{{loadingHeading}}
{{loadingSubHeading}}
healthcare financial management association

HFMA empowers healthcare financial professionals with the tools and resources they need to overcome today's toughest challenges.

Already a Member?
- Review Benefits
Connect with your healthcare finance community online or in-person.
- Access online community
- Find my Chapter
- Data + Insights
- MAP Initiative
- Peer Review
- Marketing & Sponsorship Opportunities
- Renew Membership
- Refer a Colleague
- My E-Learning
- Review Subscriptions

Sign up for HFMA`s monthly e-newsletter, The Buzz.
E-Newsletter Subscriptions
Member benefits delivered to your inbox!
Healthcare finance content, event info and membership offers delivered to your inbox.
Check out our specialized e-newsletters for healthcare finance pros.
Member benefits delivered to your inbox! Check out our specialized e-newsletters for healthcare finance pros.

Get trusted analysis and direction from the experts at HFMA.
- Regulatory & Accounting
- Healthcare Dollars & Sense
- Value Project
- Patient Friendly Billing
- Healthcare 2030
- Curing Payment Confusion
- Research & Trends
- Claim Integrity
- TLR Reports
- Healthcare Financial Practices Staff
- Sponsored Resources

All the healthcare finance news and information you need to stay current.
- Accounting & Financial Reporting
- Cost Effectiveness of Health
- Finance & Business Strategy
- Healthcare Blame Game
- Leadership & Professional Development
- Legal & Regulatory Compliance
- Operations Management
- Payment, Reimbursement & Managed Care
- Price Transparency
- Revenue Cycle
- Expert Reviewed
- Sponsored Content
- Press Releases

In-person, online. Professional development designed with you in mind.
- Live Events
- Certifications
- Digital Badging
- Organizational Learning

Supporting your career, every step of the way.
- Compensation Benchmarks
- Career Pathways
- Career Self-Assessment
8 healthcare trends for 2024: A guide for health system leaders and their boards
Healthcare providers faced many transformational challenges in 2023, including the continued advancement of payers into the provider space and the challenge of managing merger and acquisition activity.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to email a link to a friend (Opens in new window)
As health systems progress through 2024, they will require effective governance to successfully navigate the rising headwinds. As they plan and execute initiatives, their leaders and boards should remain informed about eight key trends that will have a growing impact on the industry and the future success of their organizations.
1 Continued big technology M&A
The year 2023 saw many technology-focused mergers and acquisitions (M&A) of health systems, for-profit organizations and provider groups, as well as many technology-focused M&A. In 2024, we will see continued focus on Big Tech merger activity in the healthcare space as these companies align their technology and data with patient care service offerings. Companies such as Amazon, Apple and Microsoft will continue to advance their presence in 2024, as will health plans such as UnitedHealthcare and Humana.
Insight for health system leaders. Leaders must understand their vulnerabilities around technology and data and identify capital to invest either in building their infrastructure or in forming strategic relationships with other organizations. Such advancements in technologies will reduce costs and support financial performance.
Insight for boards. Boards should challenge leadership to fully understand the organization’s technology and data growth plan and how it will enhance market position, recognizing that potential vulnerability from Big Tech or other for-profit corporations in their market could impact payment rates and/or patient access.
2 Vertical clinical integration among payer and retail corporations
Payers and retail corporations remained active in 2023, investing in primary care and other vertically aligned services (e.g., CVS’s acquisition of Oak Street Health, Amazon’s acquisition of One Medical and UnitedHealth Group’s various acquisitions). Given the cost of capital and financial challenges facing the remaining large primary care-based medical groups, acquisitions in 2024 may slow but will still impact health system market share and influence consumer behaviors.
Insight for health system leaders. As nontraditional providers expanded their footprint, the relationship between health systems and consumers changed. Branding will not be enough. Leaders should consider three other responses:
- Launching consumer-focused initiatives that provide a retail mindset where vertically integrated services are available
- Expanding primary service access
- Investing in capabilities that provide more control over the premium dollar
Insight for boards. An important competitive response to market disruptors and new market entrants is to strengthen the health system’s relationships with providers and employers. While considering local market and organizational factors, health system boards should consider nontraditional strategies to leverage the health system’s brand and influence consumers with a vertically integrated clinical service model, such as a direct-to-employer program, provider-sponsored plan or payer partnership.
3 Expansion of AI and technology solutions
In 2023, we saw an explosion of AI across the entire technology ecosystem. This year will bring new capabilities and solutions in healthcare driven by the use of data and AI. The challenge for health systems will be to prioritize the possibilities and identify immediate opportunities versus long-term strategic positioning.
Insight for health system leaders. As leaders consider the many cadres of new AI solutions in 2024, they should understand the fiscal impact to guide their decisions. New AI technologies will not only provide real revenue enhancement or cost-saving opportunities but also require significant investment. As health systems improve their financial performance in 2024, it is critical that their AI technology investments support that effort by realizing a tangible ROI.
Insight for boards. Boards will need to see proposed new AI technologies integrated with their organizations’ strategic technology road maps. It is not just about approving capital funds to launch new AI; it is about creating an AI- and technology-integrated infrastructure to strategically position the health system for success.
4 Pushback on MA contracts
According to CMS, Medicare Advantage (MA) enrollment grew by 8% or about 2.3 million beneficiaries in 2023, bringing the total enrollment to 31.6 million. As enrollment increased, hospitals were challenged with flat payment (based on Medicare rates) and growing administrative MA product challenges, resulting in increased claim denials and write-offs and decreased profits. In response, many ended their participation in MA. With expected MA growth in 2024, healthcare organizations will continue to push back on commercial MA payers regarding denied services and administrative requirements and will pressure CMS and Congress to act.
Insight for health system leaders. Community hospitals are challenged to end participation in MA. Instead, they should collaborate closely with their commercial payers to negotiate precertification requirements, timely payment and value-based performance programs. They should find ways to educate patients regarding MA criteria so these plans are seen as favorable. By evolving their payer strategy to support a community focus, they can minimize their cost of MA while continuing to deliver optimal patient care.
Insight for boards. Given the growth of the Medicare population in most communities, the board’s approach to improving their community’s health is important. Many board members have local and state legislative relationships that can be leveraged to ensure plans behave fairly and appropriately with their provider partners and beneficiaries. Boards should consider a legislative engagement strategy to ensure their community benefit standard is maintained.
5 Growth of regional MA providers
Historically, the MA market has been dominated by a few large health plans. But as Medicare beneficiary demand for these plans grows, regional plans and startups see opportunities to enter the market. Regional plans have a strategic advantage over large plans by being able to better connect with consumers in the community. Given that they lack the shareholder pressures of the larger plans, they can provide opportunities to collaborate with provider partners, especially with case/care management, patient navigation and authorization of services.
Insight for health system leaders. Because MA enrollment will continue to grow, health system leaders should consider a strategic partnership with one or more regional MA plans. If the health system has a clinically integrated provider network or accountable care organization, a strategic partnership with a regional plan would provide opportunities to develop vertically integrated services and efficiencies in care delivery. It would also allow the health system to transition more quickly into a risk-based MA product and influence the community’s MA premium.
Insight for boards. Health system boards should present a forward-thinking approach to strengthen the health system’s and community’s focus on quality, access and clinical service for the public they serve. Boards can exert pressure on MA plans to ensure patients’ health needs are met and their health systems are fairly recognized and compensated. Boards should play a role in the health system’s payer strategy, especially in overcoming obstacles with MA plans and ensuring that community needs are addressed.
6 Financial performance of medical groups
Both employed and independent medical groups continue to focus on improving financial performance, hopefully to return to prepandemic results. Hospital-employed groups will continue to struggle with rising investment (or subsidy) per physician, compensation that is not aligned with value-based care contracts and overall physician well-being. Independent groups are also struggling with rising practice costs, increased payment pressures and growth limitations due to recruitment challenges and access problems. These financial challenges will present opportunities for medical groups to collaborate with others through strategic partnerships, M&A or external investment funding.
Insight for health system leaders. Depending on whether a group is independent or employed, leaders should align their physicians to create more integrated provider partnerships. Collaborating around integrated provider networks allows systems and physicians to position themselves for success under value-based care, integrate services vertically and expand specialty service lines to leverage resources in support of stronger financial performance.
Insight for boards. Given the financial fiduciary responsibility of the board to the health system and community, boards should promote strong physician alignment strategies. Physician alignment topics should be a significant component of discussion and planning, reflected in the strategic plan and addressed during board retreats. Boards should be open to innovative strategic partnership models that can help strengthen physician alignment and financial performance.
7 Private equity (PE) investments
Between 2012 and 2021, PE deals made for physician practices increase six-fold. a And the trend continued in 2022 and 2023, particularly with specialty groups such as orthopedics, cardiovascular, dermatology and gastroenterology. In 2024, the trend is expected to continue even with the higher cost of capital. PE investors in medical groups create increased risk to hospitals and health systems, which must be included in the strategic plan and operational initiatives. Organizations that proactively address potential PE expansion will be in a better position to manage risk factors.
Insight for health system leaders. Given market factors such as payer mix, rising community healthcare costs, population growth and lack of access, health systems may be vulnerable to PE entrants. Leaders should perform a community assessment of the vulnerabilities, risks and impacts to their organization from such entrants. The assessment will provide proactive strategic approaches such as alignment models with PE, strategic partnerships with independent specialty groups and/or expansion of the employed medical group.
Insight for boards. The entry of PE investors in the market may compromise a provider organization’s financial performance. As part of the community benefit standards established by boards, regularly assessing potential risks will allow boards to evaluate the risk and adverse impact on the community’s health needs and well-being. Reviewing community assessments allows boards to evaluate and assess risks and to inform future strategic options.
8 Growth of home-based care
Entering into 2024, care access will continue to be a focus area for primary and specialty care services to meet patient demand. The in-home care model helps health systems to expand their access model by integrating technology and home-based providers while enabling them to continue managing the cost of services. Driven by retiring baby boomers who prefer at-home care, the demand is growing, evidenced by innovative care models such as skilled nursing facility (SNF), at-home and hospital-at-home, which prompt partnerships with acute care, SNFs and home health providers.
Insight for health system leaders. To address the challenges of improving access to care and addressing increasing patient demands, leaders should consider home-based care networks to support innovative care models. Many post-acute providers are well positioned to form post-acute integrated provider networks. As hospitals and physicians manage their aging high-acuity patients, post-acute integrated provider networks can more efficiently support patient care needs while addressing issues of access, staff shortage and reimbursement.
I nsight for boards. Given fiscal challenges and patients’ changing needs, home-based care models offer health systems opportunities to further diversify services by extending longitudinal care models. Seizing such opportunities can challenge boards as they expand their focus beyond the acute hospital setting. Boards should be open to home-based care models as part of the strategic planning process to address the community’s healthcare needs.
Setting priorities through effective governance
Health system leaders and boards will have many issues to address in the coming years as the industry continues to be influenced by new market entrants, technology and AI, PE, financial pressures and the evolving needs of patients. Boards and leaders should focus on common priorities to create a unified front in addressing the issues confronting health systems, hospitals and medical groups.
Over the next two years, board meetings will tend to focus on operations in support of the strategic vision. Leadership meetings will focus on execution of strategic initiatives driven by the need for improved financial performance and better patient outcomes. Health systems will need to focus on effective governance and high-impact priorities and remain diligent in execution to realize high performance.
a. Henderson, J., “Private equity takeovers of physician practices soared over a decade,” MedPage Today , July 11, 2023.

Daniel J. Marino
is a managing partner, Lumina Health Partners, Chicago.
Related Tags
Advertisements
Recent healthcare business trends, personalized communication helps state provide the highest possible recovery and patient-satisfaction rates for clients, news briefs: a second appeals court rules against providers in the 340b contract-pharmacy dispute, a new doj task force is the latest example of intensified federal oversight of healthcare antitrust issues, for providers, application of the 2-midnight rule to medicare advantage appears to bring a revenue influx, hospital payments have been substantially affected by the change healthcare cyberattack, report finds, sign up for the buzz.
Healthcare finance content, event info and membership offers delivered to your inbox. Sign up for HFMA’s monthly e-newslettter, The Buzz.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

The FutureS of healthcare
Francesco schiavone.
a Parthenope University of Naples, Department of Management Studies & Quantitative Methods, Italy
b Paris School of Business, France
Marco Ferretti
This editorial for the special issue of FutureS is not intended to provide a comprehensive, analytical overview of the future of health care; rather, it collects the perspectives on which scholars have focused most. There is a danger that what we report will quickly become obsolete for numerous reasons; think of the speed of current technological progress or the fact that the Covid-19 pandemic could further stress health care systems around the world. However, we would like to outline some of the current topics explored in the literature and focus on the scenarios envisioned by practitioners. We write this piece being interested in the innovative impulses of all the actors belonging to the "renewed" health care ecosystem, aware of the fact that there are significant differences between the countries of the North and South of the world and, consequently, between their health care systems. What we can say with certainty is that the healthcare and life sciences are the protagonists of an unparalleled revolution. The aging population and changing needs, the increasingly common occurrence of chronic disorders, and digitization are some of the challenges facing the sector. The technological change of the fourth industrial revolution is disruptive and changes the logic of the market, not only that of healthcare but also that of adjacent markets. Because of the intensity with which insiders have to face these new trends, the topic has been the focus of interest of scholars and practitioners in recent years. The big players in consulting, as well as the scholars, have deepened the issues of healthcare of the future, focusing on what will be the major challenges in 10 years and imagining potential scenarios that will reconfigure the way health care is delivered and used.
In the next 10 years, there will be profound demographic changes and the healthcare system will necessarily have to reconfigure the supply of the necessary services and the methods of delivery (KPMG, 2018). Due to the aging of the population, there has already been a dramatic increase in chronic and degenerative diseases requiring complex treatment in recent years.
In addition, the Covid-19 pandemic that has been sweeping the world since 2019 has strained global health systems, revealed already existing weaknesses, even in the most advanced countries, and is representing an important moment of reflection for all policymakers. The whole world is questioning what will need to be done to foster greater effectiveness of national systems as well as better capacity to cope with shocks of such magnitude.
In this document we explore what practitioners and scholars consider the main future challenges and the major changes that need to be made in the healthcare sector in order to embrace a new paradigm of care, based on the centrality of the patient, on prevention and not on cure, on technologies at the side of humans.
Healthcare systems around the world have undergone profound changes, reforms, developments and improvements in recent years. There are numerous opportunities for the healthcare industry to seize while multiple challenges remain, especially in developing countries.
In general, people are healthier, financially better off, and living longer today than they did 30 years ago. Over the past 30 years, the challenges faced by the global health system have included increasing population and urbanization, the spread of chronic diseases, behavioral changes, infectious diseases, region-specific conflicts, and security in health care delivery. It is foreseeable that by 2045 ( Durrani, 2016 ), most of the world's population growth will occur in urban areas of poor countries as the rapid, unplanned and unsustainable style of urban development will make cities in developing countries the nevralgic centers for emerging environmental and health risks. All of this will necessarily require changes in hospital design, culture, and practices to better meet the needs of patients, families, and all stakeholders.
Medical and scientific advances impose significant challenges on today's health care systems. Developments in genetics, information technology, and nanotechnology are changing the approach to health care as it tends toward personalization, and increasingly moves outside the hospital setting. A shift to patient-centered care and patient empowerment has already been underway for some time.
The traditional model of care is undergoing radical transformations and will need to change further to meet the many emerging challenges ( Durrani, 2016 ).
So, what can we expect in the near future?
We explore this in the special issue of FutureS, which has collected 10 contributions on the future of healthcare. Such a call is linked to the RNI Forum on Innovation 2019 on “Innovation for Health. Innovation for Life”, hold at University of Naples Parthenope (Italy) on 17–19 July 2019. This special issue is one of the actions of the project “Dipartmento di Eccellenza” (funded by The Ministry of Education, Universities and Research - MIUR) carried out by the Department of Management Studies and Quantitative Methods (DiSAQ) of the University of Naples Parthenope (Italy). In the next few pages we will explore these contributions by connecting to possible scenarios gathered from scholars and practitioners. What they expect could be summarized in a few main aspects: a new patient-centered healthcare system; a redesigned concept of the healthcare ecosystem and the resulting redesign of roles and stakeholders; and the predominant importance of technologies in shaping the future. In a report provided by Deloitte (2021) on the challenges of the global healthcare industry, the authors systematize the major global issues that healthcare providers, policymakers, and all stakeholders who gravitate to this particular ecosystem must focus on. These are: (1) digital transformation and interoperable data, (2) socioeconomic change, (3) labor and talent, (4) care model innovation, (5) consumers and the human experience, and (6) collaboration. Further, we assert that these six issues are the ones that actually reflect problems around the world, although some countries, as we know, are running at different speeds. Surely, the healthcare system will have to balance the needs of the older population for which an "acute" type of care is foreseeable and those of the young people who will require increasingly "out of hospital" care and who have different needs and requirements in terms of a better experience for the patient, convenience and coordination between health and wellness programs. The today's and the near future's patient are increasingly taking on the guise of a consumer who has changed his or her needs and whose needs must be met quickly, on demand and 24/7, like all the other services he enjoys.
Moreover, consumer needs are variable and often difficult to understand. For this reason, large volumes of free data would be needed. According to recent studies, individuals would be willing to share their medical information if this would improve the effectiveness of the treatment, achieve better services, greater value, better experiences and greater personalisation ( KPMG, 2018 ).
In such a context the new paradigm of healthcare delivery will be supported by technological disruptors, possessing large amounts of data and a deep knowledge of the behaviour of patients - now consumers - who will play a fundamental role in the consumerization of healthcare. The patient, in fact, is increasingly assimilated to a consumer and the powerful technological tools of the industrial revolution will support this process of transition towards a consumer-centred model ( Balint, 1969 ; Castro, Van Regenmortel, Vanhaecht, Sermeus, & Van Hecke, 2016 ) in which the relationship with the patient is strengthened and, although it may seem an oxymoron, humanized. Humanisation linked to the well-being of the patient, the environment, spaces, specialist and collaborative interventions, integration with the community, the individual and the community, taking into account that each person is unique and unrepeatable and reacts differently to problems. In this sense it would be necessary to include social sciences in the training of future health workers ( De la Fuente-Martos et al., 2018 ). With these assumptions, it becomes imperative to move from a cure regime to one of care ( De Valck, Bensing, Bruynooghe, & Batenburg, 2001 ; Ciasullo, Troisi, Cosimato, & Douglas, 2018 ; Font & Sato, 2012 ).
Infact, evidence suggests that there is a close relationship between living and working conditions and health, in fact variables such as income, education, working conditions, social support can positively or negatively affect the health of individuals and communities.
Individuals are taking proactive attitudes towards a healthy lifestyle that includes diet, exercise, sleep patterns, energy levels and stress management ( KPMG, 2018 ), as such a regimen has been shown to delay the onset of the disease ( Gopal, Suter-Crazzolara, Toldo, & Eberhardt, 2019 ).
New patients are no longer understood as recipients of treatments and no longer behave that way but are themselves co-producers of health services and co-creators of value ( Palumbo, 2017 ).
The patient-medical relationship will change - from a reactive approach related to diagnosis and treatment in response to signs and symptoms, to a proactive type of health ( Waldman & Terzic, 2019 ) focused on personalized patient care based on early warning signals, predictive models related to gene analysis and continuous monitoring of a multitude of data from different sources ( Hamburg & Collins, 2010 ). Chronic diseases must be treated with the active participation of the patient and his family, in order to find the most congenial tailor-made solutions ( Accenture, 2019a , 2019b ; Deloitte, 2019a , 2019b , 2019c ; Auffray, Charron, & Hood, 2010 ; McKinsey, 2019a , 2019b , 2019c , 2019d ; Sagner et al., 2017 ). This active participation results in a co-creation process in which patients and professionals cooperate to solve problems ( Dalal et al., 2016 ; Osei-Frimpong, Wilson, & Lemke, 2018 ; Tartaglione, Cavacece, Cassia, & Russo, 2018 ).
Therefore, the healthcare system of the future will be patient-centered.
All the transformations we are witnessing, a consequence of environmental and lifestyle changes, which see health care changing from reactive to preventive and proactive, person-centered and focused on wellness and not disease, are driven and accompanied by a series of innovations in technology and business models that will change health care as we are used to understanding it within thirty years ( Aceto, Persico, & Pescapé, 2018 ).
Most of the existing contributions on healthcare and on the possible scenarios of this sector, combine the word future with the word technology. In fact, such obvious strides in technology suggest a future in which the patient journey is highly embedded and dependent on technology. A quick search on Scopus or Web of Science suggests how important technology is in this transition from the traditional model of the health care system to a new model of care delivery, whether in a developed or developing country.
The patient of today is different than the patient of 30 years ago, their needs have changed, the way they think about the hospital, the site of care, and even how they approach diseases. In addition, the tools he uses or could use are also extremely different.
The reconfiguration of the entire system also involves a reduction in traditional settings and the consequent expansion of alternative care sites. Patients will be able to receive care where and when they prefer through a variety of flexible formats, as is the case for many retail brands that leverage a variety of sales channels. In this new landscape, there will be specific care facilities depending on the target group of patients that can provide different levels of acuity, different diagnostic features and different levels of convenience. It will also be possible for each facility to be informed about the patient's medical record regardless of where the patient has requested treatment.
And if patients can receive the care they need when and where they want, why necessarily in a physical space? The disruptive technology that has emerged in recent years will allow for an increase in virtual care. We have already experienced this because of Covid-19, which required alternative and timely solutions and other forms of virtual care, regardless of geography and used strategically, enable providers to meet the needs of patients at a distance or at home, and can also provide guidance to physicians in other locations facing complicated cases.
Telemedicine is considered a solution to the current challenges of the health sector, even more so in a period of crisis such as the one following the Covid that forced us indoors for a long time; thanks to information technologies, in fact, it has been possible to bridge geographical distances, albeit minimal ( Jnr, 2020 ; Wosik et al., 2020 ). Gjellebæk, Svensson, Bjørkquist, Fladeby, and Grundén (2020 this issue) discuss its importance in their article, submitted to this special issue; they look at the difficulty in the diffusion of such technologies and study it in relation to the management strategies implemented by managers. The article suggests conditions for organizational and knowledge-based innovation in the face of future health and care needs in society. Management strategies that focus on middle managers and their use of strategies to be used in the work of facilitating learning in the workplace in relation to the introduction of technology and new ways of working are examined. The central position of middle managers in the organizational hierarchy as well as their contribution to learning and communication across organizational levels is highlighted in the article.
Another contribution of this special issue analyzes, in relation to telemedicine, its role in decreasing inequalities in access to health care. The objective of the article "The Future of Telemedicine Cabin: The Case of French Student Acceptability" by Patricia Baudier, Kondrateva, and Ammi (2020 this issue) is to determine the variables that influence student adoption of telemedicine cabins implemented within Universities, Business Schools… This targeted population, are more reluctant to consult in the event of minor health issues. Telemedicine booths could make it easier for them to access health care. The future of such solutions, in fact, must be seriously studied as Telemedicine Cabin or Teleconsultation could be a solution in case of pandemic period such as Covid-19 where all contact between doctors and patients must be avoided and reserved for critical situations. In fact, in case of severe infection, hospitals cannot treat all patients and must focus on vital emergencies. Therefore, the accessibility, availability, and ease of use of the telemedicine booth or teleconsultation can be part of the national governments' plan to reduce the level of contamination by performing remote consultations even from home.
In addition to eliminating distance and inequity a focal goal is to eliminate fragmentation of health care systems; instead, the objective should be to enjoy an integrated system that knows no physical boundaries and allows for all-round patient-centered care.
In this regard, Ciasullo, Manna, Cavallone, and Palumbo (2020 this issue) in an article of this special issue, analyzing data collected from the Eurofound database, not only shed light on the existence of five different types of systems, but also pointed out that the healthcare systems of the future should be based on a hybridization of healthcare systems: in fact, the future of healthcare will benefit from a contamination of the different types of existing healthcare systems; this will make it possible to achieve greater equity of treatment and higher financial sustainability.
In the systems of the future, as suggested by many scholars, the patient will be actively involved which will allow that they will be able to manage themselves ( Ascione, 2018 ; Bürklea, Deneckea, Lehmanna, Zetzb, & Holma, 2018 ). This is true for countries such as the United States and other economically advanced nations but also for low-income countries as they will face the same issues that will require more hospital care in comorbidities but will move some treatment pathways out of hospitals.
The leaders of the future will certainly be those organizations that will prepare the necessary measures to put the consumer at the center of the ecosystem. Practitioners all agree that those who will not be part of the change in this revolution risk playing a less central role in the future ( Accenture, 2018 , 2019a , 2019b ; KPMG, 2018 ; McKinsey, 2019a , 2019b , 2019c , 2019d ). Many of the ICT technologies we know have evolved exponentially in line with Moore's law ( Moore, 1965 ) and there have already been a significant number of disruptive innovations in the healthcare sector, but since the 1920s the pace at which these innovations have followed one another has been overwhelming.
As suggested by the disruptive changes we are witnessing in recent years, the protagonists of the change will not be biopharmaceutical companies, but technology giants such as Amazon, Apple, Google, Microsoft, Alibaba, etc. For some time, these Giants have entered the world of health care launching mainly products in the field of prevention and diagnostics; many patents have been filed in recent years and the partnerships concluded with biopharmaceutical companies are equally high. Traditional companies are aware that a revolution is underway and that a new sector, that of "health tech" ( Pwc, 2019 ), is coming to life. Such a regime of change must necessarily correspond to a cultural transformation. For digital health to enter our lives and operate in the right way it is necessary to build knowledge and attitude ( Meskó, Drobni, Bényei, Gergely, & Győrffy, 2017 ).
The fourth industrial revolution and the so-called smart technologies are revolutionizing healthcare. Ćwiklicki, Klich, and Chen (2020 this issue) , by addressing this special issue, study the adaptive capacity of the world's healthcare systems to the fourth industrial revolution. They identify key determinants of adaptive capacity, which are: 1) human capital, 2) information and communication technology, 3) social capital, 4) financial resources, 5) governance, and 6) legal norms. Their results show that among the most important determinants for smart technologies to become an integral part of the systems of the future are human capital, financial resources and legal regulations. Also among the most difficult barriers to overcome is the absence of a long-term vision. Understanding the factors that enable the acceptance of 4.0 health and those that hinder it is certainly a good starting point for improving service delivery.
Overcome reluctance, healthcare providers would then be able to predict the needs, behaviors, and attitudes of the new "patient-consumer" and with them the risks, and be able to provide timely interventions when needed, avoiding, for example, the use of the emergency room, or providing context-related solutions (an app that warns a lung patient that it's time to sit down given the temperature of the environment and other variables).
The already mentioned telemedicine, wearable devices, home monitoring devices, electronic pills, and all implantable sensors will replace, as argued by practitioners and scholars, traditional modes of care and allow greater flexibility ( Accenture, 2019a , 2019b ; Aceto et al., 2018 ).
And this flexibility goes hand in hand with effectiveness and efficiency, for example in the use of electronic medical records, which can be consulted anywhere and in real-time. The most powerful technologies are certainly the big data& analytics, quantum computing that allows to drastically improve protein folding and drug discovery through probabilistic modeling of the human body's reaction to stimuli. Through augmented reality and virtual reality, exploited for training, patient education, and treatment, it will be possible to simulate realistic scenarios able to eliminate almost all risks.
In addition, an ever-closer man-machine reality is expected. This is what results from numerous studies of major consulting firms ( Accenture, 2019a , 2019b ; Deloitte, 2019a , 2019b , 2019c ; KPMG, 2018 ). Artificial intelligence (AI) already has numerous applications ranging from decision support for physicians, drug discovery by matching biological patient information with the existing scientific literature on that specific case, to complex genomic processing to provide highly personalized care. AI is already used for the disinfection of operating rooms, to offer companionship, to assist physicians in surgeries. Robots won't take work away from human beings, but on the contrary, the value that the man-machine combination can generate is much higher than what one of the two alone could achieve. Machine learning allows the system to continuously learn from all the data it absorbs that no human being could ever store, but humans can validate the results of the technology and spend more time and effort on tasks that require problem-solving and critical thinking ( Accenture, 2019a , 2019b ; Deloitte, 2019a , 2019b , 2019c ). Workers, therefore, will not carry decades of institutional knowledge within an organization in the performance of a role. Instead, they will move between one environment and another, whether physical or virtual, working alongside technologies that can fill any gaps. Knowledge will remain within the organization itself; it will not travel together with people.
AI will help in the reconfiguration of the work environment and in the improvement of doctors' conditions - avoiding the increasing cases of burn-out ( Meskó, Hetényi, & Győrffy, 2018 ). Also, technology will assist humans thanks to drones delivering medicines, blood and organs, and autonomous vehicles such as ambulances that will improve the efficiency of the intervention, for example by optimizing the route and reducing human error.
While AI applications are attracting considerable attention in healthcare and numerous tools are already in use especially in the United States and China, multiple reticence and obstacles remain, especially in terms of regulation as well as problems with the associated costs ( Jiang et al., 2017 ).
The radical innovations brought by the aforementioned technologies, the demographic changes, the changes in lifestyles and the onset of chronic diseases converge in an approach that in the literature is defined by 4 Ps: predictive, preventive, participatory, personalized medicine ( Hood & Friend, 2011 ).
The adoption of a new approach based on these four Ps promises to reduce the burden of chronic diseases through the effective exploitation of technology and a better understanding of human-environmental interactions and of the determinants of chronic diseases. Fortunately, most chronic diseases can be prevented or delayed. The deeper we look at the issues of genomics, and thus its interaction with lifestyle, social and physical environment, and personal experiences, the more we will be able to predict the risk and prevent these diseases.
The pharmaceutical industry is also investing heavily in R&D to provide more personalized and patient-specific medicines. One of the contributions of this special issue is that by Aldieri, Bruno, Senatore, and Vinci (2020 this issue) who argue that the profound changes and transformations we are witnessing make it necessary to imagine a future in which healthcare services are more efficient. The paper combines two interesting themes in innovation research: on the one hand, the role of knowledge spillovers in the innovation process and, on the other hand, the use of contrasting scenarios to highlight the uncertainty and dynamic behavior of the pharmaceutical industry in future developments. The effects on R&D innovation productivity are a crucial point to investigate future scenarios of the pharmaceutical industry in the European Union, Japan and the United States.
As this last contribution highlights, in order to achieve a service provision as efficient and close to the patient as possible, many different actors will necessarily come into the field and work together.
Both scholars and practitioners affirm that in the future, the health care systems will be redesigned in terms of stakeholders and their roles: strong collaboration between stakeholders is needed.
Infact, healthcare systems are expected to enter into alliances with innovative biotech companies, technologists, insurance companies and other nationally important health care systems that do not compete in the same geographical areas. A deeper and deeper convergence ( Bröring & Leker, 2007 ) of sectors that are distorting the competitive logic is desirable.
It would be also desirable to form multi-stakeholder groups that, trained within communities, should create effective and innovative planning applicable at the local level. The approach will need to be systemic and interdisciplinary and will need a common language to help researchers, health professionals, and stakeholders to collaborate as efficiently as possible.
In their article, under the umbrella of the futures of healthcare’s special issue, Sophie Boutillier, Fourmentin, and Laperche (2020 this issue) show how stakeholders' positions are shaped and transformed over time, by their interactions with others. Indeed, the scholars, in their work entitled "Food additives and the future of health, an ongoing controversy on titanium dioxide" bring out the transformations of organizational routines and the consequent changes in the roles of stakeholders, highlighting the "signal role" played by scientists, transmitted by NGOs who raised the "precautionary principle". This study confirms the transition we are witnessing, highlighting another important aspect, namely that different disciplinary fields are strongly interconnected. It will also be necessary to identify opportunities for sustainable partnerships to implement change such as incubators, research centers, universities, private sector, and global health networks to make innovative project ideas concrete. Hospitals and healthcare facilities in general could also generate value through collaboration with the start-up ecosystem that could help address current business problems, rejuvenate culture, or expand into future markets. And clearly among all the figures mentioned, at the center of the ecosystem will be the patient, a new proactive player in value co-creation.
Regarding multidisciplinarity, another interesting article submitted by Pau and Hall (2021 this issue) highlights the possibility of numerous possible futures and investigate these scenarios through a participatory method involving non-experts. They have built the Collective Imagination Framework (CIF), developed through an 18-month practice-based design research project entitled "Designing for Healthcare in Space" at the Royal College of Art. The framework is designed to facilitate open and accessible contributions to the future of healthcare and broader participation beyond experts and the modern-day community of interest to address the unknowns of the future.
Non-expert images of the future can move from being used as a source of data for experts to filter, to a more equal voice in a feedback loop with experts. Healthcare, in this new perspective, leaves behind the top-down approach traditionally used and effective with infectious diseases or acute injuries.
Since many changes are contemplated in the delivery of care, it is expected that hospitals, so traditionally conceived, will also mutate in structure and design. In fact, a number of studies have demonstrated the relationship between physical environment and healing ( Huisman, Morales, van Hoof, & Kort, 2012 ).
In this sense, the environment must be designed in a way that favors the best permanence of patients, with architectures based on empathy with them, or structures that incorporate art, gardens, and landscapes to reduce the stress of patients and families ( KPMG, 2018 ); acoustics and lighting will also play an important role. Furthermore, the reformulation of the hospital concept is also observed in efforts to optimize care and efficiency in healthcare facilities. Indeed, many providers are making some strategic and structural changes to hospitals. This facilitates the coordination of the whole range of care and allows patients to access care closer to home.
Besides the defragmentation of healthcare systems, the shift of care from the hospital to the home, and the reduction of costs associated with patient services, another important goal is that of sustainability, intended in all its meanings. The current pandemic has further highlighted the urgency of transitioning our healthcare systems to make them more environmentally, economically, and socially sustainable. The issue of sustainability is a hot topic on which many are wondering. And this aspect of sustainability, critical today, as well as one of the focal points of the trends that will characterize the new paradigm of care, is addressed by the paper of the special issue of Pereno and Eriksson (2020 this issue) . The authors in their work investigate the possible futures of sustainable health care from a multistakeholder perspective. The results highlighted three main horizons and drivers for improving the socio-technical transition to a desirable scenario based on collaboration among dynamic distributed networks. In addition, this study identifies specific innovation, information, and collaboration strategies for transition at local and international levels. Jackson Williams (2021 this issue) also addresses this special issue by investigating several scenarios starting from the analysis of the potential factors of a reduction in the growth of health expenditure in the United States. In fact, the author denounces the inordinate growth of health care costs in America and provides a series of plausible scenarios in which financial sustainability is an imperative.
In such a complex context, affected by variety and variability, it is crucial to reconfigure the resources and skills of the multiple actors involved in the health care of the future. Despite the overwhelming weight of technology, we refer again to the concept of humanization that will have to be taken into account when designing roles.
Another of the characteristics of the care paradigm of the future is definitely the re-design of the skills and capabilities of healthcare professionals. In this regard, there is a high interest from scholars regarding the integration of new skills and technological capabilities by health workers. With respect to this issue, an article of great interest is the one by Kalisz, Khelladi, Castellano, and Sorio (2021 this issue) that explores the perception of healthcare professionals about the adoption and diffusion of social robots. The main objective of the article is to treat social robots as hybrid products. The study explores practitioners' perceptions of the adoption and diffusion of social robots, including features of categorical ambiguity. The analysis of this perception is crucial because it is related to the creation of a robotics solution as an alternative for future customer needs. And in addition to meeting the needs of new patient-consumers, the authors explain, their adoption would significantly reduce healthcare costs ( Kalisz et al., 2021 ).
Furthermore, it will be necessary to develop new skills in terms of alliances and collaborations with partners and suppliers, of Big Data, Artificial Intelligence, and Quantum Computing. New roles will arise such as nanomedical engineers, planners of AR/VR devices operation, as well as physical spaces design. As the patient is the heart of the system, skills in terms of consumer satisfaction regarding the patient's experience will also be required.
In conclusion, many of the most advanced economies such as the United States, China, Australia, New Zealand, Japan are already taking big steps into the future.
What we expect in the near future is definitely an integrated and patient-centric healthcare system. Technologies such as big data, AI, IoT, augmented & virtual reality will increasingly make their way into this field; this and other environmental variables will pave for the reconfiguration of ecosystems that will see new stakeholders involved. Hospitals will be rethought as a function of an increasingly tangible switch from a treatment regime to one that will allow people to cope with certain pathologies (mostly chronic) directly in their own homes. All of this necessarily requires that new knowledge and skills be acquired by healthcare professionals and that healthcare systems around the world make a collaborative effort-as suggested by the Covid crisis-in such a way that geographical distances are shortened and inequities in the use of healthcare services are reduced.
Acknowledgement
The research was funded via the research project “Dipartimento di Eccellenza 2018” funded by MUR, Italian Ministry of University.
- Accenture . 2018. Future agenda; Future of patient data, insights from multiple expert, discussion around the world. [ Google Scholar ]
- Accenture . 2019. DIGITAL HEALTH TECH VISION are you ready for what’s next in healthcare? [ Google Scholar ]
- Accenture . Accenture 2019 Digital Health consumer Survey; 2019. Today’s consumers reveal the future of healthcare. [ Google Scholar ]
- Aceto G., Persico V., Pescapé A. The role of Information and Communication Technologies in healthcare: Taxonomies, perspectives, and challenges. Journal of Network and Computer Applications. 2018; 107 :125–154. [ Google Scholar ]
- Aldieri L., Bruno B., Senatore L., Vinci C.P. The future of pharmaceuticals industry within the triad: The role of knowledge spillovers in innovation process. Futures. 2020; 122 this issue. [ Google Scholar ]
- Ascione A. 2018. Hoepli Il futuro della salute: Come la tecnologia digitale sta rivoluzionando la medicina (e la nostra vita) [ Google Scholar ]
- Auffray C., Charron D., Hood L. 2010. Predictive, preventive, personalized and participatory medicine: Back to the future. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Balint E. The possibilities of patient-centered medicine. The Journal of the Royal College of General Practitioners. 1969; 17 (82):269. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Baudier P., Kondrateva G., Ammi C. The future of Telemedicine Cabin? The case of the French students’ acceptability. Futures. 2020; 122 this issue. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Boutillier S., Fourmentin S., Laperche B. Food additives and the future of health: An analysis of the ongoing controversy on titanium dioxide. Futures. 2020; 122 this issue. [ Google Scholar ]
- Bröring S., Leker J. Industry convergence and its implications for the front end of innovation: A problem of absorptive capacity. Creativity and Innovation Management. 2007; 16 (2):165–175. [ Google Scholar ]
- Bürklea T., Deneckea K., Lehmanna M., Zetzb E., Holma J. Integrated care processes designed for the future healthcare system. IOS Press; 2018. p. 20. January. [ PubMed ] [ Google Scholar ]
- Castro E.M., Van Regenmortel T., Vanhaecht K., Sermeus W., Van Hecke A. Patient empowerment, patient participation and patient-centeredness in hospital care: A concept analysis based on a literature review. Patient Education and Counseling. 2016; 99 (12):1923–1939. [ PubMed ] [ Google Scholar ]
- Ciasullo M.V., Manna R., Cavallone M., Palumbo R. Envisioning the future of health systems: Exploratory insights from European countries. Futures. 2020; 121 this issue. [ Google Scholar ]
- Ciasullo M.V., Troisi O., Cosimato S., Douglas A. Defining health service eco-system “infection”: A critical analysis of patient surveys. Int. J. Bus. Manag. 2018; 13 :118–138. [ Google Scholar ]
- Ćwiklicki M., Klich J., Chen J. The adaptiveness of the healthcare system to the fourth industrial revolution: A preliminary analysis. Futures. 2020; 122 [ Google Scholar ]
- Dalal A.K., Dykes P.C., Collins S., Lehmann L.S., Ohashi K., Rozenblum R.…Mlaver E. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: A preliminary evaluation. Journal of the American Medical Informatics Association. 2016; 23 (1):80–87. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- De la Fuente-Martos C., Rojas-Amezcua M., Gómez-Espejo M.R., Lara-Aguayo P., Morán-Fernandez E., Aguilar-Alonso E. Humanization in healthcare arises from the need for a holistic approach to illness. Medicina Intensiva (English Edition) 2018; 42 (2):99–109. [ PubMed ] [ Google Scholar ]
- De Valck C., Bensing J., Bruynooghe R., Batenburg V. Cure-oriented versus care-oriented attitudes in medicine. Patient Education and Counseling. 2001; 45 (2):119–126. [ PubMed ] [ Google Scholar ]
- Deloitte . 2021. 2021 global healthcare outlook. Accelerating industry change. [ Google Scholar ]
- Deloitte . 2019. 2020 global health care outlook. Laying a foundation for the future. [ Google Scholar ]
- Deloitte . 2019. Healthcare and life sciences predictions 2020. A bold future? [ Google Scholar ]
- Deloitte . 2019. Prospettive, potenzialità, impatti e modelli dell’Artificial Intelligence in ambito sanitario. [ Google Scholar ]
- Durrani H. Healthcare and healthcare systems: Inspiring progress and future prospects. Mhealth. 2016; 2 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Font J.C., Sato A. Health systems futures: The challenges of technology, prevention and insurance. Futures. 2012; 44 (7):696–703. [ Google Scholar ]
- Gjellebæk C., Svensson A., Bjørkquist C., Fladeby N., Grundén K. Management challenges for future digitalization of healthcare services. Futures. 2020; 124 this issue. [ Google Scholar ]
- Gopal G., Suter-Crazzolara C., Toldo L., Eberhardt W. Digital transformation in healthcare–architectures of present and future information technologies. Clinical Chemistry and Laboratory Medicine (CCLM) 2019; 57 (3):328–335. [ PubMed ] [ Google Scholar ]
- Hamburg M.A., Collins F.S. The path to personalized medicine. The New England Journal of Medicine. 2010; 363 (4):301–304. [ PubMed ] [ Google Scholar ]
- Hood L., Friend S.H. Predictive, personalized, preventive, participatory (P4) cancer medicine. Nature Reviews Clinical Oncology. 2011; 8 (3):184–187. [ PubMed ] [ Google Scholar ]
- Huisman E.R., Morales E., van Hoof J., Kort H.S. Healing environment: A review of the impact of physical environmental factors on users. Building and Environment. 2012; 58 :70–80. [ Google Scholar ]
- Jiang F., Jiang Y., Zhi H., Dong Y., Li H., Ma S.…Wang Y. Artificial intelligence in healthcare: Past, present and future. Stroke and Vascular Neurology. 2017; 2 (4) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jnr B.A. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. Journal of Medical Systems. 2020; 44 (7):1–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kalisz D.E., Khelladi I., Castellano S., Sorio R. The adoption, diffusion & categorical ambiguity trifecta of social robots in e-health–Insights from healthcare professionals. Futures. 2021; 129 this issue. [ Google Scholar ]
- KPMG . 2018. Healthcare reimagined; Innovation trends, predictions and actions for healthcare leaders. [ Google Scholar ]
- Mckinsey . 2019. Digital health ecosystems: A payer perspective. [ Google Scholar ]
- McKinsey . 2019. McKinsey on healthcare, best of 2019. [ Google Scholar ]
- McKinsey . 2019. Next-generation member engagement during the care journey. [ Google Scholar ]
- McKinsey . 2019. The hospital is dead, is dead, long live the hospital. [ Google Scholar ]
- Meskó B., Drobni Z., Bényei É., Gergely B., Győrffy Z. Digital health is a cultural transformation of traditional healthcare. Mhealth. 2017:3. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meskó B., Hetényi G., Győrffy Z. Will artificial intelligence solve the human resource crisis in healthcare? BMC Health Services Research. 2018; 18 (1):545. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Moore G. Moore’s law. Electronics Magazine. 1965; 38 (8):114. [ Google Scholar ]
- Osei-Frimpong K., Wilson A., Lemke F. Patient co-creation activities in healthcare service delivery at the micro level: The influence of online access to healthcare information. Technological Forecasting and Social Change. 2018; 126 :14–27. [ Google Scholar ]
- Palumbo R. Springer; 2017. The bright side and the dark side of patient empowerment: Co-creation and co-destruction of value in the healthcare environment. [ Google Scholar ]
- Pau S.S.T., Hall A. New spaces for healthcare futures studies: Connecting existing theory to deeper participatory practice. Futures. 2021; 126 this issue. [ Google Scholar ]
- Pereno A., Eriksson D. A multi-stakeholder perspective on sustainable healthcare: From 2030 onwards. Futures. 2020; 122 this issue. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pwc . 2019. Driving the future of health. How biopharma can defend and grow its business in an era of digitally enabled healthcare. [ Google Scholar ]
- Sagner M., McNeil A., Puska P., Auffray C., Price N.D., Hood L.…McEwen B.S. The P4 health spectrum–a predictive, preventive, personalized and participatory continuum for promoting healthspan. Progress in Cardiovascular Diseases. 2017; 59 (5):506–521. [ PubMed ] [ Google Scholar ]
- Tartaglione A.M., Cavacece Y., Cassia F., Russo G. The excellence of patient-centered healthcare. The TQM Journal. 2018 [ Google Scholar ]
- Waldman S.A., Terzic A. Healthcare evolves from reactive to proactive. Clinical Pharmacology and Therapeutics. 2019; 105 (1):10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams J. Unsustainable health care spending in the USA: How will it end? Futures. 2021; 126 [ Google Scholar ]
- Wosik J., Fudim M., Cameron B., Gellad Z.F., Cho A., Phinney D.…Tcheng J. Telehealth transformation: COVID-19 and the rise of virtual care. Journal of the American Medical Informatics Association. 2020; 27 (6):957–962. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Healthcare’s next chapter: What’s ahead for the US healthcare industry
Uncertainty has been the norm in healthcare in 2023, and that’s not likely to change in 2024. A presidential election year looms in the context of pressure on federal government finances from large budget deficits and the impact of higher interest rates on federal debt servicing costs. In addition, the healthcare industry faces uncertainty about the financing of Medicare and Medicaid; regulation, including views about horizontal and vertical integration; and overall industry economics.
In the face of this uncertainty—some might call it opacity—discerning senior management teams can act on a few trends that are clearer. Some of the trends and possible responses germane to strategy and performance of healthcare organizations in 2024 are highlighted below.
What’s ahead for healthcare players: An overview
We outlined in 2022 how the gathering storm fueled by inflation and workforce shortages would put pressure on healthcare over the next few years. Indeed, the pressure on healthcare leaders continues unabated. In response, industry players will have to consider repositioning their businesses as well as gearing up to ensure superior business performance:
- Hospital systems face a 200-basis point gap between reimbursement rates and cost inflation, according to McKinsey analysis. The gap could require performance transformations on the part of health systems, including more outsourcing, ramping up digital and automation efforts, and business rationalization.
- In 2024, employers are facing rising health insurance premiums well above their comfort zone of annual increases of less than 4 percent. 1 Kathryn Mayer, “Aon report: Big increase projected for 2024 employer health care costs,” SHRM, August 29, 2023. As payers see continued increases in medical costs and accelerating prescription drug costs, this pressure will require health plans to renew focus on medical and administrative cost control.
- These cost pressures offer many opportunities for tech-enabled services companies that can show customers near-term return on investment from their products. At the same time, many healthcare services and technology companies without demonstrable return will face severe downside to their businesses.
- Higher interest rates and less liquidity in the financial markets have raised the hurdle rate for private equity (PE) and venture capital firms. In these circumstances, private investors must ensure their portfolio companies deliver bottom-line performance, produce organic growth backed by proven business models, and have the ability to make any inorganic growth accretive based on robust capabilities. Large, well-capitalized healthcare companies will find a favorable valuation environment for acquiring PE portfolio companies as well as for forming strategic partnerships with private investors.
What’s ahead for payers
Payer value creation continues to shift from administering health benefits and providing insurance to managing care and capturing delivery and pharmacy economics. Partnering with and enabling physicians, likely in risk-based arrangements, will continue to gain in importance relative to other models of utilization management.
As pressure from rising medical and prescription costs mount, scaling proven physician partnership models (for example, primary care–centered value-based care) as well as innovating new ones (specialty benefit management and specialty value-based care) will grow in importance. Enhancing health outcomes and members’ care experience, prompted by both the incentives in government programs but also rising demand from employers, will be important priorities.
Finally, a renewed focus on reducing administrative costs will be high on the agenda for payers to ensure sustainable margins, offer a better experience for members and clinicians, and to free up resources to invest in strategic capabilities.
What’s ahead for health systems
Healthcare delivery will continue its restructuring. The definition of at-scale systems has changed in the past few years; today, it takes more than $13 billion to be a top-20 system by revenue, and many have reached their current position through inorganic growth, according to McKinsey analysis. The recent wave of M&A, however, is distinct from its predecessors. It is characterized by cross-geography deals designed to create value by scaling investments in platform capabilities across digital, analytics, shared services, and workforce management.
Beyond scale, sites of care have shifted increasingly from the hospital to ambulatory, home, and virtual care. This trend was playing out before the COVID-19 pandemic and was certainly accelerated by it. But the pivot toward ambulatory sites has been slower than expected, given the impact such a transition has on health system revenue, among other structural issues. Disruptors are vying to meet consumers’ demand for convenient access, but patients can be stuck navigating a complex system of healthcare organizations when their needs become more acute.
In parallel, health systems have struggled to fill their clinical workforce needs. The nursing shortage has become more acute: more than 100,000 nurses left the profession from 2019 to 2022, and health systems could face a shortage of 200,000 to 450,000 nurses by 2025. 2 Gretchen Berlin, Meredith Lapointe, Mhoire Murphy, and Joanna Wexler, “ Assessing the lingering impact of COVID-19 on the nursing workforce ,” McKinsey, May 11, 2022. Anticipated physician shortages are also an issue, though health system employment of physicians has slowed. Regulation (for example, price transparency and the 340B drug pricing program) and rising costs of capital (due to macroeconomic factors as well as ratings trajectories) will continue to create uncertainty.
While health system performance has generally improved over the past year as the industry emerges from the pandemic, a subset of players is really shining. Those that appear to be breaking away are hyperfocused on resilience, taking a multilever approach to growth while continuing to identify and take actions to ensure sustainable margins.
What’s ahead for artificial intelligence in healthcare
Generative artificial intelligence (gen AI) has created considerable excitement in the industry. Gen AI could be catalytic in accelerating the application of digital and automation in healthcare, thereby offering some answers to the twin challenges of affordability and workforce availability. For example, adopting currently available technology (including but not limited to automation, AI, and gen AI) could allow payers to reduce administrative costs by 13 to 25 percent, reduce medical costs by 5 to 11 percent, and increase revenue by 3 to 12 percent.
However, healthcare has lagged behind other industries in adoption of AI. For several reasons, the industry has had a hard time adopting the technology. For example, AI requires time-consuming and often manual preparation of clean and structured data; well-planned, narrow use cases (such as predicting a specific event or outcome); modern infrastructure; and hard-to-hire talent (such as data scientists and data engineers).
Given the need for empathetic and intelligent interactions in a service industry such as healthcare, the recognition, comprehension, and content creation capabilities of gen AI represent a major opportunity. It is particularly appealing in its simplicity: gen AI thrives on unstructured data, which is plentiful in healthcare; it is pretrained; and it is broadly understood by people across the organization. The potential use cases for gen AI cross every domain and function. Gen AI use cases, in addition to existing analytics use cases, could help address real burdens, including reducing preparation time and improving quality of clinical documentation, modernizing outdated or legacy applications, and personalizing patient and member outreach at scale.
Unlocking this value will be a leadership challenge. Senior healthcare executives will need to educate their boards, leadership teams, and employees; attract talent; drive adoption; and pursue change management initiatives such as workflow shifts. Scaling pilots to production-scale solutions with concurrent process changes will be important differentiators in 2024.

What’s ahead in prescription drugs
GLP-1 drugs hold the promise of treating type 2 diabetes (in 11 percent of the US population; 38 percent of the population has prediabetes 3 National Diabetes Statistics Report , Centers for Disease Control and Prevention, accessed November 20, 2023. ) and obesity (42 percent of adults 4 “Adult obesity facts,” Centers for Disease Control and Prevention, accessed November 20, 2023. ), potentially helping to avoid many other ailments, such as heart and chronic kidney disease. The population of patients meeting clinical eligibility criteria for GLP-1s is one of the largest of any new drug class in the past 20 to 30 years.
Although there is much to be excited about, experience shows that taking advantage of medical advances is often elusive in healthcare. GLP-1s must be taken consistently to maintain weight loss; however, initial studies indicate persistency and adherence to therapy is poor (32 percent of members remain persistent at one year and 27 percent during the second year 5 “Real-world analysis of glucagon-like peptide-1 antagonist (GLP-1a) obesity treatment one-year cost-effectiveness and therapy adherence,” Prime Therapeutics and MagellanRx Management, July 11, 2023. ).
Nonetheless, the shift in care and financing models that accompany GLP-1 drugs are likely to be material. The growth of the GLP-1 market has amplified the conversation around preventive care and demonstrated the impact of media awareness and consumer-driven demand in treatment decisions. Its expansion has also fueled the rise of telehealth providers, broadening access points for consumers.
The growth of the GLP-1 market presents cost challenges in the near term because benefits will accrue over time. The annual wholesale acquisition cost per patient ranges from $12,000 to $16,000. The high cost of the therapy raises complex coverage decisions for payers and plan sponsors, made even harder by the potential spending waste from therapy discontinuation.
GLP-1 drugs are not the only broad population drugs emerging or in the late-stage pipeline; others include treatments for Alzheimer’s and non-alcoholic fatty liver disease. New drugs have the potential to not only improve patients’ health but also heighten the need for better therapy and cost management. The resulting business model changes across the healthcare value chain are likely to be meaningful.
We hear from many healthcare leaders that this is an unnerving time given the relentless pressure and uncertain outlook they face. They also tell us that this is an exciting time that presents opportunities for innovation to improve members’ and patients’ health and lives, to reimagine current organizations, and build new capabilities and businesses. We would suggest healthcare leaders address known trends and avoid trying to predict future trends, given the considerable uncertainty ahead. Building resilient and agile organizations capable of rapidly adapting to new challenges as they emerge will be important to succeed in this environment.
Shubham Singhal is the global leader of McKinsey’s Social, Healthcare, and Public Entities (SHaPE) Practice in McKinsey’s Detroit office, and Drew Ungerman is the global leader of McKinsey’s Healthcare Practice and the McKinsey Health Institute in the Dallas office.
Explore a career with us
Related articles.

2024 payers outlook: Opportunities abound

2024 healthcare services outlook: Challenges and opportunities

2024 health systems outlook: A host of challenges ahead
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
What has the pandemic revealed about the US health care system — and what needs to change?
Press contact :.

Previous image Next image
With vaccinations for Covid-19 now underway across the nation, MIT SHASS Communications asked seven MIT scholars engaged in health and health care research to share their views on what the pandemic has revealed about the U.S. health care system — and what needs to change. Representing the fields of medicine, anthropology, political science, health economics, science writing, and medical humanities, these researchers articulate a range of opportunities for U.S. health care to become more equitable, more effective and coherent, and more prepared for the next pandemic.
Dwaipayan Banerjee , associate professor of science, technology, and society
On the heels of Ebola, Covid-19 put to rest a persistent, false binary between diseases of the rich and diseases of the poor. For several decades, health care policymakers have labored under the impression of a great epidemiological transition. This theory holds that the developed world has reached a stage in its history that it no longer needs to worry about communicable diseases. These "diseases of the poor" are only supposed to exist in distant places with weak governments and struggling economies. Not here in the United States.
On the surface, Covid-19 made clear that diseases do not respect national boundaries. More subtly, it tested the hypothesis that the global north no longer need concern itself with communicable disease. And in so doing, it undermined our assumptions about global north health-care infrastructures as paradigmatically more evolved. Over the last decades, the United States has been focused on developing increasingly sophisticated drugs. While this effort has ushered in several technological breakthroughs, a preoccupation with magic-bullet cures has distracted from public health fundamentals. The spread of the virus revealed shortages in basic equipment and hospitals beds, the disproportionate effects of disease on the marginalized, the challenge of prevention rather than cure, the limits of insurance-based models to provide equitable care, and our unacknowledged dependence on the labor of underpaid health care workers.
To put it plainly, the pandemic did not create a crisis in U.S. health care. For many in the United States, crisis was already a precondition of care, delivered in emergency rooms and negotiated through denied insurance claims. As we begin to imagine a "new normal," we must ask questions about the old. The pandemic made clear that the "normal" had been a privilege only for a few well-insured citizens. In its wake, can we imagine a health-care system that properly compensates labor and recognizes health care as a right, rather than a privilege only available to the marginalized when an endemic crisis is magnified by a pandemic emergency?
Andrea Campbell , professor of political science
No doubt, the pandemic reveals the dire need to invest in public-health infrastructure to better monitor and address public-health threats in the future, and to expand insurance coverage and health care access. To my mind, however, the pandemic’s greatest significance is in revealing the racism woven into American social and economic policy.
Public policies helped create geographic and occupational segregation to begin with; inadequate racist and classist public policies do a poor job of mitigating their effects. Structural racism manifests at the individual level, with people of color suffering worse housing and exposure to toxins, less access to education and jobs, greater financial instability, poorer physical and mental health, and higher infant mortality and shorter lifespans than their white counterparts. Residential segregation means many white Americans do not see these harms.
Structural racism also materializes at the societal level, a colossal waste of human capital that undercuts the nation’s economic growth, as social and economic policy expert Heather McGhee shows in her illuminating book, "The Sum of Us." These society-wide costs are hidden as well; it is difficult to comprehend the counterfactual of what growth would look like if all Americans could prosper. My hope is that the pandemic renders this structural inequality visible. There is little point in improving medical or public-health systems if we fail to address the structural drivers of poor health. We must seize the opportunity to improve housing, nutrition, and schools; to enforce regulations on workplace safety, redlining, and environmental hazards; and to implement paid sick leave and paid family leave, among other changes. It has been too easy for healthy, financially stable, often white Americans to think the vulnerable are residual. The pandemic has revealed that they are in fact central. It’s time to invest for a more equitable future.
Jonathan Gruber , Ford Professor of Economics
The Covid-19 pandemic is the single most important health event of the past 100 years, and as such has enormous implications for our health care system. Most significantly, it highlights the importance of universal, non-discriminatory health insurance coverage in the United States. The primary source of health insurance for Americans is their job, and with unemployment reaching its highest level since the Great Depression, tens of millions of workers lost, at least temporarily, their insurance coverage.
Moreover, even once the economy recovers, millions of Americans will have a new preexisting condition, Covid-19. That’s why it is critical to build on the initial successes of the Affordable Care Act to continue to move toward a safety net that provides insurance options for all without discrimination.
The pandemic has also illustrated the power of remote health care. The vast majority of patients in the United States have had their first experience with telehealth during the pandemic and found it surprisingly satisfactory. More use of telehealth can lead to increased efficiency of health care delivery as well as allowing our system to reach underserved areas more effectively.
The pandemic also showed us the value of government sponsorship of innovation in the health sciences. The speed with which the vaccines were developed is breathtaking. But it would not have been possible without decades of National Institute of Health investments such as the Human Genome Project, nor without the large incentives put in place by Operation Warp Speed. Even in peacetime, the government has a critical role to play in promoting health care innovation
The single most important change that we need to make to be prepared for the next pandemic is to recognize that proper preparation is, by definition, overpreparation. Unless we are prepared for the next pandemic that doesn’t happen, we won’t possibly be ready for the next pandemic that does.
This means working now, while the memory is fresh, to set up permanent, mandatorily funded institutions to do global disease surveillance, extensive testing of any at-risk populations when new diseases are detected, and a permanent government effort to finance underdeveloped vaccines and therapeutics.
Jeffrey Harris , professor emeritus of economics and a practicing physician The pandemic has revealed the American health care system to be a non-system. In a genuine system, health care providers would coordinate their services. Yet when Elmhurst Hospital in Queens was overrun with patients, some 3,500 beds remained available in other New York hospitals. In a genuine system, everyone would have a stable source of care at a health maintenance organization (HMO). While our country has struggled to distribute the Covid-19 vaccine efficiently and equitably, Israel, which has just such an HMO-based system, has broken world records for vaccination.
Germany, which has all along had a robust public health care system, was accepting sick patients from Italy, Spain, and France. Meanwhile, U.S. hospitals were in financial shock and fee-for-service-based physician practices were devastated. We need to move toward a genuine health care system that can withstand shocks like the Covid-19 pandemic. There are already models out there to imitate. We need to strengthen our worldwide pandemic and global health crisis alert systems. Despite concerns about China’s early attempts to suppress the bad news about Covid-19, the world was lucky that Chinese investigators posted the full genome of SARS-CoV-2 in January 2020 — the singular event that triggered the search for a vaccine. With the recurrent threat of yet another pandemic — after H1N1, SARS, MERS, Ebola, and now SARS-Cov-2 — along with the anticipated health consequences of global climate change, we can’t simply cross our fingers and hope to get lucky again.
Erica Caple James , associate professor of medical anthropology and urban studies The coronavirus pandemic has revealed some of the limits of the American medical and health care system and demonstrated many of the social determinants of health. Neither the risks of infection nor the probability of suffering severe illness are equal across populations. Each depends on socioeconomic factors such as type of employment, mode of transportation, housing status, environmental vulnerability, and capacity to prevent spatial exposure, as well as “preexisting” health conditions like diabetes, obesity, and chronic respiratory illness.
Such conditions are often determined by race, ethnicity, gender, and “biology,” but also poverty, cultural and linguistic facility, health literacy, and legal status. In terms of mapping the prevalence of infection, it can be difficult to trace contacts among persons who are regular users of medical infrastructure. However, it can be extraordinarily difficult to do so among persons who lack or fear such visibility, especially when a lack of trust can color patient-clinician relationships.
One’s treatment within medical and health care systems may also reflect other health disparities — such as when clinicians discount patient symptom reports because of sociocultural, racial, or gender stereotypes, or when technologies are calibrated to the norm of one segment of the population and fail to account for the severity of disease in others.
The pandemic has also revealed the biopolitics and even the “necropolitics” of care — when policymakers who are aware that disease and death fall disproportionately in marginal populations make public-health decisions that deepen the risks of exposure of these more vulnerable groups. The question becomes, “Whose lives are deemed disposable?” Similarly, which populations — and which regions of the world — are prioritized for treatment and protective technologies like vaccines and to what degree are such decisions politicized or even racialized?
Although no single change will address all of these disparities in health status and access to treatment, municipal, state, and federal policies aimed at improving the American health infrastructure — and especially those that expand the availability and distribution of medical resources to underserved populations — could greatly improve health for all.
Seth Mnookin , professor of science writing
The Covid-19 pandemic adds yet another depressing data point to how the legacy and reality of racism and white supremacy in America is lethal to historically marginalized groups. A number of recent studies have shown that Black, Hispanic, Asian, and Native Americans have a significantly higher risk of infection, hospitalization, and death compared to white Americans.
The reasons are not hard to identify: Minority populations are less likely to have access to healthy food options, clean air and water, high-quality housing, and consistent health care. As a result, they’re more likely to have conditions that have been linked to worse outcomes in Covid patients, including diabetes, hypertension, and obesity.
Marginalized groups are also more likely to be socioeconomically disadvantaged — which means they’re more likely to work in service and manufacturing industries that put them in close contact with others, use public transportation, rely on overcrowded schools and day cares, and live in closer proximity to other households. Even now, more vaccines are going to wealthier people who have the time and technology required to navigate the time-consuming vaccine signup process and fewer to communities with the highest infection rates.
This illustrates why addressing inequalities in Americans’ health requires addressing inequalities that infect every part of society. Moving forward, our health care systems should take a much more active role in advocating for racial and socioeconomic justice — not only because it is the right thing to do, but because it is one of the most effective ways to improve health outcomes for the country as a whole.
On a global level, the pandemic has illustrated that preparedness and economic resources are no match for lies and misinformation. The United States, Brazil, and Mexico have, by almost any metric, handled the pandemic worse than virtually every other country in the world. The main commonality is that all three were led by presidents who actively downplayed the virus and fought against lifesaving public health measures. Without a global commitment to supporting accurate, scientifically based information, there is no amount of planning and preparation that can outflank the spread of lies.
Parag Pathak , Class of 1922 Professor of Economics The pandemic has revealed the strengths and weaknesses of America’s health care systems in an extreme way. The development and approval of three vaccines in roughly one year after the start of the pandemic is a phenomenal achievement. At the same time, there are many innovations for which there have been clear fumbles, including the deployment of rapid tests and contact tracing. The other aspect the pandemic has made apparent is the extreme inequality in America’s health systems. Disadvantaged communities have borne the brunt of Covid-19 both in terms of health outcomes and also economically. I’m hopeful that the pandemic will spur renewed focus on protecting the most vulnerable members of society. A pandemic is a textbook situation in economics of externalities, where an individual’s decision has external effects on others. In such situations, there can be major gains to coordination. In the United States, the initial response was poorly coordinated across states. I think the same criticism applies globally. We have not paid enough attention to population health on a global scale. One lesson I take from the relative success of the response of East Asian countries is that centralized and coordinated health systems are more equipped to manage population health, especially during a pandemic. We’re already seeing the need for international cooperation with vaccine supply and monitoring of new variants. It will be imperative that we continue to invest in developing the global infrastructure to facilitate greater cooperation for the next pandemic.
Prepared by MIT SHASS Communications Editor and designer: Emily Hiestand Consulting editor: Kathryn O'Neill
Share this news article on:
Related links.
- Program in Science, Technology and Society
- Graduate Program in Science Writing
- MIT Anthropology
- Department of Economics
- Department of Political Science
- Department of Urban Studies and Planning
Related Topics
- Anthropology
- Political science
- Program in STS
- Science writing
- Public health
- Health care
- Diversity and inclusion
- Science, Technology, and Society
- School of Humanities Arts and Social Sciences
Related Articles

Reflecting on a year of loss, grit, and pulling together
Building equity into vaccine distribution.

In online vigil, MIT community shares grief, anger, and hope
Previous item Next item
More MIT News

A new way to spot life-threatening infections in cancer patients
Read full story →

Technique improves the reasoning capabilities of large language models

A creation story told through immersive technology
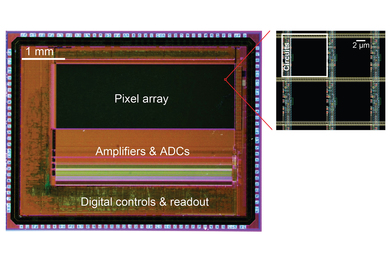
With programmable pixels, novel sensor improves imaging of neural activity

Featured video: Researchers discuss queer visibility in academia
Scientists preserve DNA in an amber-like polymer
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram

IMAGES
VIDEO
COMMENTS
Below, we provide a perspective on how these changes have affected payers, health systems, healthcare services and technology, and pharmacy services, and what to expect in 2024 and beyond.
The authors discuss gaps and barriers in the current design of health and health systems, and the needed escalation of transformation including transition from hospital-based systems to primary...
8 healthcare trends for 2024: A guide for health system leaders and their boards. Healthcare providers faced many transformational challenges in 2023, including the continued advancement of payers into the provider space and the challenge of managing merger and acquisition activity. Daniel J. Marino. March 23, 2024 8:33 am. Print.
Few papers discussed healthcare professionals’ behaviour, and those available focused on technology-led changes perspective. In this view, individual acceptance of change within the healthcare context resulted being undeveloped and offers rooms for further analyses.
Medical and scientific advances impose significant challenges on today's health care systems. Developments in genetics, information technology, and nanotechnology are changing the approach to health care as it tends toward personalization, and increasingly moves outside the hospital setting.
The US healthcare industry faces demanding conditions in 2023, including recessionary pressure, continuing high inflation rates, labor shortages, and endemic COVID-19. But players are not standing still.
What’s ahead for healthcare players: An overview. We outlined in 2022 how the gathering storm fueled by inflation and workforce shortages would put pressure on healthcare over the next few years. Indeed, the pressure on healthcare leaders continues unabated.
With vaccinations for Covid-19 now underway across the nation, MIT SHASS Communications asked seven MIT scholars engaged in health and health care research to share their views on what the pandemic has revealed about the U.S. health care system — and what needs to change.
1. Surging healthcare spend and investment. Global healthcare spend is thought to have grown more than 40% between 2018 and 2022, reaching $12 trillion.
The COVID-19 pandemic brought about health, economic, political and environmental challenges and exposed global disparities caused by income, age, race, sex and geography, but it also allowed for innovation in science and medicines development, distribution and delivery.