

Coronavirus Disease 2019
How the pandemic changed family dynamics, the potential impact of covid-19 on adolescents’ social development..
Posted August 2, 2021 | Reviewed by Abigail Fagan
- The social effects of quarantine hit younger adolescents particularly hard, derailing typical development.
- During COVID-19, family was more influential than friends during a developmental period when the opposite would normally be true.
- Siblings may have functioned as a buffer against the social effects of quarantine for older adolescents.
The social landscape has looked wildly different over the past year and a half. Because of the quarantines and social restrictions made necessary by the COVID-19 pandemic, in-person social interactions were greatly reduced in 2020 as many found themselves spending the majority of their time at home with family, and away from friends and colleagues. Previous research has already connected quarantine and increased mental health issues that have been observed during the pandemic (e.g., Chahal et al., 2020; Ghebreyesus et al., 2020).
Adolescence is a time of social exploration where peers begin to play a greater role than parents as teens move toward independence, so the disruption of this normative timeline, and particularly interactions with friends, is cause for concern (Ellis et al., 2020; Orben, Tomova, Blakemore, 2020). Cross-sectional studies on the effects of COVID-19 have shown that maintaining friendships is something children and adolescents were bothered by and that while online social connections can be beneficial, in-person interactions are more effective (Ellis et al., 2020; Orben et al., 2020).

A recent study led by Dr. Reuma Gadassi-Polack in our lab expanded what is known about the effects of COVID-19 quarantine by looking at adolescents’ social interactions and depressive symptoms before and during the pandemic (Gadassi Polack et al., in press). Researchers collected data from kids using short questionnaires completed daily, a year before COVID and again at the beginning of the pandemic. Each day, participants reported both positive and negative interactions with family members and peers and their depressive symptoms.
The study looked at 112 participants (age 8-15) who completed daily questionnaires in both the initial pre-COVID data collection (Wave 1) and the data collection during COVID (Wave 2). Researchers were able to capture information about both individual relationships and how they affect one another via “spillover,” a concept that will be discussed further below.
COVID Had Greater Negative Effects on Younger Adolescents
In typical development, we would expect to see uniform increases in interactions with peers alongside decreases in interactions with parents (e.g., Lam et al., 2012; Larson et al., 1991; Larson et al., 1996). Instead, younger (but not older) participants had significantly fewer positive interactions with peers during COVID compared to pre-COVID. For participants 13 and older, significantly more positive interactions with siblings were seen during COVID vs. before. This led to a greater negative impact on younger adolescents, who lost positive interactions with peers without gaining any positive interactions with siblings like older adolescents. In fact, younger adolescents had more negative interactions with siblings than friends or parents.

For both age groups, negative interactions with friends significantly decreased while there were no other significant decreases in other relationships. This finding presents a different facet of the move to online school: for some, this was an opportunity to escape a negative environment.
Altogether, the lack of the expected increase in interactions with friends suggests that the COVID-19 pandemic has derailed the typical trajectory of social development. The larger effect can potentially be credited to less social development as younger adolescents are experiencing the same effects earlier in development, with less social skills in place. A further implication of these results is that in-person interactions cannot be neatly substituted with virtual interaction.
Family Members Were More Influential than Friends During the Early Stages of COVID-19
Looking at a process named “spillover” allowed researchers to understand the connections within the family, family subsystems, and peer relationships. The concept of spillover is grounded in the idea that our social world is made up of subsystems, including those within the family: the mother and father is a subsystem, as is the parent and child, or the siblings. These subsystems are of course connected (e.g., the mother-father relationship is related to the mother-child relationship), but not without some boundaries . When these boundaries become weaker, interactions in one subsystem can affect interactions in other subsystems via spillover (e.g., Chung et al., 2011; Flook & Fuligni, 2008; Kaufman et al., 2020; Krishnakumar & Buehler, 2000; Mastrotheodoros et al., 2020).

For example, an argument between parents can cause each parent to be more likely to argue with their child. What began as a negative interaction in the mother-father relationship has then spilled over into the parent-child relationship. This example would be considered negative spillover, where negative occurrences in one subsystem lead to negative interactions or feelings in another. Positive spillover occurs when the same thing happens with positive occurrences. For example, being praised by their mother might cause a child to be kinder to their sibling . Then, a positive interaction in the mother-child relationship has spilled over into the sibling relationship.
COVID-19 appeared to create a more closed family system, with fewer spillover effects from outside and more inside. In other words, interactions with family members impacted interactions with friends to a lesser degree during COVID. Separate interactions with family and friends are expected to affect each other less as adolescents develop typically. However, in the context of the pandemic, this was particularly detrimental for those who already had more negative family relationships prior to COVID as there was less day-level positive spillover and increased negative spillover on the individual level.

Increase in Depressive Symptoms Related to Family Interactions
Changes were not only seen in interactions, but also in levels of depressive symptoms. Depressive symptoms increased significantly by almost 40 percent during COVID-19, regardless of age. This signifies the severity of COVID-19’s impact on adolescent mental health, above and beyond any increase in depression typically seen in development (e.g., Salk et al., 2016). The occurrence of less positive and more negative interactions with family members significantly predicted depressive symptoms during COVID-19.
More Positive than Negative Interactions and a New Role for Siblings
The effects of the social changes wrought by the COVID-19 pandemic were not wholly negative, however. Overall, most kids reported five times more positive interactions than negative interactions. Importantly, having more positive interactions with family members was associated with smaller increases in depressive symptoms during COVID.

The effect of the pandemic on sibling relationships was also more positive. Few would be surprised to hear siblings had a high number of negative interactions – much higher compared to any other relationship. However, increased positive interactions without an increase in negative interactions with siblings was seen in older adolescents, suggesting that siblings can compensate at least somewhat for the decrease in in-person peer interactions.
Combined with prior research on siblings’ positive effects on mental health and loneliness (McHale, Updegraff, & Whiteman, 2012; Wikle, Ackert, & Jenson, 2019), these results suggest that the presence of siblings is beneficial during a time of social isolation .
In general, this research shines a light on how important peer interactions are for normative development and the necessity of ensuring children and adolescents are given opportunities to spend time, especially in-person, with peers.
Take-Home Points
- Family negativity predicted the increase in depressive symptoms during COVID-19. In families with more positive interactions, there was less of an increase.
- Siblings potentially functioned as a buffer for the social effects of quarantine for older adolescents.
Anna Leah Davis, a Yale undergraduate, contributed to the writing of this blog post.
Chahal, R., Kirshenbaum, J. S., Miller, J. G., Ho, T. C., & Gotlib, I. H. (2020). Higher executive control network coherence buffers against puberty-related increases in internalizing symptoms during the COVID-19 pandemic. Biological Psychiatry. https://doi.org/10.1016/j.bpsc.2020.08.010
Chung, G. H., Flook, L., & Fuligni, A. J. (2011). Reciprocal associations between family and peer conflict in adolescents' daily lives. Child Development, 82, 1390–1396. https://doi.org/10.1111/j.1467-8624.2011.01625.x
Ellis, W. E., Dumas, T. M., & Forbes, L. M. (2020). Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science, 52, 177-187. http://dx.doi.org/10.1037/cbs0000215
Flook, L., & Fuligni, A. J. (2008). Family and school spillover in adolescents’ daily lives. Child Development, 79, 776-787. https://doi.org/10.1111/j.1467-8624.2008.01157.x
Gadassi Polack, R. Sened, H., Aubé, S., Zhang, A., Joormann, J., & Kober, H. (in press) Connections during Crisis: Adolescents’ social dynamics and mental health during COVID-19. Developmental Psychology.
Ghebreyesus, T.A. (2020). Addressing mental health needs: an integral part of COVID-19 response. World Psychiatry, 19, 129–130. https://doi.org/10.1002/wps.20768
Hankin, B. L., Stone, L., & Wright, P. A. (2010). Corumination, interpersonal stress generation, and internalizing symptoms: accumulating effects and transactional influences in a multiwave study of adolescents. Development and Psychopathology, 22, 217–235. https://doi.org/10.1017/S0954579409990368
Kaufman, T. M., Kretschmer, T., Huitsing, G., & Veenstra, R. (2020). Caught in a vicious cycle? Explaining bidirectional spillover between parent-child relationships and peer victimization. Development and Psychopathology, 32, 11-20. doi: 10.1017/S0954579418001360.
Krishnakumar, A., & Buehler, C. (2000). Interparental conflict and parenting behaviors: A meta‐analytic review. Family Relations, 49, 25-44. https://doi.org/10.1111/j.1741-3729.2000.00025.x
Lam, C. B., McHale, S. M., & Crouter, A. C. (2012). Parent–child shared time from middle childhood to late adolescence: Developmental course and adjustment correlates. Child Development, 83, 2089-2103. DOI: 10.1111/j.1467-8624.2012.01826.x
Larson, R., & Richards, M. H. (1991). Daily companionship in late childhood and early adolescence: Changing developmental contexts. Child Development, 62, 284-300. https://doi.org/10.2307/1131003
Larson, R. W., Richards, M. H., Moneta, G., Holmbeck, G., & Duckett, E. (1996). Changes in adolescents' daily interactions with their families from ages 10 to 18: Disengagement and transformation. Developmental Psychology, 32, 744–754. https://doi.org/10.1037/0012-1649.32.4.744
Mastrotheodoros, S., Van Lissa, C. J., Van der Graaff, J., Deković, M., Meeus, W. H., & Branje, S. J. (2020). Day-to-day spillover and long-term transmission of interparental conflict to adolescent–mother conflict: The role of mood. Journal of Family Psychology. doi: 10.1037/fam0000649.
McHale, S. M., Updegraff, K. A., & Whiteman, S. D. (2012). Sibling Relationships and Influences in Childhood and Adolescence. Journal of Marriage and the Family, 74, 913–930. https://doi.org/10.1111/j.1741-3737.2012.01011.x
Orben, A., Tomova, L., & Blakemore, S. J. (2020). The effects of social deprivation on adolescent development and mental health. The Lancet Child & Adolescent Health. https://doi.org/10.1016/ S2352-4642(20)30186-3
Salk, R. H., Petersen, J. L., Abramson, L. Y., & Hyde, J. S. (2016). The contemporary face of gender differences and similarities in depression throughout adolescence: Development and chronicity. Journal of Affective Disorders, 205, 28-35. http://dx.doi.org/10.1016/j.jad.2016.03.071
Wikle, J. S., Ackert, E., & Jensen, A. C. (2019). Companionship patterns and emotional states during social interactions for adolescents with and without siblings. Journal of Youth and Adolescence, 48, 2190–2206. https://doi.org/10.1007/s10964-019-01121-z

Jutta Joormann, Ph.D ., is a professor of psychology at Yale University who studies risk factors for depression and anxiety disorders.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Rochester News
- Science & Technology
- Society & Culture
- Campus Life
- University News
How does the pandemic affect families who were already struggling?

- Facebook Share on Facebook
- X/Twitter Share on Twitter
- LinkedIn Share on LinkedIn
Rochester psychologists have been awarded federal funding to study the pandemic’s long-term effects on family cohesion and child well-being.
About a year and a half after COVID-19 rapidly spread around the globe, scientists have begun to examine the pandemic’s long-term societal effects. University of Rochester psychologists and the University’s Mt. Hope Family Center have been awarded a $3.1 million grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development ( NICHD ) to study the pandemic’s implications for American families and parenting.
The study’s principal coinvestigators, psychology professors Melissa Sturge-Apple and Patrick Davies , expect acute negative effects on family functioning and family cohesion to last for years, especially in families that already experienced high levels of difficulties prior to the pandemic.
While scientifically sound, measures to slow the pandemic—such as stay-at-home orders, remote instruction, and limited public gatherings—had negative repercussions on families.
“The pandemic has been extremely stressful for families with significant worries about the health of family members, financial instability, food uncertainty, social isolation, and increased caregiving burdens associated with having children at home,” says Sturge-Apple, who is also the University’s vice provost and dean of graduate education. “The study seeks to identify factors that helped families cope, in order to inform best interventions for families at risk.”
How and why COVID amplifies family conflict
During the pandemic, the incidence of domestic violence in the US surged, with estimates ranging between a 21 to 35 percent increase. These statistics are particularly distressing in the context of already high levels of harsh parenting , as documented in Davies and Sturge-Apple’s work, even before the pandemic.
“By following families before, during, and after the pandemic, we will be able to assess more precisely how and why COVID-19 may amplify conflict between parents that then spills over into the way they care for their children,” says Davies. “Our study will examine a number of different mechanisms at neurobiological, familial, and extrafamilial levels.”
What helped secure the NICHD funding was the existence of a recent three-year family study at Mt. Hope Family Center immediately prior to the onset of the pandemic, which provides a baseline against which the additional COVID-19 stressors and effects can be measured. The teams plan on three additional annual waves of data collection.
Understanding the public health significance is crucial for developmental scientists, clinicians, and public policy advocates in order to develop evidence-based treatments and interventions that help struggling families.
The NICHD will award the grant funding over five years.

The Mt. Hope Family Center sits on a two-way street. Its researchers and clinicians have provided evidence-based services to at-risk families, while training the next generation of clinicians and research scientists.

New grants recognize the center’s success in addressing complex challenges among vulnerable children and their families.

A new study shows that early experiences of environmental harshness, in combination with personal temperament, can shape the child’s problem-solving abilities later in life.
More in Society & Culture

Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:

In Their Own Words, Americans Describe the Struggles and Silver Linings of the COVID-19 Pandemic
The outbreak has dramatically changed americans’ lives and relationships over the past year. we asked people to tell us about their experiences – good and bad – in living through this moment in history..
Pew Research Center has been asking survey questions over the past year about Americans’ views and reactions to the COVID-19 pandemic. In August, we gave the public a chance to tell us in their own words how the pandemic has affected them in their personal lives. We wanted to let them tell us how their lives have become more difficult or challenging, and we also asked about any unexpectedly positive events that might have happened during that time.
The vast majority of Americans (89%) mentioned at least one negative change in their own lives, while a smaller share (though still a 73% majority) mentioned at least one unexpected upside. Most have experienced these negative impacts and silver linings simultaneously: Two-thirds (67%) of Americans mentioned at least one negative and at least one positive change since the pandemic began.
For this analysis, we surveyed 9,220 U.S. adults between Aug. 31-Sept. 7, 2020. Everyone who completed the survey is a member of Pew Research Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. This way nearly all U.S. adults have a chance of selection. The survey is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
Respondents to the survey were asked to describe in their own words how their lives have been difficult or challenging since the beginning of the coronavirus outbreak, and to describe any positive aspects of the situation they have personally experienced as well. Overall, 84% of respondents provided an answer to one or both of the questions. The Center then categorized a random sample of 4,071 of their answers using a combination of in-house human coders, Amazon’s Mechanical Turk service and keyword-based pattern matching. The full methodology and questions used in this analysis can be found here.
In many ways, the negatives clearly outweigh the positives – an unsurprising reaction to a pandemic that had killed more than 180,000 Americans at the time the survey was conducted. Across every major aspect of life mentioned in these responses, a larger share mentioned a negative impact than mentioned an unexpected upside. Americans also described the negative aspects of the pandemic in greater detail: On average, negative responses were longer than positive ones (27 vs. 19 words). But for all the difficulties and challenges of the pandemic, a majority of Americans were able to think of at least one silver lining.
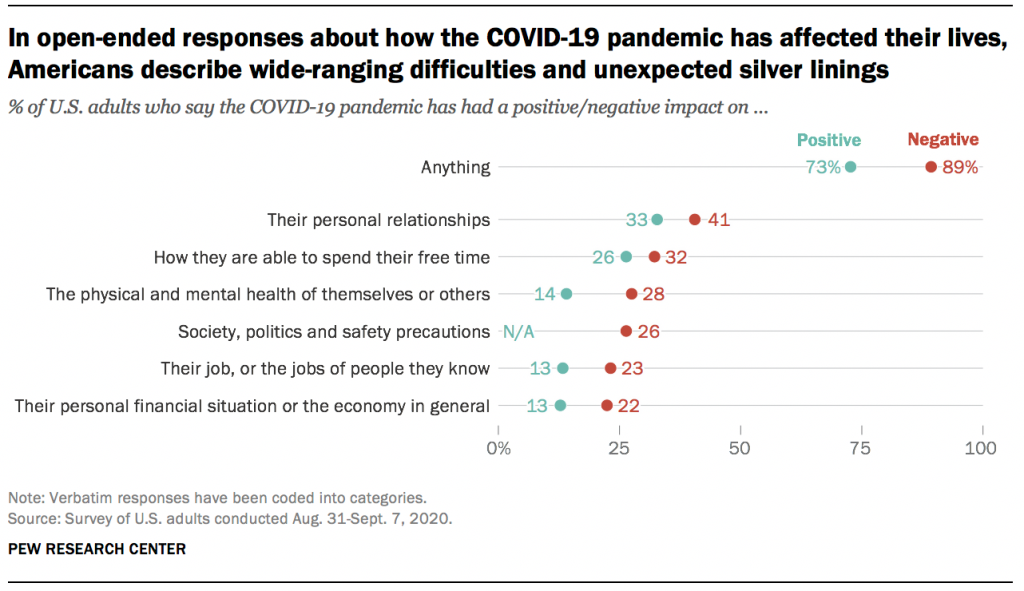
Both the negative and positive impacts described in these responses cover many aspects of life, none of which were mentioned by a majority of Americans. Instead, the responses reveal a pandemic that has affected Americans’ lives in a variety of ways, of which there is no “typical” experience. Indeed, not all groups seem to have experienced the pandemic equally. For instance, younger and more educated Americans were more likely to mention silver linings, while women were more likely than men to mention challenges or difficulties.
Here are some direct quotes that reveal how Americans are processing the new reality that has upended life across the country.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
- Open access
- Published: 30 November 2020
Family perspectives of COVID-19 research
- Shelley M. Vanderhout 1 ,
- Catherine S. Birken 2 ,
- Peter Wong 3 ,
- Sarah Kelleher 4 ,
- Shannon Weir 4 &
- Jonathon L. Maguire 1 , 5
Research Involvement and Engagement volume 6 , Article number: 69 ( 2020 ) Cite this article
186k Accesses
20 Citations
3 Altmetric
Metrics details
The COVID-19 pandemic has uniquely affected children and families by disrupting routines, changing relationships and roles, and altering usual child care, school and recreational activities. Understanding the way families experience these changes from parents’ perspectives may help to guide research on the effects of COVID-19 among children.
As a multidisciplinary team of child health researchers, we assembled a group of nine parents to identify concerns, raise questions, and voice perspectives to inform COVID-19 research for children and families. Parents provided a range of insightful perspectives, ideas for research questions, and reflections on their experiences during the pandemic.
Including parents as partners in early stages of COVID-19 research helped determine priorities, led to more feasible data collection methods, and hopefully has improved the relevance, applicability and value of research findings to parents and children.
Peer Review reports
Plain English summary
Understanding the physical, mental, and emotional impacts of the COVID-19 pandemic for children and families will help to guide approaches to support families and children during the pandemic and after. As a team of child health researchers in Toronto, Canada, we assembled a group of parents and clinician researchers during the COVID-19 pandemic to identify concerns, raise questions, and voice perspectives to inform COVID-19 research for children and families. Parents were eager to share their experience of shifting roles, priorities, and routines during the pandemic, and were instrumental in guiding research priorities and methods to understand of the effects of COVID-19 on families. First-hand experience that parents have in navigating the COVID-19 pandemic with their families contributed to collaborative relationships between researchers and research participants, helped orient research about COVID-19 in children around family priorities, and offered valuable perspectives for the development of guidelines for safe return to school and childcare. Partnerships between researchers and families in designing and delivering COVID-19 research may lead to a better understanding of how health research can best support children and their families during the COVID-19 pandemic.
Children and families have been uniquely affected by the COVID-19 pandemic. While children appear to experience milder symptoms from COVID-19 infection than older individuals [ 1 ], sudden changes in routines, resources, and relationships as a result of restrictions on physical interaction have resulted in major impacts on families with young children. In the absence of school, child care, extra-curricular activities and family gatherings, children’s social and support networks have been broadly disrupted. Stress from COVID-19 has been compounded by additional responsibilities for parents as they adapt to their new roles as educators and playmates while balancing full-time caregiving with their own stressful changes to work, financial and social situations. On the contrary, families with greater parental support and perceived control have had less perceived stress during COVID-19 [ 2 ].
The COVID-19 pandemic has rapidly sparked research activity across the globe. Patient and family voices are increasingly considered essential to research agenda and priority setting [ 3 ]. Understanding the physical, mental, and emotional consequences of the COVID-19 pandemic for families will inform approaches to support parents and children during the pandemic and after. In this unusual time, patient and family voices can be valuable in informing health research priorities, study designs, implementation plans and knowledge translation strategies that directly affect them [ 4 ].
As a multidisciplinary team of child health researchers with expertise in general paediatrics, nutrition and mental health, we assembled a group of nine parents to identify concerns, raise questions, and voice perspectives to inform COVID-19 research for children and families. Parents were recruited from the TARGet Kids! primary care research network [ 5 ], which is a collaboration between applied health researchers at the SickKids and St. Michael’s Hospitals, primary care providers from the Departments of Pediatrics and Family and Community Medicine at the University of Toronto, and families. Parents were contacted by email and invited to voluntary meetings on April 7 and 23, 2020 via Zoom [ 6 ] for 3 h. In an unstructured discussion, we asked how parents imagined research about COVID-19 could make an impact on child and family well-being. Parents were encouraged to share their lived experience and perspectives on the anticipated effects of COVID-19 and social distancing policies on their children and families, and opinions to inform how research on child mental and physical health during and after the pandemic could best be conducted. Parents had opportunities to review proposed data collection tools such as smartphone apps and serology testing devices, and provided feedback about the feasibility and meaningfulness of each. Content, frequency and organization of questionnaires were also reviewed by parents to ensure they were appropriate in length and feasible to complete.
Parent perspectives
Parents were optimistic that research would provide an understanding of the effects of COVID-19 on families and deliver solutions to minimize negative effects and bolster positive effects. Parents wondered about several questions which they hoped research would answer including: What will be the effects of physical distancing and disrupted routines for my children? How can I help my children develop healthy coping habits? How can I appropriately talk about the virus with my children? What factors might predict resiliency against negative effects of the pandemic among children and families, and how can these be strengthened?
Parents speculated what risks children might face as a result of schoolwork transitioning to home, educational activities provided online, child care being limited or unavailable, social relationships changing, sports and extra-curricular activities being cancelled, and stress and anxiety increasing at home. Some parents reflected on feeling some relief from not having to coordinate usual extracurricular activities. However, they expressed frustration in finding high quality educational activities and resources to support physical and mental health for their children during physical isolation. Parents voiced a need for a centralized, accessible hub with peer reviewed, high quality resources to keep children entertained and supported while spending more time indoors, away from usual activities and school. They hoped for resources to help families adjust to new routines and roles, as well as answer children’s questions in truthful ways that would not increase anxiety.
Parents were curious about studying the impact of COVID-19 on children and families. How would researchers use information about children who are affected physically, mentally, or socially by the pandemic? What could be the possible implications of testing for COVID-19 on social relationships and parents’ employment? This question generated discussion about difficult positions families of lower socio-economic status, who may need to maintain attendance at work but have a suspected COVID-19 infected household member. Would health and social care for children going forward reflect the unique ways they had been impacted by changes in their daily routines and relationships? How can families return to school and everyday routines with a minimum of disruption? What will be done to prepare children and families for emergency situations in the future? Considering these questions may lead child health researchers to study relevant and contemporary concepts to families during the COVID-19 pandemic.
When presented with options to include more measures on other family members, parents maintained that the focus of our COVID-19 research should be on children. Parents provided essential feedback about the length and frequency of questionnaires, to ensure they were appropriate given the limited time available for completing them. Parent involvement early in the research process helped to direct research priorities, informed data collection strategies and hopefully has increased the relevance of research conducted for children and families. Conducting a follow-up meeting with parents was important to understand shifting concerns and ensure data collection was reflecting current routines, habits and policies affecting families.
Conclusions
As researchers who are seeking to understand the impact of COVID-19 on children and families, we felt it important to involve families in designing and implementing new research. First-hand experience that parents have in navigating the COVID-19 pandemic with their children contributed to co-building between researchers and research participants. Parents were generous with their time and provided insightful, honest suggestions for how researchers could create knowledge that would be directly relevant to them. Next steps will include expanding our dialogue with a more diverse group of parents in terms of gender, as all parents in our meetings were women, and ethnicity to better represent the diversity of Toronto. Other researchers conducting COVID-19 research among children and families may consider engaging parents and caregivers in preliminary stages to identify priorities, understand lived experiences and help guide all stages of the research process. This presents value in focusing research on the most important priorities for families and developing data collection methods which are feasible in the context of the COVID-19 pandemic. As the nature of the COVID-19 pandemic is dynamic, ongoing communication between researchers and parents to understand changing perspectives and concerns is important to respond to family needs. We hope that ongoing partnerships between parents and researchers will promote leadership among parents as co-investigators in COVID-19 research, and result in research which addresses the needs of parents and children during the COVID-19 pandemic. Ideally, engaging with families in COVID-19 research will result in findings that will be valuable to families, assist them in developing collective resilience, and provide a foundation for family-oriented research throughout the COVD-19 pandemic and beyond.
Availability of data and materials
Not applicable.
Lee PI, Hu YL, Chen PY, Huang YC, Hsueh PR. Are children less susceptible to COVID-19? J Microbiol Immunol Infect. 2020;53(3):371.
Article CAS Google Scholar
Brown SM, Doom JR, Lechuga-Pena S, Watamura SE, Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse Negl. 2020;1:104699.
Article Google Scholar
Manafo E, Petermann L, Vandall-Walker V, Mason-Lai P. Patient and public engagement in priority setting: a systematic rapid review of the literature. PLoS One. 2018;13(3):e0193579.
Strategy for Patient Oriented Research. Strategy for Patient-Oriented Research - Patient Engagement Framework. http://www.cihr-irsc.gc.ca/e/48413.html-a7 . Published 2019. Accessed 2020.
Carsley S, Borkhoff CM, Maguire JL, et al. Cohort profile: the applied research Group for Kids (TARGet kids!). Int J Epidemiol. 2014;44(3):776.
Zoom [computer program]. Version 2.0.02020.
Download references
Acknowledgements
We thank the TARGet Kids! Parent And Clinician Team for their generous contribution of time and participation in discussions about COVID-19 in children and families.
Ethical approval and consent to participate
There is no funding source for this paper.
Author information
Authors and affiliations.
Li Ka Shing Knowledge Institute of St. Michael’s Hospital, Unity Health Toronto, 209 Victoria St, Toronto, ON, M5B 1T8, Canada
Shelley M. Vanderhout & Jonathon L. Maguire
Division of Paediatric Medicine and the Paediatric Outcomes Research Team, The Hospital for Sick Children, 555 University Avenue, Toronto, Ontario, M5G 1X8, Canada
Catherine S. Birken
Child Health Evaluative Sciences, The Hospital for Sick Children, Peter Gilgan Centre for Research & Learning, 686 Bay Street, 11th floor, Toronto, Ontario, M5G 0A4, Canada
Patient partners, Toronto, Canada
Sarah Kelleher & Shannon Weir
Toronto, Canada
Jonathon L. Maguire
You can also search for this author in PubMed Google Scholar
Contributions
Shelley Vanderhout, Catherine Birken, Peter Wong, Shannon Weir, Sarah Kelleher and Jonathon Maguire participated in the concept and design, drafting and revising of the manuscript. All authors approved the manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Correspondence to Jonathon L. Maguire .
Ethics declarations
Consent for publication, competing interests.
The authors have no competing interest to disclose.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Vanderhout, S.M., Birken, C.S., Wong, P. et al. Family perspectives of COVID-19 research. Res Involv Engagem 6 , 69 (2020). https://doi.org/10.1186/s40900-020-00242-1
Download citation
Received : 18 August 2020
Accepted : 24 November 2020
Published : 30 November 2020
DOI : https://doi.org/10.1186/s40900-020-00242-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Research Involvement and Engagement
ISSN: 2056-7529
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 27 January 2021
The effects of social isolation on well-being and life satisfaction during pandemic
- Ruta Clair ORCID: orcid.org/0000-0001-9828-9911 1 ,
- Maya Gordon 1 ,
- Matthew Kroon 1 &
- Carolyn Reilly 1
Humanities and Social Sciences Communications volume 8 , Article number: 28 ( 2021 ) Cite this article
98k Accesses
148 Citations
161 Altmetric
Metrics details
- Health humanities
The SARS-CoV-2 pandemic placed many locations under ‘stay at home” orders and adults simultaneously underwent a form of social isolation that is unprecedented in the modern world. Perceived social isolation can have a significant effect on health and well-being. Further, one can live with others and still experience perceived social isolation. However, there is limited research on psychological well-being during a pandemic. In addition, much of the research is limited to older adult samples. This study examined the effects of perceived social isolation in adults across the age span. Specifically, this study documented the prevalence of social isolation during the COVID-19 pandemic as well as the various factors that contribute to individuals of all ages feeling more or less isolated while they are required to maintain physical distancing for an extended period of time. Survey data was collected from 309 adults who ranged in age from 18 to 84. The measure consisted of a 42 item survey from the Revised UCLA Loneliness Scale, Measures of Social Isolation (Zavaleta et al., 2017 ), and items specifically about the pandemic and demographics. Items included both Likert scale items and open-ended questions. A “snowball” data collection process was used to build the sample. While the entire sample reported at least some perceived social isolation, young adults reported the highest levels of isolation, χ 2 (2) = 27.36, p < 0.001. Perceived social isolation was associated with poor life satisfaction across all domains, as well as work-related stress, and lower trust of institutions. Higher levels of substance use as a coping strategy was also related to higher perceived social isolation. Respondents reporting higher levels of subjective personal risk for COVID-19 also reported higher perceived social isolation. The experience of perceived social isolation has significant negative consequences related to psychological well-being.
Similar content being viewed by others

Loneliness trajectories over three decades are associated with conspiracist worldviews in midlife

Determinants of behaviour and their efficacy as targets of behavioural change interventions
Mechanisms linking social media use to adolescent mental health vulnerability
Introduction.
In March 2020, the World Health Organization declared the COVID-19 outbreak a global pandemic, prompting most governors in the United States to issue stay-at-home orders in an effort to minimize the spread of COVID-19. This was after several months of similar quarantine orders in countries throughout Asia and Europe. As a result, a unique situation arose, in which most of the world’s population was confined to their homes, with only medical staff and other essential workers being allowed to leave their homes on a regular basis. Several studies of previous quarantine episodes have shown that psychological stress reactions may emerge from the experience of physical and social isolation (Brooks et al., 2020 ). In addition to the stress that might arise with social isolation or being restricted to your home, there is also the stress of worrying about contracting COVID-19 and losing loved ones to the disease (Brooks et al., 2020 ; Smith and Lim, 2020 ). For many families, this stress is compounded by the challenge of working from home while also caring for children whose schools had been closed in an effort to slow the spread of the disease. While the effects of social isolation has been reported in the literature, little is known about the effects of social isolation during a global pandemic (Galea et al., 2020 ; Smith and Lim, 2020 ; Usher et al., 2020 ).
Social isolation is a multi-dimensional construct that can be defined as the inadequate quantity and/or quality of interactions with other people, including those interactions that occur at the individual, group, and/or community level (Nicholson, 2012 ; Smith and Lim, 2020 ; Umberson and Karas Montez, 2010 ; Zavaleta et al., 2017 ). Some measures of social isolation focus on external isolation which refers to the frequency of contact or interactions with other people. Other measures focus on internal or perceived social isolation which refers to the person’s perceptions of loneliness, trust, and satisfaction with their relationships. This distinction is important because a person can have the subjective experience of being isolated even when they have frequent contact with other people and conversely they may not feel isolated even when their contact with others is limited (Hughes et al., 2004 ).
When considering the effects of social isolation, it is important to note that the majority of the existing research has focused on the elderly population (Nyqvist et al., 2016 ). This is likely because older adulthood is a time when external isolation is more likely due to various circumstances such as retirement, and limited physical mobility (Umberson and Karas Montez, 2010 ). During the COVID-19 pandemic the need for physical distancing due to virus mitigation efforts has exacerbated the isolation of many older adults (Berg-Weger and Morley, 2020 ; Smith et al., 2020 ) and has exposed younger adults to a similar experience (Brooks et al., 2020 ; Smith and Lim, 2020 ). Notably, a few studies have found that young adults report higher levels of loneliness (perceived social isolation) even though their social networks are larger (Child and Lawton, 2019 ; Nyqvist et al., 2016 ; Smith and Lim, 2020 ); thus indicating that age may be an important factor to consider in determining how long-term distancing due to COVID-19 will influence people’s perceptions of being socially isolated.
The general pattern in this research is that increased social isolation is associated with decreased life satisfaction, higher levels of depression, and lower levels of psychological well-being (Cacioppo and Cacioppo, 2014 ; Coutin and Knapp, 2017 ; Dahlberg and McKee, 2018 ; Harasemiw et al., 2018 ; Lee and Cagle, 2018 ; Usher et al., 2020 ). Individuals who experience high levels of social isolation may engage in self-protective thinking that can lead to a negative outlook impacting the way individuals interact with others (Cacioppo and Cacioppo, 2014 ). Further, restricting social networks and experiencing elevated levels of social isolation act as mediators that result in elevated negative mood and lower satisfaction with life factors (Harasemiw et al., 2018 ; Zheng et al., 2020 ). The relationship between well-being and feelings of control and satisfaction with one’s environment are related to psychological health (Zheng et al., 2020 ). Dissatisfaction with one’s home, resource scarcity such as food and self-care products, and job instability contribute to social isolation and poor well-being (Zavaleta et al., 2017 ).
Although there are fewer studies with young and middle aged adults, there is some evidence of a similar pattern of greater isolation being associated with negative psychological outcomes for this population (Bergin and Pakenham, 2015 ; Elphinstone, 2018 ; Liu et al., 2019 ; Nicholson, 2012 ; Smith and Lim, 2020 ; Usher et al., 2020 ). There is also considerable evidence that social isolation can have a detrimental impact on physical health (Holt-Lunstad et al., 2010 ; Steptoe et al., 2013 ). In a meta-analysis of 148 studies examining connections between social relationships and risk of mortality, Holt-Lunstad et al. ( 2010 ) concluded that the influence of social relationships on the risk for death is comparable to the risk caused by other factors like smoking and alcohol use, and greater than the risk associated with obesity and lack of exercise. Likewise, other researchers have highlighted the detrimental impact of social isolation and loneliness on various illnesses, including cardiovascular, inflammatory, neuroendocrine, and cognitive disorders (Bhatti and Haq, 2017 ; Xia and Li, 2018 ). Understanding behavioral factors related to positive and negative copings is essential in providing health guidance to adult populations.
Feelings of belonging and social connection are related to life satisfaction in older adults (Hawton et al., 2011 ; Mellor et al., 2008 ; Nicholson, 2012 ; Victor et al., 2000 ; Xia and Li, 2018 ). While physical distancing initiatives were implemented to save lives by reducing the spread of COVID-19, these results suggest that social isolation can have a negative impact on both mental and physical health that may linger beyond the mitigation orders (Berg-Weger and Morley, 2020 ; Brooks et al., 2020 ; Cava et al., 2005 ; Smith et al., 2020 ; Usher et al., 2020 ). It is therefore important that we document the prevalence of social isolation during the COVID-19 pandemic as well as the various factors that contribute to individuals of all ages feeling more or less isolated, while they are required to maintain physical distancing for an extended period of time. It was hypothesized that perceived social isolation would not be limited to an older adult population. Further, it was hypothesized that perceived social isolation would be related to individual’s coping with the pandemic. Finally, it was hypothesized that the experience of social isolation would act as a mediator to life satisfaction and basic trust in institutions for individuals across the adult lifespan. The current study was designed to examine the following research questions:
Are there age differences in participants’ perceived social isolation?
Do factors like time spent under required distancing and worry about personal risk for illness have an association with perceived social isolation?
Is perceived social isolation due to quarantine and pandemic mitigation efforts related to life satisfaction?
Is there an association between perceived social isolation and trust of institutions?
Is there a difference in basic stressors and coping during the pandemic for individuals experiencing varying levels of perceived social isolation?
Participants
Participants were adults age 18 years and above. Individuals younger than 18 years were not eligible to participate in the study. There were no limitations on occupation, education, or time under mandatory “stay at home” orders. The researchers sought a sample of adults that was diverse by age, occupation, and ethnicity. The researchers sought a broad sample that would allow researchers to conduct a descriptive quantitative survey study examining factors related to perceived social isolation during the first months of the COVID-19 mitigation efforts.
Participants were asked to complete a 42-item electronic survey that consisted of both Likert-type items and open-ended questions. There were 20 Likert scale items, 3 items on a 3-point scale (1 = Hardly ever to 3 = Often) and 17 items on a 5-point scale (1 = Not at all satisfied to 4 = very satisfied, 0 = I don’t know), 11 multiple choice items, one of which had an available short response answer, and 11 short answer items.
Items were selected from Measures of Social Isolation (Zavaleta et al., 2017 ) that included 27 items to measure feelings of social isolation through the proxy variables of stress, trust, and life satisfaction. Trust was measured for government, business, and media. Life satisfaction examined overall feelings of satisfaction as well as satisfaction with resources such as food, housing, work, and relationships. Three items related to social isolation were chosen from the Revised UCLA Loneliness Scale. Hughes et al. ( 2004 ) reported that these three items showed good psychometric validity and reliability for the construct of Loneliness.
There were a further 12 items from the authors specifically about circumstances regarding COVID-19 at the time of the survey. Participants answered questions about the length of time spent distancing from others, level of compliance with local regulations, primary news sources, whether physical distancing was voluntary or mandatory, how many people are in their household, work availability, methods of communication, feelings of personal risk of contracting COVID-19, possible changes in behavior, coping methods, stressors, and whether there are children over the age of 18 staying in the home.
This study was submitted to the Cabrini University Institutional Review Board and approval was obtained in March 2020. Researchers recruited a sample of people that varied by age, gender, and ethnicity by identifying potential participants across academic and non-academic settings using professional contact lists. A “snowball” approach to data gathering was used. The researchers sent the survey to a broad group of adults and requested that the participants send the survey to others they felt would be interested in taking part in research. Recipients received an email that contained a description of the purpose of the study and how the data would be used. Included at the end of the email was a link to the online survey that first presented the study’s consent form. Participants acknowledged informed consent and agreed to participate by opening and completing the survey.
At the end of the survey, participants were given the opportunity to supply an email to participate in a longitudinal study which consists of completing surveys at later dates. In addition, the sample was asked to forward the survey to their contacts who might be interested. Overall, the study took ~10 min to complete.
Demographics
Participants were 309 adults who ranged in age from 18 to 84 ( M = 38.54, s = 18.27). Data was collected beginning in 2020 from late March until early April. At the time of data collection distancing mandates were in place for 64.7% and voluntary for 34.6% of the sample, while 0.6% lived in places which had not yet outlined any pandemic mitigation policies. The average length of time distancing was slightly more than 2 weeks ( M = 14.91 days, s = 4.5) with 30 days as the longest reported time.
The sample identified mostly as female (80.3%), with males (17.8%) and those who preferred not to answer (1.9%) representing smaller numbers. The majority of the sample identified as Caucasian (71.5%). Other ethnic identities reported by participants included Hispanic/Latinx, African-American/Black, Asian/East Asian, Jewish/Jewish White-Passing, Multiracial/Multiethnic, and Country of Origin (Table 1 ). Individuals resided in the United States and Europe.
The majority of the sample lived in households with others (Fig. 1 ). More than one-third (36.7%) lived with one other person, 19.7% lived with two others, and 21% lived with three other people. People living alone comprised 12.1% of the sample. When asked about the presence of children under 18 years of age in the home, 20.5% answered yes.
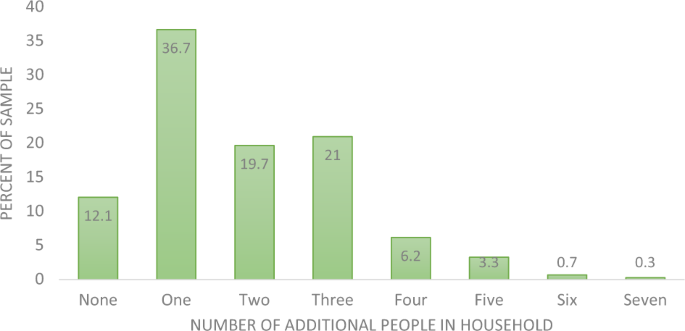
Figure shows how many additional individuals live in the participant’s household in March 2020.
The highest level of education attained ranged from completion of lower secondary school (0.3%) to doctoral level (6.8%). Two thirds of the sample consisted of individuals with a Bachelor’s degree or above (Table 2 ).
Participants were asked to provide their occupation. The largest group identified themselves as professionals (26.5%), while 38.6% reported their field of work (Table 3 ). Students comprised 23.1% of the sample, while 11.1% reported that they were retired. Some of the occupations reported by the sample included nurses and physicians, lawyers, psychologists, teachers, mental health professionals, retail sales, government work, homemakers, artists across types of media, financial analysts, hairdresser, and veterinary support personnel. One person indicated that they were unemployed prior to the pandemic.
Social isolation and demographics
Spearman’s rank-order correlations were used to examine relationships between the three Likert scale items from the Revised UCLA Loneliness Scale that measure social isolation. Feeling isolated from others was significantly correlated with lacking companionship ( r s = 0.45, p < 0.001) and feeling left out ( r s = 0.43, p < 0.001). The items related to lacking companionship and feeling left out were also significantly correlated ( r s = 0.39, p < 0.001).
Kruskal–Wallis tests were conducted to determine if the variables of time in required distancing and age were each related to the three levels of social isolation (hardly, sometimes, often). There were no significant findings between perceived social isolation and length of time in required distancing, χ 2 (2) = 0.024, p = 0.98.
A significant relationship was found between perceived social isolation and age, χ 2 (2) = 27.36, p < 0.001). Subsequently, pairwise comparisons were performed using Dunn’s procedure with a Bonferroni correction for multiple comparisons. Adjusted p values are presented. Post hoc analysis revealed statistically significant differences in age between those with high levels of social isolation (Mdn = 25) and some social isolation (Mdn = 31) ( p = <0.001) and low isolation (Mdn = 46) ( p = 0.002). Higher levels of social isolation were associated with younger age.
Age was then grouped (18–29, 30–49, 50–69, 70+) and a significant relationship was found between social isolation and age, χ 2 (3) = 13.78, p = 0.003). Post hoc analysis revealed statistically significant differences in perceived social isolation across age groups. The youngest adults (age 18–29) reported significantly higher social isolation (Mdn = 2.4) than the two oldest groups (50–69 year olds: Mdn = 1.6, p = 004); age 70 and above: Mdn = 1.57), p = 0.01). The difference between the youngest adults and the next youngest (30–49) was not significant ( p = 0.09).
When asked if participants feel personally at risk for contracting SARS-CoV-2 61.2% reported that they feel at risk. A Mann–Whitney U test was conducted to compare social isolation experienced by those who reported feeling at risk and those who did not feel at risk. Individuals who feel at risk for infection reported more social isolation (Mdn = 2.0) than those that do not feel at risk (Mdn = 1.75), U = 9377, z = −2.43, p = 0.015.
Social isolation and life satisfaction
The relationship between level of social isolation and overall life satisfaction were examined using Kruskal–Wallis tests as the measure consisted of Likert-type items (Table 4 ).
Overall life satisfaction was significantly lower for those who reported greater social isolation ( χ 2 (2) = 50.56, p < 0.001). Post hoc analysis revealed statistically significant differences in life satisfaction scores between those with high levels of social isolation (Mdn = 2.82) and some social isolation (Mdn = 3.04) ( p ≤ 0.001) and between high and low isolation (Mdn = 3.47) ( p ≤ 0.001), but not between high levels of social isolation and some social isolation ( p = 0.09).
The pandemic added concern about access to resources such as food and 68% of the sample reported stress related to availability of resources. A significant relationship was found between social isolation and satisfaction with access to food, χ 2 (2) = 21.92, p < 0.001). Individuals reporting high levels of social isolation were the least satisfied with their food situation. Statistical difference were evident between high social isolation (Mdn = 3.28) and some social isolation (Mdn = 3.46) ( p = 0.003) and between high and low isolation (Mdn = 3.69) ( p < 0.001). Reporting higher levels of social isolation is associated with lower satisfaction with food.
As a result of stay at home orders, many participants were spending more time in their residences than prior to the pandemic. A significant relationship was found between social isolation and housing satisfaction, χ 2 (2) = 10.33, p = 0.006). Post hoc analysis revealed statistically a significant difference in housing satisfaction between those with high levels of social isolation (Mdn = 3.49) and low social isolation (Mdn = 3.75) ( p = 0.006). Higher levels of social isolation is associated with lower levels of satisfaction with housing.
Work life changed for many participants and 22% of participants reported job loss as a result of the pandemic. A significant relationship was found between social isolation and work satisfaction, χ 2 (2) = 21.40, p < 0.001). Post hoc analysis revealed individuals reporting high social isolation reported much lower satisfaction with work (Mdn = 2.53) than did those reporting low social isolation (Mdn = 3.27) ( p < 0.001) and moderate social isolation (Mdn = 3.03) ( p = 0.003).
Social isolation and trust of institutions
The relationship between social isolation and connection to community was measured using a Kruskal–Wallis test. A significant relationship was found between feelings of social isolation and connection to community ( χ 2 (2) = 13.97, p = 0.001. Post hoc analysis revealed a statistically significant difference in connection to community such that the group reporting higher social isolation (Mdn = 2.27, p = 0.001) reports less connection to their community than the group reporting low social isolation (Mdn = 2.93).
A significant relationship was found between social isolation and trust of central government institutions, χ 2 (2) = 10.46, p = 0.005). Post hoc analysis revealed a statistically significant difference in trust of central government between individuals reporting low social isolation (Mdn = 2.91) and those reporting high social isolation (Mdn = 2.32) ( p = 0.008) and moderate social isolation (Mdn = 2.48) ( p = 0.03). There was less trust of central government for the group reporting high social isolation. However, distrust of central government did not extend to local government institutions. There was no significant difference in trust of local government for low, moderate, and high social isolation groups, χ 2 (2) = 5.92, p = 0.052.
Trust levels of business was significantly different between groups that differed in feelings of social isolation, χ 2 (2) = 9.58, p = 0.008). Post hoc analysis revealed more trust of business institutions for the low social isolation group (Mdn = 3.10) compared to the group reporting high social isolation (Mdn = 2.62) ( p = 0.007).
Sixty-seven participants reported loss of a job as a result of COVID-19. A Mann–Whitney U test was conducted to compare social isolation experienced by those who had lost their job to those who had not. Individuals who experienced job loss reported more social isolation (Mdn = 2.26) than those that did not lose their job (Mdn = 1.80), U = 5819.5, z = −3.66 , p < 0.001.
Stress related to caring for an elderly family member was identified by 12% of the sample. A Mann–Whitney U test was conducted to compare social isolation experienced by those who reported that caring for an elderly family member is a stressor to those who had not. There was no significant finding, U = 4483, z = −1.28, p = 0.20. Similarly, there was no significant effect for caring for a child, U = 3568.5, z = −0.48, p = 0.63.
Coping strategies
Participants were asked to check off whether they were using virtual communication, exercise, going outdoors, and/or substances in order to cope with the challenges of distancing during pandemic. A Mann–Whitney U test was conducted to compare social isolation experienced by those who used substances as a coping strategy and those that did not. Individuals who reported substance use reported more social isolation (Mdn = 2.12) than those that did not (Mdn = 1.80), U = 6724, z = −2.01, p = 0.04.
There was no significant difference on Mann–Whitney U test for social isolation between those individuals who went outdoors to cope with pandemic versus those that did not, U = 5416, z = −0.72, p = 0.47. Similarly, there was no difference in social isolation between those individuals who used exercise as a coping tool and those that did not. Finally, there was no difference in social isolation between those that used virtual communication tools and those that did not, U = 7839.5, z = −0.56, p = 0.58. The only coping strategy which was significantly associated with social isolation was substance use.
While research has explored the subjective experience of social isolation, the novel experience of mass physical distancing as a result of the SARS-CoV-2 pandemic suggests that social isolation is a significant factor in the public health crisis. The experience of social isolation has been examined in older populations but less often in middle-age and younger adults (Brooks et al., 2020 ; Smith and Lim, 2020 ). Perceived social isolation is related to numerous negative outcomes related to both physical and mental health (Bhatti and Haq, 2017 ; Holt-Lunstad et al., 2010 , Victor et al., 2000 ; Xia and Li, 2018 ). Our findings indicate that younger adults in their 20s reported more social isolation than did those individuals aged 50 and older during physical distancing. This supports the findings of Nyqvist et al. ( 2016 ) that found teenagers and young adults in Finland reported greater loneliness than did older adults.
The experience of social isolation is related to a reduction in life satisfaction. Previous research has shown that feelings of social connection are related to general life satisfaction in older adults (Hawton et al., 2011 , Hughes et al., 2004 , Mellor et al., 2008 ; Victor et al., 2000 , Xia and Li, 2018 ). These findings indicate that perceived social isolation can be a significant mediator in life satisfaction and well-being across the adult lifespan during a global health crisis. Individuals reporting higher levels of social isolation experience less satisfaction with the conditions in their home.
During mandated “stay-at-home” conditions, the experience of work changed for many people. For many adults work is an essential aspect of identity and life satisfaction. The experience of individuals reporting elevated social isolation was also related to lower satisfaction with work. This study included a wide span of occupations involving both individuals required to work from home and essential workers continuing to work outside the home. Further, ~22% of the sample ( n = 67) reported job loss as a stressor related to the SARS-CoV-2 pandemic and reported elevated social isolation. As institutions and businesses consider whether remote work is an economically viable alternative to face-to-face offices once physical distancing mandates are ended, the needs of workers for social interaction should be considered.
Further, individuals reporting higher social isolation also indicated less connection to their community and lower satisfaction with environmental factors such as housing and food. Findings indicate that higher perceived social isolation is associated with broad dissatisfaction across social and life domains and perceptions of personal risk from COVID-19. This supports research that identified a relationship between social isolation and health-related quality of life outcomes (Hawton et al., 2011 , Victor et al., 2000 ). Perceptions of elevated social isolation are related to lower life satisfaction in functional and social domains.
Perceived social isolation is likewise related to trust of some institutions. While there was no effect for local government, individuals with higher perceived social isolation reported less trust of central government and of business. There is an association between higher levels of perceived social isolation and less connection to the community, lower life satisfaction, and less trust of large-scale institutions such as central government and businesses. As a result, the individuals who need the most support may be the most suspicious of the effectiveness of those institutions.
Coping strategies related to exercise, time spent outdoors, and virtual communication were not related to social isolation. However, individuals who reported using substances as a coping strategy reported significantly higher social isolation than did the group who did not indicate substance use as a coping strategy. Perceived social isolation was associated with negative coping rather than positive coping. This study shows that clinicians and health care providers should ask about coping strategies in order to provide effective supports for individuals.
There are several limitations that may limit the generalizability of the findings. The study is heavily female and this may have an effect on findings. In addition, the majority of the sample has a post-secondary degree and, as such, this study may not accurately reflect the broad experience of individuals during pandemic. Further, it cannot be ruled out that individuals reporting high levels of perceived social isolation may have experienced some social isolation prior to the pandemic.
Conclusions
In conclusion, this study suggests that perceived social isolation is a significant element of health-related quality of life during pandemic. Perceived social isolation is not just an issue for older adults. Indeed, young adults appear to be suffering greatly from the distancing required to reduce the spread of SARS-CoV-2. The experience of social isolation is associated with poor life satisfaction across domains, work-related stress, lower trust of institutions such as central government and business, perceived personal risk for COVID-19, and higher levels of use of substances as a coping strategy. Measuring the degree of perceived social isolation is an important addition to wellness assessments. Stress and social isolation can impact health and immune function and so reducing perceived social isolation is essential during a time when individuals require strong immune function to fight off a novel virus. Further, it is anticipated that these widespread effects may linger as the uncertainty of the virus continues. As a result, we plan to follow participants for at least a year to examine the impact of SARS-CoV-2 on the well-being of adults.
Data availability
The dataset generated during and analyzed during the current study is not publicly available due to ethical restrictions and privacy agreements between the authors and participants.
Berg-Weger M, Morley J (2020) Loneliness and social isolation in older adults during the COVID-19 pandemic: implications for gerontological social work. J Nutr Health Aging 24(5):456–458
Article CAS Google Scholar
Bergin A, Pakenham K (2015) Law student stress: relationships between academic demands, social isolation, career pressure, study/life imbalance, and adjustment outcomes in law students. Psychiatry Psychol Law 22:388–406
Article Google Scholar
Bhatti A, Haq A (2017) The pathophysiology of perceived social isolation: effects on health and mortality. Cureus 9(1):e994. https://doi.org/10.7759/cureus.994
Article PubMed PubMed Central Google Scholar
Brooks S, Webster R, Smith L, Woodland L, Wesseley S, Greenberg N, Rubin G (2020) The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395:912–920
Cacioppo JT, Cacioppo S (2014) Social relationships and health: the toxic effects of perceived social isolation. Soc Personal Psychol Compass 8(2):58–72. https://doi.org/10.1111/spc3.12087
Cava M, Fay K, Beanlands H, McCay E, Wignall R (2005) The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs 22(5):398–406
Child ST, Lawton L (2019) Loneliness and social isolation among young and late middle age adults: associations with personal networks and social participation. Aging Mental Health 23:196–204
Coutin E, Knapp M (2017) Social isolation, loneliness, and health in old age. Health Soc Care Community 25:799–812
Dahlberg L, McKee KJ (2018) Social exclusion and well-being among older adults in rural and urban areas. Arch Gerontol Geriatrics 79:176–184
Elphinstone B (2018) Identification of a suitable short-form of the UCLA-Loneliness Scale. Austral Psychol 53:107–115
Galea S, Merchant R, Lurie N (2020) The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med 180(6):817–818
Harasemiw O, Newall N, Mackenzie CS, Shooshtari S, Menec V (2018) Is the association between social network types, depressive symptoms and life satisfaction mediated by the perceived availability of social support? A cross-sectional analysis using the Canadian Longitudinal Study on Aging. Aging Mental Health 23:1413–1422
Hawton A, Green C, Dickens A, Richards C, Taylor R, Edwards R, Greaves C, Campbell J (2011) The impact of social isolation on the health status and health-related quality of life of older people. Qual Life Res 20:57–67
Holt-Lunstad J, Smith TB, Layton JB (2010) Social relationships and mortality risk: a meta-analytic review. PLoS Med 7:1–20
Hughes M, Waite L, Hawkley L, Cacioppo J (2004) A short scale of measuring loneliness in large surveys: results from two population-based studies. Res Aging 26(6):655–672
Lee J, Cagle JG (2018) Social exclusion factors influencing life satisfaction among older adults. J Poverty Soc Justice 26:35–50
Liu H, Zhang M, Yang Q, Yu B (2019) Gender differences in the influence of social isolation and loneliness on depressive symptoms in college students: a longitudinal study. Soc Psychiatry Psychiatr Epidemiol 55:251–257. https://doi.org/10.1007/s00127-019-01726-6
Article PubMed Google Scholar
Mellor D, Stokes M, Firth L, Hayashi Y, Cummins R (2008) Need for belonging, relationship satisfaction, loneliness, and life satisfaction. Personal Individ Differ 45(2008):213–218
Nicholson N (2012) A review of social isolation: an important but underassessed condition in older adults. J Prim Prev 33(2–3):137–152. https://doi.org/10.1007/s10935-012-0271-2
Nyqvist F, Victor C, Forsman A, Cattan M (2016) The association between social capital and loneliness in different age groups: a population-based study in Western Finland. BMC Public Health 16:542. https://doi.org/10.1186/s12889-016-3248-x
Smith B, Lim M (2020) How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res Pract 30(2):e3022008. https://doi.org/10.17061/phrp3022008
Smith M, Steinman L, Casey EA (2020). Combatting social isolation among older adults in the time of physical distancing: the COVID-19 social connectivity paradox. Front Public Health https://doi.org/10.3389/fpubh.2020.00403
Steptoe A, Shankar A, Demakakos P, Wardle J (2013) Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA 110(15):5797–5801. https://doi.org/10.1073/pnas.1219686110
Article ADS CAS PubMed Google Scholar
Umberson D, Karas Montez J (2010) Social relationships and health: a flashpoint for health policy. J Health Soc Behav 51:S54–66. https://doi.org/10.1177/0022146510383501
Usher K, Bhullar N, Jackson D (2020). Life in the pandemic: social isolation and mental health. J Clin Nurs https://doi.org/10.1111/jocn.15290
Victor C, Scambler S, Bond J, Bowling A (2000) Being alone in later life: loneliness, social isolation and living alone. Rev Clin Gerontol 10(4):407–417. https://doi.org/10.1017/S0959259800104101
Xia N, Li H (2018) Loneliness, social isolation, and cardiovascular health. Antioxid Redox Signal 28(9):837–851
Zavaleta D, Samuel K, Mills CT (2017) Measures of social isolation. Soc Indic Res 131(1):367–391
Zheng L, Miao M, Gan Y (2020). Perceived control buffers the effects of the covid-19 pandemic on general health and life satisfaction: the mediating role of psychological distance. Appl Psychol https://doi.org/10.1111/aphw.12232
Download references
Author information
Authors and affiliations.
Cabrini University, Radnor, USA
Ruta Clair, Maya Gordon, Matthew Kroon & Carolyn Reilly
You can also search for this author in PubMed Google Scholar
Contributions
All authors jointly supervised and contributed to this work.
Corresponding author
Correspondence to Ruta Clair .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Clair, R., Gordon, M., Kroon, M. et al. The effects of social isolation on well-being and life satisfaction during pandemic. Humanit Soc Sci Commun 8 , 28 (2021). https://doi.org/10.1057/s41599-021-00710-3
Download citation
Received : 29 August 2020
Accepted : 07 January 2021
Published : 27 January 2021
DOI : https://doi.org/10.1057/s41599-021-00710-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Assessing the impact of covid-19 on self-reported levels of depression during the pandemic relative to pre-pandemic among canadian adults.
- Rasha Elamoshy
- Marwa Farag
Archives of Public Health (2024)
Associations between social networks, cognitive function, and quality of life among older adults in long-term care
- Laura Dodds
- Carol Brayne
- Joyce Siette
BMC Geriatrics (2024)
Locked Down: The Gendered Impact of Social Support on Children’s Well-Being Before and During the COVID-19 Pandemic
- Jasper Dhoore
- Bram Spruyt
- Jessy Siongers
Child Indicators Research (2024)
Life Satisfaction during the Second Lockdown of the COVID-19 Pandemic in Germany: The Effects of Local Restrictions and Respondents’ Perceptions about the Pandemic
- Lisa Schmid
- Pablo Christmann
- Carolin Thönnissen
Applied Research in Quality of Life (2024)
From the table to the sofa: The remote work revolution in a context of crises and its consequences on work attitudes and behaviors
- Humberto Batista Xavier
- Suzana Cândido de Barros Sampaio
- Kathryn Cormican
Education and Information Technologies (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, the impact of the covid-19 pandemic on families: young people’s experiences in estonia.

- 1 Institute of Social Studies, University of Tartu, Tartu, Estonia
- 2 Institute of Cultural Research, University of Tartu, Tartu, Estonia
This articles reflects the impacts of the COVID-19 pandemic on the everyday lives of children and their families in Estonia during lockdown in spring 2020 and 2021. The data corpus is based on diaries compiled by children during the first lockdown in 2020 for a collection at the Estonian Literary Museum, and on a series of semi-structured interviews with children documenting their experiences during lockdown in spring 2021. The study draws on literature from the “new sociology of childhood” and applies Bronfenbrenner’s social ecological model to an analysis of young people’s experiences when their mobility outside the home was restricted, and they were forced to reorganise their time use. The findings show how the pandemic extended the social contexts in which children and their families are embedded and highlighted the role played by socio-cultural factors in shaping children’s coping capacities. In combination, analysis of the two datasets demonstrated the differential effects of lockdown on young children. The accounts from the first wave of the pandemic in 2020 suggested that positive family environments could smooth the negative effects of lockdown and help them cope with unexpected changes in their everyday lives. The interviews during the second outbreak of the pandemic revealed how the emerging weariness and boredom reported by some children strained family relationships. The amount of time that children spent online both modified and expanded their experiences of technology-supported interactive spaces. Their reports showed that the interactive contexts in which they were operating through social media extended beyond national borders to an interest in transnational and global events. Online communication did not, however, compensate for the loss of real-life contacts with friends, which became a major concern for young people in Estonia. In the concluding discussion, the authors consider policy responses that address the main issues identified in the research.
Introduction
The World Health Organisation declared a state of international public health emergency on 30 January 2020 and a global pandemic on 11 March 2020. Lockdown was promptly proclaimed in the Baltic States: in Estonia and Latvia on 12 March 2020, and in Lithuania four days later. From an economic perspective, the situation of the three Baltic States differed to a certain extent. Before the outbreak of the pandemic, Lithuania had experienced steady economic growth, while growth in Estonia and Latvia was slowing down and went into decline in the first quarter of 2020. The second quarter of 2020 was difficult in all three Baltic States, but the decline in GDP remained well below the EU27 average of −14%: it was lowest in Estonia (−4.6%) and highest in Latvia (−8.9%). A similar trend occurred in the unemployment rate: it increased least in Estonia and most in Latvia, while remaining below the EU average ( Parliament of Estonia Foresight Centre, 2020b ). The Bank of Latvia ( Parliament of Estonia Foresight Centre, 2020a ) noted that during the first wave of the pandemic, Estonia had disbursed more in support measures than Latvia and Lithuania, and furlough support was also more generous: 0.9% of GDP compared to 0.8% in Lithuania and 0.3% in Latvia.
In mid-October 2020, Estonia, Latvia and Lithuania were among the EU member states with the lowest COVID-19 infection and death rates in the EU. Estonia also reported the lowest numbers among the Baltic States ( Our World in Data, 2021 ). Like most other Central and Eastern European countries, all three Baltic States had been relatively untouched by the first wave of the pandemic in March−April 2020. The second outbreak started in late October 2020 and peaked on 25 December 2020 in Lithuania and on 17 March 2021 in Estonia. Rates in Latvia fluctuated between the two dates. By June 2021, the number of confirmed new cases per million inhabitants had fallen to 130 in Latvia, 119 in Lithuania and 68 in Estonia; the deaths rates (rolling 7-days average) had fallen to 3.3 for both Latvia and Lithuania and 1.4 for Estonia.
The COVID-19 pandemic not only halted economic growth, it also constituted a huge challenge to health care capacity. Until the onslaught of the pandemic, Baltic societies had not experienced any major public health problems in recent years. As in other Western countries, the pandemic gave a new prominence to the role of scientists in informing political decisions and the ways in which government policies were communicated to the public.
The first lockdown was proclaimed on 12 March 2020 and was due to last until 1 May 2020 but was then extended to 17 May 2020. The second lockdown was in force from 11 March 2021 to 25 May 2021. Lockdown during the two waves of the pandemic involved substantively the same measures, although they were applied with different degrees of stringency and were not perceived as having the same impacts on the everyday lives of young people. During both waves schools switched to distance learning. Shopping centres, theatres, cinemas and other places of entertainment were closed. Social distancing was compulsory in public places. Wearing masks was recommended in 2020 and compulsory in 2021. The 2 + 2 rule was introduced, allowing meetings of two people from two different households out-of-doors. Government rules did not apply to the private sphere. Although private gatherings were not recommended, no restrictions were placed on meetings between friends. Nor were children of separated parents prevented from moving between households. Parents who commuted across borders for work were hit by border closures and by restrictions introduced in neighbouring countries.
During the lockdown in spring 2020, the government’s intention was to limit the impact of the pandemic on public health facilities by keeping society as closed as possible. Evidence of the harm caused by lockdown restrictions to economic and social life, in combination with greater knowledge about the virus, the introduction of effective vaccines and the adaptative capacity of the health services, persuaded the government to apply a lower level of stringency in 2021.
Drawing on data collected over more than a year of living with the COVID-19 pandemic, the authors of this article reflect on how children in families in Estonia coped with the severe disruptions it caused to their everyday lives. Estonia was selected for an exploratory study because it managed the pandemic relatively well, compared to many other EU member states. Estonia also stands out as a country that had benefitted fully from technological developments in the post-Soviet era. In a small economy with good recovery capacity, the IT sector proved to be an important factor in the successful management of everyday life during periods of severe restrictions on mobility and social interaction. IT-based services for schoolwork and online study, as well as other e-services such as digital medical prescriptions, were already an integral part of everyday life. Estonians were technically relatively well prepared to study and work from home.
During the first lockdown in spring 2020, the Estonian research team carried out new empirical work based on a corpus of diaries compiled by young people aged 12–13 and 17–18. The diaries were the result of a public data collection campaign organised by the Estonian Literary Museum. A year later in spring 2021, the research team at Tartu University conducted a series of semi-structured interviews with a different sample of children aged 8–15, documenting their experiences during lockdown. The researchers contextualised the two datasets by drawing on international statistics, policy documents, data from public opinion surveys and public discourse. Data concerning Latvia and Lithuania provided a backcloth for situating developments in Estonia.
First, the article provides a brief overview of literature about the impacts of the pandemic on young people’s lives. Then follows a description of the methodology for the empirical work and a presentation of the findings. The discussion and conclusions indicate how the research was used to inform policy development.
TRACKING THE IMPACT OF COVID-19 ON YOUNG PEOPLE’S Lives
Young people interact in different life domains, including family, friendship groups, school, community and via technology, all of which were affected by and had an impact on well-being during the COVID-19 crisis. Social and human science researchers around the world have explored the effects of the COVID-19 pandemic and ensuing lockdowns on young people’s lives. In the United States, for example, based on the reports of adolescents concerning their experiences of the pandemic, a qualitative study by psychologists ( Scott et al., 2021 ) identified 14 thematic fields where the pandemic had affected everyday life. They included mental and physical health, family relations, friendships, social connections and community, attendance at important events, socio-economic performance, routines, observance of COVID rules, exposure to COVID risks, and the adoption of technologies. Psychologists in Spain ( Idoiaga et al., 2020 ) explored children’s social and emotional representations of the pandemic and analysed how children coped during the crisis.
Studies in child psychiatry, psychology and public health in different parts of the world have shown that the pandemic increased child vulnerability and endangered mental health, resulting in a decline in subjective well-being ( Fegert et al., 2020 ; Gadermann et al., 2021 ; O’Sullivan et al., 2021 ). In a wide-ranging review article, Chaturvedi and Pasipanodya (2021) highlight disruptions to school and social life as the main factors determining child vulnerability. Other researchers identify COVID-19 related stressors, such as high levels of anxiety and depressive symptoms, associated with perceptions of parental stress within families, causing new problems in parenting that influenced children’s ability to cope with the pandemic ( Brown et al., 2020 ; Spinelli et al., 2020 ).
The COVID-19 pandemic caused momentous changes in patterns of interaction, due to the implementation of lockdowns and policies on social distancing in children’s lives. Family sociologists in Poland ( Markowska-Manista and Zakrzewska-Olędzka, 2020 ) studied changes in family life caused by restrictions and limitations on mobility and social relationships. Comparative evidence from Switzerland, Canada and Estonia showed how the pandemic exacerbated inequalities between children across different life domains, especially within families, at school, with friends and in access to public services ( Stoecklin et al., 2021 ). While increasing the importance of virtual spaces, government measures in these countries were found to limit physical interaction with friends, teachers and relatives by closing access to schools, playgrounds, and recreational activities.
From a sociological perspective, children’s experiences can be best understood by setting them within what has been described as a “social ecological framework” ( Bronfenbrenner, 1979 ; Bronfenbrenner and Morris, 2006 ; Sallis et al., 2008 ). Bronfenbrenner’s model provides an appropriate theoretical and methodological framework for the present study by capturing children’s experiences through the mutual interactions between a child, her or his immediate environmental settings, and the wider socio-cultural contexts in which she or he is embedded ( Scott et al., 2021 ). This approach considers children as dynamic social actors and reliable sources of information about their own lives ( Casas et al., 2013 ; Mason and Danby, 2011 ).
Methodology
This section describes the data collection and analysis in the two distinct phases of the project covering the periods in 2020 and 2021 when schools were closed, many families were confined to their homes, and the participants were distance learning at home.
Data Collection and Analysis
The data corpus for the research was compiled from two sources: children’s diaries during the first lockdown in spring 2020 and semi-structured interviews with children documenting young people’s assessments and reflections on their lives during the lockdown in spring 2021.
On 18 March 2021, the Estonian Literary Museum launched a public collection initiative of lockdown experiences in the form of diaries. Such an initiative is not unique and was replicated in several countries: for example, the Koronakevät initiative by the Finnish Literature Society, the Pandemic Diary Project in Latvia, and the Pandemic Diary Research Project in Poland. In Estonia, the call stemmed from a tradition of collecting life stories, starting in the late 1980s and early 1990s, that laid the foundation for the life-story archive of the Estonian Literary Museum, which today holds over 4,000 life narratives. The collection is viewed as a cultural resource of (national) memory and is archived for an indefinite period. The material was not collected with concrete research objectives in mind but has provided a basis for a wide range of research projects carried out by scholars with a background in literary/narrative studies, ethnology, folklore studies, and history. Preservation and access to the materials in the Cultural History Archive are governed by archival laws and regulations (see http://www.folklore.ee/era/eng/procedure.htm ).
Schoolchildren of all ages were invited to keep a daily record of their lockdown experiences, paying attention to changes in everyday life, and in their relationships with family members and wider society. They were encouraged to write about their fears and hopes as well as commenting on how lockdown was being handled by the authorities, and the support, if any, offered by national and local governing bodies. The call did not specify a minimal number of entries, their length or the required duration. It was published on the homepage of the Estonian Literary Museum and also promoted through online, social and traditional media. Schools were asked to create student assignments based on the call requiring participants to keep a lockdown diary or to write a memoir.
The data corpus for spring 2020 included 19 diaries by children aged 12–13 (grade six; 10 girls and 9 boys), and 20 personal narratives by upper secondary school students aged 17–18 (grade 12; 14 girls and 6 boys), that the students wrote as a school assignment. No personal data were collected about the diarists other than their grade at school, name and gender. The diaries covered the period from 18 March to 15 May 2020, with one diary entry per day. Some diaries included illustrations. The length of the entries varied, ranging from 50 to 200 words each. The diaries were handwritten in regular school notebooks. Personal records by older students were loosely based on the questions in the public call. They contained longer reflections (300–800 words) on the lockdown period and were submitted in digital form. With the consent of their parents, the children offered their diaries and reflections to the museum on a voluntary basis. For the purposes of the present article, the children’s identities were anonymised: only the first initials of their first names, sex and age group are indicated in the analysis.
The second data source contains transcripts of 24 semi-structured interviews, each lasting about 15–20 min, with children aged 8–15 (7 girls, 4 boys, 13 gender not specified), carried out as a practical fieldwork assignment for students attending a course on Children and Childhoods (3 ECTS) at the University of Tartu. The interviews document experiences of lockdown in spring 2021. The students were allowed to apply a convenience sampling method to find interviewees among children whom they knew, combined with an element of purposive sampling. Alongside the objective of carrying out a training exercise, the intention was to analyse the experiences of schoolchildren from different age groups, loosely defined. The purposive sampling method had the advantage of providing a mosaic of young people’s reactions to the pandemic across a wide age span, while contributing to the overall objectives of the training exercise. It had the disadvantage of not producing a representative sample of specific age groups as would have been possible in a larger-scale more quantitative study using a more rigorous sampling method.
The fieldwork process was supervised by the first author of the article in her capacity as course director. The interviews were carried out online or by telephone. A few interviews took place face-to-face observing social distancing rules. The interview frame was very simple: the children were asked what had changed in their lives compared to the situation pre-lockdown, what had improved or got worse. Children’s names and other personal data were not used. The children participated in the interviews on a voluntary basis and with parental informed consent: the interviewers approached the parents by telephone or by e-mail.
The authors were granted access to the handwritten and digital diaries. The interviews were first transcribed, and the interviewers wrote short fieldwork reports as part of their course assignment. The authors undertook in-depth analyses of the interview transcripts and diaries using a directed content analysis method consistent with the Bronfenbrenner’s social ecological framework ( Hsieh and Shannon, 2005 ). The two datasets covered different phases in the pandemic. They were not directly comparable since the diaries were child-driven, and the interviews were led by adults. The combined evidence from the two data sources do, however, provide valuable insights into the cumulative effects of the pandemic, as it progressed, on family life in Estonia as experienced by children.
ANALYSIS OF CHILDREN’S DIARIES: SPRING 2020
Before the outbreak in March 2020, COVID-19 was perceived by the public as something happening elsewhere in the world, mostly in Asia, that would never reach Estonia, as was the case with the H1N1 influenza virus in 2009. Since the introduction of lockdown on 12 March 2020, the rate of new infections had remained relatively low, around 20 for 100,000 inhabitants. As in the rest of the world, Estonian society was, nonetheless, exposed to an unprecedented situation generating the feeling of loss of control over everyday life, and causing anxiety and insecurity. Lockdown altered lifestyles and disrupted the enjoyment of living in a society that had become used to a high level of social protection and general well-being. For families, lockdown meant that many parents were unable to go to work due to temporary closure of their workplaces. Unless they were able to switch to teleworking, in most cases they were entitled to compensation from the government for loss of income. School closures resulted in children moving overnight to distance learning.
In Estonia, households with children form one fourth of all households and close to one fifth of children living with a single parent ( Statistics Estonia, 2021 ). The majority of children living with a single parent maintain some contact with their other parent. Many children have visiting orders that had been agreed by the parents, a child protection specialist or court, which had to be followed by the child. The strong recommendation to stay at home served as a pretext not to follow the visiting order. In addition to the general disruption to routines that this caused, some children had to stay longer than they would have wished with one of their parents. Although data were not collected about individual living arrangements, it was clear from some of the comments in the diaries that different family constellations and socio-economic circumstances influenced how children coped with the impact of lockdown.
The Impact of the Pandemic on Family Practices
Analysis of the diary entries suggested that the pandemic had diverse effects on children’s subjective well-being and development. Many homes turned into over-populated multifunctional places 24/7, with both positive and negative impacts on relationships. The children’s diaries indicate that they fully understood the seriousness of the crisis. Several diaries contain statistics about the spread of the virus in Estonia and elsewhere in the world. Boys more often than girls documented COVID-19 statistics in their diaries. Girls focused rather on describing relationships and activities with family members and friends. One boy’s report showed awareness of the pandemic crossing country borders and continents on a daily basis:
There are more than 200 cases of corona in Estonia so far and it is quite horrifying since the number has doubled since yesterday (16 March). Today there was the first corona death in Estonia (25 March). Today there was a new record in Italy but this is very sad record; 1,000 people died during the last 24 hours (27 March). Corona has taken over almost the whole world by now except a few countries in Africa (30 March). (Ka, boy, grade 6)
The diaries of both younger (grade 6) and older (grade 12) students recorded the responses of their family members to information about the spread of the virus, demonstrating feelings of fear and insecurity. One upper school student was concerned about the health and well-being of his father who had to commute between different countries during lockdown. He wrote: “That night I got very little sleep because my father told me that his … sleep routine was all messed up.” (Ma, boy, grade 12) For him, an additional source of tension was the fear that the father could transmit the virus. He was upset by his mother’s perception of the father as a potential source of health risk to the family and the self-isolation measures that she thought necessary. Other boys expressed concerns about transmission of the disease:
The elderly care home is in quarantine … it is quite scary that it is so close. We don’t know if it is only life threatening for older people or whether younger people also die. (Ol, boy, grade 6)
The diaries and personal reflections commented on different safety measures that the children and their families followed. They expressed concern about people who did not follow the rules. The diary entries suggest that the public message requiring everyone to help keep the virus under control by following the rules was taken seriously by both the children and their families. One student wrote that he wished:
…people would stay at home, because this is in the best interests of their health and that of the others. The longer we put up with staying at home, the faster we get out again. (Sv, boy, grade 12)
Children of all ages expressed a positive attitude and understanding as to why lockdown and stringent restrictions were necessary. Children described, for example, how they followed the rule about social distancing:
With my friend we wanted to go to Lossimäed [a nice park] but there were people there. We waited for them to leave but they did not, and so we ended up not going at all. (Ro, boy, grade 6)
A male upper school student commented on changes in the public health instructions, stating that: “Before leaving home we need to clean our hands and wash them right away after returning home.” (Sv, boy, grade 12) He and several other upper school students mentioned postponing or cancelling visits to older family members. One girl, whose grandmother lived with the family, and who used to have friends come to her home, wrote: “My mother has established a rule that no one can visit us right now. I respect my mother’s rule and my grandmother’s health.” (Gr, girl, grade 12) Another upper school diarist commented:
It is really sad to witness that there are still people who throw parties or ignore the restrictions.… We all need to do what we are asked to do and follow all instructions, then we can all successfully manage this situation together. (An, girl, grade 12)
Older children analysed the role of different media in spreading information about the virus and government measures:
When the situation became more serious, global panic started … that was, of course, spread by social media … At times of crisis like that, leaders and governments can show how weak or strong they are. (Ti, boy, grade 12)
Some older students expressed frustration with news that focused only on negative events, resulting in them giving up following the news altogether (Ka, girl, grade 12). However, most students in the older age range did not report perceiving very high risks to their own safety or those of their family members. One girl reported that, although the number of infected people had risen to 679, with 3 corona deaths:
I know that there are few corona deaths in Estonia. My strong immune system would cope well with the virus. In my family, people are protected and the possibility of them getting the virus is small. (Ma, girl, grade 12)
In the older age group, children who stayed at a school dormitory during term time enjoyed being at home with family members, doing gardening and maintenance work around the house, and helping younger siblings to manage their schoolwork. While younger students frequently mentioned new family activities such as going for a jog together, doing puzzles or trying out new recipes, they occasionally became frustrated with their siblings and conflicts developed. About a third of the children reported an increase in anxiety and tension in relationships at home. One girl in grade 6 wrote:
We fought with my brother against our sister for half an hour or so. I got some bruises. But in the end, everything worked out [and] we made up. (Kr, girl, grade 6)
Younger children often developed conflicts with their siblings; they were usually solved very quickly, and normal friendly socialising continued. A girl whose father was commuting to work wrote: “My father has worked in Virumaa [North-East Estonia] the whole 3 weeks. I cannot stand my mother and brother alone anymore. Hell.” (An, girl, grade 12) Some children also mentioned problems with their parents:
I was too tired to get up right away. When I was getting dressed, my stepfather shouted that I need to feed my cat right away or he will take it to the shelter. (Be, girl, grade 6)
Children in the younger age group whose parents were separated wrote about missing the parent with whom they did not live on a daily basis: “I’d like to spend the last week of school with my real father.” (Sa, boy, grade 6) Some of the younger boys also mentioned suffering from being separated from their grandparents: “Grandparents wanted to visit us, but our parents did not allow that, it was such a pity.” (Ol, boy, grade 6).
Lockdown was generally associated with greater stability and more opportunities to share leisure activities or do housework and small household repairs together, thereby generating greater closeness and more dialogue and new routines within families. Children described growing closer to their families but also suffering from having to live in such close proximity all the time, especially with younger siblings. Some children also wrote about tensions and feelings of isolation in the home, not being able to share personal matters in a trusting atmosphere, being pressed to do too many home chores on top of managing schoolwork, and missing out on parental attention. They regretted not being able to see close relatives, including grandparents, parents who were living apart from them or who had to travel to work, and were concerned about their welfare.
The Impact of the Pandemic on School Life and Social Contacts
Schools in Estonia had already been using web applications such as eKool and Stuudium to facilitate teaching and learning several years before the pandemic, and collections of online study materials were freely accessible for all students, for example Opiq. These tools were used for assigning tasks, feedback and grading, monitoring progress, communicating with students and parents, posting study materials and submitting assignments. Nevertheless, neither children and parents nor teachers had a clear vision of how full-time e-learning would work. Children’s experience of distance learning varied. New learning environments and requirements challenged children who previously had learning difficulties, those with special educational needs and those where internet access was limited. The pandemic erased the distinction between school time and free time, cancelling extracurricular hobbies or moving them online, thereby considerably constraining the range of free-time activities. Although few children felt they could not handle e-learning at all, relatively few did not experience some problems with distance schooling. Moving schools to distance learning was the protective measure that the children raised as posing the greatest challenges for them.
Young people in both age groups commented in their diaries on positive aspects such as being able to sleep longer and having greater freedom in managing their time. Upper school students, in particular, appreciated being in charge of their time and able to study independently. One girl pointed out that she no longer felt exhausted at the end of the school day since she “managed to plan her school day more productively than when she was at school”, and she was able to “think independently” (Vi, girl, grade 12).
In the younger age group, boys reported more positive attitudes to distance learning: “Most of us are glad about that, me included. You can sleep longer in the morning and study whenever you want.” (Ka, boy, grade 6) Another boy noted that distance learning seemed easier: “I like … to study in my own room. I can also take whatever I want to eat from the kitchen.” (Ol, boy, grade 6) Students in different age groups mentioned as a positive aspect of staying at home more varied and better tasting meals, indicating that families were finding time to support their children during lockdown.
Children in both age groups found it difficult, and physically straining, to sit at the computer all day. They complained about problems with self-motivation, considered school assignments monotonous and missed the contrast between time spent in and outside school:
Why do we have so much homework? Where has my motivation gone? As I could not sleep at night, I take a nap, then start doing schoolwork at about 4 pm and end at 2 in the morning. (Ja, girl, grade 12)
Some of the diarists mentioned experiencing mental health problems, the failure of parents to understand their problems, and the need to seek online professional psychological counselling.
Several younger students expressed their frustration with distance learning. A male diarist complained: “I am so tired of distance learning, since I couldn’t get out of the house and meet up with my friends. This routine is getting on my nerves.” (Ma, boy, grade 6) Particularly in the younger age group, sleep problems were quite frequent and could be viewed as a major effect of the pandemic and the change of routine, as admitted by one girl:
Though studying is necessary, studying during lockdown upsets me and even drives me crazy. I woke up at six o’clock again. I contemplated starting to get going with my schoolwork, but nevertheless fell asleep again ... [At night] our parents asked us to put the lights off and the laptop away and go to sleep. We put the laptop away and the lights off but did not go to sleep. (Kr, girl, grade 6)
Some younger students wrote about skipping a whole night’s sleep or even reported not sleeping for several nights in a row. For upper school students, not knowing whether they would be able to graduate with good results and continue their education was the greatest source of distress, far exceeding fear of the virus. By contrast, some younger students noted that the less stringent demands being made on them by distance learning made it more tolerable:
I even like [distance learning] now, because, firstly, I can sleep longer and, secondly, I don’t need to take everything so seriously and, thirdly, in some subjects we...simply get pass or fail. (Ka, boy, grade 6)
A sociological study among teachers, parents and children in Estonia in 2020 revealed that about one third of children were satisfied with distance learning, another third had difficulties in adapting to it, and the rest said that it made no difference for them ( Lauristin et al., 2020 ). Distance learning challenged children’s self-regulation skills. Some children enjoyed it because of the relative independence to introduce their own daily time schedules and distinguish between school, hobbies and leisure. But other children missed the pre-pandemic ways of teaching and learning and were not able to adapt to new forms of schooling without the atmosphere in the classroom and opportunities for open and direct discussions, questions and answers.
Children in both age groups commented that social distancing from friends was the most difficult challenge they faced. Many children, especially in the younger age group, wrote about missing friends and opportunities to hang out with them:
I miss my friends; it seems I haven’t seen them for years. I miss school. I wish the virus would go away so that regular routine can continue. (Ca, girl, grade 6)
I would so much like to go back to school as I have nothing to do at home. (Ro, boy, grade 6)
I miss school, first of all, all my friends. Also, schoolwork progresses much faster at school. (Ol, boy, grade 6)
Younger children also missed teachers and the school atmosphere for which online classes were no substitute. Although younger students rarely recorded difficulties in managing schoolwork, they clearly preferred face-to-face learning.
The reflections of older students showed that friends played a central role in handling problems and maintaining a positive outlook on life. One diarist, who was suffering from forced separation from her boyfriend and problems with managing schoolwork, mentioned the communication channels she and her friends adopted, while admitting that this format of communication was not an adequate substitute for those used in pre-pandemic times. In her life, problems piled up, but her mother was aware of them and was supportive:
Life within these walls in these conditions without good friends is nothing short of a catastrophe. At least [friends] check up on me via phone and messages. [When my] Mom … sees that I’m messed up, she gives me a break with schoolwork and chores at home. (An, girl, grade 12)
Girls and boys, particularly in the younger age group, described taking up new hobbies or rediscovering old ones, as well as finding ideas for activities on the internet: “In the evening I watched different YouTube videos on things to do during lockdown and got a lot of new ideas.” (Me, girl, grade 6) Other diarists found photography tips (Kr, girl, grade 6), instructions for making wrist bands (La, girl, grade 6), for playing the piano and composing (Ma, boy, grade 6), or they used the time at home to pursue other artistic activities: “I have had more time to practice my guitar and … out of utter boredom I even messed around with watercolours a bit!” (An, girl, grade 12).
The diaries demonstrated that young people reacted and adapted to the challenges they perceived in their everyday lives in many different ways. In the majority of cases, they displayed resourcefulness, flexibility and effective coping strategies. They appreciated the support they were given at home and by their schools. Yet, the diaries revealed a number of problems, the most important for both age groups being the lack of direct contact and face-to-face socialising with friends, teachers and schoolmates.
ANALYSIS OF THE INTERVIEWS WITH CHILDREN: SPRING 2021
Although COVID-19 death rates remained relatively low by international standards, a new lockdown was imposed on Estonian society between March and June 2021 in response to rising rates of infection ( Our World in Data, 2021 ). Schools reverted to distance learning, shopping centres, theatres, cinemas and all places of entertainment were closed, wearing masks was compulsory in public places, the 2 + 2 rule was reintroduced. Local governments decided to distribute food packages through schools to compensate for the loss of free lunches, previously offered at school to all students. Compared to the first lockdown in Spring 2020, the government tried to keep the society as open as possible. As a result, the lockdown introduced on 11 March 2021 was criticised for coming too late to prevent the peak for new cases being reached on the 17 March 2021. The government’s priority was to avoid the collapse of the healthcare system. In public discourse, young people were blamed for transmitting the virus while being unprotected against it because they had not been vaccinated. The economic coping capacities of families were endangered because central government had decided to end the income-loss compensation scheme despite rising unemployment in the second half of the lockdown. After a year living with the pandemic, the level of anxiety experienced during the first wave had lessened, but weariness and discontent with the regulations were contributing to emerging mental health problems among young children as reported in the interviews.
The interviews with children showed that their attitudes towards the virus and their patterns of behaviour were largely determined by the way their families handled the pandemic. As in the diaries, in the interviews children recalled that they had felt frightened and insecure a year earlier in spring 2020. They told how they had followed the very strict self-isolation measures, for example by staying indoors for months, and/or avoiding all public places. At the time of the interviews in April 2021, the whole society was better prepared for living with the virus than they had been during the first wave of the pandemic. Children felt safer and expressed the belief that the danger could be minimised if all the safety measures were followed. They considered themselves to be well informed about the risks and safety measures.
The interviews confirmed that most of the children were continuing to follow safety regulations. One child recounted: “When my older brother comes to visit us from Tallinn where he goes to school, he wears a mask at home.” (boy, aged 9) A few parents or family members did not consider it important to follow any safety measures or even acknowledge the existence of the pandemic: “I don’t care one bit about the virus, my father said that there is no such thing as the virus.” (boy, aged 14) In the interview, he made clear that, in his everyday life, he followed safety measures loosely; for example, he talked about meeting up with friends on a regular basis, whereas most other interviewees noted that they had few opportunities to see their friends and were suffering from the lack of regular contacts, because they considered it important to follow the safety precautions.
Compared to the accounts in the diaries, the interviewees more often spoke about weariness and strain in family relationships. They complained about having to spend time with their family members 24/7, resulting in tensions and arguments and occasional conflicts with younger siblings. But most children were content with their lives, reflecting their subjective assessment of how they were adapting to the new reality. Many children described being able to manage schoolwork and felt they had the necessary support. In cases where significant changes had taken place in their parents’ lives, due to the considerable reduction in income, loss of employment, or fatigue and frustration resulting from the additional responsibilities at work and at home, children did not necessarily observe a worsening of their home environments. In some instances, they talked about noticing the greater workload on their parents, but were supportive and appreciative of the way their parents were coping. Where the family’s income made it possible to procure extra services, the children rated their quality of life highly. For example, one family had hired a private teacher who came to their house and helped the family’s two children with schoolwork 3 days a week.
As in the diaries from spring 2020, the children mentioned family activities − going for walks and outings and cooking together − as well as new activities that helped them to endure lockdown. They also remarked on holidays and birthday celebrations being scaled down, admitting that they preferred bigger gatherings and outings on festive occasions.
When asked about their recent experiences during lockdown in April 2021, the children described the pandemic as having lasted one and a half years. For adults, the period under consideration at that time was perceived as having lasted for a calendar year; for children, it represented three school terms that had been lost because they had been studying at home or moving in and out of lockdown, making them miss contact hours at school. They therefore perceived time spent remotely as lasting longer than the time spent at school.
The schooling situation differed from that in spring 2020 since students, teachers and parents had, meanwhile, developed skills in handling distance teaching and learning. Schools were also technically better equipped, and teachers had adopted more effective online teaching techniques. During distance learning periods, the number of videoed classes increased considerably, often equalling the number of regular classes. The interviews with children showed that, in general, they believed distance learning was progressing smoothly. Most children described managing distance learning relatively well and even expressed the hope that, in the future, distance learning (e-learning) would be integrated more thoroughly into daily learning schedules. As noted in the diaries, the interviewees valued the greater degree of independence and self-management opportunities made possible by distance learning.
Yet, some children felt the need for more support from individual teachers if they perceived that they were lagging behind with schoolwork and lacked help to get back on track. The interviews showed that children of primary and lower school age (7–15) were often relying heavily on their parents’ support and/or the support of older siblings, sometimes to a greater extent than on help from school. These children pointed out that schoolwork had become more mechanical, and that they did not have enough time to focus properly. They admitted that they often cheated, for example by handing in school tasks that someone else had completed. The children were, consequently, worried about their results.
The most widely reported and strongly felt impact of the pandemic was on social contacts. This effect had clearly worsened considerably since spring 2020. Most children said that they felt estranged from their friends and admitted that virtual communication did not make up for regular face-to-face contact. Some children said that they had lost all their friends and were now completely alone. Children also observed changes in the behaviour of their friends and classmates. They noticed other children around them becoming more nervous, getting frustrated and more easily upset. In some cases, children detected mental health problems among their friends, including the infliction of self-harm (cutting). Children who had been active in playing sports (group gymnastics and basketball), or some other hobby that could not take place online, suffered from the cancellation of these activities and the associated loss of opportunities to socialise, including participating in competitions. Almost all the interviewees felt tired and bored. Many expressed fears that the world might never return to the way it was before the pandemic, and that they might never get back to their normal, regular lives.
Discussion and Conclusions
An important aim of the empirical research described in this article was to understand how findings from a study of the impacts of the COVID-19 pandemic on children’s lives in Estonia might be used to track the interactive process between policy as promulgated in lockdown measures and as reported in the behaviour of young people. Published reports, opinion polls and grey literature provided background evidence about the wider socio-political factors shaping government responses to the health crisis and, in turn, influencing young people’s perception of the effects of lockdown on their lives.
The impact of school and workplace closures, combined with measures restricting mobility, social and physical contact, on the socio-psychological climate of families with children was immediate and profound. It transformed the reality of everyday life. In all the Baltic States, the workload for parents assisting children with online learning and taking care of pre-school children increased markedly. In addition, parents who commuted across borders for work in the Baltic States were hit by restrictions on border crossings and by border closures.
A national study of students, teachers and parents in Estonia during the first lockdown in 2020 indicated that, depending on the type of work, 36% of parents were using their homes as offices, and 44% reported an accumulation of responsibilities and increased stress levels, especially for parents with small children and families with several children ( Lauristin et al., 2020 ). Lithuania registered more than a doubling of the level of anxiety and a marked deterioration in the emotional climate during the 2020 lockdown ( Eriksonas, 2020 ).
Income inequality between families increased markedly during the pandemic: in late May 2020, 55% of the population reported a decrease in their own or their family’s income level, and 36% of the unemployed said they had lost their job during the crisis ( Riigikantselei, 2020 ). A year later, when unemployment support schemes were withdrawn, 25% of the population reported problems with coping financially ( Riigikantselei, 2021 ). Young people’s diary entries during the first wave of the pandemic in 2020 suggested that a positive family environment could alleviate the negative effects of the lockdown and help them to cope with unexpected changes in their everyday lives. Stable family life encouraged communal activities, such as table talk, board games and outdoor activities as a family group, although the children were already expressing concern about the effects of lockdown measures on their interaction with friends and the wider community. The restrictive measures in spring 2020 had been introduced so rapidly that it was not possible to capture their impact, making it difficult to predict how they would be perceived by children. The voices of parents and teachers became increasingly audible in policies and public debates presenting the problems of coping with distance learning and other impacts of the pandemic on everyday lives.
Analysis of the interviews in spring 2021 suggested that, over time, working from home and living in close proximity increased boredom and strain in family relationships, impacting negatively on subjective well-being. The children were particularly affected by the loss of physical and social space due to confinement at home and the limits imposed on mobility and social interactions, even if these conditions were partially mitigated, at least initially, for children because they were able to spend more time with family members.
Problems of domestic violence were not mentioned in the diaries or interviews, although they were being widely discussed in public debate in early 2021. Social workers and psychologists acknowledged that, during lockdown when family members were living in close proximity, such cases had become more prevalent, but that the victims seemed to be too frightened to report abuse. One psychologist described how the presence of other family members threatened children’s privacy and made it difficult for them to speak about personal experiences of abusive behaviour ( Haldre, 2020 ).
The restrictive measures posing the greatest challenges to children according to the accounts in the diaries and interviews resulted from having to reorganise their studies and to forego most of their regular socialising activities. Both in spring 2020 and 2021, distance learning was introduced universally, with teachers providing daily schedules of classes to enable children to structure their day. By spring 2021, the capacity of schools to carry out distance learning had increased considerably. On both occasions, densely populated areas with high infection rates were treated similarly to sparsely populated rural areas with low rates. The adverse effects of distance learning were greatest for children who were most dependent on direct communication with the teacher in a real classroom for motivation and encouragement whether they lived in an urban or rural setting.
In line with the findings from the diaries and interviews, educationalists became increasingly concerned about the loss of learning, particularly for children in the most deprived families. In spring 2021, ideas were being sought to enable children to catch up at the end of the school year. A proposal that found fruitful political soil and public support was the organisation of “summer learning camps” for children at an educational disadvantage as a result of the pandemic ( Otsmaa, 2021 ). On 27 May 2021, the Minister for Education and Research announced its decision to support student camps aimed at stimulating interest in learning and “re-socialising” in preparation for the return to school. Funding was also made available for schools to provide additional support for pupils and for the purchase of laptops to loan to students, and for improving internet access, speed and reliability.
Following a suggestion from the Scientific Advisory Board in May 2021, the Minister for Education and Research (2021) stated in an interview that grades one to six and upper school classes should, in future, be closed only during extreme circumstances. It seemed likely that the combination of distance and in-person learning would find support across the educational landscape and that formal and non-formal education would become more closely integrated ( Estonia Education Forum, 2021 ). The analysis of children’s perspectives on distance learning in the two phases of the research demonstrated that online communication did not compensate for real-life classes, although the children in the study were not averse to the adoption of blended solutions.
A study carried out in spring 2020 had revealed that 10–15% of children were likely to be severely disadvantaged by distance learning ( Lauristin et al., 2020 ). The diary entries provided evidence of how the socio-economic and cultural inequalities between children in their everyday lives had been exacerbated by government policies. The interviews indicated that the lockdown measures presented significantly greater risks and challenges for the mental health of families and children during the second wave of the pandemic in 2021, even though they were less stringent.
The inclusion in the study of two different age groups demonstrated that the main challenges arising from the lockdown measures—limited social contacts and distance learning—were shared by both age groups but with different effects. Children in the younger age group saw socialising as an important part of schooling, whereas the main concern for the older children was the insecurity of their prospects for continuing their education. Markers of mental health issues were present in both age groups, but only children in the older age group were aware of the problem and ready to seek professional help.
Analysis of the diary entries had shown that some children recognised that they were at an advantage because their homes were well equipped with technological resources, and their parent(s) possessed the knowledge and skills needed to assist in schoolwork and were able to spend more time on family activities than before the pandemic. These children felt safe and protected, even though they missed direct social contacts with friends. The interviews, and to some extent the diaries, showed that the children who did not share these advantages experienced difficulty with self-motivation, failing friendships and deteriorating mental health. They were most likely to be suffering from the lack of parental support with their schoolwork and face-to-face socialising with friends, to feel isolated and excluded from the wider community. When they encountered problems with schoolwork, they felt that they would have benefitted greatly from more direct contact with teachers.
An Estonia Education Forum (2021) confirmed that these disadvantaged children needed direct interaction with teachers and other children in the classroom to advance their educational outcomes, as well as their social skills. The impact of social distancing on children’s mental health served as a warning sign. To deal with the deteriorating mental health situation in spring 2021, at the time when the interviews were being carried out, psychologists and therapists launched online counselling sessions and public campaigns to draw attention to strategies for coping with mental health problems resulting from social distancing. Compared to the lockdown in 2020, children gained more visibility in policies during the lockdown in 2021 mediated by educationalists and psychologists.
Although, compared to other countries, national surveys found Estonian adults to be more satisfied with the decisions taken by the government ( Ahrendt et al., 2021 ; Riigikantselei, 2021 ), our findings showed that the children were critical of government responses, in particular rules on social distancing. However, they also understood the need for them. Evidence from the diaries and interviews reported in this article suggests that political decisions affecting the delivery of, and access to, any of the services provided by local authorities could have severe implications for children both by exacerbating the negative impacts of the pandemic on their well-being and by increasing the social inequalities between them. The pandemic impinged on the wider socio-economic and cultural contexts in which children and their families are embedded. Although the decrease in GDP was relatively small in Estonia, confirming the flexibility of a small economy, as the crisis was prolonged, the increase in national debt threw into sharp relief the sustainability of public services and the risk of austerity. The increase in the education budget was designed to mitigate the negative impact of the pandemic on children’s education.
The diaries and interviews confirmed the value of Bronfenbrenner’s social ecological model ( Bronfenbrenner, 1979 ) in helping to understand children’s experiences during the pandemic within the multiple interactive contexts of family, school and the wider community. They demonstrated bi-directional influences between child and context. At the micro-level, the pandemic challenged the children’s capacities of self-regulation and self-confidence, endangering their identity and self-worth; it also modified their interactions with other family members by creating the risk of isolation while giving a new impetus to mutual relationships.
Major modifications in the interactions between children and the wider community occurred in the educational environment, where a direct social constructionist learning process in a shared reality was replaced with online distance learning. Not only the study process but also children’s relationships went online, thereby totally modifying and transforming the process into “friendships from a distance”, causing major protests among children. Time spent on the web was modified and expanded to enable greater access to technology-supported interactive spaces. The children accused the pandemic regulations of taking away their autonomy and freedom. Some direct forms of interaction—maintaining friendships and effective learning—became indirect, mediated by the internet, while some previously indirect interactions mediated by family units within the wider community—managing the health crisis and government restrictions—became everyday practices for children.
This study has analysed the impact of national lockdown measures on children’s familial, educational and social lives in Estonia. The accounts of young people’s experiences of the pandemic showed that they were aware of the need for protective measures and prepared to comply with them. The analysis in the article has also considered the role played by policies introduced by central government to mitigate and reverse the short- and longer-term effects of the restrictive measures on children’s well-being. The adequacy of these policies remains to be seen. More could be done, for example, to improve the targeting of support measures for children, including access to mental health counselling. Whatever the outcome in the longer term, the findings from the study confirm the value of listening to young people and of taking their experiences seriously throughout the interactive policymaking process.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
The author DK had a lead role in formulating the research questions. She framed and supervised the qualitative interviewing and primary analysis of data collected in spring 2021. The co-author LK-K organised the collection of children’s diaries and donation to the Estonian Literary Museum in spring 2020 and negotiated the use of the diaries in this study. The authors contributed equally to the data analysis and drafting of the article.
The research carried out for this publication was supported by a grant from the Estonian Research Council (Grant No. PRG700) and by the European Union through the European Regional Development Fund, Centre of Excellence in Estonian Studies.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank all the children who donated their diaries and personal narratives as school assignments to the Estonian Literary Museum as well as those who agreed to be interviewed and students who carried out the interviews. We thank the Estonian Literary Museum for the permission to use children’s diaries and narratives as source material for the present study. We are grateful to the reviewers for their constructive comments on the article.
Ahrendt, D., Mascherini, M., Nivakoski, S., and Sándor, E. (2021). Living, Working and COVID-19 (Update April 2021): Mental Health and Trust Decline across EU as Pandemic Enters Another Year. Eurofound Report . Luxembourg: Publications Office of the European Union . Available at: https://www.eurofound.europa.eu/publications/report/2021/living-working-and-covid-19-update-april-2021-mental-health-and-trust-decline-across-eu-as-pandemic .
Bronfenbrenner, U., and Morris, P. A. (2006). The Bioecological Model of Human Development, In Handbook of Child Psychology . Theoretical Models of Human Development . 6th Edn, Editors W. Damon, and R. M. Lerner, (New York: John Wiley ), Vol. 1, 793–828.
Google Scholar
Bronfenbrenner, U. (1979). The Ecology of Human Development: Experiments by Nature and Design . Cambridge, MA: Harvard University Press .
Brown, S. M., Doom, J. R., Lechuga-Peña, S., Watamura, S. E., and Koppels, T. (2020). Stress and Parenting during the Global COVID-19 Pandemic. Child. Abuse Negl. 110 (2), 104699. doi:10.1016/j.chiabu.2020.104699
PubMed Abstract | CrossRef Full Text | Google Scholar
Casas, F., Bello, A., González, M., and Aligué, M. (2013). Children's Subjective Well-Being Measured Using a Composite Index: What Impacts Spanish First-Year Secondary Education Students' Subjective Well-Being?. Child. Ind. Res. 6 (3), 433–460. doi:10.1007/s12187-013-9182-x
CrossRef Full Text | Google Scholar
Chaturvedi, S., and Pasipanodya, T. E. (2021). A Perspective on Reprioritizing Children's' Wellbeing amidst COVID-19: Implications for Policymakers and Caregivers. Front. Hum. Dyn. 2. doi:10.3389/fhumd.2020.615865
Eriksonas, L. (2020). Lithuania Social Briefing: The Coronavirus Stirs up the Negative Emotions in the Society under Quarantine. China-CEE Institute Weekly Briefing. Available at: https://china-cee.eu/wp-content/uploads/2020/05/2020s04_Lithuania.pdf . (Accessed 25 June 2021).
Estonia Education Forum (2021). Eesti Hariduse Tulevikuvaated − EHF25 [Future Perspectives of Education in Estonia] . 11 June 2021. Tartu, Estonia . Available at: https://haridusfoorum.ee/suurfoorumid/alates-2015/suurfoorum-2021 (Accessed 25 June 2021).
Fegert, J. M., Vitiello, B., Plener, P. L., and Clemens, V. (2020). Challenges and Burden of the Coronavirus 2019 (COVID-19) Pandemic for Child and Adolescent Mental Health: A Narrative Review to Highlight Clinical and Research Needs in the Acute Phase and the Long Return to Normality. Child. Adolesc. Psychiatry Ment. Health 14 (20), 20. doi:10.1186/s13034-020-00329-3
Gadermann, A. C., Thomson, K. C., Richardson, C. G., Gagné, M., McAuliffe, C., Hirani, S., et al. (2021). Examining the Impacts of the COVID-19 Pandemic on Family Mental Health in Canada: Findings from a National Cross-Sectional Study. BMJ Open 11 (1), e042871. doi:10.1136/bmjopen-2020-042871
Haldre, L. (2020). Uus Normaalsus COVID-ga Läbi Psühholoogi Pilgu [New Normality with COVID through the Lens of a Psychologist]. Presentation at Lõuna-Eesti Heaolufoorum Maailm Algab Sinust [South-Estonia Health Forum]. 2 November 2020. Tartu, Estonia. Available at: https://media.voog.com/0000/0046/3854/files/Uus%20normaalsus%20COVID-ga%20l%C3%A4bi%20ps%C3%BChholoogi%20pilgu%20(002).pdf . (Accessed 25 June 2021).
Hsieh, H. F., and Shannon, S. E. (2005). Three Approaches to Qualitative Content Analysis, Qual. Health Res. , 15. 1277–1288. doi:10.1177/1049732305276687
Idoiaga, N., Berasategi, N., Eiguren, A., and Picaza, M. (2020). Exploring Children's Social and Emotional Representations of the COVID-19 Pandemic. Front. Psychol. 11, 1952. doi:10.3389/fpsyg.2020.01952
Lauristin, M., Loogma, K., Erss, M., Vernik-Tuubel, E.-M., and ja Sarv, E.-S. (2020). Õpilaste, Õpetajate Ja Lastevanemate Toimetulek Koroonakriisi Aegses Kaugõppes [Coping of Students, Teachers and Parents with Distance Learning during Lockdown]. Eesti Haridusfoorum. 1 August 2020. Available at: https://haridusfoorum.ee/images/2020/Distantsppe_uuring_EHF_250720.pdf . (Accessed 25 June 2021).
Markowska-Manista, U., and Zakrzewska-olędzka, D. (2020). Family with Children in Times of Pandemic - what, where, How? Dilemmas of Adult-Imposed Prohibitions and Orders. Sr 4 (3), 89–110. doi:10.14746/sr.2020.4.3.05
Mason, J., and Danby, S. (2011). Children as Experts in their Lives: Child Inclusive Research. Child. Ind. Res. 4 (2), 185–189. doi:10.1007/s12187-011-9108-4
O’Sullivan, K., Clark, S., McGrane, A., Rock, N., Burke, L., Boyle, N., et al. (2021). A Qualitative Study of Child and Adolescent Mental Health during the COVID-19 Pandemic in Ireland. Ijerph 18 (3), 1062. doi:10.3390/ijerph18031062
Otsmaa, S. (2021). Baltic Education Ministers Shared Experience on Exiting COVID-19 Crisis. Republic of Estonia Ministry of Education and Research. Available at: https://www.hm.ee/en/news/baltic-education-ministers-shared-experience-exiting-covid-19-crisis . (Accessed 25 June 2021).
Our World in Data (2021). Coronavirus Explorer. Available at: https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&Metric=Confirmed+cases&Interval=7-day+rolling+average&Relative+to+Population=true&Align+outbreaks=false&country=EST∼LVA∼LTU . (Accessed 25 June 2021).
Parliament of Estonia Foresight Centre, (2020a). A Comparative Review of Socio-economic Implications of the Coronavirus Pandemic (COVID-19) in the Baltic States . Tallinn: Forsight Centre . Available at: https://www.riigikogu.ee/wpcms/wp-content/uploads/2020/11/Baltic-Assembly_final_02.11.2020.pdf . (Accessed 25 June 2021).
Parliament of Estonia Foresight Centre, (2020b). The Impact of the Virus Crisis on the Estonian Economy. Scenarios up to 2030 . Tallinn: Forsight Centre . Available at: https://www.riigikogu.ee/wpcms/wp-content/uploads/2021/02/2020_viiruskriisi_m6ju_eng_web.pdf . (Accessed 25 June 2021).
Riigikantselei, (2020). COVID-19 Teemalise Küsitluse Raportid. 10. Küsitlusvooru (19.-20.05.2020) Üldraport [COVID-19 Monitoring Reports. Wave 10, 19–20. Available at: https://riigikantselei.ee/uuringud . (Accessed 25 June 2021).
Riigikantselei, (2021). COVID-19 Teemalise Küsitluse Raportid. 30. Küsitlusvooru (21.-23.05.2021) Üldraport [COVID-19 Monitoring Reports. Wave 30, 21–23. Available at: https://riigikantselei.ee/uuringud . (Accessed 25 June 2021).
Sallis, J. F., Owen, N., and Fisher, E. B. (2008). Ecological Models of Health Behavior. In K. Glanz, B. K. Rimer, and K. Viswanath (Eds), Health Behavior and Health Education: Theory, Research, and Practice . San Francisco, CA: Jossey-Bass , pp. 465–486.
Scott, S. R., Rivera, K. M., Rushing, E., Manczak, E. M., Rozek, C. S., and Doom, J. R. (2021). “I Hate This”: A Qualitative Analysis of Adolescents' Self-Reported Challenges during the COVID-19 Pandemic. J. Adolesc. Health 68(2), 262–269. doi:10.1016/j.jadohealth.2020.11.010
Spinelli, M., Lionetti, F., Pastore, M., and Fasolo, M. (2020). Parents' Stress and Children's Psychological Problems in Families Facing the COVID-19 Outbreak in Italy. Front. Psychol. 11. doi:10.3389/fpsyg.2020.01713
Statistics Estonia, (2021). Online Statistical Database. Available at: https://andmed.stat.ee/en/stat . (Accessed 25 June 2021).
Stoecklin, D., Gervais, C., Kutsar, D., and Heite, C. (2021). Lockdown and Children's Well-Being: Experiences of Children in Switzerland, Canada and Estonia. Child. Vulnerability 29. doi:10.1007/s41255-021-00015-2
Keywords: children’s perspectives on COVID-19, distance learning, family dynamics, impact of lockdown, social contacts, young people’s subjective well-being
Citation: Kutsar D and Kurvet-Käosaar L (2021) The Impact of the COVID-19 Pandemic on Families: Young People’s Experiences in Estonia. Front. Sociol. 6:732984. doi: 10.3389/fsoc.2021.732984
Received: 29 June 2021; Accepted: 06 August 2021; Published: 25 August 2021.
Reviewed by:
Copyright © 2021 Kutsar and Kurvet-Käosaar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dagmar Kutsar, [email protected]
This article is part of the Research Topic
Families and COVID-19: an interactive relationship
The Short-term Impact of COVID-19 on Families

The recent COVID-19 pandemic has changed numerous things about our daily lives. Much of the public focus has naturally been on the health and safety of individuals, families, and society. Others have focused on the economic impact of both the virus and the various policies implemented to slow its spread and “flatten the curve.” Social distancing has changed almost all aspects of our daily interactions.
One common consequence of these measures for families has been increased time spent together in the home. This increased time together has likely benefited many families. Long dormant relationships have perhaps been rekindled as priorities have been reassessed.
Some whose work-related stressors have kept them out of the home may have a newfound passion for their family relationships. Many parents are finding increased opportunity to interact and draw close to their children.
Other families are getting the opportunity to create new traditions and family rituals, often to fend off boredom but in the meantime creating meaningful interactions that are fostering closeness and unity.
But there are other ways in which families may be struggling during this time of uncertainty. These struggles may not make the news headlines the way other topics do, but they are just as important for the long-term sustainability and health of our society and culture. In the social sciences, classic stress theory provides some important insights into what many of these short-term stressors may be for families.
Families are “stressed” when they encounter changes in their environment, and they cope with that stress based on their available resources. For example, when an appliance, let’s say a dishwasher, breaks down (change), the family may feel stress. They may then hire someone to fix the appliance, turning to financial and time resources to cope with the stressor. They could also look to each other as resources to wash the dishes by hand until the appliance can be fixed.
The COVID-19 pandemic and the associated societal changes have elevated the felt stress of most families by increasing change in their lives while decreasing resources. With families losing income and losing access to institutional resources (school systems, gyms, parks, etc.), most individuals and families have fewer coping resources to deal with the elevated stress and anxiety during this time of crisis. A long history of social science suggests that this elevated individual and family stress will translate into what I call an exaggeration effect of negative outcomes. That means that any underlying negative behaviors or issues that families were dealing with prior to the pandemic will be exaggerated during it. From Fargo to New Jersey , we have already seen news reports of elevated child and domestic abuse, an easy illustration of this principle.
Other negative family outcomes, less enticing to reporters but equally important, are also happening. Social scientists have noted that web traffic to pornography sites has increased during the pandemic, suggesting that risk-taking behaviors and compulsive pornography use are increasing. The National Institute on Drug Abuse has issued caution about the impact the pandemic might have on drug abuse. Scholars have already warned about the increases likely to be seen in both depression and anxiety and the CDC has been so concerned about mental health during the pandemic, they launched a new section of their website strictly dedicated to mental health resources. The list goes on and on.
Many of these issues predated COVID-19, but in some families, the pandemic has shined a spotlight on these issues and caused them to both accelerate and become aggregated problems in their daily lives.
So, what can families do if they find themselves struggling with the realities of these issues? What if a family is physically healthy, but struggling with unique conflicts and relational issues that have been brought to the surface due to the changes over the last few months? The immediate need for most families is an increase of available resources.
Given the circumstances, digital and online resources are increasingly important. Luckily, while most families are often unaware of these resources, they do exist. For example, online resources are available to help combat mental health problems and domestic violence .
What about those families that aren’t suffering with major stressors but simply need better parenting or couple resources to cope with increased tension or fighting? Often one of the most important resources for families is to recapture the structure that school and work schedules forced on many prior to the pandemic. Sit down with your partner or family and map out a daily schedule and routine. For many families, this creates a sense of normalcy that can help alleviate some of the conflicts and stresses that have popped up.
Another important resource for families to remember during times of crisis is maintaining and/or establishing family rituals and traditions. This might be a great time to start a few new family traditions. Research has found that such rituals improve closeness and foster healthy family relationships. Consider starting a weekly dessert bar or a family movie night.
Find new ways to interact through board games or an art project. These events will serve to destress your family and provide the needed breaks from the daily challenges of living in close proximity to each other.
In addition to finding ways to strengthen your own family, consider reaching out to families around you who may be struggling in the shadows of their own home. Despite our need to socially distance, social resources are especially vital for families that are struggling. You never know how even a friendly voice, or a reassuring comment might help lift up and support families around us.
Most current pandemic related policy is aimed at either health or economic outcomes, the two most concerning issues for the vast majority of the country. In the meantime, while many families are thriving in an environment that is forcing family time and closeness, many others, especially those who were already struggling with underlying family issues before the pandemic, are suffering silently (or not so silently on some social media outlets).
We are truly in a unique moment in time when it comes to family interaction. This is both an opportunity and a challenge for families. Old problems might pop back up or new problems might arise. Seeking out and being proactive in building your family resources—and reaching out to those whose resources are even less adequate—can be a critical part of your survival plan for the current pandemic.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 11, Issue 1
- Examining the impacts of the COVID-19 pandemic on family mental health in Canada: findings from a national cross-sectional study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-6947-1052 Anne C Gadermann 1 , 2 ,
- http://orcid.org/0000-0002-4508-2463 Kimberly C Thomson 1 , 2 ,
- http://orcid.org/0000-0002-7641-7027 Chris G Richardson 2 , 3 ,
- http://orcid.org/0000-0002-3220-7351 Monique Gagné 1 , 2 ,
- http://orcid.org/0000-0002-7868-564X Corey McAuliffe 4 ,
- http://orcid.org/0000-0003-1084-3039 Saima Hirani 4 ,
- http://orcid.org/0000-0003-4649-2904 Emily Jenkins 4
- 1 Human Early Learning Partnership, School of Population and Public Health, University of British Columbia , Vancouver , British Columbia , Canada
- 2 Centre for Health Evaluation and Outcome Sciences, Providence Health Care Research Institute , Vancouver , British Columbia , Canada
- 3 School of Population and Public Health , University of British Columbia , Vancouver , British Columbia , Canada
- 4 School of Nursing , University of British Columbia , Vancouver , British Columbia , Canada
- Correspondence to Dr Anne C Gadermann; anne.gadermann{at}ubc.ca
Objectives In the first wave of the COVID-19 pandemic, social isolation, school/child care closures and employment instability have created unprecedented conditions for families raising children at home. This study describes the mental health impacts of the COVID-19 pandemic on families with children in Canada.
Design, setting and participants This descriptive study used a nationally representative, cross-sectional survey of adults living in Canada (n=3000) to examine the mental health impacts of the COVID-19 pandemic. Outcomes among parents with children <18 years old living at home (n=618) were compared with the rest of the sample. Data were collected via an online survey between 14 May to 29 May 2020.
Outcome measures Participants reported on changes to their mental health since the onset of the pandemic and sources of stress, emotional responses, substance use patterns and suicidality/self-harm. Additionally, parents identified changes in their interactions with their children, impacts on their children’s mental health and sources of support accessed.
Results 44.3% of parents with children <18 years living at home reported worse mental health as a result of the COVID-19 pandemic compared with 35.6% of respondents without children <18 living at home, χ 2 (1, n=3000)=16.2, p<0.001. More parents compared with the rest of the sample reported increased alcohol consumption (27.7% vs 16.1%, χ 2 (1, n=3000)=43.8, p<0.001), suicidal thoughts/feelings (8.3% vs 5.2%, χ 2 (1, n=3000)=8.0, p=0.005) and stress about being safe from physical/emotional domestic violence (11.5% vs 7.9%, χ 2 (1, n=3000)=8.1, p=0.005). 24.8% (95% CI 21.4 to 28.4) of parents reported their children’s mental health had worsened since the pandemic. Parents also reported more frequent negative as well as positive interactions with their children due to the pandemic (eg, more conflicts, 22.2% (95% CI 19.0 to 25.7); increased feelings of closeness, 49.7% (95% CI 45.7 to 53.7)).
Conclusions This study identifies that families with children <18 at home have experienced deteriorated mental health due to the pandemic. Population-level responses are required to adequately respond to families’ diverse needs and mitigate the potential for widening health and social inequities for parents and children.
- mental health
- public health
- community child health
- epidemiology
Data availability statement
Data are available upon reasonable request.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-042871
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
Survey items were informed by a longitudinal COVID-19 mental health survey, first commissioned by the UK Mental Health Foundation and developed in consultation with people with lived experience of mental health conditions; adaptations were made for the Canadian context and to support analyses focussed on issues of equity.
The large sample size enabled subgroup analyses in mental health according to gender, age, pre-existing mental health conditions, disabilities and household demographics.
Targeted sampling supported participation from families of diverse backgrounds.
Cross-sectional observational design and lack of adjustment for potential confounding prohibits causal inference.
Introduction
The COVID-19 pandemic has led to unprecedented global morbidity and mortality, with population mental health impacts recognised as a growing concern, 1 and particular risks identified within the family context. 2–4 Specifically, the COVID-19 pandemic has posed new threats to families through social isolation due to physical distancing measures, school/child care closures, financial and employment insecurity, housing instability and changes to health and social care access. 3–5 These shifts have profoundly interrupted the systems and structures that previously operated to both support the mental health and well-being of families and mitigate the risks that contribute to health and social inequities.
During the pandemic, many parents have experienced increased pressures and erosions to social supports, with implications for their mental health. In a US survey, the majority of parents expressed that during the pandemic, concerns about finances, social isolation, criticism from others, as well as emotional experiences of sadness and loneliness were affecting their parenting. 6 Globally, school and child care closures and the hiatus of after-school activities has added to parental pressure to balance responsibilities, including becoming the sole providers of supervision and education for their children—all while experiencing heightened financial and emotional stress. 7 Families, generally, are affected by the disruptions of the pandemic. However, these pressures disproportionately affect families who experience health and social inequities, including fewer financial and social resources, crowded homes and limited technology and Internet access. 7–9 The collision of these stressors has contributed to increases in domestic violence, 10 11 and emerging studies have shown increased frequency of shouting and physical punishment of children since the pandemic began. 6
In Canada, federal and provincial governments began implementing lockdown measures mid-March 2020 including border closures and restricted travel, restrictions on group gatherings, school/child care closures, mandatory working from home and temporary suspension of non-essential health and public services. 12 National COVID-19 incidence rates first peaked in April 2020 with nearly 3000 new cases confirmed daily. 13 By early May 2020, incidence rates were decreasing and provinces began easing lockdown measures including re-opening businesses and encouraging rehiring of employees. 12 However, there were indications that the pandemic was already impacting the mental health and well-being of Canadian children. 1 For example, by April 2020, reports showed a dramatic surge in calls documented by Kids Help Phone, a national helpline for young people, with a 48% increase in calls about social isolation, a 42% increase in calls about anxiety and stress and a 28% increase in calls about physical abuse. 14 Experts raised alarms that disruptions to routines and services, combined with increased family stressors, social isolation and domestic violence, were creating conditions that risked increasing child mental health problems on an unprecedented scale, with children from marginalised and socioeconomically disadvantaged backgrounds likely to be disproportionately affected. 15 16 Thus, while young people initially appear to be less susceptible to the physical effects of the virus, they are experiencing significant challenges, likely resulting from the social and economic impacts of the pandemic within their family contexts. 4 17 This is particularly concerning as research consistently demonstrates that children’s early exposures to stress can have lasting effects. 18–21
Families and children are furthermore supported by a social ecological system that has been forced to adapt quickly to support families’ needs, often with limited information or evaluation. School and child care closures due to the pandemic are concerning not only for the disruption to typical classroom learning, but also for the loss of systems-level safeguards such as nutrition programmes, after-school care, school health and counselling services and vaccination clinics 22 23 that seek to mitigate some consequences of health and social inequities among structurally vulnerable children and families. And yet, even as schools and workplaces started to re-open, concerns were raised about the health risks of returning to populated spaces (including public transit) disproportionally affecting families with lower incomes, fewer resources and with limited options for returning to work. 24 Furthermore, families, child care settings and schools are nested within health authorities and government structures that determine many of the policies, services and financial and employment supports available to parents as well as the availability of these supports beyond the pandemic.
This paper presents findings on the impact of the COVID-19 pandemic on families from the first wave of a nationally representative cross-sectional survey monitoring the mental health of people living in Canada. The study aimed to answer three questions: (1) How is the COVID-19 pandemic affecting the mental health of parents and children and what subgroups are most impacted by the pandemic? (2) How have parent–child interactions changed due to the pandemic? and (3) What are the factors that support mental health in the family context? The findings provide critical evidence to inform rapid, data-driven public health responses to meet the mental health needs of families and children in the context of the COVID-19 pandemic and beyond.
Survey development and approach
This investigation focusses on data from the initial wave of our cross-sectional survey, ‘Assessing the Impacts of COVID-19 on Mental Health’. The study represents a unique collaboration between academic researchers from the University of British Columbia, the Canadian Mental Health Association (Canada) and by an international research partnership with the Mental Health Foundation (UK).
Patient and public involvement
Survey items were informed by a longitudinal survey first commissioned by the Mental Health Foundation in March 2020 and developed in consultation with people with lived experience of mental health conditions via a citizen’s jury participatory methodology process. The citizen’s jury was a collaborative process that engaged people with diverse experiences and backgrounds in the development and interpretation of the research to enhance its relevance and impact, including insights on stressors, coping strategies and mental health. 25 26 Items on family mental health were adapted from previously developed community survey items related to the COVID-19 pandemic from the University of Michigan. 6 Modifications were made by the research team in consultation with collaborators from the Canadian Mental Health Association to reflect the Canadian context, aimed at examining indicators of mental health, stress and coping related to the COVID-19 pandemic among the Canadian population. Modifications included adding items on the impacts on young people’s mental health, potential sources of support, family dynamics, financial interventions introduced by the Government of Canada in response to the pandemic (eg, Canada Emergency Response Benefit) and food security systems. Survey items are provided in online supplemental file 1 .
Supplemental material
Data were collected between 14 May to 29 May 2020, via a rapid online survey distributed by polling vendor Maru/Matchbox. Maru/Matchbox maintains the Maru Voice Canada panel consisting of approximately 125 000 adults. Panel participants were recruited through direct email, with targeted sampling through affiliate community partners to increase inclusion of populations that may be difficult to reach via the Internet (eg, older adults, racialized populations). 27 Surveys were distributed to 3558 panel members to reach a total of 3000 respondents, yielding an invitation-to-response rate of 84%. Members of the panel were randomly invited by Maru/Matchbox to participate in the survey using Canadian national census informed stratifications defined by sociodemographic characteristics (age, gender, household income and region) with adjustments for response propensity to generate a representative sample by age, gender, income and region. 27 The data collection period captured the first phases of ‘re-opening’ across many Canadian provinces and territories, emerging from approximately 2 months of mandated physical distancing, school/child care and work closures and related disruptions.
All participants completed an online consent process prior to beginning the survey and were provided with a small honorarium through Maru/Matchbox to compensate for their time.
Measures and analyses
This investigation focusses on a subsample of participants who identified as parents with children <18 years old currently living at home (n=618). Changes in mental health due to the pandemic were compared between this parent subsample and the rest of the sample (ie, respondents who were not parents with children <18 living at home). Comparisons were also conducted within the subsample of parents. Participants completed sociodemographic questions as well as questions about their mental health, emotional responses to the pandemic, changes in substance use, experiences of suicidal thoughts and self-harm. Parents also completed questions on changes to parent–child interactions, impacts of the pandemic on their children’s mental health and were asked to identify sources of stress and support for themselves and their children.
Descriptive and bivariate analyses (frequencies, χ 2 tests) were used to examine self-reported changes in mental health since the onset of the pandemic across groups defined by gender, age, disability and pre-existing mental health conditions, as well as frequently identified stressors, supports and changes in parent–child interactions. Data were analysed using SPSS V.26. 28 The maximum margin of error for proportions derived from the parent subsample was ±3.9% at a 95% level of confidence. This was a complete case analysis. In χ 2 analyses, ‘don’t know’, ‘not applicable’ and ‘prefer not to answer’ responses were treated as ‘not yes’.
Sample description
Of the 3000 respondents, 618 identified as parents to a child <18 living at home. 2 The average age of the parent subsample was 43.0 years (SD=9.0 years) and 52.4% identified as women. Further sample characteristics are presented in table 1 .
- View inline
Sociodemographic characteristics of the parent subsample (n=618)
Pandemic-related changes in parent mental health
Parents identified more pandemic-related risks and vulnerabilities compared with respondents without children <18 years living at home across a number of mental health constructs. Since the onset of the COVID-19 pandemic, a significantly higher proportion of parents reported deteriorated mental health (44.3%) compared with 35.6% among their counterparts without children <18 years at home, χ 2 (1, n=3000)=16.2, p<0.001. Changes to mental health furthermore varied across sociodemographic characteristics within the parent subsample. Table 2 presents the proportions of parents reporting deteriorated mental health since the pandemic according to parent gender, age, pre-existing mental health conditions, disabilities, child age and employment and financial circumstances. Among parents with children at home, deteriorated mental health was significantly more prevalent among women, parents under age 35, parents with a pre-existing mental health condition, parents with a disability, parents of younger children (≤4 years) and parents reporting financial stress. When asked about their emotions in the past 2 weeks as a result of the COVID-19 pandemic, the most frequent response from parents was anxious and worried (51.9%; 95% CI 47.9 to 55.9), followed by stressed (46.1%; 95% CI 42.1 to 50.1) and bored (39.5%; 95% CI 35.6 to 43.5).
Changes in parent self-reported mental health since the onset of the COVID-19 pandemic
Overall, 8.3% of parents reported experiencing suicidal thoughts/feelings as a result of the COVID-19 pandemic in the past 2 weeks compared with 5.2% among their counterparts without children at home, χ 2 (1, n=3000)=8.0, p=0.005. Furthermore, 2.6% of parents reported deliberately hurting themselves as a result of the pandemic in the past 2 weeks compared with 1.3% among their counterparts, χ 2 (1, n=3000)=4.8, p=0.028.
As a means of coping with deteriorations in mental health and stressors of the pandemic, many parents identified an increase in alcohol use. Specifically, 27.7% of parents reported increased alcohol consumption compared with 16.1% among those without children at home, χ 2 (1, n=3000)=43.8, p<0.001. Within the parent subsample, increased alcohol consumption was more prevalent among men (32.3%) compared with women (23.5%), χ 2 (1, n=618)=6.0, p=0.014.
Pandemic-related stressors
As shown in figure 1 , when asked about stressors and worries resulting from the COVID-19 pandemic in the past 2 weeks, parents frequently reported mental health impacts, physical health threats related to the pandemic and relational and financial concerns. Being able to cope with uncertainty (59.2%; 95% CI 55.2 to 63.1), fear of a family member getting sick or dying (58.9%; 95% CI 54.9 to 62.8) and being separated from friends and family (58.7%; 95% CI 54.7 to 62.7) were the most frequent responses. A large proportion also reported being stressed about financial concerns (45.6%; 95% CI 41.2 to 49.7), losing/loss of job (31.4%; 95% CI 27.8 to 35.2) and having enough food to meet their household’s basic needs (20.4%; 95% CI 17.3 to 23.8). Further, 36.9% (95% CI 33.1 to 40.8) of parents reported being stressed about looking after children while continuing to work and 27.8% (95% CI 24.3 to 31.6) were stressed that the pandemic would make their existing mental health problems worse.
- Download figure
- Open in new tab
- Download powerpoint
Parent stressors in the past 2 weeks as a result of the COVID-19 pandemic. Note: Maximum margin of error for proportions was ±3.9% at a 95% level of confidence.
Relationship challenges were also a prominent concern among parents. For example, 28.3% (95% CI 24.8 to 32.1) of parents reported being stressed about experiencing relationship challenges with their partner and 11.5% (95% CI 9.1 to 14.3) reported being stressed about being safe from physical or emotional domestic violence during the 2 weeks prior. This proportion identifying concern about being safe from domestic violence was significantly higher among parents compared with the rest of the sample (7.9%), χ 2 (1, n=3000)=8.1, p=0.005. Within the parent subsample, a higher proportion of men (14.6%) reported being stressed about being safe from physical or emotional domestic violence compared with women (8.6%), χ 2 (1, n=618)=5.4, p=0.020.
Child mental health and parent–child interactions
The majority of parents (59.7%; 95% CI 55.7 to 63.6) reported their children’s mental health had stayed the same since the onset of the COVID-19 pandemic; however, 24.8% (95% CI 21.4 to 28.4) indicated that their children’s mental health had worsened.
Overall, due to the COVID-19 pandemic, parents reported more negative interactions with their children, including more conflicts (22.2%; 95% CI 19.0 to 25.7), yelling/shouting (16.7%; 95% CI 13.8 to 19.8), disciplining (16.0%; 95% CI 13.2 to 19.2) and using harsh words (10.7%; 95% CI 8.4 to 13.4). However, overall, parents also reported that they experienced increased positive interactions with their children, including having more quality time (65.4%; 95% CI 61.5 to 69.1), feeling closeness (49.7%; 95% CI 45.7 to 53.7), showing love or affection to their children (44.5%; 95% CI 40.5 to 48.5) and observing increased resilience (strength and perseverance) in their children (38.2%; 95% CI 34.3 to 42.2). Parents often reported increases in both negative and positive interactions due to the COVID-19 pandemic. For example, a higher proportion of parents who reported more conflicts with children also reported increased feelings of closeness (59.1%) compared with parents who did not report more conflicts with children (47.0%), χ 2 (1, n=618)=6.3, p=0.012.
Changes in parent–child interactions also varied according to salient sources of stress (ie, financial concerns and worries that the pandemic would make existing mental health problems worse). A higher proportion of parents reported increased harsh words with children when they were stressed about finances (13.8%) compared with parents who did not report this stressor (8.0%), χ 2 (1, n=618)=5.4, p=0.020. Parents who reported stress that the pandemic would make an existing mental health problem worse, compared with parents without this stressor, also more frequently reported increased harsh words with children since the pandemic (20.9% vs 6.7%), as well as increased discipline (23.8% vs 13.0%), conflicts (33.1% vs 17.9%) and yelling/shouting (31.4% vs 11.0%), χ 2 (1, n=618)=10.8 to 37.2, p ’s ≤0.001.
Interestingly, a higher proportion of parents stressed about financial concerns, compared with parents who did not report this stressor, also reported increased quality time with children (71.6% vs 60.1%), showing more love and affection to their children (49.3% vs 40.5%) and observing resilience in their children (43.3% vs 33.9%), χ 2 (1, n=618)=4.82 to 8.98, p’s <0.028. A higher proportion of parents stressed about an existing mental health problem also reported showing more love and affection to children as a result of the pandemic (53.5%) compared with parents without this stressor (41.0%), χ 2 (1, n=618)=7.8, p<0.005.
Sources of support
Figure 2 presents sources of support identified by parents that had helped them cope with stress related to the COVID-19 pandemic in the past 2 weeks. Parents most frequently identified going for a walk/exercise (59.1%; 95% CI 55.1 to 63.0), connecting with family and friends via phone and video chat (50.5%; 95% CI 46.5 to 54.5), connecting with those in their household (47.6%; 95% CI 43.6 to 51.6) and maintaining a healthy lifestyle (37.9%; 95% CI 34.0 to 41.8) as strategies that had helped them.
Parent-identified supports for coping with stress related to the COVID-19 pandemic in the past 2 weeks. Note: Maximum margin of error for proportions was ±3.9% at a 95% level of confidence.
Figure 3 presents sources of support identified by parents that had helped their children cope with stress related to the pandemic in the past 2 weeks. Parents most frequently identified these same strategies, as well as maintaining family routines (53.9%; 95% CI 49.9 to 57.9), playing inside (47.2%; 95% CI 43.2 to 51.3) and playing outdoors (45.8%; 95% CI 41.8 to 49.8) as having helped their children. Furthermore, 34.0% (95% CI 30.3 to 37.9) of parents identified staying in touch with teachers, school adults and child care workers as a source of support during the pandemic, and 5.8% (95% CI 4.1 to 8.0) identified accessing virtual educational or self-help mental health resources (eg, websites, applications) as a strategy that had helped their children. Additionally, 4.2% (95% CI 2.8 to 6.1) of parents had contacted a school or community-based mental health worker or counsellor virtually (eg, via phone or video chat).
Parent-identified supports for helping their children cope with stress related to the COVID-19 pandemic in the past 2 weeks. Note: Maximum margin of error for proportions was ±3.9% at a 95% level of confidence.
Regarding structural supports, a significantly higher proportion of parents (23.3%) identified having a supportive employer as a factor that helped their stress related to the pandemic in the past 2 weeks, compared with respondents without children at home (14.1%), χ 2 (1, n=3000)=30.9, p<0.001. Although overall access of structural supports was low, a significantly higher proportion of parents reported accessing federal financial benefits to help cope with stress in the past 2 weeks (13.6%) compared with the rest of the sample (9.2%), χ 2 (1, n=3000)=10.2, p=0.001. When restricted to parents stressed about financial concerns due to the COVID-19 pandemic (n=282), this proportion increased to 19.1% (95% CI 14.7 to 24.2). Finally, a significantly higher proportion of parents (7.9%) reported that they or a member of their household had accessed a food-based community programme since the onset of the pandemic such as the Food Bank, free meal programmes, community kitchens or food vouchers from a charity, compared with the rest of the sample (4.4%), χ 2 (1, n=3000)=12.5, p<0.001. When restricted to parents stressed about having enough food to meet household needs due to the COVID-19 pandemic (n=126), this proportion increased to 17.5% (95% CI 11.3 to 25.2).
This study identifies that following the first lockdown phase in Canada, 44.3% of parents of children <18 living at home reported worse mental health as a result of the pandemic. This aligns with research in the US identifying similar deteriorations in family mental health due to the COVID-19 pandemic. 29 International studies monitoring mental health trends in the general population throughout the first 5 months of the pandemic estimated prevalence rates of up to 51% for anxiety symptoms, up to 48% for depressive symptoms and up to 54% for symptoms of psychological distress. 30 Within parts of Canada during the same period, the prevalence of depressive symptoms in the general population had more than doubled compared with previous national estimates, 31 with experts projecting national increases in suicide based on trends in unemployment. 32 To our knowledge, the current study is the first national Canadian survey to identify that parents of children <18 living at home are a group at disproportionate risk of worsened mental health due to the COVID-19 pandemic. Compared with the rest of the population, a larger proportion of parents with children <18 at home reported increased alcohol consumption as a result of the pandemic, and suicidal thoughts or feelings, self-harm and stress about being safe from physical or emotional domestic violence in the past 2 weeks. These data validate early public health concerns regarding these mental health consequences of the pandemic. 2 10 33 Within our parent subsample, women, younger parents, parents of small children, those living with a disability and those with a pre-existing mental health condition reported worsened mental health since the start of the pandemic compared with other parents.
Within the subsample of parents with children living at home, more men reported increased alcohol use and being stressed about domestic violence compared with women. This gender difference in alcohol use aligns with pre-pandemic research findings that men generally consume more alcohol than women and are more likely than women to externalise distress through increased alcohol consumption. 34 35 However, the finding that men reported greater worry and stress from domestic violence than women is contrary to pre-pandemic studies showing that women are disproportionately affected by domestic violence. 36 37 Our survey question specifically asked about stress/worries about being safe from physical or emotional domestic violence as a result of the COVID-19 pandemic, which may not be comparable to the examination of this experience in other studies. This necessitates further research to unpack this association in the context of social isolation, financial stress and parenting responsibilities.
Parents with children <18 at home reported unique pressures, including worrying about their children’s health, mental health, education and being stressed about looking after children while continuing to work. A high proportion of parents reported being stressed about financial concerns (45.6%), about the pandemic making their existing mental health problems worse (27.8%) and about having enough food to meet their household’s basic needs (20.4%). A larger proportion of parents indicating stress about financial concerns or worsening of existing mental health problems due to the pandemic reported increased negative interactions with their children, including increased conflicts, discipline, use of harsh words and yelling/shouting compared with parents without these stressors. This aligns with other research showing that children have been relatively overlooked as a population vulnerable to the impacts of the COVID-19 virus, but are particularly vulnerable to stressful conditions exacerbated by the pandemic including financial stress, food insecurity, domestic violence and disrupted systems of care and education. 38 39
However, the majority of parents also reported increased positive interactions at home, including having more quality time together, feeling closeness, showing love and affection and observing resilience in their children. Parents often reported increases in both negative and positive interactions with children due to the COVID-19 pandemic, possibly due to increased opportunities for family interactions overall. Furthermore, a larger proportion of parents stressed about financial concerns due to the pandemic reported having more quality time, showing more love and affection and observing resilience in their children. A larger proportion of parents stressed about worsening mental health problems reported showing more love and affection with their children. Increased time and flexibility at home has created conditions for families to engage in more conversations and activities together. 40 41 Previous research has found that while parenting pressures during the pandemic have increased, so have opportunities to strengthen family connectedness. 7 Our results indicate that strengthened connectedness may be particularly salient for families experiencing heightened stress due to the pandemic, although the specific mechanisms underlying these associations are unclear.
Free digital technologies have furthermore facilitated connecting with others outside the home, as well as tools for managing parenting stress and enabling children to participate in school and child-friendly activities online. 7 8 41 However, digital technologies and online learning are not easily accessible for everyone, particularly for families with limited Internet or digital device access and language barriers, and for children with learning difficulties and special needs. In the current study, fewer than 6% of families reported accessing virtual mental health supports as strategies for addressing children’s stress related to the pandemic. Although online mental health services have been found to be effective, feasible and acceptable among adults and youth, 42 real-world uptake and retention has generally been found to be low. 43 44 Early COVID-specific research from China has found that uptake of any mental health services since the start of the pandemic has been as low as 3.7%, with concerns raised that online mental health services may still not address present needs due to existing digital divides, appropriateness for all populations and quality assurance. 45
Considering the needs of diverse families, as well as issues of health equity, early examinations of the COVID-19 pandemic have also emphasised the importance of community organisations and governments in providing access to economic and social supports. 46 47 In the current study, a significantly greater proportion of parents with children <18 living at home compared with the rest of the population had relied on supportive employers and government financial supports in the past 2 weeks, and had accessed food programmes since the start of the pandemic. Parents also frequently identified school, community and government supports that had helped them and their children cope with stress related to the COVID-19 pandemic. Other studies have also identified supports such as paid emergency leave, unemployment insurance, rent protection and access to safe and secure housing and outdoor spaces as critical in supporting parents to have the time and resources necessary to care for their children. 46 47 Although these policies and relief systems may not have been designed specifically for families and children, they hold the potential to help address some of the underlying causes 48 of compromised parent and child mental health at the population level, including family financial stress, employment and food insecurity, stigma, overcrowding and violence. The effectiveness of these policies, however, will depend on the human resources to organise, distribute and implement services when workforces are already overloaded. For example, in the current study, fewer than one in five families with financial stress or concerns about having enough food to meet their household basic needs had recently accessed federal benefits or food programmes, respectively, warranting further investigation into the ease of access to these services. 49 Furthermore, many of these underlying causes of health inequities will remain after the COVID-19 crisis has subsided, 50 suggesting that many of these interventions should be sustained irrespective of the pandemic.
Strengths and limitations
A notable strength of this study was the large, nationally representative sample that enabled population subgroup analyses to examine disparities in mental health for parents and across parent subgroups. The study was designed to include participation from families of diverse backgrounds, although small numbers of parents identifying as Indigenous or LGBT2Q+ ((lesbian, gay, bisexual, transgender, two-spirit and queer) prohibited us from examining these populations of interest. We also did not have a reliable measure of single parent status to investigate mental health trends among this group. Although strategies including oversampling and community partnerships were used to minimise selection bias and reduce possible technology barriers, it is possible that survey respondents differed from survey non-respondents on key measures of interest including mental health, financial security or family conflict, which may have affected our estimates. The study design was cross-sectional, therefore we cannot determine if outcomes such as parent–child interactions and parent stressors were causally related, only that they were associated. We also did not control for potential confounding variables that might have introduced bias; further in-depth investigations would complement this study by providing more understanding of these associations. This study did not measure the prevalence of specific mental health outcomes or include clinical assessments of mental illness which may limit comparability with other research. This study also did not take into account baseline measures of mental health or multiple comorbidities and was specific to the Canadian context during the first re-opening phase of the COVID-19 pandemic. It will be important to monitor the impact of the pandemic on family mental health over time and in different contexts. We were also unable to assess the impact of the pandemic from the perspectives of children and youth themselves, including children’s reactions to parents’ stress during the pandemic and children’s reported supports including use of mental health services. This is a critical knowledge gap for future research to address. The purpose of the current study was to assess preliminary impacts of the COVID-19 pandemic on families’ general mental health at a community level and to provide early data to inform relevant policy and programming actions. Examining specific impacts on the prevalence of mental health disorders and effective clinical responses is an important focus for future research.
Conclusions and implications
In response to the COVID-19 pandemic, policymakers and service providers globally have been faced with the challenge of having to make rapid decisions that will have immediate and long-term effects on the mental health and well-being of families and children. In the early days of the first ‘re-opening’ phase in Canada, nearly two in every five people reported worse mental health since the pandemic began, with this proportion increasing to nearly one in every two people for parents with children <18 living at home. Schools/child care, communities and government systems play an essential role in protecting and supporting parents and children, particularly for families without reliable access to the Internet or virtual technologies. While pressure is put on parents, it is important to remember that families exist within a social ecosystem with opportunities to promote child and youth mental health. Supports such as affordable child care, low barrier Internet access, publicly-funded stepped care and psychotherapy and easily available financial supports are interventions that can directly benefit families. 41 51 Continuations of financial interventions beyond the pandemic have also been suggested, including the idea of a universal basic income. 52 The effectiveness of these systems further depends on intersectoral communication, collaboration and action, and therefore seeking feedback and advice from community stakeholders will be critical for monitoring whether these systems are working for families and children during the remainder of the pandemic and beyond.
Ethics statements
Patient consent for publication.
Not required.
Ethics approval
Ethics approval was provided by the Behavioural Research Ethics Board at the University of British Columbia (H20-01273).
Acknowledgments
We are appreciative of the support and partnership we received in mobilising this project from the Canadian Mental Health Association (CMHA) and Mental Health Foundation. We are grateful for the financial support provided by CMHA to fund Maru/Matchbox to deploy the survey. AG and EJ would also like to thank the Michael Smith Foundation for Health Research for financial support (Scholar Awards) and KT would like to thank the Canadian Institutes of Health Research and Michael Smith Foundation for Health Research for financial support (Fellowship Awards). Special thanks to Katherine Janson, Margaret Eaton and Jonathan Morris (CMHA) for facilitating study communications and government relations outreach and to Jacqueline Campbell, Neesha Mathew and Stacey Kinley (Maru/Matchbox) for supporting survey deployment and data preparation. We also thank Dr Antonis Kousoulis for his role in the early conceptualisations of the study, including survey design.
- Jenkins E ,
- McAuliffe C ,
- Hirani S , et al
- Holmes EA ,
- O'Connor RC ,
- Perry VH , et al
- Coller RJ ,
- Gassman-Pines A ,
- Ananat EO ,
- Fitz-Henley J
- Canadian Human Rights Commission
- Lachman JM ,
- Sherr L , et al
- Pfefferbaum B ,
- Kofman YB ,
- Children First Canada
- Fegert JM ,
- Vitiello B ,
- Plener PL , et al
- Waddell C ,
- Schwartz C ,
- Barican J ,
- Gray-Grant D
- Russell BS ,
- Hutchison M ,
- Tambling R , et al
- Shonkoff JP ,
- Garner AS ,
- Siegel BS , et al
- Hertzman C ,
- Benner AD ,
- Armitage R ,
- Golberstein E ,
- Gonzales G ,
- Kousoulis A ,
- Crepaz-Keay D , et al
- Patrick SW ,
- Henkhaus LE ,
- Zickafoose JS , et al
- Lipsitz O ,
- Nasri F , et al
- Schmitz N ,
- Meng X , et al
- McIntyre RS ,
- Gunnell D ,
- Appleby L ,
- Arensman E , et al
- Palmer RHC ,
- Hopfer CJ , et al
- Bronte-Tinkew J ,
- Matthews G , et al
- Winstok Z ,
- Melton HC ,
- Bennett D ,
- Taylor-Robinson DC
- Chanchlani N ,
- Buchanan F ,
- Bashshur RL ,
- Shannon GW ,
- Bashshur N , et al
- Edan S , et al
- Fleming T ,
- Lucassen M , et al
- Benfer EA ,
- Merchant RM ,
- Canadian Mental Health Association
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Correction notice This article has been corrected since it first published. The provenance and peer review statement has been included.
Contributors AG, KT, MG, EJ and CM co-led the conceptualisation of this investigation. AG directed the data analyses, interpretation and writing of this manuscript. KT conducted the data analyses and contributed to data interpretation and writing of this manuscript. EJ, CGR, MG, CM and SH contributed to the interpretation and writing of this manuscript.
Funding The Canadian Mental Health Association (CMHA) funded survey data collection through national polling vendor, Maru/Matchbox. Collaborators from CMHA also contributed to the survey development. CMHA had no further role in the study design, data collection, data analysis or interpretation.
Conflict of Interest Declaration CGR reports receiving personal fees from the University of British Columbia during the conduct of this study. All other authors report no competing interests.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
↵ For the context of this study, children are defined as children and youth below the age of 18.
↵ In the following when we refer to parents, these are parents living with children <18 years old unless otherwise specified.
Read the full text or download the PDF:
- Introduction
- Conclusions
- Article Information
eTable. Unadjusted and Adjusted Odds Ratios of Family Economic Hardship by COVID-19 Exposure, Restricting COVID-19 Diagnoses to Those Told They “Definitely had COVID-19”
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Hair NL , Urban C. Association of Severe COVID-19 and Persistent COVID-19 Symptoms With Economic Hardship Among US Families. JAMA Netw Open. 2023;6(12):e2347318. doi:10.1001/jamanetworkopen.2023.47318
Manage citations:
© 2024
- Permissions
Association of Severe COVID-19 and Persistent COVID-19 Symptoms With Economic Hardship Among US Families
- 1 Department of Health Services Policy and Management, University of South Carolina Arnold School of Public Health, Columbia
- 2 Department of Economics, Montana State University, Bozeman
Question Are COVID-19 outcomes, including severe COVID-19 and persistent COVID-19 symptoms, associated with economic hardship among US families?
Findings In this cohort study of 6932 families, the odds of reporting economic hardship were higher for families headed by an adult with persistent COVID-19 symptoms and, to a lesser extent, families headed by an adult with previous severe COVID-19 compared with families with no history of COVID-19. Families with lower income before the pandemic were more vulnerable to employment disruptions and earnings losses associated with an adult family member’s COVID-19 illness.
Meaning Policy actions to mitigate the household financial hardship of post–COVID-19 conditions merit continued discussion.
Importance Little is known about the association of severe COVID-19 and post–COVID-19 conditions with household finances.
Objective To examine associations between COVID-19 outcomes, pandemic-related economic hardship, and prepandemic socioeconomic status among families in the US.
Design, Setting, and Participants This cohort study used data from the Panel Study of Income Dynamics (PSID), a nationally representative, longitudinal study. Data included 6932 families active in the PSID in both 2019 and 2021.
Exposures Ordinal exposure categories were defined based on whether the reference person or spouse or partner reported a positive COVID-19 diagnosis and (1) persistent COVID-19 symptoms, (2) previous severe COVID-19, or (3) previous moderate, mild, or asymptomatic COVID-19. Families with no history of COVID-19 served as the reference group.
Main Outcomes and Measures Outcomes included whether a resident family member was laid off or furloughed, lost earnings, or had any financial difficulties due to the COVID-19 pandemic.
Results In this cohort study of 6932 families (772 Hispanic families [weighted, 13.5%; 95% CI, 12.4%-14.6%], 2725 non-Hispanic Black families [weighted, 13.1%; 95% CI, 12.3%-14.1%], and 3242 non-Hispanic White families [weighted, 66.8%; 95% CI, 65.2%-68.3%]), close to 1 in 4 (2222 [weighted, 27.0%; 95% CI, 25.6%-28.6%]) reported income below 200% of the US Census Bureau poverty threshold. In survey-weighted regression models adjusted for prepandemic sociodemographic characteristics and experiences of economic hardship, the odds of reporting pandemic-related economic hardship were 2.0 to 3.7 times higher among families headed by an adult with persistent COVID-19 symptoms (laid off or furloughed: adjusted odds ratio [AOR], 1.98 [95% CI, 1.37-2.85]; lost earnings: AOR, 2.86 [95% CI, 2.06-3.97]; financial difficulties: AOR, 3.72 [95% CI, 2.62-5.27]) and 1.7 to 2.0 times higher among families headed by an adult with previous severe COVID-19 (laid off or furloughed: AOR, 1.69 [95% CI, 1.13-2.53]; lost earnings: AOR, 1.99 [95% CI, 1.37-2.90]; financial difficulties: AOR, 1.87 [95% CI, 1.25-2.80]) compared with families with no history of COVID-19. Families headed by an adult with persistent COVID-19 symptoms had increased odds of reporting financial difficulties due to the pandemic regardless of prepandemic socioeconomic status (families with lower income: AOR, 3.71 [95% CI, 1.94-7.10]; families with higher income: AOR, 3.74 [95% CI, 2.48-5.63]). Previous severe COVID-19 was significantly associated with financial difficulties among families with lower income (AOR, 2.59 [95% CI, 1.26-5.31]) but was not significantly associated with financial difficulties among those with high income (OR, 1.56 [95% CI, 0.95-2.56]).
Conclusions and Relevance This cohort study suggests that persistent COVID-19 symptoms and, to a lesser extent, previous severe COVID-19 were associated with increased odds of pandemic-related economic hardship in a cohort of US families. The economic consequences of COVID-19 varied according to socioeconomic status; families with lower income before the pandemic were more vulnerable to employment disruptions and earnings losses associated with an adult family member’s COVID-19 illness.
More than 5.9 million COVID-19–associated hospital admissions have been recorded among US adults. 1 It is estimated that at least 3 million to 5 million US adults are currently living with activity-limiting post–COVID-19 conditions (PCCs) and that approximately 15% of the US adult population (approximately 39 million adults) have, at some point, experienced PCCs. 2 , 3 Beyond significant personal health effects, there is accumulating evidence that patients with severe COVID-19 and PCCs face considerable economic consequences. Symptoms of PCCs can adversely affect daily functioning and have been associated with a lower likelihood of working full time and a higher likelihood of being unemployed. 4 , 5 COVID-19–associated hospitalizations have been similarly associated with job loss. 6 In addition to the direct associations with patients’ work and earnings, household finances may be further stressed by out-of-pocket medical expenses and lost caretaker productivity. 6 - 9 The consequences may be even more severe for families with low income who have fewer resources available to buffer against COVID-19–related financial shocks but appear to be more likely to experience severe or long-term health effects from COVID-19. 10 , 11
This study used data from the Panel Study of Income Dynamics (PSID), a long-running, nationally representative household panel survey with interviews conducted both before and during the COVID-19 pandemic, to examine associations between COVID-19 exposure and economic hardship at the family level and, furthermore, whether these associations vary according to a family’s prepandemic socioeconomic status. We hypothesized (1) that COVID-19 exposure would be positively associated with experiences of economic hardship, (2) that the strength of these associations would vary according to the duration and severity of COVID-19 symptoms, and (3) that the economic sequelae of COVID-19 would be most pronounced among families with lower income before the pandemic.
This cohort study was deemed exempt from review by the Office of Research Compliance, an administrative office that supports the University of South Carolina Institutional Review Board, because it involved secondary analysis of publicly available, deidentified data. We followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline for cohort studies. 12
We used unrestricted public use data from the PSID, a nationally representative, longitudinal study of families in the US. 13 The core PSID survey, fielded biennially, collects detailed information on income, employment, wealth, and family composition. The PSID collects detailed information for the family’s reference person (RP) and, if present, their spouse or partner (SP). Fewer details are collected for other family members. In 2021, the PSID added questions to assess the outcome of the COVID-19 pandemic on study families, including COVID-19–related health outcomes and pandemic-related financial difficulties. The PSID-2021 survey was fielded from March 19 to December 31, 2021.
The PSID-2021 Early Release file includes data collected from a balanced panel of 8468 families who were active in the PSID in both 2019 and 2021. We merged postpandemic measures of family economic hardship and COVID-19–related health outcomes collected in the PSID-2021 survey with prepandemic sociodemographic characteristics collected in the PSID-2019 survey. We excluded families with incomplete sociodemographic or economic information (n = 259) or indeterminate COVID-19 exposure (n = 1277). The study cohort comprised 6932 families.
We examined 3 indicators of family-level economic hardship reported by the RP in the PSID-2021 survey. They were (1) resident family member laid off or furloughed due to the pandemic, (2) resident family member lost earnings due to the pandemic, and (3) resident family member had financial difficulties due to the pandemic.
Information related to COVID-19 infection and severity and duration of COVID-19 symptoms was collected for the RP and SP (if present). The RP was asked if they or their SP had “talked to a doctor or other health care professional about whether [they] may have had COVID-19.” An affirmative response was followed by, “Did they say that [you/your SP] definitely had COVID-19, probably had it, may have had it, probably did not have it, or definitely did not have COVID-19?” If the RP reported that they or their SP were told that they definitely or probably had COVID-19, they were considered to have a positive COVID-19 diagnosis. Follow-up questions ascertained whether the RP or their SP was admitted to a hospital because of COVID-19 (yes or no); had experienced any COVID-19 symptoms (yes or no) and, if so, how bad or bothersome these symptoms were at their worst (mild, moderate, severe, or very severe); or were currently experiencing lingering physical or mental health effects from COVID-19 (yes or no). Families headed by at least 1 adult (RP and/or SP) with a COVID-19 diagnosis were assigned to 1 of 3 ordinal exposure categories:
Persistent COVID-19: families headed by at least 1 adult who, at the time of the survey, was currently experiencing lingering health effects from COVID-19;
Severe COVID-19: families with no indication of persistent COVID-19 headed by at least 1 adult who was hospitalized or experienced severe or very severe symptoms due to COVID-19; and
Moderate, mild, or asymptomatic COVID-19: families with no indication of severe or persistent COVID-19 headed by at least 1 adult who had moderate, mild, or no symptoms associated with their previous COVID-19 illness.
If the RP reported that they or their SP had not talked to a health care professional or were told that they may, probably did not, or definitely did not have COVID-19, they were asked if they had “symptoms or exposure… that led [them] to believe [they] had COVID-19” and, when applicable, about the severity and duration of symptoms. Families with no history of COVID-19 illness (ie, no COVID-19 diagnosis and no self-reported COVID-19 symptoms or lingering health effects) were assigned to a reference group. Families with indeterminate COVID-19 exposure (eg, incomplete data on COVID-19 health outcomes or self-reported COVID-19 symptoms or lingering health effects without a corresponding COVID-19 diagnosis) were excluded.
We included the following sociodemographic characteristics collected in the PSID-2019: any children younger than 16 years in the family (yes or no), age of the RP, self-reported race and ethnicity of the RP (Hispanic, non-Hispanic Black, non-Hispanic White, or other [including non-Hispanic Alaska Native, American Indian, Asian, or Pacific Islander persons or individuals who reported other race]), highest level of education completed by the RP or SP (less than college, some college, or college graduate), total family income relative to US Census Bureau poverty thresholds 14 (income below or above 200% of the poverty threshold), whether any family member went without health insurance in the past 2 years (yes or no), geographic region (northeast, north central, south, or west), and residence in a nonmetropolitan area (yes or no). For each outcome of interest, we also identified a closely related indicator of economic hardship collected in the PSID-2019: whether the RP or SP missed work because they were temporarily laid off (yes or no), total family labor income, or whether any family member had credit card or store card debt (yes or no).
First, we estimated a multinomial logistic regression model to assess correlations between families’ sociodemographic characteristics and experiences of economic hardship at baseline and COVID-19 exposure. The no COVID-19 exposure category served as the reference outcome. Results are presented as adjusted relative risk ratios (ARRRs) with 95% CIs.
Next, we estimated logistic regression models to examine associations between COVID-19 exposure (persistent; severe; or moderate, mild, or asymptomatic COVID-19 vs no COVID-19) and 3 indicators of pandemic-related economic hardship (laid off or furloughed, lost earnings, and financial difficulties) among US families. Separate models were fit for each economic outcome. Results are presented as unadjusted odds ratios (ORs) or adjusted ORs (AORs) with 95% CIs. Adjusted models included a range of potentially confounding sociodemographic characteristics and, to account for the possibility that COVID-19 exposure may be associated with economic hardship at baseline, a closely related economic indicator collected in the PSID-2019 ( Table 1 ). We further examined whether associations between COVID-19 exposure and economic hardship varied by prepandemic socioeconomic status. Differences across subgroups were evaluated by fitting separate regression models stratified by prepandemic family income (below vs above 200% of the poverty threshold).
All analyses were conducted using the survey commands in Stata, version 16 (StataCorp LLC) to apply family weights provided by the PSID. Estimates were considered statistically significant if 95% CIs did not include 1 (equivalent to 2-sided P < .05).
Table 1 presents unweighted frequencies and weighted percentages for sample characteristics. The study cohort comprised 6932 families. Of these, 1340 (17.0% [95% CI, 15.9%-18.3%]), 1780 (23.0% [95% CI, 21.7%-24.4%]), and 1489 (16.8% [95% CI, 15.6%-18.0%]) reported that a resident family member had been laid off or furloughed, lost earnings, or had financial difficulties, respectively, due to the COVID-19 pandemic. A total of 15.4% (95% CI, 14.3%-16.5%) of families were headed by an adult (RP and/or SP) with a COVID-19 diagnosis, including 303 (4.4% [95% CI, 3.8%-5.1%]), 243 (3.1% [95% CI, 2.6%-3.7%]), and 601 (7.9% [95% CI, 7.2%-8.8%]) with a history of persistent COVID-19, severe COVID-19, or moderate, mild, or asymptomatic COVID-19, respectively. Close to 1 in 4 households (28.4% [95% CI, 24.8%-32.1%]) headed by an adult with a prior COVID-19 diagnosis reported symptoms consistent with PCCs. The remaining 5785 in-sample families (84.6% [95% CI, 83.4%-85.7%]) had no history of COVID-19 illness.
The sample was racially and ethnically diverse; 772 families (13.5% [95% CI, 12.4%-14.6%]) were headed by a Hispanic RP, 2725 (13.1% [95% CI, 12.3%-14.1%]) by a non-Hispanic Black RP, and 3242 (66.8% [95% CI, 65.2%-68.3%]) by a non-Hispanic White RP ( Table 1 ). Nearly 25% of families (2388 families [23.2%; 95% CI, 22.0%-24.5%]) included at least 1 resident child younger than 16 years. Close to 75% of families (4863 families [70.4%; 95% CI, 68.9%-72.0%]) were headed by an adult (RP or SP) with at least some college education, including 2286 families (36.8% [95% CI, 35.3%-38.4%]) headed by a college graduate. Close to 1 in 4 families (2222 families [27.0%; 95% CI, 25.6%-28.6%]) reported total family income below 200% of the poverty threshold; 1218 families (14.2% [95% CI, 13.1%-15.4%]) had at least 1 member who went without health insurance in the past 2 years, and 1040 (15.8% [95% CI, 14.7%-17.0%]) resided in a nonmetropolitan area.
Table 2 presents results from a multinomial logistic regression in which the reference outcome is no COVID-19 exposure. Accounting for baseline family characteristics, prepandemic experiences of economic hardship were associated with COVID-19 exposure. Families headed by an adult who missed work because they were temporarily laid off or furloughed were at higher risk of persistent COVID-19 symptoms (ARRR, 2.82 [95% CI, 1.34-5.93]), while families with credit card or store card debt (an indicator of financial difficulties) were at higher risk of moderate, mild, or asymptomatic COVID-19 infection (ARRR, 1.58 [95% CI, 1.25-2.00]).
Table 3 presents results from unadjusted and adjusted logistic regression models. Compared with families with no history of COVID-19, families headed by an adult with persistent COVID-19 symptoms had at least a 2-fold greater odds of having a resident family member who was laid off or furloughed (OR, 2.31 [95% CI, 1.64-3.25]; AOR, 1.98 [95% CI, 1.37-2.85]) or lost earnings (OR, 3.07 [95% CI, 2.24-4.21]; AOR, 2.86 [95% CI, 2.06-3.97]) and a more than 3-fold greater odds of reporting any financial difficulties (OR, 3.82 [95% CI, 2.77-5.27]; AOR, 3.72 [95% CI, 2.62-5.27]) due to the pandemic. Associations between acute COVID-19 symptoms (ie, COVID-19 symptoms resolved by the time of the PSID-2021 survey) and indicators of economic hardship were generally less strong but varied significantly by symptom severity. The odds of a resident family member being laid off or furloughed (OR, 2.03 [95% CI, 1.35-3.05]; AOR, 1.69 [95% CI, 1.13-2.53]), losing earnings (OR, 2.30 [95% CI, 1.57-3.36]; AOR, 1.99 [95% CI, 1.37-2.90]), or having financial difficulties (OR, 2.28 [95% CI, 1.53-3.39]; AOR, 1.87 [95% CI, 1.25-2.80]) due to the pandemic were 1.7 to 2.0 times greater among families headed by an adult with previous severe COVID-19 compared with families with no history of COVID-19. In unadjusted models, a history of moderate, mild, or asymptomatic COVID-19 infection was associated with greater odds of a resident family member losing earnings due to the pandemic (OR, 1.41 [95% CI, 1.09-1.82]); however, the association was no longer statistically significant after adjusting for baseline family characteristics (AOR, 1.21 [95% CI, 0.92-1.58]). We found no statistically significant association between previous moderate, mild, or asymptomatic COVID-19 and a resident family member either being laid off or furloughed (OR, 1.22 [95% CI, 0.91-1.62]; AOR, 1.05 [95% CI, 0.78-1.42]) or experiencing financial difficulties (OR, 1.05 [95% CI, 0.78-1.40]; AOR, 0.91 [95% CI, 0.67-1.24]) due to the pandemic. In sensitivity analyses, results were similar when we considered only those who were told by a health care professional that they definitely had COVID-19 as having a COVID-19 diagnosis (eTable in Supplement 1 ).
Table 4 presents results separately for families with a prepandemic income below or above 200% of the poverty threshold. Among families with lower income, the odds of experiencing economic hardship due to the pandemic were 2.5 to 4.9 times greater for families headed by an adult with persistent COVID-19 symptoms (laid off or furloughed: AOR, 2.46 [95% CI, 1.25-5.28]; lost earnings: AOR, 4.88 [95% CI, 2.62-9.11]; financial difficulties: AOR, 3.71 [95% CI, 1.94-7.10]) or with previous severe COVID-19 (laid off or furloughed: AOR, 2.76 [95% CI, 1.29-5.90]; lost earnings: AOR, 4.61 [95% CI, 2.34-9.06]; financial difficulties: AOR, 2.59 [95% CI, 1.26-5.31]) than for families with no history of COVID-19. In addition, compared with families with lower income and no history of COVID-19, families with lower income headed by an adult with previous moderate, mild, or asymptomatic COVID-19 had a close to 2-fold greater odds of having a resident family member who lost earnings (AOR, 1.86 [95% CI, 1.02-3.39]) due to the pandemic; positive associations with a family member being laid off or furloughed (AOR, 1.68 [95% CI, 0.91-3.07]) or experiencing financial difficulties (AOR, 1.06 [95% CI, 0.61-1.84]) were not statistically significant.
Among families with higher income, the odds of a resident member being laid off or furloughed (AOR, 1.81 [95% CI, 1.19-2.75]), losing earnings (AOR, 2.37 [95% CI, 1.62-3.46]), or having financial difficulties (AOR, 3.74 [95% CI, 2.48-5.63]) due to the pandemic were 1.8 to 3.7 times greater for families headed by an adult with persistent COVID-19 symptoms than for families with no COVID-19 ( Table 4 ). Positive associations between previous severe COVID-19 and pandemic-related economic hardship (laid off or furloughed: AOR, 1.36 [95% CI, 0.84-2.19]; lost earnings: AOR, 1.44 [95% CI, 0.93-2.24]; financial difficulties: AOR, 1.56 [95% CI, 0.95-2.56]) were not statistically significant among families with higher income. We found no statistically significant associations between previous moderate, mild, or asymptomatic COVID-19 and experiences of economic hardship (laid off or furloughed: AOR, 0.92 [95% CI, 0.65-1.30]; lost earnings: AOR, 1.10 [95% CI, 0.81-1.50]; financial difficulties: AOR, 0.85 [95% CI, 0.58-1.25]) among families with higher income.
This cohort study contributes timely, policy-relevant information on how COVID-19 and PCCs may be associated with families’ economic well-being. Using data from a long-running, nationally representative household panel survey with interviews conducted both before and during the COVID-19 pandemic, we found that persistent COVID-19 symptoms and, to a lesser extent, previous (resolved) severe COVID-19 were associated with increased odds of pandemic-related economic hardship among US families. In regression models adjusted for prepandemic sociodemographic characteristics and experiences of economic hardship, the odds of a resident family member being laid off or furloughed, losing earnings, or having financial difficulties were 2.0 to 3.7 times higher among families headed by an adult with persistent COVID-19 symptoms and 1.7 to 2.0 times higher among families headed by an adult with previous severe COVID-19 compared with families with no history of COVID-19. We found no statistically significant association in the overall sample between moderate, mild, or asymptomatic COVID-19 and indicators of family economic hardship.
Compared with similar families with no history of COVID-19, families headed by an adult with persistent COVID-19 symptoms had increased odds of experiencing economic hardship regardless of their prepandemic financial status. In contrast, an adult family member’s severe COVID-19 illness was more strongly associated with indicators of economic hardship among families with lower income. On balance, families with lower income before the pandemic (ie, families who had fewer resources available to buffer against COVID-19–related financial shocks) were more vulnerable to employment disruptions and earnings losses associated with an adult family member’s COVID-19 illness. Individuals living in economically vulnerable households are more likely to hold essential jobs, which have been associated with increased employment-related exposure and risk of severe COVID-19 among workers and their household members. 15 , 16 Low-wage essential workers, who typically do not have the ability to work from home, are also least likely to have access to paid leave. 17 , 18 Our results highlight the extent to which the economic sequelae of COVID-19 vary according to socioeconomic status and, consequently, may compound preexisting inequalities.
A total of 15.4% of households in our sample were headed by an adult with a prior COVID-19 diagnosis. Of those, close to 1 in 4 (weighted 28.4%; 4.4% of the overall sample) reported persistent symptoms consistent with PCCs. Although point prevalence estimates of PCCs vary across studies, populations, and settings, our findings are in line with prior work that estimates 13% to 30% of those who have had COVID-19 are currently experiencing PCCs or associated conditions. 2 , 19 - 21 At least 3 million to 5 million US adults are currently living with activity-limiting PCCs. 3 Given the significant economic consequences of COVID-19 and the expectation that PCCs will continue to affect individuals and their families over the long term, policy actions to mitigate the household financial impact of PCCs (eg, expanded paid sick leave, improved workplace accommodations, and wider access to disability insurance) merit continued discussion. 22 - 24
This study has some limitations. First, we cannot definitively rule out the possibility that the increased odds of economic hardship we observed among families headed by an adult with previous severe COVID-19 or persistent COVID-19 symptoms were associated with factors other than COVID-19 illness. However, leveraging the longitudinal nature of PSID data, we were able to adjust for a range of potentially confounding factors measured prior to the pandemic. The absence of a strong association between economic hardship and previous moderate, mild, or asymptomatic COVID-19 further strengthens our interpretation of the study findings. Second, measures of economic hardship, COVID-19 diagnosis, and severity and duration of COVID-19 symptoms were self-reported and thus subject to recall and misclassification bias. Third, we excluded those with possible symptoms of COVID-19 who did not talk to a health care professional. Fourth, the PSID-2021 survey was fielded from March to December 2021, so our results may not reflect later phases of the pandemic.
This cohort study suggests that persistent COVID-19 symptoms and, to a lesser extent, severe COVID-19 were associated with increased odds of pandemic-related economic hardship among a cohort of US families. The economic consequences of COVID-19 varied according to socioeconomic status; families with lower income before the pandemic were more vulnerable to employment disruptions and earnings losses associated with an adult family member’s COVID-19 illness.
Accepted for Publication: October 30, 2023.
Published: December 12, 2023. doi:10.1001/jamanetworkopen.2023.47318
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Hair NL et al. JAMA Network Open .
Corresponding Author: Nicole L. Hair, PhD, Department of Health Services Policy and Management, University of South Carolina Arnold School of Public Health, 915 Greene St, Columbia, SC 29208 ( [email protected] ).
Author Contributions: Drs Hair and Urban had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Both authors.
Acquisition, analysis, or interpretation of data: Both authors.
Drafting of the manuscript: Both authors.
Critical review of the manuscript for important intellectual content: Both authors.
Statistical analysis: Both authors.
Obtained funding: Both authors.
Administrative, technical, or material support: Urban.
Conflict of Interest Disclosures: None reported.
Funding/Support: This project was supported by grant 5 RDR18000001-05-00 from the US Social Security Administration (SSA) (Dr Hair). The collection of data used in this study was partly supported by the National Institutes of Health under grant numbers R01 HD069609 and R01 AG040213 and the National Science Foundation under award numbers SES 1157698 and 1623684.
Role of the Funder/Sponsor: The funder reviewed the manuscript for inaccurate descriptions of SSA policy or procedure. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The research reported herein was performed pursuant to a grant from the SSA funded as part of the Retirement and Disability Consortium. The opinions and conclusions expressed are solely those of the author(s) and do not represent the opinions or policy of the SSA or any agency of the federal government. Neither the US government nor any agency thereof, nor any of their employees, makes any warranty, express or implied, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of the contents of this report. Reference herein to any specific commercial product, process, or service by trade name, trademark, manufacturer, or otherwise does not necessarily constitute or imply endorsement, recommendation, or favoring by the US government or any agency thereof.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
How to Write About Coronavirus in a College Essay
Students can share how they navigated life during the coronavirus pandemic in a full-length essay or an optional supplement.
Writing About COVID-19 in College Essays

Getty Images
Experts say students should be honest and not limit themselves to merely their experiences with the pandemic.
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many – a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.
Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them – and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic – and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
10 Ways to Discover College Essay Ideas

Tags: students , colleges , college admissions , college applications , college search , Coronavirus
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
College Admissions: Get a Step Ahead!
Sign up to receive the latest updates from U.S. News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
Ask an Alum: Making the Most Out of College
You May Also Like
Federal vs. private parent student loans.
Erika Giovanetti May 9, 2024

14 Colleges With Great Food Options
Sarah Wood May 8, 2024

Colleges With Religious Affiliations
Anayat Durrani May 8, 2024

Protests Threaten Campus Graduations
Aneeta Mathur-Ashton May 6, 2024

Protesting on Campus: What to Know
Sarah Wood May 6, 2024

Lawmakers Ramp Up Response to Unrest
Aneeta Mathur-Ashton May 3, 2024

University Commencements Must Go On
Eric J. Gertler May 3, 2024

Where Astronauts Went to College
Cole Claybourn May 3, 2024

College Admitted Student Days
Jarek Rutz May 3, 2024

Universities, the Police and Protests
John J. Sloan III May 2, 2024

Impact of the COVID-19 Crisis on Family Dynamics in Economically Vulnerable Households

The COVID-19 crisis and its reverberations resulted in levels of economic distress unprecedented since the 1930s. But COVID was a seismic social shock even for families that lost no income, due at least in part to abrupt school closures and the widespread threat of illness and death. The COVID-19 crisis will not affect all families equally, but may cause particular harm to children of low-income and less-educated parents and for preschool age children, who are especially sensitive to developmental inputs. We surveyed 572 low income families with preschool-age children in Chicago to understand family dynamics following the economic and social restrictions imposed by the pandemic. We separately examine the associations between economic hardship, exposure to the virus, and pandemic-induced increases in childcare time on parental mental health and stress, parent-child interaction, and children’s adjustment. We find both positive and negative effects: Parental job and income losses are strongly associated with parents’ depressive symptoms, stress, diminished sense of hope, and negative interactions with children. However, these ill effects do not occur for parents who lose jobs but do not experience concomitant income losses. In fact, job losses without income losses are associated with more positive parent-child interactions. Parents’ exposure to COVID-19 is associated with less positive parent-child interactions and more child behavior problems. In contrast, parents who report spending substantially more time in childcare as a consequence of the pandemic report more positive parent-child interaction. We discuss the implications of these results for policy and practice.
More Research From These Scholars
Welfare reform and the quality of young children’s home environments, the education gradient in maternal enjoyment of time in childcare, making a song and dance about it: the effectiveness of teaching children vocabulary with animated music videos.
Exploring the interplay between individual and family functioning during the COVID-19 pandemic: a cross-sectional study
- Open access
- Published: 07 May 2024
Cite this article
You have full access to this open access article

- Valentina Lucia La Rosa ORCID: orcid.org/0000-0002-6619-6777 1 ,
- Miriana Tornatore 1 &
- Elena Commodari ORCID: orcid.org/0000-0002-7647-8743 1
138 Accesses
Explore all metrics
Family relationships are central to an individual’s development and influence their emotional, relational, and social trajectories. Optimal family functioning, encompassing emotional connections, communication patterns, and coping mechanisms, is pivotal to the well-being of individual family members, especially during challenging periods such as the COVID-19 pandemic. From this perspective, this study, conducted during the second wave of the COVID-19 pandemic in Italy, assessed the interplay between individual and family functioning. Utilizing Hill's ABC-X model, we explored how the pandemic (stressor) impacted family dynamics (resources), perceived individual affectivity and family efficacy (perception), thereby influencing family quality of life (outcome). Four hundred and four participants completed a battery of standardized questionnaires to evaluate perceived individual affectivity during the pandemic, family quality of life, family dynamics (cohesion, flexibility, and communication), family conflict, family efficacy, and family coping strategies. Positive affectivity was associated with better family quality of life and more adaptive family coping strategies. The sample reported a low family quality of life and low family cohesion, flexibility, and communication during the pandemic. A positive sense of family cohesion, flexibility, and communication was associated with better individual well-being, better family quality of life and efficacy, and less conflict. Family communication was the strongest predictor of family quality of life in the study sample. In conclusion, our results emphasize the importance of strengthening family and individual resilience in transforming post-pandemic challenges into psychological and familial growth opportunities.
Similar content being viewed by others
Pandemic-Related Disruption and Positive Adaptation: Profiles of Family Function at the Onset of the Pandemic
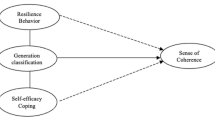
Intergenerational differences on resilience, sense of coherence, and self-efficacy coping of family during covid19 crisis: a salutogenic perspective

Impacts of COVID-19 and partial lockdown on family functioning, intergenerational communication and associated psychosocial factors among young adults in Singapore
Avoid common mistakes on your manuscript.
Human development encompasses physical, cognitive, and psychosocial growth throughout an individual's life cycle (Bornstein, 2018 ). Changes in one of these developmental areas often impact the other throughout life as they are interconnected and overlap (Sigelman & Rider, 2018 ).
Family relationships play a pivotal role in individual development, influencing the emotional, relational, and social trajectories (Morris et al., 2007 ; Shigeto & Voltaire, 2020 ; Sigelman & Rider, 2018 ). A supportive family fosters harmonious development from infancy through adulthood, affecting everything from early social skills to resilience against psychopathological disorders in later life stages (Butler et al., 2022 ; Chu et al., 2010 ). The family remains a cornerstone for support and development throughout the lifespan, from childhood through adolescence to adulthood (Bonnie et al., 2019 ; Shigeto & Voltaire, 2020 ; Wood et al., 2018 ). From this perspective, optimal family functioning, covering emotional bonds, communication, and coping strategies, is fundamental to individual psychological well-being (Bornstein, 2018 ; Olson, 2011 ). In a positive family environment, members work together as an interconnected unit to overcome difficult situations and conflicts, activating coping and resilience skills, especially in times of crisis (Kao & Caldwell, 2017 ).
From a developmental perspective, the COVID-19 pandemic can be considered a non-normative life event, that is, a life event that is significant, unpredictable, and unexpected and that does not follow a predetermined developmental pattern of the life cycle (e.g., natural disasters, death of a family member, illness) (Koulenti & Anastassiou-Hadjicharalambous, 2011 ). From this perspective, the pandemic has disrupted the regular course of individual and family dynamics (Fernandes et al., 2021 ). As global lockdowns reshaped social interactions, there were profound implications for mental health and interpersonal relationships (Luttik et al., 2020 ; Passavanti et al., 2021 ). While confinement-strained, family ties also underscored the importance of family cohesion in navigating shared traumas (Luttik et al., 2020 ).
According to the Family Stress Model (FSM), as formulated by Hill ( 1949 ), families experience stress when encountering various life events or challenges, such as financial difficulties, health issues, or interpersonal conflicts. These stressors can disrupt equilibrium within the family and lead to a series of reactions and adjustments. Hill's theory emphasizes that families strive to maintain stability and adapt to stress through coping strategies and support networks (McKenry & Price, 2005 ). Family quality of life is deeply influenced by the individual well-being and satisfaction of its members, making it a crucial outcome to assess (Brown & Brown, 2014 ). Therefore, studying the interplay between individual family members and their broader social contexts is essential for understanding how stress affects family dynamics and relationships. From this perspective, a pandemic can be considered an external stressor that affects the family system. To cope with the challenges of the pandemic, families need to actively balance external pressures with their coping strategies and belief in their ability to address challenges, thus developing resilient strategies and ultimately achieving family well-being (Crandall et al., 2022 ; Wu & Xu, 2020 ).
Several studies have evaluated the main dimensions of family functioning during the COVID-19 pandemic. A recent study on family functioning in Portuguese families showed that some families are more vulnerable to stress than others (Fernandes et al., 2021 ). In particular, family functioning was enhanced among the members who maintained balanced levels of cohesion and adaptability. These individuals can adapt and shift between different levels during crises, unlike those at the most extreme levels, which are deemed unbalanced (Fernandes et al., 2021 ). Other studies have underlined two opposite consequences of the pandemic on family quality of life: family conflict increased, but family cohesion represented an essential protective factor that could mitigate stress consequences and protect family well-being and resilience (Zeng et al., 2021 ). Communication is another dimension of family functioning that can relieve stress and represents an effective strategy for facing the COVID-19 pandemic (Hall et al., 2022 ; Zeng et al., 2021 ). Family coping is also an important construct to be investigated during critical periods such as the COVID-19 pandemic to understand how the family responds to stressors and adverse life events and how such coping strategies affect family functioning and the well-being of family members (Fogel et al., 2022 ). Recent studies have reported that family members may employ various coping strategies to deal with the stressors of the pandemic (Kusnadi et al., 2022 ). Some opt for cognitive or appraisal-centered approaches to shift their perspective on COVID-19 and re-evaluate how it affects their families’ daily lives. Others have used problem-focused coping techniques to address the challenges posed by the pandemic within their families (Wu & Xu, 2020 ). In particular, using positive coping strategies empowers family members to enhance their capacity to withstand distress and to improve their families’ quality of life. Fogel et al. ( 2022 ) showed that positive cognitive appraisal was a protective factor against a significant decrease in family quality of life during the pandemic.
Although the link between individual and family functioning is well established, there is a noticeable gap in research on understanding these dynamics during unprecedented events, such as pandemics. Most studies conducted during the COVID-19 pandemic have approached this issue from an individual perspective; however, a comprehensive exploration encompassing both individual and family dimensions in the context of a global crisis is scarce. Moreover, few studies have investigated the coping construct in the family dimension, as most have focused on individual coping (Kusnadi et al., 2022 ). Therefore, studies on this topic are critical to understanding the relationship between pandemic stressors and family quality of life.
In light of these considerations, it is essential to investigate how families coped with COVID-19 and their relationships with their functioning and quality of life. Furthermore, it is also relevant to assess the interplay between family functioning and the individual well-being of family members during a global crisis such as the pandemic.
Theoretical framework of the study
This study was guided by the FSM, which offers a comprehensive framework for understanding family dynamics under stress, particularly during the COVID-19 pandemic (Reich et al., 2023 ). More specifically, Hill's ABC-X model helps examine how families navigate COVID-19-related stress, delineating the interplay between the stressor event (A), the family's internal and external resources (B) to manage the crisis, the family's perception and interpretation of the stressor (C) and the resulting crisis outcome (X).
Several recent studies have effectively utilized Hill's FSM to analyze the impact of the COVID-19 pandemic on family structures and dynamics (McGill et al., 2022 ; Prime et al., 2020 ; Reich et al., 2023 ; von Suchodoletz et al., 2023 ). This growing research has demonstrated the model's robust applicability and relevance in contemporary contexts. Aligning with these research trends, our study employed Hill's model to explore the various outcomes (X) observed in families during the pandemic.
In the context of our study, as shown in Fig. 1 , the COVID-19 pandemic serves as the stressor event (A), fundamentally altering families' daily lives and routines. Our investigation focused on how families mobilize their resources (B), including cohesion, flexibility, communication, conflict, and coping strategies, to confront the challenges of the pandemic. Moreover, we examine the critical role of perceived family efficacy and pandemic-related individual affectivity (C), significantly shaping family responses and coping strategies for dealing with the crisis. Finally, we considered X (crisis outcomes) as the specific way in which family quality of life has been affected by the COVID-19 pandemic, resulting from the interplay between the stressor event (A), the family's resources (B), and the perception of the stressor (C).
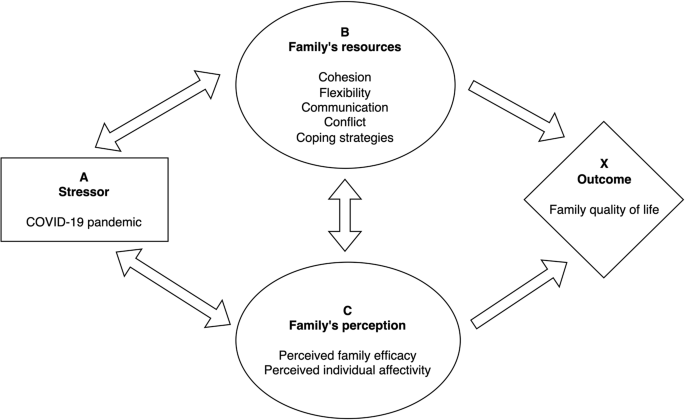
Application of Hill's Family Stress Model to the COVID-19 pandemic
Study aims and hypotheses
This study aimed to analyze family and individual functioning during the COVID-19 pandemic in Italy using Hill's ABC-X model. We focused on the interplay between the pandemic as a stressor (A), family dynamics such as cohesion, flexibility, communication, conflict, and coping strategies as resources (B), and perceived family efficacy and individual affectivity during the pandemic (C). In particular, this study explored how these factors collectively impact family quality of life (X).
Based on these study's aims, the following hypotheses were formulated as follows:
H1: Family dynamics (B)–cohesion, communication, flexibility, and conflict–positively influence family quality of life (X). More robust family dynamics predict better family quality of life.
H2: Perceived pandemic-related individual affectivity (C) correlates with family quality of life (X) and family dynamics (B). Positive pandemic-related individual affectivity is associated with better family quality of life and healthier family dynamics, while negative affectivity is linked to higher conflict and avoidance coping.
H3: Robust family functioning domains (B), positive perceived pandemic-related individual affectivity and high perceived family efficacy (C) lead to higher family quality of life (X), showcasing effective adaptation to pandemic stressors (A).
Materials and methods
Study design and participants.
This cross-sectional study was conducted during the second wave of the COVID-19 pandemic in Italy. During this period, the restriction measures varied according to the virus spread rates in different regions, vaccination status, and possession of the Green Pass (a certificate required in Italy to gain access to specific activities and attest to COVID-19 vaccination, recovery from disease or a negative COVID test). The participants were subjects who resided in Italy and agreed to respond to an online survey distributed through the main social networks. Exclusion criteria included individuals not living in Italy, under 18 years of age, unable or unwilling to provide informed consent, and with diagnosed psychiatric disorders. Participation in the study was voluntary, anonymous, and without remuneration. Online informed consent was obtained before participants answered the questionnaire.
The study protocol was drafted according to the Declaration of Helsinki, the Ethics Code for Italian psychologists (l. 18.02.1989, n. 56), Italian law for data privacy (dlgs 196/2003), and the Ethics Code for Psychological Research (March 27, 2015) approved by the Italian Psychologists Association. Furthermore, the Institutional Review Board of the Department of Educational Sciences of the University [omitted for peer review] approved this study.
The online questionnaire comprised 71 multiple-choice questions, and its completion required approximately 15 min.
The first section of the questionnaire consisted of 11 sociodemographic questions about gender, age, marital status, education, employment, online work during the pandemic, contracting COVID-19, COVID-19 cases in the family, hospitalization for COVID-19 of participants and family members, and family bereavements due to COVID-19.
The second section consisted of 60 items. Participants were asked to respond to items drawn from validated questionnaires using an approach already adopted in psychological and health research (Lanza et al., 2010 ; Mantziki et al., 2014 ; McGee et al., 2015 ).
In selecting the items to be included in the survey, the objectives of the study were clearly defined, with a focus on assessing the impact of the COVID-19 pandemic on family and individual well-being, and an extensive review of the existing literature was undertaken to identify validated questionnaires assessing the constructs of interest.
Criteria for item selection were established based on the research objectives and constructs of interest. These criteria included the relevance of each item to the pandemic context, the ability to represent best the underlying constructs, and consideration of survey length and respondent burden. Subject matter experts in family psychology were engaged to review the selection of items to ensure content validity, providing insight into the appropriateness and relevance of the selected items to the measured constructs, particularly in the context of the pandemic.
Using the established criteria and expert feedback, a preliminary selection of items was made from the identified validated questionnaires. Where necessary, selected items were adapted to fit the context of the pandemic and the study population better. To ensure the construct validity of the adapted scales, confirmatory factor analysis (CFA) was performed, and Cronbach's alpha was calculated for each scale to ensure that the selected items consistently measured the intended constructs.
Perceived individual affectivity during the COVID-19 pandemic was assessed using the Questionnaire on positive and negative emotions related to the experience of the COVID-19 pandemic , which has already been validated in adolescents and young adults (Commodari & La Rosa, 2020 ; Commodari et al., 2021 ). Participants were asked to complete a Likert-type scale that focused on their personal feelings regarding their cognitive, physiological, and behavioral states. Each item (e.g., “In this period in which I must stay at home, I feel well physically”; “In this period in which I must stay home, I am tense and I feel tight”) was scored on a five-point Likert-type scale ranging from 1 ( not at all ) to 5 ( most of the time ). The scale measures two affective dimensions: “ negative affectivity ” and “ positive affectivity.” A high score corresponds to an increased perception of negative or positive feelings. Confirmatory factor analysis was also performed to assess the validity of the structure of the questionnaire. Regarding the model for the “negative feelings,” all the goodness of fit values were satisfactory (RMSEA =. 08; SRMR = 0.04; CFI = 0.93; TLI = 0.91). The same result was obtained for the model of the “positive feelings” (RMSEA = 0.06; SRMR = 0.03; CFI = 0.96; TLI = 0.93). Furthermore, both scales showed good reliability in the study sample (negative feelings: Cronbach’s α = 0.81; positive feelings: Cronbach’s α = 0.75).
Eight items on individual perception of family quality of life were formulated based on the Italian version of the Family Quality of Life Survey (Brown et al., 2006 ) and adapted to the context of the COVID-19 pandemic. Specifically, the items included in the questionnaire were related to the impact of family members' health status, support received from health services, and relationships within the family on family quality of life (“ I consider my family's health important to my quality of life and that of other family members ,” “ I worry about the health status of my family members ,” “ I am overall satisfied with the health status of my family members ,” “ I consider the support provided by the National Health Service to be important for my family's quality of life ,” “ I am overall satisfied with the support provided to my family by the National Health Service ,” “ I consider family relationships important for my family’s quality of life ,” “ I believe that the members of my family are committed to maintaining good relations with each other ,” “ I am overall satisfied with the relationships within my family ”). Each item was scored on a five-point Likert-type scale ranging from 1 ( not at all ) to 5 ( most of the time ). A high score indicates a high level of family quality of life. Confirmatory factor analysis showed that the factor structure of the questionnaire was appropriate (RMSEA = 0.06; SRMR = 0.08; CFI = 0.95; TLI = 0.94). The scale's reliability in this study was also good (Cronbach’s α = 0.80).
Sixteen items on the three main dimensions of family functioning were selected from the Italian adaptation of the Flexibility and Cohesion Evaluation Scale – IV Edition (Olson, 2011 ; Visani et al., 2014 ), which consists in its original version of 42 items. Specifically, the items with highest factor loadings for each dimension were selected: six items assessed cohesion, defined as the emotional bond between family members (e.g., “In my family, we support each other, especially in difficult moments,” “We feel too close to each other”); six items assessed flexibility, defined as the quality and expression of leadership and organizations, role relationships, and relationship rules (e.g., “In my family, rules are established together,” “In my family, it is important to follow the rules”); four items assessed communication, defined as the positive communication skills used within the family system (e.g., “I feel I can freely express my problems to my family,” “Each of us tries to understand the feelings of other family members”). Each item is rated on a five-point scale ranging from 1 ( not at all ) to 5 ( most of the time ). The goodness-of-fit measures for all dimensions were satisfactory (cohesion: RMSEA = 0.03, SRMR = 0.05, CFI = 0.98, TLI = 0.98; flexibility: RMSEA = 0.03, SRMR = 0.05, CFI = 0.99, TLI = 0.99; communication: RMSEA = 0.05, SRMR = 0.02, CFI = 0.97, TLI = 0.91). Furthermore, all subscales showed good internal consistency in our sample (cohesion: Cronbach’s α = 0.86; flexibility: Cronbach’s α = 0.83; communication: Cronbach’s α = 0.84).
Four items on family conflict were selected from the Brief Family Relationship Scale (Fok et al., 2011 ), which consists in its original version of 19 items. Specifically, the items with the highest discrimination parameters were selected to represent best the underlying construct (“ In our family, we lose our tempers a lot ,” “ In our family, we often put down each other ,” “ In our family, we are really mad at each other a lot ,” “ In our family, we raise our voice when we are mad ”). Then, the selected items were adapted to the pandemic context. Each item was rated on a five-point scale ranging from 1 ( not at all ) to 5 ( most of the time ). The scale showed satisfactory goodness of fit (RMSEA = 0.04, SRMR = 0.04, CFI = 0.92, TLI = 0.98) and good reliability (Cronbach’s α = 0.78) in the study sample.
Ten items on family coping strategies were adapted from the Coping Orientations To Problem Experienced—New Italian Version (Sica et al., 2008 ), which consists in its original version of 60 items assessing individual coping strategies. Specifically, the core items for each coping style were selected and then adapted to the family context during the pandemic. Items were chosen as follows: two items for social support strategies, which consist of sharing the resolution of problems with both family members and the external environment (“ We seek support from each other ,” “ We ask for help from those who have had similar experiences to ours ”); two items for avoidance strategies, which consist of behavioral and mental detachment to escape the critical situations (“ We recognize that we cannot deal with the situation and abandon all attempts to act to solve the problem ,” “ We pretend it did not happen ”); two items for positive attitude strategies, which consist of the attitude of acceptance and positive reinterpretation of stressful events (“ We try to learn something from experience ,” “ We try to find something positive in what happens ”); two items for problem orientation strategies, which consist of planning and using appropriate problem solving strategies (“ We are deeply committed to cope with the problem ,” “ We try to devise strategies on what to do ”); two items for transcendent orientation strategies, which consist of using humor and religion to cope with difficult situations (“ We try to find comfort in religion ,” “ We joke about the situation ”). Participants responded to each item on a 5-point Likert scale ranging from 1 ( not at all ) to 5 ( most of the time ). Confirmatory factor analysis showed a good questionnaire structure (RMSEA = 0.06, SRMR = 0.06, CFI = 0.97, TLI = 0.93). The scale's reliability in the study sample was also acceptable (Cronbach’s α = 0.77).
Four items on individual perception of family efficacy were adapted from the General Self-Efficacy Scale (Schwarzer & Jerusalem, 1995 ), which consists in its original version of 10 items assessing individual self-efficacy. In particular, we selected the items that had the highest discrimination parameters best representing the underlying construct (“ Thanks to our resourcefulness, we can handle unforeseen situations” ; “ We are confident that we could deal efficiently with unexpected events”; “We can remain calm when facing difficulties because we can rely on our coping abilities”; “If we are in trouble, we can think of a good solution” ) and adapted them to the family context during the pandemic. Each item was rated on a five-point scale ranging from 1 ( not at all ) to 5 ( most of the time ). Confirmatory factor analysis showed that the factor structure of the questionnaire was appropriate (RMSEA = 0.03; SRMR = 0.04; CFI = 0.94; TLI = 0.94). The reliability of the scale in this study was also good (Cronbach’s α = 0.86).
Statistical analyses
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 25.0 (IBM Corporation, Armonk, NY). The study methodology adhered to the Journal Article Reporting Standards (Kazak, 2018 ). The materials and analysis code for this study are available by emailing the corresponding author. The study design and analysis were not pre-registered.
No data were excluded from the analyses, and no outliers were identified. The necessary sample size was calculated using G*Power 3.1, targeting power of 0.90, with 19 predictors (the maximum number included in the multiple linear regression), and α set at 0.05. The aim was to detect a minimum effect size of f 2 = 0.15, which was indicative of a medium effect, as outlined by Cohen ( 1988 ).
A CFA was performed to test the measurement model for each scale. The goodness of fit was evaluated using the Root Mean Square Error of Approximation (RMSEA < 0.05), the Standardized Root Mean Square Residual (SRMR < 0.08), and the Comparative Fit Index and the Tucker-Lewis Index (CFI and TLI > 0.90). Cronbach’s α was used to assess the reliability of the scales and was considered acceptable when > 0.70.
The scale scores were obtained by summing the answers given to the individual items. Higher scores represent higher levels of the variables. Median cut-off points were used to distinguish between low and high scores for each variable.
The Kolmogorov–Smirnov test was used to assess the normal distribution of the variables. Continuous variables with normal distribution are presented as mean (M) and standard deviation (SD), while frequencies and percentages describe categorical variables. The scores were divided into high and low, assuming the median was the cut-off.
Correlations between continuous variables were evaluated using Pearson’s correlation coefficient. In addition, a multivariate analysis of variance (MANOVA) was performed to explore the relationship between sociodemographic variables, individual affectivity, and family functioning. Finally, a multiple regression model was run to identify family quality of life predictors during the COVID-19 pandemic. Specifically, family quality of life was the dependent variable in the regression model. The predictors entered into the model were sociodemographic variables, family functioning, and individual affectivity.
Sample characteristics
In total, 404 participants completed the questionnaire. Of the participants, 65.6% were women, and the mean age was 36.52 ( SD = 15.43, range = 18–76). Most of the participants had a high school diploma (43.8%) or a degree (40.6%) and were students (34.7%). Furthermore, 54.0% of the sample were single, and 40.8% were married or cohabiting. Only 14.9% had contracted COVID-19 during the study period, and only five were hospitalized. In contrast, 33.9% reported cases of COVID-19 in their families, of which 27 were hospitalized. Finally, 7.7% experienced family losses due to COVID-19. Table 1 reports all the sociodemographic characteristics of the sample.
Questionnaire scores and correlations between study variables
Based on the median cut-off points of the questionnaire scores, most participants reported low family quality of life, family functioning, and family efficacy. Most of the sample reported low levels of family conflict (70.0%). Regarding pandemic-related individual affectivity, 62.1% reported low positive affectivity, whereas 47.0% reported high negative affectivity.
All variables investigated were significantly correlated (Table 2 ). In particular, the most significant correlations were observed between the family quality of life and family communication ( r = 0.554, p < 0.001), family quality of life and family efficacy ( r = 0.507, p < 0.001), family cohesion and family flexibility ( r = 0.591, p < 0.001), family communication and family efficacy ( r = 0.680, p < 0.001), family communication and social support coping strategies ( r = 0.592, p < 0.001), family communication and problem orientation coping strategies ( r = 0.559, p < 0.001), and family efficacy and adaptive coping strategies (social support: r = 0.659, p < 0.001; positive attitude: r = 0.628, p < 0.001; problem orientation: r = 0.731, p < 0.001).
Individual affectivity, family well-being and dimensions of family structure
Three-way MANOVA showed significant main effects of cohesion [(F (10, 387) = 4.88, p < 0.001, η 2 = 0.11)], flexibility [(F (10, 387) = 4.87, p < 0.001, η 2 = 0.11)], and communication [(F (10, 387) = 15.98, p < 0.001, η 2 = 0.29)] on individual affectivity and family well-being. However, this interaction effect was not statistically significant.
Table 3 reports the differences in scores of individual well-being, family quality of life, conflict, efficacy, and coping based on the dimensions of family functioning. Higher family cohesion, flexibility, and communication levels are associated with better individual well-being, higher quality of life and family efficacy, and lower family conflict.
Individual affectivity and family variables
The two-way MANOVA test showed significant main effects of positive affectivity [(F (11, 390) = 6.18, p < 0.001, η 2 = 0.15)] and negative affectivity [(F (11, 390) = 6.72, p < 0.001, η 2 = 0.16)] on family quality of life. However, the interaction effect was not statistically significant [(F (11, 390) = 0.50, p = 0.90)].
Analyzing the specific scores, participants with high positive affectivity reported significantly higher scores for family quality of life ( p < 0.001), cohesion ( p = 0.003), flexibility ( p = 0.006), communication ( p < 0.001), and efficacy ( p < 0.001). Furthermore, participants with high positive affectivity showed significantly higher scores for social support ( p < 0.001), positive attitudes ( p < 0.001), problem orientation ( p < 0.001), and transcendent orientation ( p = 0.001) than participants with low positive affectivity.
Participants with high negative affectivity reported lower scores for family cohesion ( p < 0.001) and flexibility ( p = 0.005) and higher scores for family conflict ( p < 0.001) than participants with low negative affectivity. Furthermore, high negative affectivity was associated with higher scores on the coping avoidance strategy ( p < 0.001) and lower scores on the positive attitude coping strategy ( p = 0.02).
Family functioning and sociodemographic characteristics
The results of two-way MANOVA showed a significant overall main effect of gender [(F (6, 393) = 4.96, p < 0.001, η 2 = 0.07)] and age groups [(F (12, 788) = 2.19, p = 0.01, η 2 = 0.03)] on family functioning variables. However, the interaction effect between gender and age groups was not statistically significant [F (12, 786) = 1.45, p = 0.14]. Specifically, women reported higher scores for family quality of life ( p < 0.001), family communication ( p = 0.03), and family efficacy ( p < 0.001) than did men. Furthermore, women reported lower scores for family conflict ( p = 0.007) than men. Regarding age groups, the Bonferroni post-hoc test showed that the 18–28 age group reported lower scores for family cohesion than the 29–49 ( p = 0.002) and the > 50 ( p = 0.03) groups and lower scores for family flexibility and communication than the 29–49 age group ( p < 0.001). Finally, they reported higher scores for family conflict than the 29–49 age group ( p < 0.001).
MANOVA also showed a significant overall main effect for gender [(F (5, 394) = 4.64, p < 0.001, η 2 = 0.06)] but not for age groups [(F (10, 790) = 2.19, p = 0.61, η 2 = 0.01)] on family coping strategies. However, the interaction effect between gender and age groups was not statistically significant [F (10, 788) = 0.94, p = 0.50]. In particular, women reported higher scores for social support ( p = 0.005), positive attitude ( p = 0.002), and problem orientation ( p = 0.03) than did men. Furthermore, women reported lower scores for avoiding coping strategies ( p = 0.007) than men.
Regarding marital status, the MANOVA results showed a significant main effect on family functioning variables [(F(18, 1117) = 2.44, p = 0.001, η 2 = 0.04)] but not on family coping strategies [(F(15, 1093) = 0.73, p = 0.76)]. In particular, the Bonferroni post-hoc test showed that single people reported lower family cohesion scores than married or cohabiting people ( p = 0.003). Furthermore, family communication scores were significantly lower for single people than married or cohabiting people ( p = 0.02). Finally, single people reported higher scores for family conflict than married or cohabiting people ( p = 0.03).
No significant differences regarding the educational level and employment were found.
Family functioning and COVID-19 variables
MANOVA tests showed significant differences in family variables between participants affected by COVID-19 and those without the disease [(F (6, 397) = 2.36, p = 0.03, η 2 = 0.03)]. Specifically, people who contracted COVID-19 reported higher scores on family flexibility ( p = 0.003) and communication ( p = 0.017) than those who did not contract the disease. Furthermore, regarding family coping strategies [(F (5, 398) = 3.22, p = 0.007, η 2 = 0.04)], people who contracted COVID-19 reported higher scores for positive attitudes ( p = 0.002) and problem orientation ( p = 0.02) than people who had not contracted the virus.
Furthermore, people who had cases of COVID-19 in their families reported higher positive attitude scores than people who did not ( p = 0.03). No other significant differences were found in the presence of cases of COVID-19 in the family. The presence of bereavements in the family due to COVID-19 was also not associated with significant differences in the study variables.
Predictors of family quality of life in the study sample
Multiple regression analyses were used to investigate the study sample's family quality of life predictor variables. Preliminary analyses were conducted to ensure that the assumptions of normality, linearity, multicollinearity, and homoscedasticity assumptions were not violated.
The regression model explained 41% of the variance (R 2 = 0.410, F = 12.54; p < 0.001). The independent variables that contributed the most to explaining the family quality of life score were family communication ( β = 0.32, p < 0.001), positive affectivity ( β = 0.19, p < 0.001), gender ( β = 0.12, p = 0.006), and avoidance coping strategy ( β = -0.11, p = 0.038). Table 4 shows all the regression analysis results and the contribution of each independent variable.
This study aimed to explore the interplay between individual affectivity and family functioning within the framework of Hill's Family Stress Model during the COVID-19 pandemic, trying to understand how the non-normative event of the pandemic changed the family structure and the quality of family relationships and how these changes affected the psychological well-being of family members.
As hypothesized, our results underlined the role of the pandemic as a significant stressor (A) that alters family dynamics and individual well-being. Furthermore, the pivotal role of family resources (B) – cohesion, flexibility, and communication – has been confirmed in managing the impact of the pandemic. Consistent with our hypotheses, stronger family dynamics (good cohesion, flexibility, and communication levels) were correlated with better individual and family well-being, supporting the model's emphasis on resources in crisis management. This finding aligns with the ABC-X model, demonstrating that robust family dynamics can mitigate the adverse effects of stressors.
The influence of individual affectivity on family functioning is also evident. In fact, positive affectivity was associated with better family quality of life and adaptive coping strategies, while negative affectivity was correlated with increased family conflict and avoidance strategies. These findings illustrate factor C of the model, in which individual perceptions and emotional responses shape family crisis outcomes (X). Furthermore, these data are in line with a developmental perspective that considers individuals and families as interconnected systems and individual development and well-being as the result of multiple variables, including the functioning of the family system (Kail & Cavanaugh, 2018 ; Morris et al., 2007 ; Shigeto & Voltaire, 2020 ; Sigelman & Rider, 2018 ).
Most of our sample reported a low family quality of life and low family cohesion, flexibility, and communication. Furthermore, the levels of family efficacy in our sample were low, confirming a reduced sense of family cohesion during the pandemic that does not allow the family to work collectively to achieve shared goals (Kao & Caldwell, 2017 ). When comparing the mean scores on the questionnaire, people with COVID-19 reported lower scores on perceived family flexibility and communication. The pandemic, especially the direct experience of COVID-19 within the family, seems to have a significant impact on the family organization due to uncertainty and new rules to be observed and on communication between family members, which is more difficult due to tension and fear over the possible outcomes of the disease (Prime et al., 2020 ; Soejima, 2021 ). Furthermore, participants who had contracted COVID-19 reported less use of adaptive family coping strategies, such as positive attitudes and problem orientation, confirming that the disease also affects family ways of coping with stress, with negative consequences on the well-being of both the individual and the entire family system (Prime et al., 2020 ). Instead, people who had cases of COVID-19 among their family members reported higher positive attitude scores than those who did not. This result may seem counterintuitive, but likely, households that have had to cope with cases of COVID-19 have probably had to adapt, acquire more knowledge about the disease, and provide mutual support during the healing process (Au et al., 2023 ). This communal struggle may lead to an increased competence and a more positive outlook on overcoming future obstacles. Indeed, it is possible to suppose that increased family resilience in the face of the pandemic may contribute to this positive attitude: in particular, the direct impact of COVID-19 within a family could stimulate a 'fight or flight' response, where the choice is often to fight back through positive thinking and resilience-building practices (Gayatri & Irawaty, 2021 ). Also, we found a significant positive correlation in our sample between positive attitude and social support, so we can hypothesize that an adequate social support network may contribute to a more positive attitude in coping with cases of COVID-19 in the family. However, this coping style was not found to be as significant as positive attitude. Therefore, other variables not explicitly investigated in this study, such as resilience, positive thinking, optimism, and social support, may significantly predict the use of more adaptive coping mechanisms, as widely highlighted in several studies conducted during the COVID-19 pandemic (Budimir et al., 2021 ; Lasota & Mróz, 2021 ; Lee, 2023 ; Leslie-Miller et al., 2021 ). Future research should address this point in greater detail.
The presence of grief in the family for COVID-19 did not seem to be significantly associated with the variables investigated in our study. This result contrasts with data from the literature that underlines how the family experience of grief was profoundly altered during the pandemic, especially during the lockdown (van Schaik et al., 2022 ). In the early stages of the pandemic, family members infected with COVID-19 died alone, and funerals were forbidden for some time. Therefore, families were prevented from sharing their grief and elaborating on it through symbolic rituals (Burrell & Selman, 2020 ; Imber‐Black, 2020 ). However, the relatively small number of reported bereavements in our sample may have influenced our results and limited their generalizability beyond the study sample. Furthermore, the study was carried out later in the pandemic when funeral bans were no longer in force, favoring more adaptive management of family grief.
Contrary to expectations, our sample's perceived family conflict level was low. This finding contrasts the literature on the topic, which shows that lockdowns and long periods of forced family cohabitation are responsible for a significant increase in family conflict (Fosco et al., 2021 ; Sinko et al., 2021 ). A possible interpretation of this finding is that the family coping strategies used in our sample were mainly adaptive, representing a protective factor against the risk of escalation of family conflict.
Other significant findings concern the role of sociodemographic variables such as gender and age. Regarding gender, women reported a higher family efficacy and quality of life and fewer family conflicts than men. Furthermore, women reported more adaptive family coping strategies than did men. However, at the same time, being female was associated with lower levels of positive affectivity and higher levels of negative affectivity. Therefore, the perceptions of family and individual well-being were contradictory among the women in our sample. In this regard, our study aligns with the findings of Rania et al. ( 2022 ), which highlight the critical role of gender in shaping family well-being. Women in our Italian sample, similar to the Italian sample of the study by Rania and colleagues, reported high family efficacy and quality of life, highlighting their central role in maintaining family stability during the crisis. However, this apparent family resilience came at a personal cost, as the same women experienced lower positive affectivity and higher negative affectivity. The contradiction between subjective well-being and family functioning may reflect a socio-cultural dynamic in which women's increased family responsibilities during the lockdown may have exacerbated personal stress despite the outward appearance of effective family coping strategies (Epifanio et al., 2021 ). For this reason, women in our sample might perceive a lower individual psychological well-being but good family functioning during the pandemic and use more adaptive family coping strategies than men. These findings suggest a complex interplay between gender roles and family dynamics during this pandemic, which deserves further study.
Regarding the role of age, our findings contrast with those reported by Fernandes et al. ( 2021 ). Specifically, in our sample, participants in the 18–28 age group reported higher levels of negative affectivity and worse perceived family functioning and quality of life. However, this finding is consistent with the literature on the psychological consequences of the pandemic, highlighting the more detrimental impact on young people who experience greater uncertainty about their future than on adults. More specifically, this finding may be due to the increased pressures this age group faces, which includes many new parents who are dealing with the challenges of raising children in such uncertain times (Rania et al., 2022 ). On the other side, the same study by Rania et al. shows a significant percentage of young people over the age of 18 still living with their parents (30.1%), underlining the tendency of young Italians to live with their families for longer due to the greater difficulties in joining the labor market compared to young people in other countries (Manacorda & Moretti, 2006 ; Menniti et al., 2000 ). This delay in the outflow from the family of origin by young Italians could explain their more negative perception of family relationships and higher levels of conflict within the family during the pandemic.
Single people reported lower family cohesion and communication scores than married or cohabiting people. Furthermore, they reported more family conflict than married or cohabiting people. These data confirm the findings of Fernandes et al. ( 2021 ), according to which Portuguese singles reported lower family functioning values during the COVID-19 pandemic. This result can also be explained by considering the family structure of countries such as Italy and Portugal. In these countries, the family is characterized by strong ties based on the mutual aid of all its members. Family units are very different but tend to be small and nuclear (Amaro & Neves, 2016 ). Therefore, this may explain the worse perception of the quality of family relationships in single people than in married or cohabiting people. These data should also be further investigated by comparing them with those from countries characterized by different family cultures.
In the context of Hill's ABC-X model, our findings showed that family quality of life (X) was intricately linked to how families navigate the stressor of the pandemic (A), the resources (B) they possess or lack, and their perception (C) of the crisis. According to the regression model results, family quality of life was significantly predicted by high levels of family communication, positive perceived individual affectivity, and low use of avoidance coping strategies, which indicates effective management of the pandemic's stress and partially confirms our hypothesis. These results underscore the model's assertion that the outcome (X) is not merely a result of the stressor itself but a complex interplay of family dynamics, resources, and perceptions, highlighting the nuanced nature of family adaptation and resilience during crises.
Strengths and limitations
This study has several strengths. First, it explored a timely topic considering the significant psychosocial impact of the COVID-19 pandemic on both individuals and families. At the same time, this study adopted a developmental perspective aimed at investigating the interdependence between individual and family well-being and identifying not only risk factors but also protective factors that can transform the pandemic event into an opportunity for individual and family development and empowerment. Second, we used a battery of questionnaires with good psychometric properties in our sample. Furthermore, the study was conducted in a period characterized by the adoption of less stringent restrictive measures than during the first wave of the pandemic in Italy. Therefore, the results allow us to take a snapshot of individual and family well-being during this transition and adaptation phase after the total closure of the first COVID-19 lockdown.
However, this study had some limitations. The first notable limitation of this study was the absence of a pre-pandemic baseline for comparison. This baseline would have provided a clearer picture of the pandemic's impact on family dynamics beyond what can be inferred from the absence of a traditional control group. Another significant limitation of this study is its cross-sectional design, which does not allow causal relationships between variables or capture changes in variables over time. However, convenience sampling did not allow for an adequate sample balance concerning sociodemographic variables such as gender, marital status, and employment. In particular, females prevailed significantly over males in the study sample. This finding may be related to the sampling strategy used in the study and the more active role of women within families, which is typical of Italian culture.
Regarding the measurement tools used, the study used a modified version of existing scales to better fit the specific context and objectives of the research. Although these modifications were made with rigorous methodological considerations, they nevertheless introduce potential limitations in terms of the validity and reliability of the scales. Consequently, the results of this study should be interpreted with caution when considering their generalizability to other contexts or their comparability with studies using fully validated scales. Future research should aim to validate these modified scales further in different settings to increase their robustness and applicability. In addition, comparisons with other studies using the original versions of these scales should be made carefully considering the potential differences introduced by the modifications.
Finally, using an online questionnaire may have introduced bias by excluding older individuals who face more significant challenges in using electronic devices. Furthermore, although the study focused on participants' perceptions of their family relationships, it did not compare evaluations from individuals within the same households. Further studies are needed to better investigate family functioning during the COVID-19 pandemic, considering the role of additional psychological variables such as resilience, optimism, and perceived social support, as well as of sociodemographic variables such as the presence of children, family members with physical and/or intellectual disabilities, and older people to care for.
Theoretical and practical implications
The results of our study highlight the complex dynamics of family resilience and individual psychological responses in the context of a global health crisis. The fact that individuals with COVID-19-affected family members exhibited positive attitudes suggests a complex interplay between adaptive perceptions and coping mechanisms. These adaptations may stem from increased empathy, solidarity, and shared purpose within families, promoting resilience and a positive outlook in the face of adversity. Theoretically, our findings highlight the importance of social support systems and adaptive coping strategies in mitigating the psychological impact of pandemics. In practice, these findings have profound implications for developing targeted interventions to enhance family resilience. Policymakers and practitioners can use this understanding to design community support programs that strengthen family cohesion and individual coping strategies during health crises.
Future research should explore the longitudinal effects of family-based resilience strategies and their effectiveness in different socio-economic and cultural contexts. The role of virtual support networks and digital communication tools in maintaining family cohesion and individual well-being during periods of isolation deserves further exploration. We recommend developing public health policies prioritizing mental health services and support for families affected by COVID-19. Educational programs that equip families with stress management and communication tools may further empower individuals to cope more effectively with the challenges posed by the pandemic.
In conclusion, our study places the COVID-19 pandemic within Hill's ABC-X Model as a significant stressor that has led to varied outcomes in family and individual well-being. However, in addition to being considered a traumatic and stressful event, the COVID-19 pandemic might also be a critical transitional event that can promote the maturation of the individual and their family, as it allows the reorganization of relationships and the development of new and more adaptive ways of coping with stress. Therefore, from a life-cycle wellness promotion perspective, the pandemic event can be considered an opportunity to mobilize novel coping and resilience skills rather than only a traumatic event associated with adverse psychological outcomes.
Our findings emphasize the importance of further research on the long-term psychological impact of the pandemic, focusing on how family resources and perceptions influence coping and resilience. Such insights are crucial in designing interventions that bolster family and individual resilience and transform the pandemic's challenges into psychological and familial growth opportunities.
Data availability
The dataset generated and analyzed during the current study is not publicly available because of the Department's privacy policies but is available from the corresponding author upon reasonable request.
Amaro, F., & Neves, B. B. (2016). Portugal, Families in. In Encyclopedia of Family Studies (pp. 1–5). Wiley. https://doi.org/10.1002/9781119085621.wbefs213
Au, A. K. Y., Ng, J. C. K., Wu, W. C. H., & Chen, S. X. (2023). Who do we trust and how do we cope with COVID-19? A mixed-methods sequential exploratory approach to understanding supportive messages across 35 cultures. Humanities and Social Sciences Communications, 10 (1). https://doi.org/10.1057/s41599-023-01747-2
Bonnie, R. J., Backes, E. P., & National Academies of Sciences Engineering and Medicine (U.S.). (2019) Committee on the neurobiological and socio-behavioral science of adolescent development and its applications. The promise of adolescence: realizing opportunity for all youth . National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK545481/
Bornstein, M. H. (2018). The SAGE Encyclopedia of Lifespan Human Development . https://doi.org/10.4135/9781506307633
Brown, I., Brown, R. I., Baum, N., Isaacs, B., Myerscough, T., Neikrug, S. M., Roth, D., Shearer, J., & Wang, M. (2006). Family Quality of Life Survey: Main caregivers of people with intellectual or developmental disabilities . Surrey Place Centre.
Google Scholar
Brown, R. I., & Brown, I. (2014). Family quality of life. In Encyclopedia of Quality of Life and Well-Being Research (pp. 2194–2201). https://doi.org/10.1007/978-94-007-0753-5_1006
Budimir, S., Probst, T., & Pieh, C. (2021). Coping strategies and mental health during COVID-19 lockdown. Journal of Mental Health, 30 (2), 156–163. https://doi.org/10.1080/09638237.2021.1875412
Article PubMed Google Scholar
Burrell, A., & Selman, L. E. (2020). How do funeral practices impact bereaved relatives’ mental health, grief and bereavement? A mixed methods review with implications for COVID-19. OMEGA - Journal of Death and Dying, 85 (2), 345–383. https://doi.org/10.1177/0030222820941296
Butler, N., Quigg, Z., Bates, R., Jones, L., Ashworth, E., Gowland, S., & Jones, M. (2022). The contributing role of family, school, and peer supportive relationships in protecting the mental wellbeing of children and adolescents. School Mental Health, 14 (3), 776–788. https://doi.org/10.1007/s12310-022-09502-9
Article PubMed PubMed Central Google Scholar
Chu, P. S., Saucier, D. A., & Hafner, E. (2010). Meta-analysis of the relationships between social support and well-being in children and adolescents. Journal of Social and Clinical Psychology, 29 (6), 624–645. https://doi.org/10.1521/jscp.2010.29.6.624
Article Google Scholar
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Routledge.
Commodari, E., La Rosa, V. L., Carnemolla, G., & Parisi, J. (2021). The psychological impact of the lockdown on Italian university students during the first wave of COVID-19 pandemic: psychological experiences, health risk perceptions, distance learning, and future perspectives. Mediterranean Journal of Clinical Psychology, 9 (2). https://doi.org/10.13129/2282-1619/mjcp-3009
Commodari, E., & La Rosa, V. L. (2020). Adolescents in quarantine during COVID-19 pandemic in Italy: Perceived health risk, beliefs, psychological experiences and expectations for the future. Frontiers in Psychology, 11 , 559951. https://doi.org/10.3389/fpsyg.2020.559951
Crandall, A., Daines, C., Hanson, C. L., & Barnes, M. D. (2022). The effects of COVID-19 stressors and family life on anxiety and depression one-year into the COVID-19 pandemic. Family Process, 62 (1), 336–351. https://doi.org/10.1111/famp.12771
Epifanio, M. S., Andrei, F., Mancini, G., Agostini, F., Piombo, M. A., Spicuzza, V., Riolo, M., Lavanco, G., Trombini, E., & La Grutta, S. (2021). The impact of COVID-19 pandemic and lockdown measures on quality of life among italian general population. Journal of Clinical Medicine, 10 (2), 289. https://doi.org/10.3390/jcm10020289
Fernandes, C. S., Magalhães, B., Silva, S., & Edra, B. (2021). Adaptability and cohesion of families in times of the COVID-19 pandemic. Nursing Practice Today, 8 (3), 234–243. https://doi.org/10.18502/npt.v8i3.5938
Fogel, Y., Sela, Y., & Hen-Herbst, L. (2022). Coping strategies of families and their relationships with family quality of life during Covid-19 pandemic. PLoS ONE, 17 (9), e0273721. https://doi.org/10.1371/journal.pone.0273721
Fok, C. C. T., Allen, J., Henry, D., People Awakening Team. (2011). The brief family relationship scale: A brief measure of the relationship dimension in family functioning. Assessment, 21 (1), 67–72. https://doi.org/10.1177/1073191111425856
Fosco, G. M., Sloan, C. J., Fang, S., & Feinberg, M. E. (2021). Family vulnerability and disruption during the COVID-19 pandemic: Prospective pathways to child maladjustment. Journal of Child Psychology and Psychiatry, 63 (1), 47–57. https://doi.org/10.1111/jcpp.13458
Gayatri, M., & Irawaty, D. K. (2021). Family resilience during COVID-19 pandemic: A literature review. The Family Journal, 30 (2), 132–138. https://doi.org/10.1177/10664807211023875
Hall, E. D., Earle, K., Silverstone, J., Immel, M., Carlisle, M., & Campbell, N. (2022). Changes in family communication during the COVID-19 pandemic: The role of family communication patterns and relational distance. Communication Research Reports, 39 (1), 56–67. https://doi.org/10.1080/08824096.2021.2025045
Hill, R. (1949). Families under stress: Adjustment to the crises of war separation and reunion . Harper and Brothers.
Imber-Black, E. (2020). Rituals in the time of COVID-19: Imagination, responsiveness, and the human spirit. Family Process, 59 (3), 912–921. https://doi.org/10.1111/famp.12581
Kail, R. V., & Cavanaugh, J. C. (2018). Human development: A life-span view . Cengage Learning.
Kao, T.-S.A., & Caldwell, C. H. (2017). Family efficacy within ethnically diverse families: A qualitative study. Family Process, 56 (1), 217–233. https://doi.org/10.1111/famp.12149
Kazak, A. E. (2018). Editorial: Journal article reporting standards. American Psychologist, 73 (1), 1–2. https://doi.org/10.1037/amp0000263
Koulenti, T., & Anastassiou-Hadjicharalambous, X. (2011). Non-normative life events. In Goldstein, S. & Naglieri, J. A. (Eds.), Encyclopedia of Child Behavior and Development (pp. 1018–1020). https://doi.org/10.1007/978-0-387-79061-9_1977
Kusnadi, A. P., Putri, H. M., Riyantono, E. R., & Kristiana, I. F. (2022). Family’s coping strategies in the COVID-19 pandemic: Systematic literature review. Proceedings of International Conference on Psychological Studies (ICPSYCHE), 3 , 416–426.
Lanza, I., Ajslev, T. A., Andersen, C. S., Ingstrup, K. G., Nohr, E. A., & Sørensen, T. I. A. (2010). Maternal postpartum distress and childhood overweight. PLoS One , 5 (6). https://doi.org/10.1371/journal.pone.0011136
Lasota, A., & Mróz, J. (2021). Positive psychology in times of pandemic—Time perspective as a moderator of the relationship between resilience and meaning in life. International Journal of Environmental Research and Public Health, 18 (24). https://doi.org/10.3390/ijerph182413340
Lee, S. (2023). Exploring the role of resilience and optimism during the COVID-19 pandemic in older European adults. Research on Aging, 45 (9–10), 643–653. https://doi.org/10.1177/01640275231152570
Leslie-Miller, C. J., Waugh, C. E., & Cole, V. T. (2021). Coping with COVID-19: The benefits of anticipating future positive events and maintaining optimism. Frontiers in Psychology, 12 . https://doi.org/10.3389/fpsyg.2021.646047
Luttik, M. L. A., Mahrer-Imhof, R., García-Vivar, C., Brødsgaard, A., Dieperink, K. B., Imhof, L., Østergaard, B., Svavarsdottir, E. K., & Konradsen, H. (2020). The COVID-19 pandemic: A family affair. Journal of Family Nursing, 26 (2), 87–89. https://doi.org/10.1177/1074840720920883
Manacorda, M., & Moretti, E. (2006). Why do most Italian youths live with their parents? Intergenerational transfers and household structure. Journal of the European Economic Association , 4 (4), 800–829. http://www.jstor.org/stable/40004818
Mantziki, K., Vassilopoulos, A., Radulian, G., Borys, J.-M., du Plessis, H., Gregório, M. J., Graça, P., de Henauw, S., Handjiev, S., Visscher, T. L. S., & Seidell, J. C. (2014). Promoting health equity in European children: Design and methodology of the prospective EPHE (Epode for the Promotion of Health Equity) evaluation study. BMC Public Health, 14 (1). https://doi.org/10.1186/1471-2458-14-303
McGee, C. E., Trigwell, J., Fairclough, S. J., Murphy, R. C., Porcellato, L., Ussher, M., & Foweather, L. (2015). Influence of family and friend smoking on intentions to smoke and smoking-related attitudes and refusal self-efficacy among 9–10 year old children from deprived neighbourhoods: a cross-sectional study. BMC Public Health, 15 (1). https://doi.org/10.1186/s12889-015-1513-z
McGill, M. G., Purkey, E., Davison, C. M., Watson, A., & Bayoumi, I. (2022). Financial stress during COVID-19: implications for parenting behaviour and child well-being. BMJ Paediatr Open , 6 (1). https://doi.org/10.1136/bmjpo-2022-001569
McKenry, P. C., & Price, S. J. (2005). Families and change: Coping with stressful events and transitions . Sage.
Menniti, A., Misiti, M., & Savioli, M. (2000). Italian ‘Stay at Home’ Children: Attitudes and Constraints . Retrieved March 1, 2023 from https://www.demogr.mpg.de/papers/workshops/000906_paper01.pdf
Morris, A. S., Silk, J. S., Steinberg, L., Myers, S. S., & Robinson, L. R. (2007). The role of the family context in the development of emotion regulation. Social Development, 16 (2), 361–388. https://doi.org/10.1111/j.1467-9507.2007.00389.x
Olson, D. (2011). FACES IV and the circumplex model: Validation study. Journal of Marital and Family Therapy, 37 (1), 64–80. https://doi.org/10.1111/j.1752-0606.2009.00175.x
Passavanti, M., Argentieri, A., Barbieri, D. M., Lou, B., Wijayaratna, K., Foroutan Mirhosseini, A. S., Wang, F., Naseri, S., Qamhia, I., Tangerås, M., Pelliciari, M., & Ho, C.-H. (2021). The psychological impact of COVID-19 and restrictive measures in the world. Journal of Affective Disorders, 283 , 36–51. https://doi.org/10.1016/j.jad.2021.01.020
Prime, H., Wade, M., & Browne, D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75 (5), 631–643. https://doi.org/10.1037/amp0000660
Rania, N., Coppola, I., Lagomarsino, F., & Parisi, R. (2022). Family well-being during the COVID-19 lockdown in Italy: Gender differences and solidarity networks of care. Child & Family Social Work, 27 (1), 1–10. https://doi.org/10.1111/cfs.12867
Reich, S. M., Liu, Y., Tulagan, N., Martin, E., Dahlin, M., & Cabrera, N. (2023). Applying a family stress model to understand U.S. families’ patterns of stress, media use, and child behavior during the COVID-19 pandemic. Journal of Children and Media, 17 (2), 246–265. https://doi.org/10.1080/17482798.2023.2187853
Schwarzer, R., & Jerusalem, M. (1995). Generalized Self-Efficacy scale. In Weinman, J., Wright, S., & Johnston, M. (Eds.), Measures in health psychology: A user’s portfolio. Causal and control beliefs (pp. 35–37). NFER-NELSON.
Shigeto, A., & Voltaire, M. (2020). Role of the family in personality development, The. In Encyclopedia of Personality and Individual Differences (pp. 4504–4512). https://doi.org/10.1007/978-3-319-24612-3_1932
Sica, C., Magni, C., Ghisi, M., Altoè, G., Sighinolfi, C., Chiri, L. R., & Franceschini, S. (2008). Coping orientation to problems experienced-nuova versione Italiana (COPE-NVI): Uno strumento per la misura degli stili di coping. Psicoterapia Cognitiva e Comportamentale, 14 (1), 27–53.
Sigelman, C. K., & Rider, E. A. (2018). Life-span human development . Cengage Learning.
Sinko, L., He, Y., Kishton, R., Ortiz, R., Jacobs, L., & Fingerman, M. (2021). “The stay at home order is causing things to get heated up”: Family conflict dynamics during COVID-19 From the perspectives of youth calling a national child abuse hotline. Journal of Family Violence, 37 (5), 837–846. https://doi.org/10.1007/s10896-021-00290-5
Soejima, T. (2021). Impact of the coronavirus pandemic on family well-being: A rapid and scoping review. Open Journal of Nursing, 11 (12), 1064–1085. https://doi.org/10.4236/ojn.2021.1112085
van Schaik, T., Brouwer, M. A., Knibbe, N. E., Knibbe, H. J. J., & Teunissen, S. C. C. M. (2022). The Effect of the COVID-19 pandemic on grief experiences of bereaved relatives: An overview review. OMEGA - Journal of Death and Dying . https://doi.org/10.1177/00302228221143861
Visani, E., Di Nuovo, S., & Loriedo, C. (2014). Il Faces IV. Il modello circonflesso di Olson nella clinica e nella ricerca . Franco Angeli.
von Suchodoletz, A., Belanger, J., Bryan, C., Ali, R., & Al Nuaimi, S. R. (2023). COVID-19’s shadow on families: A structural equation model of parental stress, family relationships, and child wellbeing. PLoS ONE, 18 (10), e0292292. https://doi.org/10.1371/journal.pone.0292292
Wood, D., Crapnell, T., Lau, L., Bennett, A., Lotstein, D., Ferris, M., & Kuo, A. (2018). Emerging adulthood as a critical stage in the life course. In Halfon, N., Forrest, C. B., Lerner, R. M., & Faustman, E. M. (Eds.), Handbook of Life Course Health Development (pp. 123–143). https://doi.org/10.1007/978-3-319-47143-3_7
Wu, Q., & Xu, Y. (2020). Parenting stress and risk of child maltreatment during the COVID-19 pandemic: A family stress theory-informed perspective. Developmental Child Welfare, 2 (3), 180–196. https://doi.org/10.1177/2516103220967937
Zeng, Y., Ye, B., Zhang, Y., & Yang, Q. (2021). Family cohesion and stress consequences among Chinese college students during COVID-19 pandemic: A moderated mediation model. Frontiers in Public Health, 9 , 703899. https://doi.org/10.3389/fpubh.2021.703899
Download references
Open access funding provided by Università degli Studi di Catania within the CRUI-CARE Agreement. The work was not supported by any fund/grant.
Author information
Authors and affiliations.
Department of Educational Sciences, University of Catania, Via Biblioteca 4, 95124, Catania, Italy
Valentina Lucia La Rosa, Miriana Tornatore & Elena Commodari
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Valentina Lucia La Rosa and Miriana Tornatore. The first draft of the manuscript was written by Valentina Lucia La Rosa and Elena Commodari, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Valentina Lucia La Rosa .
Ethics declarations
Research involving human participants and/or animals.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all subjects.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Lucia La Rosa, V., Tornatore, M. & Commodari, E. Exploring the interplay between individual and family functioning during the COVID-19 pandemic: a cross-sectional study. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-06058-6
Download citation
Accepted : 26 April 2024
Published : 07 May 2024
DOI : https://doi.org/10.1007/s12144-024-06058-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Family functioning
- Family quality of life
- Family coping
- Find a journal
- Publish with us
- Track your research

Thousands Believe Covid Vaccines Harmed Them. Is Anyone Listening?
All vaccines have at least occasional side effects. But people who say they were injured by Covid vaccines believe their cases have been ignored.
Shaun Barcavage, 54, a nurse practitioner in New York City, said that ever since his first Covid shot, standing up has sent his heart racing. Credit... Hannah Yoon for The New York Times
Supported by
- Share full article

By Apoorva Mandavilli
Apoorva Mandavilli spent more than a year talking to dozens of experts in vaccine science, policymakers and people who said they had experienced serious side effects after receiving a Covid-19 vaccine.
- Published May 3, 2024 Updated May 4, 2024
Within minutes of getting the Johnson & Johnson Covid-19 vaccine, Michelle Zimmerman felt pain racing from her left arm up to her ear and down to her fingertips. Within days, she was unbearably sensitive to light and struggled to remember simple facts.
She was 37, with a Ph.D. in neuroscience, and until then could ride her bicycle 20 miles, teach a dance class and give a lecture on artificial intelligence, all in the same day. Now, more than three years later, she lives with her parents. Eventually diagnosed with brain damage, she cannot work, drive or even stand for long periods of time.
“When I let myself think about the devastation of what this has done to my life, and how much I’ve lost, sometimes it feels even too hard to comprehend,” said Dr. Zimmerman, who believes her injury is due to a contaminated vaccine batch .
The Covid vaccines, a triumph of science and public health, are estimated to have prevented millions of hospitalizations and deaths . Yet even the best vaccines produce rare but serious side effects . And the Covid vaccines have been given to more than 270 million people in the United States, in nearly 677 million doses .
Dr. Zimmerman’s account is among the more harrowing, but thousands of Americans believe they suffered serious side effects following Covid vaccination. As of April, just over 13,000 vaccine-injury compensation claims have been filed with the federal government — but to little avail. Only 19 percent have been reviewed. Only 47 of those were deemed eligible for compensation, and only 12 have been paid out, at an average of about $3,600 .
Some scientists fear that patients with real injuries are being denied help and believe that more needs to be done to clarify the possible risks.
“At least long Covid has been somewhat recognized,” said Akiko Iwasaki, an immunologist and vaccine expert at Yale University. But people who say they have post-vaccination injuries are “just completely ignored and dismissed and gaslighted,” she added.

In interviews and email exchanges conducted over several months, federal health officials insisted that serious side effects were extremely rare and that their surveillance efforts were more than sufficient to detect patterns of adverse events.
“Hundreds of millions of people in the United States have safely received Covid vaccines under the most intense safety monitoring in U.S. history,” Jeff Nesbit, a spokesman for the Department of Health and Human Services, said in an emailed statement.
But in a recent interview, Dr. Janet Woodcock, a longtime leader of the Food and Drug Administration, who retired in February, said she believed that some recipients had experienced uncommon but “serious” and “life-changing” reactions beyond those described by federal agencies.
“I feel bad for those people,” said Dr. Woodcock, who became the F.D.A.’s acting commissioner in January 2021 as the vaccines were rolling out. “I believe their suffering should be acknowledged, that they have real problems, and they should be taken seriously.”
“I’m disappointed in myself,” she added. “I did a lot of things I feel very good about, but this is one of the few things I feel I just didn’t bring it home.”
Federal officials and independent scientists face a number of challenges in identifying potential vaccine side effects.
The nation’s fragmented health care system complicates detection of very rare side effects, a process that depends on an analysis of huge amounts of data. That’s a difficult task when a patient may be tested for Covid at Walgreens, get vaccinated at CVS, go to a local clinic for minor ailments and seek care at a hospital for serious conditions. Each place may rely on different health record systems.
There is no central repository of vaccine recipients, nor of medical records, and no easy to way to pool these data. Reports to the largest federal database of so-called adverse events can be made by anyone, about anything. It’s not even clear what officials should be looking for.
“I mean, you’re not going to find ‘brain fog’ in the medical record or claims data, and so then you’re not going to find” a signal that it may be linked to vaccination, Dr. Woodcock said. If such a side effect is not acknowledged by federal officials, “it’s because it doesn’t have a good research definition,” she added. “It isn’t, like, malevolence on their part.”
The government’s understaffed compensation fund has paid so little because it officially recognizes few side effects for Covid vaccines. And vaccine supporters, including federal officials, worry that even a whisper of possible side effects feeds into misinformation spread by a vitriolic anti-vaccine movement.
‘I’m Not Real’
Patients who believe they experienced serious side effects say they have received little support or acknowledgment.
Shaun Barcavage, 54, a nurse practitioner in New York City who has worked on clinical trials for H.I.V. and Covid, said that ever since his first Covid shot, merely standing up sent his heart racing — a symptom suggestive of postural orthostatic tachycardia syndrome , a neurological disorder that some studies have linked to both Covid and, much less often, vaccination .
He also experienced stinging pain in his eyes, mouth and genitals, which has abated, and tinnitus, which has not.
“I can’t get the government to help me,” Mr. Barcavage said of his fruitless pleas to federal agencies and elected representatives. “I am told I’m not real. I’m told I’m rare. I’m told I’m coincidence.”
Renee France, 49, a physical therapist in Seattle, developed Bell’s palsy — a form of facial paralysis, usually temporary — and a dramatic rash that neatly bisected her face. Bell’s palsy is a known side effect of other vaccines, and it has been linked to Covid vaccination in some studies.
But Dr. France said doctors were dismissive of any connection to the Covid vaccines. The rash, a bout of shingles, debilitated her for three weeks, so Dr. France reported it to federal databases twice.
“I thought for sure someone would reach out, but no one ever did,” she said.
Similar sentiments were echoed in interviews, conducted over more than a year, with 30 people who said they had been harmed by Covid shots. They described a variety of symptoms following vaccination, some neurological, some autoimmune, some cardiovascular.
All said they had been turned away by physicians, told their symptoms were psychosomatic, or labeled anti-vaccine by family and friends — despite the fact that they supported vaccines.
Even leading experts in vaccine science have run up against disbelief and ambivalence.
Dr. Gregory Poland, 68, editor in chief of the journal Vaccine, said that a loud whooshing sound in his ears had accompanied every moment since his first shot, but that his entreaties to colleagues at the Centers for Disease Control and Prevention to explore the phenomenon, tinnitus, had led nowhere.
He received polite responses to his many emails, but “I just don’t get any sense of movement,” he said.
“If they have done studies, those studies should be published,” Dr. Poland added. In despair that he might “never hear silence again,” he has sought solace in meditation and his religious faith.
Dr. Buddy Creech, 50, who led several Covid vaccine trials at Vanderbilt University, said his tinnitus and racing heart lasted about a week after each shot. “It’s very similar to what I experienced during acute Covid, back in March of 2020,” Dr. Creech said.
Research may ultimately find that most reported side effects are unrelated to the vaccine, he acknowledged. Many can be caused by Covid itself.
“Regardless, when our patients experience a side effect that may or may not be related to the vaccine, we owe it to them to investigate that as completely as we can,” Dr. Creech said.
Federal health officials say they do not believe that the Covid vaccines caused the illnesses described by patients like Mr. Barcavage, Dr. Zimmerman and Dr. France. The vaccines may cause transient reactions, such as swelling, fatigue and fever, according to the C.D.C., but the agency has documented only four serious but rare side effects .
Two are associated with the Johnson & Johnson vaccine, which is no longer available in the United States: Guillain-Barré syndrome , a known side effect of other vaccines , including the flu shot; and a blood-clotting disorder.
The C.D.C. also links mRNA vaccines made by Pfizer-BioNTech and Moderna to heart inflammation, or myocarditis, especially in boys and young men. And the agency warns of anaphylaxis, or severe allergic reaction, which can occur after any vaccination.
Listening for Signals
Agency scientists are monitoring large databases containing medical information on millions of Americans for patterns that might suggest a hitherto unknown side effect of vaccination, said Dr. Demetre Daskalakis, director of the C.D.C.’s National Center for Immunization and Respiratory Diseases.
“We toe the line by reporting the signals that we think are real signals and reporting them as soon as we identify them as signals,” he said. The agency’s systems for monitoring vaccine safety are “pretty close” to ideal, he said.

Those national surveillance efforts include the Vaccine Adverse Event Reporting System (VAERS). It is the largest database, but also the least reliable: Reports of side effects can be submitted by anyone and are not vetted, so they may be subject to bias or manipulation.
The system contains roughly one million reports regarding Covid vaccination, the vast majority for mild events, according to the C.D.C.
Federal researchers also comb through databases that combine electronic health records and insurance claims on tens of millions of Americans. The scientists monitor the data for 23 conditions that may occur following Covid vaccination. Officials remain alert to others that may pop up, Dr. Daskalakis said.
But there are gaps, some experts noted. The Covid shots administered at mass vaccination sites were not recorded in insurance claims databases, for example, and medical records in the United States are not centralized.
“It’s harder to see signals when you have so many people, and things are happening in different parts of the country, and they’re not all collected in the same system,” said Rebecca Chandler, a vaccine safety expert at the Coalition for Epidemic Preparedness Innovations.
An expert panel convened by the National Academies concluded in April that for the vast majority of side effects, there was not enough data to accept or reject a link.
Asked at a recent congressional hearing whether the nation’s vaccine-safety surveillance was sufficient, Dr. Peter Marks, director of the F.D.A.’s Center for Biologics Evaluation and Research, said, “I do believe we could do better.”
In some countries with centralized health care systems, officials have actively sought out reports of serious side effects of Covid vaccines and reached conclusions that U.S. health authorities have not.
In Hong Kong, the government analyzed centralized medical records of patients after vaccination and paid people to come forward with problems. The strategy identified “a lot of mild cases that other countries would not otherwise pick up,” said Ian Wong, a researcher at the University of Hong Kong who led the nation’s vaccine safety efforts.
That included the finding that in rare instances — about seven per million doses — the Pfizer-BioNTech vaccine triggered a bout of shingles serious enough to require hospitalization.
The European Medicines Agency has linked the Pfizer and Moderna vaccines to facial paralysis, tingling sensations and numbness. The E.M.A. also counts tinnitus as a side effect of the Johnson & Johnson vaccine, although the American health agencies do not. There are more than 17,000 reports of tinnitus following Covid vaccination in VAERS.
Are the two linked? It’s not clear. As many as one in four adults has some form of tinnitus. Stress, anxiety, grief and aging can lead to the condition, as can infections like Covid itself and the flu.
There is no test or scan for tinnitus, and scientists cannot easily study it because the inner ear is tiny, delicate and encased in bone, said Dr. Konstantina Stankovic, an otolaryngologist at Stanford University.
Still, an analysis of health records from nearly 2.6 million people in the United States found that about 0.04 percent , or about 1,000, were diagnosed with tinnitus within three weeks of their first mRNA shot. In March, researchers in Australia published a study linking tinnitus and vertigo to the vaccines .
The F.D.A. is monitoring reports of tinnitus, but “at this time, the available evidence does not suggest a causal association with the Covid-19 vaccines,” the agency said in a statement.
Despite surveillance efforts, U.S. officials were not the first to identify a significant Covid vaccine side effect: myocarditis in young people receiving mRNA vaccines. It was Israeli authorities who first raised the alarm in April 2021. Officials in the United States said at the time that they had not seen a link.
On May 22, 2021, news broke that the C.D.C. was investigating a “relatively few” cases of myocarditis. By June 23, the number of myocarditis reports in VAERS had risen to more than 1,200 — a hint that it is important to tell doctors and patients what to look for.
Later analyses showed that the risk for myocarditis and pericarditis, a related condition, is highest after a second dose of an mRNA Covid vaccine in adolescent males aged 12 to 17 years.
In many people, vaccine-related myocarditis is transient. But some patients continue to experience pain, breathlessness and depression, and some show persistent changes on heart scans . The C.D.C. has said there were no confirmed deaths related to myocarditis, but in fact there have been several accounts of deaths reported post-vaccination .
Pervasive Misinformation
The rise of the anti-vaccine movement has made it difficult for scientists, in and out of government, to candidly address potential side effects, some experts said. Much of the narrative on the purported dangers of Covid vaccines is patently false, or at least exaggerated, cooked up by savvy anti-vaccine campaigns.
Questions about Covid vaccine safety are core to Robert F. Kennedy Jr.’s presidential campaign. Citing debunked theories about altered DNA, Florida’s surgeon general has called for a halt to Covid vaccination in the state.
“The sheer nature of misinformation, the scale of misinformation, is staggering, and anything will be twisted to make it seem like it’s not just a devastating side effect but proof of a massive cover-up,” said Dr. Joshua Sharfstein, a vice dean at Johns Hopkins University.
Among the hundreds of millions of Americans who were immunized for Covid, some number would have had heart attacks or strokes anyway. Some women would have miscarried. How to distinguish those caused by the vaccine from those that are coincidences? The only way to resolve the question is intense research .
But the National Institutes of Health is conducting virtually no studies on Covid vaccine safety, several experts noted. William Murphy, a cancer researcher who worked at the N.I.H. for 12 years, has been prodding federal health officials to initiate these studies since 2021.
The officials each responded with “that very tired mantra: ‘But the virus is worse,’” Dr. Murphy recalled. “Yes, the virus is worse, but that doesn’t obviate doing research to make sure that there may be other options.”
A deeper understanding of possible side effects, and who is at risk for them, could have implications for the design of future vaccines, or may indicate that for some young and healthy people, the benefit of Covid shots may no longer outweigh the risks — as some European countries have determined.
Thorough research might also speed assistance to thousands of Americans who say they were injured.
The federal government has long run the National Vaccine Injury Compensation Program , designed to compensate people who suffer injuries after vaccination. Established more than three decades ago, the program sets no limit on the amounts awarded to people found to have been harmed.
But Covid vaccines are not covered by that fund because Congress has not made them subject to the excise tax that pays for it. Some lawmakers have introduced bills to make the change.
Instead, claims regarding Covid vaccines go to the Countermeasures Injury Compensation Program . Intended for public health emergencies, this program has narrow criteria to pay out and sets a limit of $50,000, with stringent standards of proof.
It requires applicants to prove within a year of the injury that it was “the direct result” of getting the Covid vaccine, based on “compelling, reliable, valid, medical, and scientific evidence.”
The program had only four staff members at the beginning of the pandemic, and now has 35 people evaluating claims. Still, it has reviewed only a fraction of the 13,000 claims filed, and has paid out only a dozen.
Dr. Ilka Warshawsky, a 58-year-old pathologist, said she lost all hearing in her right ear after a Covid booster shot. But hearing loss is not a recognized side effect of Covid vaccination.
The compensation program for Covid vaccines sets a high bar for proof, she said, yet offers little information on how to meet it: “These adverse events can be debilitating and life-altering, and so it’s very upsetting that they’re not acknowledged or addressed.”
Dr. Zimmerman, the neuroscientist, submitted her application in October 2021 and provided dozens of supporting medical documents. She received a claim number only in January 2023.
In adjudicating her claim for workers’ compensation, Washington State officials accepted that Covid vaccination caused her injury, but she has yet to get a decision from the federal program.
One of her therapists recently told her she might never be able to live independently again.
“That felt like a devastating blow,” Dr. Zimmerman said. “But I’m trying not to lose hope there will someday be a treatment and a way to cover it.”
Apoorva Mandavilli is a reporter focused on science and global health. She was a part of the team that won the 2021 Pulitzer Prize for Public Service for coverage of the pandemic. More about Apoorva Mandavilli
Advertisement

IMAGES
VIDEO
COMMENTS
A growing body of research demonstrates that COVID-19 has had a profound impact on family functioning and well-being in a range of countries. The fear and uncertainty of the health risks, in addition to the stress from ensuing restrictions and constraints on everyday life caused major disruptions, impacting the financial, emotional, and physical well-being of adults and children alike.
The effects of the social changes wrought by the COVID-19 pandemic were not wholly negative, however. Overall, most kids reported five times more positive interactions than negative interactions ...
What helped secure the NICHD funding was the existence of a recent three-year family study at Mt. Hope Family Center immediately prior to the onset of the pandemic, which provides a baseline against which the additional COVID-19 stressors and effects can be measured. The teams plan on three additional annual waves of data collection.
The outbreak has dramatically changed Americans' lives and relationships over the past year. We asked people to tell us about their experiences - good and bad - in living through this moment in history. Pew Research Center has been asking survey questions over the past year about Americans' views and reactions to the COVID-19 pandemic.
Background The COVID-19 pandemic has uniquely affected children and families by disrupting routines, changing relationships and roles, and altering usual child care, school and recreational activities. Understanding the way families experience these changes from parents' perspectives may help to guide research on the effects of COVID-19 among children. Main body As a multidisciplinary team ...
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the ...
In "Impact of the COVID-19 Crisis on Family Dynamics in Economically Vulnerable Households," Ariel Kalil, Susan E. Mayer, and Rohen Shah find that there are, indeed, negative effects for mothers (and their work is largely focused on mothers), many of whom are experiencing increased levels of stress. ... Taken together, these papers offer ...
COVID-19 and Family Dynamics 2 Abstract The COVID-19 crisis and its reverberations resulted in levels of economic distress unprecedented since the 1930s. But COVID was a seismic social shock even for families that lost no income, due at least in part to abrupt school closures and the widespread threat of illness and death.
ABSTRACT. This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery.
While physical distancing initiatives were implemented to save lives by reducing the spread of COVID-19, these results suggest that social isolation can have a negative impact on both mental and ...
When the COVID-19 pandemic hit in early 2020, many families found themselves suddenly isolated together at home. A year later, new research has linked this period with a variety of large ...
The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty, while the number of ...
This articles reflects the impacts of the COVID-19 pandemic on the everyday lives of children and their families in Estonia during lockdown in spring 2020 and 2021. The data corpus is based on diaries compiled by children during the first lockdown in 2020 for a collection at the Estonian Literary Museum, and on a series of semi-structured interviews with children documenting their experiences ...
April 22, 2020 09:00 AM. The recent COVID-19 pandemic has changed numerous things about our daily lives. Much of the public focus has naturally been on the health and safety of individuals, families, and society. Others have focused on the economic impact of both the virus and the various policies implemented to slow its spread and "flatten ...
Objectives In the first wave of the COVID-19 pandemic, social isolation, school/child care closures and employment instability have created unprecedented conditions for families raising children at home. This study describes the mental health impacts of the COVID-19 pandemic on families with children in Canada. Design, setting and participants This descriptive study used a nationally ...
Importance Little is known about the association of severe COVID-19 and post-COVID-19 conditions with household finances.. Objective To examine associations between COVID-19 outcomes, pandemic-related economic hardship, and prepandemic socioeconomic status among families in the US.. Design, Setting, and Participants This cohort study used data from the Panel Study of Income Dynamics (PSID ...
Writing About COVID-19 in College Essays. Experts say students should be honest and not limit themselves to merely their experiences with the pandemic. The global impact of COVID-19, the disease ...
The COVID-19 crisis and its reverberations resulted in levels of economic distress unprecedented since the 1930s. But COVID was a seismic social shock even for families that lost no income, due at least in part to abrupt school closures and the widespread threat of illness and death. The COVID-19 crisis will not affect all families equally, but ...
Family relationships are central to an individual's development and influence their emotional, relational, and social trajectories. Optimal family functioning, encompassing emotional connections, communication patterns, and coping mechanisms, is pivotal to the well-being of individual family members, especially during challenging periods such as the COVID-19 pandemic. From this perspective ...
We nd that the substantial variation in the impact of COVID-19 on students tracked with existing socioeconomic divides. For example, compared to their more a uent peers, lower-income students are 55% more likely to delay graduation due to COVID-19 and are 41% more likely to report that COVID-19 impacted their major choice.
Family farms play a key role in food production, natural resources stewardship, and economic development in the United States (US). Therefore, family farms' resilience (i.e., their capacity to deal with disturbances or shocks and recover from their negative impacts) is crucial for sustainability goals. The COVID-19 crisis posed several challenges to already strained family farms opening an ...
The F.D.A. is monitoring reports of tinnitus, but "at this time, the available evidence does not suggest a causal association with the Covid-19 vaccines," the agency said in a statement.
It is shown that patients with COVID infection have more severe pancreato-biliary disease and worse post-ERCP outcomes, including longer length of stay and higher mortality rate. BACKGROUND Viral infections are known to impact the pancreato-biliary system; however, there are limited data showing that the same is true of COVID-19. Endoscopic retrograde cholangiopancreatography (ERCP) can safely ...
The quality of human development depends on the level of fulfillment of their needs in the fields of health, education, and per capita spending. The government as a driver of development activities has a vital role in human development, especially after the pandemic era which previously had a negative impact on people's quality of life. Through an effective regional budget allocation, the ...
Objective: Cannabis use is common among college students and many students use cannabis to cope with negative affect. The COVID-19 pandemic was a particularly stressful time for college students. Subsequently, the present study compared college students who reported increases in anxiety/depression symptoms since COVID-19 stay at home orders to those who reported no change in anxiety/depression ...
Background: SARS-CoV-2 pandemic has caused an impact on healthcare systems worldwide, leading to inevitable negative consequences for health epidemiological indicators and diseases. Consequently, there is currently a lack of understanding the new trends and benchmarks needed to define guidelines for the prevention and control of diseases ...