The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.

How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Critical thinking in nursing clinical practice, education and research: From attitudes to virtue
Affiliations.
- 1 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, Consolidated Research Group Quantitative Psychology (2017-SGR-269), University of Barcelona, Barcelona, Spain.
- 2 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, Consolidated Research Group on Gender, Identity and Diversity (2017-SGR-1091), University of Barcelona, Barcelona, Spain.
- 3 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, University of Barcelona, Barcelona, Spain.
- 4 Multidisciplinary Nursing Research Group, Vall d'Hebron Research Institute (VHIR), Vall d'Hebron Hospital, Barcelona, Spain.
- PMID: 33029860
- DOI: 10.1111/nup.12332
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing profession. In this context, the ethics of virtue is a theoretical framework that becomes essential for analyse the critical thinking concept in nursing care and nursing science. Because the ethics of virtue consider how cultivating virtues are necessary to understand and justify the decisions and guide the actions. Based on selective analysis of the descriptive and empirical literature that addresses conceptual review of critical thinking, we conducted an analysis of this topic in the settings of clinical practice, training and research from the virtue ethical framework. Following JBI critical appraisal checklist for text and opinion papers, we argue the need for critical thinking as an essential element for true excellence in care and that it should be encouraged among professionals. The importance of developing critical thinking skills in education is well substantiated; however, greater efforts are required to implement educational strategies directed at developing critical thinking in students and professionals undergoing training, along with measures that demonstrate their success. Lastly, we show that critical thinking constitutes a fundamental component in the research process, and can improve research competencies in nursing. We conclude that future research and actions must go further in the search for new evidence and open new horizons, to ensure a positive effect on clinical practice, patient health, student education and the growth of nursing science.
Keywords: critical thinking; critical thinking attitudes; nurse education; nursing care; nursing research.
© 2020 John Wiley & Sons Ltd.
PubMed Disclaimer
Similar articles
- Teaching strategies and outcome assessments targeting critical thinking in bachelor nursing students: a scoping review protocol. Westerdahl F, Carlson E, Wennick A, Borglin G. Westerdahl F, et al. BMJ Open. 2020 Feb 2;10(1):e033214. doi: 10.1136/bmjopen-2019-033214. BMJ Open. 2020. PMID: 32014875 Free PMC article. Review.
- Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. Eddy K, Jordan Z, Stephenson M. Eddy K, et al. JBI Database System Rev Implement Rep. 2016 Apr;14(4):96-137. doi: 10.11124/JBISRIR-2016-1843. JBI Database System Rev Implement Rep. 2016. PMID: 27532314 Review.
- Student and educator experiences of maternal-child simulation-based learning: a systematic review of qualitative evidence protocol. MacKinnon K, Marcellus L, Rivers J, Gordon C, Ryan M, Butcher D. MacKinnon K, et al. JBI Database System Rev Implement Rep. 2015 Jan;13(1):14-26. doi: 10.11124/jbisrir-2015-1694. JBI Database System Rev Implement Rep. 2015. PMID: 26447004
- Ethics in nursing education: learning to reflect on care practices. Vanlaere L, Gastmans C. Vanlaere L, et al. Nurs Ethics. 2007 Nov;14(6):758-66. doi: 10.1177/0969733007082116. Nurs Ethics. 2007. PMID: 17901186 Review.
- Strategies to overcome obstacles in the facilitation of critical thinking in nursing education. Mangena A, Chabeli MM. Mangena A, et al. Nurse Educ Today. 2005 May;25(4):291-8. doi: 10.1016/j.nedt.2005.01.012. Epub 2005 Apr 12. Nurse Educ Today. 2005. PMID: 15896414
- Higher Vocational Nursing Students' Clinical Core Competence in China: A Cross-Sectional Study. Wang S, Huang S, Yan L. Wang S, et al. SAGE Open Nurs. 2024 Mar 1;10:23779608241233147. doi: 10.1177/23779608241233147. eCollection 2024 Jan-Dec. SAGE Open Nurs. 2024. PMID: 38435341 Free PMC article.
- Effect of the case-based learning method combined with virtual reality simulation technology on midwifery laboratory courses: A quasi-experimental study. Zhao L, Dai X, Chen S. Zhao L, et al. Int J Nurs Sci. 2023 Dec 16;11(1):76-82. doi: 10.1016/j.ijnss.2023.12.009. eCollection 2024 Jan. Int J Nurs Sci. 2023. PMID: 38352279 Free PMC article.
- Translation, validation and psychometric properties of the Albanian version of the Nurses Professional Competence Scale Short form. Duka B, Stievano A, Caruso R, Prendi E, Ejupi V, Spada F, De Maria M, Rocco G, Notarnicola I. Duka B, et al. Acta Biomed. 2023 Aug 3;94(4):e2023197. doi: 10.23750/abm.v94i4.13575. Acta Biomed. 2023. PMID: 37539614 Free PMC article.
- A study of the effects of blended learning on university students' critical thinking: A systematic review. Haftador AM, Tehranineshat B, Keshtkaran Z, Mohebbi Z. Haftador AM, et al. J Educ Health Promot. 2023 Mar 31;12:95. doi: 10.4103/jehp.jehp_665_22. eCollection 2023. J Educ Health Promot. 2023. PMID: 37288404 Free PMC article. Review.
- Multilevel Modeling of Individual and Group Level Influences on Critical Thinking and Clinical Decision-Making Skills among Registered Nurses: A Study Protocol. Zainal NH, Musa KI, Rasudin NS, Mamat Z. Zainal NH, et al. Healthcare (Basel). 2023 Apr 19;11(8):1169. doi: 10.3390/healthcare11081169. Healthcare (Basel). 2023. PMID: 37108003 Free PMC article.
- Alfaro-Lefevre, R. (2019). Critical thinking, clinical reasoning and clinical judgment. A practical approach, 7th ed. Elsevier.
- Armstrong, A. (2006). Towards a strong virtue ethics for nursing practice. Nursing Philosophy, 7(3), 110-124.
- Armstrong, A. (2007). Nursing ethics. A virtue-based approach. Palgrave Macmillian.
- Banks-Wallace, J., Despins, L., Adams-Leander, S., McBroom, L., & Tandy, L. (2008). Re/Affirming and re/conceptualizing disciplinary knowledge as the foundations for doctoral education. Advances in Nursing Sciencies, 31(1), 67-78. https://doi.org/10.1097/01.ANS.0000311530.81188.88
- Banning, M. (2008). Clinical reasoning and its application to nursing: Concepts and research studies. Nurse Education in Practice, 8(3), 177-183.
- Search in MeSH
Grants and funding
- PREI-19-007-B/School of Nursing. Faculty of Medicine and Health Sciences. University of Barcelona
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Critical Thinking in Nursing
- First Online: 02 January 2023
Cite this chapter

- Şefika Dilek Güven 3
Part of the book series: Integrated Science ((IS,volume 12))
1169 Accesses
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered. Nurses should develop their critical thinking skills so that they can analyze the problems of the current century, keep up with new developments and changes, cope with nursing problems they encounter, identify more complex patient care needs, provide more systematic care, give the most appropriate patient care in line with the education they have received, and make clinical decisions. The present chapter briefly examines critical thinking, how it relates to nursing, and which skills nurses need to develop as critical thinkers.
Graphical Abstract/Art Performance

Critical thinking in nursing.
This painting shows a nurse and how she is thinking critically. On the right side are the stages of critical thinking and on the left side, there are challenges that a nurse might face. The entire background is also painted in several colors to represent a kind of intellectual puzzle. It is made using colored pencils and markers.
(Adapted with permission from the Association of Science and Art (ASA), Universal Scientific Education and Research Network (USERN); Painting by Mahshad Naserpour).
Unless the individuals of a nation thinkers, the masses can be drawn in any direction. Mustafa Kemal Atatürk
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Thinking Critically About the Quality of Critical Thinking Definitions and Measures

Criticality in Osteopathic Medicine: Exploring the Relationship between Critical Thinking and Clinical Reasoning

Clinical Decision Making
Bilgiç Ş, Kurtuluş Tosun Z (2016) Birinci ve son sınıf hemşirelik öğrencilerinde eleştirel düşünme ve etkileyen faktörler. Sağlık Bilimleri ve Meslekleri Dergisi 3(1):39–47
Article Google Scholar
Kantek F, Yıldırım N (2019) The effects of nursing education on critical thinking of students: a meta-analysis. Florence Nightingale Hemşirelik Dergisi 27(1):17–25
Ennis R (1996) Critical thinking dispositions: their nature and assessability. Informal Logic 18(2):165–182
Riddell T (2007) Critical assumptions: thinking critically about critical thinking. J Nurs Educ 46(3):121–126
Cüceloğlu D (2001) İyi düşün doğru karar ver. Remzi Kitabevi, pp 242–284
Google Scholar
Kurnaz A (2019) Eleştirel düşünme öğretimi etkinlikleri Planlama-Uygulama ve Değerlendirme. Eğitim yayın evi, p 27
Doğanay A, Ünal F (2006) Eleştirel düşünmenin öğretimi. In: İçerik Türlerine Dayalı Öğretim. Ankara Nobel Yayınevi, pp 209–261
Scheffer B-K, Rubenfeld M-G (2000) A consensus statement on critical thinking in nursing. J Nurs Educ 39(8):352–359
Article CAS Google Scholar
Rubenfeld M-G, Scheffer B (2014) Critical thinking tactics for nurses. Jones & Bartlett Publishers, pp 5–6, 7, 19–20
Gobet F (2005) Chunking models of expertise: implications for education. Appl Cogn Psychol 19:183–204
Ay F-A (2008) Mesleki temel kavramlar. In: Temel hemşirelik: Kavramlar, ilkeler, uygulamalar. İstanbul Medikal Yayıncılık, pp 205–220
Birol L (2010) Hemşirelik bakımında sistematik yaklaşım. In: Hemşirelik süreci. Berke Ofset Matbaacılık, pp 35–45
Twibell R, Ryan M, Hermiz M (2005) Faculty perceptions of critical thinking in student clinical experiences. J Nurs Educ 44(2):71–79
The Importance of Critical Thinking in Nursing. 19 November 2018 by Carson-Newman University Online. https://onlinenursing.cn.edu/news/value-critical-thinking-nursing
Suzanne C, Smeltzer Brenda G, Bare Janice L, Cheever HK (2010) Definition of critical thinking, critical thinking process. Medical surgical nursing. Lippincott, Williams & Wilkins, pp 27–28
Profetto-McGrath J (2003) The relationship of critical thinking skills and critical thinking dispositions of baccalaureate nursing students. J Adv Nurs 43(6):569–577
Elaine S, Mary C (2002) Critical thinking in nursing education: literature review. Int J Nurs Pract 8(2):89–98
Brunt B-A (2005) Critical thinking in nursing: an integrated review. J Continuing Educ Nurs 36(2):60–67
Carter L-M, Rukholm E (2008) A study of critical thinking, teacher–student interaction, and discipline-specific writing in an online educational setting for registered nurses. J Continuing Educ Nurs 39(3):133–138
Daly W-M (2001) The development of an alternative method in the assessment of critical thinking as an outcome of nursing education. J Adv Nurs 36(1):120–130
Edwards S-L (2007) Critical thinking: a two-phase framework. Nurse Educ Pract 7(5):303–314
Rogal S-M, Young J (2008) Exploring critical thinking in critical care nursing education: a pilot study. J Continuing Educ Nurs 39(1):28–33
Worrell J-A, Profetto-McGrath J (2007) Critical thinking as an outcome of context-based learning among post RN students: a literature review. Nurse Educ Today 27(5):420–426
Morrall P, Goodman B (2013) Critical thinking, nurse education and universities: some thoughts on current issues and implications for nursing practice. Nurse Educ Today 33(9):935–937
Raymond-Seniuk C, Profetto-McGrath J (2011) Can one learn to think critically?—a philosophical exploration. Open Nurs J 5:45–51
Download references
Author information
Authors and affiliations.
Nevşehir Hacı Bektaş Veli University, Semra ve Vefa Küçük, Faculty of Health Sciences, Nursing Department, 2000 Evler Mah. Damat İbrahim Paşa Yerleşkesi, Nevşehir, Turkey
Şefika Dilek Güven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Şefika Dilek Güven .
Editor information
Editors and affiliations.
Universal Scientific Education and Research Network (USERN), Stockholm, Sweden
Nima Rezaei
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Güven, Ş.D. (2023). Critical Thinking in Nursing. In: Rezaei, N. (eds) Brain, Decision Making and Mental Health. Integrated Science, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-031-15959-6_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-15959-6_10
Published : 02 January 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-15958-9
Online ISBN : 978-3-031-15959-6
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
What is Problem-Solving in Nursing? (With Examples, Importance, & Tips to Improve)
Whether you have been a nurse for many years or you are just beginning your nursing career, chances are, you know that problem-solving skills are essential to your success. With all the skills you are expected to develop and hone as a nurse, you may wonder, “Exactly what is problem solving in nursing?” or “Why is it so important?” In this article, I will share some insight into problem-solving in nursing from my experience as a nurse. I will also tell you why I believe problem-solving skills are important and share some tips on how to improve your problem-solving skills.
What Exactly Is Problem-Solving In Nursing?
5 reasons why problem-solving is important in nursing, reason #1: good problem-solving skills reflect effective clinical judgement and critical thinking skills, reason #2: improved patient outcomes, reason #3: problem-solving skills are essential for interdisciplinary collaboration, reason #4: problem-solving skills help promote preventative care measures, reason #5: fosters opportunities for improvement, 5 steps to effective problem-solving in nursing, step #1: gather information (assessment), step #2: identify the problem (diagnosis), step #3: collaborate with your team (planning), step #4: putting your plan into action (implementation), step #5: decide if your plan was effective (evaluation), what are the most common examples of problem-solving in nursing, example #1: what to do when a medication error occurs, how to solve:, example #2: delegating tasks when shifts are short-staffed, example #3: resolving conflicts between team members, example #4: dealing with communication barriers/lack of communication, example #5: lack of essential supplies, example #6: prioritizing care to facilitate time management, example #7: preventing ethical dilemmas from hindering patient care, example #8: finding ways to reduce risks to patient safety, bonus 7 tips to improve your problem-solving skills in nursing, tip #1: enhance your clinical knowledge by becoming a lifelong learner, tip #2: practice effective communication, tip #3: encourage creative thinking and team participation, tip #4: be open-minded, tip #5: utilize your critical thinking skills, tip #6: use evidence-based practices to guide decision-making, tip #7: set a good example for other nurses to follow, my final thoughts, list of sources used for this article.

- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Margaret McCartney:...
Nurses are critical thinkers
Rapid response to:
Margaret McCartney: Nurses must be allowed to exercise professional judgment
- Related content
- Article metrics
- Rapid responses
Rapid Response:
The characteristic that distinguishes a professional nurse is cognitive rather than psychomotor ability. Nursing practice demands that practitioners display sound judgement and decision-making skills as critical thinking and clinical decision making is an essential component of nursing practice. Nurses’ ability to recognize and respond to signs of patient deterioration in a timely manner plays a pivotal role in patient outcomes (Purling & King 2012). Errors in clinical judgement and decision making are said to account for more than half of adverse clinical events (Tomlinson, 2015). The focus of the nurse clinical judgement has to be on quality evidence based care delivery, therefore, observational and reasoning skills will result in sound, reliable, clinical judgements. Clinical judgement, a concept which is critical to the nursing can be complex, because the nurse is required to use observation skills, identify relevant information, to identify the relationships among given elements through reasoning and judgement. Clinical reasoning is the process by which nurses observe patients status, process the information, come to an understanding of the patient problem, plan and implement interventions, evaluate outcomes, with reflection and learning from the process (Levett-Jones et al, 2010). At all times, nurses are responsible for their actions and are accountable for nursing judgment and action or inaction.
The speed and ability by which the nurses make sound clinical judgement is affected by their experience. Novice nurses may find this process difficult, whereas the experienced nurse should rely on her intuition, followed by fast action. Therefore education must begin at the undergraduate level to develop students’ critical thinking and clinical reasoning skills. Clinical reasoning is a learnt skill requiring determination and active engagement in deliberate practice design to improve performance. In order to acquire such skills, students need to develop critical thinking ability, as well as an understanding of how judgements and decisions are reached in complex healthcare environments.
As lifelong learners, nurses are constantly accumulating more knowledge, expertise, and experience, and it’s a rare nurse indeed who chooses to not apply his or her mind towards the goal of constant learning and professional growth. Institute of Medicine (IOM) report on the Future of Nursing, stated, that nurses must continue their education and engage in lifelong learning to gain the needed competencies for practice. American Nurses Association (ANA), Scope and Standards of Practice requires a nurse to remain involved in continuous learning and strengthening individual practice (p.26)
Alfaro-LeFevre, R. (2009). Critical thinking and clinical judgement: A practical approach to outcome-focused thinking. (4th ed.). St Louis: Elsevier
The future of nursing: Leading change, advancing health, (2010). https://campaignforaction.org/resource/future-nursing-iom-report
Levett-Jones, T., Hoffman, K. Dempsey, Y. Jeong, S., Noble, D., Norton, C., Roche, J., & Hickey, N. (2010). The ‘five rights’ of clinical reasoning: an educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’ patients. Nurse Education Today. 30(6), 515-520.
NMC (2010) New Standards for Pre-Registration Nursing. London: Nursing and Midwifery Council.
Purling A. & King L. (2012). A literature review: graduate nurses’ preparedness for recognising and responding to the deteriorating patient. Journal of Clinical Nursing, 21(23–24), 3451–3465
Thompson, C., Aitken, l., Doran, D., Dowing, D. (2013). An agenda for clinical decision making and judgement in nursing research and education. International Journal of Nursing Studies, 50 (12), 1720 - 1726 Tomlinson, J. (2015). Using clinical supervision to improve the quality and safety of patient care: a response to Berwick and Francis. BMC Medical Education, 15(103)
Competing interests: No competing interests

ANA Nursing Resources Hub
Search Resources Hub

Problem Solving in Nursing: Strategies for Your Staff
4 min read • September, 15 2023
Problem solving is in a nurse manager’s DNA. As leaders, nurse managers solve problems every day on an individual level and with their teams. Effective leaders find innovative solutions to problems and encourage their staff to nurture their own critical thinking skills and see problems as opportunities rather than obstacles.
Health care constantly evolves, so problem solving and ingenuity are skills often used out of necessity. Tackling a problem requires considering multiple options to develop a solution. Problem solving in nursing requires a solid strategy.
Nurse problem solving
Nurse managers face challenges ranging from patient care matters to maintaining staff satisfaction. Encourage your staff to develop problem-solving nursing skills to cultivate new methods of improving patient care and to promote nurse-led innovation .
Critical thinking skills are fostered throughout a nurse’s education, training, and career. These skills help nurses make informed decisions based on facts, data, and evidence to determine the best solution to a problem.
Problem-Solving Examples in Nursing
To solve a problem, begin by identifying it. Then analyze the problem, formulate possible solutions, and determine the best course of action. Remind staff that nurses have been solving problems since Florence Nightingale invented the nurse call system.
Nurses can implement the original nursing process to guide patient care for problem solving in nursing. These steps include:
- Assessment . Use critical thinking skills to brainstorm and gather information.
- Diagnosis . Identify the problem and any triggers or obstacles.
- Planning . Collaborate to formulate the desired outcome based on proven methods and resources.
- Implementation . Carry out the actions identified to resolve the problem.
- Evaluation . Reflect on the results and determine if the issue was resolved.
How to Develop Problem-Solving Strategies
Staff look to nurse managers to solve a problem, even when there’s not always an obvious solution. Leaders focused on problem solving encourage their team to work collaboratively to find an answer. Core leadership skills are a good way to nurture a health care environment that supports sharing concerns and innovation .
Here are some essentials for building a culture of innovation that encourages problem solving:
- Present problems as opportunities instead of obstacles.
- Strive to be a positive role model. Support creative thinking and staff collaboration.
- Encourage feedback and embrace new ideas.
- Respect staff knowledge and abilities.
- Match competencies with specific needs and inspire effective decision-making.
- Offer opportunities for continual learning and career growth.
- Promote research and analysis opportunities.
- Provide support and necessary resources.
- Recognize contributions and reward efforts .

Embrace Innovation to Find Solutions
Try this exercise:
Consider an ongoing departmental issue and encourage everyone to participate in brainstorming a solution. The team will:
- Define the problem, including triggers or obstacles.
- Determine methods that worked in the past to resolve similar issues.
- Explore innovative solutions.
- Develop a plan to implement a solution and monitor and evaluate results.
Problems arise unexpectedly in the fast-paced health care environment. Nurses must be able to react using critical thinking and quick decision-making skills to implement practical solutions. By employing problem-solving strategies, nurse leaders and their staff can improve patient outcomes and refine their nursing skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart
- Who We Insure
- Insurance Products
- About Berxi
Topics on this page:
The importance of critical thinking in nursing.
Topics on this page

While not every decision is an immediate life-and-death situation, there are hundreds of decisions nurses must make every day that impact patient care in ways small and large.
“Being able to assess situations and make decisions can lead to life-or-death situations,” said nurse anesthetist Aisha Allen . “Critical thinking is a crucial and essential skill for nurses.”
The National League for Nursing Accreditation Commission (NLNAC) defines critical thinking in nursing this way: “the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief-based. This is demonstrated in nursing by clinical judgment, which includes ethical, diagnostic, and therapeutic dimensions and research.”
Why Critical Thinking in Nursing Is Important
An eight-year study by Johns Hopkins reports that 10% of deaths in the U.S. are due to medical error — the third-highest cause of death in the country.
“Diagnostic errors, medical mistakes, and the absence of safety nets could result in someone’s death,” wrote Dr. Martin Makary , professor of surgery at Johns Hopkins University School of Medicine.
Everyone makes mistakes — even doctors. Nurses applying critical thinking skills can help reduce errors.
“Question everything,” said pediatric nurse practitioner Ersilia Pompilio RN, MSN, PNP . “Especially doctor’s orders.” Nurses often spend more time with patients than doctors and may notice slight changes in conditions that may not be obvious. Resolving these observations with treatment plans can help lead to better care.
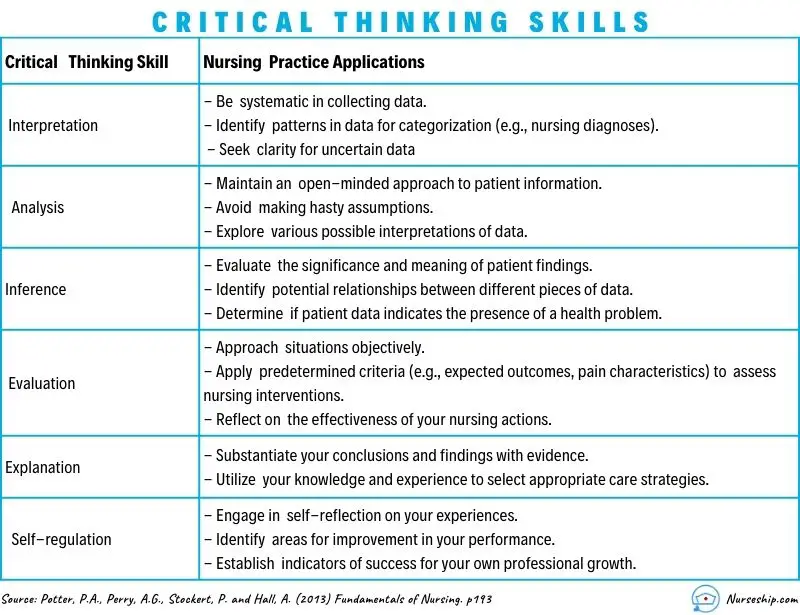
Key Nursing Critical Thinking Skills
Some of the most important critical thinking skills nurses use daily include interpretation, analysis, evaluation, inference, explanation, and self-regulation.
- Interpretation: Understanding the meaning of information or events.
- Analysis: Investigating a course of action based on objective and subjective data.
- Evaluation: Assessing the value of information and its credibility.
- Inference: Making logical deductions about the impact of care decisions.
- Explanation: Translating complicated and often complex medical information to patients and families in a way they can understand to make decisions about patient care.
- Self-Regulation: Avoiding the impact of unconscious bias with cognitive awareness.
These skills are used in conjunction with clinical reasoning. Based on training and experience, nurses use these skills and then have to make decisions affecting care.
It’s the ultimate test of a nurse’s ability to gather reliable data and solve complex problems. However, critical thinking goes beyond just solving problems. Critical thinking incorporates questioning and critiquing solutions to find the most effective one. For example, treating immediate symptoms may temporarily solve a problem, but determining the underlying cause of the symptoms is the key to effective long-term health.
8 Examples of Critical Thinking in Nursing
Here are some real-life examples of how nurses apply critical thinking on the job every day, as told by nurses themselves.
Example #1: Patient Assessments
“Doing a thorough assessment on your patient can help you detect that something is wrong, even if you're not quite sure what it is,” said Shantay Carter , registered nurse and co-founder of Women of Integrity . “When you notice the change, you have to use your critical thinking skills to decide what's the next step. Critical thinking allows you to provide the best and safest care possible.”
Example #2: First Line of Defense
Often, nurses are the first line of defense for patients.
“One example would be a patient that had an accelerated heart rate,” said nurse educator and adult critical care nurse Dr. Jenna Liphart Rhoads . “As a nurse, it was my job to investigate the cause of the heart rate and implement nursing actions to help decrease the heart rate prior to calling the primary care provider.”
Nurses with poor critical thinking skills may fail to detect a patient in stress or deteriorating condition. This can result in what’s called a “ failure to rescue ,” or FTR, which can lead to adverse conditions following a complication that leads to mortality.
Example #3: Patient Interactions
Nurses are the ones taking initial reports or discussing care with patients.
“We maintain relationships with patients between office visits,” said registered nurse, care coordinator, and ambulatory case manager Amelia Roberts . “So, when there is a concern, we are the first name that comes to mind (and get the call).”
“Several times, a parent called after the child had a high temperature, and the call came in after hours,” Roberts said. “Doing a nursing assessment over the phone is a special skill, yet based on the information gathered related to the child's behavior (and) fluid intake, there were several recommendations I could make.”
Deciding whether it was OK to wait until the morning, page the primary care doctor, or go to the emergency room to be evaluated takes critical thinking.
Example #4: Using Detective Skills
Nurses have to use acute listening skills to discern what patients are really telling them (or not telling them) and whether they are getting the whole story.
“I once had a 5-year-old patient who came in for asthma exacerbation on repeated occasions into my clinic,” said Pompilio. “The mother swore she was giving her child all her medications, but the asthma just kept getting worse.”
Pompilio asked the parent to keep a medication diary.
“It turned out that after a day or so of medication and alleviation in some symptoms, the mother thought the child was getting better and stopped all medications,” she said.
Example #5: Prioritizing
“Critical thinking is present in almost all aspects of nursing, even those that are not in direct action with the patient,” said Rhoads. “During report, nurses decide which patient to see first based on the information gathered, and from there they must prioritize their actions when in a patient’s room. Nurses must be able to scrutinize which medications can be taken together, and which modality would be best to help a patient move from the bed to the chair.”
A critical thinking skill in prioritization is cognitive stacking. Cognitive stacking helps create smooth workflow management to set priorities and help nurses manage their time. It helps establish routines for care while leaving room within schedules for the unplanned events that will inevitably occur. Even experienced nurses can struggle with juggling today’s significant workload, prioritizing responsibilities, and delegating appropriately.
Example #6: Medication & Care Coordination
Another aspect that often falls to nurses is care coordination. A nurse may be the first to notice that a patient is having an issue with medications.
“Based on a report of illness in a patient who has autoimmune challenges, we might recommend that a dose of medicine that interferes with immune response be held until we communicate with their specialty provider,” said Roberts.
Nurses applying critical skills can also help ease treatment concerns for patients.
“We might recommend a patient who gets infusions come in earlier in the day to get routine labs drawn before the infusion to minimize needle sticks and trauma,” Robert said.
Example #7: Critical Decisions
During the middle of an operation, the anesthesia breathing machine Allen was using malfunctioned.
“I had to critically think about whether or not I could fix this machine or abandon that mode of delivering nursing anesthesia care safely,” she said. “I chose to disconnect my patient from the malfunctioning machine and retrieve tools and medications to resume medication administration so that the surgery could go on.”
Nurses are also called on to do rapid assessments of patient conditions and make split-second decisions in the operating room.
“When blood pressure drops, it is my responsibility to decide which medication and how much medication will fix the issue,” Allen said. “I must work alongside the surgeons and the operating room team to determine the best plan of care for that patient's surgery.”
“On some days, it seems like you are in the movie ‘The Matrix,’” said Pompilio. “There's lots of chaos happening around you. Your patient might be decompensating. You have to literally stop time and take yourself out of the situation and make a decision.”
Example #8: Fast & Flexible Decisions
Allen said she thinks electronics are great, but she can remember a time when technology failed her.
“The hospital monitor that gives us vitals stopped correlating with real-time values,” she said. “So I had to rely on basic nursing skills to make sure my patient was safe. (Pulse check, visual assessments, etc.)”
In such cases, there may not be enough time to think through every possible outcome. Critical thinking combined with experience gives nurses the ability to think quickly and make the right decisions.
Improving the Quality of Patient Care
Nurses who think critically are in a position to significantly increase the quality of patient care and avoid adverse outcomes.
“Critical thinking allows you to ensure patient safety,” said Carter. “It’s essential to being a good nurse.”
Nurses must be able to recognize a change in a patient’s condition, conduct independent interventions, anticipate patients and provider needs, and prioritize. Such actions require critical thinking ability and advanced problem-solving skills.
“Nurses are the eyes and ears for patients, and critical thinking allows us to be their advocates,” said Allen.
Image courtesy of iStock.com/ davidf
Last updated on Jan 05, 2024 .
Originally published on Aug 25, 2021 .
The views expressed in this article are those of the author and do not necessarily reflect those of Berxi™ or Berkshire Hathaway Specialty Insurance Company. This article (subject to change without notice) is for informational purposes only, and does not constitute professional advice. Click here to read our full disclaimer
Delegation in Nursing: Steps, Skills, & Solutions for Creating Balance at Work
The 7 Most Common Nursing Mistakes (And What You Can Do If You Make One)
Resource topics.

What is Critical Thinking in Nursing? (Explained W/ Examples)
Last updated on August 23rd, 2023
Critical thinking is a foundational skill applicable across various domains, including education, problem-solving, decision-making, and professional fields such as science, business, healthcare, and more.
It plays a crucial role in promoting logical and rational thinking, fostering informed decision-making, and enabling individuals to navigate complex and rapidly changing environments.
In this article, we will look at what is critical thinking in nursing practice, its importance, and how it enables nurses to excel in their roles while also positively impacting patient outcomes.
What is Critical Thinking?
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
It’s a mental activity that goes beyond simple memorization or acceptance of information at face value.
Critical thinking involves careful, reflective, and logical thinking to understand complex problems, consider various perspectives, and arrive at well-reasoned conclusions or solutions.
Key aspects of critical thinking include:
- Analysis: Critical thinking begins with the thorough examination of information, ideas, or situations. It involves breaking down complex concepts into smaller parts to better understand their components and relationships.
- Evaluation: Critical thinkers assess the quality and reliability of information or arguments. They weigh evidence, identify strengths and weaknesses, and determine the credibility of sources.
- Synthesis: Critical thinking involves combining different pieces of information or ideas to create a new understanding or perspective. This involves connecting the dots between various sources and integrating them into a coherent whole.
- Inference: Critical thinkers draw logical and well-supported conclusions based on the information and evidence available. They use reasoning to make educated guesses about situations where complete information might be lacking.
- Problem-Solving: Critical thinking is essential in solving complex problems. It allows individuals to identify and define problems, generate potential solutions, evaluate the pros and cons of each solution, and choose the most appropriate course of action.
- Creativity: Critical thinking involves thinking outside the box and considering alternative viewpoints or approaches. It encourages the exploration of new ideas and solutions beyond conventional thinking.
- Reflection: Critical thinkers engage in self-assessment and reflection on their thought processes. They consider their own biases, assumptions, and potential errors in reasoning, aiming to improve their thinking skills over time.
- Open-Mindedness: Critical thinkers approach ideas and information with an open mind, willing to consider different viewpoints and perspectives even if they challenge their own beliefs.
- Effective Communication: Critical thinkers can articulate their thoughts and reasoning clearly and persuasively to others. They can express complex ideas in a coherent and understandable manner.
- Continuous Learning: Critical thinking encourages a commitment to ongoing learning and intellectual growth. It involves seeking out new knowledge, refining thinking skills, and staying receptive to new information.
Definition of Critical Thinking
Critical thinking is an intellectual process of analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
What is Critical Thinking in Nursing?
Critical thinking in nursing is a vital cognitive skill that involves analyzing, evaluating, and making reasoned decisions about patient care.
It’s an essential aspect of a nurse’s professional practice as it enables them to provide safe and effective care to patients.
Critical thinking involves a careful and deliberate thought process to gather and assess information, consider alternative solutions, and make informed decisions based on evidence and sound judgment.
This skill helps nurses to:
- Assess Information: Critical thinking allows nurses to thoroughly assess patient information, including medical history, symptoms, and test results. By analyzing this data, nurses can identify patterns, discrepancies, and potential issues that may require further investigation.
- Diagnose: Nurses use critical thinking to analyze patient data and collaboratively work with other healthcare professionals to formulate accurate nursing diagnoses. This is crucial for developing appropriate care plans that address the unique needs of each patient.
- Plan and Implement Care: Once a nursing diagnosis is established, critical thinking helps nurses develop effective care plans. They consider various interventions and treatment options, considering the patient’s preferences, medical history, and evidence-based practices.
- Evaluate Outcomes: After implementing interventions, critical thinking enables nurses to evaluate the outcomes of their actions. If the desired outcomes are not achieved, nurses can adapt their approach and make necessary changes to the care plan.
- Prioritize Care: In busy healthcare environments, nurses often face situations where they must prioritize patient care. Critical thinking helps them determine which patients require immediate attention and which interventions are most essential.
- Communicate Effectively: Critical thinking skills allow nurses to communicate clearly and confidently with patients, their families, and other members of the healthcare team. They can explain complex medical information and treatment plans in a way that is easily understood by all parties involved.
- Identify Problems: Nurses use critical thinking to identify potential complications or problems in a patient’s condition. This early recognition can lead to timely interventions and prevent further deterioration.
- Collaborate: Healthcare is a collaborative effort involving various professionals. Critical thinking enables nurses to actively participate in interdisciplinary discussions, share their insights, and contribute to holistic patient care.
- Ethical Decision-Making: Critical thinking helps nurses navigate ethical dilemmas that can arise in patient care. They can analyze different perspectives, consider ethical principles, and make morally sound decisions.
- Continual Learning: Critical thinking encourages nurses to seek out new knowledge, stay up-to-date with the latest research and medical advancements, and incorporate evidence-based practices into their care.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed.
It’s a dynamic process that enhances clinical reasoning , problem-solving, and overall patient outcomes.
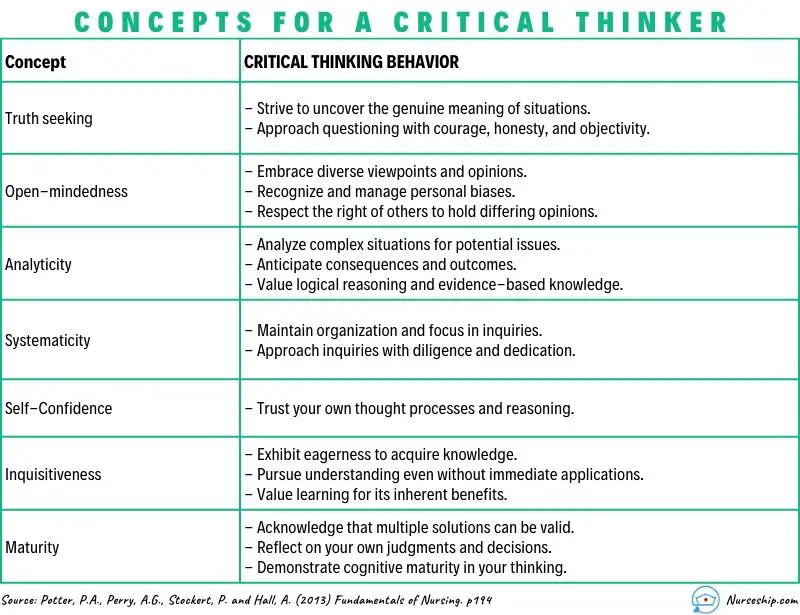
What are the Levels of Critical Thinking in Nursing?
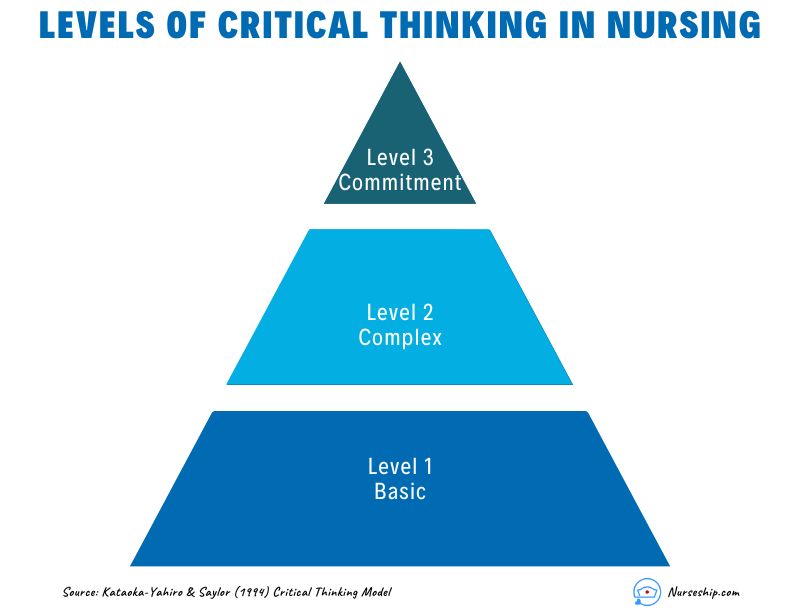
The development of critical thinking in nursing practice involves progressing through three levels: basic, complex, and commitment.
The Kataoka-Yahiro and Saylor model outlines this progression.
1. Basic Critical Thinking:
At this level, learners trust experts for solutions. Thinking is based on rules and principles. For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted.
2. Complex Critical Thinking:
Learners start to analyze choices independently and think creatively. They recognize conflicting solutions and weigh benefits and risks. Thinking becomes innovative, with a willingness to consider various approaches in complex situations.
3. Commitment:
At this level, individuals anticipate decision points without external help and take responsibility for their choices. They choose actions or beliefs based on available alternatives, considering consequences and accountability.
As nurses gain knowledge and experience, their critical thinking evolves from relying on experts to independent analysis and decision-making, ultimately leading to committed and accountable choices in patient care.
Why Critical Thinking is Important in Nursing?
Critical thinking is important in nursing for several crucial reasons:
Patient Safety:
Nursing decisions directly impact patient well-being. Critical thinking helps nurses identify potential risks, make informed choices, and prevent errors.
Clinical Judgment:
Nursing decisions often involve evaluating information from various sources, such as patient history, lab results, and medical literature.
Critical thinking assists nurses in critically appraising this information, distinguishing credible sources, and making rational judgments that align with evidence-based practices.
Enhances Decision-Making:
In nursing, critical thinking allows nurses to gather relevant patient information, assess it objectively, and weigh different options based on evidence and analysis.
This process empowers them to make informed decisions about patient care, treatment plans, and interventions, ultimately leading to better outcomes.
Promotes Problem-Solving:
Nurses encounter complex patient issues that require effective problem-solving.
Critical thinking equips them to break down problems into manageable parts, analyze root causes, and explore creative solutions that consider the unique needs of each patient.
Drives Creativity:
Nursing care is not always straightforward. Critical thinking encourages nurses to think creatively and explore innovative approaches to challenges, especially when standard protocols might not suffice for unique patient situations.
Fosters Effective Communication:
Communication is central to nursing. Critical thinking enables nurses to clearly express their thoughts, provide logical explanations for their decisions, and engage in meaningful dialogues with patients, families, and other healthcare professionals.
Aids Learning:
Nursing is a field of continuous learning. Critical thinking encourages nurses to engage in ongoing self-directed education, seeking out new knowledge, embracing new techniques, and staying current with the latest research and developments.
Improves Relationships:
Open-mindedness and empathy are essential in nursing relationships.
Critical thinking encourages nurses to consider diverse viewpoints, understand patients’ perspectives, and communicate compassionately, leading to stronger therapeutic relationships.
Empowers Independence:
Nursing often requires autonomous decision-making. Critical thinking empowers nurses to analyze situations independently, make judgments without undue influence, and take responsibility for their actions.
Facilitates Adaptability:
Healthcare environments are ever-changing. Critical thinking equips nurses with the ability to quickly assess new information, adjust care plans, and navigate unexpected situations while maintaining patient safety and well-being.
Strengthens Critical Analysis:
In the era of vast information, nurses must discern reliable data from misinformation.
Critical thinking helps them scrutinize sources, question assumptions, and make well-founded choices based on credible information.
How to Apply Critical Thinking in Nursing? (With Examples)
Here are some examples of how nurses can apply critical thinking.
Assess Patient Data:
Critical Thinking Action: Carefully review patient history, symptoms, and test results.
Example: A nurse notices a change in a diabetic patient’s blood sugar levels. Instead of just administering insulin, the nurse considers recent dietary changes, activity levels, and possible medication interactions before adjusting the treatment plan.
Diagnose Patient Needs:
Critical Thinking Action: Analyze patient data to identify potential nursing diagnoses.
Example: After reviewing a patient’s lab results, vital signs, and observations, a nurse identifies “ Risk for Impaired Skin Integrity ” due to the patient’s limited mobility.
Plan and Implement Care:
Critical Thinking Action: Develop a care plan based on patient needs and evidence-based practices.
Example: For a patient at risk of falls, the nurse plans interventions such as hourly rounding, non-slip footwear, and bed alarms to ensure patient safety.
Evaluate Interventions:
Critical Thinking Action: Assess the effectiveness of interventions and modify the care plan as needed.
Example: After administering pain medication, the nurse evaluates its impact on the patient’s comfort level and considers adjusting the dosage or trying an alternative pain management approach.
Prioritize Care:
Critical Thinking Action: Determine the order of interventions based on patient acuity and needs.
Example: In a busy emergency department, the nurse triages patients by considering the severity of their conditions, ensuring that critical cases receive immediate attention.
Collaborate with the Healthcare Team:
Critical Thinking Action: Participate in interdisciplinary discussions and share insights.
Example: During rounds, a nurse provides input on a patient’s response to treatment, which prompts the team to adjust the care plan for better outcomes.
Ethical Decision-Making:
Critical Thinking Action: Analyze ethical dilemmas and make morally sound choices.
Example: When a terminally ill patient expresses a desire to stop treatment, the nurse engages in ethical discussions, respecting the patient’s autonomy and ensuring proper end-of-life care.
Patient Education:
Critical Thinking Action: Tailor patient education to individual needs and comprehension levels.
Example: A nurse uses visual aids and simplified language to explain medication administration to a patient with limited literacy skills.
Adapt to Changes:
Critical Thinking Action: Quickly adjust care plans when patient conditions change.
Example: During post-operative recovery, a nurse notices signs of infection and promptly informs the healthcare team to initiate appropriate treatment adjustments.
Critical Analysis of Information:
Critical Thinking Action: Evaluate information sources for reliability and relevance.
Example: When presented with conflicting research studies, a nurse critically examines the methodologies and sample sizes to determine which study is more credible.

Making Sense of Critical Thinking Skills
What is the purpose of critical thinking in nursing.
The purpose of critical thinking in nursing is to enable nurses to effectively analyze, interpret, and evaluate patient information, make informed clinical judgments, develop appropriate care plans, prioritize interventions, and adapt their approaches as needed, thereby ensuring safe, evidence-based, and patient-centered care.
Why critical thinking is important in nursing?
Critical thinking is important in nursing because it promotes safe decision-making, accurate clinical judgment, problem-solving, evidence-based practice, holistic patient care, ethical reasoning, collaboration, and adapting to dynamic healthcare environments.
Critical thinking skill also enhances patient safety, improves outcomes, and supports nurses’ professional growth.
How is critical thinking used in the nursing process?
Critical thinking is integral to the nursing process as it guides nurses through the systematic approach of assessing, diagnosing, planning, implementing, and evaluating patient care. It involves:
- Assessment: Critical thinking enables nurses to gather and interpret patient data accurately, recognizing relevant patterns and cues.
- Diagnosis: Nurses use critical thinking to analyze patient data, identify nursing diagnoses, and differentiate actual issues from potential complications.
- Planning: Critical thinking helps nurses develop tailored care plans, selecting appropriate interventions based on patient needs and evidence.
- Implementation: Nurses make informed decisions during interventions, considering patient responses and adjusting plans as needed.
- Evaluation: Critical thinking supports the assessment of patient outcomes, determining the effectiveness of intervention, and adapting care accordingly.
Throughout the nursing process , critical thinking ensures comprehensive, patient-centered care and fosters continuous improvement in clinical judgment and decision-making.
What is an example of the critical thinking attitude of independent thinking in nursing practice?
An example of the critical thinking attitude of independent thinking in nursing practice could be:
A nurse is caring for a patient with a complex medical history who is experiencing a new set of symptoms. The nurse carefully reviews the patient’s history, recent test results, and medication list.
While discussing the case with the healthcare team, the nurse realizes that the current treatment plan might not be addressing all aspects of the patient’s condition.
Instead of simply following the established protocol, the nurse independently considers alternative approaches based on their assessment.
The nurse proposes a modification to the treatment plan, citing the rationale and evidence supporting the change.
This demonstrates independent thinking by critically evaluating the situation, challenging assumptions, and advocating for a more personalized and effective patient care approach.
How to use Costa’s level of questioning for critical thinking in nursing?
Costa’s levels of questioning can be applied in nursing to facilitate critical thinking and stimulate a deeper understanding of patient situations. The levels of questioning are as follows:
| Level 1: Gathering | 1. What are the common side effects of the prescribed medication? 2. When was the patient’s last bowel movement? 3. Who is the patient’s emergency contact person? 4. Describe the patient’s current level of pain. 5. What information is in the patient’s medical record? |
| 1. What would happen if the patient’s blood pressure falls further? 2. Compare the patient’s oxygen saturation levels before and after administering oxygen. 3. What other nursing interventions could be considered for wound care? 4. Infer the potential reasons behind the patient’s increased heart rate. 5. Analyze the relationship between the patient’s diet and blood glucose levels. | |
| 1. What do you think will be the patient’s response to the new pain management strategy? 2. Could the patient’s current symptoms be indicative of an underlying complication? 3. How would you prioritize care for patients with varying acuity levels in the emergency department? 4. What evidence supports your choice of administering the medication at this time? 5. Create a care plan for a patient with complex needs requiring multiple interventions. |
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
- Nursing Concept Map (FREE Template)
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
Critical thinking in nursing is the foundation that underpins safe, effective, and patient-centered care.
Critical thinking skills empower nurses to navigate the complexities of their profession while consistently providing high-quality care to diverse patient populations.
Reading Recommendation
Potter, P.A., Perry, A.G., Stockert, P. and Hall, A. (2013) Fundamentals of Nursing
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Healthcare (Basel)
- PMC10779280

Teaching Strategies for Developing Clinical Reasoning Skills in Nursing Students: A Systematic Review of Randomised Controlled Trials
Associated data.
Data are contained within the article.
Background: Clinical reasoning (CR) is a holistic and recursive cognitive process. It allows nursing students to accurately perceive patients’ situations and choose the best course of action among the available alternatives. This study aimed to identify the randomised controlled trials studies in the literature that concern clinical reasoning in the context of nursing students. Methods: A comprehensive search of PubMed, Scopus, Embase, and the Cochrane Controlled Register of Trials (CENTRAL) was performed to identify relevant studies published up to October 2023. The following inclusion criteria were examined: (a) clinical reasoning, clinical judgment, and critical thinking in nursing students as a primary study aim; (b) articles published for the last eleven years; (c) research conducted between January 2012 and September 2023; (d) articles published only in English and Spanish; and (e) Randomised Clinical Trials. The Critical Appraisal Skills Programme tool was utilised to appraise all included studies. Results: Fifteen papers were analysed. Based on the teaching strategies used in the articles, two groups have been identified: simulation methods and learning programs. The studies focus on comparing different teaching methodologies. Conclusions: This systematic review has detected different approaches to help nursing students improve their reasoning and decision-making skills. The use of mobile apps, digital simulations, and learning games has a positive impact on the clinical reasoning abilities of nursing students and their motivation. Incorporating new technologies into problem-solving-based learning and decision-making can also enhance nursing students’ reasoning skills. Nursing schools should evaluate their current methods and consider integrating or modifying new technologies and methodologies that can help enhance students’ learning and improve their clinical reasoning and cognitive skills.
1. Introduction
Clinical reasoning (CR) is a holistic cognitive process. It allows nursing students to accurately perceive patients’ situations and choose the best course of action among the available alternatives. This process is consistent, dynamic, and flexible, and it helps nursing students gain awareness and put their learning into perspective [ 1 ]. CR is an essential competence for nurses’ professional practice. It is considered crucial that its development begin during basic training [ 2 ]. Analysing clinical data, determining priorities, developing plans, and interpreting results are primary skills in clinical reasoning during clinical nursing practise [ 3 ]. To develop these skills, nursing students must participate in caring for patients and working in teams during clinical experiences. Among clinical reasoning skills, we can identify communication skills as necessary for connecting with patients, conducting health interviews, engaging in shared decision-making, eliciting patients’ concerns and expectations, discussing clinical cases with colleagues and supervisors, and explaining one’s reasoning to others [ 4 ].
Educating students in nursing practise to ensure high-quality learning and safe clinical practise is a constant challenge [ 5 ]. Facilitating the development of reasoning is challenging for educators due to its complexity and multifaceted nature [ 6 ], but it is necessary because clinical reasoning must be embedded throughout the nursing curriculum [ 7 ]. Such being the case, the development of clinical reasoning is encouraged, aiming to promote better performance in indispensable skills, decision-making, quality, and safety when assisting patients [ 8 ].
Nursing education is targeted at recognising clinical signs and symptoms, accurately assessing the patient, appropriately intervening, and evaluating the effectiveness of interventions. All these clinical processes require clinical reasoning, and it takes time to develop [ 9 ]. This is a significant goal of nursing education [ 10 ] in contemporary teaching and learning approaches [ 6 ].
Strategies to mitigate errors, promote knowledge acquisition, and develop clinical reasoning should be adopted in the training of health professionals. According to the literature, different methods and teaching strategies can be applied during nursing training, as well as traditional teaching through lectures. However, the literature explains that this type of methodology cannot enhance students’ clinical reasoning alone. Therefore, nursing educators are tasked with looking for other methodologies that improve students’ clinical reasoning [ 11 ], such as clinical simulation. Clinical simulation offers a secure and controlled setting to encounter and contemplate clinical scenarios, establish relationships, gather information, and exercise autonomy in decision-making and problem-solving [ 12 ]. Different teaching strategies have been developed in clinical simulation, like games or case studies. Research indicates a positive correlation between the use of simulation to improve learning outcomes and how it positively influences the development of students’ clinical reasoning skills [ 13 ].
The students of the 21st century utilise information and communication technologies. With their technological skills, organisations can enhance their productivity and achieve their goals more efficiently. Serious games are simulations that use technology to provide nursing students with a safe and realistic environment to practise clinical reasoning and decision-making skills [ 14 ] and can foster the development of clinical reasoning through an engaging and motivating experience [ 15 ].
New graduate nurses must possess the reasoning skills required to handle complex patient situations. Aware that there are different teaching methodologies, with this systematic review we intend to discover which RCTs published focus on CR in nursing students, which interventions have been developed, and their effectiveness, both at the level of knowledge and in increasing clinical reasoning skills. By identifying the different techniques used during the interventions with nursing students in recent years and their effectiveness, it will help universities decide which type of methodology to implement to improve the reasoning skills of nursing students and, therefore, obtain better healthcare results.
This study aims to identify and analyse randomised controlled trials concerning clinical reasoning in nursing students. The following questions guide this literature review:
Which randomised controlled trials have been conducted in the last eleven years regarding nursing students’ clinical reasoning? What are the purposes of the identified RCTs? Which teaching methodologies or strategies were used in the RCTs studies? What were the outcomes of the teaching strategies used in the RCTs?
2. Materials and Methods
This review follows the PRISMA 2020 model statement for systematic reviews. That comprises three documents: the 27-item checklist, the PRISMA 2020 abstract checklist, and the revised flow diagram [ 16 ].
2.1. Search Strategy
A systematic literature review was conducted on PubMed, Scopus, Embase, and the Cochrane Controlled Register of Trials (CENTRAL) up to 15th October 2023.
The PICOS methodology guided the bibliographic search [ 17 ]: “P” being the population (nursing students), “I” the intervention (clinical reasoning), “C” comparison (traditional teaching), “O” outcome (dimension, context, and attributes of clinical reasoning in the students’ competences and the results of the teaching method on nursing students), and “S” study type (RCTs).
The search strategy used in each database was the following: (“nursing students” OR “nursing students” OR “pupil nurses” OR “undergraduate nursing”) AND (“clinical reasoning” OR “critical thinking” OR “clinical judgment”). The filters applied were full text, randomised controlled trial, English, Spanish, and from 1 January 2012 to 15 October 2023. The search strategy was performed using the same process for each database. APP performed the search, and AZ supervised the process.
During the search, the terms clinical reasoning, critical thinking, and clinical judgement were used interchangeably since clinical judgement is part of clinical reasoning and is defined by the decision to act. It is influenced by an individual’s previous experiences and clinical reasoning skills [ 18 ]. Critical thinking and clinical judgement involve reflective and logical thinking skills and play a vital role in the decision-making and problem-solving processes [ 19 ].
The first search was conducted between March and September 2022, and an additional search was conducted during October 2023, adding the new articles published between September 2022 and September 2023, following the same strategy. The search strategy was developed using words from article titles, abstracts, and index terms. Parallel to this process, the PRISMA protocol was used to systematise the collection of all the information presented in each selected article. This systematic review protocol was registered in the international register PROSPERO: CRD42022372240.
2.2. Eligibility Criteria and Study Selection
The following inclusion criteria were examined: (a) clinical reasoning, clinical judgment, and critical thinking in nursing students as a primary aim; (b) articles published in the last eleven years; (c) research conducted between January 2012 and September 2023; (d) articles published only in English and Spanish; and (e) RCTs. On the other hand, the exclusion criteria were studies conducted with students from other disciplines other than nursing, not random studies or review articles.
2.3. Data Collection and Extraction
After this study selection, the following information was extracted from each article: bibliographic information, study aims, teaching methodology, sample size and characteristics, time of intervention, and conclusions.
2.4. Risk of Bias
The two reviewers, APP and AZ, worked independently to minimise bias and mistakes. The titles and abstracts of all papers were screened for inclusion. All potential articles underwent a two-stage screening process based on the inclusion criteria. All citations were screened based on title, abstract, and text. Reviewers discussed the results to resolve minor discrepancies. All uncertain citations were included for full-text review. The full text of each included citation was obtained. Each study was read thoroughly and assessed for inclusion following the inclusion and exclusion criteria explained in the methodology. The CASP tool was utilised to appraise all included studies. The CASP Randomized Controlled Trial Standard Checklist is an 11-question checklist [ 20 ], and the components assessed included the appropriateness of the objective and aims, methodology, study design, sampling method, data collection, reflexivity of the researchers, ethical considerations, data analysis, rigour of findings, and significance of this research. These items of the studies were then rated (“Yes” = with three points; “Cannot tell” = with two points; “No” = with one point). The possible rates for every article were between 0 and 39 points.
2.5. Ethical Considerations
Since this study was a comprehensive, systematic review of the existing published literature, there was no need for us to seek ethical approval.
3.1. Search Results
The initial search identified 158 articles using the above-mentioned strategy (SCOPUS ® n = 72, PUBMED ® n = 56, CENTRAL ® n = 23, and EMBASE ® n= 7), and the results are presented in Figure 1 . After retrieving the articles and excluding 111, 47 were selected for a full reading. Finally, 17 articles were selected. To comply with the methodology, the independent reviewers analysed all the selected articles one more time after the additional search, and they agreed to eliminate two of them because this study sample included nursing students as well as professional nurses. Therefore, to have a clear outcome focused on nursing students, two articles were removed, and the very final sample size was fifteen articles, following the established selection criteria ( Figure 1 ). The reasons for excluding studies from the systematic review were: nurses as targets; other design types of studies different from RCTs; focusing on other health professionals such as medical students; review studies; and being published in full text in other languages other than Spanish or English.

Flowchart of screening of clinical reasoning RCTs that underwent review.
3.2. Risk of Bias in CASP Results
All studies included in the review were screened with the CASP tool. Each study was scored out of a maximum of 39 points, showing the high quality of the randomised control trial methodology. The studies included had an average score of 33.1, ranging from 30 to 36 points. In addition, this quantitative rate of the items based on CASP, there were 13 studies that missed an item in relation to assessing/analysing outcome/s ‘blinded or not’ or not, and 11 studies that missed the item whether the benefits of the experimental intervention outweigh the harms and costs.
3.3. Data Extraction
Once the articles had undergone a full reading and the inclusion criteria were applied, data extraction was performed with a data extraction table ( Appendix A ). Their contents were summarised into six different cells: (1) CASP total points result, (2) purpose of this study, (3) teaching strategy, (4) time of intervention, (5) sample size, and (6) author and year of publication. After the review by the article’s readers, fifteen RCTs were selected. Of the fifteen, the continent with the highest number of studies was Asia, with 53.33% of the studies (n = 8) (Korea n = 4, Taiwan n = 2, and China n = 2), followed by Europe with 26.66% (n = 4) (Turkey n = 2, Paris n = 1, and Norway n = 1), and lastly South America with 20% (n = 3), all of them from Brazil.
3.4. Teaching Strategies
Different teaching strategies have been identified in the reviewed studies: simulation methods (seven articles) and learning programmes (eight articles). There are also two studies that focus on comparing different teaching methodologies.
3.4.1. Clinical Simulation
The simulation methods focused on in the studies were virtual simulation (based on mobile applications), simulation games, and high-fidelity clinical simulation. Of the total number of nursing students in the studies referring to clinical simulations, 43.85% were in their second year, while 57.1% were senior-year students. The most used method in the clinical simulation group was virtual simulation, and 57.14% of studies included only one-day teaching interventions.
Virtual simulations were used to increase knowledge about medication administration and nasotracheal suctioning in different scenarios [ 21 ], to evaluate the effect of interactive nursing skills, knowledge, and self-efficacy [ 11 ], and to detect patient deterioration in two different cases [ 22 ]. Simulation game methodology was used to improve nursing students’ cognitive and attention skills, strengthen judgment, time management, and decision-making [ 14 ].
Clinical simulation was used to develop nursing students’ clinical reasoning in evaluating wounds and their treatments [ 12 ], to evaluate and compare the perception of stressors, with the goal of determining whether simulations promote students’ self-evaluation and critical-thinking skills [ 23 ], and also to evaluate the impact of multiple simulations on students’ self-reported clinical decision-making skills and self-confidence [ 24 ].
3.4.2. Learning Programs
Different types of learning programmes have been identified in this systematic review: team-based learning, reflective training programs, person-centred educational programmes, ethical reasoning programmes, case-based learning, mapping, training problem-solving skills, and self-instructional guides. Of the total number of nursing students in the studies referring to learning programs, 57.1% were junior-year students, while 43.85% were in their senior year.
Team-based learning is a learner-centred educational strategy that promotes active learning to improve students’ problem-solving, knowledge, and practise performance. It can be implemented in small or large groups divided into teams with an instructor and reading material based on case scenarios [ 25 ]. Reflective training is based on a new mentoring practise to explore, think about, and solve problems actively during an internship. During the reflective training program, the mentors lead students to uncover clinical nursing problems through conversations with them and discussing feedback for their professional portfolios [ 26 ]. The person-centred educational programme focuses on how nursing students perceive individualised care, using design thinking to improve their perception. The use of design thinking gave the students opportunities to apply their theoretical knowledge of the person-centred program to plan innovative solutions that may effectively resolve real-life situations [ 27 ]. Another educational programme identified is the ethical reasoning program, and the aim of this is to improve nursing students’ handling of ethical decision-making situations [ 28 ], engaging the students in complex ethical clinical situations based on real cases.
Case-based learning was used to explore and demonstrate the feasibility of implementing unfolding cases in lectures to develop students’ critical-thinking abilities [ 29 ]. The web-based concept mapping of nursing students was also investigated to determine its impact on critical-thinking skills [ 30 ]. Training problem-solving skills were used to find out how it affected the rate of self-handicapping among nursing students [ 31 ]. And the last article evaluated the effect of the self-instructional guide to improve clinical reasoning skills on diagnostic accuracy in undergraduate nursing students [ 32 ].
4. Discussion
Although 158 studies were initially identified, only 15 articles were finally included in this review. The excluded articles were mainly from other disciplines other than nursing and used a less rigorous study design than RCT.
The three longest interventions were developed in Asia [ 26 , 28 , 29 ]. The longest was 300 h in duration, through one year [ 30 ]. These interventions were based on learning programs, case-based learning, person-centred care (PCC), and reflective training programs. However, it is important to take into account that Asian nursing curriculum programmes are different from European or United States curriculum because their internship is carried out only during the last academic degree year, while in Europe, following the European directive 2005/36/CE, 2013/55/UE nursing education requirements of 4600 h (2300 h of clinical practice) is carried out along the 3–4 years of the academic degree [ 33 ]. On the other hand, the intervention with the biggest sample was 419 nursing students [ 30 ], 210 in the experimental group, and 209 in the control group, and the one with the lowest sample was 51, with 24 students in the control group and 27 in the intervention group [ 32 ]. Therefore, all the included studies had a good sample size.
This systematic review has detected different methodologies to help nursing students improve their reasoning and decision-making skills. Virtual simulation was the most frequently used teaching method, both as a mobile application and as a serious game. In terms of its effectiveness in a study carried out in Taiwan, the use of a mobile application resulted in significantly higher knowledge scores, better skill performance, and higher satisfaction in students than traditional paper materials [ 21 ]. Virtual simulation [ 11 , 14 , 21 ] has also proven to be an effective tool for enhancing knowledge and confidence in recognising and responding to rapidly deteriorating patients, but studies that combined two educational strategies were more effective [ 29 ], like clinical simulation combined with another teaching strategy such as lectures or videos [ 12 ].
An interactive learner-centred nursing education mobile application with systematic contents effectively allowed students to experience positive practical nursing skills [ 11 ]. However, in a study comparing serious game simulation versus traditional teaching methods, no significant difference was found immediately or in the month following the training [ 22 ], but serious games can improve nursing students’ cognitive skills to detect patient deterioration and to make safe decisions about patient care [ 14 ]. Although the innovative teaching method was well received by the students, who expressed higher levels of satisfaction and motivation [ 22 ]. We can affirm that the development of a mobile application and its application can be effectively used by nursing students at all levels [ 11 ]. However, the performance of all these studies was measured on its short-term outcomes, only 40 min [ 21 ], 2 h [ 22 ], and 1 week [ 11 , 14 ] of intervention, and was performed with a mean sample size of 97 nursing students.
The data obtained in a study developed in Brazil [ 12 ] confirm that clinical simulation is effective for the development of nursing students’ clinical reasoning in wound evaluation and treatment and that clinical simulation in conjunction with other educational methods promotes the acquisition of knowledge by facilitating the transition from what the student knows to rational action. Moreover, the high-fidelity simulation strategy increases the perception of stressors related to a lack of competence and interpersonal relationships with patients, multidisciplinary teams, and colleagues compared with the conventional practice class in the skill laboratory. This increase was related to the students’ capacity for self-evaluation and critical reflection, concerning their learning responsibility and the need to acquire the required skills for patient care [ 23 ]. However, in the case of the effect of multiple simulations on students, there are no differences found between the double-versus single-scenario simulations [ 24 ]. The intervention time in these three studies was 30 min [ 23 ], 3.5 h [ 12 ], and 4 days [ 24 ]; then the time used to implement the intervention can determine the results obtained.
The different learning methods have an impact on various learning outcomes and students’ variables. Team-based learning [ 25 ], reflective training [ 26 ], the person-centred education programme [ 27 ], web-based concept mapping [ 30 ], and teaching cognitive-behavioural approaches [ 31 ] have proven to be effective in enhancing problem-solving abilities, knowledge, and reasoning processes and consequently improving the quality of nursing practical education. Team-based learning increased problem-solving ability scores significantly, while those in the control group decreased [ 25 ]. Reflective training, developed in China based on the new mentoring approach, was effective in encouraging nursing students to explore, think about, and solve problems actively during an internship, consequently improving their disposition for critical thinking [ 26 ]. A person-centred education programme using design thinking can effectively improve how nursing students perceive individualised care. Using design thinking allowed the students to apply their theoretical knowledge of the programme to plan innovative solutions that may effectively resolve real health problems [ 27 ]. These programmes were developed in 5 or 6 days [ 27 , 31 ], 1 week or 3 weeks [ 25 , 30 ], and 1 year [ 26 ].
The education programme focused on improving ethical decision-making had statistically significant improvements in nursing students’ self-efficacy in communication confidence, complex ethical decision-making skills, and decreased communication difficulty [ 28 ]. Case-based learning was more effective with lectures than without them in developing students’ critical thinking abilities [ 29 ]. This study was one of the longest developed with 300 h during one school year. This long-term learning intervention could have a positive impact on this study sample. Therefore, the time of the learning intervention could be a limitation in the studied RCTs. The one-time self-instruction guide was ineffective in impacting students’ diagnostic accuracy in solving case studies [ 32 ], and it is possible that only one day of intervention is not enough.
Studies have shown that problem- and team-based learning [ 25 , 31 ] are more beneficial than traditional teaching [ 29 ], as they enhance nursing skills and improve problem-solving abilities, clinical performance, communication competencies, critical thinking, and self-leadership.
Researchers generally agree that clinical reasoning is an important ability and one of the most important competencies for good nursing practise to ensure optimal patient outcomes [ 29 ] and to recognise and address patient deterioration effectively. However, effective communication is crucial in clinical reasoning. It is required to establish a rapport with patients, conduct health evaluations, make collaborative decisions, and discuss clinical cases with colleagues and supervisors. Developing clinical reasoning skills during training is essential to improving nursing professionals’ practice. To enhance clinical reasoning abilities, nursing schools should integrate simulations at every level of education to ultimately improve patient care. Improving nursing students’ preparation will impact the quality of patient care. In addition, new innovative teaching methodologies based on the use of technology could be a motivational driver in nursing clinical reasoning [ 22 ].
5. Limitations
This systematic review did not perform a search on CINAHL. Although most of the journals included in this database are included in MEDLINE, this should be addressed in the future because of the relevance of the database to nursing research. The results of the included studies could have also been influenced by the different times of the interventions and the different contexts. In addition, the reviewers have identified other studies published in languages other than those required by the inclusion criteria. It seems that many articles are published by Asian researchers, but some of them are not in English, so they cannot be analysed.
6. Conclusions
As society progresses, the new generation of nursing students poses a challenge; new technologies are ingrained in their daily lives with access to increasingly advanced technologies like artificial intelligence, and we must adapt training to capture their interest and increase their learning skills. The utilisation of mobile apps, digital simulations, and learning games has a positive impact on the clinical reasoning abilities of nursing students and their motivation. Incorporating new technologies into problem-solving-based learning and decision-making can also enhance nursing students’ reasoning skills. As a result, it is crucial to incorporate these tools into the learning process to maintain students’ interest, motivation, and satisfaction in education. Clinical simulation is particularly important in the training of students in terms of clinical performance. Still, it is necessary to add another teaching method to increase the efficacy of clinical simulations. Therefore, nursing schools should evaluate their current teaching methods and consider integrating or modifying new technologies and methodologies that can help enhance students’ learning, improve their clinical reasoning and cognitive skills, and potentially improve nursing students’ ability to affect patient care positively. By doing so, students will be better equipped to provide high-quality patient care in the future.
| Study | Sample Size | Time Intervention | Teaching Strategies | Purpose of the RCTs | CASP |
|---|---|---|---|---|---|
| Maurício et al., 2022 [ ] | n = 51 | 1 day | Self-Instructional Guide | To evaluate the effect of the Self-Instructional Guide for Clinical Reasoning on the diagnostic accuracy of undergraduate nursing students. | 36 |
| Calik and Kapucu 2022 [ ] | n = 60 | 1 week | Simulation game | Evaluated the efficacy of serious games using pre- and post-tests. | 36 |
| Zhang et al., 2017 [ ] | n = 157 | 12 months | Reflective training program | To evaluate the effects of reflective training for nursing students on their critical thinking disposition. | 35 |
| Chang et al., 2021 [ ] | n = 110 | 40 min | Mobile application | To test the hypothesis that nursing students who used a mobile learning app would have significantly higher levels of knowledge about nasotracheal suctioning and medication administration and a better development of skill performance in medication administration. | 35 |
| (Virtual simulation) | |||||
| Blanié et al., 2020 [ ] | n= 146 | 2 h | Gaming and traditional methods | To compare a traditional teaching method with gaming to improve the clinical reasoning skills necessary to help nursing students detect patient deterioration. | 35 |
| Bilik et al., 2020 [ ] | n = 419 | 1 week | Web-based concept mapping education | To investigate the impact of web-based concept mapping education on nursing students’ critical-thinking and concept-mapping skills. | 34 |
| Zarshenas et al., 2019 [ ] | n = 90 | 2 h for 6 days | Problem-solving | To investigate how training problem-solving skills affected the rate of self-handicapping among nursing students. | 33 |
| Svellingen et al., 2021 [ ] | n = 146 | 4 days in 3 years | Clinical simulation | To evaluate the impact of multiple simulations on students’ self-reported clinical decision-making skills and self-confidence. | 33 |
| Kim and Suh 2018 [ ] | n = 72 | 1 week | Mobile application | To determine if a mobile application improved students’ skills and knowledge. | 33 |
| (virtual simulation) | |||||
| Park et al., 2021 [ ] | n = 105 | 2 h for 5 days | Education program | To develop a feasibility programme for providing foundational knowledge and skills about patient-centred care to fourth-year undergraduate nursing students using the design-thinking approach. | 32 |
| Pai et al., 2022 [ ] | n = 101 | 8 h for 14 weeks | Person-centred education program | To investigate the impact of an ethical decision-making framework on ethical decision-making and communication self-efficacy in nursing students. | 32 |
| Silva et al., 2020 [ ] | n = 78 | 3.5 h for one day | Clinical simulation | To analyse the effect of clinical simulation on the development of clinical reasoning and on nursing students’ acquisition of knowledge of wound evaluation and treatment. | 31 |
| Boostel et al., 2018 [ ] | n = 52 | 30 min | Clinical simulation | To compare and evaluate the perception of stressors by nursing students before and after a high-fidelity conventional laboratory practise class or clinical simulation. | 30 |
| Hong and Yu, 2017 [ ] | n = 122 | 300 h | Cased-based learning | To compare and explore the effectiveness of two styles of case-based learning methods, unfolding nursing cases and unusual nursing cases, implemented in lectures for developing nursing students’ critical-thinking abilities. | 30 |
| Kim et al., 2016 [ ] | n = 63 | 2 h weekly for 3 weeks | Team-based learning | To examine the effects of TBL on learning outcomes and the problem-solving ability (knowledge and clinical performance) of Korean nursing students. | 30 |
Funding Statement
This research received external funding from the European programme Eramus +2021-1-BE02-KA220-HED-000023194.
Author Contributions
Conceptualisation, A.P.-P. and A.Z.; methodology, A.P.-P. and A.Z.; formal analysis, A.P.-P.; writing—original draft preparation, A.P.-P.; writing—review and editing, A.Z.; visualisation, A.Z.; supervision, A.Z. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Creative Ways to Enhance and Assess Critical Thinking in Nursing Students
Parker, Kimberly C.
About the Author Kimberly C. Parker, DNP, RN, is a clinical instructor, University of Alabama Capstone College of Nursing, Tuscaloosa, Alabama. For more information, contact her at [email protected] .
The author has declared no conflict of interest.
Nursing students should be challenged to implement critical thinking decisions regarding conclusions they implement for patient care. This article reinforces common techniques and introduces new practices to teach critical thinking. Many ways are currently recognized utilizing an assortment of techniques. The concepts from an escape room are a great way to deliver opportunities for students to practice this skill and can be provided economically and easily. Being creative in managing these concepts will offer an exciting chance to introduce critical thinking for your students.
Full Text Access for Subscribers:
Individual subscribers.

Institutional Users
Not a subscriber.
You can read the full text of this article if you:
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Escape room: innovative teaching strategy to stimulate critical..., an integrative review of clinical reasoning teaching strategies and outcome..., can you escape nursing school educational escape room in nursing education, reconstructing a nursing skills lab: a quality improvement project, strengthening critical thinking skills in associate degree nursing students....
- ACN FOUNDATION
- SIGNATURE EVENTS
- SCHOLARSHIPS
- POLICY & ADVOCACY
- ACN MERCHANDISE
- MYACN LOGIN
- THE BUZZ LOGIN
- STUDENT LOGIN

- Celebrating 75 years
- ACN governance and structure
- Work at ACN
- Contact ACN
- NurseClick – ACN’s blog
- Media releases
- Publications
- ACN podcast
- Men in Nursing
- NurseStrong
- Recognition of Service
- Free eNewsletter
- Areas of study
- Graduate Certificates
- OSCE – Preparation for Objective Structured Clinical Examination
- Nursing (Re-entry)
- Continuing Professional Development
- Immunisation courses
- Single units of study
- Transition to Practice Program
- Refresher programs
- Principles of Emergency Care
- Medicines Management Course
- Professional Practice Course
- Endorsements
- Student support
- Student policies
- Clinical placements
- Career mentoring
- Indemnity insurance
- Legal advice
- ACN representation
- Affiliate membership
- Undergraduate membership
- Retired membership
- States and Territories
- ACN Fellowship
- Referral discount
- Health Minister’s Award for Nursing Trailblazers
- Emerging Nurse Leader program
- Emerging Policy Leader Program
- Emerging Research Leader Program
- Nurse Unit Manager Leadership Program
- Nurse Director Leadership Program
- Nurse Executive Leadership Program
- The Leader’s Series
- Nurse Executive Capability Framework
- Thought leadership
- Other leadership courses
- National Nursing Forum
- History Faculty Conference
- Next Generation Faculty Summit
- Virtual Open Day
- National Nursing Roadshow
- Policy Summit
- Nursing & Health Expo
- National Nurses Breakfast
- Event and webinar calendar
- Grants and awards
- External nursing scholarships
- Assessor’s login
- ACN Advocacy and Policy
- Position Statements
- Submissions
- White Papers
- Clinical care standards
- Aged Care Solutions Expert Advisory Group
- Nurses and Violence Taskforce
- Parliamentary Friends of Nursing
- Aged Care Transition to Practice Program
- Immunisation
- Join as an Affiliated Organisation
- Our Affiliates
- Our Corporate Partners
- Events sponsorship
- Advertise with us
- Career Hub resources
- Critical Thinking
Q&A: What is critical thinking and when would you use critical thinking in the clinical setting?
(Write 2-3 paragraphs)
In literature ‘critical thinking’ is often used, and perhaps confused, with problem-solving and clinical decision-making skills and clinical reasoning. In practice, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and critiquing solutions.
Critical thinking has been defined in many ways, but is essentially the process of deliberate, systematic and logical thinking, while considering bias or assumptions that may affect your thinking or assessment of a situation. In healthcare, the clinical setting whether acute care sector or aged care critical thinking has generally been defined as reasoned, reflective thinking which can evaluate the given evidence and its significance to the patient’s situation. Critical thinking occasionally involves suspension of one’s immediate judgment to adequately evaluate and appraise a situation, including questioning whether the current practice is evidence-based. Skills such as interpretation, analysis, evaluation, inference, explanation, and self-regulation are required to interpret thinking and the situation. A lack of critical thinking may manifest as a failure to anticipate the consequences of one’s actions.
Critical thinking is that mode of thinking – about any subject, content, or problem — in which the thinker improves the quality of his or her thinking by skillfully taking charge of the structures inherent in thinking and imposing intellectual standards upon them.
The Paul-Elder framework has three components:
- The elements of thought (reasoning)
- The intellectual standards that should be applied to the elements of reasoning
- The intellectual traits associated with a cultivated critical thinker that result from the consistent and disciplined application of the intellectual standards to the elements of thought.
Critical thinking can be defined as, “the art of analysing and evaluating thinking with a view to improving it”. The eight Parts or Elements of Thinking involved in critical thinking:
- All reasoning has a purpose (goals, objectives).
- All reasoning is an attempt to figure something out, to settle some question, to solve some problem .
- All reasoning is based on assumptions (line of reasoning, information taken for granted).
- All reasoning is done from some point of view.
- All reasoning is based on data, information and evidence .
- All reasoning is expressed through, and shaped by, concepts and ideas .
- All reasoning contains inferences or interpretations by which we draw conclusions and give meaning to data.
- All reasoning leads somewhere or has implications and consequence.
Q&A: To become a nurse requires that you learn to think like a nurse. What makes the thinking of a nurse different from a doctor, a dentist or an engineer?
It is how we view the health care consumer or aged care consumer, and the type of problems nurses deal with in clinical practice when we engage in health care patient centred care. To think like a nurse requires that we learn the content of nursing; the ideas, concepts, ethics and theories of nursing and develop our intellectual capacities and skills so that we become disciplined, self-directed, critical thinkers.
As a nurse you are required to think about the entire patient/s and what you have learnt as a nurse including; ideas, theories, and concepts in nursing. It is important that we develop our skills so that we become highly proficient critical thinkers in nursing.
In nursing, critical thinkers need to be:
Nurses need to use language that will clearly communicate a lot of information that is key to good nursing care, for handover and escalation of care for improving patient safety and reducing adverse outcomes, some organisations use the iSoBAR (identify–situation–observations–background–agreed plan–read back) format. Firstly, the “i”, for “identify yourself and the patient”, placed the patient’s identity, rather than the diagnosis, in primary position and provided a method of introduction. (This is particularly important when teams are widely spread geographically.) The prompt, “S” (“situation”) “o” for “observations”, was included to provide an adequate baseline of factual information on which to devise a plan of care. and “B” (“background”), “A” “agreed plan” and “R” “read back” to reinforce the transfer of information and accountability.
In clinical practice experienced nurses engage in multiple clinical reasoning episodes for each patient in their care. An experienced nurse may enter a patient’s room and immediately observe significant data, draw conclusions about the patient and initiate appropriate care. Because of their knowledge, skill and experience the expert nurse may appear to perform these processes in a way that seems automatic or instinctive. However, clinical reasoning is a learnt skill.
Key critical thinking skills – the clinical reasoning cycle / critical thinking process
To support nursing students in the clinical setting, breakdown the critical thinking process into phases;
- Decide/identify
This is a dynamic process and nurses often combine one or more of the phases, move back and forth between them before reaching a decision, reaching outcomes and then evaluating outcomes.
For nursing students to learn to manage complex clinical scenarios effectively, it is essential to understand the process and steps of clinical reasoning. Nursing students need to learn rules that determine how cues shape clinical decisions and the connections between cues and outcomes.
Start with the Patient – what is the issue? Holistic approach – describe or list the facts, people.
Collect information – Handover report, medical and nursing, allied health notes. Results, patient history and medications.
- New information – patient assessment
Process Information – Interpret- data, signs and symptoms, normal and abnormal.
- Analyse – relevant from non-relevant information, narrow down the information
- Evaluate – deductions or form opinions and outcomes
Identify Problems – Analyse the facts and interferences to make a definitive diagnosis of the patients’ problem.
Establish Goals – Describe what you want to happen, desired outcomes and timeframe.
Take action – Select a course of action between alternatives available.
Evaluate Outcomes – The effectiveness of the actions and outcomes. Has the situation changed or improved?
Reflect on process and new learning – What have you learnt and what would you do differently next time.
Scenario: Apply the clinical reasoning cycle, see below, to a scenario that occurred with a patient in your clinical practice setting. This could be the doctor’s orders, the patient’s vital signs or a change in the patient’s condition.
(Write 3-5 paragraphs)

Important skills for critical thinking
Some skills are more important than others when it comes to critical thinking. The skills that are most important are:
- Interpreting – Understanding and explaining the meaning of information, or a particular event.
- Analysing – Investigating a course of action, that is based upon data that is objective and subjective.
- Evaluating – This is how you assess the value of the information that you have. Is the information relevant, reliable and credible?
This skill is also needed to determine if outcomes have been fully reached.
Based upon those three skills, you can use clinical reasoning to determine what the problem is.
These decisions have to be based upon sound reasoning:
- Explaining – Clearly and concisely explaining your conclusions. The nurse needs to be able to give a sound rationale for their answers.
- Self-regulating – You have to monitor your own thought processes. This means that you must reflect on the process that lead to the conclusion. Be on alert for bias and improper assumptions.
Critical thinking pitfalls
Errors that occur in critical thinking in nursing can cause incorrect conclusions. This is particularly dangerous in nursing because an incorrect conclusion can lead to incorrect clinical actions.
Illogical Processes
A common illogical thought process is known as “appeal to tradition”. This is what people are doing when they say it’s always been done like this. Creative, new approaches are not tried because of tradition.
All people have biases. Critical thinkers are able to look at their biases and not let them compromise their thinking processes.
Biases can complicate decision making, communication and ultimately effect patient care.
Closed Minded
Being closed-minded in nursing is dangerous because it ignores other team members points of view. Essential input from other experts, as well as patients and their families are also ignored which ultimately impacts on patient care. This means that fewer clinical options are explored, and fewer innovative ideas are used for critical thinking to guide decision making.
So, no matter if you are an intensive care nurse, community health nurse or a nurse practitioner, you should always keep in mind the importance of critical thinking in the nursing clinical setting.
It is essential for nurses to develop this skill: not only to have knowledge but to be able to apply knowledge in anticipation of patients’ needs using evidence-based care guidelines.
American Management Association (2012). ‘AMA 2012 Critical Skills Survey: Executive Summary’. (2012). American Management Association. http://playbook.amanet.org/wp-content/uploads/2013/03/2012-Critical-Skills-Survey-pdf.pdf Accessed 5 May 2020.
Korn, M. (2014). ‘Bosses Seek ‘Critical Thinking,’ but What Is That?,’ The Wall Street Journal . https://www.wsj.com/articles/bosses-seek-critical-thinking-but-what-is-that-1413923730?tesla=y&mg=reno64-wsj&url=http://online.wsj.com/article/SB12483389912594473586204580228373641221834.html#livefyre-comment Accessed 5 May 2020.
School of Nursing and Midwifery Faculty of Health, University of Newcastle. (2009). Clinical reasoning. Instructors resources. https://www.newcastle.edu.au/__data/assets/pdf_file/0010/86536/Clinical-Reasoning-Instructor-Resources.pdf Accessed 11 May 2020
The Value of Critical Thinking in Nursing + Examples. Nurse Journal social community for nurses worldwide. 2020. https://nursejournal.org/community/the-value-of-critical-thinking-in-nursing/ Accessed 8 May 2020.
Paul And Elder (2009) Have Defined Critical Thinking As: The Art of Analysing And Evaluating …
https://www.chegg.com/homework-help/questions-and-answers/paul-elder-2009-defined-critical-thinking-art-analyzing-evaluating-thinking-view-improving-q23582096 Accessed 8 May 2020 .
Cody, W.K. (2002). Critical thinking and nursing science: judgment, or vision? Nursing Science Quarterly, 15(3), 184-189.
Facione, P. (2011). Critical thinking: What it is and why it counts. Insight Assessment , ISBN 13: 978-1-891557-07-1.
McGrath, J. (2005). Critical thinking and evidence- based practice. Journal of Professional Nursing, 21(6), 364-371.
Porteous, J., Stewart-Wynne, G., Connolly, M. and Crommelin, P. (2009). iSoBAR — a concept and handover checklist: the National Clinical Handover Initiative. Med J Aust 2009; 190 (11): S152.
Related posts
Planning your career 5 November 2021

Active Listening 4 November 2021
Ethical Leadership 4 November 2021
We use cookies on our website to support technical features that enhance your user experience, and to help us improve our website. By continuing to use this website, you accept our privacy policy .
- Student Login
- No-Cost Professional Certificates
- Call Us: 888-549-6755
- 888-559-6763
- Search site Search our site Search Now Close
- Request Info
Skip to Content (Press Enter)
Why Critical Thinking Skills in Nursing Matter (And What You Can Do to Develop Them)
By Hannah Meinke on 07/05/2021
The nursing profession tends to attract those who have natural nurturing abilities, a desire to help others, and a knack for science or anatomy. But there is another important skill that successful nurses share, and it's often overlooked: the ability to think critically.
Identifying a problem, determining the best solution and choosing the most effective method to solve the program are all parts of the critical thinking process. After executing the plan, critical thinkers reflect on the situation to figure out if it was effective and if it could have been done better. As you can see, critical thinking is a transferable skill that can be leveraged in several facets of your life.
But why is it so important for nurses to use? We spoke with several experts to learn why critical thinking skills in nursing are so crucial to the field, the patients and the success of a nurse. Keep reading to learn why and to see how you can improve this skill.
Why are critical thinking skills in nursing important?
You learn all sorts of practical skills in nursing school, like flawlessly dressing a wound, taking vitals like a pro or starting an IV without flinching. But without the ability to think clearly and make rational decisions, those skills alone won’t get you very far—you need to think critically as well.
“Nurses are faced with decision-making situations in patient care, and each decision they make impacts patient outcomes. Nursing critical thinking skills drive the decision-making process and impact the quality of care provided,” says Georgia Vest, DNP, RN and senior dean of nursing at the Rasmussen University School of Nursing.
For example, nurses often have to make triage decisions in the emergency room. With an overflow of patients and limited staff, they must evaluate which patients should be treated first. While they rely on their training to measure vital signs and level of consciousness, they must use critical thinking to analyze the consequences of delaying treatment in each case.
No matter which department they work in, nurses use critical thinking in their everyday routines. When you’re faced with decisions that could ultimately mean life or death, the ability to analyze a situation and come to a solution separates the good nurses from the great ones.
How are critical thinking skills acquired in nursing school?
Nursing school offers a multitude of material to master and upholds high expectations for your performance. But in order to learn in a way that will actually equip you to become an excellent nurse, you have to go beyond just memorizing terms. You need to apply an analytical mindset to understanding course material.
One way for students to begin implementing critical thinking is by applying the nursing process to their line of thought, according to Vest. The process includes five steps: assessment, diagnosis, outcomes/planning, implementation and evaluation.
“One of the fundamental principles for developing critical thinking is the nursing process,” Vest says. “It needs to be a lived experience in the learning environment.”
Nursing students often find that there are multiple correct solutions to a problem. The key to nursing is to select the “the most correct” solution—one that will be the most efficient and best fit for that particular situation. Using the nursing process, students can narrow down their options to select the best one.
When answering questions in class or on exams, challenge yourself to go beyond simply selecting an answer. Start to think about why that answer is correct and what the possible consequences might be. Simply memorizing the material won’t translate well into a real-life nursing setting.
How can you develop your critical thinking skills as a nurse?
As you know, learning doesn’t stop with graduation from nursing school. Good nurses continue to soak up knowledge and continually improve throughout their careers. Likewise, they can continue to build their critical thinking skills in the workplace with each shift.
“To improve your critical thinking, pick the brains of the experienced nurses around you to help you get the mindset,” suggests Eileen Sollars, RN ADN, AAS. Understanding how a seasoned nurse came to a conclusion will provide you with insights you may not have considered and help you develop your own approach.
The chain of command can also help nurses develop critical thinking skills in the workplace.
“Another aid in the development of critical thinking I cannot stress enough is the utilization of the chain of command,” Vest says. “In the chain of command, the nurse always reports up to the nurse manager and down to the patient care aide. Peers and fellow healthcare professionals are not in the chain of command. Clear understanding and proper utilization of the chain of command is essential in the workplace.”
How are critical thinking skills applied in nursing?
“Nurses use critical thinking in every single shift,” Sollars says. “Critical thinking in nursing is a paramount skill necessary in the care of your patients. Nowadays there is more emphasis on machines and technical aspects of nursing, but critical thinking plays an important role. You need it to understand and anticipate changes in your patient's condition.”
As a nurse, you will inevitably encounter a situation in which there are multiple solutions or treatments, and you'll be tasked with determining the solution that will provide the best possible outcome for your patient. You must be able to quickly and confidently assess situations and make the best care decision in each unique scenario. It is in situations like these that your critical thinking skills will direct your decision-making.
Do critical thinking skills matter more for nursing leadership and management positions?
While critical thinking skills are essential at every level of nursing, leadership and management positions require a new level of this ability.
When it comes to managing other nurses, working with hospital administration, and dealing with budgets, schedules or policies, critical thinking can make the difference between a smooth-running or struggling department. At the leadership level, nurses need to see the big picture and understand how each part works together.
A nurse manager , for example, might have to deal with being short-staffed. This could require coaching nurses on how to prioritize their workload, organize their tasks and rely on strategies to keep from burning out. A lead nurse with strong critical thinking skills knows how to fully understand the problem and all its implications.
- How will patient care be affected by having fewer staff?
- What kind of strain will be on the nurses?
Their solutions will take into account all their resources and possible roadblocks.
- What work can be delegated to nursing aids?
- Are there any nurses willing to come in on their day off?
- Are nurses from other departments available to provide coverage?
They’ll weigh the pros and cons of each solution and choose those with the greatest potential.
- Will calling in an off-duty nurse contribute to burnout?
- Was this situation a one-off occurrence or something that could require an additional hire in the long term?
Finally, they will look back on the issue and evaluate what worked and what didn’t. With critical thinking skills like this, a lead nurse can affect their entire staff, patient population and department for the better.
Beyond thinking
You’re now well aware of the importance of critical thinking skills in nursing. Even if you already use critical thinking skills every day, you can still work toward strengthening that skill. The more you practice it, the better you will become and the more naturally it will come to you.
If you’re interested in critical thinking because you’d like to move up in your current nursing job, consider how a Bachelor of Science in Nursing (BSN) could help you develop the necessary leadership skills.
EDITOR’S NOTE: This article was originally published in July 2012. It has since been updated to include information relevant to 2021.
- Share on Facebook
- Share on Twitter
- Share on Pinterest
- Share on LinkedIn
Request More Information
Talk with an admissions advisor today. Fill out the form to receive information about:
- Program Details and Applying for Classes
- Financial Aid and FAFSA (for those who qualify)
- Customized Support Services
- Detailed Program Plan
There are some errors in the form. Please correct the errors and submit again.
Please enter your first name.
Please enter your last name.
There is an error in email. Make sure your answer has:
- An "@" symbol
- A suffix such as ".com", ".edu", etc.
There is an error in phone number. Make sure your answer has:
- 10 digits with no dashes or spaces
- No country code (e.g. "1" for USA)
There is an error in ZIP code. Make sure your answer has only 5 digits.
Please choose a School of study.
Please choose a program.
Please choose a degree.
The program you have selected is not available in your ZIP code. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
The program you have selected requires a nursing license. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
Rasmussen University is not enrolling students in your state at this time.
By selecting "Submit," I authorize Rasmussen University to contact me by email, phone or text message at the number provided. There is no obligation to enroll. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
About the author
Hannah Meinke

Posted in General Nursing
- nursing education
Related Content

Brianna Flavin | 05.07.2024

Brianna Flavin | 03.19.2024

Robbie Gould | 11.14.2023

Noelle Hartt | 11.09.2023
This piece of ad content was created by Rasmussen University to support its educational programs. Rasmussen University may not prepare students for all positions featured within this content. Please visit www.rasmussen.edu/degrees for a list of programs offered. External links provided on rasmussen.edu are for reference only. Rasmussen University does not guarantee, approve, control, or specifically endorse the information or products available on websites linked to, and is not endorsed by website owners, authors and/or organizations referenced. Rasmussen University is accredited by the Higher Learning Commission, an institutional accreditation agency recognized by the U.S. Department of Education.
- Nursing Science
- nursing students
Fostering Nursing Students' Critical Thinking and Problem Solving Skills in Online Discussion Forums
- Journal of Nursing Education 62(6):376-376
- 62(6):376-376

- Texas A&M University - Corpus Christi
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- D. A. Lestari
- A. I. Agusty

- Chin-Lan Yang
- Hsiu-Ju Jen

- Psychol Sci Publ Interest

- Sherry S. Chesak
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Open access
- Published: 11 June 2024
Using unfolding case studies to develop critical thinking for Graduate Entry Nursing students: an educational design research study
- Rachel Macdiarmid ORCID: orcid.org/0000-0003-4791-7417 1 ,
- Eamon Merrick ORCID: orcid.org/0000-0003-4269-6360 2 , 3 &
- Rhona Winnington ORCID: orcid.org/0000-0002-6504-2856 1
BMC Nursing volume 23 , Article number: 399 ( 2024 ) Cite this article
217 Accesses
Metrics details
Graduate Entry Nursing (GEN) programmes have been introduced as another entry point to nurse registration. In the development of a new GEN programme, a problem-based approach to learning was used to develop critical thinking and clinical reasoning skills of motivated and academically capable students.
To explore and evaluate the design and delivery of course material delivered to GEN students embedded in authentic learning pedagogy from the perspectives of both GEN students and academic staff using an unfolding case study approach.
An educational design research approach was used to explore the learning experiences of GEN students using an unfolding case study approach situated in experiential pedagogy and the teaching experiences of the academics who designed it. Data were collected through semi-structured interviews with students once they had finished the course and weekly reflective diary recordings by academic staff throughout implementation. Thematic analysis was used to analyse the data.
Student reflections highlighted that this cohort had insight into how they learned and were comfortable voicing their needs to academic staff. While the unfolding case studies were not liked by all participants, for some it offered a unique learning opportunity; particularly when scaffolded with podcasts, simulation labs, tutorials and clinical placements. Staff reflections primarily aligned with student experiences.
The gaps highlighted in the delivery of the course suggest that a blended pedagogical approach to graduate entry nurse education is required. Specifically, GEN students are aware of the learning needs and are happy to express these to academic staff, thus suggesting that engaging with a co-design curriculum approach will benefit future cohorts.
Peer Review reports
Graduate entry nursing students begin their degrees as experienced learners and must develop critical thinking skills within the shortened degree time frame.
What is already known
Graduate entry students are experienced and academically capable learners who begin with a diverse range of life and career experiences.
What this paper adds
Graduate entry students would benefit by being involved in curriculum design to acknowledge the unique skill set that they bring.
Introduction
Graduate Entry Nursing (GEN) degrees, or second degrees leading to eligibility for nursing registration, have recently been introduced to New Zealand. GEN students are known to be academically capable, motivated, and driven, bringing with them a range of life experiences, and have often had significant careers before enrolment [ 1 , 2 ]. Previous research has identified that teaching and learning methods must be carefully planned and innovative [ 1 ].
Pre-registration nursing education programmes prepare nursing students to provide safe nursing care with crucial skills expected of nursing graduates, including critical thinking and clinical reasoning. Clinical reasoning enables students to approach clinical issues with a problem-solving lens that relies on gathering assessment data and intervening and evaluating the patient’s response to the intervention [ 3 ].
Problem-Based Learning (PBL) aligns with the fundamental elements of authentic learning approaches [ 4 ], where learning is situated in real-world contexts [ 5 ]. Problem-based learning is considered to be an experiential teaching and learning approach that helps students develop a critical lens and clinical reasoning skills [ 6 , 7 ]. The use of PBL in nursing education is well established with previous research focused on students’ experiences and satisfaction [ 8 ]; factors that facilitate or hinder students' learning [ 9 ]; and the development of critical thinking skills [ 10 ].
Graduate entry nursing students report enjoyment of the active learning sets that enabled discussion surrounding case studies, scenarios, and practice issues [ 11 ]. Cangelosi’s [ 12 ] phenomenological study found that although time-poor, GEN students welcomed learning opportunities that were not traditional and facilitated their development and growth.
However, there is conflicting evidence regarding the effectiveness of PBL in nursing. For example, McCormick et al. [ 13 ] compared undergraduate student performance using differing teaching approaches, such as unfolding simulation scenarios versus recorded lectures and found these to be of benefit to students. Carter and Welch [ 14 ] compared the results of associate degree nursing students who attended lectures to those whose learning was informed by an unfolding case study. In contrast to McCormick’s et al.’s [ 13 ] earlier positive results, these authors found both groups of students performed worse in the post-test.
As previous research has identified that new graduate nurses do not always have critical thinking skills, using an unfolding case study approach can reflect the reality of clinical practice where not all the relevant information is known at the first encounter with the patient [ 14 , 15 , 16 ].
Nonetheless, while several studies have investigated the use of unfolding case studies in undergraduate preregistration programmes there is little evidence that supports the use of these with more academically capable GEN students. This article reports on a qualitative interpretivist study that used an educational design methodology to explore the experiences of GEN students who participated in the programme of learning and the experiences of the academics who designed it.
Educational Design Research (EDR) is an iterative, pragmatic, and reflective methodology well suited to small projects [ 17 ]. It has arisen from design-based research and can include both quantitative and qualitative data collection methods. EDR was selected as it fitted with our desire to develop new ways of teaching alongside gaining feedback from both academic staff and students. In the first phase of this research, we redesigned the teaching and learning strategies for a component of the GEN programme [ 18 ].
EDR has four phases (Table 1 ) [ 17 ]:
Aims and objectives
The study aimed to explore and evaluate the design and delivery of course material delivered to GEN students embedded in authentic learning pedagogy from the perspectives of both GEN students and academic staff using an unfolding case study approach.
Theoretical framework
To enable the development of clinical reasoning skills a scaffolded learning approach was implemented that involved unfolding case studies designed to represent the health needs of the New Zealand population, thus, encouraging critical thinking. Unfolding case studies reflective of situations that students might face in the future were used to encourage students to consider and analyse information, provoke further questioning and identify the information required to narrow their inquiries [ 14 , 15 ]. Supported by this evidence the academic staff built a learning environment where a regular teaching schedule (two days of lectures and one day of clinical labs per week), was complemented with online resources. Initial questions about the case study were provided on the learning management system. Students attended simulations where they responded to the case and answered questions critical to unpacking the ‘patients’ reality. Alongside the unfolding case studies were podcasts where experts were interviewed on topics related to the case. Tutorials enabled students to collaboratively construct answers and share their perspectives; at the end of each week students shared their answers in an online discussion forum.
Methods and setting
This study was conducted at an education facility in New Zealand offering undergraduate and GEN programmes. The participants are academics involved in the design and delivery of the course and one cohort of students of the GEN programme. This article reports on Phase 2 and 3 of the EDR approach, the academic staff’s reflective diary during course delivery, and students' feedback after the course was completed the first time. The methods were reported using the Consolidated Criteria for Reporting Qualitative Studies (COREQ) [ 19 ].
Participants
Purposeful sampling was used as the researchers were keen to explore the experiences of a specific GEN cohort [ 20 ]. Academic staff involved in the weekly reflective diaries are also the research team ( n = 3). All students in the identified cohort ( n = 7) were invited to participate, totalling ten possible participants. Student participants were approached via an advertisement on the university’s learning management system. Students were asked to contact the research assistant, who was separate from the academic staff and was not involved in the delivery of the GEN programme; five students agreed to participate. A $20 petrol voucher was offered to those who participated.
Data collection and analysis
In keeping with education design methodology, the authors met weekly to reflect on their experiences of delivering the content and guiding students. The weekly reflective conversations, between 60–90 min in length, followed a simple format of ‘what worked, what didn’t work, and what would we (as academic staff) change?’ Face to face student interviews were conducted by the research assistant at a time and place convenient to the students using semi-structured questions that were developed by the research team (see Additional file 1 ).
The semi-structured interviews ( n = 5) and reflective meetings ( n = 9) were recorded and transcribed verbatim by a research assistant who had signed a confidentiality agreement. All identifying information was deleted from the transcripts by the research assistant before the research team reviewed the data; each recording and transcript was allocated a unique identifier, for example ‘participant one’.
Thematic analysis [ 21 , 22 ] was used to analyse the data. First, the research team independently read the transcribed interviews to familiarise themselves with the data and identified initial codes. Second, the researchers met and reviewed all transcripts to identify themes and reached consensus on the themes emerging from the data. Themes were established once more than 50% of the participants stated the same issue/thought/perception. A matrix was developed whereby common themes were identified, with quotes demonstrating the themes collated to establish an audit trail.
Reflexivity
Central to this study given the proximity of staff to this student cohort, a reflexive stance was essential. Reflexivity is an engendered practice and was used in this instance not to influence the direction and outcome of the research but to allow the researchers to engage in the data to produce viable and valuable outcomes for future staff and students. Specifically, this reflexive practice provided a means for the research to be rigorous through the consideration of the vulnerability of the participating student cohort, thus inciting reflection-before-action [ 23 ].
Ethical considerations
Ethical approval for this study was obtained from the Auckland University of Technology Ethics Committee (AUTEC) (19/233). Given the potential power differential in the student/staff relationship present, participants were approached via an online advertisement and followed up by an independent research assistant. This is key to the success of the project, as such research undertakings have the potential for conflict of interest to exist [ 24 ]. The academic staff recordings were also undertaken with the knowledge that these would remain confidential to the participants and transcriber only, with a memorandum of understanding completed to this effect. Participant information sheets were given to students interested in joining the study to ensure they knew what it entailed and how their safety and identity would be managed. Written consent was obtained before the interviews were undertaken, with oral consent obtained at the beginning of each interview.
Three dominant themes emerged, which focused on the experiences of both GEN students and teaching staff. These were:
Reflective learning: Students and staff ability to clarify what worked and what did not work
Evaluation of learning: Students and staff being insightful about their ways of learning and needs
Challenges: Planning and delivering appropriate content for GEN students is challenging for teaching staff.
Within these overarching themes, subthemes were developed and will be presented in the following data results (Table 2 ).
Reflective learning
The exploration of student and staff experiences and responses to the unfolding case studies unearths what worked and what was problematic for both parties.
Unfolding case study as problem-based approach
The student experiences of using an unfolding case study approach were divided. Some students enjoyed the case scenarios but did not necessarily find them beneficial in terms of knowledge advancement as.
“ I personally, like the case studies but personally I didn’t really find that they enhanced my learning in like the clinical setting ” (P1)
or that they were relevant to clinical practice in that.
“… some of it was definitely relatable but I just found it was very different in the clinical setting compared with doing this theoretical case setting ” (P1).
A second student supported this idea that the case studies did not add practical clinical knowledge value as.
“ I mean for me the case studies weren’t challenging…I didn’t think the case studies added anything extra into my practice, they didn’t challenge my clinical reasoning or anything like that ” (P2).
Of note was that those students with previous professional healthcare backgrounds found the use of an unfolding case study approach problematic in that.
“ I found that quite a challenge. I think because with my clinical background I was sort of going straight into, yeah like I wanted more information so you know I probably would have preferred…to have a different case study every week or have all the information…and I’d be like well what about this, what about that? ” (P5).
Participant One, however, noted that while the case studies may not have added knowledge value, they were helpful at times as.
“ …one example is we learnt about arterial blood gases and then I was on placement I came across that literally [on] day one, so was really nice to be able to put something that I’d learnt in class into practice ” (P1).
While some students were less keen on the case study approach and found them hard work, others thought they provided opportunities to encourage discussion, clinical reasoning, and autonomous thinking as.
“ there was no right or wrong answer, you just had to prove your point to say I think it is this because of this, and someone else can say something else and just kind of still prove it because it was a quite grey [area] but I actually found that it really got us thinking ” (P3).
Moreover, the same participant acknowledged that.
“…I think that’s the whole idea of the course [GEN Programme] because at this level they shouldn’t be spoon-feeding you…you should be able to think for yourself and reason things out ” (P3).
Although some discord was present with regard to the case study approach, one participant did acknowledge the value of being able to break down a huge scenario into manageable sections to enhance understanding and clinical decision-making, as.
“ when you break it down it makes it easier to kind of work out what you’re going to do and what steps you’re going to do ” (P4), and that “ because you start looking at the smaller things that you need to do rather than just the big bits ” (P4).
It appears, however, that staff involved in the programme of learning were pleased with the overall notion that problem-based learning approach offered a ‘practical’ means through which to discuss what is the hands-on job of nursing. Specifically,
“ the second session around child abuse and recognising child abuse…took me a bit by surprise as I wasn’t expecting that to go very well and it went extraordinarily well, mostly because it was case based again and story based ” (L1).
Moreover, with regard to encouraging discussion and clinical reasoning at a postgraduate level,
“ I think we’ve really pulled out the difference [of] what we’re expecting of them [GEN students] as opposed to what they may have been used to” (L1).
Use of podcasts
While the use of technology is not necessarily a completely new strategy in tertiary education, here we have linked podcasts recorded with experts in their fields which related to the unfolding case studies, Again, however, there was division in the value of podcast recordings, with some students really enjoying them, saying.
“ I liked the podcasts yeah, I found the podcasts really good especially when there was [sic] different people talking about it, yeah...podcasts are good, like to just chuck on in the car or at the gym ” (P2).
Moreover, some found them easy to listen to because.
“… it’s a different way to learn because like you’ve got YouTube videos and you’ve got books and stuff but podcasts are kind of like easy ” (P2).
Some students found the podcasts particularly engaging saying.
…I just remember listening to it and I think I was in the car and I had stopped because I was on my way home…and I was still listening to it in the garage like when I was home and I was like oh this is a really interesting podcast ” (P2).
Participant three also thought podcasts a positive addition to the resources saying.
“ yeah they were helpful…there was one I listened to…they were talking about dying…I know that [one of the lecturers’] kind of research is kind of talking about death, euthanasia and all this kind of thing, and for some reasons, I don’t know why, maybe that’s why I still remember, I can say it’s the only podcast I really listened to and it was really good because it gave me a good insight as to what is happening… ” (P3)
This positive response was also noted in face-to-face class time as one staff member reported that.
“ they [the students] loved the person who was interviewed, and the feedback was it was really nice to hear a conversation about different perspectives ” (L1).
Yet, not all students were of this opinion, with some advising the podcasts were too long (approximately 60 min each), that they can be distracting, that they preferred videos and images or an in-person discussion, saying.
“ I find podcasts…I tend to switch off a bit, a bit quicker than if I was watching something, I would probably prefer, rather than watching a podcast [sic] I’d rather have an in-class discussion with the person” (P4).
Participant one said that they too struggled with podcasts because.
“ I’m more visual so I like to look at things and see like a slide I guess or what they’re talking about or, so I sort of zone out when it’s just talking and nothing to look at, so that’s what I personally struggle with, they [podcasts] are helpful it’s just I’m more a visual learner ” (P1).
While there were some negative responses to the podcasts, another participant acknowledged their value but offered their own solutions to learning, saying that.
“ I listened to a few podcasts that were put up, because they’re just easy to listen to ” (P2).
but felt that overall there were insufficient resources made available to students and therefore.
“ just went to YouTube and just, any concepts that I was unfamiliar with or stuff in class that we went over and when I went home I was like [I have] no idea what they talked about, I just found my own videos on YouTube… ” (P2).
Evaluation of learning
Learning experiences are unique to each GEN student, as are those experienced by the teaching staff. The data collected highlighted this clearly from both perspectives, offering a particularly strong insight into how this cohort of students’ function.
Approaches to learning
It was evident that these GEN students were aware of their approach to learning and that perhaps the structure of the teaching module did not align with their needs as.
“ I’m not really the best at utilising online things I’m a really hands on learner and things like a lecture…but you know if it’s yeah, more like class time, it’s sort of more my, my learning style [I] guess ” (P5).
A number of students were able to identify that they were visual learners as.
“ I use videos more because I guess I’m more of a visual learner as well and I learn better by seeing things instead of reading a huge article, I think that [videos] it helps me a bit more” (P4).
Another student, however, preferred a discussion based approach as opposed to either videos or podcasts saying that.
“ if it’s interesting, if it’s a topic that you can like relate to [through a podcast] or something it’s fine, but for me I just switch off not really taking a lot of the information [in] whereas in a discussion setting you can ask questions and you can interact with the person, yeah I find that would be a bit more helpful ” (P4).
This approach to learning through discussion was also noted when the teaching staff reflected on their experiences in that in one teaching session the GEN students.
“ were engaged, they were round a table with the second speaker talking and what I think enabled the discussion was that she [the speaker] was using her data as stories and so she was reading them, actually she got them [the students] to read them out” (L3).
The notion of learning styles, however, was not as linear as being visual or auditory or practical, as one student noted that a combination of styles was preferable to enhance learning, saying that.
“ if we weren’t able to have lectures like a recorded lecture so that there was a PowerPoint and just someone actually talking you through it, like I know there’s the YouTube videos…some of them were a little bit helpful, but like I just felt that sometimes we missed the teaching aspect of it. There’s a lot of self-directed stuff but definitely like a recorded lecture every week to go along with the readings and extra videos to watch ” (P5).
Students as insightful and engaged
While GEN students are known for their tenacity and ability to cope with the pressure and fast paced delivery, some students discovered that this did not necessarily equate with their preferred approach to learning. This cohort of GEN students were insightful in terms of their strengths and weaknesses in relation to knowledge acquisition. The use of the unfolding case studies, however, caused some frustrations as.
“ for me it was challenging in the fact that I felt I actually got frustrated because I’m thinking well I want to know this, I want to know that and yeah not getting all the information that I wanted at the time ” (P5).
This participant went further, saying that.
“ I definitely found that difficult [lack of information] I felt like [I] wasn’t getting as much information as I wanted to be able to make my clinical decisions ” (P5),
however this may have been due to the student’s background as their.
“my background is in paramedicine ” where “ we get a lot of information in a very short amount of time ” (P5).
Some fundamental issues were raised by the participants in terms of how much study is required for them to acquire the new knowledge. As one student highlighted,
“ I have a really terrible memory, so I kind of need to listen to things a few times or write it down and then watch a video and do some more reading and then like it’s good having another element to get into your brain you know ” (P2).
For one student, a solution to this was to ensure they did their preparation before attending class as.
“ you’re supposed to have read these things before coming to class, some people don’t but my kind of person, I’d read before coming to class and I tended to answer those questions so the critical, analytical part of me would be trying to find out and come up with a reasonable answer…” (P3).
For another participant, they took an alternative pathway to learning as they.
“ I just watch it and I don’t take [it in], it just sits in the back of my head because sometimes it’s building on top of previous knowledge so just, I just watch it to see if I can gain anything from that, I don’t necessarily take down notes or anything, but I just watch it so that it’s there you know ” (P4).
The pace of content delivery appeared problematic for some students, especially in relation to the practical sessions, with one student highlighting that.
“ personally I didn’t’ really like it and most of the time they were rushing, I was always like can I write this down to go back home to like really make sense of it and then sometimes obviously, sometimes I would have to say can I stay back and practice this thing again [as] I didn’t grab it as quickly as others did and the essence of the labs is that it’s grab all of these things ” (P3).
Challenges: Teaching staff experiences of GEN student learning
While on the whole the teaching staff were able to gauge the learning needs of this GEN cohort, the expectations of both parties did not always align, with one staff member reporting that.
“ the two biggest challenges was [sic] getting them [the students] to unpack already learned behaviour and [to] acknowledge their own limitations or bias ” (L1),
however by the end of the semester the same staff member reported that.
“ I think we made a lot of progress in getting them to acknowledge how they learn ” (L1).
Moreover, the challenges anticipated in teaching GEN students were not those that transpired in that.
“ I actually thought going into the first paper I was pretty excited as to how it was going to roll out, the problems I encountered were not the problems I anticipated ” (L3).
The vocality of this cohort was tangible, however, when content did not meet their needs, interest or expectations with the students saying,
“ that they didn’t do the materials because it wasn’t of interest to them and requested other teaching very much related to the assignment as opposed to anything else …” (L1).
It was expected that the GEN students would be participatory both in class and online irrespective of their ways of learning, but there was a difference in both responses and comfort with this form of engagement. One student that talked about the unfolding case study and the online component of assessment as being problematic said that.
“.. we had to put up about 250 words of something related to the case study every week and then we spoke to someone else, [I] didn’t really like the responses…I didn’t really like having to respond to someone else ” (P3).
Yet in contrast to this statement, the teaching staff were delighted that.
“…actually I got some fantastic questions from one of the students…emailed to me on Monday night about the case that was online for them, questions that I didn’t talk about in [the] lecture, I didn’t introduce the concept…they’re talking about concepts that are currently undergoing international clinical trials” (L1).
This study explored the experiences of both GEN students and academics using unfolding case studies situated in experiential learning pedagogy. The use of unfolding case studies supported with podcasts embraced our idea of developing content situated in real-life contexts. Learning was scaffolded using different teaching approaches such as podcasts, and experiential simulated learning, to offer learners multiple ways of engaging with content. Scaffolding is recognised as learning material being broken into smaller chunks of learning and in this way aligns with case-based learning [ 25 ]. In this way, we hoped that not only would students engage in problem-solving, and develop clinical decision-making skills [ 26 , 27 ], but that they would also achieve deep and lifelong learning and ultimately have an ‘aha’ moment when it all made sense.
Reflections on using an unfolding case study approach
Findings were divided, with some students enjoying the unfolding case studies and others describing them as not sufficiently challenging. The scaffolded learning approach that we developed incorporated a range of teaching approaches that enabled them to engage with the content in a way that fitted in with their lifestyle, even if the teaching method did not align with their individual learning preferences. Students reported differing views about the case studies; some enjoyed the unfolding nature while others wanted more context and direction to feel that they could make an informed clinical decision. Nonetheless, even though they did not like information being presented in smaller chunks one student recognised it meant they analysed the information they received more deeply.
Other learning tools such as podcasts were not always valued by participants and yet, the fact that students were able to provide feedback on their use does indicate that they at least attempted to engage with them.
Student reflections indicate that perhaps the use of unfolding case studies as a learning approach is not the solution to engagement, and that often more traditional teaching methods were preferred Indeed, Hobbs and Robinson’s [ 28 ] study of undergraduate nursing students in the US supported Carter and Welch’s [ 14 ] findings that the use of unfolding case studies were of no direct benefit, whilst Ellis et al.’s., [ 29 ] study confirmed that for final year nurse practitioner students unfolding case studies were beneficial in developing critical thinking and stimulating clinical reasoning. Considering these two conflicting findings, further consideration is needed of how to engage highly motivated GEN students.
As such, our results suggest it can be difficult to predict the needs of the GEN students given the diversity of their previous academic qualifications, career, and often significant life experience they bring to the programme [ 30 , 31 ]. Interestingly students in this study simultaneously demonstrated insight into their needs supporting their previous academic study experience and felt sufficiently secure to voice them, which supports evidence found in D’Antonio et al.’s [ 32 ] study. This suggests that GEN students’ capabilities need to be embraced and incorporated when planning curriculum and scaffolding learning. Anecdotally, we have found that students embrace experiential learning such as that offered in simulation labs whether this involves the use of simulated manikins or not, it seems the hands-on learning offers not only the opportunity to experience simulated reality but also fosters collaboration and problem solving with peers that enables them to dwell in learning of what it is to be a nurse.
Graduate entry students recognised as experienced learners
Our students were not overwhelmingly supportive of the pedagogical approach of unfolding case studies we adopted. As previously recognised GEN students are experienced learners and whilst having differing educational backgrounds bring individual experience and knowledge of their own approach to their learning. Nonetheless, the value of their previous learning experience appears problematic in that those learned behaviours and attitudes need to be refocused to engage with learning how to become a nurse, as demonstrated in the academic staff reflections. Despite this background experience and perceived confidence, some students reflected that online engagement that involved exploring the case studies in discussion forums with colleagues was uncomfortable. This was surprising to the academic staff and contrasted sharply with their reflections on the activity but has been previously noted by Boling et al., [ 33 ].
Implications
Given the disparity that exists between student and academic staff experiences, as demonstrated in our study, co-designing content delivery may offer a progressive solution. By engaging ‘students as partners’ it offers them a much deeper level of involvement in future teaching delivery through collaboration and reciprocation of ideas, thus culminating in appropriate curriculum design [ 34 ]. Collaborating with students in course design might facilitate students learning as they become cognisant of the active engagement of academic staff [ 9 , 10 , 35 ]. In the future, we aim to involve students in any curriculum review and course development to ensure their perspectives influence curriculum design and content delivery.
Even so, our initial intention of scaffolding learning by offering different ways for students to engage with content is supported by recent research by Dong et al. [ 36 ] who found that students performed better academically in a flipped classroom. This point, in association with our findings, suggests that the best approach to content delivery for graduate entry nursing students is to ensure students are involved in curriculum and course design alongside the delivery of learning experiences that are well facilitated and supported by faculty so that students are aware of the expectations, required of them, and importantly how they will be assessed.
Limitations
We acknowledge that the sample size in this study is small in terms of generalisability. However, our findings offer interesting, detailed and in-depth insights into the experiences and needs of both GEN students and the academic staff involved in the development and delivery of educational material. Further work needs to be undertaken to evaluate the experiences of GEN students from a range of educational providers. A longitudinal study has been undertaken to explore the motivations and experiences of GEN students in Australasia [ 37 ], which will also support these findings regarding the learning needs of GEN students.
This study has provided a platform through which academics and GEN students can share their insights of teaching and learning experiences. The results offer a clear insight into what these students expect and need to expedite their learning and how teaching staff must respond. While participants' views were somewhat mixed in relation to the use of unfolding case studies and scaffolded learning these results demonstrate how GEN students are aware of their personal ways of learning and how this translates in terms of education needs. The sharing of these experiences provides an insightful lens through which to re-evaluate pedagogical approaches for GEN students. As such, we suggest that to meet the needs of GEN student’s not only is a blended pedagogical approach appropriate but expanding education design boundaries further through a co-design focused approach to GEN programme design.
Availability for data and materials
The datasets generated and analysed during the current study are not publicly available due privacy and ethical restrictions of the participants, but are available from the corresponding author on reasonable request.
Downey KM, Asselin ME. Accelerated master’s programs in nursing for non-nurses: An integrative review of students’ and faculty’s perceptions. J Prof Nurs. 2015;31(3):215–25. Available from: https://doi.org/10.1016/j.profnurs.2014.10.002 .
Pellico LH, Terrill E, White P, Rico J. Integrative review of graduate entry programs. J Nursg Educ. 2012;51(1):29–37. Available from: https://doi.org/10.3928/01484834-20111130-01 .
Article Google Scholar
Levett-Jones T, Hoffman K, Dempsey J, Jeong SYS, Noble D, Norton CA, et al. The ‘five rights’ of clinical reasoning: An educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’ patients. Nurse Educ Today. 2010;30(6):515–20.
Article PubMed Google Scholar
Smith SB, Kennedy S. Authentic teaching to promote active learning: Redesign of an online RN to BSN evidence-based practice nursing course. J Prof Nurs. 2020;36(2):56–61. Available from: https://doi.org/10.1016/j.profnurs.2019.07.005 .
Herrington J, Reeves TC, Oliver R. Authentic Learning Environments. In: Spector J, Merrill M, Elen J, Bishop M, editors. Handbook of Research on Educational Communications and Technology. New York: Springer; 2014. p. 401–12.
Chapter Google Scholar
Herrington J, Reeves TC, Oliver R. A guide to authentic e-learning. London and New York: Routledge; 2009.
Book Google Scholar
Merisier S, Larue C, Boyer L. How does questioning influence nursing students’ clinical reasoning in problem-based learning? A scoping review. Nurse Educ Today. 2018;65:108–15.
Spiers JA, Williams B, Gibson B, Kabotoff W, McIlwraith D, Sculley A, et al. Graduate nurses’ learning trajectories and experiences of problem-based learning: A focused ethnography study. Int J Nurs Stud. 2014;51(11):1462–71. Available from: https://doi.org/10.1016/j.ijnurstu.2014.03.002 .
Article CAS PubMed Google Scholar
Svensson J, Axén A, Andersson EK, Hjelm M. Nursing students’ experiences of what influences achievement of learning outcomes in a problem-based learning context: A qualitative descriptive study. Nurs Open. 2021;8(4):1863–9. Available from: https://doi.org/10.1002/nop2.842 .
Article PubMed PubMed Central Google Scholar
Martyn J, Terwijn R, Kek MYCA, Huijser H. Exploring the relationships between teaching, approaches to learning and critical thinking in a problem-based learning foundation nursing course. Nurse Educ Today. 2014;34(5):829–35. Available from: https://doi.org/10.1016/j.nedt.2013.04.023 .
Maddison C, Strang G. Do action learning sets facilitate collaborative, deliberative learning?: A focus group evaluation of Graduate Entry Pre-registration Nursing (GEN) students’ experience. Nurse Educ Pract. 2018;28:285–91. Available from: https://doi.org/10.1016/j.nepr.2017.10.023 .
Cangelosi PR. Voices of graduates from second-degree baccalaureate nursing programmes. J Prof Nurs. 2007;23(2):91–7.
McCormick MJ, de Slavy JR, Fuller B. Embracing technology: Using an unfolding case simulation to enhance nursing students’ learning about Parkinson Disease. J Neurosci Nurs. 2013;45(1):14–20. Available from: https://doi.org/10.1097/JNN.0b013e318275b220 .
Carter JT, Welch S. The effectiveness of unfolding case studies on ADN nursing students’ level of knowledge and critical thinking skills. Teach Learn Nurs. 2016;11:143–6. Available from: https://doi.org/10.1016/j.teln.2016.05.004 .
Carr KC. Using the unfolding case study in midwifery education. J Midwifery Womens Health. 2015;60:283–90. Available from: https://doi.org/10.1111/jmwh.12293 .
Yousey YK. The use of unfolding case studies: Innovation in online undergraduate nursing education. J Nurs EducPract. 2013;3(4):21–9. Available from: https://doi.org/10.5430/jnep.v3n4p21 .
McKenney S, Reeves T. Conducting Educational Design Research. 2nd ed. New York: Routledge; 2018. Available from: http://ebookcentral.proquest.com .
Macdiarmid R, Winnington R, Cochrane T, Merrick E. Using educational design research to develop authentic learning for graduate entry students in New Zealand. Nurse Educ Prac. 2021; 51(01) Available from: https://doi.org/10.1016/j.nepr.2021.102965
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Parahoo K. Nursing Research: principles, process and issues. 3rd ed. London: Palgrave MacMillan; 2014.
Braun V, Clarke V, Hayfield N, Terry G. Thematic analysis. In: Liamputtong P, editor. Handbook of Research Methods in Health Social Sciences. Singapore: Springer; 2019. p. 843–60.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. Available from: https://doi.org/10.1191/1478088706qp063oa .
Edwards S. Reflecting differently. New dimensions: reflection-before-action and reflection-beyond-action. Int Prac Dev J. 2017;7(1):1–14. Available from: https://doi.org/10.19043/ipdj.71.002 .
Ferguson LM, Yonge O, Myrick F. Students’ involvement in faculty research: Ethical and methodological issues. Int J Qual Methods. 2004;3(4):56–8.
Coffman S, Iommi M, Morrow K. Scaffolding as active learning in nursing education. Teach Learn Nurs. 2023;18(1):232–7.
Bowman K. Use of online unfolding case studies to foster critical thinking. J Nurs Educ. 2017;56(11):701–2.
Gonslaz L, Nielsen A, Lasatar K. Developing students clinical reasoning skills: A faculty guide. J Nurse Educ. 2021;60(9):485–93. Available from: https://doi.org/10.3928/01484834-20210708-01 .
Hobbs J, Robinson C. Learning and Transfer Effects of an Unfolding Case Study in an Adult Health Nursing Course. Nurs Educ Perspect. 2022;43(1):47–8. Available from: https://doi.org/10.1097/01.NEP.0000000000000801 .
Ellis M, Hampton D, Makowski A, Falls C, Tovar E, Scott L, et al. Using unfolding case scenarios to promote clinical reasoning for nurse practitioner students. J Am Assoc Nurse Pract. 2023;35(1):55–62. Available from: https://doi.org/10.1097/JXX.0000000000000806 .
Macdiarmid R, Turner R, Winnington R, McClunie-Trust P, Donaldson A, et al. What motivates people to commence a graduate entry nursing programme: a mixed method scoping review. BMC Nurs. 2021;20:47. Available from: https://doi.org/10.1186/s12912-021-00564-9 .
Winnington R, Shannon K, Turner R, Jarden R, McClunie-Trust P, Merrick E, Donaldson A, Macdiarmid R. Learning experiences of first year graduate entry nursing students in New Zealand and Australia: a qualitative case study. BMC Nurs. 2023;22:74. Available from: https://doi.org/10.1186/s12912-023-01233-9 .
D’Antonio P, Beal MW, Underwood PW, Ward FR, McKelvey M, Guthrie B, et al. Great expectations: points of congruencies and discrepancies between incoming accelerated second-degree nursing students and faculty. J Nurs Educ. 2010;49(12):713–7. Available from https://doi.org/10.3928/01484834-20100831-08 .
Boling EC, Hough M, Krinsky H, Saleem H, Stevens M. Cutting the distance in distance education: Perspective on what promotes positive online learning experiences. Int Higher Educ. 2012;15(2):118–26. Available from: https://doi.org/10.1016/j.iheduc.2011.11.006 .
Bovill C. Co-creation in learning and teaching: the case for a whole-class approach in higher education. High Educ. 2020;79:1023–37. https://doi.org/10.1007/s10734-019-00453-w .
Paige JB, Smith RO. Nurse faculty experiences in problem-based learning: An interpretive phenomenologic analysis. Nurs Educ Perspect. 2013;34(4):233–9.
PubMed Google Scholar
Dong Y, Yin H, Du S, Wang A. The effects of flipped classroom characterized by situational and collaborative learning in a community nursing course: A quasi-experimental design. Nurse Educ Today. 2021;105. Available from: https://doi.org/10.1016/j.nedt.2021.105037
Macdiarmid R, McClunie-Trust P, Shannon K, Winnington R, Donaldson A, Jarden R, et al. What Motivates People to Start a Graduate Entry Nursing Programme: An Interpretive Multi-Centred Case Study. SAGE Open Nursing. 2021;7. Available from: https://doi.org/10.1177/23779608211011310 .
Download references
Acknowledgements
Not applicable.
The corresponding author received funding from Faculty of Health and Environmental Science at AUT.
Author information
Authors and affiliations.
Department of Nursing, Faculty of Health and Environmental Science, Auckland University of Technology, 90 Akoranga Drive, Northcote, Auckland, 0627, New Zealand
Rachel Macdiarmid & Rhona Winnington
Nursing and Midwifery Directorate NSLHD, Royal North Shore Hospital, Level 7 Kolling Building, St Leonards, NSW, 2065, Australia
Eamon Merrick
Nursing Faculty of Health, University of Technology Sydney, Sydney, Australia
You can also search for this author in PubMed Google Scholar
Contributions
RM*: Conceptualisation, methodology, investigation, formal analysis, writing original draft and review/editing. EM: Conceptualisation, methodology, investigation, formal analysis, writing original draft and review/editing. RW: Conceptualisation, methodology, investigation formal analysis, writing original draft and review/editing. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Rachel Macdiarmid .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval and consent to participate was obtained from Auckland University of Technology Ethics Committee (19/233). All methods were carried out in accordance with relevant guidelines and policies as per the ethical approval obtained. The authors can confirm that informed consent was obtained from all subjects prior to interviews occurring. Consent was both written and verbal.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Macdiarmid, R., Merrick, E. & Winnington, R. Using unfolding case studies to develop critical thinking for Graduate Entry Nursing students: an educational design research study. BMC Nurs 23 , 399 (2024). https://doi.org/10.1186/s12912-024-02076-8
Download citation
Received : 06 December 2023
Accepted : 06 June 2024
Published : 11 June 2024
DOI : https://doi.org/10.1186/s12912-024-02076-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Graduate entry nursing
- Nursing education
- Problem-based learning
- Unfolding case-study
- Experiential pedagogy
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

A Pathway for the Registered Nurse: Discover RN Programs
Nursing is an art and a science - helping others harmonize with the science of the human body. While challenging, it is also one of the most rewarding careers available. Becoming an RN is, for many, the best decision ever made.

Nursing Degree Pathways
Education at every step. Browse nursing schools and programs by degree level and educational background.
Entry Level Programs
No prior nursing education or experience? Learn how to become a CNA , LPN/LVN , Medical Assistant , or other entry-level allied healthcare professional.
Traditional RN Programs
ADN and BSN programs are traditional RN program routes; the BSN is considered the gold standard of nursing degrees. Find out more about traditional ADN , BSN , MSN degree programs.
Bridge Programs
If you have some nursing experience and wish to go further, check out nursing bridge programs such as the RN to BSN , LPN to RN , RN to MSN , and more.
Nurse Practitioner & APRN Programs
Already a seasoned RN looking to advance? Nurse Practitioner programs and other APRN pathways are available, such as FNP , ACNP , AGNP , PMHNP , WHNP , Pediatric-NP programs and more.
See All Programs
Search Nursing Programs
Select your education background and program of interest and see all the accredited nursing programs available for you.
Latest Nursing School & Program Rankings
RegisteredNursing.org is proud to highlight the best in nursing education through our detailed rankings. Find the top schools and programs in the specialty and state of your choosing below, and visit our Rankings Methodology to learn more about our process.
- 2024 - Best BSN to DNP Programs
- 2024 - Best Dual MSN/MBA Programs
- 2024 - Best Master’s in Executive Nurse Leadership Programs
- 2024 - Best Online FNP Programs
- 2024 - Best Nurse Educator Programs
- 2024 - Best MSN in Nursing Administration Programs
- 2024 - Best DNP Programs
- 2024 - Best Ph.D. in Nursing Programs
- 2024 - Best Neonatal Nurse Practitioner Programs
- 2024 - Best MSN Public Health Nurse Programs
- 2024 - Best Nursing Informatics Programs
- 2024 - Best Clinical Nurse Specialist (CNS) Programs
Is An Online Nursing Program Right For You?
A nursing education – your way. Learn more about flexible online and hybrid nursing degree programs.
Online Nursing Programs

Nursing Resources
Whether you are just starting out or looking to expand your nursing practice, our helpful resources will give you the scoop on everything from exams, licensure, certifications, salary expectations, and so much more.
Latest Articles & Guides
One of the keys to success as a registered nurse is embracing lifelong learning. Our articles and guides address hot topics and current events in nursing, from education to career mobility and beyond. No matter where you are on your nursing journey, there’s an article to help you build your knowledge base.
Browse our latest articles, curated specifically for modern nurses.
See All Articles

- Skip to main content
Update your browser for the best possible experience
As of January 1st, 2020, Internet Explorer (versions 11 and below) is no longer supported by Evolve. To get the best possible experience using Evolve, we recommend that you use another web browser. For HESI iNet users click here .

IMAGES
VIDEO
COMMENTS
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills. ... Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate ...
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as "necessary for problem-solving and decision-making by healthcare providers.
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
Critical thinking in Nursing: Decision-making and Problem-solving WWW.RN.ORG® Reviewed December, 2021, Expires December, 2023 Provider Information and Specifics available on our Website Unauthorized Distribution Prohibited ©2021 RN.ORG®, S.A., RN.ORG®, LLC By Wanda Lockwood, RN, BA, MA The purpose of this course is to explain processes of
Critical thinking/problem-solving skills should emphasize self-examination. It should teach an individual to accomplish this using a series of steps that progress in a logical fashion, stressing that critical thinking is a progression of logical thought, not an unguided process. ... Alfaro-LeFevre R. Critical thinking in nursing: a practical ...
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses' continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues ...
Lastly, we show that critical thinking constitutes a fundamental component in the research process, and can improve research competencies in nursing. We conclude that future research and actions must go further in the search for new evidence and open new horizons, to ensure a positive effect on clinical practice, patient health, student ...
Problem-solving in nursing is the vital foundation that makes up a nurse's clinical judgment and critical thinking skills. Having a strong problem-solving skillset is pertinent to possessing the ability and means to provide safe, quality care to a variety of patients. Nurses must rely on their clinical judgment and critical thinking skills to ...
Nurses are critical thinkers. The characteristic that distinguishes a professional nurse is cognitive rather than psychomotor ability. Nursing practice demands that practitioners display sound judgement and decision-making skills as critical thinking and clinical decision making is an essential component of nursing practice.
Nurses can implement the original nursing process to guide patient care for problem solving in nursing. These steps include: Assessment. Use critical thinking skills to brainstorm and gather information. Diagnosis. Identify the problem and any triggers or obstacles. Planning. Collaborate to formulate the desired outcome based on proven methods ...
However, critical thinking goes beyond just solving problems. Critical thinking incorporates questioning and critiquing solutions to find the most effective one. For example, treating immediate symptoms may temporarily solve a problem, but determining the underlying cause of the symptoms is the key to effective long-term health.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed. It's a dynamic process that enhances clinical reasoning, problem-solving, and overall patient outcomes.
Since critical thinking is an essential part of nurses' professional responsibility and clinical problem solving, it is important to focus on how this capacity is taught to nursing students, both in educational and clinical settings and how these teaching strategies are experienced.
The effectiveness of PBL in promoting critical thinking in nursing students has been studied extensively with mixed results. ... The effectiveness of problem based learning in improving critical thinking, problem-solving and self-directed learning in first-year medical students: a meta-analysis. PLoS One. 2022;17(11):e0277339. doi:10.1371 ...
Providing nursing care requires critical thinking and problem solving skills. Occupational and environ mental health nurses practice these skills uncon sciously with each client interaction, as well as when the nurse interfaces with management and other members of the health team. This article presents a framework for critical thinking.
To investigate the impact of web-based concept mapping education on nursing students' critical-thinking and concept-mapping skills. 34: Zarshenas et al., 2019 : n = 90: 2 h for 6 days: Problem-solving: To investigate how training problem-solving skills affected the rate of self-handicapping among nursing students. 33: Svellingen et al., 2021 ...
The concepts from an escape room are a great way to deliver opportunities for students to practice this skill and can be provided economically and easily. Being creative in managing these concepts will offer an exciting chance to introduce critical thinking for your students. Nursing Education Perspectives42 (6):E145-E146, November/December 2021.
In practice, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and critiquing solutions. ... Errors that occur in critical thinking in nursing can cause incorrect conclusions. This is particularly dangerous in nursing because an ...
Why Critical Thinking Skills in Nursing Matter (And What You Can Do to Develop Them) By Hannah Meinke on 07/05/2021. This piece of ad content was created by Rasmussen University to support its educational programs. Rasmussen University may not prepare students for all positions featured within this content.
Problem solving also fosters critical thinking, creativity, and practical skills essential for active participation in society (Akinsanya & Ojotule, 2022; Luo, 2023). One of the fundamental ...
Graduate Entry Nursing (GEN) programmes have been introduced as another entry point to nurse registration. In the development of a new GEN programme, a problem-based approach to learning was used to develop critical thinking and clinical reasoning skills of motivated and academically capable students. To explore and evaluate the design and delivery of course material delivered to GEN students ...
Critical thinking is the cornerstone of effective problem solving in nursing. It involves analyzing situations, evaluating evidence, and making judgements based on a logical reasoning process.
One of the keys to success as a registered nurse is embracing lifelong learning. Our articles and guides address hot topics and current events in nursing, from education to career mobility and beyond. No matter where you are on your nursing journey, there's an article to help you build your knowledge base.
Skip to main content