics and more — for students to try at home.

By Natalie Proulx
The coronavirus has transformed life as we know it. Schools are closed, we’re confined to our homes and the future feels very uncertain. Why write at a time like this?
For one, we are living through history. Future historians may look back on the journals, essays and art that ordinary people are creating now to tell the story of life during the coronavirus.
But writing can also be deeply therapeutic. It can be a way to express our fears, hopes and joys. It can help us make sense of the world and our place in it.
Plus, even though school buildings are shuttered, that doesn’t mean learning has stopped. Writing can help us reflect on what’s happening in our lives and form new ideas.
We want to help inspire your writing about the coronavirus while you learn from home. Below, we offer 12 projects for students, all based on pieces from The New York Times, including personal narrative essays, editorials, comic strips and podcasts. Each project features a Times text and prompts to inspire your writing, as well as related resources from The Learning Network to help you develop your craft. Some also offer opportunities to get your work published in The Times, on The Learning Network or elsewhere.
We know this list isn’t nearly complete. If you have ideas for other pandemic-related writing projects, please suggest them in the comments.
In the meantime, happy writing!
Journaling is well-known as a therapeutic practice , a tool for helping you organize your thoughts and vent your emotions, especially in anxiety-ridden times. But keeping a diary has an added benefit during a pandemic: It may help educate future generations.
In “ The Quarantine Diaries ,” Amelia Nierenberg spoke to Ady, an 8-year-old in the Bay Area who is keeping a diary. Ms. Nierenberg writes:
As the coronavirus continues to spread and confine people largely to their homes, many are filling pages with their experiences of living through a pandemic. Their diaries are told in words and pictures: pantry inventories, window views, questions about the future, concerns about the present. Taken together, the pages tell the story of an anxious, claustrophobic world on pause. “You can say anything you want, no matter what, and nobody can judge you,” Ady said in a phone interview earlier this month, speaking about her diary. “No one says, ‘scaredy-cat.’” When future historians look to write the story of life during coronavirus, these first-person accounts may prove useful. “Diaries and correspondences are a gold standard,” said Jane Kamensky, a professor of American History at Harvard University and the faculty director of the Schlesinger Library at the Radcliffe Institute. “They’re among the best evidence we have of people’s inner worlds.”
You can keep your own journal, recording your thoughts, questions, concerns and experiences of living through the coronavirus pandemic.
Not sure what to write about? Read the rest of Ms. Nierenberg’s article to find out what others around the world are recording. If you need more inspiration, here are a few writing prompts to get you started:
How has the virus disrupted your daily life? What are you missing? School, sports, competitions, extracurricular activities, social plans, vacations or anything else?
What effect has this crisis had on your own mental and emotional health?
What changes, big or small, are you noticing in the world around you?
For more ideas, see our writing prompts . We post a new one every school day, many of them now related to life during the coronavirus.
You can write in your journal every day or as often as you like. And if writing isn’t working for you right now, try a visual, audio or video diary instead.
2. Personal Narrative
As you write in your journal, you’ll probably find that your life during the pandemic is full of stories, whether serious or funny, angry or sad. If you’re so inspired, try writing about one of your experiences in a personal narrative essay.
Here’s how Mary Laura Philpott begins her essay, “ This Togetherness Is Temporary, ” about being quarantined with her teenage children:
Get this: A couple of months ago, I quit my job in order to be home more. Go ahead and laugh at the timing. I know. At the time, it was hitting me that my daughter starts high school in the fall, and my son will be a senior. Increasingly they were spending their time away from me at school, with friends, and in the many time-intensive activities that make up teenage lives. I could feel the clock ticking, and I wanted to spend the minutes I could — the minutes they were willing to give me, anyway — with them, instead of sitting in front of a computer at night and on weekends in order to juggle a job as a bookseller, a part-time gig as a television host, and a book deadline. I wanted more of them while they were still living in my house. Now here we are, all together, every day. You’re supposed to be careful what you wish for, but come on. None of us saw this coming.
Personal narratives are short, powerful stories about meaningful life experiences, big or small. Read the rest of Ms. Philpott’s essay to see how she balances telling the story of a specific moment in time and reflecting on what it all means in the larger context of her life.
To help you identify the moments that have been particularly meaningful, difficult, comical or strange during this pandemic, try responding to one of our writing prompts related to the coronavirus:
Holidays and Birthdays Are Moments to Come Together. How Are You Adapting During the Pandemic?
Has Your School Switched to Remote Learning? How Is It Going So Far?
Is the Coronavirus Pandemic Bringing Your Extended Family Closer Together?
How Is the Coronavirus Outbreak Affecting Your Life?
Another option? Use any of the images in our Picture Prompt series to inspire you to write about a memory from your life.
Related Resource: Writing Curriculum | Unit 1: Teach Narrative Writing With The New York Times

People have long turned to creative expression in times of crisis. During the coronavirus pandemic, artists are continuing to illustrate , play music , dance , perform — and write poetry .
That’s what Dr. Elizabeth Mitchell, an emergency room doctor in Boston, did after a long shift treating coronavirus patients. Called “ The Apocalypse ,” her poem begins like this:
This is the apocalypse A daffodil has poked its head up from the dirt and opened sunny arms to bluer skies yet I am filled with dark and anxious dread as theaters close as travel ends and grocery stores display their empty rows where toilet paper liquid bleach and bags of flour stood in upright ranks.
Read the rest of Dr. Mitchell’s poem and note the lines, images and metaphors that speak to you. Then, tap into your creative side by writing a poem inspired by your own experience of the pandemic.
Need inspiration? Try writing a poem in response to one of our Picture Prompts . Or, you can create a found poem using an article from The Times’s coronavirus outbreak coverage . If you have access to the print paper, try making a blackout poem instead.
Related Resources: 24 Ways to Teach and Learn About Poetry With The New York Times Reader Idea | How the Found Poem Can Inspire Teachers and Students Alike
4. Letter to the Editor
Have you been keeping up with the news about the coronavirus? What is your reaction to it?
Make your voice heard by writing a letter to the editor about a recent Times article, editorial, column or Opinion essay related to the pandemic. You can find articles in The Times’s free coronavirus coverage or The Learning Network’s coronavirus resources for students . And, if you’re a high school student, your school can get you free digital access to The New York Times from now until July 6.
To see examples, read the letters written by young people in response to recent headlines in “ How the Young Deal With the Coronavirus .” Here’s what Addie Muller from San Jose, Calif., had to say about the Opinion essay “ I’m 26. Coronavirus Sent Me to the Hospital ”:
As a high school student and a part of Generation Z, I’ve been less concerned about getting Covid-19 and more concerned about spreading it to more vulnerable populations. While I’ve been staying at home and sheltering in place (as was ordered for the state of California), many of my friends haven’t been doing the same. I know people who continue going to restaurants and have been treating the change in education as an extended spring break and excuse to spend more time with friends. I fear for my grandparents and parents, but this article showed me that we should also fear for ourselves. I appreciated seeing this article because many younger people seem to feel invincible. The fact that a healthy 26-year-old can be hospitalized means that we are all capable of getting the virus ourselves and spreading it to others. I hope that Ms. Lowenstein continues spreading her story and that she makes a full recovery soon.
As you read, note some of the defining features of a letter to the editor and what made these good enough to publish. For more advice, see these tips from Thomas Feyer, the letters editor at The Times, about how to write a compelling letter. They include:
Write briefly and to the point.
Be prepared to back up your facts with evidence.
Write about something off the beaten path.
Publishing Opportunity: When you’re ready, submit your letter to The New York Times.
5. Editorial
Maybe you have more to say than you can fit in a 150-word letter to the editor. If that’s the case, try writing an editorial about something you have a strong opinion about related to the coronavirus. What have you seen that has made you upset? Proud? Appreciative? Scared?
In “ Surviving Coronavirus as a Broke College Student ,” Sydney Goins, a senior English major at the University of Georgia, writes about the limited options for students whose colleges are now closed. Her essay begins:
College was supposed to be my ticket to financial security. My parents were the first ones to go to college in their family. My grandpa said to my mom, “You need to go to college, so you don’t have to depend on a man for money.” This same mentality was passed on to me as well. I had enough money to last until May— $1,625 to be exact — until the coronavirus ruined my finances. My mom works in human resources. My dad is a project manager for a mattress company. I worked part time at the university’s most popular dining hall and lived in a cramped house with three other students. I don’t have a car. I either walked or biked a mile to attend class. I have student debt and started paying the accrued interest last month. I was making it work until the coronavirus shut down my college town. At first, spring break was extended by two weeks with the assumption that campus would open again in late March, but a few hours after that email, all 26 colleges in the University System of Georgia canceled in-person classes and closed integral parts of campus.
Read the rest of Ms. Goins’s essay. What is her argument? How does she support it? How is it relevant to her life and the world?
Then, choose a topic related to the pandemic that you care about and write an editorial that asserts an opinion and backs it up with solid reasoning and evidence.
Not sure where to start? Try responding to some of our recent argumentative writing prompts and see what comes up for you. Here are a few we’ve asked students so far:
Should Schools Change How They Grade Students During the Pandemic?
What Role Should Celebrities Have During the Coronavirus Crisis?
Is It Immoral to Increase the Price of Goods During a Crisis?
Or, consider essential questions about the pandemic and what they tell us about our world today: What weaknesses is the coronavirus exposing in our society? How can we best help our communities right now? What lessons can we learn from this crisis? See more here.
As an alternative to a written essay, you might try creating a video Op-Ed instead, like Katherine Oung’s “ Coronavirus Racism Infected My High School. ”
Publishing Opportunity: Submit your final essay to our Student Editorial Contest , open to middle school and high school students ages 10-19, until April 21. Please be sure to read all the rules and guidelines before submitting.
Related Resource: An Argumentative-Writing Unit for Students Doing Remote Learning
Are games, television, music, books, art or movies providing you with a much-needed distraction during the pandemic? What has been working for you that you would recommend to others? Or, what would you caution others to stay away from right now?
Share your opinions by writing a review of a piece of art or culture for other teenagers who are stuck at home. You might suggest TV shows, novels, podcasts, video games, recipes or anything else. Or, try something made especially for the coronavirus era, like a virtual architecture tour , concert or safari .
As a mentor text, read Laura Cappelle’s review of French theater companies that have rushed to put content online during the coronavirus outbreak, noting how she tailors her commentary to our current reality:
The 17th-century philosopher Blaise Pascal once wrote: “The sole cause of people’s unhappiness is that they do not know how to stay quietly in their rooms.” Yet at a time when much of the world has been forced to hunker down, French theater-makers are fighting to fill the void by making noise online.
She continues:
Under the circumstances, it would be churlish to complain about artists’ desire to connect with audiences in some fashion. Theater, which depends on crowds gathering to watch performers at close quarters, is experiencing significant loss and upheaval, with many stagings either delayed indefinitely or canceled outright. But a sampling of stopgap offerings often left me underwhelmed.
To get inspired you might start by responding to our related Student Opinion prompt with your recommendations. Then turn one of them into a formal review.
Related Resource: Writing Curriculum | Unit 2: Analyzing Arts, Criticizing Culture: Writing Reviews With The New York Times
7. How-to Guide
Being stuck at home with nowhere to go is the perfect time to learn a new skill. What are you an expert at that you can you teach someone?
The Times has created several guides that walk readers through how to do something step-by-step, for example, this eight-step tutorial on how to make a face mask . Read through the guide, noting how the author breaks down each step into an easily digestible action, as well as how the illustrations support comprehension.
Then, create your own how-to guide for something you could teach someone to do during the pandemic. Maybe it’s a recipe you’ve perfected, a solo sport you’ve been practicing, or a FaceTime tutorial for someone who’s never video chatted before.
Whatever you choose, make sure to write clearly so anyone anywhere could try out this new skill. As an added challenge, include an illustration, photo, or audio or video clip with each step to support the reader’s understanding.
Related Resource: Writing Curriculum | Unit 4: Informational Writing
8. 36 Hours Column
For nearly two decades, The Times has published a weekly 36 Hours column , giving readers suggestions for how to spend a weekend in cities all over the globe.
While traveling for fun is not an option now, the Travel section decided to create a special reader-generated column of how to spend a weekend in the midst of a global pandemic. The result? “ 36 Hours in … Wherever You Are .” Here’s how readers suggest spending a Sunday morning:
8 a.m. Changing routines Make small discoveries. To stretch my legs during the lockdown, I’ve been walking around the block every day, and I’ve started to notice details that I’d never seen before. Like the fake, painted window on the building across the road, or the old candle holders that were once used as part of the street lighting. When the quarantine ends, I hope we don’t forget to appreciate what’s been on a doorstep all along. — Camilla Capasso, Modena, Italy 10:30 a.m. Use your hands Undertake the easiest and most fulfilling origami project of your life by folding 12 pieces of paper and building this lovely star . Modular origami has been my absolute favorite occupational therapy since I was a restless child: the process is enthralling and soothing. — Laila Dib, Berlin, Germany 12 p.m. Be isolated, together Check on neighbors on your block or floor with an email, text or phone call, or leave a card with your name and contact information. Are they OK? Do they need something from the store? Help with an errand? Food? Can you bring them a hot dish or home-baked bread? This simple act — done carefully and from a safe distance — palpably reduces our sense of fear and isolation. I’ve seen the faces of some neighbors for the first time. Now they wave. — Jim Carrier, Burlington, Vt.
Read the entire article. As you read, consider: How would this be different if it were written by teenagers for teenagers?
Then, create your own 36 Hours itinerary for teenagers stuck at home during the pandemic with ideas for how to spend the weekend wherever they are.
The 36 Hours editors suggest thinking “within the spirit of travel, even if many of us are housebound.” For example: an album or a song playlist; a book or movie that transports you; a particular recipe you love; or a clever way to virtually connect with family and friends. See more suggestions here .
Related Resources: Reader Idea | 36 Hours in Your Hometown 36 Hours in Learning: Creating Travel Itineraries Across the Curriculum
9. Photo Essay

Daily life looks very different now. Unusual scenes are playing out in homes, parks, grocery stores and streets across the country.
In “ New York Was Not Designed for Emptiness ,” New York Times photographers document what life in New York City looks like amid the pandemic. It begins:
The lights are still on in Times Square. Billboards blink and storefronts shine in neon. If only there were an audience for this spectacle. But the thoroughfares have been abandoned. The energy that once crackled along the concrete has eased. The throngs of tourists, the briskly striding commuters, the honking drivers have mostly skittered away. In their place is a wistful awareness that plays across all five boroughs: Look how eerie our brilliant landscape has become. Look how it no longer bustles. This is not the New York City anyone signed up for.
Read the rest of the essay and view the photos. As you read, note the photos or lines in the text that grab your attention most. Why do they stand out to you?
What does the pandemic look like where you live? Create your own photo essay, accompanied by a written piece, that illustrates your life now. In your essay, consider how you can communicate a particular theme or message about life during the pandemic through both your photos and words, like in the article you read.
Publishing Opportunity: The International Center of Photography is collecting a virtual archive of images related to the coronavirus pandemic. Learn how to submit yours here.
10. Comic Strip
Sometimes, words alone just won’t do. Visual mediums, like comics, have the advantage of being able to express emotion, reveal inner monologues, and explain complex subjects in ways that words on their own seldom can.
If anything proves this point, it is the Opinion section’s ongoing visual diary, “ Art in Isolation .” Scroll through this collection to see clever and poignant illustrations about life in these uncertain times. Read the comic “ Finding Connection When Home Alone ” by Gracey Zhang from this collection. As you read, note what stands out to you about the writing and illustrations. What lessons could they have for your own piece?
Then, create your own comic strip, modeled after the one you read, that explores some aspect of life during the pandemic. You can sketch and color your comic with paper and pen, or use an online tool like MakeBeliefsComix.com .
Need inspiration? If you’re keeping a quarantine journal, as we suggested above, you might create a graphic story based on a week of your life, or just a small part of it — like the meals you ate, the video games you played, or the conversations you had with friends over text. For more ideas, check out our writing prompts related to the coronavirus.
Related Resource: From Superheroes to Syrian Refugees: Teaching Comics and Graphic Novels With Resources From The New York Times
11. Podcast
Modern Love Podcast: In the Midst of the Coronavirus Pandemic, People Share Their Love Stories
Are you listening to any podcasts to help you get through the pandemic? Are they keeping you up-to-date on the news? Offering advice? Or just helping you escape from it all?
Create your own five-minute podcast segment that responds to the coronavirus in some way.
To get an idea of the different genres and formats your podcast could take, listen to one or more of these five-minute clips from three New York Times podcast episodes related to the coronavirus:
“ The Daily | Voices of the Pandemic ” (1:15-6:50)
“ Still Processing | A Pod From Both Our Houses ” (0:00-4:50)
“ Modern Love | In the Midst of the Coronavirus Pandemic, People Share Their Love Stories ” (1:30-6:30)
Use these as models for your own podcast. Consider the different narrative techniques they use to relate an experience of the pandemic — interviews, nonfiction storytelling and conversation — as well as how they create an engaging listening experience.
Need ideas for what to talk about? You might try translating any of the writing projects above into podcast form. Or turn to our coronavirus-related writing prompts for inspiration.
Publishing Opportunity: Submit your finished five-minute podcast to our Student Podcast Contest , which is open through May 19. Please read all the rules and guidelines before submitting.
Related Resource: Project Audio: Teaching Students How to Produce Their Own Podcasts
12. Revise and Edit
“It doesn’t matter how good you think you are as a writer — the first words you put on the page are a first draft,” Harry Guinness writes in “ How to Edit Your Own Writing .”
Editing your work may seem like something you do quickly — checking for spelling mistakes just before you turn in your essay — but Mr. Guinness argues it’s a project in its own right:
The time you put into editing, reworking and refining turns your first draft into a second — and then into a third and, if you keep at it, eventually something great. The biggest mistake you can make as a writer is to assume that what you wrote the first time through was good enough.
Read the rest of the article for a step-by-step guide to editing your own work. Then, revise one of the pieces you have written, following Mr. Guinness’s advice.
Publishing Opportunity: When you feel like your piece is “something great,” consider submitting it to one of the publishing opportunities we’ve suggested above. Or, see our list of 70-plus places that publish teenage writing and art to find more.
Natalie Proulx joined The Learning Network as a staff editor in 2017 after working as an English language arts teacher and curriculum writer. More about Natalie Proulx
- CBSE Class 10th
- CBSE Class 12th
- UP Board 10th
- UP Board 12th
- Bihar Board 10th
- Bihar Board 12th
- Top Schools in India
- Top Schools in Delhi
- Top Schools in Mumbai
- Top Schools in Chennai
- Top Schools in Hyderabad
- Top Schools in Kolkata
- Top Schools in Pune
- Top Schools in Bangalore
Products & Resources
- JEE Main Knockout April
- Free Sample Papers
- Free Ebooks
- NCERT Notes
- NCERT Syllabus
- NCERT Books
- RD Sharma Solutions
- Navodaya Vidyalaya Admission 2024-25
- NCERT Solutions
- NCERT Solutions for Class 12
- NCERT Solutions for Class 11
- NCERT solutions for Class 10
- NCERT solutions for Class 9
- NCERT solutions for Class 8
- NCERT Solutions for Class 7
- JEE Main 2024
- MHT CET 2024
- JEE Advanced 2024
- BITSAT 2024
- View All Engineering Exams
- Colleges Accepting B.Tech Applications
- Top Engineering Colleges in India
- Engineering Colleges in India
- Engineering Colleges in Tamil Nadu
- Engineering Colleges Accepting JEE Main
- Top IITs in India
- Top NITs in India
- Top IIITs in India
- JEE Main College Predictor
- JEE Main Rank Predictor
- MHT CET College Predictor
- AP EAMCET College Predictor
- GATE College Predictor
- KCET College Predictor
- JEE Advanced College Predictor
- View All College Predictors
- JEE Main Question Paper
- JEE Main Cutoff
- JEE Main Advanced Admit Card
- AP EAPCET Hall Ticket
- Download E-Books and Sample Papers
- Compare Colleges
- B.Tech College Applications
- KCET Result
- MAH MBA CET Exam
- View All Management Exams
Colleges & Courses
- MBA College Admissions
- MBA Colleges in India
- Top IIMs Colleges in India
- Top Online MBA Colleges in India
- MBA Colleges Accepting XAT Score
- BBA Colleges in India
- XAT College Predictor 2024
- SNAP College Predictor
- NMAT College Predictor
- MAT College Predictor 2024
- CMAT College Predictor 2024
- CAT Percentile Predictor 2023
- CAT 2023 College Predictor
- CMAT 2024 Admit Card
- TS ICET 2024 Hall Ticket
- CMAT Result 2024
- MAH MBA CET Cutoff 2024
- Download Helpful Ebooks
- List of Popular Branches
- QnA - Get answers to your doubts
- IIM Fees Structure
- AIIMS Nursing
- Top Medical Colleges in India
- Top Medical Colleges in India accepting NEET Score
- Medical Colleges accepting NEET
- List of Medical Colleges in India
- List of AIIMS Colleges In India
- Medical Colleges in Maharashtra
- Medical Colleges in India Accepting NEET PG
- NEET College Predictor
- NEET PG College Predictor
- NEET MDS College Predictor
- NEET Rank Predictor
- DNB PDCET College Predictor
- NEET Admit Card 2024
- NEET PG Application Form 2024
- NEET Cut off
- NEET Online Preparation
- Download Helpful E-books
- Colleges Accepting Admissions
- Top Law Colleges in India
- Law College Accepting CLAT Score
- List of Law Colleges in India
- Top Law Colleges in Delhi
- Top NLUs Colleges in India
- Top Law Colleges in Chandigarh
- Top Law Collages in Lucknow
Predictors & E-Books
- CLAT College Predictor
- MHCET Law ( 5 Year L.L.B) College Predictor
- AILET College Predictor
- Sample Papers
- Compare Law Collages
- Careers360 Youtube Channel
- CLAT Syllabus 2025
- CLAT Previous Year Question Paper
- NID DAT Exam
- Pearl Academy Exam
Predictors & Articles
- NIFT College Predictor
- UCEED College Predictor
- NID DAT College Predictor
- NID DAT Syllabus 2025
- NID DAT 2025
- Design Colleges in India
- Top NIFT Colleges in India
- Fashion Design Colleges in India
- Top Interior Design Colleges in India
- Top Graphic Designing Colleges in India
- Fashion Design Colleges in Delhi
- Fashion Design Colleges in Mumbai
- Top Interior Design Colleges in Bangalore
- NIFT Result 2024
- NIFT Fees Structure
- NIFT Syllabus 2025
- Free Design E-books
- List of Branches
- Careers360 Youtube channel
- IPU CET BJMC
- JMI Mass Communication Entrance Exam
- IIMC Entrance Exam
- Media & Journalism colleges in Delhi
- Media & Journalism colleges in Bangalore
- Media & Journalism colleges in Mumbai
- List of Media & Journalism Colleges in India
- CA Intermediate
- CA Foundation
- CS Executive
- CS Professional
- Difference between CA and CS
- Difference between CA and CMA
- CA Full form
- CMA Full form
- CS Full form
- CA Salary In India
Top Courses & Careers
- Bachelor of Commerce (B.Com)
- Master of Commerce (M.Com)
- Company Secretary
- Cost Accountant
- Charted Accountant
- Credit Manager
- Financial Advisor
- Top Commerce Colleges in India
- Top Government Commerce Colleges in India
- Top Private Commerce Colleges in India
- Top M.Com Colleges in Mumbai
- Top B.Com Colleges in India
- IT Colleges in Tamil Nadu
- IT Colleges in Uttar Pradesh
- MCA Colleges in India
- BCA Colleges in India
Quick Links
- Information Technology Courses
- Programming Courses
- Web Development Courses
- Data Analytics Courses
- Big Data Analytics Courses
- RUHS Pharmacy Admission Test
- Top Pharmacy Colleges in India
- Pharmacy Colleges in Pune
- Pharmacy Colleges in Mumbai
- Colleges Accepting GPAT Score
- Pharmacy Colleges in Lucknow
- List of Pharmacy Colleges in Nagpur
- GPAT Result
- GPAT 2024 Admit Card
- GPAT Question Papers
- NCHMCT JEE 2024
- Mah BHMCT CET
- Top Hotel Management Colleges in Delhi
- Top Hotel Management Colleges in Hyderabad
- Top Hotel Management Colleges in Mumbai
- Top Hotel Management Colleges in Tamil Nadu
- Top Hotel Management Colleges in Maharashtra
- B.Sc Hotel Management
- Hotel Management
- Diploma in Hotel Management and Catering Technology
Diploma Colleges
- Top Diploma Colleges in Maharashtra
- UPSC IAS 2024
- SSC CGL 2024
- IBPS RRB 2024
- Previous Year Sample Papers
- Free Competition E-books
- Sarkari Result
- QnA- Get your doubts answered
- UPSC Previous Year Sample Papers
- CTET Previous Year Sample Papers
- SBI Clerk Previous Year Sample Papers
- NDA Previous Year Sample Papers
Upcoming Events
- NDA Application Form 2024
- UPSC IAS Application Form 2024
- CDS Application Form 2024
- CTET Admit card 2024
- HP TET Result 2023
- SSC GD Constable Admit Card 2024
- UPTET Notification 2024
- SBI Clerk Result 2024
Other Exams
- SSC CHSL 2024
- UP PCS 2024
- UGC NET 2024
- RRB NTPC 2024
- IBPS PO 2024
- IBPS Clerk 2024
- IBPS SO 2024
- Top University in USA
- Top University in Canada
- Top University in Ireland
- Top Universities in UK
- Top Universities in Australia
- Best MBA Colleges in Abroad
- Business Management Studies Colleges
Top Countries
- Study in USA
- Study in UK
- Study in Canada
- Study in Australia
- Study in Ireland
- Study in Germany
- Study in China
- Study in Europe
Student Visas
- Student Visa Canada
- Student Visa UK
- Student Visa USA
- Student Visa Australia
- Student Visa Germany
- Student Visa New Zealand
- Student Visa Ireland
- CUET PG 2024
- IGNOU B.Ed Admission 2024
- DU Admission 2024
- UP B.Ed JEE 2024
- LPU NEST 2024
- IIT JAM 2024
- IGNOU Online Admission 2024
- Universities in India
- Top Universities in India 2024
- Top Colleges in India
- Top Universities in Uttar Pradesh 2024
- Top Universities in Bihar
- Top Universities in Madhya Pradesh 2024
- Top Universities in Tamil Nadu 2024
- Central Universities in India
- CUET Exam City Intimation Slip 2024
- IGNOU Date Sheet
- CUET Mock Test 2024
- CUET Admit card 2024
- CUET PG Syllabus 2024
- CUET Participating Universities 2024
- CUET Previous Year Question Paper
- CUET Syllabus 2024 for Science Students
- E-Books and Sample Papers
- CUET Exam Pattern 2024
- CUET Exam Date 2024
- CUET Syllabus 2024
- IGNOU Exam Form 2024
- IGNOU Result
- CUET City Intimation Slip 2024 Live
Engineering Preparation
- Knockout JEE Main 2024
- Test Series JEE Main 2024
- JEE Main 2024 Rank Booster
Medical Preparation
- Knockout NEET 2024
- Test Series NEET 2024
- Rank Booster NEET 2024
Online Courses
- JEE Main One Month Course
- NEET One Month Course
- IBSAT Free Mock Tests
- IIT JEE Foundation Course
- Knockout BITSAT 2024
- Career Guidance Tool
Top Streams
- IT & Software Certification Courses
- Engineering and Architecture Certification Courses
- Programming And Development Certification Courses
- Business and Management Certification Courses
- Marketing Certification Courses
- Health and Fitness Certification Courses
- Design Certification Courses
Specializations
- Digital Marketing Certification Courses
- Cyber Security Certification Courses
- Artificial Intelligence Certification Courses
- Business Analytics Certification Courses
- Data Science Certification Courses
- Cloud Computing Certification Courses
- Machine Learning Certification Courses
- View All Certification Courses
- UG Degree Courses
- PG Degree Courses
- Short Term Courses
- Free Courses
- Online Degrees and Diplomas
- Compare Courses
Top Providers
- Coursera Courses
- Udemy Courses
- Edx Courses
- Swayam Courses
- upGrad Courses
- Simplilearn Courses
- Great Learning Courses
Covid 19 Essay in English
Essay on Covid -19: In a very short amount of time, coronavirus has spread globally. It has had an enormous impact on people's lives, economy, and societies all around the world, affecting every country. Governments have had to take severe measures to try and contain the pandemic. The virus has altered our way of life in many ways, including its effects on our health and our economy. Here are a few sample essays on ‘CoronaVirus’.
100 Words Essay on Covid 19
200 words essay on covid 19, 500 words essay on covid 19.
COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very short period of time. It has affected lives, economies and societies across the world, leaving no country untouched. The virus has caused governments to take drastic measures to try and contain it. From health implications to economic and social ramifications, COVID-19 impacted every part of our lives. It has been more than 2 years since the pandemic hit and the world is still recovering from its effects.
Since the outbreak of COVID-19, the world has been impacted in a number of ways. For one, the global economy has taken a hit as businesses have been forced to close their doors. This has led to widespread job losses and an increase in poverty levels around the world. Additionally, countries have had to impose strict travel restrictions in an attempt to contain the virus, which has resulted in a decrease in tourism and international trade. Furthermore, the pandemic has put immense pressure on healthcare systems globally, as hospitals have been overwhelmed with patients suffering from the virus. Lastly, the outbreak has led to a general feeling of anxiety and uncertainty, as people are fearful of contracting the disease.
My Experience of COVID-19
I still remember how abruptly colleges and schools shut down in March 2020. I was a college student at that time and I was under the impression that everything would go back to normal in a few weeks. I could not have been more wrong. The situation only got worse every week and the government had to impose a lockdown. There were so many restrictions in place. For example, we had to wear face masks whenever we left the house, and we could only go out for essential errands. Restaurants and shops were only allowed to operate at take-out capacity, and many businesses were shut down.
In the current scenario, coronavirus is dominating all aspects of our lives. The coronavirus pandemic has wreaked havoc upon people’s lives, altering the way we live and work in a very short amount of time. It has revolutionised how we think about health care, education, and even social interaction. This virus has had long-term implications on our society, including its impact on mental health, economic stability, and global politics. But we as individuals can help to mitigate these effects by taking personal responsibility to protect themselves and those around them from infection.
Effects of CoronaVirus on Education
The outbreak of coronavirus has had a significant impact on education systems around the world. In China, where the virus originated, all schools and universities were closed for several weeks in an effort to contain the spread of the disease. Many other countries have followed suit, either closing schools altogether or suspending classes for a period of time.
This has resulted in a major disruption to the education of millions of students. Some have been able to continue their studies online, but many have not had access to the internet or have not been able to afford the costs associated with it. This has led to a widening of the digital divide between those who can afford to continue their education online and those who cannot.
The closure of schools has also had a negative impact on the mental health of many students. With no face-to-face contact with friends and teachers, some students have felt isolated and anxious. This has been compounded by the worry and uncertainty surrounding the virus itself.
The situation with coronavirus has improved and schools have been reopened but students are still catching up with the gap of 2 years that the pandemic created. In the meantime, governments and educational institutions are working together to find ways to support students and ensure that they are able to continue their education despite these difficult circumstances.
Effects of CoronaVirus on Economy
The outbreak of the coronavirus has had a significant impact on the global economy. The virus, which originated in China, has spread to over two hundred countries, resulting in widespread panic and a decrease in global trade. As a result of the outbreak, many businesses have been forced to close their doors, leading to a rise in unemployment. In addition, the stock market has taken a severe hit.
Effects of CoronaVirus on Health
The effects that coronavirus has on one's health are still being studied and researched as the virus continues to spread throughout the world. However, some of the potential effects on health that have been observed thus far include respiratory problems, fever, and coughing. In severe cases, pneumonia, kidney failure, and death can occur. It is important for people who think they may have been exposed to the virus to seek medical attention immediately so that they can be treated properly and avoid any serious complications. There is no specific cure or treatment for coronavirus at this time, but there are ways to help ease symptoms and prevent the virus from spreading.
Applications for Admissions are open.

JEE Main Important Physics formulas
As per latest 2024 syllabus. Physics formulas, equations, & laws of class 11 & 12th chapters

ALLEN Digital Scholarship Admission Test (ADSAT)
Register FREE for ALLEN Digital Scholarship Admission Test (ADSAT)

Aakash iACST Scholarship Test 2024
Get up to 90% scholarship on NEET, JEE & Foundation courses

JEE Main Important Chemistry formulas
As per latest 2024 syllabus. Chemistry formulas, equations, & laws of class 11 & 12th chapters

PACE IIT & Medical, Financial District, Hyd
Enrol in PACE IIT & Medical, Financial District, Hyd for JEE/NEET preparation

ALLEN JEE Exam Prep
Start your JEE preparation with ALLEN
Download Careers360 App's
Regular exam updates, QnA, Predictors, College Applications & E-books now on your Mobile
Certifications
We Appeared in
MINI REVIEW article
Covid-19: emergence, spread, possible treatments, and global burden.

- 1 Department of Pharmacology, Manipal College of Pharmaceutical Sciences, Manipal Academy of Higher Education, Manipal, India
- 2 Department of Health Sciences, School of Education and Health, Cape Breton University, Sydney, NS, Canada
The Coronavirus (CoV) is a large family of viruses known to cause illnesses ranging from the common cold to acute respiratory tract infection. The severity of the infection may be visible as pneumonia, acute respiratory syndrome, and even death. Until the outbreak of SARS, this group of viruses was greatly overlooked. However, since the SARS and MERS outbreaks, these viruses have been studied in greater detail, propelling the vaccine research. On December 31, 2019, mysterious cases of pneumonia were detected in the city of Wuhan in China's Hubei Province. On January 7, 2020, the causative agent was identified as a new coronavirus (2019-nCoV), and the disease was later named as COVID-19 by the WHO. The virus spread extensively in the Wuhan region of China and has gained entry to over 210 countries and territories. Though experts suspected that the virus is transmitted from animals to humans, there are mixed reports on the origin of the virus. There are no treatment options available for the virus as such, limited to the use of anti-HIV drugs and/or other antivirals such as Remdesivir and Galidesivir. For the containment of the virus, it is recommended to quarantine the infected and to follow good hygiene practices. The virus has had a significant socio-economic impact globally. Economically, China is likely to experience a greater setback than other countries from the pandemic due to added trade war pressure, which have been discussed in this paper.
Introduction
Coronaviridae is a family of viruses with a positive-sense RNA that possess an outer viral coat. When looked at with the help of an electron microscope, there appears to be a unique corona around it. This family of viruses mainly cause respiratory diseases in humans, in the forms of common cold or pneumonia as well as respiratory infections. These viruses can infect animals as well ( 1 , 2 ). Up until the year 2003, coronavirus (CoV) had attracted limited interest from researchers. However, after the SARS (severe acute respiratory syndrome) outbreak caused by the SARS-CoV, the coronavirus was looked at with renewed interest ( 3 , 4 ). This also happened to be the first epidemic of the 21st century originating in the Guangdong province of China. Almost 10 years later, there was a MERS (Middle East respiratory syndrome) outbreak in 2012, which was caused by the MERS-CoV ( 5 , 6 ). Both SARS and MERS have a zoonotic origin and originated from bats. A unique feature of these viruses is the ability to mutate rapidly and adapt to a new host. The zoonotic origin of these viruses allows them to jump from host to host. Coronaviruses are known to use the angiotensin-converting enzyme-2 (ACE-2) receptor or the dipeptidyl peptidase IV (DPP-4) protein to gain entry into cells for replication ( 7 – 10 ).
In December 2019, almost seven years after the MERS 2012 outbreak, a novel Coronavirus (2019-nCoV) surfaced in Wuhan in the Hubei region of China. The outbreak rapidly grew and spread to neighboring countries. However, rapid communication of information and the increasing scale of events led to quick quarantine and screening of travelers, thus containing the spread of the infection. The major part of the infection was restricted to China, and a second cluster was found on a cruise ship called the Diamond Princess docked in Japan ( 11 , 12 ).
The new virus was identified to be a novel Coronavirus and was thus initially named 2019-nCoV; later, it was renamed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) ( 13 ), and the disease it causes is now referred to as Coronavirus Disease-2019 (COVID-19) by the WHO. The virus was suspected to have begun its spread in the Huanan seafood wholesale market in the Wuhan region. It is possible that an animal that was carrying the virus was brought into or sold in the market, causing the spread of the virus in the crowded marketplace. One of the first claims made was in an article published in the Journal of Medical Virology ( 14 ), which identified snakes as the possible host. A second possibility was that pangolins could be the wild host of SARS-CoV-2 ( 15 ), though the most likely possibility is that the virus originated from bats ( 13 , 16 – 19 ). Increasing evidence and experts are now collectively concluding the virus had a natural origin in bats, as with previous such respiratory viruses ( 2 , 20 – 24 ).
Similarly, SARS and MERS were also suspected to originate from bats. In the case of MERS, the dromedary camel is an intermediate host ( 5 , 10 ). Bats have been known to harbor coronaviruses for quite some time now. Just as in the case of avian flu, SARS, MERS, and possibly even HIV, with increasing selection and ecological pressure due to human activities, the virus made the jump from animal to man. Humans have been encroaching increasingly into forests, and this is true over much of China, as in Africa. Combined with additional ecological pressure due to climate change, such zoonotic spillovers are now more common than ever. It is likely that the next disease X will also have such an origin ( 25 ). We have learned the importance of identification of the source organism due to the Ebola virus pandemic. Viruses are unstable organisms genetically, constantly mutating by genetic shift or drift. It is not possible to predict when a cross-species jump may occur and when a seemingly harmless variant form of the virus may turn into a deadly strain. Such an incident occurred in Reston, USA, with the Reston virus ( 26 ), an alarming reminder of this possibility. The identification of the original host helps us to contain future spreads as well as to learn about the mechanism of transmission of viruses. Until the virus is isolated from a wild animal host, in this case, mostly bats, the zoonotic origin will remain hypothetical, though likely. It should further be noted that the virus has acquired several mutations, as noted by a group in China, indicating that there are more than two strains of the virus, which may have had an impact on its pathogenicity. However, this claim remains unproven, and many experts have argued otherwise; data proving this are not yet available ( 27 ). A similar finding was reported from Italy and India independently, where they found two strains ( 28 , 29 ). These findings need to be further cross-verified by similar analyses globally. If true, this finding could effectively explain why some nations are more affected than others.
Transmission
When the spread of COVID-19 began ( Figure 1 ), the virus appeared to be contained within China and the cruise ship “Diamond Princess,” which formed the major clusters of the virus. However, as of April 2020, over 210 countries and territories are affected by the virus, with Europe, the USA, and Iran forming the new cluster of the virus. The USA ( Figure 2 ) has the highest number of confirmed COVID-19 cases, whereas India and China, despite being among the most population-dense countries in the world, have managed to constrain the infection rate by the implementation of a complete lockdown with arrangements in place to manage the confirmed cases. Similarly, the UK has also managed to maintain a low curve of the graph by implementing similar measures, though it was not strictly enforced. Reports have indicated that the presence of different strains or strands of the virus may have had an effect on the management of the infection rate of the virus ( 27 – 29 ). The disease is spread by droplet transmission. As of April 2020, the total number of infected individuals stands at around 3 million, with ~200,000 deaths and more than 1 million recoveries globally ( 30 , 34 ). The virus thus has a fatality rate of around 2% and an R 0 of 3 based on current data. However, a more recent report from the CDC, Atlanta, USA, claims that the R 0 could be as high as 5.7 ( 35 ). It has also been observed from data available from China and India that individuals likely to be infected by the virus from both these countries belong to the age groups of 20–50 years ( 36 , 37 ). In both of these countries, the working class mostly belongs to this age group, making exposure more likely. Germany and Singapore are great examples of countries with a high number of cases but low fatalities as compared to their immediate neighbors. Singapore is one of the few countries that had developed a detailed plan of action after the previous SARS outbreak to deal with a similar situation in the future, and this worked in their favor during this outbreak. Both countries took swift action after the outbreak began, with Singapore banning Chinese travelers and implementing screening and quarantine measures at a time when the WHO recommended none. They ordered the elderly and the vulnerable to strictly stay at home, and they ensured that lifesaving equipment and large-scale testing facilities were available immediately ( 38 , 39 ). Germany took similar measures by ramping up testing capacity quite early and by ensuring that all individuals had equal opportunity to get tested. This meant that young, old, and at-risk people all got tested, thus ensuring positive results early during disease progression and that most cases were mild like in Singapore, thus maintaining a lower death percentage ( 40 ). It allowed infected individuals to be identified and quarantined before they even had symptoms. Testing was carried out at multiple labs, reducing the load and providing massive scale, something which countries such as the USA did quite late and India restricted to select government and private labs. The German government also banned large gatherings and advocated social distancing to further reduce the spread, though unlike India and the USA, this was done quite late. South Korea is another example of how a nation has managed to contain the spread and transmission of the infection. South Korea and the USA both reported their first COVID-19 cases on the same day; however, the US administration downplayed the risks of the disease, unlike South Korean officials, who constantly informed their citizens about the developments of the disease using the media and a centralized messaging system. They also employed the Trace, Test, and Treat protocol to identify and isolate patients fast, whereas the USA restricted this to patients with severe infection and only later broadened this criterion, like many European countries as well as India. Unlike the USA, South Korea also has universal healthcare, ensuring free diagnostic testing.
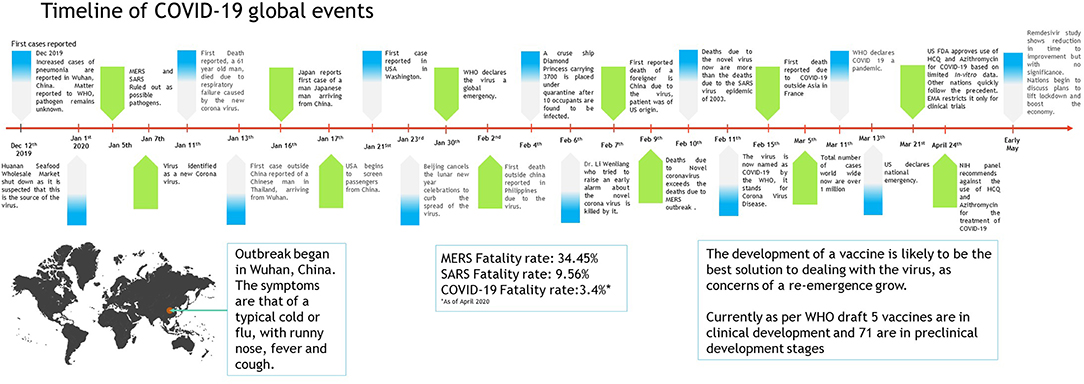
Figure 1 . Timeline of COVID-19 progression ( 30 – 32 ).
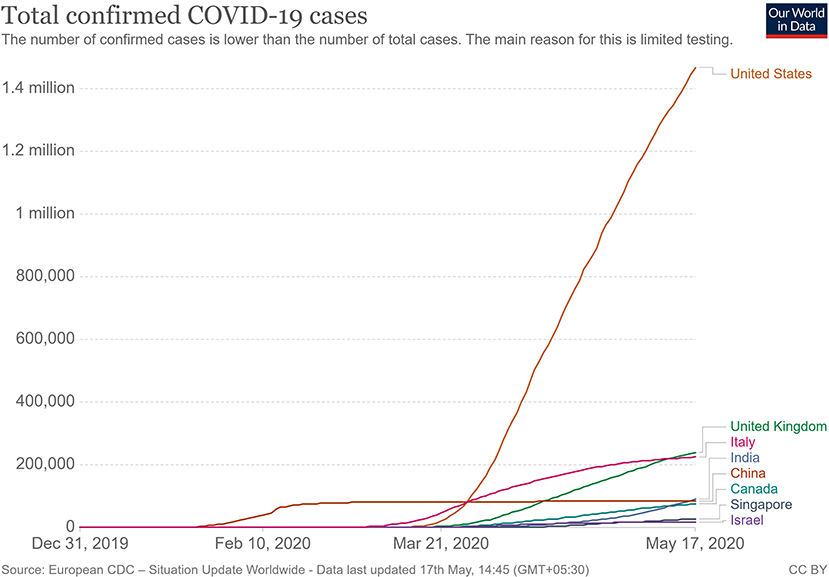
Figure 2 . Total confirmed COVID 19 cases as of May 2020 ( 33 ).
The main mode of transmission of 2019-nCoV is human to human. As of now, animal-to-human transfer has not yet been confirmed. Asymptomatic carriers of the virus are at major risk of being superinfectors with this disease, as all those infected may not develop the disease ( 41 ). This is a concern that has been raised by nations globally, with the Indian government raising concerns on how to identify and contain asymptomatic carriers, who could account for 80% of those infected ( 42 ). Since current resources are directed towards understanding the hospitalized individuals showing symptoms, there is still a vast amount of information about asymptomatic individuals that has yet to be studied. For example, some questions that need to be answered include: Do asymptomatic individuals develop the disease at any point in time at all? Do they eventually develop antibodies? How long do they shed the virus for? Can any tissue of these individuals store the virus in a dormant state? Asymptomatic transmission is a gray area that encompasses major unknowns in COVID-19.
The main route of human-to-human transmission is by droplets, which are generated during coughing, talking, or sneezing and are then inhaled by a healthy individual. They can also be indirectly transmitted to a person when they land on surfaces that are touched by a healthy individual who may then touch their nose, mouth, or eyes, allowing the virus entry into the body. Fomites are also a common issue in such diseases ( 43 ).
Aerosol-based transmission of the virus has not yet been confirmed ( 43 ). Stool-based transmission via the fecal-oral route may also be possible since the SARS-CoV-2 has been found in patient feces ( 44 , 45 ). Some patients with COVID-19 tend to develop diarrhea, which can become a major route of transmission if proper sanitation and personal hygiene needs are not met. There is no evidence currently available to suggest intrauterine vertical transmission of the disease in pregnant women ( 46 ).
More investigation is necessary of whether climate has played any role in the containment of the infection in countries such as India, Singapore, China, and Israel, as these are significantly warmer countries as compared with the UK, the USA, and Canada ( Figure 2 ). Ideally, a warm climate should prevent the virus from surviving for longer periods of time on surfaces, reducing transmissibility.
Pathophysiology
On gaining entry via any of the mucus membranes, the single-stranded RNA-based virus enters the host cell using type 2 transmembrane serine protease (TMPRSS2) and ACE2 receptor protein, leading to fusion and endocytosis with the host cell ( 47 – 49 ). The uncoated RNA is then translated, and viral proteins are synthesized. With the help of RNA-dependant RNA polymerase, new RNA is produced for the new virions. The cell then undergoes lysis, releasing a load of new virions into the patients' body. The resultant infection causes a massive release of pro-inflammatory cytokines that causes a cytokine storm.
Clinical Presentation
The clinical presentation of the disease resembles beta coronavirus infections. The virus has an incubation time of 2–14 days, which is the reason why most patients suspected to have the illness or contact with an individual having the illness remain in quarantine for the said amount of time. Infection with SARS-CoV-2 causes severe pneumonia, intermittent fever, and cough ( 50 , 51 ). Symptoms of rhinorrhoea, pharyngitis, and sneezing have been less commonly seen. Patients often develop acute respiratory distress syndrome within 2 days of hospital admission, requiring ventilatory support. It has been observed that during this phase, the mortality tends to be high. Chest CT will show indicators of pneumonia and ground-glass opacity, a feature that has helped to improve the preliminary diagnosis ( 51 ). The primary method of diagnosis for SARS-CoV-2 is with the help of PCR. For the PCR testing, the US CDC recommends testing for the N gene, whereas the Chinese CDC recommends the use of ORF lab and N gene of the viral genome for testing. Some also rely on the radiological findings for preliminary screening ( 52 ). Additionally, immunodiagnostic tests based on the presence of antibodies can also play a role in testing. While the WHO recommends the use of these tests for research use, many countries have pre-emptively deployed the use of these tests in the hope of ramping up the rate and speed of testing ( 52 – 54 ). Later, they noticed variations among the results, causing them to stop the use of such kits; there was also debate among the experts about the sensitivity and specificity of the tests. For immunological tests, it is beneficial to test for antibodies against the virus produced by the body rather than to test for the presence of the viral proteins, since the antibodies can be present in larger titers for a longer span of time. However, the cross-reactivity of these tests with other coronavirus antibodies is something that needs verification. Biochemical parameters such as D-dimer, C-reactive protein, and variations in neutrophil and lymphocyte counts are some other parameters that can be used to make a preliminary diagnosis; however, these parameters vary in a number of diseases and thus cannot be relied upon conclusively ( 51 ). Patients with pre-existing diseases such as asthma or similar lung disorder are at higher risk, requiring life support, as are those with other diseases such as diabetes, hypertension, or obesity. Those above the age of 60 have displayed the highest mortality rate in China, a finding that is mirrored in other nations as well ( Figure 3 ) ( 55 ). If we cross-verify these findings with the population share that is above the age of 70, we find that Italy, the United Kingdom, Canada, and the USA have one of the highest elderly populations as compared to countries such as India and China ( Figure 4 ), and this also reflects the case fatality rates accordingly ( Figure 5 ) ( 33 ). This is a clear indicator that aside from comorbidities, age is also an independent risk factor for death in those infected by COVID-19. Also, in the US, it was seen that the rates of African American deaths were higher. This is probably due to the fact that the prevalence of hypertension and obesity in this community is higher than in Caucasians ( 56 , 57 ). In late April 2020, there are also claims in the US media that young patients in the US with COVID-19 may be at increased risk of stroke; however, this is yet to be proven. We know that coagulopathy is a feature of COVID-19, and thus stroke is likely in this condition ( 58 , 59 ). The main cause of death in COVID-19 patients was acute respiratory distress due to the inflammation in the linings of the lungs caused by the cytokine storm, which is seen in all non-survival cases and in respiratory failure. The resultant inflammation in the lungs, served as an entry point of further infection, associated with coagulopathy end-organ failure, septic shock, and secondary infections leading to death ( 60 – 63 ).
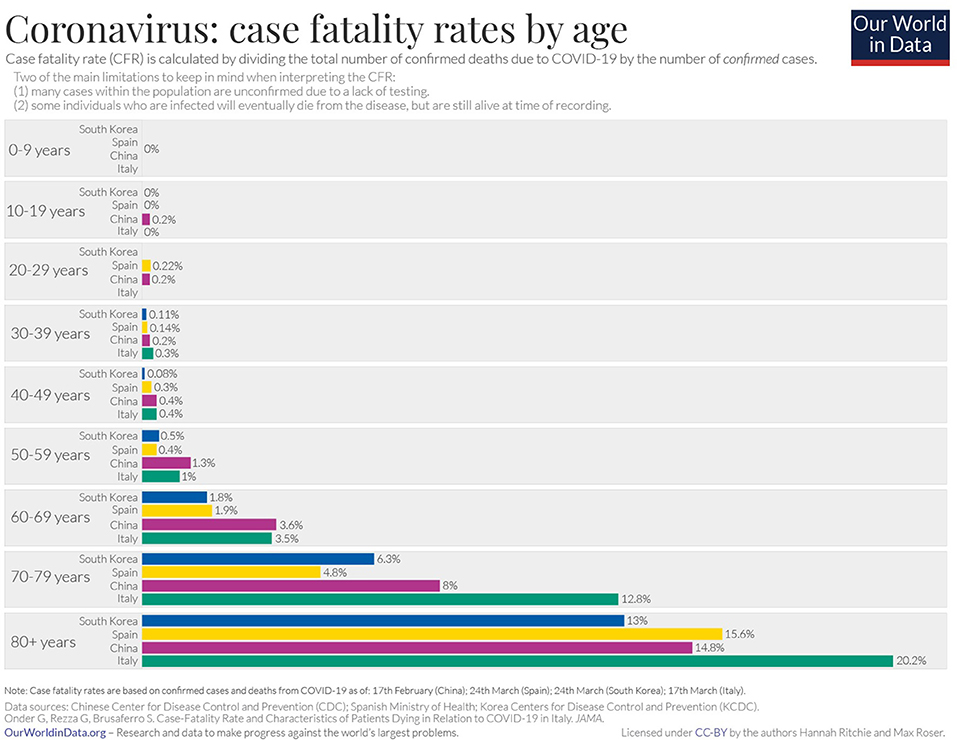
Figure 3 . Case fatality rate by age in selected countries as of April 2020 ( 33 ).
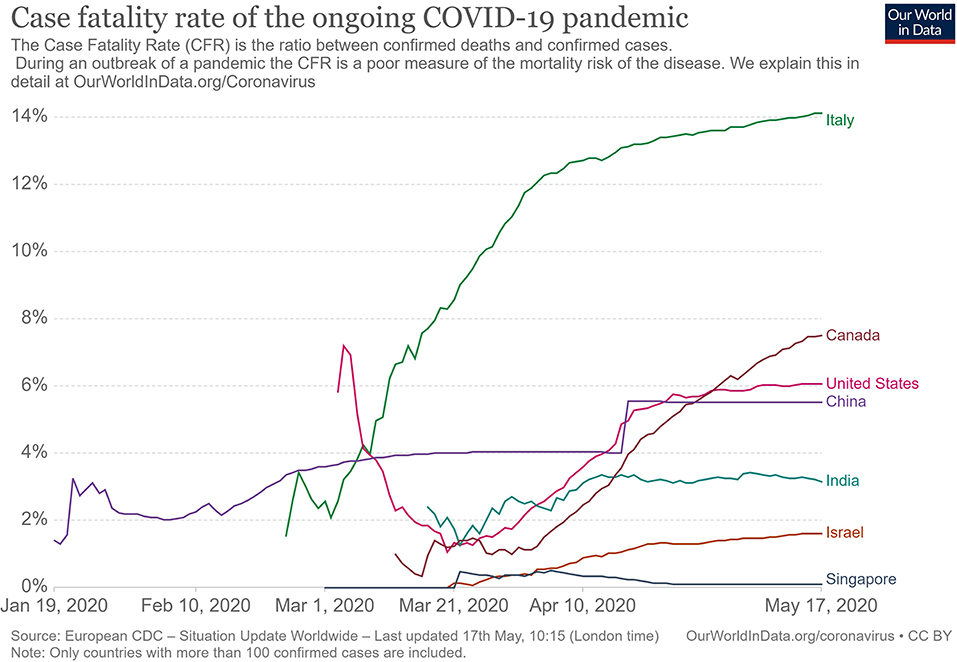
Figure 4 . Case fatality rate in selected countries ( 33 ).
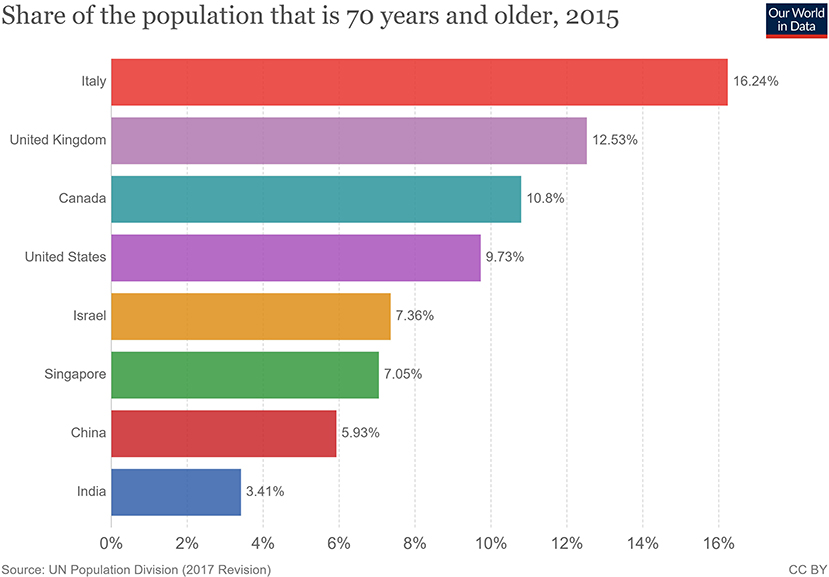
Figure 5 . Population share above 70 years of age ( 33 ).
For COVID-19, there is no specific treatment available. The WHO announced the organization of a trial dubbed the “Solidarity” clinical trial for COVID-19 treatments ( 64 ). This is an international collaborative study that investigates the use of a few prime candidate drugs for use against COVID-19, which are discussed below. The study is designed to reduce the time taken for an RCT by over 80%. There are over 1087 studies ( Supplementary Data 1 ) for COVID-19 registered at clinicaltrials.gov , of which 657 are interventional studies ( Supplementary Data 2 ) ( 65 ). The primary focus of the interventional studies for COVID-19 has been on antimalarial drugs and antiviral agents ( Table 1 ), while over 200 studies deal with the use of different forms of oxygen therapy. Most trials focus on improvement of clinical status, reduction of viral load, time to improvement, and reduction of mortality rates. These studies cover both severe and mild cases.
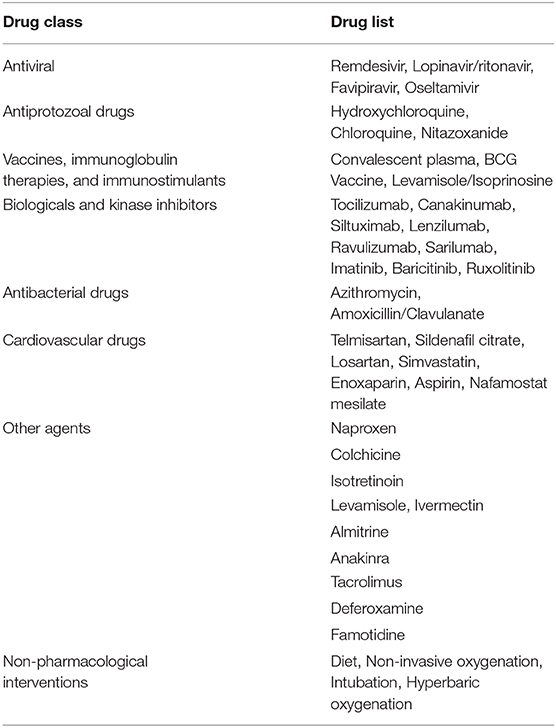
Table 1 . List of therapeutic drugs under study for COVID-19 as per clinical trials registered under clinicaltrials.gov .
Use of Antimalarial Drugs Against SARS-CoV-2
The use of chloroquine for the treatment of corona virus-based infection has shown some benefit in the prevention of viral replication in the cases of SARS and MERS. However, it was not validated on a large scale in the form of a randomized control trial ( 50 , 66 – 68 ). The drugs of choice among antimalarials are Chloroquine (CQ) and Hydroxychloroquine (HCQ). The use of CQ for COVID-19 was brought to light by the Chinese, especially by the publication of a letter to the editor of Bioscience Trends by Gao et al. ( 69 ). The letter claimed that several studies found CQ to be effective against COVID-19; however, the letter did not provide many details. Immediately, over a short span of time, interest in these two agents grew globally. Early in vitro data have revealed that chloroquine can inhibit the viral replication ( 70 , 71 ).
HCQ and CQ work by raising the pH of the lysosome, the cellular organelle that is responsible for phagocytic degradation. Its function is to combine with cell contents that have been phagocytosed and break them down eventually, in some immune cells, as a downstream process to display some of the broken proteins as antigens, thus further enhancing the immune recruitment against an antigen/pathogen. The drug was to be administered alone or with azithromycin. The use of azithromycin may be advocated by the fact that it has been seen previously to have some immunomodulatory role in airway-related disease. It appears to reduce the release of pro-inflammatory cytokines in respiratory illnesses ( 72 ). However, HCQ and azithromycin are known to have a major drug interaction when co-administered, which increases the risk of QT interval prolongation ( 73 ). Quinine-based drugs are known to have adverse effects such as QT prolongation, retinal damage, hypoglycemia, and hemolysis of blood in patients with G-6-PD deficiency ( 66 ). Several preprints, including, a metanalysis now indicate that HCQ may have no benefit for severe or critically ill patients who have COVID-19 where the outcome is need for ventilation or death ( 74 , 75 ). As of April 21, 2020, after having pre-emptively recommended their use for SARS-CoV-2 infection, the US now advocates against the use of these two drugs based on the new data that has become available.
Use of Antiviral Drugs Against SARS-CoV-2
The antiviral agents are mainly those used in the case of HIV/AIDS, these being Lopinavir and Ritonavir. Other agents such as nucleoside analogs like Favipiravir, Ribavirin, Remdesivir, and Galidesivir have been tested for possible activity in the prevention of viral RNA synthesis ( 76 ). Among these drugs, Lopinavir, Ritonavir, and Remdesivir are listed in the Solidarity trial by the WHO.
Remdesivir is a nucleotide analog for adenosine that gets incorporated into the viral RNA, hindering its replication and causing chain termination. This agent was originally developed for Ebola Virus Disease ( 77 ). A study was conducted with rhesus macaques infected with SARS-CoV-2 ( 78 ). In that study, after 12 h of infection, the monkeys were treated with either Remdesivir or vehicle. The drug showed good distribution in the lungs, and the animals treated with the drug showed a better clinical score than the vehicle group. The radiological findings of the study also indicated that the animals treated with Remdesivir have less lung damage. There was a reduction in viral replication but not in virus shedding. Furthermore, there were no mutations found in the RNA polymerase sequences. A randomized clinical control study that became available in late April 2020 ( 79 ), having 158 on the Remdesivir arm and 79 on the placebo arm, found that Remdesivir reduced the time to recovery in the Remdesivir-treated arm to 11 days, while the placebo-arm recovery time was 15 days. Though this was not found to be statistically significant, the agent provided a basis for further studies. The 28-days mortality was found to be similar for both groups. This has now provided us with a basis on which to develop future molecules. The study has been supported by the National Institute of Health, USA. The authors of the study advocated for more clinical trials with Remdesivir with a larger population. Such larger studies are already in progress, and their results are awaited. Remdesivir is currently one of the drugs that hold most promise against COVID-19.
An early trial in China with Lopinavir and Ritonavir showed no benefit compared with standard clinical care ( 80 ). More studies with this drug are currently underway, including one in India ( 81 , 82 ).
Use of Convalescent Patient Plasma
Another possible option would be the use of serum from convalescent individuals, as this is known to contain antibodies that can neutralize the virus and aid in its elimination. This has been tried previously for other coronavirus infections ( 83 ). Early emerging case reports in this aspect look promising compared to other therapies that have been tried ( 84 – 87 ). A report from China indicates that five patients treated with plasma recovered and were eventually weaned off ventilators ( 84 ). They exhibited reductions in fever and viral load and improved oxygenation. The virus was not detected in the patients after 12 days of plasma transfusion. The US FDA has provided detailed recommendations for investigational COVID-19 Convalescent Plasma use ( 88 ). One of the benefits of this approach is that it can also be used for post-exposure prophylaxis. This approach is now beginning to be increasingly adopted in other countries, with over 95 trials registered on clinicaltrials.gov alone, of which at least 75 are interventional ( 89 ). The use of convalescent patient plasma, though mostly for research purposes, appears to be the best and, so far, the only successful option for treatment available.
From a future perspective, the use of monoclonal antibodies for the inhibition of the attachment of the virus to the ACE-2 receptor may be the best bet. Aside from this, ACE-2-like molecules could also be utilized to attach and inactivate the viral proteins, since inhibition of the ACE-2 receptor would not be advisable due to its negative repercussions physiologically. In the absence of drug regimens and a vaccine, the treatment is symptomatic and involves the use of non-invasive ventilation or intubation where necessary for respiratory failure patients. Patients that may go into septic shock should be managed as per existing guidelines with hemodynamic support as well as antibiotics where necessary.
The WHO has recommended that simple personal hygiene practices can be sufficient for the prevention of spread and containment of the disease ( 90 ). Practices such as frequent washing of soiled hands or the use of sanitizer for unsoiled hands help reduce transmission. Covering of mouth while sneezing and coughing, and disinfection of surfaces that are frequently touched, such as tabletops, doorknobs, and switches with 70% isopropyl alcohol or other disinfectants are broadly recommended. It is recommended that all individuals afflicted by the disease, as well as those caring for the infected, wear a mask to avoid transmission. Healthcare works are advised to wear a complete set of personal protective equipment as per WHO-provided guidelines. Fumigation of dormitories, quarantine rooms, and washing of clothes and other fomites with detergent and warm water can help get rid of the virus. Parcels and goods are not known to transmit the virus, as per information provided by the WHO, since the virus is not able to survive sufficiently in an open, exposed environment. Quarantine of infected individuals and those who have come into contact with an infected individual is necessary to further prevent transmission of the virus ( 91 ). Quarantine is an age-old archaic practice that continues to hold relevance even today for disease containment. With the quarantine being implemented on such a large scale in some countries, taking the form of a national lockdown, the question arises of its impact on the mental health of all individuals. This topic needs to be addressed, especially in countries such as India and China, where it is still a matter of partial taboo to talk about it openly within the society.
In India, the Ministry of Ayurveda, Yoga, and Naturopathy, Unani, Siddha and Homeopathy (AYUSH), which deals with the alternative forms of medicine, issued a press release that the homeopathic, drug Arsenicum album 30, can be taken on an empty stomach for 3 days to provide protection against the infection ( 92 ). It also provided a list of herbal drugs in the same press release as per Ayurvedic and Unani systems of medicine that can boost the immune system to deal with the virus. However, there is currently no evidence to support the use of these systems of medicine against COVID-19, and they need to be tested.
The prevention of the disease with the use of a vaccine would provide a more viable solution. There are no vaccines available for any of the coronaviruses, which includes SARS and MERS. The development of a vaccine, however, is in progress at a rapid pace, though it could take about a year or two. As of April 2020, no vaccine has completed the development and testing process. A popular approach has been with the use of mRNA-based vaccine ( 93 – 96 ). mRNA vaccines have the advantage over conventional vaccines in terms of production, since they can be manufactured easily and do not have to be cultured, as a virus would need to be. Alternative conventional approaches to making a vaccine against SARS-CoV-2 would include the use of live attenuated virus as well as using the isolated spike proteins of the virus. Both of these approaches are in progress for vaccine development ( 97 ). Governments across the world have poured in resources and made changes in their legislation to ensure rapid development, testing, and deployment of a vaccine.
Barriers to Treatment
Lack of transparency and poor media relations.
The lack of government transparency and poor reporting by the media have hampered the measures that could have been taken by healthcare systems globally to deal with the COVID-19 threat. The CDC, as well as the US administration, downplayed the threat and thus failed to stock up on essential supplies, ventilators, and test kits. An early warning system, if implemented, would have caused borders to be shut and early lockdowns. The WHO also delayed its response in sounding the alarm regarding the severity of the outbreak to allow nations globally to prepare for a pandemic. Singapore is a prime example where, despite the WHO not raising concerns and banning travel to and from China, a country banned travelers and took early measures, thus managing the outbreak quite well. South Korea is another example of how things may have played out had those measures by agencies been taken with transparency. Increased transparency would have allowed the healthcare sector to better prepare and reduced the load of patients they had to deal with, helping flatten the curve. The increased patient load and confusion among citizens arising from not following these practices has proved to be a barrier to providing effective treatments to patients with the disease elsewhere in the world.
Lack of Preparedness and Protocols
Despite the previous SARS outbreak teaching us important lessons and providing us with data on a potential outbreak, many nations did not take the important measures needed for a future outbreak. There was no allocation of sufficient funds for such an event. Many countries experienced severe lack of PPE, and the lockdown precautions hampered the logistics of supply and manufacturing of such essential equipment. Singapore and South Korea had protocols in place and were able to implement them at a moment's notice. The spurt of cases that Korea experienced was managed well, providing evidence to this effect. The lack of preparedness and lack of protocol in other nations has resulted in confusion as to how the treatment may be administered safely to the large volume of patients while dealing with diagnostics. Both of these factors have limited the accessibility to healthcare services due to sheer volume.
Socio-Economic Impact
During the SARS epidemic, China faced an economic setback, and experts were unsure if any recovery would be made. However, the global and domestic situation was then in China's favor, as it had a lower debt, allowing it to make a speedy recovery. This is not the case now. Global experts have a pessimistic outlook on the outcome of this outbreak ( 98 ). The fear of COVID-19 disease, lack of proper understanding of the dangers of the virus, and the misinformation spread on the social media ( 99 ) have caused a breakdown of the economic flow globally ( 100 ). An example of this is Indonesia, where a great amount of fear was expressed in responses to a survey when the nation was still free of COVID-19 ( 101 ). The pandemic has resulted in over 2.6 billion people being put under lockdown. This lockdown and the cancellation of the lunar year celebration has affected business at the local level. Hundreds of flights have been canceled, and tourism globally has been affected. Japan and Indonesia are estimated to lose over 2.44 billion dollars due to this ( 102 , 103 ). Workers are not able to work in factories, transportation in all forms is restricted, and goods are not produced or moved. The transport of finished products and raw materials out of China is low. The Economist has published US stock market details indicating that companies in the US that have Chinese roots fell, on average, 5 points on the stock market as compared to the S&P 500 index ( 104 ). Companies such as Starbucks have had to close over 4,000 outlets due to the outbreak as a precaution. Tech and pharma companies are at higher risk since they rely on China for the supply of raw materials and active pharmaceutical ingredients. Paracetamol, for one, has reported a price increase of over 40% in India ( 104 – 106 ). Mass hysteria in the market has caused selling of shares of these companies, causing a tumble in the Indian stock market. Though long-term investors will not be significantly affected, short-term traders will find themselves in soup. Politically, however, this has further bolstered support for world leaders in countries such as India, Germany, and the UK, who are achieving good approval ratings, with citizens being satisfied with the government's approach. In contrast, the ratings of US President Donald Trump have dropped due to the manner in which the COVID-19 pandemic was handled. These minor impacts may be of temporary significance, and the worst and direct impact will be on China itself ( 107 – 109 ), as the looming trade war with the USA had a negative impact on the Chinese and Asian markets. The longer production of goods continues to remain suspended, the more adversely it will affect the Chinese economy and the global markets dependent on it ( 110 ). If this disease is not contained, more and more lockdowns by multiple nations will severely affect the economy and lead to many social complications.
The appearance of the 2019 Novel Coronavirus has added and will continue to add to our understanding of viruses. The pandemic has once again tested the world's preparedness for dealing with such outbreaks. It has provided an outlook on how a massive-scale biological event can cause a socio-economic disturbance through misinformation and social media. In the coming months and years, we can expect to gain further insights into SARS-CoV-2 and COVID-19.
Author Contributions
KN: conceptualization. RK, AA, JM, and KN: investigation. RK and AA: writing—original draft preparation. KN, PN, and JM: writing—review and editing. KN: supervision.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to acknowledge the contributions made by Dr. Piya Paul Mudgal, Assistant Professor, Manipal Institute of Virology, Manipal Academy of Higher Education towards inputs provided by her during the drafting of the manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.00216/full#supplementary-material
Supplementary Data 1, 2. List of all studies registered for COVID-19 on clinicaltrials.gov .
1. McIntosh K, Dees JH, Becker WB, Kapikian AZ, Chanock RM. Recovery in tracheal organ cultures of novel viruses from patients with respiratory disease. Proc Natl Acad Sci USA. (1967) 57:933–40. doi: 10.1073/pnas.57.4.933
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Esper F, Weibel C, Ferguson D, Landry ML, Kahn JS. Evidence of a novel human coronavirus that is associated with respiratory tract disease in infants and young children. J Infect Dis. (2005) 191:492–8. doi: 10.1086/428138
3. Stöhr K. A multicentre collaboration to investigate the cause of severe acute respiratory syndrome. Lancet. (2003) 361:1730–3. doi: 10.1016/S0140-6736(03)13376-4
4. Peiris JSM, Lai ST, Poon LLM, Guan Y, Yam LYC, Lim W, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. (2003) 361:1319–25. doi: 10.1016/S0140-6736(03)13077-2
5. Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet. (2015) 386:995–1007. doi: 10.1016/S0140-6736(15)60454-8
6. Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus ADME, Fouchier RAM. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. (2012) 367:1814–20. doi: 10.1056/NEJMoa1211721
7. Perlman S, Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nat Rev Microbiol. (2009) 7:439–50. doi: 10.1038/nrmicro2147
8. Li W, Moore MJ, Vasllieva N, Sui J, Wong SK, Berne MA, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. (2003) 426:450–4. doi: 10.1038/nature02145
9. Ge X-Y, Li J-L, Yang X-L, Chmura AA, Zhu G, Epstein JH, et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature. (2013) 503:535–8. doi: 10.1038/nature12711
10. Wang M, Hu Z. Bats as animal reservoirs for the SARS coronavirus: Hypothesis proved after 10 years of virus hunting. Virol Sin. (2013) 28:315–7. doi: 10.1007/s12250-013-3402-x
11. Diamond Princess Cruise Ship in Japan Confirms 99 New Coronavirus Cases | World news | The Guardian. Available online at: https://www.theguardian.com/world/2020/feb/17/coronavirus-japan-braces-for-hundreds-more-cases-as-another-china-city-locked-down (accessed February 17, 2020).
Google Scholar
12. Diamond Princess Coronavirus & Quarantine Updates - Notices & Advisories - Princess Cruises. Available online at: https://www.princess.com/news/notices_and_advisories/notices/diamond-princess-update.html (accessed February 17, 2020).
13. Gorbalenya AE, Baker SC, Baric RS, Groot RJ, de Drosten C, Gulyaeva AA, et al. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. (2020) 5:536–44. doi: 10.1038/s41564-020-0695-z
14. Ji W, Wang W, Zhao X, Zai J, Li X. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross-species transmission from snake to human. J Med Virol . (2020) 7:jmv.25682. doi: 10.1002/jmv.25682
15. Cyranoski D. Did pangolins spread the China coronavirus to people? Nature . (2020) doi: 10.1038/d41586-020-00364-2
CrossRef Full Text | Google Scholar
16. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. (2020) 395:565–74. doi: 10.1016/S0140-6736(20)30251-8
17. Wassenaar TM, Zou Y. 2019_nCoV: Rapid classification of betacoronaviruses and identification of traditional Chinese medicine as potential origin of zoonotic coronaviruses. Lett Appl Microbiol. (2020) 70:324–48. doi: 10.1111/lam.13285
18. Velavan TP, Meyer CG. The Covid-19 epidemic. Trop Med Int Heal . (2020) 25:278–80. doi: 10.1111/tmi.13383
19. Guarner J. Three Emerging Coronaviruses in Two Decades. Am J Clin Pathol . (2020) 153:420–21. doi: 10.1093/ajcp/aqaa029
20. Li W, Shi Z, Yu M, Ren W, Smith C, Epstein JH, et al. Bats are natural reservoirs of SARS-like coronaviruses. Science. (2005) 310:676–9. doi: 10.1126/science.1118391
21. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. (2020) 579:270–3. doi: 10.1038/s41586-020-2012-7
22. Menachery VD, Yount BL, Debbink K, Agnihothram S, Gralinski LE, Plante JA, et al. A SARS-like cluster of circulating bat coronaviruses shows potential for human emergence. Nat Med. (2015) 21:1508–13. doi: 10.1038/nm.3985
23. COVID-19 Coronavirus Epidemic has a Natural Origin—ScienceDaily. Available online at: https://www.sciencedaily.com/releases/2020/03/200317175442.htm (accessed April 22, 2020).
24. Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med . (2020) 26:450–2. doi: 10.1038/s41591-020-0820-9
25. Prioritizing Diseases for Research and Development in Emergency Contexts. Available online at: https://www.who.int/activities/prioritizing-diseases-for-research-and-development-in-emergency-contexts (accessed April 22, 2020).
26. Albariño CG, Guerrero LW, Jenks HM, Chakrabarti AK, Ksiazek TG, Rollin PE, et al. Insights into Reston virus spillovers and adaption from virus whole genome sequences. PLoS ONE. (2017) 12:e0178224. doi: 10.1371/journal.pone.0178224
27. Yao H, Lu X, Chen Q, Xu K, Chen Y, Cheng L, et al. Patient-derived mutations impact pathogenicity of SARS-CoV-2. medRxiv. (2020). doi: 10.2139/ssrn.3578153
28. Stefanelli P, Faggioni G, Lo Presti A, Fiore S, Marchi A, Benedetti E, et al. Whole genome and phylogenetic analysis of two SARS-CoV-2 strains isolated in Italy in January and February 2020: additional clues on multiple introductions and further circulation in Europe. Eurosurveillance. (2020) 25:2000305. doi: 10.2807/1560-7917.ES.2020.25.13.2000305
29. Yadav P, Potdar V, Choudhary M, Nyayanit D, Agrawal M, Jadhav S, et al. Full-genome sequences of the first two SARS-CoV-2 viruses from India. Indian J Med Res. (2020) 151:200–9. doi: 10.4103/ijmr.IJMR_663_20
30. WHO | Coronavirus disease 2019 (COVID-19) Situation Report – 26. Beijing (2020). Available online at: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml (accessed February 16, 2020).
31. WHO | Middle East Respiratory Syndrome Coronavirus (MERS-CoV). World Health Organization (2020).
32. WHO | Summary of Probable SARS Cases With Onset of Illness From 1 November 2002 to 31 July 2003. World Health Organization (2015).
33. Worldometer. Coronavirus cases. Worldometer. (2020) 1−22.
34. Update on the Outbreak of New Coronavirus Pneumonia as of 24 hours on 15 February. Beijing (2020). Available online at: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml (accessed February 16, 2020).
35. Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. (2020) 26. doi: 10.3201/eid2607.200282
36. 83% of India's Coronavirus Patients Are Below the Age of 50: Health ministry data - India News. Available online at: https://www.indiatoday.in/india/story/83-of-india-s-coronavirus-patients-are-below-the-age-of-50-health-ministry-data-1663314-2020-04-04 (accessed April 23, 2020).
37. 42% of Coronavirus Patients in 21-40 age bracket: Govt. Available online at: https://economictimes.indiatimes.com/news/politics-and-nation/42-of-coronavirus-patients-in-21-40-age-bracket-govt/articleshow/74987254.cms (accessed April 23, 2020).
38. Why COVID-19 Case Counts Are so Low in Singapore Hong Kong and Taiwan | Advisory Board Daily Briefing. Available online at: https://www.advisory.com/daily-briefing/2020/03/19/asian-countries (accessed April 29, 2020).
39. Coronavirus: Why so Few Deaths Among Singapore's 14000 Covid-19 Infections? | South China Morning Post. Available online at: https://www.scmp.com/weekasia/health-environment/article/3081772/coronavirus-why-so-few-deaths-among-singapores-14000 (accessed April 29, 2020).
40. Stafford N. Covid-19: Why Germany's case fatality rate seems so low. BMJ. (2020) 7:369. doi: 10.1136/bmj.m1395
41. Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-NCOV infection from an asymptomatic contact in Germany. N Engl J Med . (2020) 382:970–1. doi: 10.1056/NEJMc2001468
42. Coronavirus pandemic | 80% of COVID-19 Cases Either Asymptomatic or Show Mild Symptoms. Health ministry - Moneycontrol.com. Available online at: https://www.moneycontrol.com/news/india/coronavirus-pandemic-80-of-covid-19-cases-either-asymptomatic-or-show-mild-symptoms-health-ministry-5170631.html (accessed April 24, 2020).
43. WHO | Q&A on Coronaviruses. Available online at: https://www.who.int/news-room/q-a-detail/q-a-coronaviruses (accessed February 16, 2020).
44. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med . (2020) 382:929–36. doi: 10.1056/NEJMoa2001191
45. Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. (2020) 5:335–37. doi: 10.1016/S2468-1253(20)30048-0
46. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. (2020) 395:809–15. doi: 10.1016/S0140-6736(20)30360-3
47. Fehr AR, Perlman S. Coronaviruses: An overview of their replication and pathogenesis. In: Coronaviruses: Methods and Protocols (New York: Springer), 1–23. doi: 10.1007/978-1-4939-2438-7_1
48. Chen Y, Liu Q, Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol. (2020) 92:418–23. doi: 10.1002/jmv.25681
49. Hoffmann M, Kleine-Weber H, Schroeder S, Mü MA, Drosten C, Pö S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. (2020) 181:271–80. doi: 10.1016/j.cell.2020.02.052
50. Cheng VCC, Chan JFW, To KKW, Yuen KY. Clinical management and infection control of SARS: Lessons learned. Antiviral Res. (2013) 100:407–19. doi: 10.1016/j.antiviral.2013.08.016
51. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
52. Udugama B, Kadhiresan P, Kozlowski HN, Malekjahani A, Osborne M, Li VYC, et al. Diagnosing COVID-19: the disease and tools for detection. ACS Nano . (2020) 14:3822–35. doi: 10.1021/acsnano.0c02624
53. Testing, | CDC,. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/testing/index.html (accessed April 29, 2020).
54. Advice on the Use of Point-of-Care Immunodiagnostic Tests for COVID-19. Available online at: https://www.who.int/news-room/commentaries/detail/advice-on-the-use-of-point-of-care-immunodiagnostic-tests-for-covid-19 (accessed April 29, 2020).
55. Zhang Yanping. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) — China, 2020. (2020) Available online at: http://weekly.chinacdc.cn/en/article/id/e53946e2-c6c4-41e9-9a9bfea8db1a8f51 (accessed February 18, 2020).
56. Petersen R, Pan L, Blanck HM. Racial and ethnic disparities in adult obesity in the United States: CDC's tracking to inform state and local action. Prev Chronic Dis. (2019) 16:180579. doi: 10.5888/pcd16.180579
57. Wang L, Southerland J, Wang K, Bailey BA, Alamian A, Stevens MA, et al. Ethnic differences in risk factors for obesity among adults in California, the United States. (2017) 2017:2427483. doi: 10.1155/2017/2427483
58. Covid-19 Causes Sudden Strokes in Young Adults Doctors Say - CNN. Available online at: https://edition.cnn.com/2020/04/22/health/strokes-coronavirus-young-adults/index.html (accessed April 24, 2020).
59. Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK, Veress LA, et al. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost . (2020) 1–4. doi: 10.1111/jth.14828
60. Lancet T, Medicine R. Comment Understanding pathways to death in patients with. Lancet Respir Med. (2020) 2019:2019–21. doi: 10.1016/S2213-2600(20)30165-X
61. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA . (2020) 323:1775–6. doi: 10.1001/jama.2020.4683
62. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3
63. Doctors Warn COVID-19 Might Cause Strokes in Young Adults. Available online at: https://nypost.com/2020/04/23/doctors-warn-covid-19-might-cause-strokes-in-young-adults/ (accessed April 24, 2020).
64. “Solidarity” Clinical Trial for COVID-19 Treatments. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-clinical-trial-for-covid-19-treatments (accessed April 23, 2020).
65. Search, of: COVID-19 - List Results - ClinicalTrials.gov . Available online at: https://www.clinicaltrials.gov/ct2/results?cond=COVID-19&term=&cntry=&state=&city=&dist= (accessed May 1, 2020).
66. De Wilde AH, Jochmans D, Posthuma CC, Zevenhoven-Dobbe JC, Van Nieuwkoop S, Bestebroer TM, et al. Screening of an FDA-approved compound library identifies four small-molecule inhibitors of Middle East respiratory syndrome coronavirus replication in cell culture. Antimicrob Agents Chemother. (2014) 58:4875–84. doi: 10.1128/AAC.03011-14
67. Tai DYH. Pharmacologic treatment of SARS: current knowledge and recommendations. Ann Acad Med Singapore. (2007) 36:438–43.
PubMed Abstract | Google Scholar
68. Sheahan TP, Sims AC, Leist SR, Schäfer A, Won J, Brown AJ, et al. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. (2020) 11:222. doi: 10.1038/s41467-019-13940-6
69. Gao J, Tian Z, Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends. (2020) 14:72–73. doi: 10.5582/bst.2020.01047
70. Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. (2020) 30:269–71. doi: 10.1038/s41422-020-0282-0
71. Vincent MJ, Bergeron E, Benjannet S, Erickson BR, Rollin PE, Ksiazek TG, et al. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J. (2005) 2:1–0. doi: 10.1186/1743-422X-2-69
72. Cramer CL, Patterson A, Alchakaki A, Soubani AO. Immunomodulatory indications of azithromycin in respiratory disease: a concise review for the clinician. Postgrad Med. (2017) 129:493–9. doi: 10.1080/00325481.2017.1285677
73. Plaquenil™ Hydroxychloroquine Sulfate Tablets USP Description. Available online at: http://www.cdc.gov/malaria (accessed April 21, 2020).
74. Magagnoli J, Narendran S, Pereira F, Cummings T, Hardin JW, Sutton SS, et al. Outcomes of hydroxychloroquine usage in United States veterans hospitalized with Covid-19. medRxiv. (2020) doi: 10.1101/2020.04.16.20065920
75. Shamshirian A, Hessami A, Heydari K, Alizadeh-Navaei R, Ebrahimzadeh MA, Ghasemian R, et al. Hydroxychloroquine Versus COVID-19: A Rapid Systematic Review and Meta-Analysis. medRxiv. (2020) doi: 10.1101/2020.04.14.20065276
76. Li G, De Clercq E. Therapeutic options for the 2019 novel coronavirus (2019-nCoV). Nat Rev Drug Discov . (2020) 19:149–50. doi: 10.1038/d41573-020-00016-0
77. Warren TK, Jordan R, Lo MK, Ray AS, Mackman RL, Soloveva V, et al. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature. (2016) 531:381–5. doi: 10.1038/nature17180
78. Williamson BN, Feldmann F, Schwarz B, Meade-White K, Porter DP, Schulz J, et al. Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. bioRxiv. (2020) doi: 10.1101/2020.04.15.043166
79. Wang Y, Zhang D, Du G, Du R, Zhao J, Jin Y, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. (2020) 395:1569–78. doi: 10.1016/S0140-6736(20)31022-9
80. Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe covid-19. N Engl J Med . (2020) 382:1787–99. doi: 10.1056/NEJMoa2001282
81. Search, of: Lopinavir, Ritonavir, | COVID - List Results - ClinicalTrials.gov . Available online at: https://clinicaltrials.gov/ct2/results?term=Lopinavir%2CRitonavir&cond=COVID&draw=4&rank=22#rowId21 (accessed April 23, 2020).
82. Bhatnagar T, Murhekar M, Soneja M, Gupta N, Giri S, Wig N, et al. Lopinavir/ritonavir combination therapy amongst symptomatic coronavirus disease 2019 patients in India: protocol for restricted public health emergency use. Indian J Med Res. (2020) 151:184–9. doi: 10.4103/ijmr.IJMR_502_20
83. Yeh K-M, Chiueh T-S, Siu LK, Lin J-C, Chan PKS, Peng M-Y, et al. Experience of using convalescent plasma for severe acute respiratory syndrome among healthcare workers in a Taiwan hospital. J Antimicrob Chemother. (2005) 56:919–22. doi: 10.1093/jac/dki346
84. Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, et al. Treatment of 5 critically Ill patients with COVID-19 with convalescent plasma. JAMA . (2020) 323:1582–9. doi: 10.1001/jama.2020.4783
85. Cao W, Liu X, Bai T, Fan H, Hong K, Song H, et al. High-dose intravenous immunoglobulin as a therapeutic option for deteriorating patients with coronavirus disease 2019. Open Forum Infect Dis . (2020) 7:1–6. doi: 10.1093/ofid/ofaa102
86. Bloch EM, Shoham S, Casadevall A, Sachais BS, Shaz B, Winters JL, et al. Deployment of convalescent plasma for the prevention and treatment of COVID-19. J Clin Invest . (2020) 138745:1–22. doi: 10.1172/JCI138745
87. Ye M, Fu D, Ren Y, Wang F, Wang D, Zhang F, et al. Treatment with convalescent plasma for COVID-19 patients in Wuhan, China. J Med Virol. (2 020) doi: 10.1002/jmv.25882
88. Recommendations for Investigational COVID-19 Convalescent Plasma | FDA. Available online at: https://www.fda.gov/vaccines-blood-biologics/investigational-new-drug-ind-or-device-exemption-ide-process-cber/recommendations-investigational-covid-19-convalescent-plasma (accessed April 23, 2020).
89. Search, of: plasma | Interventional Studies | COVID - List Results - ClinicalTrials.gov . Available online at: https://clinicaltrials.gov/ct2/results?term=plasma&cond=COVID&Search=Apply&age_v=&gndr=&type=Intr&rslt= (accessed April 23, 2020).
90. Infection Prevention and Control. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control (accessed February 17, 2020).
91. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med . (2020) 27:taaa020. doi: 10.1093/jtm/taaa020
92. Press Information Bureau AYUSH Advisory for Corona virus. Press Inf Bereau. Available online at: https://pib.gov.in/PressReleasePage.aspx?PRID=1600895 (accessed February 17, 2020).
93. CanSino, Biologics : China Announces First Human Trials of Covid-19 Vaccine | MarketScreener,. Available online at: https://www.marketscreener.com/CANSINO-BIOLOGICS-INC-59318312/news/CanSino-Biologics-China-announces-first-human-trials-of-Covid-19-vaccine-30183232/ (accessed April 7, 2020).
94. Safety, and Immunogenicity Study of 2019-nCoV Vaccine (mRNA-1273) for Prophylaxis SARS CoV-2 Infection - Full Text View - ClinicalTrials.gov . Available online at: https://clinicaltrials.gov/ct2/show/NCT04283461 (accessed April 7, 2020).
95. NIH, Clinical Trial of Investigational Vaccine for COVID-19 Begins | National Institutes of Health (NIH),. Available at: https://www.nih.gov/news-events/news-releases/nih-clinical-trial-investigational-vaccine-covid-19-begins (accessed April 7, 2020).
96. Novel, Coronavirus vaccine manufacturing contract signed — The Jenner Institute,. Available online at: https://www.jenner.ac.uk/about/news/novel-coronavirus-vaccine-manufacturing-contract-signed (accessed April 7, 2020).
97. Xie L, Sun C, Luo C, Zhang Y, Zhang J, Yang J, et al. SARS-CoV-2 and SARS-CoV Spike-RBD structure and receptor binding comparison and potential implications on neutralizing antibody and vaccine development. bioRxiv [Preprint]. (2020). doi: 10.1101/2020.02.16.951723
98. The Global Economic Impact of the Coronavirus Outbreak – Harvard Gazette. Available online at: https://news.harvard.edu/gazette/story/2020/02/the-global-economic-impact-of-the-coronavirus-outbreak/ (accessed February 17, 2020).
99. Shimizu K. 2019-nCoV, fake news, and racism. Lancet . (2020) 395:685–6. doi: 10.1016/S0140-6736(20)30357-3
100. ROHDE RODNEY. 2019 Novel Coronavirus (2019-nCoV) Update: Uncoating the Virus. Am Soc Microbiol. (2020). Available online at: https://asm.org/Articles/2020/January/2019-Novel-Coronavirus-2019-nCoV-Update-Uncoating
101. Virus-free Indonesia more threatened by COVID-19 than Singapore Malaysia: Survey - World - The Jakarta Post. Available online at: https://www.thejakartapost.com/news/2020/02/18/virus-free-indonesia-more-threatened-by-covid-19-than-singapore-malaysia-survey.html (accessed February 18, 2020).
102. Japan, May Lose $1,.29 Billion in Tourism Revenue Due to COVID-19 Outbreak | The Japan Times. Available online at: https://www.japantimes.co.jp/news/2020/02/16/business/economy-business/japan-lose-billion-tourism-revenue-covid19-outbreak/#.XkvxX0fitPY (accessed February 18, 2020).
103. Coronavirus's Effect on Tourism Will Carry Into 2021 Experts Say - Bloomberg. Available online at: https://www.bloomberg.com/news/articles/2020-02-13/coronavirus-s-effect-on-tourism-will-carry-into-2021-experts-say (accessed February 18, 2020).
104. The, week in charts - The cost of covid-19 | Graphic detail | The Economist,. Available online at: https://www.economist.com/graphic-detail/2020/02/14/the-cost-of-covid-19 (accessed February 17, 2020).
105. coronavirus: Covid-19 Impact: Pharma Companies Feel the Pain as Prices of Key Inputs Shoot Up - The Economic Times. Available online at: https://economictimes.indiatimes.com/industry/healthcare/biotech/pharmaceuticals/covid-19-impact-pharma-companies-feel-the-pain-as-prices-of-key-inputs-shoot-up/articleshow/74144044.cms?from=mdr (accessed February 17, 2020).
106. Coronavirus Outbreak: Paracetamol Prices Jump 40% In India As Coronavirus Shuts Down China. Available online at: https://www.ndtv.com/india-news/coronavirus-outbreak-paracetamol-prices-jump-40-in-india-as-coronavirus-shuts-down-china-2181480 (accessed February 18, 2020).
107. The coronavirus could cripple China's economy for longer than Wall Street wants to believe | Business Insider India. Available online at: https://www.businessinsider.in/international/news/the-coronavirus-could-cripple-chinas-economy-for-longer-than-wall-street-wants-to-believe/articleshow/74162183.cms (accessed February 17, 2020).
108. Viral Slowdown - How China's Coronavirus Epidemic Could Hurt the World Economy | Leaders | The Economist. Available online at: https://www.economist.com/leaders/2020/02/13/how-chinas-coronavirus-epidemic-could-hurt-the-world-economy (accessed February 17, 2020).
109. China's Economic Battle With COVID-19 | The ASEAN Post. Available online at: https://theaseanpost.com/article/chinas-economic-battle-covid-19 (accessed February 17, 2020).
110. The Coronavirus Could Cost China's Economy $60 Billion this Quarter. - CNN. Available online at: https://edition.cnn.com/2020/01/31/economy/china-economy-coronavirus/index.html (accessed February 18, 2020).
Keywords: 2019-nCoV, COVID-19, SARS-CoV-2, coronavirus, pandemic, SARS
Citation: Keni R, Alexander A, Nayak PG, Mudgal J and Nandakumar K (2020) COVID-19: Emergence, Spread, Possible Treatments, and Global Burden. Front. Public Health 8:216. doi: 10.3389/fpubh.2020.00216
Received: 21 February 2020; Accepted: 11 May 2020; Published: 28 May 2020.
Reviewed by:
Copyright © 2020 Keni, Alexander, Nayak, Mudgal and Nandakumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Krishnadas Nandakumar, mailnandakumar77@gmail.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Newsletters
Site search
- Israel-Hamas war
- Home Planet
- 2024 election
- Supreme Court
- All explainers
- Future Perfect
Filed under:
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
Share this story
- Share this on Facebook
- Share this on Twitter
- Share this on Reddit
- Share All sharing options
Share All sharing options for: Read these 12 moving essays about life during coronavirus
/cdn.vox-cdn.com/uploads/chorus_image/image/66606035/1207638131.jpg.0.jpg)
The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
Will you support Vox today?
We believe that everyone deserves to understand the world that they live in. That kind of knowledge helps create better citizens, neighbors, friends, parents, and stewards of this planet. Producing deeply researched, explanatory journalism takes resources. You can support this mission by making a financial gift to Vox today. Will you join us?
We accept credit card, Apple Pay, and Google Pay. You can also contribute via
Next Up In Culture
Sign up for the newsletter today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
Thanks for signing up!
Check your inbox for a welcome email.
Oops. Something went wrong. Please enter a valid email and try again.

America’s misunderstood border crisis, in 8 charts

So, what was the point of John Mulaney’s live Netflix talk show?

UFOs, God, and the edge of understanding

Israel’s other war

What we know about the police killing of Black Air Force member Roger Fortson

Inside the bombshell scandal that prompted two Miss USAs to step down
Governments today are facing serious, seemingly intractable public management issues in the aftermath of COVID-19 that go to the core of effective governance and leadership, testing the very form, structure, and capacity required to meet these problems head-on. Leaders have found it necessary to go beyond established parameters and institutional structures, working across organizational boundaries in pursuit of multilayered, networked approaches that better respond to system and societal shocks brought by the pandemic.
In fall 2020, the IBM Center for The Business of Government initiated a Challenge Grant competition soliciting essays from academics and practitioners describing how government can best transform the way it works, operates, and delivers services to the public in light of the impact of the COVID-19 pandemic. Edited by Center Leadership Fellow Michael J. Keegan, COVID-19 and its Impact: Seven Essays on Reframing Government Management, features selected commentary on sustaining transformation and increasing resilience. ICMA's Tad McGalliard, director of research and development, and Laura Goddeeris, director of survey research, are among the contributing authors. Their essay draws upon ICMA survey research in exploring which pandemic-driven innovations and operational changes might prevail in a post-pandemic environment.
Expert Insight
"The key to transformation is not to lose momentum and fall back on the old ways, when potentially innovative practices and programs are still evolving from the crisis." -- Tad McGalliard, ICMA director of research and development
Key takeaways from this report include:
- The pandemic accelerated changes in the way government works and delivers services that were already underway. This change has unlocked opportunities to build a new civic future.
- Local leaders will need to address numerous policy issues raised by these changes in work environments and service delivery. Fostering a more flexible and outcome-driven culture will contribute to a new model of success for government.
- Expectations of individuals and communities will focus on access to continued online services even after conditions merit reopening of government facilities. Building a hybrid operating model to engage with citizens that adopts consistent standards for customer experience will be necessary for successful government performance.
- Cities and counties across the country are leading the way in understanding how to deliver COVID and other services to communities in need, who suffer disproportionately during the pandemic.
- Governments must anticipate risks and develop data-driven programs to mitigate risks, respond to events, and be resilient in the aftermath of inevitable threats—physical and cyber—that face agencies at all levels.
- Unprecedented demand on public procurement in response to the COVID-19 pandemic reveal significant vulnerabilities in government supply chains and procurement processes. The pandemic offers the opportunity to consider how governments can make contracting more resilient going forward.
Essays featured in this compendium:
- Five Ways COVID-19 Changes How Local Governments Do Business, by Richard Feiock
- The Future of Work in Local Governments Beyond COVID-19, by Sherri Greenberg
- Transforming Local Government Service Delivery in the Wake of COVID-19, by Tad McGalliard and Laura Goddeeris
- Community Driven Government—Reimagining Systems in a Pandemic, by Maya McKenzie and Gurdeep Gill
- COVID-19 and the Resilience Imperative in Public Procurement: Building Back Better, by Zach Huitink
- Achieving Supply Chain Immunity: Planning, Preparation, and Coordination in National Emergency Response, by Rob Handfield
- Trust and Resilience: How Public Service Principles Encouraged Compliance with COVID-19 Public Health Guidelines in New Zealand, by Rodney Scott and Eleanor Merton
You may be interested in related resources from ICMA survey research:
- COVID-19 Impacts on Local Governments (complete survey summary), July 2020
- New ICMA Survey Shows Depth of Economic Downturn for Cities and Counties, July 2020
- New Data Estimates Local Governments Will Spend Up to $20 Billion On COVID-19 Actions, March 2020
- Government Technology Solutions Survey (complete survey summary), 2017
New, Reduced Membership Dues
A new, reduced dues rate is available for CAOs/ACAOs, along with additional discounts for those in smaller communities, has been implemented. Learn more and be sure to join or renew today!
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Roger Ware Brockett, 84

Providing community support

A change of mind, heart, and soul
So how do you track spread of disease by the numbers.

Kris Snibbe/Harvard Staff Photographer
Anne J. Manning
Harvard Staff Writer
Ivan Specht decided to employ his love of math during pandemic, which led to contact-tracing app, papers, future path
Part of the commencement 2024 series.
A collection of stories covering Harvard University’s 373rd Commencement.
Ivan Specht started at Harvard on track to study pure mathematics. But when COVID-19 sent everyone home, he began wishing the math he was doing had more relevance to what was happening in the world.
Specht, a New York City native, expanded his coursework, arming himself with statistical modeling classes, and began to “fiddle around” with simulating ways diseases spread through populations. He got hooked. During the pandemic, he became one of only two undergraduates to serve on Harvard’s testing and tracing committee, eventually developing a prototype contact-tracing app called CrimsonShield.
Specht took his curiosity for understanding disease propagation to the lab of computational geneticist Pardis Sabeti , professor in Organismic and Evolutionary Biology at Harvard and member of the Broad Institute, known for her work sequencing the Ebola virus in 2014 . Specht, now a senior, has since co-authored several studies around new statistical methods for analyzing the spread of infectious diseases, with plans to continue that work in graduate school.
“Ivan is absolutely brilliant and a joy to work with, and his research accomplishments already as an undergraduate are simply astounding,” Sabeti said. “He is operating at the level of a seasoned postdoc.”
His senior thesis, “Reconstructing Viral Epidemics: A Random Tree Approach,” described a statistical model aimed at tackling one of the most intractable problems that plague infectious disease researchers: determining who transmitted a given pathogen to whom during a viral outbreak. Specht was co-advised by computer science Professor Michael Mitzenmacher, who guided the statistical and computational sections of his thesis, particularly in deriving genomic frequencies within a host using probabilistic methods.
Specht said the pandemic made clear that testing technology could provide valuable information about who got sick, and even what genetic variant of a pathogen made them sick. But mapping paths of transmission was much more challenging because that process was completely invisible. Such information, however, could provide crucial new details into how and where transmission occurred and be used to test things such as vaccine efficacy or the effects of closing schools.
Specht’s work exploited the fact that viruses leave clues about their transmission path in their phylogenetic trees, or lines of evolutionary descent from a common ancestor. “It turns out that genome sequences of viruses provide key insight into that underlying network,” said the joint mathematics and statistics concentrator.
Uncovering this transmission network goes to the heart of how single-stranded RNA pathogens survive: Once they infect their host, they mutate, producing variants that are marked by slightly different genetic barcodes. Specht’s statistical model determines how the virus spreads by tracking the frequencies of different viral variants observed within a host.
As the centerpiece of his thesis, he reconstructed a dataset of about 45,000 SARS-CoV-2 genomes across Massachusetts, providing insights into how outbreaks unfolded across the state.
Specht will take his passion for epidemiological modeling to graduate school at Stanford University, with an eye toward helping both researchers and communities understand and respond to public health crises.
A graphic designer with experience in scientific data visualization, Specht is focused not only on understanding outbreaks, but also creating clear illustrations of them. For example, his thesis contains a creative visual representation of those 45,000 Massachusetts genomes, with colored dots representing cases, positioned nearby other “dots” they are likely to have infected.
Specht’s interest in graphics began in middle school when, as an enthusiast of trains and mass transit, he started designing imagined subway maps for cities that lack actual subways, like Austin, Texas . At Harvard, he designed an interactive “subway map” depicting a viral outbreak.
As a member of the Sabeti lab, Specht taught an infectious disease modeling course to master’s and Ph.D. students at University of Sierra Leone last summer. His outbreak analysis tool is also now being used in an ongoing study of Lassa fever in that region. And he co-authored two chapters of a textbook on outbreak science in collaboration with the Moore Foundation.
Over the past three years, Specht has been lead author of a paper in Scientific Reports and another in Cell Patterns , and co-author on two others, including a cover story in Cell . His first lead-author paper, “The case for altruism in institutional diagnostic testing,” showed that organizations like Harvard should allocate COVID-19 testing capacity to their surrounding communities, rather than monopolize it for themselves. That work was featured in The New York Times .
During his time at Harvard, Specht lived in Quincy House and was design editor of the Harvard Advocate, the University’s undergraduate literary magazine. In his free time he also composes music, and he still considers himself a mass transit enthusiast.
In the acknowledgements section of his thesis, he credited Sabeti with opening his eyes to the “many fascinating problems at the intersection of math, statistics, and computational biology.”
“I could fill this entire thesis with reasons I am grateful for Professor Sabeti, but I think they can be summarized by the sense of wonder and inspiration I feel every time I set foot in her lab.”
Share this article
You might like.
Memorial Minute — Faculty of Arts and Sciences

Harvard Allston Partnership Fund awards grants to 26 Allston-Brighton nonprofits

Choosing Harvard took LyLena Estabine down an uncertain path. The former student co-president has no regrets.
Epic science inside a cubic millimeter of brain
Researchers publish largest-ever dataset of neural connections
Excited about new diet drug? This procedure seems better choice.
Study finds minimally invasive treatment more cost-effective over time, brings greater weight loss
How far has COVID set back students?
An economist, a policy expert, and a teacher explain why learning losses are worse than many parents realize
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Perspective
When pto stands for 'pretend time off': doctors struggle to take real breaks.
Mara Gordon

A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off. Wolfgang Kaehler/LightRocket via Getty Images hide caption
A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off.
A few weeks ago, I took a vacation with my family. We went hiking in the national parks of southern Utah, and I was blissfully disconnected from work.
I'm a family physician, so taking a break from my job meant not seeing patients. It also meant not responding to patients' messages or checking my work email. For a full week, I was free.
Taking a real break — with no sneaky computer time to bang out a few prescription refill requests — left me feeling reenergized and ready to take care of my patients when I returned.
But apparently, being a doctor who doesn't work on vacation puts me squarely in the minority of U.S. physicians.
Research published in JAMA Network Open this year set out to quantify exactly how doctors use their vacation time — and what the implications might be for a health care workforce plagued by burnout, dissatisfaction and doctors who are thinking about leaving medicine.
"There is a strong business case for supporting taking real vacation," says Dr. Christine Sinsky , the lead author of the paper. "Burnout is incredibly expensive for organizations."

Shots - Health News
Health workers know what good care is. pandemic burnout is getting in the way.
Researchers surveyed 3,024 doctors, part of an American Medical Association cohort designed to represent the American physician workforce. They found that 59.6% of American physicians took 15 days of vacation or less per year. That's a little more than the average American: Most workers who have been at a job for a year or more get between 10 and 14 days of paid vacation time , according to the U.S. Bureau of Labor Statistics.
However, most doctors don't take real vacation. Over 70% of doctors surveyed said they worked on a typical vacation day.
"I have heard physicians refer to PTO as 'pretend time off,'" Sinsky says, referring to the acronym for "paid time off."
Sinsky and co-authors found that physicians who took more than three weeks of vacation a year had lower rates of burnout than those who took less, since vacation time is linked to well-being and job satisfaction .
And all those doctors toiling away on vacation, sitting poolside with their laptops? Sinsky argues it has serious consequences for health care.
Physician burnout is linked to high job turnover and excess health care costs , among other problems.
Still, it can be hard to change the culture of workaholism in medicine. Even the study authors confessed that they, too, worked on vacation.
"I remember when one of our first well-being papers was published," says Dr. Colin West , a co-author of the new study and a health care workforce researcher at the Mayo Clinic. "I responded to the revisions up at the family cabin in northern Minnesota on vacation."
Sinsky agreed. "I do not take all my vacation, which I recognize as a delicious irony of the whole thing," she says.
She's the American Medical Association's vice president of professional satisfaction. If she can't take a real vacation, is there any hope for the rest of us?
I interviewed a half dozen fellow physicians and chatted off the record with many friends and colleagues to get a sense of why it feels so hard to give ourselves a break. Here, I offer a few theories about why doctors are so terrible at taking time off.
We don't want to make more work for our colleagues
The authors of the study in JAMA Network Open didn't explore exactly what type of work doctors did on vacation, but the physicians I spoke to had some ideas.
"If I am not doing anything, I will triage my email a little bit," says Jocelyn Fitzgerald , a urogynecologist at the University of Pittsburgh who was not involved in the study. "I also find that certain high-priority virtual meetings sometimes find their way into my vacations."
Even if doctors aren't scheduled to see patients, there's almost always plenty of work to be done: dealing with emergencies, medication refills, paperwork. For many of us, the electronic medical record (EMR) is an unrelenting taskmaster , delivering a near-constant flow of bureaucratic to-dos.
When I go on vacation, my fellow primary care doctors handle that work for me, and I do the same for them.
But it can sometimes feel like a lot to ask, especially when colleagues are doing that work on top of their normal workload.
"You end up putting people in kind of a sticky situation, asking for favors, and they [feel they] need to pay it back," says Jay-Sheree Allen , a family physician and fellow in preventive medicine at the Mayo Clinic.
She says her practice has a "doctor of the day" who covers all urgent calls and messages, which helps reduce some of the guilt she feels about taking time off.
Still, non-urgent tasks are left for her to complete when she gets back. She says she usually logs in to the EMR when she's on vacation so the tasks don't pile up upon her return. If she doesn't, Allen estimates there will be about eight hours of paperwork awaiting her after a week or so of vacation.
"My strategy, I absolutely do not recommend," Allen says. But "I would prefer that than coming back to the total storm."
We have too little flexibility about when we take vacation
Lawren Wooten , a resident physician in pediatrics at the University of California San Francisco, says she takes 100% of her vacation time. But there are a lot of stipulations about exactly how she uses it.
She has to take it in two-week blocks — "that's a long time at once," she says — and it's hard to change the schedule once her chief residents assign her dates.
"Sometimes I wish I had vacation in the middle of two really emotionally challenging rotations like an ICU rotation and an oncology rotation," she says, referring to the intensive care unit. "We don't really get to control our schedules at this point in our careers."
Once Wooten finishes residency and becomes an attending physician, it's likely she'll have more autonomy over her vacation time — but not necessarily all that much more.
"We generally have to know when our vacations are far in advance because patients schedule with us far in advance," says Fitzgerald, the gynecologist.
Taking vacation means giving up potential pay
Many physicians are paid based on the number of patients they see or procedures they complete. If they take time off work, they make less money.
"Vacation is money off your table," says West, the physician well-being researcher. "People have a hard time stepping off of the treadmill."
A 2022 research brief from the American Medical Association estimated that over 55% of U.S. physicians were paid at least in part based on "productivity," as opposed to earning a flat amount regardless of patient volume. That means the more patients doctors cram into their schedules, the more money they make. Going on vacation could decrease their take-home pay.
But West says it's important to weigh the financial benefits of skipping vacation against the risk of burnout from working too much.
Physician burnout is linked not only to excess health care costs but also to higher rates of medical errors. In one large survey of American surgeons , for example, surgeons experiencing burnout were more likely to report being involved in a major medical error. (It's unclear to what extent the burnout caused the errors or the errors caused the burnout, however.)
Doctors think they're the only one who can do their jobs
When I go on vacation, my colleagues see my patients for me. I work in a small office, so I know the other doctors well and I trust that my patients are in good hands when I'm away.

Doctors have their own diagnosis: 'Moral distress' from an inhumane health system
But ceding that control to colleagues might be difficult for some doctors, especially when it comes to challenging patients or big research projects.
"I think we need to learn to be better at trusting our colleagues," says Adi Shah , an infectious disease doctor at the Mayo Clinic. "You don't have to micromanage every slide on the PowerPoint — it's OK."
West, the well-being researcher, says health care is moving toward a team-based model and away from a culture where an individual doctor is responsible for everything. Still, he adds, it can be hard for some doctors to accept help.
"You can be a neurosurgeon, you're supposed to go on vacation tomorrow and you operate on a patient. And there are complications or risk of complications, and you're the one who has the relationship with that family," West says. "It is really, really hard for us to say ... 'You're in great hands with the rest of my team.'"
What doctors need, says West, is "a little bit less of the God complex."
We don't have any interests other than medicine
Shah, the infectious disease doctor, frequently posts tongue-in-cheek memes on X (formerly known as Twitter) about the culture of medicine. Unplugging during vacation is one of his favorite topics, despite his struggles to follow his own advice.
His recommendation to doctors is to get a hobby, so we can find something better to do than work all the time.
"Stop taking yourself too seriously," he says. Shah argues that medical training is so busy that many physicians neglect to develop any interests other than medicine. When fully trained doctors are finally finished with their education, he says, they're at a loss for what to do with their newfound freedom.
Since completing his training a few years ago, Shah has committed himself to new hobbies, such as salsa dancing. He has plans to go to a kite festival next year.
Shah has also prioritized making the long trip from Minnesota to see his family in India at least twice a year — a journey that requires significant time off work. He has a trip there planned this month.
"This is the first time in 11 years I'm making it to India in summer so that I can have a mango in May," the peak season for the fruit, Shah says.
Wooten, the pediatrician, agrees. She works hard to develop a full life outside her career.
"Throughout our secondary and medical education, I believe we've really been indoctrinated into putting institutions above ourselves," Wooten adds. "It takes work to overcome that."
Mara Gordon is a family physician in Camden, N.J., and a contributor to NPR. She's on X as @MaraGordonMD .
- American Medical Association
- Entertainment
CMO denies overreaching into department headed by Stormont leaders
Sir Michael McBride was asked at the Covid-19 Inquiry about an email in which he asked to ‘clear’ Executive Office papers during the pandemic.

Northern Ireland’s chief medical officer has denied overreaching on his responsibilities by asking to “clear” briefing papers sent to Stormont leaders during the coronavirus pandemic.
Giving evidence to the UK Covid-19 Inquiry in Belfast, Professor Sir Michael McBride was asked to comment on an email he sent to an official in The Executive Office in early 2020 about a paper that was being prepared for the then First Minister Arlene Foster and deputy First Minister Michelle O’Neill providing an update on the developing health emergency.
The paper’s purpose was to inform the ministers about the discussions at the latest UK-wide Cobra meeting on the situation.
Dr McBride, who works within the Department of Health (DoH), not The Executive Office (TEO), wrote in the email to the TEO official that “given the professional and technical nature of these papers, as CMO I will wish to clear all future Executive papers while DOH remains the lead government department”.

Lead counsel for the inquiry Clair Dobbin KC questioned the CMO over the intervention.
“That might be thought or might appear to the outside eye to be a clear example of overreach into the Executive Office on your part,” she said.
Dr McBride insisted he was only asking to give clearance on the “professional and technical” advice within the paper.
However, he conceded his email was “not well worded” and could lead to the interpretation drawn by Ms Dobbin.
“I don’t think it’s a question of interpretation,” replied the inquiry’s counsel.
“I mean, I think it’s a question of you as CMO inserting yourself into the processes of The Executive Office, so that the officials couldn’t provide an update without, as you saying, wishing to clear, and it’s not just this, (it’s) clearing all future Executive papers whilst the Department of Health remains the lead government department.”
Dr McBride again insisted he had only been referring to the professional and technical advice.
“I think it was entirely appropriate that I was assured of the completeness of professional and technical advice to the First Minister and deputy First Minister,” he said.
The CMO made clear he had “no role” in clearing the entirety of Executive papers.

“I think it would have been a dereliction of my responsibilities as chief medical officer were I not to assure myself of the accuracy of the information that was being provided on the professional and technical aspects of that,” Dr McBride added.
“I have no role in clearing Executive papers, none, and never have had, and did not have throughout the pandemic and that would have been understood, I understood that and officials in TEO would have understood that.”
Ms Dobbin also questioned Dr McBride on an email he wrote to all Stormont departments at the start of February about Covid-19.
In the letter, he said the Department of Health was “closely monitoring” the situation. He asked public bodies to make sure staff were across their contingency plans for dealing with infectious diseases but said no further action was required at that point.
The inquiry’s counsel suggested the letter lacked urgency.
“It might be thought that that’s hardly sounding alarm bells for either Northern Ireland government departments or to all of the public authorities that they sponsored,” she said.
Dr McBride said the email was only a “scene setter” ahead of a planned meeting with departments to outline the potential risks.
“This letter was not meant or intended to explain or set out the level of risk or the level of concern, it was an enabler to facilitate a meeting which had been suggested… (at) which there would be an update provided.”

Coseley factory fire blamed on coal dust two years after similar blaze on same road Coseley | 4 hours ago
31 photos as clock rolls back to the 1950s at the Black Country Living Museum Dudley entertainment | 8 hours ago
Traditional pub given new life by couple who call it their life Plus Wednesfield | 15 hours ago
Third man arrested on suspicion of murder in connection with fatal Wolverhampton house blaze Crime | 8 hours ago
Carlos Corberan's feelings on "equal" West Brom and Southampton play-off draw and 'emotional' atmosphere Plus West Bromwich Albion | 3 hours ago

COMMENTS
When writing a persuasive essay about the Covid-19 pandemic, it's important to consider how you want to present your argument. To help you get started, here are some example essays for you to read: Covid-19 and its Impacts. Covid19, also known as Coronavirus, is an infectious disease that has had a major impact on the world. Since its ...
rodaranches. report flag outlined. Answer: COVID-19 is a pandemic. Thousands of people are being affected and millions of people are being infected. We can't go outside and play, school is closed and we can't visit family and friends. The novel coronavirus has caused many loved ones to be mourned and missed.
COVID-19 has reached to more than 150 nations, including China, and has caused WHO to call the disease a worldwide pandemic. By the time of 2nd week of April 2020, this COVID-19 cases exceeded 18,738,58, although more than 1,160,45 deaths were recorded worldwide and United States of America became the global epicentre of coronavirus.
Writing About COVID-19 in College Essays. Experts say students should be honest and not limit themselves to merely their experiences with the pandemic. The global impact of COVID-19, the disease ...
Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. "The way I dress, the way I love, and the way I carry ...
The CDC reports that the percentage of adults who reported symptoms of anxiety of depression in the past 7 days increased from 36.4 to 41.5 % from August 2020 to February 2021. Other reports show that having COVID-19 may contribute, too, with its lingering or long COVID symptoms, which can include "foggy mind," anxiety, depression, and post ...
The COVID-19 pandemic has exposed the inadequacy of public health systems worldwide, casting a shadow that we could not have imagined even a year ago. As the fog of confusion lifts and we begin to ...
The spread of the "Severe Acute Respiratory Coronavirus 2" (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [].The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [], causing massive economic strain ...
The COVID‑19 pandemic is a singular disaster, and it is reasonable for society—and scientists—to prioritize it. ... And published COVID‑19 papers had 19 percent fewer women as first ...
During the coronavirus pandemic, artists are continuing to illustrate, play music, ... Calif., had to say about the Opinion essay "I'm 26. Coronavirus Sent Me to the Hospital":
The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty, while the number of ...
100 Words Essay on Covid 19. COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very ...
COVID-19: Emergence, Spread, Possible Treatments, and Global Burden. The Coronavirus (CoV) is a large family of viruses known to cause illnesses ranging from the common cold to acute respiratory tract infection. The severity of the infection may be visible as pneumonia, acute respiratory syndrome, and even death.
Nearly every 100 years, humans collectively face a pandemic crisis. After the Spanish flu, now the world is in the grip of coronavirus disease 2019 (COVID-19). First detected in 2019 in the Chinese city of Wuhan, COVID-19 causes severe acute respiratory distress syndrome. Despite the initial evidence indicating a zoonotic origin, the contagion ...
Read these 12 moving essays about life during coronavirus. Artists, novelists, critics, and essayists are writing the first draft of history. A woman wearing a face mask in Miami. Alissa Wilkinson ...
COVID 19. Coronavirus is the latest epidemic that has broken out in the world jeopardizing the lives of human beings on the planet. The first case of a person infected with this virus was reported from Wuhan, China, on 31 December 2019. The situation in China is quite critical; as many as 244,988 people have been reported dead with this virus ...
The doctors had warned that although his father had regained the ability to speak, he could only repeat what was said to him. Advertisement. "It's me," said my husband. "It's me," said ...
COVID-19 (Coronavirus) has affected day to day life and is slowing down the global economy. This pandemic has affected thousands of peoples, who are either sick or are being killed due to the spread of this disease. The most common symptoms of this viral infection are fever, cold, cough, bone pain and breathing problems, and ultimately leading ...
Loved by our community. Answer: The covid-19 virus spreads primarily through droplets of saliva or discharge from the nose when an infected person coughs or sneezes, so it's important that you also practice respiratory etiquette. Protect yourself and others from infection. Explanation:
A special report, COVID19 and its Impact: Seven Essays on Reframing Government Management and Operations with essays from academic and government experts around the country. Governments today are facing serious, seemingly intractable public management issues in the aftermath of COVID-19 that go to the core of effective governance and leadership ...
james920. report flag outlined. Answer:my experience during covid 19 pandemic is very challenging but. it helps me to be responsible and helps me consintrate more in my studies but there are many people suffering in this kind of pandemic and it makes me think of how can i help them there are more people who needs help but for now the only thing ...
At Harvard, he designed an interactive "subway map" depicting a viral outbreak. As a member of the Sabeti lab, Specht taught an infectious disease modeling course to master's and Ph.D. students at University of Sierra Leone last summer. His outbreak analysis tool is also now being used in an ongoing study of Lassa fever in that region.
Findings: Results showed an increase in HRT until the onset of the pandemic in March 2020, followed by a significant decline at the beginning of the COVID-19 pandemic. After the first decline, structural breaks systematically demonstrate an increase in HRT rates, reaching levels not seen in the last 9 years.
This essay serves as the introduction to TVNM's special issue on "Pandemic TV," an analysis of the ways in which the COVID-19 pandemic affected principally anglophone television and television-watching in 2020 to 2021 (including television's response to corresponding events such as the summer 2020 Black Lives Matter uprisings and the fall 2020 U.S. presidential election).
This paper examines the findings of a small qualitative study focusing on two virtual discussions facilitated by the Social Workers' Association Nepal (SWAN) in May and June 2020 and follow-up interviews conducted with the participants during June 2020. The aim of these discussions and follow-up interviews was to examine the role of social workers in responding to the COVID-19 pandemic in Nepal.
In the era of the Covid-19 Pandemic as a form of national disaster that must receive special attention, because the condition of the Covid-19 Pandemic greatly affects the health and economy of the community. The community's economy as a result of the Covid-19 pandemic, has an impact on finance companies where debtors have difficulty in paying debt obligations. The implementation of the ...
Semantic Scholar extracted view of "The Impacts of COVID-19 Pandemic on Bus Transit Demand: A 30-month Naturalistic Observation in Jiading, Shanghai, China" by Weihan Bi et al. ... Semantic Scholar's Logo. Search 218,356,333 papers from all fields of science. Search. Sign In Create Free Account. DOI: 10.1016/j.ijtst.2024.04.012;
"I remember when one of our first well-being papers was published," says Dr. Colin West, a co-author of the new study and a health care workforce researcher at the Mayo Clinic. "I responded to the ...
The recent COVID-19 pandemic inflicted wide-ranging impacts on all sectors globally. Malaysia was no exception. The purpose of this retrospective study is to explore the well-being status of Malaysian university lecturers who conducted online teaching activities during the pandemic and the effective coping strategies they adopted to maintain their wellbeing.
Sir Michael McBride was asked at the Covid-19 Inquiry about an email in which he asked to 'clear' Executive Office papers during the pandemic. Published Just now Coronavirus - Wed Nov 24, 2021