5 ways to strengthen our health systems for the future

New possibilities are emerging to ensure stronger, more resilient health systems for the future. Image: REUTERS/Ajeng Dinar Ulfiana

.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Genya Dana
Kelly mccain, matthew oliver.

.chakra .wef-9dduvl{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-9dduvl{font-size:1.125rem;}} Explore and monitor how .chakra .wef-15eoq1r{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;color:#F7DB5E;}@media screen and (min-width:56.5rem){.chakra .wef-15eoq1r{font-size:1.125rem;}} Global Health is affecting economies, industries and global issues

.chakra .wef-1nk5u5d{margin-top:16px;margin-bottom:16px;line-height:1.388;color:#2846F8;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-1nk5u5d{font-size:1.125rem;}} Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:, healthy futures.
Listen to the article
- Health systems around the world have been hit hard by the pandemic, with 90% of countries reporting disruptions to essential health services.
- As we get back on track, new possibilities are emerging to address a wide range of health issues.
- Through data and technology, along with the co-creation of health services with communities and new entrants in the health and healthcare field, we have the potential to transform healthcare for the future.
In September 2019, a group of experts working together as part of the Global Preparedness Monitoring Board (GPMB) published a report stating that the world was grossly unprepared for a lethal respiratory pathogen pandemic like what the world faced in 1918 with influenza. The cost to the modern economy of such a pandemic, they reported, could be up to $3 trillion.
The GPMB’s estimates, it turned out, were far too conservative.
The IMF in October 2021 projected that the cost to the global economy of the COVID-19 pandemic, until 2024, would be around $ 12.5 trillion . The Economist described the economic impact as “incalculable”. The toll on human health is greater still.
Health systems face enormous challenges as they seek to recover from the pandemic. Efforts to eliminate HIV, TB, malaria and hepatitis have been set back decades, while 23 million children missed basic vaccines in 2020, an increase of nearly 20% on the previous year. Waiting times for diagnosis and treatment of cancer have spiralled in many parts of the world. Further out, an aging global population means that by 2050, 1 in 6 individuals will be over the age of 65 , making a resilient health system all the more critical.
How can we possibly hope to deal with any one of these seemingly intractable challenges – let alone find solutions to them all?
5 common themes for the future of health systems
The World Economic Forum’s Health and Healthcare Platform works with stakeholders from private industry, governments, academics, civil society and patient advocates on a wide range of health issues from hepatitis and tuberculosis , to cancer and diabetes , and a number of cross-cutting initiatives. Across the breadth of these issues, we see five common themes that we believe have the potential to transform how healthcare works in the future, and ensure for stronger, more resilient health systems globally.
1. There’s a new appreciation of the importance of health.
Late last year, Dr. Tedros Ghebreyesus, Director-General of the World Health Organization (WHO), said: “The time has come for a new narrative that sees health not as a cost, but an investment that is the foundation of productive, resilient and stable economies.”
That is exactly what we have seen from our partners. On an unprecedented scale, companies want to be engaged in matters relating to health. From the C-suite down deep into supply chains, there is a recognition that health underpins wealth – and nearly everyone is keen to play a part. We’ve seen new partnerships brokered outside of the health and healthcare industry, such as DP World – a leader in global end-to-end supply chain logistics headquartered in the United Arab Emirates – partnering with UNICEF to support the global distribution of COVID-19 vaccines and critical immunization supplies in low- and lower-middle-income countries.
2. Improving the health system means supporting the local community.
The pandemic saw health services delivered in the community in an unprecedented way through the deployment of mobile testing units and pop-up vaccination centres. In the US, the YMCA partnered with CVS Health to establish vaccination sites in communities in six cities without pharmacy access to help ensure more equitable access to COVID-19 vaccines. This trend will continue, making access to care easier, more local (including in workplaces ) and more affordable, in addition to freeing up critical resources within health systems to manage emergent care.

3. The global health workforce needs care, too.
COVID-19 exacerbated the global shortage of healthcare workers and the challenges they face. In the US alone, nearly 1 in 5 healthcare workers quit their jobs during the pandemic. With women representing 70% of the healthcare workforce, gender-based policies are needed to protect and support them. We must replace aging healthcare workforces, and care for our healthcare professionals traumatized by the pandemic. Healthcare should be reimagined based on the challenges of the COVID-19 pandemic – and healthcare workers should be leading health policy work.

4. Deployment of novel technologies in the health system is critical.
A range of new technologies are starting to reach mainstream use, promising to make care more equitable and cheaper. From a collaboration by Pfizer, BioNTech and Zipline for long-range drone delivery of COVID-19 vaccines requiring ultra-cold-chain in Ghana, to the use of AI to diagnose lung conditions via X-ray, to the breakthrough use of mRNA technology and the promise it represents in fighting other challenging health conditions , exciting novel technologies can make care cheaper, more effective and more equitable.
5. A new age of diagnostics has begun.
Before the pandemic, many who worked in diagnostics felt that their contributions were undervalued. Now, everyone understands the importance of testing, with “PCRs”, “lateral flows”, “antigens” and “antibodies” becoming part of daily language. At the outset of the pandemic, only two countries in Africa could screen for coronaviruses; now, nearly all can. This carries hope for finding the “missing millions” in HIV, TB, malaria and hepatitis. There’s a new focus on genomic sequencing and the importance of sentinel surveillance. The pandemic has also shown that health data can be collected in real-time from all over the world. With more, earlier testing, we can catch health conditions sooner and get better health outcomes.
The application of “precision medicine” to save and improve lives relies on good-quality, easily-accessible data on everything from our DNA to lifestyle and environmental factors. The opposite to a one-size-fits-all healthcare system, it has vast, untapped potential to transform the treatment and prediction of rare diseases—and disease in general.
But there is no global governance framework for such data and no common data portal. This is a problem that contributes to the premature deaths of hundreds of millions of rare-disease patients worldwide.
The World Economic Forum’s Breaking Barriers to Health Data Governance initiative is focused on creating, testing and growing a framework to support effective and responsible access – across borders – to sensitive health data for the treatment and diagnosis of rare diseases.
The data will be shared via a “federated data system”: a decentralized approach that allows different institutions to access each other’s data without that data ever leaving the organization it originated from. This is done via an application programming interface and strikes a balance between simply pooling data (posing security concerns) and limiting access completely.
The project is a collaboration between entities in the UK (Genomics England), Australia (Australian Genomics Health Alliance), Canada (Genomics4RD), and the US (Intermountain Healthcare).
COVID-19 has generated an opportunity for stakeholders – from the public and private sectors, to governments, to communities – to reimagine collaboration in the pursuit of more sustainable, equitable and resilient health systems. Through more strategic use of data and technology, along with the co-creation of health services with communities and new entrants in the health and healthcare field, we have the opportunity to enable our health and healthcare systems to learn, adapt and prepare for a future that is sure to come.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Related topics:
The agenda .chakra .wef-n7bacu{margin-top:16px;margin-bottom:16px;line-height:1.388;font-weight:400;} weekly.
A weekly update of the most important issues driving the global agenda
.chakra .wef-1dtnjt5{display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;} More on Forum Institutional .chakra .wef-nr1rr4{display:-webkit-inline-box;display:-webkit-inline-flex;display:-ms-inline-flexbox;display:inline-flex;white-space:normal;vertical-align:middle;text-transform:uppercase;font-size:0.75rem;border-radius:0.25rem;font-weight:700;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;line-height:1.2;-webkit-letter-spacing:1.25px;-moz-letter-spacing:1.25px;-ms-letter-spacing:1.25px;letter-spacing:1.25px;background:none;padding:0px;color:#B3B3B3;-webkit-box-decoration-break:clone;box-decoration-break:clone;-webkit-box-decoration-break:clone;}@media screen and (min-width:37.5rem){.chakra .wef-nr1rr4{font-size:0.875rem;}}@media screen and (min-width:56.5rem){.chakra .wef-nr1rr4{font-size:1rem;}} See all

Day 2 #SpecialMeeting24: Key insights and what to know
Gayle Markovitz
April 28, 2024

Day 1 #SpecialMeeting24: Key insights and what just happened
April 27, 2024

#SpecialMeeting24: What to know about the programme and who's coming
Mirek Dušek and Maroun Kairouz

Climate finance: What are debt-for-nature swaps and how can they help countries?
Kate Whiting
April 26, 2024
What to expect at the Special Meeting on Global Collaboration, Growth and Energy for Development
Spencer Feingold and Gayle Markovitz
April 19, 2024

From 'Quit-Tok' to proximity bias, here are 11 buzzwords from the world of hybrid work
April 17, 2024
All Content
10 strategies for delivering a great presentation.
- Justin Roesch, MD;
- Patrick A. Rendon, MD
It’s noon on Tuesday, and James, a new PGY-2 resident, begins his presentation on COPD. After five minutes, you notice half of the residents playing Words with Friends, the “ortho-bound” medical student talking with a buddy in the back, and the attendings looking on with innate skepticism.

Dr. Patrick A. Rendon
Your talk on atrial fibrillation is next month, and just watching James brings on palpitations of your own. So what do you do?
Introduction
Public speaking is a near certainty for most of us regardless of training stage. A well-executed presentation establishes the clinician as an institutional authority, adroitly educating anyone around you.
Dr. Justin Roesch
So how can you deliver that killer update on atrial fibrillation? Here, we provide you with 10 tips for preparing and delivering a great presentation.
Preparation
1. Consider the audience and what they already know. No matter how interesting we think we are, if we don’t present with the audience’s needs in mind, we might as well be talking to an empty room. Consider what the audience may or may not know about the topic; this allows you to decide whether to give a comprehensive didactic on atrial fibrillation for trainees or an anticoagulation update for cardiologists. Great presenters survey their audience early on with a question such as, “How many of you here know the results of the AFFIRM trial?” This allows you to make small alterations to meet the needs of your audience.
2. Visualize the stage and setting. Understanding the stage helps you anticipate and address barriers to learning. Imagine for a moment the difference in these two scenarios: a discussion of hyponatremia with a group of medical students at 4 p.m. in a dark room versus a discussion on principles of atrial fibrillation management at 11 a.m. in an auditorium. Both require interaction, although an auditorium-based presentation requires testing your audio-visual equipment in advance.
3. Determine your objectives. To determine your objectives, begin with the end in mind. If you were to visualize your audience members at the end of the talk, what would they know (knowledge), be able to do (behavior), or have a new outlook on (attitude)? The objectives will determine the content you deliver and the activities for learning. For a one-hour presentation, identifying three to five objectives is a good rule of thumb.
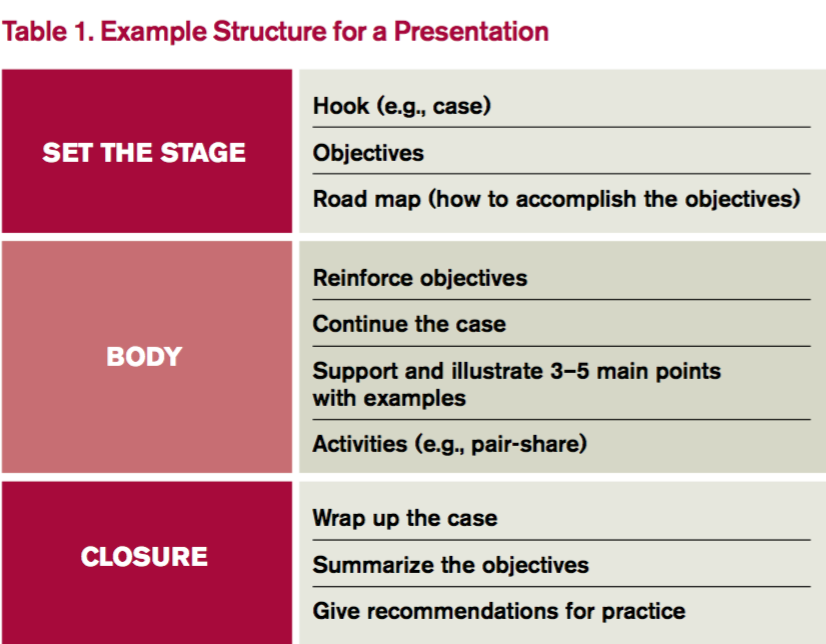
4. Build your presentation. Whether using PowerPoint, Prezi, or a white board, “build” the presentation from the objectives. Table 1 outlines one example format; Figure 1 outlines some best practices of PowerPoint.
Humans evolved to interpret visual imagery, not read text, so try to use pictures instead of bullet points. Consider first building slides with text and then using an internet search engine to convert words to pictures. For example, “atrial rate 200 bpm” is better displayed with an actual ECG.
5. Practice. Practicing helps you become more comfortable with the content itself as well as how to present that content. If you can, practice with a colleague and receive feedback to sharpen your material. No time to spare? Practice the introduction and any major point that you want to get across. Audiences decide within the first five minutes whether your talk is worth listening to before pulling out their cellphones to open up Facebook.
1. Confront nervousness. Many of us become nervous when speaking in front of an audience. To address this, it’s perfectly reasonable to rehearse a presentation at home or in a quiet call room ahead of time. If you feel extremely nervous, breathe deeply for five- to 10-second intervals. During the presentation itself, find friendly or familiar faces in the audience and look them in the eyes as you speak. This eases nerves and improves your technique.
Share:
Comment on this article cancel reply.
Your email address will not be published. Required fields are marked *

Undergraduate Program
- Overview and Welcome
- How Do I Apply?
- Our Degrees
- Research and Internships
Improving the health system and providing better healthcare
- Adopting healthier lifestyles - more exercise, checkups, and health screenings
- Disaster preparedness
- Public Health Society (PHS)
Primary-care doctors, specialists, hospitals, community health clinics – all provide care to people in need. We can make big improvements in the health of the most vulnerable people in our communities by helping everyone get better access to healthcare, improving the quality of the care they receive and making sure it is provided at a reasonable price. But doing so is not easy, and requires addressing a number of challenging questions, including:
- Why does the structure of the U.S. health system contributes to increased health disparities and what can be done to reduce those disparities?
- Why does the U.S. system costs so much compared to the rest of the world and what can be done to lower costs?
- Why are there variations across hospitals and regions in the type and quality of care people receive, and what can we do to ensure everyone has access to quality services?
The field of h ealth services research (HSR) addresses all these issues. HSR examines how people get access to healthcare, how much care costs and what happens to patients as a result of this care.
The main goals of health services research are to identify the most effective ways to organize, manage, finance and deliver high-quality care; reduce medical errors; and improve patient safety (Agency for Healthcare Research and Quality, 2002). HSR tends to be multidisciplinary, and with researchers coming from a variety of disciplines, including:
- Clinical fields of medicine, nursing, dentistry and allied health
- Social and behavioral sciences
- Human factors engineering
- Epidemiology and biostatistics
- Multidisciplinary perspectives from healthcare policy, research, administration and management
Health services researchers investigate how various factors — including social forces, financing mechanisms, organizational processes and structures, evolving health technologies and individual behavior — act separately and together to affect the delivery of healthcare and, ultimately, the health and well being of people.
They pursue careers in many settings, including academia, professional organizations, health policy groups, clinical settings, and in federal, state and local agencies. Examples of topics explored by HSR include:
Additional Links
- Executive Leadership
- University Library
- School of Engineering
- School of Natural Sciences
- School of Social Sciences, Humanities & Arts
- Ernest & Julio Gallo Management Program
- Division of Graduate Education
- Division of Undergraduate Education
Administration
- Office of the Chancellor
- Office of Executive Vice Chancellor and Provost
- Equity, Justice and Inclusive Excellence
- External Relations
- Finance & Administration
- Physical Operations, Planning and Development
- Student Affairs
- Research and Economic Development
- Office of Information Technology
University of California, Merced 5200 North Lake Rd. Merced, CA 95343 Telephone: (209) 228-4400

- © 2024
- About UC Merced
- Privacy/Legal
- Site Feedback
- Accessibility
'Improve health systems' presentation slideshows
Improve health systems - powerpoint ppt presentation.
eHealth: Global perspective
eHealth: Global perspective. S. Yunkap Kwankam Coordinator eHealth World Health Organization, Geneva. Outline of presentation. Six point agenda and health system framework WHO eHealth priorities WHO collaboration mechanisms Conclusion.
514 views • 34 slides
View Improve health systems PowerPoint (PPT) presentations online in SlideServe. SlideServe has a very huge collection of Improve health systems PowerPoint presentations. You can view or download Improve health systems presentations for your school assignment or business presentation. Browse for the presentations on every topic that you want.
Public Health Systems & Best Practices

Protecting the public's health depends on strengthening the public health system and implementing proven strategies to improve health outcomes.
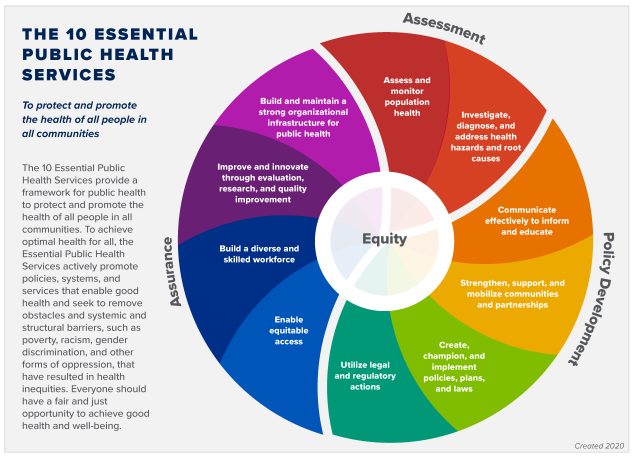
The 10 Essential Public Health Services (EPHS) describe the public health activities that all communities should undertake. On September 9, 2020, a revised EPHS framework and graphic was released. The revised EPHS is intended to bring the framework in line with current and future public health practice.

Social determinants of health describe conditions in the places where people live, learn, work, and play that affect a wide range of health risks and outcomes. Differences in these conditions lead to health inequities.
In partnership with the Robert Wood Johnson Foundation, CDC is supporting the implementation of a national voluntary accreditation program for state, tribal, local, and territorial health departments.
- Accredited Health Departments
Public health governance varies from state to state, as do the relationships between state and regional or local agencies. Explore this page to determine how agencies collaborate to protect the public’s health in your state.
In public health settings, performance and quality tools are being promoted and supported as an opportunity to increase the effectiveness of public health agencies, systems, and services.
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- Resources in Surgical Educ...
- RISE Articles
- Six Steps to Engage Reside...
Six Steps to Engage Residents in Quality Improvement Education
Neha R. Malhotra, MD; Ashley Vavra, MD; Robert E. Glasgow, MD; Brigitte K. Smith, MD
January 1, 2020
Health care systems are becoming increasingly complex and the United States continues to lag behind other industrialized nations in health outcomes relative to the amount spent. 1–2 We owe it to our patients to foster innovation and improve delivery of care. To do this, we must engage our students, residents, and fellows to understand, develop, and, ultimately, lead the movement to improve quality in health care.
This RISE article reviews the basic tenets of quality in health care and the importance of these concepts to the practice of surgery in the current health care system. We discuss barriers to effective quality improvement (QI) education, including the difference between QI and research. Finally, we outline key components for success when designing QI curricula for trainees so that they are prepared to work within complex systems of care and to make significant contributions to improving the quality of care they provide to their patients.
Establishing a Shared Mental Model of Health Care Quality
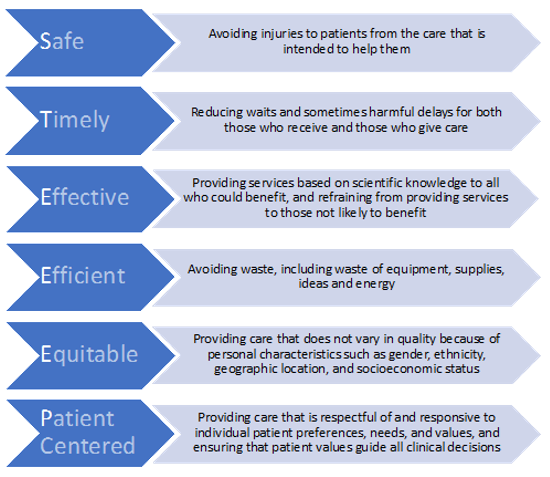
Twenty years ago, the Institute of Medicine’s landmark publication, Crossing the Quality Chasm , helped define critical disparities between the current and ideal state of quality health care in the United States (Figure 1). 2 Since then, health care practitioners are increasingly being evaluated based on the quality of care they provide. As a result, health care has evolved from quality assurance to QI, where defects are examined in order to implement change and prevent errors. 3 Surgeons today need to be capable of interventions that will achieve sustained improvement in the quality of surgical care. It is essential the principles of QI and health systems thinking be incorporated into training for students and residents. Effective educational programs in QI are needed to enable trainees to achieve competency targets and enter the workforce prepared to actively improve the quality of surgical care delivery in their own practice and local institution. 4–6
Challenges and Barriers
Developing effective approaches for teaching QI principles and methodology can be challenging. It is further complicated by the lack of consensus around the definition of quality and how QI differs from research. While both research and QI are essential to ensuring high-quality health care, there are several distinct features of QI that must be recognized and defined.
QI vs Research: What’s the Difference?
Simply stated, QI involves improving processes of care, while research seeks to improve clinical evidence. The main goals of health services research (HSR) are to identify the most effective ways to organize, manage, finance, and deliver high-quality care, reduce medical errors, and improve patient safety. Similarly, outcomes research seeks to understand the factors in health care delivery that are primarily responsible for differential results, such as mortality or quality of life. 7
HSR and outcomes research share features common to all research: biases are carefully controlled for using randomization, unequivocal outcomes are measured and significance thresholds are set, classic biostatistics are utilized to analyze data at the end of the project, and the work is powered to definitively answer a question. QI, on the other hand, seeks to operationalize best practices with a series of small changes. Data need only be sufficient to meet confidence thresholds for action or decision, are analyzed in real-time, and trends influence next steps (Table 1).
Table 1. The differences between research and quality improvement
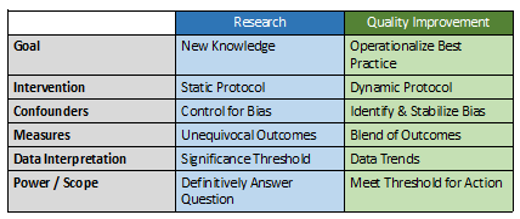
In order to design effective QI interventions, surgeons must be knowledgeable about the factors that influence the outcome of interest—the HSR and outcomes literature. QI interventions are based on knowledge generated from research, but the process of QI does not itself follow the tenets of research. Practice guidelines and standards derived from research often take years to reach implementation, while QI efforts are held to a more immediate and actionable time frame. For QI interventions to be successful, surgeons must also understand and apply principles of change management and team leadership. Change management is the science of preparing and supporting individuals and teams in the face of implementing new concepts, programs, and routines. Understanding these differences is a critical first step to help surgical educators set expectations for resident-led QI projects.
Barriers to Resident Engagement
Engaging residents in meaningful QI efforts is a significant challenge for surgical educators. Residents across specialties have struggled with overload and the challenge of adding yet another component to their curriculum, as well as lack of a shared vision for how to conduct QI and poor clarity of curricular content. 8 Residents have expressed frustration with contributing to improving local health care systems without feeling that their efforts are acknowledged or valued. Educators must address these barriers if QI curricula are to be successful.
Optimizing QI Education in Surgical Residencies
The conditions and contexts for learning are critical to the development and outcomes of QI curricula, as QI efforts occur within the clinical setting of increasingly complex health care systems. Conditions for learning include the content of the curriculum, instructional methods, learning sites, faculty, time, facilities, and health care teams and systems. Contexts for learning include faculty role-modeling, institutional values, culture and politics, and socio-political-economic forces. 9 The six tips that follow incorporate and address issues within this framework.
Establish a Formal Curriculum
While we acknowledge that many programs struggle with limited resources to expand existing curricula, the importance of establishing a complete curriculum, including goals, objectives, and assessment of learning outcomes, cannot be overstated. Residents across specialties have expressed confusion about what is being taught, what is expected of them for participation and outcomes, and the purpose of learning QI. 8 Providing clarity through a comprehensive curriculum is the first step to addressing these barriers. We have found that formalizing a program for learning QI skills helps to mitigate the sense that QI projects are simply checking a box. Rather, residents should know that they are learning a valuable skill set that they will use in their future practice. Additionally, our experience suggests residents are more likely to view QI curricula positively and engage in the when institutional and departmental leadership, program directors and other faculty show explicit support. The American College of Surgeons Quality in Training Initiative Primer is an excellent curricular resource that can be readily implemented within surgical residency programs. 10
Optimize Instructional Methods
The Institute for Healthcare Improvement (IHI) Open School online modules are a popular instructional method to deliver core content on QI to residents 11 ; however, for curricula on QI principles and their application to be effective, instructional methods must go beyond online modules. Experts in medical education and adult learning principles have suggested that a combination of didactic and experiential learning is the optimal approach to effective instruction in QI. 12 The didactic component of the curriculum should provide clarity on the concept of quality, identify differences between QI and research, and outline practical steps for leading QI initiatives. Online modules are excellent resources to deliver content, however, in-person discussions are critical to ensuring improved quality and safety are adopted as lifelong goals, rather than just a box to be checked.
Once residents haven a proven understanding of the QI curriculum, they must “show how,” by demonstrating knowledge and competence in practice by leading QI projects. 13 In our experience, the primary focus of QI project involvement should be learning and practicing the principles, not project outcomes. QI work is messy and fraught with barriers and challenges, many of which are out of the control of the average resident. Therefore, understanding fundamental QI principles with ongoing engagement in QI should be the goal.
Address Institutional Culture and Values
Management guru, Peter Drucker, is attributed as saying, “culture eats strategy for breakfast.” This is as true in establishing effective QI curricula as in the business sector. The most well-considered QI curriculum will miss the mark if institutional culture surrounding QI is not identified and addressed. The values of the institution influence residents’ ability to implement change through QI processes. Furthermore, Adult Learning Theory posits that residents will learn best when they see a need to acquire knowledge and skills in a particular domain. 14 This suggests that residents are unlikely to develop an intrinsic motivation to learn and apply QI skills without appropriate faculty role modeling of its importance. Changes in culture come from the top and it is critical to engage high level stakeholders when implementing a QI program. By engaging senior leadership first, the culture of quality will permeate all aspects of resident training, not just the siloed QI curriculum.
Support Faculty QI Champions
Our current trainees are faced with mandates to learn something for which there are exceedingly few teachers and even fewer experts. 15 For any QI curricula to succeed, faculty development is critical. (See Appendix for opportunities for advanced training in quality improvement and patient safety.) Residents should have the opportunity to interact with a faculty champion or curriculum director as they learn foundational principles, as well as a faculty coach or mentor as they work through a QI project. Educational leaders in QI have suggested that resident projects fail for two reasons: (1) burnout of the few faculty who are qualified to coach projects, and (2) lack of faculty engagement to ensure QI project success. 16 Interested faculty should be identified and encouraged to obtain training in QI through a variety of certificate programs that are now available institutionally and nationally. 16–19 Finally, QI principles are universal across specialties and health care professions, so seeking teachers and coaches outside of the department of surgery is an important avenue to consider.
Integrate and Align with the Hospital System
Hospital operations and graduate medical education (GME) alignment need to be addressed to support QI curriculum development and implementation. Implementation of effective QI curricula requires access to infrastructure and resources such as data, project management, IT support, and process improvement expertise, which are likely to reside within clinical operations. A QI initiative is more likely to gain access to these resources if it falls in line with the hospital’s strategic priorities, particularly if the resident is able to present a business case that estimates savings for the institution. However, GME and clinical operations leadership and their missions typically exist in silos and are not routinely aligned. In order to improve alignment, residents are encouraged to develop relationships with hospital quality leaders. GME-wide house staff councils are one way to facilitate this. 20 Appointing resident representatives to institutional QI councils and committees can also improve communication and collaboration between residents and hospital leaders. 21 Projects that are derived from partnership with the hospital are also more likely to affect day-to-day experience of those involved and can increase engagement of residents and faculty who are able to see the problem and results of their efforts in real time.
Celebrate Successes and Make QI Efforts Visible
Celebrating resident QI efforts is critical to achieve buy-in from the residents and promote success of the QI curriculum. Residents should be given the opportunity to share their work at conferences, such as grand rounds. 22 The University of Utah has established an annual Department Value Symposium where residents present abstracts of their QI work and a keynote speaker is invited, similar to resident research days that are commonplace across programs. Furthermore, QI is not unique to surgery and engagement with other specialties, as well as administration, can be leveraged to establish QI symposia or learning days outside the department of surgery. In addition to demonstrating appreciation for the residents’ work, this serves as an opportunity for faculty development.
Residents should present successful projects directly to the administration. These presentations will expand QI discussion, improve patient care, and show residents their research is valued. Previous work in medical fields suggests that residents may view QI as a lot of extra work, and we must remember to recognize and applaud their efforts. 8 Encourage residents to present their work at local and national meetings. As the field of patient safety and QI grows, there is great room for scholarship in this realm. Presenting at QI meetings should be encouraged and valued in line with support of research presentations and conference attendance.
Continuous improvement in the quality of care we deliver can only be achieved by continuous, frontline efforts. Effective QI curricula in residency will empower surgeons to participate in QI efforts in their clinical practice. Taking a cue from the business world on total quality management—a program aimed at increasing quality and productivity—we must “institute a vigorous program of education” and realize that quality transformation is everyone’s work. 23
- Davis K, Stremikis K, Schoen C, Squires D. Mirror, Mirror on the Wall, 2014 Update: How the U.S. Health Care System Compares Internationally . The Commonwealth Fund; June 2014. https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_fund_report_2014_ jun_1755_davis_mirror_mirror_2014.pdf . Accessed January 28, 2020.
- Institute of Medicine Committee on Quality Health Care in America. Craossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press, 2001.
- Module 4. Approaches to Quality Improvement. AHRQ. https://www.ahrq.gov/professionals/prevention-chronic-care/improve/system/pfhandbook/mod4.html . Published May 2013. Accessed June 30, 2019.
- Purnell SM, Wolf LM, Millar MM, Smith BK. A National Survey of Integrated Vascular Surgery Residents' Experiences with and Attitudes about Quality Improvement During Residency. J Surg Educ. 2020;77(1):158–165.
- Medbery RL, Sellers MM, Ko CY, Kelz RR. The unmet need for a national surgical quality improvement curriculum: A systematic review. J Surg Ed . 2014;71:613–631.
- Kelz RR, Sellers MM, Reinke CE, Medbery RL, Morris J, Ko C. Quality in-training initiative—A solution to the need for education in quality improvement: Results from a survey of program directors. J Am Coll Surg . 2013,217:1126–1132.
- Kuy S, Greenberg CC, Gusani NJ, Dimick JB, Kao LS, Brasel KJ. Health services research resources for surgeons. J Surg Res . 2011;171(1):e69–73.
- Butler JM, Anderson KA, Supiano MA, Weir CR. "It Feels Like a Lot of Extra Work": Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System. Acad Med. 2017;92(7):984–990.
- Bordage G, Harris I. Making a difference in curriculum reform and decision-making processes. Med Educ. 2011;45(1):87–94.
- American College of Surgeons National Surgical Quality Improvement Project. Practical QI: The basics of quality improvement education. ACS Quality In-Training Initiative; 2017. https://qiti.acsnsqip.org/ACS_NSQIP_2017_QITI_Curriculum.pdf . Accessed January 28, 2020.
- IHI Open School Home: IHI—Institute for Healthcare Improvement. IHI. http://www.ihi.org/education/IHIOpenSchool/Pages/default.aspx . Accessed January 28, 2020.
- Goldman J, Kuper A,Wong BM. How Theory Can Inform Our Understanding of Experiential Learning in Quality Improvement Education. Acad Med . 2018;93(12):1784–1790.
- Miller GE. The assessment of clinical skills/competence/rerformance. Acad Med. 1990;65(9 Suppl):S63–67.
- Jones AC, Shipman SA, Ogrinc G. Key characteristics of successful quality improvement curricula in physician education: A realist review. BMJ Qual Saf . 2015;24:77–88.
- Mosser G, Frisch KK, Skarda PK, Gertner E. Addressing the challenges in teaching quality improvement. Am J Med . 2009;122(5):487–491.
- Wong BM, Goldman J, Goguen JM, et al. Faculty-Resident “Co-Learning”: A Longitudinal Exploration Of An Innovative Model For Faculty Development In Quality Improvement. Acad Med . 2017; 92(8):1151–1159.
- Baxley EG, Lawson L, Garrison HG, et al. The Teachers Of Quality Academy: A Learning Community Approach To Preparing Faculty To Teach Health Systems Science. Acad Med. 2016; 91(12):1655–1660.
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators Academy: Fulfilling an unmet need for faculty development. Am J Med Qual . 2014; 29(1):5–12.
- Stille CJ, Savageau JA, McBride J, Alper EJ. Quality Improvement “201”: Context-relevant quality improvement leadership training for the busy clinician-educator. Am J Med Qual . 2012; 27(2):98–105.
- Tevis SE, Ravi S, Buel L, Clough B, Goelzer S. Blueprint for a Successful Resident Quality and Safety Council. J Grad Med Educ . 2016;8(3):328–331.
- Tess A, Vidyarthi A, Yang J, Myers JS. Bridging the Gap: A Framework and Strategies for Integrating the Quality and Safety Mission of Teaching Hospitals and Graduate Medical Education. Acad Med . 2015;90:1251–1257.
- Sellers MM, Hanson K, Schuller M, et al. Development and participant assessment of a practical quality improvement educational initiative for surgical residents. J Am Coll Surg . 2013;216:1207–1213.
- Deming WE. Out of the Crisis. Cambridge, MA: Massachusetts Institute of Technology, Center for Advanced Engineering Study; 1986.
Institute for Healthcare Improvement Open School Online—Basic Certificate in Quality & Safety
Coursera—Leading Healthcare Quality and Safety (Certificate available for a fee, course materials free)
Tuition Required—Certificate Programs
University of Washington—Certificate Program in Patient Safety and Quality
American Institute for Healthcare Quality— Certificate in Healthcare Quality
American Institute for Healthcare Quality— Certificate in Lean Six Sigma (Green Belt)
American Society for Quality—Quality Improvement Associate Certification
American Society of Health Care Risk Management— Patient Safety Certificate Program
University of Tennessee Health Science Center— Healthcare Quality Improvement, Certificate
Georgetown University—Executive Certificate for Patient Safety & Quality
George Washington University—Graduate Certificate in Health Care Corporate Compliance
University of Pittsburgh—Graduate Certificate in Health Systems Leadership and Management
University of Alabama—Graduate Certificate in Health Care Quality and Safety
University of Pennsylvania—Certificate in Health Care Quality and Safety
Johns Hopkins Medicine—Online Patient Safety Certificate
Northwestern University-Certificate in Health services Contemporary Issues and Methodology
Graduate Degrees
Thomas Jefferson University—Healthcare Quality and Safety Master’s (Online)
Nova Southeastern University—Master of Health Science: Health Care Risk Management, Patient Safety and Compliance Concentration
Franklin University—Master of Healthcare Administration—Healthcare Quality Management
Drexel University—MS in Quality, Safety and Risk Management in Healthcare (Online)
University of Illinois Chicago—Master of Science in Patient Safety Leadership (Online)
University of Alabama at Birmingham—Master of Science in Healthcare Quality and Safety (Online)
Western Governors University—Master of Health Leadership-Healthcare Quality (Online)
Georgetown University—Executive Master’s in Clinical Quality, Safety & Leadership
The George Washington University—Master of Health Sciences in Healthcare Quality (Online)
Mary Baldwin University—Master of Healthcare Administration in Quality and Systems Safety
Johns Hopkins University—Master of Applied Science in Patient Safety and Healthcare Quality (Online)
Northwestern University—Master of Science Healthcare Quality and Patient Safety and Masters of Science in Health Services and Outcomes Research
About the Authors
Neha R. Malhotra, MD, is a division of urology fellow at the University of Utah Department of Surgery in Salt Lake City.
Ashley Vavra, MD , is an assistant professor in the division of vascular surgery at Northwestern University in Evanston, IL.
Robert E. Glasgow, MD, is a professor, vice chair of clinical operation and quality, and the chief value officer in the department of surgery at the University of Utah in Salt Lake City.
Brigitte K. Smith, MD, is an assistant professor, vice chair of education, and director of resident value curriculum in the department of surgery’s division of vascular surgery at University of Utah in Salt Lake City.
The most effective ways to improve the health system presentation
Related posts.

Which components should be included in an effective message of appreciation?

Keep on Making Ways For Me

What are the 5 ways to make our food safer?

Name two ways to determine if a solution is acidic.

In what ways is meiosis II similar to and different from mitosis of a diploid cell?

Which of the following is least effective when building a sustainable competitive advantage?

All of the following are ways to reassure or calm a child during a haircutting service except:

What are three ways to put out a grease fire?

What are 5 ways food can be contaminated?

Which of the following is not one of the ways that angiotensin ii increases arterial blood pressure?

How fast does hair grow per day

Which of the following allows different operating systems to coexist on the same physical computer?

What is being defined as the degree to which something is related or useful to what is happening or being talked about?

Which of the following is NOT a pathway in the oxidation of glucose

Juan is the person employees go to when knowledge of a topic was needed. juan holds ________ power.

Which of the following is not a standard mounting dimension for an electric motor? select one:

Which set of characteristics will produce the smallest value for the estimated standard error?

Is a program that assesses and reports information about various computer resources and devices.


How much energy is needed to move one electron through a potential difference of 1.0 102 volts

Includes procedures and techniques that are designed to protect a computer from intentional theft
- Advertising
LATEST NEWS
What brand of castor oil is best for hair, what are control charts based on, vscode no server install found in wsl, needs x64, how do you get to motion settings on iphone, how long is a furlong in horse, replace the underlined word with the correct form, how many spinach plants per person, bread clip in wallet when traveling, what aisle is heavy cream on, how do you play roblox on a chromebook without downloading it.
- Privacy Policy
- Terms of Services
- Cookie Policy
- Knowledge Base
- Remove a question

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Institute of Medicine (US) Committee on Future Directions for the National Healthcare Quality and Disparities Reports; Ulmer C, Bruno M, Burke S, editors. Future Directions for the National Healthcare Quality and Disparities Reports. Washington (DC): National Academies Press (US); 2010.
Future Directions for the National Healthcare Quality and Disparities Reports.
- Hardcopy Version at National Academies Press
6 Improving Presentation of Information
The NHQR and NHDR can be forward-looking documents that not only present historical trend data but also convey a story of the potential for progress and the health benefits to the nation of closing quality and disparity gaps. To serve as catalysts for improvement, the Future Directions committee envisions that the reports will extrapolate rates of change to indicate when gaps between current and recommended care might be closed and will present benchmarks on best-in-class performance. The committee makes sug gestions for organizing report content to tell a more complete quality improvement story, realize greater integration between quality improvement and disparities elimination, improve takeaway messages and data displays, and achieve a better match between the AHRQ products and potential audiences.
The NHQR and NHDR provide an enormous amount of data—principally presented in graphs—about how the United States is performing on various measures of health care and how performance has bettered or worsened over time. Although these data are useful, the NHQR and NHDR have potential beyond reporting on historical trends; the reports can also illuminate realistic levels of performance for all to strive toward and provide information on how long it will take to close gaps between current and recommended care at the current pace of improvement.
In this chapter, the committee expands on its vision that future versions of the NHQR and NHDR should tell a more complete story of how to move toward achieving a high-quality, high-value health care system. To make the information presented in the NHQR and NHDR more forward-looking and action-oriented, the committee recommends that AHRQ make greater use of benchmarking and suggests improvements to data displays and the general organization of the NHQR and NHDR. Helping audiences for the NHQR and NHDR better understand gaps in the quality of U.S. health care—whether between actual performance and receiving the recommended standard of care, or between population groups or geographic regions—and better understand the benefits of closing those gaps would provide audiences with stronger evidence and rationales for improving quality.
The chapter begins by reviewing the Future Directions committee’s suggestions for how AHRQ’s lineup of products could better serve current and expanded audiences. The committee underscores the importance of integrating disparities reduction into quality improvement by enhancing the relationship between the structure of the two national healthcare reports. Finally, suggestions are made on improving data displays and the statistical quality of quality reporting.
- MATCHING PRODUCTS TO AUDIENCE NEEDS
At present, the national healthcare reports and related products are consulted by a variety of stakeholders, many of which have different interest areas (e.g., heart disease, rural health, racial disparities, delivery settings) and different levels of sophistication for data interpretation and analysis. The 2001 IOM report Envisioning the National Health Care Quality Report stated that the NHQR was not to be a “single static report, but rather a collection of annual reports tailored to the needs and interests of particular constituencies” (IOM, 2001, p. 6). The committee believes that AHRQ needs to expand and refine its quality reporting product line to provide products and data that are useful and understandable for a variety of audiences. Therefore, the committee recommends the following:
Recommendation 6: AHRQ should ensure that the content and presentation of its national health care reports and related products (print and online) become more actionable, advance recognition of equity as a quality of care issue, and more closely match the needs of users by:
- incorporating priority areas, goals, benchmarks, and links to promising practices;
- redesigning print and online versions of the NHQR and NHDR to be more integrated by recognizing disparities in the NHQR and quality benchmarks in the NHDR;
- taking advantage of online capability to build customized fact sheets and mini-reports; and
- enhancing access to the data sources for the reports.
The committee’s suggested products, along with their potential audiences, are reviewed in Table 6-1 .
Tailoring Products to Meet the Needs of Multiple Audiences.
Refining the Organization of the NHQR and NHDR
Integrating efforts to improve quality with efforts to eliminate disparities increases opportunities to positively affect change. Presenting the same organizational framework and measures in both reports reinforces users’ understanding of the relationship between overall health care quality and the depth of health care disparities. But currently, the two reports are not well linked beyond presenting the same measures.
Changing the Highlights Section of the Reports
The committee proposes that AHRQ present the same Highlights section in both the NHQR and NHDR to underscore the relationship between health care quality and equity. The text of the Highlights section should be developed so that the section can be published as a stand-alone document that could be the subject of dissemination events targeted to relevant stakeholder audiences. The document could:
- Spotlight areas with the greatest potential for quality improvement impact and provide detail on what the value of closing quality gaps would be to population health and equity.
- Feature progress on priority areas and toward any established national goals.
- Discuss evidence-based policies and best practices that may enhance quality improvement or factors that hinder progress as informed by data within the body of the report.
- Emphasize takeaway messages directed to different audiences (e.g., policy makers, health care providers, and the public) on what they can do to improve health care quality on prioritized topics and measures.
- Include a summary of state performance and the state of disparities.
The committee believes that a summary of state performance should be part of the Highlights section of the reports and would be of interest to legislators and policy makers at the state and national levels. A one- to two-page summary of state performance, perhaps in a scorecard fashion, should be included, and AHRQ could compile this from the information it already provides in the State Snapshots (e.g., ratings from very strong to very weak on overall health care quality, preventive measures, acute care measures, chronic measures, hospital care measures, cancer care measures). Currently, the State Snapshots are not available until several months after the reports have been released; the committee urges AHRQ to include this information in the Highlights section even if the detailed Snapshots are not posted online at the same time. Additionally, a summary on the state of disparities should be included.
Although the Highlights document proposed by the committee would be longer than the current Highlights section, sharing the same Highlights section should streamline AHRQ staff efforts.
Organizing the NHQR and NHDR by the Framework Components
The framework for health care quality and disparities measurement (see Chapter 3 ) is both a tool to assess whether balance is achieved in the selection of quality measures and a way to organize the reports. Table 6-2 suggests chapters (or sections) for future iterations of the NHQR and NHDR. To increase parallelism across both national healthcare reports, access to care, a topic currently addressed only in the NHDR, should also be included in future NHQRs. After carefully considering whether efficiency and health systems infrastructure should be featured in both reports, the committee concludes, as discussed in Chapter 3 , that efficiency measures of overuse and underuse are of interest for populations included in the NHDR and infrastructure is also applicable to equity concerns. Given the limited nature of measures at this time, however, the same efficiency and infrastructure measures may not always be available to include in both reports.
Sections Recommended for Future National Healthcare Reports.
Incorporating Equity into the NHQR
Based on interviews with current and potential users, the committee finds that, to some extent, the NHQR and NHDR have different audiences. There is one school of thought that improving health care performance overall will ameliorate the problem of disparities in health care; this view tends to neglect the reality that disparities in health care usually persist even as overall performance levels improve. The committee believes that closing equity gaps is one of the most important factors in raising overall health care quality (Chin and Chien, 2006; Clarke et al., 2004). For that reason, the NHQR should incorporate the concept of equity by including an additional section focusing on disparities elimination.
Quantifying the impact of disparities on overall quality performance may be one way to define the connection between health care quality and disparities in the Highlights section of the reports. Furthermore, the commentary on each measure within the NHQR could reflect the degree to which disparities remain or are growing even as quality improves so that conclusions on the state of quality are not misleading. An HIV/AIDS measure reported in the 2008 NHQR provides a concrete example of a situation where the nation as a whole is performing well but data in the NHQR mask disparities shown in the NHDR (AHRQ, 2009d, p. 65, 2009e, p. 63).
Presenting Data on Priority Populations
The NHDR is required by the 1999 federal law under which it was established to report on “prevailing disparities in health care delivery as it relates to racial factors and socioeconomic factors in priority populations.” 1 Priority populations were defined in the authorizing legislation with respect to the agency’s full portfolio of activities (research, evaluation, and demonstration projects): low-income groups, minority groups, women, children, the elderly, and individuals with special health care needs, including individuals with disabilities and individuals who need chronic care or end-of-life health care. AHRQ’s overall activities are also to address inner-city and rural areas. The fourth chapter of the NHDR, “Priority Populations,” includes limited supplemental measures specific to each priority population.
AHRQ has presented data on priority populations in the NHDR by offering: (1) summaries of the findings presented earlier in the report on access and on the core measures the NHDR shares with the NHQR (e.g., Tables 4.2 and 4.3 in the 2008 NHDR), and (2) occasional additional measures of particular interest for specific populations (e.g., hospital admissions for uncontrolled diabetes for American Indian and Alaska Native populations). The committee encourages more comprehensive treatment of the priority populations both within the reports and through other vehicles (e.g., alternate year treatment of priority populations in the reports, spinoff mini-reports with additional detail, customization of data via NHQRDRnet). The national reports should convey key measures that address top health concerns of the priority populations if they are not already part of the AHRQ set of core measures; inclusion would depend on passing the same rigorous evaluation process for measures outlined in Chapter 4 .
Given the limitations in the length of a print version of the NHDR, other vehicles can provide additional opportunities for more in-depth treatment. Specialized products for audiences interested in specific priority populations may garner more attention than solely expanding the priority population sections within the NHQRs and NHDRs. These derivative products could be published over time, perhaps in conjunction with partners who have a particular interest in care related to a topic or population.
While “women,” “children,” and the “elderly” are priority populations, they do not belong solely in the NHDR. At a minimum, the committee believes a summary of findings for these populations should be available in the NHQR. Moving to the NHQR much of this material, which is now in the NHDR, would open up space in the NHDR. The committee expects further inclusion of children’s quality measures in the future as a result of the findings from AHRQ’s National Advisory Council Subcommittee on Quality Measures for Children in Medicaid and Children’s Health Insurance Programs, and the ongoing AHRQ- and CMS-funded IOM study of Pediatric Health and Health Care Quality Measures (AHRQ, 2009c; IOM, 2010). The full number of metrics and the various analyses that might be performed will likely exceed the capacity of the print NHQRs and NHDRs; as noted earlier, more detailed treatment could be accomplished through a special topic report, alternating in-depth sections in the NHQR or NHDR, and/or an ability to customize reports through Web-based capabilities.
Bridging the NHQR and NHDR
An inherent problem in having two separate reports is that data on a subject (e.g., cancer, heart disease, a priority population) are split between the NHQR and NHDR. Moreover, in the NHDR, data on a subject are often hard to find because information is dispersed between different sections (see Box 6-1 ). This fragmentation of information will continue to exist, but adding an index at the end of each book would help users find information more readily.
How Do I Find Disease-Specific Information in the NHDR? When examining a health topic or specific population in the NHDR, the information is often difficult to find. For example, if one aims to look at colorectal cancer, one is unable to access all of (more...)
The committee also notes that introductory page(s) for the same topic in the NHQR and NHDR tend to cover the same types of information but are laid out differently; this requires unnecessary effort on the part of AHRQ staff and leads to confusion by readers. For example, the pages on effectiveness of cancer screening in the NHQR (AHRQ, 2009e, pp. 32-33) and NHDR (AHRQ, 2009d, p. 39) contain similar yet not identical information. The committee finds it logical to convey the same information in both locations.
Expanding and Sustaining Interest Through Derivative Products
AHRQ provides online access to the national healthcare reports and State Snapshots, to a few report-related fact sheets, and to an online data query system (NHQRDRnet); the Future Directions committee suggests changes to each of these products (see Table 6-1 , presented earlier in this chapter).
Fact Sheets and Mini-Reports
AHRQ has previously developed three fact sheets to supplement the NHQR and NHDR. The fact sheets have addressed the subjects of children and adolescents (AHRQ, 2005b, 2008a, 2009b), women’s health (2005c), and rural health (2005a). These fact sheets are not easily accessible on the national healthcare report-related websites; instead they are listed on AHRQ’s Measuring Quality website.
Concise fact sheets are a way to expand AHRQ’s reach of NHQR and NHDR findings and are useful for reaching new audiences. Timing the release of fact sheets to specific events (e.g., heart disease or breast cancer awareness months) could help sustain interest in the national healthcare reports throughout the year. Currently, Internet traffic to the NHQR and NHDR tends to decrease about two months after the report release date. Periodic releases of fact sheets could direct Internet traffic to the reports.
There may be times when a derivative product elaborating on a specific topic (e.g., a mini-report) could provide information beyond what can be contained in a fact sheet. The committee believes that such mini-reports could provide expanded treatment of priority populations. Priority population-specific derivative products would allow fuller exploration, for example, of the particular health care concerns of a priority population (e.g., children, women) or the diversity of health care experiences of different granular ethnicity groups within a race category (e.g., the Asian American population, for instance, is made up of persons of Japanese, Korean, and Cambodian heritage, among other granular ethnicity groups).
State Snapshots
In 2006, using data collected for the NHQR, AHRQ created the Web-based State Snapshots to fulfill the needs for state-level information of members of Congress, state officials, health care providers, and purchasers. As noted by previous IOM guidance, “analyses such as state-by-state comparisons on health care are familiar and meaningful to members of Congress, other policy makers, and consumers” (IOM, 2002, p. 5). The committee finds AHRQ’s Web-based State Snapshots to be a valuable addition to the NHQR and NHDR and recognizes recent improvements to the State Snapshots website. Nevertheless, the committee urges further development. For example, the State Snapshots do not show any data on access measures, and the committee believes these data are important to have at the state-level.
Health care report cards provide information about the quality of care by geographic regions, health plans, hospitals and other institutions, and even individual practitioners (Epstein, 1995). Report cards use various systems of scoring and passing judgment on quality, whether the end result is to grade national health performance, rank a state’s health care quality against all others, compare head-to-head the quality of care delivered in cities across the country, or to develop a list of best value hospitals (Brooke et al., 2008; Chernew and Scanlon, 1998; Davies et al., 2002; Hibbard and Jewett, 1997; Romano et al., 1999). A 2006 qualitative study conducted by AcademyHealth indicated that users of the State Snapshots suggested a rank ordering of states so that states could compare their performance against all others (Martinez-Vidal and Brodt, 2006). Currently, in the State Snapshots, each state is ranked on 18 selected measures. The committee’s view is that state-by-state ratings should be more clearly available so that states know what the best attained level of quality performance is, and then they could contact and learn from states with the best rates on specific quality measures. Additionally, it would be useful if state data and rankings were easily sortable for high-profile sets of metrics such as AHRQ core or HEDIS (Healthcare Effectiveness Data and Information Set) measures, given the almost 200 measures that AHRQ tracks for states.
AHRQ displays average regional performance on measures in the State Snapshots, but state audiences have indicated that adjoining states are not always peers. AHRQ has provided a graphical “dial” to show states how they fit on a spectrum of contextual factors (i.e., demographics, health status, etc.), but states have noted that they would like flexibility to be able to identify a different coterie of peer states (for example, states that have the same degree of contextual factors). Then, for example, a state policy maker could assess state performance against states that have a comparable extent of persons below the poverty level.
Users of the NHQR and NHDR suggest that their needs for information tend to be topic specific and episodic; most users of the national healthcare reports are unlikely to read the reports from cover to cover. Additionally, the reports are viewed and downloaded online more than they are used in hard copy. 2 Thus, improving the ability of users to find needed information online is an important aim. In 2008, AHRQ added an online interactive tool called NHQRDRnet that can be used to query and search the databases behind the NHQR and NHDR by content areas (quality, access, patient safety, priority populations), clinical conditions, care type or settings, and dimensions of access (e.g., insurance coverage, usual source of care, utilization).
The committee applauds AHRQ’s intent to facilitate searching for content in the national healthcare reports but finds navigating the NHQRDRnet website difficult. The committee also observes that it takes fewer steps to gain similar information from the more straightforward and easier to use Appendix D of the NHQR and NHDR. AHRQ recently commissioned a usability survey that queried current users of the national healthcare reports about their experience with and impressions of the NHQR and NHDR and related Web content (Social & Scientific Systems and UserWorks, 2009). Comments from survey participants regarding ease of using the website and clarity of information echoed the committee’s findings (e.g., difficulty finding the reports using a basic Web search, organization of report, and Web content not matching user expectations).
The major change the Future Directions committee suggests for the NHQRDRnet is the development of a tool or sorting function that would allow users to customize their own reports. Now, one can search for all data related to a topic—for example, cancer—and all data files since 2002 are displayed for download; the search does not yield a fact sheet or summarization of the current content on the subject of interest. At a minimum, links to relevant text of the current year’s NHQR and NHDR would enhance the site’s usability and ability to tell a more comprehensive story. Additionally, one- or two-page fact sheets or more in-depth mini-reports on topics (whether individual clinical conditions, framework components, or something more specific, such as quality and disparities issues of specific interest to Hispanic persons) would be useful. AHRQ’s partnerships with other stakeholders would be assisted by having prepackaged collections of information in its NHQRDRnet index.
Web-based products, in addition to the NHQRDRnet, can be configured to make it easier to guide readers to other AHRQ or non-AHRQ resources that may help with quality improvement. For example, future online versions of the NHQRs and NHDRs could link to interventions highlighted in the AHRQ Health Care Innovations Exchange or other related resources (e.g., CMS, entities utilizing measures for which data at the national level are still aspirational). This linking capacity should also be available through the Web-based version of the NHQR and NHDR without the reader having to go through the NHQRDRnet.
Online Access to Data Used in the NHQR and NHDR
The committee discussed the extent to which the NHQR and NHDR should provide data for geographic areas below the state level. Various stakeholders have noted that the national healthcare reports contain information that is too “high level” for making decisions at the local or practice level. Consequently, the reports may be of less use to some health care providers, local policy makers, or some researchers than if the performance data were stratified to show performance at more local or organizational levels and provided in a timelier manner. State-based data are a unit of analysis that policy makers as well as the public can easily relate to and use for comparative purposes. Given the interest in substate variation (e.g., the Dartmouth Atlas, the University of Wisconsin/Robert Wood Johnson Foundation county-by-county health rankings), these data would be useful to develop over time (The Dartmouth Institute for Health Policy & Clinical Practice, 2010; RWJF and the University of Wisconsin, 2010). The NHQR and NHDR could also include linkages to other HHS data resources on community health status indicators (HHS, 2010).
The data included in the NHQR and NHDR may be reported nearly a year or more after they have been submitted to AHRQ because of the processes involved with compiling data sources, cleaning the data, analyzing it, reviewing the reports at the departmental level, and submitting the work for production. For entities that are evaluating performance in real time (daily, weekly, monthly), such data may have limited use. Still, there are groups that do not have day-to-day access to performance measurement data and would benefit from the wider availability of nationally collected data at a more local level (Kerr et al., 2004). For example, AHRQ has made available county-level data on the number of Hispanic Medicare beneficiaries with diabetes who did not have an eye exam so that one area’s community aging agencies could focus intervention efforts (Moy, 2009).
In deciding whether to recommend that AHRQ provide more locally based data, the committee balanced the usefulness of local data, its timeliness, its reliability, and the additional workload for AHRQ staff. AHRQ staff indicated that it is possible to drill down to at least the larger Metropolitan Statistical Areas for about half of the State Snapshot measures, but that smaller Metropolitan Statistical Areas and counties would be more difficult because, for instance, some datasets are likely to require special permissions to present the data in these ways. 3 The committee encourages AHRQ to explore the feasibility and value of drilling down for at least some high-impact measures. When summarized in the reports, the Highlights section, or the proposed guide to using the NHQR and NHDR (discussed below), more localized data can inform readers about variation within states. Such detail could be presented in the State Snapshots to show substate variation, particularly when it is readily available in the datasets AHRQ already uses, and perhaps as a derivative product similar to the Atlas of Mortality (Pickle et al., 1996), depending on the availability of data for coverage of the United States. Links could be made to the HHS Community Health Status indicators site if it eventually included health care-related metrics and not just health status.
Individuals wanting to work with primary data are often not satisfied with the data available through the national healthcare reports’ website. AHRQ provides Excel files with the data points reflected in its graphs and text, but it does not provide access to the original datasets. Although AHRQ does not have in-house all of the databases it uses in the NHQR and NHDR, most of the data AHRQ uses are from federally sponsored datasets. The committee believes that data access could be expanded so that researchers can download the full dataset to manipulate it as needed. This is consistent with the efforts of data.gov , a website currently under development that will house all federal executive branch datasets, to “increase public access to high value, machine readable datasets generated by the Executive Branch of the Federal Government.” 4 AHRQ is among the agencies contributing data, as are other federal agencies whose data AHRQ acquires (e.g., the Centers for Disease Control and Prevention, CMS). Because the website is still under construction, the committee is unable to discern which of AHRQ’s datasets will be made available. Nonetheless, the committee feels that making available datasets that support findings in the NHQR and NHDR would be a service to providers and health services researchers.
The committee encourages AHRQ and its partners to provide access to the data in a timely fashion, even prior to its publication in the NHQR and NHDR, to allow those with the capacity for analysis to use it for their own needs. Such data access was previously recommended to AHRQ by the IOM in the 2001 report Envisioning the National Health Care Quality Report . Further, AHRQ should provide tools for analysts who want to replicate AHRQ’s methods to produce comparative data for their locale or population cohort. Until such tools are available, analytic methods will need to be clearly specified in methodology descriptions.
Proposed Development of a Guide to Using the NHQR and NHDR
Given the diversity of resources that AHRQ now offers and the potential for greater direct data access, the committee suggests that AHRQ develop a guide to using the NHQR and NHDR. As envisioned by the committee, this technical assistance product would review the resources that the print NHQR and NHDR and websites have to offer and, more importantly, would provide examples of how different stakeholder groups can apply the knowledge to action (e.g., Hispanic elders diabetes project). The guide to using the NHQR and NHDR would go beyond telling someone how to navigate a website. Instead, it would tells users how to access the data resources, provide tools for manipulating data for analyses, explain the methods used by AHRQ in its analyses, and offer suggestions for meaningful analyses. This guide, when it becomes available, should be referenced in the Highlights section of the NHQR and NHDR.
Dissemination Strategies
The committee proposes communicating the findings of the NHQR and NHDR to diverse audiences through a series of new products and modifications to existing documents. The goal of expanded dissemination efforts should be to raise awareness, visibility, and use of the reports. Between 2003 and 2008, AHRQ distributed approximately 24,000 print copies of the NHQR and NHDR. 5 The annual release of the NHQR and NHDR should be more widely publicized in advance, and momentum from the release of the reports should not be permitted to dwindle. The committee sought input on dissemination and media strategies for the NHQR and NHDR, as well as sample fact sheets, from Ketchum, a public relations and communications firm. 6
Ketchum suggested ways to repackage the wealth of information contained in the NHQR and NHDR throughout the year so that findings can be made continually relevant. AHRQ could, for example, produce succinct derivative materials that convey targeted messages (e.g., mini-reports and fact sheets), and link distribution and media outreach to appropriate audiences (e.g., advocacy groups for specific clinical conditions or population groups). In addition to relying on traditional media outreach (e.g., participating in roundtables, telebriefings, radio media tours, outreach around editorial calendars), AHRQ could take advantage of wide-reaching and increasingly common Web-based tools (e.g., blogs, advanced search engine options, inbound linking programs, social media such as Facebook and Twitter).
In Chapter 5 , the committee emphasizes that a patient’s language need is relevant to health care quality and disparities. Communicating information about quality and disparities in languages other than English is one way to reach diverse audiences. The committee acknowledges the potential resource burdens of document translation and does not intend for AHRQ to translate the entire NHQR and NHDR. When derivative products are specifically geared to audiences that may have limited English proficiency, AHRQ may wish to consider translation. HHS’ Office of Minority Health Resource Center provides technical assistance in communications and outreach to other HHS agencies (HHS, 2009b). As AHRQ expands dissemination of the reports and their derivative products to diverse stakeholder audiences, the Health Resource Center may provide valuable capacity-building support.
- TELLING A STORY IN THE NHQR AND NHDR
The committee recommends that the NHQR and NHDR tell a clear and compelling story about the impact of making progress—or of not making progress. The ways in which information is presented and summarized in the reports and related products can enhance or impede users’ understanding of the messages the reports are meant to convey. For that reason, the committee believes that AHRQ should move the reports from their current chartbook format to make them less a catalog of data and more of a comprehensive story that conveys key messages through text, graphs, and displays. 7 The committee believes that doing this effectively requires enhancing the presentation of takeaway messages on the state of quality and disparities, focusing attention on closing gaps in performance, including benchmarks to allow comparisons with high-quality performance, identifying ways to affect change, and providing information that contributes to the development of the national health care data infrastructure ( Box 6-2 ).
Key Elements of Telling a Story in the NHQR and NHDR. Enhancing Takeaway Messages that Address Closing the Performance Gap “At the current rate of change, it will take ‘X’ years to close the gap between current practice and the (more...)
Enhancing the Presentation of Takeaway Messages
In the Healthcare Research and Quality Act of 1999 , 8 Congress directed AHRQ to submit “an annual report on national trends in the quality of health care,” and AHRQ has interpreted this as needing to present “assessments of change over time” (Moy et al., 2005). Although documenting the past performance of the U.S. health care system is important and historical data certainly play a role in forming a comprehensive picture of health care quality and disparities, users of the national healthcare reports have indicated that the performance of past years (especially more than 5 years ago) is not necessarily helpful for assessing where and how quality improvements can be made today (Lansky, 2009; Martinez-Vidal and Brodt, 2006). The committee believes it would be more useful for AHRQ to interpret national trends as a way to inform the future, using available historical data to inform readers of the likelihood of closing gaps in health care quality at the current pace. Forward-looking messages regarding national trends for the future could be determined using the following central pieces of information:
- the nation’s current level of performance (expressed using means and standard errors);
- how the nation has achieved the current level of performance (expressed by the historical annual rate of change and standard error of the estimated change); and
- how far the nation has to go to close the performance gap between current practice and the recommended standard of care (goal or the benchmark)—the number of years to achieving the desired performance level based on the historical annual rate of change and corresponding interval estimate.
Using this strategy, AHRQ could transform its wealth of available trend data into an informative direction for the future. Possible templates for presenting rates of change and years to closing quality and disparity gaps are offered in Appendix H .
As previously described in Chapter 4 , the impact of closing the gap would be determined as part of the measure selection/ranking process, and data gleaned (e.g., reduction in clinically preventable burden, increase in net health benefit, and cost-effectiveness) in determining the relative ranking of measures are useful and should be presented for each measure in the reports. Additionally, the benefit to the country—if, for example, all states were performing at the level of the highest one—would also be key information.
Presenting Benchmarks and Other Data
To better convey key messages, data displays should present benchmarks. The committee believes benchmarking is a key tool for continuous quality improvement. Thus, it is expected that benchmarks will change over time depending on the frequency of obtaining updated data from the sources for the national healthcare reports. Goals, on the other hand, tend to be fixed for a longer period and set by an advisory body or at the direction of some entity such as the Secretary of HHS. (See Chapter 2 for committee definitions of goals, benchmarks, and targets.) In the context of the national healthcare reports and AHRQ’s role, the Future Directions committee emphasizes the use of benchmarks rather than goals because the committee believes the presentation of performance data, but not the setting of national goals, is within AHRQ’s purview. Benchmarks reflect empirical facts. On the other hand, the committee believes that the setting of goals for health care quality improvement (e.g., for priority areas and/or measures) requires the direction of the Secretary of HHS.
Goals or fixed targets for measures can complement benchmarks and could be set at various levels of attainment. For example, they may be aspirational—“All patients shall receive.” Goals might be set at a lower level if a finding from the measure selection assessment shows that there is little gain in health benefit beyond 85 percent of the target population receiving a service. Or a goal might be set for all states to achieve the rate of the best performing state.
Data illuminating who is delivering care and where care is delivered are necessary to identify opportunities for system change; these accountable units may be states, types of payers (e.g., Medicare, Medicaid, private insurance), or delivery systems. The committee encourages the development and presentation of these data in the reports and State Snapshots. This topic is addressed more fully in Chapter 2 .
Identifying Ways to Affect Improvements in the Health Care System
Although the reports by themselves do not affect change, they can link to entities that have improved quality and reduced or eliminated disparities. For policy makers and those engaged in measurement and improvement, having the reports illustrate actual, effective quality improvement interventions alongside comparative data would be useful. As previously discussed, AHRQ’s NHQRDRnet site links to AHRQ’s Health Innovation Exchange, and this type of connection should also be included in the online version of the reports through embedded hyperlinks. Additionally, AHRQ should consider qualitatively highlighting “islands of excellence” (whether health systems, hospitals, or geographic regions) that consistently deliver recommended care that is less costly, more efficient, and produces better outcomes (Fisher et al., 2008). Such better performing communities or entities can be showcased in textboxes and sidebars.
Currently, AHRQ links State Snapshots to other measure report cards in specific states and should continue such nonfederal linkages. In addition to the Health Innovation Exchange, AHRQ might link with sources such as the Robert Wood Johnson Foundation’s (RWJF’s) Finding Answers: Disparities Research for Change program ( www.SolvingDisparities.org ), The Commonwealth Fund’s “Why Not the Best?” quality improvement resource ( http://whynotthebest.org ), and the Institute for Healthcare Improvement’s (IHI) website ( www.ihi.org ). These sources, among others, offer multiple strategies for hospitals, providers, and other actors to improve the quality of health care. The links should be accompanied by an expressed caveat that the links are intended to highlight known best or promising practices, and that their inclusion should not be construed as an endorsement of the program or entity by AHRQ.
- USING BENCHMARKS TO SHOW ACHIEVEMENT
Benchmarks are one method of comparing data in order to improve the efficiency and the quality of health care (Deming, 1994). In Chapter 2 , the committee defined a benchmark as the quantifiable highest level of performance achieved to date. (Some additional definitions of benchmarking are shown in Table 6-3 .) Presenting performance data in the context of benchmarks stimulates debate around policy priorities, promotes transparency, fosters accountability, indicates what needs to be done, and supplies concrete milestones for evaluation and identification of areas to improve (Gawande et al., 2009; van Herten and Gunning-Schepers, 2000a,b).
Definitions of Benchmarking from Various Sources.
Benchmarks identify “demonstrably attainable,” superior performance and encourage others to emulate the practices by which this is achieved (Kiefe et al., 1998, p. 443). The original idea of using benchmarks in Continuous Quality Improvement and Total Quality Management (CQI/TQM) was that organizations could learn from the processes of an organization with better outcomes and adapt those processes, as appropriate, to their own circumstances (Dattakumar and Jagadeesh, 2003; McKeon, 1996). Benchmarking is not a static process; ideally, the level of best performance will continually evolve as positive progress is made, and the benchmark will move accordingly. At each successive stage—or in each publication year of the NHQR or NHDR—a different entity has the potential to take the role of “best-in-class,” which may engender a “race to the top” (Weissman et al., 1999).
The committee proposes approaches to benchmarking that AHRQ could incorporate into the NHQR, NHDR, and related products. The benchmarking approaches proposed by the committee do not require AHRQ to develop targets that must be attained by a specific endpoint (as has been done for Healthy People 2010); rather these strategies use benchmarks to highlight standards of care that are reported in data available to AHRQ.
The Current Use of Benchmarks in the National Healthcare Reports
The NHQR and NHDR were initially envisioned as a means to provide policy makers with snapshots of quality and disparities over time and to allow “providers and payers” to “assess their performance relative to national benchmarks” (Moy et al., 2005, p. 377). The hope was that government agencies, communities, and providers would turn to the NHQR and NHDR to compare their own health care data against national progress. Until recently, AHRQ used only an implicit benchmark—namely, the need to strive for better-than-average performance. Displays in the reports imply that states with rates below average performance should aim to achieve performance rates better than average. In a 2006 review of AHRQ’s presentation of state data, state policy makers indicated that presenting performance relative to the national average was misleading: while a state may have been doing better than average on a given measure, if the average was low compared to the recommended standard of care, the level of performance could be taken out of context to indicate that the state need not focus quality improvement efforts in that area (Martinez-Vidal and Brodt, 2006).
For a limited number of measures in the 2008 NHQR and NHDR, AHRQ reports targets established for Healthy People 2010. Partially because Healthy People focuses on measuring health improvement rather than health care improvement, these targets are not available for all measures presented in the NHQR and NHDR. The Healthy People targets are not tied to actual performance achieved by providers and health care organizations, and most targets are consequently viewed as aspirational. 9 According to the committee’s definition, a benchmark should be demonstrated as being attained by some defined entity, not just as being aspirational. For this reason, Healthy People targets tend not to be the ideal source of benchmarks for the national healthcare reports. While the inclusion of these targets may be useful and warranted as one point of information, they should be presented in conjunction with more realistic benchmarks.
Presenting Best-in-Class Benchmarks
One of the most common and easily understood methods of benchmarking is to provide comparisons relative to top performing nations, states, geographic regions, or health care entities. A key issue in benchmarking is whose performance is being measured and to which audiences the benchmark is relevant. In health care quality improvement, best practices can occur at various levels of the health care system, including at the individual physician level (Kiefe et al., 2001); at the service provision level, such as in intensive care units (Zimmerman et al., 2003); at the health care system level; or at the state level (Reintjes et al., 2007). The committee also explored establishing benchmarks at discrete levels of the health care system (e.g., top decile of hospitals), as well as at the state level. Defining a benchmark can depend on the “class” from which the measure is derived. For example, a benchmark might provide information on the best performance rate among states, the best performance rate among hospitals, the best performance rate among large hospitals, or the best performance rate for care received by Hispanics in any state.
Although it is technically true that AHRQ could choose any “class” from which it would designate a “bestin-class” benchmark, the committee finds that in the context of the national healthcare reports, where much of the analysis is done at the state level, setting benchmarks by state may appeal to a number of relevant audiences and may be most feasible given data availability. State-level data are generally available to AHRQ, and thus state-level benchmarking units can be determined for many, although not all, measures in the NHQR and NHDR. This approach could satisfy the needs of congressional and state policy makers, principal audiences to which the reports are geared. A 2004 AHRQ publication A Resource Guide for State Action was designed to help states assess the quality of care in their states and develop strategies to address gaps in quality. The Resource Guide advised that the “rate for the top State or top tier of States” may be “assumed to be a feasible goal for States to achieve” (Coffey et al., 2004).
Figure 6-1 shows that it is possible to display a best-in-class benchmark (a state in this instance) along with the national performance average and the Healthy People target. The committee does not intend that the style, format, and layout of this figure be adopted by AHRQ; rather, the committee presents this figure to show the relationship of a benchmark relative to the type of performance data that are in the domain of the NHQR or NHDR. From the perspective of the NHQR, which tends to provide state-based data as well as national average performance, the highest performing state, Oregon, provides a benchmark that could be applied across both reports.
Oregon’s performance rate for pneumococcal vaccination sets a national benchmark for other states to strive to achieve. No race, Hispanic ethnicity, or income group on a national level achieves the vaccination rate of Oregon. NOTE: Percentage (more...)
The committee recognizes that some measures and their corresponding data sources may be amenable to choosing a different benchmarking “class” than a state. A measure that uses only HEDIS data may, for instance, lend itself to analyzing data by health plans. Thus, AHRQ could present a best performing plan as the benchmark. Similarly, AHRQ might decide that the hospitals comprising the HCUP datasets constitute a comparable set of observations and could present a best performing hospital as the benchmark.
Denoting a best-in-class benchmark is as important for measures in the NHDR as it is for measures in the NHQR, and the committee concludes that for each measure, the benchmark used in the NHDR should mirror the benchmark used in the NHQR. The goal of quality improvement efforts should not be to strive just for the Hispanic population to receive care at the rate of the non-Hispanic population. Rather, quality improvement efforts should aim to improve the quality of care for all populations. In the case of the NHDR, different disparity populations would be compared against the quality benchmark in addition to being compared against the best performing population. For example, AHRQ may establish a state-based benchmark for a specific measure of lipid control and use this same benchmark in both the NHQR and NHDR. The committee recognizes that reporting in the NHDR which state has the best rate on lipid control by specific populations would be useful (e.g., reporting that X state has the highest performance level for Hispanics and Y state has the highest performance level for African Americans), but such data are not always available. Adopting a separate benchmark based on the best performing population group within a “class” can prove difficult as there are multiple population groups studied in the NHDR and detailed data are not always available or sample sizes may be too small to stratify population data by hospital, health plan, or even state. Ideally, data would be available for sociodemographic descriptors within whichever class a benchmark was being set; when they are not, this leads to looking to an alternate solution for presenting a benchmark in the NHDR. The committee advises AHRQ that the benchmark can be the best performing state or can come from the class of units compared in the measure’s data source. When the data are available, the committee encourages AHRQ to present multiple population-specific benchmarks (i.e., a benchmark that is uniform with the NHQR as well as other benchmarks that are population specific). When multiple achievement levels are available, alternatives to presenting the data graphically may be needed (e.g., listing in textboxes).
The committee encourages the analysis of performance data by accountable units (e.g., states, health plans, hospitals). When it is feasible for AHRQ to analyze data for a measure by multiple accountable units, there is the possibility for multiple benchmarks of attained performance for one specific measure. Presenting multiple benchmarks might add clutter to graphs, so AHRQ may choose to present the multiple achievement levels in a sidebar text box.
The Future Directions committee believes benchmarks provide a means to supply concrete milestones for comparison and evaluation. For comparative purposes, having a uniform benchmarking unit such as a state may be useful, although other classes (e.g., plans, hospitals) may be informative for entities implementing programs to improve quality and eliminate disparities. Thus, the committee recommends:
Recommendation 7: To the extent that the data are available, the reporting of each measure in the NHQR and NHDR measure set should include routinely updated benchmarks that represent the best known level of performance that has been attained.
Data Limitations in Benchmarking
As discussed above, AHRQ could present data on a high-performing entity for which data are available (e.g., the best performing health plans based on data from the National Committee for Quality Assurance). This approach, however, may require particular attention to issues of statistical reliability. The population distribution from which a benchmark is derived must be considered carefully so that entities are not evaluated against a population that is not well-matched to their particular case-mix, geography, or other relevant factors (Linderman et al., 2006). When the population of analysis includes high-performing entities that have a small number of cases, the analysis must be corrected to account for the small-numbers problem (Normand et al., 2007). There are techniques—including the Achievable Benchmarks of Care method, which uses a Bayesian estimator to reduce the impact of entities with a small number of eligible patients—that AHRQ could use to adjust for the small denominator problem (i.e., if a plan had only one qualifying patient, then the performance of that plan could be either 0 percent or 100 percent) (Weissman et al., 1999).
As an additional consideration, data on state performance may be unavailable for all measures. Although the State Snapshot website does not include state data for 26 of AHRQ’s 46 core measures, the committee finds it feasible for AHRQ to obtain state data for some of these (e.g., access measures, measures from Centers for Disease Control and Prevention data). 10 Furthermore, for measures in which data on the best performing state are available, not all states may have reported on the measure or been included in analysis (e.g., the Healthcare Cost and Utilization Project). Therefore, the best performing state may actually be the “reported best performing state.” AHRQ may consider recognizing this in either introductory text or in a footnote.
For many measures of health care quality, even the highest performing state, population, or provider does not deliver the level of care recommended in guidelines. Benchmarking within a field of low performers may result in further underperformance because low performance is seen as normal (Reinertsen and Schellekens, 2005). AHRQ should take this into consideration when determining the class from which to derive a benchmark and should ensure the benchmark represents a desirable level of performance.
- REFINING THE PRESENTATION OF DATA
The success of the NHQR and NHDR in reaching various audiences and spurring action depends on the presentation of information. The products developed by AHRQ have the potential to tell a more complete quality improvement story, provided the products are accessible, engaging, and informative.
Improving the Presentation of Graphic Displays
Graphic displays in the NHQR and NHDR document historical trends, present geographic variation using maps, and stratify measures by demographic characteristics. Communicating information through the simultaneous presentation of words, numbers, and, in some cases, pictures, requires that the displays be as effective as possible (Tufte, 1983). Therefore, visual design problems can undermine the usefulness of data being presented (Few, 2006). To assess the quality of graphic displays in the two reports, the committee commissioned input from Howard Wainer, an expert on data display. 11 The suggestions presented to AHRQ are only one way of enhancing data displays, but they represent well-regarded, theory-based practice.
Documenting Historical Trend Data
As noted earlier, the committee finds there should be less reliance in the NHQR and NHDR on trended data displays unless the trends inform future activities rather than solely document the past. Currently, most trend data take up substantial space in the documents without being particularly informative other than to reinforce a repeated message—that the pace of change is slow. These trend graphs are often visually cluttered with overlapping lines and many numbers over-written on a graph (see Box 6-3 ).
A Suggested Approach to Improving Data Displays. Figure A (both before and after ) presents data on patients with tuberculosis who completed treatment, but the original Figure A (below left) is visually cluttered: the graph contains a multitude of data (more...)
Captioning and Labeling
Captions for each display should be informative and focused. A good graph can be made even stronger by having an informative and interpretive caption or figure heading. Captions that explicitly relay the principal point of the display have benefits: the reader can discover the point of the display more easily and less helpful displays are eliminated. Additionally, strong graphical displays avoid legends whenever possible because legends require the viewer to learn the legend and apply it to the display. This requires two moments of perception and makes the viewer read the display rather than see it (Green, 1998). See Boxes 6-4 and 6-5 for examples.
A Suggested Approach to Improving the Labeling of Graphic Data. Figure B (both before and after ) presents data on rates of pressure sores among nursing home residents. The original figure (below left) could better convey its key finding (that although (more...)
An Example of a Complex Data Display. An informative heading or caption should explain what constitutes better performance. The measure captions currently used as headings in the NHQR and NHDR do not always indicate whether better performance is associated (more...)
The choice of x- and y-axis scales can influence the readability and interpretability of a graph. The x- and y-axis should place observed differences on a scale that acknowledges the range of possible clinically important differences. In a series of experiments conducted at AT&T Bell Laboratories, Cleveland and colleagues determined that scales should be chosen so that the data fill as much of the scale-line rectangle as possible (Cleveland, 1994a,b). A separate issue that must be considered is the choice of the ratio of the x- and y-axis scales. Altering the ratio of the scale can modify a person’s perception of the data (Cooper et al., 2003; Schriger and Cooper, 2001). The committee encourages AHRQ to choose an aspect ratio that appropriately conveys the data.
Alternative Data Displays
In addition to displaying trend data in graphs, AHRQ might consider utilizing alternate visual displays. For example, Figure 6-2 below, which was created by the CDC, succinctly presents information to readers, including readers who may not be data experts. The figure could be further improved by specifying whether the symbols represent absolute numbers of infected people or a rate ratio. In creating the figure, CDC likely meant for the figure to represent a rate ratio; however, readers may draw the conclusion that seven times more African Americans are infected than Whites (an absolute count). The display could be made clearer by including 100 small symbols for each group, and coloring in 7 for the African American population, 2.5 for the Hispanic population, and 1 for the White population.
Example of an alternate visual display. SOURCE: HHS, 2009a.
The committee recognizes that there are benefits to readers in using a small number of graphic formats with the same type of display from page-to-page, so that readers do not have to learn to interpret a new type of graph, but finds that some diversity of presentation can enhance a report. Alternative displays might be particularly useful for the Highlights section and fact sheets.
The legends on the maps in the NHQR and NHDR are often uninformative as they are simply above aver age , average , below average , and no data . For ease of comprehension, the labels might, at a minimum, contain numeric values (averages and ranges). Additionally, ordering by performance level achieved makes a coherent visual impact and suggests an implicit underlying structure. For example, gradations of a single color would better show performance levels on maps (see Figure 6-3 below). A sequence of “increasing darkness” of a single color can assist the reader in identifying increasing or decreasing rates, as utilized by Pickle and colleagues over five gradients (Pickle et al., 1996). Additionally, colors should be chosen to avoid common color vision deficiencies and so that no single color visually dominates (Pickle et al., 1996). In the NHQR and NHDR maps, the color black represents better performance and AHRQ’s use of two other colors (green and blue) does not have the visual impact of a single color gradient. Examples of such visual displays abound, and the committee believes that AHRQ may benefit from additional professional consultation on how to better present its data.
Illustration of a gradient shading scheme. SOURCE: Pickle et al., 1996.
Enhancing the Supporting Text for Data Displays
The text supporting a data display should convey information gleaned from data analysis, such as analysis not captured in the figure and implications of significant findings. Currently, supporting text for displays in the NHQR and NHDR describes what the graph depicts. The text refrains from providing additional analyses and provides minimal direction on methods that could be used to improve quality or eliminate disparities.
Refining the Presentation of Summarized Information
Summary and composite measures are useful tools for conveying information about complex constructs, such as the multiple elements of appropriate care for a stage of life (e.g., end-of-life care) or a condition that is inadequately portrayed through a single measure (e.g., diabetes). To be consistent with AHRQ’s use of the terms composite and summary measures , this report defines composite measures as the bundling of two or more measures that look at different aspects of care for a specific clinical condition (AHRQ, 2008b). 12 As an example, the composite measure on diabetes care is the percentage of adults age 40 and over with diabetes who received all three recommended services (hemoglobin A1c measurement, dilated eye examination, foot examination).
Summary measures bundle a number of conceptually similar specific measures of health care services or outcomes across multiple conditions or health care settings in order to present a single metric for a given aspect of health care delivery (e.g., combining performance rates for all prevention measures). AHRQ’s State Snapshots present such summary measures to report the performance of single and combined states on measures for different types of care (i.e., preventive, acute treatment, chronic care) and settings of care (i.e., home health, hospital, nursing home, ambulatory) (AHRQ, 2009a). Similarly, AHRQ summarizes measures in the Highlights section by core measure totals, types of settings, and types of clinical measures (including some clinical conditions across composite and individual measures).
The committee’s purpose is not to recommend specific composite or summary measures for inclusion in the national healthcare reports; rather, the committee considers desirable properties that AHRQ may consider when evaluating the way in which such measures are reported. A principal consideration in the use of a composite or summary measure is the quality of the individual measures being inputted and the relationship of these measures to one another (Murray et al., 2000). The weight of the measures that comprise the composite or summary measure may need to be considered. AHRQ does not use differential weights in its composite and summary measures; rather, it weighs every component measure equally. Implicit in choosing weights are subjective judgments about the relative clinical significance and prioritization of the component measures. AHRQ should clearly denote that composite and summary measures use equal weights and provide the denominators for each component measure (in an appendix, for instance) so that users of the data can perform their own analyses using differential weights, if they so choose (Martinez-Vidal and Brodt, 2006).
Presenting the Methodology of Summary and Composite Measures
Several standard pieces of information should accompany any composite or summary measure. While such information need not be displayed in the main body of a report, it should appear at least as an appendix, including:
- the methodological considerations taken into account when creating a composite or summary measure (e.g., how the measure is weighted);
- a description of the individual constituent measures that make up the composite or summary measure, their data source, and the distribution (e.g., means, standard deviations, ranges, floor and ceiling effects);
- a summary description of the psychometric properties of the composite measure, including how the component measures relate to each other (i.e., the pair-wise correlation coefficients of the individual quality measures or a coefficient alpha); and
- the standard error of the composite measure, in addition to the estimated composite measure.
The general methodology for the composite measures presented in the 2008 NHQR is discussed in the print report (AHRQ, 2009e, p. 20), and some measure specifications for composites included in the NHQR and NHDR are provided via online appendixes. 13 However, the appendixes do not contain all of the information outlined above. For instance, data on the individual constituent measures for the reported composite measures are sometimes unavailable or not easily accessible. Likewise, some methodological information is provided online for the summary measures used in the State Snapshots, 14 but much of the above information is also missing for those measures.
For example, the first figure presented in the 2008 NHQR (AHRQ, 2009e, p. 3) pools trend data from quality measures to quantify the overall change in quality for the health care system according to the measures AHRQ has chosen to profile. The median annual rate of change from baseline to most recent data year is reported as 1.4 percent. The NHQR does not, however, report the distribution of the underlying rates of change across measures, including the distribution and variability of the underlying rates. While it is important to know how many indicators are getting better and how many are getting worse, standard errors and correlations in rates of change are essential to identifying which measures tend to improve or worsen together.
The committee recognizes the benefits of using composite measures and summarization techniques, and AHRQ staff should continue to identify measurement areas that can benefit from such presentation. However, the committee finds that AHRQ needs to be more transparent in its methods. Methodological information may be presented in the print and online reports, although such detail may be more appropriate for appendixes where researchers who need such facts can obtain them.
Enhancing the Summary Dashboards of the State Snapshots
Dashboards are a valuable tool for efficiently and effectively communicating summarized information (Few, 2006). AHRQ utilizes this technique to provide a picture of how a state is performing relative to other states on “overall health care quality” and for 12 topics across types of care (i.e., prevention, acute, and chronic), settings of care, and clinical conditions. 15 Despite the intended purpose of simplistically conveying information, the state dashboards may confuse users. For instance, Montana appears to be doing worse today than in the baseline year, although performance may or may not be better than in the past. The Montana dashboard does not say the arrows on the meters are reflecting relative performance, nor does it have a statement such as, “Montana’s overall perfor mance is better in the most recent data year than its baseline performance, but other states have improved more, so its overall performance ranks lower than previously.”
In the State Snapshots, Arkansas is positively rated for having a low disparity rate. 16 This rating, however, may not reflect better outcomes. The low disparity rate is principally because the performance metrics of Arkansas’s White population are lower than the corresponding data for the White population in other states. Meanwhile, the quality data attributed to Arkansas’s Black or African American population are in line with the corresponding national measures. Thus, lower quality metrics associated with both White and Black individuals in Arkansas results in a smaller difference between the two populations (and thus a smaller disparity). 17
Statistical Quality of Data Reporting
Given the volume and numerous sources of reported measures, there are challenges in providing clear and useful information to readers. However, clearly stating the analytic methodology for the reports and making this methodology more readily available is important for the researchers, as they may seek to manipulate the data for their own purposes, or look to replicate such measurement reporting. Providing such methodological information also enhances the transparency of the NHQR and NHDR.
For three sections of the NHQR or NHDR, the committee assessed (1) measurement properties and definitions of quality indicators, (2) the description and use of analytical adjustments, (3) methods of summarization, (4) selection and use of benchmarks, and (5) use of prediction rules. (See Appendix H for additional information.) The committee’s review indicated that, when possible, AHRQ should make available online the following supplementary information to inform the research community:
- Data quality. Information regarding who collected the data, the reliability and validity of collected data, limitations of the data, and the extent of missing data should be reported. While this information may be difficult to gather, the quality of the NHQR and NHDR hinge on the quality of the data. A standard template could be constructed and populated, and when information cannot be determined, at a minimum, this fact could be stated.
- Description and use of analytical adjustments. Key features of analytical adjustment are required for readers to understand and correctly interpret findings. These features include a clear definition of the outcome (including the units of measurement); the observed covariates and definitions used in adjustment; justification for adjustment and how the adjustment was made; the sample sizes or weights used in the analysis; the reference population used; and how well the statistical model performed (fit) for adjustment.
- Summary measures. The choice and definition of methods of summarization should be made explicit. For example, if the summary measure is a change in performance from one time period to the next, the time periods need to be stated; the estimate should be defined (regression-based coefficient or difference in means); and the statistical significance or other metric for displaying uncertainty in the estimate should be provided.
- Prediction rules. In some instances, prediction inferences for when a particular goal will be achieved are made. In such instances, the statistical model used for the prediction should be stated, its fit assessed relative to reasonable competitor models, and the statistical uncertainty surrounding the prediction should be reported. One prediction would be the number of years to reach a particular benchmark at the current rate of change.
Conclusions on Data Presentation
Taking advantage of the full power of data displays and concise summarization will be critical for AHRQ to continue to streamline a vast amount of information. To strengthen data presentation in the reports, the committee recommends:
Recommendation 8: AHRQ should engage experts in communications and in presentation of statisti cal and graphical information to ensure that more actionable messages are clearly communicated to intended audiences, summarization methods and the use of graphics are meaningful and easily understood, and statistical methods are available for researchers using data.
The data presented in the NHQR, NHDR, and their related products need to provide clear and coherent messages about the state of health care and the level of quality that has been achieved. The reports should strive to promote actionability by relaying realistic benchmarks and leading users to resources that illuminate methods of quality improvement and disparities elimination. As discussed, AHRQ can explore various dissemination strategies to ensure the messages are effectively conveyed to relevant audiences. By employing the messaging and presentation strategies discussed in this chapter, the NHQR and NHDR may be more valuable to a wider spectrum of users while still presenting data and methods useful to researchers in the field.
- AHRQ (Agency for Healthcare Research and Quality). 2005. a. Fact sheet: Health care disparities in rural areas: Selected findings from the 2004 National Healthcare Disparities Report . Rockville, MD: Agency for Healthcare Research and Quality.
- ———. 2005. b. Fact sheet: Selected findings on child and adolescent health care from the 2004 National Healthcare Quality/Disparities Re ports . Rockville, MD: Agency for Healthcare Research and Quality.
- ———. 2005. c. Fact sheet: Women’s health care in the United States: Selected findings from the 2004 National Healthcare Quality and Dispari ties Reports . Rockville, MD: Agency for Healthcare Research and Quality.
- ———. 2008. a. Fact sheet: Selected findings on child and adolescent health care from the 2007 National Healthcare Quality and Disparities Reports . Rockville, MD: Agency for Healthcare Research and Quality.
- ———. 2008. b. National Healthcare Quality Report, 2007 . Rockville, MD: Agency for Healthcare Research and Quality.
- ———. 2009. a. 2008 State Snapshots . http: //statesnapshots .ahrq.gov/snaps08/index.jsp (accessed July 22, 2009).
- ———. 2009. b. Fact sheet: Disparities in children’s health care quality: Selected examples from the National Healthcare Quality and Dispari ties Reports, 2008 . Rockville, MD: Agency for Healthcare Research and Quality.
- ———. 2009. c. Introductory remarks and charge to the subcommittee: Slide 9 . Agency for Healthcare Research and Quality. Presentation to the AHRQ NAC Subcommittee on Children’s Healthcare Quality Measures for Medicaid and CHIP Programs, July 22, 2009. Rockville, MD.
- ———. 2009. d. National Healthcare Disparities Report, 2008 . Rockville, MD: Agency for Healthcare Research and Quality.
- ———. 2009. e. National Healthcare Quality Report, 2008 . Rockville, MD: Agency for Healthcare Research and Quality.
- Brooke, B. S., B. A. Perler, F. Dominici, M. A. Makary, and P. J. Provonost. 2008. Reduction of in-hospital mortality among California hospitals meeting Leapfrog evidence-based standards for abdominal aortic aneurysm repair . Journal of Vascular Surgery 47(6):1155-1164. [ PubMed : 18514832 ]
- Camp, R. 1998. Benchmarking: The search for industry best practices that lead to superior performance . Milwaukee, WI: American Society for Quality Press.
- Chernew, M., and D. P. Scanlon. 1998. Health plan report cards and insurance choice . Inquiry 35(1):9-22. [ PubMed : 9597014 ]
- Chin, M. H., and A. T. Chien. 2006. Reducing racial and ethnic disparities in health care: An integral part of quality improvement scholarship . Quality and Safety in Health Care 15(2):79-80. [ PMC free article : PMC2464839 ] [ PubMed : 16585103 ]
- Clarke, C. L., J. Reed, D. Wainwright, S. McClelland, V. Swallow, J. Harden, G. Walton, and A. Walsh. 2004. The discipline of improvement: Something old, something new? Journal of Nursing Management 12(2):85-96. [ PubMed : 15009624 ]
- Cleveland, W. S. 1994. a. The elements of graphing data . Summit, NJ: Hobart Press.
- ———. 1994. b. Visualizing data . Summit, NJ: Hobart Press.
- Coffey, R. M., T. L. Matthews, and K. McDermott. 2004. Diabetes care quality improvement: A resource guide for state action . Rockville, MD: Agency for Healthcare Research and Quality.
- Cook, S. 1995. Practical benchmarking: A manager’s guide to creating a competitive advantage . London: Kogan Page.
- Cooper, R. J., D. L. Schriger, R. C. Wallace, V. J. Mikulich, and M. S. Wilkes. 2003. The quantity and quality of scientific graphs in pharmaceutical advertisements . Journal of General Internal Medicine 18(4):294-297. [ PMC free article : PMC1494849 ] [ PubMed : 12709097 ]
- The Dartmouth Institute for Health Policy & Clinical Practice. 2010. The Dartmouth Atlas of Health Care . http://www .dartmouthatlas.org/ (accessed February 23, 2010).
- Dattakumar, R., and R. Jagadeesh. 2003. A review of literature on benchmarking . Benchmarking: An International Journal 10(3):176-209.
- Davies, H. T., A. E. Washington, and A. B. Bindman. 2002. Health care report cards: Implications for vulnerable patient groups and the organizations providing them care . Journal of Health Politics, Policy and Law 27(3):379-400. [ PubMed : 12092674 ]
- Deming, W. E. 1994. The new economics for industry, education, government—2nd Edition . Cambridge, MA: Massachusetts Institute of Technology Center for Advanced Engineering Study.
- Epstein, A. 1995. Performance reports on quality—prototypes, problems, and prospects . New England Journal of Medicine 333(1):57-61. [ PubMed : 7777000 ]
- Few, S. 2006. Information dashboard design: The effective visual communication of data . Sebastopol, CA: O’Reilly Media.
- Fisher, E. S., D. C. Goodman, and A. Chandra. 2008. Regional and racial variation in health care among Medicare beneficiaries: A brief report of the Dartmouth Atlas Project . Princeton, NJ: Robert Wood Johnson Foundation.
- Gawande, A., D. Berwick, E. Fisher, and M. McClellan. 2009. 10 steps to better health care . The New York Times , August 13, 2009, A27.
- Gold, M., and R. Nyman. 2004. Evaluation of the development process of the National Healthcare Quality Report . Washington, DC: Mathematica Policy Research, Inc.
- Green, M. 1998. Toward a perceptual science of multidimensional data visualization: Bertin and beyond . http://graphics .stanford .edu/courses/cs448b-06-winter /papers/Green_Towards.pdf (accessed May 13, 2010).
- HHS (U.S. Department of Health and Human Services). 2009. a. . http://www .healthreform .gov/reports/healthdisparities /disparities_final.pdf (accessed February 18, 2010).
- ———. 2009. b. Office of Minority Health Resource Center . http: //raceandhealth .hhs.gov/templates/browse .aspx?lvl=1&lvlID=8 (accessed February 4, 2010).
- ______. 2010. Community health status indicators project . http://www .communityhealth.hhs.gov (accessed March 26, 2010).
- Hibbard, J., and J. Jewett. 1997. Will quality report cards help consumers? Health Affairs 16(3):218-228. [ PubMed : 9141339 ]
- IOM (Institute of Medicine). 2001. Envisioning the National Healthcare Quality Report . Washington, DC: National Academy Press.
- ———. 2002. Guidance for the National Healthcare Disparities Report . Washington, DC: The National Academies Press. [ PubMed : 25057628 ]
- ———. 2010. Pediatric health and health care quality measures . http://www .iom.edu/Activities /Quality/PediatricQualityMeasures.aspx (accessed January 4, 2010).
- Kerr, E. A., E. A. McGlynn, J. Adams, J. Keesey, and S. M. Asch. 2004. Profiling the quality of care in twelve communities: Results from the CQI study . Health Affairs 23(3):247-256. [ PubMed : 15160823 ]
- Kiefe, C. I., N. W. Weissman, J. J. Allison, R. Farmer, M. Weaver, and O. D. Williams. 1998. Identifying achievable benchmarks of care: Concepts and methodology . International Journal for Quality in Health Care 10(5):443-447. [ PubMed : 9828034 ]
- Kiefe, C. I., J. J. Allison, O. D. Williams, S. D. Person, M. T. Weaver, and N. W. Weissman. 2001. Improving quality improvement using achievable benchmarks for physician feedback: A randomized controlled trial . Journal of the American Medical Association 285(22):2871-2879. [ PubMed : 11401608 ]
- Kleine, B. 1994. Benchmarking for continuous performance improvement: Tactics for success . Total Quality Environmental Management 3(3):283-295.
- Lansky, D. 2009. Priorities for quality improvement and ways to leverage collected information: An employer perspective . Pacific Business Group on Health. Presentation to the IOM Committee on Future Directions for the National Healthcare Quality and Disparities Reports, March 12, 2009. Newport Beach, CA. PowerPoint Presentation.
- Linderman, K., R. G. Schroeder, and A. S. Choo. 2006. Six Sigma: The role of goals in improvement teams . Journal of Operations Manage ment 24(6):779-790.
- Martinez-Vidal, E., and A. Brodt. 2006. State recommendations for revisions to the AHRQ Snapshots . Washington, DC: AcademyHealth.
- McKeon, T. 1996. Benchmarks and performance indicators: Two tools for evaluating organizational results and continuous quality improvement efforts . Journal of Nursing Care Quality 10(3):12-17. [ PubMed : 8634466 ]
- Moy, E. 2009. Lessons learned in developing NHQR and NHDR . Agency for Healthcare Research and Quality. Presentation to the IOM Committee on Future Directions for the National Healthcare Quality and Disparities Reports, February 9, 2009. Washington, DC. PowerPoint Presentation.
- Moy, E., E. Dayton, and C. M. Clancy. 2005. Compiling the evidence: The National Healthcare Disparities Reports . Health Affairs 24(2): 376-387. [ PubMed : 15757921 ]
- Murray, C. J., J. A. Salomon, and C. Mathers. 2000. A critical examination of summary measures of population health . Bulletin of the World Health Organization 78(8):981-994. [ PMC free article : PMC2560826 ] [ PubMed : 10994282 ]
- Normand, S. L., R. E. Wolf, J. Z. Ayanian, and B. J. McNeil. 2007. Assessing the accuracy of hospital clinical performance measures . Medical Decision Making 27(1):9-20. [ PubMed : 17237448 ]
- Pickle, L. W., M. Mungiole, G. K. Jones, and A. A. White. 1996. Atlas of United States mortality . Hyattsville, MD: National Center for Health Statistics.
- Reinertsen, J., and W. Schellekens. 2005. 10 powerful ideas for improving patient care: What every healthcare executive should know . Chicago, IL: Health Administrative Press.
- Reintjes, R., M. Thelen, R. Reiche, and Á. Csohán. 2007. Benchmarking national surveillance systems: A new tool for the comparison of communicable disease surveillance and control in Europe . European Journal of Public Health 17(4):375-380. [ PubMed : 17142827 ]
- Romano, P. S., J. A. Rainwater, and D. Antonius. 1999. Grading the graders: How hospitals in California and New York perceive and interpret their report cards . Medical Care 37(3):295-305. [ PubMed : 10098573 ]
- RWJF (Robert Wood Johnson Foundation) and the University of Wisconsin Population Health Institute. 2010. County health ratings . http://www .countyhealthrankings.org/ (accessed February 23, 2010).
- Schriger, D. L., and R. J. Cooper. 2001. Achieving graphical excellence: Suggestions and methods for creating high-quality visual displays of experimental data . Annals of Emerging Medicine 37(1):75-87. [ PubMed : 11145777 ]
- Social & Scientific Systems, and UserWorks. 2009. Final report: Usability evaluation of the Agency for Healthcare Research and Quality (AHRQ) QRDR web sites . Silver Spring, MD: Social & Scientific Systems, Inc. and UserWorks, Inc.
- Tufte, E. R. 1983. The visual display of quantitative information . Cheshire, CT: Graphics Press.
- van Herten, L. M., and L. J. Gunning-Schepers. 2000. a. Targets as a tool in health policy. Part II: Guidelines for application . Health Policy 53(1):13-23. [ PubMed : 10940460 ]
- ———. 2000. b. Targets as a tool in health policy: Lessons learned . Health Policy 53(1):1-11. [ PubMed : 10940459 ]
- Vaziri, K. 1992. Using competitive benchmarking to set goals . Quality Progress 25(10):81-85.
- Weissman, N. W., J. J. Allison, C. I. Kiefe, R. Farmer, M. T. Weaver, O. D. Williams, I. G. Child, J. H. Pemberton, K. C. Brown, and S. Baker. 1999. Achievable benchmarks of care: The ABCs of benchmarking . Journal of Evaluation in Clinical Practice 5(3):269-281. [ PubMed : 10461579 ]
- Zimmerman, J. E., C. Alzola, and K. T. Von Rueden. 2003. The use of benchmarking to identify top performing critical care units: A preliminary assessment of their policies and practices . Journal of Critical Care 18(2):76-86. [ PubMed : 12800117 ]
Healthcare Research and Quality Act of 1999 , Public Law 106-129, 106th Cong., 1st sess. (November 19, 1999).
Personal communication, Farah Englert, Agency for Healthcare Research and Quality, November 12, 2009.
Personal communication, Ernest Moy, Agency for Healthcare Research and Quality, November 18, 2009. AHRQ staff estimate that data for large Metropolitan Statistical Areas (MSAs) could be provided for more than 50 percent of the State Snapshots measures. All CMS Compare systems could support MSA-level estimates. The Behavioral Risk Factor Surveillance System (BRFSS) could be used for MSA-level analyses for the top 150 MSAs. Other data sources, such as vital statistics data and hospital data from Healthcare Cost and Utilization Project (HCUP) states, would require special permissions in order to analyze and publish data at the MSA-level.
The data.gov website is accessible at http://www .data.gov/ (accessed December 12, 2009).
Personal communication, Farah Englert, Agency for Healthcare Research and Quality, November 16, 2009.
Copies of the sample media and communication plan and sample fact sheets developed by Ketchum were provided directly to AHRQ staff and archived in the IOM public access file for the Future Directions project.
In 2004, AHRQ was advised to use a chartbook format for future iterations of the NHQR (Gold and Nyman, 2004).
Healthcare Research and Quality Act of 1999 , Public Law 106-129 § 902(g) and § 913(b)(2), 106th Cong., 1st sess. (November 19, 1999).
The HealthyPeople 2010 targets are, in almost all cases, higher than the currently achieved national progress or even the best performing state. For some measures presented in the NHQR and NHDR, however, performance is at or above the Healthy People target. For example, the composite measure for children ages 19-35 months who received all recommended vaccines includes the Healthy People target of 80 percent attainment. The national average for this measure was at 80.6 percent, achieving this target.
Because the State Snapshots were initially developed to supplement measures in only the NHQR, access measures are not included in the State Snapshots; in accordance with the committee’s recommendation to integrate access in the quality portfolio of measures, it is important for AHRQ to include access measures in the State Snapshots.
Howard Wainer’s paper, “Commentaries on the 2008 National Healthcare Quality Report, the 2008 National Healthcare Disparities Report and State Snapshots,” was provided directly to AHRQ staff and archived in the IOM public access file for the Future Directions project.
Ten out of the 12 reported composite measures in the reports involve the bundling of process measures, while the other 2 involve outcome measures for surgical procedures.
The 2008 measure specifications are accessible at http://www .ahrq.gov/qual /qrdr08/measurespec/ (accessed January 15, 2010).
Accessible by visiting the Methods section of the State Snapshots at http: //statesnapshots .ahrq.gov/snaps08/Methods .jsp?menuId=58&state =#stateSummary (accessed January 15, 2010).
See the Montana dashboard at http: //statesnapshots .ahrq.gov/snaps08/dashboard .jsp?menuId=4&state =MT&level=0 (accessed December 8, 2009).
See Arkansas: Focus on Disparities at http: //statesnapshots .ahrq.gov/snaps08/disparities .jsp?menuId =47&state=AR&level=83 (accessed December 20, 2009).
Personal communication, William Golden, University of Arkansas for Medical Sciences and Arkansas Medicaid, Department of Human Services, December 8, 2009.
- Cite this Page Institute of Medicine (US) Committee on Future Directions for the National Healthcare Quality and Disparities Reports; Ulmer C, Bruno M, Burke S, editors. Future Directions for the National Healthcare Quality and Disparities Reports. Washington (DC): National Academies Press (US); 2010. 6, Improving Presentation of Information.
- PDF version of this title (2.9M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Improving Presentation of Information - Future Directions for the National Healt... Improving Presentation of Information - Future Directions for the National Healthcare Quality and Disparities Reports
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
What It Takes to Give a Great Presentation
- Carmine Gallo

Five tips to set yourself apart.
Never underestimate the power of great communication. It can help you land the job of your dreams, attract investors to back your idea, or elevate your stature within your organization. But while there are plenty of good speakers in the world, you can set yourself apart out by being the person who can deliver something great over and over. Here are a few tips for business professionals who want to move from being good speakers to great ones: be concise (the fewer words, the better); never use bullet points (photos and images paired together are more memorable); don’t underestimate the power of your voice (raise and lower it for emphasis); give your audience something extra (unexpected moments will grab their attention); rehearse (the best speakers are the best because they practice — a lot).
I was sitting across the table from a Silicon Valley CEO who had pioneered a technology that touches many of our lives — the flash memory that stores data on smartphones, digital cameras, and computers. He was a frequent guest on CNBC and had been delivering business presentations for at least 20 years before we met. And yet, the CEO wanted to sharpen his public speaking skills.
- Carmine Gallo is a Harvard University instructor, keynote speaker, and author of 10 books translated into 40 languages. Gallo is the author of The Bezos Blueprint: Communication Secrets of the World’s Greatest Salesman (St. Martin’s Press).
Partner Center

How it works
Transform your enterprise with the scalable mindsets, skills, & behavior change that drive performance.
Explore how BetterUp connects to your core business systems.
We pair AI with the latest in human-centered coaching to drive powerful, lasting learning and behavior change.
Build leaders that accelerate team performance and engagement.
Unlock performance potential at scale with AI-powered curated growth journeys.
Build resilience, well-being and agility to drive performance across your entire enterprise.
Transform your business, starting with your sales leaders.
Unlock business impact from the top with executive coaching.
Foster a culture of inclusion and belonging.
Accelerate the performance and potential of your agencies and employees.
See how innovative organizations use BetterUp to build a thriving workforce.
Discover how BetterUp measurably impacts key business outcomes for organizations like yours.
A demo is the first step to transforming your business. Meet with us to develop a plan for attaining your goals.

- What is coaching?
Learn how 1:1 coaching works, who its for, and if it's right for you.
Accelerate your personal and professional growth with the expert guidance of a BetterUp Coach.
Types of Coaching
Navigate career transitions, accelerate your professional growth, and achieve your career goals with expert coaching.
Enhance your communication skills for better personal and professional relationships, with tailored coaching that focuses on your needs.
Find balance, resilience, and well-being in all areas of your life with holistic coaching designed to empower you.
Discover your perfect match : Take our 5-minute assessment and let us pair you with one of our top Coaches tailored just for you.

Research, expert insights, and resources to develop courageous leaders within your organization.
Best practices, research, and tools to fuel individual and business growth.
View on-demand BetterUp events and learn about upcoming live discussions.
The latest insights and ideas for building a high-performing workplace.
- BetterUp Briefing
The online magazine that helps you understand tomorrow's workforce trends, today.
Innovative research featured in peer-reviewed journals, press, and more.
Founded in 2022 to deepen the understanding of the intersection of well-being, purpose, and performance
We're on a mission to help everyone live with clarity, purpose, and passion.
Join us and create impactful change.
Read the buzz about BetterUp.
Meet the leadership that's passionate about empowering your workforce.

For Business
For Individuals
6 presentation skills and how to improve them

Jump to section
What are presentation skills?
The importance of presentation skills, 6 presentation skills examples, how to improve presentation skills.
Tips for dealing with presentation anxiety
Learn how to captivate an audience with ease
Capturing an audience’s attention takes practice.
Over time, great presenters learn how to organize their speeches and captivate an audience from start to finish. They spark curiosity, know how to read a room , and understand what their audience needs to walk away feeling like they learned something valuable.
Regardless of your profession, you most likely use presentation skills on a monthly or even weekly basis. Maybe you lead brainstorming sessions or host client calls.
Developing effective presentation skills makes it easier to contribute ideas with confidence and show others you’re someone to trust. Although speaking in front of a crowd sometimes brings nerves and anxiety , it also sparks new opportunities.
Presentation skills are the qualities and abilities you need to communicate ideas effectively and deliver a compelling speech. They influence how you structure a presentation and how an audience receives it. Understanding body language , creating impactful visual aids, and projecting your voice all fall under this umbrella.
A great presentation depends on more than what you say. It’s about how you say it. Storytelling , stage presence, and voice projection all shape how well you express your ideas and connect with the audience. These skills do take practice, but they’re worth developing — especially if public speaking makes you nervous.
Engaging a crowd isn’t easy. You may feel anxious to step in front of an audience and have all eyes and ears on you.
But feeling that anxiety doesn’t mean your ideas aren’t worth sharing. Whether you’re giving an inspiring speech or delivering a monthly recap at work, your audience is there to listen to you. Harness that nervous energy and turn it into progress.
Strong presentation skills make it easier to convey your thoughts to audiences of all sizes. They can help you tell a compelling story, convince people of a pitch , or teach a group something entirely new to them. And when it comes to the workplace, the strength of your presentation skills could play a part in getting a promotion or contributing to a new initiative.
To fully understand the impact these skills have on creating a successful presentation, it’s helpful to look at each one individually. Here are six valuable skills you can develop:
1. Active listening
Active listening is an excellent communication skill for any professional to hone. When you have strong active listening skills, you can listen to others effectively and observe their nonverbal cues . This helps you assess whether or not your audience members are engaged in and understand what you’re sharing.
Great public speakers use active listening to assess the audience’s reactions and adjust their speech if they find it lacks impact. Signs like slouching, negative facial expressions, and roaming eye contact are all signs to watch out for when giving a presentation.
2. Body language
If you’re researching presentation skills, chances are you’ve already watched a few notable speeches like TED Talks or industry seminars. And one thing you probably noticed is that speakers can capture attention with their body language.
A mixture of eye contact, hand gestures , and purposeful pacing makes a presentation more interesting and engaging. If you stand in one spot and don’t move your body, the audience might zone out.

3. Stage presence
A great stage presence looks different for everyone. A comedian might aim for more movement and excitement, and a conference speaker might focus their energy on the content of their speech. Although neither is better than the other, both understand their strengths and their audience’s needs.
Developing a stage presence involves finding your own unique communication style . Lean into your strengths, whether that’s adding an injection of humor or asking questions to make it interactive . To give a great presentation, you might even incorporate relevant props or presentation slides.
4. Storytelling
According to Forbes, audiences typically pay attention for about 10 minutes before tuning out . But you can lengthen their attention span by offering a presentation that interests them for longer. Include a narrative they’ll want to listen to, and tell a story as you go along.
Shaping your content to follow a clear narrative can spark your audience’s curiosity and entice them to pay careful attention. You can use anecdotes from your personal or professional life that take your audience along through relevant moments. If you’re pitching a product, you can start with a problem and lead your audience through the stages of how your product provides a solution.
5. Voice projection
Although this skill may be obvious, you need your audience to hear what you’re saying. This can be challenging if you’re naturally soft-spoken and struggle to project your voice.
Remember to straighten your posture and take deep breaths before speaking, which will help you speak louder and fill the room. If you’re talking into a microphone or participating in a virtual meeting, you can use your regular conversational voice, but you still want to sound confident and self-assured with a strong tone.
If you’re unsure whether everyone can hear you, you can always ask the audience at the beginning of your speech and wait for confirmation. That way, they won’t have to potentially interrupt you later.
Ensuring everyone can hear you also includes your speed and annunciation. It’s easy to speak quickly when nervous, but try to slow down and pronounce every word. Mumbling can make your presentation difficult to understand and pay attention to.

6. Verbal communication
Although verbal communication involves your projection and tone, it also covers the language and pacing you use to get your point across. This includes where you choose to place pauses in your speech or the tone you use to emphasize important ideas.
If you’re giving a presentation on collaboration in the workplace , you might start your speech by saying, “There’s something every workplace needs to succeed: teamwork.” By placing emphasis on the word “ teamwork ,” you give your audience a hint on what ideas will follow.
To further connect with your audience through diction, pay careful attention to who you’re speaking to. The way you talk to your colleagues might be different from how you speak to a group of superiors, even if you’re discussing the same subject. You might use more humor and a conversational tone for the former and more serious, formal diction for the latter.
Everyone has strengths and weaknesses when it comes to presenting. Maybe you’re confident in your use of body language, but your voice projection needs work. Maybe you’re a great storyteller in small group settings, but need to work on your stage presence in front of larger crowds.
The first step to improving presentation skills is pinpointing your gaps and determining which qualities to build upon first. Here are four tips for enhancing your presentation skills:
1. Build self-confidence
Confident people know how to speak with authority and share their ideas. Although feeling good about your presentation skills is easier said than done, building confidence is key to helping your audience believe in what you’re saying. Try practicing positive self-talk and continuously researching your topic's ins and outs.
If you don’t feel confident on the inside, fake it until you make it. Stand up straight, project your voice, and try your best to appear engaged and excited. Chances are, the audience doesn’t know you’re unsure of your skills — and they don’t need to.
Another tip is to lean into your slideshow, if you’re using one. Create something colorful and interesting so the audience’s eyes fall there instead of on you. And when you feel proud of your slideshow, you’ll be more eager to share it with others, bringing more energy to your presentation.
2. Watch other presentations
Developing the soft skills necessary for a good presentation can be challenging without seeing them in action. Watch as many as possible to become more familiar with public speaking skills and what makes a great presentation. You could attend events with keynote speakers or view past speeches on similar topics online.
Take a close look at how those presenters use verbal communication and body language to engage their audiences. Grab a notebook and jot down what you enjoyed and your main takeaways. Try to recall the techniques they used to emphasize their main points, whether they used pauses effectively, had interesting visual aids, or told a fascinating story.

3. Get in front of a crowd
You don’t need a large auditorium to practice public speaking. There are dozens of other ways to feel confident and develop good presentation skills.
If you’re a natural comedian, consider joining a small stand-up comedy club. If you’re an avid writer, participate in a public poetry reading. Even music and acting can help you feel more comfortable in front of a crowd.
If you’d rather keep it professional, you can still work on your presentation skills in the office. Challenge yourself to participate at least once in every team meeting, or plan and present a project to become more comfortable vocalizing your ideas. You could also speak to your manager about opportunities that flex your public speaking abilities.
4. Overcome fear
Many people experience feelings of fear before presenting in front of an audience, whether those feelings appear as a few butterflies or more severe anxiety. Try grounding yourself to shift your focus to the present moment. If you’re stuck dwelling on previous experiences that didn’t go well, use those mistakes as learning experiences and focus on what you can improve to do better in the future.
Tips for dealing with presentation anxiety
It’s normal to feel nervous when sharing your ideas. In fact, according to a report from the Journal of Graduate Medical Education, public speaking anxiety is prevalent in 15–30% of the general population .
Even though having a fear of public speaking is common, it doesn’t make it easier. You might feel overwhelmed, become stiff, and forget what you were going to say. But although the moment might scare you, there are ways to overcome the fear and put mind over matter.
Use these tactics to reduce your stress when you have to make a presentation:
1. Practice breathing techniques
If you experience anxiety often, you’re probably familiar with breathing techniques for stress relief . Incorporating these exercises into your daily routine can help you stop worrying and regulate anxious feelings.
Before a big presentation, take a moment alone to practice breathing techniques, ground yourself, and reduce tension. It’s also a good idea to take breaths throughout the presentation to speak slower and calm yourself down .
2. Get organized
The more organized you are, the more prepared you’ll feel. Carefully outline all of the critical information you want to use in your presentation, including your main talking points and visual aids, so you don’t forget anything. Use bullet points and visuals on each slide to remind you of what you want to talk about, and create handheld notes to help you stay on track.
3. Embrace moments of silence
It’s okay to lose your train of thought. It happens to even the most experienced public speakers once in a while. If your mind goes blank, don’t panic. Take a moment to breathe, gather your thoughts, and refer to your notes to see where you left off. You can drink some water or make a quick joke to ease the silence or regain your footing. And it’s okay to say, “Give me a moment while I find my notes.” Chances are, people understand the position you’re in.

4. Practice makes progress
Before presenting, rehearse in front of friends and family members you trust. This gives you the chance to work out any weak spots in your speech and become comfortable communicating out loud. If you want to go the extra mile, ask your makeshift audience to ask a surprise question. This tests your on-the-spot thinking and will prove that you can keep cool when things come up.
Whether you’re new to public speaking or are a seasoned presenter, you’re bound to make a few slip-ups. It happens to everyone. The most important thing is that you try your best, brush things off, and work on improving your skills to do better in your next presentation.
Although your job may require a different level of public speaking than your favorite TED Talk , developing presentation skills is handy in any profession. You can use presentation skills in a wide range of tasks in the workplace, whether you’re sharing your ideas with colleagues, expressing concerns to higher-ups, or pitching strategies to potential clients.
Remember to use active listening to read the room and engage your audience with an interesting narrative. Don’t forget to step outside your comfort zone once in a while and put your skills to practice in front of a crowd. After facing your fears, you’ll feel confident enough to put presentation skills on your resume.
If you’re trying to build your skills and become a better employee overall, try a communications coach with BetterUp.
Elevate your communication skills
Unlock the power of clear and persuasive communication. Our coaches can guide you to build strong relationships and succeed in both personal and professional life.
Elizabeth Perry, ACC
Elizabeth Perry is a Coach Community Manager at BetterUp. She uses strategic engagement strategies to cultivate a learning community across a global network of Coaches through in-person and virtual experiences, technology-enabled platforms, and strategic coaching industry partnerships. With over 3 years of coaching experience and a certification in transformative leadership and life coaching from Sofia University, Elizabeth leverages transpersonal psychology expertise to help coaches and clients gain awareness of their behavioral and thought patterns, discover their purpose and passions, and elevate their potential. She is a lifelong student of psychology, personal growth, and human potential as well as an ICF-certified ACC transpersonal life and leadership Coach.
The 11 tips that will improve your public speaking skills
The importance of good speech: 5 tips to be more articulate, show gratitude with “thank you for your leadership and vision” message examples, learn types of gestures and their meanings to improve your communication, why it's good to have a bff at work and how to find one, why we need to reframe potential into readiness, love them or hate them, meetings promote social learning and growth, what is a career path definition, examples, and steps for paving yours, goal-setting theory: why it’s important, and how to use it at work, similar articles, how to write a speech that your audience remembers, 8 tip to improve your public speaking skills, impression management: developing your self-presentation skills, 30 presentation feedback examples, your guide to what storytelling is and how to be a good storyteller, how to give a good presentation that captivates any audience, 8 clever hooks for presentations (with tips), how to make a presentation interactive and exciting, stay connected with betterup, get our newsletter, event invites, plus product insights and research..
3100 E 5th Street, Suite 350 Austin, TX 78702
- Platform Overview
- Integrations
- Powered by AI
- BetterUp Lead
- BetterUp Manage™
- BetterUp Care™
- Sales Performance
- Diversity & Inclusion
- Case Studies
- Why BetterUp?
- About Coaching
- Find your Coach
- Career Coaching
- Communication Coaching
- Life Coaching
- News and Press
- Leadership Team
- Become a BetterUp Coach
- BetterUp Labs
- Center for Purpose & Performance
- Leadership Training
- Business Coaching
- Contact Support
- Contact Sales
- Privacy Policy
- Acceptable Use Policy
- Trust & Security
- Cookie Preferences

IMAGES
VIDEO
COMMENTS
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
1. There's a new appreciation of the importance of health. Late last year, Dr. Tedros Ghebreyesus, Director-General of the World Health Organization (WHO), said: "The time has come for a new narrative that sees health not as a cost, but an investment that is the foundation of productive, resilient and stable economies.". That is exactly ...
SBM-R (Standards-Based Management and Recognition) • SBM-R is a management method developed by Jhpiego that aims to improve quality of care by improving health worker performance. • It adapts the four main elements of the continuous quality improvement cycle (plan, do, study, act) to standardize, do, study, and reward • 1.Assessment ...
Very few people seek out jobs based on public speaking opportunities — and that's particularly true for medical professionals. But while life-saving research and discovery is some of the most important work medical teams will do, they also need to know how to share what they've learned.. Presentations are an effective way of unveiling new findings within scientific communities, training ...
Health is a core element in people's well-being and happiness. Health is an important enabler and a prerequisite for a person's ability to reach his/her goals and aspirations, and for society to reach many of the societal goals (Minister of Social Affairs and Health, Finland, 2013: 3). Health communication has been a part of development communication or communication for development for ...
Delivery. 1. Confront nervousness. Many of us become nervous when speaking in front of an audience. To address this, it's perfectly reasonable to rehearse a presentation at home or in a quiet call room ahead of time. If you feel extremely nervous, breathe deeply for five- to 10-second intervals.
The main goals of health services research are to identify the most effective ways to organize, manage, finance and deliver high-quality care; reduce medical errors; and improve patient safety (Agency for Healthcare Research and Quality, 2002). HSR tends to be multidisciplinary, and with researchers coming from a variety of disciplines ...
By following the right strategies and keeping certain tips in mind, public health professionals launching health communication campaigns can achieve success. 1. Know the Issue. Before coming up with goals or plans, it's important to develop a layered understanding of the issue.
Visual Communication Resources. Visuals, such as pictures, drawings, charts, graphs and diagrams, can be effective tools for communicating health information. Visuals can make the presentation of complex information easier to comprehend and more attractive. They can also reinforce written or spoken health messages.
Here's how it works: After you build your slide, use the shift key while clicking the objects on your slide, in the order that you want to talk about them. Once you select everything, go to the Add Animations button on the Animations tab in the ribbon to add a Fade entrance animation.
eHealth: Global perspective. S. Yunkap Kwankam Coordinator eHealth World Health Organization, Geneva. Outline of presentation. Six point agenda and health system framework WHO eHealth priorities WHO collaboration mechanisms Conclusion. ★ ★ ★ ★ ★
9. Take the stairs. The next time you're going to a higher floor, bypass the elevator and climb the stairs instead. You'll get your blood pumping, exercise your lungs and work the muscles in your lower body. It's a great way to add physical activity to your day without having to block out time to exercise.
Speak clearly: Don't be too quiet or speak in a monotone. Be sure to emphasize the most important parts of your presentation and pause between important points to let the data sink in. Be aware of body language: Smile, maintain an upright but relaxed posture, and avoid tapping your feet or swaying.
The 10 Essential Public Health Services (EPHS) describe the public health activities that all communities should undertake. On September 9, 2020, a revised EPHS framework and graphic was released. The revised EPHS is intended to bring the framework in line with current and future public health practice. Learn More.
Dissemination Strategies. Dissemination is the targeted distribution of information and intervention materials to a specific public health or clinical practice audience. The intent is to spread knowledge and the associated evidence-based interventions. 4,5 Dissemination occurs through a variety of channels, social contexts, and settings. Evidence dissemination has several very broad goals: (1 ...
Health care systems are becoming increasingly complex and the United States continues to lag behind other industrialized nations in health outcomes relative to the amount spent. 1-2 We owe it to our patients to foster innovation and improve delivery of care. To do this, we must engage our students, residents, and fellows to understand, develop, and, ultimately, lead the movement to improve ...
If your organization wants to improve quality healthcare this is the place to start: Be as rigorous about tracking patient wellness as you are about tracking billing. Use EHRs, outcomes studies, patient satisfaction surveys, and other data sources to closely monitor the health, outcomes, overall wellness, and costs for individual patients ...
Background. Evidence-based health care practices have been promoted within healthcare systems internationally [], as the use of evidence informed practice has been linked to improved patient health outcomes [].Clinical guidelines, developed from the best available evidence aim to improve the patient outcomes, quality of care, reduce practice variation and/or reduce cost by providing clinicians ...
Results and experience. Reduced fragmentation resulting from the reforms decreased the management costs of internationally funded projects from an average of 28% in 2005 to 9% in 2011. Between 2009 and 2014, better coordination resulted in savings of more than US$ 56 million.
The NHQR and NHDR can be forward-looking documents that not only present historical trend data but also convey a story of the potential for progress and the health benefits to the nation of closing quality and disparity gaps. To serve as catalysts for improvement, the Future Directions committee envisions that the reports will extrapolate rates of change to indicate when gaps between current ...
1) The starting point will need to be to put older people at the centre of health care. This will require focusing on their unique needs and preferences, and including them as active participants in care planning and in managing their health states. But changes are needed to systems, too.
Here are a few tips for business professionals who want to move from being good speakers to great ones: be concise (the fewer words, the better); never use bullet points (photos and images paired ...
To fully understand the impact these skills have on creating a successful presentation, it's helpful to look at each one individually. Here are six valuable skills you can develop: 1. Active listening. Active listening is an excellent communication skill for any professional to hone.
prepare your new DPIA, if it covered a similar processing operation. Seek advice from . your organisation's designated safeguarding children professional, the Data Protection or Information Governance leads (e.g., Data Protection Officer), Caldicott Guardian, Professional Regulator (if applicable) or your organisation's relevant policy or legal